Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 15/108/02. The contractual start date was in January 2017. The draft report began editorial review in January 2020 and was accepted for publication in July 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2021. This work was produced by Linaker et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2021 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Scientific background and rationale for the research
Chronic pain is that which troubles a person all or most of the time over months/years and is defined as pain that persists beyond the normal period of healing, usually taken as 3 months (with a 6-month cut-off point used for research purposes). It is a major public health problem associated with mental illness, job loss, impaired function and poor quality of life. Epidemiological studies suggest that 31% of men and 37% of women have chronic pain at any point in time and that prevalence increases with age. 1 Chronic pain is more common and more severe among those with poorer socioeconomic status. Mental illness, including depression and anxiety, is significantly increased among people with chronic pain, with prevalence rates as high as 70% among those with more severe pain. Between 20% and 27% of people of working age with chronic pain are unable to participate in their usual activities, including work, because of their pain. 2 Health-care costs associated with chronic pain are high. It has been estimated that chronic pain patients consult their general practitioner (GP) up to five times more frequently than other patients, with almost 5 million GP appointments annually. 3 The costs of chronic back pain, for example, have been estimated at £12.3B per year. 4 In addition to direct medical costs, it has been estimated that as much as 48–88% of the total cost burden of chronic pain can be attributed to indirect costs arising from restricted productivity, sick leave, disability benefits and other aspects of work disability. 5 Importantly, 3 of the top 10 conditions that impact productivity are painful disorders (e.g. back/neck pain, other chronic pain and arthritic conditions). 1 In a national audit, as many as 40% of people attending UK pain clinics were prevented from working (paid or voluntary) by pain. 5
Prolonged unemployment, for any reason, causes additional health problems. 6 Those who lose their job suffer from worse mental health,7 have poorer life expectancy,8 attend health-care consultations more frequently with physical symptoms and report higher levels of pain. 9 Moreover, these effects transfer to the next generation, such that the children of unemployed people also have poorer mental health and themselves experience higher rates of unemployment. 10 Taken together, these findings illustrate the potential public health impact of rehabilitating people with chronic pain back into work.
There have been calls in the UK for improved services for chronic pain. For example, chronic pain was a focus of the Chief Medical Officer’s Annual Report 2008,2 which emphasised the need for improved holistic pain services. In addition, the Royal College of General Practitioners named chronic pain a clinical priority area in 2011–14. 11 A particular area of need highlighted by patient representative groups12 was the poor availability of information and support from health-care professionals regarding employment.
Chronic pain is one of the major causes of health-related incapacity for work in the UK, with marked impact on the individual, their family, health-care providers and society. There is little evidence showing effectiveness of traditional ‘train and place’ rehabilitation interventions for chronic pain patients in the UK, partly because return to work (RTW) is rarely the principal outcome. The results of one published study suggested that occupational rehabilitation can be integrated with pain management programmes, producing a 38% RTW rate at 6 months,13 and showed that those already unemployed need a different approach from that used for those currently in work.
People unemployed with chronic pain have a number of compounding problems, including diminished self-esteem and confidence; progressive loss of fitness and stamina through inactivity; outdated vocational skills; lack of suitable, sustainable employment opportunities; poor availability of ‘tailored’ job-seeking and occupational advice; and potential prejudice from employers against people with poor sickness records. These problems exactly parallel those faced by people with severe mental illnesses, in whom rates of unemployment as high as 95% have been reported. 14 Among people with severe mental illness, the traditional ‘train and place’ model of rehabilitation has been shown to have little success, with many patients obtaining employment in sheltered workshops only. Being in paid work, as compared with being in supported work, is associated with higher self-esteem and higher levels of hope and optimism among people with mental illness, and is clearly the outcome of choice. 15 Therefore, a new approach was developed in the USA in which the emphasis was on direct job placements, plus support to patient and employer, the so-called ‘place-and-train’ model. The model of ‘place-and-train’ that has been researched most intensively is individualised placement and support (IPS). 13,16–23 IPS is a systematic approach to helping people with severe mental illness obtain competitive employment. It involves the allocation of carefully trained vocational advisers to people who wish to RTW and equipping them with skills and health support as required. It relies on eight principles: (1) it aims towards competitive employment; (2) it is open to all those who want to work; (3) it tries to find jobs consistent with people’s preferences; (4) it works quickly; (5) it brings employment specialists into clinical teams; (6) employment specialists develop relationships with employers based on a person’s work preferences; (7) it provides time-unlimited, individualised support for the person and their employer; and (8) benefits counselling is included. 13 Although originally developed and tested in the USA, IPS has since been shown to be effective in European countries,16 despite very different systems of welfare and diverse job markets. It has been shown to translate to mental health patients in the UK,16,23 provided that it is implemented effectively23 and a high rate of adherence to the fidelity principles is achieved. 24 Pooled data from a 2012 systematic review suggest that up to 47% of those unemployed in Europe because of severe mental illness can be returned to meaningful employment using IPS. 23
Given its success for severe mental illness, IPS might work for chronic pain patients who suffer similar disability, social isolation and rates of unemployment, and for those who have high levels of psychological comorbidity. Indeed, in an uncontrolled pilot study performed by members of our research team, IPS was offered through Remploy (Leicester, UK) to 17 patients attending the local pain clinic. The results showed excellent employment rates and high rates of patient satisfaction, with a social return on investment of between £5.01 and £6.77 for every £1 invested. 25 However, long-term funding for this service could not be secured after the pilot study because of a lack of evidence from randomised controlled trials (RCTs) and insufficient data on cost-effectiveness to justify its widespread adoption.
Individualised placement and support programmes are already being offered patchily in the UK by private sector and local authority schemes. Given that IPS was manualised for a different patient group, providers will be approaching adaptation in different ways, particularly in relation to integration with pain management services. Although IPS is, in the main, a set of practical interventions in support of people seeking work, it may be that some people in pain are not ready for behavioural change, in terms of psychological and/or systemic factors. In this respect, IPS may be supported by well-evidenced psychological interventions that centre around engaging people in the process of change. Two such interventions are motivational interviewing26 and values-based work (which is described in the context of contextual cognitive–behavioural therapy). 27 The research process allows for the development of the IPS intervention to include those components that are associated with cognitive and behavioural change, and establish a basis for integration of pain management.
It is important that IPS be evaluated for chronic pain patients and that the validity of the fidelity principles for people with chronic pain be explored, given that high levels of adherence to these principles is associated with better outcomes in severe mental illness. Crucially, a high-quality clinical effectiveness and cost-effectiveness analysis is needed if we are to justify the widespread adoption of this approach in this prevalent group of patients.
This research aimed to test the feasibility of adopting IPS for people unemployed with chronic pain to lay the groundwork for a definitive RCT.
Patient and public involvement
Prior to submission of our funding application, 20 patient and public representatives participated in three workshops to review and inform our proposal. Participants were male and female, aged 20–86 years and all were diagnosed with chronic pain conditions. They included individuals who were currently working, retired from professional/managerial work, not working on the grounds of ill health and currently signed off sick from work, in addition to those actively seeking work/voluntary work. The public and patient involvement (PPI) representatives were involved in the development of the final protocol and commented on the Plain English summary.
A further two workshops were held, which included eight patient and public representatives, during the first phase of the research [alongside work packages (WPs) 1–3]. These groups reviewed all aspects of WPs 1–4 and commented on all patient-facing documentation, including the invitation letter, patient information leaflets, consent form and questionnaires. The groups iteratively helped the research management team to develop and improve procedures for recruitment and to devise the treatment-as-usual (TAU) booklet. With their proactive support, the TAU booklets were designed to be patient friendly and informative, with up-to-date information about local services for pain and employment (see www.journalslibrary.nihr.ac.uk/programmes/hta/1510802/#/documentation; accessed January 2021).
At the end of the study, two further PPI groups were held, involving six people with chronic pain (people who were employed, unemployed, retired through ill-health and retired not for health reasons) to reflect on the study findings, lessons learned and recommendations for future development work.
Lay co-applicant
Our application included a lay co-applicant who was a former local small business employer, as well as an adviser to local health charities. He proved invaluable throughout the process of the research, from original application to this report. He provided continuity by attending the Trial Management Group meetings and participating as a lay representative to the Trial Steering Committee (TSC).
Data collection tools
During this research, we piloted the use of questionnaires at baseline and follow-up, which were developed from a range of potentially suitable validated tools for evaluating an employment intervention on pain, function and quality of life. Their acceptability was evaluated qualitatively and quantitatively, and, based on our findings, they will be suitable for adaptation for any future definitive trial.
Treatment-as-usual booklet
Together with our PPI representatives, we developed and piloted a TAU booklet, which was found highly acceptable by participants and the Research Ethics Committee. Although specific to the location of this research, these would make a good prototype to be adapted for any larger-scale trial.
Chapter 2 Trial design and methods
Objectives
The specific objectives were to answer questions in the following areas.
Recruitment/retention
-
Can patients who are unemployed with chronic pain be identified efficiently from primary care?
-
Would sufficient numbers of eligible participants consent to take part in a trial?
-
What rates of dropout occur during follow-up?
-
How acceptable would such patients find randomisation?
-
What are the barriers to patients’ and health-care providers’ participation in a future RCT (e.g. practical, financial, motivational)?
-
What would be the risk of ‘contamination’ if individual-level randomisation were used?
Intervention
-
In practice, what is needed to manualise IPS for chronic pain patients?
-
What adaptations are needed?
-
How do the fidelity principles perform and can they be translated across to IPS for chronic pain patients?
-
What training/support is needed for employment support workers (ESWs) to integrate with pain services?
-
How feasible is it that this complex intervention can be delivered within the NHS?
Comparator
-
What is TAU?
-
What information should be in a booklet provided to ‘control’ subjects?
Outcomes
-
What should be the primary outcome measure in a definitive trial (e.g. employment, health related or economic)?
-
In addition to competitive employment outcomes, which in trials of IPS for severe mental health conditions have consistently found to have been improved, what do:
-
patients think are the important outcome measures?
-
employers think are the most important outcomes measures?
-
-
What is the distribution of the relevant outcome measures to calculate power for the trial?
The research was carried out over 39 months and was led by a multidisciplinary team (that included expertise in chronic pain management, delivering a programme of IPS, epidemiology, occupational medicine, research methods, primary care, public health, health economics, qualitative psychological research and local employment circumstances). The research involved mixed methods and comprised six WPs, which aimed to pave the way for a definitive RCT of IPS by addressing the below objectives.
Work package 1
Work package 1 involved qualitative work with a group of individuals with long-term health conditions and at least 24 months’ unemployment who had recently engaged with IPS [as part of the 2-year funded Solent Jobs Programme (SJP) in the cities of Southampton and Portsmouth]. We aimed to understand their views about participating in research (specifically in a trial involving IPS), whether or not they thought people would wish to, and would be able to, take part in a trial, and their individual experience of undertaking the IPS programme.
Work package 2
Work package 2 involved qualitative research with local ESWs, who were delivering IPS as part of the local SJP, to gain insight into their experiences of IPS. In addition, we enquired about their knowledge of and attitudes to people with chronic pain and their specific learning needs to implement IPS tailored to such individuals.
Work package 3
In WP 3, we undertook focus groups with primary care-based health-care professionals (PCPs) to understand their views about a trial of IPS for people with chronic pain and gain their insight as to how to develop recruitment strategies to identify people who are unemployed and have chronic pain within primary care. Furthermore, we sought their views about the acceptability of a trial of this nature and what the most important relevant outcome measures would be, and asked them to comment on the development of study materials (e.g. the TAU booklet) for WP 4.
Work package 4
Work package 4 involved a pilot primary care-based longitudinal study [i.e. the Individualised Support To Employment Participation (InSTEP) trial] to develop the RCT protocol in a small sample of individuals to:
-
test methods of recruitment and evaluate the acceptability of procedures for consent and randomisation to the IPS intervention or TAU
-
develop and ultimately manualise IPS for people with chronic pain by developing training for ESWs, creating shared documentation and integrating pain management planning by a pain specialist in conjunction with the ESWs
-
measure adherence to the study protocol and rates of attrition with follow-up of all participants using postal questionnaires at 3, 6 and 12 months
-
evaluate the acceptability of questionnaires in terms of whether or not participants can and do complete them as intended
-
inform the choice of primary outcome measures (e.g. competitive employment, quality of life, health and health economics) for a definitive trial.
In doing this, we aimed to assess any unforeseen impact on the NHS from trying to place chronic pain patients back into employment to gain an indication of the success levels and what should be measured in a definitive trial, so as to ensure that a more efficient, cost-effective trial to fully test the intervention might be ultimately conducted.
Work package 5
Work package 5 involved qualitative work to evaluate the experience and views of all stakeholders (i.e. ESWs, participants, employers and PCPs) during the pilot trial and to identify barriers to a definitive trial. From the participants, we wished to assess their motivation for participation and their perceptions of the benefits that they experienced and how those benefits might best be captured as outcome measures. In addition, we wanted to seek their views about participation in any future trial and any perceived barriers. From the ESWs, we wished to seek views about the IPS service, about integration with pain services and about important outcome measures. In addition, we hoped to understand what further training needs they perceived for working with chronic pain patients and to facilitate integration of IPS with pain management planning. From employers, we wished to understand opinions about the IPS service, providing a placement and employing someone with chronic pain and what they regarded as important outcome measures. For PCPs, we wished to evaluate the ease and success of identification and referral of people with chronic pain from primary care, and also their capacity to develop effective health plans to support these individuals. We explored the risks of contamination and any barriers to being involved with a trial. We also asked PCPs for suggestions to refine and optimise the protocol for a future trial.
Work package 6
In WP 6 we aimed to manualise the IPS intervention for chronic pain patients and review fidelity principles, in addition to refining the study protocol for a definitive trial.
Ethics approval and research governance
Ethics approval to conduct WPs 1–3 was granted by the University of Southampton Faculty of Medicine Ethics Committee on 19 December 2016 (Integrated Research Application System ID 215081) and Health Research Authority approval was given on 11 January 2017 (reference 17/HRA/0035). Approval to conduct WPs 4–6 was granted by the South Central-Hampshire Area Research Ethics Committee on 22 September 2017 (Integrated Research Application System ID 226125) and Health Research Authority approval was given on 9 October 2017 (reference 17/SC/0398).
