Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 15/69/16. The contractual start date was in April 2016. The draft report began editorial review in May 2017 and was accepted for publication in November 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Tara Renton is a stakeholder for the National Institute for Health and Care Excellence appraisal associated with this publication.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Hounsome et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Description of health problem
The four hindmost molars, known as the third molars (3Ms) or wisdom teeth, are the last teeth to erupt in the upper (maxillary) and lower (mandibular) jaws; this usually happens during young adulthood between the ages of 18 and 24 years. Third molars can be either impacted or non-impacted, and an impacted third molar (I3M) can be classed as erupted, partially erupted or unerupted. Impaction occurs when the eruption of the tooth is blocked by either soft tissue (gum) or bone.
For some patients, 3Ms erupt fully, whereas, for others, 3Ms could remain unerupted and impacted throughout the life of the tooth. Third molars can be potentially problematic to the individual by causing pain and disease; however, many 3Ms are asymptomatic (trouble free) or disease free/pathology free. There has been significant debate over the past few decades surrounding the management of 3Ms; historically, the practice has been to surgically extract 3Ms prophylactically to avoid potential problems in the future. However, 3M surgery is not without risk to the patient. Despite the substantial amount of literature dedicated to the debate on whether or not to prophylactically remove 3Ms, there is still disagreement and controversy among dentists and oral surgeons as to what constitutes best practice. 1 Current National Institute for Health and Care Excellence (NICE) guidance2 advises against the routine prophylactic removal of 3M teeth.
Kandasamy et al. 3 assert that, although there is extensive literature regarding the extraction of 3Ms, ‘[t]here is a large individual variation and a multitude of practitioners’ beliefs and biases relating to the extraction of especially asymptomatic and pathology-free third molars . . . [w]ith the current emphasis in dentistry being placed on clinicians to make evidence-based decisions.’3
There is a disagreement on the operational definition of what constitutes an asymptomatic or pathology-/trouble-/disease-free 3M. In part, this is due to some inconsistent and misleading use of vague terminology. 1,4 In some studies ‘asymptomatic’ denotes teeth that have no associated pathology, whereas in others it denotes an absence of symptoms. 4 There is a significant difference between disease free and asymptomatic: asymptomatic does not equal disease free. It is argued that pathology always precedes symptoms, so it is therefore prudent for decision-makers to assume the development of pathology if teeth are symptomatic. 1 The terminology that is used in clinical research studies needs to convey the precise condition that is being described (i.e. the presence or absence of pathology) otherwise inconsistent findings will always be reported. 4
To be clear, in this report, prophylactic removal of I3Ms is considered to relate to the removal of pathology-free 3Ms to avoid potential problems in the future.
Aetiology, pathology and prognosis
Impacted third molars are classified on the basis of their location (mandibular or maxillary), eruption status, nature of impaction, angulation of impaction and depth of impaction relative to the adjacent tooth. An impacted tooth can be visible in the mouth, can be explored with a periodontal probe or may be observed only through radiographic assessment. 5 Eruption status is described in Table 1.
| Eruption status | ||
|---|---|---|
| Erupted | Partially erupted | Unerupted |
Crown is visible in mouth:
|
Part of crown is visible in mouth:
|
Crown not visible but:
|
The nature of the impaction can be when the tooth is covered only by soft tissue and is referred to as ‘soft-tissue impaction’. The tooth can also be covered by bone; this is known as ‘partial bony impaction’ when partially erupted or as ‘complete bony impaction’ when unerupted and not communicating with the mouth.
The nature of angulation can be based on Winter’s classification,6 whereby the 3M could be:
-
mesioangular [angled towards the second molar (2M)]
-
distoangular (angled away from the 2M)
-
horizontal
-
vertical
-
buccal (angled towards the cheek)
-
lingual (angled towards the tongue).
Based on Pell and Gregory’s7 classification relating to depth, the I3M can be class 1, 2, or 3 according to the amount of tooth covered by the mandibular ramus, or A, B, or C depending on the depth of the impacted tooth compared with the 2M.
Pathological changes
Impacted third molars may be associated with pathological changes such as infection (pericoronitis), periodontal (gum) disease, dental caries, destruction of adjacent teeth and cysts and tumours. According to Worrall et al. ,8 the prevalence of pathological changes in I3Ms is higher in impacted mandibular third molars (IM3Ms) than in impacted maxillary 3Ms.
Pericoronitis
Pericoronitis is an infection of the soft tissue surrounding the crown of the tooth and is caused by an accumulation of bacteria and debris beneath the soft tissue. This can result in inflammation and pain. When 3Ms are impacted, an area is created that is difficult to clean properly with a toothbrush, which makes the molar in front of the 3M, as well as the 3M itself, vulnerable to plaque accumulation, inflammation and infection. It is reported that 20–30% of partially erupted teeth and 10% of completely unerupted teeth are associated with pericoronitis. Partial soft bony impaction and vertical or distal angulation are additional risk factors for pericoronitis. 9
Gum/periodontal disease
The early stages of gum disease include red and swollen gums and bleeding gums after tooth-brushing, which is known as gingivitis. More advanced disease, known as periodontal disease or periodontitis, can lead to bad breath, loose teeth and gum abscesses. Periodontal disease/gum disease is caused by bacteria in the mouth, which, when not removed by tooth-brushing, can lead to chronic gum inflammation that can affect the bone that supports the teeth in the mouth.
Dental caries (decay)
Dental caries or decay is the demineralisation of tooth enamel or dentine that is caused by bacteria that metabolise sugar in the diet to form acids. A longitudinal study10 in the USA followed patients with at least one 3M below the occlusal plane at baseline that had erupted during the follow-up period (median follow-up period 5.1 years). The study found that, of the 49 patients who had no 3M caries at baseline, 36 (73%) had no caries experience at follow-up and 13 (27%) had at least one 3M with caries. 10
Pathology in adjacent teeth
There is some evidence to suggest that horizontal or mesioangular I3Ms may increase the risk of decay and cause possible damage to adjacent teeth. 11 Longitudinal data from a study12 of 1231 non-veteran volunteers revealed that the presence of a 3M that was soft-tissue impacted increased the risk of incident 2M pathology by 4.88-fold [95% confidence interval (CI) 2.62 to 9.08]; however, the prevalence of soft-tissue impaction in the study population was only 3%. The relative risk for pathology in the 2M was 39.6% for those with absent 3Ms, 52.8% for those with erupted 3Ms and 56.6% for those with bony impaction. 12 There appears to be a link, therefore, between the presence of 3Ms and the development of 2M distal cervical caries (DCC), particularly with mesioangular 3Ms. 13
Cysts and tumours
Cysts and tumours may develop around I3Ms, although research has shown that the risk is low and reduces with age. 14 A study of surgically removed asymptomatic I3Ms found that histological examination of the dental follicles showed the following pathological conditions: dentigerous cysts (14.1%), calcifying odontogenic cysts (6.6%) and odontogenic keratocysts (2.5%). 15
Natural history with no treatment
Little is known about the natural history of I3Ms left in situ. This is due, in part, to the historical routine extraction of I3Ms, which means that we have limited data on which to make reliable estimates of the onset of pathology when the asymptomatic teeth are left in place. 3 Collecting the required data is also problematic in the UK, as clinical reporting systems are not sensitive enough to capture information relating to 3M management. 16 In addition, it would be costly to conduct a non-interventional/observational study to gather data on untreated I3Ms, as it would take decades because of the size of the study cohort needed to determine the occurrence of pathological conditions. 4
Epidemiology
The prevalence of I3Ms in the UK is unknown. Internationally, the prevalence of I3Ms is reported to range from 18% to 68%. 17 According to the results of a 2016 meta-analysis18 of 49 studies (83,484 individuals), the prevalence of 3M impaction worldwide in individuals aged > 17 years is 24.4% (95% CI 18.97% to 30.80%). The authors18 also found that the risk of having IM3Ms was higher than having impacted maxillary 3Ms (57.6%, 95% CI 43.3% to 68.3%; p < 0.0001), and that there was no difference in the incidence of impaction between men and women (18.6%, 95% CI –4.9% to 48.0%; p = 0.12). The most common angulation of impaction was found to be mesioangular (41.2%, 95% CI 33.8% to 49.0%).
The UK National Third Molar project8 was a cross-sectional survey that was set up in 1997 to assess the management of 3Ms in UK clinical practice. Clinical data were collected prospectively from all of the patients who were referred for assessment of 3Ms to oral and maxillofacial consultant surgeons during July 1995. 8 Completed questionnaires were returned from 181 consultants and 8298 patients (with 25,001 3Ms) who were referred to a hospital for assessment. Details of the eruption and symptom status of all 3Ms at the time of presentation are shown in Table 2. In the data available/recorded, the majority of mandibular third molars (M3Ms) (69.4%) were impacted, whereas maxillary 3Ms were more likely to be classified as ‘present and functional’ or ‘absent’.
| Status | 3M teeth (%) | |||
|---|---|---|---|---|
| Maxillary | Mandibular | |||
| Right (n = 5191) | Left (n = 5700) | Left (n = 7049) | Right (n = 7061) | |
| Present and functional | 18.9 | 19.4 | 8.5 | 4.2 |
| Absent | 34.7 | 40.5 | 16.6 | 6.1 |
| Impacted and symptomatic | 12.6 | 13.3 | 17.6 | 11.3 |
| Impacted and asymptomatic | 4.1 | 4.1 | 41.9 | 24.4 |
| Buried | 7.9 | 8.2 | 4.2 | 2.7 |
| Unrecorded | 22.0 | 14.7 | 11.3 | 51.5 |
The authors of the study8 reported that, after assessment, a total of 19,971 (80%) of the 25,001 3Ms were extracted and M3Ms were more likely to be extracted than maxillary 3Ms (87% vs. 71%, respectively). The most frequent indication for extraction was prophylactic removal (n = 8772, 44%), followed by pericoronitis (n = 7896, 40%). There were differences in the rates of and reasons for extraction between mandibular and maxillary 3Ms: 22% of M3Ms were extracted prophylactically compared with 79% of maxillary 3Ms, whereas 60% of M3Ms were removed as a result of pericoronitis, compared with 8% of maxillary 3Ms.
The results of the UK National Third Molar project8 showed that the most common age for the removal of 3Ms was between 21 and 25 years. However, in 2012, McArdle and Renton19 reported that the mean age of patients having 3Ms removed had increased from 25 years in 2000 to 32 years in 2010, with the most common age increasing from 26 to 29 years (CIs not reported).
Impact of the health problem
Prior to the introduction of the NICE guidance in 2000,2 the removal of 3Ms was one of the most common of all surgical procedures performed in the UK, with > 36,000 inpatient and 60,000 day-case admissions for ‘surgical removal of tooth’ in the period 1994–5. 20 During this period, the cost to the NHS in England of 3M surgery was estimated to be £30M per year, with additional estimated costs of £20M in the private sector. 20
The authors of a 2012 study19 investigating the effects of the NICE guidance2 on the management of 3Ms reported that, since the introduction of the NICE guidance,2 the number of 3M removals in secondary care (inpatient/day case) had reduced from ≈ 60,000 in the 1990s to ≈ 40,000 in 2003. However, since 2003, the number of removals appeared to have increased to ≈ 65,000 during 2009/10 (inpatient/day case only).
Information provided to NICE in the British Dental Association (BDA) (McArdle LW, British Dental Association, 2016, NICE submission) and the Faculty of General Dental Practice (FGDP) (Renton T, FGDP, 2016, NICE submission) submissions suggested that the prophylactic removal of 3Ms prevents future harm to patients. These organisations argue that the introduction of the NICE guidance2 initially resulted in a reduction in the number of 3Ms extracted; however, this figure has since increased. It is argued that, irrespective of the NICE guidance in 2000,2 the need for surgical extraction was not negated but postponed until a later date. It is further argued that patients aged > 25 years are at a higher risk of surgical morbidity relating to 3M extraction (Renton T, NICE submission). Another possible explanation for the increase in 3M extractions could be that patients who may have more than one I3M undergo multiple treatment episodes as and when other 3Ms become problematic (McArdle LW, NICE submission).
Current service provision
Management of disease
The treatment options for people with I3Ms are surgical removal or standard care without prophylactic removal of 3Ms.
Surgical removal
A report21 by the Royal College of Surgeons of England states that 3M surgical procedures are generally suitable for day case management, and that it is recognised that treatment under local anaesthesia, with or without sedation, is associated with reduced complication rates.
Removal of I3Ms can be carried out by a dentist, or patients can be referred to an oral surgeon if the degree of impaction or position of the tooth indicates that a more complex surgical procedure is required. If general anaesthetic is required, the surgical removal is conducted in hospital.
Generally, recovery from surgery for the removal of 3Ms is straightforward. The immediate side effects of 3M surgery, such as pain and swelling, resolve within a few days and jaw stiffness usually subsides within 1–2 weeks. 22 However, there may be potential additional complications associated with the removal of I3Ms, including damage to surrounding teeth, infection and dry socket (which can manifest as a throbbing pain in the gum or jaw and also cause bad breath). Furthermore, nerve damage may occur; this is a serious complication that can cause short- and long-term pain or a tingling sensation and numbness in the tongue, lower lip, chin, teeth and gums.
Overall, the rate of complications following the surgical removal of 3Ms is reported to vary between 2.6% and 30.9%. 23 The removal of M3Ms (regardless of eruption status) is much more likely to be associated with post-surgical complications than the removal of maxillary 3Ms. 24 The risk of infection following extraction of I3Ms is approximately 10% in healthy patients; however, it may be up to 25% in patients with low immunity. 25 Dry socket occurs in 5–10% of patients who have undergone a 3M removal and presents within 3–5 days after the initial pain from surgery has subsided. Nerve damage occurs in up to 2% of patients and is generally temporary, but in 0.5% (1 in 200) of patients, the damage is permanent. 22 The risk of nerve injury is more common if the IM3M is located close to the inferior alveolar nerve, with 20% of patients likely to then have temporary nerve damage and 2% likely to experience permanent damage. 22
Standard care without prophylactic removal
The alternative to surgical removal of an I3M is standard care without removal of the tooth. Standard care is typically patient centred and comprises regular oral health reviews, oral health advice, dental care plans and a decision on the time between recalls. 26 Standard care is carried out without the removal of the I3M. However, without the removal of the I3M, there is a risk that pathological changes, as previously described, could lead to future surgical removal of the impacted tooth.
Indications for removal or retention
The decision to remove or retain an I3M depends on whether or not it is asymptomatic (pathology or trouble free). When there are pathological changes, current NICE guidance2 states that the I3M should be removed.
Variation in services and/or uncertainty about best practice
Internationally, there is a vast quantity of published literature relating to the management of 3Ms and many published international guidelines with recommendations for best practice relating to asymptomatic or disease-free 3Ms. However, there is still debate and it remains a contentious subject. According to the FGDP submission (Renton T, NICE submission), there are differences of opinion between professionals in the UK relating to best practice. However, the submission authors assert that most UK dentists believe that erupted, non-functional, low-risk M3Ms should be removed at a young age to prevent increased surgical morbidity in older age and to prevent future harm to the patient (Renton T, NICE submission).
There is significant geographical variation in current practice when international guidelines are examined. 21,27–34 The American31 guidelines recommend a more interventional approach to 3M management. In the UK NHS setting, there is a ‘no-intervention’ policy unless there are distinct therapeutic indications, although there are differences of opinion between professionals.
There is variation between services relating to the use of either general anaesthesia or local anaesthesia and sedation. There are published data35 that illustrate that only 3% of IM3M cases in a London teaching hospital required general anaesthetic, with 40% of cases requiring intravenous sedation. However, our clinical advisor has pointed out that not all district general hospitals offer sedation services for dental extractions; therefore, the proportion of patients who receive higher-risk general anaesthetic is greater. In terms of service provision, many dental practices in the UK do not provide intravenous sedation, which results in patients of these practices being referred to hospital to undergo surgical extraction under general anaesthetic. There is also considerable variation in the perioperative care provided; for example, the provision of informed consent, the provision of patient information, the provision of pre-operative mouth rinses, the provision of analgesia and the rates of antibiotic prescription (Renton T, NICE submission).
Relevant UK guidelines
The NICE technology appraisal 1 (TA1)20 was completed in 2000; the resultant NICE guidance2 informed that the prophylactic removal of pathology-free I3Ms was not recommended (Box 1).
-
The practice of prophylactic removal of pathology-free impacted third molars should be discontinued in the NHS.
-
The standard routine programme of dental care by dental practitioners and/or paraprofessional staff, need be no different, in general, for pathology-free impacted third molars (those requiring no additional investigations or procedures).
-
Surgical removal of impacted third molars should be limited to patients with evidence of pathology. Such pathology includes unrestorable caries, non-treatable pulpal and/or periapical pathology, cellulitis, abscess and osteomyelitis, internal/external resorption of the tooth or adjacent teeth, fracture of tooth, disease of follicle including cyst/tumour, tooth/teeth impeding surgery or reconstructive jaw surgery, and when a tooth is involved in or within the field of tumour resection.
-
Specific attention is drawn to plaque formation and pericoronitis. Plaque formation is a risk factor but is not in itself an indication for surgery. The degree to which the severity or recurrence rate of pericoronitis should influence the decision for surgical removal of a third molar remains unclear. The evidence suggests that a first episode of pericoronitis, unless particularly severe, should not be considered an indication for surgery. Second or subsequent episodes should be considered the appropriate indication for surgery.
© NICE 2000 Guidance on the Extraction of Wisdom Teeth. 2 Available from www.nice.org.uk/guidance/ta1. All rights reserved. Subject to Notice of rights. NICE guidance is prepared for the National Health Service in England. All NICE guidance is subject to regular review and may be updated or withdrawn. NICE accepts no responsibility for the use of its content in this product/publication.
A review of the existing NICE guidance,2 via a review proposal in 2014, concluded that no new trial data on this topic were available. As a result, a decision was made that the NICE guidance2 did not need to be revisited and that the topic should remain on the static list. However, as the recommendations set out in the NICE guidance2 were increasingly being perceived as controversial by the dental profession, a NICE consultation with relevant stakeholders was then undertaken. Consultation responses highlighted that additional pertinent trial data were available, and therefore should be assessed. In response, NICE instructed that the current guidance2 should be partially updated (i.e. prophylactic indications only) via the multiple technology appraisal (MTA) process.
Description of the technology under assessment
Summary of the intervention
The surgical extraction of IM3Ms with evidence of pathology (see Box 1) can be undertaken in primary care, secondary care and specialist clinics. The NHS commissioning oral surgery pathway36 clearly outlines social, medical and dental factors that dictate the optimal setting (Renton T, NICE submission).
Specialist radiographic equipment and assessment may be required for risk assessment of IM3Ms, including panoral radiography and cone beam computerised tomography, which requires the input of a radiologist. For a patient who requires sedation (primary care), specialist nursing is required. Intravenous sedation services require additional staff training, the correct facilities and indemnity costs.
Identification of important subgroups
There is intrapatient variance in the presentation of I3Ms, that is a single patient can have multiple 3Ms (i.e. maxillary as well as mandibular and bilateral presence) with different types of impaction (i.e. vertical, horizontal, distoangular and mesioangular). These are the most common impaction types considered as subgroups, although a smaller proportion of patients may have ectopic impactions. The variability of 3M impactions results in different secondary disease distribution, which is dependent on the nature of the impaction (McArdle LW, NICE submission).
Patients with high-risk M3Ms (the roots cross the inferior dental canal) could be 10 times more likely to develop temporary or permanent inferior alveolar nerve injury (Renton T, NICE submission).
Chapter 2 Definition of the decision problem
The remit of this review was to appraise the clinical effectiveness and cost-effectiveness of the prophylactic removal of IM3Ms.
Decision problem
This MTA has been conducted in line with the decision problem issued by NICE in the final scope. 11 This is reproduced in Table 3.
| Criteria | Inclusion criteria |
|---|---|
| Interventions | Prophylactic removal of third molars |
| Population | People with pathology-free or trouble-free impacted mandibular third molars |
| Comparators | Standard care without prophylactic removal of third molars |
| Outcomes | The outcome measures to be considered include:
|
| Economic analysis |
The reference case stipulates that the cost-effectiveness of treatments should be expressed in terms of incremental cost per quality-adjusted life-year The reference case stipulates that the time horizon for estimating clinical effectiveness and cost-effectiveness should be sufficiently long to reflect any differences in costs or outcomes between the technologies that are being compared Costs will be considered from an NHS and Personal Social Services perspective |
| Other considerations | If evidence allows, consideration may be given to people with mesioangular or horizontally impacted third molars |
Overall aims of assessment
The aim of this assessment report is to synthesise the clinical effectiveness and cost-effectiveness of the prophylactic removal of IM3Ms, compared with standard care without prophylactic removal.
What is not included in the assessment
It is beyond the remit of this assessment report to comment on or to draw conclusions relating to the wider topic of the management of 3Ms; this assessment report focusses primarily on summarising the relevant evidence relating to the surgical extraction or retention of asymptomatic IM3Ms.
It is worth noting that the aims of the original assessment report conducted by Song et al. ,20 which contributed to the NICE guidance2 issued in 2000, were not exactly the same as the aims of this assessment, which is a partial update of TA1. Song et al. 20 aimed to ‘provide a summary of existing evidence on prophylactic removal of impacted wisdom teeth, in terms of the incidence of surgical complications associated with prophylactic removal, and the morbidity associated with retention.’
Chapter 3 Assessment of clinical effectiveness
Methods for reviewing effectiveness
Identification of studies
Search strategy
The assessment group (AG) identified relevant clinical studies, systematic reviews (SRs) and decision analyses by searching the following major medical databases from 1999 onwards: MEDLINE, EMBASE, The Cochrane Library, NHS Economic Evaluation Database (NHS EED) and EconLit. The search strategies used are presented in Appendix 1.
In addition to the electronic databases, information on studies that were in progress were sought by searching the International Standard Randomised Controlled Trial Number registry.
Citation-searching was conducted using all references in key articles and all identified SRs. The sources referenced in the professional stakeholder submissions received as part of the standard NICE process were cross-checked to identify relevant references.
A database of the published literature was assembled from the aforementioned sources and was held in the EndNote X7 software package [Clarivate Analytics (formerly Thomson Reuters), Philadelphia, PA, USA].
Inclusion and exclusion criteria
Two out of the three reviewers (JH, GP and RD) independently screened all of the titles and abstracts identified by the initial search using Covidence (Melbourne, VIC, Australia). Full-text copies of any titles/abstracts that may have been eligible were obtained and assessed for inclusion by two reviewers (JH and GP) according to the inclusion and exclusion criteria listed in Table 4. Discrepancies were resolved by consultation with a third reviewer/clinical advisor. Studies that did not meet the inclusion criteria were excluded and the reasons for exclusion were summarised. For studies that were identified as not meeting the criteria at the data abstraction stage, the bibliographic details and reasons for exclusion were summarised.
| Criteria | ||
|---|---|---|
| Inclusion | Exclusion | |
| Study design |
|
|
| Patient population | People with IM3Ms | |
| Intervention | Prophylactic removal of IM3Ms (as defined by study authors) | |
| Comparator | Standard care without prophylactic removal of IM3Ms | |
| Outcomes | The outcome measures to be considered included:
|
|
| Setting/location |
|
|
| Other considerations | If evidence allows, consideration may be given to people with mesioangular or horizontally I3Ms | |
| Limits |
|
|
The eligibility criteria reflected the decision problem from NICE;11 additional criteria were that studies were based in settings with a similar dental system to that in the UK (i.e. Europe, North America, Australasia), English-language papers (owing to a lack of resources to translate non-English-language papers) and the time frame of 1999 onwards, because this was a partial update of the previous NICE guidance. 2 The inclusion criteria for SRs were necessarily broader and were not restricted to those looking at IM3Ms only.
Data abstraction strategy
Data relating to study characteristics and outcomes were extracted by one of two reviewers (Joanne Fisher or Juliet Hounsome) and were independently checked for accuracy by a second reviewer (Joanne Fisher or Juliet Hounsome). Disagreement was resolved through consensus; when necessary, a third reviewer was consulted. Study data that were reported in multiple publications were extracted and reported as a single study.
Critical appraisal strategy
The quality of the included studies was assessed by one reviewer (Juliet Hounsome or Joanne Fisher) and independently checked for agreement by a second reviewer (Juliet Hounsome or Joanne Fisher). Disagreements were resolved through consensus. The quality of the cohort studies was assessed using an adapted version of the Newcastle–Ottawa Scale for assessing the quality of cohort studies37 and SRs were assessed according to criteria outlined by the Centre for Reviews and Dissemination. 38
Methods of data synthesis
The results of the data extraction and quality assessment for each included study are presented in structured tables (see Tables 5–9 and Appendices 3 and 4) and as a narrative summary (see following section).
Results
Quantity and quality of research available
The results of the electronic searches (conducted on 4 April 2016) and the application of the inclusion criteria are shown in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram in Figure 1.
FIGURE 1.
The PRISMA flow diagram: clinical evidence review.

In total, 22 citations,20,39–59 reporting the results of nine SRs20,40,42–46,50,56 and four cohort studies,47,48,58,59 were included in the review. No randomised controlled trials (RCTs) were identified.
The reasons for excluding papers at the full-text review stage are summarised in Appendix 2.
As shown in Figure 1, a total of 72 papers were initially included at full-text review. However, on further inspection, no relevant data for the specific population of interest for this review were available for 50 papers; these papers were subsequently excluded. The bibliographic details, with the reasons for exclusion, for these 50 studies are also reported in Appendix 2.
One study58 reported on outcomes both for standard care with and standard care without prophylactic removal of IM3Ms. Four papers39,47,48,57 reported on two studies that assessed the outcomes of standard care without prophylactic removal of IM3Ms, and one paper59 reported on a study that assessed prophylactic removal of IM3Ms. A further 16 papers20,40–46,49–56 reported on nine SRs that assessed whether or not I3Ms should be removed prophylactically.
Quality assessment: cohort studies
The quality of the four included cohort studies47,48,58,59 was assessed using an adapted version of the Newcastle–Ottawa Scale;37 the results are tabulated in Table 5.
| Characteristic | Study | |||
|---|---|---|---|---|
| Vares and Kyyak, 201458 | Fernandes et al., 201048 | Hill and Walker, 200647 | Petsos et al., 201659 | |
| Representative of cohort | No description | Truly representative | Truly representative | Truly representative |
| Ascertainment of exposure | Clinical records | Clinical records | Clinical records | Clinical records |
| Outcome present at start | Yes | Yes | Yes | Yes |
| Assessment | No description | Record linkage | Record linkage | Record linkage |
| Length of follow-up | Adequate | Adequate | Adequate | Adequate |
| Attrition rate (%) | No description | 31 | 9 | 14 |
All of the studies, with the exception of the Vares and Kyyak58 study, included patients who were representative of the population of interest. Clinical records were used in all four studies47,48,58,59 to ascertain whether or not patients were ‘exposed’ to the intervention (either retention and standard care or prophylactic removal) and all studies demonstrated that the outcome of interest (e.g. pathology) was not present at the start of the study and that the assessment of the outcome was through clinical assessment. None of the studies used a blinded assessment, as this was not possible. The length of follow-up was adequate in all studies. The attrition rates differed between three studies: 9%,47 14%59 and 31%. 48 No details of study attrition were reported by Vares and Kyyak. 58 To conclude, the AG considered all but one58 of the studies to be generally good-quality cohort studies. However, missing information in the Vares and Kyyak58 paper meant that it was not possible to adequately assess the quality of this study.
Quality assessment: systematic reviews
The quality of the nine SRs20,40,42–46,50,56 was assessed in accordance with criteria outlined by the Centre for Reviews and Dissemination. 38 The results of the quality assessment are shown in Appendix 3.
Seven of the SRs had defined clear review questions in terms of population, interventions, comparators and outcomes;20,40,42–44,46,50 however, these details were missing in two SRs. 45,56 Only three reviews20,45,46 had an adequate search strategy without language or date restrictions. Two reviews were limited by language only: one review to English, Dutch, French or German40 and one review to English. 44 One review43 was restricted by both language (English, Danish, Norwegian or Swedish) and date (1999–2003). Another review was restricted by date only (1999–2003). 50 The search terms used were not reported in the clinical evidence publications56 or in the Canadian Agency for Drugs and Technologies in Health (CADTH) SR,42 which were also restricted by date and language. Three SRs20,40,46 provided adequate information to facilitate the assessment of whether or not preventative steps had been taken to minimise bias and errors in the selection process. Four SRs20,40,45,46 reported adequate methods for assessing the quality of included studies. One SR43 reported using a recognised quality assessment tool, but did not provide details on how it was used. The remaining four SRs42,44,50,56 did not report whether or not they had conducted a quality assessment of the included studies. Adequate details of the primary studies were presented in seven of the SRs. 20,40,43,44,46,50,56 In the CADTH publication,42 details were presented only narratively for each primary study; although Costa et al. 45 presented some details of the primary studies, no details of the outcomes of the primary studies were presented. Statistical data synthesis was not appropriate for any of the SRs; instead, the authors of two SRs44,56 reported a narrative synthesis, three SRs20,40,42 summarised each study individually and one SR46 did not include any studies. Costa et al. 45 reported the results of the quality assessment only and Suska et al. 43 did not provide any synthesis. It was not possible to assess the Senter for Medisinsk Metodevurdering report for this item (were appropriate methods used for data synthesis?). 50
Assessment of the effectiveness of the included studies
Prophylactic removal versus retention and standard care
One study58 reported on outcomes for both the surgical complications of the prophylactic removal of asymptomatic IM3Ms and standard care without prophylactic removal of asymptomatic IM3Ms. The study was an observational cohort study and was conducted in Ukraine between 2009 and 2013. It was designed to develop and assess a pre-operative assessment and to create a rationale for the prophylactic removal of asymptomatic IM3Ms. The assessment included clinical and roentgenological parameters; the 84 patients who were included were assigned to one of three groups: (1) requiring removal and subsequently having the tooth removed (n = 52), (2) requiring removal but the patient refused (n = 7) and (3) those not requiring removal as determined by the assessment (n = 25). The first group (n = 52) was then separated further into three age groups: 18–25 years (n = 41), 25–45 years (n = 10) and one patient of 68 years. Patients were followed up annually for 5 years.
