Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 16/11/03. The contractual start date was in March 2017. The draft report began editorial review in November 2018 and was accepted for publication in June 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Rachel Churchill was part of a Systematic Reviews Programme Advisory Group. Simon Gilbody is/was a member of the following committees: Health Technology Assessment (HTA) Clinical Trials Board (2008–14), HTA Commissioning Board (2016–19), HTA Efficient Study Designs (2015–16), HTA End of Life Care and Add on Studies (2016), HTA Funding Boards Policy Group (formerly CSG) (2017–20), HTA Funding Teleconference Members (2015–16) and HTA Post-board Funding Teleconference (2017–20). Peter Coventry is a member of the following committees: HTA General Board (2018–19) and Health Services and Delivery Research Funding Committee Members (2019–22).
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Melton et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Background
Trauma- and stressor-related disorders and their relevance to complex traumatic events
Trauma- and stressor-related disorders, also known as reactions to severe stress and adjustment disorders, are mental health problems directly related to exposure to a traumatic event or series of traumatic events. Post-traumatic stress disorder (PTSD) is among the most common mental health disorders to occur after experiencing (or witnessing) a major traumatic event. Typical symptoms include involuntary re-experiencing of the traumatic event in a vivid and distressing way (e.g. flashbacks, nightmares), avoidance of activities reminiscent of the trauma, persistent numbness, emotional blunting and detachment from other people and previously significant activities, along with hyperarousal in the presence of reminders of the trauma (including hypervigilance, difficulty sleeping, irritability, poor concentration and an exaggerated startle response). People with PTSD may also experience comorbid psychological problems including substance use disorders, depression (with increased risk of suicide) and other anxiety disorders (e.g. panic disorders), and functional somatic syndromes, which can further impair social, educational and occupational functioning.
Post-traumatic stress disorder can occur at any age and it is relatively common, with a lifetime prevalence of 7.8%;1 12-month prevalence ranges from 3% to 4%. 2 Rates vary depending on the type of stressor experienced; for example, physical assaults in women are associated with a lifetime prevalence of 29%, combat experience in men is associated with a lifetime prevalence of 39% and lifetime prevalence is 15.4% in people exposed to war and displacement. 3
It is argued, however, that the PTSD symptom clusters described in the current and previous versions of the Diagnostic and Statistical Manual of Mental Disorders (DSM) and the International Classification of Diseases, Tenth Revision (ICD-10), do not adequately capture the full range of clinical symptoms exhibited by those who experience complex trauma (i.e. developmentally adverse interpersonal trauma such as prolonged domestic or community violence, childhood abuse, torture or exploitation). 4 People who experience complex trauma especially, but not exclusively or necessarily in formative periods, are more at risk of other psychiatric disorders. Complex PTSD (CPTSD) and disorders of extreme stress not otherwise specified (DESNOS) are labels that have been used to define syndromes that involve, in addition to core PTSD symptoms, pathological disassociation, emotional dysregulation, somatisation and altered core schemas about the self, relationships and sustaining beliefs. 5
Recent empirical work using latent class analysis in people exposed to different types of acute and chronic stress has gone some way to endorse the distinction (to be included in ICD-11)6 between PTSD and CPTSD, with the CPTSD class scoring highest for symptoms related to affective dysregulation, negative self-concept and interpersonal problems. 7,8 The symptom profile of CPTSD is thus characterised by the loss of emotional, social, cognitive and psychological skills, because either the person’s development has been interrupted during a formative phase or they have been seriously impaired owing to exposure to complex trauma. Beyond the prototypical case of childhood sexual abuse, complex trauma experiences have also come to embrace ‘other types of catastrophic, deleterious and entrapping traumatisation occurring in childhood and/or adulthood, such as repeated domestic violence, trafficking and exploitation, and being forcibly displaced’. 9 Compared with single-event PTSD, complex trauma is characterised by sustained or repeated instances of trauma of an interpersonal nature that are ‘extremely threatening or horrific and from which escape is difficult or impossible due to physical, psychological, maturational, family/environmental, or social constraints’. 10
Impact and burden of complex trauma
Mass conflict, persecution, generalised violence and human rights violations pose a critical threat to global mental health. By the end of 2014, 59.5 million people across the world were forcibly displaced (19.5 million refugees, 1.8 million asylum seekers and 38.2 million internally displaced persons) and this figure has certainly been surpassed owing to exceptional numbers fleeing conflict in the Middle East. 11 Asylum trends show that there has been a huge increase in applications in industrialised countries, with 80% being lodged in European countries (82% of these in EU countries); the UK saw a 5% increase in asylum applications from 2013 to 2014. 12
Among forcibly displaced people, 30.6% are affected by PTSD; reported torture is consistently the strongest population risk factor associated with PTSD in this group. 3 Depression and anxiety occur as frequently as, if not more often than, PTSD among refugees and asylum seekers, with rates as high as 40% observed among some displaced groups. 13 Similarly, human trafficking (i.e. recruitment and movement of individuals by force, coercion or deception for exploitative purposes) is associated with high levels of physical and mental health problems. 14 Worldwide, up to 2.5 million people are known to be in conditions of forced labour and are exposed to high levels of physical and sexual violence, economic restrictions and controlling behaviour. 15 The risk of depression, anxiety and PTSD is significantly higher in women who have been exploited for ≥ 6 months compared with the general population,16 and higher in women trafficked for sexual exploitation than in women trafficked for labour exploitation. 17
Other critical cases of complex trauma are associated with exposure to childhood sexual and physical abuse. Although under-reported (one in three cases are not reported), 1 in 20 children has been sexually abused in the UK. 18 Victims of child abuse are three times more likely to experience PTSD over their lifetime. Rates of PTSD and alcohol dependence are especially high in women who have experienced childhood abuse and related interpersonal violence. In total, the cost of physical and mental health (depression and PTSD) and substance abuse to the UK is estimated to be £3.2B per year, in part owing to under- and unemployment and the high spend in the criminal justice system, as well as costs attributed to the use of mental health services. 19 Stigma, discrimination and depression similarly affect victims of childhood abuse and severely impair their quality of life.
Treating mental health problems in people affected by complex trauma
Existing international guidance makes no distinction between more complex variants of PTSD and recommends the use of trauma-focused therapies for people with comorbidities and PTSD. However, many of the trials included in existing systematic reviews [on which National Institute for Health and Care Excellence (NICE) guidance is based]20 were carried out in North American or Western European countries where the type and severity of trauma experienced by participants may not be comparable to settings and scenarios with a higher risk of prolonged exposure to complex interpersonal trauma. In addition, the World Health Organization (WHO) guideline excluded systematic reviews based on trials of treatment of PTSD in refugee populations. 21 As such, it is unclear if treatments that are effective for people with single-event PTSD are equally effective for people exposed to complex traumatic events, who have significantly greater psychological comorbidity and functional impairment than the former group. Standard cognitive and behavioural therapies and exposure-based treatments for PTSD might have limited utility and might be harmful if used prematurely for people with psychological problems following complex traumatic events. 22 Many people with CPTSD have high levels of disassociation and psychological comorbidities that might limit their capacity to engage in exposure-based therapies, and findings from effectiveness studies in single-event PTSD cannot be generalised to people with complex trauma. 23 Compared with brief trauma-focused treatments, phase-based approaches or sequential interventions that first focus on stabilisation (ensuring individuals’ safety, resolving symptoms – including dissociative symptoms – and increasing emotional, social and psychological competencies), followed by processing unresolved aspects of individuals’ trauma, with an emphasis on consolidation of treatment gains to facilitate re-engagement with social, educational or occupational relationships, can be effective in more complex presentations of PTSD following childhood sexual abuse. 24
However, the quality of the evidence for the CPTSD expert consensus guidelines is mixed: two studies were not randomised controlled trials (RCTs); only three included an active control and none included head-to-head comparisons with trauma-focused therapies; three studies did not follow up with participants; and all of the evidence was drawn from populations exposed to childhood sexual abuse and no other types of complex trauma, which limits the validity and generalisability of the conclusions. 25 Indeed, patients with a history of complex traumatic events might benefit from existing evidence-based psychological and pharmacological treatments. Crumlish and O’Rourke identified 10 trials (n = 528) in a review of psychotherapy for refugees and asylum seekers. 26 Cognitive–behavioural therapy (CBT) and narrative exposure therapy (NET) emerged as candidate interventions for reducing core PTSD symptoms, but small sample sizes, inadequate allocation concealment and the use of different comparisons limit the conclusions. Similarly, Palic and Elklit, in a review of 25 experimental and non-experimental studies (n = 1113) of psychosocial treatments for PTSD among refugees, identified CBT as the most effective therapy for reducing PTSD symptoms. 27 Trauma-focused therapies such as CBT and NET appear to be equally efficacious across different types of trauma too, including repeated traumatisation. Powers et al. , in a review of 13 trials (n = 675), showed that there was no significant difference in effect sizes for prolonged exposure therapy across types of trauma (combat/terror, childhood sexual abuse, rape, mixed; p = 0.14). 28
More complex presentations of PTSD include psychiatric comorbidities and there is growing evidence that existing non-phase-based approaches are effective in this group. A wide-ranging review with a meta-analysis that included 148 anxiety-disordered treatment samples (47 in PTSD; combined n = 3534) showed that effect sizes post treatment or at follow-up were generally unrelated to psychiatric comorbidity (for comparisons with active and non-active psychological or pharmacotherapy treatments). 29 However, in cases of PTSD, there was a positive association between the presence of comorbidities and the treatment outcome: people with comorbidities did better. More specifically, there is emerging evidence that PTSD symptoms in patients with comorbid dissociation, depression, substance abuse and/or mild borderline personality disorder can be successfully and safely treated with existing evidence-based trauma-focused therapies, and their outcomes are comparable with those for patients without these comorbidities. 30 CBT is also possibly the most effective approach for PTSD symptoms when compared with multicomponent interventions that seek to first address additional social and psychological problems in refugees. 31
In addition, consistent with NICE guidance, trauma-focused therapies that target PTSD symptoms can have a positive impact on comorbidities. A review of 93 studies with 116 comparisons showed that there was a strong correlation between effect sizes for PTSD and depression outcomes, suggesting that psychological and pharmacological therapies are equally efficacious for PTSD and depressive symptoms. 32
Rationale and aims of this review
In summary, there is expert consensus that phase-based approaches effectively treat symptoms associated with CPTSD in adults, but the evidence on which this consensus is based is methodologically weak and exclusively based on studies that recruited participants with childhood abuse; findings might not translate to other populations with complex trauma histories. These consensus guidelines also did not review evidence about the effectiveness of pharmacological interventions in CPTSD. There is accumulating evidence that trauma-focused psychological therapies can reduce PTSD symptoms in people exposed to complex traumatic events who have psychiatric comorbidities. These treatments can also reduce comorbid illness in people with PTSD and can be used safely without a stabilisation phase. However, existing reviews of the use of trauma-focused therapies in people with complex trauma histories have focused on narrowly defined population subgroups and we still do not know how effective psychological therapies are across all populations with complex trauma. The comparative effectiveness of psychological interventions for mental health outcomes is also unknown for people with complex trauma histories in all settings. The acceptability of psychological interventions, either phased based or trauma focused, has been less well studied. There are also no comprehensive overviews of the effectiveness of pharmacological interventions in people who have been exposed to complex traumatic events. As such, a broad synthesis of evidence is needed to build on and extend the findings from previous reviews, but uncertainties and questions remain about which interventions warrant further evaluation. Furthermore, both pharmacological and psychological interventions should be included across a wide range of populations with a history of complex traumatic events.
Chapter 2 Methods of the effectiveness review and meta-analysis
Parts of this chapter are based on Coventry et al. 33 © 2020 Coventry et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Aims and objectives
The aim of this review was to provide a broad synthesis of evidence about the effectiveness of psychological and/or pharmacological interventions to treat mental health problems (with or without PTSD symptoms) in people exposed to complex traumatic events. In addition, where feasible, the review aimed to identify and synthesise qualitative and quantitative evidence about the acceptability and uptake of delivering mental health interventions for people with a history of complex traumatic events. Together, these syntheses aimed to offer estimates of the clinical effectiveness and acceptability of existing and novel treatments and to describe uncertainties about the strength of this evidence to inform a broader understanding about which interventions are likely to be candidates for testing in future definitive trials.
More specifically, the objectives of this review were as follows.
-
Descriptive synthesis: to provide an overview of existing RCTs and non-RCTs of psychological and/or pharmacological interventions for mental health problems in people with a history of complex traumatic events with specific reference to participant characteristics, intervention format and content, and the outcomes measured.
-
Clinical effectiveness: narratively and quantitatively, with a meta-analysis if feasible, to report on the clinical effectiveness of interventions delivered to adults aged 18 years and over with trauma and stressor disorders after exposure to complex traumatic events.
-
Comparative effectiveness: to provide evaluations of comparative clinical effectiveness of psychological interventions (e.g. phase-based vs. conventional trauma-focused therapies) and different pharmacological interventions using a network meta-analysis.
-
Acceptability and feasibility: to identify, appraise and synthesise narratively qualitative and quantitative data that address service user and provider perspectives about the acceptability and feasibility of using psychological and/or pharmacological interventions to treat mental health problems after complex traumatic events.
-
Research priorities: to identify candidate interventions that could feasibly be tested and used in the NHS and to make recommendations to the Health Technology Assessment programme about future research priorities.
Literature searches
Literature searches of the following databases were conducted:
-
Cumulative Index to Nursing and Allied Health Literature (CINAHL) via EBSCOhost (1937 onwards; search date: 20 April 2017).
-
Cochrane Central Register of Controlled Trials (CENTRAL) via The Cochrane Library (from inception; search date: 21 April 2017).
-
EMBASE via Ovid (1974 to 2017 Week 16; search date: 19 April 2017).
-
International Pharmaceutical Abstracts via ProQuest (1970 onwards; search date: 30 August 2017).
-
MEDLINE Epub Ahead of Print and In-Process & Other Non-Indexed Citations, Ovid MEDLINE Daily and Ovid MEDLINE via Ovid (1946 to present; search date: 18 April 2017).
-
Published International Literature On Traumatic Stress (PILOTS) via ProQuest (1987 onwards; search date: 2 May 2017).
-
PsycINFO via Ovid (1806 to April Week 2 2017; search date: 18 April 2017).
-
Science Citation Index via Web of Science (1900 onwards; search date: 20 April 2017).
The full search strategies used are available in Appendix 1.
Inclusion and exclusion criteria
Population
Neither DSM-IV nor ICD-10 distinguishes between PTSD and CPTSD. DSM-V does include a dissociative subtype, but it is unlikely that many studies have yet been conducted using this approach. ICD-11 criteria that will include CPTSD are not yet published and few studies will have used these criteria, making it difficult to identify studies using this diagnostic label. Our goal was therefore to identify studies based primarily on trauma history rather than diagnostic criteria.
We included adults > 18 years of age who had been exposed to complex interpersonal traumatic events, which were defined as follows:
. . . deliberate and premeditated event or series of events of an extreme and prolonged or repetitive nature that is experienced as extremely threatening or horrific and from which escape is difficult or impossible due to physical, psychological, maturational, family/environmental, or social constraints.
Cloitre et al. 10
This included (but was not limited to) adults exposed to childhood physical and/or sexual abuse, being a victim of or witnessing domestic violence, forcibly displaced persons (refugees, asylum seekers, internally displaced persons), torture survivors, those recruited into armed conflict as a child, those who had experienced ongoing armed conflict and combat, and those who had been relocated through human trafficking.
Studies were identified primarily based on trauma history rather than diagnostic criteria, and only those with adults > 18 years of age were included. The interpersonal trauma experience may have occurred at any age, but only studies of adults were included. Inclusion in the review was not restricted based on psychiatric comorbidities, with the exception of substance misuse disorders.
If studies included a mix of participants with complex interpersonal trauma history and single-event trauma history, studies were included if > 75% of participants had experienced complex interpersonal trauma (unless the data were presented separately).
Studies examining preventative therapies or interventions in populations not yet exhibiting psychological problems following complex traumatic events were excluded.
Interventions
Psychological interventions
Studies that evaluated any first- or second-line psychological therapy aimed at improving symptoms (including comorbidities) of trauma- and stressor-related disorders delivered either to individuals or in a group were included. Complementary and alternative therapeutic interventions were excluded from this review. As per the protocol registered with PROSPERO34 and in keeping with the classification used by NICE,20 the following interventions were considered:
-
trauma-focused CBT that included one or more of the following types of treatment techniques: exposure, cognitive therapy, stress management
-
eye movement desensitisation and reprocessing (EMDR)
-
other psychological treatments used to treat trauma survivors and victims but that predominantly use non-CBT techniques: supportive therapy and non-directive counselling, psychodynamic therapies including interpersonal psychotherapy (IPT), hypnotherapy, mindfulness and compassion-focused therapies, acceptance and commitment therapies, accelerated resolution, and sensorimotor therapies.
A more detailed study categorisation was undertaken to better describe the volume of evidence (see Subgroup analyses: categorising interventions).
Where possible, analyses of group trauma-focused CBT and group non-trauma-focused CBT were considered, as planned. The approach used is detailed in Meta-regression analyses: predictors of treatment effectiveness. The volume of evidence permitted further superordinate categorisation (see Subgroup analyses: categorising interventions).
Pharmacological interventions
All drug treatments subjected to experimental testing in the context of the treatment of mental health problems in people with a history of complex trauma were considered for inclusion. The following categories of pharmacotherapy were considered: selective serotonin reuptake inhibitors (SSRIs), antidepressants as a whole, antipsychotics, anticonvulsants and other medications typically used in the context of managing the symptoms of trauma and stressor disorders.
Comparators
Psychological interventions
Psychological interventions were compared with the following:
-
waitlist
-
treatment as usual (defined as non-experimental active treatments that conform to best and/or clinical guideline recommended care and that are ordinarily made available to patients)
-
no intervention
-
symptom monitoring
-
repeated assessment or other minimal attention control group akin to psychological placebo
-
alternative psychological treatment
-
pharmacological treatment.
Pharmacological interventions
Pharmacological interventions were compared with the following:
-
placebo
-
other medication
-
no intervention
-
psychological therapy.
Head-to-head comparisons
Comparisons of two or more active interventions were included. Differences in comparators were taken into account during data summary and analyses. Network meta-analyses were conducted to provide comparisons of all interventions within a connected network (including comparisons of active interventions not originally evaluated in the included trials).
Outcomes
The outcomes measured were core symptoms related to trauma- and stressor-related disorders and outcomes associated with psychological and psychiatric comorbidities even in the absence of PTSD. However, all outcomes reported within studies were extracted to gain a comprehensive overview of all commonly reported outcomes.
Primary outcomes
-
Reduction in severity of traumatic stress symptoms as measured using a validated and standardised clinician-rated scale.
-
Reduction in symptoms of difficulties with emotion regulation (e.g. Difficulties with Emotion Regulation Scale35) and interpersonal relationship problems (e.g. Inventory of Interpersonal Problems36).
Secondary outcomes
-
Severity of self-reported traumatic stress symptoms using a standardised measure (e.g. Modified PTSD Symptom Scale37).
-
Reduction in depressive and/or anxiety symptoms measured using validated clinician-rated instruments (e.g. Hamilton Depression Rating Scale38) or validated patient self-reported instruments (e.g. Hospital Anxiety and Depression Scale39).
-
Reduction in symptoms of panic disorder.
-
Reduction in symptoms of disassociation.
-
Reduction in symptoms of functional somatic syndromes.
-
Reduction in substance misuse.
-
Acceptability measured in terms of intervention uptake, adherence and withdrawal (dropouts).
-
Adverse events and harms from trial data (e.g. worsening of traumatic stress symptoms).
-
Suicidal ideation, attempts and completion.
-
Functioning, disability and quality of life measured by validated clinician-rated scales (e.g. Global Assessment of Functioning) or validated self-reported scales (e.g. Short Form questionnaire-36 items).
-
Study designs.
-
RCTs and cluster RCTs (where relevant).
Because CPTSD and complex trauma make up an emerging and relatively new diagnostic category, we proposed to also identify and include non-randomised controlled studies so as to capture data on emerging treatments and treatments tested in more pragmatic settings that might not have been tested in the context of a RCT. Studies undertaken in any country and setting (i.e. both low and middle-income countries and high-income countries) were included. Single-group before-and-after studies, uncontrolled observational studies, single-subject designs, case studies, opinion papers, descriptive studies and editorials were excluded.
Study selection
The selection criteria and process were independently checked by an advisory group (see Advisory group). Three researchers (Julie Jones-Diette, Hollie Melton and Holly Dale) independently screened titles and abstracts. The EndNote library was split evenly between those involved in screening, but, to ensure the distribution was not weighted to any particular year or author groups, each reviewer screened a cross-section of the library across dates and authors. To ensure that the inclusion criteria were consistently applied, a 10% sample of records was first double screened based on the title and abstract by pairs of researchers. Consensus meetings with the rest of the research team were held at regular intervals to resolve unclear decisions at the title and abstract screening phase. Full-text records were similarly screened with consensus meetings used to resolve disagreements.
Advisory group
We convened a study advisory group that comprised the principal investigator (Peter Coventry) and co-investigator (Rachel Churchill), along with content and clinical experts in trauma studies, PTSD and CPTSD. The advisory group provided independent advice about the strategic direction and scientific and policy relevance of the research undertaken by the INCiTE (INterventions for Complex Traumatic Events) review team. The broad aim of the advisory group was to ensure that the INCiTE study met its objectives and to maximise the impact and benefit of the review to end-users. The chairperson of the advisory group shared with the INCiTE team search terms and preliminary results associated with an update of a review of treatments for PTSD. Our search was shared with the advisory group and vetted for accuracy and credibility. Following the first advisory group meeting, the INCiTE team was advised to modify the inclusion criteria to include populations with a history of complex traumatic events who also had psychosis. In addition, feedback from the clinical content experts suggested that screening decisions should include combat trauma of all kinds because of the increased likelihood that veterans who present with PTSD may have encountered other traumatic events prior to military service and that it is the experience of multiple forms of trauma resulting in symptoms associated with CPTSD.
Data extraction
Data extraction was piloted on a small sample of studies by three researchers independently. Both RCTs and non-RCTs were extracted using the same template and were managed in separate Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) spreadsheets. After consensus checking, the included records were split between three reviewers to singly extract, owing to the volume of evidence. Uncertainties were resolved by consultation between reviewers tasked with data extraction or by deferring to the wider review team. Extracted data across domains related to study and participant characteristics and outcomes were compiled in a spreadsheet. When they were presented, intention-to-treat data were extracted instead of complete cases.
If an included study was published across multiple manuscripts, we used the primary publication as the main source of information. New and follow-up data were taken from subsequent publications but the unit of allocation remained the study rather than numbers of publications.
Risk of bias
Randomised controlled studies of clinical effectiveness
Studies were evenly distributed between researchers tasked with data extraction and each study was singly assessed for risk of bias. A subset of studies was used to pilot the Cochrane risk-of-bias tool. This tool assessed each study against domains known to be associated with bias in RCTs: selection, performance, detection, attrition, reporting and other biases (which were applied based on the specific context). Each study was assessed as being at ‘low’, ‘unclear’ or ‘high’ risk of bias across each of these domains. Attrition bias was used as an independent variable in the sensitivity analysis; this domain was checked by a further reviewer after all of the original appraisals had been made.
Selection bias was assessed by considering random sequence generation and allocation concealment; when these were not reported with sufficient detail, they were graded as at unclear risk. Performance bias considered the blinding of participants and personnel; when this was not possible owing to intervention type (e.g. comparing a psychological intervention with a waitlist), studies were graded as high risk. Detection bias was assessed by considering the blinding of outcomes assessors. The attrition bias domain took account of incomplete outcome data and how they were managed. When attrition was unequal, in high frequency or not appropriately managed by study authors, this was graded as high risk. Reporting bias was appraised by considering the risk of selective reporting. Generally, studies without a registered protocol were graded as being an unclear risk, while studies that favoured significant outcomes or obscured results were graded as high risk. Finally, other biases were assessed and descriptively reported if there were possible concerns not addressed by the existing domains of the tool.
Non-randomised controlled intervention studies
Non-randomised controlled intervention studies that were subject to the same piloting and agreement process as RCTs were included. Two reviewers piloted the Risk Of Bias In Non-randomized Studies – of Interventions (ROBINS-I),40 the Newcastle–Ottawa Scale41 and the NICE quality appraisal checklist. 42 After piloting these tools, the pragmatic decision was taken to use a modified version of the NICE quality appraisal checklist42 used in public health guidance. There were few non-randomised controlled studies but the resources needed to use the ROBINS-I tool would have outstripped capacity in the team and compromised the schedule allocated for extracting data from the large volume of included RCTs.
Reviewers singly appraised the quality of each included non-randomised controlled intervention study. The checklist was originally developed based on the ‘Graphical Appraisal Tool for Epidemiological studies’ (GATE) tool43 and includes domains of population bias, allocation, outcomes and analyses, as well as summary judgements for internal and external validity. Ten items were not directly relevant to the included studies, so were graded as ‘not applicable’ (items 2.3, 2.5, 3.2, 3.4, 3.5, 3.6, 4.3, 4.5 and 4.6). Each study was graded ‘++’ indicating minimal risk of bias, ‘+’ indicating potential sources of bias or ‘–’ indicating significant sources of bias. The additional grade ‘NR’ was used when studies did not report information and ‘NA’ was used when an item was not applicable to the given study design.
Data analysis
Meta-analyses of clinical effectiveness and attrition
Random-effects pairwise meta-analyses were conducted using Stata® 15 (StataCorp LP, College Station, TX, USA). We decided to use a frequentist approach for the pairwise meta-analyses, as this remains the standard approach in the literature.
Control conditions were grouped into two categories: controls (which included a waitlist or other controls with no or minimal therapeutic input) and active controls (including attention controls or treatment as usual with non-systematic psychological intervention input).
If multiple intervention groups were included in the study, we analysed the data in the following way:
-
If one of the groups did not meet criteria for our review, we did not combine across groups but used data from the group that met our review criteria.
-
If studies included two intervention groups that met criteria for the same intervention classification, we combined them together. For example, if a study included a prolonged exposure group and a cognitive processing therapy group, we combined them together into one group for the trauma-focused CBT analyses.
-
However, of course, if a study included a mindfulness arm and a trauma-focused CBT arm, we did not combine them but included them in their appropriate subgroups.
Most outcomes were continuous. If all studies used the same scale, we calculated mean differences and their 95% confidence interval (CI). If studies used different scales to measure a particular outcome, we calculated standardised mean differences (SMDs) and their 95% CI. In keeping with established cut-off points of effect in behavioural medicine, SMDs of 0.56 to 1.2 were categorised as large, effect sizes of 0.33 to 0.55 were categorised as moderate and effect sizes ≤ 0.32 were categorised as small. For dichotomous outcomes, such as attrition, we calculated odds ratios (ORs) and their 95% CI.
Heterogeneity assessment was based on visual inspection of forest plots and the I2 statistic. 44 A Q-value (approximating chi-squared distribution) of p < 0.1 indicated statistically significant heterogeneity. Statistical heterogeneity was explored using subgroup analyses, meta-regression and components network meta-analyses.
Subgroup analyses: categorising interventions
Given the substantial and inherent heterogeneity expected from our broad research questions, we conducted a range of subgroup analyses.
First, we conducted meta-analyses including all psychological interventions versus controls or active controls in all populations.
Second, we grouped these meta-analyses of all psychological interventions into the following populations based on descriptions in the study and through discussion with clinical experts: veterans, people who had experienced childhood sexual abuse, refugees, people who had experienced domestic violence and war-affected civilians.
Third, we grouped the data according to intervention categories commonly reported in the literature based on reporting from the original papers and discussion with clinical experts: trauma-focused CBT, EMDR therapy, non-trauma-focused CBT, mindfulness, dialectical behaviour therapy (DBT) and IPT. We assessed the effectiveness of these intervention categories in the same populations as described above: all psychological interventions, veterans, childhood sexual abuse, refugees, domestic violence and war.
Fourth, we further grouped the data into three superordinate intervention categories:
-
single-component trauma-focused interventions: any trauma-focused intervention that includes a single therapeutic approach (e.g. trauma-focused CBT, EMDR)
-
multicomponent trauma-focused interventions: any intervention that is primarily trauma-focused but also includes elements of other theoretical approaches, such as mindfulness, present-centred therapy or counselling [e.g. Skills Training in Affect and Interpersonal Regulation (STAIR)]
-
single-component non-trauma-focused interventions: any non-trauma-focused intervention including a single theoretical approach (e.g. non-trauma-focused CBT, mindfulness, IPT, present-centred therapy).
These intervention categories were then grouped according to the populations listed above (i.e. all psychological interventions, veterans, childhood sexual abuse, refugees, domestic violence and war).
Meta-regression analyses: predictors of treatment effectiveness
Mixed-effects meta-regression analyses were conducted using the ‘metareg’ package in Stata 15 to examine the impact of differences in population and intervention components on the effectiveness of psychological interventions (using SMD as the outcome measure) for reducing trauma outcomes in all populations (number of trials = 46). We used a frequentist approach to supplement and compare with the more complex Bayesian approach used for the components network meta-analyses.
The impact of the following populations was explored based on the same categories described above for the subgroup analyses: veterans, people who had experienced childhood sexual abuse, refugees, people who had experienced domestic violence and war-affected civilians.
Intervention components were identified on the basis of study descriptions in the published manuscripts, accessing treatment manuals where available, and in discussion with clinical experts with experience of delivering these types of interventions. The following intervention components were included, as long as they had sufficient data to be included as covariates in the meta-regression: support, psychoeducation, relaxation, cognitive restructuring, in vivo exposure, imaginal exposure, virtual reality exposure, mindfulness and phased based.
We also assessed the impact of the following methods of intervention delivery on effectiveness: individual versus group, face to face versus other and duration of intervention (< 12 weeks, 12 weeks, > 12 weeks).
Components network meta-analyses
We sought to further explore the impact of different combinations of intervention components using network meta-analyses. We used a Bayesian approach, as this allows greater flexibility in fitting more complex models and, therefore, a more thorough exploration of heterogeneity.
As with the meta-regression analyses above, we began by conducting the component network meta-analyses using SMDs that combined different trauma outcomes and all populations. However, there were difficulties with compiling the model. Given the greater complexity of the network meta-analysis models, we judged that it would be appropriate to simplify the analyses by focusing on mean differences for the Clinician-Administered PTSD Scale (CAPS; i.e. the most frequently reported trauma outcome reporting scale; number of trials = 16) in all populations for this outcome.
We fitted models using WinBUGS 1.4.3 (MRC Biostatistics Unit, Cambridge, UK) based on the components network meta-analyses approach proposed by Welton et al. 45 and an adaptation of the WinBUGS code reported in Freeman et al. 46 All models used a normal likelihood for continuous outcomes and vague priors for treatment effect and between-trial standard deviation. Convergence was assessed based on visual assessment of trace plots, the Brooks–Gelman–Rubin statistic and autocorrelation plots using three Markov chain Monte Carlo methods. All models were judged to have reached convergence after 50,000 iterations. These iterations were then discarded and all results were based on a further 50,000 iterations.
Goodness of fit to the observed data was assessed using total residual deviance and the deviance information criterion (DIC). Total residual deviance approximately equal to the number of data points was considered to indicate acceptable fit. 47 Greater than 5 points on the DIC was considered a substantial difference in goodness of fit between models. 48
We compared four models:
-
Model 1 included the intervention categories used in the pairwise meta-analyses (trauma-focused CBT, EMDR, non-trauma-focused CBT, mindfulness and IPT) compared with either control or active control.
-
Model 2 included all intervention components originally assessed in the meta-regression analyses discussed above (support, psychoeducation, relaxation, cognitive restructuring, in vivo exposure, imaginal exposure, virtual reality exposure, mindfulness and phased based). In addition to these, it was also assumed that all active treatments and attention controls included a placebo component. We also took into account the effect of the control group (waitlist vs. active control). Each component had a separate effect and assumed the total effect of the intervention was a sum of these separate effects.
-
Model 3 included all intervention components in model 2 plus all available pairs of components. Seven pairs of intervention components were reported in two or more included studies and were therefore included in the analyses: support + psychoeducation, psychoeducation + relaxation, psychoeducation + cognitive restructuring, psychoeducation + imaginal exposure, relaxation + mindfulness, relaxation + cognitive restructuring and relaxation + imaginal exposure. This model allowed for interactions between pairs of interventions above or below what would be expected from the sum of their components.
-
Model 4 included all possible combinations of intervention components.
Acceptability sensitivity analyses
For the attrition outcome, we were concerned that any differences between interventions and the control may be confounded by study design characteristics. Therefore, we conducted sensitivity analyses on attrition outcomes including only studies with a low risk of attrition bias and compared these findings with all included studies.
Chapter 3 Methods of the qualitative acceptability review
Objective
The aim of this element of the review was to identify, appraise and synthesise narratively qualitative data that addressed service user and provider perspectives about the acceptability and feasibility of using psychological and/or pharmacological interventions to treat mental health problems after complex traumatic events.
Literature searches
Literature searches of the following databases were conducted: CINAHL, EMBASE, MEDLINE and PsycINFO. The searches identified 4289 records, which were downloaded, imported into EndNote [Clarivate Analytics (formerly Thomson Reuters), Philadelphia, PA, USA] bibliographic software and de-duplicated to leave 1574 unique records. The full qualitative search strategy is available in Appendix 2.
Study selection
Qualitative research was defined as those studies that collected data using specific qualitative techniques such as unstructured interviews, semistructured interviews or focus groups, either as a stand-alone methodology or as a discrete part of a larger mixed-method study, and analysed qualitatively. Studies that collected data using qualitative methods but then analysed these data using quantitative methods were therefore excluded.
For qualitative evaluations, the inclusion criteria for population, intervention and comparisons were largely unchanged from those used to identify studies for the effectiveness syntheses. In addition, to ensure that we identified non-trial-based qualitative evaluations of acceptability of psychological and/or pharmacological interventions, we also included stand-alone studies not specifically linked to RCTs.
Population
As per the effectiveness review.
Interventions
As per the effectiveness review.
Comparators
As per the effectiveness review.
Outcomes
The outcomes were qualitative thematic and verbatim data related to service user and/or provider experiences of psychological and/or pharmacological interventions for mental health problems in the presence of complex trauma histories.
Data extraction
The findings and supporting quotations from the nine qualitative studies included were extracted into a standardised template designed for the purpose of the review. For each study, the key themes, as reported by the study authors, were first categorised according to whether they addressed issues related to the ‘acceptability’ or ‘feasibility’ of interventions. Themes were then further coded into three subcategories: (1) uptake and adherence, (2) service experience and (3) professional competencies/training. New thematic categories were created, where necessary, for any data that did not fit into the three main groupings.
Quality assessment
Following the lead established by the GRADE Working Group49 and the Cochrane Qualitative and Implementation Methods Group,50 we used the CERQual (certainty of the qualitative evidence) approach51 to assess both the methodological limitations of individual studies and the coherence of our review findings. CERQual assessment offers a framework to evaluate the certainty of evidence, addressing questions beyond the effectiveness of interventions, such as acceptability. Methodological limitations were assessed with the Critical Appraisal Skills Programme (CASP) checklist. 52 The elements of the CASP assessment, questions 1 to 9, were assessed and scored as either ‘yes’, ‘no’ or ‘cannot say’. When a question was assessed as meeting the criteria describing a suitable methodological rigour, the question was scored as ‘yes’; conversely, if the methodology did not meet the expected level of methodological rigour or the information was not apparent from the methods, the study was scores as ‘no’ or ‘cannot say’, respectively. A ‘yes’ received a numeric score of 1.0, a ‘no’ scored 0 and ‘cannot say’ scored 0.5. Therefore, the maximum score, namely if each of the nine questions was allocated a ‘yes’ for methodological rigour, would be 9.0.
The coherence of the review was assessed by identifying patterns across the data that were contributed to by each of the individual included studies, for example by combining findings across multiple settings or different subgroups. The certainty of the evidence in each individual study was rated as ‘no concerns’, ‘minimal concerns’, ‘moderate concerns’ or ‘significant concerns’ by considering the CASP assessment and ranked according to the methodological limitations and coherence of each finding.
Data analysis
A narrative synthesis approach was used to summarise the research findings of the studies included. This approach allows the creation of a description and map of findings from the studies included for interpretation, but also allows the identification of both common and emergent themes (a thematic analysis) within and between studies. This methodology provides a broader perspective on solutions and recommendations that are relevant to end-users.
Chapter 4 Results of the effectiveness review
Flow of the studies included
The searches identified 16,552 records, which were downloaded, imported into EndNote bibliographic software and de-duplicated to leave 10,212 unique records. In addition, 42 records were identified from International Pharmaceutical Abstracts. A total of 10,254 titles and/or abstracts were screened.
Approximately 10% of the titles and abstracts were pilot screened to achieve consistency and agreement between researchers. Full-text records were double screened at the following stage, and 328 were excluded for the reasons summarised in Figure 1.
FIGURE 1.
The PRISMA flow diagram indicating the flow of studies through the review process.
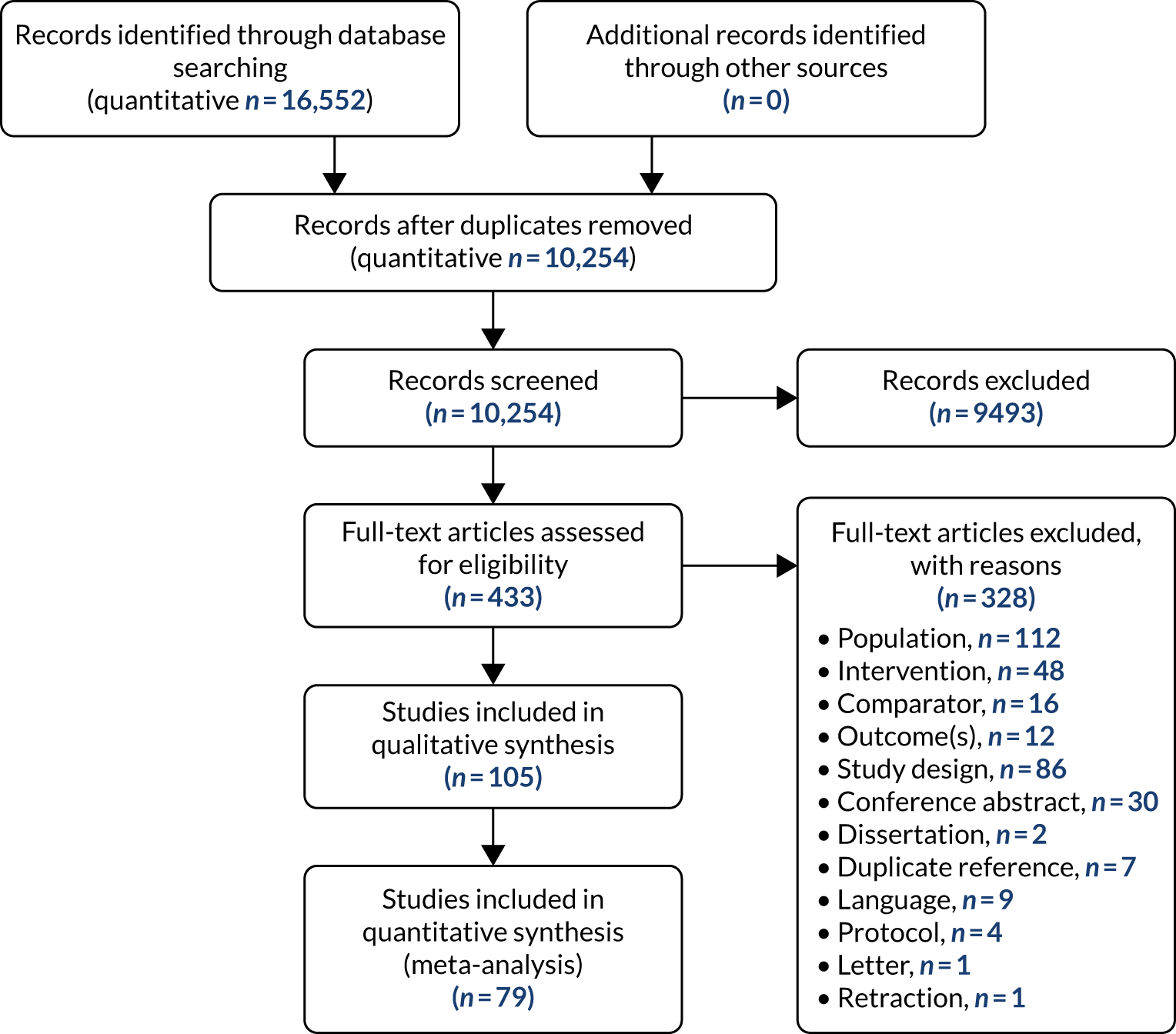
Studies included
Overall, we included 105 papers, comprising 96 reports53–147 of RCTs (95 unique trials) and nine non-randomised trials. 148–156 A table of the studies excluded, with rationale for their exclusion, can be found in Appendix 3.
Characteristics of the randomised controlled trials included
Of the RCTs, the vast majority of trials were conducted in the USA (n = 6258–60,64,66,68–76,78,79,81,82,84,85,87,89–91,93–95,97–102,104–107,109,110,112,115–117,120–133,135,137,140–142,146), followed by countries in Europe [Germany (n = 455,88,92,136), Denmark (n = 363,77,103,134), the Netherlands (n = 2138,139), Croatia (n = 180), Kosovo (n = 1143), Portugal (n = 183), Romania (n = 161) and Sweden (n = 1119)], countries in the Middle East [Iran (n = 456,57,111,118), Iraq/Iraqi Kurdistan (n = 362,144), Turkey/Syria (n = 353,54,65), Egypt (n = 1108) and Israel (n = 1147)] and countries in Africa [Uganda (n = 2113,114), Burundi (n = 1145) and the Democratic Republic of the Congo (n = 186)]. One study took place in South Korea67 and another took place remotely in Germany96 while its participants were located in Iraq. No studies were conducted in the UK. Appendix 3 details the comparisons in each study, as well as their characteristics.
In terms of the types of trauma that participants were exposed to, the vast majority of participants’ exposure related to their status as veterans (n = 47 studies56,58–60,64,65,67,71–74,78,80–85,88,91,94,95,97,99,102,104,105,107,110–112,115,118,120–124,126,128–130,135,137,140,142,147), followed by refugees (n = 1753–55,63,87,89,90,108,113,114,116,119,133,134,136,138,139), those who experienced childhood sexual abuse (n = 1466,68–70,75–77,92,98,103,106,117,127,131,132,146), those who experienced war-related trauma (n = 1057,61,62,86,96,109,143–145), those who experienced mixed trauma (n = 379,93,141) and those who experienced domestic violence (n = 3100,101,125).
Of the 95 trials included, all trial arms with active interventions were categorised for analysis. For psychological interventions this included trauma-focused CBT (n = 4155,60–63,66,71,79,81,83,84,86,87,89,90,92–94,96,100,101,105–107,109,113,114,117,119,124,126,128,136,140,143,144), EMDR (n = 1153,54,64,74,76,88,91,130,138,139), mindfulness (n = 757,95,115,120,121,142), non-trauma-focused CBT (n = 662,78,131,132,137), DBT (n = 469,70), other psychotherapy (n = 1293,103,106,114,120,124,125,128,145,146), exposure only (n = 360,119,130) and IPT (n = 2,98,108 n = 2 for each non-trauma-focused non-CBT64,111 and stabilisation,138,139 and n = 1 for both biofeedback102 and other psychological interventions). 142 Classen et al. 68 conducted a trial in two interventions (trauma-focused therapy and psychotherapy) but presented combined results, so these were not included in the categorisation. The pharmacological interventions compared in the studies included were categorised as antidepressant (n = 15,59,65,67,73,82,112,116,118,133,141,147 of which 10 were SSRIs65,67,82,112,116,118,133,141,147), antipsychotic (n = 658,85,99,110,127,135) and anticonvulsant (n = 272,104), as well as prazosin (n = 384,122,123) and rivastigmine (n = 156). There were also a number of combined treatments: antidepressant and trauma-focused CBT (n = 6,63,97,116,134 of which there were three SSRI and trauma-focused CBT interventions63,116,134), SSRI and other psychotherapy (n = 263,80), antidepressant and other psychotherapy (n = 180), benzodiazepine and trauma-focused CBT (n = 1129) and d-cycloserine and trauma-focused CBT (n = 1129).
Psychological interventions were then grouped into superordinate classifications (as described in the methods), which were single-component trauma-focused (n = 4153–55,60–62,64,74,76,79,81,83,86,87,89–91,93,94,96,106,107,109,113,114,117,119,124,126,128,136,138,139,144,145), single-component non-trauma-focused (n = 2757,62,64,78,95,98,106,108,111,114,115,120,121,124,125,128,131,132,137–139,142,146), multicomponent trauma-focused (n = 1760,66,69–71,84,88,92,100,101,105,130,140,143–145) and multicomponent non-trauma-focused (n = 470,93,103).
Characteristics of the non-randomised controlled trials included
A total of nine non-RCTs were included in the review; eight compared psychological interventions with a control group148–153,155,156 and one compared a pharmacological intervention with placebo154 (see Appendix 6). Studies were conducted in a range of regions [Canada (n = 2152,156), Croatia (n = 1154), Germany (n = 1149), Iran (n = 1153), Israel (n = 1150), Palestine (n = 1155), Sweden (n = 1151) and the USA (n = 1148)], presenting a diverse selection of health-care systems that may differ from that in the UK. Studies were published between 1999152,153,156 and 2016,150 with one-third being published in 1999.
The population subgroups included in the non-RCTs were veterans (n = 3148,150,154), childhood sexual abuse (n = 3151,152,156), war affected (n = 2153,155) and refugees (n = 1149). When reported, the mean age of participants ranged from 30 to 60 years old. Across studies, there was largely equal representation of majority female149,151,152,156 and majority male populations. 150,154,155 Further detail about the characteristics of populations of the studies included can be found in Appendix 7.
The majority of studies were compared with an inactive control (no intervention, waitlist or placebo), with the exception of two direct comparison studies,150,154 and effect sizes were not calculated for these. Another study included treatment as usual, which was considered to be an alternative active psychological intervention and so was narratively synthesised as a direct comparison. 148 Intervention details are outlined in Appendix 4.
Quality of the studies included
Randomised controlled trials
The quality of the RCTs included was assessed using the Cochrane Collaboration’s risk-of-bias tool, as described in Chapter 2, Randomised controlled studies of clinical effectiveness. The grading of each study across six domains can be found in Appendix 8.
Overall, reporting was quite variable, with a large proportion of responses being graded as ‘unclear’. Five of the six domains were largely assessed as being at an unclear or high risk of bias. This indicated that studies reported insufficient detail to make a clear decision about the risk of bias across these domains or, in most cases, that the study designs did not appropriately account for sources of bias. The exception to this was the domain of ‘other bias’, which was graded as a low risk of bias for over 80% of studies.
A small proportion of trials were rated as being at a high risk of selection bias. The majority of studies were unclear in reporting on selection bias (Figure 2). However, less than 20% were considered as at a low risk of bias based on allocation concealment and less than 50% were at a low risk based on random sequence generation.
FIGURE 2.
Proportional distribution of the risk-of-bias grades across the RCTs included per domain of bias.
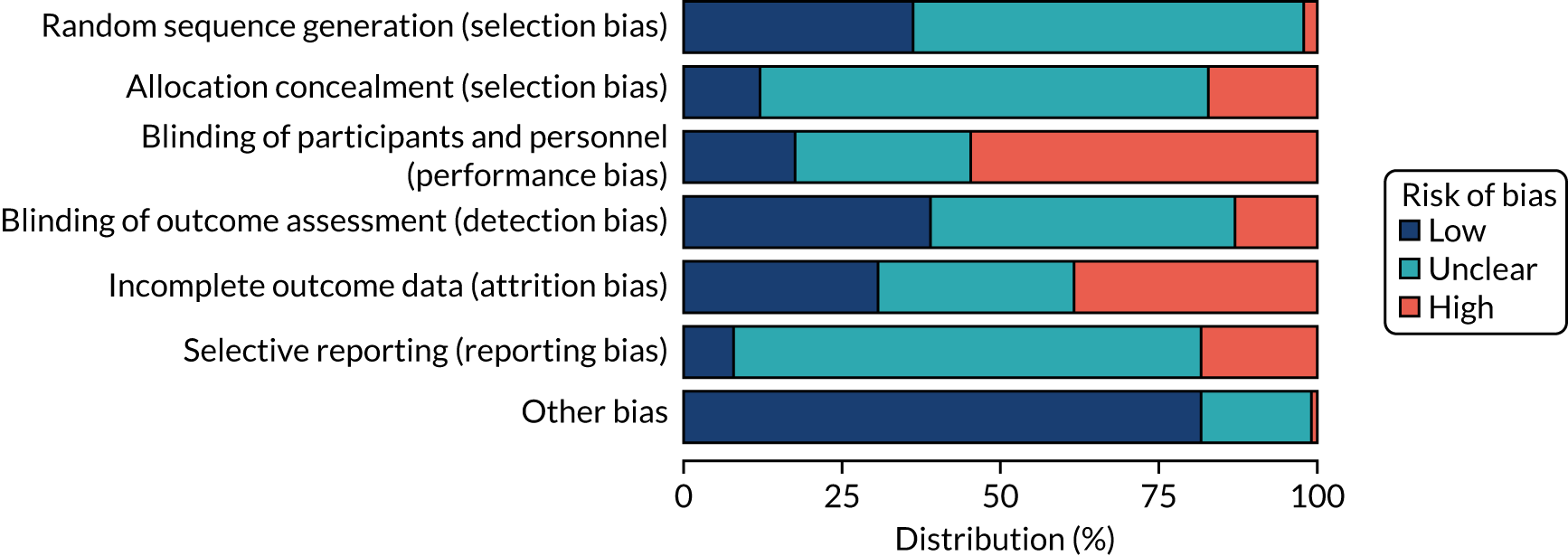
Over half of the trials were rated as being at high risk of performance bias because the blinding of participants and personnel was inadequate or infeasible. The latter was especially true in the case of most psychological interventions, in which the nature of the allocated intervention could not easily be disguised.
Detection bias was generally considered as low risk or unclear for the majority of trials, with a slightly larger proportion being rated as unclear than low risk. This was indicative of the outcome assessment being blinded effectively or reported unclearly. Approximately 10% of studies were considered as being at high risk of detection bias.
In terms of attrition bias, gradings of low risk, high risk or unclear bias were almost equally prevalent across studies. This suggested that the majority of studies experienced high dropout and did not handle it appropriately or did not report sufficiently on the number of participants and withdrawals.
Selective reporting was assessed via the reporting bias domain, for which a large majority of studies were graded as being unclear, typically owing to a lack of preregistration (see Figure 2). Close to 10% were considered as low risk in this domain of bias, and nearly 20% were considered as high risk.
Finally, there was generally a low risk of bias from other sources across the large majority of studies. The remainder of studies were graded as having an unclear risk of bias from sources not covered within the other domains. Just one study was graded as high risk from other sources of bias. 100
Non-randomised controlled trials
The quality of the nine non-randomised trials included was assessed using the NICE (2012)42 tool as described in Chapter 2, Methods, Non-randomised controlled intervention studies; the grading is presented in Table 1. Overall, methods were reported adequately to make summary judgements on studies. Notable exceptions were the availability of information to grade contamination (domain 2.6; present in only three studies148,152,156) and information regarding the similarity of other interventions across study arms (domain 2.7; clearly reported in four studies148,149,151,156).
| Authors (year) | Population bias | Allocation | Outcomes | Analyses | Summary | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1.1: Is the source population or source area well described? | 1.2: Is the eligible population or area representative of the source population or area? | 1.3: Do the selected participants or areas represent the eligible population or area? | 2.1: Allocation to intervention (or comparison). How was selection bias minimised? | 2.2: Were interventions (and comparisons) well described and appropriate? | 2.4: Were participants or investigators blind to exposure and comparison? | 2.6: Was contamination acceptably low? | 2.7: Were other interventions similar in both groups? | 2.8: Were all participants accounted for at study conclusion? | 2.10: Did the intervention or control comparison reflect usual UK practice? | 3.1: Were outcome measures reliable? | 3.3: Were all important outcomes assessed? | 4.1: Were exposure and comparison groups similar at baseline? If not, were these adjusted? | 4.2: Was intention-to-treat analysis conducted? | 4.4: Were the estimates of effect size given or calculable? | 5.1: Are the study results internally valid (i.e. unbiased)? | 5.2: Are the findings generalisable to the source population (i.e. externally valid)? | |
| King et al. (2013)148 | ++ | ++ | + | + | ++ | – | ++ | ++ | ++ | NA | + | + | ++ | + | ++ | + | + |
| Levi et al. (2016)150 | ++ | ++ | + | – | ++ | – | NR | NR | + | NA | + | + | ++ | + | ++ | – | + |
| Morgan and Cummings (1999)152 | + | + | + | + | – | ++ | NR | ++ | NA | + | – | + | + | + | + | + | |
| Saxe and Johnson (1999)156 | + | + | ++ | + | + | – | ++ | – | + | NA | + | – | ++ | – | ++ | – | + |
| Pivac et al. (2004)154 | + | + | NR | NR | + | – | NR | NR | NR | NA | + | + | + | NR | – | NR | + |
| Lundqvist et al. (2006)151 | + | + | + | – | – | – | NR | – | + | NA | + | – | + | – | + | – | + |
| Salo et al. (2008)155 | ++ | + | ++ | – | + | NR | NR | NR | – | ++ | ++ | ++ | – | – | ++ | + | ++ |
| Narimani et al. (2008)153 | – | + | ++ | + | ++ | NR | NR | NR | – | ++ | + | + | NR | NR | – | + | – |
| Kruse et al. (2009)149 | ++ | + | ++ | + | ++ | NR | NR | + | – | ++ | ++ | + | ++ | – | ++ | + | ++ |
Generally, population bias domains were well reported, with minimal or some potential sources of bias.
Allocation bias domains presented the largest subset of quality assessment and were also the most poorly reported. Investigator blinding (domain 2.4) was the highest risk domain, with a high risk of bias across all studies that reported sufficient detail to make a judgement. 148,150–152,154,156
Outcome domains were also well reported, with most studies attaining a ‘+’ grading indicating some potential sources of bias, but not high risk.
Domains regarding analyses were mostly well reported, with baseline similarities between study arms (domain 4.1) and estimates of effect being given or calculable (domain 4.4), mostly showing low or some sources of bias.
Finally, summary grades of the overall risk of bias were mostly indicative of designs attempting to address sources of bias, with some potential risks. External validity showed minimal risk of bias; just one study was graded as high risk. 153 By contrast, internal validity was not considered low risk in any study; three trials were judged to be high risk150,151,156 and one did not report sufficient detail. 154
Meta-analyses of clinical effectiveness
Of the 104 RCTs and non-RCTs included in the systematic review, 79 included effectiveness data that could be meta-analysed. 53–56,58,59,62,64–67,69,71–74,76,78,79,81,82,84–92,94–96,98–101,104–113,115,118,121–123,125–127,131,132,135,137–140,142–147 All of these studies were RCTs. We conducted a series of meta-analyses to investigate the effectiveness of psychological and pharmacological interventions on the primary outcome and, when the data permitted, a number of secondary outcomes. In summary, the comparisons that were meta-analysed were:
-
psychological interventions versus control for all populations combined
-
psychological interventions versus control in veteran populations
-
psychological interventions versus control in war-affected populations
-
psychological interventions versus control in childhood sexual abuse populations
-
psychological interventions versus control in refugee populations
-
psychological interventions versus control in domestic violence populations
-
pharmacological interventions versus placebo in veteran and childhood sexual abuse populations.
When the data permitted, the following outcomes were meta-analysed:
-
PTSD symptoms
-
CPTSD symptoms
-
emotional dysregulation
-
interpersonal problems
-
negative self-concept
-
-
depression symptoms
-
anxiety symptoms
-
quality of life
-
sleep quality.
All populations and trauma exposure combined
Post-traumatic stress disorder total symptoms
A summary of meta-analyses of the effectiveness of psychological interventions across all populations for PTSD symptoms is shown in Appendix 9, Table 34. Overall, when all eligible trials were combined (39 trials, n = 2506)53–55,62,66,69,74,76,78,81,86,88,89,91,92,94–96,98,100,101,106–109,121,126,131,132,140,142–146,157–159 across all populations, psychological interventions were associated with a large and significant post-treatment effect in favour of a reduction in PTSD total symptoms (Figure 3).
FIGURE 3.
Meta-analysis of post-treatment effect size (ES) for PTSD total symptoms, comparing all psychological interventions with control. CETA, common elements treatment approach; CPT, cognitive processing therapy.
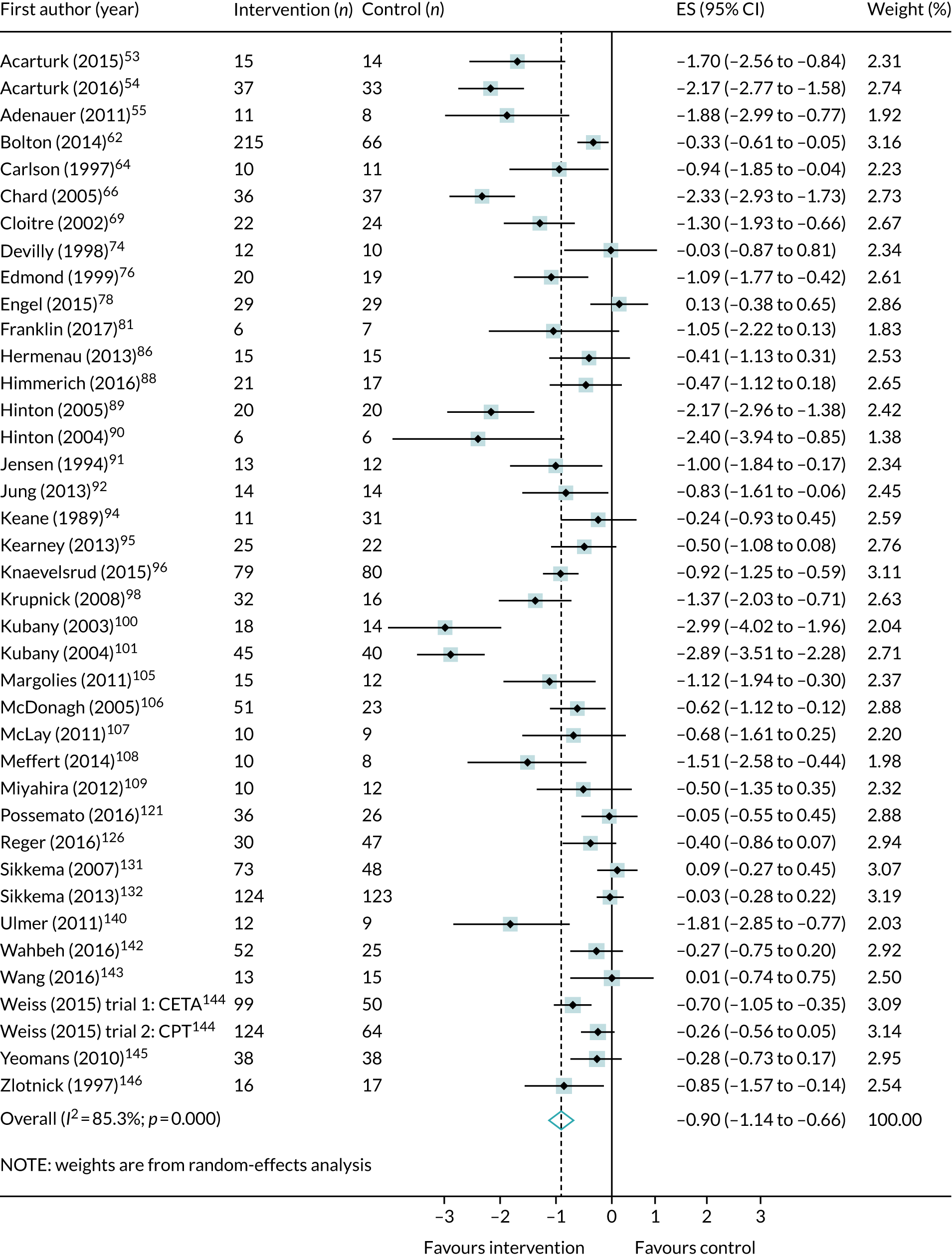
Of the six trials (n = 259)71,84,87,113,137–139,160 that compared psychological interventions with an active control, the post-treatment effect size was smaller and in favour of a reduction in total PTSD symptoms, but not significantly (SMD –0.35, 95% CI –0.72 to 0.03; I2 = 47.0%). Ten trials (n = 738)78,81,92,95,98,121,132 measured outcomes after < 6 months and showed that psychological interventions were associated with a medium and significant effect in favour of a reduction in PTSD total symptoms (SMD –0.38, 95% CI –0.68 to –0.08; I2 = 79.4%).
When treatment effects were meta-analysed by intervention type, we showed that IPT was associated with the largest post-treatment effect on total PTSD symptoms (SMD –1.41, 95% CI –1.97 to –0.85; I2 = 0%). This result is based on two small studies (n = 66)98,108 and associated with a high degree of uncertainty, as indicated by the wide CIs for the individual and combined point estimates (see Appendix 10, Figure 27).
There was strong evidence from 21 trials (n = 1283)55,62,66,81,86,92,94–96,100,101,106,107,109,126,140,143,144,158,159 that trauma-focused CBT is effective for reducing PTSD total symptoms (see Appendix 10, Figure 28). Four trials (n = 206)81,87,92,113 that tested trauma-focused CBT measured outcomes at follow-up after < 6 months and were associated with a large and significant treatment effect (SMD –0.64, 95% CI –1.10 to –0.18; I2 = 44.9%). However, we did not find evidence of the effectiveness of trauma-focused CBT versus active controls.
Evidence from seven trials (n = 244)53,54,74,76,88,91,157 showed that EMDR was similarly effective at reducing PTSD symptoms post treatment (see Appendix 10, Figure 29). Two trials (n = 71)138,139 compared EMDR with an active control. Post-treatment effects were in favour of a small reduction in PTSD total symptoms, but this result was non-significant (SMD –0.15, 95% CI –0.62 to 0.32; I2 = 0%).
Mindfulness (three trials, n = 183)95,121,142 was associated with a small non-significant effect in favour of symptom reduction when compared with control post treatment (see Appendix 10, Figure 30). In two trials95,121 that measured outcomes at follow-up after < 6 months, mindfulness was not effective for PTSD symptoms (SMD –0.08, 95% CI –1.56 to –0.32; I2 = 59%).
Non-trauma-focused CBT (three trials, n = 548)62,78,131,132 was associated with small non-significant effects in favour of symptom reduction when compared with control post treatment (see Appendix 10, Figure 31). Treatment effects were also non-significant for non-trauma-focused CBT for PTSD outcomes in two trials78,132 that measured outcomes after < 6 months (SMD –0.02, 95% CI –0.25 to 0.20; I2 = 0%).
When interventions from 22 trials (n = 1191)53–55,62,66,74,76,81,86,89,91,92,94,96,100,101,106,107,109,126,144,157,158 were grouped using composite intervention categories, we showed that single-component and trauma-focused interventions based on a single theoretical approach were associated with a large and significant treatment effect in favour of a reduction in PTSD symptoms (see Appendix 10, Figure 32). A large effect was also observed in a meta-analysis of five trials (n = 276)54,78,81,95,98,132 that measured outcomes at follow-up after < 6 months (SMD –0.94, 95% CI –1.56 to –0.32; I2 = 77.6%).
Seven trials (n = 440)69,88,140,143–145,159 delivered multicomponent and trauma-focused interventions (DBT, EMDR, trauma-focused CBT and other psychotherapeutic approaches) and were associated with a large and significant effect in favour of a reduction in PTSD symptoms (see Appendix 10, Figure 32).
There was evidence (11 trials, n = 936)62,78,95,98,106,108,121,131,132,142,146 that single-component non-trauma-focused interventions (CBT, mindfulness, counselling, IPT and other psychotherapeutic approaches) were associated with a significant and moderate treatment effect in favour of a reduction in PTSD symptoms post treatment (see Appendix 10, Figure 34). In five trials (n = 462)78,95,98,121,132 that measured outcomes after < 6 months, the treatment effect for single-component non-trauma-focused interventions was small and non-significant (SMD –0.05, 95% CI –0.23 to 0.14; I2 = 0%). When compared with an active control (two trials, n = 62),137,160 single-component non-trauma-focused interventions were associated with a non-significant large treatment effect in favour of a reduction in PTSD symptoms (SMD –0.64, 95% CI –1.82 to 0.53; I2 = 76.9%).
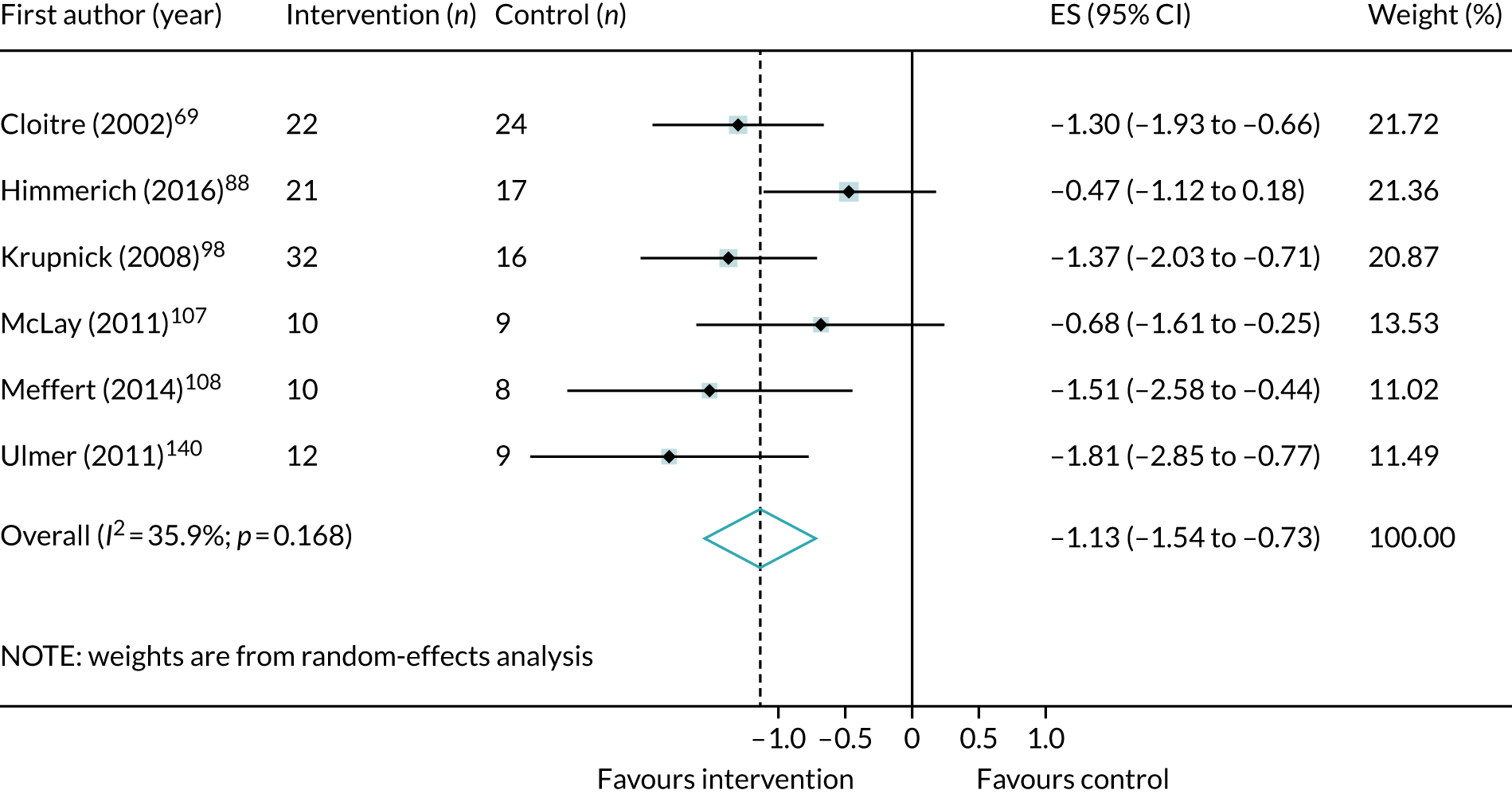
Figure 4 shows the results of a meta-analysis that compared phase-based psychological interventions with control. Only six studies (n = 190)69,88,98,107,108,140 were coded as phased based for PTSD outcomes. The results show that a variety of trauma- and non-trauma-focused interventions (DBT, EMDR, IPT and trauma-focused CBT) are associated with a large and significant improvement in PTSD symptoms when delivered as part of a phase-based approach with a stabilisation component.
FIGURE 4.
Meta-analysis of post-treatment effect size (ES) for PTSD total symptoms, comparing phase-based psychological interventions with control.
Complex post-traumatic stress disorder symptoms
A summary of meta-analyses of the clinical effectiveness of psychological interventions across all populations for CPTSD symptoms is shown in Appendix 9, Table 35.
Emotional dysregulation
Seven studies (n = 289)69,79,86,98,106,108,142 included data about symptoms of emotional dysregulation that could be meta-analysed across populations and trauma exposure. Figure 5 shows the results of a meta-analysis that compared all psychological interventions with control as regards a reduction in symptoms of emotional dysregulation at the end of treatment. The results favoured the interventions but did not reach statistical significance.
FIGURE 5.
Meta-analysis of post-treatment SMD for emotional dysregulation, comparing all psychological interventions with control.
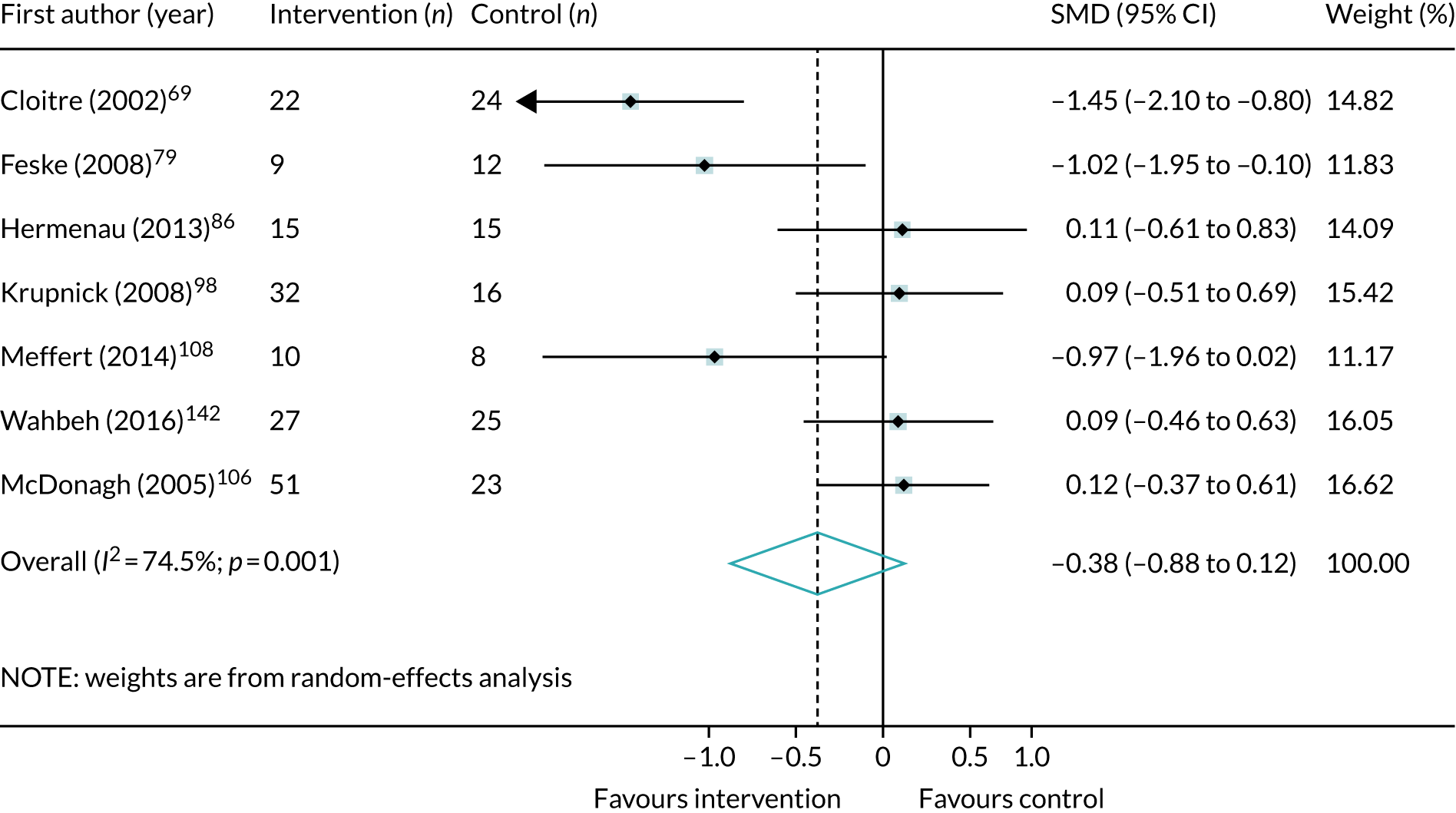
Of these seven trials, three compared trauma-focused CBT with control. 79,86,106 At the end of treatment, trauma-focused CBT was associated with a small effect in favour of a reduction in symptoms of emotional dysregulation, but this result did not reach statistical significance (see Appendix 10, Figure 35). Two small studies (n = 51)79 that compared trauma-focused CBT with control measured outcomes after < 6 months and were associated with a medium but non-significant treatment effect (SMD –0.42, 95% CI –1.53 to 0.69; I2 = 72.3%).
Four studies (n = 163)98,106,108,142 compared single-component and non-trauma-focused interventions with control. At the end of treatment, the meta-analysis showed that single-component and non-trauma interventions were not significantly associated with a reduction in symptoms of emotional dysregulation (see Appendix 10, Figure 36).
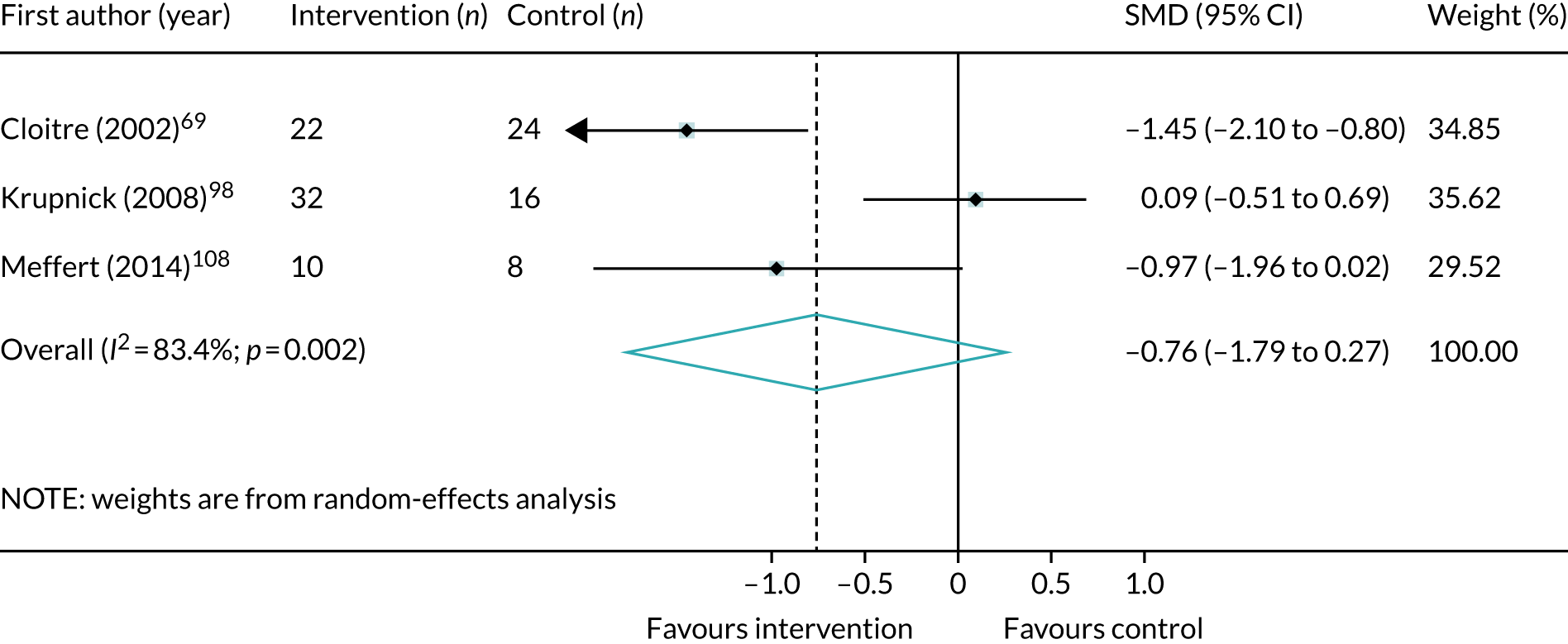
The largest treatment effect for emotional dysregulation was associated with three studies (n = 112)69,98,108 that tested interventions that can be characterised as phased based. However, while the large treatment effect favoured a reduction in symptoms of emotional dysregulation, it was statistically non-significant (Figure 6).
FIGURE 6.
Meta-analysis of post-treatment SMD for emotional dysregulation, comparing phase-based psychological interventions with control.
Negative self-concept
Five studies (n = 215)92,100,101,125,142 included data about symptoms of negative self-concept that could be meta-analysed. Figure 7 shows the results of a meta-analysis that compared all psychological interventions with control as regards a reduction in symptoms of negative self-concept at the end of treatment. When combined, psychological interventions were associated with a large treatment effect in favour of a reduction in symptoms of negative self-concept, albeit with a high degree of uncertainty and heterogeneity.
FIGURE 7.
Meta-analysis of post-treatment SMD for negative self-concept, comparing all psychological interventions with control (positive SMD equals improvement in symptoms).
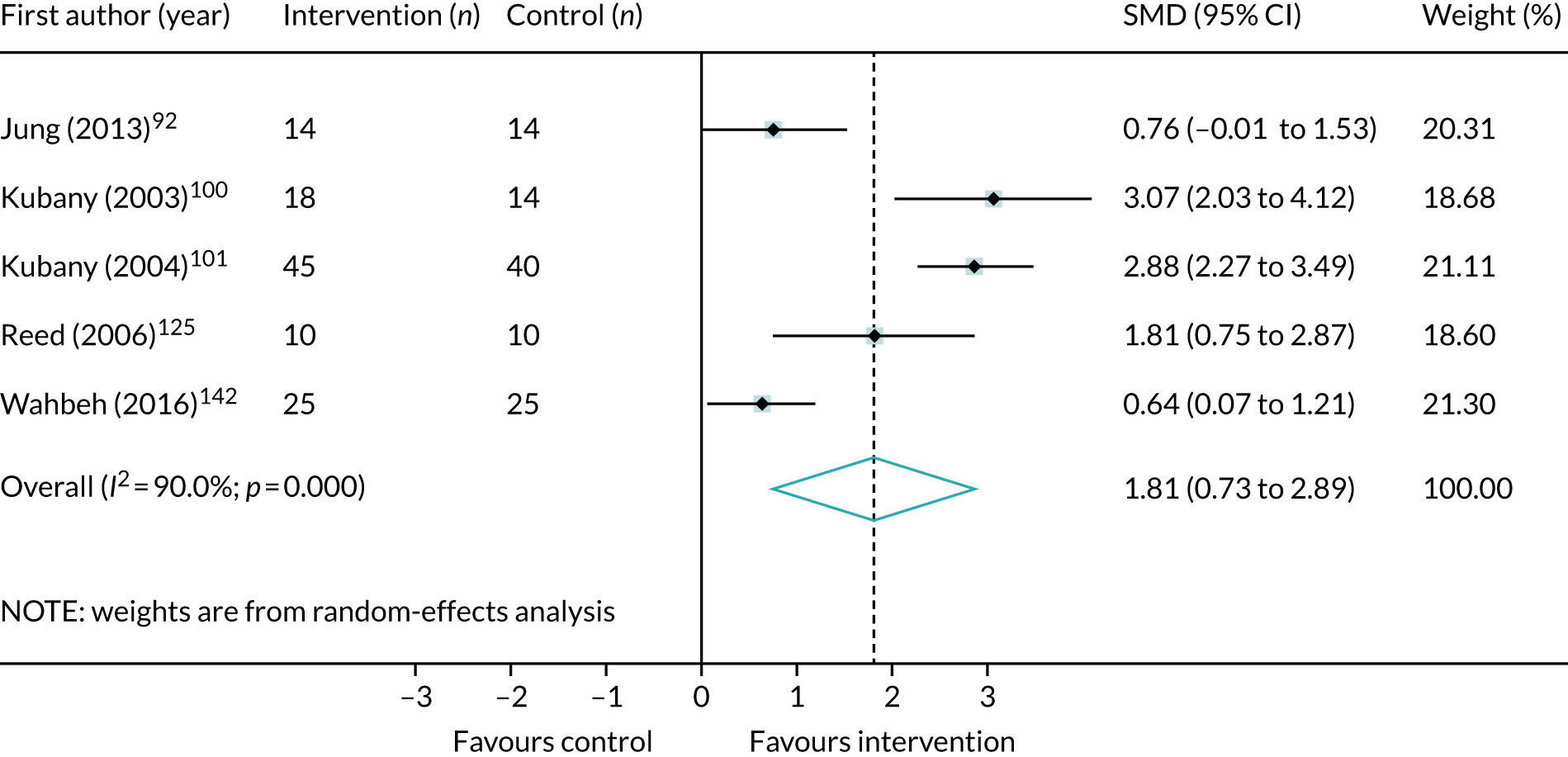
Figure 37 (see Appendix 10) shows that, when only the trauma-focused CBT studies were meta-analysed (three trials, n = 145),92,100,101 the effect size was very large and significant but with high degree of uncertainty about the combined point estimate and high levels of heterogeneity (SMD 2.22, 95% CI 0.75 to 3.70; I2 = 90.4%).
A more homogeneous and significantly large treatment effect was associated with the two studies (n = 117)100,101 that were characterised as comparing multicomponent and trauma-focused interventions with control (SMD 2.93, 95% 2.40 to 3.45; I2 = 0%; see Appendix 10, Figure 38).
Single-component non-trauma-focused interventions (two studies; n = 70)125,142 were also associated with large and significant effects in favour of improvement in negative self-concept, but the overall point estimate had a high degree of uncertainty (SMD 1.14, 95% CI 0.01 to 2.27; I2 = 72.6%; see Appendix 10, Figure 39).
Interpersonal problems
Only two studies (n = 94),69,98 both testing phase-based interventions, were identified that included outcome data for interpersonal problems that could be meta-analysed. The overall treatment effect was large and in favour of a reduction in symptoms associated with interpersonal problems, but did not reach significance (SMD –0.59, 95% CI –1.28 to 0.11; I2 = 61.9%; see Appendix 10, Figure 40).
Depression symptoms
A summary of meta-analyses of the clinical effectiveness of psychological interventions across all populations for depression symptoms is shown in Appendix 9, Table 36. Figure 8 shows the results of the meta-analysis of the 31 studies (n = 1866)53–55,62,69,74,76,81,92,95,96,98,100,101,106,108,109,111,121,125,137,140,142,144,157–159 that compared all psychological interventions with control post treatment for depression symptoms. The results show that interventions were associated with a large effect in favour of a reduction in depression symptoms. When all psychological interventions were compared with control at follow-up after < 6 months, there was a medium and still significant effect in favour of a reduction in depression symptoms (SMD –0.51, 95% CI –0.80 to –0.22; I2 = 48%; nine trials, n = 410). 54,78,81,87,92,95,98,111,121
FIGURE 8.
Meta-analysis of post-treatment effect size (ES) for depression symptoms, comparing all psychological interventions with control. CETA, common elements treatment approach; CPT, cognitive treatment therapy.

When interventions were meta-analysed by type, studies that tested trauma-focused CBT were the most numerous. Fifteen studies (n = 1115)62,81,92,96,100,101,106,109,126,140,143,144,159 compared trauma-focused CBT with control post treatment. Figure 41 (see Appendix 10) shows that trauma-focused CBT was associated with a large and significant effect in favour of a reduction in depression symptoms. There was also a positive effect in the three studies (n = 104)81,87,92 that compared post-treatment outcomes at follow-up after < 6 months, although the point estimate was associated with considerable uncertainty (SMD –0.72, 95% CI –1.43 to –0.01; I2 = 56.6%).
Large and significant treatment effects in favour of a reduction of depression symptoms were also similarly observed in a meta-analysis (five trials, n = 182)53,54,74,76,157 that compared EMDR with control post treatment (see Appendix 10, Figure 42). In the two studies (n = 72)138,139 that compared EMDR with an active control, at the end of treatment the effect on depression symptoms favoured the intervention, but did not reach significance (SMD –0.32, 95% CI –1.23 to 0.59; I2 = 47.8%).
There was also some evidence from two small studies (n = 66)98,108 that IPT compared with control was effective at reducing symptoms of depression (see Appendix 10, Figure 43).
Three studies (n = 186),95,121,142 all of which included veteran populations, compared mindfulness with control post treatment. Mindfulness interventions were associated with a medium effect size in favour of a reduction in depression symptoms (see Appendix 10, Figure 44). In the two studies95,121 that measured outcomes at follow-up after < 6 months, mindfulness was also associated with a medium and significant treatment effect (SMD –0.41, 95% CI –0.79 to –0.02; I2 = 0%).
Non-trauma-focused interventions78,137 were not effective in reducing depression symptoms (see Appendix 10, Figure 45).
Using composite intervention categories, we showed that single-component and trauma-focused interventions (17 studies; n = 1034)53–55,62,74,76,81,92,96,100,101,106,109,126,144,157,158 based on a single theoretical approach were associated with a large and significant treatment effect in favour of a reduction in depression symptoms (see Appendix 10, Figure 46). A large and significant effect was also observed in the four studies (n = 174)53,81,87,92 that compared outcomes at follow-up after < 6 months (SMD –0.85, 95% –1.42 to –0.29; I2 = 62.5%).
Six studies (n = 340)69,140,143,144,159 compared multicomponent and trauma-focused interventions with control and were associated with a similarly large and significant effect in favour of a reduction in depression symptoms (see Appendix 10, Figure 47).
A smaller but still significant and favourable treatment effect was observed in the 10 studies (n = 594)62,78,95,98,106,108,111,121,137,142 that compared single-component and non-trauma-focused interventions with control post treatment (see Appendix 10, Figure 48). There was a small and non-significant effect in the five studies (n = 236)78,95,98,111,121 that measured outcomes at follow-up after < 6 months (SMD –0.30, 95% –0.56 to 0.04; I2 = 0%).
Figure 9 shows that, post treatment, compared with control, phase-based interventions were associated with a large and significant treatment effect in favour of a reduction in depression symptoms, although this result is based on just four small studies. 69,98,108,140
FIGURE 9.
Meta-analysis of post-treatment effect size (ES) for depression symptoms, comparing phase-based interventions with control.
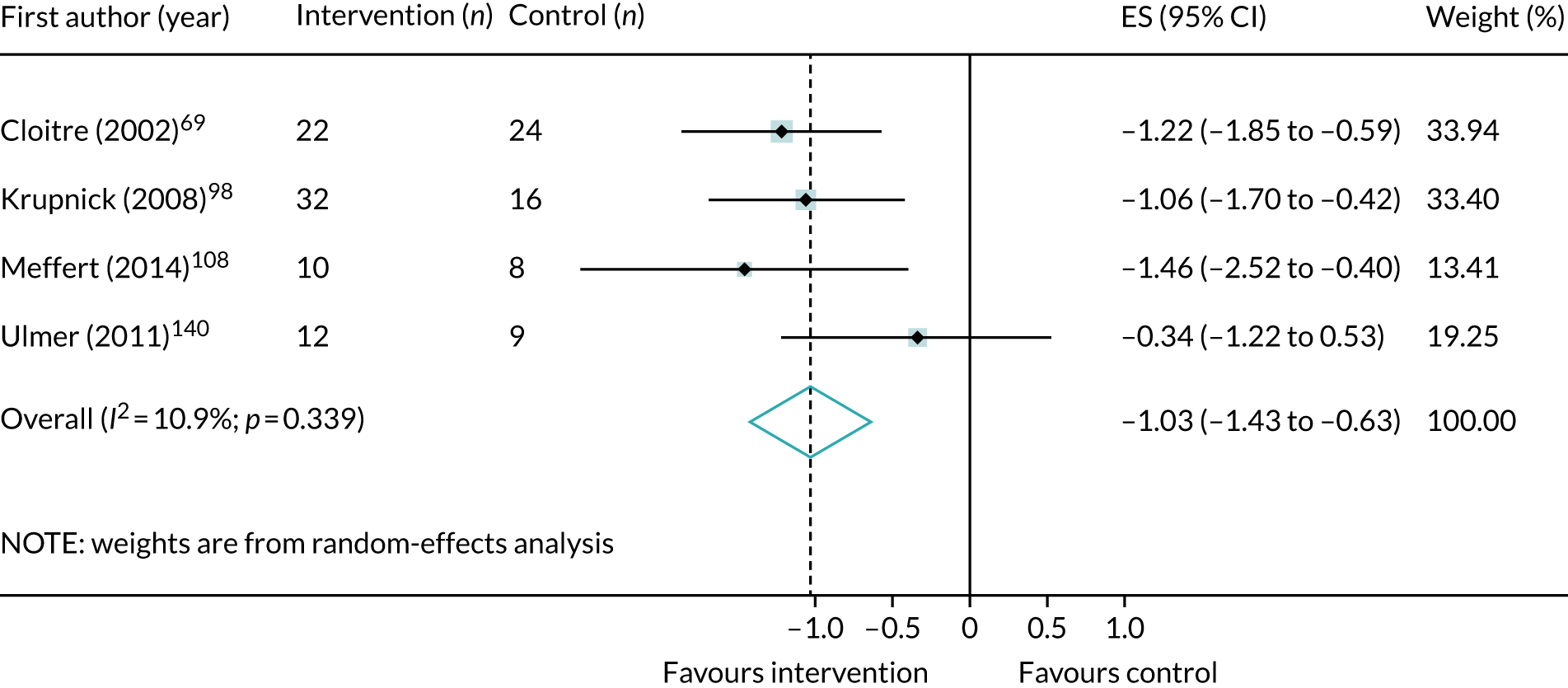
Anxiety symptoms
A summary of meta-analyses of the clinical effectiveness of psychological interventions across all populations for anxiety symptoms is shown in Appendix 9, Table 37. Figure 10 shows the result of a meta-analysis of 13 studies (n = 1136)62,69,74,76,81,91,96,126,143,144,157 that compared all psychological interventions with control post treatment. Interventions were associated with a large and significant treatment effect in favour of a reduction in anxiety symptoms.
FIGURE 10.
Meta-analysis of post-treatment effect size (ES) for anxiety symptoms, comparing all psychological interventions with control. CETA, common elements treatment approach; CPT, cognitive treatment therapy.
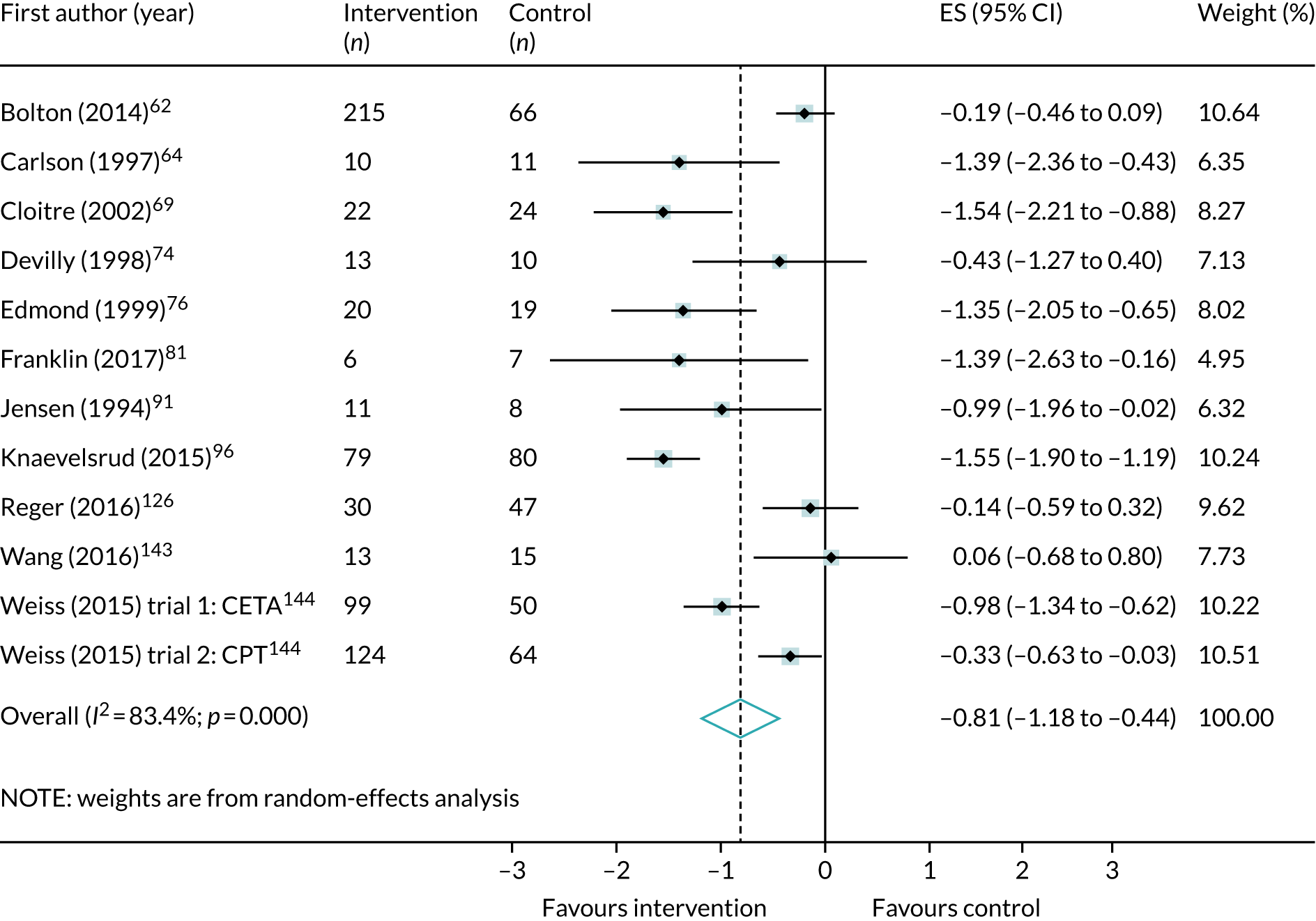
The majority of the studies (eight studies; n = 7)62,81,96,106,126,143,144 that included data about anxiety symptoms tested trauma-focused CBT. When compared with control post treatment, meta-analysis showed that trauma-focused CBT was associated with a large and significant effect in favour of a reduction in anxiety symptoms (Figure 11).
FIGURE 11.
Meta-analysis of post-treatment effect size (ES) for anxiety symptoms, comparing trauma-focused CBT with control. CETA, common elements treatment approach; CPT, cognitive treatment therapy.

The largest effects in favour of a reduction in anxiety symptoms were observed in a meta-analysis of four studies (n = 102)74,76,91,157 that compared EMDR with control post treatment (see Appendix 10, Figure 49).
There were no data that could be meta-analysed that compared mindfulness or non-trauma-focused CBT with either control or an active control.
Using composite intervention categories, we showed in a meta-analysis that single-component and trauma-focused interventions (10 studies; n = 757)62,74,76,81,91,96,106,126,144,157 were associated with a large and significant treatment effect in favour of a reduction in anxiety symptoms (see Appendix 10, Figure 50).
Compared with control, multicomponent and trauma-focused interventions were associated with the largest treatment effect in favour of a reduction of anxiety symptoms (SMD –0.85, 95% CI –1.60 to –0.10; I2 = 80.4%). 69,143,144 This meta-analysis included studies that tested a phase-based intervention and trauma-focused CBT (see Appendix 10, Figure 51).
Only two studies (n = 225)62,106 compared single-component and non-trauma-focused interventions with control post treatment: one tested a counselling intervention and one tested non-trauma-focused CBT. Although the treatment effect favoured a reduction in anxiety symptoms, the effect was small and did not reach significance (see Appendix 10, Figure 52).
Quality of life
A summary of meta-analyses of the clinical effectiveness of psychological interventions across all populations for quality of life is shown in Appendix 9, Table 38. We identified five trials (n = 307)95,96,106,109,143 that included quality-of-life data that could be meta-analysed. Figure 12 shows the result of a meta-analysis that compared all psychological interventions with control post treatment.
FIGURE 12.
Meta-analysis of post-treatment effect size (ES) for quality of life, comparing all psychological interventions with control (positive ES favours intervention).
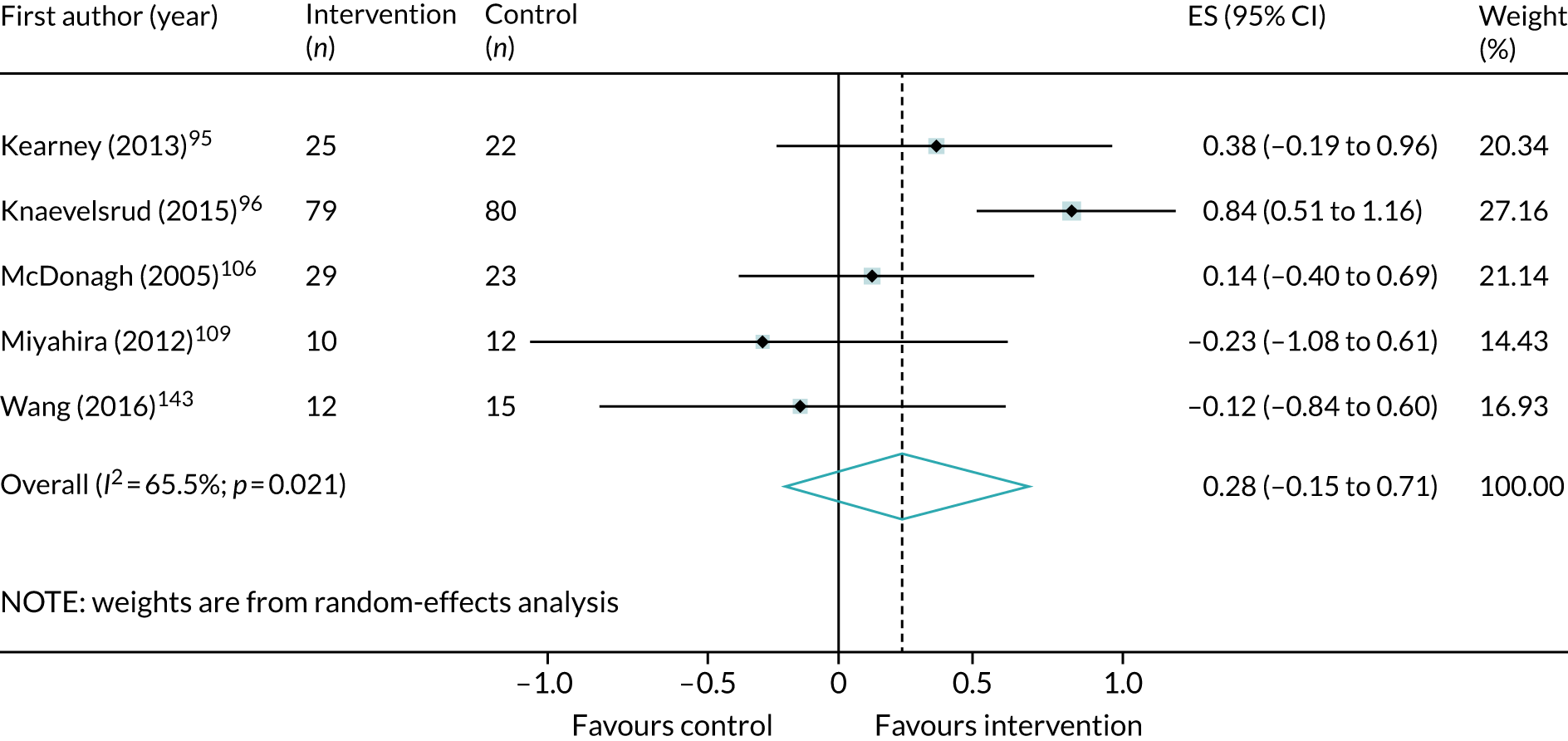
Four of these five studies (n = 260)96,106,109,143 compared trauma-focused CBT with control post treatment. Although interventions favoured a small improvement in quality of life, the effect size did not reach significance (SMD 0.23, 95% CI –0.33 to 0.79; I2 = 73.9%; see Appendix 10, Figure 53).
Sleep quality
A summary of meta-analyses of the clinical effectiveness of psychological interventions across all populations for sleep quality is shown in Appendix 9, Table 39. Only three studies (n = 111)140,142,159 included data about sleep quality that could be meta-analysed. When compared with control post treatment, all psychological interventions were associated with a large and significant effect on sleep quality (SMD –1.00, 95% CI –1.49 to –0.51; I2 = 28.8%; see Appendix 10, Figure 54). A larger and significant treatment effect in favour of improved sleep quality was observed in a meta-analysis of just two small studies140,159 that compared trauma-focused CBT with control post treatment (SMD –1.30, 95% CI –1.87 to –0.73; I2 = 0%; see Appendix 10, Figure 55).
Psychological interventions versus control
A summary of all of the clinical effectiveness meta-analyses undertaken within each trauma exposure can be found in Appendix 9.
Veterans
A summary of meta-analyses of the clinical effectiveness of psychological interventions in veterans for PTSD, depression and anxiety symptoms is shown in Appendix 9, Table 40. Twenty-three trials were identified that included data about veteran populations. Five trials were not included in the meta-analysis: three compared head-to-head interventions,120,124,128 one compared trauma-focused CBT with exposure alone60 and one did not include extractable data. 83
Post-traumatic stress disorder symptoms
Figure 13 shows the result of a meta-analysis (14 trials, n = 502)74,78,81,88,91,94,95,107,121,126,140,142,157,159 that compared all psychological interventions with control post treatment. The medium treatment effect favours a significant reduction in PTSD symptoms.
FIGURE 13.
Meta-analysis of post-treatment SMD for total PTSD symptoms, comparing all psychological interventions with control in veteran populations.
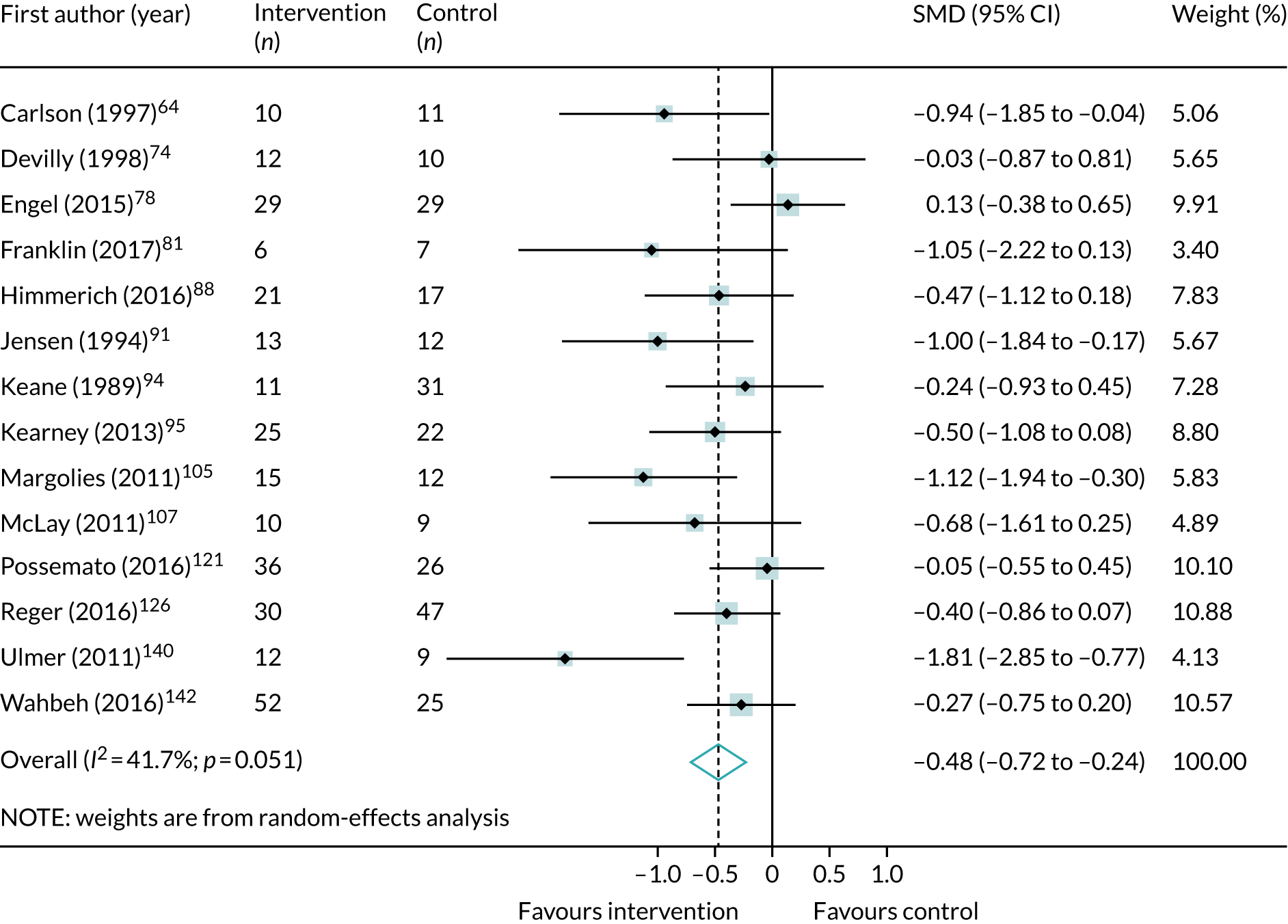
Four trials (n = 180)78,95,121 measured PTSD outcomes at follow-up after < 6 months and, while psychological interventions were associated with a small treatment effect in favour of interventions, this did not reach significance (SMD –0.20, 95% –0.72 to 0.33; I2 = 63.1%).
Six trials (n = 106)81,94,100,107,126,159 compared trauma-focused CBT with control post treatment. Trauma-focused CBT was associated with a large and significant treatment effect in favour of a reduction in PTSD total symptoms (SMD –0.77, 95% CI –1.20 to –0.33; I2 = 44.6%; see Appendix 10, Figure 56).
A meta-analysis of four trials (n = 106)74,88,91,157 showed that EMDR was associated with a smaller but still significant treatment effect when compared with control post treatment (see Appendix 10, Figure 57).
Studies that included veterans95,121,142 provided all of the data in the previous meta-analysis that compared mindfulness with control post treatment and at follow-up after < 6 months (see Appendix 10, Figure 58).
No studies that included veterans compared non-trauma-focused CBT with either a control or an active control group.
Figure 59 (see Appendix 10) shows the results of a meta-analysis (seven trials, n = 219)74,81,91,94,107,157 that compared single-component and trauma-focused interventions with control post treatment. This shows that single-component and trauma-focused interventions were associated with a medium and significant effect in favour of a reduction in PTSD symptoms. The size of the effect was about half that observed in the equivalent analysis for all populations and trauma exposures pooled.
The largest effect was observed in a meta-analysis of three small studies (n = 86)88,140,159 that compared multicomponent and trauma-focused interventions with control post treatment (see Appendix 10, Figure 60).
Single-component and non-trauma-focused interventions were not associated with a significant treatment effect in favour of a reduction in PTSD symptoms post treatment in veterans (see Appendix 10, Figure 61). 78,95,121,142
Four trials compared psychological interventions with active control (sleep and nightmare management, placebo and psychoeducation). 71,84,137,160 It was unclear if psychological interventions as a whole (SMD –0.44, 95% CI –0.98 to 0.10; I2 = 64%; four trials, n = 188) or trauma-focused CBT (SMD –0.26, 95% CI –0.88 to 0.35; I2 = 51.1%; two trials, n = 126) were effective for PTSD symptoms.
Depression
Figure 14 shows the results of a meta-analysis (11 trials; 445)74,78,81,95,111,121,126,137,140,142,157,159 that compared all psychological interventions with control post treatment. The size of the treatment effect is smaller than the effect observed in the equivalent analysis that pooled PTSD outcomes across all populations and trauma exposures. In five studies (n = 201)78,81,95,111,121 that measured outcomes at follow-up after < 6 months, all psychological interventions were associated with a medium effect in favour of a reduction in depression symptoms, but this effect was not significant (SMD –0.38, 95% CI –0.78 to 0.01; I2 = 42.3%).
FIGURE 14.
Meta-analysis of post-treatment SMD for total depression symptoms, comparing all psychological interventions with control in veteran populations.
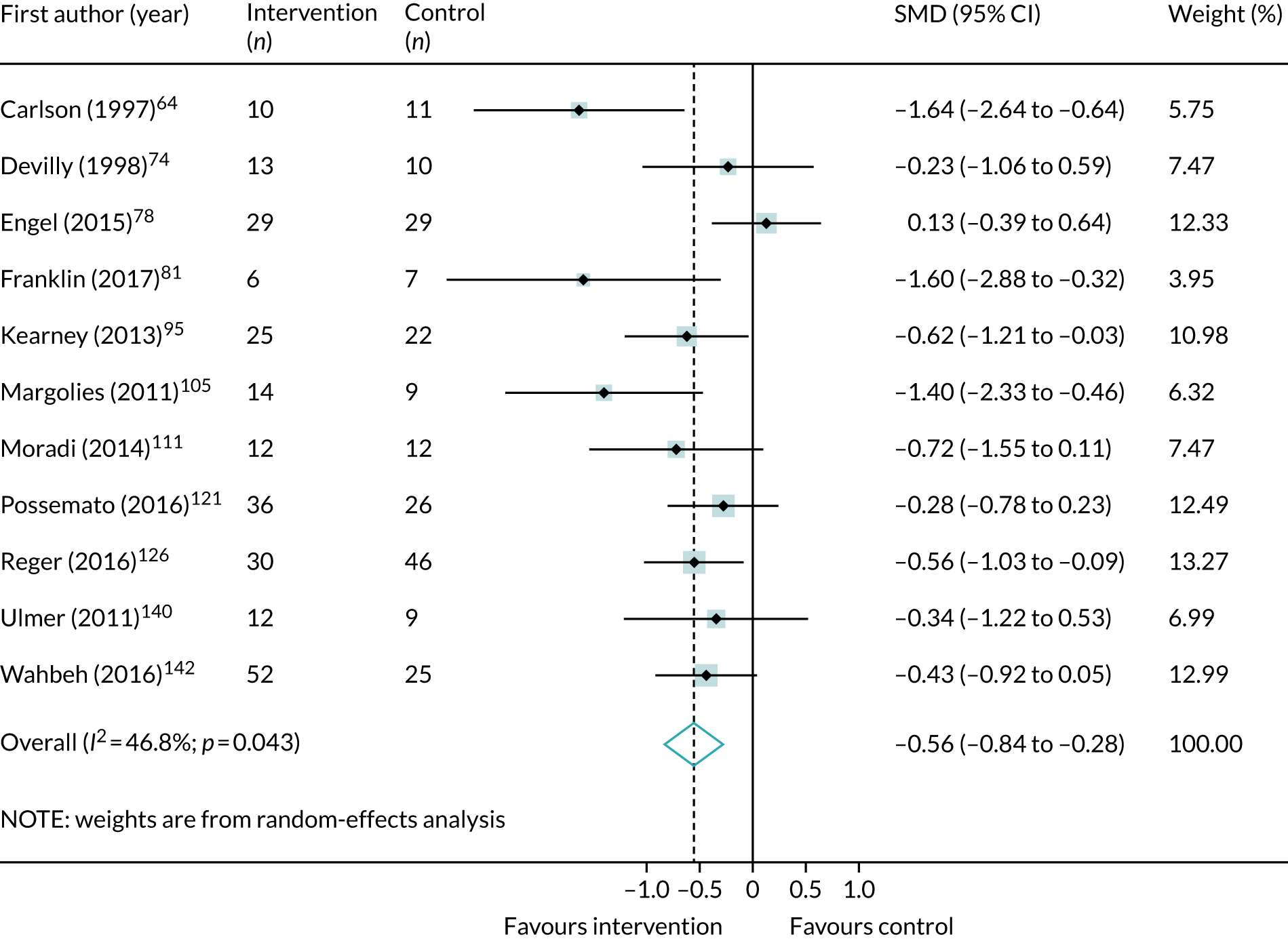
When only those studies that compared trauma-focused CBT with control post treatment were considered, the meta-analysis (three trials, n = 112)81,126,159 showed that interventions were associated with a large and significant treatment effect in favour of a reduction of depression symptoms (see Appendix 10, Figure 62). There was, however, no evidence of a significant difference between trauma-focused CBT and active control (SMD –0.04, 95% CI –0.55 to 0.48; I2 = 38.7%; two trials, n = 128). 71,84
Compared with control post treatment, EMDR was similarly associated with large effects in favour of a reduction in depression symptoms, but the overall point estimate was non-significant and associated with considerable uncertainty (see Appendix 10, Figure 63). 74,157
The pooled population meta-analysis that compared mindfulness with control post treatment and after < 6 months included only studies with veterans and is shown in Appendix 10, Figure 64. 95,121,142
No studies that included veteran populations compared non-trauma-focused CBT with control for depression symptoms.
Single-component and trauma-focused interventions were associated with large and significant effects in favour of a reduction in depression symptoms (see Appendix 10, Figure 65). 74,81,126,157
There was less evidence in favour of multicomponent and trauma-focused interventions, which were not significantly associated with a reduction in depression symptoms in a meta-analysis that included only two small trials (see Appendix 10, Figure 66). 140,159
By contrast, a meta-analysis that included five studies (n = 268)78,95,111,121,142 that compared single-component and non-trauma-focused interventions showed that interventions were associated with a medium but significant effect in favour of a reduction in depression symptoms (see Appendix 10, Figure 67). Four of these studies (n = 188)78,95,111,121 measured outcomes after < 6 months, but the effect was not significant (SMD –0.27, 95% CI –0.56 to 0.02; I2 = 0%).
Anxiety
There was less evidence for using psychological interventions for managing anxiety symptoms than other symptoms in veteran populations. We identified five studies (n = 153)74,81,91,126,157 that showed, in a meta-analysis, that overall, when pooled together, psychological interventions compared with control were associated with a large and significant effect in favour of a reduction in anxiety symptoms (Figure 15).
FIGURE 15.
Meta-analysis of post-treatment SMD for total anxiety symptoms, comparing all psychological interventions with control in veteran populations.