Methods
Work packages 1–3
Common methodological elements
In these WPs, qualitative interviews were carried out by one of two trained interviewers who were research assistants in psychology and who had prior qualitative research experience. All participants gave written, informed consent to be interviewed, for the interview to be recorded and transcribed, and for the analysis of their comments. All were made aware that their comments were confidential and would be non-attributable. In each WP, the interviewers followed a semistructured topic guide (Table 1) to allow participants to tell the story of their own experiences. 28,29 Neither interviewer had any prior relationship with any of the participants. Questions and prompts were developed in advance to aid the interviewer, but the topic guide was intentionally flexible to allow for natural discussion throughout the process. Interviews were recorded and field notes were made by the interviewer during and immediately after data collection.
| Clients | ESWs | PCPs |
|---|---|---|
|
|
|
Data analysis
Recorded interviews were transcribed verbatim by the interviewers and all text was entered into NVivo qualitative data analysis software version 11 (QSR International, Warrington, UK) for analysis. The data were analysed thematically and independently by both researchers as an iterative process alongside data collection. 30
-
All data were coded inductively by both researchers.
-
Codes were examined for patterns and refined.
-
Relationships and refined patterns between initial codes were identified and themes were developed into higher-level categories following discussion between both researchers.
-
Themes were described with representative data that supported each theme. This methodology enabled thorough exploration and detailed description of clients’ views. 31,32 Quotations were selected from the arising themes to best describe the findings, with non-identifiable identification numbers allocated to participants. The study findings were reported in accordance with the COnsolidated criteria for REporting Qualitative research (COREQ). 33
Participants and recruitment to work packages 1–3
Work package 1
Work package 1 involved a sample of people with chronic health conditions (including pain) who had been unemployed for at least 24 months and had been, therefore, recruited for and attended the SJP IPS intervention in the cities of Portsmouth and Southampton in the preceding 12 months.
Clients who were potentially eligible to take part were identified by the ESWs and managers of the IPS service in the city councils. We provided the ESWs with a participant information sheet that explained the nature and purpose of our research. The leaflet explained that we were seeking willing volunteers to take part in qualitative research, what was required of participants, that their expressed views would be confidential, anonymised and non-attributable, and that they could withdraw their consent at any time. Individuals who expressed interest in participating were asked to give consent for their contact information to be passed to the qualitative researchers. Potential participants were then contacted via telephone by the researchers to arrange an interview. Interviews were conducted at a time that suited the clients and they were offered the choice of an interview by telephone or face to face (arranged in their local job centre). It was explained to each client that the interviewer was independent of the IPS programme and that they were part of a research team investigating whether or not high-quality employment services could be of benefit to people who were unemployed and affected by long-term health conditions. Clients were assured that their comments would be strictly confidential and no one from the SJP IPS programme would be present during the interview. Travel expenses incurred by the clients were remunerated and participants were sent a high street shopping voucher after their interview to thank them for their assistance.
Work package 2
Work package 2 involved ESWs currently working in the SJP IPS intervention in the cities of Portsmouth and Southampton.
All eight ESWs involved in the SJP IPS intervention in the cities of Portsmouth and Southampton were eligible to participate. Eligible individuals were given a written information sheet by their managers, which explained the purpose of the study, emphasising that participation was voluntary and that comments would be confidential, anonymised and non-attributable, and that they could withdraw their consent at any time. Semistructured interviews were arranged at the convenience of the ESW at their place of work and travel expenses incurred by ESWs were remunerated. Written, informed consent was obtained from ESWs to record their interview and for the analysis of their views.
Work package 3
Work package 3 involved qualitative focus groups with members of the primary health-care team who were familiar with chronic pain patients (i.e. PCPs). PCPs were contacted via the local Clinical Research Network, which advertised the study to research-active general practices. Practices that expressed interest in the study were then provided with written information about the purpose of the study and what was required. Any member of the practice team involved in the care of chronic pain patients was eligible to participate.
Practices that expressed interest were contacted by a member of the research team by telephone to explain what was involved in the research and, if agreeable, a suitable time was arranged to conduct a focus group within the practice premises. Focus groups were chosen to facilitate interaction between participants and enable them to bounce ideas off each other,34 and also for convenience to minimise the total clinical time of the PCPs taken up by the research. It was emphasised that all expressed views would be confidential, anonymised and non-attributable, and that they could withdraw their consent at any time. Written, informed consent to participate, for recording and for the analysis of their views was obtained from all PCPs prior to the start of the focus group. Participating general practices were remunerated so that they could backfill the time required.
Results
Work packages 1–3
Data collection for all three WPs took place in 2017. The following sections describe those who participated.
Work package 1: participants in the Solent Jobs Programme individualised placement and support
In 2017, approximately 50 people per month were referred to the SJP IPS programme, of whom just under half agreed to participate. A total of 20 potential clients were identified and registered their interest to participate in our qualitative research. However, five clients proved uncontactable by telephone and six failed to attend an interview at an agreed time. Ultimately, a total of nine clients were interviewed. In each case, the interviews lasted a maximum of 45 minutes.
Work package 2: employment support workers
All ESWs at the two SJP IPS sites in Portsmouth and Southampton were given written information about the research. Six ESWs expressed interest in participating. However, because of work commitments, one was unable to do so. A total of five interviews were conducted and all lasted a maximum of 45 minutes.
Work package 3: health-care professionals in primary care
A total of 11 PCPs from two general practices took part in two focus groups. The PCPs included four GPs, an advanced nurse practitioner, three practice nurses, a health-care assistant, a practice manager and a medicines manager. Focus groups were arranged to make the groups as inclusive and accessible as possible, and lasted a maximum of 1 hour.
Themes identified
Quotations have been selected from the arising themes to best describe the findings, with non-identifiable identification numbers allocated. The results are presented under the key themes.
Undertaking a research trial involving individualised placement and support
The PCPs were extremely positive about the idea of a trial of an employment intervention for people unemployed with chronic pain:
I think the intentions are brilliant.
PCP1
Likewise, all ESWs were very positive about the SJP IPS programme and enthusiastic about research to show its benefits. They were keen to share success stories and highlight the benefits of the intervention that they had observed.
Primary care-based health-care professionals stated that they had observed patients who were trying to RTW and find employment, and that such individuals would be interested and engaged in a trial. However, they voiced concern that some individuals might not wish to RTW and that differences in motivation might prove problematic in terms of study trial recruitment:
And it’s the individuals, there are some people who actually like to work as we would like to see that, but there are those who just wanna get the money and the money is just easier if you are just sitting on your backside sometimes.
PCP1
The PCPs expressed concern that some patients may not want to seek employment and that it would be important to identify and measure motivation as part of the study.
One client saw the benefit of conducting the proposed research trial but, similarly, expressed concerns about the purpose and how that purpose would be communicated (e.g. about the wording of the information sheet that stated that the research aim was to ‘improve the health of people who are unemployed through long-term health problems’). She felt that this could be considered derogatory, feeling that she was not ‘unemployed’ but ‘unable to work’. At the end of the interview, she voiced apprehensions about the future research being used to force individuals to work even if they were unable to do so:
I think this is a really interesting study. I think that, it’s important, but I also think in the wrong hands, it could be used to be malicious and force people with pain into work.
C5
Overall, clients were very positive about the SJP IPS programme with which they were engaged. However, we found that they had difficulty in discussing a potential research trial that is distinct from their own personal experiences of their IPS programme. Even after clarification, some clients found the concept of a research trial difficult to understand and their answers were inherently linked to their individual experience of IPS. For example, clients seemed anxious that recruitment to a trial would mean an increased workload for their ESWs, who, they perceived, already had limited time available, without them being further burdened by new clients in a research trial:
I mean at the end of the day they’ve got 25–30, erm, clients, and you’ve only got four advisors maybe five advisors. And to be totally honest, they are also doing more interviews at the job centre in [location] and [location] and that to get more people on this course. So you are limited to the amount of time you can have with them.
C2
Recruitment to a randomised controlled trial of individualised placement and support
One client expressed concern about recruitment in health-care settings:
I don’t think . . . if I got a letter like that from my GP, I think I would just shove it in the bin. Or I would . . . I wouldn’t be very happy.
C5
In contrast, other clients felt that this method of recruitment could be a positive way to identify people who might benefit from the intervention:
That sounds like a good idea, because in a way when I was put on my antidepressants the doctor who gave me the antidepressants and telling me what to do, he told me that I needed to be part of a support programme, you are not gonna be able to do this alone, you’ve got your church, you’ve got your wife but you are gonna need more than that. You need someone to steer you in the right direction, which I have done and I continue to do.
C4
One of the core precepts of IPS is that participation is voluntary and dictated by client choice. Even so, our interviewees appeared confused about whether their enrolment in the SJP IPS programme was voluntary or mandatory. Although the ESWs explained at the outset that the programme was completely voluntary, some clients stated that they did not feel they had a choice about participation, particularly if they were referred by the job centre (which was the case for the SJP, but would not be the case in the planned pilot study). This uncertainty about their freedom of choice regarding employment services was particularly unhelpful when trying to elicit their engagement with employment-related research and when explaining the voluntary nature of research participation:
Even the advisors say it’s ‘voluntary’ it’s not voluntary . . . when you go to see the advisor at the job centre they said ‘you’re on the work activity group, you must be doing something’ so they put you on [IPS programme]. And then when you come here, they say it’s all voluntary. But it’s not voluntary; the job centre put you on this course for a reason.
C3
Clients also commented on the large volume of paperwork that arose from participation in the programme and evaluations of the IPS (i.e. evaluations of the SJP and unrelated to the current research) and that the need for this was not apparently explained to them. One client did not understand the purpose of the volume and content of questions asked in evaluations:
Yeah it’s like these [consent forms and information sheets]. Tick this thing on the computer. Tick, tick, tick. One question was did you have school dinners as a child? Yeah what’s that about?
C3
One ESW hypothesised that individuals recruited in different settings may differ from the clients who were currently being offered IPS:
. . . the referral would be different, it would be interesting to see those clients coming from a doctor’s surgery that are told to speak to someone, ’cause their mentality might be different, to people that are in the process of referrals coming often from the job centre.
ESW5
Primary care-based health-care professionals discussed recruiting eligible patients from health-care settings. They felt that it would be possible to undertake database searches using the Read codes. Read codes are the standard clinical terminology system used in general practice in the UK. 35 They provide a hierarchical clinical coding system for the purpose of reporting research decision-making and allow data to be shared reliably between different computer systems. They have been used previously for chronic pain. 36 However, the PCPs recognised that currently no Read code for unemployment exists, and so searches would identify patients with pain and certified sickness absence, but not unemployment. PCPs suggested that Read codes for chronic pain conditions could be used in conjunction with medication codes (e.g. opioids or gabapentinoids) to identify potential participants.
The PCPs also believed that they could personally identify individuals who would benefit from the programme based on regular contact through primary care services.
About the nature of the individualised placement and support intervention
Employment support workers were in agreement with offering IPS after only 3 months of unemployment, which they thought would be particularly beneficial. The clients made the same point, suggesting that the sooner after losing their job someone could enter the programme, the better it would be:
Because everybody needs that helping hand, if you think about it, if somebody’s just come out of work, for 3 months and they’ve got nothing, that’s where they’re starting to lose the point, ‘I’m unemployed, I’m signing on, I’ve gotta do this, I’ve gotta do that . . . you know where do I go next?’ We don’t want that person to go 3 months after that, 6 months unemployed and still going nowhere, they need to be somewhere where they get the support, yeah I totally agree with that.
C4
Likewise, the PCPs emphasised the importance of early intervention after unemployment:
I think the sooner you can get someone back to work, the better.
PCP4
The ESWs felt that IPS should continue to be available for longer than 1 year, as the process of preparing someone for work and securing employment could be lengthy. Clients, likewise, reported that it could take time to get someone ready for employment and into the workplace.
The pivotal role of their individual ESW in successful IPS was emphasised by the clients and, in their view, this relationship was crucial in finding clients suitable employment. On the other hand, some clients described a lack of continuity in the programme and felt that they had not developed a relationship with a single ESW, having met multiple different ones, which had negatively affected their experience of the programme:
I’ve just been moved from one advisor to another advisor, to a new one.
C2
Clients reported that ESWs asked about their potential needs and barriers to creating an individualised plan. One client recalled that the specific details of her condition had not been considered, but rather a very general discussion of her disability and illness:
So, for people with chronic pain, or anybody with mental health, or, you know, or anything that’s specific, I think what would improve this service is having an advisor who specialised in that condition. Or in a couple of things. It’s having that understanding, it bridges that gap.
C5
It seemed to the clients that personalised advice and a holistic approach were key features of the IPS intervention. Likewise, ESWs discussed the importance of tailoring IPS to each individual client. This was usually achieved by discussion with clients, as the ESW had limited knowledge about the impact and management of specific conditions:
. . . you should have advisers that have training around chronic pain and there should be a fully comprehensive directory of signposting people.
ESW4
Clients were aware of the existence of other employment interventions available for unemployed people. However, IPS was felt to be the best approach for patients with chronic pain, as other employment interventions were seen as not appropriate for individuals with complex issues:
. . . the other programme, they understood my problems but they didn’t do anything about it.
C4
The ‘control’ intervention was mentioned by the PCPs. The PCPs reviewed the draft TAU booklet that would be provided to all subjects. They reviewed the booklet positively and, in particular, highlighted the vernacular language used throughout and the reader-friendly style in which it addressed commonly asked questions without overwhelming the reader with excessive information:
I think it’s very useful, I think it will help people . . . I think patients will find it quite useful.
PCP8
The PCPs reported willingness to randomise patients to both the IPS and control interventions. One PCP explained that in previous studies participants had been unhappy if they had been randomised to a control group, and felt that it would be important to explain the benefit of both interventions:
I tend to . . . not sell it if it’s a non-intervention or control, but actually saying . . . you are actually really important in this study as well. They are part of it and they are helping. If we get to the actually nitty gritty and we are actually recruiting patients, then they’ve got that far, and we’ve talked about it, and we’ve consented them, then hopefully they are still on board.
