Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 16/104/15. The contractual start date was in July 2017. The draft report began editorial review in May 2019 and was accepted for publication in December 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Rodgers et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Autism spectrum disorder
Autism spectrum disorder (ASD) (henceforth referred to as autism) is a lifelong neurodevelopmental condition, characterised by impairments in reciprocal social communication and a pattern of restricted, repetitive behaviours, interests and activities. 1 The prevalence of diagnosed autism in the UK is around 1% of the population and is higher (2%) in men than in women (0.3%). 2,3 A feature of autism is that individuals present with a combination of strengths and difficulties, which can vary considerably over time and between individuals.
Furthermore, the presence of additional difficulties, including general or specific learning disabilities, other neurodevelopmental conditions, and mental and physical health conditions, may have additional detrimental impacts on everyday life. 4 The nature of the skills and needs of autistic people, their families and the consequences for the wider society is highly variable but, for some, the behavioural characteristics of a possible autism diagnosis may be evident from an early age, often in the preschool years. Those who are diagnosed in early childhood are typically those with more severe symptomatology5,6 and appear more likely to have an intellectual impairment,7 although this assertion is complicated by other factors, such as geographical region,5 consistency of care,6 language delay8 and socioeconomic status. 7
Autism in childhood
The developmental trajectory of autistic children is varied and complex, and they may experience improvements over time in some areas but not in others. 9 The literature highlights some characteristics potentially associated with a more positive trajectory, such as milder autism symptoms, better social and linguistic skills,10 and higher cognitive ability [intelligence quotient (IQ)]. 11 However, no clear predictive factors have emerged. In one recent study11 assessing children at age 2 years and again in middle childhood, one-third of children experienced significant improvements in intellectual abilities. In contrast, other studies have reported that a similar proportion of autistic children do not develop sufficient useful speech to meet their daily communication needs. 12
As autistic children move into social networks beyond their family, there is evidence to suggest they are at increased risk of victimisation and bullying, and social and emotional exclusion,13 compared with typically developing children. Furthermore, it has been reported that autistic children who are able to communicate their experiences identify feeling lonely significantly more frequently than children without autism. 14
Autism in adulthood
Impairments in social reciprocity, communication and behaviour may have a profound effect on children’s social development into adulthood. 15,16 However, to date, relatively little is known about the everyday experiences of autistic adults and there have been few well-conducted studies of adult outcomes. 17 The available evidence suggests that autistic adults (including those of average intellectual ability) are likely to experience poorer educational attainment, lower rates of employment, are less likely to be living independently, and experience higher rates of mental and physical health problems, compared with both the general population and adults with other disabilities. 18–20 Additionally, relatively few autistic adults report that they are married, in long-term relationships or have at least one friend, compared with the general population. 16 However, evidence suggests that the experiences of autistic adults vary considerably. For example, an examination of cohort studies reported that the average percentage of autistic adults in some form of employment (paid, sheltered or voluntary) or educational programmes was 49%, but this percentage ranged between 6% and 94% between cohorts. 16,17
Early interventions for autism
The relatively high prevalence of autism,2,3,21,22 and the range and impact of possible impairments,21 means that autism has significant economic and social impacts for individuals, their families and wider society. The estimated total costs to the UK of supporting people with autism and related conditions has been estimated at £34B per year, with high lifetime care costs reported for individuals with co-occurring intellectual disability. 23 Thus, an effective treatment that can support the child before they reach school age (defined in the review as ‘early’), maximise the child’s strengths, enhance quality of life and reduce factors associated with less favourable outcomes in the short-, medium- and especially the longer-term course of autism could have considerable benefits. 24,25
Early intensive behavioural intervention (EIBI), first described by Lovaas,26 is a well-established, early intervention based on the theoretical principles of applied behaviour analysis (ABA). These principles promote a range of techniques (such as the breaking down of skills into their basic components) that emphasise discrimination, learning and positive reinforcement. This intensive approach is often delivered on a one-to-one basis, for 20–50 hours per week. 27 However, criticisms have been made of this approach. These include concerns that the use of highly structured, primarily adult-led sessions could increase the risk of behaviours that challenge. In addition, it may reduce opportunities to encourage a child’s spontaneity and interactive communication, resulting in an over-reliance on prompts, with the potential to further restrict the child’s capacity to develop generalisation skills. 28 Additionally, it has been suggested by some in the autistic community29 that the rigid nature of ABA-based interventions could potentially increase the risk of later additional mental health problems,30 although this has yet to be effectively researched and there is little reliable published evidence confirming this. 31
In response to these concerns, a number of adaptations of the original model have been developed, which incorporate the principles of ABA within a more naturalistic and developmentally informed framework. Known collectively as naturalistic developmental behavioural interventions (NDBIs),28 these interventions include child-led and incidental training opportunities. Prominent examples of these models are pivotal response treatment (PRT)32 and the Denver model33 and its derivative the early start Denver model (ESDM). 34 These models still encompass the fundamentals of ABA methodology, such as discrete trial training, and take a comprehensive approach to skills development. However, their proponents assert that the revisions create a more multifaceted intervention able to meet the individual needs of autistic children and their families. 28 Throughout this report the term ‘early intensive ABA-based interventions’ is used as an umbrella term to describe both EIBI and NDBI approaches.
Early interventions for autism in the UK
In the UK, there is little in the way of published literature to delineate what is usual UK practice for access to early interventions for preschool autistic children. Advice from clinical experts and service providers within local authorities, obtained through our advisory group (see Appendix 1), suggests that the majority of preschool autistic children currently receive a combination of generic or autism-specific early years health- and education-based interventions. These can be delivered in a nursery or home setting, with input from generic community health-care and specialist services, such as speech and language therapists, educational psychologists, occupational therapists, mental health workers and third-sector organisations, such as the National Autistic Society (NAS) or locally organised parent support groups.
In some areas, there has been demand for early intensive ABA-based interventions, although these interventions are not specifically recommended in National Institute for Health and Care Excellence (NICE) guidelines. 35 In some areas, ABA schools for both preschool and school-aged children, as well as dedicated ABA classrooms in both special and mainstream school settings, have been established. 36 Availability of funding and places is highly variable and dependent on the local authority. There are also a number of private providers delivering ABA-based intervention services in the home, as well as providing training to enable parent- and carer-mediated therapy. 37–39 The parents of some children have used litigation through the local education authority appeals process to secure funding for ABA-based provision. 40
Existing evidence on clinical effectiveness and cost-effectiveness
The existing research evidence evaluating the clinical effectiveness of early intensive ABA-based interventions derives from both comparative and non-comparative studies, often using opportunistic samples. There is a large body of published research based on single-case experimental designs to investigate the techniques and practices employed in ABA-based interventions. This methodology has the advantage that it enables the operationalisation (defining variables into measurable factors) of specific behaviours, settings and participants, which in turn provides a framework for tracking the progress of individual children. 41 However, operationalisation to this degree may impinge on the ability to generalise these findings to broader research questions. Together with the strong potential for publication bias in this type of research, larger adequately powered controlled studies are required to understand the overall effectiveness of the wide range of published manualised early intensive ABA-based interventions. Controlled studies are necessary to estimate how much of the change on an outcome can be attributed to the intervention of interest. Without a comparator group, it would not be possible to determine the extent to which an outcome is attributable to developmental or other changes.
Several well-conducted systematic reviews of published studies comparing early intensive ABA-based interventions with treatment as usual (TAU) or other interventions have been published. 4,24,25,42–49 These have, in general, reported early intensive ABA-based interventions to be beneficial for autistic children, suggesting improvements in developmental functioning, decreased maladaptive behaviour and reduced symptom severity. 4,24,25,42–45,47–49 These findings have been heavily caveated by the review authors for a variety of reasons, including the potential difference in supervision and training between groups,42 the need for more randomised controlled trial (RCT)-based evidence,24,25,42,45,47 the poor range of consistently reported outcome measures,4,24,49 the meaningfulness of cognitive ability as an outcome measure24 and the small sample sizes of the included studies. 4 One caveat to these findings, of particular relevance, is the considerable variation in the reported outcome scores both within and between studies. 24,42,45
An approach common to all of these reviews is that they have used a narrow interpretation of early intervention models and focused on either EIBI4,24,25,42–48 or ESDM alone. 49 To the best of our knowledge, to date, there are no systematic reviews that have evaluated the effectiveness of the broad range of early intensive ABA-based interventions available and none that have compared the relative effectiveness of different early intensive ABA-based interventions. Furthermore, most of these reviews have not investigated the considerable variation in the response of children to the intervention. Of those that investigated factors that may influence the response to the interventions, child characteristics such as age, IQ, adaptive behaviour and verbal ability at intake were cited as possible moderators of effectiveness. 4,24,44,47,48 However, these analyses were based on limited aggregate data, with little power to detect differences and the potential to mislead, instead of a more detailed approach using individual participant data (IPD). One review collected IPD, providing an opportunity to examine potential effect modifiers in more detail,42 but the authors requested only four data items (age, IQ and adaptive behaviour scores at intake and after 2 years). Using these data, the authors were unable to isolate potential moderators of the treatment effect.
As well as systematic reviews assessing comparative effects, a small number of economic evaluations of early intensive ABA-based interventions have been undertaken. These evaluations have been relatively simplistic and have drawn data on intervention effects from a limited sample of studies. They also tended to focus on costs and, in general, ignored value generated via improvements in health-related quality of life (HRQoL) and other important outcomes. 44,50–54 To our knowledge, no previous studies have assessed value in a UK context.
Chapter 2 Aims and objectives
The aim of this study was to evaluate the clinical effectiveness and cost-effectiveness of early intensive ABA-based interventions for preschool autistic children and to estimate the value of undertaking additional research in this area.
The key objectives were to:
-
evaluate the effects of early intensive ABA-based interventions in young autistic children by conducting a systematic review and IPD meta-analyses of data from all available comparative studies
-
use the collected IPD to investigate potential study- and participant-level modifiers of treatment effect
-
evaluate the cost-effectiveness of early intensive ABA-based interventions in young autistic children by developing a new economic model
-
identify uncertainties in the evidence base, highlight important areas for future research and estimate the value of further research.
Chapter 3 Collaboration details
SCABARD
The Synthesising Comprehensive Applied Behaviour Analysis interventions – Research for children with autism spectrum Disorders (SCABARD) IPD meta-analysis was carried out as an international collaborative project.
The project was carried out on behalf of the SCABARD Advisory Group. All study investigators who shared data were active participating members of this group.
SCABARD individual participant data meta-analysis research team
The IPD meta-analysis was carried out by a research team based at the Centre for Reviews and Dissemination and Centre for Health Economics at the University of York, in collaboration with the Institute of Health & Society at Newcastle University and the School of Social and Community Medicine at the University of Bristol.
Protocol development and registration
At the start of the project, a publicly available review protocol was submitted to the international prospective register of systematic reviews (PROSPERO) (URL: www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42017068303).
Stakeholder engagement
To ensure that a wide range of views was represented during the planning, conduct and interpretation of the analyses, the research team established the SCABARD Advisory Group (see Appendix 1). This included representation from the NAS, research study investigators, parents of autistic children, autistic adults, UK-based ABA practice specialists, IPD research specialists, health economists, together with international and UK expert clinical academics from psychiatry, and clinical and educational psychology (see Appendix 1).
A Project Steering Group advised and supported the research team on strategic decisions over the course of the project.
Ethics approval
The SCABARD IPD meta-analysis utilised existing data provided by contributing studies and addressed the same clinical question to which study participants consented originally. Data contained no identifying names or numbers and were held securely under controlled access.
The chairperson of the University of York Health Sciences Research Governance Committee confirmed that additional ethics review was not required.
Author consultation
A draft report containing results of the IPD meta-analysis was made available to study investigators who provided data for analysis. Study investigators were also invited to a meeting in which preliminary results of the IPD meta-analysis were shared and interpretations of the evidence discussed.
Public and patient involvement
Patient and public involvement (PPI) has been integral to the SCABARD trial, from inception to completion. The PPI group consisted of six individuals who formed a part of the Advisory Group (see Appendix 1). The PPI group included a representative from the NAS, two parents or carers of autistic people and two autistic adults. Members were involved through the Advisory Group and had direct communication via e-mail and telephone.
The PPI group contributed at every stage of the research (as outlined below) except the data collection and analysis stage. This exception was deemed important to preserve the independence of the research team reviewers.
Design of the research
A protocol was written and circulated to the members of the PPI group prior to the first of three Advisory Group meetings. This first meeting outlined the purpose and nature of the project and sought input on the study design, as a result of which we adapted our project design by:
-
developing a list of relevant baseline characteristics that were important to include for the analyses
-
listing which outcomes were important to relevant stakeholder groups
-
further developing a definition of early intensive ABA-based treatments and narrowing the inclusion criteria
-
further developing search terms to ensure that they were comprehensive.
Design of the analyses
The original intent of the second meeting of the Advisory Group was to focus on the design of the economic model to ensure that it reflected key elements of autism and had face validity. However, we extended the remit of this meeting to give an update on progress and outline the quality of the studies, the interventions used and the types of outcomes that we were able to collect. The discussions of this group formed the basis of both the structure of the eventual analyses and the economic model.
Analysis of the results
The PPI group and the other members of the Advisory Group were not involved at the analysis stage to retain a measure of independence owing to the strong beliefs that many members of the public and service providers already held about the effectiveness of the intervention. We did, however, include them in the interpretation of these results. These results were circulated prior to the final Advisory Group meeting, which discussed the potential interpretations, how far we should extend the economic model and what scenarios to include.
Reporting of the research
Patient and public involvement members, as part of the Advisory Group, had an opportunity to contribute to drafts of the final report before submission. They provided extensive comments on the document via e-mail.
External stakeholder consultation
After submission, relevant external organisations and groups were also consulted in a consultation exercise. When possible, we have amended the report based on these comments and in the interests of full transparency we have included the unaltered feedback from these individuals and organisations in Appendix 20. We also included the comments of one member of the PPI group in this section who was not able to provide feedback at an earlier stage. Full permission has been received from those who made these comments to reproduce them in this report.
Chapter 4 Systematic review and meta-analysis of effectiveness: methods
Literature searches
The aim of the literature search was to identify comparative studies of comprehensive early intensive ABA-based interventions for children with autism and related conditions. An information specialist developed the search strategy in MEDLINE (via Ovid). No date, language, geographical or study design limits were applied to the strategy. The MEDLINE strategy was adapted for use in all resources searched.
The searches were conducted during August 2017. The following databases were searched: Cochrane Central Register of Controlled Trials (CENTRAL), Cumulative Index to Nursing and Allied Health Literature (CINAHL), EMBASE, Education Resources Information Center, MEDLINE, PsycINFO and Social Science Citation Index. Records identified from the database searches were downloaded and imported into EndNote bibliographic software (version X9, Clarivate Analytics, Philadelphia, PA, USA) and de-duplicated. Reference lists of relevant systematic reviews were also searched manually.
As publication bias has been identified as a concern in relation to early intensive ABA-based interventions in autism, we attempted to identify grey literature by searching for conference papers (using EMBASE and Conference Proceedings Citation Index) and dissertations and theses [using PsycINFO and The British Library’s Electronic Theses Online Service (EthOS) database]. Advisory Group members and authors of identified studies were asked to identify any additional potentially relevant studies, particularly those that are unpublished. ClinicalTrials.gov and the World Health Organization International Clinical Trials Registry Platform were also searched in an attempt to identify unpublished studies and any studies in progress. Full details of the search strategies are presented in Appendix 2.
Inclusion criteria
Population
Studies that included children with a diagnosis of ASD, including any of the following terms: autism, Asperger syndrome, pervasive developmental disorder – not otherwise specified (PDD-NOS), atypical ASD or ASD1 based on Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, or International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, criteria (ICD-10). Inclusion was not restricted by age, although the primary focus of the review is on children of preschool age (aged < 5 years in the UK). If studies with a broader age were identified, preschool age children could be identified within the IPD.
Intervention
Studies of early intensive interventions based on ABA principles were eligible for inclusion in the review.
Intensive behavioural interventions:
-
included > 15 hours per week of planned intervention
-
used a comprehensive approach, targeting a range of behaviours, skills and developmental domains
-
used ABA-based teaching strategies as the core components
-
were delivered face to face by qualified or trained individuals
-
were delivered at least initially on a one-to-one basis
-
included qualified supervision of the therapists/trained staff/parents delivering the intervention.
Studies of interventions delivered to parents rather than children and studies of narrowly targeted interventions aimed at a single behaviour (e.g. joint attention) were excluded.
Comparators
Inclusion was not restricted by study comparator.
Relevant comparators included all other forms of early intervention, such as augmented forms of communication [e.g. the Picture Exchange Communication System (PECS)];55 other speech and language therapy interventions; support programmes led by independent providers, such as charitable and third-sector organisations; educational-based structured teaching approaches, such as Treatment and Education of Autistic and Communication related handicapped CHildren (TEACCH);56 and ‘eclectic’ approaches, as well as placebo, waiting list or TAU groups.
Outcomes
All studies that met the above criteria were included and, when available, contributed data for the prespecified IPD meta-analysis outcomes (see Chapter 6).
Study design
Prospective randomised and non-randomised controlled studies meeting all other inclusion criteria were eligible for inclusion. Non-comparative, single-arm studies were excluded.
Study selection
Two researchers independently screened all titles and abstracts retrieved from electronic databases and other searches. Full-paper publications were then obtained for potentially relevant studies. If no full paper existed and study eligibility was uncertain, study authors were contacted and asked to provide further information.
Two researchers independently assessed the relevance of each full study using the fullest available information. Any discrepancies in screening decisions were resolved by consensus and discussion with a senior team member or clinician with expertise in autism, as required. Authors were contacted for further information, when necessary. Full details of the screening criteria are presented in Appendix 4.
Data collection
Published data
Two researchers independently extracted data from published and unpublished study reports. Data were extracted on study design, intervention and comparator characteristics, baseline characteristics and results. Any discrepancies were resolved by discussion and, when necessary, cross-referencing IPD or contacting study authors.
Individual participant data
Study investigators were invited to supply data in a standardised coding format developed for SCABARD. However, data were accepted in any reasonable format and recoded as necessary by the research team. Data were requested for all recruited children, including any who were excluded from original study analyses. Study protocols were also requested from authors.
When the intervention or its components were unclear from publicly available sources, study authors were asked to provide these details alongside their IPD.
The SCABARD data dictionary, listing all data items requested, is given in Appendix 3.
We requested that all participant names and identifying numbers were removed prior to supplying data.
Secure file transfer and encrypted e-mail were offered as secure methods for transferring IPD. All data were anonymous and held in a password-protected area of the University of York servers.
Critical appraisal, data checking and quality assurance
Critical appraisal of studies
Critical appraisal of included studies was based on assessment of trial publications, protocols (if available) and by checking received data sets.
Risk of bias in RCTs was assessed using the Cochrane Risk of Bias tool. 57 Non-randomised controlled study designs were assessed using the Cochrane Risk Of Bias In Non-randomised Studies – of Interventions (ROBINS-I) tool. 58
As well as assessing aspects of bias (such as blinding and/or independence of outcome assessors), when possible, the critical appraisal also assessed the fidelity of delivered interventions to the underlying treatment model. Assessment was undertaken independently by two researchers, with any discrepancies resolved by consensus or recourse to a third researcher, if necessary.
Checking and quality assurance of individual participant data
All IPD were checked on receipt. Baseline data were tabulated and compared with the study publication, with any inconsistencies noted. Data were checked for internal consistency and integrity of randomisation (if conducted). Patterns of missing data were examined. One researcher ran data checks, which were independently cross-checked by a second researcher. Findings of all data checking were discussed with senior members of the research team.
The impact these checks had on the potential quality of the studies and data was considered (e.g. whether or not there was evidence of non-random allocation). This was used alongside the critical appraisal and could upgrade or downgrade the findings of the overall quality assessment.
Comparison of data available from published and individual participant data sources
The appraisal of included evidence was also informed by comparing the variables and outcomes collected in the IPD against those (1) requested by the SCABARD team (see Appendix 3), (2) reported in corresponding publications and (3) reported in original study protocols (if available).
Individual participant data meta-analysis methods
Analysis framework and structure
Types of intervention and control
Two general classes of early intensive interventions based on ABA emerged from the literature:
-
EIBI, including the University of California, Los Angeles (UCLA)/Lovaas model26 or intensive ABA-based adult-led interventions (e.g. discrete trial training or separate learning units with a clear beginning and end).
-
EIBI with NDBI, incorporating some aspects of the developmental social pragmatic model that seeks to reinforce social communication and interaction by engaging with child-initiated activities. The ESDM emerged as a prominent form of EIBI with NDBI.
The two key comparator interventions were:
-
‘eclectic’ treatment, which may include a range of school-, clinic- or home-based interventions, sometimes incorporating lower-intensity ABA-based approaches
-
TAU, which consisted of standard local provision or waiting list controls.
Some studies compared early intensive ABA-based interventions of differing intensity.
The main meta-analyses combined all types of early intensive ABA-based interventions and both types of control arm, assuming equivalence between intervention types, to obtain overall estimates of the effectiveness of early intensive ABA-based interventions. Clinical expertise within the SCABARD team and Advisory Group suggested that the various classes of early intensive ABA-based interventions may be essentially equivalent in methodology and efficacy, so this was considered a reasonable primary approach.
Whether or not the interventions were truly equivalent was investigated by considering each intervention and comparator separately, and conducting pairwise meta-analyses for each intervention/comparator combination. This was followed by analyses that combined interventions and comparators as follows:
-
combined comparators (eclectic and TAU), keeping interventions separate
-
combined early intensive ABA-based interventions (EIBI, EIBI and NDBI), keeping comparators separate.
These meta-analyses were performed for each outcome measure using both one- and two-stage meta-analysis methods (see Statistical details of individual participant data meta-analyses). The different meta-analyses were compared to identify whether or not there was any evidence of differences between interventions and comparators. This informed the decision of if and how to combine interventions and comparators in all subsequent analyses. Statistical significance (at 5% level) was not the sole driver of this decision; observed size of the effect estimates was also considered, so groups could potentially be kept separate even if there was no statistically significant evidence of difference.
Outcome domains
The meta-analyses focused on key domains of development in autistic children, which might be measured on a range of different scales.
These domains were:
-
adaptive behaviour
-
cognitive ability
-
language development
-
autism symptom severity
-
presence of behaviours that challenge
-
placement into mainstream or specialist schools.
The intention was to analyse these domains at 6 months, 1 and 2 years after randomisation or intervention initiation, but, given the data received, this was amended to 1 and 2 years, with limited analyses at 3, 4 and 7 years for some domains. Mean differences (MDs) [i.e. not standardised mean differences (SMDs)] between early intensive ABA and comparator arms were used as the main outcome measure, because, generally, all studies used equivalent measurement scales [e.g. Vineland Adaptive Behaviour Scale (VABS)]. 59 Analyses using SMDs were performed as a sensitivity analysis for each outcome domain.
Specific outcome measures
The outcomes analysed were the individual measurement scales from each of the main outcome domains. The included studies collected a large number of outcome measures, but most were collected in only one study or with insufficient data to assess effectiveness (i.e. collected for only one study arm or no baseline data reported).
The following outcome measures were assessed by at least one study, with sufficient data to estimate effectiveness of early intensive ABA-based interventions:
-
adaptive behaviour:
-
composite VABS59
-
each component of the VABS composite score –
-
communication
-
daily living skills
-
socialisation
-
motor skills
-
maladaptive behaviour (not always recorded)
-
-
-
cognitive ability (IQ):
-
as assessed in the study (regardless of exact test used)
-
based on specified test –
-
-
non-verbal IQ:
-
Merrill–Palmer Scale of Mental Tests (MPSMT)70
-
-
language development:
-
expressive, receptive, comprehension and overall using scales –
-
-
autism symptom severity:
-
presence of behaviours that challenge:
-
Conners’ Rating Scales – Revised80
-
-
additional outcomes:
-
other components of MSEL:
-
composite score
-
fine motor
-
visual reception.
-
-
When these outcome measures were available in two or more studies at consistent time points, they were combined in one- and two-stage meta-analyses. When available from only one study, results were tabulated. Other outcome measures were described in the protocol, but not collected by any eligible studies, so are not listed here.
Covariates modifying applied behaviour analysis effectiveness
The following potential effect modifiers were investigated to explore whether or not they altered the effectiveness of early intensive ABA-based interventions, and were specified in the protocol. These were only considered when suitable data were recorded in the IPD provided, or in publications, protocols or otherwise provided by triallists (for intervention characteristics).
Study-level intervention characteristics
-
Allocation method (parental choice, location based, cohort).
-
Delivery setting (home, school, specialist centre).
-
Parental involvement in ABA (none, encouraged, some).
-
Use of ABA methods in control intervention (none, partial).
Participant-level characteristics
-
Age at enrolment.
-
Sex.
-
Baseline IQ.
-
Baseline composite VABS score.
Other characteristics were listed in the protocol, but there were insufficient data to analyse them.
The impact that these covariates have on early intensive ABA-based intervention effectiveness was assessed by using one-stage meta-analyses with the covariate included as a treatment–covariate interaction in a regression model (see Impact of covariates on treatment effect).
A separate model was fitted for each main outcome and covariate combination, when sufficient data were available.
Statistical details of individual participant data meta-analyses
Both one- and two-stage meta-analyses were performed for each outcome, provided that data were available for at least two studies. When these thresholds were not reached, a narrative summary of study results was produced.
Two-stage meta-analysis
In a two-stage meta-analysis, estimates of intervention effect (SMD or relative risk) are estimated separately for each study and are then pooled across studies to calculate a summary effect estimate.
The main within-study analysis for continuously distributed outcomes (e.g. IQ, VABS composite score) was the analysis of covariance (ANCOVA) model,81 which adjusts the outcome at time of analysis for the baseline value. This model was used to estimate the MD in outcome between intervention and control arms [with its standard error (SE)] for use in the meta-analysis.
Results were then combined across studies using both fixed-effect and DerSimonian–Laird random-effects meta-analysis, to account for possible heterogeneity. Forest plots were produced for each meta-analysis. Effect estimates (SMDs, MDs or relative risks) and 95% confidence intervals (CIs) were calculated for each study and for the combined result. Heterogeneity was also assessed using I2. If only two studies presented data, a fixed-effect meta-analysis was used, as heterogeneity cannot be reliably estimated from only two studies.
One-stage meta-analysis
A one-stage meta-analysis takes advantage of the availability of IPD by including all data from all studies in a single regression analysis (while taking account of/stratifying by study). This enables greater flexibility in the modelling structure.
A linear regression analysis was used for continuous outcomes (e.g. VABS composite score), and proportional odds regression for categorical outcomes (school placement). As for the two-stage models, the ANCOVA approach was used to estimate MDs. The models regressed final outcome against treatment and baseline value, with random intercept and intervention effects (to account for heterogeneity).
There are currently no well-tested methods available for one-stage analyses of SMD, so only two-stage analyses of SMD were performed.
All available data from all studies were included in a regression analysis; studies were excluded when they did not include data for the outcome measure of interest. As for two-stage analyses, meta-analyses were performed provided that at least two studies, with a minimum of 50 participants, provided data for the specified outcome. If only two studies provided data, a fixed-effect regression was used.
Heterogeneity assessment
All one-stage models were fitted using mixed-effects regression, with random effects, varying by study, applied to the treatment parameter. Heterogeneity was quantified in terms of the observed statistical heterogeneity in the model (τ2 estimate).
When available, results of one- and two-stage analyses were compared.
Impact of covariates on treatment effect
Access to IPD means that the analysis can potentially go beyond looking only at whether or not early intensive ABA-based interventions are effective, to consider whether or not child-level characteristics (including parental and intervention factors specific to each child) might alter how effective the intervention is. For example, whether or not IQ at time of recruitment alters how effective EIBI is in changing outcomes. The impact the covariate may have on effectiveness is called the intervention–covariate interaction.
Two-stage analyses
For study-level characteristics (such as parental involvement in ABA provision, setting and duration), subgroup analyses were used to investigate the impact of covariates. Studies were placed into groups according to the value of the characteristic (e.g. some parental involvement, involvement encouraged or no involvement, with exact groupings decided once it was known what data were available) and meta-analyses performed, as described above, within each group. Subgroups were then compared to identify any differences in effect.
One-stage analyses
For individual-level characteristics, the one-stage regression analyses described earlier were extended to include a parameter for the covariate of interest and one for the intervention–covariate interaction. To ensure model convergence, these parameters were assumed common to all studies (i.e. a fixed effect), but models with random effects for these parameters were tested to ensure the validity of making a fixed-effect assumption. A statistically significant intervention–covariate interaction parameter in these models indicates that the covariate alters the effect of the early intensive ABA-based interventions.
These models were fitted for each possible combination of outcomes and covariate to assess the associations between intervention and covariates, provided sufficient data were available (at least two studies and 50 participants reporting both outcome and covariate).
Time of measurement
Analyses were performed at 1 and 2 years after recruitment for each outcome. A tolerance of ± 6 months was used for each analysis. This means that, for example, measurements made from between 18 and 30 months could contribute to analyses at 2 years.
In a few studies, IPD were provided at times other than 1 or 2 years. To incorporate those additional data captured at other times, repeated measures analyses were performed. Repeated measures models analyse all time points simultaneously, so there is a single model estimating effects for all reported years. They also account for the fact that each child may have repeated measurements of the same outcome over time, which are likely to be correlated, by including a correlation term for each child.
When the data permitted, exploratory analyses were performed, including an assessment of whether outcomes varied linearly or log-linearly over time (i.e. assuming a trend over time rather than separate analyses). The choice of these models depended on the results of the analyses at each specific time point.
Studies not supplying individual participant data
When studies identified as eligible for inclusion in the meta-analysis did not supply IPD to the SCABARD team, relevant outcome data were extracted from study publications. Data were extracted as means and standard deviations (SDs) in each study arm, as 2 × 2 tables (numbers of events and participants by arm) or as relative risks, odds ratios or MDs if full data were unavailable.
Mean differences or SMDs for each outcome measure were calculated from extracted data. These were combined with the results for each study estimated from the IPD in exploratory two-stage meta-analyses, following the same process as described in Statistical details of individual participant data meta-analyses.
Meta-analyses combining IPD with published data from studies not supplying IPD were treated as sensitivity analyses and used to assess whether or not there are any differences between studies that did not supply IPD and those that did.
Missing data
When a study did not examine or record an outcome measure or a covariate, the study was excluded from all relevant analyses.
If > 20% of participants in the IPD had no record for an outcome measure, a best- and worse-case analysis was planned as a sensitivity analysis. All included studies had < 20% of participants with missing outcome data (when the outcome was collected), so this analysis was not required.
Complete-case analysis (excluding all participants with missing covariate data) was used for all analyses. Imputation analyses were considered in the protocol as a way of handling missing covariates, but were not performed, given the limited number of covariate analyses that were feasible and because data were largely complete for the analyses performed.
Sensitivity analysis
Although a number of sensitivity analyses were identified in the statistical analysis plan, the limitations of the IPD meant that the only sensitivity analysis performed was one limited to an analysis of only UK-based studies.
Network meta-analysis
Network meta-analyses (NMAs) analysed all types of intervention and control simultaneously. The one-stage repeated measures meta-analysis models described above were extended to include multiple arms and incorporated random effects to account for heterogeneity. Potential network inconsistency was investigated by comparing NMA results with results from direct pairwise meta-analyses.
Multivariate meta-analysis
The analysis included many outcomes that are likely to be highly correlated both within domains (e.g. different IQ scoring methods) and between domains (e.g. VABS score and autism symptom severity). Multivariate analysis of these correlated outcomes may improve estimation, particularly in cases in which some studies do not report one outcome, but do report a correlated outcome.
One-stage models of multivariate analysis were considered. Given the limited availability of outcomes, only bivariate analyses of composite VABS score with each other outcome were feasible. These analyses were done but are not reported here, owing to uncertainty as to their validity, given data limitations, and little evidence of any difference from the main univariate analyses.
Software
All data management and meta-analyses were performed at the Centre for Reviews and Dissemination, using the R software package (2016; The R Foundation for Statistical Computing, Vienna, Austria).
Additional libraries in R were used as follows:
-
data management and manipulation: tidyr, dplyr, tidyverse libraries
-
two-stage analyses: meta and metafor libraries
-
one-stage models: lme4 library
-
forest plots: using in-house R code and meta library
-
other graphics: ggplot2 library.
Chapter 5 Systematic review and meta-analysis of effectiveness: results
Study selection
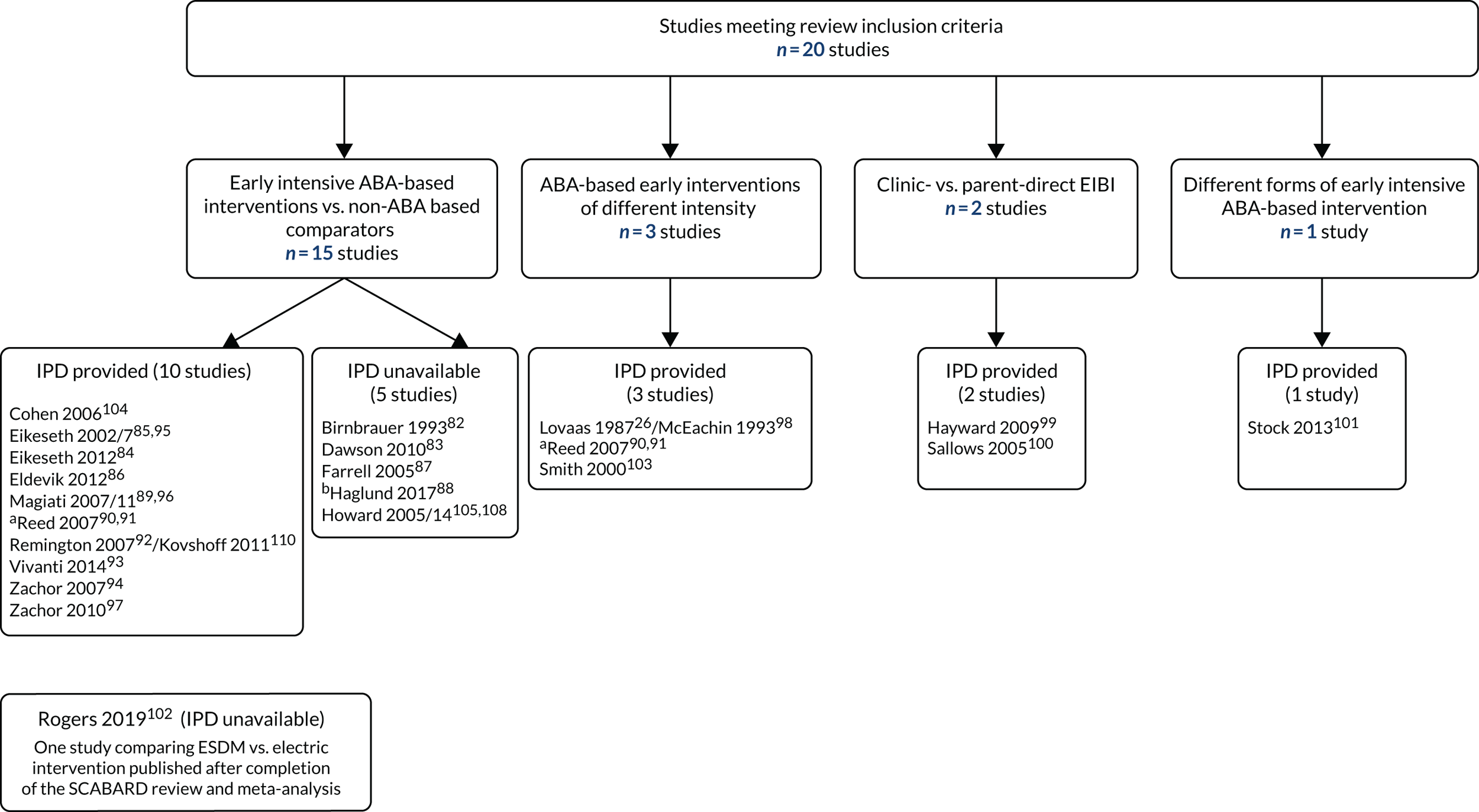
Of the 6881 records identified from the literature searches, a total of 64 studies were considered potentially eligible for inclusion on the basis of information available in record titles and abstracts. After screening full-text publications and/or contacting authors for clarification of study details, a total of 20 studies from 33 articles were included in the review (Figure 1). Studies that were not included and the reason for their rejection are included in Table 29 in Appendix 5.
FIGURE 1.
Flow of included studies.

Included studies
Figure 2 shows the included studies by treatment comparison. Fifteen studies compared some form of ABA-based early intensive intervention against a comparator treatment (typically characterised as ‘eclectic’ or TAU). 82–97,104–110 Three studies26,90,91,98,103,111 compared ABA-based early intensive interventions of different intensity, two studies99,100 compared clinic-based with parent-managed ABA-based early intensive interventions, and one study101 compared two different forms of ABA-based early intensive behavioural therapy. Table 1 summarises the characteristics of the included studies. Twenty studies (reported in 33 publications26,82–101,103–112) published between 1987 and 2017 were identified. The majority of these were published in academic journals, although one was a Doctor of Philosophy (PhD) thesis112 and another was a conference abstract that met the review inclusion criteria but did not report any results. 88 Full details of all studies are provided in Table 30 in Appendix 6.
FIGURE 2.
Studies and comparisons. a, Included multiple arms, so included in two comparisons; and b, unpublished study.
| First study author and year | Intensive ABA-based intervention name | Comparator name | Number of intervention participants (number followed up) | Number of comparator participants (number followed up) | Treatment duration (months) (SD) | Actual delivered treatment intensity (hours/week) (SD) | Mean (SD or range) age at baseline (months unless otherwise stated) | Sex (M/F) | Baseline autism symptom severity [measure] (SD) | Baseline full-scale IQ (SD) [measure] | Mean (SD) baseline VABS score |
|---|---|---|---|---|---|---|---|---|---|---|---|
| EIBI vs. TAU/eclectic intervention(s) | |||||||||||
| Birnbrauer 199382 | Murdoch Early Intervention Program | Control | 11 (9 followed up) | 8 (5 followed up) | I NR; C NR | I 18.72 (range 8.7–24.6); C NR | I 39 (32–47); C 33 (22–47) | I 4/5; C 5/0 | I NR; C NR | I 20; C 18 [BSID mental age in months] | I 18; C 17 [VABS adaptive behaviour age in months] |
| Cohen 2006104 | EIBI | TAU | 21 | 21 | I 36; C 36 | I NR; C NR | I NR; C NR | I 18/3; C 17/4 | I NR; C NR | I 61.6 (16.4); C 59.4 [BSID] | I 69.8; C 70.6 |
| Dawson 201083 | ESDM | TAU | 24 | 24 | I 24; C 24 | I 31.5 total 1 : 1 (15.2 therapist, 16.3 parent) + 5.2 other therapies (e.g. speech therapy, developmental preschool); C 18.4 (9.1 individual, 9.3 group) | I 23.9 (4.0); C 23.1 (3.9) | I NR; C 18/6 | I 7.2 (1.7); C 6.9 (1.7) [ADOS severity score] | I 61 (9.2); C 59.4 (8.6) [MSEL composite] | I 69.5 (5.7); C 69.9 (7.3) |
| Eikeseth 201284 | Community school-based EIBI | Eclectic special education teaching | 35 | 24 | I 24; C 24 | I NR; C NR | I 3.9 years; C 4.4 years | I 31/5; C 20/4 | I 37.2 (7.7); C NR [CARS] | I NR; C NR | I 67 (10.3); C 63.6 (8.1) |
| Eikeseth 2002/785,95 | EIBI | Intensive eclectic special education | 13 | 12 | I 36; C 36 | I 28 (1 year), 18 (3 years); C 29 (1 year), 16 (3 years) | I 66.31; C 65 | I 8/5; C 11/1 | I NR; C NR | I 61.92; C 65.17 [WPPSI-R, WISC-R or BSID] | I 55.77 (8.96); C 60 (13.2) |
| Eldevik 201286 | EIBI | TAU (eclectic) | 31 | 12 | I 25.1 (6.3); C 24.6 (10.8) | I 13.6 (5.3) (hours spent on weekly goals during preschool); C ≥ 5 (actual hours not specified) | I 42.2 (26–70); C 46.2 (24–67) | I 25/6; C 8/4 | I NR; C NR | I 51.6 (16.9); C 51.7 (18.1) [BSID, S–B or WPPSI] | I 62.5 (8.2); C 58.9 (7.8) |
| Farrell 200587 | EIBI | Eclectic (LUFAP) | 8 | 9 | I 26; C 20 | I NR; C NR | I NR; C NR | I 7/2; C 6/2 | I NR; C NR | I 15.6 months; C 21.8 months (BSID) | I NR; C NR |
| Haglund 201788 | CIEI | TAU | 67 | 27 | I NR; C NR | I NR; C NR | I NR; C NR | I NR; C NR | I NR; C NR [ADOS-R] | I NR; C NR [WPPSI-III] | I NR; C NR |
| Howard 2005105 | Early IBT | C1: autism educational programming – eclectic autism-specific classroom-based intervention; C2: general educational programming – generic special education classroom intervention | 29 | C1 16; C2 16 | I 14; C1 14; C2 14 | I 25–40; C1 25–30; C2 15 | I 30.86 (5.16); C1 37.44 (5.68); C2 34.56 (6.53) | I 25/4; C1 13/3; C2 16/0 | I 7.55 (1.39); C1 7.27 (1.56); C2 7.33 (2.02) [number of DSM-IV criteria met] | I 58.54 (18.15); C1 53.69 (13.5); C2 59.88 (14.85) [BSID, WPPSI or S–B] | I 70.46 (11.85); C1 69.81 (10.48); C2 71.62 (10.47) |
| Remington 200792 | EIBI | TAU | 23 | 21 | I 24; C 24 | I 25.6 (4.8); C NR | I 35.7 (4.0); C 35.7 (4.4) | I NR; C NR | I NR; C NR | I 61.43 (16.43); C 62.33 (16.64) [BSID, S–B] | I 60.22 (5.82); C 57.17 (7.05) |
| Magiati 200789 | EIBI | Autism-specific nursery (school provisions) | 28 | 16 | I 23–27; C 23–27 | I 32.4 (6.4); C 25.6 (6.4) | I 38 (7.2); C 42.5 (7.8) | I 27/1; C 12/4 | I 36.4 (6.7); C 40 (6.9) [ADI-R] | I 83 (27.9); C 65.2 (26.9) [BSID, MP, WPPSI-R] | I 59.6 (6.2); C 55.4 (5.4) |
| Vivanti 201493 | ESDM | ‘Generic’ intervention | 27 | 30 | I 11.9; C 11.8 | I 15–25; C NR | I 40.3; C 41.97 | I 23/4; C 27/3 | I 6.78; C 6.31 [ADOS calibrated score] | I 53.46; C 49.01 [MSEL total] | I 68.74; C 68.5 |
| Zachor 200794 | ‘ABA’ | Eclectic development approach | 20 | 19 | I NR; C NR | I NR; C NR | I 27.7; C 28.8 | I 19/1; C 18/1 | I NR; C NR | I NR; C NR | I NR; C NR |
| Zachor 201097 | ‘ABA’ | ‘Eclectic’ | 45 | 33 | I NR; C NR | I NR; C NR | I 25.1 (3.9); C 26.0 (4.6) | I NR; C NR | I 20.9 (4.3); C 20.1 (4.6) [ADOS new algorithm] | I 72.2 (19.2); C 73.3 (22.2) [MSEL cognitive composite] | I 66.2 (9.6); C 68.6 (6.3) |
| EIBI vs. lower-intensity ABA-based intervention | |||||||||||
| Lovaas 198726 | EIBI | Lower-intensity ABA-based treatment | 19 | 19 | I > 24 (estimated ≈ 49); C > 24 (estimated ≈ 43) | I NR; C NR | I 34.6; C 40.9 | I 16/3; C 11/8 | I NR; C NR | I mental age 18.8; C mental age 17.1 [BSID, Cattell, S–B, Gesell] | I NR; C NR |
| Smith 2000103 | IBT | Parent training | 15 | 13 | I 33.44 (11.0); C NR | I 24.52 (3.69); C NR | I 36.07 (6.0); C 35.77 (5.37) | I 12/3; C 11/2 | I NR; C NR | I 50.53 (11.18); C 50.69 (13.88) [BSID, S–B] | I 63.44 (9.35); C 65.17 (9.44) |
| Reed 200790,91 | High-intensity ABA-based interventions (Lovaas,26 CABAS and verbal behaviour) | C1 low-intensity ABA-based intervention; C2 special nursery placements (TAU); C3 portage | 14 | C1 13; C2 20; C3 16 | I 9–10; C1 9–10; C2 9; C3 9 | I 30.4 (5.0); C1 12.6 (2.3); C2 12.7 (3–23); C3 8.5 (2–15) | I 42.9 (14.8); C1 40.8 (5.6); C2 43 (41–48); C3 38 (30–45) | I 14/0; C1 13/0; C2 18/2; C3 NR | I 89.1 (14.7); C1 95.1 (11.6); C2 96.8 (10.4); C3 91.3 (14.3) [GARS] | I 57.2 (17.8); C1 49.3 (13.2); C2 51.9 (20.1); C3 53.3 (16.1) [PEP-R] | I 59.3 (10.1); C1 56.5 (4.4); C2 53 (4.6); C3 58.6 (6.0) |
| Clinic- vs. parent-managed EIBI | |||||||||||
| Hayward 200999 | EIBI: clinic managed | EIBI: parent managed | 23 | 21 | I 12; C 12 | I 37.4 (3.47); C 34.2 (5.29) | I 35.7 (6.2); C 34.4 (5.7) | I 19/4; C 15/6 | I NR; C NR | I 53.5 (15.1); C 54.1 (15.1) [BSID/WPPSI-R] | I 62.3 (6.8); C 65.1 (10.4) |
| Sallows 2005100 | Clinic-directed UCLA-based EIBI | Parent-directed UCLA-based EIBI | 13 | 10 | I 24; C 24 | I 38.6 (2.91) 1 : 1 in year 1; C 31.67 (5.81) in year 1 | I 33.23 (3.89); C 34.2 (5.06) | I 11/2; C 8/2 | I NR; C NR | I 50.85 (52.1); C 52.1 (8.98) [BSID] | I 59.54 (5.31); C 60.9 (5.94) |
| Group-based verbal behaviour intervention vs. PRT-based intervention | |||||||||||
| Stock 2013101 | Nova Scotia EIBI | Group ABA | 14 | 14 | I 12; C 12 | I NR; C 20 | I 46.7 (9.23); C 46 (8.12) | I 12/2; C 12/2 | I NR; C NR | I NR; C NR | I NR; C NR |
Children in the included studies were aged on average from 2483,106,107,112 to 6685,95 months at intake (median 37.4 months) and had a diagnosis of autism, ASD or (in some earlier studies) pervasive developmental disorder, as confirmed by the Diagnostic and Statistical Manual of Mental Disorders, Third or Fourth Edition,26,82,105,108 the ICD-10,84 the ADI-R,85,86,89,92,95,96,104,109,110 the ADOS93 or some combination of these. 83,88,94,97,99,101,106,107,112 As would be expected, the majority of participants in the included studies (from 71% to 100%) were boys. Many included studies did not record the severity of baseline autism symptoms and those that did used a range of different measures (see Chapter 6, Individual participant data received from included studies). Across all included treatment arms, mean baseline VABS composite score ranged from 55.8 to 71.6 and mean baseline standard cognitive ability scores ranged from 51 to 83 (see Table 1).
Studies recruited participants from the USA,26,83,98,100,103–108,111,112 the UK,87,89–92,96,99,109,110 Norway,84–86,88,95 Australia,82,93 Israel94,97 and Canada. 101
One additional study102 comparing an ABA-based early intensive intervention against eclectic intervention was published during the writing of the current report, after the completion of the systematic review and meta-analyses. Although there was insufficient time available to integrate this study into the body of the report, a separate description of this study and meta-analyses incorporating its aggregate outcome data can be found in Appendix 12.
Applied behaviour analysis-based early intensive intervention versus treatment as usual and eclectic comparators
Fifteen studies (14 published26,82–87,89–101,103–112 and one unpublished88) compared some form of EIBI with a TAU or eclectic intervention.
Applied behaviour analysis-based early intensive interventions of different intensity
Three studies compared EIBI with a lower-intensity variation of the same approach, requiring fewer one-to-one contact hours between child and therapist. 26,90,91,98,103,111 The original UCLA study by Lovaas26 compared 40 hours per week of EIBI against the same kind of treatment for < 10 hours per week (this study also included a retrospective cohort of children not receiving any ABA-based treatment, but insufficient data were available in either publications or IPD to inform the current meta-analysis). 26,98 A later US study compared 30 hours per week of planned intensive EIBI (plus 5 hours/week of parental treatment) against parental training in EIBI techniques alone. 103 One UK study compared 20–40 planned hours of ABA-based intervention with around 10–20 hours per week of the same approach. 90
Clinic- versus parent-directed applied behaviour analysis-based early intensive interventions
Two studies compared clinic-directed EIBI against some form of parent-directed EIBI. 99,100 In these studies, children in both treatment arms received similarly intensive intervention with therapists (30–40 hours/week), but the parent-directed groups either received less frequent supervision by senior therapists and clinical supervisors,100 or required parents to recruit and manage therapists. 99
Different forms of applied behaviour analysis-based early intensive behavioural therapy
One Canadian study, including 28 children, compared two forms of ABA-based intervention in young autistic children. 101 One treatment arm consisted of ‘Nova Scotia EIBI’, in which children received 15 hours per week of one-to-one instruction based on the PRT approach (a NDBI approach that targets ‘pivotal’ areas of a child’s development and emphasises natural reinforcement). The comparator arm was a group ABA preschool programme, based on the verbal behaviour method (a structured approach focused on teaching communication and language). Children in the group ABA group received 15–25 hours per week of training, of which 3–5 hours consisted of one-to-one discrete trial training.
Characteristics of early intensive applied behaviour analysis-based interventions
All included studies evaluated some form of early intensive ABA-based intervention. All such interventions were rooted in ABA and incorporated replications, extensions, adaptations or variations of teaching techniques originally described by Lovaas et al. at the UCLA during the 1970s and 1980s. 26,98 Early studies closely resembled the original UCLA method, although without physical aversives. 82,103 Subsequent studies have incorporated additional manualised ABA procedures into the original UCLA EIBI intervention model. 85,86,90,91,94,95,97
Several studies incorporated some or all the aspects of NDBI approach into the EIBI model. 83,84,88,92,93,99,100,104,106,107,110,112 This included approaches such as the ESDM. 83,93,106,107,112
Children in the included studies received these early intensive ABA-based interventions for a period of 9–36 months, at a planned intensity of 15–40 hours per week of mostly one-to-one teaching (when recorded). Comparator treatments were delivered for a similar duration, although treatment intensity was more variable, ranging from 2 to ≥ 30 hours per week (when recorded), with considerably less one-to-one contact.
Characteristics of comparator interventions
As stated in Chapter 4, Individual participant data meta-analysis methods, comparator treatments could be broadly classified as ‘eclectic’ or TAU. Comparators were classified as ‘eclectic’ when individual children were known to have received a mix of teaching approaches, such as TEACCH, PECS, other behavioural or development programmes, speech and language therapy, music therapy or occupational therapy. Ten studies included eclectic comparator intervention arms, eight of which were delivered in a school or nursery classroom setting84–86,89–93,95,96,105,108,110 and two of which were delivered in a university or specialist centre setting. 94,97 As well as an eclectic arm, one study included a portage treatment arm [a home-visiting educational service for preschool children with special educational needs (SEN) and disability]. 90,91
Other comparators were classified as TAU when children received non-autism-specific special education or other forms of standard local provision. Six studies included TAU arms, of which one was delivered in a school/nursery,105,108 three were delivered in a range of settings83,92,104,106,107,110,112 and two did not provide clear information about setting. 82,88 Study investigators were not typically involved in the provision of TAU comparator treatments, so often did not have detailed information on the exact interventions received by individual children (see Study quality and risk of bias).
Study quality and risk of bias
The following section illustrates some of the core issues concerning risk of bias among studies included in the review, and primarily references studies comparing early intensive ABA-based with comparator interventions as examples. A full detailed assessment of the risk of bias for each meta-analytic comparison is presented in Appendix 9.
Three included studies were RCTs83,100,103,106,107,112 and were assessed using the Cochrane Risk of Bias 2.0 tool. 57 Risk of bias in the remaining non-randomised studies was assessed using the ROBINS-I tool. 58 All non-randomised studies were rated as being at ‘serious’ or ‘high’ risk of bias for at least one outcome on one domain on the relevant assessment tool. All three randomised studies83,100,103,106,107,112 were rated as having ‘some concerns’ about risk of bias.
Bias due to a range of confounding factors
All of the non-randomised studies were at serious risk of bias due to confounding. In five studies, the type of treatment received by children was explicitly based on parental preference,82,87,92,104,105,108,110 with parents actively seeking or lobbying for early intensive ABA-based treatment and, in some cases, paying for it themselves. 87,92,110
In other studies, the type of treatment received was primarily based on location84,86,90,91 or staff availability,26,85,95,98 for which the influence of parental preference was unclear.
In some studies, baseline differences in parental education, family composition or socioeconomic status were observed between treatment groups. 89,92,96,104,105,108–110
Bias due to deviation from intended interventions
Some studies described the methods used to assess treatment fidelity in the early intensive ABA-based intervention arm. These included monitoring, observation and feedback to tutors,83,93,104–108,112 or obtaining congruent descriptions of the intervention from parents and supervisors. 90,91 In other studies, early intensive ABA-based interventions were supervised, but without explicit monitoring for treatment fidelity. Studies noted difficulties, such as high tutor turnover resulting in the intervention being delivered for fewer hours per week than intended,92,110 high proportions of children not completing the intervention,104 unreliable recording of weekly hours of EIBI,84 and families changing between different EIBI organisations or supervisors and consultants during the study period. 89,96,109
The delivery and content of comparator arms was not closely monitored in the available studies, although three studies84–86,95 did report a high proportion of children receiving ABA techniques as part of ‘eclectic’ therapy or TAU comparators.
Studies rarely recorded whether or not children received any co-interventions alongside those being evaluated. One study appeared to compare groups in terms of independently procured co-interventions, finding that children receiving EIBI received more dietary and other biological interventions, extracurricular educational interventions and alternative treatments, than children receiving TAU. 89,96,109
Bias in measurement of outcomes
Truly independent and blinded measurement of outcomes were rarely achieved in the evaluation of early intensive ABA-based intervention studies. In some cases, the participants in the ABA-based intervention and the comparison intervention arm were assessed by treatment supervisors84 or study investigators,86 sometimes with an independent second evaluator. Although some studies described employing outcome assessors who were independent of direct intervention delivery,82,85,89,92,95,96,104,105,108–110 the assessments typically involved interaction with children and parents who were not blinded to intervention. Assessors who were blinded to allocation could potentially have been unblinded by the assessment location (if this differed between intervention arms or – when delivered in the family home – provided contextual information about likely treatment allocation). Consequently, all of the included studies were considered to be at moderate or serious risk of bias for this domain.
Summary
Although randomisation is clearly feasible, most studies used convenience samples, with the allocation to early intensive ABA-based interventions being based on location or parental preference. Although some attempts were made to avoid bias in the measurement of outcomes, the nature of the intervention can make true blinded assessment difficult to achieve. There is evidence from some studies to suggest differences between the two intervention groups in terms of socioeconomic status and use of co-interventions, but this information was not consistently recorded across studies. In some cases, outcome data were missing or available for only one treatment group. It is also important to note that despite requesting them, we did not receive any protocols for the included studies. The original Lovaas study,26 in particular, was at risk of several forms of bias, including the comparator groups differing on the few available baseline variables. 26,98 Taken together, these concerns increase our uncertainty about the results observed in several included studies, making it possible that the effects observed in the meta-analysis may overestimate the true effects of early intensive ABA-based interventions.
Study variability and relevance to the current UK context
The data in the included studies were collected over a period of > 40 years (from around 1968 to 2011), during which time the understanding, diagnosis and management of autism has evolved significantly. Consequently, there is noticeable variation between individual studies in terms of the delivery of interventions and comparators, the conceptualisation of autism and the outcomes of interest. As well as differences between the studies, there may be important differences between this body of evidence and the context in which early intensive ABA-based interventions and other treatment alternatives may be delivered in the UK in the future.
Interventions
Content, delivery and expertise
The original EIBI study by Lovaas at UCLA26,98 mainly employed discrete trial training, with some generalisation activities and community outings. Contingent physical aversives (the delivery of a loud ‘no’ or slap on the thigh) were employed as a last resort. As noted in Chapter 9, later variations in early intensive ABA-based interventions have incorporated more naturalistic components in their delivery and discontinued the aversive contingencies used in the original UCLA EIBI approach. Corporal punishment has been illegal in the UK for > 30 years and physical aversives have long been abandoned as part of ABA-based intervention delivery. Although all interventions included in this review had a theoretical basis in ABA, their content and delivery has evolved over time.
The UCLA EIBI intervention was delivered by trained student therapists, overseen by the study authors who were based at a specialised university centre, ensuring a high level of resource and expertise being made available to children and their families. 26 Smith et al. 103 reported 10 years’ experience working at the UCLA Young Autism Project. Similar expertise was available in the randomised study of the ESDM, which also involved the authors who developed the intervention method. 83,106,107,112
The original narrow definition of what once constituted ‘true’ EIBI may not resemble very closely what is delivered in the current UK context, in which the intervention is more likely to be informed by more naturalistic approaches and delivered in a home or community setting, without the resources of an expert university research centre to train and supervise treatment staff.
Intensity and duration
The original UCLA EIBI was highly intensive. In addition to children receiving an average of 40 hours per week of one-to-one contact with therapists in their home, school and community for at least 2 years, parents were asked to take a year off from their current employment103 and were trained so that ‘treatment could take place for almost all of the subjects’ waking hours, 365 days a year’. 26 Although actual treatment intensity and duration data were not recorded for individuals, it would appear that children had around 4 years of treatment on average (based on reported age at recruitment and follow-up), with children who had not ‘recovered’ continuing to receive > 40 hours per week of one-to-one teaching with therapists for > 6 years. 26
As stated in Included studies, subsequent studies of early intensive ABA-based interventions were more varied in intensity and duration. Interventions rarely exceeded Lovaas’ minimum requirement of 40 weekly hours of one-to-one teaching. 26 For example, authors who had been involved in the UCLA programme have delivered forms of EIBI that are deliberately less intensive than originally proposed (30 hours/week rather than 40 hours/week, with treatment phased out after 18 months if progress was slow). 103 Other studies have shown intervention hours to substantially reduce after the first 2 years of treatment83,106,107,112 or when children started school. 85,95 Although IPD on actual intensity were largely unavailable, the average weekly hours of teaching reported in UK studies ranged from 25.692,110 to 37.499 hours per week, and ranged from 13.6 to 38.6 hours per week in other studies.
As well as a possible impact on effectiveness, the duration and intensity of ABA-based treatment has implications for resource use (e.g. staffing costs) and possibly setting. Children in the UK typically start school at 5 years of age, whereas much of the evidence included in the current meta-analysis is from countries in which the primary or elementary school starting age is 6 years (USA, Norway, Canada, Israel). So in other countries, EIBI has been delivered in home and/or nursery or preschool settings, but in the UK it may be given in a primary education environment.
Another issue is that of the intervention supervision and management model. Several EIBI studies described the intervention being delivered by tutors who received ongoing training and feedback from supervisors, who in turn were overseen by a consultant or clinic director. 26,103 However, this form of management is not always applied in the delivery of early intensive ABA-based interventions in UK practice.
Comparators
Comparator interventions for autistic children have also evolved over time, with the emergence of autism-specific rather than generic special needs care. More recently, ‘eclectic’ comparators have explicitly incorporated some ABA techniques. 83,84,86,89,93,94,96,97,105,108,109 In most studies, children in the eclectic or TAU comparator arms received fewer hours of intervention and/or less one-to-one contact. However, this was not always the case: Howard et al. 105,108 compared EIBI against an eclectic autism-specific classroom, with ≈30 hours per week of one-to-one or one-to-two intensive intervention; and Zachor et al. 94,97 reported both intervention groups receiving similar levels of funding per child, hours in preschool setting, support for parents and staff, and individual one-to-one treatments.
Although we did not restrict inclusion by comparator, all of the identified comparators were eclectic intervention or TAU; no studies compared early intensive ABA-based interventions with discrete medical or educational interventions.
It is difficult to map the comparators in the available evidence to the current UK standard provision for two reasons. First, most studies had very limited available information on the content of eclectic interventions or TAU, as the study investigators were rarely involved in their delivery. Second, there is evidence that standard provision in the UK differs substantially between local authorities, although information obtained from York local authority suggests a mix of therapies not dissimilar to those cited in the studies (Ruth Horner, City of York Council, York, 2018, personal communication).
Participants
The studies included in this review cover a period when a large increase in the annual incidence of autism has been observed (more than fivefold from 1988 to 1995). 113,114 Part of that increase has been attributed to changing and broadening diagnostic criteria,115,116 as well as increased medical and public awareness. 117 This raises concerns about whether or not children receiving early intervention ABA-based interventions in included studies are similar to those currently eligible for intervention in the UK.
The overall population of children for whom IPD were provided were young (mean age 38 months) with mild-to-moderate intellectual disability (mean IQ 57) (see Chapter 6, Individual participant data received from included studies). As all children had to have an established diagnosis of autism or related condition to participate in the included studies, the study populations ought to be comparable to those who would be eligible for treatment in the current UK context. However, some of the more highly controlled studies excluded children with comorbidities, so it is plausible that typical UK treatment populations are more heterogeneous than those in the available evidence.
Outcomes
Although we accepted any outcomes for the IPD meta-analysis, only a small number of outcome domains were consistently collected across the included studies (most commonly, verbal and non-verbal IQ, adaptive behaviour and language measures; less commonly, autism symptom severity, behaviours that challenge and school placement).
The original Lovaas study26,98 was almost entirely focused on IQ and mainstream schooling placement as measures of treatment success. Children who achieved IQ in the average range were considered ‘recovered’ and the authors made ‘considerable effort’ to keep these children in mainstream preschool. In some cases, this involved withholding the child's diagnosis of autism. The authors stated, ‘If the child became known as autistic (or as “a very difficult child”) during the first year in pre school, the child was encouraged to enrol in another, unfamiliar school (to start fresh)’. 26 Apart from any ethics and bias concerns it may raise, this excerpt shows how different the goals of early autism interventions were 30–40 years ago.
Subsequent studies incorporated behavioural measures, such as adaptive behaviour, while retaining IQ or cognitive development measures. Schooling as an outcome was only collected in a minority of studies and did not use consistent classifications. 26,89,92,96,98,103,104,109,110
Outcomes relating to social participation, well-being and quality of life were not measured among the included studies. Although measures of cognitive development and adaptive behaviour can be used to track progress and development, no studies investigated how these measures correlate with measures of well-being, either during treatment or in the long term. In fact, any measurement of outcome beyond the end of the early intervention treatment period was rare.
With the exception of one study stating that ‘no serious adverse effects related to the intervention were reported during the 2-year period’,83,106,107,112 adverse or unintended effects of intervention were not addressed in the available evidence, with no study providing IPD on adverse effects.
The selection of measurement tools used for the collected outcomes varied within and between studies. Different measures of IQ and cognitive development were used at baseline and follow-up, based on the relevant normative populations [e.g. the WPPSI-R67 or BSID scales at baseline and Wechsler Intelligence Scale for Children (WISC)65 at follow-up]. At baseline, in particular, decisions about which measure to use are also informed by children’s developmental skills and ability to meaningfully be assessed in particular tests. The IPD meta-analyses separate measures of non-verbal skills (such as the MPSMT)70 from standard intelligence tests, which include verbal and non-verbal scales, as the former are known to yield higher scores. 100
Several studies reported difficulties when using standardised measures in the evaluation of interventions in young autistic children, including floor and ceiling effects on different tests at different ages. Authors dealt with these difficulties by recording minimum or maximum scores,103 reporting age-equivalent scores,101 raw scores89,92,96,109,110 or the number of children capable of achieving a score. 92,110 Although the provision of IPD facilitated the harmonisation and synthesis of scores across some of these studies, this was not always possible or appropriate.
Most studies provided standard scores when these were available and these scores informed the IPD meta-analyses. However, although standard scores allow comparisons with typically developing populations, it has been argued that they may miss information about changes that are relevant within the autism population specifically. 118 This problem is not limited to early intensive ABA-based interventions, but is one of several barriers to valid and reliable outcome measurement in young autistic children in general. 119
Chapter 6 Results of individual participant data meta-analysis
Individual participant data received from included studies
Of the 20 studies identified, we received data from the authors of 15 studies. Of the five remaining studies, two no longer had access to the data82,87 and two declined to participate in the project. 88,105,108 The authors of one study83,106,107,112 indicated that the terms under which families consented to be in the study prevented the sharing of IPD, except through the US National Database for Autism Research (NDAR). The SCABARD research team therefore obtained the relevant data sets via NDAR (URL: www.ndar.nih.gov). However, it was not possible to identify participants from the study of interest within the wider group of participants included in the NDAR data set. The study authors reiterated that the consent terms of the study precluded them from being able to assist in identifying the participants and variables of interest.
The authors of one study94,97 indicated that they had continued to collect data following the same protocol as their included studies and therefore provided data for more participants than had been published.
Therefore, we ultimately collected 75% (669/894) of all known (published or unpublished) data from individual study participants, or 82% (654/800) of published data.
Individual participant data: participant characteristics
Table 2 shows the characteristics of participants within the studies for which IPD were available.
| First study author and year | Age at baseline (months) | Male (%) | IQa | VABS composite | ADOS CSS | % IQ < 70 | % VABS < 60 |
|---|---|---|---|---|---|---|---|
| Average by study | |||||||
| Cohen 2006104 | 31.5 | 83.3 | 60.7 | 70.2 | 73.8 | 4.9 | |
| Eikeseth 200285 | 66 | 76 | 64.5 | 57.8 | 72 | 56 | |
| Eikeseth 201284 | 49.3 | 83.1 | 65.6 | 25.4 | |||
| Eldevik 201286 | 43.3 | 76.7 | 51.6 | 61.5 | 86 | 48.8 | |
| Hayward 200999 | 35.1 | 77.3 | 54.1 | 63.6 | 79.5 | 34.1 | |
| Lovaas 198726 | 37.3 | 71.1 | 49.1 | 66.5 | 81.6 | 42.4 | |
| Magiati 200789 | 39.5 | 88.6 | 46.3 | 58.1 | 92 | 57.5 | |
| Reed 200790,91 | 41.5 | 93.7 | 52.9 | 56.5 | 87.3 | 77.8 | |
| Remington 200792 | 37.1 | 87.8 | 62.5 | 58.9 | 70.7 | 53.7 | |
| Sallows 2005100 | 32.7 | 82.6 | 50.8 | 62 | 95.7 | 43.5 | |
| Smith 2000103 | 35.9 | 82.1 | 50.6 | 60 | 89.3 | 50 | |
| Stock 2013101 | 45.8 | 89.3 | 65.8 | 32.1 | |||
| Vivanti 201493 | 41.2 | 87.7 | 68.6 | 6.5 | 22.8 | ||
| Zachor 200794 | 26.9 | 96.2 | 75 | 62.9 | 41.7 | 29.3 | |
| Zachor 201097 | 25.2 | 90.9 | 67 | 7.3 | 14.5 | ||
| Average over all studies | 37.9 | 85.6 | 56.8 | 63.3 | 7 | 77.6 | 38.3 |
| Average in ABA vs. non-ABA (main) studies | 38.4 | 87.5 | 59.4 | 63.1 | 7 | 74.2 | 37.8 |
On average across all studies, children were aged 37.9 months at intake; 86% of participants were boys. Although studies used different methods to assess IQ, all used the usual standardisation of a mean IQ of 100, with a SD of 15. Across studies, the mean baseline IQ was 56.8. The mean baseline composite VABS score was 63.3.
Studies that compared intensive ABA-based interventions with comparator early interventions had similar baseline characteristics. However, it also shows some degree of between-study variation in baseline age (from around 2 to 5.5 years) and IQ (from 46 to 65). It can be seen that autism symptom severity scores were rarely available in the IPD, with ADOS calibrated severity score values available for two studies at baseline (see Table 2).
Individual participant data meta-analysis of early intensive ABA versus treatment as usual or eclectic interventions
This section considers the main meta-analyses: those comparing early intensive ABA-based interventions (EIBI, EIBI with NDBI) with TAU or eclectic interventions. Analyses including other studies (such as low vs. high intensity) are considered in Studies making other comparisons.
Participant and study characteristics
Ten studies provided IPD for the comparison of early intensive ABA with TAU or eclectic interventions. 84–86,89–97,104,109,110 These studies reported a wide range of different eligible outcomes.
Appendix 7 shows which of the variables specified in the SCABARD data dictionary were available as IPD for each included study. The only individual-level variables that were available for every study were age at baseline, sex and assigned treatment arm. The majority of other variables were not consistently collected across studies. In some cases, study investigators clarified that these variables were not collected at all, collected for the early intensive ABA-based intervention arm only, or were otherwise unavailable. However, in most cases, variables were absent from the IPD data sets, without any definitive explanation being provided.
For a comparison of the outcome domains and measures in the IPD with those in the published literature, see Appendix 8.
A variety of scales were used to measure IQ and cognitive development, most commonly versions of the BSID62 S–B,69 WISC65 and Wechsler Preschool and Primary Scale of Intelligence (WPPSI). 67 When different scales were used in studies, this was typically due to the need to select an age-appropriate scale. As all these scales were standardised (to an average IQ of 100 with SD of 15), in the primary analysis of IQ we have not differentiated between the methods and consider them as equivalent.
Non-verbal intelligence was most commonly measured using the MPSMT70 and autism symptom severity with the ADOS. 78 Although adaptive behaviour was consistently measured using the VABS,59 language was measured using a variety of scales, most commonly the RDLS74 and the expressive and receptive subscales of MSEL. 76 Parental outcomes were not measured frequently or consistently across studies, and school placement IPD were available for only one study. 89,96,109
Data were provided at baseline and at least one follow-up time (as required for meta-analysis) for only a minority of outcomes. Table 3 summarises the outcomes recorded across studies. This shows that, for most outcomes and outcome domains, there were few studies and limited data for meta-analysis. For a comparison of the outcome domains and measures in the IPD against those in the published literature, see Appendix 8.
| Outcome domain | Outcome | Cohen 2006104 | Eikeseth 200285 | Eldevik 201286 | Magiati 200789 | Vivanti 201493 | Eikeseth 201284 | Reed 200790,91 | Remington 200792 | Zachor 200794 | Zachor 201097 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Autism symptom severity | ADOS repetitive behaviours | No | No | No | No | Yes | No | No | No | No | Yes |
| ADOS severity score | No | No | No | No | Yes | No | No | No | No | Yes | |
| IQ | IQ any scale | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | No |
| IQ BSID scale | No | Yes | No | Yes | No | No | No | No | No | No | |
| Non-verbal IQ (MPSMT) | Yes | Yes | No | Yes | No | No | No | No | No | No | |
| Language | MSEL expressive | No | No | No | No | Yes | No | No | No | No | Yes |
| MSEL receptive | No | No | No | No | Yes | No | No | No | No | Yes | |
| RDLS comprehension | Yes | Yes | No | Yes | No | No | No | No | No | No | |
| RDLS expressive | Yes | Yes | No | Yes | No | No | No | No | No | No | |
| Adaptive behaviour | VABS communication | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes |
| VABS composite | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| VABS DLS | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | |
| VABS maladaptive | No | Yes | No | No | No | Yes | No | No | No | No | |
| VABS motor skills | No | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | |
| VABS socialisation | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | |
| School placement | School placement | No | No | No | Yes | No | No | No | No | No | No |
| Other | MSEL composite | No | No | No | No | Yes | No | No | No | No | Yes |
| MSEL fine motor | No | No | No | No | Yes | No | No | No | No | Yes | |
| MSEL visual reception | No | No | No | No | Yes | No | No | No | No | Yes |
A further issue is that studies were not consistent in the times at which outcomes were recorded. Table 4 shows the number of studies reporting at each time for the outcomes listed in Table 3. This shows that, although several studies reported an outcome, not all studies reported it at consistent times. For example, several outcomes were reported only in one study, and only one study reported data at 7 years (precluding any meta-analysis).
| Outcome | Time of reporting | |||
|---|---|---|---|---|
| Baseline (10 studies84–86,89–97,104,109,110) | 1 year (eight studies84,85,90–95,97,104) | 2 years (eight studies84–86,89,92,94–97,104)a | 7 years (one study96) | |
| ADOS repetitive behaviours | 2 | 2 | 1 | 0 |
| ADOS severity score | 2 | 2 | 1 | 0 |
| IQ BSID scale | 2 | 1 | 2 | 1 |
| IQ MPSMT | 3 | 2 | 3 | 1 |
| IQ any scale | 7 | 5 | 6 | 1 |
| MSEL composite | 2 | 2 | 1 | 0 |
| MSEL expressive | 2 | 2 | 1 | 0 |
| MSEL fine motor | 2 | 2 | 1 | 0 |
| MSEL receptive | 2 | 2 | 1 | 0 |
| MSEL visual reception | 2 | 2 | 1 | 0 |
| RDLS comprehension | 3 | 2 | 3 | 1 |
| RDLS expressive | 3 | 2 | 3 | 1 |
| VABS communication | 9 | 7 | 8 | 1 |
| VABS composite | 10 | 8 | 8 | 1 |
| VABS DLS | 9 | 7 | 8 | 1 |
| VABS maladaptive | 2 | 2 | 1 | 1 |
| VABS motor skills | 8 | 6 | 7 | 1 |
| VABS socialisation | 9 | 7 | 8 | 1 |
Meta-analyses by outcome domains
This section presents results of meta-analyses for each outcome domain. Given the small numbers of studies involved, meta-analyses of any early intensive ABA-based intervention compared with TAU or eclectic interventions are presented.
Adaptive behaviour
Adaptive behaviour was assessed using the VABS composite and component scores, with results available for all 10 included studies. 84–86,89–97,104,109,110 Here, we consider the meta-analyses of the composite VABS score. The complete data on the composite score are shown in Figure 3. The points show the scores for each child, with the lines connecting each child’s score over time. Figure 4 shows the mean (average) change in score from baseline.
FIGURE 3.
Reported VABS composite scores for each child, by study and intervention.

FIGURE 4.
Mean change in VABS composite score from baseline, by study and intervention.
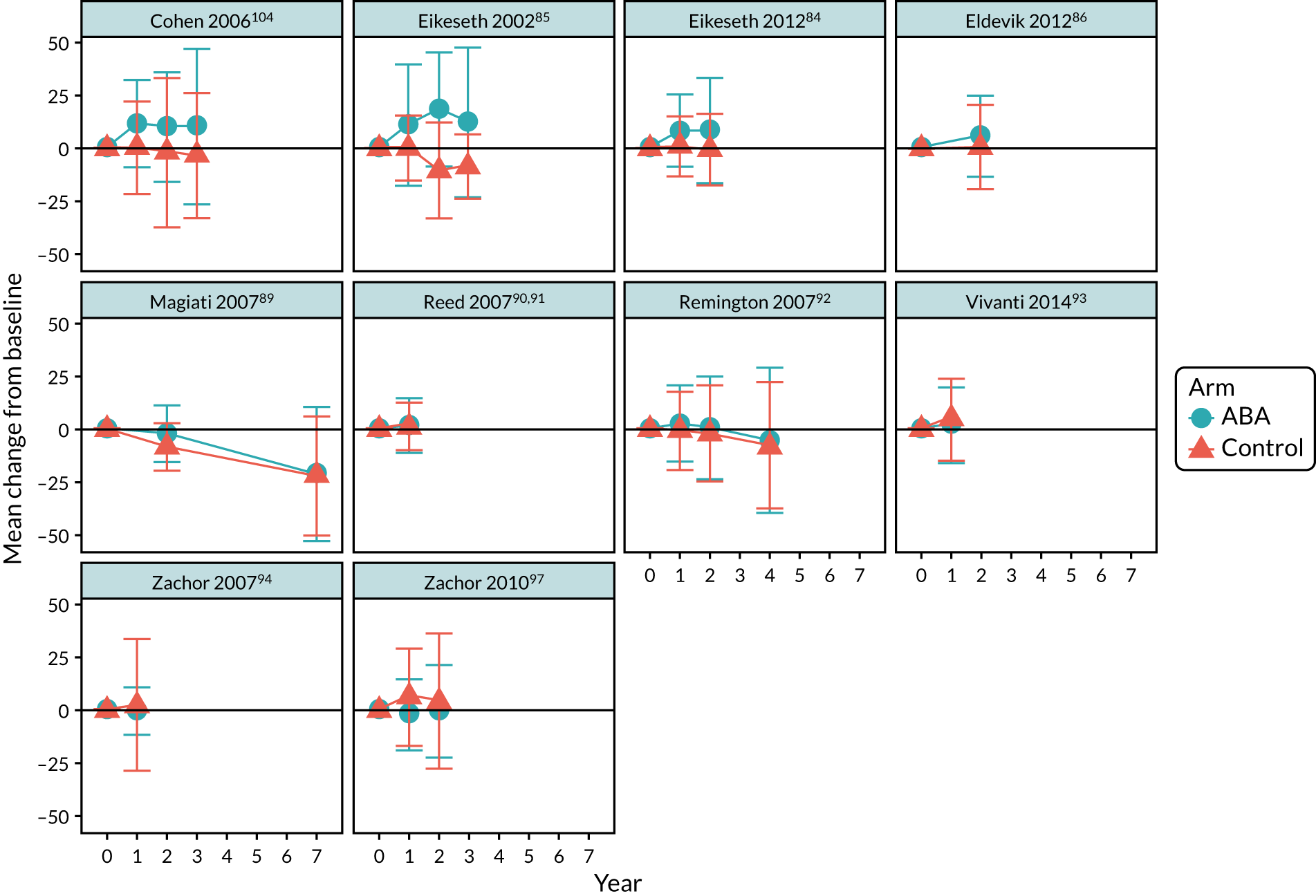
These plots suggest no consistent trend in scores across studies. Indeed, there is considerable variation in how VABS changes over time. In some studies, scores remained largely unchanged over time, in some there was little change in the control arm but increases in early intensive ABA-based interventions, and in some the scores decreased in both arms.
The meta-analyses of VABS composite score at 1 and 2 years are shown in Figures 5 and 6, respectively. These showed no clear evidence of a benefit of early intensive ABA-based interventions after 1 year, with substantial heterogeneity (MD 1.82, 95% CI –2.79 to 6.43, I2 = 80%), and a 7-point difference in favour of the ABA-based intervention (half of a SD) after 2 years, with less heterogeneity (MD 7.74, 95% CI 1.87 to 13.61, I2 = 72%). Studies varied substantially in their estimated MDs. One extreme outlier, with seven children, found a 32-point difference in favour of early intensive ABA-based interventions. In the opposite direction, one trial found a 5-point difference in favour of TAU or eclectic interventions.
FIGURE 5.
Meta-analysis of composite VABS score at 1 year.

FIGURE 6.
Meta-analysis of composite VABS score at 2 years.

Data beyond 2 years were limited. Only two small studies95,104 reported outcomes at 3 years and one study at 4 years,110 and so forest plots are not presented here. The data at 7 years came from only one study,96 which found no difference between groups at 7 years (MD –0.99, 95% CI –12.80 to 10.83).
Cognitive ability
Intelligence quotient (measured using any scoring method) was reported in the majority of studies. 85,86,89–92,94,96,104,109,110 We analysed IQ scores whatever assessment method was used.
Figure 7 shows the mean change from baseline in IQ, by study and intervention. As for VABS score, the pattern of changes varied across trials. Some trials had IQ improvements with both early intensive ABA-based and comparator groups, some showed improvement only with the early intensive ABA-based interventions and some showed no improvement at all.
FIGURE 7.
Mean change in IQ score from baseline, by study and intervention.

The meta-analyses of IQ at 1 and 2 years are shown in Figures 8 and 9, respectively. These show clear evidence of a difference in favour of early intensive ABA-based interventions of around 10 IQ points after 1 year (two-thirds of a SD, MD 10.12, 95% CI 5.81 to 14.44, I2 = 0) and after 2 years (MD 11.97, 95% CI 6.74 to 17.20, I2 = 15%).
FIGURE 8.
Meta-analysis of IQ at 1 year.

FIGURE 9.
Meta-analysis of IQ at 2 years.

