Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 12/194/01. The contractual start date was in June 2014. The draft report began editorial review in June 2018 and was accepted for publication in February 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Crispin Day is the lead developer of two parenting programmes used in this report: Helping Families Programme (HFP) and Empowering Parents Empowering Communities. Mike J Crawford has previously received research grant funding from the National Institute for Health Research. Lucy Harris is a co-developer of the Helping Families Programme. Mary McMurran was an author of the Psychoeducation plus Problems Solving (PEPS) intervention for adults with personality disorder. PEPS helped to inform the modified HFP. Paul Moran reports personal fees from a talk given at the fourth Bergen International Conference on Forensic Psychiatry, 2016, outside the submitted work. He led the development of the Standardised Assessment of Personality – Abbreviated Scale (SAPAS), the personality disorder screen used in this study.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Day et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Child mental health and parenting
There are 10.5 million children in the UK, approximately 1 million of whom experience significant emotional and behavioural disorders that interfere with their developmental progress, family life and school achievement, and increase their long-term risks of poor adult mental health, unemployment and offending. 1–5
Understanding of early life and parenthood has grown rapidly, resulting in a better, albeit imperfect, understanding of the ways in which a range of biological and environmental factors combine to influence physical, psychological and social development throughout childhood. 6–8
The most influential factors are typically located within the individual child and are the characteristics of their immediate parenting and care environment. 9 Children’s parenting environment is, in turn, influenced by the characteristics and life circumstances of each family, such as their health, mental health, life events, developmental history and social support, as well as broader social and economic conditions, such as employment, education and housing. 7
Affectionate, responsive, authoritative parenting has been consistently linked to better child outcomes. Parents are more developmentally effective when they use open, participative communication; have a sensitive and involved understanding of their child’s individual and personal needs; maintain household and relationship consistency; have routines and structure; and use flexible, problem-centred coping styles to manage parenting and its demands. 10
Effective parenting intervention as a means to improve child developmental outcomes is a significant policy and service priority in England. 11–13 Implementation to date has mainly focused on the provision of existing evidence-based programmes to generalised populations rather than to parents and children with multiple and specific mental health risks and needs. This is mainly because the evidence for specialised parenting programmes has been underdeveloped.
This research focused on the development of a specialised parenting programme for parents with severe personality difficulties who have children with emotional and behavioural problems.
Severe parent personality difficulties and disorders
The likelihood of severe and persistent child mental health problems increases when a parent is affected by significant personality difficulties, characterised by problematic interpersonal relationships, emotional arousal and regulation, impulse control, ways of perceiving and thinking, and style of relating to others and social functioning. 14,15
Personality difficulties are dimensional by nature and increasing severity is associated with greater impairment and poorer outcomes. 16,17 Severe personality difficulties include the diagnosis of personality disorders. These are common, long-term mental disorders that are characterised by significant impairments in self and interpersonal functioning that do not reflect an individual’s developmental stage, sociocultural environment, the physiological effects of a substance or a general medical condition. 18
Such difficulties are relatively stable over time: enduring, pervasive and clearly maladaptive to a broad range of personal and social situations. Difficulties are likely to emerge during childhood and persist into adulthood. They are associated with considerable personal distress and adverse life outcomes, including poorer physical and mental health, reduced life expectancy, social isolation, unemployment, intimate partner violence and exposure to substance misuse. 19,20
There are numerous biological, psychological and social risk factors that vary according to personality disorder type, the individual affected, and their past and current circumstances. Overall, findings show that genetic disposition and life experiences play a key role in the development of personality disorders. 6 Exposure to early childhood adversities, including emotional neglect, family chaos, family conflict and parental mental health difficulties, as well as specific trauma and abuse, has persistently been associated with the subsequent development of severe interpersonal difficulties and personality disorders. 6,20–23
In the UK, > 4% of the general population meet the diagnostic criteria for a personality disorder. Among users of mental health services, the prevalence of personality disorders has been estimated to be as high as 40% and, of this population, about 25% are parents. 24–26
Personality disorders, parenting and child outcomes
The inter-related mental health needs of children and their parents, and the associations between family functioning and wider disadvantage, have been highlighted in recent policy and practice recommendations. 13,27–29
Personality disorders, particularly borderline personality disorder, are associated with an extensive range of difficulties that may impair parenting. They can affect parents’ capacity to offer the stable, responsive care and nurture required for healthy child development. 30 They may result in more frequent insensitive, intrusive and overprotective interactions with children, and greater difficulties in reading children’s feelings. 31–37 Family environments are more frequently characterised by higher levels of hostility and less cohesion, as well as more inconsistent and unpredictable family routines and organisation. 38–40 The parents affected may feel more stressed in their parenting role, less competent and less satisfied. 31,32,39,40
As a consequence, children affected are at greater risk of enduring mental health problems, child maltreatment and abuse. Offspring are more likely to experience a range of negative emotional, social, behavioural and cognitive outcomes from infancy onwards, including parent–child relationship difficulties, disrupted attachment styles, poorer theory of mind, difficulties in labelling and understanding the causes of common emotions, depression, behaviour problems and attention deficit disorder. 40–49
Parenting a child with significant emotional and behavioural difficulties is stressful in itself and it may worsen a vulnerable parent’s own mental health. 49
Psychoeducational parent training programmes
Psychoeducation is an evidence-based psychotherapeutic modality used across a wide range of health conditions, including child emotional and behavioural disorders and adult personality disorders. 5,50,51 The strongest effects for psychoeducational parenting programmes are obtained for disruptive child behaviour problems. 51,52 Psychoeducational approaches are also available for children with anxiety and other internalising difficulties, but the evidence base is more limited. 53
Parenting programmes are usually delivered in individual or multifamily group formats. They generally aim to increase parental knowledge and insight about the nature, cause and management of their child’s difficulties, improve parents’ use of effective parenting strategies and mobilise their coping resources in order to improve parenting, child and parent outcomes.
Typically, psychoeducational parenting programmes use structured, manualised approaches with clearly specified content and methods. Parenting programmes are usually attended by parents only, though some include children and/or teachers. Standard parenting programmes are typically delivered over 8–12 weekly sessions, each lasting 1–2 hours.
Content is usually derived from social learning, relationship and communication theories. Methods include group discussion, skills rehearsal, role play and video modelling of effective parent–child communication, interaction and relationship methods, together with the use of positive parenting and discipline strategies.
Typically, there is little adaptation and tailoring for parents affected by mental health difficulties. As a consequence, standard parenting programmes may achieve lower engagement, lower completion rates and poorer outcomes for families with co-occurring child and parental psychopathology than for parents without co-occurring difficulties. 54
Specialised parenting programmes have been developed for families with more complex difficulties, such as parents experiencing drug misuse, young mothers, and parents whose children have been excluded from primary school. 55–57 Delivered over a longer period, specialised programmes are more likely to use an individual, personalised format, consisting of multiple components that address the inter-relationship between adult psychosocial difficulties, parenting and the children’s developmental needs.
The NHS and other costs of child mental health problems and adult personality disorders
The strongest evidence for the cost-effectiveness of child mental health interventions relates to parenting programmes for severe child disruptive behaviour. 11,58 These interventions cost approximately £1200 per parent participant, producing potential societal savings of approximately £16,500 per family over a 25-year period. 59 Potentially higher savings over the longer term of approximately £5B may accrue through parenting interventions for families at high risk of multiple, adverse mental health and social outcomes. 60
The annual direct treatment costs in the UK for adults with personality disorders exceed £70M, with wider societal costs estimated at £8B per year in England. 61 This reflects the considerable demands placed on a range of services, including emergency departments, social services and the criminal justice system.
Potentially improved treatments that lead to even small reductions in personality-related problems and child behaviour problems could lead to substantial savings in personal and service costs.
Current clinical and service challenges for coexisting parent and child mental health problems
Despite the high risk of poor child, parent and family outcomes across a range of domains, and the associated high service, social and economic costs, the treatment of coexistent child and parent mental health difficulties currently poses a serious challenge to mental health services. Despite policy initiatives advocating integration and care co-ordination, much current mental health provision offers fragmented care that focuses on the needs of either the adult or the child. 62
Many parents with severe personality difficulties may be reluctant to disclose these problems to practitioners, owing to the stigma associated with personality disorder diagnosis and a fear of safeguarding procedures. 63 Parents diagnosed with a personality disorder may be especially aware of enduring negative attitudes among some clinical staff. 64–67
As a consequence, the presence of severe personality difficulties may be under-recognised and their consequent effects on parenting may remain unaddressed, which may lead to an escalation in difficulties, resulting in a mental health crisis and a child protection intervention. 41
Development and evaluation of a specialised psychoeducational parenting intervention
At the time of commission, no evidence-based parenting programme existed that was specifically designed to meet the needs of parents affected by personality disorders. 68
Complex intervention
A specialised parenting programme of this type was likely to be complex to develop and deliver for the following reasons.
-
The specialised parenting programme would need to concurrently address multimorbidity across parenting, child and parent outcomes.
-
Target parents are affected by a mental health condition associated with a known stigma.
-
Parents affected by severe personality difficulties, including personality disorders, are more likely to find programme engagement and participation problematic.
-
There is a recognised gap in routine parenting programme provision for the target population.
-
The specialised parenting programme would be likely to consist of several interacting components delivered over multiple contacts and would be likely to require tailoring and personalisation.
-
Programme delivery would be likely to require highly specialist skills and knowledge.
Manualisation
Programme manualisation increases the likelihood of reliable implementation with fidelity and consistent replication across individuals and over time. 69 Manualisation is particularly important for the proposed intervention given the complexity of the target population and the intervention content.
Manualisation required the specification of the rationale, theory and goals of the parenting programme, as well as a description of the intervention materials, methods and procedures, mode and location of delivery, practitioner characteristics, therapist training and implementation requirements.
Phased development
A phased and iterative approach to the systematic design and evaluation of this type of complex and specialised parenting intervention was recommended to include the following. 69,70
-
Use of best available theory and evidence from existing manualised interventions and systematic reviews to establish a differentiated conceptual model of parenting for adults affected by severe personality difficulties.
-
Production of the novel intervention manual with content and methods that have the potential to improve parenting, parent, child and family functioning while attending to safeguarding needs.
-
Feasibility and pilot testing to examine key uncertainties and generate quantitative and qualitative evidence about:
-
Manual content and intervention methods including acceptability, compliance, intervention intensity, tailoring and personalisation, fidelity methods and adherence.
-
Research design and methods, including comparison conditions, primary and secondary outcomes, measurement, recruitment, retention, and effect size (ES) estimates.
-
Intervention implementation, subjective participant experience and relevant contextual factors.
-
-
Evidence synthesis from feasibility and pilot testing to inform subsequent research, potentially including a large-scale definitive trial, and improvements to the routine care and treatment of the target population and other high-risk, underserved parent and child populations.
In practice, these tasks are typically non-linear and iterative because evidence and experience from multiple sources is acquired and assimilated. 71–73 These tasks often require synthesis of evidence from rapid reviews and in-depth service user and clinician consultations. The rationale, aims and objectives of pilot and feasibility randomised trials are distinct and differ from those of other randomised trials. 71
Decision-making regarding the transition from a feasibility to a definitive trial can be a complex process. 73 It requires the systematic and transparent identification and realistic appraisal of evidence that:
-
supports preliminary design and evaluation decisions
-
identifies problems that may undermine the acceptability and delivery of the proposed trial intervention and the conduct of the evaluation
-
identifies potential solutions to the intervention and research design difficulties
-
informs the viability of the best available future options, including recommendations for the design of a full-scale, definitive evaluation.
Conclusion
This research programme aimed to advance scientific and clinical knowledge for a population of parents and children whose needs are not currently well met by existing services and where specialised early intervention is strongly indicated but rarely tested. Its phased, iterative approach was intended to generate knowledge about the design, delivery and initial evaluation of a complex psychoeducational parenting programme for parents who are often marginalised by conventional parenting programmes. The immediate patient and NHS benefits were intended to be improved child and parental mental health, with a longer-term potential to reduce the entrenched burden of psychosocial adversity and intergenerational transmission of mental disorders within families.
Chapter 2 The development, feasibility testing and evaluation of a new psychoeducational parenting programme: Helping Families Programme
Context
In 2013, the National Institute for Health Research (NIHR) Health Technology Assessment (HTA) programme announced a commissioned call for a research programme to develop and evaluate psychoeducational support for parents affected by personality disorders who have children with severe emotional and behavioural problems and were attending or being considered for referral to child and adolescent mental health services. Applicants were advised to define exact parent inclusion criteria. A study design was advised that (1) incorporated feasibility work to develop and manualise the process for identifying and selecting parental caregivers with personality disorders and to develop the therapeutic intervention, leading to (2) a small pilot randomised controlled trial (RCT) to test the feasibility of a trial. The comparator was expected to be usual care. Consideration was to be given to any existing mental health care that parents were receiving and the logistics of linking it to child and adult services.
Key research outcomes and outputs of the research programme were envisaged to be (1) the development and manualisation of a process for identifying and treating parental caregivers who would be eligible for the intervention, including acceptability of selection and randomisation; (2) the development of an intervention tailored to parents with personality disorders or the manualisation of an existing intervention; (3) the pre/post measurement of appropriate child and parent outcomes; and (4) an estimation of the parameters for a substantive study. 74 The ethics considerations of diagnosing personality disorders in people who may not have sought a diagnosis were also to be explored.
Research programme design
A pragmatic, mixed-methods research programme was planned to address these HTA requirements that involved three inter-related phases. 74
-
Phase 1: intervention and research evaluation development – to produce a draft manualised psychoeducational intervention and screening process for parents with personality disorders who have children with emotional or behavioural disorders.
-
Phase 2: pre-trial feasibility testing – to assess the acceptability to clinicians and service users of the proposed psychoeducational parenting programme and screening manual, the viability of their implementation and a description of usual care.
-
Phase 3: feasibility RCT and process evaluation – to generate quantitative and qualitative evidence about intervention implementation, research design and methods, and ES estimates to inform recommendations about a subsequent research evaluation. 5
The phased design was intended to produce research findings that would be concurrently and sequentially combined to inform the development and refinement of the new health technology and its evaluation. 74 Each phase involved staff and service users of child and adult services across two NHS mental health trusts in order to gain a better understanding of the intervention and evaluation methods across varied service circumstances.
Research programme plan and milestones
The programme plan involved three phases, as follows. 74
-
Phase 1: intervention and research evaluation development (months 1–9), including –
-
project set-up; distillation of intervention components
-
conduct of parent and clinician consultation groups; production of draft psychoeducational parenting intervention and screening manuals
-
completion of the phase 2 research protocol, ethics and service approvals.
-
-
Phase 2: pre-trial feasibility work (months 10–18), including –
-
selection and training of the research therapists for the new psychoeducational parenting intervention
-
completion of the planned pre-trial case series
-
revision of the psychoeducational parenting intervention and screening manuals; completion of the phase 3 research protocol, ethics and service approvals.
-
-
Phase 3: randomised feasibility trial and process evaluation (months 19–37), including –
-
completion of the planned randomised feasibility trial and process evaluation
-
undertaking of the follow-up evaluation
-
completion of the analysis and write-up.
-
Delays in phase 2 ethics approval, case series and trial recruitment required an 8-month no-cost extension to the original timetable.
Existing manualised interventions
The research programme used two existing manualised interventions as the basis for the development of the new psychoeducational parenting programme. These existing interventions were the Helping Families Programme (HFP) and Psycho-Education with Problem-Solving (PEPS).
Helping Families Programme
The HFP had previously shown promise as a specialised psychoeducational programme for parents with complex psychosocial needs, including parents with school-excluded children and children subject to safeguarding. 55,75–78 The programme had been field tested in several NHS Child and Adolescent Mental Health Services (CAMHS) and local authority children’s social care services.
The HFP’s manualised methods combined parenting psychoeducation with cognitive, behavioural and interpersonal strategies intended to:5
-
improve parent–child relationships and interpersonal conflicts
-
promote effective parenting and parental coping with daily stress
-
implement effective parent mood regulation strategies and promote parental warmth and consistency
-
minimise parental harm from substance misuse
-
build family social support.
The intervention had three main therapeutic components:
-
Collaborative relationships – this focused on promoting parent engagement, shared ecological assessment and the development of personalised action plans using methods derived from the evidence-based Family Partnership Model. 79
-
Parenting groundwork – this focused on intervention to improve parent characteristics that may interfere with parenting capacity such as emotional dysregulation, interpersonal hostility, and erratic and inconsistent behavioural patterns.
-
Parenting strategies – this focused on helping parents to use more effective, consistent and safer parenting behaviours, improve communication skills and parent–child interaction methods and optimise emotional nurture.
Results from real-world cohort studies demonstrated good service user acceptability and effects on a range of child and parent outcomes. 75–78
The HFP’s flexible, modular structure and goal-directed approach had strong potential to form the basis of the new, specialised psychoeducational intervention. Modification to the HFP’s existing theory, methods and content was potentially required to achieve closer alignment with the specific needs of the target population.
Psychoeducation with problem solving
Drawing on existing examples of manualised psychoeducational interventions within the field of personality disorders, PEPS was a feasible candidate intervention to provide psychoeducational content specifically designed for the target population. 80–83
Developed for adults with personality disorders, PEPS used structured clinical assessment and psychoeducational methods to explore the meaning of personality disorder diagnosis and linked this to personal difficulties in social functioning and relationships. In common with the HFP, personal goals were then formulated and addressed using focused problem-solving methods. In recognition that people with personality disorders often have difficulties maintaining participation in treatment,84 PEPS also used well-defined theory and methods to optimise participant motivation and therapeutic rapport. 85,86 Although a Phase III clinical trial of PEPS did not show evidence of improved mental health or social functioning, many recipients valued the information that they received about their condition, and uptake of the psychoeducational component of the intervention was high. 87
Research locations
Two NHS trusts participated in the research programme, South London and Maudsley NHS Foundation Trust (SLAM) and Central and North-West London NHS Foundation Trust (CNWL), which were site 1 and site 2, respectively. These sites were selected because both NHS trusts serve large and diverse populations with high rates of adult and child mental health problems. Additional fieldwork was undertaken with coterminous local authority children’s social services.
South London and Maudsley NHS Foundation Trust (site 1)
With a total catchment population of approximately 1.2 million people, SLAM provides mental health services to four London boroughs (Southwark, Lambeth, Lewisham and Croydon) together with several regional and national specialist services.
At the time of the research, adult mental health services were configured into clinical academic groups (CAGs) centred on distinct disorder clusters. The mood, anxiety and personality (MAP) CAG included eight community teams offering assessment and case management for adults aged 18–65 years with a range of emotional and personality problems. The MAP CAG had a further three specialist outpatient services offering a range of individual and group therapies and a service-user-led support network.
The CAMHS CAG had four borough community services that worked with children and adolescents aged 0–18 years, experiencing a range of emotional, behavioural, neurodevelopmental and other disorders. Additional specialist regional and national teams provided assessment and treatment centred on specific treatment modalities and clinical criteria.
Central and North-West London NHS Foundation Trust (site 2)
Central and North-West London NHS Foundation Trust provides services to a catchment area of 1.45 million people across five London boroughs (Brent, Harrow, Hillingdon, Kensington and Chelsea, and Westminster) and Milton Keynes. At the time of the research, adults with personality disorders primarily received care from seven community recovery teams. A specialist personality disorder service provided an 18-month group-based treatment programme for adult service users from Kensington and Chelsea and Westminster.
Community CAMHS teams were located in each of the CNWL boroughs and Milton Keynes, providing multidisciplinary assessment and treatment to children and adolescents aged 0–18 years. In addition, a specialist parental mental health service was operated jointly by the trust and the National Society for the Prevention of Cruelty to Children in the Royal London Borough of Kensington and Chelsea.
Research population
The target population was parents and their children who had coexisting mental health difficulties. Initially, parent caregivers were required to fulfil diagnostic criteria for one or more personality disorders. Based on feasibility evidence acquired during the research, this criterion was subsequently redefined to include parents with severe personality difficulties, including personality disorders. Index children had severe emotional and behavioural problems and were either attending or being considered for referral to routine CAMHS.
In advance of the research programme, examination of SLAM MAP CAG electronic patient records identified 556 adults (16.0%) with a diagnosis of personality disorder and a further 900 recorded personality disorder cases in CNWL. Case audit data indicated that approximately one-quarter of service users in CNWL’s specialist personality disorder service were parents with dependent children. Although no specific routine monitoring data were available from either trust, extrapolated estimates suggested that approximately 350 service users across both trusts were parents with a recorded diagnosis of personality disorder, only a minority of whom may have been receiving parenting interventions. 85
A large proportion of these parents would be expected to have children with mental health problems. Precise figures were unavailable, but the rates of mental disorders in offspring of parents with Axis I diagnoses are in the region of 30–50% and may be even higher where a parent has a personality disorder. 88–90
Examination of SLAM CAMHS CAG electronic patient records identified 1650 (24%) service users for whom parental mental health needs had been recorded in brief risk screens. It was estimated that around 40% may have been parents whose difficulties would meet the criteria for a personality disorder. Half of the identified children were likely to have been referred for significant emotional and behavioural difficulties. Similar rates were expected to apply to the CNWL CAMHS service user population of 4200. Across the two participating trusts, these estimates suggested a combined eligible CAMHS population of approximately 500 families where a parent may be affected by a personality disorder and the child may have emotional and behavioural difficulties.
Governance
The research team included established expert researchers, clinicians and a service user consultant with specialist experience of people affected by personality disorders. 5,74
The chief investigator (CD) had overall managerial responsibility for the research programme. He was accountable for project objectives and milestones and ensured that the research was run in accordance with agreed procedures and protocols. An operational research team, directed by Crispin Day and consisting over time of Lucy Harris, Daniel Michelson, Paul Ramchandani and Jackie Briskman, was responsible for the day-to-day co-ordination of research activity across the two NHS trusts, the supervision of research workers and the clinical supervision of research therapists (LH).
A project management group (PMG), chaired by Crispin Day and consisting of all co-applicants, met quarterly to oversee the research, monitor project achievements, review generated findings and formulate actions required to address significant issues related to project progress. A manualisation working group (MWG), including lead developers of the HFP (CD, LH) and PEPS (MM), led the development of the new psychoeducational parenting programme and the synthesis of findings across phases 1 and 2.
Trial Steering Committee
The chief investigator reported to an independent Trial Steering Committee (TSC), which ensured the scientific integrity of the trial. The TSC, convened in June 2014, was chaired by Professor Peter Fonagy, head of the division of psychology and language sciences at University College London and chief executive of the Anna Freud National Centre for Children and Families. Members of the TSC included independent senior clinicians and academics with expertise in trials and/or families with complex interpersonal needs, together with the chief investigator and the research programme’s service user lead. The TSC met formally every 6 months to monitor and review progress.
The TSC reviewed and approved research protocols and research ethics applications for each research phase. It reviewed and supported the approved phases 2 and 3 no-cost extensions.
Data Monitoring and Ethics Committee
The Data Monitoring and Ethics Committee (DMEC) monitored the research programme’s safety and efficacy data. The DMEC was established in parallel with the TSC and met on an annual basis. The chair was Professor Philip Graham, Emeritus Professor of Child Psychiatry at the University College London Great Ormond Street Institute of Child Health, London. Other members were experts in the assessment and treatment of personality disorders and quantitative statistics. The TSC would liaise with the DMEC should safety, ethics or efficacy issues emerge that had implications for continuing, modifying or stopping the trial. The DMEC reviewed and approved research protocols and research ethics applications for each phase of the research programme.
Independent ethics review
Professor Richard Ashcroft (Professor of Bioethics, Queen Mary University of London) independently reviewed the ethics dimensions of the original research proposal and the iterative development of the new psychoeducational parenting programme.
Patient and public involvement
The research programme’s service user expert from 2014 to 2017 was Lou Morgan, executive director of Emergence (Emergence Plus CIC, London, UK), a service user-led organisation supporting people affected by personality disorder. As chairperson of the Service User Advisory Panel (SUAP), she led service user involvement in the design, management and governance of the research programme. She sat on the PMG and the TSC. Following the administrative closure of Emergence in 2017, Lisa Foote was appointed to lead the programme’s service user involvement on behalf of the McPin Foundation (The McPin Foundation, London, UK), which exists to transform mental health research by putting the lived experiences of people affected by mental health problems at the heart of research methods and the research agenda.
The SUAPs were convened during phases 1 and 2 to ensure that research design, conduct and dissemination accurately reflected the priorities and experiences of families affected by coexisting child and parental mental health difficulties. The initial intention was to convene both parent and youth advisory panels. Only the former was formally convened, as parent users were the sole focus and target of the proposed psychoeducational parenting programme and research participation.
The parent service user advisory panel comprised parents with relevant lived experience. It provided feedback and constructive review across each research phase, including draft psychoeducational content and methods, research design and methods, review of generated findings, design of participant information resources and dissemination of materials. Practical support, expenses and access to relevant training were provided in accordance with good practice guidelines from INVOLVE. 91
Before taking over service user leadership, an experienced service user researcher (LF) was involved in the design, facilitation and analysis of phase 1 focus groups, phase 2 design, data collection and analysis, phase 3 analysis and validation. Service user leads were involved in the dissemination of programme findings across each research phase.
Conclusion
A pragmatic, mixed-methods research programme was planned to develop and evaluate a new specialised psychoeducational parenting programme for parents affected by a personality disorder and their children with severe emotional and behavioural problems.
The iterative design was intended to produce a more precise theoretical model to describe the inter-relationship between parental personality difficulties, parenting, child development and environmental contexts. Based on the integration of two existing interventions, the new psychoeducational parenting programme, if practical and acceptable, had the potential to have an impact on the immediate and longer-term effects of personality disorders on parenting, family function, child development and associated societal costs. The planned mixed-methods evaluation aimed to examine the feasibility of research design and procedures used to evaluate the acceptability, the impact and the health economics of the new intervention.
Chapter 3 Phase 1: intervention and research evaluation development
Phase 1 aim and objectives
The main aim was to develop the new manualised psychoeducational parenting intervention and the related screening and evaluation methods. 74 The phase 1 objectives were to:
-
produce a modified version of the HFP, the Helping Families Programme-Modified (HFP-M), incorporating content from PEPS
-
produce draft screening methods for the identification and recruitment of eligible parents from the target population
-
distil, synthesise and incorporate findings from a scoping review of relevant research and consultation groups with service users and clinicians into the production of the modified HFP manual and screening process.
Phase 1 design
Phase 1 involved four concurrent and inter-related activities:
-
iterative production of the modified HFP manual and associated screening and evaluation methods
-
a rapid scoping review of relevant evidence
-
consultation with services users from the target population
-
consultation with clinicians working in mental health and children’s social care services.
Development of the Helping Families Programme-Modified manual
The MWG used the template for the intervention description and replication (TIDieR) checklist to guide the synthesis of the content and methods from the two existing intervention manuals to produce the modified HFP manual and concurrent evaluation methods. 69 The TIDieR checklist consists of the following nine areas:
-
characteristics of the target population, including the intended HFP-M recipients, current patterns of service use, and eligibility criteria for research evaluation
-
conceptual model and intervention rationale, including concepts and theories underpinning the HFP-M intervention, its aims and its purpose
-
intervention organisation and delivery, including the HFP-M therapist characteristics, training and supervision, and service structures that are required to deliver the intervention
-
service and keyworker engagement and social marketing, including methods to optimise routine service and keyworker interest and enthusiasm for the HFP-M and its research evaluation, intended service user and service benefits, and management of potential barriers
-
identification of intervention recipients and research participants, including feasible, accurate identification of target service users, and related clinical and research processes
-
engagement of service users in the HFP-M and its research evaluation, including effective ways of describing the HFP-M and its evaluation so that services users can make informed choices about participation
-
case co-ordination and integration with usual care, including the use of the HFP-M to augment or replace routine clinical practice and related case co-ordination
-
intervention format, including optimal structure, frequency and duration of the HFP-M intervention sessions, materials, and intersession activities
-
intervention content, including the HFP-M psychoeducational topics, methods to optimise recipient engagement, content and delivery, personalisation and fidelity monitoring.
Rapid scoping review of relevant research
Design
Scoping reviews are appropriate when the topic of interest is complex and comprehensive reviews are unavailable. 92,93 The methodology provided a feasible mechanism to summarise and distribute relevant research findings to the MWG. Scoping reviews are typically based on broadly defined research questions, eligibility criteria and quality criteria.
The purpose was to rapidly identify and distil research findings to inform the MWG’s use of the predefined features of the TIDieR checklist to inform manual development and research design. 69 The primary research question for the rapid evidence review was:
What is known from the existing literature about (a) the rationale, engagement and participation in interventions designed for parents affected by personality disorders who have children with mental health problems, and (b) the identification, screening and recruitment of such parents to research studies?
Method
PsycINFO and PubMed were searched from September 2014 to December 2014, using the terms [parenting OR personality disorder] AND [screening OR intervention OR treatment]. Manual searches were completed of all relevant narrative and systematic reviews and individual studies. Further papers were identified by co-applicants, professional networks and relevant user organisations. Initial searches identified 2427 potentially relevant papers. Articles from the searches were screened using titles and abstracts, with studies not meeting the following inclusion criteria discarded:
-
studies reported findings in one or more of the predefined features areas of the MWG TIDieR checklist
-
participant parents were aged ≥ 18 years with a personality disorder and/or children with mental health disorders
-
articles were published in English.
Full articles were obtained for 80 studies that met the selection criteria, nine of which were discarded as they did not represent a ‘best fit’ with the research question. Data were extracted by two researchers based on the topic areas of the MWG TIDieR checklist (DM and Ruth Wilson).
Results
Characteristics of the target population
As outlined in Chapter 1, personality disorders are associated with substantial behavioural, emotional, social and cognitive impairments of parenting. They are also associated with significant personal, social and economic adversity, both current and past, that is likely to undermine parental competence and parenting capacity. 6,20–23 Parents affected by personality disorders are more frequently exposed to negative life events. 96
People affected by personality disorders more frequently experience feelings of alienation from services, which leads to disengagement and being more likely to be subject to negative staff attitudes and behaviours. 97–99 As a result of interpersonal difficulties, poor impulse control, instability, relationship conflict and multiple life problems, people affected with personality disorders may feel antagonistic, avoidant and reluctant to engage with services. They may attribute their difficulties to factors that are outside their control, and have low self-belief and efficacy as well as having few reliable social and family resources.
Helping Families Programme conceptual model and intervention rationale
The Multiple Determinants of Parenting (MDP) conceptual model100 is a well-established framework that specifies how the interaction between child characteristics and parenting is influenced by the multiple impacts of parents’ personality, couple relations, family and social networks and work experiences (Figure 1). According to the model, parents’ own proximal and distal developmental history shapes their personality including behaviour, cognition, attitudes, values, emotional regulation and coping. The MDP model illustrates the central role that parenting has in influencing child outcomes as well as its role in mediating the effects of other parent factors that influence child outcomes.
FIGURE 1.
Modified multiple determinants of parenting model.
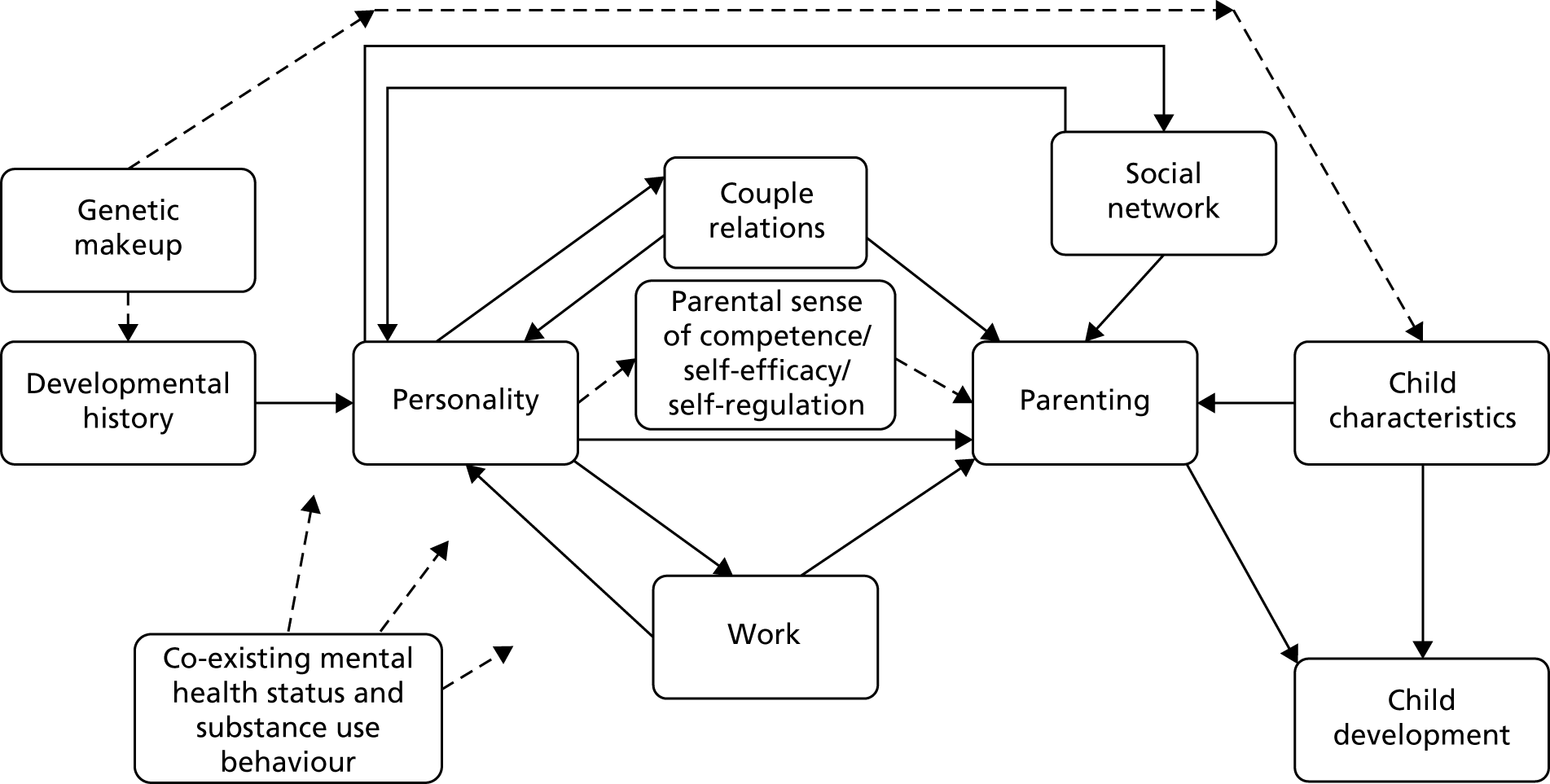
Additional factors, identified since the initial development of the MDP conceptual model, that may have particular salience for parents with severe personality difficulties include the impact and transmission of heritable characteristics and the multiple impacts across the MDP model of coexisting mental health and substance use problems.
The MDP model offered a useful conceptual framework to underpin the HFP-M because:
-
The genetic transmission of some personality disorder characteristics may increase children’s inherent vulnerability to developing prodromal personality difficulties and other mental health problems. 101
-
The persistent, pervasive and problematic interpersonal difficulties associated with personality disorders are likely to have a direct effect on the child’s parenting environment. 14,16,20,30
-
Parents affected by a personality disorder are at increased risk of parenting behaviours, emotional regulation, interactions and relationships, and cognition, that have a detrimental impact on child outcomes. These include harsh, neglectful and abusive parenting practices; emotional hostility and intrusiveness; critical, dismissive and intrusive interaction; inconsistent and unpredictable parental routines, responses and reactions; over-involvement and protectiveness; and difficulties in accurately identifying and responding sensitively to children’s emotional and developmental needs. 31–49
-
Parents affected by severe personality difficulties may be aware of normative, positive parenting but their efforts may be undermined by their personality and interpersonal functioning. 49
-
Parents affected by personality disorders are at an increased risk of coexisting mental health conditions, particularly depression and substance misuse. 17,19,24–26
-
Parents themselves may have developmental histories characterised by poor attachment, neglect and life crises. 6,21,23
-
Personality disorders are associated with personal, social and economic adversity including interpersonal conflict, intimate partner and other violence, lone parenthood, social isolation, worklessness and insecure employment. 24,93,102
Organisation and intervention delivery
The organised provision of parenting interventions is heterogeneous and it occurs across multiple types of services. 103 Parents often value community-based provision. Practitioner qualification level and type varies considerably across delivery. Practitioner skill level may improve parent initial engagement, continuing intervention participation and outcome. 104
Challenges for staff working with service users affected by personality disorders are well documented. 105 Regular supervision for staff is an integral part of specialist therapies designed for service users affected by personality disorders. 106,107
Although implementation is inconsistent, family-focused approaches in adult mental health services are advocated to improve the engagement of hard-to-reach parents and families. 28 CAMHS tend to focus on the needs of children and do not frequently integrate the treatment of parental mental health difficulties into routine provision.
Service attendance may be affected by service users’ greater exposure to adverse life events and their response to them. 96
Routine service and clinician engagement and social marketing
Personality disorders are associated with known stigma, pejorative clinician beliefs and an expectancy to receive negative treatment. Adult mental health practitioners have concerns that discussing children’s difficulties with parent service users may detrimentally affect their mental health and may lead to increased service use. 108 Conversely, clinicians are also concerned that discussion of parenting may discomfort parents and lead to therapeutic disengagement. 109
Clinicians expressed reservations about the intervention effectiveness for this target population and were concerned about additional burdens of case management that may result from multiple service involvement. 110
Identification of potential intervention recipients and research participants
Accurate identification of parental mental health difficulties within child mental health care and the identification of child emotional and behavioural problems within adult mental health services varies considerably. It may depend on individual clinician characteristics, such as perceived role, confidence and competence rather than operational procedures. 108,109,111
Practitioner concerns about diagnosing personality disorders are well documented. 110 Many adult mental health staff members have not undertaken training in child development and the assessment and treatment of child mental health difficulties.
Well-established, psychometrically robust screening instruments are available to identify personality disorders and child mental health disorders. For example, the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV), Axis II Disorders (SCID-II) is a gold standard tool for the diagnosis of personality disorders. 112 Inter-rater reliability scores for the SCID-II are excellent,113 with no significant differences between experienced and recently trained interviewers. 114 The Standardised Assessment of Personality – Abbreviated Scale (SAPAS) is a very brief interviewer-administered, structured screening tool designed to identify individuals with a potential personality disorder. 115 It does not screen for specific subtypes of personality disorders; rather, increasing scores indicate increasing likelihood that an individual has any personality disorder.
Candidate screening tools for child mental disorders include the Development and Well-Being Assessment (DAWBA), intended for children aged 5–16 years. The Pre-School Age Psychiatric Assessment (PAPA) can be used for children aged 3–4 years. Both are well-validated standardised tools completed by interview or computer for assessing child emotional and behavioural disorders. 116,117 The DAWBA covers common emotional, behavioural and hyperactivity disorders without neglecting less, but sometimes more severe, disorders. The Strengths and Difficulties Questionnaire (SDQ) is a brief behavioural screening questionnaire for 3- to 16-year-olds that is used extensively to identify common mental health problems. 118 The 25 items are divided between five scales that measure emotional, conduct, hyperactivity/inattention and peer relationship problems together with prosocial behaviour.
Engagement of service users and their interest in Helping Families Programme-Modified and its research evaluation
Time demands, flexibility and scheduling concerns are a significant barrier to participation in parenting programmes. 119 Parent and children involvement in concurrent intensive mental health, health, social care and education appointments may hinder participation.
Treatment trial participants have expressed concerns about (1) the burden of assessments and research procedures, (2) participation in interventions with unproven effects and (3) poor quality of information about potential risks and benefits. 120
Some parent service users may be reluctant to be open about difficulties, owing to fears about involvement of child protection services. 104
Case co-ordination and integration of Helping Families Programme-Modified with treatment as usual
A large-scale systematic review of trial data suggested that treatment as usual was often poorly defined and highly variable for service users affected by personality disorders. 119 Evidence from RCTs showed that better planned and organised non-specialist treatments may be comparable in effect to specialist treatments for people with borderline personality disorder. 121–125 Effective components may include experienced therapists, supportive therapeutic process, life problem focus, non-intensive format and case management integration.
Consistent with good standards of clinical practice, evidence suggests that research clinicians should retain ongoing contact with referring practitioners. Evidence from research trials showed that changes in participant functioning are important to communicate to routine services and failure to do so may have negative consequences for care co-ordination. 120
Intervention format
Session number and frequency of parenting programmes vary. Commonly, between 8 and 12 sessions and up to 16 weekly sessions can be provided. 51,54 Individualised programme formats are often superior for families with complex psychosocial needs. 51
Barriers to parenting programme participation include location accessibility, parent treatment expectancies and intervention burden. 126 Some parents are discouraged by longer programmes, whereas others are willing to engage in longer programmes when there is a known benefit. 127,128
For either format, structured, focused, meaningful content including practical activities and written information will probably increase parent engagement. 129 The volume of intersession activity undertaken by participants of parenting programmes does not appear to predict larger ESs for child outcomes and parenting skills. 130 Parents’ actual use of positive parenting techniques with their child has been found to predict larger ESs for child behavioural problems and parenting skills. 130
Evidence-based interventions for personality disorders tend to be delivered over extended time periods. 131
Intervention content
Parenting programmes are usually designed according to children’s developmental stages, with parenting content tailored accordingly. Programmes addressing wide developmental ranges are uncommon. Significant reductions in child behavioural difficulties have been widely demonstrated in studies involving parents of children aged 3–11 years. 51,132 Though feasible for parents with adolescents, the evidence base is small and further outcome research is required. 133,134
Much psychosocial treatment evidence for personality disorders is based on interventions for people affected by borderline personality disorder. Intervention characteristics associated with increased effectiveness include structured, goal-orientated methods; information provision and psychoeducational content; focus on managing current life situations; active, responsive and validating therapeutic experiences; active service user participation and agency; and limited therapeutic intensity and therapist consistency. 106,135,136
As described above, parents affected by personality disorders may have impairments across a range of parenting functions. Established parenting programmes typically have a narrow focus on parenting skills, parent–child interaction and communication. 51,137,138 There is generally less focus on therapeutic process, parent engagement and personalisation in many group format programmes. Larger ESs are associated with positive parent–child interactions, developing parent emotional communication skills, learning consistent parental responding, and learning ‘time out’ as a disciplinary skill. 130
Personalising intervention content to individual characteristics is recommended for programmes aimed at families with complex psychosocial needs. 54,55 For example, specialised programmes for depressed parents that include topics to address parental mental health have been found to be effective in modestly improving child outcomes. 54
Intervention fidelity procedures improve the accurate interpretation of manual content and may reduce the influence of possible confounders. 139 Key fidelity components include manualised intervention format, methods and content; intervention training; monitoring intervention delivery; and monitoring of intervention receipt. 140
Consultation with service users
Design
The purpose was to obtain advice and guidance from service users with relevant lived experience about (1) scoping review evidence, (2) key characteristics of the proposed parenting intervention and screening methods, and (3) the contents and methods of the draft HFP-M and screening manual. 74 Two initial consultation groups were held between September 2014 and October 2014, with a follow-up group to verify findings. A small group discussion format was used as the most effective way to generate ideas and encourage service users to share experiences and opinions.
Method
Participants
Participants were parents with relevant lived experience of personality and child mental health disorders attending the mental health services of SLAM and CNWL. Recruitment used the pre-existing networks of the study investigators and collaborating services using word of mouth, clinician recommendation, posters and leaflets. A total of eight service users, seven females and one male, participated. Participants received an explanation of the aims and purpose of the consultation group prior to attendance and gave written consent for participation and recording.
Format and procedure
Consultation groups were held in service settings familiar to the participants. Each group lasted 60–90 minutes. Moderators sought to create a welcoming and informal atmosphere. Refreshments were available throughout the sessions.
A semistructured format moderated by a service user researcher and a clinical researcher was used to guide participants through an open-ended discussion of the following topics:
-
rationale, aims, structure and content of the proposed programme
-
methods for introducing the research programme to potential participant parents
-
screening and consent methods
-
compatibility of parent programme participation alongside other care.
Moderators presented information accompanied by written handouts and PowerPoint® (Microsoft Corporation, Redmond, WA, USA) slides. Open, exploratory prompts were used to encourage discussion, elicit and clarify service users’ ideas, and develop researcher understanding. Generated findings from the first consultation group were shared with the subsequent group to stimulate and enrich discussion. Groups ended with a summary of the research team’s next steps and a debrief about the participants’ experience.
Analysis
Each consultation group was recorded and transcribed verbatim. Group moderators initially read transcripts together with contemporaneous notes in order to identify generated themes, key recommendations and advice offered by the service user participants. Researchers identified areas of consensus in participant opinions as well as variations.
Service user views were organised in relation to the nine predefined features of the MWG TIDieR checklist. 69 The MWG were responsible for distilling and synthesising findings in conjunction with those from the scoping review and clinician consultation.
Findings
Characteristics of the target population and conceptual model
Participants described their lived experience of stigma associated with the term ‘personality disorder’, which most felt would potentially affect engagement in the intervention and research evaluation. There were also some concerns expressed about the development of a ‘special programme for [parents affected by] personality disorder’ [service user (SU) 1] and the potential for activating ‘blame and guilt’ (SU 2) in parents.
