Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 14/29/01. The contractual start date was in January 2016. The draft report began editorial review in March 2019 and was accepted for publication in March 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2020. This work was produced by Abel et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2020 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Extent of the problem
Better care means that people of reproductive age who suffer from a mental illness are more likely to start families and become parents. 1 Consequently, the number of children and adolescents living with experience of significant parental mental illness may be increasing. Population data from the UK seem to bear this out. Abel et al. 2 report a significant increase in the prevalence of children and adolescents living with serious parental mental illness (CAPRI) in the last 30 years. In 2007, the number of children in the UK exposed to a mother with a mental illness diagnosed in primary care was 22.2%. By 2017, this figure had increased to 25.1%. Over the same period, the proportion of children exposed to maternal non-affective psychotic disorder such as schizophrenia increased from 0.16% to 0.20%, and the proportion living with maternal affective psychotic disorders increased by 50% (from 0.25% to 0.37%). Currently, by the time a child reaches the age of 16 years, there is a 53% chance that their mother will have experienced a mental illness that has come to services’ attention. 2
These findings suggest that parental mental illness is an increasingly common factor in the lives of children in the UK (note that these figures exclude paternal mental disorder burden). Therefore, given the scope and magnitude of the problem, and with similar estimates reported elsewhere (e.g. Australia,3 the USA,4 Canada5), the need for better information and more resources to support these young people has never been greater.
Improving the lives of CAPRI has become an urgent public health priority. 6,7 This vulnerable group is likely to experience significant difficulties on a daily basis and throughout their lives,8–10 as a result of which they are likely to suffer a poorer quality of life and utilise services more than children living with ‘healthy’ parents. 11,12 Recent epidemiological data13 show that CAPRI average one more general practitioner (GP) or nurse consultation per year than their peers, and the excess health utilisation cost to the NHS has been estimated at £652M per year. These combined facts present a strong public health argument for better early and preventative care.
Mechanisms of risk
As a group, CAPRI have, overall, been reported to show poorer outcomes than their peers across a range of domains. 14 Mechanisms of this effect vary depending on the outcome, but include social influences of multiple deprivation and life stressors,14 lack of parental support15 and parental difficulties in combining the management of their own mental health with caregiving for their children. 16,17 Such environmental effects interact with genetics,18 as well as with in utero19 and obstetric events;20 consistent reports find an association between prenatal maternal conditions, including psychopathology, and offspring neurodevelopmental abnormalities. 21 Direct effects of parental mental illness may vary and may be less detrimental than the social adversities associated with mental illness, such as poverty, multiple deprivations, living in a single-parent family and repeated parent–child separations. 22,23 Greater exposure to family discord and parental hostility is also reported to increase risk;24 one study25 reports that children of depressed mothers with antisocial personalities fare much worse than children of mothers with depression alone. Other important factors, such as parentification, neglect, maltreatment and domestic violence, compound unmet developmental needs. 6,26
Although it remains unclear how age interacts with CAPRI risks, timing of parental mental illness and associated adversity across a child’s life is likely to be important; early exposure may mean that children are exposed for longer, whereas exposure during adolescence may influence critical developmental periods. Evidence suggests that vulnerability exists during pregnancy,27 infancy,28 throughout childhood and adolescence24,29 and into adulthood. 30,31 This means that CAPRI may be exposed to a clustering of multiple adverse influences over time22,26,32 and, in many cases, effects are additive or interactive with independent direct effects of parental mental illness. 25,33,34 But the well-being of these young people should not be seen as corresponding to ‘the ebb and flow of parental mental health’, as child difficulties may persist long after parental symptoms abate,24 although risk heightens when the parent experiences hospitalisation or an acute phase of illness. 35 This especially affects children who do not have another parent or relative to look after them when this occurs. 3,35,36
Most research on the relationship between parental mental illness and adverse child outcomes revolves around the mentally ill mother,37 but evidence on the independent effects of paternal psychopathology is increasing. 38,39 For example, in their early years, children with depressive fathers are twice as likely as unaffected children to develop behavioural and emotional problems. 40 In adolescence, the effect of having a father with depression either parallels41 or outstrips the effect of having a mother with the same condition, the latter being more influential earlier on in terms of shaping child outcomes. 42
It should be noted that, even with this evidence, we cannot assume that all the same factors act as promoters or protectors in relation to all outcomes in all individuals. Rather, it is likely that many individuals show resilience across a range of circumstances and across a range of outcomes, whereas some show little resilience in few and not in all circumstances (for further discussion see Rutter,43,44 and Cicchetti and Curtis45).
Implications for CAPRI lives
With these caveats in mind, evidence suggests that CAPRI do less well across a range of life outcomes than their peers. 7 These outcomes include poorer physical health46–49 and more behavioural and emotional difficulties,9,10 which also contribute to poorer educational outcomes. 50–52 Entering adulthood, there is greater susceptibility to socioeconomic difficulties, alcohol/substance misuse and premature death. 31,53 Health care and mental health service utilisation is significantly higher among CAPRI. 11,12 Whether this always reflects greater ill health or more need for support by parents is unclear.
Living with parental mental illness also places a demonstrable strain on quality of life. CAPRI frequently grow up in environments of high family conflict,54 stress,55 and maltreatment and neglect,6,26 all of which amplify risks for impaired social functioning. 56 Several studies demonstrate that CAPRI experience more severe interpersonal difficulties than their peers, including rejection, victimisation and not being liked. 30,31,57 This vulnerable group is reported to show higher levels of internalisation of problems (manifesting as, for example, anxiety, crying, withdrawal or quietness) that make socialisation difficult and can lead to stigmatisation or bullying by other children. 56,58 In addition, CAPRI suffer socially because of parents’ potential inability (or unwillingness) to support their child’s engagement in social activities. This may deprive children of opportunities not only to make friends, but also to take part in school/afterschool activities or sports teams that would improve their interpersonal skills. 56,59,60 CAPRI may assimilate maladaptive social parental behaviours, which influence interactions with their peers outside the home. 61 Higher rates of autism62 and other neurodevelopmental disorders63 may also contribute to the social problems that they experience. Social difficulties experienced by CAPRI are neither specific nor exclusive to their parental mental illness exposure and are similarly associated with parental physical illness, parental incarceration and premature parental death. 24 Notwithstanding, the particular stigma of having a parent with mental illness is specific and may lead children and adolescents to fear developing a mental illness themselves.
But risk and resilience cannot be viewed as constant general traits among children exposed to parental mental illness. Resilience following adversity may be found for one outcome but not every outcome, or indeed any outcome of relevance to children themselves. 43,44 Thus, our approach to improving health-related quality of life (HRQoL) is based on the following premises: first, that we must ask CAPRI themselves what their needs are in relation to HRQoL; second, all CAPRI (including those not expressing risks such as mental illness or behavioural problem as detailed in literature) will benefit from such a CAPRI-informed intervention to improve HRQoL; and, third, such an intervention requires a public health approach that is scalable to all in the risk subset (i.e. all children with parental mental illness).
In summary, most CAPRI will not develop a mental illness; many will perform well in school and sustain relationships,8,15 and not all children living in the same affected family will be influenced in the same way. 64 However, multiple factors contribute to variance in risk versus resilience for a range of outcomes in individual children;65 for example, the availability of alternative familial, social, health and cognitive resources appears to benefit children. 66 The severity and duration of parental mental illness are consistently strong predictors of outcomes; children of parents with enduring and severe disorders exhibit the highest risks expression. 10,24 Children are less likely to experience problems if they have access to a healthy parent, one who acts as a ‘buffer’ between the child and the behavioural and emotional difficulties of the ill parent. 67 Mental health literacy, social connectedness and self-efficacy also equip children with internal resources to manage difficulties associated with parental mental illness on a day-to-day basis. 66
Thus, the evidence paints a picture of CAPRI as vulnerable, but with a heterogeneous set of needs that vary widely between individuals, between circumstances and over time, which means that some children require significantly more help than others. Services must understand such heterogeneity and variation in the planning of their response to unmet needs. For more complex interventions to be effective and cost-efficient, such understanding and targeting is essential. 18 No interventions currently target quality of life (QoL) in CAPRI and virtually none has been child, as opposed to parent or family, centred. 68 Currently, poorer intervention efficacy/cost-effectiveness is attributed to limited resources, budgetary restraints and skill limitations among practitioners, whereas inadequate screening and assessment processes are likely to contribute significantly. 26 Importantly for future planning, lack of multiagency collaboration between adult mental health services, Child and Adolescent Mental Health Services (CAMHS), social care and child protection services means that support lacks co-ordination and leadership. 17,68
Although many parents want to consult with professionals about their children,69 some are reluctant to do so because they fear that they may be judged or lose their children to care. 70 Such factors are likely to mean that CAPRI remain hidden because, unless they come forward themselves, they may not be identified as having a need by services whose focus remains the ill parent/parents. 17 We agree that a ‘fundamental paradigm shift is required at all levels of service development, delivery and policy’71 lest the needs of these children remain unmet. However, unlike these writers, our perspective is specifically focused on prevention for non-clinical unmet need and aligned with enhancing daily HRQoL across childhood for all CAPRI and not simply those at highest risk.
Background and rationale for the Young SMILES programme
The European Union’s (EU) Child and Adolescent Mental Health in Enlarged Europe initiative urged a change in political systems, legislative systems and health and social care systems to acknowledge and attend to the needs of CAPRI. 72 This initiative also called for better information on CAPRI and how to target vulnerable groups before their life trajectories are disrupted. 72 However, in spite of adequate policy guidance50,73 and a strong case for early intervention to support these young people,74 little reliable or child-centred evidence for intervention was available to take the process forward. 68,75 Therefore, the National Institute for Health Research (NIHR) Health Technology Assessment (HTA) programme posted call 14/29, which posed the following question to researchers:
Is it possible to develop a community-based intervention to enhance the health-related quality of life (HRQoL) of children who live with a primary carer with serious mental illness, and would it be suitable for a future trial?
This report examines whether or not the Young Simplifying Mental Illness plus Life Enhancement Skills (SMILES) programme achieved its primary aim to answer that question.
The 14/29 call for interventions aimed at enhancing HRQoL among CAPRI derived, in part, from our HTA-funded systematic review. 68 This had shown that there is little or no community-based provision for CAPRI, let alone any high-quality evidence or child-centred approaches to HRQoL. The likelihood of these young people developing mental illness, although greater than that of their unexposed peers, is outweighed by the likely influence on QoL of daily hardship and multiple deprivation. 7 Thus, the rationale for creating and piloting a novel intervention to improve CAPRI HRQoL was driven by this understanding alongside the knowledge of the significant and growing numbers of exposed and vulnerable young people in the UK today. 7 In the UK and the wider EU, we were aware of only two models aimed at supporting CAPRI directly, as opposed to supporting their parents. 76 Our task, therefore, was to create, with stakeholders, a viable approach to a significant public health problem with a view to improving resilience and reducing long-term effects of poor HRQoL in children and adolescents with serious parental mental illness.
The 2014 NIHR HTA programme call drew broadly on our own HTA systematic review of interventions for CAPRI. 68 This review had been widely informed by three focus groups with 19 different stakeholders: eight representatives from the children’s charities Barnardo’s, Young Minds, the National Children’s Bureau, the National Society for the Prevention of Cruelty to Children (NSPCC) and the Fairbridge Trust; five independent parents (four mothers and one father); and six CAPRI. 6,68,76 Key elements specified in the original HTA call were that the intervention should be community based and delivered to children across the age range living with severe parental mental illness with the express intention of improving HRQoL.
Quality of life in CAPRI
As suggested above, the HRQoL model may reflect the needs and priorities of CAPRI better than other health-related outcomes, such as mental and behavioural disorders. It is increasingly recognised that ‘well-being’ refers to more than absence of disease, with QoL being increasingly seen as a valid clinical outcome for services. 77 With recent UK50,73 and European72 policies highlighting the need for clinicians to consider young people’s perceptions of their own life experience within the context of their personal goals, expectations and priorities, a HRQoL model is anchored in the lived realities of children, rather than being service driven with disease-specific outcome measures. 6 Bee et al. 68 highlight five core life domains in QoL measures for children: (1) physical health, (2) emotional health, (3) social function, (4) material well-being and (5) environmental well-being. However, evidence is needed for a HRQoL that specifically captures the experiences of children living with a mentally ill parent. 74
Evidence for interventions to improve health-related quality of life in CAPRI
Existing interventions concerned with parental mental illness usually target the affected parent. 68 They include various modes of service delivery, including individual support78 and peer support groups,78 online courses79 and psychoeducational programmes. 80 The aim of these interventions is to enhance protective behaviours in the parent, usually the mother. 68 Recently, there has been a shift away from parent-based interventions to interventions centring on the needs and preferences of the family. 68,76 Numerous interventions with a family-centric model of delivery report positive outcomes for child well-being. 9,58,81,82 Although encouraging, such evidence should be treated with circumspection as studies reporting the largest effect sizes are invariably poorest in quality. 75 High-quality studies are still in the minority, but also consistently report modest effect sizes. Furthermore, only few studies contain any analyses of longitudinal effects, making it difficult to monitor effectiveness over time. 75,83
Reliable data on the efficacy of child-centred interventions are conspicuously lacking. 68 Most data derive from small, biased samples reporting effects too small to enable them to be considered cost-effective. 75 Efficacy might be underestimated or go undetected by aggregating effects produced by interventions across at-risk and resilient children18 (i.e. high- and low-risk individuals within the risk subset). Furthermore, most follow-up in studies is limited to < 1 year from baseline; monitoring effects over extended periods allows ascertainment of whether or not an intervention is acting to prevent difficulties in children who are at risk. 84 Potential effect moderators need to be explored; adequately powered samples might then identify which subgroups will be more responsive or sensitive to an intervention. Such moderators may include a child’s sex, age, parental diagnosis, and socioeconomic status. 84,85
Similar methodological problems apply to interventions aiming to improve the HRQoL in CAPRI. Bee et al. 68 demonstrated a lack of reliable evidence to support the effectiveness of any existing interventions. Many included studies were conducted over 20 years ago, mainly outside UK or European settings, which limits their generalisability to the NHS. Furthermore, most studies focused on parents with mild to moderate (postnatal) depression; only three considered parental serious mental illness (SMI). Interventions were not child centred and did not consider young people’s QoL; all focused exclusively on parental outcomes. 68
The review concluded that further work is needed to develop and evaluate child-centred interventions that improve HRQoL in these young people. 68 However, the challenges implicit in this recommendation are numerous and complex. One such challenge is deciding when, where and how best to intervene, while demonstrating clinical effectiveness, cost-effectiveness and the potential for non-stigmatising and non-threatening delivery of specific interventions for CAPRI. In our view, interventions should place emphasis on mental health promotion and early intervention (i.e. public health approaches), while putting young people’s preferences and priorities at the centre of service delivery. 6,17,68,76 Such preventative and early interventions should use models that are strength based and focus on resilience and, as such, better reflect CAPRI’s short- and long-term goals. Delivery should take place within community settings, such as schools, community centres, the home and other venues embedded within the child’s routine. 76
Developing the model for Young SMILES
We considered the two existing models of working with families with parental mental illness, KidsTime and Family SMILES, not only because of their suitability for adaptation, but also to take account of expert reviewer and HTA Board comments from the original grant proposal, and because of the 3-year time scale of the proposed call. We knew that both of these group-based interventions ran successfully with CAPRI families in community settings but that neither had been evaluated and that they were not designed explicitly to enhance CAPRI HRQoL. Consultation with stakeholders and NSPCC collaborators provided us with permission to adapt Family SMILES to focus on a more child-centred approach and to work alongside the NSPCC to develop a non-NHS platform of delivery through the third sector. This was important for us because we recognised that the need for a new service fell into a preventative rather than direct health care domain and, therefore, potentially sat outside a CAMHS or NHS remit. This meant that the feasibility study needed to consider willingness to pay for, arguably, a public mental health approach in an increasingly large group of children and adolescents, most of whom, at least from a mental health perspective, would remain well. We were asked to test the suitability of the new intervention for a future trial. This meant that the intervention we developed needed to be manualised, staff needed to be trained, participants needed to be randomised with a control group and, where possible, assessors needed to be blinded. With an eye to future cost-effectiveness and sustainability in community settings, which we anticipated would not be traditional NHS settings, it was agreed that the established national network of family centres offered by our NSPCC collaborators represented an ideal setting to fulfil the brief of the 14/29 call.
We saw the need to design an intervention that responded to the changing shape of service provision and stood a chance of sustainability and scalability in economically stringent environments. To this end, we determined that delivering an intervention in different community settings and to different age groups would best be achieved by partnering with established third-sector community providers and with NHS Improving Access to Psychological Therapies (IAPT), which was beginning to broaden its remit to work with children and families.
Chapter 2 provides an overview of the policy landscape behind a drive towards better HRQoL for CAPRI and, in this context, sets out the aims and objectives of the final Young SMILES programme against which we report.
Chapter 2 Aims and objectives of the feasibility study
Current policy and initiatives
As far back as 1999, the Department of Health and Social Care made perinatal mental health a priority in the NHS Plan; in the recent Implementing the Five Year Forward View for Mental Health paper,86 NHS England included perinatal mental health as the only element of focus on women’s mental health. As a result, resources have been directed to support adults with mental illness in their parenting roles, particularly women with postnatal mental illness. 87 In addition, an increase in whole-family assessments and recovery plans stems from national outcome strategies that tackle mental health across the lifespan as well as the transgenerational transmission of psychiatric morbidities. 88,89 And deeper integration between child and adult mental health services is now advocated, alongside earlier interventions for troubled families. 87,90,91
Despite this, CAPRI are neglected by social and health care services. 50,92 For a range of reasons, parents with mental illness experience greater exclusion from general health and social care services, restricting the monitoring and support available to their children. 50,93 Collectively, extant publications outline the roles and responsibilities services should take when supporting CAPRI in their daily lives. 17
Thus, in 2015, the Department of Health and Social Care and NHS England published Future in Mind,94 outlining a 5-year strategy to make it easier for children and young people (CYP) to access high-quality mental health services in recognition of the treatment gap of around 25–35% among children and young people with a diagnosable mental health condition. It proposed a step change from a ‘tiered model of care’ (i.e. a system defined in terms of what services organisations provide) to one that responds to the needs of CYP as well as their families’ needs. Greater flexibility and leadership at a more regional level was recommended to allow different services to develop to suit local needs. Developing a ‘better offer’ for the most vulnerable children was also proposed,94 contributing to a growing body of literature highlighting the importance and gaps in provision identifying and supporting at-risk children. 95
In Addressing Adversity: Prioritising Adversity and Trauma-informed Care for Children and Young People in England,96 Young Minds recommended investment in trauma-informed models of care with development of a common framework to identify at-risk children, reducing heterogeneity in how ‘vulnerable’ is defined across services, and proposed that adverse childhood experiences (ACE)/childhood adversity become a local commissioning priority. In response, new legislative requirements have been placed on local authorities, Clinical Commissioning Groups (CCGs), schools, police, and other organisations and agencies to work collaboratively to provide early identification and help for vulnerable young people, specifically mentioning children exposed to parental mental illness. 97
Thus, successive policy reflects a gradual understanding that CAPRI are unlikely to get the help they need simply as a by-product of their parents’ care, and recognition across different countries that a framework of responses dedicated to them is required (Table 1).
| Publication | Year | Author |
|---|---|---|
| Child and Adolescent Mental Health in Enlarged Europe98 | 2007 | The EU |
| Child Welfare Act99 | 2007 | Ministry of Social Affairs and Health (Finland) |
| NSW Children of Parents with a Mental Illness (COPMI) Framework for Mental Health Services 2010–2015 100 | 2010 | Department of Health (Australia) |
| Social and Emotional Wellbeing for Children and Young People 73 | 2011 | National Institute for Health and Care Excellence (UK) |
| Think Child, Think Parent, Think Family: A Guide to Parental Mental Health and Child Welfare 50 | 2011 | Social Care Institute for Excellence (UK) |
| Children First: National Guidance for the Protection and Welfare of Children 101 | 2011 | Department of Children and Young People (Ireland) |
| Working with Troubled Families: A Guide to the Evidence and Good Practice 88 | 2012 | Department for Communities and Local Government (UK) |
| Future In Mind94 (guidance outlining aims for transforming how CAMHS services are delivered nationally) | 2015 | Department of Health and Social Care (UK) |
| Children’s and Young People’s Strategy 2017–2027 102 | 2016 | Department of Education (Northern Ireland) |
Although mental health services are becoming more accessible to CYP,103 CAPRI are often not mentally ill. Instead, they are in need of recognition for the challenges they face day-to-day, of monitoring and of recourse to non-stigmatised help when they need it. 6,15,68
One possible avenue for such provision is the Improving Access to Psychological Therapies for Children and Young People service or IAPT-CYP. 104 NHS England aims to upskill these and other workforces involved in the care of CYP and to strengthen the collaboration between existing services. IAPT-CYP also promotes more evidence-based practice and robust outcome monitoring in routine services. 103,104 However, there remain challenges to increasing the accessibility of a service for CYP who commonly do not have a mental health problem when CAMHS is being prioritised, hence the need to consider other supports within non-clinical settings.
Aims and objectives of the feasibility study
This research responded to the 2014 NIHR HTA programme call to answer the related questions of whether or not (1) it is possible to develop a community-based intervention to enhance the HRQoL of children and adolescents who live with a primary carer with SMI, and (2) such an intervention is suitable for a future trial.
The initial study protocol set out our aim and preliminary objectives [available on the project web page: www.journalslibrary.nihr.ac.uk/programmes/hta/142901/#/ (accessed 1 March 2020)]. These objectives were revised prior to commencing recruitment and published in our updated protocol paper. 105
For clarity, Table 2 presents the original preliminary objectives, the subsequently revised objectives from that paper and the rationale for any changes alongside each.
| Preliminary objectives (HTA, 2014) | Revised objectives105 | Justification for change |
|---|---|---|
| A. To randomise children, adolescents and their parents to the intervention or treatment as usual pathways in a wait-list control design | 1. Using a feasibility RCT comparing the intervention developed in our earlier work with usual care to determine uptake, adherence and follow-up rates | Waiting list control was mooted as a comparator in much earlier versions of the protocol as requested by reviewers. However, it was rejected because study sites were not able to deliver twice the number of Young SMILES groups – once for the intervention group and once for the control group – within the given time frame and costs. Thus, the comparator was always usual care and not waiting list, as stated in objective A. In objective B, the comparator is stated as usual care |
| B. To estimate uptake, intervention adherence and retention to follow-up rates in a RCT comparing the intervention with usual care | Preliminary objective B was merged with objective A to make a revised objective 1 | |
| C. To determine which child/adolescent self-completed outcome measures are able to capture the effects of the intervention over time, especially in the primary outcome measures identified as important by the stakeholders | 2. To determine, from a battery of outcome measures, the most appropriate primary outcomes with which to assess any effects of the intervention over time, considering the areas identified as important by the stakeholders | The preliminary and revised objectives are the same |
| D. To obtain estimates of intervention effects and measures of variability on the selected outcome measures to inform sample size calculations for a definitive trial | Preliminary objective D was removed as inappropriate because in our feasibility trial we are not powered to estimate intervention effects | |
| E. To optimise and pilot a data collection tool to capture the most relevant aspects of families’ resource utilisation (including Young SMILES) over time | 3. To develop and pilot a data collection tool relevant to family resource use over time | Preliminary objective E and revised objective 3 remained the same |
| 4. To determine if the intervention is acceptable to CAPRI, their parents and the practitioners delivering the intervention | Objective 4 was added as part of the revised objectives (there was no corresponding one in the preliminary objectives). This is because assessing the intervention’s acceptability via qualitative work was a major aspect of the feasibility study and the preliminary objectives did not reflect this | |
| 5. To establish if the intervention can be implemented successfully within third-sector and NHS settings | Objective 5 was added as part of the revised objectives (there was no corresponding preliminary objectives). This is because the study had two distinct implementation models (NHS and third sector) and the preliminary objectives did not reflect this |
This report includes a set of final objectives, which are reproduced with permission from Gellatly et al. 105 (This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text includes minor additions and formatting changes to the original text), and are worded differently to help with the presentation of our results across the report, our ability to make judgements about whether or not we have delivered against these objectives and, furthermore, whether or not a full randomised controlled trial (RCT) is feasible.
Table 3 presents the final objectives for this report and maps them on to our published objectives. 105
| Final objectives in HTA report | Mapping onto Gellatly et al.105 objectives |
|---|---|
| A. To co-produce (with stakeholders) an intervention that was acceptable to families and feasible to deliver in the NHS and in the community with support from health and non-health professionals | This objective captures the primary aim of the study (as stated in the original 14/29 HTA call) and also incorporates published objectives 4 and 5 |
| 4. To determine if the intervention is acceptable to CAPRI, their parents and the practitioners delivering the intervention | |
| 5. To establish if the intervention can be implemented successfully within third-sector and NHS settings | |
| B. To determine the rates of intervention uptake and adherence, and of completed follow-up measures | This is the same as published objective 1 |
| 1. Using a feasibility RCT to compare the intervention developed in our earlier work with usual care to determine uptake, adherence and follow-up rates | |
| C. To identify appropriate outcome measures and estimate their data missingness | This is a revised version of objective 2. We cannot assess intervention effects on specific outcomes in a feasibility study. Therefore, we describe our objective more accurately here in terms of feasibility of completion of outcome collection at baseline and follow-up (assessed by data missingness) |
| 2. To determine, from a battery of outcome measures, the most appropriate primary outcomes with which to assess any effects of the intervention over time, considering the areas identified as important by the stakeholders | |
| D. To develop a child resource utilisation questionnaire and estimate its data missingness | This is the same as objective 3 below, revised to include ‘data missingness’ as a more accurate objective of feasibility for data collection. The final objective also specifies that resource utilisation refers to the child and not the family |
| 3. To develop and pilot a data collection tool relevant to family resource use over time | |
| E. To capture the experiences of children and parents who participated in the intervention and of professionals who referred or supported families to participate in the intervention | This is an objective that maps onto objectives 4 and 5 of Gellatly et al.105 that conveys the qualitative work that was a large part of this study to determine acceptability and feasibility |
| 4. To determine if the intervention is acceptable to CAPRI, their parents and the practitioners delivering the intervention | |
| 5. To establish if the intervention can be implemented successfully within third-sector and NHS settings |
Report roadmap
The final objectives, which we address in this report, remain focused on the basic feasibility criteria of being able to recruit and randomise participants (CAPRI and their parents) to the newly co-created Young SMILES intervention, as well as to be able to maintain participation of recruited individuals up to, and including, follow-up data collection. The final objectives place greater emphasis on participant and staff experiences as indicators of acceptability of Young SMILES and of its deliverability inside and outside the NHS.
These objectives can be broadly divided across the quantitative and qualitative aspects of the research report. The first 18 months of work is described in Chapter 3. It included study set-up and recruitment of sites, a process delayed significantly by coinciding with the newly formed Health Research Authority and by changes in the organisation of our NSPCC partner, as described in detail in Appendix 1. Subsequently, development, manualisation and training of NHS and non-NHS staff in the new, child-centred intervention (i.e. Young SMILES) was completed with significant input from children, young people and their parents. Chapter 3 describes the development and manualisation of the intervention with stakeholders over a 12-month period. Training was undertaken across three sites in Warrington, Coventry and Newcastle.
The feasibility study, testing our ability to deliver the new intervention, is described in Chapters 4–6 and constituted the second part of the 3-year study of two halves. However, the fact that the original timeline for recruitment was foreshortened by 11 months as a result of delays beyond the study team’s control (and described in detail in Appendix 1, Table 31) is, in our view, central to our final reporting of results and our recommendations about what future research activity should look like (i.e. the feasibility of a future trial).
Of note, progression criteria were not a part of the current study design.
Chapter 8 uses a matrix to present the study’s findings and to make a judgement as to whether or not a future full RCT is feasible based on established norms of uptake, adherence and follow-up rates, and also based on the reported experiences of children, parents and staff.
Chapter 3 discusses the modelling phase of an intervention called Young SMILES, which drew on qualitative and co-production methods to put children’s HRQoL needs at the centre of service delivery considerations.
Chapter 3 Intervention development
Phase 1 of the feasibility trial entailed the development of the intervention through an iterative process of integrating the existing evidence base with stakeholder consultation. This is in line with the developmental stage of the MRC Complex Intervention Framework. 106 What follows is a summary of an article published in Frontiers Psychiatry by Gellatly et al. 107 that describes the generation and co-development of the intervention. Copyright © 2019 Gellatly, Bee, Kolade, Hunter, Gega, Callender, Hope and Abel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms. The text below includes minor additions and formatting changes to the original text.
Introduction
Current evidence provides a compelling case for the theoretical development, delivery and evaluation of effective interventions that support CAPRI’s HRQoL. In view of this, we co-developed an intervention called Young SMILES during the modelling stage (Phase I) of the feasibility trial. This intervention builds on the NSPCC’s existing intervention Family SMILES, which was based on the Australian Simplifying Mental Illness plus Life Enhancement Skills (SMILES) programme. Family SMILES targeted families affected by parental mental illness. The intervention demonstrated potential to reach broader demographics in the context of the NHS, with a more clinical focus on CYP’s QoL.
Using a ‘bottom-up approach’, we explored the primary development foundations of such an intervention by utilising qualitative and co-production methods. Our aim was to put children and adolescent’s HRQoL needs at the forefront of co-refinement and co-development work, underlining the primacy of their voice by considering avenues to support CAPRI directly, and separately, from the experiences and needs of their parents. We anticipated that this evaluative process would culminate in an acceptable and feasible child-centred, community-based intervention that improves CAPRI’s HRQoL.
Methods
Semistructured interviews and focus groups were conducted with CYP (n = 14), parents (n = 7), and practitioners from social, educational and health-related sectors (n = 31), considering five key areas: (1) experiences of previous support, (2) unmet needs, (3) barriers to and facilitators of receiving/delivering support, (4) gaps in current provision and (5) what an ideal intervention would look like. Every interview was transcribed and subsequently thematically analysed. Thereafter, key findings and a summation of current evidence were presented to stakeholders, which informed a consensus exercise to underpin the preferred structure and primary components of the intervention.
Key findings
There was some consensus between parents and professional stakeholders about the perceived needs of CYP, but neither went into detail about specific requirements or their need for routine care on a daily basis. Mental health literacy, communication and problem-solving skills emerged as common themes throughout the qualitative work; however, CAPRI frequently disclosed a need for more peer-focused support, as well as more advice on how to better understand and respond to their parent’s difficulties in their own space (i.e. separate from their parents). Isolation was a recurrent problem reported by CAPRI, which was furthered by a lack of understanding from schools about their situation. Sensitively helping parents make sense of how and when their difficulties detrimentally affect their children was a need that was also identified (see Figure 1 for more details). All views were discussed at the consensus exercise and discrepancies were dealt with in group discussion. All views were taken into account but focus was specifically paid to those that did not diverge from the aims and objectives of Young SMILES (i.e. those highlighting the needs of CYP and opportunities to improve their HRQoL).
Young SMILES
These findings informed the co-development of a manualised intervention for CYP aged 6–16 years and their parents called Young SMILES. The intervention was developed within an existing delivery framework and lasted 8 weeks. Additional training materials for professionals were also included. Sessions were delivered on a weekly basis by two highly trained facilitators, each lasting 2 hours. They were group based and peer focused, including fun activities and snack times with parents. There were two age groups: children aged 6–11 years in one group and young people aged 12–16 years in another. Sessions were designed to be delivered in small groups of four to six CYP. Parents’ sessions were delivered separately from the child sessions, commencing after the fourth week of the intervention. For both the parent and the child sessions, although each had its own distinct learning objective, they were all informed by common themes of mental health literacy, communication and problem-solving skills. The venue was located within the community, which was accessible and acceptable to the child and the parent. Referral pathways were embedded within NHS and voluntary sector organisations, which identified potential families. Children’s services, mental health services, schools and voluntary organisations also supported the referral pathway.
Theory of change
A theory of change developed through consultation and consensus-building work is presented in Appendix 2, Figure 2. Primarily, this conceptualises Young SMILES in view of the problems faced by CAPRI, Young SMILES inputs and change mechanisms, primary outcome(s) for children and the impact that this has on associated risk of negative outcomes.
Conclusion
Through consultation with professional stakeholders, children and their parents, we identified a need for a more child-centred, community-based approach towards supporting CAPRI in their daily lives. In response, we have co-developed an intervention that accommodates a diversity of need for CAPRI, which can be validated with quantifiable child-centred outcome measures. This is the first multicontext intervention to improve the HRQoL among this vulnerable group in the UK.
Chapter 4 Trial design and methods
Trial design
Young SMILES is a two-arm, pragmatic, randomised controlled feasibility trial, with a 2 : 1 allocation ratio. Randomisation was considered the most appropriate response to the original NIHR HTA programme 14/29 call that specified having two arms, a control arm and an intervention arm, and that the study design followed the Medical Research Council (MRC) Complex Intervention Guidance. The MRC Complex Intervention Guidance states that ‘Experimental designs are preferred to observational designs in most circumstances’. 106 Therefore, consenting families with CYP aged 6–16 years and a parent/carer with a SMI were randomised to receive either:
-
Young SMILES – a manualised, 8-week intervention for CYP with concurrent 5-week parent sessions adapted from the Family SMILES intervention, which was developed and evaluated by the NSPCC. If eligible, families were given an initial baseline assessment prior to randomisation. Then 4- and 6-month follow-up appointments were completed with an optional feedback interview. Families referred to the NSPCC were also assessed for safeguarding concerns and suitability for the programme.
-
Treatment as usual (TAU) – families continue to use the same services as before, while receiving the baseline, 4- and 6-month assessments.
Protocol changes
Throughout the feasibility process, a number of protocol changes were made. Applications to the Research Ethics Committee (REC)/Health Research Authority (HRA) were made and the following changes were approved for all changes outlined:
-
Primary outcome point – there was a change from a 3-month to a 4-month primary outcome point, without altering the 6- and 12-month time points. This was to assist with family availability and referral rates and to ensure that the number of ‘useful data’ was maximised.
-
Data collection – a demographic questionnaire for referrers was subsequently produced to capture the variety of professional backgrounds involved in the referral process.
-
Randomisation – the ratio was altered from 1 : 1 to 2 : 1 randomisation allocation procedures (two Young SMILES intervention to one control) to expedite the formation of intervention groups. This amendment took place 8 months into recruitment, which, after numerous recruitment difficulties, expedited the start of the intervention in the two sites where most referrals were received: Newcastle (32 families referred) and Warrington (16 families referred).
-
Randomisation method – there was a change from using the Sealed Envelope system (www.sealedenvelope.com) to online randomisation software [www.randomisation.com (accessed 1 March 2020)], as the former system would not meet our requirements in relation to sample size and the ability to stratify by age and site without incurring costs.
-
Inclusion of siblings – it was initially agreed that inclusion of siblings within the same group may have a negative effect on the group dynamics. After further consideration, this was changed to allow siblings within the same group (if in the same age band), which would also expedite the formation of groups.
-
Travel – some families preferred the young person to travel to the group alone. For safeguarding, a travel consent form was developed for parents/carers to consent to the child/adolescent travelling to the intervention venue alone.
-
Participant communication – following participant feedback, we simplified the participant information sheets to enable a better understanding of the aims and objectives of the trial.
Participant eligibility
Families were considered eligible if they met the following criteria:
-
Children and adolescents aged 6–16 years whose parent had serious mental illness.
-
Parents/carers with SMI and their partners, the latter of whom may or may not have had any mental health problems. SMI is defined as a severe psychiatric disorder that requires intervention, hospitalisation or ongoing treatment; parents with a diagnosis of schizophrenia or related disorder, schizoaffective disorder, bipolar disorder, severe recurrent unipolar depression, psychotic depression, severe anxiety, obsessive–compulsive disorder and post-traumatic stress disorder were sought. Parents with a current diagnosis of a severe psychiatric disorder with a minimum requirement of scheduled follow-up with secondary care services were eligible for study inclusion. The focus of our project was the children and adolescents and their outcomes, rather than the parents. Therefore, we did not intend to carry out full clinical interviews with the parents or to report diagnostic codes. We accepted the primary and secondary diagnoses reported by a key health professional, such as the GP, care co-ordinator and key worker, as most of these parents were likely to receive secondary care or be monitored in primary care. This could be gleaned during professional referral into the study or, in the case of a self-referral by the parent, we obtained the diagnosis by contacting the parent’s appropriate care co-ordinator (e.g. GP or community psychiatric nurse) after gaining the parent’s permission to do so.
-
Children and adolescents had to have at least 10 hours of contact per week with the parent/carer with SMI. (The child/adolescent did not have to live with a mentally ill parent necessarily.)
-
The parents/carers/guardians understood the purpose and remit of the intervention for themselves and their child/adolescent and consented to their attendance and completion of outcome measures and interviews.
-
Children/adolescents had to have some awareness of the parent’s mental illness, as confirmed by the parent and/or the appropriate care co-ordinator. If they had no awareness of the parent’s illness, we discussed how the parent and care co-ordinator could prepare the children/adolescents before they started group work.
Families were excluded if they exhibited the following criteria:
-
Children/adolescents of parents diagnosed with common mental health problems (e.g. mild–moderate depression) or with primary substance misuse, rather than with a primary diagnosis of SMI as defined in inclusion criterion 2, above.
-
The children/adolescents had significant cognitive impairment or a learning disability or major mental illness or behavioural problems (as verified by their GP or other health professionals involved in the family’s care) that made it impossible or unsafe for them to participate in group work.
-
The parent was extremely mentally ill at the time of eligibility assessment, which made it difficult or unsafe for them to participate in group or individual work. (It was acknowledged that these children/adolescents might be those especially in need of support and therefore this was judged on a case-by-case basis by experienced practitioners.)
-
The children/adolescents had already participated in Family SMILES (which is not applicable in the north-east of England, where Family SMILES is not available).
Trial sites
The study was conducted at the following sites:
-
North East – Northumberland Tyne and Wear (NTW) Trust, conducted by the local Family Therapy Service and the Barnardo’s Young Carer’s team for Newcastle upon Tyne.
-
North West – NSPCC Warrington, delivered by NSPCC practitioners at the Peace Centre, Warrington. The facilitators came mainly from a social work background and had significant experience of working with vulnerable CYP.
A third locality in NSPCC Coventry had been identified to provide Young SMILES groups; however, there were recruitment problems and so no groups were run in this area (see Appendix 1, Table 31).
Recruitment and consent
Families were identified through practitioners working in CYP services, CAMHS, Adult Mental Health services and education services. Referral sources were broadened by close co-operation with NHS practitioners and services. The NIHR’s Clinical Research Network was used to assist with recruitment and identification of suitable families via GP registers, community mental health and inpatient teams, and rehabilitation units. Posters and flyers were distributed to relevant NHS and third-sector organisations and schools. In addition, practitioners working in the community were informed of the study to assist with direct opportunistic referrals.
Two methods of identifying families were deployed:
-
Recruitment gatekeepers (e.g. community nurses, care co-ordinators and young carer’s workers) identified people from their caseload who may be eligible for the trial.
-
A member of the trial team acquired permission from the gatekeeper to screen their caseload for eligible families first, and provided a list of families to the gatekeeper.
In each case, the gatekeeper gave the potential family a study information pack (an invitation letter, information sheet and consent-to-contact form). Separate packs containing the same information were provided to CYP and parents. If a family was interested in participating, they returned the consent-to-contact form, detailing their preferred method(s) of contact. Alternatively, the family could provide verbal consent to be contacted to the gatekeeper, who would then inform the study team. Here, a verbal consent-to-contact form was completed by the gatekeeper to confirm that they had received consent.
All families that were on the caseload of the services involved in the delivery of the trial were considered to be potential participants. In addition, caseloads of services within NTW Trust were also screened for participants with the permission of the professional holding the caseload.
After gaining consent to contact, the research team contacted the family, determined eligibility and received confirmation of desire to participate, which was usually received from the mentally ill parent, but could also be from the healthy parent. If the latter, the only additional factor that had to be ascertained was that the child had at least 10 hours per week of contact with the mentally ill parent. This number was considered to be an appropriate and readily measurable amount of time to ensure that the ill parent could be fully informed about what was happening and be able to support the child.
If eligible, families were informed that they would be contacted at a later stage to arrange to complete a face-to-face baseline interview. Dates for baseline interviews were contingent on the research team receiving enough referrals from the same age group at one site (based on the minimum feasible group size of four children). Families were telephoned fortnightly during the waiting period by the research team. They were informed of progress in organising groups and given an opportunity to ask any additional questions. A one-off home visit to discuss the study was also offered.
When multiple children were recruited from the same family, for the main analysis we identified an index child and included data from only that child in the analysis. We asked the parents to nominate the index child, which was always determined by which child experienced the most difficulties in responding to parental mental illness.
At baseline, the family were given the opportunity to ask any further questions and written consent was taken. The CYP were asked to give assent to participate. Consent from their parents/carers was also obtained in support of their child’s participation. Separate consent was obtained for parents/carers. It was clarified to both that they could withdraw at any point without detriment to their care. If a parent was to withdraw, their child/children could still participate with their consent. If the parent had more than one child, all children in the family were eligible to participate but were not required to do so.
After obtaining consent, family members were asked to complete the baseline measures. All measures are standardised and designed as self-complete, with the researcher present to offer assistance. Outcome measure booklets were age-dependent. Families received a total of £50 of shopping vouchers over the data collection time points for their participation in the study (£20 at baseline and £15 for each of the 4- and 6-month follow-ups). On every visit, trial researchers identified if any adverse events had occurred and reported these as per the agreed procedures. Outcome measure visits took place at a time/location convenient for the participant, which was invariably at the family’s home.
Intervention design
Comparator: treatment as usual
The control group received TAU. This was defined as access to any services or resources to which CYP and their families would usually be referred or have access. Participation in the trial did not preclude access to these services.
At the NSPCC site, there were no other services that would be a natural alternative to Young SMILES. The two other services that were on offer at the same time as the Young SMILES study were a therapeutic service for children who have been sexually abused and an assessment and a treatment programme for children who display harmful sexual behaviour.
At the NHS site, the type of TAU offered to the children depended on how they were recruited. Some children received usual family therapy support (in the form of home visits by a systemic practitioner), some received assessment and advice relevant to their role as ‘young carers’ (by practitioners in Barnardo’s) and others did not receive any specific intervention as they were children of parents who were looked after by a care co-ordinator in a community mental health team (CMHT) (these teams focus on the parent with SMI with no routine provision for their children).
Intervention: Young SMILES
Young SMILES is an 8-week group programme (four to six CYP per group) delivered by two trained practitioners. Age groups were 6–11 years or 12–16 years. At week 4, five parallel sessions were offered to the parent/carer. CYP and parent sessions lasted 2 hours each, including time for a short break and refreshments during and after the group session. Where possible, the sessions were held in non-stigmatising venues, such as a community-based location. Hospital clinics or schools were, therefore, avoided.