Only two studies (n = 90)81,126 compared trauma-focused CBT with control post treatment in veterans. Meta-analysis showed that interventions favoured a reduction in anxiety symptoms, but this effect was not significant and was associated with a high degree of uncertainty (see Appendix 10, Figure 68).
By contrast, EMDR compared with control was associated in a meta-analysis (three trials, n = 63)74,91,157 with a large treatment effect in favour of a reduction in anxiety symptoms post treatment (see Appendix 10, Figure 69). The size of this effect was marginally smaller than that observed in the meta-analysis that pooled all populations and that included more studies.
War-affected populations
A summary of meta-analyses of the clinical effectiveness of psychological interventions across war-affected populations for PTSD, depression and anxiety symptoms is shown in Appendix 9, Table 41. Ten studies that included war-affected populations were identified; eight were included in the meta-analyses. Azad Marzabadi and Hashemi Zadeh57 did not report outcomes that were sufficiently similar to other studies (i.e. they only reported on the WHO Quality of Life questionnaire) and Bichescu et al. 61 compared head-to-head interventions; therefore, these were not meta-analysed.
Post-traumatic stress disorder total symptoms
Figure 16 shows the results of a meta-analysis that compared all psychological interventions (eight trials, n = 933)62,86,96,109,143–145 with control post treatment. The results show that psychological interventions were associated with a medium effect size in favour of a reduction in total PTSD symptoms. The size of this effect was comparable to that observed for veteran populations.
FIGURE 16.
Meta-analysis of post-treatment effect size (ES) for total PTSD symptoms, comparing all psychological interventions with control in war-affected populations. CETA, common elements treatment approach; CPT, cognitive treatment therapy.

The majority of the studies (seven trials, n = 743)62,86,96,109,143,144 in war-affected populations compared trauma-focused CBT with control post treatment. Figure 70 (see Appendix 10) shows that trauma-focused interventions were associated with a medium and significant effect in favour of reducing PTSD symptoms in war-affected populations.
A very similar result was found when single-component and trauma-focused interventions were compared in a meta-analysis (five trials, n = 566)62,86,96,109,144 with control post treatment (SMD –0.51, 95% CI –0.80 to –0.23; I2 = 55.9%).
Three studies delivered therapies as part of a multicomponent and trauma-focused intervention. 143–145 When meta-analysed, these three studies (n = 253) showed that multicomponent and trauma-focused interventions were associated with a medium effect size in favour of a reduction in PTSD symptoms post treatment, but the overall point estimate was more uncertain than in the other meta-analyses in this population subgroup (see Appendix 10, Figure 71).
Depression symptoms
Six trials (n = 827)62,96,109,143,144 were identified that included data that could be meta-analysed for depression symptoms in the war-affected subgroup. All of these studies compared trauma-focused CBT with control post treatment. When meta-analysed together, Figure 17 shows that trauma-focused CBT is associated with a medium and significant effect size in favour of a reduction in depression symptoms.
FIGURE 17.
Meta-analysis of post-treatment effect size (ES) for total depression symptoms, comparing all trauma-focused CBT interventions with control in war-affected populations. CETA, common elements treatment approach; CPT, cognitive treatment therapy.

When trauma-focused CBT was delivered as part of a single-component intervention and compared with control, the meta-analysis (four trials, n = 536)62,96,109,144 shows that the intervention was associated with a similarly medium and significant effect size in favour of a reduction in depression symptoms (see Appendix 10, Figure 72). However, in the two studies that tested trauma-focused CBT as part of a multicomponent intervention, the meta-analysis (n = 177)143,144 shows that the treatment effect favoured a reduction in depression symptoms but did not reach significance (see Appendix 10, Figure 73).
Anxiety symptoms
Five trials (n = 691)62,96,143,144 were identified that included data that could be meta-analysed for depression symptoms in the war-affected subgroup. All of these studies compared trauma-focused CBT with control post treatment. When meta-analysed together, Figure 18 shows that trauma-focused CBT is associated with a large and significant effect size in favour of a reduction in anxiety symptoms.
FIGURE 18.
Meta-analysis of post-treatment effect size (ES) for total anxiety symptoms, comparing trauma-focused CBT with control in war-affected populations. CETA, common elements treatment approach; CPT, cognitive treatment therapy.