Data beyond 2 years were limited. Only two small studies104 reported outcomes at 3 years and one reported outcomes at 4 years,92,110 and so forest plots are not presented here. The data at 7 years comes from only one study,96 which found no evidence of a difference between groups at 7 years (MD –1.92, 95% CI –15.17 to 11.32).
Autism symptom severity
Only two studies reported data on autism symptom severity,93,97 in terms of ADOS calibrated severity score. Meta-analyses of these two studies could be performed only at 1 year after intervention initiation. The meta-analysis (see Appendix 11, Figure 24) suggests a possible effect with both studies favouring TAU or eclectic intervention (MD 0.27, 95% CI –0.19 to 0.73), but the sample size is small and results are not statistically significant.
Language development
Two different language tools were used: RDLS and MSEL (expressive and receptive language subscales). No studies used both tools. Results were inconsistent between studies using RDLS, which generally showed a benefit of early intensive ABA-based intervention, and those using MSEL, for which there was no evidence of a benefit on language. Given the risk of confounding that would arise from combining these two different scales in a single meta-analysis, we decided not to perform a joint meta-analysis of language development. For meta-analyses of these scales separately, see Impact of study-level covariates.
Presence of behaviours that challenge
As only one study90 reported data on behaviours that challenge, no meta-analysis was performed. It reported results at 1 year using the Conners’ Rating Scales – Revised measure.
School placement
As only one comparative study89,96,109 reported sufficient data on school placement, no meta-analysis was performed. See School placement for an analysis of all data on school placement.
Meta-analyses of all outcome measures
This section considers the meta-analysis of all reported outcomes for which there were sufficient data for a meta-analysis comparing any early intensive ABA-based interventions with TAU or eclectic interventions (see Tables 2 and 4). This includes meta-analyses of subscales, such as the subscales of VABS.
Given the large number of analyses, only summary results from the one-stage repeated measures meta-analyses are presented here. Forest plots for all meta-analyses are available on request.
Figure 10 presents a summary of the results of the one-stage repeated measures meta-analyses. Each subplot represents a separate outcome scale (e.g. ADOS repetitive behaviours in the top left). The vertical axis shows the MD in effect between early intensive ABA-based interventions and TAU or eclectic interventions, and the horizontal axis indicates the year after recruitment at which each meta-analysis was performed. Each dot is the summary MD in effect between the interventions from the relevant one-stage analysis of variance meta-analysis, with the vertical line being its 95% CI. Note that each dot and line represents an independent meta-analysis for each year; no time trends are assumed or modelled here.
FIGURE 10.
Repeated measures meta-analysis of all outcomes. a, Reduction in ADOS score is considered a positive result. For all other scales, increased scores are considered positive. DLS, daily living skills.
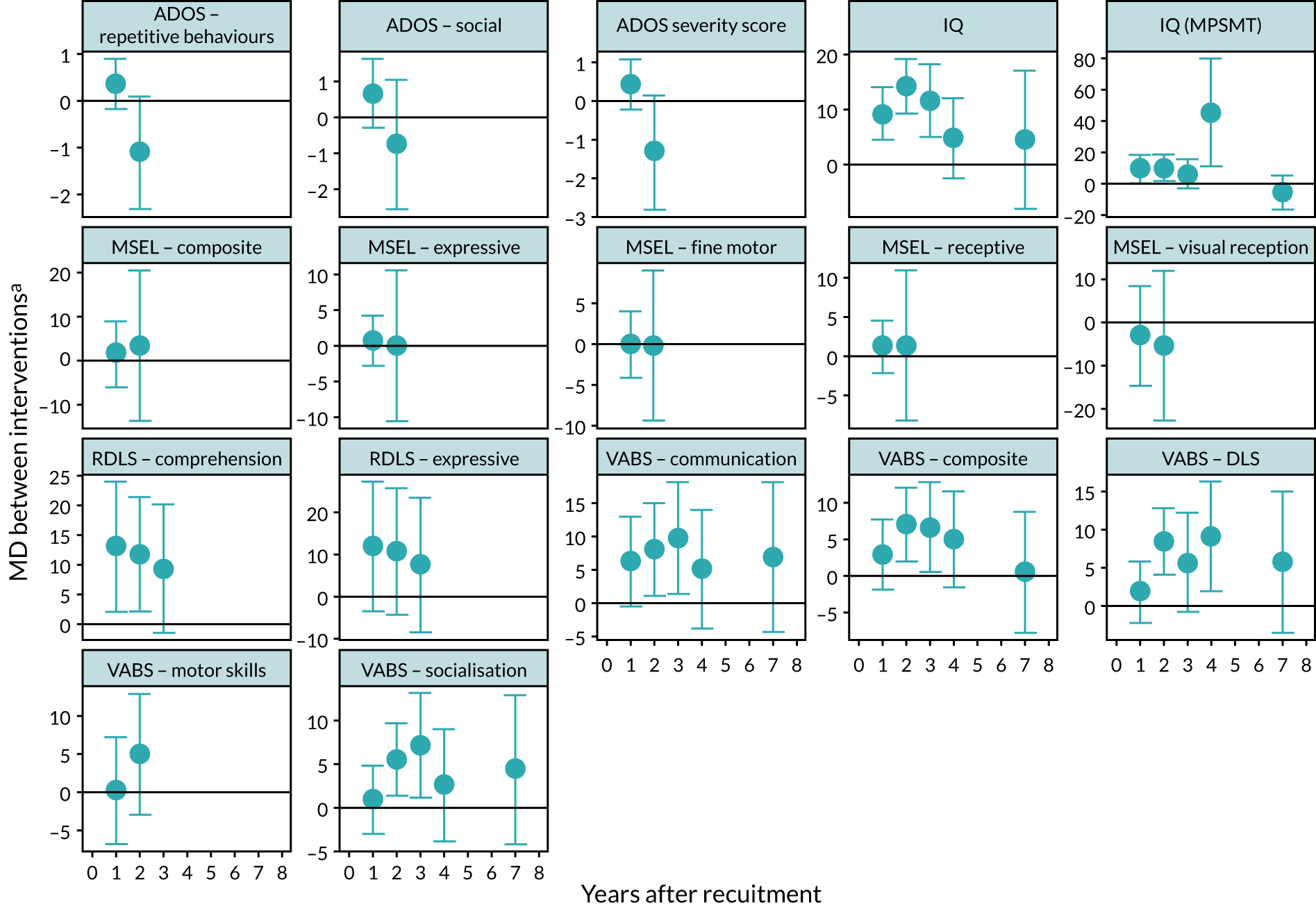
A positive result (above the blue line) indicates results favouring the early intensive ABA-based intervention, except for ADOS scores, for which results below the line favour the early intensive ABA-based intervention.
The results for VABS composite score, IQ and ADOS severity score in Figure 10 are broadly similar to those shown in the forest plots in Meta-analyses by outcome domains (see Figures 5, 6, 8, 9 and 24).
For IQ 1 year after follow-up, the meta-analysis favoured the early intensive ABA-based intervention, with a MD between groups of around 9 points (MD 9.16, 95% CI 4.38 to 13.93). After 2 years, this increased to a 134-point difference (MD 14.13, 95% CI 9.16 to 19.10).
Results after 7 years are presented here for ease of reference, but are based on only one study. 17 This study found no statistically significant evidence of a difference between interventions at 7 years (MD 4.39, 95% CI –8.17 to 16.95).
The meta-analysis results for non-verbal IQ measured using the MPSMT approach were broadly similar to general IQ at both 1 year (MD 9.45, 95% CI 0.33 to 18.59) and 2 years (MD 10.13, 95% CI 1.58 to 18.68), with MDs between groups of around 10 points after 2 years.
Composite VABS score showed no clear evidence of a difference between groups at 1 year (MD 2.93, 95% CI –1.90 to 7.76) and a statistically significant difference of around 7 points in favour of the early intensive ABA-based intervention after 2 years (MD 7.00, 95% CI 1.95 to 12.06). VABS subscale scores followed the same pattern. Socialisation and daily living scores showed no clear evidence of a difference at 1 year, and about a 5- to 8-point difference in favour of early intensive ABA-based interventions at 2 years. Communication showed a 6- to 8-point difference in favour of early intensive ABA-based interventions after 1 and 2 years (at 2 years: MD 8.03, 95% CI 1.11 to 14.97). Results for motor skills were inconclusive. The single study17 reporting data after 7 years found no difference between interventions.
For ADOS severity score, there was a MD of about 0.4 points between arms, with results favouring TAU or eclectic interventions at 1 year, but this was not statistically significant (MD 0.43, 95% CI –0.23 to 1.08). Results at 2 years were based on a single study, but showed a non-significant MD of about 1 point between arms, with results favouring early intensive ABA-based interventions (MD –1.33, 95% CI –2.81 to 0.14). There were similar results for the repetitive behaviour and social subscales.
For language development, RDLS comprehension scores after 1 year had a MD of about 12 points between arms, with results favouring early intensive ABA-based interventions (MD 12.96, 95% CI 2.01 to 23.91) and similarly at 2 years (MD 11.78, 95% CI 2.12 to 21.45). Results were similar for expressive language, although these did not achieve statistical significance. By contrast, MSEL receptive and expressive language subscales showed no evidence of any difference between early intensive ABA-based interventions and control arms after 1 or 2 years. Similarly, there was no evidence of any effect of early intensive ABA when assessed using composite MSEL score, or its fine motor or visual reception subscales.
The figure includes some estimates of effect at 3 and 4 years. These are derived from limited data from three studies,95,104,110 so should be treated with caution, but are generally consistent with effect estimates at other times, with similar estimated MDs. The exception is a large effect on non-verbal IQ (MPSMT) after 4 years, but this is based on one study110 with very few children.
Impact of child-level covariates
As described in the methods section (see Chapter 4, Impact of covariates on treatment effect), we intended to explore a range of child- and parent-level covariates. Unfortunately, the IPD supplied from most studies were too limited to permit investigation of child-level covariates. The only covariates with sufficient data for analysis were age and sex. To these covariates, we added baseline IQ and baseline composite VABS score.
To assess whether or not these covariates alter the effectiveness of early intensive ABA-based interventions, the repeated measures models were extended to include the relevant covariates and the interaction between covariate and early intensive ABA-based interventions, as set out in Chapter 4, One-stage analyses. It should be noted that these analyses test whether or not the MD between interventions varies with the covariate of interest (e.g. is the difference between VABS scores using early intensive ABA-based interventions compared with using TAU or eclectic interventions larger in girls than in boys?). We are not investigating whether or not the actual values of the outcomes vary with the covariates (e.g. if children with higher initial IQ have greater improvements in IQ or VABS after intervention). The results of these analyses for the outcomes IQ and composite VABS score (where there are most data) are shown in Table 5. Full results from all outcomes are given in Appendix 11 (see Table 45). The main point to note from these results is that CIs are very wide, spanning no effect (a value of zero), and so all p-values are well above 0.05. Therefore, there is no clear evidence of any interaction between these factors and either IQ or VABS score (e.g. no evidence that older children gain greater benefit from early intensive ABA-based interventions than with alternative interventions than younger children).
| Outcome | Interacting factor | Variation in MD | 95% CI | p-value |
|---|---|---|---|---|
| IQ | Age at recruitment | 0.08 | –0.26 to 0.42 | 0.64 |
| Sex | –1.3 | –13.36 to 10.76 | 0.83 | |
| IQ at baseline | 0.09 | –0.13 to 0.31 | 0.44 | |
| VABS at baseline | –0.11 | –0.58 to 0.35 | 0.63 | |
| VABS composite | Age at recruitment | –0.05 | –0.29 to 0.18 | 0.65 |
| Sex | 3.28 | –3.08 to 9.65 | 0.31 | |
| IQ at baseline | 0.09 | –0.06 to 0.23 | 0.24 | |
| VABS at baseline | –0.05 | –0.28 to 0.18 | 0.66 |
Impact of study-level covariates
A number of study-level covariates were investigated to determine if they had any impact on the effectiveness of early intensive ABA-based interventions. Owing to the large numbers of possible analyses, we considered only two outcomes, IQ and composite VABS score, at 1 and 2 years after recruitment, as these were the only outcomes with sufficient studies for reliable analysis.
Categorical covariates were assessed using subgroup analyses. Factors considered were:
-
allocation method (parental choice, location based, cohort)
-
delivery setting (home, school, specialist centre)
-
parental involvement in ABA (none, encouraged, some)
-
use of ABA methods in control intervention (none, partial).
Table 6 presents a summary of these subgroup analyses for outcomes at 2 years. For IQ, all p-values are > 0.05 and there are no clear patterns of variation in treatment effect across analyses. For VABS composite score, all p-values are < 0.1, but these are a consequence of extreme results in a single subgroup, driven by extreme results in a single trial,85,95 and are unlikely to represent genuine differences between subgroups.
| Outcome | Factor | Subgroup | MD | 95% CI | p-value of interaction |
|---|---|---|---|---|---|
| IQ | ABA in control arm | No | 14.72 | 6.84 to 22.61 | 0.53 |
| Partially | 10.99 | 2.49 to 19.5 | |||
| Allocation | Cohort | 14.44 | 5.57 to 23.31 | 0.52 | |
| Other | 20.49 | 3.72 to 37.27 | |||
| Parental choice | 10.2 | 1.97 to 18.43 | |||
| Delivery setting | Home | 10.2 | 1.97 to 18.43 | 0.62 | |
| School | 15.91 | 7.95 to 23.86 | |||
| Specialist centre | 10.82 | –35.91 to 57.56 | |||
| Parental involvement | 4 hours/week | 20.49 | 3.72 to 37.27 | 0.52 | |
| Encouraged | 14.58 | 5.54 to 23.61 | |||
| Some | 10.2 | 1.97 to 18.43 | |||
| VABS composite | ABA in control arm | No | 6.22 | –2.98 to 15.42 | 0.09 |
| Partially | 11.31 | 2.66 to 19.97 | |||
| Unclear | –4.79 | –16.34 to 6.76 | |||
| Allocation | Cohort | 2.77 | –11.29 to 16.84 | 0 | |
| Location | 5.13 | 0.38 to 9.87 | |||
| Other | 31.89 | 18.73 to 45.05 | |||
| Delivery setting | Parental choice | 5.73 | 0.84 to 10.62 | 0 | |
| Home | 5.73 | 0.84 to 10.62 | |||
| School | 14.34 | 0.8 to 27.87 | |||
| Specialist centre | –4.79 | –16.34 to 6.76 | 0.1 | ||
| Parental involvement | 10 hours/week | 5.13 | 0.38 to 9.87 | ||
| 4 hours/week | 31.89 | 18.73 to 45.05 | |||
| Encouraged | 2.77 | –11.29 to 16.84 | |||
| Some | 5.73 | 0.84 to 10.62 |
Continuously distributed covariates were assessed using meta-regression. Covariates considered were:
-
planned duration of early intensive ABA-based intervention
-
planned intensity (hours/week) of early intensive ABA-based intervention
-
year of study publication (to test for variation in effects over time).
Table 7 presents the results of the meta-regression analyses at 2 years. There is some suggestion that older studies had larger effects on the VABS composite scale than more recent studies (by 1.82 points on the VABS scale/year). This might suggest biased results in early studies, or that changes in how early intensive ABA-based interventions are given has led to changes in effectiveness. There was no evidence to support an impact of any other of the covariates on the effectiveness of early intensive ABA-based interventions. It should, however, be remembered that these analyses are based on few studies, and may be prone to bias.
| Outcome | Factor | Slope | 95% CI | p-value |
|---|---|---|---|---|
| IQ | Duration (planned, per year) | –1.61 | –12.24 to 9.02 | 0.77 |
| Intensity (planned, hours/week) | –0.11 | –1.39 to 1.17 | 0.87 | |
| Publication year | –0.21 | –2.29 to 1.86 | 0.84 | |
| VABS composite | Duration (planned, per year) | –1.59 | –11.99 to 8.82 | 0.77 |
| Intensity (planned, hours/week) | –0.46 | –1.54 to 0.62 | 0.4 | |
| Publication year | –1.82 | –3.65 to 0.01 | 0.05 |
Sensitivity analyses
The main analyses combined all forms of high-intensity early intensive ABA-based interventions compared with TAU or eclectic interventions. Subgroup analyses were performed to compare studies using TAU as a control with those using eclectic treatments, and to compare studies using EIBI only (e.g. Lovaas/UCLA model) with those using EIBI with NDBI. A summary of the results for IQ and VABS composite score at 2 years is shown in Table 8.
| Outcome | Analysis | Group | MD | 95% CI | p-value for interaction |
|---|---|---|---|---|---|
| IQ | Control arm | Eclectic only | 10.99 | 2.49 to 19.5 | 0.53 |
| TAU only | 14.72 | 6.84 to 22.61 | |||
| Intervention | EIBI only | 10.99 | 2.49 to 19.5 | 0.53 | |
| EIBI and NDBI only | 14.72 | 6.84 to 22.61 | |||
| VABS composite | Control arm | Eclectic only | 8.57 | 0.49 to 16.65 | 0.71 |
| TAU only | 6.22 | –2.98 to 15.42 | |||
| Intervention | EIBI only | 10.03 | –2.11 to 22.16 | 0.49 | |
| EIBI and NDBI only | 5.45 | 1.22 to 9.69 |
There was no clear evidence that the type of intervention or the type of control used leads to different results. In theory, results may be confounded as studies using only EIBI were generally compared with ‘eclectic’ control, whereas studies using EIBI with NDBI were generally compared with TAU. However, as noted previously, these comparator labels can be used somewhat interchangeably.
UK-based studies
Three of the included studies were conducted in the UK. 89–92,96,109,110 To assess whether or not the performance of early intensive ABA-based interventions in the UK was consistent with the overall meta-analysis, we performed a sensitivity analysis in the UK-based studies, repeating the main one-stage repeated measures analysis from Figure 10. The results of this analysis are shown in Figure 11, restricted to IQ and VABS subscales, as there were insufficient data for analysis of other outcomes.
FIGURE 11.
Repeated measures meta-analysis of the three UK-based studies. DLS, daily living skills.
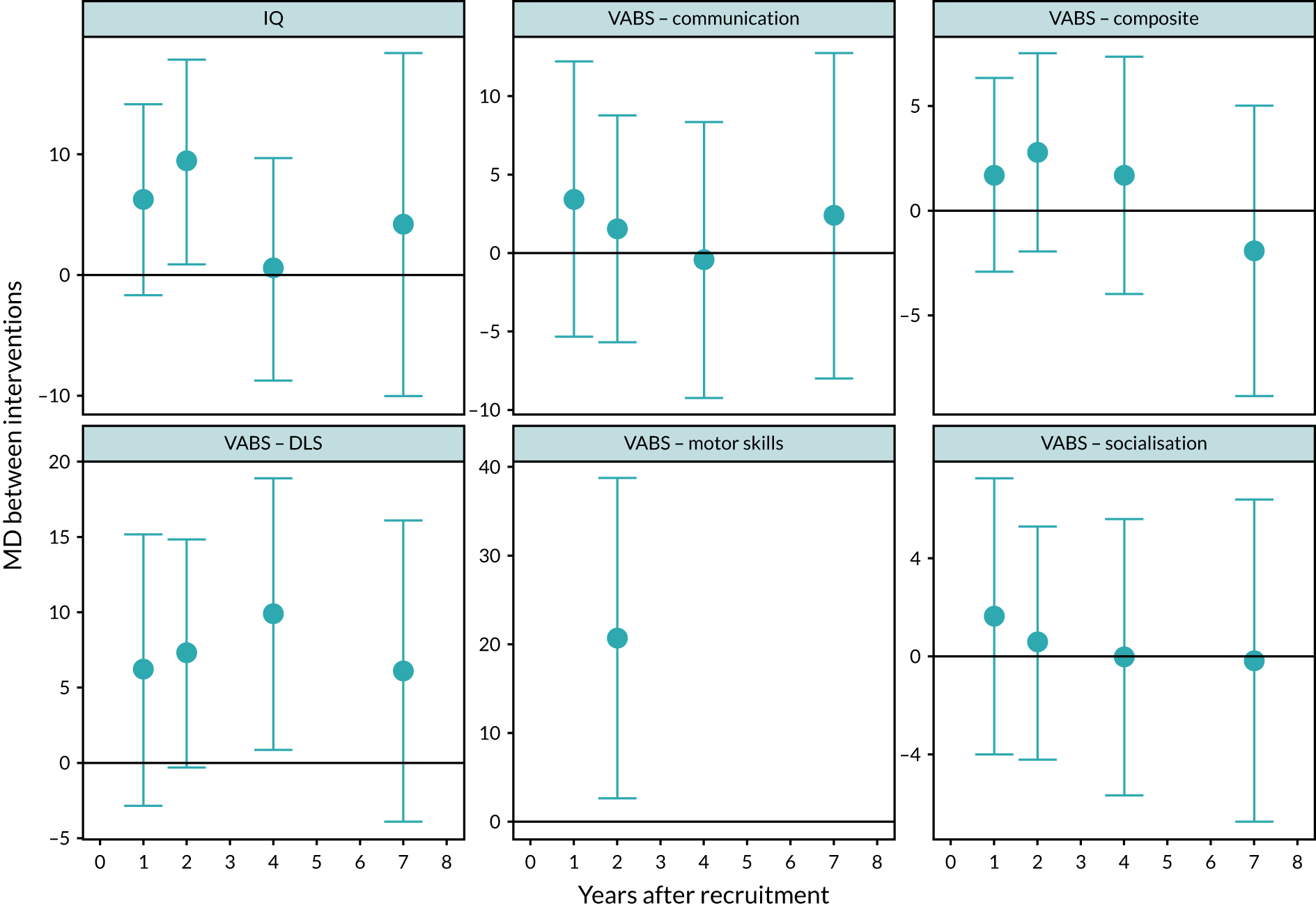
The results suggest slightly smaller effects in the UK-based studies, particularly for composite VABS score, for which the MD between early intensive ABA-based and comparator arms at 2 years was 2.78 (95% CI –1.98 to 7.54), compared with 6.33 in the main analysis. For IQ, at 2 years the MD was 9.34 (95% CI 0.91 to 17.86) in the UK studies, compared with 13.64 in the main analysis. The smaller sample size also means that CIs were wider and results were not generally statistically significant.
Longer-term data at 4 and 7 years were reported in only one study in each case. At 7 years there was no evidence of any difference between early intensive ABA-based intervention and control, as discussed in Adaptive behaviour and Cognitive ability, with most effect estimates close to 1 and no statistically significant results. 96 At 4 years, there was similarly no evidence of any difference, except for VABS daily living score (MD 9.89, 95% CI 0.87 to 18.91). 110
However, there is insufficient evidence to assert that UK studies are different from others, and the reasons for observed differences may be varied and not due to study location.
Standardised mean difference
All meta-analyses presented above have used the MD between early intensive ABA-based arms and comparator arms as the outcome. This assumes that all studies are using the same scale to measure the outcome; however, for example, studies used different IQ tests. To investigate whether or not studies were consistent when different tests were used, the meta-analyses were repeated using SMDs (i.e. Cohen’s d).
Appendix 11 includes the results of two-stage ANCOVA meta-analyses of all outcomes using SMD (see Figure 25). The results are consistent with the MD analyses. For example, IQ showed results favouring early intensive ABA at both 1 year (SMD 0.61, 95% CI 0.32 to 0.91; I2 = 13%) and 2 years (SMD 0.76, 95% CI 0.46 to 1.035; I2 = 0). Composite VABS score showed no difference between early intensive ABA-based interventions and control interventions at 1 year (SMD 0.18, 95% CI –0.35 to 0.71; I2 = 80%), but results favoured early intensive ABA at 2 years (SMD 0.95, 95% CI 0.30 to 1.61; I2 = 64%).
Inclusion of studies not providing individual participant data
Of the five studies that did not provide IPD, four have been published82,83,87,105–108 and collected a similar variety of outcome domains and measures as studies that provided IPD. Additional outcomes included measures of repetitive behaviours, shared positive affect, gesture use, and the visual reception and fine motor subscales of the MSEL (see Appendix 8).
Two of the studies did not report outcome data in a form that could be used in the meta-analysis. 82,87 Two studies comparing high-intensity ABA-based interventions with comparator interventions have published usable outcome data. 83,105–108,112 Included also is one study that was published after IPD collection had closed. 102 To investigate the impact of these studies on the meta-analyses we extracted data from their publications and combined them with the IPD to perform two-stage change-from-baseline meta-analyses (in which the mean change in outcome between observation time and baseline is analysed). The full results are presented in Appendix 11 (see Figures 27–32 and Table 42). Figures 12 and 13 show the forest plots for IQ and composite VABS score at 2 years. These forest plots present sensitivity meta-analyses, in which the two studies with data extracted from publications are analysed with studies that provided IPD.
FIGURE 12.
Intelligence quotient at 2 years, including studies not providing IPD.

FIGURE 13.
Composite VABS score at 2 years, including studies not providing IPD.
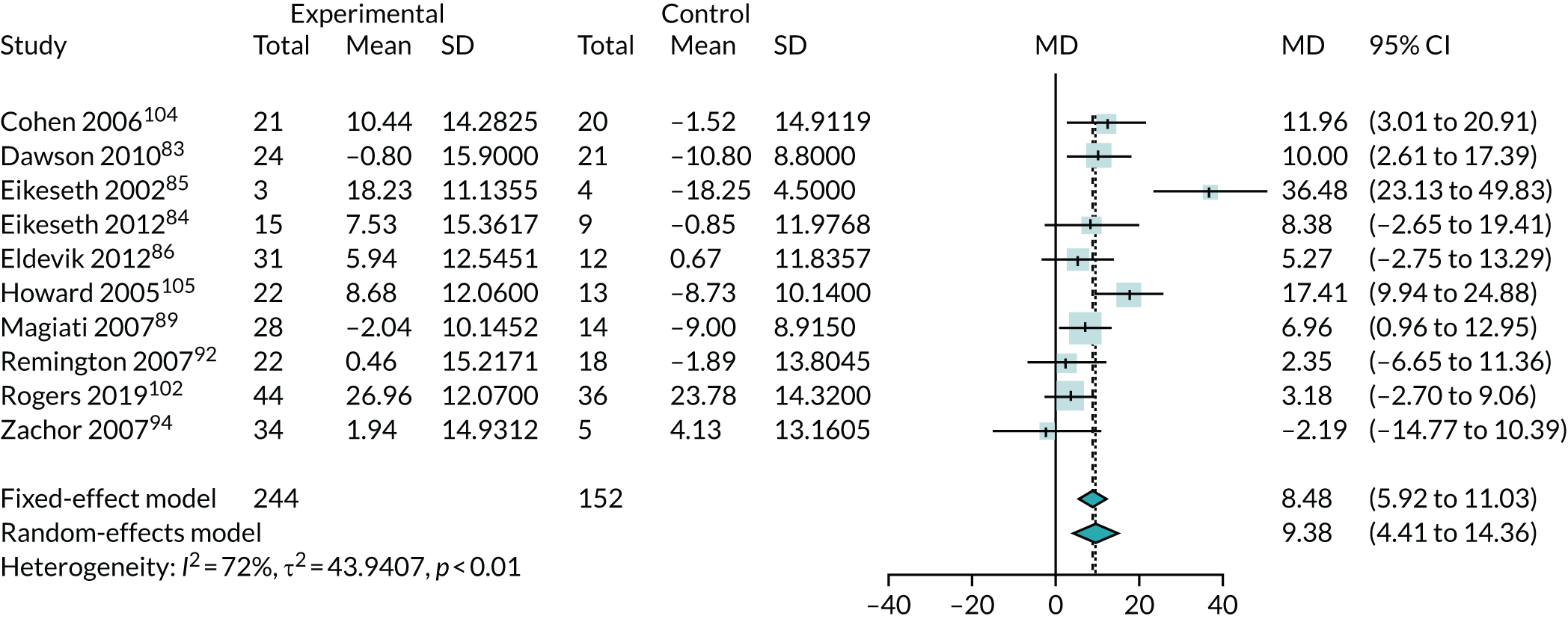
Both analyses produce larger differences between the two groups in favour of early intensive ABA-based interventions than observed in the main analyses using only IPD (see Figures 6 and 9). This is because of the very large effects found by Howard et al.,105 which are approximately double those estimated from the IPD meta-analysis. The other studies that did not provide IPD83,102 had results more consistent with the IPD meta-analysis.
Narrative synthesis of other outcomes
Meta-analyses were performed for all outcomes reported by at least two studies at a common follow-up time. There were a number of other outcomes reported in only one study, or in two studies at inconsistent times. The results of these further outcomes are summarised in Appendix 11 (see Table 43).
Data on these outcomes are too limited to draw any meaningful conclusions. However, most results were in the direction of favouring early intensive ABA-based interventions, suggesting small reductions in autism symptom severity, behaviours that challenge, and improvements in IQ and language development. These are consistent with the meta-analyses of other outcomes.
Studies making other comparisons
Some of the included studies did not compare high-intensity ABA-based interventions with a TAU or eclectic intervention, instead comparing it with lower-intensity EIBI. These studies are considered in this section.
High- versus low-intensity early intensive behavioural intervention
Three studies compared high-intensity EIBI (> 15 hours/week) with lower-intensity EIBI. 26,90,91,98,103 IQ was the only outcome recorded consistently in all three studies. A repeated measures meta-analysis of IQ comparing high- with low-intensity early ABA-based intervention is shown in Figure 14. This suggests that high-intensity ABA-based interventions produced much larger improvements in IQ than low-intensity ABA-based interventions, with differences of between 10 and 20 points from 1 to 4 years after recruitment, although results are not statistically significant at 1 and 3 years.
FIGURE 14.
Mean difference in IQ between high- and low-intensity EIBI. DLS, daily living skills.
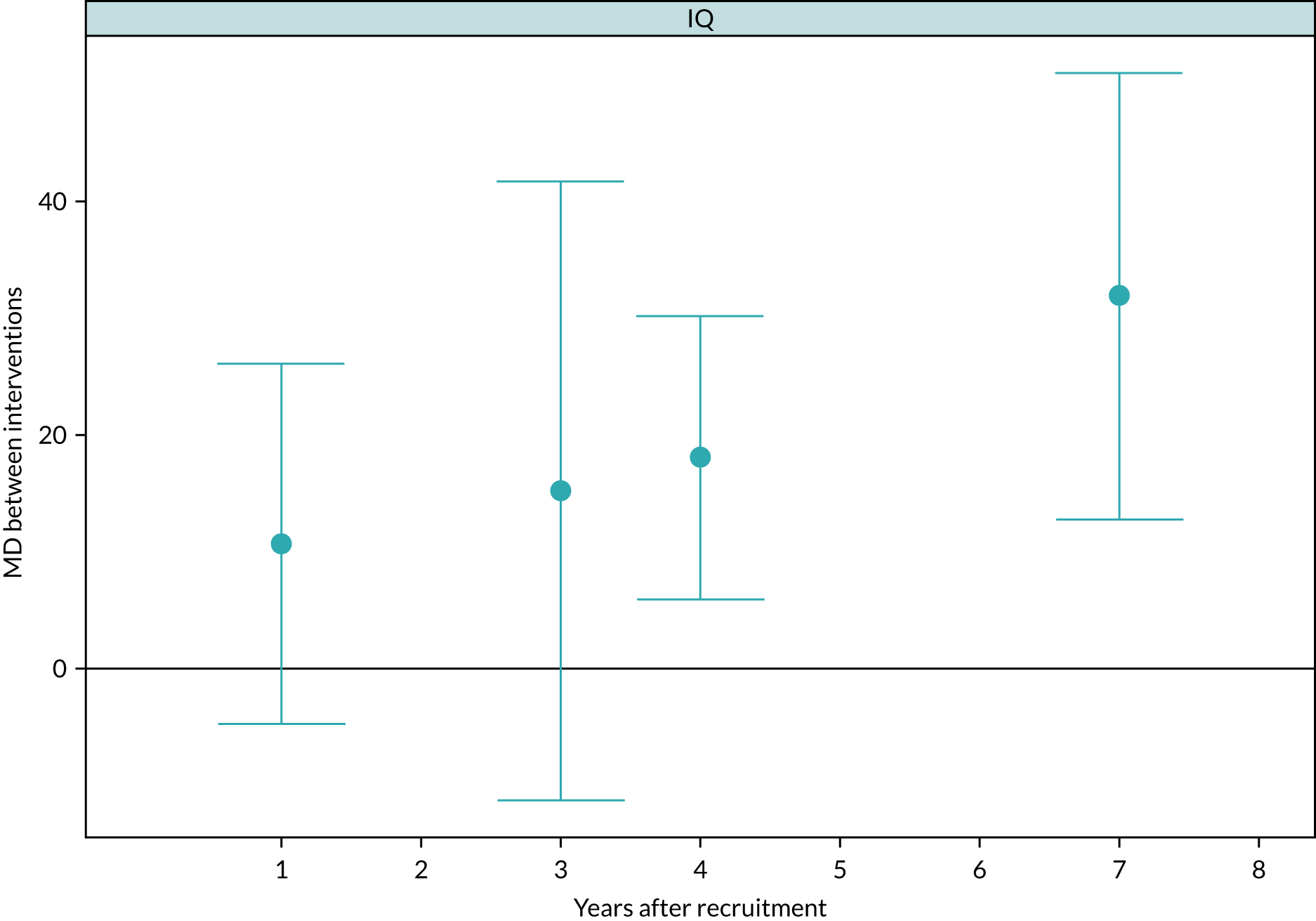
Parental-managed compared with other applied behaviour analysis
Two studies compared parent-directed or managed early intensive ABA-based interventions (specifically EIBI with NDBI) with clinician or other management of the same intervention. 99,100 The repeated measures meta-analysis of these two studies is summarised in Figure 15. There is no indication of difference in any outcome, with all CIs including no effect and effect estimates are inconsistent in the direction of effect. There is therefore little evidence based on these data that parental management of early intensive ABA-based intervention alters its effectiveness.
FIGURE 15.
Meta-analysis of parent managed compared with other management of ABA. DLS, daily living skills.

Other comparisons
One study (28 participants) specifically compared two forms of ABA-based early intervention: PRT-based intervention (Nova Scotia EIBI) compared with a group-based verbal behaviour intervention (group ABA).
Over 1 year, results for cognitive development, receptive and expressive language, adaptive behaviour, problem behaviour and parenting stress, all indicated small and statistically non-significant differences between the two treatment arms (see Table 41 in Appendix 10).
School placement
Three studies provided IPD on the school placement of children. 26,89,96,98,103,109 Only the study by Magiati et al. compared early intensive ABA-based interventions with TAU or eclectic interventions;89,96,109 the other two studies compared high- with low-intensity EIBI. 26,98,103 To analyse school placement we considered low-intensity EIBI to be equivalent to eclectic treatment (see Network meta-analysis for the justification for this).
The results suggest that generally only children receiving high-intensity EIBI proceed to mainstream education. Children receiving low-intensity or eclectic interventions are more likely to go to specialist schools.
The regression model found very large and statistically significant odds in favour of going to more mainstream education with high-intensity intervention. These odds appear implausibly large. Further regression models adjusting for IQ and VABS composite score (results not shown) found that, even after adjusting for these factors, there were substantial odds in favour of going to more mainstream education with high-intensity intervention. This suggests that school placement is not dependent on improvements in IQ or behaviour. So difference in school placement could potentially be driven by knowledge of the intervention received and by parental selection, values, preferences and priorities, among other factors. Therefore, it is not clear whether or not high-intensity ABA-based intervention improves chances of going to a mainstream school.
Figure 16 shows the distribution of school placement by study and intervention arm. Figure 17 shows the result of a proportional odds regression to estimate the odds of being placed in a ‘more mainstream’ school if receiving high-intensity ABA-based intervention. The results suggest that generally only children receiving high-intensity ABA-based intervention proceed to mainstream education and children receiving low-intensity or eclectic interventions are more likely to go to specialist schools.
FIGURE 16.
School placement of children.

FIGURE 17.
Proportional odds regression for school placement.

Network meta-analysis
A one-stage repeated measures NMA model was fitted to compare all the various intervention arms included in the review (EIBI, EIBI with NDBI, ESDM, eclectic, TAU, portage, low-intensity EIBI and parent-managed EIBI). The baseline intervention for comparison was taken to be eclectic treatment. Figure 18 shows the results of this analysis for IQ and composite VABS score. Results for all outcomes are available in Appendix 11 (see Figure 26 and Table 44).
FIGURE 18.
Network meta-analysis of IQ and composite VABS score.

There was considerable variation across the results, but they did suggest that, overall, children receiving any form of high-intensity ABA-based early intervention (EIBI, EIBI with NDBI, parent-managed EIBI) have greater gains than eclectic treatment (after 1 year for IQ, but after 2 years for VABS score), and different forms of high-intensity ABA-based early intervention are of similar effectiveness to each other. Similarly, all lower-intensity interventions (TAU, portage and low-intensity ABA-based intervention) appeared to be similar to, or possibly less effective than, eclectic intervention.
The results of this NMA agreed with previous analyses, including finding no evidence of difference between traditional EIBI and EIBI with NDBI, no difference between eclectic treatment and TAU, and no difference between patient-managed and other forms of EIBI. As with earlier analyses, there was evidence that high-intensity ABA-based intervention was more effective than low-intensity EIBI.
High- compared with low-intensity intervention
Given the evidence from the NMA that, in general, all high-intensity interventions appear to have similar effectiveness (likewise, for all low-intensity interventions), we performed a further post hoc meta-analysis of all studies comparing any high-intensity intervention with any low-intensity intervention. This allowed the studies comparing high- and low-intensity ABA-based interventions to be meta-analysed along with those comparing high-intensity ABA-based interventions with alternative interventions, increasing the sample size.
The results of one-stage repeated measures meta-analyses are shown in Figure 19. They were generally very similar to the meta-analysis presented in Figure 10. The MD in IQ between high-intensity interventions and low-intensity interventions is around 17 points (at 2 years: MD 16.76, 95% CI 10.60 to 22.93). Communication, as measured by the VABS subscale, also favoured high-intensity intervention from 1 year (MD 8.18, 95% CI 0.54 to 15.85). For other VABS components, results favoured high-intensity ABA from 2 years onwards, with a MD compared with low-intensity ABA of around 5–8 points (VABS composite at 2 years: MD 8.60, 95% CI 2.86 to 14.34).
FIGURE 19.
Repeated measures meta-analysis of high- compared with low-intensity intervention studies. DLS, daily living skills.

As in the main meta-analyses (see Figure 10), results favoured high-intensity intervention for language comprehension measured using RDLS (comprehension at 2 years: MD 11.66, 95% CI 2.00 to 21.33). There was no evidence of any difference between high- and low-intensity intervention if using the MSEL expressive and receptive language subscales. There remains little evidence on autism symptom severity, but there was a suggestion (not statistically significant) that results favoured high-intensity intervention at 2 years (ADOS severity score at 3 years: MD –1.34, 95% CI –2.82 to 0.14).
Summary of the individual participant data meta-analysis
Intelligence quotient and Vineland Adaptive Behaviour Scale
The main conclusion from all the meta-analyses is that receiving early high-intensity ABA-based intervention leads to somewhat greater improvements in IQ and VABS scores than if receiving low-intensity, TAU or eclectic interventions. IQ scores were higher by at least 9 points (about 0.6 of a SD) from 1 year after initiation of intervention onwards (MD 9.16, 95% CI 4.38 to 13.93). Scores on the VABS components were higher in the ABA intervention arms by 6–8 points on average (0.8 of a SD) after 2 years (composite score: MD 7.00, 95% CI 1.95 to 12.06). Improvements at 1 year appeared to be smaller and were not generally statistically significant.
Heterogeneity, estimated by I2, was generally low, but this was a consequence of the small size of most included studies, which makes it difficult to conclusively identify heterogeneity. There was, however, considerable variation in effect estimates across studies for some outcome measures. For example, MDs in composite VABS at 2 years ranged from –4.79 to > 33. There was also variation across studies in how the outcome measures changed over time. This raises some concerns of whether or not studies are comparable.
There were few data on the longer-term impact of early intensive ABA-based interventions beyond the end of the main intervention period. Only one study reported results at 7 years after initiation, which found no difference between early intensive ABA-based and comparator arms. It is therefore not possible to determine the long-term impact of early intensive ABA-based interventions, including whether or not any benefits observed at 2 years persist.
Other outcomes
Results for other outcomes were limited due to the small numbers of studies reporting them. Data on autism symptom severity were too limited to be conclusive, with no clear evidence that early intensive ABA-based interventions improved the severity of autism compared with TAU or eclectic interventions. There were, similarly, limited data on language comprehension. Three studies85,89,104 that used the RDLS scale found some evidence that language scores favoured the early intensive ABA-based group compared with TAU or eclectic interventions by around 11 points (RDLS comprehension at 2 years: MD 11.78, 95% CI 2.12 to 21.44). By contrast, two studies93,97 that reported the MSEL expressive and receptive language subscales found no difference in scores between the two groups. There were insufficient data on behaviours that challenge to permit any meta-analysis. The limited data from one study90 suggested that early intensive ABA-based interventions could reduce behaviours that challenge, but results were not statistically significant.
School placement was available in only one study89 comparing early intensive ABA-based interventions with TAU and eclectic interventions, and in two studies26,103 comparing high- with low-intensity ABA-based interventions. These studies suggested that children receiving a high-intensity ABA-based intervention were much more likely to be in mainstream education (possibly with support) than children receiving TAU, eclectic or low-intensity ABA-based interventions. This analysis, however, may be confounded by parental preference for early intensive ABA-based treatment and mainstream schooling placement, and the practice in Lovaas26 of encouraging children to change school if teachers became aware of their autism. 26 Consequently, there is no good-quality evidence to suggest that early intensive ABA-based interventions independently influences school placement.
Participant and study characteristics
Studies reported limited data on child and parent characteristics, or details of how early intensive ABA-based interventions were administered. It was therefore not possible to investigate most of the protocol-specified covariates and how they might influence the effectiveness of early intensive ABA-based interventions. We found no conclusive evidence that age, sex, baseline IQ or baseline VABS score had any impact on the effectiveness of early intensive ABA-based interventions when compared with other interventions.
There was no generally clear evidence that study-level covariates, including delivery setting, allocation, parental involvement, duration and intensity of early intensive ABA-based treatment, had any clear or observable impact on the MDs between these interventions and comparator groups. A possible exception was that trials from earlier years found larger impacts on VABS composite score than later trials, although the power to detect such differences was limited as there were few studies in the analysis.
Comparison of applied behaviour analysis-based interventions
Sensitivity analyses and the NMA both found no evidence of any difference in effectiveness between TAU and eclectic interventions or any difference in effectiveness between different types of ABA-based early intervention (EIBI alone or with NDBI). There was no evidence that parent-managed interventions differed in effectiveness from other forms of management.
There was some evidence that high-intensity EIBI may be more effective than low-intensity EIBI, and that high-intensity ABA-based intervention, in general, may be more effective than low-intensity interventions (whether low-intensity ABA based or eclectic interventions). This may suggest that it is the high intensity of the intervention that causes the greater benefits, rather than the precise nature of the intervention received.
Chapter 7 Economic analysis
Overview
This section outlines the development of a new economic model assessing the cost-effectiveness of implementing early intensive ABA-based interventions in a UK context.
The cost-effectiveness model built on the IPD meta-analysis presented in Chapter 6, using its results to inform the model parameters for the effectiveness of early intensive ABA-based interventions. Most of the available evidence focused on cognitive ability (IQ) and adaptive behaviour (VABS), with few data on other outcomes. In developing the model, we therefore sought to link these two outcomes to both cost and benefits.
This narrow focus on these two outcomes has important implications for the interpretation of the economic model. It means that the model does not account for effects on other outcomes and may not fully capture the benefits of early intensive ABA-based interventions. The economic model is therefore only valid to the extent that the benefits of early intensive ABA-based interventions can be captured by changes in cognitive ability and adaptive behaviour scores.
The IPD meta-analysis also identified a number of important limitations in the effectiveness data. In particular, the review raised concerns about the reliability of treatment effect estimates, given the weakness in the methods used in the primary studies. The interventions and comparators assessed also varied and it not clear how well they reflect how early intensive ABA-based interventions or other interventions are used in the UK.
In consequence of these limitations, the presented economic model should not be viewed as a comprehensive assessment of the cost-effectiveness of early ABA-based therapy, as the data currently available are insufficient to make inferential judgements. Instead, it is more appropriate to view the model as an exploratory analysis that provides a vehicle with which to explore key drivers of cost-effectiveness, while also providing indicative results of any potential cost-effectiveness of early intensive ABA-based interventions.
Economic evaluation of interventions in autism
Evaluation of cost-effectiveness examines the cost and benefits of interventions that are directly relevant to decision-makers, with the aim of informing policy decisions. Within conventional health technology assessment (HTA), which evaluates the effectiveness and value of implementing health-care interventions, it is typically assumed that decisions are taken from a health-care perspective. The perspective of economic analysis is important, as it determines the boundaries of an analysis, and which benefits and costs will be considered. In health care, these are typically costs to the NHS or social care and benefits are measured in terms of HRQoL.
Autism is defined as a long-term neurodevelopmental disability and, as such, the approach of focusing exclusively on a health perspective may be too narrow because the relative costs and benefits of interventions are likely to extend beyond the health-care system. This is demonstrated in the previous economic evaluations of early intensive ABA-based interventions44,50–54 (see Appendix 13 for a review of these studies), all of which highlighted significant cost offsets outside the health-care system (e.g. in education provision). Similarly, defining benefits in terms of HRQoL may also be too restrictive, as there are a range of non-health outcomes that may be important to decision-makers, including those related to education, the employment market and other relevant dimensions, such as changes in well-being and quality of life (not related directly to health).
Figure 20 illustrates how an intervention, such as early intensive ABA-based interventions, may impact on both health and non-health outcomes, and how it may have wider implications than those summarised by the cost per quality-adjusted life-year (QALY) metric typically used as an outcome measure in HTAs. In the context of autism, it is also worth noting that both health and non-health effects are likely to impact not only on the autistic individual, but also on families and carers. For example, there is significant literature on parental stress. 120–125
FIGURE 20.
Possible impact of ASD on health and non-health outcomes.

Building on the list of potential outcomes presented in Figure 20, Figure 21 illustrates how the impact of early intensive ABA-based interventions may fall on different sectors. In Figure 21, three perspectives are defined: (1) a health and social services perspective, (2) a public sector perspective and (3) a societal perspective. The health and social services perspective includes all health benefits along with costs incurred by the health sector; this would include any costs incurred by the NHS, such as direct medical costs, speech and language provision and social care (e.g. day care or drop-in centres). The public sector perspective adds all costs borne by the state, as well as benefits that can be attributable to a function of the state. These may include, for example, the costs of providing education, as well as any benefits received by autistic people or their families. Finally, a societal perspective includes all costs and benefits of early intensive ABA-based interventions regardless of where they accrue; this includes productivity losses that may result from care requirements for autistic children and out-of-pocket expenses incurred (e.g. travel costs for appointments).
FIGURE 21.
Categorisation of impacts of intervention.