PCP4
Outcomes to be assessed in a future trial
Participants appreciated that the outcome of the programme would be entry to employment, although they indicated that a client may well not have found employment within the relatively short length of the proposed intervention (i.e. 6–12 months). At the time of interview, none of the clients on the SJP IPS programme had secured paid employment, but all were keen to discuss the progress they had made. They highlighted the skills they had gained from the programme that made them qualified for employment, with ‘job-readiness’ seen as a potential outcome for a future study:
I feel a lot better about starting now, I don’t expect anything to happen until I’ve been here a few months or so, one thing at a time, I need some solid ground to stand on.
C7
Some clients also described a boost in their confidence since starting the programme and reported that they were being more active in daily life:
. . . it gets me out of the house and that you know what I mean, well . . . I’m out and about every day.
C6
Employment support workers recognised that the likely principal outcome of IPS would be entry to employment. However, they also recognised the probability that clients may not yet have secured employment by the end of the intervention. ESWs were keen to talk about the success stories of the IPS programme, notably client improvement in several quality-of-life domains.
The ESWs highlighted the skills that clients had acquired from the programme, which had enabled them to consider a work placement in the future. ‘Job-readiness’ was therefore proposed as a potential outcome for a future study. The importance of building clients’ confidence was also noted:
The knee jerk reaction, which throws up the barriers in the first place. So you’ve got to get those down. And by doing that, when people talk about it, when you are chatting with the client and I’ll say ‘but if you are doing that, why don’t you take it. it’s the same thing but you are on a different’, and they go ‘ohhh right’. Erm, so you are getting those kind of barriers down. At the same time as doing that, ’cause you actually understand, it builds their confidence. And ‘maybe I could do that, maybe I could plan’.
ESW3
Similar to the ESWs, PCPs speculated about the importance of the intervention in building clients’ confidence. Participants also discussed changing clients’ attitudes and views about work.
The PCPs postulated a number of benefits of employment for individuals with chronic pain. For example, they suggested that employment could increase physical activity, which in turn might reduce pain levels. In addition, they highlighted the link between chronic pain and mental health, stating that improving social interaction and sense of achievement through work could improve depression. It was thought that employment could improve patients’ overall quality of life:
So then at least these sort of work based programmes are starting to tackle that, helping people to get out of the house regularly, introducing some sort of ‘maybe I could do something’, a degree of hopefulness, where there is a degree of hopelessness.
PCP8
A summary of all of the barriers to and facilitators of a future trial of IPS for people unemployed with chronic pain that were identified from WPs 1–3 is shown in Table 2.
| Specifics of trial design | Barrier | Facilitator |
|---|---|---|
| Doing a trial | Is it voluntary to take part or compulsory?Client | This is a good thing to test. It is importantClient, PCP, ESW |
| Recruitment to a trial | Recruitment might be challenging in primary care as our GPs do not know that we are employed/not employedClientI would not be happy if my GP wrote to me about a job interventionClientThere is a risk of sending a lot of letters to people with chronic pain who currently are in workPCP | Lots of opportunities to find unemployed people with chronic pain: job centre, from other employment programmes, chronic pain services, physiotherapists, rheumatologists, support groups, community groups, librariesClientI would be more likely to consider this if my GP recommended it for meClientWe can find people using Read code searches of the primary care database. Although no code for ‘unemployed’, we can use chronic pain and medications (e.g. opioids)PCPWe know who these patients are personallyPCPRecruiting from places other than the Job centres might bring in people who are different and perhaps better motivatedESW |
| Acceptability of the intervention | It needs to be clear that it is a choice to go on the programme that it is not mandatory and that you are not being ‘forced’ into work by anybodyClientClients need to be motivated to want to work for this intervention to be possibleESWClients sometimes need more than 12 months’ support to be ready to apply for competitive employmentESW | A trial offering this support earlier after you have lost your job would be likely to be much better for people before they have lost confidence, etc.Client |
| Delivering the intervention | ESWs would need extra training in chronic painClientWe would need to know more about chronic pain and chronic pain services and management to do thisESW | The relationship with the ESW is crucial for this and it works best when you have continuity and build a relationshipClient |
| Process | There is a lot of paperwork already involved in IPS assessmentsClient | |
| Acceptability of the TAU | The booklet provided for treatment as usual is brilliantClient, PCP, ESWI think it would be very helpful and would be happy to recommend patients if they could have this or the treatmentPCP | |
| Outcomes that are important | Motivation to work will be an in important factor determining outcomePCP | Although your main reason for attending is to get a job, you get so much more out of it, for example confidence, increased social interactionClientThe benefits will include less pain, more exercise, less depression, better quality of life, not just a jobPCPThe clients develop over time; they are not all ‘ready’ for a job at the same stage but you see them benefiting in other ways to begin with. ‘Readiness for work’ could be an important outcomeESW |
Discussion work packages 1–3
In general, all three groups were enthusiastic about the proposal of a future trial of IPS for people unemployed with chronic pain. Compared with other employment interventions, both clients and ESWs favoured the choice of IPS because of its personalised approach. Everybody thought that employment could pose future health benefits. Clients and ESWs felt that they would need additional training to enable them to provide IPS for people with chronic pain. It was viewed as important that motivation to work was measured and that clients should feel that they have the choice to participate. The importance of a longer-term relationship with the ESW was emphasised by clients, something previously reported from another qualitative study undertaken among mental health IPS patients in a RCT. 37 Early intervention shortly after unemployment was thought to be key. Likewise, it was considered important that the duration of intervention could be flexible, as not everyone will achieve employment within a fixed time. Finally, although employment rates were an essential outcome, the parties all identified a number of other relevant and important outcomes that could be modified by this intervention, including confidence, mental health, increased physical activity and quality of life.
The opportunity for the current research arose from the existing SJP-funded pilot of IPS available through local job centres for anyone who was unemployed ≥ 2 years with a long-term health condition. Therefore, the clients had all experienced very long-term unemployment. It is insightful and interesting that clients pointed to the importance of offering IPS early after unemployment and they were extremely positive about the InSTEP pilot study recruiting after just 3 months’ unemployment. Re-employment rates are known to be considerably lower after prolonged unemployment because of a complex array of factors, including physical and mental health impacts, loss of confidence and self-efficacy, de-skilling and financial dependence on welfare benefits. 37–42 There may also be a strong selection effect (i.e. those best able to RTW will tend to do so sooner). It is important in planning any trial to consider how to best time the intervention to provide the greatest benefit. The views expressed by our interviewees reinforce our own view that consideration needs to be given to offering IPS as soon as possible after unemployment. Notably, there is a Norwegian trial currently underway that is recruiting individuals with more than 2 years' unemployment. 43
Clients were positive about the relevance and importance of a future trial that would recruit unemployed individuals with chronic pain. However, we encountered challenges framing research in this field to clients who struggled to comment on a hypothetical trial without referencing it to their own IPS engagement. In particular, we found that recent SJP clients were uncertain as to how voluntary the nature of their engagement in the IPS programme was, and this appeared to lead to further confusion when the concept of research was introduced. Our findings highlighted that trial participants may need additional support and explanation of the purpose of the research and their rights to give or withhold consent to participate, including withdrawing their consent at any time. Clients appeared to feel that they were compelled to engage in the IPS programme, fearing that if they did not they would be at risk of compromising their welfare benefit payments. Perhaps because of cultural differences, or differences in national health and welfare systems, no such problems were reported in the recent Norwegian pilot study. 43 In developing a UK trial, researchers will need to be sensitive to this complexity, and make every effort to ensure that participants have understood the voluntary nature of participation in IPS and research about IPS. This issue will also need careful consideration when defining the content of the patient information leaflet and will need taking into account in a situation where IPS is not widely available (i.e. deciding whether or not it is ethical to offer IPS to only those who give consent to take part in the trial).
A key challenge identified was the lack of employment status information in existing UK health-care databases and a lack of availability of linkage between health-care databases and employment databases. PCPs saw this as having important implications in terms of future trial design (i.e. a lower level of recruitment and higher attrition than might be observed in a different population, and the need to consider specific strategies to enable ongoing participation both with the IPS intervention and with the research trial).
The study highlighted an important challenge for a future definitive trial in terms of obtaining and maintaining engagement with this client group. To try to maximise participation, a choice of a face-to-face interview or a telephone interview was offered. Despite this, we found that a number of those who had agreed to participate were unavailable at the agreed time and place. This may be because individuals with chronic pain frequently have complex problems, including low self-efficacy, poor organisational or health literacy, unpredictable symptoms and comorbid conditions (e.g. depression and anxiety44). It was interesting that the PCPs also alluded to potential difficulties in undertaking research with this population because of their complex problems. These issues, however, are very similar among people with severe mental health conditions, for whom IPS has shown excellent efficacy. Therefore, design of any trial will need to take account of these issues, perhaps predicting a lower level of recruitment and a poorer rate of retention than that seen in other client groups. The design should also consider specific strategies to enable ongoing participation, both with regard to the intervention and the research. Interestingly, however, such challenges may not differ markedly from those reported in a trial of IPS for people with serious mental illness. 45
The findings do need to be considered alongside some limitations. First, although care was taken not to provide too detailed an explanation about the research aims to the ESWs who identified possible client participants, it is possible that clients who agreed to take part in WP 1 differed from other clients, and may have been more positively disposed to research and derived more benefit from the SJP IPS intervention compared with those who declined an interview. Unfortunately, the study design did not provide the opportunity to explore the views of those who did not wish to participate. Second, the views of the PCPs were elicited from two general practices that had volunteered to take part. There is therefore the possibility that the views expressed by the PCPs were generally more positive about our research aims than those of a wider sample of PCPs.
In conclusion, WPs 1–3 identified a number of barriers to and facilitators of a future trial of IPS for people unemployed with chronic pain. The insights from clients, ESWs and PCPs fed directly into the design of WP 4, the questionnaires at baseline and follow-up, and the design of the intervention and the pilot trial.
Work package 4: the InSTEP pilot trial
Study design
Work package 4 was a pilot primary care-based longitudinal study (i.e. the InSTEP pilot trial), which tested the feasibility of a RCT, with follow-up at 3, 6 and 12 months.
Research question
The research question was:
-
Among people of working age who are unemployed for > 3 months with chronic pain but wish to work, how feasible is it to undertake a RCT to test the clinical effectiveness and cost-effectiveness of IPS compared with a control, and what should be the outcome for a definitive trial?
The study aimed to:
-
test methods of recruitment and evaluate the acceptability of procedures for consent and randomisation to the IPS intervention or TAU
-
develop and ultimately manualise IPS for people with chronic pain by developing training for ESWs, creating shared documentation and integrating pain management planning by a pain specialist in conjunction with the ESWs
-
measure adherence to the study protocol and rates of attrition with follow-up of all participants using postal questionnaires at 3, 6 and 12 months
-
evaluate the acceptability of questionnaires in terms of whether or not participants can and do complete them as intended
-
inform the choice of primary outcome measures (e.g. competitive employment, quality of life, health and health economics) for a definitive trial.
In doing this, we aimed to assess any unforeseen impact on the NHS from trying to place chronic pain patients back into employment to gain an indication of the success levels and what should be measured in a definitive trial, so as to ensure that a more efficient, cost-effective trial to fully test the intervention might be ultimately conducted.
Study process
Supported by the Clinical Research Network, we advertised the research to identify practices willing to recruit for the study. Interested practices were asked to test the different methods of recruitment we had devised from WPs 1–3, including displaying posters for self-referral, Read code searches followed by a mailshot to those identified, opportunistic recruitment during appointments and opportunistic screening after hand-searching records.
All potential participants identified by any strategy were sent a study pack provided by the research team. The pack comprised a personalised invitation letter, an information sheet explaining the purpose of the study, a reply slip and a pre-paid envelope in which to return the reply slip to the study co-ordinator. Interested individuals were offered a number of ways by which they might contact the research study co-ordinator (i.e. telephone, e-mail or by completing and posting a reply slip in the pre-paid envelope).
Pre-assessment screening
All individuals who returned a reply slip were subsequently telephoned by the study co-ordinator at their convenience. This provided the opportunity to discuss the study and address any questions that the individual might have had. If agreeable, the study co-ordinator completed a brief eligibility screening form with the individual over the telephone to confirm that they:
-
were able to provide written, informed consent
-
had not previously been referred to, or had taken part in, the IPS programme via Southampton or Portsmouth city councils
-
had chronic pain (i.e. pain continuing for > 3 months)
-
had completed the diagnostic pathway for their chronic pain
-
did not anticipate recovery within the coming 12 months
-
wished to RTW.
Following satisfactory completion of the screening form, the individual was asked to give verbal consent to randomisation by the study co-ordinator. If agreeable, the participant was then randomly allocated by computer-generated algorithm (block 1 : 1) to either the active IPS intervention arm of the study or the TAU control arm.
Finally, the study co-ordinator informed the participant regarding the next (baseline visit) stage of the study. If randomised to the TAU arm, the research co-ordinator herself telephoned to make the baseline appointment at their general practice. If randomised to the intervention, the local ESW telephoned the participant to arrange the baseline appointment at the local city council premises.
Treatment as usual/control arm
There was no evidence-based NHS alternative to IPS available and suitable for use as a ‘control’ for the pilot trial. However, a number of services are available and are provided by the Department for Work and Pensions, local government and the voluntary sector, and individuals may self-refer to these services or can be referred by health-care professionals. Although the nature and type of services varies widely by region in the UK. It is not known what proportion of patients with chronic pain discuss their employment status with their GP or other member of the primary care team. It is also not known how comprehensively the PCPs keep themselves up to date about the availability of appropriate services in their area. A significant hindrance for this patient group is that they frequently lack confidence, skills and self-efficacy as a result of their chronic pain and comorbidities, such as depression and anxiety. Therefore, for the pilot trial, NHS TAU was supplemented with a standardised booklet to signpost participants to local employment and health-care services. We chose this approach both for ethical reasons and to encourage participation.