At the end of the 5 years, the study58 authors reported that there were ‘no considerable intra- or post-operative complications in the first subgroup’,58 only ‘minor complications in the second subgroup’ and, ‘in the case of 68-year-old patient surgery, all complications were related to considerable bone atrophy of the operated area’. 58
Of the seven patients who refused extraction, five required the tooth to be extracted within the 5 years’ follow-up. Of the 25 patients who were assessed at baseline as not requiring extraction, none had the tooth extracted during the 5 years’ follow-up.
The study58 authors concluded that ‘the low-to-no percentage of intra- and post-operative complications does not give any reason to leave a wisdom tooth with minor clinical manifestations or an asymptomatic wisdom tooth with bad prognosis in place, since early surgical procedures generate fewer complications, having shorter operative time and post-operative period’. 58
Further details of the study characteristics and outcomes are reported in Appendix 4.
Retention and standard care
We included two studies, Fernandes et al. 48 and Hill and Walker47 (reported in four publications39,47,48,57), that reported relevant outcomes for the comparator of standard care without prophylactic removal of IM3Ms. Both studies were single-cohort studies with follow-up periods of 1 year48 and 5 years. 47 Both studies were conducted in the UK; the number of patients with trouble-free IM3Ms was 421 in one study48 and 153 in the other. 47 The number of trouble-free IM3Ms examined was reported in one study only (n = 676). 48 Participants in one study47 were aged 16–30 years (median age 23 years); in the other study,48 participants were aged 18–70 years (18–34.9 years, n = 400; 35–49.9 years, n = 149; and 50–70 years, n = 64). 48 The percentage of males was 41% in one study48 and 34% in the other study47 (Table 6). Further study and participant characteristics are reported in Appendix 4.
| Study | Characteristic | |||
|---|---|---|---|---|
| Setting | Follow-up period | Description of I3Ms and patients | Participant demographics | |
| Fernandes et al., 201048 | Multicentre, Scotland, UK (primary care setting) | 1 year | IM3Ms (n = 676). 613 patients assessed at baseline, 583 patients eligible, 421 patients with follow-up |
|
| Hill and Walker, 200647 | Unclear but likely single centre, Cardiff, UK | 5 years | IM3Ms. 153 patients had no history of pericoronitis |
|
Outcomes were assessed by Hill and Walker47 using a questionnaire or telephone call every 6 months and a clinical examination every year, if the patient were willing to attend. A research dentist questioned and assessed the clinical outcomes of patients at the 1-year follow-up in Fernandes et al. 48
Both studies reported the rates of extraction during the study period, the reasons for extraction and the rate of the IM3M surviving asymptomatically. A summary of these outcomes is shown in Table 7. Fernandes et al. 48 reported an extraction rate over 1 year of 5.5%, whereas Hill and Walker47 reported an extraction rate over 5 years of 31.4% for those without a history of pericoronitis. The reasons for extraction also differed between the studies. Fernandes et al. 48 reported that the reason for removal was unknown by patients in 46% of cases, but that, for those patients who knew the reason, pain was the most common reason for removal (27%, 50% of known reasons), followed by pericoronitis (13.5%, 25% of known reasons). Hill and Walker47 reported that pericoronitis was the most common reason for removal (62.5%), followed by cosmetic/orthodontic reasons (12.5%). Both studies reported the number of patients having teeth removed as a result of caries in the 2M: 2.7% in one study48 and 8.3% in the other. 47
| Outcomes assessed | Rate, n/N (%) |
|---|---|
| Extraction rate | |
| aFernandes et al.48 | 37/676 (5.5) |
| Hill and Walker47 | |
| Without a history of pericoronitis | 48/153 (31.4) |
| With a history of pericoronitis | 23/66 (34.8) |
| Reasons for extraction | |
| aFernandes et al. 201048 | |
| Pericoronitis | 5/37 (13.5) |
| Pain | 10/37 (27.0) |
| Caries in distal of adjacent molar | 1/37 (2.7) |
| Caries in the 3M | 2/37 (5.4) |
| Contralateral | 2/37 (5.4) |
| Unknown | 17/37 (46.0) |
| aHill and Walker 200647 (without a history of pericoronitis) | |
| Pericoronitis after start of study | 30/48 (62.5) |
| Cosmetic/orthodontic | 6/48 (12.5) |
| Food impacted/difficult to clean | 4/48 (8.3) |
| Early caries in 2M | 4/48 (8.3) |
| Painful when eating | 2/48 (4.2) |
| Earache/TMJ pain | 2/48 (4.2) |
| Survived asymptomatically | |
| Fernandes et al. 201048 | |
| From any symptom | 562/676 (83.1) |
| From SIGN symptoms only | 623/676 (92.2) |
| Hill and Walker 200647 | 150/222b (67.6) |
| Symptoms developed by tooth | |
| Fernandes et al. 201048 | |
| Pericoronitis | 15/114 (13.2) |
| Severe pain (SIGN) | 16/114 (14.0) |
| Mild pain (SIGN) | 22/114 (19.3) |
| Discomfort/irritation (non-SIGN) | 54/114 (47.4) |
| Food stagnation (non-SIGN) | 7/114 (6.1) |
The number of patients who did not experience any symptoms over the period of the studies was 83.1% in one study48 and 67.6% in the other. 47 Fernandes et al. 48 reported the number of patients who did not experience symptoms that indicated the need for removal according to the Scottish Intercollegiate Guidelines Network (SIGN) guidelines34 as 92.2%. The authors also reported the rates for the different symptoms, with discomfort/irritation, which is not a symptom that SIGN includes as a reason for removal, being the most frequently reported reason (47.4%). 48
Fernandes et al. 48 also investigated the relationship between symptoms and several factors. The authors found that there was a statistically significant relationship between the presence of symptoms and age, angulation, eruption status and the reason for the last visit to the general dental practitioner. They found no relationship between the presence of symptoms and sex, average number of teeth, maximum basic periodontal examination score, average Gingival Index (GI), ‘average mean plaque’, education after minimum school-leaving age, employment status, frequency of brushing teeth, occasional use of mouthwashes, occasional teeth flossing, frequency of dental appointments, length of time since patient last visited the dentist, smoking, drinking > 14 units per week or deprivation category.
Prophylactic removal
The final included study, by Petsos et al. ,59 assessed the effects of the prophylactic removal of trouble-free IM3Ms. It was identified during forward citation-searching, as it was published after the date of the review searches. Details of the study, patient characteristics and outcomes are reported in Appendix 4.
The study59 was a prospective cohort study conducted in Germany that was self-funded and recruited patients over 5 months in 2014 after they underwent extraction of asymptomatic IM3Ms. The study59 was designed to assess the changes in the periodontal health of adjacent 2Ms 6 months after the removal of the asymptomatic IM3Ms. Results from 78 patients were included in the analyses. Of these 78 patients, 58 had a submucosal IM3M removed and 20 had a fully impacted M3M. The mean age of patients was 16 years and 37% of patients were male. Only four patients were smokers. At baseline, the plaque index, GI, probing pocket depth (PPD) and probing attachment level (PAL) were measured, with measurements being obtained at six sites around the 2M (i.e. mesiobuccal, buccal, distobuccal, distolingual, lingual, mesiolingual).
To assess the change in the periodontal health of the 2M at follow-up, the mean PPD and PAL scores at the three sites located closest to the distovestibular incision (buccal, distobuccal, distolingual) were used.
Although no significant change was reported in the plaque index and GI scores, the mean PPD score of the three sites improved from 3.25 ± 0.65 (range 2–5.7) to 2.57 ± 0.5 (range 1.3–3.7); this was a statistically significant reduction. Similarly, the mean PAL score across the three sites significantly improved, with a reduction from 2.96 ± 0.53 (range 2.0–5.0) to 2.55 ± 0.5 (range 1.3–3.7). 59
The surgical complications following the prophylactic removal of the IM3Ms were recorded. A total of 20 patients (25.6%) reported complications. Intense pain for > 1 day was the most frequent complication, which was reported by 12 patients. A further five patients (6.4%) reported post-operative infection (infiltrate or abscess), and the remaining three patients experienced wound dehiscence. No incidences of secondary bleeding or nerve damage were reported. 59
The authors59 concluded that ‘young patients may benefit from an early removal of mandibular M3, especially in the presence of certain cofactors’.
Systematic reviews
Nine SRs,20,40,42–46,50,56 reported in 16 publications,20,40–46,49–56 met the review inclusion criteria and their details are summarised in Tables 8 and 9, with further details shown in Appendix 4.
| Study | Characteristic | ||
|---|---|---|---|
| Publication type; date of search | Objective/research questions | Inclusion criteria | |
|
Bouloux et al. 201544 AAOMS M3Taskforce |
SR; NR | To determine, clinically, whether or not young adults who elect to retain their asymptomatic 3Ms have a risk of undergoing one or more 3M extractions in the future |
|
| CADTH 201042 | Rapid review/HTA; 2000–10 | What is the evidence for the clinical benefit of prophylactic removal of asymptomatic wisdom teeth compared with retention of asymptomatic wisdom teeth?What are the evidence-based guidelines for the prophylactic removal of asymptomatic wisdom teeth?Reproduced with permission from CADTH422010Canadian Agency for Drugs and Technologies in Healthhttps://www.cadth.ca/sites/default/files/pdf/l0202_removal_wisdom_teeth_htis_2.pdf |
|
| Clinical evidence41,51–56 | SR (updated yearly); 1966–2014 | Should asymptomatic and disease-free impacted wisdom teeth be removed prophylactically? |
|
| Costa et al. 201345 | SR; up to 30 August 2012 | To investigate whether or not there is evidence justifying the prophylactic extraction of 3Ms |
|
| Mettes et al. 201246 | SR; 1950 to 30 March 2012 | To evaluate the effect of prophylactic removal of asymptomatic impacted wisdom teeth in adolescents and adults compared with the retention (conservative management) of these wisdom teeth |
|
| Senter for Medisinsk Metodevurdering 200350 | SR/HTA (English summary only); 1999–2003 | To evaluate the evidence on the incidence of surgical complications following the prophylactic removal of I3Ms, and the morbidity, quality-of-life and economic aspects associated with retention of I3Ms | NR in English summary |
| Song et al. 200020 | SR/HTA/clinical guidance; 1984–99 | To provide a summary of the existing evidence on prophylactic removal of impacted wisdom teeth, in terms of the incidence of surgical complications associated with prophylactic removal, and the morbidity associated with retention |
|
| Stordeur and Eyssen 201240 | Rapid assessment; December 2010 to March 2011 | To present the existing scientific evidence on the prophylactic extraction of 3Ms in the absence of local disease, and to formulate clinically relevant recommendationsWhat are the benefits and risks (complications) of prophylactic extraction of pathology-free wisdom teeth (3Ms) in adolescents and adults in the absence of local disease?What is the related good clinical practice for the prophylactic removal of pathology-free wisdom teeth? |
|
| Suska et al. 201043 | HTA/SR; May 2003 to December 2009. Based on the Norwegian HTA, so searches conducted after 2003 only | Does removal of 3M teeth reduce the risk of infections and other local disease/pathological conditions in patients with asymptomatic or symptomatic I3Ms compared with no intervention? |
|
| Study | Number/type of studies included | Author conclusions as quoted in publications |
|---|---|---|
| Bouloux et al. 201544 | Cohort studies, n = 7 | The cumulative risk of 3M extraction for young adults with asymptomatic 3Ms is sufficiently high to warrant its consideration when reviewing the risks and benefits of 3M retention as a management strategy |
| CADTH 201042 |
SRs, n = 4 Non-RCTs, n = 1 Guidelines, n = 2 |
Based on evidence and guidelines from the past ten years of evidence identified for inclusion in this review, there is currently insufficient evidence supporting or refuting the practice of prophylactic removal of asymptomatic third molars. Regarding clinical practice, the decision to remove asymptomatic wisdom teeth appears to be best based on careful consideration by practitioners of the potential risks and benefits for individual patients, as well as their attitude towards a potentially unnecessary surgical procedureReproduced with permission from CADTH422010Canadian Agency for Drugs and Technologies in Healthhttps://www.cadth.ca/sites/default/files/pdf/l0202_removal_wisdom_teeth_htis_2.pdf |
| Clinical evidence41,51–56 |
Extraction of asymptomatic I3Ms: SR, n = 5 Active surveillance of asymptomatic I3Ms: no studies |
When managing asymptomatic, disease-free wisdom teeth, no RCT data are available to guide therapeutic choices. Consistent with the application of evidence-based medicine principles, after a thorough review of the risks and benefits of the treatment alternatives, patient preference should be the factor driving the clinical decision56 |
| Costa et al. 201345 |
SR, n = 1 RCT, n = 3 |
The results of the present review indicate a lack of scientific evidence to justify the indication of the prophylactic extraction of third molars |
| Mettes et al. 201246 | RCT, n = 1 |
Insufficient evidence was found to support or refute routine prophylactic removal of asymptomatic impacted wisdom teeth in adults The single RCT compared removal with retention of asymptomatic impacted wisdom teeth and reported only one relevant outcome (late lower incisor crowding at 5 years). No difference was found Watchful monitoring of asymptomatic third molar teeth may be a more prudent strategy |
| Senter for Medisinsk Metodevurdering 200350 |
Patient series, n = 13 Cohort studies, n = 3 Case–control studies, n = 2 Cross-sectional studies, n = 6 Decision analysis, n = 1 |
Removal of asymptomatic fully retained wisdom teeth is not recommended. However, Norwegian dentists recommend prophylactic removal of 3Ms when the likelihood of 3Ms causing problems in the future is high and the incidence of post-operative complications is low (including partially erupted wisdom teeth). Because this report is based on studies that are not optimal, the patient’s preferences need to be decisive |
| Song et al. 200020 |
RCT, n = 2 Decision analysis, n = 4 Literature reviews, n = 34 |
There is no reliable research evidence to support the prophylactic removal of disease-free impacted third molars. Available evidence suggests that retention may be more effective and cost-effective than prophylactic removal, at least in the short to medium term |
| Stordeur and Eyssen 201240 |
SRs, n = 2 HTAs, n = 2 CPG, n = 1 |
There is mostly little debate on the fact that third molars associated with clinical and/or radiological pathology, such as unrestorable caries, should be removed. However, there is a lack of proven benefit from the systematic prophylactic removal of pathology-free third molars, impacted or not, in all adolescents or (young) adults, and the procedure is not free of risk. Preventative actions at the level of the population are only recommended if the benefits outweigh the disadvantages, and if this is not the case it is preferable not to intervene. If there is no scientific evidence that an intervention is beneficial, the largely accepted principle of medicine: ‘primum non nocere’, ‘first, do no harm’, should be respectedReproduced with permission from the Belgian Health Care Knowledge Centre. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by-nd/4.0/), which permits reproduction, provided the original author and source are credited2012Belgian Health Care Knowledge Centre |
| Suska et al. 201043 |
HTA report/SRs, n = 2 Case series, n = 16 (none reported on asymptomatic teeth) |
A systematic literature search and review of published data has revealed that there is still no scientific documentation available to either support or refute routine prophylactic removal of asymptomatic impacted wisdom teeth in adultsReproduced with permission from HTA-centrum2010HTA-centrum |
Two reports40,42 were rapid reviews that applied SR methodology. All but one review44 attempted to assess the evidence for the prophylactic removal of 3Ms compared with standard care without prophylactic removal. Bouloux et al. 44 assessed only whether or not retention of asymptomatic 3Ms led to future extraction.
No review restricted the population to trouble-free IM3Ms. Instead, four reviews40,42,44,45 included all trouble-free 3Ms regardless of their impaction status or location, two reviews46,56 included trouble-free I3Ms regardless of their location, one review20 included all 3Ms regardless of whether or not there were symptoms and one review43 included I3Ms regardless of their symptoms or location. A further review was published in Norwegian and had an English summary only,50 so the specific population was unclear. Different types of study design were included across the SRs: five40,42,43,45,56 included SRs and five42–44,50,56 included non-RCTs (e.g. cohort studies and case series). One46 SR limited inclusion to RCTs and another44 limited inclusion to cohort studies only. One20 review also included literature reviews and the dates of the searches ranged from 195046 to 2014. 56
The different inclusion criteria adopted by the SRs meant that the studies identified and included in the SRs differed. In total, 84 studies were identified across the nine SRs, with only seven studies20,49,50,60–63 being identified by more than one review:
-
Mettes et al. 49 (SR) was included in five SRs. 40,42,43,45,56
-
Harradine et al. 61 (RCT) was included in four SRs. 20,45,46,56
-
NICE guidance2/Song et al. 20,64 publications were identified by three SRs. 40,42,56
-
The Senter for Medisinsk Metodevurdering50 report was included in three SRs. 42,43,56
-
Lindqvist and Thilander63 (RCT) was included in three SRs. 45,49,56
-
Edwards et al. 60 (decision analysis) was included in two SRs. 20,50
-
Kruger et al. 62 (cohort study) was included in two SRs. 44,50
Despite the differences in inclusion criteria across the SRs, the conclusions were similar. Seven SRs20,40,42,43,45,46,56 stated that there was insufficient evidence to support or refute the prophylactic removal of trouble-free 3Ms. Two42,56 SRs recommended that the decision to remove an asymptomatic 3M should be based on careful consideration of the risks and benefits and that patient preferences should be taken into account. Two20,40 SRs recommended that, in the light of insufficient evidence, retention/‘first do no harm’ may be appropriate. Watchful monitoring was recommended in the Cochrane review by Mettes et al. 46 The Senter for Medisinsk Metodevurdering report50 recommended the prophylactic removal of 3Ms when the likelihood of 3Ms causing problems in the future is high and the incidence of post-operative complications are low. They restrict this to partially erupted 3Ms and state that this approach is not recommended for people with fully retained (i.e. complete bony impacted) teeth. They also state that patient preferences should be decisive.
The one44 SR that looked at the risk of future extraction following the retention of trouble-free 3Ms found that the mean incidence rate of future extraction was 3.0% annually (range 1–9%), leading to a cumulative incidence rate of 5% at 1 year and 64% at 18 years. The reasons for extraction were caries, periodontal disease and other inflammatory conditions. The authors concluded that ‘the cumulative risk of M3 extraction for young adults with asymptomatic M3s is sufficiently high to warrant its consideration when reviewing the risks and benefits of M3 retention as a management strategy’. 44
Additional evidence
References from included systematic reviews
We reviewed all of the references included in the identified SRs for inclusion in this review. Of the 84 cited references, nine met our inclusion criteria and all of the references had been identified through our searches. However, the AG feels that another nine of these references warrant further discussion, as they are papers often cited in the debate on the management of 3Ms. Therefore, study details and summaries of these nine studies are provided in Appendix 5.
Professional stakeholder’s submissions
As part of the NICE process, three submissions from professional stakeholders were received: the first on behalf of the BDA; the second was a combined submission on behalf of the Faculty of Dental Surgery (FDS), the FGDP and the British Association of Oral Surgeons (BAOS); and the third on behalf of the British Association of Oral and Maxillofacial Surgeons.
The submission forms that are provided by NICE to professional stakeholders enable health-care professionals to provide their perspectives on the technology in the context of clinical practice, and include questions in a predefined template to prompt and guide the process. The submissions can also include references to additional sources of evidence that may not be found by a technology-focused SR. This could be information on recent and informal unpublished evidence, registry and audit data. The information must include sufficient detail to allow a judgement to be made as to the quality of the evidence and to determine any potential sources of bias.
The information from the submissions was reviewed to ascertain whether or not they included any data that could inform this appraisal report.
Much of the content of the submissions was professional opinions and perspectives, and the full submissions are available for the committee to consider. In terms of the references provided, no additional studies meeting our review inclusion criteria were identified and many were excluded from this review as they did not meet all of our inclusion criteria. A summary of the more pertinent papers is provided for information in Appendix 5.
The key points from each submission are summarised in the following sections.
The British Dental Association submission
The BDA highlights that the treatment of 3Ms should be undertaken in a holistic manner, rather than for each 3M in isolation. It is argued that NICE guidance,2 which does not recommend the prophylactic removal of I3Ms, has led to an increase in the rate of 3M removal overall, which causes a financial burden to the NHS and disadvantages patients. The submission authors suggest that savings could be realised if repeat treatment episodes were reduced by removing potentially problematic 3Ms at the same time as treating the symptomatic 3M.
The Faculty of Dental Surgery, Faculty of General Dental Practice and British Association of Oral Surgeons submission
The key points highlighted in the submission are that, as a result of NICE guidance,2 patients are retaining M3Ms, which results in problems for the surrounding teeth. There is variation in surgical techniques used, in the sedation and anaesthetic used for patients and in the quality of follow-up care after the surgical removal of IM3Ms.
The British Association of Oral and Maxillofacial Surgeons submission
The key points highlighted in the submission are that, as a result of NICE guidance,2 there is little difference in clinical practice in the UK regarding the removal of 3Ms; however, there is a difference in opinion between professionals in how these teeth should be managed. The Finnish longitudinal study,65 often cited to advocate the interventional removal of 3Ms to prevent problems, does not report the rationale for removal in the study and weakens the rationale for interventional removal of 3Ms. Two subgroups with different prognoses are described (i.e. those taking antiresorptive or antiangiogenic drugs and those who are to receive radiotherapy to the head and neck). The routine prophylactic removal of 3Ms would put significant strain on NHS resources in both primary and secondary care.
Summary of clinical results
Searching major electronic databases identified 14,472 citations; after screening and the application of inclusion/exclusion criteria, 13 studies from 22 publications were included in the SR (nine SRs20,40–46,49–56 and four cohort studies39,47,48,57–59).
Of the four cohort studies, one investigated the prophylactic removal of pathology-free or asymptomatic IM3Ms in comparison with the standard care and retention of these pathology-free or asymptomatic IM3Ms,58 two studies investigated the standard care and retention of pathology of asymptomatic IM3Ms without a comparison group47,48 and one study investigated the prophylactic removal of pathology-free or asymptomatic IM3Ms. 59 All of the studies described teeth as asymptomatic. All four studies were European, and the two studies looking at the standard care and retention of pathology-free or asymptomatic IM3Ms, without a comparison group, were UK based. 47,48 Follow-up across the studies varied from 6 months to 5 years, with outcomes assessed through clinical assessment. In the two studies reporting on surgical complications,59,60 no serious complications were reported, although intense pain and post-operative infection were reported in one study. The pathological changes due to retention of pathology-free or asymptomatic IM3Ms were reported in three studies. 47,48,59 The extraction rate for retained teeth varied from 5.5%48 to 31.4%,47 although this variation can be explained by the differing follow-up periods (1 and 5 years, respectively).
Discussion of clinical effectiveness results
This SR aimed to identify and appraise the relevant evidence relating to the clinical effectiveness of the prophylactic removal of IM3Ms, compared with standard care without the removal of IM3Ms. The rationale for the prophylactic removal of I3Ms is much debated in the published literature in the UK and worldwide, with variation as to what is considered the best approach to the treatment of I3Ms. There are dental professionals who advocate for the prophylactic removal of 3Ms and those who argue for a more conservative approach. There is a plethora of literature debating the controversies surrounding the prophylactic removal of 3Ms1,3,4,16,66–69 and there are a number of international clinical guidelines2,21,27–34,41–43,70 that make recommendations on this topic. These clinical guidelines focus on the management of 3Ms in general and report indications for removal rather than reviewing the evidence for the prophylactic removal of asymptomatic, pathology-free 3Ms. The SR literature is consistent in reporting a lack of evidence for or against the prophylactic removal of these teeth. The results of this review have been limited by the decision problem set by NICE, focusing on people with pathology-free or trouble-free IM3Ms, which represents a more specific population than the populations of all patients with 3Ms or I3Ms that were considered in much of the relevant literature on the management of 3Ms.
Discussion of the results of the cohort studies is hampered by the different outcomes reported by the studies, as different approaches to 3M management require different outcome measures (e.g. the rate of infection of retained IM3Ms and the rate of surgical complications following removal of IM3Ms). This means that the different interventions cannot be directly compared. However, from the included studies it appears that retention of asymptomatic IM3Ms may lead to future symptoms and consequential extraction at a rate of between 6% and 31% over a period of 1–5 years. For participants who had asymptomatic IM3Ms removed, no major surgical complication rates were reported, although intense pain and infection were reported at rates of 15% and 6%. 59
None of the nine SRs that were identified by this SR restricted their research question to pathology-free or trouble-free IM3Ms; however, most were restrictive in the time periods covered and/or languages included. The inclusion criteria for the SRs also differed, especially in relation to the study design. This led to a disparate collection of studies being included, with 73 of the 84 studies being included in one SR only. This heterogeneity reflects the heterogeneity in the literature in general and the lack of robust primary evidence. Despite these differences, most reviews concluded that there was insufficient evidence to make a decision, regardless of how inclusive an approach was used.
In conclusion, our findings are consistent with previous SRs in that there is no available RCT evidence to support or refute the practice of the prophylactic removal of asymptomatic/pathology-free IM3Ms. However, the review did identify evidence from longitudinal studies demonstrating what happens when asymptomatic IM3Ms are left in situ.
Chapter 4 Assessment of cost-effectiveness
Systematic review of existing cost-effectiveness evidence
This section presents the methods and results of a SR of the published literature comparing the cost-effectiveness of prophylactic removal of I3Ms with that of no prophylactic removal.
Search strategy
The search strategy developed for the clinical searches (see Appendix 1), with the addition of an economics filter, was used to identify studies reporting the costs and benefits associated with extracting/retaining I3Ms. As part of the search strategy, NHS EED, which is located within The Cochrane Library, and EconLit (EBSCOhost) were also searched. All databases were searched on 29 April 2016. The results were entered into an EndNote X7.4 library, de-duplicated and exported into Covidence.
Informal searching activities were carried out to identify economic evaluations relevant to the decision problem. These included contacting experts in the field and a search of Google Scholar (Google Inc., Mountain View, CA, USA). The Google Scholar search was updated on 1 February 2017 and revealed no relevant results.
The two clinical submissions from professional stakeholders that were submitted to NICE as part of the MTA process were also checked for cost-effectiveness data.
Study selection and inclusion criteria
Studies were selected based on their relevance to the decision problem and on the specific economic criteria displayed in Table 10. Two reviewers (AB and SB) independently examined the titles and abstracts of all of the studies identified by the search to find potentially eligible publications (stage 1). In the next stage (stage 2), two reviewers (AB and SB) examined the full texts of studies that were identified as being potentially relevant at stage 1. During stage 2, two modifications were made to the inclusion criteria:
-
Owing to limited information about UK costs being available, studies that included any costs were included in the review.
-
Papers reporting short-term health-related quality-of-life (HRQoL) outcomes were excluded from the review (i.e. papers with only long-term HRQoL outcomes were included) to align HRQoL outcomes with the outcomes reported in the clinical papers.
| Criteria | Inclusion |
|---|---|
| Patient population | People with I3Ms |
| Costs | UK costs |
| Outcomes | Any health outcomes, health-related quality of life |
| Study design | All study designs |
| Date | 2000 to present |
| Language | English language only |
Disagreements about inclusion were resolved through discussion and, in all cases, a consensus was reached; it was, therefore, not necessary to consult a third reviewer during the screening and selection process.
Quantity of included evidence
From the main searches, the AG identified 493 potentially relevant papers for inclusion in the review of economic evidence. Of these, 34 papers were considered for inclusion after stage 1. As shown in Figure 2, eight studies17,20,71–76 were initially included at stage 2. However, on further inspection, five71–75 of the eight studies did not include information that was relevant to the population of interest; these papers were, therefore, subsequently excluded from the review. Bibliographic details and summary data from these five studies71–75 are available in Appendix 2. Of the 34 papers considered for inclusion after stage 1, 31 were excluded during stage 2, which left three papers17,20,76 to be included in the review. The reasons for excluding the 31 studies are listed in Table 11.
FIGURE 2.
The PRISMA flow diagram: economic evidence review.