Service users raised doubts about whether or not children needed to be already involved with CAMHS in order for their parent to be eligible for the intervention.
Organisation and intervention delivery
Participants highlighted that clinicians delivering the proposed intervention should have a good understanding of personality disorders, their individual effects and the potential personal impact of the proposed psychoeducational programme, for example, ‘. . . they have to have a good understanding of borderline because it is so easy to trigger somebody’ (SU 2).
Service users typically underlined the importance of offering the programme within the context of a ‘trusting therapeutic relationship’ (SU 4) because of the guilt experienced by many parents affected by personality disorders.
Participants gave support to the structural location of the proposed intervention in both child and adult mental health services. Participants expressed some concern about locating it in children’s social care provision.
Routine service and clinician engagement and social marketing
Participants suggested that clinicians should understand the importance of improving support for parents affected by personality disorders but they did not make any specific recommendations about the optimal ways of engaging mental health staff in the research evaluation.
Identification of potential intervention recipients and research participants
Service users questioned the value of relying on clinicians’ judgement in the identification of potentially eligible parents. Some suggested that practitioners may not be knowledgeable about the parenting difficulties experienced by service users.
Participants did not provide feedback on the examples of screening tools shared by the group leaders. These included the Structured Clinical Interviews for DSM-IV Axis II Disorders (SCID-II), the SAPAS, the DAWBA and the SDQ. However, they raised a broader concern that parents ‘wouldn’t necessarily give all their information at once’ (SU 3), suggesting that the accuracy in referral and screening processes may vary accordingly.
Participants felt that identification, engagement and access to the intervention would be easier when a parent was already ‘in the system’ (SU 3) as an identified service user.
Engagement of service users and their interest in the Helping Families Programme-Modified and its research evaluation
Service users felt that the primary motivation for parents to participate in the intervention was to help and support their children. Engagement was likely to be affected by parents’ level of awareness of the impact of their own mental health difficulties on their parenting and on the outcomes of their child. Parent engagement may be greater when it is focused on ‘what you can do, rather than what you haven’t done’ (SU 7) as a parent.
Participants felt that parents would be highly sensitive to clinicians’ use of ‘judgemental’ (SU 8) language. They recommended that the offer to participate in research should be introduced by a practitioner whom the parent trusted. Participants advocated a ‘softly, softly’ (SU 1) approach that avoided activating parents’ underlying guilt. Service users expressed concerns about the involvement of children’s social services ‘at any stage’ (SU 7).
Participants promoted the importance of clear, non-patronising, plain English explanations of the intervention and research that were tailored to the needs of the individual and their circumstances with ‘no therapy speak or ‘psychobabble’ (SU 1).
Case co-ordination and integration of Helping Families Programme-Modified with usual care
Participants held differing views about participation in the proposed intervention alongside attending existing treatment services. Some service users felt that it could be ‘overwhelming and confusing’ (SU 3), whereas others felt that it should be determined by the needs and the resilience of the individual service user, and the frequency of attendance and the emotional intensity of other interventions. For example, some day care services for people affected by personality disorders require multiple attendances each week and can be ‘emotionally demanding’ (SU 8). However, ‘just seeing a psychologist for an hour a week as well as taking part in a parenting programme was more manageable’ (SU 7). Consultees felt that parents of younger children and those with other carer responsibilities may find it difficult to consistently attend appointments outside their home.
Service users advocated the inclusion of crisis plans in case co-ordination so that programme participants would know whom to contact between appointments and in the event of emergencies.
Service users were uncertain about what constituted treatment as usual for parents affected by personality disorders, with one commenting that ‘there isn’t a lot of support out there for me yet’ (SU 6).
Intervention format
Service users advocated a flexible approach to programme delivery and duration that was tailored to individual needs. For example, additional sessions may be required to take account of some parents ‘going at a slower pace, depending on how they have received the therapy’ (SU 1). Programme delivery would also need to be adjusted to account for parents’ other commitments, such as school holidays and other medical and school appointments. The option of receiving ongoing telephone support as part of the psychoeducational programme was considered useful.
Participants recommended several strategies for retaining parents’ participation in the proposed programme. These included therapists ‘having a very good understanding of the issues that affect people with personality disorder’ (SU 2), building ‘effective partnerships with parents’ (SU 7), reflecting on ‘parents’ past achievements’ (SU 4), ‘working at the parent’s pace’ (SU 1), ‘having a very good understanding of the parent’s issues in order to be realistic and use incremental goal-setting’ (SU 1) and ‘encouraging and being patient in supporting the parent in their goals’ (SU 2). Service users also recommended that intervention participants should be able to change therapists, if necessary.
Intervention content
Participants considered that a parenting programme based on a psychoeducational approach would be welcomed and would be likely to increase participants’ self-awareness, reflection and skills acquisition, particularly when tailored to an individual's needs and experiences associated with the personality disorder. Given the anticipated complexity of participants’ lives, service users felt that programme delivery would inevitably require ‘a balance between a “therapeutic element” and directing service users back to the parenting’ (SU 3).
An overly didactic, expert approach that relied on instructing parents what to do risked alienating parents and inducing negative reactions. For example, one parent said ‘I already feel guilty because I do know the list of strategies, I do know I am meant to be ignoring, rewarding, doing this doing that, but because of where I am in my depression or where I am with my disorder it means I can’t always draw upon those skills. It feels even worse. So, I don’t know how you solve that, but I just think “no”, I don’t want another list. Sorry.’ (SU 3).
A more collaborative approach based on shared understanding, respect and problem-solving was considered to be a more effective way of engaging parents. Participants felt that therapists should show flexibility in relation to the specific parenting strategies contained in the programme content. These should be tailored to individual parents’ knowledge, experience and circumstances, taking into account ‘what has and hasn’t worked in the past’ (SU 1).
Participants advocated the inclusion of programme content that focused on managing crises, for example the HFP-M Firefighting module. However, participants did recognise the challenges of using such methods when ‘a parent is stuck in a crisis’ (SU 2).
Descriptions of the methods, contents and materials of the HFP Parenting Groundwork and Parenting Strategies content received positive support, particularly topics which focused on forming a positive relationship with your child, understanding a child’s perspective, having fun with your child, boundaries, and learning how to play with your child.
Service users felt that care should reflect and be tailored to the needs of the individual. They did not make explicit recommendations about the best ways that clinicians could maintain the fidelity of specific intervention methods.
Consultation with service clinicians and managers
Design
The purpose was to obtain advice and guidance on key characteristics of the proposed parenting intervention and screening methods from clinicians and service managers working in relevant adult and child mental health services. 74 Two initial consultation groups were held between September 2014 and October 2014, with a follow-up group to share findings using a similar format and methods to those described above.
Method
Participants
Participants were all clinicians and managers working in mental health services across the two sites. Twenty-six participants were recruited through existing service networks using word of mouth, peer recommendations and e-mail invitations to team leaders. Participants received an explanation of the aims of the consultation and gave written consent for participation and audio-recording.
Format and procedure
The consultation groups were held in routine service settings. The sessions lasted between 60 and 90 minutes. Refreshments were available throughout the sessions. Each group used a semistructured format moderated by researchers (DM and Ruth Wilson) covering the same topics as the service user consultation groups. After creating a welcoming and informal atmosphere, moderators led participants through an open-ended discussion of key topics derived from the TIDieR checklist. Moderators presented information accompanied by handouts and PowerPoint slides. The groups ended with a summary of the research team’s next steps and a debrief about the participants’ experience of the consultation group.
Analysis
The same procedures as the service user consultation groups were used to identify key themes, recommendations and advice offered by service consultees, which were then categorised into the nine predefined features of the MWG checklist. The MWG synthesised these findings with other phase 1 findings.
Findings
Characteristics of the target population and conceptual model
Participants considered that research therapists’ management of the interpersonal challenges involved in working with the target population ‘would be key’ (SLAM group 1) to the success of their implementation of the proposed programme.
Supervision was considered to be a crucial support component for the research therapists.
Organisation and intervention delivery
Some staff expressed concerns about ‘helicoptering’ (CNWL group 1) specialist research therapists into routine services to deliver the intervention, as opposed to the provision of the intervention by routine staff. Staff were concerned that poorly co-ordinated care may hinder the transition when involvement in the proposed programme ended and that it may also disrupt existing ‘support networks’ (CNWL group 1).
Staff expressed concerns about ‘bridging the gap’ (CNWL group 1) that often exists between adult and child mental health services. Staff considered that there was equal value in siting the proposed intervention in both child and adult mental health services. Some staff advocated the creation of parental mental health services with a crossover between current adult and child services.
Routine service and clinician engagement and social marketing
Staff felt that ‘there is a need for this intervention’ (SLAM group 2) and could readily identify service users who would meet programme criteria and who would potentially benefit from the intervention. Introductory discussions about the proposed programme would depend on a service clinician’s confidence to talk about children’s difficulties as well as the parents’ own personal difficulties. Competence and confidence to do this varied between practitioners.
Staff recommended the use of individual clinical judgement in raising the programme with parents. They also recommended training sessions on introducing the programme and research evaluation as well as printed information to support initial discussions, including the potential benefits and challenges of participation.
Staff were unsure about how the proposed programme would complement other existing interventions available for the target population. Staff expressed concern about the potentially ‘destabilising effects that may occur’ (SLAM group 1) with parents’ programme participation and the risks that routine service clinicians could be ‘picking up the pieces’ (SLAM group 1).
Identification of potential intervention recipients and research participants
Staff were concerned that the existing structure of services and patient information systems would make it difficult for practitioners to identify eligible families. Child mental health staff were not routinely aware of all parents’ mental health status and service use. Adult mental health staff who were involved would not routinely have information about child mental health status but felt that they would have sufficient information to make recommended referrals. Some existing procedures, such as completion of the SLAM Child Risk Screen, would support initial identification. Identification of potentially eligible families would probably rely on the examination of individual caseloads.
Brief training in identification of eligible families was recommended, as well as further training for adult mental health staff in child and adolescent mental health. Some staff welcomed the use of tools to aid identification of eligible parents, whereas others felt that they could rely on their professional judgement. Positive feedback was given about the SAPAS as a screening tool.
Owing to the difficulties in accessing care, some staff raised concerns about eligibility criteria that required referral and/or attendance at CAMHS.
Engagement of service users and their interest in the Helping Families Programme-Modified and its research evaluation
Participants emphasised the importance of personalised discussions between service clinicians and eligible parents. Clinicians were concerned that parents may be ‘defensive’ (SLAM group 2) about discussing the impact of their own difficulties on their children. They were also concerned about the subsequent adverse effect on their relationships with referred service users. Most of the staff did not want to use a specific script for introducing the research programme but they wanted information sheets and guides that included suggested words and phrasing.
Although introducing the research programme would be easier for parents with existing personality disorder diagnoses, staff raised concerns about whether or not a diagnosis of personality disorder was necessary for inclusion in the programme, particularly given the associated stigma. Concerns were expressed about parents’ ability to distinguish between ‘a research and a clinical diagnosis’ (SLAM group 1) of a personality disorder, the risk of false positives, and the treatment options available for parents identified through the screening process as meeting the criteria for a research diagnosis. This was of particular concern for parent service users without an established personality disorder diagnosis who might be referred from CAMHS and subsequently allocated to a treatment-as-usual condition.
Case co-ordination and integration of Helping Families Programme-Modified with usual care
Staff explained that treatment as usual varied considerably both between and within adult and child mental health services. Staff expressed mixed views about the involvement of programme participants in other intensive interventions. They felt that the programme complemented many other available treatments, although some members of staff were concerned that participation in concurrent treatments may be ‘too much’ (SLAM group 2) and that families may become ‘overloaded’ (CNWL group 1).
Views on case co-ordination for parents involved in the proposed programme varied. Staff advocated an active role for keyworkers to introduce the research therapist to eligible parents. Some staff were concerned that eligible parents may be discharged from routine services once accepted on the research programme. Staff saw the potential for integrating the proposed programme into service user care plans and for it to become part of existing clinical pathways.
Intervention format
Some staff were uncertain about the duration of the proposed programme on the basis that interventions with service users affected by personality disorders may often be of considerable duration. They also thought that considerable time may be required to build effective therapeutic relationships.
Most of the staff advocated delivery of the programme in individual, rather than group, format. They felt that this would increase engagement and personalisation and promote change. Some staff suggested that home-based interventions may be subject to more threats to fidelity that clinic-based treatments.
Intervention content
Participants emphasised the importance of working within the defined and structured approach of the HFP sessions while maintaining some degree of flexibility to optimise engagement and delivery of programme content. Staff supported the use of structured manual content to help parents manage adverse life events and crises. These methods would help participants to focus on immediate needs while recognising that, without careful therapist guidance and boundaries, personal and family crises may become the primary focus of sessions for parents who struggle with impact regulation. Thus, the parenting content may then be missed.
The contents of the HFP Parenting Groundwork and Parenting Strategies methods were supported, particularly the breadth of topics covered in the Groundwork module and the proposed sequencing of relational parenting strategies prior to the use of discipline strategies.
Staff underlined the importance of sensitively broaching the topic of parenting and the effects of parents’ difficulties on their children’s mental health. Suggestions were made about whether to begin initial exploration on parental personality, parent–child relationship, parenting or parents’ own early experiences. Consensus supported the HFP methods and processes designed to constructively tailor the initial exploration of family ecology, including each of these key elements, with the development of a shared understanding of these issues between the parents and the research therapist.
Staff considered that personalisation was difficult to define, likely to be reliant on the individual skills practitioners and, therefore, difficult to reliably assess.
Synthesis of phase 1 findings and implications
The synthesis of phase 1 findings across the TIDieR framework used by the MWG established the following principles that underpinned the modification of the HFP-M and its logic model.
Characteristics of the target population
-
Research and clinical evidence consistently underlined that severe personality difficulties, including personality disorders, can significantly impair parenting and child outcomes.
-
Parents affected by severe personality difficulties, including personality disorders, are less likely to engage and gain benefit from standard, evidence-based psychoeducational programmes that are currently available.
-
Prevalence estimates and multigenerational effects warrant the development and evaluation of a specialised psychoeducational parenting programme.
Conceptual model and intervention rationale for Helping Families Programme-Modified
-
The modified MDP model was consistent with the ecological framework underpinning the HFP-M and consistent with views of consultees.
-
A narrow psychoeducational approach simply providing accurate information and advice was unlikely to lead to significant parenting change in the target population.
-
The HFP-M should be modified to focus on reducing the concurrent impact of adverse personality characteristics on parental behaviour, emotional regulation and cognition.
-
The HFP-M should not seek to target improvements in personality functioning per se.
-
The psychoeducational content and methods of the HFP-M should be modified to help parents improve their parenting in the context of their daily stresses and challenging personality and interpersonal difficulties.
-
The multiple interactions between MDP model factors are difficult to predict in practice and are likely to vary between individuals. The content of the HFP-M required personalisation methods to match the varying parenting and personality difficulties of parents and their child’s mental health problems.
-
Parenting programmes are more likely to be effective when targeting specific developmental periods. The best evidence supports their use during early and middle childhood, age 3–11 years.
Intervention organisation and delivery
-
There are significant limitations to the evidence base for specialised parenting interventions for the target population.
-
Adult and child mental health services do not routinely provide specialised assessments and interventions that focus on improving parenting outcomes. Routine care is highly variable and unpredictable.
-
Delivery and evaluation of the HFP-M are likely to be complex given the established needs of the population and the current organisation of child and adult mental health care.
-
Initial service and service user uncertainty and doubts need to be addressed in order to mobilise engagement and referral.
-
There was no strong evidence for a preferred location for the HFP-M in either adult or child mental health services.
-
Referral and recruitment pathways should be developed across both child and adult services. Pathways should not initially be tested in children’s social care services.
Routine service and clinician engagement and social marketing
-
Service clinicians and managers generally supported the development and testing of the HFP-M.
-
Confidence and competence to identify and engage eligible parents are likely to vary across individual practitioners.
-
Clinicians are concerned about additional service burden and adverse impacts.
-
Significant resources would be needed to engage services and develop referrer confidence to identify and engage potential participants.
Identification of intervention recipients and research participants
-
Recruitment is likely to vary across practitioners and services.
-
Variations in care, case note recording and patient information systems are likely to make identification of eligible parents more difficult.
-
Routine clinical staff require ongoing guidance, training and supporting materials to effectively identify eligible parents and support informed decision-making.
-
The use of an eligibility criterion based on personality disorder diagnosis might improve internal validity but could lead to practical challenges and ethics issues, particularly for parents without a pre-existing diagnosis.
-
Stigma and treatment expectations associated with personality disorders may affect identification and engagement.
-
The feasibility of screening procedures needs testing. Relevant tools could include brief keyworker-rated assessment measures of personality disorders and child mental health as well as in-depth diagnostic assessments based on a parent interview.
Engagement of service users in Helping Families Programme-Modified and its research evaluation
-
Identification, informed decision-making and gaining informed consent may be lengthy and influenced by parents’ insight and life circumstances and the clinical skills of routine clinical staff.
-
Potential barriers to be examined include the stigma associated with personality disorders, and the practical and psychological demands of programme participation in addition to existing service receipt.
Case co-ordination and integration of Helping Families Programme-Modified with usual care
-
The HFP-M should augment rather than replace treatment as usual.
-
Keyworkers referring the programme should openly discuss the implications of programme participation with parents.
-
Research therapists should monitor the potential burden of the intervention for participating parents and routine services.
-
Robust methods should be developed to guide the co-ordination of care between research therapists and routine clinicians.
Intervention format
-
The feasibility should be examined of the HFP-M format based on the provision of 16 individualised, home-based sessions, with each session module covering specific manualised content.
-
The HFP-M should be delivered by trained and experienced research clinicians who have the interpersonal skills and relationship qualities to engage and maintain parents’ participation.
Intervention content
-
The HFP-M content should be designed for parents of children aged 3–11 years rather than the wider age range envisaged by the commissioned call.
-
In the light of phase 1 findings, the main modifications of the HFP that were required were:
-
greater emphasis on the inter-relationship between key parent, personality functioning and parenting factors within its ecological assessment and formulation frameworks
-
intervention content and methods focused on key personality disorder characteristics likely to have most influence on parenting, that is, negative parent–child interaction/relationships, negative emotional arousal in response to child behaviour and emotions, difficulties in parental emotional regulation and impulse control in relation to parenting tasks, and negative ways of perceiving and thinking about the parenting role, the self as parent and the parent’s children
-
increased integration, rather than sequencing, of parenting groundwork content (focused on parent interpersonal functioning and emotional regulation) with parenting strategies content (focused on effective parenting skills, emotional warmth and reflective function).
-
-
The existing HFP content to be used within the HFP-M intervention included:
-
quick wins to promote parental confidence, motivation and commitment
-
structured helping processes to develop a shared understanding of family ecology, highlight parenting strengths and challenges, and set realistic parenting goals
-
parenting groundwork module content to manage the effects of personality difficulties on parenting in combination with the parenting strategies module content to enable parents to acquire accurate knowledge about child development, set realistic parenting expectations, and improve consistent use of positive parenting practices, including sensitive and supportive parent–child interactions, listening and communication skills, emotional warmth, sensitivity and availability, empathy and reflective function
-
the Firefighting module, to enhance adaptive coping with adverse life events and interpersonal crises so that they do not undermine parenting
-
goal and therapeutic engagement review to identify benefits and manage challenges as they arise.
-
-
The HFP-M methods for personalisation need to be sufficiently clear to ensure that fidelity can be assessed, including intervention monitoring, case formulation, goal specification, therapist supervision and therapist reflective practice.
This synthesis of phase 1 findings was used to produce the screening methods and the modified HFP-M intervention used in phase 2 pre-trial feasibility testing, the content and methods of which are described in Chapter 4. A detailed overview of the screening methods is given in Report Supplementary Material 1 and Report Supplementary Material 2. An overview of the manual and example manual content are provided in Report Supplementary Material 3.
Conclusion
Findings from the phase 1 scoping review and stakeholder consultation were used by the MWG to modify the existing HFP and PEPS manualised interventions to create a specialised psychoeducational intervention (HFP-M) for parents with severe personality difficulties, including personality disorders. Findings were also used to develop a preliminary screening process for the identification and recruitment of eligible parents from the target population, which is described in Chapter 4.
Chapter 4 Phase 2: pre-trial feasibility testing
Reproduced from Wilson et al. 141 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Phase 2 aim and objectives
Phase 2 aimed to examine the initial feasibility and acceptability to service users and keyworkers of the HFP-M psychoeducational parenting intervention, to examine the proposed research screening and recruitment procedures, and to develop a more detailed description of usual care for the target population. 74
Phase 2 objectives were to:
-
test preliminary referral and recruitment pathways in candidate mental health services in sites 1 and 2
-
assess initial feasibility and acceptability of the HFP-M and planned screening procedures to clinicians and service users
-
implement the HFP-M research therapist selection, training and fidelity methods
-
implement the HFP-M and planned screening procedures in a series of clinical case studies, including the assessment of clinicians’ and users’ experiences and perceived impact
-
obtain a detailed description of usual care to inform the description of the phase 3 trial comparator arm
-
obtain independent ethics scrutiny of the issues raised in the case studies and the descriptive study of usual care.
Phase 2 findings were used to refine the HFP-M, propose evaluation methods and develop the protocol for the planned phase 3 feasibility trial.
Phase 2 design
The following activities were undertaken to fulfil the objectives described above:74
-
development of parent identification, engagement and case co-ordination guidance and materials for keyworkers and services at sites 1 and 2
-
engagement events with candidate services at sites 1 and 2 to establish preliminary referral pathways for the planned case series
-
thematic review of relevant clinical policies and guidance together with a case note audit to produce a more detailed description of usual care for the target population
-
pre-trial case series to examine the initial feasibility and acceptability of the HFP-M intervention and recruitment procedures.
Development of guidance and information to assist identification and case management of eligible parents
Drawing on phase 1 findings and formative feedback from the SUAP, the research team developed the following materials to assist keyworkers and service managers to identify and case manage eligible parents:
-
Helping Families Programme-Modified: parent identification and referral decision process algorithm.
-
Introducing the Helping Families Programme-Modified: a keyworker guide.
-
Helping Families Programme-Modified Joint Working Protocol.
These materials were included in the HFP-M briefing pack (see Report Supplementary Material 1) along with the case series’ participant information sheet (PIS) and printed publicity materials.
Helping Families Programme-Modified: parent identification and referral decision process algorithm
This case identification algorithm described the procedures for keyworkers to identify and refer eligible parents to the HFP-M case series. The algorithm included participant eligibility criteria, decision rules and contraindications for identification and referral. To improve efficiency and to avoid approaching ineligible parents unnecessarily, the procedures included optional use of two standardised decision support tools to assist initial identification of potential participants: the Standardised Assessment of Personality – Abbreviated Scale: Informant (SAPAS-INF) and SDQ-Impact Supplement (SDQ-IS). Completion was not a prerequisite for case series eligibility nor were the tools meant to be used as parent self-report instruments.
Introducing the Helping Families Programme-Modified: a keyworker guide
Developed in conjunction with the SUAP, this keyworker guide offered recommendations about engaging parents in the HFP-M research case series.
Keyworkers were advised to carefully consider for each parent the relative benefits and risks of participating in the planned screening procedures, particularly in relation to parents’ learning about personality disorder research diagnosis status.
Keyworkers were encouraged to initiate sensitive, exploratory discussions with each parent about their personality difficulties, their child’s emotional and behavioural health and parenting. Keyworkers were advised to first establish sufficient rapport and common understanding with prospective participants and only then introduce the broad aims and purpose of the research case series, its eligibility criteria and screening procedures.
Helping Families Programme-Modified Joint Working Protocol
The HFP-M was intended to augment rather than replace usual care. The HFP-M Joint Working Protocol was developed in conjunction with service managers, clinicians, safeguarding leads and service users and with reference to relevant site, NHS and local authority procedures.
The protocol described the roles and responsibilities of research staff and keyworkers. It set out procedures for:
-
co-ordination and continuity of care for parents receiving the HFP-M and their children
-
effective management of existing and arising safeguarding concerns for children whose parents were in receipt of the HFP-M
-
information-sharing procedures between the HFP-M researchers, research therapists, keyworkers and other professionals involved in the care of parents receiving the HFP-M, and their children.
Primary case management responsibility remained with the referring keyworker and their service. The protocol was activated when eligible parents consented to case series participation and it ended with their completion of the research intervention.
Service site and keyworker engagement
The research team identified 28 adult and child mental health teams of varying size and function across site 1 (n = 18) and site 2 (n = 10). These included specialist teams for adults with personality disorders, generic adult mental health and CAMHS teams. Engagement events were held with 25 (89.3%; SLAM, n = 16; CNWL, n = 9) teams, usually as an adjunct to routine meetings.
Engagement events were attended by between 8 and 20 clinicians from a range of multidisciplinary backgrounds including psychiatrists, psychologists, psychiatric nurses, psychiatric social workers and occupational therapists. The format and content of the engagement events were based on previous staff workshops developed by the research team to support personality disorder trials and disseminate the HFP. 77,85 The engagement events were supported by printed materials and a PowerPoint presentation, and discussed the following:
-
teams’ experiences of the needs of parents affected by severe personality difficulties, including personality disorders, whose children had significant emotional and behavioural difficulties; currently available parenting resources; and related service demands
-
development of the HFP-M and proposed research evaluation, including phase 1 findings
-
the HFP-M intervention rationale, aims, content and methods
-
pre-trial case series aims and procedures, including participant identification and screening, informed consent and data collection procedures
-
summary of the HFP-M briefing pack contents.
Each individual clinician received a copy of the HFP-M briefing pack. The engagement response from the 25 teams was considered sufficient to meet recruitment requirements for the planned case series.
Thematic review of policy guidance and case note audit
Aim and objectives
This thematic review and case note audit aimed to provide a more detailed description of relevant usual-care recommendations and practices with the objective of informing the HFP-M Joint Working Protocol, case series process evaluation, and the planned feasibility trial comparator arm. 74
Thematic review of South London and Maudsley NHS Foundation Trust clinical and patient safety policies
Design
A non-experimental descriptive design was used to conduct a rapid scoping review of relevant clinical and patient safety policy documents relating to care processes and methods for parents affected by personality disorders whose children experience emotional and behavioural difficulties. 74 Limited research resources and better access to documentation meant that the review centred on the SLAM (site 1) policies.
Method
The research team sought to identify current clinical and patient safety policy documents located on the SLAM staff intranet website that referred to personality disorders, child mental health and parental mental health. Eligible documents were searched for relevant text using the following terms: (1) ‘child’ and/or ‘adult’ and/or ‘parent’ and/or ‘family’, and (2) ‘personality disorder’ and/or ‘emotional and behavioural’ and/or ‘mental health’ and/or ‘safeguarding’ and/or ‘child protection’, and (3) ‘care’ and/or ‘assessment, and/or ‘treatment’ and/or ‘referral’, and (4) ‘policy’ and/or ‘guidance’ and/or ‘practice’.
Data extraction and analysis
The SLAM internal website was searched between March 2015 and June 2015. Identified documents were screened for relevance and text was extracted from 34 relevant documents. Thematic content analysis was used to identify key common practice recommendations related to usual care for the target population.
Results
No specific relevant parenting pathways or recommended parenting interventions for the target population were documented in the extracted data. Analysis revealed three key themes relevant to usual-care practices.
Theme 1: identification of coexisting child and parent needs
Identification and clear documentation of coexisting child and parent needs were recommended as usual practice for clinicians working with parents diagnosed with personality disorders who have children with emotional and behavioural problems. Adult service policies recommended documenting the names and ages of all children for whom service users had parental responsibility, together with identifying any additional services providing care to other family members. CAMHS practitioners were recommended to actively identify coexistent parent and carer mental health problems as part of the mental health assessment of the individual child.
Theme 2: parenting responsibilities addressed
In the care plans for parent service users, policy guidance recommends that parenting responsibilities should be recorded, together with consideration of the mental health, social, educational and safeguarding needs of the child. These should be documented alongside the completion of the SLAM child risk screen.
All services should support parents in their parenting role and advise parents about the potential impact of mental health difficulties on their children. Each care plan should specify strategies to address the parenting needs of adult service users as well as their children.
The review of the CAMHS care plan should consider changes in family circumstances over time, including changes in parental mental health functioning, and personal and family goals. Care plan reviews were recommended to involve both child and adolescent service users as well as their parents/carers.
Theme 3: sharing information and joint working
Following the identification of coexisting parent and child mental health difficulties, appropriate steps should be taken to ensure that information is shared appropriately between all service providers involved in the assessment, the case management and the treatment of identified families. Referrals to additional services should be made when necessary to address individual and collective family needs, including safeguarding concerns.
Conclusion
Consistent with phase 1 findings, this thematic review revealed no specific parenting pathways and interventions for the target population within the NHS trust concerned. Policy guidance supported an inclusive and co-ordinated approach to the identification, assessment and care of parents with significant mental health difficulties and their children.
Clinical case note audit
The aim of the clinical case note audit was to undertake a granular examination of the parenting care, support and interventions recorded in individual service user care plans, clinical notes and referral documents of:
-
parents affected by personality disorders whose children, aged 3–11 years, experienced emotional and behavioural difficulties, and
-
children, aged 3–11 years, experiencing emotional and behavioural difficulties whose parents were affected by personality disorders.
Method
The SLAM Clinical Record Interactive Service (CRIS) system (www.maudsleybrc.nihr.ac.uk/facilities/clinical-record-interactive-search-cris/, accessed 31 July 2019) was used to identify and extract relevant anonymised data from the SLAM Patient Journeys System (SLAM PJS) of a cohort (n = 25) of relevant parent service user cases and a cohort (n = 25) of relevant child service user cases.
A CRIS data extraction script was generated using the following terms: ‘personality disorder’, ‘dependant’, ‘child emotional and behavioural problems’, ‘child mental health problems’, ‘family issues’, ‘family problems’, ‘child behaviour’, ‘child problems’, ‘child difficulties’, ‘CAMHS’, ‘child and adolescent mental health service’ and ‘parental mental health’.
Data extraction and analysis
Case note audit data were extracted in September 2015. A researcher (Ruth Wilson), under direction from the chief investigator, used a pre-existing audit tool, Meeting the Needs of Families Affected by Parental Mental Illness (MNFAPMI) (see Appendix 1),142 to benchmark extracted data. The MNFAPMI audit tool was derived from published evidence-based approaches for parents with mental health problems.
Results
The CRIS system identified case notes of 532 adult service users in which child mental health was referenced. Thirty-two case notes referenced both adult personality disorder and child mental health. Of these, 28 case notes met the criteria for parent personality disorder and child receipt of mental health service care. Scrutiny of extracted case note data revealed that none contained documented evidence that the parent service user had received any type of specified evidence-based parenting support.
Further audit of an additional set of 10 case notes, randomly selected from the original cohort of 532 service user case notes, found no other documented evidence of parenting support receipt.
The CRIS system identified 956 CAMHS users where there was documented reference to a childhood emotional and/or behavioural disorder and coexisting parental mental health difficulties. None of these case notes referred to any search terms associated with parental personality disorder. No further action was undertaken to extract information about parenting interventions.
Conclusion
The case note audit provided no further detailed information about the content of parenting support available to service users receiving usual-care practices. The lack of documented parenting support appeared to be at variance with the policy recommendations identified by the thematic review.
It is possible that the results under-reported the support that was available. Data extraction was hampered by the constraints of the SLAM PJS system, where case records are indexed on an individual basis and records of immediate family members are not structurally linked. Furthermore, case note recordings may not have been of sufficient quality and specificity to have extracted relevant enough parenting support information using the specified CRIS search terms or benchmarking by the MNFAPMI audit tool.
While methodologically limited, the findings may have otherwise reflected the underidentification and under-recording of parenting support needs in the target population identified during phase 1. The findings may have also reflected the limited routine use of evidence-based parenting support in usual care.
Phase 2 Modified Helping Families Programme case series
Aims and objectives
This case series aimed to assess the initial feasibility and acceptability of the HFP-M and the related screening and evaluation methods. 74,141 The specific objectives were to:
-
test the feasibility of preliminary recruitment pathways in candidate services in sites 1 and 2
-
examine implementation of the HFP-M, proposed evaluation methods, participant and referring keyworker experiences, and perceived impacts.
Design
A mixed-methods case series design was used with a sample of 12 participant parents74,141 (see www.journalslibrary.nihr.ac.uk/programmes/hta/1219401/#/documentation; accessed July 2019). Qualitative and quantitative data were collected from the participant parents and referring keyworkers.
The qualitative design used an interpretative phenomenological analysis (IPA) to develop a fine-grained understanding of the subjective, lived experiences of participating parents and referring keyworkers. 141,143,144
Setting
Referral pathways were agreed with 25 CAMHS and adult mental health teams across sites 1 and 2.
Participants
The target population was parents with personality disorders whose children (aged 3–11 years) had emotional and/or behavioural disorders. 74,141
The inclusion criteria were:
-
Parent – being aged 18–65 years, being the primary parental caregiver for the index child, the presence of any personality disorder, being proficient in written and spoken English and having capacity to consent to participation.
-
Index child – being aged 3–11 years, living at home with index parent, the presence of an emotional or behavioural disorder and attending or being considered for CAMHS.
The exclusion criteria were:
-
Parent – presence of psychosis, being currently engaged in another structured parenting intervention, receiving inpatient care and/or insufficient language or cognitive abilities affecting consent and full participation in trial procedures.
-
Index child – presence of a neurodevelopmental disorder (e.g. autistic spectrum disorder, learning disability, traumatic brain injury or psychosis, such as schizophrenia), not residing with the index parent and/or currently being considered for/subject to an application for care or supervision proceedings.
Sampling
The aim was to recruit 12 eligible parents and conduct qualitative interviews with each parent participant and referring keyworker.
Screening procedures
There was a two-stage process involving initial keyworker identification followed by formal screening. 74,141
Identification
Keyworkers in co-operating teams were requested to review their case lists against the study eligibility criteria. 74,141 Keyworkers used the parent identification and referral decision process algorithm, including use of the SAPAS and the SDQ-IS115,118 where necessary, to guide participant identification (see Report Supplementary Material 1). Keyworkers also had access to ongoing liaison and consultation about parent eligibility from the research team.
Consent
After the initial positive identification of a parent who may meet the eligibility criteria, each keyworker determined whether or not it was appropriate for a parent to be approached by the research team. 74,141 A clinically experienced research therapist then offered a face-to-face meeting to discuss the case series and provide a PIS (see www.journalslibrary.nihr.ac.uk/programmes/hta/1219401/#/documentation; accessed July 2019).
Referring keyworkers were also invited to participate in a qualitative interview about their experiences of the research (see www.journalslibrary.nihr.ac.uk/programmes/hta/1219401/#/documentation; accessed July 2019). All participants were fully informed, verbally and in writing, of study procedures. Informed written consent was required from parents prior to full diagnostic screening.
Parents had the opportunity to consider and seek further advice about the implications of participation for themselves and their children prior to consent, with a minimum of 7 days to decide. Research therapists used parent meetings to confirm basic eligibility criteria.
Formal screening and debriefing
The use of gold standard assessment instruments was intended to limit the risk of misdiagnosis. Parental personality disorder was formally assessed by researchers using the SCID-II112 (see Report Supplementary Material 2). All personality disorder types, and combinations thereof, were eligible because the disorders typically co-occur. There is scant evidence that parenting difficulties are more significantly related to any single, specific personality disorder. Child inclusion and exclusion diagnoses were assessed by parent interviews using one of two well-validated, standardised instruments: the DAWBA, for parents of children aged 5–11 years,116 and the PAPA, for parents of children aged 3–4 years. 117 Research therapists were fully trained to use these instruments.
Separate debriefing sessions with parents took place to review and explore the diagnostic assessment outcome (see Report Supplementary Material 2). Debriefing session content and methods were designed with advice from members of the SUAP and from clinicians highly experienced in the assessment and clinical management of people affected by personality disorders.
Participants could withdraw from the study at any time with no consequences for their care. Regardless of eligibility, parents could discuss usual-care options in local adult and child mental health services. Parents received £10 reimbursement in vouchers at each data collection point.
Measures and data collection procedures
Participant demographics
A specially designed proforma was used to collect descriptive baseline data from parents participating in the case series including parent/child age, sex and ethnicity, family household composition and family socioeconomic status.
Feasibility parameters
Rates of participant identification, consent and eligibility were routinely collected.
Clinical outcomes
The following validated, parent-report measures were completed prior to the intervention starting and after completion of the final session.
Concerns About My Child
Concerns About My Child (CAMC)132 is a visual analogue scale (0–100) that requires parents to nominate, prioritise and rate up to three key concerns about their child, providing a sensitive, individualised index of change. A community sample of parents seeking intervention had a mean pre-intervention score of 53.0. 132
Strengths and Difficulties Questionnaire
The SDQ is a 25-item questionnaire115 that assesses emotional and behavioural problems in 3- to 16-year-olds and was used to obtain a broad measure of child mental health. It produces a total difficulties score (0–40) and four problem subscale scores (emotional problems, conduct problems, hyperactivity/inattention, peer relationship problems), with higher scores indicating more dysfunction. A score of ≥ 17 indicates abnormal caseness. 115
Eyberg Child Behaviour Inventory
The Eyberg Child Behaviour Inventory (ECBI)145 is a 36-item questionnaire that assesses the intensity and number of disruptive behaviour problems in 2- to 16-year-olds, providing a comprehensive measure of child behaviour difficulties. An Intensity Scale (range 36–252) score of ≥ 131 suggests that behaviour problems are of significant severity. Problem Scale (range 0–36) scores of ≥ 15 indicate a significant number of behaviour problems. 145
Child Behavior Checklist-Internalising Scale
The Child Behavior Checklist-Internalising Scale (CBCL-Int)146 is a 32-item questionnaire that assesses emotional problems in 6- to 18-year-olds (school-age version), with an alternative 36-item version available for children aged 1.5–5 years (preschool version). Standardised t-scores are used to combine results from both versions and provide a comprehensive measure of child emotional difficulties. A score of ≥ 60 indicates clinical caseness. 146
Arnold–O’Leary Parenting Scale
The Arnold–O’Leary Parenting Scale (PS)147 is a 30-item questionnaire that assesses dysfunctional discipline styles in parents of children aged 2–16 years. It correlates significantly with more time-consuming observational ratings of parenting behaviour (r = 84). A total factor score is calculated by dividing the total score (range 30–210) by the number of items. A factor score of ≥ 3.2 differentiates between clinic-referred and non-referred groups of children. 147
Kansas Parental Satisfaction Scale
The Kansas Parental Satisfaction Scale (KPSS)148 is a three-item scale that provides a brief measure of stress and dissatisfaction in the parenting role. A seven-point Likert response scale is used, and the scores for all three items are summed to yield a total parenting satisfaction score (range 3–21). The KPSS has been found to have internal consistency reliability coefficients ranging from 0.78 to 0.95. 148
Symptom checklist-27
The Symptom Checklist-27 (SCL-27)149 is a 27-item questionnaire that assesses psychological symptoms in adults. Total score ranges from 0 to 108. The measure’s global severity index (GSI) provides a broad measure of adult mental health and is calculated as a mean of all 27 items. The GSI of the SCL-27 and the SCL-90-R (Symptom Checklist-90-Revised) show correlations above 0.90. 149
Therapeutic alliance
Therapeutic alliance was measured post intervention using the Working Alliance Inventory-Short Revised (WAI-SR) questionnaire. 150
Working Alliance Inventory-Short Revised
This is a 12-item questionnaire150 that assesses the quality of therapeutic relationships developed by trial therapists. Each item was rated on a seven-point Likert scale, yielding a total score ranging from 12 to 84.
Qualitative interviews
Semistructured topic guides were used for informant interviews. 141 Development was informed by concepts underpinning IPA. Content focused on exploring the subjective meaning and significance of parents’ and keyworkers’ experiences and perspectives on case series recruitment, screening, participation and intervention. Content and probes were developed iteratively by experienced qualitative and service user researchers (CD, LF and TW). Interviews were conducted by a white British female university graduate (Ruth Wilson), aged < 30 years, who had no clinical responsibility for participants and was trained in qualitative interview skills. 151 The researcher used topic guides to build a rapport and to encourage open description of parent and keyworker subjective experiences. 143 All interviews were audio-recorded and transcribed verbatim.
Parent interviews
Parents who consented to screening were eligible for a qualitative interview. 141 The parent topic guide covered parents’ experiences of (1) the invitation to participate in the HFP-M and research processes, (2) screening, consent procedures and assessments, (3) the HFP-M intervention content and methods, (4) the impact on the parents, child and family, including negative effects, and (5) concurrent involvement with other services (see Appendix 2). All interviews took place within the family home after participation in the HFP-M intervention was complete.
Keyworker interviews
Interviews were undertaken with referring keyworkers of parents who participated in the qualitative interviews described in Parent interviews. 141 The keyworker topic guide covered keyworker experiences of (1) offering usual care to parents affected by personality disorders whose children have emotional and behavioural difficulties, (2) identifying parents to participate in the HFP-M case series and related research procedures, (3) keyworkers’ perceptions of parents’ response to screening procedures and participation in the HFP-M, and (4) care co-ordination alongside the HFP-M (see Appendix 3).
Helping Families Programme-Modified intervention procedures
The HFP-M involved 16 weekly appointments, each lasting from 60 to 90 minutes; a session module overview and example materials are given in Report Supplementary Material 3. Each appointment covered specific manualised session module content. Appointments took place on a one-to-one basis with referred participants. Other caregivers could participate in sessions when appropriate. The HFP-M appointments took place in the family home and in the local community setting clinics when preferred by the parent. The index child and other siblings were not direct recipients.
The HFP-M rationale and aims intended to help parents to:
-
identify the ways that parent personality traits and functioning impact individual parenting and impact the index child’s development
-
identify mutually agreed goals for parenting change
-
use a range of evidence-based parenting methods to improve parenting, child mental health problems and parent–child relationships
-
use a range of evidence-based strategies to improve parental emotion regulation and coping
-
improve parents’ social resources.
The HFP-M used a relational, goal-orientated helping process to:79
-
optimise collaborative, therapeutic engagement and reduce parental alienation and stigma
-
complete an ecological assessment of each parent’s interpersonal difficulties, their parent–child relationship, their child’s emotional and behavioural difficulties, and their wider family and life circumstances
-
develop a shared understanding of static and dynamic family risk and protective factors that affect engagement, participation and progress towards agreed priorities
-
generate hope, manage adverse life circumstances and facilitate parenting change
-
encourage parents’ emotional, cognitive and behavioural readiness to make changes to their parenting
-
develop a shared understanding of warm, safe and authoritative parenting and the effect of their interpersonal difficulties on parenting and their children
-
encourage parents to use a future-orientated approach to focus on a small number of key parenting goals supported by a clear implementation of plan-based specific strategies
-
assist parents to develop and strengthen their emotional, cognitive and behavioural skills so that they can interact in warm, safe and authoritative ways with their children
-
support parents to select and utilise strategies to strengthen parent–child relationships, reinforce positive child behaviour and manage a child’s disruptive behaviour and emotional dysregulation
-
encourage parents’ use of learnt skills in daily parenting activities.
Routinely monitor therapeutic progress and alliance to identify impact, strengthen engagement and address emergent difficulties
Research therapist requirements
Four research therapists, two from each site, were selected based on their clinical expertise in adult mental health and personality disorders, child mental health and parenting, as well as their experience of delivering manualised interventions.
Three of the research therapists held band 7 NHS posts (occupational therapist/dialectical behaviour therapist, family therapist, family and systemic psychotherapist) and one held a band 8a post (clinical psychologist). All worked part-time on the study.
Research therapist training
Research therapists received eight 3-hour training sessions that included:
-
background and context to the research trial and phase 1 findings
-
case series recruitment procedures
-
SCID-II, DAWBA and PAPA training
-
the HFP-M manual, including rationale, aims, format and content
-
good practice in working with parents affected by personality disorders
-
understanding child emotional and behavioural difficulties
-
co-working and lone working processes including the HFP-M joint-working protocol
-
working with risk in community settings.
Training was provided by the research therapist supervisor (LH), two expert co-applicants (MM and PM) and a safeguarding lead nurse.
Research therapist supervision
Research therapists received fortnightly group supervision. Each session lasted 2.5 hours, under the direction of an experienced HFP supervisor and the co-developer of the HFP-M (LH). Content focused on case series recruitment procedures, fidelity monitoring and reflective case supervision of the HFP-M implementation. Reflective case supervision reviewed the clinical focus and application of the HFP-M with participating parents, therapeutic progress, management of emergent clinical challenges, therapist safety and the emotional impact of the HFP-M implementation.
Risk and ethics issues
Safe and effective care
The well-being and safety of the participating parents and their children were paramount. The following procedures were implemented to support safe and effective provision of the HFP-M.
Case co-ordination
The HFP-M augmented usual care. In line with the HFP-M Joint Working Protocol, primary case management responsibility remained with the referring keyworker. As described above, the Joint Working Protocol set out the agreed roles and responsibilities, clinical working practices and co-ordination between the HFP-M research therapists and the routine service practitioners.