Two booklets were co-designed with our PPI group (i.e. one for each city involved). The resultant booklets were professional looking, informative and tailored to the particular location (i.e. Portsmouth or Southampton), with specific information about local services for pain management and job support, including voluntary and third-sector organisations and health-related advice. The PPI group suggested that pages should be included for participants to make their own notes and to construct a list of goals that was structured towards ultimately enabling gainful employment. The booklets also promoted positive messages about self-efficacy and the value of employment in enhancing health and well-being. It was envisaged that the booklet might be an appropriate vehicle to facilitate discussion with their GP about enhancing their health sufficiently for them to RTW using existing services, and provide clear guidance about local services that might help them seek employment.
Participants randomised to TAU were contacted and offered an appointment, at their convenience, with the study co-ordinator (who had a background as a health-care professional, but had no formal occupational rehabilitation training). At the appointment, any questions about the research were answered, written, informed consent for participation was obtained and the baseline questionnaire was completed (taking approximately 20 minutes). Subsequently, the study co-ordinator spent approximately 10 minutes guiding the participant through the booklet and encouraged them to take it home and read it at their leisure. Travel costs incurred were reimbursed. No further appointments were made.
Individualised placement and support intervention/active arm
Participants allocated to the active arm of the study attended a baseline appointment with the council-employed ESW at the local city council premises, which lasted approximately 1 hour. The ESW confirmed with the individual that they were willing to participate, addressed any further questions that they might have and then obtained their written, informed consent to take part in the study and in IPS. The participant was asked to complete the baseline questionnaire (which took approximately 20 minutes) and was also given a copy of the TAU booklet. The participant was encouraged to take the booklet home and read it at their leisure. Travel costs incurred by participants were reimbursed.
Adapting individualised placement and support for chronic pain patients
Based on the results of WP 3, the ESWs were provided with initial training by the specialist pain team before recruitment commenced. The content of this training focused on what chronic pain is, how it presents in practice, the types of medication used to manage the pain (and their side effects) and common approaches to enable functioning used by pain experts.
Furthermore, all participants recruited to the trial and randomised to IPS were seen by their assigned ESW and the community pain occupational therapist (OT) together for one of their initial appointments. Some standardised integrated documentation was developed, including those domains that both parties usually covered in their initial consultations, which it was agreed would be shared subsequently with the study team. The focus of these joint appointments was on assessment of the participants’ pain and current pain management strategies, with the possibility of specific counselling and support from the OT, signposting to other relevant services or follow-up by the pain team. The ESWs were invited to integrate as much as possible with the local pain services and attend multidisciplinary team meetings, and follow-up pain service use was available to any participant.
Active arm: individualised placement and support (subsequent follow-up appointments)
Following local procedures for IPS, and alongside people participating in the SJP, pilot trial participants met with the ESW as frequently as required to support and develop their employment plans. Fundamentally, this process fell into three stages: (1) assessing preparedness for work, (2) preparing for work and (3) choice of and allocation to, a competitive paid work placement.
Questionnaires
Questionnaires were developed for baseline and reassessment at 3, 6 and 12 months of the pilot trial. The baseline questionnaire was completed with the support of the ESWs or study co-ordinator (during attendance at the baseline visit). The three follow-up questionnaires were posted to allow participants to complete and return the form at their leisure. A pre-paid envelope accompanied the questionnaire. If no response was received after 4 weeks, a reminder letter and a further copy of the questionnaire were sent. On receipt of each completed questionnaire, a £10 shopping voucher was sent to the participant to thank them for their assistance.
Analysis
Our analysis focused on the acceptability of the questionnaire, and the rates of missing data in returned questionnaires and the attrition of participants in both arms. Another aim was to scope the most suitable outcome measures for a definitive trial and define the size of change to carry out power calculations. The questionnaires therefore asked about demographics, past employment history, current employment aims, comorbidities, health-care utilisation and health literacy. The validated tools that were included were the Brief Pain Inventory (BPI), the EuroQol-5 Dimensions, five-level version (EQ-5D-5L), health-care utilisation, the Return-to-Work Self-Efficacy Scale, the Warwick–Edinburgh Mental Wellbeing Scale (WEMWBS), Waddell’s Fear-Avoidance Beliefs Questionnaire, the Patient Health Questionnaire-9 items (PHQ-9), self-rated health and Rosenberg’s Self-Esteem Scale. At follow-up, we additionally asked about interviews that the participants may have had for jobs and any new employment that they had taken up.
Data analysis
Descriptive statistics were used to summarise the:
-
proportion of people identified in primary care who were eligible for the study
-
proportion who agreed to take part
-
rates of attrition in each arm of the trial
-
rates of satisfactory completion of questionnaires in each arm
-
distribution of potential outcome measures through analysis of the questionnaire responses among participants in the control arm.
These data informed the choice of primary and secondary outcome measures for a future RCT. Time-specific differences in self-efficacy measures between the two trial arms were explored using t-tests. Changes over time were explored using random intercept linear and logistic regression modelling for continuous and binary outcomes, respectively, after adjusting for intervention arm. Analyses were carried out using Stata® version 12 (StataCorp LP, College Station, TX, USA).
Changes over time in self-rated health were explored using random intercept logistic regression modelling after adjusting for intervention arm.
Results
Recruitment
Our original estimate was that four general practices would be needed to recruit a maximum of 80 pilot study patients. However, to recruit the final sample, we needed to widen our sampling frame to include nine general practices in Southampton and Portsmouth (covering an estimated 200,000 people).
We trialled all of the approaches to primary care recruitment suggested in WPs 1–3 to understand (1) which was most effective and (2) which was most efficient. Table 3 summarises the outcomes of the approaches we made to patients identified through the different recruitment methods.
| Recruitment method | Number approached | Number identified but ineligible | Number recruited |
|---|---|---|---|
| Database search (GP) | 1017 | 31 | 26 |
| Hand-searching records | 6 | 0 | 6 |
| Posters in general practices | Unknown | 2 | 0a |
| Opportunistic (GP) | 5 | 5 | |
| Opportunistic (pain services) | 13 | 13 | |
| Total | 50 |
Read code database searches were undertaken by all nine of the participating practices (Box 1). Once they had been carried out, GPs were asked to review the generated lists to exclude anybody who they felt should not be contacted (e.g. because of recent bereavement or terminal illness). After screening, the practice mailed study packs to all those identified to ensure patient privacy and to minimise any concerns a participant may have about disclosure to others.
Exclusions: cancer, palliative, severe enduring mental health condition (as these are eligible for IPS through mental health services).
Drugs search strategyA prescription over the past 3 years, including one or more than one of tricyclics, gabapentinoids or analgesics.
(Rationale for restriction: chronic pain may have resolved if not active prescription drug users.)
Exclude-
Acute migraine treatment.
-
Analgesics: buprenorphine hydrochloride; naloxone hydrochloride (SUBOXONE® (Indivior UK Ltd, Hull, UK)) or methadone, fentanyl > 50 µg, buprenorphine (TRANSTEC®; Napp Pharmaceuticals Ltd, Cambridge, UK) > 70 mg and morphine sulfate (Zomorph®, Ethypharm UK Ltd, High Wycombe, UK) > 120 mg (on grounds upper limits of safe dosing).
-
Neuropathic pain medications: ketamine, sodium valproate (used largely in palliative care) and phenytoin sodium (rarely used in chronic pain patients).
Study information packs were posted by each practice between November 2017 and September 2018. In total, 1017 packs were mailed. In response, 57 patients made contact with the research team after receiving a pack, of whom more than half did not meet the eligibility criteria (e.g. retired, already in paid work, no longer had chronic pain). Great interest in the study was shown by those who made contact and disappointment was expressed by those who were not eligible to participate. In particular, a number of people who made contact with us reported that they were currently working but having difficulties caused by their pain and were keen to have employment support (n = 10). Unfortunately, we were not able to offer this type of support within the terms of the current research project. A further five individuals expressed interest by returning a reply slip to the research team, but were not contactable (this was because an incorrect contact number was provided or messages were left by the study co-ordinator, but no response could be obtained, despite multiple attempts).
Opportunistic screening was carried out through hand-searching of GP records (in one practice) or during GP appointments (at another practice). Using these approaches, those identified were 100% eligible and were all recruited. However, this approach proved to be slow and resource intensive (e.g. the hand-searching took approximately 2 weeks of research nurse time to yield the final six recruited patients).
Posters advertising the study were displayed in all nine practices involved, but yielded only two telephone calls from patients, both of which unfortunately came after recruitment closed.
Despite all efforts, recruitment via primary care was proving challenging and very slow; therefore, with the approval of the TSC, we approached the community pain services in April 2018 to enlist their assistance with recruitment. A targeted face-to-face opportunistic approach was again found to yield a high rate of eligible participants who went on to be successfully recruited (n = 13), but these participants were recruited over a total of 5 months, showing that even with such a personalised approach, the number of patients suitable for the trial was relatively small per head of patient attending pain services.
Ultimately, a total of 50 individuals were successfully recruited to the study using all the different approaches described. Personalised approaches were the most successful and, during the pilot trial, this was achieved most efficiently in community pain services.
Randomisation
Given the delays experienced with recruitment from primary care, block randomisation was compromised by the availability of the IPS intervention until a fixed time point (i.e. until the end of September 2019 and so the final recruit to the active arm was required by September 2018 to achieve the 12-month follow-up). Therefore, after random allocation initially, we subsequently allocated as many of the earlier recruits as possible to IPS until it was no longer available, and the remainder were thereafter allocated to TAU. Importantly, all those recruited from one large practice early on (n = 13) were randomly allocated 1 : 1 so that an assessment of the risk of contamination could be made. In all cases, the participants were recruited to a RCT and gave written informed consent to be allocated randomly to either arm. Nobody in either trial arm expressed dissatisfaction with randomisation or their allocation, and nobody dropped out after allocation or before their first appointment.
Contamination
Although the number of participants involved was small, the risk of contamination was assessed to be low, given that study participants viewed their employment as of limited relevance to their health care and held the same belief about the interest of their GP. GPs were not directly involved with any aspect of the trial and all trial information (including the TAU booklets) was provided by the study team directly and not distributed by practice staff members.
Characteristics of study participants from baseline questionnaires
Table 4 describes the baseline characteristics of those recruited to the pilot study, overall and by allocation. More women than men were recruited and participants were mostly white. A relatively high proportion were single/divorced (n = 21/50). The mean age at which participants left school was 16 years and approximately half attended further education or university. A small minority (n = 4) had university degrees and more than half (n = 30) had vocational qualifications. Interestingly, three participants had never held a paid job. Of the remainder, all had previously stopped working in a paid job, mainly or partly because of their health. When asked to indicate the type of health condition that had led to job loss, responses included chronic pain, but comorbid mental health/stress and ‘other’ diagnoses were also described by participants. Comorbidities were well reported by participants and revealed very high levels of anxiety/depression (n = 33 ‘yes’; n = 3 ‘not sure’). Most of those recruited (n = 41) were looking for part-time rather than full-time work and wanted to work < 24 hours per week.
| Characteristic | All | Trial arm | |
|---|---|---|---|
| IPS | TAU | ||
| Sex, n (%) | |||
| Male | 20 (40) | 10 (45) | 10 (36) |
| Female | 30 (60) | 12 (54) | 18 (64) |
| Ethnic origin, n (%) | |||
| White | 46 (92) | 20 (91) | 26 (93) |
| Black Caribbean | 1 (2) | 1 (5) | 0 (0) |
| Black African | 0 (0) | 0 (0) | 0 (0) |
| Black other | 1 (2) | 1 (5) | 0 (0) |
| Indian | 2 (4) | 0 (0) | 2 (7) |
| Pakistani | 0 (0) | 0 (0) | 0 (0) |
| Bangladeshi | 0 (0) | 0 (0) | 0 (0) |
| Chinese | 0 (0) | 0 (0) | 0 (0) |
| Marital status, n (%) | |||
| Married | 27 (54) | 8 (36) | 19 (68) |
| Single | 13 (26) | 10 (45) | 3 (11) |
| Civil partnership | 0 (0) | 0 (0) | 0 (0) |
| Widowed | 0 (0) | 0 (0) | 0 (0) |
| Divorced | 8 (16) | 3 (14) | 5 (18) |
| Living with a partner | 2 (4) | 1 (5) | 1 (4) |
| Age (years) left school (two missing values) | |||
| Mean (SD) | 16.0 (1.1) | 15.9 (1.3) | 16.1 (1.1) |
| Median (IQR) | 16 (15.5–16) | 16 (15–16) | 16 (16–16) |
| Further education/university, n (%) | |||
| No | 24 (48) | 10 (45) | 14 (50) |
| Yes | 26 (52) | 12 (55) | 14 (50) |
| Educational level, n (%) | |||
| O levels/GCSEs (or equivalents) | 38 (76) | 15 (68) | 23 (82) |
| A levels (or equivalents) | 9 (18) | 3 (14) | 6 (21) |
| Vocational training certificate(s) | 30 (60) | 10 (45) | 20 (71) |
| University degree(s) or HND | 4 (8) | 2 (9) | 2 (7) |
| Higher professional qualifications | 4 (8) | 1 (5) | 3 (11) |
| Ever in paid job, n (%) | |||
| No | 2 (4) | 1 (5) | 1 (4) |
| Yes | 48 (96) | 21 (95) | 27 (96) |
| Time (years) since last in paid work | |||
| Median (IQR) | 3.0 (1.3–5.5) | 2.8 (1.3–4.1) | 3.2 (1.3–16.1) |
| Missing, n | 11 | 4 | 7 |
| Leaving job because of health, n (%) | |||
| No | 3 (6) | 1 (5) | 2 (7) |
| Yes, mainly because of health | 34 (68) | 16 (73) | 18 (64) |
| Yes, partly because of health | 11 (22) | 4 (18) | 7 (25) |
| Missing | 2 (4) | 1 (5) | 1 (4) |
| HRJL (type of health problem), n (%) | |||
| Chronic pain | 24 (48) | 14 (64) | 10 (36) |
| Back, neck, arm, shoulder or leg | 34 (68) | 13 (59) | 21 (75) |
| Mental health problem or stress | 15 (30) | 5 (23) | 10 (36) |
| Heart or lungs | 2 (4) | 1 (5) | 1 (4) |
| Other | 6 (12) | 3 (14) | 3 (11) |
| N/A (no HRJL) | 3 (6) | 1 (5) | 2 (7) |
| Future work prospect, n (%) | |||
| Part time | 41 (82) | 17 (77) | 24 (86) |
| Full time | 9 (18) | 5 (23) | 4 (14) |
| Hours wanted in part-time future job, n (%) | |||
| 0–8 | 10 (20) | 5 (23) | 5 (18) |
| 9–15 | 13 (26) | 4 (18) | 9 (32) |
| 16–24 | 13 (26) | 6 (27) | 7 (25) |
| > 25 | 3 (6) | 2 (9) | 1 (4) |
| N/A | 9 (18) | 5 (23) | 4 (14) |
| Missing | 2 (4) | 0 (0) | 2 (7) |
| Comorbidities reported, n (%) | |||
| High blood pressure | |||
| No | 36 (72) | ||
| Yes | 9 (18) | ||
| Not sure | 5 (10) | ||
| Heart problems | |||
| No | 47 (94) | ||
| Yes | 3 (6) | ||
| Not sure | 0 (0) | ||
| Diabetes | |||
| No | 46 (92) | ||
| Yes | 4 (8) | ||
| Not sure | 0 (0) | ||
| Kidney disease | |||
| No | 49 (98) | ||
| Yes | 1 (2) | ||
| Not sure | 0 (0) | ||
| Previous stroke or TIA | |||
| No | 48 (96) | ||
| Yes | 2 (4) | ||
| Not sure | 0 (0) | ||
| Arthritis | |||
| No | 27 (54) | ||
| Yes | 19 (38) | ||
| Not sure | 3 (6) | ||
| Missing | 1 (2) | ||
| Asthma or other lung problems | |||
| No | 37 (74) | ||
| Yes | 12 (24) | ||
| Not sure | 1 (2) | ||
| Anxiety or depression | |||
| No | 14 (28) | ||
| Yes | 33 (66) | ||
| Not sure | 3 (6) | ||
| GI or other stomach problems | |||
| No | 37 (74) | ||
| Yes | 10 (20) | ||
| Not sure | 3 (6) | ||
Although study eligibility allowed for any period of unemployment > 3 months, we recruited people with a wide diversity of periods of unemployment (see Table 4). Twenty-eight of the 50 participants had been unemployed < 2 years and, therefore, would not have been eligible for SJP IPS. The median period of unemployment was 3.0 [interquartile range (IQR) 1.3–5.5] years, and this was quite similar in both arms (2.8 years for IPS and 3.2 years for TAU). However, we did find that there were four participants with a very long period of unemployment prior to baseline (> 20–30 years) and all four participants were allocated to TAU (Figure 1). The reason for this is likely to be the change in recruitment strategy in the last 6 months of the pilot (i.e. having opened up recruitment from pain services) because IPS became unavailable in the last 3 months. In exploring changes and distribution of outcome measures over time, this potential allocation bias needs to be borne in mind. In all other characteristics, however, the two groups seemed similar.