Reflecting the above, the main analyses were undertaken using an NHS and social care perspective, as well as a public sector perspective. The public sector perspective included local authorities and other government agencies not covered by an NHS and social care perspective. We also sought to implement a scenario analysis considering societal perspective, but we were unable to find appropriate data to implement this analysis. Evidence from Barrett et al. ,126 however, suggests that out-of-pocket expenses are small for very young children and, therefore, although potentially important to affected families, these are unlikely to be a driver of any decision about cost-effectiveness. To simplify these analyses, it was assumed that the costs of providing early intensive ABA-based interventions are incurred by the health sector, although, in reality, therapy costs may be borne by multiple sectors. It is our understanding that current provision for young children is covered by education, health and social care budgets. Furthermore, it is also common for some families to seek private provision to supplement that provided by the public sector.
Model development
In developing the new economic model our three broad aims were to:
-
adopt a cost–utility approach, that value judgements could be based not only on costs, but also on any benefits generated
-
include all benefits and costs, including those falling outside the health sector
-
model the effects of the intervention based on the results of IPD meta-analysis.
In committing to these aims, the central challenge of economic analysis was to link the results of the IPD meta-analysis to relevant measures of benefits and costs. As described in Chapter 6, the outcomes reported in the effectiveness studies did not include quality-of-life or other holistic measures and, therefore, there is no direct evidence to inform wider benefits. To capture such benefits within the model, it was therefore necessary to try to link the outcomes reported in the effectiveness studies to more holistic measures that could be used to inform policy. To do this, a systematic review of relevant quality-of-life studies was conducted (details of which are presented in Appendix 14). This review identified a large number of studies, including a small number that measure preference-based measures of HRQoL. Of the studies identified, only one reported HRQoL in a way that could be linked meaningfully with the outcomes reported in the IPD meta-analysis. This study, Payakachat et al. ,127 recruited 224 children (aged 4–17 years) with autism and related conditions, including children with co-existing intellectual disability. Its aim was to map outcomes, such as VABS, to the Health Utilities Index Mark 3 (HUI3) quality-of-life measure. See Appendix 14 for further details of the population recruited and the algorithms developed. The Payakachat et al. 127 algorithm therefore formed the basis of our model structure and was used to map changes in cognitive ability (IQ) and adaptive behaviour (VABS) scores to HRQoL.
An implication of this approach was that it was necessary to track the two outcome domains, cognitive ability and adaptive behaviour scores, over time. However, one of the key limitations of the available effectiveness data is that there are very few studies with long-term follow-up data. In previous economic evaluations,50–54 this issue has been solved by assuming trajectory effects on the basis of short-term outcomes reported in the effectiveness studies (see Appendix 13 for further details). However, this is a very strong assumption, given the limited long-term follow-up in the effectiveness studies and the limitations of the supporting epidemiological evidence, which provides only evidence of correlations between childhood outcomes and adult outcomes. This issue is further compounded by the evidence available in the epidemiological and observational studies, which report on the prognostic value of only a small number of outcomes (primarily measures of cognitive ability and language comprehension, but not adaptive behaviour scores). See Appendix 15 for an overview of the relevant epidemiological and observational studies.
Given the substantial uncertainty of extrapolating short-term benefits identified in the IPD meta-analysis into later childhood and adulthood, two assumptions were agreed with our Advisory Group.
First, it was agreed that the primary (base-case) analysis would use a time horizon of 15.5 years, the model therefore covers the period from early childhood, ages 3–18.5 years, rather than a longer lifetime horizon, which may be more appropriate given autism is a lifelong condition. This assumption reflects strongly held views within the Advisory Group that we should not seek to extrapolate any potential benefits of early intensive ABA-based interventions over TAU or eclectic interventions into adulthood, unless there was appropriate supporting evidence to do so. The age threshold of 18.5 years was selected as this represents when children transition to adult services. To explore the potential for early intensive ABA-based interventions to continue to provide benefits over TAU or eclectic interventions in the long term, an exploratory scenario analysis is presented in which a lifetime time horizon is adopted using evidence from observational studies to link childhood outcomes to adult outcomes; see Sensitivity and scenario analyses for details.
Second, because assumptions about long-term effectiveness are likely to be important drivers of cost-effectiveness, two scenarios were explored within the base-case analysis: (1) an optimistic one, in which the observed benefits of early intensive ABA-based interventions were assumed to persist; and (2) a pessimistic one, in which the suggested benefits dissipate over time.
In the previous economic analyses of early intensive ABA-based interventions, educational placement was a significant driver of cost-effectiveness and the main way in which cost offsets were generated in childhood. Educational placement is a potentially important source of costs (savings), as there is considerable additional costs associated with the providing of specialist services required by some autistic children. 128 Capturing the potential cost offsets in the education sector was therefore considered to be central to accurately estimating the cost-effectiveness of early intensive ABA-based interventions and consistent with the public sector perspective adopted. Of the studies identified in the IPD meta-analysis, only three26,89,103 reported directly on educational placement (type of school attended), one89 that compared early intensive ABA-based interventions with TAU or eclectic interventions and two26,103 that compared early intensive ABA-based interventions with low-intensity ABA-based therapy. The evidence to support the effects of early intensive ABA-based interventions on education placements was therefore very limited. Furthermore, as explained in Chapter 6, the observed treatment effects appear to be implausibly large and may be driven by knowledge of the intervention received and parental and family values and priorities about the education settings their child would attend, rather than any benefits gained from intervention. An alternative approach was therefore taken to model educational placement, in which the impact of early intensive ABA-based interventions is mediated through changes in cognitive ability and adaptive behaviour. This approach, outlined further in Model structure, was adopted to mitigate the impact of any bias in the effectiveness studies and is also a more consistent approach, as it avoids one set of studies being used to predict quality of life and non-education costs, while another set is used to predict educational placement.
Model structure
The economic model was constructed in Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) and uses a simple cohort model to capture changes in outcomes over time. It uses a cycle length of 1 month; no half-cycle correction was applied in the calculation of outcomes given the short cycle length relative to the time horizon. In line with the NICE methods guide,129 the decision model uses a discount rate of 3.5% per annum for both costs and benefits.
As explained in Model development, the model structure is based on cognitive ability (IQ) and adaptive behaviour (VABS) scores which are used to predict per cycle benefits (QALYs) and costs. Changes in the outcome measures (cognitive ability and adaptive behaviour) are incorporated as mean changes in each measure per month (Figure 22). Changes in outcomes are based on the IPD meta-analysis; see Treatment effect for details. As outcome data included in the IPD meta-analysis were available only at 1 and 2 years, a simple linear interpolation was used to estimate between-group differences at intervening time points.
FIGURE 22.
Model structure.
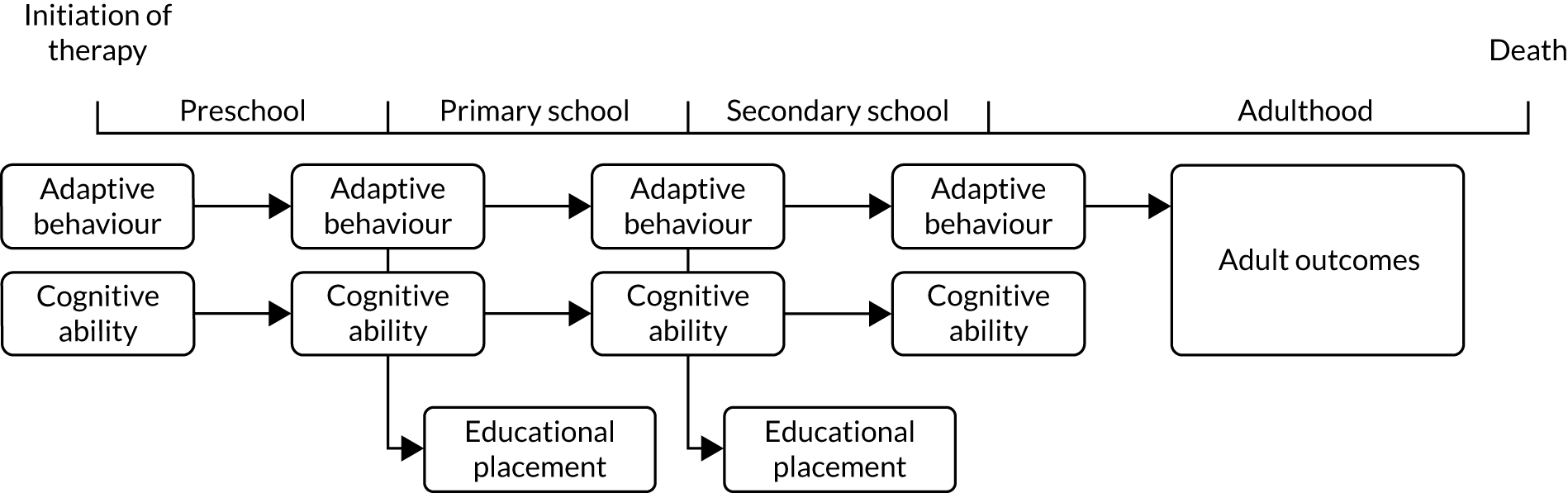
The time horizon in the main analysis is divided into two phases, representing different stages of an individual’s childhood. The first phase ‘preschool’ (up to age 4.5 years) reflects the period when early interventions are delivered, whereas the second ‘school age’ phase covers the period in which children attend primary (age 4.5–11.5 years) and secondary education (age 11.5–18.5 years). To accommodate educational placement and the associated resource implications, the model distinguishes between three education settings: (1) mainstream, (2) mainstream with support and (3) special education provision. Estimation of the proportion of children receiving each type of education is based on cognitive ability and adaptive behaviour; see Education for details.
Scenario analysis exploring adult outcomes
Although the main (base-case) analysis limits the time horizon to childhood (15.5 years), an exploratory scenario analysis considered the potential impact of incorporating adult outcomes into the model. In this scenario, an additional phase is added to the model structure. The adult phase of the model is a distinct phase in which a different model structure is used. This was done because the costs of care for autistic adults are very different from those for autistic children.
In several of the economic evaluations identified in the cost-effectiveness review (see Appendix 13), adult outcomes were defined in terms of levels of independence, often with three levels defined (e.g. independent, semi-independent and dependent). The definitions attached to each of these levels varied across the different models, but generally adopted one of two approaches. In the first most commonly used approach, levels of independence were defined with reference to special education and in some cases special education needs were also used to predict adult outcomes. The second approach used evidence from the epidemiological and observational literature, which has categorised adult outcomes based on normative evaluations of independence and social outcomes (see Appendix 13 for an overview of these studies).
This approach has important strengths, as it focuses on the support an individual needs and therefore the categorisation systems are useful in terms of reflecting costs. For example, Penner et al. 54 use a classification system reported in Howlin et al. ,15 which is widely adopted within the epidemiological and observational literature. This classification system is useful because it describes a number of important elements of care, with the definitions for each category, including references to residential status and daily needs, both of which are significant drivers of cost in adulthood. In the context of the Penner et al. 54 model, this also allowed them to link the short-term outcomes reported in the effectiveness studies to long-term adult outcomes.
This approach, however, has important limitations, as several studies have noted poor correlations between HRQoL and indicators of independence in autistic populations. 130 Furthermore, a number of studies have been critical of this type of categorisation of adult outcomes, noting that a more nuanced approach is needed to best define ‘standard concepts of what constitutes a “good” social outcome, [as these] may not always be relevant for people with ASD’. 131
The structure adopted in the adult scenario was therefore based on the classification system developed in Howlin et al. ,15 similar to the approach used in Penner et al. 54 However, noting the cited limitations, and in an attempt to mitigate these, independence levels are only used to indicate care needs and costs in adulthood. HRQoL, instead, continues to be based on the Payakachat et al. 127 algorithm used to estimate quality of life in children.
The structure adopted in the adult phase to estimate costs is based on five levels of independence: (1) ‘completely independent’, (2) ‘mostly independent’, (3) ‘some independence’, (4) ‘mostly dependent’ and (5) ‘completely dependent’. The definitions used for each category are based on those used in Howlin et al. 15 and are described in Table 9, and the costs attached to each independence level are described in Resource use.
| Independence level | Description |
|---|---|
| Completely independent | Achieving a high level of independence; has some friends/acquaintances; maintained reciprocal relationships; employed at some level (worked on voluntary/supported basis), now or in the past |
| Mostly independent | Achieving a good level of independence, but may require some support in daily living; has some friends/acquaintances; maintained reciprocal relationships; likely to be employed at some level (worked on voluntary/supported basis), now or in the past |
| Some independence | Some degree of independence, but requires support and supervision; does not need specialist residential provision; no close friends but some acquaintances; reciprocal relationships with reduced sharing; may have been employed now or in the past |
| Mostly dependent | Specialist residential provision/high level of support; no friends outside of residence; no enduring relationships; never in paid employment |
| Completely dependent | Needs high-level hospital care; no friends; no autonomy; never in paid employment |
Independence levels are determined on entering the adult phase of the model based on adaptive behaviour scores at 18.5 years of age. Owing to limitations in the epidemiological and observational evidence base, the adult phase of the model is static (i.e. once individuals enter the adult part of the model, the same level of independence is assumed throughout adulthood). This simplifying assumption is made because of lack of data regarding changes in independence over time. This may or may not reflect real life, and does not include any consideration of an individual’s potential for change or the impact of any additional health or mental health needs, life events or changes in the wider family or social community. This assumption therefore necessarily represents an important limitation of this scenario.
Model inputs
The following sections outline the key assumptions and data sources used to populate the model structure outlined above. In addition to data drawn from the IPD meta-analysis, modelled assumptions and inputs were primarily informed by three literature reviews. These included a review of observational studies to help characterise the prognosis of autistic children and adults; a utilities review to identify studies reporting on the HRQoL of autistic children and adults; and a resource review to identify resource and cost data relating to the care needs of autistic children. Details of all three of these reviews, including searches undertaken, inclusion criteria and findings, can be found in Appendices 14–16.
Furthermore, additional searches of the literature were also undertaken to identify any other input parameters not covered by these three reviews. Inputs were also informed by discussions with UK ABA practitioners, clinical academic experts, autistic adults and parents of autistic children, who provided feedback on the model assumptions, including current provision of services for autistic children, the delivery of ABA-based therapies in the UK and resource use. Information was also obtained from social care teams in several local authorities (York, Leeds and Newcastle) to ensure that we accurately reflected the current provision of services for autistic children and adults.
Treatment effect
In the TAU and eclectic arm of the model, changes in cognitive ability and adaptive behaviour scores are modelled using autism-specific natural history data to predict changes over time. To model the treatment effect, in the early intensive ABA-based arm, cognitive ability and adaptive behaviour scores are modelled by applying the treatment effect derived from the IPD meta-analysis. Outcome scores in the early intensive ABA-based interventions arm of the model are therefore the sum of the score predicted from the natural history data plus the treatment effect.
Natural history
To model changes in cognitive ability and adaptive behaviour scores over time, data were extrapolated from four studies95,96,107,110 identified in the systematic review with extended follow-up. These data were used to estimate change in baseline scores on usual care over time and were extrapolated assuming a simple linear trend. The studies identified in the systematic review of effectiveness studies was used in favour of data reported in observational studies, because few children with intellectual disability were recruited to the observational studies reporting changes in both cognitive ability and adaptive behaviour scores. See Appendix 15 for details of the review of observational evidence. The data from the effectiveness studies were therefore considered more consistent with the population modelled, although both sources reported similar patterns of change. To explore the impact of this assumption on model outcomes, sensitivity analyses were conducted using alternative rates of change in cognitive ability and adaptive behaviour scores. The mean changes in cognitive ability and adaptive behaviour scores used in the base case are presented in Table 10.
| Outcome measure | Mean | SE |
|---|---|---|
| Adaptive behaviour | –0.28 | 1.24 |
| Cognitive ability | –2.69 | 1.27 |
Treatment effect
The treatment effect was modelled in two phases: (1) a short-term phase, covering the first 2 years, and (2) a long-term phase, covering 2 years and onwards. This distinction is made to reflect the fact that most of the studies included in the IPD meta-analysis had a follow-up of ≤ 2 years.
Short-term treatment effect
In the first 2 years of the model (up to cycle 24), the treatment effect applied was drawn from the IPD meta-analysis and was based on analyses conducted at 1 and 2 years (Table 11). As discussed in Chapter 6, UK-based studies, the average treatment effect observed in the UK studies was somewhat smaller than that observed when combining all studies, and although these differences are not statistically significant, it is plausible that, because of either the differences in setting or the precise interventions compared, the benefits of early intensive ABA-based interventions may differ in the UK from those observed elsewhere in the world. A scenario analysis was therefore conducted using treatment effectiveness data drawn only from the UK studies.
| Outcome measure | Base case (all studies with IPD) | UK scenario | ||||||
|---|---|---|---|---|---|---|---|---|
| Year 1 | Year 2 | Year 1 | Year 2 | |||||
| MD | SE | MD | SE | MD | SE | MD | SE | |
| Adaptive behaviour | 2.92 | 2.46 | 7.00 | 2.58 | 1.70 | 2.36 | 2.78 | 2.42 |
| Cognitive ability | 9.16 | 2.44 | 14.13 | 2.54 | 6.27 | 4.04 | 9.39 | 4.32 |
Long-term treatment effect
Evidence on the longer-term effects of early intensive ABA-based interventions on cognitive ability and adaptive behaviour scores, and in particular the degree to which any early benefits are sustained, is very limited, with few studies reporting outcomes post end of therapy; see Chapter 6, Individual participant data meta-analysis of early intensive ABA versus treatment as usual or eclectic interventions.
Given the lack of evidence on long-term effects, it was not felt that following the norm of developing a single base-case analysis would be reasonable. Two scenarios were therefore explored:
-
an optimistic scenario, which assumed that the treatment effect persists throughout the time horizon of the model
-
a pessimistic scenario, which assumed that the treatment effect dissipates over time, such that at 7 years no treatment effect remains.
In both scenarios, these increases or decreases in the size of the treatment effect are modelled as a linear trend, as evidence from intermediate time points is unavailable. Furthermore, no changes in the size of the treatment effect are assumed after 7 years. This time limit reflects the maximum follow-up of Magiati et al. ,96 which was the study with the longest follow-up, and attempts to acknowledge that any further changes in the treatment effect are unknown. Pragmatically, it also prevents the magnitude of the treatment effect trending to extreme values (e.g. negative scores).
Mapping childhood outcomes to levels of independence used in the adult scenario analysis
Evidence linking adult levels of independence (see Appendix 15) to childhood cognitive ability and adaptive behaviour is somewhat limited. Although a number of studies report strong correlations between adult cognitive ability, adaptive behaviour scores and adult levels of independence,15,131–134 none reports results in a way that would allow contemporaneous predictions about adult outcomes (e.g. an appropriate regression analysis). However, one study, Farley et al. ,134 does report mean adaptive behaviour scores for several of the independence levels described in Scenario analysis exploring adult outcomes (see also Appendix 18 for further details).
To generate an algorithm with which to predict independence levels, the summary data reported in Farley et al. 134 were used to simulate IPD; details of methods used to do this are reported in Appendix 18. An ordinal logistic regression was then implemented to generate a regression model that could be used to predict adult outcomes. The coefficients generated from this analysis are reported in Table 12, along with the appropriate cut-off points.
| Parameter | Coefficient | SE |
|---|---|---|
| Adaptive behaviour | 0.07 | 0.01 |
| Cut-off point 1 (very poor) | 0.98 | 0.29 |
| Cut-off point 2 (poor) | 2.74 | 0.51 |
| Cut-off point 3 (fair) | 4.51 | 0.77 |
| Cut-off point 4 (good) | 6.55 | 1.05 |
Education
Few studies identified in the IPD meta-analysis reported educational placement and there is significant potential that this outcome was subject to significant bias, as predicted effects were implausibly large (see Model development). We therefore modelled educational outcomes indirectly by using regression models to predict educational placement using cognitive ability and adaptive behaviour scores.
Two regression models were generated, one to predict primary educational placement and a second to predict secondary educational placement. The proportion of children attending each of the three types of school described in Model structure is therefore determined at two points in the model, once in cycle 3 (age 4.5 years) and again in cycle 10 (age 11.5 years), with the probabilities of attending each type of educational placement estimated using two separate data sets.
The first regression model, used to predict primary educational placement, was based on pooled data from two of the studies identified in IPD meta-analysis: Smith et al. 103 and Magiati et al. 31 Secondary placement was based on data from Barret et al. ,135 a costing study identified in the resource review. As data from Barret et al. 135 were not reported in a form that allowed cognitive ability and adaptive behaviour to be linked with educational placement, we requested IPD, which were kindly provided by the authors to allow appropriate reanalysis. Both analyses used ordinal logistic analysis, with appropriate adjustments for repeated measures. Regression coefficients from these analyses are reported in Table 13.
| Parameter | Primary school | Secondary school | ||
|---|---|---|---|---|
| Coefficient | SE | Coefficient | SE | |
| Adaptive behaviour | –0.08 | 0.02 | –0.04 | 0.02 |
| Cognitive ability | –0.02 | 0.01 | –0.06 | 0.02 |
| Cut-off point 1 (mainstream with support) | –8.75 | 0.02 | –9.37 | 1.58 |
| Cut-off point 2 (specialist schooling) | –6.10 | 0.86 | –6.60 | 1.39 |
To acknowledge the potential impact of utilising an indirect approach to estimating the impact of early intensive ABA-based interventions on educational placement, a scenario analysis used the direct evidence available in the three effectiveness studies26,89,103 reporting subsequent educational placement. In this scenario analysis, children are assumed to attend the same type of education throughout childhood (see Appendix 18 for the proportions used).
Adverse effects
Adverse effects of ABA-based interventions were not reported in the studies included in the IPD meta-analysis and available information from other sources is limited, and largely anecdotal. 30,31,136 It was therefore not possible to include adverse effects in the economic model.
Mortality
A number of epidemiological studies have shown that autistic people experience reduced life expectancy compared with the general population. 137–142
To account for this reduction in life expectancy, mortality rates were estimated by applying a relative risk drawn from Hirvikoski et al. 138 to general population mortality rates adjusted for age and sex from UK life tables. 143 This study was selected because it is the largest study identified in the literature and included 27,122 autistic people and a further 2,672,185 controls. For males without intellectual disability (IQ ≥ 70), a relative risk of 1.69 was applied and a relative risk of 7.71 was applied for those with intellectual disability. For females without intellectual disability (IQ ≥ 70), a relative risk of 2.47 was applied and a relative risk of 4.75 for those with intellectual disability.
Mortality was not linked to intervention effectiveness. Given the observed effects of early intensive ABA-based interventions on cognitive ability scores and the observed differences in mortality rates in autistic people with and without intellectual disability, it is possible that early intensive ABA-based interventions may influence mortality. However, as agreed with our Advisory Group, extending any impact of early intensive ABA-based interventions to mortality was considered too strong an assumption, given the lack of evidence, and therefore no such benefits were included within the model.
Modelled population
In line with the IPD meta-analysis, the modelled population was assumed to consist of preschool children with a diagnosis of autism. Baseline characteristics modelled included age and sex, as well as the following outcome measures: autism symptom severity (ADOS), cognitive ability (IQ) and adaptive behaviour (VABS). Baseline characteristics were drawn from a pooled analysis of the studies comparing early intensive ABA-based interventions with TAU or eclectic interventions. 84–86,89–94,97,104 The exception to this is age, which was rounded down from 38 months to 36 months to ensure that the time horizon is a constant 15.5 years (this has a negligible impact on the predictions of the model). Note that because the model assumes that children will receive early intensive ABA-based interventions for 2 years, the starting age implies that some children will receive early intensive ABA-based interventions in place of regular schooling. Children in the UK are mandated to attend school by their fifth birthday144 but typically start in the September after their fourth birthday. This assumption was validated by the authors of the effectiveness studies and experts within our Advisory Group, who agreed that at least a proportion of children would receive early intensive ABA-based interventions in a school setting. In a scenario analysis in which effectiveness data were drawn from only UK studies, baseline characteristics were (when possible) drawn from the UK studies only. Starting characteristics used in the base-case analysis and in the UK studies only scenario are summarised in Table 14.
| Characteristic | Base case (10 studies84–86,89–97,104,109,110) | UK scenario (three studies89–92,96,109,110) | ||
|---|---|---|---|---|
| Mean | SE | Mean | SE | |
| Proportion male (%) | 87.57 | 1.47 | 91.59 | 2.70 |
| Proportion with intellectual disability (IQ < 70) (%) | 59.43 | 1.08 | 82.95 | 3.32 |
| Age (months) | 36 | 0 | 36 | 0 |
| Adaptive behaviour (VABS) | 63.19 | 0.43 | 57.60 | 0.55 |
| Cognitive ability (IQ) | 59.43 | 1.08 | 54.66 | 1.50 |
| Autism symptom severity (ADOS)a | 6.98 | 0.18 | 6.98 | 0.18 |
Subgroup analysis
The results of the subgroup analysis presented in Chapter 6 show little evidence of differential effects in the groups investigated. The economic model therefore does not explore subgroups any further.
Intervention and comparators
Reflecting the main comparison in the IPD meta-analysis, the model compares early intensive ABA-based interventions with TAU or eclectic interventions.
Early intensive applied behaviour analysis-based interventions
Modelled early intensive ABA-based interventions reflected our understanding of current UK provision following advice from the authors of the effectiveness studies and several UK practitioners. Data were also sourced from a UK study by Griffith et al. ,36 which described provision of ABA-based therapy in 14 UK ABA schools. In the base-case analysis it was therefore assumed that children will receive 30 hours of early intensive ABA-based interventions per week for a period of 24 months. Intensity was based on a consultation exercise with study authors and UK practitioners, who, although not in complete consensus, suggested that 30 hours would represent a typical programme. This also aligns with the average of 27 hours per week reported by the effectiveness studies and data reported in Griffith et al. 36 Duration of therapy was conservatively assumed to be 24 months on the basis that this aligns with the maximum follow-up period for the bulk of the available effectiveness evidence. However, consultation with study authors and data reported in Griffith et al. 36 suggest that it is common for children to continue receiving intensive ABA-based therapy in a school setting and the number of previous economic evaluations assumed a longer duration of therapy. A scenario analysis was therefore run assuming that children receive an intervention for a period of 36 months.
Comparator interventions
Comparator interventions included in the IPD meta-analysis were very diverse and the wider literature reveals few details about service provision in the UK. Advice from expert advisors suggested significant variability in current provision and highlighted that it usually consists of a mixture of activities delivered in a nursery or home setting. These services may also be supplemented by additional input from specialist services, such as speech and language therapists, educational psychologists, occupational therapists and mental health workers. To help provide further details on TAU and eclectic interventions, service providers in York and Newcastle local authorities kindly provided insight into provision in these areas, suggesting that TEACCH and PECS are used regularly, and that approximately one-third of children attend specialist nurseries, with the remainder supported in local authority mainstream nurseries. The model defined TAU and eclectic interventions based on York and Newcastle local authority provision, with costs also based on funding provided in these localities.
Health-related quality-of-life data used in cost-effectiveness analysis
As described in Model development, a systematic review was undertaken to identify appropriate utility data with which to populate the model. The studies identified in this review led to the adoption of a statistical algorithm developed in Payakachat et al. 127 to predict HRQoL benefits.
Application of the Payakachat and colleagues algorithm
Quality of life was estimated at each time point in the model based on the algorithms presented in the Payakachat et al. 127 study, using adaptive behaviour, age, baseline cognitive ability (IQ scores) and baseline autism symptom severity (ADOS scores). Quality-of-life scores therefore changed in accordance with changes in cognitive ability and adaptive behaviour scores, and with increasing age over time. Table 15 gives the coefficients applied in the model.
| Parameter | Scenario analysis | |
|---|---|---|
| Coefficient | SE | |
| Constant | −0.2438 | 0.2015 |
| Age | 0.0119 | 0.0186 |
| Age79 | 0.0003 | 0.0010 |
| ADOS score | 0.0079 | 0.0078 |
| IQ (log) | 0.0304 | 0.0478 |
| VABS composite score | 0.0103 | 0.0016 |
Quality of life for autistic adults (scenario analysis only)
Health-related quality of life in adulthood is also based on the Payakachat et al. 127 algorithm, with two adjustments made to reflect the fact that the algorithm is based on a paediatric population. The age parameter is held constant at 18.5 years and age-related decrements are applied to account for the natural effects of ageing on HRQoL. These decrements were calculated based on Szende et al. ,145 which described the health utilities of healthy populations of adults for different age groups. Decrements were applied as multiplier to the mean utility of the cohort from the age of 25 years onwards (see Appendix 18).
Quality of life for parents and carers
A number of studies reported lower (health-related) quality of life in parents and carers of autistic children compared either with parents of typically developing children or with population norms. 120–125 This literature has shown that child behavioural difficulties and lack of social support are particularly important drivers of quality of life in parents of children with autism and related conditions. The evidence in the IPD meta-analysis provides only very limited evidence that early intensive ABA-based interventions have any comparative advantage over other early interventions on problem behaviours, with few studies recording appropriate outcomes. Furthermore, the quality-of-life literature does not show any consistent relationship between other clinical outcomes, such as child cognitive ability,123,125 adaptive behaviour121 and autism symptom severity. 121,123–125 It is therefore not clear what, if any, effect early intensive ABA-based interventions has on parent and carer quality of life. The economic analysis therefore does not include any analysis of any possible impact of early intensive ABA-based interventions, either positive or negative, on parent or carer quality of life, although it is acknowledged that these potentially exist.
Resource use
Relevant costs and resources were identified in a systematic review of the literature and appropriate routine sources, such as Personal Social Services Research Unit (PSSRU). 146 The studies identified in this review were used to assign appropriate costs associated with the delivery and care of autistic children and adults. Information on the precise description of resources required for each individual therapy was partially based on data derived from the IPD review, and augmented with further information obtained from relevant experts and data sourced from local authorities. The price year of the analysis was 2016/17, as this was the most recent year of publication for PSSRU146 and inflation indices for 2017/18 were not available at the time of writing. Prices reported in alternative cost years were inflated using inflation indices reported in PSSRU. 146
Intervention and comparator costs
Costs of early intensive applied behaviour analysis-based interventions
Costs of early intensive ABA-based interventions were derived from a number of sources. To estimate staffing costs, data reported in Griffith et al. 36 were used to estimate staff pupil ratios. This study collected data from 14 schools delivering ABA-based interventions and recorded both the number of children attending and the numbers of teaching staff. Four types of staff were recorded: (1) consultants (senior staff members who are responsible for overall ABA programmes), (2) lead ABA tutors (staff members who are in an ABA supervisory role within a classroom), (3) ABA tutors (staff members who provide ABA therapy for children) and (4) non-ABA staff (professionals and teachers whose primary role is not ABA based, such as specialist music teachers and speech and language therapists). For each type of staff, the number of full-time equivalents per pupil was estimated, assuming that part-time members of staff worked 50% time. Staff costs were estimated using NHS and social care pay scales reported in PSSRU. 146 The appropriate point on the salary scale was selected for each of the four staff types by matching advertised salaries for relevant job vacancies listed on Indeed.co.uk to NHS and social care pay scales reported in PSSRU. 146 Only salary, national insurance and pension contributions were included from PSSRU,146 as other costs were estimated separately. Table 16 summaries the assumptions and cost data used to estimate staff costs per child per year.
| Staff type | FTE staff/child | Salary band assumed | Salary (£) | Salary oncosts (£) | Cost per child (£) |
|---|---|---|---|---|---|
| Consultant | 0.11 | 7 | 38,550 | 9605 | 5506.09 |
| Supervisor | 0.23 | 4 | 20,279 | 4602 | 5834.50 |
| ABA tutors | 0.86 | 3 | 18,777 | 4179 | 19,663.86 |
| Others | 0.14 | 4 | 20,279 | 4602 | 3375.33 |
| Total staff | 1.34 | n/a | n/a | n/a | 34,379.78 |
Capital costs and other indirect costs were estimated from costing information reported by the Department for Education, which estimates non-teaching staff costs per primary aged pupil to be £2303. The total cost of providing early intensive ABA-based interventions was therefore estimated at £36,682.78 per annum. This cost was considered to be in line with expectation from clinical experts and aligned with pricing from private providers, which typically advertise programmes at a cost of £35,000–50,000 per year. 37–39
Costs of treatment as usual
Costs of TAU and eclectic interventions were primarily based on national funding structures and information obtained from York and Leeds local authorities on SEN funding. In the UK, SEN funding is based on a three-tiered system. Element 1 refers to funding for mainstream places and in the context of early years provision refers to 30 hours of free teaching for 38 weeks per year. The amount paid is dependent on age and is derived from a national funding formula. For the 2017/18 year, this formula paid £5.39 per hour for 2-year-olds and £4.88 per hour for 3- to 4-year-olds. Element 2 is to support children with SEN and is paid either from local authority or the education funding agency. This funding is, however, not available for preschool children. Element 3 funding is top-up funding provided by the local authority for children with the highest needs, and is based on the needs of the child and is often determined through an additional banding system that classifies children according to levels of disability. Figures obtained on preschool autistic children known to York local authority suggest that 45% of children will receive element 3 funding, with the remainder receiving only element 1 funding. Of the children receiving element 3 funding, 43% received additional support as part of enhanced resource provision, which is attendance at a specialist centre, such as a specialist nursery, whereas the remainder received additional support via an education and health-care plan. Neither local authority was able to provide precise figures on funding attached to these forms of support, but provided broad estimates of £5000 per annum for enhanced resource provision and £8000 per annum for education, health and care plans (EHCP). Based on these figures, estimated nursery provision cost was £8634.33 per annum and the model assumed that two in every three children would be aged ≥ 3 years.
Costs of autism in childhood
Aligning with the model structure outlined in Model structure, costs in the model were split between education costs and those accruing to other sectors, including the health sector.
Education costs
Costs associated with each type of education were drawn from a reanalysis of IPD obtained from Barret et al. ,135 who recorded education costs in a sample of adolescents with autism and Asperger syndrome. Costs applied per annum for each education type are summarised in Table 17. These costs were applied throughout childhood despite being drawn from adolescent-aged children, as no education costs were identified in primary-aged children. Provision of education services is, however, based on the same costing formula, regardless of the age of the child, and therefore costs of providing primary-aged education are likely to be broadly similar to those of providing secondary education.
| Education type | Cost per annum (£) |
|---|---|
| Mainstream education | 4417.70 |
| Mainstream with support | 8689.78 |
| Special education | 15,702.78 |
Social care and health-care costs
Costs accruing to social and medical (NHS) care were also drawn from a reanalysis of IPD obtained from Barret et al. 135 Costs were linked to outcomes in the model using a regression equation in which cognitive ability and adaptive behaviour scores were used to predict total social care and medical costs. As with education costs, social care and medical costs were applied throughout childhood despite being drawn from an adolescent population, due to the lack of other appropriate sources. Coefficients from this analysis are reported in Table 18.
| Education type | Cost per annum (£) |
|---|---|
| Intercept | 1900.09 |
| Adaptive behaviour | –8.78 |
| Cognitive ability | –7.81 |
It is plausible that social care and medical costs change throughout childhood; however, the impact of this is likely to be minimal, as total costs accruing to social care and the NHS are small, relative to education costs. Furthermore, mean predicted social care and medical costs for the TAU and eclectic arm were comparable to those estimated in the Barret et al. 126 study, which reported mean care costs for preschool- and primary school-aged children. Note that access to the IPD from Barret et al. 126 was made available to the research team; however, this was not utilised, as costs could not be linked with VABS and IQ scores and these were not recorded in this data set.
Care costs in adulthood
Care costs in adulthood were identified in the resource review (see Appendix 16). This review identified a limited number of sources of resource use and cost data. The most comprehensive was a study by Knapp et al. ,147 later updated in Buescher et al. ,23 which estimated the full costs of autism and related conditions in the UK. This study drew on data from 185 adults and was supplemented by routinely collected data and figures reported in other research studies. The Knapp et al. 147 and Buescher et al. 23 studies outlined several cost categories that showed the economic impact of autism on a range of sectors. These were accommodation; social services, including day services, respite care, employment support and education services; and medical costs, including both primary and secondary care.
These categories were adopted to characterise adult care costs within the model, using the resource use and costing data reported in Knapp et al. ,147 and were mapped to the five adult health states described in Scenario analysis exploring adult outcomes. To ensure that assumptions made about resource use were appropriate, advice was sought from service delivery providers in York local authority, with additional resource and costing data drawn from PSSRU. 146
Total costs, including and excluding productivity losses and family out-of-pocket expenses for each level of independence, are reported in Table 19. Details of sources and assumptions made to assign costs are presented in Appendix 18.
| Resource type | Completely independent (£) | Mostly independent (£) | Some independence (£) | Mostly dependent (£) | Completely dependent (£) |
|---|---|---|---|---|---|
| Accommodation | |||||
| Own home/parents | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Supported: low intensity | 0.00 | 0.00 | 17,758.29 | 0.00 | 0.00 |
| Supported: high intensity | 0.00 | 0.00 | 33,112.15 | 49,668.22 | 49,668.22 |
| Residential | 0.00 | 0.00 | 0.00 | 57,776.50 | 57,776.50 |
| Social services | |||||
| Day services | 0.00 | 17,728.57 | 5850.43 | 0.00 | 0.00 |
| Respite care | 0.00 | 1927.00 | 635.91 | 0.00 | 0.00 |
| Employment support | 169.48 | 169.48 | 169.48 | 0.00 | 0.00 |
| Adult education | 1800.00 | 1800.00 | 1067.00 | 4159.00 | 4159.00 |
| Medical costs | |||||
| Hospital | 109.00 | 109.00 | 188.00 | 43.00 | 43.00 |
| Other health services | 887.00 | 887.00 | 587.00 | 726.00 | 726.00 |
| Societal costs | |||||
| Family expenses | 2731.00 | 2731.00 | 901.23 | 0.00 | 0.00 |
| Lost employment (parents) | 3840.75 | 3840.75 | 1280.25 | 0.00 | 0.00 |
| Lost employment (person with autism) | 17,351.07 | 17,351.07 | 17,351.07 | 29,689.61 | 29,689.61 |
| Total NHS and social | 2965.48 | 22,621.05 | 59,368.26 | 112,372.72 | 112,372.72 |
| Total societal costs | 26,888.30 | 46,543.87 | 78,900.81 | 142,062.33 | 142,062.33 |
Budget impact
The budget impact of implementing early intensive ABA-based interventions was estimated for a period of 5 years using the estimated unit costs and resource savings predicted by the cost-effectiveness model. The budget impact model was run for both the optimistic and the pessimistic assumptions about the long-term effects of early intensive ABA-based interventions. Costs and resource savings were classified based on the budget they accrue to and allocated to education or social services and NHS budgets.
The budget impact analysis assumed that all children diagnosed with autism before the age of 4 years would be eligible to receive early intensive ABA-based interventions. To model uptake of early intensive ABA-based interventions, data were drawn from a US study of early intensive ABA-based interventions services in an insured population,148 in which 94.6% of children aged < 5 years received ABA-based therapy. Expansion of early intensive ABA-based services in the UK is also likely to take some time; therefore, the budget impact model assumed a linear increase in the provision of early intensive ABA-based interventions over time, from 18.9% of eligible children in year 1 to 94.6% of eligible children in year 5.
Eligible population
The prevalence of diagnosed autism was estimated to be 3.8 per 1000 for boys and 1.5 per 1000 for girls, with estimates drawn from Taylor et al. 149 Taylor et al. 149 estimated the prevalence of diagnosed autism using data from a large and representative sample of UK general practices. Note that this is lower than estimated prevalence of autism at about 1%,1 as this figure is based on adults and includes undiagnosed cases. The Taylor et al. 149 study estimated prevalence at 8 years of age; therefore, to estimate the proportion of these children who would be diagnosed before the age of 4 years, data on diagnosis patterns were drawn from Brett et al. 150 This was combined with the prevalence rate reported in Taylor et al. 149 by assuming that diagnosis was log-normally distributed, with mean and SD based on data reported in Brett et al. 150 This exercise predicted prevalence of diagnosed autism in children aged < 4 years of 2.5 per 1000 boys and 0.8 per 1000 for girls.
The incident population each month was estimated as one-twelfth of the prevalent population, assuming that children are diagnosed at equal rates throughout the year, with constant prevalence over time.
The total number of children aged < 4 years was drawn from Office for National Statistics mid-2018 population30 estimates, with no population growth assumed for future years.
Validation
Excel formulas, model logic and input data were verified for accuracy as part of quality control procedures by a health economist not involved in the project. This included the use of a checklist to carry out a series of black-box tests and to evaluate the internal validity of the model, and pressure testing, when parameters were set to extreme values to ascertain whether or not the changes were consistent with expectations. The code of the model was also examined for potential errors. This included tracking how the parameters fed into the model and an examination of the main calculation sheets, with a view to understanding how the QALYs and costs were accumulated in the model.
To ensure external validity, the model’s predictions were compared with observed data and epidemiological reporting on the medium- and long-term costs and outcomes of autistic children.
Analytical approach, and scenario and sensitivity analyses
Although the economic analysis developed is purely exploratory, given the substantial limitations in the available data, it is necessary to consider how to interpret the results, particularly given that, as a neurodisability, autism impacts on multiple sectors. In health-care decision-making in the UK, a decision rule is often employed (based on methods developed by NICE) to provide an objective basis on which to determine the value of implementing a new intervention. This decision rule sets a willingness to pay for additional health benefits.
The benefits of an intervention are usually quantified in terms of QALYs gained, a measure of health incorporating improvements in both length and quality of life. The willingness to pay is a threshold that must be met for an intervention to be considered cost-effective. In assessments made by NICE, this is generally £20,000–30,000 per QALY gained. 129
For a technology or intervention to be considered cost-effective, it must generate 1 additional QALY per £20,000–30,000 of additional cost. Metrics of cost-effectiveness are measured in terms of the incremental costs of generating an additional QALY and is estimated as an incremental cost-effectiveness ratio (ICER), which is the ratio of incremental costs to incremental QALYs.
The threshold used by NICE can be interpreted as the opportunity costs of generating benefits in the health sector (i.e. the efficiency with which the NHS is capable of generating health per £1 spent). However, as discussed in Economic evaluation of interventions in autism, the impacts of early intensive ABA-based interventions are likely to be realised in multiple sectors, not just the health sector. This complicates the interpretation of an ICER, as the opportunity cost of generating benefits and, by extension, the implied cost-effectiveness threshold, may differ across sectors. For example, the opportunity cost of generating benefits in the health sector may not be the same as the opportunity costs of generating benefits in the education sector. This issue is further complicated by the fact that it is not clear how opportunity costs differ across sectors. In the light of this uncertainty, and for simplicity, it is assumed that benefits and costs are valued equally across sectors, implying a common threshold.
Two types of economic analysis were performed: (1) a deterministic analysis and (2) a probabilistic analysis. A deterministic analysis calculates the result using point estimates for all the parameters in the model, whereas in a probabilistic analysis values are entered as distributions. This allows uncertainty around model parameters to be incorporated into the model, reflecting that the inputs used in the model are measured with uncertainty. Relevant distributions for each parameter input were informed by the IPD meta-analysis, additional literature and expert opinion. The probabilistic analysis ran the model 10,000 times, with each iteration making random draws from the distributions used to describe input parameters. An incremental cost-effectiveness analysis was conducted based on the estimated costs and QALYs, as described above.
The probability that early intensive ABA-based intervention is a cost-effective intervention at a particular cost-effectiveness threshold was estimated by calculating the proportion of simulations in which the ICER was below the willingness-to-pay threshold. A cost-effectiveness frontier was also produced, which presents the probability of early intensive ABA-based interventions being cost-effective at different cost-effectiveness thresholds.
Sensitivity and scenario analyses
To explore the impact of alternative model assumptions and the sensitivity of results to changes in parameter inputs, a series of scenario and sensitivity analyses were performed. These scenarios were considered important by the project Advisory Group. The specific analyses undertaken have been introduced throughout this section and are listed below. Details of the assumptions made in each of these analyses are presented in Chapter 8.
Scenario analysis
-
UK evidence used to estimate short-term intervention effect.
-
Time horizon extended to a lifetime time horizon to incorporate adult outcomes.
-
Educational placement estimated directly from the effectiveness studies.
-
Duration of early intensive ABA-based intervention increased to 36 months.
Sensitivity analysis
-
Change in cognitive ability and adaptive behaviour natural history scores per annum.
-
Effects of early intensive ABA-based interventions (cognitive ability and adaptive behaviour scores) at 2 years.
-
Costs of early intensive ABA-based interventions and TAU and eclectic interventions per annum.
-
Costs of education categories, supported placement and specialist schooling.
Value-of-information analysis
One of the aims of the economic analysis was to identify key uncertainties in the evidence base and to implement a value-of-information analysis to consider the value of carrying out further research to address these uncertainties. Implementation of value-of-information analysis, however, relies on being able to adequately parameterise the uncertainty associated with any decision. In the present context, this is very difficult to do. First, the potential for bias in the underlying effectiveness studies means that the reported CIs are overly narrow and do not represent the true uncertainty in effectiveness estimates. Second, as described in Overview, there are a number of structural uncertainties relating to the appropriateness and completeness of the outcome measures modelled, as well as issues relating to the long-term impact of early intensive ABA-based interventions. Any estimate of the decision uncertainty based on the presented model structure and reported CI would therefore be likely to represent an underestimate of the true level of decision uncertainty and, thus, the value of further research. For these reasons, it was decided not to implement a value-of-information analysis, but instead to present a purely qualitative assessment of the future research needs.
Chapter 8 Cost-effectiveness and budget impact results
This section outlines the results for the developed cost-effectiveness model and budget impact analysis.
Base-case results
This section presents the results of the base-case analysis for the deterministic and probabilistic models. These analyses set out the most plausible estimates of cost-effectiveness, given the limited evidence available and taking the results of the IPD meta-analysis at face value. As described in Chapter 7, Long-term treatment effect, there is significant uncertainty about the long-term benefits of early intensive ABA-based interventions. Therefore, two scenarios are presented in the base-case analysis: an optimistic scenario, in which the comparative advantage of early intensive ABA-based interventions are assumed to persist throughout the time horizon of the model, and a pessimistic scenario, in which the treatment effect dissipates to zero.
Deterministic results
Initial results are presented assuming a narrow health-care perspective and therefore only costs and benefits accruing to the health-care system are included. Results of this analysis are presented in Table 20. Full results with a break down of costs are presented in Appendix 19.
| Scenario | Therapy | Cost (£) | QALYs | Incremental cost (£) | Incremental QALYs | ICER (£) |
|---|---|---|---|---|---|---|
| Pessimistic | ABA | 76,622 | 4.61 | 57,879 | 0.24 | 236,837 |
| TAU/eclectic | 18,743 | 4.37 | ||||
| Optimistic | ABA | 75,976 | 5.21 | 57,233 | 0.84 | 68,362 |
| TAU/eclectic | 18,743 | 4.37 |
In the pessimistic scenario, early intensive ABA-based interventions are associated with £57,879 in additional costs and generates 0.24 additional QALYs. The resulting ICER is £236,837 per additional QALY. In the optimistic scenario, early intensive ABA-based interventions are associated with £57,233 in additional costs and generates 0.84 additional QALYs. The resulting ICER is £68,362 per additional QALY. Using NICE decision rules to benchmark the results of the cost-effectiveness analysis and adopting a £30,000 per QALY threshold, these results indicate that for early intensive ABA-based interventions to be considered cost-effective in the pessimistic scenario, it would be necessary for there to be a further 1.68 QALYs or £50,547 in additional cost savings not captured by the economic model. In the optimistic scenario, early intensive ABA-based interventions would be cost-effective at a threshold of £30,000 per QALY if there were a further 1.07 QALYs or £32,117 in additional cost savings not captured by the model.
A comparison of the incremental costs in the pessimistic and optimistic scenarios shows only a relatively small difference. This reflects the lack of scope for early intensive ABA-based interventions to generate significant cost savings in the health service sector. This similarity in incremental costs, however, contrasts with a comparison of health benefits produced, which are significantly larger in the optimistic scenario.
Building on this initial scenario, Table 21 presents results considering a wider public sector perspective.
| Scenario | Therapy | Cost (£) | QALYs | Incremental cost (£) | Incremental QALYs | ICER (£) |
|---|---|---|---|---|---|---|
| Pessimistic | ABA | 195,310 | 4.61 | 43,940 | 0.24 | 179,799 |
| TAU/eclectic | 151,370 | 4.37 | ||||
| Optimistic | ABA | 187,612 | 5.21 | 36,242 | 0.84 | 43,289 |
| TAU/eclectic | 151,370 | 4.37 |
In the pessimistic scenario, early intensive ABA-based interventions are associated with £43,940 in additional costs and generates 0.24 additional QALYs. The resulting estimated ICER is £179,799 per additional QALY. In the optimistic scenario, early intensive ABA-based interventions are associated with £36,242 in additional costs and generates 0.84 additional QALYs. The resulting estimated ICER is £43,289 per additional QALY. The adoption of a public sector perspective has a significant impact on incremental costs in both the pessimistic and optimistic scenarios, with incremental costs falling by £13,939 and £20,991, respectively. This is because improvements in cognitive ability and adaptive behaviour could have a large impact in public sector cost savings, which are predominantly caused by changes in education placement.
These differences in incremental costs have a significant impact on the resulting ICER, which fall appreciably in both the pessimistic and optimistic scenarios. However, in both scenarios they remain firmly above the NICE threshold of £20,000–30,000 per QALY. Assuming a threshold of £30,000 per QALY, and making pessimistic assumptions about the long-term treatment effect, it would be necessary for early intensive ABA-based interventions to generate either a further 1.22 QALYs worth of additional health or non-health benefits, or a further £36,608 in additional costs savings. In the optimistic scenario these fall to either a 0.37 QALYs worth of benefits or £11,126 in cost savings.
Probabilistic results
A probabilistic sensitivity analysis was conducted to account for the effects of parameter uncertainty and cost-effectiveness acceptability generated. The base-case results for the probabilistic model are shown in Table 22.
| Scenario | Therapy | Cost (£) | QALYs | Incremental cost (£) | Incremental QALYs | ICER (£) |
|---|---|---|---|---|---|---|
| NHS and social services perspective | ||||||
| Pessimistic | ABA | 76,587 | 5.02 | 58,940 | 0.24 | 240,868 |
| TAU/eclectic | 17,648 | 4.77 | ||||
| Optimistic | ABA | 76,341 | 5.60 | 58,630 | 0.85 | 69,385 |
| TAU/eclectic | 17,711 | 4.75 | ||||
| Public sector perspective | ||||||
| Pessimistic | ABA | 191,264 | 5.00 | 46,103 | 0.24 | 189,122 |
| TAU/eclectic | 145,161 | 4.75 | ||||
| Optimistic | ABA | 184,411 | 5.61 | 39,233 | 0.84 | 46,768 |
| TAU/eclectic | 145,178 | 4.77 | ||||
The results of the probabilistic analysis broadly correspond with those of the deterministic analysis and indicate that further health or non-health benefits or cost savings would need to be generated for early intensive ABA-based interventions to be cost-effective at a threshold of £30,000 per QALY. Assuming a public sector perspective, in the pessimistic scenario it would be necessary for early intensive ABA-based interventions to generate either a further 1.29 additional QALYs or produce £38,790 in additional cost savings. In the optimistic scenario, these values fall to 0.47 additional QALYs and £14,066 in additional cost savings.
Assuming an NHS and social services perspective, the probabilistic results indicate that the probability of early intensive ABA-based interventions being cost-effective at a threshold of £30,000 per QALY is < 1% in the pessimistic scenario and 2.6% in the optimistic scenario. The probability that early intensive ABA-based interventions are cost-effective when assuming a public sector perspective is < 1% in the pessimistic scenario and 23% in the optimistic scenario. Taken at face value, these probabilities of cost-effectiveness indicate that there is relatively little chance that early intensive ABA-based therapy is cost-effective when pessimistic assumptions are made about the long-term effectiveness of early intensive ABA-based interventions, and a modest probability in the scenario when optimistic assumptions are made. Care should, however, be taken not to overinterpret these results, given the limitations of the economic model and the scope for further benefits or cost saving to alter this result.
The degree of decision uncertainty is illustrated in Figure 23, which presents the cost-effectiveness acceptability curve taking an NHS and social services perspective and a public sector perspective, respectively. The probability that early intensive ABA-based interventions are cost-effective when taking an NHS and social services perspective remains close to zero up to a threshold of £84,000 per QALY in the pessimistic scenario and up to £25,000 per QALY in the optimistic scenario. When a public sector perspective is adopted, the probability that early intensive ABA-based interventions are cost-effective begins to depart from zero at a threshold of around £30,000 per QALY under the pessimistic scenario and £1000 per QALY in the optimistic scenario.
FIGURE 23.
Cost-effectiveness acceptability curve.
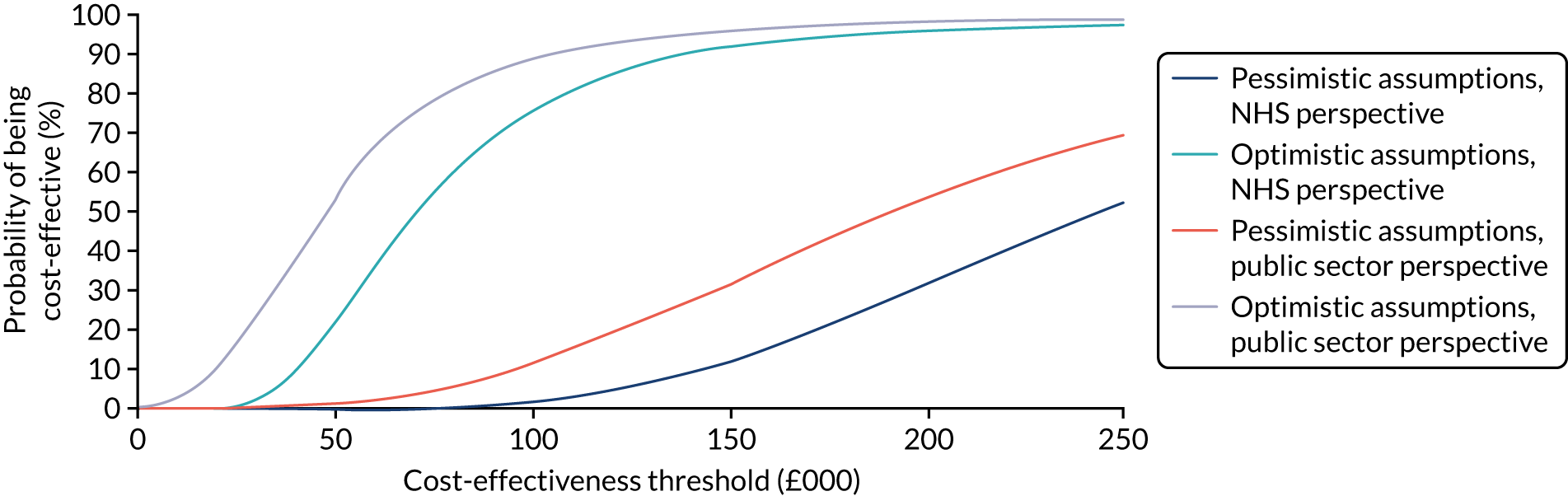
Scenario and sensitivity analysis results
To explore the impact of alternative inputs and assumptions on the results, a range of sensitivity and scenario analyses were undertaken. These sensitivity and scenario analyses were conducted using the deterministic model and assumed a public sector perspective. As in the base-case analysis, scenarios were run making both pessimistic and optimistic assumptions about the long-term treatment effect.
Scenario analysis
Four scenario analyses were undertaken:
-
UK evidence used to estimate short-term intervention effect
-
time horizon extended to a lifetime time horizon to incorporate adult outcomes
-
educational placement estimated directly from the effectiveness studies
-
duration of early intensive ABA-based intervention increased to 36 months.
In each scenario a key model parameter or assumption was varied, with all other parameters fixed at base-case values. Each scenario is presented in turn, along with a short summary of the impact the analysis had on the base-case results. Results of the scenario analysis are summarised in Table 23.
| Scenario | Therapy | Cost (£) | QALYs | Incremental cost (£) | Incremental QALYs | ICER (£) |
|---|---|---|---|---|---|---|
| Scenario 1: UK evidence | ||||||
| Pessimistic | ABA | 200,257 | 4.48 | 48,887 | 0.11 | 449,488 |
| TAU/eclectic | 151,370 | 4.37 | ||||
| Optimistic | ABA | 196,181 | 4.73 | 44,811 | 0.36 | 124,945 |
| TAU/eclectic | 151,370 | 4.37 | ||||
| Scenario 2: adult outcomes | ||||||
| Pessimistic | ABA | 1,800,040 | 6.87 | 43,940 | 0.24 | 179,799 |
| TAU/eclectic | 1,756,100 | 6.62 | ||||
| Optimistic | ABA | 1,705,806 | 8.49 | –50,294 | 1.86 | Dominant |
| TAU/eclectic | 1,756,100 | 6.62 | ||||
| Scenario 3: educational outcomes | ||||||
| Pessimistic | ABA | 170,113 | 4.61 | 12,325 | 0.24 | 50,435 |
| TAU/eclectic | 157,788 | 4.37 | ||||
| Optimistic | ABA | 169,467 | 5.21 | 11,680 | 0.84 | 13,951 |
| TAU/eclectic | 157,788 | 4.37 | ||||
| Scenario 4: duration of therapy equal to 36 months | ||||||
| Pessimistic | ABA | 222,892 | 4.61 | 71,522 | 0.24 | 292,664 |
| TAU/eclectic | 151,370 | 4.37 | ||||
| Optimistic | ABA | 213,603 | 5.21 | 62,233 | 0.84 | 74,335 |
| TAU/eclectic | 151,370 | 4.37 | ||||
Scenario 1: UK evidence
A substantial proportion of the evidence identified on the relative effectiveness of early intensive ABA-based interventions was from non-UK studies. Scenario 1 therefore draws baseline and short-term (years 1 and 2) treatment effects from a pooled IPD analysis of the UK studies only.
Using data from only UK studies results in the ICER increasing to £449,488 per QALY when pessimistic assumptions are made regarding the long-term treatment effect, whereas in the optimistic scenario the ICER increases to £124,945 per QALY. The results of this scenario analysis highlight the sensitivity of the model to even relatively small changes in the size of treatment effect and the importance of uncertainties in the generalisability of the results of the non-UK based studies to a UK setting.
Scenario 2: extending to include adult outcomes
Owing to the substantial uncertainty regarding the long-term impact of early intensive ABA-based interventions and the weak evidence linking childhood outcomes to adult outcomes, the base-case analysis uses a time horizon of ≈15 years. It is, however, plausible that the effects of early intensive ABA-based interventions extend beyond childhood into adulthood. Scenario 2 therefore implements an exploratory analysis to consider the potential impacts of early intensive ABA-based therapy on adult outcomes and further extends the time horizon to a lifetime horizon (77 years), allowing the cohort to transition to the adult phase of the model.
The impact of extending the time horizon depends substantially on the assumptions made about the long-term treatment effect. In the pessimistic scenario, the ICER does not change from the one generated in the base-case analysis, as this scenario assumes no further benefit of early intensive ABA-based interventions beyond 7 years. In the optimistic scenario, this scenario produces substantially different results from the base-case analysis, with early intensity ABA-based interventions generating substantially more QALYs and greater cost savings. A substantial change to both incremental QALYs and costs. The changes to incremental costs are so large that early intensive ABA-based interventions now dominates TAU and eclectic interventions (i.e. it generates greater benefits at lower cost). These results highlight the sensitivity of the model results to the assumptions made regarding the long-term benefits of early intensive ABA-based interventions and the potential for significant benefits and cost savings to be generated in adulthood (should the effects of interventions persist into adulthood and alter the life paths of autistic people). It is also notable that these results very broadly match those reported in the previous economic evaluations of early intensive ABA-based interventions. These previous economic evaluations similarly reported costs savings from implementing early intensive ABA-based interventions, although the estimated savings were much greater in the previous analyses (see Appendix 13 for an overview of these studies).
Scenario 3: changing educational outcomes
The available evidence linking early intensive ABA-based interventions with schooling outcomes is very limited, as this was rarely available for the studies included in the IPD meta-analysis. The base-case model therefore takes an indirect approach to modelling schooling outcomes by using cognitive ability and adaptive behaviour scores to predict schooling outcomes, rather than using the direct evidence reported in the effectiveness studies. Scenario 3 therefore explores this assumption by using the effects estimates generated directly by the effectiveness studies.
The impact of using the direct evidence is significant in both the pessimistic and the optimistic scenarios, resulting in substantially lower incremental costs in both. In the pessimistic scenario using the direct evidence on educational placement reduces the ICER to £50,435 per additional QALY, whereas in the optimistic scenario it lowers the ICER to £13,951 per additional QALY. These large changes suggest that an indirect approach to model school outcomes may not capture some of the benefits of ABA-based therapy on schooling outcomes, or alternatively that the potential selection biases documented in Chapter 6 have a very significant impact on schooling outcomes.
Scenario 4: increasing duration of the intervention
One of the key assumptions made in the base-case model is that children in the early intensive ABA-based interventions arm receive therapy for a fixed period of 24 months. Scenario 4 extends the duration of therapy to 36 months. This increases incremental costs significantly for both the pessimistic and the optimistic scenarios. This is because early intensive ABA-based interventions are implemented for longer, resulting in substantially higher therapy costs. The ICER increases to £292,664 per additional QALY when pessimistic assumptions are made and £74,335 per QALY when optimistic assumptions are made.
Two-way sensitivity analysis
Two-way and multiway sensitivity analyses were undertaken to explore uncertainty in key input values. This analysis allows assessment of the impact of changing two parameters in the model at the same time. Four analyses were conducted, each considering the following pairs of parameter values:
-
change in cognitive ability and adaptive behaviour natural history scores per annum
-
effects of early intensive ABA-based interventions (cognitive ability and adaptive behaviour scores) at 2 years
-
costs of early intensive ABA-based interventions and TAU or eclectic interventions per annum
-
costs of education categories, supported placement and specialist schooling.
For each analysis, a heat map was generated, depicting the parameter space over which early intensive ABA-based interventions would be considered cost-effective based on NICE thresholds. Cells shaded light blue display ICERs < £20,000 per QALY, orange shading displays ICERs between £20,000 and £30,000 per QALY and purple shading displays ICERs > £30,000 per QALY.
Sensitivity analysis 1: change in natural history of outcomes
The two-way scenario analysis reporting ICERs for per annum cognitive ability and adaptive behaviour natural history scores is presented in Table 24. The results of this analysis show that the model is largely insensitive to these input parameters and even the most extreme values do not impact sizably on the resulting ICER. This is because changing these values does not have a direct impact on the size of the benefits of early intensive ABA-based therapy.
| Pessimistic | Natural history: VABS (£) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| –4.69 | –4.19 | –3.69 | –3.19 | –2.69a | –2.19 | –1.69 | –1.19 | –0.69 | ||
| Natural history: IQ | –2.28 | 182,228 | 181,324 | 180,464 | 179,650 | 178,882 | 178,171 | 177,509 | 176,899 | 176,340 |
| –1.78 | 182,450 | 181,556 | 180,706 | 179,903 | 179,148 | 178,449 | 177,800 | 177,203 | 176,656 | |
| –1.28 | 182,645 | 181,760 | 180,921 | 180,130 | 179,387 | 178,701 | 178,065 | 177,480 | 176,946 | |
| –0.78 | 182,814 | 181,940 | 181,112 | 180,333 | 179,603 | 178,930 | 178,307 | 177,735 | 177,214 | |
| –0.28a | 182,962 | 182,099 | 181,283 | 180,516 | 179,799 | 179,139 | 178,529 | 177,970 | 177,462 | |
| 0.22 | 183,091 | 182,238 | 181,434 | 180,681 | 179,976 | 179,330 | 178,733 | 178,187 | 177,691 | |
| 0.72 | 183,203 | 182,362 | 181,570 | 180,829 | 180,138 | 179,505 | 178,921 | 178,389 | 177,905 | |
| 1.22 | 183,300 | 182,471 | 181,691 | 180,964 | 180,286 | 179,667 | 179,096 | 178,576 | 178,105 | |
| 1.72 | 183,384 | 182,567 | 181,800 | 181,086 | 180,422 | 179,816 | 179,259 | 178,752 | 178,293 | |
| Optimistic | Natural history: VABS (£) | |||||||||
| –4.69 | –4.19 | –3.69 | –3.19 | –2.69a | –2.19 | –1.69 | –1.19 | –0.69 | ||
| Natural history: IQ | –2.28 | 48,846 | 48,185 | 47,482 | 46,738 | 45,949 | 45,129 | 44,276 | 43,403 | 42,525 |
| –1.78 | 48,698 | 47,959 | 47,178 | 46,355 | 45,493 | 44,610 | 43,709 | 42,809 | 41,930 | |
| –1.28 | 48,343 | 47,526 | 46,668 | 45,776 | 44,856 | 43,933 | 43,015 | 42,126 | 41,290 | |
| –0.78 | 47,811 | 46,920 | 45,997 | 45,053 | 44,101 | 43,171 | 42,276 | 41,443 | 40,696 | |
| –0.28a | 47,126 | 46,173 | 45,205 | 44,238 | 43,289 | 42,395 | 41,569 | 40,838 | 40,222 | |
| 0.22 | 46,322 | 45,332 | 44,349 | 43,397 | 42,497 | 41,684 | 40,972 | 40,380 | 39,923 | |
| 0.72 | 45,437 | 44,443 | 43,487 | 42,595 | 41,789 | 41,100 | 40,536 | 40,109 | 39,819 | |
| 1.22 | 44,526 | 43,570 | 42,686 | 41,900 | 41,232 | 40,696 | 40,300 | 40,040 | 39,907 | |
| 1.72 | 43,650 | 42,779 | 42,012 | 41,370 | 40,864 | 40,498 | 40,267 | 40,159 | 40,153 | |
Sensitivity analysis 2: change in the effect of applied behaviour analysis-based intervention
Table 25 displays the analysis exploring different treatment effects at 2 years. The results show that the model results are particularly sensitivity to these parameters. In particular, they show that when optimistic assumptions are made about the long-term treatment effect, there is a large and plausible parameter space over which early intensive ABA-based interventions could be considered cost-effective at NICE thresholds. Notably, the changes to the size of treatment required for the ICER to drop below £30,000 per QALY are well within the CIs for cognitive ability and adaptive behaviour scores generated by the IPD meta-analysis, as well as being well within the range of treatment effects observed in the individual studies. The scenarios in which pessimistic assumptions are made, by contrast, paint a much bleaker picture and show that there is no plausible treatment effect that would enable early intensive ABA-based interventions to be considered cost-effective at NICE thresholds on the basis of the captured benefits and costs.
| Pessimistic | Treatment effect: VABS (£) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1.95 | 3.22 | 4.48 | 5.74 | 7.00a | 8.27 | 9.53 | 10.79 | 12.06 | ||
| Treatment effect: IQ | 9.16 | 500,438 | 362,233 | 280,965 | 227,469 | 189,601 | 161,400 | 139,598 | 122,252 | 108,133 |
| 10.40 | 489,669 | 355,790 | 276,573 | 224,227 | 187,079 | 159,363 | 137,907 | 120,819 | 106,898 | |
| 11.64 | 479,310 | 349,540 | 272,290 | 221,056 | 184,605 | 157,362 | 136,244 | 119,407 | 105,681 | |
| 12.88 | 469,335 | 343,473 | 268,112 | 217,952 | 182,179 | 155,397 | 134,608 | 118,018 | 104,481 | |
| 14.13a | 459,721 | 337,580 | 264,035 | 214,913 | 179,799 | 153,465 | 132,998 | 116,649 | 103,298 | |
| 15.37 | 450,447 | 331,852 | 260,054 | 211,937 | 177,462 | 151,565 | 131,414 | 115,300 | 102,131 | |
| 16.61 | 441,494 | 326,281 | 256,165 | 209,022 | 175,169 | 149,698 | 129,854 | 113,971 | 100,981 | |
| 17.85 | 432,844 | 320,862 | 252,366 | 206,165 | 172,916 | 147,861 | 128,318 | 112,660 | 99,846 | |
| 19.10 | 424,479 | 315,585 | 248,651 | 203,364 | 170,704 | 146,054 | 126,805 | 111,369 | 98,726 | |
| Optimistic | Treatment effect: VABS (£) | |||||||||
| 1.95 | 3.22 | 4.48 | 5.74 | 7.00a | 8.27 | 9.53 | 10.79 | 12.06 | ||
| Treatment effect: IQ | 9.16 | 161,532 | 106,506 | 78,010 | 60,581 | 48,819 | 40,349 | 33,959 | 28,969 | 24,967 |
| 10.40 | 155,504 | 103,086 | 75,681 | 58,831 | 47,423 | 39,189 | 32,968 | 28,105 | 24,200 | |
| 11.64 | 149,709 | 99,746 | 73,387 | 57,099 | 46,036 | 38,034 | 31,980 | 27,241 | 23,434 | |
| 12.88 | 144,127 | 96,482 | 71,126 | 55,383 | 44,658 | 36,885 | 30,994 | 26,379 | 22,668 | |
| 14.13a | 138,741 | 93,288 | 68,897 | 53,684 | 43,289 | 35,741 | 30,012 | 25,520 | 21,904 | |
| 15.37 | 133,539 | 90,161 | 66,700 | 52,001 | 41,930 | 34,602 | 29,034 | 24,663 | 21,142 | |
| 16.61 | 128,506 | 87,098 | 64,533 | 50,334 | 40,580 | 33,470 | 28,060 | 23,809 | 20,383 | |
| 17.85 | 123,631 | 84,096 | 62,395 | 48,685 | 39,241 | 32,345 | 27,091 | 22,959 | 19,627 | |
| 19.10 | 118,906 | 81,154 | 60,288 | 47,052 | 37,913 | 31,227 | 26,128 | 22,114 | 18,875 | |
Sensitivity analysis 3: change in intervention costs
The impact of varying the costs of early intensive ABA-based interventions, TAU and eclectic interventions is explored in Table 26. When pessimistic assumptions are made about the long-term treatment effect, the results of this analysis show that even substantial changes to the costs of early intensive ABA-based interventions, TAU and eclectic interventions do not bring the ICER < £30,000 per QALY. Therefore, even in the most extreme of these scenarios, early intensive ABA-based interventions would need to generate either substantial further benefits or cost savings. This contrasts with the analysis making optimistic assumptions. In this scenario, there is a sizable and plausible range of values under which early intensive ABA-based therapy would be considered cost-effective at NICE thresholds. This is important, as there is considerable variation in the models of early intensive ABA-based interventions assessed in the IPD meta-analysis, specifically in a number of factors that would have a direct impact on the costs of providing early intensive ABA-based interventions (e.g. intensity and staffing ratios). These results therefore suggest that if similar treatment effect sizes could be obtained either at lower intensity or with lower staff-to-child ratios, then it is plausible that early intensive ABA-based interventions could be cost-effective on the basis of captured benefits and costs.
| Pessimistic | ABA therapy costs (£) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 18,341 | 22,927 | 27,512 | 32,097 | 36,683a | 41,268 | 45,853 | 50,439 | 55,024 | ||
| TAU/eclectic costs (£) | 4317 | 60,815 | 97,005 | 133,195 | 169,385 | 205,576 | 241,766 | 277,956 | 314,146 | 350,336 |
| 5396 | 54,370 | 90,561 | 126,751 | 162,941 | 199,131 | 235,322 | 271,512 | 307,702 | 343,892 | |
| 6476 | 47,926 | 84,116 | 120,307 | 156,497 | 192,687 | 228,877 | 265,068 | 301,258 | 337,448 | |
| 7555 | 41,482 | 77,672 | 113,862 | 150,053 | 186,243 | 222,433 | 258,623 | 294,814 | 331,004 | |
| 8634a | 35,038 | 71,228 | 107,418 | 143,608 | 179,799 | 215,989 | 252,179 | 288,369 | 324,560 | |
| 9714 | 28,594 | 64,784 | 100,974 | 137,164 | 173,354 | 209,545 | 245,735 | 281,925 | 318,115 | |
| 10,793 | 22,149 | 58,340 | 94,530 | 130,720 | 166,910 | 203,100 | 239,291 | 275,481 | 311,671 | |
| 11,872 | 15,705 | 51,895 | 88,086 | 124,276 | 160,466 | 196,656 | 232,846 | 269,037 | 305,227 | |
| 12,951 | 9261 | 45,451 | 81,641 | 117,832 | 154,022 | 190,212 | 226,402 | 262,592 | 298,783 | |
| Optimistic | ABA therapy costs (£) | |||||||||
| 18,341 | 22,927 | 27,512 | 32,097 | 36,683a | 41,268 | 45,853 | 50,439 | 55,024 | ||
| TAU/eclectic costs (£) | 4317 | 8558 | 19,122 | 29,686 | 40,250 | 50,814 | 61,378 | 71,942 | 82,506 | 93,070 |
| 5396 | 6676 | 17,241 | 27,805 | 38,369 | 48,933 | 59,497 | 70,061 | 80,625 | 91,189 | |
| 6476 | 4795 | 15,359 | 25,924 | 36,488 | 47,052 | 57,616 | 68,180 | 78,744 | 89,308 | |
| 7555 | 2914 | 13,478 | 24,042 | 34,606 | 45,171 | 55,735 | 66,299 | 76,863 | 87,427 | |
| 8634a | 1033 | 11,597 | 22,161 | 32,725 | 43,289 | 53,853 | 64,418 | 74,982 | 85,546 | |
| 9714 | Dominant | 9716 | 20,280 | 30,844 | 41,408 | 51,972 | 62,536 | 73,101 | 83,665 | |
| 10,793 | Dominant | 7835 | 18,399 | 28,963 | 39,527 | 50,091 | 60,655 | 71,219 | 81,783 | |
| 11,872 | Dominant | 5954 | 16,518 | 27,082 | 37,646 | 48,210 | 58,774 | 69,338 | 79,902 | |
| 12,951 | Dominant | 4073 | 14,637 | 25,201 | 35,765 | 46,329 | 56,893 | 67,457 | 78,021 | |
Sensitivity analysis 4: change in education costs
Table 27 presents a two-way sensitivity analysis exploring different costs of providing special needs education. As in sensitivity analyses 2 and 3, the results of this analysis very much depend on the assumptions made with respect to the long-term benefits of early intensive ABA-based interventions. In the pessimistic analysis, no value set results in early intensive ABA-based interventions being cost-effective on the basis of captured benefits and costs. In the optimistic scenario, however, there is a parameter space in which early intensive ABA-based interventions would be considered cost-effective. The results show that this is most likely when the costs of supported placements are low and the costs of specialist education are high. This is because it is the difference between the costs of supported placements and specialist education that matter. This occurs because the main impact of early intensive ABA-based interventions on schooling placement in the model is to shift children from specialist education to supported placements.
| Pessimistic | Supported placement costs (£) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 4345 | 5431 | 6517 | 7604 | 8690a | 9776 | 10,862 | 11,948 | 13,035 | ||
| Special education costs (£) | 7851 | 211,015 | 213,041 | 215,067 | 217,093 | 219,119 | 221,145 | 223,172 | 225,198 | 227,224 |
| 9814 | 201,185 | 203,211 | 205,237 | 207,263 | 209,289 | 211,315 | 213,341 | 215,368 | 217,394 | |
| 11,777 | 191,354 | 193,381 | 195,407 | 197,433 | 199,459 | 201,485 | 203,511 | 205,537 | 207,564 | |
| 13,740 | 181,524 | 183,550 | 185,577 | 187,603 | 189,629 | 191,655 | 193,681 | 195,707 | 197,733 | |
| 15,703a | 171,694 | 173,720 | 175,746 | 177,773 | 179,799 | 181,825 | 183,851 | 185,877 | 187,903 | |
| 17,666 | 161,864 | 163,890 | 165,916 | 167,942 | 169,969 | 171,995 | 174,021 | 176,047 | 178,073 | |
| 19,628 | 152,034 | 154,060 | 156,086 | 158,112 | 160,138 | 162,165 | 164,191 | 166,217 | 168,243 | |
| 21,591 | 142,204 | 144,230 | 146,256 | 148,282 | 150,308 | 152,334 | 154,361 | 156,387 | 158,413 | |
| 23,554 | 132,373 | 134,400 | 136,426 | 138,452 | 140,478 | 142,504 | 144,530 | 146,557 | 148,583 | |
| Optimistic | Supported placement costs (£) | |||||||||
| 4345 | 5431 | 6517 | 7604 | 8690a | 9776 | 10,862 | 11,948 | 13,035 | ||
| Special education costs (£) | 7851 | 56,918 | 58,573 | 60,227 | 61,882 | 63,537 | 65,191 | 66,846 | 68,500 | 70,155 |
| 9814 | 51,856 | 53,511 | 55,166 | 56,820 | 58,475 | 60,129 | 61,784 | 63,439 | 65,093 | |
| 11,777 | 46,795 | 48,449 | 50,104 | 51,758 | 53,413 | 55,068 | 56,722 | 58,377 | 60,031 | |
| 13,740 | 41,733 | 43,387 | 45,042 | 46,697 | 48,351 | 50,006 | 51,660 | 53,315 | 54,970 | |
| 15,703a | 36,671 | 38,326 | 39,980 | 41,635 | 43,289 | 44,944 | 46,599 | 48,253 | 49,908 | |
| 17,666 | 31,609 | 33,264 | 34,918 | 36,573 | 38,228 | 39,882 | 41,537 | 43,191 | 44,846 | |
| 19,628 | 26,548 | 28,202 | 29,857 | 31,511 | 33,166 | 34,820 | 36,475 | 38,130 | 39,784 | |
| 21,591 | 21,486 | 23,140 | 24,795 | 26,449 | 28,104 | 29,759 | 31,413 | 33,068 | 34,722 | |
| 23,554 | 16,424 | 18,079 | 19,733 | 21,388 | 23,042 | 24,697 | 26,351 | 28,006 | 29,661 | |
Budget impact analysis
The estimated budget impact of implementing early intensive ABA-based interventions is summarised in Table 28. As with the cost-effectiveness analysis, two competing scenarios are run, making pessimistic and optimistic assumptions about the long-term effects of early intensive ABA-based interventions.
| Scenario | Year | ||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | |
| Pessimistic | |||||
| Total costs of ABA (£) | 5,649,222 | 13,178,526 | 18,826,751 | 26,357,052 | 33,887,354 |
| Savings to education budget (£) | 0 | –927,606 | –1,471,944 | –2,403,755 | –3,492,183 |
| Savings to NHS and social care (£) | –4052 | –15,990 | –34,000 | –56,820 | –83,967 |
| Net budget impact (£) | 4,323,570 | 11,684,606 | 16,787,185 | 23,942,596 | 31,258,953 |
| Cumulative net budget impact (£) | 4,323,570 | 16,008,177 | 32,795,362 | 56,737,958 | 87,996,911 |
| Optimistic | |||||
| Total costs of ABA (£) | 5,649,222 | 13,178,526 | 18,826,751 | 26,357,052 | 33,887,354 |
| Savings to education budget (£) | 0 | –927,606 | –1,476,480 | –2,414,335 | –3,511,829 |
| Savings to NHS and social care (£) | –4052 | –15,990 | –35,431 | –62,799 | –98,967 |
| Net budget impact (£) | 4,323,570 | 11,684,606 | 16,793,152 | 23,959,156 | 31,293,599 |
| Cumulative net budget impact (£) | 4,323,570 | 16,008,177 | 32,801,328 | 56,760,484 | 88,054,084 |
Results of the budget impact model show that assumptions about long-term effectiveness have little impact on the results of the budget impact model. This occurs because the impact of these assumptions on benefits and costs begin to take effect only over longer time horizons than the 5 years used in the budget impact model. The results of the budget impact analysis show that expenditure on ABA-based interventions increases significantly over time, from just £5.6M in year 1 to £33.9M in year 5. This increase largely reflects the increase in assumed uptake over time. Cost offsets from early intensive ABA-based interventions almost exclusively accrue to the education sector and increase from £0.9M in year 2 to £3.5M in year 5. Total net budget impact is estimated to be £4.3M in the first year, rising to ≈£31.2M per year in year 5. Total cumulative budget after 5 years is ≈£88M.
Summary of cost-effectiveness and budget impact analysis
In this section, a series of analyses exploring the potential cost-effectiveness of early intensive ABA-based interventions are presented. The base-case analysis was run considering two perspectives: (1) an NHS and social services perspective, and (2) a wider public sector perspective. As outlined in Chapter 7, Economic evaluation of interventions in autism, this reflects the fact that the impacts of early intensive ABA-based interventions are likely to include both health and non-health benefits, as well as cost savings for both the health service and other sectors. Assuming an NHS and social services perspective, the results of cost-effectiveness analysis suggest an ICER of £240,868 per QALY when pessimistic assumptions are made about long-term effects and an ICER of £69,386 per QALY when optimistic assumptions are made. When a broader public sector perspective was adopted, the ICER in respective scenarios was £189,122 per QALY and £46,768 per QALY (reported figures based on probabilistic analysis).
Care should be taken when drawing inferences from this analysis owing to significant limitations in the available effectiveness evidence and the contrasting possibilities that additional benefits or cost savings are not captured by the model, or that effect estimates generated by the IPD meta-analysis and used in the model may be inflated owing to bias in the included studies.
The results of the scenario analyses identified a number of drivers of value and showed that early intensive ABA-based intervention was more likely to be cost-effective if the benefits of therapy continued into adulthood or, alternatively, if it could have significant impact on the type of school attended. Little empirical evidence is available to support or refute the assumptions made in these scenarios, which are subject to significant limitations in the underlying data. More generally, the results of the scenario and sensitivity analysis highlight that early intensive ABA-based interventions must produce lasting benefits if they are to be cost-effective.
Chapter 9 Discussion
Statement of principal findings
Systematic review and individual participant data meta-analysis
We identified 20 studies, including a total of 894 participants, comparing early intensive ABA-based interventions with alternative interventions (mostly ‘eclectic’ treatment or TAU). Fifteen studies,26,84–86,89–99,103,104 representing 82% of published IPD (n = 654), were received and recoded to a common format, as set out in the project data dictionary, and then reanalysed in accordance with a prespecified analysis plan. One additional study,102 identified in initial searches but not published until after completion of our analyses, was also incorporated into aggregate meta-analyses (see Appendix 12 for details).
All children in the included studies had a diagnosis of autism, ASD or (in some earlier studies) pervasive developmental disorder, and were aged between 24 and 66 months at baseline. The majority of studies recruited participants from the USA, with studies also conducted in the UK, Norway, Australia and Canada. The most commonly reported outcomes were measures of cognitive ability (both verbal and non-verbal) and adaptive behaviour measured using VABS. Studies also less frequently reported measures of autism symptom severity, language comprehension and educational placement.
All of the included studies were at risk of bias on at least one domain using the Cochrane Risk of Bias or ROBINS-I tools,58 with the majority of studies at risk of bias in multiple domains. Randomisation was possible (as shown in a minority of studies) but rarely conducted. Most studies used convenience samples, with allocation to early intensive ABA-based interventions often based on parental preference. There is evidence to suggest that the use of convenience samples may have led to imbalances in participant characteristics between the intervention and comparator groups, with differences in terms of socioeconomic status and the use of co-interventions noted in some studies.
The nature of the interventions meant that blinding of education staff and participants was not possible, but outcome assessors were also often not blinded to intervention. This is particularly problematic when parent-reported measures were used, as the use of convenience samples often meant that parents had actively sought for their child to receive early intensive ABA-based interventions and in some studies parents may also be the source of funding for the intervention. As such, they are likely to have pre-existing expectations about the effectiveness of early intensive ABA-based interventions, which may influence their assessment of parent-reported outcome measures.
It was not possible to assess whether or not these issues and others have had an impact on the results of the included studies or, indeed, the direction of any biases. However, there is a risk that the magnitude of effects observed in our IPD meta-analysis may overestimate the true effects of early intensive ABA-based interventions.
Compared with ‘eclectic’ intervention or TAU, early intensive ABA-based interventions had minimal or no impact on parent-reported adaptive behaviour scores after 1 year (MD 2.93, 95% CI –1.90 to 7.76), but showed an average 7-point difference after 2 years (MD 7.00, 95% CI 1.95 to 12.06). This effect was, however, variable across studies, with treatment effects ranging from a 32-point difference in favour of early intensive ABA-based interventions to a 5-point advantage for TAU and eclectic comparators.
An average improvement in measures of cognitive ability of around 10 points was observed at 1 year (MD 9.16, 95% CI 4.38 to 13.93) and 2 years (MD 14.13, 95% CI 9.16 to 19.10) for early intensive ABA-based interventions relative to TAU and eclectic comparators. Only one study96 provided longer-term follow-up, reporting outcomes at 7 years. In this study no differences between early intensive ABA-based interventions and eclectic treatment were observed on adaptive behaviour (parent-rated VABS) or cognitive ability (IQ) scores.
Results for other outcomes were limited owing to the small numbers of studies reporting them. Autism symptom severity was not measured in most studies and therefore the data available were too limited to be conclusive, with no clear evidence of a difference between early intensive ABA-based interventions and TAU and eclectic groups. There were similarly limited data on language (comprehension and/or expression). Three studies that used the RDLS scale found some evidence that comprehension scores improved by around 12 points when using early intensive ABA-based interventions (MD 11.78, 95% CI 2.12 to 21.45), relative to TAU and eclectic interventions. By contrast, two studies that used the MSEL scale found no difference in scores between early intensive ABA-based arms and TAU or eclectic arms. Only one study90 reported data on behaviours that challenge. The limited data available from this single study showed no clear evidence of any benefit.
A small number of studies reported primary education placement and suggested that children receiving early high-intensity ABA-based intervention were much more likely to be in mainstream education (possibly with support) than children receiving TAU or eclectic interventions or low-intensity ABA-based interventions. However, there is a possibility that this finding was biased by study procedures, such as in Lovaas,26 in which all children receiving early intensive ABA-based interventions were placed in mainstream schools and major efforts were made to avoid authorities subsequently moving them to specialist education placements. Parental choice may also have influenced educational placement, and so these results may also be biased by parental expectations of ABA-based interventions. Additionally, local contextual detail was not available for most studies, so we could not establish the extent to which, for example, inclusive education policies would influence school placement outcomes. This raises questions about the usefulness of school placement as an outcome.
Interpreting the meaningfulness of these observed effects in terms of their impact on the everyday lives of autistic children and parents is not straightforward. Reference to conventions in interpreting effect sizes would imply that the observed effects on both cognitive ability and adaptive behaviour represent small to medium effects. Furthermore, it should be noted that the outcome measures included were considered by the stakeholders in our Advisory Group to be limited in terms of both their ability to reflect benefits and their relevance to practice.
The results of this meta-analysis were consistent with results in previous reviews. For example, Reichow et al. ,45 a recent review published by the Cochrane and Campbell Collaborations, identified similar statistically significant effects on both cognitive ability and adaptive behaviour, and a lack of evidence to support treatment effects on other measures, including behaviours that challenge and autism symptom severity. Similar findings have also been reported in other previous reviews. 4,24,42–44,46–49
A major advantage of conducting IPD meta-analysis is the ability to examine potential moderators of the treatment effect. There were, however, sufficient baseline data to examine only a few factors, namely age, sex, IQ at baseline and VABS composite score at baseline, and, at the study level, classification of intervention type (clinic or community), delivery setting, planned treatment intensity and duration, and year of publication. There was no evidence that any factor moderated any outcome at any time point. This result may reflect the limited data available to detect such effects. However, the magnitude of effects estimates did not suggest that any factor could be a potential moderating factor. Analysis of only UK-based studies suggested smaller treatment effects in these studies. These differences were, however, not statistically significant and could be due to a variety of factors other than location.
Cost-effectiveness
The limitations in the evidence available to the IPD meta-analysis had an important role in shaping the economic model, as a number of potentially relevant outcomes were not captured in the included studies. The structure of the model was therefore designed around the two most commonly measured outcomes, (1) cognitive ability and (2) adaptive behaviour, and so may have missed costs or benefits associated with other outcomes. The economic model adopted a cohort approach to capture changes in these measures and drew on the IPD meta-analysis results to link these outcomes to HRQoL and costs. Furthermore, given the limited evidence about long-term effectiveness, the model explored two scenarios: (1) an optimistic scenario, in which the observed benefits of early intensive ABA-based interventions were assumed to persist; and (2) a pessimistic scenario, in which the proposed benefits dissipate over time.
Given that the implementation of an effective early intensive ABA-based intervention for young autistic children would be likely to have an impact across multiple sectors, the model considered several perspectives relevant to a UK setting, including a health-care and social services perspective and a broader public sector perspective, which included costs falling on the local authority and education sector.
In line with the results of the IPD meta-analysis, the results of the cost-effectiveness model indicated that early intensive ABA-based intervention is more effective (higher incremental QALYs) than TAU or eclectic interventions. The model also indicated that it is more costly. Interpretation of whether or not these additional costs represent value is not straightforward, as the typical decision rules commonly employed in the context of health-care decision-making do not necessarily apply to autism owing to its impact on multiple sectors. These decision rules do, however, provide a useful benchmark against which the results of the cost-effectiveness analysis can be compared. On this basis, and adopting a public sector perspective, the results of the cost-effectiveness analysis indicate that early intensive ABA-based interventions would not meet the decision criteria for implementation used by NICE. This is irrespective of what assumptions are made about the long-term effectiveness of early intensive ABA-based interventions. For early intensive ABA-based interventions to be considered cost-effective according to these criteria, they would need to generate either further benefits or cost savings beyond those captured by the model. In monetary terms, the value of these benefits would need to be £38,790 when pessimistic assumptions were made and £14,066 when optimistic assumptions were made. Care, however, should be taken not to overinterpret the results, as the limitations of the available evidence may mean that it is plausible that uncaptured costs and benefits could alter this result.
The results of the scenario analyses identified a number of drivers of value and showed that early intensive ABA-based interventions would be cost-effective at NICE thresholds only if either significant benefits were accrued in adulthood or the intervention could significantly affect the type of school attended, as was observed in a small number of the effectiveness studies. 17,26,103 The value generated by early intensive ABA-based interventions is, however, contingent on treatment effects persisting for the time horizon of the model and it is much less likely that early intensive ABA-based interventions represent value for money if benefits are realised for only a short period of time.
The magnitude of gains in both cognitive ability and adaptive behaviour scores predicted by the IPD meta-analysis was also a significant driver of cost-effectiveness. This may be of significance when interpreting the results of the economic analysis, given both the significant variations in treatment effects observed across studies included in the IPD meta-analysis and the concerns about bias in these studies. The scenario analysis conducted showed that, conditional on treatment effects persisting, early intensive ABA-based interventions could represent value for money (at thresholds used by NICE) if treatment effect sizes were in line with the more positive studies included in the IPD meta-analysis. Equally, if treatment effects align with the less positive studies or have been exaggerated by confounding and other biases, it is unlikely that early intensive ABA-based interventions represent value for money.
Strengths
To the best of our knowledge, the IPD meta-analysis presented here is the most comprehensive investigation of the comparative evidence on the effects of early intensive ABA-based interventions for young autistic children to date, and only the second review and meta-analysis to use IPD. It is the only systematic review and meta-analysis to have been conducted by an international collaboration of investigators, including original study authors and an Advisory Group (with representation from autistic people, and parents and practitioners), and the only one to have been carried out in tandem with development of a cost-effectiveness model, which was informed by the IPD meta-analysis results.
The IPD meta-analysis is based on 75% of all known IPD, including data from 669 participants (with sensitivity analyses incorporating aggregate data generated from a further 93 participants in published analyses). The SCABARD requested data on 41 demographic and outcome variables, and provides a detailed assessment of the risk of bias for all included studies. By obtaining IPD, we have been able to benefit from access to the raw study data and from contact with the study authors. This has allowed us to ensure greater consistency in outcome measures and we have been able to adopt a consistent and more appropriate statistical approach to analysing the available data. Furthermore, it has also allowed us to clarify the extent of any unpublished data, as well as to consult with the authors of original studies to confirm study details.
The principal strength of the cost-effectiveness analysis was the ability to draw on the most comprehensive and up-to-date effectiveness data for early intensive ABA-based interventions. The model developed and reported in this report is, to the best of our knowledge, the first assessment of value in a UK context, drawing on both international and UK data, and supplementing these with expertise in the research team, in the Advisory Group and from UK service providers.
The thorough searches for relevant literature to populate the model and development of the economic model around the available effectiveness evidence highlighted specific areas of uncertainty, as well as drivers of cost-effectiveness. Explicit assumptions were made about the impact that early intensive ABA-based intervention may have on HRQoL and costs and, in particular, the impact that assumptions about the persistence of any treatment effect are likely to have on estimates of cost-effectiveness. The identification of these key uncertainties and drivers represents an important first step in defining what research is needed to more fully address whether or not early intensive ABA-based interventions are cost-effective.
To ensure that conclusions were unbiased, the SCABARD analyses were undertaken by an independent research team who were not involved in the original studies and did not have a pre-existing position on the effects of early intensive ABA-based interventions in autism. Throughout the project, the research team consulted a project Advisory Group, who provided a wide range of expertise and viewpoints. To capture the widest possible range of perspectives, all participants were encouraged to contribute to Advisory Group meetings, regardless of their background, experiences or perceptions of the interventions being evaluated. No major decision about the conduct of the project was undertaken without first consulting with, and taking into account the views of, the Advisory Group. All decisions were nonetheless taken by the project team.
To further engage with the diversity of opinions about early intensive ABA-based interventions in autism, we also conducted a wider consultation on the draft project report during the period that it was under funder peer review. This consultation process included interested groups or individuals who contacted the research team during the course of the project, as well as other groups identified by the project team as likely to have an interest in the project findings. To ensure transparency, the full responses of all consultees are included in Appendix 20.
Limitations
Despite our best efforts, we were not able to obtain data from five of the identified studies, representing 18% of participants with published outcomes. For two of these studies, data had been lost and therefore were no longer available82,87 (36 participants). Two authors declined to participate: one declined early in the project105,108 (61 participants) without further explanation, and another declined after several months of participation88 (94 participants), as they wanted to await full publication of their study. The final study83,107,112 (48 participants) deposited data in the US NDAR, to which we gained access. However, IPD for the participants of interest could not be separated from a much larger data set (and the study investigators felt unable to share which individuals in the larger data set were the study participants). In addition to these studies, we were not able to obtain IPD on the Rogers et al. 102 trial, which was published during the writing of this report. However, details of this study based on the publicly available information are included in Appendix 12.
The limitations of the economic analysis largely reflect the limitations of available research evidence. Robust evidence was lacking for several of the key model parameters. In particular, there was limited evidence to link outcomes reported in the effectiveness studies with adult outcomes and we had to rely on data from a single US cohort,134 which may not reflect outcomes in a typical UK setting. This is important in the context of interpreting scenario analyses, which illustrated the potential significance of adult outcomes on the cost-effectiveness of early intensive ABA-based interventions. Lack of robust data on the costs of standard care in the UK was also a significant barrier, and, although estimates were generated from data kindly provided by a number of local authorities, it is not clear how representative these are of wider current practice across the UK.
Further to the above, the systematic review and cost-effectiveness are somewhat limited by their focus on early intensive ABA-based interventions, as opposed to other models of ABA-based intervention aimed at primary aged children or other groups of children. This focus reflected the scope of the National Institute for Health Research (NIHR) commissioning call, but does mean that some evidence on the effectiveness of less individually intensive ABA-based interventions were excluded from the review (e.g. data from studies that focused exclusively on group-based interventions or data in a school setting). The latter may be of particular relevance to decision-makers in the UK owing to the fact that children in the UK start school at a younger age than in many other countries and therefore opportunities to deliver interventions in preschool settings are likely to be more limited.
Limitations and uncertainties in the identified evidence
Many of the limitations of this study reflected the limitations of the primary studies identified in the systematic review and included in the IPD meta-analysis. These are discussed in turn below.
Study quality
As discussed above, most studies were rated as being at risk of bias on one or more domains of the Cochrane Risk of Bias or ROBINS-I tools. 58 In particular, most studies were not randomised, with intervention assignment often based on parental preference. Studies rarely conducted blinded outcome assessments, and other steps that safeguard against bias, such as prospective registration and/or publication of study protocols, were also not undertaken (many studies pre-date the era when registration became established practice); we requested but did not receive any protocols for the studies providing IPD. The potential impact of these weaknesses in study design is difficult to ascertain, but they are particularly concerning given the results of a recently published randomised trial replicating the ESDM evaluation by Dawson et al. 83 This study is notable as the trial design and conduct addresses some (but not all) of the concerns about risk of bias in earlier studies. 102 The results of this trial are less favourable towards the early intensive ABA-based intervention, reporting only nominal statistically non-significant effects on measures of cognitive ability and adaptive behaviour. As a result, even within the narrow context of cognitive ability and adaptive behaviour, we cannot be certain of the comparative effectiveness of early intensive ABA-based interventions. Nor can we rule out the possibility that the observed effects could be either partly or entirely attributable to bias in the effectiveness studies.
Importantly, concerns about the validity of the results from the identified studies carry through to the economic modelling, which is based on the results of the IPD meta-analysis. The results of both the IPD meta-analysis and the economic model should therefore be interpreted in the context of these limitations in the effectiveness evidence, noting the potential that the observed intervention effects may partially or completely reflect weaknesses in methodology.
Outcomes measured
Despite our considerable efforts and success in obtaining full IPD from the majority of the studies, data on only a small number of outcomes were collected consistently across the primary studies (most commonly verbal and non-verbal IQ, adaptive behaviour, as measured using parent-rated VABS, and language development). Other outcome domains, such as autism symptom severity, presence of co-occurring conditions, including behaviours that challenge, and education placement, were infrequently collected. Early studies focused on IQ, whereas later studies more commonly measured language development and adaptive behaviour measures, such as VABS. Other outcomes, such as early communication, social interaction and emerging play skills, were not prioritised in the included comparative studies. Furthermore, the vast majority of the participant, family, treatment and data handling variables listed in the SCABARD data dictionary were not collected in the identified studies or were otherwise missing from the available IPD. The absence of IPD on key variables severely curtailed our ability to conduct our proposed analyses of potential moderators of effect.
The narrow focus on a limited number of outcome domains also had significant implications for the economic analysis and forced us to adopt a model structure based only on changes in cognitive ability and adaptive behaviour scores. Although links were created between these scores to both HRQoL and costs, it is plausible that other individual participant domains, such as autism symptom severity, co-occurring conditions, behaviours that challenge and language comprehension, are equally or more important drivers of both (health-related) quality of life and costs. The relative importance of these aspects of functioning together with the need for information about other relevant family and contextual factors were emphasised by the members of the Advisory Group. The lack of information on such domains means that their impact cannot be captured within the economic analysis. To the extent that early intensive ABA-based interventions may have an impact on these domains of function, the economic model may under- or overestimate benefits.
Limitations of outcome measurement tools
The tools utilised to measure each outcome domain varied, both across studies and within studies. This was often, but not always, because certain measures were appropriate only for certain developmental ages. When appropriate, we combined data measured using different tools but measuring the same underlying outcome domain in the meta-analyses. However, such decisions are not necessarily straightforward [e.g. Wechsler scales, S–B and British Ability Scales provide a cognitive ability quotient expected theoretically to stay stable over time; the MSEL and Psychoeducational Profile – Revised (PEP-R) tools list a number of competencies that accrue with age; and the BSID are structured as an ‘IQ’ measure but are used in very young children]. Furthermore, although the SCABARD data dictionary allowed study authors to provide outcome values in the form in which they were available, without restriction, most investigators provided derived scores at domain and subdomain levels, rather than raw scores. Both raw and domain scores have limitations when applied to the longitudinal evaluation of interventions for young autistic children. Raw scores can be problematic when age is differently distributed between the groups being compared or when comparing outcomes collected at different time points. Conversely, although standard scores allow comparisons against peers in the general population, some included studies reported difficulties in obtaining standard scores (including floor and ceiling effects) for certain outcomes. Although the provision of IPD facilitated the harmonisation and synthesis of scores across some of these studies, this was not always possible or appropriate.
Duration of follow-up
It has been suggested in the literature that the aim of early intensive ABA-based intervention is not specifically to effect change over these short time horizons, but instead to build core skills that can allow children to continue to progress and achieve more developmentally appropriate trajectories. 26,151,152 Evidence investigating longer-term outcomes are, however, notably missing, with most of the studies identified in the systematic review and IPD meta-analysis measuring only outcomes from intake to the end of the initial early intervention treatment period (mostly between 1 and 2 years). Furthermore, the only study with longer-term follow-up showed no clear evidence of initial comparative benefits persisting. This is of particular concern when reflecting on the results of economic analysis, as the persistence of short-term benefits is central to establishing whether or not investment in early intensive ABA-based interventions is likely to represent value for money.
Weakness in the epidemiological and observation literature further compounds the problems of establishing long-term effects of early intervention. Although a number of studies have sought to characterise patterns of change in important clinical characteristics over time, the considerable heterogeneity in longer-term outcomes for autistic individuals means that uncertainties remain, perhaps most particularly for young children with significant impairment. 17 There remains limited understanding of prognostic factors and how changes in clinical outcomes in early childhood impact on long-term trajectories. 17 Importantly, the evidence from the epidemiological and observational literature has not been able to establish links between proximal behavioural measures and the types of long-term outcomes that might be valued by autistic adolescents and adults, such as well-being, quality of life, autonomy, independence, relationships and employment. 17 This severely limits any assessment of how early interventions might impact on individuals beyond their childhood and prevents a robust characterisation of long-term effects.
Relevance of studies to current UK practice
The available data were collected over a relatively long time period (children were recruited from 1968 to 2011), during which the understanding and management of autism evolved significantly and estimates of diagnosed autism and related conditions increased significantly. 2,153 For example, in the later studies, more naturalistic components were incorporated into the delivery of early intensive ABA-based interventions and the aversive contingencies used in the original UCLA EIBI approach had long since been abandoned. Comparator treatments also evolved during this period, with the emergence of psychoeducational support for families with young autistic children, psychosocial interventions focusing on the core social communication symptoms and a range of autism-specific educational interventions in addition to the generic special needs care provision.
There are also uncertainties about the generalisability of the overall results to the current UK context, as most of the available evidence to date is from other countries. Although the included study populations are likely to be similar to young children diagnosed with autism in the early preschool period in the UK, additional child-related factors or parental attitudes, particularly those relating to education provision, may differ. Similarly, differences in the models of delivery of early intensive ABA-based interventions and what constitutes eclectic intervention or TAU in a UK setting may well be important contextual factors. For example, our Advisory Group suggested that UK ABA-based services are likely to focus on ‘problem-solving’ of day-to-day challenges, rather than necessarily addressing core autism symptoms. This approach aligns more with the subset of early intensive ABA-based interventions studies included in the systematic review, which are informed by naturalistic approaches. However, the interventions included in the research studies – unlike UK community provision – were often resourced by an expert university clinic and/or the originators of the intervention were available to train and supervise the staff delivering the interventions.
Interventions and comparators assessed
The broad scope of this review, which included any form of early intensive ABA-based intervention, also exposes other uncertainties. The studies included in the IPD meta-analysis assessed a heterogeneous set of interventions that varied in terms of setting, intensity and duration. Indeed, when we asked the authors and UK practitioners to define early intensive ABA-based interventions, we received a range of different responses, which perhaps indicates that the term is now used to cover a variety of interventions based on the original underpinning psychological behavioural principles. It has also become clear that there are other differences, with some studies evaluating early intensive ABA-based intervention services that include highly structured hierarchies of oversight from senior practitioners and therapists, whereas in other studies much less detail is provided about the training, maintenance of fidelity and delivery of the intervention. However, whether or not these differences between interventions are important is largely unknown.
The NMA and meta-regression analysis undertaken in this study do not provide any evidence that one form or intensity is superior to another. These analyses are, however, constrained by the very small sample sizes and other differences between the studies. This means that there remain important questions, not only about whether or not early intensive ABA-based interventions are more effective than more generic interventions (such as those included in the TAU/eclectic arms of the identified studies), but also about which components of early intensive ABA-based interventions may potentially drive effects. Furthermore, we do not know if other individual participant characteristics, family or other contextual factors (such as the impact of any co-interventions) may be relevant as potential moderators of effect. All this information is important when considering cost-effectiveness, as some of these factors have significant implications for costs, particularly intensity and staffing ratios, as well as how to target children and families most likely to respond and, perhaps most importantly, what might be the optimal duration of the interventions.
Evidence on adverse effects
Almost no data were collected in the identified studies on possible adverse effects of intervention and comparator therapies, with none of the included studies systematically collecting data on adverse effects. This is potentially an important omission, as some members of the autism community have raised concerns about the possible long-term mental health consequences of early intensive ABA-based interventions. However, in the absence of any systematically collected data, the nature and extent of any potential risks, adverse effects or harms of early intensive ABA-based intervention in the short, medium or longer term cannot currently be determined.
Chapter 10 Conclusions
Implications for service provision
The existing evidence cannot provide service providers with clear guidance on the value of implementing early intensive ABA-based interventions alongside, or in place of, current practice. Although the IPD meta-analyses have shown small to moderate improvements in child cognitive ability and adaptive behaviour for early intensive ABA-based interventions relative to TAU or eclectic interventions, all of the identified studies were at risk of bias, limiting the conclusions that can be drawn from these results. Furthermore, individual study results varied considerably, with some showing no relative benefit of early intensive ABA-based interventions compared with TAU or eclectic interventions. Crucially, there is also a paucity of reliable longer-term follow-up data from children who have received early intensive ABA-based interventions. There is no clear evidence on whether or not any comparative benefits of intervention are retained through childhood, if interventions alter the course of a child’s education, or if it has any impact in adulthood. Using the limited data available, none of the tested individual participant characteristics moderated the size of the intervention effect, meaning that there is no strong evidence to identify subgroups of children who might benefit more or less from early intensive ABA-based interventions.
Concerns about potential bias, together with the other limitations in the available evidence, mean that the cost-effectiveness of early intensive ABA-based interventions cannot be estimated reliably. The restricted range of outcomes addressed in existing research studies required that the economic model focus on cognitive ability and adaptive behaviour scores, which is of particular concern and may mean that the results of the economic analysis do not fully reflect the impact of early intensive ABA-based interventions on outcomes and costs. Taken at face value, however, the results of the main economic analysis indicate that early intensive ABA-based interventions are unlikely to represent value for money, based on thresholds typically adopted by NICE. In interpreting the findings of this study, service providers and funders should consider whether or not their priorities align with the outcomes used in the economic analysis; whether or not the interventions and comparators described in the economic analysis match with the intervention options that are available; and whether or not early intensive ABA-based therapy represents good value for money, given the likely extra costs associated with its implementation.
Sensitivity and scenario analyses identified a number of drivers of value and highlighted the need for early intensive ABA-based interventions that produce lasting benefits, as estimates of incremental cost-effectiveness were very high across a range of scenarios when only short-term benefits were assumed.
Further implications of this research are constrained by the lack of high-quality evidence to support the clinical effectiveness and cost-effectiveness of early intensive ABA-based interventions. Service providers, families with young autistic children, the autism community and those funding the provision of services need access to better evidence to inform decision-making. New high-quality research studies comparing early intensive ABA-based interventions with other early interventions are needed to establish which interventions achieve good outcomes for young autistic children in the short, medium and longer term.
Suggested research priorities
As discussed above, no strong conclusions should be drawn from the results of the existing evidence owing to considerable uncertainty in estimates of effects and high risk of bias.
Researchers may therefore wish to consider further evaluations of early intensive ABA-based interventions compared with TAU or eclectic approaches; however, whether or not this is an appropriate next step should be carefully considered, given both the findings from the recent Rogers et al. 102 RCT and the range of alternative preschool autism interventions that fall outside the scope of this review. The relative effectiveness of the various different behavioural and developmental–social–pragmatic interventions both to each other and to early intensive ABA-based interventions is not clear. However, implementation of many of these other interventions requires substantially less resource and, as a result, may represent better value. 154–156 Future research might therefore more productively focus on which interventions have the best evidence of effectiveness and which are worthy of further investigation. Before conducting any new comparative primary studies, a high-quality systematic review might be able to identify the most promising candidate interventions.
Future research should also consider whether or not the focus of the existing literature on questions about comparative effectiveness of early ABA-based therapy and TAU or eclectic approaches is helpful. The existing literature is heavily focused on whether early intensive ABA-based therapy is more effective than TAU or eclectic approaches; however, the heterogeneous nature of both populations, interventions and methods used in previous studies makes the interpretation of such evidence difficult, as the generalisability of results from such studies is often not clear. Alternative approaches may therefore be warranted. For example, both early intensive ABA-based interventions and eclectic interventions have multiple components, yet there is no clear evaluative evidence on which components are important. An approach such as that discussed in Green et al. ,157 whereby greater focus is placed on mechanisms of action and components of interventions rather than just on whether or not a treatment worked, may therefore be appropriate and could help provide insights that aid the development of new and better optimised interventions.
Should future studies evaluating the effects of early intensive ABA-based interventions relative to TAU and eclectic approaches be required, these would need to address the methodological limitations of the existing evidence. Such a study would preferably include a RCT design with prespecified agreed outcome measures collected by trained researchers blind to intervention received, and data collected on both fidelity to treatment received (in both arms) and withdrawals. As well as being methodologically rigorous, any future trial should adhere to the standards of governance laid out in the NIHR’s Clinical Trials Toolkit [URL: www.ct-toolkit.ac.uk/ (accessed 30 January 2020)].
Any future evaluation of early intensive ABA-based interventions should also take into account the UK context. The UK does not have a long history of using early intensive ABA-based interventions and, therefore, any planned effectiveness trial would need to be designed to evaluate a contemporary, fully specified and appropriately tailored version of early intensive ABA-based intervention suitable for delivery in the UK. This could mean, for example, a home- or an education-based format. Similarly, comparator interventions should reflect current best practice. It should be noted that consensus on current or usual practice may be difficult to establish, considering that current provision varies considerably across the country.
In designing any evaluations in early autism, careful consideration should be given to both measures of the baseline characteristics of children and their families and to the outcomes collected to ensure that the measures are relevant to children, families and decision-makers. Current studies have focused primarily on cognitive ability and adaptive behaviour, and, although future studies may also want to collect further evidence in relation to these outcomes, it is clear from our consultations with the autism community, experts, researchers and practitioners that these measures are limited in terms of both their ability to reflect benefits and their relevance to practice. This issue reflects a wider problem of measurement of progress and outcomes in young autistic children and is not limited to the evaluation of early intensive ABA-based interventions. Groups such as the Core Outcome Measures in Effectiveness Trials (COMET) initiative have sought to promote the development of core outcome sets that represent the minimum that should be measured and reported in all clinical trials of a specific condition. The development of such a core outcome set would be hugely beneficial in the context of autism research and we note that work has been done in studies, such as the Measurement in Autism Spectrum disorder Under Review (MeASURe),119 to develop such a set of core outcomes, although no agreed set of core outcomes exists presently.
The length of follow-up of any future studies of early intervention in autism also needs to be considered carefully, as there is substantial uncertainty regarding the durability of early benefits. Ideally, the longest possible follow-up in any future studies of effectiveness is desirable, but there are both financial and pragmatic constraints that prevent studies from collecting very long follow-up information. Other types of research may therefore need to be employed to address these uncertainties. This may include planned follow-ups of children recruited to existing effectiveness studies, or retrospective case–control-type analyses looking at any early intervention received. Work on prognostic factors and potential mediators and moderators of effect may also be of benefit. Such studies also need to carefully consider outcomes, as the literature focusing on autistic adolescents and adults has primarily adopted the use of social normative valuations of independence and social outcomes to characterise what constitutes a ‘good outcome’. However, such an approach has significant limitations, not only because quality of life does not necessarily correlate well with such characterisation, but also because it does not include any consideration of how best to define a nuanced approach to help us understand what constitutes successful achievements for different individuals across the autism spectrum. This is particularly true for people with intellectual impairment and/or a limited capacity to express their own needs and ambitions.
Future studies of any interventions in autistic children should include assessment of potential adverse effects or harms. Studies should record and document evidence of possible adverse effects. Consideration of harms in the context of future effectiveness studies alone, however, may be insufficient owing to the long time frames over which they may become apparent. Alternative designs may be more appropriate, such as case–control studies looking at rates of mental health issues in autistic children who have received early interventions.
Acknowledgements
We would like to thank the following individuals for their support in delivering this project:
-
Claire Rothery, Peter Murphy and Matthew Walton, who supported the development of the economic analysis
-
Ruth Horner, Lynne Johns, Rachel Thistlewood and Amber Burton, who provided expertise and data on current provision for young autistic children
-
Barbara Barrett and Sarah Byford, who kindly provided IPD on the costs of care for autistic children in the UK
-
Mike Clarke, Bernard Fleming, Patricia Howlin, Emma Jenner, Helen McConachie, Anne McLaren, Dean McMillan, Damian Milton, Roo Philip, Peter Szatmari, Emma Truelove, Colin Wilson, Anne-Marie Wood and Suzy Yardley, who all provided support as part of our Advisory Group
-
Esther Ben-Itzchak, Svein Eikeseth, Sigmund Eldevik, Hanna Kovshoff, Iliana Magiati, John McEachin, Phil Reed, Richard Stock, Giacomo Vivanti and Ditza Zachor, who kindly provided IPD.
Special thanks to Tristram Smith, who sadly passed away part-way through this project. Tristram both provided advice as part of our Advisory Group and helped us to acquire a number of the IPD data sets.
Contributions of authors
Mark Rodgers (https://orcid.org/0000-0002-5196-9239) (Research Fellow) oversaw the completion of the systematic review and IPD meta-analysis, wrote all sections pertaining to the systematic review, with the exception of the results of the meta-analysis, and contributed to the writing of all sections of the report.
David Marshall (https://orcid.org/0000-0001-5969-9539) (Research Fellow) performed data extraction and quality assessment, was the lead contact with all study authors, wrote the background section to the report and contributed to the writing of all sections of the report.
Mark Simmonds (https://orcid.org/0000-0002-1999-8515) (Senior Research Fellow) performed the statistical analyses, wrote all sections of the report pertaining to those analyses and contributed to the writing of all sections of the report.
Ann Le Couteur (https://orcid.org/0000-0001-9991-3608) (Emeritus Professor of Child and Adolescent Psychiatry) oversaw the project as a whole, provided clinical expertise, commented on drafts of the protocol and this report and contributed to the writing of all sections of the report.
Mousumi Biswas (https://orcid.org/0000-0001-6781-7400) (Research Fellow) led on the literature reviews supporting the economic analysis, contributed to the development of the economic analysis and commented on drafts of the protocol and this report.
Kath Wright (https://orcid.org/0000-0002-9020-1572) (Information Service Manager) prepared and performed all database searches for the systematic review.
Dheeraj Rai (https://orcid.org/0000-0002-7239-3523) (Consultant Senior Lecturer in Psychiatry) provided clinical expertise and commented on drafts of the protocol and this report.
Stephen Palmer (https://orcid.org/0000-0002-7268-2560) (Professor of Health Economics and Deputy Director of the Team for Economic Evaluation and Health Technology Assessment) provided expert advice and commented on drafts of the protocol and this report.
Lesley Stewart (https://orcid.org/0000-0003-0287-4724) (Professor of Evidence Synthesis) provided expert advice and commented on drafts of the protocol and this report.
Robert Hodgson (https://orcid.org/0000-0001-6962-2893) (Research Fellow) oversaw the project as a whole, developed and built the economic analysis, wrote all sections of the report pertaining to the economic analysis and contributed to the writing of all sections of the report.
Data-sharing statement
Requests for access to data should be addressed to the corresponding author. Data will be shared if the authors of the included primary studies agree to the request.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care.
References
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders: DSM-5 2013. https://doi.org/10.1176/appi.books.9780890425596.
- Baird G, Simonoff E, Pickles A, Chandler S, Loucas T, Meldrum D, et al. Prevalence of disorders of the autism spectrum in a population cohort of children in South Thames: the Special Needs and Autism Project (SNAP). Lancet 2006;368:210-15. https://doi.org/10.1016/S0140-6736(06)69041-7.
- Brugha TS, McManus S, Bankart J, Scott F, Purdon S, Smith J, et al. Epidemiology of autism spectrum disorders in adults in the community in England. Arch Gen Psychiatry 2011;68:459-65. https://doi.org/10.1001/archgenpsychiatry.2011.38.
- Makrygianni MK, Reed P. A meta-analytic review of the effectiveness of behavioural early intervention programs for children with autistic spectrum disorders. Res Autism Spect Dis 2010;4:577-93. https://doi.org/10.1016/j.rasd.2010.01.014.
- Zwaigenbaum L, Duku E, Fombonne E, Szatmari P, Smith IM, Bryson SE, et al. Developmental functioning and symptom severity influence age of diagnosis in Canadian preschool children with autism. Paediatr Child Health 2019;24:e57-e65. https://doi.org/10.1093/pch/pxy076.
- Emerson ND, Morrell HER, Neece C. Predictors of age of diagnosis for children with autism spectrum disorder: the role of a consistent source of medical care, race, and condition severity. J Autism Dev Disord 2016;46:127-38. https://doi.org/10.1007/s10803-015-2555-x.
- Shattuck PT, Durkin M, Maenner M, Newschaffer C, Mandell DS, Wiggins L, et al. Timing of identification among children with an autism spectrum disorder: findings from a population-based surveillance study. J Am Acad Child Adolesc Psychiatry 2009;48:474-83. https://doi.org/10.1097/CHI.0b013e31819b3848.
- Jónsdóttir SL, Saemundsen E, Antonsdóttir IS, Sigurdardóttir S, Ólason D. Children diagnosed with autism spectrum disorder before or after the age of 6 years. Res Autism Spect Dis 2011;5:175-84. https://doi.org/10.1016/j.rasd.2010.03.007.
- Szatmari P, Georgiades S, Duku E, Bennett TA, Bryson S, Fombonne E, et al. Developmental trajectories of symptom severity and adaptive functioning in an inception cohort of pre school children with autism spectrum disorder. JAMA Psychiatry 2015;72:276-83. https://doi.org/10.1001/jamapsychiatry.2014.2463.
- Hudry K, McConachie H, Le Couteur A, Howlin P, Barrett B, Slonims V. Predictors of reliable symptom change: secondary analysis of the Preschool Autism Communication Trial. Autism Dev Lang Impair 2018;3:1-12. https://doi.org/10.1177/2396941518764760.
- Solomon M, Iosif AM, Reinhardt VP, Libero LE, Nordahl CW, Ozonoff S, et al. What will my child’s future hold? Phenotypes of intellectual development in 2–8-year-olds with autism spectrum disorder. Autism Res 2018;11:121-32. https://doi.org/10.1002/aur.1884.
- Noens I, van Berckelaer-Onnes I, Verpoorten R, van Duijn G. The ComFor: an instrument for the indication of augmentative communication in people with autism and intellectual disability. J Intellect Disabil Res 2006;50:621-32. https://doi.org/10.1111/j.1365-2788.2006.00807.x.
- Rowley E, Chandler S, Baird G, Simonoff E, Pickles A, Loucas T, et al. The experience of friendship, victimization and bullying in children with an autism spectrum disorder: associations with child characteristics and school placement. Res Autism Spect Dis 2012;6:1126-34. https://doi.org/10.1016/j.rasd.2012.03.004.
- Bauminger N, Kasari C. Loneliness and friendship in high-functioning children with autism. Child Dev 2000;71:447-56. https://doi.org/10.1111/1467-8624.00156.
- Howlin P, Goode S, Hutton J, Rutter M. Adult outcome for children with autism. J Child Psychol Psychiatry 2004;45:212-29. https://doi.org/10.1111/j.1469-7610.2004.00215.x.
- Howlin P, Moss P. Adults with autism spectrum disorders. Can J Psychiatry 2012;57:275-83. https://doi.org/10.1177/070674371205700502.
- Magiati I, Tay XW, Howlin P. Cognitive, language, social and behavioural outcomes in adults with autism spectrum disorders: a systematic review of longitudinal follow-up studies in adulthood. Clin Psychol Rev 2014;34:73-86. https://doi.org/10.1016/j.cpr.2013.11.002.
- Croen LA, Zerbo O, Qian Y, Massolo ML, Rich S, Sidney S, et al. The health status of adults on the autism spectrum. Autism 2015;19:814-23. https://doi.org/10.1177/1362361315577517.
- Rai D, Heuvelman H, Dalman C, Culpin I, Lundberg M, Carpenter P, et al. Association between autism spectrum disorders with or without intellectual disability and depression in young adulthood. JAMA Netw Open 2018;1. https://doi.org/10.1001/jamanetworkopen.2018.1465.
- Selten JP, Lundberg M, Rai D, Magnusson C. Risks for nonaffective psychotic disorder and bipolar disorder in young people with autism spectrum disorder: a population-based study. JAMA Psychiatry 2015;72:483-9. https://doi.org/10.1001/jamapsychiatry.2014.3059.
- Lyall K, Croen L, Daniels J, Fallin MD, Ladd-Acosta C, Lee BK, et al. The changing epidemiology of autism spectrum disorders. Annu Rev Public Health 2017;38:81-102. https://doi.org/10.1146/annurev-publhealth-031816-044318.
- NHS Digital . Autism Spectrum Disorders in Adults Living in Households Throughout England – Report From the Adult Psychiatric Morbidity Survey 2007.
- Buescher AV, Cidav Z, Knapp M, Mandell DS. Costs of autism spectrum disorders in the United Kingdom and the United States. JAMA Pediatr 2014;168:721-8. https://doi.org/10.1001/jamapediatrics.2014.210.
- Howlin P, Magiati I, Charman T. Systematic review of early intensive behavioral interventions for children with autism. Am J Intellect Dev Disabil 2009;114:23-41. https://doi.org/10.1352/2009.114:23;nd41.
- Reichow B, Wolery M. Comprehensive synthesis of early intensive behavioral interventions for young children with autism based on the UCLA young autism project model. J Autism Dev Disord 2009;39:23-41. https://doi.org/10.1007/s10803-008-0596-0.
- Lovaas OI. Behavioral treatment and normal educational and intellectual functioning in young autistic children. J Consult Clin Psychol 1987;55:3-9. https://doi.org/10.1037//0022-006x.55.1.3.
- Dawson G. Early behavioral intervention, brain plasticity, and the prevention of autism spectrum disorder. Dev Psychopathol 2008;20:775-803. https://doi.org/10.1017/S0954579408000370.
- Schreibman L, Dawson G, Stahmer AC, Landa R, Rogers SJ, McGee GG, et al. Naturalistic developmental behavioral interventions: empirically validated treatments for autism spectrum disorder. J Autism Dev Disord 2015;45:2411-28. https://doi.org/10.1007/s10803-015-2407-8.
- Milton DEM. So what exactly are autism interventions intervening with?. Good Autism Pract 2014;15:6-14.
- Kupferstein H. Evidence of increased PTSD symptoms in autistics exposed to applied behavior analysis. Adv Autism 2018;4:19-2. https://doi.org/10.1108/AIA-08-2017-0016.
- Leaf JB, Ross RK, Cihon JH, Weiss MJ. Evaluating Kupferstein’s claims of the relationship of behavioral intervention to PTSS for individuals with autism. Adv Autism 2018;4:122-9. https://doi.org/10.1108/AIA-02-2018-0007.
- Koegel LK, Koegel RL, Harrower JK, Carter CM. Pivotal response intervention I: overview of approach. Res Pract Persons Severe Disabil 1999;24:174-85. https://doi.org/10.2511/rpsd.24.3.174.
- Rogers SJ, Herbison JM, Lewis HC, Pantone J, Reis K. An approach for enhancing the symbolic, communicative, and interpersonal functioning of young children with autism or severe emotional handicaps. J Early Interv 1986;10:135-48. https://doi.org/10.1177/105381518601000205.
- Rogers SJ, Dawson G. Early Start Denver Model for Young Children with Autism: Promoting Language, Learning, and Engagement. New York, NY: Guilford Press; 2010.
- National Institute for Health and Care Excellence (NICE) . Autism Spectrum Disorder in Under 19s: Support and Management 2013.
- Griffith GM, Fletcher R, Hastings RP. A national UK census of applied behavior analysis school provision for children with autism. Res Autism Spect Dis 2012;6:798-805. https://doi.org/10.1016/j.rasd.2011.10.014.
- Beam ABA services . Beam ABA Services 2018. https://ourprices.beamaba.com/ (accessed 20 November 2018).
- Eikeseth S, Hayward D, Gale C. UK Young Autism Project: Information Pack 2018. www.ukyap.org/_userfiles/pages/file/02%20Information%20Pack%20June%202017.pdf (accessed 20 November 2018).
- The Owl Centre . The Owl Centre for Children’s Independent Therapy 2018. https://theowltherapycentre.co.uk/fees-enquiry (accessed 21 February 2020).
- ABA4ALL . ABA4ALL 2018. www.abaa4all.com/aba-in-the-uk (accessed 20 November 2018).
- Horner RH, Carr EG, Halle J, McGee G, Odom S, Wolery M. The use of single-subject research to identify evidence-based practice in special education. Except Child 2005;71:165-79. https://doi.org/10.1177/001440290507100203.
- Eldevik S, Hastings RP, Hughes JC, Jahr E, Eikeseth S, Cross S. Meta-analysis of early intensive behavioral intervention for children with autism. J Clin Child Adolesc Psychol 2009;38:439-50. https://doi.org/10.1080/15374410902851739.
- Eikeseth S. Outcome of comprehensive psycho-educational interventions for young children with autism. Res Dev Disabil 2009;30:158-78. https://doi.org/10.1016/j.ridd.2008.02.003.
- Peters-Scheffer N, Didden R, Korzilius H, Matson J. Cost comparison of early intensive behavioral intervention and treatment as usual for children with autism spectrum disorder in the Netherlands. Res Dev Disabil 2012;33:1763-72. https://doi.org/10.1016/j.ridd.2012.04.006.
- Reichow B, Barton EE, Boyd BA, Hume K. Early intensive behavioral intervention (EIBI) for young children with autism spectrum disorders (ASD): a systematic review. Campbell Syst Rev 2014;9. https://doi.org/10.4073/csr.2014.9.
- Spreckley M, Boyd R. Efficacy of applied behavioral intervention in preschool children with autism for improving cognitive, language, and adaptive behavior: a systematic review and meta-analysis. J Pediatr 2009;154:338-44. https://doi.org/10.1016/j.jpeds.2008.09.012.
- Virués-Ortega J. Applied behavior analytic intervention for autism in early childhood: meta-analysis, meta-regression and dose–response meta-analysis of multiple outcomes. Clin Psychol Rev 2010;30:387-99. https://doi.org/10.1016/j.cpr.2010.01.008.
- Warren Z, McPheeters ML, Sathe N, Foss-Feig JH, Glasser A, Veenstra-Vanderweele J. A systematic review of early intensive intervention for autism spectrum disorders. Pediatrics 2011;127:e1303-11. https://doi.org/10.1542/peds.2011-0426.
- Waddington H, van der Meer L, Sigafoos J. Effectiveness of the early start Denver model: a systematic review. J Autism Dev Disord 2016;3:93-106. https://doi.org/10.1007/s40489-015-0068-3.
- Chasson GS, Harris GE, Neely WJ. Cost comparison of early intensive behavioral intervention and special education for children with autism. J Child Fam Stud 2007;16:401-13. https://doi.org/10.1007/s10826-006-9094-1.
- Cidav Z, Munson J, Estes A, Dawson G, Rogers S, Mandell D. Cost offset associated with Early Start Denver Model for children with autism. J Am Acad Child Adolesc Psychiatry 2017;56:777-83. https://doi.org/10.1016/j.jaac.2017.06.007.
- Jacobson JW, Mulick JA, Green G. Cost-benefit estimates for early intensive behavioral intervention for young children with autism – general model and single state case. Behav Interv 1998;13:201-26. https://doi.org/10.1002/(SICI)1099-078X(199811)13:43.0.CO;2-R.
- Motiwala SS, Gupta S, Lilly MB, Ungar WJ, Coyte PC. The cost-effectiveness of expanding intensive behavioural intervention to all autistic children in Ontario. Healthc Policy 2006;1:135-51. https://doi.org/10.12927/hcpol.2006.17884.
- Penner M, Rayar M, Bashir N, Roberts SW, Hancock-Howard RL, Coyte PC. Cost-effectiveness analysis comparing pre-diagnosis autism spectrum disorder (ASD)-targeted intervention with Ontario’s Autism Intervention Program. J Autism Dev Disord 2015;45:2833-47. https://doi.org/10.1007/s10803-015-2447-0.
- Carr D, Felce J. The effects of PECS teaching to phase III on the communicative interactions between children with autism and their teachers. J Autism Dev Disord 2007;37:724-37. https://doi.org/10.1007/s10803-006-0203-1.
- Mesibov GB, Shea V. The TEACCH program in the era of evidence-based practice. J Autism Dev Disord 2010;40:570-9. https://doi.org/10.1007/s10803-009-0901-6.
- Cochrane Methods Group . Risk of Bias 2.0 Tool n.d. https://methods.cochrane.org/risk-bias-20-tool (accessed 28 February 2019).
- Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;355. https://doi.org/10.1136/bmj.i4919.
- Sparrow SS, Balla DA, Cicchetti DV, Harrison PL. Vineland Adaptive Behavior Scales. Circle Pines, MN: American Guidance Service; 1984.
- Bayley N. Bayley Scales of Infant Development: Birth to Two Years. San Antonio, TX: Psychological Corporation; 1969.
- Bayley N. Bayley Scales of Infant Development: Manual. San Antonio, TX: Psychological Corporation; 1993.
- Bayley N. Bayley Scales of Infant and Toddler Development – Third Edition. J Psychoeduc Assess 2006;25:180-90. https://doi.org/10.1177/0734282906297199.
- Wechsler D. Wechsler Intelligence Scale for Children. San Antonio, TX: Psychological Corporation; 1949.
- Wechsler D. WISC-III: Test de Inteligencia Para Niños/Wechsler Intelligence Scale for Children. San Antonio, TX: Psychological Corporation; 1993.
- Wechsler D. Wechsler Intelligence Scale for Children – Revised. San Antonio, TX: Psychological Corporation; 1974.
- Wechsler D. Wechsler Preschool and Primary Scale of Intelligence – Fourth Edition. San Antonio, TX: Psychological Corporation; 2012.
- Wechsler D. WPPSI-R: Wechsler Preschool and Primary Scale of Intelligence-Revised. San Antonio, TX: Psychological Corporation; 1989.
- Wechsler D. Wechsler Preschool and Primary Scale of Intelligence – Third Edition (WPPSI – III). San Antonio, TX: Psychological Corporation; 2002.
- Roid GH, Pomplun M. The Stanford–Binet Intelligence Scales. New York, NY: Guilford Press; 2012.
- Roid GH, Sampers JL. Merrill–Palmer-Revised Scales of Development. Wood Dale, IL: Stoelting; 2004.
- Gardner MF. Expressive One-Word Picture Vocabulary Test, Revised: EO-WPVT-R. Novato, CA: Academic Therapy Publications; 1990.
- Brownell R. Expressive One-Word Picture Vocabulary Test: Manual. Novato, CA: Academic Therapy Publications; 2000.
- Dunn LM, Dunn LM, Whetton C, Burley J. British Picture Vocabulary Scale 2nd Edition (BPVS-II). Windsor: NFER-Nelson; 1997.
- Reynell J, Huntley M. Reynell Developmental Language Scale – Revised Manual. 2nd revision. Slough: National Foundation for Educational Research; 1985.
- Edwards S, Garman M, Hughes A, Letts C, Sinka I. The Reynell Developmental Language Scales III (RDLS) manual. Int J Lang Commun Disord 1997;34:151-91. https://doi.org/10.1080/136828299247487.
- Mullen EM. Mullen Scales of Early Learning. Circle Pines, MN: AGS Publishing; 1995.
- Lord C, Rutter M. Social Communication Questionnaire (SCQ). Torrance, CA: WPS; 2003.
- Lord C, Risi S, Lambrecht L, Cook EH, Leventhal BL, DiLavore PC, et al. The autism diagnostic observation schedule-generic: a standard measure of social and communication deficits associated with the spectrum of autism. J Autism Dev Disord 2000;30:205-23. https://doi.org/10.1023/A:1005592401947.
- Rutter M, Le Couteur A, Lord C. Autism Diagnostic Interview – Revised. Los Angeles, CA: Western Psychological Services; 2003.
- Conners CK. Conners’ Rating Scales – Revised: CRS-R. North Tonawanda, NJ: Multi-Health Systems; 2001.
- Riley RD, Kauser I, Bland M, Thijs L, Staessen JA, Wang J, et al. Meta-analysis of randomised trials with a continuous outcome according to baseline imbalance and availability of individual participant data. Stat Med 2013;32:2747-66. https://doi.org/10.1002/sim.5726.
- Birnbrauer JS, Leach DJ. The Murdoch early intervention program after 2 years. Behav Change 1993;10:63-74. https://doi.org/10.1017/S0813483900005556.
- Dawson G, Rogers S, Munson J, Smith M, Winter J, Greenson J, et al. Randomized, controlled trial of an intervention for toddlers with autism: the Early Start Denver Model. Pediatrics 2010;125:e17-23. https://doi.org/10.1542/peds.2009-0958.
- Eikeseth S, Klintwall L, Jahr E, Karlsson P. Outcome for children with autism receiving early and intensive behavioral intervention in mainstream preschool and kindergarten settings. Res Autism Spectr Disord 2012;6:829-35. https://doi.org/10.1016/j.rasd.2011.09.002.
- Eikeseth S, Smith T, Jahr E, Eldevik S. Intensive behavioral treatment at school for 4- to 7-year-old children with autism. A 1-year comparison controlled study. Behav Modif 2002;26:49-68. https://doi.org/10.1177/0145445502026001004.
- Eldevik S, Hastings RP, Jahr E, Hughes JC. Outcomes of behavioral intervention for children with autism in mainstream pre-school settings. J Autism Dev Disord 2012;42:210-20. https://doi.org/10.1007/s10803-011-1234-9.
- Farrell P, Trigonaki N, Webster D. An exploratory evaluation of two early intervention programmes for young children with autism. Educ Child Psychol 2005;22.
- Haglund N, Dahlgren S, Rastam M, Gustafsson P, Kallen K. Improvement of autism symptoms after comprehensive intensive early interventions in a clinical setting. Eur Psychiatry 2017;41. https://doi.org/10.1016/j.eurpsy.2017.01.1940.
- Magiati I, Charman T, Howlin P. A two-year prospective follow-up study of community-based early intensive behavioural intervention and specialist nursery provision for children with autism spectrum disorders. J Child Psychol Psychiatry 2007;48:803-12. https://doi.org/10.1111/j.1469-7610.2007.01756.x.
- Reed P, Osborne LA, Corness M. Brief report: relative effectiveness of different home-based behavioral approaches to early teaching intervention. J Autism Dev Disord 2007;37:1815-21. https://doi.org/10.1007/s10803-006-0306-8.
- Reed P, Osborne LA, Corness M. The real-world effectiveness of early teaching interventions for children with autism spectrum disorder. Except Child 2007;73:417-33. https://doi.org/10.1177/001440290707300402.
- Remington B, Hastings RP, Kovshoff H, degli Espinosa F, Jahr E, Brown T, et al. Early intensive behavioral intervention: outcomes for children with autism and their parents after two years. Am J Ment Retard 2007;112:418-38. https://doi.org/10.1352/0895-8017(2007)112[418:EIBIOF]2.0.CO;2.
- Vivanti G, Paynter J, Duncan E, Fothergill H, Dissanayake C, Rogers SJ. Victorian ASELCC Team . Effectiveness and feasibility of the Early Start Denver Model implemented in a group-based community childcare setting. J Autism Dev Disord 2014;44:3140-53. https://doi.org/10.1007/s10803-014-2168-9.
- Zachor DA, Ben-Itzchak E, Rabinovich A-L, Lahat E. Change in autism core symptoms with intervention. Res Autism Spect Dis 2007;1:304-17. https://doi.org/10.1016/j.rasd.2006.12.001.
- Eikeseth S, Smith T, Jahr E, Eldevik S. Outcome for children with autism who began intensive behavioral treatment between ages 4 and 7: a comparison controlled study. Behav Modif 2007;31:264-78. https://doi.org/10.1177/0145445506291396.
- Magiati I, Moss J, Charman T, Howlin P. Patterns of change in children with autism spectrum disorders who received community based comprehensive interventions in their pre-school years: a seven year follow-up study. Res Autism Spectr Disord 2011;5:1016-27. https://doi.org/10.1016/j.rasd.2010.11.007.
- Zachor DA, Ben Itzchak E. Treatment approach, autism severity and intervention outcomes in young children. Res Autism Spect Dis 2010;4:425-32. https://doi.org/10.1016/j.rasd.2009.10.013.
- McEachin JJ, Smith T, Lovaas OI. Long-term outcome for children with autism who received early intensive behavioral treatment. Am J Ment Retard 1993;97:359-72.
- Hayward D, Eikeseth S, Gale C, Morgan S. Assessing progress during treatment for young children with autism receiving intensive behavioural interventions. Autism 2009;13:613-33. https://doi.org/10.1177/1362361309340029.
- Sallows GO, Graupner TD. Intensive behavioral treatment for children with autism: four-year outcome and predictors. Am J Ment Retard 2005;110:417-38. https://doi.org/10.1352/0895-8017(2005)110[417:IBTFCW]2.0.CO;2.
- Stock R, Mirenda P, Smith IM. Comparison of community-based verbal behavior and pivotal response treatment programs for young children with autism spectrum disorder. Res Autism Spect Dis 2013;7:1168-81. https://doi.org/10.1016/j.rasd.2013.06.002.
- Rogers SJ, Estes A, Lord C, Munson J, Rocha M, Winter J, et al. A multisite randomized controlled two-phase trial of the Early Start Denver Model compared to treatment as usual. J Am Acad Child Adolesc Psychiatry 2019;58:853-65. https://doi.org/10.1016/j.jaac.2019.01.004.
- Smith T, Groen AD, Wynn JW. Randomized trial of intensive early intervention for children with pervasive developmental disorder. Am J Ment Retard 2000;105:269-85. https://doi.org/10.1352/0895-8017(2000)105<0269:RTOIEI>2.0.CO;2.
- Cohen H, Amerine-Dickens M, Smith T. Early intensive behavioral treatment: replication of the UCLA model in a community setting. J Dev Behav Pediatr 2006;27:145-55. https://doi.org/10.1097/00004703-200604002-00013.
- Howard JS, Sparkman CR, Cohen HG, Green G, Stanislaw H. A comparison of intensive behavior analytic and eclectic treatments for young children with autism. Res Dev Disabil 2005;26:359-83. https://doi.org/10.1016/j.ridd.2004.09.005.
- Dawson G, Jones EJ, Merkle K, Venema K, Lowy R, Faja S, et al. Early behavioral intervention is associated with normalized brain activity in young children with autism. J Am Acad Child Adolesc Psychiatry 2012;51:1150-9. https://doi.org/10.1016/j.jaac.2012.08.018.
- Estes A, Munson J, Rogers SJ, Greenson J, Winter J, Dawson G. Long-term outcomes of early intervention in 6-year-old children with autism spectrum disorder. J Am Acad Child Adolesc Psychiatry 2015;54:580-7. https://doi.org/10.1016/j.jaac.2015.04.005.
- Howard JS, Stanislaw H, Green G, Sparkman CR, Cohen HG. Comparison of behavior analytic and eclectic early interventions for young children with autism after three years. Res Dev Disabil 2014;35:3326-44. https://doi.org/10.1016/j.ridd.2014.08.021.
- Howlin P, Magiati I, Charman T. Early intensive behavioural intervention vs specialist nursery provision for pre school children with autism spectrum disorders. J Intellect Disabil Res 2007;51.
- Kovshoff H, Hastings RP, Remington B. Two-year outcomes for children with autism after the cessation of early intensive behavioral intervention. Behav Modif 2011;35:427-50. https://doi.org/10.1177/0145445511405513.
- Smith T, Groen AD, Wynn JW, Feldman MA. Early Intervention: The Essential Readings. Malden: Blackwell Publishing; 2004.
- Sullivan K. The Early Start Denver Model: outcomes and moderators of an intervention for toddlers with autism. Diss Abstr Int 2014.
- Jick H, Kaye JA, Black C. Changes in risk of autism in the U.K. for birth cohorts 1990–1998. Epidemiology 2003;14:630-2. https://doi.org/10.1097/01.EDE.0000082044.88833.c4.
- Hagberg KW, Jick H. Autism in the UK for birth cohorts 1988–2001. Epidemiology 2010;21:426-7. https://doi.org/10.1097/EDE.0b013e3181d61dd9.
- King M, Bearman P. Diagnostic change and the increased prevalence of autism. Int J Epidemiol 2009;38:1224-34. https://doi.org/10.1093/ije/dyp261.
- Fisch GS. Nosology and epidemiology in autism: classification counts. Am J Med Genet Part C Semin Med Genet 2012;160:91-103. https://doi.org/10.1002/ajmg.c.31325.
- Taylor B. Vaccines and the changing epidemiology of autism. Child Care Health Dev 2006;32:511-19. https://doi.org/10.1111/j.1365-2214.2006.00655.x.
- Weitlauf AS, McPheeters ML, Peters B, Sathe N, Travis R, Aiello R, et al. Therapies for Children with Autism Spectrum Disorder. Rockville, MD: Agency for Healthcare Research and Quality; 2014.
- McConachie H, Parr JR, Glod M, Hanratty J, Livingstone N, Oono IP, et al. Systematic review of tools to measure outcomes for young children with autism spectrum disorder. Health Technol Assess 2015;19. https://doi.org/10.3310/hta19410.
- Hoefman R, Payakachat N, van Exel J, Kuhlthau K, Kovacs E, Pyne J, et al. Caring for a child with autism spectrum disorder and parents’ quality of life: application of the CarerQol. J Autism Dev Disord 2014;44:1933-45. https://doi.org/10.1007/s10803-014-2066-1.
- McStay RL, Trembath D, Dissanayake C. Stress and family quality of life in parents of children with autism spectrum disorder: parent gender and the double ABCX model. J Autism Dev Disord 2014;44:3101-18. https://doi.org/10.1007/s10803-014-2178-7.
- Vasilopoulou E, Nisbet J. The quality of life of parents of children with autism spectrum disorder: a systematic review. Res Autism Spect Dis 2016;23:36-49. https://doi.org/10.1016/j.rasd.2015.11.008.
- Kuhlthau K, Payakachat N, Delahaye J, Hurson J, Pyne JM, Kovacs E, et al. Quality of life for parents of children with autism spectrum disorders. Res Autism Spect Dis 2014;8:1339-50. https://doi.org/10.1016/j.rasd.2014.07.002.
- Tung LC, Huang CY, Tseng MH, Yen HC, Tsai YP, Lin YC, et al. Correlates of health-related quality of life and the perception of its importance in caregivers of children with autism. Res Autism Spect Dis 2014;8:1235-42. https://doi.org/10.1016/j.rasd.2014.06.010.
- Totsika V, Hastings RP, Emerson E, Berridge DM, Lancaster GA. Behavior problems at 5 years of age and maternal mental health in autism and intellectual disability. J Abnorm Child Psychol 2011;39:1137-47. https://doi.org/10.1007/s10802-011-9534-2.
- Barrett B, Byford S, Sharac J, Hudry K, Leadbitter K, Temple K, et al. Service and wider societal costs of very young children with autism in the UK. J Autism Dev Disord 2012;42:797-804. https://doi.org/10.1007/s10803-011-1306-x.
- Payakachat N, Tilford JM, Kuhlthau KA, van Exel NJ, Kovacs E, Bellando J, et al. Predicting health utilities for children with autism spectrum disorders. Autism Res 2014;7:649-63. https://doi.org/10.1002/aur.1409.
- Rogge N, Janssen J. The economic costs of autism spectrum disorder: a literature review. J Autism Dev Disord 2019;49:2873-900. https://doi.org/10.1007/s10803-019-04014-z.
- National Institute for Health and Care Excellence (NICE) . Guide to the Methods of Technology Appraisal 2013 2013.
- Khanna R, Jariwala-Parikh K, West-Strum D, Mahabaleshwarkar R. Health-related quality of life and its determinants among adults with autism. Res Autism Spect Dis 2014;8:157-67. https://doi.org/10.1016/j.rasd.2013.11.003.
- Howlin P, Magiati I. Autism spectrum disorder: outcomes in adulthood. Curr Opin Psychiatry 2017;30:69-76. https://doi.org/10.1097/YCO.0000000000000308.
- Cederlund M, Hagberg B, Billstedt E, Gillberg IC, Gillberg C. Asperger syndrome and autism: a comparative longitudinal follow-up study more than 5 years after original diagnosis. J Autism Dev Disord 2008;38:72-85. https://doi.org/10.1007/s10803-007-0364-6.
- Esbensen AJ, Bishop S, Seltzer MM, Greenberg JS, Taylor JL. Comparisons between individuals with autism spectrum disorders and individuals with Down syndrome in adulthood. Am J Intellect Dev Disabil 2010;115:277-90. https://doi.org/10.1352/1944-7558-115.4.277.
- Farley MA, McMahon WM, Fombonne E, Jenson WR, Miller J, Gardner M, et al. Twenty-year outcome for individuals with autism and average or near-average cognitive abilities. Autism Res 2009;2:109-18. https://doi.org/10.1002/aur.69.
- Barrett B, Mosweu I, Jones CR, Charman T, Baird G, Simonoff E, et al. Comparing service use and costs among adolescents with autism spectrum disorders, special needs and typical development. Autism 2015;19:562-9. https://doi.org/10.1177/1362361314536626.
- Kirkham P. ‘The line between intervention and abuse’ – autism and applied behaviour analysis. Hist Hum Sci 2017;30:107-26. https://doi.org/10.1177/0952695117702571.
- Bilder D, Botts EL, Smith KR, Pimentel R, Farley M, Viskochil J, et al. Excess mortality and causes of death in autism spectrum disorders: a follow up of the 1980s Utah/UCLA autism epidemiologic study. J Autism Dev Disord 2013;43:1196-204. https://doi.org/10.1007/s10803-012-1664-z.
- Hirvikoski T, Mittendorfer-Rutz E, Boman M, Larsson H, Lichtenstein P, Bölte S. Premature mortality in autism spectrum disorder. Br J Psychiatry 2016;208:232-8. https://doi.org/10.1192/bjp.bp.114.160192.
- Mouridsen SE, Brønnum-Hansen H, Rich B, Isager T. Mortality and causes of death in autism spectrum disorders: an update. Autism 2008;12:403-14. https://doi.org/10.1177/1362361308091653.
- Pickett J, Xiu E, Tuchman R, Dawson G, Lajonchere C. Mortality in individuals with autism, with and without epilepsy. J Child Neurol 2011;26:932-9. https://doi.org/10.1177/0883073811402203.
- Schendel DE, Overgaard M, Christensen J, Hjort L, Jørgensen M, Vestergaard M, et al. Association of psychiatric and neurologic comorbidity with mortality among persons with autism spectrum disorder in a Danish population. JAMA Pediatr 2016;170:243-50. https://doi.org/10.1001/jamapediatrics.2015.3935.
- Shavelle RM, Strauss DJ, Pickett J. Causes of death in autism. J Autism Dev Disord 2001;31:569-76. https://doi.org/10.1023/A: 1013247011483.
- Office for National Statistics (ONS) . National Life Tables, UK: 2015 to 2017 2018.
- GOV.UK . School Attendance and Absence 2018. www.gov.uk/school-attendance-absence (accessed 17 November 2018).
- Szende A, Janssen B, Cabases J. Self-Reported Population Health: An International Perspective Based on EQ-5D. New York, NY: Springer; 2014.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2017. Canterbury: Personal Social Services Research Unit, University of Kent; 2017.
- Knapp M, Romeo R, Beecham J. Economic cost of autism in the UK. Autism 2009;13:317-36. https://doi.org/10.1177/1362361309104246.
- Croen LA, Shankute N, Davignon M, Massolo ML, Yoshida C. Demographic and clinical characteristics associated with engagement in behavioral health treatment among children with autism spectrum disorders. J Autism Dev Disord 2017;47:3347-57. https://doi.org/10.1007/s10803-017-3247-5.
- Taylor B, Jick H, Maclaughlin D. Prevalence and incidence rates of autism in the UK: time trend from 2004–2010 in children aged 8 years. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2013-003219.
- Brett D, Warnell F, McConachie H, Parr JR. Factors affecting age at ASD diagnosis in UK: no evidence that diagnosis age has decreased between 2004 and 2014. J Autism Dev Disord 2016;46:1974-84. https://doi.org/10.1007/s10803-016-2716-6.
- Rogers SJ. Neuropsychology of autism in young children and its implications for early intervention. Ment Retard Dev D R 1998;4:104-12. https://doi.org/10.1002/(SICI)1098-2779(1998)4:23.0.CO;2-P.
- Smith T, Iadarola S. Evidence base update for autism spectrum disorder. J Clin Child Adolesc Psychol 2015;44:897-922. https://doi.org/10.1080/15374416.2015.1077448.
- Rutter M. Incidence of autism spectrum disorders: changes over time and their meaning. Acta Paediatr 2005;94:2-15. https://doi.org/10.1111/j.1651-2227.2005.tb01779.x.
- Green J, Charman T, McConachie H, Aldred C, Slonims V, Howlin P, et al. Parent-mediated communication-focused treatment in children with autism (PACT): a randomised controlled trial. Lancet 2010;375:2152-60. https://doi.org/10.1016/S0140-6736(10)60587-9.
- McConkey R, Truesdale-Kennedy M, Crawford H, McGreevy E, Reavey M, Cassidy A. Pre-schoolers with autism spectrum disorders: evaluating the impact of a home-based intervention to promote their communication. Early Child Dev Care 2010;180:299-315. https://doi.org/10.1080/03004430801899187.
- Yoder P, Stone WL. Randomized comparison of two communication interventions for pre-schoolers with autism spectrum disorders. J Consult Clin Psychol 2006;74:426-35. https://doi.org/10.1037/0022-006X.74.3.426.
- Green J. Editorial: Process to progress? Investigative trials, mechanism and clinical science. J Child Psychol Psychiatry 2015;56:1-3. https://doi.org/10.1111/jcpp.12377.
- World Health Organization (WHO) . ICD-10 Classifications of Mental and Behavioural Disorder: Clinical Descriptions and Diagnostic Guidelines 1992.
- Lovaas OI, Ackerman A, Alexander D, Firestone P, Perkins M, Young DB. Teaching Developmentally Disabled Children: The ME Book. Austin, TX: Pro-Ed; 1981.
- Lovaas OI, Leaf RL. Five Videotapes for Teaching Developmentally Disabled Children. Austin, TX: Pro-Ed; 1981.
- Schopler E, Lansing M, Waters L. Individualized Assessment and Treatment for Autistic and Developmentally Disabled Children: Vol. 3. Teaching Activities for Autistic Children. Austin, TX: Pro-Ed; 1983.
- Ayres AJ. Sensory Integration and Learning Disorders. Los Angeles, CA: Western Psychological Services; 1972.
- Leaf R, McEachin J. A Work in Progress. New York, NY: DRL Books; 1999.
- Lovaas OI. Teaching Individuals with Developmental Delays: Basic Intervention Techniques. Austin, TX: Pro-Ed; 2003.
- Maurice C, Green G, Luce SC. Behavioral Intervention for Young Children with Autism: A Manual for Parents and Professionals. Austin, TX: Pro-Ed; 1996.
- Sundberg ML, Partington JW. Teaching Language to Children with Autism or Other Developmental Disabilities. Danville, CA: Behavior Analysts, Inc.; 1998.
- Philips Z, Bojke L, Sculpher M, Claxton K, Golder S. Good practice guidelines for decision-analytic modelling in health technology assessment: a review and consolidation of quality assessment. PharmacoEconomics 2006;24:355-71. https://doi.org/10.2165/00019053-200624040-00006.
- Freeman BJ. Guidelines for evaluating intervention programs for children with autism. J Autism Dev Disord 1997;27:641-51. https://doi.org/10.1023/a: 1025850715183.
- Rogers SJ, Estes A, Lord C, Vismara L, Winter J, Fitzpatrick A, et al. Effects of a brief Early Start Denver Model (ESDM)-based parent intervention on toddlers at risk for autism spectrum disorders: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry 2012;51:1052-65. https://doi.org/10.1016/j.jaac.2012.08.003.
- Bourke-Taylor H, Pallant JF, Law M, Howie L. Predicting mental health among mothers of school-aged children with developmental disabilities: the relative contribution of child, maternal and environmental factors. Res Dev Disabil 2012;33:1732-40. https://doi.org/10.1016/j.ridd.2012.04.011.
- Chuang IC, Tseng MH, Lu L, Shieh JY, Cermak SA. Predictors of the health-related quality of life in pre-school children with autism spectrum disorders. Res Autism Spectr Disord 2014;8:1062-70. https://doi.org/10.1016/j.rasd.2014.05.015.
- Clark BG, Magill-Evans JE, Koning CJ. Youth with autism spectrum disorders: self- and proxy-reported quality of life and adaptive functioning. Focus Autism Other Dev Disabil 2015;30:57-64. https://doi.org/10.1177/1088357614522289.
- Domellöf E, Hedlund L, Ödman P. Health-related quality of life of children and adolescents with functional disabilities in a northern Swedish county. Qual Life Res 2014;23:1877-82. https://doi.org/10.1007/s11136-013-0613-4.
- de Vries M, Geurts H. Influence of autism traits and executive functioning on quality of life in children with an autism spectrum disorder. J Autism Dev Disord 2015;45:2734-43. https://doi.org/10.1007/s10803-015-2438-1.
- Delahaye J, Kovacs E, Sikora D, Hall TA, Orlich F, Clemons TE, et al. The relationship between health-related quality of life and sleep problems in children with autism spectrum disorders. Res Autism Spectr Disord 2014;8:292-303. https://doi.org/10.1016/j.rasd.2013.12.015.
- Egilson ST, Ólafsdóttir LB, Leósdóttir T, Saemundsen E. Quality of life of high-functioning children and youth with autism spectrum disorder and typically developing peers: self- and proxy-reports. Autism 2017;21:133-41. https://doi.org/10.1177/1362361316630881.
- Forsyth R, Colver A, Alvanides S, Woolley M, Lowe M. Participation of young severely disabled children is influenced by their intrinsic impairments and environment. Dev Med Child Neurol 2007;49:345-9. https://doi.org/10.1111/j.1469-8749.2007.00345.x.
- Forsyth R, McNally R, James P, Crossland K, Woolley M, Colver A. Variation at local government level in the support for families of severely disabled children and the factors that affect it. Dev Med Child Neurol 2010;52:e259-66. https://doi.org/10.1111/j.1469-8749.2010.03778.x.
- Jahan MU, Karim MR, Rahman A, Akhter S. Cognitive functions and health related quality of life of institutional autism spectrum disorder children in Dhaka city. Bangladesh Med Res Counc Bull 2015;41:151-9. https://doi.org/10.3329/bmrcb.v41i3.29973.
- Kose S, Erermis S, Ozturk O, Ozbaran B, Demiral N, Bildik T, et al. Health related quality of life in children with autism spectrum disorders: the clinical and demographic related factors in Turkey. Res Autism Spectr Disord 2013;7:213-20. https://doi.org/10.1016/j.rasd.2012.09.009.
- Kuhlthau K, Kovacs E, Hall T, Clemmons T, Orlich F, Delahaye J, et al. Health-related quality of life for children with ASD: associations with behavioral characteristics. Res Autism Spectr Disord 2013;7:1035-42. https://doi.org/10.1016/j.rasd.2013.04.006.
- Kuhlthau K, Orlich F, Hall TA, Sikora D, Kovacs EA, Delahaye J, et al. Health-Related Quality of Life in children with autism spectrum disorders: results from the Autism Treatment Network. J Autism Dev Disord 2010;40:721-9. https://doi.org/10.1007/s10803-009-0921-2.
- Lai CJ, Chen CL, Chen CH, Chen CY, Chen HC, Chuang CY, et al. Health related quality of life in pre-school children with autism spectrum disorder of different cognition functions. Arch Phys Med Rehabil 2016;97. https://doi.org/10.1016/j.apmr.2016.08.321.
- Lavelle TA. Examining health and economic outcomes associated with pediatric medical conditions in the United States. Diss Abstr Int 2012;73.
- Limbers CA, Heffer RW, Varni JW. Health-related quality of life and cognitive functioning from the perspective of parents of school-aged children with Asperger’s syndrome utilizing the PedsQL™. J Autism Dev Disord 2009;39:1529-41. https://doi.org/10.1007/s10803-009-0777-5.
- Meral BF, Fidan A. Measuring the impact of feeding covariates on health-related quality of life in children with autism spectrum disorder. Res Autism Spectr Disord 2015;10:124-30. https://doi.org/10.1016/j.rasd.2014.11.009.
- Ozturk O, Erermis S, Ercan ES, Gulen F, Basay BK, Basay O, et al. Does the quality of life in autism spectrum disorder differ from other chronic disorders and healthy children?. Anadolu Psikiyatri Dergisi 2016;17:419-26. https://doi.org/10.5455/apd.185269.
- Petrou S, Johnson S, Wolke D, Hollis C, Kochhar P, Marlow N. Economic costs and preference-based health-related quality of life outcomes associated with childhood psychiatric disorders. Br J Psychiatry 2010;197:395-404. https://doi.org/10.1192/bjp.bp.110.081307.
- Potvin M-C. Participation in recreational activities in school age children with high functioning autism and their peers. Diss Abstr Int 2011;73.
- Potvin MC, Snider L, Prelock PA, Wood-Dauphinee S, Kehayia E. Health-related quality of life in children with high-functioning autism. Autism 2015;19:14-9. https://doi.org/10.1177/1362361313509730.
- Sheldrick RC, Neger EN, Shipman D, Perrin EC. Quality of life of adolescents with autism spectrum disorders: concordance among adolescents’ self-reports, parents’ reports, and parents’ proxy reports. Qual Life Res 2012;21:53-7. https://doi.org/10.1007/s11136-011-9916-5.
- Shipman DL, Sheldrick RC, Perrin EC. Quality of life in adolescents with autism spectrum disorders: reliability and validity of self-reports. J Dev Behav Pediatr 2011;32:85-9. https://doi.org/10.1097/DBP.0b013e318203e558.
- Sikora DM, Vora P, Coury DL, Rosenberg D. Attention-deficit/hyperactivity disorder symptoms, adaptive functioning, and quality of life in children with autism spectrum disorder. Pediatrics 2012;130:91-7. https://doi.org/10.1542/peds.2012-0900G.
- Stokes MA, Kornienko L, Scheeren AM, Koot HM, Begeer S. A comparison of children and adolescent’s self-report and parental report of the PedsQL among those with and without autism spectrum disorder. Qual Life Res 2017;26:611-24. https://doi.org/10.1007/s11136-016-1490-4.
- Tavernor L, Barron E, Rodgers J, McConachie H. Finding out what matters: validity of quality of life measurement in young people with ASD. Child Care Health Dev 2013;39:592-601. https://doi.org/10.1111/j.1365-2214.2012.01377.x.
- Tilford JM, Payakachat N, Kovacs E, Pyne JM, Brouwer W, Nick TG, et al. Preference-based health-related quality-of-life outcomes in children with autism spectrum disorders: a comparison of generic instruments. PharmacoEconomics 2012;30:661-79. https://doi.org/10.2165/11597200-000000000-00000.
- Tilford JM, Payakachat N, Kuhlthau KA, Pyne JM, Kovacs E, Bellando J, et al. Treatment for sleep problems in children with autism and caregiver spillover effects. J Autism Dev Disord 2015;45:3613-23. https://doi.org/10.1007/s10803-015-2507-5.
- van Steensel FJ, Bögels SM, Dirksen CD. Anxiety and quality of life: clinically anxious children with and without autism spectrum disorders compared. J Clin Child Adolesc Psychol 2012;41:731-8. https://doi.org/10.1080/15374416.2012.698725.
- Van Steensel FJA, Dirksen CD, Bogels SM. Cost-effectiveness of cognitive-behavioral therapy versus treatment as usual for anxiety disorders in children with autism spectrum disorder. Res Autism Spectr Disord 2014;8:127-37. https://doi.org/10.1016/j.rasd.2013.11.001.
- Varni JW, Handen BL, Corey-Lisle PK, Guo Z, Manos G, Ammerman DK, et al. Effect of aripiprazole 2 to 15 mg/d on health-related quality of life in the treatment of irritability associated with autistic disorder in children: a post hoc analysis of two controlled trials. Clin Ther 2012;34:980-92. https://doi.org/10.1016/j.clinthera.2012.02.023.
- Viecili MA, Weiss JA. Reliability and validity of the Pediatric Quality of Life Inventory with individuals with intellectual and developmental disabilities. Am J Intellect Dev Disabil 2015;120:289-301. https://doi.org/10.1352/1944-7558-120.4.289.
- Bishop-Fitzpatrick L, Smith DaWalt L, Greenberg JS, Mailick MR. Participation in recreational activities buffers the impact of perceived stress on quality of life in adults with autism spectrum disorder. Autism Res 2017;10:973-82. https://doi.org/10.1002/aur.1753.
- Helles A, Gillberg IC, Gillberg C, Billstedt E. Asperger syndrome in males over two decades: quality of life in relation to diagnostic stability and psychiatric comorbidity. Autism 2017;21:458-69. https://doi.org/10.1177/1362361316650090.
- Hong J, Bishop-Fitzpatrick L, Smith LE, Greenberg JS, Mailick MR. Factors associated with subjective quality of life of adults with autism spectrum disorder: self-report versus maternal reports. J Autism Dev Disord 2016;46:1368-78. https://doi.org/10.1007/s10803-015-2678-0.
- Jariwala-Parikh KM. Quality of life and healthcare utilization and costs among adults with autism. Diss Abstr Int 2016;76.
- Jennes-Coussens M, Magill-Evans J, Koning C. The quality of life of young men with Asperger syndrome: a brief report. Autism 2006;10:403-14.
- Kamio Y, Inada N, Koyama T. A nationwide survey on quality of life and associated factors of adults with high-functioning autism spectrum disorders. Autism 2013;17:15-26. https://doi.org/10.1177/1362361312436848.
- Kamp-Becker I, Schröder J, Remschmidt H, Bachmann CJ. Health-related quality of life in adolescents and young adults with high functioning autism-spectrum disorder. Psychosoc Med 2010;7. https://doi.org/10.3205/psm000065.
- Khanna R, Jariwala K, West-Strum D. Validity and reliability of the Medical Outcomes Study Short-Form Health Survey version 2 (SF-12v2) among adults with autism. Res Dev Disabil 2015;43–44:51-60. https://doi.org/10.1016/j.ridd.2015.06.006.
- Moss P, Mandy W, Howlin P. Child and adult factors related to quality of life in adults with autism. J Autism Dev Disord 2017;47:1830-7. https://doi.org/10.1007/s10803-017-3105-5.
- Ahmad MM, Dardas LA. The hidden patients: fathers of children with autism spectrum disorder. J Intellect Dev Disabil 2015;40:368-75. https://doi.org/10.3109/13668250.2015.1064879.
- Dardas LA, Ahmad MM. Quality of life among parents of children with autistic disorder: a sample from the Arab world. Res Dev Disabil 2014;35:278-87. https://doi.org/10.1016/j.ridd.2013.10.029.
- Kousha M, Attar HA, Shoar Z. Anxiety, depression, and quality of life in Iranian mothers of children with autism spectrum disorder. J Child Health Care 2016;20:405-14. https://doi.org/10.1177/1367493515598644.
- Amirian H, Solimani S, Maleki F, Ghasemi SR, Reshadat S, Gilan NR. A study on health-related quality of life, depression, and associated factors among parents of children with autism in Kermanshah, Iran. Iran J Psychiatry Behav Sci 2017;11. https://doi.org/10.5812/ijpbs.7832.
- Aral A, Usta MB, Karaosman T. Behavioral problems in pre-school and school-aged autism spectrum disorder children; associations with parent functional and psychological health: preliminary study. Klinik Psikofarmakoloji Bulteni 2015;25.
- Benjak T, Mavrinac GV, Simetin IP, Kolaric B. A comparative study on self-perceived health and quality of life of parents of children with autism spectrum disorders and parents of non disabled children in Croatia. Dev Med Child Neurol 2011;53:7-8. https://doi.org/10.1111/j.1469-8749.2011.04011.x.
- Forouzanfar S, Babakhani N, Sodagar S. Health related quality of life among mothers of children with autism spectrum disorder and its predictors. Indian J Public Health Res Dev 2016;7:209-14. https://doi.org/10.5958/0976-5506.2016.00095.4.
- Johnson N, Frenn M, Feetham S, Simpson P. Autism spectrum disorder: parenting stress, family functioning and health-related quality of life. Fam Syst Health 2011;29:232-52. https://doi.org/10.1037/a0025341.
- Johnson NL. Understanding relationships in health related quality of life of parents of children with autism spectrum disorder. Diss Abstr Int 2009;70.
- Ji B, Zhao I, Turner C, Sun M, Yi R, Tang S. Predictors of health-related quality of life in Chinese caregivers of children with autism spectrum disorders: a cross-sectional study. Arch Psychiatr Nurs 2014;28:327-32. https://doi.org/10.1016/j.apnu.2014.06.001.
- Ji B, Sun M, Yi R, Tang S. Multidisciplinary parent education for caregivers of children with autism spectrum disorders. Arch Psychiatr Nurs 2014;28:319-26. https://doi.org/10.1016/j.apnu.2014.06.003.
- Khanna R, Madhavan SS, Smith MJ, Patrick JH, Tworek C, Becker-Cottrill B. Assessment of health-related quality of life among primary caregivers of children with autism spectrum disorders. J Autism Dev Disord 2011;41:1214-27. https://doi.org/10.1007/s10803-010-1140-6.
- Kheir N, Ghoneim O, Sandridge AL, Al-Ismail M, Hayder S, Al-Rawi F. Quality of life of caregivers of children with autism in Qatar. Autism 2012;16:293-8. https://doi.org/10.1177/1362361311433648.
- Lee GK, Lopata C, Volker MA, Thomeer ML, Nida RE, Toomey JA, et al. Health-related quality of life of parents of children with high-functioning autism spectrum disorders. Focus Autism Other Dev Disabil 2009;24:227-39. https://doi.org/10.1177/1088357609347371.
- Yamada A, Kato M, Suzuki M, Suzuki M, Watanabe N, Akechi T, et al. Quality of life of parents raising children with pervasive developmental disorders. BMC Psychiatry 2012;12. https://doi.org/10.1186/1471-244X-12-119.
- Khanna R, Jariwala K, Bentley JP. Health utility assessment using EQ-5D among caregivers of children with autism. Value Health 2013;16:778-88. https://doi.org/10.1016/j.jval.2013.04.007.
- Allik H, Larsson JO, Smedje H. Health-related quality of life in parents of school-age children with Asperger syndrome or high-functioning autism. Health Qual Life Outcomes 2006;4. https://doi.org/10.1186/1477-7525-4-1.
- Steinhausen HC, Mohr Jensen C, Lauritsen MB. A systematic review and meta-analysis of the long-term overall outcome of autism spectrum disorders in adolescence and adulthood. Acta Psychiatr Scand 2016;133:445-52. https://doi.org/10.1111/acps.12559.
- Howlin P, Moss P, Savage S, Rutter M. Social outcomes in mid- to later adulthood among individuals diagnosed with autism and average nonverbal IQ as children. J Am Acad Child Adolesc Psychiatry 2013;52:572-81. https://doi.org/10.1016/j.jaac.2013.02.017.
- Gillespie-Lynch K, Sepeta L, Wang Y, Marshall S, Gomez L, Sigman M, et al. Early childhood predictors of the social competence of adults with autism. J Autism Dev Disord 2012;42:161-74. https://doi.org/10.1007/s10803-011-1222-0.
- Gray K, Keating C, Taffe J, Brereton A, Einfeld S, Tonge B. Trajectory of behavior and emotional problems in autism. Am J Intellect Dev Disabil 2012;117:121-33. https://doi.org/10.1352/1944-7588-117-2.121.
- Billstedt E, Gillberg IC, Gillberg C, Gillberg C. Autism after adolescence: population-based 13- to 22-year follow-up study of 120 individuals with autism diagnosed in childhood. J Autism Dev Disord 2005;35:351-60. https://doi.org/10.1007/s10803-005-3302-5.
- Billstedt E, Gillberg IC, Gillberg C. Autism after adolescence: population-based 13- to 22-year follow-up study of 120 individuals with autism diagnosed in childhood. J Autism Dev Disord 2007;37. https://doi.org/10.1007/s10803-006-0082-5.
- Billstedt E, Gillberg IC, Gillberg C. Aspects of quality of life in adults diagnosed with autism in childhood: a population-based study. Autism 2011;15:7-20. https://doi.org/10.1177/1362361309346066.
- Szatmari P, Bryson S, Duku E, Vaccarella L, Zwaigenbaum L, Bennett T, et al. Similar developmental trajectories in autism and Asperger syndrome: from early childhood to adolescence. J Child Psychol Psychiatry 2009;50:1459-67. https://doi.org/10.1111/j.1469-7610.2009.02123.x.
- Eaves LC, Ho HH. Young adult outcome of autism spectrum disorders. J Autism Dev Disord 2008;38:739-47. https://doi.org/10.1007/s10803-007-0441-x.
- McGovern CW, Sigman M. Continuity and change from early childhood to adolescence in autism. J Child Psychol Psychiatry 2005;46:401-8. https://doi.org/10.1111/j.1469-7610.2004.00361.x.
- Howlin P, Mawhood L, Rutter M. Autism and developmental receptive language disorder – a follow-up comparison in early adult life. II: Social, behavioural, and psychiatric outcomes. J Child Psychol Psychiatry 2000;41:561-78. https://doi.org/10.1111/1469-7610.00643.
- Bishop SL, Farmer C, Thurm A. Measurement of nonverbal IQ in autism spectrum disorder: scores in young adulthood compared to early childhood. J Autism Dev Disord 2015;45:966-74. https://doi.org/10.1007/s10803-014-2250-3.
- Anderson DK, Liang JW, Lord C. Predicting young adult outcome among more and less cognitively able individuals with autism spectrum disorders. J Child Psychol Psychiatry 2014;55:485-94. https://doi.org/10.1111/jcpp.12178.
- Marriage S, Wolverton A, Marriage K. Autism spectrum disorder grown up: a chart review of adult functioning. J Can Acad Child Adolesc Psychiatry 2009;18:322-8.
- Gray KM, Keating CM, Taffe JR, Brereton AV, Einfeld SL, Reardon TC, et al. Adult outcomes in autism: community inclusion and living skills. J Autism Dev Disord 2014;44:3006-15. https://doi.org/10.1007/s10803-014-2159-x.
- Ballaban-Gil K, Rapin I, Tuchman R, Shinnar S. Longitudinal examination of the behavioral, language, and social changes in a population of adolescents and young adults with autistic disorder. Pediatr Neurol 1996;15:217-23. https://doi.org/10.1016/S0887-8994(96)00219-6.
- Bebbington A, Beecham J. Social services support and expenditure for children with autism. Autism 2007;11:43-61. https://doi.org/10.1177/1362361307070911.
- Byford S, Cary M, Barrett B, Aldred CR, Charman T, Howlin P, et al. Cost-effectiveness analysis of a communication-focused therapy for pre-school children with autism: results from a randomised controlled trial. BMC Psychiatry 2015;15. https://doi.org/10.1186/s12888-015-0700-x.
- Järbrink K, Knapp M. The economic impact of autism in Britain. Autism 2001;5:7-22. https://doi.org/10.1177/1362361301005001002.
- Järbrink K, Fombonne E, Knapp M. Measuring the parental, service and cost impacts of children with autistic spectrum disorder: a pilot study. J Autism Dev Disord 2003;33:395-402. https://doi.org/10.1023/a: 1025058711465.
- Mavranezouli I, Megnin-Viggars O, Cheema N, Howlin P, Baron-Cohen S, Pilling S. The cost-effectiveness of supported employment for adults with autism in the United Kingdom. Autism 2014;18:975-84. https://doi.org/10.1177/1362361313505720.
- McGill P, Poynter J. High cost residential placements for adults with intellectual disabilities. J Appl Res Intellect Disabil 2012;25:584-7. https://doi.org/10.1111/j.1468-3148.2012.00689.x.
- Preece D, Jordan R. Short breaks services for children with autistic spectrum disorders: factors associated with service use and non-use. J Autism Dev Disord 2007;37:374-85. https://doi.org/10.1007/s10803-006-0174-2.
- Russell G, Ford T, Steer C, Golding J. Identification of children with the same level of impairment as children on the autistic spectrum, and analysis of their service use. J Child Psychol Psychiatry 2010;51:643-51. https://doi.org/10.1111/j.1469-7610.2010.02233.x.
- Wright B, Marshall D, Adamson J, Ainsworth H, Ali S, Allgar V, et al. Social Stories™ to alleviate challenging behaviour and social difficulties exhibited by children with autism spectrum disorder in mainstream schools: design of a manualised training toolkit and feasibility study for a cluster randomised controlled trial with nested qualitative and cost-effectiveness components. Health Technol Assess 2016;20. https://doi.org/10.3310/hta20060.
- Yuan JX, McGowan M, Hadjikoumi I, Pant B. Do children with neurological disabilities use more inpatient resources: an observational study. Emerg Themes Epidemiol 2017;14. https://doi.org/10.1186/s12982-017-0059-1.
- MacDonald RD, Parry-Cruwys, Dupere S, Ahearn W. Assessing progress and outcome of early intensive behavioral intervention for toddlers with autism. Res Dev Disabil 2014;35:3632-44. https://doi.org/10.1016/j.ridd.2014.08.036.
- Barbeau EB, Soulières I, Dawson M, Zeffiro TA, Mottron L. The level and nature of autistic intelligence III: inspection time. J Abnorm Psychol 2013;122:295-301. https://doi.org/10.1037/a0029984.
Appendix 1 Advisory Group membership
| Name | Role | Organisation |
|---|---|---|
| Mike Clarke | Academic advisor (IPD and statistics) | Queen’s University Belfast |
| Bernard Fleming | NAS representative | NAS |
| Patricia Howlin | Academic advisory (autism research) | Institute of Psychiatry, King’s College London |
| Emma Jenner | Parent | n/a |
| Helen McConachie | Academic advisory (autism research) | Newcastle University |
| Anne McLaren | Parent | n/a |
| Dean McMillan | Clinical academic | University of York |
| Damian Milton | Representative with ASD/NAS representative | NAS |
| Roo Philip | ABA practitioner | Tailor Ed Foundation |
| Tristram Smith | Clinical academic and expert in ABA therapy | University of Rochester Medical Center |
| Peter Szatmari | Academic advisory (autism research) | McMaster University |
| Emma Truelove | Education psychologist | York City Council |
| Colin Wilson | Representative with ASD | n/a |
| Anne-Marie Wood | Parent | n/a |
| Suzy Yardley | ABA practitioner | Child Autism UK |
Appendix 2 Clinical effectiveness search strategies
Early intensive applied behaviour analysis-based interventions effectiveness literature searching
Searched August 2017.
Databases searched: CENTRAL, CINAHL, Conference Papers Citation Index, EMBASE, Education Resources Information Center, Electronic Theses Online Service (EthOS) (British Library Dissertations database), MEDLINE, PsycINFO, Social Sciences Citation Index.
Trials registers searched: ClinicalTrials.gov and World Health Organization International Clinical Trials Registry Platform.
A total of 10,843 records identified. After importing into EndNote bibliographic software and deduplicating, there were a total of 6698 records.
Cochrane Central Register of Controlled Trials via Wiley’s The Cochrane Library
Search date: 3 August 2017.
Date range searched: inception to 3 August 2017.
Records retrieved: 193.
Search name: ABA autism.
Last saved: 3 August 2017.
Search strategy
#1 MeSH descriptor: [Autistic Disorder] explode all trees
#2 MeSH descriptor: [Autism Spectrum Disorder] explode all trees
#3 MeSH descriptor: [Asperger Syndrome] explode all trees
#4 autism or autistic or ASD or ASDs or ASC or AAC:ti,ab,kw (Word variations have been searched)
#5 asperger*:ti,ab,kw (Word variations have been searched)
#6 #1 or #2 or #3 or #4 or #5
#7 MeSH descriptor: [Applied Behavior Analysis] explode all trees
#8 MeSH descriptor: [Early Intervention (Education)] explode all trees
#9 MeSH descriptor: [Behavior Therapy] explode all trees
#10 “early intervention therapy”:ti,ab,kw or :early intervention therapies”:ti,ab,kw (Word variations have been searched)
#11 intensive* near/2 (analys* or behavior* or behaviour* or intervention* or program* or therap* or treat*):ti,ab,kw or intensity near/2 (analys* or behavior* or behaviour* or intervention* or program* or therap* or treat*):ti,ab,kw or high-intensity near/2 (analys* or behavior* or behaviour* or intervention* or model* or program* or therap* or treat*):ti,ab,kw or low-intensity near/2 (analys* or behavior* or behaviour* or intervention* or model* or program* or therap* or treat*):ti,ab,kw (Word variations have been searched)
#12 “high intensity” near/2 (analys* or behavior* or behaviour* or intervention* or model* or program* or therap* or treat*):ti,ab,kw or “low intensity” near/2 (analys* or behavior* or behaviour* or intervention* or model* or program* or therap* or treat*):ti,ab,kw or “intensive behavior*” near/2 (analys* or intervention* or model* or program* or therap* or treat*):ti,ab,kw or “intensive behaviour*” near/2 (analys* or intervention* or model* or program* or therap* or treat*):ti,ab,kw (Word variations have been searched)
#13 “early behavior*” near/2 (analys* or intervention* or model* or program* or therap* or treat*):ti,ab,kw or “early behaviour*” near/2 (analys* or intervention* or model* or program* or therap* or treat*):ti,ab,kw or “comprehensive behavior*” near/2 (analys* or intervention* or model* or program* or therap* or treat*):ti,ab,kw or “comprehensive behaviour*” near/2 (analys* or intervention* or model* or program* or therap* or treat*):ti,ab,kw (Word variations have been searched)
#14 “applied behavior*” near/2 (analy* or intervention* or model* or program* or therap* or treat*):ti,ab,kw or “applied behaviour*” near/2 (analy* or intervention* or model* or program* or therap* or treat*):ti,ab,kw or ABA* near/2 (analy* or intervention* or model* or program* or therap* or treat*):ti,ab,kw (Word variations have been searched)
#15 NDBI*:ti,ab,kw or “Naturalistic Developmental Behav* Intervention*”:ti,ab,kw or IBI or EIBI or ABA:ti,ab,kw or Lovaas*:ti,ab,kw (Word variations have been searched)
#16 “Early Start Denver Model”:ti,ab,kw or “Denver Model”:ti,ab,kw or ESDM or ESDM-I or ESDM-PD or P-ESDM:ti,ab,kw (Word variations have been searched)
#17 “Pivotal Response” near/2 (treat* or train* or program*):ti,ab,kw or “PRT train*” or “PRT program*” or “PRT model*”:ti,ab,kw or “discrete trial train*”:ti,ab,kw (Word variations have been searched)
#18 #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17
#19 #6 and #18
Cumulative Index to Nursing and Allied Health Literature via EBSCOhost
Search date: 8 August 2017.
Date range searched: inception to 8 August 2017.
Records retrieved: 1530.
Search strategy
| Search term | Search option | Result |
|---|---|---|
| S1 | (MH “Autistic Disorder”) | 16,208 |
| S2 | (MH “Asperger Syndrome”) | 1328 |
| S3 | TX (autism or autistic or ASD or ASDs or ASC or AAC) OR asperger* | 25,580 |
| S4 | S1 OR S2 OR S3 | 25,580 |
| S5 | (MH “Applied Behavior Analysis”) | 3 |
| S6 | (MH “Early Childhood Intervention”) OR (MH “Early Intervention”) | 13,508 |
| S7 | (MH “Behavior Therapy”) | 8718 |
| S8 | TX “early intervention therap*” | 19 |
| S9 | TX intensive* N2 (analys* or behavior* or behaviour* or intervention* or program* or therap* or treat*) | 8836 |
| S10 | TX intensity N2 (analys* or behavior* or behaviour* or intervention* or program* or therap* or treat*) | 4820 |
| S11 | TX high-intensity N2 (analys* or behavior* or behaviour* or intervention* or model* or program* or therap* or treat*) | 544 |
| S12 | TX low-intensity N2 (analys* or behavior* or behaviour* or intervention* or model* or program* or therap* or treat*) | 535 |
| S13 | TX “high intensity” N2 (analys* or behavior* or behaviour* or intervention* or model* or program* or therap* or treat*) | 544 |
| S14 | TX “low intensity” N2 (analys* or behavior* or behaviour* or intervention* or model* or program* or therap* or treat*) | 534 |
| S15 | TX “intensive behavior*” N2 (analys* or intervention* or model* or program* or therap* or treat*) | 173 |
| S16 | TX “intensive behaviour*” N2 (analys* or intervention* or model* or program* or therap* or treat*) | 24 |
| S17 | TX “early behavior*” N2 (analys* or intervention* or model* or program* or therap* or treat*) | 18 |
| S18 | TX “early behaviour*” N2 (analys* or intervention* or model* or program* or therap* or treat*) | 4 |
| S19 | TX “comprehensive behavior*” N2 (analys* or intervention* or model* or program* or therap* or treat*) | 41 |
| S20 | TX “comprehensive behaviour*” N2 (analys* or intervention* or model* or program* or therap* or treat*) | 5 |
| S21 | TX “applied behavior*” N2 (analy* or intervention* or model* or program* or therap* or treat*) | 238 |
| S22 | TX “applied behaviour*” N2 (analy* or intervention* or model* or program* or therap* or treat*) | 36 |
| S23 | TX ABA* N2 (analys* or intervention* or model* or program* or therap* or treat*) | 750 |
| S24 | TX NDBI* OR TX “Naturalistic Developmental Behav* Intervention* “ OR TX (IBI or EIBI or ABA) OR TX Lovaas* OR TX “Early Start Denver Model” OR TX “Denver Model” OR TX (ESDM or ESDM-I or ESDM-PD or P-ESDM) | 1441 |
| S25 | TX (“Pivotal Response” N2 (treat* or train* or program*)) OR TX (“PRT train*” or “PRT program*” or “PRT model*”) OR TX “discrete trial train*” | 73 |
| S26 | S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 | 37,370 |
| S27 | S4 AND S26 | 1530 |
Conference Papers Citation Index via Web of Science
Search date: 8 August 2017.
Date range searched: inception to 8 August 2017.
Records retrieved: 46.
Search strategy
| Set | Results | Search options |
|---|---|---|
| # 7 | 46 |
#6 AND #1 Indexes = CPCI-S Timespan = All years |
| # 6 | 11,151 |
#5 OR #4 OR #3 OR #2 Indexes = CPCI-S Timespan = All years |
| # 5 | 27 |
TOPIC: (Lovaas*) OR TOPIC: (“Early Start Denver Model”) OR TOPIC: (“Denver Model”) OR TOPIC: (ESDM or ESDM-I or ESDM-PD or P-ESDM) OR TOPIC: (“Pivotal Response” NEAR/2 (treat* or train* or program*)) OR TOPIC: (“PRT train*” or “PRT program*” or “PRT model*”) OR TOPIC:(“discrete trial train*”) Indexes = CPCI-S Timespan = All years |
| # 4 | 3285 |
TOPIC: (“applied behavior*” NEAR/2 (analy* or intervention* or model* or program* or therap* or treat*)) OR TOPIC: (“applied behaviour*” NEAR/2 (analy* or intervention* or model* or program* or therap* or treat*)) OR TOPIC: (ABA* NEAR/2 (analys* or intervention* or model* or program* or therap* or treat*)) OR TOPIC: (NDBI) OR TOPIC: (“Naturalistic Developmental Behav* Intervention*”) OR TOPIC: (IBI or EIBI or ABA) Indexes = CPCI-S Timespan = All years |
| # 3 | 29 |
TOPIC: (“intensive behavior*” NEAR/2 (analys* or intervention* or model* or program* or therap* or treat*)) OR TOPIC: (“intensive behaviour*” NEAR/2 (analys* or intervention* or model* or program* or therap* or treat*)) OR TOPIC: (“early behavior*” NEAR/2 (analys* or intervention* or model* or program* or therap* or treat*)) OR TOPIC: (“early behaviour*” NEAR/2 (analys* or intervention* or model* or program* or therap* or treat*)) OR TOPIC: (“comprehensive behavior*” NEAR/2 (analys* or intervention* or model* or program* or therap* or treat*)) OR TOPIC: (“comprehensive behaviour*” NEAR/2 (analys* or intervention* or model* or program* or therap* or treat*)) Indexes = CPCI-S Timespan = All years |
| # 2 | 7833 |
TOPIC: (“early intervention therap*”) OR TOPIC: (intensive* NEAR/2 (analys* or behavior* or behaviour* or intervention* or program* or therap* or treat*)) OR TOPIC: (intensity NEAR/2 (analys* or behavior* or behaviour* or intervention* or program* or therap* or treat*)) OR TOPIC: (high-intensity NEAR/2 (analys* or behavior* or behaviour* or intervention* or model* or program* or therap* or treat*)) OR TOPIC: (low-intensity NEAR/2 (analys* or behavior* or behaviour* or intervention* or model* or program* or therap* or treat*)) OR TOPIC: (“high intensity” NEAR/2 (analys* or behavior* or behaviour* or intervention* or model* or program* or therap* or treat*)) OR TOPIC: (“low intensity” NEAR/2 (analys* or behavior* or behaviour* or intervention* or model* or program* or therap* or treat*)) Indexes = CPCI-S Timespan = All years |
| # 1 | 7148 |
TOPIC: (autism or autistic or ASD or ASDs or ASC or AAC) OR TOPIC: (asperger*) Indexes = CPCI-S Timespan = All years |
EMBASE via OVID
Search date: 3 August 2017.
Date range searched: inception to 3 August 2017.
Date range searched: 1974 to 2017 week 31.
Records retrieved: 2127.
Search strategy
-
Autism/(47,419)
-
Asperger Syndrome/(4044)
-
(autism or autistic or ASD or ASDs or ASC or AAC).ti,ab. (68,497)
-
Asperger$.ti,ab. (2656)
-
1 or 2 or 3 or 4 (79,183)
-
Behavior Modification/(7275)
-
Behavior Therapy/(41,005)
-
early intervention therap$.ti,ab. (78)
-
(intensive$ adj2 (analys$ or behavior$ or behaviour$ or intervention$ or program$ or therap$ or treat$)).ti,ab. (36,345)
-
(intensity adj2 (analys$ or behavior$ or behaviour$ or intervention$ or program$ or therap$ or treat$)).ti,ab. (10,909)
-
(high-intensity adj2 (analys$ or behavior$ or behaviour$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (1466)
-
(low-intensity adj2 (analys$ or behavior$ or behaviour$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (1364)
-
(high intensity adj2 (analys$ or behavior$ or behaviour$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (1466)
-
(low intensity adj2 (analys$ or behavior$ or behaviour$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (1364)
-
(intensive behavior$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (339)
-
(intensive behaviour$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (66)
-
(early behavior$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (58)
-
(early behaviour$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (13)
-
(comprehensive behavior$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (145)
-
(comprehensive behaviour$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (21)
-
(applied behavior$ adj2 (analy$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (391)
-
(applied behaviour$ adj2 (analy$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (74)
-
(ABA$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (4837)
-
NDBI$.ti,ab. (13)
-
Naturalistic Developmental Behav$ Intervention$.ti,ab. (5)
-
(IBI or EIBI or ABA).ti,ab. (9873)
-
Lovaas$.ti,ab. (43)
-
(Early Start Denver Model or Denver Model).ti,ab. (54)
-
(ESDM or ESDM-I or ESDM-PD or P-ESDM).ti,ab. (65)
-
(Pivotal Response adj2 (treat$ or train$ or program$)).ti,ab. (58)
-
(PRT train$ or PRT program$ or PRT model$).ti,ab. (66)
-
discrete trial train$.ti,ab. (35)
-
6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 (107,960)
-
5 and 33 (2173)
Education Resources Information Center via EBSCOhost
Search date: 8 August 2017.
Date range searched: inception to 8 August 2017.
Records retrieved: 2070.
Search strategy
| Search term | Search option | Result |
|---|---|---|
| S1 | (DE “Autism” or DE “Asperger Syndrome”) | 11,905 |
| S2 | (DE “Pervasive Developmental Disorders”) | 5920 |
| S3 | TX (autism or autistic or ASD or ASDs or ASC or AAC) OR asperger* | 14,033 |
| S4 | S1 OR S2 OR S3 | 14,161 |
| S5 | (DE “Early Intervention”) | 7149 |
| S6 | (DE “Behavior Modification”) | 9498 |
| S7 | TX “early intervention therap*” | 8 |
| S8 | TX intensive* N2 (analys* or behavior* or behaviour* or intervention* or program* or therap* or treat*) | 2510 |
| S9 | TX intensity N2 (analys* or behavior* or behaviour* or intervention* or program* or therap* or treat*) | 404 |
| S10 | TX high-intensity N2 (analys* or behavior* or behaviour* or intervention* or model* or program* or therap* or treat*) | 39 |
| S11 | TX low-intensity N2 (analys* or behavior* or behaviour* or intervention* or model* or program* or therap* or treat*) | 31 |
| S12 | TX “high intensity” N2 (analys* or behavior* or behaviour* or intervention* or model* or program* or therap* or treat*) | 39 |
| S13 | TX “low intensity” N2 (analys* or behavior* or behaviour* or intervention* or model* or program* or therap* or treat*) | 31 |
| S14 | TX “intensive behavior*” N2 (analys* or intervention* or model* or program* or therap* or treat*) | 209 |
| S15 | TX “intensive behaviour*” N2 (analys* or intervention* or model* or program* or therap* or treat*) | 9 |
| S16 | TX “early behavior*” N2 (analys* or intervention* or model* or program* or therap* or treat*) | 19 |
| S17 | TX “early behaviour*” N2 (analys* or intervention* or model* or program* or therap* or treat*) | 3 |
| S18 | TX “comprehensive behavior*” N2 (analys* or intervention* or model* or program* or therap* or treat*) | 27 |
| S19 | TX “comprehensive behaviour*” N2 (analys* or intervention* or model* or program* or therap* or treat*) | 0 |
| S20 | TX “applied behavior*” N2 (analy* or intervention* or model* or program* or therap* or treat*) | 2099 |
| S21 | TX “applied behaviour*” N2 (analy* or intervention* or model* or program* or therap* or treat*) | 44 |
| S22 | TX ABA* N2 (analys* or intervention* or model* or program* or therap* or treat*) | 251 |
| S23 | TX NDBI* OR TX “Naturalistic Developmental Behav* Intervention* “ OR TX (IBI or EIBI or ABA) OR TX Lovaas* OR TX “Early Start Denver Model” OR TX “Denver Model” OR TX (ESDM or ESDM-I or ESDM-PD or P-ESDM) | 477 |
| S24 | TX (“Pivotal Response” N2 (treat* or train* or program*)) OR TX (“PRT train*” or “PRT program*” or “PRT model*”) OR TX “discrete trial train*” | 125 |
| S25 | S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 | 20,716 |
| S26 | S4 AND S25 | 2070 |
Electronic Theses Online Service (The British Library)
Search date: 2 August 2017.
Date range searched: inception to 2 August 2017.
URL: http://ethos.bl.uk/Home.do
Search strategy
-
Intensive behavioural analysis (5)
-
Applied behavioural analysis (10)
-
1 and 2 (15)
MEDLINE via OVID
Search date: 3 August 2017.
Date range searched: inception to 3 August 2017.
Records retrieved: 1626 (after deduplication).
Search strategy
-
Autistic Disorder/ (18,816)
-
Autism Spectrum Disorder/ (2942)
-
Asperger Syndrome/ (1735)
-
(autism or autistic or ASD or ASDs or ASC or AAC).ti,ab. (52,030)
-
Asperger$.ti,ab. (1995)
-
1 or 2 or 3 or 4 or 5 (55,402)
-
Applied Behavior Analysis/ (5)
-
“Early Intervention (Education)”/ (2461)
-
Behavior Therapy/ (26,715)
-
early intervention therap$.ti,ab. (40)
-
(intensive$ adj2 (analys$ or behavior$ or behaviour$ or intervention$ or program$ or therap$ or treat$)).ti,ab. (26,198)
-
(intensity adj2 (analys$ or behavior$ or behaviour$ or intervention$ or program$ or therap$ or treat$)).ti,ab. (7977)
-
(high-intensity adj2 (analys$ or behavior$ or behaviour$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (1064)
-
(low-intensity adj2 (analys$ or behavior$ or behaviour$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (1102)
-
(high intensity adj2 (analys$ or behavior$ or behaviour$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (1064)
-
(low intensity adj2 (analys$ or behavior$ or behaviour$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (1102)
-
(intensive behavior$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (244)
-
(intensive behaviour$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (49)
-
(early behavior$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (39)
-
(early behaviour$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (13)
-
(comprehensive behavior$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (119)
-
(comprehensive behaviour$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (14)
-
(applied behavior$ adj2 (analy$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (452)
-
(applied behaviour$ adj2 (analy$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (39)
-
(ABA$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (3478)
-
NDBI$.ti,ab. (12)
-
Naturalistic Developmental Behav$ Intervention$.ti,ab. (5)
-
(IBI or EIBI or ABA).ti,ab. (10137)
-
Lovaas$.ti,ab. (37)
-
(Early Start Denver Model or Denver Model).ti,ab. (33)
-
(ESDM or ESDM-I or ESDM-PD or P-ESDM).ti,ab. (31)
-
(Pivotal Response adj2 (treat$ or train$ or program$)).ti,ab. (45)
-
(PRT train$ or PRT program$ or PRT model$).ti,ab. (46)
-
discrete trial train$.ti,ab. (33)
-
7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 (75,387)
-
6 and 35 (1717)
PsycINFO via OVID
Search date: 3 August 2017.
Date range searched: 1806 to July week 5 2017.
Records retrieved: 2248.
Search strategy
-
Autism Spectrum Disorder/ (35,797)
-
(autism or autistic or ASD or ASDs or ASC or AAC).ti,ab. (43,559)
-
Asperger$.ti,ab. (3376)
-
1 or 2 or 3 (45,868)
-
Behavior Modification/ (10,208)
-
Behavior Therapy/ (13,232)
-
early intervention therap$.ti,ab. (18)
-
(intensive$ adj2 (analys$ or behavior$ or behaviour$ or intervention$ or program$ or therap$ or treat$)).ti,ab. (5950)
-
(intensity adj2 (analys$ or behavior$ or behaviour$ or intervention$ or program$ or therap$ or treat$)).ti,ab. (1911)
-
(high-intensity adj2 (analys$ or behavior$ or behaviour$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (177)
-
(low-intensity adj2 (analys$ or behavior$ or behaviour$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (334)
-
(high intensity adj2 (analys$ or behavior$ or behaviour$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (177)
-
(low intensity adj2 (analys$ or behavior$ or behaviour$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (334)
-
(intensive behavior$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (381)
-
(intensive behaviour$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (64)
-
(early behavior$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (81)
-
(early behaviour$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (13)
-
(comprehensive behavior$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (140)
-
(comprehensive behaviour$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (9)
-
(applied behavior$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (1683)
-
(applied behaviour$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (118)
-
(ABA$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (847)
-
NDBI$.ti,ab. (3)
-
Naturalistic Developmental Behav$ Intervention$.ti,ab. (4)
-
(IBI or EIBI or ABA).ti,ab. (1410)
-
Lovaas$.ti,ab. (123)
-
(Early Start Denver Model or Denver Model).ti,ab. (44)
-
(ESDM or ESDM-I or ESDM-PD or P-ESDM).ti,ab. (35)
-
(Pivotal Response adj2 (treat$ or train$ or program$)).ti,ab. (127)
-
(PRT train$ or PRT program$ or PRT model$).ti,ab. (17)
-
discrete trial train$.ti,ab. (97)
-
5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 (33,512)
-
34 and 32 (2248)
Social Science Citation Index via Web of Science
Search date: 8 August 2017.
Date range searched: inception to 8 August 2017.
Records retrieved: 978.
Search strategy
| Set | Results | Search options |
|---|---|---|
| # 7 | 978 |
#6 AND #1 Indexes = SSCI Timespan = All years |
| # 6 | 11,712 |
#5 OR #4 OR #3 OR #2 Indexes = SSCI Timespan = All years |
| # 5 | 250 |
TOPIC: (Lovaas*) OR TOPIC: (“Early Start Denver Model”) OR TOPIC: (“Denver Model”) OR TOPIC: (ESDM or ESDM-I or ESDM-PD or P-ESDM) OR TOPIC: (“Pivotal Response” NEAR/2 (treat* or train* or program*)) OR TOPIC: (“PRT train*” or “PRT program*” or “PRT model*”) OR TOPIC:(“discrete trial train*”) Indexes = SSCI Timespan = All years |
| # 4 | 2864 |
TOPIC: (“applied behavior*” NEAR/2 (analy* or intervention* or model* or program* or therap* or treat*)) OR TOPIC: (“applied behaviour*” NEAR/2 (analy* or intervention* or model* or program* or therap* or treat*)) OR TOPIC: (ABA* NEAR/2 (analys* or intervention* or model* or program* or therap* or treat*)) OR TOPIC: (NDBI) OR TOPIC: (“Naturalistic Developmental Behav* Intervention*”) OR TOPIC: (IBI or EIBI or ABA) Indexes = SSCI Timespan = All years |
| # 3 | 584 |
TOPIC: (“intensive behavior*” NEAR/2 (analys* or intervention* or model* or program* or therap* or treat*)) OR TOPIC: (“intensive behaviour*” NEAR/2 (analys* or intervention* or model* or program* or therap* or treat*)) OR TOPIC: (“early behavior*” NEAR/2 (analys* or intervention* or model* or program* or therap* or treat*)) OR TOPIC: (“early behaviour*” NEAR/2 (analys* or intervention* or model* or program* or therap* or treat*)) OR TOPIC: (“comprehensive behavior*” NEAR/2 (analys* or intervention* or model* or program* or therap* or treat*)) OR TOPIC: (“comprehensive behaviour*” NEAR/2 (analys* or intervention* or model* or program* or therap* or treat*)) Indexes = SSCI Timespan = All years |
| # 2 | 8714 |
TOPIC: (“early intervention therap*”) OR TOPIC: (intensive* NEAR/2 (analys* or behavior* or behaviour* or intervention* or program* or therap* or treat*)) OR TOPIC: (intensity NEAR/2 (analys* or behavior* or behaviour* or intervention* or program* or therap* or treat*)) OR TOPIC: (high-intensity NEAR/2 (analys* or behavior* or behaviour* or intervention* or model* or program* or therap* or treat*)) OR TOPIC: (low-intensity NEAR/2 (analys* or behavior* or behaviour* or intervention* or model* or program* or therap* or treat*)) OR TOPIC: (“high intensity” NEAR/2 (analys* or behavior* or behaviour* or intervention* or model* or program* or therap* or treat*)) OR TOPIC: (“low intensity” NEAR/2 (analys* or behavior* or behaviour* or intervention* or model* or program* or therap* or treat*)) Indexes = SSCI Timespan = All years |
| # 1 | 36,199 |
TOPIC: (autism or autistic or ASD or ASDs or ASC or AAC) OR TOPIC: (asperger*) Indexes = SSCI Timespan = All years |
Searches of trials registers
ClinicalTrials.gov
Via: https://clinicaltrials.gov/ct2/home
Search date: 8 August 2017.
Date range searched: inception to 8 August 2017.
Ran a series of searches, downloaded records and deduplicated within EndNote bibliographic software.
Search strategy
Autism AND applied behavioural analysis = 20 records
Autism spectrum disorder AND applied behaviour analysis = 13 records
Autism AND ABA = 12 studies
Autism spectrum disorder AND ABA = 8 studies
Asperger syndrome AND applied behaviour analysis = 0
Asperger syndrome AND ABA = 0
Total of 53 records, deduplicated to 22 unique records.
World Health Organization International Clinical Trials Registry Platform
Via: http://apps.who.int/trialsearch/Default.aspx.
Search date: 8 August 2017.
Date range searched: inception to 8 August 2017.
Ran a series of searches, downloaded records and deduplicated within EndNote bibliographic software.
Search strategy
Autism AND applied behavior analysis = 2 records
Autism AND applied behaviour analysis = 1 record
Autism AND ABA = 2 studies
Asperger AND applied behaviour analysis = 0
Asperger syndrome AND ABA = 0
Total of five records, deduplicated to three unique records.
Appendix 3 Data coding dictionary
Sheet 1: participant and family characteristics and treatment details
If possible, please complete the ‘participant, family, treatment’ spreadsheet using the suggested coding below (this coding can also be found in comments on the relevant variable names in the spreadsheet itself).
If you use an alternative coding format please provide details of the coding used.
Please provide information on all study participants, even if individuals were excluded from analysis.
| Variable | Variable name in data file | Suggested coding | |
|---|---|---|---|
| Participant characteristic | Participant ID | ChildID | Any unique coding may be used |
| Date of randomisation or allocation to treatment | DateRandom | Date in dd/mm/yyyy format | |
| Age at baseline | AgeBaseline |
Numeric value (in months) 777 = not collected in trial 999 = missing for this participant |
|
| Sex | Sex |
1 = male 2 = female 777 = not collected in trial 999 = missing for this participant |
|
| Ethnicity | Ethnicity |
11 = African-American 12 = Afro-Caribbean 13 = African or other black ethnicity 21 = East Asian (e.g. Chinese/Japanese) 22 = South Asian (e.g. Indian/Pakistani) 31 = Hispanic or Latino 32 = Hispanic black 33 = Hispanic white 41 = Middle Eastern or North African 51 = Native American or First Nations 52 = Pacific Islander 61 = white European or North American 62 = other Caucasian/white 81 = mixed ethnicity (any) 82 = other 777 = not collected in trial 999 = missing for this participant |
|
| Diagnosis of ASD | ASDDiagnosis |
1 = ASD (DSM-5 or unspecified) 2 = Autistic disorder/childhood autism (DSM-IV/ICD-10) 3 = Asperger’s disorder/Asperger’s syndrome (DSM-IV/ICD-10) 4 = PDD-NOS/atypical autism/other pervasive developmental disorders (DSM-IV/ICD-10) 777 = not collected in trial 999 = missing for this participant |
|
| Age (in months) at ‘first mention’ diagnosis | AgefirstDiag |
Numeric value (in months) 777 = not collected in trial 999 = missing for this participant |
|
| Age (in months) at final confirmed diagnosis | AgeConfDiag |
Numeric value (in months) 777 = not collected in trial 999 = missing for this participant |
|
| Intellectual impairment at baseline | ASDIntel |
0 = no 1 = yes 777 = not collected in trial 999 = missing for this participant |
|
| Language impairment at baseline | ASDLang |
0 = no 1 = yes 777 = not collected in trial 999 = missing for this participant |
|
| Comorbidities at baseline | Comorbid |
1 = anxiety disorders 2 = mood disorders 3 = attention deficit hyperactivity disorder 4 = obsessive compulsive disorder/tic disorders (e.g. Tourette’s syndrome) 5 = oppositional defiant disorder/conduct disorder 6 = psychosis 7 = recognised genetic disorders, including chromosomal disorders 8 = seizures/epilepsy 9 = sensory sensitivities 10 = sleep disorders 11 = gastrointestinal symptoms (including feeding difficulties and food selectivity) 12 = other physical health problems (asthma, diabetes, immune disorders, etc) 13 = other (not mentioned above); please specify 777 = not collected in trial 888 = none/participants with comorbidities were excluded 999 = missing for this participant |
|
| Participant nursery/education setting | ChildEdu |
1 = mainstream setting (without specialist support) 2 = mainstream setting with specialist support 3 = specialist setting 4 = home educated 5 = none 777 = not recorded in trial 999 = missing for this participant |
|
| Family variable | Number of parents in the household | ParN |
Numeric value 777 = not collected in trial 999 = missing for this participant |
| Number of siblings in the household | SiblingN |
Numeric value 777 = not collected in trial 999 = missing for this participant |
|
| Parent conditions (present for any parent) | ParCond |
1 = ASD/Asperger’s syndrome 2 = intellectual disability 3 = depression or anxiety disorder 4 = other mental health condition 5 = physical health condition 6 = none 777 = not recorded in trial 999 = missing for this participant |
|
| Sibling conditions (present for any sibling) | SiblingCond |
1 = ASD/Asperger’s syndrome 2 = intellectual disability 3 = other developmental disorder 4 = depression or anxiety disorder 5 = other mental health condition 6 = physical health condition 7 = none 777 = not recorded in trial 999 = missing for this participant |
|
| Parental education (highest level for any parent in the household) | ParEdu |
1 = high school/secondary school 2 = post-secondary vocational or professional education 3 = Bachelor’s degree or equivalent level 4 = Master’s degree or equivalent level 5 = Doctoral degree or equivalent level 777 = not recorded in trial 999 = missing for this participant |
|
| Parental employment | ParWork |
1 = higher managerial, administrative or professional 2 = intermediate managerial, administrative or professional 3 = supervisory or clerical and junior managerial, administrative or professional 4 = skilled manual occupations 5 = semi-skilled and unskilled manual occupations 6 = casual or lowest grade occupations, pensioners and others who depend on the welfare state for their income 777 = not recorded in trial 999 = missing for this participant |
|
| Treatment variable | Treatment arm assigned | Arm |
0 = comparator 1 = ABA-based arm 1 2 = ABA-based arm 2 (if applicable) 3 = ABA-based arm 3 (if applicable) 999 = missing for this participant |
| Did the child receive discrete trial training techniques? | DTT |
0 = no 1 = yes 777 = not done in trial 999 = missing for this participant |
|
| Did the child receive incidental training techniques? | IT |
0 = no 1 = yes 777 = not done in trial 999 = missing for this participant |
|
| Did the child receive verbal behaviour techniques? | VB |
0 = no 1 = yes 777 = not done in trial 999 = missing for this participant |
|
| Did the child receive PRT techniques? | PRT |
0 = no 1 = yes 777 = not done in trial 999 = missing for this participant |
|
| Did the child receive CABAS techniques? | CABAS |
0 = no 1 = yes 777 = not done in trial 999 = missing for this participant |
|
| Did the child receive aversive techniques? | Aversive |
0 = no 1 = yes 777 = not done in trial 999 = missing for this participant |
|
| Number of interventionists (paid, professional, parental or volunteer) delivering the treatment to the child | InterN |
Numeric value 777 = not collected in trial 999 = missing for this participant |
|
| Who delivered the intervention? | InterDeliv |
1 = professional/specialist delivery alone 2 = parental delivery alone 3 = joint specialist/parental delivery 777 = not recorded in trial 999 = missing for this participant |
|
| Primary interventionist qualifications/experience (highest level for anyone delivering the intervention) | InterQual |
1 = RBT or equivalent 2 = BCaBA/relevant degree-level training or equivalent 3 = BCBA/relevant masters-level training or equivalent 4 = Doctoral-level BCBA-D/relevant PhD or equivalent 777 = not recorded in trial 999 = missing for this participant |
|
| Were interventionist(s) supervised? | Supervision |
0 = no 1 = yes 777 = not collected in trial 999 = missing for this participant |
|
| Supervisor qualification | SuperQual |
1 = RBT or equivalent 2 = BCaBA/relevant degree-level training or equivalent 3 = BCBA/relevant masters-level training or equivalent 4 = Doctoral-level BCBA-D/relevant PhD or equivalent 5 = parental supervision 6 = joint parental and professional supervision 777 = not recorded in trial 999 = missing for this participant |
|
| Average weekly treatment intensity (hours/week) | Intensity |
Numeric value (in hours/week) 777 = not collected in trial 999 = missing for this participant |
|
| Total number of hours of treatment received (over the entire treatment period) | TotalHours |
Numeric value (total hours of active treatment) 777 = not collected in trial 999 = missing for this participant |
|
| Total number of hours of treatment delivered by interventionist(s) (over the entire treatment period) | InterHours |
Numeric value (hours of active treatment) 777 = not collected in trial 999 = missing for this participant |
|
| Total number of hours of treatment delivered by parent(s) (over the entire treatment period) | ParentHours |
Numeric value (hours of active treatment) 777 = not collected in trial 888 = not applicable (no patient delivery) 999 = missing for this participant |
|
| Length of time over which the intervention was delivered to the child in the study (total number of weeks) | Duration |
Numeric value (total in weeks) 777 = not collected in trial 999 = missing for this participant |
|
| Treatment setting | Setting |
1 = home exclusively 2 = school exclusively 3 = clinic or specialist setting exclusively 4 = clinic and home 5 = school and home 6 = multiple settings 777 = not recorded in trial 999 = missing for this participant |
|
| Were co-intervention(s) received alongside treatment? | CoIntYN |
0 = no 1 = yes 777 = not collected in trial 999 = missing for this participant |
|
| Which co-interventions were received? | CoIntDetail |
Free text (150 characters maximum) For example, speech and language therapy; respite |
|
| Discontinuation of study treatment | DiscontinueTreat |
0 = no discontinuation 1 = discontinued due to lack of efficacy 2 = discontinued for reason other than lack of efficacy 3 = discontinued but reason not known 777 = not recorded in trial 999 = missing for this participant |
|
| Data handling | Whether or not participant was excluded from original study analysis | Exclusion |
0 = not excluded 1 = excluded 999 = unknown |
| Reason for exclusion | ReasonExcluded |
Free text (50 characters maximum). Please give brief description of reason for exclusion (e.g. lost to follow-up) 888 = not applicable (participant was not excluded) |
|
Sheets 2 and 3: baseline and outcome data (with key to collected outcomes)
Please describe the measures and types of scores that were used to collect baseline and follow-up data in the ‘key to collected outcomes’ spreadsheet. Please then add the values for these outcomes in the corresponding cells in the ‘baseline and outcome data’ sheet.
An illustration for each of these is given below and in the Excel workbook.
Illustration A: study-level details
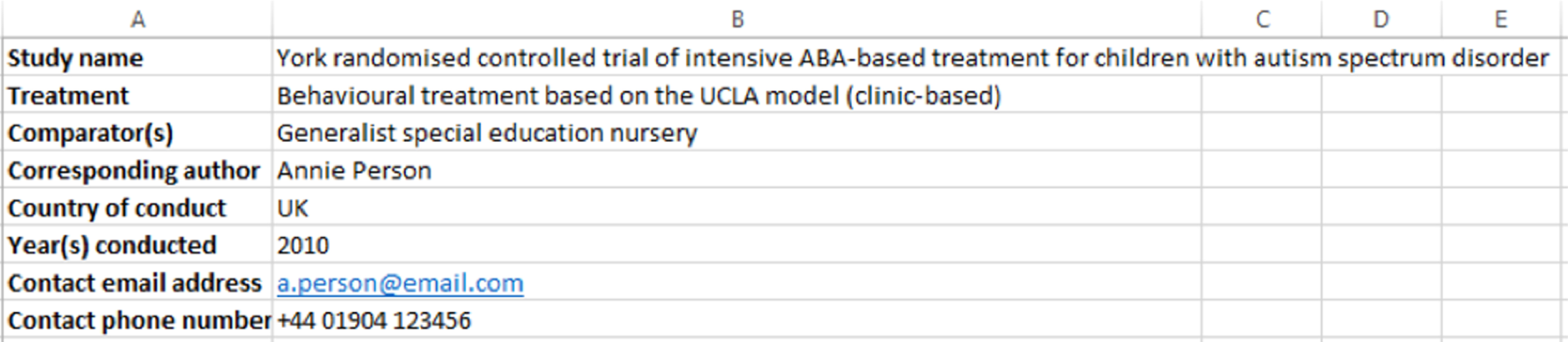
Illustration B: participant, family and treatment characteristics at baseline