When trauma-focused CBT was delivered as part of a single-component intervention and compared with control, the meta-analysis (three trials, n = 514)62,96,144 shows that the intervention was associated with a large effect size in favour of a reduction in anxiety symptoms, but this effect did not reach significance (see Appendix 10, Figure 74). Similarly, in the two studies143,144 that tested trauma-focused CBT as part of a multicomponent intervention, the meta-analysis (n = 177) shows that the treatment effect favoured a reduction in depression symptoms but did not reach significance and was associated with considerable uncertainty (see Appendix 10, Figure 75).
Childhood sexual abuse
A summary of meta-analyses of the clinical effectiveness of psychological interventions across populations exposed to childhood sexual abuse for PTSD, depression and anxiety symptoms is shown in Appendix 9, Table 42. Thirteen of these studies included data that could be meta-analysed in the childhood sexual abuse subgroup; nine studies (n = 687)66,69,76,92,98,106,131,132,146 were included in the meta-analyses. Those excluded from the meta-analyses were Cloitre et al. ,69 which was a deconstruction trial; Lau and Kristensen,103 which compared analytic with systemic group therapy; Classen et al. ,68 which combined data from trauma-focused CBT and present-centred therapy groups, making it difficult to separate out and interpret the intervention effects; and Owens et al. ,117 which only reported loss of PTSD diagnosis (an outcome not reported in any other study in this population).
Post-traumatic stress disorder total symptoms
Figure 19 shows the results of a meta-analysis (nine trials, n = 687)66,69,76,92,98,106,131,132,146 that compared all psychological interventions with control post treatment. The treatment effect was large and significant and about twice the size of the comparable result in the meta-analysis that assessed the effectiveness of all psychological interventions across all populations. Three studies (n = 323)92,98,132 measured outcomes at follow-up after < 6 months. The meta-analysis of these three studies showed that the treatment effect still favoured a reduction in PTSD symptoms, but it did not reach significance (SMD –0.27, 95% CI –0.71 to 0.17; I2 = 53.6%).
FIGURE 19.
Meta-analysis of post-treatment SMD for total PTSD symptoms, comparing all psychological interventions with control in childhood sexual abuse populations.
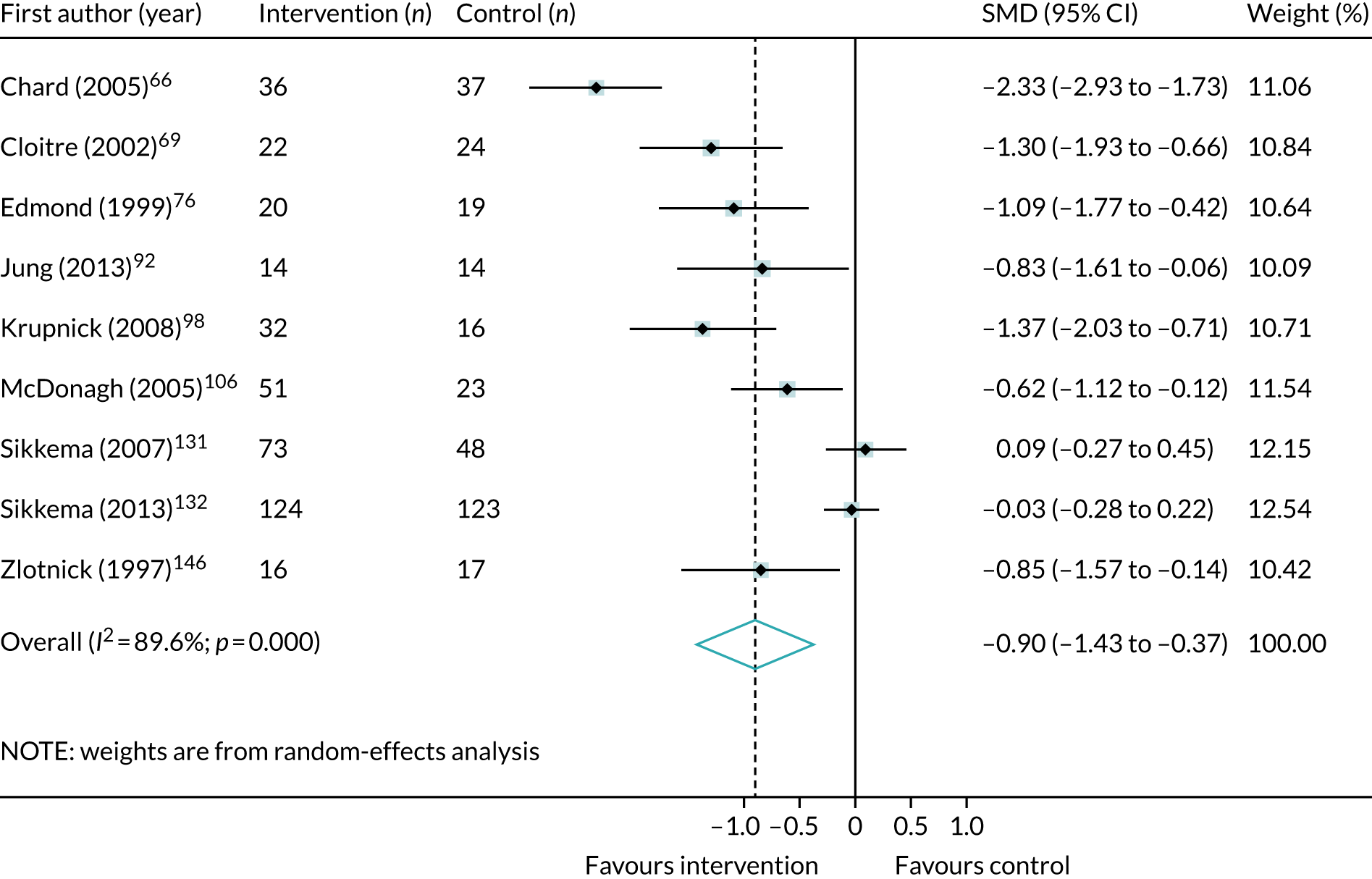
Three studies (n = 153)66,92,106 compared trauma-focused CBT with control post treatment. The meta-analysis shows that trauma-focused CBT was the most effective intervention in this subgroup. Figure 76 (see Appendix 10) shows that this intervention was associated with a large effect in favour of a reduction in PTSD symptoms, but the wide CIs suggest that this result is particularly uncertain.
By contrast, non-trauma-focused CBT, meta-analysed in two studies (n = 368),131,132 did not favour the intervention when compared with control post treatment (see Appendix 10, Figure 77).
When studies (three trials, n = 119)66,76,92,106 were grouped using the composite categories, we showed that single-component and trauma-focused interventions were associated with a large and significant effect in favour of a reduction in PTSD symptoms (see Appendix 10, Figure 78).
Larger and significant effects in favour of a reduction in PTSD symptoms were observed in the meta-analysis that compared multicomponent and trauma-focused interventions with control post treatment, but the treatment estimate was associated with considerable uncertainty (SMD –1.82, 95% CI –2.83 to –0.81; I2 = 81.3%; two trials, n = 122). Single-component and non-trauma-focused interventions (five trials, n = 494)98,106,131,132,146 were shown, in a meta-analysis, to be associated with a medium and significant effect that favoured a reduction in PTSD symptoms (see Appendix 10, Figure 79). This analysis included a phase-based study of IPT that was associated with a large and significant effect. 98 Two of these trials measured outcomes at follow-up after < 6 months and a meta-analysis shows that there was no significant difference between interventions and control (SMD –0.08, 95% CI –0.31 to 0.15; I2 = 0%). 98,132
Depression
Figure 20 shows the result of a meta-analysis (six trials, n = 307)69,76,92,98,106 that compared all psychological interventions with control post treatment. Psychological interventions were associated with a large and significant effect in favour of a reduction in depression symptoms.
FIGURE 20.
Meta-analysis of post-treatment SMD for depression symptoms, comparing all psychological interventions with control in childhood sexual abuse populations.
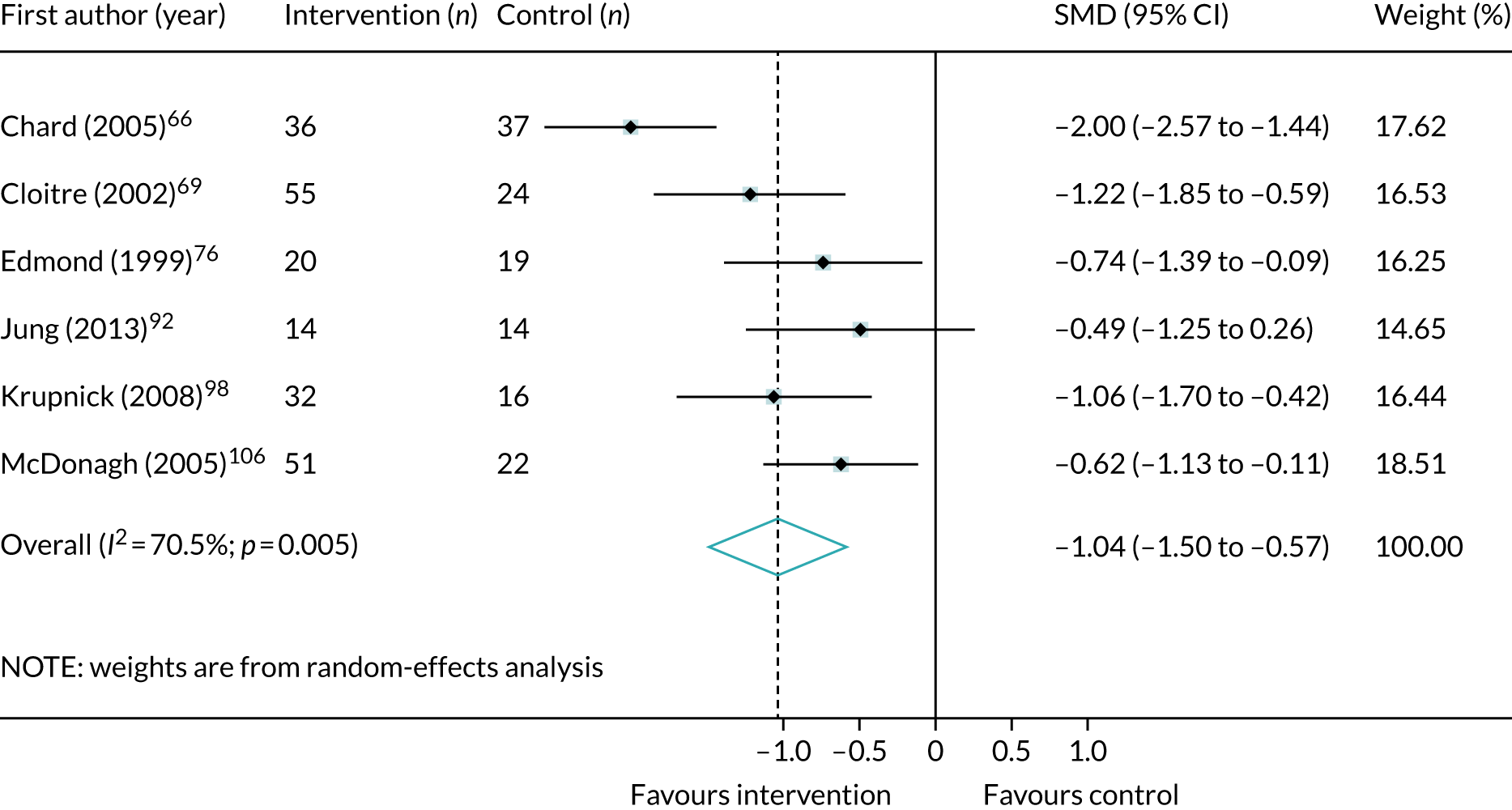
Two of these six trials measured outcomes at follow-up after < 6 months; the treatment effect still favoured interventions and was significant (SMD –0.52, 95% CI –0.99 to –0.04; I2 = 0%). 92,98
Figure 80 (see Appendix 10) shows that trauma-focused CBT, when compared with control post treatment, is associated with a large but non-significant effect size in favour of a reduction in depression symptoms. This analysis was based on three small studies (n = 152) and there is considerable uncertainty regarding the overall point estimate.
There was some tentative evidence from a meta-analysis of three studies (n = 118)76,92,106 that single-component and trauma-focused interventions were similarly associated with a large and significant effect size (see Appendix 10, Figure 81).
Single-component and non-trauma-focused interventions were associated with a medium and significant effect in favour of a reduction in depression symptoms in this subgroup (see Appendix 10, Figure 82). This analysis was based on three small studies (n = 118). 76,92,106
Larger and significant effects in favour of a reduction in depression symptoms were observed in the meta-analysis that compared multicomponent and trauma-focused interventions with control post treatment, but the treatment estimate was associated with considerable uncertainty (SMD –1.63, 95% CI –2.40 to –0.85; I2 = 69.7%; two trials, n = 122).
Anxiety symptoms
Only two studies (n = 90)76,106 included anxiety outcome data that could be meta-analysed. Figure 83 (see Appendix 10) shows that single-component and trauma-focused interventions (one testing EMDR, one testing trauma-focused CBT) are associated with a large effect in favour of a reduction in anxiety symptoms, but the effect did not reach significance.
Refugee populations
A summary of meta-analyses of the clinical effectiveness of psychological interventions across refugee populations for PTSD, depression and anxiety symptoms is shown in Appendix 9, Table 43. Twelve studies that included refugee populations were identified; however, few meta-analyses were possible. The following trials did not appear in any meta-analyses:
-
Neuner et al. 114 compared trauma-focused CBT, supportive counselling and psychoeducation and there was no comparison with a control group.
-
Paunovic and Ost119 compared trauma-focused CBT with an exposure-only intervention.
-
In Stenmark et al. ,136 trauma-focused CBT data were not extractable.
Post-traumatic stress disorder symptoms
Figure 21 shows the results of a meta-analysis (six trials, n = 188)53–55,89,108,136,158 that compared all psychological interventions with control post treatment. Interventions were associated with a very large and significant effect size in favour of a reduction in PTSD symptoms. Three studies (n = 235)54,87,113 measured outcomes at follow-up after < 6 months and, in the meta-analysis, the treatment effect was large and significant at follow-up (SMD –0.66, 95% CI –1.22 to –0.09; I2 = 72.7%).
FIGURE 21.
Meta-analysis of post-treatment SMD for total PTSD symptoms, comparing all psychological interventions with control in refugee populations.
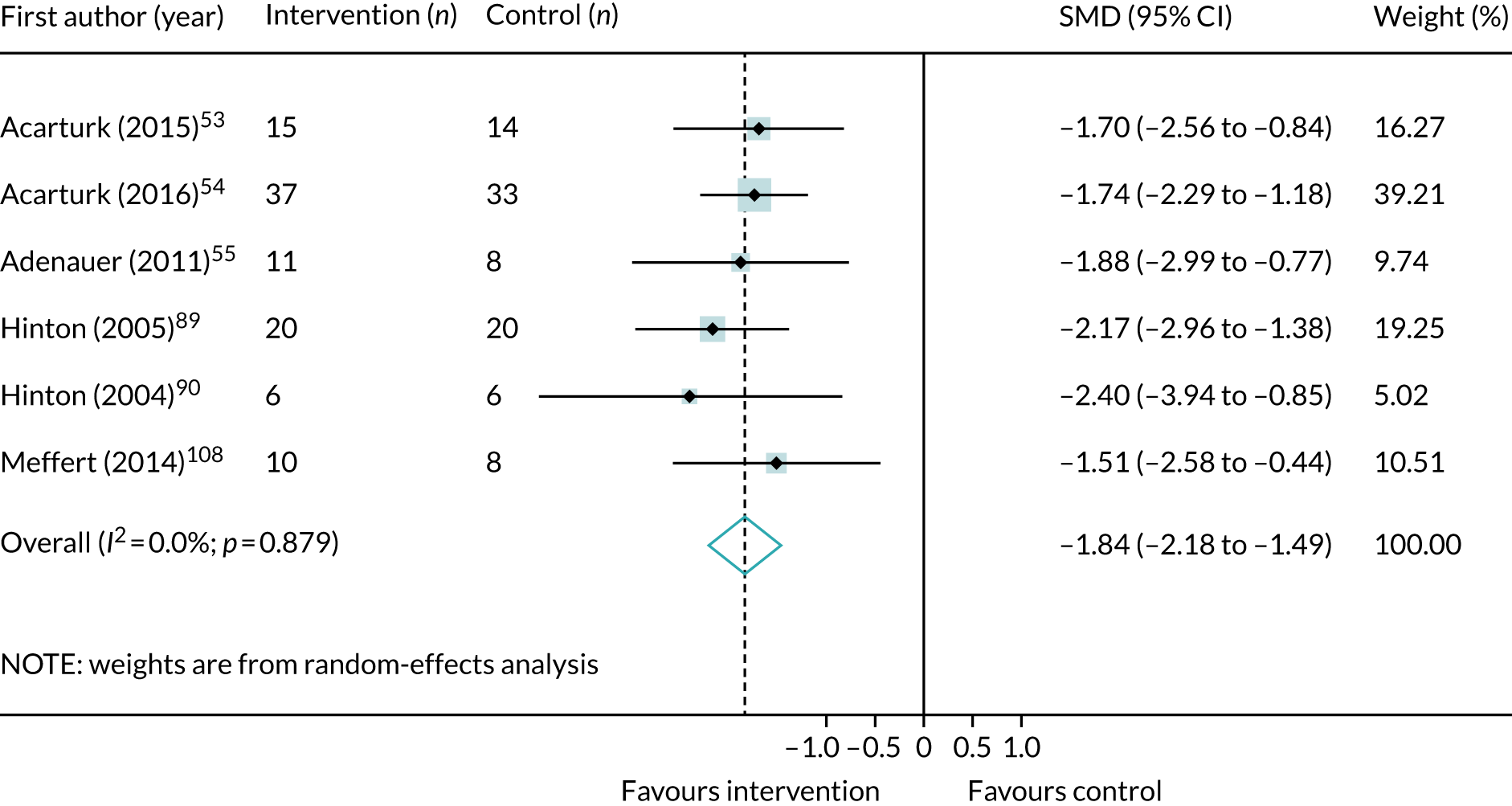
Three small studies (n = 71)55,89,158 compared trauma-focused CBT with control post treatment and were associated in a meta-analysis with a very large and significant treatment effect in favour of a reduction in PTSD symptoms (see Appendix 10, Figure 83). Two larger studies (n = 165)87,113 that compared trauma-focused CBT with control measured outcomes at follow-up after < 6 months. The meta-analysis of these two studies showed that the treatment effect favoured interventions but did not reach significance (SMD –0.40, 95% CI –0.87 to 0.06; I2 = 86.3%).
There was some evidence, based on two small trials (n = 99),53,54 that EMDR, when compared with control post treatment, was effective at reducing total PTSD symptoms (see Appendix 10, Figure 85).
A large and significant effect in favour of a reduction in total PTSD symptoms was observed in a meta-analysis (five trials, n = 170)53–55,89,158 that compared single-component and trauma-focused interventions with control post treatment (see Appendix 10, Figure 86). Two studies (n = 133)54,87 measured outcomes at follow-up after < 6 months and, in a meta-analysis, the treatment effect favoured the interventions but did not reach significance (SMD –0.67, 95CI% –1.65 to 0.32; I2 = 86.3%).
In addition to the comparisons with control, two studies (n = 71)138,139 compared EMDR with stabilisation only. There was insufficient evidence to conclude that EMDR was more effective post treatment (SMD –0.15, 95% CI –0.62 to 0.32; I2 = 0%) and at follow-up after < 6 months (SMD –0.15, 95% CI –0.80 to 0.49; I2 = 22.4%).
Depression symptoms
Figure 22 shows the results of a meta-analysis (five trials, n = 148)53–55,108,158 that compared all psychological interventions with control post treatment. There is evidence that psychological interventions are effective in reducing symptoms of depression in refugee populations.
FIGURE 22.
Meta-analysis of post-treatment SMD for depression symptoms, comparing all psychological interventions with control in refugee populations.
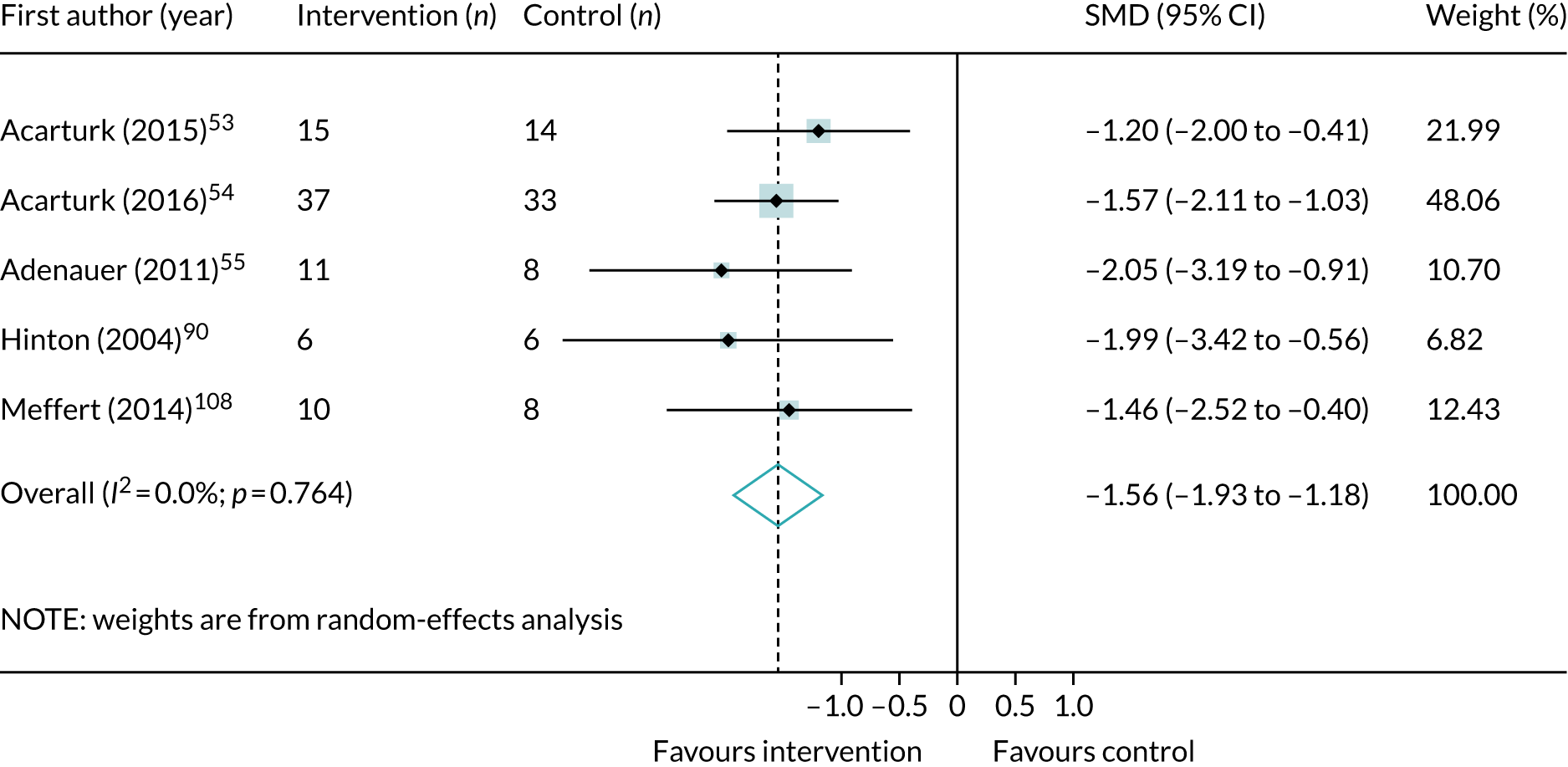
There was only modest evidence from a meta-analysis of two small trials (n = 31)55,158 that trauma-focused CBT when compared with control is associated with large and significant treatment effects in favour of a reduction in depression symptoms; the wide CIs suggest this result is uncertain (see Appendix 10, Figure 87). Two other trials (n = 133)54,87 measured outcomes at follow-up after < 6 months and a meta-analysis shows that the treatment effect favoured interventions but did not reach significance (SMD –0.73, 95% CI –1.57 to 0.10; I2 = 81.3%).
Evidence to support the use of EMDR for managing depression in this population was also based only on data from two small trials (n = 99). 53,54 When compared with control post treatment, EMDR was associated with a large and significant treatment effect in favour of a reduction in depression symptoms (see Appendix 10, Figure 88).
Taken together, single-component and trauma-focused interventions that included trauma-focused CBT and EMDR were effective at reducing depression in refugee populations. A meta-analysis (four trials, n = 130)53–55,158 showed that, overall, these interventions are associated with a large and significant treatment effect (see Appendix 10, Figure 89).
Two studies also compared EMDR with stabilisation only. 138,139 There was insufficient evidence to conclude that EMDR was more effective post treatment (SMD –0.32, 95% CI –1.23 to 0.59; I2 = 47.8%; two trials, n = 72) or at follow-up after < 6 months (SMD –0.01, 95% CI –0.47 to 0.45; I2 = 0%; two trials, n = 73).
Anxiety symptoms
Only data from two studies that compared EMDR with stabilisation included data on anxiety symptoms that could be extracted. 138,139 There was no evidence that EMDR was effective in reducing anxiety symptoms in refugee populations post treatment (SMD –0.36, 95% CI –0.82 to 0.11; I2 = 0%; two trials, n = 73) or at follow-up after < 6 months (SMD –0.43, 95% CI –1.21 to 0.35; I2 = 35.1%; two trials, n = 73).
Domestic violence
A summary of meta-analyses of the clinical effectiveness of psychological interventions across populations exposed to domestic violence for PTSD, depression and anxiety symptoms is shown in Appendix 9, Table 44.
Post-traumatic stress disorder symptoms
Three trials were identified that measured PTSD symptoms in populations affected by domestic violence. Two of the three trials were included in the meta-analyses that compared trauma-focused CBT with control post treatment and interventions were associated with a large and significant treatment effect (SMD –2.92, 95% CI –3.45 to –2.39; I2 = 0%; two trials, n = 117). 100,101
The other trial in this subgroup compared forgiveness therapy with an alternative treatment including anger validation, assertiveness and interpersonal skills training and could not be meta-analysed. 125
Depression symptoms
The same two trials that compared trauma-focused CBT with control also reported post-treatment outcomes for depression. A meta-analysis showed that interventions were associated with a large and significant treatment effect, but there is a high degree of uncertainty about the overall point estimate (SMD –3.24, 95% CI –4.40 to –2.09; I2 = 66.6%; two trials, n = 117). 125
Pharmacological interventions versus placebo
Nineteen trials were identified that compared pharmacological interventions with placebo. Rezaei Ardani et al. 56 tested rivastigmine augmentation and this study was not included in the meta-analyses because there were no other comparable interventions to combine it with. Two other studies were excluded from the meta-analyses because they compared head-to-head interventions, with no placebo group. 65,67 All the trials (n = 16)58,59,72,73,82,84,85,99,104,110,112,118,122,123,135,147 included in the meta-analyses, except one trial in childhood sexual abuse, were in veteran populations.
Total post-traumatic stress disorder symptoms
A summary of meta-analyses of the clinical effectiveness of pharmacological interventions for PTSD symptoms is shown in Appendix 9, Table 45. A meta-analysis of six trials (n = 338)59,73,82,112,118,147 compared antidepressants with placebo post treatment. The results show that there was a medium treatment effect in favour of antidepressants, but this did not reach significance (see Appendix 10, Figure 90).
Four trials (n = 293)82,112,118,147 were included in a meta-analysis that compared SSRIs with placebo. Figure 91 (see Appendix 10) shows that SSRIs were associated with a large effect in favour of a reduction in total PTSD symptoms, but this did not reach significance.
Data about the effectiveness of antipsychotics were meta-analysed in five trials (n = 365). 58,85,99,110,135 Antipsychotics were associated with a medium and significant treatment effect in favour of a reduction in total PTSD symptoms post treatment (see Appendix 10, Figure 92).
Only two trials that compared anticonvulsants with placebo were meta-analysed and there was little evidence that these classes of drugs were effective at reducing total PTSD symptoms (see Appendix 10, Figure 93). 72,104
Three trials (n = 110) compared prazosin with placebo and a meta-analysis showed that this sympatholytic medication is associated with a medium treatment effect post treatment in favour of reducing total PTSD symptoms (see Appendix 10, Figure 94). 84,122,123
Depression symptoms
A summary of meta-analyses of the clinical effectiveness of pharmacological interventions for depression symptoms is shown in Appendix 9, Table 46. Antidepressant medication was compared with placebo post treatment in a meta-analysis that included three trials (n = 220). 59,73,82 The results were inconclusive, with no evidence that these classes of drugs were effective in reducing depression symptoms in veteran populations (see Appendix 10, Figure 95).
There was some evidence drawn from two trials (n = 266)99,135 that antipsychotic medication compared with placebo post treatment favoured the intervention, but the treatment effect did not reach significance (see Appendix 10, Figure 96).
There was very little evidence that anticonvulsants compared with placebo post treatment were effective in reducing depression symptoms. A meta-analysis of two trials (n = 106)72,104 showed that the treatment effect marginally favoured the placebo group (see Appendix 10, Figure 97).
In a meta-analysis of two trials (n = 76)84,123 that compared prazosin with placebo post treatment, the treatment effect favoured prazosin but did not reach significance.
There were insufficient data to assess the effectiveness of SSRIs. Only one study that compared SSRIs with placebo reported a depression outcome. 82 Among the other studies that tested SSRIs, one study did not report depression outcomes separately and instead presented combined depression and anxiety data using the Hospital Anxiety and Depression Scale total,112 and two other trials did not report any depression outcome data. 118,147
Anxiety symptoms
No meta-analyses were possible for anxiety outcomes.
Psychosis symptoms
A summary of meta-analyses of the clinical effectiveness of pharmacological interventions for psychosis symptoms is shown in Appendix 9, Table 47. All of the trials included in the meta-analyses that compared antipsychotic medication with placebo tested risperidone. Three trials were identified that included post-treatment outcome data related to symptoms of psychosis; all used the Positive and Negative Syndrome Scale (PANSS). 58,85,99
There was no good evidence that antipsychotic medication reduces symptoms of psychosis in veteran and childhood sexual abuse populations.
In a meta-analysis of three trials (n = 329),58,85,99 risperidone was associated with a reduction in positive psychotic symptoms on the PANSS, but the treatment effect did not reach significance and the overall point estimate was very uncertain (see Appendix 10, Figure 98).
In a meta-analysis of one small and one medium-sized trial, the treatment effect did not favour risperidone for either negative or total scores on the PANSS, although the effects were not significant (see Appendix 10, Figures 99 and 100). 85,99 In the same meta-analysis, there was some evidence that risperidone favoured an improvement on the general psychopathology scale of the PANSS, but the effect did not reach significance (see Appendix 10, Figure 101).
Sleep quality
A summary of meta-analyses of the clinical effectiveness of pharmacological interventions for sleep quality is shown in Appendix 8, Figure 26. Prazosin was the only pharmacological intervention with sufficient data to conduct meta-analyses; it was more effective than placebo (mean difference –2.53, 95% CI –3.82 to 1.23; I2 = 0%; three trials, n = 109). 84,122,123
Meta-analysis of attrition
Of the RCTs included, 46 studies representing 47 trials in psychological interventions reported attrition data. 53,55,62,64,66,69,71,76,78,79,81,83,84,86–92,94–96,98,100,105–109,111,115,121,125,126,128,131,132,135–140,144,145 Thirteen RCTs reported attrition data for pharmacological interventions. 56,58,72,73,82,84,85,99,104,110,118,127,141 We conducted meta-analyses to investigate the odds of attrition from psychological and pharmacological interventions. Owing to a subset of trials reporting zero attrition, ORs were not calculable for eight trials;88–91,94,111,125,138 therefore, these were excluded from the analyses presented. The comparisons meta-analysed for odds of attrition from psychological interventions were considered two ways:
-
psychological interventions versus control for all populations combined, reported by intervention category
-
all psychological interventions versus control, reported by trauma experience.
All pharmacological interventions included in this analysis were in veteran populations, with the exception of one study in individuals with a history of childhood sexual abuse;127 therefore, veterans-only pharmacological intervention attrition meta-analyses were undertaken (see Veterans).
Intervention categories
Trauma-focused cognitive–behavioural therapy
Twenty-one studies (n = 1557)55,62,66,79,81,83,86,87,92,96,100,105–107,109,126,128,136,140,144 reported attrition figures in trauma-focused CBT across all populations, and indicated participation in a trauma-focused CBT intervention was significantly associated with a reduction in the odds of dropout compared with controls (Figure 23).
FIGURE 23.
Meta-analysis of ORs of attrition for trauma-focused CBT interventions compared with control. CETA, common elements treatment approach; CPT, cognitive treatment therapy.
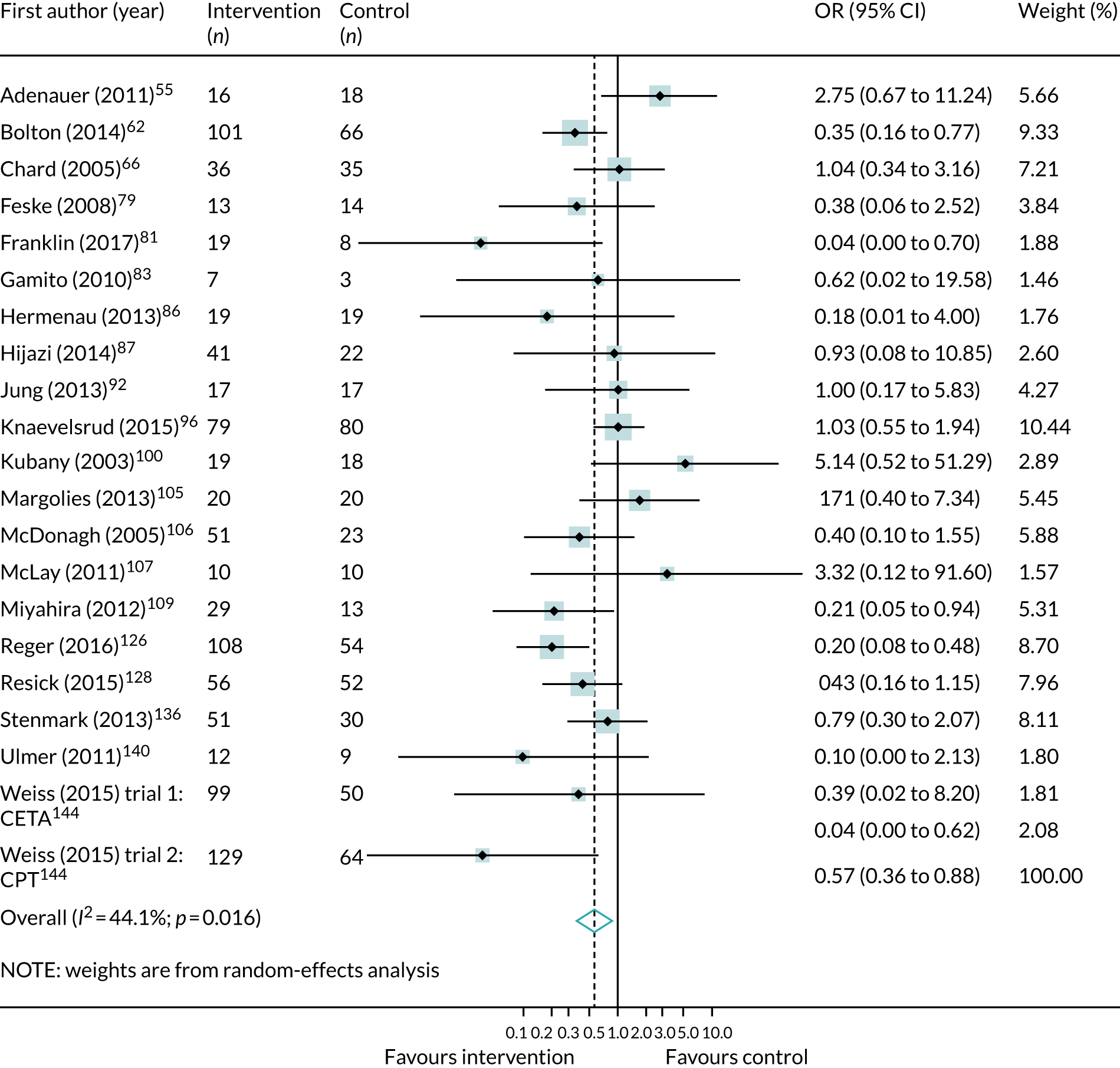
Four trials stood out owing to ORs that favoured increased attrition from the intervention; these had smaller sample sizes (< 20 participants per arm) and did not have a common trauma population (including veterans,105,107 domestic violence populations100 and refugees55).
Eye movement desensitisation and reprocessing
Few controlled EMDR trials reported attrition data (three trials, n = 179). 53,64,76 All favoured increased odds of attrition in the intervention group, with a non-significant pooled estimate suggesting uncertainty (OR 1.79, 95% CI 0.79 to 4.07; I2 = 0.0%). Trials included within this analysis were each from different populations (refugees,53 veterans64 and those with a history of childhood sexual abuse76).
Mindfulness
There were also few mindfulness trials reporting attrition (three trials, n = 141). 57,95,121 The pooled estimate suggested that the odds of attrition of individuals in mindfulness interventions were one-third those of individuals on a waitlist, but this finding did not reach significance (OR 0.29, 95% CI 0.05 to 1.74; n = 141). There was also moderate heterogeneity in the sample with the CI including 1, suggesting mindfulness interventions could also have greater odds of attrition than waitlists.
Non-trauma-focused cognitive–behavioural therapy
There were insufficient data comparing non-trauma-focused CBT with an inactive control to perform analyses.
Trauma populations
Meta-analyses were carried out according to each intervention category within populations in which there were multiple studies present. The results for each of these can be found in Appendix 10. The following sections give the results of attrition from any psychological intervention within each population and highlight notable contrasts due to the sparsity of data in grouped meta-analyses.
Veterans
Twelve trials (n = 616)66,78,81,83,95,105–107,109,121,128,157 were included in this meta-analysis, which compared psychological intervention with a control (see Appendix 10, Figure 102). Veterans receiving any psychological intervention had less than half the odds of attrition as those on a waitlist (OR 0.49, 95% CI 0.26 to 0.92; I2 = 41.8%), a statistically significant result. This suggests that it is likely that psychological therapies experience favourable dropout in comparison with waitlists or non-interventions in veteran populations.
Four trials (n = 225) compared psychological interventions with an active control71,84,115,137 and also showed reduced attrition among veterans receiving psychological intervention (OR 0.34, 95% CI 0.17 to 0.68; I2 = 0.0%; see Appendix 10, Figure 103).
Pharmacological interventions
A sufficient number of pharmacological trials in veterans reported attrition to analyse the odds of dropout in antidepressant intervention, including three studies of SSRIs82,118,141 (OR 0.56, 95% CI 0.29 to 1.07; I2 = 24.9%; four studies, n = 345; see Appendix 10, Figure 104)73,82,118,141 and antipsychotics (OR 0.46, 95% CI 0.14 to 1.56; I2 = 56.5%; four studies, n = 414; see Appendix 10, Figure 105). 58,85,99,110 Two studies reported attrition for the use of anticonvulsants72,104 (see Appendix 10, Figure 106).
Although all had an OR that favoured reduced attrition in the intervention group, none was significant.
Childhood sexual abuse
Based on five trials (n = 414),69,92,98,131,140 individuals with experience of childhood sexual abuse and receiving psychological therapy had almost one-quarter the odds of dropout as inactive controls (OR 0.24, 95% CI 0.08 to 0.75; I2 = 26.5%; see Appendix 10, Figure 107). Three of the five studies in the analysis were also phased based. 69,98,140
One trial reported attrition data for a pharmacological intervention, comparing antipsychotics with placebo; therefore, an OR was not calculated for these data. 127
Refugee populations
Evidence for attrition in refugee populations was mixed. Five studies (n = 298)53,55,87,108,136 were associated with psychological intervention having greater odds of attrition than controls, a finding that was not significant (OR 1.21, 95% CI 0.69 to 2.12; I2 = 0.0%; see Appendix 10, Figure 108). Across trials, odds were not consistent in favouring increased or decreased odds of attrition, resulting in a wide CI for the pooled estimate.
Domestic violence
There were only two studies on psychological interventions for individuals exposed to domestic violence. 62,100 Both investigated individual therapies and they had opposing directions of effect for attrition (see Appendix 10, Figure 109).
War-affected populations
Six trials of psychological interventions gave a pooled OR that suggested reduced attrition for psychological intervention (when compared with inactive controls) in war-related trauma populations (OR 0.66, 95% CI 0.27 to 1.60; I2 = 36.7%; n = 695). 57,86,96,144,145 However, the CI includes 1, while an equivalent number of trials favour both reduced and increased odds of attrition. There is large uncertainty as regards the direction of effect, despite low to moderate heterogeneity (see Appendix 10, Figure 110).
Meta-regression analyses: predictors of treatment effectiveness
We conducted meta-regression analyses for any validated trauma outcome measure (using SMDs) and in all populations.
Model 1: predictors of treatment effectiveness by population type
Table 2 shows the results of the univariable analyses. Interventions delivered in studies that included veterans were less likely to be effective than interventions delivered in studies in other populations. In addition, interventions delivered in studies that included people who had experienced domestic violence were more effective than studies that included other populations. However, there were few studies of people exposed to domestic violence and therefore it is unclear if further studies will consistently show greater effectiveness for people who have experienced domestic violence.
| Populations | Coefficient (standard error) | p-value |
|---|---|---|
| Veterans | 0.56 (0.23) | 0.02 |
| Childhood sexual abuse | –0.04 (0.30) | 0.89 |
| Refugees | –0.36 (0.28) | 0.21 |
| Domestic violence | –2.19 (0.52) | < 0.001 |
| War affected | 0.25 (0.45) | 0.59 |
In multivariable analyses both remained statistically significant: studies of veterans [coefficient 0.41, standard error (SE) 0.20; p = 0.049] and studies of people experiencing domestic violence (coefficient –2.01, SE 0.51; p < 0.001). The multivariable model was statistically significant [F2,42 = 11.51; p < 0.001) and explained some of the heterogeneity (adjusted R2 = 38.96%); however, a substantial proportion of heterogeneity remained unexplained (I2 residual = 79%).
Model 2: predictors of treatment effectiveness by intervention components
When covariates for intervention content were assessed, only imaginal exposure was found to have a statistically significant association with effectiveness, but psychoeducation had a borderline statistically significant effect (Table 3). Therefore, both covariates were included in the multivariable analysis; psychoeducation was no longer statistically significant (coefficient –0.39, SE 0.23; p = 0.1) and imaginal exposure was borderline statistically significant (coefficient –0.44, SE 0.24; p = 0.07). The multivariable model as a whole was statistically significant (F2,42 = 3.88; p = 0.03) and explained some of the heterogeneity (adjusted R2 = 15.78%), but a substantial proportion of heterogeneity remained unexplained (I2 residual = 81.19%).
| Components | Coefficient (SE) | p-value |
|---|---|---|
| Support | –0.12 (0.33) | 0.71 |
| Psychoeducation | –0.47 (0.23) | 0.052 |
| Relaxation | –0.06 (0.27) | 0.83 |
| Mindfulness | –0.13 (0.36) | 0.73 |
| Cognitive | –0.03 (0.25) | 0.91 |
| In vivo exposure | –0.04 (0.45) | 0.92 |
| Virtual reality exposure | 0.36 (0.49) | 0.47 |
| Imaginal exposure | –0.51 (0.24) | 0.04 |
| Phased based | –0.36 (0.37) | 0.33 |
Model 3: treatment effectiveness by delivery method
Studies that tested individually delivered interventions reported improved outcomes compared with studies that tested interventions delivered in a group (Table 4). Since almost all interventions were delivered face to face, it was not possible to confirm if there was a difference in effectiveness compared with other modalities. There was no evidence that the duration of intervention had an impact on effectiveness.
| Delivery method | Coefficient (SE) | p-value |
|---|---|---|
| Face to face vs. other | –0.47 (0.39) | 0.74 |
| Individual vs. group | –0.67 (0.28) | 0.02 |
| < 12 weeks vs. 12 weeks | 0.12 (0.32) | 0.70 |
| > 12 weeks vs. 12 weeks | 0.20 (0.44) | 0.66 |
Only studies that used individually delivered psychological interventions were statistically significantly associated with greater effectiveness compared with group-delivered psychological interventions explaining a small proportion of the heterogeneity (adjusted R2 = 12.72%; I2 residual = 81.54%). No multivariable analyses were conducted.
Components network meta-analyses
We fitted four models to assess the impact of different combinations of interventions on reducing trauma. Owing to the instability of models when assessing different trauma scales combined, we conducted all analyses on the CAPS (the most frequently reported trauma scale). Figure 24 shows all of the combinations of intervention components extracted from the studies included. The thickness of the lines for each node are weighted by the number of studies (i.e. the thicker the line, the more studies comparing a particular combination of components with an active control or a waitlist).
FIGURE 24.
Network plot for all combinations of components extracted from the studies included.
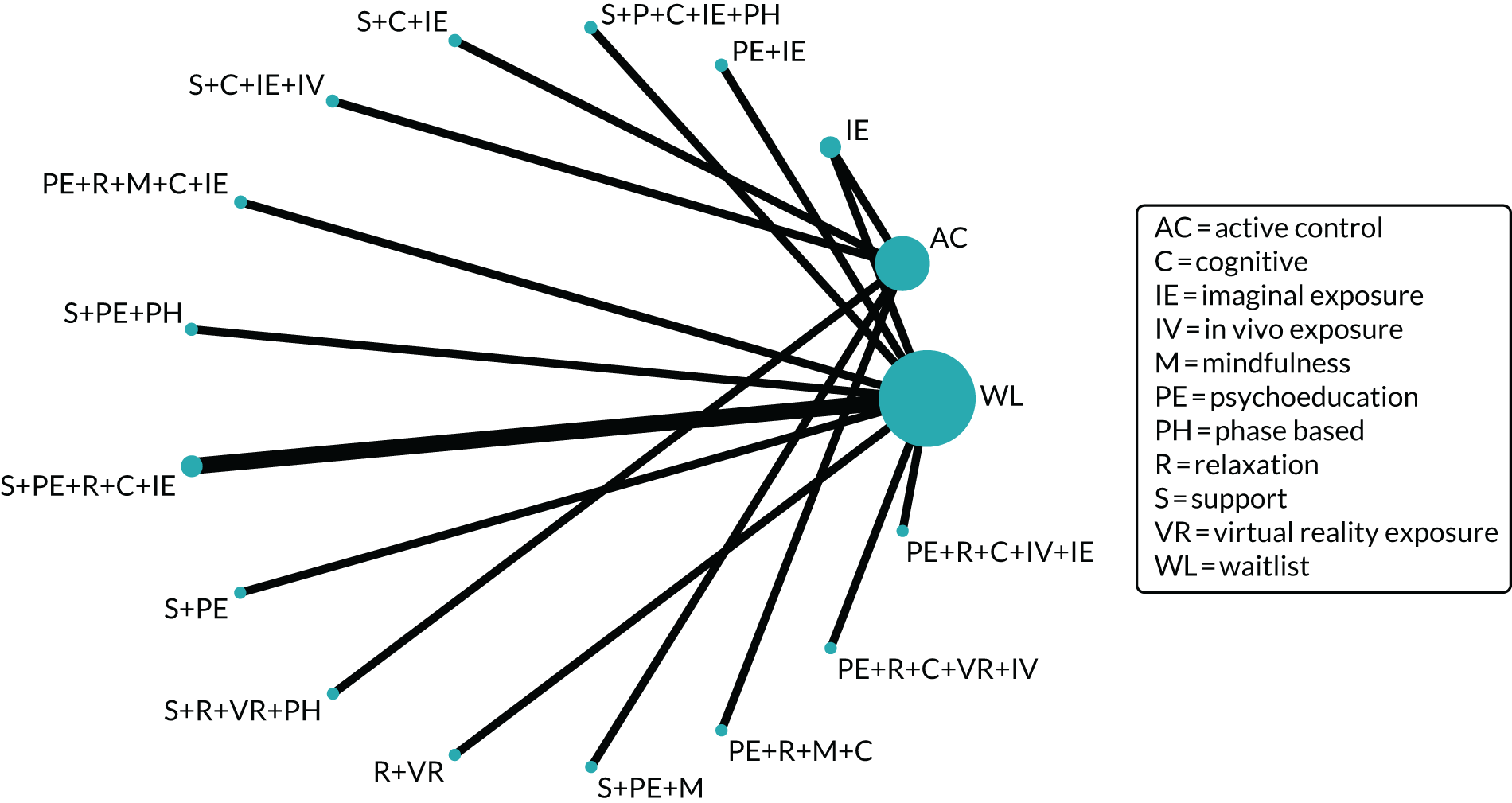
Model selection
Models 1, 2 and 4 did not fit the data well, reflected by the very high total residual deviance found for each of these models. Model 3 had an acceptable goodness of fit (total residual deviance = 36.33) and the DIC was substantially lower than in other models. Therefore, further analyses were conducted using model 3 (Table 5).
| Model | Posterior mean deviance | DIC | Total residual deviance | τ |
|---|---|---|---|---|
| Model 1: waitlist, active control, trauma-focused CBT, EMDR, mindfulness, DBT, IPT | 25.72 | 252.99 | 70.03 | 0.043 |
| Model 2: waitlist, placebo, support, psychoeducation, relaxation, cognitive restructuring, in vivo exposure, imaginal exposure, virtual reality exposure, mindfulness, phased based | 28.60 | 267.93 | 70.57 | 0.042 |
| Model 3: waitlist, placebo, support, psychoeducation, relaxation, cognitive restructuring, in vivo exposure, imaginal exposure, virtual reality exposure, phased based, support + psychoeducation, psychoeducation + relaxation, psychoeducation + cognitive restructuring, psychoeducation + imaginal exposure, relaxation + mindfulness, relaxation + cognitive restructuring, relaxation + imaginal exposure | 30.94 | 235.45 | 36.33 | 0.13 |
| Model 4: full interaction model | 30.56 | 264.89 | 66.09 | 0.04 |
Findings from the intervention component network meta-analysis (model 3)
The intervention components with evidence of effectiveness and sufficiently precise credible intervals were mindfulness, cognitive restructuring, phase-based approaches, relaxation + imaginal exposure and relaxation + cognitive restructuring (Table 6).
| Intervention component | Mean difference vs. waitlist (95% CI) |
|---|---|
| Active control | –0.07 (–61.71 to 62.21) |
| Placebo | –27.6 (–57.76 to 2.60) |
| Support | 16.78 (–13.07 to 47.08) |
| Psychoeducation | –0.24 (–30.23 to 29.76) |
| Relaxation | 24.32 (–12.12 to 60.56) |
| Mindfulness | –32.22 (–53.18 to –10.52) |
| Cognitive restructuring | –39.24 (–54.05 to –23.88) |
| Virtual reality exposure | –8.6 (–42.08 to 25.84) |
| Imaginal exposure | –1.18 (–32.16 to 29.76) |
| Phased based | –26.95 (–41.59 to –11.96) |
| In vivo exposure | 14.45 (–32.74 to 61.39) |
| Support + psychoeducation | 21.3 (–10.29 to 52.64) |
| Psychoeducation + relaxation | 32.09 (–6.64 to 70.77) |
| Psychoeducation + cognitive restructuring | 10.56 (–8.07 to 29.29) |
| Psychoeducation + imaginal exposure | 18.28 (–13.0 to 49.48) |
| Relaxation + mindfulness | 28.03 (–17.44 to 73.86) |
| Relaxation + cognitive restructuring | –28.29 (–47.56 to –8.79) |
| Relaxation + imaginal exposure | –45.34 (–70.86 to –19.52) |
| Mindfulness + cognitive restructuring | 28.41 (–16.96 to 74.14) |
| Cognitive restructuring + in vivo exposure | 14.31 (–32.8 to 61.41) |
| In vivo exposure + imaginal exposure | 15.42 (–18.72 to 49.73) |
Acceptability sensitivity analyses
Estimates of attrition in intervention and control groups are likely to be effected by both the acceptability of the intervention and attrition bias. To try to disentangle these factors, we conducted sensitivity analyses including only studies judged to be at a low risk of attrition bias. Table 7 shows the OR of attrition for psychological interventions compared with controls, as presented in Trauma populations earlier, and the OR of attrition for psychological interventions compared with controls for only those trials graded as at a low risk of attrition bias.
| Population | OR (95% CI) | |
|---|---|---|
| All studies | Low risk of attrition bias | |
| All | 0.56 (0.40 to 0.80) | 0.39 (0.21 to 0.73) |
| Veterans | 0.49 (0.26 to 0.92) | 0.44 (0.06 to 3.54) |
| Childhood sexual abuse | 0.24 (0.08 to 0.75) | 0.18 (0.03 to 1.00) |
| Refugee | 1.21 (0.69 to 2.12) | 2.10 (0.62 to 7.14) |
| Domestic violence | Insufficient data | Insufficient data |
| War affected | 0.66 (0.27 to 1.60) | 0.11 (0.01 to 1.27) |
| Mixed | Insufficient data | Insufficient data |
Overall, studies with a low risk of attrition bias were associated with reduced odds of dropout from psychological interventions in comparison with controls in all populations combined (14 trials). 55,62,64,78,87,92,98,121,126,131,132,140,144 This trend was seen across trauma experiences (when data were available), although differences between interventions and controls were not always statistically significant. The exception was refugee populations, in which people assigned to psychological interventions were more likely to drop out than those in controls.
Trauma populations that demonstrated a reduced likelihood of dropout in psychological interventions saw a further decrease in the likelihood of dropout when considering only those trials with a low risk of attrition bias. These populations were veterans (three trials),64,78,121 childhood sexual abuse populations (four trials)92,98,131,140 and war-affected populations (two trials),144 but none was statistically significant. In the case of veterans and childhood sexual abuse populations, the reduced odds of dropout were statistically significant when considering trials of all risk-of-bias gradings. Therefore, the lack of statistical significance is most likely explained by the reduced statistical power resulting from including only a subset of the data.
In refugee populations, the odds of dropout from psychological interventions were greater than from controls and increased when considering only those trials with a low risk of attrition bias (based on two trials);55,87 however, neither of the pooled ORs was statistically significant.
Adverse events for pharmacological interventions
All of the data relating to adverse events and pharmacological interventions were collated (Table 8). All reporting of further information regarding reasons for withdrawal and adverse events were from veteran populations. Withdrawal owing to adverse events was common across studies, but with relatively small numbers. Practical issues resulting in withdrawal were more frequently reported; there was insufficient detail to infer acceptability from this.
| Intervention category | Authors (year), population | Reasons for withdrawal | Adverse events |
|---|---|---|---|
| Antidepressants (including SSRIs) | Becker et al. (2007),59 veterans | Bupropion and control overall: allergic reaction (n = 1), transportation difficulties (n = 1), no further interest (n = 1), lost to contact (n = 2) | Overall: allergic reaction (n = 1) |
| Chung et al. (2004),67 veterans |
Mirtazapine: lack of efficacy (n = 3), personal reasons (n = 3), side effects (n = 1) Sertraline: lack of efficacy (n = 5), personal reasons (n = 1) |
NR | |
| Davis et al. (2004),73 veterans |
Nefazodone: adverse effects (n = 5), medication ineffective (n = 2), lost to follow-up (n = 4), non-compliance (n = 1) Placebo: adverse effects (n = 1), medication ineffective (n = 2), lost to follow-up (n = 1), no reason given (n = 2) |
Nefazodone: drowsiness, dizziness, agitation, gastrointestinal distress, fatigue, orthostatic hypotension, headaches Placebo: insomnia, irritability |
|
| Panahi et al. (2011),118 veterans |
Sertraline: adverse events (n = 2), protocol violation (n = 1) Placebo: adverse event (n = 1), protocol violation (n = 2), other (of own accord) (n = 2) |
Sertraline: headache (31%), insomnia (31%), nausea (31%), restlessness (25%), diarrhoea (22%), dry mouth (19%), drowsiness (16%), asthenia (16%), decreased appetite (16%), constipation (16%), decreased libido (13%) Placebo: headache (20%), insomnia (13%), nausea (17%), restlessness (17%), diarrhoea (13%), dry mouth (17%), drowsiness (7%), asthenia (7%), decreased appetite (10%), constipation (10%), decreased libido (7%) |
|
| Zohar et al. (2002),147 veterans | NR |
Sertraline: nausea (35%), headache (26%), drowsiness (26%), asthenia (17%), increased appetite (13%), dry mouth (13%), decreased appetite (13%) Placebo: nausea (21%), headache (16%), drowsiness (16%), asthenia (15%), increased appetite (10%), dry mouth (10%), decreased appetite (5%) |
|
| Antipsychotics | Bartzokis et al. (2005),58 veterans |
Risperidone: adverse effects (n = 11), unrelated medical condition (n = 1), alcohol abuse (n = 1), discontinuing medication (n = 1), lost to follow-up (n = 5) Placebo: adverse effects (n = 6), alcohol abuse (n = 1), lost to follow-up (n = 3) |
NR |
| Monnelly et al. (2003),110 veterans | Risperidone: episode of urinary retention (n = 1) |
Risperidone: mild adverse event (n = 4) Placebo: mild adverse event (n = 2), moderate adverse event (n = 1) |
|
| Stein et al. (2002),135 veterans |
Olanzapine: (early protocol terminations) somnolence (n = 2), unspecified (n = 1) Placebo: lack of efficacy (n = 1) |
Olanzapine: weight gain change of +13.2 lb (SD 5.9 lb) Placebo: –3 lb (SD 6.5 lb) |
|
| Anticonvulsants | Davis et al. (2008),72 veterans |
Divalproex: adverse events (n = 3), serious but unrelated adverse event (n = 1), failure to return (n = 2), lost to follow-up (n = 4) Placebo: adverse event (n = 1), lack of efficacy (n = 1), lost to follow-up (n = 4) |
NR |
| Lindley et al. (2007),104 veterans |
Topiramate: adverse events (n = 6), clinician withdrew because of adverse event (n = 2), significant worsening of symptoms (n = 1), left residential treatment (n = 1), discharged by clinical staff owing to behaviour (n = 1) Placebo: adverse event (n = 1), clinician withdrew because of adverse event (n = 1), left residential treatment (n = 12), discharged by clinical staff owing to behaviour (n = 1) |
Topiramate: reported in 17 patients Placebo: reported in 16 patients |
|
| Prazosin | Raskind et al. (2013),123 veterans |
Prazosin: adverse event (n = 1), opted for open-label prazosin (n = 1), too busy (n = 1), lost contact (n = 1) Placebo: opted for open-label prazosin (n = 1), too busy (n = 2), lost contact (n = 3) |
Prazosin: hospitalisation for suicidal ideation (n = 1), suicide attempt with non-lethal overdose of oxycodone/acetaminophen (n = 1); syncope (3%), light-headedness (25%), nasal congestion (22%), palpitations (6%), drowsiness (3%), muscle weakness (3%), headaches (3%) Placebo: light-headedness (20%), nasal congestion (11%), lack of energy (3%), palpitations (3%), drowsiness (9%), depression (6%), headaches (23%) |
Non-randomised studies of clinical effectiveness
Post-traumatic stress disorder symptoms
Six of the nine non-randomised studies reported PTSD outcomes. 148–150,152,155,156 Effect sizes were calculated for four of these studies (representing five interventions), as they used inactive control comparators (Table 9). 149,152,155,156
| Authors (year) | Population | Intervention (category) | Control | Scale | Post-treatment effect, SMD (95% CI) | n |
|---|---|---|---|---|---|---|
| Kruse et al. (2009)149 | Refugees | Trauma-focused psychotherapy (non-trauma-focused CBT) | Treatment as usual | HTQ | –2.54 (–3.21 to –1.88) | 64 |
| Morgan and Cummings (1999)152 | Childhood sexual abuse | Group therapy (multicomponent trauma-focused intervention) | No intervention | DSM-III subscales | –0.18 (–0.62 to 0.26) | 80 |
| Salo et al. (2008)155 | War affected | Individual therapy (trauma-focused CBT) | Waitlist | HTQ: re-experiencing | 0.00 (–0.50 to 0.50) | 95 |
| HTQ: avoidance | –1.22 (–1.75 to –0.69) | 95 | ||||
| HTQ: hyperarousal | –1.50 (–2.04 to –0.95) | 95 | ||||
| Group therapy (multicomponent non-trauma-focused intervention) | HTQ: re-experiencing | 0.32 (–0.18 to 0.81) | 96 | |||
| HTQ: avoidance | 2.66 (2.04 to 3.28) | 96 | ||||
| HTQ: hyperarousal | 0.74 (0.24 to 1.25) | 96 | ||||
| Saxe and Johnson (1999)156 | Childhood sexual abuse | ‘Victim to survivor’ group therapy (trauma-focused CBT) | No intervention | IES intrusion subscale | –0.09 (–0.58 to 0.41) | 63 |
| IES avoidance subscale | –1.01 (–1.53 to –0.48) | 63 |
Trauma-focused interventions
Two studies in trauma-focused CBT saw a significant reduction in PTSD avoidance symptoms. 155,156 One study investigated ‘victim to survivor’ group therapy in a childhood sexual abuse population156 (SMD –1.01, 95% CI –1.53 to –0.48; n = 63) and the other investigated individual therapy in a war-affected population155 (SMD –1.22, 95% CI –1.75 to –0.69; n = 95). Individual therapy in a war-affected population also showed a large and significant effect in reducing PTSD hyperarousal symptoms (SMD –1.50, 95% CI –2.04 to –0.95; n = 95), but was equivalent to the waitlist at reducing PTSD re-experiencing symptoms. 155
One study examined a multicomponent trauma-focused intervention delivered in a group format to a childhood sexual abuse population. 152 A small reduction in PTSD symptoms was found, but this was not significant.
Non-trauma-focused interventions
Non-trauma-focused CBT was investigated in one study in a refugee population and showed a large and significant effect favouring group intervention for reducing PTSD symptoms (SMD –2.54, 95% CI –3.21 to –1.88; n = 64). 149
Multicomponent non-trauma-focused therapy was investigated in just one study of war-affected individuals155 and showed significant effects favouring controls for PTSD hyperarousal (SMD 0.74, 95% CI 0.24 to 1.25; n = 96) and avoidance symptoms (SMD 2.66, 95% CI 2.04 to 3.28; n = 96). A small, insignificant effect on PTSD re-experiencing symptoms also favoured the control group.
Head-to-head comparisons
Two148,150 of the non-randomised studies reporting PTSD outcomes were head-to-head comparisons conducted in veteran populations.
One comparison of trauma-focused CBT versus psychodynamic psychotherapy reported a significant reduction in PTSD symptoms (clinician- and patient-rated), with no significant difference between interventions. 150
A comparison of mindfulness-based cognitive therapy with a mixed comparator of active interventions reported a significant reduction in PTSD symptoms for those undergoing mindfulness-based cognitive therapy, but not the mixed comparator. 148
Depression
Five non-randomised studies150–153,156 reported depression outcomes. Of these, four studies150–152,156 used inactive comparators. Effect sizes were calculated for three studies (constituting four interventions); outcome reporting prohibited this for one study,153 so it is described as published (Table 10).
| Authors (year) | Population | Intervention | Control | Scale | Post-treatment effect, SMD (95% CI) | n |
|---|---|---|---|---|---|---|
| Lundqvist et al. (2006)151 | Childhood sexual abuse | Group therapy (trauma-focused CBT) | Waitlist | SCL-90: depression | –0.31 (–1.00 to 0.38) | 52 |
| Short-term therapy (trauma-focused CBT) | SCL-90: depression | 0.11 (–0.66 to 0.89) | 28 | |||
| Morgan and Cummings (1999)152 | Childhood sexual abuse | Group therapy (multicomponent trauma-focused intervention) | No intervention | BDI | –0.43 (–0.88 to 0.01) | 80 |
| Saxe and Johnson (1999)156 | Childhood sexual abuse | ‘Victim to survivor’ group therapy (trauma-focused CBT) | Waitlist | BDI | –1.53 (–2.09 to –0.97) | 63 |
| CES-D | –1.19 (–1.73 to –0.65) | 63 |
Trauma-focused interventions
All studies for which SMDs were calculated were trauma-focused interventions, delivered in a group format, to childhood sexual abuse populations.
Two studies reported depression outcomes for three trauma-focused CBT interventions. In one study,151 a short-term therapy demonstrated an insignificant and small effect of increasing depression (compared with control); the same study found an insignificant and small effect of group therapy reducing depression. Another study156 of trauma-focused CBT in group therapy showed a large and significant effect for decreasing depression symptoms on two scales: the Beck Depression Inventory (–1.53, 95% CI –2.09 to –0.97; n = 63) and the Center for Epidemiologic Studies Depression Scale (–1.19, 95% CI –1.73 to –0.65; n = 63).
Based on one study,152 multicomponent trauma-focused group therapy was associated with a moderate treatment effect in favour of a reduction of depression and this was of borderline significance (SMD –0.43, 95% CI –0.88 to 0.01; n = 80).
In one study,153 a SMD was not calculated owing to outcome reporting. This compared both EMDR and trauma-focused CBT with a control in a war-affected population. The reported results stated that both interventions significantly reduced depression symptoms with no significant difference between EMDR and CBT, suggesting effectiveness.
Head-to-head comparisons
One study150 reported a direct comparison of trauma-focused CBT with psychodynamic therapy in veterans. A significant reduction in depression symptoms was reported following treatment, with equivalent effectiveness between therapies.
Anxiety
One151 of the nine non-randomised studies included in this review reported anxiety outcomes for two interventions. The findings are presented in Table 11.
| Authors (year) | Population | Intervention | Control | Scale | Post-treatment effect, SMD (95% CI) | n |
|---|---|---|---|---|---|---|
| Lundqvist et al. (2006)151 | Childhood sexual abuse | Group therapy (trauma-focused CBT) | Waitlist | SCL-90 anxiety | –0.16 (–0.85 to 0.53) | 52 |
| Short-term therapy (trauma-focused CBT) | SCL-90 anxiety | 0.16 (–0.62 to 0.93) | 28 |
Trauma-focused interventions
Two trauma-focused CBT interventions were both compared with control in a childhood sexual abuse population. 151 Group therapy was associated with a small reduction in anxiety symptoms, while short-term therapy was associated with a small increase compared with control. Neither finding was significant.
Quality of life
None of the non-randomised studies included reported quality-of-life outcomes.
Sleep quality
None of the non-randomised studies included reported sleep quality outcomes.
Attrition
Six148–151,155,156 of the non-randomised trials included reported attrition data for eight comparisons. All were compared with a control group, with the exception of one active control trial148 and one head-to-head comparison. 150 ORs were calculated for all controlled trials and are presented in Table 12.
| Authors (year) | Trauma population | Intervention category vs. control | OR of attrition (95% CI) | n |
|---|---|---|---|---|
| Kruse et al. (2009)149 | Refugees | Non-trauma-focused CBT | 2.06 (0.19 to 23.83) | 70 |
| Lundqvist et al. (2006)151 | Childhood sexual abuse | (Group) trauma-focused CBT | 0.58 (0.03 to 12.08) | 55 |
| (Short-term) trauma-focused CBT | 0.20 (0.01 to 4.01) | 32 | ||
| Salo et al. (2008)155 | War affected | Trauma-focused CBT | 0.02 (0.00 to 0.36) | 106 |
| Multicomponent non-trauma-focused intervention | 0.00 (0.00 to 0.08) | 106 | ||
| Saxe and Johnson (1999)156 | Childhood sexual abuse | Trauma-focused CBT | 0.51 (0.16 to 1.61) | 108 |
Only one trial,155 investigating two interventions, reached significance. There was a reduced likelihood of dropout in both the trauma-focused CBT and the multicomponent non-trauma-focused intervention compared with control in a war-affected population.
Three trauma-focused CBT interventions in a childhood sexual abuse population had reduced odds of attrition among those receiving the intervention, but large CIs resulting in uncertain estimates. 151,156 A non-trauma-focused CBT intervention in a refugee population showed increased odds of dropout among those receiving the intervention compared with those in the control; this finding also had wide CIs and was not significant. 149
Chapter 5 Results of the qualitative acceptability review
Studies included
In total, 1609 titles and abstracts were screened and 1560 were excluded. In addition, 49 full-text papers were screened and 41 were excluded, with the reasons summarised in Figure 25. We included nine papers, constituting eight unique studies, that were found to use qualitative methods or a mixed-methods approach with a strong qualitative component. Qualitative components included data collection using interviews (unstructured or semistructured) and focus groups, and the data were analysed following a qualitative methodology, with methods such as thematic analysis, ethnography or a phenomenological approach.
FIGURE 25.
The PRISMA diagram of the flow of records through the review process.
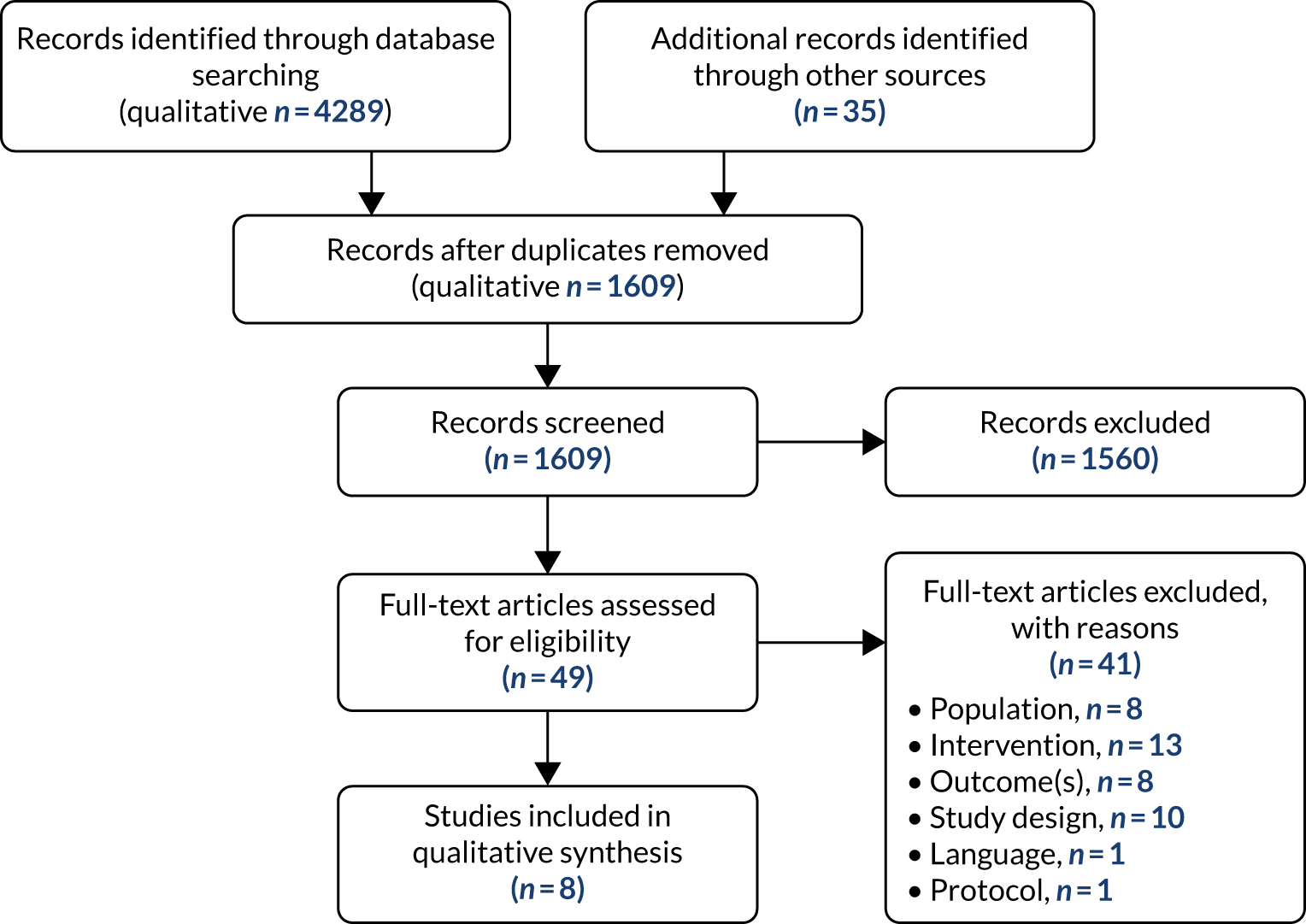
Of the studies selected for inclusion in the qualitative review, the majority were from North America (n = 7); two studies were performed in Canada but most of the research was performed in the USA (n = 5). The other studies were performed in Bangladesh (n = 1) and the UK (n = 1).
In terms of the types of trauma that participants were exposed to, four studies involved participants exposed to intimate partner violence,161–164 of which two are linked. 163,164 Two studies involved veterans,165,166 two studies involves participants exposed to childhood sexual abuse167,168 and one study involved asylum seekers. 169
The intervention classifications include group mindfulness-based stress reduction (MBSR; n = 3163–165), motivational interviewing (n = 1162), prolonged exposure (n = 1166), mental health counselling (n = 1161), group healing or group treatments (n = 2167,168) and trauma-focused CBT (n = 2166,169), which, in one case, was a combined treatment with prolonged exposure (n = 1166). Table 13 provides details of all of the studies included.
| Research question | Authors (year) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Hundt et al. (2017)166 | Martinez et al. (2015)165 | aBermudez et al. (2013)163 | aDutton et al. (2013)164 | Hughes and Rasmussen (2010)162 | Naved et al. (2009)161 | Palmer et al. (2007)167 | Parker et al. (2007)168 | Vincent et al. (2013)169 | |
| 1. Was there a clear statement of the aims of the research? | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 2. Was a qualitative methodology appropriate? | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 3. Was the research design appropriate to address the aims of the research? | Y | Y | Y | Y | Y | C | Y | Y | Y |
| 4. Was the recruitment strategy appropriate to the aims of the research? | Y | Y | Y | Y | N | N | C | Y | Y |
| 5. Were the data collected in a way that addressed the research issue? | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 6. Has the relationship between researcher and participants been adequately considered? | C | C | C | Y | Y | Y | Y | Y | C |
| 7. Have ethical issues been taken into consideration? | Y | Y | Y | C | Y | Y | C | Y | Y |
| 8. Was the data analysis sufficiently rigorous? | Y | Y | Y | Y | C | C | Y | Y | C |
| 9. Is there a clear statement of findings? | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 10. How valuable is the research? | Score 8.5 | Score 8.5 | Score 8.5 | Score 8.5 | Score 7.5 | Score 7.5 | Score 8.0 | Score 9.0 | Score 8.0 |
Quality of the studies included: Critical Appraisal Skills Programme assessment
Methodological limitations were assessed with the CASP qualitative checklist to facilitate the assessment of both study design and implementation, as described in the GRADE-CERQual recommendations. 51 The studies included were assessed for methodological limitations using a modified version of the CASP in which the individual elements for the quality assessment (see Table 13 for the CASP checklist) were used in conjunction with a scoring system. A full score of 9.0 for the CASP assessment allowed a CERQual score of ‘no concerns’ as regards the methodological limitations of the studies included, as well as the relevance and coherence of data with regard to integration across the review themes.
The majority of the studies were allocated less than the maximum score of 9.0, as information was not clearly apparent in the methods of the paper. This contributed to a CERQual assessment of ‘minimal concerns’ for the integration of research findings for this review. When no score was given, the CERQual score was registered as ‘significant concerns’; the only instance of this was attributed to selection bias for the participant selection, as many studies experienced difficulties in recruiting participants and, as such, studies enrolled a small number of participants or a convenience sample.
Table 13 presents the findings of the CASP assessment and the tables in Appendix 9 provides additional information on the study details and their methodological assessments.
Narrative synthesis
All of the studies included offered in-depth accounts of service user experiences of psychological interventions either delivered in health- or social-care or settings or by voluntary agencies. Population subgroups included veterans, people with a history of childhood sexual abuse, people with a history of domestic violence and asylum seekers. Using acceptability and feasibility as organising meta-themes, we identified three core subthemes across these populations:
-
therapeutic context
-
skills strengthening
-
self-efficacy and reward.
Therapeutic context
Group-based therapies
This theme captured data that spoke to service users’ perspectives on the merits of engaging in therapeutic interventions in groups and how feasibly these group-based approaches aligned with the therapeutic orientation and goals of the intervention. For non-trauma-focused interventions such as mindfulness, there was an understanding that delivering interventions in groups was potentially a safe and advantageous way to connect with others who have had similar traumatic experiences without fear of re-traumatisation. This was especially true of women with a history of domestic violence: ‘Having had common traumas made it easy to relate to other participants. I was able to revisit traumatic situations without judgement.’163
However, this perspective was not universally shared, with a contrary finding among veterans, whose overall perception of mindfulness was positive but was layered with misgivings about taking part in groups. For some participants, groups were less acceptable because their PTSD symptom profile made them feel ‘uncomfortable in groups’, with the risk that interactions with other group members were counterproductive to the therapeutic goals of achieving serenity and non-judgemental self-awareness: ‘I had such issues with certain people and one of them couldn’t sit still. I would turn around and he kept staring at me. I was not comfortable.’165
Women with a history of childhood sexual abuse also voiced similar concerns about the negative impact of taking part in groups as part of more trauma-focused interventions:
[I] found it hard to break through the barriers that I’d already set up . . . a lot of trust issues with the group . . . I was still just breaking the ice . . . about my sexuality . . . I saved it right up to the very last day.
Palmer et al. 167
The idea that group approaches were not always an acceptable platform to engage people with complex trauma histories was also linked to concerns that group-based activities that focused on trauma experiences risked re-traumatising participants: ‘I would come out of [the process groups] exhausted, even if I didn’t say anything . . . just listening to other people’s stories was very draining.’167
Scheduling and setting
Another key feature of the therapeutic context that underpinned perceptions about the acceptability and feasibility of interventions was that scheduling and the setting of treatments were important determinants of participants’ satisfaction and engagement with therapy. Veterans that were signed up to mindfulness noted that scheduling could be a practical barrier to attendance. 165 More critically, among women with a history of domestic violence, there were widely voiced concerns that waiting times and the length of treatment sessions for counselling could increase the risk of further abuse at home if they returned late. 161 This highlighted the importance of providing treatment in a safe and caring environment that offered participants sanctuary and the security to engage in treatment, as reported by women with a history of domestic violence who were given classes in motivational interviewing at a shelter: ‘You deserve the caring, and you deserve to be treated well.’162
The need for additional wraparound care to help facilitate engagement with treatment was especially salient among women exposed to domestic violence who had children and felt frustrated that their family needs were not often met:
I was takto [irritated/annoyed] . . . I was annoyed that I left my child in the corridor. They took me to another room . . . The child was crying.
Naved et al. 161
Skills strengthening
Participants’ ratings about the acceptability of interventions were also associated with the extent to which they perceived interventions as strengthening their personal and interpersonal skills. This was especially true among participants who had experience of non-trauma-focused interventions such as mindfulness and motivational interviewing. MBSR was particularly earmarked by women with a history of domestic violence as conferring opportunities to use newly acquired skills in self-compassion and self-awareness to regulate their emotions and manage their stress more effectively, because they ‘felt they had learned how to quiet their minds’. 163,164
Beyond the recognition that non-trauma-focused interventions can bring about positive steps towards self-actualisation through personal development, there were also signals that treatment acceptability hinged on the broader impact on participants’ interpersonal skills. Women with a history of domestic violence voiced how taking part in motivational interviewing had enabled them to more effectively engage in other treatment services. In addition, for some participants, these interpersonal benefits spilled over into the domestic sphere, positively affecting the way that they interacted with partners and underpinning a newly derived confidence to engage in family life:
My confidence has gone up a great deal . . . Even though I came in self-confident in some areas of my life, I think that when it comes to specifically how I relate with my husband in that area, it’s boosted it up completely. I think that I’m capable.
Hughes and Rasmussen162
Self-efficacy and reward
Related to the notion that interventions were more acceptable if they led to strengthening of personal and interpersonal skills was the finding that participants tended to favour interventions that made intuitive sense, rewarded persistence and were demonstrably effective. In this sense, the more self-efficacious participants felt about fulfilling the requirement of treatment sessions, the more likely they were to persist with treatment; this bi-directional relationship was also reinforced by visible signs of recovery. Dropout and attrition were more common among participants who engaged in interventions that they struggled to identify with and master, with mindfulness being singled out by veterans, among the non-trauma-focused interventions, as challenging:
I just didn’t get it. I was so stupid when I first went to it the last time. I didn’t even realise what I was supposed to be doing . . . I felt ignorant and embarrassed so that’s why I quit.
Martinez et al. 165
By contrast, although trauma-focused interventions such as prolonged exposure and cognitive processing therapy could initially lead to a worsening of symptoms, veteran participants recognised that it was likely to be ultimately effective and ‘worth it’. 166
In part, participants’ willingness to stay the course in trauma-focused treatment stemmed from a ‘commitment to finish’, born from a realisation that their time had come to ‘turn things around’, to paraphrase a male veteran, a theme that was voiced by other veterans engaged in cognitive processing therapy:
Yes, I did [consider dropping out] because I was avoiding having to write out my traumatic experience but I knew I had to do it . . . I can’t keep burying my head in the sand.
Hundt et al. 166
For others, participation in trauma-focused work was made feasible only through engagement with a supportive therapist. In this context, a positive therapeutic alliance conferred the means to stay focused on treatment goals:
I loved [therapist name]; she was great and she was patient and she helped keep me focused . . . that made it a little bit easier to show up.
Hundt et al. 166
The tone of participants’ ratings about trauma-focused interventions differed depending on their circumstances, with asylum seekers, who feared deportation, more likely push themselves to take up treatment on the grounds that it will be effective:
I used to force myself to do it just because I feel that it’s going to help me.
Vincent et al. 169
Despite ongoing fears of repatriation and a sense of creeping fatalism among asylum seekers, there were participants whose ability to see signs of progress encouraged them to continue to push themselves to take up therapy:
. . . I started maybe feeling a bit of difference. That’s when I used to force myself ‘You have to go. No, be strong, go and they are helping you’, so I end up going.
Vincent et al. 169
Summary
In summary, the acceptability of interventions was associated with how congruent they were with participants’ therapeutic needs and social contexts, and the means by which the interventions were able to provide participants with opportunities to engage in personal and interpersonal improvement and confer demonstrable improvements. The feasibility of interventions hinged on more instrumental features, such as the scheduling and timing of treatment sessions.
Chapter 6 Patient and public involvement and the research prioritisation exercise
Although the overarching focus and framework of the current review was prespecified by the commissioned brief, we recognise that patient and public involvement (PPI) in systematic reviews is a critical means to ensure that the research process and products are more accessible, relevant and meaningfully used through active involvement of service users (known as ‘experts by experience’) and key stakeholders. 170 However, there is a broad range of conceptual models of service user involvement in systematic reviews, from one-off consultation to ongoing collaboration, and early engagement with potential contributors at a conceptual level is likely to shape the content and style of user involvement. 171
Our strategy was informed by an understanding that knowledge mobilisation is a dynamic and interactive process that is reliant on forming equitable transactional relationships with patients, the public and stakeholders. 172 Our user engagement strategy was informed by an understanding that experts by experience can bring critical insights and perspectives that can add value to contextualising the findings of our review and contribute to enhancing the reach of dissemination activities, especially in relation to setting future research priorities.
Aims
Our PPI strategy had three broad aims:
-
to consult with experts by experience about the focus and design of the review
-
to contribute to identifying research priorities
-
to contribute to dissemination of the findings of the review, including the research priorities.
Aim 1: consultation on the overall aims and design of the review
Methods
To identify people with a history of complex traumatic events, we approached The Retreat hospital, York, or service user groups that were known to us through our clinical experience of working in the field. We have not named the groups involved in this consultation exercise to protect the identity of the service users.
Participants
Ten people (six women and four men) who had used inpatient and secondary care mental health services, all with a history of complex trauma, took part in the focus groups. Trauma histories included childhood sexual abuse, sexual assault as adults, self-harm and domestic violence. Some had experienced homelessness and had been offenders; comorbidities and symptom profiles included drug and alcohol addictions, suicidality and dissociated identities. All of the service users identified were all currently using or had recently used NHS mental health services and/or third-sector mental health services. None of the subjects was approached within an NHS setting or directly through NHS services.
Research governance approval to contact and identify eligible service users who had been patients at The Retreat was granted on 31 July 2017 by Dr Mark McFetridge, Chairperson of the Clinical Governance Group at The Retreat, York.
Format and timing of focus groups
Interviewing people who are currently using mental health services or who are still acutely affected by their symptoms is difficult owing to the sometimes chaotic nature of engagement with services, as well as the sensitivity and care needed to avoid causing harm to these subjects. An expert by experience (the Involvement Lead at The Retreat) and a specialist trauma psychotherapist (IS) carried out the interviews so that the risk of re-traumatisation was minimised. Following the interviews, all of the subjects had access to mental health nursing staff or support workers with whom they had an existing relationship.
Four focus groups were conducted between May and July 2018. Where possible, focus groups were carried out at times when the service users were already planning to meet so that the researchers could align the focus groups with an existing structured timetable, thereby minimising disturbance to the service users’ schedule.
Topic guide
A structured topic guide was used to ensure that each focus group addressed similar issues pertinent to the review process. Participants were given copies of lay summaries of the project protocol that specified and explained the criteria for the population, interventions, comparisons and outcomes used to determine inclusion within and exclusion from the eligible studies. In addition, participants were given lay summaries of the descriptive results of the effectiveness review that characterised the number of studies included, the types of populations included and the characteristics of the interventions included. The following questions and prompts were used to elicit responses about the aims and focus of the review, with a view to generating feedback about the scope of the current review and future research priorities:
-
Which populations should be included in the study?
-
Do you feel this is an accurate representation of populations with a history of trauma?
-
What other groups do you think should be included?
-
Do you think this is the right balance of studies on each population?
-
-
What types of therapies should be included in the review?
-
Is this an accurate representation of the therapies available for people with a history of trauma?
-
Do you know of any therapies for trauma that have not been included here?
-
Do you think this is a good balance of therapies included in the systematic review?
-
Are there any additional psychological interventions that should be included?
-
Do you think any of the therapies included to date require further research?
-
-
Which medicines should be included in the review?
-
What other types of medicine are prescribed to individuals with complex trauma?
-
What do you think about the balance of studies on each type of medication included in the systematic review?
-
Results
Theme 1: under- or over-representation of populations of interest
There were a number of responses that clustered around discussions of certain population groups exposed to complex trauma being either under- or over-represented in the review: ‘It’s important to include all populations to get the scale of it’.
In general, participants suggested that female populations were seen as under-represented within population groups that might typically be associated with males, such as veterans: ‘. . . it’s strange; it’s [the review] so male dominated because most domestic abuse happens to women’.
Respondents suggested that groups such as people in drug and alcohol services and those that foster children should be included. In addition, participants who had experienced treatment in inpatient settings suggested that studies that evaluated treatments among inpatients were under-represented and pointed to the complexity of their symptoms as indicative of the need for a broader formulation of what complex trauma is: ‘. . . people associate trauma with war, but PTSD is not the same as complex trauma’ and ‘. . . it can be a fine line between stress and trauma’.
Theme 2: mind and body separation
Participants highlighted that the review was possibly focused on a narrow range of symptoms associated with mental health alone, with too little focus on understanding the impact of complex trauma on physical functioning: ‘why does it just include psychological therapies? There is a mind–body separation here’.
This awareness of a mind–body separation was reflected by participants acknowledging that the therapies included in the review were prescriptive and manualised psychological interventions, with a focus on mental health symptom management rather than more humanistic and integrative therapies, such as transactional analysis and Gestalt, which look to overcome such mind–body dualism: ‘. . . are trauma-focused CBT and exposure therapies really integrative therapies? . . . humanistic therapies should be added as a category of their own’.
Similarly, participants noted that there is also scope to learn more about the effectiveness of therapies that address the somatic impact of complex trauma, such as alternative and complimentary therapies such as yoga and kinesiology: ‘. . . lots of trauma relates to the body’.
There was also a sense that future research should address the effectiveness of therapies for people who had limited access to existing evidence-based treatments owing to learning difficulties and language barriers.
Theme 3: further work on pharmacological therapies
Fewer studies about pharmacological interventions have been included in the current review and service users’ own experiences were predominantly drawn from their experience of psychological interventions. However, there was an awareness that, in the current review, many of the studies that evaluated the effectiveness of medications were focused on medications used for severe and enduring mental health problems (such as personality disorder rather than PTSD) and it was not clear if there was sufficient understanding about the role of a broader range of medications in managing symptoms across the complex trauma experience.
Aims 2 and 3: setting research priorities and disseminating findings
Process
A stakeholder research prioritisation day was held on 9 July 2018 to present preliminary quantitative and qualitative findings. The goal was to identify research priorities and co-produce with stakeholders a ranked list of future research questions. Attendees were practitioners with interest and experience in complex trauma, voluntary and third-sector providers of services to people affected by complex trauma, and experts by experience.
The team from Beyond The Room (http://beyondtheroom.net/) facilitated online voting and online public engagement via social media. A Twitter account was set up (@UoY_INCiTE) and a hashtag for the project (#INCiTEstudy) was also active throughout the day, alongside the Beyond The Room social media account, to disseminate information being shared at the event and to invite non-participants on the day to engage in the voting.
Future research priorities were co-produced in a workshop format, following the presentation of results. Three break-out groups discussed their perspectives on the range of evidence presented and identified important unanswered questions. The role of the review team was to help facilitate development of research questions and offer guidance about appropriate methodologies that could be feasibly used to address the questions identified within the groups.
Research priorities were then collated online using MentiMeter (www.mentimeter.com), an online voting platform provided by the Beyond The Room team. This platform enabled online voting among participants in the room but also facilitated wider engagement with voting on research priorities from those not present but following the discussions on the INCiTE Twitter account. Each participant was awarded 100 points to allocate to the long-list of research questions.
Participants were encouraged to promote further engagement in the voting exercise by advertising the voting link with interested people in their networks. Voting was open for 1 week following the event and closed on 16 July 2018.
Results
On the day, there were 16 attendees (plus the review team) who were from:
-
The Retreat, York
-
Tees, Esk and Wear Valleys NHS Foundation Trust, Darlington
-
Combat Stress, Surrey
-
Home-Start, York
-
IDAS (Independent Domestic Abuse Services), York
-
University of Manchester, Manchester
-
University of York, York.
The research priorities developed during the prioritisation event are listed in Table 14. A total of 68 people took part in the online vote. The proportional share of points awarded to each priority is also shown.
| Research priority | Vote share (%) |
|---|---|
| Conduct a definitive trial of the effectiveness of interventions in complex trauma, with long-term follow-up (e.g. 24 months) | 15.91 |
| Understand the lived experience of people with experience of complex traumatic events: a peer researcher exercise | 14.80 |
| Conduct a qualitative study exploring the patient perspective on key outcomes, preferred therapies, acceptability and delivery format of interventions (e.g. group or individual) | 12.48 |
| Develop holistic and biopsychosocial assessment, prioritising a mind–body approach | 10.46 |
| Understand what the core outcomes for patients, families and health-care providers are (e.g. appropriate outcome domains and measures, including adverse outcomes) | 7.55 |
| Understand how best you engage populations with experience of complex traumatic events | 6.43 |
| Understand what the key outcomes that should be included in trials are | 6.28 |
| What are the key components of an effective multicomponent intervention? (e.g. support in engaging in work, debt management) | 5.83 |
| Test the feasibility of social prescribing for wraparound care for people with complex traumatic experiences | 5.68 |
| Understand what the core components and domains of interventions and integrated approaches are (e.g. individual vs. group plus individual therapy) | 4.71 |
| Understand how we can define good practice. Use a Delphi survey to capture perspectives on positive recovery stories and barriers to and facilitators of retaining patients in care | 3.74 |
| Understand how we best taper off psychological interventions | 3.14 |
| Understand what the optimal duration of treatment is | 2.99 |
A majority of the points were awarded to just 4 of the 13 research priorities, accumulating over 10% each. A definitive trial of the effectiveness of interventions with a long-term follow-up and a peer researcher exercise to understand the lived experience of people with experience of complex trauma were the two most favoured priorities, with both having a similar percentage of vote share.
Chapter 7 Discussion
Summary of results across all populations with complex trauma for post-traumatic stress disorder
We included 104 studies in the effectiveness review and reported 37 comparisons using meta-analysis across 79 RCTs. There were a total of nine non-RCTs that included five comparisons for PTSD, four comparisons for depression and two comparisons for anxiety. The number of non-RCTs included in the review was much lower than anticipated and we identified a greater volume of trial evidence than was anticipated. This may have been because we adopted a strategy that favoured including studies based on trauma exposure rather than diagnostic criteria and thereby we were able to identify a much broader range of studies pertaining to complex trauma. However, the merit of including data from non-RCTs was diminished by the fact that these studies rarely reported the same intervention types or outcomes, making meta-analyses less possible. Overall, the quality of the available evidence was unclear, with the lowest risk observed in domains related to detection bias, random sequence generation and other risks of bias and the highest risk of bias observed in performance bias and attrition domains. The majority of studies were at high risk of performance bias, partially explained by the predominance of psychological interventions included in the review and the challenges of blinding their delivery. When pooled across all populations with complex trauma, psychological interventions were proven to be effective at reducing PTSD symptoms when compared with control post treatment. There was less evidence that this finding held when treatment effects were measured up to 6 months post treatment, with only trauma-focused CBT and single-component trauma-focused interventions showing positive effects over the longer term. There was no significant difference in the effectiveness of psychological interventions for PTSD symptoms when compared with active controls.
The bulk of the evidence across all populations for reducing PTSD symptoms favoured trauma-focused CBT when compared with control post treatment and at follow-up after up to 6 months. There was no evidence of the effectiveness of trauma-focused CBT versus active controls and this is a weakness of the set of trials analysed. IPT and EMDR were also superior to control post treatment but there was less evidence that mindfulness improves PTSD symptoms in the presence of complex trauma. Non-trauma-focused CBT was not effective at any time point. These findings were reflected in the meta-analysis that showed that single-component and trauma-focused interventions were more effective than control post treatment and at follow-up and outperformed multicomponent and trauma-focused interventions post treatment. Collectively, single-component non-trauma-focused interventions that included approaches beyond CBT were effective post treatment, but these approaches were the least best option for managing PTSD symptoms across all populations.
Few studies addressed the symptom cluster associated with CPTSD and, of those that did, the majority focused on emotional dysregulation. We found no evidence that either trauma- or non-trauma-focused psychological interventions were superior to control in improving emotional dysregulation or interpersonal problems post treatment. By contrast, psychological interventions post treatment were associated with large and positive effect sizes for improving negative self-concept, with multicomponent trauma-focused interventions outperforming all other approaches. There was some evidence that phase-based approaches that allow for stabilisation work to be done before exposure to trauma-focused interventions are the most promising candidate intervention for managing emotional dysregulation and interpersonal problems, although the superiority of these approaches over control was not statistically significant.
Summary of results for psychological interventions across populations for depression and anxiety
Collectively, psychological interventions were shown to be superior to control, but not to active control, both post treatment and at follow-up for managing associated symptoms of depression in all populations with complex trauma. There was strong evidence that trauma-focused CBT post treatment was a highly effective treatment for managing depression in people exposed to complex trauma, but there was less evidence that these effects are present at 6 months’ follow-up. IPT and EMDR were similarly associated with large treatment effects for reducing depression when compared with control, but not active control, post treatment, but evidence in favour of these approaches was thin. Mindfulness was also superior to control post treatment; it was also effective at 6 months’ follow-up, but evidence for this finding is inconclusive. While single-component non-trauma-focused interventions that included mindfulness-based approaches were effective in reducing depression symptoms post treatment, the most consistent and largest effects for depression post treatment and at 6 months’ follow-up were observed in trials that tested single-component and trauma-focused interventions.
A similar set of results were returned in the meta-analyses that assessed the effectiveness of psychological interventions across all populations for reducing associated symptoms of anxiety. All analyses for this outcome were conducted post treatment. Trauma-focused CBT emerged as a leading candidate intervention for reducing anxiety symptoms in the presence of any type of complex trauma, with interventions associated with medium to large effect sizes. The largest effects were observed in trials that compared EMDR with control, albeit this finding was based on relatively few trials. In summary, trauma-focused approaches, when delivered as either a single-component or a multicomponent intervention, were superior to control for anxiety symptoms when effects were pooled across all populations.
We found no evidence that psychological interventions in general, and trauma-focused CBT in particular, were effective in improving quality of life across all populations. There was a modest amount of evidence in favour of trauma-focused CBT for managing sleep problems when results were pooled across all populations.
Summary of population subgroup analyses
Veterans
Among veterans, psychological trauma-focused CBT and EMDR emerged as the most effective individual psychological interventions for reducing PTSD symptoms post treatment. There was little evidence to show that mindfulness was an effective therapeutic strategy in this group and, overall, single-component non-trauma-focused interventions were not superior to control either post treatment or at follow-up. Multicomponent and trauma-focused interventions were the most effective approaches among veterans for managing PTSD symptoms.
Psychological interventions, in general, are effective for managing depression in veterans exposed to complex trauma. When effects were pooled across all interventions, the SMD post treatment represented a medium and positive effect in favour of reducing depression, but this effect was about half the size observed in the analysis across any type of trauma exposure. The most effective interventions for depression among veterans were trauma-focused CBT and EMDR, and these positive and large effects held when trauma-focused interventions were delivered as either a single-component or a multicomponent approach. Limited evidence from non-RCTs suggested that trauma-focused CBT and psychodynamic therapy had equivalent positive effects for depression in veterans. The least effective but still positive approaches for depression in veterans were mindfulness and single-component non-trauma-focused interventions, which yielded moderate treatment effects.
Similarly, psychological interventions were, on the whole, effective at reducing associated anxiety symptoms in veterans exposed to complex trauma post treatment. There was less evidence to draw on by comparison with studies that measured depression. However, EMDR and trauma-focused CBT were superior to control post treatment and were associated with large and positive effects in favour of reducing anxiety.
Childhood sexual abuse
People exposed to childhood sexual abuse formed the next largest complex trauma subgroup. We showed that psychological interventions overall were associated with large and positive treatment effects for reducing PTSD in this subgroup post treatment only. As was the case with veterans, individual trauma-focused CBT was the most effective individual treatment for PTSD in people exposed to childhood sexual abuse. In addition, evidence gleaned from the non-RCTs showed that trauma-focused CBT was superior to control in reducing PTSD avoidance symptoms, suggesting that this approach was among the most effective in this group. Moreover, while single-component and trauma-focused interventions were collectively superior to control post treatment, it is clear that larger and positive effects were observed in trials that tested multicomponent and trauma-focused interventions in the childhood sexual abuse subgroup.
A similar pattern emerged for associated depression symptoms in this subgroup. When pooled together, psychological interventions in general were associated with large and positive effects for reducing depression post treatment; there was only modest evidence that these effects were positive at follow-up. Individual trauma-focused CBT and, collectively, single-component and trauma-focused interventions were superior to control for reducing depression post treatment. Consistent with the findings for veterans, the single-component and non-trauma-focused interventions were also superior to control post treatment for depression. Furthermore, the largest treatment effects for depression symptoms observed in the childhood sexual abuse subgroup were associated with multicomponent and trauma-focused interventions. With veteran and childhood sexual abuse being prototypical exposures for CPTSD, it might be that, among these populations, PTSD and associated depression symptoms are more effectively managed with multicomponent approaches that also include non-trauma-focused work. There was, however, no strong evidence in any direction for which types of psychological interventions might be most effective for reducing anxiety symptoms in this subgroup.
War-affected populations
War-affected populations comprised the next largest subgroup. All analyses in this subgroup were conducted post treatment. Although psychological interventions of any type were superior to control for PTSD symptoms, the sizes of the SMDs were small in comparison with all other subgroups except for veterans. Individual trauma-focused CBT interventions were the most efficacious for reducing PTSD symptoms in war-affected populations. In addition, evidence gleaned from the non-RCTs showed that trauma-focused CBT was superior to control in reducing PTSD avoidance symptoms, suggesting that this approach was among the most effective in this group. Single-component and trauma-focused interventions were marginally more effective than multicomponent and trauma-focused interventions, but both approaches yielded medium and positive treatment effects in favour of reducing PTSD symptoms. Evidence from non-RCTs suggested that multicomponent interventions were in fact inferior to control for PTSD symptoms, but this finding was not endorsed by the meta-analyses of trials.
Comparable medium and positive treatment effects were observed for individual trauma-focused CBT in this subgroup for associated depression symptoms. Single-component, but not multicomponent, trauma-focused interventions were superior to control post treatment for depression symptoms. There was less evidence to judge the effectiveness of psychological interventions for anxiety symptoms in war-affected populations. Individual trauma-focused CBT was the only class of intervention associated with significant and positive effects in favour of reducing anxiety.
Refugees
Few meta-analyses were possible among studies that included refugees. Any psychological intervention was vastly superior to control post treatment and also at follow-up for PTSD symptoms in refugees. In keeping with a recent review of treatments in refugees and asylum seekers,173 we found that very large and positive treatment effects for PTSD were observed in studies that compared trauma-focused CBT and EMDR with control post treatment, but these effects were not sustained at follow-up. A similar picture was shown when psychological interventions were compared with control for associated depression symptoms: trauma-focused CBT and EMDR emerged as being better than control post treatment, but these findings were based on scarce evidence and it is not possible to judge if these effects are maintained at follow-up. Based on limited evidence from non-RCTs, it is possible that non-trauma-focused interventions could be effective for PTSD in refugees, but this finding was not observed in the meta-analyses of the trials. There was insufficient evidence to determine if psychological interventions were effective for anxiety symptoms in refugees.
Domestic violence
There was very limited evidence to draw on to make firm conclusions about the effectiveness of psychological interventions in the subgroup of trials that included people exposed to domestic violence. Individual trauma-focused CBT was associated with very large and positive effects in favour of reducing PTSD and associated depression symptoms in this subgroup post treatment only. However, these findings were associated with high levels of uncertainty and based on few studies of variable quality.
Summary of results of pharmacological interventions
The pooled results for pharmacological interventions in veterans showed that only antipsychotic medication was effective in reducing PTSD symptoms post treatment. The SMD for antipsychotics was equivalent to that observed in a comparable analysis in veterans that compared psychological interventions as a whole with control, but less than half the size of that observed in the analysis that compared multicomponent and trauma-focused interventions with control. There was also a small amount of evidence to signal that blood pressure medicine (prazosin) can reduce PTSD symptoms in veterans. Curiously, in veterans, antipsychotic medication was not effective in reducing symptoms of psychosis.
These findings might suggest that, in veterans at least, pharmacological interventions alone are not as effective as using multicomponent and trauma-focused interventions for PTSD symptoms. Moreover, additional strategies might be warranted to more effectively manage symptoms of psychosis in veterans in the presence of complex trauma.
Heterogeneity
The I2 statistic and chi-squared tests for the pooled results across all populations demonstrated substantial and significant heterogeneity at the 0.10 level for all classes of psychological interventions for PTSD symptoms. A similar picture was seen in the forest plots for the pooled results across all populations for associated symptoms of depression and anxiety. Although this might be mainly attributed to clinical diversity among the populations, it is also known that there is a link between meta-analysis size and heterogeneity levels and the high levels detected in our review might also thus be a function of the size of the review.
We explored these high levels of heterogeneity by undertaking subgroup analyses of the effectiveness of interventions by population. For the primary outcome, the pooled results for psychological interventions as a whole were associated with much less heterogeneity in the veteran and war-affected subgroups, with I2 results (between 42 and 50%) suggesting lower levels of between-study variability, but chi-squared results were still significant suggesting inconsistency between study results.
However, the pooled results for PTSD symptoms by intervention type among the veteran and war-affected subgroups returned considerably lower levels of heterogeneity. It might be that subgrouping by population and then by intervention appears to explain much of the heterogeneity in veteran and war-effected groups but not in others (e.g. childhood sexual abuse groups). This trend was not duplicated in the childhood sexual abuse subgroup, in which the pooled results across all psychological interventions and for specific classes of psychological interventions were still associated with high and significant levels of heterogeneity, making it more difficult to be confident about the true size and direction of effects in this subgroup. There was negligible and non-significant levels of heterogeneity for the pooled results for PTSD for all and any class of psychological intervention in the refugee and domestic violence subgroups. We might suggest that the lower and nil levels of heterogeneity returned in the subgroup analyses can partly be explained by less clinical variability and fewer trials within each subgroup. However, it is worth noting that, among the veteran, war-affected and childhood sexual abuse subgroups, heterogeneity was still more apparent in the pooled results that compared composite intervention categories with control. This was especially true for the pooled results that compared multicomponent and trauma-focused interventions with control and it might be that, in these analyses, heterogeneity was partly driven by variability among intervention components as well as by any residual clinical diversity.
In addition, we can conclude on the basis of the meta-regression results that population type partly moderated the effectiveness of psychological interventions for PTSD symptoms, with interventions doing less well in veterans and war-affected populations and significantly better in those exposed to domestic violence. In this sense, clinical diversity accounted for a modest amount of the heterogeneity observed in the pooled results across all populations, but there was still significant levels of residual heterogeneity that remained unexplained. Similarly, while the meta-regression was able to model the moderating effects of intervention content on the effectiveness for PTSD symptoms, results were fairly inconclusive, with the multivariable model that included only imaginal exposure and psychoeducation accounting for a fraction of heterogeneity and between-study inconsistencies.
Component network meta-analysis
We further explored the treatment effects of different components of the composite complex interventions included by using component network meta-analysis. The results of the component network meta-analysis showed that the components of standard trauma-focused CBT – cognitive restructuring, imaginal exposure and relaxation – appear to be effective for PTSD symptoms. This is consistent with the results of the population subgroup analyses. There were strong interaction effects between relaxation, cognitive restructuring and imaginal exposure in part because most of these components were used together.
Mindfulness was treated as a component and, in that sense, it was an approach identified in studies that primarily tested a mindfulness intervention as well as in studies in which mindfulness was a component of a broader CBT intervention. However, there were limitations to categorising mindfulness interventions owing to the variability of reporting, especially when mindfulness was but one of several components as part of a broader CBT package. There is scope here for future work to tease apart differences in the effectiveness of mindfulness when delivered as a stand-alone therapy and mindfulness as part of a composite psychological intervention.
The analyses of phase-based approaches presented even greater challenges. The phase-based approaches included in this review comprised combinations of multicomponent trauma-focused CBT, DBT, EMDR and IPT. Pragmatically, these approaches were categorised for the network meta-analysis in terms of the components included, for example imaginal exposure or mindfulness. However, we also coded these interventions as phased based if the components were phased in such a way that allowed for stabilisation before working on the trauma. It is unclear if the phasing itself constitutes an intervention or if it is a higher order theoretical construct, but phasing of these components, as well as the intervention content, appears to be one of the factors having an impact on effectiveness. There is a need for future work on phase-based approaches to reach a consensus on how phasing is conceptualised in the presence of composite interventions.
Attrition
Across all populations, trauma-focused CBT was associated with reduced odds of attrition compared with control. There was less evidence to draw firm conclusions about the attrition rate for other interventions, although there was some suggestion that across all populations EMDR incurred a greater attrition rate than control. When attrition was analysed across population subgroups, we found that veterans who received any type of psychological intervention were half as likely to drop out than those on a waitlist or in the active control. In studies that tested psychological interventions in people exposed to childhood sexual abuse, the attrition rate for any psychological intervention was one-quarter of that observed in the control groups. There was a mixed picture among studies that included refugees, with some evidence that there were greater rates of attrition among those given a psychological intervention than in the control, suggesting that it is a challenge for displaced populations to adhere to psychological treatment protocols. Why this might be is not clear and future work could focus on the acceptability and feasibility of psychological interventions in this group. There was insufficient evidence to determine the odds of attrition in war-affected and domestic abuse populations.
Acceptability and feasibility of interventions: qualitative findings
The narrative synthesis of the subset of qualitative studies identified three core themes related to patient ratings about the acceptability and feasibility of interventions: therapeutic context, skills strengthening, and self-efficacy and reward. These themes cut across patient perceptions about both trauma- and non-trauma-focused therapies. Specifically, where and how interventions were delivered were seen to be important factors that determined acceptability and feasibility. Group delivery could be advantageous in some contexts, for example for the delivery of non-trauma-focused interventions such as mindfulness, but there were risks of vicarious re-traumatisation for those attending group-based therapies with a focus on trauma reprocessing. Perceptions about the acceptability of different therapeutic approaches were split between instrumental perceptions about the capacity for interventions to confer life skills and perceptions about how likely interventions were to aid symptomatic recovery. For those primarily engaged with non-trauma-focused interventions, there was a sense of these approaches equipping them with practical skills that made using other health- and social-care services more feasible. By contrast, among those who had experience of trauma-focused interventions, their willingness to persist with treatment was linked with their belief that they were going to feel better and the emergence of vital signs that were indeed feeling better.
Comparison with other reviews and guidance
We have shown that existing psychological treatments for PTSD are effective for people with a history of complex traumatic events. The strongest evidence was in favour of trauma-focused therapies such as trauma-focused CBT and EMDR delivered either as stand-alone therapies or as part of single-component and trauma-focused interventions. This finding mirrors that of a Cochrane review for psychological therapies for the treatment of chronic PTSD and is consistent with the NICE guideline that recommends the use of trauma-focused psychological treatment for PTSD for ≥ 3 months. 20,174 While there was less good evidence in favour of non-trauma-focused interventions, we did show that IPT and mindfulness were effective, to varying degrees, across all populations for PTSD symptoms and to a lesser extent for depression too. This breaks with the NICE guideline, which suggests that non-trauma-focused interventions should not be routinely offered to people with chronic PTSD for > 3 months. We were not able to identify sufficient evidence about adverse events associated with psychological treatments to make judgements about the safety of these approaches in people with complex trauma. However, we showed that dropout was lower in people offered psychological interventions and this might suggest that existing trauma-focused interventions are at least acceptable and feasible, as well as effective, in the presence of complex trauma.
Consistent with the International Society for Traumatic Stress Studies (ISTSS) expert consensus guidelines for CPTSD, we also showed that phase-based interventions that drew on a variety of trauma-focused (CBT, EMDR) and non-trauma-focused (DBT, IPT) approaches and included stabilisation and skills strengthening were effective across all populations for PTSD symptoms. 175 However, unlike the ISTSS expert guidelines, our review includes only evidence from RCTs and we were able to also show that phasing of interventions moderated effectiveness, making our findings more robust and trustworthy.
Current NICE guidance suggests that, when several problems need to be addressed, especially in the presence of multiple traumatic events or when presented with comorbid problems, trauma-focused interventions should perhaps be extended and wrapped around a broader care plan. However, we showed that unmodified and existing trauma-focused treatments delivered individually or as part of multicomponent packages were also shown to be effective for managing associated symptoms of depression and anxiety in people exposed to complex trauma.
Although the underlying findings from the pooled results across all complex trauma populations show that trauma-focused interventions are effective for PTSD and associated mental disorder comorbidities, the effects were less pronounced in veterans and war-affected populations. A recent rapid review of service provision for UK armed forces veterans with PTSD included a meta-review of seven systematic reviews and concluded that there was limited and low-quality evidence in favour of EMDR, cognitive processing therapy, trauma-focused CBT and exposure-based therapies for PTSD symptoms and depression. 176 In addition, this rapid review also found evidence in favour of a broad range of pharmacotherapies for PTSD and depression in veterans. Previous reviews have shown that SSRIs are superior to placebo for PTSD in a wide range of populations with PTSD, including those exposed to combat trauma. 177 By contrast, our findings showed that only antipsychotics were effective for reducing PTSD symptoms in veterans, suggesting that pharmacotherapy might not be a candidate for first-line therapy in the presence of complex trauma.
Although adjacent to and in some senses part of the same broader class of people affected by humanitarian crises, we undertook separate subgroup analyses of war-affected populations and of refugees. Among the war-affected populations, we showed that trauma-focused CBT was effective for reducing PTSD but there was little support for other approaches. Similarly, Purgato et al. 178 have shown in a Cochrane review that psychological therapies, many with a trauma focus, are effective at reducing PTSD among people affected by humanitarian crises. The pooled treatment effect for PTSD identified by Purgato et al. 178 was twice that identified in our review and this might be accounted for by their exclusive focus on low- to middle-income countries and the inclusion of studies of children and adolescents. Our findings and those of Purgato et al. 178 were very similar, however, when assessing the impact of psychological interventions on depression and anxiety in adults alone.
Dorrepaal et al. 179 have previously shown that trauma-focused therapies, especially those that include exposure, can benefit people with a history of childhood sexual abuse. Of note in our review was that single-component and non-trauma-focused interventions were the most effective for associated depression symptoms among childhood sexual abuse populations, suggesting that different combinations of therapies that include non-trauma- as well as trauma-focused approaches might be warranted in this population.
Among refugees and asylum seekers resettled in high-income countries, manualised and brief narrative exposure therapies based on CBT have been shown to be effective for PTSD symptoms. 180 There is a strong argument that treatment provision for conflict-affected and displaced populations should be provided as part of multiagency care and extend beyond PTSD symptoms. 181 In the absence of such integrated and multiagency care, our review at least confirms that trauma-focused interventions are superior to control for PTSD and can also be effective for depression too.
A review based on 21 studies (11 of which measured PTSD) showed that brief psychological interventions that are tailored to meet the additional needs of people exposed to intimate partner domestic violence are effective for PTSD, depression, increased self-esteem and functioning. 182 The most effective classes of interventions were CBT and IPT. Our findings partially concur, but are based on a very narrow and limited data set drawn from few studies. In the light of the thin evidence base, there is a consensus that further well-designed and controlled studies of the effectiveness of interventions for survivors of intimate partner violence are needed, especially with a focus on how setting moderates effectiveness.
There was a less clear picture about the effectiveness of treatments for the CPTSD symptom cluster. Conventional stand-alone trauma-focused interventions were not effective in treating emotional dysregulation or interpersonal problems, but did have a positive impact on negative self-concept. In keeping with the ISTSS expert consensus guidelines for CPTSD, we identified phase-based approaches as a leading candidate intervention for managing emotional dysregulation, although the evidence was based on only three trials and the result was of borderline significance. More robust evidence was gleaned from the component network meta-analysis, which identified phasing as a key moderating component of the effectiveness of both trauma- and non-trauma-focused interventions.
Taken together, the fact that trauma-focused interventions do less well in certain populations with complex trauma, and only have a modest impact on disturbances of self-organisation, suggests that our review findings endorse the current diagnostic distinction between CPTSD and PTSD. This is an important argument that has implications for research and practice. We explicitly eschewed a diagnostic approach to the inclusion of studies in this review, but, nonetheless, we would suggest that our findings converge with comparable reviews that have opted to use the new ICD-11 diagnostic CPTSD category as an organising feature of their inclusion criteria. 183 Accordingly, because CPTSD exerts symptoms over and above PTSD extending to disturbances of self-organisation, there is merit in exploring ways to harness existing trauma- and non-trauma-focused interventions more effectively, with phase-based interventions among the leading candidate approaches.
Strengths and limitations
Our review has a number of strengths that enhance the robustness of the findings. By taking a non-diagnostic approach, we were able to develop and operationalise broad inclusion criteria for the population of interest based on exposure to traumatic events that could be defined as complex using the ICD-11 criteria for CPTSD, but which need not have been diagnosed as CPTSD. In doing so, our search was not tied to a narrowly defined group of studies that exclusively evaluated interventions in populations with the as yet untested diagnostic label of CPTSD, but rather captured a broader set of studies salient to more complex trauma rather than a single event and not of an interpersonal nature. In addition, our approach conferred a level of scientific independence from the clinical community actively involved in research in CPTSD and, as such, we feel confident that the process of screening and inclusion was as free from bias as possible. However, to ensure that our review linked with but did not duplicate other ongoing evidence syntheses in the field, we convened a study advisory group that included content and clinical experts in chronic PTSD and CPTSD. The advisory group offered indispensable advice about how to ensure that our review retained an independent identity outside existing evidence syntheses on CPTSD, provided scientific scrutiny about the process of the review, and supported and enabled dissemination activities within the broader trauma studies community.
Our broad approach also extended to including both randomised and non-randomised evaluations of psychological interventions, evaluations of pharmacological interventions and qualitative evaluations of acceptability of interventions, making this review the largest and most comprehensive assessment of treatment effectiveness and acceptability of interventions in complex trauma. This approach was facilitated by conducting an extensive search across key electronic databases, as well as searching specialist fee-for-service libraries and hand searching existing systematic reviews. Although we did not double screen all titles and abstracts, we did run a pilot screening exercise whereby members of the research team double screened a sample of abstracts and titles to familiarise themselves with the PICO. At the title and abstract screening phase, all uncertain decisions were resolved by a consensus meeting, thus minimising the risk of excluding relevant studies.
Additional strengths of the review include the application of robust and innovative approaches to understanding treatment effectiveness and moderators of effectiveness. We not only completed a broad range of meta-analyses, including subgroup analyses by population, but also explored moderators using multivariable meta-regression. By searching extensively and adopting a broad approach to inclusion, we were able to assemble a much larger data set than in previous reviews, enhancing our ability to quantify and explore heterogeneity with a greater level of statistical power and reducing the chance of spurious findings. 184 Many of the meta-analyses exhibited high levels of estimated heterogeneity, but this is a positive finding, as it appears that heterogeneity levels are being consistently underestimated in meta-analyses. 185 Because there is a link between meta-analysis size and heterogeneity levels, we anticipated that we might detect high levels given the size of our review, but the large between-study variability suggests that there might be other study- or patient-level variables that could explain some of it. Individual patient data meta-analysis is likely to confer considerable advantages to accounting for such residual heterogeneity associated with patient-level characteristics.
We were not able to fully undertake all planned PPI activities as specified in the protocol. Specifically, we were unable to recruit service users with experience of complex trauma to join the study advisory group. Our initial plan was to use The Retreat hospital in York to identify eligible candidates for the advisory group, but the length of time that elapsed between applying for and securing research governance permissions meant that opportunities to do this were prohibitively curtailed. However, during this down time, we worked with the Involvement Lead and Iram Shah from The Retreat to offer experts by experience from a voluntary organisation run by service users for people affected by mental health problems to contribute to a series of telephone and face-to-face focus groups. These groups, in lieu of lay membership of the advisory group, contributed critical thinking about the focus of our review and generated data that informed the scope of the research prioritisation exercise. In addition, via our network with the Tees, Esk and Wear Valleys NHS Foundation Trust, we invited service users by experience (as well as key stakeholders from the scientific and clinical communities with an interest in trauma and stress research) to attend and contribute to the research prioritisation day. We also engaged a wider group of stakeholders and service users in the research prioritisation exercise via our social media presence. In these ways, we were still able to build PPI into our review in ways that aligned with established best practice for user involvement in systematic reviews. 186
We originally committed to using the ROBINS-I40 tool for assessing the risk of bias in non-RCTs, but ultimately we opted for a more parsimonious approach afforded by a quality appraisal checklist widely used by NICE in public health guidelines. Although the ROBINS-I tool has emerged as the most likely gold standard method for assessing the risk of bias in non-randomised studies of interventions, it was decided that the tool operated at too high a level of resolution for the purposes of our review and the resource needed to use this tool appropriately would have outstripped capacity within the team at a time when the emphasis was on data extraction and assessing the risk of bias in over 100 RCTs. Future studies that intend on including both non-RCTs and RCTs should ensure that there is sufficient capacity within the review team to use the ROBINS-I tool.
Despite using an extensive search strategy and applying broad inclusion criteria, there is an under-representation of studies in our review with a focus on complex trauma populations drawn from prison settings and survivors of torture and forced migrant labour, otherwise known as modern slavery. Future work should look to identify ways to ensure these populations are not overlooked. In addition, our search did not capture a critical mass of studies that included outcomes related to comorbid psychiatric states such as borderline personality disorder. This might have been off set had we adopted a more clinical and diagnostic approach to our inclusion criteria, but we have previously explained that our review set out to explicitly avoid running searches around diagnostic labels. Finally, while we did include populations with comorbidities, including psychiatric disorders and common mental health problems, we excluded those with dual diagnosis of complex trauma and substance and alcohol misuse on the grounds that these populations are likely to require care that is different from and more specialist than that typically provided in the context of PTSD. However, recent work among ex-serving regular personnel deployed to combat roles in Iraq or Afghanistan has highlighted that populations with dual diagnoses (e.g. mental health problems and alcohol misuse) are an important feature following exposure to complex trauma. 187
A further limitation relates to the use of standard frequentist approaches to random-effects meta-analyses. When there are few studies included in the meta-analyses, there is the potential for bias in estimating the heterogeneity parameter.
Conclusions and implications for research
The funder called for a review to identify the most promising front runners that the Health Technology Assessment programme could then consider for future primary research in complex trauma as part of a separate call.
We have identified that trauma-focused CBT and other trauma-focused interventions, including EMDR, delivered as single-component or multicomponent approaches are superior to control for PTSD symptoms and associated mental comorbidities. However, the size of these positive treatment effects was not equivalent across populations exposed to complex trauma, with treatments being least effective among veterans. Phase-based interventions, along with non-trauma-focused intervention components including mindfulness and relaxation, are potentially among the most effective approaches for PTSD symptoms in people with a history of complex trauma, such as childhood sexual abuse. In addition, there was inconclusive evidence that existing trauma-focused interventions are effective in treating the symptom cluster associated with disturbances of self-organisation typically seen in CPTSD. There is scope to identify if phase-based approaches are more effective than non-phase-based approaches for PTSD and the broader symptom profile associated with complex trauma. There was little evidence of effectiveness of pharmacological interventions for PTSD or for associated mental comorbidities, and no trial that tested the effectiveness of pharmacological interventions for outcomes related to disturbances of self-organisation.
Going forward, we can synthesise the findings from our meta-analyses and from the stakeholder and service user research prioritisation event and draw up a long-list of research questions for consideration in future funding calls. These research questions come under five main topic domains: (1) the effectiveness of psychological and/or pharmacological interventions, (2) the process and implementation of care, (3) understanding the lived experience of complex trauma, (4) the safety and adverse event profile of interventions and (5) methodological considerations about trials in complex trauma.
-
studies about the effectiveness of interventions
-
definitive and fully powered evaluations of the effectiveness of interventions in complex trauma with long-term follow-up (i.e. at least 12 months), especially in veterans, childhood sexual abuse populations and populations affected by humanitarian crises
-
phase-based versus non-phase-based interventions
-
trauma-focused versus non-trauma-focused interventions (including IPT, DBT, mindfulness and relaxation)
-
integrated and multiagency care packages versus control
-
pharmacological interventions versus placebo.
-
-
-
studies about the process and implementation of care
-
qualitative and quantitative process evaluations that draw on best practice for understanding the relationship between intervention and programme theory and anticipated outputs and trial results (Medical Research Council guidance)
-
measuring fidelity and adherence to interventions
-
understanding if contexts (e.g. setting, timing of delivery) moderate outcomes
-
assessing what was delivered (i.e. intervention content) and how it was delivered (e.g. individual vs. group) with a view to drawing conclusions about drivers of effectiveness
-
-
qualitative evaluations of the acceptability and feasibility of interventions among people exposed to complex interventions to inform barriers to and facilitators of treatment uptake, especially in refugees and asylum seekers.
-
-
studies about understanding the lived experience of people with a history of complex trauma
-
qualitative evaluations that draw on a phenomenological perspective to elicit in-depth narratives of the day-to-day lived experience of people with a history of complex trauma
-
ethnographic research to illustrate commonalities and differences in the lived experience of complex trauma across population subgroups.
-
-
studies about the safety and adverse event profile of interventions for people with a history of complex trauma
-
evaluations of adverse events associated with trauma- and non-trauma-focused psychological interventions (e.g. rates of re-traumatisation)
-
evaluations of adverse events associated with pharmacological treatments in all complex trauma populations.
-
-
studies about methodological considerations in trials among people with a history of complex traumatic events
-
developing a core outcome set for trials in complex trauma that include outcomes related to disturbances of self-organisation and mental comorbidities
-
testing the validity of the new ICD-11 diagnostic category for CPTSD to identify and recruit eligible participants to experimental studies.
-
Acknowledgements
Contributions of authors
Hollie Melton (https://orcid.org/0000-0003-3837-510X) (Research Fellow, evidence synthesis) screened titles, abstracts and full-text papers, led the data extraction and risk-of-bias assessment, undertook attrition meta-analyses, led the writing up of the risk-of-bias assessment for randomised controlled intervention studies and non-randomised controlled intervention studies, led the synthesis of non-randomised intervention studies, led the research prioritisation exercise and ran the INCiTE social media account.
Nick Meader (https://orcid.org/0000-0001-9332-6605) (Research Fellow, evidence synthesis and statistics) contributed to the research prioritisation exercise, was principally responsible for the methodological aspects of the effectiveness review and led the meta-analyses, meta-regression and component network meta-analysis.
Holly Dale (https://orcid.org/0000-0002-6553-7939) (Research Training Fellow, evidence synthesis) screened titles, abstracts and full-text papers, contributed to the research prioritisation exercise, contributed to data extraction and contributed to writing up the risk-of-bias assessment for randomised controlled intervention studies.
Kath Wright (https://orcid.org/0000-0002-9020-1572) (Information Service Manager, Information Specialist) was principally responsible for compiling and running database searches and building and maintaining the EndNote libraries.
Julie Jones-Diette (https://orcid.org/0000-0003-1769-8612) (Research Fellow, evidence synthesis and PROSPERO manager) contributed to the research prioritisation exercise and led the data extraction and appraisal of qualitative data.
Melanie Temple (https://orcid.org/0000-0002-4496-3437) (Consultant Psychiatrist, complex trauma) contributed to the research prioritisation exercise, data extraction and meta-analyses of phase-based interventions.
Iram Shah (https://orcid.org/0000-0002-7868-601X) (Consultant Trauma Psychotherapist, trauma) contributed to the research prioritisation exercise, led the service user engagement, ran the focus groups to support delivery of the PPI strategy and led the writing up of the focus group results.
Karina Lovell (https://orcid.org/0000-0001-8821-895X) (Professor of Mental Health, psychological therapies and PPI) contributed to the research prioritisation exercise and supported the development of the PPI engagement strategy.
Dean McMillan (https://orcid.org/0000-0002-2901-8410) (Reader, mental health services research) contributed to intervention coding, meta-analyses and protocol development.
Rachel Churchill (https://orcid.org/0000-0002-1751-0512) (Professor of Evidence Synthesis, knowledge mobilisation) contributed to the research prioritisation exercise and was a full member of the study advisory group.
Corrado Barbui (https://orcid.org/0000-0003-1073-9282) (Professor of Psychiatry, psychiatry and global mental health) contributed to writing the protocol and search terms and to identifying ongoing studies.
Simon Gilbody (https://orcid.org/0000-0002-8236-6983) (Professor of Health Services Research, psychological medicine) contributed to writing the protocol and the research prioritisation exercise.
Peter Coventry (https://orcid.org/0000-0003-0625-3829) (Senior Lecturer, health services research) had overall responsibility for the project, chaired the review group meetings, was a full member of the advisory group, supervised the review team, contributed to the research prioritisation exercise and took primary responsibility for the drafting of the report.
All authors contributed to the report and approved the final version.
Contributions of others
We would like to express our gratitude to the members of the study advisory group – Professor Jon Bisson (Cardiff University), Professor Thanos Karatzias (Edinburgh Napier University), Dr Marylene Cloitre (New York University School of Medicine) and Dr Neil Roberts (Cardiff University) – for their support and contribution to undertaking this review. Their top-rate critical thinking and wealth of knowledge in the field of trauma studies has been immensely helpful to the review team and our approach to this review has been significantly improved by their guidance. Any errors or omissions in the review are, however, the responsibility of the review team and not the study advisory group.
We thank Dr Jane Dalton (previously of the Centre for Reviews and Dissemination, University of York) for her contributions to screening and data extraction and we also want to thank Gary Raine (the Centre for Reviews and Dissemination, University of York) for early work on the qualitative acceptability review.
We also thank all contributors to the research prioritisation exercise: Professor Joe Reilly [Tees, Esk and Wear Valleys NHS Foundation Trust (TEWV)], Lindsay Jones (TEWV), Simon Hughes (TEWV), Amanda Hall (TEWV), Madeleine Rowlinson (TEWV), Dr Mark McFetridge (The Retreat, York), Emily Herbert (The Retreat, York), Trish Horner (Independent Domestic Abuse Services, York), Dr Dominic Murphy (Combat Stress/King’s College London), Maria O’Keefe (Home-Start, York) and Debra Hilton (Home-Start, York). Special thanks go to Vanessa Garrity (Beyond The Room) for facilitating the event and promoting INCiTE on social media and to André Tomlin (The Mental Elf/Beyond The Room) for providing support via The Mental Elf and organising the format of the prioritisation day and the online voting.
Publication
Coventry P, Meader N, Melton H, Temple M, Dale H, Wright K, et al. Psychological and pharmacological interventions for posttraumatic stress disorder and comorbid mental health problems following complex traumatic events: systematic review and component network meta-analysis. PLOS Med 2020;17:e1003262.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care.
References
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1995;52:1048-60. https://doi.org/10.1001/archpsyc.1995.03950240066012.
- Karam EG, Andrews G, Bromet E, Petukhova M, Ruscio AM, Salamoun M, et al. The role of criterion A2 in the DSM-IV diagnosis of posttraumatic stress disorder. Biol Psychiatry 2010;68:465-73. https://doi.org/10.1016/j.biopsych.2010.04.032.
- Steel Z, Chey T, Silove D, Marnane C, Bryant RA, van Ommeren M. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: a systematic review and meta-analysis. JAMA 2009;302:537-49. https://doi.org/10.1001/jama.2009.1132.
- Friedman MJ, Resick PA, Bryant RA, Brewin CR. Considering PTSD for DSM-5. Depress Anxiety 2011;28:750-69. https://doi.org/10.1002/da.20767.
- Herman JL. Complex PTSD: a syndrome in survivors of prolonged and repeated trauma. J Trauma Stress 1992;5:377-91. https://doi.org/10.1002/jts.2490050305.
- Maercker A, Brewin CR, Bryant RA, Cloitre M, van Ommeren M, Jones LM, et al. Diagnosis and classification of disorders specifically associated with stress: proposals for ICD-11. World Psychiatry 2013;12:198-206. https://doi.org/10.1002/wps.20057.
- Cloitre M, Garvert DW, Weiss B, Carlson EB, Bryant RA. Distinguishing PTSD, complex PTSD, and borderline personality disorder: a latent class analysis. Eur J Psychotraumatol 2014;5. https://doi.org/10.3402/ejpt.v5.25097.
- Knefel M, Garvert DW, Cloitre M, Lueger-Schuster B. Update to an evaluation of ICD-11 PTSD and complex PTSD criteria in a sample of adult survivors of childhood institutional abuse by Knefel. Lueger-Schuster (2013): a latent profile analysis. Eur J Psychotraumatol 2015;6. https://doi.org/10.3402/ejpt.v6.25290.
- Courtois CA. Complex trauma, complex reactions: assessment and treatment. Psychotherapy (Chic) 2004;41:412-25. https://doi.org/10.1037/0033-3204.41.4.412.
- Cloitre M, Garvert DW, Brewin CR, Bryant RA, Maercker A. Evidence for proposed ICD-11 PTSD and complex PTSD: a latent profile analysis. Eur J Psychotraumatol 2013;4. https://doi.org/10.3402/ejpt.v4i0.20706.
- UNHCR . UNHCR Mid-Year Trends 2015 2015. www.unhcr.org/56701b969.html (accessed 22 October 2019).
- UNHCR . Asylum Trends, First Half 2014. Levels and Trends in Industrialized Countries 2014. www.unhcr.org/uk/statistics/unhcrstats/551128679/asylum-levels-trends-industrialized-countries-2014.html (accessed 10 January 2020).
- Turrini G, Purgato M, Ballette F, Nosè M, Ostuzzi G, Barbui C. Common mental disorders in asylum seekers and refugees: umbrella review of prevalence and intervention studies. Int J Ment Health Syst 2017;11. https://doi.org/10.1186/s13033-017-0156-0.
- Oram S, Stöckl H, Busza J, Howard LM, Zimmerman C. Prevalence and risk of violence and the physical, mental, and sexual health problems associated with human trafficking: systematic review. PLOS Med 2012;9. https://doi.org/10.1371/journal.pmed.1001224.
- International Labour Organization . A Global Alliance Against Forced Labour 2005.
- Hossain M, Zimmerman C, Abas M, Light M, Watts C. The relationship of trauma to mental disorders among trafficked and sexually exploited girls and women. Am J Public Health 2010;100:2442-9. https://doi.org/10.2105/AJPH.2009.173229.
- Tsutsumi A, Izutsu T, Poudyal AK, Kato S, Marui E. Mental health of female survivors of human trafficking in Nepal. Soc Sci Med 2008;66:1841-7. https://doi.org/10.1016/j.socscimed.2007.12.025.
- Radford L, Corral S, Bradley C, Fisher H, Bassett C, Howat N, et al. Child Abuse and Neglect in the UK Today. London: National Society for the Prevention of Cruelty to Children; 2011.
- Saied-Tessier A. Estimating the Costs of Child Sexual Abuse in the UK. London: National Society for the Prevention of Cruelty to Children; 2014.
- National Collaborating Centre for Mental Health . The Management of PTSD in Adults and Children in Primary and Secondary Care 2005.
- World Health Organization . WHO Guidelines on Conditions Specifically Related To Stress 2013.
- van Minnen A, Hendriks L, Olff M. When do trauma experts choose exposure therapy for PTSD patients? A controlled study of therapist and patient factors. Behav Res Ther 2010;48:312-20. https://doi.org/10.1016/j.brat.2009.12.003.
- McDonnell M, Robjant K, Katona C. Complex posttraumatic stress disorder and survivors of human rights violations. Curr Opin Psychiatry 2013;26:1-6. https://doi.org/10.1097/YCO.0b013e32835aea9d.
- Cloitre M, Courtois CA, Charuvastra A, Carapezza R, Stolbach BC, Green BL. Treatment of complex PTSD: results of the ISTSS expert clinician survey on best practices. J Trauma Stress 2011;24:615-27. https://doi.org/10.1002/jts.20697.
- De Jongh A, Resick PA, Zoellner LA, van Minnen A, Lee CW, Monson CM, et al. Critical analysis of the current treatment guidelines for complex PTSD in adults. Depress Anxiety 2016;33:359-69. https://doi.org/10.1002/da.22469.
- Crumlish N, O’Rourke K. A systematic review of treatments for post-traumatic stress disorder among refugees and asylum-seekers. J Nerv Ment Dis 2010;198:237-51. https://doi.org/10.1097/NMD.0b013e3181d61258.
- Palic S, Elklit A. Psychosocial treatment of posttraumatic stress disorder in adult refugees: a systematic review of prospective treatment outcome studies and a critique. J Affect Disord 2011;131:8-23. https://doi.org/10.1016/j.jad.2010.07.005.
- Powers MB, Halpern JM, Ferenschak MP, Gillihan SJ, Foa EB. A meta-analytic review of prolonged exposure for posttraumatic stress disorder. Clin Psychol Rev 2010;30:635-41. https://doi.org/10.1016/j.cpr.2010.04.007.
- Olatunji BO, Cisler JM, Tolin DF. A meta-analysis of the influence of comorbidity on treatment outcome in the anxiety disorders. Clin Psychol Rev 2010;30:642-54. https://doi.org/10.1016/j.cpr.2010.04.008.
- van Minnen A, Harned MS, Zoellner L, Mills K. Examining potential contraindications for prolonged exposure therapy for PTSD. Eur J Psychotraumatol 2012;3. https://doi.org/10.3402/ejpt.v3i0.18805.
- Nickerson A, Bryant RA, Silove D, Steel Z. A critical review of psychological treatments of posttraumatic stress disorder in refugees. Clin Psychol Rev 2011;31:399-417. https://doi.org/10.1016/j.cpr.2010.10.004.
- Ronconi JM, Shiner B, Watts BV. A meta-analysis of depressive symptom outcomes in randomized, controlled trials for PTSD. J Nerv Ment Dis 2015;203:522-9. https://doi.org/10.1097/NMD.0000000000000322.
- Coventry P, Meader N, Melton H, Temple M, Dale H, Wright K, et al. Psychological and pharmacological interventions for posttraumatic stress disorder and comorbid mental health problems following complex traumatic events: systematic review and component network meta-analysis. PLOS Med 2020;17. https://doi.org/10.1371/journal.pmed.1003262.
- Coventry P, Churchill R, Gilbody S, Lovell K, Barbui C, Meader N, et al. INterventions for Complex Traumatic Events – INCiTE. PROSPERO 2017:CRD42017055523 n.d. www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42017055523 (accessed 3 December 2019).
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J Psychopathol Behav Assess 2004;26:41-54. https://doi.org/10.1023/B:JOBA.0000007455.08539.94.
- Pilkonis PA, Kim Y, Proietti JM, Barkham M. Scales for personality disorders developed from the Inventory of Interpersonal Problems. J Personal Disord 1996;10:355-69. https://doi.org/10.1521/pedi.1996.10.4.355.
- Falsetti SA, Resnick HS, Resick PA, Kilpatrick DG. The Modified PTSD Symptom Scale: a brief self-report measure of posttraumatic stress disorder. Behav Ther 1993;16:161-2.
- Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry 1960;23:56-62. https://doi.org/10.1136/jnnp.23.1.56.
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361-70. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x.
- Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;355. https://doi.org/10.1136/bmj.i4919.
- Wells G, Shay B. Data Extraction for Non-randomised Systematic Reviews. Ottawa, ON: University of Ottawa; n.d.
- Methods for the Development of NICE Public Health Guidance. London: NICE; 2012.
- Jackson R, Ameratunga S, Broad J, Connor J, Lethaby A, Robb G, et al. The GATE frame: critical appraisal with pictures. Evid Based Med 2006;11:35-8. https://doi.org/10.1136/ebm.11.2.35.
- Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539-58. https://doi.org/10.1002/sim.1186.
- Welton NJ, Caldwell DM, Adamopoulos E, Vedhara K. Mixed treatment comparison meta-analysis of complex interventions: psychological interventions in coronary heart disease. Am J Epidemiol 2009;169:1158-65. https://doi.org/10.1093/aje/kwp014.
- Freeman SC, Scott NW, Powell R, Johnston M, Sutton AJ, Cooper NJ. Component network meta-analysis identifies the most effective components of psychological preparation for adults undergoing surgery under general anesthesia. J Clin Epidemiol 2018;98:105-16. https://doi.org/10.1016/j.jclinepi.2018.02.012.
- Dias S, Sutton AJ, Ades AE, Welton NJ. Evidence synthesis for decision making 2: a generalized linear modeling framework for pairwise and network meta-analysis of randomized controlled trials. Med Decis Making 2013;33:607-17. https://doi.org/10.1177/0272989X12458724.
- Spiegelhalter DJ, Best NG, Carlin BP, Van Der Linde A. Bayesian measures of model complexity and fit. J R Stat Soc Series B Stat Methodol 2002;64:583-639. https://doi.org/10.1111/1467-9868.00353.
- GRADE n.d. www.gradeworkinggroup.org (accessed 3 December 2019).
- Cochrane Qualitative & Implementation Methods Group n.d. https://methods.cochrane.org/qi/ (accessed 3 December 2019).
- Lewin S, Booth A, Glenton C, Munthe-Kaas H, Rashidian A, Wainwright M, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings: introduction to the series. Implement Sci 2018;13. https://doi.org/10.1186/s13012-017-0688-3.
- Critical Appraisal Skills Programme . CASP Qualitative Checklist 2018. https://casp-uk.net/casp-tools-checklists/ (accessed 20 April 2017).
- Acarturk C, Konuk E, Cetinkaya M, Senay I, Sijbrandij M, Cuijpers P, et al. EMDR for Syrian refugees with posttraumatic stress disorder symptoms: results of a pilot randomized controlled trial. Eur J Psychotraumatol 2015;6. https://doi.org/10.3402/ejpt.v6.27414.
- Acarturk C, Konuk E, Cetinkaya M, Senay I, Sijbrandij M, Gulen B, et al. The efficacy of eye movement desensitization and reprocessing for post-traumatic stress disorder and depression among Syrian refugees: results of a randomized controlled trial. Psychol Med 2016;46:2583-93. https://doi.org/10.1017/S0033291716001070.
- Adenauer H, Catani C, Gola H, Keil J, Ruf M, Schauer M, et al. Narrative exposure therapy for PTSD increases top-down processing of aversive stimuli – evidence from a randomized controlled treatment trial. BMC Neurosci 2011;12. https://doi.org/10.1186/1471-2202-12-127.
- Rezaei Ardani A, Hosseini G, Fayyazi Bordbar MR, Talaei A, Mostafavi Toroghi H. Effect of rivastigmine augmentation in treatment of male patients with combat-related chronic posttraumatic stress disorder: a randomized controlled trial. J Clin Psychopharmacol 2017;37:54-60. https://doi.org/10.1097/JCP.0000000000000624.
- Azad Marzabadi E, Hashemi Zadeh SM. The effectiveness of mindfulness training in improving the quality of life of the war victims with post traumatic stress disorder (PTSD). Iran J Psychiatry 2014;9:228-36.
- Bartzokis G, Lu PH, Turner J, Mintz J, Saunders CS. Adjunctive risperidone in the treatment of chronic combat-related posttraumatic stress disorder. Biol Psychiatry 2005;57:474-9. https://doi.org/10.1016/j.biopsych.2004.11.039.
- Becker ME, Hertzberg MA, Moore SD, Dennis MF, Bukenya DS, Beckham JC. A placebo-controlled trial of bupropion SR in the treatment of chronic posttraumatic stress disorder. J Clin Psychopharmacol 2007;27:193-7. https://doi.org/10.1097/JCP.0b013e318032eaed.
- Beidel DC, Frueh BC, Uhde TW, Wong N, Mentrikoski JM. Multicomponent behavioral treatment for chronic combat-related posttraumatic stress disorder: a randomized controlled trial. J Anxiety Disord 2011;25:224-31. https://doi.org/10.1016/j.janxdis.2010.09.006.
- Bichescu D, Neuner F, Schauer M, Elbert T. Narrative exposure therapy for political imprisonment-related chronic posttraumatic stress disorder and depression. Behav Res Ther 2007;45:2212-20. https://doi.org/10.1016/j.brat.2006.12.006.
- Bolton P, Bass JK, Zangana GA, Kamal T, Murray SM, Kaysen D, et al. A randomized controlled trial of mental health interventions for survivors of systematic violence in Kurdistan, Northern Iraq. BMC Psychiatry 2014;14. https://doi.org/10.1186/s12888-014-0360-2.
- Buhmann CB, Nordentoft M, Ekstroem M, Carlsson J, Mortensen EL. The effect of flexible cognitive-behavioural therapy and medical treatment, including antidepressants on post-traumatic stress disorder and depression in traumatised refugees: pragmatic randomised controlled clinical trial. Br J Psychiatry 2016;208:252-9. https://doi.org/10.1192/bjp.bp.114.150961.
- Carlson JG, Chemtob CM, Rusnak K, Hedlund NL, Muraoka MY. Eye movement desensitization and reprocessing (EMDR) treatment for combat-related posttraumatic stress disorder. Jpn J Biofeedback Res 1997;24:50-64. https://doi.org/10.20595/jjbf.24.0_50.
- Celik C, Ozdemir B, Ozmenler KN, Yelboga Z, Balikci A, Oznur T, et al. Efficacy of paroxetine and amitriptyline in posttraumatic stress disorder: an open-label comparative study. Klinik Psikofarmakol Bulteni 2011;21:179-85. https://doi.org/10.5455/bcp.20110627111141.
- Chard KM. An evaluation of cognitive processing therapy for the treatment of posttraumatic stress disorder related to childhood sexual abuse. J Consult Clin Psychol 2005;73:965-71. https://doi.org/10.1037/0022-006X.73.5.965.
- Chung MY, Min KH, Jun YJ, Kim SS, Kim WC, Jun EM. Efficacy and tolerability of mirtazapine and sertraline in Korean veterans with posttraumatic stress disorder: a randomized open label trial. Hum Psychopharmacol 2004;19:489-94. https://doi.org/10.1002/hup.615.
- Classen C, Koopman C, Nevill-Manning K, Spiegel D. A preliminary report comparing trauma-focused and present-focused group therapy against a wait-listed condition among childhood sexual abuse survivors with PTSD. J Aggression Maltreat Trauma 2001;4:265-88. https://doi.org/10.1300/J146v04n02_12.
- Cloitre M, Koenen KC, Cohen LR, Han H. Skills training in affective and interpersonal regulation followed by exposure: a phase-based treatment for PTSD related to childhood abuse. J Consult Clin Psychol 2002;70:1067-74. https://doi.org/10.1037/0022-006X.70.5.1067.
- Cloitre M, Stovall-McClough KC, Nooner K, Zorbas P, Cherry S, Jackson CL, et al. Treatment for PTSD related to childhood abuse: a randomized controlled trial. Am J Psychiatry 2010;167:915-24. https://doi.org/10.1176/appi.ajp.2010.09081247.
- Cook JM, Harb GC, Gehrman PR, Cary MS, Gamble GM, Forbes D, et al. Imagery rehearsal for posttraumatic nightmares: a randomized controlled trial. J Trauma Stress 2010;23:553-63. https://doi.org/10.1002/jts.20569.
- Davis LL, Davidson JR, Ward LC, Bartolucci A, Bowden CL, Petty F. Divalproex in the treatment of posttraumatic stress disorder: a randomized, double-blind, placebo-controlled trial in a veteran population. J Clin Psychopharmacol 2008;28:84-8. https://doi.org/10.1097/JCP.0b013e318160f83b.
- Davis LL, Jewell ME, Ambrose S, Farley J, English B, Bartolucci A, et al. A placebo-controlled study of nefazodone for the treatment of chronic posttraumatic stress disorder: a preliminary study. J Clin Psychopharmacol 2004;24:291-7. https://doi.org/10.1097/01.jcp.0000125685.82219.1a.
- Devilly GJ, Spence SH, Rapee RM. Statistical and reliable change with eye movement desensitization and reprocessing: treating trauma within a veteran population. Behav Ther 1998;29:435-55. https://doi.org/10.1016/S0005-7894(98)80042-7.
- Edmond T, Rubin A. Assessing the long-term effects of EMDR: results from an 18-month follow-up study with adult female survivors of CSA. J Child Sex Abus 2004;13:69-86. https://doi.org/10.1300/J070v13n01_04.
- Edmond T, Rubin A, Wambach KG. The effectiveness of EMDR with adult female survivors of childhood sexual abuse. Social Work Res 1999;23:103-16. https://doi.org/10.1093/swr/23.2.103.
- Elkjaer H, Kristensen E, Mortensen EL, Poulsen S, Lau M. Analytic versus systemic group therapy for women with a history of child sexual abuse: 1-year follow-up of a randomized controlled trial. Psychol Psychother 2014;87:191-208. https://doi.org/10.1111/papt.12011.
- Engel CC, Litz B, Magruder KM, Harper E, Gore K, Stein N, et al. Delivery of self training and education for stressful situations (DESTRESS-PC): a randomized trial of nurse assisted online self-management for PTSD in primary care. Gen Hosp Psychiatry 2015;37:323-8. https://doi.org/10.1016/j.genhosppsych.2015.04.007.
- Feske U. Treating low-income and minority women with posttraumatic stress disorder: a pilot study comparing prolonged exposure and treatment as usual conducted by community therapists. J Interpers Violence 2008;23:1027-40. https://doi.org/10.1177/0886260507313967.
- Franćišković T, Suković Z, Janović S, Stevanović A, Nemćić-Moro I, Ronćević-Gržeta I, et al. Tianeptine in the combined treatment of combat related posttraumatic stress disorder. Psychiatr Danub 2011;23:257-63.
- Franklin CL, Cuccurullo LA, Walton JL, Arseneau JR, Petersen NJ. Face to face but not in the same place: a pilot study of prolonged exposure therapy. J Trauma Dissociation 2017;18:116-30. https://doi.org/10.1080/15299732.2016.1205704.
- Friedman MJ, Marmar CR, Baker DG, Sikes CR, Farfel GM. Randomized, double-blind comparison of sertraline and placebo for posttraumatic stress disorder in a Department of Veterans Affairs setting. J Clin Psychiatry 2007;68:711-20. https://doi.org/10.4088/JCP.v68n0508.
- Gamito P, Oliveira J, Rosa P, Morais D, Duarte N, Oliveira S, et al. PTSD elderly war veterans: a clinical controlled pilot study. Cyberpsychol Behav Soc Netw 2010;13:43-8. https://doi.org/10.1089/cyber.2009.0237.
- Germain A, Richardson R, Moul DE, Mammen O, Haas G, Forman SD, et al. Placebo-controlled comparison of prazosin and cognitive-behavioral treatments for sleep disturbances in US Military Veterans. J Psychosom Res 2012;72:89-96. https://doi.org/10.1016/j.jpsychores.2011.11.010.
- Hamner MB, Faldowski RA, Ulmer HG, Frueh BC, Huber MG, Arana GW. Adjunctive risperidone treatment in post-traumatic stress disorder: a preliminary controlled trial of effects on comorbid psychotic symptoms. Int Clin Psychopharmacol 2003;18:1-8. https://doi.org/10.1097/00004850-200301000-00001.
- Hermenau K, Hecker T, Schaal S, Maedl A, Elbert T. Addressing post-traumatic stress and aggression by means of narrative exposure: a randomized controlled trial with ex-combatants in the eastern DRC. J Aggression Maltreat Trauma 2013;22:916-34. https://doi.org/10.1080/10926771.2013.824057.
- Hijazi AM, Lumley MA, Ziadni MS, Haddad L, Rapport LJ, Arnetz BB. Brief narrative exposure therapy for posttraumatic stress in Iraqi refugees: a preliminary randomized clinical trial. J Trauma Stress 2014;27:314-22. https://doi.org/10.1002/jts.21922.
- Himmerich H, Willmund GD, Zimmermann P, Wolf JE, Bühler AH, Kirkby KC, et al. Serum concentrations of TNF-α and its soluble receptors during psychotherapy in German soldiers suffering from combat-related PTSD. Psychiatr Danub 2016;28:293-8.
- Hinton DE, Chhean D, Pich V, Safren SA, Hofmann SG, Pollack MH. A randomized controlled trial of cognitive-behavior therapy for Cambodian refugees with treatment-resistant PTSD and panic attacks: a cross-over design. J Trauma Stress 2005;18:617-29. https://doi.org/10.1002/jts.20070.
- Hinton DE, Pham T, Tran M, Safren SA, Otto MW, Pollack MH. CBT for Vietnamese refugees with treatment-resistant PTSD and panic attacks: a pilot study. J Trauma Stress 2004;17:429-33. https://doi.org/10.1023/B:JOTS.0000048956.03529.fa.
- Jensen JA. An investigation of eye movement desensitization and reprocessing (EMD/R) as a treatment for posttraumatic stress disorder (PTSD) symptoms of Vietnam combat veterans. Behav Ther 1994;25:311-25. https://doi.org/10.1016/S0005-7894(05)80290-4.
- Jung K, Steil R. A randomized controlled trial on cognitive restructuring and imagery modification to reduce the feeling of being contaminated in adult survivors of childhood sexual abuse suffering from posttraumatic stress disorder. Psychother Psychosom 2013;82:213-20. https://doi.org/10.1159/000348450.
- Katz LS, Douglas S, Zaleski K, Williams J, Huffman C, Cojucar G. Comparing holographic reprocessing and prolonged exposure for women veterans with sexual trauma: a pilot randomized trial. J Contemp Psychother 2014;44:9-19. https://doi.org/10.1007/s10879-013-9248-6.
- Keane TM, Fairbank JA, Caddell JM, Zimering RT. Implosive (flooding) therapy reduces symptoms of PTSD in Vietnam combat veterans. Behav Ther 1989;20:245-60. https://doi.org/10.1016/S0005-7894(89)80072-3.
- Kearney DJ, McDermott K, Malte C, Martinez M, Simpson TL. Effects of participation in a mindfulness program for veterans with posttraumatic stress disorder: a randomized controlled pilot study. J Clin Psychol 2013;69:14-27. https://doi.org/10.1002/jclp.21911.
- Knaevelsrud C, Brand J, Lange A, Ruwaard J, Wagner B. Web-based psychotherapy for posttraumatic stress disorder in war-traumatized Arab patients: randomized controlled trial. J Med Internet Res 2015;17. https://doi.org/10.2196/jmir.3582.
- Kosten TR, Krystal JH, Giller EL, Frank J, Dan E. Alexithymia as a predictor of treatment response in post-traumatic stress disorder. J Trauma Stress 1992;5:563-73. https://doi.org/10.1002/jts.2490050406.
- Krupnick JL, Green BL, Stockton P, Miranda J, Krause E, Mete M. Group interpersonal psychotherapy for low-income women with posttraumatic stress disorder. Psychother Res 2008;18:497-50. https://doi.org/10.1080/10503300802183678.
- Krystal JH, Rosenheck RA, Cramer JA, Vessicchio JC, Jones KM, Vertrees JE, et al. Adjunctive risperidone treatment for antidepressant-resistant symptoms of chronic military service-related PTSD: a randomized trial. JAMA 2011;306:493-502. https://doi.org/10.1001/jama.2011.1080.
- Kubany ES, Hill EE, Owens JA. Cognitive trauma therapy for battered women with PTSD: preliminary findings. J Trauma Stress 2003;16:81-9. https://doi.org/10.1023/A:1022019629803.
- Kubany ES, Hill EE, Owens JA, Iannce-Spencer C, McCaig MA, Tremayne KJ, et al. Cognitive trauma therapy for battered women with PTSD (CTT-BW). J Consult Clin Psychol 2004;72:3-18. https://doi.org/10.1037/0022-006X.72.1.3.
- Lande RG, Williams LB, Francis JL, Gragnani C, Morin ML. Efficacy of biofeedback for post-traumatic stress disorder. Complement Ther Med 2010;18:256-9. https://doi.org/10.1016/j.ctim.2010.08.004.
- Lau M, Kristensen E. Outcome of systemic and analytic group psychotherapy for adult women with history of intrafamilial childhood sexual abuse: a randomized controlled study. Acta Psychiatr Scand 2007;116:96-104. https://doi.org/10.1111/j.1600-0447.2006.00977.x.
- Lindley SE, Carlson EB, Hill K. A randomized, double-blind, placebo-controlled trial of augmentation topiramate for chronic combat-related posttraumatic stress disorder. J Clin Psychopharmacol 2007;27:677-81. https://doi.org/10.1097/jcp.0b013e31815a43ee.
- Margolies SO, Rybarczyk B, Lynch J, Vrana S. Efficacy of a cognitive-behavioral treatment for insomnia among Afghanistan and Iraq (OEF/OIF) veterans with PTSD. Sleep 2011;34:A253-A4.
- McDonagh A, Friedman M, McHugo G, Ford J, Sengupta A, Mueser K, et al. Randomized trial of cognitive-behavioral therapy for chronic posttraumatic stress disorder in adult female survivors of childhood sexual abuse. J Consult Clin Psychol 2005;73:515-24. https://doi.org/10.1037/0022-006X.73.3.515.
- McLay RN, Wood DP, Webb-Murphy JA, Spira JL, Wiederhold MD, Pyne JM, et al. A randomized, controlled trial of virtual reality-graded exposure therapy for post-traumatic stress disorder in active duty service members with combat-related post-traumatic stress disorder. Cyberpsychol Behav Soc Netw 2011;14:223-9. https://doi.org/10.1089/cyber.2011.0003.
- Meffert SM, Abdo AO, Alla OAA, Elmakki YOM, Omer AA, Yousif S, et al. A pilot randomized controlled trial of interpersonal psychotherapy for Sudanese refugees in Cairo, Egypt. Psychol Trauma 2014;6:240-9. https://doi.org/10.1037/a0023540.
- Miyahira SD, Folen RA, Hoffman HG, Garcia-Palacios A, Spira JL, Kawasaki M. The effectiveness of VR exposure therapy for PTSD in returning warfighters. Stud Health Technol Inform 2012;181:128-32.
- Monnelly EP, Ciraulo DA, Knapp C, Keane T. Low-dose risperidone as adjunctive therapy for irritable aggression in posttraumatic stress disorder. J Clin Psychopharmacol 2003;23:193-6. https://doi.org/10.1097/00004714-200304000-00012.
- Moradi AR, Moshirpanahi S, Parhon H, Mirzaei J, Dalgleish T, Jobson L. A pilot randomized controlled trial investigating the efficacy of MEmory Specificity Training in improving symptoms of posttraumatic stress disorder. Behav Res Ther 2014;56:68-74. https://doi.org/10.1016/j.brat.2014.03.002.
- Naylor JC, Dolber TR, Strauss JL, Kilts JD, Strauman TJ, Bradford DW, et al. A pilot randomized controlled trial with paroxetine for subthreshold PTSD in Operation Enduring Freedom/Operation Iraqi Freedom era veterans. Psychiatry Res 2013;206:318-20. https://doi.org/10.1016/j.psychres.2012.11.008.
- Neuner F, Onyut PL, Ertl V, Odenwald M, Schauer E, Elbert T. Treatment of posttraumatic stress disorder by trained lay counselors in an African refugee settlement: a randomized controlled trial. J Consult Clin Psychol 2008;76:686-94. https://doi.org/10.1037/0022-006X.76.4.686.
- Neuner F, Schauer M, Klaschik C, Karunakara U, Elbert T. A comparison of narrative exposure therapy, supportive counseling, and psychoeducation for treating posttraumatic stress disorder in an African refugee settlement. J Consult Clin Psychol 2004;72:579-87. https://doi.org/10.1037/0022-006X.72.4.579.
- Niles BL, Klunk-Gillis J, Ryngala DJ, Silberbogen AK, Paysnick A, Wolf EJ. Comparing mindfulness and psychoeducation treatments for combat-related PTSD using a telehealth approach. Psychol Trauma 2012;4:538-47. https://doi.org/10.1037/a0026161.
- Otto MW, Hinton D, Korbly NB, Chea A, Ba P, Gershuny BS, et al. Treatment of pharmacotherapy-refractory posttraumatic stress disorder among Cambodian refugees: a pilot study of combination treatment with cognitive-behavior therapy vs sertraline alone. Behav Res Ther 2003;41:1271-6. https://doi.org/10.1016/S0005-7967(03)00032-9.
- Owens GP, Pike JL, Chard KM. Treatment effects of cognitive processing therapy on cognitive distortions of female child sexual abuse survivors. Behav Ther 2001;32:413-24. https://doi.org/10.1016/S0005-7894(01)80028-9.
- Panahi Y, Moghaddam BR, Sahebkar A, Nazari MA, Beiraghdar F, Karami G, et al. A randomized, double-blind, placebo-controlled trial on the efficacy and tolerability of sertraline in Iranian veterans with post-traumatic stress disorder. Psychol Med 2011;41:2159-66. https://doi.org/10.1017/S0033291711000201.
- Paunovic N, Ost LG. Cognitive-behavior therapy vs exposure therapy in the treatment of PTSD in refugees. Behav Res Ther 2001;39:1183-97. https://doi.org/10.1016/S0005-7967(00)00093-0.
- Polusny MA, Erbes CR, Thuras P, Moran A, Lamberty GJ, Collins RC, et al. Mindfulness-based stress reduction for posttraumatic stress disorder among veterans: a randomized clinical trial. JAMA 2015;314:456-65. https://doi.org/10.1001/jama.2015.8361.
- Possemato K, Bergen-Cico D, Treatman S, Allen C, Wade M, Pigeon W. A randomized clinical trial of primary care brief mindfulness training for veterans with PTSD. J Clin Psychol 2016;72:179-93. https://doi.org/10.1002/jclp.22241.
- Raskind MA, Peskind ER, Hoff DJ, Hart KL, Holmes HA, Warren D, et al. A parallel group placebo controlled study of prazosin for trauma nightmares and sleep disturbance in combat veterans with post-traumatic stress disorder. Biol Psychiatry 2007;61:928-34. https://doi.org/10.1016/j.biopsych.2006.06.032.
- Raskind MA, Peterson K, Williams T, Hoff DJ, Hart K, Holmes H, et al. A trial of prazosin for combat trauma PTSD with nightmares in active-duty soldiers returned from Iraq and Afghanistan. Am J Psychiatry 2013;170:1003-10. https://doi.org/10.1176/appi.ajp.2013.12081133.
- Ready DJ, Gerardi RJ, Backscheider AG, Mascaro N, Rothbaum BO. Comparing virtual reality exposure therapy to present-centered therapy with 11 U.S. Vietnam veterans with PTSD. Cyberpsychol Behav Soc Netw 2010;13:49-54. https://doi.org/10.1089/cyber.2009.0239.
- Reed GL, Enright RD. The effects of forgiveness therapy on depression, anxiety, and posttraumatic stress for women after spousal emotional abuse. J Consult Clin Psychol 2006;74:920-9. https://doi.org/10.1037/0022-006X.74.5.920.
- Reger GM, Koenen-Woods P, Zetocha K, Smolenski DJ, Holloway KM, Rothbaum BO, et al. Randomized controlled trial of prolonged exposure using imaginal exposure vs. virtual reality exposure in active duty soldiers with deployment-related posttraumatic stress disorder (PTSD). J Consult Clin Psychol 2016;84:946-59. https://doi.org/10.1037/ccp0000134.
- Reich DB, Winternitz S, Hennen J, Watts T, Stanculescu C. A preliminary study of risperidone in the treatment of posttraumatic stress disorder related to childhood abuse in women. J Clin Psychiatry 2004;65:1601-6. https://doi.org/10.4088/JCP.v65n1204.
- Resick PA, Wachen JS, Mintz J, Young-McCaughan S, Roache JD, Borah AM, et al. A randomized clinical trial of group cognitive processing therapy compared with group present-centered therapy for PTSD among active duty military personnel. J Consult Clin Psychol 2015;83:1058-68. https://doi.org/10.1037/ccp0000016.
- Rothbaum BO, Price M, Jovanovic T, Norrholm SD, Gerardi M, Dunlop B, et al. A randomized, double-blind evaluation of D-cycloserine or alprazolam combined with virtual reality exposure therapy for posttraumatic stress disorder in Iraq and Afghanistan War veterans. Am J Psychiatry 2014;171:640-8. https://doi.org/10.1176/appi.ajp.2014.13121625.
- Rogers S, Silver SM, Goss J, Obenchain J, Willis A, Whitney RL. A single session, group study of exposure and eye movement desensitization and reprocessing in treating posttraumatic stress disorder among Vietnam War veterans: preliminary data. J Anxiety Disord 1999;13:119-30. https://doi.org/10.1016/S0887-6185(98)00043-7.
- Sikkema KJ, Hansen NB, Kochman A, Tarakeshwar N, Neufeld S, Meade CS, et al. Outcomes from a group intervention for coping with HIV/AIDS and childhood sexual abuse: reductions in traumatic stress. AIDS Behav 2007;11:49-60. https://doi.org/10.1007/s10461-006-9149-8.
- Sikkema KJ, Ranby KW, Meade CS, Hansen NB, Wilson PA, Kochman A. Reductions in traumatic stress following a coping intervention were mediated by decreases in avoidant coping for people living with HIV/AIDS and childhood sexual abuse. J Consult Clin Psychol 2013;81:274-83. https://doi.org/10.1037/a0030144.
- Smajkic A, Weine S, Djuric-Bijedic Z, Boskailo E, Lewis J, Pavkovic I. Sertraline, paroxetine, and venlafaxine in refugee posttraumatic stress disorder with depression symptoms. J Trauma Stress 2001;14:445-52. https://doi.org/10.1023/A:1011177420069.
- Sonne C, Carlsson J, Bech P, Elklit A, Mortensen EL. Treatment of trauma-affected refugees with venlafaxine versus sertraline combined with psychotherapy – a randomised study. BMC Psychiatry 2016;16. https://doi.org/10.1186/s12888-016-1081-5.
- Stein MB, Kline NA, Matloff JL. Adjunctive olanzapine for SSRI-resistant combat-related PTSD: a double-blind, placebo-controlled study. Am J Psychiatry 2002;159:1777-9. https://doi.org/10.1176/appi.ajp.159.10.1777.
- Stenmark H, Catani C, Neuner F, Elbert T, Holen A. Treating PTSD in refugees and asylum seekers within the general health care system. A randomized controlled multicenter study. Behav Res Ther 2013;51:641-7. https://doi.org/10.1016/j.brat.2013.07.002.
- Teng EJ, Bailey SD, Chaison AD, Petersen NJ, Hamilton JD, Dunn NJ. Treating comorbid panic disorder in veterans with posttraumatic stress disorder. J Consult Clin Psychol 2008;76:704-10. https://doi.org/10.1037/0022-006X.76.4.710.
- Ter Heide FJ, Mooren TM, Kleijn W, de Jongh A, Kleber RJ. EMDR versus stabilisation in traumatised asylum seekers and refugees: results of a pilot study. Eur J Psychotraumatol 2011;2. https://doi.org/10.3402/ejpt.v2i0.5881.
- Ter Heide FJ, Mooren TM, van de Schoot R, de Jongh A, Kleber RJ. Eye movement desensitisation and reprocessing therapy v. stabilisation as usual for refugees: randomised controlled trial. Br J Psychiatry 2016;209:311-18. https://doi.org/10.1192/bjp.bp.115.167775.
- Ulmer CS, Edinger JD, Calhoun PS. A multicomponent cognitive-behavioral intervention for sleep disturbance in veterans with PTSD: a pilot study. J Clin Sleep Med 2011;7:57-68.
- van der Kolk BA, Dreyfuss D, Michaels M, Shera D, Berkowitz R, Fisler R, et al. Fluoxetine in posttraumatic stress disorder. J Clin Psychiatry 1994;55:517-22.
- Wahbeh H, Goodrich E, Goy E, Oken BS. Mechanistic Pathways of Mindfulness Meditation in Combat Veterans With Posttraumatic Stress Disorder. J Clin Psychol 2016;72:365-83. https://doi.org/10.1002/jclp.22255.
- Wang SJ, Bytyçi A, Izeti S, Kallaba M, Rushiti F, Montgomery E, et al. A novel bio-psycho-social approach for rehabilitation of traumatized victims of torture and war in the post-conflict context: a pilot randomized controlled trial in Kosovo. Confl Health 2016;10. https://doi.org/10.1186/s13031-016-0100-y.
- Weiss WM, Murray LK, Zangana GA, Mahmooth Z, Kaysen D, Dorsey S, et al. Community-based mental health treatments for survivors of torture and militant attacks in Southern Iraq: a randomized control trial. BMC Psychiatry 2015;15. https://doi.org/10.1186/s12888-015-0622-7.
- Yeomans PD, Forman EM, Herbert JD, Yuen E. A randomized trial of a reconciliation workshop with and without PTSD psychoeducation in Burundian sample. J Trauma Stress 2010;23:305-12. https://doi.org/10.1002/jts.20531.
- Zlotnick C, Shea TM, Rosen K, Simpson E, Mulrenin K, Begin A, et al. An affect-management group for women with posttraumatic stress disorder and histories of childhood sexual abuse. J Trauma Stress 1997;10:425-36. https://doi.org/10.1002/jts.2490100308.
- Zohar J, Amital D, Miodownik C, Kotler M, Bleich A, Lane RM, et al. Double-blind placebo-controlled pilot study of sertraline in military veterans with posttraumatic stress disorder. J Clin Psychopharmacol 2002;22:190-5. https://doi.org/10.1097/00004714-200204000-00013.
- King AP, Erickson TM, Giardino ND, Favorite T, Rauch SA, Robinson E, et al. A pilot study of group mindfulness-based cognitive therapy (MBCT) for combat veterans with posttraumatic stress disorder (PTSD). Depress Anxiety 2013;30:638-45. https://doi.org/10.1002/da.22104.
- Kruse J, Joksimovic L, Cavka M, Wöller W, Schmitz N. Effects of trauma-focused psychotherapy upon war refugees. J Trauma Stress 2009;22:585-92. https://doi.org/10.1002/jts.20477.
- Levi O, Bar-Haim Y, Kreiss Y, Fruchter E. Cognitive-Behavioural Therapy and Psychodynamic Psychotherapy in the Treatment of Combat-Related Post-Traumatic Stress Disorder: A Comparative Effectiveness Study. Clin Psychol Psychother 2016;23:298-307. https://doi.org/10.1002/cpp.1969.
- Lundqvist G, Svedin CG, Hansson K, Broman I. Group therapy for women sexually abused as children: mental health before and after group therapy. J Interpers Violence 2006;21:1665-77. https://doi.org/10.1177/0886260506294986.
- Morgan T, Cummings AL. Change experienced during group therapy by female survivors of childhood sexual abuse. J Consult Clin Psychol 1999;67:28-36. https://doi.org/10.1037/0022-006X.67.1.28.
- Narimani M, Sadeghieh Ahari S, Rajabi S. Comparison of efficacy of eye movement desensitization and reprocessing and cognitive behavioral therapy therapeutic methods for reducing anxiety and depression of Iranian combatant afflicted by post traumatic stress disorder. J Appl Sci 2008;8:1932-7. https://doi.org/10.3923/jas.2008.1932.1937.
- Pivac N, Kozaric-Kovacic D, Muck-Seler D. Olanzapine versus fluphenazine in an open trial in patients with psychotic combat-related post-traumatic stress disorder. Psychopharmacology 2004;175:451-6.
- Salo J, Punamaki R-L, Qouta S, El Sarraj E. Individual and group treatment and self and other representations predicting posttraumatic recovery among former political prisoners. Traumatology 2008;14:45-61. https://doi.org/10.1177/1534765608319079.
- Saxe BJ, Johnson SM. An empirical investigation of group treatment for a clinical population of adult female incest survivors. J Child Sexual Abuse 1999;8:67-88. https://doi.org/10.1300/J070v08n01_05.
- Carlson JG, Chemtob CM, Rusnak K, Hedlund NL, Muraoka MY. Eye movement desensitization and reprocessing (EDMR) treatment for combat-related posttraumatic stress disorder. J Trauma Stress 1998;11:3-24. https://doi.org/10.1023/A:1024448814268.
- Hinton D, Pich V, Chhean D, Pollack M. Olfactory-triggered panic attacks among Khmer refugees: a contextual approach. Transcult Psychiatry 2004;41:155-99. https://doi.org/10.1177/1363461504043564.
- Margolies SO, Rybarczyk B, Vrana SR, Leszczyszyn DJ, Lynch J. Efficacy of a cognitive-behavioral treatment for insomnia and nightmares in Afghanistan and Iraq veterans with PTSD. J Clin Psychol 2013;69:1026-42. https://doi.org/10.1002/jclp.21970.
- Niles B, Seligowski A, Silberbogen A. Measuring mindfulness: which aspects of mindfulness change following a brief telehealth intervention for PTSD?. BMC Complement Altern Med 2012;12. https://doi.org/10.1186/1472-6882-12-S1-P191.
- Naved RT, Rimi NA, Jahan S, Lindmark G. Paramedic-conducted mental health counselling for abused women in rural Bangladesh: an evaluation from the perspective of participants. J Health Popul Nutr 2009;27:477-91. https://doi.org/10.3329/jhpn.v27i4.3391.
- Hughes MJ, Rasmussen LA. The utility of motivational interviewing in domestic violence shelters: a qualitative exploration. J Aggression Maltreat Trauma 2010;19:300-22. https://doi.org/10.1080/10926771003705213.
- Bermudez D, Benjamin MT, Porter SE, Saunders PA, Myers NA, Dutton MA. A qualitative analysis of beginning mindfulness experiences for women with post-traumatic stress disorder and a history of intimate partner violence. Complement Ther Clin Pract 2013;19:104-8. https://doi.org/10.1016/j.ctcp.2013.02.004.
- Dutton MA, Bermudez D, Matas A, Majid H, Myers NL. Mindfulness-based stress reduction for low-income, predominantly African American women with PTSD and a history of intimate partner violence. Cogn Behav Pract 2013;20:23-32. https://doi.org/10.1016/j.cbpra.2011.08.003.
- Martinez ME, Kearney DJ, Simpson T, Felleman BI, Bernardi N, Sayre G. Challenges to enrollment and participation in mindfulness-based stress reduction among veterans: a qualitative study. J Altern Complement Med 2015;21:409-21. https://doi.org/10.1089/acm.2014.0324.
- Hundt NE, Barrera TL, Arney J, Stanley MA. ‘It’s worth it in the end’: veterans’ experiences in prolonged exposure and cognitive processing therapy. Cogn Behav Pract 2017;24:50-7. https://doi.org/10.1016/j.cbpra.2016.02.003.
- Palmer S, Stalker CA, Harper K, Gadbois S. Balancing positive outcomes with vicarious traumatization: participants’ experiences with group treatment for long-term effects of childhood abuse. Soc Work Groups 2007;30:59-77. https://doi.org/10.1300/J009v30n04_05.
- Parker A, Fourt A, Langmuir JI, Dalton EJ, Classen CC. The experience of trauma recovery: a qualitative study of participants in the Women Recovering from Abuse Program (WRAP). J Child Sex Abus 2007;16:55-77. https://doi.org/10.1300/J070v16n02_04.
- Vincent F, Jenkins H, Larkin M, Clohessy S. Asylum-seekers’ experiences of trauma-focused cognitive behaviour therapy for post-traumatic stress disorder: a qualitative study. Behav Cogn Psychother 2013;41:579-93. https://doi.org/10.1017/S1352465812000550.
- Braye S, Preston-Shoot M. Emerging from out of the shadows? Service user and carer involvement in systematic reviews. Evid Policy 2005;1:173-94. https://doi.org/10.1332/1744264053730743.
- Smith E, Donovan S, Beresford P, Manthorpe J, Brearley S, Sitzia J, et al. Getting ready for user involvement in a systematic review. Health Expect 2009;12:197-208. https://doi.org/10.1111/j.1369-7625.2009.00535.x.
- Rushmer RK, Cheetham M, Cox L, Crosland A, Gray J, Hughes L, et al. Research utilisation and knowledge mobilisation in the commissioning and joint planning of public health interventions to reduce alcohol-related harms: a qualitative case design using a cocreation approach. Health Serv Deliv Res 2015;3. https://doi.org/10.3310/hsdr03330.
- Thompson CT, Vidgen A, Roberts NP. Psychological interventions for post-traumatic stress disorder in refugees and asylum seekers: a systematic review and meta-analysis. Clin Psychol Rev 2018;63:66-79. https://doi.org/10.1016/j.cpr.2018.06.006.
- Bisson JI, Roberts NP, Andrew M, Cooper R, Lewis C. Psychological therapies for chronic post-traumatic stress disorder (PTSD) in adults. Cochrane Database Syst Rev 2013;12. https://doi.org/10.1002/14651858.CD003388.pub4.
- Cloitre M, Courtois CA, Ford JD, Green BL, Alexander P, Briere J, et al. The ISTSS Expert Consensus Treatment Guidelines for Complex PTSD in Adults 2012. www.istss.org/ISTSS_Main/media/Documents/ISTSS-Expert-Concesnsus-Guidelines-for-Complex-PTSD-Updated-060315.pdf (accessed 10 January 2020).
- Dalton J, Thomas S, Melton H, Harden M, Eastwood A. The provision of services in the UK for UK armed forces veterans with PTSD: a rapid evidence synthesis. Health Serv Deliv Res 2018;6. https://doi.org/10.3310/hsdr06110.
- Hoskins M, Pearce J, Bethell A, Dankova L, Barbui C, Tol WA, et al. Pharmacotherapy for post-traumatic stress disorder: systematic review and meta-analysis. Br J Psychiatry 2015;206:93-100. https://doi.org/10.1192/bjp.bp.114.148551.
- Purgato M, Gastaldon C, Papola D, van Ommeren M, Barbui C, Tol WA. Psychological therapies for the treatment of mental disorders in low- and middle-income countries affected by humanitarian crises. Cochrane Database Syst Rev 2018;7. https://doi.org/10.1002/14651858.CD011849.pub2.
- Dorrepaal E, Thomaes K, Hoogendoorn AW, Veltman DJ, Draijer N, van Balkom AJ. Evidence-based treatment for adult women with child abuse-related Complex PTSD: a quantitative review. Eur J Psychotraumatol 2014;5. https://doi.org/10.3402/ejpt.v5.23613.
- Nosè M, Ballette F, Bighelli I, Turrini G, Purgato M, Tol W, et al. Psychosocial interventions for post-traumatic stress disorder in refugees and asylum seekers resettled in high-income countries: systematic review and meta-analysis. PLOS ONE 2017;12. https://doi.org/10.1371/journal.pone.0171030.
- Tol WA, Purgato M, Bass JK, Galappatti A, Eaton W. Mental health and psychosocial support in humanitarian settings: a public mental health perspective. Epidemiol Psychiatr Sci 2015;24:484-94. https://doi.org/10.1017/S2045796015000827.
- Arroyo K, Lundahl B, Butters R, Vanderloo M, Wood DS. Short-term interventions for survivors of intimate partner violence: a systematic review and meta-analysis. Trauma Violence Abuse 2017;18:155-71. https://doi.org/10.1177/1524838015602736.
- Karatzias T, Murphy P, Cloitre M, Bisson J, Roberts N, Shevlin M, et al. Psychological interventions for ICD-11 complex PTSD symptoms: systematic review and meta-analysis. Psychol Med 2019;49:1761-75. https://doi.org/10.1017/S0033291719000436.
- Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 1996;49:1373-9. https://doi.org/10.1016/S0895-4356(96)00236-3.
- Kontopantelis E, Springate DA, Reeves D. A re-analysis of the Cochrane Library data: the dangers of unobserved heterogeneity in meta-analyses. PLOS ONE 2013;8. https://doi.org/10.1371/journal.pone.0069930.
- Vale CL, Tierney JF, Spera N, Whelan A, Nightingale A, Hanley B. Evaluation of patient involvement in a systematic review and meta-analysis of individual patient data in cervical cancer treatment. Syst Rev 2012;1. https://doi.org/10.1186/2046-4053-1-23.
- Stevelink SAM, Jones M, Hull L, Pernet D, MacCrimmon S, Goodwin L, et al. Mental health outcomes at the end of the British involvement in the Iraq and Afghanistan conflicts: a cohort study. Br J Psychiatry 2018;213:690-7. https://doi.org/10.1192/bjp.2018.175.
- Abramowitz EG, Barak Y, Ben-Avi I, Knobler HY. Hypnotherapy in the treatment of chronic combat-related PTSD patients suffering from insomnia: a randomized, zolpidem-controlled clinical trial. Int J Clin Exp Hypn 2008;56:270-80. https://doi.org/10.1080/00207140802039672.
- Acierno R, Gros DF, Ruggiero KJ, Hernandez-Tejada BM, Knapp RG, Lejuez CW, et al. Behavioral activation and therapeutic exposure for posttraumatic stress disorder: a noninferiority trial of treatment delivered in person versus home-based telehealth. Depress Anxiety 2016;33:415-23. https://doi.org/10.1002/da.22476.
- Aderka IM, Gillihan SJ, McLean CP, Foa EB. The relationship between posttraumatic and depressive symptoms during prolonged exposure with and without cognitive restructuring for the treatment of posttraumatic stress disorder. J Consult Clin Psychol 2013;81:375-82. https://doi.org/10.1037/a0031523.
- Adler AB, Bliese PD, McGurk D, Hoge CW, Castro CA. Battlemind debriefing and battlemind training as early interventions with soldiers returning from Iraq: randomization by platoon. J Consult Clin Psychol 2009;77:928-40. https://doi.org/10.1037/a0016877.
- Alderman CP, Condon JT, Gilbert AL. An open-label study of mirtazapine as treatment for combat-related PTSD. Ann Pharmacother 2009;43:1220-6. https://doi.org/10.1345/aph.1M009.
- Alderman CP, McCarthy LC, Condon JT, Marwood AC, Fuller JR. Topiramate in combat-related posttraumatic stress disorder. Ann Pharmacother 2009;43:635-41. https://doi.org/10.1345/aph.1L578.
- Allan NP, Short NA, Albanese BJ, Keough ME, Schmidt NB. Direct and mediating effects of an anxiety sensitivity intervention on posttraumatic stress disorder symptoms in trauma-exposed individuals. Cogn Behav Ther 2015;44:512-24. https://doi.org/10.1080/16506073.2015.1075227.
- Allon M. EMDR group therapy with women who were sexually assaulted in the Congo. J EMDR Pract Res 2015;9:28-34. https://doi.org/10.1891/1933-3196.9.1.28.
- Alvarez J, McLean C, Harris AH, Rosen CS, Ruzek JI, Kimerling R. The comparative effectiveness of cognitive processing therapy for male veterans treated in a VHA posttraumatic stress disorder residential rehabilitation program. J Consult Clin Psychol 2011;79:590-9. https://doi.org/10.1037/a0024466.
- Amin M, Gold M, Gold AR. The effect of nasal continuous positive airway pressure (Nasal CPAP) treatment on post traumatic stress disorder (PTSD) symptoms among veterans population. Sleep 2013;36.
- Angelo FN, Miller HE, Zoellner LA, Feeny NC. ‘I need to talk about it’: a qualitative analysis of trauma-exposed women’s reasons for treatment choice. Behav Ther 2008;39:13-21. https://doi.org/10.1016/j.beth.2007.02.002.
- Arntz A, Tiesema M, Kindt M. Treatment of PTSD: a comparison of imaginal exposure with and without imagery rescripting. J Behav Ther Exp Psychiatry 2007;38:345-70. https://doi.org/10.1016/j.jbtep.2007.10.006.
- Ayoughi S, Missmahl I, Weierstall R, Elbert T. Provision of mental health services in resource-poor settings: a randomised trial comparing counselling with routine medical treatment in North Afghanistan (Mazar-e-Sharif). BMC Psychiatry 2012;12. https://doi.org/10.1186/1471-244X-12-14.
- Baños RM, Guillen V, Quero S, García-Palacios A, Alcañiz M, Botella C. A virtual reality system for the treatment of stress-related disorders: a preliminary analysis of efficacy compared to a standard cognitive behavioral program. Int J Hum Comput Stud 2011;69:602-13. https://doi.org/10.1016/j.ijhcs.2011.06.002.
- Basharpoor S, Narimani M, Gamari-Give H, Abolgasemi A, Molavi P. Effect of cognitive processing therapy and holographic reprocessing on reduction of posttraumatic cognitions in students exposed to trauma. Iran J Psychiatry 2011;6:138-44.
- Bass JK, Annan J, McIvor Murray S, Kaysen D, Griffiths S, Cetinoglu T, et al. Controlled trial of psychotherapy for Congolese survivors of sexual violence. N Engl J Med 2013;368:2182-91. https://doi.org/10.1056/NEJMoa1211853.
- Batka C, Tanielian T, Woldetsadik MA, Farmer C, Jaycox LH. Stakeholder experiences in a stepped collaborative care study within U.S. army clinics. Psychosomatics 2016;57:586-97. https://doi.org/10.1016/j.psym.2016.05.008.
- Benedek DM. Posttraumatic stress disorder from Vietnam to today: the evolution of understanding during Eugene Brody’s tenure at the journal of nervous and mental disease. J Nerv Ment Dis 2011;199:544-52. https://doi.org/10.1097/NMD.0b013e318225f0e9.
- Bensimon M, Amir D, Wolf Y. A pendulum between trauma and life: group music therapy with post-traumatized soldiers. Arts Psychother 2012;39:223-33. https://doi.org/10.1016/j.aip.2012.03.005.
- Betancourt TS, McBain R, Newnham EA, Akinsulure-Smith AM, Brennan RT, Weisz JR, et al. A behavioral intervention for war-affected youth in Sierra Leone: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry 2014;53:1288-97. https://doi.org/10.1016/j.jaac.2014.09.011.
- Bisson JI. Trauma-focused group psychotherapy is not effective for posttraumatic stress disorder in Vietnam veterans. Evid Based Ment Health 2003;6. https://doi.org/10.1136/ebmh.6.4.124.
- Bisson JI. Eye movement desensitisation and reprocessing reduces PTSD symptoms compared with fluoxetine at six months post-treatment. Evid Based Ment Health 2007;10. https://doi.org/10.1136/ebmh.10.4.118.
- Blevins D, Roca J, Spencer T. Life guard: evaluation of an ACT-based workshop to facilitate reintegration of OIF/OEF veterans. Prof Psychol Res Pr 2011;42:32-9. https://doi.org/10.1037/a0022321.
- Bohus M, Dyer AS, Priebe K, Krüger A, Kleindienst N, Schmahl C, et al. Dialectical behaviour therapy for post-traumatic stress disorder after childhood sexual abuse in patients with and without borderline personality disorder: a randomised controlled trial. Psychother Psychosom 2013;82:221-33. https://doi.org/10.1159/000348451.
- Bolton P, Lee C, Haroz EE, Murray L, Dorsey S, Robinson C, et al. A transdiagnostic community-based mental health treatment for comorbid disorders: development and outcomes of a randomized controlled trial among Burmese refugees in Thailand. PLOS Med 2014;11. https://doi.org/10.1371/journal.pmed.1001757.
- Bomyea J, Stein MB, Lang AJ. Interference control training for PTSD: a randomized controlled trial of a novel computer-based intervention. J Anxiety Disord 2015;34:33-42. https://doi.org/10.1016/j.janxdis.2015.05.010.
- Bormann JE, Thorp S, Wetherell JL, Golshan S. A spiritually based group intervention for combat veterans with posttraumatic stress disorder: feasibility study. J Holist Nurs 2008;26:109-16. https://doi.org/10.1177/0898010107311276.
- Bormann JE, Thorp SR, Wetherell JL, Golshan S, Lang AJ. Meditation-based mantram intervention for veterans with posttraumatic stress disorder: a randomized trial. Psychol Trauma 2013;5:259-67. https://doi.org/10.1037/a0027522.
- Bormann J, Beck D, Glickman M, Zhao S, Osei-Bonsu P, Johnston J, et al. Meditation-based mantram repetition program for veterans with PTSD: a randomized controlled trial in the VA healthcare system. J Altern Complement Med 2014;20. https://doi.org/10.1089/acm.2014.5022.abstract.
- Bradley RG, Follingstad DR. Group therapy for incarcerated women who experienced interpersonal violence: a pilot study. J Trauma Stress 2003;16:337-40. https://doi.org/10.1023/A:1024409817437.
- Brady K, Pearlstein T, Asnis GM, Baker D, Rothbaum B, Sikes CR, et al. Efficacy and safety of sertraline treatment of posttraumatic stress disorder: a randomized controlled trial. JAMA 2000;283:1837-44. https://doi.org/10.1001/jama.283.14.1837.
- Bremner JD, Mletzko T, Welter S, Siddiq S, Reed L, Williams C, et al. Treatment of posttraumatic stress disorder with phenytoin: an open-label pilot study. J Clin Psychiatry 2004;65:1559-64. https://doi.org/10.4088/JCP.v65n1120.
- Bremner JD, Afzal N, Vaccarino V, Carmody J, Divitale S. Mindfulness based stress reduction (MBSR) in the treatment of Iraq combat-related PTSD. Psychosom Med 2011;73.
- Brown AJ, Bollini AM, Craighead LW, Astin MC, Norrholm SD, Bradley B. Self-monitoring of reexperiencing symptoms: a randomized trial. J Trauma Stress 2014;27:519-25. https://doi.org/10.1002/jts.21950.
- Bryan CJ, Clemans TA, Hernandez AM, Mintz J, Peterson AL, Yarvis JS, et al. Evaluating potential iatrogenic suicide risk in trauma-focused group cognitive behavioral therapy for the treatment of PTSD in active duty military personnel. Depress Anxiety 2016;33:549-57. https://doi.org/10.1002/da.22456.
- Bui A, Bishop TM, Heffner K, Cerulli C, Crean H, Pigeon WR. Brief CBT-I disproportionally reduces depression, posttraumatic stress, and insomnia severity among survivors of intimate partner violence who are objective short sleepers. Sleep 2016;39:A220-A1.
- Byers MG, Allison KM, Wendel CS, Lee JK. Prazosin versus quetiapine for nighttime posttraumatic stress disorder symptoms in veterans: an assessment of long-term comparative effectiveness and safety. J Clin Psychopharmacol 2010;30:225-9. https://doi.org/10.1097/JCP.0b013e3181dac52f.
- Byers MG. Long-term effectiveness of prazosin for PTSD. Brown Univ Psychopharmacol Update 2010;21.
- Campbell M, Decker KP, Kruk K, Deaver SP. Art therapy and cognitive processing therapy for combat-related PTSD: a randomized controlled trial. Art Ther 2016;33:169-77. https://doi.org/10.1080/07421656.2016.1226643.
- Carr C, d’Ardenne P, Sloboda A, Scott C, Wang D, Priebe S. Group music therapy for patients with persistent post-traumatic stress disorder – an exploratory randomized controlled trial with mixed methods evaluation. Psychol Psychother 2012;85:179-202. https://doi.org/10.1111/j.2044-8341.2011.02026.x.
- Castillo DT, Chee CL, Nason E, Keller J, C’de Baca J, Qualls C, et al. Group-delivered cognitive/exposure therapy for PTSD in women veterans: a randomized controlled trial. Psychol Trauma 2016;8:404-12. https://doi.org/10.1037/tra0000111.
- Cates ME, Bishop MH, Davis LL, Lowe JS, Woolley TW. Clonazepam for treatment of sleep disturbances associated with combat-related posttraumatic stress disorder. Ann Pharmacother 2004;38:1395-9. https://doi.org/10.1345/aph.1E043.
- Chemtob CM, Novaco RW, Hamada RS, Gross DM. Cognitive-behavioral treatment for severe anger in posttraumatic stress disorder. J Consult Clin Psychol 1997;65:184-9. https://doi.org/10.1037/0022-006X.65.1.184.
- Chen JA, Keller SM, Zoellner LA, Feeny NC. ‘How will it help me?’ Reasons underlying treatment preferences between sertraline and prolonged exposure in posttraumatic stress disorder. J Nerv Ment Dis 2013;201:691-7. https://doi.org/10.1097/NMD.0b013e31829c50a9.
- Dempsey C, Chesney M, Lao L, Vegella P, Magyari T, Robertson MB, et al. Acupuncture and mindfulness-based stress reduction among female child abuse survivors: a randomized waitlist-controlled pilot study. J Altern Complement Med 2014;20. https://doi.org/10.1089/acm.2014.5229.abstract.
- Church D, Hawk C, Brooks AJ, Toukolehto O, Wren M, Dinter I, et al. Psychological trauma symptom improvement in veterans using emotional freedom techniques: a randomized controlled trial. J Nerv Ment Dis 2013;201:153-60. https://doi.org/10.1097/NMD.0b013e31827f6351.
- Church D. Reductions in pain, depression, and anxiety symptoms after PTSD remediation in veterans. Explore 2014;10:162-9. https://doi.org/10.1016/j.explore.2014.02.005.
- Clark RD, Cañive JM, Calais LA, Qualls CR, Tuason VB. Divalproex in posttraumatic stress disorder: an open-label clinical trial. J Trauma Stress 1999;12:395-401. https://doi.org/10.1023/A:1024797014210.
- Classen CC, Palesh OG, Cavanaugh CE, Koopman C, Kaupp JW, Kraemer HC, et al. A comparison of trauma-focused and present-focused group therapy for survivors of childhood sexual abuse: a randomized controlled trial. Psychol Trauma 2011;3:84-93. https://doi.org/10.1037/a0020096.
- Cloitre M, Koenen KC. The impact of borderline personality disorder on process group outcome among women with posttraumatic stress disorder related to childhood abuse. Int J Group Psychother 2001;51:379-98. https://doi.org/10.1521/ijgp.51.3.379.49886.
- Cole KL, Sarlund-Heinrich P, Brown L. Developing and assessing effectiveness of a time-limited therapy group for incarcerated women survivors of childhood sexual abuse. J Trauma Dissociation 2007;8:97-121. https://doi.org/10.1300/J229v08n02_07.
- Connolly S, Sakai C. Brief trauma intervention with Rwandan genocide-survivors using thought field therapy. Int J Emerg Ment Health 2011;13:161-72.
- Cort NA, Cerulli C, Poleshuck EL, Bellenger KM, Yinglin X, Xin T, et al. Interpersonal psychotherapy for depressed women with histories of intimate partner violence. Psychol Trauma 2014;6:700-7. https://doi.org/10.1037/a0037361.
- Coulter S. Systemic family therapy for families who have experienced trauma: a randomised controlled trial. Br J Soc Work 2010;41:502-19. https://doi.org/10.1093/bjsw/bcq132.
- Crespo M, Arinero M. Assessment of the efficacy of a psychological treatment for women victims of violence by their intimate male partner. Span J Psychol 2010;13:849-63. https://doi.org/10.1017/S113874160000250X.
- David D, De Faria L, Mellman TA. Adjunctive risperidone treatment and sleep symptoms in combat veterans with chronic PTSD. Depress Anxiety 2006;23:489-91. https://doi.org/10.1002/da.20187.
- Davidson JR, Kudler HS, Saunders WB, Erickson L, Smith RD, Stein RM, et al. Predicting response to amitriptyline in posttraumatic stress disorder. Am J Psychiatry 1993;150:1024-9. https://doi.org/10.1176/ajp.150.7.1024.
- Davidson J, Pearlstein T, Londborg P, Brady KT, Rothbaum B, Bell J, et al. Efficacy of sertraline in preventing relapse of posttraumatic stress disorder: results of a 28-week double-blind, placebo-controlled study. Am J Psychiatry 2001;158:1974-81. https://doi.org/10.1176/appi.ajp.158.12.1974.
- Davidson JR, Rothbaum BO, van der Kolk BA, Sikes CR, Farfel GM. Multicenter, double-blind comparison of sertraline and placebo in the treatment of posttraumatic stress disorder. Arch Gen Psychiatry 2001;58:485-92. https://doi.org/10.1001/archpsyc.58.5.485.
- Davis LL, Nugent AL, Murray J, Kramer GL, Petty F. Nefazodone treatment for chronic posttraumatic stress disorder: an open trial. J Clin Psychopharmacol 2000;20:159-64. https://doi.org/10.1097/00004714-200004000-00007.
- Davis JL, Rhudy JL, Pruiksma KE, Byrd P, Williams AE, McCabe KM, et al. Physiological predictors of response to exposure, relaxation, and rescripting therapy for chronic nightmares in a randomized clinical trial. J Clin Sleep Med 2011;7:622-31. https://doi.org/10.5664/jcsm.1466.
- Dawson KS, Schafer A, Anjuri D, Ndogoni L, Musyoki C, Sijbrandij M, et al. Feasibility trial of a scalable psychological intervention for women affected by urban adversity and gender-based violence in Nairobi. BMC Psychiatry 2016;16. https://doi.org/10.1186/s12888-016-1117-x.
- Dieperink E, Leskela J, Dieperink ME, Evans B, Thuras P, Ho SB. The effect of pegylated interferon-α2b and ribavirin on posttraumatic stress disorder symptoms. Psychosomatics 2008;49:225-9. https://doi.org/10.1176/appi.psy.49.3.225.
- Difede J, Cukor J, Wyka K, Olden M, Hoffman H, Lee FS, et al. D-cycloserine augmentation of exposure therapy for post-traumatic stress disorder: a pilot randomized clinical trial. Neuropsychopharmacology 2014;39:1052-8. https://doi.org/10.1038/npp.2013.317.
- Dorrepaal E, Thomaes K, Smit JH, van Balkom AJ, Veltman DJ, Hoogendoorn AW, et al. Stabilizing group treatment for complex posttraumatic stress disorder related to child abuse based on psychoeducation and cognitive behavioural therapy: a multisite randomized controlled trial. Psychother Psychosom 2012;81:217-25. https://doi.org/10.1159/000335044.
- Dorrepaal E, Thomaes K, Smit JH, Veltman DJ, Hoogendoorn AW, van Balkom AJ, et al. Treatment compliance and effectiveness in complex PTSD patients with co-morbid personality disorder undergoing stabilizing cognitive behavioral group treatment: a preliminary study. Eur J Psychotraumatol 2013;4. https://doi.org/10.3402/ejpt.v4i0.21171.
- Doruk A, Yetkin S, Aydin H. The efficacy of sertraline on post-traumatic stress disorder. Klinik Psikofarmakol Bulteni 1999;9:47-52.
- Dougherty MJ. Client satisfaction survey of inpatient trauma and dissociative disorders program. J Trauma Dissociation 2002;3:97-105. https://doi.org/10.1300/J229v03n02_06.
- Drozdek B. Follow-up study of concentration camp survivors from Bosnia-Herzegovina: three years later. J Nerv Ment Dis 1997;185:690-4. https://doi.org/10.1097/00005053-199711000-00007.
- Droždek B, Bolwerk N. Evaluation of group therapy with traumatized asylum seekers and refugees—The Den Bosch Model. Traumatology 2010;16:117-27. https://doi.org/10.1177/1534765610388298.
- Drožđek B, Kamperman AM, Bolwerk N, Tol WA, Kleber RJ. Group therapy with male asylum seekers and refugees with posttraumatic stress disorder: a controlled comparison cohort study of three day-treatment programs. J Nerv Ment Dis 2012;200:758-65. https://doi.org/10.1097/NMD.0b013e318266f860.
- Duffy JD, Malloy PF. Efficacy of buspirone in the treatment of posttraumatic stress disorder: an open trial. Ann Clin Psychiatry 1994;6:33-7. https://doi.org/10.3109/10401239409148837.
- Duffy M, Gillespie K, Clark DM. Post-traumatic stress disorder in the context of terrorism and other civil conflict in Northern Ireland: randomised controlled trial. BMJ 2007;334. https://doi.org/10.1136/bmj.39021.846852.BE.
- Dunn NJ, Rehm LP, Schillaci J, Souchek J, Mehta P, Ashton CM, et al. A randomized trial of self-management and psychoeducational group therapies for comorbid chronic posttraumatic stress disorder and depressive disorder. J Trauma Stress 2007;20:221-37. https://doi.org/10.1002/jts.20214.
- Durham RC, Chambers JA, Power KG, Sharp DM, Macdonald RR, Major KA, et al. Long-term outcome of cognitive behaviour therapy clinical trials in central Scotland. Health Technol Assess 2005;9. https://doi.org/10.3310/hta9420.
- Echeburúa E, de Corral P, Zubizarreta I, Sarasua B. Psychological treatment of chronic posttraumatic stress disorder in victims of sexual aggression. Behav Modif 1997;21:433-56. https://doi.org/10.1177/01454455970214003.
- Echeburúa E, Sarasua B, Zubizarreta I. Individual versus individual and group therapy regarding a cognitive-behavioral treatment for battered women in a community setting. J Interpers Violence 2014;29:1783-801. https://doi.org/10.1177/0886260513511703.
- Edmond TE, Sloan L, McCarty D. Sexual abuse survivors’ perceptions of the effectiveness of EMDR and eclectic therapy. Res Soc Work Pract 2004;14:259-72. https://doi.org/10.1177/1049731504265830.
- Ekstrom M, Carlsson J, Sonne C, Mortensen EL. Stress management versus cognitive restructuring: a randomized clinical study on traumatized refugees. Eur Psychiatry 2016;33:S399-S400. https://doi.org/10.1016/j.eurpsy.2016.01.1437.
- Ekstrom M, Sonne C, Carlsson J, Bech P, Elklit A. The treatment of traumatised refugees with sertraline versus venlafaxine in combination with psychotherapy – a randomised clinical study. Eur Psychiatry 2016;33. https://doi.org/10.1016/j.eurpsy.2016.01.1438.
- Elkjaer H, Kristensen E, Mortensen EL, Poulsen S, Lau M. Efficacy of specialized incest group psychotherapy in reducing symptoms of PTSD: 5 year follow-up of a randomized trial. Eur Psychiatry 2012;27. https://doi.org/10.1016/S0924-9338(12)75304-X.
- Ertl V, Pfeiffer A, Schauer E, Elbert T, Neuner F. Community-implemented trauma therapy for former child soldiers in northern Uganda: a randomized controlled trial. JAMA 2011;306:503-12. https://doi.org/10.1001/jama.2011.1060.
- Esala JJ, Taing S. Testimony therapy with ritual: a pilot randomized controlled trial. J Trauma Stress 2017;30:94-8. https://doi.org/10.1002/jts.22163.
- Falsetti SA, Erwin BA, Resnick HS, Davis J, Combs-Lane AM. Multiple channel exposure therapy of PTSD: impact of treatment on functioning and resources. J Cogn Psychother 2003;17:133-47. https://doi.org/10.1891/jcop.17.2.133.57439.
- Farchi M, Gidron Y. The effects of ‘psychological inoculation’ versus ventilation on the mental resilience of Israeli citizens under continuous war stress. J Nerv Ment Dis 2010;198:382-4. https://doi.org/10.1097/NMD.0b013e3181da4b67.
- Fiorillo D, McLean C, Pistorello J, Hayes SC, Follette VM. Evaluation of a web-based acceptance and commitment therapy program for women with trauma-related problems: a pilot study. J Contextual Behav Sci 2017;6:104-13. https://doi.org/10.1016/j.jcbs.2016.11.003.
- Foa EB, Rothbaum BO, Riggs DS, Murdock TB. Treatment of posttraumatic stress disorder in rape victims: a comparison between cognitive-behavioral procedures and counseling. J Consult Clin Psychol 1991;59:715-23. https://doi.org/10.1037/0022-006X.59.5.715.
- Foa EB, Dancu CV, Hembree EA, Jaycox LH, Meadows EA, Street GP. A comparison of exposure therapy, stress inoculation training, and their combination for reducing posttraumatic stress disorder in female assault victims. J Consult Clin Psychol 1999;67:194-200. https://doi.org/10.1037/0022-006X.67.2.194.
- Foa EB, Hembree EA, Cahill SP, Rauch SA, Riggs DS, Feeny NC, et al. Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: outcome at academic and community clinics. J Consult Clin Psychol 2005;73:953-64. https://doi.org/10.1037/0022-006X.73.5.953.
- Forbes D, Phelps A, McHugh T. Treatment of combat-related nightmares using imagery rehearsal: a pilot study. J Trauma Stress 2001;14:433-42. https://doi.org/10.1023/A:1011133422340.
- Forbes D, Lewis V, Parslow R, Hawthorne G, Creamer M. Naturalistic comparison of models of programmatic interventions for combat-related post-traumatic stress disorder. Aust N Z J Psychiatry 2008;42:1051-9. https://doi.org/10.1080/00048670802512024.
- Forbes D, Lloyd D, Nixon RD, Elliott P, Varker T, Perry D, et al. A multisite randomized controlled effectiveness trial of cognitive processing therapy for military-related posttraumatic stress disorder. J Anxiety Disord 2012;26:442-52. https://doi.org/10.1016/j.janxdis.2012.01.006.
- Ford JD, Steinberg KL, Zhang W. A randomized clinical trial comparing affect regulation and social problem-solving psychotherapies for mothers with victimization-related PTSD. Behav Ther 2011;42:560-78. https://doi.org/10.1016/j.beth.2010.12.005.
- Fortney JC, Pyne JM, Kimbrell TA, Hudson TJ, Robinson DE, Schneider R, et al. Telemedicine-based collaborative care for posttraumatic stress disorder: a randomized clinical trial. JAMA Psychiatry 2015;72:58-67. https://doi.org/10.1001/jamapsychiatry.2014.1575.
- Fortney JC, Pyne JM, Kimbrell TA, Hudson TJ, Robinson DE, Schneider R, et al. ‘Telemedicine-based collaborative care for posttraumatic stress disorder: a randomized clinical trial’: correction. JAMA Psychiatry 2015;72. https://doi.org/10.1001/jamapsychiatry.2014.1575.
- Frommberger U, Stieglitz RD, Nyberg E, Richter H, Novelli-Fischer U, Angenendt J, et al. Comparison between paroxetine and behaviour therapy in patients with posttraumatic stress disorder (PTSD): a pilot study. Int J Psychiatry Clin Pract 2004;8:19-23. https://doi.org/10.1080/13651500310004803.
- Galovski TE, Monson C, Bruce SE, Resick PA. Does cognitive-behavioral therapy for PTSD improve perceived health and sleep impairment?. J Trauma Stress 2009;22:197-204. https://doi.org/10.1002/jts.20418.
- Galovski TE, Blain LM, Mott JM, Elwood L, Houle T. Manualized therapy for PTSD: flexing the structure of cognitive processing therapy. J Consult Clin Psychol 2012;80:968-81. https://doi.org/10.1037/a0030600.
- Gamito P, Oliveira J, Morais D, Oliveira S, Duarte N, Saraiva T, et al. Virtual reality therapy controlled study for war veterans with PTSD. Preliminary results. Stud Health Technol Inform 2009;144:269-72.
- Garfield DA, Fichtner CG, Leveroni C, Mahableshwarkar A. Open trial of nefazodone for combat veterans with posttraumatic stress disorder. J Trauma Stress 2001;14:453-60. https://doi.org/10.1023/A:1011148304140.
- Gatz M, Brown VB, Hennigan K, Rechberger E, O’Keefe M, Rose T, et al. Effectiveness of an integrated, trauma-informed approach to treating women with co-occurring disorders and histories of trauma: the Los Angeles site experience. J Community Psychol 2007;35:863-78. https://doi.org/10.1002/jcop.20186.
- Gebler FA, Maercker A. Expressive writing and the existential dimension in coping with traumatic experiences: a randomized controlled pilot study. Trauma Und Gewalt 2007;1:264-72.
- Gelpin E, Bonne O, Peri T, Brandes D, Shalev AY. Treatment of recent trauma survivors with benzodiazepines: a prospective study. J Clin Psychiatry 1996;57:390-4.
- Gillin JC, Smith-Vaniz A, Schnierow B, Rapaport MH, Kelsoe J, Raimo E, et al. An open-label, 12-week clinical and sleep EEG study of nefazodone in chronic combat-related posttraumatic stress disorder. J Clin Psychiatry 2001;62:789-96. https://doi.org/10.4088/JCP.v62n1007.
- Ginsberg DL. Prazosin reduces nightmares in posttraumatic stress disorder. Prim Psychiatry 2003;10.
- Ginzburg K, Butler LD, Giese-Davis J, Cavanaugh CE, Neri E, Koopman C, et al. Shame, guilt, and posttraumatic stress disorder in adult survivors of childhood sexual abuse at risk for human immunodeficiency virus: outcomes of a randomized clinical trial of group psychotherapy treatment. J Nerv Ment Dis 2009;197:536-42. https://doi.org/10.1097/NMD.0b013e3181ab2ebd.
- Glover H. A preliminary trial of nalmefene for the treatment of emotional numbing in combat veterans with post-traumatic stress disorder. Isr J Psychiatry Relat Sci 1993;30:255-63.
- Glynn SM, Eth S, Randolph ET, Foy DW, Urbaitis M, Boxer L, et al. A test of behavioral family therapy to augment exposure for combat-related posttraumatic stress disorder. J Consult Clin Psychol 1999;67:243-51. https://doi.org/10.1037/0022-006X.67.2.243.
- Goldberg JF, Cloitre M, Whiteside JE, Han H. An open-label pilot study of divalproex sodium for posttraumatic stress disorder related to childhood abuse. Curr Ther Res Clin Exp 2003;64:45-54. https://doi.org/10.1016/S0011-393X(03)00003-1.
- Gosselin A, Shlik J, Christie K. Comparison of two conceptually different methods for treating PTSD and insomnia among Canadian military veterans: CBTi vs. MBSR. Sleep 2016;39:A397-A8.
- Graham-Bermann SA, Miller LE. Intervention to reduce traumatic stress following intimate partner violence: an efficacy trial of the Moms’ Empowerment Program (MEP). Psychodyn Psychiatry 2013;41:329-49. https://doi.org/10.1521/pdps.2013.41.2.329.
- Gray MJ, Schorr Y, Nash W, Lebowitz L, Amidon A, Lansing A, et al. Adaptive disclosure: an open trial of a novel exposure-based intervention for service members with combat-related psychological stress injuries. Behav Ther 2012;43:407-15. https://doi.org/10.1016/j.beth.2011.09.001.
- Gros DF, Strachan M, Ruggiero KJ, Knapp RG, Frueh BC, Egede LE, et al. Innovative service delivery for secondary prevention of PTSD in at-risk OIF-OEF service men and women. Contemp Clin Trials 2011;32:122-8. https://doi.org/10.1016/j.cct.2010.10.003.
- Gros DF, Yoder M, Tuerk PW, Lozano BE, Acierno R. Exposure therapy for PTSD delivered to veterans via telehealth: predictors of treatment completion and outcome and comparison to treatment delivered in person. Behav Ther 2011;42:276-83. https://doi.org/10.1016/j.beth.2010.07.005.
- Gutner CA, Casement MD, Stavitsky Gilbert K, Resick PA. Change in sleep symptoms across cognitive processing therapy and prolonged exposure: a longitudinal perspective. Behav Res Ther 2013;51:817-22. https://doi.org/10.1016/j.brat.2013.09.008.
- Hall BJ, Bolton PA, Annan J, Kaysen D, Robinette K, Cetinoglu T, et al. The effect of cognitive therapy on structural social capital: results from a randomized controlled trial among sexual violence survivors in the Democratic Republic of the Congo. Am J Public Health 2014;104:1680-6. https://doi.org/10.2105/AJPH.2014.301981.
- Hamner MB. Clozapine treatment for a veteran with comorbid psychosis and PTSD. Am J Psychiatry 1996;153. https://doi.org/10.1176/ajp.153.6.841.
- Hamner MB, Deitsch SE, Brodrick PS, Ulmer HG, Lorberbaum JP. Quetiapine treatment in patients with posttraumatic stress disorder: an open trial of adjunctive therapy. J Clin Psychopharmacol 2003;23:15-20. https://doi.org/10.1097/00004714-200302000-00003.
- Harris JI, Erbes CR, Engdahl BE, Thuras P, Murray-Swank N, Grace D, et al. The effectiveness of a trauma focused spiritually integrated intervention for veterans exposed to trauma. J Clin Psychol 2011;67:425-38. https://doi.org/10.1002/jclp.20777.
- Haynes P, Kelly MR, Parthasarathy S, Bootzin R. A randomized controlled trial of cognitive behavioral social rhythm group therapy (CBSRT) for male veterans with PTSD, major depressive disorder, and sleep problems. Sleep 2012;35. https://doi.org/10.21236/ADA574704.
- Hébert M, Bergeron M. Efficacy of a group intervention for adult women survivors of sexual abuse. J Child Sex Abus 2007;16:37-61. https://doi.org/10.1300/J070v16n04_03.
- Held P, Owens GP. Effects of self-compassion workbook training on trauma-related guilt in a sample of homeless veterans: a pilot study. J Clin Psychol 2015;71:513-26. https://doi.org/10.1002/jclp.22170.
- Hensel-Dittmann D, Schauer M, Ruf M, Catani C, Odenwald M, Elbert T, et al. Treatment of traumatized victims of war and torture: a randomized controlled comparison of narrative exposure therapy and stress inoculation training. Psychother Psychosom 2011;80:345-52. https://doi.org/10.1159/000327253.
- Hertzberg MA, Feldman ME, Beckham JC, Kudler HS, Davidson JR. Lack of efficacy for fluoxetine in PTSD: a placebo controlled trial in combat veterans. Ann Clin Psychiatry 2000;12:101-5. https://doi.org/10.3109/10401230009147096.
- Hertzberg MA, Feldman ME, Beckham JC, Moore SD, Davidson JR. Three- to four-year follow-up to an open trial of nefazodone for combat-related posttraumatic stress disorder. Ann Clin Psychiatry 2002;14:215-21. https://doi.org/10.3109/10401230209147460.
- Hijazi A, Ziadni M, Arnetz BB, Haddad L, Lumley M. Narrative exposure therapy to treat traumatic stress in middle eastern refugees: a clinical trial. Psychosom Med 2013;75.
- Hobfoll SE, Blais RK, Stevens NR, Walt L, Gengler R. Vets prevail online intervention reduces PTSD and depression in veterans with mild-to-moderate symptoms. J Consult Clin Psychol 2016;84:31-42. https://doi.org/10.1037/ccp0000041.
- Holliday R, Williams R, Bird J, Mullen K, Surís A. The role of cognitive processing therapy in improving psychosocial functioning, health, and quality of life in veterans with military sexual trauma-related posttraumatic stress disorder. Psychol Serv 2015;12:428-34. https://doi.org/10.1037/ser0000058.
- Hopton JL, Huta V. Evaluation of an intervention designed for men who were abused in childhood and are experiencing symptoms of posttraumatic stress disorder. Psychol Men Masc 2013;14:300-13. https://doi.org/10.1037/a0029705.
- Igreja V, Kleijn WC, Schreuder BJ, Van Dijk JA, Verschuur M. Testimony method to ameliorate post-traumatic stress symptoms. Community-based intervention study with Mozambican civil war survivors. Br J Psychiatry 2004;184:251-7. https://doi.org/10.1192/bjp.184.3.251.
- Ironson G, Freund B, Strauss JL, Williams J. Comparison of two treatments for traumatic stress: a community-based study of EMDR and prolonged exposure. J Clin Psychol 2002;58:113-28. https://doi.org/10.1002/jclp.1132.
- Ivarsson D, Blom M, Hesser H, Carlbring P, Enderby P, Nordberg R, et al. Guided internet-delivered cognitive behavior therapy for post-traumatic stress disorder: a randomized controlled trial. Internet Interventions 2014;1:33-40. https://doi.org/10.1016/j.invent.2014.03.002.
- Iverson KM, Gradus JL, Resick PA, Suvak MK, Smith KF, Monson CM. Cognitive-behavioral therapy for PTSD and depression symptoms reduces risk for future intimate partner violence among interpersonal trauma survivors. J Consult Clin Psychol 2011;79:193-202. https://doi.org/10.1037/a0022512.
- Jaberghaderi N, Greenwald R, Rubin A, Dalatabadi S, Zand SO. A comparison of CBT and EMDR for sexually abused Iranian girls. Clin Psychol Psychother 2002;11:358-68. https://doi.org/10.1002/cpp.395.
- Jain S, McMahon GF, Hasen P, Kozub MP, Porter V, King R, et al. Healing Touch with Guided Imagery for PTSD in returning active duty military: a randomized controlled trial. Mil Med 2012;177:1015-21. https://doi.org/10.7205/MILMED-D-11-00290.
- Jenkins MM, Drummond SP, Straus LD, Nappi CM. Examining the efficacy of adding sleep-specific therapies to an empirically validated trauma treatment in veterans with PTSD. Sleep 2014;37.
- Jerud AB, Zoellner LA, Pruitt LD, Feeny NC. Changes in emotion regulation in adults with and without a history of childhood abuse following posttraumatic stress disorder treatment. J Consult Clin Psychol 2014;82:721-30. https://doi.org/10.1037/a0036520.
- Jetly R, Heber A, Fraser G, Boisvert D. The efficacy of nabilone, a synthetic cannabinoid, in the treatment of PTSD-associated nightmares: A preliminary randomized, double-blind, placebo-controlled cross-over design study. Psychoneuroendocrinology 2015;51:585-8. https://doi.org/10.1016/j.psyneuen.2014.11.002.
- Johnson DM, Zlotnick C, Perez S. Cognitive behavioral treatment of PTSD in residents of battered women’s shelters: results of a randomized clinical trial. J Consult Clin Psychol 2011;79:542-51. https://doi.org/10.1037/a0023822.
- Kaiser EM, Gillette CS, Spinazzola J. A controlled pilot-outcome study of sensory integration (SI) in the treatment of complex adaptation to traumatic stress. J Aggression Maltreat Trauma 2010;19:699-720. https://doi.org/10.1080/10926771.2010.515162.
- Karatzias T, Ferguson S, Gullone A, Cosgrove K. Group psychotherapy for female adult survivors of interpersonal psychological trauma: a preliminary study in Scotland. J Ment Health 2016;25:512-19. https://doi.org/10.3109/09638237.2016.1139062.
- Kaslow NJ, Leiner AS, Reviere S, Jackson E, Bethea K, Bhaju J, et al. Suicidal, abused African American women’s response to a culturally informed intervention. J Consult Clin Psychol 2010;78:449-58. https://doi.org/10.1037/a0019692.
- Kelly MR, Haynes PL, Parthasarathy S, Bootzin RR, Perkins S. Negative mood regulation expectancies and trauma symptoms following a randomized controlled trial of cognitive behavioral social rhythm group therapy for male veterans with PTSD, major depressive disorder, and sleep problems. Sleep 2016;39.
- Kelly A, Garland EL. Trauma-informed mindfulness-based stress reduction for female survivors of interpersonal violence: results from a stage I RCT. J Clin Psychol 2016;72:311-28. https://doi.org/10.1002/jclp.22273.
- Khazaie H, Nasouri M, Ghadami MR. Prazosin for trauma nightmares and sleep disturbances in combat veterans with post-traumatic stress disorder. Iran J Psychiatry Behav Sci 2016;10. https://doi.org/10.17795/ijpbs-2603.
- King A, Giardino N, Rauch S, Rebecca S, Hu JY, Liberzon I. Pilot study of mindfulness-based exposure therapy for PTSD in OEF/OIF veterans: preliminary clinical outcomes and pre-post fMRI neuroimaging. Neuropsychopharmacology 2011;36.
- King AP, Block SR, Sripada RK, Rauch S, Giardino N, Favorite T, et al. Altered Default Mode Network (DMN) resting state functional connectivity following a mindfulness-based exposure therapy for posttraumatic stress disorder (PTSD) in combat veterans of Afghanistan and Iraq. Depress Anxiety 2016;33:289-99. https://doi.org/10.1002/da.22481.
- King AP, Block SR, Sripada RK, Rauch SA, Porter KE, Favorite TK, et al. A pilot study of mindfulness-based exposure therapy in OEF/OIF combat veterans with PTSD: altered medial frontal cortex and amygdala responses in social-emotional processing. Front Psychiatry 2016;7. https://doi.org/10.3389/fpsyt.2016.00154.
- Kip KE, Rosenzweig L, Hernandez DF, Shuman A, Sullivan KL, Long CJ, et al. Randomized controlled trial of accelerated resolution therapy (ART) for symptoms of combat-related post-traumatic stress disorder (PTSD). Mil Med 2013;178:1298-309. https://doi.org/10.7205/MILMED-D-13-00298.
- Kip KE, Rosenzweig L, Hernandez DF, Shuman A, Diamond DM, Girling SA, et al. Accelerated Resolution Therapy for treatment of pain secondary to symptoms of combat-related posttraumatic stress disorder. Eur J Psychotraumatol 2014;5. https://doi.org/10.3402/ejpt.v5.24066.
- Kluepfel L, Ward T, Yehuda R, Dimoulas E, Smith A, Daly K. The evaluation of mindfulness-based stress reduction for veterans with mental health conditions. J Holist Nurs 2013;31:248-55. https://doi.org/10.1177/0898010113495975.
- Koehn CV. Women’s perceptions of power and control in sexual abuse counseling. J Child Sex Abus 2007;16:37-60. https://doi.org/10.1300/J070v16n01_03.
- Kozarić-Kovacić D, Pivac N, Mück-Seler D, Rothbaum BO. Risperidone in psychotic combat-related posttraumatic stress disorder: an open trial. J Clin Psychiatry 2005;66:922-7. https://doi.org/10.4088/JCP.v66n0716.
- Kozaric-Kovacic D, Pivac N. Quetiapine treatment in an open trial in combat-related post-traumatic stress disorder with psychotic features. Int J Neuropsychopharmacol 2007;10:253-61. https://doi.org/10.1017/S1461145706006596.
- Kozel FA, Didehbani N, Motes MA, Jones P, Schraufnagel CD, DeLaRosa B, et al. Augmenting cognitive processing therapy with RTMS in combat veterans of recent conflicts with PTSD. Biol Psychiatry 2016;79.
- Krakow B, Hollifield M, Schrader R, Koss M, Tandberg D, Lauriello J, et al. A controlled study of imagery rehearsal for chronic nightmares in sexual assault survivors with PTSD: a preliminary report. J Trauma Stress 2000;13:589-60. https://doi.org/10.1023/A:1007854015481.
- Krakow B, Hollifield M, Johnston L, Koss M, Schrader R, Warner TD, et al. Imagery rehearsal therapy for chronic nightmares in sexual assault survivors with posttraumatic stress disorder: a randomized controlled trial. JAMA 2001;286:537-45. https://doi.org/10.1001/jama.286.5.537.
- Kreidler M. Group therapy for survivors of childhood sexual abuse who have chronic mental illness. Arch Psychiatr Nurs 2005;19:176-83. https://doi.org/10.1016/j.apnu.2005.05.003.
- Krüger A, Ehring T, Priebe K, Dyer AS, Steil R, Bohus M. Sudden losses and sudden gains during a DBT-PTSD treatment for posttraumatic stress disorder following childhood sexual abuse. Eur J Psychotraumatol 2014;5. https://doi.org/10.3402/ejpt.v5.24470.
- Kuckertz JM, Amir N, Boffa JW, Warren CK, Rindt SE, Norman S, et al. The effectiveness of an attention bias modification program as an adjunctive treatment for post-traumatic stress disorder. Behav Res Ther 2014;63:25-3. https://doi.org/10.1016/j.brat.2014.09.002.
- Labrador FJ, Fernandez-Velasco MdR, Rincon PP. Efficacy of a brief individual treatment program for the posttraumatic stress disorder in women victims of domestic violence. Int J Clin Health Psychol 2006;6:527-47.
- Lampe A, Mitmansgruber H, Gast U, Schüssler G, Reddemann L. Treatment outcome of psychodynamic trauma therapy in an inpatient setting. Neuropsychiatr 2008;22:189-97.
- Lang AJ, Schnurr PP, Jain S, Raman R, Walser R, Bolton E, et al. Evaluating transdiagnostic treatment for distress and impairment in veterans: a multisite randomized controlled trial of acceptance and commitment therapy. Contemp Clin Trials 2012;33:116-23. https://doi.org/10.1016/j.cct.2011.08.007.
- Lange A, van de Ven JP, Schrieken B, Emmelkamp PM. Interapy, treatment of posttraumatic stress through the internet: a controlled trial. J Behav Ther Exp Psychiatry 2001;32:73-90. https://doi.org/10.1016/S0005-7916(01)00023-4.
- Lange A, Rietdijk D, Hudcovicova M, van de Ven JP, Schrieken B, Emmelkamp PM. Interapy: a controlled randomized trial of the standardized treatment of posttraumatic stress through the internet. J Consult Clin Psychol 2003;71:901-9. https://doi.org/10.1037/0022-006X.71.5.901.
- Lange A, van de Ven JP, Schrieken B. Interapy: treatment of post-traumatic stress via the internet. Cogn Behav Ther 2003;32:110-24. https://doi.org/10.1080/16506070302317.
- Largo-Marsh LK. The Relationships Among Expectancy, Hypnotizability, and Treatment Outcome Associated With Eye Movement Desensitization in the Treatment of Post-Traumatic Stress Disorder 1996.
- Liebling H, Davidson L, Akello GF, Ochola G. The experiences of survivors and trauma counselling service providers in northern Uganda: Implications for mental health policy and legislation. Int J Law Psychiatry 2016;49:84-92. https://doi.org/10.1016/j.ijlp.2016.06.012.
- Liedl A, Müller J, Morina N, Karl A, Denke C, Knaevelsrud C. Physical activity within a CBT intervention improves coping with pain in traumatized refugees: results of a randomized controlled design. Pain Med 2011;12:234-45. https://doi.org/10.1111/j.1526-4637.2010.01040.x.
- Lim K, Erbes C, Thuras P, Rodman J, Sponheim S, Polusny M. Meditation interventions for treatment of PTSD in veterans. Neuropsychopharmacology 2014;39:S375-S6.
- Littleton H, Grills AE, Kline KD, Schoemann AM, Dodd JC. The From Survivor to Thriver program: RCT of an online therapist-facilitated program for rape-related PTSD. J Anxiety Disord 2016;43:41-5. https://doi.org/10.1016/j.janxdis.2016.07.010.
- Litz BT, Engel CC, Bryant RA, Papa A. A randomized, controlled proof-of-concept trial of an Internet-based, therapist-assisted self-management treatment for posttraumatic stress disorder. Am J Psychiatry 2007;164:1676-83. https://doi.org/10.1176/appi.ajp.2007.06122057.
- Litz BT, Salters-Pedneault K, Steenkamp MM, Hermos JA, Bryant RA, Otto MW, et al. A randomized placebo-controlled trial of D-cycloserine and exposure therapy for posttraumatic stress disorder. J Psychiatr Res 2012;46:1184-90. https://doi.org/10.1016/j.jpsychires.2012.05.006.
- Long ME, Hammons ME, Davis JL, Frueh BC, Khan MM, Elhai JD, et al. Imagery rescripting and exposure group treatment of posttraumatic nightmares in Veterans with PTSD. J Anxiety Disord 2011;25:531-5. https://doi.org/10.1016/j.janxdis.2010.12.007.
- Macdonald A, Monson CM, Doron-Lamarca S, Resick PA, Palfai TP. Identifying patterns of symptom change during a randomized controlled trial of cognitive processing therapy for military-related posttraumatic stress disorder. J Trauma Stress 2011;24:268-76. https://doi.org/10.1002/jts.20642.
- Macklin ML, Metzger LJ, Lasko NB, Berry NJ, Orr SP, Pitman RK. Five-year follow-up study of eye movement desensitization and reprocessing therapy for combat-related posttraumatic stress disorder. Compr Psychiatry 2000;41:24-7. https://doi.org/10.1016/S0010-440X(00)90127-5.
- Manteghi AA, Hebrani P, Mortezania M, Haghighi MB, Javanbakht A. Baclofen add-on to citalopram in treatment of posttraumatic stress disorder. J Clin Psychopharmacol 2014;34:240-3. https://doi.org/10.1097/JCP.0000000000000089.
- Martenyi F, Brown EB, Zhang H, Prakash A, Koke SC. Fluoxetine versus placebo in posttraumatic stress disorder. J Clin Psychiatry 2002;63:199-206. https://doi.org/10.4088/JCP.v63n0305.
- Martenyi F, Soldatenkova V. Fluoxetine in the acute treatment and relapse prevention of combat-related post-traumatic stress disorder: Analysis of the veteran group of a placebo-controlled, randomized clinical trial. Eur Neuropsychopharmacol 2006;16:340-9. https://doi.org/10.1016/j.euroneuro.2005.10.007.
- Matud MP, Padilla V, Medina L, Fortes D. Efficacy of an intervention program for battered women. Terapia Psicologica 2016;34:199-208. https://doi.org/10.4067/S0718-48082016000300004.
- Mauritz MW, Van Gaal BG, Jongedijk RA, Schoonhoven L, Nijhuis-van der Sanden MW, Goossens PJ. Narrative exposure therapy for posttraumatic stress disorder associated with repeated interpersonal trauma in patients with severe mental illness: a mixed methods design. Eur J Psychotraumatol 2016;7. https://doi.org/10.3402/ejpt.v7.32473.
- McFall M, Saxon AJ, Thompson CE, Yoshimoto D, Malte C, Straits-Troster K, et al. Improving the rates of quitting smoking for veterans with posttraumatic stress disorder. Am J Psychiatry 2005;162:1311-19. https://doi.org/10.1176/appi.ajp.162.7.1311.
- McGlinchey R, Rosenblatt A, Mercado R, Esterman M, DeGutis J. Internet-based cognitive training enhances attention and functional outcomes in OEF/OIF/OND veterans. Brain Inj 2014;28:624-5.
- McWhirter PT. Differential therapeutic outcomes of community-based group interventions for women and children exposed to intimate partner violence. J Interpers Violence 2011;26:2457-82. https://doi.org/10.1177/0886260510383026.
- Mehling W, Chesney M, Metzler TJ, Goldstein LA, Maguen S, Geronimo C, et al. Integrative exercise reduces posttraumatic stress symptoms in war veterans: the VGX study. J Altern Complement Med 2016;22.
- Mehta A, Wohlgemuth WK, Malphurs JE, Claude LB, Gonzalez C, David D. Mindfullness-based stress reduction improves total sleep time in veterans with PTSD. Sleep 2012;35.
- Mello MF, Yeh MS, Barbosa Neto J, Braga LL, Fiks JP, Mendes DD, et al. A randomized, double-blind, placebo-controlled trial to assess the efficacy of topiramate in the treatment of post-traumatic stress disorder. BMC Psychiatry 2009;9. https://doi.org/10.1186/1471-244X-9-28.
- Mithoefer MC, Wagner MT, Mithoefer AT, Jerome L, Doblin R. The safety and efficacy of ±3,4-methylenedioxymethamphetamine-assisted psychotherapy in subjects with chronic, treatment-resistant posttraumatic stress disorder: the first randomized controlled pilot study. J Psychopharmacol 2011;25:439-52. https://doi.org/10.1177/0269881110378371.
- Monson CM, Schnurr PP, Resick PA, Friedman MJ, Young-Xu Y, Stevens SP. Cognitive processing therapy for veterans with military-related posttraumatic stress disorder. J Consult Clin Psychol 2006;74:898-907. https://doi.org/10.1037/0022-006X.74.5.898.
- Monson CM, Fredman SJ, Macdonald A, Pukay-Martin ND, Resick PA, Schnurr PP. Effect of cognitive-behavioral couple therapy for PTSD: a randomized controlled trial. JAMA 2012;308:700-9. https://doi.org/10.1001/jama.2012.9307.
- Morland LA, Greene CJ, Rosen CS, Foy D, Reilly P, Shore J, et al. Telemedicine for anger management therapy in a rural population of combat veterans with posttraumatic stress disorder: a randomized noninferiority trial. J Clin Psychiatry 2010;71:855-63. https://doi.org/10.4088/JCP.09m05604blu.
- Morland LA, Hynes AK, Mackintosh MA, Resick PA, Chard KM. Group cognitive processing therapy delivered to veterans via telehealth: a pilot cohort. J Trauma Stress 2011;24:465-9. https://doi.org/10.1002/jts.20661.
- Morland LA, Mackintosh MA, Greene CJ, Rosen CS, Chard KM, Resick P, et al. Cognitive processing therapy for posttraumatic stress disorder delivered to rural veterans via telemental health: a randomized noninferiority clinical trial. J Clin Psychiatry 2014;75:470-6. https://doi.org/10.4088/JCP.13m08842.
- Morland LA, Mackintosh MA, Rosen CS, Willis E, Resick P, Chard K, et al. Telemedicine versus in-person delivery of cognitive processing therapy for women with posttraumatic stress disorder: a randomized noninferiority trial. Depress Anxiety 2015;32:811-20. https://doi.org/10.1002/da.22397.
- Moser JS, Cahill SP, Foa EB. Evidence for poorer outcome in patients with severe negative trauma-related cognitions receiving prolonged exposure plus cognitive restructuring: implications for treatment matching in posttraumatic stress disorder. J Nerv Ment Dis 2010;198:72-5. https://doi.org/10.1097/NMD.0b013e3181c81fac.
- Mughal U, Carrasco D, Brown R, Ayers S. Rehabilitating civilian victims of war through psychosocial intervention in Sierra Leone. J Appl Soc Psychol 2015;45:593-601. https://doi.org/10.1111/jasp.12322.
- Murray H, Merritt C, Grey N. Clients’ experiences of returning to the trauma site during PTSD treatment: an exploratory study. Behav Cogn Psychother 2016;44:420-30. https://doi.org/10.1017/S1352465815000338.
- Muzik M, Rosenblum KL, Alfafara EA, Schuster MM, Miller NM, Waddell RM, et al. Mom Power: preliminary outcomes of a group intervention to improve mental health and parenting among high-risk mothers. Arch Womens Ment Health 2015;18:507-21. https://doi.org/10.1007/s00737-014-0490-z.
- Nacasch N, Foa EB, Huppert JD, Tzur D, Fostick L, Dinstein Y, et al. Prolonged exposure therapy for combat- and terror-related posttraumatic stress disorder: a randomized control comparison with treatment as usual. J Clin Psychiatry 2011;72:1174-80. https://doi.org/10.4088/JCP.09m05682blu.
- Nagy LM, Morgan CA, Southwick SM, Charney DS. Open prospective trial of fluoxetine for posttraumatic stress disorder. J Clin Psychopharmacol 1993;13:107-13. https://doi.org/10.1097/00004714-199304000-00004.
- Nakamura Y, Lipschitz DL, Landward R, Kuhn R, West G. Two sessions of sleep-focused mind-body bridging improve self-reported symptoms of sleep and PTSD in veterans: A pilot randomized controlled trial. J Psychosom Res 2011;70:335-45. https://doi.org/10.1016/j.jpsychores.2010.09.007.
- Neuner F, Kurreck S, Ruf M, Odenwald M, Elbert T, Schauer M. Can asylum-seekers with posttraumatic stress disorder be successfully treated? A randomized controlled pilot study. Cogn Behav Ther 2010;39:81-9. https://doi.org/10.1080/16506070903121042.
- Neylan TC, Metzler TJ, Schoenfeld FB, Weiss DS, Lenoci M, Best SR, et al. Fluvoxamine and sleep disturbances in posttraumatic stress disorder. J Trauma Stress 2001;14:461-7. https://doi.org/10.1023/A:1011100420978.
- Neylan TC, Lenoci M, Maglione ML, Rosenlicht NZ, Leykin Y, Metzler TJ, et al. The effect of nefazodone on subjective and objective sleep quality in posttraumatic stress disorder. J Clin Psychiatry 2003;64:445-50. https://doi.org/10.4088/JCP.v64n0415.
- Nijdam MJ, Gersons BP, Reitsma JB, de Jongh A, Olff M. Brief eclectic psychotherapy v. eye movement desensitisation and reprocessing therapy for post-traumatic stress disorder: randomised controlled trial. Br J Psychiatry 2012;200:224-31. https://doi.org/10.1192/bjp.bp.111.099234.
- Niles BL, Vujanovic AA, Silberbogen AK, Seligowski AV, Potter CM. Changes in mindfulness following a mindfulness telehealth intervention. Mindfulness 2013;4:301-10. https://doi.org/10.1007/s12671-012-0130-5.
- Nishith P, Weaver TL, Resick PA, Uhlmansiek MH, Williams LM, Banyard VL. Trauma & Memory. Thousand Oaks, CA: SAGE Publications, Inc.; 1999.
- Nishith P, Mueser KT, Morse GA. A brief intervention for posttraumatic stress disorder in persons with a serious mental illness. Psychiatr Rehabil J 2015;38:314-19. https://doi.org/10.1037/prj0000158.
- Ochsner Margolies S, Rybarczyk B, Vrana S, Lynch J. Efficacy of a cognitive-behavioral treatment for insomnia among Afghanistan and Iraq (OEF/OIF) veterans with PTSD. Sleep 2012;35:A240-A1.
- Oman D, Bormann JE. Mantram repetition fosters self-efficacy in veterans for managing PTSD: a randomized trial. Psycholog Relig Spiritual 2015;7:34-45. https://doi.org/10.1037/a0037994.
- Padala PR. Risperidone for PTSD in abused women. Brown Univ Psychopharmacol Update 2006;17:3-4.
- Padala PR, Madison J, Monnahan M, Marcil W, Price P, Ramaswamy S, et al. Risperidone monotherapy for post-traumatic stress disorder related to sexual assault and domestic abuse in women. Int Clin Psychopharmacol 2006;21:275-80. https://doi.org/10.1097/00004850-200609000-00005.
- Paivio SC, Jarry JL, Chagigiorgis H, Hall I, Ralston M. Efficacy of two versions of emotion-focused therapy for resolving child abuse trauma. Psychother Res 2010;20:353-66. https://doi.org/10.1080/10503300903505274.
- Paunovic N. Exposure inhibition therapy as a treatment for chronic posttraumatic stress disorder: a controlled pilot study. Psychology 2011;2:605-14. https://doi.org/10.4236/psych.2011.26093.
- Peskind ER, Bonner LT, Hoff DJ, Raskind MA. Prazosin reduces trauma-related nightmares in older men with chronic posttraumatic stress disorder. J Geriatr Psychiatry Neurol 2003;16:165-71. https://doi.org/10.1177/0891988703256050.
- Petty F, Brannan S, Casada J, Davis LL, Gajewski V, Kramer GL, et al. Olanzapine treatment for post-traumatic stress disorder: an open-label study. Int Clin Psychopharmacol 2001;16:331-7. https://doi.org/10.1097/00004850-200111000-00003.
- Pigeon WR, May PE, Perlis ML, Ward EA, Lu N, Talbot NL. The effect of interpersonal psychotherapy for depression on insomnia symptoms in a cohort of women with sexual abuse histories. J Trauma Stress 2009;22:634-8. https://doi.org/10.1002/jts.20456.
- Pigeon WR, Cerulli C, Crean H, Gallegos A, Nelson L, Casey C, et al. Cognitive-behavioral therapy for insomnia for survivors of interpersonal violence who subsequently receive cognitive processing therapy. Sleep 2015;38.
- Pivac N, Kozarić-Kovacić D. Pharmacotherapy of treatment-resistant combat-related posttraumatic stress disorder with psychotic features. Croat Med J 2006;47:440-51.
- Pokhariyal GP, Rono RC, Munywoki S. Analysis of treatment methods for victims of torture in Kenya and east Africa region. Traumatology 2012;19:107-17. https://doi.org/10.1177/1534765612451341.
- Pollack MH, Hoge EA, Worthington JJ, Moshier SJ, Wechsler RS, Brandes M, et al. Eszopiclone for the treatment of posttraumatic stress disorder and associated insomnia: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry 2011;72:892-7. https://doi.org/10.4088/JCP.09m05607gry.
- Possemato K, Ouimette P, Knowlton P. A brief self-guided telehealth intervention for post-traumatic stress disorder in combat veterans: a pilot study. J Telemed Telecare 2011;17:245-50. https://doi.org/10.1258/jtt.2011.100909.
- Possemato K, Kuhn E, Johnson E, Hoffman JE, Owen JE, Kanuri N, et al. Using PTSD Coach in primary care with and without clinician support: a pilot randomized controlled trial. Gen Hosp Psychiatry 2016;38:94-8. https://doi.org/10.1016/j.genhosppsych.2015.09.005.
- Price C. Body-oriented therapy in recovery from child sexual abuse: an efficacy study. Altern Ther Health Med 2005;11:46-57.
- Price C. Body-oriented therapy in sexual abuse recovery: a pilot-test comparison. J Bodyw Mov Ther 2006;10:58-64. https://doi.org/10.1016/j.jbmt.2005.03.001.
- Pruiksma KE, Davis J, Cranston C. A randomized controlled trial of exposure, relaxation, and rescripting therapy (ERRT) versus relaxation training (RT) for chronic nightmares in trauma-exposed persons: preliminary findings. Sleep 2012;35:A252-A3.
- Pruiksma KE, Taylor DJ, Resick PA, Wachen JS, Mintz J, Young-McCaughan S. Do sleep disturbances remain after PTSD treatments?. Sleep 2013;36:A305-A6.
- Ragsdale KG, Cox RD, Finn P, Eisler RM. Effectiveness of short-term specialized inpatient treatment for war-related posttraumatic stress disorder: a role for adventure-based counseling and psychodrama. J Trauma Stress 1996;9:269-83. https://doi.org/10.1002/jts.2490090209.
- Rahman A, Hamdani SU, Awan NR, Bryant RA, Dawson KS, Khan MF, et al. Effect of a multicomponent behavioral intervention in adults impaired by psychological distress in a conflict-affected area of Pakistan: a randomized clinical trial. JAMA 2016;316:2609-17. https://doi.org/10.1001/jama.2016.17165.
- Randall PK, Bremner JD, Krystal JH, Nagy LM, Heninger GR, Nicolaou AL, et al. Effects of the benzodiazepine antagonist flumazenil in PTSD. Biol Psychiatry 1995;38:319-24. https://doi.org/10.1016/0006-3223(94)00306-N.
- Raskind MA, Peskind ER, Kanter ED, Petrie EC, Radant A, Thompson CE, et al. Reduction of nightmares and other PTSD symptoms in combat veterans by prazosin: a placebo-controlled study. Am J Psychiatry 2003;160:371-3. https://doi.org/10.1176/appi.ajp.160.2.371.
- Raskind MA, Peterson K, Williams T, Peskind ER. A trial of prazosin for combat trauma PTSD with nightmares in active duty soldiers returned from Iraq and Afghanistan. Neuropsychopharmacology 2012;38. https://doi.org/10.1037/e533652013-069.
- Raskind M. Update on the use of alpha-1 adrenoreceptor antagonists for PTSD. Int J Neuropsychopharmacol 2014;17:20-1.
- Rauch S, Sripada R, King A, Abelson J, Rothbaum B, Liberzon I. Extinction and change in cognitions and cortisol activity in posttraumatic stress disorder treatment. Neuropsychopharmacology 2014;39:S356-S7.
- Rauch SA, King AP, Abelson J, Tuerk PW, Smith E, Rothbaum BO, et al. Biological and symptom changes in posttraumatic stress disorder treatment: a randomized clinical trial. Depress Anxiety 2015;32:204-12. https://doi.org/10.1002/da.22331.
- Ready DJ, Pollack S, Rothbaum BO, Alarcon RD. Virtual reality exposure for veterans with posttraumatic stress disorder. J Aggression Maltreat Trauma 2006;12:199-220. https://doi.org/10.1300/J146v12n01_11.
- Reed GL. A Forgiveness Intervention With Post-Relationship Psychologically Abused Women 2004.
- Renner W, Banninger-Huber E, Peltzer K. Culture-Sensitive and Resource Oriented Peer (CROP)-groups as a community based intervention for trauma survivors: a randomized controlled pilot study with refugees and asylum seekers from Chechnya. Australasian J Disaster Trauma Stud 2011;1:1-13.
- Resick PA, Schnicke MK. Cognitive processing therapy for sexual assault victims. J Consult Clin Psychol 1992;60:748-56. https://doi.org/10.1037/0022-006X.60.5.748.
- Resick PA, Nishith P, Weaver TL, Astin MC, Feuer CA. A comparison of cognitive-processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. J Consult Clin Psychol 2002;70:867-79. https://doi.org/10.1037/0022-006X.70.4.867.
- Resick PA, Nishith P, Griffin MG. How well does cognitive-behavioral therapy treat symptoms of complex PTSD? An examination of child sexual abuse survivors within a clinical trial. CNS Spectr 2003;8:340-55. https://doi.org/10.1017/S1092852900018605.
- Resick PA, Galovski TE, Uhlmansiek MO, Scher CD, Clum GA, Young-Xu Y. A randomized clinical trial to dismantle components of cognitive processing therapy for posttraumatic stress disorder in female victims of interpersonal violence. J Consult Clin Psychol 2008;76:243-58. https://doi.org/10.1037/0022-006X.76.2.243.
- Resick PA, Wachen JS, Dondanville KA, Pruiksma KE, Yarvis JS, Peterson AL, et al. Effect of group vs individual cognitive processing therapy in active-duty military seeking treatment for posttraumatic stress disorder: a randomized clinical trial. JAMA Psychiatry 2017;74:28-36. https://doi.org/10.1001/jamapsychiatry.2016.2729.
- Rimane E, Rosner R. Developmentally Adapted Cognitive Processing Therapy for Adolescents and Young Adults With PTSD Symptoms After Physical and Sexual Abuse 2013. www.drks.de/DRKS00004787 (accessed 31 July 2017).
- Robert S, Hamner MB, Durkalski VL, Brown MW, Ulmer HG. An open-label assessment of aripiprazole in the treatment of PTSD. Psychopharmacol Bull 2009;42:69-80.
- Rodgman C, Verrico CD, Holst M, Thompson-Lake D, Haile CN, De La Garza R, et al. Doxazosin XL reduces symptoms of posttraumatic stress disorder in veterans with PTSD: a pilot clinical trial. J Clin Psychiatry 2016;77:e561-5. https://doi.org/10.4088/JCP.14m09681.
- Rosenbaum S, Sherrington C, Tiedemann A. Exercise augmentation compared with usual care for post-traumatic stress disorder: a randomized controlled trial. Acta Psychiatr Scand 2015;131:350-9. https://doi.org/10.1111/acps.12371.
- Rothbaum BO. A controlled study of eye movement desensitization and reprocessing in the treatment of posttraumatic stress disordered sexual assault victims. Bull Menninger Clin 1997;61:317-34.
- Rothbaum BO, Hodges LF, Ready D, Graap K, Alarcon RD. Virtual reality exposure therapy for Vietnam veterans with posttraumatic stress disorder. J Clin Psychiatry 2001;62:617-22. https://doi.org/10.4088/JCP.v62n0808.
- Rothbaum BO, Astin MC, Marsteller F. Prolonged Exposure versus Eye Movement Desensitization and Reprocessing (EMDR) for PTSD rape victims. J Trauma Stress 2005;18:607-16. https://doi.org/10.1002/jts.20069.
- Rothbaum BO, Davidson JR, Stein DJ, Pedersen R, Musgnung J, Tian XW, et al. A pooled analysis of gender and trauma-type effects on responsiveness to treatment of PTSD with venlafaxine extended release or placebo. J Clin Psychiatry 2008;69:1529-39. https://doi.org/10.4088/JCP.v69n1002.
- Ryan M, Nitsun M, Gilbert L, Mason H. A prospective study of the effectiveness of group and individual psychotherapy for women CSA survivors. Psychol Psychother 2005;78:465-79. https://doi.org/10.1348/147608305X42226.
- Sachsse U, Vogel C, Leichsenring F. Results of psychodynamically oriented trauma-focused inpatient treatment for women with complex posttraumatic stress disorder (PTSD) and borderline personality disorder (BPD). Bull Menninger Clin 2006;70:125-44. https://doi.org/10.1521/bumc.2006.70.2.125.
- Sack M, Spieler D, Wizelman L, Epple G, Stich J, Zaba M, et al. Intranasal oxytocin reduces provoked symptoms in female patients with posttraumatic stress disorder despite exerting sympathomimetic and positive chronotropic effects in a randomized controlled trial. BMC Med 2017;15. https://doi.org/10.1186/s12916-017-0801-0.
- Salloum A, Dorsey CS, Swaidan VR, Storch EA. Parents’ and children’s perception of parent-led trauma-focused cognitive behavioral therapy. Child Abuse Negl 2015;40:12-23. https://doi.org/10.1016/j.chiabu.2014.11.018.
- Sautter FJ, Glynn SM, Cretu JB, Senturk D, Vaught AS. Efficacy of structured approach therapy in reducing PTSD in returning veterans: a randomized clinical trial. Psychol Serv 2015;12:199-212. https://doi.org/10.1037/ser0000032.
- Schaal S, Elbert T, Neuner F. Narrative exposure therapy versus interpersonal psychotherapy. A pilot randomized controlled trial with Rwandan genocide orphans. Psychother Psychosom 2009;78:298-306. https://doi.org/10.1159/000229768.
- Schnurr PP, Friedman MJ, Foy DW, Shea MT, Hsieh FY, Lavori PW, et al. Randomized trial of trauma-focused group therapy for posttraumatic stress disorder: results from a department of veterans affairs cooperative study. Arch Gen Psychiatry 2003;60:481-9. https://doi.org/10.1001/archpsyc.60.5.481.
- Schnurr PP, Friedman MJ, Engel CC, Foa EB, Shea MT, Chow BK, et al. Cognitive behavioral therapy for posttraumatic stress disorder in women: a randomized controlled trial. JAMA 2007;297:820-30. https://doi.org/10.1001/jama.297.8.820.
- Schnurr PP, Lunney CA, Forshay E, Thurston VL, Chow BK, Resick PA, et al. Sexual function outcomes in women treated for posttraumatic stress disorder. J Womens Health 2009;18:1549-57. https://doi.org/10.1089/jwh.2008.1165.
- Schnurr PP, Lunney CA. Differential effects of prolonged exposure on posttraumatic stress disorder symptoms in female veterans. J Consult Clin Psychol 2015;83:1154-60. https://doi.org/10.1037/ccp0000031.
- Schnurr PP, Lunney CA. Symptom benchmarks of improved quality of life in PTSD. Depress Anxiety 2016;33:247-55. https://doi.org/10.1002/da.22477.
- Seppälä EM, Nitschke JB, Tudorascu DL, Hayes A, Goldstein MR, Nguyen DT, et al. Breathing-based meditation decreases posttraumatic stress disorder symptoms in U.S. military veterans: a randomized controlled longitudinal study. J Trauma Stress 2014;27:397-405. https://doi.org/10.1002/jts.21936.
- Sezgin U, Punamäki R. Effectiveness of group psychotherapy among women with multiple traumatic life events: a pilot study in the southeast Anatolian region. J Loss Trauma 2008;13:557-75. https://doi.org/10.1080/15325020802173694.
- Shearing V, Lee D, Clohessy S. How do clients experience reliving as part of trauma-focused cognitive behavioural therapy for posttraumatic stress disorder?. Psychol Psychother 2011;84:458-75. https://doi.org/10.1111/j.2044-8341.2010.02012.x.
- Short NP. Vocal heroes: the views of two people who experienced a cognitive behavioural approach for their difficulties. Their narratives are accompanied by a commentary from the therapist. J Psychiatr Ment Health Nurs 2005;12:574-81. https://doi.org/10.1111/j.1365-2850.2005.00877.x.
- Silver SM, Brooks A, Obenchain J. Treatment of Vietnam War veterans with PTSD: a comparison of eye movement desensitization and reprocessing, biofeedback, and relaxation training. J Trauma Stress 1995;8:337-42. https://doi.org/10.1002/jts.2490080212.
- Skinhoj KT, Larsson S, Helweg-Joergensen S, Hansen EH. Experiences of long-term tranquillizer use: a psychodynamic perspective. Subst Use Misuse 2001;36:1165-86. https://doi.org/10.1081/JA-100106222.
- Smith PN, Gamble SA, Cort NA, Ward EA, He H, Talbot NL. Attachment and alliance in the treatment of depressed, sexually abused women. Depress Anxiety 2012;29:123-30. https://doi.org/10.1002/da.20913.
- Spence J, Titov N, Johnston L, Jones MP, Dear BF, Solley K. Internet-based trauma-focused cognitive behavioural therapy for PTSD with and without exposure components: a randomised controlled trial. J Affect Disord 2014;162:73-80. https://doi.org/10.1016/j.jad.2014.03.009.
- Spiegel D, Classen C, Thurston E, Butler L, Koenig LJ, Doll LS, et al. From Child Sexual Abuse to Adult Sexual Risk: Trauma, Revictimization, and Intervention. Washington, DC: American Psychological Association; 2004.
- Stade K, Skammeritz S, Hjortkjær C, Carlsson J. ‘After all the traumas my body has been through, I feel good that it is still working.’ – Basic Body Awareness Therapy for traumatised refugees. Torture 2015;25:33-50.
- Stalker CA, Fry R. A comparison of short-term group and individual therapy for sexually abused women. Can J Psychiatry 1999;44:168-74. https://doi.org/10.1177/070674379904400208.
- Steil R, Dyer A, Priebe K, Kruger A, Bohus M. Dialectical-behavior-therapy for severe posttraumatic stress disorder after childhood sexual abuse: a randomized controlled trial. Eur J Psychotraumatol 2011;24:102-6.
- Stein DJ, van der Kolk BA, Austin C, Fayyad R, Clary C. Efficacy of sertraline in posttraumatic stress disorder secondary to interpersonal trauma or childhood abuse. Ann Clin Psychiatry 2006;18:243-9. https://doi.org/10.1080/10401230600948431.
- Steinert C, Bumke PJ, Hollekamp RL, Larisch A, Leichsenring F, Mattheß H, et al. Resource activation for treating post-traumatic stress disorder, co-morbid symptoms and impaired functioning: a randomized controlled trial in Cambodia. Psychol Med 2017;47:553-64. https://doi.org/10.1017/S0033291716002592.
- Steuwe C, Rullkötter N, Ertl V, Berg M, Neuner F, Beblo T, et al. Effectiveness and feasibility of Narrative Exposure Therapy (NET) in patients with borderline personality disorder and posttraumatic stress disorder – a pilot study. BMC Psychiatry 2016;16. https://doi.org/10.1186/s12888-016-0969-4.
- Stovall-McClough KC, Cloitre M. Reorganization of unresolved childhood traumatic memories following exposure therapy. Ann N Y Acad Sci 2003;1008:297-9. https://doi.org/10.1196/annals.1301.036.
- Su H, Wang JT, Lou ZS, Lu HT. Cognitive-exposure therapy for post-traumatic stress disorder. J Clin Rehab Tissue Eng Res 2007;11:7783-6.
- Sulejmanpasic-Arslanagic G, Bise Srebrenka B. Olanzapine augmentation in alleviating treatment-resistant nightmares and insomnia in patients with combat-related PTSD. Eur Neuropsychopharmacol 2015;25:S570-S1. https://doi.org/10.1016/S0924-977X(15)30799-9.
- Surís A, North C, Adinoff B, Powell CM, Greene R. Effects of exogenous glucocorticoid on combat-related PTSD symptoms. Ann Clin Psychiatry 2010;22:274-9.
- Surís A, Link-Malcolm J, Chard K, Ahn C, North C. A randomized clinical trial of cognitive processing therapy for veterans with PTSD related to military sexual trauma. J Trauma Stress 2013;26:28-37. https://doi.org/10.1002/jts.21765.
- Swanson LM, Favorite TK, Horin E, Arnedt JT. A combined group treatment for nightmares and insomnia in combat veterans: a pilot study. J Trauma Stress 2009;22:639-42. https://doi.org/10.1002/jts.20468.
- Taing S, Strasser J, Chhim S. Culturally sensitive trauma treatment for Khmer Rouge survivors. Asian J Psych 2011;4. https://doi.org/10.1016/S1876-2018(11)60136-6.
- Talbot NL, Chaudron LH, Ward EA, Duberstein PR, Conwell Y, O’Hara MW, et al. A randomized effectiveness trial of interpersonal psychotherapy for depressed women with sexual abuse histories. Psychiatr Serv 2011;62:374-80. https://doi.org/10.1176/ps.62.4.pss6204_0374.
- Talbot LS, Maguen S, Metzler TJ, Schmitz M, McCaslin SE, Richards A, et al. Cognitive behavioral therapy for insomnia in posttraumatic stress disorder: a randomized controlled trial. Sleep 2014;37:327-41. https://doi.org/10.5665/sleep.3408.
- Tan G, Dao TK, Farmer L, Sutherland RJ, Gevirtz R. Heart rate variability (HRV) and posttraumatic stress disorder (PTSD): a pilot study. Appl Psychophysiol Biofeedback 2011;36:27-35. https://doi.org/10.1007/s10484-010-9141-y.
- Tarquinio C, Brennstuhl M, Rydberg J, Schmitt A, Mouda F, Lourel M, et al. Eye movement desensitization and reprocessing (EMDR) therapy in the treatment of victims of domestic violence: a pilot study. Eur Rev Appl Psychol 2012;62:205-12. https://doi.org/10.1016/j.erap.2012.08.006.
- Tarrier N, Sommerfield C. Treatment of chronic PTSD by cognitive therapy and exposure: 5-Year follow-up. Behav Ther 2004;35:231-46. https://doi.org/10.1016/S0005-7894(04)80037-6.
- Thomaes K, Dorrepaal E, van Balkom AJ, Veltman DJ, Smit JH, Hoogendoorn AW, et al. Complex PTSD following early-childhood trauma: emotion-regulation training as addition to the PTSD guideline. Tijdschr Psychiatr 2015;57:171-82.
- Thorp SR, Stein MB, Jeste DV, Patterson TL, Wetherell JL. Prolonged exposure therapy for older veterans with posttraumatic stress disorder: a pilot study. Am J Geriatr Psychiatry 2012;20:276-80. https://doi.org/10.1097/JGP.0b013e3182435ee9.
- Tourigny M, Guillor M-L, Morissette P. Effectiveness of a group intervention for men sexually molested during childhood. Can J Behav Sci 2005;37:97-109. https://doi.org/10.1037/h0087248.
- Truijens FL, Van Emmerik AAP. Visual feedback in written imaginal exposure for posttraumatic stress: a preliminary study. J Loss Trauma 2014;19:403-15. https://doi.org/10.1080/15325024.2013.794664.
- van den Berg DP, van der Gaag M. Treating trauma in psychosis with EMDR: a pilot study. J Behav Ther Exp Psychiatry 2012;43:664-71. https://doi.org/10.1016/j.jbtep.2011.09.011.
- van der Kolk BA, Spinazzola J, Blaustein ME, Hopper JW, Hopper EK, Korn DL, et al. A randomized clinical trial of eye movement desensitization and reprocessing (EMDR), fluoxetine, and pill placebo in the treatment of posttraumatic stress disorder: treatment effects and long-term maintenance. J Clin Psychiatry 2007;68:37-46. https://doi.org/10.4088/JCP.v68n0105.
- van Emmerik AA, Kamphuis JH, Emmelkamp PM. Treating acute stress disorder and posttraumatic stress disorder with cognitive behavioral therapy or structured writing therapy: a randomized controlled trial. Psychother Psychosom 2008;77:93-100. https://doi.org/10.1159/000112886.
- Vera M, Reyes-Rabanillo ML, Juarbe D, Pérez-Pedrogo C, Olmo A, Kichic R, et al. Prolonged exposure for the treatment of Spanish-speaking Puerto Ricans with posttraumatic stress disorder: a feasibility study. BMC Res Notes 2011;4. https://doi.org/10.1186/1756-0500-4-415.
- Villarreal G, Calais LA, Cañive JM, Lundy SL, Pickard J, Toney G. Prospective study to evaluate the efficacy of aripiprazole as a monotherapy in patients with severe chronic posttraumatic stress disorder: an open trial. Psychopharmacol Bull 2007;40:6-18.
- Villarreal G, Cañive JM, Calais LA, Toney G, Smith AK. Duloxetine in military posttraumatic stress disorder. Psychopharmacol Bull 2010;43:26-34.
- Vitriol VG, Ballesteros ST, Florenzano RU, Weil KP, Benadof DF. Evaluation of an outpatient intervention for women with severe depression and a history of childhood trauma. Psychiatr Serv 2009;60:936-42. https://doi.org/10.1176/ps.2009.60.7.936.
- Weine S, Kulauzovic Y, Klebic A, Besic S, Mujagic A, Muzurovic J, et al. Evaluating a multiple-family group access intervention for refugees with PTSD. J Marital Fam Ther 2008;34:149-64. https://doi.org/10.1111/j.1752-0606.2008.00061.x.
- Wells A, Colbear JS. Treating posttraumatic stress disorder with metacognitive therapy: a preliminary controlled trial. J Clin Psychol 2012;68:373-81. https://doi.org/10.1002/jclp.20871.
- Westbury E, Tutty LM. The efficacy of group treatment for survivors of childhood abuse. Child Abuse Negl 1999;23:31-44. https://doi.org/10.1016/S0145-2134(98)00109-4.
- Wood DP, Webb-Murphy J, McLay RN, Wiederhold BK, Spira JL, Johnston S, et al. Reality graded exposure therapy with physiological monitoring for the treatment of combat related post traumatic stress disorder: a pilot study. Stud Health Technol Inform 2011;163:696-702.
- Yeh MS, Mari JJ, Costa MC, Andreoli SB, Bressan RA, Mello MF. A double-blind randomized controlled trial to study the efficacy of topiramate in a civilian sample of PTSD. CNS Neurosci Ther 2011;17:305-10. https://doi.org/10.1111/j.1755-5949.2010.00188.x.
- Yehua R. Skills training plus exposure therapy may reduce post traumatic stress in women who experienced childhood abuse. Evid Based Ment Health 2003;6. https://doi.org/10.1136/ebmh.6.2.50.
- Yehuda R, Bierer LM, Pratchett LC, Lehrner A, Koch EC, Van Manen JA, et al. Cortisol augmentation of a psychological treatment for warfighters with posttraumatic stress disorder: Randomized trial showing improved treatment retention and outcome. Psychoneuroendocrinology 2015;51:589-97. https://doi.org/10.1016/j.psyneuen.2014.08.004.
- Yuen EK, Gros DF, Price M, Zeigler S, Tuerk PW, Foa EB, et al. Randomized controlled trial of home-based telehealth versus in-person prolonged exposure for combat-related PTSD in veterans: preliminary results. J Clin Psychol 2015;71:500-12. https://doi.org/10.1002/jclp.22168.
- Ziemba SJ, Bradley NS, Landry LA, Roth CH, Porter LS, Cuyler RN. Posttraumatic stress disorder treatment for Operation Enduring Freedom/Operation Iraqi Freedom combat veterans through a civilian community-based telemedicine network. Telemed J E Health 2014;20:446-50. https://doi.org/10.1089/tmj.2013.0312.
- Zimmermann P, Guse U, Barre K, Biesold K. EMDR in the German Armed Forces – therapeutic impact of inpatient therapy of posttraumatic stress disorder. Krankenhauspsychiatrie 2005;16:57-63. https://doi.org/10.1055/s-2004-830275.
- Zimmermann P, Biesold KH, Barre K, Lanczik M. Long-term course of post-traumatic stress disorder (PTSD) in German soldiers: effects of inpatient eye movement desensitization and reprocessing therapy and specific trauma characteristics in patients with non-combat-related PTSD. Mil Med 2007;172:456-60. https://doi.org/10.7205/MILMED.172.5.456.
- Zisook S, Chentsova-Dutton YE, Smith-Vaniz A, Kline NA, Ellenor GL, Kodsi AB, et al. Nefazodone in patients with treatment-refractory posttraumatic stress disorder. J Clin Psychiatry 2000;61:203-8. https://doi.org/10.4088/JCP.v61n0310.
- Zlotnick C, Capezza NM, Parker D. An interpersonally based intervention for low-income pregnant women with intimate partner violence: a pilot study. Arch Womens Ment Health 2011;14:55-6. https://doi.org/10.1007/s00737-010-0195-x.
- Zoellner LA, Feeny NC, Fitzgibbons LA, Foa EB. Response of African American and Caucasian women to cognitive behavioral therapy for PTSD. Behav Ther 1999;30:581-95. https://doi.org/10.1016/S0005-7894(99)80026-4.
- Shapiro F. Three Day Training Course (Levels 1 and 2) in EMDR. Gold Coast, QLD; 1992.
Appendix 1 Literature search strategies for the effectiveness review
Literature searches of the following databases were conducted: CINAHL, CENTRAL, EMBASE, International Pharmaceutical Abstracts, MEDLINE, PILOTS, PsycINFO and Science Citation Index.
The original searches carried out in April and May 2017 identified 17,177 records, which were downloaded, imported into EndNote bibliographic software and de-duplicated to leave 10,212 unique records.
CINAHL via EBSCOhost
Search date: 20 April 2017.
Records retrieved: 1919.
Date range searched: 1937 onwards.
| Search terms | Search options |
|---|---|
| S1 | (MH “Violence”) OR (MH “Exposure to Violence”) |
| S2 | TX violence |
| S3 | (MH “Domestic Violence”) OR (MH “Intimate Partner Violence”) OR (MH “Dating Violence”) |
| S4 | TX (batter$ N2 (wife* or wive* or woman or women or men or husband* or partner*)) OR TX (physical* N2 (abus* or assault* or violen* or aggress*)) OR TX emotional N2 abus* |
| S5 | (MH “Rape”) |
| S6 | TX rape OR TX (sexual* N2 (assault* or abus* or violen* or aggress*)) |
| S7 | (MH “Child Abuse, Sexual”) OR (MH “Child Abuse Survivors”) OR (MH “Sexual Abuse”) OR (MH “Child Abuse”) |
| S8 | TX “child* sexual abuse” |
| S9 | TX child* N2 exploit* OR TX child* N2 neglect* OR TX child* N2 trauma* OR TX (“non accidental injur*” or “non-accidental injur*” or “nonaccidental injur*”) |
| S10 | TX “human rights abuse*” |
| S11 | (MH “Human Trafficking”) |
| S12 | TX ((human or person* or people) N2 (traffick* or exploit*)) OR TX ((forced or exploit*) N2 labour*) |
| S13 | organ N2 traffick* |
| S14 | TX slavery or slaves or “slave trade” |
| S15 | (MH “Torture”) OR (MH “Torture Survivors”) |
| S16 | (MH “Prostitution”) |
| S17 | TX (prostitut* or brothel*) OR TX (sex* N2 (exploit* or traffick*)) |
| S18 | (MH “Terrorism”) |
| S19 | TX (terrorism or terrorist*) OR TX “political terror*” |
| S20 | (MH “War”) OR (MH “War Crimes”) |
| S21 | (MH “Holocaust”) |
| S22 | TX ethnic* N2 cleans* OR TX genocide OR TX (civil N2 (unrest or conflict* or disturb* or war or wars or warfare)) OR TX (persecution or victimisation or victimization) OR TX (captivity or imprison*) OR TX concentration camp* |
| S23 | (MH “Disasters”) OR (MH “Natural Disasters”) OR (MH “Mass Casualty Incidents”) |
| S24 | catastrophe* or (“catastrophic event*”) or (“catastrophic experience*”) |
| S25 | (MH “Survivors+”) |
| S26 | (MH “Refugees”) |
| S27 | TX refugee* OR TX “asylum seek*” OR TX migrant* OR TX ((forcibly or internally) N2 displaced) OR TX (displace* N2 (people or person* or civilian*)) |
| S28 | (MH “Crime Victims”) OR (MH “Victims”) |
| S29 | (MH “Prisoners”) |
| S30 | (MH “Veterans”) |
| S31 | TX ((expose* or exposure) N2 (abuse or assault* or disaster* or terror* or torture* or trauma* or rape or violen* or war or warfare)) OR TX (survivor* N2 (abuse or assault* or disaster* or terror* or torture* or trauma* or rape or violen* or war or warfare)) OR TX (victim* N2 (abuse or assault* or crime or disaster* or rape or terror* or torture* or trauma* or violen* or war or warfare)) OR TX (witness* N2 (abuse or assault* or disaster* or rape or terror* or torture* or trauma* or violen* or war or warfare)) |
| S32 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 (143,422) |
| S33 | (MH “Stress Disorders, Post-Traumatic+”) |
| S34 | TX (PTSD or CPTSD) OR TX posttrauma* OR TX post-trauma* OR TX “post trauma*” OR TX “post traumatic stress” OR TX “combat stress*” OR TX “combat disorder*” OR TX DESNOS OR TX “complex trauma*” OR TX complex N3 trauma* OR TX “traumatic stress” OR TX “traumatic memor*” |
| S35 | TX traumatisation OR TX traumatization OR TX (trauma* N3 (expos* or event* or experienc*)) |
| S36 | S33 OR S34 OR S35 (28,298) |
| S37 | (MH “Cognitive Therapy+”) OR TX “cognitive behaviour* therap*” OR TX “cognitive behavior* therap*” OR TX “cognitive restructuring” OR TX “cognitive rescripting” OR TX “cognitive processing therap*” OR TX (CPT or CBT or TFCBT) OR TX “cognitive therap*” OR TX “cognitive behavioural treat*” OR TX “cognitive behavioral treat*” OR TX “cognitive trauma therap*” OR TX “trauma focus* CBT” |
| S38 | (MH “Behavior Therapy”) OR TX (behavior* N2 (therap* or treat* or modif*)) OR TX (behavior* N2 (therap* or treat* or modif*)) OR TX ((dialectical behavio*) N1 (therap* or treat*)) OR TX (biofeedback or neurofeedback or (“sensory feedback”)) OR TX psychological N2 desensiti#ation OR TX (“eye movement desensiti#ation reprocessing”) OR TX EMDR OR TX (exposure N1 (therap* or treat*)) OR TX “live exposure” OR TX “imaginal exposure” OR TX “prolonged exposure therapy” |
| S39 | TX “imaginal flooding” OR TX “exposure inhibition therap*” OR TX “implosive therap*” OR TX “image habituation” OR TX “inoculation training” |
| S40 | ((MH “Acceptance and Commitment Therapy”)) OR TX acceptance N2 therap* OR TX commitment N2 therap* |
| S41 | (MH “Biofeedback”) |
| S42 | (MH “Feedback”) |
| S43 | (MH “Eye Movement Desensitization and Reprogramming”) |
| S44 | (MH “Virtual Reality Exposure Therapy”) |
| S45 | (MH “Hypnosis”) |
| S46 | TX hypnosis or hypnotherap* |
| S47 | (MH “Mindfulness”) |
| S48 | TX mindfulness |
| S49 | TX “supportive therap*” OR TX (non-directive N1 (counselling or counseling)) OR TX ((non directive) N1 (counselling or counseling)) |
| S50 | ((MH “Psychotherapy”) OR (MH “Psychotherapy, Brief”) OR (MH “Psychotherapy, Group”) OR (MH “Psychotherapy, Psychodynamic”)) OR TX psychodynamic N1 therap* OR TX “inter personal psychotherap*” OR TX “interpersonal psychotherap*” OR TX IPT OR TX “compassion therap*” OR TX “accelerated resolution*” OR TX “sensorimotor therap*” OR TX “schema therap*” OR TX stress N2 manag* |
| S51 | (MH “Counseling”) OR TX “non-directive counsel*” OR TX “non directive counsel*” OR TX “nondirective counsel*” OR “compassion therap*” |
| S52 | S37 OR S38 OR S39 OR S40 OR S41 OR S42 OR S43 OR S44 OR S45 OR S46 OR S47 OR S48 OR S49 OR S50 OR S51 (99,780) |
| S53 | ((MH “Hypnotics and Sedatives”)) OR TX (alprazolam or amobarbital or azaperone or barbital or bromisovalum or “chloral hydrate” or chloralose or chlordiazepoxide or chlormethiazole or dexmedetomidine or diazepam or diphenhydramine or eszopiclone or ethchlorvynol or etomidate or etorphine or flurazepam or glutethimide or hexobarbital or lorazepam or medazepam or medetomidine or mephobarbital or meprobamate or methapyrilene or methaqualone or midazolam or nitrazepam or oxazepam or paraldehyde or pentobarbital or phenobarbital or propofol or secobarbital or temazepam or thiamylal or thiopental or xylazine) OR TX “z drugs” |
| S54 | (MH “Antianxiety Agents+”) OR (bromazepam or buspirone or chlormezanone or “clorazepate dipotassium” or estazolam or flunitrazepam or fluvoxamine or nordazepam or ondansetron or oxprenolol or prazepam or pregabalin or ritanserin or tranylcypromine or trazodone or triazolam or zolazepam or benzodiazepines or benzodiazepinones or “sedative antihistamine*” or promethazine) |
| S55 | (MH “Antidepressive Agents+”) OR TX (benactyzine or clorgyline or deanol or “desvenlafaxine succinate” or “duloxetine hydrochloride” or iproniazid or isocarboxazid or “lithium carbonate” or “lithium compounds” or moclobemide or nialamide or phenelzine or pizotyline or rolipram or sertraline or tranylcypromine or “vilazodone hydrochloride” or Imipramine or mirtazapine) |
| S56 | (MH “Antipsychotic Agents+”) OR TX (acepromazine or aripiprazole or azaperone or benperidol or butaclamol or chlorpromazine or chlorprothixene or clopenthixol or clozapine or droperidol or etazolate or flupenthixol or fluphenazine or fluspirilene or haloperidol or loxapine or “lurasidone hydrochloride” or mesoridazine or methiothepin or methotrimeprazine or molindone or ondansetron or “paliperidone palmitate” or penfluridol or perazine or perphenazine or pimozide or prochlorperazine) OR TX (promazine or “quetiapine fumarate” or raclopride or remoxipride or reserpine or risperidone or ritanserin or spiperone or sulpiride or thioridazine or thiothixene or “tiapride hydrochloride” or trifluoperazine or trifluperidol or triflupromazine or olanzapine) |
| S57 | (MH “Anticonvulsants+”) OR TX (anticonvulsants or acetazolamide or bromides or carbamazepine or clonazepam or “clorazepate dipotassium” or diazepam or dimethadione or estazolam or ethosuximide or flunarizine or lorazepam or “magnesium sulfate” or medazepam or mephenytoin or mephobarbital or meprobamate or nitrazepam or paraldehyde or phenobarbital or phenytoin or pregabalin or primidone or riluzole or thiopental or tiletamine or trimethadione or “valproic acid” or vigabatrin) |
| S58 | (MH “Antimanic Agents+”) OR TX (“lithium chloride” or “lithium compounds” or lamotrigine or topiramate) |
| S59 | (MH “Monoamine Oxidase Inhibitors+”) OR TX (chlorphenamidine or clorgyline or cuprizone or furazolidone or harmaline or harmine or isocarboxazid or moclobemide or monocrotophos or pargyline or selegiline or tranylcypromine or Prazosin or N-Methyl-3,4-methylenedioxyamphetamine or MDMA or ecstasy) |
| S60 | S53 OR S54 OR S55 OR S56 OR S57 OR S58 OR S59 (68,988) |
| S61 | S32 AND S36 AND S52 (1786) |
| S62 | S32 AND S36 AND S60 (229) |
| S63 | S61 OR S62 (1936) |
| S64 | S61 OR S62 (1919) 1992 ONWARDS |
CENTRAL via The Cochrane Library
Search date: 21 April 2017.
Records retrieved: 637.