Potential adverse events
Each researcher and clinical research contact incorporated a brief review of potential adverse reactions, including (1) deterioration in parent/child outcomes, (2) acute adverse events, for example self-harm, and (3) adverse effects and/or harm attributed directly to the HFP-M and research procedures. Any adverse events identified by participants, research staff and service clinicians were to be reported to the chief investigator and research therapist supervisor (LH) to assess significance and ensure that appropriate and timely actions were taken in accordance with the agreed study and NHS procedures. A serious adverse event form was to be completed when adverse events fell into predetermined risk categories.
Adverse events were to be reported promptly to the programme’s DMEC, as per governance requirements of the sponsor and funder.
Ethics review and site permissions
All key case series documents and procedures were reviewed internally by the SUAP, TSC, DMEC and the independent ethics consultant (Richard Ashcroft, Professor of Bioethics, Queen Mary, University of London) prior to external review by the National Research Ethics Service (NRES) Committee London (Camberwell St Giles).
External NRES approval required two full submissions. This delayed the start of the case series recruitment. The major focus of concern for the NRES committee was the potential adverse reactions stemming from the inclusion of parents who had not previously sought a personality disorder diagnosis and the associated participant information.
Ethics approval for the study was obtained from the NRES Committee London (Camberwell St Giles 15/LO/0079). Relevant NHS site research and development approvals were provided.
Data analysis
Feasibility and outcome data
Descriptive statistics were used to describe the feasibility of recruitment, consent, screening procedures and individual case outcomes.
Qualitative data
Verbatim transcripts obtained for analysis were downloaded to NVivo 10 (QSR International, Warrington, UK), a computer package for the management, classification and analysis of text-based data. Parent and keyworker data were initially analysed separately and then triangulated. 141
Data were analysed using the methods of IPA and they were coded at three levels. 143,144 Initially, the researcher (Ruth Wilson) familiarised herself with each transcript, attaching descriptive codes containing initial observations and reflections to data. The researcher then developed second-level descriptive labels which were coded and organised into conceptual categories. Interpretations at this analytic stage intended to capture the subjective value attributed by the participant parents and keyworkers to generated categories. For example, the theme ‘experience of parenthood’ incorporated the subcodes containing emotional responses (e.g. frustration) and parenting behaviours (e.g. seeking support and negative experiences of parenting programmes). Finally, generated results were explored and verified in shared meetings with Crispin Day and Timothy Weaver, who were familiar with data transcripts. The codes, categories and themes generated from the two respondent groups were examined and connections were explored.
Results were subject to validation with a parent and a clinician participant. These procedures verified the generated findings.
Results
Feasibility findings
Sites and participants
Recruitment to the case series was initially planned to take place over a 6-month period. Ethics approval coincided with school summer holidays, which delayed recruitment because many referred parents did not want to be screened while their child was on holiday. Recruitment and intervention delivery took place from July 2015 to February 2016. Seventeen out of 25 teams (68.0%) referred parents. Modal team referral was one parent (range 1–3).
Twenty-six parents were referred to the case series (site 1, n = 18, 69.2%; site 2, n = 8, 30.8%) as shown in the Consolidated Standards of Reporting Trials (CONSORT) flow diagram in Figure 2. Fourteen (53.9%) parents were referred by adult mental health keyworkers, eight (30.8%) from CAMHS and a further four (15.3%) from parental mental health keyworkers.
FIGURE 2.
Case series recruitment CONSORT flow diagram.

Four of the parents from the referred cohort who met all of the eligibility criteria were offered and accepted to take part in the research intervention. 141 The main reasons for exclusion were evenly distributed: parents who declined participation (n = 5, 19.2%), parents whom researchers were unable to contact (n = 5, 19.2%), parents who did not meet eligibility criteria or were unable to participate owing to acute mental health crises and/or life circumstances (n = 5, 19.2%), and children who did not meet the eligibility criteria (n = 7, 26.9%).
In total, eight of the referred parents were unable to be contacted by researchers or declined participation. Children of three parents were placed on child protection plans during the recruitment and screening process and a further three parents were not able to participate because of acute personal and family crises.
Contact with referred parents
Detailed records of the contact processes between researchers, referring keyworkers and parents were maintained. Researchers contacted referred parents by telephone, text and e-mail, when acceptable. The modal number of completed contacts with parents to agree consent and arrange screening appointments was 6 (range 1–7). The mean duration between referral and agreeing consent was 41.3 days (range 15–76 days). Delays were mainly a result of parent factors, including busy family schedules, school holidays, family health, education appointments, and referrer factors, such as incorrect contact information.
Screening procedures
Researchers contacted 19 parents who gave informed consent to participate in the case series. Further in-depth discussion with these parents about the research project led to the exclusion of nine parents prior to screening for the reasons given in Figure 2.
Ten parents (52.6%) who gave consent for participation completed screening procedures, of whom six were then excluded. Of these, two parents did not meet criteria for the SCID-II research diagnosis of personality disorders, and children of three parents did not meet the DAWBA criteria. Screening was started but not completed for one consenting parent owing to repeated cancelled appointments.
Parents who participated in the screening procedures reported that the screening procedures were lengthy; completion of the SCID-II and the DAWBA generally took two or three 1- to 2-hour appointments.
Measure acceptability and completion
Three parents completed all measures at time 1 (T1) and time 2 (T2). One parent did not complete T2 measures because she could not be contacted. There were no missing data items on any completed questionnaire.
Participant feedback indicated that the measures were acceptable, although lengthy, to complete. Some items needed assistance from the researcher to explain, particularly in questionnaires using American English.
Participant characteristics
Demographic information
All four case series participants were mothers (Table 1). 141 Index children were aged 3–11 years, three of whom were boys. Participant mothers had no postschool qualifications. Only one mother was in part-time employment. Two mothers were not working by choice. None of the participants had partners who shared parenting responsibilities.
| Outcome | Case series participant | |||
|---|---|---|---|---|
| Parent 1 | Parent 2 | Parent 3 | Parent 4 | |
| Parent | ||||
| Gender | Female | Female | Female | Female |
| Relationship to child | Biological mother | Biological mother | Biological mother | Biological mother |
| Highest level of education | Left school at 16 years with qualifications | Other qualifications | Attended secondary education aged 16–18 years | Attended secondary education aged 16–18 years |
| Employment status | No | Not in employment by choice | Not in employment by choice | Part-time employment |
| Ethnicity group | White British | Black UK/African-Caribbean | White British | – |
| First language | English | English | English | English |
| Partner | ||||
| Partner who shares parenting responsibilities | No | No | No | No |
| Child | ||||
| Gender | Female | Male | Male | Male |
| Age (years) | 11 | 7 | 10 | 3 |
| Number of children in the home | 3 | 3 | 3 | 1 |
Intervention acceptability
All parents meeting the eligibility criteria accepted the proposed intervention. The mean number of days between completing screening and starting the HFP-M was 49.3 days. The main reasons for delay were a result of parent factors, including busy family schedules, reluctance to participate in the intervention during school holidays, and delays in replying to telephone calls and texts from the research therapist.
For three participants, the WAI-SR data were available and each parent reported high ratings for almost all items (Table 2). These data suggest that parents established positive therapeutic alliances with their HFP-M therapist in relation to the goals and outcomes of the intervention, the therapeutic tasks involved and the quality of the therapeutic relationship.
| Parent | Total WAI-SR score | Items rated very often/always (%) |
|---|---|---|
| 1 | 83 | 100 |
| 2 | 80 | 100 |
| 3 | 73 | 83.3 |
| 4 | – | – |
Clinical outcome findings
Outcome data
Three out of the four parents completed outcome measures pre and post intervention. Scrutiny of descriptive data showed a pattern of child improvement across the CAMC, the SDQ-Total, the ECBI and the CBCL-Int measures (Table 3). A similar pattern of improvement was shown for parenting behaviour and confidence across the PS and the KPSS measures (Table 4).
| Outcome | Measure | Case series participant | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Parent 1 | Parent 2 | Parent 3 | Parent 4 | ||||||
| T1 | T2 | T1 | T2 | T1 | T2 | T1 | T2 | ||
| Child | CAMC 1 | 92 | 56 | 74 | 60 | 99 | 87 | 90 | – |
| CAMC 2 | 91 | 45 | 88 | 25 | 88 | 98 | 74 | – | |
| CAMC 3 | 92 | 0 | 59 | 50 | 72 | 71 | 84 | – | |
| SDQ-Total | 26 | 23 | 17 | 7 | 31 | 20 | 12 | – | |
| SDQ caseness | Very high | Very high | High | Close to average | Very high | Very high | Close to average | – | |
| ECBI problem | 22 | 22 | 24 | 14 | 31 | 25 | 19 | – | |
| ECBI intensity | 194 | 179 | 157 | 102.86 | – | 171 | 134 | – | |
| CBCL-Int | 73 | 73 | 61 | 50 | 79 | 73 | 62 | – | |
| Outcome | Measure | Case series participant | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Parent 1 | Parent 2 | Parent 3 | Parent 4 | ||||||
| T1 | T2 | T1 | T2 | T1 | T2 | T1 | T2 | ||
| Parenting | PS | 4.0 | 2.9 | 4.1 | 3.6 | 3.9 | 4.0 | 2.8 | – |
| KPSS | 5 | 14 | 11 | 17 | 8 | 12 | 13 | – | |
| Parent | SCL-27 GSI | 3.1 | 2.6 | 0.7 | 0.4 | 2.2 | 2.1 | 2.7 | – |
Parent 1 reported improvements in the intensity of child behaviour problems and parental child concerns, and consistent improvements in parent functioning. No other noteworthy improvements in child outcomes were reported. Parent 2 reported consistent improvements across all child and parenting measures, with the index child SDQ caseness reported as ‘close to average’. Parent 3 reported a reduction in the level of child behaviour problems and the SDQ score, although caseness remained ‘high’. Parent outcomes at T2 showed little change. Two parents reported reductions in adult distress measured by the SCL-27.
Qualitative findings
Five out of the nine parents who completed the case series screening procedures agreed to interview. 141 Two parents could not be contacted and two declined participation. Three interviewed parents participated in the intervention. Of the remainder, one parent had declined the intervention as she was pregnant. The other parent had a clinical diagnosis of personality disorder, but did not meet the SCID-II criteria for a research diagnosis.
All were mothers, three of whom were lone parents. All parents had a clinical diagnosis of personality disorder. All interviewed parents were referred by CAMHS keyworkers (site 1, n = 4; site 2, n = 1). All five referring keyworkers were interviewed.
Although smaller than planned, the parent and keyworker sample sizes were consistent with recommendations for IPA data collection and its ideographic focus. Parent data analysis revealed four key themes and clinician data analysis revealed three themes.
Parent themes
Theme 1: the experience of parenthood
Parents reported a history of persistent, problematic and distressing interactions with their children, which had an impact on family life. 141 Parents described their frustration over the difficulties and a sense of helplessness:
. . I’m hitting my head up against a brick wall because I just don’t know what else to do.
Parent 3
These daily challenges appeared to define participants’ experience of parenthood. Parents experienced a sense of desperation and voiced a willingness to try whatever support was offered. This expressed interest was despite parents’ previous negative experiences of parenting interventions, which were variously described as ‘ineffective’, ‘inappropriate’ and ‘patronising’.
Theme 2: being a parent affected by a personality disorder
Parents sensed that their own experience of being a parent affected by a personality disorder appeared to mediate many encounters with professionals. 141 They described how professionals appeared to assume that a personality disorder diagnosis automatically meant that they would be a ‘bad parent’:
They were trying to say, ‘oh it’s down to your parenting, you were this, you were that . . . it’s you that has given it to him’. . . I felt like they were blaming me.
Parent 1
Parents described how they felt that clinicians did not take their parenting experiences seriously, perceiving them to be a function of the parents’ interpersonal difficulties. As a consequence, parents had the experience of feeling ‘unheard’, ‘judged’ and ‘blamed’ by clinicians, and feeling unable to communicate their sense of desperation and helplessness.
Despite their discomfort with these clinical interactions, parents felt that they often had to consent to and comply with professional advice and intervention, otherwise they would be perceived as ‘unco-operative’.
Theme 3: experience of Helping Families Programme-Modified
Despite initial pessimism, participant parents mostly described family life as ‘more manageable’ and their parenting challenges as ‘slightly easier’ post intervention. 141 Parents described successfully using the HFP-M parenting strategies, including boundary setting, use of routines and spending time with the child. Participant parents felt that they had a greater awareness of the impact of their own parenting behaviour on their child. They also felt that they had developed a greater interest and appreciation of their child’s own subjective experiences:
If I’m calmer and settled then obviously he’s gonna be a bit more calm and settled.
Parent 1
As a result, parents felt a greater sense of agency in their parenting behaviour, more confidence and an increased sense of hope:
I can see that it has worked and see the changes.
Parent 2
Theme 4: qualities of helping
Parents valued their experience of the interpersonal qualities of their research therapist, variously described as ‘encouraging’, ‘non-judgemental’, ‘open’, ‘honest’, ‘not patronising’ and ‘patient’. 141 In contrast to previous parenting and clinical experiences, parents also felt ‘listened to’, ‘understood’ and, as a result, ‘more encouraged’, with a greater sense of personal control during their appointments with the research therapist.
Keyworker themes
Theme 1: challenges in addressing parental needs
Referring keyworkers described the challenges that they experienced in meeting the needs of parents affected by personality disorders whose children had behavioural and emotional problems. 141 They attributed some of these difficulties to systemic service issues, such as ‘funding’, ‘workload’, ‘high thresholds’, and the organisational and cultural separation of CAMHS and adult services:
. . . they’re like two different worlds in what we provide.
Clinician 2
Keyworkers described the clinical challenges involved in working with the target population. As keyworkers in CAMHS, they felt that parents’ psychological needs may become ‘a secondary focus’ to the needs of their child. The keyworkers also felt ‘less confident’ to assess and manage parental mental health difficulties.
Despite clinical limitations, keyworkers felt that they often continued to support children whose parents had severe personality difficulties because of their ongoing concerns about family functioning. Keyworkers questioned the value of standard parenting programmes for parents affected by personality disorders, because they felt that the commonly used group formats could potentially exacerbate parents’ emotional and interpersonal difficulties.
Theme 2: engaging parents in the Helping Families Programme-Modified case series
Keyworkers felt that the term personality disorder could be used in pejorative ways and its use could have a detrimental impact on their therapeutic relationship with parents. 141 Keyworkers described situations in which they encountered parents becoming ‘defensive and disengaged’ when the keyworker raised issues about parental personality and interpersonal functioning.
Even with care and sensitivity, keyworkers expressed misgivings about raising the issue of personality disorder with parents who they considered eligible:
I’ve worked with her for quite a while and I was aware of the pattern that we’d been having in terms of we suggest a service, we get completely shut down . . . there’s no way she’s actually gonna come round to this.
Clinician 1
Theme 3: limited involvement during the Helping Families Programme-Modified intervention
Keyworkers felt that they had little contact with the referred parent while they were participating in the case series. 141 This was mainly a result of caseload ‘pressure’. Participation in the HFP-M meant that keyworkers felt ‘less immediate concern’ than with other families on their caseload. As a consequence, keyworkers felt that they had limited knowledge of the HFP-M’s specific impacts. They were nevertheless generally positive about its potential value:
She’s [mother] not got in touch with me. That’s a massive difference . . . just really for this parent to have someone else to speak to and to understand her . . . it’s definitely a benefit to her.
Clinician 1
Triangulation of parent and keyworker themes
Parents had previously felt that their concerns about their child’s difficulties were frequently unheard by past clinicians and services. 141 Parents often felt stigmatised because of their personality disorder diagnosis and they felt blamed for their child’s difficulties. Keyworkers described their difficulties in talking openly and effectively with parents about their personality difficulties. This led, at times, to parental over-compliance, clinician avoidance and, as a consequence, unresolved differences about the nature and cause of family difficulties.
Parents had experienced negative experiences with previous parenting interventions, of which keyworkers were often aware. 141 These experiences had the contradictory effect of increasing parents’ helplessness and desperation as well as their sense of pessimism over whether or not family life could be improved. Prior to participation, this resulted in parents and their referring keyworker feeling largely sceptical about the potential benefits of engaging in the HFP-M. In contrast, parents’ subsequent experiences of participation in the programme, the relationship with their research therapist and the programme’s impact were largely experienced as positive. 141
Case series conclusion
Notwithstanding its small sample size and the risk of selection bias, the case series provided initial evidence about the preliminary recruitment and screening procedures used and the HFP-M’s implementation and acceptability. 141 The qualitative findings, sufficient to meet IPA methodological recommendations for sample size,143,144 provided some initial insights into parent and keyworker experiences of recruitment and participation in the HFP-M.
Recruitment and screening
Recruitment proved to be more challenging and less effective than anticipated, with a lower referral rate of eligible parents than that projected in the research protocol.
Delays in ethics approval foreshortened the embedding of preliminary recruitment procedures in clinical services. Case series findings also pointed to specific challenges for keyworkers and parents to participate in the recruitment and screening procedures.
Participant identification
The recruitment cohort was small and findings should be treated with caution. Nevertheless, the case series provided evidence of specific service and parent factors that, if more widely held, may hamper recruitment flow.
These included negative parenting intervention expectancies, keyworker topic avoidance and the stigma associated with personality disorders. Interviewed parents described profound despondency about their family circumstances and their parenting role. They also expressed initial scepticism about participation in the HFP-M as a result of previous clinical and parenting support experiences.
Given the recruitment flow and the fact that the majority of referrals did not receive the HFP-M, it is unlikely that referring keyworkers’ exposure to the case series and the positive impact reported by recipient parents would have been sufficient to challenge the negative perspectives described by parents and keyworkers. Despite the development of the Joint Working Protocol, interviewed keyworkers described little subsequent contact with parents during the case series, again reducing the likelihood of learning about potential parent benefit.
Despite engagement events and access to detailed briefing packs, a significant number of referred parents proved to be ineligible prior to screening. Referring keyworkers may have not understood eligibility criteria, were unable to operationalise them accurately, or were keen to refer parents irrespective of their status.
Personality disorder criteria
Generated findings raised questions about the feasibility and acceptability of personality disorder eligibility criteria. Keyworkers, particularly those in child mental health services, found explicit discussion of the diagnostic category difficult with potentially eligible parents. Parents explained that diagnostic status often seemed to be used by clinicians as a generalised explanation of their parenting difficulties and the difficulties of their children. This resulted in parents feeling misunderstood, blamed and acquiescent. Parents expressed concern about the time required to complete the SCID-II and the DAWBA diagnostic screening interviews, which often took two or three appointments.
The research ethics review gave lengthy and detailed consideration to the proposed screening procedures. The research ethics committee (REC) was concerned about the inclusion of parents who did not have an existing personality disorder diagnosis, an objective in the research programme’s commissioning brief. The committee was keen to ensure the clearest possible informed consent procedures for these individuals, including any potentially undesirable consequences in receiving the research diagnosis. Modifications to research information materials to meet research ethics requirements were made in consultation with service user researchers and the SUAP. On review, the SUAP felt that the revised research information materials may have been experienced as daunting and potentially stigmatising by potential participants.
Complex life circumstances
A significant proportion of parents did not complete screening procedures. This was primarily a result of difficulties in contacting referred parents and serious changes in their circumstances. The length of time and the multiple contacts required by researchers to meet the referred parents were substantial. The recruitment and screening process highlighted the complex and fragile life circumstances of the target population. Unrelated to the research procedures, the children of three referred parents were subject to child protection procedures and three other parents were subject to acute mental health and/or life events.
Intervention feasibility
All four eligible parents accepted the HFP-M. The limited evidence available from the case series suggested that the HFP-M may be a feasible intervention in its current format and content. Though not methodologically robust, the small cohort of parents described positive engagement and beneficial outcomes that were consistent with published findings, including changes to their parental behaviour, reflective function and emotional regulation. 55,141
Parents appeared to value the programme’s personalised and flexible approach, contrasting this with experience of previous parenting interventions. Emergent WAI-SR and qualitative findings offered initial evidence to support the HFP-M’s model of relational therapeutic practice. The HFP-M appeared to promote sensitive, secure parental engagement and shared decision-making. There was also preliminary evidence of its potential to generate changes in parenting with participants who expressed initial ambivalence about involvement.
The programme’s Firefighting strategies appeared to help parents and research therapists to manage adverse life events and crises, while not significantly distracting from the main psychoeducational purpose of the programme.
Participants in receipt of the HFP-M provided initial endorsement of its psychoeducational content and methods. Impacts reported by parents were consistent with the aims and the content of Parenting Strategies and with the Groundwork content of the programme.
Phase 2 public and patient involvement
The research programme’s service user co-applicant (LM) and the SUAP made significant contributions to the development and revision of phase 2 recruitment and screening methods These included advice on the Joint Working Protocol, the post-screening diagnostic debriefing protocol, and the HFP-M briefing pack for keyworkers. They also advised on the research ethics application, including participant information resources and responses to REC amendment requests. The service user co-applicant (LM) and the SUAP were involved in the review of findings from the case series and contributed to revisions of eligibility criteria and screening methods.
Synthesis of phase 2 findings and implications
Phase 2 produced initial evidence about the feasibility of preliminary referral and recruitment pathways in candidate mental health services, including methods to facilitate parent engagement, identification and subsequent case co-ordination. Phase 2 also produced initial evidence about the acceptability and use of the HFP-M with eligible parents, implementation by trained and supervised research therapists as well as an account of usual parenting support for the target population.
The MWG used the TIDieR checklist to synthesise phase 2 findings in order to identify key issues of feasibility and acceptability, potential solutions and ongoing uncertainties. The MWG’s synthesis was informed by contributions from service user advisors, topic experts and the programme’s independent ethics consultant.
Specific implications drawn from the MWG synthesis were:
Characteristics of the target population
-
Parents may have previous negative experiences of parenting support that may exacerbate their difficulties and hinder help-seeking.
-
There may be significant variations in parenting support available to the target population through usual care with a low probability of receiving a specialised psychoeducational parenting intervention.
Conceptual model and intervention rationale
-
The modified MDP model used by the HFP-M provided a pragmatic, differentiated ecological description of the inter-relationship between parent, child, parenting and wider circumstances for the target population.
-
The modified MDP model may offer a more acceptable and plausible explanation to parents of their family difficulties than the narrower linear causal formulations commonly available in usual care.
Intervention organisation and delivery
-
The HFP-M is a complex and highly specialised intervention to organise and deliver that should augment rather replace usual care.
-
The research programme’s limited research therapist resources restricted the locations of the research intervention in specific teams and services.
-
The inclusion of a brief parenting support session in the usual-care arm of the planned trial may help to address potential ethics and methodological concerns.
-
The brief parenting session may provide an additional form of parenting support to parent participants randomised to the usual-care arm in the planned trial, who may otherwise receive limited or no specific parenting support.
Service and keyworker engagement and social marketing
-
Teams from children’s social care should be engaged alongside additional child and adult mental health teams in order to augment the participant flow required for the planned feasibility trial, particularly given the additional requirement for randomisation.
-
Research information and materials should be revised to differentiate trial interventions from standardised parenting programmes.
Identification of intervention recipients and research participants
-
When used in the context of recruitment to a parenting intervention, the use of a research diagnosis of personality disorder may impede recruitment and engagement of eligible parents.
-
The inclusion of parents without prior personality disorder diagnosis may be particularly problematic to implement.
-
Equivalent brief, valid non-diagnostic screening instruments may be more efficient than the SCID-II, the DAWBA and the PAPA.
-
Using existing electronic patient record systems to obtain eligible caseload may be subject to significant error.
Engagement of service users in the Helping Families Programme-Modified and its research evaluation
-
Parent engagement and recruitment may be time-consuming and affected by keyworker ambivalence and parents’ life circumstances.
-
Keyworkers may need additional guidance and skills to promote parent engagement.
Case co-ordination and integration of the Helping Families Programme-Modified with treatment as usual
-
The Joint Working Protocol reflected recommended good practice; however, keyworker caseload demands and usual-care practices resulted in its inconsistent use during the case series.
-
Research therapists will require multiple channels of communication with other professionals to ensure effective case co-ordination.
-
Research participation may lead to a reduction in keyworker involvement.
The Helping Families Programme-Modified format
-
The HFP-M’s individual format and home-based approach appeared to be consistent with the expressed preferences and needs of parents.
-
The HFP-M methods appeared to promote parent engagement but consistent weekly appointments may be challenging to deliver.
-
Fidelity monitoring needs to take account of fluctuations in participant family circumstances and programme personalisation.
Intervention content
-
The HFP-M alliance methods may promote participant engagement and participation.
-
The HFP-M Quick Wins may promote confidence, hope and commitment in the context of participants’ complex life circumstances and previous help-seeking experiences.
-
Participants may use the combined HFP-M Groundwork and Parenting Strategies modules to implement changes in parenting.
-
The HFP-M Firefighting module was validated as a method to help parents manage their life difficulties in the context of the programme’s main aims.
Conclusion
The findings broadly supported the rationale and the aims of the HFP-M research programme. The case series provided preliminary support for the HFP-M format and content acceptability. The findings suggested some changes to preliminary recruitment and screening methods, particularly in relation to eligibility criteria and screening methods, extension of recruitment to include children’s social care teams and threats to the programme delivery, such as fluctuating life circumstances of the target population. Phase 2 findings provided sufficient basis for proceeding to the conduct of the planned feasibility trial.
The planned randomised feasibility trial would test the viability of revised research procedures, including randomisation, expanded recruitment and intervention delivery. It would provide the opportunity to further explore the influence of parent, service and other contextual factors identified in phase 2. It would also produce variance, implementation and cost estimates to inform the further development and evaluation of the HFP-M.
Chapter 5 Phase 3: randomised feasibility trial and process evaluation
Parts of this chapter are reproduced from Day et al. 5 Crown Copyright © 2017. Published by Elsevier Inc. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/BY-NC-ND/4.0/).
Phase 3 aim and objectives
The aim was to assess feasibility of a full clinical trial of the HFP-M. 5,74,152 Phase 3 objectives were to:
-
assess feasibility of the revised research procedures and the HFP-M delivery
-
explore parent, service and other contextual factors on the implementation and impact of the HFP-M and its research evaluation
-
obtain ESs and variance estimates for child and parent outcomes necessary to power a full-scale trial, with child behaviour nominated as the primary clinical outcome
-
measure intervention costs and make preliminary estimates of cost-effectiveness
-
make recommendations on further development and evaluation of the HFP-M.
Phase 3 design
Phase 3 consisted of the following activities:
-
Revision of the phase 2 eligibility criteria and screening methods to improve acceptability and feasibility.
-
Development of a brief parent information and support session for inclusion in the usual-care arm of the randomised feasibility trial.
-
Development of recruitment pathways in local authority children’s social care teams and engagement of additional site 1 and 2 child and adult mental health teams.
-
Conduct of a feasibility randomised control trial of the HFP-M.
Reformulation of eligibility criteria and revision of screening procedures
Phase 2 evidence suggested that research diagnosis of personality disorder as an eligibility criterion may have hindered participant identification and recruitment. The associated screening procedures were lengthy and challenging to implement.
Consistent with the phase 1 scoping review and consultation evidence, keyworkers in phase 2 expressed concern about the stigmatising effects of the diagnostic term, particularly when used in the context of recruiting to a novel parenting intention. Keyworkers appeared reluctant to broach the topic of research participation when eligibility required diagnostic assessment of personality disorder.
Parents expressed concerns about the way in which personality disorder diagnosis could be used as a narrow explanation for their children’s emotional and behavioural difficulties, which may reduce parent engagement and the likelihood of trial participation.
Phase 2 research ethics review drew attention to concerns about the inclusion of parents without an existing clinical diagnosis of personality disorder. Phase 2 research information amendments were acceptable to independent ethics review but may have had the unintended consequence of making these materials more daunting and onerous for referred parents.
The personality disorder eligibility criterion was amended with support from topic experts, the TSC and the SUAP. The revised criterion was to include parents experiencing enduring and pervasive interpersonal and personality difficulties assessed by a score of ≥ 3 on the self-administered SAPAS. 113 The revised criterion sought to include parents likely to be affected by features of one or more personality disorders without requiring a formal research diagnosis.
The self-administered SAPAS is a very brief, psychometrically robust screening measure that provides a categorical assessment of personality difficulties with good sensitivity and specificity. The SAPAS was reviewed in phase 1 keyworker and service user consultation groups and was included in the phase 2 HFP-M: parent identification and referral decision process algorithm.
Considerably less concern was expressed about screening for child mental disorders, other than the lengthy procedure involved. The research team replaced the DAWBA with the SDQ,116,118 which was subject to phase 1 consultation and was included as a phase 2 outcome measure. The SDQ is available in parallel parent-, teacher- and youth-reported versions, and it provides an overall index of mental health symptom severity by summing subscale on emotional difficulties, conduct problems, hyperactivity/inattention problems and peer relationship problems. It is probably the most widely used measure of its kind with well-demonstrated feasibility and psychometric properties.
Revision to research information and materials
All research information, materials and communication were amended to reflect the revised eligibility criteria and screening methods. Information about the HFP-M was amended to reflect phase 2 parent engagement findings.
A total of 60 mental health and children’s social care teams were contacted about referral participation in the planned trial. Engagement and information events were held with 52 teams (86.7%), including 17 teams that referred parents to the phase 2 case series. Meetings varied in size from large-scale local authority events involving over 50 social care staff members to small meetings with team representatives. Revised briefing packs were distributed to all referring keyworkers. Keyworkers were encouraged to engage parents in ways that were consistent with phase 2 findings.
Phase 3 usual-care condition
In the absence of clear evidence of a consistent parenting pathway in usual-care practices, a brief parent information and support session was developed in line with phase 2 findings. This was intended to augment usual care received by research participants randomised to the usual-care arm of the feasibility trial.
The brief usual-care parenting session was developed in conjunction with the Empowering Parents Empowering Communities (EPEC) team, in SLAM. The psychoeducational content was derived from the evidence-based EPEC parenting programme, ‘Being a Parent’. 132 The Being a Parent programme has well-validated effects on child, parent and parenting outcomes, and high levels of participant acceptability. 132,153
The Being a Parent session was adapted by two experienced EPEC facilitators from the original eight-session curriculum with support from the SUAP and access to phase 1 findings. The session content included:
-
brief exploration of parent and child needs, parents’ experience of parenting, emotional and practical support available to the parent from family and friends, and identification of parent priorities and goals
-
selection of one topic worksheet related to primary parent goal: Exploring Parenting, Playing Together, Being Good Enough, Listening to My Child, Praising My Child, Taking Care of Myself, Understanding My Child’s Behaviour or My Child’s Emotion.
The Being a Parent session was piloted with five parents who provided favourable feedback on its acceptability and face validity; see Report Supplementary Material 4 for example content.
Randomised feasibility trial
Design
A mixed-methods, two-arm, parallel feasibility trial with random allocation of consenting parents in a one-to-one ratio to the:5,152
-
intervention arm – HFP-M, 16-session module psychoeducational parenting intervention plus usual services from mental health and social care providers
-
usual-care arm – usual services plus the Being a Parent parenting session.
Quantitative data were intended to be collected at baseline (T1), post intervention (T2) and at the 6-month follow-up [time 3 (T3)] by research staff blind to group allocation. A parallel process evaluation collected observational and qualitative interview data to develop a fine-grained understanding of parent and keyworker experience of trial procedures and interventions (see www.journalslibrary.nihr.ac.uk/programmes/hta/1219401/#/documentation; accessed July 2019).
Eligibility criteria
Eligibility for the trial depended on the parent and index child meeting the following inclusion criteria:5,152
-
Parent – being aged 18–65 years, being the primary parental caregiver for the index child, experiencing severe personality difficulties assessed by a score of ≥ 3 on the self-administered SAPAS,14 being proficient in written and spoken English and having capacity to provide informed consent to participation.
-
Index child – being aged 3–11 years, living at home with the index parent and experiencing significant emotional and/or behavioural difficulties indicated by a score of ≥ 17 on the SDQ Total Difficulties scale. 118
The exclusion criteria were:
-
Parent – presence of coexisting psychosis, being currently engaged in another structured parenting intervention, receiving inpatient mental health care and/or insufficient language or cognitive abilities affecting consent and full participation in trial procedures.
-
Index child – presence of neurodevelopmental disorder (e.g. autistic spectrum disorder, learning disability, traumatic brain injury or psychosis, such as schizophrenia), not residing with the index parent and/or currently being considered for/subject to local authority proceedings/supervision.
Interventions
Intervention arm
The HFP-M format and content were the same as summarised in Chapter 4 and Report Supplementary Material 3. 5 This intervention was designed to work collaboratively with parents to:
-
explore ways in which severe parental personality difficulties, including personality disorders, have an impact on parenting and child functioning
-
identify meaningful and realistic goals for improved parenting and child outcomes
-
use evidence-based parenting and parent self-care strategies to improve parenting, child and parent functioning.
The intervention was intended to be delivered over 16 sessions. Each session contained specific manualised content. Six specially trained and supervised trial therapists, two of whom participated in the phase 2 case series, delivered the HFP-M according to a detailed manual. Research therapists were selected, trained and supervised according to the same procedures used in the case series (see Chapter 4). The intervention primarily involved one-to-one sessions with the primary parental caregiver, although other family members were involved when appropriate.
Usual-care arm
Participants in the usual-care arm continued to receive routine care, augmented by the Being a Parent session. 5 The Being a Parent session was delivered by three trained and experienced EPEC facilitators. Parents were also provided with details of sources for additional support and information.
Concomitant interventions
Trial interventions were delivered in conjunction with medical, psychosocial and educational support and treatment services used by participant parents and their families, supported by the HFP-M Joint Working Protocol (see Report Supplementary Material 1).
Measures
Participant characteristics
Descriptive data were collected on parent and child age, gender, ethnicity, family household composition, participant diagnostic status and family socioeconomic status. Basic information on keyworkers including professional background and service type was also collected.
Feasibility evaluation
Structured record sheets were used to document key feasibility parameters related to trial procedures and intervention delivery. 5 Relevant fields were completed prospectively by research staff and trial therapists, as appropriate, to obtain the rates of:
-
participant identification, including initial approach by keyworker and verbal consent for contact by research staff
-
trial participation, including screening, eligibility, informed written consent, randomisation and reasons for non-participation
-
data collection at baseline and at follow-up, including reasons for missing data
-
intervention use, including uptake, session attendance, retention and reasons for missed sessions and dropout.
Clinical evaluation
Validated parent-report measures with well-established psychometric properties were used to assess clinical acceptability and health-economic outcomes. 5 These measures had been previously reviewed by service user representatives to ensure relevance, comparative ease of use and that they had been tested in the phase 2 case series. Outcomes were to be measured at three time points: T1, pre-randomisation baseline; T2, post-intervention follow-up, approximately 4 months from baseline; and T3, 6-month follow-up, approximately 10 months from baseline. Measures were collected by researchers who were blind to the group allocation.
Clinical outcome measures
Concerns About My Child
The CAMC132 is a visual analogue scale (0–100) that required parents to nominate, prioritise and rate up to three key concerns about their child. The same concerns nominated at baseline were re-rated at follow-up to provide a sensitive, individualised index of change. 5
Eyberg Child Behaviour Inventory
The ECBI145 is a 36-item questionnaire that assesses intensity and number of disruptive behaviour problems in 2- to 16-year-olds, providing a comprehensive measure of child behaviour difficulties. An Intensity Scale (range 36–252) score of ≥ 131 suggests behaviour problems are of significant severity. Problem Scale (range 0–36) scores of ≥ 15 indicate a significant number of behaviour problems. 5
Child Behaviour Checklist-Internalising Scale
The CBCL-Int146 is a 32-item questionnaire that assesses internalising problems in 6- to 18-year-olds (school-age version) with an alternative 36-item version for children aged 1.5–5 years (preschool version). Standardised t-scores were used to combine results from both versions and to provide a comprehensive measure of child emotional difficulties. A score of ≥ 60 indicates clinical caseness. 5
Arnold–O’Leary Parenting Scale
The PS147 is a 30-item questionnaire that assesses dysfunctional discipline styles in parents of children aged 2–16 years. It correlates significantly with more time-consuming observational ratings of parenting behaviour (r = 84). A score of ≥ 3.2 differentiates between clinic-referred and non-referred groups of children. 5
Intervention acceptability: parent-research therapist alliance measure
Therapeutic alliance was measured at T2 using the WAI-SR. 5,150
Working Alliance Inventory-Short Revised
The WAI-SR150 is a 12-item questionnaire that assesses participants’ rating of the quality of therapeutic relationships. It consists of three subscales. The goals subscale measures the extent to which a service user and therapist agree on the goals and outcomes that are the target of the intervention. The tasks subscale measures the extent to which a service user and a therapist agree on the behaviours and thoughts underpinning the intervention process. The bond subscale measures the extent to which a service user and a therapist possess mutual trust, acceptance and confidence. 5
Economic evaluation measures
The economic evaluation was conducted from the UK NHS/Personal Social Services (PSS) perspective and societal perspectives. Intervention costs were estimated by combining data on the number of screening and intervention sessions provided with the unit costs derived from local data on service expenditure and activity. Costs included therapist time, on-costs, overheads and capital. Estimates of staff training and supervision costs were also included. 5
Resource use and economic outcome information for parents and children was intended to be collected at each assessment point using the Client Service Receipt Inventory (CSRI) and EuroQol-5 Dimensions (EQ-5D)5.
Client Service Receipt Inventory
A modified version of the CSRI,154 developed especially for the trial, was used to measure resource use. It was used to measure parent-/carer-reported resource use immediately post intervention (T2), and at 6 months post intervention (T3). Versions of the CSRI have been used in > 300 research studies in the UK and internationally with adults and children. Services included in the modified CSRI included primary and secondary health care, social care, school-related services (including educational psychologists and other educational support), early years help, and youth and criminal justice services. 5 Additional activities recorded by the CSRI included time spent by parents accompanying their children to use services, days off work as a result of health problems and days out of school for children. Resource use data were combined with appropriate national unit costs based on 2016/17 GBP figures to calculate the total service costs using the Personal Social Services Research Unit (PSSRU) Unit Costs of Health and Social Care155 (2017 figures) and the NHS Improvement 2016–17 reference cost data. 156 The unit costs for prescribed medication were obtained from the British National Formulary via Medicines Complete. 157 These costs were added to the costs of the intervention to generate total health-care-related costs per participant. Parental time lost from work was valued using median wage rates. 5,158
EuroQol-5 Dimensions
The EQ-5D group159,160 develops a standardised measure of health status that provides a simple, generic measure of health for clinical and economic appraisal. For the cost–utility analysis, cost data were combined with quality-adjusted life-years (QALYs) derived from the EQ-5D. Two versions of the EQ-5D questionnaire were used: for parents/carers the EuroQol-5 Dimensions, five-level version (EQ-5D-5L); for children, the EQ-5D-Y.
Parent qualitative data
Qualitative interviews were conducted with parent participants following the T2 follow-up assessment. 5
Interview content, data collection and analytical methods were grounded in IPA. 143,144 The use of IPA was intended to focus on parents’ subjective, lived experience of, and reactions to, participation in the trial’s research methods and interventions rather than parents’ broader perspectives.
Interviews were conducted using a semistructured topic guide (see Appendix 4). These were employed flexibly and were subject to iterative development in order to reflect and explore generated themes in subsequent interviews. The guide used an open-ended approach that enabled interviewers to explore designated topics and respond flexibly to the conversational leads of interviewees as experts of their own experience. Research interviewers aimed to develop a comfortable space in which participants felt free to talk openly and honestly about their experiences.
All participants who completed T2 data collection (n = 32) were invited to interviews. Twenty-seven participants consented and five declined, owing to fatigue following completion of questionnaires or concerns about audio-recording. Fourteen participants had received the HFP-M and 13 participants had received usual care. Demographic information about qualitative interviewees is provided in Appendix 5.
Twenty-six interviews were conducted in participants’ homes. One was conducted in a café that offered sufficient privacy. Four interviews were conducted with a significant other present. A total of 26 out of 27 interviews were audio-recorded. One participant did not want to be recorded but dictated data to the interviewer.
Interviewer characteristics
Most interviews (n = 25) were undertaken by Liberty Mosse, a white British female researcher and mother of two, educated to MSc level and with professional experience of providing mental health care in NHS settings and lived experience of mental health problems. She was committed to the involvement of people with lived experience of mental health problems in research and its impact on services, participants and researchers. Alongside her research role, Liberty Mosse campaigned to undermine stigma in mental health and is a member of a mental health SUAP. When appropriate, Liberty Mosse shared information about her identity to promote rapport and lessen potential power imbalance in an interview. Two interviews were conducted by a white British male (Alex McGookin), a psychology graduate in his 20s with experience of providing mental health care in NHS services for adults affected by personality disorders. Parents were reimbursed £20 in vouchers for their time.
Keyworker qualitative data
Keyworkers were selected based on their involvement in recruitment and case management of parent participants. Interview content, data collection and analytical methods were grounded in Thematic Content Analysis. 157 The purpose was to obtain a broad understanding of the professional and service factors affecting keyworkers’ involvement in trial procedures and their perspectives on interventions provided.
A semistructured topic guide (see Appendix 6) used an open-ended, exploratory approach that was designed to explore specific topics of interest. Interviewers responded flexibly to the responses and content provided by interviewees. Interviews were conducted by telephone and audio-recorded.
Of the 27 referring keyworkers who were selected, 12 consented and completed the interview. Those not taking part in the interviews were on maternity leave, no longer employed or not responsive to the interview invitation.
Interviewer characteristics
Seven interviews were conducted by Liberty Mosse (see above). The remaining interviews were conducted by Nadine Kendall, a white British female graduate and mother of two.
Sample size
A confidence interval (CI) approach was used to calculate a sample size of n = 70 based on key feasibility objectives for the trial. 5 It was decided a priori that the single most important feasibility criterion would be a T2 trial treatment retention rate of at least 65%. 84 Using a 95% CI for the proportion of parents who completed treatment and an expected completion rate of 80% based on previous evaluations of the HFP, it was determined that a sample size of n = 35 in the intervention arm would enable a sufficiently precise estimate of this feasibility objective (95% CI 0.67 to 0.93). Further attrition was expected to occur over the subsequent follow-up period. With a sample size of n = 70 across both groups, there was 95% confidence that the anticipated 6-month follow-up rate of 70% would be estimated to be within ± 10.7%. A sample size of n = 70 was also sufficient to obtain stable estimates of population variances for future power calculations for which at least 30 participants were recommended to estimate a parameter. 161
The process evaluation involved qualitative interviews with samples of parent and keyworker participants. The precise number of participants was determined by data saturation.
Recruitment and consent procedures
Settings
Recruitment took place in sites 1 and 2 mental health services as well as concomitant local authority children’s social care services (see Chapter 2). 5
Identification
Keyworkers were encouraged to use their professional judgement in undertaking an exploratory discussion about the research with potentially eligible participants. 5 Keyworkers were advised to carefully consider the participation risks and benefits for both parents and their families. Parents were provided with verbal and written information about the trial by keyworkers. Following discussion, keyworkers determined whether or not a parent was agreeable to being contacted by a researcher.
Keyworkers provided the research team with telephone contact details for potential participants who had provided initial verbal consent. 5 The referring keyworker was informed if contact could not be made. When contact was successful, more detailed information about the study aims, eligibility criteria and procedures was given verbally by researchers to referred parents. Parents also received a PIS by post and/or e-mail, according to their preference (see www.journalslibrary.nihr.ac.uk/programmes/hta/1219401/#/documentation; accessed July 2019). Parents were encouraged to discuss the PIS with family members, keyworkers and other professionals in their network, as appropriate.
Parents were contacted again by their preferred means of communication 1 week after anticipated receipt of the PIS. When contact was successful, a researcher sought to answer any further parent questions about the research. The potential risks and benefits of being involved in the study were discussed, along with confidentiality issues, randomisation procedures and the right to withdraw from the study at any stage. During this conversation, the researcher established whether the parent (1) was willing and able to participate, (2) was unwilling/unable to participate or (3) required additional time/information to decide.
Consent
Following parent agreement, researchers arranged a face-to-face meeting with each referred parent at a convenient time and location to obtain informed written consent. This meeting reviewed the PIS as well as parents’ understanding of the research, and addressed any outstanding questions and concerns. When the parent was agreeable, the researcher obtained two signed copies of the consent forms, one of which was held by the research team and one was retained by the participant.
Allocation and randomisation
Participants were allocated a unique, anonymised identification (ID) number by the trial co-ordinator. Details were entered into the Independent Randomisation Service, an independently monitored computer system of allocation managed by the accredited Clinical Trials Unit at King’s College, London. 5 Trial participants were randomised in equal numbers to one of the two trial arms between 11 May 2016 and 29 March 2017.
Allocation outcome for each participant was communicated confidentially to the feasibility trial senior clinical supervisor (LH), who arranged for either an intervention arm HFP-M therapist or a usual-care arm Being a Parent facilitator to contact the allocated participant as appropriate. Other members of the research team including the chief investigator, statistician and research workers remained blind to participant allocation status.
Intervention delivery in both arms of the trial was planned to begin as soon as possible after allocation.
Data collection
Screening and time 1 assessments
Following receipt of parent consent, researchers arranged to administer two brief parent-report screening measures at a convenient time and location. 5 Participants received telephone and text message reminders about screening and initial baseline assessment. A reminder text message was sent 24 hours before scheduled meetings.