| Study | Reason for exclusion |
|---|---|
| Aravena and Cartes-Velasquez 201177 | Literature review describing the signs and symptoms used to evaluate post-operative complications in 3M surgery. Abstract only |
| Bienstock et al. 201178 | Short-term study of the duration of disability after 3M surgery (mean 1.4 ± 1.8 days) and risk factors associated with prolonged recovery (maximum 26 days) |
| Bienstock 201279 | Indirect costs (mean number of work days missed and risk factors associated with prolonged return to work after 3M surgery) |
| Chuang et al. 200780 | Estimates of post-surgery complication rates and risk factors after removal of 3Ms |
| Chuang et al. 200881 | Risk factors for post-surgery inflammatory complications after removal of 3Ms |
| Colorado-Bonnin et al. 200682 | Short-term (7-day) post-operative HRQoL data |
| Conrad et al. 199983 | Short-term (14-day) patients’ perceptions of recovery after 3M surgery |
| Deepti et al. 200984 | Short-term (7-day) post-operative HRQoL data after I3M removal |
| Edwards et al. 199960 | Data were included in the HTA review by Song et al.20 that informed TA1 |
| Gutierrez-Perez 200485 | Signs and symptoms of 3M infections. Written in Spanish |
| Inverso et al. 201486 | The value of telephone vs. clinical follow-up after 3M surgery |
| Inverso et al. 201471 | No information relating to I3Ms |
| Koumaras 201272 | No information relating to I3Ms |
| Kunkel et al. 200674 | No information relating to I3Ms |
| Kunkel et al. 200773 | No information relating to I3Ms |
| Liedholm et al. 201087 | No figures relating to I3Ms were specifically reported |
| Leidholm et al. 200575 | No information relating to I3Ms |
| Matijević et al. 201488 | Comparison of the effect on patient-reported HRQoL of detailed written and oral instructions vs. written instruction only about treatment after surgical removal of a lower 3M |
| Offenbacher et al. 201289 | A study of visible 3Ms and probing depths |
| Osunde et al. 201190 | A review of literature on different modalities for minimising inflammatory complications associated with 3M surgery |
| Pandurić et al. 200991 | Short-term (14-day) post-operative HRQoL data reported for patients (after 3M surgery) in Croatia |
| Phillips et al. 200392 | Short-term (14-day) diary designed to assess a patient’s perception of recovery after removal of all four 3Ms |
| Phillips et al. 201093 | Short-term (14-day) diary used to study the effect of age and sex on recovery after 3M surgery |
| Ruvo et al. 200594 | Short-term (14-day) outcomes after removal of all four 3Ms |
| Sancho-Puchades et al. 201295 | Short-term (7-day) study of HRQoL after 3M surgery when using conscious sedation |
| Sato et al. 200996 | Short-term (7-day) outcomes: data about post-operative signs and symptoms collected daily from patients and surgeons |
| Shugars and White 200397 | Editorial linked to McGrath et al.76 paper: no rates, frequencies or other statistics provided |
| Shugars et al. 200698 | Short-term (14-day) HRQoL outcomes collected using two different instruments |
| Slade et al. 200499 | Short-term (pre and 7 days post) oral health outcomes after removal of 3Ms |
| White et al. 2003100 | Short-term (14-day) clinical and HRQoL outcomes after removal of all four 3Ms |
| White 2004101 | List of citations (with comments) summarising clinical and HRQoL outcomes after 3M surgery |
The three papers17,20,76 that were included in the review are listed in Table 12. Two studies17,20 provided information on costs and one study76 provided information on patient HRQoL. The characteristics of these studies are presented in Table 13.
| Study | Title |
|---|---|
| Cost and cost-effectiveness | |
| Anjrini et al. 201517 | Cost-effectiveness modelling of a ‘watchful monitoring strategy’ for impacted third molars vs prophylactic removal under general anaesthetic: an Australian perspective |
| Song et al. 200020 | The effectiveness and cost-effectiveness of prophylactic removal of wisdom teeth |
| HRQoL | |
| McGrath et al. 200376 | 6-month study of patients’ perceptions of oral HRQoL after removal of impacted 3Ms |
| Study | Country | 3Ms or I3Ms | Study design/purpose | Comparators | Reported measures | Cost/outcome source | Time horizon | Cost year |
|---|---|---|---|---|---|---|---|---|
| Anjrini et al. 201517 | Australia | I3Ms | National cost model | Watchful monitoring strategy for I3Ms vs. prophylactic removal of I3Ms under GA | Number of hospitalisations for impacted wisdom teeth (population aged 15–34 years); direct, indirect and total costs of hospitalisation | Australian Refined Diagnosis Related Group costs from private and public hospitals | 20 years | 2009 (unless otherwise stated) |
| Song et al. 200020 | UK | I3Ms | SR (and decision analysis) | NA | NA | NHS | NA | NA |
| McGrath et al. 200376 | UK | I3Ms | Evaluation of patients’ perceptions of changes in (OHRQoL) over a 6-month period after I3M surgery | Patients awaiting I3M surgery | Change in OHRQoL as measured by OHIP-14 and OHRQoL-UK scores | Patient questionnaires and patient ‘recovery log’ diaries | From the day of the I3M surgery until 7 days after I3M surgery | NA |
Quality of the included evidence
Contrary to the review protocol, the AG made the decision not to quality assess the papers included in the review of cost-effectiveness evidence using a cost-effectiveness checklist. This decision was made because only one paper20 directly considers the cost-effectiveness of prophylactic removal of I3Ms in a UK setting [and a summary of this paper and its quality are located in the clinical evidence section of this report (see Tables 8 and 9 and Appendix 4)].
Economic review: overview of included papers
The AG concludes that relevant data on I3Ms are limited to three studies. 17,20,76 Two of the papers report details about the cost-effectiveness of the prophylactic removal of I3Ms. The review by Song et al. 20 includes details about the cost-effectiveness from a UK NHS perspective, whereas the material presented in the study by Anjrini et al. 17 is of less direct relevance as estimates are based on the Australian health-care system and the results are presented in Australian dollars. The third paper76 reports findings that relate to an assessment of oral HRQoL after the removal of I3Ms.
Key results: cost-effectiveness of prophylactic removal of impacted third molars
Cost-effectiveness: Song et al.20
This publication by Song et al. 20 is the AG’s report for TA1 (The effectiveness and cost-effectiveness of prophylactic removal of wisdom teeth). 1 It includes a summary of the findings from a study reported by Edwards et al. ,60 who estimated the cost-effectiveness of removal and retention of disease-free 3Ms and concluded that the cost of prophylactic removal of I3Ms was approximately 33% higher than the cost of retention. The report by Song et al. 20 also includes findings from a paper by Walters,102 who identified that the compensation awarded for permanent nerve damage after 3M surgery ranged from £4000 to £14,000 per case, or higher.
Song et al. 20 concluded that, in the short to medium term, based on available evidence, retention of I3Ms may be more cost-effective than prophylactic removal.
Cost-effectiveness: Anjrini et al.17
The objective of the study reported by Anjrini et al. 17 was to develop a model to compare the direct (and indirect) costs associated with a watchful monitoring strategy for I3Ms with the costs associated with prophylactic removal under general anaesthetic. Data were obtained from the Western Australian Hospital Morbidity Data system. All of the episodes of discharge from all hospitals (private and public) in Western Australia for the financial year 2008–9 for the removal of impacted or embedded teeth as the principal oral condition were included. The rate calculations for Western Australian hospitalisation were measured using Australian population 2006 data.
The annual direct cost to the state for I3M removal in hospital was estimated to be AUS$259M, which equates to a direct cost of AUS$2644 for each hospitalisation (i.e. £1536 using the conversion rate of 22 August 2016). The time frame for the analysis was 20 years. The average watchful waiting strategy cost per participant was AUS$1077. This cost included the clinical examinations (AU$60.30) and panoramic radiographs (AUS$47.40), both of which were undertaken every 2 years. Thus, the estimated annual cost was AUS$53.80 per individual, which is approximately 1% of the estimated cost of removal. The authors conclude that ‘with no evidence to support the prophylactic removal of asymptomatic wisdom teeth, a proposed watchful monitoring strategy is a more cost effective alternative in the Australian context’. 17
Health-related quality of life: McGrath et al.76
The study by McGrath et al. 76 in 2003 assessed oral HRQoL in patients after the removal of their I3Ms over a period of 6 months using two specific oral HRQoL tools and a patient diary. Patients in the study were a mix of people with asymptomatic (n = 19) and symptomatic (n = 69) 3Ms. Study results demonstrated that people who had previously reported having pericoronitis symptoms achieved greater oral HRQoL gains after I3M surgery than people who had not; the authors considered the findings to be both statistically significant and clinically significant.
Cost-effectiveness review: conclusions
As there is very limited clinical effectiveness evidence comparing the prophylactic removal of I3M with a ‘watchful waiting’ strategy, it is unsurprising that economic evidence relating to this comparison is also limited. There are only two published cost-effectiveness studies17,20 that directly consider this comparison and, in both cases, the authors conclude that there is currently no economic evidence to support the prophylactic removal of I3Ms. However, Song et al. 20 restrict their conclusion to a short- to medium-term time frame.
Independent economic assessment
To our knowledge, there are no existing cost–utility analyses that are relevant to the decision problem and generalisable to the NHS in England. For these reasons, the AG constructed a de novo economic model to determine the cost-effectiveness of the prophylactic removal of IM3Ms compared with standard care, where standard care refers to what is currently being carried out (i.e. no prophylactic removal, referred to as ‘watchful waiting’) in a population with pathology-free or trouble-free IM3Ms.
The model perspective is that of the UK NHS only, as Personal Social Services costs are not relevant to the decision problem. Outcomes were measured in quality-adjusted life-years (QALYs) and both costs and QALYs were discounted at an annual rate of 3.5%, as recommended by NICE. 103
In the AG’s model, in line with the age of the youngest patient recruited to the Fernandes et al. 48 study, the AG chose to use a starting age of 20 years in the base case; sensitivity analyses are used to explore the impact of using starting ages of 30, 40 and 50 years.
In the AG’s model, the base-case time horizon is 80 years (i.e. up to the point when people reach the age of 100 years, when < 1% of patients are still alive). The time horizon is varied in scenario analyses (10, 20, 30, 40 and 50 years) to assess the impact that this change has on model outputs.
Model pathways
The elements of both the intervention (prophylactic removal) and the comparator (watchful waiting) pathways were determined through consultation with clinical experts and examination of clinical data identified via the AG’s SR of clinical effectiveness evidence. Clinical consultation was conducted through a combination of face-to-face meetings, telephone conversations and comments on draft versions of the report.
In the NHS watchful waiting pathway, there are many different points at which an IM3M may, or should, be extracted. For example, the decision to extract an IM3M may be determined by a specific number of instances of pericoronitis, the degree of severity of pericoronitis, a decayed adjacent tooth or the amount of tooth pain. Following several searches of the literature and consultation with experts, the AG concluded that data to populate the current watchful waiting pathway with extraction driven by, for example, a decayed adjacent tooth or number of instances of pericoronitis are absent and clinical advice to the AG was that patient preference would probably play a significant role in the decision to extract.
The AG has, therefore, chosen to design an economic model that is based on what actually happens in terms of the current extraction rates of IM3Ms (i.e. use available data) rather than on what might or should happen under a watchful waiting pathway following symptom development. This approach minimises the use of assumptions around when extraction occurs and allows analysis of the true current situation in the NHS against a change in extraction rates if prophylactic removal was recommended. However, how far the results can be interpreted as a comparison of a watchful waiting strategy with strict adherence to extraction only after certain symptom-related criteria is met, against a prophylactic removal strategy, is unclear.
A visual representation of the intervention pathway (prophylactic removal) is shown in Figure 3. The pathway is modelled as a combination of a Markov model process to move people between different IM3M health states, with decision trees to determine the probability of complications and severity of complications at each cycle and to determine the outcomes from the extraction of an IM3M.
FIGURE 3.
Prophylactic removal of the IM3M model pathway. M2M, mandibular second molar; RoCT, root canal treatment.
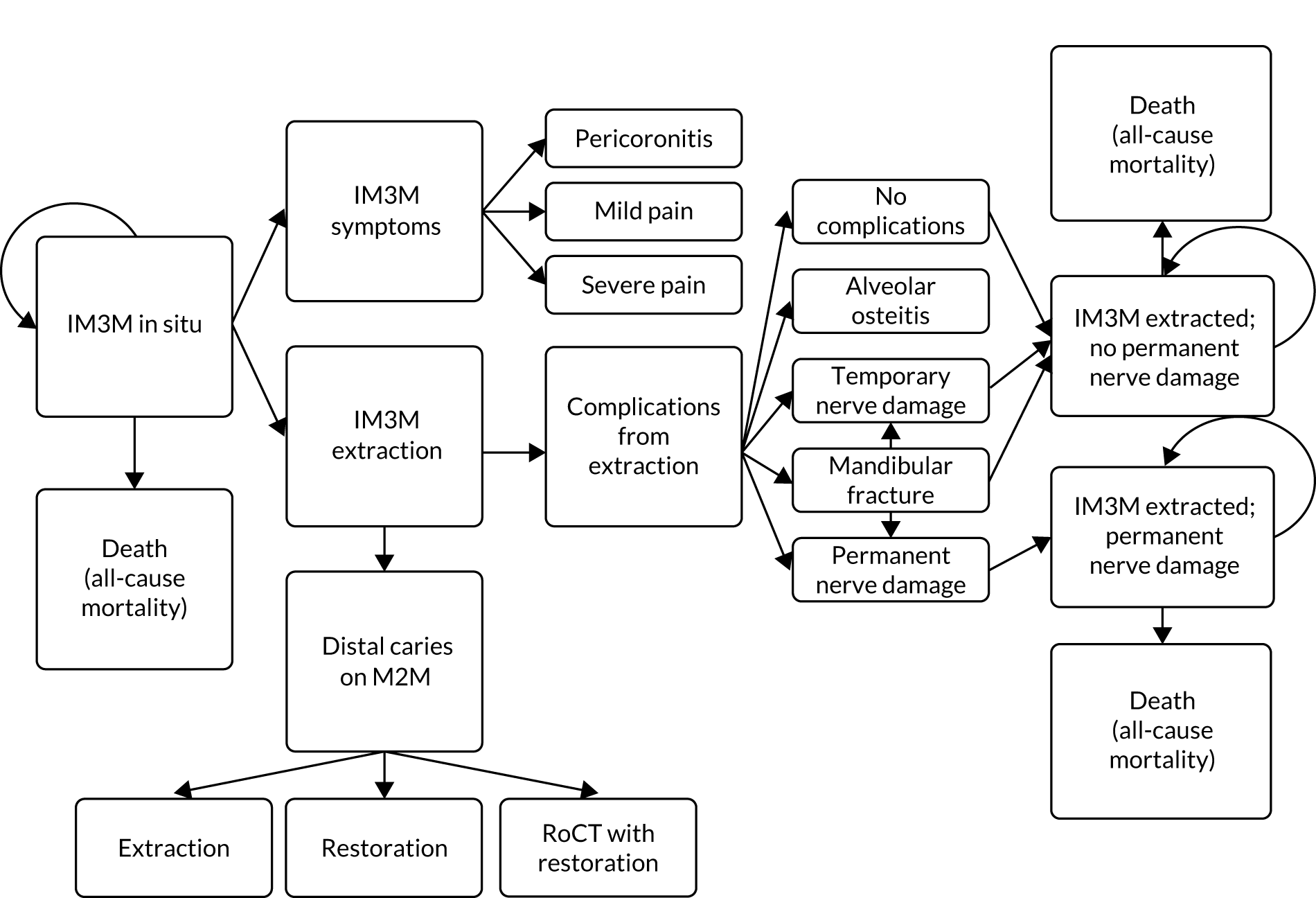
The cycle length is 1 year. In each cycle, a person can develop IM3M symptoms (the severity of which is determined by decision trees) but not have the IM3M extracted, have the IM3M extracted (either with or without complications, determined by decision trees), remain in a post-extraction state (with or without permanent nerve damage) or die from any cause.
For every person with an IM3M in situ, there is a probability that, in each cycle, the person will die (from any cause), their IM3M will develop symptoms and/or their IM3M will be extracted. The probability of extraction is independent of symptom development. The possible symptoms are pericoronitis, mild pain and severe pain, which is determined in the model by a decision tree. If a person has only symptoms in a cycle without extraction, they remain in the ‘IM3M in situ’ state.
When a tooth is extracted, the person might be found by the dental surgeon to have developed a DCC in the adjacent mandibular second molar (M2M). The AG has assumed that the probability of extraction of an IM3M is independent of the development of a M2M DCC. This assumption has been made because the data that are available describe the proportion of people with M2M DCC in a population who had an IM3M extracted only, and not on whether or not this was the reason for the extraction. 104 If M2M DCC is present, the tooth can be extracted, be simply restored or have more complex restoration, including root canal treatment.
Extraction of an IM3M can be complication free or result in mandibular fracture, temporary nerve damage, permanent nerve damage or alveolar osteitis (‘dry socket’). If a person has IM3M extraction in a given cycle, these events are determined by a decision tree. After extraction, people can enter either an ‘extracted with permanent nerve damage’ state or an ‘extracted with no nerve damage’ state. They will then remain in either of these states for the lifetime of the model or until death.
Based on the pathway, a model was constructed in Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) that captured the cost and benefits of 1000 patients transitioning through the intervention and comparator pathways.
Model transition probabilities
The transition probabilities used in the AG’s model have been drawn from published studies identified in the clinical evidence review and from evidence identified by clinical experts.
Evidence presented by Fernandes et al. 48 has been used to represent the annual rate of tooth extraction and the development of symptoms for people who have asymptomatic IM3Ms. In this 1-year prospective cohort study, the authors collected data from patients with at least one IM3M. All of the participants were registered with general dental practices in Scotland, where SIGN guidelines34 recommending a watchful waiting pathway have been in place since 2000. The AG considered that these data were generalisable to an English NHS setting.
In the paper by Fernandes et al.,48 the annual rate of extraction (5.47%) was found to be independent of age. The inclusion criterion in terms of the age of the cohort studied by Fernandes et al. 48 was 18–70 years, but only those aged 20–63 years were actually recruited to the study. This determined the model start age of 20 years. It was assumed that the annual rate of extraction continued at 5.47% after the age of 63 years. A scenario analysis explored a scenario in which no extractions were undertaken after the age of 63 years.
Although the Fernandes et al. 48 study is a prospective cohort study, the AG considered that it was well designed with a large sample and provided a satisfactory evidence base to estimate the annual rate of extraction of IM3Ms in a UK NHS setting. The annual rate of extraction of 5.47% that was reported by Fernandes et al. 48 gives a 5-year extraction rate of 24.5%, which is lower than, but of a similar order to, that reported by Hill and Walker47 (31.4%). Given that Hill and Walker47 report on extraction from a different part of the UK to Fernandes et al. 48 and the two studies suggest similar annual extraction rates, this supports the generalisability of the findings from Fernandes et al. 48 to the wider NHS. To check the effect of varying the annual rate of extraction, the upper (7.39% per annum, equivalent to a 5-year extraction rate of 32.0%) and lower (3.94% per annum) bounds of the 95% CI quoted in the paper by Fernandes et al48 were used in the AG’s sensitivity analysis.
For the prophylactic removal pathway, the AG’s base-case assumption is that not all people will accept the recommendation that the IM3M(s) should be extracted and, therefore, these teeth will remain in situ. Fernandes et al. 48 reports that 45.9% of patients who had their IM3Ms extracted did not know why the tooth had been extracted, and so the extraction could have been prophylactic (despite the SIGN guideline34 recommendation). Based on this finding, the AG chose a base-case value of 46.95% to represent the proportion of people who would accept prophylactic removal of asymptomatic IM3Ms, if it were offered to them. The AG recognises that it is likely that this figure overestimates the true rate of non-prophylactic removal, as it is unlikely that all of the 45.9% of patients who could not recall why their IM3M was extracted had their tooth extracted when the IM3M was asymptomatic. However, it could also be an underestimate if future guidelines were to suggest that prophylactic removal is recommended. Owing to these uncertainties, the AG carried out sensitivity analyses to explore the impact of different levels of acceptance of prophylactic removal (10%, 25%, 50%, 75% and 100%).
Findings from the Fernandes et al. 48 study suggest that symptom development is age dependent (at least up to the age of 63 years), declining as a patient ages. In the base case, the AG assumes that the rate of symptom development follows a linear trend from the ages of 53 to 63 years, and that this trend is applied beyond the age of 63 years. A scenario analysis explores the impact of symptom development no longer occurring past the age of 63 years. The probabilities, by age, of experiencing symptoms can be found in Appendix 6.
The probability of a person who, on having an IM3M extracted, is found to have associated M2M DCC, and the likelihoods of the M2M being extracted, simply restored or undergoing complex restoration, have been taken from the a study by McArdle et al. 104 In this study, the investigators undertook a retrospective review of 339 people in England, across two cohorts from 2006 to 2014, who had IM3Ms removed as a result of having M2M DCC.
The probabilities of specific complications that are associated with tooth extraction were derived from Chuang et al. 80 Chuang et al. 80 also reported an odds ratio (OR) for all complications (OR 1.46) for patients aged ≥ 25 years compared with those aged < 25 years. The AG has adjusted the individual complication rates reported by Chuang et al. 80 using this OR to estimate the probability of specific complications for those aged < 25 years and for those aged ≥ 25 years.
One complication for which there is no evidence available in the study by Chuang et al. 80 is the rate of permanent nerve damage. The AG has used a value reported by Valmaseda-Castellón et al. 105 This value has been adjusted for age (aged < 25 years and aged ≥ 25 years) using the OR reported by Chuang et al. 80
Table 14 shows a full list of probabilities used in the AG’s model. Rates for death from any cause have been taken from the Office for National Statistics’ life tables. 106
| Parameters | Probability (%) | Study |
|---|---|---|
| Symptoms | ||
| Pericoronitis | 13.16 | Fernandes et al. 201048 |
| Severe pain | 14.04 | |
| Mild pain | 19.30 | |
| DCC of M2M on extraction of IM3M | ||
| DCC of M2M | 15.00 | McArdle et al. 2018104 |
| M2M extracted | 42.00 | |
| M2M restored | 42.00 | |
| M2M root canal treatment and restored | 16 | |
| IM3M extraction complications | ||
| Mandibular fracture (aged < 25 years) | 0.019 | Chuang et al. 200780 |
| Mandibular fracture (aged ≥ 25 years) | 0.03 | |
| Permanent nerve damage (< 25 years) | 0.22 | Valmaseda-Castellón et al. 2001105 |
| Permanent nerve damage (≥ 25 years) | 0.33 | Chuang et al. 200780 |
| Temporary nerve damage (< 25 years) | 2.89 | Chuang et al. 200780 |
| Temporary nerve damage (≥ 25 years) | 4.16 | |
| Alveolar osteitis (< 25 years) | 5.61 | |
| Alveolar osteitis (≥ 25 years) | 7.98 | |
The use of annual transition probabilities for symptom development in the AG’s model results in a person being able to experience IM3M symptoms only once per year for each tooth. Given that people may develop symptoms more than once per year in each IM3M, the model may underestimate the actual annual symptom burden for people with IM3Ms. This will result in the AG’s model underestimating the annual cost of treating IM3M symptoms and the impact of IM3M symptoms on HRQoL.
As a watchful waiting strategy leaves people with more IM3Ms in situ than prophylactic removal does, the results of the AG’s model will underestimate the potential reduction in costs and gains in HRQoL from reductions in IM3M symptoms when these two pathways are compared. The incremental cost-effectiveness ratio (ICER) per QALY gained generated by the model for prophylactic removal compared with watchful waiting will therefore be an overestimate, as people can develop IM3M symptoms more than once per year.
By designing the model around the available data and excluding the complicated pathology that can occur if IM3Ms are left in situ, the model is biased towards generating more favourable results for a watchful waiting strategy. For example, with an IM3M left in situ, pericoronitis can develop into a severe infection that can spread to the throat and lead to severe cellulitis, which causes airway blockage resulting in hospitalisation, intensive care unit admission and, in some cases, death. Pericoronitis can also lead to abscess formation and is accompanied by a potential risk of developing sepsis.
No published data could be found to estimate the risk of these serious events occurring. However, one of the AG’s clinical experts reported treating one person per month who had been admitted to the intensive care unit with life-threatening cellulitis that was due to having had an IM3M. Although there is no way to generalise this experience into a probability that can be included in the AG’s model, if such a complication were to be included, it would result in a reduction in QALYs and an increase in costs for the watchful waiting strategy.
Resource use and unit cost estimation
The total number of patients with IM3M extractions each year in the NHS is unknown. However, McArdle et al. 104 have estimated that, in 2014/15, there were 152,000 people with IM3M extractions: 67,000 (44.1%) extractions were carried out during inpatient admissions, 38,000 (25.0%) during outpatient attendances and 47,000 (30.9%) during a primary care appointment. The AG has used these estimates as the basis for estimating the cost to the NHS of IM3M extractions. The unit costs of extraction in an acute setting have been taken from the NHS Reference Costs 2015 to 2016. 107 The cost of an extraction in primary care is a band 2 treatment and is charged to the NHS as 3 units of dental activity (UDAs).
The AG has assumed that 75% of M2Ms with DCC are extracted at the same time as the IM3M, at no additional cost. For those M2Ms extracted independently, the cost of extraction is assumed to be the same as the estimated cost of IM3M extraction. Sensitivity analyses have been used to explore the impact of this assumption on model results. Values of concurrent IM3M and M2M extractions of between 0% and 100% have been used in these analyses.
To estimate the cost associated with pericoronitis and severe pain, in the absence of any published information or clinical advice, the AG has assumed that 25% of people will self-medicate and that symptoms will resolve without the need for dental or medical intervention. For the 75% of people who require treatment, dental care will be required. Based on clinical advice, this dental care would comprise band 2 treatment (3 UDAs) plus an antibiotic prescription for erythromycin (a further 0.75 UDAs for issuing a prescription). For the 75% of patients with severe pain, the AG has assumed that an emergency dental appointment will be required (1.2 UDAs) and that people will be prescribed an analgesic (codeine, which incurs a further 0.75 UDAs for issuing a prescription). The AG has undertaken sensitivity analyses to explore the impact on model results of varying the proportion of people self-treating from 0% to 100%.
The cost of a UDA varies across England. In the base case, the AG has used a figure of £25. The BDA quotes this figure as being the mean UDA cost across England. 108 The AG has undertaken sensitivity analyses to explore the impact of lower and higher UDA costs on model results. The figures used in the sensitivity analyses are based on a freedom of information request1 made in 2009 and ranged from £11.08 to £105.58.
Antibiotic and analgesic prescription costs have been sourced from Prescription Cost Analysis, England 2015 data. 109 The AG has assumed that the cost of all other aspects of treatment is covered either by the relevant NHS reference cost or by the payments received for UDAs.
The AG has assumed that mild pain does not result in any cost being incurred by the NHS and that the treatment of alveolar osteitis is included in the cost of the initial extraction. For more serious complications following extraction, the AG has assumed that everyone with permanent nerve damage will receive surgery to try to correct the damage and that no one with temporary nerve damage will receive corrective surgery. No litigation costs from permanent nerve damage are included in the model. However, as it is likely that some people with permanent nerve damage will receive compensation and that some people with temporary nerve damage will receive surgery (indeed, the nerve damage may be only temporary because of corrective surgery), these assumptions mean that the AG’s model will underestimate the true cost to the NHS that arises from nerve damage. For mandibular fracture, the NHS Reference Cost107 for fixation of jaw following fracture was used.
With the exception of the costs of antibiotics and analgesia, the AG has undertaken sensitivity analyses to explore the impact of varying these costs on model results. For those costs based on the NHS Reference Costs 2015 to 2016,107 upper and lower quartile figures have been used in these analyses.