In Newcastle, groups were delivered in an NHS organisation, utilising a co-delivery model where one facilitator was from the NHS (Family Therapy Service) and the other was from a third-sector organisation (Barnardo’s). Third-sector organisation facilitators had a mix of professional backgrounds, which included social work, children’s services and occupational therapy.
In Warrington, the intervention was delivered by NSPCC practitioners at the Peace Centre, which is an accessible, award-winning venue embedded within the local community. The facilitators came mainly from a social work background and had significant experience of working with vulnerable CYP.
The training manual for facilitators provided an overview of the feasibility trial and development of Young SMILES. It incorporated details about service and intervention delivery. It provided a manual to support trainers to ‘teach’ practitioners aspects of the model and how it should be delivered, as well as an ongoing guide/reference for practitioners who delivered the service.
Children and young people’s group sessions
Every session had specific aims and objectives, which for both age groups remained consistent throughout (Table 4). However, activities and communication style varied depending on the abilities of the CYP. Adapting to the learning styles of the CYP in the group was also an important role of the facilitators. The themes traversing all sessions were mental health literacy, communication and problem-solving skills. The outcome of each session was facilitated through the creation of an ‘imaginary family’ for younger children (made from cardboard cut-outs/cartoon characters created electronically and printed) and a ‘graffiti wall family’ for older children. A normal session included a ‘getting to know you’ (first session)/’welcome back’ and a ‘check-in’ on previous week, ‘ice-breaker’ activity, activities based on the session aims and snack time. A ‘weekly challenge’ at the end of each session was included to orientate and tether the CYP to the next session in order to optimise engagement.
| Session | Objectives |
|---|---|
| 1: Welcome to Young SMILES | Understand the aims of the group and introduce key themes (e.g. the fictitious family) |
| 2: All about me | Understand a sense of self, and identify personal strengths and qualities |
| 3: What happens in my family? | Understand mental illness and the impact that it can have on a young person’s family |
| 4: Things we worry about | Identify the sources of feelings and understand healthy and unhealthy responses to them |
| 5: Our world | Identify the key sources of stress and the building blocks needed for a foundation of feeling good |
| 6: Where do I go when I need help? | Identify support networks and learn how to access help from professionals |
| 7: Enjoying being me | Understand personal strengths and aspirations, recognise which aspirations they can shape |
| 8: Moving on together | Celebrate progress, consolidate relationships and plan for the future |
Parent/carer group sessions
The focus of the parent/carer sessions was determined during the CYP session in the previous week (Table 5). This was to retain the child-centred basis of the intervention. CYP and parents came together in the final ‘Moving on together’ session to review progress and for the last few activities that focus on hopes and fears, achievements and moving forward. Activities for each session were standardised, but not prescriptive. As long as they met the overall objectives of the sessions and were consistent with the ethos of the Young SMILES programme the facilitator was afforded the freedom of action to change their approach to better suit the different needs and learning styles within the group.
| Session | Objectives |
|---|---|
| 1: Welcome | General introduction and welcome parents |
| 2: What our children do well | Develop insights into how parents/carers can (and do) encourage and support their children to do well and feel good about themselves |
| 3: What our children worry about | Identify sources of stress in their children and understand healthy and unhealthy responses |
| 4: How we support our children | Identify obstacles to successful family communication and identify support networks |
| 5: Moving on together | Celebrate progress, consolidate relationships and plan for the future |
Practitioner training
The Development and Impact Manager from NSPCC Children’s Services held a 2-day Young SMILES intervention training event, which was held in Newcastle (1 and 2 March 2017) for NTW NHS Foundation Trust and Barnardo’s Newcastle practitioners, and in Warrington (20 and 21 March 2017) for NSPCC Warrington and NSPCC Coventry practitioners. The training provided practitioners with the following: the study context, the feasibility study, intervention format and guidance, delivery location context and referral pathways, the incorporation of the imaginary family and problem-solving.
Four half-day sessions were also arranged to work through the intervention activities (11, 12 and 18 July 2017 and 5 September 2017), ensuring that practitioners felt confident supporting CYP and their parents/carers. Practitioners also identified the need to gain more of an understanding about SMI in adults. This was covered in the training in Newcastle and additionally in two sessions for Warrington and Coventry NSPCC staff (5 and 6 July 2017).
Outcome assessment
A list of the primary and secondary outcomes and tools used can be found in Table 6. A description of each measure and how scores were calculated can be located in Appendix 3. Although measures were available for all ages, some CYP experienced difficulties completing certain measures. In this instance, researchers were responsive to the CYP’s needs, supporting the CYP to ensure completion of the self-report measures. The following demographic details were also collected: age, sex, sexual identity (if aged ≥ 16 years), ethnicity, nationality, religion, education, employment and current living arrangements.
| Outcome | Measured by/using |
|---|---|
| Primary outcome | |
| HRQoL | PedsQL108 |
| KIDSCREEN™109 | |
| Secondary outcomes | |
| Child psychopathology and prosocial behaviour | SDQ110 |
| Symptoms of common mental health problems | RCADS111 |
| Knowledge and perceptions about SMI (mental health literacy) | MHLq112,113 |
| Parenting competencies | Arnold–O’Leary Parenting Scale114 |
| Degree and cause of stress in parent–child relationships | PSI-SF115 |
| Incremental health gain in quality-adjusted life-years | CHU-9D116 |
| Resource use | Child and Adolescent Service Use Schedule [see the project web page: www.journalslibrary.nihr.ac.uk/programmes/hta/142901/#/ (accessed 1 March 2020)] |
| CYP, parent, facilitator acceptability | Qualitative interviews |
Outcome measures
Outcome measures are summarised by trial arm at baseline and follow-up. As efficacy is not within the scope of a feasibility trial, estimated effect sizes are not presented. Completeness and variability of the outcome measures will be used to inform future trial design. In cases where multiple children were recruited from the same family, parents were asked to nominate an index child for inclusion in the main analysis. Other sibling(s) were still offered the opportunity to attend Young SMILES (if their family was randomised to the intervention group). Parents were not present for any data collection from their child/children. The number of families with multiple children is presented and summaries of demographics are presented for index children and all children.
Resource utilisation
Collection of child resource utilisation data was piloted using the Child and Adolescent Service Use Schedule (CA-SUS). We aimed to develop a resource use collection tool that captures the most important aspects of resource utilisation and assess the feasibility of collecting child resource utilisation.
The CA-SUS was adapted for our study setting in consultation with Professor Sarah Byford, the designer of the CA-SUS questionnaire. This adaptation involved removing the sections on out-of-pocket expenses and employment, removing the question on education type, removing the follow-on questions asking name of hospital for the hospital service use questions, removing complementary therapist (e.g. homeopath) from the list of community services, adding NHS walk-in services and NHS Direct to the list of community services, and simplifying the questions in the criminal justice services section. A copy of the CA-SUS version used for data collection was submitted alongside this report [see project web page: www.journalslibrary.nihr.ac.uk/programmes/hta/142901/#/documentation (accessed April 2020)].
Resource utilisation data were collected retrospectively using participant recall. The adapted version of the CA-SUS records resource use in the following categories: accommodation, education, hospital services, community services, medication and criminal justice services. Resource utilisation data were collected at three time points: baseline (recalling use over the previous 6 months), 4-month follow-up (recalling use since baseline) and 6-month follow-up (recalling use since the last interview).
As the aim was to assess the feasibility of collecting resource utilisation data to inform data collection methods in a future trial, reporting of results is purely descriptive. No statistical testing was performed.
Qualitative interviews
Acceptability is a key priority in the design, implementation and evaluation phases of complex interventions. 117 It is perceived as a necessary but not sufficient condition concerning the effectiveness of an intervention. Broadly speaking, acceptability is a construct that examines the degree to which an intervention is accepted by those delivering and/or receiving it. 117,118 Definitions have varied considerably, depending on what theoretical perspective the researcher adopts. For example, two studies119,120 investigate acceptability in the terms of patient attitude or satisfaction, whereas other work121,122 conflates the construct with patient behaviours, such as engagement and adherence to treatment. This lack of consensus has served to undermine the credibility of acceptability as a valid assessment instrument. 117
A post-intervention qualitative evaluation of Young SMILES was conducted with CYP, parents/carers and eligible referrers. This was to determine acceptability among those that received the intervention, as well as to assess how practitioners and potential referrers were able to deliver the intervention. These studies (four in total) took place after the primary outcome point. Interviews with CYP and parents/carers focused on, inter alia, barriers to and facilitators of attending, what they liked and disliked, and if they thought Young SMILES helped their family. Referrer and practitioner interviews explored which factors facilitated or hindered the implementation of Young SMILES (see Chapters 5 and 6 for a description of the methods and analysis). 123
Sample size in all of the qualitative studies conducted was governed by the numbers of eligible participants referring, delivering or taking part in the intervention, rather than by traditional concepts of data saturation. In qualitative research, saturation is reported as a criterion for achieving an adequate sample size, and thus no additional information is expected to enhance or change the findings. However, this is an inappropriate quality marker where sample sizes are limited by other factors, including trial participation. In such studies, information power is a more appropriate concept,123 with the final sampling frame guided by the study aim. A less extensive sample is needed when participants taking part are targeted because of their characteristics that are aligned with the study aim, in this case trial (and intervention) participation. Recruitment ceased when all intervention facilitators and participants had been invited for interview. Data analysis in the context of this feasibility study was focused on achieving key insights that contributed to or challenged current understandings of intervention acceptability.
Sample size
Formal power calculations for between-group effects were not conducted as is appropriate for a feasibility study, which is primarily aimed at developing and piloting a new intervention and training package. The study that was piloted examined the feasibility of the Young SMILES intervention training and the acceptability of delivering this to young people in a RCT design in two different settings. The original sample size proposed at the outset was 60 randomised families (30 per group, as recommended for pilot studies124). This was deemed sufficient to facilitate the main study aims [e.g. determining feasibility of recruitment and estimating standard deviations (SDs) of the outcome measures to perform a future power calculation]. The aim was to run a minimum of three sets of CYP groups, alongside three parallel parent groups in the two recruitment sites during the recruitment period. The new target sample size was 35–40 families, following challenges during the study that significantly restricted our recruitment and follow-up periods (see Appendix 1, Table 31).
Randomisation
The randomisation ratio for the final three groups was 2 : 1. Randomisation lists were stratified by age group and site, prepared using Stata® 15 (StataCorp LP, College Station, TX, USA) by an independent statistician with the command ralloc, using random blocks of size 3 and 6.
Blinding
Randomisation was conducted by the study co-ordinator to maintain blinding of the statistician and research team, thereby reducing detection bias. To facilitate blinding, the research team adhered to the following: (1) that families knew that they could contact the study co-ordinator should they have any queries about their allocation or Young SMILES arrangements and (2) the researcher conducting the data collection visits reminded families to refrain from revealing their allocation during follow-up visits. Should a researcher become aware of any allocations, this was recorded and reported.
Statistics
The overall focus is on summaries of the key indicators of success of the study: recruitment and participant flow. Data are reported in line with the feasibility and pilot extension of the Consolidated Standards of Reporting Trials (CONSORT) statement. 125 The numbers of participants who dropped out from the intervention, withdrew their consent and did not provide follow-up outcome data are also reported.
Adverse events
During the baseline and subsequent follow-up visits, trial researchers identified if any adverse events occurred and reported, as per standard operating procedures (SOPs) [see additional files (www.journalslibrary.nihr.ac.uk/programmes/hta/142901/#/documentation; accessed April 2020)]. The Trial Steering Committee monitored participant safety during the trial and was responsible for reviewing any serious adverse events occurring as part of the trial.
Public involvement
The research team actively consulted with young people and practitioners about what the intervention would comprise. This included the structure of the group and the activities within the groups. Young people and practitioners were also consulted on the outcome measures that would be used to calculate the time taken to complete the outcome measure booklets.
Young people, parents/carers, referrers and practitioners were all interviewed to provide feedback on the trial recruitment procedures, their experience in the group and what effect the Young SMILES intervention had on experiences outside the group.
Chapter 5 Quantitative results
This chapter examines and reports data on the feasibility of the recruitment of CAPRI and the delivery of the Young SMILES intervention. This entails reporting the number of families approached, the number of eligible children within the approached group, the number that were recruited from that eligible population and the number finally randomised and who took part. This chapter will also report on the number of children in each group (randomised to Young SMILES or to TAU) who completed data collection at each follow-up time point. Thereafter, as evidence of feasibility of delivery, we report on how many children and adolescents randomised to Young SMILES (as opposed to TAU) adhered to the intervention and how many sessions they completed.
In addition, we provide evidence on the feasibility of collecting data from children of all age groups (6–16 years) and their parents, using the chosen measures within the protocol. We present data that help to assess whether or not the chosen measures can capture change in the population over the time periods of use. The Young SMILES protocol and study design is neither tasked nor designed to estimate the effect of our intervention. As a result, we shall not make between-group comparisons in the chosen measures over the time periods of data collection. Such an examination will be undertaken in an appropriately powered and designed efficacy study.
Participant flow
The first pathway of recruitment into the study relied on NHS staff identifying eligible families through screening their patient caseloads and patient records within adult community mental health NHS teams, as well as contacting relevant care co-ordinators of patients with a diagnosis of severe mental illness who had children aged 6–16 years. Care co-ordinators were asked to contact their patients to pass on information about the study. Once their patient has confirmed their interest in the study, the care co-ordinator would either complete a verbal-consent-to-contact form and send it to the address of the research team, or encourage the patient to complete and send a consent-to-contact form to the same address. Adult community mental health services in the NHS routinely focus on adults. They are therefore not concerned with their children, unless there is a risk of harm to the child or a mental illness diagnosed for the child.
The second recruitment pathway followed an opportunistic approach of identifying families who came into contact with children’s charities during the period of the study’s recruitment. We relied on charity workers who assessed the child to identify whether or not their parent had severe mental illness, thereby gauging the potential eligibility of the child for Young SMILES. Charities, such as the NSPCC, focus on children and involve parents/carers who are well; they do not customarily assess or work with the mentally ill parent.
At the NSPCC sites, we do not have information about how many families NSPCC staff approached. Overall, 18 families reported an interest in participating and were screened for eligibility by phone, 15 of these were recruited via an NSPCC professional who had first seen each family and three via self-referral in response to a public advert or via signposting by a non-NSPCC professional. Three families had to be withdrawn by the research team because their children were eligible for the 12- to 16-year age group only, which did not get the chance to assemble because of recruitment difficulties for this cohort. In the NHS, out of the 1963 patient records that were screened by NHS staff, 162 (8%) families were considered potentially eligible. The research team asked the care co-ordinators to approach these 162 families. Care co-ordinators reported that a total of 33 families had expressed an interest, a response we took at face value, assuming that they had indeed approached all 162 potentially eligible families. One hypothesis is that front-line clinical staff could have acted as barriers to participant recruitment. This happens either by staff making decisions about the suitability of research on their client’s behalf or by gatekeeping access to research studies in other ways. This is likely to be a significant problem and to skew apparent recruitment uptake. Therefore, we cannot be sure how many of the 162 families were approached, or if care co-ordinators endorsed the study to the families they did approach.
However, we can reliably report that, of the 33 families whose details were provided to us by NHS care co-ordinators, 31 were screened by telephone but two were uncontactable. From the NSPCC, 18 families were screened by telephone. Out of a total of 49 families screened, 35 (71%) met inclusion criteria and received a face-to-face assessment and subsequent randomisation; nearly one-third of those (n = 12) were recruited in the NSPCC sites and two-thirds (n = 23) in the NHS. Out of the 35 randomised families, 33 families (18 in the Young SMILES group and 15 in the TAU group) provided baseline data. Of those families, 28 gave follow-up data at the primary end point (4 months post baseline): 15 out of 20 (75%) in the intervention group and 13 out of 15 (87%) in the control group.
When multiple children were recruited from the same family, only the index child’s data were included in analyses. Siblings were still offered the opportunity to attend Young SMILES (if their family was randomised to the intervention group). The index child was determined by the parent only. The parent was asked by the research team to choose which child they wanted to have their measures collected. The research team discovered that in all instances the parent’s decision was based on their perceptions of which sibling experiences the most difficulties in responding to parental mental illness. Only 6 out of the 20 families who were randomised to the intervention had children (seven in total) other than the index child of an age eligible to participate (aged 6–16 years). Baseline data are presented both for index children and for all children. Figure 1 presents participant flow from identification to follow-up.
FIGURE 1.
The CONSORT participant flow diagram.
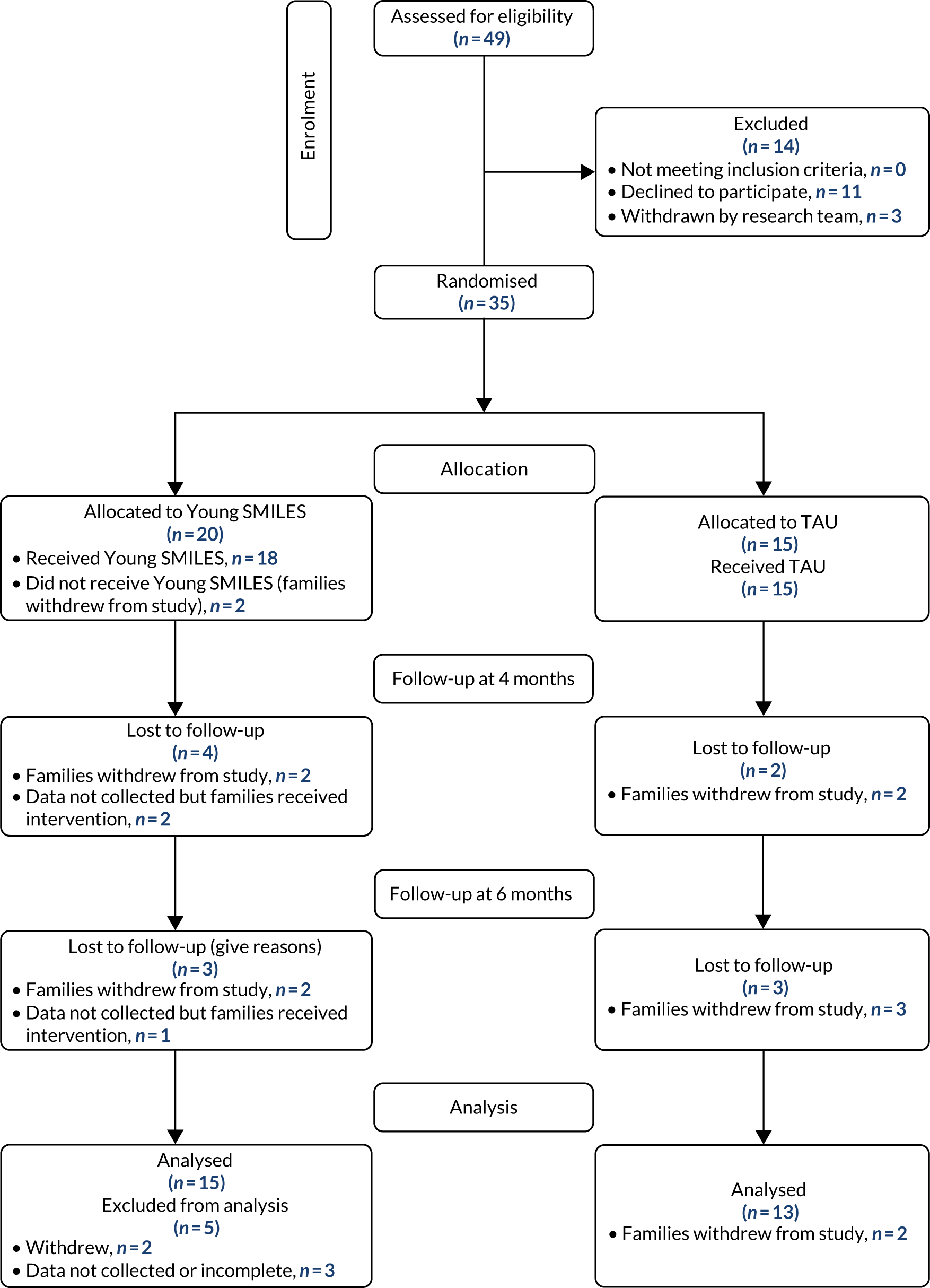
Participant characteristics
The group of children that received Young SMILES (n = 18) was split into two age groups: 6- to 11-year-olds (n = 14, mean 9.2, SD 1.2) and 12–16 year olds (n = 4, mean 13.8, SD 1.7). The mean age of the children (n = 15) in the control group was 11 years (SD 2.7 years). The female-to-male ratio was 3 : 2 in both groups. All children were living with their parents. Most children (13/18, 72%, in the intervention group and 12/15, 80%, in the control group) were aware that their parent had severe mental illness. In total, 31 out of 33 parents checked the box as ‘living with a partner’ at baseline, which would suggest that the majority (81.8%) were unmarried parents. Table 7 details demographic characteristics for participating children in each group.
| Characteristic | Index children (N = 33) | All children (N = 40) | ||
|---|---|---|---|---|
| Young SMILES (n = 18) | TAU (n = 15) | Young SMILES (n = 24) | TAU (n = 16) | |
| Age, years (range 7–16), mean (SD) | ||||
| Whole group | 10.2 (2.3) | 11.1 (2.7) | 10.2 (2.1) | 10.9 (2.7) |
| 6–11 | 9.2 (1.2) | 9.4 (1.1) | 9.4 (1.3) | 9.3 (1.1) |
| 12–16 | 13.8 (1.7) | 14.4 (1.3) | 13.4 (1.7) | 14.4 (1.3) |
| Age, years (range 7–16), n (%) | ||||
| 6–11 | 14 (78) | 10 (67) | 19 (79) | 11 (69) |
| 12–16 | 4 (22) | 5 (33) | 5 (21) | 5 (31) |
| Sex, n (%) | ||||
| Female | 10 (56) | 9 (60) | 12 (50) | 9 (56) |
| Male | 8 (44) | 6 (40) | 12 (50) | 7 (44) |
| Total | 18 (100) | 15 (100) | 24 (100) | 16 (100) |
| Living with parents, n (%) | ||||
| Yes | 18 (100) | 15 (100) | 24 (100) | 16 (100) |
| No | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Number of siblings, n (%) | ||||
| 1 | 4 (22) | 5 (33) | 4 (17) | 5 (31) |
| 2 | 5 (28) | 3 (20) | 8 (33) | 3 (19) |
| 3 | 2 (11) | 1 (7) | 2 (8) | 1 (6) |
| 4 | 4 (22) | 2 (13) | 5 (21) | 3 (19) |
| 5 | 2 (11) | 4 (27) | D2 (8) | 4 (25) |
| 6 | 1 (6) | 0 (0) | 3 (13) | 0 (0) |
| Total | 18 (100) | 15 (100) | 24 (100) | 16 (100) |
| Knowledge of parental SMI, n (%) | ||||
| Yes | 13 (72) | 12 (80) | 18 (75) | 12 (75) |
| No | 5 (28) | 3 (20) | 6 (25) | 4 (25) |
| Total | 18 (100) | 15 (100) | 24 (100) | 16 (100) |
The majority of the parents in the participating families across both groups were mothers (30/33), white British (30/33), not in active employment (32/33) and aged 25–44 years (27/33). Families lived either in their own homes (10/33), in rented accommodation (8/33) or in social housing (12/33). Self-reported types of mental illness experienced by the parents included bipolar affective disorder, alcoholism, depression, anxiety, personality disorder, schizophrenia, panic disorder, substance abuse and phobia. In most cases, parents experienced a combination of these. Table 8 provides a breakdown of characteristics for the participating parents in each group (control and intervention).
| Characteristic | Young SMILES (N = 18) | TAU (N = 15) |
|---|---|---|
| Age (years), n (%) | ||
| 25–44 | 14 (78) | 13 (87) |
| 45–64 | 4 (22) | 2 (13) |
| Sex, n (%) | ||
| Female | 17 (94) | 13 (87) |
| Male | 1 (6) | 2 (13) |
| Ethnicity, n (%) | ||
| White British | 16 (89) | 14 (93) |
| Asian | 2 (11) | 0 (0) |
| Missing | 0 (0) | 1 (7) |
| Education, n (%) | ||
| Secondary school | 7 (40) | 10 (67) |
| Further education | 8 (44) | 2 (13) |
| University | 2 (11) | 0 (0) |
| Postgraduate | 0 (0) | 2 (13) |
| Missing | 0 (0) | 1 (7) |
| Accommodation, n (%) | ||
| Owner occupied | 7 (39) | 3 (20) |
| Rented | 3 (17) | 5 (33) |
| Social housing | 7 (39) | 5 (33) |
| Other | 1 (6) | 0 (0) |
| Self-reported mental illness, n (%) | ||
| Bipolar | 6 (33) | 6 (40) |
| Alcoholism | 7 (39) | 8 (53) |
| Depression | 10 (56) | 8 (53) |
| Anxiety | 8 (44) | 6 (40) |
| Personality disorder | 4 (22) | 0 (0) |
| Schizophrenia | 2 (11) | 1 (7) |
| Panic disorder | 3 (17) | 2 (13) |
| Substance abuse | 9 (50) | 6 (40) |
| Phobia | 1 (6) | 1 (7) |
| No diagnosis | 3 (17) | 4 (27) |
| Do not know | 1 (6) | 0 (0) |
| Other | 3 (17) | 3 (20) |
The number of attended sessions by all children (n = 23) and their parents (n = 19) was not normally distributed (Table 9), so the median and interquartile range (IQR) were calculated in place of the mean and SD. The majority of children attended seven out of the eight sessions offered (IQR 6–8 sessions) and typically parents attended three out of the five sessions offered (IQR 2–5 sessions).
| Participant | Total number of sessions | Median | IQR | Minimum | Maximum |
|---|---|---|---|---|---|
| Child | 23 | 7 | 6–8 | 0 | 8 |
| Parent | 19 | 3 | 2–5 | 0 | 5 |
Outcomes
Table 10 provides an overview of the outcome measures we used in the study, along with their interpretation of scores and established cut-off points. See Appendix 3 for a more detailed description of every measure used.
| Measure | Interpretation of scores | Established cut-off points |
|---|---|---|
| PedsQL (child self-report and parent-proxy) | Higher scores better HRQoL | One SD below the population mean = at risk of poor QoL |
| KIDSCREEN (child self-report) | Higher scores better HRQoL | No established cut-offs |
| CHU-9D (child self-report) | Higher scores better HRQoL | Utility values:
|
| RCADS (child self-report and parent-proxy) | Higher scores more severe anxiety and depression | 0–64 = no clinical need |
| 65–69 = borderline clinical need | ||
| ≥ 70 = clinical need | ||
| SDQ (child self-report and parent-proxy) | Higher scores greater child difficulties | No established cut-off points |
| MHLq (child self-report) | Higher scores better child’s mental health literacy | No established cut-off points |
| Arnold–O’Leary Parenting Scale (parent self-report) | Higher scores less helpful parenting style | Mother may need support if:
|
| Parent Stress Index (parent self-report) | Higher scores worse parent–child relationship | Family may need support if:
|
We present QoL outcomes as self-reported by children and proxy-reported by parents using the Paediatric Quality of Life Inventory™ (PedsQL™)108 and KIDSCREEN™ (a health-related quality of life questionnaire for children and young people and their parents). 126 We present outcome data from the indexed children only. As there were only six families who had more than one child, we did not estimate a family cluster intraclass correlation coefficient, because this would have been large and would have had very low precision. Little power would be gained from including multiple children per family, so our results are presented, as per protocol, using the index children as our sample, with no design effect of siblings who may have participated in the intervention. Parents’ outcomes (both proxy for their children and self-reported for themselves) are treated as a separate independent sample.
Paediatric Quality of Life Inventory
For all 23 items across both groups at all time points, total mean scores for child report ranged from 73.3 to 87.3 and for parent report ranged from 62.6 to 74.9. SDs ranged from 9.6 to 19.6 for child report and 7.1 to 23.4 for parent report. For the 15 items of psychosocial health, mean values ranged from 65.4 to 81.2 (SD 15.6 to 21.6) for self-report and from 56.1 to 66.8 (SD 14.3 to 21.1) for parent report. Furthermore, for the eight items of physical health, mean values ranged from 76.1 to 94.0 (SD 8.3 to 26.4) for self-report and from 63.5 to 83.0 (SD 12.4 to 27.6) for parent report (Table 11).
A meaningful cut-off point to identify those at risk of poor QoL has been proposed as one SD below the population mean. 127 Most literature on child QoL is from medical settings (e.g. diabetes, cancer, asthma). Estimates of the minimum clinically important difference (MCID) for PedsQL total scores are available for children with diabetes: these estimates lie between 6.27 points (parent proxy-report) and 4.72 points (child self-report). 128
| Child reported | Parent reported | |||
|---|---|---|---|---|
| Young SMILES, n (mean); SD | TAU, n (mean); SD | Young SMILES, n (mean); SD | TAU, n (mean); SD | |
| PedsQL total (0–100) | ||||
| Baseline | 18 (74.0); 19.6 | 15 (83.2); 11.2 | 18 (67.5); 22.1 | 15 (69.4); 7.1 |
| 4 months | 15 (79.0); 18.8 | 12 (86.2); 12.9 | 13 (67.3); 20.2 | 10 (69.5); 11.4 |
| 6 months | 14 (73.3); 18.9 | 13 (87.3); 9.6 | 14 (74.9); 15.5 | 12 (62.6); 23.4 |
| PedsQL domains (0–100) | ||||
| Psychological | ||||
| Baseline | 18 (65.4); 18.7 | 15 (72.7); 20.0 | 18 (62.9); 20.2 | 15 (56.1); 12.7 |
| 4 months | 15 (74.6); 21.6 | 12 (78.3); 20.9 | 13 (61.8); 20.5 | 10 (57.8); 14.3 |
| 6 months | 14 (70.5); 16.4 | 13 (81.2); 15.6 | 14 (66.8); 20.1 | 12 (61.7); 21.1 |
| Physical | ||||
| Baseline | 18 (82.5); 22.0 | 15 (93.8); 8.8 | 18 (72.0); 27.6 | 15 (82.7); 12.4 |
| 4 months | 15 (83.5); 17.2 | 12 (94.0); 13.1 | 13 (72.8); 22.0 | 10 (81.3); 17.6 |
| 6 months | 14 (76.1); 26.4 | 13 (93.5); 8.3 | 14 (83.0); 13.7 | 12 (63.5); 28.7 |
KIDSCREEN-52
The 52-measure KIDSCREEN126 was completed by children aged 8–16 years in our sample as a self-report measure of their QoL and by their parents as a proxy-report measure of their children’s QoL. The KIDSCREEN-52 is not validated for 7-year-olds, so data for children of that age in our sample are available only from their parent’s proxy-report.
Child self-report KIDSCREEN mean scores across all 10 domains at all time points ranged from 42.7 to 64.5 (SD 8.8 to 17.5) in the TAU group and from 45.1 to 55.4 (SD 8.4 to 14.3) in the Young SMILES group. Parent proxy-report KIDSCREEN mean scores across all 10 domains ranged from 34.9 to 54.7 (SD 6.8 to 16.8) for the TAU group and 40.2 to 50.9 (SD 8.0 to 15.7) for the Young SMILES group.
The two randomised groups (Young SMILES vs. TAU) were comparable (< 1 point apart) at baseline scores in only three KIDSCREEN domains: self-perception (50.6 vs. 51.0) and autonomy (50.4 vs. 49.7) in the child self-report version, and physical health (43.0 vs. 42.8) in the parent proxy-report version. The widest gap in baseline scores between Young SMILES and TAU were in the child self-report for school (51.4 vs. 58.9) and in the parent proxy-report for bullying (44.6 vs. 36.4).
Child self-report scores across all KIDSCREEN domains were consistently higher than their corresponding parent proxy-report scores at all time points. We visually inspected the gaps between child and parent scores to identify KIDSCREEN domains with high discordance. In the Young SMILES group, we looked for scores that were at least 7.15 points apart [i.e. half the maximum SD (14.3) noted across all domains in the Young SMILES group]. In the TAU group, we looked for scores that were at least 8.75 points apart [i.e. half the maximum SD (17.5) noted across all domains in the TAU group].
In the Young SMILES group, we observed high discordance (at least 7.15 points) between child and parent scores in four domains: mood and emotion at 4 months and 6 months, autonomy at baseline and 4 months, parent relations at 4 months, and bullying at 4 months. In the TAU group, there was high discordance (at least 8.75 points) between child and parent scores in six domains: physical health at 6 months, psychological health at baseline and 6 months, mood and emotion at all time points, self-perception at 6 months, school at 4 and 6 months, and bullying at 4 and 6 months. One domain, mood and emotion, had high discordance between child and parent scores across all time points and in both Young SMILES and TAU groups (Table 12).
| Child reported | Parent reported | |||
|---|---|---|---|---|
| Young SMILES, n (mean); SD | TAU, n (mean); SD | Young SMILES, n (mean); SD | TAU, n (mean); SD | |
| Physical | ||||
| Baseline | 17 (47.0); 13.5 | 13 (50.2); 10.3 | 17 (43.0); 12.7 | 14 (42.8); 10.0 |
| 4 months | 14 (51.1); 11.1 | 11 (52.2); 10.3 | 14 (50.0); 13.2 | 11 (48.6); 10.5 |
| 6 months | 13 (52.4); 14.3 | 12 (54.8); 10.4 | 14 (50.7); 14.9 | 12 (44.5); 9.3 |
| Psychological | ||||
| Baseline | 17 (48.9); 11.4 | 14 (51.1); 10.5 | 18 (44.9); 12.8 | 15 (41.6); 8.0 |
| 4 months | 14 (53.1); 8.4 | 11 (49.5); 13.7 | 14 (46.0); 12.1 | 11 (43.6); 8.5 |
| 6 months | 13 (50.8); 11.7 | 11 (59.3); 8.8 | 14 (44.9); 14.2 | 12 (49.0); 9.9 |
| Mood/emotion | ||||
| Baseline | 17 (48.0); 8.9 | 14 (51.3); 11.6 | 17 (43.4); 14.5 | 14 (40.5); 6.8 |
| 4 months | 14 (53.8); 10.7 | 11 (53.2); 13.7 | 13 (45.0); 12.6 | 11 (41.3); 8.8 |
| 6 months | 13 (49.3); 8.4 | 12 (56.1); 17.5 | 14 (40.4); 13.2 | 12 (38.0); 12.0 |
| Self-perception | ||||
| Baseline | 17 (50.6); 11.0 | 14 (51.0); 10.8 | 18 (48.3); 13.9 | 15 (45.2); 11.9 |
| 4 months | 14 (51.9); 10.4 | 11 (51.6); 9.2 | 13 (45.9); 15.7 | 11 (44.4); 11.1 |
| 6 months | 13 (50.1); 10.8 | 12 (54.8); 11.7 | 13 (50.6); 15.0 | 12 (43.1); 8.7 |
| Autonomy | ||||
| Baseline | 17 (50.4); 11.3 | 14 (49.7); 16.0 | 18 (43.1); 10.5 | 15 (49.0); 9.5 |
| 4 months | 14 (53.6); 9.9 | 11 (54.0); 17.5 | 13 (45.7); 11.7 | 11 (49.4); 13.1 |
| 6 months | 13 (51.0); 11.8 | 12 (56.6); 13.8 | 14 (48.6); 14.9 | 12 (51.4); 9.7 |
| Parent relations | ||||
| Baseline | 17 (51.1); 8.7 | 14 (54.3); 10.4 | 18 (44.8); 8.7 | 15 (48.4); 10.0 |
| 4 months | 14 (54.3); 8.8 | 10 (55.6); 12.8 | 13 (46.0); 11.7 | 11 (47.9); 10.2 |
| 6 months | 13 (51.3); 12.3 | 12 (58.2); 10.1 | 14 (49.0); 13.3 | 12 (49.8); 10.4 |
| Financial | ||||
| Baseline | 16 (47.1); 9.4 | 12 (51.7); 10.4 | 16 (48.5); 14.1 | 15 (47.4); 9.7 |
| 4 months | 13 (52.4); 10.6 | 11 (55.6); 9.1 | 13 (49.2); 14.6 | 10 (51.2); 11.9 |
| 6 months | 13 (48.3); 11.4 | 12 (54.4); 12.5 | 13 (46.9); 14.9 | 12 (50.2); 10.2 |
| Peers | ||||
| Baseline | 17 (46.3); 12.3 | 14 (49.7); 10.0 | 17 (40.2); 8.0 | 14 (45.1); 13.0 |
| 4 months | 14 (45.5); 13.5 | 11 (53.3); 11.1 | 13 (41.9); 14.0 | 11 (51.2); 14.4 |
| 6 months | 13 (46.4); 10.1 | 12 (54.7); 13.5 | 14 (50.9); 14.6 | 12 (47.3); 8.4 |
| School | ||||
| Baseline | 17 (51.4); 9.5 | 14 (58.9); 11.4 | 18 (48.5); 14.4 | 14 (52.4); 11.1 |
| 4 months | 14 (55.4); 13.3 | 11 (62.4); 10.1 | 13 (49.2); 14.3 | 11 (50.1); 11.4 |
| 6 months | 13 (50.8); 11.7 | 12 (64.5); 13.1 | 14 (49.5); 13.9 | 12 (54.7); 11.3 |
| Bullying | ||||
| Baseline | 17 (45.1); 13.5 | 14 (42.7); 13.9 | 18 (44.6); 12.7 | 15 (36.4); 10.8 |
| 4 months | 14 (52.2); 8.7 | 11 (46.9); 14.9 | 13 (43.8); 12.2 | 11 (34.9); 18.0 |
| 6 months | 13 (52.1); 9.7 | 12 (49.8); 13.0 | 14 (46.0); 13.5 | 12 (41.0); 16.8 |
Child Health Utility 9D
To inform a future economic evaluation, we used the Child Health Utility 9D (CHU-9D). 116 This is validated for children aged 7–17 years to estimate incremental health gain in quality-adjusted life-years (QALYs). By visually inspecting the results, means ranged from 0.7 to 0.9 and SDs from 0.1 to 0.2. With the caveat of small sample sizes, children in the TAU sample had ‘excellent’ QoL that remained so at all measurement time points. By contrast, QoL fluctuated from ‘good’ (baseline) to ‘excellent’ (4-month follow-up) and ‘very good’ (6-month follow-up) for the Young SMILES group. Notably, some children in the Young SMILES group had CHU-9D scores as low as 0.2, whereas the lowest score for the TAU group was 0.6 (Table 13).
| Time point | Young SMILES | TAU | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Responses (n) | Mean | SD | Min. | Max. | Responses (n) | Mean | SD | Min. | Max. | |
| Baseline | 18 | 0.7 | 0.2 | 0.2 | 1 | 14 | 0.9 | 0.1 | 0.6 | 1 |
| 4 months | 15 | 0.9 | 0.1 | 0.6 | 1 | 13 | 0.9 | 0.1 | 0.6 | 1 |
| 6 months | 14 | 0.8 | 0.2 | 0.3 | 1 | 11 | 0.9 | 0.1 | 0.8 | 1 |
| QALYs | 11 | 0.410 | 0.073 | – | – | 11 | 0.475 | 0.076 | – | – |
| n | Median | IQR | Min. | Max. | n | Median | IQR | Min. | Max. | |
| Days between baseline and 4-month follow-up | 15 | 130 | 105–141 | 92 | 152 | 12 | 133 | 106.5–140 | 91 | 163 |
| Days between 4- and 6-month follow-ups | 11 | 64 | 54–74 | 35 | 92 | 12 | 72 | 49.5–78.5 | 41 | 116 |
Revised Child Anxiety and Depression Scale-25
Revised Child Anxiety and Depression Scale-25 (RCADS-25) scores across all groups and time points were in the non-clinical range. There were imbalances in baseline scores for Young SMILES versus TAU from both child-reported data (total, 47.5 vs. 42.2; anxiety, 47.6 vs. 42.6; depression, 47.8 vs. 43.2) and parent-reported data (total, 61.1 vs. 56.4; anxiety, 59.0 vs. 54.6; depression, 61.7 vs. 57.4), with scores consistently lower in the TAU group. Follow-up scores across all groups and all scales ranged from 39.3 to 62.4. SDs ranged from 10.0 to 20.2 at baseline and from 8.2 to 17.5 at follow-up.
Parent proxy-reported scores for both Young SMILES and TAU groups were much higher than the corresponding child self-reported scores across all time points. Using the established cut-off score of 65, the parents’ scores are approaching a proxy-reported clinical need for their children, whereas the children’s self-reported scores are much below the clinical threshold (Table 14).
| Child reported | Parent reported | |||
|---|---|---|---|---|
| Young SMILES, n (mean); SD | TAU, n (mean); SD | Young SMILES, n (mean); SD | TAU, n (mean); SD | |
| RCADS-25 total | ||||
| Baseline | 17 (47.5); 14.3 | 14 (42.2); 12.5 | 18 (61.1); 20.2 | 15 (56.4); 10.0 |
| 4 months | 14 (42.0); 10.3 | 11 (39.3); 9.3 | 14 (57.6); 14.2 | 11 (59.3); 17.5 |
| 6 months | 13 (44.7); 13.8 | 12 (40.1); 17.4 | 14 (56.9); 17.0 | 12 (52.3); 9.5 |
| RCADS domains | ||||
| Anxiety | ||||
| Baseline | 17 (47.6); 13.2 | 14 (42.6); 12.0 | 18 (59.0); 19.3 | 15 (54.6); 10.1 |
| 4 months | 14 (43.3); 11.0 | 11 (40.6); 8.6 | 14 (56.4); 14.0 | 11 (54.8); 17.5 |
| 6 months | 13 (43.8); 11.1 | 12 (40.6); 14.9 | 14 (55.3); 16.6 | 12 (49.0); 9.8 |
| Depression | ||||
| Baseline | 17 (47.8); 14.1 | 14 (43.2); 11.2 | 18 (61.7); 18.5 | 15 (57.4); 11.3 |
| 4 months | 14 (41.6); 8.4 | 11 (39.9); 9.6 | 14 (57.7); 13.9 | 11 (62.4); 14.3 |
| 6 months | 13 (46.8); 14.6 | 12 (41.7); 17.4 | 14 (58.1); 16.7 | 12 (56.3); 8.2 |
Strengths and Difficulties Questionnaire
There were imbalances at baseline scores between Young SMILES and TAU for the Strengths and Difficulties Questionnaire (SDQ), which were > 1 point in the SDQ total score and in the emotional domain score. This is perhaps not surprising, given the small sample of children who provided self-report data. Despite these imbalances, the mean scores (rounded to the nearest integer) in total and across all domains denoted the same level of difficulties between the two groups (i.e. average, slightly raised, high or very high). Parent proxy-report mean scores at baseline were similar between Young SMILES and TAU in total and across all SDQ domains.