Date range searched: from inception.
| #1 MeSH descriptor: [Violence] explode all trees |
| #2 violence:ti,ab,kw (Word variations have been searched) |
| #3 MeSH descriptor: [Domestic Violence] explode all trees |
| #4 MeSH descriptor: [Intimate Partner Violence] explode all trees |
| #5 MeSH descriptor: [Battered Women] explode all trees |
| #6 batter* near/2 (wife* or wive* or woman or women or men or husband* or partner*):ti,ab,kw (Word variations have been searched) |
| #7 physical* near/2 (abus* or assault* or violen* or aggress*):ti,ab,kw (Word variations have been searched) |
| #8 emotional* near/2 abus*:ti,ab,kw (Word variations have been searched) |
| #9 MeSH descriptor: [Rape] explode all trees |
| #10 rape:ti,ab,kw or sexual* near/2 (abus* or assault* or violen* or aggress*):ti,ab,kw (Word variations have been searched) |
| #11 MeSH descriptor: [Child Abuse, Sexual] explode all trees |
| #12 child* sexual abuse:ti,ab,kw (Word variations have been searched) |
| #13 child* near/2 (exploit* or neglect* or trauma*):ti,ab,kw (Word variations have been searched) |
| #14 non accidental injur*:ti,ab,kw or non-accidental injur*:ti,ab,kw or nonaccidental injur*:ti,ab,kw (Word variations have been searched) |
| #15 MeSH descriptor: [Human Rights Abuses] explode all trees |
| #16 MeSH descriptor: [Human Trafficking] explode all trees |
| #17 (human or person or people) near/2 (traffick* or exploit*):ti,ab,kw (Word variations have been searched) |
| #18 (forced or exploit*) near/2 labour:ti,ab,kw (Word variations have been searched) |
| #19 MeSH descriptor: [Organ Trafficking] explode all trees |
| #20 MeSH descriptor: [Slavery] explode all trees |
| #21 MeSH descriptor: [Torture] explode all trees |
| #22 slavery or enslave* or torture*:ti,ab,kw (Word variations have been searched) |
| #23 MeSH descriptor: [Sex Workers] explode all trees |
| #24 MeSH descriptor: [Prostitution] explode all trees |
| #25 prostitut* or brothel*:ti,ab,kw (Word variations have been searched) |
| #26 sex* near/2 (exploit* or traffick*):ti,ab,kw (Word variations have been searched) |
| #27 MeSH descriptor: [Terrorism] explode all trees |
| #28 terrorism or terrorist*:ti,ab,kw (Word variations have been searched) |
| #29 political terror*:ti,ab,kw (Word variations have been searched) |
| #30 MeSH descriptor: [Torture] explode all trees |
| #31 MeSH descriptor: [Warfare] explode all trees |
| #32 MeSH descriptor: [Armed Conflicts] explode all trees |
| #33 MeSH descriptor: [War Crimes] explode all trees |
| #34 MeSH descriptor: [Genocide] explode all trees |
| #35 MeSH descriptor: [Holocaust] explode all trees |
| #36 MeSH descriptor: [Ethnic Cleansing] explode all trees |
| #37 civil near/2 (unrest or conflict* or disturbance* or war or wars or warfare):ti,ab,kw (Word variations have been searched) |
| #38 persecution or victimization or victimisation:ti,ab,kw (Word variations have been searched) |
| #39 captivity or imprison* or concentration camp*:ti,ab,kw (Word variations have been searched) |
| #40 MeSH descriptor: [Disasters] explode all trees |
| #41 MeSH descriptor: [Earthquakes] explode all trees |
| #42 MeSH descriptor: [Tsunamis] explode all trees |
| #43 natural disaster*:ti,ab,kw (Word variations have been searched) |
| #44 earthquake* or tsunami*:ti,ab,kw (Word variations have been searched) |
| #45 humanitarian near/1 (crisis or crises):ti,ab,kw (Word variations have been searched) |
| #46 catastrophe* or catastrophic event* or catastrophic experience*:ti,ab,kw (Word variations have been searched) |
| #47 MeSH descriptor: [Survivors] explode all trees |
| #48 MeSH descriptor: [Refugees] explode all trees |
| #49 asylum seeker* or refugee* or migrant*:ti,ab,kw (Word variations have been searched) |
| #50 (forcibly or internally) near/2 displace*:ti,ab,kw (Word variations have been searched) |
| #51 displace* near/2 (people or person* or civilian*):ti,ab,kw (Word variations have been searched) |
| #52 MeSH descriptor: [Crime Victims] explode all trees |
| #53 MeSH descriptor: [Adult Survivors of Child Abuse] explode all trees |
| #54 MeSH descriptor: [Disaster Victims] explode all trees |
| #55 MeSH descriptor: [Prisoners] explode all trees |
| #56 MeSH descriptor: [Prisoners of War] explode all trees |
| #57 MeSH descriptor: [Slaves] explode all trees |
| #58 MeSH descriptor: [Veterans] explode all trees |
| #59 MeSH descriptor: [Military Personnel] explode all trees |
| #60 exposure near/2 (abuse or assault* or disaster* or terror* or torture* or trauma* or rape or violen* or war or warfare):ti,ab,kw (Word variations have been searched) |
| #61 exposed near/2 (abuse or assault* or disaster* or terror* or torture* or trauma* or rape or violen* or war or warfare):ti,ab,kw (Word variations have been searched) |
| #62 survivor* near/2 (abuse or assault* or disaster* or terror* or torture* or trauma* or rape or violen* or war or warfare):ti,ab,kw (Word variations have been searched) |
| #63 victim* near/2 (abuse or assault* or crime or disaster* or rape or terror* or torture* or trauma* or violen* or war or warfare):ti,ab,kw (Word variations have been searched) |
| #64 witness* near/2 (abuse or assault* or disaster* or rape or terror* or torture* or trauma* or violen* or war or warfare):ti,ab,kw (Word variations have been searched) |
| #65 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 or #30 or #31 or #32 or #33 or #34 or #35 or #36 or #37 or #38 or #39 or #40 or #41 or #42 or #43 or #44 or #45 or #46 or #47 or #48 or #49 or #50 or #51 or #52 or #53 or #54 or #55 or #56 or #57 or #58 or #59 or #60 or #61 or #62 or #63 or #64 |
| #66 MeSH descriptor: [Stress Disorders, Post-Traumatic] explode all trees |
| #67 PTSD or CPTSD:ti,ab,kw (Word variations have been searched) |
| #68 posttrauma*:ti,ab,kw (Word variations have been searched) |
| #69 post-trauma*:ti,ab,kw (Word variations have been searched) |
| #70 post trauma*:ti,ab,kw (Word variations have been searched) |
| #71 “post traumatic stress”:ti,ab,kw (Word variations have been searched) |
| #72 combat stress:ti,ab,kw (Word variations have been searched) |
| #73 combat disorder*:ti,ab,kw (Word variations have been searched) |
| #74 DESNOS:ti,ab,kw (Word variations have been searched) |
| #75 extreme distress:ti,ab,kw (Word variations have been searched) |
| #76 complex near/3 trauma:ti,ab,kw (Word variations have been searched) |
| #77 traumatic stress:ti,ab,kw (Word variations have been searched) |
| #78 traumatic memories:ti,ab,kw (Word variations have been searched) |
| #79 traumatization:ti,ab,kw (Word variations have been searched) |
| #80 “traumatisation”:ti,ab,kw (Word variations have been searched) |
| #81 trauma near/3 (expos* or event* or experienc*):ti,ab,kw (Word variations have been searched) |
| #82 #66 or #67 or #68 or #69 or #70 or #71 or #72 or #73 or #74 or #75 or #76 or #77 or #78 or #79 or #80 or #81 |
| #83 #65 and #82 |
| #84 MeSH descriptor: [Cognitive Therapy] explode all trees |
| #85 cognitive near/2 therap*:ti,ab,kw (Word variations have been searched) |
| #86 “cognitive restructuring”:ti,ab,kw (Word variations have been searched) |
| #87 cognitive rescripting:ti,ab,kw (Word variations have been searched) |
| #88 “cognitive processing therapy”:ti,ab,kw (Word variations have been searched) |
| #89 CPT:ti,ab,kw (Word variations have been searched) |
| #90 cognitive near/2 treat*:ti,ab,kw (Word variations have been searched) |
| #91 CBT or TFCBT:ti,ab,kw (Word variations have been searched) |
| #92 MeSH descriptor: [Behavior Therapy] explode all trees |
| #93 behavior* near/2 (therap* or treat* or modif*):ti,ab,kw (Word variations have been searched) |
| #94 behaviour* near/2 (therap* or treat* or modif*):ti,ab,kw (Word variations have been searched) |
| #95 MeSH descriptor: [Biofeedback, Psychology] explode all trees |
| #96 MeSH descriptor: [Feedback, Sensory] explode all trees |
| #97 MeSH descriptor: [Neurofeedback] explode all trees |
| #98 biofeedback:ti,ab,kw (Word variations have been searched) |
| #99 “neurofeedback”:ti,ab,kw (Word variations have been searched) |
| #100 “sensory feedback”:ti,ab,kw (Word variations have been searched) |
| #101 MeSH descriptor: [Eye Movement Desensitization Reprocessing] explode all trees |
| #102 MeSH descriptor: [Implosive Therapy] explode all trees |
| #103 MeSH descriptor: [Virtual Reality Exposure Therapy] explode all trees |
| #104 psychological near/2 desensit*:ti,ab,kw (Word variations have been searched) |
| #105 “Eye Movement Desensitization Reprocessing”:ti,ab,kw or “Eye Movement Desensitisation Reprocessing”:ti,ab,kw (Word variations have been searched) |
| #106 EMDR:ti,ab,kw (Word variations have been searched) |
| #107 exposure near/1 (therap* or treat*):ti,ab,kw (Word variations have been searched) |
| #108 “live exposure”:ti,ab,kw (Word variations have been searched) |
| #109 “imaginal exposure”:ti,ab,kw (Word variations have been searched) |
| #110 “prolonged exposure therapy”:ti,ab,kw (Word variations have been searched) |
| #111 “imaginal flooding”:ti,ab,kw (Word variations have been searched) |
| #112 “exposure inhibition therapy”:ti,ab,kw (Word variations have been searched) |
| #113 “implosive therapy”:ti,ab,kw (Word variations have been searched) |
| #114 “image habituation”:ti,ab,kw (Word variations have been searched) |
| #115 “inoculation training”:ti,ab,kw (Word variations have been searched) |
| #116 MeSH descriptor: [Acceptance and Commitment Therapy] explode all trees |
| #117 acceptance near/2 therap*:ti,ab,kw (Word variations have been searched) |
| #118 commitment near/2 therap*:ti,ab,kw (Word variations have been searched) |
| #119 MeSH descriptor: [Hypnosis] explode all trees |
| #120 hypnosis:ti,ab,kw (Word variations have been searched) |
| #121 hypnotherap*:ti,ab,kw (Word variations have been searched) |
| #122 MeSH descriptor: [Mindfulness] explode all trees |
| #123 mindfulness:ti,ab,kw (Word variations have been searched) |
| #124 supportive near/1 therap*:ti,ab,kw (Word variations have been searched) |
| #125 non-directive near/1 counsel*:ti,ab,kw (Word variations have been searched) |
| #126 nondirective near/2 counsel*:ti,ab,kw (Word variations have been searched) |
| #127 “non directive” near/1 counsel*:ti,ab,kw (Word variations have been searched) |
| #128 MeSH descriptor: [Psychotherapy] explode all trees |
| #129 MeSH descriptor: [Psychotherapy, Brief] explode all trees |
| #130 MeSH descriptor: [Cognitive Therapy] explode all trees |
| #131 MeSH descriptor: [Psychotherapy, Group] explode all trees |
| #132 MeSH descriptor: [Psychotherapy, Multiple] explode all trees |
| #133 MeSH descriptor: [Psychotherapy, Psychodynamic] explode all trees |
| #134 MeSH descriptor: [Psychotherapy, Rational-Emotive] explode all trees |
| #135 psychodynamic near/1 therap*:ti,ab,kw (Word variations have been searched) |
| #136 interpersonal near/1 psychotherap*:ti,ab,kw (Word variations have been searched) |
| #137 compassion near/2 therap*:ti,ab,kw (Word variations have been searched) |
| #138 “accelerated resolution”:ti,ab,kw (Word variations have been searched) |
| #139 sensorimotor near/2 therap*:ti,ab,kw (Word variations have been searched) |
| #140 schema near/1 therap*:ti,ab,kw (Word variations have been searched) |
| #141 MeSH descriptor: [Counseling] explode all trees |
| #142 #84 or #85 or #86 or #87 or #88 or #89 or #90 or #91 or #92 or #93 or #94 or #95 or #96 or #97 or #98 or #99 or #100 or #101 or #102 or #103 or #104 or #105 or #106 or #107 or #108 or #109 or #110 or #111 or #112 or #113 or #114 or #115 or #116 or #117 or #118 or #119 or #120 or #121 or #122 or #123 or #124 or #125 or #126 or #127 or #128 or #129 or #130 or #131 or #132 or #133 or #134 or #135 or #136 or #137 or #138 or #139 or #140 or #141 |
| #143 MeSH descriptor: [Hypnotics and Sedatives] explode all trees |
| #144 MeSH descriptor: [Alprazolam] explode all trees |
| #145 MeSH descriptor: [Amobarbital] explode all trees |
| #146 MeSH descriptor: [Azaperone] explode all trees |
| #147 MeSH descriptor: [Barbital] explode all trees |
| #148 MeSH descriptor: [Bromisovalum] explode all trees |
| #149 MeSH descriptor: [Chloral Hydrate] explode all trees |
| #150 MeSH descriptor: [Chloralose] explode all trees |
| #151 MeSH descriptor: [Chlordiazepoxide] explode all trees |
| #152 MeSH descriptor: [Chlormethiazole] explode all trees |
| #153 MeSH descriptor: [Dexmedetomidine] explode all trees |
| #154 MeSH descriptor: [Diazepam] explode all trees |
| #155 MeSH descriptor: [Diphenhydramine] explode all trees |
| #156 MeSH descriptor: [Eszopiclone] explode all trees |
| #157 MeSH descriptor: [Ethchlorvynol] explode all trees |
| #158 MeSH descriptor: [Etomidate] explode all trees |
| #159 MeSH descriptor: [Etorphine] explode all trees |
| #160 MeSH descriptor: [Flurazepam] explode all trees |
| #161 MeSH descriptor: [Glutethimide] explode all trees |
| #162 MeSH descriptor: [Hexobarbital] explode all trees |
| #163 MeSH descriptor: [Lorazepam] explode all trees |
| #164 MeSH descriptor: [Medazepam] explode all trees |
| #165 MeSH descriptor: [Medetomidine] explode all trees |
| #166 MeSH descriptor: [Mephobarbital] explode all trees |
| #167 MeSH descriptor: [Meprobamate] explode all trees |
| #168 MeSH descriptor: [Methapyrilene] explode all trees |
| #169 MeSH descriptor: [Methaqualone] explode all trees |
| #170 MeSH descriptor: [Midazolam] explode all trees |
| #171 MeSH descriptor: [Nitrazepam] explode all trees |
| #172 MeSH descriptor: [Oxazepam] explode all trees |
| #173 MeSH descriptor: [Paraldehyde] explode all trees |
| #174 MeSH descriptor: [Pentobarbital] explode all trees |
| #175 MeSH descriptor: [Phenobarbital] explode all trees |
| #176 MeSH descriptor: [Propofol] explode all trees |
| #177 MeSH descriptor: [Secobarbital] explode all trees |
| #178 MeSH descriptor: [Temazepam] explode all trees |
| #179 MeSH descriptor: [Thiamylal] explode all trees |
| #180 MeSH descriptor: [Thiopental] explode all trees |
| #181 MeSH descriptor: [Xylazine] explode all trees |
| #182 #143 or #144 or #145 or #146 or #147 or #148 or #149 or #150 or #151 or #152 or #153 or #154 or #155 or #156 or #157 or #158 or #159 or #160 or #161 or #162 or #163 or #164 or #165 or #166 or #167 or #168 or #169 or #170 or #171 or #172 or #173 or #174 or #175 or #176 or #177 or #178 or #179 or #180 or #181 |
| #183 “z drugs”:ti,ab,kw (Word variations have been searched) |
| #184 MeSH descriptor: [Anti-Anxiety Agents] explode all trees |
| #185 MeSH descriptor: [Bromazepam] explode all trees |
| #186 MeSH descriptor: [Buspirone] explode all trees |
| #187 MeSH descriptor: [Chlormezanone] explode all trees |
| #188 MeSH descriptor: [Estazolam] explode all trees |
| #189 MeSH descriptor: [Flunitrazepam] explode all trees |
| #190 MeSH descriptor: [Fluvoxamine] explode all trees |
| #191 MeSH descriptor: [Nordazepam] explode all trees |
| #192 MeSH descriptor: [Ondansetron] explode all trees |
| #193 MeSH descriptor: [Oxprenolol] explode all trees |
| #194 MeSH descriptor: [Prazepam] explode all trees |
| #195 MeSH descriptor: [Pregabalin] explode all trees |
| #196 MeSH descriptor: [Ritanserin] explode all trees |
| #197 MeSH descriptor: [Tranylcypromine] explode all trees |
| #198 MeSH descriptor: [Trazodone] explode all trees |
| #199 MeSH descriptor: [Triazolam] explode all trees |
| #200 MeSH descriptor: [Zolazepam] explode all trees |
| #201 MeSH descriptor: [Benzodiazepines] explode all trees |
| #202 MeSH descriptor: [Benzodiazepinones] explode all trees |
| #203 sedative near/1 antihistamine*:ti,ab,kw (Word variations have been searched) |
| #204 MeSH descriptor: [Promethazine] explode all trees |
| #205 #183 or #184 or #185 or #186 or #187 or #188 or #189 or #190 or #191 or #192 or #193 or #194 or #195 or #196 or #197 or #198 or #199 or #200 or #201 or #202 or #203 or #204 |
| #206 MeSH descriptor: [Antidepressive Agents] explode all trees |
| #207 MeSH descriptor: [Benactyzine] explode all trees |
| #208 MeSH descriptor: [Clorgyline] explode all trees |
| #209 MeSH descriptor: [Deanol] explode all trees |
| #210 MeSH descriptor: [Desvenlafaxine Succinate] explode all trees |
| #211 MeSH descriptor: [Duloxetine Hydrochloride] explode all trees |
| #212 MeSH descriptor: [Iproniazid] explode all trees |
| #213 MeSH descriptor: [Isocarboxazid] explode all trees |
| #214 MeSH descriptor: [Lithium Compounds] explode all trees |
| #215 MeSH descriptor: [Moclobemide] explode all trees |
| #216 MeSH descriptor: [Nialamide] explode all trees |
| #217 MeSH descriptor: [Phenelzine] explode all trees |
| #218 MeSH descriptor: [Pizotyline] explode all trees |
| #219 MeSH descriptor: [Rolipram] explode all trees |
| #220 MeSH descriptor: [Sertraline] explode all trees |
| #221 MeSH descriptor: [Tranylcypromine] explode all trees |
| #222 MeSH descriptor: [Vilazodone Hydrochloride] explode all trees |
| #223 MeSH descriptor: [Imipramine] explode all trees |
| #224 #206 or #207 or #208 or #209 or #210 or #211 or #212 or #213 or #214 or #215 or #216 or #217 or #218 or #219 or #220 or #221 or #222 or #223 |
| #225 MeSH descriptor: [Antipsychotic Agents] explode all trees |
| #226 MeSH descriptor: [Acepromazine] explode all trees |
| #227 MeSH descriptor: [Aripiprazole] explode all trees |
| #228 MeSH descriptor: [Azaperone] explode all trees |
| #229 MeSH descriptor: [Benperidol] explode all trees |
| #230 MeSH descriptor: [Butaclamol] explode all trees |
| #231 MeSH descriptor: [Chlorpromazine] explode all trees |
| #232 MeSH descriptor: [Chlorprothixene] explode all trees |
| #233 MeSH descriptor: [Clopenthixol] explode all trees |
| #234 MeSH descriptor: [Clozapine] explode all trees |
| #235 MeSH descriptor: [Droperidol] explode all trees |
| #236 MeSH descriptor: [Etazolate] explode all trees |
| #237 MeSH descriptor: [Flupenthixol] explode all trees |
| #238 MeSH descriptor: [Fluphenazine] explode all trees |
| #239 MeSH descriptor: [Fluspirilene] explode all trees |
| #240 MeSH descriptor: [Haloperidol] explode all trees |
| #241 MeSH descriptor: [Loxapine] explode all trees |
| #242 MeSH descriptor: [Mesoridazine] explode all trees |
| #243 MeSH descriptor: [Methiothepin] explode all trees |
| #244 MeSH descriptor: [Methotrimeprazine] explode all trees |
| #245 MeSH descriptor: [Molindone] explode all trees |
| #246 MeSH descriptor: [Paliperidone Palmitate] explode all trees |
| #247 MeSH descriptor: [Penfluridol] explode all trees |
| #248 MeSH descriptor: [Perazine] explode all trees |
| #249 MeSH descriptor: [Perphenazine] explode all trees |
| #250 MeSH descriptor: [Pimozide] explode all trees |
| #251 MeSH descriptor: [Prochlorperazine] explode all trees |
| #252 MeSH descriptor: [Promazine] explode all trees |
| #253 MeSH descriptor: [Quetiapine Fumarate] explode all trees |
| #254 MeSH descriptor: [Raclopride] explode all trees |
| #255 MeSH descriptor: [Remoxipride] explode all trees |
| #256 MeSH descriptor: [Reserpine] explode all trees |
| #257 MeSH descriptor: [Risperidone] explode all trees |
| #258 MeSH descriptor: [Ritanserin] explode all trees |
| #259 MeSH descriptor: [Spiperone] explode all trees |
| #260 MeSH descriptor: [Sulpiride] explode all trees |
| #261 MeSH descriptor: [Thioridazine] explode all trees |
| #262 MeSH descriptor: [Thiothixene] explode all trees |
| #263 MeSH descriptor: [Tiapride Hydrochloride] explode all trees |
| #264 MeSH descriptor: [Trifluoperazine] explode all trees |
| #265 MeSH descriptor: [Trifluperidol] explode all trees |
| #266 MeSH descriptor: [Triflupromazine] explode all trees |
| #267 “olanzapine”:ti,ab,kw (Word variations have been searched) |
| #268 #225 or #226 or #227 or #228 or #229 or #230 or #231 or #232 or #233 or #234 or #235 or #236 or #237 or #238 or #239 or #240 or #241 or #242 or #243 or #244 or #245 or #246 or #247 or #248 or #249 or #250 or #251 or #252 or #253 or #254 or #255 or #256 or #257 or #258 or #259 or #260 or #261 or #262 or #263 or #264 or #265 or #266 or #267 |
| #269 MeSH descriptor: [Anticonvulsants] explode all trees |
| #270 MeSH descriptor: [Acetazolamide] explode all trees |
| #271 MeSH descriptor: [Bromides] explode all trees |
| #272 MeSH descriptor: [Carbamazepine] explode all trees |
| #273 MeSH descriptor: [Clonazepam] explode all trees |
| #274 MeSH descriptor: [Clorazepate Dipotassium] explode all trees |
| #275 MeSH descriptor: [Diazepam] explode all trees |
| #276 MeSH descriptor: [Dimethadione] explode all trees |
| #277 MeSH descriptor: [Estazolam] explode all trees |
| #278 MeSH descriptor: [Ethosuximide] explode all trees |
| #279 MeSH descriptor: [Flunarizine] explode all trees |
| #280 MeSH descriptor: [Lorazepam] explode all trees |
| #281 MeSH descriptor: [Magnesium Sulfate] explode all trees |
| #282 MeSH descriptor: [Medazepam] explode all trees |
| #283 MeSH descriptor: [Mephenytoin] explode all trees |
| #284 MeSH descriptor: [Mephobarbital] explode all trees |
| #285 MeSH descriptor: [Meprobamate] explode all trees |
| #286 MeSH descriptor: [Nitrazepam] explode all trees |
| #287 MeSH descriptor: [Paraldehyde] explode all trees |
| #288 MeSH descriptor: [Phenobarbital] explode all trees |
| #289 MeSH descriptor: [Phenytoin] explode all trees |
| #290 MeSH descriptor: [Pregabalin] explode all trees |
| #291 MeSH descriptor: [Primidone] explode all trees |
| #292 MeSH descriptor: [Riluzole] explode all trees |
| #293 MeSH descriptor: [Thiopental] explode all trees |
| #294 MeSH descriptor: [Tiletamine] explode all trees |
| #295 MeSH descriptor: [Trimethadione] explode all trees |
| #296 MeSH descriptor: [Valproic Acid] explode all trees |
| #297 MeSH descriptor: [Vigabatrin] explode all trees |
| #298 #269 or #270 or #271 or #272 or #273 or #274 or #275 or #276 or #277 or #278 or #279 or #280 or #281 or #282 or #283 or #284 or #285 or #286 or #287 or #288 or #289 or #290 or #291 or #292 or #293 or #294 or #295 or #296 or #297 |
| #299 MeSH descriptor: [Antimanic Agents] explode all trees |
| #300 MeSH descriptor: [Lithium Chloride] explode all trees |
| #301 “lamotrigine”:ti,ab,kw (Word variations have been searched) |
| #302 “topiramate”:ti,ab,kw (Word variations have been searched) |
| #303 MeSH descriptor: [Monoamine Oxidase Inhibitors] explode all trees |
| #304 MeSH descriptor: [Chlorpheniramine] explode all trees |
| #305 MeSH descriptor: [Clorgyline] explode all trees |
| #306 MeSH descriptor: [Cuprizone] explode all trees |
| #307 MeSH descriptor: [Furazolidone] explode all trees |
| #308 MeSH descriptor: [Harmaline] explode all trees |
| #309 MeSH descriptor: [Harmine] explode all trees |
| #310 MeSH descriptor: [Isocarboxazid] explode all trees |
| #311 MeSH descriptor: [Moclobemide] explode all trees |
| #312 MeSH descriptor: [Monocrotophos] explode all trees |
| #313 MeSH descriptor: [Pargyline] explode all trees |
| #314 MeSH descriptor: [Selegiline] explode all trees |
| #315 MeSH descriptor: [Tranylcypromine] explode all trees |
| #316 MeSH descriptor: [Prazosin] explode all trees |
| #317 MeSH descriptor: [N-Methyl-3,4-methylenedioxyamphetamine] explode all trees |
| #318 MDMA:ti,ab,kw or ecstasy:kw (Word variations have been searched) |
| #319 #299 or #300 or #301 or #302 or #303 or #304 or #305 or #306 or #307 or #308 or #309 or #310 or #311 or #312 or #313 or #314 or #315 or #316 or #317 or #318 |
| #320 #182 or #205 or #224 or #268 or #298 or #319 |
| #321 #83 and #142 |
| #322 #83 and #320 |
| #323 #321 or #322 |
EMBASE via Ovid
Search date: 19 April 2017.
Records retrieved: 5473.
Date range searched: 1974 to 2017 week 16.
| 1 exp Violence/ (127,415) |
| 2 violence.ti,ab. (42,364) |
| 3 Exposure to Violence/ (299) |
| 4 Domestic Violence/(8799) |
| 5 Sexual Violence/ (1468) |
| 6 Battered Woman/ (3115) |
| 7 (batter$ adj2 (wife$ or wive$ or woman or women or men or husband$ or partner$)).ti,ab. (973) |
| 8 (physical$ adj2 (abus$ or assault$ or violen$ or aggress$)).ti,ab. (12,350) |
| 9 (emotional$ adj2 abus$).ti,ab. (2304) |
| 10 Rape/(7255) |
| 11 Sexual Assault/ (1440) |
| 12 rape.ti,ab. (7034) |
| 13 (sexual$ adj2 (abus$ or assault$ or violen$ or aggress$)).ti,ab. (23,249) |
| 14 Child Sexual Abuse/ (8661) |
| 15 child$ sexual abuse.ti,ab. (4983) |
| 16 Child Abuse/ (27,390) |
| 17 (child$ adj2 exploit$).ti,ab. (221) |
| 18 child neglect.ti,ab. (490) |
| 19 (child$ adj2 trauma).ti,ab. (6375) |
| 20 (non accidental injur$ or non-accidental injur$ or nonaccidental injury).ti,ab. (755) |
| 21 Human Rights Abuse/ (1442) |
| 22 Human Trafficking/(259) |
| 23 ((human or person or people) adj2 (traffick$ or exploit$)).ti,ab. (907) |
| 24 ((forced or exploit$) adj2 labour).ti,ab. (62) |
| 25 Organ Trafficking/ (190) |
| 26 Slavery/ (115) |
| 27 Torture/ (2635) |
| 28 (slavery or enslave$ or torture$).ti,ab. (2768) |
| 29 Prostitution/ (8919) |
| 30 (prostitut$ or brothel$).ti,ab. (3430) |
| 31 (sex$ adj2 (exploit$ or traffick$)).ti,ab. (618) |
| 32 exp Terrorism/ (9017) |
| 33 (terrorism or terrorist$).ti,ab. (6169) |
| 34 political terror$.ti,ab. (19) |
| 35 Torture/ (2635) |
| 36 exp warfare/ (18,460) |
| 37 War crime/ (174) |
| 38 Genocide/ (334) |
| 39 Holocaust/ (369) |
| 40 Ethnic Conflict/ (58) |
| 41 (civil adj (unrest or conflict$ or disturbance$ or war or wars or warfare)).ti,ab. (1866) |
| 42 (persecution or victimization or victimisation).ti,ab. (7768) |
| 43 (captivity or imprison$ or concentration camp$).ti,ab. (6611) |
| 44 exp Disasters/ (27,191) |
| 45 natural disaster$.ti,ab. (3220) |
| 46 (earthquake$ or tsunami$).ti,ab. (8306) |
| 47 (humanitarian adj (crisis or crises)).ti,ab. (230) |
| 48 (catastrophe$ or catastrophic event$ or catastrophic experience$).ti,ab. (7315) |
| 49 exp Survivor/ (65,046) |
| 50 Refugee/ (9945) |
| 51 (asylum seeker$ or refugee$ or migrant$).ti,ab. (22,105) |
| 52 ((forcibly or internally) adj2 displace$).ti,ab. (518) |
| 53 (displace$ adj2 (people or person$ or civilian$)).ti,ab. (769) |
| 54 Crime Victim/(1526) |
| 55 exp Childhood Trauma Survivor/ (209) |
| 56 Disaster Victim/ (296) |
| 57 exp Prisoner/ (15,304) |
| 58 Prisoner of War/ (396) |
| 59 Slave/ (82) |
| 60 Veteran/ (24,063) |
| 61 Soldier/ (29,325) |
| 62 ((expose$ or exposure) adj2 (abuse or assault$ or disaster$ or terror$ or torture$ or trauma$ or rape or violen$ or war or warfare)).ti,ab. (8060) |
| 63 (survivor$ adj2 (abuse or assault$ or disaster$ or terror$ or torture$ or trauma$ or rape or violen$ or war or warfare)).ti,ab. (2541) |
| 64 (victim$ adj2 (abuse or assault$ or crime or disaster$ or rape or terror$ or torture$ or trauma$ or violen$ or war or warfare)).ti,ab. (9275) |
| 65 (witness$ adj2 (abuse or assault$ or disaster$ or rape or terror$ or torture$ or trauma$ or violen$ or war or warfare)).ti,ab. (1147) |
| 66 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49 or 50 or 51 or 52 or 53 or 54 or 55 or 56 or 57 or 58 or 59 or 60 or 61 or 62 or 63 or 64 or 65 (372,799) |
| 67 Posttraumatic Stress Disorder/ (48,288) |
| 68 (PTSD or CPTSD).ti,ab. (22,853) |
| 69 posttrauma$.ti,ab. (35,543) |
| 70 post-trauma$.ti,ab. (32,384) |
| 71 “post trauma$”.ti,ab. (32,384) |
| 72 post traumatic stress.ti,ab. (12,118) |
| 73 post traumatic stress.kw. (2904) |
| 74 combat stress$.ti,ab. (414) |
| 75 combat disorder$.ti,ab. (19) |
| 76 DESNOS.ti,ab. (37) |
| 77 “Disorders of Extreme Distress Not Otherwise Specified”.ti,ab. (0) |
| 78 complex trauma$.ti,ab. (468) |
| 79 (complex adj3 trauma$).ti,ab. (1446) |
| 80 traumatic stress.ti,ab. (14,496) |
| 81 traumatic memor$.ti,ab. (767) |
| 82 traumatization.ti,ab. (1253) |
| 83 traumatisation.ti,ab. (258) |
| 84 (trauma$ adj3 (expos$ or event$ or experienc$)).ti,ab. (20,684) |
| 85 67 or 68 or 69 or 70 or 71 or 72 or 73 or 74 or 75 or 76 or 77 or 78 or 79 or 80 or 81 or 82 or 83 or 84 (99,034) |
| 86 66 and 85 (29,961) |
| 87 exp Cognitive Therapy/ (44,498) |
| 88 cognitive behaviour$ therapy.ti,ab. (5617) |
| 89 cognitive behavior$ therapy.ti,ab. (10,869) |
| 90 cognitive restructuring.ti,ab. (1117) |
| 91 cognitive rescripting.ti,ab. (0) |
| 92 cognitive processing therapy.ti,ab. (197) |
| 93 CPT.ti,ab. (15,303) |
| 94 cognitive therapy.ti,ab. (3567) |
| 95 cognitive behavioural treatment$.ti,ab. (569) |
| 96 cognitive behavioral treatment$.ti,ab. (1915) |
| 97 (CBT or TFCBT).ti,ab. (11,649) |
| 98 cognitive trauma therapy.ti,ab. (7) |
| 99 trauma focus$ CBT.ti,ab. (48) |
| 100 87 or 88 or 89 or 90 or 91 or 92 or 93 or 94 or 95 or 96 or 97 or 98 or 99 (65,898) |
| 101 exp Behavior Therapy/ (42,878) |
| 102 (behavior$ adj2 (therap$ or treat$ or modif$)).ti,ab. (35,788) |
| 103 (behaviour$ adj2 (therap$ or treat$ or modif$)).ti,ab. (13,871) |
| 104 (dialectical behavio$ adj (therap$ or treat$)).ti,ab. (829) |
| 105 biofeedback, psychology/or feedback, sensory/or neurofeedback/ (21,789) |
| 106 (biofeedback or neurofeedback or sensory feedback).ti,ab. (11,442) |
| 107 eye movement desensitization reprocessing/or implosive therapy/or virtual reality exposure therapy/ (414) |
| 108 (psychological adj2 desensiti$).ti,ab. (9) |
| 109 eye movement desensiti?ation reprocessing.ti,ab. (39) |
| 110 EMDR.ti,ab. (560) |
| 111 (exposure adj (therap$ or treat$)).ti,ab. (2851) |
| 112 live exposure.ti,ab. (16) |
| 113 imaginal exposure.ti,ab. (183) |
| 114 prolonged exposure therapy.ti,ab. (120) |
| 115 imaginal flooding.ti,ab. (27) |
| 116 exposure inhibition therap$.ti,ab. (0) |
| 117 implosive therap$.ti,ab. (58) |
| 118 image habituation.ti,ab. (4) |
| 119 inoculation training.ti,ab. (114) |
| 120 101 or 102 or 103 or 104 or 105 or 106 or 107 or 108 or 109 or 110 or 111 or 112 or 113 or 114 or 115 or 116 or 117 or 118 or 119 (107,793) |
| 121 “Acceptance and Commitment Therapy”/ (780) |
| 122 (acceptance adj2 therap$).ti,ab. (384) |
| 123 (commitment adj2 therap$).ti,ab. (858) |
| 124 Hypnosis/ (14,590) |
| 125 (hypnosis or hypnotherap$).ti,ab. (9008) |
| 126 Mindfulness/ (3696) |
| 127 mindfulness.ti,ab. (5250) |
| 128 supportive therap$.ti,ab. (5535) |
| 129 (non-directive adj (counselling or counseling)).ti,ab. (118) |
| 130 (nondirective adj (counselling or counseling)).ti,ab. (51) |
| 131 (non directive adj (counselling or counseling)).ti,ab. (118) |
| 132 Psychotherapy/or Group Therapy/or Psychodynamic Psychotherapy/ (104,777) |
| 133 psychodynamic therap$.ti,ab. (636) |
| 134 inter personal psychotherap$.ti,ab. (1) |
| 135 interpersonal psychotherap$.ti,ab. (940) |
| 136 IPT.ti,ab. (2383) |
| 137 (compassion adj2 therap$).ti,ab. (58) |
| 138 accelerated resolution.ti,ab. (120) |
| 139 sensorimotor therap$.ti,ab. (24) |
| 140 schema therapy.ti,ab. (180) |
| 141 (stress adj2 manag$).ti,ab. (6629) |
| 142 supportive therap$.ti,ab. (5535) |
| 143 Counseling/ (75,492) |
| 144 (non-directive counsel$ or non directive counsel$ or nondirective counsel$).ti,ab. (170) |
| 145 compassion therap$.ti,ab. (2) |
| 146 121 or 122 or 123 or 124 or 125 or 126 or 127 or 128 or 129 or 130 or 131 or 132 or 133 or 134 or 135 or 136 or 137 or 138 or 139 or 140 or 141 or 142 or 143 or 144 or 145 (209,736) |
| 147 100 or 120 or 146 (330,152) |
| 148 hypnotic sedative agent/or alprazolam/or amobarbital/or azaperone/or barbital/or bromisovalum/or chloral hydrate/or chloralose/or chlordiazepoxide/or chlomethiazole/or dexmedetomidine/or diazepam/or diphenhydramine/or eszopiclone/or ethchlorvynol/or etomidate/or etorphine/or flurazepam/or glutethimide/or hexobarbital/or lorazepam/or medazepam/or medetomidine/or methylphenobarbital/or meprobamate/or methapyrilene/or methaqualone/or midazolam/or nitrazepam/or oxazepam/or paraldehyde/or pentobarbital/or phenobarbital/or propofol/or secobarbital/or temazepam/or thiamylal/or thiopental/or xylazine/ (321,753) |
| 149 z drugs.ti,ab. (207) |
| 150 anxiolytic agent/or bromazepam/or buspirone/or chlormezanone/or clorazepate dipotassium/or estazolam/or flunitrazepam/or fluvoxamine/or nordazepam/or ondansetron/or oxprenolol/or prazepam/or pregabalin/or ritanserin/or tranylcypromine/or trazodone/or triazolam/or zolazepam/ (100,358) |
| 151 benzodiazepine derivative/ (40,227) |
| 152 sedative antihistamine$.ti,ab. (114) |
| 153 promethazine/ (13,661) |
| 154 antidepressive agent/or benactyzine/or clorgyline/or deanol/or desvenlafaxine/or duloxetine/or iproniazid/or isocarboxazid/or lithium carbonate/or lithium derivative/or moclobemide/or nialamide/or phenelzine/or pizotifen/or rolipram/or sertraline/or tranylcypromine/or vilazodone/ (147,901) |
| 155 Imipramine/ (34,101) |
| 156 mirtazapine/ (10,903) |
| 157 neuroleptic agent/or acepromazine/or aripiprazole/or azaperone/or benperidol/or butaclamol/or chlorpromazine/or chlorprothixene/or clopenthixol/or clozapine/or droperidol/or etazolate/or flupentixol/or fluphenazine/or fluspirilene/or haloperidol/or loxapine/or lurasidone/or mesoridazine/or metitepine/or methotrimeprazine/or molindone/or ondansetron/or paliperidone/or penfluridol/or perazine/or perphenazine/or pimozide/or prochlorperazine/or promazine/or quetiapine/or raclopride/or remoxipride/or reserpine/or risperidone/or ritanserin/or spiperone/or sulpiride/or thioridazine/or tiothixene/or tiapride/or trifluoperazine/or trifluperidol/or triflupromazine/ (250,352) |
| 158 olanzapine/ (30,419) |
| 159 anticonvulsive agent/or acetazolamide/or bromides/or carbamazepine/or clonazepam/or clorazepate dipotassium/or diazepam/or dimethadione/or estazolam/or ethosuximide/or flunarizine/or lorazepam/or magnesium sulfate/or medazepam/or mephenytoin/or methylphenobarbital/or meprobamate/or nitrazepam/or paraldehyde/or phenobarbital/or phenytoin/or pregabalin/or primidone/or riluzole/or thiopental/or tiletamine/or trimethadione/or valproic acid/or vigabatrin/ (370,923) |
| 160 tranquilizer/or lithium chloride/or lithium derivative/ (25,358) |
| 161 lamotrigine/ (21,972) |
| 162 topiramate/ (18,900) |
| 163 monoamine oxidase inhibitor/or chlorphenamidine/or clorgyline/or cuprizone/or furazolidone/or harmaline/or harmine/or isocarboxazid/or moclobemide/or monocrotophos/or pargyline/or selegiline/or tranylcypromine/ (44,538) |
| 164 Prazosin/ (22,822) |
| 165 3,4 methylenedioxyamphetamine/ (2221) |
| 166 (MDMA or ecstasy).ti,ab. (6467) |
| 167 148 or 149 or 150 or 151 or 152 or 153 or 154 or 155 or 156 or 157 or 158 or 159 or 160 or 161 or 162 or 163 or 164 or 165 or 166 (904,230) |
| 168 86 and 147 (4620) |
| 169 86 and 167 (1616) |
| 170 168 or 169 (5607) |
| 171 limit 170 to yr=“1992 -Current” (5473) |
International Pharmaceutical Abstracts via ProQuest
Search date: 30 August 2017.
The initial search identified 625 records.
Date range searched: 1970 onwards.
| (SU.EXACT(“Stress disorders”)) OR (PTSD or CPTSD) OR (posttrauma* or post-trauma*) OR (“post traumatic stress”) OR (“combat disorder*”) OR (“combat stress”) OR DESNOS OR (traumatisation OR traumatization) OR (complex NEAR/3 trauma*) OR (trauma* NEAR/3 (expos* or event* or experienc*)) |
MEDLINE via Ovid
Search date: 18 April 2017.
Records retrieved: 2818.
Database: Ovid MEDLINE Epub Ahead of Print and In-Process & Other Non-Indexed Citations, Ovid MEDLINE Daily and Ovid MEDLINE.
Date range searched: 1946 to present.
| 1 exp Violence/ (84,653) |
| 2 violence.ti,ab. (38,287) |
| 3 Domestic Violence/ (5769) |
| 4 Intimate Partner Violence/ (716) |
| 5 Battered Women/ (2579) |
| 6 (batter$ adj2 (wife$ or wive$ or woman or women or men or husband$ or partner$)).ti,ab. (870) |
| 7 (physical$ adj2 (abus$ or assault$ or violen$ or aggress$)).ti,ab. (10,464) |
| 8 (emotional$ adj2 abus$).ti,ab. (1749) |
| 9 Rape/ (6157) |
| 10 rape.ti,ab. (6600) |
| 11 (sexual$ adj2 (abus$ or assault$ or violen$ or aggress$)).ti,ab. (19,466) |
| 12 Child Sexual Abuse/ (9551) |
| 13 child$ sexual abuse.ti,ab. (4339) |
| 14 (child$ adj2 exploit$).ti,ab. (200) |
| 15 child neglect.ti,ab. (468) |
| 16 (child$ adj2 trauma).ti,ab. (4689) |
| 17 (non accidental injur$ or non-accidental injur$ or nonaccidental injury).ti,ab. (533) |
| 18 Human Rights Abuses/ (734) |
| 19 Human Trafficking/ (177) |
| 20 ((human or person or people) adj2 (traffick$ or exploit$)).ti,ab. (818) |
| 21 ((forced or exploit$) adj2 labour).ti,ab. (56) |
| 22 Organ Trafficking/ (33) |
| 23 Slavery/ (45) |
| 24 Torture/ (1996) |
| 25 (slavery or enslave$ or torture$).ti,ab. (2480) |
| 26 Sex Work/ (5675) |
| 27 (prostitut$ or brothel$).ti,ab. (3946) |
| 28 (sex$ adj2 (exploit$ or traffick$)).ti,ab. (561) |
| 29 Terrorism/ (4718) |
| 30 (terrorism or terrorist$).ti,ab. (5408) |
| 31 political terror$.ti,ab. (16) |
| 32 Torture/ (1996) |
| 33 exp warfare/ (35,511) |
| 34 exp Armed Conflicts/ (8467) |
| 35 War crimes/ (1197) |
| 36 Genocide/ (84) |
| 37 Holocaust/ (782) |
| 38 Ethnic Cleansing/ (0) |
| 39 (civil adj (unrest or conflict$ or disturbance$ or war or wars or warfare)).ti,ab. (1859) |
| 40 (persecution or victimization or victimisation).ti,ab. (7276) |
| 41 (captivity or imprison$ or concentration camp$).ti,ab. (6151) |
| 42 exp Disasters/ (67,463) |
| 43 Earthquakes/ (3095) |
| 44 Tsunamis/ (708) |
| 45 natural disaster$.ti,ab. (2928) |
| 46 (earthquake$ or tsunami$).ti,ab. (7947) |
| 47 (humanitarian adj (crisis or crises)).ti,ab. (221) |
| 48 (catastrophe$ or catastrophic event$ or catastrophic experience$).ti,ab. (5922) |
| 49 exp Survivors/ (22,782) |
| 50 Refugees/ (8204) |
| 51 (asylum seeker$ or refugee$ or migrant$).ti,ab. (21,535) |
| 52 ((forcibly or internally) adj2 displace$).ti,ab. (476) |
| 53 (displace$ adj2 (people or person$ or civilian$)).ti,ab. (763) |
| 54 Crime Victims/ (7200) |
| 55 Adult Survivors of Child Abuse/ (1437) |
| 56 Disaster Victims/ (96) |
| 57 Prisoners/ (15,110) |
| 58 Prisoners of War/ (469) |
| 59 Slaves/ (31) |
| 60 Veterans/ (13,136) |
| 61 Military Personnel/ (35,416) |
| 62 ((expose$ or exposure) adj2 (abuse or assault$ or disaster$ or terror$ or torture$ or trauma$ or rape or violen$ or war or warfare)).ti,ab. (7019) |
| 63 (survivor$ adj2 (abuse or assault$ or disaster$ or terror$ or torture$ or trauma$ or rape or violen$ or war or warfare)).ti,ab. (2319) |
| 64 (victim$ adj2 (abuse or assault$ or crime or disaster$ or rape or terror$ or torture$ or trauma$ or violen$ or war or warfare)).ti,ab. (8160) |
| 65 (witness$ adj2 (abuse or assault$ or disaster$ or rape or terror$ or torture$ or trauma$ or violen$ or war or warfare)).ti,ab. (1041) |
| 66 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49 or 50 or 51 or 52 or 53 or 54 or 55 or 56 or 57 or 58 or 59 or 60 or 61 or 62 or 63 or 64 or 65 (331,505) |
| 67 Stress Disorders, Post Traumatic/ (26,733) |
| 68 (PTSD or CPTSD).ti,ab. (18,107) |
| 69 posttrauma$.ti,ab. (30,066) |
| 70 post-trauma$.ti,ab. (25,637) |
| 71 “post trauma$”.ti,ab. (25,637) |
| 72 post traumatic stress.ti,ab. (9289) |
| 73 post traumatic stress.kw. (88) |
| 74 combat stress$.ti,ab. (343) |
| 75 combat disorder$.ti,ab. (15) |
| 76 DESNOS.ti,ab. (31) |
| 77 “Disorders of Extreme Distress Not Otherwise Specified”.ti,ab. (0) |
| 78 complex trauma$.ti,ab. (403) |
| 79 (complex adj3 trauma$).ti,ab. (1217) |
| 80 traumatic stress.ti,ab. (10,740) |
| 81 traumatic memor$.ti,ab. (579) |
| 82 traumatization.ti,ab. (990) |
| 83 traumatisation.ti,ab. (192) |
| 84 (trauma$ adj3 (expos$ or event$ or experienc$)).ti,ab. (16,288) |
| 85 67 or 68 or 69 or 70 or 71 or 72 or 73 or 74 or 75 or 76 or 77 or 78 or 79 or 80 or 81 or 82 or 83 or 84 (75,076) |
| 86 66 and 85 (24,059) |
| 87 exp Cognitive Therapy/ (22,441) |
| 88 cognitive behaviour$ therapy.ti,ab. (3982) |
| 89 cognitive behavior$ therapy.ti,ab. (8052) |
| 90 cognitive restructuring.ti,ab. (723) |
| 91 cognitive rescripting.ti,ab. (0) |
| 92 cognitive processing therapy.ti,ab. (178) |
| 93 CPT.ti,ab. (10,770) |
| 94 cognitive therapy.ti,ab. (2397) |
| 95 cognitive behavioural treatment$.ti,ab. (403) |
| 96 cognitive behavioral treatment$.ti,ab. (1378) |
| 97 (CBT or TFCBT).ti,ab. (7996) |
| 98 cognitive trauma therapy.ti,ab. (6) |
| 99 trauma focus$ CBT.ti,ab. (31) |
| 100 87 or 88 or 89 or 90 or 91 or 92 or 93 or 94 or 95 or 96 or 97 or 98 or 99 (40,659) |
| 101 exp Behavior Therapy/ (64,582) |
| 102 (behavior$ adj2 (therap$ or treat$ or modif$)).ti,ab. (26,789) |
| 103 (behaviour$ adj2 (therap$ or treat$ or modif$)).ti,ab. (9862) |
| 104 (dialectical behavio$ adj (therap$ or treat$)).ti,ab. (581) |
| 105 biofeedback, psychology/or feedback, sensory/or neurofeedback/ (9330) |
| 106 (biofeedback or neurofeedback or sensory feedback).ti,ab. (8461) |
| 107 eye movement desensitization reprocessing/or implosive therapy/or virtual reality exposure therapy/ (1347) |
| 108 (psychological adj2 desensiti$).ti,ab. (4) |
| 109 eye movement desensiti?ation reprocessing.ti,ab. (25) |
| 110 EMDR.ti,ab. (372) |
| 111 (exposure adj (therap$ or treat$)).ti,ab. (2282) |
| 112 live exposure.ti,ab. (11) |
| 113 imaginal exposure.ti,ab. (147) |
| 114 prolonged exposure therapy.ti,ab. (99) |
| 115 imaginal flooding.ti,ab. (13) |
| 116 exposure inhibition therap$.ti,ab. (0) |
| 117 implosive therap$.ti,ab. (43) |
| 118 image habituation.ti,ab. (3) |
| 119 inoculation training.ti,ab. (78) |
| 120 101 or 102 or 103 or 104 or 105 or 106 or 107 or 108 or 109 or 110 or 111 or 112 or 113 or 114 or 115 or 116 or 117 or 118 or 119 (90,057) |
| 121 “Acceptance and Commitment Therapy”/ (184) |
| 122 (acceptance adj2 therap$).ti,ab. (257) |
| 123 (commitment adj2 therap$).ti,ab. (603) |
| 124 Hypnosis/ (8730) |
| 125 (hypnosis or hypnotherap$).ti,ab. (7561) |
| 126 Mindfulness/ (1325) |
| 127 mindfulness.ti,ab. (4005) |
| 128 supportive therap$.ti,ab. (3906) |
| 129 (non-directive adj (counselling or counseling)).ti,ab. (100) |
| 130 (nondirective adj (counselling or counseling)).ti,ab. (54) |
| 131 (non directive adj (counselling or counseling)).ti,ab. (100) |
| 132 Psychotherapy/or Psychotherapy, Brief/or Psychotherapy, Group/or Psychotherapy, Multiple/or Psychotherapy, Psychodynamic/or Psychotherapy, Rational-emotive/ (65,822) |
| 133 psychodynamic therap$.ti,ab. (431) |
| 134 inter personal psychotherap$.ti,ab. (1) |
| 135 interpersonal psychotherap$.ti,ab. (778) |
| 136 IPT.ti,ab. (1907) |
| 137 (compassion adj2 therap$).ti,ab. (39) |
| 138 accelerated resolution.ti,ab. (86) |
| 139 sensorimotor therap$.ti,ab. (21) |
| 140 schema therapy.ti,ab. (106) |
| 141 (stress adj2 manag$).ti,ab. (5168) |
| 142 supportive therap$.ti,ab. (3906) |
| 143 Counseling/(32,854) |
| 144 (non-directive counsel$ or non directive counsel$ or nondirective counsel$).ti,ab. (155) |
| 145 compassion therap$.ti,ab. (1) |
| 146 121 or 122 or 123 or 124 or 125 or 126 or 127 or 128 or 129 or 130 or 131 or 132 or 133 or 134 or 135 or 136 or 137 or 138 or 139 or 140 or 141 or 142 or 143 or 144 or 145 (122,017) |
| 147 100 or 120 or 146 (211,031) |
| 148 “hypnotics and sedatives”/or alprazolam/or amobarbital/or azaperone/or barbital/or bromisovalum/or chloral hydrate/or chloralose/or chlordiazepoxide/or chlormethiazole/or dexmedetomidine/or diazepam/or diphenhydramine/or eszopiclone/or ethchlorvynol/or etomidate/or etorphine/or flurazepam/or glutethimide/or hexobarbital/or lorazepam/or medazepam/or medetomidine/or mephobarbital/or meprobamate/or methapyrilene/or methaqualone/or midazolam/or nitrazepam/or oxazepam/or paraldehyde/or pentobarbital/or phenobarbital/or propofol/or secobarbital/or temazepam/or thiamylal/or thiopental/or xylazine/ (114,648) |
| 149 z drugs.ti,ab. (120) |
| 150 anti-anxiety agents/or bromazepam/or buspirone/or chlormezanone/or clorazepate dipotassium/or estazolam/or flunitrazepam/or fluvoxamine/or nordazepam/or ondansetron/or oxprenolol/or prazepam/or pregabalin/or ritanserin/or tranylcypromine/or trazodone/or triazolam/or zolazepam/ (33,101) |
| 151 benzodiazepines/or benzodiazepinones/ (23,660) |
| 152 sedative antihistamine$.ti,ab. (61) |
| 153 promethazine.ti,ab. (2061) |
| 154 antidepressive agents/or benactyzine/or clorgyline/or deanol/or desvenlafaxine succinate/or duloxetine hydrochloride/or iproniazid/or isocarboxazid/or lithium carbonate/or lithium compounds/or moclobemide/or nialamide/or phenelzine/or pizotyline/or rolipram/or sertraline/or tranylcypromine/or vilazodone hydrochloride/ (55,533) |
| 155 Imipramine/ (9832) |
| 156 mirtazapine.ti,ab. (1765) |
| 157 antipsychotic agents/or acepromazine/or aripiprazole/or azaperone/or benperidol/or butaclamol/or chlorpromazine/or chlorprothixene/or clopenthixol/or clozapine/or droperidol/or etazolate/or flupenthixol/or fluphenazine/or fluspirilene/or haloperidol/or loxapine/or lurasidone hydrochloride/or mesoridazine/or methiothepin/or methotrimeprazine/or molindone/or ondansetron/or paliperidone palmitate/or penfluridol/or perazine/or perphenazine/or pimozide/or prochlorperazine/or promazine/or quetiapine fumarate/or raclopride/or remoxipride/or reserpine/or risperidone/or ritanserin/or spiperone/or sulpiride/or thioridazine/or thiothixene/or tiapride hydrochloride/or trifluoperazine/or trifluperidol/or triflupromazine/(114,997) |
| 158 olanzapine.ti,ab. (7555) |
| 159 anticonvulsants/or acetazolamide/or bromides/or carbamazepine/or clonazepam/or clorazepate dipotassium/or diazepam/or dimethadione/or estazolam/or ethosuximide/or flunarizine/or lorazepam/or magnesium sulfate/or medazepam/or mephenytoin/or mephobarbital/or meprobamate/or nitrazepam/or paraldehyde/or phenobarbital/or phenytoin/or pregabalin/or primidone/or riluzole/or thiopental/or tiletamine/or trimethadione/or valproic acid/or vigabatrin/ (129,932) |
| 160 antimanic agents/or lithium chloride/or lithium compounds/ (9229) |
| 161 lamotrigine.ti,ab. (4632) |
| 162 topiramate.ti,ab. (4045) |
| 163 monoamine oxidase inhibitors/or chlorphenamidine/or clorgyline/or cuprizone/or furazolidone/or harmaline/or harmine/or isocarboxazid/or moclobemide/or monocrotophos/or pargyline/or selegiline/or tranylcypromine/ (17,953) |
| 164 Prazosin/ (7567) |
| 165 N-Methyl-3,4-methylenedioxyamphetamine/ (3644) |
| 166 (MDMA or ecstasy).ti,ab. (5232) |
| 167 148 or 149 or 150 or 151 or 152 or 153 or 154 or 155 or 156 or 157 or 158 or 159 or 160 or 161 or 162 or 163 or 164 or 165 or 166 (407,459) |
| 168 86 and 147 (2717) |
| 169 86 and 167 (405) |
| 170 168 or 169 (3004) |
| 171 limit 170 to yr=“1992 -Current” (2818) |
PILOTS via ProQuest
Search date: 2 May 2017.
Two separate searches were conducted: one for psychological interventions and a second for pharmacological interventions.
Total records retrieved: 1981.
Date range searched: 1987 onwards.
| Set | Search | Results |
|---|---|---|
| Psychological interventions search strategy | ||
| S1 | (SU.EXACT(“Dating Violence”) OR SU.EXACT(“Interpersonal Violence”) OR SU.EXACT(“Family Violence”)) OR (batter* NEAR/2 (wife* OR wive* OR woman OR women OR men OR husband* OR partner*)) OR (physical* NEAR/2 (abus* OR assault* OR violen* OR aggress*)) OR (emotional* NEAR/1 abus*) OR (SU.EXACT(“Acquaintance Rape”) OR SU.EXACT(“Acquaintance Rape” OR “Partner Rape” OR “Rape”) OR SU.EXACT(“Partner Rape”)) OR (sexual* NEAR/2 (abus* OR assault* OR violen* OR aggress*)) OR SU.EXACT(“Child Abuse”) OR (child* NEAR/2 (abus* OR assault* OR violen* OR aggress*)) OR (child* NEAR/2 (exploit* OR neglect* OR trauma*)) OR (“non accidental injur*” OR “non-accidental injur*” OR “nonaccidental injur*”) OR SU.EXACT(“Human Trafficking”) OR ((human OR person OR people) NEAR/2 (traffick* OR exploit*)) OR ((forced OR exploit*) NEAR/2 labour) OR SU.EXACT(“Slavery”) OR SU.EXACT(“Torture”) OR (slavery OR enslave* OR torture*) OR SU.EXACT(“Prostitution”) OR (prostitution* OR brothel*) OR (sex* NEAR/2 (exploit* OR traffick*)) OR SU.EXACT(“Terrorism”) OR SU.EXACT(“Chemical Warfare” OR “Civil Warfare” OR “Humanitarian Intervention” OR “Military Intervention” OR “War”) OR SU.EXACT(“Genocide”) OR (SU.EXACT(“War Neuroses”) OR SU.EXACT(“War Imprisonment”)) OR SU.EXACT(“Persecution”) OR (civil NEAR/1 (unrest OR conflict* OR disturbance* OR war OR wars OR warfare)) OR (persecution OR victimization OR victimisation) OR (captivity OR imprison*) OR SU.EXACT(“Concentration Camps”) OR (SU.EXACT(“Avalanches” OR “Blizzards” OR “Drought” OR “Earthquakes” OR “Epidemics” OR “Epizootics” OR “Famine” OR “Floods” OR “Hurricanes” OR “Landslides” OR “Lightning” OR “Natural Disasters” OR “Tornadoes” OR “Tsunamis” OR “Volcanoes”) OR SU.EXACT(“Accidents” OR “Agent Orange” OR “Air Traffic Accidents” OR “Avalanches” OR “Blizzards” OR “Building Collapse” OR “Disasters” OR “Drought” OR “Earthquakes” OR “Epidemics” OR “Epizootics” OR “Explosions” OR “Famine” OR “Fires” OR “Floods” OR “Home Accidents” OR “Hurricanes” OR “Industrial Accidents” OR “Landmines” OR “Landslides” OR “Lightning” OR “Motor Traffic Accidents” OR “Natural Disasters” OR “Nuclear Accidents” OR “Nuclear Testing” OR “Oil Spills” OR “Pedestrian Accidents” OR “Railroad Accidents” OR “Ship Accidents” OR “Technological Disasters” OR “Tornadoes” OR “Toxic Contamination” OR “Tsunamis” OR “Volcanoes”)) OR (humanitarian NEAR/1 (crisis OR crises)) OR (catastrophe OR catastrophic) OR SU.EXACT(“Survivors”) OR SU.EXACT(“Asylum Seekers” OR “Refugees”) OR ((forcibly OR internally) NEAR/1 displace*) OR (displace* NEAR/1 (people OR person* OR civilian*)) OR (victim* NEAR/2 (crime* OR disaster*)) OR (SU.EXACT(“Political Prisoners”) OR SU.EXACT(“Prisoners of War”)) OR SU.EXACT(“Military Personnel”) OR ((expose* OR exposure) NEAR/2 (abuse OR assault* OR disaster* OR terror* OR torture* OR trauma* OR rape OR violen* OR war OR warfare)) OR (survivor* NEAR/2 (abuse OR assault* OR disaster* OR terror* OR torture* OR trauma* OR rape OR violen* OR war OR warfare)) OR (victim* NEAR/2 (abuse OR assault* OR crime OR disaster* OR rape OR terror* OR torture* OR trauma* OR violen* OR war OR warfare)) OR (witness* NEAR/2 (abuse OR assault* OR crime OR disaster* OR rape OR terror* OR torture* OR trauma* OR violen* OR war OR warfare)) | 43,537° |
| S2 | (cognitive N2 therap*) OR (cognitive N2 treat*) OR (cognitive N1 rescript*) OR (cognitive N1 restructur*) OR CPT OR CBT OR TFCBT OR (trauma N2 CBT) | 812° |
| S4 | (behav* N2 therap*) OR (behav* N2 treat*) OR (behav* N2 modif*) OR biofeedback OR neurofeedback OR “sensory feedback” OR “eye movement desensitization reprocessing” OR “eye movement desensitisation reprocessing” OR EMDR | 1077° |
| S6 | (exposure N2 therap*) OR (exposure N2 treat*) OR “live exposure” OR “imaginal exposure” OR “imaginal flooding” OR “exposure inhibition therapy” OR (implosive N2 therap*) OR “image habituation” OR “inoculation training” | 223° |
| S8 | (acceptance N2 therap*) OR (commitment N2 therap*) OR hypnosis OR hypnotherap* OR mindfulness OR (supportive N2 therap*) OR (non-directive N2 counsel*) OR (nondirective N2 counsel*) OR psychotherapy OR “group therapy” | 6900° |
| S9 | (psychodynamic N1 therap*) OR (interpersonal psychotherap*) OR IPT OR (compassion N2 therap*) OR “accelerated resolution” OR (sensorimotor N1 therap*) OR (schema N1 therap*) | 756° |
| S10 | ((cognitive N2 therap*) OR (cognitive N2 treat*) OR (cognitive N1 rescript*) OR (cognitive N1 restructur*) OR CPT OR CBT OR TFCBT OR (trauma N2 CBT)) OR ((behav* N2 therap*) OR (behav* N2 treat*) OR (behav* N2 modif*) OR biofeedback OR neurofeedback OR “sensory feedback” OR “eye movement desensitization reprocessing” OR “eye movement desensitisation reprocessing” OR EMDR) OR ((exposure N2 therap*) OR (exposure N2 treat*) OR “live exposure” OR “imaginal exposure” OR “imaginal flooding” OR “exposure inhibition therapy” OR (implosive N2 therap*) OR “image habituation” OR “inoculation training”) OR ((acceptance N2 therap*) OR (commitment N2 therap*) OR hypnosis OR hypnotherap* OR mindfulness OR (supportive N2 therap*) OR (non-directive N2 counsel*) OR (nondirective N2 counsel*) OR psychotherapy OR “group therapy”) OR ((psychodynamic N1 therap*) OR (interpersonal psychotherap*) OR IPT OR (compassion N2 therap*) OR “accelerated resolution” OR (sensorimotor N1 therap*) OR (schema N1 therap*)) | 8207° |
| S11 | ((SU.EXACT(“Dating Violence”) OR SU.EXACT(“Interpersonal Violence”) OR SU.EXACT(“Family Violence”)) OR (batter* NEAR/2 (wife* OR wive* OR woman OR women OR men OR husband* OR partner*)) OR (physical* NEAR/2 (abus* OR assault* OR violen* OR aggress*)) OR (emotional* NEAR/1 abus*) OR (SU.EXACT(“Acquaintance Rape”) OR SU.EXACT(“Acquaintance Rape” OR “Partner Rape” OR “Rape”) OR SU.EXACT(“Partner Rape”)) OR (sexual* NEAR/2 (abus* OR assault* OR violen* OR aggress*)) OR SU.EXACT(“Child Abuse”) OR (child* NEAR/2 (abus* OR assault* OR violen* OR aggress*)) OR (child* NEAR/2 (exploit* OR neglect* OR trauma*)) OR (“non accidental injur*” OR “non-accidental injur*” OR “nonaccidental injur*”) OR SU.EXACT(“Human Trafficking”) OR ((human OR person OR people) NEAR/2 (traffick* OR exploit*)) OR ((forced OR exploit*) NEAR/2 labour) OR SU.EXACT(“Slavery”) OR SU.EXACT(“Torture”) OR (slavery OR enslave* OR torture*) OR SU.EXACT(“Prostitution”) OR (prostitution* OR brothel*) OR (sex* NEAR/2 (exploit* OR traffick*)) OR SU.EXACT(“Terrorism”) OR SU.EXACT(“Chemical Warfare” OR “Civil Warfare” OR “Humanitarian Intervention” OR “Military Intervention” OR “War”) OR SU.EXACT(“Genocide”) OR (SU.EXACT(“War Neuroses”) OR SU.EXACT(“War Imprisonment”)) OR SU.EXACT(“Persecution”) OR (civil NEAR/1 (unrest OR conflict* OR disturbance* OR war OR wars OR warfare)) OR (persecution OR victimization OR victimisation) OR (captivity OR imprison*) OR SU.EXACT(“Concentration Camps”) OR (SU.EXACT(“Avalanches” OR “Blizzards” OR “Drought” OR “Earthquakes” OR “Epidemics” OR “Epizootics” OR “Famine” OR “Floods” OR “Hurricanes” OR “Landslides” OR “Lightning” OR “Natural Disasters” OR “Tornadoes” OR “Tsunamis” OR “Volcanoes”) OR SU.EXACT(“Accidents” OR “Agent Orange” OR “Air Traffic Accidents” OR “Avalanches” OR “Blizzards” OR “Building Collapse” OR “Disasters” OR “Drought” OR “Earthquakes” OR “Epidemics” OR “Epizootics” OR “Explosions” OR “Famine” OR “Fires” OR “Floods” OR “Home Accidents” OR “Hurricanes” OR “Industrial Accidents” OR “Landmines” OR “Landslides” OR “Lightning” OR “Motor Traffic Accidents” OR “Natural Disasters” OR “Nuclear Accidents” OR “Nuclear Testing” OR “Oil Spills” OR “Pedestrian Accidents” OR “Railroad Accidents” OR “Ship Accidents” OR “Technological Disasters” OR “Tornadoes” OR “Toxic Contamination” OR “Tsunamis” OR “Volcanoes”)) OR (humanitarian NEAR/1 (crisis OR crises)) OR (catastrophe OR catastrophic) OR SU.EXACT(“Survivors”) OR SU.EXACT(“Asylum Seekers” OR “Refugees”) OR ((forcibly OR internally) NEAR/1 displace*) OR (displace* NEAR/1 (people OR person* OR civilian*)) OR (victim* NEAR/2 (crime* OR disaster*)) OR (SU.EXACT(“Political Prisoners”) OR SU.EXACT(“Prisoners of War”)) OR SU.EXACT(“Military Personnel”) OR ((expose* OR exposure) NEAR/2 (abuse OR assault* OR disaster* OR terror* OR torture* OR trauma* OR rape OR violen* OR war OR warfare)) OR (survivor* NEAR/2 (abuse OR assault* OR disaster* OR terror* OR torture* OR trauma* OR rape OR violen* OR war OR warfare)) OR (victim* NEAR/2 (abuse OR assault* OR crime OR disaster* OR rape OR terror* OR torture* OR trauma* OR violen* OR war OR warfare)) OR (witness* NEAR/2 (abuse OR assault* OR crime OR disaster* OR rape OR terror* OR torture* OR trauma* OR violen* OR war OR warfare))) AND (((cognitive N2 therap*) OR (cognitive N2 treat*) OR (cognitive N1 rescript*) OR (cognitive N1 restructur*) OR CPT OR CBT OR TFCBT OR (trauma N2 CBT)) OR ((behav* N2 therap*) OR (behav* N2 treat*) OR (behav* N2 modif*) OR biofeedback OR neurofeedback OR “sensory feedback” OR “eye movement desensitization reprocessing” OR “eye movement desensitisation reprocessing” OR EMDR) OR ((exposure N2 therap*) OR (exposure N2 treat*) OR “live exposure” OR “imaginal exposure” OR “imaginal flooding” OR “exposure inhibition therapy” OR (implosive N2 therap*) OR “image habituation” OR “inoculation training”) OR ((acceptance N2 therap*) OR (commitment N2 therap*) OR hypnosis OR hypnotherap* OR mindfulness OR (supportive N2 therap*) OR (non-directive N2 counsel*) OR (nondirective N2 counsel*) OR psychotherapy OR “group therapy”) OR ((psychodynamic N1 therap*) OR (interpersonal psychotherap*) OR IPT OR (compassion N2 therap*) OR “accelerated resolution” OR (sensorimotor N1 therap*) OR (schema N1 therap*))) | 5986° |
| S12 | SU.EXACT(“Complex PTSD”) OR SU.EXACT(“PTSD”) | 18,871° |
| S13 | (((SU.EXACT(“Dating Violence”) OR SU.EXACT(“Interpersonal Violence”) OR SU.EXACT(“Family Violence”)) OR (batter* NEAR/2 (wife* OR wive* OR woman OR women OR men OR husband* OR partner*)) OR (physical* NEAR/2 (abus* OR assault* OR violen* OR aggress*)) OR (emotional* NEAR/1 abus*) OR (SU.EXACT(“Acquaintance Rape”) OR SU.EXACT(“Acquaintance Rape” OR “Partner Rape” OR “Rape”) OR SU.EXACT(“Partner Rape”)) OR (sexual* NEAR/2 (abus* OR assault* OR violen* OR aggress*)) OR SU.EXACT(“Child Abuse”) OR (child* NEAR/2 (abus* OR assault* OR violen* OR aggress*)) OR (child* NEAR/2 (exploit* OR neglect* OR trauma*)) OR (“non accidental injur*” OR “non-accidental injur*” OR “nonaccidental injur*”) OR SU.EXACT(“Human Trafficking”) OR ((human OR person OR people) NEAR/2 (traffick* OR exploit*)) OR ((forced OR exploit*) NEAR/2 labour) OR SU.EXACT(“Slavery”) OR SU.EXACT(“Torture”) OR (slavery OR enslave* OR torture*) OR SU.EXACT(“Prostitution”) OR (prostitution* OR brothel*) OR (sex* NEAR/2 (exploit* OR traffick*)) OR SU.EXACT(“Terrorism”) OR SU.EXACT(“Chemical Warfare” OR “Civil Warfare” OR “Humanitarian Intervention” OR “Military Intervention” OR “War”) OR SU.EXACT(“Genocide”) OR (SU.EXACT(“War Neuroses”) OR SU.EXACT(“War Imprisonment”)) OR SU.EXACT(“Persecution”) OR (civil NEAR/1 (unrest OR conflict* OR disturbance* OR war OR wars OR warfare)) OR (persecution OR victimization OR victimisation) OR (captivity OR imprison*) OR SU.EXACT(“Concentration Camps”) OR (SU.EXACT(“Avalanches” OR “Blizzards” OR “Drought” OR “Earthquakes” OR “Epidemics” OR “Epizootics” OR “Famine” OR “Floods” OR “Hurricanes” OR “Landslides” OR “Lightning” OR “Natural Disasters” OR “Tornadoes” OR “Tsunamis” OR “Volcanoes”) OR SU.EXACT(“Accidents” OR “Agent Orange” OR “Air Traffic Accidents” OR “Avalanches” OR “Blizzards” OR “Building Collapse” OR “Disasters” OR “Drought” OR “Earthquakes” OR “Epidemics” OR “Epizootics” OR “Explosions” OR “Famine” OR “Fires” OR “Floods” OR “Home Accidents” OR “Hurricanes” OR “Industrial Accidents” OR “Landmines” OR “Landslides” OR “Lightning” OR “Motor Traffic Accidents” OR “Natural Disasters” OR “Nuclear Accidents” OR “Nuclear Testing” OR “Oil Spills” OR “Pedestrian Accidents” OR “Railroad Accidents” OR “Ship Accidents” OR “Technological Disasters” OR “Tornadoes” OR “Toxic Contamination” OR “Tsunamis” OR “Volcanoes”)) OR (humanitarian NEAR/1 (crisis OR crises)) OR (catastrophe OR catastrophic) OR SU.EXACT(“Survivors”) OR SU.EXACT(“Asylum Seekers” OR “Refugees”) OR ((forcibly OR internally) NEAR/1 displace*) OR (displace* NEAR/1 (people OR person* OR civilian*)) OR (victim* NEAR/2 (crime* OR disaster*)) OR (SU.EXACT(“Political Prisoners”) OR SU.EXACT(“Prisoners of War”)) OR SU.EXACT(“Military Personnel”) OR ((expose* OR exposure) NEAR/2 (abuse OR assault* OR disaster* OR terror* OR torture* OR trauma* OR rape OR violen* OR war OR warfare)) OR (survivor* NEAR/2 (abuse OR assault* OR disaster* OR terror* OR torture* OR trauma* OR rape OR violen* OR war OR warfare)) OR (victim* NEAR/2 (abuse OR assault* OR crime OR disaster* OR rape OR terror* OR torture* OR trauma* OR violen* OR war OR warfare)) OR (witness* NEAR/2 (abuse OR assault* OR crime OR disaster* OR rape OR terror* OR torture* OR trauma* OR violen* OR war OR warfare))) AND (((cognitive N2 therap*) OR (cognitive N2 treat*) OR (cognitive N1 rescript*) OR (cognitive N1 restructur*) OR CPT OR CBT OR TFCBT OR (trauma N2 CBT)) OR ((behav* N2 therap*) OR (behav* N2 treat*) OR (behav* N2 modif*) OR biofeedback OR neurofeedback OR “sensory feedback” OR “eye movement desensitization reprocessing” OR “eye movement desensitisation reprocessing” OR EMDR) OR ((exposure N2 therap*) OR (exposure N2 treat*) OR “live exposure” OR “imaginal exposure” OR “imaginal flooding” OR “exposure inhibition therapy” OR (implosive N2 therap*) OR “image habituation” OR “inoculation training”) OR ((acceptance N2 therap*) OR (commitment N2 therap*) OR hypnosis OR hypnotherap* OR mindfulness OR (supportive N2 therap*) OR (non-directive N2 counsel*) OR (nondirective N2 counsel*) OR psychotherapy OR “group therapy”) OR ((psychodynamic N1 therap*) OR (interpersonal psychotherap*) OR IPT OR (compassion N2 therap*) OR “accelerated resolution” OR (sensorimotor N1 therap*) OR (schema N1 therap*)))) AND (SU.EXACT(“Complex PTSD”) OR SU.EXACT(“PTSD”)) | 1955° |
| S14 | (((SU.EXACT(“Dating Violence”) OR SU.EXACT(“Interpersonal Violence”) OR SU.EXACT(“Family Violence”)) OR (batter* NEAR/2 (wife* OR wive* OR woman OR women OR men OR husband* OR partner*)) OR (physical* NEAR/2 (abus* OR assault* OR violen* OR aggress*)) OR (emotional* NEAR/1 abus*) OR (SU.EXACT(“Acquaintance Rape”) OR SU.EXACT(“Acquaintance Rape” OR “Partner Rape” OR “Rape”) OR SU.EXACT(“Partner Rape”)) OR (sexual* NEAR/2 (abus* OR assault* OR violen* OR aggress*)) OR SU.EXACT(“Child Abuse”) OR (child* NEAR/2 (abus* OR assault* OR violen* OR aggress*)) OR (child* NEAR/2 (exploit* OR neglect* OR trauma*)) OR (“non accidental injur*” OR “non-accidental injur*” OR “nonaccidental injur*”) OR SU.EXACT(“Human Trafficking”) OR ((human OR person OR people) NEAR/2 (traffick* OR exploit*)) OR ((forced OR exploit*) NEAR/2 labour) OR SU.EXACT(“Slavery”) OR SU.EXACT(“Torture”) OR (slavery OR enslave* OR torture*) OR SU.EXACT(“Prostitution”) OR (prostitution* OR brothel*) OR (sex* NEAR/2 (exploit* OR traffick*)) OR SU.EXACT(“Terrorism”) OR SU.EXACT(“Chemical Warfare” OR “Civil Warfare” OR “Humanitarian Intervention” OR “Military Intervention” OR “War”) OR SU.EXACT(“Genocide”) OR (SU.EXACT(“War Neuroses”) OR SU.EXACT(“War Imprisonment”)) OR SU.EXACT(“Persecution”) OR (civil NEAR/1 (unrest OR conflict* OR disturbance* OR war OR wars OR warfare)) OR (persecution OR victimization OR victimisation) OR (captivity OR imprison*) OR SU.EXACT(“Concentration Camps”) OR (SU.EXACT(“Avalanches” OR “Blizzards” OR “Drought” OR “Earthquakes” OR “Epidemics” OR “Epizootics” OR “Famine” OR “Floods” OR “Hurricanes” OR “Landslides” OR “Lightning” OR “Natural Disasters” OR “Tornadoes” OR “Tsunamis” OR “Volcanoes”) OR SU.EXACT(“Accidents” OR “Agent Orange” OR “Air Traffic Accidents” OR “Avalanches” OR “Blizzards” OR “Building Collapse” OR “Disasters” OR “Drought” OR “Earthquakes” OR “Epidemics” OR “Epizootics” OR “Explosions” OR “Famine” OR “Fires” OR “Floods” OR “Home Accidents” OR “Hurricanes” OR “Industrial Accidents” OR “Landmines” OR “Landslides” OR “Lightning” OR “Motor Traffic Accidents” OR “Natural Disasters” OR “Nuclear Accidents” OR “Nuclear Testing” OR “Oil Spills” OR “Pedestrian Accidents” OR “Railroad Accidents” OR “Ship Accidents” OR “Technological Disasters” OR “Tornadoes” OR “Toxic Contamination” OR “Tsunamis” OR “Volcanoes”)) OR (humanitarian NEAR/1 (crisis OR crises)) OR (catastrophe OR catastrophic) OR SU.EXACT(“Survivors”) OR SU.EXACT(“Asylum Seekers” OR “Refugees”) OR ((forcibly OR internally) NEAR/1 displace*) OR (displace* NEAR/1 (people OR person* OR civilian*)) OR (victim* NEAR/2 (crime* OR disaster*)) OR (SU.EXACT(“Political Prisoners”) OR SU.EXACT(“Prisoners of War”)) OR SU.EXACT(“Military Personnel”) OR ((expose* OR exposure) NEAR/2 (abuse OR assault* OR disaster* OR terror* OR torture* OR trauma* OR rape OR violen* OR war OR warfare)) OR (survivor* NEAR/2 (abuse OR assault* OR disaster* OR terror* OR torture* OR trauma* OR rape OR violen* OR war OR warfare)) OR (victim* NEAR/2 (abuse OR assault* OR crime OR disaster* OR rape OR terror* OR torture* OR trauma* OR violen* OR war OR warfare)) OR (witness* NEAR/2 (abuse OR assault* OR crime OR disaster* OR rape OR terror* OR torture* OR trauma* OR violen* OR war OR warfare))) AND (((cognitive N2 therap*) OR (cognitive N2 treat*) OR (cognitive N1 rescript*) OR (cognitive N1 restructur*) OR CPT OR CBT OR TFCBT OR (trauma N2 CBT)) OR ((behav* N2 therap*) OR (behav* N2 treat*) OR (behav* N2 modif*) OR biofeedback OR neurofeedback OR “sensory feedback” OR “eye movement desensitization reprocessing” OR “eye movement desensitisation reprocessing” OR EMDR) OR ((exposure N2 therap*) OR (exposure N2 treat*) OR “live exposure” OR “imaginal exposure” OR “imaginal flooding” OR “exposure inhibition therapy” OR (implosive N2 therap*) OR “image habituation” OR “inoculation training”) OR ((acceptance N2 therap*) OR (commitment N2 therap*) OR hypnosis OR hypnotherap* OR mindfulness OR (supportive N2 therap*) OR (non-directive N2 counsel*) OR (nondirective N2 counsel*) OR psychotherapy OR “group therapy”) OR ((psychodynamic N1 therap*) OR (interpersonal psychotherap*) OR IPT OR (compassion N2 therap*) OR “accelerated resolution” OR (sensorimotor N1 therap*) OR (schema N1 therap*)))) AND (SU.EXACT(“Complex PTSD”) OR SU.EXACT(“PTSD”))Limits applied | |
| Pharmacological interventions search strategy | ||
| S1 | (SU.EXACT(“Dating Violence”) OR SU.EXACT(“Interpersonal Violence”) OR SU.EXACT(“Family Violence”)) OR (batter* NEAR/2 (wife* OR wive* OR woman OR women OR men OR husband* OR partner*)) OR (physical* NEAR/2 (abus* OR assault* OR violen* OR aggress*)) OR (emotional* NEAR/1 abus*) OR (SU.EXACT(“Acquaintance Rape”) OR SU.EXACT(“Acquaintance Rape” OR “Partner Rape” OR “Rape”) OR SU.EXACT(“Partner Rape”)) OR (sexual* NEAR/2 (abus* OR assault* OR violen* OR aggress*)) OR SU.EXACT(“Child Abuse”) OR (child* NEAR/2 (abus* OR assault* OR violen* OR aggress*)) OR (child* NEAR/2 (exploit* OR neglect* OR trauma*)) OR (“non accidental injur*” OR “non-accidental injur*” OR “nonaccidental injur*”) OR SU.EXACT(“Human Trafficking”) OR ((human OR person OR people) NEAR/2 (traffick* OR exploit*)) OR ((forced OR exploit*) NEAR/2 labour) OR SU.EXACT(“Slavery”) OR SU.EXACT(“Torture”) OR (slavery OR enslave* OR torture*) OR SU.EXACT(“Prostitution”) OR (prostitution* OR brothel*) OR (sex* NEAR/2 (exploit* OR traffick*)) OR SU.EXACT(“Terrorism”) OR SU.EXACT(“Chemical Warfare” OR “Civil Warfare” OR “Humanitarian Intervention” OR “Military Intervention” OR “War”) OR SU.EXACT(“Genocide”) OR (SU.EXACT(“War Neuroses”) OR SU.EXACT(“War Imprisonment”)) OR SU.EXACT(“Persecution”) OR (civil NEAR/1 (unrest OR conflict* OR disturbance* OR war OR wars OR warfare)) OR (persecution OR victimization OR victimisation) OR (captivity OR imprison*) OR SU.EXACT(“Concentration Camps”) OR (SU.EXACT(“Avalanches” OR “Blizzards” OR “Drought” OR “Earthquakes” OR “Epidemics” OR “Epizootics” OR “Famine” OR “Floods” OR “Hurricanes” OR “Landslides” OR “Lightning” OR “Natural Disasters” OR “Tornadoes” OR “Tsunamis” OR “Volcanoes”) OR SU.EXACT(“Accidents” OR “Agent Orange” OR “Air Traffic Accidents” OR “Avalanches” OR “Blizzards” OR “Building Collapse” OR “Disasters” OR “Drought” OR “Earthquakes” OR “Epidemics” OR “Epizootics” OR “Explosions” OR “Famine” OR “Fires” OR “Floods” OR “Home Accidents” OR “Hurricanes” OR “Industrial Accidents” OR “Landmines” OR “Landslides” OR “Lightning” OR “Motor Traffic Accidents” OR “Natural Disasters” OR “Nuclear Accidents” OR “Nuclear Testing” OR “Oil Spills” OR “Pedestrian Accidents” OR “Railroad Accidents” OR “Ship Accidents” OR “Technological Disasters” OR “Tornadoes” OR “Toxic Contamination” OR “Tsunamis” OR “Volcanoes”)) OR (humanitarian NEAR/1 (crisis OR crises)) OR (catastrophe OR catastrophic) OR SU.EXACT(“Survivors”) OR SU.EXACT(“Asylum Seekers” OR “Refugees”) OR ((forcibly OR internally) NEAR/1 displace*) OR (displace* NEAR/1 (people OR person* OR civilian*)) OR (victim* NEAR/2 (crime* OR disaster*)) OR (SU.EXACT(“Political Prisoners”) OR SU.EXACT(“Prisoners of War”)) OR SU.EXACT(“Military Personnel”) OR ((expose* OR exposure) NEAR/2 (abuse OR assault* OR disaster* OR terror* OR torture* OR trauma* OR rape OR violen* OR war OR warfare)) OR (survivor* NEAR/2 (abuse OR assault* OR disaster* OR terror* OR torture* OR trauma* OR rape OR violen* OR war OR warfare)) OR (victim* NEAR/2 (abuse OR assault* OR crime OR disaster* OR rape OR terror* OR torture* OR trauma* OR violen* OR war OR warfare)) OR (witness* NEAR/2 (abuse OR assault* OR crime OR disaster* OR rape OR terror* OR torture* OR trauma* OR violen* OR war OR warfare)) | 43,537° |
| S12 | SU.EXACT(“Complex PTSD”) OR SU.EXACT(“PTSD”) | 18,871° |
| S13 | ((SU.EXACT(“Dating Violence”) OR SU.EXACT(“Interpersonal Violence”) OR SU.EXACT(“Family Violence”)) OR (batter* NEAR/2 (wife* OR wive* OR woman OR women OR men OR husband* OR partner*)) OR (physical* NEAR/2 (abus* OR assault* OR violen* OR aggress*)) OR (emotional* NEAR/1 abus*) OR (SU.EXACT(“Acquaintance Rape”) OR SU.EXACT(“Acquaintance Rape” OR “Partner Rape” OR “Rape”) OR SU.EXACT(“Partner Rape”)) OR (sexual* NEAR/2 (abus* OR assault* OR violen* OR aggress*)) OR SU.EXACT(“Child Abuse”) OR (child* NEAR/2 (abus* OR assault* OR violen* OR aggress*)) OR (child* NEAR/2 (exploit* OR neglect* OR trauma*)) OR (“non accidental injur*” OR “non-accidental injur*” OR “nonaccidental injur*”) OR SU.EXACT(“Human Trafficking”) OR ((human OR person OR people) NEAR/2 (traffick* OR exploit*)) OR ((forced OR exploit*) NEAR/2 labour) OR SU.EXACT(“Slavery”) OR SU.EXACT(“Torture”) OR (slavery OR enslave* OR torture*) OR SU.EXACT(“Prostitution”) OR (prostitution* OR brothel*) OR (sex* NEAR/2 (exploit* OR traffick*)) OR SU.EXACT(“Terrorism”) OR SU.EXACT(“Chemical Warfare” OR “Civil Warfare” OR “Humanitarian Intervention” OR “Military Intervention” OR “War”) OR SU.EXACT(“Genocide”) OR (SU.EXACT(“War Neuroses”) OR SU.EXACT(“War Imprisonment”)) OR SU.EXACT(“Persecution”) OR (civil NEAR/1 (unrest OR conflict* OR disturbance* OR war OR wars OR warfare)) OR (persecution OR victimization OR victimisation) OR (captivity OR imprison*) OR SU.EXACT(“Concentration Camps”) OR (SU.EXACT(“Avalanches” OR “Blizzards” OR “Drought” OR “Earthquakes” OR “Epidemics” OR “Epizootics” OR “Famine” OR “Floods” OR “Hurricanes” OR “Landslides” OR “Lightning” OR “Natural Disasters” OR “Tornadoes” OR “Tsunamis” OR “Volcanoes”) OR SU.EXACT(“Accidents” OR “Agent Orange” OR “Air Traffic Accidents” OR “Avalanches” OR “Blizzards” OR “Building Collapse” OR “Disasters” OR “Drought” OR “Earthquakes” OR “Epidemics” OR “Epizootics” OR “Explosions” OR “Famine” OR “Fires” OR “Floods” OR “Home Accidents” OR “Hurricanes” OR “Industrial Accidents” OR “Landmines” OR “Landslides” OR “Lightning” OR “Motor Traffic Accidents” OR “Natural Disasters” OR “Nuclear Accidents” OR “Nuclear Testing” OR “Oil Spills” OR “Pedestrian Accidents” OR “Railroad Accidents” OR “Ship Accidents” OR “Technological Disasters” OR “Tornadoes” OR “Toxic Contamination” OR “Tsunamis” OR “Volcanoes”)) OR (humanitarian NEAR/1 (crisis OR crises)) OR (catastrophe OR catastrophic) OR SU.EXACT(“Survivors”) OR SU.EXACT(“Asylum Seekers” OR “Refugees”) OR ((forcibly OR internally) NEAR/1 displace*) OR (displace* NEAR/1 (people OR person* OR civilian*)) OR (victim* NEAR/2 (crime* OR disaster*)) OR (SU.EXACT(“Political Prisoners”) OR SU.EXACT(“Prisoners of War”)) OR SU.EXACT(“Military Personnel”) OR ((expose* OR exposure) NEAR/2 (abuse OR assault* OR disaster* OR terror* OR torture* OR trauma* OR rape OR violen* OR war OR warfare)) OR (survivor* NEAR/2 (abuse OR assault* OR disaster* OR terror* OR torture* OR trauma* OR rape OR violen* OR war OR warfare)) OR (victim* NEAR/2 (abuse OR assault* OR crime OR disaster* OR rape OR terror* OR torture* OR trauma* OR violen* OR war OR warfare)) OR (witness* NEAR/2 (abuse OR assault* OR crime OR disaster* OR rape OR terror* OR torture* OR trauma* OR violen* OR war OR warfare))) AND (SU.EXACT(“Complex PTSD”) OR SU.EXACT(“PTSD”)) | 13,010° |
| S14 | alprazolam or amobarbital or azaperone or barbital or bromisovalum or chloral hydrate or chloralose or chlordiazepoxide or chlormethiazole or dexmedetomidine or diazepam or diphenhydramine or eszopiclone or ethchlorvynol or etomidate or etorphine or flurazepam or glutethimide or hexobarbital or lorazepam or medazepam or medetomidine or mephobarbital or meprobamate or methapyrilene or methaqualone or midazolam or nitrazepam or oxazepam or paraldehyde or pentobarbital or phenobarbital or propofol or secobarbital or temazepam or thiamylal or thiopental or xylazine | 77° |
| S15 | bromazepam or buspirone or chlormezanone or clorazepate dipotassium or estazolam or flunitrazepam or fluvoxamine or nordazepam or ondansetron or oxprenolol or prazepam or pregabalin or ritanserin or tranylcypromine or trazodone or triazolam or zolazepam | 84° |
| S16 | benzodiazepines or benzodiazepinones or promethazine or benactyzine or clorgyline or deanol or desvenlafaxine succinate or duloxetine hydrochloride or iproniazid or isocarboxazid or lithium carbonate or lithium compounds or moclobemide or nialamide or phenelzine or pizotyline or rolipram or sertraline or tranylcypromine or vilazodone hydrochloride or Imipramine or mirtazapine | 547° |
| S17 | acepromazine or aripiprazole or azaperone or benperidol or butaclamol or chlorpromazine or chlorprothixene or clopenthixol or clozapine or droperidol or etazolate or flupenthixol or fluphenazine or fluspirilene or haloperidol or loxapine or lurasidone hydrochloride or mesoridazine or methiothepin or methotrimeprazine or molindone or ondansetron or paliperidone palmitate or penfluridol or perazine or perphenazine or pimozide or prochlorperazine or promazine or quetiapine fumarate or raclopride or remoxipride or reserpine or risperidone or ritanserin or spiperone or sulpiride or thioridazine or thiothixene or tiapride hydrochloride or trifluoperazine or trifluperidol or triflupromazine or olanzapine | 107° |
| S18 | acetazolamide or bromides or carbamazepine or clonazepam or clorazepate dipotassium or diazepam or dimethadione or estazolam or ethosuximide or flunarizine or lorazepam or magnesium sulfate or medazepam or mephenytoin or mephobarbital or meprobamate or nitrazepam or paraldehyde or phenobarbital or phenytoin or pregabalin or primidone or riluzole or thiopental or tiletamine or trimethadione or valproic acid or vigabatrin or lithium chloride or lithium compounds or lamotrigine or topiramate | 145° |
| S19 | monoamine oxidase inhibitors or chlorphenamidine or clorgyline or cuprizone or furazolidone or harmaline or harmine or isocarboxazid or moclobemide or monocrotophos or pargyline or selegiline or tranylcypromine or Prazosin or N-Methyl-3,4-methylenedioxyamphetamine or MDMA or ecstasy | 197° |
| S20 | hypnotics OR (hypnotic drugs) OR sedatives OR (sedative drugs) OR “anti-anxiety drug*” OR “anti-anxiety agent*” OR “antidepressive agent*” OR “antidepressive drug*” OR “antipsychotic agent*” OR “antipsychotic drug*” | 413° |
| S21 | “antimanic agent*” OR “antimanic drug*” OR anticonvulsants OR “anticonvulsant drug*” OR “z drug*” | 176° |
| S22 | (alprazolam or amobarbital or azaperone or barbital or bromisovalum or chloral hydrate or chloralose or chlordiazepoxide or chlormethiazole or dexmedetomidine or diazepam or diphenhydramine or eszopiclone or ethchlorvynol or etomidate or etorphine or flurazepam or glutethimide or hexobarbital or lorazepam or medazepam or medetomidine or mephobarbital or meprobamate or methapyrilene or methaqualone or midazolam or nitrazepam or oxazepam or paraldehyde or pentobarbital or phenobarbital or propofol or secobarbital or temazepam or thiamylal or thiopental or xylazine) OR (bromazepam or buspirone or chlormezanone or clorazepate dipotassium or estazolam or flunitrazepam or fluvoxamine or nordazepam or ondansetron or oxprenolol or prazepam or pregabalin or ritanserin or tranylcypromine or trazodone or triazolam or zolazepam) OR (benzodiazepines or benzodiazepinones or promethazine or benactyzine or clorgyline or deanol or desvenlafaxine succinate or duloxetine hydrochloride or iproniazid or isocarboxazid or lithium carbonate or lithium compounds or moclobemide or nialamide or phenelzine or pizotyline or rolipram or sertraline or tranylcypromine or vilazodone hydrochloride or Imipramine or mirtazapine) OR (acepromazine or aripiprazole or azaperone or benperidol or butaclamol or chlorpromazine or chlorprothixene or clopenthixol or clozapine or droperidol or etazolate or flupenthixol or fluphenazine or fluspirilene or haloperidol or loxapine or lurasidone hydrochloride or mesoridazine or methiothepin or methotrimeprazine or molindone or ondansetron or paliperidone palmitate or penfluridol or perazine or perphenazine or pimozide or prochlorperazine or promazine or quetiapine fumarate or raclopride or remoxipride or reserpine or risperidone or ritanserin or spiperone or sulpiride or thioridazine or thiothixene or tiapride hydrochloride or trifluoperazine or trifluperidol or triflupromazine or olanzapine) OR (acetazolamide or bromides or carbamazepine or clonazepam or clorazepate dipotassium or diazepam or dimethadione or estazolam or ethosuximide or flunarizine or lorazepam or magnesium sulfate or medazepam or mephenytoin or mephobarbital or meprobamate or nitrazepam or paraldehyde or phenobarbital or phenytoin or pregabalin or primidone or riluzole or thiopental or tiletamine or trimethadione or valproic acid or vigabatrin or lithium chloride or lithium compounds or lamotrigine or topiramate) OR (monoamine oxidase inhibitors or chlorphenamidine or clorgyline or cuprizone or furazolidone or harmaline or harmine or isocarboxazid or moclobemide or monocrotophos or pargyline or selegiline or tranylcypromine or Prazosin or N-Methyl-3,4-methylenedioxyamphetamine or MDMA or ecstasy) OR (hypnotics OR (hypnotic drugs) OR sedatives OR (sedative drugs) OR “anti-anxiety drug*” OR “anti-anxiety agent*” OR “antidepressive agent*” OR “antidepressive drug*” OR “antipsychotic agent*” OR “antipsychotic drug*”) OR (“antimanic agent*” OR “antimanic drug*” OR anticonvulsants OR “anticonvulsant drug*” OR “z drug*”) | 1302° |
| S23 | (((SU.EXACT(“Dating Violence”) OR SU.EXACT(“Interpersonal Violence”) OR SU.EXACT(“Family Violence”)) OR (batter* NEAR/2 (wife* OR wive* OR woman OR women OR men OR husband* OR partner*)) OR (physical* NEAR/2 (abus* OR assault* OR violen* OR aggress*)) OR (emotional* NEAR/1 abus*) OR (SU.EXACT(“Acquaintance Rape”) OR SU.EXACT(“Acquaintance Rape” OR “Partner Rape” OR “Rape”) OR SU.EXACT(“Partner Rape”)) OR (sexual* NEAR/2 (abus* OR assault* OR violen* OR aggress*)) OR SU.EXACT(“Child Abuse”) OR (child* NEAR/2 (abus* OR assault* OR violen* OR aggress*)) OR (child* NEAR/2 (exploit* OR neglect* OR trauma*)) OR (“non accidental injur*” OR “non-accidental injur*” OR “nonaccidental injur*”) OR SU.EXACT(“Human Trafficking”) OR ((human OR person OR people) NEAR/2 (traffick* OR exploit*)) OR ((forced OR exploit*) NEAR/2 labour) OR SU.EXACT(“Slavery”) OR SU.EXACT(“Torture”) OR (slavery OR enslave* OR torture*) OR SU.EXACT(“Prostitution”) OR (prostitution* OR brothel*) OR (sex* NEAR/2 (exploit* OR traffick*)) OR SU.EXACT(“Terrorism”) OR SU.EXACT(“Chemical Warfare” OR “Civil Warfare” OR “Humanitarian Intervention” OR “Military Intervention” OR “War”) OR SU.EXACT(“Genocide”) OR (SU.EXACT(“War Neuroses”) OR SU.EXACT(“War Imprisonment”)) OR SU.EXACT(“Persecution”) OR (civil NEAR/1 (unrest OR conflict* OR disturbance* OR war OR wars OR warfare)) OR (persecution OR victimization OR victimisation) OR (captivity OR imprison*) OR SU.EXACT(“Concentration Camps”) OR (SU.EXACT(“Avalanches” OR “Blizzards” OR “Drought” OR “Earthquakes” OR “Epidemics” OR “Epizootics” OR “Famine” OR “Floods” OR “Hurricanes” OR “Landslides” OR “Lightning” OR “Natural Disasters” OR “Tornadoes” OR “Tsunamis” OR “Volcanoes”) OR SU.EXACT(“Accidents” OR “Agent Orange” OR “Air Traffic Accidents” OR “Avalanches” OR “Blizzards” OR “Building Collapse” OR “Disasters” OR “Drought” OR “Earthquakes” OR “Epidemics” OR “Epizootics” OR “Explosions” OR “Famine” OR “Fires” OR “Floods” OR “Home Accidents” OR “Hurricanes” OR “Industrial Accidents” OR “Landmines” OR “Landslides” OR “Lightning” OR “Motor Traffic Accidents” OR “Natural Disasters” OR “Nuclear Accidents” OR “Nuclear Testing” OR “Oil Spills” OR “Pedestrian Accidents” OR “Railroad Accidents” OR “Ship Accidents” OR “Technological Disasters” OR “Tornadoes” OR “Toxic Contamination” OR “Tsunamis” OR “Volcanoes”)) OR (humanitarian NEAR/1 (crisis OR crises)) OR (catastrophe OR catastrophic) OR SU.EXACT(“Survivors”) OR SU.EXACT(“Asylum Seekers” OR “Refugees”) OR ((forcibly OR internally) NEAR/1 displace*) OR (displace* NEAR/1 (people OR person* OR civilian*)) OR (victim* NEAR/2 (crime* OR disaster*)) OR (SU.EXACT(“Political Prisoners”) OR SU.EXACT(“Prisoners of War”)) OR SU.EXACT(“Military Personnel”) OR ((expose* OR exposure) NEAR/2 (abuse OR assault* OR disaster* OR terror* OR torture* OR trauma* OR rape OR violen* OR war OR warfare)) OR (survivor* NEAR/2 (abuse OR assault* OR disaster* OR terror* OR torture* OR trauma* OR rape OR violen* OR war OR warfare)) OR (victim* NEAR/2 (abuse OR assault* OR crime OR disaster* OR rape OR terror* OR torture* OR trauma* OR violen* OR war OR warfare)) OR (witness* NEAR/2 (abuse OR assault* OR crime OR disaster* OR rape OR terror* OR torture* OR trauma* OR violen* OR war OR warfare))) AND (SU.EXACT(“Complex PTSD”) OR SU.EXACT(“PTSD”))) AND ((alprazolam or amobarbital or azaperone or barbital or bromisovalum or chloral hydrate or chloralose or chlordiazepoxide or chlormethiazole or dexmedetomidine or diazepam or diphenhydramine or eszopiclone or ethchlorvynol or etomidate or etorphine or flurazepam or glutethimide or hexobarbital or lorazepam or medazepam or medetomidine or mephobarbital or meprobamate or methapyrilene or methaqualone or midazolam or nitrazepam or oxazepam or paraldehyde or pentobarbital or phenobarbital or propofol or secobarbital or temazepam or thiamylal or thiopental or xylazine) OR (bromazepam or buspirone or chlormezanone or clorazepate dipotassium or estazolam or flunitrazepam or fluvoxamine or nordazepam or ondansetron or oxprenolol or prazepam or pregabalin or ritanserin or tranylcypromine or trazodone or triazolam or zolazepam) OR (benzodiazepines or benzodiazepinones or promethazine or benactyzine or clorgyline or deanol or desvenlafaxine succinate or duloxetine hydrochloride or iproniazid or isocarboxazid or lithium carbonate or lithium compounds or moclobemide or nialamide or phenelzine or pizotyline or rolipram or sertraline or tranylcypromine or vilazodone hydrochloride or Imipramine or mirtazapine) OR (acepromazine or aripiprazole or azaperone or benperidol or butaclamol or chlorpromazine or chlorprothixene or clopenthixol or clozapine or droperidol or etazolate or flupenthixol or fluphenazine or fluspirilene or haloperidol or loxapine or lurasidone hydrochloride or mesoridazine or methiothepin or methotrimeprazine or molindone or ondansetron or paliperidone palmitate or penfluridol or perazine or perphenazine or pimozide or prochlorperazine or promazine or quetiapine fumarate or raclopride or remoxipride or reserpine or risperidone or ritanserin or spiperone or sulpiride or thioridazine or thiothixene or tiapride hydrochloride or trifluoperazine or trifluperidol or triflupromazine or olanzapine) OR (acetazolamide or bromides or carbamazepine or clonazepam or clorazepate dipotassium or diazepam or dimethadione or estazolam or ethosuximide or flunarizine or lorazepam or magnesium sulfate or medazepam or mephenytoin or mephobarbital or meprobamate or nitrazepam or paraldehyde or phenobarbital or phenytoin or pregabalin or primidone or riluzole or thiopental or tiletamine or trimethadione or valproic acid or vigabatrin or lithium chloride or lithium compounds or lamotrigine or topiramate) OR (monoamine oxidase inhibitors or chlorphenamidine or clorgyline or cuprizone or furazolidone or harmaline or harmine or isocarboxazid or moclobemide or monocrotophos or pargyline or selegiline or tranylcypromine or Prazosin or N-Methyl-3,4-methylenedioxyamphetamine or MDMA or ecstasy) OR (hypnotics OR (hypnotic drugs) OR sedatives OR (sedative drugs) OR “anti-anxiety drug*” OR “anti-anxiety agent*” OR “antidepressive agent*” OR “antidepressive drug*” OR “antipsychotic agent*” OR “antipsychotic drug*”) OR (“antimanic agent*” OR “antimanic drug*” OR anticonvulsants OR “anticonvulsant drug*” OR “z drug*”)) | 199° |
PsycINFO via Ovid
Search date: 18 April 2017.
Records retrieved: 2658.
Date range searched: 1806 to April week 2 2017.
| 1 exp Violence/ (66,551) |
| 2 Exposure to Violence/ (509) |
| 3 violence.ti,ab. (60,703) |
| 4 Domestic Violence/ (10,282) |
| 5 Intimate Partner Violence/ (5917) |
| 6 Battered Females/ (3011) |
| 7 Partner Abuse/ (4576) |
| 8 (batter$ adj2 (wife$ or wive$ or woman or women or men or husband$ or partner$)).ti,ab. (2311) |
| 9 Physical Abuse/ (5465) |
| 10 (physical$ adj2 (abus$ or assault$ or violen$ or aggress$)).ti,ab. (14,559) |
| 11 Emotional Abuse/ (2267) |
| 12 (emotional$ adj2 abus$).ti,ab. (2704) |
| 13 Rape/ (5043) |
| 14 rape.ti,ab. (7403) |
| 15 (sexual$ adj2 (abus$ or assault$ or violen$ or aggress$)).ti,ab. (30,943) |
| 16 Child Abuse/ (26,161) |
| 17 Sexual Abuse/ (18,589) |
| 18 child$ sexual abuse.ti,ab. (8393) |
| 19 Incest/ (2526) |
| 20 (child$ adj2 exploit$).ti,ab. (354) |
| 21 Child Neglect/ (3628) |
| 22 child neglect.ti,ab. (642) |
| 23 (child$ adj2 trauma).ti,ab. (4693) |
| 24 (non accidental injur$ or non-accidental injur$ or nonaccidental injur$).ti,ab. (48) |
| 25 Human Trafficking/ (595) |
| 26 ((human or person or people) adj2 (traffick$ or exploit$)).ti,ab. (543) |
| 27 ((forced or exploit$) adj2 labour).ti,ab. (40) |
| 28 Slavery/ (215) |
| 29 Torture/ (1151) |
| 30 (slavery or torture$ or enslave$).ti,ab. (3946) |
| 31 Prostitution/ (2998) |
| 32 (prostitut$ or brothel$).ti,ab. (2805) |
| 33 (sex$ adj2 (exploit$ or traffick$)).ti,ab. (1080) |
| 34 Terrorism/ (6711) |
| 35 (terrorism or terrorist$).ti,ab. (7151) |
| 36 political terror$.ti,ab. (71) |
| 37 Torture/ (1151) |
| 38 War/ (12,259) |
| 39 Combat Experience/ (2479) |
| 40 Genocide/ (899) |
| 41 Holocaust/ (1199) |
| 42 Mass Murder/ (84) |
| 43 (civil adj (unrest or conflict$ or disturbance$ or war or wars or warfare)).ti,ab. (1682) |
| 44 (persecution or victimization or victimisation).ti,ab. (15,549) |
| 45 (captivity or imprison$ or concentration camp$).ti,ab. (5516) |
| 46 exp Disasters/ (7760) |
| 47 Natural Disasters/ (4227) |
| 48 natural disaster$.ti,ab. (2344) |
| 49 (earthquake$ or tsunami$).ti,ab. (2820) |
| 50 (humanitarian adj (crisis or crises)).ti,ab. (106) |
| 51 (catastrophe$ or catastrophic event$ or catastrophic experience$).ti,ab. (1943) |
| 52 exp Survivors/ (11,959) |
| 53 Holocaust Survivors/ (1105) |
| 54 Refugees/ (4568) |
| 55 (asylum seeker$ or refugee$ or migrant$).ti,ab. (13,548) |
| 56 ((forcibly or internally) adj displace$).ti,ab. (237) |
| 57 (displace$ adj (people or person$ or civilian$)).ti,ab. (408) |
| 58 Crime Victims/ (4167) |
| 59 Victimization/ (18,276) |
| 60 Prisoners/ (9692) |
| 61 “Prisoners of War”/ (472) |
| 62 Slavery/ (215) |
| 63 Military Veterans/ (10,341) |
| 64 ((expose$ or exposure) adj2 (abuse or assault$ or disaster$ or terror$ or torture$ or trauma$ or rape or violen$ or war or warfare)).ti,ab. (9024) |
| 65 (survivor$ adj2 (abuse or assault$ or disaster$ or terror$ or torture$ or trauma$ or rape or violen$ or war or warfare)).ti,ab. (4321) |
| 66 (victim$ adj2 (abuse or assault$ or crime or disaster$ or rape or terror$ or torture$ or trauma$ or violen$ or war or warfare)).ti,ab. (9727) |
| 67 (witness$ adj2 (abuse or assault$ or disaster$ or rape or terror$ or torture$ or trauma$ or violen$ or war or warfare)).ti,ab. (1747) |
| 68 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49 or 50 or 51 or 52 or 53 or 54 or 55 or 56 or 57 or 58 or 59 or 60 or 61 or 62 or 63 or 64 or 65 or 66 or 67 (213,458) |
| 69 exp Posttraumatic Stress Disorder/ (27,018) |
| 70 Complex PTSD/ (123) |
| 71 DESNOS/ (15) |
| 72 “Disorders of Extreme Distress Not Otherwise Specified”.ti,ab. (0) |
| 73 (PTSD or CPTSD).ti,ab. (25,381) |
| 74 posttrauma$.ti,ab. (26,998) |
| 75 post-trauma$.ti,ab. (11,564) |
| 76 “post trauma$”.ti,ab. (11,564) |
| 77 post traumatic stress.ti,ab. (8923) |
| 78 post traumatic stress.id. (2783) |
| 79 combat stress$.ti,ab. (497) |
| 80 combat disorder$.ti,ab. (12) |
| 81 DESNOS.ti,ab. (54) |
| 82 complex trauma$.ti,ab. (515) |
| 83 (complex adj2 trauma$).ti,ab. (689) |
| 84 traumatic stress.ti,ab. (11,630) |
| 85 traumatic memor$.ti,ab. (1290) |
| 86 traumatization.ti,ab. (1511) |
| 87 traumatisation.ti,ab. (154) |
| 88 (trauma adj2 (expos$ or event$ or experienc$)).ti,ab. (6634) |
| 89 69 or 70 or 71 or 72 or 73 or 74 or 75 or 76 or 77 or 78 or 79 or 80 or 81 or 82 or 83 or 84 or 85 or 86 or 87 or 88 (47,567) |
| 90 68 and 89 (25,142) |
| 91 exp Cognitive Therapy/ (12,639) |
| 92 cognitive behaviour$ therapy.ti,ab. (3854) |
| 93 cognitive behavior$ therapy.ti,ab. (13,015) |
| 94 cognitive restructuring.ti,ab. (2074) |
| 95 cognitive rescripting.ti,ab. (0) |
| 96 cognitive processing therapy.ti,ab. (272) |
| 97 CPT.ti,ab. (1922) |
| 98 cognitive therapy.ti,ab. (5335) |
| 99 cognitive behavioural treatment$.ti,ab. (520) |
| 100 cognitive behavioral treatment$.ti,ab. (2997) |
| 101 (CBT or TFCBT).ti,ab. (10,616) |
| 102 cognitive trauma therapy.ti,ab. (8) |
| 103 trauma focus$ CBT.ti,ab. (57) |
| 104 91 or 92 or 93 or 94 or 95 or 96 or 97 or 98 or 99 or 100 or 101 or 102 or 103 (33,767) |
| 105 exp Behavior Therapy/ (18,509) |
| 106 (behavior$ adj2 (therap$ or treat$ or modif$)).ti,ab. (41,822) |
| 107 (behaviour$ adj2 (therap$ or treat$ or modif$)).ti,ab. (7365) |
| 108 (dialectical behavio$ therap$ or dialectical behavio$ treat$).ti,ab. (1461) |
| 109 DBT.ti,ab. (1135) |
| 110 biofeedback, psychology/or feedback, sensory/or neurofeedback/ (1205) |
| 111 (biofeedback or neurofeedback or sensory feedback).ti,ab. (6695) |
| 112 desensitization, psychologic/or eye movement desensitization reprocessing/or implosive therapy/or virtual reality exposure therapy/ (421) |
| 113 (psychological adj2 desensiti$).ti,ab. (5) |
| 114 Eye Movement Desensitization Therapy/ (1230) |
| 115 eye movement desensiti?ation reprocessing.ti,ab. (61) |
| 116 EMDR.ti,ab. (1346) |
| 117 Exposure Therapy/ (1979) |
| 118 (exposure adj (therap$ or treat$)).ti,ab. (2200) |
| 119 prolonged exposure therap$.ti,ab. (151) |
| 120 live exposure.ti,ab. (22) |
| 121 imaginal exposure.ti,ab. (280) |
| 122 imaginal flooding.ti,ab. (35) |
| 123 exposure inhibition therap$.ti,ab. (1) |
| 124 implosive therap$.ti,ab. (143) |
| 125 image habituation.ti,ab. (5) |
| 126 inoculation training.ti,ab. (292) |
| 127 105 or 106 or 107 or 108 or 109 or 110 or 111 or 112 or 113 or 114 or 115 or 116 or 117 or 118 or 119 or 120 or 121 or 122 or 123 or 124 or 125 or 126 (65,864) |
| 128 (acceptance adj2 therap$).ti,ab. (376) |
| 129 (commitment adj2 therap$).ti,ab. (1501) |
| 130 Hypnosis/ (7091) |
| 131 (hypnosis or hypnotherap$).ti,ab. (11,623) |
| 132 Mindfulness/ (6583) |
| 133 mindfulness.ti,ab. (8091) |
| 134 (supportive adj (therap$ or psychotherap$)).ti,ab. (1490) |
| 135 (non-directive adj (counselling or counseling)).ti,ab. (81) |
| 136 (nondirective adj (counselling or counseling)).ti,ab. (113) |
| 137 (non directive adj (counselling or counseling)).ti,ab. (81) |
| 138 psychodynamic therap$.ti,ab. (1317) |
| 139 inter personal psychotherap$.ti,ab. (1) |
| 140 interpersonal psychotherap$.ti,ab. (1197) |
| 141 interpersonal therapy.ti,ab. (512) |
| 142 IPT.ti,ab. (974) |
| 143 (compassion adj2 therap$).ti,ab. (105) |
| 144 accelerated resolution.ti,ab. (8) |
| 145 sensorimotor therap$.ti,ab. (11) |
| 146 schema therapy.ti,ab. (312) |
| 147 Stress Management/ (4566) |
| 148 Supportive Psychotherapy/ (480) |
| 149 Group Psychotherapy/ (18,367) |
| 150 Counseling/ (21,293) |
| 151 (non-directive counsel$ or non directive counsel$ or nondirective counsel$).ti,ab. (197) |
| 152 compassion therap$.ti,ab. (4) |
| 153 128 or 129 or 130 or 131 or 132 or 133 or 134 or 135 or 136 or 137 or 138 or 139 or 140 or 141 or 142 or 143 or 144 or 145 or 146 or 147 or 148 or 149 or 150 or 151 or 152 (71,049) |
| 154 104 or 127 or 153 (140,028) |
| 155 hypnotic drugs/or amobarbital/or apomorphine/or barbital/or chloral hydrate/or codeine/or flurazepam/or glutethimide/or hexobarbital/or meprobamate/or methaqualone/or nitrazepam/or pentobarbital/or phenobarbital/or secobarbital/or thalidomide/or thiopental/or triazolam/ (5588) |
| 156 hypnotics.ti,ab. (1574) |
| 157 hypnotic drug$.ti,ab. (399) |
| 158 z drug$.ti,ab. (43) |
| 159 tranquilizing drugs/or amitriptyline/or benactyzine/or doxepin/or haloperidol/or meprobamate/or minor tranquilizers/or neuroleptic drugs/or phenothiazine derivatives/or pimozide/or thiothixene/ (27,445) |
| 160 exp benzodiazepines/ (9874) |
| 161 sedative antihistamine$.ti,ab. (13) |
| 162 promethazine.ti,ab. (184) |
| 163 antidepressant drugs/or bupropion/or citalopram/or fluoxetine/or fluvoxamine/or iproniazid/or isocarboxazid/or lithium carbonate/or methylphenidate/or mianserin/or moclobemide/or molindone/or nefazodone/or nialamide/or nomifensine/or paroxetine/or phenelzine/or pheniprazine/or pipradrol/or serotonin norepinephrine reuptake inhibitors/or sertraline/or sulpiride/or tranylcypromine/or trazodone/or tricyclic antidepressant drugs/or venlafaxine/or zimeldine/ (31,904) |
| 164 Imipramine.ti,ab. (3980) |
| 165 mirtazapine.ti,ab. (1112) |
| 166 neuroleptic drugs/or aripiprazole/or clozapine/or molindone/or nialamide/or olanzapine/or quetiapine/or reserpine/or risperidone/or spiroperidol/or sulpiride/or tetrabenazine/ (28,386) |
| 167 mood stabilizers/or anticonvulsive drugs/or carbamazepine/or lithium/or valproic acid/ (13,520) |
| 168 mood stabilisers.ti,ab. (141) |
| 169 antiepileptics.ti,ab. (305) |
| 170 lamotrigine.ti,ab. (1792) |
| 171 topiramate.ti,ab. (1494) |
| 172 valproate.ti,ab. (2781) |
| 173 monoamine oxidase inhibitors/or iproniazid/or isocarboxazid/or moclobemide/or nialamide/or pargyline/or phenelzine/or pheniprazine/or tranylcypromine/ (2188) |
| 174 antihypertensive drugs/or alpha methylparatyrosine/or captopril/or chlorpromazine/or clonidine/or guanethidine/or hexamethonium/or hydralazine/or mecamylamine/or methyldopa/or phenoxybenzamine/or quinpirole/ (4387) |
| 175 alpha blocker anti-hypertensive$.ti,ab. (0) |
| 176 alpha blocker antihypertensive$.ti,ab. (0) |
| 177 prazosin.ti,ab. (618) |
| 178 Methylenedioxymethamphetamine/ (1923) |
| 179 (mdma or ecstasy).ti,ab. (3061) |
| 180 155 or 156 or 157 or 158 or 159 or 160 or 161 or 162 or 163 or 164 or 165 or 166 or 167 or 168 or 169 or 170 or 171 or 172 or 173 or 174 or 175 or 176 or 177 or 178 or 179 (99,763) |
| 181 90 and 154 (2588) |
| 182 90 and 180 (306) |
| 183 181 or 182 (2861) |
| 184 limit 183 to human (2798) |
| 185 limit 184 to yr=“1992 -Current” (2658) |
Science Citation Index via Web of Science
Search date: 20 April 2017.
Records retrieved: 1066.
Date range searched: 1900 onwards.
| #16 | 1066 |
#15 OR #11 Indexes=SCI-EXPANDED Timespan=1992-2017 |
| #15 | 204 |
#14 AND #7 Indexes=SCI-EXPANDED Timespan=1992-2017 |
| #14 | 352,711 |
#13 OR #12 Indexes=SCI-EXPANDED Timespan=1992-2017 |
| #13 | 188,961 |
TS=((hypnotic or sedative) NEAR/1 (drug$ or agent$)) OR TS=(hypnotics or sedatives) OR TS=(alprazolam or amobarbital or azaperone or barbital or bromisovalum or “chloral hydrate” or chloralose or chlordiazepoxide or chlormethiazole or dexmedetomidine or diazepam or diphenhydramine or eszopiclone or ethchlorvynol or etomidate or etorphine or flurazepam or glutethimide or hexobarbital or lorazepam or medazepam or medetomidine or mephobarbital or meprobamate or methapyrilene or methaqualone or midazolam or nitrazepam or oxazepam or paraldehyde or pentobarbital or phenobarbital or propofol or secobarbital or temazepam or thiamylal or thiopental or xylazine) OR TS=(“z drug$”) OR TS=(“anti-anxiety agent$” or “anti-anxiety drug$”) OR TS=(“antianxiety agent$” or “antianxiety drug$”) OR TS=(“anti anxiety agent$” or “anti anxiety drug$”) OR TS=(“anxiolytic agent$” or “anxiolytic drug$” or anxiolytics) OR TS=(bromazepam or buspirone or chlormezanone or “clorazepate dipotassium” or estazolam or flunitrazepam or fluvoxamine or nordazepam or ondansetron or oxprenolol or prazepam or pregabalin or ritanserin or tranylcypromine or trazodone or triazolam or zolazepam or benzodiazepines or benzodiazepinones or “sedative antihistamine$” or promethazine) OR TS=(“antidepressive agent$” or “antidepressive drug$” or antidepressives) OR TS=(“anti-depressive agent$” or “anti-depressive drug$” or antidepressives) OR TS=(“anti depressive agent$” or “anti depressive drug$” or antidepressives) OR TS=(benactyzine or clorgyline or deanol or “desvenlafaxine succinate” or “duloxetine hydrochloride” or iproniazid or isocarboxazid or “lithium carbonate” or “lithium compounds” or moclobemide or nialamide or phenelzine or pizotyline or rolipram or sertraline or tranylcypromine or “vilazodone hydrochloride” or imipramine or mirtazapine) OR TS=(“antipsychotic agent$” or “antipsychotic drug$” or antipsychotics) OR TS=(“anti-psychotic agent$” or “anti-psychotic drug$” or anti-psychotics) OR TS=(“anti psychotic agent$” or “anti psychotic drug$” or anti psychotics) OR TS=(acepromazine or aripiprazole or azaperone or benperidol or butaclamol or chlorpromazine or chlorprothixene or clopenthixol or clozapine or droperidol or etazolate or flupenthixol or fluphenazine or fluspirilene or haloperidol or loxapine or lurasidone hydrochloride or mesoridazine or methiothepin or methotrimeprazine or molindone or ondansetron or “paliperidone palmitate” or penfluridol or perazine or perphenazine or pimozide or prochlorperazine or promazine or quetiapine fumarate or raclopride or remoxipride or reserpine or risperidone or ritanserin or spiperone or sulpiride or thioridazine or thiothixene or “tiapride hydrochloride” or trifluoperazine or trifluperidol or triflupromazine or olanzapine) Indexes=SCI-EXPANDED Timespan=1992-2017 |
| #12 | 202,663 |
TS=(“anticonvulsants agent$” or “anticonvulsant drug$” or anticonvulsants) OR TS=(“anti-convulsants agent$” or “anti-convulsant drug$” or anti-convulsants) OR TS=(“anti convulsants agent$” or “anti convulsant drug$” or anti convulsants) OR TS=(acetazolamide or bromides or carbamazepine or clonazepam or “clorazepate dipotassium” or diazepam or dimethadione or estazolam or ethosuximide or flunarizine or lorazepam or magnesium sulfate or medazepam or mephenytoin or mephobarbital or meprobamate or nitrazepam or paraldehyde or phenobarbital or phenytoin or pregabalin or primidone or riluzole or thiopental or tiletamine or trimethadione or “valproic acid” or vigabatrin) OR TS=(“antimanic agent$” or “antimanic drug$”) OR TS=(“anti-manic agent$” or “anti-manic drug$”) OR TS=(“anti manic agent$” or “anti manic drug$”) OR TS=(“lithium chloride” or “lithium compounds” or lamotrigine or topiramate) OR TS=(“monoamine oxidase inhibitors” or chlorphenamidine or clorgyline or cuprizone or furazolidone or harmaline or harmine or isocarboxazid or moclobemide or monocrotophos or pargyline or selegiline or tranylcypromine or Prazosin or “N-Methyl-3 4-methylenedioxyamphetamine” or MDMA or ecstasy) Indexes=SCI-EXPANDED Timespan=1992-2017 |
| #11 | 915 |
#10 AND #7 Indexes=SCI-EXPANDED Timespan=1992-2017 |
| #10 | 130,643 |
#9 OR #8 Indexes=SCI-EXPANDED Timespan=1992-2017 |
| #9 | 75,396 |
TS=(acceptance NEAR/2 therap$) OR TS=(commitment NEAR/2 therap$) OR TS=(hypnosis or hypnotherap$) OR TS=(mindfulness) OR TS=(“supportive therapy”) OR TS=(non-directive NEAR/1 (counselling or counseling)) OR TS=(nondirective NEAR/1 (counselling or counseling)) OR TS=(“non directive” NEAR/1 (counselling or counseling)) OR TS=(psychotherapy or “brief psychotherapy” or “group psychotherapy” or “psychodynamic psychotherapy”) OR TS=(“rational emotive psychotherapy”) OR TS=(“rational-emotive psychotherapy”) OR TS=(“psychodynamic therap$”) OR TS=(“inter personal psychotherap$” or “interpersonal psychotherap$” or “inter-personal psychotherap$”) OR TS=((compassion or schema or sensorimotor) NEAR/2 therap$) OR TS=(counseling or counselling) OR TS=(“accelerated resolution”) Indexes=SCI-EXPANDED Timespan=1992-2017 |
| #8 | 60,687 |
TS=(cognitive NEAR/3 (therap$ or treat$ or restructur$ or rescript$)) OR TS=(CBT or CPT or TFCBT) OR TS=(“trauma focus$ CBT”) OR TS=(behavior$ NEAR/2 (therap$ or treat$ or modif$)) OR TS=(behaviour$ NEAR/2 (therap$ or treat$ or modif$)) OR TS=(biofeedback or neurofeedback or “sensory feedback”) OR TS=(“implosive therapy”) OR TS=(“virtual reality therapy”) OR TS=(psychological NEAR/2 desensiti$) OR TS=(“eye movement desensitisation reprocessing” or “eye movement desensitization reprocessing”) OR TS=(EMDR) OR TS=(exposure NEAR/2 (imaginal or live or prolonged or therap$ or treat$)) OR TS=(“imaginal flooding”) OR TS=(“image habituation”) OR TS=(“inoculation training”) Indexes=SCI-EXPANDED Timespan=1992-2017 |
| #7 | 9164 |
#6 AND #5 Indexes=SCI-EXPANDED Timespan=1992-2017 |
| #6 | 29,452 |
TOPIC: (“posttraumatic stress disorder*”) OR TOPIC: (“post-traumatic stress disorder*”) OR TOPIC: (“post traumatic stress disorder*”) OR TOPIC: (“posttraumatic stress*”) OR TOPIC: (“post-traumatic stress*”) OR TOPIC: (“post traumatic stress*”) OR TOPIC: (“traumatic stress*”) OR TOPIC: (posttrauma$ or post-trauma$ or “post trauma$”) OR TOPIC: (“combat stress” or “combat disorder”) OR TOPIC: (DESNOS) OR TOPIC: (“extreme distress”) OR TOPIC: (“complex trauma”) OR TOPIC: (complex NEAR/3 trauma) OR TOPIC: (traumatic NEAR/2 (stress or memor$)) OR TOPIC: (traumatization or traumatisation) OR TOPIC: (trauma$ NEAR/3 (expos$ or event$ or experienc$)) Indexes=SCI-EXPANDED Timespan=1992-2017 |
| #5 | 288,605 |
#4 OR #3 OR #2 OR #1 Indexes=SCI-EXPANDED Timespan=1992-2017 |
| #4 | 29,766 |
TOPIC: (victim$) OR TOPIC: (prisoner$) OR TOPIC: (soldier$ or veteran$) AND TOPIC: ((expose$ or exposure) NEAR/2 (abuse or assault$ or disaster$ or terror$ or torture$ or trauma$ or rape or violen$ or war or warfare)) AND TOPIC: (survivor$ NEAR/2 (abuse or assault$ or disaster$ or terror$ or torture$ or trauma$ or rape or violen$ or war or warfare)) AND TOPIC: (victim$ NEAR/2 (abuse or assault$ or crime or disaster$ or rape or terror$ or torture$ or trauma$ or violen$ or war or warfare)) AND TOPIC: (witness$ NEAR/2 (abuse or assault$ or disaster$ or rape or terror$ or torture$ or trauma$ or violen$ or war or warfare)) Indexes=SCI-EXPANDED Timespan=1992-2017 |
| #3 | 202,637 |
TOPIC: (disaster$ or earthquake$ or tsunami$) OR TOPIC: (“natural disaster$”) OR TOPIC: (humanitarian NEAR/2 (crisis or crises)) OR TOPIC: (catastrophe$ or “catastrophic event$” or “catastrophic experience$”) OR TOPIC: (survivor*) OR TOPIC: (refugee$ or “asylum seeker$” or migrant$) OR TOPIC: ((forcibly or internally) NEAR/2 displace$) OR TOPIC: (displace$ NEAR/2 (people or person$ or civilian$)) Indexes=SCI-EXPANDED Timespan=1992-2017 |
| #2 | 25,515 |
TOPIC: (“human rights abuse*”) OR TOPIC: ((human or person or people) NEAR/2 (traffick$ or exploit$)) OR TOPIC: ((forced or exploit$) NEAR/2 labour) OR TOPIC: (“organ traffick$”) OR TOPIC: (slavery or “slave trade$” or enslave$) OR TOPIC: (torture$) OR TOPIC: (prostitution or “sex work$” or brothel$) OR TOPIC: (sex NEAR/2 (exploit$ or traffick$)) OR TOPIC: (terrorism or terrorist$ or “political terror$”) OR TOPIC: (warfare or “war crime$” or “armed conflict$” or “civil conflict” or “civil war$” or “civil unrest”) OR TOPIC: (“ethnic conflict$” or “ethnic unrest” or “ethnic cleans*” or genocide or holocaust) OR TOPIC: (persecution or victimization or victimisation) OR TOPIC: (imprison$ or “concentration camp”) Indexes=SCI-EXPANDED Timespan=1992-2017 |
| #1 | 47,352 |
TS=(violence) OR TS=(batter* NEAR/2 (wife$ or wive$ or woman or women or men or husband$ or partner$)) OR TS=(physical$ NEAR/2 (abus$ or assault$ or violen$ or aggress$)) OR TS=(emotional near/2 abus*) OR TS=(rape) OR TS=(sexual$ NEAR/2 (abus$ or assault$ or violen$ or aggress$)) OR TS=(child$ NEAR/2 (abus$ or exploit or maltreat$ or neglect$ or trauma$)) OR TS=(“non accidental injur$” or “non-accidental injur$” or “nonaccidental injur$”) Indexes=SCI-EXPANDED Timespan=1992-2017 |
Appendix 2 Literature search strategies for the qualitative acceptability review
The original searches were carried out in June 2017 using the following databases: CINAHL, EMBASE, MEDLINE and PsycINFO. Results were restricted to 1992 onwards.
The numbers of records identified in each database are as follows:
-
CINAHL: 470
-
EMBASE: 1749
-
MEDLINE: 1151
-
PsycINFO: 919.
The total number of records identified before de-duplication was 4289; after de-duplication, 3162 records were left.
This set was subsequently de-duplicated against the results of the effectiveness searches to leave a total of 1574 records.
CINAHL via EBSCOhost
Search date: 1 June 2017.
| Search terms | Search options | |
|---|---|---|
| S1 | (MH “Stress Disorders, Post-Traumatic+”) | |
| S2 | TX (PTSD or CPTSD) OR TX posttrauma* OR TX post-trauma* OR TX “post trauma*” OR TX “post traumatic stress” OR TX “combat stress*” OR TX “combat disorder*” OR TX DESNOS OR TX “complex trauma*” OR TX “complex N3 trauma*” OR TX “traumatic stress” OR TX “traumatic memor*” | |
| S3 | TX traumatisation OR TX traumatization OR TX (trauma* N3 (expos* or event* or experienc*)) | |
| S4 | S1 OR S2 OR S3 | |
| S5 | (MH “Cognitive Therapy+”) OR TX “cognitive behaviour* therap*” OR TX “cognitive behavior* therap*” OR TX “cognitive restructuring” OR TX “cognitive rescripting” OR TX “cognitive processing therap*” OR TX (CPT or CBT or TFCBT) OR TX “cognitive therap*” OR TX “cognitive behavioural treat*” OR TX “cognitive behavioral treat*” OR TX “cognitive trauma therap*” OR TX “trauma focus* CBT” | |
| S6 | (MH “Behavior Therapy”) OR TX (behavior* N2 (therap* or treat* or modif*)) OR TX (behavior* N2 (therap* or treat* or modif*)) OR TX ((“dialectical behavio*”) N1 (therap* or treat*)) OR TX (biofeedback or neurofeedback or “sensory feedback”) OR TX psychological N2 desensiti#ation OR TX “eye movement desensiti#ation reprocessing” OR TX EMDR OR TX (exposure N1 (therap* or treat*)) OR TX “live exposure” OR TX “imaginal exposure” OR TX “prolonged exposure therapy” | |
| S7 | TX “imaginal flooding” OR TX “exposure inhibition therap*” OR TX “implosive therap*” OR TX “image habituation” OR TX “inoculation training” | |
| S8 | ((MH “Acceptance and Commitment Therapy”)) OR TX acceptance N2 therap* OR TX commitment N2 therap* | |
| S9 | (MH “Biofeedback”) | |
| S10 | (MH “Feedback”) | |
| S11 | (MH “Eye Movement Desensitization and Reprogramming”) | |
| S12 | (MH “Virtual Reality Exposure Therapy”) | |
| S13 | (MH “Hypnosis”) | |
| S14 | TX hypnosis or hypnotherap* | |
| S15 | (MH “Mindfulness”) | |
| S16 | TX mindfulness | |
| S17 | TX “supportive therap*” OR TX (non-directive N1 (counselling or counseling)) OR TX (“non directive” N1 (counselling or counseling)) | |
| S18 | ((MH “Psychotherapy”) OR (MH “Psychotherapy, Brief”) OR (MH “Psychotherapy, Group”) OR (MH “Psychotherapy, Psychodynamic”)) OR TX psychodynamic N1 therap* OR TX “inter personal psychotherap*” OR TX “interpersonal psychotherap*” OR TX IPT OR TX “compassion therap*” OR TX “accelerated resolution*” OR TX “sensorimotor therap*” OR TX “schema therap*” OR TX stress N2 manag* | |
| S19 | (MH “Counseling”) OR TX “non-directive counsel*” OR TX “non directive counsel*” OR TX “nondirective counsel*” OR “compassion therap*” | |
| S20 | S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 | |
| S21 | ((MH “Hypnotics and Sedatives”)) OR TX (alprazolam or amobarbital or azaperone or barbital or bromisovalum or “chloral hydrate” or chloralose or chlordiazepoxide or chlormethiazole or dexmedetomidine or diazepam or diphenhydramine or eszopiclone or ethchlorvynol or etomidate or etorphine or flurazepam or glutethimide or hexobarbital or lorazepam or medazepam or medetomidine or mephobarbital or meprobamate or methapyrilene or methaqualone or midazolam or nitrazepam or oxazepam or paraldehyde o... | |
| S22 | (MH “Antianxiety Agents+”) OR (bromazepam or buspirone or chlormezanone or “clorazepate dipotassium” or estazolam or flunitrazepam or fluvoxamine or nordazepam or ondansetron or oxprenolol or prazepam or pregabalin or ritanserin or tranylcypromine or trazodone or triazolam or zolazepam or benzodiazepines or benzodiazepinones or “sedative antihistamine*” or promethazine) | |
| S23 | (MH “Antidepressive Agents+”) OR TX (benactyzine or clorgyline or deanol or “desvenlafaxine succinate” or “duloxetine hydrochloride” or iproniazid or isocarboxazid or “lithium carbonate” or “lithium compounds” or moclobemide or nialamide or phenelzine or pizotyline or rolipram or sertraline or tranylcypromine or “vilazodone hydrochloride” or Imipramine or mirtazapine) | |
| S24 | (MH “Antipsychotic Agents+”) OR TX (acepromazine or aripiprazole or azaperone or benperidol or butaclamol or chlorpromazine or chlorprothixene or clopenthixol or clozapine or droperidol or etazolate or flupenthixol or fluphenazine or fluspirilene or haloperidol or loxapine or “lurasidone hydrochloride” or mesoridazine or methiothepin or methotrimeprazine or molindone or ondansetron or “paliperidone palmitate” or penfluridol or perazine or perphenazine or pimozide or prochlorperazine) OR TX (p... | |
| S25 | (MH “Anticonvulsants+”) OR TX (anticonvulsants or acetazolamide or bromides or carbamazepine or clonazepam or “clorazepate dipotassium” or diazepam or dimethadione or estazolam or ethosuximide or flunarizine or lorazepam or “magnesium sulfate” or medazepam or mephenytoin or mephobarbital or meprobamate or nitrazepam or paraldehyde or phenobarbital or phenytoin or pregabalin or primidone or riluzole or thiopental or tiletamine or trimethadione or “valproic acid” or vigabatrin) | |
| S26 | (MH “Antimanic Agents+”) OR TX (“lithium chloride” or “lithium compounds” or lamotrigine or topiramate) | |
| S27 | (MH “Monoamine Oxidase Inhibitors+”) OR TX (chlorphenamidine or clorgyline or cuprizone or furazolidone or harmaline or harmine or isocarboxazid or moclobemide or monocrotophos or pargyline or selegiline or tranylcypromine or Prazosin or N-Methyl-3, 4-methylenedioxyamphetamine or MDMA or ecstasy) | |
| S28 | S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 | |
| S29 | S4 AND S20 | (3665) |
| S30 | S4 AND S28 | (820) |
| S31 | S29 OR S30 | (4259) |
| S32 | (MH “Qualitative Studies”) | (74,214) |
| S33 | (MH “Interviews”) OR (MH “Unstructured Interview”) OR (MH “Semi-Structured Interview”) | (156,659) |
| S34 | (MH “Ethnographic Research”) | (6044) |
| S35 | (MH “Grounded Theory”) | (11,936) |
| S36 | (MH “Thematic Analysis”) | (41,678) |
| S37 | (MH “Observational Methods”) OR (MH “Participant Observation”) | (16,594) |
| S38 | (MH “Field Notes”) | (6623) |
| S39 | (MH “Narratives”) | (11,936) |
| S40 | (MH “Field Studies”) | (2485) |
| S41 | (MH “Audiorecording”) | (36,402) |
| S42 | (MH “Focus Groups”) | (31,284) |
| S43 | (MH “Descriptive Research”) | (60,598) |
| S44 | (MH “Case Studies”) | (16,717) |
| S45 | (MH “Discourse Analysis”) | (3490) |
| S46 | (MH “Exploratory Research”) | (29,405) |
| S47 | (MH “Phenomenology”) | (2577) |
| S48 | (MH “Naturalistic Inquiry”) | (929) |
| S49 | (MH “Open-Ended Questionnaires”) | (3206) |
| S50 | (MH “Videorecording”) | (22,181) |
| S51 | (MH “Anthropology, Cultural”) | (1713) |
| S52 | “conversation* analysis” OR “comparative method*” OR hermeneutic* OR participatory OR in-depth OR key informant* OR narration* | (45,445) |
| S53 | S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 OR S43 OR S44 OR S45 OR S46 OR S47 OR S48 OR S49 OR S50 OR S51 OR S52 | (325,689) |
| S54 | S31 AND S53 | (470) |
EMBASE via Ovid
Search date: 1 June 2017.
Date range searched: 1980 to 2017 week 22.
| 1 Posttraumatic Stress Disorder/ (45,884) |
| 2 (PTSD or CPTSD).ti,ab. (22,707) |
| 3 posttrauma$.ti,ab. (34,058) |
| 4 post-trauma$.ti,ab. (30,965) |
| 5 “post trauma$”.ti,ab. (30,965) |
| 6 post traumatic stress.ti,ab. (12,036) |
| 7 post traumatic stress.kw. (2854) |
| 8 combat stress$.ti,ab. (405) |
| 9 combat disorder$.ti,ab. (18) |
| 10 DESNOS.ti,ab. (39) |
| 11 “Disorders of Extreme Distress Not Otherwise Specified”.ti,ab. (0) |
| 12 complex trauma$.ti,ab. (454) |
| 13 (complex adj3 trauma$).ti,ab. (1408) |
| 14 traumatic stress.ti,ab. (14,416) |
| 15 traumatic memor$.ti,ab. (768) |
| 16 traumatization.ti,ab. (1152) |
| 17 traumatisation.ti,ab. (242) |
| 18 (trauma$ adj3 (expos$ or event$ or experienc$)).ti,ab. (20,405) |
| 19 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 (95,383) |
| 20 exp Cognitive Therapy/ (42,280) |
| 21 cognitive behaviour$ therapy.ti,ab. (5626) |
| 22 cognitive behavior$ therapy.ti,ab. (10,664) |
| 23 cognitive restructuring.ti,ab. (1093) |
| 24 cognitive rescripting.ti,ab. (0) |
| 25 cognitive processing therapy.ti,ab. (197) |
| 26 CPT.ti,ab. (15,122) |
| 27 cognitive therapy.ti,ab. (3508) |
| 28 cognitive behavioural treatment$.ti,ab. (571) |
| 29 cognitive behavioral treatment$.ti,ab. (1879) |
| 30 (CBT or TFCBT).ti,ab. (11,500) |
| 31 cognitive trauma therapy.ti,ab. (7) |
| 32 trauma focus$ CBT.ti,ab. (46) |
| 33 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 (64,373) |
| 34 exp Behavior Therapy/ (40,674) |
| 35 (behavior$ adj2 (therap$ or treat$ or modif$)).ti,ab. (33,760) |
| 36 (behaviour$ adj2 (therap$ or treat$ or modif$)).ti,ab. (13,506) |
| 37 (dialectical behavio$ adj (therap$ or treat$)).ti,ab. (811) |
| 38 biofeedback, psychology/or feedback, sensory/or neurofeedback/ (20,411) |
| 39 (biofeedback or neurofeedback or sensory feedback).ti,ab. (10,762) |
| 40 eye movement desensitization reprocessing/or implosive therapy/or virtual reality exposure therapy/ (438) |
| 41 (psychological adj2 desensiti$).ti,ab. (6) |
| 42 eye movement desensiti?ation reprocessing.ti,ab. (38) |
| 43 EMDR.ti,ab. (559) |
| 44 (exposure adj (therap$ or treat$)).ti,ab. (2781) |
| 45 live exposure.ti,ab. (16) |
| 46 imaginal exposure.ti,ab. (180) |
| 47 prolonged exposure therapy.ti,ab. (111) |
| 48 imaginal flooding.ti,ab. (20) |
| 49 exposure inhibition therap$.ti,ab. (0) |
| 50 implosive therap$.ti,ab. (36) |
| 51 image habituation.ti,ab. (4) |
| 52 inoculation training.ti,ab. (115) |
| 53 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49 or 50 or 51 or 52 (102,846) |
| 54 “Acceptance and Commitment Therapy”/ (709) |
| 55 (acceptance adj2 therap$).ti,ab. (363) |
| 56 (commitment adj2 therap$).ti,ab. (838) |
| 57 Hypnosis/ (12,985) |
| 58 (hypnosis or hypnotherap$).ti,ab. (8081) |
| 59 Mindfulness/ (3457) |
| 60 mindfulness.ti,ab. (5257) |
| 61 supportive therap$.ti,ab. (5309) |
| 62 (non-directive adj (counselling or counseling)).ti,ab. (114) |
| 63 (nondirective adj (counselling or counseling)).ti,ab. (50) |
| 64 (non directive adj (counselling or counseling)).ti,ab. (114) |
| 65 Psychotherapy/or Group Therapy/or Psychodynamic Psychotherapy/ (93,420) |
| 66 psychodynamic therap$.ti,ab. (627) |
| 67 inter personal psychotherap$.ti,ab. (1) |
| 68 interpersonal psychotherap$.ti,ab. (930) |
| 69 IPT.ti,ab. (2387) |
| 70 (compassion adj2 therap$).ti,ab. (62) |
| 71 accelerated resolution.ti,ab. (112) |
| 72 sensorimotor therap$.ti,ab. (22) |
| 73 schema therapy.ti,ab. (174) |
| 74 (stress adj2 manag$).ti,ab. (6583) |
| 75 supportive therap$.ti,ab. (5309) |
| 76 Counseling/ (52,136) |
| 77 (non-directive counsel$ or non directive counsel$ or nondirective counsel$).ti,ab. (165) |
| 78 compassion therap$.ti,ab. (2) |
| 79 54 or 55 or 56 or 57 or 58 or 59 or 60 or 61 or 62 or 63 or 64 or 65 or 66 or 67 or 68 or 69 or 70 or 71 or 72 or 73 or 74 or 75 or 76 or 77 or 78 (174,613) |
| 80 33 or 53 or 79 (291,814) |
| 81 19 and 80 (10,397) |
| 82 hypnotic sedative agent/or alprazolam/or amobarbital/or azaperone/or barbital/or bromisovalum/or chloral hydrate/or chloralose/or chlordiazepoxide/or chlomethiazole/or dexmedetomidine/or diazepam/or diphenhydramine/or eszopiclone/or ethchlorvynol/or etomidate/or etorphine/or flurazepam/or glutethimide/or hexobarbital/or lorazepam/or medazepam/or medetomidine/or methylphenobarbital/or meprobamate/or methapyrilene/or methaqualone/or midazolam/or nitrazepam/or oxazepam/or paraldehyde/or pentobarbital/or phenobarbital/or propofol/or secobarbital/or temazepam/or thiamylal/or thiopental/or xylazine/ (276,213) |
| 83 z drugs.ti,ab. (207) |
| 84 anxiolytic agent/or bromazepam/or buspirone/or chlormezanone/or clorazepate dipotassium/or estazolam/or flunitrazepam/or fluvoxamine/or nordazepam/or ondansetron/or oxprenolol/or prazepam/or pregabalin/or ritanserin/or tranylcypromine/or trazodone/or triazolam/or zolazepam/ (91,974) |
| 85 benzodiazepine derivative/ (36,147) |
| 86 sedative antihistamine$.ti,ab. (115) |
| 87 promethazine/ (11,286) |
| 88 antidepressive agent/or benactyzine/or clorgyline/or deanol/or desvenlafaxine/or duloxetine/or iproniazid/or isocarboxazid/or lithium carbonate/or lithium derivative/or moclobemide/or nialamide/or phenelzine/or pizotifen/or rolipram/or sertraline/or tranylcypromine/or vilazodone/ (131,288) |
| 89 Imipramine/ (29,724) |
| 90 mirtazapine/ (10,727) |
| 91 neuroleptic agent/or acepromazine/or aripiprazole/or azaperone/or benperidol/or butaclamol/or chlorpromazine/or chlorprothixene/or clopenthixol/or clozapine/or droperidol/or etazolate/or flupentixol/or fluphenazine/or fluspirilene/or haloperidol/or loxapine/or lurasidone/or mesoridazine/or metitepine/or methotrimeprazine/or molindone/or ondansetron/or paliperidone/or penfluridol/or perazine/or perphenazine/or pimozide/or prochlorperazine/or promazine/or quetiapine/or raclopride/or remoxipride/or reserpine/or risperidone/or ritanserin/or spiperone/or sulpiride/or thioridazine/or tiothixene/or tiapride/or trifluoperazine/or trifluperidol/or triflupromazine/ (221,511) |
| 92 olanzapine/ (29,757) |
| 93 anticonvulsive agent/or acetazolamide/or bromides/or carbamazepine/or clonazepam/or clorazepate dipotassium/or diazepam/or dimethadione/or estazolam/or ethosuximide/or flunarizine/or lorazepam/or magnesium sulfate/or medazepam/or mephenytoin/or methylphenobarbital/or meprobamate/or nitrazepam/or paraldehyde/or phenobarbital/or phenytoin/or pregabalin/or primidone/or riluzole/or thiopental/or tiletamine/or trimethadione/or valproic acid/or vigabatrin/ (323,161) |
| 94 tranquilizer/or lithium chloride/or lithium derivative/ (21,662) |
| 95 lamotrigine/ (21,528) |
| 96 topiramate/ (18,511) |
| 97 monoamine oxidase inhibitor/or chlorphenamidine/or clorgyline/or cuprizone/or furazolidone/or harmaline/or harmine/or isocarboxazid/or moclobemide/or monocrotophos/or pargyline/or selegiline/or tranylcypromine/(38,999) |
| 98 Prazosin/ (21,809) |
| 99 3,4 methylenedioxyamphetamine/ (1999) |
| 100 (MDMA or ecstasy).ti,ab. (6408) |
| 101 82 or 83 or 84 or 85 or 86 or 87 or 88 or 89 or 90 or 91 or 92 or 93 or 94 or 95 or 96 or 97 or 98 or 99 or 100 (796,293) |
| 102 19 and 101 (6845) |
| 103 81 or 102 (15,327) |
| 104 qualitative research/ (44,728) |
| 105 unstructured interview/or semi structured interview/or interview/ (180,660) |
| 106 ethnography/ (1859) |
| 107 grounded theory/ (4097) |
| 108 thematic analysis/ (6983) |
| 109 observational method/ (1260) |
| 110 participant observation/ (4400) |
| 111 narrative/ (5915) |
| 112 field study/ (2893) |
| 113 audio recording/ (1997) |
| 114 descriptive research/ (14,116) |
| 115 discourse analysis/ (760) |
| 116 hermeneutics/ (167) |
| 117 naturalistic inquiry/ (459) |
| 118 phenomenology/ (8633) |
| 119 participatory research/ (3550) |
| 120 recording/ (41,930) |
| 121 cultural anthropology/ (48,605) |
| 122 case stud$.ti,ab. (92,088) |
| 123 comparative method$.ti,ab. (2818) |
| 124 field notes.ti,ab. (1743) |
| 125 focus group$.ti,ab. (39,224) |
| 126 conversation$ analysis.ti,ab. (506) |
| 127 exploratory stud$.ti,ab. (13,200) |
| 128 open-ended.ti,ab. (12,795) |
| 129 in-depth.ti,ab. (55,739) |
| 130 key informant$.ti,ab. (5832) |
| 131 narration.ti,ab. (644) |
| 132 104 or 105 or 106 or 107 or 108 or 109 or 110 or 111 or 112 or 113 or 114 or 115 or 116 or 117 or 118 or 119 or 120 or 121 or 122 or 123 or 124 or 125 or 126 or 127 or 128 or 129 or 130 or 131 (505,231) |
| 133 103 and 132 (1259) |
| 134 (accept$ or adherence or attitude$ or belief$ or believ$ or choice$ or choos$ or drop out$ or experienc$ or feasib$ or opinion$ or perceiv$ or percept$ or prefer$ or uptake or view$ or withdraw$).ti. (761,456) |
| 135 103 and 134 (637) |
| 136 133 or 135 (1799) |
| 137 limit 136 to yr=“1992 -Current” (1749) |
MEDLINE via Ovid
Search date: 1 June 2017.
Database: Ovid MEDLINE Epub Ahead of Print and In-Process & Other Non-Indexed Citations, Ovid MEDLINE Daily and Ovid MEDLINE.
Date range searched: 1946 to present.
| 1 Stress Disorders, Post Traumatic/ (27,020) |
| 2 (PTSD or CPTSD).ti,ab. (18,404) |
| 3 posttrauma$.ti,ab. (30,457) |
| 4 post-trauma$.ti,ab. (25,925) |
| 5 “post trauma$”.ti,ab. (25,925) |
| 6 post traumatic stress.ti,ab. (9454) |
| 7 post traumatic stress.kw. (96) |
| 8 combat stress$.ti,ab. (348) |
| 9 combat disorder$.ti,ab. (15) |
| 10 DESNOS.ti,ab. (30) |
| 11 “Disorders of Extreme Distress Not Otherwise Specified”.ti,ab. (0) |
| 12 complex trauma$.ti,ab. (409) |
| 13 (complex adj3 trauma$).ti,ab. (1224) |
| 14 traumatic stress.ti,ab. (10,931) |
| 15 traumatic memor$.ti,ab. (594) |
| 16 traumatization.ti,ab. (1004) |
| 17 traumatisation.ti,ab. (192) |
| 18 (trauma$ adj3 (expos$ or event$ or experienc$)).ti,ab. (16,547) |
| 19 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 (75,969) |
| 20 exp Cognitive Therapy/ (22,774) |
| 21 cognitive behaviour$ therapy.ti,ab. (4058) |
| 22 cognitive behavior$ therapy.ti,ab. (8246) |
| 23 cognitive restructuring.ti,ab. (728) |
| 24 cognitive rescripting.ti,ab. (0) |
| 25 cognitive processing therapy.ti,ab. (181) |
| 26 CPT.ti,ab. (10,875) |
| 27 cognitive therapy.ti,ab. (2427) |
| 28 cognitive behavioural treatment$.ti,ab. (408) |
| 29 cognitive behavioral treatment$.ti,ab. (1406) |
| 30 (CBT or TFCBT).ti,ab. (8178) |
| 31 cognitive trauma therapy.ti,ab. (6) |
| 32 trauma focus$ CBT.ti,ab. (31) |
| 33 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 (41,296) |
| 34 exp Behavior Therapy/ (65,175) |
| 35 (behavior$ adj2 (therap$ or treat$ or modif$)).ti,ab. (27,210) |
| 36 (behaviour$ adj2 (therap$ or treat$ or modif$)).ti,ab. (9995) |
| 37 (dialectical behavio$ adj (therap$ or treat$)).ti,ab. (587) |
| 38 biofeedback, psychology/or feedback, sensory/or neurofeedback/ (9410) |
| 39 (biofeedback or neurofeedback or sensory feedback).ti,ab. (8547) |
| 40 eye movement desensitization reprocessing/or implosive therapy/or virtual reality exposure therapy/ (1375) |
| 41 (psychological adj2 desensiti$).ti,ab. (4) |
| 42 eye movement desensiti?ation reprocessing.ti,ab. (25) |
| 43 EMDR.ti,ab. (376) |
| 44 (exposure adj (therap$ or treat$)).ti,ab. (2318) |
| 45 live exposure.ti,ab. (11) |
| 46 imaginal exposure.ti,ab. (149) |
| 47 prolonged exposure therapy.ti,ab. (101) |
| 48 imaginal flooding.ti,ab. (13) |
| 49 exposure inhibition therap$.ti,ab. (0) |
| 50 implosive therap$.ti,ab. (43) |
| 51 image habituation.ti,ab. (3) |
| 52 inoculation training.ti,ab. (79) |
| 53 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49 or 50 or 51 or 52 (91,074) |
| 54 “Acceptance and Commitment Therapy”/ (187) |
| 55 (acceptance adj2 therap$).ti,ab. (262) |
| 56 (commitment adj2 therap$).ti,ab. (615) |
| 57 Hypnosis/ (8767) |
| 58 (hypnosis or hypnotherap$).ti,ab. (7616) |
| 59 Mindfulness/ (1406) |
| 60 mindfulness.ti,ab. (4162) |
| 61 supportive therap$.ti,ab. (3938) |
| 62 (non-directive adj (counselling or counseling)).ti,ab. (100) |
| 63 (nondirective adj (counselling or counseling)).ti,ab. (54) |
| 64 (non directive adj (counselling or counseling)).ti,ab. (100) |
| 65 Psychotherapy/or Psychotherapy, Brief/or Psychotherapy, Group/or Psychotherapy, Multiple/or Psychotherapy, Psychodynamic/or Psychotherapy, Rational-emotive/ (66,081) |
| 66 psychodynamic therap$.ti,ab. (435) |
| 67 inter personal psychotherap$.ti,ab. (1) |
| 68 interpersonal psychotherap$.ti,ab. (788) |
| 69 IPT.ti,ab. (1934) |
| 70 (compassion adj2 therap$).ti,ab. (41) |
| 71 accelerated resolution.ti,ab. (86) |
| 72 sensorimotor therap$.ti,ab. (22) |
| 73 schema therapy.ti,ab. (113) |
| 74 (stress adj2 manag$).ti,ab. (5239) |
| 75 supportive therap$.ti,ab. (3938) |
| 76 Counseling/ (33,064) |
| 77 (non-directive counsel$ or non directive counsel$ or nondirective counsel$).ti,ab. (155) |
| 78 compassion therap$.ti,ab. (1) |
| 79 54 or 55 or 56 or 57 or 58 or 59 or 60 or 61 or 62 or 63 or 64 or 65 or 66 or 67 or 68 or 69 or 70 or 71 or 72 or 73 or 74 or 75 or 76 or 77 or 78 (122,833) |
| 80 33 or 53 or 79 (212,817) |
| 81 “hypnotics and sedatives”/or alprazolam/or amobarbital/or azaperone/or barbital/or bromisovalum/or chloral hydrate/or chloralose/or chlordiazepoxide/or chlormethiazole/or dexmedetomidine/or diazepam/or diphenhydramine/or eszopiclone/or ethchlorvynol/or etomidate/or etorphine/or flurazepam/or glutethimide/or hexobarbital/or lorazepam/or medazepam/or medetomidine/or mephobarbital/or meprobamate/or methapyrilene/or methaqualone/or midazolam/or nitrazepam/or oxazepam/or paraldehyde/or pentobarbital/or phenobarbital/or propofol/or secobarbital/or temazepam/or thiamylal/or thiopental/or xylazine/ (115,279) |
| 82 z drugs.ti,ab. (129) |
| 83 anti-anxiety agents/or bromazepam/or buspirone/or chlormezanone/or clorazepate dipotassium/or estazolam/or flunitrazepam/or fluvoxamine/or nordazepam/or ondansetron/or oxprenolol/or prazepam/or pregabalin/or ritanserin/or tranylcypromine/or trazodone/or triazolam/or zolazepam/ (33,247) |
| 84 benzodiazepines/or benzodiazepinones/ (23,792) |
| 85 sedative antihistamine$.ti,ab. (61) |
| 86 promethazine.ti,ab. (2067) |
| 87 antidepressive agents/or benactyzine/or clorgyline/or deanol/or desvenlafaxine succinate/or duloxetine hydrochloride/or iproniazid/or isocarboxazid/or lithium carbonate/or lithium compounds/or moclobemide/or nialamide/or phenelzine/or pizotyline/or rolipram/or sertraline/or tranylcypromine/or vilazodone hydrochloride/ (55,863) |
| 88 Imipramine/ (9836) |
| 89 mirtazapine.ti,ab. (1789) |
| 90 antipsychotic agents/or acepromazine/or aripiprazole/or azaperone/or benperidol/or butaclamol/or chlorpromazine/or chlorprothixene/or clopenthixol/or clozapine/or droperidol/or etazolate/or flupenthixol/or fluphenazine/or fluspirilene/or haloperidol/or loxapine/or lurasidone hydrochloride/or mesoridazine/or methiothepin/or methotrimeprazine/or molindone/or ondansetron/or paliperidone palmitate/or penfluridol/or perazine/or perphenazine/or pimozide/or prochlorperazine/or promazine/or quetiapine fumarate/or raclopride/or remoxipride/or reserpine/or risperidone/or ritanserin/or spiperone/or sulpiride/or thioridazine/or thiothixene/or tiapride hydrochloride/or trifluoperazine/or trifluperidol/or triflupromazine/ (115,485) |
| 91 olanzapine.ti,ab. (7626) |
| 92 anticonvulsants/or acetazolamide/or bromides/or carbamazepine/or clonazepam/or clorazepate dipotassium/or diazepam/or dimethadione/or estazolam/or ethosuximide/or flunarizine/or lorazepam/or magnesium sulfate/or medazepam/or mephenytoin/or mephobarbital/or meprobamate/or nitrazepam/or paraldehyde/or phenobarbital/or phenytoin/or pregabalin/or primidone/or riluzole/or thiopental/or tiletamine/or trimethadione/or valproic acid/or vigabatrin/ (130,525) |
| 93 antimanic agents/or lithium chloride/or lithium compounds/ (9289) |
| 94 lamotrigine.ti,ab. (4677) |
| 95 topiramate.ti,ab. (4081) |
| 96 monoamine oxidase inhibitors/or chlorphenamidine/or clorgyline/or cuprizone/or furazolidone/or harmaline/or harmine/or isocarboxazid/or moclobemide/or monocrotophos/or pargyline/or selegiline/or tranylcypromine/ (18,012) |
| 97 Prazosin/ (7586) |
| 98 N-Methyl-3,4-methylenedioxyamphetamine/ (3654) |
| 99 (MDMA or ecstasy).ti,ab. (5261) |
| 100 81 or 82 or 83 or 84 or 85 or 86 or 87 or 88 or 89 or 90 or 91 or 92 or 93 or 94 or 95 or 96 or 97 or 98 or 99 (409,556) |
| 101 19 and 80 (5684) |
| 102 19 and 100 (1860) |
| 103 101 or 102 (7197) |
| 104 Qualitative Research/ (34,279) |
| 105 interview/ (27,920) |
| 106 Grounded Theory/ (570) |
| 107 Personal Narratives/ (2920) |
| 108 Focus Groups/ (23,242) |
| 109 Hermeneutics/ (122) |
| 110 Anthropology, Cultural/ (5645) |
| 111 interview$.ti,ab. (295,531) |
| 112 ethnog$.ti,ab. (8787) |
| 113 case stud$.ti,ab. (75,187) |
| 114 grounded theory.ti,ab. (9150) |
| 115 thematic analysis.ti,ab. (9942) |
| 116 observational method$.ti,ab. (584) |
| 117 comparative method$.ti,ab. (2606) |
| 118 field notes.ti,ab. (1605) |
| 119 participant observation.ti,ab. (2952) |
| 120 narrative$.ti,ab. (26,469) |
| 121 field stud$.ti,ab. (12,896) |
| 122 audio recording.ti,ab. (240) |
| 123 focus group$.ti,ab. (34,349) |
| 124 conversation$ analysis.ti,ab. (454) |
| 125 descriptive stud$.ti,ab. (22,097) |
| 126 discourse analysis.ti,ab. (1338) |
| 127 exploratory stud$.ti,ab. (11,645) |
| 128 Hermeneutic.ti,ab. (2283) |
| 129 naturalistic.ti,ab. (8879) |
| 130 Phenomenolog$.ti,ab. (21,696) |
| 131 Participatory.ti,ab. (9369) |
| 132 Open-ended.ti,ab. (10,984) |
| 133 in-depth.ti,ab. (49,756) |
| 134 semi-structured.ti,ab. (29,761) |
| 135 key informant$.ti,ab. (5436) |
| 136 tape record$.ti,ab. (3069) |
| 137 narration.ti,ab. (467) |
| 138 104 or 105 or 106 or 107 or 108 or 109 or 110 or 111 or 112 or 113 or 114 or 115 or 116 or 117 or 118 or 119 or 120 or 121 or 122 or 123 or 124 or 125 or 126 or 127 or 128 or 129 or 130 or 131 or 132 or 133 or 134 or 135 or 136 or 137 (546,383) |
| 139 103 and 138 (951) |
| 140 (accept$ or adherence or attitude$ or belief$ or believ$ or choice$ or choos$ or drop out$ or experienc$ or feasib$ or opinion$ or perceiv$ or percept$ or prefer$ or uptake or view$ or withdraw$).ti. (680,726) |
| 141 103 and 140 (344) |
| 142 139 or 141 (1212) |
| 143 limit 142 to yr=“1992 -Current” (1151) |
PsycINFO via Ovid
Search date: 1 June 2017.
Date range searched: 1987 to May Week 4 2017.
| 1 exp Posttraumatic Stress Disorder/ (26,903) |
| 2 Complex PTSD/ (130) |
| 3 DESNOS/ (15) |
| 4 “Disorders of Extreme Distress Not Otherwise Specified”.ti,ab. (0) |
| 5 (PTSD or CPTSD).ti,ab. (25,512) |
| 6 posttrauma$.ti,ab. (26,670) |
| 7 post-trauma$.ti,ab. (11,375) |
| 8 “post trauma$”.ti,ab. (11,375) |
| 9 post traumatic stress.ti,ab. (8922) |
| 10 post traumatic stress.id. (2822) |
| 11 combat stress$.ti,ab. (450) |
| 12 combat disorder$.ti,ab. (12) |
| 13 DESNOS.ti,ab. (54) |
| 14 complex trauma$.ti,ab. (527) |
| 15 (complex adj2 trauma$).ti,ab. (699) |
| 16 traumatic stress.ti,ab. (11,652) |
| 17 traumatic memor$.ti,ab. (1271) |
| 18 traumatization.ti,ab. (1431) |
| 19 traumatisation.ti,ab. (155) |
| 20 (trauma adj2 (expos$ or event$ or experienc$)).ti,ab. (6690) |
| 21 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 (46,932) |
| 22 exp Cognitive Therapy/ (11,610) |
| 23 cognitive behaviour$ therapy.ti,ab. (3892) |
| 24 cognitive behavior$ therapy.ti,ab. (12,974) |
| 25 cognitive restructuring.ti,ab. (1765) |
| 26 cognitive rescripting.ti,ab. (0) |
| 27 cognitive processing therapy.ti,ab. (277) |
| 28 CPT.ti,ab. (1871) |
| 29 cognitive therapy.ti,ab. (5079) |
| 30 cognitive behavioural treatment$.ti,ab. (521) |
| 31 cognitive behavioral treatment$.ti,ab. (2909) |
| 32 (CBT or TFCBT).ti,ab. (10,696) |
| 33 cognitive trauma therapy.ti,ab. (8) |
| 34 trauma focus$ CBT.ti,ab. (57) |
| 35 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 (32,467) |
| 36 exp Behavior Therapy/ (11,576) |
| 37 (behavior$ adj2 (therap$ or treat$ or modif$)).ti,ab. (33,755) |
| 38 (behaviour$ adj2 (therap$ or treat$ or modif$)).ti,ab. (6941) |
| 39 (dialectical behavio$ therap$ or dialectical behavio$ treat$).ti,ab. (1477) |
| 40 DBT.ti,ab. (1136) |
| 41 biofeedback, psychology/or feedback, sensory/or neurofeedback/ (1224) |
| 42 (biofeedback or neurofeedback or sensory feedback).ti,ab. (4469) |
| 43 desensitization, psychologic/or eye movement desensitization reprocessing/or implosive therapy/or virtual reality exposure therapy/ (152) |
| 44 (psychological adj2 desensiti$).ti,ab. (3) |
| 45 Eye Movement Desensitization Therapy/ (1241) |
| 46 eye movement desensiti?ation reprocessing.ti,ab. (61) |
| 47 EMDR.ti,ab. (1367) |
| 48 Exposure Therapy/ (1988) |
| 49 (exposure adj (therap$ or treat$)).ti,ab. (2129) |
| 50 prolonged exposure therap$.ti,ab. (153) |
| 51 live exposure.ti,ab. (21) |
| 52 imaginal exposure.ti,ab. (267) |
| 53 imaginal flooding.ti,ab. (21) |
| 54 exposure inhibition therap$.ti,ab. (1) |
| 55 implosive therap$.ti,ab. (29) |
| 56 image habituation.ti,ab. (5) |
| 57 inoculation training.ti,ab. (226) |
| 58 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49 or 50 or 51 or 52 or 53 or 54 or 55 or 56 or 57 (51,566) |
| 59 (acceptance adj2 therap$).ti,ab. (347) |
| 60 (commitment adj2 therap$).ti,ab. (1499) |
| 61 Hypnosis/(3983) |
| 62 (hypnosis or hypnotherap$).ti,ab. (6655) |
| 63 Mindfulness/ (6716) |
| 64 mindfulness.ti,ab. (8233) |
| 65 (supportive adj (therap$ or psychotherap$)).ti,ab. (1186) |
| 66 (non-directive adj (counselling or counseling)).ti,ab. (40) |
| 67 (nondirective adj (counselling or counseling)).ti,ab. (52) |
| 68 (non directive adj (counselling or counseling)).ti,ab. (40) |
| 69 psychodynamic therap$.ti,ab. (1267) |
| 70 inter personal psychotherap$.ti,ab. (1) |
| 71 interpersonal psychotherap$.ti,ab. (1175) |
| 72 interpersonal therapy.ti,ab. (502) |
| 73 IPT.ti,ab. (963) |
| 74 (compassion adj2 therap$).ti,ab. (107) |
| 75 accelerated resolution.ti,ab. (9) |
| 76 sensorimotor therap$.ti,ab. (9) |
| 77 schema therapy.ti,ab. (321) |
| 78 Stress Management/ (4239) |
| 79 Supportive Psychotherapy/ (461) |
| 80 Group Psychotherapy/ (12,925) |
| 81 Counseling/ (15,966) |
| 82 (non-directive counsel$ or non directive counsel$ or nondirective counsel$).ti,ab. (92) |
| 83 compassion therap$.ti,ab. (4) |
| 84 59 or 60 or 61 or 62 or 63 or 64 or 65 or 66 or 67 or 68 or 69 or 70 or 71 or 72 or 73 or 74 or 75 or 76 or 77 or 78 or 79 or 80 or 81 or 82 or 83 (53,717) |
| 85 35 or 58 or 84 (108,582) |
| 86 21 and 85 (5589) |
| 87 hypnotic drugs/or amobarbital/or apomorphine/or barbital/or chloral hydrate/or codeine/or flurazepam/or glutethimide/or hexobarbital/or meprobamate/or methaqualone/or nitrazepam/or pentobarbital/or phenobarbital/or secobarbital/or thalidomide/or thiopental/or triazolam/ (3430) |
| 88 hypnotics.ti,ab. (1260) |
| 89 hypnotic drug$.ti,ab. (286) |
| 90 z drug$.ti,ab. (44) |
| 91 tranquilizing drugs/or amitriptyline/or benactyzine/or doxepin/or haloperidol/or meprobamate/or minor tranquilizers/or neuroleptic drugs/or phenothiazine derivatives/or pimozide/or thiothixene/ (21,857) |
| 92 exp benzodiazepines/ (7742) |
| 93 sedative antihistamine$.ti,ab. (13) |
| 94 promethazine.ti,ab. (125) |
| 95 antidepressant drugs/or bupropion/or citalopram/or fluoxetine/or fluvoxamine/or iproniazid/or isocarboxazid/or lithium carbonate/or methylphenidate/or mianserin/or moclobemide/or molindone/or nefazodone/or nialamide/or nomifensine/or paroxetine/or phenelzine/or pheniprazine/or pipradrol/or serotonin norepinephrine reuptake inhibitors/or sertraline/or sulpiride/or tranylcypromine/or trazodone/or tricyclic antidepressant drugs/or venlafaxine/or zimeldine/ (28,111) |
| 96 Imipramine.ti,ab. (2559) |
| 97 mirtazapine.ti,ab. (1118) |
| 98 neuroleptic drugs/or aripiprazole/or clozapine/or molindone/or nialamide/or olanzapine/or quetiapine/or reserpine/or risperidone/or spiroperidol/or sulpiride/or tetrabenazine/ (25,765) |
| 99 mood stabilizers/or anticonvulsive drugs/or carbamazepine/or lithium/or valproic acid/ (11,793) |
| 100 mood stabilisers.ti,ab. (144) |
| 101 antiepileptics.ti,ab. (281) |
| 102 lamotrigine.ti,ab. (1802) |
| 103 topiramate.ti,ab. (1501) |
| 104 valproate.ti,ab. (2716) |
| 105 monoamine oxidase inhibitors/or iproniazid/or isocarboxazid/or moclobemide/or nialamide/or pargyline/or phenelzine/or pheniprazine/or tranylcypromine/ (1627) |
| 106 antihypertensive drugs/or alpha methylparatyrosine/or captopril/or chlorpromazine/or clonidine/or guanethidine/or hexamethonium/or hydralazine/or mecamylamine/or methyldopa/or phenoxybenzamine/or quinpirole/ (2481) |
| 107 alpha blocker anti-hypertensive$.ti,ab. (0) |
| 108 alpha blocker antihypertensive$.ti,ab. (0) |
| 109 prazosin.ti,ab. (579) |
| 110 Methylenedioxymethamphetamine/ (1926) |
| 111 (mdma or ecstasy).ti,ab. (2879) |
| 112 87 or 88 or 89 or 90 or 91 or 92 or 93 or 94 or 95 or 96 or 97 or 98 or 99 or 100 or 101 or 102 or 103 or 104 or 105 or 106 or 107 or 108 or 109 or 110 or 111 (83,790) |
| 113 21 and 112 (1054) |
| 114 86 or 113 (6545) |
| 115 Qualitative Research/ (7366) |
| 116 exp INTERVIEWS/ (9209) |
| 117 exp ETHNOGRAPHY/ (7251) |
| 118 exp Grounded Theory/ (3212) |
| 119 exp Observation Methods/ (3079) |
| 120 exp NARRATIVES/ (16,768) |
| 121 exp Audiotapes/ (250) |
| 122 exp Discourse Analysis/ (7393) |
| 123 conversation/ (7816) |
| 124 exp HERMENEUTICS/ (1857) |
| 125 exp PHENOMENOLOGY/ (10,792) |
| 126 exp Participation/ (11,842) |
| 127 exp Informants/ (734) |
| 128 anthropology/ (4659) |
| 129 case stud$.ti,ab. (74,204) |
| 130 thematic analysis.ti,ab. (7137) |
| 131 comparative method$.ti,ab. (1958) |
| 132 field notes.ti,ab. (3029) |
| 133 audio recording.ti,ab. (214) |
| 134 focus group$.ti,ab. (27,182) |
| 135 conversation$ analysis.ti,ab. (1659) |
| 136 descriptive study.ti,ab. (5331) |
| 137 exploratory stud$.ti,ab. (12,989) |
| 138 naturalistic.ti,ab. (11,518) |
| 139 (open-ended or in-depth).ti,ab. (52,099) |
| 140 semi-structured.ti,ab. (26,340) |
| 141 key informant$.ti,ab. (2662) |
| 142 tape record$.ti,ab. (1949) |
| 143 narration.ti,ab. (1417) |
| 144 115 or 116 or 117 or 118 or 119 or 120 or 121 or 122 or 123 or 124 or 125 or 126 or 127 or 128 or 129 or 130 or 131 or 132 or 133 or 134 or 135 or 136 or 137 or 138 or 139 or 140 or 141 or 142 or 143 (271,473) |
| 145 114 and 144 (652) |
| 146 (accept$ or adherence or attitude$ or belief$ or believ$ or choice$ or choos$ or drop out$ or experienc$ or feasib$ or opinion$ or perceiv$ or percept$ or prefer$ or uptake or view$ or withdraw$).ti. (288,349) |
| 147 114 and 146 (346) |
| 148 145 or 147 (947) |
| 149 limit 148 to yr=“1992 -Current” (919) |
Appendix 3 List of studies excluded, with reasons
| Authors (year) | Reason for exclusion |
|---|---|
| Abramowitz et al. (2008)188 | Intervention did not meet criteria |
| Acierno et al. (2016)189 | Intervention did not meet criteria |
| Aderka et al. (2013)190 | Population did not meet criteria |
| Adler et al. (2009)191 | Intervention did not meet criteria |
| Alderman et al. (2009)192 | Study design did not meet criteria |
| Alderman et al. (2009)193 | Study design did not meet criteria |
| Allan et al. (2015)194 | Study design did not meet criteria |
| Allon (2015)195 | Population did not meet criteria |
| Alvarez et al. (2011)196 | Study design did not meet criteria |
| Amin et al. (2013)197 | Article is a conference abstract |
| Angelo et al. (2008)198 | Study design did not meet criteria |
| Arntz et al. (2007)199 | Population did not meet criteria |
| Ayoughi et al. (2012)200 | Study design did not meet criteria |
| Baños et al. (2011)201 | Population did not meet criteria |
| Basharpoor et al. (2011)202 | Population did not meet criteria |
| Bass et al. (2013)203 | Population did not meet criteria |
| Batka et al. (2016)204 | Intervention did not meet criteria |
| Benedek (2011)205 | Study design did not meet criteria |
| Bensimon et al. (2012)206 | Intervention did not meet criteria |
| Betancourt et al. (2014)207 | Population did not meet criteria |
| Bisson (2003)208 | Study design did not meet criteria |
| Bisson (2007)209 | Population did not meet criteria |
| Blevins et al. (2011)210 | Intervention did not meet criteria |
| Bohus et al. (2013)211 | Population did not meet criteria |
| Bolton et al. (2014)212 | Population did not meet criteria |
| Bomyea et al. (2015)213 | Population did not meet criteria |
| Bormann et al. (2008)214 | Intervention did not meet criteria |
| Bormann et al. (2013)215 | Intervention did not meet criteria |
| Bormann et al. (2014)216 | Article is a conference abstract |
| Bradley and Follingstad (2003)217 | Population did not meet criteria |
| Brady et al. (2000)218 | Population did not meet criteria |
| Bremner et al. (2004)219 | Study design did not meet criteria |
| Bremner et al. (2011)220 | Article is a conference abstract |
| Brown et al. (2014)221 | Intervention did not meet criteria |
| Bryan et al. (2016)222 | Study design did not meet criteria |
| Bui et al. (2016)223 | Article is a conference abstract |
| Byers et al. (2010)224 | Study design did not meet criteria |
| Byers (2010)225 | Study design did not meet criteria |
| Campbell et al. (2016)226 | Intervention did not meet criteria |
| Carlson et al. (1998)157 | Duplicate article |
| Carr et al. (2012)227 | Intervention did not meet criteria |
| Castillo et al. (2016)228 | Population did not meet criteria |
| Cates et al. (2004)229 | Study design did not meet criteria |
| Celik et al. (2011)65 | Duplicate article |
| Chemtob et al. (1997)230 | Population did not meet criteria |
| Chen et al. (2013)231 | Outcomes did not meet criteria |
| Chesney et al. (2014)232 | Article is a conference abstract |
| Church et al. (2013)233 | Intervention did not meet criteria |
| Church (2014)234 | Study design did not meet criteria |
| Clark et al. (1999)235 | Study design did not meet criteria |
| Classen et al. (2011)236 | Population did not meet criteria |
| Cloitre and Koenen (2001)237 | Study design did not meet criteria |
| Cole et al. (2007)238 | Population did not meet criteria |
| Connolly and Sakai (2011)239 | Intervention did not meet criteria |
| Cort et al. (2014)240 | Study design did not meet criteria |
| Coulter (2010)241 | Intervention did not meet criteria |
| Crespo and Arinero (2010)242 | Population did not meet criteria |
| David et al. (2006)243 | Study design did not meet criteria |
| Davidson et al. (1993)244 | Study design did not meet criteria |
| Davidson et al. (2001)245 | Population did not meet criteria |
| Davidson et al. (2001)246 | Population did not meet criteria |
| Davis et al. (2000)247 | Study design did not meet criteria |
| Davis et al. (2004)73 | Duplicate article |
| Davis et al. (2008)72 | Duplicate article |
| Davis et al. (2011)248 | Population did not meet criteria |
| Dawson et al. (2016)249 | Population did not meet criteria |
| Dempsey et al. (2014)233 | Article is a conference abstract |
| Dieperink et al. (2008)250 | Intervention did not meet criteria |
| Difede et al. (2014)251 | Population did not meet criteria |
| Dorrepaal et al. (2012)252 | Population did not meet criteria |
| Dorrepaal et al. (2013)253 | Outcomes did not meet criteria |
| Doruk et al. (1999)254 | Non-English language article |
| Dougherty (2002)255 | Population did not meet criteria |
| Drozdek (1997)256 | Study design did not meet criteria |
| Droždek and Bolwerk (2010)257 | Intervention did not meet criteria |
| Drožđek et al. (2012)258 | Intervention did not meet criteria |
| Duffy and Malloy (1994)259 | Study design did not meet criteria |
| Duffy et al. (2007)260 | Population did not meet criteria |
| Dunn et al. (2007)261 | Population did not meet criteria |
| Durham et al. (2005)262 | Study design did not meet criteria |
| Echeburúa et al. (1997)263 | Population did not meet criteria |
| Echeburúa et al. (2014)264 | Comparator did not meet criteria |
| Edmond et al. (2004)265 | Outcomes did not meet criteria |
| Ekstrom et al. (2016)266 | Article is a conference abstract |
| Ekstrom et al. (2016)267 | Article is a conference abstract |
| Elkjaer et al. (2012)268 | Article is a conference abstract |
| Ertl et al. (2011)269 | Population did not meet criteria |
| Esala et al. (2017)270 | Intervention did not meet criteria |
| Falsetti et al. (2003)271 | Population did not meet criteria |
| Farchi and Gidron (2010)272 | Intervention did not meet criteria |
| Fiorillo et al. (2017)273 | Study design did not meet criteria |
| Foa et al. (1991)274 | Population did not meet criteria |
| Foa et al. (1999)275 | Population did not meet criteria |
| Foa et al. (2005)276 | Population did not meet criteria |
| Forbes et al. (2001)277 | Study design did not meet criteria |
| Forbes et al. (2008)278 | Population did not meet criteria |
| Forbes et al. (2012)279 | Population did not meet criteria |
| Ford et al. (2011)280 | Population did not meet criteria |
| Fortney et al. (2015)281 | Intervention did not meet criteria |
| Fortney et al. (2015)282 | Intervention did not meet criteria |
| Frommberger et al. (2004)283 | Population did not meet criteria |
| Galovski et al. (2009)284 | Study design did not meet criteria |
| Galovski et al. (2012)285 | Population did not meet criteria |
| Gamito et al. (2009)286 | Study design did not meet criteria |
| Garfield et al. (2001)287 | Study design did not meet criteria |
| Gatz et al. (2007)288 | Population did not meet criteria |
| Gebler and Maercker (2007)289 | Non-English language article |
| Gelpin et al. (1996)290 | Population did not meet criteria |
| Gillin et al. (2001)291 | Study design did not meet criteria |
| Ginsberg (2003)292 | Study design did not meet criteria |
| Ginzburg et al. (2009)293 | Outcomes did not meet criteria |
| Glover (1993)294 | Study design did not meet criteria |
| Glynn et al. (1999)295 | Intervention did not meet criteria |
| Goldberg et al. (2003)296 | Study design did not meet criteria |
| Gosselin et al. (2016)297 | Article is a conference abstract |
| Graham-Bermann and Miller (2013)298 | Intervention did not meet criteria |
| Gray et al. (2012)299 | Study design did not meet criteria |
| Gros et al. (2011)300 | Comparator did not meet criteria |
| Gros et al. (2011)301 | Comparator did not meet criteria |
| Gutner et al. (2013)302 | Population did not meet criteria |
| Hall et al. (2014)303 | Outcomes did not meet criteria |
| Hamner (1996)304 | Article is a letter to the editor |
| Hamner et al. (2003)305 | Study design did not meet criteria |
| Harris et al. (2011)306 | Intervention did not meet criteria |
| Haynes et al. (2012)307 | Article is a conference abstract |
| Hébert and Bergeron (2007)308 | Population did not meet criteria |
| Held and Owens (2015)309 | Population did not meet criteria |
| Hensel-Dittmann et al. (2011)310 | Population did not meet criteria |
| Hertzberg et al. (2000)311 | Population did not meet criteria |
| Hertzberg et al. (2002)312 | Study design did not meet criteria |
| Hijazi et al. (2013)313 | Article is a conference abstract |
| Hobfoll et al. (2016)314 | Population did not meet criteria |
| Holliday et al. (2015)315 | Population did not meet criteria |
| Hopton and Huta (2013)316 | Population did not meet criteria |
| Hughes and Rasmussen (2010)162 | Study design did not meet criteria |
| Igreja et al. (2004)317 | Intervention did not meet criteria |
| Ironson et al. (2002)318 | Population did not meet criteria |
| Ivarsson et al. (2014)319 | Population did not meet criteria |
| Iverson et al. (2011)320 | Outcomes did not meet criteria |
| Jaberghaderi et al. (2002)321 | Population did not meet criteria |
| Jain et al. (2012)322 | Intervention did not meet criteria |
| Jenkins et al. (2014)323 | Article is a conference abstract |
| Jerud et al. (2014)324 | Population did not meet criteria |
| Jetly et al. (2015)325 | Study design did not meet criteria |
| Johnson et al. (2011)326 | Population did not meet criteria |
| Kaiser et al. (2010)327 | Outcomes did not meet criteria |
| Karatzias et al. (2016)328 | Study design did not meet criteria |
| Kaslow et al. (2010)329 | Population did not meet criteria |
| Kelly et al. (2016)330 | Article is a conference abstract |
| Kelly and Garland (2016)331 | Population did not meet criteria |
| Khazaie et al. (2016)332 | Population did not meet criteria |
| King et al. (2011)333 | Article is a conference abstract |
| King et al. (2016)334 | Population did not meet criteria |
| King et al. (2016)335 | Population did not meet criteria |
| Kip et al. (2013)336 | Population did not meet criteria |
| Kip et al. (2014)337 | Outcomes did not meet criteria |
| Kluepfel et al. (2013)338 | Population did not meet criteria |
| Koehn (2007)339 | Study design did not meet criteria |
| Kozarić-Kovacić et al. (2005)340 | Study design did not meet criteria |
| Kozaric-Kovacic and Pivac (2007)341 | Study design did not meet criteria |
| Kozel et al. (2016)342 | Article is a conference abstract |
| Krakow et al. (2000)343 | Population did not meet criteria |
| Krakow et al. (2001)344 | Population did not meet criteria |
| Kreidler (2005)345 | Population did not meet criteria |
| Krüger et al. (2014)346 | Population did not meet criteria |
| Krystal et al. (2011)99 | Population did not meet criteria |
| Kuckertz et al. (2014)347 | Population did not meet criteria |
| Labrador et al. (2006)348 | Non-English language article |
| Lampe et al. (2008)349 | Non-English language article |
| Lang et al. (2012)350 | Article is a study protocol |
| Lange et al. (2001)351 | Population did not meet criteria |
| Lange et al. (2003)352 | Population did not meet criteria |
| Lange et al. (2003)353 | Population did not meet criteria |
| Largo-Marsh (1996)354 | Article is a dissertation |
| Liebling et al. (2016)355 | Intervention did not meet criteria |
| Liedl et al. (2011)356 | Retracted study |
| Lim et al. (2014)357 | Article is a conference abstract |
| Littleton et al. (2016)358 | Population did not meet criteria |
| Litz et al. (2007)359 | Population did not meet criteria |
| Litz et al. (2012)360 | Population did not meet criteria |
| Long et al. (2011)361 | Study design did not meet criteria |
| Macdonald et al. (2011)362 | Population did not meet criteria |
| Macklin et al. (2000)363 | Study design did not meet criteria |
| Manteghi et al. (2014)364 | Study design did not meet criteria |
| Margolies et al. (2013)159 | Duplicate article |
| Martenyi et al. (2002)365 | Population did not meet criteria |
| Martenyi et al. (2006)366 | Study design did not meet criteria |
| Matud et al. (2016)367 | Non-English language article |
| Mauritz et al. (2016)368 | Article is a study protocol |
| McFall et al. (2005)369 | Intervention did not meet criteria |
| McGlinchey et al. (2014)370 | Intervention did not meet criteria |
| McWhirter (2011)371 | Population did not meet criteria |
| Mehling et al. (2016)372 | Article is a conference abstract |
| Mehta et al. (2012)373 | Article is a conference abstract |
| Mello et al. (2009)374 | Article is a study protocol |
| Mithoefer et al. (2011)375 | Population did not meet criteria |
| Monson et al. (2006)376 | Population did not meet criteria |
| Monson et al. (2012)377 | Intervention did not meet criteria |
| Morland et al. (2010)378 | Comparator did not meet criteria |
| Morland et al. (2011)379 | Comparator did not meet criteria |
| Morland et al. (2014)380 | Comparator did not meet criteria |
| Morland et al. (2015)381 | Comparator did not meet criteria |
| Moser et al. (2010)382 | Comparator did not meet criteria |
| Mughal et al. (2015)383 | Intervention did not meet criteria |
| Murray et al. (2016)384 | Outcomes did not meet criteria |
| Muzik et al. (2015)385 | Intervention did not meet criteria |
| Nacasch et al. (2011)386 | Population did not meet criteria |
| Nagy et al. (1993)387 | Study design did not meet criteria |
| Nakamura et al. (2011)388 | Intervention did not meet criteria |
| Neuner et al. (2010)389 | Population did not meet criteria |
| Neylan et al. (2001)390 | Study design did not meet criteria |
| Neylan et al. (2003)391 | Study design did not meet criteria |
| Nijdam et al. (2012)392 | Population did not meet criteria |
| Niles et al. (2012)160 | Article is a conference abstract |
| Niles et al. (2013)393 | Outcomes did not meet criteria |
| Nishith et al. (1999)394 | Population did not meet criteria |
| Nishith et al. (2015)395 | Study design did not meet criteria |
| Ochsner Margolies et al. (2012)396 | Article is a conference abstract |
| Oman and Bormann (2015)397 | Intervention did not meet criteria |
| Padala (2006)398 | Study design did not meet criteria |
| Padala et al. (2006)399 | Population did not meet criteria |
| Paivio et al. (2010)400 | Comparator did not meet criteria |
| Paunovic (2011)401 | Population did not meet criteria |
| Peskind et al. (2003)402 | Study design did not meet criteria |
| Petty et al. (2001)403 | Study design did not meet criteria |
| Pigeon et al. (2009)404 | Study design did not meet criteria |
| Pigeon et al. (2015)405 | Article is a conference abstract |
| Pivac and Kozarić-Kovacić (2006)406 | Study design did not meet criteria |
| Pokhariyal et al. (2012)407 | Population did not meet criteria |
| Pollack et al. (2011)408 | Population did not meet criteria |
| Possemato et al. (2011)409 | Intervention did not meet criteria |
| Possemato et al. (2016)410 | Comparator did not meet criteria |
| Price (2005)411 | Intervention did not meet criteria |
| Price (2006)412 | Intervention did not meet criteria |
| Pruiksma et al. (2012)413 | Article is a conference abstract |
| Pruiksma et al. (2013)414 | Article is a conference abstract |
| Ragsdale et al. (1996)415 | Population did not meet criteria |
| Rahman et al. (2016)416 | Population did not meet criteria |
| Randall et al. (1995)417 | Study design did not meet criteria |
| Raskind et al. (2003)418 | Study design did not meet criteria |
| Raskind et al. (2012)419 | Article is a conference abstract |
| Raskind et al. (2013)123 | Duplicate article |
| Raskind (2014)420 | Article is a conference abstract |
| Rauch et al. (2014)421 | Article is a conference abstract |
| Rauch et al. (2015)422 | Population did not meet criteria |
| Ready et al. (2006)423 | Study design did not meet criteria |
| Reed (2004)424 | Article is a dissertation |
| Renner et al. (2011)425 | Intervention did not meet criteria |
| Resick and Schnicke (1992)426 | Population did not meet criteria |
| Resick et al. (2002)427 | Population did not meet criteria |
| Resick et al. (2003)428 | Study design did not meet criteria |
| Resick et al. (2008)429 | Comparator did not meet criteria |
| Resick et al. (2017)430 | Comparator did not meet criteria |
| Rimane and Rosner (2013)431 | Article is a study protocol |
| Robert et al. (2009)432 | Study design did not meet criteria |
| Rodgman et al. (2016)433 | Study design did not meet criteria |
| Rosenbaum et al. (2015)434 | Intervention did not meet criteria |
| Rothbaum (1997)435 | Population did not meet criteria |
| Rothbaum et al. (2001)436 | Study design did not meet criteria |
| Rothbaum et al. (2005)437 | Population did not meet criteria |
| Rothbaum et al. (2008)438 | Study design did not meet criteria |
| Rothbaum et al. (2014)129 | Study design did not meet criteria |
| Ryan et al. (2005)439 | Intervention did not meet criteria |
| Sachsse et al. (2006)440 | Study design did not meet criteria |
| Sack et al. (2017)441 | Outcomes did not meet criteria |
| Salloum et al. (2015)442 | Intervention did not meet criteria |
| Sautter et al. (2015)443 | Intervention did not meet criteria |
| Schaal et al. (2009)444 | Comparator did not meet criteria |
| Schnurr et al. (2003)445 | Population did not meet criteria |
| Schnurr et al. (2007)446 | Population did not meet criteria |
| Schnurr et al. (2009)447 | Outcomes did not meet criteria |
| Schnurr and Lunney (2015)448 | Study design did not meet criteria |
| Schnurr and Lunney (2016)449 | Study design did not meet criteria |
| Seppälä et al. (2014)450 | Intervention did not meet criteria |
| Sezgin and Punamäki (2008)451 | Study design did not meet criteria |
| Shearing et al. (2011)452 | Population did not meet criteria |
| Short (2005)453 | Study design did not meet criteria |
| Silver et al. (1995)454 | Study design did not meet criteria |
| Skinhoj et al. (2001)455 | Study design did not meet criteria |
| Smith et al. (2012)456 | Study design did not meet criteria |
| Spence et al. (2014)457 | Population did not meet criteria |
| Spiegel et al. (2004)458 | Study design did not meet criteria |
| Stade et al. (2015)459 | Intervention did not meet criteria |
| Stalker and Fry (1999)460 | Study design did not meet criteria |
| Steil et al. (2011)461 | Article is a conference abstract |
| Stein et al. (2006)462 | Study design did not meet criteria |
| Steinert et al. (2017)463 | Population did not meet criteria |
| Steuwe et al. (2016)464 | Study design did not meet criteria |
| Stovall-McClough and Cloitre (2003)465 | Study design did not meet criteria |
| Su et al. (2007)466 | Non-English language article |
| Sulejmanpasic-Arslanagic and Bise Srebrenka (2015)467 | Article is a conference abstract |
| Surís et al. (2010)468 | Intervention did not meet criteria |
| Surís et al. (2013)469 | Population did not meet criteria |
| Swanson et al. (2009)470 | Study design did not meet criteria |
| Taing et al. (2011)471 | Article is a conference abstract |
| Talbot et al. (2011)472 | Population did not meet criteria |
| Talbot et al. (2014)473 | Population did not meet criteria |
| Tan et al. (2011)474 | Comparator did not meet criteria |
| Tarquinio et al. (2012)475 | Population did not meet criteria |
| Tarrier and Sommerfield (2004)476 | Population did not meet criteria |
| Thomaes et al. (2015)477 | Non-English language article |
| Thorp et al. (2012)478 | Study design did not meet criteria |
| Tourigny et al. (2005)479 | Non-English language article |
| Truijens and Van Emmerik (2014)480 | Population did not meet criteria |
| van den Berg and van der Gaag (2012)481 | Population did not meet criteria |
| van der Kolk et al. (2007)482 | Population did not meet criteria |
| van Emmerik et al. (2008)483 | Population did not meet criteria |
| Vera et al. (2011)484 | Population did not meet criteria |
| Villarreal et al. (2007)485 | Study design did not meet criteria |
| Villarreal et al. (2010)486 | Study design did not meet criteria |
| Vitriol et al. (2009)487 | Intervention did not meet criteria |
| Weine et al. (2008)488 | Intervention did not meet criteria |
| Wells and Colbear (2012)489 | Population did not meet criteria |
| Westbury and Tutty (1999)490 | Intervention did not meet criteria |
| Wood et al. (2011)491 | Study design did not meet criteria |
| Yeh et al. (2011)492 | Population did not meet criteria |
| Yehua (2003)493 | Study design did not meet criteria |
| Yehuda et al. (2015)494 | Population did not meet criteria |
| Yuen et al. (2015)495 | Comparator did not meet criteria |
| Ziemba (et al. 2014)496 | Comparator did not meet criteria |
| Zimmermann et al. (2005)497 | Non-English language article |
| Zimmermann et al. (2007)498 | Study design did not meet criteria |
| Zisook et al. (2000)499 | Study design did not meet criteria |
| Zlotnick et al. (2011)500 | Population did not meet criteria |
| Zoellner et al. (1999)501 | Population did not meet criteria |
| Zohar et al. (2002)147 | Duplicate article |
Appendix 4 Characteristics of randomised controlled trials included
| Authors (year) | Intervention(s) | Intervention category; superordinate category | Control(s) | Intensity (duration, frequency and length of sessions) | Delivery (method, setting and type of professional) |
|---|---|---|---|---|---|
| Acarturk et al. (2015)53 | EMDR | EMDR; SCTF | Waitlist |
Duration: NR Frequency: NR Length of sessions: seven sessions, 90 minutes each |
Face to face; community/refugee camp; Turkish psychologists trained at level 1 EMDR, supervised by EMDR institute accredited trainer |
| Acarturk et al. (2016)54 | EMDR | EMDR; SCTF | Waitlist |
Duration: 5 weeks Frequency: NR Length of sessions: NR |
Face to face/online; community/refugee camp; psychologists trained in EMDR |
| Adenauer et al. (2011)55 | NET | TFCBT; SCTF | Waitlist |
Duration: NR Frequency: weekly or biweekly Length of sessions: 12 sessions, average length 108 minutes (SD 17 minutes) |
Face to face; setting NR; clinical psychologists |
| Azad Marzabadi and Hashemi Zadeh (2014)57 | MBSR | Mindfulness; SCNTF | Waitlist/continued treatment |
Duration: 4 weeks Frequency: twice a week Length of sessions: eight sessions, 90 minutes each |
Face to face; hospital; psychologist |
| Bichescu et al. (2007)61 | NET | TFCBT; MCTF | Psychoeducation |
Duration: 5 weeks Frequency: weekly or biweekly Length of sessions: 120 minutes |
Face to face, individual; setting NR; trained PhD psychology student |
| Beidel et al. (2011)60 | Trauma management therapy with exposure | TFCBT; MCTF |
Duration: 17 weeks Frequency: exposure three times per week; social and emotional rehabilitation twice a week (2 weeks), weekly for 10 weeks Length of sessions: 14 sessions of exposure, length NR. Social and emotional rehabilitation 90 minutes |
Face to face, individual and group; setting NR; doctoral-level therapists | |
| Exposure-only therapy | Exposure only |
Duration: 17 weeks Frequency: three times per week Length of sessions:14 sessions of exposure, 14 sessions of psychoeducation |
|||
| Bolton et al. (2014)62 | Behavioural activation treatment for depression | NTFCBT; SCNTF | Waitlist |
Duration: NR Frequency: NR Length of sessions: 12 sessions, length NR |
Face to face, individual; primary health clinics and one outpatient clinic; community mental health workers (nurses, pharmacist assistants or physician assistants) with a mental health background |
| CPT | TFCBT; SCTF |
Duration: NR Frequency: NR Length of sessions: 12 sessions, length NR |
|||
| Buhmann et al. (2016)63 | CBT | TFCBT; NA | Waitlist |
Duration: 6 months Frequency: weekly Length of sessions: 16 sessions, length NR |
Face to face; mental health clinic; doctors and therapists with mental health background |
| Carlson et al. (1997)64 | EMDR biofeedback relaxation | EMDR; SCTF | Waitlist |
Duration: 6 weeks Frequency: twice a week Length of sessions: 12 sessions, 60–75 minutes each |
Face to face, individual; clinic based; experienced therapists, EMDR trained therapists with research and clinical backgrounds |
| Biofeedback relaxation | NTFCBT; SCNTF |
Duration: 6 weeks Frequency: twice a week Length of sessions: 12 sessions, 40 minutes each |
Face to face, individual; clinic based; experienced therapists with behavioural, psychodynamic and biofeedback backgrounds | ||
| Chard (2005)66 | CPT for sexual abuse survivors | TFCBT; MCTF | Waitlist |
Duration: 17 weeks Frequency: weekly individual and group sessions Length of sessions: group sessions 90 minutes, individual sessions 60 minutes |
Face to face, individual and group; Centre for Traumatic Stress Studies; graduate psychology students with background in behavioural interventions and mental health |
| Classen et al. (2001)68 | Trauma-focused therapy | NA; NA (data were presented together) | Waitlist |
Duration: 24 weeks Frequency: weekly Length of sessions: 90 minutes |
Face to face, group; setting NR; experienced group leaders supervised by an expert in trauma (therapists included psychologists and one licensed MFCC) |
| Present-centred therapy |
Duration: 24 weeks Frequency: weekly Length of sessions: 90 minutes |
||||
| Cloitre et al. (2002)69 | STAIR-modified PE | DBT; MCTF | Minimal attention waitlist and support/exposure |
Duration: 12 weeks Frequency: weekly STAIR/twice weekly modified PE Length of sessions: 16 sessions, STAIR 60 minutes, modified PE 90 minutes |
Face to face, individual; setting NR; clinical psychologist |
| STAIR/exposure | DBT; MCTF |
Duration: 16 weeks Frequency: weekly Length of sessions: NR |
Face to face, individual; setting NR; master’s/doctorate psychologist/social work staff/expert clinicians with mental health backgrounds | ||
| STAIR/support | DBT; MCNTF |
Duration: 16 weeks Frequency: weekly Length of sessions: NR |
Face to face, individual; setting NR; master’s/doctorate psychologist/social work staff/expert clinicians with mental health backgrounds | ||
| Cook et al. (2010)71 | Imagery rehearsal therapy | TFCBT; MCTF |
Duration: 6 weeks Frequency: weekly Length of sessions: 90 minutes |
Face to face, group; setting NR; psychologists and psychiatric nurse | |
| Sleep and nightmare management |
Duration: 6 weeks Frequency: weekly Length of sessions: 90 minutes |
||||
| Devilly et al. (1998)74 | EMDR | EMDR; SCTF | Standard psychiatric support |
Duration: NR Frequency: NR Length of sessions: two sessions, 90 minutes |
Face to face, individual; setting NR; active clinician trained by Shapiro502 |
| Reactive eye dilatation desensitisation and reprocessing | EMDR; SCTF |
Duration: NR Frequency: NR Length of sessions: two sessions, 90 minutes |
|||
| Edmond et al. (1999)76 | EMDR | EMDR; SCTF | Delayed treatment |
Duration: 6 weeks Frequency: weekly Length of sessions: 90 minutes |
Face to face; setting NR; white female master’s-level therapists |
| Routine individual treatment |
Duration: 6 weeks Frequency: weekly Length of sessions: 90 minutes |
||||
| Engel et al. (2015)78 | Delivery of self training and education for stressful situations (DESTRESS-PC) | NTFCBT; SCNTF | Optimised usual care |
Duration: 6 weeks Frequency: three times per week Length of sessions: 18 sessions, log in 15–30 minutes, homework 30 minutes |
Computer/telephone; remote setting; online/nurse support |
| Feske (2008)79 | PE | TFCBT; SCTF | Treatment as usual |
Duration: 12 weeks Frequency: weekly Length of sessions: 9–12 total sessions, PE 90 minutes, treatment as usual 60 minutes |
Face to face, individual (individual and group for controls); community clinic setting; trained master’s-level social workers and a nurse with a mental health background |
| Franklin et al. (2017)81 | PE by iPhone (Apple Inc., Cupertino, CA, USA) | TFCBT; SCTF | Treatment as usual |
Duration: 10 weeks Frequency: 10 sessions within 12 weeks Length of sessions: NR |
iPhone-based video chat; teleconference at community VA centre; psychologists |
| PE by computer-based teleconferencing | TFCBT; SCTF | Treatment as usual |
Duration: 10 weeks Frequency: 10 sessions within 12 weeks Length of sessions: NR |
Computer-based teleconference; teleconference at community VA centre; psychologists | |
| Gamito et al. (2010)83 | Virtual reality exposure therapy | TFCBT; SCTF | Waitlist |
Duration: NR Frequency: NR Length of sessions: 12 sessions, length NR |
Face to face, individual; setting NR; professional NR |
| Exposure in imagination | TFCBT; SCTF |
Duration: NR Frequency: NR Length of sessions: 12 sessions, length NR |
Computer-based teleconference; teleconference at community VA centre; psychologists | ||
| Germain et al. (2012)84 | Behavioural sleep intervention | TFCBT; MCTF | Placebo |
Duration: 8 weeks Frequency: weekly Length of sessions: eight sessions, 45 minutes each |
Face to face; setting NR; master’s-level therapist with mental health background |
| Hermenau et al. (2013)86 | NET for forensic offender rehabilitation (FORNET) | TFCBT; SCTF | No intervention |
Duration: 2 weeks Frequency: approximately every other day Length of sessions: 1–2 hours |
Face to face (individual and group); non-governmental organisation reintegration centre for war-affected young people; therapists with a mental health background |
| Hijazi et al. (2014)87 | Brief NET | TFCBT; SCTF | Waitlist |
Duration: 3 weeks Frequency: weekly Length of sessions: 60–90 minutes |
Face to face; private room setting according to participant preference (e.g. own home, church, community centre); therapists trained by a licensed psychologist with expertise in exposure therapies |
| Himmerich et al. (2016)88 | Inpatient psychotherapy | EMDR; MCNTF | Outpatient clinical management |
Duration: 6 weeks Frequency: NR Length of sessions: inpatient |
Face to face; hospital; professionals NR, but with mental health background |
| Hinton et al. (2004)90 | CBT | TFCBT; SCTF | Delayed treatment |
Duration: 11 weeks Frequency: weekly Length of sessions: NR |
Face to face, individual; setting NR; trained CBT therapist with cultural facilitators |
| Hinton et al. (2005)89 | CBT | TFCBT; SCTF | Delayed treatment |
Duration: 12 weeks Frequency: weekly Length of sessions: NR |
Face to face, individual; setting NR; psychiatrist |
| Jensen (1994)91 | EMDR | EMDR; SCTF | Treatment as usual with option of delayed EMDR |
Duration: NR Frequency: NR Length of sessions: NR |
Face to face; setting NR; trained therapist with mental health background |
| Jung and Steil (2013)92 | Cognitive restructuring and imagery modification | TFCBT; MCTF | Waitlist |
Duration: NR Frequency: NR Length of sessions: two sessions, treatment 90 minutes, booster 50 minutes |
Face to face/use of internet; specialist PTSD outpatient centres; one at university and two at large psychiatric hospitals; therapist supervised by senior therapist (both authors) |
| Katz et al. (2014)93 | Holographic reprocessing | Other psychotherapy; MCNTF | Person-centred control |
Duration: 10 weeks Frequency: weekly Length of sessions: NR |
Face to face, individual; setting NR; psychologist, clinical social workers, psychology post-docs, marriage and family therapist trainees and psychiatry residents, with mental health backgrounds |
| PE | TFCBT; SCTF | Waitlist | Face to face/use of internet; specialist PTSD outpatient centres; one at university and two at large psychiatric hospitals; therapist supervised by senior therapist (both authors) | ||
| Keane et al. (1989)94 | Implosive (flooding) therapy | TFCBT; SCTF | Waitlist |
Duration: NR Frequency: NR Length of sessions: 14 sessions (plus an additional two sessions if deemed appropriate by therapist), 90 minutes |
Face to face (individual); VA medical centre; therapist with mental health background |
| Kearney et al. (2013)95 | MBSR and treatment as usual | Mindfulness; SCNTF | Treatment as usual |
Duration: 8 weeks Frequency: weekly Length of sessions: 2.5 hours (plus 7-hour retreat) |
Face to face (group); VA medical centre; professional instructors with mental health backgrounds |
| King et al. (2013)148 | Mindfulness-based cognitive therapy group | Treatment as usual (PTSD psychoeducation and skills group or imagery rehearsal therapy group) |
Duration: 8 weeks Frequency: weekly Length of sessions: 8 hours |
Face to face (group); PTSD outpatient clinic (for veterans); therapists with a mental health background, including clinical psychologists | |
| Knaevelsrud et al. (2015)96 | Internet-based CBT | TFCBT; SCTF | Waitlist |
Duration: 5 weeks Frequency: twice a week Length of sessions: not fixed |
Computer; remote (web-based) setting; psychotherapists or psychiatrists |
| Krupnick et al. (2008)98 | IPT | IPT; SCNTF | Waitlist |
Duration: 16 weeks Frequency: weekly Length of sessions: 2 hours |
Face to face, group; setting NR; clinical psychologists |
| Kubany et al. (2004)100 | Cognitive trauma therapy for battered women | TFCBT; MCTF | Waitlist |
Duration: 4 weeks Frequency: NR Length of sessions: 1.5 hours, 8.5 mean total sessions |
Face to face (individual); setting NR; therapist |
| Kubany et al. (2004)101 | Cognitive trauma therapy for battered women | TFCBT; MCTF | Delayed treatment |
Duration: 4–6 weeks Frequency: twice a week Length of sessions: 60 minutes, 8–11 total sessions |
Face to face, individual; setting NR; professionals included clinical psychologist, advanced degree nurses, master’s in counselling psychology, victim witness advocate, baccalaureate degree and several years of experience in domestic violence counselling |
| Lande et al. (2010)102 | Biofeedback and treatment as usual | Biofeedback; NA | Treatment as usual |
Duration: 3 weeks Frequency: twice a week Length of sessions: 20 minutes |
Face to face (individual) via computer; specialist psychiatric outpatient clinic; computer, professional NR |
| Lau and Kristensen (2007)103 | Analytic group psychotherapy | Other psychotherapy; MCNTF | Treatment as usual |
Duration: 52 weeks Frequency: weekly Length of sessions: 2.25 hours |
Face to face (group); outpatient mental health services; therapists with a mental health background |
| Systemic group psychotherapy | Other psychotherapy; MCNTF | ||||
| Margolies et al. (2011)105 | CBT for insomnia with imagery rehearsal therapy | TFCBT; MCTF | Minimal attention waitlist and waitlist |
Duration: 8 weeks Frequency: NR Length of sessions: 60 minutes; four individual sessions, with break between second and third sessions |
Face to face, individual; VA medical centre; clinical psychologist |
| McDonagh et al. (2005)106 | CBT | TFCBT; SCTF | Minimal attention waitlist |
Duration: 14 weeks Frequency: weekly Length of sessions: 2 hours for first seven sessions, 1.5 hours for final seven sessions |
Face to face, individual; setting NR; psychologists and master’s-level clinical social workers |
| Present-centred therapy | Other psychotherapy; MCNTF |
Duration: 14 weeks Frequency: weekly Length of sessions: 2 hours for first seven sessions, 1.5 hours for final seven sessions |
|||
| McLay et al. (2011)107 | Virtual reality graded exposure therapy | TFCBT; SCTF | Waitlist |
Duration: 10 weeks Frequency: up to twice a week, closer to weekly Length of sessions: NR |
Face to face, individual; navy medical facilities; psychologist |
| Meffert et al. (2014)108 | IPT | IPT; SCNTF | Waitlist |
Duration: 3 weeks Frequency: twice a week Length of sessions: NR |
Face to face; private rooms of community-based support organisation; members of Sudanese community without mental health background |
| Miyahira et al. (2012)109 | Add-on virtual reality exposure | TFCBT; SCTF | Minimal attention |
Duration: 5 weeks Frequency: twice a week Length of sessions: NR |
Face to face; setting NR; therapist with training on manualised CBT treatment protocol with virtual reality exposure |
| Moradi et al. (2014)111 | Memory specificity training | NTFCBT; SCNTF | Treatment as usual |
Duration: 4 consecutive weeks Frequency: weekly Length of sessions: four sessions, one hour |
Face to face/group/individual; specialist military hospital; clinical psychologist |
| Neuner et al. (2008)113 | NET | TFCBT; SCTF | Monitoring |
Duration: 3 weeks Frequency: twice a week Length of sessions: 2 hours |
Face to face; setting NR; lay counsellors without mental health background |
| Trauma counselling | TFCBT; SCTF |
Duration: 3 weeks Frequency: twice a week Length of sessions: 2 hours |
|||
| Neuner et al. (2004)114 | NET | TFCBT; SCTF | Psychoeducation |
Duration: 3 weeks Frequency: four sessions in 3 weeks Length of sessions: 90 minutes (up to 120 minutes in exceptional circumstances) |
Face to face (individual); setting NR; doctoral-level psychologists or graduate students with experience in other therapies (e.g. counselling) |
| Supportive counselling | TFCBT; SCTF |
Duration: 3 weeks Frequency: four sessions in 3 weeks Length of sessions: 90 minutes (up to 120 minutes in exceptional circumstances) |
|||
| Niles et al. (2012)115 | Mindfulness | Mindfulness; SCNTF | Psychoeducation |
Duration: 8 weeks Frequency: weekly Length of sessions: 45 minutes in-person sessions, 20 minutes telephone sessions |
Remotely (individual); mostly home-based; two female clinicians with PhDs in clinical psychology served as therapists |
| Owens et al. (2001)117 | CPT for sexual abuse | TFCBT; SCTF | Minimal attention |
Duration: 17 weeks Frequency: NR Length of sessions: NR |
Face to face, individual and group; setting NR; professionals NR |
| Paunovic and Ost (2001)119 | CBT | TFCBT; SCTF | Minimal attention |
Duration: 4–5 months Frequency: weekly Length of sessions: NR |
Face to face, individual; setting NR; clinical psychology doctoral student |
| Exposure-only therapy | Exposure only; SCTF |
Duration: 4–5 months Frequency: weekly Length of sessions: 20 minutes |
|||
| Polusny et al. (2015)120 | MBSR | Mindfulness; SCNTF |
Duration: 9 weeks Frequency: weekly Length of sessions: 2.5 hours |
Face to face, group; VA medical centre; instructors and doctoral-level clinicians | |
| Present-centred therapy | Other psychotherapy; SCNTF |
Duration: 9 weeks Frequency: weekly Length of sessions: 1.5 hours |
|||
| Possemato et al. (2016)121 | Primary care brief mindfulness training | Mindfulness; SCNTF | Primary care treatment as usual |
Duration: 4 weeks Frequency: weekly Length of sessions: 1.5 hours |
Face to face individual/group; VA medical centre; physicians expert in MBSR practitioners and certified instructors |
| Ready et al. (2010)124 | Virtual reality exposure | TFCBT; SCTF |
Duration: NR Frequency: NR Length of sessions: 90 minutes, 10 sessions |
Face to face, individual; setting NR; professional NR | |
| Present-centred therapy | Other psychotherapy; SCNTF |
Duration: NR Frequency: NR Length of sessions: 90 minutes, 10 sessions |
|||
| Reed and Enright (2006)125 | Forgiveness therapy | Other psychotherapy; SCNTF | Alternative therapy |
Duration: 5–12 months Frequency: weekly Length of sessions: 1 hour, average duration 7.95 months |
Face to face, individual; setting NR; trained psychiatric nurse |
| Reger et al. (2016)126 | Virtual reality exposure | TFCBT; SCTF | Waitlist |
Duration: 5 weeks Frequency: weekly or twice weekly Length of sessions: 1.5–2 hours, 10 sessions in total |
Face to face (individual); army military installation; doctoral-level clinicians |
| PE | TCBT; SCTF |
Duration: 5 weeks Frequency: weekly or twice weekly Length of sessions: 1.5–2 hours, 10 sessions in total |
|||
| Resick et al. (2015)128 | CPT – cognitive-only version | TFCBT; SCTF |
Duration: NR Frequency: twice a week Length of sessions: 90 minutes, 12 sessions in total |
Face to face, group; setting NR; civilian therapists with mental health background | |
| Present-centred therapy | Other psychotherapy; SCNTF |
Duration: NR Frequency: twice a week Length of sessions: 90 minutes, 12 sessions in total |
|||
| Rogers et al. (1999)130 | EMDR | EMDR; SCTF |
Duration: one session Frequency: once Length of sessions: 60–90 minutes |
Face to face, individual; setting NR; trained therapist with mental health background | |
| Exposure (implosive flooding) | Exposure only; SCTF |
Duration: one session Frequency: once Length of sessions: 60–90 minutes |
|||
| Sikkema et al. (2007)131 | HIV and trauma coping group | NTFCBT; SCNTF | Waitlist |
Duration: 15 weeks Frequency: weekly Length of sessions: 90 minutes |
Face to face; community clinics; clinical psychologists/clinical social workers |
| Support group | NTFCBT; SCNTF |
Duration: 15 weeks Frequency: weekly Length of sessions: 90 minutes |
|||
| Sikkema et al. (2013)132 | Coping skills programme | NTFCBT; SCNTF | HIV support group |
Duration: 15 weeks Frequency: weekly Length of sessions: 90 minutes |
Face to face (group); community health centre; therapists with a mental health background |
| Stenmark et al. (2013)136 | NET | TFCBT; SCTF | Treatment as usual |
Duration: 10 weeks Frequency: weekly Length of sessions: 90 minutes |
Face to face, individual; setting NR; professionals included psychologists, psychiatrists, psychiatric nurses, occupational therapists, drama therapists, clinical social workers |
| Teng et al. (2008)137 | Panic control treatment | NTFCBT; SCNTF | Psychoeducational supportive treatment (PE-SUP) |
Duration: 10 weeks Frequency: weekly Length of sessions: 1 hour |
Face to face (individual); VA hospital; master’s-level clinicians |
| Ter Heide et al. (2011)138 | EMDR | EMDR; SCTF |
Duration: 11 weeks Frequency: weekly Length of sessions: 90 minutes (60 minutes dedicated to EMDR) |
Face to face, individual; centre for psychotrauma; psychotherapists, psychiatrist, health-care psychologists | |
| Stabilisation | EMDR; SCNTF |
Duration: 11 weeks Frequency: weekly Length of sessions: 60 minutes |
Face to face, individual; centre for psychotrauma; clinical psychologist, physician/psychotherapist, physician, social-psychiatric nurses | ||
| Ter Heide et al. (2016)139 | EMDR | EMDR; SCTF |
Duration: 9 weeks Frequency: NR Length of sessions: 12 hours overall |
Face to face (individual); treatment centre for CPTSD; clinical psychologists and psychotherapists | |
| Stabilisation as usual | Stabilisation; SCNTF |
Duration: 9 weeks Frequency: NR Length of sessions: 12 hours overall |
|||
| Ulmer et al. (2011)140 | Sleep intervention for PTSD | TFCBT; MCTF | Usual care |
Duration: 12 weeks Frequency: fortnightly Length of sessions: 1 hour |
Face to face, individual; setting NR; clinical psychologist |
| Wahbeh et al. (2016)142 | Mindfulness meditation | Mindfulness; SCNTF | Sitting quietly |
Duration: 6 weeks Frequency: weekly Length of sessions: 20 minutes |
Face to face and remote, individual; setting NR; research assistant |
| Slow breathing with biofeedback device (mindfulness meditation and slow breathing) | Biofeedback; SCNTF |
Duration: 6 weeks Frequency: weekly Length of sessions: 20 minutes |
|||
| Slow breathing | Other psychological intervention; SCNTF |
Duration: 6 weeks Frequency: weekly Length of sessions: 20 minutes |
|||
| Wang et al. (2016)143 | Biofeedback-supported CBT and group therapy (physiotherapy and exercises) | TFCBT; MCTF | Waitlist |
Duration: 10 weeks Frequency: twice a week Length of sessions: group sessions 60–90 minutes, individual sessions 90 minutes (60 minutes for CBT intervention, 15- to 20-minute period of breathing training using a biofeedback device, 10–15 minutes for reviewing and note taking) |
Face to face (individual and group); rehabilitation centre (for torture victims); therapists and physiotherapists with mental health backgrounds |
| Weiss et al. (2015), trial 1: CETA144 | CETA | TFCBT; MCTF | Waitlist |
Duration: 8–12 weeks Frequency: weekly Length of sessions: 50–60 minutes, 8–12 sessions in total |
Face to face, individual; community; community mental health workers |
| Weiss et al. (2015), trial 2: CPT144 | CPT | TFCBT; SCTF | Waitlist |
Duration: 12 weeks Frequency: weekly Length of sessions: NR |
Face to face, individual; community; community mental health workers |
| Yeomans et al. (2010)145 | Workshop with psychoeducation | Other psychotherapy; MCTF | Waitlist |
Duration: 4 days Frequency: 3 consecutive days and 1-month follow-up Length of sessions: day long |
Face to face, group; community; local facilitators without a mental health background |
| Workshop without psychoeducation | Other psychotherapy; SCTF |
Duration: 4 days Frequency: 3 consecutive days and 1-month follow-up Length of sessions: day long |
|||
| Zlotnick et al. (1997)146 | Affect management | Waitlist |
Duration: 15 weeks Frequency: weekly Length of sessions: 2 hours |
Face to face (group); setting NR; therapist with mental health background |
| Author (year) | Intervention(s) | Intervention category | Control(s) | Intensity (duration, frequency and dose) |
|---|---|---|---|---|
| Rezaei Ardani et al. (2017)56 | Rivastigmine augmented therapy | Rivastigmine | Placebo (in combination with citalopram and sodium valproate) |
Rivastigmine augmented therapy of citalopram and sodium valproate Duration: 12 weeks Frequency: twice a day Dose: Weeks 1–4 1.5 mg twice a day, Week 5 3 mg twice a day in addition to citalopram 40 mg/day and sodium valproate 20 mg/kg/day |
| No intervention | ||||
| Bartzokis et al. (2005)58 | Risperidone | Antipsychotic | Placebo |
First 4 weeks delivered in conjunction with an inpatient psychosocial programme. The remainder of the intervention was delivered as an outpatient programme. Duration: 16 weeks Frequency: NR Dose: initiated at 1 mg, increased to 3 mg bedtime dose (over 2 weeks); maintained at 3 mg |
| Becker et al. (2007)59 | Bupropion SR | Antidepressant | Placebo |
Duration: 8 weeks Frequency: once or twice a day Dose: 100 mg/day for 2 weeks. Dose increased to 100 mg twice a day as indicated. No significant improvement at 4 weeks resulted in a maximum dose of 150 mg twice a day |
| Celik et al. (2011)65 | Paroxetine | SSRI/antidepressant |
Duration: 8 weeks Frequency: once a day Dose: initiated at 10 mg/day for Week 1, then increased to 20 mg for Weeks 2 and 3, 30 mg for Weeks 4 and 5, 40 mg for Weeks 6 and 7 and 60 mg for Weeks 8–12 (if tolerated/clinically indicated) |
|
| Amitriptyline | Antidepressant |
Duration: 8 weeks Frequency: once a day Dose: initiated at 75 mg/day for Weeks 1–3 (initial dose of 25 mg for Days 1–3, 50 mg for Days 4–7 and 75 mg for Days 8–21), then increased to 100 mg from Week 4 (as necessary) and up to 200 mg or down to 75 mg from Week 5 (as necessary) |
||
| Chung et al. (2004)67 | Mirtazapine | Antidepressant |
Duration: 6 weeks Frequency: daily Dose: initiated at mean dose of 19.1 ± 8.53 mg/day, Weeks 1–2 31.5 ± 9.13 mg/day, Weeks 2–6 38.5 ± 12.10 mg/day |
|
| Sertraline | SSRI/antidepressant |
Duration: 6 weeks Frequency: daily Dose: initiated at 58.2 ± 24.15 mg/day, Weeks 1–2 89.8 ± 23.89 mg/day and Weeks 2–6 115.3 ± 36.02 mg/day Mean daily dose: mirtazapine 34.1 mg, sertraline 101.5 mg |
||
| Davis et al. (2004)73 | Nefazodone | Antidepressant | Placebo |
Duration: 12 weeks Frequency: twice a day Dose: initiated at 100 mg, increased by 100 mg every 4 days as tolerated, up to a maximum benefit (not exceeding 600mg/day) |
| Davis et al. (2008)72 | Divalproex | Anticonvulsant | Placebo |
Duration: 8 weeks Frequency: twice a day Dose: initiated at 500 mg twice a day, increased by 500 mg as tolerated to a maximum of 3000 mg/day |
| Friedman et al. (2007)82 | Sertraline | SSRI/antidepressant | Placebo |
Duration: 12 weeks Frequency: daily Dose: initiated at 25 mg/day, Week 2 increased dose to 50 mg/day where dose-limiting adverse events did not present. Subjects who failed to respond received titrated weekly increment of 50 mg up to a maximum of 200 mg/day |
| Germain et al. (2012)84 | Prazosin | Prazosin | Placebo |
Duration: 8 weeks Frequency: daily Dose/length of sessions: initiated at 1 mg, increasing over the following weeks to 2 mg, 4 mg, 6 mg, 10 mg and 15 mg. Final mean dose 8.9 mg |
| Hamner et al. (2003)85 | Adjunctive risperidone | Antipsychotic | Placebo |
Risperidone added to regimen of antidepressant treatment (fluoxetine, nefazadone, paroxetine, sertraline, buprioprion) Duration: 5 weeks Frequency: daily Dose: initiated at 1 mg/day, increased to a maximum of 6 mg/day |
| Krystal et al. (2011)99 | Adjunctive risperidone | Antipsychotic | Placebo |
Adjunctive risperidone with ongoing pharmacotherapy Duration: 24 weeks Frequency: daily Dose: initiated at 1 mg at night. Increased by 1 mg/week to 3 mg. After 4 weeks, a further 1 mg increase could be made if tolerated and clinically indicated |
| Lindley et al. (2007)104 | Topiramate | Anticonvulsant | Placebo |
Duration: 7 weeks Frequency: daily Dose: initiated at 25 mg, increased by 50 mg each week until maximum toleration or 200 mg/day |
| Monnelly et al. (2003)110 | Risperidone | Antipsychotic | Placebo |
Duration: 6 weeks Frequency: daily Dose: initiated at 0.5 mg, increased fortnightly to maximum 2 mg/day |
| Naylor et al. (2013)112 | Paroxetine | SSRI/antidepressant | Placebo |
Duration: 12 weeks Frequency: daily Dose: flexible dosing 10–40 mg/day depending on tolerance and response |
| Otto et al. (2003)116 | Sertraline | SSRI/antidepressant | Compared with SSRI/antidepressant with TFCBT; see Table 30 |
Duration: NR Frequency: daily Dose/length of sessions: sertraline initiated at 25 mg, titrated 50 mg each week to maximum 200 mg. Mean final dose 125 mg/day |
| Panahi et al. (2011)118 | Sertraline | SSRI/antidepressant | Placebo |
Duration: 10 weeks Frequency: daily Dose: initiated at 50 mg/day, flexible adjustment fortnightly to a maximum of 200 mg/day |
| Raskind et al. (2007)122 | Prazosin | Prazosin | Placebo |
Duration: 8 weeks Frequency: daily Dose: initiated at 1 mg/nightly for 3 days. Days 3–7 increased to 2 mg/day based on response. Persistence of traumatic nightmares increased dose to 2 mg per week up to 10 mg/day at Day 28. Persistent lack of response allowed additional 5 mg to a maximum of 15 mg/day. Mean daily dose of prazosin was 13 (3) mg and of placebo capsules was 14 (2) mg |
| Raskind et al. (2013)123 | Prazosin | Prazosin | Placebo |
Duration: 15 weeks Frequency: once or twice daily Dose: titrated 1–2 mg/day, depending on gender. Week 2: males (AM 1 mg, PM 4 mg), females (AM 1 mg, PM 2 mg); Week 3: males (AM 2 mg, PM 6 mg), females (AM 1 mg, PM 2 mg); Week 4: males (AM 2 mg, PM 10 mg), females (AM 2 mg, PM 6 mg); Week 5: males (AM 5 mg, PM 15 mg), females (AM 2 mg, PM 10 mg); Week 6: males (AM 5 mg, PM 20 mg), females (AM 2 mg, PM 10 mg) |
| Reich et al. (2004)127 | Risperidone | Antipsychotic | Placebo |
Duration: 8 weeks Frequency: daily (can be divided into two or three doses) Dose: initiated at 0.5 mg/day, increased to 1 mg/day at 3 days, then increased by 1 mg/day for 1 week up to target dose of 4 mg/day until symptom relief reported. Dosage increased to maximum of 8 mg/day if lack of response by Week 5 |
| Smajkic et al. (2001)133 | Paroxetine | SSRI/antidepressant |
Duration: 6 weeks Frequency: daily Dose: 20 mg once daily for 14 days then, if tolerated at 2 weeks, the dosage was continued |
|
| Sertraline | SSRI/antidepressant |
Duration: 6 weeks Frequency: daily Dose: 50 mg once daily for 14 days then, if tolerated at 2 weeks, 100 mg once daily |
||
| Venlafaxine | Antidepressant |
Duration: 6 weeks Frequency: twice a day Dose: 37.5 mg twice daily for 14 days then, if tolerated at 2 weeks, 75 mg twice daily |
||
| Stein et al. (2002)135 | Adjunctive olanzapine | Antipsychotic | Placebo |
Adjunctive olanzapine for subjects minimally responsive to SSRIs at maximally tolerated doses Duration: 8 weeks Frequency: daily Dose: initiated at 10 mg, increased to 20 mg after 2 weeks if clinically indicated and tolerated |
| van der Kolk et al. (1994)141 | Fluoxetine | SSRI/antidepressant | Placebo |
Duration: 5 weeks Frequency: daily Dose: initiated at 20 mg/day, increased weekly to a maximum of 60 mg |
| Zohar et al. (2002)147 | Sertraline | SSRI/antidepressant | Placebo |
Duration: 10 weeks Frequency: daily Dose: initiated at 50 mg/day, flexible titration in 50 mg increments fortnightly up to a maximum of 200 mg |
| Authors (year) | Intervention(s) | Intervention categories | Control(s) | Intensity (duration, frequency and strength of dose/length of sessions) | Delivery (method, setting and type of professional) |
|---|---|---|---|---|---|
| Buhmann et al. (2016)63 | Sertraline, psychoeducation and CBT | SSRI/antidepressant and TFCBT | Waitlist |
Duration: 6 months Frequency: psychoeducation and CBT weekly, sertraline daily Dose/length of sessions: 10 consultations and 16 sessions of CBT Sertraline increased by 25–50 mg to a maximum dose of 200 mg. Mianserin given at 10–30 mg, titrated weekly by 10 mg |
Face to face; mental health clinic; doctors and therapists with mental health background |
| Sertraline and psychoeducation | SSRI/antidepressant and other psychotherapy |
Duration: 6 months Frequency: psychoeducation weekly, sertraline daily Dose/length of sessions: 10 sessions of psychoeducation, length NR |
|||
| Franćišković et al. (2011)80 | Tianeptine and group therapy | Antidepressant and other psychotherapy |
Duration: 6 months Frequency: group therapy twice weekly, tianeptine daily Dose/length of sessions: 37.5 mg/day, NR for group therapy |
Face to face; setting NR; psychiatrist and psychologist with mental health backgrounds Drugs prescribed by physician |
|
| Fluoxetine and group therapy | SSRI/antidepressant and other psychotherapy |
Duration: 6 months Frequency: group therapy twice weekly, fluoxetine daily Dose/length of sessions: 40 mg/day, NR for group therapy |
|||
| Kosten et al. (1992)97 | Phenelzine and psychotherapy | Antidepressant and TFCBT | Placebo and psychotherapy |
Duration: NR Frequency: psychotherapy weekly, imipramine daily Dose/length of sessions: dose of drug and length of sessions NR. Mean maximal dose 68 ± 20 mg |
Face to face; setting NR; master’s-level psychologist with mental health background. Drug delivery NR |
| Imipramine and psychotherapy | Antidepressant and TFCBT |
Duration: NR Frequency: psychotherapy weekly, imipramine daily Dose/length of sessions: dose of drug and length of sessions NR. Mean maximal dose 225 ± 55 mg |
|||
| Otto et al. (2003)116 | CBT and sertraline | SSRI/antidepressant and TFCBT | Compared with SSRI/antidepressant; see Table 29 |
Duration: NR Frequency: CBT NR, sertraline daily Dose/length of sessions: CBT 10 sessions, length NR Sertraline initiated at 25 mg, titrated by 50 mg each week to a maximum of 200 mg. Mean final dose 100 mg/day |
Face to face; otherwise NR. Drug delivery NR |
| Rothbaum et al. (2014)129 | D-cycloserine and virtual reality exposure therapy | D-cycloserine and TFCBT | Placebo and exposure therapy |
Duration: 6 weeks Frequency: weekly Dose/length of sessions: introductory session, five therapeutic sessions, 90 minutes each D-cycloserine delivered at 50 mg 30 minutes before exposure |
Face to face; setting NR; doctoral-level clinicians with a mental health background. Drug delivery supervised within sessions |
| Alprazolam and virtual reality exposure therapy | Benzodiazepine and TFCBT |
Duration: 6 weeks Frequency: weekly Dose/length of sessions: introductory session, five therapeutic sessions, 90 minutes each Alprazolam delivered at 0.25 mg 30 minutes before exposure |
|||
| Sonne et al. (2016)134 | Venlafaxine and CBT | Antidepressant and TFCBT |
Duration: 20–24 weeks Frequency: venlafaxine daily, CBT weekly Dose/length of sessions: 10 sessions with a psychiatrist, 16 sessions with a psychologist Venlafaxine initiated at 37.5–75 mg/day, increased weekly by 37.5–75 mg for 6 weeks. Rest of trial, monthly increases up to a maximum of 375 mg |
Face to face; psychiatry centre; psychiatrist | |
| Sertraline and CBT | SSRI/antidepressant and TFCBT |
Duration: 20–24 weeks Frequency: venlafaxine daily, CBT weekly Dose/length of sessions: 10 sessions with a psychiatrist, 16 sessions with a psychologist Sertraline initiated at 25–50 mg/day, increased weekly by 25–50 mg for 6 weeks. Rest of trial, monthly increases up to a maximum of 200 mg |
Appendix 5 Population characteristics of included randomised controlled trials
| Authors (year) | Trauma experience category | Country | Age of males, years (SD) | Gender (% male) | Ethnicity | Type(s) of trauma experienced | Current comorbidities | PTSD diagnosis at baseline (yes/no) |
|---|---|---|---|---|---|---|---|---|
| Acarturk et al. (2015)53 | Refugee | Turkey/Syria | I = 35.27 (13.21), C = 37.92 (9.06) | 24.14 | NR | NR | NR | No |
| Acarturk et al. (2016)54 | Refugee | Turkey/Syria | I = 33.32, C = 34.04 | 26 | NR | Syrian refugees (100%) | NR | Yes |
| Adenauer et al. (2011)55 | Refugee | Germany | I = 30.3 (9.2), C = 36.4 (9.9) | I = 56.3, C = 55.6 |
I = Middle East (50%), Central East (13%), Africa (38%) C = Middle East (61%), Central East (6%), The Balkans (17%), Africa (11%) |
Refugees and asylum seekers (100%) | Unclear (mention of depression) | Yes (100%) |
| Rezaei Ardani et al. (2017)56 | Veterans | Iran | I = 50.08 (4.5), Placebo = 51.5 (6.4), No intervention = 49.08 (6.13) | 100 | NR | Veterans of the Iraq–Iran war (100%) | NR | Yes (100%) |
| Azad Marzabadi and Hashemi Zadeh (2014)57 | War affected | Iran | Range: I = 35–45 (57.1%), 46–55 (35.8%), 56–60 (7.1%); C = 35–45 (35.7%), 46–55 (64.3%) | 100 | NR | War victims from the Iran–Iraq war | NR | |
| Bartzokis et al. (2005)58 | Veteran | USA | 51.6 (4.2) | 100 | White (n = 44), African American (n = 19), other (n = 2) | Veterans | NR | Yes |
| Becker et al. (2007)59 | Veteran | USA | 50.39 (7.46) | 79 | African American (64%), white (29%), other (7%) | War trauma (50%), domestic violence (7%), rape (3.5%), motor vehicle accident (7%), homicide (7%), medical illness (11%), death/suicide of a loved one (7%), childhood sexual or physical abuse (7%) | NR | Yes |
| Beidel et al. (2011)60 | Veteran | USA | I = 58.93, C = 59.76 | 100 | White (100%) | Veterans (100%) | NR | Yes (100%) |
| Bichescu et al. (2007)61 | War affected | Romania | I = 68.9 (4.4), C = 69.8 (6.0) | I = 100, C = 88.9 | NR | Former political detainees (100%) | NR | Yes (100%) |
| Bolton et al. (2014)62 | War affected | Iraqi Kurdistan | BADT = 36.9 (12.4), CPT = 41.5 (13.7), C = 42.3 (12.5) | BADT = 43, CPT = 42, C = 41 | NR | Victims of systematic violence (including physical torture, imprisonment, gas attacks, other military attacks) | Depression: 100% (was a necessary condition of inclusion) | NR |
| Buhmann et al. (2016)63 | Refugee | Denmark | Medication + psychoeducation + CBT = 45 (10), medication + psychoeducation = 43 (9), CBT = 46 (8), waitlist = 47 (8) | 59 | NR | Refugees (including those who had experienced torture, a refugee camp/asylum centre or were an ex-combatant) | Of completers (217), 94% had depression, 27% had a personality change (ICD-10 code F62.0), 9% were psychotic and 36% were in treatment for somatic disorder. About one-third reported a traumatic brain injury | Yes |
| Carlson et al. (1997)64 | Veteran | USA | EMDR = 52.7 (8.6), RXT = 46.9 (4.0), C = 45.4 (3.5) | 100 | EMDR = white (60%), RXT = white (54%), C = white (50%) | Veterans (100%) | NR | Yes (100%) |
| Celik et al. (2011)65 | Veteran | Turkey | I = 32.5 (4.7), C = 29.1 (7.4) | NR | NR | Veterans (100%) | On average, both groups met the cut-off for depression and anxiety based on baseline scores | Yes |
| Chard (2005)66 | Childhood sexual abuse | USA | 32.77 (8.87) | 0 | African American (14%), white (81.4%), Hispanic, Latin or Mexican (3.5%), other (1%) | Childhood sexual abuse (100%) | Current major depression (40%) | Yes (100%) |
| Chung et al. (2004)67 | Veteran | South Korea | I = 59.1 (6.04), C = 60.59 (6.70) | 100 | NR | Veterans (100%) |
Major depressive disorder: I = 11 (21.6%), C = 6 (14.3%) Dysthymia: I = 37 (72.6%), C = 42 (81.6%) Major depressive disorder and dysthymia: I = 3 (6.1%), C = 1 (2.04%) |
Yes |
| Classen et al. (2001)68 | Childhood sexual abuse | USA | 38.4 (11.7) | 0 | White/European American (64%), Hispanic/Latina (15%), black/African American (8%), native American (4%), other (10%) | Childhood sexual abuse (100%) | NR | Yes |
| Cloitre et al. (2002)69 | Childhood sexual abuse | USA | 34 (7.22) | 0 | White (46%), African American (20%), Hispanic (15%), other (19%) | Childhood sexual/physical abuse (100%): sexual and physical abuse (48%), sexual abuse (39%), physical abuse (13%) | Major depression (45%), anxiety disorders (79%), generalised anxiety disorder (48%) | Yes (100%) |
| Cloitre et al. (2010)70 | Childhood sexual abuse | USA | STAIR/expsoure = 33.2, STAIR/support = 37.1, support/exposure = 38.7 | 0 |
STAIR/support = white (33–37%), African American (24%), Hispanic (30%), other (9%) STAIR/exposure = white (37%), African American (21%), Hispanic (29%), other (11%) Support/exposure = white (33%), African American (39%), Hispanic (18%), other (9%) |
Childhood abuse (100%). The large majority also experienced interpersonal abuse as adults (including domestic violence, sexual abuse and other interpersonal abuse) |
Axis I diagnosis: STAIR/support = 84.8%, STAIR/exposure = 92.1%, support/exposure = 87.9% Axis II diagnosis: STAIR/support = 48.5%, STAIR/exposure = 52.6%, support/exposure = 60.6% |
Yes (100%) |
| Cook et al. (2010)71 | Veteran | USA | I = 59.79 (3.18), C = 59.06 (3.86) | 100 |
I = white (44.3%), African American (49.2%), other (6.6%) C = white (39.7%), African American (54%), other (6.4%) |
Vietnam veterans (100%) |
I = depressive disorder (57.4%), anxiety disorder (57.4%) C = depressive disorder (55.6%), anxiety disorder (49.2%) |
Yes (100%) |
| Davis et al. (2004)73 | Veteran | USA | I = 53.8 (8.7), C = 53.8 (7.1) | 97.6 |
I = white (54%), African American (46%) C = white (53%), African American (47%) |
Combat (97.6%), sexual trauma (2.4%) I = combat (96%), sexual trauma (4%) C = combat (100%), sexual trauma (0%) |
I = major depression (42%), dysthymia (27%), panic with agoraphobia (4%) C = major depression (40%), dysthymia (27%), panic without agoraphobia (13%) |
Yes (100%) |
| Davis et al. (2008)72 | Veteran | USA | 55.2 (6.8) | 98 | NR | Combat-related trauma (95%) | NR | Yes (100%) |
| Devilly et al. (1998)74 | Veteran | USA | 50.1 (6.48) | 100 | NR | Veterans (100%) | NR | Yes (100%) |
| Edmond et al. (1999);76 Edmond and Rubin (2004)75 | Childhood sexual abuse | USA | 35; follow-up = 36 (range 18–51) | 0 | White (85%), follow-up = 83% | Childhood sexual abuse: 100%, childhood physical abuse 58%, adult re-victimisation (including domestic violence and rape 66%) | NR | NR |
| Engel et al. (2015)78 | Veteran | USA | I = 36.2 (7.75), C = 36.7 (9.75) | I = 79.1, C = 83.8 |
I = white, not Hispanic (53.5%) C = white, not Hispanic (56.8%) |
Recently deployed military service members and veterans | NR | Yes (100%) |
| Feske (2008)79 | Mixed | USA | 43.1 (range 29–55) | 0 | African American (95.2%), white (4.8%) |
Multiple traumas (100%), including childhood sexual abuse (85.7%) Index traumas: adult sexual assault (47.6%), domestic violence (23.8%), child sexual abuse (19%), child physical abuse (4.8%), witnessed murder (4.8%) |
Current comorbid Axis-I (95.2%) [including major depression (66.7%), panic disorder (38.1%), social phobia (28.6%), generalised anxiety disorder (23.8%), borderline personality disorder (52.4%)] | Yes (100%) |
| Franćišković et al. (2011)80 | Mixed | Croatia | Median = 48 (range 37–60) | 100 | NR | Veterans with combat experience from the Homeland War in Croatia (100%), torture and imprisonment (9.3%), refugees (6.9%) | NR | Yes (100%) |
| Franklin et al. (2017)81 | Veteran | USA | 46.1 (15.5) | 92.6 | Euro-American (69.2%), African American (23.1%), ‘other’ (7.7%) | Veterans (7.4% reported as having no war zone experience) | NR | Yes (100%) |
| Friedman et al. (2007)82 | Veteran | USA | I = 45, C = 46 | I = 79, C = 81 | White: I = 67%, C = 75% | Primary exposure: being in war or combat (I = men 85.3%, women 11.1%; C = men 88.1%, women 6.3%), physical or sexual assault (I = men 2.9%, women 66.7%; C = men 3%, women 62.5%) |
Major depression: I = men (50%), women (56%); C = men (40%), women (56%) Anxiety disorder: I = men (22%), women (22%); C = men (13%) women (25%) |
Yes |
| Gamito et al. (2010)83 | Veteran | Portugal | NR | 100 | Unclear | Veterans of Portuguese Colonial War (100%) | NR | Yes (100%) |
| Germain et al. (2012)84 | Veteran | USA | BSI = 40 (14.1), prazosin = 39.4 (11.9), C = 43.6 (14.0) | BSI = 82.4, prazosin = 88.9, placebo = 100 | Caucasian: BSI = 70.6%, prazosin = 83.3%, placebo = 93.3% | Veterans of various wars (100%) |
BSI = generalised anxiety disorder (5.9%), major depressive disorder (5.9%), insomnia (41.2%) Prazosin = generalised anxiety disorder (5.6%), insomnia (16.7%) Placebo = insomnia (33.3%) |
Yes (BSI = 41.2%, prazosin = 72.2%, placebo = 60%) |
| Hamner et al. (2003)85 | Veteran | USA | I = 50.8 (4.9), C = 53.7 (7.6) | 100 |
I = white (53%), African American (47%) C = white (39%), African American (61%) |
Veterans of the Vietnam war | Major depressive episodes 86%, other anxiety disorder 41%, number of psychotic symptoms: I = 3.7 (SD 1.6), C = 4.1 (SD 0.9) | Yes |
| Hermenau et al. (2013)86 | War affected | Democratic Republic of the Congo | 19 (2.02) | 100 | NR | Former child soldiers and ex-combatants | NR | NR |
| Hijazi et al. (2014)87 | Refugee | USA | 48.2 (8.9) | 44.4 | Iraqi (100%) | Oppressed because of race/ethnicity/religion (92.1%), combat exposure (92.1%), witnessed destruction of religious shrines (74.6%), witnessed murder (68.3%), witnessed someone physically harmed (66.7%), property looted/confiscated/destroyed (65.1%), murder/violent death of family or friends (65.1%), witnessed rotten corpses (60.3%), kidnapping of family/friends (58.7%), witnessed arrest/torture/execution of religious leaders (46%), witnessed torture (41.3%), physically harmed (38.1%), imprisoned arbitrarily (28.6%), witnessed mass execution (27%), kidnapped (27%), tortured (25.4%), serious physical injury from combat/mine (25.4%), taken hostage (17.5%), sexually abused/raped (6.3%) | NR | Yes |
| Himmerich et al. (2016)88 | Veteran | Germany | I = 29 (7.62), C = 28.8 (3.4) | 100 | NR | Soldiers (100%) | NR | NR |
| Hinton et al. (2004)90 | Refugee | USA | NR | I = 50, C = 50 | Vietnamese (100%) | Refugees (100%). All men were ex-political detainees (former Southern Vietnamese military, police or political officials imprisoned by Northern Vietnamese) | NR | Yes (100%) |
| Hinton et al. (2005)89 | Refugee | USA | I = 50.9 (6.11), C = 52.7 (7.43) | I = 40, C = 40 | Cambodian refugees | Cambodian refugees living in the USA (100%) | NR | Yes (100%) |
| Jensen (1994)91 | Veteran | USA | 43.1 (2.84) | 100 | NR | Veterans | 40% had received a recent veteran’s affairs diagnosis of alcohol abuse or alcohol dependence, but owing to 88% of subjects being in current receipt of inpatient, outpatient or domiciliary services, subjects were considered to not have ingested alcohol or other non-prescribed drugs during the study | Yes |
| Jung and Steil (2013)92 | Childhood sexual abuse | Germany | 37.18 (range: 19–61) | 0 | Total sample: white (89%), Asian (11%) | Childhood sexual abuse (100%) | Major depressive disorder (57.1%), eating disorders (32.1%), borderline personality disorder (32.1%) | Yes |
| Katz et al. (2014)93 | Mixed | USA | HR = 45, PE = 36, C = 42 | 0 |
HR = white (41%), African American (24%), Hispanic (6%), other/missing data (29%) PE = white (41%), African American (12%), Hispanic (12%), other/missing data (35%) C (control) = white (47%), African American (24%), Hispanic (17%), other/missing data (12%) |
Sexual trauma history: veterans (100%) Military sexual trauma (HR = 82%, PE = 82%, PC = 94%) Domestic violence (HR = 76%, PE = 71%, C = 65%) Child abuse (HR = 100%, PE = 59%, C = 82%) Adult abuse (HR = 71%, PE = 47%, C = 41%) |
NR | Yes (100%) |
| Keane et al. (1989)94 | Veteran | USA | I = 34.7 (4.3), C = 34.5 (2.1) | 100 |
I = white (91%), Hispanic (9%) C = white (69%), black (31%) |
Veterans | NR | Yes |
| Kearney et al. (2013)95 | Veteran | USA | I = 52 (13.4), C = 52 (11.7) | 79 |
I = white (76%), African American (20%) C = white (59%), African American (9%), other (27%) |
Veterans | NR | Yes |
| Knaevelsrud et al. (2015)96 | War affected | Iraq/Germany (remote) | 28.1 (7.43) | 28 | Iraqi | War related (including bomb attacks and torture) and sexual abuse | Depression, anxiety | Yes |
| Kosten et al. (1992)97 | Veteran | USA | 39 (2.3) | 100 | Non-white (12%) | Vietnam veterans with PTSD (100%) | Minor depression (47.4%) | Yes (100%) |
| Krupnick et al. (2008)98 | Childhood sexual abuse | USA | 32.1 (10.2) | 0 | African American (75%), Hispanic black (4.2%), Afro-Caribbean (2.1%), Latina (8.3%), non-Hispanic white (6.2%), Asian American (4.2%) |
I = mean of 6.8 (SD = 4.2), different types of interpersonal traumas C = mean of 5.7 (SD = 3.5), different types of interpersonal traumas Sexual trauma (97.1%, of which 97.9% were before 12 years of age), physical assault before 12 years of age (95.9%) |
NR | Yes (100%) |
| Krystal et al. (2011)99 | Veteran | USA | I = 54.2 (10.8), C = 54.5 (10.6) | 96.6 |
Means (SD) White (not Hispanic): I = 84 (63.2), C = 93 (69.4) Black (not Hispanic): I = 25 (18.8), C = 25 (18.7) Hispanic: I = 16 (12.0), C = 11 (8.2) Other: I = 8 (6), C = 5 (3.7) |
Combat trauma (78.3%) | NR | Yes |
| Kubany et al. (2003)100 | Domestic violence | USA | 36.4 (9.1) | 0 | White (n = 18), Asian (n = 10), Pacific Islander (n = 6), black and Puerto Rican (n = 3) | Battered women (physical domestic abuse) | NR | Yes |
| Kubany et al. (2004)101 | Domestic violence | USA | 42.2 (10.1) | 0 | White (52.8%), Native Hawaiian (8.8%), Filipino (7.2%), Japanese (6.4%), black (4.8%), Samoan (4.8%), American Indian (1.6%), other or mixed ethnicity (13.6%) | All physically, sexually and/or psychologically abused by intimate romantic partner. Physically hurt more than five times (68%), physically hurt by more than one intimate partner (51%) | NR | Yes (100%) |
| Lande et al. (2010)102 | Veteran | USA | Range: 18–25 (35.9%), 26–35 (33.3%), ≥ 36 (30.7%) | 85 | NR | Veterans | NR | Yes |
| Lau and Kristensen (2007);103 Elkjaer et al. (2014)77 | Childhood sexual abuse | Denmark | I = 34.2 (10.5), C = 32.4 (8.8) | 0 | NR | Childhood sexual abuse (intrafamilial) |
Females aged 30–39 years: affective disorders Females aged 40–41 years: anxiety disorders Females aged 42 and 44–49 years: other nervous diseases Females aged 50–59 years: behavioural syndromes Females aged 60–62 years: personality disorders |
Yes: I = 16%, C = 29% |
| Lindley et al. (2007)104 | Veteran | USA | I = 52.9 (0.7), C = 53.9 (0.4) | 100 | White (62.5%), African American (17.5%), Hispanic (16%), other (5%) | Veterans (100%) | Most patients had comorbid depression | Yes (100%) |
| Margolies et al. (2011)105 | Veteran | USA | I = 36.43 (9.3), C = 39.11 (8.9) | I = 90, C = 90 |
I = white (40%), black (60%) C = white (40%), black (60%) |
Operation Enduring Freedom/Operation Iraqi Freedom veterans | NR | Yes (100%) |
| McDonagh et al. (2005)106 | Childhood sexual abuse | USA | CBT = 39.8 (9.9), PCT = 39.6 (9.6), C = 42 (9.8) | 0 |
CBT = white (90%), African American (0%), Native American (10%), other (0%) PCT = white (95%), African American (5%), Native American (0%), other (0%) Waitlist = white (96%), African American (0%), Native American (0%), other (4%) |
Childhood sexual abuse (100%), characteristics: CBT = life threat (34.5%), injured (41.4%), penetrated (72.4%), mean age at onset = 6.1(2) PCT = life threat (5%), injured (31.8%), penetrated (59.1%), mean age at onset = 7.6(2.8) Waitlist = life threat (26.1%), injured (27.3%), penetrated (56.5%), mean age at onset = 6.1(2.9) CBT = childhood physical abuse (82.8%), adult physical abuse (58.6%), adult sexual trauma (44.8%), mean number of trauma types = 3.3 (1) PCT = childhood physical abuse (81.8%), adult physical abuse (68.2%), adult sexual trauma (63.6%), mean number of trauma types = 3.1 (1.3) Waitlist = childhood physical abuse (73.9%), adult physical abuse (60.9%), adult sexual trauma (43.5%), mean number of trauma types = 3.4 (0.9) |
NR | Yes (100%) |
| McLay et al. (2011)107 | Veteran | USA | I = 28 (range: 22–43), C = 28.8 (range: 21–45) | I = 90, C = 100 | NR |
Active duty service members with PTSD (100%) I = shot (10%), ambush (20%), improvised explosive device blast (20%), mortar attack (20%), suicide bomber (10%), firefight (10%), military medical trauma (10%) C = improvised explosive device blast (30%), close combat (10%), firefight (20%), suicide bomber (10%), civilian casualties (20%), bridge collapse (10%) |
NR | Yes (100%) |
| Meffert et al. (2014)108 | Refugee | Egypt | I = 31.3, C = 30.4 | 19 | Sudanese | Refugees (no further detail) | NR | Yes |
| Miyahira et al. (2012)109 | War affected | USA | NR | NR | NR | Returning war fighters from Iraq or Afghanistan | NR | Yes |
| Monnelly et al. (2003)110 | Veteran | USA | I = 48.9 (8.3), C = 53.5 (3.0) | 100 | White (80%), black (13.3%), Hispanic (6.7%) | Combat (100%) |
I = major depression (26.7%), dysthymic disorder (6.7%), generalised anxiety disorder (13.3%), panic disorder (6.7%) C = major depression (40%), dysthymia (6.7%), generalised anxiety disorder (6.7%) |
Yes (100%) |
| Moradi et al. (2014)111 | Veteran | Iran | I = 45.25 (3.86), C = 45.33 (3.80) | 100 | Iranian | War trauma (mixed) | NR | Yes |
| Naylor et al. (2013)112 | Veteran | USA | I = 39.21 (4.7), C = 35.86 (9.69) | NR | NR | Combat-related (41.6%), non-combat related with a history of combat (41.6%) and non-combat related with no combat experience (16.7%) | C = obsessive compulsive disorder, generalised anxiety disorder and agoraphobia (8.3%), major depressive episode (8.3%), agoraphobia (8.3%) | Yes (partial PTSD = 100%) |
| Neuner et al. (2004)114 | Refugee | Uganda | NET = 31.9 (6.7), supportive counselling = 33.8 (7.9), psychoeducation = 34.2 (6.9) | 37 | Sudanese | Refugees (including those who had witnessed killings and experienced torture) | NR | Yes |
| Neuner et al. (2008)113 | Refugee | Uganda | NET = 34.4 (12.2), trauma counselling = 35.2 (12.8), C = 35.6 (14.0) | 48.7 | Somalian (45.1%), Rwandan (54.9%) | 13.1–14.5 types of traumatic events in groups. Majority of the refugees in Nakivale fled civil conflict | NR | NR |
| Niles et al. (2012)115 | Veteran | USA | 52.0 (13.0) | 100 | White, not Hispanic (76%, n = 25), black, not Hispanic (15%, n = 5), white, Hispanic (6%, n = 2) and ‘other’ (3%, n = 1) | Veterans | NR | Yes |
| Otto et al. (2003)116 | Refugee | USA | 47.2 | 0 | Cambodian (100%) | Refugees (100%) | High unreported psychiatric comorbidity | Yes (100%) |
| Owens et al. (2001)117 | Childhood sexual abuse | USA | 33 (9.15) | 0 | African American (11%), white (87%), Hispanic/Latino/Mexican American (2%) | Childhood sexual abuse (100%). Sexual abuse events reported: vaginal and/or anal penetration, kissing, fondling and oral sexual contact | NR | Yes (100%) |
| Panahi et al. (2011)118 | Veteran | Iran | I = 46.5 (5.4), C = 44.6 (5.1) | 100 | NR | Iranian Iran–Iraq war veterans (100%) | NR | Yes (100%) |
| Paunovic and Ost (2001)119 | Refugee | Sweden | 37.9 (7.6) | 85 | NR | Refugees (100%). Experienced more than one traumatic event (70%). Primary traumatic events (assumed to be based on 16 completers): torture = 6, combat = 6, physical assault in civilian life = 5, witnessing murder of significant others = 4, witnessing massacre = 3, assault with weapon in civilian life = 2, transportation accident = 2, witnessing physical assault in civilian life = 2, witnessing assault with weapon in civilian life = 2, witnessing sudden violent death = 2, witnessing murder of strangers = 2, death threats against family = 2, threat of torture = 1, sexual assault = 1, exposure to toxic substance = 1, death threats with a weapon in civilian life = 1 | NR | Yes (100%) |
| Polusny et al. (2015)120 | Veteran | USA | I = 57.6 (10.4), C = 59.4 (9.2) | MBSR = 79, PCT = 90 |
MBSR = white (81%), black (5%), other (4%), mixed (10%) PCT = white (86%), black (10%), other (4%), mixed (0%) |
Veterans (100%), lifetime traumas: I = combat exposure (68%), sexual trauma (37%), physical assault (68%), disaster exposure (44%), serious injury event (67%), life-threatening illness/injury (60%), other (97%) C = combat exposure (80%), sexual trauma (19%), physical assault (63%), disaster exposure (43%), serious injury event (61%), life-threatening illness/injury (56%), other (93%) |
I = mood disorder (44.8%) C = mood disorder (39.7%) No other comorbidities reported as measured |
Yes (full PTSD = 97.4%, subthreshold PTSD = 2.6%). Per group: full PTSD (I = 98.3%, C = 96.6%), subthreshold PTSD (I = 1.7%, C = 3.4%) |
| Possemato et al. (2016)121 | Veteran | USA | I = 46.3 (16.4), C = 47.4 (16.2) | 87.1 | White (82.3%) | Veterans | NR | Yes (48.4%) |
| Raskind et al. (2007)122 | Veteran | USA | 56 (9) | 95 |
White (n = 26), African American (n = 11), Asian American (n = 1), Hispanic (n = 1) and Native American (n = 1) Overall (40) |
Veterans | Depression | Yes |
| Raskind et al. (2013)123 | Veteran | USA | I = 30.0 (6.6), C = 30.8 (6.5) | I = 81, C = 89 |
I = African American (13%), Asian (3%), Caucasian (66%), Hispanic (16%), other (3%) C = African American (14%), Caucasian (60%), Hispanic (9%), Native American (6%), other (11%) |
Active duty soldiers returned from Afghanistan and Iraq (100%) I = mean number of deployments 2.6 (SD 4.0), combat experiences scale score 10.9 (SD 3.8) C = mean number of deployments 1.9 (SD 1.2), combat experiences scale score 11.9 (SD 3.6) |
I = major depression (34%), C = major depression (43%) | Yes (100%) |
| Ready et al. (2010)124 | Veteran | USA | Virtual reality exposure = 57 (range: 53–61), PCT = 58 (range: 55–62) | 100 | White (54.5%), African American (45.5%) | Vietnam veterans | NR | Yes (100%) |
| Reed and Enright (2006)125 | Domestic violence | USA | 44.95 (7.01) | 100 | European Americans (90%), Hispanic American (5%), Native American (5%) | Romantic partner emotional abuse: criticising (90%), ridiculing (100%), jealous control (75%), purposeful ignoring (100%), threats of abandonment (25%), threats of personal harm (30%), threats of harm to property or pets (20%), sexual abuse (30%: n = 5 ridicule followed by demands for sexual favours, n = 1 threats of physical harm combined with demands for sexual favours) | NR | NR |
| Reger et al. (2016)126 | Veteran | USA | Virtual reality exposure = 29.52 (6.47), PE = 30.89 (7.09), C = 30.39 (6.45) | > 95 | White (59.9%), black (9.3%), Hispanic (17.3%) | Veterans | NR | Yes |
| Reich et al. (2004)127 | Childhood sexual abuse | USA | I = 30.6, C = 24.2 | 0 |
White: I = 75%, C = 100% African American: I = 16.7%, C = 0% Asian American: I = 8.3%, C = 0% |
Trauma related to childhood: emotional (I = 66.7%, C = 54.5%), verbal (I = 50%, C = 77.8%), physical (I = 50%, C = 44.4%), sexual abuse (I = 83.3%, C = 66.7%) |
Major depression (I = 66.6%, C = 55.5%) Dysthymia (I = 8.3%, C = 0%) Panic disorder (I = 25%, C = 11.1%) Agoraphobia with panic disorder (I = 16.6%, C = 0%) Agoraphobia without panic disorder (I = 8.3%, C = 0%) Generalised anxiety disorder (I = 8.3%, C = 22.2%) Simple phobia (I = 25%, C = 0%) Social phobia (I = 0%, C = 11.1%) Eating disorder not otherwise specified (I = 8.3%, C = 0%) Obsessive–compulsive disorder (I = 0%, C = 11.1%) Somatisation disorder (I = 8.3%, C = 0%) |
Yes |
| Resick et al. (2015)128 | Veteran | USA | I = 31.8 (7.3), C = 32.4 (7.9) | CPT-C = 93, PCT = 92 |
CPT-C = black (20%), Hispanic (9%), white (63%), other (9%) PCT = black (21%), Hispanic (19%), white (52%), other (8%) |
Active duty military with criterion A traumatic event (100%) | NR | Yes (100%) |
| Rogers et al. (1999)130 | Veteran | USA | Range: 47–53 | 100 | NR | Vietnam veterans (100%) | NR | Yes (100%) |
| Rothbaum et al. (2014)129 | Veteran | USA | D-cycloserine + PE = 34.9, alprazolam + PE = 36.2, C = 34.3 | 95 | Black (50.6%), white (41.6%), Hispanic (5%) | Veterans | 27.5% had a comorbid mood disorder | Yes |
| Sikkema et al. (2007)131 | Childhood sexual abuse | USA | Female = 43.18 (6.99), male = 41.75 (6.99) | 46 | Total sample: white (11.3%), African American (68.6%), Hispanic-Latino (16%), other (4.1%) | Primarily childhood sexual abuse. 62% of women and 43% of men also experienced rape as adults | HIV-positive sero-status; meets DSM-IV criteria for PTSD: women (37%), men (43%) | Yes |
| Sikkema et al. (2013)132 | Childhood sexual abuse | USA | 42.3 (6.8) | 47 | Overall: African American (68%), Hispanic (17%), white (10%) | Childhood sexual abuse | NR | Yes (40%) |
| Smajkic et al. (2001)133 | Refugee | USA | 51.34 (10.11) | Venlafaxine = 100, sertraline = 40, paroxetine = 25 | Bosnian (100%) | Refugees (100%) | NR | Yes (100%) |
| Sonne et al. (2016)134 | Refugee | Denmark | I = 43.2 (9.6), C = 44 (9.7) | Venlafaxine = 62.2, sertraline = 58.3 | Origin: venlafaxine = ex-Yugoslavia (11.2%), Iran (13.3%), Iraq (34.7%), Afghanistan (10.2%), Lebanon (12.6%), other (18.4%); sertraline = ex-Yugoslavia (8.3%), Iran (13.9%), Iraq (34.4%), Afghanistan (16.7%), Lebanon (13%), other (13.9%) | Refugees (100%): venlafaxine = imprisonment (58.8%), torture (55.1%), refugee camp (22.9%); sertraline = imprisonment (48.6%), torture (41.7%), refugee camp (27.5%) | Venlafaxine = depression (97.96%), enduring personality change after catastrophic experience (41.3%), other psychiatric disorder (12.24%); sertraline = depression (99.08%), enduring personality change after catastrophic experience (40.38%), other psychiatric disorder (11.1%) | Yes (100%) |
| Stein et al. (2002)135 | Veteran | USA | I = 55.2 (6.6), C = 51.1 (8.1) | 100 | NR | Military veterans (n = 3 Vietnam-related) | All subjects had depression and pronounced sleep problems | Yes |
| Stenmark et al. (2013)136 | Refugee | Germany | I = 34.5 (11.1), C = 36.6 (11.0) | I = 67, C = 73 | Region of origin: I = Afghanistan (14%), Iraq (29%), Middle East (remaining countries) (16%), Africa (25%), other countries (16%); C = Afghanistan (17%), Iraq (23%), Middle East (remaining countries) (17%), Africa (26%), other countries (17%) | Refugees and asylum seekers with PTSD (100%). Mean number of traumatic events: I = 8.3 (2.2), C = 7.9 (2.9) | NR | Yes (100%) |
| Teng et al. (2008)137 | Veteran | USA | I = 52.00 (8.13), C = 51.87 (9.07) | 86 | African American (42.9%), white (42.9%), Hispanic (14.2%) | Veterans | Panic disorder (13.3%), panic disorder with agoraphobia (86.7%), specific phobia (23.3%), obsessive–compulsive disorder (13.3%), acute stress disorder (3.3%), generalised anxiety disorder (26.7%), major depressive disorder (60.0%), dysthymic disorder (30.0%) | Yes |
| Ter Heide et al. (2016)139 | Refugee | The Netherlands | I = 43.1 (10.7), C = 39.8 (11.9) | 69 | The vast majority of refugees came from Iraq, Afghanistan or countries in Africa (ethnicities were NR). Other origin countries included Former Yugoslavia and other Middle-Eastern countries | Refugees (including asylum seekers and illegal immigrants) | 77.8% had comorbid depression | Yes |
| Ter Heide et al. (2011)138 | Refugee | The Netherlands | I = 40 (9.31), C = 43 (7.93) | I = 50, C = 70 | Origin: Afghanistan (20%), Algeria (5%), Bosnia (20%), Iran (10%), Iraq (30%), Lebanon (5%), Turkey (5%) | Asylum seekers and refugees. Experienced 10 separate events, on average, including: murder/unnatural death of family or friend (95%), physical or psychological torture (70%) | Depression (I = 80%, C = 50%) | NR |
| Ulmer et al. (2011)140 | Veteran | USA | I = 47.0 (9.5), C = 50.2 (11.6) | I = 66.7, C = 55.6 |
I = African American (33.3%), white (33.3%), other (33.3%) C = African American (33.3%), white (33.3%), other (33.3%) |
Veterans with PTSD | NR | Yes (100%) |
| van der Kolk et al. (1994)141 | Mixed | USA | I = 40.8 (6.4), C = 39.9 (7.8) | 30 | NR | 31/64 were veterans, 33 were non-veterans (20/33 had experienced childhood sexual abuse) | Depression (54.8%) | Yes |
| Wahbeh et al. (2016)142 | Veteran | USA | MM = 53.3 (12.6), SB = 52.2 (12.5), MM + SB = 50 (12.8), SQ = 53 (11.8) | MM = 93, SB = 92, MM + SB = 96, SQ = 96 | White (MM = 85%, SB = 88%, MM + SB = 88%, SQ = 84%) |
Combat veterans with PTSD (100%) Combat exposure: MM = 24.1 (9.4), SB = 22.5 (8.5), MM + SB = 26.6 (10.3), SQ = 25.8 (9.8) Lifetime trauma (Life Events Checklist): MM = 32.2 (7.8), SB = 33.7 (5.7), MM + SB = 32.7 (6.3), SQ = 31.3 (8.1) |
NR | Yes (100%) |
| Wang et al. (2016)143 | War affected | Kosovo | I = 46.8 (10.4), C = 48.8 (10.9) | 55 | NR | Victims of torture and war (civilians) | Depression = 92.9%, anxiety disorders = 89.3% | Yes (50%) |
| Weiss et al. (2015), trial 1: CETA144 | War affected | Iraq | I = 41.6 (11.3), C = 45.16 (11.1) | Male: I = (67.7), C = (32.3) | NR | Survivors of systemic violence: having witnessed or experienced physical torture or militant attacks | NR | NR |
| Weiss et al. (2015), trial 2: CPT144 | War affected | Iraq | I = 40 (12.3), C = 41 (9.5) | I = 67.4, C = 62.5 | NR | Survivors of systemic violence: having witnessed or experienced physical torture or militant attacks | NR | NR |
| Yeomans et al. (2010)145 | War affected | Burundi | 38.6 (12.8) | 65.6 | Hutu (52.4%), Tutsi (47.6%) |
Witnessed: mixed (e.g. rape, serious injury owing to combat) Experienced: combat (98.8%), forced to hide (97.1%), unnatural death of family member (96.7%), lack of food/water (95%), narrowly escaping death (91.7%), lack of shelter (90.4%), ill health without medical care (86.2%), loss of personal property (81.9%), confined indoors owing to danger (79.5%), betrayed and placed at risk of death (41.7%), serious physical injury from combat (35%), forced to hide among the dead (27.5%), imprisonment (23.8%); other |
NR | NR |
| Zlotnick et al. (1997)146 | Childhood sexual abuse | USA | 39 (9.59) | 0 | 99% white (n = 1: Native American) | Childhood sexual abuse | Extreme stress (100%) | Yes |
| Zohar et al. (2002)147 | Veteran | Israel | I = 41 (6), C = 38 (9) | I = 83, C = 95 | NR | Veterans (100%) | NR | Yes (100%) |
Appendix 6 Characteristics of included non-randomised controlled studies
| Authors (year) | Intervention(s) | Control(s) | Intensity (duration, frequency and strength of dose/length of sessions) | Delivery (method, setting and type of professional) |
|---|---|---|---|---|
| King et al. (2013)148 | Mindfulness-based cognitive therapy | Treatment as usual |
Duration: 8 weeks Frequency: weekly Dose/length of sessions: 8 hours Unclear for treatment as usual group |
Face to face (group); outpatient veterans’ affairs clinic; doctoral- and master’s-level clinicians with mental health backgrounds |
| Kruse et al. (2009)149 | Trauma-focused psychotherapy | Treatment as usual |
Duration: NR Frequency: weekly (first 3 months), fortnightly (remainder) Dose/length of sessions: 50 minutes, 25 hours total |
Face to face (individual); setting NR; trained psychotherapists |
| Levi et al. (2016)150 | CBT |
Duration: 24 weeks Frequency: weekly Dose/length of sessions: NR |
Face to face (individual); army PTSD treatment centre; psychiatrists, clinical psychologists and social workers | |
| Psychodynamic psychotherapy |
Duration: 50 weeks Frequency: weekly Dose/length of sessions: NR |
|||
| Lundqvist et al. (2006)151 | Group therapy | Waitlist |
Duration: 2 years (phase 1, 5 months; phase 2, 4 months; phase 3, 1 year) Frequency: twice a week (phase 1), weekly (phase 2), monthly (phase 3) Dose/length of sessions: NR |
Face to face (group); hospital psychiatric outpatient unit; female group leaders, unknown training |
| Short-term focused therapy |
Duration: 2 years (phase 1, 5 months; phase 2, 4 months; phase 3, 1 year) Frequency: twice a week (phase 1), weekly (phase 2), monthly (phase 3) Dose/length of sessions: NR |
|||
| Morgan and Cummings (1999)152 | Group psychotherapy | No intervention |
Duration: 20 weeks Frequency: weekly Dose/length of sessions: NR |
Face to face (group); community social services; psychotherapists |
| Narimani et al. (2008)153 | EMDR | Waitlist |
Duration: 70 days (typically) Frequency: NR Dose/length of sessions: 90 minutes |
Face to face (individual); setting NR; trained therapists |
| CBT |
Duration: 70 days Frequency: NR Dose/length of sessions: 60–120 minutes |
|||
| Pivac et al. (2004)154 | Olanzapine |
Duration: 6 weeks Frequency: once or twice daily Dose/length of sessions: 5–10 mg |
Drug intervention; delivered by hospital for PTSD; psychiatrists | |
| Fluphenazine |
Duration: 6 weeks Frequency: once or twice daily Dose/length of sessions: 5–10 mg |
|||
| Salo et al. (2008)155 | Individual therapy | No intervention |
Duration: 1 year Frequency: weekly Dose/length of sessions: NR |
Face to face (individual); setting NR; master’s-level social workers and psychologists |
| Group therapy |
Duration: 1 year Frequency: weekly Dose/length of sessions: NR |
Face to face (group); setting NR; therapists with a baccalaureate degree in psychology and social work with mental health backgrounds | ||
| Saxe and Johnson (1999)156 | ‘Victim to survivor’ group therapy | Waitlist |
Duration: 20 weeks Frequency: weekly Dose/length of sessions: NR |
Face to face (group); community mental health agency; experienced mental health social workers |
Appendix 7 Population characteristics of included non-randomised controlled studies
| Authors (year) | Trauma experience category | Country | Age of males, years (SD) | Gender (% male) | Ethnicity | Type(s) of trauma experienced | Current comorbidities | PTSD diagnosis at baseline? |
|---|---|---|---|---|---|---|---|---|
| King et al. (2013)148 | Veteran | USA | I = 60.1 (9.7), C = 58.3 (8.3) | NR | NR | Veterans | 65% of participants from the treatment group and 76% from the control had a current major depressive disorder | Yes |
| Kruse et al. (2009)149 | Refugee | Germany | I = 44.7 (9.0), C = 44.3 (12.2) | I = 35.3%, C = 30% | Bosnian (100%) |
Bosnian refugees (100%). Highly stressful war-related events: I = close to death (97%), forced separation (82.3%), murder of family/friends (70.6%), murder of strangers (67.7%), physical torture (70.6%), combat situation (50%), rape/sexual abuse (41.2%), brainwashed (85.3%), lack of food/water (67.7%), unnatural death of friends (58.8%), lost/kidnapped (64.7%), lack of medical care (70.6%), no shelter (79.4%), imprisoned (55.9%), serious injury (70.6%), isolation (41.2%); number of events 10.7 (SD 4.4) C = close to death (100%), forced separation (93.3%), murder of family/friends (83.3%), murder of strangers (83.3%), physical torture (93.4%), combat situation (63.4%), rape/sexual abuse (50%), brainwashed (96.7%), lack of food/water (86.6%), unnatural death of friends (80%), lost/kidnapped (86.6%), lack of medical care (70%), no shelter (96.7%), imprisoned (80%), serious injury (90%), isolation (66.7%); number of events 13.5 (SD 3.2) |
NR | Yes (100%) |
| Levi et al. (2016)150 | Veteran | Israel | I = 30.8 (11.4), C = 33.4 (11.45) | 100% | NR | Veterans | NR | Yes |
| Lundqvist et al. (2006)151 | Childhood sexual abuse | Sweden | Group therapy = 34 (range: 20–54), short-term focused therapy = 39 (range: 25–54), C = 41 (range: 28–55) | 0% (100% female) | NR | Childhood sexual abuse | NR | NR |
| Morgan and Cummings (1999)152 | Childhood sexual abuse | Canada | I = 36.92 (8.01), C = 33.05 (10.27) | 0% (100% female) | NR | Childhood sexual abuse | NR | NR |
| Narimani et al. (2008)153 | War affected | Iran | Overall: 47.95 (5.07) | NR | Iranian (100%) | Combatants afflicted and hospitalised at psychiatric/psychological hospital (100%) | NR | NR |
| Pivac et al. (2004)154 | Veteran | Croatia | I = 37.2 (4.5), C = 38.1 (4.8) | 100% | NR | Veterans | All participants had comorbid psychotic symptoms: 37 (68%) had psychotic depression with auditory hallucinations or auditory and visual hallucinations; 18 (37%) had delusional paranoid symptoms | Yes |
| Salo et al. (2008)155 | War affected | Palestine | Individual treatment = 32.36 (1.44), group treatment = 30.45 (1.40), C = 30.82 (0.72) | 100% | Palestinian (100%) | Former political prisoners (100%). Most common experiences of torture/ill treatment: different types of beatings such as by gun or baton (87.8%), psychological abuse such as sham execution (75.5%); classic torture methods less common: burning with cigarettes (13.8%), pain by electricity (11%) | NR | NR |
| Saxe and Johnson (1999)156 | Childhood sexual abuse | Canada | NR | 0% (100% female) | NR | Childhood sexual abuse (incest) | NR | NR |
Appendix 8 Risk-of-bias gradings of included randomised controlled trials
FIGURE 26.
Risk-of-bias ratings across the domains of the Cochrane tool for all included RCTs.
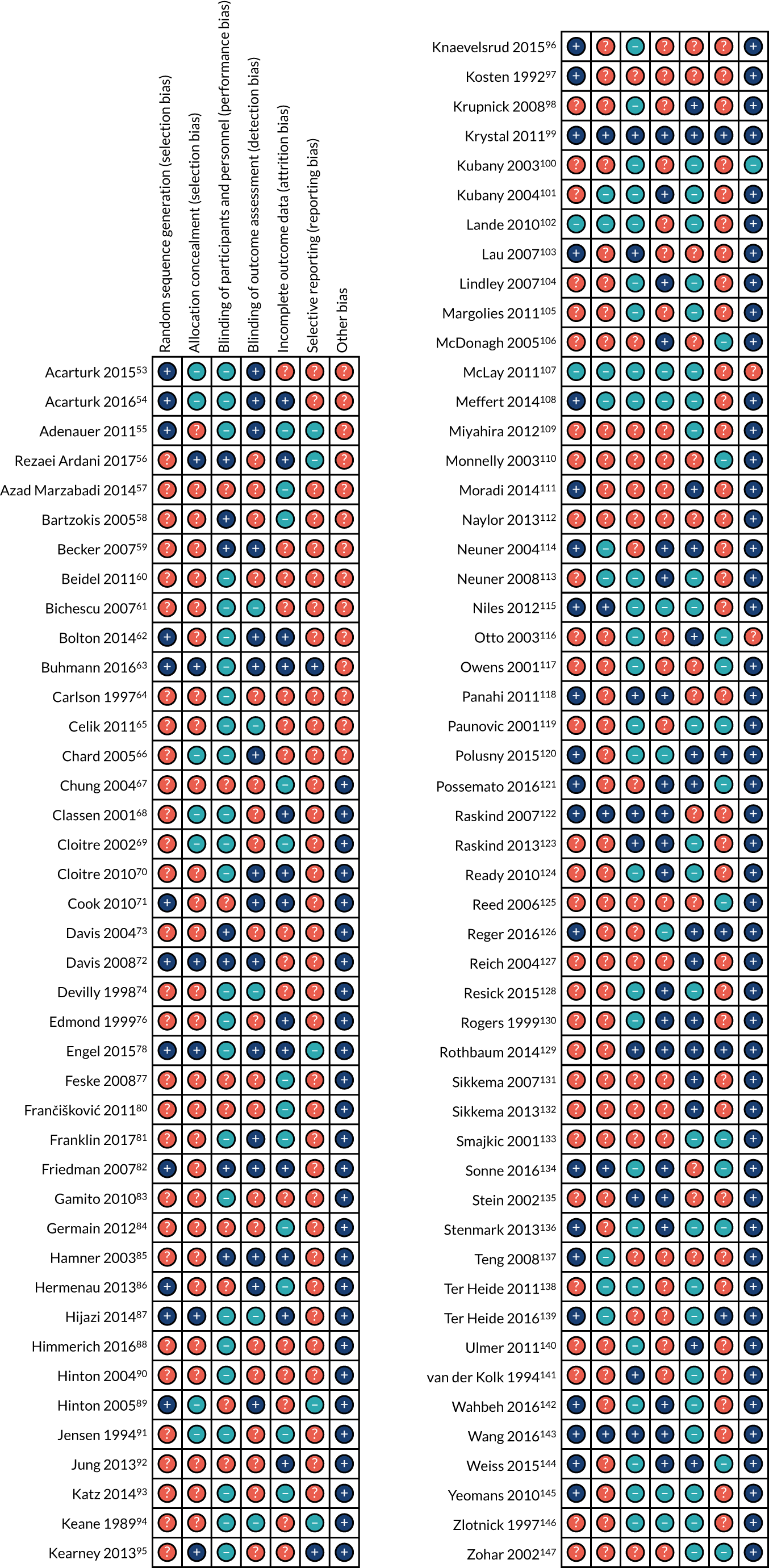
Appendix 9 Summary tables of clinical effectiveness analyses
Effectiveness of psychological interventions across all populations
Post-traumatic stress disorder outcomes
| Psychological interventions vs. control | Control | Active control | ||
|---|---|---|---|---|
| Post treatment | Follow-up after < 6 months | Post treatment | Follow-up after < 6 months | |
| All | SMD –0.90 (95% CI –1.14 to –0.66), I2 = 85.3%, number of trials = 39, n = 2506 | SMD –0.45 (95% CI –0.82 to –0.08), I2 = 79.4%, number of trials = 10, n = 738 | SMD –0.35 (95% CI –0.72, 0.03), I2 = 47.0%, number of trials = 6, n = 259 | – |
| Trauma-focused CBT | SMD –1.09 (95% CI –1.44 to –0.75), I2 = 86%, number of trials = 21, n = 1283 | SMD –0.64 (95% CI –1.10 to –0.18), I2 = 44.9%, number of trials = 4, n = 206 | – | – |
| EMDR | SMD –1.07 (95% CI –1.65 to –0.50), I2 = 75.4%, number of trials = 7, n = 244 | – | SMD –0.15 (95% CI –0.62, 0.32), I2 = 0%, number of trials = 2, n = 71 | – |
| IPT | SMD –1.41 (95% CI –1.97 to –0.85), I2 = 0%, number of trials = 2, n = 66 | – | – | – |
| Mindfulness | SMD –0.26 (95% CI –0.55, 0.04), I2 = 0%, number of trials = 3, n = 183 | SMD –0.08 (95% CI –0.68, 0.52), I2 = 59%, number of trials = 2, n = 109 | – | – |
| Non-trauma-focused CBT | SMD –0.05 (95% CI –0.23, 0.13), I2 = 0%, number of trials = 3, n = 548 | SMD –0.02 (95% CI –0.25, 0.20), I2 = 0%, number of trials = 2, n = 305 | – | – |
| Single-component and trauma-focused interventions | SMD –1.16 (95% CI –1.52 to –0.81), I2 = 86.2%, number of trials = 23, n = 1264 | SMD –0.94 (95% CI –1.56 to –0.32), I2 = 77.6%, number of trials = 5, n = 276 | – | – |
| Multicomponent and trauma-focused interventions | SMD –0.73 (95% CI –1.11 to –0.35), I2 = 62.3%, number of trials = 7, n = 385 | – | – | – |
| Single-component non-trauma-focused interventions | SMD –0.39 (95% CI –0.66 to –0.12), I2 = 69.6%, number of trials = 11, n = 936 | SMD –0.05, (95% CI –0.23, 0.14), I2 = 0%, number of trials = 5, n = 462 | SMD –0.64 (95% CI –1.82, 0.53), I2 = 76.9%, number of trials = 2, n = 62 | – |
| Phase-based interventions | Effect size –1.13 (95% CI –1.54 to –0.73), I2 = 35.9%, number of trials = 6, n = 190 | – | – | – |
Complex post-traumatic stress disorder outcomes
| CPTSD symptom cluster | Psychological interventions vs. control | Control | Active control | ||
|---|---|---|---|---|---|
| End of treatment | Follow-up after < 6 months | End of treatment | Follow-up after < 6 months | ||
| Emotional dysregulation | All | SMD –0.38 (95% CI –0.88 to 0.12), I2 = 74.5%, number of trials = 7, n = 289 | SMD –0.42 (95% CI –1.53 to 0.69), I2 = 72.3%, number of trials = 2, n = 51 | – | – |
| Trauma-focused CBT | SMD –0.17 (95% CI –0.82 to 0.49), I2 = 60.6%, number of trials = 3, n = 103 | SMD –0.42 (95% CI –1.53 to 0.69), I2 = 72.3%, number of trials = 2, n = 51 | – | – | |
| Single-component and trauma-focused interventions | – | – | – | – | |
| Multicomponent and trauma-focused interventions | – | – | – | – | |
| Single-component and non-trauma-focused interventions | SMD –0.04 (95% CI –0.41 to 0.33), I2 = 23.9%, number of trials = 4, n = 163 | – | – | – | |
| Phase-based interventions | SMD –0.76 (95% CI –1.79 to 0.27), I2 = 83.4%, number of trials = 3, n = 118 | – | – | – | |
| Interpersonal problems | All | SMD –0.59 (95% CI –1.28 to 0.11), I2 = 61.9%, number of trials = 2, n = 94 | – | – | – |
| Trauma-focused CBT | – | – | – | – | |
| Single-component and trauma-focused interventions | – | – | – | – | |
| Multicomponent and trauma-focused interventions | – | – | – | – | |
| Single-component and non-trauma-focused interventions | – | – | – | – | |
| Phase-based interventions | SMD –0.59 (95% CI –1.28 to 0.11), I2 = 61.9%, number of trials = 2, n = 94 | – | – | – | |
| Negative self-concept | All | SMD 1.81 (95% CI 0.73 to 2.89), I2 = 90%, number of trials = 5, n = 215 | – | – | – |
| Trauma-focused CBT | SMD 2.22 (95% CI 0.75 to 3.70), I2 = 90.4%, number of trials = 3, n = 145 | – | – | – | |
| Single-component and trauma-focused interventions | – | – | – | – | |
| Multicomponent and trauma-focused interventions | SMD 2.93 (95% CI 2.40 to 3.45), I2 = 0%, number of trials = 2, n = 117 | – | – | – | |
| Single-component and non-trauma-focused interventions | SMD 1.14 (95% CI 0.01 to 2.27), I2 = 72.6%, number of trials = 2, n = 70 | – | – | – | |
| Phase-based interventions | – | – | – | – | |
Depression
| Psychological interventions vs. control | Control | Active control | ||
|---|---|---|---|---|
| Post treatment | Follow-up after < 6 months | Post treatment | Follow-up after < 6 months | |
| All | SMD –0.89 (95% CI –1.15 to –0.64), I2 = 81.3%, number of trials = 30, n = 1793 | SMD –0.51 (95% CI –0.80 to –0.22), I2 = 48%, number of trials = 9, n = 410 | SMD –0.32 (95% CI –1.23 to 0.59), I2 = 47.8%, number of trials = 2, n = 72 | – |
| Trauma-focused CBT | SMD –0.91 (95% CI –1.31 to –0.51), I2 = 87.3%, number of trials = 14, n = 1042 | SMD –0.72 (95% CI –1.43 to –0.01), I2 = 56.6%, number of trials = 3, n = 104 | – | – |
| EMDR | SMD –1.12 (95% CI –1.68 to –0.55), I2 = 65.2%, number of trials = 5, n = 182 | – | SMD –0.32 (95% CI –1.23 to 0.59), I2 = 47.8%, number of trials = 2, n = 72 | – |
| IPT | SMD –1.17 (95% CI –1.71 to –0.62), I2 = 0%, number of trials = 2, n = 66 | – | – | – |
| Mindfulness | SMD –0.43 (95% CI –0.73 to –0.13), I2 = 0%, number of trials = 3, n = 186 | SMD –0.41 (95% CI –0.79 to –0.02), I2 = 0%, number of trials = 2, n = 109 | – | – |
| Non-trauma-focused CBT | SMD –0.05 (95% CI –0.48 to 0.39), I2 = 10%, number of trials = 2, n = 93 | – | – | – |
| Single-component and trauma-focused interventions | SMD –1.14 (95% CI –1.54 to –0.74), I2 = 86.6%, number of trials = 17, n = 1034 | SMD –0.85 (95% CI –1.42 to –0.29), I2 = 62.5%, number of trials = 4, n = 174 | – | – |
| Multicomponent and trauma-focused interventions | SMD –0.75 (95% CI –1.22 to –0.29), I2 = 58.6%, number of trials = 5, n = 267 | – | – | – |
| Single-component non-trauma-focused interventions | SMD –0.48 (95% CI –0.72 to –0.25), I2 = 42.0%, number of trials = 10, n = 594 | SMD –0.30, (95% CI –0.56 to –0.04), I2 = 0%, number of trials = 5, n = 236 | – | – |
| Phase-based interventions | Effect size –1.03 (95% CI –1.43 to –0.63), I2 = 10.9%, number of trials = 4, n = 133 | – | – | – |
Anxiety
| Psychological interventions vs. control | Control | Active control | ||
|---|---|---|---|---|
| Post treatment | Follow-up after < 6 months | Post treatment | Follow-up after < 6 months | |
| All | SMD –0.81 (95% CI –1.18 to –0.46), I2 = 83.4%, number of trials = 13, n = 1136 | – | – | – |
| Trauma-focused CBT | SMD –0.60 (95% CI –1.01 to –0.19), I2 = 85.5%, number of trials = 8, n = 832 | – | – | – |
| EMDR | SMD –1.05 (95% CI –1.50 to –0.61), I2 = 9.2%, number of trials = 4, n = 102 | – | – | – |
| IPT | – | – | – | – |
| Mindfulness | – | – | – | – |
| Non-trauma-focused CBT | – | – | – | – |
| Single-component and trauma-focused interventions | SMD –0.76 (95% CI –1.15 to –0.37), I2 = 81.5%, number of trials = 10, n = 757 | – | – | – |
| Multicomponent and trauma-focused interventions | SMD –0.85 (95% CI –1.60 to –0.10), I2 = 80.4%, number of trials = 3, n = 223 | – | – | – |
| Single-component non-trauma-focused interventions | SMD –0.18 (95% CI –0.53 to 0.17), I2 = 26.9%, number of trials = 2, n = 225 | – | – | – |
| Phase-based interventions | – | – | – | – |
Quality of life
| Psychological interventions vs. control | Control | Active control | ||
|---|---|---|---|---|
| Post treatment | Follow-up after < 6 months | Post treatment | Follow-up after < 6 months | |
| All | SMD 0.28 (95% CI –0.15 to 0.71), I2 = 65.5%, number of trials = 5, n = 307 | – | – | – |
| Trauma-focused CBT | SMD 0.23 (95% CI –0.33 to 0.79), I2 = 73.9%, number of trials = 4, n = 260 | – | – | – |
| EMDR | – | – | – | – |
| IPT | – | – | – | – |
| Mindfulness | – | – | – | – |
| Non-trauma-focused CBT | – | – | – | – |
| Single-component and trauma-focused interventions | – | – | – | – |
| Multicomponent and trauma-focused interventions | – | – | – | – |
| Single-component non-trauma-focused interventions | – | – | – | – |
| Phase-based interventions | – | – | – | – |
Sleep quality
| Psychological interventions vs. control | Control | Active control | ||
|---|---|---|---|---|
| Post treatment | Follow-up after < 6 months | Post treatment | Follow-up after < 6 months | |
| All | SMD –1.00 (95% CI –1.49 to –0.51), I2 = 28.8%, number of trials = 3, n = 111 | – | – | – |
| Trauma-focused CBT | SMD –1.30 (95% CI –1.87 to –0.73), I2 = 0%, number of trials = 2, n = 59 | – | – | – |
| EMDR | – | – | – | – |
| IPT | – | – | – | – |
| Mindfulness | – | – | – | – |
| Non-trauma-focused CBT | – | – | – | – |
| Single-component and trauma-focused interventions | – | – | – | – |
| Multicomponent and trauma-focused interventions | – | – | – | – |
| Single-component non-trauma-focused interventions | – | – | – | – |
| Phase-based interventions | – | – | – | – |
Effectiveness of psychological interventions by trauma exposure
Veterans
| Outcome | Psychological interventions vs. control | Control | Active control | ||
|---|---|---|---|---|---|
| Post treatment | Follow-up after < 6 months | Post treatment | Follow-up after < 6 months | ||
| PTSD symptoms | All | SMD –0.48 (95% CI –0.72 to –0.24), I2 = 41.7%, number of trials = 14, n = 502 | SMD –0.20 (95% CI –0.72 to 0.33), I2 = 63.1%, number of trials = 4, n = 180 | SMD –0.44 (95% CI –0.98 to 0.10), I2 = 64%, number of trials = 4, n = 188 | – |
| Trauma-focused CBT | SMD –0.77 (95% CI –1.20 to –0.33), I2 = 44.6%, number of trials = 5, n = 199 | – | SMD –0.26 (95% CI –0.88 to 0.35), I2 = 51.1%, number of trials = 2, n = 126 | – | |
| EMDR | SMD –0.58 (95% CI –1.00 to –0.16), I2 = 11.1%, number of trials = 4, n = 106 | – | – | – | |
| IPT | – | – | – | – | |
| Mindfulness | SMD –0.26 (95% CI –0.55 to 0.04), I2 = 0%, number of trials = 3, n = 186 | SMD –0.08 (95% CI –0.68 to 0.52), I2 = 59%, number of trials = 2, n = 109 | – | – | |
| Non-trauma-focused CBT | – | – | – | – | |
| Single-component and trauma-focused interventions | SMD –0.51 (95% CI –0.79 to –0.23), I2 = 0%, number of trials = 7, n = 219 | – | – | – | |
| Multicomponent and trauma-focused interventions | SMD –1.05 (95% CI –1.80 to –0.30), I2 = 59.4%, number of trials = 3, n = 86 | – | – | – | |
| Single-component non-trauma-focused interventions | SMD –0.16 (95% CI –0.42 to 0.10), I2 = 0%, number of trials = 4, n = 244 | SMD 0.01 (95% CI –0.36 to 0.36), I2 = 28.1%, number of trials = 3, n = 167 | – | – | |
| Phase-based interventions | – | – | – | – | |
| Depression symptoms | All | SMD –0.56 (95% CI –0.84 to –0.28), I2 = 46.8%, number of trials = 11, n = 445 | SMD –0.38 (95% CI –0.78 to 0.01), I2 = 42.3%, number of trials = 5, n = 201 | – | – |
| Trauma-focused CBT | SMD –1.02 (95% CI –1.72 to –0.32), I2 = 51%, number of trials = 3, n = 112 | – | – | – | |
| EMDR | SMD –0.91 (95% CI –2.28 to 0.47), I2 = 77.7%, number of trials = 2, n = 44 | – | – | – | |
| IPT | – | – | – | – | |
| Mindfulness | SMD –0.43 (95% CI –0.73 to –0.13), I2 = 0%, number of trials = 3, n = 186 | SMD –0.41 (95% CI –0.79 to –0.02), I2 = 0%, number of trials = 2, n = 109 | – | – | |
| Non-trauma-focused CBT | – | – | – | – | |
| Single-component and trauma-focused interventions | SMD –0.87 (95% CI –1.50 to –0.24), I2 = 56%, number of trials = 4, n = 133 | – | – | – | |
| Multicomponent and trauma-focused interventions | SMD –0.86 (95% CI –1.89 to 0.17), I2 = 61.4%, number of trials = 2, n = 44 | – | – | – | |
| Single-component non-trauma-focused interventions | SMD –0.33 (95% CI –0.61 to –0.05), I2 = 20.7%, number of trials = 5, n = 268 | SMD –0.27 (95% CI –0.56 to 0.02), I2 = 0%, number of trials = 4, n = 188 | – | – | |
| Phase-based interventions | – | – | – | – | |
| Anxiety symptoms | All | SMD –0.74 (95% CI –1.29 to –0.18), I2 = 54%, number of trials = 5, n = 153 | – | – | – |
| Trauma-focused CBT | SMD –0.63 (95% CI –1.83 to 0.57), I2 = 71.3%, number of trials = 2, n = 90 | – | – | – | |
| EMDR | SMD –0.89 (95% CI –1.45 to –0.33), I2 = 10.6%, number of trials = 3, n = 63 | – | – | – | |
| IPT | – | – | – | – | |
| Mindfulness | – | – | – | – | |
| Non-trauma-focused CBT | – | – | – | – | |
| Single-component and trauma-focused interventions | – | – | – | – | |
| Multicomponent and trauma-focused interventions | – | – | – | – | |
| Single-component non trauma-focused interventions | – | – | – | – | |
| Phase-based interventions | – | – | – | – | |
War-affected populations
| Outcome | Psychological interventions vs. control | Control | Active control | ||
|---|---|---|---|---|---|
| Post treatment | Follow-up after < 6 months | Post treatment | Follow-up after < 6 months | ||
| PTSD symptoms | All | SMD –0.46 (95% CI –0.68 to –0.25), I2 = 50.4%, number of trials = 8, n = 933 | – | – | – |
| Trauma-focused CBT | SMD –0.48 (95% CI –0.82 to –0.15), I2 = 74.8%, number of trials = 6, n = 713 | – | – | – | |
| EMDR | – | – | – | – | |
| IPT | – | – | – | – | |
| Mindfulness | – | – | – | – | |
| Non-trauma-focused CBT | – | – | – | – | |
| Single-component and trauma-focused interventions | SMD –0.51 (95% CI –0.80 to –0.23), I2 = 55.9%, number of trials = 5, n = 566 | – | – | – | |
| Multicomponent and trauma-focused interventions | SMD –0.41 (95% CI –0.80 to –0.02), I2 = 48.3%, number of trials = 3, n = 253 | – | – | – | |
| Single-component non-trauma-focused interventions | – | – | – | – | |
| Phase-based interventions | – | – | – | – | |
| Depression symptoms | All | – | – | – | – |
| Trauma-focused CBT | SMD –0.48 (95% CI –0.82 to –0.15), I2 = 74.8%, number of trials = 6, n = 827 | – | – | – | |
| EMDR | – | – | – | – | |
| IPT | – | – | – | – | |
| Mindfulness | – | – | – | – | |
| Non-trauma-focused CBT | – | – | – | – | |
| Single-component and trauma-focused interventions | SMD –0.47 (95% CI –0.89 to –0.05), I2 = 79.1%, number of trials = 4, n = 536 | – | – | – | |
| Multicomponent and trauma-focused interventions | SMD –0.44 (95% CI –1.34 to 0.45), I2 = 79.1%, number of trials = 2, n = 177 | – | – | – | |
| Single-component non-trauma-focused interventions | – | – | – | – | |
| Phase-based interventions | – | – | – | – | |
| Anxiety symptoms | All | – | – | – | – |
| Trauma-focused CBT | SMD –0.64 (95% CI –1.18 to –0.10), I2 = 90.4%, number of trials = 5, n = 691 | – | – | – | |
| EMDR | – | – | – | – | |
| IPT | – | – | – | – | |
| Mindfulness | – | – | – | – | |
| Non-trauma-focused CBT | – | – | – | – | |
| Single-component and trauma-focused interventions | SMD –0.70 (95% CI –1.48 to 0.08), I2 = 94.3%, number of trials = 3, n = 514 | – | – | – | |
| Multicomponent and trauma-focused interventions | SMD –0.52 (95% CI –1.53 to 0.50), I2 = 83.7%, number of trials = 2, n = 177 | – | – | – | |
| Single-component non-trauma-focused interventions | – | – | – | – | |
| Phase-based interventions | – | – | – | – | |
Childhood sexual abuse
| Outcome | Psychological interventions vs. control | Control | Active control | ||
|---|---|---|---|---|---|
| Post treatment | Follow-up after < 6 months | Post treatment | Follow-up after < 6 months | ||
| PTSD symptoms | All | SMD –0.90 (95% CI –1.43 to –0.37), I2 = 89.6%, number of trials = 9, n = 687 | SMD –0.27 (95% CI –0.71, 0.17), I2 = 53.6%, number of trials = 3, n = 323 | – | – |
| Trauma-focused CBT | SMD –1.22 (95% CI –2.40 to –0.05), I2 = 90.3%, number of trials = 3, n = 153 | – | – | – | |
| EMDR | – | – | – | – | |
| IPT | – | – | – | – | |
| Mindfulness | – | – | – | – | |
| Non-trauma-focused CBT | SMD 0.01 (95% CI –0.20 to 0.21), I2 = 0%, number of trials = 2, n = 368 | – | – | – | |
| Single-component and trauma-focused interventions | SMD –1.19 (95% CI –2.04 to –0.35), I2 = 85.5%, number of trials = 4, n = 192 | – | – | – | |
| Multicomponent and trauma-focused interventions | – | – | – | – | |
| Single-component non-trauma-focused interventions | SMD –0.54 (95% CI –1.05 to –0.03), I2 = 83.4%, number of trials = 5, n = 494 | SMD –0.08 (95% CI –0.31 to 0.15), I2 = 0%, number of trials = 2, n = 295 | – | – | |
| Phase-based interventions | – | – | – | – | |
| Depression symptoms | All | SMD –0.82 (95% CI –1.10 to –0.55), I2 = 0%, number of trials = 5, n = 234 | SMD –0.52 (95% CI –0.99 to –0.04), I2 = 0%, number of trials = 2, n = 76 | – | – |
| Trauma-focused CBT | SMD –0.50 (95% CI –0.95 to –0.05), I2 = 0%, number of trials = 2, n = 79 | – | – | – | |
| EMDR | – | – | – | – | |
| IPT | – | – | – | – | |
| Mindfulness | – | – | – | – | |
| Non-trauma-focused CBT | – | – | – | – | |
| Single-component and trauma-focused interventions | SMD –0.58 (95% CI –0.95 to –0.21), I2 = 0%, number of trials = 3, n = 118 | – | – | – | |
| Multicomponent and trauma-focused interventions | – | – | – | – | |
| Single-component non-trauma-focused interventions | SMD –0.92 (95% CI –1.36 to –0.48), I2 = 0%, number of trials = 2, n = 93 | – | – | – | |
| Phase-based interventions | – | – | – | – | |
| Anxiety symptoms | All | – | – | – | – |
| Trauma-focused CBT | – | – | – | – | |
| EMDR | – | – | – | – | |
| IPT | – | – | – | – | |
| Mindfulness | – | – | – | – | |
| Non-trauma-focused CBT | – | – | – | – | |
| Single-component and trauma-focused interventions | SMD –0.87 (95% CI –1.76 to 0.03), I2 = 75.2%, number of trials = 2, n = 90 | – | – | – | |
| Multicomponent and trauma-focused interventions | – | – | – | – | |
| Single-component non-trauma-focused interventions | – | – | – | – | |
| Phase-based interventions | – | – | – | – | |
Refugee populations
| Outcome | Psychological interventions vs. control | Control | Active control | ||
|---|---|---|---|---|---|
| Post treatment | Follow-up after < 6 months | Post treatment | Follow-up after < 6 months | ||
| PTSD symptoms | All | SMD –1.84 (95% CI –2.18 to –1.49), I2 = 0%, number of trials = 6, n = 188 | SMD –0.66 (95% CI –1.22 to –0.09), I2 = 72.7%, number of trials = 3, n = 235 | – | – |
| Trauma-focused CBT | SMD –2.12 (95% CI –2.71 to –1.53), I2 = 0%, number of trials = 3, n = 71 | SMD –0.40 (95% CI –0.87 to 0.06), I2 = 40.1%, number of trials = 2, n = 165 | – | – | |
| EMDR | SMD –1.72 (95% CI –2.19 to –1.26), I2 = 0%, number of trials = 2, n = 99 | – | SMD –0.15 (95% CI –0.62 to 0.32), I2 = 0%, number of trials = 2, n = 71 | SMD –0.15 (95% CI –0.80 to 0.49), I2 = 22.4%, number of trials = 2, n = 71 | |
| IPT | – | – | – | – | |
| Mindfulness | – | – | – | – | |
| Non-trauma-focused CBT | – | – | – | – | |
| Single-component and trauma-focused interventions | SMD –1.87 (95% CI –2.24 to –1.51), I2 = 0%, number of trials = 5, n = 170 | SMD –0.67 (95% CI –1.65 to 0.32), I2 = 86.3%, number of trials = 2, n = 133 | – | – | |
| Multicomponent and trauma-focused interventions | – | – | – | – | |
| Single-component non-trauma-focused interventions | – | – | – | – | |
| Phase-based interventions | – | – | – | – | |
| Depression symptoms | All | SMD –1.56 (95% CI –1.93 to –1.16), I2 = 0%, number of trials = 5, n = 148 | SMD –0.73 (95% CI –1.57 to 0.10), I2 = 81.3%, number of trials = 2, n = 133 | – | – |
| Trauma-focused CBT | SMD –2.03 (95% CI –2.92 to –1.13), I2 = 0%, number of trials = 2, n = 31 | SMD –0.73 (95% CI –1.57 to 0.10), I2 = 81.3%, number of trials = 2, n = 133 | – | – | |
| EMDR | SMD –1.46 (95% CI –1.90 to –1.01), I2 = 0%, number of trials = 2, n = 99 | – | SMD –0.32 (95% CI –1.23 to 0.59), I2 = 47.8%, number of trials = 2, n = 72 | SMD –0.01 (95% CI –0.47 to 0.45), I2 = 0%, number of trials = 2, n = 73 | |
| IPT | – | – | – | – | |
| Mindfulness | – | – | – | – | |
| Non-trauma-focused CBT | – | – | – | – | |
| Single-component and trauma-focused interventions | SMD –1.57 (95% CI –1.97 to –1.17), I2 = 0%, number of trials = 4, n = 130 | SMD –0.73 (95% CI –1.57 to 0.10), I2 = 81.3%, number of trials = 2, n = 133 | – | – | |
| Multicomponent and trauma-focused interventions | – | – | – | – | |
| Single-component non-trauma-focused interventions | – | – | – | – | |
| Phase-based interventions | – | – | – | – | |
| Anxiety symptoms | All | – | – | – | – |
| Trauma-focused CBT | – | – | – | – | |
| EMDR | – | – | |||
| IPT | – | – | – | – | |
| Mindfulness | – | – | – | – | |
| Non-trauma-focused CBT | – | – | – | – | |
| Single-component and trauma-focused interventions | – | – | – | – | |
| Multicomponent and trauma-focused interventions | – | – | – | – | |
| Single-component non-trauma-focused interventions | – | – | – | – | |
| Phase-based interventions | – | – | – | – | |
Domestic violence
| Outcome | Psychological interventions vs. control | Control | Active control | ||
|---|---|---|---|---|---|
| Post treatment | Follow-up after < 6 months | Post treatment | Follow-up after < 6 months | ||
| PTSD symptoms | All | – | – | – | – |
| Trauma-focused CBT | SMD –2.92 (95% CI –3.45 to –2.39), I2 = 0%, number of trials = 2, n = 117 | – | – | – | |
| EMDR | – | – | – | – | |
| IPT | – | – | – | – | |
| Mindfulness | – | – | – | – | |
| Non-trauma-focused CBT | – | – | – | – | |
| Single-component and trauma-focused interventions | – | – | – | – | |
| Multicomponent and trauma-focused interventions | – | – | – | – | |
| Single-component non-trauma-focused interventions | – | – | – | – | |
| Phase-based interventions | – | – | – | – | |
| Depression symptoms | All | – | – | – | – |
| Trauma-focused CBT | SMD –3.24 (95% CI –4.40 to –2.09), I2 = 66.6%, number of trials = 2, n = 117 | – | – | – | |
| EMDR | – | – | – | – | |
| IPT | – | – | – | – | |
| Mindfulness | – | – | – | – | |
| Non-trauma-focused CBT | – | – | – | – | |
| Single-component and trauma-focused interventions | – | – | – | – | |
| Multicomponent and trauma-focused interventions | – | – | – | – | |
| Single-component non-trauma-focused interventions | – | – | – | – | |
| Phase-based interventions | – | – | – | – | |
| Anxiety symptoms | All | – | – | – | – |
| Trauma-focused CBT | – | – | – | – | |
| EMDR | – | – | – | – | |
| IPT | – | – | – | – | |
| Mindfulness | – | – | – | – | |
| Non-trauma-focused CBT | – | – | – | – | |
| Single-component and trauma-focused interventions | – | – | – | – | |
| Multicomponent and trauma-focused interventions | – | – | – | – | |
| Single-component non-trauma-focused interventions | – | – | – | – | |
| Phase-based interventions | – | – | – | – | |
Pharmacological interventions
All studies included in analyses were conducted in veteran populations.
Post-traumatic stress disorder
| Pharmacological interventions vs. placebo | Placebo | |
|---|---|---|
| Post treatment | Follow-up after < 6 months | |
| All | – | – |
| Antidepressants | SMD –0.50 (95% CI –1.22 to 0.22), I2 = 87%, number of trials = 6, n = 338 | – |
| SSRIs | SMD –0.61 (95% CI –1.64 to 0.41), I2 = 92.2%, number of trials = 4, n = 293 | – |
| Antipsychotics | SMD –0.45 (95% CI –0.85 to –0.05), I2 = 51.2%, number of trials = 5, n = 365 | – |
| Anticonvulsants | SMD –0.16 (95% CI –0.77 to 0.45), I2 = 45.5%, number of trials = 2, n = 106 | – |
| Prazosin | SMD –0.52 (95% CI –1.03 to –0.02), I2 = 41.4%, number of trials = 3, n = 110 | – |
Depression
| Pharmacological interventions vs. placebo | Placebo | |
|---|---|---|
| Post treatment | Follow-up after < 6 months | |
| All | – | – |
| Antidepressants | SMD 0.07 (95% CI –0.20 to 0.34), I2 = 0%, number of trials = 3, n = 220 | – |
| SSRIs | – | – |
| Antipsychotics | SMD –0.71 (95% CI –1.44 to 0.03), I2 = 58.3%, number of trials = 2, n = 266 | – |
| Anticonvulsants | SMD 0.02 (95% CI –0.37 to 0.40), I2 = 0%, number of trials = 2, n = 106 | – |
| Prazosin | SMD –0.37 (95% CI –1.21 to 0.47), I2 = 68.5%, number of trials = 2, n = 76 | – |
Psychosis
| Outcome | Pharmacological interventions vs. placebo | Placebo | |
|---|---|---|---|
| Post treatment | Follow-up after < 6 months | ||
| PANSS-positive | All | – | – |
| Antidepressants | – | – | |
| SSRIs | – | – | |
| Antipsychoticsa | Mean difference –1.75 (95% CI –4.04 to 0.54), I2 = 76.9%, number of trials = 3, n = 329 | – | |
| Anticonvulsants | – | – | |
| Prazosin | – | – | |
| PANSS-negative | All | – | – |
| Antidepressants | – | – | |
| SSRIs | – | – | |
| Antipsychoticsa | Mean difference 0.54 (95% CI –0.14 to 1.22), I2 = 0%, number of trials = 2, n = 284 | – | |
| Anticonvulsants | – | – | |
| Prazosin | – | – | |
| PANSS: total | All | – | – |
| Antidepressants | – | – | |
| SSRIs | – | – | |
| Antipsychoticsa | Mean difference 0.04 (95% CI –2.08 to 2.16), I2 = 0%, number of trials = 2, n = 284 | – | |
| Anticonvulsants | – | – | |
| Prazosin | – | – | |
| PANSS: general psychopathology | All | – | – |
| Antidepressants | – | – | |
| SSRIs | – | – | |
| Antipsychoticsa | Mean difference –0.18 (95% CI –1.39 to 1.03), I2 = 0%, number of trials = 2, n = 284 | – | |
| Anticonvulsants | – | – | |
| Prazosin | – | – | |
Sleep quality
| Pharmacological interventions vs. placebo | Placebo | |
|---|---|---|
| Post treatment | Follow-up after < 6 months | |
| All | – | – |
| Antidepressants | – | – |
| SSRIs | – | – |
| Antipsychotics | – | – |
| Anticonvulsants | – | – |
| Prazosin | SMD –0.73 (95% CI –1.12 to –0.34), I2 = 0%, number of trials = 3, n = 109 | – |
Appendix 10 Forest plots of results of effectiveness meta-analyses
Psychological interventions versus control in all trauma populations
Post-traumatic stress disorder symptoms
FIGURE 27.
Meta-analysis of post-treatment effect size (ES) for PTSD total symptoms, comparing all IPT interventions with control.