Illustration C: key to collected outcome measures
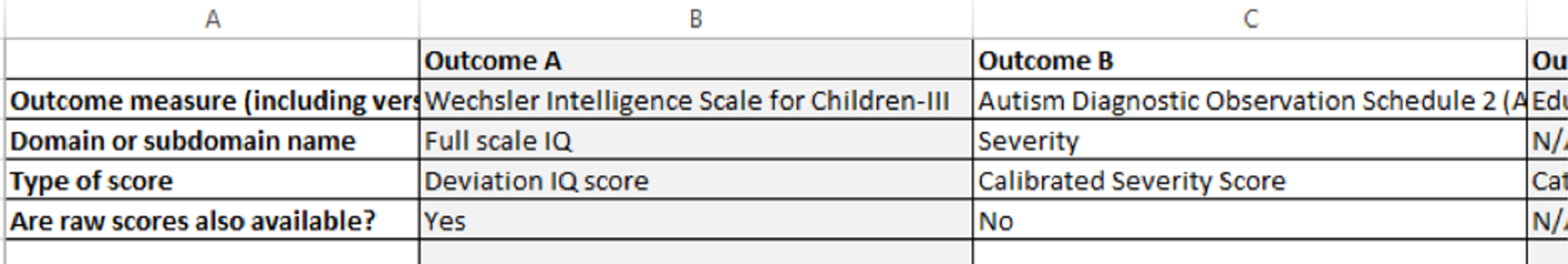
Illustration D: outcome measure values at baseline and follow-up
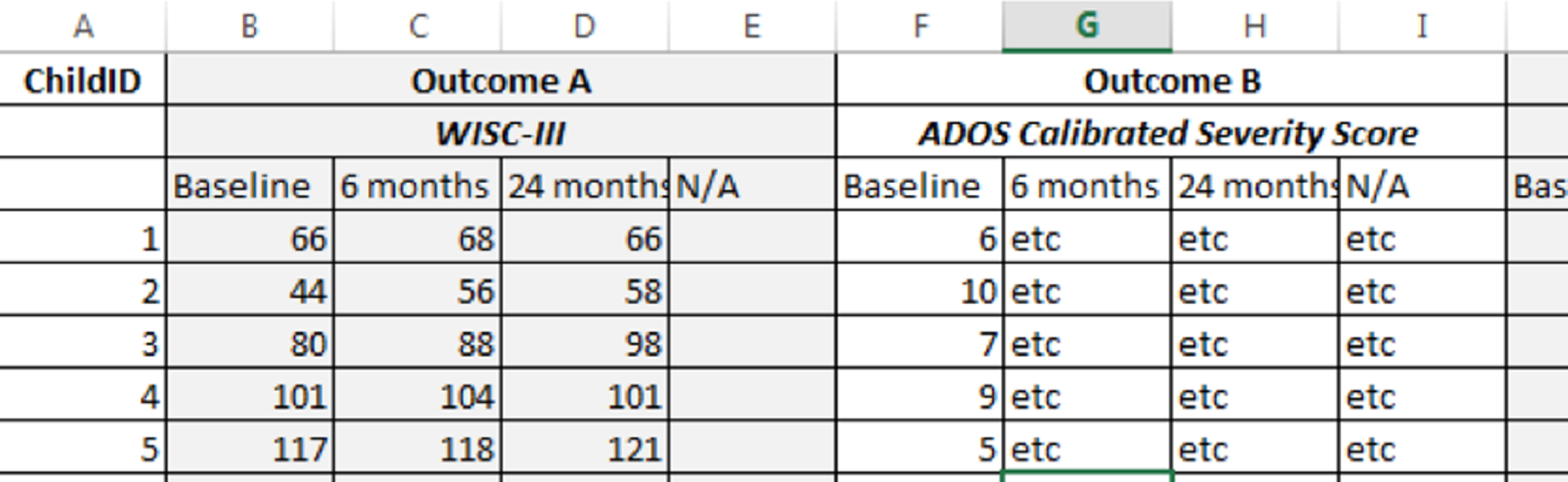
Whenever possible for continuous data, please provide exact rather than categorical values [e.g. ‘64’ rather than ‘≤70’ for WISC, Fourth Edition, full-scale IQ].
Please include the full name and version of each outcome measure that was used.
Appendix 4 Screening criteria
Participants, interventions, comparisons, outcomes, study design
Participants
Studies that include children with a diagnosis of autistic disorder, Asperger syndrome, PDD-NOS, atypical ASD or ASD.
Interventions
Intensive behavioural interventions based on ABA, defined as:
-
> 15 hours per week
-
comprehensive, targeting a range of behaviours not a single behaviour (e.g. joint attention)
-
ABA-based teaching strategies by qualified and trained staff
-
delivered at least initially on a one-to-one basis
-
qualified supervision of the therapist delivering the intervention.
Studies that involve a degree of parental involvement will be included if the other criteria are satisfied.
Comparators
Relevant comparators will include all other forms of early intervention.
Outcomes
Inclusion will not be restricted by outcome.
Study designs
Prospective RCTs and non-RCTs meeting all other inclusion criteria will be eligible for inclusion.
Coding options
-
Include: all criteria met.
-
Reject x: clearly outside scope. Give numbered reason(s) (e.g. non-comprehensive intervention = Reject 2B).
-
Borderline (explain reason): unclear based on available information. May include studies in which some but not all participants appear to meet inclusion criteria.
-
Contact: contact authors for missing information.
-
Review: systematic review.
-
Cost: potentially relevant to cost-effectiveness.
Appendix 5 Excluded studies
| Study | Reason for exclusion |
|---|---|
| Azarbehi AC. The effectiveness of early intervention programs for children with autism: A one-year follow-up study of Intensive Behavioural Intervention versus pre-school integration. Diss Abstr Int B Sci Eng 2012;73 | Abstract only and could not contact authors |
| Brian J. Evaluation of Social ABCs with Attention Training Intervention for Toddlers with Suspected Autism (NCT03215394). Bethesda, MD: ClinicalTrials.gov; 2017 | Abstract only and could not contact authors |
| Duifhuis EA, den Boer JC, Doornbos A, Buitelaar JK, Oosterling IJ, Klip H. The effect of pivotal response treatment in children with autism spectrum disorders: a non-randomized study with a blinded outcome measure. J Autism Dev Disord 2017;47:231–42 | Parent-focused intervention |
| Fava L, Strauss K, Valeri G, D’Elia L, Arima S, Vicari S. The effectiveness of a cross-setting complementary staff- and parent-mediated early intensive behavioral intervention for young children with ASD. Research Autism Spectr Disord 2011;5:1479–92 | Low-intensity intervention |
| Ghamari Kivi H, Nasoudi R. Efficacy of applied behavioral analysis in reducing symptoms of stereotyped behavior, interaction and communicational problems in autistic children. Iran J Psychiatry 2012;1:106–7 | Abstract only and could not contact authors |
| Goods KS, Ishijima E, Chang YC, Kasari C. Pre-school based JASPER intervention in minimally verbal children with autism: pilot RCT. J Autism Dev Disord 2013;43:1050–6 | Intervention did not satisfy inclusion criteria for comprehensiveness |
| Granpeesheh D, Kenzer A, Tarbox J. Comparison of Two-Year Outcomes for Children with Autism Receiving High Versus Low-Intensity Behavioral Intervention. European Psychiatry Conference: 19th European Congress of Psychiatry, EPA, 2011 | Abstract only and could not contact authors |
| Hayati M, Pelleshahi SR, Farrokhi N. Effect of multi-dimensional training program, using a combination method of TICH and ABA, on improve autistic children’s behavior. Eur Psychiatry 2017;41:S440 | Abstract only and could not contact authors |
| Howard J, Sparkman C, Cohen H, Green G, Stanislaw H. Correction concerning Howard et al. (2005). J Speech Lang Pathol Appl Behav Anal 2007;2:144–5 | Non-comparative study |
| Martin CN, Winter JM, Kim SH, Lord C. Integrated naturalistic developmental behavioral interventions for toddlers with autism: a pilot study of treatment efficacy and program feasibility within a community based setting. J Dev Behav Pediatr 2017;38:S10 | Abstract only and could not contact authors |
| Martsenkovsky I, Bikshaieva I, Vashenko O, Kazakova S. Efficacy of special early behavioral intervention (SEBI) in toddlers with autism spectrum disorders (ASD). Eur Child Adolesc Psychiatry 2011;20:S145 | Abstract only and could not contact authors |
| Mohammadzaheri F, Koegel LK, Rezaee M, Rafiee SM. A randomized clinical trial comparison between pivotal response treatment (PRT) and structured applied behavior analysis (ABA) intervention for children with autism. J Autism Develop Disord 2014;44:2769–77 | Low-intensity intervention |
| Molnar C, Eldevik S. [Behavioral intervention for pre-school children with autism – outcome of parent-based intervention.] Zeitschrift fur Kinder-und Jugendpsychiatrie und Psychotherapie 2017;45:181–91 | Non-comparative study |
| Nasoudi Ghareh Bolagh R, Zahednezhad H, Ilkhchi SV. The effectiveness of applied behavior analysis and treatment-education methods in children with autism disorders. Iran J Psychiatry 2012;1:106 | Abstract only and could not contact authors |
| Reed P, Osborne LA, Corness M. Effectiveness of special nursery provision for children with autism spectrum disorders. Autism 2010;14:67–82 | Low-intensity intervention |
| Reed P, Osborne LA, Makrygianni M, Waddington E, Etherington A, Gainsborough J. Evaluation of the Barnet early autism Model (BEAM) teaching intervention programme in a ‘real world’ setting. Res Autism Spec Disord 2013;7:631–8 | Low-intensity intervention |
| Rogers S. Intervention Effects of Intensity and Delivery Style for Toddlers with Autism (NCT02272192). Bethesda, MD: ClinicalTrials.gov; 2014 | Protocol only and could not contact authors |
| Schoneberger T. Autism research controversy: a response to Howard et al.’s (2005) defenders. J Speech Lang Pathol Appl Behav Anal 2007;2:242–50 | Non-comparative study |
| Shade-Monuteaux DM. An innovative approach for children with autism spectrum disorders: a preliminary outcome evaluation. Diss Abstr Int B Sci Eng 2003;63:6107 | Abstract only and could not contact authors |
| Sheinkopf SJ, Siegel B. Home-based behavioral treatment of young children with autism. J Autism Develop Disord 1998;28:15–23 | Non-comparative study |
| Smith T. Randomized Study of Intensive One-on-One Behavioral Treatment for Pre-School Aged Children with Autism (NCT00004449). Bethesda, MD: ClinicalTrials.gov; 1999 | Patient data already included |
| Soltanifar A, Hojati M, Mashhadi A, Reebye P. A Comparative Efficacy of HOLISTIC Multidimensional Treatment Model (HMTM) and Applied Behavioral Analysis (ABA) in the Treatment of Children with Autism Spectrum Disorder (ASD). European Psychiatry Conference, 19th European Congress of Psychiatry, EPA, 2011 | Abstract only and could not contact authors |
| Strauss K, Esposito M, Polidori G, Vicari S, Valeri G, Fava L. Facilitating play, peer engagement and social functioning in a peer group of young autistic children: comparing highly structured and more flexible behavioral approaches. Res Autism Spect Disord 2014;8:413–23 | Low-intensity intervention |
| Strauss K, Vicari S, Valeri G, D’Elia L, Arima S, Fava L. Parent inclusion in early intensive behavioral intervention: the influence of parental stress, parent treatment fidelity and parent-mediated generalization of behavior targets on child outcomes. Res Dev Disabil 2012;33:688–703 | Low-intensity intervention |
| Tang JC, Lee SH, Wang MC. The effects of pivotal response training on communicative behavior of pre-schoolers with autism. Int J Psychol 2008;43:592 | Non-comparative study |
| Wetherby AM, Guthrie W, Woods J, Schatschneider C, Holland RD, Morgan L, Lord C. Parent-implemented social intervention for toddlers with autism: an RCT. Pediatrics 2014;134:1084–93 | Parent-focused intervention |
| Xu Y, Yao J, Yang J. Application of Early Start Denver Model for early intervention on autistic children. Chin J Clin Psychol 2017;25:188–91 | Low-intensity intervention |
| Young HE, Falco RA, Hanita M. Randomized, controlled trial of a comprehensive program for young students with autism spectrum disorder. J Autism Dev Disord 2016;46:544–60 | Low-intensity intervention |
| Yuan Q, Wang RC, Wu ZF, Zhao Y, Bao XJ, Jin R. [Observation on clinical therapeutic effect of Jin’s 3-needling therapy on severe autism.] Zhongguo Zhenjiu 2009;29:177–80 | Abstract only and could not contact authors |
Appendix 6 Study characteristics tables
| General | Intervention details | Comparator details |
|---|---|---|
|
First author (year) Birnbrauer (1993)82 Sampling frame/population Children who were 24–48 months of age, met DSM-II criteria for pervasive developmental disorder or PDD-NOS, had attained intellectual and adaptive behaviour functioning levels of less than borderline and were free of sensory or physical impairments that would require special materials. Referrals were received from agencies concerned with autism and developmental disabilities, child health centres and medical practitioners in the Perth Metropolitan area When were participants recruited? NR How was autism diagnosed? Met the DSMIII-R criteria for pervasive developmental disorder autistic disorder and PDD-NOS How were participants allocated to intervention? Non-randomised. Allocated on the basis of location and when enrolled; families who met the selection criteria but lived too far away were invited to join the control group |
Intervention name Murdoch Early Intervention Program Is it based on a previous model? Yes If yes, which model is it based on? Based on Lovaas 198726 model, but differs in several aspects Was the intervention manualised? No Who delivers the intervention? Volunteer trainers with support from programme co-ordinator and mother Qualifications of the interventionist(s) Recruited from university students. On-the-job training Length of interventionist(s) experience None required Number of people delivering the intervention 24 Was the interventionist supervised? Yes Qualifications of the supervisor Experience with delivering behavioural techniques to children with disabilities Extent of parental involvement in delivery Supervisory role Where was the intervention delivered? Home based What was the planned intensity of intervention? 9–25 hours/week What was the planned duration of intervention? Approximately 24 months Were any co-interventions given? NR |
Comparator 1 name Not clearly described Is the comparator ABA based? No Is it based on a previous model? No Which model(s) is it based on? TAU Who delivers the comparator? NR Qualifications of the interventionist NR Length of interventionist experience n/a Number of people delivering the intervention n/a Extent of parental involvement in delivery n/a Where was the comparator delivered? n/a What was the planned intensity of the comparator? n/a What was the planned duration of the comparator? Approximately 24 months Were any co-interventions given? NR |
|
First author (year) Cohen (2006)104 Sampling frame/population Children with a diagnosis of autistic disorder or PDD-NOS, with a pre-treatment IQ > 35 on the BSIDR, chronological age between 18 and 42 months at diagnosis and < 48 months at treatment onset, with no severe medical limitation or illness that would preclude a child from participating and residence within 60 km of the treatment agency When were participants recruited? 1995–2000 How was autism diagnosed? Based on an evaluation by an independent licensed psychologist and confirmed by the ADI-R How were participants allocated to intervention? Parental choice |
Intervention name EIBI Is it based on a previous model? Yes If yes, which model is it based on? Lovaas/UCLA 198726 Was the intervention manualised? Yes Who delivers the intervention? Tutors were recruited from the community and were the main providers of direct services. Parents also contributed Qualifications of the interventionist(s) NR Length of interventionist(s) experience NR Number of people delivering the intervention NR Was the interventionist supervised? Yes Qualifications of the supervisor Graduate or Masters level with 2 years experience of EIBI Extent of parental involvement in delivery Weekly sessions at home Where was the intervention delivered? Primarily home based, with some peer play and classroom inclusion What was the planned intensity of intervention? 30 hours/week of one to one (20 hours with therapist, > 10 hours with parents) What was the planned duration of intervention? 3 years [17 participants completed 3 years and four did not complete (two at 6 months and two in the second year)] Were any co-interventions given? NR |
Comparator 1 name TAU (participants received a number of interventions, including an early start intervention programme, ‘home-based developmental intervention’ or public school special day class using eclectic methodology) Is the comparator ABA based? NR Is it based on a previous model? No Which model(s) is it based on? NR Who delivers the comparator? Various Qualifications of the interventionist NR Length of interventionist experience NR Number of people delivering the intervention NR Extent of parental involvement in delivery NR Where was the comparator delivered? Various What was the planned intensity of the comparator? NR What was the planned duration of the comparator? 3 years [17 participants completed 3 years and four did not complete (two at 6 months and two in the second year)] Were any co-interventions given? Speech, occupational and behavioural therapy (0–5 hours/week), brief sessions in mainstreamed education |
|
First author (year) Dawson (2010, 2012);83,106 Sullivan (2014);112 Estes (2015)107 Sampling frame/population Children aged between 18 and 30 months diagnosed with autistic disorder or PDD-NOS Exclusion criteria Neurodevelopmental disorder, significant sensory or motor impairment, major physical problems, seizures at time of entry, use of psychoactive medications, history of a serious head injury and/or neurological disease, alcohol or drug exposure during the prenatal period and ratio IQ < 35 (as measured by the MSEL) When were participants recruited? NR How was autism diagnosed? Meeting criteria for autism or ASD on the ADOS and a clinical diagnosis based on DSM-IV criteria How were participants allocated to intervention? Individually randomised, stratified by IQ and gender |
Intervention name ESDM Is it based on a previous model? Yes If yes, which model is it based on? ESDM Was the intervention manualised? Yes Who delivers the intervention? Therapist for 20 hours/week, parents for anything above that Qualifications of the interventionist(s) Bachelors degree in education or related field plus 2 months’ training Length of interventionist(s) experience NR Number of people delivering the intervention NR Was the interventionist supervised? Yes Qualifications of the supervisor Masters degree and 5 years’ experience Extent of parental involvement in delivery Minimum of 10 hours/week on top of intervention hours (actual amount was 16.3 hours) Where was the intervention delivered? Home based What was the planned intensity of intervention? 30 hours/week one to one (20 hours with therapist, > 10 hours with parents) What was the planned duration of intervention? 2 years Were any co-interventions given? 5.2 hours in other therapies (e.g. speech therapy, developmental preschool) |
Comparator 1 name ‘Assess and Monitor’ community intervention (interventions delivered by Birth-to-Three centres and individual providers delivering speech and language therapy, occupational therapy and/or ABA treatments) Is the comparator ABA based? Inconsistent Is it based on a previous model? Variety of interventions designed to ameliorate the impact of autism and enhance functioning Which model(s) is it based on? n/a Who delivers the comparator? Various Qualifications of the interventionist NR Length of interventionist experience NR Number of people delivering the intervention NR Extent of parental involvement in delivery NR Where was the comparator delivered? Various What was the planned intensity of the comparator? NR What was the planned duration of the comparator? 2 years Were any co-interventions given? NR |
|
First author (year) Eikeseth (2012)84 Sampling frame/population Children diagnosed with autism enrolled at Banyan Centre (Sweden) (intervention); total population of children diagnosed with autism at Akershus University Hospital (Nordbyhagen, Norway) (control) When were participants recruited? Intervention between March 2008 and May 2010; control between 2005 and 2010 How was autism diagnosed? An independent agency prior to referral to the centre, based on the ICD-10 criteria158 How were participants allocated to intervention? Place of diagnosis |
Intervention name Community school-based EIBI Is it based on a previous model? Yes If yes, which model is it based on? Lovaas/UCLA 198726 Was the intervention manualised? Yes Who delivers the intervention? School’s staff as therapists Qualifications of the interventionist(s) None required Length of interventionist(s) experience None required Number of people delivering the intervention NR Was the interventionist supervised? Yes Qualifications of the supervisor Bachelors or Masters degree Extent of parental involvement in delivery 10 hours/week Where was the intervention delivered? School (parents at home) What was the planned intensity of intervention? Not stated. Actual received was 15–37 hours/week plus 10 hours/week of parent involvement What was the planned duration of intervention? 2 years Were any co-interventions given? NR |
Comparator 1 name Eclectic special education teaching Is the comparator ABA based? Partially Is it based on a previous model? Yes Which model(s) is it based on? Eclectic special education teaching model. [The treatment incorporated elements from a variety of different interventions, such as alternative communication, total communication, TEACCH, sensory–motor therapies, ABA, as well as procedures derived from teachers’ own clinical experience] Who delivers the comparator? Special education teacher and teaching assistant Qualifications of the interventionist NR Length of interventionist experience None required Number of people delivering the intervention 2 Extent of parental involvement in delivery NR Where was the comparator delivered? Preschools or kindergartens What was the planned intensity of the comparator? Special education teacher worked 3–5 hours/week/child plus teaching assistant was hired to work one to one with the child (but no planned time duration was reported) What was the planned duration of the comparator? 2 years Were any co-interventions given? NR |
|
First author (year) Sampling frame/population Children from Akershus and Vestfold, Norway, with a diagnosis of childhood autism (ICD-10), with a chronological age between 4 and 7 years at the time of intake, and without any major medical conditions other than autism When were participants recruited? November 1995–November 1998 How was autism diagnosed? ADI-R and an independent child clinical psychologist How were participants allocated to intervention? Availability of qualified supervisors for behavioural treatment |
Intervention name Intensive behavoural treatment based on the UCLA treatment model (EIBI) Is it based on a previous model? Yes If yes, which model is it based on? Lovaas et al. 1981,159 and Lovaas and Leaf 1981160 Was the intervention manualised? Yes Who delivers the intervention? Therapist/special education teacher Qualifications of the interventionist(s) None required Length of interventionist(s) experience None required Number of people delivering the intervention NR Was the interventionist supervised? Yes Qualifications of the supervisor Bachelors or Masters degree Extent of parental involvement in delivery 4 hours/week Where was the intervention delivered? Public kindergartens and elementary schools What was the planned intensity of intervention? Minimum 20 hours/week What was the planned duration of intervention? 1 year Were any co-interventions given? NR |
Comparator 1 name Intensive eclectic special education Is the comparator ABA based? Partially Is it based on a previous model? Partially Which model(s) is it based on? Included elements from a variety of different interventions, such as project TEACCH (Schopler et al. 1983161), sensory–motor therapies (Ayres 1972162) and ABA (Lovaas et al. 1981159), as well as methods derived from personal experience Who delivers the comparator? Therapist/special education teacher Qualifications of the interventionist NR Length of interventionist experience NR Number of people delivering the intervention NR Extent of parental involvement in delivery NR Where was the comparator delivered? Public kindergartens and elementary schools What was the planned intensity of the comparator? Minimum 20 hours/week What was the planned duration of the comparator? 1 year Were any co-interventions given? NR |
|
First author (year) Eldevik (2012)86 Sampling frame/population Children with ASD aged between 2 and 6 years, receiving > 5 hours/week of intervention at an EIBI centre and children receiving TAU in their local mainstream school When were participants recruited? January 2000–February 2011 How was autism diagnosed? ADI-R How were participants allocated to intervention? Cohort |
Intervention name EIBI Is it based on a previous model? Yes If yes, which model is it based on? Widely used EIBI manuals (Leaf and McEachin 1999;163 Lovaas et al. 1981, 2003;159,164 Maurice et al. 1996;165 Sundberg and Partington 1998166) Was the intervention manualised? Yes Who delivers the intervention? Therapists recruited from preschool staff Qualifications of the interventionist(s) NR Length of interventionist(s) experience NR Number of people delivering the intervention Two or three Was the interventionist supervised? Yes Qualifications of the supervisor Bachelors degree and 2–10 years’ experience with EIBI Extent of parental involvement in delivery Encouraged to ensure generalisation and maintenance of skills at home Where was the intervention delivered? Mainstream preschool What was the planned intensity of intervention? NR What was the planned duration of intervention? 2 years Were any co-interventions given? NR |
Comparator 1 name TAU (eclectic) Is the comparator ABA based? Partially Is it based on a previous model? Partially Which model(s) is it based on? Eclectic special education teaching model (alternative communication, ABA, total communication, sensory–motor therapies, programmes based on the principles from TEACCH, as well as other methods that were incorporated based on the personal experience of the particular special education teacher and staff) Who delivers the comparator? Preschool staff Qualifications of the interventionist NR Length of interventionist experience NR Number of people delivering the intervention NR Extent of parental involvement in delivery NR Where was the comparator delivered? Mainstream preschool What was the planned intensity of the comparator? NR What was the planned duration of the comparator? 2 years Were any co-interventions given? NR |
|
First author (year) Farrell (2005)87 Sampling frame/population EIBI group: children whose parents had lobbied for the intervention. Comparator: children selected by educational psychologist contributing to a statutory assessment When were participants recruited? 1999 How was autism diagnosed? Educational psychologist How were participants allocated to intervention? Cohort/parental preference |
Intervention name EIBI Is it based on a previous model? Yes If yes, which model is it based on? Lovaas 198726 Was the intervention manualised? Yes Who delivers the intervention? Therapists with parental support Qualifications of the interventionist(s) NR Length of interventionist(s) experience NR Number of people delivering the intervention Up to five Was the interventionist supervised? Yes Qualifications of the supervisor NR Extent of parental involvement in delivery NR Where was the intervention delivered? Home What was the planned intensity of intervention? At least 30 hours What was the planned duration of intervention? 2 years Were any co-interventions given? NR |
Comparator 1 name Lancashire Under Fives Autism Project Is the comparator ABA based? Partially Is it based on a previous model? Yes Which model(s) is it based on? Lancashire Under Fives Autism Project Who delivers the comparator? Teaching assistants Qualifications of the interventionist NR Length of interventionist experience NR Number of people delivering the intervention NR Extent of parental involvement in delivery NR Where was the comparator delivered? School What was the planned intensity of the comparator? School full time What was the planned duration of the comparator? 2 years Were any co-interventions given? NR |
|
First author (year) Haglund (2017, conference abstract only)88 Sampling frame/population Children with ASD aged ≤ 6 years in Skane county, Sweden When were participants recruited? Autumn 1998–spring 2005 How was autism diagnosed? DSM-IV/ICD 10 How were participants allocated to intervention? Parental preference: children of parents rejecting the ABA-based intervention acted as the comparator group |
Intervention name Comprehensive intensive early interventions Is it based on a previous model? Yes If yes, which model is it based on? NDBI programme described by Schreibman et al. 28 Was the intervention manualised? Yes Who delivers the intervention? Therapists/parents Qualifications of the interventionist(s) Preschool teaching/educational background Length of interventionist(s) experience NR Number of people delivering the intervention NR Was the interventionist supervised? Yes Qualifications of the supervisor NR Extent of parental involvement in delivery Some Where was the intervention delivered? Combination What was the planned intensity of intervention? 15–25 hours/week What was the planned duration of intervention? 2 years Were any co-interventions given? NR |
Comparator 1 name TAU Is the comparator ABA based? No Is it based on a previous model? Variety of interventions designed to ameliorate the impact of autism and enhance functioning Which model(s) is it based on? None Who delivers the comparator? NR Qualifications of the interventionist NR Length of interventionist experience NR Number of people delivering the intervention NR Extent of parental involvement in delivery NR Where was the comparator delivered? NR What was the planned intensity of the comparator? NR What was the planned duration of the comparator? 2 years Were any co-interventions given? NR |
|
First author (year) Hayward (2009)99 Sampling frame/population Children who joined the UK Young Autism Project When were participants recruited? NR How was autism diagnosed? ICD-10 (confirmed with ADI-R) How were participants allocated to intervention? By catchment area |
Intervention name EIBI, clinic managed Is it based on a previous model? Yes If yes, which model is it based on? UCLA Was the intervention manualised? Yes Who delivers the intervention? Therapists Qualifications of the interventionist(s) NR Length of interventionist(s) experience NR Number of people delivering the intervention Two to five Was the interventionist supervised? Yes Qualifications of the supervisor > 3 years’ clinical experience as an EIBI tutor and senior tutor Extent of parental involvement in delivery NR Where was the intervention delivered? Home What was the planned intensity of intervention? NR (37 hours actual) What was the planned duration of intervention? 1 year Were any co-interventions given? NR |
Comparator 1 name EIBI, parent managed Is the comparator ABA based? Yes Is it based on a previous model? Yes Which model(s) is it based on? UCLA Who delivers the comparator? Therapists Qualifications of the interventionist NR Length of interventionist experience NR Number of people delivering the intervention Two to five Extent of parental involvement in delivery NR Where was the comparator delivered? Home What was the planned intensity of the comparator? NR (34 hours actual) What was the planned duration of the comparator? 1 year Were any co-interventions given? NR |
|
First author (year) Sampling frame/population Children with ASD referred by non-profit agencies under contract with the State of California Department of Developmental Services When were participants recruited? 1996–2003 How was autism diagnosed? DSM-IV by independent examiner How were participants allocated to intervention? Cohort |
Intervention name Early intensive behaviour analytic treatment Is it based on a previous model? Yes If yes, which model is it based on? UCLA Was the intervention manualised? Yes Who delivers the intervention? Trained therapists Qualifications of the interventionist(s) Undergraduate students Length of interventionist(s) experience NR Number of people delivering the intervention Four or five Was the interventionist supervised? Yes Qualifications of the supervisor Bachelor’s or Master’s degree in psychology or special education Extent of parental involvement in delivery Some Where was the intervention delivered? Combination of home, school, community What was the planned intensity of intervention? 25–40 hours/week What was the planned duration of intervention? 14 months Were any co-interventions given? NR |
Comparator 1 name Autism educational programming: eclectic autism-specific classroom-based intervention Is the comparator ABA based? Partially Is it based on a previous model? NR Which model(s) is it based on? NR Who delivers the comparator? Teaching assistants Qualifications of the interventionist NR Length of interventionist experience NR Number of people delivering the intervention Four to eight Extent of parental involvement in delivery NR Where was the comparator delivered? School What was the planned intensity of the comparator? 25–30 hours/week What was the planned duration of the comparator? 14 months Were any co-interventions given? Speech and language therapy Comparator 2 name General educational programming: generic special education classroom intervention for children with a variety of disabilities Is the comparator ABA based? No Is it based on a previous model? No Which model(s) is it based on? NR Who delivers the comparator? Teaching assistants Qualifications of the interventionist NR Length of interventionist experience NR Number of people delivering the intervention Four to eight Extent of parental involvement in delivery NR Where was the comparator delivered? School What was the planned intensity of the comparator? 15 hours/week What was the planned duration of the comparator? 14 months Were any co-interventions given? NR |
|
First author (year) Remington (2007);92 Kovshoff (2011)110 Sampling frame/population Referrals from local education authorities, through advertisements placed with the UK NAS, its regional branches and through parent groups or charities When were participants recruited? NR How was autism diagnosed? Independent assessor, confirmed by ADI-R How were participants allocated to intervention? Parental preference |
Intervention name EIBI Is it based on a previous model? Yes If yes, which model is it based on? UCLA Was the intervention manualised? Yes Who delivers the intervention? Trained tutors and parents Qualifications of the interventionist(s) NR Length of interventionist(s) experience NR Number of people delivering the intervention Three to five Was the interventionist supervised? Yes Qualifications of the supervisor ‘Substantial experience with EIBI’ Extent of parental involvement in delivery Some Where was the intervention delivered? Home What was the planned intensity of intervention? 40 hours/week What was the planned duration of intervention? 2 years Were any co-interventions given? Dietary, TEACCH, medication, vitamin supplementation, homeopathy and speech therapy |
Comparator 1 name TAU Is the comparator ABA based? No Is it based on a previous model? Variety of interventions designed to ameliorate the impact of autism and enhance functioning (including speech therapy, TEACCH, PECS, sign language or Makaton) Which model(s) is it based on? None Who delivers the comparator? NR Qualifications of the interventionist NR Length of interventionist experience NR Number of people delivering the intervention NR Extent of parental involvement in delivery n/a Where was the comparator delivered? NR What was the planned intensity of the comparator? NR What was the planned duration of the comparator? 2 years Were any co-interventions given? Dietary, medication, vitamin supplementation, homeopathy |
|
First author (year) Lovaas (1987);26 McEachin (1993)98 Sampling frame/population UCLA diagnosed When were participants recruited? NR How was autism diagnosed? Independent assessor using DSM-III criteria How were participants allocated to intervention? Staff availability (low-intensity group); historical controls (untreated group) |
Intervention name EIBI Is it based on a previous model? Yes If yes, which model is it based on? UCLA Was the intervention manualised? Yes Who delivers the intervention? Trained student therapists, parents Qualifications of the interventionist(s) Students Length of interventionist(s) experience NR Number of people delivering the intervention NR Was the interventionist supervised? NR Qualifications of the supervisor NR Extent of parental involvement in delivery Some Where was the intervention delivered? Home, school and community What was the planned intensity of intervention? 40 hours/week, one to one What was the planned duration of intervention? ≥ 2 years Were any co-interventions given? No |
Comparator 1 name Lower-intensity ABA-based treatment Is the comparator ABA based? Yes Is it based on a previous model? Yes Which model(s) is it based on? UCLA Who delivers the comparator? Trained student therapists, parents Qualifications of the interventionist Students Length of interventionist experience NR Number of people delivering the intervention NR Extent of parental involvement in delivery Some Where was the comparator delivered? Home, school and community What was the planned intensity of the comparator? < 10 hours/week, one to one What was the planned duration of the comparator? ≥ 2 years Were any co-interventions given? Small special educational classes Comparator 2 name No treatment; no further details available |
|
First author (year) Magiati (2007, 2011);89,96 Howlin (2007)109 Sampling frame/population UK-based LEAs, specialist schools, diagnostic centres and NAS When were participants recruited? July 1998–April 2000 How was autism diagnosed? Independent diagnosis confirmed by ADI-R How were participants allocated to intervention? Cohort (parental choice) |
Intervention name EIBI Is it based on a previous model? Yes If yes, which model is it based on? UCLA Was the intervention manualised? Yes Who delivers the intervention? Therapist Qualifications of the interventionist(s) Undergraduate student or graduate in psychology or special education Length of interventionist(s) experience NR Number of people delivering the intervention Nine Was the interventionist supervised? Yes Qualifications of the supervisor NR Extent of parental involvement in delivery Some Where was the intervention delivered? Home based What was the planned intensity of intervention? 18–40 hours/week, one to one What was the planned duration of intervention? 2 years Were any co-interventions given? Range of dietary, biological, educational interventions and alternative treatments |
Comparator 1 name Autism-specific nursery (school provisions) Is the comparator ABA based? Partially Is it based on a previous model? Partially Which model(s) is it based on? Eclectic Who delivers the comparator? Led by tutor Qualifications of the interventionist NR Length of interventionist experience NR Number of people delivering the intervention NR Extent of parental involvement in delivery NR Where was the comparator delivered? School based What was the planned intensity of the comparator? Nursery hours = 15–30 hours/week. One to one = 6 hours (range 1.5–25 hours/week) What was the planned duration of the comparator? 2 years Were any co-interventions given? Range of dietary, biological and educational interventions |
|
First author (year) Sampling frame/population NR When were participants recruited? NR How was autism diagnosed? NR How were participants allocated to intervention? Location |
Intervention name High-intensity ABA-based interventions Is it based on a previous model? Yes If yes, which model is it based on? UCLA, CABAS and verbal behaviour Was the intervention manualised? Yes Who delivers the intervention? Tutors Qualifications of the interventionist(s) NR Length of interventionist(s) experience NR Number of people delivering the intervention NR Was the interventionist supervised? Yes Qualifications of the supervisor NR Extent of parental involvement in delivery Some Where was the intervention delivered? Home based What was the planned intensity of intervention? 20–40 hours/week, one to one What was the planned duration of intervention? 9–10 months Were any co-interventions given? NR |
Comparator 1 name Low-intensity ABA-based intervention Is the comparator ABA based? Yes Is it based on a previous model? NR Which model(s) is it based on? NR Who delivers the comparator? Tutors Qualifications of the interventionist NR Length of interventionist experience NR Number of people delivering the intervention NR Extent of parental involvement in delivery NR Where was the comparator delivered? Home based What was the planned intensity of the comparator? 10–20 hours/week What was the planned duration of the comparator? 9–10 months Were any co-interventions given? NR Comparator 2 name Special nursery placements (TAU) Is the comparator ABA based? NR Is it based on a previous model? Partially Which model(s) is it based on? Eclectic Who delivers the comparator? Group, led by tutor Qualifications of the interventionist Teaching assistant Length of interventionist experience NR Number of people delivering the intervention NR Extent of parental involvement in delivery NR Where was the comparator delivered? School based What was the planned intensity of the comparator? 2–23 hours/week What was the planned duration of the comparator? 9 months Were any co-interventions given? NR Comparator 3 name Portage Is the comparator ABA based? No Is it based on a previous model? Yes Which model(s) is it based on? Portage Who delivers the comparator? NR Qualifications of the interventionist NR Length of interventionist experience NR Number of people delivering the intervention NR Extent of parental involvement in delivery Full Where was the comparator delivered? Home based What was the planned intensity of the comparator? 2–15 hours/week What was the planned duration of the comparator? 9 months Were any co-interventions given? NR |
|
First author (year) Sallows (2005)100 Sampling frame/population Children were recruited through local birth to three (special education) programmes When were participants recruited? 1996–7 How was autism diagnosed? DSM-IV with ADI-R How were participants allocated to intervention? RCT (matched pairs) |
Intervention name Clinic-directed UCLA-based intervention Is it based on a previous model? Yes If yes, which model is it based on? UCLA/Lovaas26 Was the intervention manualised? Yes Who delivers the intervention? Therapists Qualifications of the interventionist(s) Undergraduate level. 30 hours training, including ≥ 10 hours of one-to-one training and feedback Length of interventionist(s) experience NR Number of people delivering the intervention NR Was the interventionist supervised? Yes Qualifications of the supervisor Graduate, 1 year of experience with two or more children, 16-week internship programme modelled after UCLA model (total 2000 hours) Extent of parental involvement in delivery Some Where was the intervention delivered? Home based What was the planned intensity of intervention? 40 hours/week What was the planned duration of intervention? 2 years Were any co-interventions given? Preschool special education, speech therapy, sensory integration, auditory integration training, music therapy, horseback riding, special diets, vitamin/Dimethylglycine treatment, Nystatin (Sandoz Ltd, Surrey, UK), intravenous immune globulin (distribution between treatment groups unclear) |
Comparator 1 name Parent-directed UCLA Is the comparator ABA based? Yes Is it based on a previous model? Yes Which model(s) is it based on? UCLA Who delivers the comparator? Therapists Qualifications of the interventionist Undergraduate level. 30 hours training, including ≥ 10 hours of one-to-one training and feedback Length of interventionist experience NR Number of people delivering the intervention NR Extent of parental involvement in delivery Some [McEachin (1993)98], home-based What was the planned intensity of the comparator? 30 hours/week What was the planned duration of the comparator? 2 years Were any co-interventions given? Preschool special education, speech therapy, sensory integration, auditory integration training, music therapy, horseback riding, special diets, vitamin/Dimethylglycine treatment, Nystatin, intravenous immune globulin (distribution between treatment groups unclear) |
|
First author (year) Smith (2000)103 Sampling frame/population Referrals with autism to the UCLA Young Autism Project When were participants recruited? 1989–92 How was autism diagnosed? Independent licensed practititioners How were participants allocated to intervention? RCT (matched pairs) |
Intervention name Intensive behavioural treatment Is it based on a previous model? Yes If yes, which model is it based on? UCLA/Lovaas26 Was the intervention manualised? Yes Who delivers the intervention? Student therapist. Parents for 5 hours/week Qualifications of the interventionist(s) Undergraduate Length of interventionist(s) experience NR Number of people delivering the intervention Five or six Was the interventionist supervised? Yes Qualifications of the supervisor Graduate, programme trained, 1500 hours, one-to-one experience Extent of parental involvement in delivery 5 hours/week for the first 3 months Where was the intervention delivered? Home based for 1 year then school based What was the planned intensity of intervention? 30 hours/week What was the planned duration of intervention? 2 years Were any co-interventions given? NR |
Comparator 1 name Parent training Is the comparator ABA-based? Yes Is it based on a previous model? Yes Which model(s) is it based on? UCLA Who delivers the comparator? Parent Qualifications of the interventionist 5 hours/week training for 6–9 months Length of interventionist experience NR Number of people delivering the intervention NR Extent of parental involvement in delivery Primary therapist Where was the comparator delivered? Home based What was the planned intensity of the comparator? NR What was the planned duration of the comparator? 2 years Were any co-interventions given? Special education class for 10–15 hours per week |
|
First author (year) Stock (2013)101 Sampling frame/population Children with ASD enrolled in a private group ABA preschool programme located in a large city in western Canada and children enrolled in a government-funded autism intervention programme in Nova Scotia, Canada When were participants recruited? NR How was autism diagnosed? ADOS, ADI-R and clinical diagnosis How were participants allocated to intervention? Cohort (with selected matched pairs) |
Intervention name Nova Scotia EIBI Is the comparator ABA based? Yes Is it based on a previous model? Yes Which model(s) is it based on? PRT Who delivers the comparator? Therapist/parent Qualifications of the interventionist Early childhood educator Length of interventionist experience NR Number of people delivering the intervention NR Extent of parental involvement in delivery Encouraged Where was the comparator delivered? Home and preschool based What was the planned intensity of the comparator? 15 hours/week one to one for 12 months; or 15 hours/week one to one for 6 months; 10 hours/week for 3 months; 5 hours/week for 3 months What was the planned duration of the comparator? 12 months Were any co-interventions given? NR |
Comparator name Group ABA Is it based on a previous model? Yes If yes, which model is it based on? Verbal behaviour Was the intervention manualised? Yes Who delivers the intervention? Therapist Qualifications of the interventionist(s) Early childhood education background Length of interventionist(s) experience NR Number of people delivering the intervention NR Was the interventionist supervised? Yes Qualifications of the supervisor Masters or doctoral clinicians who were BCBAs Extent of parental involvement in delivery Encouraged Where was the intervention delivered? Preschool-like and home-based settings What was the planned intensity of intervention? 15–25 hours/week (3–5 hours/week one to one) What was the planned duration of intervention? 12 months Were any co-interventions given? NR |
|
First author (year) Vivanti (2014)93 Sampling frame/population Eligibility criteria for enrolment in two service centres in Australia that require a diagnosis of ASD from a medical professional (paediatrician or child psychiatrist) and chronological age up to 6 years When were participants recruited? NR How was autism diagnosed? ADOS How were participants allocated to intervention? Cohort |
Intervention name ESDM Is it based on a previous model? Yes If yes, which model is it based on? ESDM Was the intervention manualised? Yes Who delivers the intervention? Trained therapists/teachers Qualifications of the interventionist(s) EDSM introductory and advanced training Length of interventionist(s) experience NR Number of people delivering the intervention NR Was the interventionist supervised? NR Qualifications of the supervisor NR Extent of parental involvement in delivery Some Where was the intervention delivered? School based What was the planned intensity of intervention? 15–20 hours/week What was the planned duration of intervention? 12 months Were any co-interventions given? NR |
Comparator 1 name ‘Generic’ intervention Is the comparator ABA based? No, but included some elements Is it based on a previous model? Yes Which model(s) is it based on? Eclectic (incorporated aspects of TEACCH, PRT, other naturalistic approaches, PECS) Who delivers the comparator? Trained therapists/teachers Qualifications of the interventionist NR Length of interventionist experience NR Number of people delivering the intervention NR Extent of parental involvement in delivery Some, included regular parent training Where was the comparator delivered? School based What was the planned intensity of the comparator? 15 hours/week What was the planned duration of the comparator? 12 months Were any co-interventions given? NR |
|
First author (year) Zachor (2007)94 Sampling frame/population Children with ASD based in two centres from different counties, receiving the same budget per child from national agencies When were participants recruited? NR How was autism diagnosed? ADI-R and DSM-IV How were participants allocated to intervention? Cohort |
Intervention name ABA Is it based on a previous model? Yes If yes, which model is it based on? ‘Based on ABA principles’ Was the intervention manualised? Yes Who delivers the intervention? Skilled behavioural therapists Qualifications of the interventionist(s) NR Length of interventionist(s) experience NR Number of people delivering the intervention NR Was the interventionist supervised? Yes Qualifications of the supervisor Trained behaviour analyst Extent of parental involvement in delivery NR Where was the intervention delivered? Centre based What was the planned intensity of intervention? 35 hours/week What was the planned duration of intervention? 12 months Were any co-interventions given? NR |
Comparator 1 name Eclectic development approach Is the comparator ABA based? Partially Is it based on a previous model? Yes Which model(s) is it based on? Eclectic (developmental individual–difference relationship model; TEACCH; ABA) Who delivers the comparator? Special education teacher Qualifications of the interventionist NR Length of interventionist experience NR Number of people delivering the intervention NR Extent of parental involvement in delivery NR Where was the comparator delivered? Centre based What was the planned intensity of the comparator? Unclear (2 hours/week of individual sessions, 1 hour of group therapy from each therapist in additon to daily work in small group activities) What was the planned duration of the comparator? 12 months Were any co-interventions given? NR |
|
First author (year) Zachor (2010)97 Sampling frame/population Children with ASD from seven autism-specific early intervention community-based preschool centres, receiving the same budget per child from national agencies When were participants recruited? NR How was autism diagnosed? ADI-R and DSM-IV How were participants allocated to intervention? Cohort |
Intervention name ABA Is it based on a previous model? Yes If yes, which model is it based on? ‘Based on ABA principles’ Was the intervention manualised? Yes Who delivers the intervention? Skilled behavioural therapists Qualifications of the interventionist(s) Graduates in behavioural analysis principles, overseen by programme supervisor Length of interventionist(s) experience NR Number of people delivering the intervention Three ABA therapists, one speech and language therapist, one occupational therapist, one special education preschool teacher Was the interventionist supervised? Yes Qualifications of the supervisor Masters degree in psychology or special education and BCBA Extent of parental involvement in delivery Parents received weekly instructions for home treatment from the behaviour analyst Where was the intervention delivered? Centre based with home support What was the planned intensity of intervention? 40 hours/week in preschool, with 20 hours of one-to-one intervention What was the planned duration of intervention? 12 months Were any co-interventions given? NR |
Comparator 1 name ‘Eclectic’ Is the comparator ABA based? Unclear Is it based on a previous model? Yes Which model(s) is it based on? Eclectic (developmental model; developmental individual–difference relationship model; TEACCH) Who delivers the comparator? Clinical psychologist, speech and language therapist, occupational therapist, special education preschool teacher, music therapist, teacher’s aids Qualifications of the interventionist NR Length of interventionist experience NR Number of people delivering the intervention Five Extent of parental involvement in delivery ‘Active parental participation in the programme’ Where was the comparator delivered? Centre based What was the planned intensity of the comparator? 40 hours/week in preschool, with 19 hours of one-to-one intervention What was the planned duration of the comparator? 12 months Were any co-interventions given? NR |
Appendix 7 Individual participant data obtained from authors
| IPD | Study author (year) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cohen (2006)104 | Eikeseth (2002, 2007)85,95 | Hayward (2009)99 | Eldevik (2012)86 | Lovaas (1987, 1993)26,98 | Magiati (2007, 2011)89,96 | Smith (2000)103 | Vivanti (2014)93 | Eikeseth (2012)84 | Reed (2007)90,91 | Remington (2007)92 | Stock (2013)101 | Sallows (2005)100 | Zachor (2007)94 | Zachor (2010)97 | ||
| Participant characteristic | Participant ID | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Date of randomisation or allocation to treatment | No information | Yes | No | No information | Not coded | NC | NC | Yes | No information | No information | Not coded | No information | No information | No information | No information | |
| Age at baseline | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | NC | Yes | Yes | Yes | |
| Sex | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| Ethnicity | NC | No information | No information | No information | Not available | Yes | Yes | No information | No information | No information | NC | NC | NC | Not coded | Not coded | |
| Diagnosis of ASD | Yes | No information | No information | Yes | No information | Yes | Yes | No information | No information | No information | Not coded | Yes | Not coded | Yes | Yes | |
| Age (in months) at ‘first mention’ diagnosis | NC | No information | No information | No information | Not available | No information | NC | No information | No information | No information | NC | NC | Not coded | NC | NC | |
| Age (in months) at final confirmed diagnosis | Yes | No information | No information | No information | Not available | No information | Yes | No information | No information | No information | NC | NC | Not coded | Not coded | Not coded | |
| Intellectual impairment at baseline | Yes | No information | No information | Yes | Yes | Yes | Yes | No information | No information | Not coded | Not coded | NC | Yes | Not coded | Not coded | |
| Language impairment at baseline | Yes | No information | No information | No information | Yes | Yes | Yes | No information | No information | Not coded | Not coded | NC | Yes | NC | NC | |
| Comorbidities at baseline | NC | No information | No information | No information | Not included | Yes | NC | No information | No information | NC | NC | NC | No information | NC | NC | |
| Participant nursery/education setting | Yes | No information | No information | No information | Yes | Yes | Yes | No information | No information | No information | NC | Yes | Yes | Not coded | Not coded | |
| Family variables | Number of parents in the household | Yes | No information | No information | No information | Not available | Yes | Yes | No information | No information | No information | NC | NC | Not coded | Not coded | Not coded |
| Number of siblings in the household | NC | No information | No information | No information | Not available | Yes | Yes | No information | No information | No information | NC | NC | NC | Yes | Yes | |
| Parent conditions | NC | No information | No information | No information | NC | NC | NC | No information | No information | No information | NC | NC | NC | Yes | Yes | |
| Family variables | Sibling conditions (present for any sibling) | NC | No information | No information | No information | NC | Yes | NC | No information | No information | No information | NC | NC | NC | Yes | Yes |
| Parental education (highest level for any parent in the household) | Yes | No information | No information | No information | Not available | Yes | Yes | No information | No information | No information | Yes | NC | Not coded | Not coded | Not coded | |
| Parental employment | NC | No information | No information | No information | NC | Yes | NC | No information | No information | No information | NC | NC | Not coded | NC | NC | |
| Treatment variables | Treatment arm assigned | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Did the child receive discrete trial training techniques? | Yes | No information | No information | No information | Yes | Yes | Yes | No information | No information | Not coded | Yes | Yes | Yes | Yes | Yes | |
| Did the child receive incidental training techniques? | Yes | No information | No information | No information | Yes | NC | Yes | No information | No information | Not coded | Yes | Yes | Yes | Yes | Yes | |
| Did the child receive verbal behaviour techniques? | Yes | No information | No information | No information | Yes | NC | Yes | No information | No information | Not coded | Yes | Yes | Yes | NC | NC | |
| Did the child receive PRT techniques? | Yes | No information | No information | No information | Yes | NC | Yes | No information | No information | Not coded | Yes | Yes | Yes | NC | NC | |
| Did the child receive CABAS techniques? | Yes | No information | No information | No information | Yes | NC | Yes | No information | No information | Not coded | Yes | Yes | Yes | NC | NC | |
| Did the child receive aversive techniques? | Yes | No information | No information | No information | Yes | Yes | Yes | No information | No information | No information | NC | Yes | Yes | NC | NC | |
| Treatment variables | Number of interventionists (paid, professional, parental, or volunteer) delivering the treatment to the child | NC | No information | No information | No information | NC | Yes | Yes | No information | No information | Yes | NC | NC | NC | Not coded | Not coded |
| Who delivered the intervention? | No information | No information | No information | No information | Not coded | Yes | Not coded | No information | No information | Not coded | Not coded | Yes | No information | Not coded | Not coded | |
| Primary interventionist qualifications/experience (highest level for anyone delivering the intervention) | Yes | No information | No information | No information | Yes | Yes | Yes | No information | No information | Not coded | NC | Yes | Yes | Not coded | Not coded | |
| Were interventionists supervised? | Yes | No information | No information | No information | Yes | Yes | Yes | No information | No information | Not coded | Yes | Yes | Yes | Not coded | Not coded | |
| Supervisor qualification | Yes | No information | No information | No information | Yes | Yes | Yes | No information | No information | No information | Yes | Yes | Yes | Not coded | Not coded | |
| Average weekly treatment intensity (hours/week) | NC | No information | No information | EIBI only | NC | Yes | NC | No information | EIBI only | Yes | NC | No information | Not coded | Not coded | Not coded | |
| Total number of hours of treatment received (over the entire treatment period) | NC | No information | No information | No information | NC | Yes | Yes | No information | No information | Not coded | NC | NC | Not coded | Not coded | Not coded | |
| Total number of hours of treatment delivered by interventionist(s) (over the entire treatment period) | NC | No information | No information | No information | NC | Yes | Yes | No information | No information | Not coded | NC | NC | Not coded | Not coded | Not coded | |
| Treatment variables | Total number of hours of treatment delivered by parent(s) (over the entire treatment period) | NC | No information | No information | No information | NC | Yes | NC | No information | No information | No information | NC | NC | NC | NC | NC |
| Length of time over which the intervention was delivered to the child in the study (total number of weeks) | NC | No information | No information | Yes | NC | Yes | NC | No information | No information | Not coded | NC | Yes | NC | Not coded | Not coded | |
| Treatment setting | EIBI only | No information | No information | No information | Yes | EIBI only | Yes | No information | No information | Not coded | EIBI only | Yes | Yes | Not coded | Not coded | |
| Were co-intervention(s) received alongside treatment? | EIBI only | No information | No information | No information | Not included | Yes | Yes | No information | No information | No information | NC | NC | Yes | NC | NC | |
| Which co-interventions were received? | No information | No information | No information | No information | Not included | Yes | NC | No information | No information | No information | NC | NC | No information | NC | NC | |
| Discontinuation of study treatment | Yes | No information | No information | No information | Yes | NC | Yes | No information | No information | No information | NC | Yes | Yes | No information | No information | |
| Data handling | Whether or not participant was excluded from original study analysis | Yes | No information | No information | No information | Yes | Yes | Yes | No information | No information | Not coded | No information | Yes | Yes | Not coded | Not coded |
| Reason for exclusion | Yes | No information | No information | No information | Yes | Yes | Yes | No information | No information | Not coded | No information | Yes | Yes | Not coded | Not coded | |
Appendix 8 Outcome domains and measures
Studies providing individual participant data
Of the 15 studies that provided IPD (see Appendix 7), all reported collecting data on at least two of the following outcome domains: verbal or non-verbal IQ or cognitive development score, autism symptom severity, challenging behaviour, adaptive behaviour (as a composite score and/or communication, daily living skills, socialisation or motor skills subscores), language ability (expressive, receptive or total scores), parental outcomes and school placement. Less consistently reported outcome domains included academic achievement, symbolic play, joint attention, social communication, maladaptive behaviour, change in autism diagnosis, skill acquisition and emotional, behavioural, social or cognitive adjustment (Table 32).
| First study author (year) | IQ/cognitive development score | Non-verbal IQ | Autism symptom severity scores | Challenging behaviour | Communication | Daily living | Socialisation | Motor skills | Composite | Expressive language | Receptive language | Total | Parental outcomes | School placement | Other |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ABA vs. TAU/eclectic | |||||||||||||||
| Cohen (2006)104 | BSID-R; WPPSI | MPSMT | VABS | VABS | VABS | VABS | VABS | RDLS | RDLS | ‘Regular education classroom setting’a | |||||
| Eikeseth (2002/7)85,95 | BSID-R; WISC-R; WPPSI-R | MPSMT; WISC-R; WPPSI-R | ABCb | VABS | VABS | VABS | VABS | RDLS | RDLS | RDLS | VABS maladaptive behaviour | ||||
| Eikeseth (2012)84 | CARS (EIBI arm only) | VABS | VABS | VABS | VABS | VABS | VABS maladaptive behaviour (EIBI arm only); learning rate | ||||||||
| Eldevik (2012)86 | BSID-II/III; S–B4/5; WPPSI-R | VABS | VABS | VABS | VABS | VABS | |||||||||
| Magiati (2007,2011)89,96 | BSID; WPPSI-R; WISC-IV; WPPSI-III; MPSMT | MPSMT | ADI-R; ADOS CSS | VABS | VABS | VABS | VABS | VABS | EOWPVT | BPVS-II | School placement | ||||
| Reed (2007)90,91 | PEP-R; BAS-II | GARS | CRS-R (subscales) | VABS | VABS | VABS | VABS | VABS | |||||||
| Remington (2007);92 Kovshoff (2011)110 | BSID-IV; S–B | ADI-R | NCBRF; DBC | VABS | VABS | VABS | VABS | VABS | RDLS-3c | RDLS-3c | Stress; anxiety; depression; positive perceptions | School placement | Autism Screening Questionnaire; Early Social Communication Scales (joint attention) | ||
| Vivanti (2014)93 | MSEL | ADOS CSS | VABS | VABS | VABS | VABS | VABS | MSEL | MSEL | SCQ | |||||
| Zachor (2007)94 | BSID-II; S–B4 | ADI; ADOS | VABS | VABS | VABS | VABS | VABS | Change in autism diagnosis | |||||||
| Zachor (2010)97 | MSEL | ADI-R; ADOS | VABS | VABS | VABS | VABS | VABS | MSEL | MSEL | ||||||
| High vs. low | |||||||||||||||
| Lovaas (1987)26/McEachin (1993)98 | BSID; CIIS; GIDS; WISC-R; S–B; PPVT; WPPSI; LIPS | VABSd | VABSd | VABSd | VABSd | ‘In regular classes’ | VABS maladaptive behaviour (reported at age 8–9 years follow-up in EIBI arm only); Personality Inventory for Children; behavioural observations | ||||||||
| Smith (2009)103 | BSID-II; S–B5 | MPSMT | CBCL | VABS | VABS | VABS | VABS | RDLS | RDLS | RDLS | Family Satisfaction Questionnaire | Classroom placemente | Academic achievement (WIAT); skill acquisition (Early Learning Measure); behavioural observation | ||
| Clinic vs. parent | |||||||||||||||
| Hayward (2009)99 | BSID-R; WPPSI-R | MPSMT | ADI-R | VABS | VABS | VABS | VABS | VABS | RDLSf | RDLSf | |||||
| Sallows (2005)100 | BSID I/II; WPPSI; WISC-III | MPSMT | ADI-R | CBCL | VABS | VABS | VABS | VABS | RDLS; CELF-III | RDLS; CELF-III | School placementa | Personality Inventory for Children; academic achievement (Woodcock–Johnson III Tests of Achievement) | |||
| VB vs. PRT | |||||||||||||||
| Stock (2013)101 | S–B5; MSEL; WPPSI-III | CBCL | VABS | PLS-4 | PLS-4 | PSI | |||||||||
Across all comparisons, a variety of scales were used to measure IQ and cognitive development, most commonly versions of the BSID, S–B, WISC and WPPSI. When different scales were used within studies, this was typically due to the need to select an age-appropriate scale. Non-verbal intelligence was most commonly measured using the MPSMT and autism symptom severity with the ADOS or ADI-R. Although adaptive behaviour was consistently measured using the VABS, language was measured using a variety of scales, most commonly the RDLS. Parental outcomes were not measured frequently or consistently across studies and, although six studies collected school placement data,26,89,92,96,98,100,103,104,109,110 IPD were available for only three26,89,96,98,103,109 and the method of classification was not entirely consistent across these studies.
Outcomes reported in publications compared with outcomes available in individual participant data
The outcome measures most commonly missing from the IPD related to behaviours that challenge (three studies85,92,95,100,110), followed by autism symptom severity (two studies94,100), parental outcomes (two studies92,103,110) and school placement (two studies92,100,110). For four studies,86,89,94,96,97,109 the IPD provided by investigators included outcome data that were not reported in their associated publications.
Studies not providing individual participant data
Of the five studies82,83,87,88,105,107,112 that did not provide IPD, one study88 had not published any outcome data. The remaining four studies82,83,87,105,107,112 reported data on the following outcome domains: IQ, adaptive behaviour (as a composite score and/or communication, daily living skills, socialisation or motor skills subscores), and language ability (expressive, receptive, or total scores). Only one study83,107,112 reported autism symptom severity and behaviour that challenges and only one reported on parental stress (Table 33). Less consistently reported outcome domains included academic achievement, symbolic play, joint attention, social communication, maladaptive behaviour, change in autism diagnosis, skill acquisition and emotional, behavioural, social or cognitive adjustment (see Table 32).
| First study author (year) | IQ/cognitive development score | Non-verbal IQ | Autism symptom severity scores | Challenging behaviour | Communication | Daily living | Socialisation | Motor skills | Composite | Expressive | Receptive | Total | Parental outcomes | School placement | Other |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ABA vs. TAU/eclectic | |||||||||||||||
| Birnbrauer (1993)82 | BSID-R; PPVT; S–B5; WISC; WPPSI | LIPS | VABS | RDLS; REELS | RDLS; REELS | PSI | Personality inventory for children; behavioural observation | ||||||||
| Dawson (2010);83 Estes (2015);107 Sullivan (2014)112 | MSEL; DAS | ADOS CSS | ABCa | VABS | VABS | VABS | VABS | VABS | MSEL | MSEL | RBS-R; change in autism diagnosis; visual reception (MSEL); fine motor (MSEL); shared positive effect; gesture use | ||||
| Farrell (2005)87 | BSID | VABS | VABS | VABS | |||||||||||
| bHaglund (2017)88 | |||||||||||||||
| Howard (2005)105 | BSID-II; DP-II; DAS; WPPSI-R; S–B4; PEP-R; DAYC | MPSMT; LIPS | VABS | VABS | VABS | VABS | VABS | RDLS; REELS; EVT; EOWPVT; ITLS; PLS-3; ITDA; DP-II; SICD-R; PPVT-III | RDLS; REELS; ITLS; PLS3; ITDA; EVT; DP-II; SICD-R; PPVT-III; ROWPVT | RDLS; REELS; EVT; EOWPVT; ITLS; PLS3; ITDA; EVT; DP-II; SICD-R; PPVT-III; ROWPVT | |||||
Appendix 9 Risk-of-bias assessment
Applied behaviour analysis-based early intensive interventions compared with treatment as usual and eclectic comparators
Fourteen of the 15 included studies reported results in at least one publication, and 10 of these studies provided IPD. Just one study was randomised and was assessed using the Cochrane Risk of Bias tool. 83,106,107,112 Risk of bias in the remaining non-randomised studies was assessed using the ROBINS-I tool. 82,84,85,87–97,104,105,108–110 All studies were rated as being at ‘serious’ or ‘high’ risk of bias for at least one outcome on one domain on the relevant assessment tool (Tables 34 and 35).
| Domain | Cohen (2006)104 | Eikeseth (2002, 2007)85,95 | Eikeseth (2012)84 | |||
|---|---|---|---|---|---|---|
| Risk-of-bias judgement by outcome | Comment | Risk-of-bias judgement by outcome | Comment | Risk-of-bias judgement by outcome | Comment | |
| Bias due to confounding |
IQ: serious MPSMT: serious RDLS: serious VABS: serious Personal Inventory for Children: serious |
Parents chose intervention. Comparator children matched on unknown variables. Parents in EIBI group had significantly more education and were more likely to be living in the same household In authors’ original analysis, baseline values of dependent variables included in ANCOVA but not baseline age |
IQ: serious Performance IQ: serious Language functioning: serious VABS: serious Achenbach CBCL: serious |
Allocation by supervisor availability, so not obviously influenced by parental preference No socioeconomic or parent/family data collected No data on severity |
IQ: serious VABS: serious |
Allocation by place of diagnosis. Unclear if this was influenced by parental preference No socioeconomic or parent/family data collected |
| Bias in selection of participants into the study |
IQ: moderate MPSMT: moderate RDLS: moderate VABS: moderate Personal Inventory for Children: moderate |
Simultaneous start of comparator and follow-up not established |
IQ: moderate Performance IQ: moderate Language functioning: moderate VABS: moderate Achenbach CBCL: moderate |
Simultaneous start of comparator and follow-up not established |
IQ: moderate VABS: moderate |
Comparison groups were not entirely concurrent (eclectic special education recruited 2005–10, EIBI recruited 2008–10) Simultaneous start of comparator and follow-up not established |
| Bias in classification of interventions |
IQ: low MPSMT: low RDLS: low VABS: low Personal Inventory for Children: low |
Misclassification unlikely |
IQ: low Performance IQ: low Language functioning: low VABS: low Achenbach CBCL: low |
Misclassification unlikely |
IQ: low VABS: low |
Misclassification unlikely |
| Bias due to deviations from intended interventions |
IQ: moderate MPSMT: moderate RDLS: moderate VABS: moderate Personal Inventory for Children: moderate |
EIBI fidelity assessed Eight of 21 children did not complete EIBI No available information on co-interventions |
IQ: moderate Performance IQ: moderate Language functioning: moderate VABS: moderate Achenbach CBCL: moderate |
No data on fidelity, but EIBI was manualised and supervised 42% of children in the eclectic group received some form of ABA No available data on co-interventions |
IQ: moderate VABS: moderate |
The eclectic special education comparator incorporated aspects of ABA The authors state that data on number of weekly hours of EIBI delivered was of ‘low reliability’ No available data on co-interventions |
| Bias due to missing data/IPD |
IQ: low MPSMT: low RDLS: low VABS: low Personal Inventory for Children: low |
IPD were reasonably complete for available outcomes |
IQ: low Performance IQ: low Language functioning: low VABS: low Achenbach CBCL: low |
Some of the collected baseline and outcome measures were missing (although the amount of missing data were small, mostly from two participants) |
IQ: low VABS: low |
2-year data were only collected for 15 of 59 participants Other outcome data largely complete |
| Bias in measurement of outcomes |
IQ: moderate MPSMT: moderate RDLS: moderate VABS: moderate Personal Inventory for Children: moderate |
Outcomes assessed by independent evaluator, but truly blinded assessment unlikely |
IQ: moderate Performance IQ: moderate Language functioning: moderate VABS: moderate Achenbach CBCL: moderate |
Outcome assessors were independent of the study and were not informed of the children’s group assignment, although truly blinded assessment difficult to achieve Age-appropriate measures used throughout |
IQ: serious VABS: serious CARS: serious |
Severity data (CARS) and VABS maladaptive scores were only collected for the EIBI group (not comparator group) Outcome assessors were treatment supervisors (EIBI group) and hospital staff (comparison group). None were blinded |
| Bias in selection of the reported result |
IQ: n/a MPSMT: n/a RDLS: n/a VABS: n/a Personal Inventory for Children: n/a |
Domain not applicable when IPD have been independently analysed All outcomes measures and domains in IPD were reported in publications |
IQ: n/a Performance IQ: n/a Language functioning: n/a VABS: n/a Achenbach CBCL: n/a |
Domain not applicable when IPD have been independently analysed Achenbach Childhood Behaviour Checklist data that were reported in 2007 publication were not included in IPD data set |
IQ: n/a VABS: n/a |
Domain not applicable when IPD have been independently analysed |
| Eldevik (2012)86 | Magiati (2007, 2011)89,96 | Reed (2007)90,91 | ||||
| Risk-of-bias judgement by outcome | Comment | Risk-of-bias judgement by outcome | Comment | Risk-of-bias judgement by outcome | Comment | |
| Bias due to confounding |
IQ: serious VABS: serious |
Comparator group were children receiving TAU from a local university hospital. Role of parental preference unclear No socioeconomic or parent/family data collected Baseline age, IQ and VABS included in authors’ original ANCOVA model. No data were collected on symptom severity or language |
IQ: serious Language: serious VABS: serious Autism symptom severity: serious Play: serious |
Children enrolled in either EIBI home-based programme or autism-specific school-based nursery provision. Role of parental preference unclear EIBI families were more highly educated and tended to have higher socioeconomic status. Number of siblings was similar between groups Baseline differences in IQ and VABS (clinically small) between groups. IQ included in authors’ original ANCOVA model |
IQ: serious Educational functioning: serious Autism symptom severity: serious VABS: serious Behavioural problems/ADHD: serious |
Assignment was based on the intervention being offered in the child’s location. Authors reported that locations had socioeconomic profiles but not data collected for included families. Role of parental preference unclear |
| Bias in selection of participants into the study |
IQ: moderate VABS: moderate |
Simultaneous start of interventions and follow-up not established |
IQ: moderate Language: moderate VABS: moderate Autism symptom severity: moderate Play: moderate |
Simultaneous start of interventions and follow-up not established |
IQ: moderate Educational functioning: moderate Autism symptom severity: moderate VABS: moderate Behavioural problems/ADHD: moderate |
Simultaneous start of interventions and follow-up not established |
| Bias in classification of interventions |
IQ: low VABS: low |
Misclassification of intervention unlikely |
IQ: low Language: low VABS: low Autism symptom severity: low Play: low |
Misclassification of intervention unlikely |
IQ: low Educational functioning: low Autism symptom severity: low VABS: low Behavioural problems/ADHD: low |
Misclassification of interventions unlikely |
| Bias due to deviations from intended interventions |
IQ: moderate VABS: moderate |
No data on fidelity, but EIBI was manualised and supervised TAU included some aspects of ABA No available data on intensity of either intervention or for co-interventions |
IQ: serious Language: serious VABS: serious Autism symptom severity: serious Play: serious |
No data on fidelity, but the nature and extent of supervision/oversight varied between EIBI families. Eight of 24 families changed their EIBI organisation or supervisor/consultant at least once EIBI children received more dietary and other biological interventions, extracurricular educational interventions and alternative treatments |
IQ: moderate Educational functioning: moderate Autism symptom severity: moderate VABS: moderate Behavioural problems/ADHD: moderate |
Congruent descriptions of the intervention content by both parents and supervisors was considered sufficient to establish ‘fidelity’. Authors acknowledge the lack of direct observation may have been a limitation No available data on co-interventions |
| Bias due to missing data/IPD |
IQ: low VABS: low |
IPD were reasonably complete for collected measures |
IQ: low Language: low VABS: low Autism symptom severity: low Play: low |
IPD were extensive and included fairly complete data on a wide number of variables not available from the literature |
IQ: low Educational functioning: low Autism symptom severity: low VABS: low Behavioural problems/ADHD: low |
IPD were fairly complete for the collected outcomes |
| Bias in measurement of outcomes |
IQ: serious VABS: serious |
EIBI group included a mixture of blinded and unblinded outcome assessments. In cases when an assessment were undertaken by both the study investigator or EIBI consultant and an independent evaluator, bias was not obvious. However, the difficulties in blinding this type of comparison remain Age-inappropriate measures used throughout |
IQ: moderate Language: moderate VABS: moderate Autism symptom severity: moderate Play: moderate |
Assessments were conducted by an author and research assistant who were not blinded but were independent of treatment delivery. Inter-rater reliability was assessed When multiple measures of the same domain (e.g. IQ) were available, the most age-appropriate test was used |
IQ: moderate Educational functioning: moderate Autism symptom severity: moderate VABS: moderate Behavioural problems/ADHD: moderate |
Educational psychologist doing assessments was blinded to allocation, but helped parents complete GARS and VABS tests, and could have been unblinded by the parental interaction or assessment location |
| Bias in selection of the reported result |
IQ: n/a VABS: n/a |
Domain not applicable when IPD have been independently analysed |
IQ: n/a Language: n/a VABS: n/a Autism symptom severity: n/a Play: n/a |
Domain not applicable when IPD have been independently analysed |
IQ: n/a Educational functioning: n/a Autism symptom severity: n/a VABS: n/a Behavioural problems/ADHD: n/a |
Domain not applicable when IPD have been independently analysed |
| Remington (2007);92 Kovshoff (2011)110 | Vivanti (2014)93 | Zachor (2007, 2010)94,97 | ||||
| Risk-of-bias judgement by outcome | Comment | Risk-of-bias judgement by outcome | Comment | Risk-of-bias judgement by outcome | Comment | |
| Bias due to confounding |
IQ: serious Language: serious Autism symptom severity: serious VABS: serious Parental well-being: serious |
Allocated to treatment according to patient preference. The EIBI families had actively sought ABA-based treatment, some of whom (unknown number) paid for it themselves. Comparison group received local educational authority provision and were not actively seeking EIBI Substantially higher per cent of mothers with university education in EIBI group (81% vs. 57%) Data on potential baseline confounders collected |
Developmental level: serious Autism symptom severity: serious VABS: serious Social communication: serious |
No information on how children were allocated to treatment. Role of parental preference unclear Socioeconomic/parental data only available for ESDM group. Data on other potential baseline confounders collected |
IQ: serious Developmental level: serious Autism symptom severity: serious VABS: serious |
A governmental welfare committee decided placement of the children with a diagnosis of ASD to community-based intervention programmes based on family place of residence. Role of parental preference unclear Parental education similar between groups. Other socioeconomic factors not measured. Data on some other baseline confounders collected |
| Bias in selection of participants into the study |
IQ: moderate Language: moderate Autism symptom severity: moderate VABS: moderate Parental well-being: moderate |
Simultaneous start of interventions and follow-up not established |
Developmental level: serious Autism symptom severity: serious VABS: serious Social communication: serious |
Baseline values in IPD were collected for some participants before starting treatment, for others it was months afterwards |
IQ: moderate Developmental level: moderate Autism symptom severity: moderate VABS: moderate |
Not clear if participants were recruited consecutively. Simultaneous start of intervention and follow-up not established |
| Bias in classification of interventions |
IQ: low Language: low Autism symptom severity: low VABS: low Parental well-being: low |
Misclassification of interventions unlikely |
Developmental level: low Autism symptom severity: low VABS: low Social communication: low |
Misclassification of interventions unlikely |
IQ: low Developmental level: low Autism symptom severity: low VABS: low |
Misclassification of intervention unlikely |
| Bias due to deviations from intended interventions |
IQ: moderate Language: moderate Autism symptom severity: moderate VABS: moderate Parental well-being: moderate |
Authors stated that treatment was not manualised ‘because we chose to adopt broad inclusion criteria’, adding that ‘ . . . problems of treatment fidelity, primarily the result of tutor shortages, were far more significant than those of treatment coherence’97 No available data on co-interventions |
Developmental level: moderate Autism symptom severity: moderate VABS: moderate Social communication: moderate |
Fidelity assessed through training, monitoring and observation of ESDM therapists No available data on co-interventions |
IQ: moderate Developmental level: moderate Autism symptom severity: moderate VABS: moderate |
No data on fidelity, but EIBI was manualised and supervised Both arms included input from speech and language therapists, occupational therapists and special education preschool teachers. Other co-interventions not recorded |
| Bias due to missing data/IPD |
IQ: low Language: serious Autism symptom severity: low VABS: low Parental well-being: serious |
Values were fairly complete for outcome measures in the IPD data set IPD contained ADI-R scores that were not available in publications The IPD did not contain the following outcomes reported in publications: RDLS, Third Edition; Positive Social subscale of the Nisonger Child Behavior Rating Form; parent-report version of the Developmental Behaviour Checklist; Hospital Anxiety and Depression Scale (measure of parents’ mental health); the parent and family problems subscale of the Questionnaire on Resources and Stress (Friedrich short form); Kansas Inventory of Parental Perceptions (positive contributions subscale) |
Developmental level: low Autism symptom severity: low VABS: low Social communication: low |
Values were fairly complete for most outcomes in the IPD data set The SCQ was collected at baseline and follow-up in IPD, but not reported in publication |
IQ: low Developmental level: low Autism symptom severity: low VABS: low |
Values were fairly complete for the outcomes reported in the IPD data set. Greater loss to follow-up on VABS at 2 years among eclectic participants |
| Bias in measurement of outcomes |
IQ: moderate Language: moderate Autism symptom severity: moderate VABS: moderate Parental well-being: moderate |
2-year outcomes assessed by independent psychometrician (and co-author) not informed of group allocation. Circumstances (home assessment with families) risked unblinding. Outcome assessor was aware of group allocation at 4-year follow-up |
Developmental level: serious Autism symptom severity: serious VABS: serious Social communication: serious |
Outcome assessors were not blind to treatment allocation, but were independent of delivery. ESDM assessors were blinded to whether the assessment was pre or post treatment, although may have been unblinded by the age of the child being assessed |
IQ: serious Developmental level: serious Autism symptom severity: serious VABS: serious |
Some assessments were blinded to intervention, but those undertaken in the intervention facilities were not. None of the examiners were involved in the delivery of the interventions |
| Bias in selection of the reported result |
IQ: n/a Language: n/a Autism symptom severity: n/a VABS: n/a Parental well-being: n/a |
Domain not applicable when IPD have been independently analysed |
Developmental level: n/a Autism symptom severity: n/a VABS: n/a Social communication: n/a |
Domain not applicable when IPD have been independently analysed |
IQ: n/a Developmental level: n/a Autism symptom severity: n/a VABS: n/a |
Domain not applicable when IPD have been independently analysed |
| Birnbrauer (1993)82 | Farrell (2005)87 | Howard (2005, 2014)105,108 | ||||
| Risk-of-bias judgement by outcome | Comment | Risk-of-bias judgement by outcome | Comment | Risk-of-bias judgement by outcome | Comment | |
| Bias due to confounding |
IQ: serious Language functioning: serious VABS: serious Personality Inventory for Children: serious Behavioural observation: serious Parental stress: serious |
Allocation informed by parental preference Proportion of boys higher in comparator group than in EIBI group (100% vs. 56%) No information on socioeconomic variables. Age, language, IQ and adaptive skills measured at baseline. Only limited data reported, but evidence of some baseline imbalances No formal statistical analysis |
IQ: serious VABS: serious |
Parents in the EIBI group lobbied strongly for intervention and formed a local support group. The comparator was simply offered to parents elsewhere in the country EIBI group had 6 months more intervention than comparator group on average (26 vs. 20 months) The IQ and VABS socialisation/communication scores for children in the EIBI group were considerably worse than the comparator group at baseline No socioeconomic or family data reported No formal statistical analysis |
IQ: serious Non-verbal skills: serious Language functioning: serious VABS: serious |
‘Although educational placement decisions regarding participants in this study were made by IEP or IFSP teams, parental preferences weighed heavily’105 EIBI group were younger than comparators at diagnosis, intake and follow-up, and had more years of parental education Age at diagnosis and parent’s mean level of education were included in multiple regression analyses. Other differences were not |
| Bias in selection of participants into the study |
IQ: moderate Language functioning: moderate VABS: moderate Personality Inventory for Children: moderate Behavioural observation: moderate Parental stress: moderate |
Not clear how comparator participants were recruited Intervention and start of follow-up likely to coincide |
IQ: serious VABS: serious |
EIBI treatment started a year earlier than comparator treatment. Unclear if follow-up started a year into EIBI treatment |
IQ: serious Non-verbal skills: serious Language functioning: serious VABS: serious |
Seventeen of 78 children (21%) were excluded from the analysis for various reasons (including abandoning EIBI treatment due to poor or negative initial progress). No ITT analysis or observations carried forward |
| Bias in classification of interventions |
IQ: low Language functioning: low VABS: low Personality Inventory for Children: low Behavioural observation: low Parental stress: low |
Misclassification of intervention unlikely |
IQ: low VABS: low |
Misclassification of interventions was unlikely |
IQ: low Non-verbal skills: low Language functioning: low VABS: low |
Misclassification of interventions was unlikely |
| Bias due to deviations from intended interventions |
IQ: no information Language functioning: no information VABS: no information Personality Inventory for Children: no information Behavioural observation: no information Parental stress: no information |
Insufficient data on fidelity to make a judgement No available data on co-interventions |
IQ: no information VABS: no information |
No data available on fidelity or co-interventions |
IQ: moderate Non-verbal skills: moderate Language functioning: moderate VABS: moderate |
Although efforts were made to ensure treatment integrity (e.g. through frequent direct observation and videotaping of staff implementing procedures with children, and frequent feedback from supervisors), no formal measurement of treatment integrity was undertaken Additional services, such as occupational therapy or individual or small group therapy were provided to the children in the early intensive ABA-based treatment group. 105 No information on parent-procured co-interventions or co-interventions in comparison arms No crossover from EIBI to comparator arms, but several participants crossed over between the two comparator arms |
| Bias due to missing data/IPD |
IQ: serious Language functioning: serious VABS: serious Personality Inventory for Children: serious Behavioural observation: serious Parental stress: serious |
One in 10 EIBI and three in eight comparator participant families were lost to follow-up. Reasons not reported. Ultimately, only 14 participants with any outcome data in the whole study. For some measures, data were only available for 11 participants (seven EIBI and four comparator) |
IQ: serious VABS: serious |
Very few participants and different subsets of children gave baseline and follow-up values. Seventeen children in total, although IQ follow-up data available for only nine children (four EIBI, five comparator). The authors noted missing IQ and VABS data, citing problems in obtaining the assessment results from the outcome assessors |
IQ: serious Non-verbal skills: serious Language functioning: serious VABS: serious |
Seven participants excluded from EIBI arm, nine from comparator arms combined. Reasons for exclusion differed between arms Among the remaining participants, standard scores were missing at baseline or follow-up for between 0 % and 27.6% of participants at 14 months, depending on the outcome |
| Bias in measurement of outcomes |
IQ: moderate Language functioning: moderate VABS: moderate Personality Inventory for Children: moderate Behavioural observation: moderate Parental stress: serious |
Follow-up assessments by ‘experienced clinical psychologists who did not know the group placement of the children or how long they had been in the program’,82 although assessment was in the child’s home with their mother present, making genuine blinding difficult to achieve. Relationship of outcome assessors to authors not reported |
IQ: serious VABS: serious |
Psychometric assessments were carried out by educational psychologists in the local authority as part of their ongoing work with the child and family. No mention of blinding |
IQ: serious Non-verbal skills: serious Language functioning: serious VABS: serious |
Outcome assessors were not involved in treatment but were also not blinded to allocation |
| Bias in selection of the reported result |
IQ: serious Language functioning: serious VABS: serious Personality Inventory for Children: serious Behavioural observation: serious Parental stress: serious |
Some results reported for each of the collected measures; however, results are not reported fully or consistently across outcomes |
IQ: serious VABS: serious |
Values reported for each of the collected measures. VABS and Bayley scores were reported only as age-equivalent scores in months |
IQ: low Non-verbal skills: low Language functioning: low VABS: low |
No protocol available, but all data were reported for all outcomes mentioned in the journal articles. No clear evidence of selective reporting of measures, analyses or subgroups |
| Outcome | aDawson (2010) | aEstes (2015)107 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| MSELb | VABSb | ADOSb | RBSb | MSEL/DASc | VABSc | ADOSc | RBSc | ABC scorec | ||
| Randomisation process | 1.1: was the allocation sequence random?d | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 1.2: was the allocation sequence concealed until participants were recruited and assigned to interventions?d | PY | PY | PY | PY | PY | PY | PY | PY | PY | |
| 1.3: were there baseline imbalances that suggest a problem with the randomisation process? | No | No | No | No | No | No | No | No | No | |
| Risk-of-bias judgement | Low | Low | Low | Low | Low | Low | Low | Low | Low | |
| Deviations from intended interventions | 2.1: were participants aware of their assigned intervention during the trial? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 2.2: were carers and trial personnel aware of participants’ assigned intervention during the trial? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |
| 2.3: if yes/PY/NI to 2.1 or 2.2, were important co-interventions balanced across intervention groups? | NI | NI | NI | NI | NI | NI | NI | NI | NI | |
| 2.4: was the intervention implemented successfully?e | PY | PY | PY | PY | PY | PY | PY | PY | PY | |
| 2.5 Did study participants adhere to the assigned intervention regimen?f | PY | PY | PY | PY | PY | PY | PY | PY | PY | |
| 2.6 If N/PN/NI to 2.3, 2.4 or 2.5: Was an appropriate analysis used to estimate the effect of starting and adhering to the intervention? | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | |
| Risk-of-bias judgement | Low | Low | Low | Low | Some concerns | Some concerns | Some concerns | Some concerns | Some concerns | |
| Missing outcome data | 3.1: were outcome data available for all, or nearly all, participants randomised? | PYg | PYg | PYg | PYg | Noh | Noi | Noh | Noj | Nok |
| 3.2: if no/PN/NI to 3.1, are the proportions of missing outcome data and reasons for missing outcome data similar across intervention groups? | No | No | No | No | Nol | PNl | PNl | PNl | PNl | |
| 3.3: if no/PN/NI to 3.1, is there evidence that results were robust to the presence of missing outcome data? | n/a | n/a | n/a | n/a | Nom | Nom | NIm | Nom | Nom | |
| Risk-of-bias judgement | Low | Low | Low | Low | High | High | High | High | High | |
| Measurement of the outcome | 4.1: were outcome assessors aware of the intervention received by study participants? | PYn | PYn | PYn | PYn | PYn | PYn | PYn | PYn | PYn |
| 4.2: if yes/PY/NI to 4.1, was the assessment of the outcome likely to be influenced by knowledge of intervention received?o | PY | PY | PY | PY | PY | PY | PY | PY | PY | |
| Risk-of-bias judgement | Some concerns | Some concerns | Some concerns | Some concerns | Some concerns | Some concerns | Some concerns | Some concerns | Some concerns | |
| Selection of the reported result | 5.1: are the reported outcome data likely to have been selected, on the basis of the results, from multiple outcome measurements (e.g. scales, definitions, time points) within the outcome domain? | PN | PN | PN | PN | PYp | PN | PN | PN | PYq |
| 5.2: are the reported outcome data likely to have been selected, on the basis of the results, from multiple analyses of the data? | PN | PN | PN | PN | PN | PN | PN | PN | PN | |
| Risk-of-bias judgement | Low | Low | Low | Low | Some concernsr | Low | Low | Low | Some concerns | |
| Overall risk of bias | Overall risk-of-bias judgement | Some concerns | Some concerns | Some concerns | Some concerns | Highs | Highs | Highs | Highs | Highs |
Bias due to confounding
All of the non-randomised studies were at serious risk of bias due to confounding (see Table 34). In five studies, the type of treatment received by children was explicitly based on parental preference,82,87,92,104,105,108,110 with parents actively seeking or lobbying for ABA-based treatment, and in some cases paying for it themselves. 87,92,110 In some studies, there were differences in parental education, family composition or socioeconomic status between treatment groups. 89,92,96,104,105,108–110
In other studies, the type of treatment received was primarily based on location84,86,90,91 or staff availability,85,95 for which the influence of parental preference was unclear. Some studies suggested baseline differences in diagnosis (e.g. a higher proportion of participants in the comparison group diagnosed with PDD-NOS). 104
The treatment groups in the one randomised study by Dawson et al. 83 appeared to be balanced on baseline variables and so the study was rated as having a low risk of bias for this domain for all outcomes.
Bias in the selection of participants
Studies rarely described the procedure by which participants were recruited to the study. In most non-randomised studies, the investigators were not involved in recruiting children to the comparator treatment, as these were typically cohorts or ‘convenience’ samples in which children received ‘standard’ local or regional treatment. However, even for the early intensive ABA-based treatment arms, investigators did not typically record if all potentially eligible children were recruited prospectively and/or consecutively. Studies rarely established simultaneous initiation of treatment and follow-up, and when IPD were available, dates were inconsistently recorded across studies. In one study, baseline values in the IPD were collected before the start of treatment for some participants, and months after starting treatment for others. 93 Baseline values obtained after a period of treatment may differ from those collected before starting treatment, and when the pattern of early and late baseline collection differs between study arms there is the potential for bias.
One study excluded 21% of participants for various reasons, including those abandoning EIBI treatment due to poor or negative initial progress. 105,108 This study did not include an intention-to-treat (ITT) analysis or other method to explore the impact of excluding these participants on its findings, and IPD were not available for the SCABARD team to analyse independently.
Bias in the classification of interventions
As studies were unlikely to misclassify children in terms of the intervention they received, all were considered to be at low risk of bias for this domain.
Bias due to deviation from intended interventions
Some studies described the methods used to assess treatment fidelity in the ABA-based intervention arm. These included monitoring, observation and feedback to tutors,83,93,104–108,112 or obtaining congruent descriptions of the intervention from parents and supervisors. 90,91 Elsewhere, the ABA-based interventions were manualised and supervised, but without explicit monitoring for treatment fidelity. One study noted the problem of high tutor turnover, resulting in the intervention being delivered for fewer hours per week than intended (25.6 hours delivered vs. 40 hours intended). 92,110 Other studies noted 38% of children not completing EIBI,104 unreliable recording of weekly hours of EIBI,84 and families changing between different EIBI organisations or supervisors and consultants during the study period. 89,96,109
The delivery and content of comparator arms was not closely monitored in the available studies, although three studies did report a high proportion of children receiving ABA techniques as part of ‘eclectic’ therapy or TAU. 84–86,95
Studies rarely recorded whether or not children received any co-interventions alongside those being evaluated. One study noted that children in both early intensive ABA-based interventions and eclectic treatment arms received input from speech and language therapists, occupational therapists and special education preschool teachers;94,97 another reported no additional services, such as occupational therapy or individual or small group therapy, being provided to the early intensive ABA-based group, but did not clarify whether or not this was also true for the comparator arms. 105,108 One study appeared to collect data only on independently procured co-interventions, finding that children receiving early intensive ABA-based interventions received more dietary and other biological interventions, extracurricular educational interventions and alternative treatments. 89,96,109
Bias due to missing data
When possible, judgements about the extent of missing data were based on the content of provided IPD data sets. For the four studies for which IPD were not available, these judgements were based on all relevant publications. 82,83,87,105–108,112
As shown in Appendix 7, some outcomes domains were available in IPD data sets, publications or both sources. In most cases, when an outcome measure was available in an IPD data set, the individual values for that measure were mostly complete. When individual outcome values were missing, this was usually for a small number of participants and did not appear to follow any systematic pattern.
However, all four studies not providing IPD were at serious risk of bias due to missing data. In one study,82 data were available on only some measures for 11 of 18 participants, with reasons for loss to follow-up not reported. Another small study87 reported baseline and follow-up values for different subsets of children, citing problems in obtaining the assessment data from the outcome assessors. A larger study105,108 comparing an early intensive ABA-based intervention against both TAU and eclectic intervention reported missing values at baseline or follow-up for between 0% and 27.6% of participants, depending on the outcome. The one available randomised study83,106,107,112 reported reasonably complete data at 2 years, but missing values for between 19% and 33% of participants for outcomes measured at age 6 years. None of these four studies appeared to conduct an ITT analysis.
Bias in measurement of outcomes
Truly independent and blinded measurement of outcomes is difficult to achieve in the evaluation of intensive behavioural interventions. This was the case for most studies comparing early intensive ABA-based interventions with TAU or eclectic intervention. In some cases, early intensive ABA-based interventions were assessed by treatment supervisors84 or study investigators,86 sometimes with an independent second evaluator. Although some studies described employing outcome assessors who were independent of direct intervention delivery,82,85,89,92,95,96,104,105,108–110 the assessments typically involved interaction with children and parents who were not blinded to intervention. Assessors who were blinded to allocation could potentially have been unblinded by the assessment location (if this differed between intervention arms or – when delivered in the family home – provided contextual information about likely treatment allocation). Consequently, all the included studies were considered to be at moderate or serious risk of bias for this domain.
Bias in the selection of the reported result
For the 10 studies84–86,89–97,104,109,110 providing IPD, assessment of selective outcome reporting bias was not applicable. Although research protocols were not available to assess reported outcomes against those originally planned to be collected, study authors affirmed that all the outcome data provided in the IPD data sets are all that were available. Outcomes were then selected for meta-analysis as described in Chapter 4, Individual participant data meta-analysis methods.
The four published studies not providing IPD did not provide research protocols82,83,87,105–108,112 and two were considered to be at a serious risk of bias for partial or inconsistent reporting of results. 82,87 The one available randomised study appeared to report all collected outcomes at 2 years, although two measures (Differential Ability Scales and Aberrant Behaviour Checklist) were only reported for later follow-up periods. 83,106,107,112 The fourth study appeared to report results for all the outcomes mentioned across the available publications. 105,108
Summary
With the exception of one randomised study comparing ESDM with an eclectic intervention at 2 years,83,106,112 all studies comparing early intensive ABA-based interventions with TAU or eclectic interventions had at least one domain that was considered to be at serious or high risk of bias.
Although randomisation is clearly feasible, most studies used convenience samples, with the allocation to early intensive ABA-based interventions being based on location or parental preference. The nature of the intervention meant that outcome assessment can rarely be blinded and outcome assessors were often not independent of treatment. There is evidence from some studies to suggest differences between intervention groups in terms of socioeconomic status and use of co-interventions, but this information was not consistently recorded across studies. In some cases outcome data were missing or only available for one treatment group, and we did not receive any protocols for the included studies to allow us to understand how the studies had been planned in advance. Taken together, these concerns increase our uncertainty about the results observed in the included studies. Although it is not possible to establish for certain how these potential biases influence the direction and magnitude of the study results, given the prevalence of parental preference for early intensive ABA-based interventions in some studies and the difficulties in blinding, the effects we have observed in the meta-analysis may potentially overestimate the true effects of this intervention approach.
Applied behaviour analysis-based early interventions of different intensity
Three studies comparing higher- with lower-intensity EIBI: assessment using the Cochrane Risk of Bias tool raised some concerns for one randomised study103 and two non-randomised studies assessed were judged to have a ‘serious’ risk of bias for at least one outcome on one domain of the ROBINS-I tool26,90,91,98 (Tables 36 and 37).
| Domain | Lovaas (1987);26 McEachin (1993)98 | Reed (2007)90,91 | ||
|---|---|---|---|---|
| Risk-of-bias judgement by outcome | Comment | Risk-of-bias judgement by outcome | Comment | |
| Bias due to confounding |
IQ: serious VABS: serious Educational placement: serious ‘Psychological disturbance’: serious |
Allocation based on staff availability/distance of family from treatment centre, so no overt parental preference for high- vs. low-intensity treatment comparison. A second ‘no treatment’ control arm appears to have been retrospectively identified, for which parental preference may have been a confounder. However, no baseline data were reported for this group and no IPD were provided No formal language measures were collected On average, low-intensity group participants were 6 months older than high-intensity EIBI participants at baseline and had a lower proportion of boys (58% vs. 84%) Authors’ original analysis only included pre-treatment mental age as a baseline covariate in their analysis Participants were recruited over a period of 15 years. Potential for the interventions and/or their implementation to change over time |
IQ: serious Educational functioning: serious Autism symptom severity: serious VABS: serious Behavioural problems/ADHD: serious |
Assignment was based on the intervention being offered in the child’s location. Authors reported that locations had similar socioeconomic profiles, but no data collected for included families. Role of parental preference unclear |
| Bias in selection of participants into the study |
IQ: serious VABS: serious Educational placement: serious ‘Psychological disturbance’: serious |
At the later follow-up, the average age of the control group was 10 years and the experimental group was 13 years (because the experimental group was recruited first) Only seven children were recruited in the first 3.5 years, so most early recruited children were allocated to the experimental treatment, as therapists were available The authors suggested that the order of recruitment did not affect baseline balance in IQ. Insufficient data are available on other baseline characteristics |
IQ: moderate Educational functioning: moderate Autism symptom severity: moderate VABS: moderate Behavioural problems/ADHD: moderate |
Simultaneous start of interventions and follow-up not established |
| Bias in classification of interventions |
IQ: low VABS: low Educational placement: low ‘Psychological disturbance’: low |
Misclassification unlikely |
IQ: low Educational functioning: low Autism symptom severity: low VABS: low Behavioural problems/ADHD: low |
Misclassification of interventions unlikely |
| Bias due to deviations from intended interventions |
IQ: moderate VABS: moderate Educational placement: moderate ‘Psychological disturbance’: moderate |
No data on fidelity, but EIBI procedures followed a teaching manual No available data on co-interventions |
IQ: moderate Educational functioning: moderate Autism symptom severity: moderate VABS: moderate Behavioural problems/ADHD: moderate |
Congruent descriptions of the intervention content by both parents and supervisors was considered sufficient to establish ‘fidelity’. Authors acknowledge the lack of direct observation may have been a limitation No available data on co-interventions |
| Bias due to missing data/IPD |
IQ: moderate VABS: serious Educational placement: serious ‘Psychological disturbance’: serious |
No baseline IPD other than chronological age, mental age and IQ. No follow-up IPD other than IQ, educational placement VABS was only reported in the 1993 publication98 and only for the EIBI arm at later follow-up No IPD available on the ‘no treatment’ control group |
IQ: low Educational functioning: low Autism symptom severity: low VABS: low Behavioural problems/ADHD: low |
IPD was fairly complete for the collected outcomes |
| Bias in measurement of outcomes |
IQ: serious VABS: serious Educational placement: serious ‘Psychological disturbance’: serious |
Outcomes were assessed by project staff members (no mention of blinding or quality assurance for most participants but authors reported ‘no significant differences between staff members and outside agency raters’26) Developmentally appropriate IQ measures were used |
IQ: moderate Educational functioning: moderate Autism symptom severity: moderate VABS: moderate Behavioural problems/ADHD: moderate |
Educational psychologist doing assessments was blinded to allocation, but helped parents complete GARS and VABS tests, and could have been unblinded by the parental interaction or assessment location |
| Bias in selection of the reported result |
IQ: n/a VABS: n/a Educational placement: n/a ‘Psychological disturbance’: n/a |
Domain not applicable when IPD have been independently analysed Published studies reported data for only a subset of children for certain measures (e.g. EIBI children only at later follow-up; missing data on ‘no treatment’ group) |
IQ: n/a Educational functioning: n/a Autism symptom severity: n/a VABS: n/a Behavioural problems/ADHD: n/a |
Domain not applicable when IPD have been independently analysed |
| Outcome | aSmith 2000103 | ||||||
|---|---|---|---|---|---|---|---|
| IQ | Non-verbal IQ | Language | VABS | CBCL | Academic achievement | ||
| Randomisation process | 1.1: was the allocation sequence random?b | PY | PY | PY | PY | PY | PY |
| 1.2: was the allocation sequence concealed until participants were recruited and assigned to interventions?b | PY | PY | PY | PY | PY | PY | |
| 1.3: were there baseline imbalances that suggest a problem with the randomisation process? | No | No | No | No | No | No | |
| Risk-of-bias judgement | Low | Low | Low | Low | Low | Low | |
| Deviations from intended interventions | 2.1: were participants aware of their assigned intervention during the trial? | Yes | Yes | Yes | Yes | Yes | Yes |
| 2.2: were carers and trial personnel aware of participants’ assigned intervention during the trial? | Yes | Yes | Yes | Yes | Yes | Yes | |
| 2.3: if yes/PY/NI to 2.1 or 2.2, were important co-interventions balanced across intervention groups? | NI | NI | NI | NI | NI | NI | |
| 2.4: was the intervention implemented successfully?c | Yes | Yes | Yes | Yes | Yes | Yes | |
| 2.5 Did study participants adhere to the assigned intervention regimen? | Yes | Yes | Yes | Yes | Yes | Yes | |
| 2.6: if no/PN/NI to 2.3, 2.4 or 2.5, was an appropriate analysis used to estimate the effect of starting and adhering to the intervention? | n/a | n/a | n/a | n/a | n/a | n/a | |
| Risk-of-bias judgement | Low | Low | Low | Low | Low | Low | |
| Missing outcome data | 3.1: were outcome data available for all, or nearly all, participants randomised?d | No | No | No | No | No | No |
| 3.2: if no/PN/NI to 3.1, are the proportions of missing outcome data and reasons for missing outcome data similar across intervention groups? | No | No | No | No | No | No | |
| 3.3: if no/PN/NI to 3.1, is there evidence that results were robust to the presence of missing outcome data? | PY | PY | PY | PY | PY | PY | |
| Risk-of-bias judgement | Low | Low | Low | Low | Low | Low | |
| Measurement of the outcome | 4.1: were outcome assessors aware of the intervention received by study participants?e | PN | PN | PN | PN | PN | PN |
| 4.2: if yes/PY/NI to 4.1, was the assessment of the outcome likely to be influenced by knowledge of intervention received? | n/a | n/a | n/a | n/a | n/a | n/a | |
| Risk-of-bias judgementf | Some concerns | Some concerns | Some concerns | Some concerns | Some concerns | Some concerns | |
| Selection of the reported result | 5.1: are the reported outcome data likely to have been selected, on the basis of the results, from multiple outcome measurements (e.g. scales, definitions, time points) within the outcome domain?g | PN | PN | PN | PN | PN | PN |
| 5.2 Are the reported outcome data likely to have been selected, on the basis of the results, from multiple analyses of the data? | No | No | No | No | No | No | |
| Risk-of-bias judgement | Low | Low | Low | Low | Low | Low | |
| Overall risk-of-bias judgement | Some concerns | Some concerns | Some concerns | Some concerns | Some concerns | Some concerns | |
Bias due to confounding
As described previously, non-randomised studies were judged to have a serious risk of bias due to confounding. The original UCLA study by Lovaas26 recruited children to higher- or lower-intensity EIBI on the basis of family location and staff availability. 26,98 On average, low-intensity group participants were 6 months older than high-intensity EIBI participants at baseline and had a lower proportion of boys (58% vs. 84%). This study also included a retrospectively identified ‘no treatment’ arm, for which the role of parental preference is unknown. A second non-randomised study included three comparator treatments, of which low-intensity EIBI was one. 90,91 Assignment was based on the intervention being offered in the eligible child’s location. Authors reported that locations had similar socioeconomic profiles, although these type of data were not collected for families included in the study. A third study allocated children to high- or low-intensity treatment using matched-pair random assignment (children were matched on IQ then an independent statistician assigned treatment on the basis of a random numbers table) and the treatment groups appeared to be balanced at baseline on the collected variables. 103
Bias in the selection of participants
Concerns about participant selection were similar to those for studies comparing early intensive ABA-based with TAU and eclectic interventions. The study by Lovaas26 was conducted over a 15-year period. Only seven children were recruited in the first 3.5 years, so most early recruited children were allocated to the high-intensity intervention, as therapists were available. The authors suggested that the order of recruitment did not affect baseline balance in IQ, but insufficient data were available on other baseline measures. 26,98
Bias in the classification of interventions
As for other comparisons, studies were unlikely to misclassify children in terms of the intervention they received, so all were considered to be at low risk of bias for this domain.
Bias due to deviation from intended interventions
Although therapists in all three studies were trained, followed a teaching manual and were supervised,26,90,91,98,103 the methods used to assess treatment fidelity in the early intensive ABA-based intervention arm and data specific to treatment fidelity were not available.
None of the studies recorded whether or not children received any co-interventions alongside those being evaluated.
Bias due to missing data
All three studies provided IPD for analysis, two of which provided reasonably complete IPD for their collected outcomes. 90,91,103
For the Lovaas study,26 only chronological age, mental age and IQ were available at baseline and IQ and educational placement at follow-up. VABS data were available only for the higher-intensity intervention arm and only at longer-term follow-up. 98 (Note that no IPD were available for the ‘no treatment’ control group and baseline data were not published, so this study could not be included in any meta-analysis of early intensive ABA-based intervention compared with TAU and eclectic interventions.)
Bias in measurement of outcomes
As mentioned previously, truly independent and blinded measurement of outcomes is difficult to achieve in the evaluation of intensive behavioural interventions. However, Smith et al. 103 described efforts to keep outcome assessors blind, including testing all participants in the same location. There was also some indication of robustness when outcomes were checked by a truly external examiner. As described previously, outcomes in Reed et al. 90,91 were collected by an educational psychologist who was blinded to allocation, but helped parents complete Gilliam Autism Rating Scale and VABS tests, and could potentially have been unblinded by the parental interaction or assessment location. Lovaas26 was considered to be at a higher risk of bias, as outcomes were assessed by project staff members with no mention of blinding or quality assurance for most participants, although authors did report ‘no significant differences between staff members and outside agency raters’. 26
Bias in the selection of the reported result
All three studies26,90,91,103 provided IPD and selection for meta-analysis was based on the methods described in Chapter 4, Individual participant data meta-analysis methods. However, as for other studies, research protocols were not available to inform risk-of-bias judgments.
Summary
Three studies26,90,91,103 compared higher- and lower-intensity forms of early intensive ABA-based therapy. Although Smith et al. 103 was considered to be at low risk of bias for most domains, the other studies were considered to have a serious risk of confounding among other concerns, including a lack of data on participant characteristics and co-interventions. The original Lovaas study,26 in particular, was at risk of several forms of bias, with participants receiving treatment non-concurrently and the comparator groups differing on the few available baseline variables. Although some attempts were made to avoid bias in the measurement of outcomes, the nature of the intervention makes true blinded assessment very difficult to achieve. Consequently, any estimate of effects based on a meta-analysis of these studies will be highly uncertain.
Clinic- compared with parent-directed early intensive behavioural intervention treatment
Two studies99,100 compared clinic-directed EIBI with some form of parent-directed EIBI.
Hayward et al. 99 compared clinic-based EIBI with a parent-managed treatment model in a UK study. Like other controlled studies of early intensive ABA-based interventions, treatment allocation was decided by the eligible family’s proximity to a clinic. The authors did not indicate any overt influence of parental preference on allocation, but no socioeconomic or parent or family data were collected to determine whether or not the groups were similar on these measures at baseline. Consequently, the risk of confounding on these variables could not be ruled out (Tables 38 and 39). Like the majority of other studies, no data on co-interventions were reported and, although outcome assessors were not informed of treatment assignment, true blinding of outcome assessors would have been difficult to achieve.
| Domain | Hayward (2005)99 | |
|---|---|---|
| Risk-of-bias judgement by outcome | Comment | |
| Bias due to confounding |
IQ: serious Non-verbal IQ: serious Language functioning: serious VABS: serious |
Treatment group allocation was decided by time period and proximity to clinic, so no overt influence of parental preference on clinic or parent managed No socioeconomic or parent/family data collected |
| Bias in selection of participants into the study |
IQ: low Non-verbal IQ: low Language functioning: low VABS: low |
Start of treatment and follow-up appear to coincide Authors mention only one referral that chose a different treatment than would have been allocated (choosing parent managed rather than clinic based) Five children dropped out before 1 year and were not included in the analysis (three clinic based and two parent managed; no observations carried forward or ITT analysis) |
| Bias in classification of interventions |
IQ: low Non-verbal IQ: low Language functioning: low VABS: low |
Misclassification of intervention is unlikely |
| Bias due to deviations from intended interventions |
IQ: moderate Non-verbal IQ: moderate Language functioning: moderate VABS: moderate |
Treatment integrity was monitored using videotaped sessions No available data on co-interventions |
| Bias due to missing data/IPD |
IQ: low Non-verbal IQ: low Language functioning: low VABS: low |
Complete IPD provided for the 44 participants included in the analysis. Reasons for loss to follow-up among the five excluded participants not reported, although number lost to follow-up was small and similar between groups |
| Bias in measurement of outcomes |
IQ: moderate Non-verbal IQ: moderate Language functioning: moderate VABS: moderate |
Follow-up assessments were done by independent psychologists who were not informed of children’s group assignments, although truly blind assessment was difficult to achieve Age-appropriate measures used for IQ |
| Bias in selection of the reported result |
IQ: n/a Non-verbal IQ: n/a Language functioning: n/a VABS: n/a |
Domain not applicable when IPD have been independently analysed VABS subdomain scores were not reported by treatment group in the publication, but were available in the IPD |
| Outcome | aSallows (2005)100 | |||||
|---|---|---|---|---|---|---|
| IQ | Non-verbal IQ | Language | VABS | ADI-R | ||
| Randomisation process | 1.1: was the allocation sequence random?b | PY | PY | PY | PY | PY |
| 1.2: was the allocation sequence concealed until participants were recruited and assigned to interventions?b | NI | NI | NI | NI | NI | |
| 1.3: were there baseline imbalances that suggest a problem with the randomisation process? | PN | PN | PN | PN | PN | |
| Risk-of-bias judgementc | Some concerns | Some concerns | Some concerns | Some concerns | Some concerns | |
| Deviations from intended interventions | 2.1: were participants aware of their assigned intervention during the trial? | Yes | PY | PY | PY | PY |
| 2.2: were carers and trial personnel aware of participants’ assigned intervention during the trial? | Yes | Yes | Yes | Yes | Yes | |
| 2.3: if yes/PY/NI to 2.1 or 2.2, were important co-interventions balanced across intervention groups?d | NI | NI | NI | NI | NI | |
| 2.4: was the intervention implemented successfully? | PY | Yes | Yes | Yes | Yes | |
| 2.5: did study participants adhere to the assigned intervention regimen? | PY | PY | PY | PY | PY | |
| 2.6: if no/PN/NI to 2.3, 2.4 or 2.5, was an appropriate analysis used to estimate the effect of starting and adhering to the intervention? | n/a | n/a | n/a | n/a | n/a | |
| Risk-of-bias judgement | Low | Low | Low | Low | Low | |
| Missing outcome data | 3.1: were outcome data available for all, or nearly all, participants randomised? | Yes | Yes | Yes | Yes | Yes |
| 3.2: if no/PN/NI to 3.1, are the proportions of missing outcome data and reasons for missing outcome data similar across intervention groups? | n/a | n/a | n/a | n/a | n/a | |
| 3.3: if no/PN/NI to 3.1, is there evidence that results were robust to the presence of missing outcome data? | n/a | n/a | n/a | n/a | n/a | |
| Risk-of-bias judgement | Low | Low | Low | Low | Low | |
| Measurement of the outcome | 4.1: were outcome assessors aware of the intervention received by study participants? | PY | PY | PY | PY | PY |
| 4.2: if yes/PY/NI to 4.1, was the assessment of the outcome likely to be influenced by knowledge of intervention received?e | NI | NI | NI | NI | NI | |
| Risk-of-bias judgement | Some concerns | Some concerns | Some concerns | Some concerns | Some concerns | |
| Selection of the reported result | 5.1: are the reported outcome data likely to have been selected, on the basis of the results, from multiple outcome measurements (e.g. scales, definitions, time points) within the outcome domain?f | PN | PN | PN | PN | PN |
| 5.2 Are the reported outcome data likely to have been selected, on the basis of the results, from multiple analyses of the data?g | NI | NI | NI | NI | NI | |
| Risk-of-bias judgement | Some concerns | Some concerns | Some concerns | Some concerns | Some concerns | |
| Overall risk-of-bias judgement | Some concerns | Some concerns | Some concerns | Some concerns | Some concerns | |
This study was considered to be at low risk for the bias domains relating to selection of participants, classification of interventions and missing data (complete IPD were provided for the 44 participants included in the analysis). Although reasons for loss to follow-up for five excluded participants were not reported, the number lost was small and similar between groups. Unpublished VABS subdomain scores were available in the IPD data set.
A second study (Sallows et al. 100) randomly assigned children to receive clinic- or parent-directed EIBI. Children were randomised in matched pairs, based on age and IQ. Although the parent-directed group had a higher non-verbal IQ, most other variables appeared to be similar at baseline.
Unlike most other studies, Sallows et al. 100 reported the co-interventions received by children in the study (including special education preschool, speech therapy, sensory integration, auditory integration training, music therapy, horseback riding, special diets, vitamin/dimethylglycine treatment, Nystatin and intravenous immune globulin). However, the distribution of these co-interventions between treatment groups was not available.
Summary
The two studies comparing clinic- and parent-directed EIBI were of a similar standard to studies for other comparisons. Although the risks of bias related to the selection of participants, classification of interventions and completeness of outcome data were low, some concerns remained about the risk of confounding and bias in measurement of outcomes. These risks increase our uncertainty about the accuracy of results from these studies, although how they might influence the magnitude or direction of effects is not clear.
Different forms of applied behaviour analysis-based early intensive behavioural therapy
A single Canadian study compared a PRT approach with an intervention based on the verbal behaviour method. 101 Children in the verbal behaviour arm were compared with children taken from a separate PRT-treated cohort, matched on chronological age and cognitive score (Table 40). The role of parental preference in initial recruitment to each arm was unclear, and no socioeconomic, family or autism symptom severity data were available to compare the groups at baseline. Outcome assessors were not blind to treatment allocation and several were done in part by a co-author and active interventionist, raising serious concerns about risk of bias. Given these concerns, and the small number of participants (n = 28), the results of this comparison are highly uncertain.
| Domain | Stock (2013)101 | |
|---|---|---|
| Risk-of-bias judgement by outcome | Comment | |
| Bias due to confounding |
IQ: serious Language functioning: serious VABS: serious Challenging behaviour: serious Parental stress: serious |
Verbal behaviour arm was compared with matched children (chronological age and cognitive score) taken from a separate cohort of PRT-treated children Role of parental preference in initial recruitment to each arm unclear No socioeconomic, family or autism symptom severity data available |
| Bias in selection of participants into the study |
IQ: low Language functioning: low VABS: low Challenging behaviour: low Parental stress: low |
The investigator performing the matching was blinded to other participant variables |
| Bias in classification of interventions |
IQ: low Language functioning: low VABS: low Challenging behaviour: low Parental stress: low |
Misclassification of interventions was unlikely |
| Bias due to deviations from intended interventions |
IQ: moderate Language functioning: moderate VABS: moderate Challenging behaviour: moderate Parental stress: moderate |
Treatment fidelity of both programmes assessed by direct observation and coded videotaped sessions No information on co-interventions |
| Bias due to missing data/IPD |
IQ: low Language functioning: low VABS: low Challenging behaviour: low Parental stress: low |
IPD reasonably complete for the collected outcome measures |
| Bias in measurement of outcomes |
IQ: serious Language functioning: serious VABS: serious Challenging behaviour: serious Parental stress: serious |
Outcomes assessors were not blind to treatment allocation and several were done in part by a co-author and active interventionist |
| Bias in selection of the reported result |
IQ: n/a Language functioning: n/a VABS: n/a Challenging behaviour: n/a Parental stress: n/a |
Not applicable when IPD have been independently analysed |
Appendix 10 Stock et al.101 analysis
| Outcome | MD | SE | 95% CI |
|---|---|---|---|
| CBCL composite | –1.507 | 2.348 | –6.110 to 3.095 |
| Merrill–Palmer-Revised Developmental Index | –4.512 | 8.467 | –21.108 to 12.084 |
| Preschool Language Scale: expressive | –2.983 | 3.185 | –9.225 to 3.260 |
| Preschool Language Scale: receptive | –1.395 | 3.711 | –8.668 to 5.879 |
| Parenting Stress Index – Short Form | 2.995 | 6.138 | –9.036 to 15.026 |
| VABS: composite | –3.226 | 2.563 | –8.249 to 1.797 |
Appendix 11 Additional individual participant data meta-analyses and plots
FIGURE 24.
Analysis of covariance ADOS at 1 year.
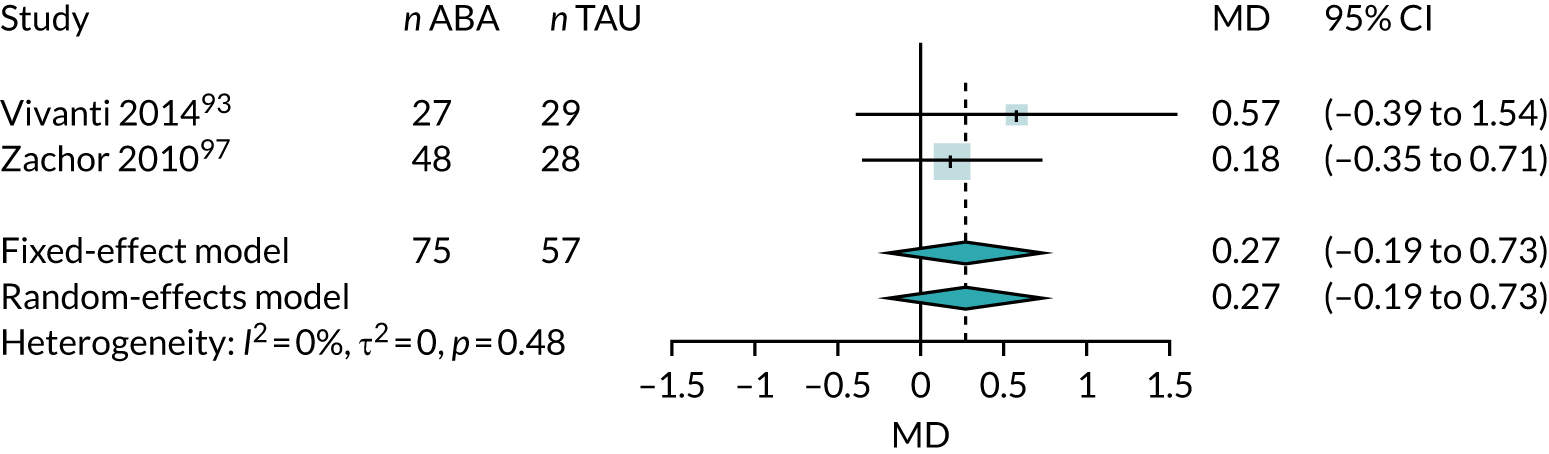
FIGURE 25.
Two-stage SMD ANCOVA. DLS, daily living skills.
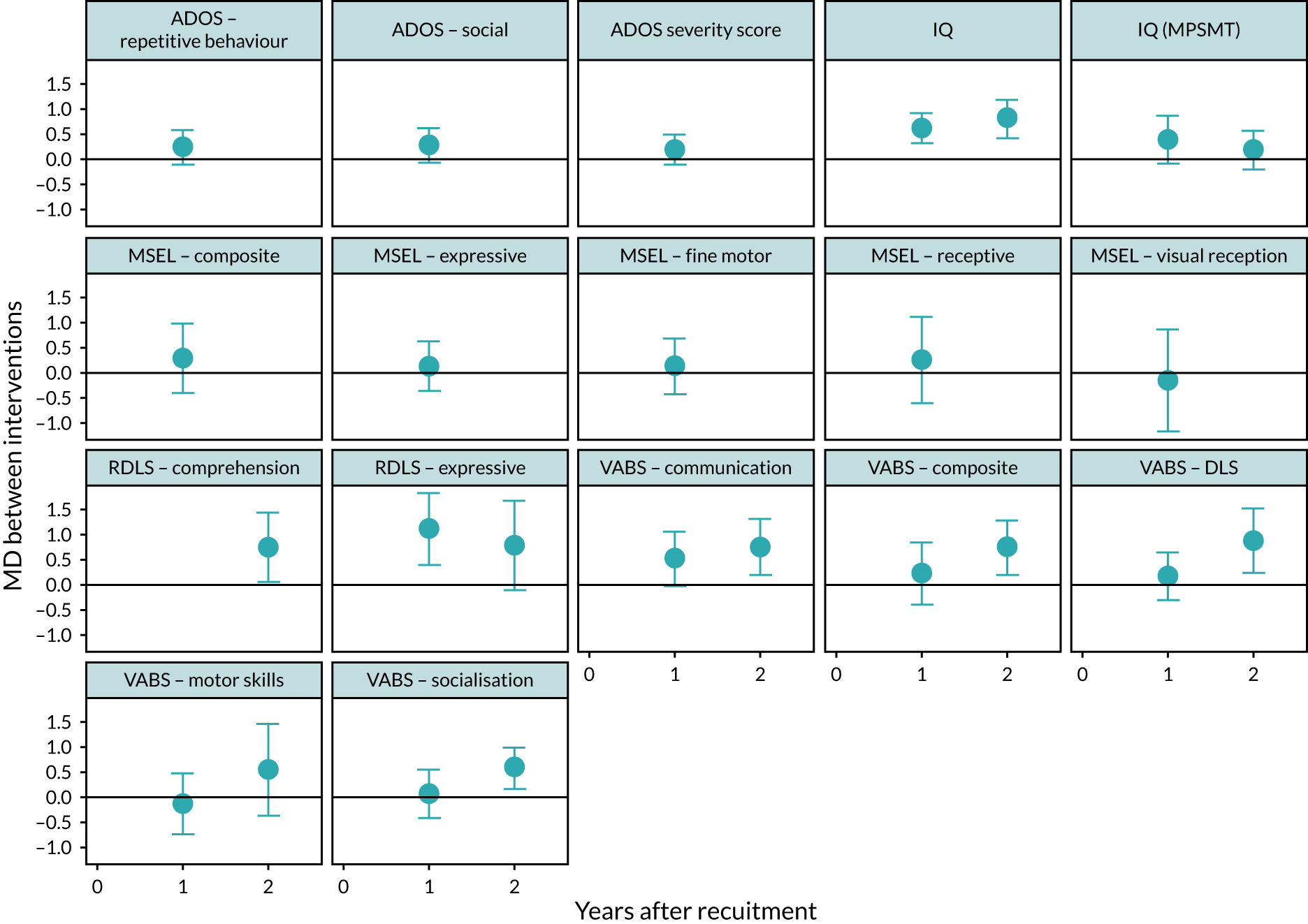
| Outcome | Year | Number of studies | Number of children | MD | 95% CI | I 2 |
|---|---|---|---|---|---|---|
| ADOS severity | 1 | 4 | 271 | –0.06 | –0.72 to 0.60 | 47 |
| 2 | 3 | 189 | –0.50 | –2.31 to 1.32 | 86 | |
| IQ | 1 | 7 | 283 | 12.37 | 7.57 to 17.17 | 0 |
| 2 | 7 | 258 | 14.10 | 8.92 to 19.29 | 0 | |
| MSEL comprehension | 1 | 3 | 216 | 4.35 | –1.55 to 10.26 | 0 |
| 2 | 2 | 109 | 1.06 | –9.80 to 11.93 | 0 | |
| MSEL expressive | 1 | 3 | 169 | 2.51 | –1.14 to 6.15 | 0 |
| 2 | 2 | 75 | 7.24 | 0.86 to 13.62 | 0 | |
| MSEL receptive | 1 | 3 | 169 | 3.87 | –1.11 to 8.85 | 44 |
| 2 | 2 | 75 | 4.46 | –8.56 to 17.48 | 41 | |
| RDLS expressive | 1 | 3 | 98 | 15.41 | 7.42 to 23.41 | 0 |
| 2 | 3 | 113 | 12.48 | –1.09 to 26.06 | 64 | |
| RDLS receptive | 1 | 1 | 41 | 14.60 | 1.38 to 27.82 | |
| 2 | 1 | 40 | 18.15 | 2.28 to 34.02 | ||
| VABS composite | 1 | 11 | 527 | 2.87 | –0.59 to 6.32 | 63 |
| 2 | 10 | 396 | 9.38 | 4.41 to 14.36 | 72 |
| Outcome domain | Outcome measure | Study | Year | Number of children | MD | 95% CI |
|---|---|---|---|---|---|---|
| Autism symptom severity | ADI composite | Magiati 200789 | 2 | 40 | –3.63 | –12.5 to 5.25 |
| Magiati 200789 | 7 | 32 | –0.45 | –12.22 to 11.32 | ||
| ADOS communication | Vivanti 201493 | 1 | 51 | 1.23 | –0.07 to 2.53 | |
| Magiati 200789 | 2 | 24 | 0.97 | –1.09 to 3.03 | ||
| Magiati 200789 | 7 | 34 | –0.61 | –1.86 to 0.64 | ||
| ADOS functional play | Vivanti 201493 | 1 | 51 | –0.6 | –1.9 to 0.71 | |
| Magiati 200789 | 2 | 24 | 0.07 | –1.67 to 1.82 | ||
| Magiati 200789 | 7 | 34 | –0.08 | –1.06 to 0.9 | ||
| ADOS unusual sensory | Vivanti 201493 | 1 | 51 | –0.35 | –1.6 to 0.89 | |
| ADOS social interaction | Vivanti 201493 | 1 | 51 | 1.12 | –0.61 to 2.86 | |
| Magiati 200789 | 2 | 24 | 0.3 | –4.92 to 5.52 | ||
| Magiati 200789 | 7 | 34 | –1.05 | –2.89 to 0.79 | ||
| GARS | Reed 200790,91 | 1 | 50 | –3.13 | –7.94 to 1.68 | |
| Language development | BVPS comprehension | Magiati 200789 | 2 | 40 | 4.73 | –7.35 to 16.8 |
| Magiati 200789 | 7 | 35 | –5.23 | –31.13 to 20.66 | ||
| Expressive one word | Magiati 200789 | 2 | 41 | 3.3 | –7.12 to 13.72 | |
| Magiati 200789 | 7 | 35 | 0.89 | –25.98 to 27.76 | ||
| MSEL general motor | Zachor 201097 | 1 | 9 | 5.5 | –11.83 to 22.83 | |
| RDLS composite | Eikeseth 200285 | 1 | 24 | 25.92 | 10.86 to 40.97 | |
| SCQ | Vivanti 201493 | 1 | 49 | 3.84 | 0.17 to 7.52 | |
| IQ | BSID | Magiati 200789 | 2 | 35 | 34.79 | 15.75 to 53.82 |
| Verbal IQ | Eikeseth 200285 | 7 | 25 | 9.15 | –10.04 to 28.35 | |
| WISC-R | Eikeseth 200285 | 7 | 22 | 5.62 | –17.82 to 29.06 | |
| Magiati 200789 | 7 | 9 | –4.21 | –28.11 to 19.68 | ||
| WPPSI-R | Eikeseth 200285 | 1 | 18 | 1.3 | –23.59 to 26.19 | |
| Magiati 200789 | 2 | 8 | –2.83 | –36.72 to 31.06 | ||
| Magiati 200789 | 7 | 15 | –5.83 | –15.98 to 4.32 | ||
| VABS subscale | Maladaptive behaviour | Eikeseth 200285 | 1 | 18 | –5.9 | –11.81 to 0.01 |
| Magiati 200789 | 2 | 40 | –7.28 | –11.54 to –3.02 | ||
| Eikeseth 200285 | 7 | 22 | –6.18 | –12.65 to 0.28 | ||
| Magiati 200789 | 7 | 31 | –5.12 | –11.79 to 1.55 | ||
| Behaviours that challenge | CRS ADHD | Reed 200790,91 | 1 | 48 | –1.53 | –6.55 to 3.49 |
| CRS cognition | Reed 200790,91 | 1 | 48 | –1.69 | –17.63 to 14.24 | |
| CRS hyperactivity | Reed 200790,91 | 1 | 48 | –1.31 | –6.03 to 3.42 | |
| CRS oppositional | Reed 200790,91 | 1 | 48 | 9.5 | 3.03 to 15.97 | |
| Other | British Abilities Scale | Reed 200790,91 | 1 | 50 | 9.48 | 1.31 to 17.65 |
| Year | Treatment | Outcome | MD vs. eclectic intervention | 95% CI | p-value |
|---|---|---|---|---|---|
| 1 | EIBI | ADOS repetitive behaviours | 1.09 | –1.65 to 3.83 | 0.44 |
| ADOS social | 1.73 | –2.35 to 5.81 | 0.41 | ||
| ADOS severity score | 0.28 | –2.88 to 3.45 | 0.86 | ||
| IQ | 4.18 | –4.28 to 12.64 | 0.33 | ||
| IQ (MPSMT) | –12.56 | –30.87 to 5.75 | 0.18 | ||
| MSEL composite | –1.48 | –25.33 to 22.36 | 0.90 | ||
| MSEL expressive | –0.14 | –15.18 to 14.91 | 0.99 | ||
| MSEL fine motor | 1.15 | –14.60 to 16.89 | 0.89 | ||
| MSEL receptive | 0.99 | –13.67 to 15.65 | 0.89 | ||
| MSEL visual reception | –8.78 | –29.66 to 12.10 | 0.41 | ||
| RDLS expressive | 19.89 | –12.26 to 52.04 | 0.23 | ||
| VABS communication | 0.56 | –6.68 to 7.79 | 0.88 | ||
| VABS composite | –0.24 | –6.68 to 6.19 | 0.94 | ||
| VABS DLS | –2.96 | –8.57 to 2.65 | 0.30 | ||
| VABS motor skills | –3.39 | –10.60 to 3.81 | 0.36 | ||
| VABS socialisation | –4.41 | –8.92 to 0.10 | 0.06 | ||
| EIBI and NDBI | IQ | 4.89 | –3.57 to 13.36 | 0.26 | |
| IQ (MPSMT) | –24.69 | –48.32 to –1.05 | 0.04 | ||
| RDLS comprehension | 16.19 | –6.60 to 38.98 | 0.16 | ||
| RDLS expressive | –9.87 | –39.22 to 19.49 | 0.51 | ||
| VABS communication | 5.47 | –1.68 to 12.63 | 0.13 | ||
| VABS composite | 3.48 | –4.48 to 11.44 | 0.39 | ||
| VABS DLS | 2.17 | –4.60 to 8.95 | 0.53 | ||
| VABS motor skills | 6.27 | –4.62 to 17.16 | 0.26 | ||
| VABS socialisation | 1.37 | –6.34 to 9.08 | 0.73 | ||
| EIBI and NDBI (PM) | IQ | 5.62 | –3.99 to 15.23 | 0.25 | |
| IQ (MPSMT) | –33.66 | –56.21 to –11.11 | 0.00 | ||
| RDLS comprehension | 15.52 | –8.95 to 39.99 | 0.21 | ||
| RDLS expressive | –9.87 | –39.18 to 19.45 | 0.51 | ||
| VABS communication | –1.97 | –14.53 to 10.59 | 0.76 | ||
| VABS composite | 2.88 | –11.43 to 17.18 | 0.69 | ||
| VABS DLS | –10.83 | –25.72 to 4.05 | 0.15 | ||
| VABS motor skills | 7.18 | –16.36 to 30.71 | 0.55 | ||
| VABS socialisation | 2.85 | –9.36 to 15.06 | 0.65 | ||
| EIBI low intensity | IQ | –5.44 | –16.91 to 6.03 | 0.35 | |
| VABS composite | –5.52 | –24.69 to 13.65 | 0.57 | ||
| ESDM | ADOS repetitive behaviours | –0.64 | –3.46 to 2.18 | 0.66 | |
| ADOS social | 0.08 | –2.90 to 3.06 | 0.96 | ||
| ADOS severity score | 1.37 | –2.09 to 4.83 | 0.44 | ||
| MSEL composite | 5.04 | –20.00 to 30.07 | 0.69 | ||
| MSEL expressive | 2.23 | –13.07 to 17.52 | 0.78 | ||
| MSEL fine motor | 2.27 | –18.31 to 22.86 | 0.83 | ||
| MSEL receptive | 1.07 | –14.80 to 16.94 | 0.90 | ||
| MSEL visual reception | 2.69 | –18.11 to 23.48 | 0.80 | ||
| VABS communication | –9.79 | –34.84 to 15.25 | 0.44 | ||
| VABS composite | –1.26 | –19.66 to 17.15 | 0.89 | ||
| VABS DLS | –12.85 | –38.77 to 13.08 | 0.33 | ||
| VABS motor skills | –5.14 | –24.29 to 14.01 | 0.60 | ||
| VABS socialisation | –5.80 | –25.39 to 13.78 | 0.56 | ||
| NDBI | IQ (MPSMT) | –49.43 | –75.91 to –22.95 | 0.00 | |
| VABS composite | 3.76 | –16.03 to 23.54 | 0.71 | ||
| Portage | IQ | –8.89 | –28.72 to 10.94 | 0.38 | |
| VABS composite | –5.85 | –24.85 to 13.16 | 0.55 | ||
| TAU | IQ | –5.63 | –18.37 to 7.11 | 0.39 | |
| IQ (MPSMT) | –46.25 | –88.69 to –3.80 | 0.03 | ||
| RDLS expressive | –26.14 | –63.21 to 10.92 | 0.17 | ||
| VABS communication | –8.59 | –23.18 to 6.00 | 0.25 | ||
| VABS composite | –3.66 | –16.51 to 9.20 | 0.58 | ||
| VABS DLS | –2.48 | –10.88 to 5.91 | 0.56 | ||
| VABS socialisation | –4.41 | –16.35 to 7.53 | 0.47 | ||
| 2 | EIBI | ADOS repetitive behaviours | –0.29 | –3.23 to 2.66 | 0.85 |
| ADOS social | 0.36 | –3.95 to 4.66 | 0.87 | ||
| ADOS severity score | –1.55 | –4.96 to 1.85 | 0.37 | ||
| IQ | 19.23 | 10.16 to 28.31 | 0.00 | ||
| IQ (MPSMT) | –9.10 | –25.58 to 7.37 | 0.28 | ||
| MSEL composite | 0.95 | –27.21 to 29.11 | 0.95 | ||
| MSEL expressive | –0.24 | –18.22 to 17.74 | 0.98 | ||
| MSEL fine motor | 1.54 | –16.02 to 19.11 | 0.86 | ||
| MSEL receptive | 2.57 | –14.52 to 19.65 | 0.77 | ||
| MSEL visual reception | –11.48 | –36.04 to 13.07 | 0.36 | ||
| RDLS comprehension | 11.77 | –22.07 to 45.61 | 0.50 | ||
| RDLS expressive | 2.81 | –26.98 to 32.60 | 0.85 | ||
| VABS communication | 7.36 | –0.47 to 15.18 | 0.07 | ||
| VABS composite | 9.39 | 2.46 to 16.32 | 0.01 | ||
| VABS DLS | 8.69 | 2.87 to 14.51 | 0.00 | ||
| VABS motor skills | 4.69 | –3.19 to 12.58 | 0.24 | ||
| VABS socialisation | 5.98 | 1.05 to 10.91 | 0.02 | ||
| EIBI and NDBI | IQ | 20.75 | 11.71 to 29.79 | 0.00 | |
| IQ (MPSMT) | –9.73 | –32.86 to 13.39 | 0.41 | ||
| RDLS comprehension | 12.61 | –12.24 to 37.46 | 0.32 | ||
| RDLS expressive | 18.69 | –6.70 to 44.08 | 0.15 | ||
| VABS communication | 10.40 | 2.29 to 18.51 | 0.01 | ||
| VABS composite | 10.50 | 1.87 to 19.14 | 0.02 | ||
| VABS DLS | 9.41 | 1.83 to 16.98 | 0.01 | ||
| VABS motor skills | 8.85 | –2.95 to 20.65 | 0.14 | ||
| VABS socialisation | 7.32 | –0.93 to 15.57 | 0.08 | ||
| EIBI and NDBI (PM) | IQ | 19.62 | 7.99 to 31.25 | 0.00 | |
| IQ (MPSMT) | –22.22 | –44.97 to 0.53 | 0.06 | ||
| RDLS comprehension | 11.86 | –14.09 to 37.80 | 0.37 | ||
| RDLS expressive | 18.69 | –7.43 to 44.81 | 0.16 | ||
| VABS communication | 8.23 | –6.25 to 22.71 | 0.27 | ||
| VABS composite | 11.35 | –4.31 to 27.01 | 0.16 | ||
| VABS DLS | –5.92 | –22.23 to 10.39 | 0.48 | ||
| VABS motor skills | 29.24 | –7.23 to 65.71 | 0.12 | ||
| VABS socialisation | 8.32 | –5.30 to 21.93 | 0.23 | ||
| EIBI low intensity | IQ | 8.89 | –6.44 to 24.21 | 0.26 | |
| TAU | IQ | 6.45 | –6.57 to 19.48 | 0.33 | |
| IQ (MPSMT) | –27.33 | –69.40 to 14.75 | 0.20 | ||
| RDLS comprehension | –3.70 | –35.81 to 28.40 | 0.82 | ||
| RDLS expressive | 4.72 | –28.19 to 37.62 | 0.78 | ||
| VABS communication | –1.25 | –16.20 to 13.70 | 0.87 | ||
| VABS composite | 1.32 | –11.86 to 14.49 | 0.84 | ||
| VABS DLS | 2.40 | –6.47 to 11.27 | 0.60 | ||
| VABS socialisation | 2.12 | –10.07 to 14.31 | 0.73 |
FIGURE 26.
Network meta-analysis. DLS, daily living skills.
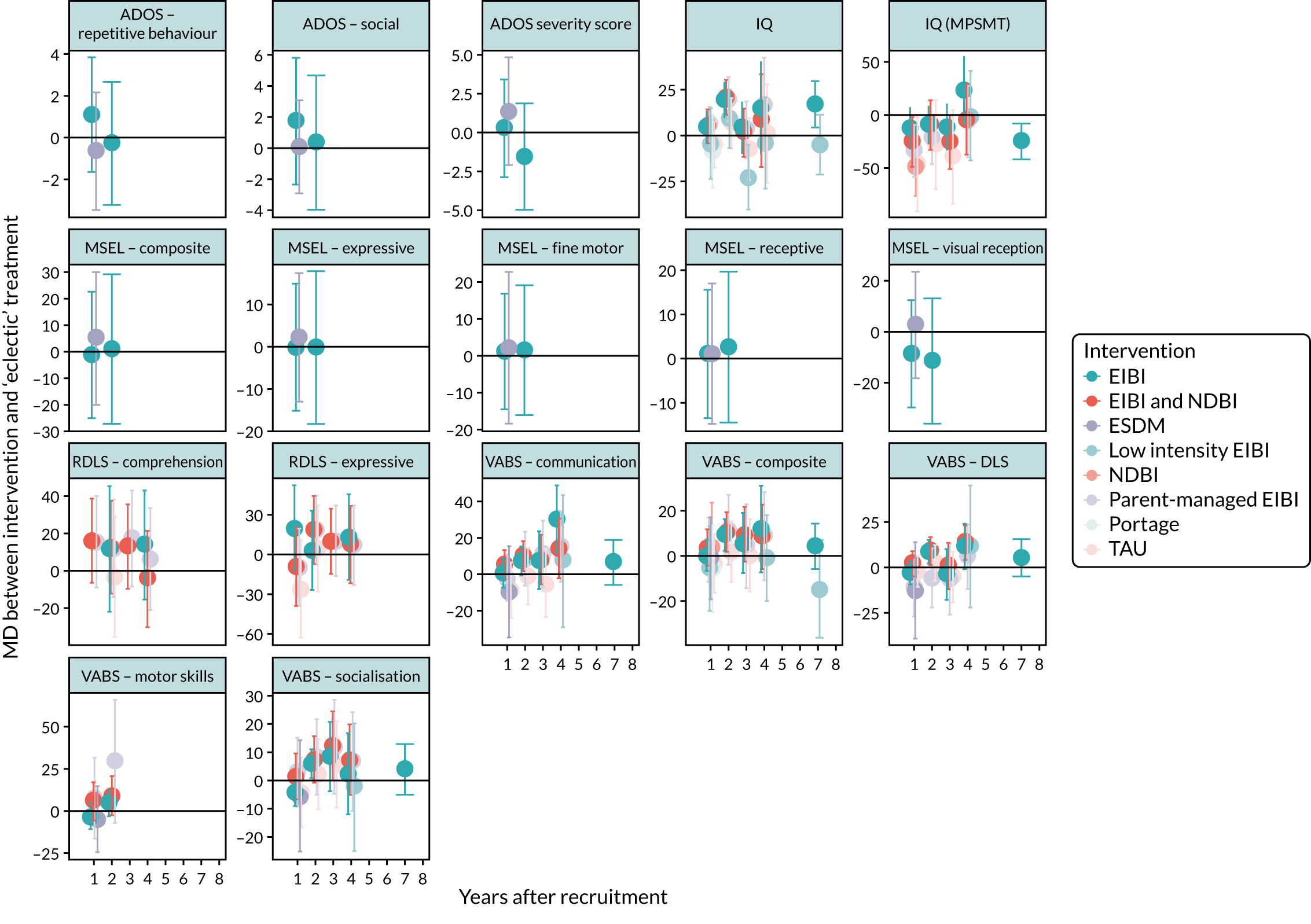
| Outcome | Factor | Variation in MD | 95% CI | p-value |
|---|---|---|---|---|
| ADOS repetitive behaviours | Age at recruitment (per month) | 0.07 | 0.02 to 0.12 | 0.01 |
| Sex | –0.15 | –1.61 to 1.32 | 0.85 | |
| VABS at baseline (per point) | –0.01 | –0.07 to 0.04 | 0.64 | |
| ADOS social | Age at recruitment (per point) | –0.03 | –0.13 to 0.06 | 0.49 |
| Sex | 2.54 | –0.37 to 5.45 | 0.09 | |
| VABS at baseline | 0.12 | 0 to 0.23 | 0.05 | |
| ADOS severity score | Age at recruitment | 0 | –0.06 to 0.05 | 0.93 |
| Sex | 1.06 | –0.52 to 2.63 | 0.19 | |
| VABS at baseline | 0.05 | –0.01 to 0.11 | 0.12 | |
| IQ (MPSMT) | Age at recruitment | –0.32 | –0.81 to 0.17 | 0.21 |
| Sex | 14.67 | –4.52 to 33.85 | 0.13 | |
| IQ at baseline | –0.12 | –0.52 to 0.29 | 0.57 | |
| VABS at baseline | –0.06 | –0.75 to 0.63 | 0.87 | |
| IQ | Age at recruitment | 0.08 | –0.26 to 0.42 | 0.64 |
| Sex | –1.3 | –13.36 to 10.76 | 0.83 | |
| IQ at baseline | 0.09 | –0.13 to 0.31 | 0.44 | |
| VABS at baseline | –0.11 | –0.58 to 0.35 | 0.63 | |
| MSEL composite | Age at recruitment | –0.28 | –0.85 to 0.28 | 0.33 |
| Sex | 27.25 | 9.77 to 44.73 | 0 | |
| VABS at baseline | 0.43 | –0.18 to 1.04 | 0.16 | |
| MSEL expressive | Age at recruitment | –0.07 | –0.44 to 0.29 | 0.7 |
| Sex | 8.8 | –2.58 to 20.18 | 0.13 | |
| VABS at baseline | 0.02 | –0.39 to 0.43 | 0.92 | |
| MSEL fine motor | Age at recruitment | 0.36 | 0.05 to 0.68 | 0.02 |
| Sex | 0.55 | –9.33 to 10.42 | 0.91 | |
| VABS at baseline | –0.19 | –0.54 to 0.16 | 0.29 | |
| MSEL receptive | Age at recruitment | 0.29 | –0.05 to 0.64 | 0.09 |
| Sex | 11.53 | 0.49 to 22.57 | 0.04 | |
| VABS at baseline | –0.18 | –0.58 to 0.22 | 0.39 | |
| MSEL visual reception | Age at recruitment | –0.03 | –0.59 to 0.52 | 0.91 |
| Sex | 7.53 | –6.97 to 22.04 | 0.31 | |
| VABS at baseline | 0.23 | –0.29 to 0.75 | 0.38 | |
| RDLS comprehension | Age at recruitment | –0.07 | –1.33 to 1.19 | 0.91 |
| Sex | 30.38 | 5.71 to 55.04 | 0.02 | |
| IQ at baseline | 0.12 | –0.4 to 0.65 | 0.64 | |
| VABS at baseline | 0.66 | –0.23 to 1.55 | 0.14 | |
| RDLS expressive | Age at recruitment | 0.13 | –0.74 to 0.99 | 0.78 |
| Sex | 30.24 | 7.17 to 53.32 | 0.01 | |
| IQ at baseline | –0.07 | –0.65 to 0.5 | 0.8 | |
| VABS at baseline | 0.18 | –0.72 to 1.09 | 0.69 | |
| VABS communication | Age at recruitment | –0.05 | –0.37 to 0.27 | 0.76 |
| Sex | 5.49 | –3.3 to 14.28 | 0.22 | |
| IQ at baseline | 0.11 | –0.11 to 0.33 | 0.33 | |
| VABS at baseline | 0 | –0.34 to 0.33 | 0.98 | |
| VABS composite | Age at recruitment | –0.05 | –0.29 to 0.18 | 0.65 |
| Sex | 3.28 | –3.08 to 9.65 | 0.31 | |
| IQ at baseline | 0.09 | –0.06 to 0.23 | 0.24 | |
| VABS at baseline | –0.05 | –0.28 to 0.18 | 0.66 | |
| VABS DLS | Age at recruitment | 0.04 | –0.19 to 0.27 | 0.72 |
| Sex | 3.91 | –3.39 to 11.2 | 0.29 | |
| IQ at baseline | 0.08 | –0.1 to 0.25 | 0.39 | |
| VABS at baseline | –0.02 | –0.28 to 0.23 | 0.86 | |
| VABS motor skills | Age at recruitment | 0.16 | –0.2 to 0.53 | 0.38 |
| Sex | 2.15 | –7.08 to 11.38 | 0.65 | |
| IQ at baseline | –0.34 | –0.76 to 0.08 | 0.11 | |
| VABS at baseline | –0.3 | –0.65 to 0.05 | 0.09 | |
| VABS socialisation | Age at recruitment | 0.07 | –0.16 to 0.29 | 0.58 |
| Sex | 4.92 | –1.74 to 11.57 | 0.15 | |
| IQ at baseline | 0.04 | –0.13 to 0.22 | 0.62 | |
| VABS at baseline | 0.02 | –0.22 to 0.26 | 0.86 |
Appendix 12 Rogers et al.102
Overview
At the time of writing the current report, a manuscript reporting the results of an additional eligible study by Rogers et al. 102 was published online. As insufficient time was available to fully integrate the study into the body of the report, it is briefly summarised here.
This study was described as a ‘single-blind randomised, multi-site, intent-to-treat study . . . designed to replicate Dawson et al. (2010) randomized controlled trial (RCT) testing effects of the Early Start Denver Model (ESDM), an intensive play- and routines-based intervention delivered in natural settings’. 102
Participants and interventions
A total of 118 children with ASD (with a baseline mean age of 20.6 months and ADOS severity score of 7.49) were randomly assigned to ESDM or community interventions for 27 months (Table 46). The study was conducted at three separate universities.
| First study author (year) | Intensive ABA-based intervention name | Comparator name | Number of intervention participants | Number of comparator participants | Treatment duration (months) | Actual delivered treatment intensity (hours/week) | Mean (SD or range) age at baseline (months unless otherwise stated) | Sex (male/female) | Baseline ASD severity [measure] | Baseline full-scale IQ [measure] | Mean (SD) baseline Vineland adaptive behaviour composite score |
|---|---|---|---|---|---|---|---|---|---|---|---|
| EIBI vs. TAU/eclectic intervention(s) | |||||||||||
| Rogers (2019)102 | ESDM | TAU | 63 | 55 | I 27; C 27 | I 0–3 months = 3.15, 3–15 months = 18.54, 15–27 months = 25.73; C 0–3 months = 5.28, 3–15 months = 14.85, 15–27 months = 20.01 | I 20.6 (3.37); C 20.7 (3.21) | I 41/14; C 51/12 | I 7.20 (1.94); C 7.83 (1.97) [ADOS severity score] | I 66.98 (18.61); C 64.52 (15.56) [MSEL developmental quotient] | I 12.8 (4.66); C 12.91 (5.79) [VABS composite ‘age equivalent’] |
Children assigned to ESDM intervention initially received 3 months of weekly parent coaching (3.15 intervention hours/week, on average). This was followed by 24 months of more intensive one-to-one intervention in homes or day care settings from supervised therapy assistants, while parents received 4 hours of coaching per month from a certified ESDM therapist (average of 18.5 intervention hours/week for months 3–15 and 25.7 hours/week for months 15–27). Treatment procedures followed published manuals and a study treatment supervisor oversaw treatment at all three sites to ensure consistency. Treatment fidelity of implementation was assessed on the basis of coded videotaped sessions.
Children in the community group continued to receive whatever interventions their parents arranged (averaging 5.28 intervention hours/week in the first 3 months, 14.9 intervention hours/week for months 3–15 and 20 hours/week for months 15–27). No further details on community intervention were available.
Co-interventions (across both intervention groups) included ABA; occupational therapy; physiotherapy; speech and language therapy; TEACCH; the developmental, individual difference, relationship-based model; play therapy; home session with infant/toddler educators; infant/toddler treatment groups; and formal preschool/educational settings, as well as study ESDM hours.
Risk of bias
Unlike previous studies, this RCT employed an independent data co-ordinating centre to undertake randomisation and data analyses, and was described by the authors as an ITT RCT (Table 47).
| Outcome | aRogers (2019)102 | ||||
|---|---|---|---|---|---|
| Language composite age-equivalent (based on MSEL) | Developmental quotient (MSEL) | VABS age-equivalent composite | ADOS severity score | ||
| Randomisation process | 1.1: was the allocation sequence random?b | Yes | Yes | Yes | Yes |
| 1.2: was the allocation sequence concealed until participants were recruited and assigned to interventions?b | Yes | Yes | Yes | Yes | |
| 1.3: were there baseline imbalances that suggest a problem with the randomisation process?c | No | No | No | No | |
| Risk-of-bias judgement | Low | Low | Low | Low | |
| Deviations from intended interventions | 2.1: were participants aware of their assigned intervention during the trial? | Yes | Yes | Yes | Yes |
| 2.2: were carers and trial personnel aware of participants’ assigned intervention during the trial? | Yes (parents) | Yes (parents) | Yes (parents) | Yes (parents) | |
| 2.3: if yes/PY/NI to 2.1 or 2.2, were there deviations from the intended intervention beyond what would be expected in usual practice? | NI | NI | NI | NI | |
| 2.4: if yes/PY to 2.3, were these deviations from intended intervention unbalanced between groups and likely to have affected the outcome?d | n/a | n/a | n/a | n/a | |
| 2.5: were any participants analysed in a group different from the one to which they were assigned?e | No | No | No | No | |
| 2.6: if yes/PY/NI to 2.5, was there potential for a substantial impact (on the estimated effect of intervention) of analysing participants in the wrong group | n/a | n/a | n/a | n/a | |
| Risk-of-bias judgement | Some concerns | Some concerns | Some concerns | Some concerns | |
| Missing outcome data | 3.1: were outcome data available for all, or nearly all, participants randomised?f | No | No | No | No |
| 3.2 if no/PN/NI to 3.1, are the proportions of missing outcome data and reasons for missing outcome data similar across intervention groups?g | No | No | No | No | |
| 3.3 if no/PN/NI to 3.1, is there evidence that results were robust to the presence of missing outcome data?h | NI | NI | NI | NI | |
| Risk-of-bias judgement | Some concerns | Some concerns | Some concerns | Some concerns | |
| Measurement of the outcome | 4.1: were outcome assessors aware of the intervention received by study participants?i | No | No | Yes | No |
| 4.2: if yes/PY/NI to 4.1, was the assessment of the outcome likely to be influenced by knowledge of intervention received? | n/a | n/a | NI | n/a | |
| Risk-of-bias judgement | Low | Low | Some concerns | Low | |
| Selection of the reported result | 5.1: are the reported outcome data likely to have been selected, on the basis of the results, from multiple outcome measurements (e.g. scales, definitions, time points) within the outcome domain?j | NI | NI | NI | NI |
| 5.2: are the reported outcome data likely to have been selected, on the basis of the results, from multiple analyses of the data?k | NI | NI | NI | NI | |
| Risk-of-bias judgement | Some concerns | Some concerns | Some concerns | Some concerns | |
| Overall risk of biasl | Negative values favour Nova Scotia EIBI | Some concerns | Some concerns | Some concerns | Some concerns |
However, despite being described as a replication of Dawson et al. ,83 this study differed from the original study in several respects, primarily relating to the collection of outcomes. The Rogers et al. 102 manuscript stated that the primary outcome was a ‘language composite age equivalent score [calculated] by averaging the Expressive Language and Receptive Language age-equivalents from the MSEL at each time point’. This specific measure was not employed in the original study and the published protocol [URL: https://clinicaltrials.gov/ct2/show/NCT00698997 (accessed 4 February 2020)] does not name a primary (or any other) outcome domain. However, the authors state that outcomes were prespecified and provided in writing to an independent Data Safety and Monitoring Board before any analyses began, and that adherence to the prespecified plan was monitored by the independent data co-ordinating centre.
Similarly, the approaches to measuring cognitive development and adaptive behaviour differed from the original study. The original Dawson et al. study83 used the MSEL composite and VABS composite standard scores. However, a quotient score was calculated for MSEL in this study ‘since many children fell below the basal standard score’, and an ‘adaptive behaviour age equivalent’ was calculated by averaging the means of the age equivalents of the four domain scores from VABS-II ‘because the manual does not provide developmental ages corresponding to total scores that could be used to construct quotient scores’. 102
At 2 years, data were available for only 69% of participants (81/118), although the authors stated that ‘data from all 118 children were used in analyses’. 102 It is unclear whether or not this means that all participants lost to follow-up were accounted for in the analyses at each time point. Although ITT would imply that this was the case, it is unclear if last observation carried forward or other methods of imputation were applied.
Although this study appears to be at lower risk of bias than earlier studies in some respects, concerns about bias remain due to a lack of clarity in the reporting of some aspects of study conduct and findings.
Results
Language composite age-equivalent score increased more over time for ESDM than community intervention in two study sites, but increased more for community intervention than ESDM at one study site. Across all three sites, age-equivalent language scores favoured ESDM (39.9 months vs. 35 months at the end of follow-up).
No significant differences were found between ESDM and community treatment in terms of autism symptom severity (ADOS), developmental quotient (MSEL) or adaptive behaviour (VABS).
Developmental quotient, baseline ADOS play score, baseline joint attention percentage scores and maternal education were investigated as potential moderating variables. With the exception of baseline developmental quotient on ADOS severity score at follow-up, no variable appeared to moderate effects on any outcome measure.
FIGURE 27.
Meta-analysis of composite VABS score at 1 year.