When both the parent and the index child were eligible, researchers established whether or not sufficient time was available to complete baseline measures. When required, a separate meeting was arranged. The T1 measures were administered in a standard sequence and took approximately 60–90 minutes to complete. Researchers helped to clarify questionnaire content and instructions when necessary. Any signs of parent discomfort were addressed sensitively and supportively. Participants were reimbursed £10 in vouchers per hour for the time involved in data completion.
Time 2 and time 3 follow-up assessments
Researchers maintained periodic contact with participants, updating them on research progress and reminding them about arrangements for completion of T2 and T3 assessments. Each participant received a telephone call from a researcher at least 1 week prior to data collection, the purpose of which was to verify the participant’s latest contact details and to review availability for the remaining research procedures. Persistent and non-intrusive efforts were made to reach each parent by telephone to arrange data collection at each time point.
Researchers remained blind to the randomisation allocation during outcome measure completion. Participants were requested not to reveal their allocation status until the point at which process evaluation interviews were conducted. The randomisation status of participants was stated in a sealed envelope, opened by researchers after they conducted the T2 follow-up outcome assessment and before conducting the qualitative interview.
Interview with keyworkers
Parent participants were informed verbally, and in the trial PIS, that the researchers may conduct a separate interview with their keyworker. 5 Keyworkers received their own PIS and Consent Form prior to taking part in a qualitative interview (see www.journalslibrary.nihr.ac.uk/programmes/hta/1219401/#/documentation; accessed July 2019). Interviews were conducted by an unblinded researcher. Keyworkers were not reimbursed for their participation.
Data management
Identifiable data, such as participant names and addresses, were removed from completed research measures. An anonymous ID was assigned to each participant to identify the questionnaires and demographic information. Personal data including participant names and contact details were transferred only electronically using encrypted USB (universal serial bus) drives and secure NHS e-mail servers.
Qualitative interviews were recorded on encrypted devices as per the requirement of the sponsor. Completed recordings were uploaded onto password-protected computers and deleted from recording devices once transcribed. Recordings were uploaded and transcribed as soon as possible after interviews were completed. Participant numbers were assigned to each interview transcript and anonymised text was used in data transcripts for names, places or any other identifiable information.
The chief investigator acted as custodian of the data in accordance with the UK Data Protection Act162 and the terms of the sponsor and funder. Personal contact details of participants were retained for the duration of the trial to enable follow-up. Other research data generated by the study will be retained for 7 years to cover contractual liability.
Analysis plan
Statistical methods
The statistical analysis was mainly descriptive. 5 It aimed to provide estimates of key trial parameters and to inform power calculations for a future definitive trial. A description of the sample was presented using means and standard deviations for continuous data, or medians and ranges where data were skewed. Frequencies and proportions were used to analyse categorical variables. Feasibility of trial retention was assessed using the proportion of a predetermined parameter and estimated 95% CIs. Because of the small number of follow-ups at T3, the original analysis plan to use multilevel models to estimate the likely range of intervention effects was revised to use analysis of covariance (ANCOVA) models with pre-randomisation values as a covariate. 163 Standardised ESs were calculated by dividing the estimated treatment effect by the standard deviation at baseline (Cohen’s d). Population variances for future power calculations were determined using the upper 80th percentile of CIs around the estimated population variance, as recommended by Browne. 164
Economic evaluation
Non-intervention service use and cost comparisons were made between the two groups at each of the follow-up time points (T2 and T3). As baseline CSRI data were not collected, the analysis could not control for baseline costs. Costs over the time points were then combined with the intervention costs and again compared between the two groups. As cost data are skewed, the analysis used bootstrapped regression models to generate 95% CIs around the differences in costs between the two groups. A cost–utility analysis was subsequently conducted by linking the cost data with QALYs. QALY gains were calculated using area under the curve methods with linear interpolation between scores, controlling for baseline utility. 165 The time intervals between the time points varied among the participants. The analysis used the time intervals that were specific to each participant. The point estimates of cost and QALYs were used to indicate whether the HFP-M was dominant, resulting in better outcomes at a lower cost, or whether each extra QALY produced by HFP-M, or usual care, was at an increased cost.
Dominance was achieved by a group if the costs were lower and the outcomes were also greater when compared with the other group. If both costs and outcomes were higher than the other group, then the incremental cost-effectiveness ratio (ICER) was calculated in order to identify the extra cost incurred per extra QALY. The ICER was produced by calculating the difference in cost between the two groups, divided by the difference in their QALYs. As the economic analysis was based over a short time period, discounting was not applied to costs and outcomes.
The non-parametric bootstrapping method was used to produce cost-effectiveness planes using 1000 cost–QALY combinations to illustrate the uncertainty surrounding the results using bootstrap regression models. This allowed the research team to determine the probability that the intervention resulted in:
-
lower costs and more QALYs
-
lower costs and fewer QALYs
-
increased costs and fewer QALYs or
-
increased costs and more QALYs than usual care.
This feasibility trial was intended to generate indicative cost-effectiveness estimates within but not beyond the study period.
Parent qualitative data analysis
Qualitative data transcripts were transcribed verbatim and downloaded to NVivo 10, a computer program that manages, classifies and analyses text-based data.
Using methods consistent with IPA,143,144 an iterative data-driven approach to analysis was used to explore and analyse parents’ subjective experiences. 5 Analysis began during data collection and progressed through a series of systematised and non-linear stages. The primary qualitative researcher (Liberty Mosse) familiarised herself with each transcript by reading each transcript thoroughly and recording initial observations and reflections. Liberty Mosse then systematically re-read transcripts, attached descriptive labels to small segments of text and then grouped similar labels together to form promising data nodes. Liberty Mosse then organised promising nodes derived from the first 11 data transcripts into a preliminary coding frame of generated themes and subthemes.
Verification of this preliminary coding frame was undertaken by a servicer user researcher (LF) who reviewed the frame, relevant transcripts and derived nodes. Liberty Mosse and Lisa Foote then reconciled their preliminary interpretations of the data available.
Remaining transcripts were uploaded to NVivo 10 as they became available. New data were analysed according to the verified coding frame. As additional analysis was undertaken, new nodes and themes were produced and the verified coding frame updated. This process was supervised by Crispin Day. Topic guide content and interviews were modified in the light of generated findings.
Final analysis was conducted by the primary qualitative researcher who coded all remaining transcripts. The resulting analysis was explored and verified by experienced qualitative researchers (CD, TW, LF). Saturation was monitored throughout data collection by examining the rate and frequency at which novel codes and themes were generated.
Interviewee characteristics are provided in Appendix 5.
Validation was undertaken by Liberty Mosse, Crispin Day and Lisa Foote with interview participants. 151
Five interviewees were invited to a group discussion of findings, three of whom attended. At the event, Liberty Mosse and Lisa Foote presented findings, using anonymised extracts to ground results in specific data, for discussion in an open and exploratory way and invited participants to reflect on the authenticity and representation of the findings (see Report Supplementary Material 5). Participants validated the structure of generated findings. Some specific themes and subthemes were renamed to improve clarity and more accurately reflect participant experience.
Keyworker qualitative data analysis
Interviews were transcribed verbatim, uploaded to NVivo 10 and analysed using thematic content analysis. 5 Thematic content analysis was undertaken in a series of iterative steps. 166
First, each transcript was read thoroughly by the primary researcher (Liberty Mosse), who generated an initial list of observations, reflections, ideas and meanings from which a provisional framework for understanding the data was developed. Based on this provisional framework Liberty Mosse re-read transcripts, attaching descriptive labels to small segments of text and creating preliminary categories in order to understand and further analyse the data. A second researcher (Nadine Kendall) re-read selected transcripts, noting observations and reflections in relation to the provisional framework and generated findings. These researchers shared their findings in order to produce a unified set of generated categories based on salient and prominent features of the data. These generated categories were shared with Crispin Day in order to establish a coherent set of themes and subthemes to describe the data.
Interviewee characteristics are described in Appendix 7.
Synthesis of findings
Findings from each of the quantitative and qualitative analyses above were combined in order to report on the principal aims of the feasibility trial.
The relevant themes and subthemes derived from each qualitative analysis, together with illustrative data quotes, are reported in relation to the feasibility, acceptability, clinical outcome and cost aims of the trial in subsequent chapters.
Interpretative phenomenological analysis of parent interview data generated three main themes, each with a number of subthemes. The overall structure of the parent qualitative results is described in Appendix 8. The main themes are listed here with the relevant trial aim in brackets:
-
theme 1 – experience of RCT methods and procedures (trial feasibility)
-
theme 2 – life circumstances, personal histories and help-seeking (trial feasibility)
-
theme 3 – experiencing a psychoeducational parenting intervention (intervention acceptability and clinical outcome).
Thematic content analysis of keyworker interview data generated four themes, each with a number of subthemes. The overall structure of the keyworker qualitative results is described in Appendix 9. The main themes are listed here with the relevant trial aim in brackets:
-
theme 1 – engaging teams and keyworkers (trial feasibility)
-
theme 2 – implementing trial methods and procedures (trial feasibility)
-
theme 3 – keyworker decision-making (trial feasibility)
-
theme 4 – intervention characteristics (intervention acceptability and clinical outcome).
Trial governance
The trial was overseen by the PMG, the TSC and the DMEC in accordance with responsibilities described in Chapter 2. 5 All key trial documents and procedures were reviewed internally by the PMG, the SUAP, the TSC and the DMEC.
Risk and ethics issues
Independent ethics review and site permissions
Ethics approval was obtained from Health Research Authority South East Coast and Brighton & Sussex Research Ethics Committee (reference: 16/LO/0199). Relevant NHS site research and development approvals were provided.
Safe and effective care
The well-being and safety of participating parents and their children were paramount. The HFP-M augmented usual care. In line with the HFP-M Joint Working Protocol, primary case management responsibility remained with the referring keyworker. As described previously, the Joint Working Protocol set out the agreed roles and responsibilities, clinical working practices and co-ordination between the HFP-M research therapists and routine service practitioners.
Potential adverse events
The chief investigator was responsible for reporting to the DMEC and to the responsible REC committee any serious adverse event that was both related to the research procedures and unexpected. Researchers carrying out interviews and assessments with participants were instructed to report any adverse circumstances to the project manager and principal investigator, no matter how minor the circumstances may appear. Therapists were required to impart information on potentially serious adverse events to their supervisor during supervision sessions and to the chief investigator at other times, if necessary. A standard form for reporting serious adverse events was used by all trial staff. No serious adverse events were reported during the study.
Access to databases
The chief investigator (CD) acted as custodian of the data in accordance with legislation and the requirements of the research sponsor (King’s College London) and the funder (NIHR, UK).
Chapter 6 Feasibility of trial methodology and sample characteristics
This chapter reports quantitative and qualitative results related to the feasibility of trial methodology and sample characteristics.
Quantitative findings report on 10 areas of recruitment and retention feasibility, the most important being the a priori feasibility criterion that the T2 treatment retention rate would be at least 65.0%. Relevant qualitative results drawn from parent and keyworker interview data are provided to give further fine-grained information about the influence of parent, service and other contextual factors on trial methods and procedures.
This chapter then reports the demographic and health characteristics of the parents in the trial, supported by relevant qualitative findings.
Recruitment and retention feasibility
Trial recruitment was planned to take 6 months; however, the actual recruitment period was 10 months. The recruitment target was originally 70 participants, which was revised to 48 owing to recruitment delays in site 2. Feasibility results are reported across 10 areas. 152
Rate of initial participant identification by keyworkers
Referring keyworkers and other service staff were not able to provide reliable estimates of the number and proportion of potentially eligible parents identified from caseloads. As a result, it was not possible to report reliably on the proportion of service users across referring teams whom keyworkers considered likely to meet trial eligibility criteria.
Rate of service user consent to be contacted by research team
The lack of accurate data on keyworker initial participant identification data meant that it was not possible to report on the proportion of service users considered eligible by keyworkers who then consented to be approached by researchers.
A total of 89 service users gave verbal consent for their contact details to be given to the research team, as shown in Figure 3. Service users were referred by a total of 70 keyworkers from 52 teams. The modal number of referrals per keyworker was 1 (range 1–10).
FIGURE 3.
Phase 3 randomised feasibility trial recruitment CONSORT flow diagram. Reproduced with permission from Day et al. 152 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The figure includes minor additions and formatting changes to the original.

A total of 65 (73.0%) service users were referred from site 1 services. The remaining 24 (27.0%) service users were referred from site 2 services. Across the sample as a whole, 30 (33.7%) service users were referred from adult mental health services, 29 (32.6%) from CAMHS and 30 (33.7%) from children’s social care services (Table 5). Site 1 participants were quite evenly spread across the three referral sources, whereas CAMHS referrals were more common in site 2 (see Table 5).
| Site | Referral source (service), n (%) | Total, n (%) | ||
|---|---|---|---|---|
| AMH | CAMHS | Children’s social care | ||
| SLAM | 23 (25.8) | 18 (20.2) | 24 (27.0) | 65 (73.0) |
| CNWL | 7 (7.9) | 11 (12.4) | 6 (6.7) | 24 (27.0) |
| Total | 30 (33.7) | 29 (32.6) | 30 (33.7) | 89 (100) |
Rate of successful contact of referred service users
Researchers made telephone contact with 87 (97.7%) referred service users. Two service users moved from the area without forwarding their contact information, before successful contact was made. The number of contact attempts per participant ranged from 1 to 13.
Rate of service user initial eligibility for screening
At initial contact, 60 (69.7%) referred service users met criteria for screening. The most common reason for ineligibility was that parents declined to participate in the trial (n = 12, 13.5%) (see Figure 3). Six referred service users were excluded for child-related reasons, most commonly because the child had a diagnosis of autism (see Figure 3).
Rate of service user informed consent for the screening procedure
Written consent for research participation and screening was obtained from all participants meeting initial eligibility criteria prior to screening (n = 60, 100.0%).
Rate of availability for the trial screening procedure
All eligible participants (n = 60, 100.0%) completed the trial screening procedure. The number of contacts to arrange screening appointments ranged from 1 to 13. Fifty-nine (98.3%) screening appointments were conducted in the service users’ homes.
Rate of screening participants meeting trial screening criteria
Both the SAPAS and the SDQ screening instruments were completed by all participants with no missing items.
A total of 48 service users met both parent (SAPAS) and child (SDQ) screening criteria. Five (8.3%) service users were excluded because they met neither parent nor child screening criteria (see Figure 3). Four (6.7%) were excluded because they did not meet the parent SAPAS criterion and three (5.0%) were excluded because they did not meet the child SDQ eligibility criterion.
All participants fulfilling all of the eligibility criteria (n = 48) agreed to enter the trial, representing 80.0% of service users who completed the screening measures. This represented 53.9% of service users initially referred to the trial and 68.6% of the originally planned trial sample of 70 participants.
A total of 36 (75.0%) participants were referred from site 1 services, as shown in Table 6. Site 1 recruitment exceeded the planned number by 2.9%. Site 2 recruitment (n = 12) was only 34.3% of the planned number. The main contributing factors for lower site 2 recruitment were a delay in starting recruitment and lower levels of team and keyworker engagement.
| Site | Referral source (service), n (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| Eligible service users | Ineligible service users | |||||||
| AMH | CAMHS | Children’s social care | Total | AMH | CAMHS | Children’s social care | Total | |
| 1 | 14 (38.9) | 10 (27.8) | 12 (33.3) | 36 (75.0) | 9 (31.3) | 8 (27.6) | 12 (41.3) | 29 (70.7) |
| 2 | 4 (33.3) | 6 (50.0) | 2 (16.7) | 12 (25.0) | 3 (25.0) | 5 (41.7) | 4 (33.3) | 12 (29.3) |
| Total | 18 (37.5) | 16 (33.3) | 14 (29.2) | 48 (100.0) | 12 (29.3) | 13 (31.7) | 16 (39.0) | 41 (100.0) |
Eighteen (37.5%) trial participants were referred from adult mental health services, 16 (33.3%) from child mental health services and 14 (29.2%) from children’s social care (see Table 6).
Randomisation to trial arm
Of the 24 eligible participants randomised to the intervention arm, 21 (87.5%) participants accepted the HFP-M and were allocated to a research therapist. The modal duration between randomisation and first intervention session was 2 weeks (range 1–23 weeks).
In total, three parents (12.5%) declined the HFP-M (Figure 4). One parent gave birth, another was in conflict with her partner about participation and a third did not respond to the invitation to participate.
FIGURE 4.
Participant data completion at T1, T2 and T3.
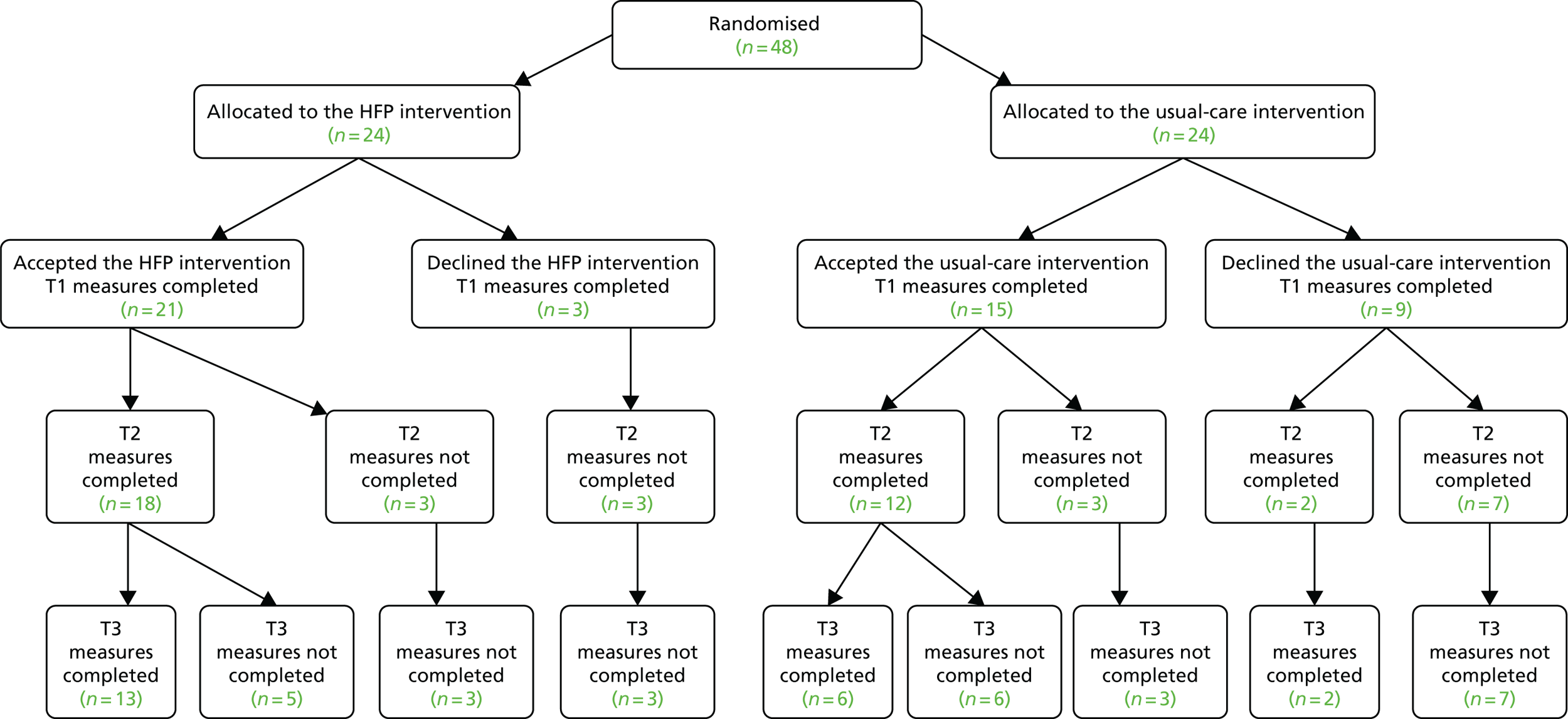
There was a significant statistical difference in the uptake of the two trial conditions [χ2 = 4.0, df = 1 (48); p < 0.05].
Fifteen (62.5%) participants randomised to usual care took up the Being a Parent psychoeducational session (see Figure 4). The most common reason for declining to participate in the sessions was that participants had hoped to be allocated to the HFP-M. The modal duration between randomisation and first intervention session was 5.5 weeks (range 1–17 weeks).
Rate of baseline (time 1) self-report measurement completion
All participants completed T1 assessment measures (Table 7). The vast majority (n = 46, 95.9%) completed these immediately after screening. Two participants chose to arrange a further appointment to complete baseline measures. There were less than 0.1% missing data items across baseline assessment questionnaires.
| Condition | Time point, n (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| T1 | T2 | T3 | |||||||
| Accepted | Declined | Total | Accepted | Declined | Total | Accepted | Declined | Total | |
| Intervention (N = 24) | 21 (87.5) | 3 (12.5) | 24 (50.0) | 18 (100.0) | 0 (0.0) | 18 (75.0) | 13 (100.0) | 0 (0.0) | 13 (54.2) |
| Control (N = 24) | 15 (62.5) | 9 (37.5) | 24 (50.0) | 12 (85.7) | 2 (14.3) | 14 (58.3) | 6 (75.0) | 2 (25.0) | 8 (33.3) |
| Total (N = 48) | 36 (75.0) | 12 (25.0) | 48 (100.0) | 30 (93.8) | 2 (6.2) | 32 (66.7) | 19 (90.8) | 2 (9.2) | 21 (43.8) |
Baseline economic data (CSRI) were not included in T1 data collection as a result of researcher error.
Rate of time 2 and 3 self-report measurement completion
At T2, 32 (66.7%, 95% CI 51.6% to 79.6%) participants completed post-intervention assessments. More HFP-M participants (75.0%) completed assessments than usual-care participants (58.3%), but this difference was not statistically significant (χ2 = 3.2, p = 0.074). Only two participants (4.2%, 95% CI 0.5% to 14.3%) who declined the allocated intervention, both from the usual-care group, completed T2 measures (see Table 7). Thirty participants (83.3%, 95% CI 67.2% to 93.6%) who accepted an intervention at randomisation completed T2 measures. The majority of participants who declined an intervention following randomisation did not complete T2 measures (n = 10, 83.3%, 95% CI 51.6% to 97.9%) (see Figure 4).
The modal number of contacts by researchers to complete T2 data collection was 3 (range 1–8). Reasons for non-completion of T2 measures included researchers being unable to contact participants (n = 5), participant declining completion (n = 5), participant life circumstances (n = 3), participant ill-health (n = 2) and child subject to safeguarding (n = 1).
Time 2 measures were completed a mean of 42 weeks [standard deviation (SD) 14.6 weeks] after T1 [intervention arm mean = 49 weeks (SD 14.2 weeks); usual-care arm mean = 32 weeks (SD 8.8 weeks)]. There were less than 0.1% missing data items across T2 assessment questionnaires. Twenty-six participants completed the T2 CSRI economic measure.
At T3, 21 (43.8%) parents accepted into the trial (intervention arm, n = 13, 54.1%; usual-care arm, n = 8, 33.3%) completed assessment measures. Twenty-one (65.6%) participants completed T3 measures after also completing T2 measures. T3 measures were completed a mean of 20 weeks (SD 8.9 weeks) after T2 assessments.
The modal number of contacts for researchers to complete T3 data collection was similar to T2.
Item completion rates at T3 were similar to the previous two time periods. Twenty participants (76.9%) provided T3 economic data. Missing data affected health economic analysis and interpretation of results.
Parent qualitative findings related to trial methodology
Theme 1: experience of randomised controlled trial procedures
Theme 1 focused on participants’ experience of trial procedures and design, and the emotional effects of undertaking trial procedures. The theme consists of three subthemes: subtheme 1 (trial procedures), subtheme 2 (trial design choice) and subtheme 3 (lived experience of trial allocation).
Subtheme 1: trial procedures
This subtheme reflected participants’ practical experience of completing the methodological procedures required for participation in the feasibility trial. Participants offered limited, but generally positive, descriptions about the information they received from keyworkers and research staff about the aims and purpose of the research:
They fully explained the whole scenario to us, so we were very aware about what was going on.
Participant 1002, paragraph 26
Views on screening and outcome questionnaire completion varied among participants. Some parents felt that questionnaire completion was useful and hoped that it provided awareness of their difficulties:
I think by us doing that questionnaire, it would kind of give you guys an insight into what kind of support [I need].
Participant 1020, paragraph 4
Other parents were more cautious about their experience of questionnaire completion, highlighting the emotional impact of answering questions about significant personal and family difficulties:
Answering those questions can have a mental impact. Can make you feel guilty or like a bad parent. When ringing to make appointments warn people that they are quite in-depth.
Participant 2011, paragraph 5
Generally, participants were complimentary about the manner, sensitivity and understanding of the researchers who conducted data collection:
Meeting [the researchers], it was really lovely . . . and very respectful and considerate of how I’m feeling and, [they] were able to recognise that if I’m upset and I need to stop . . . which I think is really, really important.
Participant 2008, paragraph 13
Subtheme 2: trial design choice
The most significant methodological design issue for participants was the use of randomisation. Some parents, usually those randomised to the intervention arm, described how they fully accepted the process of random allocation:
. . . there’s potentially this really useful programme . . . but no, I always knew there was a chance I would be in the other group . . .
Participant 1013, paragraph 45
Despite understanding the logic of the purpose and the procedures used in the trial, some parents felt that randomisation was not an appropriate procedure mainly because it presented a risk to receiving the HFP-M:
I don’t know . . . you’re doing these questionnaires and . . . you’re being truthful about it, and you’re asking for help. I don’t think it should be a computer that’s deciding whether this child or this adult needs help.
Participant 1034, paragraph 54
Parents also expressed reservations and doubts about random allocation because of the significant needs of the families involved in the trial:
I think that’s completely wrong. Because what happens if there’s a family out there who’s really struggling? And then there’s a family that’s not. And you’ve given the 16 hours to the family that’s not really struggling and you’ve given that one session to that poor family that is struggling.
Participant 2003, paragraph 85
Er, to be honest I’m not too sure, it’s kind of annoying because often maybe some of those parents that got overlooked who need the support so in that sense I’m not a terribly big fan of it.
Participant 1030, paragraph 46
Other parents, most frequently those allocated to the intervention arm, felt that, while regrettable, randomisation was necessary for service development and the advancement of research:
I don’t know, I think it’s like trial research of anything really, you’ve got to have two sides of the story . . . to know the difference of help or if you don’t get the help, I suppose I was pleased that we was one of the ones that did get it so . . . I did understand it.
Participant 1016, paragraph 13
But, I also understood that it’s research and that, that in order to do research properly you have to have um, it’s split like that, you have to have one, you know, one group doing it the same and one group doing it differently.
Participant 2008, paragraph 22
Subtheme 3: lived experience of trial allocation
Subtheme 3 focused on the emotional impact of trial allocation. For some parents, concerns about allocation began at the point at which the randomised design was explained:
When, when [the researcher] said, ‘It could be a one session or a 16 session. It depends’, I was worrying then.
Participant 1024, paragraph 58
Participants’ emotional response to the randomisation decision was broadly determined by participants’ resulting allocation. Most participants allocated to the intervention condition described a sense of relief and happiness:
Oh gosh I was elated.
Participant 1020, paragraph 21
Luckily I got the longer term, so yeah that made me quite happy.
Participant 1018, paragraph 19
Some participants, relieved to have been allocated to the HFP-M, also described the potential distress they may have felt had they been randomised to the usual-care condition:
There’s an opportunity here but, well, it might not be yours. It would have really . . . made me very low, actually . . . it would have had a very negative effect on me.
Participant 1023, paragraph 25
Some parents felt a sense of resignation about allocation to the usual-care condition, which resonated with an established pattern of disappointments in their lives:
To be honest with you, I’m very negative anyway about myself and when they were going through the questionnaires and told me that I was qualified and I would either get the one session or the 16. The first thing that came into my head was, ‘I know I’m going to get the one session’ so because . . . I’m so negative on how I think anyway, so I wasn’t really that disappointed because I always expect the worst I guess.
Participant 1015, paragraph 2
I’m trying to sort myself out and everything. What’s the point? You try but you don’t get nowhere . . . That’s alright, no one’s fault is it. It’s just life, I should have known.
Participant 1029, paragraph 69
Some parents found it difficult to understand why they had not been allocated to the trial intervention given the nature of their needs:
I was told that there was a chance that I might not be accepted onto the programme . . . I filled out all the questionnaires . . . and my score was really high . . . when I got contacted back and they said that . . . I hadn’t been accepted and I said ‘Why, because my score was really high?’
Participant 1034, paragraph 18
A significant number of parents offered detailed and emotional accounts of their disappointment and anger following allocation to usual care. For some, this resulted in a sense of alienation and withdrawal:
When I didn’t get them and I was proper disappointed and angry so I didn’t even answer the phone or reply to the e-mails . . . because I was just angry and **** off and I knew, like, one session just wouldn’t do it and because . . . in my head I got 16 sessions when I didn’t get them it . . . was upsetting because I put all my hopes on these 16 sessions fixing me.
Participant 1029, paragraph 48
Other parents carried a sense of recrimination and self-blame about the outcome of trial allocation:
Also, it should be done by the needs of the child and the parent, not random. As a mum, I personally didn’t believe that I was good enough, or my son was, to get the sessions. I thought, ‘for real, I opened up and I felt I was stressed out and my head was messed up and then no one helped’ . . . I thought they thought my problems were too much.
Participant 2011, paragraph 7
Keyworker findings related to trial methodology
Two themes generated by the thematic content analysis of keyworker interview data were most relevant to the feasibility of trial methodology: theme 1 (engaging teams and keyworkers) and theme 2 (implementing trial methods and procedures). Each theme consisted of several subthemes, described below.
Theme 1: engaging teams and keyworkers
This theme summarised keyworkers’ experience of trial communication and information that mobilised their interest in the trial and motivated them to refer parents. It consisted of subtheme 1 (clear, personal communication) and subtheme 2 (proactive, persistent contact).
Subtheme 1: clear, personal communication
Referring keyworkers usually heard about the trial either from team colleagues, most often during team meeting case discussions, or directly from researchers, during presentation visits to their team:
It was probably through the [service manager] and then I think actually [researchers] might have come to our team meeting.
Keyworker 4006, paragraph 21
Keyworkers preferred direct contact with researchers to being sent more generalised e-mail information. Face-to-face discussion allowed keyworkers to clarify and feel assured about the relevance of the research trial, its purpose and methods:
It was presented in a quite detailed way and we had opportunities personally to discuss concerns, it was quite helpful . . . Sometimes when you get information through an e-mail and it’s not the same as having people coming in to really tailor it around us, so that helped.
Keyworker 4007, paragraph 41
Although keyworkers mainly considered the trial information provided adequate for identification and referral, some keyworkers wanted better plain English summaries and more guidance about how to explain the trial interventions to parents:
I didn’t feel like I had a lot of information about the programme itself . . . I got, the gist of it . . . a mixture between a parenting programme and something that’s more therapeutic . . .
Keyworker 4002, paragraph 41
I don’t know it well enough to be able to explain it to someone. So, I think kind of guidance on that may be helpful, just how to kind of explain it in a way that doesn’t just sound . . . clinical. I think that maybe can be off-putting for people. I didn’t get that guidance.
Keyworker 4015, paragraph 35
Subtheme 2: proactive, persistent contact
Keyworkers found that frequent reminders and proactive contact from the research team helped them to keep the trial in mind, especially given the demanding context of their routine clinical work:
You have to continually promote these things for people because you know they’re very busy out and about in the community and at home visits and sometimes it’s just continually reminding people what’s out there for people.
Keyworker 4006, paragraph 63
Regular updates on the referral progress from the research team were useful, as was, although less commonly organised, a nominated link practitioner in the clinical team designated to liaise with the research team.
Theme 2: implementing trial methods and procedures
Theme 2 described keyworkers’ experience of trial methods and referral procedures, including their use of trial criteria and their reaction to the use of a randomised trial design. It consisted of subtheme 1 (trial criteria), subtheme 2 (randomisation) and subtheme 3 (referral pathway and progress).
Subtheme 1: trial criteria
Trial criteria helped the majority of keyworkers to identify parents who they thought would be suitable for the trial. Some keyworkers were disappointed that inclusion and exclusion criteria restricted access to the trial for parents whom they were concerned about and considered could benefit.
Keyworkers described giving careful consideration of multiple family mental health and other needs and their match with trial criteria:
She was struggling and it was clearly linked to the struggles within the family. A lady who was a single parent and who had many children and more than one of them displayed some difficulties, like emotional difficulties and behavioural difficulties. She seemed to have met the criteria for your research project and also, she seemed to be in need for support.
Keyworker 4014, paragraph 7
Keyworkers were not only matching parents with trial criteria, but also giving attention to parents’ capacity to engage and benefit from the trial. Some keyworkers described some referred parents’ relief that they did not meet trial criteria on screening:
. . . you know the other thing is, what is that patient’s capacity to actually benefit from and utilise what you offer?
Keyworker 4003, paragraph 37
Subtheme 2: randomisation
Keyworkers were sometimes initially wary about the consequences for service users of a trial involving randomised allocation. Keyworkers gave serious consideration to the possible negative effects of random allocation on parents and the potential consequences for the keyworker:
So, I asked lots of questions about it, at the time, because I just thought, this is really, potentially setting people up to feel distressed which, if they’re allocated into the control group, will be something that potentially care co-ordinators will have to try and work with the possible distress that that could throw up.
Keyworker 4016, paragraph 13
Half of the keyworkers expressed misgivings about the use of random allocation in the trial design. This was frequently based on their view that randomisation represented the restriction of an intervention that should, in their view, be more widely available:
It just feels such a shame, I think that’s the difficulty, that there is a treatment that’s been so optimal, that the . . . family might not get to have a trial of it.
Keyworker 4010, paragraph 68
At the same time, some keyworkers were pragmatic about randomisation, often seeing the trial as a means of offering an intervention that would otherwise not be available to all:
They just wanted some parenting support, so I don’t think they really minded the fact that it was a 50/50. No one complained about it, no one said that there was an issue.
Keyworker 4002, paragraph 59
Keyworkers described processes that helped them to discuss the trial with parents, including adopting an open and straightforward approach with parents about the trial design and the potential outcome of randomisation:
Well randomisation is always a bit fussy isn’t it, and I think, just being very clear about, you know, numbers and what might happen and what might not happen enabled me to be very clear with the person I referred, so that I could try and get her as ready as possible for, possible disappointment . . .
Keyworker 4016, paragraph 89
Keyworkers were also aware of the emotional effects that random allocation had on themselves and acknowledged that these may be different from the reactions of parents:
This family completely understood the notion of it and were very on board with understanding that they may or may not get [Helping Families Programme]. I think it was probably more concerning for me than it was for them.
Keyworker 4010, paragraph 70
These effects were moderated for some keyworkers by knowing that the usual-care condition included the single psychoeducational session:
What made it easier when she was refused the other intervention [Helping Families Programme], she was still offered something. At least she was offered something.
Keyworker 4014, paragraph 47
Subtheme 3: referral pathway and progress
Keyworkers mainly construed referral to the trial as the opportunity to seek an additional service for parents who may otherwise not be available, rather than the opportunity to participate in a research programme:
I don’t know whether all services are as good as this one, but we just seemed to . . . you all got back to me quickly.
Keyworker 4017, paragraph 85
Keyworkers largely found the trial referral pathway straightforward and responsive:
I found a pathway to yourselves very easy and smooth and accommodating of us.
Keyworker 4003, paragraph 23
They appreciated the rapid response of the research team to keyworker enquiries, which they felt helped to engage referred parents:
It was a very straightforward system and it was quick. Where you have systems that are just straightforward and not too complicated, you’re gonna get better results.
Keyworker 4002, paragraph 113
Keyworkers frequently felt well informed as parents progressed through the trial procedures and found research team feedback helpful:
Communication [was] very, very good. I received the e-mail back informing me what happened to the client, what she was offered, where she was allocated. It was very helpful.
Keyworker 4014, paragraph 43
Sample characteristics
This section reports the demographic, health and outcome characteristics of the sample at baseline. 152
Demographic characteristics
Of the 48 eligible participants, only one was male (2.1%) (Table 8). All participants were the biological parent of the index child. Parents’ mean age was 34.9 (SD 7.1) years. The majority (n = 28, 61.0%) of participants described themselves as white British/Irish (see Table 8). A smaller proportion described themselves as black/black British (n = 9, 19.6%) or of dual heritage (n = 6, 13.5%). English was the first language spoken in the majority of homes (n = 44, 91.7%). Twenty-five (55.6%) participants had completed education at 18 years or younger. Only four participants (8.9%) were graduates.
| Demographic characteristic | Baseline (T1) | ||
|---|---|---|---|
| Total (N = 48) | Intervention (N = 24) | Usual care (N = 24) | |
| Parent gender (female), n (%) | 47 (97.9) | 24 (100.0) | 23 (95.8) |
| Parent age (years), mean (SD) | 34.9 (7.1) | 34.7 (7.5) | 35.0 (6.9) |
| Received psychiatric diagnosis, n (%) | 25 (86.2) | 16 (88.9) | 19 (81.8) |
| Psychiatric diagnosis duration (years), mean (SD) | 9.7 (7.4) | 8.6 (7.0) | 10.9 (8.1) |
| Parent relationship to index child (biological parent), n (%) | 46 (100.0) | 24 (100.0) | 22 (100.0) |
| Index child gender (male), n (%) | 26 (55.3) | 12 (50.0) | 14 (60.9) |
| Index child age (years), mean (SD) | 7.8 (2.2) | 7.7 (2.0) | 7.9 (2.2) |
| Number of children at home, median (range) | 2 (1–5) | 2 (1–5) | 2 (1–5) |
| Not in paid employment, n (%) | 37 (80.4) | 19 (79.2) | 18 (81.8) |
| Lone parent, n (%) | 31 (67.4) | 14 (58.3) | 17 (77.3) |
| Partner in employment, n (%) | 9 (19.5) | 6 (25.0) | 3 (12.5) |
| Parent education, n (%) | |||
| Graduate | 4 (8.9) | 2 (8.3) | 2 (9.5) |
| University not completed | 3 (6.7) | 3 (12.5) | 0 (0.0) |
| Other (e.g. NVQ) | 13 (28.9) | 6 (25.0) | 7 (33.3) |
| Left school at 18 years | 9 (20.0) | 4 (16.7) | 5 (23.8) |
| Left school at 16 years | 7 (15.6) | 4 (16.7) | 3 (14.3) |
| Left school at < 16 years | 9 (20.0) | 5 (20.9) | 4 (19.0) |
| Ethnicity, n (%) | |||
| White UK/Irish | 28 (61.0) | 13 (54.2) | 15 (68.2) |
| Black UK/African-Caribbean | 9 (19.6) | 7 (29.2) | 2 (9.1) |
| Dual heritage | 6 (13.0) | 3 (12.5) | 3 (13.6) |
| Black UK/African | 2 (4.3) | 0 (0.0) | 2 (9.1) |
| Other | 1 (2.2) | 1 (4.2) | 0 (0.0) |
Of the participants who provided information, 25 (86.2%) parents had received a formal psychiatric diagnosis at a mean age of 25.8 years (range 13–40 years). The mean time since initial diagnosis was 9.7 (SD 7.4) years.
In total, 26 (54.2%) index children were male, with a mean age of 7.8 (SD 2.2) years. The median number of children in the home was 2 (range 1–5) (see Table 8).
The majority of participants were lone parents (n = 31, 67.4%) and were not in paid employment (n = 37, 80.4%).
Fifteen (32.6%) parents had a partner who shared parental child care responsibilities. Nine participants (19.5%) had partners in paid employment, predominantly part-time (n = 7, 15.2%). In total, there was no parent in paid employment in 30 (65.2%) of the participant households.
Family health characteristics
The majority of participants suffered significant difficulties with anxiety and/or depression (n = 22, 61.1%), 17 (47.2%) suffered significant pain and/or discomfort, with a smaller proportion experiencing difficulties in undertaking everyday activities (n = 13, 36.1%) (Table 9).
| Parent health status | Baseline (T1), n (%) | ||
|---|---|---|---|
| Total (N = 36) | Intervention (N = 17) | Usual care (N = 19) | |
| Mobility problems | 9 (25.0) | 4 (23.5) | 5 (26.4) |
| Problems in self-care washing and dressing | 3 (8.3) | 1 (5.9) | 2 (10.5) |
| Difficulties in undertaking usual activities | 13 (36.1) | 7 (41.1) | 6 (31.6) |
| Suffered pain/discomfort | 17 (47.2) | 6 (35.3) | 11 (57.9) |
| Experienced anxiety/depression | 22 (61.1) | 10 (58.8) | 12 (63.1) |
The health status of the index children was less severely affected. Six (15.8%) children were significantly affected by anxiety and/or depression and five (13.2%) children had difficulties in undertaking their usual activities (Table 10).
| Child health status | Baseline (T1), n (%) | ||
|---|---|---|---|
| Total (N = 38) | Intervention (N = 18) | Usual care (N = 20) | |
| Mobility problems | 1 (2.6) | 0 (0.0) | 1 (5.0) |
| Problems in self-care washing and dressing | 3 (7.9) | 2 (11.1) | 1 (5.0) |
| Difficulties in undertaking usual activities | 5 (13.2) | 2 (11.1) | 3 (15.0) |
| Suffered pain/discomfort | 3 (7.9) | 0 (0.0) | 3 (10.0) |
| Experienced anxiety/depression | 6 (15.8) | 2 (11.1) | 4 (20.0) |
Clinical characteristics
Baseline clinical outcome scores were consistently elevated. For the ECBI, the PS and the CBCL-Int, the means were above cut-off points for clinical severity (Table 11). 152
| Measure | Baseline (T1), mean (SD) | ||
|---|---|---|---|
| Total (N = 48) | Intervention (N = 24) | Usual care (N = 24) | |
| CAMC 1 | 85.3 (15.3) | 84.6 (16.0) | 85.9 (14.7) |
| CAMC 2 | 84.0 (17.4) | 85.0 (19.1) | 82.9 (15.7) |
| CAMC 3 | 80.0 (17.6) | 81.0 (17.0) | 78.9 (18.5) |
| ECBI problem | 22.3 (6.7) | 22.1 (7.4) | 22.4 (6.1) |
| ECBI intensity | 168.9 (33.6) | 168.3 (35.8) | 169.6 (31.8) |
| CBCL-Int (t-score) | 71.9 (10.7) | 72.9 (9.7) | 70.9 (11.9) |
| PS | 3.7 (0.7) | 3.7 (0.7) | 3.8 (0.8) |
| KPSS | 10.5 (3.0) | 10.1 (3.1) | 10.9 (2.8) |
| SCL-27 GSI | 1.6 (0.86) | 1.7 (1.0) | 1.6 (0.7) |
Over 80% of the ECBI scores exceeded cut-off points indicating clinical caseness (Table 12). Three-quarters of the parent-reported parenting behaviour exceeded the PS recommended cut-off point for clinically significant parenting behaviour difficulties.
| Measure | Baseline (T1), n (%) | ||
|---|---|---|---|
| Total (N = 48) | Intervention (N = 24) | Usual care (N = 24) | |
| ECBI problem caseness (≥ 15)a | 41 (89.1) | 21 (87.5) | 20 (90.9) |
| ECBI intensity caseness (≥ 131)a | 39 (83.0) | 19 (79.2) | 20 (83.3) |
| CBCL-Int (t-score) caseness (≥ 60)a | 45 (95.8) | 23 (95.8) | 22 (95.7) |
| PS caseness (≥ 3.2)a | 35 (74.5) | 18 (75.0) | 17 (73.9) |
Compatibility of parent concerns with trial aims content
Participants’ primary, secondary and tertiary concerns about their child, derived from CAMC data, were categorised to examine their compatibility with the aims and content of the trial aims (Table 13).
| Concern category | Concerns, n (%) | Total, n (%) | ||
|---|---|---|---|---|
| Primary | Secondary | Tertiary | ||
| Conduct problemsa | 18 (38.3) | 27 (58.7) | 24 (53.3) | 69 (50.0) |
| Parent–child relationship and communication | 16 (34.0) | 2 (4.4) | 4 (8.9) | 22 (15.9) |
| Child self regulationb | 4 (8.5) | 11 (23.9) | 7 (15.6) | 22 (15.9) |
| Emotional distressc | 8 (17.0) | 4 (8.8) | 7 (15.6) | 19 (13.8) |
| Otherd | 1 (2.1) | 2 (4.4) | 1 (2.2) | 4 (2.9) |
| School | 0 (0.0) | 0 (0.0) | 2 (4.4) | 2 (1.5) |
| Total | 47 (100) | 46 (100) | 45 (100) | 138 (100) |
The concerns identified by parents were highly compatible with the aims and content of the trial. The most common concerns were related to children’s conduct and oppositional behaviour (n = 69, 50.0%) (see Table 13). Other common concerns were related to parent–child communication, child self-regulation and emotional distress.
Parent qualitative findings related to sample characteristics
Theme 2: life circumstances, personal histories and help-seeking
This theme reflected participants’ current difficulties and complex life circumstances as well as past adverse adult and childhood experiences. Parents had frequently sought help from a variety of health, social care and parenting support services. Their experiences often affected their perceptions of subsequent help-seeking and service use. This theme consisted of subtheme 1 (life circumstances and personal histories) and subtheme 2 (help-seeking).