FIGURE 28.
Meta-analysis of post-treatment effect size (ES) for PTSD total symptoms, comparing all trauma-focused CBT interventions with control. CETA, common elements treatment approach; CPT, cognitive treatment therapy.
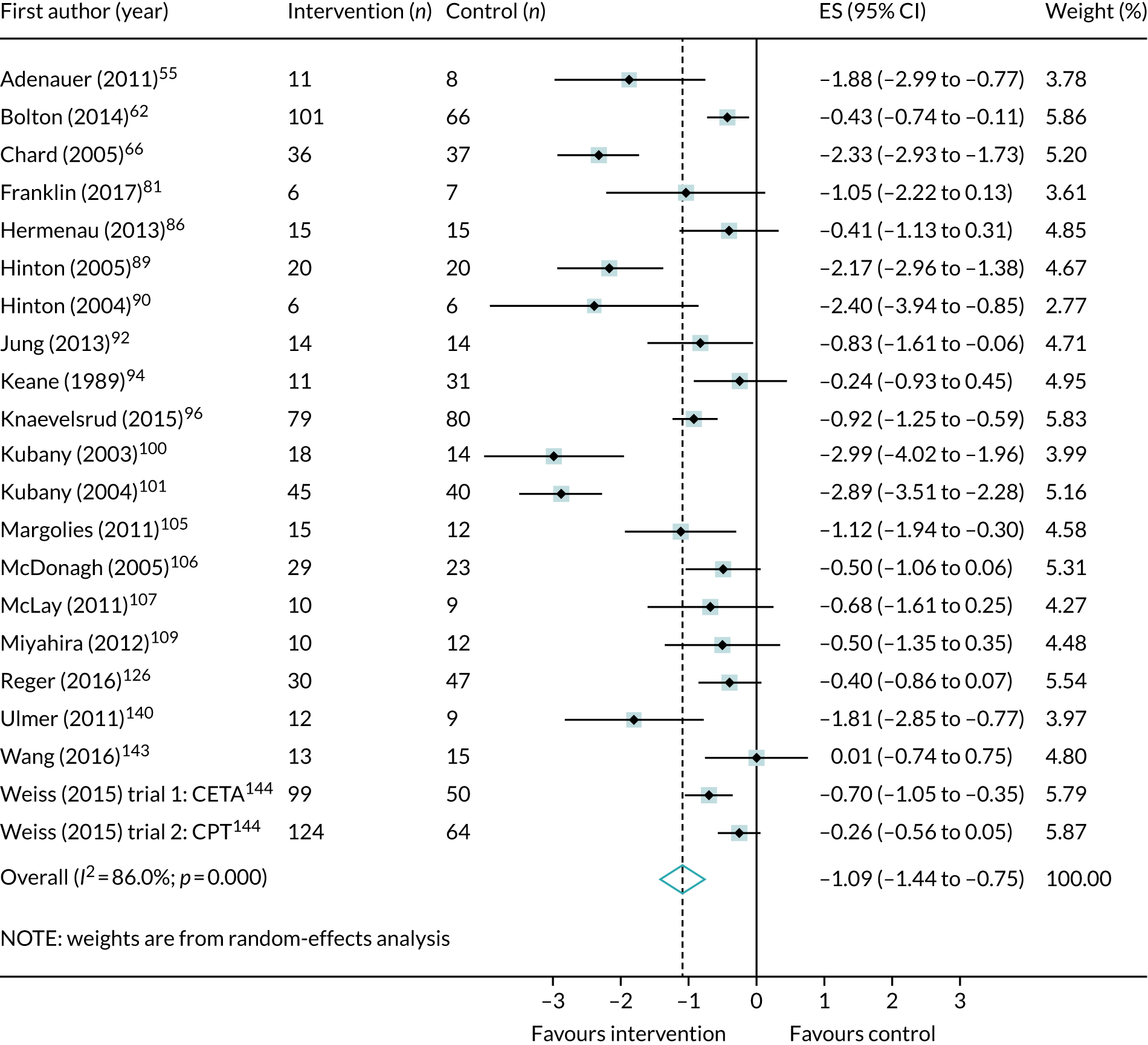
FIGURE 29.
Meta-analysis of post-treatment effect size (ES) for PTSD total symptoms, comparing all EMDR interventions with control.
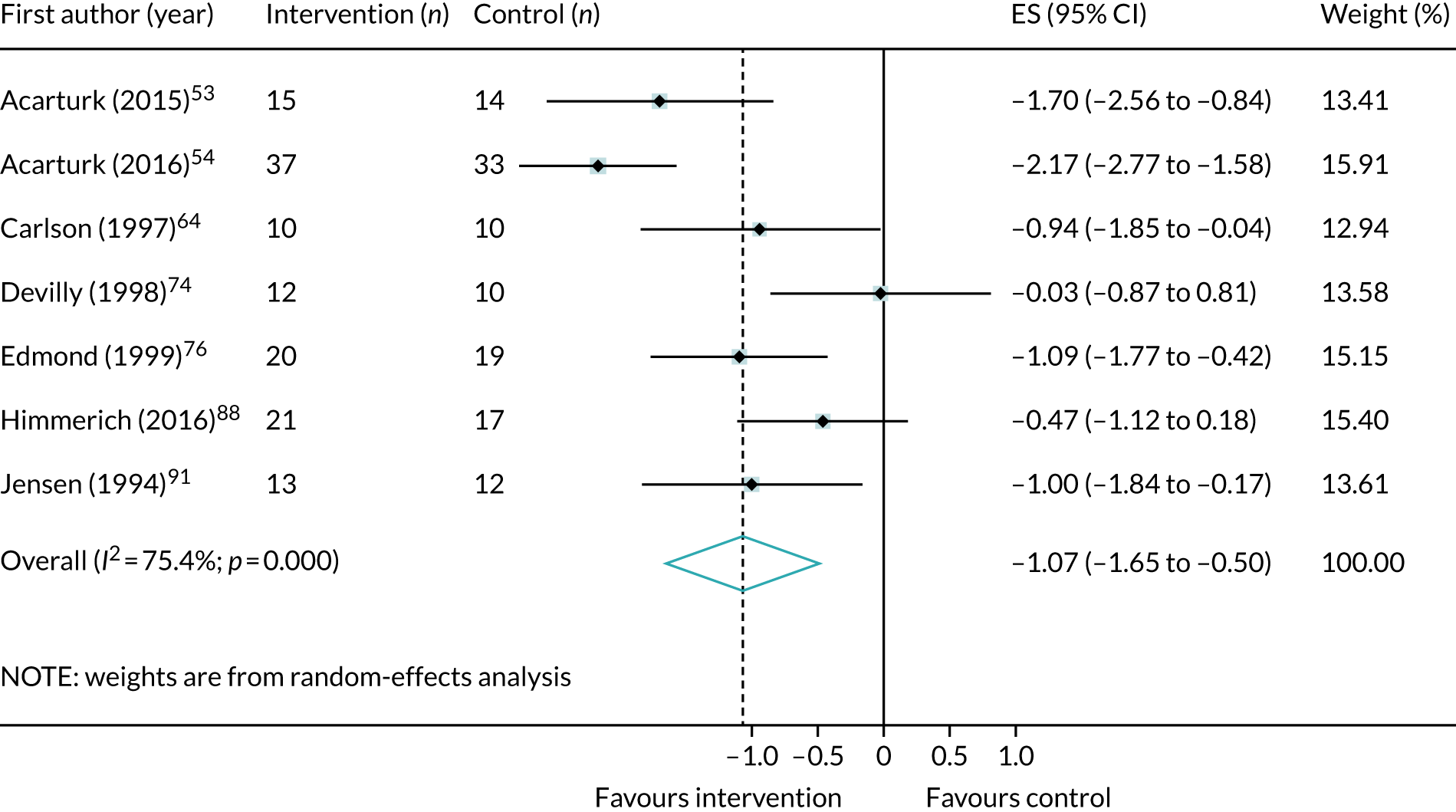
FIGURE 30.
Meta-analysis of post-treatment effect size (ES) for PTSD total symptoms, comparing all mindfulness interventions with control.