FIGURE 28.
Meta-analysis of composite VABS score at 2 years.
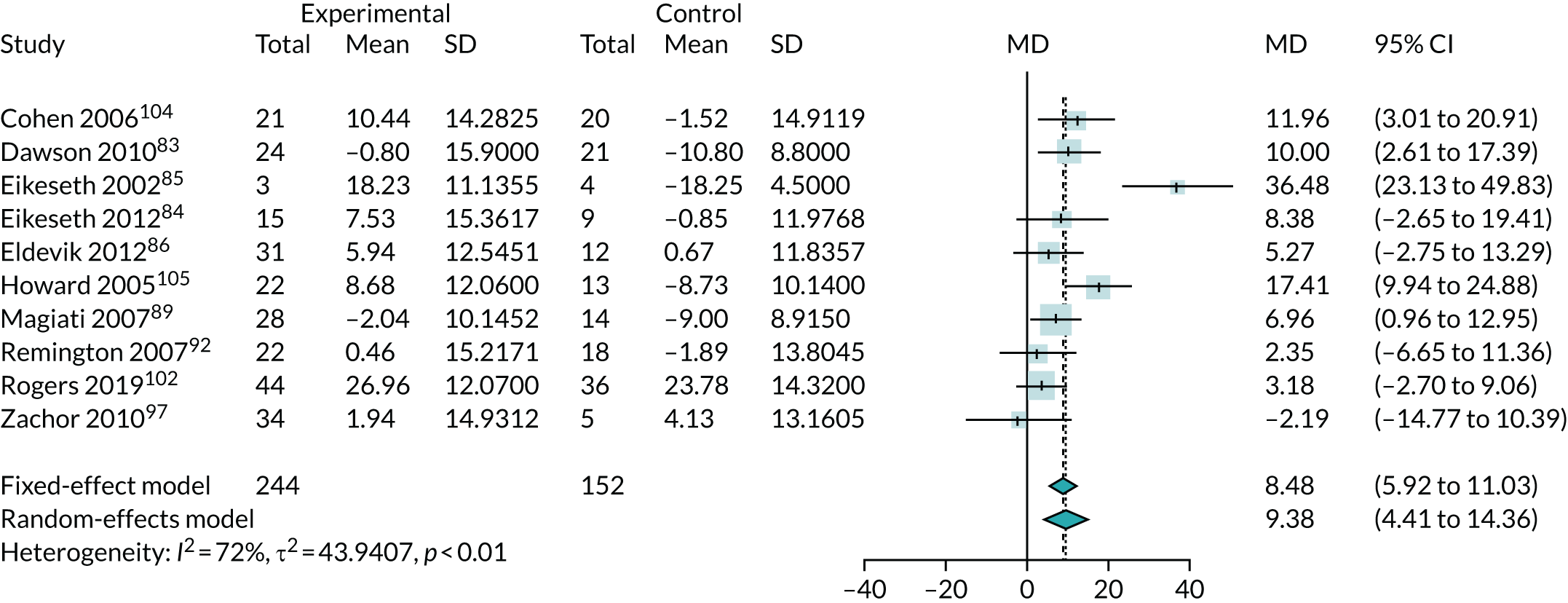
FIGURE 29.
Meta-analysis of MSEL score at 1 year.