A full list of costs used in the AG’s model is provided in Table 15.
| Cost element | Value (£) | Calculation details and source |
|---|---|---|
| UDA | 25.00 | BDA108 |
| Tooth extraction: hospital admission | 801.81 |
NHS Reference Costs 2015 to 2016 107 HRG code: major surgical removal of tooth CD04 A (weighted by activity of day case/elective inpatient/non-elective inpatient) |
| Tooth extraction: outpatient | 148.00 |
NHS Reference Costs 2015 to 2016 107 HRG code: major surgical removal of tooth CD04 A (outpatient) |
| Tooth extraction: primary care | 75.00 | Band 2 treatment (3 UDAs) |
| Average cost of tooth extraction (based on weighted average of location of extraction: used for IM3M extraction) | 413.62 | McArdle et al. 2018104 |
| Average cost of extraction of M2M with DCC | 103.41 | £413.62 divided by 4, as 75% of extractions undertaken concurrently with IM3M extraction (see source above104) |
| Pericoronitis treatment | 70.31 | 3.75 UDAs (see source above104) × 75% seeking treatment (assumption) |
| Antibiotics (for pericoronitis) | 2.25 | Prescription Cost Analysis 2015: erythrocin_B-Pack 10 Filmtab 500 mg109 |
| Severe dental pain treatment | 36.56 | 1.95 UDAs (see source above) × 75% seeking treatment (assumption) |
| Analgesic (for severe dental pain) | 3.56 | Prescription Cost Analysis 2015: codeine Phos_Tab 30 mg109 |
| Fixation of jaw following fracture (for mandibular fracture) | 2854.00 |
NHS Reference Costs 2015 to 2016 107 HRG code: reduction or fixation of jaw CA96Z (inpatient) |
| Surgery for permanent nerve damage | 5507.00 |
NHS Reference Costs 2015 to 2016 107 HRG code: complex maxillofacial procedures CA91B (inpatient) |
| Restoration of M2M | 75.00 | Band 2 treatment (3 UDAs) (assumption) |
| M2M endodontically treated and restored | 300.00 | Band 3 treatment (12 UDAs) (assumption) |
Health measurement and valuation estimation
No IM3M-specific utilities, or utility values related to IM3M symptoms or extraction complications, could be identified from a targeted search of the published literature (see search strategy in Appendix 7). Therefore, the AG used values from a working paper by Ara and Brazier110 to populate these parameters in the model. It is reported in this paper110 that people with teeth, mouth or tongue conditions in the UK have a EuroQol-5 Dimensions utility score that is 0.345 less than those who do not report having any teeth, mouth or tongue conditions. This is comparable to a utility decrement for level 3 pain based on the EuroQol-5 Dimensions, three-level version, questionnaire (‘I have extreme pain or discomfort’) of 0.386. 110
The AG’s model includes a 0.345 utility decrement to represent the experience of people with any IM3M complication(s) or any complication(s) following extraction. For people experiencing mild pain, the decrement was assumed to be 50% of 0.345 (i.e. 0.1725). Sensitivity analyses were undertaken to explore the impact of varying these figures on model results. The decrements were varied individually over the 95% CI (0.102 to 0.549) reported in the paper by Ara and Brazier. 110 The AG has assumed that M2M restoration is not associated with any loss of utility and that extraction of the M2M would result in a loss of utility only if it occurred independently of an IM3M extraction.
To generate a QALY loss when a person experiences a complication, the duration of symptoms from the complication is required. The AG was not able to identify any evidence that described the duration of symptoms associated with extraction complications. Thus, it was necessary to make a number of assumptions about the durations of symptoms; the AG’s clinical experts were contacted to verify these assumptions. The AG has undertaken sensitivity analyses to assess the impact of varying these estimates of duration on model results (duration varied by ± 50%). To reflect the declining HRQoL as people age in the model, utility declines with age in line with age-related population norms described in the paper by Ara and Brazier. 110
The details of the values used in the model to represent utility decrement, the duration of symptoms assumed and the resulting QALY loss associated with symptoms and complications are shown in Table 16.
| Cause of utility decrement | Utility decrement | Duration of symptoms | QALY loss |
|---|---|---|---|
| Symptoms | |||
| Pericoronitis | 0.345 | 9 days | 0.009 |
| Severe pain | 0.345 | 30 days | 0.028 |
| Mild pain | 0.1725 | 30 days | 0.014 |
| Extraction | |||
| IM3M or M2M | 0.345 | 7 days | 0.007 |
| Complications following IM3M extraction | |||
| Mandibular fracture | 0.345 | 42 days | 0.040 |
| Permanent nerve damage | 0.345 | Lifetime | 0.345 |
| Temporary nerve damage | 0.345 | 30 days | 0.028 |
| Alveolar osteitis | 0.345 | 9 days | 0.009 |
Analysis of uncertainty
The AG explored the uncertainty surrounding the model assumptions using deterministic sensitivity analyses and scenario analyses. Probabilistic sensitivity analysis was not undertaken, as the only parameter for which a distribution could be drawn based solely on published evidence was the annual rate of extraction. Creating distributions around the central value of other parameters would not be meaningful either because the parameter values are essentially fixed (e.g. in the case of costs) or because the central values are, at least partly, based on assumptions as a result of the lack of data (e.g. the actual utility values associated with symptoms or the duration of symptoms). Furthermore, a probabilistic sensitivity analysis could potentially lead to confounding results, as the uncertainty around most of the assumptions used in the AG’s model is not known; therefore, from a statistical perspective, this cannot be confidently modelled.
The parameter ranges explored in the deterministic sensitivity analyses are summarised in Table 17 and the scenario analyses performed are summarised in Table 18.
| Analysis | Base-case value | Range in sensitivity analysis | Range source |
|---|---|---|---|
| Utility decrement (QALY) | |||
| Pericoronitis | 0.345 | 0.102 to 0.549 | Ara and Brazier110 (95% CI) |
| Severe pain | 0.345 | 0.102 to 0.549 | |
| Mild pain | 0.1725 | 0.051 to 0.275a | |
| Alveolar osteitis | 0.345 | 0.102 to 0.549 | |
| Tooth extraction | 0.345 | 0.102 to 0.549 | |
| Mandibular fracture | 0.345 | 0.102 to 0.549 | |
| Permanent nerve damage | 0.345 | 0.102 to 0.549 | |
| Temporary nerve damage | 0.345 | 0.102 to 0.549 | |
| Duration of symptoms (days) | |||
| Pericoronitis | 9 | 4.5 to 13.5 | Assumption (base case ± 50%) |
| Severe pain | 30 | 15 to 45 | |
| Mild pain | 30 | 15 to 45 | |
| Alveolar osteitis | 9 | 4.5 to 13.5 | |
| Tooth extraction | 7 | 3.5 to 10.5 | |
| Mandibular fracture | 42 | 21 to 63 | |
| Temporary nerve damage | 30 | 15 to 45 | |
| Unit costs (£) | |||
| UDA | 25.00 | 11.08 to 105.58 | BDA108 |
| Discount rate (%) | |||
| Annual rate | 3.5 | 1.5 to 5.0 | NICE Reference Case103 |
| Proportion seeking treatment for IM3M symptoms (%) | |||
| Pericoronitis | 75 | 0 to 100 | Assumption |
| Severe dental pain | 75 | 0 to 100 | |
| Annual rate of extraction (%) | |||
| IM3M | 5.47 | 3.94 to 7.39 | Fernandes et al.48 (95% CI) |
| Extraction of M2M (%) | |||
| Percentage of patients having M2M with DCC extracted at same time as IM3M | 75 | 0 to 100 | McArdle et al.104 |
| Scenario variant | Base-case value | Value(s) used in scenario(s) |
|---|---|---|
| Vary model start age | 20 years | 30, 40 and 50 years |
| Vary model time horizon | Lifetime | 10, 20, 30, 40 and 50 years |
| No IM3M symptoms after 63 years of age | Same rate of symptoms as for those aged 53–63 years | 0 |
| No extractions after 63 years of age | 5.47% per annum | 0% per annum |
| Modifying patient acceptance of prophylactic removal | 45.95% | 10%, 25%, 50%, 75%, 100% |
| All extractions occur in primary care | 30.9% (making average cost of extraction £413.62) | 100.0% (making average cost of extraction £565.13) |
| No extractions occur in primary care | 30.9% (making average cost of extraction £413.62) | 0.0% (making average cost of extraction £75.00) |
Base-case results
Costs
For the modelled population, the AG’s model results predict that, compared with a watchful waiting strategy, a prophylactic removal strategy will result in 2.14% more people with IM3Ms having their impacted teeth removed over their lifetime. For the prophylactic removal strategy, this results in the average discounted cost of extraction per person being £71.49 higher than the watchful waiting strategy.
The AG’s model results show that a prophylactic removal strategy leads to lower rates of permanent nerve damage and jaw fracture following extraction than a watchful waiting strategy. However, the actual discounted cost of treating these extraction complications will be higher for a prophylactic removal strategy than for a watchful waiting strategy, as the costs of these complications will, predominantly, occur in the first year of the model. With a watchful waiting strategy, these costs will accrue across decades, resulting in the discounted costs being lower than for the prophylactic removal strategy, even though more complications occur with a watchful waiting strategy.
The model results show that a prophylactic removal strategy results in lower IM3M symptom treatment costs than a watchful waiting strategy. These cost savings lead to the total cost of a prophylactic removal strategy being £55.71 higher per person than a watchful waiting strategy.
The base-case costs generated by the AG’s model for a cohort of 1000 people with asymptomatic IM3Ms are shown in Table 19.
| Complication or symptom | Strategy | Difference (prophylactic removal – watchful waiting) | ||||
|---|---|---|---|---|---|---|
| Watchful waiting | Prophylactic removal | |||||
| Number | Cost (£) | Number | Cost (£) | Number | Cost (£) | |
| IM3Ms extracted | 955.4 | 258,014 | 975.9 | 329,503 | 20.5 | 71,489 |
| Permanent nerve damage | 2.9 | 9874 | 2.6 | 10,979 | –0.3 | 1106 |
| Jaw fracture | 0.2 | 428 | 0.2 | 481 | –0.02 | 52 |
| Number of M2Ms with DCC | 143.3 | 77.5 | –65.9 | |||
| M2Ms extracted | 60.2 | 4064 | 32.5 | 2196 | –27.7 | –1867 |
| M2Ms restored | 60.2 | 2947 | 32.5 | 1593 | –27.7 | –1354 |
| M2Ms RoCT and restoration | 22.9 | 4491 | 12.4 | 2427 | –10.5 | –2064 |
| Pericoronitis | 295.9 | 15,946 | 160.0 | 8620 | –135.9 | –7326 |
| Severe pain | 315.7 | 9408 | 170.7 | 5085 | –145.0 | –4322 |
Health-related quality-of-life results
More people have an IM3M extracted under a prophylactic removal strategy and more extractions happen earlier than with a watchful waiting strategy. The AG’s model predicts that the expected discounted QALY loss per person from IM3M extraction is greater with a prophylactic removal strategy than with a watchful waiting strategy. As was the case with costs, when comparing results from a prophylactic removal strategy with those from a watchful waiting strategy, although complications from extraction will be lower when a prophylactic removal strategy is employed (because these complications occur earlier in the model), the discounted QALY loss from extraction complications will be higher than with a watchful waiting strategy.
However, the QALY loss from IM3M symptoms is lower when using a prophylactic removal strategy than with a watchful waiting strategy, and outweighs the QALY loss from the greater number of IM3M extractions with prophylactic removal. This results in an overall expected QALY gain from prophylactic removal of 0.005, compared with watchful waiting.
The base-case QALY results generated by the AG’s model for a cohort of 1000 people with asymptomatic IM3Ms are shown in Table 20.
| Complication or symptom | Strategy | Difference (prophylactic removal – watchful waiting) | ||||
|---|---|---|---|---|---|---|
| Watchful waiting | Prophylactic removal | |||||
| Number | QALY loss | Number | QALY loss | Number | QALY loss | |
| IM3Ms extracted | 955.4 | 4.124 | 975.9 | 5.267 | 20.5 | 1.143 |
| Permanent nerve damage | 2.9 | 0.619 | 2.6 | 0.688 | –0.3 | 0.069 |
| Temporary nerve damage | 36.6 | 0.653 | 33.1 | 0.729 | –3.6 | 0.076 |
| Jaw fracture | 0.2 | 0.006 | 0.2 | 0.007 | –0.02 | 0.001 |
| Alveolar osteitis | 70.4 | 0.377 | 63.8 | 0.423 | –6.6 | 0.046 |
| Number of M2Ms with DCC extracted | 60.2 | 0.155 | 32.5 | 0.084 | –27.7 | –0.071 |
| Pericoronitis | 295.9 | 1.868 | 160.0 | 1.010 | –135.9 | –0.858 |
| Severe pain | 315.7 | 6.644 | 170.7 | 3.591 | –145.0 | –3.052 |
| Mild pain | 434.0 | 4.566 | 234.6 | 2.468 | –199.4 | –2.098 |
Cost-effectiveness results
Combining the cost and QALY results that were generated by the model suggests an ICER of £11,741 per QALY gained for the comparison of a prophylactic removal strategy with a watchful waiting strategy. The incremental costs and benefits for a cohort of 1000 people with asymptomatic IM3Ms are shown in Table 21.
| Total costs (£) | Total QALYs | Incremental cost (£) | Incremental QALYs | Incremental ICER per QALY gained (£) | ||
|---|---|---|---|---|---|---|
| Watchful waiting strategy | Prophylactic removal strategy | Watchful waiting strategy | Prophylactic removal strategy | |||
| 305,173 | 360,885 | 22,615 | 22,620 | 55,713 | 4.74 | 11,741 |
Deterministic sensitivity analysis
Tornado diagrams summarising the results of the one-way deterministic sensitivity analyses detailed in Table 17 are shown in Figure 4.
FIGURE 4.
Deterministic sensitivity analyses results.

The tornado diagram shows that the most important parameters that affect model results are the discount rate, the cost of a UDA, the annual extraction rate for IM3Ms, the utility decrements applied to IM3M symptoms and the duration of the symptoms.
Although the results are most sensitive to changes in the discount rate, which is to be expected given that the prophylactic strategy effectively ‘front loads’ extraction costs in the model compared with the watchful waiting strategy, which spreads those costs over many years, the ICER is still under £20,000 per QALY gained even when the discount rate is 5% per annum. The AG considers that, although the 3.5% per annum discount rate is the correct one to apply, an argument could be made that prophylactic removal constitutes a public health intervention similar to vaccination, and so a 1.5% per annum discount rate should be applied instead. At this lower rate, the model predicts an ICER of £3377 per QALY gained for the prophylactic removal strategy.
Given that there is no direct evidence on the QALY loss from symptoms of IM3Ms, it is potentially concerning that the ICER per QALY gained is sensitive to values used in the AG’s model to estimate the IM3M symptom QALY loss. However, over all of the parameter ranges considered, only the lower bound for the utility decrement for severe pain (0.102 as opposed to 0.345 in the base case) results in an ICER of > £20,000 per QALY gained for prophylactic removal (£21,469 per QALY gained).
As stated previously, there is evidence from Hill and Walker47 that the annual rate of extraction of IM3Ms is closer to the upper bound of 7.39% per annum reported by Fernandes et al. ,48 rather than the 5.47% per annum used in the base case. If the annual rate of extraction was 7.39% per annum, the ICER would be £9944 per QALY gained. However, even if the annual rate of extraction was at the lower bound, suggested by Fernandes et al. ,48 of 3.94%, the ICER would be £13,847 per QALY gained, which is still below the £20,000 per QALY gained threshold.
As stated previously, the cost of a UDA varies widely across the country. The value used in the AG’s base case (£25) is at the lower end of the potential range used in England (i.e. from £11.08 to £105.58). At the lower UDA price (£11.08), the ICER for prophylactic removal is £12,925 per QALY gained and, thus, remains below the £20,000 per QALY gained threshold. For geographical areas where the UDA price is higher than the £25 base-case value, the ICER per QALY gained increasingly favours a prophylactic removal strategy.
The AG’s model results are insensitive to several parameters for which no information was available and assumptions had to be made, for example the duration of symptoms of complications from extraction, the percentage of patients seeking treatment for pericoronitis and the percentage of patients having a M2M extraction at the same time as an IM3M extraction. This finding suggests that the lack of robust information on these parameters does not affect on the conclusions that can be drawn from the AG’s model.
Scenario analyses
The total number of patients with IM3M extractions each year in the NHS is unknown. However, McArdle et al. 104 have estimated that, in 2014/15, 152,000 people underwent IM3M extractions: 67,000 (44.1%) extractions were carried out during inpatient admissions, 38,000 (25.0%) during outpatient attendances and 47,000 (30.9%) during a primary care appointment. The AG has used these estimates as the basis for estimating the cost of IM3M extractions to the NHS. Unit costs of extraction in an acute setting have been taken from the NHS Reference Costs 2015 to 2016. 107 The cost of an extraction in primary care is a band 2 treatment and is charged to the NHS as 3 UDAs. Although the number of extractions in an acute setting was derived from published statistics, McArdle et al. 104 estimated the number of extractions in primary care from a historical data source, as primary care IM3M extractions have not been recorded since 2004/5. McArdle et al. 104 state that they believe that their estimate of 47,000 extractions in primary care is probably an underestimate. However, given the potential uncertainty around the number of primary care extractions, scenario analyses were undertaken in which (1) no extractions occurred in primary care and (2) all extractions occurred in primary care.
Proportion of extractions occurring in primary care
Increasing the proportion of people having extractions in primary care reduced the average cost of extraction per person, and vice versa.
If all extractions were to take place in primary care, the average cost per extraction decreases to £75 and the ICER per QALY gained decreases such that prophylactic removal becomes a dominant strategy compared with watchful waiting. If no extractions take place in primary care, the average cost per extraction increases to £565.13 and the ICER increases to £17,116 per QALY gained for prophylactic removal. The results of this scenario analysis are shown in Table 22.
| IM3M extractions | Total costs (£) | Total QALYs | Incremental cost (£) | Incremental QALYs | ICER per QALY gained (£) | ||
|---|---|---|---|---|---|---|---|
| Watchful waiting strategy | Prophylactic removal strategy | Watchful waiting strategy | Prophylactic removal strategy | ||||
| Base case | 305,173 | 360,885 | 22,615 | 22,620 | 55,713 | 4.74 | 11,741 |
| 100% of extractions in primary care | 90,616 | 89,331 | 22,615 | 22,620 | –1285 | 4.74 | Dominates |
| 0% of extractions in primary care | 401,173 | 482,388 | 22,615 | 22,620 | 81,215 | 4.74 | 17,116 |
Model start age
The age at which people entered the model varied between 30 years and 50 years (base case = 20 years). As the age at the start increases, so does the ICER per QALY gained for the comparison of a prophylactic removal strategy with a watchful waiting strategy. However, even when the starting age was set at 50 years, the ICER for this comparison remains below £20,000 per QALY gained. The results of these sensitivity analyses are presented in Table 23.
| Model start age | Total costs (£) | Total QALYs | Incremental cost (£) | Incremental QALYs | ICER per QALY gained (£) | ||
|---|---|---|---|---|---|---|---|
| Watchful waiting strategy | Prophylactic removal strategy | Watchful waiting strategy | Prophylactic removal strategy | ||||
| Base case (20 years) | 305,173 | 360,885 | 22,615 | 22,620 | 55,713 | 4.74 | 11,741 |
| 30 years | 303,175 | 362,483 | 20,616 | 20,620 | 59,308 | 4.36 | 13,609 |
| 40 years | 296,341 | 358,764 | 18,190 | 18,194 | 62,423 | 4.22 | 14,787 |
| 50 years | 283,219 | 351,611 | 15,335 | 15,339 | 68,392 | 3.94 | 17,348 |
Time horizon
The time horizon used in the AG’s model varied in 10-year increments between 10 years and 50 years. The results of these scenarios compared with the base-case results are shown in Table 24.
| Model time horizon | Total costs (£) | Total QALYs | Incremental cost (£) | Incremental QALYs | ICER per QALY gained (£) | ||
|---|---|---|---|---|---|---|---|
| Watchful waiting strategy | Prophylactic removal strategy | Watchful waiting strategy | Prophylactic removal strategy | ||||
| Base case (lifetime) | 305,173 | 360,885 | 22,615 | 22,620 | 55,713 | 4.74 | 11,741 |
| 10 years | 186,095 | 296,515 | 7364 | 7365 | 110,419 | 1.57 | 70,310 |
| 20 years | 259,364 | 336,122 | 13,102 | 13,106 | 76,758 | 3.72 | 20,620 |
| 30 years | 288,021 | 351,613 | 16,987 | 16,992 | 63,593 | 4.42 | 14,401 |
| 40 years | 299,141 | 357,625 | 19,538 | 19,543 | 58,484 | 4.64 | 12,598 |
| 50 years | 303,325 | 359,886 | 21,184 | 21,188 | 56,562 | 4.72 | 11,994 |
As the prophylactic removal strategy ‘front loads’ the costs of extraction compared with a watchful waiting strategy, the ICER per QALY gained is sensitive to the time horizon employed in the model. The shorter the time horizon, the fewer people in the watchful waiting strategy who have an extraction and develop symptoms as a result of their IM3Ms. By 21 years, the ICER per QALY gained for the comparison of a prophylactic removal strategy with a watchful waiting strategy has fallen below £20,000.
No impacted mandibular third molar symptoms after the age of 63 years
The assumption that people continue to have IM3M symptoms after the age of 63 years makes a minor difference to the size of the ICER per QALY gained. When comparing a prophylactic removal strategy with a watchful waiting strategy, removing the assumption so that no people experience IM3M symptoms after the age of 63 years increases the ICER per QALY gained by £51. The results of this scenario analysis are shown in Table 25.
| IM3M symptoms | Total costs (£) | Total QALYs | Incremental cost (£) | Incremental QALYs | ICER per QALY gained (£) | ||
|---|---|---|---|---|---|---|---|
| Watchful waiting strategy | Prophylactic removal strategy | Watchful waiting strategy | Prophylactic removal strategy | ||||
| Base case | 305,173 | 360,885 | 22,615 | 22,620 | 55,713 | 4.74 | 11,741 |
| No IM3M symptoms after the age of 63 years | 305,097 | 360,844 | 22,615 | 22,620 | 55,747 | 4.73 | 11,793 |
No extractions after the age of 63 years
The assumption that people continue to have IM3Ms extracted after the age of 63 years also makes only a minor difference to the value of the ICER per QALY gained. This is unsurprising as, by the age of 63 years (annual extraction rate of 5.47%), approximately 91% of patients will have had their IM3M removed with watchful waiting and both costs and benefits by this age are substantially discounted. When comparing a prophylactic removal strategy with a watchful waiting strategy, removing the assumption that people continue to have IM3Ms extracted after the age of 63 years increases the ICER per QALY gained by £437. The results of this scenario analysis are shown in Table 26.
| IM3M extractions | Total costs (£) | Total QALYs | Incremental cost (£) | Incremental QALYs | ICER per QALY gained (£) | ||
|---|---|---|---|---|---|---|---|
| Watchful waiting strategy | Prophylactic removal strategy | Watchful waiting strategy | Prophylactic removal strategy | ||||
| Base case | 305,173 | 360,885 | 22,615 | 22,620 | 55,713 | 4.74 | 11,741 |
| No IM3M extractions after the age of 63 years | 301,435 | 358,865 | 22,615 | 22,620 | 57,430 | 4.71 | 12,180 |
Proportion of people accepting prophylactic removal of impacted mandibular third molars
Varying the proportion of people who accept prophylactic removal of IM3Ms resulted in no change to the base-case cost-effectiveness results, as the increase in costs that accompanied an increase in the number of prophylactic removals resulted in a directly proportional increase in QALYs. Therefore, the ICER per QALY gained for the comparison of a prophylactic removal strategy with a watchful waiting strategy remained the same, irrespective of the proportion of patients accepting prophylactic removal.
Summary of cost-effectiveness results
The results generated by the AG’s economic model indicate that the ICER per QALY gained for the comparison of the cost-effectiveness of a prophylactic removal strategy with a watchful waiting strategy is £11,741 for people aged 20 years with asymptomatic IM3Ms. The incremental cost per person associated with prophylactic extraction is £55.71, with an incremental QALY gain of 0.005 per person. The base-case ICER per QALY gained was found to be robust when a range of one-way sensitivity analyses were carried out to test parameter uncertainty and when scenario analyses were carried out to test structural assumptions.
Discussion of cost-effectiveness results
The AG’s review of cost-effectiveness evidence identified only two published cost-effectiveness studies17,20 that directly consider the decision problem. The authors of both studies17,20 concluded that there was no economic evidence to support the prophylactic removal of IM3Ms. However, the AG notes that Song et al. 20 restrict their conclusions to a short- to medium-term time frame. More importantly, none of the studies was a cost–utility analysis; therefore, the relevance of the reported results to the decision problem is limited.
The results generated by the AG’s economic model indicated that the ICER per QALY gained for the comparison of the cost-effectiveness of a prophylactic removal strategy with a watchful waiting strategy is markedly lower than the £20,000 per QALY gained threshold widely accepted by NICE Appraisal Committees.
Although the ICER was determined to be robust when a range of scenario and one-way sensitivity analyses were carried out, uncertainty exists around the magnitude of utility loss from IM3M symptom development (either through the utility decrement or through the duration of symptoms). As no direct values for these parameters could be drawn from the published literature, parameter values had to be derived from generic studies of utility and from expert clinical opinion. This inevitably places a limit on the robustness of the AG’s model results. However, the AG’s notes that a central model assumption is that symptoms can develop only once per year, which will probably underestimate the true symptom burden arising from IM3Ms.
The ICER per QALY gained for prophylactic removal also increases as the percentage of people having an extraction in an acute setting rises. However, it is noted that the percentage of extractions in primary care in the base case of the model (30.9%) was considered to probably be an underestimate by the authors of the study (McArdle et al. 104) from which the proportions of location of extraction were derived. The greater the percentage of people who can have their IM3Ms extracted in a primary care setting, the more cost-effective prophylactic removal becomes.
In addition to the limit of developing symptoms only once per year, seven other model assumptions also suggested that the base-case ICER per QALY gained generated by the model may be conservative:
-
No serious complications arising from IM3M symptoms (e.g. from severe infection) are included in the model.
-
No disutility from M2M decay and restorative treatment (including root canal treatment) is included in the model.
-
Expert clinical advice to the AG is that tooth extraction becomes much more difficult as people age, which could result in the extraction being more complex and, therefore, more costly. The only way that this increase in difficulty is represented in the model is through an increase in the complication rate.
-
No litigation costs from permanent nerve damage and/or fracture are included in the model.
-
No surgical treatment costs for temporary nerve damage or ongoing costs of treating permanent nerve damage are included in the model.
-
No costs of additional check-ups or X-rays are included for a watchful waiting strategy. Routine dental care costs are assumed to be identical regardless of whether the IM3M is in situ.
-
Patients who develop symptoms in the model but do not have their teeth removed have the same risk of developing symptoms in future years as if they had stayed asymptomatic. It may be the case that patients who develop symptoms are inherently more prone to symptom development or that prior symptoms and treatment increase the likelihood of developing future symptoms.
The AG’s model results are ultimately driven by the finding that most individuals with asymptomatic IM3Ms will eventually have their IM3Ms extracted. This finding arises from the AG’s long-term extrapolation of the annual extraction data reported in the study by Fernandes et al. 48 In this sense, a watchful waiting strategy may be more accurately described as ‘putting off the inevitable’. The findings reported by Fernandes et al. 48 on the rate of extraction of IM3Ms are supported by the results of Hill and Walker. 47 Importantly, even if the annual rates of extraction are substantially lower than that used in the model base case, the ICER per QALY gained remains below £20,000.
Chapter 5 Discussion
Statement of principal findings
The SR of clinical evidence found no RCT data to support or refute the prophylactic removal of pathology-free/trouble-free IM3Ms. The authors of the two included studies58,59 that investigated the rate of surgical complications concluded that no serious complications were reported. The three longitudinal studies47,48,58 that assessed the outcomes of retained IM3Ms reported varying extraction rates owing to the different lengths of follow-up. No studies reported the impact of retention on the status of the 2Ms.
As there is very limited clinical effectiveness evidence comparing the prophylactic removal of I3Ms with a watchful waiting strategy, it is unsurprising that the economic evidence relating to this comparison is also limited. The two published cost-effectiveness studies17,20 that directly consider this comparison conclude that there is currently no economic evidence to support the prophylactic removal of I3Ms.
The results generated by the AG’s de novo economic model indicate that the ICER per QALY gained for the comparison of the cost-effectiveness of a prophylactic removal strategy with that of a watchful waiting strategy is £11,741 for people aged 20 years with asymptomatic IM3Ms. The incremental cost per person associated with prophylactic extraction is £55.71, with an incremental QALY gain of 0.005 per person. The base-case ICER per QALY gained was found to be robust when a range of one-way sensitivity analyses were carried out to test parameter uncertainty and when scenario analyses were carried out to test structural assumptions.
Although the available published economic evidence is limited, the findings that prophylactic removal is not cost-effective would seem to be contradicted by the findings from the results of the AG’s de novo model. There are several reasons that may explain this apparent contradiction. First, the model time horizon is important, as shown by the results of the scenario analysis in Table 24. It is unlikely that economic models that consider only the short and medium term would show that a prophylactic removal strategy was more cost-effective than a watchful waiting strategy. Second, there are data available47,48 on the annual rate of extraction and symptom development in the UK under a watchful waiting strategy that were not available at the time of the Song et al. study. 20 Additional sources of information104 are also now available on, for example, the rate of M2Ms with DCC as a result of IM3Ms. Third, the costs of extraction have now been robustly estimated and are significantly lower than those previously estimated (see, for example, Anjrini et al. 17). Lower costs of extraction will make it more likely that a prophylactic removal strategy will be more cost-effective than a watchful waiting strategy. Finally, the studies included in the review of cost-effectiveness evidence were not cost–utility analyses and so the analysis of effectiveness in these studies is fundamentally different from that considered here. The AG is, therefore, not surprised that the results generated by the de novo model differ from those published previously. 17,20
Strengths and limitations of the assessment
The main strength of this review is the breadth of literature that was considered. All clinical study designs and SRs were included in an attempt to identify all of the relevant literature. However, two limitations were the date of the search and the very specific population outlined in the decision problem. As this review was an update of the current NICE guidance2 published in 2000, the conducted searches were dated from 2000 to 2016. The population outlined in the decision problem was people with pathology-free or trouble-free impacted mandibular third molars; much of the literature cited by the professional stakeholders and the identified SRs did not provide data on the position of the tooth (maxillary or mandibular) or on whether or not teeth were impacted, and several did not provide information on the state of the tooth (i.e. pathology free or trouble free). This severely limited the number of studies relevant to this review.