FIGURE 1.
Duration of unemployment (years) prior to recruitment to InSTEP pilot trial by treatment allocation.

Having identified a possible difference between participants recruited through primary care, as compared with pain services, we explored their baseline characteristics in more detail (Table 5).
| Characteristic | All | Pain service | General practice |
|---|---|---|---|
| Sex, n (%) | |||
| Male | 19 (40) | 5 (38) | 14 (40) |
| Female | 29 (60) | 8 (62) | 21 (60) |
| Ethnic origin, n (%) | |||
| White | 44 (92) | 9 (69) | 35 (100) |
| Black Caribbean | 1 (2) | 1 (8) | 0 (0) |
| Black African | 0 (0) | 0 (0) | 0 (0) |
| Black other | 1 (2) | 1 (8) | 0 (0) |
| Indian | 2 (4) | 2 (15) | 0 (0) |
| Pakistani | 0 (0) | 0 (0) | 0 (0) |
| Bangladeshi | 0 (0) | 0 (0) | 0 (0) |
| Chinese | 0 (0) | 0 (0) | 0 (0) |
| Marital status, n (%) | |||
| Married | 26 (54) | 4 (31) | 22 (63) |
| Single | 13 (27) | 7 (54) | 6 (17) |
| Civil partnership | 0 (0) | 0 (0) | 0 (0) |
| Widowed | 0 (0) | 0 (0) | 0 (0) |
| Divorced | 7 (15) | 2 (15) | 5 (14) |
| Living with a partner | 2 (4) | 0 (0) | 2 (6) |
| Age (years) left school (two missing values) | |||
| Mean (SD) | 16.0 (1.2) | 16.3 (1.8) | 15.9 (0.8) |
| Median (IQR) | 16 (15–16) | 16 (16–16) | 16 (15–16) |
| Further education/university, n (%) | |||
| No | 23 (48) | 4 (31) | 19 (54) |
| Yes | 25 (52) | 9 (69) | 16 (46) |
| Educational level, n (%) | |||
| O levels/GCSEs (or equivalents) | 36 (75) | 10 (78) | 26 (74) |
| A levels (or equivalents) | 9 (19) | 2 (15) | 7 (20) |
| Vocational training certificate(s) | 28 (58) | 7 (54) | 21 (60) |
| University degree(s) or HND | 4 (8) | 2 (15) | 2 (6) |
| Higher professional qualifications | 4 (8) | 1 (8) | 3 (9) |
| Ever in paid job, n (%) | |||
| No | 2 (4) | 2 (15) | 0 (0) |
| Yes | 46 (96) | 11 (84) | 35 (100) |
| Leaving job because of health, n (%) | |||
| No | 2 (4) | 2 (15) | 0 (0) |
| Yes, mainly because of health | 33 (69) | 7 (54) | 26 (74) |
| Yes, partly because of health | 11 (23) | 2 (15) | 9 (26) |
| Missing | 2 (4) | 2 (15) | 0 (0) |
| Health-related job loss (type of health problem), n (%) | |||
| Chronic pain | 23 (48) | 8 (62) | 15 (43) |
| Back, neck, arm, shoulder or leg | 33 (69) | 5 (38) | 28 (80) |
| Mental health problem or stress | 15 (31) | 3 (23) | 12 (34) |
| Heart or lungs | 2 (4) | 0 (0) | 2 (6) |
| Other | 6 (13) | 1 (8) | 5 (14) |
| Future work prospect, n (%) | |||
| Part time | 40 (83) | 10 (77) | 30 (86) |
| Full time | 8 (17) | 3 (23) | 5 (14) |
| Hours wanted in part-time future job, n (%) | |||
| 0–8 | 10 (21) | 2 (15) | 8 (23) |
| 9–15 | 13 (27) | 4 (31) | 9 (26) |
| 16–24 | 12 (25) | 2 (15) | 10 (29) |
| > 25 | 3 (6) | 2 (15) | 1 (3) |
| N/A | 8 (17) | 3 (23) | 5 (14) |
| Missing | 2 (4) | 0 (0) | 2 (6) |
| Health literacy: how easy/difficult is it for you to . . ., n (%) | |||
| Judge when you need to get a second opinion from another doctor? | |||
| Very easy | 13 (27) | 4 (31) | 9 (26) |
| Easy | 17 (35) | 3 (23) | 14 (40) |
| Difficult | 13 (27) | 5 (38) | 8 (23) |
| Very difficult | 3 (6) | 1 (8) | 2 (6) |
| Missing | 2 (4) | 0 (0) | 2 (6) |
| Use information the doctor gives you to make decisions about your illness? | |||
| Very easy | 16 (33) | 4 (31) | 12 (34) |
| Easy | 18 (38) | 4 (31) | 14 (40) |
| Difficult | 12 (25) | 5 (38) | 7 (20) |
| Very difficult | 1 (2) | 0 (0) | 1 (3) |
| Missing | 1 (2) | 0 (0) | 1 (3) |
| Find information on how to manage mental health problems, such as stress and depression? | |||
| Very easy | 10 (21) | 4 (31) | 6 (17) |
| Easy | 22 (46) | 3 (23) | 19 (54) |
| Difficult | 12 (25) | 6 (46) | 6 (17) |
| Very difficult | 2 (4) | 0 (0) | 2 (6) |
| Missing | 2 (4) | 0 (0) | 2 (6) |
| Judge if the information on health risks in the media is reliable (e.g. from the television or internet)? | |||
| Very easy | 11 (23) | 4 (31) | 7 (20) |
| Easy | 15 (31) | 3 (23) | 12 (34) |
| Difficult | 18 (38) | 6 (46) | 12 (34) |
| Very difficult | 3 (6) | 0 (0) | 3 (9) |
| Missing | 1 (2) | 0 (0) | 1 (3) |
| Find out about activities that are good for your mental well-being (e.g. medication, exercise and walking)? | |||
| Very easy | 14 (29) | 4 (31) | 10 (29) |
| Easy | 25 (52) | 6 (46) | 19 (54) |
| Difficult | 7 (15) | 3 (23) | 4 (11) |
| Very difficult | 1 (2) | 0 (0) | 1 (3) |
| Missing | 1 (2) | 0 (0) | 1 (3) |
| Understand information in the media on how to get healthier (e.g. from the internet, daily or weekly magazines)? | |||
| Very easy | 13 (27) | 4 (31) | 9 (26) |
| Easy | 23 (48) | 6 (46) | 17 (49) |
| Difficult | 11 (23) | 3 (23) | 8 (23) |
| Very difficult | 0 (0) | 0 (0) | 0 (0) |
| Missing | 1 (2) | 0 (0) | 1 (3) |
| How often do you need to have someone help you when you read instructions, pamphlets or other written material from your doctor or pharmacy? | |||
| Never | 22 (46) | 5 (38) | 17 (49) |
| Rarely | 8 (17) | 2 (15) | 6 (17) |
| Sometimes | 10 (21) | 5 (38) | 5 (14) |
| Often | 4 (8) | 0 (0) | 4 (11) |
| Always | 3 (6) | 1 (8) | 2 (6) |
| Missing | 1 (2) | 0 (0) | 1 (3) |
| Score derived from all the above (three missing values)a | |||
| Mean (SD) | 14.2 (4.7) | 14.7 (5.7) | 14.1 (4.3) |
| Median (IQR) | 14 (11–18) | 17 (8–19) | 14 (11–17.5) |
We found that those participants recruited through pain services were more ethnically diverse and were very much more likely to be single (54% vs. 17%), but were somewhat more likely to have received further educational opportunities (69% vs. 46%). It appeared that those participants recruited from pain services reported somewhat lower health literacy than those recruited from general practices.
Participants showed themselves willing to provide a great deal of information about their personal circumstances, dependants, home ownership, finances and welfare benefit dependence (Table 6). Many participants (19/50) were living alone, but 16 of 46 had children aged < 18 years and the majority (n = 44) had dependants outside their household. Only 12 participants owned their home outright and most reported that they were struggling financially. Thirty of 50 participants were in receipt of welfare benefits and 41 were willing to describe their monthly income. Alcohol abuse was not reported by any participant. Fifteen participants were current cigarette smokers.
| Variable | Baseline (N = 50) |
|---|---|
| Adults in household, n (%) | |
| One | 19 (38) |
| Two | 22 (44) |
| Three | 6 (12) |
| Five | 3 (6) |
| Had children aged < 18 years, n (%) | |
| Zero | 30 (60) |
| One | 11 (22) |
| Two | 5 (10) |
| Missing | 4 (8) |
| Participant’s part of the household income, n (%) | |
| None | 17 (34) |
| Less than one-quarter | 12 (25) |
| Between one-quarter and a half | 5 (10) |
| Half or more | 16 (32) |
| Financial dependants outside household, n (%) | |
| Yes | 44 (88) |
| No | 5 (10) |
| Missing | 1 (2) |
| Housing tenure, n (%) | |
| Owned outright | 12 (24) |
| Mortgaged | 16 (32) |
| Rented | 22 (44) |
| Rent free | 0 (0) |
| Other | 0 (0) |
| Managing financially, n (%) | |
| Living comfortably | 4 (8) |
| Doing all right | 12 (24) |
| Just about getting by | 13 (26) |
| Finding it difficult | 7 (14) |
| Finding it very difficult | 14 (28) |
| Are there things that you can no longer afford?, n (%) | |
| No | 5 (10) |
| Few things | 31 (62) |
| Many things | 14 (28) |
| Are there things that friends have and you cannot afford?, n (%) | |
| No | 8 (16) |
| Few things | 28 (56) |
| Many things | 14 (28) |
| Receipt of benefits, n (%) | |
| No | 19 (38) |
| Yes | 30 (60) |
| Missing | 1 (2) |
| Which benefits, n/N | |
| Income support | 2/50 |
| Incapacity Benefit | 0/50 |
| Child Tax Credit | 3/50 |
| Disability Living Allowance (now Personal Independence Payment) | 2/50 |
| Jobseeker’s Allowance | 2/50 |
| Working Tax Credit | 1/50 |
| Housing benefit | 9/50 |
| Employment and Support Allowance | 5/50 |
| Statutory sick pay | 0/50 |
| Personal Independence Payment | 14/50 |
| Universal Credit | 14/50 |
| Carer’s Allowance | 1/50 |
| Other | 0/50 |
| Weekly money (£) from benefits, median (IQR) | 188.5 (127–260.5) |
| Missing, n | 10 |
| Total weekly income (£), n (%) | |
| 0–99 | 6 (12) |
| 100–149 | 7 (14) |
| 150–249 | 6 (12) |
| 250–349 | 7 (14) |
| 350–449 | 4 (8) |
| 450–599 | 2 (4) |
| 600–749 | 4 (8) |
| ≥ 750 | 5 (10) |
| Missing | 9 (18) |
| BMI, n (%) | |
| Underweight | 0 (0) |
| Normal | 17 (34) |
| Overweight | 16 (32) |
| Obese | 13 (26) |
| Missing | 4 (8) |
| Drinking | |
| Frequency of > 6 units if female and > 8 units if male on a single occasion, n (%) | |
| Never | 24 (48) |
| Less than monthly | 20 (40) |
| Monthly | 3 (6) |
| Weekly | 2 (4) |
| Daily | 0 (0) |
| Missing | 1 (2) |
| Frequency of failing to do what expected because of drinking, n (%) | |
| Never | 47 (94) |
| Less than monthly | 2 (4) |
| Monthly | 0 (0) |
| Weekly | 0 (0) |
| Daily | 0 (0) |
| Missing | 1 (2) |
| Smoking status, n (%) | |
| Never | 21 (42) |
| Ex-smoker | 14 (28) |
| Age when started (years) | |
| n | 14 |
| Median | 15 |
| IQR | 15–16 |
| Age when stopped (years) | |
| n | 14 |
| Median | 32.5 |
| IQR | 23–40 |
| Current | 15 (30) |
| Age when started (years) | |
| n | 15 |
| Median | 15 |
| IQR | 14–17 |
Allocation
Treatment-as-usual arm
In total, 28 participants were randomised and allocated to the ‘control’ arm. All of these participants attended their appointment with the research co-ordinator, which was arranged at their convenience in their general practice. Practices were extremely helpful in identifying a room for these appointments. Participants expressed satisfaction with the appointment and the TAU booklet. No further appointments were arranged thereafter, but follow-up questionnaires were mailed as planned at 3, 6 and 12 months.