The discordance between child and parent scores within each randomised group at all time points was large, consistently indicating that parents perceived their children’s difficulties to be greater than the children’s assessment of their own difficulties. The only two domains where children and parents agreed on the level of difficulties were hyperactivity and prosocial behaviours. For these domains, all scores across all time points in both groups were close to ‘average’. These observations come with the caveat that we had three times more data from parents than from children, because a lot of the children in our sample were younger than 11 years and did not complete the self-report questionnaire.
At baseline, in both Young SMILES and TAU groups, children assessed their total difficulties to be ‘slightly raised’, whereas parents assessed the same to be ‘high’. At follow-up, children’s self-reported total difficulties were close to ‘average’ in both Young SMILES and TAU groups, whereas parents’ scores remained in the ‘high difficulties’ range for the TAU group and fluctuated between ‘slightly raised’ (6-month follow-up) and ‘very high’ (6-month follow-up) in the Young SMILES group. For the emotional and conduct domains, across all time points in both groups the children’s scores were close to ‘average’, whereas parents’ scores ranged between ‘slightly raised’ and ‘high’. For peer relationships, the children rated their difficulties as ‘high’, whereas their parents rated them as ‘very high’ (Table 15).
| Child-reported | Parent proxy | |||
|---|---|---|---|---|
| Young SMILES, n (mean); SD | TAU, n (mean); SD | Young SMILES, n (mean); SD | TAU, n (mean); SD | |
| SDQ total (min. 0–max. 40) | ||||
| Baseline | 6 (16.5); 5.1 | 6 (15.3); 4.5 | 18 (18.0); 5.4 | 15 (18.9); 5.0 |
| 4 months | 5 (13.2); 2.2 | 4 (13.8); 4.4 | 14 (20.0); 5.2 | 11 (18.3); 6.4 |
| 6 months | 6 (13.7); 4.5 | 5 (13.8); 4.3 | 14 (16.8); 5.3 | 12 (18.9); 4.2 |
| SDQ domains (min. 0–max. 10) | ||||
| Emotional problems | ||||
| Baseline | 6 (4.3); 2.8 | 6 (3.0); 1.5 | 18 (4.6); 2.9 | 15 (4.7); 2.7 |
| 4 months | 5 (1.8); 1.6 | 4 (2.5); 1.9 | 14 (5.0); 3.2 | 11 (4.5); 2.5 |
| 6 months | 6 (3.7); 3.1 | 5 (2.6); 2.4 | 14 (4.0); 3.9 | 12 (4.5); 1.9 |
| Conduct problems | ||||
| Baseline | 6 (3.3); 1.4 | 6 (3.5); 2.0 | 18 (3.4); 1.8 | 15 (3.5); 1.7 |
| 4 months | 5 (2.0); 1.4 | 4 (1.8); 1.0 | 14 (3.6); 1.7 | 11 (3.0); 1.4 |
| 6 months | 6 (2.2); 1.0 | 5 (2.2); 1.1 | 14 (2.6); 0.9 | 12 (3.6); 1.6 |
| Hyperactivity | ||||
| Baseline | 6 (4.7); 2.2 | 6 (4.5); 1.2 | 18 (4.6); 1.6 | 15 (4.9); 1.2 |
| 4 months | 5 (4.6); 1.8 | 4 (5.0); 2.8 | 14 (5.6); 1.5 | 11 (5.4); 2.5 |
| 6 months | 6 (3.8); 1.5 | 5 (4.4); 0.5 | 14 (4.9); 1.8 | 12 (5.1); 2.1 |
| Peer problems | ||||
| Baseline | 6 (4.2); 1.5 | 6 (4.3); 1.0 | 18 (5.3); 1.6 | 15 (5.7); 1.4 |
| 4 months | 5 (4.8); 0.4 | 4 (4.5); 0.6 | 14 (5.9); 1.7 | 11 (5.4); 1.8 |
| 6 months | 6 (4.0); 0.9 | 5 (4.6); 0.9 | 14 (5.3); 1.2 | 12 (5.8); 1.4 |
| Prosocial behaviours | ||||
| Baseline | 6 (7.2); 1.7 | 6 (7.8); 1.8 | 18 (8.1); 1.8 | 15 (8.1); 2.4 |
| 4 months | 5 (7.6); 2.3 | 4 (8.5); 2.4 | 14 (8.1); 1.8 | 11 (8.3); 2.0 |
| 6 months | 6 (6.7); 2.2 | 5 (7.8); 1.5 | 14 (8.1); 2.2 | 12 (8.3); 1.7 |
Mental Health Literacy questionnaire
Total Mental Health Literacy questionnaire (MHLq) mean scores across all time points ranged from 128.0 to 131.7 (SD 8.5 to 13.7) in the TAU group and from 130.4 to 134.5 (SD 12.6 to 16.6) in the Young SMILES group. For the three MHLq subdomains and across both randomisation groups, means ranged from 41.3 to 44.5 for help-seeking and first-aid skills, from 52.7 to 56.5 for knowledge and stereotypes, and from 26.6 to 32.6 for self-help strategies. The SDs across both the Young SMILES and TAU groups ranged from 3.2 to 6.4 for help-seeking and first-aid skills, from 4.3 to 7.7 for knowledge and stereotypes, and from 2.7 to 5.5 for self-help strategies.
On total MHLq scores, our sample’s baseline means (130.5 for Young SMILES and 128.0 for TAU) and follow-up means at 6 months (130.4 for Young SMILES and 131.7 for TAU) were notably lower than the mean baseline score (133.3) in Campos et al. ’s113 group of children who were close to someone with mental illness. On the domain of the MHLq called ‘help-seeking and first-aid skills’, our sample’s baseline means (41.3 for Young SMILES and 41.7 for TAU) were marginally smaller than Campos et al. ’s113 mean score (41.9), but higher at all follow-up time points.
We note that the instructions of summing up relevant items under each subscale came from communication with the authors of the MHLq. These instructions were different from the Campos et al. 113 paper for two domains of the MHLq: knowledge and stereotypes (which included 18 items in the Campos et al. paper,113 as opposed to 15 items as we were instructed) and self-help strategies (which included five items in the Campos et al. paper,113 instead of eight as we were instructed). Therefore, we can compare Campos et al. ’s113 sample with our sample only on the total MHLq score and the subscore of ‘help-seeking and first-aid skills’ (Table 16).
| Young SMILES, n (mean); SD | TAU, n (mean); SD | |
|---|---|---|
| MHLq total (min. 33–max. 165) | ||
| Baseline | 15 (130.5); 13.2 | 13 (128.0); 13.7 |
| 4 months | 12 (134.5); 16.6 | 11 (129.5); 11.6 |
| 6 months | 14 (130.4); 12.6 | 11 (131.7); 8.5 |
| MHLq domains | ||
| Help-seeking and first-aid skills (min. 10–max. 50) | ||
| Baseline | 18 (41.3); 6.4 | 13 (41.7); 4.4 |
| 4 months | 13 (42.6); 5.4 | 11 (44.5); 3.2 |
| 6 months | 14 (42.3); 4.8 | 12 (43.8); 3.9 |
| Knowledge and stereotypes (min. 15–max. 75) | ||
| Baseline | 16 (54.0); 6.1 | 13 (52.7); 7.7 |
| 4 months | 12 (55.9); 7.5 | 11 (54.2); 7.5 |
| 6 months | 14 (54.4); 6.3 | 11 (56.5); 4.3 |
| Self-help strategies (min. 8–max. 40) | ||
| Baseline | 17 (32.0); 4.7 | 13 (29.4); 4.4 |
| 4 months | 13 (32.6); 5.5 | 11 (26.6); 2.7 |
| 6 months | 14 (29.4); 4.0 | 11 (27.5); 5.0 |
Parenting outcomes
Arnold–O’Leary parenting scale
Baseline mean scores in total and across all domains for both Young SMILES and TAU groups ranged from 4.5 (for verbosity) to 3.0 (for laxness); and SDs ranged from 0.6 to 1.2. At follow-up, mean scores in the Young SMILES group ranged from 4.1 (for verbosity) to 2.5 (for over-reactivity), while SDs ranged from 0.5 to 1.1. For the TAU group, mean scores ranged from 4.2 (for verbosity) to 2.7 (for laxness), while SDs ranged from 0.3 to 1.2.
The recommended clinical cut-off scores (for mothers, who predominated in our sample) are total score 3.2, laxness 3.6, over-reactivity 4.0 and verbosity 2.4. 114,129 Verbosity was the only domain for which parents’ scores were above the clinical cut-off point at all time points and in both groups, indicating a possible area of need in our sample’s parenting style (Table 17).
| Young SMILES, n (mean); SD | TAU, n (mean); SD | |
|---|---|---|
| Total (min. 1–max. 7)a | ||
| Baseline | 17 (3.6); 0.6 | 15 (3.3); 0.7 |
| 4 months | 14 (3.6); 0.5 | 11 (3.6); 0.3 |
| 6 months | 12 (2.9); 0.8 | 12 (3.1); 0.6 |
| Arnold–O’Leary parenting scale domains | ||
| Laxness (min. 1–max. 7) | ||
| Baseline | 16 (3.0); 1.1 | 15 (3.3); 1.2 |
| 4 months | 14 (3.1); 0.8 | 11 (3.2); 0.6 |
| 6 months | 12 (2.6); 0.8 | 12 (2.7); 0.8 |
| Over-reactivity (min. 1–max. 7) | ||
| Baseline | 16 (3.7); 1.2 | 15 (3.3); 0.8 |
| 4 months | 14 (3.6); 0.9 | 11 (3.7); 0.7 |
| 6 months | 12 (2.5); 1.1 | 12 (2.8); 1.0 |
| Verbosity (min. 1–max. 7) | ||
| Baseline | 17 (4.5); 1.1 | 15 (3.7); 1.2 |
| 4 months | 14 (4.1); 0.7 | 11 (4.2); 0.7 |
| 6 months | 12 (3.8); 1.1 | 12 (3.8); 0.9 |
We observed imbalances in baseline total scores for Parent Stress Index – Short Form (PSI-SF) between Young SMILES and TAU (107.4 ± 29.1 vs. 102.4 ± 24.7). At follow-up, the lowest mean total score was 84.9 (at 6 months for Young SMILES) and the highest was 98.2 (at 4 months for Young SMILES). SDs for the total scores ranged from 19.4 to 30.6. Mean scores and SDs for the subscales at baseline for Young SMILES and TAU, respectively, were for parental distress, 38.3 ± 12.0 and 33.3 ± 8.6; for parent–child dysfunctional interaction 32.7 ± 11.8 and 34.0 ± 12.6; and for difficult child 36.4 ± 11.8 and 37.9 ± 6.3. At follow-up, mean scores across all subscales ranged from 26.1 to 38.3 and SDs ranged from 6.3 to 12.6.
The cut-off score above which a family may need support and further services is 114 for the total score, 40 for parental distress and difficult child and 36 for parent–child dysfunctional interactions. Mean scores in total and for all subscales at all time points were lower than the cut-off point of needing support across both groups; however, the maximum total scores of 148 for the Young SMILES group and 159 for the TAU group at baseline suggest that some parents in the group experienced high parental distress (Table 18).
| Young SMILES | TAU | |||||
|---|---|---|---|---|---|---|
| n (mean); SD | Min. | Max. | n (mean); SD | Min. | Max. | |
| Total (min. 36–max. 180) | ||||||
| Baseline | 16 (107.4); 29.1 | 52 | 159 | 12 (102.4); 24.7 | 63 | 148 |
| 4 months | 13 (98.2); 20.8 | 54 | 132 | 11 (85.5); 20.1 | 50 | 118 |
| 6 months | 13 (84.9); 30.6 | 46 | 142 | 12 (90.0); 19.4 | 47 | 112 |
| Domains (min. 12–max. 60) | ||||||
| Parental distress | ||||||
| Baseline | 16 (38.3); 12.0 | 13 | 59 | 11 (33.3); 8.6 | 20 | 44 |
| 4 months | 13 (37.9); 8.3 | 25 | 52 | 11 (31.7); 9.4 | 21 | 54 |
| 6 months | 12 (32.6); 12.2 | 15 | 51 | 12 (31.4); 10.4 | 14 | 53 |
| Parent–child dysfunctional interaction | ||||||
| Baseline | 16 (32.7); 11.8 | 16 | 56 | 12 (34.0); 12.6 | 19 | 58 |
| 4 months | 13 (26.8); 7.9 | 14 | 37 | 11 (26.1); 8.3 | 13 | 37 |
| 6 months | 13 (28.0); 12.3 | 12 | 52 | 12 (27.4); 8.6 | 16 | 47 |
| Difficult child | ||||||
| Baseline | 16 (36.4); 11.8 | 17 | 59 | 12 (37.9); 6.3 | 30 | 48 |
| 4 months | 13 (33.4); 9.6 | 15 | 48 | 10 (30.5); 7.0 | 16 | 41 |
| 6 months | 13 (26.8); 10.6 | 14 | 45 | 12 (31.2); 8.2 | 13 | 41 |
A construct called ‘Defensive Responding’ is also calculated from PSI-SF. This is calculated as the sum of seven items (1, 2, 3, 7, 8, 9 and 11) and helps with quality checking and interpreting the PSI-SF scores. If a parent scores < 10 in the total sum of the defensive responding items, they may be answering defensively and not being completely forthcoming in their responses. In our sample, parents’ mean scores ranged from 18.2 to 22.4 and SDs ranged from 5.0 to 7.8. Notably, some parents scored < 10, as indicated by minimum values of defensive responding scores in the range of 7 to 9 (Table 19).
| Time point | Young SMILES | TAU | ||||
|---|---|---|---|---|---|---|
| n (mean); SD | Min. | Max. | n (mean); SD | Min. | Max. | |
| Baseline | 16 (18.3); 5.0 | 12 | 25 | 12 (22.4); 7.4 | 7 | 34 |
| 4 months | 13 (20.1); 7.0 | 11 | 35 | 10 (22.2); 5.5 | 10 | 31 |
| 6 months | 13 (18.8); 6.0 | 9 | 31 | 12 (18.2); 7.8 | 7 | 31 |
Resource use over time
The collection of child resource utilisation data was piloted using the CA-SUS. 130,131 We used the tool to identify the most important aspects of resource utilisation, as well as to assess the feasibility of collecting information on receipt of care and services from the NHS, social care, education, voluntary and third-sector organisations. We did not calculate costs for this resource use as part of this feasibility study.
The CA-SUS was adapted for our study in consultation with Professor Sarah Byford, the designer of the CA-SUS questionnaire. This adaptation involved removing the sections on out-of-pocket expenses and employment, removing the question on education type, removing the follow-on questions asking name of hospital for the hospital service use questions, removing complementary therapist (e.g. homeopath) from the list of community services, adding NHS walk-in services and NHS Direct to the list of community services, and simplifying the questions in the criminal justice services section. A copy of the CA-SUS version used in our study can be found in the additional files of this report [see the project web page: www.journalslibrary.nihr.ac.uk/programmes/hta/142901/#/documentation (accessed April 2020)].
Resource utilisation was collected retrospectively using parent recall, responding on behalf of the child. Parents completed the questionnaire on their own, but could ask the researcher for clarifications on any questions that they did not understand or found difficult to answer. The adapted version of the CA-SUS elicited information on resource use in the following categories: accommodation, education, hospital services, community services, medication and criminal justice services. Resource utilisation data were collected at three time points: baseline (recalling utilisation over the previous 6 months), 4-month follow-up (recalling utilisation since baseline) and 6-month follow-up (recalling utilisation since the last interview).
We obtained resource use data from 28 parents at baseline, 25 parents at the 4-month follow-up and 26 parents at the 6-month follow-up. This corresponds to the same number of children at each time point. Owing to the small sample size and infrequency of utilisation of many services, results are not reported separately by treatment arm.
Accommodation, education and hospital service use
Descriptive statistics for accommodation, education and the utilisation of hospital services are presented in Table 20. Results are summarised as the proportion of the sample who reported using a service during the recall period (for yes/no questions) and among those answering ‘yes’ the mean number of days/times used. The number of participants who completed the question is also reported to illustrate the completeness of data collection.
| Service type | Baseline (n = 28) | 4-month follow-up (n = 25) | 6-month follow-up (n = 26) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Number of participantsa | Mean | SD | Number of participantsa | Mean | SD | Number of participantsa | |
| Lived in domestic accommodation (yes/no) | 1.00 | 0.00 | 28 | 1.00 | 0.00 | 25 | 1.00 | 0.00 | 26 |
| Number of days absent from school/studies | 4.30 | 5.73 | 28 | 6.52 | 12.53 | 25 | 2.69 | 3.59 | 26 |
| Hospital admission (yes/no) | 0.00 | 0.00 | 28 | 0.4 | 0.20 | 25 | 0.04 | 0.20 | 26 |
| If yes, number of nights | – | – | 0 | – | – | 0 | – | – | 0 |
| Hospital outpatient appointment (yes/no) | 0.32 | 0.48 | 28 | 0.28 | 0.46 | 25 | 0.27 | 0.45 | 26 |
| If yes, number of appointments | 3.00 | 3.64 | 9 | 1.29 | 0.76 | 7 | 1.57 | 0.98 | 7 |
| Called an ambulance (yes/no) | 0.25 | 0.44 | 28 | 0.04 | 0.20 | 25 | 0.19 | 0.98 | 26 |
| If yes, number of times ambulance called | 1.83 | 0.41 | 6 | 1.00 | – | 1 | – | – | 0 |
| Attended A&E (yes/no) | 0.17 | 0.39 | 23 | 0.08 | 0.28 | 25 | 0.08 | 0.27 | 26 |
Response rates were high for the questions about accommodation, education and use of hospital services, with all respondents completing all of the initial questions. The only exception was the question about attendance at an accident and emergency (A&E) department, which was answered by only 23 out of 28 respondents at baseline. Although we cannot comment on the accuracy of the reported use, participants were willing and able to respond to questions regarding accommodation, education and use of hospital services using the CA-SUS.
All respondents reported that their child was living in domestic accommodation at all three time points. The average number of days absent from school or studies during the recall period was 4.3 at baseline, 6.5 at 4-month follow-up and 2.7 at 6-month follow-up. Hospital admission was rare, with no respondents reporting that their child had been admitted to hospital in the 6 months preceding baseline. In total, 0.04% of the sample reported being admitted to hospital at both the 4- and the 6-month follow-ups. Outpatient appointments were more common, with nearly one-third of the sample reporting their child having attended an outpatient appointment in the 6 months preceding baseline data collection. One-quarter (25%) of all respondents reported an ambulance having been called for their child in the 6 months preceding baseline, whereas 17% reported that their child attended A&E during the same period (Table 20).
Community services use
Descriptive statistics for community services use are presented in Table 21. Results are summarised as the mean number of contacts per individual. The number of participants who completed the question is also reported to illustrate the completeness of data collection.
| Service | Baseline (N = 28) | 4-month follow-up (N = 25) | 6-month follow-up (N = 26) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Number of participantsa | Mean | SD | Number of participantsa | Mean | SD | Number of participantsa | |
| GP (home visit) | 0.00 | 0.00 | 28 | 0.00 | 0.00 | 25 | 0.00 | 0.00 | 26 |
| GP (surgery) | 0.39 | 0.50 | 28 | 0.32 | 0.48 | 25 | 0.12 | 0.33 | 26 |
| GP (telephone) | 0.04 | 0.19 | 28 | 0.08 | 0.28 | 25 | 0.08 | 0.27 | 26 |
| Practice nurse | 0.11 | 0.31 | 28 | 0.04 | 0.20 | 25 | 0.04 | 0.20 | 26 |
| District nurse | 0.00 | 0.00 | 28 | 0.00 | 0.00 | 25 | 0.04 | 0.20 | 26 |
| Community paediatrician | 0.07 | 0.26 | 28 | 0.08 | 0.28 | 25 | 0.04 | 0.20 | 26 |
| Care co-ordinator, case manager, key worker | 0.14 | 0.36 | 28 | 0.04 | 0.20 | 25 | 0.04 | 0.20 | 26 |
| Psychiatrist | 0.00 | 0.00 | 28 | 0.00 | 0.00 | 25 | 0.00 | 0.00 | 26 |
| Clinical psychologist | 0.00 | 0.00 | 28 | 0.00 | 0.00 | 25 | 0.00 | 0.00 | 26 |
| CAMHS worker | 0.04 | 0.19 | 28 | 0.04 | 0.20 | 25 | 0.00 | 0.00 | 26 |
| Community psychiatric nurse | 0.00 | 0.00 | 28 | 0.00 | 0.00 | 25 | 0.00 | 0.00 | 26 |
| Counsellor | 0.04 | 0.19 | 28 | 0.08 | 0.28 | 25 | 0.04 | 0.20 | 26 |
| Family therapist | 0.04 | 0.19 | 28 | 0.00 | 0.00 | 25 | 0.00 | 0.00 | 26 |
| Art/drama/music/occupational therapy | 0.00 | 0.00 | 28 | 0.04 | 0.20 | 25 | 0.00 | 0.00 | 26 |
| Social worker | 0.11 | 0.31 | 28 | 0.13 | 0.34 | 24 | 0.08 | 0.27 | 26 |
| Family support worker | 0.14 | 0.36 | 28 | 0.04 | 0.20 | 25 | 0.04 | 0.20 | 26 |
| Social services youth worker | 0.00 | 0.00 | 28 | 0.04 | 0.20 | 25 | 0.00 | 0.00 | 26 |
| Accommodation key worker | 0.00 | 0.00 | 28 | 0.00 | 0.00 | 25 | 0.00 | 0.00 | 26 |
| Educational psychologist | 0.00 | 0.00 | 28 | 0.00 | 0.00 | 25 | 0.00 | 0.00 | 26 |
| Education welfare officer | 0.07 | 0.26 | 28 | 0.12 | 0.33 | 25 | 0.04 | 0.20 | 26 |
| Connexions | 0.00 | 0.00 | 28 | 0.16 | 0.80 | 25 | 0.00 | 0.00 | 26 |
| Mentor | 0.00 | 0.00 | 28 | 0.08 | 0.28 | 25 | 0.04 | 0.20 | 26 |
| Drug/alcohol support worker | 0.00 | 0.00 | 28 | 0.00 | 0.00 | 25 | 0.00 | 0.00 | 26 |
| Advice service (e.g. housing association) | 0.04 | 0.19 | 28 | 0.00 | 0.00 | 25 | 0.00 | 0.00 | 26 |
| Helpline (e.g. Samaritans) | 0.00 | 0.00 | 28 | 0.00 | 0.00 | 25 | 0.00 | 0.00 | 26 |
| NHS walk-in | 0.04 | 0.19 | 28 | 0.00 | 0.00 | 25 | 0.00 | 0.00 | 26 |
| NHS Direct | 0.00 | 0.00 | 28 | 0.00 | 0.00 | 25 | 0.00 | 0.00 | 26 |
Of the community services listed, GP surgery appointments were the most frequently used during all three periods. The mean number of GP surgery appointments per participant was 0.39 in the 6 months preceding baseline.
Participants reported no utilisation of the following services at any of the three data collection time points: GP home visits, psychiatrist, clinical psychologist, community psychiatric nurse, accommodation key worker, educational psychologist, drug/alcohol support worker, helpline (e.g. Samaritans) or NHS Direct.
The results from our feasibility study would suggest that these services are not used; therefore, to minimise participant burden, it may be advisable to remove some or all of these services from the list of community services questions. Alternatively, the lack of reporting could indicate problems with participant/parent recall. For a future trial, we will consult with stakeholders whether we should include or omit these community services, as well as how we can facilitate the completion of relevant items on the CA-SUS (see Table 21).
Medication and criminal justice services
Questions about medication prescriptions and interactions with criminal justice services were also included in the CA-SUS, but response rates in these sections were very low. No response data were recorded in the medical prescriptions section at any of the three time points. The criminal justice services section was also left blank by all respondents at both baseline and 4-month follow-up. At 6-month follow-up, three respondents gave answers to two of the questions asked in the criminal justice services section, covering nights spent in youth custody and being a victim of crime. As a result of the low response rate and the sensitivity of this information, these responses have not been reported in any more detail here.
Discussion
Participants
In our original protocol, we intended to recruit 60 families, equally split across two NSPCC sites (intended n = 40) and one NHS site (intended n = 20). We recruited to time and target in the NHS (actual n = 23 families), but we did not reach our intended recruitment target at the NSPCC sites (actual n = 12 families).
We have discussed in detail the reasons why recruitment was delayed by the transitioning into the new HRA process during the early months and first year of our award. This created an unforeseen and critical 11-month delay in our ability to start recruitment. During this period, the NSPCC sites that we had originally identified for recruitment were no longer available for the study or were closed. The delay also meant that, critically, recruitment start dates coincided with school holidays. Following extensive contact with NIHR, it was decided to foreshorten the recruitment period. This led to a number of protocol changes: to include 2 : 1 randomisation into the Young SMILES intervention and a new target to recruit 40 families in total. We requested an extension to the grant, but this was not feasible given the lack of costs available to support staff.
It is our view that the opportunistic recruitment method within the NSPCC was less effective at identifying suitable families than the caseload review and record screening approach of recruitment within NHS services. By the same token, relying on gatekeepers who work primarily with children was less effective than going directly to gatekeepers who work with mentally ill parents. This is important for future recruitment of families into similar studies in the NHS. Intuitively, researchers may be tempted to follow a less fruitful recruitment pathway via CAMHS to recruit children into a study that delivers an intervention for children. However, our experience taught us that we could reach more eligible families within a limited time frame by engaging with care co-ordinators from adult mental health teams, especially when risk factors for a child are associated with their family. Furthermore, the children whom we targeted did not necessarily have mental illness and, therefore, may have gone unidentified by services. Indeed, in our sample, few endorsed symptoms likely to fulfil criteria for a clinical diagnosis.
In our feasibility study, we found that only a small pool of families (8%) in NHS secondary care adult mental health services were eligible for the Young SMILES trial (i.e. had a parent with SMI and children aged 6–16 years). The NHS recruitment pathway drew from a large population (all adults who were in receipt of secondary care mental health services), but only a fraction of this population (8%) was potentially eligible. We found that adults in secondary care services either were too young to have children aged ≥ 6 years (especially in early intervention for psychosis services) or had adult children (e.g. parents with lifelong severe mental illness). Parents with severe mental illness who have school-age children are not necessarily in receipt of secondary care services, but they are looked after in primary care. Future research studies that evaluate interventions for children and families experiencing severe mental illness can boost recruitment by screening GP and pharmacy records.
The research team was able to contact just one-fifth of potentially eligible families. We cannot tell whether the remaining potentially eligible families were approached by care co-ordinators but declined participation or if the care co-ordinators did not approach these families in the first place. Once families were identified as eligible, agreed to participate and were randomised, on average, across both intervention and control groups, there was a high rate (> 80%) of completion of follow-up measures. Children typically had high adherence to the intervention by completing seven out of the eight offered sessions. The overwhelming majority of recruited parents were mothers, although there was a balance of sexes among participating CAPRI.
Outcomes
Differences in baseline scores are a useful indicator of the comparability of the intervention and the control groups, and the success of randomisation. There were visually noticeable differences in mean scores at baseline between the two randomised groups across all outcome measures. Such differences are likely to be the result of chance rather than bias, given that the randomisation was done remotely with a computer program. This is not surprising given our small sample size. The observed baseline imbalances could be the result of factors other than compromised randomisation (e.g. the children’s age). In our sample, the proportion of 6- to 11-year-olds was slightly higher in the intervention group than in the control group (78% vs. 67%). Expected imbalances at baseline are an important consideration for a future RCT’s design and outcome selection. Such imbalances can be minimised at the RCT’s design phase through stratification of participants, and further adjusted at the point of analysis by including baseline scores as covariates.
Overall, the children’s self-reported QoL and functioning were high, but their emotional and mental health needs were below the clinical threshold within each outcome measure and across all time points. By visually inspecting the outcome data at both follow-up points across all outcome measures, there are neither alarming results nor an obvious and consistent direction of scores in relation to time or outcomes, even when baseline scores were similar between the intervention and the control group.
We refrain from making statistical between-group comparisons on QoL and mental health outcomes at follow-up, because our RCT was not intended to estimate between-group differences in outcomes. Given that our sample for analysis included only 33 participants (Young SMILES, n = 18; TAU, n = 15), unsurprisingly, it was not powered to do so. Furthermore, there was an imbalance in baseline scores between the randomised groups, so any differences at follow-up would not necessarily indicate a treatment effect. For example, for the PedsQ, the means for Young SMILES versus TAU at 6-month follow-up were 73.3 and 87.2, indicating that the TAU group had a higher QoL. However, this imbalance was also reported at baseline (Young SMILES vs. TAU was 74.0 vs. 83.2, respectively), so we would be likely to see no intervention effect after controlling for baseline scores, even if we had sufficient power to justify a between-group comparison.
Parents’ proxy-reported scores consistently tended to overestimate areas of need and difficulty for their children, as well as underestimating their children’s QoL compared with the children’s corresponding self-reported scores. Discordance between child- and parent-reported scores is common in the literature for outcomes based on the PedsQL132 and KIDSCREEN. 133 Parental mental health can also influence their reports of the QoL of their children, particularly in the areas of physical well-being and social support, with elevated levels of parental depression and anxiety being associated with lower QoL scores among their children. 134 Although self-report is preferable for measuring QoL from the child’s perspective, the parent’s view of their child’s QoL is equally important as it can influence help-seeking and service utilisation. 135 It will be useful for future research studies that evaluate interventions for children and families experiencing severe mental illness to include both child self-report and parent-proxy versions of a QoL questionnaire.
Parent self-reported outcomes across all time points indicated that parents in our sample were, on average, below the cut-off scores for distress and difficulties with their children and that their parenting style was positive.
Mental health literacy
We refrain from making statistical comparisons of MHLq scores between Young SMILES and TAU because of our small sample size and the observed baseline imbalances. By visually inspecting the data, there is no sense of direction of MHLq scores in favour of either the intervention or the control. There is no information in the literature that would help us to interpret the observed differences in mental health literacy between different samples or between the intervention and control groups. The same applies to differences within the same group at different time points (e.g. by knowing what the minimal difference in MHLq scores that is important in a clinical context, similar to a MCID). We also do not know what the normative values are for MHLq, so that we can gauge whether baseline mental health literacy in our sample was ‘better’ or ‘poorer’ than in other samples or in the general population or ‘average’. Future studies need to set benchmark criteria against which we can interpret MHLq scores and a MCID for MHLq. This is needed to assess whether or not an intervention such as Young SMILES can lead to a meaningful change in mental health literacy.
Campos et al. 113 identified three predictors of better mental health literacy based on the MHLq: being female, being a teenager (as opposed to being aged < 13 years) and being close to someone with mental illness. We would expect that, on account of having a mentally ill parent, our participating children have better mental health literacy than their peers in the general population. Our sample had more girls than boys, which would act in favour of better mental health literacy. However, the average age in both Young SMILES and TAU groups was < 13 years, and this may have contributed to lower MHLq scores than in Campos et al. ’s sample. 113 Future studies of interventions that aim to improve mental health literacy in children of mentally ill parents need to consider stratification according to the children’s sex and age.
It is worth noting that the MHLq includes items that are relevant to severe mental illness, such as schizophrenia. However, it also refers to other mental illnesses, such as depression and anxiety. A scoping review of all mental health literacy measures136 identified 69 knowledge measures (e.g. assessing ability to recognise mental illness and factual knowledge of terminology, aetiology, diagnosis, prognosis and consequences of mental illness) and 35 help-seeking measures (e.g. assessing help-seeking attitudes, intentions and actual help-seeking behaviours). Despite the plethora of mental health literacy measures, it is not immediately clear which ones are more appropriate for children with severely mentally ill parents, with respect to their content.
A recent literature review of mental health literacy content for children with severely mentally ill parents137 highlighted the need for adding family-contextual content (e.g. dealing with stigma experiences, managing stress and communicating about parental mental illness) to the standard content of mental health literacy that is designed for children in the general population. This suggests that generic mental health literacy measures may not be fit for assessing the utility of an intervention for children with mentally ill parents. Future studies that aim to improve mental health literacy in children with severely mentally ill parents need to use measures that allow the addition of family-contextual content.
In the context of interventions like Young SMILES, whose ultimate aim is to improve QoL, mental health literacy is a mediating variable (i.e. a mechanism by which we expect the intervention to work to produce the desirable outcome). Therefore, not only does the intervention need to bring about meaningful change in MHLq scores, but this change should be positively correlated with a subsequent change in QoL outcomes. Our feasibility study was too small to enable us to explore associations between changes in mental health literacy and changes in QoL. Future studies that seek to explore the mediating effects of mental health literacy on children’s QoL need to estimate the sample size that will enable such a mediational analysis.
Resource utilisation
We noted high completion rates of the resource utilisation questionnaire across all time points (> 90% of all participants). Participants were willing and able to respond to questions from the CA-SUS regarding accommodation, education, hospital service utilisation and community services utilisation. However, of the 27 community services listed in the CA-SUS questionnaire, participants reported no utilisation of nine of these services at all three time points. To minimise participant burden, it may therefore be advisable to remove some or all of these services from the list of community services questions in a future trial.
Outpatient appointments were the most common type of health-care use, with nearly one-third of the parents reporting that their child had attended an outpatient appointment within the previous 6 months. Ambulance use and A&E attendance were also relatively high in our sample. Other than GP appointments and input from a social worker and a family support worker, children were scarcely reported to use any other community or social care services.
Response rates were zero for questions regarding medication prescriptions. They were also very low for questions regarding interactions with the criminal justice system. Given that these categories are important, especially if a future economic evaluation takes a societal rather than just a health and personal social services perspective, for an intervention that is likely to have an impact on resource use in these areas, we will consider alternative methods of data collection in addition to a self-report questionnaire.
Data missingness
Table 22 gives an overview of all missing data for each outcome measure within each group from baseline to the primary end point (4 months).
| Measure | Data missing Young SMILES | Data missing TAU |
|---|---|---|
| PedsQL (child self-report) | 3/18 | 2/15 |
| PedsQL (parent-proxy) | 5/18 | 5/15 |
| KIDSCREEN (child self-report) | All domains (except financial): 3/17 | Physical: 1/13 |
| Financial: 3/16 | Financial: 0/12 | |
| All other domains: 2/14 | ||
| CHU-9D (child self-report) | 3/18 | 1/14 |
| RCADS (child self-report) | 3/17 | 2/14 |
| RCADS (parent-proxy) | 4/18 | 4/15 |
| SDQ (child self-report) | 1/6 | 1/6 |
| SDQ (parent-proxy) | 4/18 | 4/18 |
| MHLq (child self-report) | 3/15 | 2/13 |
| Arnold–O’Leary parenting scale (parent self-report) | 3/17 | 4/15 |
| PSI-SF (parent self-report) | 3/16 | 1/12 |
Chapter 6 Acceptability of intervention: parent and children and young people qualitative studies
The value of qualitative research nested within clinical trials is increasingly acknowledged,138,139 especially when it pertains to complex health-related matters. 140 Rather than being seen as a mere appendage to the main trial, it is often used to explicate a deeper understanding of the perceptions of those delivering and receiving a treatment. In this respect, qualitative research not only forms a crucial part of the trial’s evaluation, but also assists in determining the meaning behind the quantitative findings. 139,141
Two qualitative studies were conducted as part of the Young SMILES trial to explore the views of those who had the opportunity to attend the intervention. The first explored the perceptions of the parents who attended the parent element of the intervention and the second explored the perceptions of the CYP who received the Young SMILES intervention.
Study 1: parent interviews
Methods
Parents were recruited through purposive sampling techniques. All parents (n = 14) allocated to the intervention arm were invited for interview. Maximum variation sampling techniques could not be deployed in this study because our study sample was too small. Between April 2018 and May 2018, the identity of the parents who received the intervention was revealed to the research team, taking place after the collection of the primary outcome measures. The parents were asked to attend a qualitative interview by the researcher in person at their last follow-up data collection meeting.
Consent was gained at trial baseline and information about the qualitative assessment was provided after the collection of the primary outcome measures. The interview took place at a time and venue most convenient to the parents, which was in their homes and in two instances a community centre. Usually only the researcher and the parent were present at the interview, but in two cases the child was present throughout because the parent had no one to look after them. The parent gave written consent before the interview commenced. No field notes were made during or after the interviews. Participation was voluntary and reimbursement was provided in the form of a £10 voucher.
Data collection
A semistructured interview schedule was developed in advance of the interview, which was based on prior knowledge of the research area,6,17,68,76 in addition to evidence gleaned during the modelling phase of the intervention. The schedule was designed with the aim of focusing on particular themes, while permitting the participant to freely raise issues that appertained to these themes. See www.journalslibrary.nihr.ac.uk/programmes/hta/142901/#/documentation (accessed April 2020) for topic guides that informed the structure and content for all qualitative interviews.
The opening section focused on what the parent thought about the trial when they first heard about it. Therein was an exploration of their initial motivations for agreeing to participate, as well as how their awareness of the trial was raised (i.e. via a service, practitioner, advertisement poster, etc.). The parent was then asked whether or not their child wanted to attend the intervention. This question was asked to gain insight into how Young SMILES appealed to children from the parents’ perspective, and whether or not additional motivation to attend was required.
The next section of the interview explored parental experiences in the group. In particular, the parent was questioned about what it was like to discuss parental mental illness with other parents encountering the same difficulties. Perceptions of how facilitators presided over discussions and activities around sensitive themes were also sought, identifying key skills that are required in such instances and whether or not they were demonstrated in sessions by the facilitators. This section of the interview was concluded with a discussion around the perceived benefits and disadvantages of being separated from the children during sessions.
The following section explored the experienced and observable effects of the intervention on the family. The object here was determine not only how Young SMILES helped the parent co-manage their mental illness alongside their parenting responsibilities, but also whether or not the intervention had a demonstrable impact on their children’s QoL. The researcher also asked if Young SMILES made any difficulties worse as a direct or inadvertent result of attending sessions. Whether or not parents disclosed negative remarks about the Young SMILES intervention, each was nonetheless asked what could be done to improve the intervention to help their family.
The parent was then asked how their experiences of receiving an intervention within the confines of a group of other parents compared with more conventional, individualised support. The interview concluded with the parent being asked to provide recommendations on how the intervention could be improved.
A male Young SMILES researcher (Adekeye Kolade), who had lived experience of parental mental illness, and whose qualifications include a master’s degree in research and a postgraduate diploma in counselling and psychotherapy, carried out all interviews. Adekeye Kolade also has experience in qualitative research, gaining informed consent and adhering to the code of conduct stipulated in the SOPs [see www.journalslibrary.nihr.ac.uk/programmes/hta/142901/#/documentation (accessed April 2020)], which ensured compliance with research governance, health and safety, informed assent/consent, transcription services, data management and dealing with potential challenges that emerge within the interview process. The one interview that Adekeye Kolade did not carry out was carried out by Craig Callender, whose qualifications include a Master of Science (MSc) in Psychology. Craig Callender also has experience of clinical settings with vulnerable groups as an assistant psychologist and support worker.
Adekeye Kolade had previously met with the parents during previous recruitment and quantitative data collection visits. Familiarity with the researcher was thought to enhance the interview process given that they had had previous opportunities to build a relationship with the researcher and the researcher was already aware of their circumstances, which eliminated the need to repeat relevant information. Adekeye Kolade informed parents that he was not involved with the delivery of the intervention and that their personal views of the Young SMILES intervention would be used only in an anonymous way. Interviews lasted from 18 to 65 minutes.
An encrypted audio-recording device was used to record parent interviews, which were then transcribed verbatim by an independent transcription company.
Data analysis
Analysis and collection of data were carried out at the same time to allow for the interview schedule to be amended for later interviews in the light of the data collected. Transcripts were subject to thematic analysis,142 commencing before knowledge of the trial’s effects were gained from the quantitative data. Transcripts were read and re-read by three members of the research team: the researcher who conducted the interviews and two other qualitative researchers (PBe and JG). NVivo (QSR International, Warrington, UK) is considered to be the best software for managing qualitative data,143 and was used to transform the qualitative data into codes, thereby ascribing multiple and variegated units of meaning to different parts of each transcribed interview. 142 Codes were then built into themes through a process of consultation.
Theory for analysis
As detailed previously, in Chapter 3, acceptability is a key priority of feasibility studies. Sekhon et al. 117 inductively synthesised the findings from an overview of systematic reviews on acceptability in health-care studies, and subsequently applied methods of deductive reasoning to better theorise the concept of acceptability. This culminated in development of the ‘Theoretical Framework of Acceptability’ (TFA), which presents the following working definition of acceptability that can be operationalised in the service of clinical research:
A multi-faceted construct that reflects the extent to which people delivering or receiving a healthcare intervention consider it to be appropriate, based on anticipated or experienced cognitive and emotional responses to the intervention.
This definition considers the different ways acceptability can be explored (i.e. cognitive and emotional responses), in addition to providing a hypothesis (i.e. cognitive and emotional responses that could affect engagement and adherence outcomes). It comprises seven components, each of which is identified and defined in Table 23.
| Construct | Meaning |
|---|---|
| Intervention coherence | The degree to which the individual understands the intervention |
| Affective attitude | How an individual feels about the intervention |
| Burden | The experienced amount of effort that is required to participate |
| Ethicality | The extent to which the intervention aligns with the values of the individual |
| Opportunity costs | The amount of benefits and values, and values that are sacrificed to participate in the intervention |
| Perceived effectiveness | The perceived likelihood that the intervention will fulfil its purpose |
| Self-efficacy | The participant’s confidence that they have the ability to perform what is required to participate in the intervention |
A key feature of the TFA is its ability to overcome the distinction between prospective and retrospective acceptability, where the component constructs of acceptability can be assessed before, during and after the delivery of the intervention. Constructs often overlap and influence each other and the extent to which they converge and diverge is an empirical question for the researcher. 117
Following open coding using thematic analysis, the TFA was used to assess acceptability of the Young SMILES intervention among parent participants in accordance with the seven constructs of the framework.