Although the quality of the four cohort studies47,48,58,59 was generally good, it should be noted that no RCTs were identified limiting the ability of the review to draw firm conclusions.
The findings of this review were in line with those from the other nine identified SRs,20,40,42–46,50,56 suggesting that the limitations of this review did not overly affect the conclusions.
The strength of the de novo economic model is the use of existing evidence48 on the annual rates of symptom development and on the annual rates of extraction of IM3Ms that are currently pathology free/trouble free. All of the assumptions employed in the model suggest that the base-case ICER per QALY gained for the comparison of prophylactic removal with watchful waiting may be conservative. An additional strength of the model is that it is robust to variations across the range of parameter values that could be considered clinically plausible.
The economic model was limited by the lack of direct utility evidence around IM3M symptoms. However, suitable proxies could be found and the cost-effectiveness findings were robust across a range of potential values that could be chosen.
Uncertainties
The AG’s model results are driven by figures reported by Fernandes et al. 48 and McArdle et al. 104 Although the results reported by Fernandes et al. 48 on the rate of extraction of IM3Ms are supported by the results reported by Hill and Walker,47 the results reported by McArdle et al. 104 on the different proportions of people having IM3Ms extracted in non-acute NHS settings have yet to be confirmed by other studies. However, even if all of the extractions were carried out in the acute setting, the size of the ICER for prophylactic removal compared with watchful waiting would still remain below £20,000 per QALY gained.
The Fernandes et al. 48 study from which IM3M symptom development and extraction rates were derived was not a clinical trial but an analysis of real-world data. As such, the study provides estimates of symptom development and extraction in a real-world setting when watchful waiting has been recommended, rather than to a strictly defined and monitored policy of watchful waiting, as would be the case in a clinical trial. Although this is a limitation of the economic model, it can also be seen as a strength, as the model findings are based on a change in potential recommendation and its impact on actual practice, rather than any specific watchful waiting strategy itself. The results of the modelling in this respect are clear – that under current extraction and symptom development rates for IM3Ms, any change in recommendations that increased the proportion of patients opting for prophylactic extraction would most likely be cost-effective.
All people with IM3Ms are treated equally in the model regardless of impaction status (i.e. whether partially erupted or a bony impaction). Expert clinical advice to the AG is that it is only partially erupted teeth that tend to cause problems. If this is the case, then both the extraction and complication rates reported by Fernandes et al. 48 (this study included people with both bony IM3Ms and partially erupted IM3Ms) would be underestimates of the rates for people with partially erupted IM3Ms. The base-case ICERs generated by the model are, therefore, overestimates for those with partially erupted IM3Ms and underestimates for those with bony impaction.
Model results show that the difference in costs between the prophylactic removal strategy and the watchful waiting strategy is £55.71 per person. With such a small difference in the cost, the level of confidence in the utility associated with the two strategies gains importance. Although the model has been shown to be robust to variations in utility values, all of the utility values used in the model are based on a figure published in the study by Ara and Brazier. 110 The utility values reported in Ara and Brazier110 were not sourced directly from patients with IM3Ms, and this is a limitation of the findings. However, the model results were insensitive to a wide range of utility values considered. This suggests that, unless the values chosen for the model were substantially different from reality, the use of the values from Ara and Brazier110 will not have influenced the conclusions drawn from the model. The limitation of the source of the utility values also has to be interpreted against the range of assumptions made by the AG as QALY gains from the model are potentially lower than would be expected in reality, for example applying no disutility M2M decay, the assumption of no serious complications arising from pericoronitis and that extraction of an IM3M does not increase in difficulty as people age.
Chapter 6 Conclusions
The findings from the clinical evidence review are consistent with previous SRs,20,40,42–46,50,56 in that there is no available RCT evidence to support or refute the practice of the prophylactic removal of asymptomatic/pathology-free IM3Ms. However, the review did identify evidence from longitudinal studies that demonstrated what happens when asymptomatic IM3Ms are left in situ.
Only two published cost-effectiveness studies17,20 that directly consider the study question were identified. In both cases, the authors conclude that there is currently no economic evidence to support the prophylactic removal of I3Ms.
The base-case results generated by the AG’s economic model indicate that the ICER per QALY gained for the comparison of the cost-effectiveness of a prophylactic removal strategy with a watchful waiting strategy is markedly lower than the £20,000 per QALY gained threshold widely accepted by NICE Appraisal Committees.
Implications for service provision
The results from the clinical studies and those generated by the economic model show that most people with IM3Ms will have their impacted teeth removed at some point and that, although prophylactic removal is probably more costly than a watchful waiting strategy (this may not be the case if, for example, compensation pay-outs for permanent nerve damage are taken into consideration), the improvements in HRQoL for people from a reduction in IM3M symptoms mean that prophylactic removal is a cost-effective strategy for the NHS.
The reintroduction of the prophylactic removal of pathology-free/trouble-free IM3Ms will have resource implications in both primary and secondary care settings, with the rate of pathology-free IM3M extractions increasing. Expert clinical advice to the AG is that it can be argued that the cost would be offset by the reduction in the number of complicated extractions being performed when people are older. There is no published evidence that this is the case, although there is evidence that complications associated with extraction increase with age. 80
Suggested research priorities
The AG was able to produce a robust economic model, despite the limited clinical evidence relating to the prophylactic removal of pathology-free/trouble-free IM3Ms by using IM3M extraction, symptom development and extraction complication rates from the literature. Utility valuation studies of patients with symptomatic IM3Ms and following extraction (with and without complications) would strengthen the economic modelling that can be undertaken in the future. However, there remains a lack of head-to-head trial evidence comparing a prophylactic removal strategy with a watchful waiting strategy. The practical difficulties (e.g. time, cost and the need for extended follow-up) associated with undertaking such studies mean that it is unlikely that this type of study will be conducted.
Future longitudinal studies on the pathology of retained I3Ms could be designed to record the impaction status and health of the retained I3M, with the results being presented separately for maxillary and mandibular teeth. Ideally these studies would include longer follow-up periods and include subgroup analyses of adults based on age to help identify the outcomes of retained IM3Ms and the pattern of extraction rate over the years. If such studies are not possible, the systematic collection of routine data collected across different countries may be beneficial; however, for further studies to be meaningful, common definitions and outcome reporting methods need to be agreed.
Acknowledgements
The authors would like to thank Paul Coulthard (Professor of Maxillofacial Surgery), Rebecca Harris (Professor/Honorary Consultant Dental Public Health) and Margaret Raison (Academic Clinical Fellow) for clinical input and Joanne Fisher (Research Assistant) for assistance with data extraction.
Contributions of authors
Juliet Hounsome (https://orcid.org/0000-0002-2026-3778) (Research Associate, Evidence synthesis) was involved in protocol development, a clinical reviewer and involved in the writing of the report.
Gerlinde Pilkington (https://orcid.org/0000-0003-0028-0746) (Research Associate, Evidence synthesis) was involved in protocol development, a clinical reviewer and involved in the writing of the report.
James Mahon (https://orcid.org/0000-0002-2187-1003) (Consultant, Health Economist) was involved in the development of de novo economic model.
Angela Boland (https://orcid.org/0000-0002-5435-8644) (Associate Director of Liverpool Reviews and Implementation Group, Evidence Synthesis) was an economic reviewer and checked the economic model.
Sophie Beale (https://orcid.org/0000-0003-0164-103X) (Senior Research Associate, Evidence Synthesis) was an economic reviewer and checked the economic model.
Eleanor Kotas (https://orcid.org/0000-0002-8410-6034) (Research Associate, Information Specialist) conducted clinical and economic searches.
Tara Renton (https://orcid.org/0000-0003-2331-4005) (Professor Oral Surgery) provided clinical advice.
Rumona Dickson (https://orcid.org/0000-0003-1416-0913) (Professor of Evidence synthesis/Director of Liverpool Reviews and Implementation Group) was involved in screening of studies, protocol development and finalising of the report.
Data-sharing statement
All available data can be obtained by contacting the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care.
References
- Rafetto LK. Controversy, evidence, and third molar management. Atlas Oral Maxillofac Surg Clin North Am 2012;20:253-61. https://doi.org/10.1016/j.cxom.2012.06.004.
- National Institute for Health and Care Excellence (NICE) . Guidance on the Extraction of Wisdom Teeth: NICE Technology Appraisal Guidance [TA1]. 2000.
- Kandasamy S, Rinchuse DJ, Rinchuse DJ. The wisdom behind third molar extractions. Aust Dent J 2009;54:284-92. https://doi.org/10.1111/j.1834-7819.2009.01152.x.
- Flick WG. The third molar controversy: framing the controversy as a public health policy issue. J Oral Maxillofac Surg 1999;57:438-44. https://doi.org/10.1016/S0278-2391(99)90285-9.
- Dodson TB, Bagheri S, Bell B, Khan H. Current Therapy in Oral and Maxillofacial Surgery. St Louis, MO: Elsevier Saunders; 2012.
- Winter GB. Impacted Mandibular Third Molar. St Louis, MO: American Medical Book Company; 1926.
- Pell GJ, Gregory BT. Impacted mandibular third molars: classification and modified techniques for removal. The Dental Digest 1933;39.
- Worrall SF, Riden K, Haskell R, Corrigan AM. UK National Third Molar project: the initial report. Br J Oral Maxillofac Surg 1998;36:14-8. https://doi.org/10.1016/s0266-4356(98)90740-9.
- Kim SJ, Hwang CJ, Park JH, Kim HJ, Yu HS. Surgical removal of asymptomatic impacted third molars: considerations for orthodontists and oral surgeons. Semin Orthod 2016;22:75-83. https://doi.org/10.1053/j.sodo.2015.10.010.
- Ahmad N, Gelesko S, Shugars D, White RP, Blakey G, Haug RH, et al. Caries experience and periodontal pathology in erupting third molars. J Oral Maxillofac Surg 2008;66:948-53. https://doi.org/10.1016/j.joms.2007.11.013.
- National Institute for Health and Care Excellence (NICE) . Third Molars (Impacted) – Prophylactic Removal [ID898]. Final Scope 2016.
- Nunn ME, Fish MD, Garcia RI, Kaye EK, Figueroa R, Gohel A, et al. Retained asymptomatic third molars and risk for second molar pathology. J Dent Res 2013;92:1095-9. https://doi.org/10.1177/0022034513509281.
- McArdle LW, McDonald F, Jones J. Distal cervical caries in the mandibular second molar: an indication for the prophylactic removal of third molar teeth? Update. Br J Oral Maxillofac Surg 2014;52:185-9. https://doi.org/10.1016/j.bjoms.2013.11.007.
- Adeyemo WL. Do pathologies associated with impacted lower third molars justify prophylactic removal? A critical review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006;102:448-52. https://doi.org/10.1016/j.tripleo.2005.08.015.
- Yildirim G, Ataoğlu H, Mihmanli A, Kiziloğlu D, Avunduk MC. Pathologic changes in soft tissues associated with asymptomatic impacted third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008;106:14-8. https://doi.org/10.1016/j.tripleo.2007.11.021.
- Toedtling V, Yates JM. Revolution vs status quo? Non-intervention strategy of asymptomatic third molars causes harm. Br Dent J 2015;219:11-2. https://doi.org/10.1038/sj.bdj.2015.525.
- Anjrini AA, Kruger E, Tennant M. Cost effectiveness modelling of a ‘watchful monitoring strategy’ for impacted third molars vs prophylactic removal under GA: an Australian perspective. Br Dent J 2015;219:19-23. https://doi.org/10.1038/sj.bdj.2015.529.
- Carter K, Worthington S. Predictors of third molar impaction: a systematic review and meta-analysis. J Dent Res 2016;95:267-76. https://doi.org/10.1177/0022034515615857.
- McArdle LW, Renton T. The effects of NICE guidelines on the management of third molar teeth. Br Dent J 2012;213. https://doi.org/10.1038/sj.bdj.2012.780.
- Song F, O’Meara S, Wilson P, Golder S, Kleijnen J. The effectiveness and cost-effectiveness of prophylactic removal of wisdom teeth. Health Technol Assess 2000;4. https://doi.org/10.3310/hta4150.
- The Royal College of Surgeons of England . Faculty of Dental Surgery: National Clinical Guidelines 1997. Management of Patients With Impacted Third Molar Teeth n.d. www.rcseng.ac.uk/-/media/files/rcs/fds/publications/ncg97.pdf?la=en (accessed 3 March 2016).
- The Royal College of Surgeons of England . Wisdom Teeth Extraction. Get Well Soon. Helping You Make a Speedy Recovery After Removal of Wisdom Teeth n.d. www.rcseng.ac.uk/patient-care/recovering-from-surgery/wisdom-teeth-extraction/ (accessed 9 March 2016).
- Bui CH, Seldin EB, Dodson TB. Types, frequencies, and risk factors for complications after third molar extraction. J Oral Maxillofac Surg 2003;61:1379-89. https://doi.org/10.1016/j.joms.2003.04.001.
- Brauer HU, Dent M, Green RA, Pynn BR. Complications During and After Surgical Removal of Third Molars 2013. www.oralhealthgroup.com/features/complications-during-and-after-surgical-removal-of-third-molars/ (accessed 10 March 2016).
- Lodi G, Figini L, Sardella A, Carrassi A, Del Fabbro M, Furness S. Antibiotics to prevent complications following tooth extractions. Cochrane Database Syst Rev 2012;11. https://doi.org/10.1002/14651858.CD003811.pub2.
- National Institute for Health and Care Excellence (NICE) . NICE Pathways. Oral and Dental Health Overview 2016.
- Agence Nationale d’Accréditation et d’Evaluation en Santé . Indications Et Non-Indications De L’avulsion Des Troisièmes Molaires Mandibulaires 1997. http://maxillorisq.com/sites/maxillorisq.com/files/Recommandation_ANDEM_avulsion_1997.pdf (accessed 3 March 2016).
- Agency for Quality in Dentistry (ZZQ) . Surgical Removal of Third Molars 2006. www3.kzbv.de/zzqpubl.nsf/7549c7b9ec54d2dfc1257018002ad508/5f184e5d59df47ebc125714d004890fa/$FILE/Leitlinie_Weish_EN.pdf (accessed 18 January 2016).
- American Academy of Pediatric Dentistry . Guideline on Adolescent Oral Health Care 2015. www.aapd.org/media/policies_guidelines/g_adoleshealth.pdf (accessed 18 January 2016).
- American Academy of Pediatric Dentistry . The Reference Manual of Pediatric Dentistry. Management Considerations for Pediatric Oral Surgery and Oral Pathology 2015. www.aapd.org/media/policies_guidelines/g_oralsurgery.pdf (accessed 18 January 2016).
- American Association of Oral and Maxillofacial Surgeons (AAOMS) . Management of Third Molar Teeth: White Paper 2016.
- Ministry of Health Malaysia (MoH) . Management of Unerupted and Impacted Third Molar Teeth n.d.
- Agency for Healthcare Research and Quality . Guidelines and Measures n.d. www.guideline.gov/content.aspx?id=47399 (accessed 3 March 2016).
- Scottish Intercollegiate Guidelines Network . Management of Unerupted and Impacted Third Molar Teeth – SIGN 43 2000.
- Devine M, Gerrard G, Renton T. Current practice in mandibular third molar surgery. A national survey of British Association of Oral Surgeons membership. Oral Surgery 2016;10:11-9. https://doi.org/10.1111/ors.12211.
- NHS England . Guide for Commissioning Oral Surgery and Oral Medicine 2015. www.england.nhs.uk/commissioning/wp-content/uploads/sites/12/2015/09/guid-comms-oral.pdf (accessed 3 March 2016).
- Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle–Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses 2014. www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed 15 August 2016).
- Centre for Reviews and Dissemination (CRD) . Systematic Reviews: CRD’s Guidance for Undertaking Reviews in Health Care 2008.
- Fernandes MJ, Ogden GR, Pitts NB, Ogston SA, Ruta DA. Incidence of symptoms in previously symptom-free impacted lower third molars assessed in general dental practice. Br Dent J 2009;207. https://doi.org/10.1038/sj.bdj.2009.804.
- Stordeur S, Eyssen M. Prophylactic Removal of Pathology-Free Wisdom Teeth: Rapid Assessment. Brussels: Belgian Health Care Knowledge Centre; 2012.
- Dodson TB, Susarla SM. Impacted wisdom teeth. BMJ Clin Evid 2010;2010.
- Canadian Agency for Drugs and Technologies in Health (CADTH) . Prophylactic Removal Of Wisdom Teeth: A Review Of The Clinical Benefit And Guidelines 2010. www.cadth.ca/sites/default/files/pdf/l0202_removal_wisdom_teeth_htis_2.pdf (accessed 17 June 2020).
- Suska F, Kjeller G, Molander A, Samuelsson O, Svanberg T, Liljegren A. Removal of impacted wisdom teeth. Gothenburg: The Regional Health Technology Assessment Centre (HTA-centrum); 2010.
- Bouloux GF, Busaidy KF, Beirne OR, Chuang SK, Dodson TB. What is the risk of future extraction of asymptomatic third molars? A systematic review. J Oral Maxillofac Surg 2015;73:806-11. https://doi.org/10.1016/j.joms.2014.10.029.
- Costa MG, Pazzini CA, Pantuzo MC, Jorge ML, Marques LS. Is there justification for prophylactic extraction of third molars? A systematic review. Braz Oral Res 2013;27:183-8. https://doi.org/10.1590/S1806-83242013000100024.
- Mettes TD, Ghaeminia H, Nienhuijs ME, Perry J, van der Sanden WJ, Plasschaert A. Surgical removal versus retention for the management of asymptomatic impacted wisdom teeth. Cochrane Database Syst Rev 2012;6. https://doi.org/10.1002/14651858.CD003879.pub3.
- Hill CM, Walker RV. Conservative, non-surgical management of patients presenting with impacted lower third molars: a 5-year study. Br J Oral Maxillofac Surg 2006;44:347-50. https://doi.org/10.1016/j.bjoms.2005.08.014.
- Fernandes MJ, Ogden GR, Pitts NB, Ogston SA, Ruta DA. Actuarial life-table analysis of lower impacted wisdom teeth in general dental practice. Community Dent Oral Epidemiol 2010;38:58-67. https://doi.org/10.1111/j.1600-0528.2009.00501.x.
- Mettes TG, Nienhuijs ME, van der Sanden WJ, Verdonschot EH, Plasschaert AJ. Interventions for treating asymptomatic impacted wisdom teeth in adolescents and adults. Cochrane Database Syst Rev 2005;2. https://doi.org/10.1002/14651858.CD003879.pub2.
- Senter for Medisinsk Metodevurdering . Prophylactic Removal of Wisdom Teeth 2003.
- Worrall S. Impacted wisdom teeth. Clin Evid 2002;7:1244-7.
- Esposito M, Coulthard P. Impacted wisdom teeth. BMJ Clin Evid 2008;2008.
- Esposito M. Impacted wisdom teeth. BMJ Clin Evid 2006;15:1868-70.
- Esposito M. Impacted wisdom teeth. BMJ Clin Evid 2005;13:1722-5.
- Esposito M. Impacted wisdom teeth. BMJ Clin Evid 2004;11:1802-5.
- Dodson TB, Susarla SM. Impacted wisdom teeth. BMJ Clin Evid 2014;2014.
- Hill CM, Walker RV. Conservative, non-surgical management of lower third molars. Br J Oral Maxillofac Surg 2007;45. https://doi.org/10.1016/j.bjoms.2007.02.009.
- Vares Y, Kyyak S. Management of asymptomatic and mandibular impacted third molars that do not present any considerable pathological changes. Dent Med Probl 2014;51:35-42.
- Petsos H, Korte J, Eickholz P, Hoffmann T, Borchard R. Surgical removal of third molars and periodontal tissues of adjacent second molars. J Clin Periodontol 2016;43:453-60. https://doi.org/10.1111/jcpe.12527.
- Edwards MJ, Brickley MR, Goodey RD, Shepherd JP. The cost, effectiveness and cost effectiveness of removal and retention of asymptomatic, disease free third molars. Br Dent J 1999;187:380-4. https://doi.org/10.1038/sj.bdj.4800285.
- Harradine NW, Pearson MH, Toth B. The effect of extraction of third molars on late lower incisor crowding: a randomized controlled trial. Br J Orthod 1998;25:117-22. https://doi.org/10.1093/ortho/25.2.117.
- Kruger E, Thomson WM, Konthasinghe P. Third molar outcomes from age 18 to 26: findings from a population-based New Zealand longitudinal study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001;92:150-5. https://doi.org/10.1067/moe.2001.115461.
- Lindqvist B, Thilander B. Extraction of third molars in cases of anticipated crowding in the lower jaw. Am J Orthod 1982;81:130-9. https://doi.org/10.1016/0002-9416(82)90037-9.
- Song F, Landes DP, Glenny AM, Sheldon TA. Prophylactic removal of impacted third molars: an assessment of published reviews. Br Dent J 1997;182:339-46. https://doi.org/10.1038/sj.bdj.4809378.
- Ventä I, Ylipaavalniemi P, Turtola L. Clinical outcome of third molars in adults followed during 18 years. J Oral Maxillofac Surg 2004;62:182-5. https://doi.org/10.1016/j.joms.2003.04.011.
- Bagheri SC, Khan HA. Extraction versus nonextraction management of third molars. Oral Maxillofac Surg Clin North Am 2007;19:15-21. https://doi.org/10.1016/j.coms.2006.11.009.
- Friedman JW. The prophylactic extraction of third molars: a public health hazard. Am J Public Health 2007;97:1554-9. https://doi.org/10.2105/AJPH.2006.100271.
- Hill CM. Removal of asymptomatic third molars: an opposing view. J Oral Maxillofac Surg 2006;64:1816-20. https://doi.org/10.1016/j.joms.2006.04.007.
- Task Force for Third Molar Summary . Summary of the third molar clinical trials: report of the AAOMS Task Force for Third Molar Summary. J Oral Maxillofac Surg 2012;70:2238-48. https://doi.org/10.1016/j.joms.2012.06.180.
- The Finnish Medical Society Duodecim . [Third Molar Current Care Guideline.] 2014.
- Inverso G, Heald R, Padwa BL. The cost of third molar management. J Oral Maxillofac Surg 2014;72:1038-9. https://doi.org/10.1016/j.joms.2013.12.009.
- Koumaras GM. What costs are associated with the management of third molars?. J Oral Maxillofac Surg 2012;70:8-10. https://doi.org/10.1016/j.joms.2012.04.023.
- Kunkel M, Kleis W, Morbach T, Wagner W. Severe third molar complications including death-lessons from 100 cases requiring hospitalization. J Oral Maxillofac Surg 2007;65:1700-6. https://doi.org/10.1016/j.joms.2007.04.014.
- Kunkel M, Morbach T, Kleis W, Wagner W. Third molar complications requiring hospitalization. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006;102:300-6. https://doi.org/10.1016/j.tripleo.2005.09.010.
- Liedholm R, Knutsson K, Lysell L, Rohlin M, Brickley M, Shepherd J. Third molar treatment outcome: a comparison of patients’ preferences in Sweden and Wales. Br Dent J 2005;199:287-91. https://doi.org/10.1038/sj.bdj.4812653.
- McGrath C, Comfort MB, Edward CM, Luo Y. Can third molar surgery improve quality of life? A 6-month cohort study. J Oral Maxillofac Surg 2003;61:759-63. https://doi.org/10.1016/S0278-2391(03)00150-2.
- Aravena P, Cartes-Velasquez R. Signs and symptoms of postoperative complications in third-molar surgery. Int J Oral Maxillofac Surg 2011;40. https://doi.org/10.1016/j.ijom.2011.07.387.
- Bienstock DA, Dodson TB, Perrott DH, Chuang SK. Prognostic factors affecting the duration of disability after third molar removal. J Oral Maxillofac Surg 2011;69:1272-7. https://doi.org/10.1016/j.joms.2010.06.211.
- Bienstock D. Work days missed following third molar surgery. J Oral Maxillofac Surg 2012;2. https://doi.org/10.1016/j.joms.2012.06.010.
- Chuang SK, Perrott DH, Susarla SM, Dodson TB. Age as a risk factor for third molar surgery complications. J Oral Maxillofac Surg 2007;65:1685-92. https://doi.org/10.1016/j.joms.2007.04.019.
- Chuang SK, Perrott DH, Susarla SM, Dodson TB. Risk factors for inflammatory complications following third molar surgery in adults. J Oral Maxillofac Surg 2008;66:2213-18. https://doi.org/10.1016/j.joms.2008.06.067.
- Colorado-Bonnin M, Valmaseda-Castellón E, Berini-Aytés L, Gay-Escoda C. Quality of life following lower third molar removal. Int J Oral Maxillofac Surg 2006;35:343-7. https://doi.org/10.1016/j.ijom.2005.08.008.
- Conrad SM, Blakey GH, Shugars DA, Marciani RD, Phillips C, White RP. Patients’ perception of recovery after third molar surgery. J Oral Maxillofac Surg 1999;57:1288-94. https://doi.org/10.1016/S0278-2391(99)90861-3.
- Deepti C, Rehan HS, Mehra P. Changes in quality of life after surgical removal of impacted mandibular third molar teeth. J Maxillofac Oral Surg 2009;8:257-60. https://doi.org/10.1007/s12663-009-0063-2.
- Gutierrez-Perez JL. Third molar infections. Med Oral Patol Oral Cir Bucal 2004;9:122-5.
- Inverso G, Desrochers HR, Padwa BL. The value of postoperative visits for third molar removal. J Oral Maxillofac Surg 2014;72:30-4. https://doi.org/10.1016/j.joms.2013.08.018.
- Liedholm R, Knutsson K, Norlund A. Economic aspects of mandibular third molar surgery. Acta Odontol Scand 2010;68:43-8. https://doi.org/10.3109/00016350903303486.
- Matijević M, Uzarević Z, Ivanisević Z, Gvozdić V, Leović D, Popić B, et al. Determining the quality of life after removing of impacted lower wisdom tooth using the principal component analysis method. Coll Antropol 2014;38:691-9.
- Offenbacher S, Beck JD, Moss KL, Barros S, Mendoza L, White RP. What are the local and systemic implications of third molar retention?. J Oral Maxillofac Surg 2012;70:58-65. https://doi.org/10.1016/j.joms.2012.04.036.
- Osunde OD, Adebola RA, Omeje UK. Management of inflammatory complications in third molar surgery: a review of the literature. Afr Health Sci 2011;11:530-7.
- Pandurić DG, Brozović J, Susić M, Katanec D, Bego K, Kobler P. Assessing health-related quality of life outcomes after the surgical removal of a mandibular third molar. Coll Antropol 2009;33:437-47.
- Phillips C, White RP, Shugars DA, Zhou X. Risk factors associated with prolonged recovery and delayed healing after third molar surgery. J Oral Maxillofac Surg 2003;61:1436-48. https://doi.org/10.1016/j.joms.2003.08.003.
- Phillips C, Gelesko S, Proffit WR, White RP. Recovery after third-molar surgery: the effects of age and sex. Am J Orthod Dentofacial Orthop 2010;138:700.e1-8. https://doi.org/10.1016/j.ajodo.2010.06.013.
- Ruvo AT, Shugars DA, White RP, Phillips C. The impact of delayed clinical healing after third molar surgery on health-related quality-of-life outcomes. J Oral Maxillofac Surg 2005;63:929-35. https://doi.org/10.1016/j.joms.2005.03.007.
- Sancho-Puchades M, Valmaseda-Castellón E, Berini-Aytés L, Gay-Escoda C. Quality of life following third molar removal under conscious sedation. Med Oral Patol Oral Cir Bucal 2012;17:e994-9. https://doi.org/10.4317/medoral.17677.
- Sato FR, Asprino L, de Araújo DE, de Moraes M. Short-term outcome of postoperative patient recovery perception after surgical removal of third molars. J Oral Maxillofac Surg 2009;67:1083-91. https://doi.org/10.1016/j.joms.2008.09.032.
- Shugars D, White RP. Can third molar surgery improve quality of life? A 6-month cohort study. J Oral Maxillofac Surg 2003;61:764-5. https://doi.org/10.1016/S0278-2391(03)00151-4.
- Shugars DA, Gentile MA, Ahmad N, Stavropoulos MF, Slade GD, Phillips C, et al. Assessment of oral health-related quality of life before and after third molar surgery. J Oral Maxillofac Surg 2006;64:1721-30. https://doi.org/10.1016/j.joms.2006.03.052.
- Slade GD, Foy SP, Shugars DA, Phillips C, White RP. The impact of third molar symptoms, pain, and swelling on oral health-related quality of life. J Oral Maxillofac Surg 2004;62:1118-24. https://doi.org/10.1016/j.joms.2003.11.014.