FIGURE 31.
Meta-analysis of post-treatment effect size (ES) for PTSD total symptoms, comparing all non-trauma-focused CBT interventions with control.

FIGURE 32.
Meta-analysis of post-treatment effect size (ES) for PTSD total symptoms, comparing all single-component trauma-focused interventions with control. CPT, cognitive processing therapy.
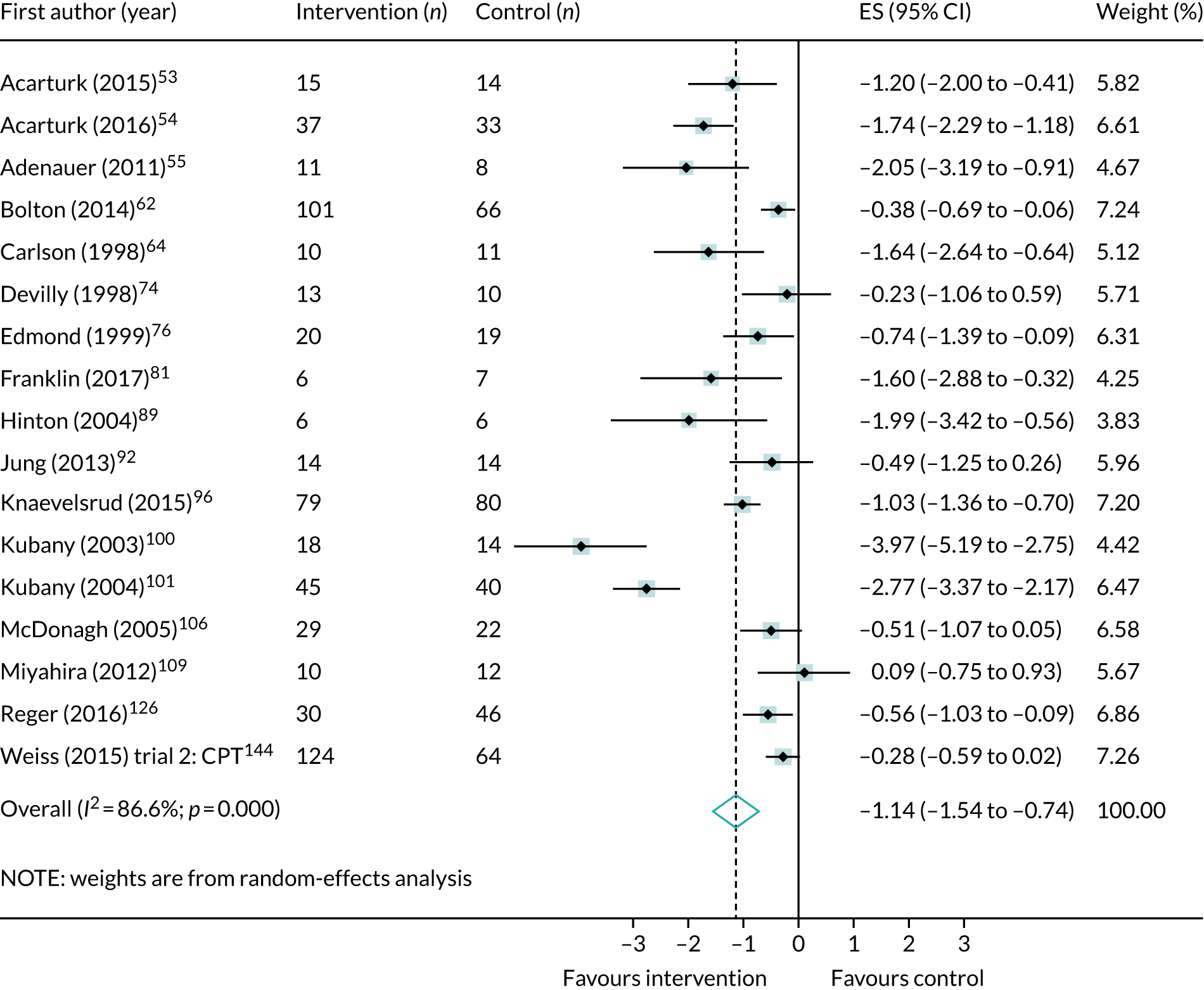
FIGURE 33.
Meta-analysis of post-treatment effect size (ES) for PTSD total symptoms, comparing all multicomponent trauma-focused interventions with control. CETA, common elements treatment approach.
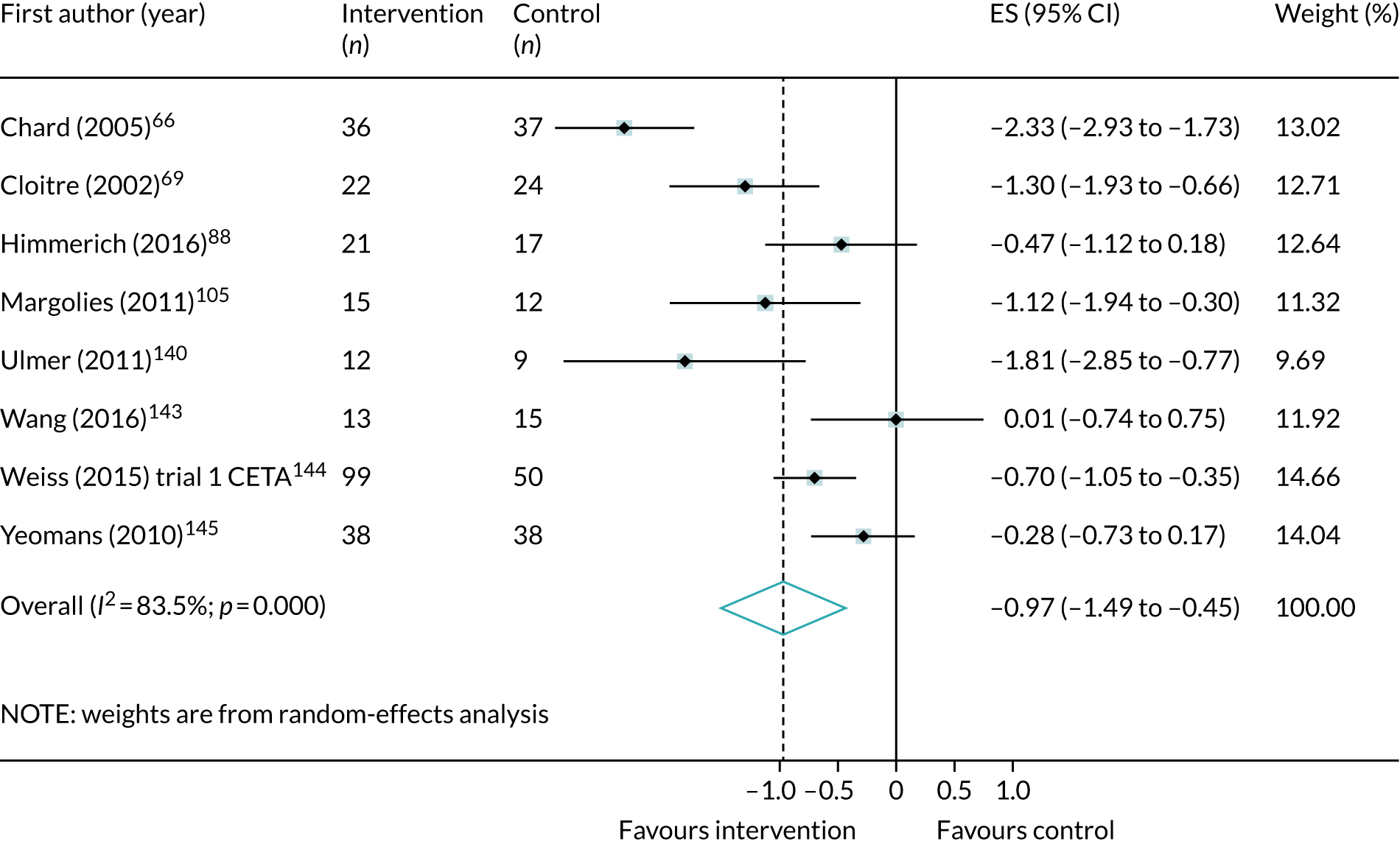
FIGURE 34.
Meta-analysis of post-treatment effect size (ES) for PTSD total symptoms, comparing all single-component non-trauma-focused interventions with control.
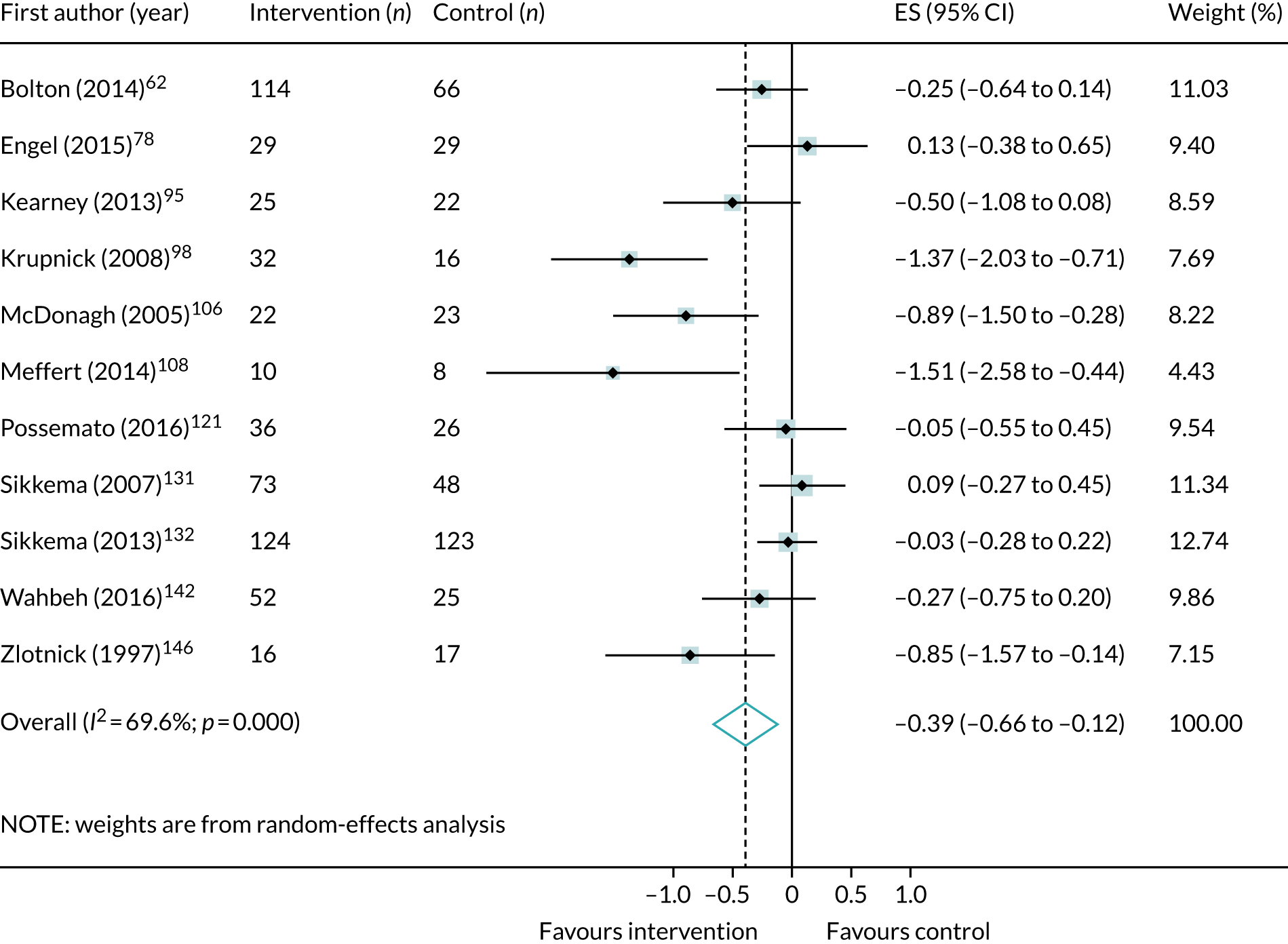
Complex post-traumatic stress disorder symptoms
FIGURE 35.
Meta-analysis of post-treatment SMD for emotional dysregulation, comparing trauma-focused CBT interventions with control.
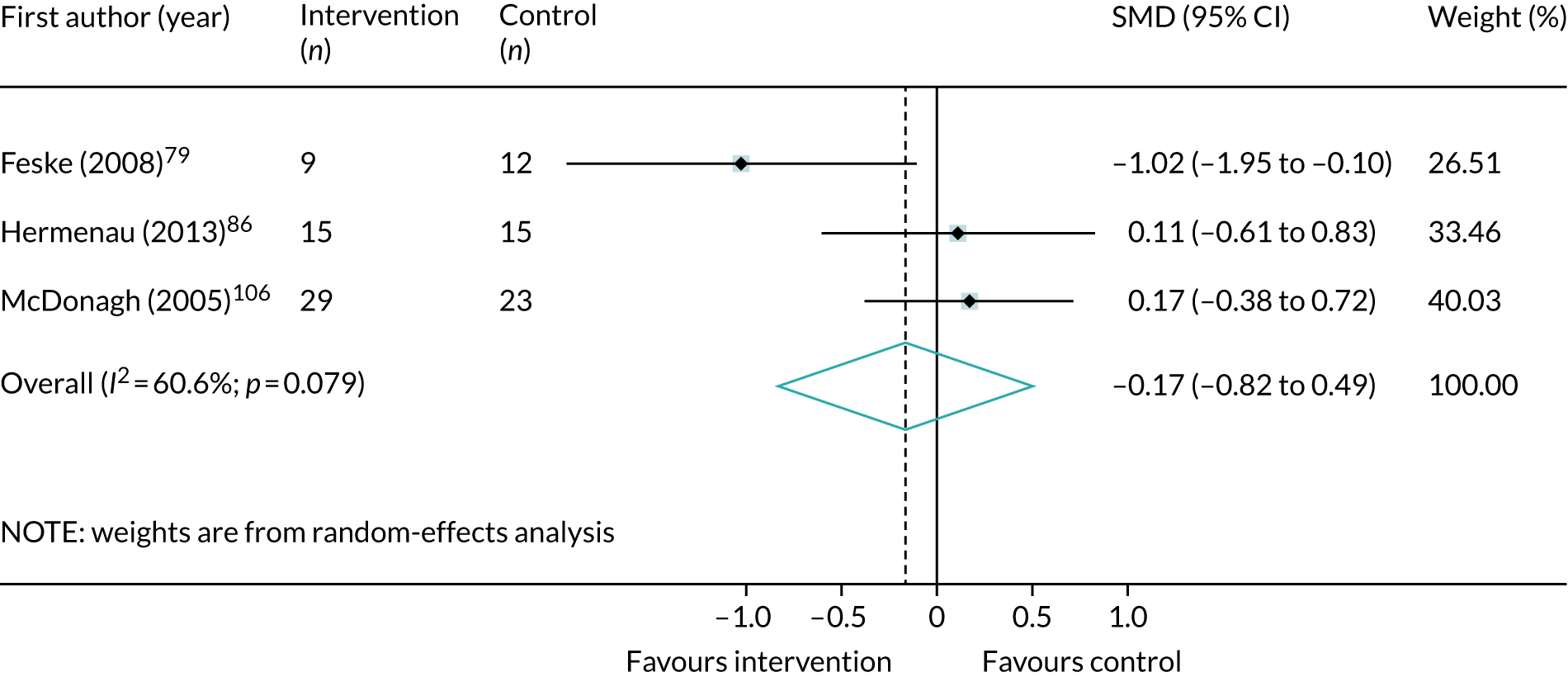
FIGURE 36.
Meta-analysis of post-treatment SMD for emotional dysregulation, comparing single-component and non-trauma-focused interventions with control.