Key findings
Demographics of the parents who took part in an interview can be found in Table 24. In total, 14 out of 20 parents who were invited consented to take part. All but one of the participants were mothers, with over two-thirds being aged < 34 years. All parents reported diagnoses of SMI; most experienced comorbid mental health conditions.
| Demographic | Total (N = 14), n |
|---|---|
| Age (years) | |
| 25–34 | 10 |
| 35–44 | 4 |
| Sex | |
| Male | 1 |
| Female | 13 |
| Diagnosisa | |
| Depression | 6 |
| Schizophrenia | 5 |
| Generalised anxiety | 4 |
| PTSD | 3 |
| Bipolar disorder | 3 |
| OCD | 2 |
| Panic disorder | 1 |
Following the open coding of all transcripts, codes were mapped on to the TFA framework. The resulting coding tree can be found in Table 25.
| Component construct | Study themes |
|---|---|
| Intervention coherence |
|
| Affective attitude |
|
| Burden |
|
| Ethicality |
|
| Opportunity costs |
|
| Perceived effectiveness | For child |
|
|
| For parent (unintended outcomes) | |
|
|
| Ineffective because of lack of focus on purpose | |
| Self-efficacy |
|
Intervention coherence
The ways in which parents understood the Young SMILES intervention varied. Some were clearly aware that the aims of the intervention were focused on the impact that their mental health difficulties were having on their children’s QoL; they highlighted the principles of a whole-family approach and how it was different from the support that had been available previously:
I’m hoping that he can take SMILES away with him and like I said before, if his friends are feeling crap and he sees that there are signs of mental health there, that he can go up to his friends and say, look you can get help, you can talk to me and what have you. I think if I was in this generation that we live in now and I was a 10-year-old and I thought my head was going a little bit cuckoo, I’d like to know that there are kids there that do understand and that they are there to help.
W17P17A1
I thought it was really great to start with. Yeah, it was really good because it kind of involves obviously the family. So obviously [child] never had sort of any – I’d call it professional intervention – at all in the past. It’s just been sort of how we try to put it into layman’s terms for her.
N33P01A1
On the other hand, several parents’ expectations were not met as they had anticipated that there would be a specific focus on the problems that they had been experiencing personally as a result of their own mental health condition. For some, the non-alignment of their expectations and experiences left them feeling unfulfilled and unable to perceive a benefit from attending the intervention:
I thought there wasn’t much discussed around mental health by yourselves from an adult’s point of view. It was mainly about sort of ‘how can you help your children?’, which is fair enough but I thought there could have been a bit more adult stuff as well because everyone in that room had some mental health problem where nobody really talked about it. I generally don’t like to tell anybody about my mental health but if I’m in a room with other people and then we’re coming, you know, with their sort of problems it might have been somewhere that I could unburden myself a little bit.
N33P01A1
I wanted help for myself because ideally how am I meant to help [child] if I’m not right myself? I’d be a bit of a hypocrite really, for you to help anybody, regardless of them being your partner, your child, whatever, you need to start on yourself.
W17P17A1
A key misunderstanding among these parents related to the parental aspect of the intervention. Many highlighted that, based on the information provided prior to attending, there were uncertainties about the reasons for attending and the way in which the parental element would be delivered. Based on their lack of awareness and understanding of the intervention, initial apprehensiveness towards attending was apparent:
[I was anxious because] I was going to a group where I wasn’t sure of who’s going to be there, what people are going to think of me, because a lot of my mental health issues is always something to deal with, in regards to what others think of me, whether I’m going to be judged or not.
W17P17A1
The way it was explained to me was, it was a thing for children, and if you wanted to go as a parent, like you were dropping them off, and you wanted to stay or whatever, it was a bit like a nursery, where you can either leave your kid or come back for it. I felt like that was the impression I was given. I could have took her and stayed and left with her, or I could have took her and left her and come back for her, or whatever. You know? And I didn’t realise that there was, I thought it was just like a chitty chatty room for the adults, I didn’t realise there was actually stuff going on.
N07P01A2
Affective attitude
Parents reflected on their motivations behind attending the Young SMILES intervention. Aligned with the aims of the intervention, developing an understanding of the value of equipping their children with an increased awareness of parental mental illness and the benefits that could bring was acknowledged. For many, the Young SMILES intervention was a unique opportunity in comparison with the support their family has previously received focusing more on equipping their children with the knowledge and awareness required to understand the ‘whys and whats’ of their illness:
I wanted him to be able to have an understanding . . . the signs of what to look out for, not even in myself, but say for his peers, amongst him and what have you and even himself . . . I was willing to give it a go and what have you, for the simple reasons, I wanted [my child] to have a bit of an understanding as to why I can be like the way I am.
W17P17A1
Yeah, well it was kind of like a relief, it was kind of like a weight had been lifted off my shoulders because whenever I’ve been in hospital in the past we’ve always told the kids, oh mum’s having her meds changed, and, mum’s having some therapy with the doctors, or, she . . . but we’ve never gone into why and what and, you know, all that.
W16P16A1
In addition to the benefits that the intervention could bring for their children, motivation to attend also concerned the potential gains they saw for themselves:
To get a better understanding of what my depression was, then I think it would be brilliant. So, I was really interested in doing it and I was quite happy when I got there.
W12P12A1
Reflecting on their experiences of attending the Young SMILES intervention, parents generally expressed positive views about how it affected them. The intervention instilled a sense of hope for the future through the recognition of the improvements that they had observed. Most were in favour of the group approach as if facilitated the ability to communicate and connect with other parents in similar situations. The value of having the opportunity to speak to other parents to whom they could relate was valued more than a one-to-one approach with a professional:
Yeah, it was, it was lovely, it was an experience that I won’t forget, hopefully one that I might improve, I might . . . if there’s another group available I might . . . now that I’ve done one group I might . . . yeah, I’ll try another group.
W11P11A1
I’ve visited psychologists and psychiatrists in the past . . . you know, there’ve been nurses and different doctors involved and hospitals involved, and stuff like that, and, you know, you get all these different people around you and you can make your problems seem a lot worse than what they are already, you know? . . . why do I need all these people involved? . . . what’s going on . . . I suffer with paranoia anyway and to have all these kind of people in your life, you know, it can be quite draining and quite scary at times . . . but going to Young SMILES and speaking to the parents there at Young SMILES and the staff at the Young SMILES I felt like my problems were halved, like I belonged there and that I . . . you know, I had . . . I’ve made some good friends and that I wasn’t this psychopath.
W16P16A1
I still find it . . . I’m under therapy at the minute and she does one-to-one on me and I struggle when it’s one-to-one sometimes because I know that she’s picking into me and she’s trying to get an understanding as to what makes me either tick or what makes me upset and things like that. So in a bit of a sense, on a one-to-one, I do keep myself guarded because it’s not necessarily, you’re in a group full of people that are going through pretty much the same stuff as you.
W17P17A1
The welcoming informal atmosphere projected when attending the intervention contributed to parents’ positive evaluation of their involvement:
Yeah, to be honest, it felt . . . the atmosphere when you walk in, when you first walked in, it didn’t feel like I wanted to be there, but like the second time it was more that I wanted to be there and then the third time it was more like a homely feeling . . . It was just in conversation or just generally making a joke, asking if you wanted a brew or coffee or whatever, asking if you wanted fruit and stuff like that.
W11P11A1
Yeah, it was lovely, like the adults and the children, and we were just all joking and mucking about, and it was just lovely: lovely atmosphere.
N29P01A2
Although attitudes to the Young SMILES intervention were generally positive, the group approach was not preferred by all. One parent felt that it led to unprofessionalism among attendees, with individuals failing to act in the ways they should:
I don’t think so much difference. They are working in same criteria but in like a different way, but the doctor and nurses way, it’s more concerned way and more professional way to comparison to Young SMILE. Young SMILE is little bit low . . . Comparison to Young SMILE they are not very professional . . . Like you are very considerate on every single point. I wish that other Young SMILE members follow this rule and regulation that you are working, they have to consider these things. Like every time you come round and you are very polite and normal, you are not very strict, but you are normal and kind and understand everything. So, that’s the main thing.
N18Y01A2
Furthermore, there was a belief that longer and more sessions (similar to those received by their children) would have provided more opportunities to work directly with their children. Moving the focus away from their children, the purpose of the intervention, parents spoke of the benefits of providing more time to help them to overcome initial apprehensions, to develop better-quality relationships and to allow for more dialogue within the parent group:
I think they should be a little bit longer, where parents and the children are more together because there was never really any sessions where it was me and [my child].
W17P17A1
In fact the only negative thing I’ve got to say is that it wasn’t long enough . . . Yeah, because things were just getting going and things we’re just . . . you know, we were just unwinding a little bit more, a little bit more and a little bit more, you know, stuff like that. So, I think another 5 weeks and we would . . . it would have been great, you know, but it finished and then it was like, oh, nothing, you know, got nothing now to do.
N16P16A1
Burden
Parents recognised the efforts that were implemented by the facilitators to ensure ease of participation for them and their children. The opportunity to become familiar and to build relationships with some of the individuals involved in the delivery of Young SMILES prior to the group commencing was valued and considered as a means to enhance their willingness and ability to attend. The importance of relationship building was apparent throughout. Parents appreciated the facilitators’ professionalism and the positive environment that was created as a result of this, reducing burden to participate:
I’d be lying if I say I wasn’t anxious about going to the group and what have you but with [Young SMILES facilitator’s] help, she reassured me to say that pretty much everyone that’s going to be there, are in the same predicament as myself. So she made it a little bit easier to get there, yes, I was willing to give it a go.
W17P17A1
Because she [child] doesn’t like change and she likes to know . . . she likes to build a relationship with someone before she works with them . . . I think [Young SMILES facilitator] was lovely. I think her approach . . . her happy, bubbly personality, I think really took off in the group. She was very easy to talk to and any issues I’ve had outside the group, she’s been fantastic and supportive. I think that’s really good. I like the way she’s communicated with school too. I like the way that whole communication was done in school, thought it was brilliant.
W07P07A1
They [facilitators] respected everybody’s privacy and they respected everybody’s opinion, they were just really, really nice and fair and they were quite . . . they’d go into stuff, questions, in quite depth, some things and they had all the boards, so everything was written down and they would ask everybody a point, and everybody was given answers and suggestions, and everyone was getting it written down.
N29P01A2
However, there were suggestions that forging positive relationships with the facilitators alone did not ensure the acceptability of attending. A number of factors placed specific burdens on many parents. In one site, the arranged transport was, at times, unreliable, which had an impact on the accessibility of getting to the intervention venue and had notable consequences for parents and their children:
When I took him one time because he was playing around with the other kids and stuff but when the taxis were late, he was like, I don’t want to go because he knew he was going to sit in a long taxi ride, get there and then just have to sit in a long taxi ride back, to be honest with you, which isn’t a lot of fun for an 8-year-old.
N17P01A1
It’s too late to send you the taxi . . . [I felt] very, very low and I spent 1 week to recover, because my mental health is like this, if it is bad, even though it’s nothing, even it’s nothing, nothing, if it is bad, I’m not going to get forget for 1 month, why it’s happened like this.
N29P01A1
Anxieties around attending contributed to the reluctance to engage. For some these anxieties could not be overcome, resulting in the inability to attend at all. Other narratives described how such difficulties had been overcome over time by parents exposing themselves to their fears:
I probably wouldn’t have done it . . . due to like anxiety problems and being in like big crowds and stuff like that, I don’t like big crowds.
W11P11A1
At the beginning I’d be very reluctant, yeah, because I’d be . . . I’d panic about it and I’d think . . . I’d just think, oh no, no, no, but once we’d signed up and with the kids got through to the . . . I don’t know, the final however many it was then I thought, oh well, you know, we . . . it’s gone this far now so I’ll have to attend it. So, yeah.
W16P16A1
For one parent the burden of attending the Young SMILES intervention prevailed. The attendance of their children continued because of the perceived pressures being placed on them:
Because [my children] wanted me to [attend] and the NSPCC were putting quite a bit of pressure on to go as well, yeah . . . I felt really under pressure, because the [my children] weren’t going to go to the last session either, because school were a bit funny about them having time off. Because it’s coming up to their SATs [Standard Assessment Tests] and basically the NSPCC said we’re not having that and they rang the school and said, look, you’ve referred them, they’re coming, we’re having this party, you’re all coming, aren’t you? And I was, like, I felt I had to agree with them.
W01P01A1
A lack of attention and sensitivity to the cultural needs of families was observed by one parent. One participant reported that there was insufficient suitable food and that, as the only participant whose first language was not English, they did not have enough time to contribute to group discussions, leading to a negative experience:
Like when they offering a food and when they start the group they said, we’ll have a Halal food, but Halal food is very small amount.
N18P01A2
English is not my first language but I was . . . I’m . . . when I was in group I was very brave, still determined to talk to in Urdu . . . in English and still determined to give the sufficient answer, but they just step in, next, next, next . . . For example, if I am expecting from you that that’s the Urdu group and you have to talk in Urdu, stay in Urdu, that time I have to consider.
N18P01A2
Ethicality
The Young SMILES intervention was significantly aligned with parents’ value systems. They expressed a need for their children to have valuable ‘child time’, something many felt was lacking currently as a direct result of their mental illness. Separation of the child and parent sessions was valued and considered as having a positive influence on their child’s well-being and ability to normalise their personal circumstances. Personally, it provided an opportunity to be relieved of their parental responsibilities within an environment where they could express their thoughts, feelings and experiences without a child ‘clinging to their side’ (N22P01A1) and the fear of how their children would react:
I’ve never really had the opportunity. I’ve never really had much interest in doing a group myself, but the kids, I didn’t know there were groups available for . . . that would teach them about mental health, and stuff like that. So, you know, I didn’t know there were those sort of things out there for young kids. So, when it popped up at the school I was . . . I felt, yeah, that sounds good, yeah.
W16P16A1
I think it was nice because, I think, that if my kids had been sat in with me, in this group . . . you know, like when they used to ask about your feelings . . . well, name some things about [child] . . . I don’t think I could have sat there and read a list of things off about [child] in front of her. I don’t think I could have been as open as I was about my feelings in front of the kids, because I would have thought to myself, it’s not fair lumping them with all this.
W12P12A1
Although the value of separation was consistently reported, parents emphasised the desire to spend more valuable time with their children. They saw the role Young SMILES could play as a means of facilitating this:
I think the group, would have been nice if maybe it alternated, maybe 1 week separated, 1 week together, I think that would be maybe a good way of doing it.
N17P01A1
Yes, it wasn’t . . . yeah, a group thing. So I did enjoy that; but I was upset that we didn’t do any activities with my son. Yeah, that was the only thing that I would have liked to have been doing then, even if it wasn’t every week; just 1 week or 2 weeks, you know, out of the however many weeks it is, just to do something with him.
N29P01A2
The group provided a space that was positively evaluated in comparison with previous support. However, a conflict of patient versus patient narrative was apparent. In referring to what they gained from the intervention, most gains were identified as being unintended outcomes:
I know you can speak to counsellors, but I didn’t really feel comfortable speaking to a counsellor. I don’t know . . . I couldn’t tell you why, just didn’t . . . in my head, I just didn’t want to speak to a counsellor. But, then [referrer] was going on about all this and I thought, well give it a try. Because, I was at first, because I thought, oh, here we go again, [child] put me on another of these . . . trying to get me on this course.
W12P12A1
I do feel a lot better, but . . . about the judging . . . but being in that group, it was like, I can just say what I want and everyone would agree with you. They were like . . . because I said at one point, I said I used to feel awful crying and people just saying, right, I had nothing wrong with me and I was just attention-seeking. They were all like, no, no. She said . . . one of the ladies said, yes some people used to say that to me. She said it used to really upset me. I said, yes it did me, I said, but now I know . . . I said, because I’m sat here with you, all you people, I said I know that it’s not just me in the world. Which I knew it wasn’t, but it was just nice meeting these people.
W12P12A1
Recognition of such outcomes was identified as being unaligned with the values placed on reasons for attending:
I thought it was to see the mental health through my child’s eyes, I didn’t think I was there to gain self-confidence myself.
W01P01A1
The environment in which the intervention was delivered was considered an important factor in parental evaluation. Contrasting views were identified between parents across the different sites utilising different spaces:
It was the [Young SMILES venue] and it was a lovely place and it was . . . wasn’t surgical, like I said. It was like sofas and cushions and everything was just nicely planned out and everything was smooth and everything ran lovely.
W16P16A1
The hospital grounds itself is so big, so obviously it’s not like in the unit where people are, or just sort of be in residence, I guess is the best way to put it. But yeah, being on that site I was like, OK [laugh], this might be a bit difficult. But I guess after the first couple of sessions anxiety lessened, shall we say.
N33P01A1
Opportunity costs
A noticeably small number of issues were raised with respect to what personal values parents felt conflicted with the intervention. The fundamental concern expressed highlighted tensions between themselves and their children due to beliefs about the perceived difficulty attending. These issues were not necessarily developed as a direct result of the intervention:
It’s just not my thing at all. And I just feel like, rather than going, and either upsetting myself or somebody else, in turn, either embarrassing or upsetting [child], I thought it was probably best for us just for us not to go . . . After the first couple of weeks, I did feel a bit bad, but then after the first couple of weeks she was like, it’s not like they’re sitting in a gang. I think the last week she was a bit like, nobody was there for me, which I felt a bit bad, but I was just like, I don’t know, I feel like [child] can be more [child], when I’m not there . . . I don’t think it changed our relationship. She always says this, I don’t show very much enthusiasm for what she’d done.
N07Y01A2
Assessments prior to attending were regarded as too invasive and not family centred, contributing to a feeling of losing control:
But they kept coming out and they did a lot of, like, interviews in the beginning, like, screening things and that really opened a lot of worms for me and led to a decrease in my mental health and then they really got involved and were really pushy and, as I say, they rang the safeguarding people twice.
W01P01A1
The focus on the impact that parental mental illness had on children did not align with all belief systems, resulting in dissatisfaction:
[Young SMILES] points to my mental health damaging them and the whole thing seemed to centralise around my mental health damaging them.
W01P01A1
Perceived effectiveness
Perceptions of effectiveness following attendance were aligned with the principal aims of Young SMILES. Narratives highlighted the acknowledgement of specific improvements gained by their children. Post-intervention improvements in children’s well-being and behaviour were noted. Gaining insight into parental mental illness and improving mental health literacy was believed to be a key driver of the outcomes observed:
Yeah, because it’s helped him cope with his . . . what am I looking for . . . his anger issues, it’s helped him cope with that a little bit as well, so he’s not just coming home and just bursting basically into the monstrous child. He’s calming himself down, he’s going upstairs, he’s sitting on the stairs, he’ll play on his phone and then he’ll come down, if he’s had a bad day. If he’s had a good day he’ll just come in and then make jokes and things.
W11P11A1
I thought it’d be beneficial to the kids because they didn’t have any knowledge about me and my mental health, and stuff like that, and obviously I have days when I’m not myself and I have days when I’m alright. The days that . . . when I’m not myself, you know, the kids can be quite confused as to what’s going on and I just thought that it’d be good for them to have a bit of an insight into other people’s mental health disorders, and stuff, and they looked at it as some sort of disability. They thought if you had mental health you had an arm missing, or something like that. So, they were totally unaware of everything that goes on with mental health and issues, and stuff. So, I just thought that they’d benefit from it greatly . . . So, they’ve been quite sheltered from it, from my whole mental health side of me . . . So, then, you know, they had a bit more of an understanding about me and about my ways and certain things that I do and, you know, stuff like that. So, yeah, it was kind of like a relief really.
W16P16A1
Consequently, positive changes on the family environment, family relationships and cohesion were reported, specifically easing existing family tensions:
I think he was a bit better after Young SMILES, he was a bit more understanding and a bit more helpful, caring really, he understood a bit better, but I don’t know what was said to him because I haven’t had a conversation with him, about what went on in the group, just little things and I’m not going to.
N17P01A1
Yeah, I’d say it has helped my family. The kids definitely have a better understanding of me when I’m having a bad day, low day, you know, and stuff like that, and just say, don’t worry, mum, we’ll help you do this, we’ll help you through this. And, you know, they seem to know a lot more what’s going on and, you know, stuff like that. So, we . . . they . . . like if I’m getting worked up [children] will say, are you getting stressed, mum, are you a bit stressed; do you want me to make you a coffee, mum; are you alright, mum? And the . . . yeah, they’re just . . . yeah, they understand me a lot better.
W16P16A1
Parental and child respite was valued and contributed meaningfully to alleviating the pressures families faced:
I think it’s because it takes the pressure off you, and your child. Because your child is having, actually, a break, you’re having a mental break from it. And probably, that helps considerably, for me, anyway. Because it’s just chaos in my brain, like, when I’ve got, I’ve got to think for everybody, apart from [child], because she’s very, she knows what she’s doing anyway. But I’ve got to think for [child], half the time, his memory is getting worse, actually, you might have to repeat a bit.
N29P02A1
Despite recognition of the positive effects Young SMILES had upon their children and, subsequently, at a family level, the focus predominantly addressed gains from a personal perspective. Such outcomes were unintended and were not aligned with the aims of the intervention. The outcomes that were reported varied. The Young SMILES intervention created a normalising, supportive, safe space acting as a platform to discuss experiences and emotions. Many reported how this led to a reduction in the severity of their emotional and mental health symptoms:
It was nice to know that it wasn’t just me feeling sad, depressed, upset and feeling like you strangle your kids at times. Because it . . . there were some times when I was really low, when I thought to myself, right kids, I could strangle you.
W12P12A1
Well, it’s not nice to know that somebody else is suffering the same way like you do, but on the other hand, I was pleased that I wasn’t the only one.
N29P01A2
Yeah, well it was kind of like a relief, it was kind of like a weight had been lifted off my shoulders because whenever I’ve been in hospital in the past we’ve always told the kids, oh mum’s having her meds changed, and, mum’s having some therapy with the doctors, or, she . . . but we’ve never gone into why and what and, you know, all that . . . And so, it was kind of like a bit of a relief for the kids to be learning about it.
W16P16A1
It has helped, it’s got me out of a bit of a black hole, it’s got me out of the house and just pretty much trying to do things that are not necessarily, not that I’ve not wanted to do them, it’s just that I’ve not had the kick up the arse that I’ve needed.
W17P17A1
Being around similar others resulted in the reappraisal of their own life circumstances and experiences, resulting in a reduction of self-criticism, negative mood, and feelings of guilt, isolation and failure:
I felt quite lucky and I’d sometimes walk into the group feeling really down and really sad and really alone and really isolated and then I’d look at the group and think, hang on, yes, I’m like this but my life is really not that bad, even though I’ve lost all these people and I’ve been through the mill, I just don’t tend to feel sorry for myself as much . . . it’s good to know that people are in the same boat as you and it’s good to know that they criticise yourself as a parent and feel guilty because you can’t do things that other parents do . . . It’s made me feel less guilty and there’s a bit more discipline put in place, to be honest with you.
N17P01A1
That was comforting to know that other people were . . . and listening to how they spoke about their children and how their children behave at home, gave me some comfort that I’m not the only one who experiences difficulties and there were other single parents as well, which was good as well to know that you’re not alone.
W01P01A1
I would say, because it gives you all a mental break. And it makes you realise you’re not failing as a parent . . . Yes, I thought I was the only person going through this, and I do get a bit paranoid when I go out. I think people are looking at me and seeing.
N29P01A2
Recognition of outcomes extended beyond those achieved personally to those gained by other members of the group:
It was just nice being sat with other people like that, you know, in the . . . We had the support there as well, because [Young SMILES facilitator] used to say, if you’ve ever got any problems, just ring me and things like that, if you’re feeling down. It was just nice to have that in the group. We used to like recap, before we started the work for that day, what we’d all been doing in the week and how we’d been feeling. It was strange for the first week, up until like the last week, everyone say, oh I’ve been a bit down and then it was like, by the last weekend, we were saying, oh I’m feeling a lot better.
W12P12A1
Collegiality among parent group members was observable. Sharing information and advice in a group setting had noticeable benefits on a personal level and had a considerable impact upon the ability to form positive relationships with others, something parents identified as being very difficult in day-to-day life:
Just like people giving ideas about how to . . . when you were feeling a bit down and you talked to someone and . . . things like that. It’s just . . . like advise some of the people and it felt great, without someone actually saying, you’ve got to do this. It . . . well as I say, it felt like advice, it was just . . . useful information for me to take in.
W12P12A1
I really don’t know. I just say it’s . . . I think a problem shared is a problem halved and I think with them telling me their stories as well as me sharing mine own and, you know, stuff like that, I think it’s a lot easier than going in and just, you know, like telling the psychiatrist what’s been going on and what’s been happening . . . Yeah, I’m friends with them on Facebook [Facebook, Inc., Menlo Park, CA, USA] now, so I’m going to keep in contact and, you know, maybe meet up one day, or something, in town for a coffee . . . It’s really, really good. I’m made up, you know, because, like I say, me and the girls got really close, you know, and sharing our stories, and stuff like that, with each other and our personal experiences, and stuff like that.
W16P16A1
You get to know the like friendships and things, which I don’t really do easily, so . . . yeah, I’d say, I’d advise other people to do it.
W11P11A1
Some narratives differed where negative perspectives regarding outcomes were a major factor. Affiliated with the primary focus of the intervention being on improving the QoL of their children, session work was perceived as being ‘sugar-coated’ with lack of focus on developing an understanding of their children’s experiences:
That’s what it’s about, it’s about raising awareness of the impact that mental health is having on your children. I don’t think I’ve learnt anything. What was discussed with the other parents, I don’t think they would have learnt anything, because it was discussed as a group and they never said, this is how it affects them. I feel like the parents are put a bit more first, than the children. I feel like they were putting our feelings before the kids and I think they were scared of upsetting us, at what the children had mentioned about mental health. I think it should have been a bit more . . . I don’t know whether [my child] did mention anything, or whether she didn’t. But, I know I have bad days and I know it does affect the kids, not in a bad way, but I know that [my child] knows when I’ve got no energy and I just want to chill. But, I don’t know how that affects [my child] and that was what I wanted out of it.
W07P07A1
I thought it [attendance] was to see the mental health through my child’s eyes, I didn’t think I was there to gain self-confidence myself.
W01P01A1
Self-efficacy
Prior to attending Young SMILES, feelings of apprehension were prevalent. Via retrospective evaluation, for most carers, their confidence grew and initial beliefs about their ability to participate were overcome. The non-judgemental approach of facilitators and other group members was welcomed and the atmosphere was compared positively with previous support experienced, enhancing people’s ability to participate:
She said, just try it, [child]. I’m glad I did now, I’m glad that I just overcome that little bit of fear, because if I hadn’t, I would have just been, probably still moaning and crying and . . . but it has, it boosted my confidence a lot. That’s only been like over 5 weeks.
W12P12A1
We all said we all felt a bit apprehensive at first, but once we’d all met it was brilliant. So, I just loved it, being in that group, after that . . . I just loved it. I just loved being in the group and be able to talk to people. I was actually looking forward to my next week . . . not to be judged and just to be in a nice group and feel relaxed and . . . it was just like being sat at home . . . It felt like it . . . I used to love Thursday mornings, waiting for the minibus. It’s stupid. I used to get excited Wednesday night, oh Young SMILES tomorrow!
W12P12A1
Because they weren’t being judgemental or anything at all, they were listening to everybody’s opinions and everybody’s comments and there was no judgemental feedback or any comments back, why they were condemning you, whether what you said was good or bad, there was no, kind of, it was lovely, there was no animosity or no bad feeling at all, there.
N17P01A1
And the people that run the group, the women, the ones who were there, I spoke better with them than I have done with my husband and my psychologist, my psychiatrist. And so, I felt that that was really beneficial to me because, you know, it wasn’t . . . they didn’t make a big deal out of mental health. It wasn’t like an explosion. It . . . you know, it was just a subtle and dead . . . the way they did it was really heart-warming kind of thing and made you feel normal . . . You know, they weren’t patronising or they weren’t . . . you know, they weren’t judgemental, or anything like that. They were just lovely women, and men. There was a man there as well and they were all lovely. And as soon as I’d seen that they were lovely with the kids and the way they were with the kids, they were dead gentle and dead encouraging and, you know . . . and stuff like that. So, I felt safe around them, so I carried on with the sessions.
W16P16A1
Although parents considered themselves as on a ‘level playing field’ with others, the distinctive role of the facilitator stood out as a valuable part of enhancing their participation:
There was a lady called [Young SMILES facilitator]. She was lovely. She was like a mother to you and she made you feel really relaxed and really comfortable and she got everything that you needed, she did everything for you, you know, and she was . . . nothing was too much for her and she ran it really well. She . . . you know, she was a lovely . . . really, really nice person. They were all really nice people and there were no issues with any of them.
W16P16A1
Drawing on the perceived strengths of other parents in the group, such as braveness, overcoming/addressing adversities and vulnerabilities acted as a catalyst for their participation and continued attendance. The environment free of hierarchies or ascribed group roles further enhanced parental ability to identify themselves as a significant member of the group and to approach others embracing the development of a ‘new family’:
They are still parent, they are still coming in group, they are still laughing. So, one woman was laughing a lot with mental health. She’s quite middle age, like she’s kind of aunty, but when I was observing her and I learn that she’s brave . . . they discuss how they act, what is their strategy, how they use their family, friends when they’re feeling now and they say, yes, we need share with some friend who are understand and when we feeling horrible they help and support somebody at least here for us.
N18P01A1
Just because they were sharing their same experiences as me and I could see their vulnerability and it just made me feel relaxed and . . . yeah, just relaxed, I mean comfortable to talk to them, and stuff like that . . . you know, open my heart to them and they were all experiencing the same thing as me and they knew exactly where I was coming from and they were giving me advice, they give me love, they give me sympathy, they give me encouragement . . . give me everything that I needed . . . that made me feel, you know, touched . . . there were a couple of other ladies there who were . . . wouldn’t speak much and they were quite withdrawn . . . and I suppose I was the same, but as soon as we started talking and the group opened up more and, you know, we started telling our stories, and stuff like that, and we just became like a little group, little unit.
W16P16A1
Development of and participation in a collegial group was enhanced by the small group size, allowing everyone to participate:
We were kind of really lucky in a way because we did have a small group, so it did work really well in that sort of aspect. That sometimes people get scared by big groups so it could be very intimidating sometimes, but there was possibly four families that were there every, like every week. And obviously when the parent side of it kicked in, everyone was chipping in so there was nobody that was like . . . felt like they couldn’t speak out. So it seemed to work really well. And obviously you got a spin on everybody else’s, not life, but the way they deal with things, the way they explain things. And obviously everyone disagrees and agrees with some things.
N33P01A1
There was only four of us . . . It was only a small group. I don’t know how I’d cope in a bigger group, but that was like a start for me.
W12P12A1
Autonomy within the group was valued and respected, as it allowed parents to speak about what they had experienced when they wanted to without feeling that they were wasting valuable time and reduced the anxieties of those who wanted to participate minimally. Confidence to speak up was facilitated by the group environment, which allowed parents to open up about their experiences without fear of negative consequences. This subsequently led to altered beliefs about their self-worth and abilities to draw on their own experiences to help others:
I mean I know doctors, GPs, they’re all trained for all this, but it’s sometimes . . . talking to your GP, it’s not the same because you can tell they’re busy and they’re trying to get . . . they’re rushing you. But in this group, it wasn’t like that. If you wanted to talk, just talk and . . . but it was really useful and helpful and it has, it’s . . . I’d write it across the sky, I loved it.’
W12P12A1
Even if you put . . . it’s like I thought I’d asked a stupid question . . . I can’t remember what it was . . . one of the other girls went, I was thinking that but I thought . . . because I said, I think it’s a really stupid question and like [Young SMILES facilitator]’s like, no, no. One of the other girls pipes up, she went, I was going to say that but I felt stupid saying it. I said, yes, I did, but it was one of those things that I needed to get off my chest. I thought, is it going to sound like a stupid question or not. Like, I can’t even remember what it was I asked, but I must have sat there for about twenty minutes tapping my fingers, shall I say . . . and I thought, go on, bite the bullet, just say it, no one . . . laughed, laughed with them. Not laughing at you, laughing with you. It was . . . no it . . . I just felt good, talking to other people.
W12P12A1
[Young SMILES facilitators] seemed very, very pleased that I was actually coming up with a lot of ideas, so they could spur the rest of the group . . . Being recognised as a human being, I suppose. And kind of like, having good ideas, and being able to help others.
N29P02A1
Positive experiences and feeling part of a reciprocal group, however, were not present in all narratives. Disappointment by lack of meaningful conversations about personal experiences left some parents feeling isolated, like ‘a stranger at a bus stop’ (N29P01A1), whereas others felt frustration with their experience of being in a group with parents who did not contribute:
Yeah, because there’s no . . . within a group sort of situation you would expect to know a bit more about each other. Like somebody, like a chair[person] or a facilitator, or whatever you want to call it, to encourage those . . . the relationships to kind of form.
N29P01A1
I was one that spoke more. The others were quite reserved, I was quite open about situations and certain scenarios that I’d dealt with in the past and that. A lot of them didn’t speak, but I . . . I’m quite open anyway, I will tell you what . . . anything, so . . . I don’t know whether that would be beneficial to others, but it was for me . . . I’d say something and [Young SMILES facilitator] would say, do you find that? They’d just be like, no or yes and it was too quiet. Two of them were just like, no and the other one would be like, yes, but then would explain something. But, no one really spoke anything else, half of it was mainly me.
W07P07A1
Study 2: children and young people interviews
Methods
Purposive sampling was used in this study. Only those allocated to the intervention arm were invited for interview (n = 24). Between April 2018 and May 2018, the researcher was unblinded as to which children were allocated to the intervention. This took place immediately after the primary outcome measures were collected. The participants who received the intervention were invited to attend a qualitative interview by the researcher in person.
Consent was gained at trial baseline for the research team to make subsequent contact regarding additional research opportunities. Invitation letters and study information sheets were handed to the child and parent by the researcher after the primary outcome measures had been collected. This was to ensure that the researcher remained blind while collecting these measures. A time and venue for the interview was then agreed on, which was in the participant’s home or school. All interviews were conducted with the child alone except in one case where the parent was present because she did not have anywhere else to go during the interview as all other rooms in her house were occupied. Written assent was provided by the children at the time of the face-to-face interview. The parent also gave written consent before the researcher interviewed their child. No field notes were made during or after the interview. Although participation was voluntary, reimbursement was offered to each participant in the form of a £10 voucher.
Data collection
A semistructured interview schedule was developed in advance of the interview, which was based on prior knowledge of the research area, in addition to evidence collated and discussions held with key stakeholders (including CYP) during the initial development phase of the intervention. The schedule was designed with the aim of focusing on particular themes, while permitting the participant to freely raise issues that appertained to these themes.
Age-appropriate language was used to frame open-ended questions to the CYP. The opening section covered aspects related to CYP’s initial thoughts and feelings about the trial, whether or not they wanted to go, and what their original motivations were in deciding to attend. The CYP were then asked questions about their experiences of being part of a group with other children, as well as their relationship with the facilitators. The researcher then asked about the CYP’s favourite/least favourite activities, and then encouraged the CYP to speak about the reasons behind their view. Thereafter, the CYP was asked about their experience of their parent also attending sessions.
The interview then moved on to how the Young SMILES intervention differed from previous support the CYP had received, which was followed by questions about whether or not the trial helped with any difficulties that afflicted the participant’s QoL. The CYP was then asked about which areas of the Young SMILES intervention could be improved to make the intervention better, if there were any at all. The interview was concluded after the researcher gained insight into what the CYP would say to someone who is thinking about attending the Young SMILES intervention.
All interviews were carried out by a male Young SMILES researcher (Adekeye Kolade), who had lived experience of parental mental illness, and whose qualifications include a master’s degree in research and a postgraduate diploma in counselling and psychotherapy. Adekeye Kolade also has experience in qualitative research, gaining informed consent and adhered to the code of conduct stipulated in the SOPs as detailed previously [see www.journalslibrary.nihr.ac.uk/programmes/hta/142901/#/documentation (accessed April 2020)]. The one interview that Adekeye Kolade did not carry out was carried out by Craig Callender, whose qualifications include a MSc in Psychology. Craig Callender also has experience of clinical settings with vulnerable groups as an assistant psychologist and support worker.
Adekeye Kolade had previously met with the children during previous recruitment and quantitative data collection visits. Familiarity with the researcher was thought to enhance the interview process given that they had had previous opportunities to build a relationship with the researcher and the researcher was already aware of their circumstances, which eliminated the need to repeat relevant information. Adekeye Kolade informed CYP that he was not involved with the delivery of the intervention and that their personal views of the Young SMILES intervention would be used only in an anonymous way. Interviews lasted from 16 to 54 minutes.
An encrypted audio-recording device was used to record CYP interviews, which were then transcribed verbatim by an independent transcription company.
Data analysis
Data analysis mirrored the approach adopted for the parent interviews, detailed previously. Transcripts were read and re-read by three members of the research team – the researcher who conducted the interviews and two other qualitative researchers (PBe and JG). The TFA was similarly used to assess the acceptability of the Young SMILES intervention among CYP in accordance with the seven constructs of the framework: affective attitude, burden, perceived effectiveness, ethicality, intervention coherence, opportunity costs, and self-efficacy (see Table 27). To maximise data collection and sample recruitment, the analysis of the interview data did not distinguish between the index child and other siblings in families where more than one sibling had attended the intervention.
Key findings
Demographics of the CYP who took part in an interview can be found in Table 26. In total, 17 out of 24 CYP who were invited consented to take part. Relatively similar numbers of girls and boys took part. Although different age groups were represented, the majority of the CYP were aged 8–10 years.
| Demographic | Total (N = 17), n |
|---|---|
| Age (years) | |
| 7 | 2 |
| 8–10 | 9 |
| 11–12 | 4 |
| ≥ 13 | 2 |
| Sex | |
| Male | 9 |
| Female | 8 |
Codes were mapped on to the TDF framework, the results of which can be found on the coding tree seen in Table 27.
| Component construct | Study themes |
|---|---|
| Intervention coherence |
|
| Affective attitude |
|
| Burden |
|
| Ethicality |
|
| Opportunity costs |
|
| Perceived effectiveness |
|
| Self-efficacy |
|
Intervention coherence
There was a general sense of uncertainty about what participation for CYP and their parents would involve. Drawing on knowledge and awareness of other support group approaches and comparing with school experiences contributed to initial expectations. Some narratives highlighted an inability to distinguish between perceptions of participation in the trial procedures and intervention sessions and activities, leading to a negative outlook on participating:
I didn’t really have that much of an idea of what it would be like. I thought it would just generally be about like, I thought it would kind of be like a group counselling session and I haven’t done that before.
N07Y01A2
I thought it would be like there would be a lot of little babies there, and like just little kids running around . . . because I went to Little Stars [children’s centre] when I was young and there were a lot of babies there, so I thought it would be like that.
W16Y20A1
I didn’t actually feel like it was going to be good like with all the snacks and all the fun stuff. I thought it was just going to be filling forms and in doing work.
N17Y01A1
Provision of information from referrers prior to attending reduced preconceived negative perceptions of attending and expected outcomes; however, this failed to fully alleviate the concerns of some:
I knew that it was something to help children like stop what they . . . stop their worries about their parents and things. And it could actually help them if they are really worried, but I also thought it would be scary because it’s a bit . . . especially learning new things, how to do it and stuff and meeting new people, but it’s sometimes a bit worrying for me.
N33Y01A1
Recognition of the aim to improve mental health literacy, provide respite and identify support mechanisms outside Young SMILES was aligned with perceived needs:
Well, now I know more ideas of how to help my parents or get rid of some of my worries . . . basically like if I feel sad about something I can just write it down on a piece of paper or in my notepad.
N29Y01A1
Well because it teaches you and it’s a bit of fun because you have a break where you can talk or laugh.
W17Y22A1
I thought I might have like been able to learn about stuff and why my mam does stuff she does.
N29Y01A2
Expectations were at a discord however for some, with particular reference to the extent to which parental mental health issues and the impact that they have on children were discussed:
I was expecting to be talking about mental health and airing and how it might affect them and then how it might affect me and everybody else there, so maybe talk about things . . . It surprised me [that it wasn’t discussed] because I thought that was what the group was about.
W01Y01A1
The eldest member of one group further highlighted that not only was learning about parental mental illness not addressed satisfactorily, but when it was addressed it was done so at inappropriate times:
But it feels like, OK, everybody’s in the room with the same issue that we’re just not really going to address for a little bit. And then we’ll just jump in; OK, everybody is going to talk about this really personal issue, and it was a bit like, especially if people aren’t that comfortable in groups anyway and if people aren’t comfortable talking, generally it just felt a bit inappropriate.
N07Y01A1
Affective attitude
Enthusiasm about attending the Young SMILES intervention was abundant among children, who were motivated to attend in view of their own personal situations. Views aligned with the prospect of having the opportunity to speak about their parent’s difficulties and to improve their mental health literacy:
I’m always worrying about my mum and what might happen. It makes me like so, so worried about her that I start crying for some reason with how worried I am.
N33Y01A
I know how it feels because my mum can’t sleep and I just want to know what it is called, what her problems are called.
W16Y21A1
Meeting new people during their attendance, providing an environment in which their experiences were normalised and was distinctively different from a school approach, was a fundamental factor contributing to their opinion of the intervention and interest in attending:
It was exciting to talk about something private and if I didn’t want to talk about anything, to anyone else and getting to know new people and learning new things about people that have . . . some people that have mental illness.
N18Y01A1
And like in a way it was like, I know it’s not true, but you know when people are, it’s like all people have got it worse so you shouldn’t feel bad. And that’s not true but it kind of did make us feel like that but then it was like you’re in the same boat. Do you know what I mean, so like everybody’s going through, so that if I just walked past them in the street I would have no clue. Do you know what I mean? It was like everybody’s going through something. And obviously there’s just so many different ways of dealing with it. So the way I deal with things isn’t necessarily a bad way, it’s just how it is.
N07Y01A2
Young SMILES is more fun, school is weird. School is just more education.
W17Y22A1
Narratives, however, also reflected on the barriers and emotional responses to attending. Many were negative and some related specifically to the intervention content and delivery mechanisms. Others highlighted a tension between parental needs and children’s desire to attend and vice versa:
Just sometimes I find it hard to make new friends and stuff.
N29Y01A1
A little bit worried, a little bit grumpy, and a little bit . . . and I thought it was going to be very, very, very, very, very quiet . . . but then my mum said we’ll have to go on Tuesday.
N17Y01A1
Well, I don’t know. It was just a bit awkward for me but again, as I said, like I understood that that’s not her thing and that’s fine. If I felt pressured, like if I felt uncomfortable going and I was forced to go I wouldn’t like it, so it’s totally understandable. But it was just, obviously whenever I came in like by myself it really was like, you know, like looked like sympathetic and I was kind of like, do you know what I mean? . . . I think it would have been a lot more beneficial if my mum did come because she could even, even if she just reflected, obviously I’m not totally sure what they did in the parent groups but if she even reflected on that and I didn’t reflect from that there would have been, she could have applied what she learned in the household instead of me just, one-sided, do you know what I mean?
N07Y01A2
Burden
Attendance at the Young SMILES intervention sessions was affected by accessibility issues. Getting to and from the venue was an important aspect of children’s experiences. Taxis arranged on behalf of families were viewed negatively and directly affected attendance, while venue accessibility for parents caused worry for children. Some took on the responsibility of ensuring that their parent successfully navigated obstacles, whereas other narratives described the negative impact of their parents’ experience:
They’re [taxis] just unpredictable because sometimes they took like half an hour to turn up . . . just made me like not want to go as much.