FIGURE 30.
Meta-analysis of MSEL score at 2 years.

FIGURE 31.
Meta-analysis of ADOS severity score at 1 year.
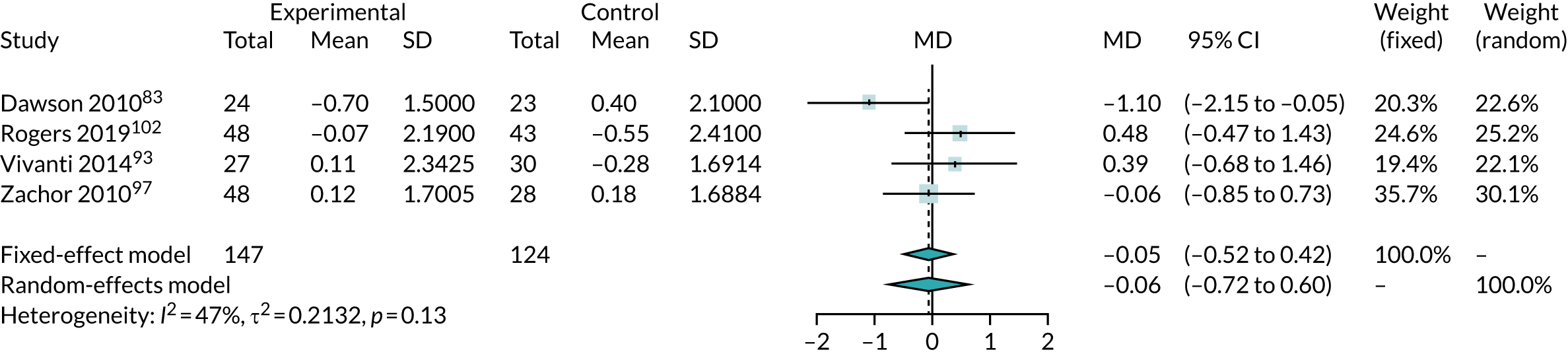
FIGURE 32.
Meta-analysis of ADOS severity score at 2 years.

Appendix 13 Cost-effectiveness review
Overview
A systematic review of studies evaluating the cost-effectiveness of early intensive ABA-based interventions was undertaken. The purpose of this review was to provide a summary of the existing cost-effectiveness evidence, and to provide an overview of modelling approaches and assumptions employed in previous economic evaluation.
Methods
To identify published economic evidence, the following databases were searched for eligible studies: MEDLINE (Ovid), EMBASE (Ovid) 1980 onwards, CINAHL (EBSCOhost), The Cochrane Library (Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effects, HTA database and CENTRAL). The searches were undertaken in November 2017. The full search strategy used is reported in Appendix 17.
Study selection
Two researchers independently undertook the screening of all titles and abstracts identified in the search. Full-paper publications were then obtained for potentially relevant studies and screened against the eligibility criteria. Disagreements between reviewers were resolved by discussion.
Studies were included in the review if they assessed the cost-effectiveness of early intensive ABA-based interventions relative to any other intervention. A broad range of studies were considered for inclusion in the assessment of cost-effectiveness, including economic evaluations conducted alongside trials, modelling studies and analyses of administrative databases. Only full economic evaluations that compared two or more options and considered both costs and consequences (including cost-effectiveness, cost–utility or cost–benefit analyses) were included.
Data extraction and quality assessment strategy
Details of eligible studies were extracted and summarised using a Microsoft Excel data extraction template. Data were extracted by one reviewer and checked by a second reviewer. Disagreements between reviewers was resolved through discussion. Data extraction included the following items: type of economic analysis, population, interventions, comparators, perspective, time horizon, structure and type of model used, clinical effectiveness data, source of quality of life (when appropriate), resource use data, unit cost data, price year, discounting and results of presented analysis, including sensitivity analyses. Quality assessment of the included studies was also undertaken as part of the extraction process using the modified Philips et al. 167 checklist.
Results
Search results
A flow diagram describing study selection is presented in Figure 33. A total of 233 studies were identified from the searches after removing duplicates. Following assessment of title and abstract, full texts were obtained for 17 studies and scrutinised against the inclusion criteria. A total of six studies44,50–54 were found to meet the eligibility criteria and were included in the review.
FIGURE 33.
Flow diagram showing study selection for the economic evaluations review.