Subtheme 1: life circumstances and personal histories
Participants often emphasised the deep connection between their experience of parenting and their own mental health difficulties:
At the time, the depression was quite hard on me . . . I was at a point where I was actually slitting my wrists. I wanted to die and I was going through it myself. I didn’t see a point in living, so it was very hard for me to parent [my child] as well as keep myself at a certain point.
Participant 1003, paragraph 20
Parenting was affected not only by parents’ mental health difficulties but also by their wider stressful circumstances:
Because at that time, with the difficulties of everything that had happened . . . my parenting skills was proving quite difficult and I was finding it extremely difficult to maybe bond and communicate and understand what was going on with the kids because I also had a lot of personal issues going on as well. Then on top of that, there was issues that were out of all our hands that were also going on for me and the kids.
Participant 2010, paragraph 127
Stress was often cumulative across a range of areas in parents’ lives, including child and family health difficulties and disability as well as social isolation and economic disadvantage:
. . . it’s just been so hard and everyone always just sees me as the person, like my birth mum’s got learning difficulties, my brother’s got learning difficulties, X [partner] has got a drinking problem, my dad’s old he’s got his drinking problem plus his wife just left him. So . . . you just have a lot and then it just like, I just feel very overwhelmed and then it’s yeah, I just feel like I’m trying to stay afloat but then I’m kind of sinking then also with having my own medical conditions.
Participant 1021, paragraph 88
My children weren’t going to school, I’d lost two children that had passed away, I was going through a bad time, I’m living in housing [that] wasn’t very good.
Participant 1036, paragraph 125
Participants also described personal histories characterised by persistent adverse childhood and adult life events, such as intimate partner violence, family instability, lack of parental involvement and neglect:
. . . a lot of things I didn’t realise had kind of like happened in my childhood not like bad things but I was practically like as a teenager left to raise myself. So, homework wasn’t checked, I put myself into college and from there I basically done my own thing. I think the problem is more with me as a parent than with my child being a child . . . ’cause I don’t feel like I was ever equipped with parenting skills.
Participant 1021, paragraph 11
I’m explaining to them look, I was abused, I’ve got issues, I need the help.
Participant 1019, paragraph 74
Stressful life circumstances and past experiences provided the foundation through which many parents made sense of their own parenting, their children’s developmental needs and contact with professionals:
[My] family have been through quite a traumatic life so far . . . I was . . . brought up by my mum so I never had any father figure. It’s always been winging it.
Participant 1002, paragraph 4
Especially if people have been like in situations like me, like domestic violence. You get a lot of mums that are on their own . . . the father’s hit the mother and it’s always the children that are going to suffer. The mother suffers . . . and I think you know children’s behaviour will change, my children’s behaviour changed because they seen me going through it.
Participant 1036, paragraph 127
I guess it’s sort of difficult because most of my mental health problems come from being badly parented, like 90% . . . that’s been my big problem. That’s why . . . I avoided having a child . . . for 20 years. Even though I desperately wanted to have a child and a partner and a happy family, I just kept choosing really inappropriate partners and, but I knew I would never have children with them because I was scared I was going to turn into my mum.
Participant 1023, paragraph 13
Subtheme 2: help-seeking
In the main, participants highlighted previous negative experiences with mental health, social care and other support services:
I remember, at one point, I was getting counselling from the family justice centre and the lady was really, really judgemental.
Participant 1020, paragraph 104
For some participants, these help-seeking experiences appeared to evoke and reinforce more deeply held beliefs about the difficult and unfair nature of their circumstances and personal histories:
The group here is absolute **** . . . they don’t want to do any referrals . . . so they stay employed . . . so, they refuse to refer me to the [specialist mental health service] . . . that deals specifically with my issues, they refused, they don’t want to refer me or to do anything more . . . I’ve lived a life-long of being angry, it’s just accepting there’s nothing one can do about it, that’s it.
Participant 1019, paragraph 82
Some parents had previously participated in psychoeducational parenting groups. Positive experiences often encouraged their further involvement in the research trial:
I was up for it, ‘cause I’d done two parenting courses . . . and I really enjoyed it . . . so, when I got told that someone would come here and we’d get some sort of help . . . I thought it would be good to sort of get up-to-date advice sort of what to do.
Participant 2003, paragraph 14
Some parents enthusiastically welcomed participation in the research intervention trial:
At the time . . . I really wanted the help actually, so I was actually really hoping I would be in the parenting group [HFP-M intervention] . . . because I was going through a lot, like with mental health and depression and I wanted some support because also my son had some anxieties as well, at the time, so I just wanted . . . to get some help around that and how to be able to work with him and his behaviours also alongside my issues as well. So yeah, I was really up for it, like I wanted, yeah.
Participant 1001, paragraph 2
For other participants, their unrewarding and sometimes futile experiences at home and with services provided motivation to seek out the new support available through the research trial:
I was just hoping that, maybe, like, even though I’m quite a strong person myself, where my [son] is concerned, well, I just wanted some help really. I’m just banging my head against a brick wall.
Participant 1034, paragraph 21
However, for other participants their hopes were tempered by caution and pessimism, often because of previous negative life and service experiences:
That something; you get to the point where you go through all these things and you’ve got that hope but you feel so sort of, like, do you know what, it’s not going to happen, I mean, but you know, deep down inside that there is a possibility of that hope, so you just push through.
Participant 1015, paragraph 26
You start believing that things aren’t going to be any different, and even if it is going make that effect or difference, you just sit there, and the way you view things, and how you think that all these things are, when they’re offered to you, it’s like, same old, same old . . .
Participant 1015, paragraph 9
Parents described a range of different hopes related to participation in the trial intervention. These included improved relationships with their children, new parenting skills (e.g. better understanding of their children’s emotional needs and more consistent family boundaries), as well as changes in children’s behaviour and emotional well-being, such as reduced aggression and lower anxiety:
The way that I parent, the way that she gets angry, the way I react to her, the way I can’t do boundaries and I’m not consistent, the way I don’t have rules, the way there’s no discipline, she talks to me like rubbish, she hits me and things like that . . .
Participant 1029, paragraph 28
To kind of cope more as a parent and not feel so negative towards my child and helping with the behaviour rather than just kind of generalising everything. So, I know I needed help because the feelings I had at the time was strong. I wouldn’t say hate but a strong dislike and I felt sad because she’s my child and no parent should feel like that. So, I was quite happy that I was going to get some help and in turn that helped me.
Participant 1030, paragraph 38
Because I wanted to improve my parenting skills and my confidence, and I was worrying about my son and I, especially . . . worry about the impact of my own illness on my children. So, I was interested to see how I could improve relationships between me and my children. And how to parent them better.
Participant 2008, paragraph 33
Keyworker findings related to sample characteristics
Theme 3: keyworker decision-making
Theme 3, keyworker decision-making, was generated by the thematic content analysis of keyworker interview data and was most relevant to the characteristics of the sample. The theme consisted of subtheme 1 (sensitive, careful deliberation), subtheme 2 (pragmatic opportunistic referral) and subtheme 3 (parent engagement).
This theme reflected the issues that keyworkers considered when they assessed the suitability of raising the research trial with parents.
Subtheme 1: sensitive, careful deliberation
Some keyworkers highlighted the importance of individualised decision-making based on sensitive consideration of individual service user needs, the potential impact of trial participation and the potential consequences for the keyworkers themselves:
So, you can reactivate . . . that sense of feeling that they’re not good enough or judgement. And then you’re going to activate what we could call a defensive reaction and often aggression and hostility.
Keyworker 4003, paragraph 37
This subtheme reflected keyworkers’ wider consideration of parents’ life circumstances and adverse experiences prior to broaching trial participation with parents. At times, this elicited a protective response from some keyworkers:
People who perhaps have some issues, perhaps are clearly less well off than other people already or have issues of not being entitled to good things. You might think twice in case they didn’t get accepted they might perceive it and feel it as a rejection.
Keyworker 4007, paragraph 37
Subtheme 2: pragmatic, opportunistic referral
Keyworkers also described a more pragmatic and opportunistic decision-making approach that sought to make the most use of the scarce therapeutic resource available through the trial:
Sometimes with research projects, people get a service they wouldn’t normally get. So, if you think it’s going to benefit who you’re referring, then that’s a positive thing by potentially getting an intervention they wouldn’t have got.
Keyworker 4006, paragraph 35
This approach mainly focused on access to the interventions available rather than the research processes:
I kind of feel, it was better than not having anything at all. All those families who went on the programme benefited and they wouldn’t have got that from anywhere else. At that point in time, we didn’t have anything else.
Keyworker 4002, paragraph 49
It often involved taking a broad caseload approach to identification and referral, examining family needs and identifying who might benefit from the interventions available:
You’re like, right, okay. What’s going on with these families? They’re vulnerable. What are the issues? How do we make a difference? And I’m literally grouping them together and identifying all those who would benefit from parenting alongside other issues and I will group them together and make referrals.
Keyworker 4002, paragraph 65
Subtheme 3: parent engagement
Keyworkers described features that helped them to discuss potential trial participation with parents. Despite some misgivings about trial design and concerns about parents’ personal difficulties, many keyworkers adopted a direct and open approach to discussing participation with parents:
It was really straightforward to just talk to them about where they’re struggling and what it would be like if the situation was better and more positive, and the service will help [to make] it a bit easier to find strategies to manage behaviour.
Keyworker 4002, paragraph 15
Introducing the trial and possibility of referral was easier when keyworkers felt that they had a positive relationship with the parent:
So, in terms of trying to introduce other aspects of help, like your service, it was relatively easy because she kind of had that trust in us.
Keyworker 4003, paragraph 31
Keyworkers also felt that the invitation of the trial was more likely to be effective when offered as a positive, strengths-based opportunity for parents rather than as a deficit, punitive or stigmatised referral:
What helps is when you have something that you can say, ‘This is not related to social services, this is just a resource to help with these particular issues and to kind of understand what your needs are . . .’
Keyworker 4007, paragraph 55
Chapter 7 Acceptability and implementation of trial interventions
This chapter reports quantitative and qualitative results related to the acceptability of trial interventions. Quantitative findings report on four areas of acceptability and implementation of the HFP-M and the Being a Parent usual-care session. 152 Further fine-grain information about the influence of parent, service and other contextual factors on acceptability and implementation is reported from the relevant themes and subthemes generated by the qualitative analysis of parent and keyworker interview data.
Acceptability of the trial interventions
Rate of trial intervention uptake
In total, 21 participants (87.5%, 95% CI 67.6% to 97.3%) accepted the HFP-M. A smaller proportion of participants (n = 15, 62.5%, 95% CI 40.6% to 81.2%) took up usual care. Rates of participation did not differ significantly between sites [χ2(1) = 0.593; p = 0.441].
A total of 13 (61.9%, 95% CI 38.4% to 81.9%) participants completed the HFP-M during the period of the trial. Six (28.6%, 95% CI 11.3% to 52.2%) participants withdrew before completion. The most common reasons for withdrawal were acute adult mental health crisis and complex family circumstances unrelated to the trial interventions.
Delays in participant recruitment and the longer duration for delivery meant that two (9.5%, 95% CI 1.2% to 30.4%) participants did not complete the HFP-M when the feasibility trial was finished.
All 15 participants allocated to usual care who accepted the Being a Parent session completed it (100%, 95% CI 78.2% to 100%).
Rate of the Helping Families Programme-Modified appointment attendance
The HFP-M consisted of 16 session modules intended to be delivered though weekly appointments. The number of appointments offered to participants varied, as did the number of session modules completed within the trial.
The delivery of the HFP-M to eight participants was affected by the unplanned absence of one full-time research therapist as a result of long-term sick leave. This research therapist was replaced by two part-time therapists, which resulted in the duplication of some intervention sessions. The repeated sessions were required to re-establish therapeutic momentum and to review content following delays in the schedule of intervention delivery. Session attendance was adjusted to take account of session duplication. Adjusted appointment results are reported here, as they more accurately reflect provision. Actual appointment data are described in Appendix 10.
The total number of adjusted intervention appointments offered across all of the HFP-M participants was 352, of which 94 (26.7%) were cancelled and rearranged and 11 (3.1%) were not attended by the participants [did not attend (DNA)] (Table 14). A total of 247 (70.2%) offered appointments were attended by participants. The total mean number of appointments attended was 15.8. Mean duration of programme delivery was 28.4 (SD 21.7) weeks.
| Site | Intervention appointments | |||||||
|---|---|---|---|---|---|---|---|---|
| Attended | Cancelled | DNA | Offered | |||||
| Total, n (% of total appointments offered) | Mean (SD) | Total, n (% of total appointments offered) | Mean (SD) | Total, n (% of total appointments offered) | Mean (SD) | Total, n (% of total appointments offered) | Mean (SD) | |
| 1 (N = 16) | 201 (71.0) | 12.6 (5.8) | 74 (26.2) | 4.6 (3.7) | 8 (2.8) | 0.5 (1.0) | 283 (80.5) | 17.5 (6.1) |
| 2 (N = 5) | 46 (66.7) | 7.7 (6.5) | 20 (28.9) | 3.3 (4.1) | 3 (4.4) | 0.5 (0.8) | 69 (19.5) | 11.3 (10.1) |
| Total (N = 21) | 247 (70.2) | 11.2 (6.3) | 94 (26.7) | 4.3 (3.9) | 11 (3.1) | 0.5 (1.0) | 352 (100.0) | 15.8 (7.7) |
Rate of trial Helping Families Programme-Modified session completion
Participants completing the HFP-M received a mean number of 12.9 (3.8) session modules of the 16-session module programme (range 7–16) (Table 15). Participants who withdrew received a mean number of 4.8 (SD 2.3) session modules of the programme (range 2–9). Two participants’ intervention was incomplete; one participant received three session modules and the other participant received six session modules. Site 2 participants received fewer total session modules (see Table 15).
| Site | Intervention status | |||||||
|---|---|---|---|---|---|---|---|---|
| Completed (N = 13) | Withdrawn (N = 6) | Incomplete (N = 2) | Total (N = 21) | |||||
| Mean (SD) n | Range | Mean (SD) n | Range | Mean (SD) n | Range | Mean (SD) n | Range | |
| 1 (N = 16) | 13.4 (4.2) 10 | 7–16 | 5.4 (2.1) 5 | 4–9 | 6.0 (0.0) 1 | 6 | 10.4 (5.2) 16 | 4–16 |
| 2 (N = 5) | 11.3 (2.1) 3 | 9–11 | 2.00 (0.0) 1 | 2 | 3 (0.0) 1 | 3 | 6.5 (5.5) 5 | 2–13 |
| Total | 12.9 (3.8) 13 | 7–16 | 4.8 (2.3) 6 | 2–9 | 4.5 (2.1) 2 | 3–6 | 9.3 (5.5) 21 | 1–16 |
The Helping Families Programme-Modified therapeutic alliance acceptability
The Helping Families Programme-Modified
A total of 18 (85.3%) participants who received the HFP-M completed the WAI-SR at T2, providing information about the quality of therapeutic relationships developed during the HFP-M.
The mean WAI-SR total score was 73.8 (SD 10.4) and mean subscales scores were consistent [WAI-SR tasks subscale score, 24.9 (SD 3.5); WAI-SR bond subscale score, 24.9 (SD 3.9); WAI-SR goals subscale score, 23.9 (SD 4.1)]. Post hoc scrutiny of the WAI-SR scores between sites suggested a possible difference in alliance quality [site 1, n = 13, WAI-SR total mean = 77.7 (SD 5.5); site 2, n = 5, WAI-SR total mean = 63.8 (SD 14.0)].
The three items most commonly receiving a rating of very often/always were Bond item ‘My therapist and I trust one another’ (n = 17, 94.5%), Goals item ‘My therapist and I are working towards mutually agreed upon goals’ (n = 16, 88.9%) and Tasks item ‘We agree on what is important for me to work on’ (n = 16, 88.9%).
Usual-care Being a Parent session
A total of six (40.0%) out of 15 usual-care participants completed the WAI-SR at T2. The mean total WAI-SR score was lower, at 56.2 (SD 18.8), for the usual-care participants. Mean subscales scores were also consistently lower than in the intervention arm [WAI-SR tasks subscale score, 17.4 (SD 7.2); WAI-SR bond subscale score, 19.8 (SD 7.1); WAI-SR goals subscale score, 19.0 (SD 7.6)].
The three WAI-SR items most commonly receiving a rating of very often/always were all from the Bond subscale: ‘I believe my therapist likes me’ (n = 4, 66.7%), ‘I feel that my therapist appreciates me’ (n = 4, 66.7%) and ‘My therapist and I trust one another’ (n = 4, 66.7%).
Comparison between the Helping Families Programme-Modified and usual-care Working Alliance Inventory-Short Revised scores
There appeared to be a substantial difference in the WAI-SR scores between the two conditions but there were insufficient usual-care data to test for a statistical difference.
Parent qualitative findings related to intervention acceptability
Theme 3: experiencing a psychoeducational parenting intervention
This theme described participants’ experiences of receiving either of the psychoeducational parenting interventions available in the trial, including their acceptability, characteristics and perceived impact. Two of the theme’s three subthemes were relevant to intervention acceptability: subtheme 1 (intervention format) and subtheme 2 (intervention content).
Subtheme 1: intervention format
This subtheme reflected participants’ experiences of the structural characteristics of the interventions provided in both arms of the trial. The majority of the HFP-M recipients found its structure engaging and appropriate. Participants were generally more critical of the usual-care session format. Participant experiences appeared to be influenced by their intervention expectations and the characteristics of the research therapist providing the intervention.
Personalised, one-to-one format
Many participants valued the tailored and personalised one-to-one approach used by both interventions. Parents mostly felt that this enabled them to receive more in-depth help that could be more easily tailored to the complexity of their personal and family circumstances:
Yeah, because . . . it’s more like a one to one and . . . she explains things more deeper. You can understand, and if you don’t understand, she’ll break it down and explain it more to you.
Participant 1024, paragraph 86
The one-to-one format was contrasted with reservations that parents held about receiving group-based psychoeducational support, where they felt that there may be less understanding and appreciation of their mental health difficulties from other group members:
It was . . . just having that very personal, sort of focused on me and my problems, and how I was going to manage my particular situation and manage me . . . when you are out in a public sphere with other parents, for example, you know, they don’t necessarily have mental health issues but I think the key thing for me was, you know, I’m trying to do all of this with the mental health issues and that, and to have my personal issues dealt with and my daughter’s personal issues, that was really important . . .
Participant 1023, paragraph 52
Parents also saw some drawbacks in the one-to-one format, such as the lack of opportunity to meet other parents, the reassurance that other parents experienced similar difficulties and the opportunity to learn successful coping and parenting strategies from other parents:
It’s quite contradicting, the fact that I wouldn’t be hearing it from another parent’s perspective, but at the same time it would be directly based on me . . . and my children. In one aspect, it’s good because it can be focused on . . . just me and just the kids, but then on the other aspects you’re not necessarily learning what has or hasn’t worked for other people. What other people has also gone through.
Participant 2010, paragraph 56
Intervention duration and frequency
The 16-session, weekly format of the HFP-M was broadly acceptable to most participants but also generated challenges for consistent, regular attendance:
We were meeting once a week and they were for an hour . . . yeah, that was good. An hour was plenty, was an enough time, and that, that was good yeah.
Participant 2008, paragraph 27
It would have been ideal obviously if you could have met every week, every other week and yet follow it up.
Participant 2004, paragraph 36
A very small number of parents felt that the individual appointment duration of the HFP-M should have been longer to allow for discussion of wider life stresses:
An hour was just not enough to cover the programme and for me to discuss how I was getting on with . . . other things that had come up during the week that weren’t in the programme . . . that’s what I also needed to do. Because ‘yes, we’re doing the programme’ but this is my life, and this is my week and this other stuff has come up and I need to sort of, deal with it now . . .’
Participant 1023, paragraph 10
Participants receiving the usual-care session were often critical of its single-session format. For many, it lacked face validity and it affected their treatment expectancies even prior to receipt:
I knew full well it wasn’t going to be effective, because one session to come into this household when you don’t really know what’s going on . . . when you’ve got a child with special needs, or complex needs, you go in one session and it’s not going to be effective. . .
Participant 1015, paragraph 62
Parents felt that an intervention of such limited duration as the usual-care session did not provide sufficient time for their complex parenting issues to be understood:
The one-off thing, no [no], ‘cause it’s so short, you know. Although she seemed to be here for ages [yeah], it was short [yeah]. You know . . . if your children’s got problems and your family’s got problems, you need sessions, not just a one-off thing.
Participant 1022, paragraph 123
Parents also felt that the single session content was too compact, preventing them from being able to focus on credible, tailored parenting solutions for their difficulties:
If you’re trying to cram one session and you’ve got all these complex needs, I think if there would have been more time . . . to focus on it, to be able to explain all the situation and all that lot, then it would have been more helpful. But you’ve got like an hour, two hours, whatever the time is, and you’re trying to cram it all in, by the time you’ve finished explaining the situation and all the complex situation and needs, you’ve hardly got any time to go through the actual situations or the programme itself to be able to sit there and see if it would help anyway.
Participant 1015, paragraph 84
The limited duration of the usual-care session also raised concerns for some parents about the absence of continuing support to help them to successfully put session content into practice:
Yeah instead of having an hour and then it’s like, then she’s gone. So, it’s like well the hours not really sort of long enough [no]. And I know you had like 20 pieces of cardboard to go through but it was, I don’t think it was good enough.
Participant 2003, paragraph 180
Proactive and persistent
The persistent determination of the HFP-M research therapists to maintain contact with parents over the duration of the intervention often had a positive emotional impact on participants:
And one time she couldn’t contact me for a few times and actually she come and put a note through my door yeah so, and I thought that that was really, really lovely.
Participant 1018, paragraph 23
Therapist persistence had the effect of participants feeling cared for and increased parental commitment to the intervention:
The determination of not giving up, making sure I’m alright, rearranging the schedule to fit in so it was like, alright she really wants to do this, **** it lets do it.
Participant 1003, paragraph 123
Intersessional support provided by the HFP-M therapists was also welcomed by participants:
I learnt [my child] . . . she needs a lot of positive attention and if you give her positive attention after she’s done something then life’s good so positive attention goes a long way and the therapist will text us two or three times a week still to this day, ‘Keep up the positive attention’ . . .
Participant 1016, paragraph 60
Despite broad support for a weekly session format, parent session cancellation was not uncommon. Participants attributed this mainly to their complex life circumstances and personal difficulties rather than intervention ambivalence:
I was going through so much and we kept sort of missing appointments. I was either out or busy or up the hospital or something or another.
Participant 1003, paragraph 59
I just don’t wanna deal with people, talk with people or interact with anyone. I get quite . . . a recluse, into my bedroom. I literally will spend days in my bedroom. Like you’ll very rarely even see me come out the house. I won’t eat . . . most I’ll have is a cup of coffee.
Participant 1003, paragraph 107
Participants often expressed a sense of regret and concern about missed sessions. They were often mindful of the impact on themselves as well as potential inconvenience for the research therapist:
I started blaming myself because I wanted to have that time, everybody wanted a piece of me and I couldn’t cope with everything that was going on around me, you know. I had them days when I just thought oh I can’t cope with this, you know, but the times that I did get to see [the research therapist], it was good.
Participant 1036, paragraph 33
I felt like I should just say to [the research therapist], ‘You know, we’ve cancelled so much I don’t want to waste your time’, that’s the only time I felt unsure of doing the programme . . .
Participant 1016, paragraph 176
Intervention location and choice
Generally, participants valued the use of non-clinical environments for the delivery of the interventions, which enabled them to feel more at ease:
Yeah I found it quite comforting [to have it at home] . . . yeah more relaxing.
Participant 1018, paragraph 129
. . . because it was in my own home, um, it’s different to being in a very clinical environment um so I do think in the home it worked well for me um I felt more comfortable being in my own home . . .
Participant 2004, paragraph 112
Parents liked being involved in the choice of venue. Most expressed a preference for comfortable, non-stigmatising and normalising environments rather than clinical settings. Most participants selected their home as the location. Some preferred using a neutral, social venue, such as a café:
Yeah it was nice to get away yeah to get away from everything what was going on in my life, just going out and being able to sit and talk it was good.
Participant 1036, paragraph 85
Multiagency care co-ordination
Parents appreciated that research therapists shared information about their participation in the HFP-M with other professionals involved in their care. They felt that this was in their interests, improved co-ordination and reduced duplication:
[The research therapist] was very much involved in the other agencies . . . involved with [my child]. I kind of wanted a lot of transparency, so everybody knew what was happening and that nothing overlaps and they kind of worked together in partnership to kind of help and that I felt was very helpful.
Participant 1030, paragraph 67
Parents felt that they had appropriate choice and involvement in the communication with other professionals:
Yeah, she asked me, ‘Is it okay if I could send this to your social worker, to let her know I touched base on bits that we’re working on and stuff?’ like so she asked me and I either said yes or no and I said yes majority of the time.
Participant 1004, paragraph 67
Supporting materials
Both interventions used printed materials. Some parents found that printed materials augmented the content of the intervention, bringing clarity and new insight to their situation and circumstances:
It just puts everything into perspective as well and helped you because when you’re doing it yourself you don’t realise everything but when you talk about it and put it on paper you can see it clearly.
Participant 1018, paragraph 171
Parents liked the process of assembling written materials into a HFP-M folder, producing an asset that parents planned to continue to use after completion of the intervention:
[The research therapist would] teach me and she give me a folder with everything in and said I ‘can add to it . . . it’s an ongoing process, I can carry on, carry on so it doesn’t stop here’. She explained a lot.
Participant 1024, paragraph 130
I wouldn’t say we’re finished because the thing is it’s like they leave this light in my life where I can reflect, I can go back and look if I see where I’m going wrong regarding my children I can go back and look at my folder and that will just remind me of my therapists. So, it’s not, it’s never finished yeah.
Participant 1020, paragraph 101
Other parents felt less enthusiastic about the use of the written materials, mainly because they were perceived to be more of an administrative task rather than therapeutically helpful:
No. I think the only thing that I found a bit long and boring was the paperwork.
Participant 1003, paragraph 307
Similarly, the perceived density of the written materials used in the usual-care session also meant that they were sometimes experienced as procedural and didactic rather than personalised:
It was run through, like, these sort of cards and ‘Right, turn the card. turn the card’. And that’s what it was like and it was so . . . regimental.
Participant 1002, paragraph 117
There was more opportunity to adjust and negotiate the use of the written materials over the longer duration of the HFP-M:
She said, ‘I’m so sorry there’s so much papers’. She said, ‘That’s just what it is’. She said ‘Maybe we can work on it next time and make it less paperwork’, she said ‘I know it’s like overwhelming’.
Participant 1018, paragraph 103
Subtheme 2: intervention content
This subtheme reflected parents’ lived experience of the psychoeducational content and therapeutic methods of the interventions offered in the trial, including the interpersonal techniques used by therapists, the helping process, the intervention strategies and the subject matter.
Therapist characteristics
Parents were sensitive to the impression made by the research therapist providing the allocated intervention. Descriptions of positive research therapist attributes were plentiful. These were particularly reported by the intervention arm participants.
Participants focused on perceived therapist qualities such as being understanding, accepting, determined and responsive. Parents not only valued them for their therapeutic effect but drew attention to the way that their characteristics affected their perception of the therapist as a person and their commitment to the intervention:
I was living in a hostel, coming from where I was, and I had to open up and tell her my life before the hostel. And, some people would look at you and judge you, ‘Oh gosh, how did she get to this’ you know what I mean, but she didn’t judge me at all, she just was really, really supportive, really supportive.
Participant 1020, paragraph 61
Parents repeatedly associated the influence of these characteristics on their engagement in the HFP-M and the therapeutic alliance formed:
If you’re a good listener, with me that makes me feel very confident, if somebody just like talks and then that’s it, you go show that you’re not that interested, after a little while I won’t ever talk to you again. I won’t talk about my problems like that, you’ll never hear me open up my mouth any more, like I might give a little bit sooner but I won’t use you, not use you I mean I won’t interact with you any more . . .
Participant 1004, paragraph 95
The first session, if I remember rightly, was just quite relaxed. It was sort of us getting to know each other, just building a basis of understanding, what help I might want? What the problems are at home? What the problems are with me? What the problems are with [my child]? Just literally back tracking, getting our feet stuck in, and comfortable with each other. Building, I suppose, a relationship . . . to be able to understand.
Participant 1003, paragraph 51
Some parents in both arms of the trial felt that their therapist was less flexible, consistent and sensitive. More often than not participants accepted these difficulties, though some felt misunderstood, somewhat judged and, as result, less engaged in the intervention:
She literally just very to a T. I suppose when you’re going round half a dozen different houses and you’re seeing different people and you’ve got to go through these things every time, it does become like that but there’s no warmth there.
Participant 1002, paragraph 148
Some participants questioned whether or not these difficulties may sometimes have been influenced by their own repeated, negative help-seeking experiences as well as specific therapist characteristics:
If you’ve got someone that doesn’t understand your situation, in my case, I’ve had a lot of people judge me for it, so I don’t know if it’s just natural reaction because so many people have judged me in the past, that I felt like she was doing it because of my anxiety, I don’t know, but I felt like she didn’t understand . . .
Participant 1015, paragraph 109
Parent–therapist partnership, choice and tailoring
Parents welcomed the extent to which they were explicitly involved in intervention choices and decision-making. This was often contrasted with previous experiences in which parents felt that they were more controlled and directed by practitioners:
And then she’d say to me, like, shall we do this bit first or would you rather do that bit? And then I’d pick like, oh, maybe we should do this first and then follow up with that bit and . . . It was different [from what I’ve done before].
Participant 1008, paragraph 43
Collaborative partnerships between parents and research therapists were more explicit and easily achieved in the HFP-M group. This had the effects of reinforcing commitment and building parental self-esteem:
It made me feel more confident, as well, because I was involved in what is happening, that is, you meet professionals and, they’re like they’re the ones there in the sessions, they’re like this is what we’re doing. [The research therapist] didn’t make it feel like that, [the research therapist] got us involved.
Participant 1030, paragraph 59
‘Cause if I don’t understand something, I’ll tell her that I don’t understand. What that means is that she’ll break it right down and say, ‘In your own words, just say it in your own words. Say it in your own words’. She said, ‘Use your own language’, you know. So, I find it more helpful. She said, ‘What language you speak?’ and I said, ‘I speak Patois’ and she says, ‘Speak it! Use it in your own words. Your own words. Use it!’ and I say, ‘Oh, that’s good’.
Participant 1024, paragraph 33
Parents appreciated the way that the HFP-M intervention as a whole was adjusted and tailored to their specific parenting and family needs and priorities. They were also aware of the way that individual session content was adjusted to reflect their immediate personal functioning and circumstances:
[The research therapist] knew exactly what I was going through and that. She could see like the difference in, even the communication difference in the sessions. Like she could see the difference in how I would be able to like . . . I wasn’t able to give as much information or I wasn’t really in there in the room with her. And she’d even say to me, ‘We can leave it for today if you want’. I’m like, ‘No, come on, just do it’.
Participant 1003, paragraph 113
Parents’ experience of the usual-care session was generally more mixed. Some parents felt that they were invited to tailor its psychoeducational content and focus. Other participants felt that the session was more strongly directed by the research therapist:
There were a few different sets of cards, erm, and I could choose what I thought would be most relevant, so I did and that was really good. It was like, 5 or 6 different sets of cards . . . she left me with all of them, so I could do the others on my own . . . I got to pick and we did the one that was most, kind of, appropriate, so that was really good.
Participant 1013, paragraph 115
Structure and clarity
Most parents were aware of the underlying structure of the trial interventions, with recipients of the HFP-M valuing its planned, goal-orientated approach:
Yeah, we set plans, and . . . there was worksheets, and the sessions were very structured on what we’d be doing and then I would have homework . . . it was structured and it was very goal-orientated, which I liked.
Participant 2008, paragraph 23
The explicit use of goals helped to provide parents with clarity about their plans:
She does a piece of paper . . . like for the goals for next week. Just the fact that you can always go back and see what you write last week and then you can work out if you done what you said you was going to do . . . so, it’s not as though it’s just all up in the air, you know what you’re doing when you’re doing it.
Participant 1016, paragraph 188
They also provided a means to collaboratively review progress and avoid drift:
We definitely kept an eye on the sort of where we was trying to get to, like if we felt we weren’t sort of staying on topic of the goal we’d sort of revert back.
Participant 1003, paragraph 285
Some parents would have preferred a clearer description of the content and expectations of the HFP-M at the beginning of the initial sessions, which would have helped them to understand its flow and overall content:
I would have given all of the information at the beginning saying, ‘This is the course information’ and then completely go through . . . each week’s session. So, the first session, this is what we’re going to talk about today and then follow it up the next time we meet.
Participant 2004, paragraph 54
In terms of the HFP-M session structure, parents valued the opportunity to ‘offload’ about the critical events and incidents going on in their lives that occurred between appointments. This made it easier for parents to focus on intervention content during sessions. It also enabled therapists to appreciate the complexity of parents’ broader lives while maintaining the focus on the aims of the HFP-M:
I liked the fact that before we started actually doing the work we had an offload session. So, whatever had gone on in the week, I could discuss with her first . . . and we could talk about it and then we could start doing the [parenting] work. Had I just . . . straight done the work, I wouldn’t have been able to focus on it properly, because I’d still have the issues that I dealt with in the week going ‘round in my head. But the fact that I was able to ‘offload’ then I could concentrate on the [parenting] work.
Participant 1008, paragraph 19
A significant number of participants felt that the usual-care session was too structured, with the effect of restricting choice and inhibiting the development of a collaborative approach:
. . . [the research therapist] was nice and polite. That wasn’t the issue. The issue was what [the research therapist] had to work inside the framework.
Participant 1002, paragraph 127
Psychoeducational content and methods
Parents provided insight into the methods used by therapists to communicate and personalise psychoeducational content of the interventions. These were more commonly described by parents participating in the HFP-M:
I would say something and she’d sort of explain to me what I said . . . and then I would say ‘Yeah that’s exactly what I mean’ so like she knows what I’m saying but how to say it. Because, I don’t really know how to say it properly. And then when she actually relays it back slightly different. It’s like ‘Oh, actually yeah’.
Participant 1018, paragraph 87
These personalised methods helped parents to develop new insight into their family difficulties in open and thoughtful ways:
. . . it . . . made me think about things in a, sort of, detailed way that I hadn’t necessarily done before, and when you do that, you sort of think ‘Actually . . . yeah, you know, they’ve got a point, this is potentially a really useful way of looking at it’. You know, you get . . . stuck in what your beliefs are and then, if something comes along to kind of, prompt you to think through it . . . I definitely kind of realised . . . I hadn’t thought of it that way, but actually that’s a really useful way of looking at it.
Participant 1013, paragraph 131
The HFP-M content was not always successful. Some parents related this to therapists’ failure to effectively deliver the psychoeducational content of the programme:
If I’m being totally honest, I didn’t get a huge amount out of the programme in the sense that the therapist I had was, she was a very friendly, nice person and easy. We would talk about the issues but I didn’t feel I got any concrete strategies or help from her to try and deal with the issues I was having.
Participant 2004, paragraph 38
Parents also related it to the extent to which psychoeducational content was relevant and tailored to their specific and complex circumstances:
The cards come more across if you’ve got, like, normal situations. Like, it’s things like a normal parenting sort of thing, it doesn’t seem like it’s based around if you’ve got a situation with a child with special needs or . . . the knock-on effect for the family.
Participant 1015, paragraph 117
I guess, I guess for me . . . a lot of questions . . . that wasn’t relevant . . . because it is quite broad as well . . . it didn’t apply to me or the kids.
Participant 2010, paragraph 44
Parents in the intervention arm more frequently attributed the failure of the content to generate improvements to the nature of their own child and parent and family difficulties, rather than the HFP-M content:
But I don’t believe that’s to do with the [intervention], it is just . . . there are underlying problems with [my child] that I don’t think have yet been discovered.
Participant 1018, paragraph 183
Keyworker qualitative findings related to intervention acceptability
Category 4: intervention characteristics
The theme intervention characteristics, generated by the thematic content analysis of keyworker interview data, reflected intervention aims, methods and content that keyworkers felt were useful and effective in meeting referred parents’ needs. Two of the theme’s three subthemes were directly relevant to intervention acceptability: subtheme 1 (clinical and service user relevance) and subtheme 2 (home-based, individualised format).
Subtheme 1: clinical and service user relevance
The aims and format of the HFP-M received strong support from interviewees. The HFP-M was frequently seen as an additional service component that complemented keyworkers’ own practice and addressed a significant gap in parenting provision:
We saw it like as an additional intervention, additional help for the family, parenting and supporting the mother . . . we do need to refer to services that will offer support for parents not just for children.
Keyworker 4009, paragraph 51
A key feature giving the HFP-M credibility was its focus on the connections between parent mental health functioning, parenting and child outcomes, combined with its specialised content:
Something that’s flexible, that will go to the parents . . . that understands the parents’ difficulties, especially with parents that have difficulties regulating their emotions and their relationships. You know you’ve got practitioners that are able to sit with that parent through that and help them think about their parenting.
Keyworker 4006, paragraph 85
It seems to fit a lot better for these parents, we just don’t have either the training, the resources or it’s just not something we offer.
Keyworker 4010, paragraph 38
Subtheme 2: home-based, individualised format
Referring keyworkers supported the home-based format of both interventions, which they felt improved engagement and was distinctly different from routinely available care:
We’d obviously tried to bring it together but if they weren’t coming that often and if only one of them could turn up it was hard. Whereas I felt the family did really well. It was because both of them could be seen in the home and so parenting differences could be discussed more frankly and things tried out that could try to do.
Keyworker 4017, paragraph 15
They also felt that a home-based format potentially offered a more authentic environment in which to help parents compared with the use of clinic locations:
Having somebody coming in, doing a parenting intervention within the home . . . you are offering that intervention, and that advice, and support in a live space, where it happens all the time. That was great.
Keyworker 4015, paragraph 17
Keyworkers saw the potential value of an individualised format being a good fit for parents with significant interpersonal difficulties and low self-confidence, who they felt may not engage in traditional group-based parenting programmes:
Not everyone likes group work and that will put a lot of parents off, if they’re struggling with their confidence, if they’re not great at managing relationships and their emotions. Sometimes going into a group is really overwhelming.
Keyworker 4006, paragraph 111
Chapter 8 Clinical outcomes and costs
This chapter reports quantitative and qualitative clinical outcomes and cost findings for the randomised feasibility trial. 152 The results include preliminary estimates of clinical ESs, intervention costs and cost-effectiveness. Relevant themes and subthemes of the qualitative analysis of parent and keyworker interview data provide further fine-grained information about the influence of parent, service and other contextual factors on outcome and costs.
Impact and outcomes
Differences at T2 follow-up were investigated in an intention-to-treat analysis using an ANCOVA model with T1 pre-randomisation scores as covariates to control for baseline imbalances and treatment arm as a categorical factor, as shown in Tables 16 and 17. Results showed mean improvements from baseline scores in a number of variables within both intervention and usual-care groups. 152 The estimated mean improvement at follow-up in the intervention group exceeded that in the usual-care arm on several outcomes, though these results should be treated with caution given the wide CIs. There was a statistically significant difference in the CAMC problem 2 (see Table 16).
| Measure | Group | Time point, mean (SD) n | Estimated mean difference at follow-up (T2) | p-value | ES (Cohen’s d) | ||
|---|---|---|---|---|---|---|---|
| T1 | T2 | T3 | |||||
| CAMC | |||||||
| Problem 1 | Intervention | 84.6 (16.0) 24 | 45.2 (27.2) 18 | 58.2 (29.5) 13 | –18.633 (95% CI –40.177 to 2.910) | 0.087 | 1.2 (0.4 to 2.0) |
| Usual care | 85.9 (14.7) 22 | 63.1 (31.1) 14 | 53.3 (34.4) 8 | ||||
| Problem 2 | Intervention | 85.0 (19.1) 24 | 51.1 (31.9) 18 | 56.4 (35.5) 13 | –22.486 (95% CI –44.318 to –0.654) | 0.044 | 1.3 (0.5 to 2.1) |
| Usual care | 82.9 (15.7) 22 | 72.5 (26.0) 14 | 66.5 (35.5) 8 | ||||
| Problem 3 | Intervention | 81.0 (17.0) 24 | 54.4 (33.8) 17 | 42.8 (35.4) 13 | –2.909 (95% CI –28.349 to 22.530) | 0.816 | 0.0 (–0.7 to 0.7) |
| Usual care | 78.9 (18.5) 22 | 57.3 (34.1) 14 | 39.6 (24.3) 8 | ||||
| ECBI | |||||||
| Problem score | Intervention | 22.1 (7.4) 24 | 17.9 (8.5) 15 | 15.3 (9.4) 13 | 0.804 (95% CI –4.948 to 6.556) | 0.776 | –0.1 (–0.73 to 0.97) |
| Usual care | 22.43 (6.2) 21 | 18.0 (11.5) 14 | 18.8 (12.3) 8 | ||||
| Intensity score | Intervention | 168.2 (35.9) 24 | 142.4 (39.3) 24 | 131.7 (43.0) 18 | –12.866 (95% CI –34.385 to 8.664) | 0.233 | 0.4 (–0.3 to 1.1) |
| Usual care | 169.5 (31.8) 23 | 155.7 (49.6) 14 | 148.9 (58.4) 8 | ||||
| CBCL-Int | |||||||
| (t-score) | Intervention | 72.9 (9.7) 24 | 69.6 (10.4) 18 | 68.2 (8.3) 13 | 1.853 (95% CI –9.023 to 5.317) | 0.601 | 0.2 (–0.5 to 0.9) |
| Usual care | 70.9 (11.9) 23 | 70.9 (9.3) 14 | 69.6 (8.6) 8 | ||||
| Measure | Group | Time point, mean (SD) n | Estimated mean difference at follow-up (T2) (CI) | p-value | ES (Cohen’s d) | ||
|---|---|---|---|---|---|---|---|
| T1 | T2 | T3 | |||||
| KPSS | Intervention | 10.1 (3.1) 24 | 12.9 (3.5) 18 | 14.9 (3.8) 13 | –1.177 (95% CI –1.260 to 3.615) | 0.331 | 0.4 (–0.3 to 1.1) |
| Usual care | 10.9 (2.8) 23 | 12.4 (3.9) 14 | 13.6 (3.9) 7 | ||||
| PS | Intervention | 111.0 (19.6) 24 | 108.7 (16.5) 18 | 98.3 (27.2) 13 | –0.210 (95% CI –14.776 to –15.196) | 0.977 | 0.0 (–0.7 to 0.7) |
| Usual care | 113.5 (24.8) 23 | 108.7 (28.9) 14 | 98.1 (26.9) 7 | ||||
| SCL-27 GSI | Intervention | 1.8 (1.1) 24 | 1.6 (0.8) 18 | 1.9 (0.8) 13 | 0.105 (95% CI –0.599 to 0.389) | 0.666 | –0.1 (–0.8 to 0.6) |
| Usual care | 1.7 (0.8) 22 | 1.7 (0.9) 14 | 1.3 (1.0) 8 | ||||
Estimated treatment ESs showed a general T2 advantage for the impact of the intervention condition on a range of outcomes. A large ES was detected for parental goal attainment (CAMC problem 1: ES 1.2, 95% CI 0.4 to 2.0; CAMC problem 2: ES 1.3, 95% CI 0.5 to 2.1). Medium ESs were detected for child behavioural problem severity (ECBI Intensity: ES 0.4, 95% CI –0.3 to 1.1) and parenting satisfaction (KPSS: ES 0.4, 95% CI –0.3 to 1.1) (see Tables 16 and 17). Caution needs to be exercised in relation to the interpretation of these results given the breadth of the ES CIs. No effects were detected for parenting behaviour and adult mental health outcomes. Again, the wide CIs suggested that these results should be treated with caution.
Scrutiny of T3 descriptive findings showed that outcome scores across both groups were generally maintained or continued to improve.
Descriptive examination of clinical caseness showed similar rates of reduction between intervention and usual-care conditions on the measures available (Table 18). T3 data may indicate a further decrease in intervention child behaviour problem caseness, with a smaller decrease in positive parenting behaviour. The usual-care group showed further improvements in positive parenting behaviour.
| Measure | Condition | Caseness, n (%) | ||
|---|---|---|---|---|
| Baseline (T1) | Post intervention (T2) | Follow-up (T3) | ||
| ECBI Problem | Intervention | 21 (87.5) | 10 (66.7) | 6 (46.2) |
| Usual care | 20 (90.9) | 9 (64.3) | 5 (62.5) | |
| ECBI Intensity | Intervention | 19 (79.2) | 11 (61.1) | 6 (46.2) |
| Usual care | 20 (87.0) | 9 (64.3) | 5 (62.5) | |
| CBCL-Int (t-score) | Intervention | 23 (95.8) | 14 (77.8) | 10 (76.9) |
| Usual care | 22 (95.7) | 12 (85.7) | 7 (87.5) | |
| PS | Intervention | 18 (78.3) | 12 (66.7) | 7 (53.8) |
| Usual care | 17 (73.9) | 9 (64.3) | 3 (37.5) | |
Economic findings
Service use data were collected not at baseline but at T2 and T3. There was a considerable number of missing data in both groups. At T2, service use data were available for 17 (71%) of the HFP-M and 9 (38%) of the usual-care participants. At T3, service use data were available for 12 (50%) of the HFP-M and 7 (29%) of the usual-care participants.