FIGURE 37.
Meta-analysis of post-treatment SMD for negative self-concept, comparing all trauma-focused CBT interventions with control (positive SMD equals improvement in symptoms).

FIGURE 38.
Meta-analysis of post-treatment SMD for negative self-concept, comparing all multicomponent and trauma-focused interventions with control (positive SMD equals improvement in symptoms).
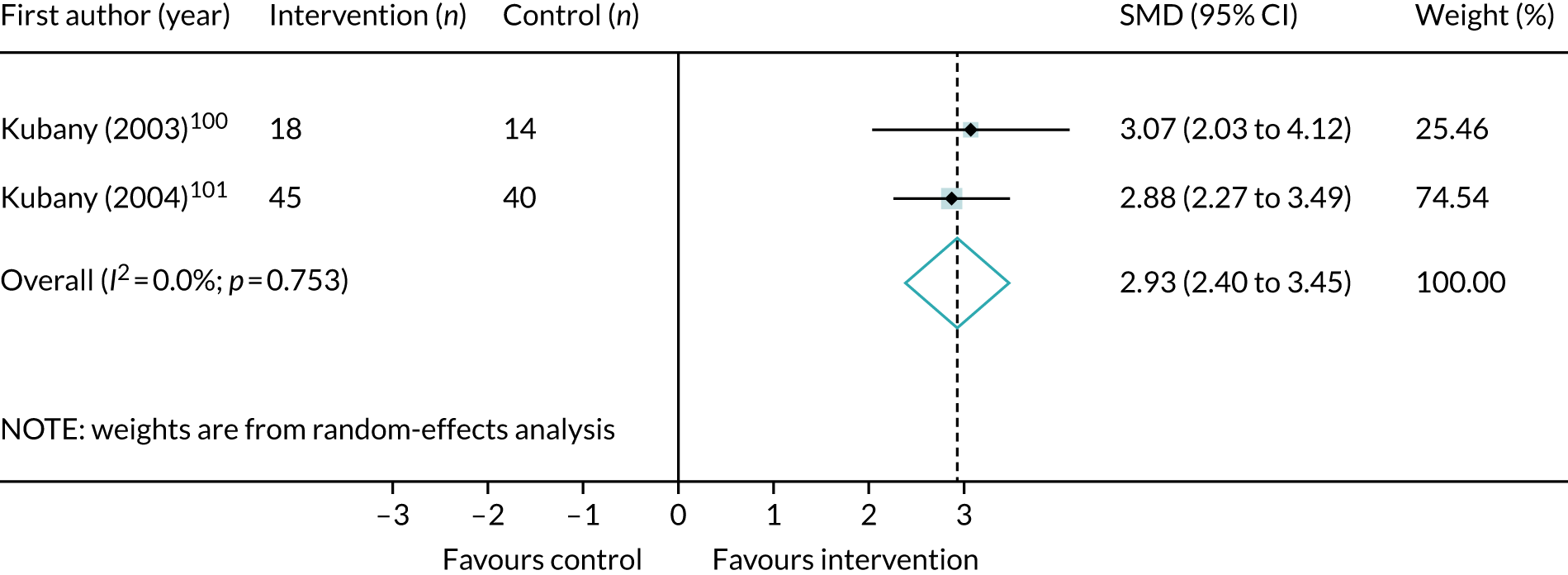
FIGURE 39.
Meta-analysis of post-treatment SMD for negative self-concept, comparing all single-component and non-trauma-focused interventions with control (positive SMD equals improvement in symptoms).

FIGURE 40.
Meta-analysis of post-treatment SMD for interpersonal problems, comparing all psychological interventions with control.
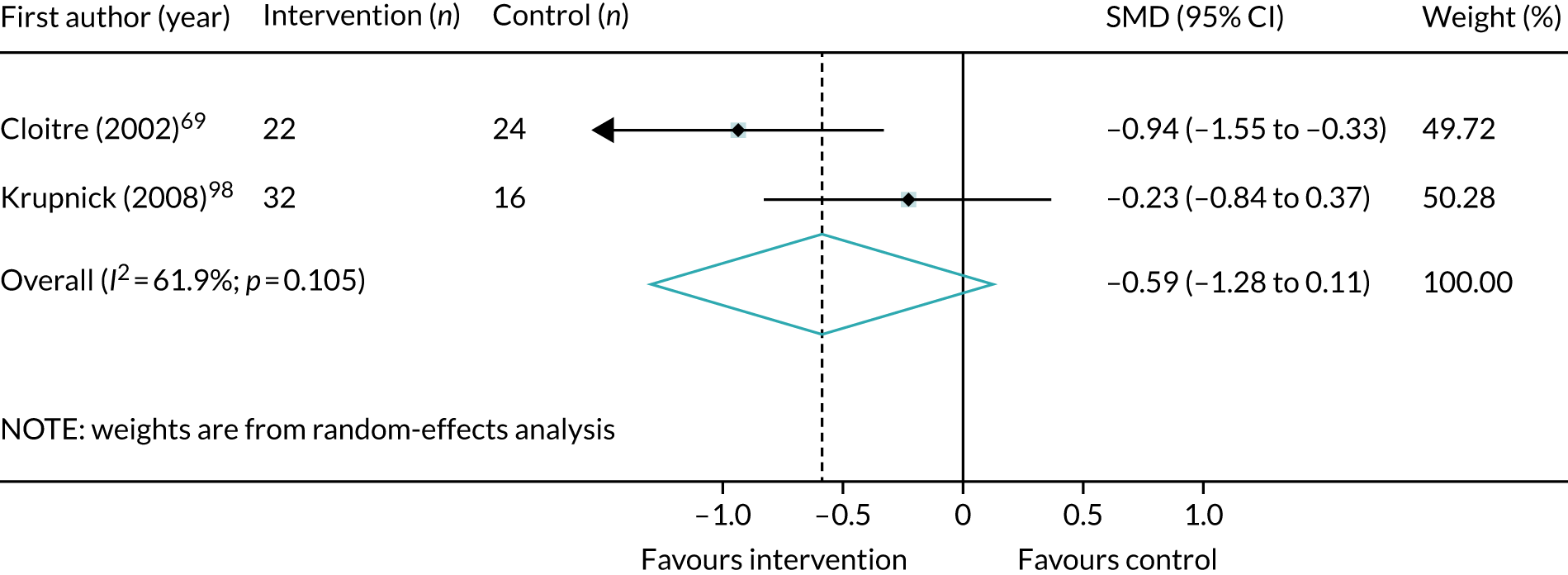
Depression symptoms
FIGURE 41.
Meta-analysis of post-treatment effect size (ES) for depression symptoms, comparing all trauma-focused CBT interventions with control. CETA, common elements treatment approach; CPT, cognitive treatment therapy.
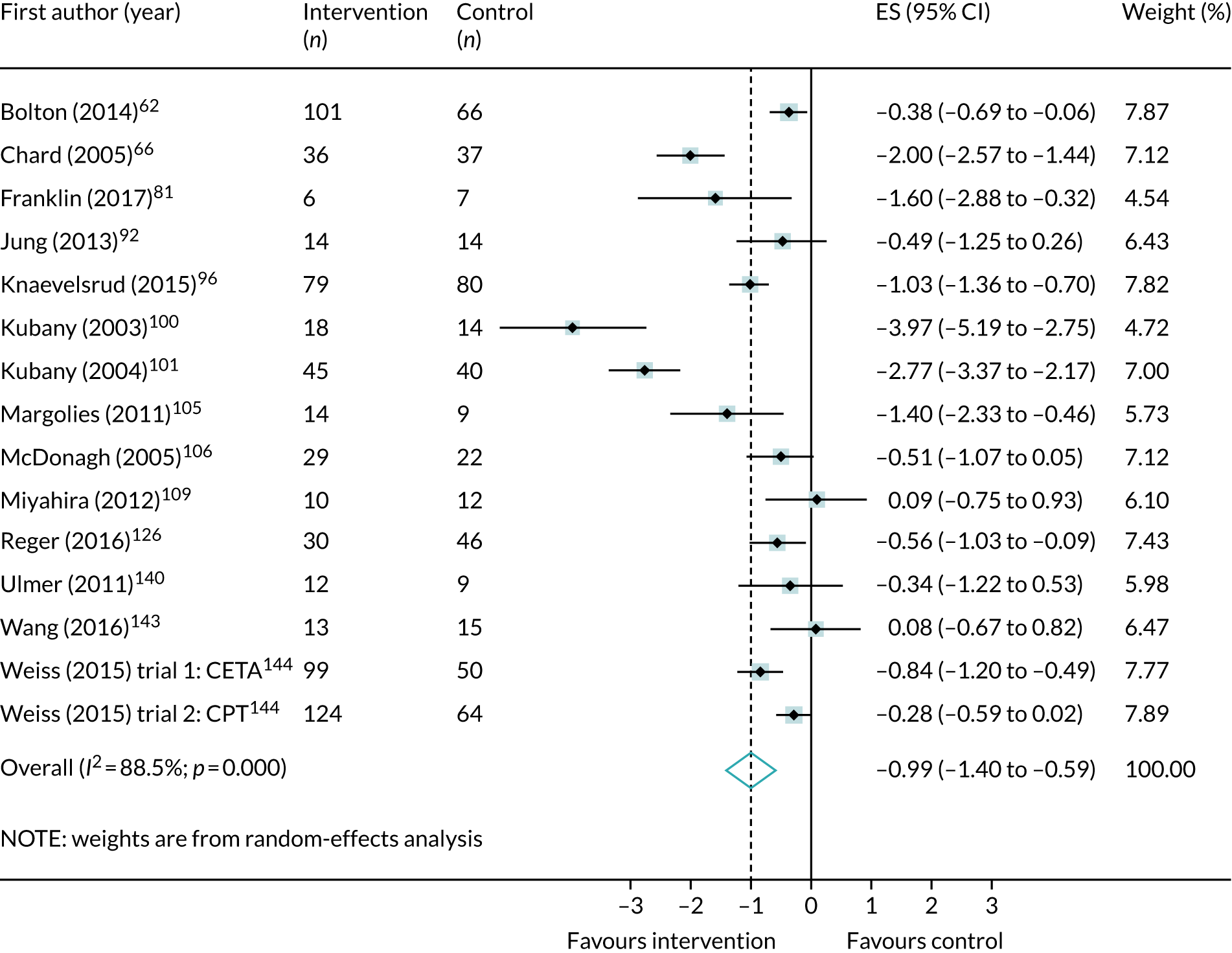
FIGURE 42.
Meta-analysis of post-treatment effect size (ES) for depression symptoms, comparing all EMDR interventions with control.
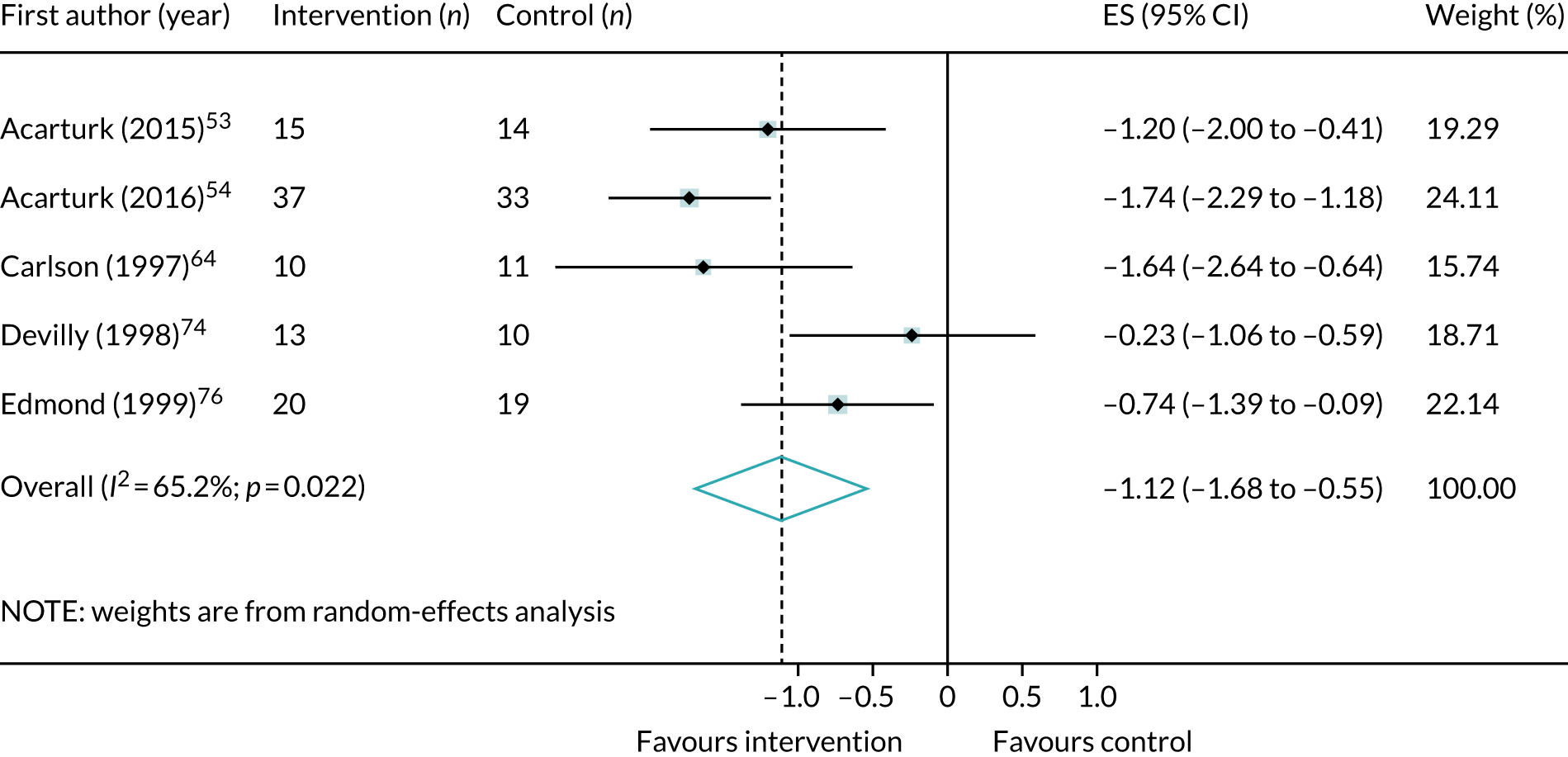
FIGURE 43.
Meta-analysis of post-treatment effect size (ES) for depression symptoms, comparing all IPT interventions with control.

FIGURE 44.
Meta-analysis of post-treatment effect size (ES) for depression symptoms, comparing all mindfulness interventions with control.
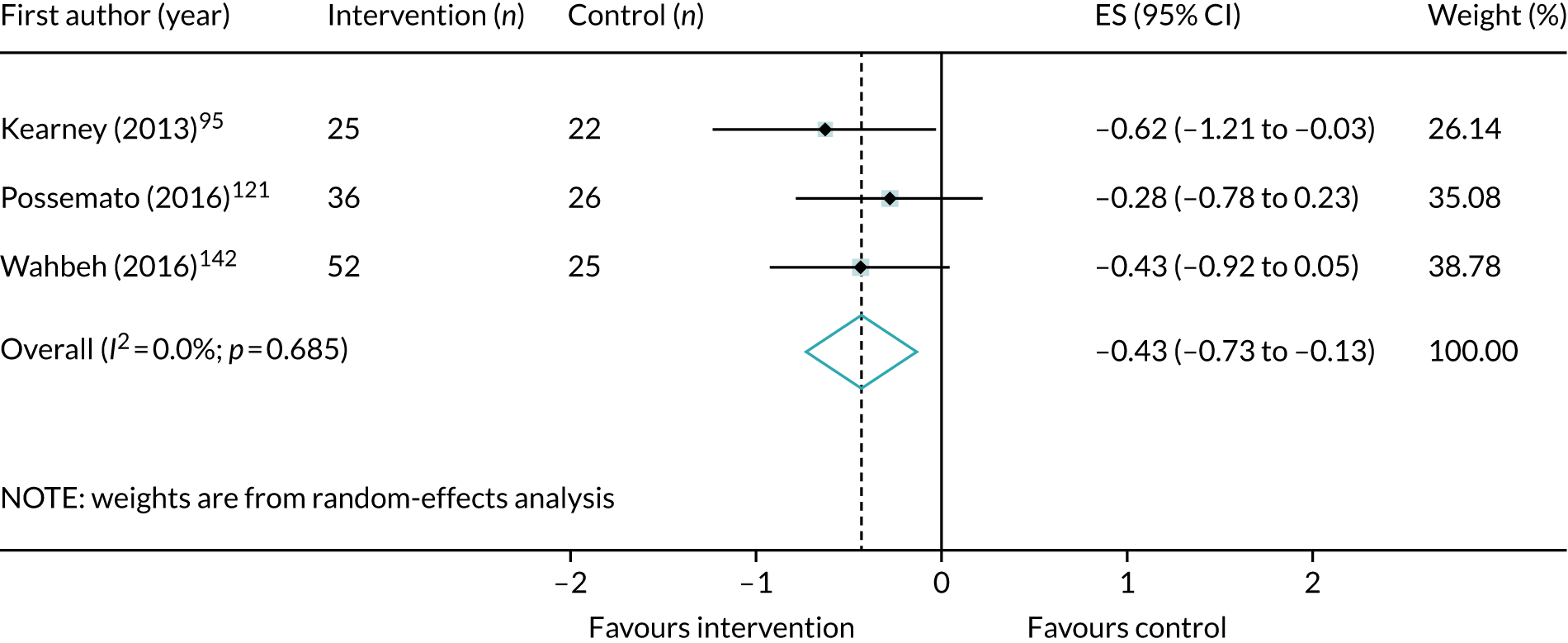
FIGURE 45.
Meta-analysis of post-treatment effect size (ES) for depression symptoms, comparing all non-trauma-focused CBT interventions with control.
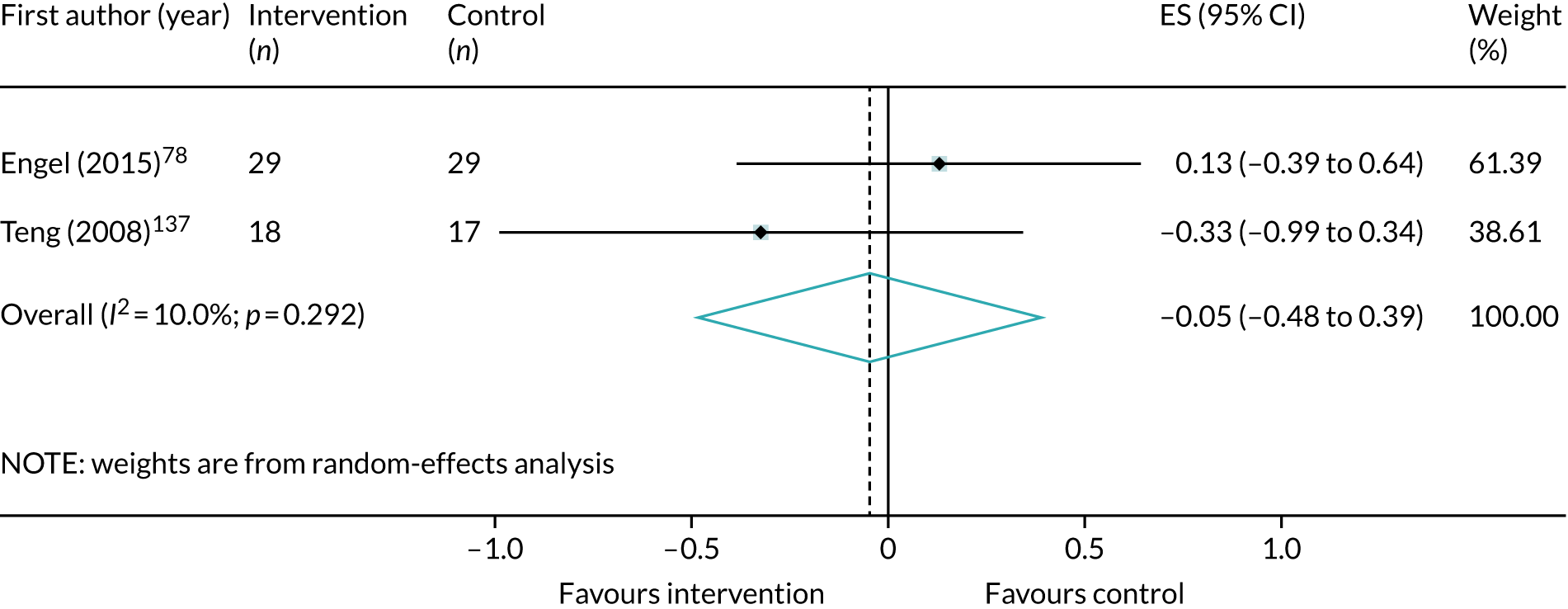
FIGURE 46.
Meta-analysis of post-treatment effect size (ES) for depression symptoms, comparing all single-component and trauma-focused CBT interventions with control. CPT, cognitive processing therapy.

FIGURE 47.
Meta-analysis of post-treatment effect size (ES) for depression symptoms, comparing all multicomponent and trauma-focused interventions with control. CETA, common elements treatment approach.
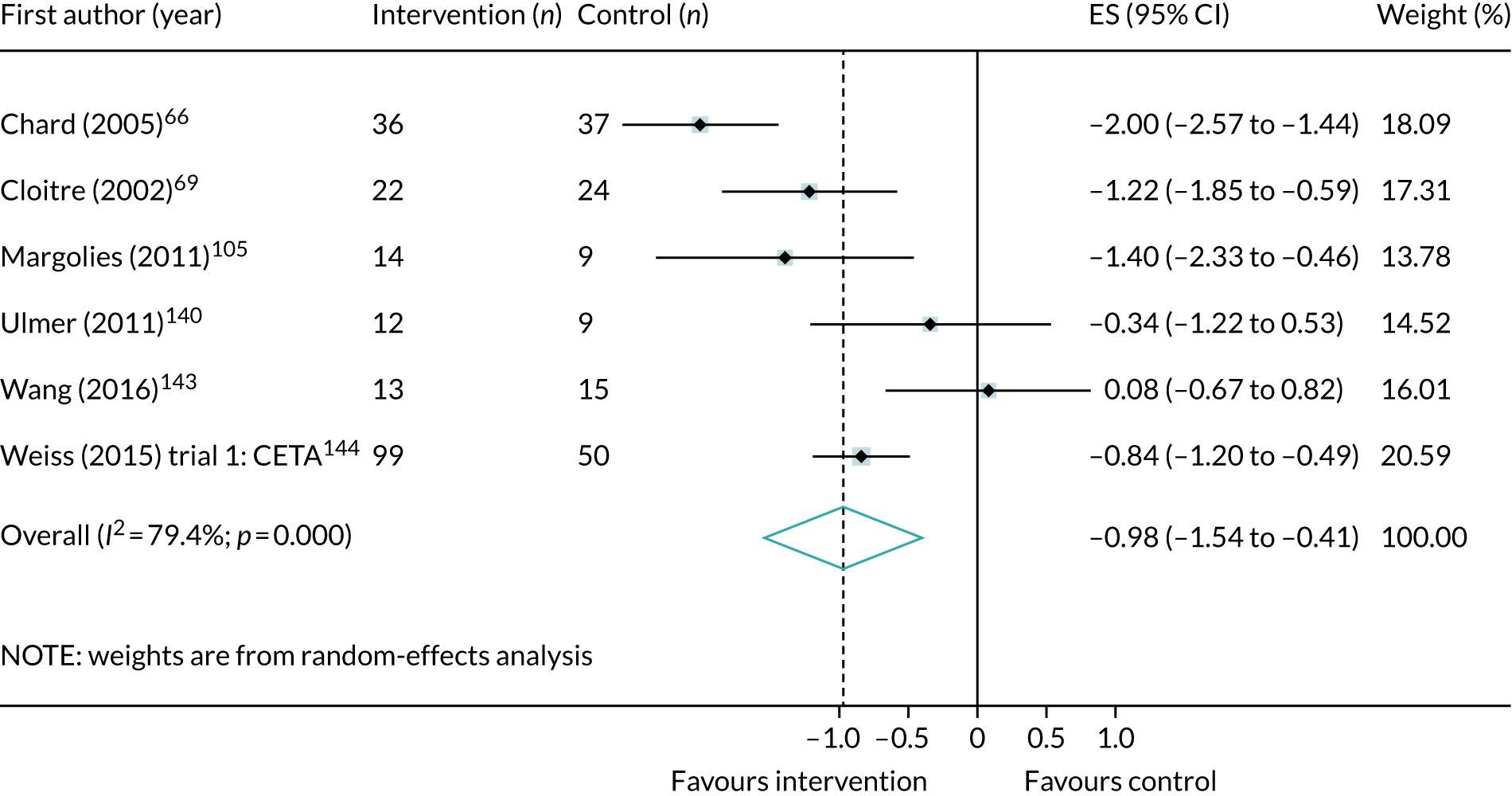
FIGURE 48.
Meta-analysis of post-treatment effect size (ES) for depression symptoms, comparing all single-component and non-trauma-focused interventions with control.

Anxiety symptoms
FIGURE 49.
Meta-analysis of post-treatment effect size (ES) for anxiety symptoms, comparing EMDR interventions with control.
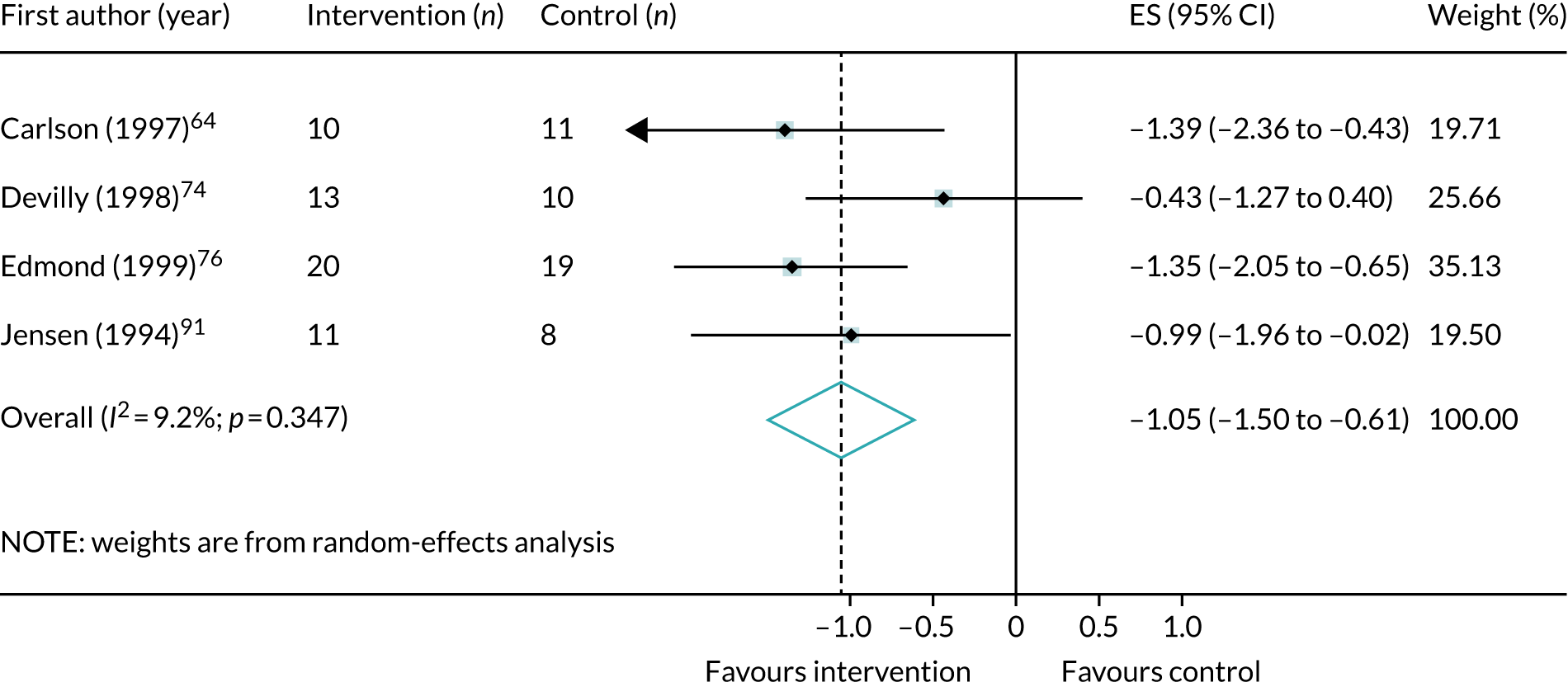
FIGURE 50.
Meta-analysis of post-treatment effect size (ES) for anxiety symptoms, comparing single-component and trauma-focused interventions with control. CPT, cognitive processing therapy.
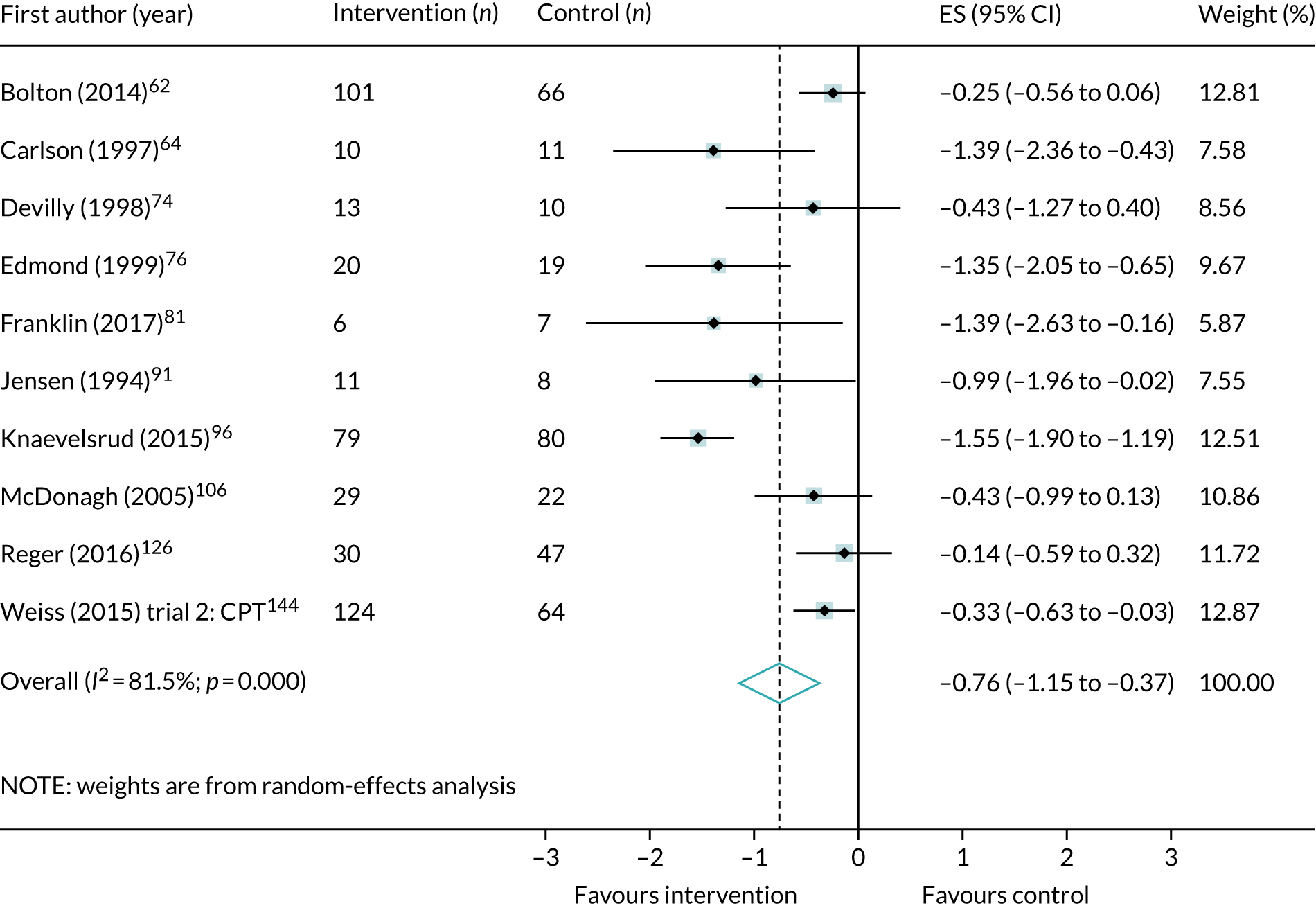
FIGURE 51.
Meta-analysis of post-treatment effect size (ES) for anxiety symptoms, comparing multicomponent and trauma-focused interventions with control. CETA, common elements treatment approach.
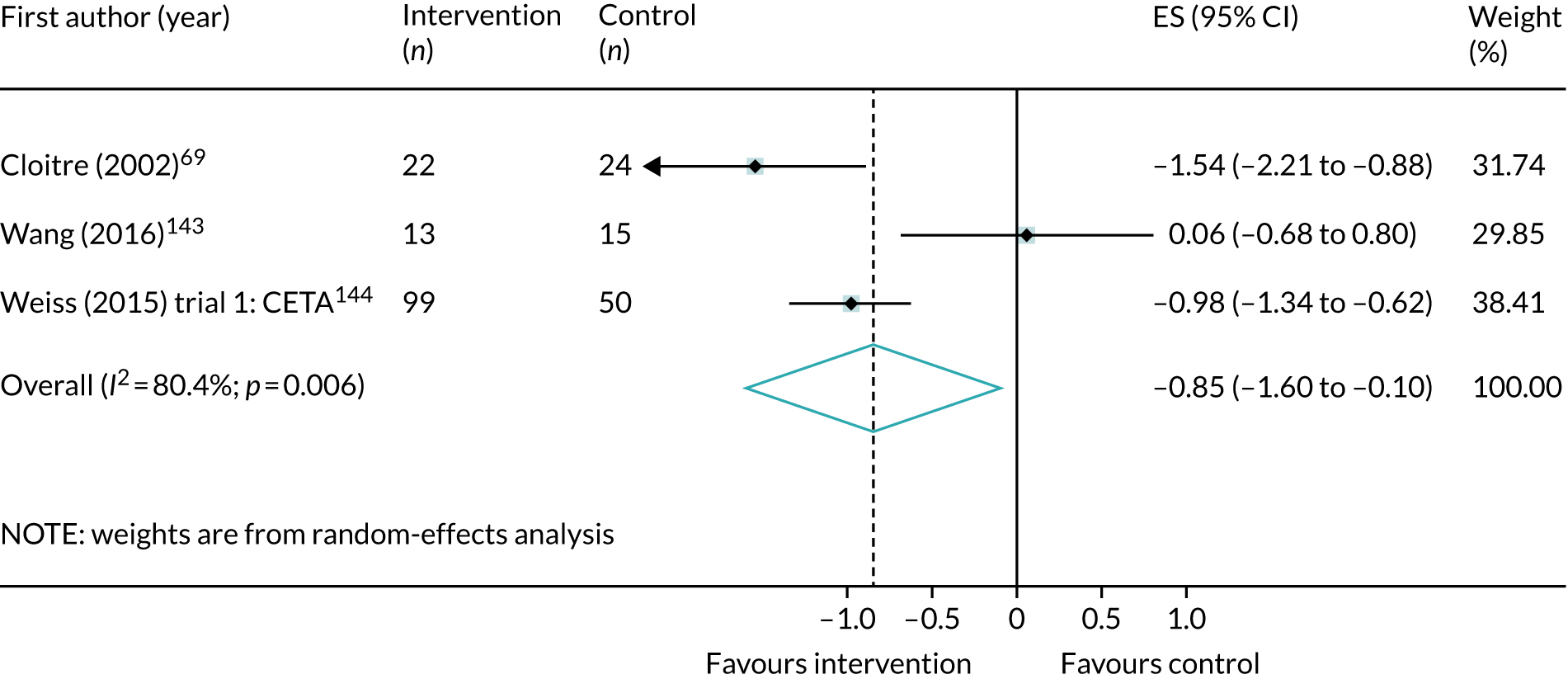
FIGURE 52.
Meta-analysis of post-treatment effect size (ES) for anxiety symptoms, comparing single-component and non-trauma-focused interventions with control.
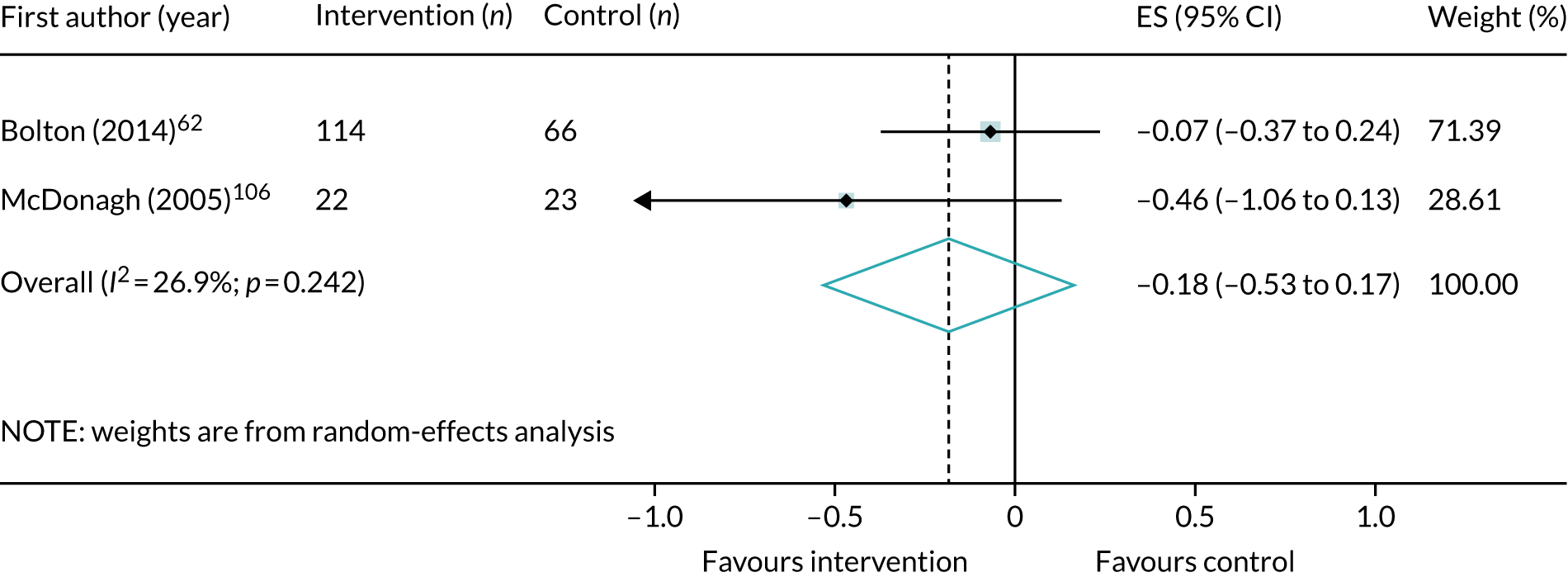
Quality of life
FIGURE 53.
Meta-analysis of post-treatment effect size (ES) for quality of life, comparing trauma-focused CBT interventions with control (positive ES favours intervention).
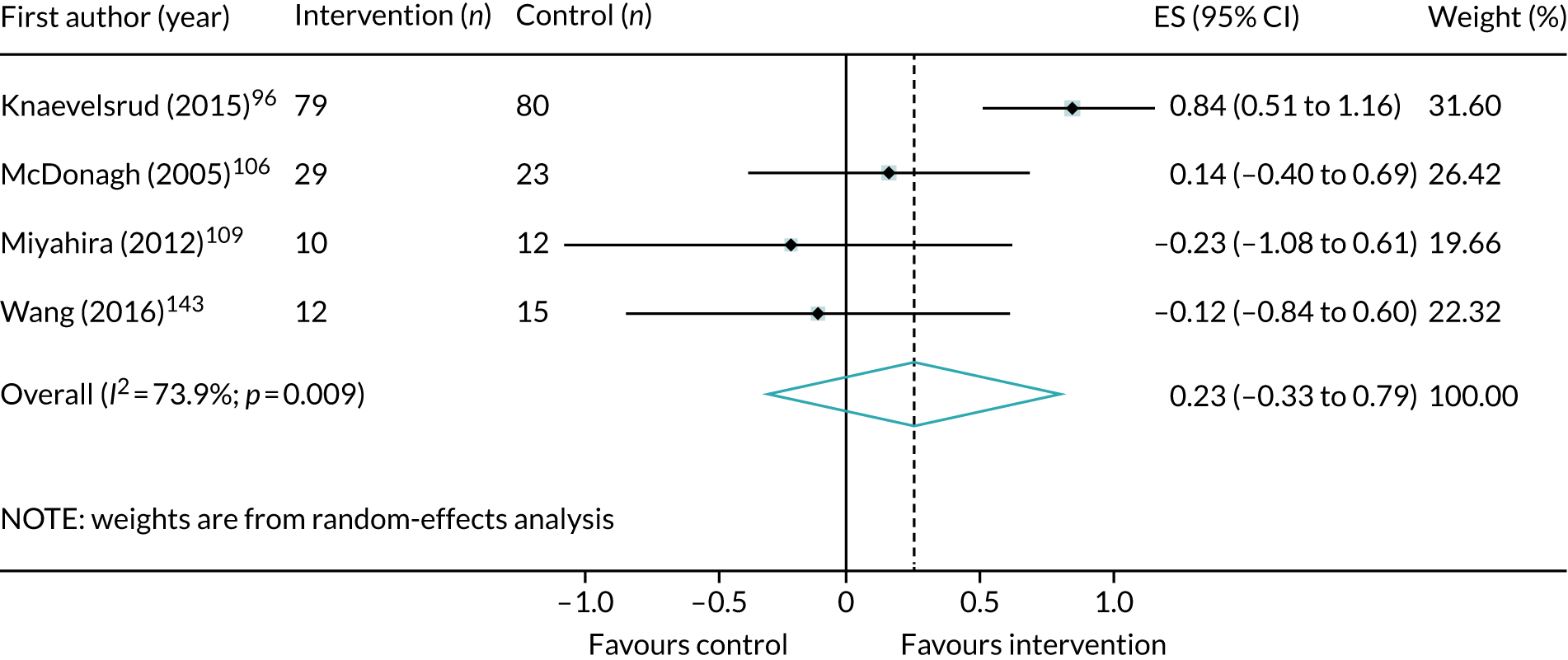
Sleep quality
FIGURE 54.
Meta-analysis of post-treatment effect size (ES) for sleep quality, comparing all psychological interventions with control.
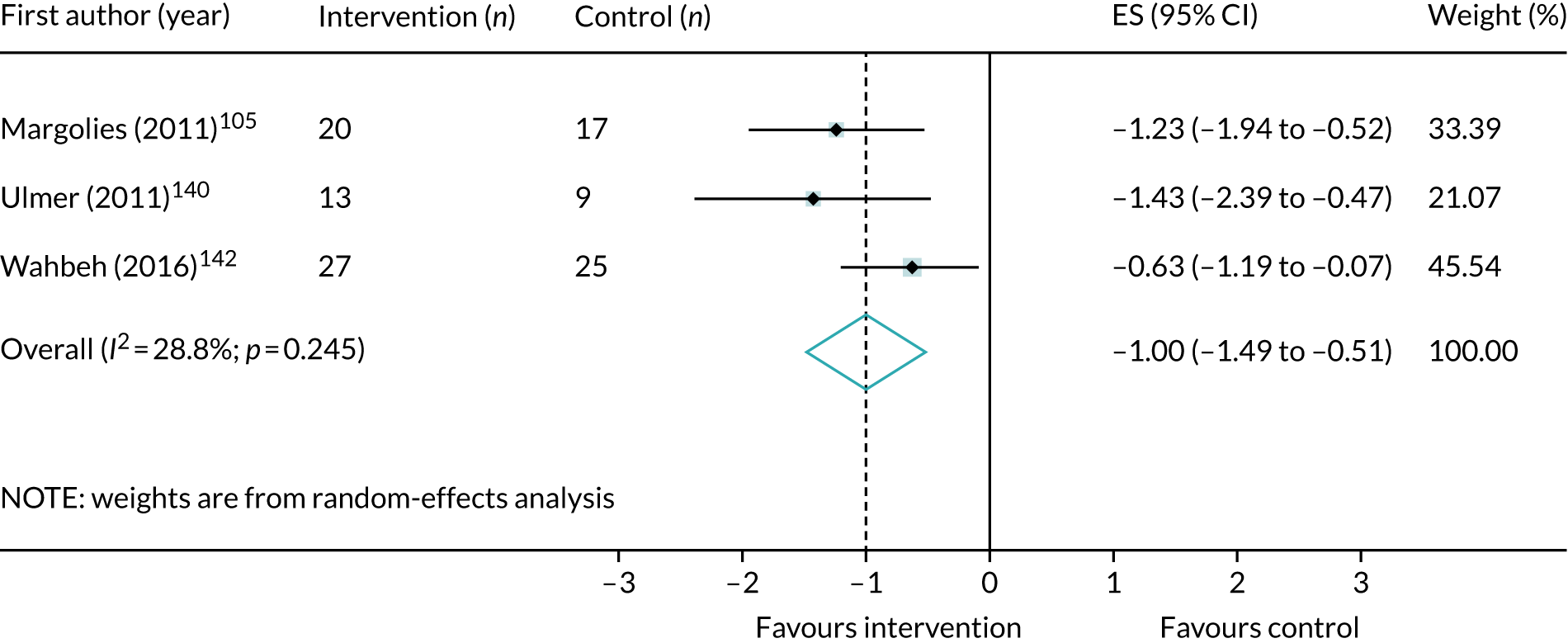
FIGURE 55.
Meta-analysis of post-treatment effect size (ES) for sleep quality, comparing trauma-focused CBT interventions with control.
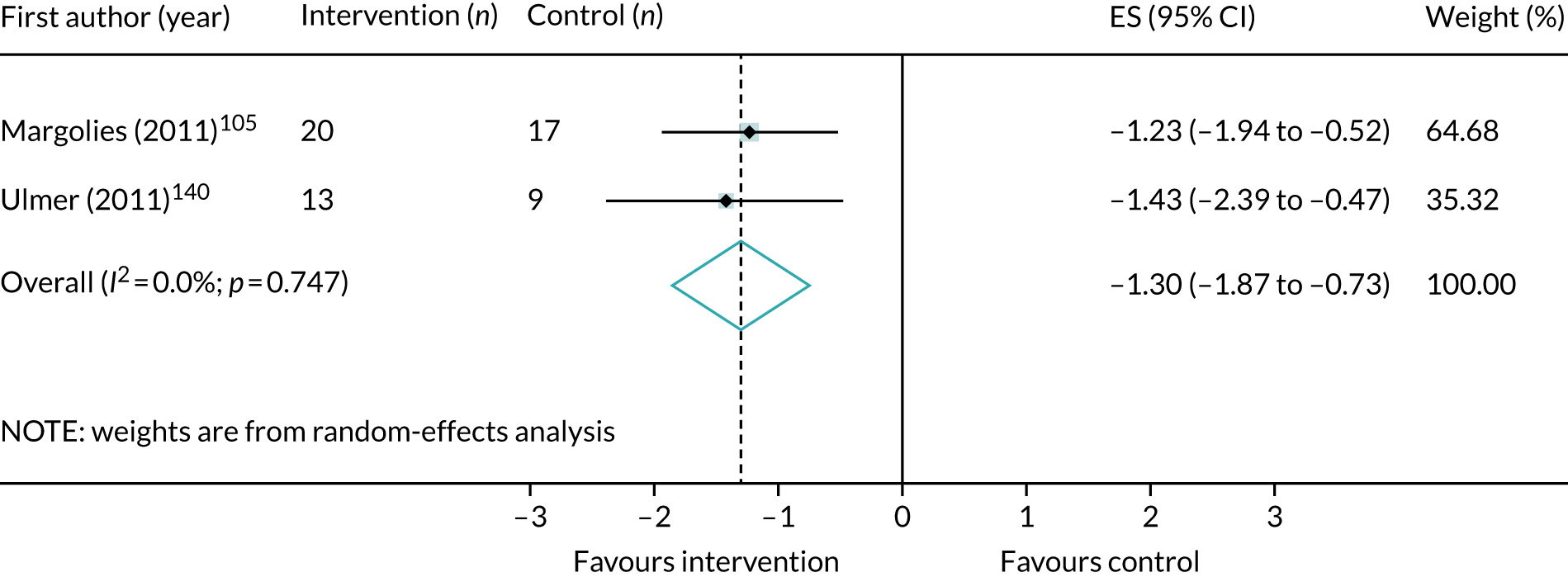
Psychological interventions versus control in trauma subgroups
Veterans
Post-traumatic stress disorder symptoms
FIGURE 56.
Meta-analysis of post-treatment SMD for total PTSD symptoms, comparing trauma-focused CBT interventions with control in veteran populations.

FIGURE 57.
Meta-analysis of post-treatment SMD for total PTSD symptoms, comparing EMDR interventions with control in veteran populations.
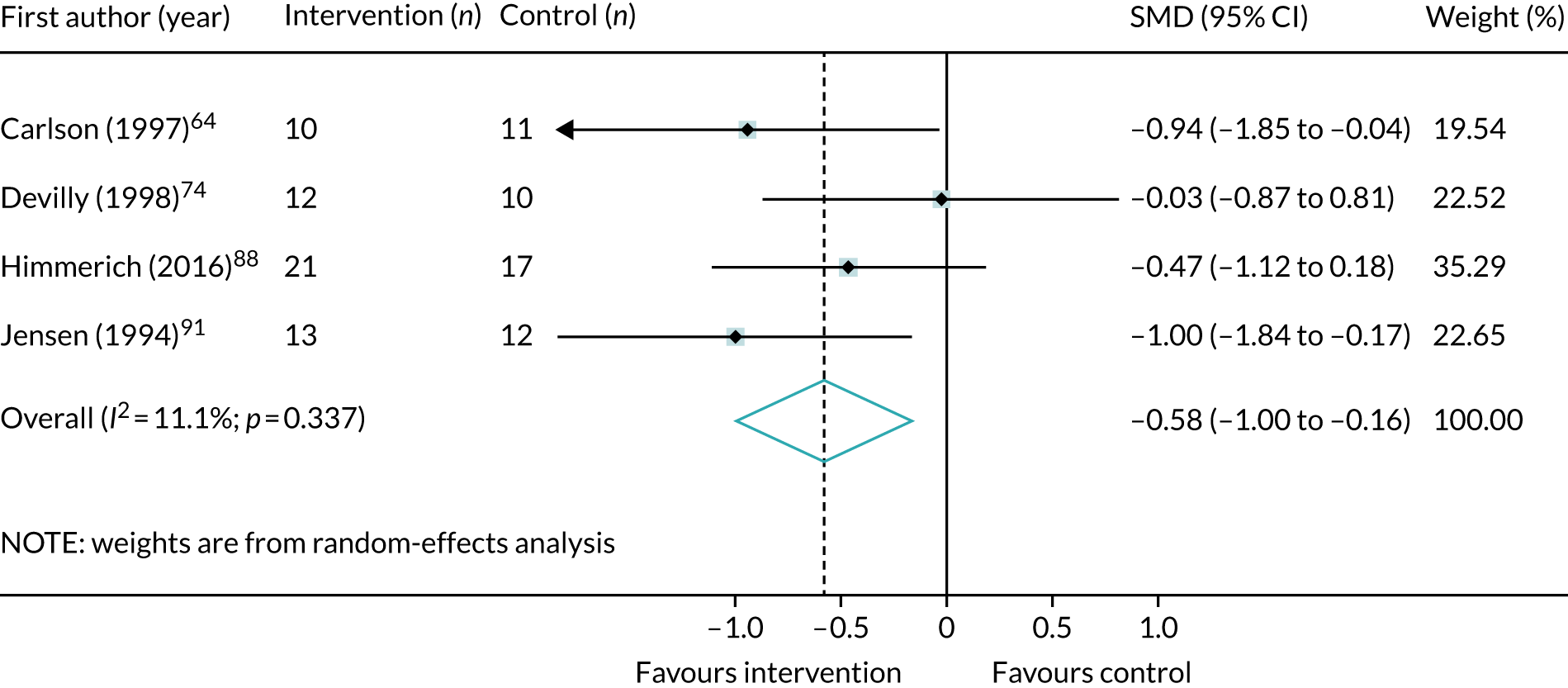
FIGURE 58.
Meta-analysis of post-treatment SMD for total PTSD symptoms, comparing mindfulness interventions with control in veteran populations.

FIGURE 59.
Meta-analysis of post-treatment SMD for total PTSD symptoms, comparing single-component and trauma-focused interventions with control in veteran populations.
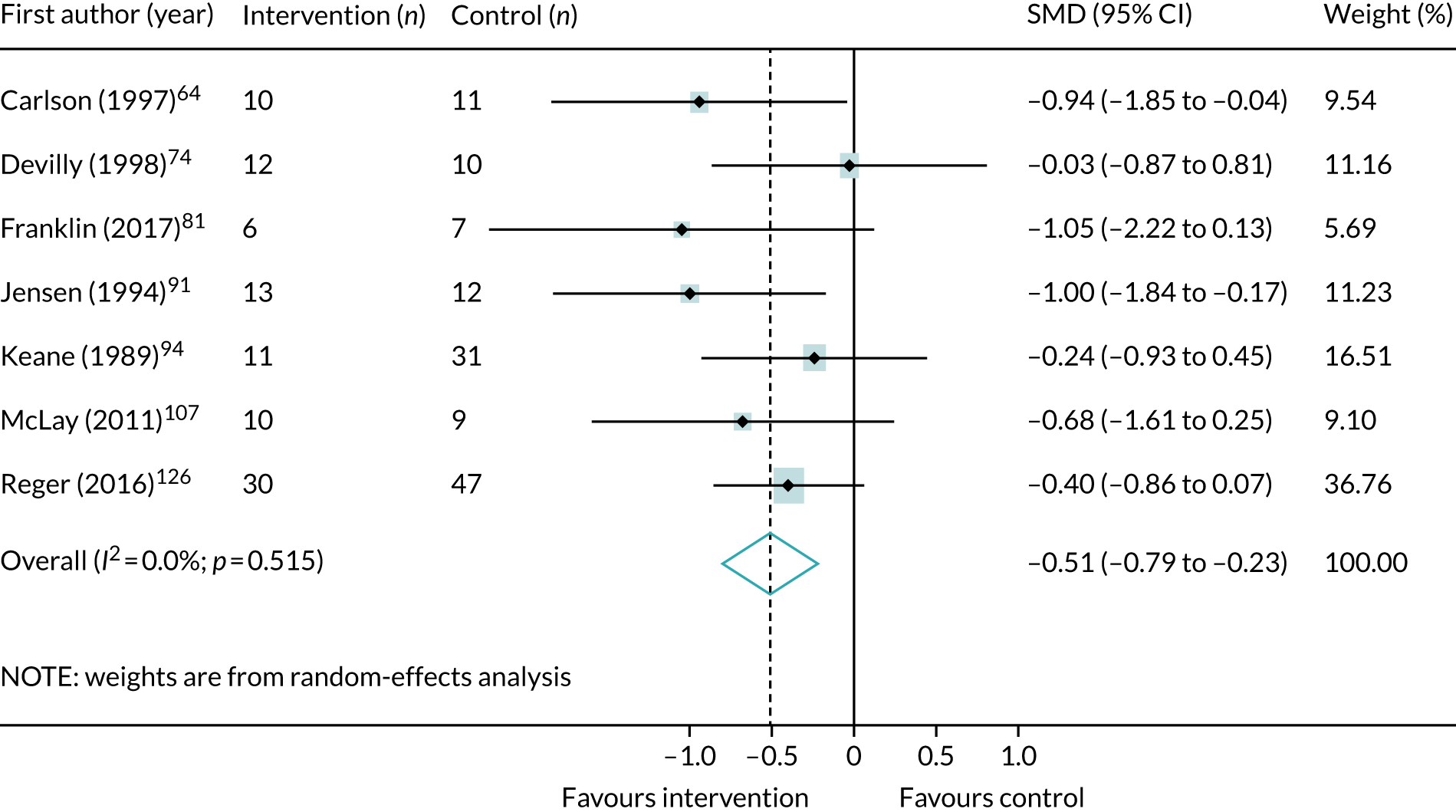
FIGURE 60.
Meta-analysis of post-treatment SMD for total PTSD symptoms, comparing multicomponent and trauma-focused interventions with control in veteran populations.
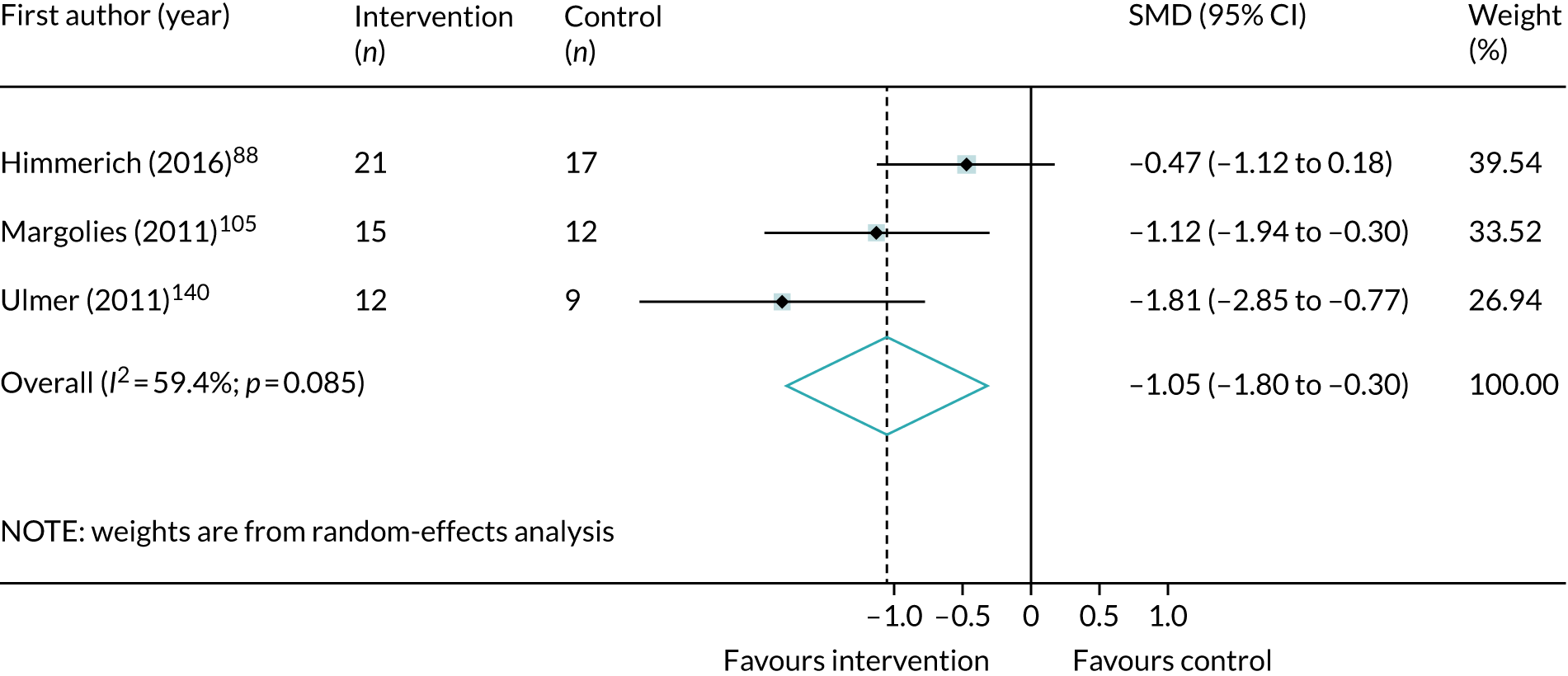
FIGURE 61.
Meta-analysis of post-treatment SMD for total PTSD symptoms, comparing single-component and non-trauma-focused interventions with control in veteran populations.