Description of included studies
The full data extraction from the six studies identified in the systematic review of cost-effectiveness is presented in Table 48, with quality assessment presented in Table 49.
| Study | Details |
|---|---|
| Jacobson (1998)52 | |
| Country | USA |
| Year of cost analysis | 1996 |
| Currency | US dollar |
| Intervention costs per year | US$32,820 (US$50,000 used in model) |
| Source | Government report |
| Decision analysis model overview | Cost–benefit analysis was conducted using decision tree (cost model) |
| Perspective | Public sector perspective |
| Discount rate: benefits and costs | Not applied, but inflation adjusted |
| Time horizon | (1) 18 years and (2) 52 years |
| Population details | Children with autism, PDD-NOS |
| Intervention vs. comparator(s) | EIBI for 3 years (Lovaas model26) vs. no EIBI |
| Primary effectiveness measure(s) | The benefits for EIBI for autism were estimated by classifying individuals into three groups: (1) normal functioning, defined as participation in regular education with little or no support, and are vocationally productive as adults; (2) children who derive sufficient benefit that they can participate in less intensive special education, and have reduced dependency in adulthood; and (3) children who still require specialised and intensive educational and adult services |
| Costs considered | Early intervention annual cost, family support services annual cost, education costs, home- and community-based services, institutional services, supplemental security income/aid to dependent children annual cost (estimate for all generic public support costs) and value of supported wages value |
| Costs source | Used Pennsylvania model – costs for services and income estimates |
| Results | Incremental costs presented at differing levels of effectiveness |
| Sensitivity analysis undertaken and results | n/a |
| Motiwala (2006)53 | |
| Country | Canada |
| Year of cost analysis | 2003 |
| Currency | Canadian Dollar |
| Intervention costs per year | CA$75,670 per child aged 2–5 years based on 23 hours/week of therapy for 3 years |
| Source | Ontario Ministry of Children’s Services and Ontario Ministry of Community (now the Ministry of Children, Community and Social Services) |
| Decision analysis model overview | Cost-effectiveness analysis using decision tree |
| Perspective | Government perspective |
| Discount rate: benefits and costs | 3.0% discount rate for costs. In sensitivity analyses, discount rates from 1.0% to 5.0% were used |
| Time horizon | Age 65 years |
| Population details | Autistic children |
| Intervention vs. comparator(s) | Expansion of EIBI services vs. status quo provision vs. no intervention. IBI based on Ontario Ministry of Children’s Services and Ontario Ministry of Community and Social Services, and assumes 23 hours/week for 3 years |
| Primary effectiveness measure(s) | Children were categorised according to their levels of functioning – normal, semi-dependent and very dependent – on completion of IBI until the age of 65 years. Efficacy rates for no intervention, the cohort that received no IBI, were based on published literature. It was assumed that 25% attain normal functioning, 25% are semi-dependent and 50% are very dependent without receiving IBI (Freeman168). The efficacy rates for expansion were assumed to be 30% normal, 50% semi-dependent and 20% very dependent. The resultant efficacy rates for status quo were 26.9% normal, 34.3% semi-dependent and 38.9% very dependent |
| Costs considered | Costs for government-funded respite services and speech and language therapy; special education costs; adult care costs; adult day programmes costs; costs of living in public residential facilities; disability support |
| Costs source | Multiple sources, including various government sectors and education department |
| Results | Incremental cost savings per individual: no intervention vs. status quo = CA$19,241; no intervention vs. expansion = CA$53,720; status quo expansion = CA$34,479 |
| Sensitivity analysis undertaken and results | Yes |
| Chasson (2007)50 | |
| Country | USA |
| Year of cost analysis | NR |
| Currency | US Dollar |
| Intervention costs per year | US$22,500 |
| Source | Assumption |
| Decision analysis model overview | Cost comparison and cost saving analysis using a simple decision tree model |
| Perspective | Government perspective |
| Discount rate – benefits and costs | None |
| Time horizon | 18 years (age range 4–22 years) |
| Population details | Children with autism |
| Intervention vs. comparator(s) | EIBI programme (Lovaas model26) delivered for 3 years vs. special education services |
| Primary effectiveness measure(s) | The benefits for EIBI were model with respect to the use of special education services, with children categorised as either mainstreaming or dependent on specialist education services. Effectiveness estimates were drawn directly from Lovaas26 and assumed 72% of children will receive a mainstream education. For children receiving special education services, it was assumed that all children would not be reliant on these services throughout their childhood |
| Costs considered | Utilised a method from Jacobson et al.52 for hypothetically comparing the costs of special education with the costs of EIBI for children with autism in Texas, USA. The formula incorporates special educations costs, EIBI costs, EIBI effectiveness, population estimates of children with autism in Texas and the expected number of years required for each type of service |
| Costs source | Various sources based on literature and reports, and assumptions based on no evidence |
| ICER | A total saving of US$84,300 per child in state-budgeted funds is achieved over the total school years. Comparing the reported actual cost of a special education programme with a 3-year EIBI programme (and a 72% special education offset) suggested savings of US$208,500 per child |
| Sensitivity analysis undertaken and results | None |
| Peters-Scheffer (2012)44 | |
| Country | Netherlands |
| Year of cost analysis | Not reported |
| Currency | Euro |
| Intervention costs per year | €33,333 |
| Source | Micro costing |
| Decision analysis model overview | A cost–offset analysis using a decision tree |
| Perspective | Public sector |
| Discount rate: benefits and costs | Not reported |
| Time horizon | Age 3–65 years |
| Population details | Children with ASD |
| Intervention vs. comparator(s) | EIBI vs. TAU. EIBI assumed to be delivered at average intensity of 32.54 hours/week for a total of 27.01 months, based on a meta-analysis of studies assessing the effectiveness of EIBI |
| Primary effectiveness measure(s) | Children were categorised into three groups according to their level of functioning. The first group comprised children who achieve normal functioning, defined as participation in regular education with little or no support, and who are vocationally productive as adults. The second group consisted of children who participate in less intensive special education and have reduced dependency in adulthood. The third group requires continuing specialised, intensive educational and adult services. Efficacy rates were based on published literature (six meta-analyses studies) |
| Costs considered |
Child cost: costs of education, parents of (semi-) dependent children aged between 3 and 18 years old receive a compensation in the costs of raising a child with a disability Adult costs: disability benefit, costs for adult living and day programmes or supported work were obtained from the Dutch government, cost of minimal support and care, cost of intensive comprehensive support and care |
| Costs source | Various sources based on literature/reports and service costs |
| Results | Long-term savings were approximately €1,103,067 |
| Sensitivity analysis undertaken and results | None |
| Penner (2015)54 | |
| Country | Canada |
| Year of cost analysis | 2013 |
| Currency | Canadian Dollar |
| Intervention costs per year | CA$56,000 |
| Source | Government report |
| Decision analysis model overview | Decision tree |
| Perspective | Government payer perspective and societal perspective |
| Discount rate: benefits and costs | 3% discount rate was applied to both cost and effectiveness |
| Time horizon | Age 65 years |
| Population details | Children with ASD |
| Intervention vs. comparator(s) | Intensive ESDM was compared with parent-delivered ESDM and EIBI. Intensive ESDM was assumed to be therapist-delivered early intensive ABA-based therapy and based on Dawson et al.83 was assumed to be delivered for 20 hours/week for 2 years. Parent-delivered ESDM was parent delivered with 1 hour of therapist training, delivered for 12 weeks. The remainder of the intervention was delivered by parents. EIBI was defined with respect to usual provision in Ontario, Canada, no details provided |
| Primary effectiveness measure(s) | Assumed that 37% of children received EIBI. In the intensive ESDM and parent-delivered ESDM, gains in IQ of 17.6 and 4.94 points were assumed, respectively. IQ outcomes were stratified into children with IQ above and below 70, from which the probability of achieving different levels of dependence was modelled. Children achieving independence were assumed to accrue 60 DFLYs and semi-dependence 30 DFLYs, whereas those remaining dependent were assumed to accrue 0 DFLYs |
| Costs considered | Costs for government-funded respite services and speech and language therapy; special education costs; adult care costs; adult day programmes costs; costs of living in public residential facilities; disability support |
| Costs source | Costs for each pathway were determined using the budget of an ESDM pilot project and government publications |
| Results | ICERs were calculated for the intensive ESDM group. Compared with the EIBI, intensive ESDM cost an additional CA$12,237 per person and generated an additional 0.53 DFLYs, resulting in an ICER of ≈CA$23,000/DFLY. Compared with the parent-delivered ESDM, intensive ESDM cost an additional CA$20,871 and generated an additional 0.36 DFLYs. The resulting ICER was ≈CA$58,000/DFLY |
| Sensitivity analysis undertaken and results | Yes |
| Cidav (2017)51 | |
| Country | USA |
| Year of cost analysis | 2015 |
| Currency | US Dollar |
| Intervention costs per year | US$60,369 (US$16,015) annual costs |
| Source | Micro costing |
| Decision analysis model overview | Trial-based cost–offset analysis |
| Perspective | Public sector |
| Discount rate: benefits and costs | Only costs were discounted on a 3% rate after the first year |
| Time horizon | Two time horizons were considered: (1) intervention period – included all service use that occurred from the onset of the intervention to the 2-year assessment, including the ESDM use; and (2) post-intervention period – included all service use that occurred from the 2-year assessment to the age 6 years assessment |
| Population details | Children with ASD or PDD-NOS |
| Intervention vs. comparator(s) | ESDM vs. community care, including ABA/EIBI. The ESDM arm received 14.8 hours/week, on average, of either ESDM or ABA/EIBI services compared with 9.4 hours/week of ABA/EIBI services in the community arm. Initial duration of therapy was 2 years, but children could continue to receive ABA/EIBI beyond this period |
| Primary effectiveness measure(s) | Clinical effectiveness parameters were not included. Annualised service use and costs during the intervention and post intervention for the two study arms were compared |
| Costs considered | Parents reported children’s service use, collected every 6 months from enrolment to final follow-up (age 6 years). Services were grouped into the following categories: ESDM, ABA/EIBI, general education (for children < 5 years of age, day care-type typical class; for children > 5 years of age, school-based typical class), occupational and physical therapy, social skills training, special education, speech therapy and other miscellaneous (biomedical therapy, music therapy, parent-focused therapy, nutritional therapy, counselling and psychological services). ‘Total health-related service use’ was defined as sum of all use of these services except general education |
| Costs source | Parents reported children’s service use which was collected alongside the trial every 6 months from enrolment to final follow-up (age 6 years) |
| Results | Total health-related cost comparison: (1) intervention period: ESDM – US$60,369 (SD US$16,015) vs. community care – US$45,975 (SD US$33,089); and (2) post-intervention period: ESDM – US$31,962 (SD US$17,220) vs. US$50,969 (SD US$37,945) |
| Sensitivity analysis undertaken and results | None |
| Quality assessment | Jacobson (1998)52 | Motiwala (2006)53 | Chasson (2007)50 | Peters-Scheffer (2012)44 | Penner (2015)54 | Cidav (2017)51 |
|---|---|---|---|---|---|---|
| Study question | ||||||
| 1. Costs and effects examined | Yes | Yes | Yes | Yes | Yes | No |
| 2. Alternatives compared | Yes | Yes | Yes | Yes | Yes | Yes |
| 3. The viewpoint(s)/perspective of the analysis is clearly stated (e.g. NHS, society) | Yes | Yes | Yes | Yes | Yes | Yes |
| Selection of alternatives | ||||||
| 4. All relevant alternatives are compared (including do-nothing if applicable) | Yes | Yes | Yes | Yes | Yes | Yes |
| 5. The alternatives being compared are clearly described (who did what, to whom, where and how often) | Yes | Yes | Yes | Yes | Yes | Yes |
| 6. The rationale for choosing the alternative programmes or interventions compared is stated | Yes | Yes | Yes | Yes | Yes | Yes |
| Form of evaluation | ||||||
| 7. The choice of form of economic evaluation is justified in relation to the questions addressed | No | Yes | No | Yes | Yes | No |
| 8. If a cost minimisation design is chosen, have equivalent outcomes been adequately demonstrated | n/a | Yes | n/a | n/a | n/a | n/a |
| Effectiveness data | ||||||
| 9. The source(s) of effectiveness estimates used are stated (e.g. single study, selection of studies, systematic review, expert opinion) | Yes | Yes | Yes | Yes | Yes | No |
| 10. Effectiveness data from a RCT or review of RCTs | No | No | No | Yes | No | No |
| 11. Potential biases identified (especially if data not from RCTs) | No | No | No | No | No | No |
| 12. Details of the method of synthesis or meta-analysis of estimates are given (if based on an overview of a number of effectiveness studies) | No | No | No | Yes | No | n/a |
| Costs | ||||||
| 13. All the important and relevant resource use included | Yes | Yes | No | Yes | Yes | Yes |
| 14. All the important and relevant resource use measured accurately (with methodology) | Yes | Yes | No | Yes | Yes | Yes |
| 15. Appropriate unit costs estimated (with methodology) | Yes | Yes | No | Yes | Yes | Yes |
| 16. Unit costs reported separately from resource use data | Yes | No | No | Yes | Yes | Yes |
| 17. Productivity costs treated separately from other costs | Yes | Yes | No | n/a | Yes | Unclear |
| 18. The year and country to which unit costs apply is stated with appropriate adjustments for inflation and/or currency conversion | Yes | Partial | No | No | Yes | Yes |
| Benefit measurement and valuation | ||||||
| 19. The primary outcome measure(s) for the economic evaluation are clearly stated | Yes | Yes | Yes | Yes | Yes | No |
| 20. Methods to value health states and other benefits are stated | No | No | No | Yes | Yes | No |
| 21. Details of the individuals from whom valuations were obtained are given | No | No | No | No | No | No |
| Decision modelling | ||||||
| 22. Details of any decision model used are given (e.g. decision tree, Markov model) | Yes | Yes | Yes | Yes | Yes | Yes |
| 23. The choice of model used and the key input parameters on which it is based are adequately detailed and justified | Yes | Yes | Yes | Yes | Yes | Yes |
| 24. All model outputs described adequately | Yes | Yes | Yes | Yes | Yes | Yes |
| Discounting | ||||||
| 25. Discount rate used for both costs and benefits | No | Yes | No | No | Yes | Unclear |
| 26. Do discount rates accord with NHS guidance | No | No | No | No | No | No |
| Time horizon | ||||||
| 27. Is the time horizon of the model sufficient to reflect all important differences between options | Yes | Yes | No | Yes | Yes | n/a |
| 28. Are the time horizon of the model, the duration of treatment and the duration of the treatment effect described and justified | Yes | Yes | Yes | Yes | Yes | n/a |
| Allowance for uncertainty | ||||||
| 29. Details of statistical tests and CIs are given for stochastic data | n/a | n/a | n/a | n/a | n/a | n/a |
| 30. Uncertainty around cost-effectiveness expressed (e.g. CI around ICER, cost-effectiveness acceptability curves) | n/a | n/a | n/a | n/a | n/a | n/a |
| 31. Are all appropriate input parameters included with uncertainty | No | No | No | No | Yes | Yes |
| 32. Is second-order uncertainty (uncertainty in means) included rather than first order (uncertainty between patients) | No | No | No | No | Yes | No |
| 33. Are the probability distributions adequately detailed and appropriate | No | No | No | No | Yes | Yes |
| 34. Sensitivity analysis used to assess uncertainty in non-stochastic variables (e.g. unit costs, discount rates) and analytic decisions (e.g. methods to handle missing data) | No | No | No | No | Yes | Yes |
| Deterministic analysis | ||||||
| 35. The approach to sensitivity analysis is given (e.g. univariate, threshold analysis, etc.) | No | Yes | No | No | Yes | n/a |
| 36. The choice of variables for sensitivity analysis is justified | No | Yes | No | No | Yes | n/a |
| 37. The ranges over which the variables are varied are stated | No | Yes | No | No | Yes | n/a |
| Presentation of results | ||||||
| 38. Incremental analysis is reported using appropriate decision rules | No | Yes | No | No | Yes | n/a |
| 39. Major outcomes are presented in a disaggregated as well as aggregated form | No | Yes | No | No | No | n/a |
| 40. Applicable to the NHS setting | No | No | No | No | No | No |
Overview
None of the six studies44,50–54 identified in the cost-effectiveness review took a UK perspective, with two studies53,54 taking a Canadian governmental perspective, three studies50–52 taking a US perspective and one study44 taking a Dutch perspective. Five44,50–53 of the six studies used a cost-minimisation approach and did not assess benefits. The only exception to this was Penner et al. ,54 in which the main outcome measure was defined in terms of dependency-free life-years. Five44,50,52–54 of the six studies took a model-based approach and one study51 was a RCT-based economic evaluation.
Model structure
The approach taken in the model-based evaluations was broadly similar across all five studies,44,50,52–54 with all five using simple decision tree or calculator type approaches. Health states were defined with respect to reliance on special needs education and other services. In four44,52–54 of the five models, a tripartite classification system was used to define levels of dependency on specialist services: normal functioning or independent (when individuals were typically assumed to require no special education or service requirements), moderate gain of functioning or semi-independent (when individuals were typically assumed to require some specialist education and adult services) and no significant gain of function or dependent (when individuals were assumed to require intensive special education and adult services). The exception to this tripartite classification was the Chasson et al. study,50 which used a binary classification system instead (normal function and fully dependent on specialist services). In the trial-based evaluation, resource use, both during and post discontinuation of the intervention, was recorded and costs assigned to estimate incremental costs.
Therapies compared
Four44,50,52,53 of the six studies compared early intensive ABA-based interventions with TAU; one study54 compared an expansion of current ABA-based provision to all infants diagnosed with autism with current provision (one-third of diagnosed children receiving ABA-based interventions) or no intervention; and one study51 compared ESDM with TAU, which included the provision of ABA-based techniques. Details of the early intensive ABA-based interventions assessed varied across studies. Two studies50,52 reported few details, but appear to be based on the early Lovaas model26 of intervention, which involved 30–40 hours therapy per week. Assumed intensity in the other four studies44,51,53,54 was based on either real-world data or trial data, with reported intensity of therapy ranging between 14.8 hours and 32.54 hours per week. One study, by Penner et al. ,54 also investigated a parent-delivered model of early intensive ABA-based intervention, with only a nominal number of hours delivered by a trained therapist. Early intensive ABA-based provision was assumed to be implemented for a period of either 2 or 3 years in all studies, although it was clear from the study by Cidav et al. 51 that the children could continue to receive the intervention beyond the initial 2-year intervention period.
Treatment effects
In two of the economic evaluations, clinical effectiveness data used to populate the models were drawn from comparative studies. Cidav et al. 51 used data from a RCT (Dawson et al. 83), whereas Penner et al. 54 used data drawn from two RCTs (Dawson et al. 83 and Rogers et al. 169). In the remaining four studies,44,50,52,53 comparative clinical effectiveness was based on unmatched comparisons. Jacobson et al. 52 and Chasson et al. 50 based outcomes in the early intensive ABA-based arm on the model of Lovaas,26 with Jacobson et al. 52 exploring a range of possible treatment effects. In both studies, children in the comparator arm were assumed to be 100% reliant on specialist service for their entire childhood (i.e. zero effectiveness). Motiwala et al. 53 adopted a similar approach to modelling outcomes in the early intensive ABA-based arm of the model, but based effects on results reported in McEachin et al. 98 and Sallows et al. 100 Comparator outcomes were assumed to be in line with an observation study by Freeman et al. 168 Peters-Scheffer et al. 44 also used Freeman et al. 168 to model comparator outcomes, but based outcomes in the early intensive ABA-based arm on a meta-analysis of relevant studies.
In the majority of the economic evaluations (four44,50,52,53 out of five), the impact of early intensive ABA-based interventions was modelled directly by using educational placement outcomes reported in the effectiveness literature to indicate current and future needs. The only exception to this was the model developed by Penner et al. ,54 in which IQ was used as an intermediate outcome, to predict future dependency on specialist services. This was done using data from an observational study by Howlin et al. ,15 which reported on the prognostic value of childhood IQ as an indicator of adult independence. The use of the effectiveness data to directly model outcomes in this way is important because, as discussed in Chapter 5, education placement is likely to be at very high risk of bias, with a strong possibility that the results of the studies are biased by study procedures, as well as the influence of parental choice on schooling placement.
A further important issue is that, due to the short follow-up in the clinical effectiveness studies evaluating early intensive ABA-based interventions, all studies assumed either (explicitly or implicitly) that the benefits of the intervention persisted over the entire time horizon of the model. Evidence to support this assumption was generally not cited, with the exception again being Penner et al. ,54 in which epidemiological evidence from Howlin et al. 15 was drawn on to extrapolate changes to IQ observed in the trial period. The importance of this assumption cannot be overstated and the lack of supporting evidence to support these assumptions is highly problematic. Even in the study by Penner et al. ,54 which used epidemiological evidence to extrapolate short-term outcomes, the assumptions made were strong. The Howlin et al. 15 study, although providing evidence to support the prognostic value of childhood cognitive ability, provided only evidence of a correlation between childhood IQ and adult outcomes. This does not necessarily imply a causal relationship that would mean that changes to childhood IQ would have an impact on future outcomes. Moreover, even if we assume that it does, it is hard to imagine a causal relationship that does not require the effects on IQ to persist over time. Furthermore, the Howlin et al. 15 study showed that outcomes were very variable and neither verbal nor performance IQ was shown to be a consistent prognostic indicator. The focus on IQ alone, therefore, may be too restrictive.
Costs considered
The costs considered largely focused on the provision of specialist schooling and the provision of adult support services, which were assumed to include residential care and assisted living services, disability support services and supported employment placements. All six analyses conducted used a public perspective; however, two studies also conducted an analysis from a broader societal perspective (Jacobson et al. 52 and Penner et al. 54). Costs of early intensive ABA-based services were estimated to be between £16,472 and £57,489 (inflated to 2017 prices) per annum, with estimated costs based on government reports in three studies52–54 and micro-costing in one study. 44 In Chasson et al. ,50 which reported the lowest annual costs, costs of ABA-based interventions were assumed to be the same as the provision of special education.
Quality of life and benefits of therapy
Only one of the studies (Penner et al. 54) considered benefits, assigning dependency-free life-years to each of the levels of independence. The value of each health state was, however, based solely on assumptions, with no evidence provided to justify the values used. Inferences about the value of benefits predicted by the Penner et al. 54 model must therefore be heavily caveated to reflect this lack of supporting evidence.
Results of identified studies
The results of all six of the economic evaluations were overwhelmingly positive, with the results of all four of the studies44,50,52,54 comparing early intensive ABA-based interventions with TAU predicting significant cost savings. In all of the analyses, these cost savings were attributable to significant cost offsets resulting from reductions in resource use, particularly specialist schooling provision and residential care.
Summary
The cost-effectiveness review identified six studies,44,50–54 five44,50,52–54 of which adopted a model-based approach. Although each of the models used different sources of data and made a variety of different assumptions, all five of the identified models adopted similar structures based primarily around educational placement and independence. Central to all models was the assumption that the effects of early intensive ABA-based interventions persisted over the entire time horizon of the model, but little evidence was reported justifying this assumption. Many of the studies also drew directly on educational placement outcomes reported in the effectiveness studies, which is problematic given the limitations of this evidence. In general, results of the previous analyses should be viewed with some caution, although they do highlight several important drivers of cost-effectiveness.
Appendix 14 Quality-of-life review
Overview
A literature review was conducted to identify studies investigating quality of life in children and autistic adults.
Methods
To identify published evidence, the following databases were searched for eligible studies: MEDLINE (Ovid), EMBASE (Ovid) 1980 onwards, NHS Economic Evaluation Database and PsycINFO. The searches were undertaken in November 2017. The full search strategy is reported in Appendix 17.
Study selection
Two researchers independently undertook the screening of all titles and abstracts identified in the searches. Full-paper publications were then obtained for potentially relevant studies and screened against the eligibility criteria. Disagreements between reviewers were resolved by discussion.
Studies were eligible if they included children or adults with a diagnosis of ASD and reported utility score or values using a validated quality-of-life questionnaire.
Data extraction
Details of eligible studies were extracted by a single reviewer and summarised using a Microsoft Excel data extraction template.
Results
Search results
A total of 1179 records were identified in the search after removing duplicates, of which 214 studies were identified as potentially relevant from their titles and/or abstracts. The full-text articles of these records were assessed for eligibility. A total of 42 studies (45 records) were found to meet the inclusion criteria. Figure 34 presents a flow diagram of the selection process.
FIGURE 34.
Flow diagram showing study selection for the quality-of-life review.

Studies conducted in children and adolescents with autistic spectrum disorder
A total of 33 studies (35 records) were identified assessing quality of life in children and/or autistic adolescents. 120,124,127,170–201 The majority of the included studies were cross-sectional survey studies, except two studies199,200 which conducted trials in autistic children. Neither of these trials were of ABA-based interventions. A range of methods were employed to collect the data, using mostly mail surveys. Most of the studies used parents or primary caregivers as proxy; however, a few studies elicited values directly from children. 172,173,176,189–192,194,198,199 A total of seven different quality-of-life measures were used across the 33 identified studies. The most commonly reported were the Pediatric Quality of Life Inventory™ (PedsQL™) measure, used in 15 studies;170,174,175,179,180,182,185,187,189–195,200,201 the Health Utilities Index measure, used in seven studies;120,127,177,178,188,196,197 and the KIDSCREEN measure, used in four studies. 172,176,186,195 A detailed description of participants and results of the included studies are presented in Table 50.
| Study | Participants | Subgroup/trial arms | n | Male % | Age (years), mean (SD) | Symptom severity measure, mean (SD) | IQ, mean (SD) | Respondent | Utility measure(s), mean score (SD) |
|---|---|---|---|---|---|---|---|---|---|
| Cross-sectional studies | |||||||||
| Kuhlthau (2013)181 | Children with ASD | n/a | 71 | 87.0 | 7.9 | PDDBI, 43.6 (21.4) | NR | Parent | CHIP-CE resilience, 42.3 (13.8); comfort, 46.1 (9.6); risk avoidance, 40.7 (10.5); satisfaction, 39.1 (10.9); achievement, 33.3 (11.4) |
| Domellöf (2014)173 | Children and adolescents with ASD | n/a | 61 | 86.9 | 12.0 (3) | NR | NR | Child (37.7%); parent (27.9%); not stated (34.4%) | EQ-5D-Y VAS, 80.7 (18.8) |
| van Steensel (2012)198 | Children with high-functioning ASD and comorbid anxiety disorders | n/a | 115 | 78.3 | 11.37 (2.63) | NR | NR | Parent and child | EQ-5D, NR (NR) |
| Forsyth (2007)177 | Young children with severe disabilities | n/a | 600 | 70.0 | 2.67 (median) | NR | NR | Parent | HUI, median 0.44 (IQR 0.21–0.67) |
| Forsyth (2010)178 | Young children with severe disabilities | n/a | 5862 | 68.0 | 10.58 (3.92) | NR | NR | Parent | HUI, 0.33 (0.34) |
| Hoefman (2014)120 | Children with ASD | n/a | 224 | 87.0 | 8.4 (3.5) | NR | NR | Primary caregiver | HUI3, 0.66 (0.16); QWB-SA, 0.59 (0.16) |
| Payakachat (2014)127 | Children with ASD | n/a | 224 | 86.6 | 8.4 (3.5) | ADOS, 7.2 (1.8) | 75.7 (24.3) | Primary caregiver | HUI3, 0.66 (0.23) |
| Petrou (2010)188 | Children with ASD | n/a | 11 | NR | NR | NR | NR | Parent | HUI3, 0.61 (0.26); HUI2, 0.72 (0.15) |
| Tilford (2012)196 | Children with ASD | ASD, PDD-NOS, AS | 150 | 85.3 | 8.6 (3.3) | NR | NR | Primary caregiver | HUI3, 0.66 (0.23); QWB-SA, 0.59 (0.16) |
| Tilford (2015)197 | Children with ASD | n/a | 224 | 86.6 | 8.2 (3.5) | NR | NR | Primary caregiver | HUI3, 0.66 (0.23); QWB-SA, 0.59 (0.16) |
| Clark (2015)172 | Adolescents with ASD | n/a | 22 | 86.4 | 15.2 (1.7) | NR | NR | Child and parent | KIDSCREEN-52. Scores on all 10 dimensions vary between 40 and 50 or within 1 SD of the mean of 50 |
| Egilson (2017)176 | Children with ASD | n/a | 96 | 87.5 | 8–11, 43.8%; 12–17, 56.3% | NR | NR | Parent | KIDSCREEN-52. Scores vary on 8/10 dimensions between 45 and 50 or within half a SD of mean of 50 |
| Meral (2015)186 | Children with ASD | n/a | 379 | 78.6 | 9.57 (4.44) | NR | NR | Parent | KIDSCREEN-27, 76.52 (13.55) |
| Bourke-Taylor (2012)170 | Children with ASD | n/a | 94 | NR | 9.5 (3.7) | NR | NR | Mother | PedsQL, NR (NR) |
| de Vries (2015)174 | Children with ASD | n/a | 120 | 90.0 | 10.2 (1.3) | ADI-R age of first word, 18.5 (7.7); age of first sentence, 26.1 (9.7); language composite, 5.4 (2.1) | WISC-III, 110.9 (20.6) | Parent | PedsQL, 32.9 (11.6) |
| Delahaye (2014)175 | Children with ASD | n/a | 86 | 83.7 | 7.18 (NR) | PDDBI, 46.38 (NR) | S–B5 and MSEL composite score < 70, 61.22%; composite score ≥ 70, 38.78% | Parent | PedsQL, 64.18 (64) |
| Jahan (2015)179 | Children with ASD | n/a | 149 | 77.2 | 7.8 (3.06) | NR | PedsQL-4.0 cognitive functioning scale, 68.9 (23.4) | Parent | PedsQL, 71.38 (16.76) |
| Kose (2013)180 | Children with autism (ASD, PDD-NOS, AS) | Overall | 102 | 82.4 | 8.2 (3.7) | NR | NR | Parent | PedsQL, NR (NR) |
| ASD | 46 | 87.0 | 8.6 (3.8) | CARS, 15–29 0%; 30–36, 41.3%; 37–60, 58.7% | NR | NR | PedsQL, 50.1 (10.8) | ||
| PDD-NOS | 38 | 84.2 | 6.3 (2.5) | CARS, 15–29: 55.3%; 30–36, 34.2%; 37–60, 10.5% | NR | NR | PedsQL, 61 (15.1) | ||
| AS | 18 | 66.7 | 11.5 (2.9) | CARS 15–29, 83.3%; 30–36, 11.1%; 37–60, 5.6% | NR | NR | PedsQL, 65.1 (14.4) | ||
| Kuhlthau (2010)182 | Children with ASD | Overall | 286 | 82.5 | 2–4, 36.0%; 5–7, 26.2%; 8–12, 7.8% | SRS, 98.9 (29.3) | NR | Parent | PedsQL, 65.2 (15.9) |
| Autism | 196 | NR | NR | NR | NR | PedsQL, 63.8 (1.5) | |||
| Asperger syndrome | 25 | NR | NR | NR | NR | PedsQL, 67.7 (3.2) | |||
| PDD-NOS | 65 | NR | NR | NR | NR | PedsQL, 65.1 (2.1) | |||
| Limbers (2009)185 | Children with Asperger syndrome | n/a | 22 | 90.9 | 9.25 (2.15) | NR | PedsQL cognitive functioning scale, 41.41 (24.55) | Parent | PedsQL, 55.58 (11.52) |
| Ozturk (2016)187 | Children with ASD | n/a | 102 | 82.4 | 8.23 (3.68) | CARS, NR (NR) | NR | Parent | PedsQL, NR (NR) |
| Potvin (2011, 2015)189,190 | Children with high-functioning autism | n/a | 30 | 86.7 | 111.03 months (18.8) | NR | NR | Child and parent | PedsQL child reported, 64.14 (13.24); parent reported: 56.1 (13.58) |
| Sheldrick (2012);191 Shipman (2011)192 | Children with ASD | n/a | 39 | 73.0 | 14.8 (range 12–18) | SRS, 73.7 (NR) | NR | Child and parent | PedsQL child: 41.8 (NR); parent projected, 37.5 (NR); parent standard, 35.5 (NR) |
| Sikora (2012)193 | Children with ASD | Overall | 2020 | 84.3 | 2–5, 56.6% 6–11, 33.3% 12–18, 10.1% | NR | MSEL < 70, 34.1%; ≥ 70, 65.9% | Parent | PedsQL, NR (NR) |
| ASD | NR | NR | NR | NR | NR | PedsQL, 68.9 (NR) | |||
| ASD + ADHD | NR | NR | NR | NR | NR | PedsQL, 59.1 (NR) | |||
| Stokes (2017)194 | Children with ASD | n/a | 229 | 85.6 | 13.7 (3.1) | ADOS, 5.8 (4.1) | PPVT, 104 (12.7) | Child | PedsQL, NR (NR) |
| Tavernor (2013)195 | Children with ASD | n/a | 11 | NR | NR | NR | NR | NR | PedsQL, NR (NR); KIDSCREEN, NR (NR) |
| Viecili (2015)201 | Children with ASD | n/a | 122 | NR | NR | NR | NR | Not clear | PedsQL, 63.64 (16.6) |
| Chuang (2014)171 | Children with ASD | n/a | 106 | 84.9 | 4.53 (0.8) | CARS severe, 56.7; mild/moderate, 29.2; non-autistic, 14.1 | CPEP-3 receptive language ability, 12 (3.7); expressive language ability, 11.9 (3.5); cognition, 12.7 (8.3) | Parent | TAPQOL-C, NR |
| Lai (2016)183 | Children with ASD | Overall | 31 | NR | 50.6 months (16.9) | NR | NR | NR | TAPQOL-C, NR |
| Mild (cognition domain ≥ 4) | 11 | NR | NR | NR | NR | NR | TAPQOL-C, 73.8 (16.3) | ||
| Severe (cognition domain < 4) | 20 | NR | NR | TAPQOL-C, 64.2 (14.2) | |||||
| Lavelle (2012)184 | Children with ASD | Overall | 138 | 81.5 | 3–5 years, 8.15%; 6–10 years, 32.59%; 11–13 years, 23.70%; 14–17 years, 35.56% | NR | NR | Parent | TTO, 0.56 (NR) |
| Autism | 43 | NR | NR | NR | NR | NR | TTO, 0.55 (NR) | ||
| AS | 64 | NR | NR | NR | NR | NR | TTO, 0.53 (NR) | ||
| PDD-NOS | 29 | NR | NR | NR | NR | NR | TTO, 0.63 (NR) | ||
| Tung (2014)124 | Children with autism | n/a | 84 | 88.1 | 5.94 (2.32) | CARS, 32.05 (4.8) | NR | Caregiver | WHOQOL-BREF, NR (NR) |
| Trials | |||||||||
| Van Steensel (2014)199 | Children with ASD | CBT | 24 | 83.3 | 11 (2.62) | ADI-R, 31.88 (7.03) | NR | Child and parent | EQ-5D parent report, 0.66 (0.19); child report, 0.69 (0.12) |
| TAU | 25 | 80.0 | 10.72 (2.25) | 33.04 (8.03) | EQ-5D parent report, 0.73 (0.22); child report, 0.82 (0.26) | ||||
| Varni (2012)200 | Children with ASD | Aripiprazole (Abilify®, Otsuka Pharmaceutical, Tokyo, Japan) | 167 | 88.0 | 9.5 (3.1) | NR | NR | Parent | PedsQL, 42 (15.6) |
| Placebo | 76 | 89.5 | 9.4 (3) | PedsQL, 40.4 (15.6) | |||||
Studies conducted in adults (including young adults) with autistic spectrum disorder
A total of nine studies (10 records130,202–210) reported on quality of life in adults and young adults with autism or related conditions. As in the studies of children, the majority of the included studies were cross-sectional surveys. The range of data collection methods used in the identified studies included mail and internet surveys, with a smaller number also using face-to-face interviews. Most of the studies used self-reported measures; however, two studies202,204 elicited values from parent and carers’ perspective. Of the nine identified studies, seven202,204–208,210 used the World Health Organization Quality of Life-BREF (WHOQOL-BREF) quality-of-life measure, one203 used the Short Form questionnaire-36 items (SF-36) and one130,209 used the Short Form questionnaire-12 items (SF-12) version 2. A detailed description of participants and results of the included studies are presented in Table 51.
| Study | Participants | Subgroup/trial arms | n | Male (%) | Age years, mean (SD) | Symptom severity measure, mean (SD) | IQ, mean (SD) | Respondent | Utility measure(s), mean score (SD) |
|---|---|---|---|---|---|---|---|---|---|
| Helles (2017)203 | Adults with AS | n/a | 100 | 100 | No longer ASD, 10.9 (3.8); ASD, 10.3 (2.5); ASD plus, 12.5 (5.4) | ASSQ no longer ASD, 20.0 (7.9); ASD, 22.9 (8.0); ASD plus, 24.1 (9.0) | WAIS-III no longer ASD, 100.6 (15.0); ASD,105.1 (22.0); ASD plus, 104.3 (15.2) | Self-reported | SF-36 PCS, 54.3 (6.3); MCS, 42.0 (9.8) |
| Khanna (2014, 2015)130,209 | Adults with ASD | n/a | 291 | 60.8 | 30.76 (11.88) | AQ-10; 6.34 (2.35) | NR | Self-reported | SF-12 PCS, 49.44 (10.36); MCS, 40.77 (9.32) |
| Bishop-Fitzpatrick (2017)202 | Adults with ASD | n/a | 60 | 76.7 | 31.48 (6.75) | ADI-R, 41.22 (6.79) | NR | Self and carer | WHOQOL-BREF, 72.91 (15.68) |
| Hong (2016)204 | Adults with ASD | n/a | 60 | 76.7 | 32 (6.8) | NR | NR | Self, mother | WHOQOL-BREF, NR (NR) |
| Jariwala-Parikh (2015)205 | Adults with ASD | n/a | 265 | 55.7 | 33.1 (13.76) | AQ-10 low severity, 44%; high severity, 66% | NR | Self-reported | WHOQOL-BREF, NR (NR) |
| Jennes-Coussens (2006)206 | Adults with AS | n/a | 12 | NR | 20.3 (1.3) | NR | NR | Self-reported | WHOQOL-BRIEF, 3.7 (0.7) |
| Kamp-Becker (2010)208 | Adults with AS, high-functioning autism or atypical autism | n/a | 26 | 100 | 21.6 (3.4) | ADOS-G: NR (NR) | Wechsler, 99.3 (17.7) | Self-reported | WHOQOL-BREF, 60.6 (26.1) |
| Kamio (2013)207 | Adults with ASD | n/a | 154 | 79.9 | 27.6 (6.5) | NR | NR | Self-reported | WHOQOL-BREF psychological health raw score, 2.78 (0.74); social relationships raw score, 2.71 (0.82) |
| Moss (2017)210 | Adults with autism | Childhood | 52 | 82.7 | 6.3 (2.1) | ADI-R, 40.1 (7.4) | 89.3 (14.4) | Caregivers, self-reported | WHOQOL-BREF, NR (NR) |
| Adulthood | 47.9 (9.5) | ADI-R, 27.6 (7.8) | 69.9 (32.4) | WHOQOL-BREF, NR (NR) |
Studies conducted in carers and parents
A total of 17 studies (18 records123,211–226) were identified reporting quality-of-life measures in carers and parents of children with autism or a related condition. The majority of the included studies were cross-sectional surveys, with the exception being a trial investigating a parent-targeted education programme. 221 All of the studies elicited values directly from the carer or parent. The most commonly used tool was the SF-36, used in 11214–225 of the 17 studies. A further three studies211–213 reported WHOQOL-BREF, two studies123,226 used EuroQol-5 Dimensions, one study227 used the SF-12 and one study123 used the SF-6D. A description of participants and results of the included studies are presented in Table 52.
| Study | Participants | Subgroup/trial arms | n | Child characteristic | Respondent | Utility measure(s), mean score (SD) | |||
|---|---|---|---|---|---|---|---|---|---|
| Male (%) | Age years, mean (SD) | Symptom severity measure, mean (SD) | IQ, mean (SD) | ||||||
| Ahmad (2015)211 | Fathers of children with ASD | n/a | 101 | 85.2% | 5.0 (3.2) | NR | NR | Self-report | WHOQOL-BREF, 74.17 (13.99) |
| Allik (2006)227 | Parents of children with AS or high-functioning autism and parents of typically developing children | Overall | 61 | NR | 10.8 (range 8–12) | NR | NR | Self-report | NR |
| AS/HFA: mother | 31 | SF-12 MCS, 49.1 (11.1); PCS, 44.7 (10.8) | |||||||
| Control: mother | 30 | SF-12 MCS, 52.0 (9.6); PCS, 52.5 (7.4) | |||||||
| AS/HFA: father | 30 | SF-12 MCS, 51.3 (7.8); PCS, 49.8 (6.9) | |||||||
| Control: father | 29 | SF-12 MCS, 53.6 (6.1); PCS, 53.0 (6.8) | |||||||
| Amirian (2017)214 | Parents of children with ASD | Overall | 97 | NR | NR | NR | NR | Self-report | SF-36 MCS, 50.78 (17.08); PCS, 59.70 (21.35) |
| Fathers | 21 | SF-36 MCS, 47.92 (12.97); PCS, 59.88 (14.67) | |||||||
| Mothers | 76 | SF-36 MCS, 50.93 (18.07); PCS, 59.65 (22.94) | |||||||
| Aral (2015)215 | Families of children with ASD | n/a | 30 | NR | NR | NR | NR | Self-report | SF-36, NR (NR) |
| Benjak (2011)216 | Parents of children with ASD and typically developing children | n/a | 350 | NR | NR | NR | NR | Self-report | SF-36, NR (NR) |
| Dardas (2014)212 | Parents of children with autistic disorder | Overall | 184 | NR | 6.04 (3.05) | NR | NR | Self-report | WHOQOL-BREF, NR (NR) |
| Fathers | 70 | WHOQOL-BREF, 58.2 (9.2) | |||||||
| Mothers | 114 | WHOQOL-BREF, 83.2 (8.8) | |||||||
| Forouzanfar (2016)217 | Mothers of children with ASD | n/a | 203 | NR | 7.89 (3.3) | NR | NR | Self-report | SF-36 MCS, 43.65 (6.95); PCS, 53.25 (25.51) |
| Johnson (2009, 2011)218,219 | Parents of children with ASD | Overall | 128 | 81 | 7.8 (3.9) | NR | NR | Self-report | SF-36 MCS, 34.21 (13.11); PCS, 49.21 (11.22) |
| Fathers | 64 | SF-36 MCS, 41.60 (12.93); PCS, 51.16 (9.56) | |||||||
| Mothers | 64 | SF-36 MCS, 34.21 (13.11); PCS, 49.21 (11.22) | |||||||
| Ji (2014)220 | Caregivers of children with ASD | n/a | 273 | 81 | 4.81 (2.01) | CARS ≥ 36, 42.1%; < 36, 57.9% | NR | Self-report | SF-36 MCS, 45.58 (16.71); PCS, 58.72 (12.48) |
| Ji (2014)221 | Primary caregivers of children with ASD | Overall | 42 | 83 | 5.27 (NR) | CARS ≥ 36, 50%; < 36, 50% | NR | Self-report | SF-36, NR (NR) |
| Intervention | 22 | 81.8 | 4.93 (2.03) | CARS ≥ 36, 50%; < 36, 50% | NR | SF-36 MCS, 53.85 (9.10); PCS, 63.11 (7.42) | |||
| Waiting list control | 20 | 85.0 | 5.65 (1.74) | CARS ≥ 36, 50%; < 36, 50% | NR | SF-36 MCS, 51.00 (15.96); PCS, 63.54 (9.69) | |||
| Khanna (2011)222 | Parents of children with ASD | n/a | 305 | 82.9 | < 5, 7%; 5–10, 44.14%; 11–14, 41.4%; 15–18, 6.6% | CARS, 33.20 (9.05) | NR | Self-report | SF-36 MCS, 37.48 (11.78); PCS, 51.28 (9.6) |
| Khanna (2013)226 | Primary caregivers of children with autism | n/a | 316 | 80.1 | < 5, 16.8%; 5–10, 46.5%; 11–18, 36.1% | NR | NR | Self-report | EQ-5D 18–44 years old, 0.82 (0.16); 45–64 years old, 0.81 (0.16) |
| Kheir (2012)223 | Parents of children with ASD and typically developing children | Overall | 98 | NR | NR (range 3 –17) | NR | NR | Self-report | SF-36, NR (NR) |
| ASD | 56 | NR | NR | NR | NR | SF-36 MCS, 41.94 (11.98); PCS, 48.85 (8.14) | |||
| Typical development | 42 | NR | NR | NR | NR | SF-36 MCS, 45.14 (9.60); PCS, 49.42 (7.96) | |||
| Kousha (2016)213 | Mothers of children with ASD | n/a | 127 | 76 | 6.26 (2.82) | NR | NR | Self-report | WHOQOL-BREF, NR (NR) |
| Kuhlthau (2014)123 | Parents of children with ASD | n/a | 224 | 86.5 | 8.4 (3.5) | ADOS ≤ 5, 11%; 6 –7, 46%; ≥ 8, 43% | ≤ 70, 48%;> 70, 52% | Self-report | SF-6D, 0.74 (0.12); EQ-5D, 0.85 (0.14) |
| Lee (2009)224 | Parents of children with high-functioning autism and typically developing children | Overall | 135 | NR | NR | NR | NR | Self-report | SF-36, NR (NR) |
| HFA | 89 | 91.9 | 9.5 (2.0) | NR | NR | SF-36, NR (NR) | |||
| Typical development | 46 | 90.0 | 9.7 (2.1) | NR | NR | SF-36, NR (NR) | |||
| Yamada (2012)225 | Parents of children with PDD | Overall | 269 | 81.6 | 9.08 (2.5) | NR | > 70, 74%; 50–69, 21%; < 50, 5% | Self-report | SF-36, NR (NR) |
| Fathers | 122 | SF-36 MCS, 49.4 (8.0); PCS, 51.1 (5.5) | |||||||
| Mothers | 147 | SF-36 MCS, 42.9 (11.9); PCS, 50.3 (6.9) | |||||||
Appendix 15 Review of epidemiological and observational studies
Overview
A literature review was conducted to identify studies describing the prognosis and outcomes of autistic children and adults. This review had three objectives:
-
to characterise the natural history of children with autism and related conditions with reference to the outcome measures most commonly reported in the effectiveness studies identified as part of the IPD meta-analysis
-
to review the literature on prognostic variables, in particular the relationships between short-term measures reported in the effectiveness studies and outcomes in adulthood
-
to characterise contemporaneous relationships between outcome measures reported in the effectiveness studies and adult outcomes (e.g. the correlations between adult measures of IQ and other adult outcomes).
Methods
To address the three objectives, three related reviews were undertaken. Review 1 addressed the first objective, review 2 addressed the second and review 3 addressed the third.
To identify appropriate literature, two recent previous systematic reviews17,228 addressing similar research questions were used. The first review, Magiati et al. ,17 was a review of longitudinal studies and sought to describe both changes in commonly reported outcome measures between childhood and adulthood and the prognostic value of these measures. Magiati et al. 17 therefore addressed reviews 1 and 2. The second review used was Steinhausen et al. ,228 which sought to describe social outcomes in adulthood. This review did not address any of the review questions directly, but identified literature that could address review question 3.
To supplement and update these two literature reviews, updated searches were also undertaken to identify any literature published following the publications of these reviews. The following databases were searched as part of these update searches: MEDLINE (Ovid), EMBASE (Ovid) 1980 onwards, NHS Economic Evaluation Database and PsycINFO. The searches were undertaken in February 2018 and date limited to post 2013. The full search strategy used is reported in Appendix 17.
Study selection
A single reviewer obtained full texts of the studies identified in the two previous reviews and compared them with the inclusion criteria for each review. For the update searches, a single independent reviewer undertook the screening of all titles and abstracts identified. Full-paper publications were then obtained for potentially relevant studies before screening against the eligibility criteria. The inclusion criteria of each review are described in Table 53.
| Review | Inclusion criteria |
|---|---|
| Review 1: natural history of autism | |
| Population | Studies of autistic populations, including ASD, AS and PPD-NOS |
| Outcomes | Cognitive ability, VABS composite or component scores, ADOS severity score |
| Study type | Longitudinal studies reporting outcomes in both childhood (< 18 years of age) and adulthood (≥ 18 years of age). More than 20 participants |
| Date limit | Published after 1990 |
| Review 2: prognostic outcomes | |
| Population | Studies of autistic populations including ASD, AS and PPD-NOS |
| Outcomes | Adult social outcomes |
| Study type | Longitudinal studies reporting on the prognostic value of any childhood measures as a predictor of adult social outcomes |
| Date limit | Published after 1990 |
| Review 3: adult predictors of social outcomes | |
| Population | Studies of autistic populations including ASD, AS and PPD-NOS |
| Outcomes | Adult social outcomes |
| Study type | Any study reporting on adult outcome measures as a predictor of adult social outcomes |
| Date limit | Published after 1990 |
Data extraction
Details of eligible studies were extracted by a single reviewer and summarised using a Microsoft Excel data extraction template.
Results
Search results
A flow diagram describing study selection is presented in Figure 35. A total of 33 studies were identified in the two systematic reviews after removing duplicates and were assessed against the inclusion criteria for each review. Of the 33 studies, 15 were considered to meet the inclusion criteria for one or more reviews. The update searches identified a total of 632 unique studies. After initial screening, 70 studies were selected for full-text review, 33 identified in previous reviews and 37 through the additional searches. A total of 17 studies were included in one or more of the reviews. The total number of studies included in reviews 1–3 was 14, 11 and 5, respectively.
FIGURE 35.
Flow diagram showing study selection for the epidemiology reviews.

Overview of studies
A summary of the key characteristics for each of the 18 studies included in the three reviews are presented in Table 54. The studies identified were mostly longitudinal studies, with a minority using cross-sectional designs. The studies recruited from a range of populations, including participants diagnosed with autism, Asperger syndrome and/or PDD-NOS. Populations recruited were predominantly male, with some recruiting all-male populations. Mean IQ at baseline ranged from 52.2 to 86.3, with most studies recruiting participants with and without intellectual disability. A smaller number of studies, however, recruited from populations with IQ in the normal range only. Sample sizes varied from 20 to 119 participants. A summary of the results of the studies included in each of the reviews is presented in Table 52.
| Study | Review | n | Population characteristic | Measure reported | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Age (years) at baseline, mean (SD) [age range] | Age (years) at last follow-up, mean (SD) [age range] | IQ at baseline, mean (SD) [cut-off criteria for IQ] | IQ description | Male (%) | VABs | ADOS | IQ | Adult social outcomes | |||
| Howlin (2013)229 | 1, 2, 3 | 60 | 6.9 (2.9) | 44.2 (9.4) [29–64] | 86.3 [> 70] | Normal | 81.60 | No | No | Yes | Yes |
| Gillespie-Lynch (2012)230 | 1, 2 | 20 | 3.9 (1.2) | 26.6 (3.8) | NR | NR | 100 | Yes | No | DQ only | Yes |
| Gray (2012)231 | 1 | 119 | 8.7 (4.3) | 24.8 (4.7) | Borderline or average, 27 (22.6%); mild/moderate ID, 75 (63.1%); severe ID, 17 (14.3%) | Mixed | 82.40 | No | No | Yes (groups only) | No |
| Billsedt (2005, 2007, 2011)232–234 | 1, 2 | 108 | < 10 | 25.5 (6.4) | > 70, 98 (82%); < 70, 22 (18%) | Mixed | 71.30 | No | No | Yes | Yes |
| Farley (2009)134 | 1, 2, 3 | 41 | 7.2 (4.1) | 32.5 (5.7) | FSIQ, 83.68 (17.56) | Normal | 92.70 | Yes | No | Yes | Yes |
| Szatmari (2009)235 | 1 | 36 | 5.5 (0.98) | 17.7 (1.56) | 84.5 (16.11) [> 70] | Normal | 86.10 | Yes | No | No | No |
| Cederlund (2008)132 | 1, 2 | 70 | < 10 | Autism, 24.5 (5.4) | < 50, 39; 50–69, 31; 70–84, 10; ≥ 85, 4 | Mixed | 100 | No | No | Yes (groups only) | Yes |
| Eaves (2008)236 | 1, 2, 3 | 48 | 6.8 [3–12] | 24.0 [19–31] | VIQ > 70, 17.4%; NVIQ > 50, 61% | Mixed | 77.10 | No | No | Yes (groups only) | Yes |
| McGovern (2005)237 | 1 | 48 | 3.9 (1) | 19.0 (3.8) | 52.2 (13.3) | Mixed | 87.50 | Yes | Yes | Yes | No |
| Howlin (2004)15 | 1, 2, 3 | 68 | 7.24 (3.10) | 29.33 (7.97) | PIQ, 80.21 (19.28) | > 50 | 89.70 | No | No | Yes | Yes |
| Howlin (2000)238 | 1 | 18 | 7–8 | 23.75 (1.79) | NR | NR | 55.50 | No | No | Yes | No |
| Ballaban-Gil (1996)243 | 1 | 99 | 6.8 [0.8–20.3] | 18.1 | Severe mental retardation, 31%; mild mental retardation, 15%; normal or near-normal, 22%; indeterminate, 28% | Mixed | 71.00 | No | No | Yes (groups only) | No |
| Bishop (2015)239 | 1 | 84 | 2 | 19 | 66.3 (20.6) | Mixed | 87 | Yes | No | Yes | No |
| Anderson (2014)240 | 1 | 85 | 2 | 19 | 69.28 (NR) | Mixed | NR | Yes | No total score | Yes | Yes |
| Marriage (2009)241 | 2 | 45 | 12.4 (3.4) | 21.3 (4.0) | > 70, 33; < 70, 12 | Mixed | 82.20 | No | No | Yes (groups only) | Yes |
| Gray (2014)242 | 2 | 8.7 (4.3) | 24.8 (4.7) | Average, 9.2%; borderline, 13.4%; mild ID, 24.4%; moderate ID, 38.7%; severe ID, 14.3% | Mixed | 82.40 | No | No | Yes (groups only) | No | |
| Esbensen (2010)133 | 3 | 70 | 37.7 | NR | Mild, 25.7%; moderate, 27.1%; severe, 35.7%; profound, 8.6%; unknown, 2.9% | Mixed | NR | No | No | Yes (groups only) | Yes |
Natural history
The majority of studies included in review 1 demonstrate changes in IQ over time, with fewer (four) reporting changes in VABS (composite or component) scores and none reporting changes in ADOS scores.
Patterns of change over time varied across studies with respect to both IQ and VABS scores. With respect to IQ, 915,134,229,231,236–238,242,243 of the 14 studies15,132,134,229–234,236–240,243 reported only small changes in IQ over time, although some noted significant variations at the individual level. The remaining five studies132,230,232–234,239,240 observed declines in IQ scores, although it was not always clear as to the magnitude of these declines due to the limited reporting. There was also some evidence of greater declines in scores for participants with intellectual disability at baseline, with two studies noting differences in trajectories for those with and without intellectual disability.
In contrast to IQ, VABS (composite and component) scores show a more pronounced pattern of change over time, but with less consistency across studies. Szamatri et al. 235 observed increases in individual component scores but falls in composite scores. Other studies230,237 also report increases in component scores, but, unlike Szamatri et al. ,235 these report increases in composite scores. The reasons for these different trends are unclear, but it may be that some studies are reporting raw scores, rather than standardised scores.
Comparisons between the epidemiological data and the limited long-term effectiveness data for TAU and eclectic arms show a similar pattern of change to that in the majority of the observational literature with respect to IQ, with scores remaining broadly stable over time. With respect to VABS composite scores, the evidence from the effectiveness studies appears to align with Szamatri et al. ,235 as declines in VABS scores are observed over time.
Prognostic factors
Nearly all of the studies included in review 2 reported IQ as a prognostic factor, showing a positive association between childhood IQ and adult social outcomes. Limitations in the predictive value of IQ were, however, noted in a number of studies. 134,229 For example, Howlin et al. 229 reported substantial variations in adult social outcomes in participants who all had IQ within the normal range, and observed that neither verbal nor performance IQ was a consistent prognostic indicator. These variations aside, the identified studies consistently report that individuals with intellectual disability tend to have ‘poor’ outcomes, with the majority being highly dependent on adult social services and few leading independent lives. This may be an unsurprising finding, given the severity of disability experienced by these individuals, and may suggest more limited opportunities for people with intellectual disability to live independent lives. However, it is also clear that normal or high IQ is not sufficient to enable individuals to live independently, although the reported correlations suggested that there is potentially greater scope for them to do so.
In addition to IQ, a number of studies also reported childhood language skills as predictor of adult social outcome. This finding, however, was not consistent across studies. 229
In terms of utilising the data reported to populate the model, it is notable that no study reported on the prognostic value of VABS component or composite scores, despite this being a commonly reported outcome in the effectiveness studies.
Contemporaneous factors
Review 3 identified only six studies reporting correlations between adult outcome measures and adult social outcomes. As in review 2, IQ was the predominant measure reported and was found to be a relatively strong predictor of adult social outcomes. Other measures reported were severity (ADI-R and Childhood Autism Rating Scale), language and reading skills, and VABS composite scores. Of the six studies identified, Farley et al. 134 was notable because it reported both VABS composite and IQ scores and observed that VABS scores were the better predictor of the two (respective correlation coefficients of 0.78 and 0.55). It was also notable that none of the studies went beyond simple correlations and attempted to predict adult social outcomes (Table 55).
| Study | Review 1 | Review 2 | Review 3 | ||
|---|---|---|---|---|---|
| VABS | ADOS | IQ | |||
| Howlin (2013)229 | NR | NR | Relatively stable over time, although with some individual variation | IQ and ADI-R reported as predictors | IQ and ADI-R correlated with current social functioning |
| Gillespie-Lynch (2012)230 | Component raw scores increase overtime | NR | DQ falls over time | DQ not strongly predictive of social functioning. RJA and language predictive of social function | n/a |
| Gray (2012)231 | NR | NR | Appear relatively stable over time, but only reported by group | n/a | n/a |
| Billsedt (2005, 2007, 2011)232–234 | NR | NR | IQ appears to fall | IQ and language appear to predict social outcomes | n/a |
| Farley (2009)134 | NR | NR | Relatively stable over time, although with significant individual variation | IQ reported as predictor | VABS and IQ are correlated with current social outcomes |
| Szatmari (2009)235 | Component scores improve, whereas composite scores appear to fall | NR | NR | n/a | n/a |
| Cederlund (2008)132 | NR | NR | IQ appears to fall | n/a | IQ correlated with current social functioning |
| Eaves (2008)236 | NR | NR | IQ stable over time | IQ and CARS reported as predictors | IQ and CARS correlated with current social functioning |
| McGovern (2005)237 | Composite scores appear to increase over time | NR | IQ relatively stable over time, some evidence of decline in early adulthood | n/a | n/a |
| Howlin (2004)15 | NR | NR | Some measures report decline, others increase | IQ reported as predictor | IQ and language, reading and spelling correlated with current social functioning |
| Howlin (2000)238 | NR | NR | Some measures report decline, others increase | n/a | n/a |
| Ballaban-Gil (1996)243 | NR | NR | Relatively stable over time, although with significant individual variation | n/a | n/a |
| Bishop (2015)239 | VABS DLS increases in normal range individuals and appears to fall in those with ID | NR | IQ appears to fall | n/a | n/a |
| Anderson (2014)240 | In adults with IQ in the normal range, VABS scores increased over time. In adults with IQ below the normal range, VABS scores fell | NR | In adults with IQ in the normal range, IQ scores increased over time. In adults with IQ below the normal range, IQ scores fell | n/a | n/a |
| Marriage (2009)241 | n/a | n/a | n/a | IQ reported as predictor | n/a |
| Gray (2014)242 | NR | n/a | IQ stable over time | n/a | n/a |
| Esbensen (2010)133 | n/a | n/a | n/a | n/a | IQ correlated with current social functioning |
Appendix 16 Resource use review
Overview
A literature review was conducted to identify studies reporting on resource use and care costs in autistic children and adults.
Methods
To identify published economic evidence, the following databases were searched for eligible studies: MEDLINE (Ovid), EMBASE (Ovid) 1980 onwards, NHS Economic Evaluation Database and PsycINFO. The searches were undertaken in November 2017. The full search strategy is reported in Appendix 17.
Study selection
Two researchers independently undertook the screening of all titles and abstracts identified in the search. Full-paper publications were then obtained for potentially relevant studies and screened against the eligibility criteria. Disagreements between reviewers were resolved by discussion.
Studies were included if they reported on costs or resource use associated with the care of autistic children or adults.
Data extraction
Details of eligible studies were extracted by a single reviewer and summarised using a Microsoft Excel data extraction template.
Results
A total of 892 records were identified in the search, of which 63 studies were identified as potentially relevant from their titles and/or abstracts. The full-text articles of these records were assessed for eligibility. A total of 15 studies were found to meet the inclusion criteria. Figure 36 presents a flow diagram of the selection process.
FIGURE 36.
Flow diagram showing study selection for the resource review.