Time 2 resource use
Parent contacts
General practitioners (GPs) had the highest percentage of contacts, > 89% in both groups, followed by contacts with a social worker, > 44% in both groups (see Appendix 11). Health service costs were highest for day hospital, clinical psychologist and GP contacts in the HFP-M group. The highest costs in the usual-care group were for inpatient admissions, followed by day hospital and psychiatrist contacts. The mean numbers of contacts and days in the tables in Appendices 11 and 12 are for those participants with at least one contact and exclude participants not using any of the specific services.
Child contacts
The service most commonly used by children, reported by parents, was general practice, with > 50% of contacts for both groups (see Appendix 11). The costs of services used by children in the HFP-M group were generally higher than those for the usual-care group. There were, however, some instances where the usual-care arm had higher service costs, such as for hospital, home help support and dental services.
Time 3 resource use
Parent contacts
Over 90% of the HFP-M group had a contact with a GP, compared with 57% in the usual-care group. Overall, the HFP-M group had a greater consumption of resource use than the usual-care group and consequently higher costs (see Appendix 12).
Child contacts
When focusing on the services used by children, a similar pattern to that of parents was observed. The HFP-M group had a higher number of contacts with the majority of services than usual care and, therefore, higher costs. The services with the highest rate of use in the HFP-M group were contacts with school nurses, GPs and after-school clubs; 50% of individuals had contacts with these services. The services with the highest use in the usual-care group were contacts with dentists and GPs, with over 50% of the sample having such contacts (see Appendix 12).
Quality-adjusted life-years
Appendix 13 shows the EQ-5D scores for parents/carers and children in each group at each time point and the associated QALYs, irrespective of whether or not participants had cost data.
Parents
In the HFP-M group, an improvement was seen at each time point in terms of the EQ-5D-5L utility score (see Appendix 13, Table 21). The usual-care group experienced a small loss in utility score between T1 and T2; however, an improvement in utility score was later seen between T2 and T3. The HFP-M group was associated with higher QALYs than the usual-care group.
Children
The HFP-M group experienced slightly greater QALYs than the usual-care group. Children in the usual-care group saw an improvement in utility score at each time point (see Appendix 13, Table 22). At T2, there was a decrease in utility score for the HFP-M group; however, a larger increase in utility score was observed at T3. This is probably a result of outliers influencing the relatively small sample.
Cost-effectiveness analyses
Owing to the substantial number of missing data at T3, it was decided to display the cost-effectiveness results based on two separate analyses.
-
Analysis 1: those with CSRI and intervention costs at T2, and EQ-5D at T1 and T2, and, therefore, QALYs are based on only T1 and T2. This analysis was chosen as more participants had CSRI cost data and EQ-5D data at these time points.
-
Analysis 2: those with CSRI and intervention costs at T2 and T3, and EQ-5D at all three time points. This was a ‘complete case’ analysis. The sample size was reduced for these analyses so results have to be treated with caution.
Table 19 displays the cost-effectiveness results from analyses 1 and 2, described from NHS/PSS and societal perspectives.
| Perspective | Participant (95% CI) | Incremental cost (£) (95% CI) | Incremental QALYs (95% CI) | ICER |
|---|---|---|---|---|
| Analysis 1 | ||||
| NHS PSS perspective | Parent | –2302 (–10,300 to 4480) | 0.1367 (–0.0393 to 0.3334) | HFP dominates |
| Child | 488 (–6279 to 5827) | 0.0297 (–0.1155 to 0.1961) | £16,466 | |
| Societal perspective | Parent | –2338 (–10,284 to 4391) | 0.1367 (–0.0393 to 0.3334) | HFP dominates |
| Child | 451 (–6300 to 5769) | 0.0297 (–0.1155 to 0.1961) | £15,191.21 | |
| Analysis 2 | ||||
| NHS PSS perspective | Parent | 2547 (–8584 to 10,837.70) | 0.0249 (–0.1982 to 0.2318) | £102,083 |
| Child | 3654 (–5636 to 10,867) | –0.1250 (–0.3847 to 0.1381) | Usual care dominates | |
| Societal perspective | Parent | 2399 (–8577 to 10,571) | 0.0249 (–0.1982 to 0.2318) | £96,155 |
| Child | 3534 (–5661 to 10,791) | –0.1250 (–0.3847 to 0.1381) | Usual care dominates | |
In the results from analysis 1, using parent QALYs when controlling for baseline EQ-5D-5L scores, the HFP-M dominated usual care from both perspectives, indicating that the HFP-M is associated with lower costs and greater QALYs than usual care. Using child QALYs, having also controlled for baseline EQ-5D-3L scores, the HFP-M had higher costs and also higher QALYs than usual care from both perspectives.
Figures 5 and 6 show the uncertainty around the ICERs when controlling for baseline EQ-5D-3L scores for children from NHS/PSS and societal perspectives. The points on the cost-effectiveness planes represent a pair of incremental costs and QALYs from 1000 bootstrapped samples. The points in Figures 5 and 6 were not confined to one quadrant of the cost-effectiveness plane, indicating uncertainty around the result; however, Figures 5 and 6 show that more of the points (just over 40%) were confined to the north-east quadrant (where costs are higher and outcomes are better) than in the other quadrants. Corresponding cost-effectiveness acceptability curves are provided in Appendix 13.
FIGURE 5.
Cost-effectiveness plane based on T2 data (NHS perspective). NE, north-east; NW, north-west; SE, south-east; SW, south-west.

FIGURE 6.
Cost-effectiveness plane based on T2 data (societal perspective). NE, north-east; NW, north-west; SE, south-east; SW, south-west.

Results from analysis 2, using parent QALYs when controlling for baseline EQ-5D-5L scores, showed that the HFP-M was associated with greater costs and QALYs than usual care. Using child QALYs, having also controlled for baseline EQ-5D-3L scores, the HFP-M was dominated by usual care, as the HFP-M was associated with higher costs and fewer QALYs than usual care from both perspectives.
Parent qualitative findings related to outcomes
Theme 3: experiencing a psychoeducational parenting intervention
This theme described participants’ experiences of receiving either of the psychoeducational parenting interventions available in the trial. Two subthemes were relevant to intervention acceptability and have been reported above. The third subtheme, intervention impact and outcomes, was relevant to participant outcomes.
Subtheme 3: intervention impact and outcomes
This subtheme described the personal and family effects that parents experienced as result of participating in the trial interventions. These impacts predominantly focused on behavioural, cognitive and emotional changes in parenting, parental confidence, the index child and the parent–child relationship. Positive impacts were generally, although not consistently, described by participants who received the HFP-M. Fewer positive impacts were reported by parents in the usual-care arm.
Changes in parenting behaviour included increased parental consistency and boundary setting, and less use of physical and harsh punishments:
My daughter would watch TV [television] every morning before school . . . which meant that she wasn’t eating her breakfast, everything was taking much longer so I decided that there would be a house rule where in the morning on school days the TV wouldn’t go on to watch children’s TV. And the whole nine months, I pretty much kept to that.
Participant 2004, paragraph 58
So, before I was kind of grounding her for the whole week. And [the research therapist] kind of explained to me, like poor child . . . it’s a lot. So, if she does one thing or two things, focus on those things and give her praise for those things and kind of still address the negative. Discuss it, but make it short and then draw a line and leave it and move on. And so that was one of the things that I used that was very helpful.
Participant 1030, paragraph 85
When I used to do it [use physical punishments], I used to, you know, feel sorry . . . because that’s the last thing I want to do but when [the research therapist] talked to me and, you know, I don’t do it anymore. It makes me feel so good.
Participant 1024, paragraph 156
Parents described greater involvement with their children and increased use of positive attention and praise:
Not focusing on everything that she does bad and focusing on the good stuff as well has helped a lot . . . It was easy for her just to get bad attention . . . now she knows that the attention is there and she doesn’t have to be bad to get attention. It’s calmed down a lot.
Participant 1016, paragraph 123
The changes parents described in their children included fewer tantrums, fights and aggressive outbursts:
There’s a few things that we came up with, like dealing with [my child] and when she goes into her tantrum, and sort of things like ignoring her and that. ’Cause me and [my child] used to get into some really terrible arguments and in the last, two months’ things have really actually changed.
Participant 1003, paragraph 147
She was like constantly disrespectful, just constantly, constantly, constantly and speak back to me and it was just really hurting me. But now, I’m not saying she don’t do it but not as often and I would talk to her about it and say to her that’s not nice and things like that and she kind of understands now.
Participant 1020, paragraph 115
Parents also described changes in their relationships with their children, characterised by greater warmth, communication, role delineation and an increased emotional-cognitive capacity to more accurately understand and appreciate their children’s needs:
. . . [the research therapist] says ‘If she’s quiet, don’t just leave her be, let her know that you’re still thinking of her’ so she’s like not craving the attention, you know, she don’t feel like she has to shut herself in her bedroom and, like, play with her toys and stay away from us and plus it makes [the child] feel good, I mean, you look round and say ‘Alright babe’ and she thinks ‘Oh they’re still thinking about me’. You know, little things like that go a long way.
Participant 1016, paragraph 112
[The research therapist] . . . helped me to, kind of, understand how relationships work . . . one of the things I remember [the research therapist] saying to me ‘It’s our relationship, think of it as a plant and every day you water it and get a bit of sunshine and it will grow’. So, don’t force it, just allow it to happen and it has yeah.
Participant 1030, paragraph 101
Before I was not a mum, I was a mate to my kids, I was never a mum. I was their mate so there was no rules ‘cause I kind of lost the mum control. I became more of their friend which never worked, ever.
Participant 2009, paragraph 129
Parents, predominantly in the intervention arm, described improvements in their own emotional regulation:
When before . . . I was maybe kind of quick to get mad and just you know scream and stuff like that. Now I don’t, not as often, and I try my best to understand where they’re coming from.
Participant 1020, paragraph 115
Yeah, breathe or just come out the room for a bit and then go back.
Participant 1021, paragraph 93
You know, you just need to talk, just stick to what you say and that’s it and it works. And try and calm when you’re talking because if you’re not calm when you’re talking then you’re just going to boil up like that and you want to burst out. So, [the research therapist] said, ‘Just try and be calm and talk’.
Participant 1024, paragraph 164
This often involved parents changing their feelings about parenting tasks that they had previously found difficult as well as interpreting the needs of their children differently:
I feel like, if you’ve just come in from somewhere like work or whatever and your children are all like, ‘Oh mum this happened, that happened, oh mum can you get this? Can you do this? Can you do that?’ . . . I think you have to sort of like take a step back and think ‘Right, I’m just gonna spend 10 minutes to relax’. And then obviously, ‘cause you’re so relaxed and you’ve unwound, unwound you can then . . . deal with things better.
Participant 1008, paragraph 69
With these changes, parents often described a greater preparedness and ability to see things from their children’s perspective. This often gave parents a greater awareness of how their own behaviour affected and exacerbated their children’s difficulties:
I mean even . . . noticing things about him, . . . he’s just so angry and so rude to me . . . but I’m rude to him too and that’s probably why he’s like that and it doesn’t help, you know, and to just realise those kinds of things, which in those sessions I did, about [my child] as well . . . the dad.
Participant 1018, paragraph 171
The psychoeducational content also helped parents to gain better understandings of their parenting role, and more accurate expectations of their children’s developmental needs:
The reassurance that it’s not all my fault . . . that as a parent, sometimes, there isn’t a right thing you can do. [Knowing children’s] emotions can be just as sudden as your own. Definitely the reassurance of knowing that I’m not alone and I am doing the best that I can do as a mum.
Participant 1003, paragraph 75
This not only helped parents to adjust and change their parenting but also resulted in greater self-confidence, more positive views of themselves as parents, greater assurance about parenting as well as being more conscious of looking after their own needs:
It’s helped me to believe in myself. It’s heartening to understand how my children are feeling, it’s helped me to be able to help them, to need to be a better parent, it’s helped me. It’s opened a gate for me to be more optimistic towards my children, to understand how they feel and their feelings.
Participant 1036, paragraph 59
I feel loads better, I feel more confident . . . I just feel like I can handle more situations. So, now, where I got my confidence back and stuff, and then I learned how to say ‘no’, I learned how to say ‘no’, that was the hardest one.
Participant 2009, paragraph 129
Keyworker qualitative findings related to intervention acceptability
Theme 4: intervention characteristics
Theme 4, intervention characteristics, was generated by the thematic content analysis of keyworker interview data and it reflected intervention content and methods that keyworkers felt were useful and effective. Of the theme’s subthemes, the most relevant was subtheme 3 (parent experience and outcome).
Subtheme 3: parent experience and outcome
Based on their experience of the trial, the majority of keyworkers would have been likely to refer other parents to the trial and interventions if the opportunity arose again:
There was nothing that would put me off referring on again for the right client.
Keyworker 4014, paragraph 45
The majority of referring keyworkers described parents’ positive experiences and impacts of intervention participation:
[The participant] spoke very highly of the work that you did with her.
Keyworker 4003, paragraph 21
She was happy to have insight and support into her mental health really.
Keyworker 5002, paragraph 47
She was disappointed but she actually found that the one-off session . . . she reported back saying it had given her loads of ideas and she found it quite helpful.
Keyworker 4016, paragraph 27
However, some keyworkers were unable to assess impact as they no longer had contact with the parents and their families:
A lot of these families are now closed. I’d assume that a lot of the issues must have been addressed, because [there are] no longer had concerns.
Keyworker 4002, paragraph 69
I only saw her for an assessment and then she was allocated to a counsellor within our team. So, the only contact I had with her [was] when I . . . agreed with her that we’re going to make this referral.
Keyworker 4014, paragraph 65
Chapter 9 Randomised feasibility trial conclusion
The randomised trial conducted in phase 3 assessed the feasibility of revised research procedures and the acceptability of the HFP-M and usual-care interventions. It examined the influence of parent, service and other contextual factors affecting the conduct of the trial procedures, intervention delivery and uptake. Evidence was obtained about indicative variance estimates for parent and child outcomes, and intervention and participant service costs.
The results supported feasibility of most trial methods and provided helpful methodological and intervention insights that can be used to inform a definitive trial protocol. 152 The HFP-M proved to be acceptable to participants despite delivery duration being longer and less efficient than planned. The usual-care condition was less acceptable to participants with some associated effects on trial retention.
Outcome effects were identified across both trial arms, with some advantage for the HFP-M. There may also be some cost advantage for the HFP-M. Caution needs to be exercised in the interpretation of these results, owing to the lower than expected sample size and missing data. This was a result of recruitment difficulties in site 2 and sample attrition. Cross-sectional process evaluation provided a fine-grained understanding of key contextual factors that affected the conduct of the trial and its interventions.
Feasibility of trial methods and procedures
Initial service user identification, referral and eligibility
Parents were referred from a wide range of keyworker and service sources. Despite caution expressed in phase 1 consultation findings, recruitment was successfully extended in the feasibility trial to children’s social care teams, who provided one-third of referrals.
All referred parents consented to initial screening, which resulted in one-third of referred parents being identified as ineligible. The main reason was that parents elected not to take part in the trial. The process evaluation provided rich accounts of factors that affected keyworker referrals and parents’ participation decisions. These included the adverse impact of parents’ life circumstances on their availability to participate, previous negative service experiences and, from parent and keyworker perspectives, the paucity of similar interventions available within routine care. In common with many people who seek treatment, parents generally approached trial participation with hopeful expectations, caution and uncertainty. 167,168
The use of non-diagnostic eligibility criteria and screening measures was effective and successful, without the ethics concerns and participant burden experienced in phase 2. The trial required morbidity for both referred parent and index child. Eighty per cent of service users who completed screening measures met both parent and child eligibility criteria. The majority of excluded service users exceeded the screening cut-off point for either the parent SAPAS score or the child SDQ, but not both. At formal screening, < 10% of referred service users satisfied neither the SAPAS nor the SDQ eligibility criteria.
Site recruitment
Despite the estimated prevalence of parents and children fulfilling trial criteria and the strong evidence of detrimental impacts of parent personality difficulties on parenting and child outcomes,169,170 referral flow was lower than planned, particularly in site 2. Although not practical within the feasibility trial, successfully implementing the proposed methods to collect keyworker data on initial rates of participant identification and service user consent would have helped to shed further light on factors affecting recruitment flow.
The proportions of parents meeting criteria at each recruitment stage were similar between sites. A subsequent trial may have similar inclusion rates at each recruitment stage. Methods improving recruitment flow into a definitive trial may be necessary, including systematic routine caseload identification, in-depth training and support to improve keyworker confidence to positively engage parents, and information to reduce perceived keyworker burden. For example, evidence suggested that trial participation probably did not increase keyworker tasks and it did not lead to adverse events. Qualitative evidence suggested that keyworkers may have redirected their care to other service users once participants were in the trial.
The feasibility results demonstrated very clear site differences in referral rates. Three-quarters of trial participants were referred from site 1 services. A similar recruitment flow in site 2 would have resulted in the planned recruitment target. The lower than anticipated recruitment rate reduced power and increased CIs of outcome variance estimates generated.
The differential site recruitment rate highlighted the conditions necessary to facilitate successful trial recruitment. Site 1 could more consistently implement types of proactive, personalised researcher activities to support busy, hard-pressed practitioners identified by keyworkers in the process evaluation. Keyworker qualitative results provided helpful insights into the proactive and persistent research methods necessary to generate recruitment success.
Randomised trial allocation
Process findings suggested that participants understood the rationale of the trial’s methods. Some questioned the use of a randomised design given the level of expressed need and paucity of similar provision in routine services.
Almost all participants randomised to the HFP-M arm accepted the intervention. Those who did not, mainly declined owing to family circumstances. A greater proportion of participants declined the usual-care Being a Parent session. This post-allocation attrition represented a potential threat to the validity of a definitive trial. Consistent with the wider literature, process findings suggested that this differential take-up rate may have been affected by parent treatment expectancies, their response to trial allocation and the face validity of the usual-care session. 171 For some participants, usual-care allocation served to reinforce broader experiences common to the sample population of rejection and inequity, often provoking feelings of anger. 172
While the PIS carefully set out the purpose and methods of the trial, a definitive trial may need a greater emphasis from referring keyworkers on the importance of testing, rather than assuming, the effectiveness of the HFP-M. To address the evident allocation concerns and, possibly, to improve retention, a trial would also need to consider ways of improving the face validity of the usual-care arm without it becoming an alternative treatment condition. 173
Measure completion and sample retention
The measures used in the trial proved to be feasible, with negligible missing items at each assessment. The exception to this was the problematic completion of the CSRI, which hampered the health economic analysis. Occasionally, questionnaires were not completed, mainly as a result of participant fatigue. This was particularly the case at T2, when participants completed a lengthy qualitative interview. Parents and researchers often preferred to complete data collection on single occasions, because of difficulties in successfully rearranging appointments.
Two-thirds of trial participants completed T2 measures. This exceeded the most important a priori feasibility criterion of a trial retention rate of 65%. 84 Over 80% of participants who accepted a trial intervention in either arm completed T2 measures, similar to rates in previous HFP and PEPS evaluations. 30,83
In order to complete the trial within the agreed time frame, T3 data collection took place at around 4 months after T2 rather than 6 months later as planned. There was also a difference in the follow-up period between trial arms, owing to the time required to complete the HFP-M delivery. Two-thirds of participants completing T2 measures provided T3 data. Maintaining participant retention at T2 and T3 proved more difficult for participants who declined intervention but did not formally withdraw from the trial.
Researcher persistence to contact participants was a common feature at each data collection stage. The difficulties in contacting parents led to delays in screening and intervention uptake for some parents, and they resulted in overall delays in the trial. Negative life events and parents’ reactions to these were common reasons for delays in data collection and intervention appointment cancellations. Higher levels of research engagement activities, such as sharing trial updates and progress, may be useful to adopt in a subsequent trial given the increased frequency of major life events and disruptions in life functioning, to which the target population is exposed. 96 These are most likely to be effective when researchers use personalised, rather than generalised, methods of communication.
Trial sample characteristics
The trial procedures and eligibility criteria resulted in the recruitment of a participant sample affected by substantial levels of personal, social and economic adversity. There were no substantial differences between participants allocated to the two conditions that were likely to affect the interpretation of the trial findings.
Sample characteristics are typical of the mental health morbidity and the wider adversity experienced by the target population. 174,175 Morbidity was substantially higher than that reported by parents recruited to a community parenting intervention conducted in a similar geographical area. 132
The vast majority of participants had one or more long-standing psychiatric diagnosis. Many experienced coexisting physical health problems and disability. The majority were lone parents and only a minority of families included a parent in employment.
The trial sought to recruit both mothers and fathers. However, like the vast majority of other parenting interventions, virtually all participants were biological mothers,51 most of whom reporting substantial parenting difficulties.
Participant accounts from the process evaluation were often characterised by a sense of sadness about the ways in which parents felt that their mental health and interpersonal difficulties had combined with current and past adversity to shape, and often undermine, their sense of parental competence and parenting capacity. 6,17,19–21,23,24
Unlike the majority of parenting programmes, this trial did not specifically recruit children with behavioural difficulties; the index children recruited had substantially elevated levels of emotional, behavioural and other mental health difficulties. This is consistent with the wider literature that points towards the increased risks of a range of mental health difficulties for the offspring of parents with severe personality difficulties. 30–32,34,38,46,49,168
Many of the sample characteristics are generally associated with poorer treatment engagement and outcomes. 174 Although potentially selective, process findings reflected the participants’ largely negative previous service experiences, which are consistent with other evidence of non-therapeutic reactions of health and social care practitioners to people with personality disorders of mental health. 97,98,172
Acceptability of trial interventions
Intervention uptake and completion
Intervention uptake differed substantially between the two trial arms, with a much greater proportion of participants accepting the HFP-M. The HFP-M retention rate was consistent with evidence from personality disorder treatment trials involving service users exposed to higher levels of social adversity. 24,96,110
Intervention non-completion is frequently associated with increased risk of adverse longer-term outcomes. Participants who withdrew prematurely did so because of acute personal mental health crises and adverse family life events, rather than intervention dissatisfaction or expulsion. 110 All participants who accepted the usual-care intervention completed the session.
Intervention delivery
Participants’ uptake of the HFP-M was consistent with meaningful exposure to psychotherapeutic treatments and parenting programme interventions. 11,51,176,177 The HFP-M session module delivery took place over more appointments and with a longer duration than planned. Its home-based delivery format resulted in a very low proportion of DNAs. However, appointment cancellation affected around one in five appointments.
Cancellations represented a substantial intervention cost that may have had a detrimental effect on efficient intervention adherence and efficiency, compromising availability to other eligible participants, and it may have lowered therapist and service morale. 110
Although potentially frustrating for research therapists and problematic for trial delivery, process findings suggested that cancellations were not caused by participant disinterest. They were more likely to reflect the greater vulnerability of the sample population to negative life events and their response to them. 96 Parents regretted having missed appointments and were mindful of the effects on themselves and the inconvenience to research therapists. Process findings suggested that intersession texts and telephone messages may have reinforced parents’ perceptions of therapists’ commitment and willingness to exceed standard therapeutic requirements. 106,107
Given the complex nature of the target population, it may be necessary to incorporate assumptions about cancellations into the format of the HFP-M delivery. At the same time, other methods should be considered to improve efficiency of the HFP-M and reduce its duration, such as pre-emptive cancellation planning. 178,179 Methods to manage cancellation issues may be more likely to be successful given the stronger therapeutic bonds reported by the HFP-M participants. 171
Therapeutic alliance
Building a good therapeutic alliance has received particular attention in the personality disorder literature. This is not only because of the recognised difficulties in establishing strong alliances with those affected, but also because of the association between therapeutic alliance, engagement and outcomes for people affected by personality disorders. 106,135,174
Parents’ rating of therapeutic alliance for the two interventions differed substantially. The HFP-M participants rated highly their ability to reach agreement on the tasks and goals of the intervention as well as positive affective bonds with their research therapist. This may reflect the success of the HFP-M manual content, therapist training and supervision procedures, which included explicit methods and skills to develop collaborative, validating parent–therapist alliances.
Although it is a small sample, the lower alliance ratings given by usual-care participants may also be a function of the duration and depth of the HFP-M compared with the one-session Being a Parent intervention. The process evaluation illustrated some of the difficulties for therapists and parents to develop effective, validating therapeutic alliances in a single psychoeducational session of this type with the target population. The alliance differences may have also reflected the wider evidence that participants assigned to a control condition may be more likely to be dissatisfied. 180
The process findings suggested that the HFP-M appeared to better mobilise parents’ hopes than usual care. 180 Parents allocated to the HFP-M often responded with excitement and enthusiasm, potentially affected by treatment expectancies and paucity of effective routine provision. The duration, structure and format of the intervention had greater credibility, which parents felt offered greater depth and opportunity to address the complexity of their parenting and family difficulties.
For many participants, irrespective of group allocation, the usual-care session intervention lacked validity. Parents contrasted the complex and enduring nature of their personal, parenting and family needs with the brevity of the single session. These views may reflect a realistic appraisal of parents’ difficulties and the amount of intervention time required to achieve change. Their views may also have been affected by keyworker expectancies and assessment of the trial interventions.
Intervention format and content
The process findings suggested that parents’ experiences of the HFP-M format and content were consistent with recommended therapeutic practice for people with personality disorders. 135,171 Its goal-orientated helping process offered parents clarity about the intervention focus and methods. The HFP-M used a clear appointment structure that enabled parents to share their immediate life circumstances at the beginning of each appointment (offload) and briefly problem-solve suitable coping strategies (firefighting), if necessary. Each session module focused on specific content, supported by written materials, that built sequentially over time and was tailored to individual needs. 107,135,136 The HFP-M incorporated regular progress review that focused on outcome progress as well as the quality of the therapeutic alliance. 172
These structural and content elements were most successful when combined with specific therapist characteristics. Therapist responsiveness, including empathic validation, flexibility and collaboration, is strongly emphasised in personality disorder psychotherapy literature. 106,107,181 Process findings elaborated the WAI-SR alliance ratings. Parents’ accounts focused on therapists who they felt genuinely appreciated and understood their personal circumstances, were persistent and reliable, offered choice and flexibility, and engaged them in a collaborative and facilitative partnership. For example, parents who received the HFP-M felt that it gave greater scope to explore and develop a shared understanding of family ecology and its strengths and difficulties. This collaborative process provided the basis to validate parent experiences and flexibly tailor the HFP-M parenting content and self-care strategies to individual participant need, their family and their wider context. 172
Parents contrasted these collaborative processes with the unhelpful impact of more didactic, non-personalised and therapist-driven interactions.
Clinical outcome measurement
Personality disorders, and borderline personality disorder in particular, are associated with parenting impairments across a range of emotional, interpersonal, behavioural and social domains. 6,17,19–21,23,24,169 An aim of the feasibility trial was to produce variance estimates for parent and child outcomes that could be used to power a definitive trial. Sample size and trial retention rates affected the reliability of outcome findings.
The results from the intention-to-treat analysis suggested that child and parent clinical outcomes may have improved over time in both intervention and usual-care groups. There was evidence of a potential post-intervention advantage for the intervention condition across parental concerns about their index child (CAMC), severity of child behaviour and parenting satisfaction. There was less evidence of possible intervention-arm advantage for child internalising difficulties, positive parenting behaviours and parental mental health; these outcomes showed similar patterns of potential improvement across both groups. The T3 data were not included in the intention-to-treat analysis, because only a very small sample was available.
Overall, these post-intervention improvements are to be welcomed, particularly given the nature of the intervention population’s complex difficulties and associated negative parent and practitioner treatment expectancies identified over the course of the research and wider literature. 97–99
The results suggested that a subsequent trial should be based on an estimated small to medium ES. Overall, ES estimates varied across outcomes from large to nil, each subject to expected wide CIs. The largest effects were detected for the parental goal attainment measure, CAMC. This type of idiographic goal attainment scaling measure is strongly advocated as a means of identifying and measuring service user priorities and is typically most sensitive to change. 182 Potential medium effects on child behaviour severity and parenting satisfaction were also detected, although with similar caveats about reliability given wide CIs. Although participants reported improvements in ECBI Intensity score, the mean post-intervention score remained above the measure’s cut-off point for significant severity.
The results potentially suggested a more significant intervention impact on child behaviour problems than internalising difficulties. This is consistent with broader evidence for the efficacy of parenting interventions for child behavioural difficulties. Comparatively less evidence is available in relation to internalising difficulties. A definitive trial could narrow its intervention focus and eligibility criteria to reflect this finding. The alternative would be to review and strengthen the HFP-M content for child internalising difficulties, for example through the inclusion of content related to graded exposure, reduction of parental maintaining behaviours and improvement in child coping skills. 53
Similarly, there is evidence of an effect on parenting satisfaction, but less in relation to positive parenting behaviour as measured by the PS. This is surprising given the broader evidence supporting the effectiveness of parenting programmes with this parenting domain and parents’ qualitative accounts. 51 Process findings provided detailed participant accounts of intervention impacts on parenting, including greater parental sensitivity and lower levels of intrusiveness, more effective family boundaries and organisation, warmer and more cohesive family atmosphere and improved reflective function. Parents associated these changes with lower parental stress, improved parental competence and satisfaction. These positive changes were more often, though not exclusively, attributed to participation in the HFP-M.
Intervention costs and economic impact
Data availability was limited for the health economic analyses. Ideally, cost-effectiveness would be assessed over the entire follow-up, but here the more robust findings are those reported at T2. When considering parental QALYs, the HFP-M intervention dominated usual care. When QALYs for children were used, the HFP-M resulted in higher costs and more QALYs.
Methodological issues
The trial’s recruitment and intervention delivery were embedded in existing service frameworks, increasing its ecological validity, potential generalisability and replication of its methods. Its mixed-methods design synthesised quantitative and qualitative findings to report on trial aims. 71,72
Recruitment and retention difficulties affected final sample size, and limited trial power and the interpretation of quantitative findings. 183 The intention-to-treat analysis did not include T3 follow-up data because of the small sample available. A future trial would need to create effective methods to maintain and retain participant involvement, particularly given the post-allocation attrition in the comparison group.
A number of potential sources of bias may have affected trial findings. In particular, participants were exposed to parenting interventions across the two trial arms of significantly different duration and therapeutic intensity. Given that all participants continued to receive other interventions alongside this trial, it is possible that the potential outcome effects detected may have been a result of these factors rather than active intervention content.
Outcome measurement relied on parent self-report measures. Subsequent research should incorporate independent measures of parenting and child outcomes. Process findings included parent-reported changes in parent–child relationships, reflective function and safer parenting, none of which were included in outcome measurement. Future consideration should be given to the selection of primary and secondary outcome domains of interest in a future trial, to ensure that they are as closely aligned as possible to parent and child needs, safer parenting and child protection, as well as the intervention aims, content and effects.
Health economics
There were limitations to the health economic aspects of the study. Baseline CSRI data were not collected. As a consequence, no baseline resource use and costs were collected. It was then possible to not control for baseline costs in the subsequent analysis.
Service use data were provided by family members and recall may have not been optimal. In addition, there were some services that could not be costed for in the analysis. These were used by a small number of participants and unlikely to affect the results in a major way. The cost for time lost from school was also not included in the main analysis.
The time intervals between the CSRI collection differed for each participant. The period between T2 and T3 was originally planned as 6 months. However, study constraints reduced this to a mean of 4 months. Some participants had follow-up points that were longer than 4 months, so different intervals were used to calculate the QALYs.
The follow-up at T3 could provide only indicative results of cost-effectiveness and a future trial should have a longer follow-up, controlling for baseline resource use.
The site recruitment differences were not predicted. The findings served to highlight the site commitment and resources required to undertake this type of complex trial. Supported by keyworker process findings, an unintended consequence was that site differences potentially served to demonstrate that implementation of the trial service engagement procedures may have improved recruitment.
Process evaluation
The process evaluation used a large, robust parent sample with sufficient exposure to the trial methods and two contrasting interventions. Research interview methods resulted in parents providing rich and informative data. Systematic and transparent analytic procedures were followed, incorporating examination of data saturation and participant validation. A service user researcher was involved in key research activities and a research worker with lived experience was involved in data collection and analysis. Keyworker qualitative findings were derived from a smaller sample, with interviews conducted by telephone rather than in person, which may have affected the quality of data acquired. All qualitative interviews were based on participant recall.
Although providing in-depth accounts of parent and keyworker experiences, the process evaluation was based on inherently subjective methods of analysis that may be open to participant and interpretative bias. For example, participants may have overly attributed change to their participation in the intervention condition to which they were allocated rather than to other factors, particularly when they had had a positive experience of the intervention and of the research therapist. Only a small minority of interviewed participants declined the intervention offered.
The very nature of the interviews meant that researchers were not blinded to the participant trial allocation, which may have influenced participant content as well as subsequent analysis. There is little evidence of participant interview compliance. Parents showed a willingness to be critical as well as complimentary of trial interventions and methods.
Fidelity monitoring
More effective adherence methods would have helped to manage and report intervention fidelity. This is a challenging issue given the complex needs of the target population, their adverse life circumstances and the therapeutic requirements for personalisation that may improve engagement and impact. There are some indications in the findings that the HFP-M implementation may have varied across sites, although insufficient data were available to substantiate this.
The trial collected therapist-reported data on the extent to which parents completed the HFP-M session modules. It would have been useful to have collected further detail on parent uptake and implementation of module content. Six HFP-M therapists and three Being a Parent therapists delivered the interventions, with some possible between-site differences. Although no formal data were collected, anecdotal evidence suggests that, owing to site differences, site 1 therapists received more extensive training, supervision and support.
Adverse events
No adverse events were reported over the course of the trial. A number of participants withdrew from the intervention condition. This was most frequently because of deterioration of participant mental health and life circumstances, unrelated to trial participation. The most significant unforeseen effect was the impact of participant allocation to usual care. The disappointment expressed by participants highlighted the importance of ensuring that future participants are well informed and prepared for trial methods as well as the importance of managing the emotional impact of subsequent allocation.
Phase 3 public and patient involvement
The research programme’s service user representatives (LM and LF) and the SUAP made significant contributions to the development of phase 3 recruitment and screening methods, data analysis and interpretation. Liberty Mosse provided advice on the briefing pack for keyworkers and the Joint Working Protocol. Lisa Foote participated in phase 3 analysis of parent qualitative data and initial data interpretation, and co-facilitated the participant validation event.
Chapter 10 Conclusions and recommendations
Research programme summary
Background
This research programme was commissioned to develop and evaluate a psychoeducational intervention for parents with personality disorders whose children had severe emotional and behavioural problems, and who were attending or being considered for referral to CAMHS.
This required the development of a complex parenting intervention intended to concurrently address multimorbidities across parent, parenting and child outcomes in a population typically subject to high levels of social and economic adversity. Guided by an explicit framework, intervention development was undertaken in consultation with service users and service clinicians.
The routine identification and provision of parenting interventions to the target population typically falls outside the remit of any single established clinical service component. For example, routine mental health service provision is typically aligned to meet the needs of individual parents or children, rather than concurrently address their multimorbidities. Children’s social care services typically focus on reducing safeguarding risks to children but are unlikely to directly address parent and child mental health concerns.
Requiring specialist training and therapeutic skills, the parenting intervention, the HFP-M, developed involved components focused on parent personality and interpersonal functioning, parenting and child mental health. It took account of negative treatment expectancies, service disengagement and adverse outcomes typically experienced by the target population, and staff providing care by incorporating additional methods to promote parent engagement and personalise intervention content.
The concurrent research aimed to develop and manualise feasible methods to identify, select and engage eligible participants in a methodically robust and ethics evaluation of the innovative parenting programme.
Phased research programme
The phased design consisted of three inter-related and sequential components.
Phase 1: intervention and research evaluation development
Findings from the phase 1 scoping review, service user and keyworker consultation were used to modify the existing HFP and PEPS manualised interventions to create the specialised psychoeducational HFP-M intervention. A preliminary screening process for the identification and recruitment of parents meeting research diagnosis of personality disorder was produced.
The HFP-M manual development was guided by the TIDieR checklist, including in-depth understanding of symptomatic difficulties and experiences of the target population, use of the MDP conceptual model as a pragmatic, differentiated ecological description of the inter-relationship between parent, child and parenting outcomes for the target population, current organisation and provision of relevant care, methods to engage practitioners and eligible parents in the HFP-M and its evaluation, specification of the HFP-M format and content, and methods to co-ordinate the HFP-M with usual care.
Phase 2: pre-trial feasibility testing
Phase 2 completed a small case series to test the HFP-M with parents meeting a research diagnosis of personality disorder. Findings provided preliminary support for the rationale, aims, format and content acceptability for the HFP-M and they provided a sufficient basis on which to proceed to the planned randomised feasibility trial. Case series findings suggested changes to the proposed recruitment and screening methods, particularly the use of non-diagnostic eligibility criteria and the extension of recruitment to children’s social care teams. The case series also identified potential threats to the programme delivery, such as the often fluctuating life circumstances of the target population.
Phase 2 produced an account of usual parenting support for the target population that was used to inform feasibility trial planning. A training programme for selected research therapists was completed. A range of research information and case co-ordination materials were produced to assist identification, engagement and case management of eligible parents.
Phase 3: randomised feasibility trial and process evaluation
The final research phase completed a randomised feasibility trial that assessed revised research procedures and the acceptability of the HFP-M and usual-care Being a Parent interventions. 152
Synthesis of quantitative and qualitative results broadly supported the feasibility of trial methods and identified areas to address in a subsequent definitive trial. 71,72 The HFP-M proved to be largely acceptable to participants despite delivery duration being longer than planned. The usual-care condition was less acceptable to participants, with some associated effects on trial retention.
Effects were identified across both trial arms, with some potential advantage for the HFP-M. Results produced indicative variance estimates for parent and child outcomes and measured intervention and participant service costs. Caution was required for the interpretation of results, owing to lower than expected sample recruitment and retention. Cross-sectional process evaluation provided a fine-grained understanding of key contextual factors that affected the conduct of the trial and its interventions.
Research outputs
The research programme produced:
-
the HFP-M – a new manualised psychoeducational health technology with potential to reduce adverse risks and associated costs of severe parental personality difficulties and concurrent child mental health difficulties through improvements in parenting, child and family functioning (see Report Supplementary Material 3)
-
the Being a Parent usual care session – a new manualised single assessment and psychoeducational parenting guidance technology, with potential to reduce the variability of usual care (see Report Supplementary Material 4)
-
a systematic method, based on the TIDieR checklist, to produce theoretically grounded, evidence-informed specialised parenting interventions for parents with severe mental health difficulties69
-
fine-grained knowledge about the feasibility of evaluation methods to inform the development of a definitive trial protocol
-
fine-grained knowledge to optimise the implementation, performance and impact of the HFP-M research and routine service settings.
Helping Families Programme-Modified
The HFP-M rationale and aims were consistently endorsed by keyworkers and service users. Its availability was frequently seen as making up for gaps in existing service provision rather than as a research endeavour. In contrast to some existing assumptions, referred parents were highly receptive to the HFP-M. Research programme evidence suggested that it was possible to develop strong therapeutic alliances focused on parenting intervention with this high-need, high-risk, multimorbid population.
In contrast to some service perceptions, parents were often highly sensitive to the disruption and inconvenience caused by appointment cancellation as a result of their personal circumstances. Therapist persistence, validation and specifically designed HFP-M content reinforced parent commitment to intervention participation.
The HFP-M’s combination of persistent, validating and personalised therapeutic practice with effective parenting and parent self-care strategies is consistent with wider treatment recommendations for people affected by personality disorders. Findings suggested that well-planned, theoretically robust specialised parenting interventions for parents affected by severe personality difficulties may have the potential to become an important service asset that can support and augment routine care.
Dissemination
The research has so far resulted in two peer-reviewed publications, two conference papers and a training event (see Publications). 6,76 Findings have influenced the establishment of a Helping Families parental mental health team in one large NHS trust. Despite limitations identified in the feasibility trial, the Being a Parent materials have been subsequently field-tested by routine adult mental health clinicians as a method to support validating and purposeful assessment and discussion of parenting with service users affected by serious and enduring mental health difficulties. The research team has collaborated with service users to produce a short film for educational and training purposes about the effects of severe mental health difficulties on parenting and parents’ experiences of mental health care.
Research programme appraisal and recommendations
Transition from this feasibility research to a definitive trial of the HFP-M requires realistic appraisal of the evidence produced about the research design and evaluation methods, as well as identified, and potential future, threats to the HFP-M acceptability. Potential solutions also need to be identified. 73 This appraisal needs to take account not only of conditions that may exist in a definitive trial, but also those that pertain to the real-world contexts in which the HFP-M may be subsequently delivered.
Design and evaluation strengths, limitations and solutions
The mixed-methods trial design had good internal and external validity. Feasibility testing identified potential threats to validity. Identification methods and referral procedures for eligible parents were successful across child and adult mental health and children’s social care teams, when service managers and keyworkers were proactively engaged and supported by persistent researcher activity, informative materials, and senior clinical and service support. Threats to identification and referral included difficulties with local research and services prioritising the trial, busy keyworker caseloads and lack of confidence to engage parents, who themselves may have felt cautious about trial participation.
More effective keyworker training, additional researcher resources, and routine assessment of parental mental health and its impact on parenting and child outcomes may improve rates of initial identification of eligible parents. Keyworker identification could be augmented in a definitive trial by independent researcher caseload scrutiny and direct parent recruitment. Recruitment in a subsequent trial may inevitably include a proportion of ineligible referred parents, given the paucity of existing routine specialised parenting provision for the target population.
Non-diagnostic eligibility criteria were more effective and ethically more acceptable than the use of research diagnosis, particularly for parents without an existing personality disorder diagnosis. Trial eligibility criteria and screening procedures led to the recruitment of an appropriate, multimorbid sample.
Recruitment and other differences were evident across the two trial sites, both of which were in London. The ecological validity of a definitive trial would be improved by the inclusion of additional sites located outside London, as it would help to demonstrate the efficacy of the HFP-M across different populations and services.
A randomised design with one-to-one allocation was feasible, although challenging, for participants and referring keyworkers. It provided stronger internal validity than the use of a quasi-experimental design. Based on small to medium ES, a full trial would require a significantly larger sample. Retention of participants, particularly parents allocated to a usual-care condition, is likely to be challenging in a full trial using a similar randomised design. The target population’s complex personality difficulties and, typically, heightened sensitivity to rejection underline the importance of managing random allocation sensitively and effectively. Researchers in a definitive trial will need to maintain proactive and validating relationships with participants, particularly those allocated to usual care. Specific researcher training in key therapeutic engagement methods may assist participant retention.
Screening, outcome and process data collection was largely effective. Health economic data completion suffered as a result of participant fatigue. Given the range of parenting outcome effects, a definitive trial should consider inclusion of independent research outcome assessment as well as additional outcome domains identified by the feasibility trial process evaluation, such as parent–child relationships and parental reflective function.
The trial design enabled participants to receive meaningful exposure to the HFP-M. A definitive trial should consider methods to take account of the differential duration and intensity of the HFP-M and a usual-care condition. While maintaining the authenticity of a usual-care condition, a definitive trial could augment the use of the usual-care Being a Parent intervention with a parent self-help support and recovery group, in order to create better equipoise between conditions.
Intervention strengths, challenges and solutions
The HFP-M development was thorough, guided by an explicit framework, and consistently informed by service user and clinician perspectives. It incorporated findings from the preliminary case series and can be further refined using the feasibility findings. Development and feasibility testing were grounded in real-world contexts that reflect the HFP-M’s potential use in routine practice.
The HFP-M has effective content and methods that are consistent with recommended practice and the personalised needs of the target population. It generated meaningful therapeutic alliances from a sample population at elevated risk of service alienation and poor engagement. Feasibility trial data suggested some advantages for the HFP-M over usual-care practice augmented by a brief psychoeducation session.
The intervention took longer to deliver than planned as a result of parents’ life circumstances. Adjustments to parent introductory session modules of the HFP-M should include explicit, validating discussion with participants about the intervention duration and the potential impact of life circumstances on attendance. More concerted and proactive use of the HFP-M Firefighting module, pre-emptive cancellation plans and intersession contact may improve cancellation rates.
Personalisation and multiple components of the HFP-M require high levels of therapist adherence and fidelity monitoring. A definitive trial should consider the collection of additional fine-grained adherence and fidelity procedures to monitor protocol consistent delivery of the HFP-M.
The research team has devised methods for the selection, training and supervision of research and clinical therapists in the content and methods of the HFP-M. These would need to be replicated across sites involved in a definitive trial, together with methods for ensuring intervention quality, consistency and fidelity between research therapists and across trial sites.
Research recommendations
The Helping Families Programme-Modified: a definitive trial
This research programme improved scientific and intervention knowledge for a specific high-risk population of parents and their children exposed to significant multimorbidities.
It was effective in developing and testing feasible trial methods and an acceptable specialised psychoeducation parenting intervention. The findings usefully identified potential threats to recruitment, retention and intervention delivery that need to be taken into account in the planning of a definitive trial.
A definitive trial will be a substantial undertaking that will need realistic costing of the research and service resources required. The trial will most likely require preliminary practitioner training across trial sites, to ensure that service keyworkers have the skills and confidence to identify eligible parents, generate sufficient recruitment flow and optimise the use of available service user information systems. Active procedures will be required to reduce the risk of participant attrition and minimise the risk of missing data, particularly from the comparison condition. The trial will also require the development of a revised comparator condition that can provide equipoise and face validity without distorting usual care. The existing Being a Parent session plus an ongoing parent support group followed by access to the HFP-M on trial completion may provide the most realistic option. Further methods for increasing participant data collection at follow-up could include increased remuneration in ways that did not present an ethics risk, and the provision of booster sessions to support parents’ continued implementation of the HFP-M methods.