Depression symptoms
FIGURE 62.
Meta-analysis of post-treatment SMD for total depression symptoms, comparing trauma-focused CBT interventions with control in veteran populations.
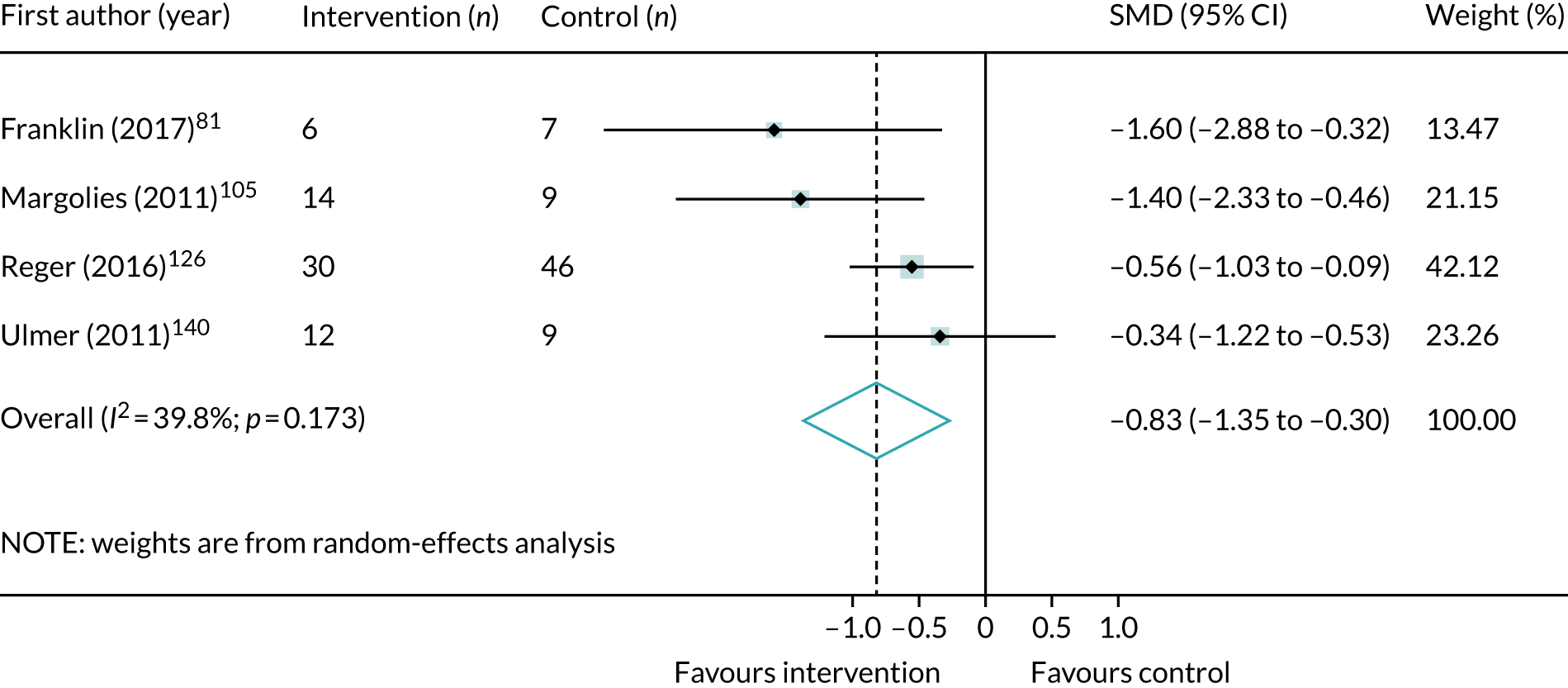
FIGURE 63.
Meta-analysis of post-treatment SMD for total depression symptoms, comparing EMDR interventions with control in veteran populations.

FIGURE 64.
Meta-analysis of post-treatment SMD for total depression symptoms, comparing mindfulness interventions with control in veteran populations.
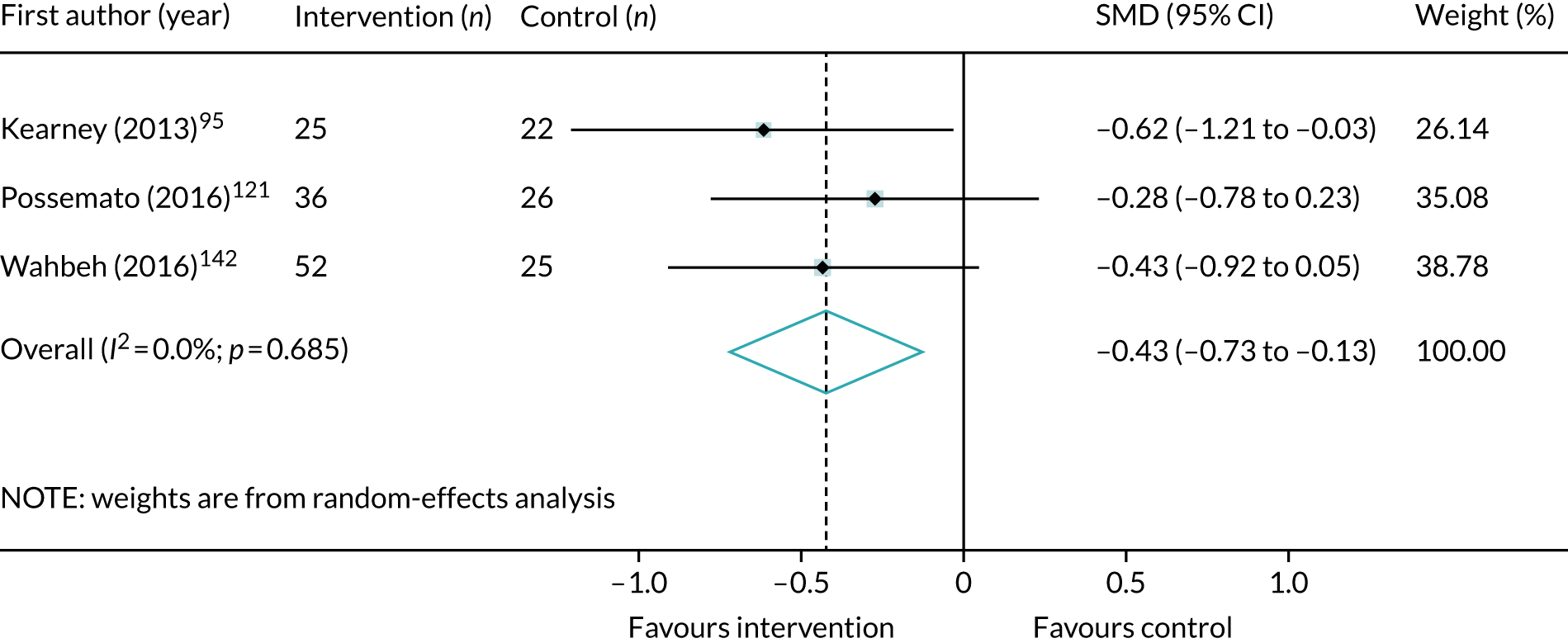
FIGURE 65.
Meta-analysis of post-treatment SMD for total depression symptoms, comparing single-component and trauma-focused interventions with control in veteran populations.
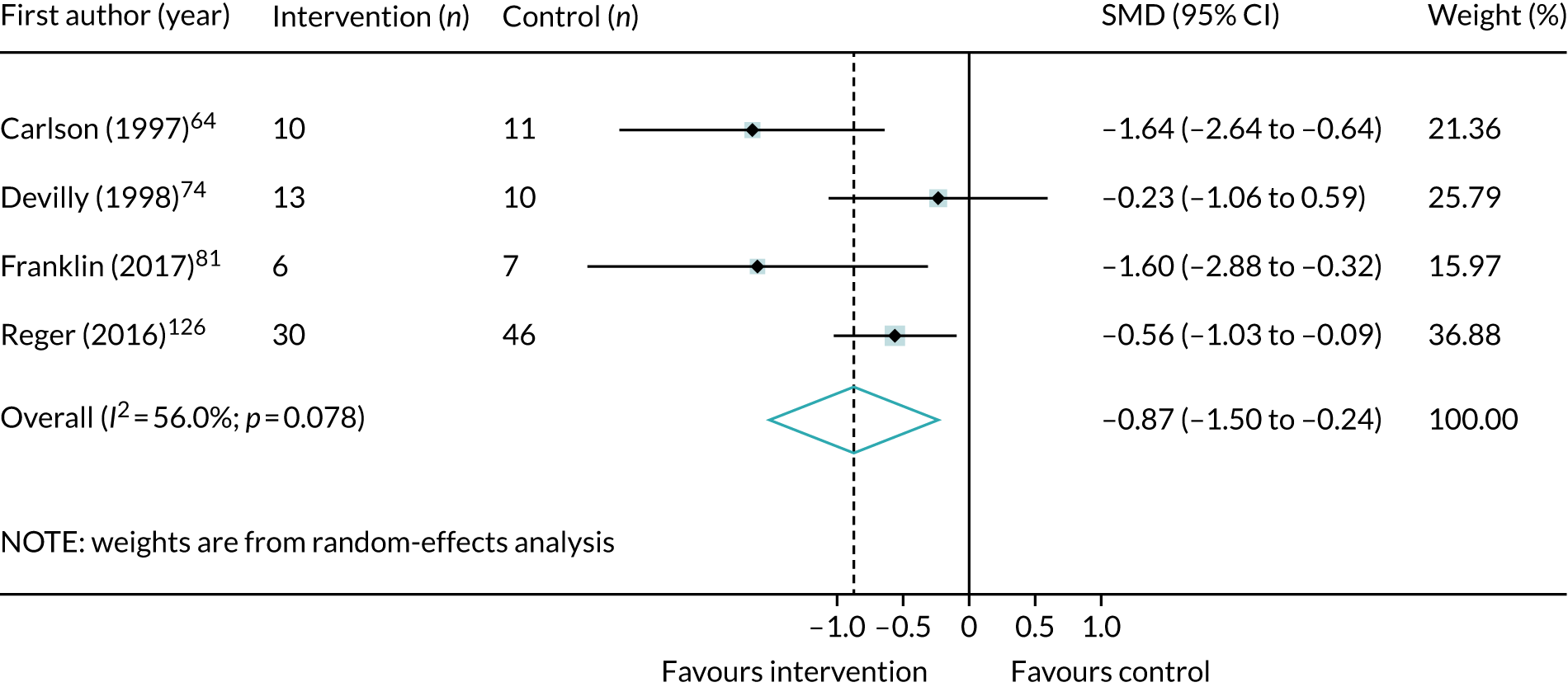
FIGURE 66.
Meta-analysis of post-treatment SMD for total depression symptoms, comparing multicomponent and trauma-focused interventions with control in veteran populations.

FIGURE 67.
Meta-analysis of post-treatment SMD for total depression symptoms, comparing single-component and non-trauma-focused interventions with control in veteran populations.
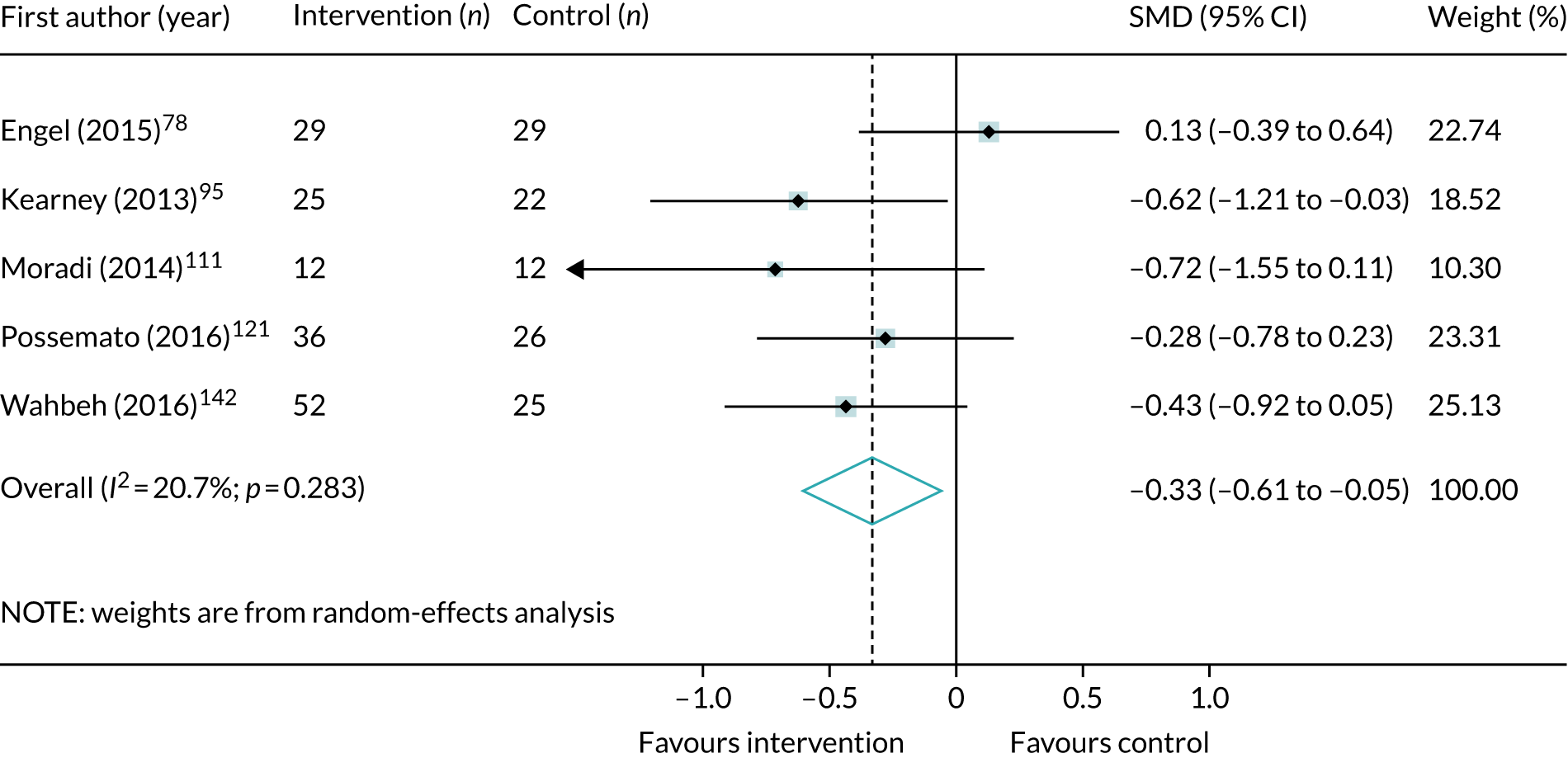
Anxiety symptoms
FIGURE 68.
Meta-analysis of post-treatment SMD for total anxiety symptoms, comparing trauma-focused CBT interventions with control in veteran populations.

FIGURE 69.
Meta-analysis of post-treatment SMD for total anxiety symptoms, comparing EMDR interventions with control in veteran populations.
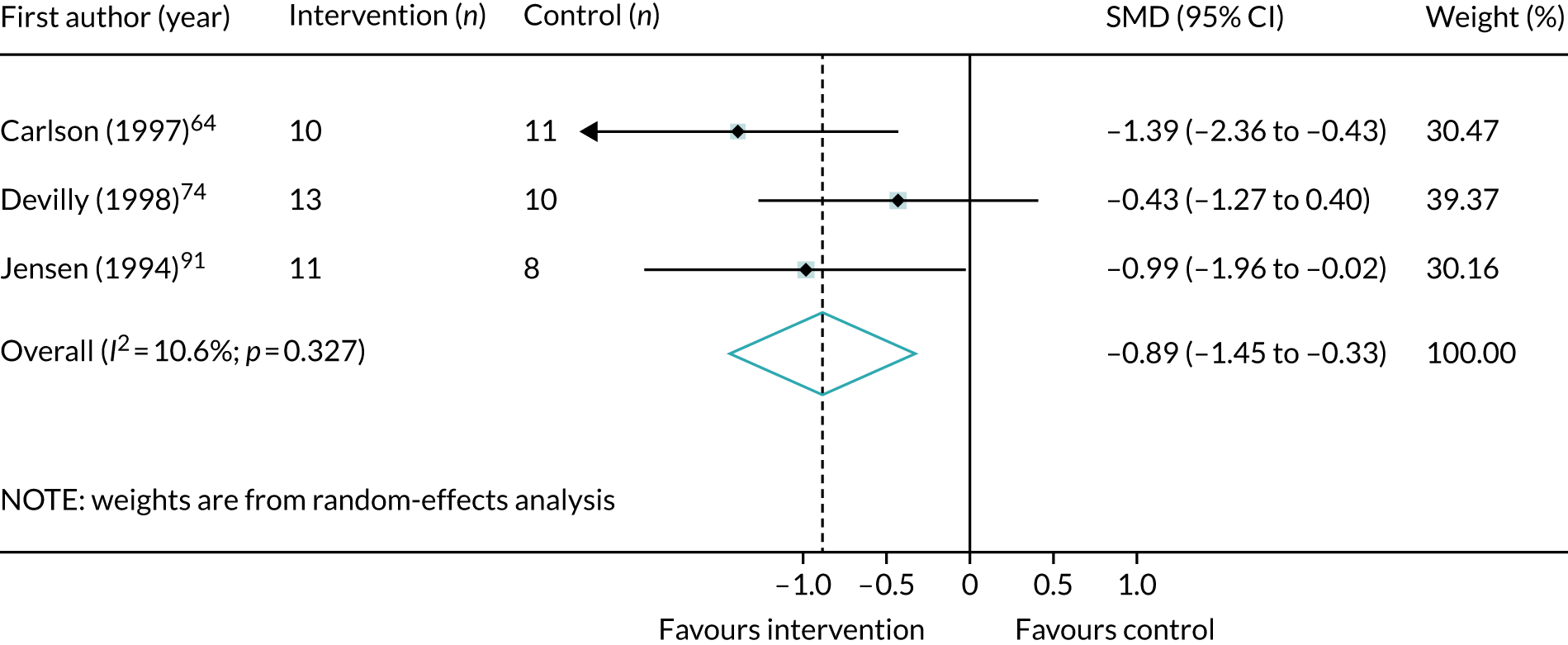
War-affected populations
Post-traumatic stress disorder symptoms
FIGURE 70.
Meta-analysis of post-treatment effect size (ES) for total PTSD symptoms, comparing trauma-focused CBT interventions with control in war-affected populations. CETA, common elements treatment approach; CPT, cognitive treatment therapy.
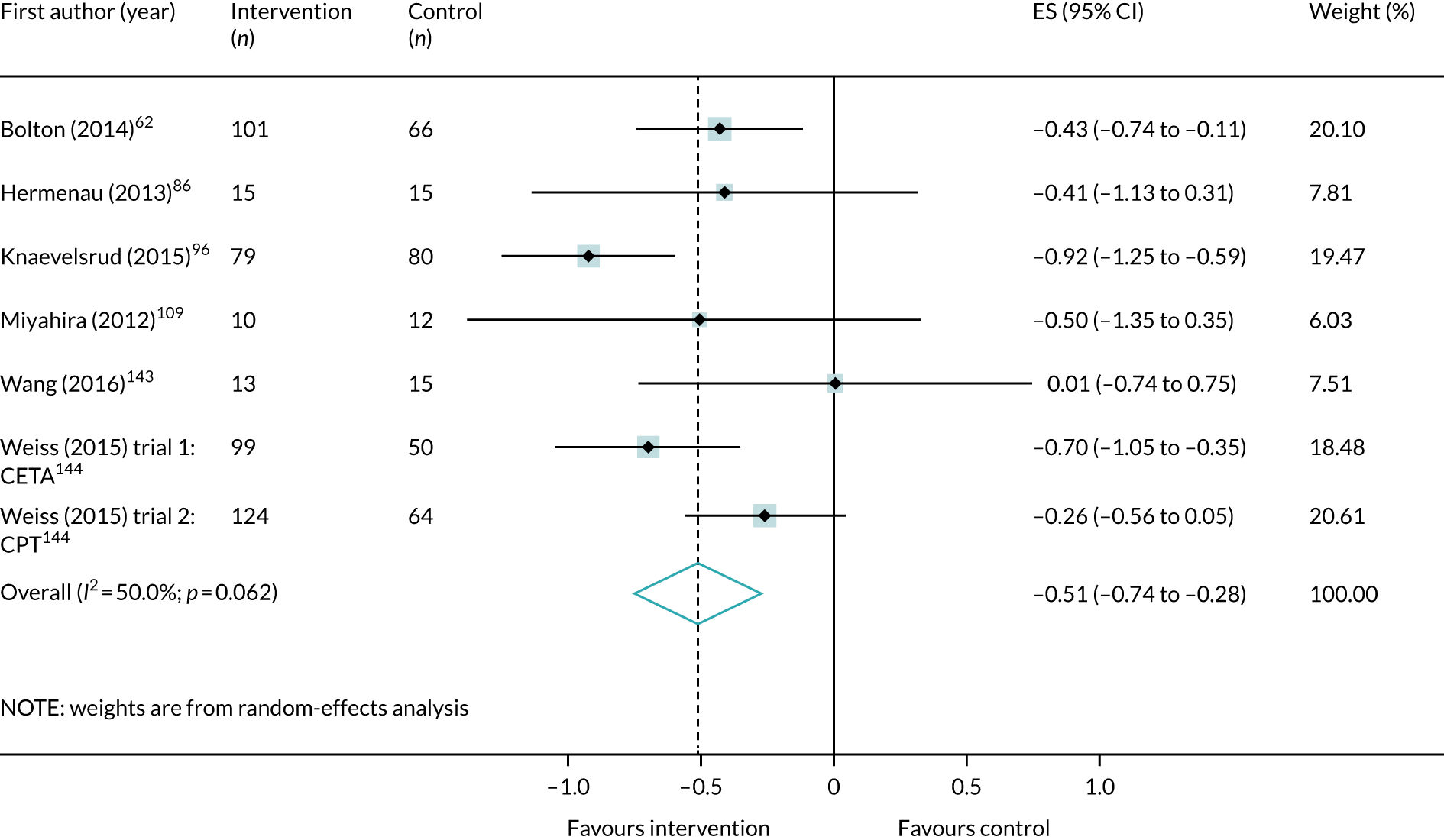
FIGURE 71.
Meta-analysis of post-treatment effect size (ES) for total PTSD symptoms, comparing multicomponent trauma-focused interventions with control in war-affected populations. CETA, common elements treatment approach.
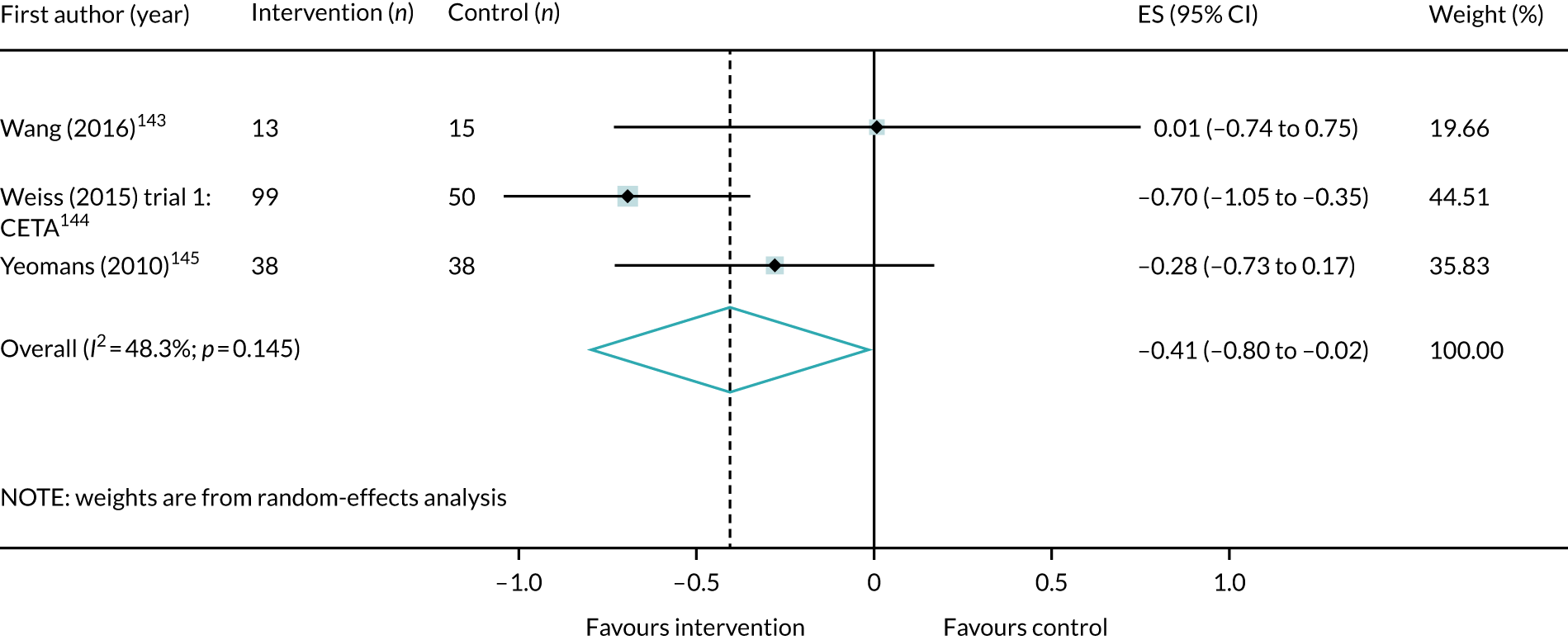
Depression symptoms
FIGURE 72.
Meta-analysis of post-treatment SMD for depression symptoms, comparing single-component and trauma-focused interventions with control in war-affected populations. CPT, cognitive processing therapy.

FIGURE 73.
Meta-analysis of post-treatment effect size (ES) for depression symptoms, comparing multicomponent and trauma-focused interventions with control in war-affected populations. CETA, common elements treatment approach.
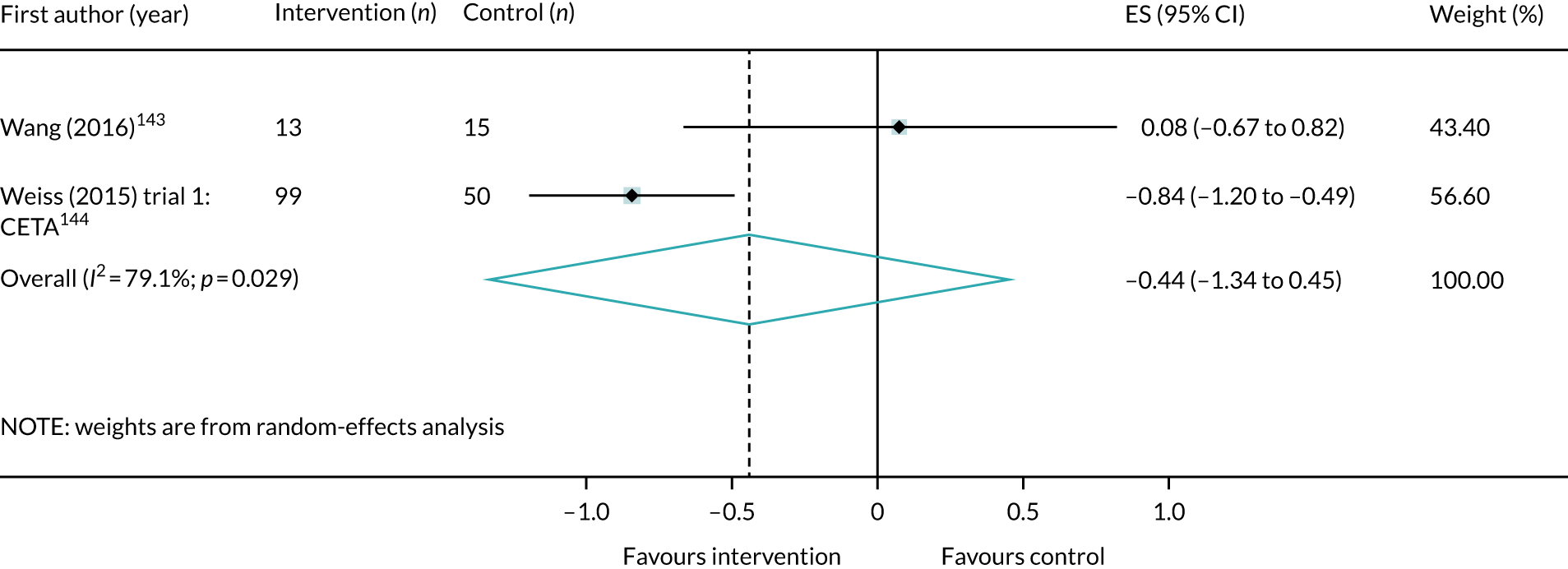
Anxiety symptoms
FIGURE 74.
Meta-analysis of post-treatment SMD for total anxiety symptoms, comparing single-component and trauma-focused interventions with control in war-affected populations. CPT, cognitive processing therapy.
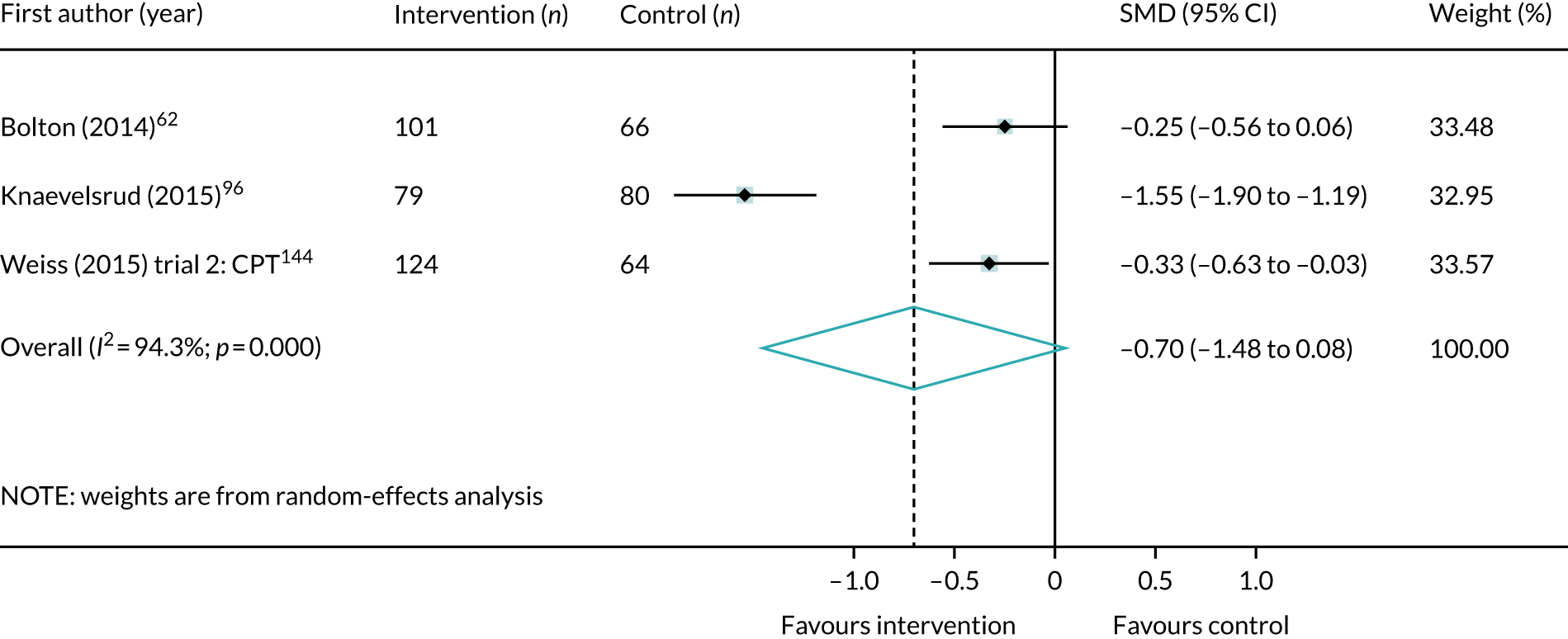
FIGURE 75.
Meta-analysis of post-treatment effect size (ES) for total anxiety symptoms, comparing multicomponent and trauma-focused interventions with control in war-affected populations. CETA, common elements treatment approach.

Childhood sexual abuse populations
Post-traumatic stress disorder symptoms
FIGURE 76.
Meta-analysis of post-treatment SMD for total PTSD symptoms, comparing trauma-focused CBT interventions with control in childhood sexual abuse populations.
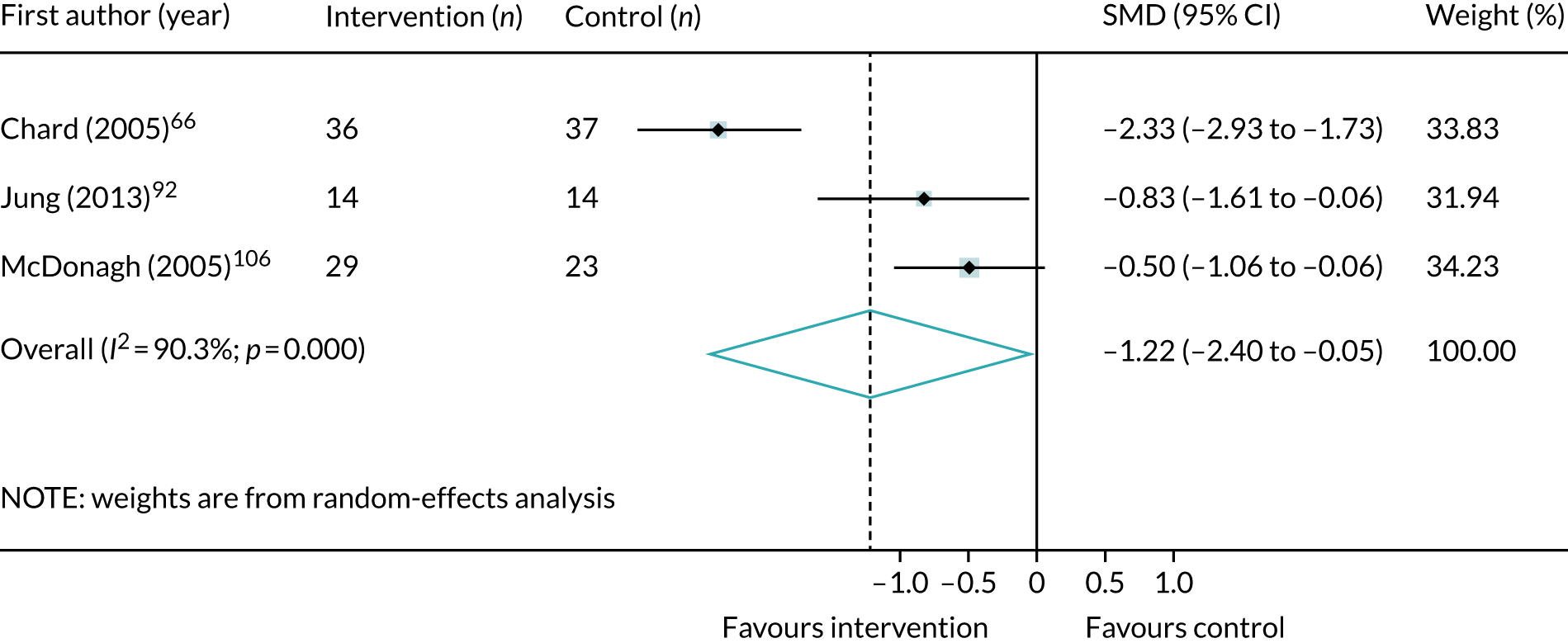
FIGURE 77.
Meta-analysis of post-treatment SMD for total PTSD symptoms, comparing non-trauma-focused CBT interventions with control in childhood sexual abuse populations.

FIGURE 78.
Meta-analysis of post-treatment SMD for total PTSD symptoms, comparing single-component and trauma-focused interventions with control in childhood sexual abuse populations.
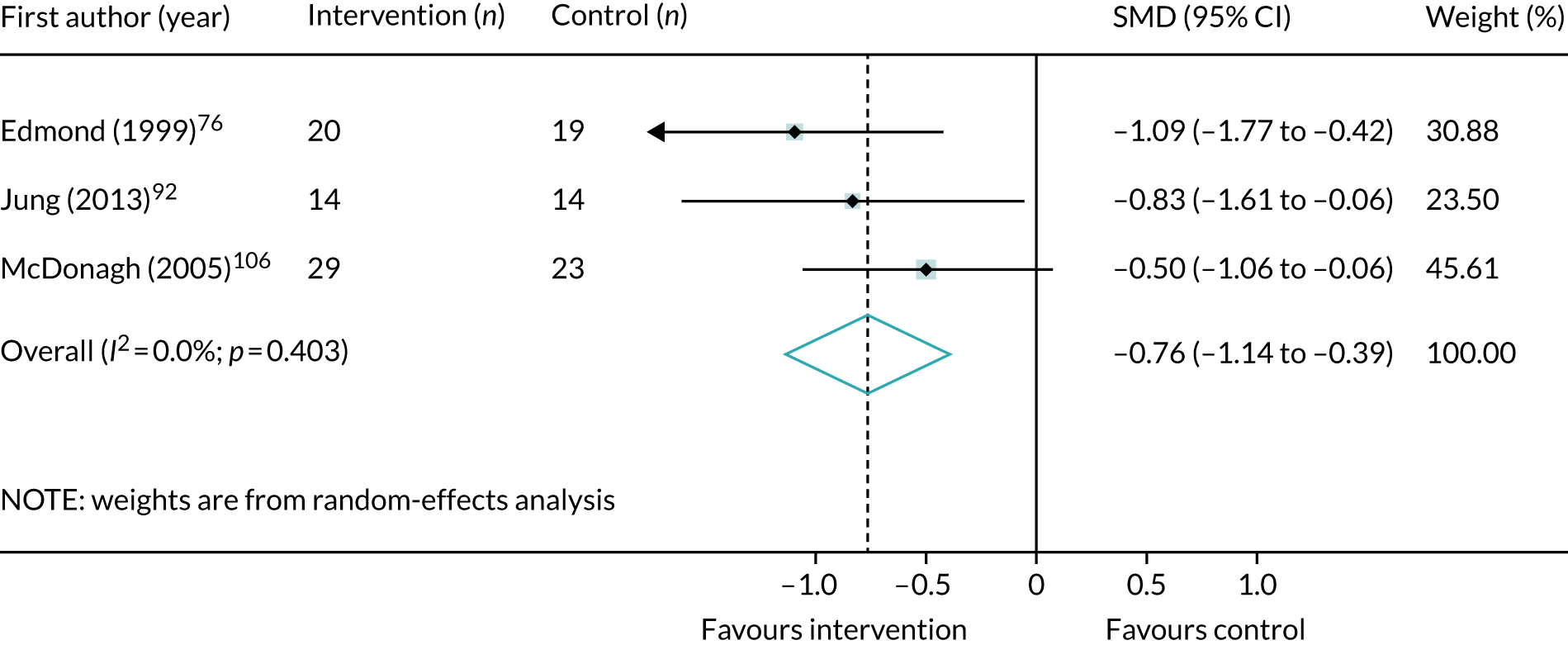
FIGURE 79.
Meta-analysis of post-treatment SMD for total PTSD symptoms, comparing single-component and non-trauma-focused interventions with control in childhood sexual abuse populations.
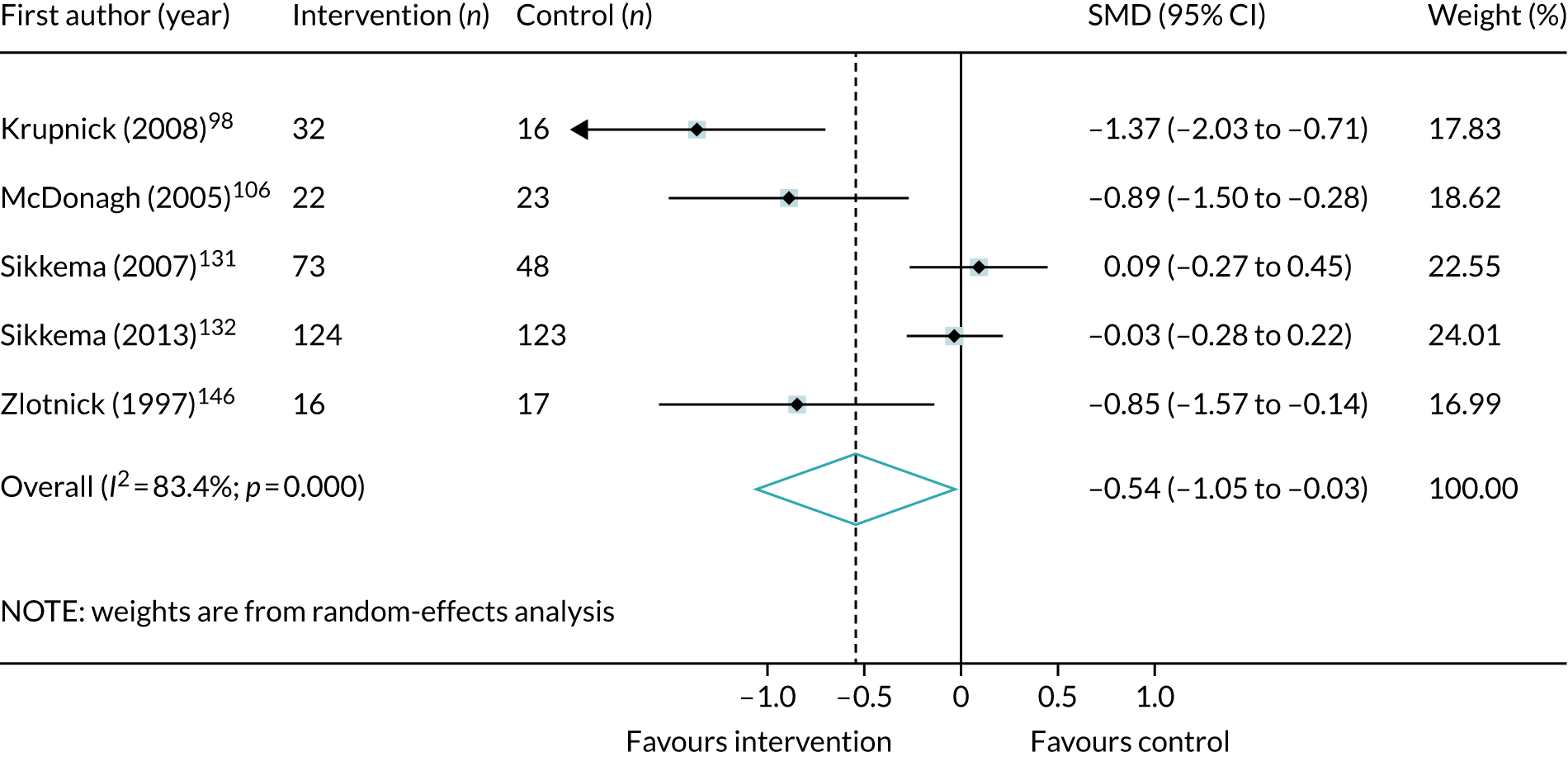
Depression symptoms
FIGURE 80.
Meta-analysis of post-treatment SMD for depression symptoms, comparing trauma-focused CBT interventions with control in childhood sexual abuse populations.
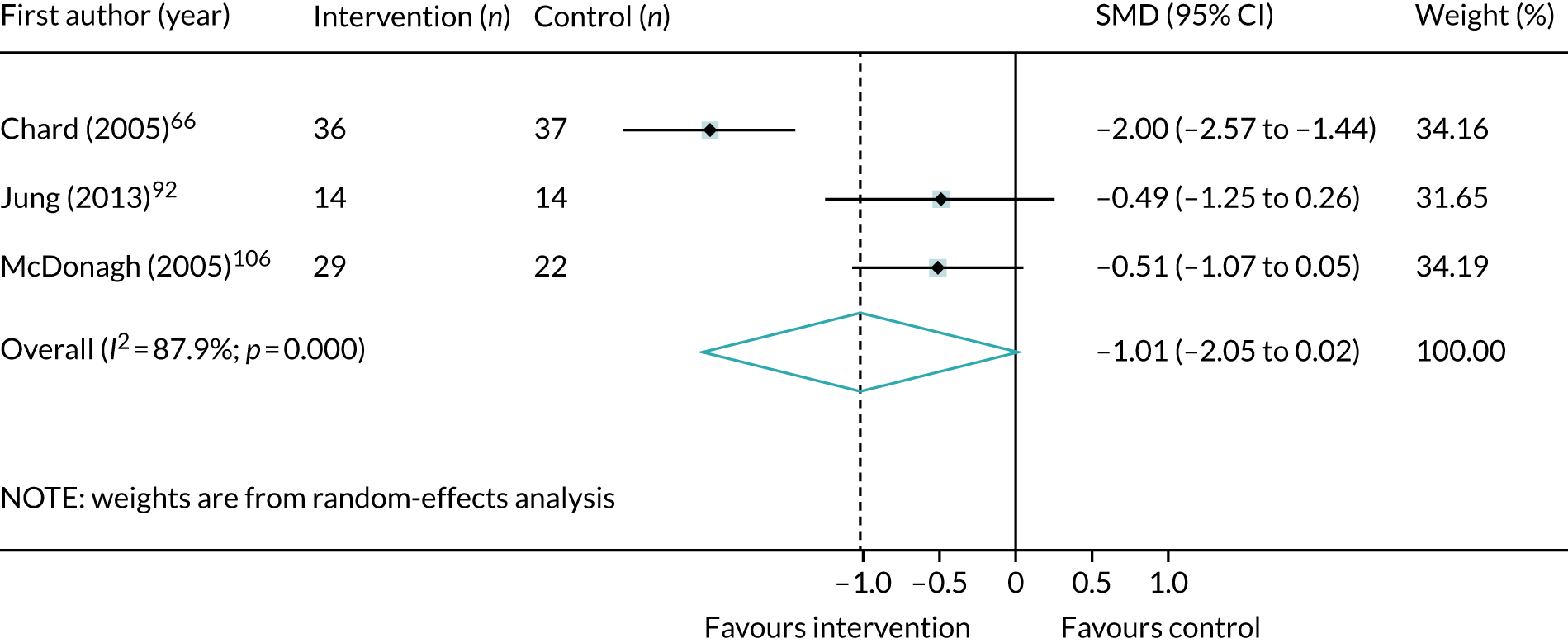
FIGURE 81.
Meta-analysis of post-treatment SMD for depression symptoms, comparing single-component and trauma-focused interventions with control in childhood sexual abuse populations.
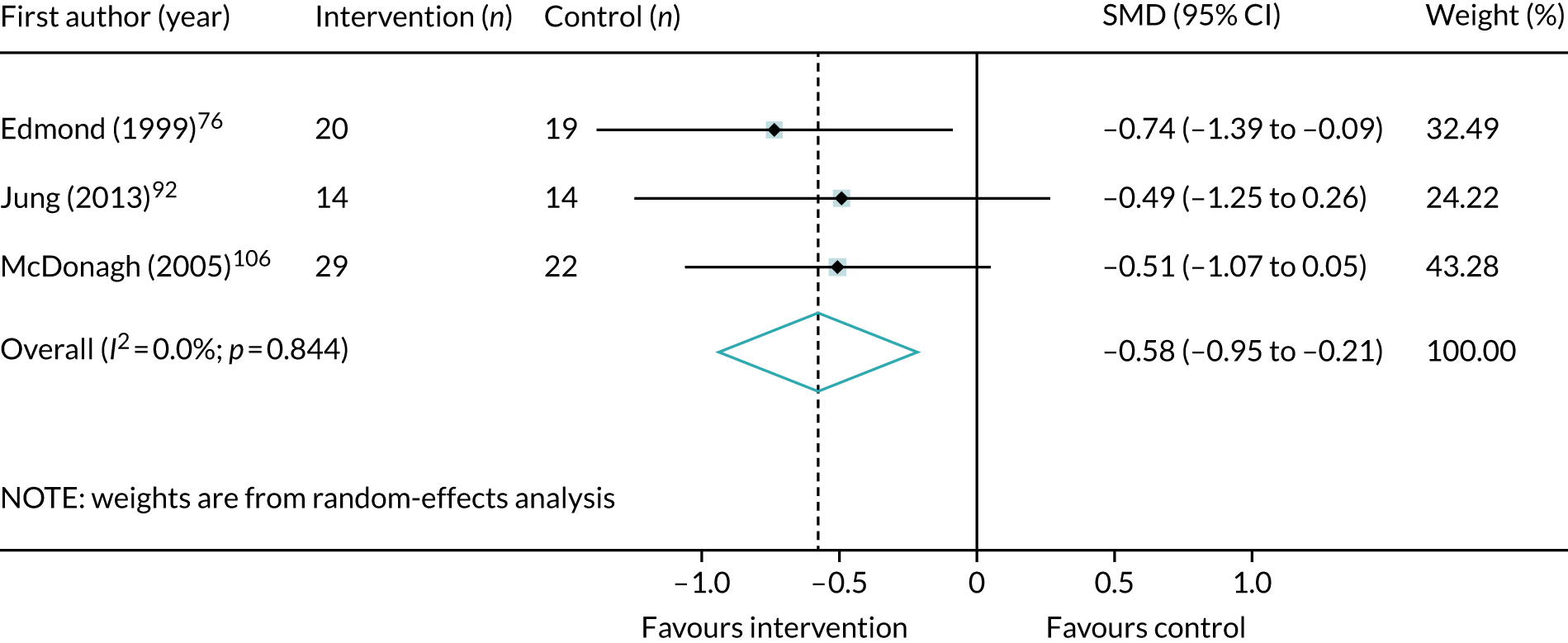
FIGURE 82.
Meta-analysis of post-treatment SMD for depression symptoms, comparing single-component and non-trauma-focused interventions with control in childhood sexual abuse populations.

Anxiety symptoms
FIGURE 83.
Meta-analysis of post-treatment SMD for anxiety symptoms, comparing single-component and trauma-focused interventions with control in childhood sexual abuse populations.
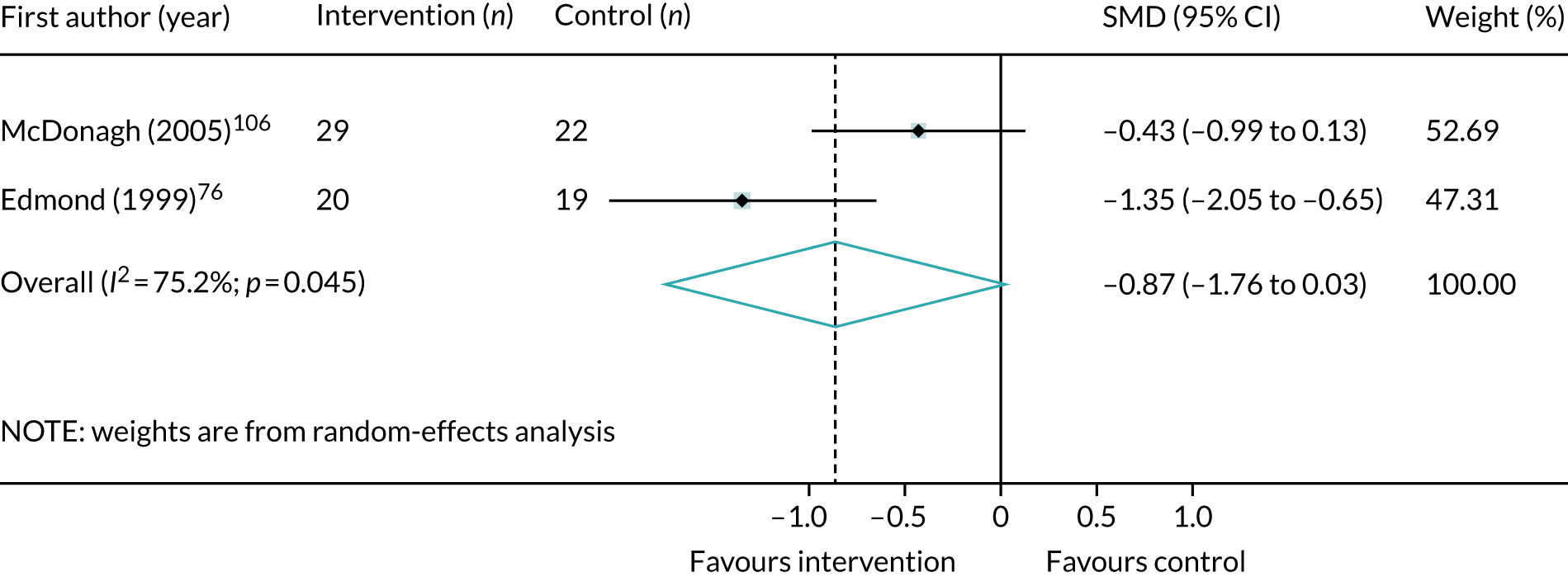
Refugee populations
Post-traumatic stress disorder symptoms
FIGURE 84.
Meta-analysis of post-treatment SMD for total PTSD symptoms, comparing trauma-focused CBT interventions with control in refugee populations.

FIGURE 85.
Meta-analysis of post-treatment SMD for total PTSD symptoms, comparing EMDR interventions with control in refugee populations.

FIGURE 86.
Meta-analysis of post-treatment SMD for total PTSD symptoms, comparing single-component and trauma-focused interventions with control in refugee populations.
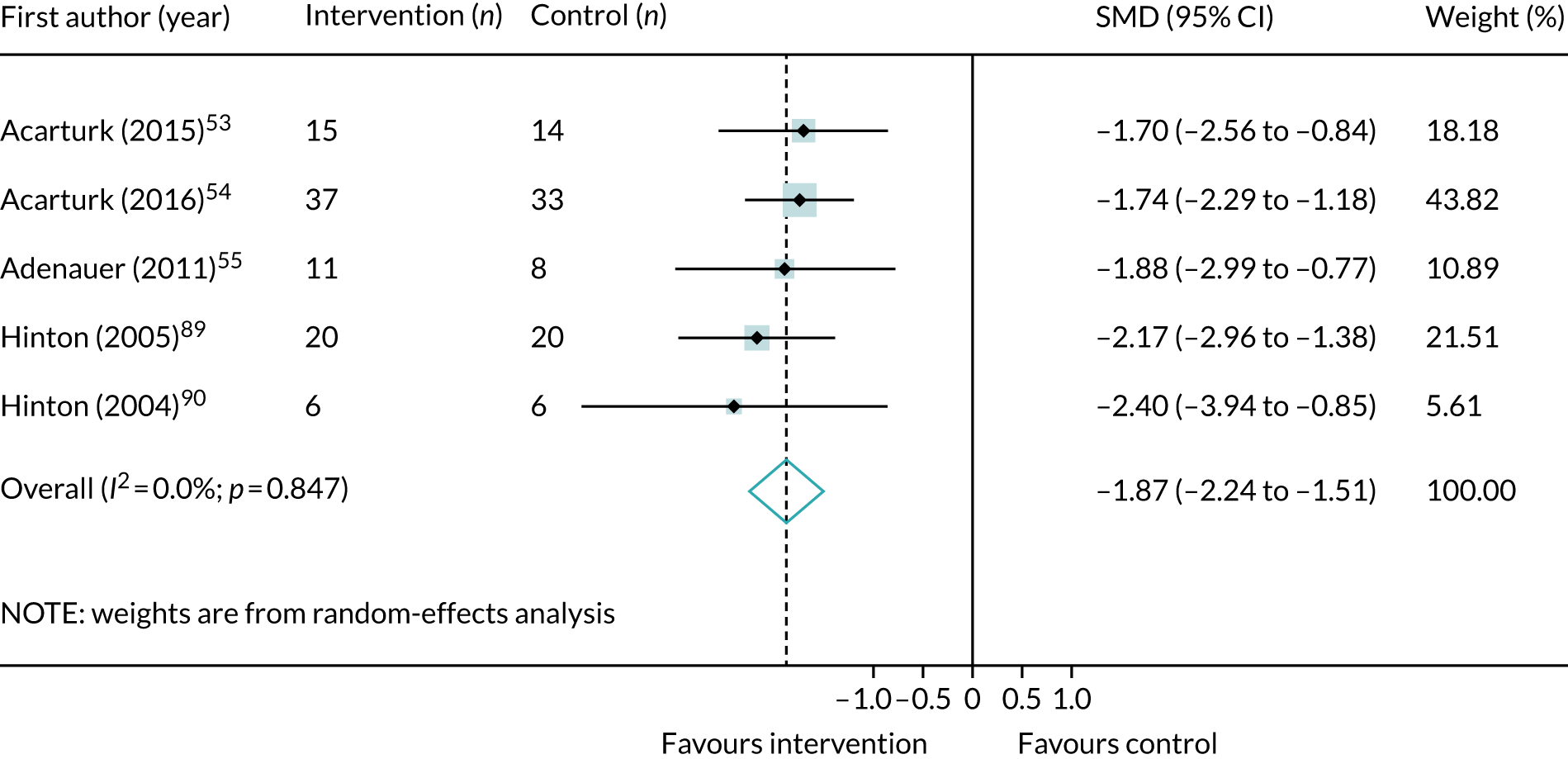
Depression symptoms
FIGURE 87.
Meta-analysis of post-treatment SMD for depression symptoms, comparing trauma-focused CBT interventions with control in refugee populations.
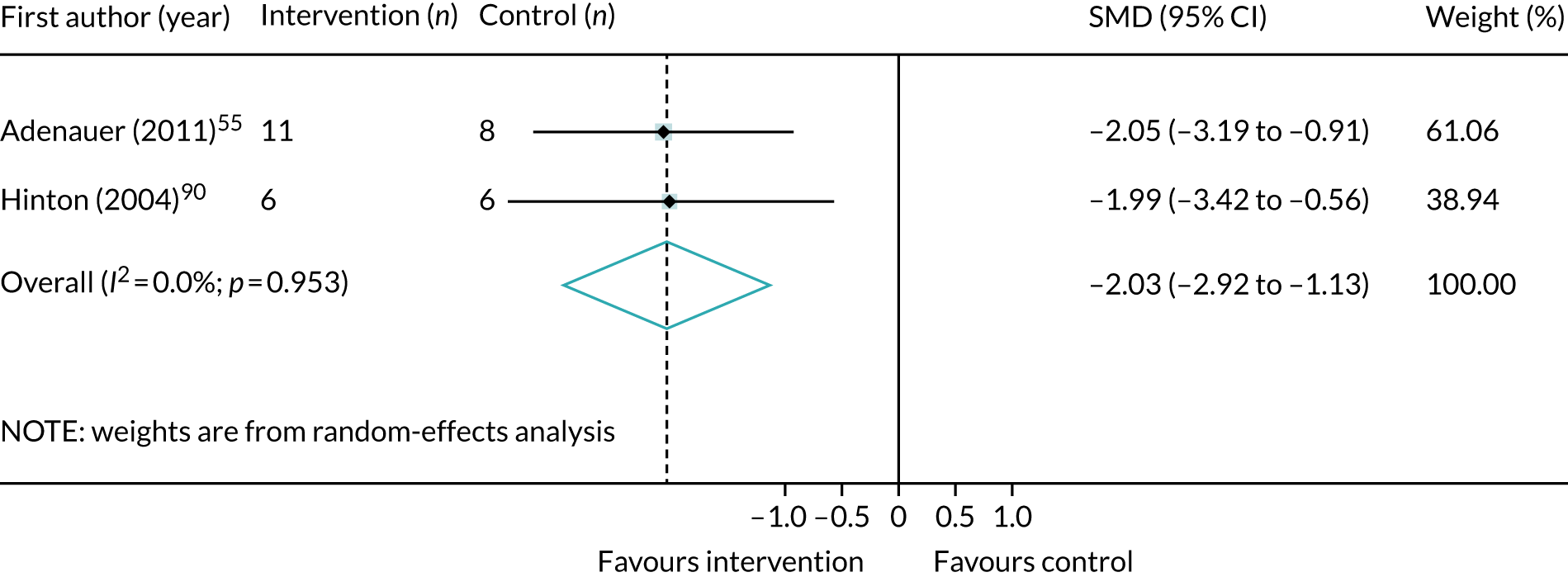
FIGURE 88.
Meta-analysis of post-treatment SMD for depression symptoms, comparing EMDR interventions with control in refugee populations.

FIGURE 89.
Meta-analysis of post-treatment SMD for depression symptoms, comparing single-component and trauma-focused interventions with control in refugee populations.
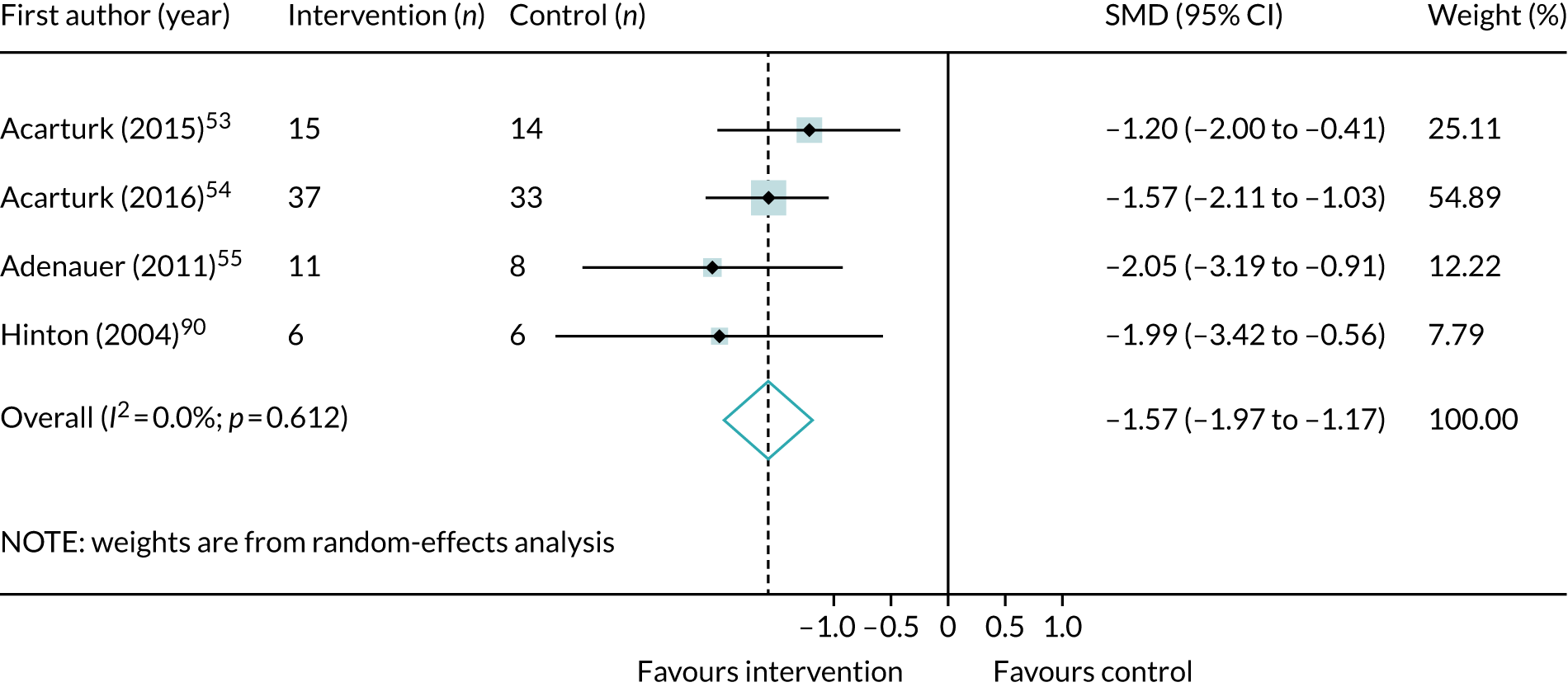
Pharmacological interventions versus placebo
Post-traumatic stress disorder symptoms
FIGURE 90.
Meta-analysis of post-treatment SMD for PTSD symptoms, comparing antidepressants with placebo.

FIGURE 91.
Meta-analysis of post-treatment SMD for PTSD symptoms, comparing SSRIs with placebo.
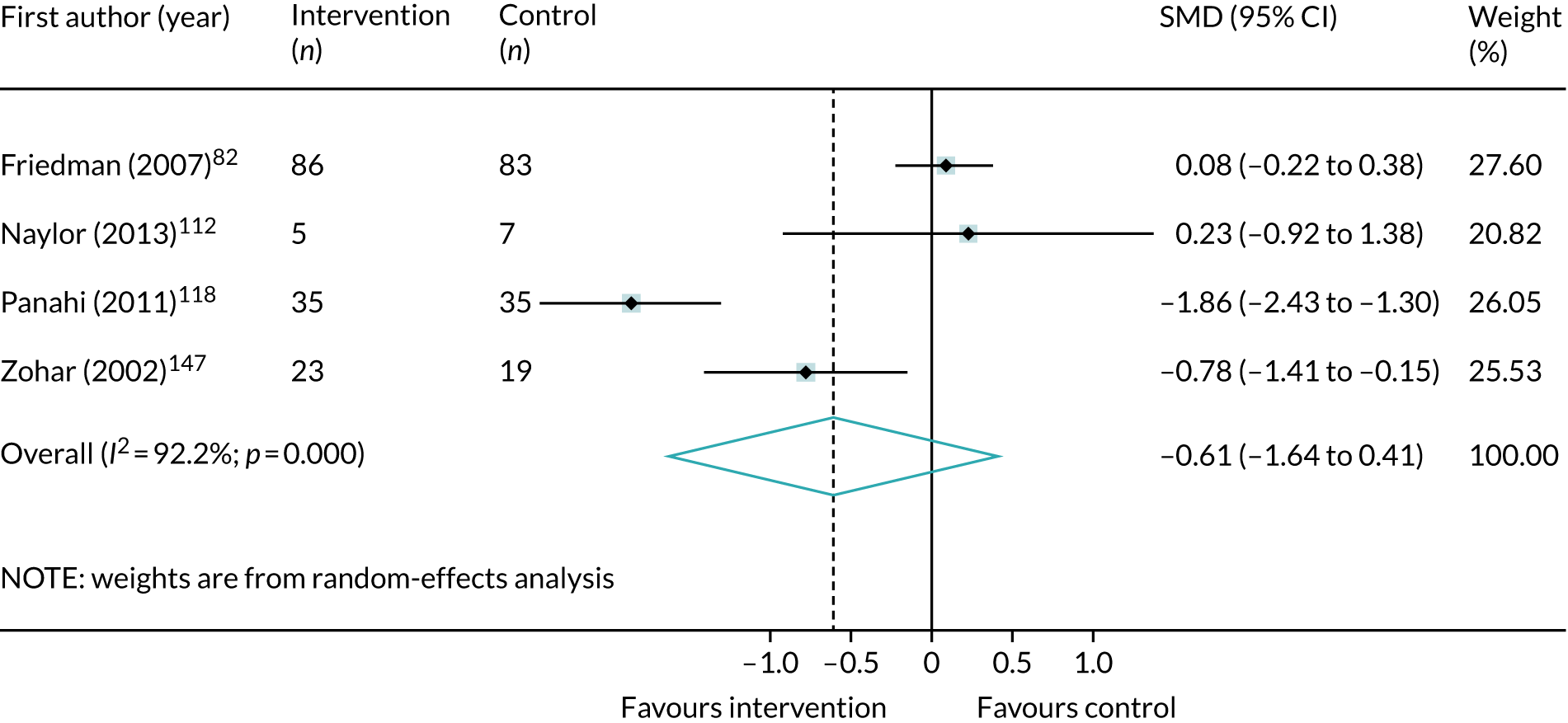
FIGURE 92.
Meta-analysis of post-treatment SMD for PTSD symptoms, comparing antipsychotics with placebo.
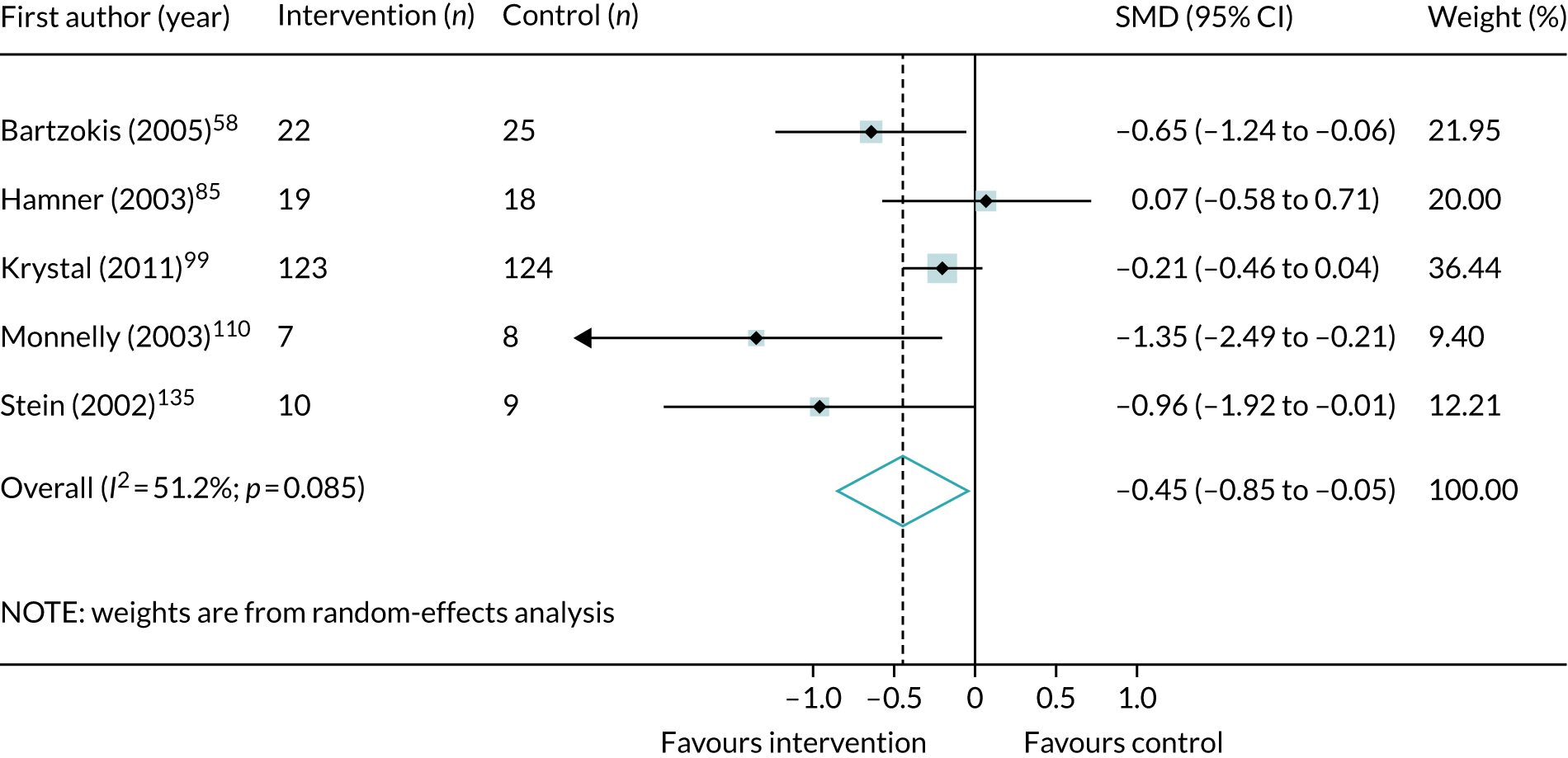
FIGURE 93.
Meta-analysis of post-treatment SMD for PTSD symptoms, comparing anticonvulsants with placebo.
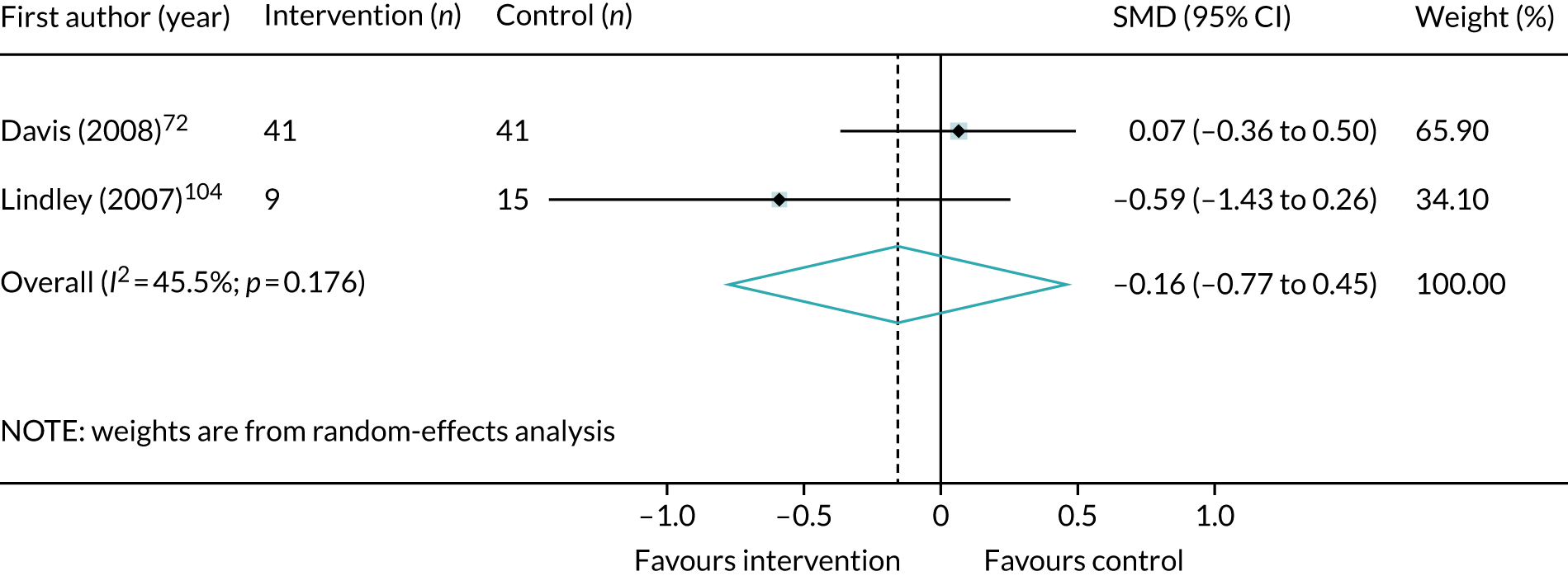
FIGURE 94.
Meta-analysis of post-treatment SMD for PTSD symptoms, comparing prazosin with placebo.

Depression symptoms
FIGURE 95.
Meta-analysis of post-treatment SMD for depression symptoms, comparing antidepressants with placebo.
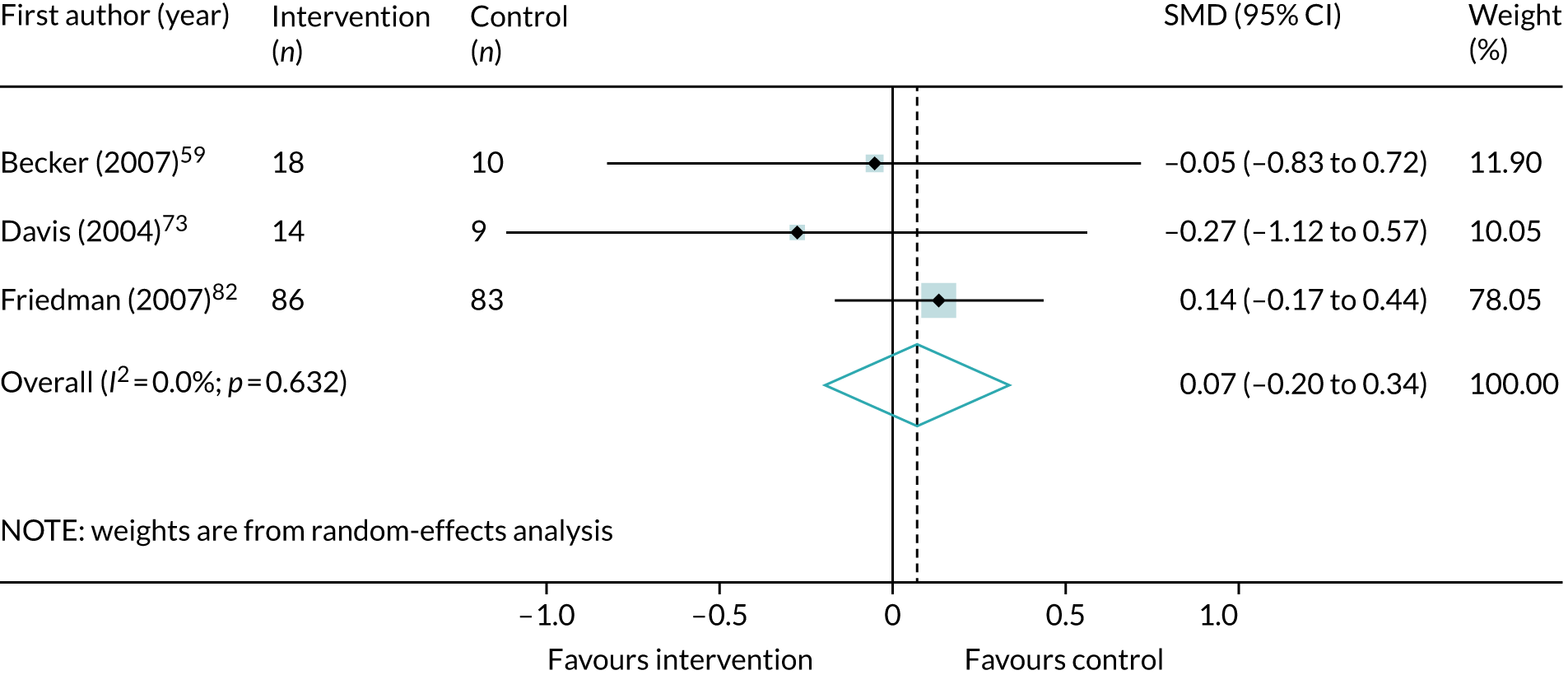
FIGURE 96.
Meta-analysis of post-treatment SMD for depression symptoms, comparing antipsychotics with placebo.
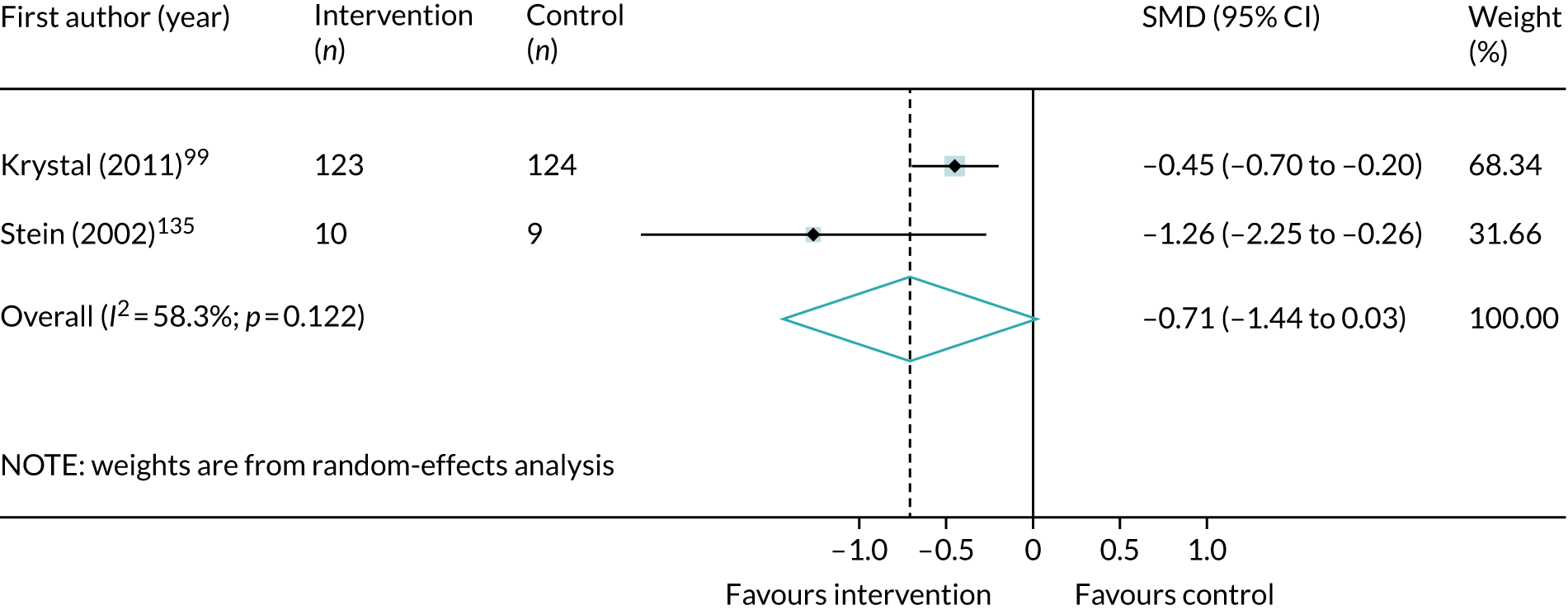
FIGURE 97.
Meta-analysis of post-treatment SMD for depression symptoms, comparing anticonvulsants with placebo.

Psychosis symptoms
FIGURE 98.
Meta-analysis of post-treatment weighted mean difference (WMD) for positive psychotic symptoms, comparing risperidone with placebo.

FIGURE 99.
Meta-analysis of post-treatment weighted mean difference (WMD) for negative psychotic symptoms, comparing risperidone with placebo.

FIGURE 100.
Meta-analysis of post-treatment weighted mean difference (WMD) for total psychotic symptoms, comparing risperidone with placebo.

FIGURE 101.
Meta-analysis of post-treatment weighted mean difference (WMD) for general psychopathology symptoms, comparing risperidone with placebo.

Attrition meta-analyses
Veterans
FIGURE 102.
Meta-analysis of OR of attrition from all psychological interventions compared with control, among a veteran population.

FIGURE 103.
Meta-analysis of OR of attrition from all psychological interventions compared with active controls, among a veteran population.
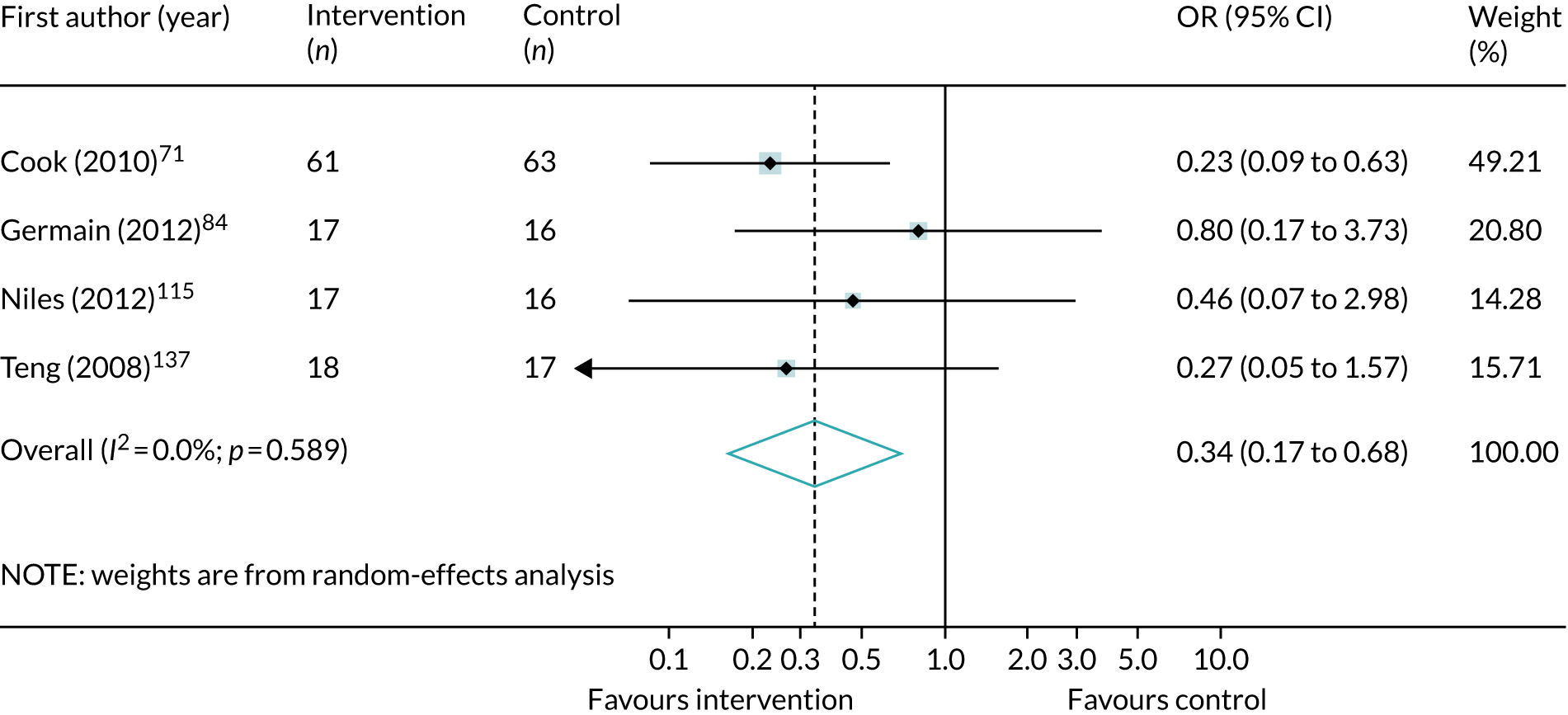
Pharmacological interventions
FIGURE 104.
Meta-analysis of OR of attrition from antidepressants compared with placebo, among a veteran population.
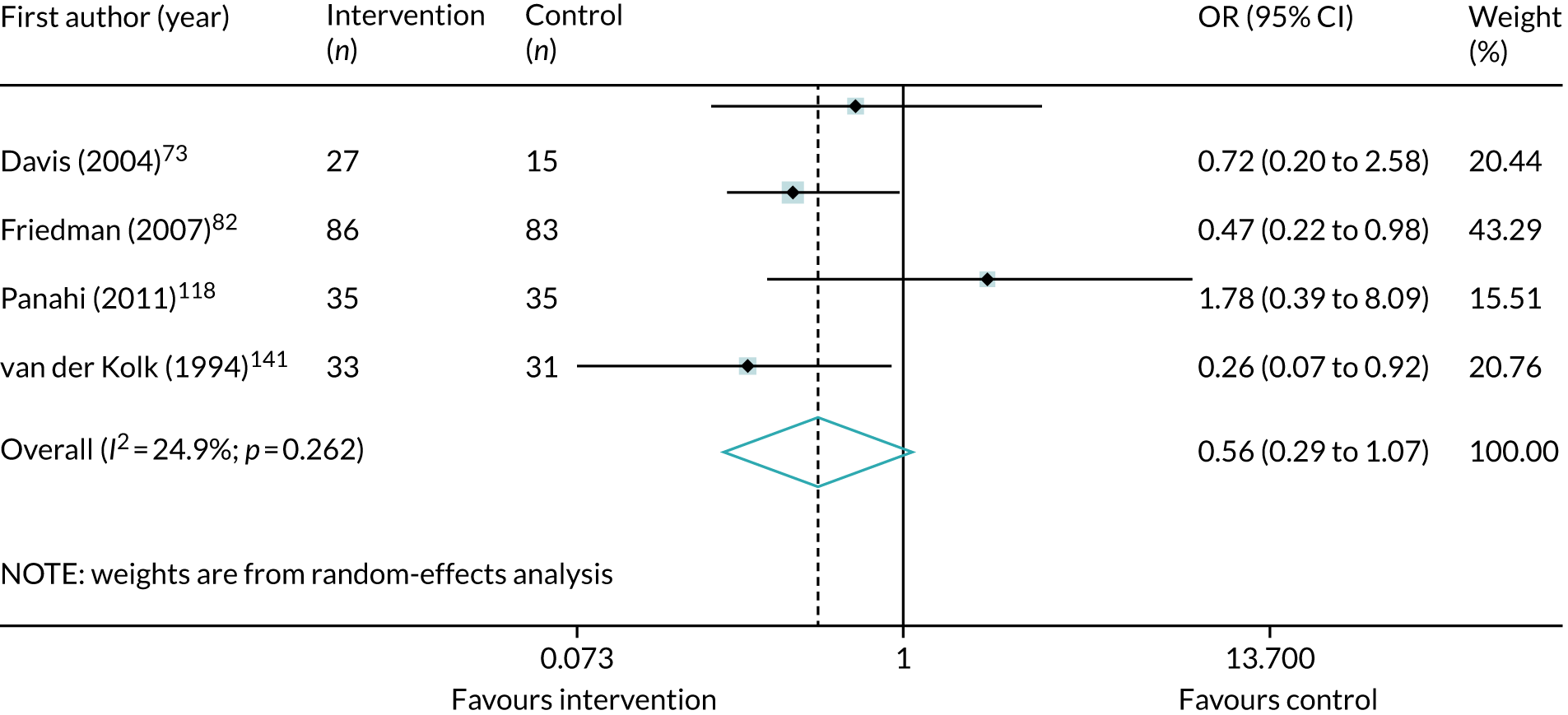
FIGURE 105.
Meta-analysis of OR of attrition from antidepsychotics compared with placebo, among a veteran population.
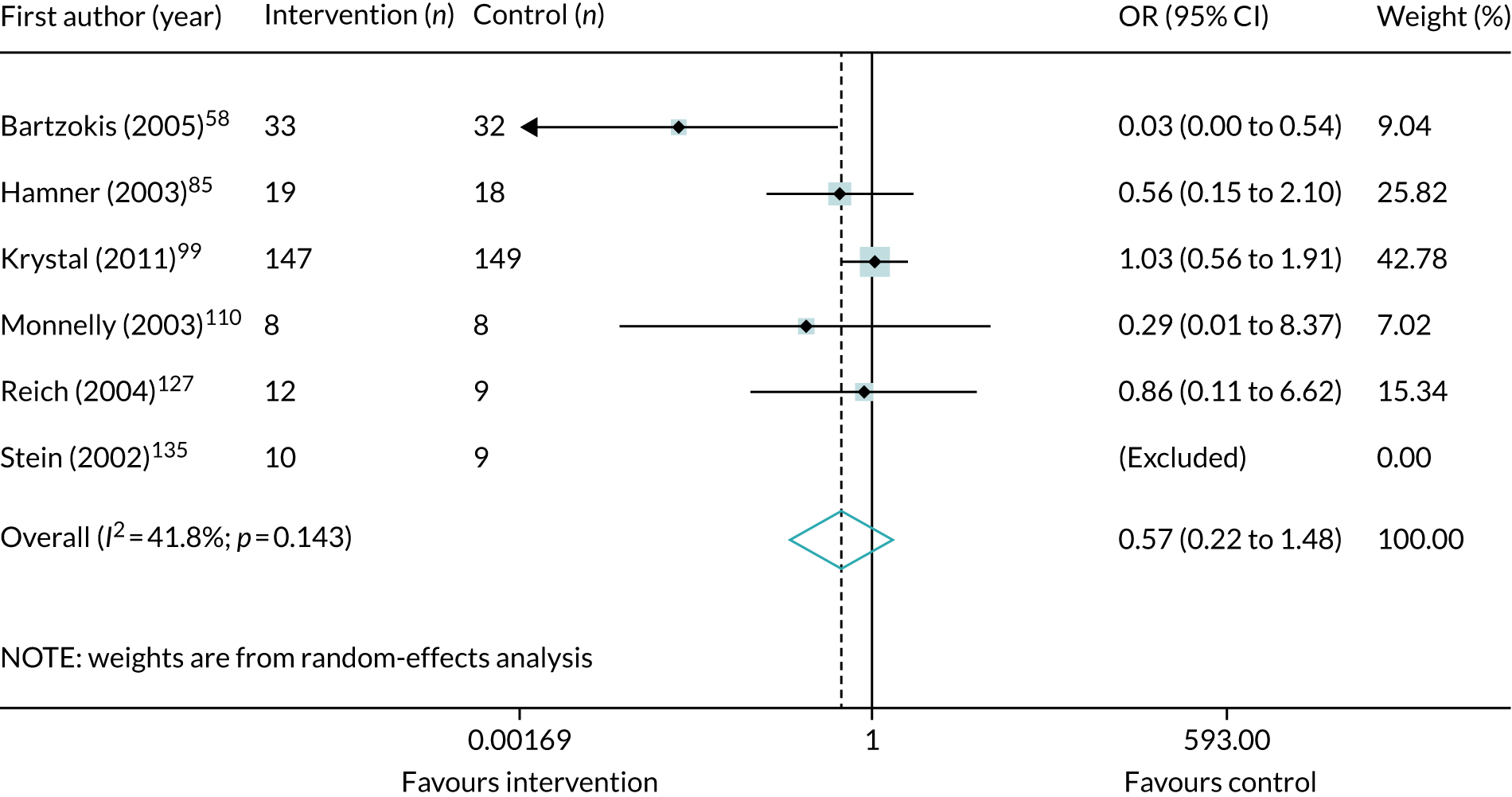
FIGURE 106.
Meta-analysis of OR of attrition from anticonvulsants compared with placebo, among a veteran population.
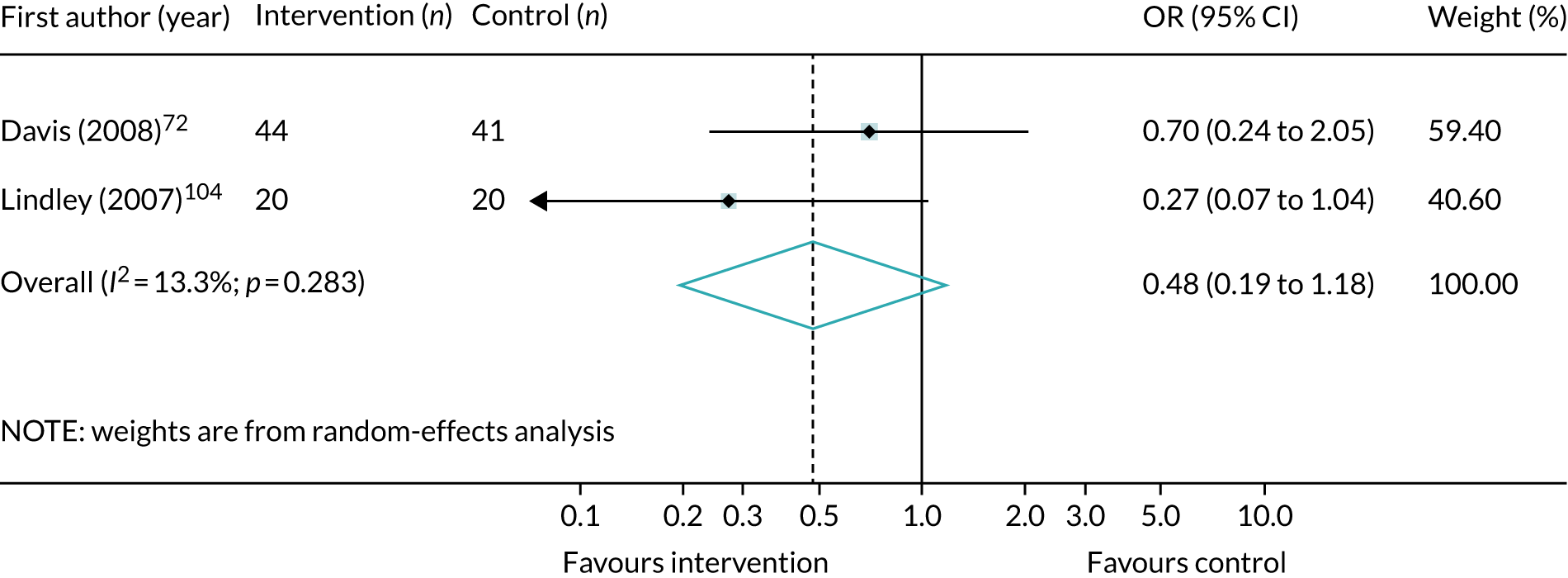
Childhood sexual abuse populations
FIGURE 107.
Meta-analysis of OR of attrition from all psychological interventions compared with control, among a childhood sexual abuse population.
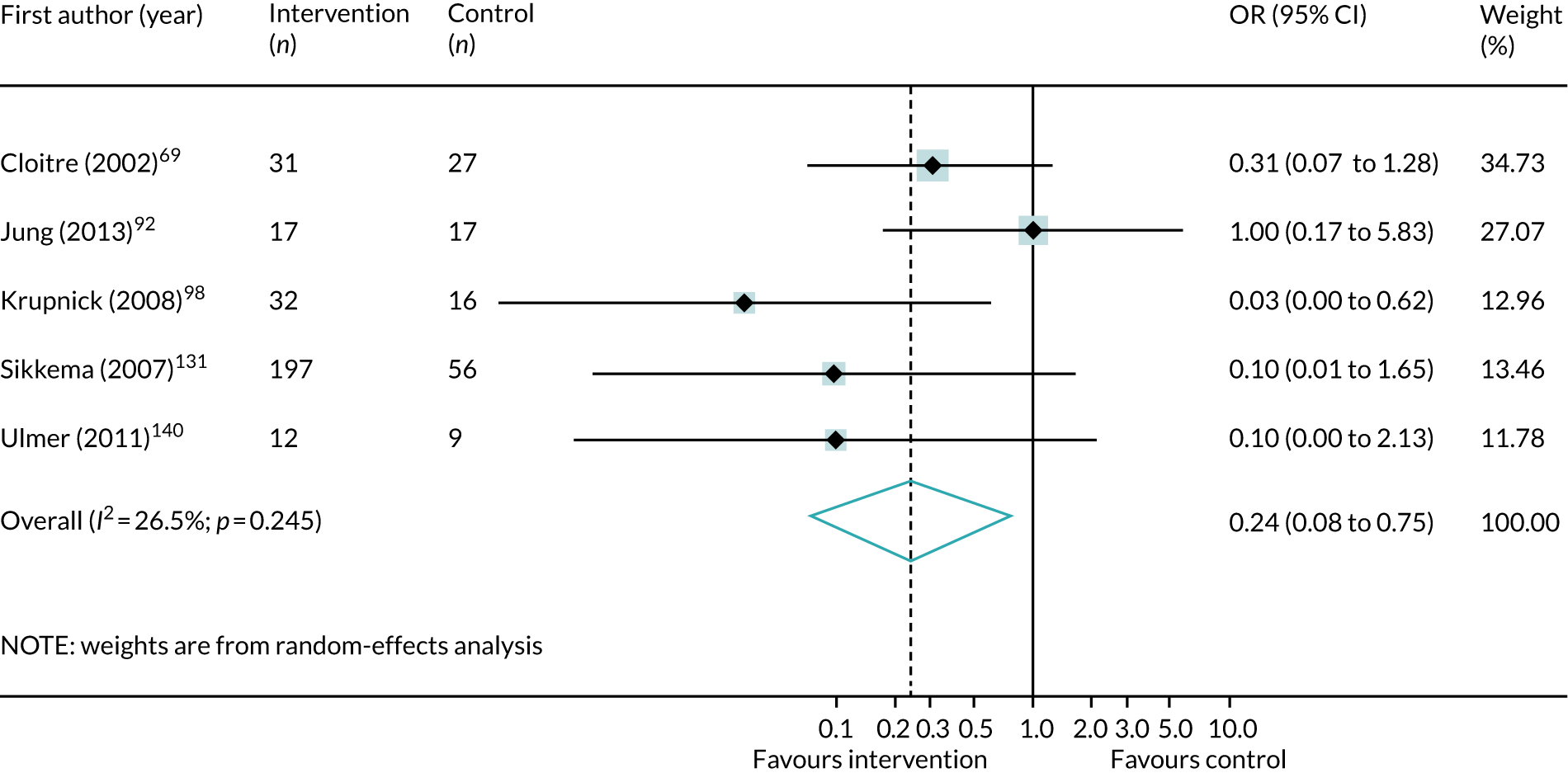
Refugee populations
FIGURE 108.
Meta-analysis of OR of attrition from all psychological interventions compared with control, among a refugee population.
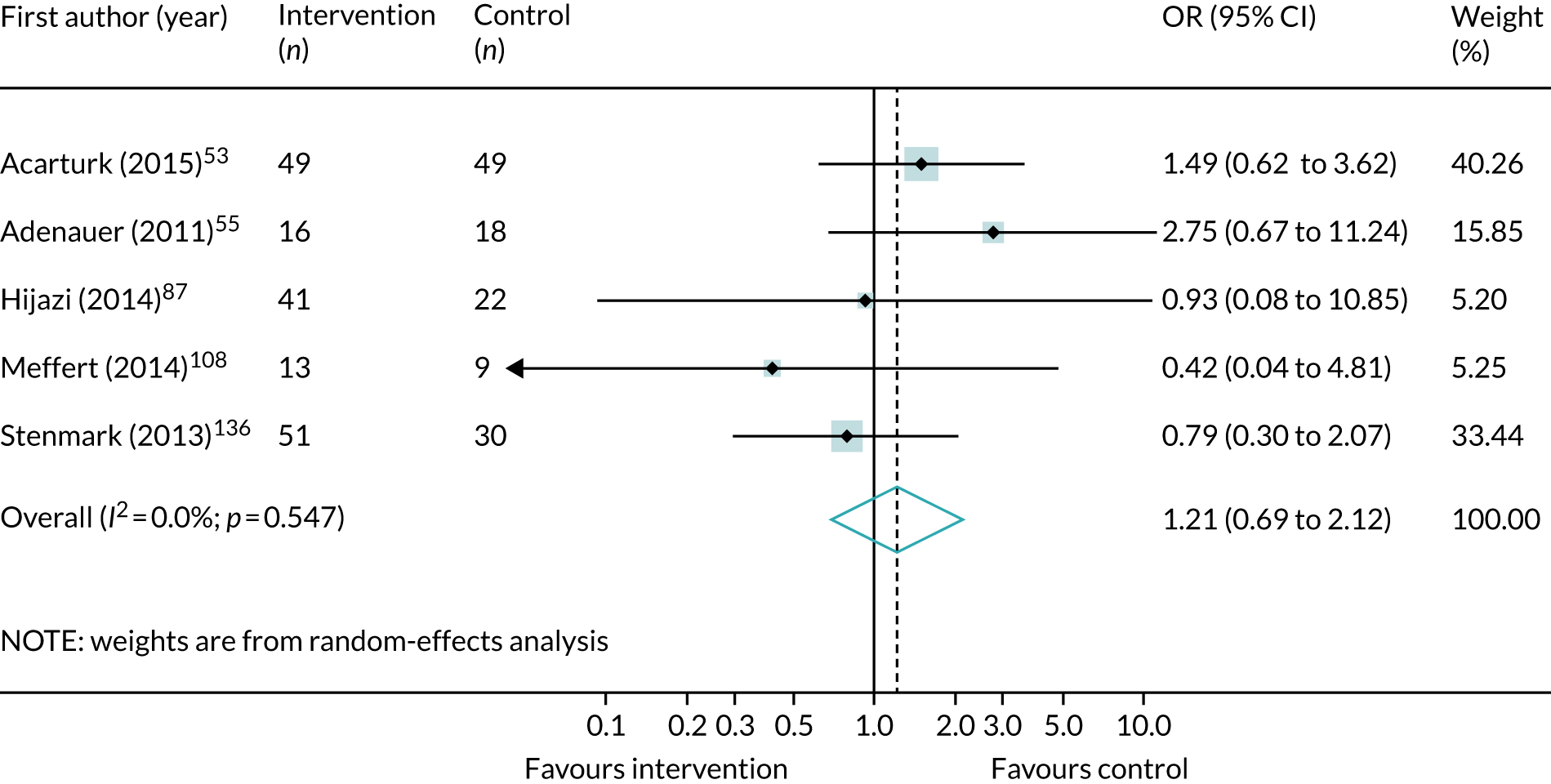
Domestic violence populations
FIGURE 109.
Meta-analysis of OR of attrition from all psychological interventions compared with control, among a domestic violence population.
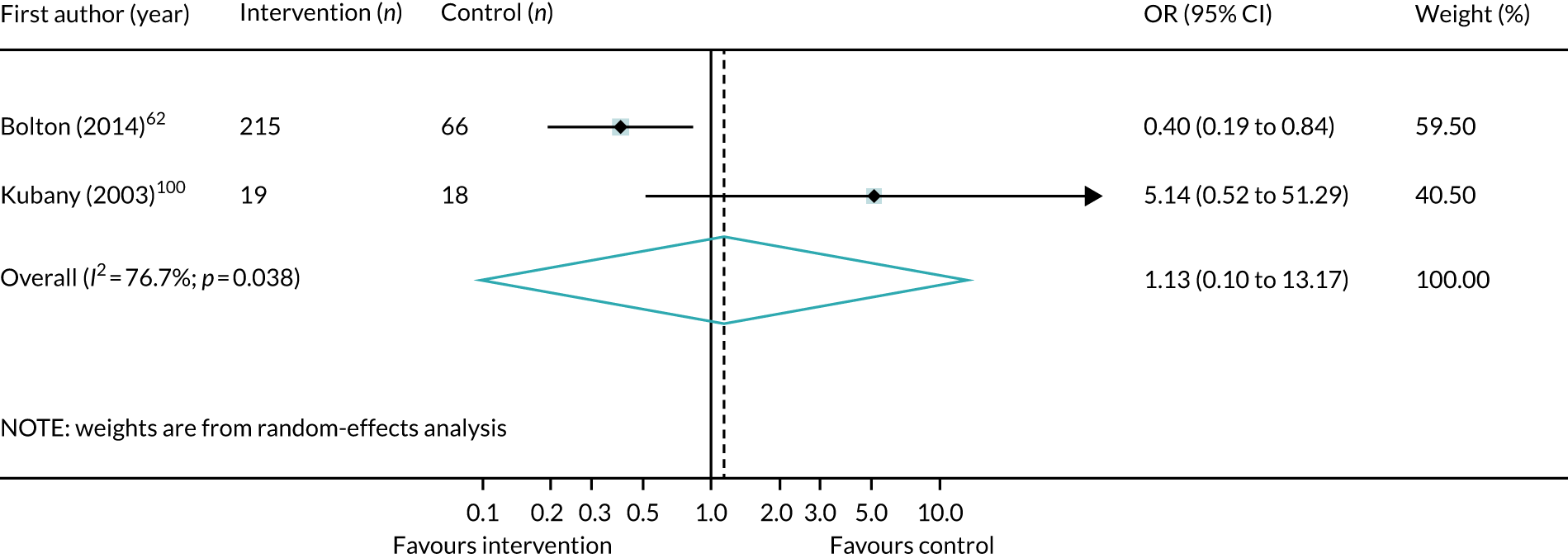
War-affected populations
FIGURE 110.
Meta-analysis of OR of attrition from all psychological interventions compared with control, among a war-affected population. CETA, common elements treatment approach; CPT, cognitive treatment therapy.

Appendix 11 Characteristics of qualitative studies included
| Authors (year), country | Aim | Population (sample size) | Intervention(s) and delivery | Outcomes | Qualitative approach and data collection | CERQual outcome |
|---|---|---|---|---|---|---|
| Bermudez et al. (2013),163 USA | An analysis of the perspectives of women with trauma exposure participating in mindfulness-based interventions over time | Low-income minority women with a PTSD history exposed to intimate partner violence (n = 10) | Group MBSR | Struggle to practise meditation, vision of growing and helping, personal and interpersonal improvement |
Semistructured interviews/focus group Thematic analysis (interpretive phenomenological analysis) |
Minimal concerns Contributes to existing knowledge, identifies areas of value to women experiencing intimate partner violence |
| Dutton et al. (2013),164 USA | The use of MBSR as a community-based intervention to reduce health disparities for low-income, predominantly African American, women with a history of intimate partner violence and PTSD | Low-income minority women with a PTSD history exposed to intimate partner violence (n = 53) | Group MBSR |
Feasibility, initial interest to participate Acceptability, congruent and relevant to participant needs Positive benefits included increased awareness; self-acceptance; self-empowerment, non-reactivity and self-care; decreased distress; increased sense of belonging and compassion |
Follow-up interviews Thematic findings |
Minimal concerns Description of method lacking Pilot study to inform future research. Offers insight into dropout rates and reasons for attrition, as well as effects of conflict within the groups |
| Hughes and Rasmussen (2010),162 USA | Study to examine the use of motivational interviewing with women receiving services at a domestic violence shelter | Women in domestic shelters who have been exposed to domestic violence. Experimental group (n = 10) and control group (n = 10) were included in the mixed-methods study but not all were included in the qualitative review (n = 6) | Motivational interviewing vs. treatment as usual | Self-perception, beliefs of abuse causation, beliefs of shelter efficacy, emotions towards abuser, specific statements, beliefs of personal strength |
Interviews/grounded theory Part of mixed-methods study |
Minimal concerns Some qualitative methods reported; results not thematic (more difficult to pick out) Pilot study. Valuable to inform future design of full study |
| Hundt et al. (2017),166 USA | Qualitative interviews to elicit first-hand accounts of veterans’ experiences in these evidence-based psychotherapies | Male and female veterans (n = 23) | Prolonged exposure, cognitive processing therapy or both | Patient experience of intervention, perceptions of treatment mechanisms |
Qualitative interviews Thematic analysis (grounded theory). Focus is qualitative |
Minimal concerns Contributes to body of evidence for patient’s satisfaction with prolonged exposure treatment and cognitive processing therapy |
| Martinez et al. (2015),165 USA | Study to better understand the unique challenges that may keep veterans referred to MBSR from enrolling and completing the programme | Male and female veterans (n = 48) | MBSR vs. no control | Barriers to enrolment and participation |
Semistructured interviews/content analysis Some qualitative methods reported and thematic findings. Focus is qualitative |
Minimal concerns Provides insight into barriers to enrolment and participation by veterans in MBSR |
| Naved et al. (2009),161 Bangladesh | Evaluation of an initiative to use paramedics as first-level mental health counsellors of abused women in rural Bangladesh (2003–2004) from the perspective of the abused women | Women in rural Bangladesh exposed to lifetime physical and sexual abuse (n = 30) | Paramedic-conducted mental health counselling | Includes patient experience of the intervention |
In-depth interviews/thematic/content analysis Part of mixed-methods design (survey and interviews) |
Significant concerns regarding recruitment and data analysis Mixed-methods design. Value in identifying barriers to participation in low-income rural areas |
| Palmer et al. (2007),167 Canada | Inpatient programme for traumatic stress recovery in which patients were interviewed after discharge about their experiences during treatment | Males and females exposed to childhood sexual abuse (n = 30) | Group 6-week inpatient programme for traumatic stress recovery. Community milieu (group healing), safety (supportive environment), addressing problematic behaviours, traumatic re-enactment | Includes patient experience of intervention |
Semistructured interviews Thematic/constant comparison/ethnography. Part of a larger quantitative study |
Minimal concerns Useful to inform participant screening and selection when designing group-based interventions |
| Parker et al. (2007),168 Canada | Qualitative study to understand how women with a history of child maltreatment experienced the ‘Women Recovering from Abuse Program’ (WRAP), an existing intensive group treatment programme | Women exposed to childhood sexual abuse (n = 7) | Group treatment | Includes patient experience of intervention |
Semistructured interviews Thematic/phenomenological approach. Focus is qualitative. Some qualitative methods reported. Thematic findings |
No concerns Useful to examine the phenomenological approach to investigate the patients’ perspective of the intervention in relation to their own personal lived experiences |
| Vincent et al. (2013),169 UK | This study considers the acceptability of trauma-focused CBT for asylum seekers with PTSD by exploring their experiences of treatment | Asylum seekers exposed to trauma (n = 7) | Trauma-focused CBT for PTSD | Includes patient experience of the intervention – acceptability |
Semistructured interviews Interpretive phenomenological analysis |
Minimal concerns Useful insight into the challenges of examining the value of interventions on asylum seekers with PTSD |
List of abbreviations
- CAPS
- Clinician-Administered PTSD Scale
- CASP
- Critical Appraisal Skills Programme
- CBT
- cognitive–behavioural therapy
- CENTRAL
- Cochrane Central Register of Controlled Trials
- CI
- confidence interval
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CPT
- cognitive processing therapy
- CPTSD
- complex post-traumatic stress disorder
- DBT
- dialectical behaviour therapy
- DESNOS
- disorders of extreme stress not otherwise specified
- DIC
- deviance information criterion
- DSM
- Diagnostic and Statistical Manual of Mental Disorders
- EMDR
- eye movement desensitisation and reprocessing
- ICD
- International Classification of Diseases
- ICD-10
- International Classification of Diseases, Tenth Revision
- INCiTE
- INterventions for Complex Traumatic Events
- IPT
- interpersonal psychotherapy
- ISTSS
- International Society for Traumatic Stress Studies
- MBSR
- mindfulness-based stress reduction
- NA
- not applicable
- NET
- narrative exposure therapy
- NICE
- National Institute for Health and Care Excellence
- NR
- did not report information
- OR
- odds ratio
- PANSS
- Positive and Negative Syndrome Scale
- PILOTS
- Published International Literature On Traumatic Stress
- PPI
- patient and public involvement
- PTSD
- post-traumatic stress disorder
- RCT
- randomised controlled trial
- ROBINS-I
- Risk Of Bias In Non-randomized Studies – of Interventions
- SE
- standard error
- SMD
- standardised mean difference
- SSRI
- selective serotonin reuptake inhibitor
- STAIR
- Skills Training in Affect and Interpersonal Regulation
- WHO
- World Health Organization