Individualised placement and support arm
In total, 22 participants were randomised and allocated to the IPS arm. For the purposes of the pilot study, IPS was provided by just two trained ESWs with experience of IPS as part of the SJP (one in Portsmouth and the other in Southampton). All 22 participants allocated to IPS attended their baseline appointments with the ESWs and provided written, informed consent to participate in the study. The baseline questionnaire was completed with the support of the ESW, if required (taking a maximum of 20 minutes of the appointment). Subsequently, all 22 IPS participants attended an appointment held jointly with the pain specialist (a single pain-trained OT took this role throughout the study) and their ESW early after recruitment, during which their pain, medication and pain management strategies were discussed. A pain management plan was constructed by all three parties. The pain OT found that participants varied widely in their needs and, therefore, a range of different interventions were recommended at this appointment. These are summarised later in this report for manualisation of IPS (see Table 14).
The ESWs found that the 22 trial participants also differed considerably in how ready and prepared they were for a work placement. As with all SJP participants, they assessed each individual based on their current needs and worked with them in aiming towards readiness for and acceptance of a supported work placement during the time available for intervention. The variation has been summarised later in this report for manualisation (see Table 14).
Withdrawals
Two participants allocated to IPS found paid work very rapidly (i.e. before the 3-month questionnaire), but the job opportunity required them to relocate (and in one case out of the UK). In consequence, both withdrew from study follow-up.
Questionnaire response rates and retention
Questionnaires were mailed out to all 48 remaining participants at 3, 6 and 12 months, with reminders posted 4 weeks later, if appropriate. In total, five participants completed only the baseline questionnaire and did not return any follow-up questionnaires. We compared the baseline characteristics of those who failed to return any questionnaires with those who returned at least one of the three questionnaires (Table 7). In particular, we were concerned with whether or not those who had not returned any questionnaires had lower levels of health literacy. The non-responders were mostly men (4/5), white (4/5) and single (4/5). They were more likely than responders to have further education (4/5). According to every parameter of health literacy, they were better off than those who completed at least one postal questionnaire.
| Characteristic | All | Followed up | Dropouts |
|---|---|---|---|
| Sex, n (%) | |||
| Male | 19 (40) | 15 (35) | 4 (80) |
| Female | 29 (60) | 28 (65) | 1 (20) |
| Ethnic origin, n (%) | |||
| White | 44 (92) | 40 (93) | 4 (80) |
| Black Caribbean | 1 (2) | 0 (0) | 1 (20) |
| Black African | 0 (0) | 0 (0) | 0 (0) |
| Black other | 1 (2) | 1 (2) | 0 (0) |
| Indian | 2 (4) | 2 (5) | 0 (0) |
| Pakistani | 0 (0) | 0 (0) | 0 (0) |
| Bangladeshi | 0 (0) | 0 (0) | 0 (0) |
| Chinese | 0 (0) | 0 (0) | 0 (0) |
| Marital status, n (%) | |||
| Married | 26 (54) | 26 (60) | 0 (0) |
| Single | 13 (27) | 9 (21) | 4 (80) |
| Civil partnership | 0 (0) | 0 (0) | 0 (0) |
| Widowed | 0 (0) | 0 (0) | 0 (0) |
| Divorced | 7 (15) | 6 (14) | 1 (20) |
| Living with a partner | 2 (4) | 2 (5) | 0 (0) |
| Age (years) left school (two missing values) | |||
| Mean (SD) | 16.0 (1.2) | 16.1 (1.2) | 15.2 (0.8) |
| Median (IQR) | 16 (15–16) | 16 (16–16) | 15 (15–16) |
| Further education/university, n (%) | |||
| No | 23 (48) | 22 (51) | 1 (20) |
| Yes | 25 (52) | 21 (49) | 4 (80) |
| Educational level, n (%) | |||
| O levels/GCSEs (or equivalents) | 36 (75) | 33 (77) | 3 (60) |
| A levels (or equivalents) | 9 (19) | 8 (19) | 1 (20) |
| Vocational training certificate(s) | 28 (58) | 26 (60) | 2 (40) |
| University degree(s) or HND | 4 (8) | 3 (7) | 1 (20) |
| Higher professional qualifications | 4 (8) | 4 (9) | 0 (0) |
| Ever in paid job, n (%) | |||
| No | 2 (4) | 1 (2) | 1 (20) |
| Yes | 46 (96) | 42 (98) | 4 (80) |
| Leaving job because of health, n (%) | |||
| No | 2 (4) | 2 (5) | 0 (0) |
| Yes, mainly because of health | 33 (69) | 30 (70) | 3 (60) |
| Yes, partly because of health | 11 (23) | 10 (23) | 1 (20) |
| Missing | 2 (4) | 1 (2) | 1 (20) |
| HRJL (type of problem), n (%) | |||
| Chronic pain | 23 (48) | 21 (49) | 2 (40) |
| Back, neck, arm, shoulder or leg | 33 (69) | 31 (72) | 2 (40) |
| Mental health problem or stress | 15 (31) | 14 (33) | 1 (20) |
| Heart or lungs | 2 (4) | 2 (5) | 0 (0) |
| Other | 6 (13) | 6 (14) | 0 (0) |
| N/A (no HRJL) | 2 (4) | 2 (5) | 0 (0) |
| Future work prospect, n (%) | |||
| Part time | 40 (83) | 35 (81) | 5 (100) |
| Full time | 8 (17) | 8 (19) | 0 (0) |
| Hours wanted in part-time future job, n (%) | |||
| 0–8 | 10 (21) | 8 (19) | 2 (40) |
| 9–15 | 13 (27) | 12 (28) | 1 (20) |
| 16–24 | 12 (25) | 12 (28) | 0 (0) |
| > 25 | 3 (6) | 1 (2) | 2 (40) |
| N/A | 8 (17) | 8 (19) | 0 (0) |
| Missing | 2 (4) | 2 (5) | 0 (0) |
| Health literacy: how easy/difficult is it for you to . . ., n (%) | |||
| Judge when you need to get a second opinion from another doctor? | |||
| Very easy | 13 (27) | 11 (26) | 2 (40) |
| Easy | 17 (35) | 14 (33) | 3 (60) |
| Difficult | 13 (27) | 13 (30) | 0 (0) |
| Very difficult | 3 (6) | 3 (7) | 0 (0) |
| Missing | 2 (4) | 2 (5) | 0 (0) |
| Use information the doctor gives you to make decisions about your illness? | |||
| Very easy | 16 (33) | 14 (33) | 2 (40) |
| Easy | 18 (38) | 15 (35) | 3 (60) |
| Difficult | 12 (25) | 12 (28) | 0 (0) |
| Very difficult | 1 (2) | 1 (2) | 0 (0) |
| Missing | 1 (2) | 1 (2) | 0 (0) |
| Find information on how to manage mental health problems, such as stress and depression? | |||
| Very easy | 10 (21) | 9 (21) | 1 (20) |
| Easy | 22 (46) | 19 (44) | 3 (60) |
| Difficult | 12 (25) | 11 (26) | 1 (20) |
| Very difficult | 2 (4) | 2 (5) | 0 (0) |
| Missing | 2 (4) | 2 (5) | 0 (0) |
| Judge if the information on health risks in the media is reliable (e.g. from the television or internet)? | |||
| Very easy | 11 (23) | 9 (21) | 2 (40) |
| Easy | 15 (31) | 13 (30) | 2 (40) |
| Difficult | 18 (38) | 17 (40) | 1 (20) |
| Very difficult | 3 (6) | 3 (7) | 0 (0) |
| Missing | 1 (2) | 1 (2) | 0 (0) |
| Find out about activities that are good for your mental well-being (e.g. medication, exercise and walking)? | |||
| Very easy | 14 (29) | 13 (30) | 1 (20) |
| Easy | 25 (52) | 22 (51) | 3 (60) |
| Difficult | 7 (15) | 6 (14) | 1 (20) |
| Very difficult | 1 (2) | 1 (2) | 0 (0) |
| Missing | 1 (2) | 1 (2) | 0 (0) |
| Understand information in the media on how to get healthier (e.g. from the internet, daily or weekly magazines)? | |||
| Very easy | 13 (27) | 12 (28) | 1 (20) |
| Easy | 23 (48) | 20 (47) | 3 (60) |
| Difficult | 11 (23) | 10 (23) | 1 (20) |
| Very difficult | 0 (0) | 0 (0) | 0 (0) |
| Missing | 1 (2) | 1 (2) | 0 (0) |
| How often do you need to have someone help you when you read instructions, pamphlets or other written material from your doctor or pharmacy? | |||
| Never | 22 (46) | 18 (42) | 4 (80) |
| Rarely | 8 (17) | 8 (19) | 0 (0) |
| Sometimes | 10 (21) | 9 (21) | 1 (20) |
| Often | 4 (8) | 4 (9) | 0 (0) |
| Always | 3 (6) | 3 (7) | 0 (0) |
| Missing | 1 (2) | 1 (2) | 0 (0) |
| Score derived from all the above (three missing values)a | |||
| Mean (SD) | 14.2 (4.7) | 14.5 (4.7) | 12.4 (4.4) |
| Median (IQR) | 14 (11–18) | 15.5 (11–18) | 13 (10–13) |
Response rates by allocation
Four of the participants who failed to return any postal questionnaires were in the IPS arm and one was in the TAU arm (see Table 7). Overall, 19 of 28 participants in the TAU arm returned all of their questionnaires, but only 10 of 20 participants in the IPS arm returned all of their questionnaires (Table 8).
| Follow-up | All, n (%) | Trial arm, n (%) | |
|---|---|---|---|
| IPS | TAU | ||
| Baseline | 5 (10) | 4 (20) | 1 (4) |
| Baseline + 3 months | 4 (8) | 2 (10) | 2 (7) |
| Baseline + 6 months | 2 (4) | 1 (5) | 1 (4) |
| Baseline + 3 months + 6 months | 7 (15) | 3 (15) | 4 (14) |
| Baseline + 3 months + 12 months | 1 (2) | 0 (0) | 1 (4) |
| Baseline + 3 months + 6 months + 12 months | 29 (60) | 10 (50) | 19 (68) |
In the control arm of the trial, there were no withdrawals and all but one participant returned at least one of the three follow-up questionnaires. We hypothesised that differential response rates in the two arms might be at least partly because of the nature of the control arm. In the control arm, the study co-ordinator met with everyone to administer the TAU booklet, and during this appointment emphasised the nature of the research and explained the importance of the follow-up questionnaires. In contrast, those participating in the IPS arm had a number of appointments with the ESWs; however, these appointments were focused on the intervention and job-readiness, and, therefore, it may be that participation in the research was eclipsed in importance. Importantly, the ESWs explained that around 55% of people referred to the SJP dropped out after the assessment visit, either because they did not wish to RTW or because they felt unable to commit to the programme. It appeared, therefore, that our pilot trial participants were more likely to remain engaged with IPS than those people recruited from job centres through SJP, possibly suggesting that we were identifying people who had been unemployed for a shorter time and who were keen to get back to work, or that having their health assessed was attractive to participants in the InSTEP pilot.