N29Y01A1
I said, do you have an elevator but they said no . . . So, I was staying behind mum in case she fell and she’d land on me.
W16Y20A1
I felt sorry for my mum because, like, when we were walking upstairs, it was hard for her, and like she had to put one foot on one step and then her foot on the same one, and then keep doing that, and she was, like, in the middle and there were like two parents behind her. And it sort of made me feel sorry for her.
W16Y21A1
Alienation was also apparent when accommodating learning styles of younger group members, which came at the cost of intellectually challenging older attendees:
Because you have to work along with other people and then some people get like a higher perspective of what mental health is and then the other people don’t really understand it. So then it kind of makes it . . . I think the people who didn’t really understand mental health should go out on a one-to-one, but people who they can understand it stay, yeah.
W01Y01A1
Ethicality
Trust played a vital role in children’s acceptability of the intervention. The Young SMILES model enhanced opportunities to meet people and develop trusting relationships. Being surrounded by other children with similar experiences of adversity accelerated the ability to trust. Underpinning their ability to trust was individuals’ ability to respect the confidential nature of group discussions:
‘Cause your like you’ve met them before the group and it . . . like, and then you knew them . . . ‘cause, like, you knew, like, when you went in they were, like, you knew them and you could trust them.
W01Y02A1
Well, some of the people in my class don’t know what I mean by those problems and don’t understand it but in Young SMILES most of them do and they experience it themselves.
N29Y01A1
Because it’s like a group and because I got to know the group and I knew that it was an own thing, a personal thing, you can talk, and I knew that it wasn’t . . . it’s not going to go out wide, loads of people are not going to know and that’s when I knew I could talk.
N18Y02A1
The intervention approach was unique for many, in comparison with previous support. Having the opportunity to spend time with parents was valued and regarded as significant in terms of outcome. It was notable, however, that opportunities to be more autonomous and to experience respite in an environment absent of parental mental illness contributed to positive experiences:
Because you get to spend time with them and I don’t really do that.
W11Y15A1
Sort of better because you won’t always be hugging your mum and stuff like that, and like you won’t always be just staying with your parents, you just feel like playing with other people.
W16Y20A1
It was kind of good because mum wouldn’t be there and she wouldn’t be seeing the stuff that we said. Not saying that in a bad way but like, she would just go ‘don’t say that’.
W16Y21A1
The informal, relaxing environment was essential. Facilitators were vital driving forces in ensuring this. Children responded positively to the laidback, outgoing style they displayed, comparing it positively with previous encounters with professionals, and describing it as meeting needs and expectations to a greater extent:
Yeah because they’re not strict and they are fun, they’re not like a party pooper . . . because they’re like fun and they’re helpful when you need it.
W07Y10A1
She was funny . . . and like making the atmosphere happy . . . with all her funny jokes.
W01Y02A1
We do learning if we ask someone in Young SMILES. If we ask the doctor, we don’t do it, they don’t show us and if we ask a teacher, they won’t show us. So, it’s different to Young SMILES because Young SMILES will show us but a teacher and a doctor or a nurse, will tell us but Young SMILES will show us . . . Like they would draw it show us it on a picture or something . . . It was better seeing it because you could understand more but if you hear it, you won’t understand it more.
W12Y17A1
They would explain what to do, they would give us some information, they would let us draw, they would let us go out and have some fresh air and I just think they were a really big help . . . They helped with my mum’s anger, they helped with me learn about more stuff, and helping other kids and they were caring for us.
W16Y21A1
Having fun and making new friends was a key meaningful element of the intervention. Children reported that the activities they took part in enhanced opportunities to make new friends, developing relationships during the process of sharing experiences, and contributed to the acceptability of the intervention. At times, this was irrespective of their beliefs about the benefits gained:
It says Young SMILES and it sounded fun like it would make you smile and it did.
W17Y23A1
The best kind of group that helped me that I’ve ever been to. It was fun, I didn’t dislike anything. The thing that I loved the most was all the different kinds of food that helped me try new things.
N33Y01A1
I enjoyed all the activities we did and making new friends . . . It was good because everyone knew each other and we was getting along really nicely.
W01Y02A1
It was just a case of going there and making friends with the people who were there, things like that . . . Probably not [did not gain anything], but at the same time it was good.
W01Y01A1
Opportunity costs
Attending Young SMILES raised some concerns among CYP. Participation in a group came at the cost of their sense of security in an emotional sense, causing nervousness due to being in a group situation, and in a practical sense because of the perceived consequences of disclosing their own and their parent’s personal experiences:
I don’t really like being in crowds with loads of people. It’s fine if I’m with five the most and the minimum of being by myself, don’t really like being by myself but I hate being in the crowd worse.
N33Y01A1
I am afraid that they might tell everyone and I am not used to new people.
W16Y20A1
I didn’t like it because I don’t like talking about my mum’s disabilities because it feels like I’ll have to and everyone will be talking about it, and they might not like us anymore . . . It felt like if I told them then they would chat to their mum and then they might chat with a different person and then that person might chat with someone else, then that other person they’ve told might tell like a social worker.
N17Y01A1
Some saw the Young SMILES intervention as a missed opportunity to spend quality time with their parents as it is something generally lacking in their family experiences:
Because you get to spend time with them and I don’t really do that.
W11Y15A1
Narratives described the factors influencing children’s attendance that they perceived as beyond their control, such as exacerbation of parental mental illness and feeling responsible for attending to maintain group numbers despite their needs not being met:
I was like, well if I go, my mum won’t know where I am, if I stay my mum knows where I am, and I don’t want to scare my mum.
W17Y22A1
It was like I’m not getting anything from this. It was just like, it just felt tedious at a lot of points and by the end of it I really didn’t want to go but I was like I feel bad because obviously the numbers and I’d said that I would go and, you know, I wanted to give it a chance.
N07Y01A2
Perceived effectiveness
Aligned with one of the core aims of the Young SMILES intervention, CYP reported improvements in mental health literacy. Developing a wider understanding of how mental health affects individuals enhanced their comprehension of how to support and respond to parental needs. Gaining insight into the manifestation and prevalence of parental mental illness to a certain extent normalised experiences:
It’s helped me out with mental health and it’s helped me out to know my mum better, like what’s happening . . . Because they told us, what it means, and my mum has got it and lots of different people and it says, if somebody out of your family has got mental health, that people in the family will help the person with mental health.
W17Y22A1
I didn’t think that before but I think I did take a lot away from that because it was kind of like, like everybody’s got something going on, whether it is caring for a parent or not, everybody’s got something going on and it’s like, you’re doing fine.
N07Y01A2
More significantly, as a direct result of improved mental health literacy, improvements in family cohesion were reported. Relationships with parents were perceived to have benefited from more understanding of their experiences, which saw a shift in their behaviour as a result:
I just felt a bit better because, like I said, I can understand my mum and dad’s illnesses and what they can and can’t do.
N29Y01A1
I have a better understanding of how my mum feels . . . [which has made their relationship] a lot better because we’re getting along a lot better now . . . We’re not arguing anymore.
W01Y02A1
So I don’t get into much arguments anymore with my dad because I’m doing more activities with him than I used to instead of getting arguments. I do get into arguments but not like I used to, so it wasn’t big ones . . . because we used to be dead mean to our mum and like we used to never help her, but now we do.
W11Y15A1
Developing knowledge and skills around how to support parents adversely affected by their mental illness was proclaimed important, and had a positive impact on their and their parent’s well-being; some reported a shift in parental attitudes:
Well, now I know more ideas of how to help my parents or get rid of some of my worries . . . basically like if I feel sad about something I can just write it down on a piece of paper or in my notepad.
N29Y01A1
She could trust me before, but not a lot, but now she trusts me a lot . . . Because me and my sister usually never play with each other, but now we do.
W16Y20A1
Like before when I said it’s helped with my behaviour, and I think it’s helped my mum as well because she’s not as stressed anymore. I’m not saying that she was like really stressed, but like her stress when . . . like when I’m stressed, and her having to deal with [child’s brother] as well. I think it’s helped with that so that she’s not as stressed because I’m not as stressed.
W07Y10A1
However, lack of engagement from parents corresponded with the development of negatively perceived outcomes and detrimental effects on child–parent relationships:
Obviously it did create that kind of like shift between me and my mum but I think that wasn’t, like there wasn’t anything the group could have done about that because that was just how it was. My mum didn’t want to go, OK, you know, that’s just what it is . . . I just think it was like, I felt there was an issue anyway although I didn’t realise it and I was just like, oh, in attitude and I was like, OK, that’s, that’s the thing. Do you know what I mean? Like I said, it just highlighted that that was an issue.
N07Y01A2
Family relationships aside, the development of new social networks was a key contributor to positive experiences of attending. The opportunity to engage with others (peers and facilitators) and make friends was an outcome not attained through other supportive mechanisms experienced. Networks provided an environment in which support and advice could be sought:
Well, I guess because I could see my friends from Young SMILES and I can’t really see my friends from Young SMILES when we go somewhere else as a family. So that seems what was different [from other services] . . . I would just say if I had any worries about it. I would just ask one of the adults there or one of my friends there and I would ask if they had any ideas and they would just tell me the idea if they had and that was it.
N29Y01A1
Strong bonds and friendships between CYP were formed; however, because of the time-limited nature of the intervention, many of these friendships were regarded as similarly time-bound:
This is what I got from [other child in group], but it’s like my half says best friends, her half says best friends . . . because we are best friends. If we ever meet again, she’ll be wearing her necklace and I should be allowed to wear my necklace, and then we’d just put it together and then we would know each other again. We’d know each other by seeing this necklace.
N33Y01A1
I [went to Young SMILES because] I wanted to make new friends . . . but like I’m never going to see them again and that’s sad.
W17Y22A1
Older participants were least enthused about the intervention, maintaining that little was gained throughout:
A bit like boring, a little because it didn’t really feel like we were doing much like for the amount of time we were there.
N29Y01A2
Self-efficacy
The Young SMILES sessions were regarded as an enabling environment. Despite some initial concerns about participating in a group, beliefs and attitudes changed relatively swiftly. Initial fears were alleviated by reflecting on meeting children in similar circumstances. The peer group environment, compared with previous one-to-one support mechanisms and day-to-day interactions with peers, helped to reduce isolation and enhance their perceived ability to participate:
Good [experience] because you all got supported by the other teachers and you all got supported by the teachers and you got supported by friends, got supported by everyone there.
W12Y16A1
Well, basically, like I just asked them how they figure out their problems and they tell me and I just tell them how I do it.
N29Y01A1
Mostly because some of them experience the same problems with their family lives so they understood . . . Well, basically just to know that they understand all my problems and I could talk about ways how they solved it so I could, kind of, well, just do the same.
N29Y01A1
Like if you were like just one person, like the facilitator and just you, you’d just feel alone . . . a bit more comfortable where there’s other people.
N29Y01A2
Some of the people in my class don’t know what I mean by those problems and don’t understand it but in Young SMILES most of them do and they experience it themselves . . . I just thought, nice to know that I can be with the children who experience the same problems as I do and I know that they can help me like with that and that the adults can too.
N17Y01A1
The Young SMILES sessions offered a safe environment devoid of perceived negative consequences. Witnessing others speak about their experiences of their parent’s mental illness was enabling, reducing feelings of being judged. The issue of anonymity beyond the confines of the group was discussed:
Because, like, everyone else it talking you can, like, understand more and you know that you’re not going to be judged . . . because, like everyone else is doing the same thing.
W01Y02A1
I wasn’t scared to say it because it’s like you’re not going to see them for a long time . . . So, like, if you go to like WWE [World Wrestling Entertainment] and stuff like that, and start shouting, you don’t need to be scared because you’re only going to be there once and you’re not . . . It’s almost 99.9% that you’re not going to see them again.
W16Y21A1
Despite their membership of a group, facilitators’ abilities and efforts in adapting to individual circumstances were key to the acceptability of the intervention and continued participation. Providing individual support when required was valued:
Well if someone was ill, they took them out straightaway, so they didn’t get embarrassed or anything, they took them out straightaway and then . . . yes, they took her out, so she wouldn’t be embarrassed.
W07Y10A1
Because I was worried that I wouldn’t know anyone’s name on the last day, apart from [Young SMILES facilitator and trial researcher] but luckily she did a name game. Every week, because I’m always, always worried about when I go and meet new people, I’m always, always worried about getting names wrong, so that’s why every time I go into a new group, they do a name game for me, so it’s easy for me to remember names.
N33Y01A1
Strengths and limitations of parent and children and young people studies
The exploration of parents’ views provides useful insight into the acceptability of delivering a child-centred intervention from the perspective of the individuals who are experiencing the difficulties that may project onto their children and that the intervention aims to overcome. As is inherent in many qualitative studies, the study was subject to a number of limitations, most specifically with respect to generalisability.
Reflecting on the data collected, it was also apparent that the sample may have been biased towards a group of mothers who were not necessarily ‘ready’ to receive an intervention directed at understanding how their mental health difficulties affected their children. Many narratives from the parents highlighted the need for a more personalised, needs-based approach centred on their experiences as opposed to their children’s.
In spite of the perceived bias in the sample, there was variation in the experiences and views obtained. There was clear support for the intervention, which was balanced by more negative views highlighting elements of the intervention that may need to be adapted further to better meet the needs of those attending.
The exploration of CYP’s views of the Young SMILES intervention provides illuminating evidence of how the intervention is seen through the eyes of those whose lives it is intended to improve. Although the inclusion of children in the acceptability study was dependent on the consent of their parent, it was not reliant on the parent taking part. Children whose parents did take part were interviewed separately; thus, they could express their views without being concerned about how their parent may react. Potentially, this enhanced our ability to obtain a more truthful insight into CYP’s experiences of attending. For older children, some narratives expressing openness about their feelings towards their parent were indicative of this.
Our sample size was confined to CYP and parents who had been randomised to the Young SMILES intervention. As this was a feasibility study, and target recruitment figures were notably small, the number of CYP and parents available to invite was limited and people who did not consent to taking part in the trial were unattainable. Individuals who did not take part in the intervention may be averse to taking part in group interventions but we were unable to explore this or any other barriers that they may face. The resulting parent sample recruited was biased towards mothers, with only one father partaking, but the CYP sample was representative of children of all ages and both sexes, with over two-thirds of the children who attended represented in this study. Despite this observation, over three-quarters of the parents who attended the intervention completed an interview. Although this is indicative of reports in previous literature, it leaves some gaps in our knowledge.
Two researchers were involved in conducting the interviews, both of whom had previously been involved in collecting baseline and follow-up measures as part of the trial. Therefore, for some, relationships may have already been built, contributing to the ease of participation for parents and CYP. However, as distinction between service delivery and trial procedures is not always apparent, participants may have been cautious about expressing negative views about the intervention if they thought that the researcher was part of the service team. Despite this possibility, a range of positive and negative experiences were collated.
We did not use the theory of change to guide the interview schedules used in the parent and CYP qualitative studies, which would have been an alternative approach. As there was a limited population from which to sample, it was inappropriate for the broader study aims. Instead we focused on intervention acceptability and perceived effectiveness of the intervention as a whole. That said, we used an established theory of acceptability that is recognised as a strategy to optimise information power. In addition, we did not present our analysis for additional comment because of the inability to recontact participants post trial.
Discussion
Qualitative work, by nature, allows us to identify potential intervention benefits on a personal level but does not guarantee that differences in outcomes quantitatively collected will be significant. Therefore, data need to be interpreted in the context of subjective effectiveness rather than objective evaluation.
Children were enthusiastic about attending the Young SMILES sessions, improving their mental health literacy and making new friends, but narratives highlighted the need for their role supporting their parent to be acknowledged. This was not clear when developing the intervention but was clear in relation to the theory of change model. For some, discourse reflected on how their learning, and subsequent understanding, from attending the Young SMILES sessions could directly affect their parent and family rather than reflecting on changes to their own QoL.
Parents, despite initial apprehensions, were motivated to attend for the benefit of their child’s well-being. However, discussions about the acceptability of the intervention, for most, focused on the benefits that they had personally achieved, moving the focus away from their children. Some views regarding what they would be discussing in sessions appeared misaligned with the aims of the Young SMILES intervention, with many expressing the need for more time to discuss their own experiences. Although parents felt that their needs were not necessarily met, they were still supportive of their children getting help independently of themselves. The Young SMILES intervention was explicitly designed to address service gaps identified in the previous review68 (i.e. child-centred psychological education). This does not preclude the need for other services. If effective, it would be nested within service provision. This intervention would be delivered as one component of a broader set of support strategies for CAPRI families.
For both children and parents, their experiences of the intervention compared favourably with other support received previously, particularly having the opportunity to spend time and share experiences with others in similar circumstances. Both recognised the importance of spending time apart to enhance the benefits gained from the intervention but also saw Young SMILES as a place where they could have spent more quality family time. The atmosphere and environment was important and, for most, was enhanced by the enabling personalities of the facilitators.
Older children’s narratives appeared to display less satisfaction than younger children. Although this may reflect a poorer fit with the intervention, it may also be that they are more able to appraise their experiences on a wider level than younger children. Older children’s views raised issues concerning the ability of a single intervention to support children in a broad age range. The same issue could be highlighted for the inclusion of parents by addressing parental ‘readiness’ and cultural needs.
Acceptability and potential long-term outcomes were compounded by the time-bounded nature of the Young SMILES intervention. Children and parents emphasised the importance of the relationships that had developed. However, only parents commented on how these could be extended (e.g. via Facebook) after completion of the intervention. Children valued the relationships and wanted them to continue and clearly noted how they came to an end as the intervention ended.
Furthermore, it should also be noted that our sample contained a disproportionately low number of families from ethnic minority backgrounds, with Asian people being the only ethnic minority represented in the trial. The low proportion of ethnic minority families and the lack of diversity among those minorities in the trial mean that generalising the results to ethnic minorities must be done with caution. Any further research could look to adopt specific strategies to encourage a more diverse sample.
Chapter 7 Intervention delivery: facilitator and referrer qualitative studies
Two qualitative studies were conducted to assess implementation of the Young SMILES intervention. Interviews and focus groups were held with individual referrers and those delivering the intervention at both trial sites.
Study 1: intervention facilitator perspectives
Our aim was to explore facilitator views of delivering the Young SMILES intervention. We obtained information about what they thought about the format and content of the intervention and if changes would need to be made to ensure sustainability and meet the needs of CAPRI.
Methods
All individuals across both sites involved in the facilitation of the Young SMILES intervention were invited to participate. Information sheets were provided by e-mail and, if individuals were interested, contact could be made with the research team. Participation in the study was voluntary and not associated with monetary or professional reward. Research team members were available by e-mail or telephone to answer questions.
Data collection
Two focus groups were conducted: one with the voluntary organisation and the other with the mixed NHS-voluntary organisation. Focus groups were conducted on each organisation’s premises. All individuals, except one, involved in facilitation of CYP and parent groups agreed to participate. Written consent forms were signed by participants at the start of the focus group prior to data collection. All agreed to the audio-recording of the group discussion.
Data collection was undertaken by the female trial manager (Judith Gellatly), who has a PhD in health services research and extensive training in qualitative methods but no prior experience of delivering Young SMILES or similar interventions. Judith Gellatly had met some of the participants previously during the intervention development and set-up phases of the Young SMILES intervention. She had delivered presentations about the purpose of the feasibility study, highlighting the importance of addressing the needs of CAPRI and Phase I methods and findings.
Focus groups followed an inductive questioning framework driven by a semistructured topic guide devised and piloted by the research team. Focus groups lasted 68–90 minutes, were digitally recorded using an encrypted digital recorder and were transcribed verbatim. Field notes were taken during focus groups as an aide-memoire but did not contribute systematically to the data analysis.
Data analysis
Data underwent thematic analysis [informed by normalisation process theory144 (NPT) and managed in NVivo] independently in two phases. First, to make sense of the data they were initially coded inductively using thematic analysis, conducted by the trial manager (Judith Gellatly) and subsequently verified by a qualitative research team member (Penny Bee). Emergent themes were coded using a method of constant comparing, classifying and refining codes across interviews until no new themes emerged. The distribution of codes was recorded and data falling outside the coding frame were re-examined to determine if important concepts were being missed.
Second, emergent themes (and constituent codes) were mapped to the NPT framework, continually checking for fit. Mapping was carried out collaboratively with ambiguities and/or differences in insight resolved via discussion with a third member of the team. Participant checking of the data coding process was not performed.
Theoretical perspective
Uptake and implementation of new health interventions is widely recognised as a complex process. NPT is a conceptual framework for understanding and evaluating the processes by which these interventions are operationalised in practice. It focuses on what individuals or groups of individuals do, instead of focusing on what they intend to do or believe, to enable interventions to become normalised. NPT offers an empirically validated framework to guide the evaluation of complex interventions144 and has been frequently used in feasibility trial evaluation. 145
Normalisation process theory consists of four constructs: coherence (the work people do to understand and make sense of a complex intervention), cognitive participation (the manner by which they engage with the intervention), collective action (the way in which they enact it) and reflexive monitoring (the work they do to appraise its effects). 144 NPT permitted a means for the inductive coding to be strengthened, enabling further understanding of the barriers and enablers faced by the facilitators when implementing the Young SMILES intervention.
Key findings
A total of 18 potential participants were invited to the study; all expressed an interest in taking part and 17 subsequently attended focus groups. In the co-delivered site focus group, six NHS staff and three voluntary organisation individuals attended; at the voluntary organisation, nine individuals took part. The participants included six children’s services practitioners, five family therapists, three young carers support workers, two team managers and one individual involved in the organisation and management of the groups at one of the sites. Of those involved, 13 (76.5%) were female. No other individuals were present during the discussions.
All the emergent themes identified in Phase I of our analysis mapped onto the NPT framework; no codes were deemed to fall outside its scope (Table 28). Therefore, we structure the presentation of our results around its four key constructs: coherence, cognitive participation, collective action and reflexive monitoring. Participants are assigned a number rather than a name or pseudonym within the text.
| NPT construct | Study themes |
|---|---|
| Coherence | Young SMILES fills an identified gap in current support for CAPRI |
| Young SMILES provides opportunities for new service developments | |
| Young SMILES builds upon existing service procedures and practitioner skills | |
| Cognitive participation | Investment required to identify participants |
| Trial procedures negatively affect implementation | |
| Parent engagement and commitment influenced by readiness for change | |
| Parental engagement enhanced by relationship building prior to the start of intervention | |
| Collective action | CYP enthusiasm influenced by delivery approaches/mechanisms |
| To ensure success, Young SMILES needs to be adaptable to needs | |
| Young SMILES is reliant on maximising existing knowledge and skills – co-organisation | |
| Young SMILES implementation requires additional resources | |
| Reflexive monitoring | Facilitators acknowledge benefits of Young SMILES for CYP |
| Opportunity of Young SMILES success influenced by time constraints | |
| Adequate resourcing of Young SMILES important to ensure sustainability | |
| Young SMILES manual requires development | |
| Support for practitioners to ensure intervention fidelity and quality required | |
| Strategies to implement within co-delivered sites need to be established |
Coherence: understanding and making sense of the Young SMILES intervention
The implementation of new interventions in services relies on those involved in their delivery developing a common understanding about their aims and values. Practitioners working across third-sector and NHS environments were consistent in positioning Young SMILES as a much needed solution to a national service gap, and as a meaningful, localised activity with potential to positively influence participant outcomes:
There are obviously a lot of families where mental health is a significant concern where it impacts on parenting, really, and it therefore impacts on children, so I think we felt it was a very valuable service. I don’t think we felt it wasn’t valuable. I think we felt it was valuable.
R8, Voluntary organisation
The Young SMILES intervention was seen as distinct from other services. Much of its value was attributed to its underlying philosophy advocating child-centred support and increased service accessibility for a broader population. Focus group participants repeatedly acknowledged the ‘hidden’ status of CAPRI and displayed a shared set of values around the moral and social imperative to ensure that support was available for subclinical, as well as clinical, populations:
I used to work in CYPS [children and young people services], child and adolescent mental health, you know, so children that had a reasonably significant mental health difficulty could get referred to a service and get a service, but maybe children that had parental mental health, but maybe were or weren’t being affected by that, there was not necessarily an identified service. So that’s what I mean about being missed.
R5, NHS-Voluntary
Additional coherence was evident in the way that the Young SMILES intervention aligned well with new care pathways that were being envisaged locally and in the way that its timely introduction supported the type of organisational and workforce development necessary for these care pathways to emerge:
Within the trust, there had been some work going on about how we identify young carers and then link young carers up with an appropriate service. But actually, we started to ask questions about, well, what do people need and how effective are the interventions that people experience . . . we heard about Young SMILES and it seemed like such a good opportunity to do something that I think ethically we felt we needed to be thinking about as a family therapy team.
R9, NHS-Voluntary
So that’s what got me excited both about Young SMILES but also the potential for a co-delivered project with Barnardo’s, I think, because Barnardo’s were telling us is that the children want more to do with adult mental health workers and we were saying, well, we want more to do with the children’s workers.
R9, NHS-Voluntary
In aligning with these local aspirations, the Young SMILES intervention navigated a unique path. Simultaneously, the intervention was upheld as something meaningful and distinct from current service provision, yet something that also drew on, and benefited from, existing skills and care philosophies:
I think that’s the kind of work that we try to do in our one-to-one sessions with the children and the parents. And we’ve not done . . . we’ve done sibling groups but it wasn’t just mental health, because we work with physical health and drug and alcohol addiction as well, but only one to one because it’s such a delicate area to go in. And you are there as a support worker, people see you as an authority, so what gives you the right to talk to people about these delicate areas of their life, or even give advice, maybe you have got an opinion but they haven’t asked for your advice. But to do it like in a group setting and peer support, and people learn from each other, it’s a lot more client-friendly, I think.
R6, NHS-Voluntary
I think that’s quite typical, isn’t it, of the way that we work already, because we have run coffee mornings, we have done other groups . . . And we know, we’ve already built up relationships with those parents before inviting them along to things. And then we support them to think about coming and sometimes give them a lift. So that is the way that we would generally work to get familiar with them.
R3, Voluntary organisation
Cognitive participation: work needed for a new community of practice
Successful implementation of any new intervention requires facilitators to foster commitment and buy-in from intervention participants and from their colleagues and peers. NPT asserts that, when a new set of practices is initiated, a core problem is often whether or not key participants are working to drive them forward. Intervention facilitators may ultimately need to organise or reorganise themselves and others to contribute collectively to the work involved in the new practices.
In the context of the Young SMILES feasibility trial, considerable interprofessional work was necessary first to identify suitable families for the intervention and then to guide them successfully through the trial referral processes. A key concern for facilitators was the inherent difficulty of identifying the target population and the potential impact of this on intervention reach. Success was perceived to rely heavily on service context and on the working processes already available (or not) at local sites:
I think that services that have been set up to think of the needs of children, like Barnardo’s, were able to identify the families relatively easily, that’s my impression, you might have something different. But actually, in an adult mental health context, I think a lot of it was about working with potential referrers to say why this is important and that it wasn’t necessarily those families who were notably struggling or where there’s difficult relational issues, that actually . . . well, we know there’s such a big wider population of need, and that unless people are taught to look for it, they don’t necessarily see it.
R9, NHS-Voluntary
One of the things that actually struck me, just the last thing I’ll say is, it was interesting the number of people who we identified on the caseload who were already known to you, which made me think, well, is that something about people are thinking about the kids, so they’re already thinking we’re a bit worried about this, that there needs to be something in place, or have they got families who are actively seeking support and intervention. We did not capture the people who we know aren’t accessing this anyway.
R9, NHS-Voluntary
Recruiting families into the feasibility trial of the Young SMILES intervention was acknowledged to be challenging. Although a key difficulty was the need to identify and reach out to families falling within intervention scope proactively, facilitators also recognised that research trial procedures had negatively affected participant enrolment. The fact that a notable proportion of families would be allocated to TAU and would not have access to the Young SMILES intervention was a study design feature that concerned those tasked with implementing the intervention and was, at times, perceived to affect families negatively:
The worry was how is that going to be displayed in the family home and what’s the outcome for the child of this is going to be? Because . . . I hope this doesn’t sound patronising . . . but there is a huge amount of work to make this family understand that this is a good thing for the child. And that took so much work. And then for that child to be randomised. And all they heard that the good thing is not going to happen for the child. And it does send the parent in a downward spiral . . . they’d be in tears when I’m telling them they’re not going.
R6, NHS-Voluntary
Every appointment I’ve had since then, every time, every time I try and contact them about having appointments, I’ve had the same thing about she hasn’t got anything, you know, why did this have to happen. And I know why, there’s an absolute . . . there’s a reason that we have to do it like that, but it was very difficult. This person was very unwell, or is very unwell.
R7, NHS-Voluntary
Many recognised conflicts between trial procedures and those implemented in their current services, where the immediacy of families’ needs was considered on an individual basis. Furthermore, facilitators reported not being involved in the composition of groups, which made it difficult to resolve anticipated challenges in group dynamics:
It’s the pressures of trying to do it when it’s being evaluated, so you’ve got to run a group now, so instead of being able to pick and choose who you wanted or saying, well, they’ll be best for the next group or they need to wait 6 months before they’re ready to move on, we’ve had to stick them all together because of the pressures of you’ve got to bring in another group now because we’re stopping it, sort of thing, so that hasn’t helped.
R7, Voluntary organisation
Because you’ve got a limited sort of pick of people and families, you’ve got no choice over the group dynamics, so some of this lot you wouldn’t want in a group ever together. It makes it impossible working, and ideally you’d assess that before and think, well, just separate them out and think . . .
R1, Voluntary organisation
Lack of individual control over intervention set-up and implementation was a key theme for facilitators and highlighted how critical it was to build communal engagement in Young SMILES, so that the process and outcomes of this new practice could be optimised and sustained. Incorporating additional procedures to ensure family engagement and understanding, with particular emphasis on parents, was strongly advocated:
. . . it’s probably something that you consider for the manual I think about engagement and the first stage of the manual, you know. So if we were running a group together, you know, would we go out and meet every family beforehand and individually, and talk about what the group was about and help prepare people to attend.
R1, NHS-Voluntary
One variable that facilitators debated at length was parental readiness for change. Although children engaged well with the Young SMILES intervention, parental engagement varied. Facilitators’ perceptions of parent readiness to change contrasted across the two sites, with those working at the health and social care interface more likely to comment on engagement challenges. Whether the difference observed between the sites was solely a reflection of true differences in group membership or was, in fact, partially influenced by professional experience, role and expectation remained unclear. What was evident was that a combination of cognitive and relational work was required with parents at intervention initiation and that this work was perceived to be the joint responsibility of intervention facilitators and intervention participants:
These parents have really severe mental health issues, most of them that are coming to them, and some of them don’t even go out, they don’t even open their door to people, so it’s been very difficult just to get in to start with some families.
R3, Voluntary organisation
They’re still not ready for group work, some are just not ready, and they’re not ready to deal with and cope with and listen to and discuss the impact on their child, because they’ve got so many issues of their own that’s blocking them from coping with their children’s feelings and emotions and so on . . .
R4, Voluntary organisation
Running a parent group with participants who were not ready to identify and explore their children’s experiences (as opposed to their own) caused some facilitators to question the ethics of this aspect of the intervention design and had a negative influence on their motivation and commitment to this role:
The children all love coming and have been very positive, but of course the parents haven’t been, and we feel like we’ll get to them and they’ll be hearing about the same rubbish, nothing will change for them in their lives, but we’ve shown them that it could be different but it’s not going to be.
R2, Voluntary organisation
Those sessions were near impossible . . . they’re very stuck, you’re constantly bringing them back and they’re just not getting it.
R2, Voluntary organisation
Despite these sentiments, the conceptual and theoretical arguments for including parents in a child-centred intervention were well understood. Clear tensions were evident between the magnitude of work that was required to engage and sustain parental input, and the perceived consequence that this would have for children if it could not be achieved. Parent engagement was considered vital not only to assist with their own understanding of their children’s experiences, but also to ensure that their children felt included in the intervention and experienced maximum socioemotional benefit:
Unless you can change the parent, and it isn’t the child in this, it is the parent. The parent has to own some responsibility, yes, the mental health is there, no denying that, we understand the mental health, but they’ve got to have the capacity to change, if that change doesn’t happen, you’re setting children up to fail.
R8, Voluntary organisation
Just observing from the children’s group, is that a child was on his own, his parents didn’t come with him to the session, and so when all the parents come in to pick them up, this child hadn’t got anyone to pick him up . . . there are things like that, and it’s that feeling of being separate, with this young child that their mum wouldn’t come to the group.
R6, Voluntary organisation
Facilitators in one site suggested that parental engagement with the Young SMILES intervention was naturally enhanced by some of the parents meeting informally before the parent sessions commenced. It was thought that meeting spontaneously while waiting to collect their children from their first sessions allowed parents to build relationships before meeting in the more formal sessions. Parents who had not had this opportunity, or who struggled to relate to their peers, were disadvantaged socially and struggled to integrate into the group. In this sense, relational work instigated by and sustained by the parent participants was upheld as an important ingredient for intervention success:
By the time [we] started the first group and we had a group contract, people knew each other already, they exchanged telephone numbers already. In a way, they did quite a bit of the work that was meant to be done in the first session, they gelled.
R6, NHS-Voluntary
And some parents seemed to get lost through the process once they’d started informally because, you know, it was an unfacilitated process that was happening, or some joined later and then relationships had formed between certain members of the group, so what it would be like to try and join the group that was already formed at that point.
R9, NHS-Voluntary
For others, more explicit solutions were necessary. This included allocating more time to precipitate parent change within the intervention and providing more dedicated opportunities for families to work through their experiences as a unit:
We talked around as well linking in some work and more sessions around changing the women’s beliefs as well, you know, how we would work with them to change their beliefs, the beliefs like I can’t cope, or my life’s over, actually changing those beliefs and getting them to change those beliefs and look at how they need to behave differently and how they need then to give those beliefs to their children, and how they’re going to do that . . . to give the best possible service, I suppose.
R3, Voluntary organisation
I think there must be more active joint activities, like you only have an hour together rather than them going there and the kids down here, I think they need to do things together so that we can see what’s going on in the kids’ heads if they do those activities together . . .
R7, Voluntary organisation
Collective action: delivering the intervention in practice
A central tenet of NPT is that any novel or modified intervention must display interactional workability in order to be taken up and integrated into routine practice. Although facilitators across both sites reported that CYP were engaged with the Young SMILES intervention, there was some recognition that CYP commitment varied depending on the approaches taken. This observation was applicable to both age groups, with facilitators consistently acknowledging that opportunities to engage the group in dynamic activities were more likely to be well received and more likely to engage participants than direct group discussion:
They weren’t verbal about not wanting to talk [laugh] but they just didn’t say anything. So we had silence. So we knew they didn’t want to do the discussion-based things because it was just really awkward and they didn’t . . . they just weren’t willing to share in front of everybody.
R3, NHS-Voluntary
They were a bit like, oh, not this again . . . I think with the little ones, it felt like we really had to keep the serious bits to a minimum, because they just got bored actually, we just lost them. So we were almost bribing them with, we’ll do this bit and then we’ll do something fun. So I think as well, to make it any kind of a worthwhile activity for them, just keep it really short.
R8, Voluntary organisation
It became apparent that, for some CYP, a major barrier to talking was the expectation that their thoughts and feelings would be shared with their parents. Fear of disclosure was closely linked to a reluctance to prioritise their own needs and a reluctance to tell their parents what they had been experiencing as a result of their parent’s mental illness:
There was a feeling of what, you know, their parent might think, put two and two together and knew that it was them that had said that. I think that’s quite a big thing for a little one to carry, isn’t it, and worry about. So, we kept things quite general at times, didn’t we, and really respected what the little ones had said.
R4, NHS-Voluntary
One important discussion point for the Young SMILES facilitators was the recommendation in the intervention manual that groups create an ‘imaginary family’. Although this tool was viewed as a useful mechanism for older children to share experiences in a non-threatening way, facilitators reported that, among younger children, the concept was not always fully understood. Younger children were typically perceived as less ‘self-conscious’ and ‘happy to talk’ directly about their own family; therefore, facilitators were forced to adopt a more flexible and adaptive approach, gauging the value of some intervention tools and exercises depending on how the group attendees responded to their introduction and use:
They used it [the imaginary family] when there was something particularly difficult, like when we were talking about what they would want to say to their parent, they found it a lot easier to think what the imaginary child would want to say, because that just gave them that chance to remove it from themselves. So it was definitely useful in some cases, but other times it did just get ignored and it felt . . . they knew why we were bringing it out, they knew it was to give them that opportunity to not talk about themselves. So I think it felt a bit false maybe.
R3, NHS-Voluntary
It’s just a reflection just because [we] did the younger children. A lot of hard work, trying to get it right. We actually didn’t use the . . . the made-up family just didn’t work with the little ones, they just didn’t get the concept . . . they were just talking about their own families, which I felt was more . . . went more successfully. So there was a lot of adapting.
R8, NHS-Voluntary
Having responsive facilitators with the necessary knowledge and expertise to facilitate child-centred groups was regarded as a vital element of the successful delivery of Young SMILES. Although it was acknowledged that intervention training, in part, fulfilled this objective, facilitators recognised the ‘hard work’ that was subsequently required to deliver the Young SMILES intervention.
For those working in the co-organisation delivery site, working alongside individuals from a different field allowed them to draw upon their differing strengths to fill in gaps in their current knowledge and experience. For NHS facilitators, this involved developing their skills and understanding of how to work with groups of children, whereas for those working in the third-sector organisation the chance to work with someone who was skilled in supporting adults with mental health problems was key. Working within a collaborative model was thought to provide an efficient solution to individual skill gaps and positively added to their ability to fulfil the needs of families attending the Young SMILES sessions:
Certainly, I mean, I couldn’t have done it without [third-sector facilitator], because it’s that expertise and knowing what’s going to work with kids and pitching things. And I really just followed your [their] with that and been able to sort of draw on lots of experience of working with people and knowing what might work, what mightn’t work, you know, that kind of thing. And just having ideas as well, creative ideas, that was great, yeah.
R1, NHS-Voluntary
I felt very reassured co-facilitating with [NHS facilitator] because I knew we had some quite unwell parents in our group, and just knowing that that’s what you do, you know, was very reassuring, yeah.
R2, NHS-Voluntary
Sharing responsibility between facilitators with complementary skill sets built accountability and maintained confidence in Young SMILES, an intervention that by design was relatively structured and manualised. Facilitators recognised the usefulness of the Young SMILES manualised approach in providing structure and coherence within and between sessions, simultaneously acknowledging that such an approach could be challenging when faced with dynamic family circumstances and differing participant needs:
It’s an age-old tension, isn’t it, you know, between how do you have a manual that allows you to do things in a relatively informed way that hopefully is linked to what proves to be helpful and effective, but also has enough room to wriggle. You know, that’s a tension with any manualised approach, isn’t it . . .
R9, NHS-Voluntary
It would be difficult but I can also see the benefit of that [open intervention], you know, I don’t know if it would allow you more flexibility for people to come and go . . . if you did have that flexibility for just people to come in and out when they were feeling well or whatever was doable for them, does that make that more accessible, rather than being very constrained, right, we have to get this done in 6 weeks and just plough through the manual, which I think maybe it felt like that at times. I think time was tight.
R4, NHS-Voluntary
Navigating the different needs and preferences of the group while maintaining intervention fidelity was an ongoing challenge in intervention delivery and required considerable sensitivity and creativity on the part of the facilitators. One facilitator recognised the ‘chaos’ that many children are experiencing in their lives and the importance of allowing time for both children and parents to work through those stressors before re-enforcing the aims of the session:
I think it was . . . chaotic. So they came in with that, you know, on the ceiling and then it was that job of bringing them back down and refocusing it again . . . it’s helpful for the child that they’re sorting that kind of thing out . . . we need to just let them voice that but then bring them back to, you know, [to] what the aim of the session was about. I think that works really well. And they heard it, didn’t they?
R4, NHS-Voluntary
. . . everyone would stick with the theme of the session but we might have to divert a little bit so that session might be, like, OK, what we need to do is go in, yes, look at them, how it felt for them when that happened, then get them to link it to their children, because, you know, obviously if they can’t, if they’re stuck and they can’t make the link, you’re going to have to go back to their stuff, get them to look at how it felt and do an exercise around that and then get them to link it, you know, and stuff like that, and you know, we’ve had to do things like that sometimes to try and shift people on a bit and stuff, so they can benefit from the programme.
R3, Voluntary organisation
Facilitators were clear that the division of labour underpinning the sessions should be weighted towards the group leader, with the onus on them to optimise intervention delivery and effect change. Homework completed by participants between sessions was piloted but was not considered viable. A key barrier was the need for CYP to have access to the necessary resources to complete the homework but, even after this was identified and resources were provided, facilitators felt that, for many children, homework was unfeasible:
They still struggled to bring it [homework] in and a lot of the same, they’ve got enough to do with the homework from school without doing this.
R6, Voluntary organisation
. . . you’ve got to take it into account, haven’t you, I mean, I’m not being funny, these are the sorts of families that won’t be doing the homework at home . . . Because the parents won’t be motivated to sort of sit and support the children with their homework, you know, and again, like I said, that comes down to some of the issues with the parents, doesn’t it, you know, so getting them to do homework for us is pointless, really.
R8, Voluntary organisation
For the parent group, homework was generally considered to be more feasible:
. . . you can sometimes in the adults group give little bits of practical homework . . . we want you to do an activity with your child and then report back to us what you did and how that went, you know, things like that are quite useful in the adult group, but for the kids, I think, you know, we need to knock that one on the head.
R8, Voluntary organisation
Reflexive monitoring: appraising and redefining the intended intervention
Reflecting on the process and outcomes of the Young SMILES intervention, most facilitators commented on the benefits it had for CYP, parents and collective family units. Third-sector representatives who retained close links with their intervention referrers provided feedback that went beyond their own observations. Reported benefits to CYP included increased confidence, concentration and self-esteem:
Some of those children were very good, weren’t they? I always remember we got some very positive feedback about how they’d seen the children’s self-esteem grow and their confidence grow, the children were able to express themselves better and the schools saw some very positive changes in the children, you know?
R8, Voluntary organisation
The schools were saying that the children were concentrating a lot better . . . I think the other thing, I think the schools were saying they were concentrating more, their self-esteem grew and I’m sure they said they felt they’d got a sense that the children were less dissociated . . . obviously we couldn’t measure that . . . remembering it back now as well about parents and schools also saying things like the children were talking more about their feelings, so that had been positive, so the children were actually saying about how they were feeling so that was then having a positive impact on their behaviours, because they were talking more about how they were feeling.