- White RP, Shugars DA, Shafer DM, Laskin DM, Buckley MJ, Phillips C. Recovery after third molar surgery: clinical and health-related quality of life outcomes. J Oral Maxillofac Surg 2003;61:535-44. https://doi.org/10.1053/joms.2003.50106.
- White RP. Recovery after third-molar surgery. Am J Orthod Dentofacial Orthop 2004;126. https://doi.org/10.1016/j.ajodo.2004.06.012.
- Walters H. Reducing lingual nerve damage in third molar surgery: a clinical audit of 1350 cases. Br Dent J 1995;178:140-4. https://doi.org/10.1038/sj.bdj.4808682.
- National Institute for Health and Care Excellence (NICE) . Guide to the Methods of Technology Appraisal 2013 2013. www.nice.org.uk/process/pmg9/resources/guide-to-the-methods-of-technology-appraisal-2013-pdf-2007975843781 (accessed 10 March 2020).
- McArdle LW, Patel N, Jones J, McDonald F. The mesially impacted mandibular third molar: the incidence and consequences of distal cervical caries in the mandibular second molar. Surgeon 2018;16:67-73. https://doi.org/10.1016/j.surge.2016.05.001.
- Valmaseda-Castellón E, Berini-Aytés L, Gay-Escoda C. Inferior alveolar nerve damage after lower third molar surgical extraction: a prospective study of 1117 surgical extractions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001;92:377-83. https://doi.org/10.1067/moe.2001.118284.
- Office for National Statistics . National Life Tables, UK: 2013 to 2015 2016. www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/lifeexpectancies/bulletins/nationallifetablesunitedkingdom/20132015 (accessed 5 December 2016).
- Department of Health and Social Care . NHS Reference Costs 2015 to 2016 2016.
- GDPUK . UDA Values Vary Hugely Across UK Claim Tories 2009. www.gdpuk.com/news/latest-news/432-uda-values-vary-hugely-across-uk-claim-tories (accessed 3 March 2016).
- NHS Digital . Prescription Cost Analysis, England 2015 2016. http://content.digital.nhs.uk/catalogue/PUB20200 (accessed 3 January 2017).
- Ara R, Brazier JE. Populating an economic model with health state utility values: moving toward better practice. Value Health 2010;13:509-18. https://doi.org/10.1111/j.1524-4733.2010.00700.x.
- Al-Belasy FA, Tozoglu S, Ertas U. Mastication and late mandibular fracture after surgery of impacted third molars associated with no gross pathology. J Oral Maxillofac Surg 2009;67:856-61. https://doi.org/10.1016/j.joms.2008.09.007.
- Allen RT, Witherow H, Collyer J, Roper-Hall R, Nazir MA, Mathew G. The mesioangular third molar – to extract or not to extract? Analysis of 776 consecutive third molars. Br Dent J 2009;206. https://doi.org/10.1038/sj.bdj.2009.517.
- The Centre for Reviews and Dissemination . Prophylactic removal of impacted third molars: is it justified?. Br J Orthod 1999;26:149-51. https://doi.org/10.1093/ortho/26.2.149.
- Baykul T, Saglam AA, Aydin U, Başak K. Incidence of cystic changes in radiographically normal impacted lower third molar follicles. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005;99:542-5. https://doi.org/10.1016/j.tripleo.2004.08.010.
- Blakey GH, Gelesko S, Marciani RD, Haug RH, Offenbacher S, Phillips C, et al. Third molars and periodontal pathology in American adolescents and young adults: a prevalence study. J Oral Maxillofac Surg 2010;68:325-9. https://doi.org/10.1016/j.joms.2009.04.123.
- Blakey GH, Golden BA, White RP, Offenbacher S, Phillips C, Haug RH. Changes over time in the periodontal status of young adults with no third molar periodontal pathology at enrollment. J Oral Maxillofac Surg 2009;67:2425-30. https://doi.org/10.1016/j.joms.2008.12.064.
- Blakey GH, Hull DJ, Haug RH, Offenbacher S, Phillips C, White RP. Changes in third molar and nonthird molar periodontal pathology over time. J Oral Maxillofac Surg 2007;65:1577-83. https://doi.org/10.1016/j.joms.2006.10.011.
- Blakey GH, Jacks MT, Offenbacher S, Nance PE, Phillips C, Haug RH, et al. Progression of periodontal disease in the second/third molar region in subjects with asymptomatic third molars. J Oral Maxillofac Surg 2006;64:189-93. https://doi.org/10.1016/j.joms.2005.10.014.
- Blakey GH, Marciani RD, Haug RH, Phillips C, Offenbacher S, Pabla T, et al. Periodontal pathology associated with asymptomatic third molars. J Oral Maxillofac Surg 2002;60:1227-33. https://doi.org/10.1053/joms.2002.35717.
- Blakey GH, Parker DW, Hull DJ, White RP, Offenbacher S, Phillips C, et al. Impact of removal of asymptomatic third molars on periodontal pathology. J Oral Maxillofac Surg 2009;67:245-50. https://doi.org/10.1016/j.joms.2008.08.022.
- Divaris K, Fisher EL, Shugars DA, White RP. Risk factors for third molar occlusal caries: a longitudinal clinical investigation. J Oral Maxillofac Surg 2012;70:1771-80. https://doi.org/10.1016/j.joms.2011.12.035.
- Phillips C, Norman J, Jaskolka M, Blakey GH, Haug RH, Offenbacher S, et al. Changes over time in position and periodontal probing status of retained third molars. J Oral Maxillofac Surg 2007;65:2011-17. https://doi.org/10.1016/j.joms.2006.11.055.
- Shugars DA, Elter JR, Jacks MT, White RP, Phillips C, Haug RH, et al. Incidence of occlusal dental caries in asymptomatic third molars. J Oral Maxillofac Surg 2005;63:341-6. https://doi.org/10.1016/j.joms.2004.11.009.
- Shugars DA, Jacks MT, White RP, Phillips C, Haug RH, Blakey GH. Occlusal caries experience in patients with asymptomatic third molars. J Oral Maxillofac Surg 2004;62:973-9. https://doi.org/10.1016/j.joms.2003.08.040.
- Bloomer CR. Alveolar osteitis prevention by immediate placement of medicated packing. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000;90:282-4. https://doi.org/10.1067/moe.2000.108919.
- Brann CR, Brickley MR, Shepherd JP. Factors influencing nerve damage during lower third molar surgery. Br Dent J 1999;186:514-16. https://doi.org/10.1038/sj.bdj.4800155.
- Chaparro-Avendaño AV, Pérez-García S, Valmaseda-Castellón E, Berini-Aytés L, Gay-Escoda C. Morbidity of third molar extraction in patients between 12 and 18 years of age. Med Oral Patol Oral Cir Bucal 2005;10:422-31.
- Cunha-Cruz J, Rothen M, Spiekerman C, Drangsholt M, McClellan L, Huang GJ. Northwest Practice-Based Research Collaborative in Evidence-Based Dentistry . Recommendations for third molar removal: a practice-based cohort study. Am J Public Health 2014;104:735-43. https://doi.org/10.2105/AJPH.2013.301652.
- Huang GJ, Cunha-Cruz J, Rothen M, Spiekerman C, Drangsholt M, Anderson L, et al. A prospective study of clinical outcomes related to third molar removal or retention. Am J Public Health 2014;104:728-34. https://doi.org/10.2105/AJPH.2013.301649.
- Dicus C, Blakey GH, Faulk-Eggleston J, Hoverstad E, Offenbacher S, Phillips C, et al. Second molar periodontal inflammatory disease after third molar removal in young adults. J Oral Maxillofac Surg 2010;68:3000-6. https://doi.org/10.1016/j.joms.2010.05.055.
- Faria AI, Gallas-Torreira M, López-Ratón M. Mandibular second molar periodontal healing after impacted third molar extraction in young adults. J Oral Maxillofac Surg 2012;70:2732-41. https://doi.org/10.1016/j.joms.2012.07.044.
- Faria AI, Gallas-Torreira M, López-Ratón M, Crespo-Vázquez E, Rodríguez-Núñez I, López-Castro G. Radiological infrabony defects after impacted mandibular third molar extractions in young adults. J Oral Maxillofac Surg 2013;71:2020-8. https://doi.org/10.1016/j.joms.2013.07.029.
- Figueiredo R, Valmaseda-Castellón E, Berini-Aytés L, Gay-Escoda C. Incidence and clinical features of delayed-onset infections after extraction of lower third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005;99:265-9. https://doi.org/10.1016/j.tripleo.2004.06.004.
- Güven O, Keskin A, Akal UK. The incidence of cysts and tumors around impacted third molars. Int J Oral Maxillofac Surg 2000;29:131-5. https://doi.org/10.1016/S0901-5027(00)80011-9.
- Hanson BP, Cummings P, Rivara FP, John MT. The association of third molars with mandibular angle fractures: a meta-analysis. J Can Dent Assoc 2004;70:39-43.
- Juhl GI, Svensson P, Norholt SE, Jensen TS. Long-lasting mechanical sensitization following third molar surgery. J Orofac Pain 2006;20:59-73.
- Juhl GI, Jensen TS, Norholt SE, Svensson P. Central sensitization phenomena after third molar surgery: a quantitative sensory testing study. Eur J Pain 2008;12:116-27. https://doi.org/10.1016/j.ejpain.2007.04.002.
- Kucukkolbasi H, Esen A, Erinanc OH. Immunohistochemical analysis of Ki-67 in dental follicle of asymptomatic impacted third molars. J Oral Maxillofac Pathol 2014;18:189-93. https://doi.org/10.4103/0973-029X.140737.
- Monaco G, Tavernese L, Agostini R, Marchetti C. Evaluation of antibiotic prophylaxis in reducing postoperative infection after mandibular third molar extraction in young patients. J Oral Maxillofac Surg 2009;67:1467-72. https://doi.org/10.1016/j.joms.2008.12.066.
- Montevecchi M, Incerti Parenti S, Checchi V, Palumbo B, Checchi L, Alessandri Bonetti G. Periodontal healing after ‘orthodontic extraction’ of mandibular third molars: a retrospective cohort study. Int J Oral Maxillofac Surg 2014;43:1137-41. https://doi.org/10.1016/j.ijom.2014.03.015.
- Naghipur S, Shah AA, Elgazzar RF. The effect of lower third molar presence and position on fracture of the mandibular angle and condyle. J Oral Maxillofac Surg 2013;71:e95-e96. https://doi.org/10.1016/j.joms.2013.06.177.
- Naghipur S, Shah A, Elgazzar RF. Does the presence or position of lower third molars alter the risk of mandibular angle or condylar fractures?. J Oral Maxillofac Surg 2014;72:1766-72. https://doi.org/10.1016/j.joms.2014.04.004.
- Ozeç I, Hergüner Siso S, Taşdemir U, Ezirganli S, Göktolga G. Prevalence and factors affecting the formation of second molar distal caries in a Turkish population. Int J Oral Maxillofac Surg 2009;38:1279-82. https://doi.org/10.1016/j.ijom.2009.07.007.
- Pepper T, Konarzewski T, Grimshaw P, Combes J. Frequency of caries in the distal surface of mandibular second molars with reference to third molar position. Br J Oral Maxillofac Surg 2012;50. https://doi.org/10.1016/j.bjoms.2012.04.188.
- Phillips C, White RP. How predictable is the position of third molars over time?. J Oral Maxillofac Surg 2012;70:11-4. https://doi.org/10.1016/j.joms.2012.04.024.
- Poeschl PW, Eckel D, Poeschl E. Postoperative prophylactic antibiotic treatment in third molar surgery – a necessity?. J Oral Maxillofac Surg 2004;62:3-8. https://doi.org/10.1016/j.joms.2003.05.004.
- Polat HB, Ozan F, Kara I, Ozdemir H, Ay S. Prevalence of commonly found pathoses associated with mandibular impacted third molars based on panoramic radiographs in Turkish population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008;105:e41-7. https://doi.org/10.1016/j.tripleo.2008.02.013.
- Sarikov R, Juodzbalys G. Inferior alveolar nerve injury after mandibular third molar extraction: a literature review. J Oral Maxillofac Res 2014;5. https://doi.org/10.5037/jomr.2014.5401.
- Şimşek-Kaya G, Melih-Ömezli M, Yapici G, Dayi E, Ertaş U. Prevalence of impacted premolars in a Turkish population and considerations for surgical treatment. Med Oral Patol Oral Cir Bucal 2011;16:e781-6. https://doi.org/10.4317/medoral.17027.
- Ventä I, Turtola L, Ylipaavalniemi P. Change in clinical status of third molars in adults during 12 years of observation. J Oral Maxillofac Surg 1999;57:386-9. https://doi.org/10.1016/S0278-2391(99)90273-2.
- Ventä I, Turtola L, Ylipaavalniemi P. Radiographic follow-up of impacted third molars from age 20 to 32 years. Int J Oral Maxillofac Surg 2001;30:54-7. https://doi.org/10.1054/ijom.2000.0002.
- Ventä I, Ylipaavalniemi P, Turtola L. Long-term evaluation of estimates of need for third molar removal. J Oral Maxillofac Surg 2000;58:288-91. https://doi.org/10.1016/S0278-2391(00)90055-7.
- Vondeling H, Maningky M, Bezemer D, Smeele LE, Baart JA, Waal I. Issues in the Design and Preliminary Results of a Randomized Controlled Trial Comparing the Effects and Costs of Preventive Removal of Third Molars Versus Removal on Indication n.d.
- von Wowern N, Nielsen HO. The fate of impacted lower third molars after the age of 20. A four-year clinical follow-up. Int J Oral Maxillofac Surg 1989;18:277-80. https://doi.org/10.1016/s0901-5027(89)80094-3.
- Garcia RI, Chauncey HH. The eruption of third molars in adults: a 10-year longitudinal study. Oral Surg Oral Med Oral Pathol 1989;68:9-13. https://doi.org/10.1016/0030-4220(89)90107-2.
- van der Sanden WJ, Mettes DG, Plasschaert AJ, Grol RP, Mulder J, Verdonschot EH. Effectiveness of clinical practice guideline implementation on lower third molar management in improving clinical decision-making: a randomized controlled trial. Eur J Oral Sci 2005;113:349-54. https://doi.org/10.1111/j.1600-0722.2005.00232.x.
- van de Waal I. Amsterdam: Free University Amsterdam Department of Oral and Maxillofacial Surgery; 1999.
- Berge TI. Incidence of chronic neuropathic pain subsequent to surgical removal of impacted third molars. Acta Odontol Scand 2002;60:108-12. https://doi.org/10.1080/000163502753509518.
- Gülicher D, Gerlach KL. Sensory impairment of the lingual and inferior alveolar nerves following removal of impacted mandibular third molars. Int J Oral Maxillofac Surg 2001;30:306-12. https://doi.org/10.1054/ijom.2001.0057.
- Hill CM, Mostafa P, Thomas DW, Newcombe RG, Walker RV. Nerve morbidity following wisdom tooth removal under local and general anaesthesia. Br J Oral Maxillofac Surg 2001;39:419-22. https://doi.org/10.1054/bjom.2001.0723.
- Rakprasitkul S. Pathologic changes in the pericoronal tissues of unerupted third molars. Quintessence Int 2001;32:633-8.
- Renton T, McGurk M. Evaluation of factors predictive of lingual nerve injury in third molar surgery. Br J Oral Maxillofac Surg 2001;39:423-8. https://doi.org/10.1054/bjom.2001.0682.
- Tay S. Third molar surgery under local anaesthesia – a clinical audit. Singapore Dent J 2000;23:11-3.
- Valmaseda-Castellón E, Berini-Aytés L, Gay-Escoda C. Lingual nerve damage after third lower molar surgical extraction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000;90:567-73. https://doi.org/10.1067/moe.2000.110034.
- White RP, Madianos PN, Offenbacher S, Phillips C, Blakey GH, Haug RH, et al. Microbial complexes detected in the second/third molar region in patients with asymptomatic third molars. J Oral Maxillofac Surg 2002;60:1234-40. https://doi.org/10.1053/joms.2002.35718.
- Yamaoka M, Furusawa K, Ikeda M, Hasegawa T. Root resorption of mandibular second molar teeth associated with the presence of the third molars. Aust Dent J 1999;44:112-16. https://doi.org/10.1111/j.1834-7819.1999.tb00211.x.
- Yoshii T, Hamamoto Y, Muraoka S, Kohjitani A, Teranobu O, Furudoi S, et al. Incidence of deep fascial space infection after surgical removal of the mandibular third molars. J Infect Chemother 2001;7:55-7. https://doi.org/10.1007/s101560170036.
- Güngörmüs M. Pathologic status and changes in mandibular third molar position during orthodontic treatment. J Contemp Dent Pract 2002;3:11-22. https://doi.org/10.5005/jcdp-3-2-11.
- Shafer DM, Frank ME, Gent JF, Fischer ME. Gustatory function after third molar extraction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999;87:419-28. https://doi.org/10.1016/S1079-2104(99)70240-4.
- Kan KW, Liu JK, Lo EC, Corbet EF, Leung WK. Residual periodontal defects distal to the mandibular second molar 6-36 months after impacted third molar extraction. J Clin Periodontol 2002;29:1004-11. https://doi.org/10.1034/j.1600-051X.2002.291105.x.
- Libersa P, Roze D, Cachart T, Libersa JC. Immediate and late mandibular fractures after third molar removal. J Oral Maxillofac Surg 2002;60:163-5. https://doi.org/10.1053/joms.2002.29811.
- Ma’aita J, Alwrikat A. Is the mandibular third molar a risk factor for mandibular angle fracture?. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000;89:143-6. https://doi.org/10.1067/moe.2000.103527.
- Perry PA, Goldberg MH. Late mandibular fracture after third molar surgery: a survey of Connecticut oral and maxillofacial surgeons. J Oral Maxillofac Surg 2000;58:858-61. https://doi.org/10.1053/joms.2000.8204.
- Punwutikorn J, Waikakul A, Ochareon P. Symptoms of unerupted mandibular third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999;87:305-10. https://doi.org/10.1016/S1079-2104(99)70213-1.
- Brickley M, Kay E, Shepherd JP, Armstrong RA. Decision analysis for lower-third-molar surgery. Med Decis Making 1995;15:143-51. https://doi.org/10.1177/0272989X9501500207.
- Tulloch JF, Antczak-Bouckoms AA. Decision analysis in the evaluation of clinical strategies for the management of mandibular third molars. J Dent Educ 1987;51:652-60.
- Tulloch JF, Antczak-Bouckoms AA, Ung N. Evaluation of the costs and relative effectiveness of alternative strategies for the removal of mandibular third molars. Int J Technol Assess Health Care 1990;6:505-15. https://doi.org/10.1017/s0266462300004177.
- Toth B. The Appropriateness of Prophylactic Extraction of Impacted Third Molars. A Review of the Literature. Bristol: Health Care Evaluation Unit, University of Bristol; 1993.
- Stephens RG, Kogon SL, Reid JA. The unerupted or impacted third molar – a critical appraisal of its pathologic potential. J Can Dent Assoc 1989;55:201-7.
- Mercier P, Precious D. Risks and benefits of removal of impacted third molars. A critical review of the literature. Int J Oral Maxillofac Surg 1992;21:17-2. https://doi.org/10.1016/s0901-5027(05)80447-3.
- Daley TD. Third molar prophylactic extraction: a review and analysis of the literature. Gen Dent 1996;44:310-20.
- Vasir NS, Robinson RJ. The mandibular third molar and late crowding of the mandibular incisors – a review. Br J Orthod 1991;18:59-66. https://doi.org/10.1179/bjo.18.1.59.
- Anderson M. Removal of asymptomatic third molars: indications, contraindications, risks and benefits. J Indiana Dent Assoc 1998;77:41-6.
- Bertrand G. La dent de sagesse. Question mise en discussion. Orthod Fr 1989;60.
- Bishara SE. Third molars: a dilemma! Or is it?. Am J Orthod Dentofacial Orthop 1999;115:628-33. https://doi.org/10.1016/S0889-5406(99)70287-8.
- Bonetti GA, Prati C, Graziani E. The third molar: evaluation of its role and indications for extraction. Dent Cadmos 1988;56:56-60.
- Bramante MA. Controversies in orthodontics. Dent Clin North Am 1990;34:91-102.
- Brokaw WC. The third molar question: when and why should we recommend removal?. Va Dent J 1991;68:18-21.
- Cade TA. Paresthesia of the inferior alveolar nerve following the extraction of the mandibular third molars: a literature review of its causes, treatment, and prognosis. Mil Med 1992;157:389-92. https://doi.org/10.1093/milmed/157.8.389.
- Chikhani L, Cartier S, Elamrani K, Guilbert F. Lésions du nerf lingual au cours de l’extraction de la dent de sagesse mandibulaire. Conséquences. Etiopathogénie. Prévention. Evolution. Aspects médicaux légaux. Rev Stomatol Chir Maxillofac 1994;95:369-73.
- Dénes J, Dénes Z, Kaán M. Indications for Preventive Removal of Impacted Third Molars 1993;86:227-30.
- Emergency Care Research Institute (ECRI) . Removal of Third Molars n.d.
- Forssel H, Miettinen J. Indications for the extraction of mandibular third molars. Suom Hammaslaakarilehti 1988;35:1078-81.
- Garattini G, Grecchi MT, Vogel G. Role of lower third molars in the development of dental malocclusion: review of the literature. Mondo Ortod 1990;15:145-50.
- Goia F, Gilardino M, Cappella M, Bruno GB. Third molar: evaluation and indications for extraction from an orthodontic point of view. Minerva Ortognatod 1990;8:135-8.
- Pajarola GF. Extraction chirurgicale des dents de sagesse inferieures (II). Schweizerische Monatsschrift für Zahnmedizin 1994;104:1531-48.
- Kugelberg CF. Third molar surgery. Curr Opin Dent 1992;2:9-16.
- Lechien P. Should we or should we not extract impacted teeth. Rev Belge Med Dent 1995;50:29-3.
- Mommaerts M, Jacobs W. Lingual nerve injury during extraction of lower wisdom teeth. Rev Belge Med Dent 1991;46:27-46.
- Peterson LJ. Rationale for removing impacted teeth: when to extract or not to extract. J Am Dent Assoc 1992;123:198-204. https://doi.org/10.14219/jada.archive.1992.0160.
- Robinson RJ, Vasir NS. The great eights debate: do the mandibular third molars affect incisor crowding? A review of the literature. Dent Update 1993;20:242-6.
- Robinson PD. The impacted lower wisdom tooth: to remove or to leave alone?. Dent Update 1994;21:245-8.
- Sands T, Pynn BR, Nenniger S. Third molar surgery: current concepts and controversies. Part 2. Oral Health 1993;83.
- Sands T, Pynn BR, Nenniger S. Third molar surgery: current concepts and controversies. Part 1. Oral Health 1993;83.
- Southard TE. Third molars and incisor crowding: when removal is unwarranted. J Am Dent Assoc 1992;123:75-9. https://doi.org/10.14219/jada.archive.1992.0224.
- Tate TE. Impactions: observe or treat?. J Calif Dent Assoc 1994;22:59-64.
- Tealdi R, Domini R. Indications for extraction of the impacted 3d molar in an orthodontic treatment program. A review of the literature. Minerva Stomatol 1986;35:461-3.
- Torres J. Bénéfices et risques des avulsions de dents de sagesse. Rev Stomatol Chir Maxillofac 1997;98:173-78.
- van der Linden WJ, Lownie JF, Cleaton-Jones PE. Should impacted third molars be removed? A review of the literature. J Dent Assoc S Afr 1993;48:235-40.
- Waite PD, Reynolds RR. Surgical management of impacted third molars. Semin Orthod 1998;4:113-23. https://doi.org/10.1016/s1073-8746(98)80008-x.
- Weisenfeld MD, Kondis SL. Prophylactic removal of impacted third molars, revisited. Gen Dent 1991;39:344-5.
- Falci SG, de Castro CR, Santos RC, de Souza Lima LD, Ramos-Jorge ML, Botelho AM, et al. Association between the presence of a partially erupted mandibular third molar and the existence of caries in the distal of the second molars. Int J Oral Maxillofac Surg 2012;41:1270-4. https://doi.org/10.1016/j.ijom.2012.03.003.
- McArdle LW, Renton TF. Distal cervical caries in the mandibular second molar: an indication for the prophylactic removal of the third molar?. Br J Oral Maxillofac Surg 2006;44:42-5. https://doi.org/10.1016/j.bjoms.2005.07.025.
- Blondeau F, Daniel NG. Extraction of impacted mandibular third molars: postoperative complications and their risk factors. J Can Dent Assoc 2007;73.
- Chang SW, Shin SY, Kum KY, Hong J. Correlation study between distal caries in the mandibular second molar and the eruption status of the mandibular third molar in the Korean population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;108:838-43. https://doi.org/10.1016/j.tripleo.2009.07.025.
- NHS Digital . Hospital Episode Statistics n.d. www.hscic.gov.uk/hes (accessed 3 March 2016).
- Kang F, Huang C, Sah MK, Jiang B. Effect of eruption status of the mandibular third molar on distal caries in the adjacent second molar. J Oral Maxillofac Surg 2016;74:684-92. https://doi.org/10.1016/j.joms.2015.11.024.
- McArdle L. NICE and the third molar debate. Fac Dental J 2013;4:166-71. https://doi.org/10.1308/204268513X13776914744718.
- Oderinu OH, Adeyemo WL, Adeyemi MO, Nwathor O, Adeyemi MF. Distal cervical caries in second molars associated with impacted mandibular third molars: a case-control study. Oral Surg Oral Med Oral Pathol Oral Radiol 2012. https://doi.org/10.1016/j.oooo.2012.03.039.
- Ozgun AN, Sherriff M, Renton T. An Assessment of Lower Third Molar Treatment Needs n.d.
- World Health Organization (WHO) . International Statistical Classification of Diseases and Related Health Problems. Tenth Revision (ICD-10) 2010.
- Haug RH, Perrott DH, Gonzalez ML, Talwar RM. The American Association of Oral and Maxillofacial Surgeons Age-Related Third Molar Study. J Oral Maxillofac Surg 2005;63:1106-14. https://doi.org/10.1016/j.joms.2005.04.022.
Appendix 1 Literature search strategies
The Cochrane Library
Cochrane Database of Systematic Reviews/Cochrane Central Register Of Controlled Trials/Database of Abstracts of Reviews of Effects (DARE)/Health Technology Assessments
Date range searched: 1999 to 29 April 2016.
Date searched: 29 April 2016.
Search strategy
| # | Search | Hits (n) |
|---|---|---|
| 1 | MeSH descriptor: [Molar, Third] explode all trees | 836 |
| 2 | ((third or three) near/1 molar*) | 1756 |
| 3 | (wisdom near/1 (tooth or teeth)) | 180 |
| 4 | (itm or itms) | 69 |
| 5 | M3 and (tooth or teeth) | 19 |
| 6 | MeSH descriptor: [Tooth, Impacted] explode all trees | 506 |
| 7 | (impact* near/1 (tooth or teeth)) | 598 |
| 8 | #1 or #2 or #3 or #4 or #5 or #6 or #7 Publication Year from 1999 | 1318 |
| 9 | age determin* | 39,875 |
| 10 | MeSH descriptor: [Age Determination by Teeth] explode all trees | 5 |
| 11 | #9 or #10 | 39,875 |
| 12 | #8 not #11 | 1206 |
MEDLINE
Date range searched: 1999 to 29 April 2016.
Date searched: 29 April 2016.
Search strategy
| # | Search | Hits (n) |
|---|---|---|
| 1 | Molar, Third/ | 5258 |
| 2 | ((third or three) adj1 molar*).tw. | 6535 |
| 3 | (wisdom adj1 (tooth or teeth)).tw. | 937 |
| 4 | Tooth, Impacted/ | 5989 |
| 5 | (impact* adj1 (tooth or teeth)).tw. | 1066 |
| 6 | (itm or itms).tw. | 491 |
| 7 | 1 or 2 or 3 or 4 or 5 or 6 | 12,952 |
| 8 | M3.tw. | 17,929 |
| 9 | (tooth or teeth).tw. | 114,879 |
| 10 | 8 and 9 | 147 |
| 11 | 7 or 10 | 13,039 |
| 12 | limit 11 to yr = “1999 -Current” | 7043 |
| 13 | animal/not human/ | 4,178,280 |
| 14 | 12 not 13 | 6746 |
| 15 | limit 14 to english language | 6312 |
| 16 | comment/or editorial/or letter/or news/ | 1,532,370 |
| 17 | 15 not 16 | 6033 |
| 18 | Age Determination by Teeth/ | 1410 |
| 19 | “age determin*”.tw. | 898 |
| 20 | 18 or 19 | 2146 |
| 21 | 17 not 20 | 5895 |
EMBASE
Date range searched: 1999 to 29 April 2016.
Date searched: 29 April 2016.