A definitive cost-effectiveness analysis should include a wider range of costs, including time lost from school. It should also use modelling methods to extrapolate costs and outcome beyond the trial period.
Improved understanding of parents with mental health disorders
The research findings provided an insight into the personal, family, social and economic adversity experienced by many families with a parent affected by severe personality difficulties. Process findings suggested that participant parents may often have been aware of the ways in which their own experiences and mental health difficulties combined to impair their parenting, resulting in parental resignation and distress. There was also preliminary evidence from the feasibility trial of parents receiving the usual-care condition reporting some outcome improvements.
The MDP model underpinned the development of the HFP-M. Further research may be warranted to develop a more detailed understanding of the role of specific parent and family factors that impair parenting, as well as how they provide resilience and protect parenting and child development.
Improved recognition and identification of parenting needs
Further research may be warranted to test methods aimed at improving the systematic assessment of parenting and child mental health for parents affected by serious and enduring mental health difficulties. Such methods could be used to better identify at-risk and impaired family functioning across routine services. Effective methods are likely to require specific assessment content of parenting, parent and child functioning for target populations. Drawing on findings from the research, assessment methods are also likely to require methods that validate service users’ parenting roles and experiences, minimise stigma and help parents to focus on feasible parenting goals. More accurate identification and assessment may be important initial stages in stepped-care approaches that could improve prevention and increase access to early and specialised parenting intervention for high-risk, multimorbid mental health populations.
Specialised parenting interventions for families affected by multiple morbidities
Effective parenting intervention as a means to improve child developmental outcomes is a significant policy and service priority in the England. 12,13 Implementation to date has mainly focused on the provision of existing evidence-based programmes to generalised populations.
Families suffering multiple and inter-related morbidities across individual members are at high risk of continuing and transgenerational adverse outcomes. The research findings provide further evidence of the significant intervention and care co-ordination challenge that these families present to services, including parent and keyworker negative parenting intervention expectancies and complex help-seeking intentions.
This research has developed and tested the feasibility of an intervention for parents and children with multiple mental health risks and needs. The HFP-M research programme and its findings are consistent with recent policy and proposals that recognise the inter-related mental needs of children and their parents, and the associations between family functioning and wider disadvantage. 12,13,27–29 The programme’s findings are also consistent with good practice recommendations in relation to whole-family approaches to parental mental health and child welfare, and clinical interventions for people affected by personality disorders. 11,29,66,135
Further research is required to evaluate the effectiveness of the HFP-M. Its target population, parents with severe personality difficulties, is not the only high-risk, multimorbid population in which parental mental health problems may impair parenting and child developmental outcomes. As further research evidence is accumulated, the methods and findings of this research programme can be used to inform the development and evaluation of further specialised parenting interventions for parents with other severe and enduring mental health difficulties, such as parents affected by psychosis.
Conclusion
This research programme successfully produced the HFP-M, a specialised parenting intervention for parents affected by severe personality difficulties and their children with significant mental health problems. Findings from the mixed-methods randomised feasibility trial endorsed the acceptability of the HFP-M and broadly supported the feasibility of trial methods. The usual-care condition was less acceptable to participants, with some associated effects on trial retention. Findings usefully identified potential threats to recruitment, retention and intervention delivery that need to be taken into account in the planning and conduct of a definitive trial.
Acknowledgements
We are indebted to the parents who took part in each stage of this research. They shared their knowledge, family experiences and personal difficulties with us. We would also like to thank the practitioners, clinicians and service managers who worked with us. They made vital contributions throughout the study.
We would particularly like to thank Sarah Inkpen, Bethan Stevenson and Chelsea McCorry for their help with the validation of the phase 3 qualitative findings.
Peter Fonagy was a wise, compassionate and determined chairperson of the TSC. It was a pleasure to work with Peter and colleagues on the TSC. Likewise, Philip Graham, Stephen Blumenthal and John Gregson were assured and insightful DMEC colleagues.
Ruth Wilson worked as a research worker on the study. She made significant contributions to the research programme in communicating with parent participants and their mental health teams. She collected and assisted in the analysis of phase 2 case series data.
Nadine Kendall collected and assisted in the analysis of phase 3 qualitative data.
Contributions of the authors
Dr Crispin Day (Head, Centre for Parent and Child Support, South London and Maudsley NHS Foundation Trust and Head, CAMHS Research Unit, King’s College London) was the chief investigator and responsible for the overall conception, design, data acquisition, analysis and interpretation of findings at each phase of this research. He is responsible for the overall content of this report.
Ms Jackie Briskman (Department of Psychology, King’s College London) was the senior research co-ordinator for phase 3 in this research and was responsible for data acquisition, analysis, interpretation, drafting findings and revising this report.
Professor Mike J Crawford (Professor in Mental Health Research, Centre for Psychiatry, Imperial College London) was a co-applicant and contributed to the overall conception, design and interpretation of findings at each phase of this research. He provided an expert contribution about personality disorder. He contributed to critically revising this report.
Ms Lisa Foote (McPin Foundation) was a service user researcher and representative in this research. She contributed to the design, data acquisition, analysis, interpretation and drafting of findings. She contributed to critically revising this report.
Dr Lucy Harris (Deputy Head, Centre for Parent and Child Support, South London and Maudsley NHS Foundation Trust) was responsible for the development and revision of Helping Families Programme-Modified and supervised phase 2 and 3 research therapists. She contributed to critically revising this report.
Ms Janet Boadu (Researcher at King’s Health Economics, King’s College London) co-conducted the health economic analysis and drafted findings for this report.
Professor Paul McCrone (Professor of Healthcare Economics, Institute of Lifecourse Development, University of Greenwich) was a co-applicant and contributed to the overall conception, design and interpretation of findings at each phase of this research. He led the health economic component of the research and contributed to critically revising this report.
Professor Mary McMurran (Professor at the Institute of Mental Health, University of Nottingham) was a co-applicant and contributed to the overall conception, design and interpretation of findings at each phase of this research. She provided an expert contribution about personality disorder. She was a member of the Manualisation Working Group, contributed to research therapist training and contributed to critically revising this report.
Dr Daniel Michelson (Senior Lecturer in Clinical Psychology, School of Psychology, University of Sussex), was a co-applicant and worked closely with the chief investigator on the overall conception and design of this research. He was senior research co-ordinator for phases 1 and 2 was responsible for data acquisition, analysis, interpretation and drafting of findings. He contributed to critically revising this report.
Professor Paul Moran (Professor of Psychiatry, Population Health Sciences, University of Bristol) was a co-applicant and contributed to the overall conception, design and interpretation of findings at each phase of this research. He provided an expert contribution about personality disorder. He contributed to research therapist training and critically revised this report.
Ms Liberty Mosse (CAMHS Research Unit, King’s College London) was a researcher worker on this study. She was responsible for phase 3 data acquisition, analysis and interpretation of findings. She completed the majority of qualitative data acquisition and led its analysis under the direction of the chief investigator. She contributed to critically revising this report.
Professor Stephen Scott (Professor of Child Health and Behaviour, King’s College London) was a co-applicant and contributed to the overall conception, design and interpretation of findings at each phase of this research. He provided an expert contribution about parenting and parenting programmes. He contributed to critically revising this report.
Dr Daniel Stahl (Reader in Biostatistics, Biostatistics and Health Informatics, King’s College London) was a co-applicant and contributed to the overall conception, design and interpretation of findings at each phase of this research. He provided an expert contribution to the design, analysis and interpretation of quantitative components of the research. He contributed to critically revising this report.
Professor Paul Ramchandani [LEGO® (LEGO®, Billund, Denmark) Professor of Play in Education, Development and Learning, Faculty of Education, University of Cambridge] was a co-applicant and contributed to the overall conception, design and interpretation of findings at each phase of this research. He provided an expert contribution about child mental health and co-ordinated the research in CNWL. He contributed to critically revising this report.
Dr Timothy Weaver (Associate Professor in Mental Health, Mental Health Social Work and Interprofessional Learning, Middlesex University) was a co-applicant and contributed to the overall conception, design and interpretation of findings at each phase of this research. He provided an expert contribution about qualitative design, data acquisition and interpretation. He contributed to critically revising this report.
Publications
Peer-reviewed journal papers
Day C, Harris L, McCrone P, McMurran M, Moran P, Morgan L, et al. Feasibility trial of a psychoeducational intervention for parents with personality difficulties: the Helping Families Programme. Contemp Clin Trials Commun 2017;8:67–74.
Wilson R, Weaver T, Michelson D, Day C. Experiences of parenting and clinical intervention for mothers affected by personality disorder: a pilot qualitative study combining parent and clinician perspectives. BMC Psychiatry 2018;18:152.
Day C, Briskman J, Crawford MJ, Foote L, Harris L, Boadu J, et al. Randomised feasibility trial of the helping families programme-modified: an intensive parenting intervention for parents affected by severe personality difficulties. BMJ Open 2020;10:e033637.
Treatment manuals
Day C, Adewole C, Dunn A, Penney C. Being a Parent: Brief Psychoeducational Materials – Usual Care. London: South London and Maudsley NHS Foundation Trust/King’s College London; 2016.
Harris L, Michelson D, McMurran M, Day C. Helping Families Programme Manual-Modified: Psychoeducational Parenting Intervention for Parents Affected by Severe Personality Difficulties. London: South London and Maudsley NHS Foundation Trust/King’s College London; 2016.
Conference presentations
Michelson D. Helping Families: Development and Feasibility Study of a New Psychoeducational Parenting Intervention for Parents with Personality Disorders. International Society for the Study of Personality Disorders Conference XIV, Montreal, 2015.
Wilson R, Michelson D, Morgan L. Involving Service Users in the Development of a New Parenting Programme for Parents with Personality Disorders: Intervention Design and Feasibility Study. Division of Clinical Psychology Annual Conference, London, 2015.
Day C. On Being a Parent. Think Family Conference. South London and Maudsley NHS Foundation Trust, London, 2017.
Day C. Transformational Parenting: Hope, Trust and Change Open the Doors. No Wrong Door, Safeguarding Conference, Epsom, 2018.
Training
Day C, Adewole C. On Being a Parent: The Theory and Practice of Supporting Parent-focussed recovery. One-day Training for Adult Mental Health Clinical Psychologists and Psychotherapists. London: South London and Maudsley NHS Foundation Trust; 2016.
Data-sharing statement
All manuals can be obtained from the corresponding author. All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care.
References
- Green H, McGinnity A, Meltzer H, Ford T, Goodman R. Mental Health of Children and Young People in Great Britain. 2004 2005. www.esds.ac.uk/doc/5269/mrdoc/pdf/5269technicalreport.pdf (accessed 16 January 2019).
- Loeber R, Farrington DP. Young children who commit crime: epidemiology, developmental origins, risk factors, early interventions, and policy implications. Dev Psychopathol 2000;12:737-62. https://doi.org/10.1017/S0954579400004107.
- Davis H, Day C, Cox A, Cutler L. Child and adolescent mental health needs assessment and service implications in an inner-city area. Clin Child Psychol Psychiatry 2000;5:169-88. https://doi.org/10.1177/1359104500005002003.
- Fergusson DM, Horwood LJ, Ridder EM. Show me the child at seven: the consequences of conduct problems in childhood for psychosocial functioning in adulthood. J Child Psychol Psychiatry 2005;46:837-49. https://doi.org/10.1111/j.1469-7610.2004.00387.x.
- Day C, Harris L, McCrone P, McMurran M, Moran P, Morgan L, et al. Feasibility trial of a psychoeducational intervention for parents with personality difficulties: the Helping Families Programme. Contemp Clin Trials Comm 2017;8:67-74. https://doi.org/10.1016/j.conctc.2017.08.002.
- Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, et al. The enduring effects of abuse and related adverse experiences in childhood. A convergence of evidence from neurobiology and epidemiology. Eur Arch Psychiatry Clin Neurosci 2006;256:174-86. https://doi.org/10.1007/s00406-005-0624-4.
- Belsky J, de Haan M. Annual research review: parenting and children’s brain development: the end of the beginning. J Child Psychol Psychiatry 2011;52:409-28. https://doi.org/10.1111/j.1469-7610.2010.02281.x.
- Bronfenbrenner U, Morris P, Lerner R, Damon W. Theoretical Models of Human Development. Hoboken, NJ: John Wiley & Sons Inc.; 2006.
- Steele H, Steele M, Busch F. Mentalization: Theoretical Considerations, Research Findings, and Clinical Implications. New York, NY: Taylor and Francis; 2008.
- O’ Connor T, Scott S. Parenting and Outcomes for Children. York: Joseph Rowntree Trust; 2007.
- National Institute for Health and Care Excellence (NICE) . Antisocial Behaviour and Conduct Disorders in Children and Young People: Recognition, Intervention and Management 2013.
- Allen G. Early Intervention: The Next Steps. London: Cabinet Office and Department for Work and Pensions; 2011.
- Mental Health Taskforce . The Five Year Forward View of Mental Health. Mental Health Taskforce 2016. www.england.nhs.uk/mentalhealth/taskforce (accessed 22 November 2018).
- Macfie J. Development in children and adolescents whose mothers have borderline personality disorder. Child Dev Perspect 2009;3. https://doi.org/10.1111/j.1750-8606.2008.00079.x.
- Reinelt E, Stopsack M, Aldinger M, Ulrich I, Grabe HJ, Barnow S. Longitudinal transmission pathways of borderline personality disorder symptoms: from mother to child?. Psychopathology 2014;47:10-6. https://doi.org/10.1159/000345857.
- McCabe JE. Maternal personality and psychopathology as determinants of parenting behavior: a quantitative integration of two parenting literatures. Psychol Bull 2014;140:722-50. https://doi.org/10.1037/a0034835.
- Yang M, Coid J, Tyrer P. Personality pathology recorded by severity: national survey. Br J Psychiatry 2010;197:193-9. https://doi.org/10.1192/bjp.bp.110.078956.
- World Health Organization . The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines 2016. www.who.int/classifications/icd/en/bluebook.pdf (accessed 25 September 2019).
- Fok ML-Y, Hayes RD, Chang CK, Stewart R, Callard FJ, Moran P. Life expectancy at birth and all-cause mortality among people with personality disorder. J Psychosom Res 2012;73:104-7. https://doi.org/10.1016/j.jpsychores.2012.05.001.
- Boucher MÈ, Pugliese J, Allard-Chapais C, Lecours S, Ahoundova L, Chouinard R, et al. Parent-child relationship associated with the development of borderline personality disorder: a systematic review. Personal Ment Health 2017;11:229-55. https://doi.org/10.1002/pmh.1385.
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1995;52:1048-60. https://doi.org/10.1001/archpsyc.1995.03950240066012.
- Teicher MH, Andersen SL, Polcari A, Anderson CM, Navalta CP. Developmental neurobiology of childhood stress and trauma. Psychiatr Clin North Am 2002;25:397-426. https://doi.org/10.1016/S0193-953X(01)00003-X.
- Pietrek C, Elbert T, Weierstall R, Müller O, Rockstroh B. Childhood adversities in relation to psychiatric disorders. Psychiatry Res 2013;206:103-10. https://doi.org/10.1016/j.psychres.2012.11.003.
- Coid J, Yang M, Tyrer P, Roberts A, Ullrich S. Prevalence and correlates of personality disorder in Great Britain. Br J Psychiatry 2006;188:423-31. https://doi.org/10.1192/bjp.188.5.423.
- Newton-Howes G, Tyrer P, Anagnostakis K, Cooper S, Bowden-Jones O, Weaver T. COSMIC study team. The prevalence of personality disorder, its comorbidity with mental state disorders, and its clinical significance in community mental health teams. Soc Psychiatry Psychiatr Epidemiol 2010;45:453-60. https://doi.org/10.1007/s00127-009-0084-7.
- Tunnard J. Parental Mental Health Problems: Messages from Research, Policy and Practice. Dartington: Research Into Practice; 2014.
- Department for Education (2017) . Transforming Children and Young People’s Mental Health Provision: A Green Paper 2018.
- Damian Green MP. Improving Lives: Helping Workless Families. London: GOV.UK; 2017.
- Social Care Institute for Excellence . Think Child, Think Parent, Think Family: A Guide to Parental Mental Health and Child Welfare 2011. www.scie.org.uk/publications/guides/guide30/summary.asp (accessed 31 May 2018).
- Johnson JG, Cohen P, Kasen S, Ehrensaft MK, Crawford TN. Associations of parental personality disorders and axis I disorders with childrearing behavior. Psychiatry 2006;69:336-50. https://doi.org/10.1521/psyc.2006.69.4.336.
- Newman LK, Stevenson CS, Bergman LR, Boyce P. Borderline personality disorder, mother-infant interaction and parenting perceptions: preliminary findings. Aust N Z J Psychiatry 2007;41:598-605. https://doi.org/10.1080/00048670701392833.
- Feldman RB, Zelkowitz P, Weiss M, Vogel J, Heyman M, Paris J. A comparison of the families of mothers with borderline and nonborderline personality disorders. Compr Psychiatry 1995;36:157-63. https://doi.org/10.1016/S0010-440X(95)90110-8.
- White H, Flanagan TJ, Martin A, Silverman J. Mother–infant interactions in women with borderline personality disorder, major depressive disorder, their co-occurrence, and healthy controls. J Reprod Infant Psyc 2011;29:223-35. https://doi.org/10.1080/02646838.2011.576425.
- Barnow S, Spitzer C, Grabe HJ, Kessler C, Freyberger HJ. Individual characteristics, familial experience, and psychopathology in children of mothers with borderline personality disorder. J Am Acad Child Adolesc Psychiatry 2006;45:965-72. https://doi.org/10.1097/01.chi.0000222790.41853.b9.
- Crandell LE, Patrick MP, Hobson RP. ‘Still-face’ interactions between mothers with borderline personality disorder and their 2-month-old infants. Br J Psychiatry 2003;183:239-47. https://doi.org/10.1192/bjp.183.3.239.
- Hobson RP, Patrick M, Crandell L, García-Pérez R, Lee A. Personal relatedness and attachment in infants of mothers with borderline personality disorder. Dev Psychopathol 2005;17:329-47. https://doi.org/10.1017/S0954579405050169.
- Kiel EJ, Gratz KL, Moore SA, Latzman RD, Tull MT. The impact of borderline personality pathology on mothers’ responses to infant distress. J Fam Psychol 2011;25:907-18. https://doi.org/10.1037/a0025474.
- Schacht R, Hammond L, Marks M, Wood M, Conroy S. The relation between mind-mindedness in mothers with borderline personality disorder and mental state understanding in their children. Infant Child Dev 2013;22:68-84. https://doi.org/10.1002/icd.1766.
- Elliot RL, Campbell L, Hunter M, Cooper G, Melville J, McCabe K, et al. When I look into my baby’s eyes . . . infant emotion recognition by mothers with borderline personality disorder. Inf Ment Health J 2014;35:21-32. https://doi.org/10.1002/imhj.21426.
- Herr NR, Hammen C, Brennan PA. Maternal borderline personality disorder symptoms and adolescent psychosocial functioning. J Pers Disord 2008;22:451-65. https://doi.org/10.1521/pedi.2008.22.5.451.
- Kim J, Cicchetti D, Rogosch FA, Manly JT. Child maltreatment and trajectories of personality and behavioral functioning: implications for the development of personality disorder. Dev Psychopathol 2009;21:889-912. https://doi.org/10.1017/S0954579409000480.
- Eyden J, Winsper C, Wolke D, Broome MR, MacCallum F. A systematic review of the parenting and outcomes experienced by offspring of mothers with borderline personality pathology: potential mechanisms and clinical implications. Clin Psychol Rev 2016;47:85-105. https://doi.org/10.1016/j.cpr.2016.04.002.
- Macfie J, Swan SA. Representations of the caregiver-child relationship and of the self, and emotion regulation in the narratives of young children whose mothers have borderline personality disorder. Dev Psychopathol 2009;21:993-1011. https://doi.org/10.1017/S0954579409000534.
- Abela JR, Skitch SA, Auerbach RP, Adams P. The impact of parental borderline personality disorder on vulnerability to depression in children of affectively ill parents. J Pers Disord 2005;19:68-83. https://doi.org/10.1521/pedi.19.1.68.62177.
- Macfie J, Swan S, Fitzpatrick K, Watkins C, Rivas E. Mothers with borderline personality and their young children: adult attachment interviews, mother–child interactions, and children’s narrative representations. Dev Psychopathol 2014;26:539-5. https://doi.org/10.1017/S095457941400011X.
- Suveg C, Jacob M, Payne M. Parental interpersonal sensitivity and youth social problems: a mediational role for child emotion dysregulation. J Child Fam Stud 2010;19:677-86. https://doi.org/10.1007/s10826-010-9354-y.
- Weiss M, Zelkowitz P, Feldman RB, Vogel J, Heyman M, Paris J. Psychopathology in offspring of mothers with borderline personality disorder: a pilot study. Can J Psychiatry 1996;41:285-90. https://doi.org/10.1177/070674379604100505.
- Pfohl B, Blum N, St John D, McCormick B, Allen J, Black DW. Reliability and validity of the Borderline Evaluation of Severity Over Time (BEST): a self-rated scale to measure severity and change in persons with borderline personality disorder. J Pers Disord 2009;23:281-93. https://doi.org/10.1521/pedi.2009.23.3.281.
- Dutton D, Denny-Keys M, Sells J. Parental personality disorder and its effects on children: a review of current literature. J Child Custod 2011;8:268-83. https://doi.org/10.1080/15379418.2011.620928.
- Lukens E, McFarlane W. Psychoeducation as evidence-based practice: considerations for practice, research, and policy. Brief Treat Crisis Interv 2004;4:205-25. https://doi.org/10.1093/brief-treatment/mhh019.
- Michelson D, Davenport C, Dretzke J, Barlow J, Day C. Do evidence-based interventions work when tested in the ‘real world?’ A systematic review and meta-analysis of parent management training for the treatment of child disruptive behavior. Clin Child Fam Psychol Rev 2013;16:18-34. https://doi.org/10.1007/s10567-013-0128-0.
- Forehand R, Jones DJ, Parent J. Behavioral parenting interventions for child disruptive behaviors and anxiety: what’s different and what’s the same. Clin Psychol Rev 2013;33:133-45. https://doi.org/10.1016/j.cpr.2012.10.010.
- Creswell C, Murray L, Stacey J, Cooper P, Silverman WK, Field AP. Anxiety Disorders in Children and Adolescents. Cambridge: Cambridge University Press; 2011.
- Reyno SM, McGrath PJ. Predictors of parent training efficacy for child externalizing behavior problems – a meta-analytic review. J Child Psychol Psychiatry 2006;47:99-111. https://doi.org/10.1111/j.1469-7610.2005.01544.x.
- Day C, Kowalenko S, Ellis M, Dawe S, Harnett P, Scott S. The Helping Families Programme: a new parenting intervention for children with severe and persistent conduct problems. Child Adol Ment Health-UK 2011;16:167-71. https://doi.org/10.1111/j.1475-3588.2010.00588.x.
- Dawe S, Harnett PH. Improving family functioning in methadone maintained families: results from a randomised controlled trial. J Subst Abuse Treat 2007;32:381-90. https://doi.org/10.1016/j.jsat.2006.10.003.
- Olds DL. Prenatal and infancy home visiting by nurses: from randomized trials to community replication. Prev Sci 2002;3:153-72. https://doi.org/10.1023/A:1019990432161.
- Stevens M. The cost-effectiveness of UK parenting programmes for preventing children’s behaviour problems – a review of the evidence. Child Fam Soc Work 2012;19:109-18. https://doi.org/10.1111/j.1365-2206.2012.00888.x.
- Bonin EM, Stevens M, Beecham J, Byford S, Parsonage M. Costs and longer-term savings of parenting programmes for the prevention of persistent conduct disorder: a modelling study. BMC Public Health 2011;11. https://doi.org/10.1186/1471-2458-11-803.
- Friedli L, Parsonage M. Mental Health Promotion: Building an Economic Case. Belfast: Northern Ireland Association for Mental Health; 2007.
- McCrone P, Dhanasiri S, Patel A, Knapp M, Lawton-Smith S. Paying the Price: The Cost of Mental Health Care in England to 2026. London: The King’s Fund; 2008.
- Armstrong H. Ministerial Foreword. Reaching Out: Think Family. London: Cabinet Office Social Exclusion Task Force; 2007.
- Ackerson B. Coping with the dual demands of severe mental illness and parenting: the parents’ perspective. Fam Soc 2003;84:109-18. https://doi.org/10.1606/1044-3894.69.
- Lewis G, Appleby L. Personality disorder: the patients psychiatrists dislike. Br J Psychiatry 1988;153:44-9. https://doi.org/10.1192/bjp.153.1.44.
- Newton-Howes G, Weaver T, Tyrer P. Attitudes of staff towards patients with personality disorder in community mental health teams. Aust N Z J Psychiatry 2008;42:572-7. https://doi.org/10.1080/00048670802119739.
- Mind . ‘Shining Lights in Dark Corners of People’s Lives’. The Consensus Statement for People With Complex Mental Health Difficulties Who Are Diagnosed With a Personality Disorder 2017. www.mind.org.uk/media/21163353/consensus-statement-final.pdf (accessed 31 May 2018).
- National Institute for Mental Health in England (NIMHE) . Personality Disorder: No Longer a Diagnosis of Exclusion. Policy Implementation Guidance for the Development of Services for People With Personality Disorder 2003.
- Stepp SD, Whalen DJ, Pilkonis PA, Hipwell AE, Levine MD. Children of mothers with borderline personality disorder: identifying parenting behaviors as potential targets for intervention. Personal Disord 2012;3:76-91. https://doi.org/10.1037/a0023081.
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348. https://doi.org/10.1136/bmj.g1687.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and Evaluating Complex Interventions: New Guidance. London: Medical Research Council; 2008.
- Eldridge SM, Chan CL, Campbell MJ, Bond CM, Hopewell S, Thabane L, et al. CONSORT 2010 statement: extension to randomised pilot and feasibility trial. BMJ 2016;355. https://doi.org/10.1136/bmj.i5239.
- O’Cathain A, Hoddinott P, Lewin S, Thomas KJ, Young B, Adamson J, et al. Maximising the impact of qualitative research in feasibility studies for randomised controlled trials: guidance for researchers. Pilot Feasibility Stud 2015;1. https://doi.org/10.1186/s40814-015-0026-y.
- Bugge C, Williams B, Hagen S, Logan J, Glazener C, Pringle S, et al. A process for Decision-making after Pilot and feasibility Trials (ADePT): development following a feasibility study of a complex intervention for pelvic organ prolapse. Trials 2013;14. https://doi.org/10.1186/1745-6215-14-353.
- Day C, Michelson D, Crawford M, Ellis M, McMurran M, Moran P, et al. Helping Families: The Systematic Development and Pilot Randomised Controlled Trial of a Psychoeducational Intervention for Parents with Personality Disorders: NIHR HTA Research Protocol V2 19.5.14 (Project Number: HTA 12/194/01). London: King’s College London; 2014.
- Day C, Ellis M, Harris L. Helping Families Programme: An innovative Parenting Intervention Developed for Families Living in complex Social Circumstances Whose Children Experience Severe and Persistent Conduct Problems. London: Centre for Parent and Child Support; 2011.
- Day C, Ellis M, Harris L. High Need Families Project: Development and Piloting a New Parenting Intervention (The Helping Families Programme) for Children with Severe and Persistent Conduct Problems. London: Department for Education; 2012.
- Ellis M, Harris L, Day C. Ealing and HFP: Feedback from 2012 Pilot. London: Centre for Parent and Child Support; 2013.
- Stevens M, Harris L, Ellis M, Day C, Beecham J. Investigating changes in use of services by high-need families following the Helping Families Programme, an innovative parenting intervention for children with severe and persistent conduct problems. Child Adol Ment H-UK 2014;19:185-91. https://doi.org/10.1111/camh.12035.
- Day C, Ellis M, Harris L. Family Partnership Model: Reflective Practice Handbook. London: South London and Maudsley NHS Foundation Trust; 2015.
- Banerjee P, D’Silva K, Huband N, Duggan C, McMurran M. Psychoeducation for People with Personality Disorder. Nottingham: Nottinghamshire Healthcare NHS Trust; 2009.
- Banerjee P, Duggan C, Huband N, Watson N. Brief psychoeducation for people with personality disorder: a pilot study. Psychol Psychother 2006;79:385-94. https://doi.org/10.1348/147608305X57987.
- Huband N, McMurran M, Evans C, Duggan C. Social problem-solving plus psychoeducation for adults with personality disorder: pragmatic randomised controlled trial. Br J Psychiatry 2007;190:307-13. https://doi.org/10.1192/bjp.bp.106.023341.
- McMurran M, Crawford MJ, Reilly JG, McCrone P, Moran P, Williams H, et al. Psycho-education with problem solving (PEPS) therapy for adults with personality disorder: a pragmatic multi-site community-based randomised clinical trial. Trials 2011;12. https://doi.org/10.1186/1745-6215-12-198.
- McMurran M, Huband N, Overton E. Non-completion of personality disorder treatments: a systematic review of correlates, consequences, and interventions. Clin Psychol Rev 2010;30:277-87. https://doi.org/10.1016/j.cpr.2009.12.002.
- Tetley A, Jinks M, Huband N, Howells K, McMurran M. Barriers to and facilitators of treatment engagement for clients with personality disorder: a Delphi survey. Personal Ment Health 2012;6:97-110. https://doi.org/10.1002/pmh.1176.
- Jinks M, McMurran M, Huband N. Engaging clients with personality disorder in treatment. Ment Health Rev J 2012;17:139-45. https://doi.org/10.1108/13619321211287229.
- Crawford M, Rutter D, Price K, Weaver T, Josson M, Tyrer P, et al. Learning the Lessons: A Multi-Method Evaluation of Dedicated Community-Based Services for People with Personality Disorder. London: National Co-ordinating Centre for NHS Service Delivery and Organisation; 2007.
- Pilowsky DJ, Wickramaratne PJ, Rush AJ, Hughes CW, Garber J, Malloy E, et al. Children of currently depressed mothers: a STAR*D ancillary study. J Clin Psychiatry 2006;67:126-36. https://doi.org/10.4088/JCP.v67n0119.
- Beidel DC, Turner SM. At risk for anxiety: I. Psychopathology in the offspring of anxious parents. J Am Acad Child Psy 1997;36:918-24. https://doi.org/10.1097/00004583-199707000-00013.
- Van Aken C, Junger M, Verhoeven M, van Aken M, Dekovic M, Denissen J. Parental personality, parenting and toddlers’ externalising behaviours. Eur J Pers 2007;21:993-1015. https://doi.org/10.1002/per.643.
- INVOLVE . Payment for Involvement: A Guide for Making Payments to Members of the Public Actively Involved in NHS, Public Health and Social Care Research 2010.
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Method 2005;8:19-32. https://doi.org/10.1080/1364557032000119616.
- Mays N, Roberts E, Popay J, Allen P, Black N, Clarke A, et al. Studying the Organisation and Delivery of Health Services: Research Methods. London: Routledge; 2001.
- Pawson R. Evidence-based policy: in search of a method. Evaluation 2002;8:157-81. https://doi.org/10.1177/1358902002008002512.
- Ritchie J, Spencer L, Bryman A, Burgess RG. Analysing Qualitative Data. London: Routledge; 1994.
- Jovev M, Jackson HJ. The relationship of borderline personality disorder, life events and functioning in an Australian psychiatric sample. J Pers Disord 2006;20:205-17. https://doi.org/10.1521/pedi.2006.20.3.205.
- Barlow J, Kirkpatrick S, Stewart-Brown S, Davis H. Hard-to-reach or out-of-reach? Reasons why women refuse to take part in early interventions. Child Soc 2005;19:199-210. https://doi.org/10.1002/chi.835.
- Cleary M, Siegfried N, Walter G. Experience, knowledge and attitudes of mental health staff regarding clients with a borderline personality disorder. Int J Ment Health Nurs 2002;11:186-91. https://doi.org/10.1046/j.1440-0979.2002.00246.x.
- Rossberg JI, Karterud S, Pedersen G, Friis S. An empirical study of countertransference reactions toward patients with personality disorders. Compr Psychiatry 2007;48:225-30. https://doi.org/10.1016/j.comppsych.2007.02.002.
- Belsky J, Jaffee SR, Cicchetti D, Cohen DJ. Developmental Psychopathology, Volume Three: Risk, Disorder and Adaptation. Hoboken, NJ: John Wiley & Sons; 2006.
- Amad A, Ramoz N, Thomas P, Jardri R, Gorwood P. Genetics of borderline personality disorder: systematic review and proposal of an integrative model. Neurosci Biobehav Rev 2014;40:6-19. https://doi.org/10.1016/j.neubiorev.2014.01.003.
- Moran P, Romaniuk H, Coffey C, Chanen A, Degenhardt L, Borschmann R, et al. The influence of personality disorder on the future mental health and social adjustment of young adults: a population-based, longitudinal cohort study. Lancet Psychiatry 2016;3:636-45. https://doi.org/10.1016/S2215-0366(16)30029-3.
- Parker G, Beresford B, Clarke S, Gridley K, Pitman R, Spiers G, et al. Research Reviews on Prevalence, Detection and Interventions in Parental Mental Health and Child Welfare: Summary Report 2008.
- Beresford B, Clarke S, Gridley K, Parker G, Pitman R, Spiers G, et al. Technical Report for SCIE Research Review on Access, Acceptability and Outcomes of Services Interventions to Support Parents With Mental Health Problems and Their Families 2008.
- National Institute for Mental Health in England . The Personality Disorder Capabilities Framework: Breaking the Cycle of Rejection 2003.
- Linehan M. Cognitive Behavioral Treatment of Borderline Personality Disorder (Diagnosis and Treatment of Mental Disorders). New York, NY: Guilford Press; 1993.
- Bateman A, Fonagy P. Psychotherapy for Borderline Personality Disorder: Mentalization-based Treatment. Oxford: Oxford University Press; 2004.
- McMurran M, Delport J, Wood K, Jenkins S, Wall M, Day F. Recruitment to personality disorder treatment trials. Ment Health Rev J 2012;17:119-27. https://doi.org/10.1108/13619321211287166.
- Creswell C, Brereton J. Community mental health services and the children of service users. Clin Psychol For 2000;144:4-6.
- Koekkoek B, van Meijel B, Hutschemaekers G. Community mental health care for people with severe personality disorder: narrative review. The Psychiatrist 2018;34:24-30. https://doi.org/10.1192/pb.bp.108.022426.
- Horsfall J, Cleary M, Hunt GE. Stigma in mental health: clients and professionals. Issues Ment Health Nurs 2010;31:450-5. https://doi.org/10.3109/01612840903537167.
- First MB, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS. User’s Guide for the Structured Clinical Interview for DSM-IV Axis II Personality Disorders SCID-II. Washington, DC: American Psychiatric Press, Inc.; 1997.
- Lobbestael J, Leurgans M, Arntz A. Inter-rater reliability of the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID I) and Axis II Disorders (SCID II). Clin Psychol Psychother 2011;18:75-9. https://doi.org/10.1002/cpp.693.
- Ventura J, Liberman RP, Green MF, Shaner A, Mintz J. Training and quality assurance with the Structured Clinical Interview for DSM-IV (SCID-I/P). Psychiatry Res 1998;79:163-73. https://doi.org/10.1016/S0165-1781(98)00038-9.
- Moran P, Leese M, Lee T, Walters P, Thornicroft G, Mann A. Standardised Assessment of Personality - Abbreviated Scale (SAPAS): preliminary validation of a brief screen for personality disorder. Br J Psychiatry 2003;183:228-32. https://doi.org/10.1192/bjp.183.3.228.
- Goodman R, Ford T, Richards H, Gatward R, Meltzer H. The Development and Well-Being Assessment: description and initial validation of an integrated assessment of child and adolescent psychopathology. J Child Psychol Psychiatry 2000;41:645-55. https://doi.org/10.1111/j.1469-7610.2000.tb02345.x.
- Egger H, Ascher B, Angold A. The Preschool Age Psychiatric Assessment: Version 1.4. Durham, NC: Center for Developmental Epidemiology, Department of Psychiatry and Behavioral Sciences, Duke University Medical Center; 2003.
- Goodman R. The extended version of the Strengths and Difficulties Questionnaire as a guide to child psychiatric caseness and consequent burden. J Child Psychol Psychiatry 1999;40:791-9. https://doi.org/10.1111/1469-7610.00494.
- Bee P, Bower P, Byford S, Churchill R, Calam R, Stallard P, et al. The clinical effectiveness, cost-effectiveness and acceptability of community-based interventions aimed at improving or maintaining quality of life in children of parents with serious mental illness: a systematic review. Health Technol Assess 2014;18. https://doi.org/10.3310/hta18080.
- Patel MX, Doku V, Tennakoon L. Challenges in recruitment of research participants. Adv Psychiatr Treat 2003;9:229-38. https://doi.org/10.1192/apt.9.3.229.
- Clarkin JF, Levy KN, Lenzenweger MF, Kernberg OF. Evaluating three treatments for borderline personality disorder: a multiwave study. Am J Psychiatry 2007;164:922-8. https://doi.org/10.1176/ajp.2007.164.6.922.
- Bateman A, Fonagy P. Randomized controlled trial of outpatient mentalization-based treatment versus structured clinical management for borderline personality disorder. Am J Psychiatry 2009;166:1355-64. https://doi.org/10.1176/appi.ajp.2009.09040539.
- McMain SF, Guimond T, Streiner DL, Cardish RJ, Links PS. Dialectical behavior therapy compared with general psychiatric management for borderline personality disorder: clinical outcomes and functioning over a 2-year follow-up. Am J Psychiatry 2012;169:650-61. https://doi.org/10.1176/appi.ajp.2012.11091416.
- McMain SF, Links PS, Gnam WH, Guimond T, Cardish RJ, Korman L, et al. A randomized trial of dialectical behavior therapy versus general psychiatric management for borderline personality disorder. Am J Psychiatry 2009;166:1365-74. https://doi.org/10.1176/appi.ajp.2009.09010039.
- Chanen AM, Jackson HJ, McCutcheon LK, Jovev M, Dudgeon P, Yuen HP, et al. Early intervention for adolescents with borderline personality disorder using cognitive analytic therapy: randomised controlled trial. Br J Psychiatry 2008;193:477-84. https://doi.org/10.1192/bjp.bp.107.048934.
- Lundahl B, Risser HJ, Lovejoy MC. A meta-analysis of parent training: moderators and follow-up effects. Clin Psychol Rev 2006;26:86-104. https://doi.org/10.1016/j.cpr.2005.07.004.
- Leung C, Tsang S, Dean S, Chow P. Development and pilot evaluation of the Hands on Parent Empowerment (HOPE) project – a parent education programme to establish socially disadvantaged parents as facilitators of pre-school children’s learning. J Child Serv 2009;4:21-32. https://doi.org/10.1108/17466660200900003.
- Spoth R, Redmond C. Research on family engagement in general population interventions: toward improved use of scientific findings in practice. J Prim Prev 2000;21:267-84. https://doi.org/10.1023/A:1007039421026.
- Sanders MR, Kirby JN. Consumer engagement and the development, evaluation, and dissemination of evidence-based parenting programs. Behav Ther 2012;43:236-50. https://doi.org/10.1016/j.beth.2011.01.005.
- Kaminski JW, Valle LA, Filene JH, Boyle CL. A meta-analytic review of components associated with parent training program effectiveness. J Abnorm Child Psychol 2008;36:567-89. https://doi.org/10.1007/s10802-007-9201-9.
- Bateman AW, Fonagy P. Effectiveness of psychotherapeutic treatment of personality disorder. Br J Psychiatry 2000;177:138-43. https://doi.org/10.1192/bjp.177.2.138.
- Day C, Michelson M, Thomson S, Penney C, Draper L. Evaluation of a peer-led parenting intervention for child behaviour problems: a community-based randomised controlled trial. BMJ 2012;344. https://doi.org/10.1136/bmj.e1107.
- Michelson D, Ben-Zion I, James AI, Draper L, Penney C, Day C. ‘Living With Teenagers’: feasibility study of a peer-led parenting intervention for socially disadvantaged families with adolescent children. Arch Dis Child 2014;99:731-7. https://doi.org/10.1136/archdischild-2013-304936.
- Medlow S, Klineberg E, Jarrett C, Steinbeck K. A systematic review of community-based parenting interventions for adolescents with challenging behaviours. J Adolesc 2016;52:60-71. https://doi.org/10.1016/j.adolescence.2016.07.003.
- Bateman A, Gunderson J, Mulder R. Treatment of personality disorder. Lancet 2015;385:735-43. https://doi.org/10.1016/S0140-6736(14)61394-5.
- Gunderson JG, Links P. Handbook of Good Psychiatric Management (GPM) for Borderline Personality Disorder. Washington, DC: American Psychiatric Press; 2014.
- Maliken AC, Katz LF. Exploring the impact of parental psychopathology and emotion regulation on evidence-based parenting interventions: a transdiagnostic approach to improving treatment effectiveness. Clin Child Fam Psychol Rev 2013;16:173-86. https://doi.org/10.1007/s10567-013-0132-4.
- Scott S, Dadds MR. Practitioner review: when parent training doesn’t work: theory-driven clinical strategies. J Child Psychol Psychiatry 2009;50:1441-50. https://doi.org/10.1111/j.1469-7610.2009.02161.x.
- Borrelli B, Sepinwall D, Ernst D, Bellg AJ, Czajkowski S, Breger R, et al. A new tool to assess treatment fidelity and evaluation of treatment fidelity across 10 years of health behavior research. J Consult Clin Psychol 2005;73:852-60. https://doi.org/10.1037/0022-006X.73.5.852.
- Gearing RE, El-Bassel N, Ghesquiere A, Baldwin S, Gillies J, Ngeow E. Major ingredients of fidelity: a review and scientific guide to improving quality of intervention research implementation. Clin Psychol Rev 2011;31:79-88. https://doi.org/10.1016/j.cpr.2010.09.007.
- Wilson R, Weaver T, Michelson D, Day C. Experiences of parenting and clinical intervention for mothers affected by personality disorder: a pilot qualitative study combining parent and clinician perspectives. BMC Psychiatry 2018;18. https://doi.org/10.1186/s12888-018-1733-8.
- Thomson S, Michelson D, Day C, Polencec M. Meeting the Needs of Families Affected by Parental Mental Illness. London: Centre for Parent and Child Support, South London and Maudsley NHS Foundation Trust; 2011.
- Smith J, Osborne M, Smith J. Qualitative Psychology: A Practical Guide to Research Methods. London: SAGE Publications Ltd; 2003.
- Smith J, Smith JA, Harré R, Van Langehove L. Rethinking Methods in Psychology. London: SAGE Publications Ltd; 1995.
- Eyberg S, Ross A. Assessment of child behaviour problems: the validation of a new inventory. J Clin Child Psychol 1978;7:113-16. https://doi.org/10.1080/15374417809532835.
- Achenbach T, Rescorla L. Manual for the ASEBA School-Age Forms and Profiles: an Integrated System of Multi-Informant Assessment. Burlington, VT: University of Vermont, Research Center for Children, Youth & Families; 2001.
- Arnold D, O’Leary S, Wolff L, Acker M. The Parenting Scale: a measure of dysfunctional parenting in discipline situations. Psychol Assessment 1993;5:137-44. https://doi.org/10.1037/1040-3590.5.2.137.
- James D, Schumm W, Kennedy C, Grigsby C, Shectman K, Nichols C. Characteristics of the Kansas parental satisfaction scale among two samples of married parents. Psychol Rep 1985;57:163-9. https://doi.org/10.2466/pr0.1985.57.1.163.
- Müller J, Postert C, Beyer T, Furniss T, Achtergarde S. Comparison of eleven short versions of the Symptom Checklist 90-Revised (SCL-90-R) for use in the assessment of general psychopathology. Psychol Assess 2010;32:246-54. https://doi.org/10.1007/s10862-009-9141-5.
- Hatcher R, Gillaspy J. Development and validation of a revised short version of the working alliance inventory. Psychother Res 2006;16:12-25. https://doi.org/10.1080/10503300500352500.
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349-57. https://doi.org/10.1093/intqhc/mzm042.
- Day C, Briskman J, Crawford MJ, Foote L, Harris L, Boadu J, et al. Randomised feasibility trial of the helping families programme-modified: an intensive parenting intervention for parents affected by severe personality difficulties. BMJ Open 2020;10. https://doi.org/10.1136/bmjopen-2019-033637.
- Day C, Kearney C, Squires F. Art, science and experience of peer support: learning from the Empowering Parents, Empowering Communities programme. IJBPE 2017;4:13-9.
- Beecham J, Knapp M, Thornicroft G. Measuring Mental Health Needs. London: Gaskell; 2001.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2017. Canterbury: Personal Social Services Research Unit, University of Kent; 2017.
- NHS Improvement . Reference Costs 2018. https://improvement.nhs.uk/resources/reference-costs/ (accessed 2 May 2018).
- Medicines Complete 2018. www.new.medicinescomplete.com/#/ (accessed 29 May 2018).