R3, Voluntary organisation
Most benefits appeared to emanate directly from children’s engagement in the group intervention. The effect of parental engagement on CYP appeared more variable. For parents, facilitators felt that the manualised activities were successful, enabling some parents to improve their understanding and insight into their child’s experiences to a ‘significant and remarkable’ extent. For others, the benefits were not so apparent and not as long-lived:
It’s very powerful [sharing information from CYP], and the timing of it is key . . . you knew instantly those that had connected because they went quiet, their body language told you and some of them became a bit tearful . . . I remember one of the parents said I’m parenting how my mum parented me’, and I thought, oh my god, and that was like a light bulb, that’s when we knew she had it, because she actually thought she wasn’t her mum and when she looked and she was able to do the flip, she just was very . . . you could see it in her face . . . And that was kind of . . . and you could tell that when we went to see her at home, it was very different, there was a shift, an evident shift . . .
R4, Voluntary organisation
All the children wrote down the impact on them so their parents would hear from them, and then we got the adults to look at it, and they said it was really hard-hitting. It did stop them in their tracks for about 2 seconds, you know? And then they started making excuses and banging on again, but I do think it is potentially quite powerful, that. They do go, oh, they’re sad, look at that, someone’s sad, whose child is sad? It just dropped, like a realisation, but then there was the cover-up of the feelings and then it’s their fault, they should know what my feelings are like, they should look after me. If that had been a bit longer, then we could have explored that with them, but there’s just not the time.
R4, Voluntary organisation
Time constraints on the Young SMILES intervention were frequently discussed. Reflecting on the time available, facilitators focused on three core aspects of the intervention: (1) time allocated to conduct initial assessments, (2) time dedicated to the intervention itself and (3) time available to optimise communication between the CYP and parent sessions.
Voluntary organisation staff were clear in emphasising the importance of the initial family assessment and in highlighting that the time dedicated to this assessment was less than that available for the assessments that they routinely conducted for other comparable interventions delivered by their organisation. Lack of time in the assessment period was perceived to limit the depth of information that could be shared and to affect relationship quality at a critical time for participant engagement. Much of the practitioners’ concern about assessment of the family appeared to link to parent-focused approaches with which they may have been more familiar:
We would say there needs to be a longer assessment period, so there needs to be a longer assessment period and more opportunity to do a more thorough assessment at the beginning, really, because I think we felt we were having to rush to do those assessments, and that’s not ideal, really, you know? So I think we would feel that that would need looking at, really.
R8, Voluntary organisation
You can’t go in, can you, and say tell us about your childhood experiences, well, that’s fine, move onto the next thing now. Obviously you’ve got to deal with that in a sensitive, responsive way . . . those sorts of issues aren’t quick issues that you can turn around within 1 week, you know? So I think it’s more that, even what we were saying, you know, for us to do a proper job and for us to sort of do this well, we would have appreciated a bit more time, really.
R8, Voluntary organisation
The desire to have more time allocated to assessment indicated a broader preference for a time-rich intervention. A time-limited intervention lasting only 8 weeks was generally viewed as too short, with one facilitator emphasising the potential negative effects that such a short length of time may have on CYP and on the coherence of the intervention for other members of the family:
Yes, and we know especially for the children it goes really quick and then we’re just leaving them, that’s what it feels like, we’re just dropping them and it doesn’t seem fair on them.
R5, Voluntary organisation
And I found that that bit was really rushed, it was all jammed together; and then the end was also rushed. Because we prepared and we told parents, this is a celebration event, but they had to do a really hard piece of work, which is goal-setting. And if it had been me doing that, I would have been sweating, it would not have been a celebration for me to set goals. And it really showed what people thought about this, because they all left, they all left the paperwork with us, they left it behind. And I think that was a clear sign that either we didn’t give enough time or it was too hard a task when they were expecting a celebration of eating and drinking, to think about what do I need to change and how am I going to do that?
R6, NHS-Voluntary
Across both sites, facilitators explicitly focused on the time allocated to the parent sessions, noting that parents started their sessions 3 weeks after their children and that this felt counterintuitive to intervention success:
You see, to me, systemically I think about context, you know, when we work with families rather than an individual, because the system changes and the context of somebody’s life changes over the time . . . So, if you think about a child, you know, if you think about you’re working with the parents, then the context is that they will become more aware of the child’s needs and maybe respond in different ways. That kind of makes me think it might be more important to have the parents group start at the beginning, so that there is more time and opportunity for that to develop, you know.
R5, NHS-Voluntary
Consensus among the facilitators was that additional work with the parents at the outset may have helped to enhance the outcomes of the intervention for children. Ensuring that sufficient time was available to communicate discussions from CYP to parent groups was considered a vital component of a high-quality service and something that had not been fully addressed in the Young SMILES manual or training information:
I think ideally, you know, lots of the families that we have could deal with a programme on their own first, you know, so if they had a parents programme with 8 or 10 weeks first and then we did work with them and their children, we have a children’s group and maybe some joint sessions with the parents and children together as part of the children’s programme, you know, then that will probably be a better service overall, you know . . .
R3, Voluntary organisation
Before every session, we had to spend time knowing where the children’s team is, because the adult group work relies on what is happening . . . and the information we received from the facilitators was absolutely invaluable. Without that I think it would have been really difficult.
R6, NHS-Voluntary
Support to deliver the intervention was at times perceived to be compromised by a failure to validate the resource that was required at a team and an organisational level. Concepts of resource encompassed access to the practical tools necessary to conduct activities, such as art materials, but also extended to staff. Facilitators were mindful that, at times, CYP or parents may need to be individually supported, which represented an additional burden on local systems. Having the capacity to augment or extend the intervention was recognised as fundamental to enhancing service provision, but was acknowledged to be difficult in the context of contemporary health services:
I think if it’s agreed that it’s built into somebody’s sort of job plan, you know, that that’s part of their role for however long that is, yes, otherwise things get squeezed or put to the side.
R5, NHS-Voluntary
Families also need to be supported to access the intervention; without this, many would not have engaged. However, arranging transport was a burden for facilitators across both sites and affected their ability to run the groups effectively:
The first group we kind of went with the taxis. I think I did the first when I look back, you know I would meet at a school, get in a taxi but that kind of worked, and those that lived local were fine. So that wasn’t too bad, believe it or not, and again it was time to free up . . . This one has been a logistic nightmare, but again I also think would they have come if a taxi arrived, probably some of them not. So there’s swings and roundabouts with both, and it has been hard, and kind of had to think about this because we’ve had to cancel some groups because clearly there were not enough that was coming, and all of that, and also we’ve run over the holidays. That in itself, and then the other part about that is we’ve had some of the primary children go to high school.
R2, Voluntary organisation
Facilitators recognised that, despite receiving training and being able to draw on previous experiences and skills, implementation of the Young SMILES intervention faced inherent challenges. Being involved in the development of the intervention in the earlier stage of the feasibility study was viewed as beneficial, but several uncertainties about how it would work in practice remained. Some practitioners reflected that, with hindsight, they were ‘not clear’ about what they were doing and resolving this uncertainty regularly demanded extra preparation time ahead of intervention delivery:
I think the one thing we did realise is you need a lot more time to prepare. We spent . . . we met a good couple of times, took a good couple of hours out I think to look at the manual. And then there was kind of before the group came, we had conversations. And even on the night, we were just sort of talking, actually is this working, maybe we should try something else. So there was quite a lot of that going on.
R1, NHS-Voluntary
I think sometimes it felt like we were just talking a lot rather than doing, so we had tweaked it a little bit, it’s better now than what it was originally, we kept to the model but just changed the activity to make it a little bit more engaging . . . we’ve used some activities that we’ve used before in groups with children which worked really well, but obviously with mental health . . . more arts and crafts.
R4, Voluntary organisation
All facilitators recognised potential adaptations that could be made to the Young SMILES manual and facilitator training programme to ensure success and sustainability. Some felt that the manual was not developed fully, was repetitive at times and did not provide enough information or guidance to be able to deliver the Young SMILES intervention without additional work:
I guess a manual that was more formed from the start, you know, it would have helped me. And it wasn’t really. Maybe that’s part of kind of a pilot study. And I guess connected to that, there was repetition in the manual, so there was maybe . . . yeah, a more finished product. You could have like an appendix after each session or at the end, you know, optional additional exercises for different age groups, something like that . . . pages people could refer to for seeds of ideas.
R5, NHS-Voluntary
When we first talked about this as a manualised model, I was influenced by other manualised training that I’ve had, which has been very much this is what you do within the manual. And for some of the exercises, it was difficult to know exactly what they were and we actually locally ended up arranging . . . we had four extra training, half-day training days where we went through the manual step by step and we experimented, we role-played what we might do . . .
R9, NHS-Voluntary
For those with experience of similar models, explicit permission to introduce new activities or modify activities in situ was recommended. Supervision of less experienced facilitators by more experienced personnel was advocated as one way of preserving intervention fidelity and quality, but this was not operationalised in practice:
I wonder whether reassurance as well, if there’s an activity you know of that fulfils the same purpose but you think you’re more familiar with, you can do it. Because I think I was asked a couple of times, ‘well, I’ve done this activity in this way, can I do it?’. Not that I’m the oracle on things, but I think just having that reassurance for somebody, if you were to pick up and think, have I got to follow it exactly because I don’t know. I mean, as an example, the example of volcano, don’t know how to make a volcano. But if I know how to do this and it does the same purpose, I mean something from . . . I think it would reassure people.
R7, NHS-Voluntary
Because I know there was that all that business about, wasn’t there, at one point, because when it all first started off, all that business about we were meant to be offering some supervision, and then that never happened, I don’t know what happened with it.
R8, Voluntary organisation
Further discussions about delivery in relation to future developments of the intervention focused around whether or not a co-delivered model between the NHS and the third sector would be offered. The value of this approach was, again, emphasised but concerns about governance surrounding such an approach were identified:
It’s one of the complexities of the joint model, you know. If you had a commission to do the whole of the same area as we had [in the trial], I’m guessing we would have moved groups around the areas. Because ultimately, it was staff at the end of the night who were putting potentially unaccompanied minors in taxis, and different organisations have different ideas about the expectations of that. I think there’d have to be quite clear service level agreements in place around that. There is an issue about how you influence commissioners . . . So there’s a lot of work would have to take place’.
R9, NHS-Voluntary
Strengths and limitations
This novel exploration of facilitators’ views provides a critical insight into some of the challenges inherent in developing a new child-centred intervention for children living with parents with SMI. Concomitantly, it is subject to many limitations inherent in qualitative research, especially with respect to generalisability.
Our sample size was ultimately set by the number of eligible participants available and consenting to interview. Involvement of participants from different trial sites and service backgrounds helped to maximise heterogeneity in professional experience and views.
Recruiting active facilitators from trial sites raises the potential for bias, because it may be posited that these individuals may be more engaged in evidence-based practice and service development than non-participants. Equally, it may be argued that the current study was primarily evaluating a research-driven rather than a spontaneous (naturally occurring) change. Participation in intervention delivery was, in this sense, more likely to reflect site and managerial agreement than individual preferences for any particular model of care improvement.
All but one of the facilitators involved across both intervention sites actively participated in a focus group to discuss their experiences of delivering the Young SMILES intervention. However, the focus groups conducted were site specific. As the quality of dialogue is recognised as a key component of information power, offering facilitators from the different sites the opportunity to attend a combined focus group may have provided a way to further elucidate insights raised by both groups.
The current study was nested within a feasibility trial and, as such, enables the identification of early implementation barriers to intervention uptake and delivery. We were unable to obtain ethnographic observation data on intervention delivery and, therefore, our analysis remains reflective and exploratory. Predicting potential uptake and spread of the Young SMILES intervention at a national level requires more detailed information on service contexts and working conditions, and the likely ratio of conducive to impeding factors. Quantitative or mixed-methods research capable of evaluating different models of implementation would offer an additional perspective.
Discussion
Facilitators regarded Young SMILES as a meaningful and distinctive intervention that had great potential to fill a critical gap in current services. The intervention drew on existing skills and underlying philosophies, but individuals not experienced in working with this population and/or group delivery mode needed support to fill gaps in their knowledge and perceived ability to deliver the intervention. Ensuring adequate resources and training, or co-delivery where responsibility and accountability could be shared, was key in in such circumstances. However, the challenges of working across organisations where it is important to ensure the alignment with core aims and governance protocols were acknowledged. Working contexts need to be aligned to ensure success.
Alignment with existing protocols was specifically highlighted with respect to the time constraints placed on delivery of the intervention and, notably, the time assigned to conduct initial family assessments. The lack of time to gather information and prepare families for the intervention was worrying for many and concern was focused on parents rather than children. Thus, some asked for more time to prepare ill parents who they felt were not always ready to engage with an intervention, especially one focused on their children’s needs rather than their own needs.
Facilitators also highlighted some aspects of the intervention that caused significant burden. The manual was seen as helpful but it was felt that more work is needed to ensure better implementation in practice. In particular, practitioners/facilitators with less clinical experience found that considerable effort was required to familiarise themselves with sessions and activities. There was a perception of significant repetition in the manual that may have increased their workload prior to delivering sessions. Others highlighted that further efforts were needed to ensure successful attendance by families and they reported their frustration and that of families about transport difficulties.
Acceptability of the intervention was evident but it is apparent that it is likely to be affected by the facilitator’s existing experience and skill set. Facilitators with less experience working with adults were more vocal about the concept of ‘parent readiness’, at times highlighting that this was a barrier to achieving outcomes. Those with more experience of working with whole families tended to focus more on the benefits gained by parents, viewed as an additional benefit to the CYP outcomes that the Young SMILES intervention aimed to achieve. The data allude to the requirement for additional work to be done to align intervention facilitators traditionally used to working within adult or CYP services with a new model of working. Such training needs to provide opportunities for interdisciplinary and cross-fertilisation of experience.
Study 2: referrer perspectives
The aim of this study was to explore the challenges of identifying and engaging with families about the intervention. During the trial, we were aware of challenges to recruitment, and randomisations fell short of our target sample size. Therefore, we sought qualitative analysis of perceptions of practitioners involved in establishing referrals. These data must inform recommendations about how best to identify, engage and refer this vulnerable group for future intervention.
Methods
Purposive sampling techniques were used to identify participants in one site (voluntary organisation), which was based on practitioners in the NHS, schools and the voluntary sector who agreed to refer eligible families that they worked with to the Young SMILES trial. Practitioners were approached to take part in this qualitative study after the recruitment deadline elapsed (May 2018) by the e-mail provided to our research team during a launch day to services and organisations that engage with families affected by parental mental illness. The e-mail contained a consent to contact form as well as a participant information sheet explaining the study. Participation in the qualitative study was entirely voluntary and not associated with any monetary or professional reward. Research team members were available by e-mail or telephone to answer questions. Once the consent to contact form was sent back to the researcher, the practitioner was contacted to arrange the time, date and location of the qualitative interview, offering the option of meeting in person or conducting the interview over the telephone. Non-referrers were also approached to identify the obstacles that prevented them from referring families to the trial.
Data collection
Qualitative interviews were conducted face to face and by telephone. Written consent forms were signed by participants at the start of the focus group prior to any data being collected. All agreed to the recording of the discussion. Data collection was undertaken by the trial researcher (AK) who had received qualitative training. NPT was used to inform the content of the interview semistructured schedule that was developed in advance of the interviews. The first section focused on practitioners’ initial perceptions of Young SMILES. First, the interview explored how the practitioner was made aware of the Young SMILES intervention, as well as the quality of information provided about the intervention. The interview moved to how practitioners appraised the value of the intervention. The objective of the topic guide was to facilitate exploration of (1) practitioners’ initial expectations of the trial to help their clients, (2) potential value of the intervention to the practitioners’ work, (3) differences between the intervention and other forms of available provision, (4) the impact of implementing the referral pathway on practitioners’ work schedules and their services and (5) whether or not the service they worked for was sufficiently resourced to manage the referral pathway effectively.
The second part explored practicalities and challenges of referring families to the Young SMILES intervention. The aim was to identify obstacles that undermined or prevented practitioners from referring families to the Young SMILES intervention and to explore how referral pathways differed from other services in the local area. The interview concluded with a discussion about viability of the practitioner continuing to refer families to Young SMILES if it were a permanent part of the local service provision.
Data analysis
Data underwent a thematic analysis informed by NPT. 144 Data were managed in NVivo and thematic analysis was conducted by one researcher and independently verified by another. Emergent themes were coded using a method of constant comparison comparing, classifying and refining codes across interviews until no new themes emerged. Distribution of codes was recorded and any data falling outside the coding frame were re-examined to determine if important concepts were being missed.
In the second phase of analysis, emergent themes (and constituent codes) were mapped to the NPT framework, continually checking for fit. Mapping was carried out collaboratively by two researchers, with ambiguities and/or differences in insight resolved by discussion with a third member of the team. Participant checking of the data coding process was not performed. Analysis and collection of interview data were conducted concurrently.
Key findings
A total of 33 potential participants were invited to the study; six expressed an interest in taking part and five completed a qualitative interview. The demographic characteristics of the referrers who participated can be found in Table 29.
| Characteristic | Total (n = 5) |
|---|---|
| Sex | |
| Female | 5 |
| Male | 0 |
| Referrers | 3 |
| Non-referrers | 2 |
| Occupation | |
| Primary school safeguarding officers | 3 |
| NHS school health officer | 1 |
| Recovery worker | 1 |
All of the emergent themes identified in the first phase of our analysis mapped onto the NPT framework and no codes were deemed to fall outside its scope (Table 30). Therefore, we structure the presentation of our results around its four key constructs: coherence, cognitive participation, collective action and reflexive monitoring. Participants are assigned a number rather than a name or pseudonym within the text. Participants’ sex and length of professional experience are provided.
| NPT construct | Study themes |
|---|---|
| Coherence |
|
| Cognitive participation |
|
| Collective action |
|
| Reflexive monitoring |
|
Coherence
Referrers recognised the value of the Young SMILES intervention, reporting that it aligned with the objectives of their organisations. Of particular relevance for referrers was the acknowledgement that there was a lack of services at a local and national level that take into account the impact of parental mental health on CYP. Although there was recognition of parental support and separate support for children experiencing difficulties, Young SMILES was regarded as a novel ‘whole family approach’ with the potential to fill this identified gap in services:
I think most of our families that are in similar schools to us, in similar areas to us, will all say that mental health is one of our big hot spots, so trying to be able to address family support. And you unpick a child’s, you unpick a behaviour of a child, there’s always some sort of mental health problem with a family member that we’re trying to unpick as well . . . if a family are saying that they’re struggling I think it’s and they’ve got mental health or the child has got mental health I think it’s a brilliant scheme to be able to get families in.
R3, Referrer
I can’t believe that you’ve not been inundated . . . it’s what we’ve been looking for, something to support our children who are dealing with highs and lows of parents. It’s what we’ve been looking for. There’s nothing out there.
R1, Referrer
In attending, referrers were hopeful that Young SMILES would positively contribute to children attaining insight into their parents’ experiences and, consequently, have a direct impact on aspects of their QoL:
Yeah, I suppose it would be things like regular school attendance, improved sort of . . . maybe more parents’ motivation, understanding, you know, when medication stopped, things like that, that it does impact on the children.
R2, Referrer
Yeah, I mean I’d hoped that it would achieve sort of changes really and sort of I suppose a bit of a better understanding because I suppose when parents are locked in all their own needs and sort of, you know, some quite serious mental health conditions sometimes the child’s needs can be overlooked in a way, and I suppose it’s hopefully giving them a better appreciation of that. That’s perhaps the hope maybe, and that would have then an impact on things like attendance, getting them ready for school, homework, hopefully, in some way, give them a . . . yeah.
R2, Referrer
Referrers spoke positively about the information packs that had been produced for families. They felt that the information was accessible and conveyed all aspects of the intervention and feasibility trial effectively. However, many referrers recognised that they lacked awareness of some of the research processes that may have influenced how the trial was explained to families, highlighting a tension between the research design and the referral pathway. Some mistook the mechanism by which families were included and randomised, highlighting the fact that some families would not be offered anything:
Really clear [information pack] and I just want to say that it was that clear that the meetings that I had I took the pack into the meeting and some of our parents can’t access long words, lengthy documents, all that kind of thing but it was easy accessible for the parents that struggle with reading, things like that. So I would share it in a meeting with them and they’d be like, oh, yes, yes, this is something I want to do . . . The only thing, I was a bit like, so who’s going to be delivering it? Why are we sending it to Manchester? I was a bit like . . . I don’t get that side of it but do you know what, I’m going to send the referral in anyway . . . Maybe again on my behalf, I didn’t fully understand that so I didn’t get them ready for . . . I thought once the referral had gone in, if you’d got past that stage you were in.
R1, Referrer
We had others that were interested but I think there was some complications with some people getting in and some people not receiving anything . . . It was something to do with being research, wasn’t it? That some families get the service and some don’t to see if works or not.
R5, Non-referrer
Cognitive participation
Referrers demonstrated their commitment to ensuring that family access to the Young SMILES intervention was a smooth time-efficient process. They regarded themselves as responsible for ensuring the successful engagement of families with this process, with some assuming accountability for the resultant outcome(s):
Once a parent has said they’ll do it, I like to try and get it in straight away because then it’s done and dusted really. And it’s not hanging round like, saying, well come in next week and we’ll fill the form in. It’s like it’s getting them here again.
R3, Referrer
Referrers recognised that families generally want support and that Young SMILES could serve as an alternative support mechanism. For some, persuading families to participate in the trial was straightforward. However, it was acknowledged that, in spite of their own commitment, they would have to invest time and effort to ensure the commitment of many of the families they encountered. Overcoming parental barriers to engaging with mental health services led to low expectations of getting families to engage:
It’s not going to be an easy sell ever I think because it’s quite a commitment isn’t it for that family to take on. I think it’s much needed but I think it was one that was, once you sort of got over being able to talk about it, because some parents just want to deal with it in isolation and not bring the children into it because they, they, my children doesn’t know about my mental health.
R3, Referrer
Further difficulties were anticipated when trying to engage families where the parent is not committed to invest in their own recovery. Poor parental engagement was regarded as a generalised problem, but not one that was necessarily restricted to mental health research or interventions:
I just feel like some of the parents who we have contact with, we struggle getting them to attend . . . to take their children to their own health appointments and to even access health appointments for themselves, without them committing to do something that’s a course, just statistically, we tend to have quite poor engagement with parents. They’ll contact . . . we’ll have a good one-to-one and we can have that contact but for them to actually attend things, it’s really hard.
R4, Non-referrer
Referrers acknowledged that non-engagement did not reflect the parent’s lack of interest in supporting their children’s needs; parents had a genuine interest in trying to improve the lives of their children, but were often hampered by the mental health difficulties they were experiencing. It was clear that parent engagement was difficult across numerous services, not just those with a specific family focus. It was thought that parents may have been more persuaded by the value of the Young SMILES intervention if their participation was not required:
I think most parents genuinely want the best for their children and they want the children’s needs met and their emotional needs met. So I think most parents wouldn’t have an issue with the children or young people being referred but the actual commitment of them to have to attend something, I don’t think a lot of them have that ability, due to their poor mental health, if that makes sense? . . . I’d say I tried on three or four occasions about support for the child or young person and the parent seemed keen initially and then as soon as you suggest that it’s something that they might have to attend, they weren’t interested.
R4, Non-referrer
Parents’ apprehension about their problems becoming known to social services conflicted with their desire to participate:
I suppose for . . . the concern is that the parents, because of sometimes lack of engagement and the way that, you know, mental health can be where you can sort of bury your head a bit really, if you like, stop taking your medication, not engage with people in the outside world, and things, that that would . . . could have an impact where they think, well I don’t want to . . . I can see the benefits but I’m not going to do that, you know? . . . they’re the ones that . . . they’re the ones you want to help because they’re the ones whose children aren’t coming in and aren’t doing their homework, and all the things that the impact . . . don’t engage in, other things with school, and, you know? . . . But obviously they’re scared, saying, oh, my children are going to be taken off me, I don’t want that . . . because people don’t quite know how . . . what the response will be to them or them disclosing something about their . . . particular things around self-harm and children being . . . you know, all that kind of stuff is, yeah.
R2, Referrer
Despite their enthusiasm for the Young SMILES intervention and their identification of the gap in current services that the intervention has the potential to fill, at times referrers were apprehensive about promoting involvement in the trial as they were unable to sell the benefits of the intervention in the face of this being an early-phase trial and, therefore, coming before a supportive evidence base. Initial caution about the Young SMILES intervention was apparent. The gap in current knowledge about the Young SMILES intervention had a direct effect on the attitudes of referrers and their anticipated belief that the parents they approached would be happy to participate. Gathering knowledge about the outcomes and experience of families who have been involved in the Young SMILES intervention increased referrers’ optimism about the anticipated engagement of families. Having the opportunity to communicate directly with other families who had participated was regarded as a potentially effective mechanism to legitimise the intervention and ensure commitment from future families:
If I refer young people onto things, I normally have evidence of, it might be something that you don’t engage in, it might be something that you don’t feel of benefit to, but I’ve usually got evidence, or I’ve got some proof that this has worked before and once something is up and running, I am confident, as a practitioner, to recommend and refer that person onto the service.
R4, Non-referrer
Once we’ve got this family through I think it will definitely have a snowball effect and we’ll be able to get through families, more families through. Even more me, you know what I mean as, because I’d have more of a sort of, know what it’s about . . . it’s having knowledge of, you’ve had a family that’s gone through it and then you can sort of really say how the impact of that on that family. It’s good to have one to say, I know a family that have done this project, they’ve got this, this and this out of it and I think it would be a really good one for you. I think that’s a good sell.
R3, Referrer
I think, you know, parents saying to other parents who, because best will in the world those parents will talk to parents with similar needs and they will sort of say, well, we’ve done this project. It was brilliant. We really got this, this and this out of it. Go and have a chat with [member of staff]. That’s how I find a lot of my things come. I get more from parents selling it to other parents than me trying to sell it to other parents.
R3, Referrer
Collective action
Having conceived the Young SMILES intervention as a beneficial addition to the services that already existed, referrers reported the ease of endorsing it in practice for the identification of families to participate. Many reported that their day-to-day roles facilitated the process of engaging with CYP or families whom the trial may benefit. Existing systems to flag concerns about children were easily utilised to refer to the Young SMILES intervention and the identification of suitable families was also enhanced where there was an existing awareness of parental mental illness influencing family life:
We can refer clients quite quickly after they have first engaged with our service . . . they’re normally really happy to let you get on with your job like that. If they come to you asking for help it makes your job of supporting them so much easier.
R5, Non-referrer
We have a system called CPOMS [software application] in school, so it’s a way of writing down. So, all staff have access to that, to write down if the child’s got a concern, if you’re concerned and that gets flagged to myself and the head, who then will look at ways of what we need to do next . . . So, it might be the PANTS programme [NSPCC framework], the programme that we might need to do with the child and the best people to do that was the class teacher, or it might be a referral to CAMHS, and we’re thinking well if we stick a CAMHS referral in we might as well stick a Young SMILES one. You know to me it’s that sort of look at things really.
R2, Referrer
Referrers all identified that success in identifying suitable families and their subsequent engagement with the trial relied on them having established relationships with families, particularly with parents. Such families were open to discussions about their mental health, which removed some of the concerns that some parents had about opening up about difficulties they are experiencing:
Well, because of the relationship I have with the families that go to our school, I mean, the thing is I’m . . . Because of the relationship I have with them I’m outside morning and night. They tell me what they’ve had for breakfast, that relationship is, you know, how many lagers they had last night. Even if they’re going to get in trouble with me they tell me. So by me saying to them, look, there’s this course, it’s about mental health, they wouldn’t think, God, she thinks I’m going crazy. It’s not . . . because I said to you we talk about the mental health every single day so it’s not a swear word. It’s not a, oh my God, they’re going to take my kids off me. We talk about it so they don’t take it as, I’m not doing that because they’re going to take my kids. They think, oh, yes, brilliant that, brilliant.
R1, Referrer
Challenges were faced where potential families were recognised but relationships did not already exist. Referrers acknowledged that they were more likely to prioritise referral of those already familiar to them. Developing a level of trust with families was considered vital prior to suggesting routes to support:
If I went to a family that started at our school last week and said, oh, I’ve got this course about mental health, they’d go, on your bike, because, yes, I haven’t built up that relationship.
R1, Referrer
Following identification, the process of referring families to the trial was reported as being straightforward. It aligned well with existing referral protocols and, at times, was actually a less convoluted process than the demands associated with referring to other services. Referrers spoke about how easy the trial and intervention was to discuss with families. In aiming to convince families to participate they used the study pack and highlighted their methods of giving families time before following up to gauge interest:
I thought it was an easy one. You know, there’s an easy referral form to get in. It was pretty straightforward, it certainly wasn’t like other referrals. It wasn’t that, it wasn’t pages and pages, which always puts people off. Yeah, it was, you know, it was a quick one-sided thing and talking to the family, them agreeing to it and then you sort of made contact with the family. That’s the only thing I thought that may be a sticky wicket with some of our families, because they don’t answer the phone very well.
R3, Referrer
Sometimes when you initially say to parents that, what about a bit of a referral to this? It’s, you sort of do that once and then you walk . . . have a think about. Then you come back to it and you say, what do you think about it? And it’s sort of that drip feed into there and sort of talking about the project.
R2, Referrer
It was just dead easy. That’s why I couldn’t understand you weren’t inundated because it was so easy, so easy and the families thought it was so easy. I was able to give them a leaflet, talk through it in a meeting, take this leaflet home, have a read, come back tomorrow and if you still want it we’ll fill the form in and that’s how quick and easy it was.
R1, Referrer
After being made aware of the Young SMILES intervention, all practitioners reportedly integrated into their daily routines the business of referring families to the research team straight away and without too much difficulty. This was because of how the referral pathway fitted into their existing work without any reported difficulty:
I’m always keen to refer people onto good quality services that I feel that they’re going to benefit from. So I do feel . . . because I have a drop-in service within one of my . . . I’ve got a high school, so my high school, I’m in my high school for 4 to 5 hours a week.
R4, Non-referrer
I do an awful lot of referring into different, to different, to different companies for different things and it’s trying to find one that will help that certain family sort of thing. So I found it was, I’m quite open about talking about mental health . . .
R2, Referrer
Referrers stated that they worked independently to embed the referral pathway into their existing work-based settings, requiring little or no consultation with others to do so. However, there was recognition that a number of key individuals were involved in the process of obtaining support for CYP and that raising and widening the awareness of the existence of new interventions would enhance the decision-making process:
I wouldn’t need much help in referring families as it is an easy thing to do . . . I mean it doesn’t take much time at all. It would be good if the period you could refer families was longer . . . we had other families that could have been referred . . . as you know [laughs].
R5, Non-referrer
Although the referral process was straightforward, adding little or no burden to current procedures, one referrer took responsibility for following up the progress of a family through the recruitment and intervention process. This aligned with their views that once a referral had been made this did not mean that all responsibility for that family had been passed on. They wanted to retain a role in the process, taking time to support ongoing procedures if needed:
To be honest, that’s why I went that extra mile because when I refer a family it’s not like I fill a piece of paper in and then it’s your business. As far as I’m concerned when I’m referring someone I’m buying into that as well. So when you [researcher] rang me back and said, can’t get hold of . . . it’s not, oh, well, I’m sorry you can’t get hold of . . . I think that’s . . . I’m the referrer so I need to make sure that’s happening. That’s why I did the extra bits to make sure that happened . . . if I got a message off the NSPCC saying it’s been postponed or whatever, I would make sure I spoke to those families that morning and if they weren’t on the playground I’d ring them but when you talk about taking up time in my day, I would say that’s part of my job. It’s part of my job to make sure my families know when the course that I’ve referred on is going to start.
R1, Referrer
This approach of chasing up referral progress and re-engaging with parents, however, was a personal choice and not one practised by others and thus it was not considered vital to the implementation of the Young SMILES intervention. For some, because the Young SMILES trial was voluntary, they did not want to seem like they were forcing parents into it:
I’m more, I do, I do the playground every morning so parents will predominantly come and speak to me about their days and it’s just an informal way of me getting on that playground to see parents and see families and see how they tick. And to sort of say, how’s it going? How’s your day? How’s this week been? Do you need anything? Where are you up to? And to sort of say, well don’t forget we’ve had a chat about that. Don’t forget if you want to do it, if you need the paperwork again come and see me. I’ll print it off and we can go through it again.
R3, Referrer
Reflexive monitoring
Referrers were all interested in developing insight into the experiences of the children they referred to the trial. No formalised ways of obtaining that feedback had been implemented, but referrers reporting seeking feedback during any communication opportunities with the children of parents that arose, for example during scheduled or unscheduled telephone calls or meetings. For the majority, reported outcomes were positive. Children were also offered support after attending sessions, but it was never required:
When I have a parent ask to see me at the front that, I mean, she was one of the ones that we had to keep chasing and rearranging and all that, when I have a parent come to me at the front and say, Young SMILES has changed my life, that’s enough for me.
R1, Referrer
The feedback from the children, the feedback from the parents, after a Thursday was amazing; absolutely amazing. I sent kids on there that had anxiety. I sent children on there that don’t like to be with anybody that they don’t know and they were amazing. They came back, ate their dinner, no worries, no crying, no . . . As a safeguarding manager I left time in my day on a Thursday to give them children support when they came back in case; they didn’t need it.
R1, Referrer
In addition to the feedback received, referrers observed changes in the behaviour of CYP who opened up about talking about mental health after attending the Young SMILES intervention, sharing their learning with other CYP who did not attend:
One of the girls that went on the course, she’s in a group that I do in school as well and she said to me, am I allowed to share things that was on the Young SMILES? I said to her, well, you’re not allowed to share things with names, but you can share . . . if you think that would help our group or it’s a strategy that you could use, and a number of times she shared strategies with a group of children suffering with anxiety.
R1, Referrer
Despite recognising the benefits of the intervention, parents expressed scepticism:
No, I’ve read lots of course details. I’ve read lots of programme details and my families say to me, it’s just the same thing over and over again. They’re just telling us the same things. You just think my parenting’s rubbish. You think this. You think . . . So I thought if I start low, if I get one thing or a parent gets one thing from this course my job has been worth referring.
R3, Referrer
In reflecting on the referral process and how it could be enhanced, the importance of building collaborative supportive relationships between referrers, their organisations and the delivering organisation to involve key individuals at early stages of the process was highlighted. Referrers demonstrated their commitment to making this work and discussed the possibility of developing ‘working parties’ to ensure that barriers or unexpected challenges (particularly those not aligned with their working protocols) are challenged and resolved:
About the taxis, I mean, I think the people who were setting it up, without being horrible to anybody, don’t work in the school so the logistics of a child getting in a taxi is massive. So like the [voluntary organisation] was ringing me and saying, right, yes, OK, we’ll put taxis on. So I said, OK, so what about when that parent goes that child’s in the taxi with them, fine. What about if that parent doesn’t turn up? I can’t send that child with somebody else’s parent because we haven’t had an acceptance with that. Oh, right, well, we’ll have to look into that. So I think the people who designed the programme, fantastic. I think the people of the set-up need to be aware of the policies and procedures in school because I can’t just let somebody go in a taxi with somebody else’s parent.
R1, Referrer
Enhancing engagement with CYP and their parents was something that referrers indicated that they had failed to do to a great extent and something that they felt in the future could enhance engagement and experience:
I think it might be better if there’s a few, a few of us sort of talking it through. And I think it would be better if, to be able to have an open morning, thinking like the, and your, the people are coming here. I’m going to invite a few to come and sort of sell it to them that way. That’s always gone pretty well with getting services in; and I think it’s that knock on effect if others, of other families in the area doing it as well. And then you sort of say, oh well they’re and if they’re not even in primary, some sort of youth service, that type of thing and sort of saying, you know, get those in. Drugs and alcohol maybe that’s the need. So, it’s a bit more of a crossover of people and doing referrals in.
R3, Referrer
In hindsight as a . . . if you were to run it again, that where you put the poster in the thing where all parents can see and . . . things, or maybe on the newsletter. I don’t know. We’ve done that about other things. We didn’t on this occasion. I think it was new. They came in and did it and, yeah, perhaps with more thought if you knew it better you could do that . . . So, it . . . I suppose it’s giving them opportunity to see that this programme’s on offer, and that’s probably where it’s . . . the shortfall’s been maybe, looking at it, but I didn’t even think of it until you come today . . . Early help maybe, yeah, preventative stuff are the ones what we’ve perhaps not targeted, and it’s probably a variety of . . . the time limit you get, someone coming in, oh, we’ve got this project. Great, I’ll refer in. And it’s the ones who immediately come to your head that you refer rather than thinking, right, I’ll think this through and I’ll put the poster up.
R2, Referrer
Referrers acknowledged that incorporating Young SMILES referrals had little effect on their workload but identified that aspects of its implementation could be modified to ensure the well-being of users and enhance experiences including removing the waiting list group, increasing the window of time for receiving referrals and reliable information about waiting times. Despite positive views about outcome, randomisation of some families to usual care was perceived to have detrimental effects and could be challenging for referrers to respond to. Eliminating the option of being referred to nothing was considered an important future approach to overcome such negative effects:
It was hard. It was like [parent] came in and she was like, look, I’m not even good enough for that, because at the time as well she was having job interviews and she’d been knocked back from two of them so she was just like, see, I’m not even good enough. You’re telling me that . . . so it was all that. So I had quite a heated meeting with her and I was like, yes, you are, and had to bring her back down to, look, this is about . . . I did say to her then, this is about a screen with names on, tick numbers, if you’ve got enough ticks you go through. If you’re not right for this scheme you’ll go on the next one maybe. I didn’t know what would happen next and I just needed to come to a plan with her that she didn’t feel low self-esteem and that she’d been let down.
R1, Referrer
Having a longer time period to introduce the value of the Young SMILES intervention to families could improve the referral pathway and have a significant effect on awareness and use of the service:
If it was a longer-term project it is something that could, sort of you can roll out to staff in school. So I could talk, we do safeguarding days. So September we always have a safeguarding day, so we would re-hash all the things that we stand for and we do in our school and we will talk about, I talk about projects like parenting referrals and all those sort of things. So at that point, you know, I would probably stand up and say, we’ve got this new project come in. If any parents, you’re thinking parents will address it or want to talk about it, tell them to come and have a chat with somebody about it. Or they’ll come and bring them down.
R3, Referrer
Reliable information about processes that could be communicated to families was a vital part of sustaining the engagement of families. Referrers reported gaps in their knowledge about some aspects of the process, particularly in relation to waiting times that were of unknown length, which had an impact on the work of the referrer:
Yes, you see my parents do as I say, a little bit. So I say to them, it starts then, and then I go back to them and say, it’s not starting this week so don’t worry, I’ll let you know, so it was all that. So they’re really good but I’ve never come up with a problem that they say, oh, you told me last week, I’m not going on it now. I haven’t come up with that because they do listen and I say, look, it’s been postponed, don’t worry I’ll come back to you. This is when it’s going to start, and they just listen to my word. Again, I think that’s because of the relationship but I could do one next time and if it’s put back put back, put back, they might be, oh, I’m not going on it now.
R1, Referrer
Although acknowledging that referring families to the Young SMILES intervention was not complicated or a burden on referrers’ time, it was suggested that referral rates could be enhanced via adult services where work is focused directly on the parents:
I mean we can sell something to parents and as I say and to families, maybe it’s something that should be sold more with adult services, who the parents are engaging with. Maybe it’s to get adult services, when they have contact with parents to say, this would be really good for your child to attend, I don’t know.
R4, Non-referrer
Strengths and limitations
The small sample size in the referrer study is noted as a considerable limitation. Having increased representation from both referrers and non-referrers would have been beneficial. It is also disappointing that the sample lacks representation of the individuals and organisations that had the opportunity to refer families to the Young SMILES intervention. However, as this study was added as an additional way of exploring the difficulties experienced with recruitment and the development of referral pathways in the voluntary organisation site, it does provide helpful insights into some of the difficulties faced when referring families into a research trial and some suggestions for future work with this sample.
Despite not referring any families to the Young SMILES intervention, non-referrers, albeit a non-representative sample, were extremely positive about the intervention. Owing to the small sample size and positive attitudes, little exploration of this issue was enabled. However, it is anticipated that the non-referrers may not have wished to disclose their lack of referral as it was influenced partly by their own values on research participation. Given their awareness of family needs, it was evident that some referrers feared negative consequences for families should they not be allocated to the intervention. This needs consideration with respect to future evaluations of the Young SMILES intervention based on RCT methodology.
Focus group methodology, rather than individual interviews, may have revealed individual values focused on communal attitudes and barriers related to referral to the Young SMILES intervention rather than individual practices and values.
Discussion
For referrers (and non-referrers), it was apparent that barriers to referring families primarily related not to the implementation of Young SMILES within current working service models, but to research trial restrictions/procedures, as observed in facilitator interviews. Uncertainties surrounding when the intervention was going to start caused communication difficulties between the referrer and the families. For some, this related to the fact that families gathered interest in taking part and then subsequently were saddened when randomised to usual care.
Recognition needs to be given to the fact that, in a trial setting, research processes of referral and recruitment using third-party representatives have a potential two-way effect, affecting not only trial recruitment numbers but also relationships between referrer and potential participants (families). To enhance referral rates, effort may need to go into co-developing training and support mechanisms/resources to explain trial procedures and preserve existing relationships between referrers and participants. These concerns may be less salient at service roll-out, when referrers would be able to draw on evidence of effect and guarantee evidence of eligibility and access to intervention.
As recruitment strategies were different in the co-delivered NHS–voluntary organisation site where it was possible to target lists of families currently receiving support, explorations of referrer views were not sought as the families were targeted and invited directly by a trial researcher employed within the NHS. Speaking to members of the other site may have helped to explore how learning from different recruitment procedures could enhance recruitment and referral pathway development at other sites.
Chapter 8 Summary of findings and assessment of feasibility
This series of feasibility studies addressed the research question of whether it was possible to co-develop an intervention to enhance the HRQoL of CAPRI and whether or not such an intervention would be suitable for future trial.
The following provides a summary of the final objectives and the criteria for success for whether or not they are achieved. Under each tabled objective, we discuss the evidence for their delivery; this evidence is then considered in the final chapter on conclusions and recommendations about whether or not a future trial is needed and feasible.
Objective 1
Co-produce (with stakeholders) an intervention that was acceptable to families and feasible to deliver in the NHS and in the community with support from health and non-health professionals
Chapter 2 of this report provides definitive evidence that we successfully co-developed a standardised intervention called Young SMILES (including staff and service user manuals and resources) for CAPRI. We did this in collaboration with service users, NHS and non-NHS stakeholders at every stage of the process. We also developed training for staff facilitators that was tailored to the differing needs of NHS, Barnardo’s and NSPCC staff. This training was standardised and included a manual for practitioners delivering the intervention and a compendium of resources, including craft materials for activities and relevant literature.