Search strategy
| # | Search | Hits (n) |
|---|---|---|
| 1 | Molar, Third/ | 24,449 |
| 2 | ((third or three) adj1 molar*).tw. | 7130 |
| 3 | (wisdom adj1 (tooth or teeth)).tw. | 1068 |
| 4 | Tooth, Impacted/ | 16,122 |
| 5 | (impact* adj1 (tooth or teeth)).tw. | 1162 |
| 6 | (itm or itms).tw. | 825 |
| 7 | 1 or 2 or 3 or 4 or 5 or 6 | 42,489 |
| 8 | M3.tw. | 34,492 |
| 9 | (tooth or teeth).tw. | 123,929 |
| 10 | 8 and 9 | 231 |
| 11 | 7 or 10 | 42,616 |
| 12 | limit 11 to yr = “1999 -Current” | 20,887 |
| 13 | animal/not human/ | 1,297,895 |
| 14 | 12 not 13 | 19,854 |
| 15 | limit 14 to english language | 18,383 |
| 16 | comment/or editorial/or letter/or news/ | 1,398,219 |
| 17 | 15 not 16 | 17,982 |
| 18 | Age Determination by Teeth/ | 5092 |
| 19 | (age adj2 (determin* or estimat*)).tw. | 15,389 |
| 20 | 18 or 19 | 18,641 |
| 21 | 17 not 20 | 17,719 |
| 22 | limit 21 to embase | 6238 |
EconLit
Search strategy
| # | Search | Hits (n) |
|---|---|---|
| S1 | ((third or three) N1 molar*) | 0 |
| S2 | (wisdom N1 (tooth or teeth)) | 0 |
| S3 | (impact* N1 (tooth or teeth)) | 0 |
| S4 | (itm or itms) | 32 |
| S5 | M3 AND (teeth or tooth) | 0 |
| S6 | S1 OR S2 OR S3 OR S4 OR S5 | 32 |
| S7 | age determination on teeth | 0 |
| S8 | “age determin*” | 6 |
| S9 | (S7 OR S8) | 6 |
| S10 | (S6 NOT S9) | 32 |
NHS Economic Evaluation Database
Date searched: 29 April 2016.
Search strategy
| # | Search | Hits (n) |
|---|---|---|
| 1 | mandibular wisdom teeth | 3 |
Appendix 2 Excluded studies
Reasons for exclusion of clinical studies excluded at full-text review
| Reason for exclusion | Number of studies |
|---|---|
| Wrong design | 61 |
| Non-SR | 24 |
| Non-English language | 8 |
| Wrong setting | 87 |
| No relevant outcomes | 20 |
| Not M3M | 24 |
| Not impacted | 13 |
| Not pathology free or trouble free | 114 |
| Total | 351 |
Reasons for exclusion of clinical studies excluded at data abstraction
| Reason for exclusion | Number of studies |
|---|---|
| Ahmad et al. 200810 | Not impacted |
| Al-Belasy et al. 2009111 | Not pathology free or trouble free |
| Allen et al. 2009112 | No data for impacted pathology free/trouble free |
| The Centre for Review on Dissemination 1999113 | Reprint of an article based on Song et al. 199764 |
| Baykul et al. 2005114 | Not pathology free or trouble free |
| Blakey et al. 2010115 | Not all impacted, not all M3Ms, no relevant outcomes reported for IM3Ms |
| Blakey et al. 2009116 | |
| Blakey et al. 2007117 | |
| Blakey et al. 2006118 | |
| Blakey et al. 2002119 | |
| Blakey et al. 2009120 | |
| Divaris et al. 2012121 | |
| Phillips et al. 2007122 | |
| Shugars et al. 2005123 | |
| Shugars et al. 2004124 | |
| Bloomer 2000125 | Not pathology free or trouble free |
| Brann et al. 1999126 | Not pathology free or trouble free |
| Chaparro-Avendaño et al. 2005127 | No results for impacted pathology free or trouble free |
| Cunha-Cruz et al. 2014128 | Not all impacted pathology-free or trouble-free M3Ms |
| Huang et al. 2014129 | |
| Dicus et al. 2010130 | Not results for impacted, mandibular pathology-free or trouble-free teeth |
| Faria et al. 2012131 | No relevant outcomes |
| Faria et al. 2013132 | |
| Figueiredo et al. 2005133 | Not pathology free or trouble free |
| Güven et al. 2000134 | No results for impacted pathology free or trouble free |
| Hanson et al. 2004135 | Not impacted |
| Juhl et al. 2006136 | Not pathology free or trouble free |
| Juhl et al. 2008137 | Not pathology free or trouble free |
| Kucukkolbasi et al. 2014138 | No relevant outcomes |
| Monaco et al. 2009139 | Not pathology free or trouble free |
| Montevecchi et al. 2014140 | Not pathology free or trouble free |
| Naghipur et al. 2013141 | Not pathology free or trouble free |
| Naghipur et al. 2014142 | Not pathology free or trouble free |
| Nunn et al. 201312 | No results for impacted pathology-free or trouble-free M3Ms |
| Ozeç et al. 2009143 | No results for impacted pathology free or trouble free |
| Pepper et al. 2012144 | Not pathology free or trouble free |
| Phillips et al. 200392 | No relevant outcomes |
| Phillips et al. 2012145 | No relevant outcomes |
| Poeschl et al. 2004146 | 94% impacted but not pathology free/trouble free |
| Polat et al. 2008147 | Not pathology free or trouble free |
| Sarikov and Juodzbalys 2014148 | Not pathology free or trouble free |
| Şimşek-Kaya et al. 2011149 | Premolars |
|
Ventä et al. 1999150 Ventä et al. 2001151 Ventä et al. 2000152 Ventä et al. 200465 |
No relevant outcomes reported by impacted M3Ms |
| Vondeling et al. 1999153 | Not impacted |
| Yildirim et al. 200815 | No relevant outcomes |
Bibliographic details and data summaries of five studies initially included in the economic evidence review and subsequently excluded
| Study | Country | 3Ms or I3Ms | Study design/purpose | Comparators | Reported measures | Cost/outcome source | Time horizon | Cost year |
|---|---|---|---|---|---|---|---|---|
| Inverso et al. 201471 | USA | 3Ms | Microcosting analysis | S1: extraction of four symptom-free, disease-free 3Ms. S2: active surveillance of four symptom-free, disease free 3Ms | S1: average time and cost by visit type (consultation, operative and post-operative) for extraction of four 3Ms; S2: cost of surveillance visit by an oral and maxillofacial surgeon every 2 years | Private health care | 10, 20 and 30 years for S2 | 2013 estimates |
| Koumaras 201272 | USA | 3Ms and I3Ms | Financial analysis of claims data | Operative vs. non-operative management of asymptomatic, disease-free 3Ms and I3Ms | S1: retention of asymptomatic, disease-free 3Ms for 20 years; S2: removal of asymptomatic, disease-free I3Ms; S3: removal of previously asymptomatic, disease-free I3M that was monitored for 10 years | Insurance claims data | S1: 20 years. S2: not provided. S3: 10 years | Services provided in the 2009 calendar year |
| Kunkel et al. 200674 | Germany | 3Ms | Prospective cohort study of patients who were admitted to hospital for management of 3M-associated complications | A: Prophylactic 3M removal. B: non-elective 3M removal. C: 3M present at time of admission | Infection parameters, treatment costs, length of hospital stay, days of disability, post-operative complications (A and B) were compared with complications based on pericoronitis | German NHS: diagnostic-related group rates for hospital treatment | Patients presenting over a 2-year period | 2004–5 |
| Kunkel et al. 200773 | NA | |||||||
| Liedholm et al. 200575 | Sweden and Wales (UK) | 3Ms | Comparison of patient preferences using the multiattribute utility method | Patients referred (1997/8) for removal of one or both of their M3Ms | Home and social life; general health and well-being; job and studies; health and comfort of mouth, teeth and gums; appearance | Patient interviews | Interviews took place in the clinic immediately after consultation | NA |
Appendix 3 Quality assessment
Quality assessment of systematic reviews
| Study question | Study | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Bouloux et al. 201544 | Clinical evidence56 | CADTH 201042 | Costa et al. 201345 | Mettes et al. 201246 | aSenter for Medisinsk Metodevurdering50 | Song et al. 200020 | Stordeur and Eyssen 201240 | Suska et al. 201043 | |
| Was the review question clearly defined in terms of population, interventions, comparators, outcomes and study designs? | Yes | Partially | Yes | Partially | Yes | Unclear | Yes | Yes | Yes |
| Was the search strategy adequate and appropriate? Were there any restrictions on language, publication status or publication date? | Partially | Partially | No | Yes | Yes | Partially | Yes | Partially | Partially |
| Were preventative steps taken to minimise bias and errors in the study selection process? | Unclear | Unclear | Unclear | Unclear | Yes | Unclear | Yes | Yes | Unclear |
| Were appropriate criteria used to assess the quality of the primary studies, and were preventative steps taken to minimise bias and errors in the quality assessment process? | Unclear | Unclear | Unclear | Yes | Yes | Unclear | Yes | Yes | Partially |
| Were preventative steps taken to minimise bias and errors in the data extraction process? | Yes | NS | NS | Yes | Yes | Unclear | Yes | Yes | Unclear |
| Were adequate details presented for each of the primary studies? | Yes | Yes | Partially | Partially | Yes | Yes | Yes | Yes | Yes |
| Were appropriate methods used for data synthesis? Were differences between studies assessed? Were the studies pooled, and if so was it appropriate and meaningful to do so? | Yes | Yes | No | No | NA | Unclear | No | No | No |
| Do the authors’ conclusions accurately reflect the evidence that was reviewed? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
Appendix 4 Data abstraction tables
Characteristics of the study comparing prophylactic removal with retention and standard care
| Characteristic | Study |
|---|---|
| Vares and Kyyak 201458 | |
| Aim | The aim of our investigation was to systematize a scheme of objective preoperative clinical and roentgenological assessment of mandibular impacted symptom-free ‘wisdom teeth’ to create a rationale for their prophylactic removal |
| Conclusion | The low-to-no percentage of intra- and postoperative complications does not give any reason to leave a wisdom tooth with minor clinical manifestations or an asymptomatic wisdom tooth with bad prognosis in place, since early surgical procedures generate less number of complications, having shorter operative time and postoperative period |
| Design | Prospective cohort study |
| Setting | Department of Surgical Dentistry and Maxillofacial Surgery of Lviv Danylo Halytsky National Medical University, Ukraine |
| Recruitment period/follow-up | 2009–13/annual follow-up, 5 years |
| Sponsorship/conflict of interests | NR/NR |
| Power | NR |
| Description of IM3Ms, total | 84 patients with asymptomatic IM3Ms with no considerable pathological changes |
| Inclusion/exclusion criteria | NR |
| Demographics | NR |
| Baseline assessments (assessment of requirement for removal) |
|
| Results of assessment and description of groups |
|
| Details of surgery/anaesthesia/surgeon | The third molar removal was conducted using the surgical bur technique. In accordance with the severity of impaction, a proper incision and tooth sectioning were made following the strict conventional scheme and with a minimisation of the distal bone removal and the operative time |
Outcomes of prophylactic removal versus retention and standard care study
| Group | Outcomes | Results |
|---|---|---|
| Removal (n = 52) | Surgical complications | NRNo considerable intra- or post-operative complications in the first subgroup (41 cases of patients 18–25 years old); minor complications in the second subgroup (10 cases of 25–45 year old patients). In the case of 68 year-old patient, all complications were related to considerable bone atrophy of the operated area |
| Retention though requiring removal (n = 7) | Removed during follow-up because of the appearance of indications | 5/7 teeth |
| Retention (n = 25) | Removed during follow-up because of the appearance of indications | 0/25 teeth |
Study characteristics of retention and standard care studies
| Study | Characteristic | |||||||
|---|---|---|---|---|---|---|---|---|
| Aim | Conclusion | Design | Setting | Recruitment period; follow-up | Sponsorship; conflict of interests | Power | Outcomes | |
| Fernandes et al. 201048 |
|
Older patients are less likely to develop the symptoms studied. In addition the authors believe that there is evidence to suggest that general dental practitioners might not be following current guidelines when deciding whether or not to extract an impacted lower third molar in the centres studied | Prospective cohort study | Multicentre, Scotland, UK (primary care setting) | 1995–2002; 12 months | The Wellcome Trust (061636/HS/SH/MW/sf). Professor Pitts acknowledges support from the Chief Scientist Office, which core funds the Dental Health Services Research Unit | NR |
|
| Hill and Walker 200647 | Find out what happened over a period of 5 years to fully or partially impacted M3Ms that were left alone |
|
Prospective cohort study | Unclear but likely single centre, Cardiff, UK | NR; 5 years | Partly funded by a grant from the Leeds Oral Surgery Trust | Based on various assumptions about the incidence of pericoronitis, a minimum of 200 patients would be needed to complete the study |
|
Participant characteristics of retention and standard care studies
| Study | Characteristic | |||
|---|---|---|---|---|
| Description of I3Ms (n) | Inclusion/exclusion criteria | Demographics | Baseline assessments | |
| Fernandes et al. 201048 | n = 421 (69% of 613 assessed at baseline); lower I3Ms examined, n = 676 | Inclusion:
|
|
Clinical characteristics (reported by sex and age group):
|
| Hill 200668 |
|
Inclusion:
|
|
|
Outcomes of retention and standard care studies
| Study | Outcomes assessed | Rate, n (%) (unless otherwise stated) | p-value | How it was measured; timing; analysis |
|---|---|---|---|---|
| Fernandes et al. 201048 | Teeth extracted | 37 (5.47) | Questions and assessed by research dentist; 1 year; NA | |
| Reasons for extraction | ||||
| Pericoronitis | 5 (13.5) | |||
| Pain | 10 (27.0) | |||
| Caries in distal of adjacent molar | 1 (2.7) | |||
| Caries in the 3M | 2 (5.4) | |||
| Contralateral | 2 (5.4) | |||
| Unknown | 17 (46.0) | |||
| Survived asymptomatically, n/N (%) | 562/676 (83.1) | |||
| Symptoms developed by tooth | ||||
| Pericoronitis (SIGN) | 15 (13.2) | |||
| Severe pain (SIGN) | 16 (14.0) | |||
| Mild pain (SIGN) | 22 (19.3) | |||
| Discomfort/irritation (non-SIGN) | 54 (47.4) | |||
| Food stagnation (non-SIGN) | 7 (6.1) | |||
| Distribution of lower I3Ms according to survival and the development of symptoms in 1 year | ||||
| Survived symptom free | 552 (81.7) | |||
| Survived with symptoms (SIGN) | 31 (4.6) | |||
| Survived with symptoms (non-SIGN) | 55 (8.1) | |||
| Extracted symptom free | 10 (1.5) | |||
| Extracted with symptoms (SIGN) | 23 (3.4) | |||
| Extracted with symptoms (non-SIGN) | 5 (0.7) | |||
| Some form of symptoms | ||||
| 18–34.9 years of age | 83 (22.6) | p = 0.0028 | Questioned and assessed by research dentist; 1 year; Pearson chi-squared test | |
| 35–49.9 years of age | 28 (20.9) | |||
| ≥ 50 years of age | 3 (5) | |||
| Sex | NR | p > 0.05 | ||
| Vertical angulation | 34 (22.7) | p ≤ 0.001 | ||
| Mesial angulation | 43 (13.15) | |||
| Distal angulation | 31 (30.7) | |||
| Horizontal angulation | 6 (6.5) | |||
| Unerupted (%) | 10.49 | p ≤ 0.001 | ||
| Partially erupted (%) | 23.05 | |||
| Average number of teeth | NR | p > 0.05 | Questioned and assessed by research dentist; 1 year; NR | |
| Maximum BPE scores | NR | p > 0.05 | ||
| Average GI | NR | p > 0.05 | ||
| Average mean plaque | NR | p > 0.05 | ||
| Reason for last visit to the general dental practitioner | NR | p = 0.041 | Questioned and assessed by research dentist; 1 year; t-test | |
| Education after minimum school-leaving age | NR | p = 0.191 | ||
| Employment status | NR | p = 0.560 | ||
| Frequency of brushing teeth | NR | p = 0.305 | ||
| Occasional use of mouthwashes | NR | p = 0.116 | ||
| Occasional teeth flossing | NR | p = 0.124 | ||
| Frequency of dental appointments | NR | p = 0.133 | ||
| Length of time since patient last visited the dentist | NR | p = 0.335 | ||
| Smoking | NR | p = 0.291 | ||
| Drinking > 14 units of alcohol per week | NR | p = 0.447 | ||
| Deprivation category | NR | p = 0.058 | ||
| Symptoms as SIGN symptoms only (infection, severe pain and caries) (%) | ||||
| Vertical angulation | 10.29 | p ≤ 0.001 | Questioned and assessed by research dentist; 1 year; Pearson χ2 test | |
| Mesial angulation | 5.48 | |||
| Distal angulation | 24.69 | |||
| Horizontal angulation | 3.34 | |||
| Unerupted | NR | p = 0.004 | ||
| Partially erupted | NR | |||
| Hill 200668 | Extraction rates (per patient) | No history of pericoronitis: 48/153; history of pericoronitis: 23/66 | Questionnaire/telephone (every 6 months); clinical examination (or telephone) | |
| Reasons for extraction, n/N (%) | ||||
| Pericoronitis after start of study | 30/48 (62.5) | Every year; NA | ||
| Cosmetic/orthodontic | 6/48 (12.5) | |||
| Food impacted/difficult to clean | 4/48 (8.3) | |||
| Early caries in 2M | 4/48 (8.35) | |||
| Painful when eating | 2/48 (4.2) | |||
| Earache/TMJ pain | 2/48 (4.2) | |||
| Clinical factors | ||||
| Visible plaque | NR | Clinical examination (or telephone call); every year; NA | ||
| Depth of pocket distal to the 2M | NR | |||
| Bleeding on probing | NR | |||
| Intrabony defect | NR | |||
| Evaluation of the position of the upper 3M | NR | |||
| Any evidence of resorption | 0 | |||
| Radiographic measurement of the follicular space | NR | |||
| Remained symptomless (n/N) | 150/228 | |||
Study and participant characteristics of the prophylactic removal study
| Characteristic | Study |
|---|---|
| Petsos et al. 201659 | |
| Aim | To investigate the effect of M3M removal on the periodontal health of adjacent 2Ms. PPD and PAL have been described for primary outcome. As cofactors involved, sex, complications, two suture materials and two types of impaction were chosen as secondary outcomes |
| Conclusion | Young patients may benefit from an early removal of M3M, especially in the presence of certain cofactors |
| Design | Prospective cohort study |
| Setting | Unclear on number of sites, Germany |
| Recruitment period/follow-up | 2 June to 31 October 2014/6 months |
| Sponsorship/conflict of interests | Self-funded/no conflicts |
| Power | NR |
| Description of IM3Ms, n | 78/91 recruited patients with a randomly selected 78/148 removed teeth selected for analysis; submucosal, n = 58, fully impacted, n = 20 |
| Inclusion/exclusion criteria |
|
| Demographics |
|
| Baseline assessments |
|
| Details of surgery/anaesthesia/surgeon/other interventions |
|
Outcomes for the prophylactic removal study
| Outcomes assessed by Pestos et al. 201659 | Rate | p-value |
|---|---|---|
| PII | ||
| Baseline | NR | > 0.5 |
| 6 months | NR | |
| GI | ||
| Baseline | NR | > 0.05 |
| 6 months | NR | |
| PPD (mm) of 3 sites,a mean ± SD (range) | ||
| Baseline | 3.25 ± 0.65 (2–5.7) | < 0.05 |
| 6 months | 2.57 ± 0.5 (1.3–3.7) | |
| PAL (mm) of 3 sites,a mean ± SD (range) | ||
| Baseline | 2.96 ± 0.53 (2.0–5.0) | < 0.05 |
| 6 months | 2.55 ± 0.5 (1.3–3.7) | |
| Any complication, n/N | 20/78 | |
| Intense pain for > 1 day | 12/78 | |
| Post-operative infection (infiltrate or abscess) | 5/78 | |
| Wound dehiscence | 3/78 | |
| Secondary bleeding | 0/78 | |
| Nerve damage | 0/78 | |
Systematic reviews
Systematic review characteristics
| Study | Characteristic | ||||
|---|---|---|---|---|---|
| Publication type; date of search | Objective | Inclusion criteria | Outcomes reported | Other study variables | |
|
Bouloux et al. 201544 AAOMS M3Taskforce |
SR; NR | To determine clinically whether or not young adults who elect to retain their asymptomatic 3Ms have a risk of undergoing one or more 3M extractions in the future |
|
|
|
| CADTH 201042 | Rapid review; 9 July 2010 | What is the evidence for the clinical benefit of prophylactic removal of asymptomatic wisdom teeth compared with retention of asymptomatic wisdom teeth?What are the evidence-based guidelines for the prophylactic removal of asymptomatic wisdom teeth?Reproduced with permission from CADTH422010Canadian Agency for Drugs and Technologies in Healthhttps://www.cadth.ca/sites/default/files/pdf/l0202_removal_wisdom_teeth_htis_2.pdfNote: this rapid review did not restrict to impacted teeth |
|
Clinical outcomes summarised narratively | Each study was summarised narratively |
| Clinical evidence41,51–56 |
SR (updated yearly) 1966–2014 |
Should asymptomatic and disease-free impacted wisdom teeth be removed prophylactically? |
|
|
NR |
| Costa et al. 201345 | SR; up to 30 August 2012 | To investigate whether or not there is evidence justifying the prophylactic extraction of 3Ms |
|
|
NR |
| Mettes et al. 201246 | SR; 1950 – 30 March 2012 | To evaluate the effect of prophylactic removal of asymptomatic impacted wisdom teeth in adolescents and adults compared with the retention (conservative management) of these wisdom teeth |
|
Primary outcome:
|
|
| Senter for Medisinsk Metodevurdering 200350 | SR (English summary only); 1999–2003 | To evaluate the evidence on the incidence of surgical complications following the prophylactic removal of I3Ms, and the morbidity, quality-of-life and economic aspects associated with retention of I3Ms | NR in English summary |
|
|
| Song et al. 200020 | Clinical guidance/SR; 1984–99 | To provide a summary of existing evidence on prophylactic removal of impacted wisdom teeth, in terms of the incidence of surgical complications associated with prophylactic removal and the morbidity associated with retention | Study design:
|
Narrative description of included studies | RCTs:
|
| Stordeur and Eyssen 201240 | Rapid assessment; no restriction to December 2010/March 2011 | To present the existing scientific evidence on the prophylactic extraction of 3Ms in the absence of local disease and to formulate clinically relevant recommendationsWhat are the benefits and risks (complications) of prophylactic extraction of pathology-free wisdom teeth (3Ms) in adolescents and adults in the absence of local disease?What is the related good clinical practice for the prophylactic removal of pathology-free wisdom teeth?Reproduced with permission from the Belgian Health Care Knowledge Centre. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by-nd/4.0/), which permits reproduction, provided the original author and source are credited2012Belgian Health Care Knowledge Centre |
English, French, German and Dutch languages Study design: |
NR |
SRs and HTAs: CPGs: |
| Suska et al. 201043 | May 2003 to December 2009; based on the Norwegian HTA so searches conducted after 2003 only | Does removal of 3M teeth reduce the risk of infections and other local disease/pathological conditions in patients with asymptomatic or symptomatic I3Ms compared with no intervention?Reproduced with permission from HTA-centrum2010HTA-centrum |
|
Primary: infection Secondary: |
|
Systematic review results
| Study | Characteristic | |||
|---|---|---|---|---|
| Number/type of studies included | Summary of population characteristics | Summary of results | Author conclusions | |
|
Bouloux et al. 201544 AAOMS M3Taskforce |
Cohort studies: n = 7 |
|
|
The cumulative risk of 3M extraction for young adults with asymptomatic 3Ms is sufficiently high to warrant its consideration when reviewing the risks and benefits of 3M retention as a management strategy |
| CADTH 201042 | SRs: n = 4
|
NR | Overall, seven relevant articles were identified from the electronic search of databases and grey literature. This included four SRs, one non-randomised study and two CPGs. No relevant HTA reports or RCTs were identified | Based on evidence and guidelines from the past 10 years of evidence identified for inclusion in this review, there is currently insufficient evidence supporting or refuting the practice of prophylactic removal of asymptomatic 3Ms. Regarding clinical practice, the decision to remove asymptomatic wisdom teeth appears to be best based on careful consideration by practitioners of the potential risks and benefits for individual patients, as well as their attitude towards a potentially unnecessary surgical procedureReproduced with permission from CADTH422010Canadian Agency for Drugs and Technologies in Healthhttps://www.cadth.ca/sites/default/files/pdf/l0202_removal_wisdom_teeth_htis_2.pdf |
| Clinical evidence41,51–56 |
|
Extraction:
|
We found five SRs evaluating the extraction of impacted wisdom teeth, which, between them, identified one RCT that met Clinical Evidence inclusion criteria | When managing asymptomatic, disease-free wisdom teeth, no RCT data are available to guide therapeutic choices. Consistent with the application of evidence-based medicine principles, after a thorough review of the risks and benefits of the treatment alternatives, patient preference should be the factor driving the clinical decision |
| Costa et al 201345 | SR, n = 1:
|
|
Four papers qualified for the final analysisA medium degree of quality and methodological consistency was found in three studies, and low quality was found in one study. No studies showed a high degree of consistency. The most significant flaw was an inadequate sample size | The results of the present review indicate a lack of scientific evidence to justify the indication of the prophylactic extraction of third molars |
| Mettes et al. 201246 | RCT, n = 1:
|
Maxillary only Sample size: n = 164 Completed trial: n = 77 Mean length of follow-up: 66 months ± 12.6 months Mean age: 14 years and 10 months % male: 45 |
One RCT was identified that compared removal with retention of asymptomatic impacted wisdom teeth. This study was restricted to adolescents and the only relevant outcome measured was the effect on late lower incisor crowding This study, at high risk of bias, provided no evidence that extraction of wisdom teeth had an effect on lower incisor crowding over 5 years |
Insufficient evidence was found to support or refute routine prophylactic removal of asymptomatic impacted wisdom teeth in adults The single RCT compared removal with retention of asymptomatic impacted wisdom teeth and reported only one relevant outcome (late lower incisor crowding at 5 years). No difference was found Watchful monitoring of asymptomatic third molar teeth may be a more prudent strategy |
| Senter for Medisinsk Metodevurdering 200350 | Patient series, n = 13 (11 reported in summary):
|
Studies on complications related to prophylactic removal report low incidences of: But report relatively high prevalence of deep residual periodontal defects at the distal surface of the mandibular 2M after the surgical extraction of the adjacent impacted 3M Studies on complications related to retention report low incidence of: But report a relatively high incidence of pericoronitis and caries, with higher incidence of pericoronitis related to partially erupted third molars compared to fully retained |
Removal of asymptomatic fully retained wisdom teeth is not recommended. However, Norwegian dentists recommend prophylactic removal of 3Ms when the likelihood of 3Ms causing problems in the future is high and the incidence of post-operative complications is low (including partially erupted wisdom teeth). As this report is based on studies that are not optimal, the patient’s preferences need to be decisive | |
| Song et al. 200020 |
RCT, n = 2Decision analysis studies, n = 4 Brickley et al. 1995175 Edwards et al. 199960 Tulloch and Antczack-Bouckoms 1987176 Tulloch et al. 1990177 Literature reviews, n = 34 |
Only available for Harradine 1998.61
|
One RCT in the UK focused on the effects of retained 3Ms on incisor crowding (predominantly a cosmetic problem) in patients who had previously undergone orthodontic treatment. The results of this trial suggested that the removal of 3Ms to prevent late incisor crowding cannot be justified. Another ongoing RCT in Denmark compares the effects and costs of prophylactic removal of 3Ms with removal according to morbidity. So far, this trial has recruited 200 participants, and preliminary results indicate that watchful waiting may be a promising strategy. However, more data and longer follow-up of patients are needed to conclude which treatment strategy is the most cost-effective. It is also known that a trial is ongoing in the USA, but no results are available so farThe methodological quality of the literature reviews was generally poor, and none of the reviews was systematic. Conclusions from nine reviews on anterior crowding suggested that there was only a weak association between retention of 3Ms and crowding. Six out of 21 reviews with a more general scope also concluded that the prophylactic removal of 3Ms was unjustified. Twelve general reviews did not conclude with a clear message about the management of 3Ms. Three reviews suggested that prophylactic removal of 3Ms is appropriate, but these reviews were rated as being of poorer methodological quality than the majority of other reviews. Three out of four papers focusing on surgical management expressed uncertain conclusions relating to the prophylactic extraction of 3Ms. It is difficult to compare prophylactic removal of I3Ms with retention in the absence of disease, partly because these two strategies are related to different types of outcomes. By using utility methods, four decision analyses made it possible to compare different outcomes directly in the coherent models. Although there were important differences in the structure and methods for estimating input values, the findings of the decision analyses (by two groups of researchers) consistently suggested that retention of 3Ms was cost saving and more cost-effective than prophylactic removal of I3Ms | There is no reliable research evidence to support the prophylactic removal of disease-free I3Ms. Available evidence suggests that retention may be more effective and cost-effective than prophylactic removal, at least in the short to medium term |
| Stordeur and Eyssen 201240 | SRs, n = 2:HTAs, n = 2:CPG, n = 1:
|
NA | Evidence of good quality in this domain is sparse. The methodological quality of the primary studies is rated as being low to very low. The three RTCs that could be included are more than 10 years old, but a search for primary (randomised or not) controlled clinical trials of more recent date yielded no results. Most of the included studies explicitly focus on impacted wisdom teeth onlyReproduced with permission from the Belgian Health Care Knowledge Centre. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by-nd/4.0/), which permits reproduction, provided the original author and source are credited2012Belgian Health Care Knowledge CentreThe message emerging from this evidence is that prophylactic removal of pathology-free impacted wisdom teeth for orthodontic reasons in adolescents neither reduces nor prevents late problems of front teeth misalignment. The single RCT dealing with the management of non-orthodontic indications concludes that watchful waiting might be the more beneficial approach. The SR dealing with non-orthodontic indications concludes that existing reviews favouring prophylactic removal are generally of poorer methodological quality than those concluding that prophylactic removal is unjustified. Two HTA reports conclude that there is still no scientific documentation available to either support or reject routine prophylactic removal of pathology-free wisdom teethDecision-analysis models compare prophylactic with symptomatic extraction for I3Ms, including frequencies and ratings of severity of complications in both cases. They consistently suggest that patients’ well-being is maximised if surgical removal is confined to wisdom teeth with pathological changes. Several of the included publications stress the importance of clear communication with patients about expected benefits and potential side effects and complications of the prophylactic removal of pathology-free 3Ms | There is mostly little debate on the fact that 3Ms associated with clinical and/or radiological pathology, such as unrestorable caries, should be removed. However, there is a lack of proven benefit from the systematic prophylactic removal of pathology-free 3Ms, impacted or not, in all adolescents or (young) adults, and the procedure is not free of risk. Preventative actions at the level of the population are only recommended if the benefits outweigh the disadvantages, and, if this is not the case, it is preferable not to intervene. If there is no scientific evidence that an intervention is beneficial, the largely accepted principle of medicine: ‘primum non nocere’, ‘first, do no harm’, should be respectedReproduced with permission from the Belgian Health Care Knowledge Centre. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by-nd/4.0/), which permits reproduction, provided the original author and source are credited2012Belgian Health Care Knowledge Centre |
| Suska et al. 201043 | HTA/SRs, n = 2:Case series, n = 16: none reported on asymptomatic teeth | NR | The literature search did not find any randomised or non-randomised, adequately controlled trial in which prophylactic removal of 3M teeth has been compared with no interventionThe level of evidence of prophylactic removal of asymptomatic 3M teeth as well as for removal of symptomatic 3M teeth is very low according to the GRADE systemNone of the case series reported the distribution of asymptomatic and symptomatic patients or the outcome of the extraction according to the presence or absence of symptoms at the time of the procedureReproduced with permission from HTA-centrum2010HTA-centrum | A systematic literature search and review of published data has revealed that there is still no scientific documentation available to either support or refute routine prophylactic removal of asymptomatic impacted wisdom teeth in adultsReproduced with permission from HTA-centrum2010HTA-centrum |
Appendix 5 Additional excluded studies
As mentioned earlier, many of the references included in previously published SRs and the submissions from the BDA and the FDS, FGDP and BAOS were excluded from this review. However, as a result of the paucity of information available, the AG feels that it would be pertinent to discuss and summarise the results from some of these studies. The studies we have summarised here are studies that nearly met our inclusion criteria but did not specifically report results for the specific population of interest to this review (i.e. trouble-free IM3Ms).