- Office for National Statistics . Annual Survey of Hours and Earnings: 2017 Provisional and 2016 Revised Results 2017. www.ons.gov.uk/employmentandlabourmarket/peopleinwork/earningsandworkinghours/bulletins/annualsurveyofhoursandearnings/2017provisionaland2016revisedresults (accessed 29 May 2018).
- van Reenen M, Janssen B. EQ-5D-5L User Guide. Version 2.1 2015. https://euroqol.org/wp-content/uploads/2016/09/EQ-5D-5L_UserGuide_2015.pdf (accessed 29 May 2018).
- Wille N, Badia X, Bonsel G, Burström K, Cavrini G, Devlin N, et al. Development of the EQ-5D-Y: a child-friendly version of the EQ-5D. Qual Life Res 2010;19:875-86. https://doi.org/10.1007/s11136-010-9648-y.
- Hertzog MA. Considerations in determining sample size for pilot studies. Res Nurs Health 2008;31:180-91. https://doi.org/10.1002/nur.20247.
- Great Britain . UK Data Protection Act 2018. www.gov.uk/government/collections/data-protection-act-2018 (accessed 5 August 2019).
- Brown H, Prescott R. Applied Mixed Models in Medicine. New York, NY: John Wiley & Sons; 2007.
- Browne RH. On the use of a pilot sample for sample size determination. Stat Med 1995;14:1933-40. https://doi.org/10.1002/sim.4780141709.
- Fenwick E, Byford S. A guide to cost-effectiveness acceptability curves. Br J Psychiatry 2005;187:106-8. https://doi.org/10.1192/bjp.187.2.106.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Bartholomew T, Scheel M, Cole B. Development and validation of the Hope for Change through Counseling Scale. Couns Psychol 2015;43:671-702. https://doi.org/10.1177/0011000015589190.
- Frank JD, Frank JB. Persuasion and Healing: A Comparative Study of Psychotherapy. Baltimore, MD: Johns Hopkins University Press; 1991.
- Petfield L, Startup H, Droscher H, Cartwright-Hatton S. Parenting in mothers with borderline personality disorder and impact on child outcomes. Evid Based Ment Health 2015;18:67-75. https://doi.org/10.1136/eb-2015-102163.
- Laporte L, Paris J, Zelkowitz P. Estimating the prevalence of borderline personality disorder in mothers involved in youth protection services. Personal Ment Health 2018;12:49-58. https://doi.org/10.1002/pmh.1398.
- Cooper AA, Conklin LR. Dropout from individual psychotherapy for major depression: A meta-analysis of randomized clinical trials. Clin Psychol Rev 2015;40:57-65. https://doi.org/10.1016/j.cpr.2015.05.001.
- McMain S, Boritz T, Leybman M. Common strategies for cultivating a positive therapy relationship in the treatment of borderline personality disorder. J Psychother Integr 2015;25:20-9. https://doi.org/10.1037/a0038768.
- Stines LR, Feeny NC. Unique Ethical Concerns in Clinical Trials Comparing Psychosocial and Psychopharmalogical Interventions. Ethics Behav 2008;18:234-46. https://doi.org/10.1080/10508420802064333.
- Barnicot K, Katsakou C, Marougka S, Priebe S. Treatment completion in psychotherapy for borderline personality disorder: a systematic review and meta-analysis. Acta Psychiatr Scand 2011;123:327-38. https://doi.org/10.1111/j.1600-0447.2010.01652.x.
- Singleton N, Bumpstead R, O’Brien M, Lee A, Meltzer H. Psychiatric Morbidity Among Adults Living in Private Households 2002.
- Anderson E, Lambert M. Short-term dynamically oriented psychotherapy: a review and meta-analysis. Clin Psychol Rev 1995;15:503-14. https://doi.org/10.1016/0272-7358(95)00027-M.
- Hansen N, Lambert M, Forman E. The psychotherapy dose–response effect and its implications for treatment delivery services. Clin Psychol Sci Pract 2002;9:329-43. https://doi.org/10.1093/clipsy/9.3.329.
- Bornovalova M, Daughters S. How does dialectical behaviour therapy facilitate treatment retention among individuals with comorbid borderline personality disorders and substance use disorders?. Clin Psychol Rev 2007;27:923-43. https://doi.org/10.1016/j.cpr.2007.01.013.
- Ogrodniczuk JS, Joyce AS, Lynd LD, Piper WE, Steinberg PI, Richardson K. Predictors of premature termination of day treatment for personality disorder. Psychother Psychosom 2008;77:365-71. https://doi.org/10.1159/000151390.
- Lindström D, Sundberg-Petersson I, Adami J, Tönnesen H. Disappointment and drop-out rate after being allocated to control group in a smoking cessation trial. Contemp Clin Trials 2010;31:22-6. https://doi.org/10.1016/j.cct.2009.09.003.
- Larsen D, Stege R. Client accounts of hope in early counselling sessions: a qualitative study. J Couns Dev 2012;90:45-54. https://doi.org/10.1111/j.1556-6676.2012.00007.x.
- Wolpert M. Commentary: why measuring clinical change at the individual level is challenging but crucial –commentary on Jensen and Corralejo (2017). Child Adolesc Ment Health 2017;22:167-9. https://doi.org/10.1111/camh.12228.
- Yang M, Maxwell SE. Treatment effects in randomized longitudinal trials with different types of nonignorable dropout. Psychol Methods 2014;19:188-210. https://doi.org/10.1037/a0033804.
Appendix 1 Meeting the Needs of Families Affected by Parental Mental Illness audit tool
Appendix 2 Phase 2: case series parent semistructured interview topic guide
Appendix 3 Phase 2: case series keyworker semistructured interview topic guide
Appendix 4 Phase 3: randomised feasibility trial parent semistructured interview topic guide
Appendix 5 Phase 3: qualitative interview parent participant characteristics
| Trial arm | Participant ID | Site | Parent age (years) | Parent ethnicity | Index child gender | Index child age (years) | Intervention status | Intervention sessions completed (n) |
|---|---|---|---|---|---|---|---|---|
| HFP-M | 1003 | 1 | 28 | White UK/Irish | Female | 9 | Completed | 7 |
| 1004 | 1 | 24 | Dual Heritage | Male | 3 | Completed | 8 | |
| 1008 | 1 | 39 | White UK/Irish | Male | 8 | Completed | 16 | |
| 1016 | 1 | 26 | White UK/Irish | Female | 7 | Completed | 7 | |
| 1018 | 1 | 27 | White UK/Irish | Male | 6 | Withdrew | 9 | |
| 1020 | 1 | 44 | Black UK | Female | 7 | Completed | 16 | |
| 1021 | 1 | 28 | Black UK | Female | 7 | Withdrew | 4 | |
| 1023 | 1 | 49 | White UK/Irish | Female | 8 | Completed | 16 | |
| 1024 | 1 | 40 | Black UK | Male | 8 | Completed | 16 | |
| 1030 | 1 | 33 | Black UK | Female | 6 | Completed | 16 | |
| 1036 | 1 | 37 | White UK/Irish | Female | 11 | Incomplete | 6 | |
| 2004 | 2 | 36 | White UK/Irish | Female | 7 | Completed | 13 | |
| 2008 | 2 | 38 | White UK/Irish | Male | 8 | Withdrew | 2 | |
| 2009 | 2 | 29 | White UK/Irish | Male | 9 | Incomplete | 3 | |
| Usual care | 1001 | 1 | 27 | Dual heritage | Male | 10 | Completed | N/A |
| 1002 | 1 | 44 | White UK/Irish | Female | 10 | Completed | N/A | |
| 1013 | 1 | 39 | White UK/Irish | Female | 8 | Completed | N/A | |
| 1015 | 1 | 37 | White UK/Irish | Male | 7 | Completed | N/A | |
| 1017 | 1 | 37 | White UK/Irish | Male | 7 | Completed | N/A | |
| 1019 | 1 | 32 | Black UK | Female | 3 | Completed | N/A | |
| 1022 | 1 | 47 | Black African | Male | 10 | Completed | N/A | |
| 1029 | 1 | 42 | White UK/Irish | Female | 6 | Declined | N/A | |
| 1034 | 1 | 47 | White UK/Irish | Female | 8 | Completed | N/A | |
| 1035 | 1 | 29 | Black UK | Male | 8 | Declined | N/A | |
| 2003 | 2 | Female | 9 | Completed | N/A | |||
| 2010 | 2 | 29 | Black African | Female | 11 | Completed | N/A | |
| 2011 | 2 | 33 | White UK/Irish | Male | 10 | Completed | N/A |
Appendix 6 Phase 3: randomised feasibility trial keyworker semistructured interview topic guide
Appendix 7 Phase 3: qualitative interview keyworker participant characteristics
| Participant ID | Service | Role | Referral number | Gender | Age (years) | Ethnicity |
|---|---|---|---|---|---|---|
| 4002 | Early Help Hub | Locality school and community early help advisor | 10 | Female | 38 | African-Caribbean |
| 4003 | Specialist Personality Disorder Service | Psychotherapist | 1 | Male | 50 | White Scottish |
| 4005 | Specialist Personality Disorder Service | Psychotherapist | 1 | Female | 40 | White British |
| 4006 | Parental Mental Health Team | Team manager | 2 | Female | 40 | White British |
| 4007 | Integrated Psychological Therapies Service | Principal clinical psychologist | 1 | Female | 50 | South American |
| 4009 | CAMHS | Specialty doctor | 1 | Female | ||
| 4010 | CAMHS | Clinical psychologist | 1 | Female | 47 | White British |
| 4014 | Primary Care Adult Mental Health | High-intensity cognitive therapist | 1 | Female | 35 | White other |
| 4015 | CAMHS Early Intervention | CAMHS practitioner (Qualified Mental Health Nurse) | 1 | Male | 31 | White British |
| 4016 | Adult Mental Health Service | DBT therapist | 1 | Female | 54 | White British |
| 4017 | CAMHS | CAMHS practitioner | 3 | Female | ||
| 5002 | Early Help Service | Senior early help practitioner | 1 | Female | 49 | White British |
Appendix 8 Phase 3: parent qualitative results – main themes and subthemes
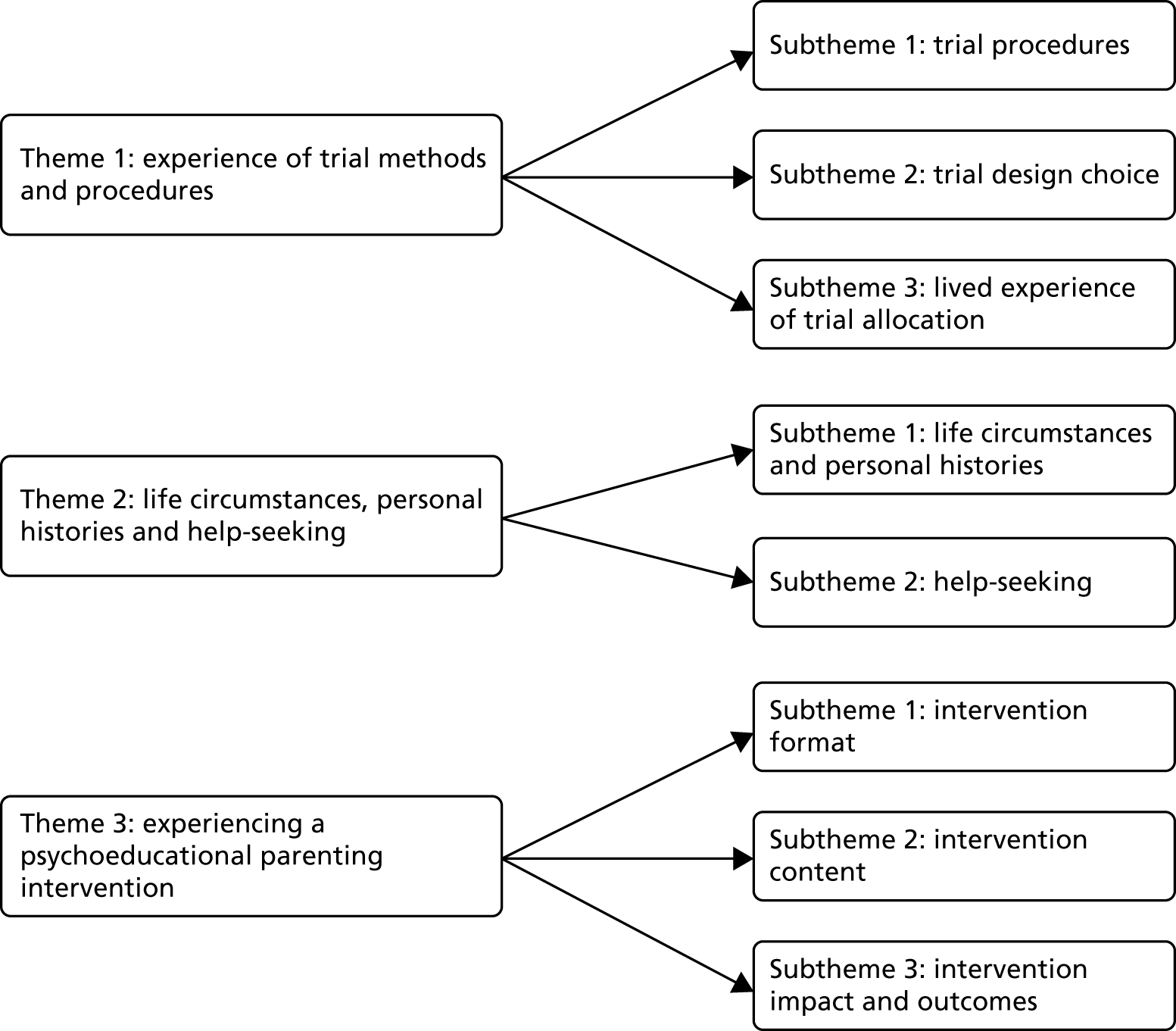
Appendix 9 Phase 3: keyworker qualitative results – main themes and subthemes
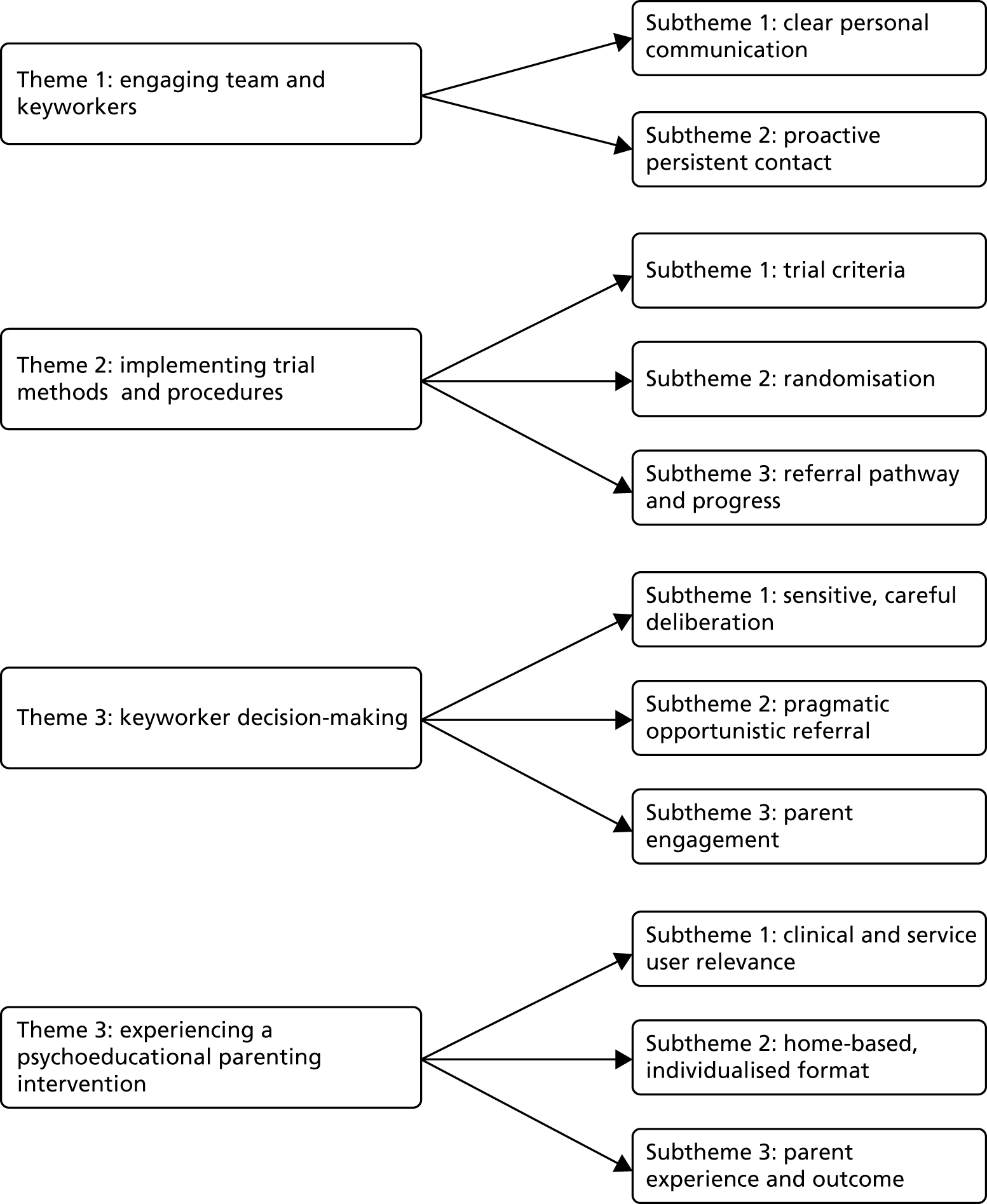
Appendix 10 Phase 3: Helping Families Programme-Modified actual appointment attendance, cancellation and did not attends
A total of 385 intervention appointments were offered, of which 108 (25.9%) were cancelled and rearranged and 12 (3.0%) were not attended by the participant (DNA) (Table 20). A total of 265 (68.8%) of the offered appointments were attended by participants.
| Site | Intervention appointments | |||||||
|---|---|---|---|---|---|---|---|---|
| Attended | Cancelled | DNA | Offered | |||||
| Total, n (%) | Mean (SD) | Total, n (%) | Mean (SD) | Total, n (%) | Mean (SD) | Total, n (%) | Mean (SD) | |
| 1 (N = 16) | 219 (69.8) | 12.6 (5.8) | 87 (27.7) | 5.4 (3.7) | 8 (3.0) | 0.5 (1.0) | 314 (81.6) | 19.6 (6.1) |
| 2 (N = 5) | 46 (64.7) | 9.2 (6.5) | 21 (29.7) | 4.2 (4.1) | 4 (5.6) | 0.8 (0.8) | 71 (18.4) | 14.2 (9.7) |
| Total | 265 (68.8) | 12.6 (6.3) | 108 (25.9) | 5.1 (3.8) | 12 (3.0) | 0.6 (0.9) | 385 (100.0) | 18.3 (7.6) |
The mean number of total appointments offered per participant was 18.3 (SD 7.6) and the mean number of appointments attended was 12.6 (SD 6.3). The mean number of appointments cancelled was 5.1 (SD 3.8). The overall pattern of appointment uptake, cancellation and DNA activity was similar between the two sites (see Table 20). However, site 2 participants received substantially fewer appointments. This was mainly as a result of the late recruitment in site 2 and under-resourced provision of research therapists during the trial.
Appendix 11 Phase 3: economic results – service use, lost employment and costs (£ 2016–17) at time 2 by group
| Service type | Group | |||||
|---|---|---|---|---|---|---|
| Intervention (HFP-M) (N = 17) | Control (usual care) (N = 9) | |||||
| Number of sample, n (%) | Contacts/days, mean (SD) | Cost (£), mean (SD) | Number of sample, n (%) | Contacts/days, mean (SD) | Cost (£), mean (SD) | |
| Face-to-face contacts with professionals | ||||||
| General practitioner | 17 (100) | 9.6 (13.9) | 431.90 (444.80) | 8 (89) | 8.9 (12.7) | 444.80 (744.70) |
| Psychiatrist | 5 (29) | 7.4 (9.6) | 220.80 (588.80) | 2 (22) | 26.5 (36.1) | 636.00 (1867.80) |
| Other medical professional | 4 (24) | 3.5 (3.0) | 72.20 (165.70) | 2 (22) | 8.5 (10.6) | 293.30 (654.80) |
| Psychologist | 6 (35) | 26.6 (31.2) | 497.60 (1155.90) | 1 (11) | 52.0 (0.0) | 306.20 (918.70) |
| Drug and alcohol advisor | 2 (12) | 10.0 (7.1) | 140.00 (447.70) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Other counsellor/therapist | 3 (18) | 25.0 (9.5) | 233.80 (550.50) | 2 (22) | 24.0 (0.0) | 235.60 (467.40) |
| Home treatment/crisis team member | 2 (12) | 27.5 (17.7) | 66.70 (188.60) | 1 (11) | 1.0 (0.0) | 0.40 (1.10) |
| Assertive outreach team member | 1 (6) | 5.0 (0.0) | 11.20 (46.10) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Early intervention team member | 4 (24) | 5.7 (3.7) | 59.20 (132.70) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Social worker | 8 (47) | 14.0 (14.5) | 395.30 (705.60) | 4 (44) | 9.3 (8.9) | 140.90 (251.40) |
| Mental health nurse | 1 (6) | 20.0 (0.0) | 51.80 (213.40) | 1 (11) | 6.0 (0.0) | 29.30 (88.00) |
| Occupational therapist | 1 (6) | 2.0 (0.0) | 5.30 (21.80) | 1 (11) | 8.0 (0.0) | 30.00 (90.00) |
| Accident and emergency service | 4 (24) | 2.0 (1.4) | 69.60 (157.80) | 1 (11) | 1.0 (0.0) | 16.40 (49.30) |
| Day-care services | ||||||
| Drug/alcohol service | 2 (12) | 5.5 (0.7) | 77.60 (220.20) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Community mental health centre | 0 (0) | 0.0 (0.0) | 0.00 (0.00) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Day-care centre/day hospital | 2 (12) | 185.5 (260.9) | 854.40 (3498.40) | 1 (11) | 157.0 (0.0) | 680.30 (2041.00) |
| Drop-in centre | 2 (12) | 13.0 (17.0) | 59.60 (236.10) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Self-help/support group | 3 (18) | 8.7 (5.5) | 59.60 (153.00) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Class/group at a leisure centre | 1 (6) | 17.0 (0.0) | 44.00 (181.40) | 1 (11) | 17.0 (0.0) | 0.00 (0.00) |
| Adult education class | 4 (24) | 24.5 (19.2) | 224.80 (528.70) | 1 (11) | 17.0 (0.0) | 73.70 (221.00)a |
| Other day-care activity | 1 (6) | 24.0 (0.0) | 55.10 (227.00) | 1 (11) | 17.0 (0.0) | 73.70 (221.00)a |
| Inpatient admissions | ||||||
| Days as an inpatient | 1 (6) | 9.0 (0.0) | 332.50 (1370.80) | 1 (11) | 13.0 (0.0) | 907.10 (2721.30) |
| Police contacts | ||||||
| Victim | 5 (29) | 2.4 (1.7) | N/A | 2 (22) | 6.5 (7.8) | N/A |
| Witness | 0 (0) | 0.0 (0.0) | N/A | 2 (22) | 2.5 (0.7) | N/A |
| Unknown | 3 (18) | 2.0 (1.7) | N/A | 0 (0) | 0.0 (0.0) | N/A |
| Prescribed medicationb | ||||||
| Receipt of prescription | 12 (71) | N/A | 136.40 (328.40) | 6 (67) | N/A | 413.20 (355.60) |
| Are you a student/pupil at school or college? | ||||||
| Lost education owing to health problems (days) | 2 (12) | 2.0 (0.0) | N/A | 2 (22) | 0.5 (0.7) | N/A |
| Employment | ||||||
| Days off work (owing to health problems) | 4 (24) | 1.3 (1.2) | 30.20 (85.20) | 2 (22) | 4.0 (1.4) | 56.90 (118.80) |
| Service type | Number of sample, n (%) | Weeks, mean (SD) | Cost (£), mean (SD) | Number of sample, n (%) | Weeks, mean (SD) | Cost (£), mean (SD) |
| Benefits | ||||||
| Income support | 3 (18) | 42.7 (23.5) | N/A | 1 (11) | 17.0 (0.0) | N/A |
| Incapacity benefit | 2 (12) | 32.5 (9.2) | N/A | 1 (11) | 52.0 (0.0) | N/A |
| Disability living allowance care component | 2 (12) | 29.0 (26.9) | N/A | 5 (56) | 33.6 (15.1) | N/A |
| Disability living allowance mobility component | 0 (0) | 0.0 (0.0) | N/A | 3 (33) | 34.7 (15.0) | N/A |
| Disabled person’s tax credit | 0 (0) | 0.0 (0.0) | N/A | 2 (22) | 39.0 (18.4) | N/A |
| Severe disablement allowance | 0 (0) | 0.0 (0.0) | N/A | 1 (11) | 52.0 (0.0) | N/A |
| Council tax benefit | 6 (35) | 34.7 (17.0) | N/A | 6 (67) | 34.4 (13.1) | N/A |
| Housing benefit | 11 (65) | 42.4 (12.7) | N/A | 6 (67) | 33.0 (13.6) | N/A |
| Jobseeker’s allowance | 1 (6) | 65.0 (0.0) | N/A | 0 (0) | 0.0 (0.0) | N/A |
| Working tax credit | 2 (12) | 54.0 (21.2) | N/A | – | – | N/A |
| Statutory sick pay | 0 (0) | 0.0 (0.0) | N/A | 0 (0) | 0.0 (0.0) | N/A |
| State retirement pension | 0 (0) | 0.0 (0.0) | N/A | 0 (0) | 0.0 (0.0) | N/A |
| Other benefits | ||||||
| Carer’s allowance | 3 (18) | – | N/A | 2 (22) | – | N/A |
| Employment support allowance | 4 (24) | – | N/A | 3 (33) | – | N/A |
| Universal credit | 6 (35) | – | N/A | 1 (11) | – | N/A |
| Child tax credit | 3 (18) | – | N/A | 1 (11) | – | N/A |
| Child tax | 1 (6) | – | N/A | 0 (0) | – | N/A |
| Incapacity support | 1 (6) | – | N/A | 0 (0) | – | N/A |
| Personal independence payment | 3 (18) | – | N/A | 1 (11) | – | N/A |
| Service type | Number of sample, n (%) | Contacts/days, mean (SD) | Cost (£), mean (SD) | Number of sample, n (%) | Contacts/days, mean (SD) | Cost (£), mean (SD) |
| Child section services | ||||||
| School nurse | 9 (53) | 23.6 (48.3) | 736.30 (2138.20) | 3 (33) | 1.7 (1.2) | 32.80 (59.80) |
| Health visitor | 2 (12) | 1.0 (0.0) | 6.90 (19.60) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Dentist | 7 (41) | 1.5 (0.5) | 77.40 (102.80) | 4 (44) | 3.5 (4.4) | 195.10 (406.80) |
| General practitioner | 13 (76) | 4.1 (2.4) | 134.10 (112.80) | 5 (56) | 2.8 (1.6) | 93.30 (115.30) |
| Paediatrician | 4 (24) | 1.7 (0.9) | 77.70 (165.60) | 3 (33) | 1.0 (0.0) | 66.10 (99.10) |
| Optician | 9 (53) | 1.1 (0.3) | 63.70 (66.90) | 4 (44) | 1.0 (0.0) | 48.10 (57.10) |
| Child development centre | 2 (12) | 24.0 (0.0) | 149.60 (422.40) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Child and adolescent mental health services | 5 (29) | 5.3 (4.0) | 147.90 (290.80) | 3 (33) | 5.7 (7.2) | 144.20 (332.60) |
| Speech therapy out of school | 2 (12) | 1.0 (0.0) | 11.50 (32.50) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Hearing specialist | 2 (12) | 1.0 (0.0) | 9.80 (33.30) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Counselling | ||||||
| Family therapist | 1 (6) | 5.0 (0.0) | 25.90 (106.70) | 1 (11) | 2.0 (0.0) | 19.60 (58.70) |
| Individual therapy | 3 (18) | 15.7 (21.2) | 227.80 (851.00) | 2 (22) | 7.5 (9.2) | 123.90 (339.80) |
| Other counselling | 3 (18) | 1.0 (0.0) | 38.80 (86.40) | 3 (33) | 34.0 (14.0) | 756.10 (1458.60) |
| Support | ||||||
| Home help/care worker | 4 (24) | 15.3 (15.5) | 85.00 (232.70) | 1 (11) | 30.0 (0.0) | 583.30 (1750.00) |
| Day-care centre | 1 (6) | 24.0 (0.0) | 52.60 (216.80) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Social services nursery school place | 1 (6) | 1.0 (0.0) | 3.50 (14.30) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| After-school club | 11 (65) | 78.8 (78.2) | N/A | 4 (44) | 13.8 (13.7) | N/A |
| Other service | 2 (12) | 29.0 (15.6) | N/A | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Hospital services | ||||||
| Contacts | 2 (12) | 1.0 (0.0) | 80.60 (195.10) | 2 (22) | 46.0 (45.3) | 1873.30 (5115.90) |
| Days off school | ||||||
| Days | 14 (82) | 9.7 (13.3) | N/A | 6 (67) | 9.7 (10.7) | N/A |
Appendix 12 Phase 3: economic results – service use, lost employment and costs (£ 2016–17) at time 3 by group
| Service type | Group | |||||
|---|---|---|---|---|---|---|
| Intervention (HFP-M) (N = 12) | Control (usual care) (N = 7) | |||||
| Number of sample, n (%) | Contacts/days, mean (SD) | Cost (£), mean (SD) | Number of sample, n (%) | Contacts/days, mean (SD) | Cost (£), mean (SD) | |
| Face-to-face contacts with professionals | ||||||
| General practitioner | 11 (92) | 4.2 (1.8) | 235.30 (182.30) | 4 (57) | 5.8 (3.6) | 156.10 (192.70) |
| Psychiatrist | 5 (42) | 7.4 (5.1) | 315.00 (497.00) | 1 (14) | 2.0 (0.0) | 30.90 (81.60) |
| Other medical professional | 1 (8) | 1.0 (0.0) | 30.00 (103.90) | 1 (14) | 1.0 (0.0) | 8.60 (22.70) |
| Psychologist | 3 (25) | 4.3 (2.5) | 53.00 (113.00) | 1 (14) | 4.0 (0.0) | 30.30 (80.10) |
| Drug and alcohol advisor | 1 (8) | 8.0 (0.0) | 79.30 (274.80) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Other counsellor/therapist | 5 (42) | 4.8 (4.7) | 90.50 (195.90) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Home treatment/crisis team member | 0 (0) | 0.0 (0.0) | 0.00 (0.00) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Assertive outreach team member | 0 (0) | 0.0 (0.0) | 0.00 (0.00) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Early intervention team member | 0 (0) | 0.0 (0.0) | 0.00 (0.00) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Social worker | 5 (42) | 6.6 (5.6) | 155.90 (247.10) | 3 (43) | 10.0 (0.0) | 209.70 (325.80) |
| Mental health nurse | 1 (8) | 8.0 (0.0) | 14.70 (50.80) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Occupational therapist | 1 (8) | 1.0 (0.0) | 1.90 (6.50) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Accident and emergency service | 4 (33) | 3.8 (4.3) | 184.80 (428.00) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Day-care services | ||||||
| Drug/alcohol service | 1 (8) | 6.0 (0.0) | 60.00 (207.80) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Community mental health centre | 0 (0) | 0.0 (0.0) | 0.00 (0.00) | 1 (14) | 0.0 (0.0) | 0.00 (0.00) |
| Day-care centre/day hospital | 0 (0) | 0.0 (0.0) | 0.00 (0.00) | 1 (14) | 6.0 (0.0) | 33.40 (88.40) |
| Drop-in centre | 2 (17) | 2.0 (1.4) | 13.00 (34.60) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Self-help/support group | 1 (8) | 1.0 (0.0) | 3.30 (11.30) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Class/group at a leisure centre | 1 (8) | 3.0 (0.0) | 10.80 (37.20) | 2 (29) | 54.5 (9.2) | 0.00 (0.00) |
| Adult education class | 2 (17) | 6.0 (7.1) | 9.80 (33.80) | 1 (14) | 48.0 (0.0) | 607.30 (1047.40) |
| Other NHS day-care activity | 2 (17) | 6.5 (4.9) | 0.30 (1.10) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Inpatient admissions | ||||||
| Days as inpatient | 3 (25) | 12.3 (15.3) | 1936.30 (5392.00) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Police contacts | ||||||
| Victim | 1 (8) | 3.0 (0.0) | N/A | 1 (14) | 3.0 (0.0) | N/A |
| Witness | 0 (0) | 0.0 (0.0) | N/A | 0 (0) | 0.0 (0.0) | N/A |
| Unknown | 0 (0) | 0.0 (0.0) | N/A | 1 (14) | 2.0 (0.0) | N/A |
| Prescribed medication | ||||||
| Receipt of prescription | 10 (83) | N/A | 107.90 (132.60) | 6 (86) | N/A | 295.00 (374.40) |
| Are you a student/pupil at school or college? | ||||||
| Lost education as a result of health problems (days) | 2 (17) | 5.0 (7.1) | N/A | 1 (14) | 0.0 (0.0) | N/A |
| Employment | ||||||
| Days off work as a result of health problems | 3 (25) | 5.7 (6.4) | 131.30 (410.00) | 2 (29) | 3.5 (3.5) | 46.90 (86.00) |
| Service type | Group | |||||
| Intervention (HFP-M) (N = 12) | Control (usual care) (N = 7) | |||||
| Number of sample, n (%) | Weeks, mean (SD) | Cost (£), mean (SD) | Number of sample, n (%) | Weeks, mean (SD) | Cost (£), mean (SD) | |
| Benefits | ||||||
| Income support | 2 (17) | 17.5 (6.4) | N/A | 2 (29) | 37.0 (15.6) | N/A |
| Incapacity benefit | 1 (8) | 0.0 (0.0) | N/A | 0 (0) | 0.0 (0.0) | N/A |
| Disability living allowance care component | 5 (42) | 16.0 (3.9) | N/A | 4 (57) | 28.3 (14.5) | N/A |
| Disability living allowance mobility component | 0 (0) | 0.0 (0.0) | N/A | 2 (29) | 18.5 (7.8) | N/A |
| Disabled person’s tax credit | 0 (0) | 0.0 (0.0) | N/A | 2 (29) | 26.0 (0.0) | N/A |
| Severe disablement allowance | 0 (0) | 0.0 (0.0) | N/A | 0 (0) | 0.0 (0.0) | N/A |
| Council tax benefit | 3 (25) | 16.3 (4.9) | N/A | 4 (57) | 28.3 (14.5) | N/A |
| Housing benefit | 5 (42) | 15.8 (3.8) | N/A | 5 (71) | 22.4 (7.1) | N/A |
| Jobseeker’s allowance | 0 (0) | 0.0 (0.0) | N/A | 0 (0) | 0.0 (0.0) | N/A |
| Working tax credit | 1 (8) | 17.0 (0.0) | N/A | 0 (0) | 0.0 (0.0) | N/A |
| Statutory sick pay | 0 (0) | 0.0 (0.0) | N/A | 0 (0) | 0.0 (0.0) | N/A |
| State retirement pension | 0 (0) | 0.0 (0.0) | N/A | 0 (0) | 0.0 (0.0) | N/A |
| Other | ||||||
| Carer’s allowance | 1 (8) | – | N/A | 1 (14) | N/A | – |
| Child tax | 1 (8) | – | N/A | 0 (0) | N/A | – |
| Employment and support allowance | 0 (0) | – | N/A | 3 (43) | N/A | – |
| Personal independence payment | 1 (8) | – | N/A | 0 (0) | N/A | – |
| Universal | 0 (0) | – | N/A | 1 (14) | N/A | – |
| Universal credit | 4 (33) | – | N/A | 1 (14) | N/A | – |
| Service type | Group | |||||
| Intervention (HFP-M) (N = 12) | Control (usual care) (N = 7) | |||||
| Number of sample, n (%) | Contacts/days, mean (SD) | Cost (£), mean (SD) | Number of sample, n (%) | Contacts/days, mean (SD) | Cost (£), mean (SD) | |
| Child section-services | ||||||
| School nurse | 6 (50) | 8.4 (13.8) | 247.80 (607.20) | 2 (29) | 1.0 (0.0) | 19.70 (30.50) |
| Health visitor | 0 (0) | 0.0 (0.0) | 0.00 (0.00) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Dentist | 2 (17) | 1.0 (0.0) | 20.90 (48.80) | 4 (57) | 1.0 (0.0) | 83.60 (64.80) |
| General practitioner | 6 (50) | 1.4 (0.5) | 34.60 (42.30) | 4 (57) | 1.5 (0.6) | 42.70 (39.70) |
| Paediatrician | 2 (17) | 1.0 (0.0) | 33.00 (77.10) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Optician | 2 (17) | 1.0 (0.0) | 18.00 (42.10) | 1 (14) | 1.0 (0.0) | 18.00 (44.20) |
| Child development centre | 0 (0) | 0.0 (0.0) | 0.00 (0.00) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Child and adolescent mental health services | 3 (25) | 18.0 (16.1) | 438.60 (980.20) | 3 (43) | 2.0 (0.0) | 72.50 (108.10) |
| Speech therapy out of school | 1 (8) | 1.0 (0.0) | 8.20 (28.30) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Hearing specialist | 2 (17) | 1.0 (0.0) | 19.60 (45.90) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Counselling | ||||||
| Family therapist | 1 (8) | 12.0 (0.0) | 66.00 (228.60) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Individual therapy | 2 (17) | 18.0 (0.0) | 264.00 (616.60) | 1 (14) | 2.0 (0.0) | 29.30 (65.60) |
| Other counselling | 4 (33) | 13.0 (7.8) | 288.20 (495.90) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Support | ||||||
| Home help/care worker | 2 (17) | 12.5 (13.4) | 59.10 (133.40) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Day-care centre | 0 (0) | 0.0 (0.0) | 0.00 (0.00) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| Social services nursery school place | 0 (0) | 0.0 (0.0) | 0.00 (0.00) | 0 (0) | 0.0 (0.0) | 0.00 (0.00) |
| After-school club | 6 (50) | 26.3 (21.9) | N/A | 0 (0) | 0.0 (0.0) | N/A |
| Other service | 1 (8) | 10.0 (0.0) | N/A | 0 (0) | 0.0 (0.0) | N/A |
| Hospital services | ||||||
| Contacts | 0 (0) | 0.0 (0.0) | 0.00 (0.00) | 1 (14) | 2.0 (0.0) | 66.10 (161.80) |
| Days off school | ||||||
| Days off | 12 (100) | 3.1 (4.7) | N/A | 5 (71) | 7.0 (7.2) | N/A |
Appendix 13 Phase 3: economic outcomes
| Time point | Group | ||||
|---|---|---|---|---|---|
| Intervention (HFP-M) (N = 24) | Control (usual care) (N = 24) | Difference (SD) | |||
| Participants, n (%) | Mean (SD) | Participants, n (%) | Mean (SD) | ||
| 1 | 17 (71) | 0.5826 (0.3163) | 19 (79) | 0.6576 (0.3288) | –0.0751 (0.6529) |
| 2 | 18 (75) | 0.6672 (0.2967) | 14 (58) | 0.6490 (0.3506) | 0.0182 (0.6475) |
| 3 | 13 (54) | 0.7550 (0.2516) | 8 (33) | 0.7368 (0.3160) | 0.0182 (0.5705) |
| QALYs (T3) | 10 (42) | 0.6322 (0.2804) | 7 (29) | 0.5934 (0.3550) | 0.0373 (0.3947) |
| Time point | Group | ||||
|---|---|---|---|---|---|
| Intervention (HFP-M) (N = 24) | Control (usual care) (N = 24) | Difference (SD) | |||
| Participants, n (%) | Mean (SD) | Participants, n (%) | Mean (SD) | ||
| 1 | 18 (75) | 0.6407 (0.2841) | 20 (83) | 0.5752 (0.3130) | 0.0655 (0.6002) |
| 2 | 18 (75) | 0.5894 (0.3773) | 13 (54) | 0.6910 (0.2810) | –0.1016 (0.6906) |
| 3 | 12 (50) | 0.8777 (0.2183) | 8 (33) | 0.8716 (0.1468) | 0.0060 (0.3953) |
| QALYs (T3) | 9 (38) | 0.7355 (0.3140) | 7 (29) | 0.7309 (0.1991) | –0.1560 (0.4831) |
Figures 7 and 8 present the cost-effectiveness acceptability curves and a range of cost-effectiveness threshold values from analysis 1 using child QALYs from a NHS/PSS and societal perspective, respectively. At a cost-effectiveness threshold of £30,000 per QALY the probability of being cost-effective was 52% from both perspectives.
FIGURE 7.
Analysis 1: child QALYs – NHS/PSS perspective.

FIGURE 8.
Analysis 1: child QALYs – societal perspective.

Glossary
- Child and adolescent mental health services
- Services that assess and treat children and young people with emotional, behavioural and other mental health difficulties. Child and adolescent mental health services teams are made up of nurses, therapists, psychologists, psychiatrists, support workers and other relevant professionals.
- Childhood emotional and behavioural problems/difficulties
- Common examples of these are disruptive behaviour, aggression, overactivity and anxiety. These problems often interfere with family life, friendships and school achievements and they increase the chances of poor mental health in adulthood.
- Children’s social care services
- Services that have a statutory obligation to safeguard and promote the welfare of vulnerable children and that provide a wide range of services to children and their parents, typically within the family home environment and co-ordinated by a social worker.
- Keyworker
- Every service user referred to the mental health services is allocated a keyworker. The keyworker may be a psychiatrist, mental health nurse, occupational therapist, psychologist or other mental health worker. In this report, we use the term to include children’s social workers and family support workers.
- Psychoeducational intervention
- A systematic method that helps service users and carers to learn about the health condition that affects them and to learn useful ways of managing its symptoms and improving outcomes. In this report, we focus on a psychoeducational intervention for parenting problems and personality difficulties.
- Randomised feasibility trial
- A type of trial whose primary aim is to assess the viability and practicality of conducting a future definitive randomised controlled trial. A definitive trial aims to assess effectiveness or efficacy.
- Severe personality difficulties
- The enduring, persistent and pervasive problems that some people have in managing their feelings and relationships. Personality disorder refers to a cluster of psychiatric diagnoses used to classify such difficulties.
List of abbreviations
- ANCOVA
- analysis of covariance
- CAG
- clinical academic group
- CAMC
- Concerns About My Child
- CAMHS
- Child and Adolescent Mental Health Services
- CBCL-Int
- Child Behavior Checklist-Internalising Scale
- CI
- confidence interval
- CNWL
- Central and North-West London NHS Foundation Trust
- CONSORT
- Consolidated Standards of Reporting Trials
- CRIS
- Clinical Record Interactive Service
- CSRI
- Client Service Receipt Inventory
- DAWBA
- Development and Well-Being Assessment
- DMEC
- Data Monitoring and Ethics Committee
- DNA
- did not attend
- DSM-IV
- Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition
- ECBI
- Eyberg Child Behaviour Inventory
- EPEC
- Empowering Parents Empowering Communities
- EQ-5D
- EuroQol-5 Dimensions
- EQ-5D-3L
- EuroQol-5 Dimensions, three-level version
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- ES
- effect size
- GP
- general practitioner
- GSI
- global severity index
- HFP
- Helping Families Programme
- HFP-M
- Helping Families Programme-Modified
- HTA
- Health Technology Assessment
- ICER
- incremental cost-effectiveness ratio
- ID
- identification number
- IPA
- interpretative phenomenological analysis
- KPSS
- Kansas Parental Satisfaction Scale
- MAP
- mood, anxiety and personality
- MDP
- Multiple Determinants of Parenting
- MNFAPMI
- Meeting the Needs of Families Affected by Parental Mental Illness
- MWG
- manualisation working group
- NIHR
- National Institute for Health Research
- NRES
- National Research Ethics Service
- PAPA
- Pre-School Age Psychiatric Assessment
- PEPS
- Psycho-Education with Problem-Solving
- PIS
- participant information sheet
- PMG
- project management group
- PS
- Arnold-O’Leary Parenting Scale
- PSS
- Personal Social Services
- PSSRU
- Personal Social Services Research Unit
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- REC
- research ethics committee
- SAPAS
- Standardised Assessment of Personality – Abbreviated Scale
- SAPAS-INF
- Standardised Assessment of Personality – Abbreviated Scale: Informant
- SCID-II
- Structured Clinical Interviews for DSM-IV Axis II Disorders
- SCL-27
- Symptom checklist-27
- SD
- standard deviation
- SDQ
- Strengths and Difficulties Questionnaire
- SDQ-IS
- Strengths and Difficulties Questionnaire-Impact Supplement
- SLAM
- South London and Maudsley NHS Foundation Trust
- SLAM PJS
- South London and Maudsley NHS Foundation Trust Patient Journeys System
- SUAP
- Service User Advisory Panel
- T1
- time 1
- T2
- time 2
- T3
- time 3
- TIDieR
- template for intervention description and replication
- TSC
- Trial Steering Committee
- WAI-SR
- Working Alliance Inventory-Short Revised
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/hta24140).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