Completeness of data over the follow-up questionnaires at 3, 6 and 12 months
The questionnaires, despite being quite lengthy (18 sides in total), were well completed by those who returned them. (However, the absence of returns in the IPS arm and, in particular, at 12 months should be noted.) Table 9 describes the extent of missing data for key potential outcome measures at each of the four time points. In particular, EQ-5D-5L, self-rated health and BPI pain scores were extremely well completed by those who returned questionnaires (possibly because the respondents thought them most relevant).
| Outcome variable | Domain | Baseline (N = 50), n | 3 months (N = 41), n | 6 months (N = 38), n | 12 months (N = 30), n |
|---|---|---|---|---|---|
| Return-to-Work Self-Efficacy Scale score | 5 | 4 | 3 | 2 | |
| Self-rated health | 1 | 0 | 0 | 0 | |
| WEMWBS | 1 | 3 | 0 | 0 | |
| EQ-5D-5L | Mobility | 0 | 0 | 0 | 0 |
| Self-care | 0 | 0 | 0 | 0 | |
| Usual activities | 1 | 0 | 0 | 0 | |
| Pain/discomfort | 0 | 0 | 0 | 0 | |
| Anxiety/depression | 0 | 0 | 0 | 0 | |
| Combined score | 1 | 0 | 0 | 0 | |
| VAS | 0 | 0 | 0 | 0 | |
| PHQ-9 | 1 | 1 | 3 | 0 | |
| Rosenberg’s Self-Esteem Scale score | 0 | 2 | 0 | 2 | |
| Pain interfered with work | 1 | 1 | 3 | 0 | |
| BPI pain scores | Worst | 0 | 0 | 0 | 0 |
| Least | 0 | 0 | 0 | 0 | |
| Average | 0 | 0 | 0 | 0 |
Distribution and responsiveness of potential outcome measures
Self-efficacy for return to work
Self-efficacy for RTW does not currently have a consensus scoring system and three different approaches have been published. 46–48 The scale developed by Brouwer and colleagues46 was particularly attractive for use in the current research project, as it included four items that specifically enquired about pain and RTW. However, subsequent to publication of this measure, Black and colleagues,49–51 attempted to incorporate the two pre-existing instruments of Brouwer and colleagues46 and Lagerveld and colleagues48 (Lagerveld and colleagues48 include items about the social aspects of returning to work) into one new measure, which they have validated. 49–51 Their final scale [i.e. the Return-to-Work Self-Efficacy Scale (RTW-SE)] includes 11 items, four of which were derived directly from Brouwer and colleagues. 46 Given this similarity and the potential importance of self-efficacy for RTW as a primary outcome for a definitive trial, we chose to include the questions for measuring both scales. The Brouwer and colleagues46 scale includes 10 items rated from 1 to 5 (‘not at all certain’ to ‘completely certain’). In contrast, the Black and colleagues49–51 RTW-SE uses 11 items, also rated from 1 to 5, but the responses are ‘strongly agree’, ‘agree’, ‘neither agree or disagree’, ‘disagree’ and ‘strongly disagree’. To maximise their utility for our research, we incorporated the additional items from Black and colleagues’ research, but did so by changing the questions and responses so that they could be included alongside the Brouwer and colleagues’ items, with the same heading and response choices. For example, the statement ‘If I resumed my work fully tomorrow, I could discuss any limitations I have to my co-workers’ with original responses graded ‘strongly agree’ to ‘strongly disagree’ became instead ‘Thinking about starting a new job, how certain are you that you would be able to explain your physical limitations to co-workers?’ with response options ‘not at all certain’ through to ‘completely certain’. In total, therefore, we asked 17 questions from the two tools. The 10 items from Brouwer and colleagues46 were analysed as a total score (scaled 0–10) and in three domains: (1) ‘supervisor’ (four items), (2) ‘pain’ (four items) and (3) ‘co-worker’ (two items), each of which were also scaled separately as a score out of 10. The RTW-SE was analysed as a total scale (i.e. including the 11 items and scaled 0–10) and also for its three different domains: (1) work completion beliefs (three items), (2) affective work beliefs (five items) and (3) work social support beliefs (three items), again each scaled 0–10. In all cases, a low score indicates poorer self-efficacy (Table 10).
| Self-efficacy score | Time point | Response to item | IPS | TAU | Time-specific difference between IPS and TAU | |||
|---|---|---|---|---|---|---|---|---|
| Complete, n | Missing, n | Mean (SD) | Median (IQR) | Mean (SD) | Median (IQR) | |||
| Overall (N = 49) | Baseline | 44 | 4 | 6.4 (2.1) | 6.8 (4.3–8.5) | 5.1 (2.2) | 5.0 (4.0–6.8) | 0.056 |
| 3 months | 36 | 4 | 5.2 (2.7) | 5.4 (3.8–6.5) | 3.9 (2.5) | 4.6 (1.8–5.5) | 0.125 | |
| 6 months | 27 | 3 | 5.2 (2.6) | 5.3 (3.6–6.9) | 2.7 (2.6) | 2.5 (0.0–4.3) | 0.019 | |
| 12 months | 26 | 2 | 5.7 (2.7) | 5.5 (4.0–7.3) | 3.4 (2.2) | 3.3 (2.5–5.0) | 0.031 | |
| Supervisor (N = 49) | Baseline | 45 | 3 | 7.4 (2.5) | 7.5 (5.6–10.0) | 6.0 (2.3) | 6.3 (4.4–7.5) | 0.049 |
| 3 months | 40 | 0 | 6.1 (2.9) | 6.9 (5.0–7.5) | 4.2 (2.9) | 5.0 (2.5–7.5) | 0.055 | |
| 6 months | 27 | 3 | 5.5 (2.8) | 6.3 (3.1–7.2) | 3.0 (3.2) | 2.5 (0.0–5.0) | 0.044 | |
| 12 months | 26 | 7 | 6.1 (3.1) | 6.3 (3.8–8.1) | 3.6 (3.0) | 5.0 (0.0–5.0) | 0.062 | |
| Pain (N = 49) | Baseline | 46 | 2 | 5.6 (2.3) | 5.6 (4.1–7.2) | 4.7 (2.2) | 5.0 (3.8–6.3) | 0.225 |
| 3 months | 39 | 2 | 4.2 (3.2) | 5.0 (0.6–6.3) | 3.7 (2.8) | 3.8 (1.3–5.9) | 0.611 | |
| 6 months | 28 | 3 | 4.6 (3.1) | 4.7 (2.5–7.2) | 3.1 (3.0) | 2.5 (0.3–5.3) | 0.187 | |
| 12 months | 26 | 2 | 5.1 (3.1) | 5.0 (2.5–6.9) | 3.1 (2.3) | 2.5 (1.3–5.0) | 0.068 | |
| Co-worker (N = 49) | Baseline | 45 | 3 | 5.9 (2.4) | 6.3 (3.8–7.5) | 4.1 (2.9) | 4.4 (2.5–6.3) | 0.033 |
| 3 months | 39 | 2 | 4.9 (2.8) | 5.0 (3.8–7.5) | 3.5 (3.1) | 3.8 (0.0–6.3) | 0.173 | |
| 6 months | 28 | 3 | 5.6 (2.3) | 5.6 (5.0–6.3) | 2.7 (3.1) | 1.9 (0.0–4.4) | 0.010 | |
| 12 months | 26 | 2 | 6.0 (2.0) | 6.3 (5.0–6.3) | 3.7 (2.8) | 5.0 (0.0–5.0) | 0.038 | |
| Work: social support beliefs (N = 51) | Baseline | 45 | 3 | 6.5 (2.3) | 7.5 (5.0–8.3) | 4.8 (2.4) | 5.0 (3.3–6.7) | 0.022 |
| 3 months | 39 | 2 | 5.3 (2.9) | 5.0 (4.2–7.5) | 3.8 (2.9) | 3.3 (1.7–5.8) | 0.132 | |
| 6 months | 28 | 3 | 5.5 (2.4) | 5.0 (4.6–6.7) | 2.8 (3.1) | 2.1 (0.0–4.6) | 0.020 | |
| 12 months | 26 | 2 | 6.0 (2.3) | 5.8 (4.2–7.5) | 3.6 (2.6) | 4.2 (1.7–5.0) | 0.032 | |
| Work: completion beliefs (N = 51) | Baseline | 45 | 3 | 5.5 (2.3) | 5.8 (3.3–7.5) | 4.5 (2.1) | 5.0 (2.5–5.8) | 0.106 |
| 3 months | 38 | 2 | 3.9 (3.3) | 4.2 (0.8–7.5) | 3.8 (2.8) | 4.2 (0.8–6.7) | 0.890 | |
| 6 months | 28 | 3 | 4.1 (3.1) | 3.3 (2.1–6.7) | 3.1 (3.1) | 2.5 (0.0–5.8) | 0.396 | |
| 12 months | 26 | 2 | 5.0 (3.3) | 4.2 (2.5–7.5) | 3.2 (2.4) | 4.2 (0.8–5.0) | 0.134 | |
| Affective work beliefs (N = 51) | Baseline | 45 | 3 | 5.7 (1.9) | 6.0 (4.0–7.0) | 4.4 (2.3) | 4.8 (3.0–6.0) | 0.055 |
| 3 months | 40 | 1 | 4.5 (2.8) | 5.0 (3.0–5.5) | 4.2 (2.6) | 4.5 (2.5–6.0) | 0.721 | |
| 6 months | 29 | 2 | 5.3 (2.4) | 5.0 (4.5–6.3) | 2.8 (2.9) | 2.5 (0.0–4.0) | 0.025 | |
| 12 months | 26 | 2 | 5.3 (2.1) | 5.0 (4.5–5.5) | 3.3 (2.7) | 3.0 (0.0–5.0) | 0.063 | |
| RTW-SE (N = 51) | Baseline | 44 | 4 | 5.9 (1.9) | 6.1 (4.5–7.5) | 4.5 (2.1) | 4.7 (3.2–6.1) | 0.028 |
| 3 months | 37 | 3 | 4.8 (2.6) | 5.0 (3.6–6.1) | 3.9 (2.7) | 3.9 (2.5–6.1) | 0.343 | |
| 6 months | 28 | 3 | 5.0 (2.4) | 4.5 (4.1–6.3) | 3.0 (2.9) | 2.5 (0.8–4.9) | 0.062 | |
| 12 months | 26 | 2 | 5.4 (2.3) | 5.0 (4.1–6.1) | 3.4 (2.2) | 3.2 (2.5–5.0) | 0.036 | |
These data suggested that people allocated to each arm started with different levels of RTW self-efficacy, with the scores better among those in the IPS arm. In the TAU arm, RTW self-efficacy generally declined over 12 months of follow-up. In contrast, although there were withdrawals and non-responders in the IPS arm (two of whom had attained employment), self-efficacy scores remained fairly stable in this arm and were generally substantially better (and in many cases statistically significantly better) than those in the TAU arm. Even despite our lack of data from non-responders, we believe that RTW self-efficacy could be a primary outcome for a future trial.
Self-rated health
As a general health measure, we included self-rated health. This is a widely used item that is a strong and consistent predictor of mortality in epidemiological studies. 52 Among the 50 participants, 30 reported that their self-rated health was fair or poor at baseline (Tables 11 and 12).
| Self-rated health | Baseline (N = 50), n (%) |
|---|---|
| Excellent | 2 (4) |
| Very good | 4 (8) |
| Good | 13 (26) |
| Fair | 15 (30) |
| Poor | 15 (30) |
| Missing | 1 (2) |
| Change from baseline | Time point, OR (95% CI); p-value | ||
|---|---|---|---|
| 3 months | 6 months | 12 months | |
| Poor or fair self-rated health | 3.25 (0.88 to 11.96); 0.077 | 1.60 (0.46 to 5.60); 0.459 | 0.74 (0.19 to 2.83); 0.661 |
| Poor self-rated health | 0.69 (0.15 to 3.14); 0.633 | 0.81 (0.17 to 3.81); 0.788 | 0.67 (0.13 to 3.58); 0.641 |
The data show that self-rated health scores generally declined slightly over time among all participants. This measure does not appear useful for a primary outcome.
Brief Pain Inventory pain severity scores
We included the BPI as the pain instrument53 in line with the recent IMMPACT (Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials) recommendation that this tool should be used for clinical trials involving patients with chronic pain. 52 Every participant reported pain (other than everyday kinds of pain) at baseline, one participant in the IPS arm reported no pain at 3 months, four participants (again all in the IPS arm) reported no pain at 6 months and only one participant (again in the IPS arm) reported no pain at 12 months. The number of body sites affected ranged from one (in two participants) to 13 (also in two participants). Pain severity at its best was rated at a median intensity of 4 (IQR 2–5) at baseline and at 3 months in both arms, and these scores increased in both arms to a median intensity of 5 (IQR 4–6) at 12 months. Pain severity at its worst was rated at a median intensity of 7 (IQR 6–9) at baseline and 3 months, increasing to median intensity of 8 (IQR 6–9) at 6 months and returning to a median intensity of 7 (IQR 6–9) at 12 months. Pain, on average, was rated at a median intensity of 5 (IQR 4–7) at baseline, but was rated at a median intensity of 6 (IQR 5–6) at all follow-ups. It does not appear that pain scores were altered by this intervention or that they could be recommended as a primary outcome measure.
Brief Pain Inventory pain interference scores
As part of the pain interference section of the BPI, one question enquires about ‘pain interfering with normal work’. At baseline and at all three follow-up time points, participants scored a median of 7 (IQR 5–8) for this question. There was a reduction in these scores, but the size of the effects appeared to be small, and certainly too small to recommend this as a primary outcome measure.
Rosenberg’s Self-Esteem Scale
At baseline, the median Rosenberg’s Self-Esteem Scale score54 for participants was 16 (IQR 12–21). The scores improved slightly in both study arms at 3, 6 and 12 months [the score in the IPS group at 12 months was 19 (IQR 14–21) and in the TAU arm it was 16.5 (IQR 15–18)]. This measure may be a useful secondary outcome measure for a definitive trial.
Patient Health Questionnaire-9 items depression score
At baseline, the median PHQ-955 score for depression was 10 (IQR 7–16) (score ranges from 0 to 27, with higher scores more indicative of depression). Very little change in the scores was observed during the follow-up period. If anything, scores tended to increase (but by < 1 unit) and, therefore, the difference is too small to recommend as a primary outcome measure.
Warwick–Edinburgh Mental Wellbeing Scale
The WEMWBS56 was explored as a measure of well-being. The median score at baseline for WEMWBS was 41 (IQR 37–52). Scores changed minimally over the follow-up, with a final median score of 42 (IQR 37–48). This implies that WEMWBS scores tended to improve during the trial, but the difference appears too small to recommend this as a primary outcome measure.
EuroQol-5 Dimensions, five-level version
The median EQ-5D-5L combined score was 0.6 (IQR 0.3–0.7) at baseline. Over time, these scores did not appear to change very much [with a median of 0.7 (IQR 0.2–0.8) at 12 months]. However, when we explored the visual analogue scale score of the EQ-5D-5L as a continuous measure, the median score at baseline [i.e. 50 (IQR 40–70)] appeared to increase slightly at 6 and 12 months among those in the IPS arm [a median of 54 (IQR 40–78) at 6 months and a median of 52.5 (IQR 40–80) at 12 months], whereas no changes were seen in the TAU participants. Although encouraging, these findings suggest that the EQ-5D-5L should remain a secondary outcome for assessment of quality-adjusted life-years, but not be recommended as a primary outcome measure.