Young SMILES broadened the scope and content of the existing Family SMILES NSPCC intervention to make it:
-
specific to families whose parents have SMI – schizophrenia, bipolar affective disorder or severe depression or personality disorder
-
in line with current NHS priorities and service structures
-
deliverable in different practice settings by a varied staff skill mix, including NHS IAPT practitioners and NSPCC third-sector providers
-
age appropriate to a wide age range of children
-
accessible to all CAPRI and not only those with identified risk of maltreatment/neglect or childhood mental health problems.
The early stages of our qualitative evaluation prioritised already established frameworks of acceptability and implementation for intervention development rather than identifying critical change mechanisms. Shaping our intervention using our intervention theory of change would have been an alternative approach; however, our qualitative studies evidenced multiple examples of the change mechanisms postulated at the start of the feasibility study.
Strongly endorsed theory of change mechanisms (see Appendix 2, Figure 2) included improving parent–child communication, normalising mental health and improving children’s social networks. Others will require further consideration at intervention refinement stages, including practising mindfulness.
Objective 2
Determine the rates of intervention uptake and adherence, and of completed follow-up measures
One-fifth of eligible families who were approached by their care co-ordinators showed an interest in participating. Out of the total 49 families who were assessed by telephone (via the NHS, n = 31; via the NSPCC, n = 18) for eligibility, 35 (71%) met inclusion criteria and received a face-to-face assessment and subsequent randomisation; nearly one-third of those (n = 12) were recruited in the NSPCC sites and two-thirds (n = 23) in the NHS.
Children typically had very high adherence to the intervention, completing seven out of the eight offered sessions. The overwhelming majority of recruited parents were mothers, although there was a balance of sexes among participating CAPRI.
Quantitative data revealed that CYP had a high adherence to the intervention, attending seven out of the eight offered sessions (see Chapter 4). Treatment uptake by parents mirrored previous experience for Family SMILES,146 which similarly found it more difficult to recruit parents than: Family SMILES included three or four assessments with parents prior to the intervention and, in general, was significantly parent focused compared with our child-centred approach. This is notable given that NSPCC facilitators and referrers raised particular concerns (see Chapters 5 and 6) about the relative lack of parent assessment within Young SMILES and attributed parent difficulties in engaging with the process to this. A key misunderstanding among these parents related to the parental aspect of the intervention and the fact that their needs were not the focus of sessions, which many had difficulty with and were not used to.
Qualitative feedback reported in Chapter 5 was provided by 17 children (from different families) and by 14 parents who underwent Young SMILES. Feedback from CAPRI randomised to Young SMILES was primarily from younger children, equally divided between girls and boys. Both parents and children initially expressed reservations about what the intervention was for and about transport difficulties. However, feedback from both was largely positive with key areas for refinement/adaptation. However, there was no clear pattern of positive/negative views by demographic group (e.g. about the nature of the intervention and their experience of attending the sessions). Children highlighted the benefits of having learnt more about mental health and what some of the experiences of their parents were like. They also valued making new friends and the fact that the Young SMILES intervention acknowledged their roles in supporting their parents, which they felt needed more attention from services. Children said that attending the Young SMILES sessions provided learning and subsequent understanding that they felt could affect their parent and family directly rather than changing their QoL directly.
Despite initial apprehension, parents were motivated to attend for the benefit of their child’s well-being. For many, the Young SMILES intervention offered a unique opportunity compared with the support that their family had previously received, instilling a sense of hope through recognition of improvements they observed in their relationship with their children and facilitating communication and connection with their children and with other parents in similar situations. They expressed difficulties with attendance focusing on their anxieties about exposing their difficulties to professionals and about practical aspects of arranging transport or having the time to attend. Notwithstanding this, parents all asked for more sessions (i.e. the same number of sessions as their children) and for more preparation for groups (akin to Family SMILES146). In other words, parental feedback about adherence was contradictory.
Only three of the older children provided feedback. They expressed concerns about a ‘one size fits all’ approach in sessions. In spite of this, participation and adherence among older children was uniformly excellent.
Chapter 6 reflected facilitator and referrer feedback about if and how the Young SMILES intervention met the expectations and needs of the target group. It was clear that it provided a much needed approach for a group of children who these stakeholders viewed as vulnerable, in need and significant in number with one referrer commenting ‘I can’t believe that you’ve not been inundated . . . it’s what we’ve been looking for’ (WR1). However, they identified the need for further development to create efficient, safe referral pathways with better mechanisms for working across organisations.
Combining evidence from CAPRI, parents, facilitators and referrers, we propose that Young SMILES represents a standardised intervention that does indeed meet many, if not all, the varied and complex needs of participating families. We also conclude that the Young SMILES intervention needs to be tailored and adapted to address the criticisms described in this report. Some of these changes include:
-
more training about the randomisation process for referrers and services
-
developing an orientation for parents and children prior to their involvement to clarify the purpose of the Young SMILES intervention
-
using simplified packs that we developed for referrers and parents
-
describing elements of the content more clearly for facilitators with more resources and exemplars in the manuals
-
further development of the Young SMILES intervention for the older age groups and to meet the diverse needs of different families and children.
Overall, participants’ perceptions following attendance suggested that the intervention aligned well with the principal aims of the Young SMILES intervention. In particular, narratives highlighted specific improvements gained by children. Post-intervention improvements in children’s well-being and behaviour were particularly noted through narrative accounts by a range of stakeholders and children, who said that they had gained insight into parental mental illness and improved their mental health literacy.
The NSPCC practitioners had a high level of skill and experience of working with children in group work settings, and the NSPCC assessment for suitability, completed on receipt of the referral, provided essential information to help the practitioners respond to the child’s needs within the group and on an individual basis. NSPCC practitioners were also experienced in delivering and achieving intervention outcomes via creative activities.
Out of the 35 randomised families, 33 families (Young SMILES group, n = 18; TAU group, n = 15) provided baseline data. Of those families, 28 gave follow-up data at the primary end point (4 months post baseline): 15 out of 20 (75%) in the intervention group and 13 out of 15 in the control group (87%). Across both intervention group and control group, once randomised, there was a high rate of > 80% completion of follow-up measures. Complete or near-complete outcome measures were collected from CYP at baseline and the two follow-up time points (i.e. 4 and 6 months) for the primary outcomes of HRQoL and for our secondary outcomes. Researchers reported the ease with which they collected measures from CYP, who, in the main, demonstrated considerable enthusiasm when engaging with the research process. For parents, there were slightly more missing data by the 6-month follow-up as more parents had dropped out. This reflects not only the experience of the Family SMILES intervention in earlier studies, but also reflects better engagement and adherence by CAPRI compared with their parents overall.
Objective 3
Identify appropriate outcome measures and estimate their data missingness
From a battery of standardised questionnaires, we identified two primary outcome measures for child HRQoL: the PedsQL127 and the KIDSCREEN. 126 We explored each measure’s sensitivity to change and ability to capture key areas of HRQoL for CAPRI. Outcome measures also included the SDQ,110 which is routinely used by IAPT-CYP and NSPCC services, and the RCADS. 111 We also measured parenting skills and child–parent relationships using the Arnold–O’Leary parenting scale114 and the PSI-SF. 115
We noted high completion rates (> 80%) of the child-reported outcomes measures at the primary end point (4 months). Parent-completed questionnaires had more data missing (up to one-third) for child-proxy outcomes and for parent outcomes (up to one-quarter missing). We were not able to capture any change or a sense of direction for change in the measured outcomes because of the sample’s small size and large heterogeneity.
Our systematic review, which underpinned the original HTA 14/29 call, found that there were no interventions to improve HRQoL aimed at recent populations of exposed children. 6,68 Similarly, there is little or no evidence available about the HRQoL of these children. However, accumulating high-quality evidence reports that children living with parental mental illness in the UK in 2020 are more likely to live in the lowest socioeconomic quintile and, therefore, more likely to be exposed to multiple deprivation and experience significant unmet needs. Furthermore, although population data suggest that the majority of CAPRI do not develop mental illness, or other adverse outcomes, their relative risk across almost all outcomes (e.g. mortality, injuries, broader physical health, mental health, health-care use, vaccination uptake, as well as school leaving grades and employment) suggests that they do relatively badly compared with their peers without parental mental illness. Taken together, we would expect more unmet needs, as well as worse QoL in CAPRI. This was not picked up in our small sample using the available, age-appropriate, HRQoL measures developed for the general population.
Our view about this is as follows: either future research needs to develop better ways of measuring QoL specific to the experiences of this population and QoL is likely to fluctuate over time and any such outcomes need to reflect this fluctuation, or QoL may not be the most appropriate construct to use as a measure of the vulnerabilities experienced by this group of young people and is, therefore, inappropriate to target in any future interventions to improve their life outcomes. With this is mind, we have reflected that assessment of unmet needs across a broad array of experiences in the home, their social lives and school may be a more sensitive guide to the repeatedly evidenced vulnerability of children living with parental mental illness. We are also of the view that such needs are likely to vary over time and to depend on circumstances within and outside the family (e.g. exams or bullying) not just the state of the parent’s health.
Bearing these challenges in mind, it is our view that improving the lives of CAPRI requires a public health approach (because the vulnerabilities evidenced are described across the population of exposed offspring) that is scalable, affordable and responsive to changes in individual needs across time. We believe that such an intervention is likely to be digital and our preliminary discussions with stakeholders suggest that many of the valued elements of the Young SMILES intervention can be repurposed to this end.
Objective 4
Develop a child resource utilisation questionnaire and estimate its data missingness
We developed a resource use data collection tool. We did this by adapting the CA-SUS130 for our study setting in consultation with Professor Sarah Byford, the designer of the original CA-SUS questionnaire. This adaptation involved removing the sections on out-of-pocket expenses and employment, removing the question on education type, removing the follow-on questions asking name of hospital for the hospital service use questions, removing complementary therapist (e.g. homeopath) from the list of community services, adding NHS walk-in services and NHS Direct to the list of community services, and simplifying the questions in the criminal justice services section.
We then piloted the collection of resource utilisation data using this adapted version of the CA-SUS. Resource utilisation was collected retrospectively during this piloting using participant recall.
From this piloting exercise we found that participants were willing and able to respond to questions from the CA-SUS regarding accommodation, education, hospital service utilisation and community services utilisation. However, of the 27 community services listed in the CA-SUS questionnaire, participants reported no utilisation of nine of these services at all three time points. To minimise participant burden it may therefore be advisable to remove some or all of these services from the list of community services questions in a future trial.
Response rates were zero for questions regarding medication prescriptions, and very low for questions regarding interactions with the criminal justice system. For a future trial, a decision must be made about the likely importance of these categories for this patient group. If it is hypothesised that the intervention is likely to have an impact on resource use in these areas then alternative methods of data collection may be necessary. The importance of criminal justice service use will also depend on the perspective of any future evaluation, and may be excluded if taking only a national health and personal social services perspective.
Objective 5
Capture the experiences of children and parents who participated in the intervention and of professionals who referred or supported families
Content co-development was within the limitations of the target population. The aim was not to co-design from the start. The outcome of the intervention (i.e. HRQoL) was determined a priori by previous literature identifying evidence gaps. Thus, intervention development may be more closely aligned with stakeholder co-refinement and co-development of format and content, rather than co-production across the piece. The aim of the qualitative aspect of the feasibility trial was to seek further CYP input for amendments and adaptations in future iterations of the intervention.
Although children were unable to contribute to intervention content directly, their views were gathered through qualitative work in Phase I and represented during presentations at the consensus exercise. Professionals involved were not restricted to those working in health, allowing for varied views from different capacities and organisations to support the development of the Young SMILES intervention.
Children and young people who provided their views (and who subsequently took part in the Young SMILES intervention) lacked representation of older CAPRI (12–16 years). This is discussed as a limitation in Chapter 9.
We assessed acceptability as per the TFA framework criteria detailed in Table 23. A key misunderstanding among parents related to the parental aspect of the intervention. There were uncertainties about the reasons for attending and the way in which the parental element would be delivered with a clear tension between child and parental needs and outcomes evident. In comparison to previous support, Young SMILES was favourable with improvements to family environment, relationships and cohesion recognised as important outcomes.
The views of CAPRI were generally favourable towards the Young SMILES intervention: atmosphere, environment and facilitator personality were all reported as important contributors to a positive experience. Some concern was expressed about the ability of the Young SMILES intervention to support such a broad age range. In any future interventions, work may be needed to ensure the successful support and integration of older children to reduce alienation. Increasing opportunities for developing social networks may also enhance the experiences of young people.
Individuals referring in to and delivering the intervention recognised the opportunity for the Young SMILES intervention to fill an identified gap in service provision for CAPRI. The Young SMILES intervention was felt to be well aligned with organisational aims and objectives but needs to be adaptable to individual needs. In the current model, this depends on experienced facilitators being able to draw on others’ experiences in a collaborative approach, and when this was achieved in the groups it was valued. Strategies to implement the Young SMILES intervention in co-delivered sites requires exploration, and adequate resourcing would be necessary for the successful implementation and sustainability of the Young SMILES intervention. Parental readiness was identified as a factor that could influence the implementation and success of the Young SMILES intervention; further work is needed to maximise young people’s outcomes.
In the children’s groups, facilitators introduced self-esteem and confidence-building work as this was judged necessary for their group; this was not included in the Young SMILES programme. The imaginary family was a useful tool that the group did use, but sometimes the group was more comfortable referring to their own family’s experiences. Most of the exercises in the manual had two versions, one for the younger children and one for the older children, but, at times, facilitators had to pitch the exercises somewhere in between. In the parents’ groups, self-esteem work was also incorporated, as the facilitators felt that the parents needed this to enable them to engage with the group. The facilitators also allowed additional time for parents to talk about the impact that their mental health has on their children, as this was an emotive and important issue for them. Parents dealing with guilt and shame needed extra time to discuss and reflect on this during and after the sessions.
Some of the issues identified in the qualitative work, specifically parental readiness, highlight that further exploration of this issue is necessary to add to the current existing knowledge gap; if the Young SMILES intervention becomes routine, this potentially will have a larger impact. Families would need to be assessed to identify when they are ‘ready’ to engage in the intervention to ensure that child outcomes are maximised.
One adverse event was recorded throughout the entire study. A mother reportedly experienced distress after a Young SMILES facilitator took her comments about the welfare of her family too literally, contacting social services and reporting it as a safeguarding concern. The parent made a formal complaint to the research team, which was handled appropriately and responded to by the NSPCC after an investigation was conducted. The mother accepted the verdict of investigation, which saw evidence of malpractice.
Chapter 9 Conclusions and recommendations for a future trial
There remains a pressing public health imperative to support CAPRI
Recent papers from the UK2 and Sweden147 provide robust indicators of the increasing prevalence of children with parental mental illness. These authors also suggest that more ill mothers are receiving treatment and this should improve the circumstances for their children. However, children’s needs must be distinguished from their parents’ needs, which are clearly quite different. 42 Underlying environmental factors, such as poverty or violence in the home, are important additional sources of hardship for CAPRI. 43,44 Similarly, the most common likely consequences, such as social and educational difficulties and reduced QoL,45 are unlikely to be addressed in the very limited services tailored to these young people. Mental health services (adult, child and adolescent) are available only at the point when children become ill themselves. Furthermore, we know that the absolute risk of developing SMI, even when both parents have a SMI diagnosis, is low;46 therefore, solely increasing mental health provision is unlikely to meet their needs over time.
Children and adolescents of parents with SMI are an easily identifiable group of at-risk young people. Reliable, detailed information about the numbers, ages, regional variation and types of illness to which they are exposed over time is vital for policy-makers, clinical commissioners, education and health service providers. In our minds, the increasing prevalence and lack of resources make clear the ongoing need for appropriate and timely approaches to support CAPRI QoL. Yet it is clear from our findings that HRQoL specifically is an inappropriate measure of these young people’s needs. Most are physically fit, so the questions on PedsQL or EuroQoL-5 Dimensions do not engage with the problems that they face. The lack of recognition of need in these children,49 combined with a gap in dedicated provision for them and growth in the number of mothers diagnosed and treated for mental illness over time, suggests that they are a substantial population with unmet needs but this does not appear to be accessed by measuring HRQoL. Future planned linkages to the hospital records of CAPRI will better describe their needs and provide valuable evidence of how to address them, which aligns well with UK Department of Health and Social Care initiatives to make health care more focused on prevention. 48 These concerns should not be confined to the UK; this population is increasingly recognised as in need of greater attention and better support across the European region, and studies in North America and Australia have also demonstrated that many children are exposed to maternal mental illness. 2 CAPRI represent a challenge to the global health community.
Interventions and support must take account of children’s concerns about stigma at the same time as recognising their particular needs and providing them with the care they require separately and independently from the care of their parents. 50
Around 2.5 million children in the UK live with difficult family circumstances, such as poverty, poor parental mental health and addiction. 2 Loss of preventative public health and early intervention provision from local authority commissioning alongside specialist CAMHS raising their thresholds and eligibility criteria to manage demand, as well as geographical variation in the availability of services, has led to increasing numbers of children, young people and families reaching crisis point. 148,149
NHS England’s Implementing the Five Year Forward View for Mental Health86 places greater emphasis on prevention, integration of services and building the resilience of young people. The goal is to provide an extra 70,000 children with access to evidence-based interventions each year and move towards services that are tailored to the needs of the community. Identified areas of good practice from Future In Mind94 (guidance outlining aims for transforming how CAMHS are delivered nationally) include the need to involve CYP and their families and carers, where appropriate, at every level: from service design to commissioning, recruitment and decisions about care. The Department of Health and Social Care prioritises the creation of services that are sensitive to area, which engage across service boundaries, but also that work to reduce stigma for young people.
Our work fulfils most of these demands as well as the government’s 2018 requirement for services to respond to ACE and to focus on identifying risk and prevention. 96 Addressing Adversity: Prioritising Adversity and Trauma-informed Care for Children and Young People in England96 presents the latest direction on how services can strengthen resilience and support recovery extending the Vulnerable Groups and Inequalities Task and Finish Group, co-chaired by the main author, Sarah Brennan, who served on the independent taskforce that created Future in Mind. 94,96 The report seldom mentions CAPRI, but its recommendations clearly demonstrate that the Young SMILES intervention fits well into a wider national scheme on how services and organisations respond to ACE by investing in adversity-informed models of care. This includes building individual/social resources, wider resiliency and connections to support in the community. Importantly, we have also provided evidence that the Young SMILES intervention significantly aligned with parents’ value systems. They expressed a need for their children to have valuable ‘child time’, something that many felt was lacking as a direct result of their own mental illness.
A sum of £1.25B has now been made available by the government for child and adolescent mental health and, to access this, CCGs must develop a local transformation plan (LTP) showing how they will improve access to mental health provision for CYP. In many cases, local areas do not record potential risk factors such as parental mental illness, making early intervention difficult. Early intervention services have been the target of cuts as a result of financial constraints: only 1 in 10 local areas intended to commission a new service in their LTP. 150
Within the current national context, therefore, we conclude that there is a strong argument that future development of the Young SMILES intervention represents a valuable, evidence-based, co-developed basis to preventative approaches in at-risk children. Referrers, service providers and facilitators in NHS-IAPT and in the third sector (e.g. NSPCC and Barnardo’s) provide clear evidence that the Young SMILES intervention fills an acknowledged gap in current provision across the sector. It was noted by multiple stakeholders that, although LTPs include new provision for CAMHS and tier 4 services, LTPs do not address need below a clinical threshold. CAPRI and parents both agreed that there remains a pressing need for intervention; and children particularly reinforced the positive experience of having something directed at them and for them. Children welcomed recognition of their role as carers and a focus on their needs rather than their parents’ needs. They relished the respite away from family and separate from school classrooms, as well as the relationships they could make with other young people experiencing similar difficulties. School referrers noted changes in children’s concentration in class, and greater happiness and less distress in children attending sessions.
Is a future trial feasible?
We have no doubt that the population of interest – CAPRI – remains in need of an intervention to improve their HRQoL. This small first-phase study has successfully developed an acceptable intervention with meaningful input from CYP and other stakeholders. Moreover, this intervention was successfully manualised, and staff from NHS and non-NHS settings were trained successfully to deliver it. We have also demonstrated the feasibility of recruiting and retaining families within this, especially CAPRI themselves.
However, we think a future RCT needs to reconsider both the outcome of interest and the mechanism of such delivery. The Young SMILES intervention needs more detailed specification for the facilitators to clarify what is and what is not within the intervention bounds. Recruitment pathways need revising: we believe that a future recruitment strategy should focus on primary care and NHS services including IAPT-CYP. We would also recommend social media and self-referral. We highly value the collaboration with NSPCC partners, but they have decided that further involvement is unlikely to fit their future service remit and priorities. There needs to be a formal process evaluation of what does and does not work within a structured but flexible intervention – possibly delivered, in part, through virtual workshops. A future trial delivery would see all Young SMILES intervention sessions recorded. This would include the possibility to analyse the ways in which people delivering the course use the balance between structure and tailoring; permitting standardisation without being prescriptive. Furthermore, the outcome specified in the original NIHR HTA programme call was HRQoL. In our relatively small sample of CAPRI, we did not find evidence of significantly reduced HRQoL at baseline. This belies the consistent evidence from population data of poor outcomes across a range of health and social domains for CAPRI. It is our concern that the standardised HRQoL measures available for the age groups studied were not fit for purpose to address the probably unmet need of these young people.
Recommendations for future research
Taken together, the reservations we outline above mean that we would not recommend that the evidence is sufficient for a fully powered trial of the Young SMILES intervention in the near future. In our view, the core outcome of the intervention should be reconsidered and either (1) a new measure of HRQoL should be co-developed that is sensitive to the challenges CAPRI tell us they face in their daily lives; or (2) a measure of unmet need should be developed as the primary outcome and then this should be used to inform further development of the intervention.
We also consider that future work in this domain should focus more on a digital approach as outlined above and in Chapter 8, Objective 3. This could include sessions with parents that are delivered via virtual workshops.
Of note, the original NIHR HTA commissioning brief called for consideration to be given to family socioeconomic status, and this may be particularly important. The number of mothers with mental illness being diagnosed in primary care in Britain today is considerable and significantly associated with area level deprivation and indices of poverty. 7 In this sense, we feel that focusing our efforts in poorer northern regions of the UK is appropriate; London and South East regions have the lowest morbidity and highest level of services for vulnerable families and other services for vulnerable families. This includes the greatest provision of perinatal mental health specialist services and children’s services, for example Young Minds and Barnardo’s. This regional approach sits well with evidence from a recent mapping of mental health need and research activity. 151
Providing mental health services is expensive, with most of the ongoing cost of mental health services being used to maintain a team of trained clinical staff to deliver a service and paying them to deliver it. We seek to develop a wholly different and much broader public health approach and one with a flexible, personalisable digital focus. A public health approach to the intervention may be best because most of these young people remain well most of the time, and so, although their absolute risks are low across outcomes (and most will remain resilient most of the time), consistent population estimates find their relative risk to be high across a range of outcomes compared with those without mentally ill parents. Thus, because the Young SMILES intervention expressly occupies a non-clinical domain, as CAPRI are often not mentally ill (only one in five children presenting to CAMHS is estimated to have a mentally ill parent in secondary care8), a public health approach to the intervention can be tailored to the changing needs of CAPRI, and can be agile to these needs so that it can respond to fluctuations over time.
We recognise the potential cost in QALYs that the absence of an intervention either to improve HRQoL or to meet the broader needs of CAPRI implies over time. 152 We also recognise that CAPRI are a growing group of CYP at higher risk overall of developing illness and mental illness as adults than their peers who do not have a parent with a SMI. Although our intervention was designed to improve HRQoL in all children with mentally ill parents, irrespective of their own mental health status, the Young SMILES intervention will not be best placed within CAMHS – where children already have mental health or behavioural problems. We believe that any future approach to supporting these vulnerable young people is best set in schools, community services or adult CMHTs who look after mentally ill parents. Family therapy teams in the NHS that are part of adult CMHTs will be well placed to use any future intervention. Third-sector organisations that see young carers or children at risk of adversity will also be appropriate settings for a future Young SMILES intervention.
Acknowledgements
First, we would like to acknowledge the generous involvement of the many CYP, CAPRI and their parents who took the time and displayed the courage to become involved with this project. We are indebted to them for their contribution and wish them all the very best for the future. We acknowledge the fantastic contribution of NHS, Barnardo’s and NSPCC staff in delivering the groups and having the flexibility and dedication to undertake an unfamiliar new programme for this study, as well as all support staff in the services referring to the Young SMILES intervention, without whom the research would not have been possible.
Contributions of authors
Kathryn M Abel (https://orcid.org/0000-0003-3538-8896) (Professor, Psychological Medicine and Reproductive Psychiatry) conceived the study and managed and led both the research team and the trial management team. She also conceived and co-developed the intervention, contributed to publications, prepared the results and data analyses for publication, and led report writing.
Penny Bee (https://orcid.org/0000-0002-5600-0400) (Professor, Mental Health Nursing) conceived and supervised the qualitative analyses and other qualitative aspects of the study. She also contributed to the trial management team and co-authored the qualitative chapters of the report and qualitative papers for publication.
Lina Gega (https://orcid.org/0000-0003-2902-9256) (Reader, Mental Health Nursing and Psychological Therapies) co-led the quantitative studies, supervised the Newcastle research assistant, contributed to the trial management team and co-led preparation of the quantitative data and analyses for publication and report writing.
Judith Gellatly (https://orcid.org/0000-0002-5134-5581) (Research Fellow) was the programme manager. She supervised protocol development, data collection and qualitative data collection, analysed the qualitative findings and co-authored qualitative chapters of the report.
Adekeye Kolade (https://orcid.org/0000-0003-1352-7680) (Research Assistant) undertook quantitative and qualitative interviews, entered quantitative data and organised follow-up contacts. In addition, he analysed qualitative findings, organised and contributed to the trial management team, and contributed to the writing of the report.
Diane Hunter (https://orcid.org/0000-0002-0135-0884) (Manager of Family SMILES Programme) contributed to development of the Young SMILES intervention, managed and advised on NSPCC site working. She also contributed to the trial management team and the writing of the report.
Craig Callender (https://orcid.org/0000-0002-8073-6274) (Research Assistant) undertook quantitative and qualitative interviews, entered quantitative data and organised follow-up contacts and contributed to the writing of the report.
Lesley-Anne Carter (https://orcid.org/0000-0002-1193-8681) (Lecturer in Biostatistics) undertook quantitative data analyses and co-authored biostatistical elements of the report.
Rachel Meacock (https://orcid.org/0000-0001-8933-5058) (Senior Lecturer in Health Economics) co-designed resource use data collection protocol and analysed and authored health economic elements of report.
Peter Bower (https://orcid.org/0000-0001-9558-3349) (Professor in Health Services Research) contributed to trial design, development and the trial management team, as well as to manuscript and report writing.
Nicky Stanley (https://orcid.org/0000-0002-7644-1625) (Professor in Social Work) advised on safeguarding, CYP and parental mental illness, as well as contributing to protocol development, the trial management team and report writing.
Rachel Calam (https://orcid.org/0000-0002-4385-1687) (Professor of Psychology) contributed to the trial management team, protocol development and the writing of the report.
Miranda Wolpert (https://orcid.org/0000-0002-7463-4976) (Professor at Anna Freud Centre and University College London) contributed to protocol and intervention development, supported the children’s groups and dissemination and contributed to the trial management team.
Paul Stewart (https://orcid.org/0000-0002-3058-8787) (NSPCC Business Manager) liaised with NSPCC teams and contributed to the development of the Young SMILES intervention and the trial management team.
Richard Emsley (https://orcid.org/0000-0002-1218-675X) (Professor of Biostatistics) contributed to trial design and protocol development and advised on randomisation procedures and amendments, and was part of the trial management team.
Kim Holt (https://orcid.org/0000-0003-3407-8300) (Professor of Social Work) oversaw the development of recruitment pathways.
Holly Linklater (https://orcid.org/0000-0001-7927-5506) provided overall expertise and guidance on the educational landscape. She advised specifically on aspects of linking with schools and teachers for recruitment and for transporting children to Young SMILES after school.
Simon Douglas (https://orcid.org/0000-0002-1336-0131) (Research Manager) supervised NHS staff in family services for provision of the Young SMILES intervention.
Bryony Stokes-Crossley (https://orcid.org/0000-0002-7265-6223) (Research Assistant) contributed to recruitment and qualitative and quantitative data collection.
Jonathan Green (https://orcid.org/0000-0002-0143-181X) (Professor of Child and Adolescent Mental Health) advised on protocol development and contributed to manuscript and report writing.
Publications
Gellatly J, Bee P, Gega L, Bower P, Hunter D, Stewart P, et al. A community-based intervention (Young SMILES) to improve the health-related quality of life of children and young people of parents with serious mental illness: randomised feasibility protocol. Trials 2018;19:550.
Gellatly J, Bee P, Kolade A, Hunter D, Gega L, Callender C, et al. Developing an intervention to improve the health related quality of life in children and young people with serious parental mental illness. Front Psychiatry 2019;10:155.
Data-sharing statement
We shall make data available to the scientific community with as few restrictions as feasible, while retaining exclusive use until the publication of major outputs. Some of the qualitative secondary data may not be suitable for sharing but these can equally be discussed with the corresponding author.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care.
References
- Castle DJ, Abel KM. Comprehensive Women’s Mental Health. Cambridge: Cambridge University Press; 2016.
- Abel KM, Hope H, Swift E, Parisi R, Ashcroft DM, Kosidou K, et al. Prevalence of maternal mental illness among children and adolescents in the UK between 2005 and 2017: a national retrospective cohort analysis. Lancet Public Health 2019;4:e291-300. https://doi.org/10.1016/S2468-2667(19)30059-3.
- Maybery D, Reupert A. Parental mental illness: a review of barriers and issues for working with families and children. J Psychiatr Ment Health Nurs 2009;16:784-91. https://doi.org/10.1111/j.1365-2850.2009.01456.x.
- Stambaugh LF, Forman-Hoffman V, Williams J, Pemberton MR, Ringeisen H, Hedden SL, et al. Prevalence of serious mental illness among parents in the United States: results from the National Survey of Drug Use and Health, 2008–2014. Ann Epidemiol 2017;27:222-4. https://doi.org/10.1016/j.annepidem.2016.12.005.
- Bassani DG, Padoin CV, Philipp D, Veldhuizen S. Estimating the number of children exposed to parental psychiatric disorders through a national health survey. Child Adolesc Psychiatry Ment Health 2009;3. https://doi.org/10.1186/1753-2000-3-6.
- Bee P, Berzins K, Calam R, Pryjmachuk S, Abel KM. Defining quality of life in the children of parents with severe mental illness: a preliminary stakeholder-led model. PLOS ONE 2013;8. https://doi.org/10.1371/journal.pone.0073739.
- Abel KM, Hope H, Swift E, Parisi R, Ashcroft DM, Kosidou K, et al. Prevalence of maternal mental illness among children and adolescents in the UK between 2005 and 2017: a national retrospective cohort analysis. Lancet Public Health 2019;4:e291-e300.
- Dean K, Stevens H, Mortensen PB, Murray RM, Walsh E, Pedersen CB. Full spectrum of psychiatric outcomes among offspring with parental history of mental disorder. Arch Gen Psychiatry 2010;67:822-9. https://doi.org/10.1001/archgenpsychiatry.2010.86.
- Siegenthaler E, Munder T, Egger M. Effect of preventive interventions in mentally ill parents on the mental health of the offspring: systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry 2012;51:8-17.e8. https://doi.org/10.1016/j.jaac.2011.10.018.
- van Santvoort F, Hosman CM, Janssens JM, van Doesum KT, Reupert A, van Loon LM. The impact of various parental mental disorders on children’s diagnoses: a systematic review. Clin Child Fam Psychol Rev 2015;18:281-99. https://doi.org/10.1007/s10567-015-0191-9.
- Olfson M, Marcus SC, Druss B, Alan Pincus H, Weissman MM. Parental depression, child mental health problems, and health care utilization. Med Care 2003;41:716-21. https://doi.org/10.1097/01.MLR.0000064642.41278.48.
- Anderson LN, Campbell MK, daSilva O, Freeman T, Xie B. Effect of maternal depression and anxiety on use of health services for infants. Can Fam Physician 2008;54:1718-19.
- Hope H, Abel KM, Evans, Osam S, Swift E, Ashcroft D, . The Health Utilisation and Costs of Children Exposed to Parental Mental Illness in the UK n.d.
- Manning C, Gregoire A. Effects of parental mental illness on children. Psychiatry 2006;5:10-2. https://doi.org/10.1383/psyt.2006.5.1.10.
- Gladstone BM, Boydell KM, Seeman MV, McKeever PD. Children’s experiences of parental mental illness: a literature review. Early Interv Psychiatry 2011;5:271-89. https://doi.org/10.1111/j.1751-7893.2011.00287.x.
- Ackerson BJ. Parents with serious and persistent mental illness: issues in assessment and services. Soc Work 2003;48:187-94. https://doi.org/10.1093/sw/48.2.187.
- Gellatly J, Bee P, Gee L, Hunter D, Abel KM. Parental Mental Health and Child Welfare. Shoreham-by-Sea: Pavilion; 2016.
- Bakermans-Kranenburg MJ, van IJzendoorn MH. The hidden efficacy of interventions: Gene× environment experiments from a differential susceptibility perspective. Annu Rev Psychol 2015;66:381-409. https://doi.org/10.1146/annurev-psych-010814-015407.
- Cattaneo A, Malpighi C, Cattane N, Provencal N, Pariante C. 126. Prenatal depression exposure and enhanced stress responses in the offspring: role of the glucocorticoid-mediated epigenetic changes. Biol Psychiatry 2018;83:S51-2. https://doi.org/10.1016/j.biopsych.2018.02.144.
- Brand SR, Brennan PA. Impact of antenatal and postpartum maternal mental illness: how are the children?. Clin Obstet Gynecol 2009;52:441-55. https://doi.org/10.1097/GRF.0b013e3181b52930.
- Field T. Prenatal depression effects on early development: a review. Infant Behav Dev 2011;34:1-14. https://doi.org/10.1016/j.infbeh.2010.09.008.
- Howe D, Batchelor S, Bochynska K. Estimating consumer parenthood within mental health services: a census approach. AeJAMH 2009;8:231-41. https://doi.org/10.5172/jamh.8.3.231.
- Hall A, Göpfert M, Webster J, Seeman MV. Parental Psychiatric Disorder: Distressed Parents and their Families. Cambridge: Cambridge University Press; 2004.
- Rutter M, Quinton D. Parental psychiatric disorder: effects on children. Psychol Med 1984;14:853-80. https://doi.org/10.1017/s0033291700019838.
- Kim-Cohen J, Caspi A, Rutter M, Tomás MP, Moffitt TE. The caregiving environments provided to children by depressed mothers with or without an antisocial history. Am J Psychiatry 2006;163:1009-18. https://doi.org/10.1176/ajp.2006.163.6.1009.
- Steer S, Reupert A, Maybery D. Programs for children of parents who have a mental illness: referral and assessment practices. ‘One size fits all’?. Aust Soc Work 2011;64:502-14. https://doi.org/10.1080/0312407X.2011.594901.
- Kinsella MT, Monk C. Impact of maternal stress, depression and anxiety on fetal neurobehavioral development. Clin Obstet Gynecol 2009;52:425-40. https://doi.org/10.1097/GRF.0b013e3181b52df1.
- Murray L, Cooper P, Hipwell A. Mental health of parents caring for infants. Arch Womens Ment Health 2003;6:71-7. https://doi.org/10.1007/s00737-003-0007-7.
- Smith M. Parental mental health: disruptions to parenting and outcomes for children. Child Fam Soc Work 2004;9:3-11. https://doi.org/10.1111/j.1365-2206.2004.00312.x.
- Weissman MM, Warner V, Wickramaratne P, Moreau D, Olfson M. Offspring of depressed parents. 10 years later. Arch Gen Psychiatry 1997;54:932-40. https://doi.org/10.1001/archpsyc.1997.01830220054009.
- Weissman MM, Wickramaratne P, Nomura Y, Warner V, Pilowsky D, Verdeli H. Offspring of depressed parents: 20 years later. Am J Psychiatry 2006;163:1001-8. https://doi.org/10.1176/ajp.2006.163.6.1001.
- Riebschleger J, Grove C, Costello S, Cavanaugh D. Mental health literacy for children with a parent with a mental illness. J Parent Fam Ment Health 2018;3. https://doi.org/10.7191/parentandfamily.1006.
- Havinga PJ, Boschloo L, Hartman CA, Schoevers RA. Paternal and maternal depression and offspring risk: additive effects or worse?. Lancet Psychiatry 2018;5:107-8. https://doi.org/10.1016/S2215-0366(18)30013-0.
- Lewis G, Neary M, Polek E, Flouri E, Lewis G. Paternal and maternal depression and offspring risk: additive effects or worse? – Authors’ reply. Lancet Psychiatry 2018;5. https://doi.org/10.1016/S2215-0366(18)30014-2.
- Fudge E, Mason P. Consulting with young people about service guidelines relating to parental mental illness. AeJAMH 2004;3:50-8. https://doi.org/10.5172/jamh.3.2.50.
- Reupert A, Maybery D. Families affected by parental mental illness: a multiperspective account of issues and interventions. Am J Orthopsychiatry 2007;77:362-9. https://doi.org/10.1037/0002-9432.77.3.362.
- Wilson S, Durbin CE. Effects of paternal depression on fathers’ parenting behaviors: a meta-analytic review. Clin Psychol Rev 2010;30:167-80. https://doi.org/10.1016/j.cpr.2009.10.007.
- Fisher SD, Brock RL, O’Hara MW, Kopelman R, Stuart S. Longitudinal contribution of maternal and paternal depression to toddler behaviors: interparental conflict and later depression as mediators. Couple Family Psychol 2015;4. https://doi.org/10.1037/cfp0000037.
- Flouri E. Fathers’ behaviors and children’s psychopathology. Clin Psychol Rev 2010;30:363-9. https://doi.org/10.1016/j.cpr.2010.01.004.
- Ramchandani P, Stein A, Evans J, O’Connor TG. ALSPAC study team . Paternal depression in the postnatal period and child development: a prospective population study. Lancet 2005;365:2201-5. https://doi.org/10.1016/S0140-6736(05)66778-5.
- Jacobs RH, Talati A, Wickramaratne P, Warner V. The influence of paternal and maternal major depressive disorder on offspring psychiatric disorders. J Child Fam Stud 2015;24:2345-51. https://doi.org/10.1007/s10826-014-0037-y.
- Connell AM, Goodman SH. The association between psychopathology in fathers versus mothers and children’s internalizing and externalizing behavior problems: a meta-analysis. Psychol Bull 2002;128:746-73. https://doi.org/10.1037/0033-2909.128.5.746.
- Rutter M. Resilience as a dynamic concept. Dev Psychopathol 2012;24:335-44. https://doi.org/10.1017/S0954579412000028.
- Rutter M. Implications of resilience concepts for scientific understanding. Ann NY Acad Sci 2006;1094:1-12. https://doi.org/10.1196/annals.1376.002.
- Cicchetti D, Curtis WJ. Multilevel perspectives on pathways to resilient functioning. Dev Psychopathol 2007;19:627-9. https://doi.org/10.1017/s0954579407000314.
- Santos IS, Matijasevich A, Domingues MR, Barros AJ, Barros FC. Long-lasting maternal depression and child growth at 4 years of age: a cohort study. J Pediatr 2010;157:401-6. https://doi.org/10.1016/j.jpeds.2010.03.008.
- Giallo R, Bahreinian S, Brown S, Cooklin A, Kingston D, Kozyrskyj A. Maternal depressive symptoms across early childhood and asthma in school children: findings from a longitudinal Australian population based study. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0121459.
- Letourneau NL, Kozyrskyj AL, Cosic N, Ntanda HN, Anis L, Hart MJ, et al. Maternal sensitivity and social support protect against childhood atopic dermatitis. Allergy Asthma Clin Immunol 2017;13. https://doi.org/10.1186/s13223-017-0199-4.
- Pierce M, Hope H, Kolade A, Gellatly J, Osman SO, Abel KM. The Physical Health of Children with Parental Mental Illness: A Systematic Review and Meta-analysis. Manchester: University of Manchester; 2019.
- Diggins M. Think Child, Think Parent, Think Family: A Guide to Parental Mental Health and Child Welfare. London: Social Care Institute for Excellence; 2011.
- Tabak I, Zabłocka-Żytka L, Ryan P, Poma SZ, Joronen K, Viganò G, et al. Needs, expectations and consequences for children growing up in a family where the parent has a mental illness. Int J Ment Health Nurs 2016;25:319-29. https://doi.org/10.1111/inm.12194.
- Farahati F, Marcotte DE, Wilcox-Gök V. The effects of parents’ psychiatric disorders on children’s high school dropout. Econ Educ Rev 2003;22:167-78. https://doi.org/10.1016/S0272-7757(02)00031-6.
- Stanley N, Penhale B, Riordan D, Barbour RS, Holden S. Working on the interface: identifying professional responses to families with mental health and child-care needs. Health Soc Care Community 2003;11:208-18. https://doi.org/10.1046/j.1365-2524.2003.00428.x.
- Hipwell AE, Murray L, Ducournau P, Stein A. The effects of maternal depression and parental conflict on children’s peer play. Child Care Health Dev 2005;31:11-23. https://doi.org/10.1111/j.1365-2214.2005.00448.x.
- Feurer C, Hammen CL, Gibb BE. Chronic and episodic stress in children of depressed mothers. J Clin Child Adolesc Psychol 2016;45:270-8. https://doi.org/10.1080/15374416.2014.963859.
- Breslend NL, Parent J, Forehand R, Peisch V, Compas BE. Children of parents with a history of depression: the impact of a preventive intervention on youth social problems through reductions in internalizing problems. Dev Psychopathol 2019;31:219-31. https://doi.org/10.1017/S0954579417001821.
- Beardselee WR, Versage EM, Giadstone TR. Children of affectively ill parents: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry 1998;37:1134-41. https://doi.org/10.1097/00004583-199811000-00012.
- Compas BE, Forehand R, Thigpen JC, Keller G, Hardcastle EJ, Cole DA, et al. Family group cognitive-behavioral preventive intervention for families of depressed parents: 18- and 24-month outcomes. J Consult Clin Psychol 2011;79:488-99. https://doi.org/10.1037/a0024254.
- Dodge KA, Bates JE, Pettit GS. Mechanisms in the cycle of violence. Science 1990;250:1678-83. https://doi.org/10.1126/science.2270481.