References from included systematic reviews
Of the 84 references reported in the included SRs, only nine reviews2,20,41,43,45,47–50 met the inclusion criteria for this review, meaning that 75 references, previously included in SRs, were excluded. For 41 of these references,61,63,64,154,155,175–184,186–211 the date of publication was prior to 1999 and the studies were therefore published prior to the date limits of this SR. The remaining 34 references and the reasons for exclusion are shown in Table 27. Nine of these references did not meet our specific inclusion criteria but warrant further discussion as they are papers often cited in the debate. The details of the study aims, the results and conclusions are summarised narratively and in Table 28.
| Study | Design and reason for exclusion |
|---|---|
| Agency for Quality in Dentistry (ZZQ) 200628 |
|
| Berge 2002158 |
|
| Bishara 1999185 |
|
| Blakey et al. 2002119 |
|
| Conrad et al. 199983 |
|
| Edwards et al. 199960 |
|
| Flick 19994 | Literature review |
| Gülicher and Gerlach 2001159 |
|
| Güngörmüs 2002168 |
|
| Güven et al. 2000134 |
|
| Hill et al. 2001160 |
|
| Kan et al. 2002170 |
|
| Kruger et al. 200162 |
|
| Kunkel et al. 200773 |
|
| Libersa et al. 2002171 |
|
| Ma’aita and Alwrikat 2000172 |
|
| Perry and Goldberg 2000173 |
|
| Punwutikorn et al. 1999174 |
|
| Rakprasitkul 2001161 |
|
| Renton and McGurk 2001162 |
|
| Shafer et al. 1999169 |
|
| Tay 2000163 |
|
| Valmaseda-Castellón et al. 2000164 and Valmaseda-Castellón et al. 2001105 |
|
| van de Waal 1999157 |
|
| van der Sanden et al. 2005156 | Decision-making tool |
| Ventä et al. 1999150 |
|
| Ventä et al. 2000152 |
|
| Ventä et al. 2001151 |
|
| Ventä et al. 200465 |
|
| Vondeling et al. 1999153 |
|
| White et al. 2002165 |
|
| Yamaoka et al. 1999166 |
|
| Yoshii et al. 2001167 |
|
| Study | Reason for exclusion | Aims | Conclusions |
|---|---|---|---|
| Blakey et al. 2002119 |
|
To report the prevalence of PD as a clinical measure of the extent of periodontitis associated with asymptomatic 3Ms at the initial examination in a cohort of patients enrolled in an institutional review board-approved longitudinal clinical trial | Our data indicating that 25% of patients with retained asymptomatic 3Ms have considerable periodontal pathology in the 3M region were unexpectedNational epidemiological surveys indicate a much lower rate of periodontitis in the population younger than 35 years |
| White et al. 2002165 |
|
Our goal was to report the detection and levels of pathogenic bacteria in subgingival plaque samples taken from the distal of all 2Ms in 295 patients with asymptomatic 3Ms | The clinical findings of increased PDs and PAL coupled with colonisation of periodontal pathogens support the concept that clinical and microbial changes associated with the initiation of periodontitis may present first in the 3M region in young adults |
| Ventä et al. 1999150 |
|
To follow the clinical changes in 3M status during a 12-year period in patients aged 20 to 32 years | 3Ms undergo continuous clinical change at least up to the age of 32 years |
| Ventä et al. 2000152 |
Not all impacted and mandibular and no relevant outcomes reported However, details on symptoms are reported |
The aim of this study was to evaluate the estimates on need for 3M removals made at age 20 after 12 years | Because need for surgical removal decreases during early adulthood, routine prophylactic extraction of asymptomatic 3Ms in young adults cannot be recommended. Well-defined indications for prophylactic removals are needed |
| Ventä et al. 2001151 |
|
To examine radiographic changes in I3Ms in adults from 20 to 32 years, with special interest on sagittal changes in inclination | Considerable radiographic changes, without notable symptoms, may occur involving inclination of the tooth and state of impaction in I3Ms after the usual age of eruption |
| Ventä et al. 200465 |
|
The aim of the present study was to follow the clinical changes in 3M status during an 18-year period in patients aged 20 to 38 years | 3Ms undergo continuous clinical change on a reduced scale at least up to the age of 38 years |
| Edwards et al. 199960 | Not impacted | The study was undertaken to identify the least costly, most effective and most cost-effective management strategy for asymptomatic, disease-free M3Ms | M3M retention is less costly to the NHS, more effective for the patient and more cost-effective to both parties than removal. However, should the likelihood of developing pericoronitis, periodontal disease and caries increase substantially then removal becomes the more cost-effective strategy |
| van de Waal 1999157 |
|
NR | NR |
| Vondeling et al. 1999153 |
An ongoing trial identified by Song et al. 20 No further results have been published and we have not been able to access the conference abstract identified by Song et al. 20 |
NR | NR |
Blakey et al. 119 is one in a series of publications that report on a longitudinal clinical trial including patients between 14 and 45 years of age who had four asymptomatic 3Ms with adjacent 2Ms. The Blakey et al. 119 paper assessed the periodontal probing depth (PD) of these molars at enrolment and found that 64 out of the 329 patients had a PD of ≥ 5 mm on any 3M, 35 of which were on the M3M only. However, two-thirds of all 3Ms in patients studied were erupted to the occlusal plane (i.e. not impacted or partially erupted/unerupted). Moreover, these fully erupted teeth were found to be just as likely as teeth below the occlusal plane to exhibit a change in probing depth. The White et al. 165 paper is also part of this series of papers and reports on the detection and levels of pathogenic bacteria in subgingival plaque of the same patients. The authors165 reported results in relation to position and angulation. However, the results section did not include outcomes separately for mandibular and maxillary 3Ms.
The papers by Ventä et al. 65,150–152 are based on a longitudinal study that followed 181 first-year students at the University of Helsinki. Participants’ teeth were clinically examined and panoramic radiographs were taken at baseline and 18 years later, at the end of the study (n = 118). Some students were also examined at 6 years and 12 years (n = 81). Not all of the teeth were impacted and both mandibular and maxillary 3Ms were included. Not all were pathology free or trouble free, although two of the published papers do report the results of a questionnaire in which students were asked about symptoms. The authors of the studies conclude that 3Ms ‘undergo continuous clinical change on a reduced scale at least up to the age of 38 years’ and that ‘considerable radiographic changes, without notable symptoms, may occur involving inclination of the tooth and state of impaction in I3Ms after the usual age of eruption’. One paper152 reporting the results of the need for removal reported that 33 out of 54 3Ms that were removed were asymptomatic and concluded that ‘because need for surgical removal decreases during early adulthood, routine prophylactic extraction of asymptomatic third molars in young adults cannot be recommended. Well-defined indications for prophylactic removals are needed’.
The study by Edwards et al. 60 is a decision analysis that was identified by two SRs. 20,50 The study aimed to identify the ‘least costly, most effective and most cost-effective management strategy for asymptomatic, disease free mandibular third molars’. Although the authors did conduct a review to identify information to populate the model, no details on the results of the clinical review are reported. The study did not restrict analyses to I3Ms. Further details on the cost-effectiveness elements of the study are discussed in Chapter 4.
It was not possible to access any published data on either the van de Waal157 or the Vondeling et al. 153 papers. However, both reported on discontinued trials, according to the SRs citing them. The van de Waal157 citation was a reference to an ongoing trial and was identified in the original Cochrane review by Mettes et al. ,49 but van de Waal157 is also listed as an author of the Vondeling et al. 153 abstract. As both have similar titles, it is possible that the citations are for the same study, which has been discontinued, and so no results have been published. From the details reported in the citing SRs,49,202 neither of the studies was restricted to I3Ms.
References from submissions
The main reference lists included in the submissions (n = 26) were checked by the AG to ensure that a complete and thorough review of the available evidence could be conducted. Three references had already been included by the AG. The remaining 23 references did not meet the criteria for inclusion in this review; a list of these references, with comprehensive reasons for exclusion is supplied in Table 29.
There were five references13,112,143,212,213 included in the submissions that partially met the inclusion criteria for this SR and that warrant further discussion. In addition to the main submission forms, the additional sources provided in the combined FDS, FGDP and BAOS submission were also checked and a further nine references65,80,81,118,122,147,150,152,214 were identified, which also fell into this category. The AG has therefore summarised these 14 studies13,65,80,81,112,118,122,143,147,150,152,212–214 in Table 30.
| Study | Design and reason for exclusion |
|---|---|
| AAOMS 201631 | Wrong study design |
| Allen et al. 2009112 |
|
| Chang et al. 2009215 |
|
| Devine et al. 201635 | Wrong study design |
| Falci et al. 2012212 |
|
| Draft FDS RCS M3M Guidancea | Wrong study design |
| Finnish Guidelines 201470 | Wrong study design |
| Hospital Episode Statistics 216 | Wrong study design |
| Internal Audit GSTT Dept of Oral Surgery, 2016b | Wrong study design |
| Kang et al. 2016217 |
|
| McArdle and Renton 2006213 |
|
| McArdle and Renton 201219 | Wrong study design |
| McArdle 2013218 | Wrong study design |
| McArdle et al. 201413 |
|
| McArdle et al. 2018104 |
Retrospective cohort All IM3Ms Unclear whether or not all 3Ms were pathology free/trouble free |
| McArdle PhD data | No access to reference |
| Oderinu et al. 2012219 |
|
| National Life Tables, UK: 2013 to 2015 106 | Wrong study design |
| Ozeç et al. 2009143 |
|
| Ozgun et al.220 |
|
| SIGN 200034 | Wrong study design |
| World Health Organization 2010221 | Wrong study design |
| Worrall et al. 19988 | Pre 1999 |
| Study | Reason for exclusion | Aims | Conclusions |
|---|---|---|---|
| Allen et al. 2009112 |
|
To identify the prevalence of caries in lower 3Ms and the distal aspect of corresponding lower 2M in patients referred for lower 3M assessment | Distal caries in lower 2M related to a mesioangular 3M is a common finding in oral and maxillofacial patients in secondary care, especially if the 3M is fully or partially erupted. If such a 3M is left in situ, close monitoring and regular bitewing radiographs are recommended |
| Blakey et al. 2006118 |
|
To assess the change in periodontal status over time by PD in the 3M region | Increased PDs of ≥ 2 mm were often found in the 3M region for asymptomatic patients with at least one PD of ≥ 4 mm at enrolment, clinical measures that indicated increased periodontal pathology, and a deteriorating periodontal condition |
| Blondeau and Daniel 2007214 |
|
To evaluate the incidence of various complications, including alveolitis, infection and paraesthesia of the inferior alveolar nerve, in association with removal of IM3Ms | Surgical removal of IM3Ms should be carried out well before the age of 24 years, especially for female patients. Older patients are at greater risk of post-operative complications and permanent sequelae. A surgeon’s lack of experience could also be a major factor in the development of post-operative complications |
| Chuang et al. 200881 | Not all mandibular or impacted or pathology free or trouble free | To estimate the frequency of inflammatory complications (surgical site infection and alveolar osteitis) following 3M extraction and identify risk factors for such complications | Level of impaction, pre-existing infection and pathology were associated with increased risk for post-operative inflammatory complications following 3M surgery |
| Chuang et al. 200780 |
|
The purpose of this study was to estimate the frequency of complications after 3M surgery, with age as the primary risk factor | The results of these analyses suggest that increased age (> 25 years) appears to be associated with a higher complication rate for 3M extractions |
| Falci et al. 2012212 | Unclear whether or not all patients pathology free/trouble free | The objective of this study was to verify, using periapical radiographs, whether a partially erupted M3M is a factor in the presence of dental caries on the distal surface of the adjacent 2M | The results indicate that the presence of a partially erupted M3M with an angulation of 31 degrees or more, is a risk factor for caries on the distal surface of the mandibular 2Ms |
| McArdle and Renton 2006213 | Unclear whether or not all patients pathology free/trouble free | DCC in M2M teeth are responsible for the removal of up to 5% of all M3Ms. Our aim was to identify the clinical features of these patients | DCC is a late phenomenon and has been reported only in association with impacted 3Ms. The early or prophylactic removal of a partially erupted mesioangular 3M could prevent DCC forming in the mandibular 2M |
| McArdle et al. 201413 | Unclear whether or not all patients pathology free/trouble free | The aim of this follow-up study was to find out whether the findings in a new group of patients corroborate those of our previous study | The prophylactic removal of a partially erupted mesioangular 3M will prevent distal cervical caries forming in the 2M tooth |
| Ozeç et al. 2009143 | Not all patients pathology free/trouble free | The aim was to evaluate the prevalence of DCC 2M in a Turkish population and to determine the factors that affect it | The results revealed that DCC 2M justifies prophylactic 3M removal and partially erupted 3Ms that have an angulation of 30–90° with a contact point on the amelocemental junction should be removed to prevent DCC 2M |
| Phillips et al. 2007122 |
Not all mandibular and impacted Results unclear |
To assess changes over time in 3M position relative to the occlusal plane and in the periodontal probing status of 3Ms in asymptomatic patients who had at least one 3M below the occlusal plane at baseline and retained all 3Ms to follow-up | The anatomic position of 3Ms was not static over time even if patients were older than 25 years. Thus, unerupted 3Ms should be monitored for changes in position and periodontal pathology as long as the teeth are retained |
| Polat et al. 2008147 | Not pathology free/trouble free | To determine the association between commonly found pathological conditions and angulations and impaction depths of lower 3M teeth | Horizontal and mesioangular impactions were found with more pathological situations; especially in class A impaction depth. Angulation and impaction depth of the IM3M should be taken into consideration when making a decision whether or not to extract an IM3M |
| Ventä et al. 1999150 |
|
The aim of the study was to follow the clinical changes in 3M status during a 12-year period in patients aged 20 to 32 years | 3Ms undergo continuous clinical change at least up to the age of 32 years |
| Ventä et al. 2000152 |
|
The aim of this study was to evaluate the estimates on need for 3M removals made at age 20 after 12 years | Because need for surgical removal decreases during early adulthood, routine prophylactic extraction of asymptomatic 3Ms in young adults cannot be recommended. Well-defined indications for prophylactic removals are needed |
| Ventä et al. 200465 |
|
The aim of the present study was to follow the clinical changes in 3M status during an 18-year period in patients aged 20 to 38 years | 3Ms undergo continuous clinical change on a reduced scale at least up to the age of 38 years |
Six studies13,112,143,147,212,213 were retrospective in design, five publications65,118,122,150,152 reported the outcomes of longitudinal studies and three publications80,81,214 reported outcomes of prospective cohort studies. Six of the studies13,112,143,147,212,213 reported outcomes relating to DCC in the 2M. The position of 3Ms and probing depth or clinical changes were reported in three publications. 118,122,150 Clinical complications of 3M surgery were reported by three studies80,81,214 and one study152 reported the estimation of the need for removal of 3Ms.
The publications by Blakey et al. 118 and Phillips et al. 122 report on different outcomes from the same longitudinal study conducted in the USA at the University of Kentucky and the University of North Carolina. Two other linked publications119,165 from the same longitudinal study were discussed in the previous section and are not repeated here. Blakey et al. 118 assessed the changes in periodontal health over time and it was concluded that, for asymptomatic patients with at least one PD of ≥ 4 mm at enrolment, there were increased PDs of ≥ 2 mm often found in the 3M region. Phillips et al. 122 reported on the changes over time in the position of 3Ms relative to the occlusal plane and concluded that the anatomical position of 3Ms was not static over time; therefore, unerupted 3Ms should be monitored for changes in position and periodontal pathology.
There were also three linked publications by Venta et al. 65,150,152 that report on outcomes from a longitudinal study conducted in Finland, at the University of Helsinki, which were also discussed in detail in the previous section. Briefly, Ventä et al. 150 followed the clinical changes in 3M status in patients aged 20–32 years and, similar to Phillips et al. ,122 found that 3Ms undergo continuous clinical change. During the follow-up period, it was reported that 22% of 3Ms had erupted and 42% of 3Ms were removed. In a subsequent publication,152 it was reported that 67% of patients had one or more 3Ms removed during the follow-up period.
The publications by Chuang et al. 80,81 are linked to a series of publications78,79,222 that report the outcomes of the American Association of Oral and Maxillofacial Surgeons Age-Related Third Molar Study,222 a prospective cohort study. Chuang et al. 80 reports on the frequency of complications following 3M surgery, and it was concluded from the results that increased age appears to be associated with a higher rate of complications: patients aged 25–35 years were statistically significantly more likely to have a complication than patients aged < 25 years (OR 1.63; 95% CI 1.12 to 2.37; p = 0.01). The level of impaction, evidence of periodontal condition and pathology were also associated with an increased risk of complications. Chuang et al. 81 reported the frequencies of inflammatory complications after 3M surgery, and it was found that the level of impaction, pre-existing infection and pathology were associated with inflammatory complications. Fully bony impacted teeth (OR 6.01; 95% CI 4.7 to 7.7), followed by partially bony impacted teeth (OR 4.7; 95% CI 3.6 to 6.1) and soft-tissue impacted teeth (OR 2.5; 95% CI 1.7 to 3.7) were more likely to have inflammatory complications than erupted teeth. Blondeau and Daniel214 evaluated the incidence of post-surgical complications and reported that the overall complication rate differed significantly between men and women (2.2% and 10.2%, respectively; χ2 = 13; p = 0.0003).
Six studies13,112,143,147,212,213 reported outcomes relating to DCC in the 2M; all of the studies reported a relationship between I3Ms, in particular mesioangular I3Ms, and the presence of 2M DCC. Allen et al. 112 concluded that, if 3Ms are left in situ, there is a need for close monitoring and regular bitewing radiographs. McArdle et al. 13,213 and Ozeç et al. 143 recommend prophylactic removal of the 3M to prevent DDC of the 2M.
Appendix 6 Transition probabilities used in the model
| Age (years) | Mortality rate active | Probability of symptoms |
|---|---|---|
| 20 | 0.0003165 | 0.196694 |
| 21 | 0.000328486 | 0.19048 |
| 22 | 0.000324472 | 0.184418 |
| 23 | 0.000372943 | 0.178507 |
| 24 | 0.000357425 | 0.172744 |
| 25 | 0.000375412 | 0.16713 |
| 26 | 0.000414361 | 0.161663 |
| 27 | 0.000424342 | 0.156341 |
| 28 | 0.00046136 | 0.151162 |
| 29 | 0.000475787 | 0.146125 |
| 30 | 0.000525243 | 0.141229 |
| 31 | 0.000569221 | 0.13647 |
| 32 | 0.000572207 | 0.131847 |
| 33 | 0.000626161 | 0.127357 |
| 34 | 0.000677156 | 0.122999 |
| 35 | 0.00074904 | 0.118769 |
| 36 | 0.000776518 | 0.114666 |
| 37 | 0.000864864 | 0.110687 |
| 38 | 0.00097521 | 0.106829 |
| 39 | 0.001062676 | 0.10309 |
| 40 | 0.00116042 | 0.099467 |
| 41 | 0.001236812 | 0.095958 |
| 42 | 0.0013093 | 0.092561 |
| 43 | 0.001457008 | 0.089271 |
| 44 | 0.001580834 | 0.086088 |
| 45 | 0.00175737 | 0.083007 |
| 46 | 0.001809657 | 0.080027 |
| 47 | 0.002005622 | 0.077145 |
| 48 | 0.002094736 | 0.074359 |
| 49 | 0.002342629 | 0.071665 |
| 50 | 0.002514115 | 0.069062 |
| 51 | 0.002791667 | 0.066546 |
| 52 | 0.003009129 | 0.064116 |
| 53 | 0.003313748 | 0.061769 |
| 54 | 0.003623468 | 0.059502 |
| 55 | 0.003987477 | 0.057313 |
| 56 | 0.004297595 | 0.0552 |
| 57 | 0.004825849 | 0.05316 |
| 58 | 0.005308646 | 0.051192 |
| 59 | 0.005923238 | 0.049293 |
| 60 | 0.006400301 | 0.047461 |
| 61 | 0.007057382 | 0.045694 |
| 62 | 0.007728454 | 0.043989 |
| 63 | 0.008281076 | 0.042345 |
| 64 | 0.009066209 | 0.040778235 |
| 65 | 0.009661762 | 0.03926944 |
| 66 | 0.010460394 | 0.037816471 |
| 67 | 0.011719073 | 0.036417262 |
| 68 | 0.012927631 | 0.035069823 |
| 69 | 0.014311085 | 0.033772239 |
| 70 | 0.015800852 | 0.032522667 |
| 71 | 0.017563933 | 0.031319328 |
| 72 | 0.02002717 | 0.030160513 |
| 73 | 0.02188925 | 0.029044574 |
| 74 | 0.024206902 | 0.027969925 |
| 75 | 0.026799934 | 0.026935037 |
| 76 | 0.029680244 | 0.025938441 |
| 77 | 0.032715119 | 0.024978719 |
| 78 | 0.03680341 | 0.024054506 |
| 79 | 0.041100184 | 0.023164489 |
| 80 | 0.046894523 | 0.022307403 |
| 81 | 0.05270411 | 0.021482029 |
| 82 | 0.059299519 | 0.020687194 |
| 83 | 0.066956709 | 0.019921768 |
| 84 | 0.075685636 | 0.019184663 |
| 85 | 0.084829623 | 0.01847483 |
| 86 | 0.095257973 | 0.017791261 |
| 87 | 0.106315742 | 0.017132985 |
| 88 | 0.118288053 | 0.016499064 |
| 89 | 0.1331211 | 0.015888599 |
| 90 | 0.146901404 | 0.015300721 |
| 91 | 0.161803302 | 0.014734594 |
| 92 | 0.184076189 | 0.014189414 |
| 93 | 0.197660796 | 0.013664406 |
| 94 | 0.210945629 | 0.013158823 |
| 95 | 0.230126836 | 0.012671946 |
| 96 | 0.260778283 | 0.012203084 |
| 97 | 0.279505262 | 0.01175157 |
| 98 | 0.301488605 | 0.011316762 |
| 99 | 0.324712845 | 0.010898042 |
| 100 | 0.335866615 | 0.010494814 |
Appendix 7 Search strategy (impacted mandibular third molar-specific utilities)
MEDLINE
Date searched: 10 March 2016.
Search strategy
| # | Search term |
|---|---|
| 1 | Pericoronitis/ |
| 2 | Toothache/ |
| 3 | exp Dental Caries/ |
| 4 | Dry Socket/ |
| 5 | Tooth Extraction/ |
| 6 | jaw fractures/or mandibular fractures/or maxillary fractures/ |
| 7 | Facial Paralysis/ |
| 8 | (Pericoronit* or toothache* or dry socket or tooth extract* or jaw fracture*).tw. |
| 9 | ((tooth or dental) adj1 (decay* or caries)).tw. |
| 10 | ((mandibular or maxillary) adj2 fracture*).tw. |
| 11 | ((Facial or face) adj2 nerve* adj2 damage*).tw. |
| 12 | ((Facial or face) adj2 paralysis*).tw. |
| 13 | or/1-12 |
| 14 | (multiattribute$ or multi attribute$).ti,ab,kf. |
| 15 | utility.ab./freq = 2 |
| 16 | utilities.ti,ab,kf. |
| 17 | disutili$.ti,ab,kf. |
| 18 | (standard gamble$ or sg).ti,ab,kf. |
| 19 | (time trade off$1 or time tradeoff$1 or tto or timetradeoff$1).ti,ab,kf. |
| 20 | (utility adj3 (score$1 or scoring or valu$ or measur$ or evaluat$ or scale$1 or instrument$1 or weight or weights or weighting or information or data or unit or units or health$ or life or estimat$ or elicit$ or disease$ or mean or cost$ or expenditure$1 or gain or gains or loss or losses or lost or analysis or index$ or indices or overall or reported or calculat$ or range$ or increment$ or state or states or status)).ti,ab,kf. |
| 21 | or/14-20 |
| 22 | 13 and 21 |
Glossary
- Decision analysis
- A systematic, quantitative and interactive method used to address and evaluate important choices confronted by decision-makers.
- Distal cervical caries
- Decay of the back surface of the neck of the tooth.
- Dry socket
- Dry socket (alveolar osteitis) occurs when a blood clot fails to develop (or is dislodged) in the tooth socket as a normal part of healing and can cause a dull, aching pain in the gum or jaw. It can also cause a bad taste or smell to come from the tooth socket.
- Impacted third molar
- A third molar that has failed to erupt completely as a result of being blocked by another tooth, bone or tissue.
- Mandibular
- Relating to the lower jaw.
- Maxillary
- Relating to the upper jaw.
- Roentgenology
- Branch of medicine dealing with diagnosis and therapy through X-rays.
- Treatment episode
- Period of time between the first treatment and the last treatment for a given diagnosis.
List of abbreviations
- 2M
- second molar
- 3M
- third molar
- AG
- assessment group
- BAOS
- British Association of Oral Surgeons
- BDA
- British Dental Association
- CADTH
- Canadian Agency for Drugs and Technologies in Health
- CI
- confidence interval
- DCC
- distal cervical caries
- FDS
- Faculty of Dental Surgery
- FGDP
- Faculty of General Dental Practice
- GI
- Gingival Index
- HRQoL
- health-related quality of life
- I3M
- impacted third molar
- ICER
- incremental cost-effectiveness ratio
- IM3M
- impacted mandibular third molar
- M2M
- mandibular second molar
- M3M
- mandibular third molar
- MTA
- multiple technology appraisal
- NHS EED
- NHS Economic Evaluation Database
- NICE
- National Institute for Health and Care Excellence
- OR
- odds ratio
- PAL
- probing attachment level
- PD
- periodontal probing depth
- PPD
- probing pocket depth
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- SIGN
- Scottish Intercollegiate Guidelines Network
- SR
- systematic review
- TA
- technology appraisal
- UDA
- unit of dental activity