Description of included studies
A summary of key characteristics of the 15 identified studies23,126,135,147,188,244–252 is presented in Table 56. A range of methods were used to collect data, including surveys of respondents, as well as secondary analysis of data collected by local authorities and other providers. Of the 15 identified studies, eight23,126,135,147,245,246,248,252 provided a comprehensive assessment of public sector service costs for autistic children or adults. In the studies of children, education costs were consistently reported as the most significant driver of total public sector costs, with health and other social care costs making up the majority of the remainder. In studies of autistic adults, care costs were dominated by residential care costs and costs of day care services. A summary of the resource data collected by study is outlined in Table 57.
| Study | Participants | Subgroup/trial arm | n | Male (%) | Age years, mean (SD) | Objective of study | Year of costing | Source of data |
|---|---|---|---|---|---|---|---|---|
| Barret (2012)126 | Young children with autism | n/a | 152 | 91 | 3.74 (0.66) | To describe service use in young children with autism | 2006–7 | Service use for the 6 months prior to interview |
| Barret (2015)135 | Adolescents with autism, autism-related conditions, other SEN and typically developing children | Autism | 51 | 94 | 15.70 (0.54) | To describe service use in four groups of adolescents: (1) adolescents with autism, (2) adolescents with other ASDs, (3) adolescents with other SEN, and (4) typically developing adolescents | 2007–8 | Service use for the 6 months prior to interview |
| Broader ASD | 45 | 87 | 15.44 (0.38) | |||||
| SEN | 24 | 88 | 15.46 (0.38) | |||||
| Typical development | 28 | 100 | 15.62 (0.68) | |||||
| Bebbington (2007)244 | Children with autism | n/a | 6310 | 80 | 0–16 | To describe social service use in children with autism and the costs of providing these services | Unclear | Children in Need survey 2001 |
| Buescher (2014)23 | People with ASD | n/a | n/a | n/a | n/a | To update estimates of age-specific, direct, indirect, and lifetime societal economic costs associated with autism. Update to the Knapp et al. study147 | 2010–11 | Published evidence used (combination of UK, USA and Australia) |
| Byford (2015)245 | Preschool children with autism | PACT + TAU group | 74 | 92 | Median 4 (range 2–5) | To assess the cost-effectiveness of a preschool intervention for children with autism carried out within the Preschool Autism Communication Trial | 2006–7 | Total resource used and costs per participant over the 13-month follow-up estimated |
| TAU group | 69 | 90 | Median 4 (range 2–5) | |||||
| Järbrink (2001)246 | People with autism | n/a | n/a | n/a | n/a | To assess the economic impact of autism in the UK | 1998–9 | Published evidence |
| Järbrink (2003)247 | Children with ASD | n/a | 17 children; 15 parents | n/a | 7.8 (n/a) | To assess the feasibility of research instrument developed specifically to collect cost information for individuals with ASD | 1999–2000 | Questionnaire and diary survey |
| Knapp (2009)147 | People with ASD | n/a | n/a | n/a | n/a | To estimate direct, indirect and lifetime societal economic costs associated with autism | 2005–6 | Published evidence used (combination of UK, USA and Australia) |
| Mavranezouli (2014)248 | Adults with autism | n/a | n/a | n/a | n/a | To assess the cost-effectiveness of supported employment compared with standard care (day services) for adults with autism | 2011–12 | Published evidence, authors’ assumptions |
| McGill (2012)249 | Adults in residential care | n/a | 70 | 73 | 33 (NR) | To characterise the highest cost residential placements in the south-east of England | 2010 | Survey of local authorities |
| Petrou (2010)188 | Any autistic disorder | n/a | 11 | NR | NR | To estimate costs and preference-based health-related quality-of-life outcomes (health utilities) associated with a broad range of childhood psychiatric disorders during the eleventh year of life | 2006–7 | Parent-reported questionnaire survey |
| Preece (2007)250 | ASD | n/a | 155 | NR | NR | To examine the use of short break services in the UK and their association with informal support networks and child level of dependence | n/a | Postal survey |
| Russell (2010)251 | ASD | n/a | 71 | NR | NR | To compare resource use in children with diagnosed autism and those with undiagnosed autism | n/a | The Avon Longitudinal Study of Parents and Children |
| Wright (2016)252 | Children with ASD | Social stories (intervention arm) vs. TAU (comparator arm) | 52 | NR | NR | Feasibility RCT; the feasibility of collecting data on resource use measures for cost-effectiveness analysis in a fully powered trial | Unclear | Resource used over 6-week period |
| Yuan (2017)253 | Children with or without neurological disabilities | n/a | 942 | NR | 6.5 (NR) | To compare inpatient resource use in children with and without neurological disabilities | n/a | HES data |
| Study | Resource utilisation collected/included | ||||||
|---|---|---|---|---|---|---|---|
| Accommodation | Hospital-based health services | Community health, social and voluntary services | Medication | Education and childcare | Disability living allowance | Other | |
| Barret (2012)126 | Yes | Yes | Yes | Yes | Yes | No | Out-of-pocket expenses, productivity losses |
| Barret (2015)135 | Yes | Yes | Yes | Yes | Yes | No | n/a |
| Bebbington (2007)244 | Yes | No | Yes | No | No | No | n/a |
| Buescher (2014)23 | Yes | Yes | Yes | Yes | Yes | No | Employment support |
| Byford (2015)245 | Yes | Yes | Yes | Yes | Yes | No | Parental productivity losses and informal care |
| Järbrink (2001)246 | Yes | Yes | Yes | Yes | Yes | Living support | Lost productivity, family members’ time cost, family expenses, sheltered work |
| Järbrink (2003)247 | No | Yes | Yes | Yes | Yes | No | Informal care and out-of-pocket expenses, income losses |
| Knapp (2009)147 | Yes | Yes | Yes | Yes | Yes | No | Employment support |
| Mavranezouli (2014)248 | Yes | Yes | Yes | Yes | Yes | No | n/a |
| McGill (2012)249 | Yes | No | No | No | No | No | n/a |
| Petrou (2010)188 | No | Yes | Yes | Yes | Yes | No | n/a |
| Preece (2007)250 | No | No | Short break services | No | No | No | n/a |
| Russell (2010)251 | No | No | No | No | Yes | No | n/a |
| Wright (2016)252 | Yes | Yes | Yes | Yes | Yes | No | n/a |
| Yuan (2017)253 | No | Inpatient resource use | No | No | No | No | n/a |
Appendix 17 Searches implemented to inform economic analysis
Cost-effectiveness searches
Searches were implemented to identify previous economic evaluations of early intensive ABA-based interventions.
Databases searched included EMBASE, HTA database, MEDLINE, NHS Economic Evaluation Database and PsycINFO.
The searches identified 379 records.
EMBASE via OVID
Date searched: 11 November 2017.
Date range searched: 1974 to 9 November 2017.
Search strategy
-
Autism/ (49,006)
-
Asperger Syndrome/ (4129)
-
(autism or autistic or ASD or ASDs or ASC or AAC).ti,ab. (70,967)
-
Asperger$.ti,ab. (2685)
-
1 or 2 or 3 or 4 (81,926)
-
Behavior Modification/ (7370)
-
Behavior Therapy/ (41,427)
-
early intervention therap$.ti,ab. (80)
-
(intensive$ adj2 (analys$ or behavior$ or behaviour$ or intervention$ or program$ or therap$ or treat$)).ti,ab. (37,176)
-
(intensity adj2 (analys$ or behavior$ or behaviour$ or intervention$ or program$ or therap$ or treat$)).ti,ab. (11,460)
-
(high-intensity adj2 (analys$ or behavior$ or behaviour$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (1558)
-
(low-intensity adj2 (analys$ or behavior$ or behaviour$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (1425)
-
(high intensity adj2 (analys$ or behavior$ or behaviour$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (1558)
-
(low intensity adj2 (analys$ or behavior$ or behaviour$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (1425)
-
(intensive behavior$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (351)
-
(intensive behaviour$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (67)
-
(early behavior$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (59)
-
(early behaviour$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (13)
-
(comprehensive behavior$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (154)
-
(comprehensive behaviour$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (23)
-
(applied behavior$ adj2 (analy$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (401)
-
(applied behaviour$ adj2 (analy$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (75)
-
(ABA$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (5001)
-
NDBI$.ti,ab. (13)
-
Naturalistic Developmental Behav$ Intervention$.ti,ab. (5)
-
(IBI or EIBI or ABA).ti,ab. (10,120)
-
Lovaas$.ti,ab. (45)
-
(Early Start Denver Model or Denver Model).ti,ab. (57)
-
(ESDM or ESDM-I or ESDM-PD or P-ESDM).ti,ab. (68)
-
(Pivotal Response adj2 (treat$ or train$ or program$)).ti,ab. (61)
-
(PRT train$ or PRT program$ or PRT model$).ti,ab. (67)
-
discrete trial train$.ti,ab. (35)
-
6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 (110,230)
-
5 and 33 (2217)
-
health economics/ (35,525)
-
exp economic evaluation/ (268,818)
-
exp health care cost/ (258,306)
-
exp pharmacoeconomics/ (189,269)
-
or/35-38 (583,319)
-
(economic$ or cost or costs or costly or costing or price or prices or pricing or pharmacoeconomic$).ti,ab. (836,568)
-
(expenditure$ not energy).ti,ab. (33,161)
-
(value adj2 money).ti,ab. (2009)
-
budget$.ti,ab. (32,261)
-
(or/40) or 41 or 42 or 43 (867,818)
-
39 or 44 (1,177,243)
-
letter.pt. (998,943)
-
editorial.pt. (552,823)
-
note.pt. (695,192)
-
46 or 47 or 48 (2,246,958)
-
45 not 49 (1,073,110)
-
(metabolic adj cost).ti,ab. (1278)
-
((energy or oxygen) adj cost).ti,ab. (3825)
-
((energy or oxygen) adj expenditure).ti,ab. (27,346)
-
51 or 52 or 53 (31,456)
-
50 not 54 (1,066,753)
-
exp animal/ (23,945,891)
-
exp animal experiment/ (2,180,860)
-
nonhuman/ (5,376,119)
-
(rat or rats or mouse or mice or hamster or hamsters or animal or animals or dog or dogs or cat or cats or bovine or sheep).ti,ab,sh. (4,500,617)
-
56 or 57 or 58 or 59 (25,649,733)
-
exp human/ (19,181,630)
-
exp human-experiment/ (398,342)
-
61 or 62 (19,183,186)
-
60 not (60 and 63) (6,467,566)
-
55 not 64 (977,661)
-
634 and 65 (131)
MEDLINE In-Process & Other Non-Indexed Citations via OVID
Date searched: 11 November 2017.
Date range searched: 1946 to present.
Search strategy
-
Autistic Disorder/ (22,034)
-
Autism Spectrum Disorder/ (4163)
-
Asperger Syndrome/ (2146)
-
(autism or autistic or ASD or ASDs or ASC or AAC).ti,ab. (58,960)
-
Asperger$.ti,ab. (2384)
-
1 or 2 or 3 or 4 or 5 (62,676)
-
Applied Behavior Analysis/ (13)
-
“Early Intervention (Education)”/ (2699)
-
Behavior Therapy/ (28,032)
-
early intervention therap$.ti,ab. (44)
-
(intensive$ adj2 (analys$ or behavior$ or behaviour$ or intervention$ or program$ or therap$ or treat$)).ti,ab. (27,769)
-
(intensity adj2 (analys$ or behavior$ or behaviour$ or intervention$ or program$ or therap$ or treat$)).ti,ab. (8610)
-
(high-intensity adj2 (analys$ or behavior$ or behaviour$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (1177)
-
(low-intensity adj2 (analys$ or behavior$ or behaviour$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (1189)
-
(high intensity adj2 (analys$ or behavior$ or behaviour$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (1177)
-
(low intensity adj2 (analys$ or behavior$ or behaviour$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (1189)
-
(intensive behavior$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (265)
-
(intensive behaviour$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (50)
-
(early behavior$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (42)
-
(early behaviour$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (14)
-
(comprehensive behavior$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (127)
-
(comprehensive behaviour$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (16)
-
(applied behavior$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (469)
-
(applied behaviour$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (40)
-
(ABA$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (3842)
-
NDBI$.ti,ab. (13)
-
Naturalistic Developmental Behav$ Intervention$.ti,ab. (5)
-
(IBI or EIBI or ABA).ti,ab. (11,310)
-
Lovaas$.ti,ab. (48)
-
(Early Start Denver Model or Denver Model).ti,ab. (40)
-
(ESDM or ESDM-I or ESDM-PD or P-ESDM).ti,ab. (37)
-
(Pivotal Response adj2 (treat$ or train$ or program$)).ti,ab. (56)
-
(PRT train$ or PRT program$ or PRT model$).ti,ab. (50)
-
discrete trial train$.ti,ab. (39)
-
7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 (80,416)
-
6 and 35 (2018)
-
economics/(27,492)
-
exp “costs and cost analysis”/or Cost Allocation/or Cost-Benefit Analysis/or Cost Control/or Cost of Illness/or Cost Sharing/or Health Care Costs/or Health Expenditures/ (224,837)
-
economics, dental/ (1905)
-
exp “economics, hospital”/or Hospital Charges/or Hospital Costs/ (23,580)
-
economics, medical/ (9205)
-
economics, nursing/ (4019)
-
economics, pharmaceutical/ (3002)
-
(economic$ or cost$ or price or prices or pricing or pharmacoeconomic$).tw. (717,189)
-
(expenditure$ not energy).tw. (26,209)
-
(value adj1 money).tw. (34)
-
budget$.tw. (26,294)
-
37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 (863,345)
-
((energy or oxygen) adj cost).ti,ab. (3935)
-
(metabolic adj cost).ti,ab. (1287)
-
((energy or oxygen) adj expenditure).ti,ab. (23,489)
-
or/49-51 (27,725)
-
48 not 52 (856,916)
-
letter.pt. (1,033,891)
-
editorial.pt. (469,249)
-
historical article.pt. (358,123)
-
54 or 55 or 56 (1,843,012)
-
53 not 57 (822,035)
-
exp animals/not humans/(4,741,624)
-
58 not 59 (762,726)
-
36 and 60 (85)
PsycINFO via OVID
Date searched: 11 November 2017.
Date range searched: 1806 to November week 1 2017.
Search strategy
-
Autism Spectrum Disorder/ (36,543)
-
(autism or autistic or ASD or ASDs or ASC or AAC).ti,ab. (44,595)
-
Asperger$.ti,ab. (3398)
-
1 or 2 or 3 (46,929)
-
Behavior Modification/ (10,223)
-
Behavior Therapy/ (13,276)
-
early intervention therap$.ti,ab. (18)
-
(intensive$ adj2 (analys$ or behavior$ or behaviour$ or intervention$ or program$ or therap$ or treat$)).ti,ab. (6049)
-
(intensity adj2 (analys$ or behavior$ or behaviour$ or intervention$ or program$ or therap$ or treat$)).ti,ab. (1956)
-
(high-intensity adj2 (analys$ or behavior$ or behaviour$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (184)
-
(low-intensity adj2 (analys$ or behavior$ or behaviour$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (341)
-
(high intensity adj2 (analys$ or behavior$ or behaviour$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (184)
-
(low intensity adj2 (analys$ or behavior$ or behaviour$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (341)
-
(intensive behavior$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (393)
-
(intensive behaviour$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (64)
-
(early behavior$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (81)
-
(early behaviour$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (13)
-
(comprehensive behavior$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (143)
-
(comprehensive behaviour$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (9)
-
(applied behavior$ adj2 (analyS$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (1678)
-
(applied behaviour$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (115)
-
(ABA$ adj2 (analys$ or intervention$ or model$ or program$ or therap$ or treat$)).ti,ab. (864)
-
NDBI$.ti,ab. (3)
-
Naturalistic Developmental Behav$ Intervention$.ti,ab. (4)
-
(IBI or EIBI or ABA).ti,ab. (1454)
-
Lovaas$.ti,ab. (126)
-
(Early Start Denver Model or Denver Model).ti,ab. (47)
-
(ESDM or ESDM-I or ESDM-PD or P-ESDM).ti,ab. (38)
-
(Pivotal Response adj2 (treat$ or train$ or program$)).ti,ab. (130)
-
(PRT train$ or PRT program$ or PRT model$).ti,ab. (18)
-
discrete trial train$.ti,ab. (102)
-
5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 (33,737)
-
4 and 32 (2275)
-
“costs and cost analysis”/ (15,176)
-
“Cost Containment”/ (539)
-
(economic adj2 evaluation$).ti,ab. (1420)
-
(economic adj2 analy$).ti,ab. (1364)
-
(economic adj2 (study or studies)).ti,ab. (679)
-
(cost adj2 evaluation$).ti,ab. (291)
-
(cost adj2 analy$).ti,ab. (3246)
-
(cost adj2 (study or studies)).ti,ab. (760)
-
(cost adj2 effective$).ti,ab. (13,368)
-
(cost adj2 benefit$).ti,ab. (3122)
-
(cost adj2 utili$).ti,ab. (1062)
-
(cost adj2 minimi$).ti,ab. (316)
-
(cost adj2 consequence$).ti,ab. (108)
-
(cost adj2 comparison$).ti,ab. (172)
-
(cost adj2 identificat$).ti,ab. (20)
-
(pharmacoeconomic$ or pharmaco-economic$).ti,ab. (294)
-
34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49 (30,824)
-
(task adj2 cost$).ti,ab,id. (530)
-
(switch$ adj2 cost$).ti,ab,id. (1116)
-
(metabolic adj cost).ti,ab,id. (90)
-
((energy or oxygen) adj cost).ti,ab,id. (257)
-
51 or 52 or 53 or 54 (1809)
-
50 not 55 (30,673)
-
(animal or animals or rat or rats or mouse or mice or hamster or hamsters or dog or dogs or cat or cats or bovine or sheep or ovine or pig or pigs).ab,ti,id,de. (327,532)
-
editorial.dt. (41,001)
-
letter.dt. (19,944)
-
dissertation abstract.pt. (450,546)
-
57 or 58 or 59 or 60 (819,492)
-
56 not 61 (26,772)
-
33 and 62 (24)
Quality-of-life searches
Databases were searched for studies reporting the quality of life of children and adults with autism and Asperger syndrome.
Databases searched included EMBASE, HTA database, MEDLINE, NHS Economic Evaluation Database and PsycINFO.
The searches identified a total of 1502 records.
EMBASE via OVID
Date searched: 11 November 2017.
Date range searched: 1974 to 9 November 2017.
Search strategy
-
Autism/ (49,006)
-
Asperger Syndrome/ (4129)
-
(autism or autistic or ASD or ASDs or ASC or AAC).ti,ab. (70,967)
-
Asperger$.ti,ab. (2685)
-
1 or 2 or 3 or 4 (81,926)
-
(utilit$ approach$ or health gain or hui or hui1 or hui2 or hui3).ti,ab. (2707)
-
(health measurement$ scale$ or health measurement$ questionnaire$).ti,ab. (75)
-
(standard gamble$ or categor$ scal$ or linear scal$ or linear analog$ or visual scal$ or magnitude estimat$).ti,ab. (6577)
-
(time trade off$ or rosser$ classif$ or rosser$ matrix or rosser$ distress$ or hrqol).ti,ab. (21,014)
-
(index of wellbeing or quality of wellbeing or qwb).ti,ab. (257)
-
(multiattribute$ health ind$ or multi attribute$ health ind$).ti,ab. (2)
-
(health utilit$ index or health utilit$ indices).ti,ab. (1022)
-
(multattribute$ theor$ or multi attribute$ theor$ or multiattribute$ analys$ or multi attribute$ analys$).ti,ab. (19)
-
(health utilit$ scale$ or classification of illness state$).ti,ab. (14)
-
health state$ utilit$.ti,ab. (954)
-
well year$.ti,ab. (31)
-
(multiattribute$ utilit$ or multi attribute$ utilit$).ti,ab. (324)
-
health utilit$ scale$.ti,ab. (13)
-
(euro qual or euro qol or eq-5d or eq5d or eq 5d or euroqual or euroqol).ti,ab. (14,223)
-
(qualy or qaly or qualys or qalys or quality adjusted life year$).ti,ab. (18,668)
-
willingness to pay.ti,ab. (6304)
-
(hye or hyes or health$ year$ equaivalent$).ti,ab. (116)
-
(person trade off$ or person tradeoff$ or time tradeoff$ or time trade off$).ti,ab. (1759)
-
theory utilit$.ti,ab. (10)
-
(sf36 or sf 36).ti,ab. (29,946)
-
(short form 36 or shortform 36 or sf thirtysix or sf thirty six or shortform thirtysix or shortform thirty six or shrt form thirtysix or short form thirty six).ti,ab. (11,583)
-
(sf 6d or sf6d or short form 6d or shortform 6d or sf six$ or shortform six$ or short form six$).ti,ab. (1213)
-
or/6-27 (88,865)
-
5 and 28 (434)
MEDLINE In-Process & Other Non-Indexed Citations via OVID
Date searched: 11 November 2017.
Date range searched: 1946 to present.
Search strategy
-
Autistic Disorder/ (22,034)
-
Autism Spectrum Disorder/ (4163)
-
Asperger Syndrome/ (2146)
-
(autism or autistic or ASD or ASDs or ASC or AAC).ti,ab. (58,960)
-
Asperger$.ti,ab. (2384)
-
or/1-5 (62,676)
-
Quality-Adjusted Life Years/ (10,851)
-
Value of Life/ (5842)
-
(qaly$ or qald$ or qale$ or qtime$).ti,ab,kf. (9018)
-
(quality adjusted or adjusted life year$).ti,ab,kf. (13,989)
-
disability adjusted life.ti,ab,kf. (2644)
-
daly$1.ti,ab,kf. (2388)
-
((index adj3 wellbeing) or (quality adj3 wellbeing) or qwb).ti,ab,kf. (584)
-
(multiattribute$ or multi attribute$).ti,ab,kf. (814)
-
(utility adj3 (score$1 or scoring or valu$ or measur$ or evaluat$ or scale$1 or instrument$1 or weight or weights or weighting or information or data or unit or units or health$ or life or estimat$ or elicit$ or disease$ or mean or cost$ or expenditure$1 or gain or gains or loss or losses or lost or analysis or index$ or indices or overall or reported or calculat$ or range$ or increment$ or state or states or status)).ti,ab,kf. (29,311)
-
utility.ab./freq = 2 (14,979)
-
utilities.ti,ab,kf. (6240)
-
disutili$.ti,ab,kf. (392)
-
(HSUV or HSUVs).ti,ab,kf. (50)
-
health$1 year$1 equivalent$1.ti,ab,kf. (49)
-
(hye or hyes).ti,ab,kf. (72)
-
(hui or hui1 or hui2 or hui3).ti,ab,kf. (1307)
-
(illness state$1 or health state$1).ti,ab,kf. (5782)
-
(euro qual or euro qual5d or euro qol5d or eq-5d or eq5-d or eq5d or euroqual or euroqol or euroqual5d or euroqol5d).ti,ab,kf. (8561)
-
(eq-sdq or eqsdq).ti,ab,kf. (1)
-
(short form$ or shortform$).ti,ab,kf. (28,850)
-
(sf36$ or sf 36$ or sf thirtysix or sf thirty six).ti,ab,kf. (20,701)
-
(sf6 or sf 6 or sf6d or sf 6d or sf six or sfsix or sf8 or sf 8 or sf eight or sfeight).ti,ab,kf. (2937)
-
(sf12 or sf 12 or sf twelve or sftwelve).ti,ab,kf. (4062)
-
(sf16 or sf 16 or sf sixteen or sfsixteen).ti,ab,kf. (24)
-
(sf20 or sf 20 or sf twenty or sftwenty).ti,ab,kf. (348)
-
(15D or 15-D or 15 dimension).ti,ab,kf. (4788)
-
(standard gamble$ or sg).ti,ab,kf. (9284)
-
(time trade off$1 or time tradeoff$1 or tto or timetradeoff$1).ti,ab,kf. (1775)
-
7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 (126,607)
-
6 and 35 (386)
PsycINFO via OVID
Date searched: 11 November 2017.
Date range searched: 1806 to November week 1 2017.
Search strategy
-
Autism Spectrum Disorder/ (36,543)
-
(autism or autistic or ASD or ASDs or ASC or AAC).ti,ab. (44,595)
-
Asperger$.ti,ab. (3398)
-
1 or 2 or 3 (46,929)
-
exp “Quality of Life”/ (37,006)
-
(qaly$ or qald$ or qale$ or qtime$).ti,ab,kf. (920)
-
(quality adjusted or adjusted life year$).ti,ab,kf. (1440)
-
disability adjusted life.ti,ab,kf. (333)
-
daly$1.ti,ab,kf. (549)
-
((index adj3 wellbeing) or (quality adj3 wellbeing) or qwb).ti,ab,kf. (374)
-
(multiattribute$ or multi attribute$).ti,ab,kf. (965)
-
(utility adj3 (score$1 or scoring or valu$ or measur$ or evaluat$ or scale$1 or instrument$1 or weight or weights or weighting or information or data or unit or units or health$ or life or estimat$ or elicit$ or disease$ or mean or cost$ or expenditure$1 or gain or gains or loss or losses or lost or analysis or index$ or indices or overall or reported or calculat$ or range$ or increment$ or state or states or status)).ti,ab,kf. (7785)
-
utility.ab./freq = 2 (5982)
-
utilities.ti,ab,kf. (1732)
-
disutili$.ti,ab,kf. (177)
-
(HSUV or HSUVs).ti,ab,kf. (3)
-
health$1 year$1 equivalent$1.ti,ab,kf. (4)
-
(hye or hyes).ti,ab,kf. (18)
-
(hui or hui1 or hui2 or hui3).ti,ab,kf. (507)
-
(illness state$1 or health state$1).ti,ab,kf. (1341)
-
(euro qual or euro qual5d or euro qol5d or eq-5d or eq5-d or eq5d or euroqual or euroqol or euroqual5d or euroqol5d).ti,ab,kf. (1641)
-
(eq-sdq or eqsdq).ti,ab,kf. (1)
-
(short form$ or shortform$).ti,ab,kf. (11,238)
-
(sf36$ or sf 36$ or sf thirtysix or sf thirty six).ti,ab,kf. (4080)
-
(sf6 or sf 6 or sf6d or sf 6d or sf six or sfsix or sf8 or sf 8 or sf eight or sfeight).ti,ab,kf. (333)
-
(sf12 or sf 12 or sf twelve or sftwelve).ti,ab,kf. (981)
-
(sf16 or sf 16 or sf sixteen or sfsixteen).ti,ab,kf. (0)
-
(sf20 or sf 20 or sf twenty or sftwenty).ti,ab,kf. (42)
-
(15D or 15-D or 15 dimension).ti,ab,kf. (221)
-
(standard gamble$ or sg).ti,ab,kf. (866)
-
(time trade off$1 or time tradeoff$1 or tto or timetradeoff$1).ti,ab,kf. (352)
-
5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 (63,306)
-
4 and 32 (605)
Prognosis and longitudinal outcomes searches
Databases were searched for studies reporting longitudinal outcomes in children and adults with autism and Asperger syndrome.
Databases searched included EMBASE, MEDLINE and PsycINFO.
Date limit was 2013 onwards.
A total of 737 records were identified.
EMBASE via OVID
Date searched: 8 February 2018.
Date range searched: 1974 to 9 November 2017.
Search strategy
-
Autism/ (23,952)
-
Asperger Syndrome/ (1563)
-
(autism or autistic or ASD or ASDs or ASC or AAC).ti,ab. (16,833)
-
Asperger$.ti,ab. (282)
-
1 or 2 or 3 or 4 (26,561)
-
6 (adult* or adolescen* or people or individual* or youth* or teenag* or “young people”).ti,ab. (278394)
-
(outcome* or prognosis or follow-up or longitudinal or long-termor predict* or change* or continuit* or trajector*).ti,ab. (40,725)
-
6 and 7 (20,524)
-
5 and 8 (220)
MEDLINE In-Process & Other Non-Indexed Citations via OVID
Date searched: 8 February 2018.
Date range searched: 1946 to present.
Search strategy
-
Autistic Disorder/ (933)
-
Autism Spectrum Disorder/ (991)
-
Asperger Syndrome/ (140)
-
(autism or autistic or ASD or ASDs or ASC or AAC).ti,ab. (1670)
-
Asperger$.ti,ab. (53)
-
or/1-5 (1912)
-
(adult* or adolescen* or people or individual* or youth* or teenag* or “young people”).ti,ab. (270,342)
-
(outcome* or prognosis or follow-up or longitudinal or long-term or predict* or change* or continuit* or trajector*).ti,ab. (25,0979)
-
7 and 8 (116,323)
-
6 and 9 (340)
PsycINFO via OVID
Date searched: 8 February 2018.
Date range searched: 1806 to November week 1 2017.
Search strategy
-
Autism Spectrum Disorder/ (16,066)
-
(autism or autistic or ASD or ASDs or ASC or AAC).ti,ab. (14,477)
-
Asperger$.ti,ab. (370)
-
1 or 2 or 3 (17,126)
-
(adult* or adolescen* or people or individual* or youth* or teenag* or “young people”).ti,ab. (113,016)
-
(outcome* or prognosis or follow-up or longitudinal or long-termor predict* or change* or continuit* or trajector*).ti,ab. (55,365)
-
5 and 6 (8582)
-
4 and 7 (177)
Resource use searches
Databases were searched for studies reporting resource and cost data for children and adults with autism and Asperger syndrome.
Databases searched included EMBASE, HTA database, MEDLINE, NHS Economic Evaluation Database and PsycINFO.
A total of 892 records were identified. We attempted to restrict to UK studies by using the NICE UK search filter.
EMBASE via OVID
Date searched: 11 November 2017.
Date range searched: 1974 to 10 November 2017.
Search strategy
-
Autism/ (49,065)
-
Asperger Syndrome/ (4134)
-
(autism or autistic or ASD or ASDs or ASC or AAC).ti,ab. (71,033)
-
Asperger$.ti,ab. (2686)
-
1 or 2 or 3 or 4 (82,010)
-
health economics/ (35,551)
-
exp economic evaluation/ (269,060)
-
exp health care cost/ (258,598)
-
exp pharmacoeconomics/ (189,432)
-
6 or 7 or 8 or 9 (583,838)
-
(economic$ or cost or costs or costly or costing or price or prices or pricing or pharmacoeconomic$).ti,ab. (837,144)
-
(expenditure$ not energy).ti,ab. (33,183)
-
(value adj2 money).ti,ab. (2011)
-
budget$.ti,ab. (32,277)
-
11 or 12 or 13 or 14 (868,410)
-
economics/ (227,601)
-
cost-benefit analys$.mp. (78,709)
-
cost minimi?ation.mp. (3812)
-
cost-effective$.mp. (208,439)
-
costeffective$.mp. (4218)
-
CEA.mp. (31,340)
-
cost utilit$.mp. (9869)
-
cost-utilit$.mp. (9869)
-
costutilit$.mp. (131)
-
CUA.mp. (1247)
-
“fees and charges”/ (15,073)
-
drug cost$.mp. (71,695)
-
healthcare cost$.mp. (13,892)
-
health care cost$.mp. (172,817)
-
hospital charges.mp. (4068)
-
hospital running costs.mp. (24)
-
hospitali?ation cost$.mp. (6336)
-
cost control.mp. (62,003)
-
budget/ (24,983)
-
“willingness to pay”.mp. (6463)
-
(HCRU or MRU).mp. (717)
-
((healthcare or health care or health resource$ or medical resource$) adj3 utili?ation).mp. (68,104)
-
((healthcare or health care or health resource$ or medical resource$) adj3 “use”).mp. (16,742)
-
(resource$ adj2 (“use$” or util$ or allocat$)).mp. (64,570)
-
((economic or health$ or resource) adj3 burden).mp. (27,185)
-
or/16-40 (824,272)
-
10 or 15 or 41 (1,430,406)
-
5 and 42 (2912)
-
United Kingdom/ (388,356)
-
(national health service* or nhs*).ti,ab,in,ad. (270,391)
-
(english not ((published or publication* or translat* or written or language* or speak* or literature or citation*) adj5 english)).ti,ab. (33,942)
-
(gb or “g.b.” or britain* or (british* not “british columbia”) or uk or “u.k.” or united kingdom* or (england* not “new england”) or northern ireland* or northern irish* or scotland* or scottish* or ((wales or “south wales”) not “new south wales”) or welsh*).ti,ab,jw,in,ad. (2,839,356)
-
(bath or “bath’s” or ((birmingham not alabama*) or (“birmingham’s” not alabama*) or bradford or “bradford’s” or brighton or “brighton’s” or bristol or “bristol’s” or carlisle* or “carlisle’s” or (cambridge not (massachusetts* or boston* or harvard*)) or (“cambridge’s” not (massachusetts* or boston* or harvard*)) or (canterbury not zealand*) or (“canterbury’s” not zealand*) or chelmsford or “chelmsford’s” or chester or “chester’s” or chichester or “chichester’s” or coventry or “coventry’s” or derby or “derby’s” or (durham not (carolina* or nc)) or (“durham’s” not (carolina* or nc)) or ely or “ely’s” or exeter or “exeter’s” or gloucester or “gloucester’s” or hereford or “hereford’s” or hull or “hull’s” or lancaster or “lancaster’s” or leeds* or leicester or “leicester’s” or (lincoln not nebraska*) or (“lincoln’s” not nebraska*) or (liverpool not (new south wales* or nsw)) or (“liverpool’s” not (new south wales* or nsw)) or ((london not (ontario* or ont or toronto*)) or (“london’s” not (ontario* or ont or toronto*)) or manchester or “manchester’s” or (newcastle not (new south wales* or nsw)) or (“newcastle’s” not (new south wales* or nsw)) or norwich or “norwich’s” or nottingham or “nottingham’s” or oxford or “oxford’s” or peterborough or “peterborough’s” or plymouth or “plymouth’s” or portsmouth or “portsmouth’s” or preston or “preston’s” or ripon or “ripon’s” or salford or “salford’s” or salisbury or “salisbury’s” or sheffield or “sheffield’s” or southampton or “southampton’s” or st albans or stoke or “stoke’s” or sunderland or “sunderland’s” or truro or “truro’s“ or wakefield or “wakefield’s” or wells or westminster or “westminster’s” or winchester or “winchester’s” or wolverhampton or “wolverhampton’s” or (worcester not (massachusetts* or boston* or harvard*)) or (“worcester’s” not (massachusetts* or boston* or harvard*)) or (york not (“new york*” or ny or ontario* or ont or toronto*)) or (“york’s” not (“new york*” or ny or ontario* or ont or toronto*))))).ti,ab,in,ad. (2,116,965)
-
(bangor or “bangor’s” or cardiff or “cardiff’s” or newport or “newport’s” or st asaph or “st asaph’s” or st davids or swansea or “swansea’s”).ti,ab,in,ad. (85,474)
-
(aberdeen or “aberdeen’s” or dundee or “dundee’s” or edinburgh or “edinburgh’s” or glasgow or “glasgow’s” or inverness or (perth not australia*) or (“perth’s” not australia*) or stirling or “stirling’s”).ti,ab,in,ad. (294,276)
-
(armagh or “armagh’s” or belfast or “belfast’s” or lisburn or “lisburn’s” or londonderry or “londonderry’s” or derry or “derry’s” or newry or “newry’s”).ti,ab,in,ad. (38,399)
-
44 or 45 or 46 or 47 or 48 or 49 or 50 or 51 (3,460,981)
-
(exp “arctic and antarctic”/or exp oceanic regions/or exp western hemisphere/or exp africa/or exp asia/or exp “australia and new zealand”/) not (united kingdom/or europe/) (2,753,727)
-
52 not 53 (3,283,935)
-
43 and 54 (433)
-
letter.pt. (999,410)
-
editorial.pt. (553,065)
-
note.pt. (695,520)
-
56 or 57 or 58 (2,247,995)
-
55 not 59 (395)
-
exp animal/ (23,958,412)
-
exp animal experiment/ (2,181,990)
-
nonhuman/ (5,379,549)
-
(rat or rats or mouse or mice or hamster or hamsters or animal or animals or dog or dogs or cat or cats or bovine or sheep).ti,ab,sh. (4,501,587)
-
61 or 62 or 63 or 64 (25,663,010)
-
exp human/ (19,192,687)
-
exp human experiment/ (398,415)
-
66 or 67 (19,194,242)
-
65 not (65 and 68) (6,469,786)
-
60 not 69 (387)
MEDLINE In-Process & Other Non-Indexed Citations via OVID
Date searched: 11 November 2017.
Date range searched: 1946 to present.
Search strategy
-
Autistic Disorder/ (22,034)
-
Autism Spectrum Disorder/ (4163)
-
Asperger Syndrome/ (2146)
-
(autism or autistic or ASD or ASDs or ASC or AAC).ti,ab. (58,960)
-
Asperger$.ti,ab. (2384)
-
or/1-5 (62,676)
-
economics/ (27,492)
-
economics, dental/ (1905)
-
exp “economics, hospital”/or Hospital Charges/or Hospital Costs/ (23,580)
-
economics, medical/ (9205)
-
economics, nursing/ (4019)
-
economics, pharmaceutical/ (3002)
-
(economic$ or cost$ or price or prices or pricing or pharmacoeconomic$).tw. (717,189)
-
exp “costs and cost analysis”/or Cost Allocation/or Cost-Benefit Analysis/or Cost Control/or Cost of Illness/or Cost Sharing/or Health Care Costs/or Health Expenditures/ (224,837)
-
“cost minimization analysis”/ (48,126)
-
economic evaluation/(77,044)
-
“cost effectiveness analysis”/ (77,044)
-
“cost utility analysis”/ (77,044)
-
cost-benefit analysis.mp. (78,658)
-
cost minimi?ation.mp. (1207)
-
economic evaluation.mp. (8554)
-
cost effective$.mp. (117,719)
-
cost-effective$.mp. (117,719)
-
costeffective$.mp. (171)
-
CEA.mp. (22,030)
-
cost utilit$.mp. (4174)
-
cost-utilit$.mp. (4174)
-
costutilit$.mp. (10)
-
CUA.mp. (1128)
-
“fees and charges”/ (9057)
-
exp drug costs/ (15,223)
-
drug cost$.mp. (17,583)
-
exp cost of illness/(24,636)
-
healthcare costs.mp. (6724)
-
health care costs.mp. (45,300)
-
hospital charges.mp. (4962)
-
hospital running costs.mp. (11)
-
hospitali?ation cost.mp. (625)
-
cost control.mp. (22,628)
-
budgets/ (11,172)
-
“willingness to pay”.mp. (4366)
-
HCRU or MRU).mp. (408)
-
((healthcare or health care or health resource$ or medical resource$) adj3 utili?ation).mp. (15,973)
-
((healthcare or health care or health resource$ or medical resource$) adj3 “use”).mp. (13,610)
-
(resource adj2 (“use$” or util$ or allocat$)).mp. (33,167)
-
((economic or health$ or resource) adj3 burden).mp. (19,031)
-
(expenditure$ not energy).tw. (26,209)
-
(value adj1 money).tw. (34)
-
budget$.tw. (26,294)
-
7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49 (936,074)
-
6 and 50 (1503)
-
United Kingdom/ (226,997)
-
(national health service* or nhs*).ti,ab,in,ad. (160,752)
-
(english not ((published or publication* or translat* or written or language* or speak* or literature or citation*) adj5 english)).ti,ab. (93,005)
-
(gb or “g.b.” or britain* or (british* not “british columbia”) or uk or “u.k.” or united kingdom* or (england* not “new england”) or northern ireland* or northern irish* or scotland* or scottish* or ((wales or “south wales”) not “new south wales”) or welsh*).ti,ab,jw,in,ad. (1,937,468)
-
(bath or “bath’s” or ((birmingham not alabama*) or (“birmingham’s” not alabama*) or bradford or “bradford’s” or brighton or “brighton’s” or bristol or “bristol’s” or carlisle* or “carlisle’s” or (cambridge not (massachusetts* or boston* or harvard*)) or (“cambridge’s” not (massachusetts* or boston* or harvard*)) or (canterbury not zealand*) or (“canterbury’s” not zealand*) or chelmsford or “chelmsford’s” or chester or “chester’s” or chichester or “chichester’s” or coventry or “coventry’s” or derby or “derby’s” or (durham not (carolina* or nc)) or (“durham’s” not (carolina* or nc)) or ely or “ely’s” or exeter or “exeter’s” or gloucester or “gloucester’s” or hereford or “hereford’s” or hull or “hull’s” or lancaster or “lancaster’s” or leeds* or leicester or “leicester’s” or (lincoln not nebraska*) or (“lincoln’s” not nebraska*) or (liverpool not (new south wales* or nsw)) or (”liverpool’s” not (new south wales* or nsw)) or ((london not (ontario* or ont or toronto*)) or (“london’s” not (ontario* or ont or toronto*)) or manchester or “manchester’s” or (newcastle not (new south wales* or nsw)) or (“newcastle’s” not (new south wales* or nsw)) or norwich or “norwich’s” or nottingham or “nottingham’s” or oxford or “oxford’s” or peterborough or “peterborough’s” or plymouth or “plymouth’s” or portsmouth or “portsmouth’s” or preston or “preston’s” or ripon or “ripon’s” or salford or “salford’s” or salisbury or “salisbury’s” or sheffield or “sheffield’s” or southampton or “southampton’s” or st albans or stoke or “stoke’s” or sunderland or “sunderland’s” or truro or “truro’s” or wakefield or “wakefield’s” or wells or westminster or “westminster’s” or winchester or “winchester’s” or wolverhampton or “wolverhampton’s” or (worcester not (massachusetts* or boston* or harvard*)) or (“worcester’s” not (massachusetts* or boston* or harvard*)) or (york not (“new york*” or ny or ontario* or ont or toronto*)) or (“york’s” not (“new york*” or ny or ontario* or ont or toronto*))))).ti,ab,in,ad. (1,283,584)
-
(bangor or “bangor’s” or cardiff or “cardiff’s” or newport or “newport’s” or st asaph or “st asaph’s” or st davids or swansea or “swansea’s”).ti,ab,in,ad. (48,661)
-
(aberdeen or “aberdeen’s” or dundee or “dundee’s” or edinburgh or “edinburgh’s” or glasgow or “glasgow’s” or inverness or (perth not australia*) or (“perth’s” not australia*) or stirling or “stirling’s”).ti,ab,in,ad. (187,571)
-
(armagh or “armagh’s” or belfast or “belfast’s” or lisburn or “lisburn’s” or londonderry or “londonderry’s” or derry or “derry’s” or newry or “newry’s”).ti,ab,in,ad. (22,619)
-
52 or 53 or 54 or 55 or 56 or 57 or 58 or 59 (2,434,713)
-
(exp “arctic and antarctic”/or exp oceanic regions/or exp western hemisphere/or exp africa/or exp asia/or exp “australia and new zealand”/) not (united kingdom/or europe/) (959,801)
-
60 not 61 (2,360,187)
-
51 and 62 (230)
PsycINFO via OVID
Date searched: 11 November 2017.
Date range searched: 1806 to November week 1 2017.
Search strategy
-
Autism Spectrum Disorder/ (36,543)
-
(autism or autistic or ASD or ASDs or ASC or AAC).ti,ab. (44,595)
-
Asperger$.ti,ab. (3398)
-
1 or 2 or 3 (46,929)
-
exp “costs and cost analysis”/ (23,667)
-
“Cost Containment”/ (539)
-
(economic adj2 evaluation$).ti,ab. (1420)
-
(economic adj2 analy$).ti,ab. (1364)
-
(economic adj2 (study or studies)).ti,ab. (679)
-
(cost adj2 evaluation$).ti,ab. (291)
-
11 (cost adj2 analy$).ti,ab. (3246)
-
(cost adj2 (study or studies)).ti,ab. (760)
-
(cost adj2 effective$).ti,ab. (13,368)
-
(cost adj2 benefit$).ti,ab. (3122)
-
(cost adj2 utili$).ti,ab. (1062)
-
(cost adj2 minimi$).ti,ab. (316)
-
(cost adj2 consequence$).ti,ab. (108)
-
(cost adj2 comparison$).ti,ab. (172)
-
(cost adj2 identificat$).ti,ab. (20)
-
(pharmacoeconomic$ or pharmaco-economic$).ti,ab. (294)
-
5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 (37,543)
-
economics/ (20,082)
-
(economic$ or cost$ or price or prices or pricing or pharmacoeconomic$).tw. (195,712)
-
Health Care Costs/or Health Care Economics/or Health Care Utilization/or Pharmacoeconomics/ (22,859)
-
cost-benefit analysis.mp. (936)
-
cost minimi?ation.mp. (109)
-
economic evaluation.mp. (1121)
-
cost effective$.mp. (13,374)
-
cost-effective$.mp. (13,374)
-
costeffective$.mp. (47)
-
CEA.mp. (1066)
-
cost utilit$.mp. (530)
-
cost-utilit$.mp. (530)
-
costutilit$.mp. (4)
-
CUA.mp. (38)
-
drug cost$.mp. (330)
-
healthcare costs.mp. (974)
-
health care costs.mp. (10,135)
-
hospital charges.mp. (101)
-
hospital running costs.mp. (0)
-
hospitali?ation cost.mp. (32)
-
cost control.mp. (201)
-
budgets/(1008)
-
“willingness to pay”.mp. (1622)
-
(HCRU or MRU).mp. (17)
-
((healthcare or health care or health resource$ or medical resource$) adj3 utili?ation).mp. (16,300)
-
((healthcare or health care or health resource$ or medical resource$) adj3 “use”).mp. (3938)
-
(resource adj2 (“use$” or util$ or allocat$)).mp. (8730)
-
((economic or health$ or resource) adj3 burden).mp. (3116)
-
(expenditure$ not energy).tw. (7202)
-
(value adj1 money).tw. (40)
-
budget$.tw. (7944)
-
22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49 or 50 or 51 or 52 (230,490)
-
4 and 21 (236)
-
4 and 53 (1113)
-
54 or 55 (1113)
-
(England or Scotland or Wales or Ireland).lo. (41,732)
-
(Great Britain or United Kingdom).lo. (75,329)
-
(national health service* or nhs*).ti,ab,in,cq. (26,199)
-
(english not ((published or publication* or translat* or written or language* or speak* or literature or citation*) adj5 english)).ti,ab. (91,766)
-
(gb or “g.b.” or britain* or (british* not “british columbia”) or uk or “u.k.” or united kingdom* or (england* not “new england”) or northern ireland* or northern irish* or scotland* or scottish* or ((wales or “south wales”) not “new south wales”) or welsh*).ti,ab,jx,in,cq. (423,302)
-
(bath or “bath’s” or ((birmingham not alabama*) or (“birmingham’s” not alabama*) or bradford or “bradford’s” or brighton or “brighton’s” or bristol or “bristol’s” or carlisle* or “carlisle’s” or (cambridge not (massachusetts* or boston* or harvard*)) or (“cambridge’s” not (massachusetts* or boston* or harvard*)) or (canterbury not zealand*) or (“canterbury’s” not zealand*) or chelmsford or “chelmsford’s” or chester or “chester’s” or chichester or “chichester’s” or coventry or “coventry’s” or derby or “derby’s” or (durham not (carolina* or nc)) or (“durham’s” not (carolina* or nc)) or ely or “ely’s” or exeter or “exeter’s” or gloucester or “gloucester’s” or hereford or “hereford’s” or hull or “hull’s” or lancaster or “lancaster’s” or leeds* or leicester or “leicester’s” or (lincoln not nebraska*) or (“lincoln’s” not nebraska*) or (liverpool not (new south wales* or nsw)) or (“liverpool’s” not (new south wales* or nsw)) or ((london not (ontario* or ont or toronto*)) or (“london’s” not (ontario* or ont or toronto*)) or manchester or “manchester’s” or (newcastle not (new south wales* or nsw)) or (“newcastle’s” not (new south wales* or nsw)) or norwich or “norwich’s” or nottingham or “nottingham’s” or oxford or “oxford’s” or peterborough or “peterborough’s” or plymouth or “plymouth’s” or portsmouth or “portsmouth’s” or preston or “preston’s” or ripon or “ripon’s” or salford or “salford’s” or salisbury or “salisbury’s” or sheffield or “sheffield’s” or southampton or “southampton’s” or st albans or stoke or “stoke’s” or sunderland or “sunderland’s” or truro or “truro’s” or wakefield or “wakefield’s” or wells or westminster or “westminster’s” or winchester or “winchester’s” or wolverhampton or “wolverhampton’s” or (worcester not (massachusetts* or boston* or harvard*)) or (“worcester’s” not (massachusetts* or boston* or harvard*)) or (york not (“new york*” or ny or ontario* or ont or toronto*)) or (“york’s” not (“new york*” or ny or ontario* or ont or toronto*))))).ti,ab,in,cq. (330,838)
-
(bangor or “bangor’s” or cardiff or “cardiff’s” or newport or “newport’s” or st asaph or “st asaph’s” or st davids or swansea or “swansea’s”).ti,ab,in,cq. (17,174)
-
(aberdeen or “aberdeen’s” or dundee or “dundee’s” or edinburgh or “edinburgh’s” or glasgow or “glasgow’s” or inverness or (perth not australia*) or (“perth’s” not australia*) or stirling or “stirling’s”).ti,ab,in,cq. (41,252)
-
(armagh or “armagh’s” or belfast or “belfast’s” or lisburn or “lisburn’s” or londonderry or “londonderry’s” or derry or “derry’s” or newry or “newry’s”).ti,ab,in,cq. (5352)
-
57 or 58 or 59 or 60 or 61 or 62 or 63 or 64 or 65 (580,416)
-
56 and 66 (198)
Appendix 18 Model inputs and assumptions
Details of Payakachat et al. study127
The study by Payakachat et al. 127 provided the algorithms used to map VABS composite and IQ scores to utility scores used in the economic analysis. The Payakachat et al. study127 is a US study, which aimed to develop a number of mapping algorithms using behavioural and other measures to predict HRQoL. The study recruited a total of 214 children aged between 4 and 17 years, all diagnosed with ASD. A summary of key baseline characteristics is presented in Table 58.
| Characteristic | Result |
|---|---|
| Age, mean (SD) [range] | 8.4 (3.5) [4.0–17.9] |
| Male (%) | 86.6 |
| Type of school attended (%) | |
| Non-specialised public schoola | 44.6 |
| Specialised public schoola | 8.2 |
| Vocational public schoola | 0.5 |
| Private school | 7.3 |
| Home school | 2.3 |
| Special education school | 26.8 |
| Other (e.g. special education programme, self-contained class) | 10.5 |
| Diagnosis (%) | |
| Autistic disorder | 73.4 |
| Asperger syndrome | 8.7 |
| Pervasive development disorder | 17.9 |
| Cognitive ability, mean (SD) [range] | 75.7 (24.3) [41–148] |
| Vineland-II composite, mean (SD) [range] | 68.4 (11.1) [25–105] |
| ADOS severity score, mean (SD) [range] | 7.2 (1.8) [2–10] |
The target measure used in the Payakachat et al. 127 study was the HUI3. The HUI3 is a measure of HRQoL and measures responses on eight domains of health, including vision, hearing, speech, ambulation, dexterity, emotion, cognition and pain. The resulting health utility scores range from –0.36 (worst possible health) to 1.0 (best possible health). All algorithms developed in Payakachat et al. 127 aimed to predict HUI3 scores using different behavioural measures. The algorithms developed were built around three measures: the Child Behaviour Checklist, Vineland-II Adaptive Behaviour Scales and PedsQL. All of the models included child’s age, cognitive ability (IQ) and ADOS severity scores as control variables. The model selected for use in the economic model was based on only the Vineland-II Adaptive Behaviour Scales composite scores, as Child Behaviour Checklist and PedsQL were not reported as outcomes in the studies identified in IPD meta-analysis.
Generation of quasi-individual participant data from Farley et al.134
Farley et al. 134 reported mean VABS composite score for a number of levels of independence (Table 59). As none of the sample was in the bottom category, completely dependent values for this category were imputed assuming a linear extrapolation of the values in the other four categories.
| Independence level | VABS |
|---|---|
| Completely independent | 102 |
| Mostly independent | 75 |
| Some independence | 51 |
| Mostly dependent | 28 |
| Completely dependent | 17a |
To generate a model with which to predict independence levels, the summary data reported in Farley et al. 134 were used to simulate an IPD set on which appropriate regression analysis could be conducted. This was done using a microsimulation approach and assumed for each independence level that VABS composite scores were normally distributed with mean score as reported in Table 4. The SD for each group was calculated using the SD reported for the whole sample, assuming that the SD for each group was the same. The simulated sample consisted of 1000 hypothetical individuals per independence level (5000 in total). An order logistic model was then run to estimate coefficients, from which the probability of each independence level could be estimated for a given VABS composite score. To estimate the uncertainty in the estimated coefficients, the simulation was run 1000 times, with mean scores for each independence level assumed to follow a beta distribution. SEs for mean VABS composite score were estimated using the estimated SD and the reported sample size for each group. Sample size for the completely dependent group was assumed to be one.
Direct evidence on school type attended
The proportion of children attending each type of schooling in this scenario analysis, in which evidence is directly drawn from the three studies17,26,103 reporting schooling outcomes, is reported in Table 60.
| School type | ABA-based therapy, % | TAU, % |
|---|---|---|
| Mainstream | 30 | 1 |
| Mainstream with support | 38 | 27 |
| Specialist school | 32 | 72 |
Adult utility decrements
To account for the impact of ageing on utilities in adulthood, decrements were applied as multiplier to the mean utility of the cohort from the age of 25 years onwards (Table 61). 145
| Parameter (age in years) | Disutility |
|---|---|
| 25–34 | 0.93 |
| 35–44 | 0.91 |
| 45–54 | 0.85 |
| 55–64 | 0.80 |
| 65–74 | 0.78 |
| ≥ 75 | 0.73 |
Details of assumptions and inputs used to characterise care costs in adulthood
This appendix outlines the assumptions and data sources used to characterise costs of care in adulthood. The care costs are assumed to fall into five categories: (1) accommodation, (2) day services, (3) respite care, (4) productivity losses and (5) other. The other category covers costs of employment support, adult education, medical costs and family out-of-pocket expenses.
Accommodation
The model distinguished between four types of accommodation: (1) own home/living with parents, (2) low-intensity supported accommodation, (3) high-intensity supported accommodation and (4) residential care. Supported accommodation was split into two groups, on the advice of service providers in York, who suggested that there was considerable variation in the levels of support provided in these types of accommodation. Unit cost for each accommodation type are summarised in Table 62.
| Accommodation | Unit costs (£) per annum | Source |
|---|---|---|
| Own home/parents | 0.00 | Assumption |
| Sheltered: low intensity | 53,274.88 | PSSRU:146 supported living homes for adults with autism and complex needs. Assumes 46 hours of care/week |
| Sheltered: high intensity | 99,336.44 | PSSRU:146 supported living homes for adults with autism and complex needs. Assumes 127 hours of care/week |
| Residential | 115,553.00 | PSSRU:146 residential care homes for adults with autism and complex needs |
The proportion of individuals residing in each type of accommodation was guided by the definitions used to define each category and assumptions agreed with service providers in York local authority. All individuals in the ‘completely independent’ or ‘mostly independent’ category were assumed to be either living in their own home or with parents, carers or families. Individuals in the ‘some independence’ category were assumed to be split equally between own home or parents, low-intensity sheltered accommodation and high-intensity sheltered accommodation. Adults in the ‘mostly dependent’ and ’completely dependent’ categories were assumed to be split equally between the high-intensity sheltered accommodation and residential care. Table 63 summarises resource use for accommodation services.
| Accommodation | Completely/mostly independent, % | Some independence, % | Completely/mostly dependent, % |
|---|---|---|---|
| Own home/parents | 100 | 33 | 0 |
| Sheltered: low intensity | 0 | 33 | 0 |
| Sheltered: high intensity | 0 | 33 | 50 |
| Residential | 0 | 0 | 50 |
Costs of living in own house and living with parents, carers or families were assumed to be zero, with remaining costs drawn from the PSSRU. 146 Costs of sheltered accommodation were based on reported costs for supported living homes for autistic adults with complex needs. As costs in the PSSRU146 were reported only for average care needs, it was assumed that individuals in low-intensity sheltered care received 46 hours of care (1 SD below the mean) and individuals in high-intensity sheltered care received 127 hours of care per week (1 SD above the mean). Other costs were assumed equal across both placements. Residential care costs were based on residential care homes for autistic adults with complex needs reported in the PSSRU. 146
Day services
Resource use was based on advice from service providers at York local authority, who suggested that the majority of adults who required support would be those living with a parent, carer or family member, or in their own home. Aligning with assumptions made regarding accommodation services, it was assumed that 100% of individuals in the ‘mostly independent’ category and 33% in the ‘some independence’ category would access day care services. Reflecting the high levels of independence of those in the ‘completely independent’ category, it was assumed that they would not require day care services.
Costs of day care services were drawn from the PSSRU. 146 Local authority own-provision day care for people requiring disability support assumed the reported mean cost per client week of £340 and multiplied by 52.14 (weeks/year) to generate an annual cost of £17,728.57.
Respite care
Aligning with the assumptions made regarding accommodation in Knapp et al. ,147 it was assumed that 100% of individuals in the ‘mostly independent’ and 33% of those in the ‘some independence’ categories would receive respite care. Adults in the ‘completely independent’ category were assumed not to receive any respite care on the basis that they are truly independent, and it was assumed that no respite care would be required in the ‘mostly dependent’ and ‘completely dependent’ categories as these individuals would reside in some form of state provided accommodation.
Costs of respite care were drawn from Knapp et al. 147 and updated using the PSSRU,146 which reports an annual cost of £1927.00.
Other costs
Employment support, adult education and medical costs were drawn from Knapp et al. 147 and PSSRU,146 and mapped to the adult outcomes. Costs in these studies were stratified according to the residential status into three groups: private households, supported people and residential care. These three groups were mapped to the five independence levels used in the model as follows: private households are equivalent to the ‘completely independent’ and ‘mostly independent’ categories, supported people are equivalent to the ‘some independence’ category and residential care is equivalent to the ‘mostly dependent’ and ‘completely dependent’ categories. Costs per annum are presented in Table 64.
| Resource type | Completely/mostly independent (£) | Some independence (£) | Completely/mostly dependent (£) |
|---|---|---|---|
| Employment support | 169.48 | 169.48 | 0.00 |
| Adult education | 1800.00 | 1067.00 | 4159.00 |
| Medical costs | 996.00 | 775.00 | 769.00 |
Appendix 19 Full model results
Tables 65–68 present the full results from the deterministic analysis presented in Tables 20 and 21.
| Outcome | ABA | TAU | Incremental |
|---|---|---|---|
| Treatment costs (£) | 70,754.11 | 12,598.85 | 58,155.26 |
| Education costs (£) | 0.00 | 0.00 | 0.00 |
| Childhood care costs (£) | 5867.40 | 6143.87 | –276.47 |
| Total costs (£) | 76,621.52 | 18,742.72 | 57,878.79 |
| Childhood QALYs | 4.61 | 4.37 | 0.24 |
| Total QALYs | 4.61 | 4.37 | 0.24 |
| Total life-years | 14.94 | 14.94 | 0.00 |
| ICER (£) | 236,837 | ||
| Outcome | ABA | TAU | Incremental |
|---|---|---|---|
| Treatment costs (£) | 70,754.11 | 12,598.85 | 58,155.26 |
| Education costs (£) | 0.00 | 0.00 | 0.00 |
| Childhood care costs (£) | 5221.65 | 6143.87 | –922.22 |
| Total costs (£) | 75,975.77 | 18,742.72 | 57,233.04 |
| Childhood QALYs | 5.21 | 4.37 | 0.84 |
| Total QALYs | 5.21 | 4.37 | 0.84 |
| Total life-years | 14.94 | 14.94 | 0.00 |
| ICER (£) | 68,362 | ||
| Outcome | ABA | TAU | Incremental |
|---|---|---|---|
| Treatment costs (£) | 70,754.11 | 12,598.85 | 58,155.26 |
| Education costs (£) | 118,688.10 | 132,627.20 | –13,939.10 |
| Childhood care costs (£) | 5867.40 | 6143.87 | –276.47 |
| Total costs (£) | 195,309.62 | 151,369.92 | 43,939.70 |
| Childhood QALYs | 4.61 | 4.37 | 0.24 |
| Total QALYs | 4.61 | 4.37 | 0.24 |
| Total life-years | 14.94 | 14.94 | 0.00 |
| ICER (£) | 179,799 | ||
| Outcome | ABA | TAU | Incremental |
|---|---|---|---|
| Treatment costs (£) | 70,754.11 | 12,598.85 | 58,155.26 |
| Education costs (£) | 111,636.23 | 132,627.20 | –20,990.97 |
| Childhood care costs (£) | 5221.65 | 6,143.87 | –922.22 |
| Total costs (£) | 187,611.99 | 151,369.92 | 36,242.07 |
| Childhood QALYs | 5.21 | 4.37 | 0.84 |
| Total QALYs | 5.21 | 4.37 | 0.84 |
| Total life-years | 14.94 | 14.94 | 0.00 |
| ICER (£) | 43,289 | ||
Appendix 20 Consultation exercise
The following text is feedback we received from a consultation exercise undertaken, in which copies of the draft report were sent to 10 stakeholder groups who had expressed an interest in the outcome of the project, but who we could not include in the Advisory Group. We received feedback from seven stakeholder groups and have reproduced these comments here. We also included comments from an autistic adult member of the Advisory Group who was unable to provide feedback on the report before this point. To minimise any potential bias and to maximise transparency, all comments have been provided unaltered, with the exception of the correction of minor spelling errors, and without response.
We would, however, like to reiterate that both the clinical review and the subsequent cost-effectiveness study are limited by the scope of the NIHR commissioning call, specifically the focus on early intensive ABA-based interventions, as opposed to other models of ABA-based intervention, aimed at primary-aged children or other groups of children. This means that some evidence of the effectiveness of less individually intensive ABA-based interventions, which may reflect current practice in the UK and have different costs, was excluded from the review (e.g. data from studies that focused exclusively on group-based interventions or data from a school setting).
Feedback from an autistic member of the Advisory Group
The report shows good efforts to balance the competing interests and strong opinions on this controversial topic. The team have responded well to the issues discussed by stakeholders in the advisory group and many of those issues have been integrated into this report and modelling, and the language and framing in the background is much improved.
I found the explanation of the risk of bias assessments easy to understand and I’m glad this was covered and the strengths and limitations of the current research base were clearly set out.
[Page 29.] Whilst aversive conditioning may be less prevalent or changed considerably from earlier forms of EIBI, this section suggests physical aversives have long been abandoned, which I am not convinced is the case. Certainly the situation in the Judge Rotenberg Center in Massachusetts, USA, springs to mind where electric shocks are still used as a behavioural intervention. Autistic people may also consider forced eye contact or focus, touching/holding or sensory cues to be quite aversive due to the way we experience and process sensory input. The large number of hours of contact time and interpersonal focus on a weekly basis and the resulting social exhaustion may also be considered aversive from an autistic perspective.
There was a very good explanation of the challenges with the current evidence to project any effects into adulthood in the economic modelling, but it is not clear how the effects were projected to the end of childhood (age 15.5 in the model) based on the included studies as few did follow-ups into mid/late childhood, are effects after average age of final follow-up given a trajectory going forward or has the effect been considered flat as with the adult projection?
Feedback on behalf of Easy Steps Limited
Alice Koriki, MSc, Board Certified Behaviour Analyst, Clinical Director
Effectiveness
The exclusion criteria, that only included studies that compared ABA interventions to other models, excluded the largest part of research that shows effectiveness in a broader range of children. The single case studies that dominate the science of applied behaviour analysis I believe provide a better way of examining the effectiveness of ABA especially when we are all aware that the children are so unique and it is very hard to assign them into groups to compare and contrast them.
Long term effects of eclectic education wasn’t clearly analysed, and there were no evidence of true long term effectiveness of eclectic education.
It wasn’t clear whether the EIBI programmes were stopped after the end of the studies, which could potentially also explain the lack of long term progress in the one study described.
EIBI programmes are more optimal when they start around the age of 2y [years]. but that has not been stressed within the current meta-analysis. A study by MacDonald et al. (2014)[254] pointed out that children who started treatment between 18–23 months of age showed the highest levels of despondence (91%) where the despondence levels dropped significantly as the children grew older.
Part of the interventions used in the eclectic groups, or control groups, also included intervention directly derived from the science of behaviour analysis, like TEACCH and PECS. Hence even the effectiveness of those intervention can to some extent be attributed to the principles of applied behaviour analysis.
ABA is an evidence based study and all of us professionals continue to develop our clinical practice using current research. The studies that you have included are somewhat dated (as you have also pointed out) and ABA today in the UK looks nothing like ABA 20 years back when I personally got into the field. Hence those meta-analysis fail to really show the effect of ABA at the present moment, which might be very misleading.
You have pointed out numerous times in the draft the need of further research. That should not be done through meta-analysis of other studies, as they don’t give the true perspective of how early intervention works in the UK. Also research should focus on the overall effectiveness and the cost of the current TAU in the UK, and also on the overall effectiveness of the current SEN special education, as there are very little information available.
Cost
As you pointed out in [page 55] the ‘present economic model should not be viewed as a comprehensive economic assessment of the cost effectiveness of early ABA-based therapy as the data currently available are insufficient to make inferential judgements’. Based on that all other evidence proposed lack robustness in my opinion.
I own the first and until very recently the only early intervention clinic in the UK providing EIBI programmes to children as young as 1 years old. Our cost at the moment, starts from £28.500 per year and doesn’t go above £49.500, and we include a multidisciplinary team around the child, that includes 1 : 1 trained ABA therapists (with RBT qualifications), a BCBA [Board Certified Behaviour Analyst], an OT [occupational therapist] and an SLT [speech and language therapist]. Hence the costs you are presenting are not as representative as described.
The cost of ABA can also be further reduced if it was more widely available as it will be better organised and managed. Making it more widely available through the NHS and Local Educational Authorities will also make it more well-regulated, and effectiveness will be more easily researched.
Final conclusion
It was very promising that you have decided to conduct this meta-analysis even though I do personally believe it has its weaknesses as pointed above. Nevertheless, further research into the effectiveness of ABA in the UK and how the system can improve to provide the children with early intervention more readily, is very important and studies like the present can be the corner stones of that. However, further research is essential and needs to be conducted sooner rather than later, as the autism population increases and the long life cost of looking after those individuals increases. Personally it surprises me that the system has accepted PBS (which is based fully on ABA) to support adults with autism, and related difficulties including behaviours issues, but has difficulty accepting EIBI and ABA interventions in children, in general.
Feedback on behalf of the UK Society for Behaviour Analysis
Dr Mecca Chiesa, Board Certified Behaviour Analyst – Doctoral, chairperson
Congratulations on bringing together such a complex and challenging research project – evaluating research on service provision(s) for autistic children and attempting to estimate short- and long-term relative costs. Given the breadth of services provided, the heterogeneous nature of autism and the inevitably individualised nature of those services, this was never going to be straightforward. However, as other systematic and equally rigorous evaluations have concluded, the SCABARD evaluation reports considerable clinical effectiveness in cognitive and adaptive behaviour outcomes for children exposed to Behaviour Analytic procedures in contrast to children exposed to ‘other’ kinds of procedures (referred to as TAU/eclectic).
A brief note re one of the TAU assumptions – PECS is included as a ‘comparator’ [p. 65]. This is an error. PECS is a systematic behaviour-analytic communication system developed in the 1980s at the Delaware Autism Project by Dr Andrew Bondy (a Behaviour Analyst) and Lori Frost (a speech and language specialist). The development of PECS was based on the functional analysis of language described and explained by B.F. Skinner in his book Verbal Behavior (1957). It is not unusual for PECS to be introduced into an ABA programme in cases where a child struggles with vocal/verbal behaviour. See https://pecsusa.com/research/ for further information.
Re–assessment of TAU costs of £8634 [p. 67] – the report focuses on local authority nursery SEN uplift costs. In the broader experience of children, families and schools I have worked/liaised with over the past 25 years, those TAU programmes also typically consist of one, some or all of the following: Sensory Integration Therapy, Occupational Therapy, SALT, Rebound Therapy, Portage, Early Bird, TEACCH, Intensive Interaction. For future reference, and to be considered more reliable, an economic analysis should include costs (actual examples of costs rather than ‘broad estimates’, [p. 67]) that include and evaluate these typically provided state-funded services. Without capturing all such services and their costs the report may be considerably underestimating the full public sector costs of the UK’s early autism offer – which would, in turn, alter the ICER figures presented. Ideally, this would form part of the ‘recommendations for further research’.
Chart 26 [p. 80] shows EIBI meeting QALY thresholds at £27,000 and indeed becoming ‘dominant’ at £18,000 which prompts a further observation: why are TAU procedures so typically provided in the UK not under scrutiny by the NHS and/or NIHR for clinical/educational/social effectiveness as well as cost-effectiveness? These procedures are funded throughout the UK, many by the NHS, others by multiple LAs [local authorities], yet there is no evidence base relating to their effectiveness. In relation to the economic analysis, TAU provisions may be ‘superior’, but they may have no advantage at all on an effectiveness analysis (with subsequent, lifelong implications). Without robust effectiveness analysis of TAU procedures the UK public (fundamentally, funders of the services) has no assurance that valuable national resources are wisely allocated. The UK’s autistic children, their families, and the public at large should be reassured, via research on all services provided, that those services are likely to result in meaningful improvements in important areas such as adaptive behaviours and cognitive functioning. Again, ideally, this would form part of the ‘recommendations for further research’.
Other economic analyses
On [p. 239] you note that ‘None of the six studies identified in the cost-effectiveness review took a UK perspective with two taking a Canadian governmental perspective, three a US perspective and one study a Dutch perspective’. Clinical effectiveness studies carried out in other countries were included in the SCABARD review. Therefore, there is no logic in not including cost effectiveness reviews carried out in other countries. If Canada, Texas and the Netherlands* (the three evaluations I am familiar with) conclude that early provision of Behaviour Analysis for autistic children results in very considerable lifetime cost savings to the state (and therefore the public) – why would those outcomes not transfer to the UK? That has not been explained. Cost savings are cost savings – whether they are in US Dollars, Canadian Dollars or Euros.
https://www.sciencedirect.com/science/article/abs/pii/S0891422212000984?via%3Dihub
Challenging behaviour
The report states there is no evidence that ABA-based interventions improve challenging behaviour (which lies at the root of many poor outcomes for autistic children and higher costs to the state – e.g. school exclusions, ATU placements etc). The Advisory Group should have examined the extensive research on Challenging Behaviour and ABA-based interventions. It has a long history in the field dating back to the early 1980s. Currently, the UK is seeing increasing uptake of ABA services in adult NHS intensive support services for challenging behaviour, and also in some CAMHS children/adolescent services. NICE guidance NG11 references behaviour analysts and the just-released QS101 refers to the need for every community to have a ‘specialist behavioural support team’. The NHS and many of the care groups in which it funds placements for autistic and/or learning disabled clients are employing PBS^ (Positive Behaviour Support) services, also an ABA-based intervention. There is no logic to the NHS adopting ABA for challenging behaviour at every age except pre school. It makes economic and social sense to tackle challenging behaviour earlier than when a crisis point is reached in the teens or adult life. That the review does not include mention of at least some of the important studies+ demonstrating ABA’s effectiveness in reducing and helping to redirect challenging behaviours is most unfortunate and misleading, see
In conclusion
Further evidence of the effectiveness of Behaviour Analysis in autism provision is not required. It exists in abundance in the form of innumerable SCD (single-case design) reports and many other highly-credible systematic reviews and meta-analyses. As noted previously, the various social and educational practices currently receiving state funding (public monies) have either little or no evidence of clinical/educational/social effectiveness or lifelong benefits. Many highly credible effectiveness and cost-effectiveness analyses (illogically dismissed from the SCABARD report), meta-analyses, systematic reviews have concluded that EIBI is highly effective in improving short and long-term outcomes for children and families, with incremental benefits to the public in terms of substantial cost-savings. There is no disputing the conclusion that autism is costly for families and society at large. The indication so far from clinical and cost-effectiveness research is that spending in the early years on evidence-based practice (EIBI) has substantial and long-term benefits for individuals, families and the state.
Feedback on behalf of Child Autism UK
We at Child Autism UK are grateful to SCABARD for performing this UK-based review of the EIBI (Early Intensive Behaviour Intervention) research. As EIBI is only one specific model that uses ABA (Applied Behaviour Analysis) based techniques, we will use the latter term here as it better represents the broader range of related UK services including the variety of approaches outlined in your report.
We are glad to see your report highlights that ABA-based techniques can increase IQ points and effectively increase adaptive skills. These areas are key in increasing crucial skills such as independence which enhance the well-being of children with autism and their families. It should also be noted that levels of independence are a key factor in reducing the huge costs of lifelong care for people with autism.
My comments aim to address common misunderstandings about ABA-based techniques which echo throughout this report. Most of these misunderstandings relate to a historical context and sadly persist more with the field of ABA than any other profession.
Section 1.4 Early interventions for Autism: The second paragraph states:
‘However, criticisms have been made of this approach. These include concerns that the use of highly structured, primarily adult-led sessions could increase the risk of behaviours that challenge. Also, that it may reduce opportunities to encourage a child’s spontaneity and interactive communication, an over-reliance on prompts, with the potential to further restrict the child’s capacity to develop generalisation skills. [28]’
It would be useful to note that again these are historical concerns. The reference used to cite these concerns[28] is a paper, by behaviour analysts, which assimilates decades of developments in ABA research and that have resulted in great progress in the areas outlined. In their paper, Schreibman et al. conclude that: ‘The field of autism early intervention has changed dramatically in the last 30 years. Since the development of the first empirically-validated and highly-structured ABA-based interventions that changed the lives of children with autism, continued research has expanded these efforts by moving towards more naturalistic interventions . . .’ The second paragraph continues with a reference to one report, from a non peer-reviewed journal, that claims that ABA-based techniques may cause mental health issues: ‘Additionally, it has been suggested, for example by the autistic community,[28] that the rigid nature of ABA-based interventions could potentially increase the risk of later additional mental health problems,[29] though this has yet to be effectively researched and there is little reliable published evidence about this. [30]’
It is misleading to refer to the ‘autistic community’ as if they are a homogenous group. We have had very positive feedback from many adults with autism that learned through ABA-based teaching with us in childhood. We have also had very positive feedback from both parents and tutors of clients who happen to also have an autism diagnosis themselves.
In relation to the suggestion that ABA-based techniques could lead to a risk of mental health problems it could more accurately be said that there was no reliable published evidence for this. The one article referenced here[29] had multiple severe methodological flaws such as not even defining ABA. [30] Your report goes on to state: ‘In response to these concerns, a number of adaptations of the original model have been developed which incorporate the principles of ABA-based techniques within a more naturalistic and developmentally informed framework. Known collectively as Naturalistic Developmental Behavioural Interventions (NDBIs),[28]’ As noted elsewhere in your report, ABA-based techniques have been evolving rapidly over the years as no interventions exist in a cultural vacuum. The changes are made due to the adaption of the science and in response to changing cultural norms.
Having the last concluding paragraph of this report devoted to side-effects and specifically mental health concerns gives too much weight to what was in effect an online survey that wasn’t even from the UK. How often ABA is held to the rigorous standards of randomised control trial research when no other institutional government funded approach to autism comes close to the level of the evidence base of ABA/EIBI.
More research into interventions for children with autism and subsequent adult mental health would be very welcome. Of-course this should be for all education and therapeutic interventions not just EIBI. For example, many children with autism without ABA-based support are unable to express their needs or are excluded from school or put into isolation. These are factors highly likely to have a negative impact on mental health. Conversely, Child Autism UK ABA-based programmes include, when needed, replacing challenging behaviour with appropriate communication, anxiety reduction, increasing problem-solving skills, assertiveness, social skills and tolerance. These are the factors likely to have a positive impact on mental health. Research is therefore needed to find out if ABA-based techniques are actually more likely to improve the mental health of those that receive it than those that don’t.
Interventions
The report has mentioned that in the original Lovaas research, aversives were used as a last resort. It also mentioned that corporal punishment is no longer used in schools. This context is crucial and it is concerning that yet again the field of ABA is dogged by these decades-old criticisms whereas other approaches are not. For example, TEACCH, which is widely used in education has a similar entry in its manual from 1980 that suggest teachers use a ‘slap’ and yet this is never mentioned. Many of the practices in health and education of the 1980s are abhorrent to any practitioner now and the field of ABA is no different. We have practitioners who remember when ABA-based programmes first came to the UK in the 90s and we can categorically say it was unheard of for anyone to slap a child or shout ‘no’. We are mystified as to why an issue which we believe has never once occurred in the UK should be brought up in this report.
Economic analysis
Child Autism UK is one of the largest providers of home programmes in the UK and our costings are very different from those outlined. This is largely because our model does not need a separate supervisor and consultant because the case manager provides both roles. This is because our case managers have an academic background in behaviour analysis due to UK Universities now providing Master’s level degrees in the subject. Another difference is due to our flexibility and willingness to work with a range of families who could benefit from our services. We provide a choice of packages such as our short-term programme which lasts 3–4 months and is a very focused intervention. This starts from £1,313 for the whole package to our long-term intervention from £5,250 per year. This starting cost is where teaching assistants are already employed by schools and we train them in ABA-based techniques. Other key variables are tutor individual costs which vary across the country and start at £15,600 per year for a full-time programme. The findings whether an ABA-based approach is economically viable is based on amounts and a model doesn’t reflect our practice or many organisations that we know.
Conclusions
It is good to see that the review found some evidence to support ABA-based techniques. Even though there was not enough data to form a conclusion about the long-term effects of ABA-based techniques, the evidence presented here still far exceeds any evidence for the eclectic approach. The report rightly highlights how much research is needed into current practices of ABA-based techniques in the UK. This also points to the urgency for the existing eclectic provision that is already funded to have research into its efficacy.
In summary
Whilst we are glad to see the important issue of ABA-based provision being examined, it is a shame that old misunderstandings are raised throughout. Any concerns about ABA-based techniques causing increases in challenging behaviours or reducing spontaneity were addressed decades ago. The several references to concerns about mental health problems caused by ABA-based techniques, from one article that has no evidence-base, is disappointing. Especially considering that good evidence from some ABA studies in peer-reviewed journals were dismissed because of lacking the gold standard of having a randomised control. In a similar vein, mentioning aversives from a bygone era, when they were routinely used in all schools, adds nothing to a paper about current ABA-based interventions in the UK. Finally, the economic analysis bears little relation to the costs of most of the programmes run by Child Autism UK and many other similar organisations. This will impact on whether EIBI does in fact meet the threshold for the NICE guidelines on cost effectiveness. We would urge that the cost analysis be re-examined using costs from a range of UK providers, and using comparison figures from a consistent geographical area. While everyone waits for even more research into ABA, the ‘treatment as usual’ approach that is currently being funded is a ‘hope for the best’ strategy, which would seem to be far less cost effective, and a gamble for children with autism and their families.
Feedback on behalf of the Focus Surrey Saturday club for children with autism
Sue Archdall, chairperson, June Goh, trustee and BCBA, Tracey Tibbals and Karolina Gburczyk, trustees
Thank you for this comprehensive report. We are very pleased to see the NHS giving such serious and independent consideration to early intervention ABA, which many parents have found incredibly helpful and sometimes life changing for their children with ASD and their families. We are responding as trustees and consultants for Focus Surrey a registered charity which runs Focus Surrey Saturday Club for children with autism in partnership with ABA professionals. Our work with families has provided evidence that a few hours of ABA has the potential to improve basic functional skills of most children and young people with ASD who have never been taught using simple ABA procedures that we believe should be universal. If the NHS can offer EIBI it would provide an essential start to learning for children with ASD and return them to their developmental trajectory that autism has impeded.
We are aware that the research about EIBI shows gains for the younger cohort of ASD children. However, we are able to show that the use of ABA methodology and principles through interactive play sessions can provide benefits and meet the outcomes for children of varying ages at our Saturday club. At Focus Surrey Saturday club sessions, children aged 3 to 13 receive 2 hours of ABA a week and parents report the benefits of the programme to their children. It is important to note that although the club accepts children from age 3 the majority of children are aged 5 and above – only two children have attended who fit the early intervention criteria. We believe that interest and knowledge about the efficacy of ABA is increasing but families in the UK still do not have clear guidance about the whole range of evidence-based methodologies for ASD. Families often find out about ABA through a small network of parents who have researched and invested in the therapy in their homes. It is another reason why Focus UK came into being; families felt that the benefits of ABA should be more widely shared in the community.
The club has been running for 6 ten-week terms since September 2016 and the findings are incredibly positive and demand remains high. We have moved from a single 4 hr session to two, 2 hr sessions for 2 age groups in our most recent term (Term 6 – Feb to May 2019) to meet demand from parents. Our waiting list is consistently more than 100 children with new parents signing up regularly. Progress towards outcomes was maintained through precisely managed sessions that offered greater intensity and consistency of input from ABA trained volunteers. For such a small-scale model where many families cannot access any ABA at all, our play sessions are stepping stones to providing parents the opportunity to gauge the effectiveness of ABA for themselves. Children do make progress (as shown by achieving the targets set for them) at Focus Surrey; of the 31 attending in Term 6, 29 children met at least one target set for them. They made progress because they have a small number of very specific individualized goals that the ABA professionals track and measure. Targets vary according to children’s abilities when they start the club. Example of targets are: Pairing – To increase the amount and type of items that are motivating; Social Skills – To request items from peers; To respond to requests from peers; To take turns with 1–2 peers with adult support. For the more advanced children targets include: Requesting – To have a conversation with a peer; Ask or Answer questions; or to play a game with a peer without adult support.
Parents can attend the tutor training and can access the free talks that are run in conjunction with the play group. One of the key points of the club for us is the dissemination of ABA though organized talks which provides information about ABA and suggests strategies to parents directly, as well as being a support network for families where they can share stories and information. Effective parent training is available so that parents themselves can also be tutors if necessary to increase the hours of ABA a child is getting as well as being able to apply ABA principles and techniques at home. Having parents as tutors has benefited parents and has meant the consultants have been able to work on issues (such as un-wanted behaviours) that they wouldn’t have otherwise been able to do with a tutor who sees them only once a week. Some parents who have seen progress at Focus Surrey have then gone on to request their own ABA home programmes. Families surveyed, overwhelmingly endorse Focus Surrey where each term children practice their social, play and communication skills while having fun with their 1 : 1 ABA trained tutors and their peers. Some parents have reported seeing ‘better eye contact’ and their child being ‘more inclined to initiate play’ and being ‘more sociable’ since attending the club. Others have seen benefits in turn taking, sharing and better ‘expression’ and ‘better play skills’ from their children. Testimonies from parents include:
‘My son has been able to accept transitions more, his tantrums are much less.’
‘My child was able to request something from his peers which he was not able to do before. He is practising more to talk louder so that others can actually hear him and he made new friends.’
‘Left to his own devices, my son doesn’t know how to play with toys or other children. But when he’s actively engaged he really enjoys playing and can be quite sociable. Focus provides a really fun set up with lots of toys and activities to enjoy with his tutor. He is also learning how to take turns with other children – a vital play skill and life skill. All overseen by professionals.’
‘My son was able to retain information that he was learning at club and using it outside of club and he started signing words that he wasn’t learning at school . . . He had language until 2.5 and then lost all of his language and then we had only had sporadic words in four years, very infrequently across that time . . . The exposure to that signing environment at the club meant that we were able to start that at home and that has made improvements for him. He gets so excited and pleased with himself when he signs . . . it encouraged us to pursue more one to one support for him . . . .’ – This child attended a local special school setting which didn’t use the principles of ABA so only received ABA at Focus Surrey and they found that he was communicating more than he had done in the past four years.
‘The club gives us a structure to the day and it gives us somewhere we can take him, where we know he’s going to get something out of it . . . taking him to normal places we get a lot of problem behaviour’.
‘The consultants’ support was amazing and their knowledge, experience and understanding of the subject matter really made the difference’, one parent volunteer said of her first term at Focus Surrey. ABA format at Focus Surrey.
At Focus Surrey the children all work towards 2 to 4 targets based on their social, play and communication skills that are assessed at the beginning of the term by 2 ABA consultants, (Tracey Tibbals and Karolina Gburczyk) qualified and certified at BCBA level with more than 35 years ABA experience between them. Tutors working with each child take performance data on the child’s progress with their individual targets that are regularly analysed by the two BCBAs and at the end of term, parents are given a report on progress. Focus Surrey charges £25 a day for the two-hour club which is subsidized by grants and fundraising. We recruit volunteers and provide training for them to work 1 to 1 with children to keep costs down. There are also opportunities for parents to be trained to work alongside their child. Last term six parents received training on ABA and learnt strategies and techniques on how to encourage social, communication and play skills with their own children at home. We believe that a holistic and consistent approach in all environments using ABA can improve long term outcomes and lead to better progress for children and this can reduce overall costs of ABA. However, we stand by the research that intensive ABA model would bring stronger gains than a part-time model of delivery. We are concerned that when we start compromising treatment based on costs the needs of the child are no longer the priority. We recognize that NHS services and treatment for all children with disabilities can be restricted by budgets. As parents of children with ASD we would like to see parity of treatment for children with autism alongside those with more physical disabilities. We would also like to see ABA offered to children beyond early years as they are able to learn more effectively using ABA methods throughout their childhood so age should not be a barrier and this would in fact discriminate against older children who should benefit equally.
Focus Surrey’s partner BCBAs Tibbals and Gburczyk are of the view that in the UK we are moving away from discreet trials at the table and rote procedures to a more flexible approach based on clinical judgement. The model is different in the UK (according to what Justin Leaf is doing in the US). UK professionals they work closely with fall under Leaf’s definition of ‘Progressive ABA’). Tibbals and Gburczyk add that, ‘It was also important to note that EIBI does not need to be 40hrs [hours] and that in the Lovaas study the 40hrs was an average with some children receiving 20 hrs and some children receiving 50+ hrs. The number of hours would be greatly dictated by the severity of the child’s autism, other learning difficulties, levels of challenging behaviour etc. In the UK, therapies such as Occupational Therapy, Speech and Language Therapy, Play Therapy and Portage (up to age 3) is available to children with ASD but for only an hour a week or less often – it is questionable as to what difference this makes at such a low level. With the added intervention of behaviour analysts and the team around the child working together these therapies can be more effective but there is still no research evidence that indicates that this is as effective as a more intense evidence-based ABA programme’.
In terms of cost, Tibbals and Gburczyk estimate that, ‘ABA programmes can be provided at a reduced cost to those mentioned in the Scabard study. For a 20–25 hr a week programme, the costs can range from £22,400–£32,400 depending if tutors cost £20/hr or £25/hr [hour]. This is for 10 months of the year. By having trained parents take on some of the tutoring costs can be reduced even more. Focus Surrey would like to see other therapies incorporate ABA principles and teams working collaboratively so that motivation and behaviour analysis are key to effective treatment and best outcomes for children with ASD. This is the model deployed by well-established ABA schools and clinics that support a multidisciplinary approach in school and on home programmes.
Feedback on behalf of ABA Access4All
Jane McCready
Thank you for this comprehensive report. Very pleased to see the NHS giving such serious and independent consideration to early ABA, which so many of us parents have found incredibly helpful for our children. I am responding on my own behalf and for my 6500-strong parent/professional ABA campaign – ABA Access4All (www.abaa4all.com). I suppose I would sum up your report’s conclusions as ‘NHS study says there’s evidence early ABA works better than the UK’s ‘treatment as usual’ on some important areas for autistic children, but it’s just too pricey’.
ABA helps kids in 4 important areas . . .
As mum to an autistic boy, this phrase on [p. xxix] really resonates: ‘Results favoured ABA-based intervention when assessing adaptive behaviour . . . after 2 years when compared to treatment as usual. In analyses of cognitive ability (IQ) results also favoured ABA by about 10 points after 1 year and 14 points after 2 years’.
Later [page 42] you break down exactly what you mean by ‘adaptive behaviour’ and that the biggest gains are in 3 Vineland areas: communication (which includes talking, reading & writing); socialisation (stuff like turn-taking, play skills, conversational skills etc) and daily living skills – which include washing, maths, toileting, telling the time – a long list. As a parent, I can tell you that this shows ABA is improving pretty much everything a child needs to learn before school starts. You do go on to say that there is little evidence that these skills improve outcomes in later life but come on, let’s inject some commonsense here? You on the research team have kids too? You teach them the skills above and their quality of life improves, any parent knows that. Why the need to constantly confirm the blinking obvious, the minute autism enters the picture?
If ABA were cheaper . . .
On [page xxix], 2nd paragraph of ‘Results’ section, you say that early ABA would need to ‘generate larger benefits or cost savings to be considered cost effective [under NHS QALY thresholds]’. But surely you need to add ‘or be provided at lower costs by providers’? We see in Table 26 that there are levels at which ABA would meet NHS thresholds, and indeed many UK providers are now charging less than your £36k p.a. estimate (which is high, particularly outside of London). I think I am right, looking at that chart, that it’s at around the £27k mark that ABA starts to look viable on NHS criteria – with orange and green cells showing a QALY at your target range of between £20–30k.
Why no urgency?
In your Conclusions section on [page xxxi], there seems to be a lack of urgency in your calls for future worldwide research to ‘establish internationally agreed core outcomes’. This sounds grand but a bit ‘pie in the sky’. At a £34bn yearly UK bill for autism, and 1% of the population diagnosed autistic, more urgency and precise research proposals would be welcome here.
‘The autistic community’ – who’s in it?
On [page 2] you refer to the views of ‘the autistic community’ about ABA’s ‘rigidity’. This surely must be changed to ‘some in the autistic community’ – unless you’ve rung round all 700,000 autistic people/their parents in the UK? Autism is so varied a condition that no one person, or even group, can speak for all the millions of different presentations of autism. This is important as we see from studies* that ‘autism research’ is increasingly not that at all, but in fact ‘demi-autism research’. This skews the debate, and omits arguably the most needy from policy and funding decisions.
Without parents’ care 24/7/365 for their autistic children, often into old age, the UK’s costs of autism would be many many times over what is described in your report. Please don’t let this report negate both the parent and the more severely autistic viewpoint. The NHS should not cleave to only one part of the vast spectrum, and indeed to a relatively privileged segment with arguably far more modest needs of its services – particularly in the early years which are the focus of this report. The note 55 you refer to at this point concerns the work of one autistic academic, who is also on your advisory group. His is just one voice though, and my campaign has featured several very pro ABA autistic voices too – e.g. https://medium.com/@craigrigden78/im-autistic-this-is-why-i-chose-applied-behavioural-analysis-for-my-2-children-with-asd-fb3698afbd98 and https://medium.com/@pmlerner2000/how-aba-saved-my-life-b468bff23a7b
Anecdote/opinion surely can’t inform this NHS study, in either direction? However on a brighter note, at the top of [page 2] I thank you for publishing in your notes not just the (fairly dodgy and anecdotal) Kupferstein ‘research’ but also the robust rebuttal of it as really more of a self-selecting survey by the US author of her like-minded online network.
* https://molecularautism.biomedcentral.com/articles/10.1186/s13229-019-0260-x
An omission?
On [page 5] your stated aim iv) is to highlight areas for future research and ‘to estimate the value of further research’. I am not sure you do actually do this? Unless I missed it? It seems a pretty important one given that autism is the single costliest condition facing the NHS – costing more than cancer, heart attack and stroke combined (Knapp et al. [147]).
On [page 6] you talk about your stakeholder engagement and ‘parents of autistic children’. Again, how much was the severely autistic voice represented? This seems important since c. 50% on the spectrum also have a learning disability, and you say at [page 2] that ‘high lifetime care costs are reported for individuals with co-occurring intellectual disability’. So this group matters a great deal in the cost effectiveness equations. If only the non learning disabled autistic voice was heard on your group, you’ve only got half the picture – and arguably the less costly/needy half too.
UK ABA looks different nowadays . . .
Thank you also at paragraph 2 on [page 65] for acknowledging that today’s UK ABA might in fact look very different from your predominantly US sample, which anyway stops at 2011. Quite a lot of new development has gone on in the UK ABA field in the last 8 years, with costs going down via economies of scale, the UK education and charity sectors embracing different and more affordable models of EIBI, and a much more naturalistic plus Verbal Behaviour ‘Skinnerian’ slant.
ATUs [assessment and treatment units]
In your Table 9 on [page 60], I feel you have missed the whole NHS ‘Transforming Care’ piece. Per Knapp,[147] the bulk of the UK’s £34bn autism bill relates to social care costs housing autistic adults who cannot live independently. We have all seen scandals such as Winterbourne View and recently Whorlton Hall. The resulting ‘post Winterbourne’ agenda is seeing ABA professionals employed by NHS adult autism/LD [learning disability] services to redirect challenging behaviour and keep folk in their communities. Why wait though for the adult crisis – intervening earlier with ABA surely makes more sense?
ABA within the state system, economies of scale . . .
On [page 65] you cite the Griffiths research into ABA schools. But it’s 7 years old and fails to capture a much more nuanced picture today, where big state special schools like Calthorpe Academy in Birmingham or Gogarth in Llandudno are incorporating EIBI classes into their schools, helping kids on a state school budget. In addition, I think the £36k figure for ABA at the bottom of [page 65] looks very high, based more on an old-style home programme model. With economies of scale, nimble new providers and state uptake of EIBI (as above) this cost is too high and may skew your model.
London weighting
I note, on [page 65], that you obtained your TAU costs from Northern-based boroughs but many of your ABA costs from private London providers. This seems unbalanced. Again on the London point, I think your school costs at page 114 need updating as special schools near me in London are more likely to be £25/30k, and standard SEN ‘high needs’ costs of £10k are more up to date. Maybe worth a check? Also, is The Owl Therapy Centre (note 62) even an ABA provider, doesn’t seem that way?
Cochrane
On [page 84] thank you for noting that your study reaches broadly the same conclusions as Cochrane re the improvements in IQ & adaptive behaviour from EIBI. You end the report with a somewhat discursive and philosophical couple of paras that veer into territory not backed up by any actual research: talk of ‘social normative valuations’ and possible harms. I think this reflects a particular agenda and ends what is otherwise a credible report on a jarring note.
Feedback from Mickey Keenan, Fellow of the British Psychological Society, Board Certified Behaviour Analyst – Doctoral, Ulster University, and Karola Dillenburger, Board Certified Behaviour Analyst – Doctoral, Health and Care Professions Council – Clinical Psychologist, Queens University Belfast
We have published many articles on misinformation on ABA in the UK over the years (e.g. https://tinyurl.com/y5jvh2wf) and this report, while well intentioned, exposes the problem yet again. Prior to the commencement of this project we wrote to Dr. Hodgson (July, 2017) and alerted him to the ethical compromise contained in a NICE report that concluded there was no evidence to support investment in the scientific discipline of Applied Behaviour Analysis. NICE has since admitted that none of its reviewers had training in Applied Behaviour Analysis to international standards, and that they were, at best, simply ‘familiar’ with it. In other words, NICE operated on the principle that anyone ‘familiar’ with a scientific discipline is to be regarded as being on a par with someone actually trained in this scientific discipline and thus competent to review its practices and evidence base. No other science would consider this practice acceptable when assessing its findings.
To his credit, Dr. Hogdson has taken these concerns on board, but not sufficiently in our opinion. Since the original e-mail correspondence with him, there are now 49 US States who have implemented legislation ensuring persons diagnosed with autism can get access to ABA-based services, not because there are no alternatives, but because of the overwhelming evidence of effectiveness. The current report had an opportunity to finally put an end to confusion in the UK about ABA but it appears it did not fully appreciate the extent of the hostile environment and the activities of various gate keepers that have blocked its uptake. In a recent Autism Europe Link magazine, for example, there was an article that discussed progress made in the past 70 years in addressing issues associated with autism (https://tinyurl.com/yyvs2tjb). There was no mention of the remarkable legislative changes in the USA, nor was there any mention of the wide variety of agencies and professional bodies that acknowledged the hundreds of publications which informed the introduction of this legislation (https://tinyurl.com/yxgd3hmz). The author of article in the Autism Europe magazine is listed as a member of the Advisory Group for the current report. When advances in ABA are underreported, when the science itself is often maligned (https://tinyurl.com/y5tby245), and when ABA professionals are excluded from participating in discussions about service provision (https://tinyurl.com/y6aldgk3), alarm bells should ring for any venture by professionals without training in the science whose evidence base they are reviewing. Given the nature of this context, it would have made sense to consult with the authorities in each of these 49 US States to examine the evidence that provided the basis of their decisions to fully endorse this scientific discipline. However, it is not clear if this was done. Furthermore, it should be noted that a significant omission from the Advisory Group, is any reference to consultation with professional ABA bodies in the USA such as The Association for Professional Behavior Analysts prior to producing a draft report.
Our brief comments on this report re-emphasis the problems that arise when talk about ABA is reduced to talk about using the scientific method as if it was something that is of questionable practice. [The linked article [https://tinyurl.com/y46chccq]] summarises how the scientific method appears in the practice of ABA. So, let’s see, is Step 1 (Select behaviour to be analysed) to be considered as being of questionable value? We would hope not because it is the only place to start when working with an individual. Even here, though, we run into problems because those critics who have not been trained in behaviour analysis often confuse their own different, shallow, definition of ‘behaviour’ with that used by behaviour analysis (https://tinyurl.com/y2rzom8k).
Step 2 (Measure the behaviour) should also be considered as being acceptable because it is needed to determine a baseline for assessing the outcomes of an intervention. Step 3 (Select treatment strategies), Step 4 (Implement the strategies) and Step 5 (Evaluate the outcomes) should also be acceptable because they describe the essence of evidence-based practice.
Is this report to be viewed as advising the NHS that there is little to be gained by training parents in the use of the scientific method as outlined here? The lack of any in-depth discussion on the topic of parent training certainly raises a question about the perceived value of educating parents, or professionals for that matter, despite the rich database of research on how to do this effectively. Parent training is about sharing the scientific method with parents because they will need it. Once they acquire the skills in evidence-based practice, this will last a lifetime, whatever the prognosis for their child after early intervention; note also, that it is not the scientific method that limits the outcomes for children. Not factoring in the value of parent training to any great extent in the sophisticated equations for defining costs is a huge omission.
Can it really be the case that the NHS is being asked to accept one review in the UK as exceeding the thoroughness of 49 different reviews in the USA where numerous ABA professionals with extensive research expertise contributed to discussions on their science? It certainly seems that way.
Apart from these comments above, we see little value in providing a commentary on any draft report. Suffice to say, that the issues raised above are extremely serious and parents who have benefited from ABA should be alert to the potential consequences. Children with autism are children with autism all over the world, and whether they come from the UK or the USA their hearts beat in the same way and they all share the ability to learn, even if it is to different degrees. They have a right to be supported with evidence-based practices so they can develop to their full potential.
We leave the final word to a parent who is a consultant in the NHS:
‘Our son D. was diagnosed as autistic before his third birthday. He was initially diagnosed by a private pediatrician we took him to. By that time I (a clinician with knowledge of autism) already knew he was autistic and had done a huge amount of research into what we could do next. We had therefore already decided on and started getting together, an ABA programme for him, by the time we got to see the NHS ‘pediatrician’ in the local child development clinic. This was actually a junior doctor who was not yet a qualified pediatrician, despite being described on the clinic letter as a consultant, he did not have the necessary qualifications to be an NHS consultant. I know this very well, because I am an NHS consultant!
After telling us our son had a diagnosis of autism, the NHS doctor could offer only one piece of advice when I asked what he would advise that we do next. He pointed to the phone number for the DLA benefits department, which was stuck up on a post-it [Post-it® (3M, Saint Paul, MN, USA)] note on the wall above his head, and told us we could apply for some benefits. That was it. I then told him that we were starting an ABA programme. He had never heard of ABA.
When D. started ABA, just after his third birthday, he had no means of communication, was behaviourally impossible to control, and banged his head literally hundreds of times a day, often hurting himself badly. Over the following year and a half of ABA, under a highly skilled BCBA and with the dedicated work of his tutors, the head-banging was brought under control and then eradicated, he learned to comply with instructions and to enjoy working with his tutors, and is now learning to read and spell. He does not talk but it seems likely that he will be able to communicate using a device he can write or type on. He is now in mainstream school part-time, with the ABA programme continuing in the afternoons. There are no behavioural problems at school and he loves it.
The stress, financial and emotional, on our family has been enormous, but I would do it all again at the drop of a hat. The stress is not because of the programme itself that has always felt like a saviour and a lifeline. The stress has been from having to pay for it all, and having to fight with the Local Authority to get them to even acknowledge that this is what he needs. And they have clearly indicated that at the end of this school year they expect him to be in school full-time and for the programme to have ceased. So the fight will, no doubt, go on . . . and on . . .’ (https://tinyurl.com/y3ezhokp)
Feedback on behalf of the National Autistic Society
Firstly, we would like to thank you for giving us the opportunity to comment on this very comprehensive, thorough and robust report. We are sure that it will act as a landmark study on this hugely important topic.
We have a few minor concerns as follows:
We are concerned that the report is not putting sufficient weight on the three RCTs. All the analysis seems to treat all 20 studies as equally strong evidence. This seems like a flaw in the whole exercise given how badly biased the other 17 are. The report should also say what the combined participant numbers are for the three RCTs and whether they sourced IPD for all of them.
We are concerned that the report really stretches the evidence for the economic model. Not just the ABA evidence but the other evidence used. Although the results are pretty damning for ABA, there are some things which proponents will latch on to and we are concerned it legitimises the evidence too much. An ICER of £45k (public sector optimistic scenario) is not a million miles away from NICE’s £30k threshold but to read from this that ABA is close to being cost effective would be inappropriate. Another example is the seductively low £11,802 in scenario 3 of the sensitivity analysis. This is based on only three studies that looked at education outcomes (were any of them RCTs?) and that’s on top of all the other flaws and assumptions in the evidence.
The report acknowledges that it has no evidence on adverse effects. This is a big weakness especially when moving to the modelling into adulthood. Could the report not model this as a scenario? For example X amount of damage to Y ABA recipients would results in Z public sector costs or loss of QALYs. What would X and Y need to be to double the ICER of ABA? Not much we suspect given the cost of poor mental health.
In the summary we think the report might be quoting the wrong ICER figure under the pessimistic scenario. £327k is for NHS and social care only (see Table 20) not whole public sector (which is actually £261k from Table 22).
Using Payakachat et al. (2014)[116] to convert IQ and VABS to HRQoL is helpful but the report could do more to acknowledge the weaknesses of using one study that found correlations of 0.3 to 0.45. Also the average age in that study was 8.4 so not a great match for ABA.
IQ measurement – we are not sure there is enough discussion of the suitability of IQ measures for autistic children. We think there’s more literature on this that might be worth citing e.g. Barbeau et al. (2012). [255]
Language – some phrases perhaps need more qualification:
‘Cost of autism’. We understand that this makes some sense in the NICE context. Others have turned it round to ‘autism dividend’ which might not work here but could they find something less emotive?
Autistic people rather than ‘People with autism’.
‘Severity’. Maybe put this in quotes?
It would be useful to know the split of participant numbers by country (especially UK), rather than just number of studies per country.
Mortality – it discusses why it did not attribute gains to ABA (quite rightly) but we are puzzled by the 77 years figure used in Scenario 2 which sound (tragically) too old.
Figure 18’s title needs changing to something like ‘potential’ or ‘hypothesised’ impacts. It is not showing actual impacts and could be taken out of context.
Glossary
- Aberrant Behaviour Checklist
- A standardised caregiver report checklist designed to assess challenging behaviours in children and adults with developmental disabilities. Its age range is 5 years to adult and it includes normative data for populations with learning disabilities.
- Adverse effect
- An abnormal or harmful effect caused by, and attributable to, exposure to an intervention, such as a medication or a psychosocial or psychoeducation intervention, which is indicated by some symptom(s), such as illness or death.
- Applied behaviour analysis
- An applied psychological approach with an established theoretical basis designed to analyse and change behaviour through an array of behavioural techniques, including operant, classical and relational conditioning.
- Autism Diagnostic Interview – Revised
- A standardised semistructured diagnostic interview for a parent or carer of individuals with suspected autism spectrum disorder. The age range is from 18 months through adulthood.
- Autism Diagnostic Observation Schedule
- A standardised structured play- and activity-based assessment for the direct observation and assessment of individuals with suspected autism spectrum disorder. It consists of four modules for children and adults of differing developmental and language levels. The age range is from 12 months through to adulthood.
- Autism spectrum disorder/autism
- A lifelong neurodevelopmental disorder characterised by impairments in social communication and a pattern of restricted, repetitive repertoire of interests, behaviours and activities.
- Child Behaviour Checklist
- A parent- or teacher-reported standardised measure that assesses for a wide range of emotional and behavioural problems in children. It has preschool and school age versions, allowing it to cover an age range of between 18 months and 18 years.
- Childhood Autism Rating Scale
- A behavioural rating scale that is widely used in the diagnosis and screening of autistic children aged ≥ 2 years.
- Confidence interval
- The confidence interval associated with a value indicates the estimated range within which the ‘true’ value (i.e. the size of the effect of an intervention) is expected to lie if sampling could be repeated a large number of times. Generally, 95% confidence intervals are reported.
- Cost-effectiveness acceptability curve
- A graph describing the impact of uncertainty on the result of a cost-effectiveness model. The graph plots a range of cost-effectiveness thresholds on the horizontal axis against the probability that the intervention will be cost-effective at that threshold on the vertical axis. It can usually be drawn directly from the results of a probabilistic sensitivity analysis.
- Cost-effectiveness model
- A cost-effectiveness or decision model seeks to answer questions about how to deploy resources in a health-care system. A model is a simplified representation of a real-world condition and treatment pathway, which aims to estimate the costs and consequences arising from making a particular policy decision (i.e. whether or not the NHS should fund a new procedure or drug). All relevant alternative courses of action and their long-term costs and consequences are compared to inform a decision on which option to adopt.
- Cost-effectiveness threshold
- Represents the maximum amount a health-care system is willing to pay to provide a new technology or intervention. National Institute for Health and Care Excellence guidance (National Institute for Health and Clinical Excellence. Guide to the Methods of Technology Appraisal 2013. London: NICE; 2013) typically considers interventions with an incremental cost-effectiveness ratio of between £20,000 and £30,000 per quality-adjusted life-year as cost-effective.
- Cycle
- The smallest period of time measured in an economic model.
- Deterministic sensitivity analysis
- Explores the impact on model results of varying one or two input parameters at a time.
- Developmental trajectory
- The rate of development of a child when compared with that of their peers.
- Diagnostic and Statistical Manual of Mental Disorders
- A publication by the American Psychiatric Association that defines the criteria for the classification of mental health disorders, including autism spectrum disorders. The fifth edition was published in 2013.
- Discrete trial training
- A highly structured training technique that requires the therapists to break down skills into small, achievable tasks or behaviours using a series of learning opportunities or trials. Each trial has a clear beginning and end, which is why it is described as discrete.
- Dominance
- In the field of health economics, a treatment option is said to be ‘dominant’ when it is both less costly and produces better health outcomes than the comparator strategy. Thus, a treatment that is both more expensive and results in poorer health outcomes is referred to as ‘dominated’.
- Early intensive applied behaviour analysis-based therapy
- The term we have used in this report to collectively describe early intensive behavioural interventions and naturalistic developmental behavioural interventions with an intensity of > 15 hours per week.
- Early intensive behavioural intervention
- An umbrella term used to describe a range of interventions that are based on the principles of applied behavioural analysis with young preschool children. The term has become most well known when linked with the work of Lovaas in the 1980s with young autistic children (Lovaas OI. Behavioral treatment and normal educational and intellectual functioning in young autistic children. J Consult Clin Psychol 1987;55:3–9).
- Early start Denver model
- An early intervention model combining developmental and behavioural approaches that is designed to help the development of very young children. It incorporates both early intensive behavioural intervention and naturalistic developmental behavioural intervention elements.
- EuroQol-5 Dimensions
- A generic measurement of quality of life used in many clinical trials. This instrument is easy to use and has been extensively validated across many disease areas. The benefit of the EuroQol-5 Dimensions is the availability of utility scores (generated through large population surveys) for each possible combination of questionnaire responses; these can be combined with the time individuals reside in particular health states to calculate the quality-adjusted life-years associated with an intervention.
- Expressive language
- The ability to put thoughts into words and sentences in a way that makes sense and is accurate. Expressive language also informs an individual’s writing.
- Gilliam Autism Rating Scale
- A developmental checklist to assist in the identification of autism, developed to discriminate individuals who are autistic from those with other developmental disabilities.
- Inclusion
- The practice of educating all or most children in the same classroom, including children with physical, mental and developmental disabilities. Inclusion classes often require a special assistant to the classroom teacher.
- Incremental cost-effectiveness ratio
- A measure that represents the economic value of an intervention compared with an alternative, and is generally the primary outcome of an economic evaluation. An incremental cost-effectiveness ratio is calculated by dividing the difference in costs between two interventions by the difference in quality-adjusted life-years. The incremental cost-effectiveness ratio is the cost of generating an additional quality-adjusted life-year using the intervention we are interested in compared with an alternative, usually current clinical practice.
- Individualised education plan
- A yearly education plan written by a multidisciplinary team and the child’s parents for school-age children who need special education. The individualised education plan attempts to address the student’s needs and outlines the educational supports and services necessary to meet those needs.
- Intellectual disability
- A condition characterised by low cognitive ability, as measured by an intelligence quotient score (< 70) and associated difficulties in adaptive functioning presenting before the age of 18 years.
- Intelligence quotient
- A score calculated from a set of standardised tests developed to assess a person’s cognitive abilities compared with others in their age group. It is calculated as the ratio of tested mental age to chronological age and expressed as a quotient multiplied by 100.
- Intention to treat
- An analysis in which all participants enrolled in a trial are analysed according to the intervention to which they were initially allocated, regardless of whether or not they went on to receive it. This type of analysis is considered best at providing an unbiased comparison of effectiveness across treatment groups.
- Leiter International Performance Scale
- A non-verbal assessment of cognitive ability through assessing fluid reasoning, visuospatial memory and attention. It is used primarily with children with communication difficulties. It gives an intelligence quotient score and has an age range of between 2 and 20 years.
- Merrill–Palmer Scale of Mental Tests
- A standardised test of intellectual ability validated for use with preschool children. Many of its range of tests consist of concrete stimuli (e.g. puzzles) and rely less on children’s language skills when assessing non-verbal intelligence quotient to other tests of cognitive ability. These factors combined with a more liberal way to determine when to end testing means it tends to yield higher scores for autistic children. Its age range is between 1 and 78 months of age.
- Meta-analysis and network meta-analysis
- Meta-analysis is a set of statistical techniques in which data from multiple studies on the effects of two interventions are combined to provide an overall estimate of the relative effects of the two interventions. Network meta-analysis is similar to standard meta-analysis, but allows comparative effects to be assessed for more than two alternative interventions.
- Mullen Scales of Early Learning
- An individually administered, multidomain measure of early development for children from birth to 68 months, assessing visual reception, receptive language, expressive language and fine motor skills.
- Naturalistic developmental behavioural intervention
- A collection of intervention models that adapt the early intensive behavioural intervention approach to incorporate the principles of applied behaviour analysis in a more naturalistic and developmentally informed framework. These interventions include child-led and incidental training opportunities. Examples of these models are pivotal response treatment, the Denver model and the Denver model’s derivative, the early start Denver model.
- Opportunity cost
- The opportunity cost associated with an intervention is the benefits we could have obtained if we spent the money elsewhere. In a health-care system with a fixed budget, existing services must be displaced to fund the new intervention; this means that the ability of the system to generate health will be reduced if the opportunity costs outweigh the benefits of the new intervention.
- Picture exchange communication system
- A visual augmentative communication system developed to help individuals quickly acquire a functional means of communication.
- Pivotal response training
- A systematic applied behaviour analysis-based approach that targets pivotal skills to produce collateral improvements across related skills, theorised to lead to improvements in the quality of social and communicative interactions. Pivotal response treatment is considered an example of the naturalistic developmental behavioural intervention approach.
- Prevalence
- A measure of the number of cases of a disorder in a defined population at a particular point in time.
- Probabilistic sensitivity analysis
- Assesses the joint uncertainty across all input parameters in the model. This is done by assigning probability distributions to each input parameter and making random draws from each of these distributions. This process is then repeated many thousands of times, resulting in a distribution of outputs that describe the uncertainty in the results of the model.
- Psychoeducational Profile – Revised
- A measure used to assess the developmental level and emerging skills of young children with autism and communication disabilities. The tool consists of a developmental scale and a behavioural scale. It has an age range of between 6 months and 7 years.
- Quality-adjusted life-year
- An index of health gain, on which survival duration is weighted or adjusted according to the patient’s quality of life over the time they are alive. Quality-adjusted life-years are based on utilities, which are valuations of quality of life measured on a scale between full health (1) and death (0). These valuations are multiplied by the number of years that an individual spends in a health state with that particular utility score, and the quality-adjusted life-years are summed over the modelled time horizon.
- Quality of life
- A broad concept incorporating all of the factors that might have an impact on an individual’s physical, mental and social well-being. Health-related quality of life refers to the specific impact a medical condition or treatment has on an individual’s functioning and general well-being. Health-related quality of life is generally measured in clinical trials alongside other outcomes to assess the impact of an intervention from a patient’s perspective, typically using questionnaires completed by patients, their families or clinicians, such as the EuroQol-5 Dimensions and Short Form questionnaire-36 items.
- Randomised controlled trial
- An experiment in which investigators randomly allocate eligible people into groups that are each assigned a different intervention, to compare their relative effectiveness and safety.
- Receptive language
- Refers to the comprehension of information provided to us and is the input system of language. It is the information we take in from what we see, hear and read.
- Reinforcement
- The provision of a pleasant consequence (positive reinforcement) or removal of an unpleasant consequence (negative reinforcement) after a behaviour to increase or maintain the likelihood of that behaviour occurring when it is preceded by a specific antecedent stimulus (the situation or context in which the behaviour occurs).
- Reynell Developmental Language Scales
- A widely used standardised assessment for identifying language development and impairment in young children. It contains subscales for both expressive and receptive language, which can be combined into a comprehensive score. Its age range is between 2 years and 7 years, 5 months.
- Scenario analysis
- A process of exploring alternative future outcomes by selection of different assumptions used in the economic model. Scenarios can represent outcomes ranging from optimistic, for which input variables are changed to their most optimistic values, to their most pessimistic. These types of analyses test the cost-effectiveness and safety of an intervention in the best and worst cases, and in other plausible ‘alternative worlds’.
- Sensitivity analysis
- In cost-effectiveness modelling, many of the parameter values are often estimated with a degree of uncertainty. Sensitivity analysis is used to explore the impact of this uncertainty. This is done by varying assumptions and inputs used in the model and recording their impact on the results.
- Short Form questionnaire-36 items
- A patient-reported set of generic, coherent and easily administered quality-of-life measures. Different combinations of answers can be assigned utility weights and used to calculate quality-adjusted life-years.
- Stanford–Binet Intelligence Scales
- A test of general cognitive ability, widely used for clinical and research purposes. The test yields a full-scale intelligence quotient, a non-verbal intelligence quotient and a verbal intelligence quotient. The age range is 2 years to adulthood.
- Statistical significance
- A result in which the reported p-value falls below the selected significance level; this value represents the probability that the observed result could have occurred due to chance alone if the ‘null hypothesis’ is true (i.e. there was no true difference between the groups).
- Time horizon
- In an economic model, the duration over which costs and health outcomes are calculated. The choice of time horizon is important and generally depends on the nature of the condition for which an intervention is being assessed. A long time horizon is preferred in chronic or long-term conditions for which there are likely to be important ongoing management costs and consequences well into the future. The use of a long-term time horizon often involves the extrapolation of short-term data into the future and the use of assumptions about the persistence of treatment effects due to a lack of long-term data.
- Treatment and Education of Autistic and Related Communication-Handicapped Children
- A model of early intervention revolving around a philosophy of recognising autism as a lifelong condition and responding to it as a culture. Teaching is designed around individual strengths, skills, interests and needs, working in collaboration with parents and families. Intervention strategies are largely based around physical and visual structure, schedules, work systems and task organisation.
- Vineland Adaptive Behaviour Scale
- A tool used extensively as a measure of adaptive behaviour in autistic people. Adaptive behaviour refers to the social, communication, behavioural and self-help skills needed by individuals to function and be self-sufficient within their everyday environments. It has an age range of birth through to adulthood.
- Wechsler Intelligence Scale for Children
- A psychological assessment that measures aspects of cognitive ability. It contains a range of tests to measure different aspects of a child’s abilities, which can be combined to yield a full-scale intelligence quotient. It has an age range of 6 to 16 years.
- Wechsler Preschool and Primary Scale of Intelligence
- A standardised assessment of cognitive ability for young children. It contains a range of subtests that yields scores for full-scale intelligence quotient, verbal intelligence quotient and performance intelligence quotient. It has an age range of 2 years, 6 months, to 7 years, 7 months.
List of abbreviations
- ABA
- applied behaviour analysis
- ADI-R
- Autism Diagnostic Interview – Revised
- ADOS
- Autism Diagnostic Observation Schedule
- ANCOVA
- analysis of covariance
- ASD
- autism spectrum disorder
- BSID
- Bayley Scales of Infant Development
- CENTRAL
- Cochrane Central Register of Controlled Trials
- CI
- confidence interval
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- EIBI
- early intensive behavioural intervention
- ESDM
- early start Denver model
- HRQoL
- health-related quality of life
- HTA
- Health Technology Assessment
- HUI3
- Health Utilities Index Mark 3
- ICD-10
- International Statistical Classification of Diseases and Related Health Problems, Tenth Revision
- ICER
- incremental cost-effectiveness ratio
- IPD
- individual participant data
- IQ
- intelligence quotient
- ITT
- intention to treat
- MD
- mean difference
- MPSMT
- Merrill–Palmer Scale of Mental Tests
- MSEL
- Mullen Scales of Early Learning
- NAS
- National Autistic Society
- NDAR
- National Database for Autism Research
- NDBI
- naturalistic developmental behavioural intervention
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- NMA
- network meta-analysis
- PDD-NOS
- pervasive developmental disorder – not otherwise specified
- PECS
- Picture Exchange Communication System
- PedsQL™
- Pediatric Quality of Life Inventory™
- PEP-R
- Psychoeducational Profile – Revised
- PPI
- patient and public involvement
- PRT
- pivotal response treatment
- PSSRU
- Personal Social Services Research Unit
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- RDLS
- Reynell Developmental Language Scales
- ROBINS-I
- Risk Of Bias In Non-randomised Studies – of Interventions
- S–B
- Stanford-Binet Intelligence Scale
- SCABARD
- Synthesising Comprehensive Applied Behaviour Analysis interventions – Research for children with autism spectrum Disorders
- SCQ
- Social Communication Questionnaire
- SD
- standard deviation
- SE
- standard error
- SEN
- special educational needs
- SF-12
- Short Form questionnaire-12 items
- SF-36
- Short Form questionnaire-36 items
- SMD
- standardised mean difference
- TAU
- treatment as usual
- TEACCH
- Treatment and Education of Autistic and Communication related handicapped CHildren
- UCLA
- University of California, Los Angeles
- VABS
- Vineland Adaptive Behaviour Scale
- WHOQOL-BREF
- World Health Organization Quality of Life-BREF
- WISC
- Wechsler Intelligence Scale for Children
- WISC-R
- Wechsler Intelligence Scale for Children – Revised
- WPPSI
- Wechsler Preschool and Primary Scale of Intelligence
- WPPSI-R
- Wechsler Preschool and Primary Scale of Intelligence – Revised