- Zahnâ Waxler C, Cummings EM, Iannotti RJ, Radkeâ Yarrow M. Young offspring of depressed parents: a population at risk for affective problems. New Dir Child Adolesc Dev 1984;1984:81-105. https://doi.org/10.1002/cd.23219842607.
- Hammen C, Brennan PA. Depressed adolescents of depressed and nondepressed mothers: tests of an interpersonal impairment hypothesis. J Consult Clin Psychol 2001;69:284-94. https://doi.org/10.1037//0022-006x.69.2.284.
- Sullivan PF, Magnusson C, Reichenberg A, Boman M, Dalman C, Davidson M, et al. Family history of schizophrenia and bipolar disorder as risk factors for autism. Arch Gen Psychiatry 2012;69:1099-103. https://doi.org/10.1001/archgenpsychiatry.2012.730.
- Shen H, Magnusson C, Rai D, Lundberg M, Lê-Scherban F, Dalman C, et al. Associations of parental depression with child school performance at age 16 years in Sweden. JAMA Psychiatry 2016;73:239-46. https://doi.org/10.1001/jamapsychiatry.2015.2917.
- Reupert AE, Cuff R, Drost L, Foster K, van Doesum KT, van Santvoort F. Intervention programs for children whose parents have a mental illness: a review. Med J Aust 2013;199:18-22. https://doi.org/10.5694/mja11.11145.
- Garber J, Little S. Predictors of competence among offspring of depressed mothers. J Adolesc Res 1999;14:44-71. https://doi.org/10.1177/0743558499141004.
- Fraser E, Pakenham KI. Resilience in children of parents with mental illness: relations between mental health literacy, social connectedness and coping, and both adjustment and caregiving. Psychol Health Med 2009;14:573-84. https://doi.org/10.1080/13548500903193820.
- Vakrat A, Apter-Levy Y, Feldman R. Fathering moderates the effects of maternal depression on the family process. Dev Psychopathol 2018;30:27-38. https://doi.org/10.1017/S095457941700044X.
- Bee P, Bower P, Byford S, Churchill R, Calam R, Stallard P, et al. The clinical effectiveness, cost-effectiveness and acceptability of community-based interventions aimed at improving or maintaining quality of life in children of parents with serious mental illness: a systematic review. Health Technol Assess 2014;18. https://doi.org/10.3310/hta18080.
- Perera DN, Short L, Fernbacher S. There is a lot to it: being a mother and living with a mental illness. Adv Ment Health 2014;12:167-81. https://doi.org/10.1080/18374905.2014.11081895.
- Angermeyer MC, Matschinger H. The stigma of mental illness: effects of labelling on public attitudes towards people with mental disorder. Acta Psychiatr Scand 2003;108:304-9. https://doi.org/10.1034/j.1600-0447.2003.00150.x.
- Reupert A, Maybery D. What do we know about families where parents have a mental illness? A systematic review. Child Youth Serv 2016;37:98-111. https://doi.org/10.1080/0145935X.2016.1104037.
- Braddick F, Carral V, Jenkins R, Jané-Llopis E. Child and Adolescent Mental Health in Europe: Infrastructures, Policy and Programmes. Luxembourg: European Communities; 2009.
- National Institute for Health and Care Excellence (NICE) . Social and Emotional Wellbeing for Children and Young People 2013.
- Crossroads Caring for Carers and Princess Royal Trust for Carers . Economic Evaluation of Young Carers’ Interventions 2008. https://pdfs.semanticscholar.org/d956/a899ff65378adad55f462ef7c2e3f53d804e.pdf (accessed 15 July 2020).
- Thanhäuser M, Lemmer G, de Girolamo G, Christiansen H. Do preventive interventions for children of mentally ill parents work? Results of a systematic review and meta-analysis. Curr Opin Psychiatry 2017;30:283-99. https://doi.org/10.1097/YCO.0000000000000342.
- Bee P. Community preventive interventions for children of parents with serious mental illness: a commentary on the evidence base. Adv Ment Health 2015;13:165-7. https://doi.org/10.1080/18387357.2015.1066945.
- Barry MM, Zissi A. Quality of life as an outcome measure in evaluating mental health services: a review of the empirical evidence. Soc Psychiatry Psychiatr Epidemiol 1997;32:38-47. https://doi.org/10.1007/bf00800666.
- Nicholson J, Sweeney EM, Geller JL. Mothers with mental illness: II. Family relationships and the context of parenting. Psychiatr Serv 1998;49:643-9. https://doi.org/10.1176/ps.49.5.643.
- van der Zanden R, Kramer J, Gerrits R, Cuijpers P. Effectiveness of an online group course for depression in adolescents and young adults: a randomized trial. J Med Internet Res 2012;14. https://doi.org/10.2196/jmir.2033.
- Lucksted A, McFarlane W, Downing D, Dixon L. Recent developments in family psychoeducation as an evidence-based practice. J Marital Fam Ther 2012;38:101-21. https://doi.org/10.1111/j.1752-0606.2011.00256.x.
- Compas BE, Forehand R, Keller G, Champion JE, Rakow A, Reeslund KL, et al. Randomized controlled trial of a family cognitive-behavioral preventive intervention for children of depressed parents. J Consult Clin Psychol 2009;77:1007-20. https://doi.org/10.1037/a0016930.
- Muñoz RF, Beardslee WR, Leykin Y. Major depression can be prevented. Am Psychol 2012;67:285-95. https://doi.org/10.1037/a0027666.
- Loechner J, Starman K, Galuschka K, Tamm J, Schulte-Körne G, Rubel J, et al. Preventing depression in the offspring of parents with depression: a systematic review and meta-analysis of randomized controlled trials. Clin Psychol Rev 2018;60:1-14. https://doi.org/10.1016/j.cpr.2017.11.009.
- Compas BE, Forehand R, Thigpen J, Hardcastle E, Garai E, McKee L, et al. Efficacy and moderators of a family group cognitive-behavioral preventive intervention for children of parents with depression. J Consult Clin Psychol 2015;83:541-53. https://doi.org/10.1037/a0039053.
- Stice E, Shaw H, Bohon C, Marti CN, Rohde P. A meta-analytic review of depression prevention programs for children and adolescents: factors that predict magnitude of intervention effects. J Consult Clin Psychol 2009;77:486-503. https://doi.org/10.1037/a0015168.
- NHS England . Implementing the Five Year Forward View for Mental Health 2016.
- Cabinet Office . Reaching Out: Think Family 2007.
- HM Goverment . Working With Troubled Families: A Guide to the Evidence and Good Practice 2012.
- Scottish Government . Towards a Mentally Flourishing Scotland: Policy and Action Plan 2009–11 2009.
- Dearden C, Becker S. Young Carers in the UK: The 2004 Report 2004.
- Afzelius M, Plantin L, Östman M. Families living with parental mental illness and their experiences of family interventions. J Psychiatr Ment Health Nurs 2018;25:69-77. https://doi.org/10.1111/jpm.12433.
- Social Exclusion Unit . Mental Health and Social Exclusion. Social Exclusion Unit Report 2004.
- Department of Health, Social Services and Public Safety . Families Matter: Supporting Families in Northern Ireland: Regional Family and Parenting Strategy 2009.
- Department of Health and Social Care (DHSC) . Future in Mind 2015.
- Public Health Wales . Adverse Childhood Experiences 2018. www.wales.nhs.uk/sitesplus/888/page/88524 (accessed 7 March 2019).
- Bush M. Addressing Adversity: Prioritising Adversity and Trauma-Informed Care for Children and Young People in England. Addressing Adversity n.d. https://youngminds.org.uk/media/2142/ym-addressing-adversity-book-web.pdf (accessed 15 July 2020).
- Department for Education . Working Together to Safeguard Children: A Guide to Inter-Agency Working to Safeguard and Promote the Welfare of Children 2018.
- Puras D, Kolaitis G, Tsiantisn J. Child and adolescent mental health in the enlarged European Union: overview of the CAMHEE Project. Int J Mental Health Promot 2010;12:3-9. https://doi.org/10.1080/14623730.2010.9721821.
- Finnish Government . Child Welfare Act 2007. http://www.finlex.fi/en/laki/kaannokset/2007/en20070417 (accessed 15 July 2020).
- NSW Government . NSW Children of Parents With a Mental Illness (COPMI) Framework for Mental Health Services 2010–15 2010. www.wslhd.health.nsw.gov.au/Redbank-House/Redbank-Services/Children-of-Parents-with-a-Mental-Illness--COPMI- (accessed 15 July 2020).
- Government of Ireland . Children First: National Guidance for the Protection and Welfare of Children 2011.
- Northern Ireland Executive . Children and Young People’s Strategy 2017–2027 2016.
- Fonagy P, Pugh K, O’Herlihy A, Skuse D, Bruce H, Dowdney L. Child Psychology and Psychiatry: Frameworks for Clinical Training and Practice. Hoboken, NJ: John Wiley & Sons; 2017.
- NHS England . Children and Young People’s Improving Access to Psychological Therapies Programme 2019. www.england.nhs.uk/mental-health/cyp/iapt/ (accessed 7 March 2019).
- Gellatly J, Bee P, Gega L, Bower P, Hunter D, Stewart P, et al. A community-based intervention (Young SMILES) to improve the health-related quality of life of children and young people of parents with serious mental illness: randomised feasibility protocol. Trials 2018;19. https://doi.org/10.1186/s13063-018-2935-6.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and Evaluating Complex Interventions: Following Considerable Development in the Field Since 2006, MRC and NIHR have Jointly Commissioned an Update of this Guidance to be Published in 2019. Southampton: Medical Research Council Lifecourse Epidemiology Unit; 2006.
- Gellatly J, Bee P, Kolade A, Hunter D, Gega L, Callender C, et al. Developing an intervention to improve the health related quality of life in children and young people with serious parental mental illness. Front Psychiatry 2019;10. https://doi.org/10.3389/fpsyt.2019.00155.
- Varni JW, Seid M, Kurtin PS. PedsQL 4.0: Reliability and validity of the Pediatric Quality of Life Inventory™ Version 4.0 Generic Core Scales in healthy and patient populations. Med Care 2001;39:800-12. https://doi.org/10.1097/00005650-200108000-00006.
- The KIDSCREEN Group Europe . The KIDSCREEN Questionnaires. Quality of Life Questionnaires for Children and Adolescents 2006.
- Strengths and Difficulties Questionnaire (SDQ) 2017. https://theshapesystem.com/resource-assessments/4118/SDQ_FINAL_11.29.17.pdf (accessed 16 February 2019).
- Chorpita BF, Ebesutani C, Spence S. Revised Children’s Anxiety and Depression Scale: User’s Guide 2015 n.d. www.childfirst.ucla.edu/wp-content/uploads/sites/163/2018/03/RCADSUsersGuide20150701.pdf (accessed 7 March 2019).
- Campos L, Dias P, Palha F. Finding space to mental health – promoting mental health in adolescents: pilot study. Educ Health 2014;32:23-9.
- Campos L, Dias P, Palha F. Finding space to mental health – promoting mental health in adolescents: pilot study. Educ Health 2014;32:23-9.
- Arnold DS, O’Leary SG, Wolff LS, Acker MM. The Parenting Scale: a measure of dysfunctional parenting in discipline situations. Psychol Assess 1993;5:137-44. https://doi.org/10.1037/1040-3590.5.2.137.
- Abidin RR, Zalaquett CP, Wood RJ. Evaluating Stress: A Book of Resources. Lanham, MD: Scarecrow Education; 1997.
- Stevens K. Valuation of the Child Health Utility 9D Index. PharmacoEconomics 2012;30:729-47. https://doi.org/10.2165/11599120-000000000-00000.
- Sekhon M, Cartwright M, Francis JJ. Acceptability of healthcare interventions: an overview of reviews and development of a theoretical framework. BMC Health Serv Res 2017;17. https://doi.org/10.1186/s12913-017-2031-8.
- Martinsen KD, Kendall PC, Stark K, Neumer S-P. Prevention of anxiety and depression in children: acceptability and feasibility of the transdiagnostic EMOTION program. Cogn Behav Pract 2016;23:1-13. https://doi.org/10.1016/j.cbpra.2014.06.005.
- Kulier R, Helmerhorst FM, Maitra N, Gülmezoglu AM. Effectiveness and acceptability of progestogens in combined oral contraceptives – a systematic review. Reprod Health 2004;1. https://doi.org/10.1186/1742-4755-1-1.
- Brooke-Sumner C, Petersen I, Asher L, Mall S, Egbe CO, Lund C. Systematic review of feasibility and acceptability of psychosocial interventions for schizophrenia in low and middle income countries. BMC Psychiatry 2015;15. https://doi.org/10.1186/s12888-015-0400-6.
- Muftin Z, Thompson AR. A systematic review of self-help for disfigurement: effectiveness, usability, and acceptability. Body Image 2013;10:442-50. https://doi.org/10.1016/j.bodyim.2013.07.005.
- El-Den S, O’Reilly CL, Chen TF. A systematic review on the acceptability of perinatal depression screening. J Affect Disord 2015;188:284-303. https://doi.org/10.1016/j.jad.2015.06.015.
- Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res 2016;26:1753-60. https://doi.org/10.1177/1049732315617444.
- Lancaster GA, Dodd S, Williamson PR. Design and analysis of pilot studies: recommendations for good practice. J Eval Clin Pract 2004;10:307-12. https://doi.org/10.1111/j.2002.384.doc.x.
- Eldridge SM, Chan CL, Campbell MJ, Bond CM, Hopewell S, Thabane L, et al. PAFS consensus group . CONSORT 2010 statement: extension to randomised pilot and feasibility trials. Pilot Feasibility Stud 2016;2. https://doi.org/10.1186/s40814-016-0105-8.
- Ravens-Sieberer U, Gosch A, Rajmil A, Erhart M, Bruil J, Duer W, et al. KIDSCREEN-52 quality of life measure for children and adolescents. Expert Rev Pharmacoecon Res 2005;5:353-64. https://doi.org/10.1586/14737167.5.3.353.
- Varni JW, Burwinkle TM, Seid M, Skarr D. The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul Pediatr 2003;3:329-41. https://doi.org/10.1367/1539-4409(2003)003<0329:TPAAPP>2.0.CO;2.
- Hilliard ME, Lawrence JM, Modi AC, Anderson A, Crume T, Dolan LM, et al. Identification of minimal clinically important difference scores of the PedsQL in children, adolescents, and young adults with type 1 and type 2 diabetes. Diabetes Care 2013;36:1891-7. https://doi.org/10.2337/dc12-1708.
- Rhoades KA, O’Leary SG. Factor structure and validity of the parenting scale. J Clin Child Adolesc Psychol 2007;36:137-46. https://doi.org/10.1080/15374410701274157.
- Byford S, Barrett B, Roberts C, Wilkinson P, Dubicka B, Kelvin RG, et al. Cost-effectiveness of selective serotonin reuptake inhibitors and routine specialist care with and without cognitive behavioural therapy in adolescents with major depression. Br J Psychiatry 2007;191:521-7. https://doi.org/10.1192/bjp.bp.107.038984.
- Byford S, Harrington R, Torgerson D, Kerfoot M, Dyer E, Harrington V, et al. Cost-effectiveness analysis of a home-based social work intervention for children and adolescents who have deliberately poisoned themselves. Results of a randomised controlled trial. Br J Psychiatry 1999;174:56-62. https://doi.org/10.1192/bjp.174.1.56.
- Yi-Frazier JP, Hilliard ME, Fino NF, Naughton MJ, Liese AD, Hockett CW, et al. Whose quality of life is it anyway? Discrepancies between youth and parent health-related quality of life ratings in type 1 and type 2 diabetes. Qual Life Res 2016;25:1113-21. https://doi.org/10.1007/s11136-015-1158-5.
- Qadeer RA, Ferro MA. Child–parent agreement on health-related quality of life in children with newly diagnosed chronic health conditions: a longitudinal study. Int J Adolesc Youth 2018;23:99-108. https://doi.org/10.1080/02673843.2017.1297242.
- Oltean II, Ferro MA. Agreement of child and parent-proxy reported health-related quality of life in children with mental disorder. Qual Life Res 2019;28:703-12. https://doi.org/10.1007/s11136-018-2026-x.
- Varni JW, Setoguchi Y. Screening for behavioral and emotional problems in children and adolescents with congenital or acquired limb deficiencies. Am J Dis Child 1992;146:103-7. https://doi.org/10.1001/archpedi.1992.02160130105030.
- Wei Y, McGrath PJ, Hayden J, Kutcher S. Mental health literacy measures evaluating knowledge, attitudes and help-seeking: a scoping review. BMC Psychiatry 2015;15. https://doi.org/10.1186/s12888-015-0681-9.
- Riebschleger J, Grové C, Cavanaugh D, Costello S. Mental health literacy content for children of parents with a mental illness: thematic analysis of a literature review. Brain Sci 2017;7. https://doi.org/10.3390/brainsci7110141.
- Moffatt S, Mackintosh J, White M, Howel D, Sandell A. The acceptability and impact of a randomised controlled trial of welfare rights advice accessed via primary health care: qualitative study. BMC Public Health 2006;6. https://doi.org/10.1186/1471-2458-6-163.
- Thomas KS, Bradshaw LE, Sach TH, Cowdell F, Batchelor JM, Lawton S, et al. Randomised controlled trial of silk therapeutic garments for the management of atopic eczema in children: the CLOTHES trial. Health Technol Assess 2017;21. https://doi.org/10.3310/hta21160.
- Grønning K, Bratås O, Steinsbekk A. Patients’ perceptions of having a good life one year after arthritis patient education: a qualitative study nested within a randomized controlled trial. Nurse Media J Nurs 2017;7:1-14. https://doi.org/10.14710/nmjn.v7i1.15123.
- Jibb LA, Stevens BJ, Nathan PC, Seto E, Cafazzo JA, Johnston DL, et al. Perceptions of adolescents with cancer related to a pain management app and its evaluation: qualitative study nested within a multicenter pilot feasibility study. JMIR Mhealth Uhealth 2018;6. https://doi.org/10.2196/mhealth.9319.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Hilal AH, Alabri SS. Using NVivo for data analysis in qualitative research. Int Interdiscip J Educ 2013;2:181-6. https://doi.org/10.12816/0002914.
- May CR, Mair F, Finch T, MacFarlane A, Dowrick C, Treweek S, et al. Development of a theory of implementation and integration: Normalization Process Theory. Implement Sci 2009;4. https://doi.org/10.1186/1748-5908-4-29.
- May CR, Cummings A, Girling M, Bracher M, Mair FS, May CM, et al. Using Normalization Process Theory in feasibility studies and process evaluations of complex healthcare interventions: a systematic review. Implement Sci 2018;13. https://doi.org/10.1186/s13012-018-0758-1.
- Margolis R, Fernandes P. Building Children’s Confidence and Improving Parents’ Protective Skills: Final Evaluation of the NSPCC Family SMILES Service. London: NSPCC; 2017.
- Nevriana, Pierce M, Dalman C, Wicks S, Hasselberg M, Hope H, et al. Association between maternal and paternal mental illness and risk of injuries in children and adolescents: nationwide register based cohort study in Sweden. BMJ 2020;369. https://doi.org/10.1136/bmj.m853.
- Young Minds . New Era for Young People’s Mental Health 2019. https://youngminds.org.uk/blog/nhs-long-term-plan-commits-to-young-peoples-mental-health/ (accessed 13 March 2019).
- House of Commons Committee of Public Accounts . Mental Health Services for Children and Young People 2019.
- Early Intervention Foundation . Realising the Potential of Early Intervention 2018.
- Bower P, Grigoroglou C, Anselmi L, Kontopantelis E, Sutton M, Ashworth M, et al. Is health research undertaken where the burden of disease is greatest? Observational study of geographical inequalities in recruitment to research in England 2013–2018. BMC Med 2020;18. https://doi.org/10.1186/s12916-020-01555-4.
- Knapp M, McDaid D, Parsonage M. Mental Health Promotion and Mental Illness Prevention: The Economic Case. London: Department of Health and Social Care; 2011.
- Upton P, Eiser C, Cheung I, Hutchings HA, Jenney M, Maddocks A, et al. Measurement properties of the UK–English version of the Pediatric Quality of Life Inventory 4.0 (PedsQL) generic core scales. Health Qual Life Outcomes 2005;3. https://doi.org/10.1186/1477-7525-3-22.
- Ravens-Sieberer U, Erhart M, Torsheim T, Hetland J, Freeman J, Danielson M, et al. HBSC Positive Health Group . An international scoring system for self-reported health complaints in adolescents. Eur J Public Health 2008;18:294-9. https://doi.org/10.1093/eurpub/ckn001.
- Chen G, Flynn T, Stevens K, Brazier J, Huynh E, Sawyer M, et al. Assessing the health-related quality of life of Australian adolescents: an empirical comparison of the child health utility 9D and EQ-5D-Y instruments. Value Health 2015;18:432-8. https://doi.org/10.1016/j.jval.2015.02.014.
- Drummond M. Introducing economic and quality of life measurements into clinical studies. Ann Med 2001;33:344-9. https://doi.org/10.3109/07853890109002088.
- Chorpita BF, Moffitt CE, Gray J. Psychometric properties of the Revised Child Anxiety and Depression Scale in a clinical sample. Behav Res Ther 2005;43:309-22. https://doi.org/10.1016/j.brat.2004.02.004.
- Goodman R. Psychometric properties of the strengths and difficulties questionnaire. J Am Acad Child Adolesc Psychiatry 2001;40:1337-45. https://doi.org/10.1097/00004583-200111000-00015.
Appendix 1 Recruitment difficulties
| Recruitment difficulties | Details |
|---|---|
| HRA approval delays | The REC/HRA approval processes for ethical amendments to Phase I took an unexpectedly long time, considerably impinging on the amount of time we had to consult with NHS and third-sector professionals about referral pathways |
| Substantial ethical amendments | The request from the HRA for an additional, separate ethics application to be submitted for Phase II further delayed the point at which we could begin recruiting families, and was compounded by Barnardo’s, Newcastle, requiring a separate ethics application (with the HRA-approved documents submitted to the Barnardo’s Research Ethical Committee) |
| NSPCC site closures | A number of the NSPCC service centres that were targeted for recruitment closed. New NSPCC recruitment sites (Warrington and Coventry) were arranged, but this further impinged on the amount of time we could allocate for recruitment to meet study targets |
| School holidays | The timing of recruitment coincided with school holidays, limiting the amount of opportunities for referrers to engage with children and their families about the study |
| HRA rejection of a fully costed extension | These unforeseen obstacles to beginning recruitment were presented to the HRA in the furtherance of obtaining a fully costed extension to Phase II of the trial. This was not approved of by the HRA, which instead offered a non-costed extension that the Trial Management Group considered financially unviable. Consequently, we had to recruit families within the original timeframe that did not account for the above delays |
| Untargeted approaches to recruitment | There was a lack of concerted effort on the part of some practitioners to ensure that information packs reached families, with several promoting the study by leaving leaflets/posters in places families may or may not have seen, rather than targeting eligible families and engaging with them verbally |
| No relationship with parent | Many practitioners worked with children only and had no professional relationship with the parents, who would be the source of consent for the child to participate. A lack of parental trust for the practitioner working with the child was also suggested as a potential source of reluctance for parents to participate |
| Gatekeeping | Few practitioners made the decision to not engage with eligible families about the study because of their interpretation of their capacity to participate |
| Deteriorating parental mental health | Several families could not participate because the parent’s mental health deteriorated after they expressed an interest in the trial to their care co-ordinators |
| Child taken into care | A few families who expressed an interest in participating could no longer do so because their child was placed into care after social services intervened |
Appendix 2 Young SMILES theory of change diagram
FIGURE 2.
Theory of change diagram.
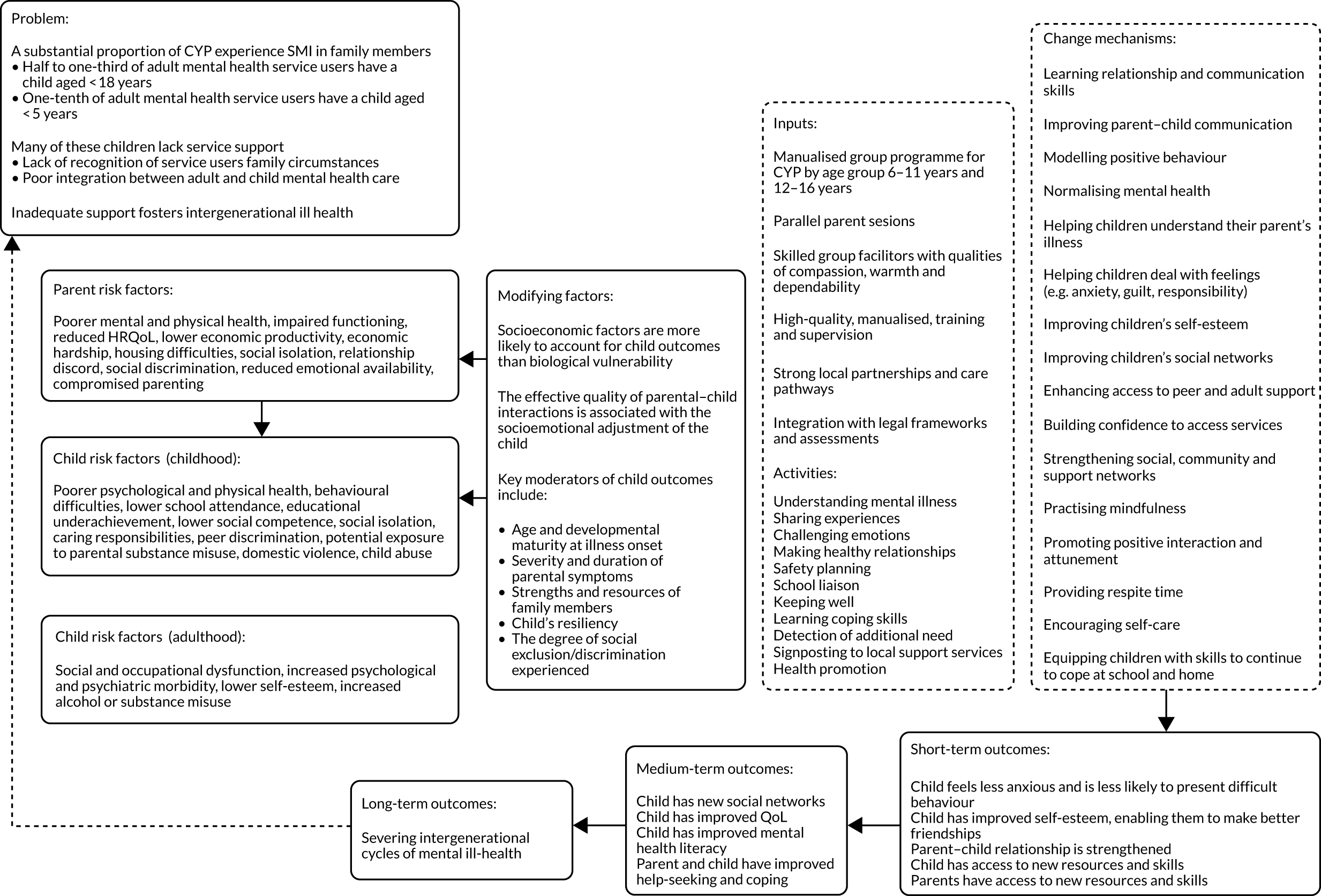
Appendix 3 Outcome descriptions
Description of primary measures
Paediatric Quality of Life Inventory
The PedsQL comprises 23 items capturing the children’s physical and emotional health and their social and school functioning. 153 Each item asks the child to indicate how much of a problem a particular aspect of life has been for them over the previous month. For example, under the section ‘My health and activities’, items include ‘It is hard for me to do chores around the house’ and ‘I hurt or ache’; under the section ‘About my feelings’, items include ‘I feel afraid or scared’ and ‘I worry about what will happen to me’. The child’s answer is scored according to the frequency with which each of the 23 problems affect them, from a choice of five options: never = 0, almost never = 1, sometimes = 2, often = 3, almost always = 4.
KIDSCREEN
The 52-measure KIDSCREEN126 was completed by children aged 8–16 years in our sample as a self-report measure of their QoL, and by their parents as a proxy-report measure of their children’s QoL. The KIDSCREEN-52 is not validated for 7-year-olds, so data for children of that age in our sample are available from their parent’s proxy-report only. The KIDSCREEN questionnaire covers 10 domains: (1) physical well-being, (2) psychological well-being, (3) mood and emotions, (4) self-perception, (5) autonomy, (6) parent relation and home life, (7) financial resources, (8) social support and peers, (9) school environment and (10) social acceptance (bullying).
Children and parents rated each item using a 1- to 5-point Likert-type scale according to the frequency (1 = never, 2 = seldom, 3 = quite often, 4 = very often, 5 = always) or intensity (1 = not at all, 2 = slightly, 3 = moderately, 4 = very, 5 = extremely) that they attributed to each statement (e.g. ‘have you felt sad?’ or ‘have you been worried about the way you look?’) over the previous week. The KIDSCREEN-52 does not provide an overall measure of general QoL, but it considers each domain separately, with higher scores indicating a better QoL in each domain.
For 14 items, scores had to be reversed so that higher scores reflected a better QoL for those items. These items were:
-
physical well-being – (1) in general, how would you say your health is? (excellent = 5, very good = 4, good = 3, fair = 2, poor = 1)
-
moods and emotions – (1) have you felt that you do everything badly? (2) have you felt sad? (3) have you felt so bad that you didn’t want to do anything? (4) have you felt that everything in your life goes wrong? (5) have you felt fed up? (6) have you felt lonely? (7) have you felt under pressure? (never = 5, seldom = 4, quite often = 3, very often = 2, always = 1)
-
self-perception – (3) have you been worried about the way you look? (4) have you felt jealous of the way other girls and boys look? (5) would you like to change something about your body? (never = 5, seldom = 4, quite often = 3, very often = 2, always = 1)
-
social acceptance (bullying) – (1) have you been afraid of other girls and boys? (2) have other girls and boys made fun of you? (3) have other girls and boys bullied you? (never = 5, seldom = 4, quite often = 3, very often = 2, always = 1).
Summary scores were calculated by adding all the scores from each participant. Only summary scores from participants with complete data, where every item of the scale was answered, were summed. Rasch person parameters (PP) were assigned to each possible summary score. 154 The PPs were transformed into t-scores with a mean of 50 and a SD of approximately 10.
Description of secondary measures
Child Health Utility 9D (children and young people only)
To inform a future economic evaluation, we used the CHU-9D,116 which is validated for children aged 7–17 years, to estimate incremental health gain in QALYs. This QoL measure was used in addition to PedsQL and KIDSCREEN, which do not have corresponding utility values and cannot be used to calculate QALYs in a future economic evaluation.
The questionnaire consists of nine domains, each with five statements (scored 1–5) that assess the child’s functioning ‘today’ across domains of worry, sadness, pain, tiredness, annoyance, school, sleep, daily routine and activities, for example 1 = I don’t feel sad today, 2 = I feel a little bit sad today, 3 = I feel a bit sad today, 4 = I feel quite sad today, 5 = I feel very sad today. The responses under the nine domains can be taken together as a description of the child’s QoL or ‘health state’ using a descriptive system that combines all responses across all items (e.g. 11232152). There are many different health states based on this descriptive system because of the different combinations of responses across the nine dimensions. Each of these health states has a utility value on a 0–1 scale, where 1 is perfect health and 0 is a state equivalent to being dead.
Completed CHU-9D questionnaires were scored and transformed into utility values using Statistical Product and Service Solutions (SPSS) syntax provided by the developers of the measure. Here, we describe the CHU-9D’s mean utility values and SDs for our sample as an indicator of the CHU-9D’s performance in capturing QoL for our population. There are suggestions in the literature that utility values of 0.9, 0.8, 0.7 and ≤ 0.6, correspond to excellent, very good, good, fair or poor general health, respectively. 155 Differences over 0.03 units in utility-based measures of QoL in adults are considered clinically important156 but there is no established MCID for equivalent measures in children.
Revised Child Anxiety and Depression Scale
The brief version of the RCADS is a 25-item questionnaire that derives from the full 47-item RCADS157 and assesses children’s depression and anxiety. It is validated as a self-completed measure for 8- to 18-year-olds and it can also be completed by their parents as a proxy-report. We had two children younger than 8 years in our sample, for whom we only obtained parent proxy-report data.
Items are rated on a four-point Likert scale from 0 to 3, where 0 = never, 1 = sometimes, 2 = often and 3 = always. Examples of items are ‘I worry when I think I have done poorly at something’ (anxiety) and ‘nothing is much fun anymore’ (depression). Raw scores are obtained by adding the scores of all the items. Missing data for raw scores for up to two missing items can be prorated using the remaining items within a scale (sum of the completed items divided by the number of the completed items, then multiplied by the total number of items and rounded to the nearest integer).
Raw scores are transformed into t-scores by matching the raw score to its corresponding age and sex normed t-scores available in the questionnaire’s user guide. 111 Clinical cut-off points for the t-scores are 0–64 pre-clinical range, 65–69 borderline clinical range and ≥ 70 clinical range. Higher scores denote greater clinical need. We analysed the t-scores as a continuous variable because the small sample size did not allow grouping the children into clinical categories.
Strengths and Difficulties Questionnaire
The 25-item SDQ110,158 is validated as a self-report measure for 11- to 16-year-olds and as a parent proxy-report measure for all ages. For children aged < 11 years in our sample, we obtained parent proxy-report data only. Over two-thirds of our sample were aged < 11 years, so we have fewer child self-report data than parent proxy-report data on the SDQ.
The SDQ assesses positive and negative attributes of a child’s behaviours and experiences over the previous 6 months under the following five domains:
-
emotional symptoms (e.g. ‘I worry a lot’); items 3, 8, 13, 16, 24
-
conduct problems (e.g. ‘I fight a lot. I can make other people do what I want’); items 5, 7, 12, 18, 22
-
hyperactivity/inattention (e.g. ‘I am constantly fidgeting or squirming’); items 2, 10, 15, 21, 25
-
peer relationship problems (e.g. ‘I am usually on my own. I generally play alone or keep to myself’); items 6, 11, 14, 19, 23
-
prosocial behaviour [e.g. ‘I often volunteer to help others (parents, teachers, children)’]; items 1, 4, 9, 17, 20.
Children or parents mark a box for ‘not true = 0, somewhat true = 1, certainly true = 2’. Items 7, 11, 14, 21 and 25 need to be reverse coded. The resultant score for each subscale is 0–10 and the total score ranges from 0 to 40. A total ‘difficulties’ score was generated by summing scores from four scales, excluding the prosocial behaviours one. If one of the four component scores is missing, then the total score is not counted. Higher mean scores for SDQ total and for the four subscales (other than prosocial behaviours scale) indicate a higher level of difficulties. For prosocial behaviours, higher mean scores indicate less difficulties. Each 1-point increase in the total difficulties score corresponds with an increase in the risk of mental health problems.
A range of scores can be used to categorise difficulties into four groups: close to average, slightly raised, high and very high. For child self-report, the corresponding range of scores are:
-
total difficulties – 0–14, 15–17, 18–19, 20–40
-
emotional problems – 0–4, 5, 6, 7–10
-
conduct problems – 0–3, 4, 5, 6–1
-
hyperactivity – 0–5, 6, 7, 8–10
-
peer problems – 0–2, 3, 4, 5–10
-
prosocial – 7–10, 6, 5, 0–4.
For parent proxy-report the range of scores are:
-
total difficulties – 0–13, 14–16, 17–19, 20–40
-
emotional problems – 0–3, 4, 5–6, 7–10
-
conduct problems – 0–2, 3, 4–5, 6–10
-
hyperactivity – 0–5, 6–7, 8, 9–10
-
peer problems – 0–2, 3, 4, 5–10
-
prosocial – 8–10, 7, 6, 0–5.
Mental Health Literacy questionnaire (children and young people only)
We computed the total MHLq score as the sum of all 33 items – the minimum possible score is 33 and the maximum possible score is 165. If any of the items on the questionnaire were missing, then we did not obtain a total score. We also computed subscores for the three MHLq domains by summing up the relevant items, that is:
-
Help seeking and first-aid skills (10 items – 1, 5, 6, 8, 10, 13, 19, 20, 24, 29). Example items – ‘If a friend of mine developed a mental disorder, I would talk to the form teacher or other teacher’; ‘If I had a mental disorder I would seek my friends’ help’. The minimum possible score is 11 and the maximum possible score is 55.
-
Knowledge/stereotypes on mental health problems (15 items – 3, 4, 7, 11, 12, 15–18, 22, 23, 25, 26, 28, 31). Example items – ‘People with schizophrenia usually have delusions (i.e. they may believe they are constantly being followed and observed)’, ‘People with mental disorders come from families with little money.’ The minimum possible score is 15 and the maximum possible score is 75.
-
Self-help strategies (8 items – 2, 9, 14, 21, 27, 30, 32, 33). ‘Good sleep helps to improve mental health’, ‘Doing something enjoyable helps to improve mental health’. The minimum possible score is 8 and the maximum possible score is 40.
Parenting scale (parents only)
Parents who completed the questionnaire described their parenting style over the previous 2 months by using a 7-point visual continuum between two polarised statements (e.g. ‘When my child misbehaves . . . I do something right away – I do something later’). Each point in the continuum receives a score of 1–7, where 7 is the ineffective/maladaptive/unhelpful end of the item. The following items have 7 on the left side: 2, 3, 6, 9, 10, 13, 14, 17, 19, 20, 23, 26, 27 and 30. The rest are reversed scored and have the 7 on the right side.
We computed the total parenting scale score by adding the scores for all the items and then dividing by the number of scored items to arrive at an average total response for parenting. We obtained subscores by calculating the average of responses on the items specific to each domain, as follows:
-
laxness – items 7, 8, 12, 15, 16, 19, 20, 21, 24, 26, 30 (11 items) (e.g. ‘I threaten to do things that . . . I’m sure I can carry out – I know I won’t actually do’)
-
over-reactivity – items 3, 6, 9, 10, 14, 17, 18, 22, 25, 28 (10 items) (e.g. When I’m upset or under stress . . . I am picky and on my child’s back – I am not more picky than usual’)
-
verbosity – items 2, 4, 7, 9, 11, 23, 29 (seven items) (e.g. ‘If my child talks back or complains when I handle a problem . . . I ignore the complaining and stick to what I said – I give my child a talk about not complaining’)
-
items not on a domain but included in the total score – items 1, 5, 13, 27 (four items) (e.g. ‘When my child pesters me . . . I can ignore the pestering – I can’t ignore the pestering’).
The Parent Stress Index – Short Form (parents only)
Out of the 36 items, 33 items use a Likert scale response option of 1 (strongly disagree) to 5 (strongly agree); for example, ‘I feel trapped by my responsibilities as a parent’. Out of the three remaining items, item 22 asks whether the parent feels that they are 1 = a very good parent, 2 = a better than average parent, 3 = an average parent, 4 = a person who has some trouble being a parent, or 5 = not very good at being a parent. Item 32 asks whether the parent found that getting their child to do something or to stop doing something was 1 = harder, 2 = somewhat harder, 3 = about as hard as, 4 = somewhat easier, or 5 = much easier than they expected. Finally, item 33 asks how many things that the child does annoy their parent and the response options were 1 = 1–3, 2 = 4–5, 3 = 6–7, 4 = 8–9, 5 = 10 +. All items in the scale are reverse-coded so that ascending PSI-SF values indicate ‘worse’ scores, except for items 22 and 33 that are already phrased in this direction and, therefore, are not reversed scored for the analysis.
Scores were calculated separately for the three subscales by summing scores of the 12 items on each subscale, with possible scores in each subscale ranging from 12 to 60. Parental distress was calculated as the sum of items 1–12, parent–child dysfunctional interaction is calculated as the sum of items 13–24 and difficult child is calculated as the sum of items 25–36. The three subscales are computed if all items are answered or if a maximum of one item is missing. A total score for the PSI-SF is calculated by summing the three subscale scores, with possible scores ranging from 36 to 180. Higher scores on the PSI-SF total and its subscales indicate greater parental stress.
Measures for resource use
Child and Adolescent Service Use Schedule
The collection of child resource utilisation data was piloted using the CA-SUS. 130,131 We used the tool to identify the most important aspects of resource utilisation and to assess the feasibility of collecting information on the receipt of care and services in relation to children’s needs and services from the NHS, social care, education, and voluntary and third-sector organisations. We did not calculate costs for this resource use as part of this feasibility study.
The CA-SUS was adapted for our study in consultation with Professor Sarah Byford, the designer of the CA-SUS questionnaire. This adaptation involved removing the sections on out-of-pocket expenses and employment; removing the question on education type; removing the follow-on questions asking name of hospital for the hospital service use questions; removing complementary therapists (e.g. homeopath) from the list of community services, adding NHS walk-in services and NHS Direct to the list of community services; and simplifying the questions in the criminal justice services section. A copy of the CA-SUS version used in our study can be found on the project web page [www.journalslibrary.nihr.ac.uk/programmes/hta/142901/#/ (accessed 1 March 2020)].
List of abbreviations
- A&E
- accident and emergency
- ACE
- adverse childhood experiences
- CAPRI
- children and adolescents of parents with serious mental illness
- CA-SUS
- Child and Adolescent Service Use Schedule
- CAMHS
- Child and Adolescent Mental Health Services
- CCG
- Clinical Commissioning Group
- CHU-9D
- Child Health Utility 9D
- CMHT
- community mental health team
- CONSORT
- Consolidated Standards of Reporting Trials
- CYP
- children and young people
- EU
- European Union
- GP
- general practitioner
- HRA
- Health Research Authority
- HRQoL
- health-related quality of life
- HTA
- Health Technology Assessment
- IAPT
- Improving Access to Psychological Therapies
- IAPT-CYP
- Improving Access to Psychological Therapies for Children and Young People
- IQR
- interquartile range
- LTP
- local transformation plan
- MCID
- minimum clinically important difference
- MHLQ
- Mental Health Literacy questionnaire
- MSc
- Master of Science
- NIHR
- National Institute for Health Research
- NPT
- normalisation process theory
- NSPCC
- National Society for the Prevention of Cruelty to Children
- NTW
- Northumberland Tyne and Wear
- PedsQL
- Paediatric Quality of Life Inventory
- PP
- person parameters
- PSI-SF
- Parent Stress Index – Short Form
- QoL
- quality of life
- QALY
- quality-adjusted life-year
- RCADS
- Revised Child Anxiety and Depression Scale
- RCT
- randomised controlled trial
- REC
- Research Ethics Committtee
- SD
- standard deviation
- SDQ
- Strengths and Difficulties Questionnaire
- SMI
- serious mental illness
- SMILES
- Simplifying Mental Illness plus Life Enhancement Skills
- SOP
- standard operating procedure
- TAU
- treatment as usual
- TFA
- Theoretical Framework of Acceptability