Employment outcomes
Among the TAU group, 14 (50%) of 28 participants returned all three follow-up questionnaires and never entered a paid job (Table 13). Three participants started a paid job during the year, but stopped working again before the final questionnaire. Another three participants reported that they were not working at the time of their last completed questionnaire. Two participants reported that they were in paid work at every follow-up point and another six reported that they were working in the last questionnaire that they returned. Therefore, at best, 8 of 28 participants of the TAU group achieved sustained work during the study and, at worst, it was 3 of 28 participants. It did seem, however, that participants became less likely to return questionnaires once they were working. This may be because they perceive that they were no longer relevant to the research or that they had more limited time for completing a questionnaire. Either way, this is an important consideration to address in any definitive trial.
| Employment status at follow-up | Questionnaire | Number | ||
|---|---|---|---|---|
| 3 months | 6 months | 12 months | ||
| Not in work or probably not in work at 12 months | Not in work | Not in work | Not in work | 14 |
| – | Working | Not in work | 1 | |
| Not in work | Working | Not in work | 1 | |
| Working | Working | Not in work | 1 | |
| Not in work | – | Not in work | 1 | |
| – | Not in work | – | 1 | |
| Not in work | Not in work | – | 1 | |
| In work or probably in work at 12 months | Working | Working | Working | 2 |
| Working | – | – | 2 | |
| Working | Working | – | 3 | |
| Not in work | Working | Working | 1 | |
| Total | 28 | |||
As stated above, 2 of the 22 participants who were allocated to IPS obtained jobs within the first 3 months; however, in both cases the jobs required that they move away and so they decided to withdraw from follow-up in the research. Another four participants in the IPS arm engaged well with the ESWs and the IPS intervention, but failed to return any follow-up questionnaires. As described above, we considered that this might be because of poorer health literacy, but our analyses suggested that this was not the case and that, in fact, the non-responders were more likely to be male, single and have a high level of educational attainment than those who did return questionnaires. Among the remaining 16 participants, five returned all three questionnaires and were never in a paid job, and two obtained work at one follow-up time point, but reported that they were not working at 12 months (Table 14). A further five participants were not working at the last time point at which they responded. Overall, two participants were in paid work at all three follow-up time points, one participant obtained work by 6 months (which was sustained at 12 months) and one participant was in paid work when they last responded (at 6 months).
| Employment status at follow-up | Questionnaire | Number | ||
|---|---|---|---|---|
| 3 months | 6 months | 12 months | ||
| Not in work or probably not in work at 12 months | Not in work | Not in work | Not in work | 5 |
| Not in work | – | – | 2 | |
| Not in work | Working | Not in work | 1 | |
| Working | Working | Not in work | 1 | |
| Not in work | Not in work | – | 3 | |
| In work or probably in work at 12 months | Working | Working | Working | 2 |
| – | Working | – | 1 | |
| Not in work | Working | Working | 1 | |
| Withdrew as found work by moving | 2 | |||
| Never returned a follow-up questionnaire | 4 | |||
| Total | 22 | |||
Employment outcomes: data from employment support workers
Additional data about employment outcomes were available for the IPS participants from the records made by the ESWs. According to these data, 8 of the 22 IPS participants attained a job by the end of the study (including the two participants who moved away to work), a further one participant was doing voluntary work, four participants were in vocational training and seven participants were actively job-seeking (with one participant having received a job offer).
This indicates a clear difficulty with this research: the questionnaire retention was poor among those receiving the IPS intervention. As a result, the follow-up questionnaire data provided an incomplete picture of the changes in actual achievement of a competitive paid job. This is a major limitation of the current pilot study and would need careful consideration for any future trial.
Job applications and job interviews
Given the rates of attrition of follow-up questionnaires, it was also difficult to comment on whether or not participants in either arm were making more job applications or attending more interviews for jobs.
Untoward incident
One individual contacted the Research Governance Office at the University of Southampton (the sponsor for the research) directly to complain about having received the study pack. The complaint was left as an answering machine message, as nobody was in the office. Despite numerous attempts to contact the person and having left numerous telephone messages, the University of Southampton research governance team were not able to speak with the individual to discuss the complaint. The general practice from which the pack had been mailed confirmed that they had not received a complaint from any individual with regard to the study. We were unable to follow this up any further, as we had no way of contacting the relevant complainant.
Discussion
In WP 4, we undertook a pilot RCT to evaluate study processes for a future trial, explore potential outcome measures and investigate, in detail, the feasibility issues raised by recruitment, randomisation, contamination and attrition over follow-up. Despite the optimism of the primary care teams in WP 1, we encountered challenges with recruitment from primary care. We trialled a range of approaches, as suggested by our PCPs, but found that Read code searches yielded large numbers of ineligible participants, creating potential for complaints from people approached who were in fact working and inconvenience for general practice staff. Approaches made after hand-searching were more successful, but this was resource intensive and yielded only relatively small numbers of participants. Opportunistic recruitment was effective but slow. The most efficient recruitment of eligible participants was achieved in the community pain services, where work is routinely discussed with all those attending, opening up the possibility of a personalised referral to employment services.
Once potential participants were identified, we achieved high rates of successful randomisation and participants seemed content with allocation to TAU, as well as to IPS. TAU was a one-to-one visit by the study co-ordinator who had no expertise in occupational rehabilitation. During this visit, the study co-ordinator worked through the TAU booklet with the participant. A high rate of attendance and satisfaction was recorded with this approach.
Individualised placement and support was adapted for the pilot study, as suggested by the ESWs in WP 2, to start with bespoke training about chronic pain, what it is, how it presents and what treatments are routinely used. Moreover, an early ESW assessment was carried out jointly by a pain OT and a ESW, and a personalised pain plan was developed to support the individual through the IPS. Rapid access return to pain services was available, but rarely used, and ESWs were integrated within the pain service team as far as possible. Otherwise, IPS was unchanged from that being offered as part of the SJP to local people with long-term health conditions. Unfortunately, the questionnaire-based follow-up of IPS participants proved challenging and yielded incomplete data. Owing to successful job-seeking, two participants moved away and were lost to follow-up and a further four participants failed to return any of the questionnaires at any time point. We also saw a particularly low level of return of the 12-month questionnaires in the IPS arm. This is an issue of considerable concern for a future trial. As the problem came to light very late in the study, we had limited opportunity to further explore approaches to maximise our retention. Data were available through the ESWs, which provided a much clearer picture as to relevant employment outcomes, but did not assist with defining rates of change of validated outcome measures. It is possible that the follow-up retention could have been significantly better if the ESWs had completed all questionnaires with the participants (either face to face or over the telephone), but this would have resource implications for a future trial and it is unclear whether or not it could bias the findings, if compared with questionnaires completed at home by those in the TAU arm. We suggest that more research is required to better understand how to maximise research retention, particularly when participants attain paid employment. One possibility is that employment outcomes could be obtained through linkage with national employment records, but this would not allow insight into health outcomes.
It is noteworthy, however, that the ESWs ‘expect’ that a significant proportion (i.e. > 50%) of people referred for IPS through other routes (in most cases through Job Centre Plus) choose not to engage after their initial assessment. Interestingly, the proportion who failed to engage after initial assessment appeared to be lower among those recruited within this pilot trial. This may be because they were recruited through health care, rather than employment services and, therefore, felt more encouraged to engage. Alternatively, it may be because our eligibility allowed for recruitment after only 3 months of unemployment, rather than the 2 years required by the SJP, meaning that some of our participants were closer to recent work and perhaps more motivated and less uncomfortable about pursuing a job placement. The ESWs did, however, report that they found a wide variation of ‘readiness to return to work’ among the participants in the trial. Although a small number of participants were able to take up a work placement quickly (and remained in work 12 months later), two-thirds of those in the IPS arm were not ready for a work placement and required more support to develop their readiness during the 6 months provided by the programme.
Follow-up was planned at 3, 6 and 12 months via postal questionnaires. Questionnaires that were returned were completed well, with few missing data. Our findings suggest that RTW self-efficacy would make a suitable primary outcome measure. We saw limited changes in scores for pain severity (i.e. between best, worst, average), pain interfering with normal work, self-rated health, Rosenberg’s Self-Esteem Scale score, PHQ-9 depression score, WEMWBS score and EQ-5D-5L overall score.
Outputs
-
Identification and recruitment of eligible participants is feasible, but time-consuming and resource-intensive in the absence of systematic recording of employment status in primary care records.
-
Questionnaires containing suitable data collection tools were developed for a future trial.
-
Randomisation is acceptable to both arms.
-
TAU as defined in this study was found to be acceptable to stakeholders and trial participants.
-
IPS can be adapted to integrate with pain management and planning, and is suitable for manualisation.
-
Significant issues were identified in retaining subjects through 12 months of follow-up, with the greatest problems in the IPS arm. It appears that attrition was greatest among those who obtained a job. Revised methodology will be required to attain significantly better follow-up in a future trial.
-
The WPs provided evidence for outcome measures suitable for a definitive RCT.
Work package 5
Aim
The aim of WP 5 was to obtain as full an understanding as possible of the views of stakeholders about the pilot trial.
Study design
The WP involved qualitative work with a target of at least eight participants in the study (from both the IPS and TAU/control arms), two ESWs and the two teams of PCPs that were directly involved with the InSTEP study; an analysis of comments from participants in the pilot trial on their questionnaires; and an analysis of informal conversations with two employers who provided work placements to IPS participants.
Methods: qualitative
All participants, ESWs and the relevant PCPs who were involved in the pilot study were eligible to take part in the qualitative research in WP 5. Eligible PCPs and ESWs were contacted by e-mail or post to invite them to take part, with a written information sheet attached, explaining the purpose of the interview or focus group, emphasising that participation was entirely voluntary and that comments would be confidential, anonymised and non-attributable, and that they could withdraw their consent at any time. A participant letter of invitation and an information sheet were posted to the home address of all participants who had taken part in both the IPS and TAU arms of the pilot trial and had consented to be contacted regarding a post-study interview (n = 30). If interested, the participants were invited to return the enclosed reply slip in a pre-paid envelope or, alternatively, to telephone or e-mail the study co-ordinator. The participants were provided with the opportunity to discuss the study further and raise any queries that they might have regarding this stage of the trial. Interested participants were then contacted by the interviewer to arrange a mutually convenient appointment during working hours at their general practice or city council premises. Non-responders to the mailing were recontacted by post on one further occasion.
If interested, the face-to-face interviews with ESWs and the focus groups with the PCPs were arranged at their respective places of work at a mutually convenient time.
Interviews with interested study participants were arranged at the individual’s convenience and conducted either by telephone or face to face during working hours at their own general practice or local city council premises. Written, informed consent to participate, and for the analysis of their views, was obtained from all participants prior to conducting all interviews or focus groups. Travel and time expenses were remunerated and participants (from both IPS and TAU arms) were given a £10 shopping voucher to thank them for their assistance with this stage of the study.
As with WP 1, the interviewer followed a semistructured topic guide to enable participants to relate their own experiences. 28,29 The interviewer had no prior relationship with participants. Questions and prompts were developed in advance to aid the interviewer, but the topic guide was intentionally flexible to allow for natural discussion throughout the process. Field notes were made by the interviewer during and immediately after data collection.
Other information collected for work package 5
Comments from pilot trial participants were sought in an ‘open space’ section of the pilot trial questionnaires at each of the 3-, 6- and 12-month follow-ups. These comments were collated and key themes were identified for WP 5. In addition, employers who had provided work placements to IPS participants in the pilot trial were asked for consent for contact by the study team. Those who gave consent for informal interviews were contacted to arrange an appointment at their workplace at a time convenient to them. Their comments have been organised into themes.
Data analysis
Data analysis involved thematic analysis of qualitative data from stakeholders (including participants, ESWs, PCPs and employers), specifically in relation to lessons learned about recruitment, participation and engagement, and outcomes.
Results
Study participants
Disappointingly, only 4 of the 48 trial participants expressed interest in participating in WP 5 (three participants from the IPS arm and one participant from the TAU arm). All of these participants provided contact details, but, despite numerous attempts, only one participant (from the IPS arm) actually proved contactable and was available to attend an interview with the qualitative researcher.
This one interview was carried out and analysed; however, the participant was nervous and rather unforthcoming, once again demonstrating some difficulty in understanding that the research objectives are separate from those of the employment intervention.
The themes that emerged from comments on the returned questionnaires covered participation in the study, content of the questionnaires, effective and less effective aspects of the IPS programme and the realities of living and working with chronic pain. The comments also highlighted the role that health-care professionals can play in worsening disability.
Participation in the study
Participants in both arms expressed gratitude for the opportunity provided within the study:
. . . thanks for your help for myself, thanks for your assistance to me. I happy had this time for my health. Thanks so much.
IPS
It has been a pleasure and hopefully I have contributed to your studies.
TAU
Questionnaire content
Two participants reflected that some questions in the questionnaires were difficult for them to answer:
There were questions I answered which I’d have answered differently if it hadn’t been a check box. There were answers I left as I didn’t know the answer.
IPS
Some of the questions are difficult to answer as they do not accurately deal with my illness.
TAU
Aspects of individualised placement and support
Positive progress was reported by an IPS participant who also reflected on the importance of the ESW’s confidence and support in that progress:
I am moving forwards slowly. When I see ESW I feel more optimistic in gaining some paid employment, however, I wave/wobble on my own. I have applied for some voluntary work. I have socialised more than over the past 3 months which has improved confidence.
IPS
Another IPS participant reflected on the role that IPS had played in their life and that the same could not have been achieved by TAU:
I couldn’t have turned myself around and regained my shattered/crushed confidence/self-esteem fundamental to a return to paid employment without your support and having seen you over the course of the last year. A paper questionnaire approach alone from the InSTEP study, would have totally failed with my type of personality/temperament. With your support I view the year’s InSTEP study and work a total success!
IPS
However, another IPS participant expressed dissatisfaction with their IPS work placement:
From the start of the programme, I have had one job through the scheme which was at a coffee shop. After 2 months it came to light that there never was going to be a permanent position for me. I get the impression that companies sign up for this scheme only use it for cheap/free labour.
IPS
Living and trying to work with their chronic pain condition
One participant from the IPS arm reflected that their pain was worsening:
I have had physio [physiotherapy] several times but it hasn’t done much good. I have also had steroid injections in my hands that also didn’t work. I shall make an appointment with the doctor as some of the pain seems to be getting worse at times.
IPS
A TAU participant described their situation at 12 months’ follow-up as follows:
I’m getting no support and have just left university because of this and another illness has made it too difficult to study or work. I can’t prove either so getting work or income support is extremely difficult.
TAU
Similar themes were expressed by another TAU participant at 12 months:
I have been given an appointment at the orthopaedic department and this can’t come soon enough. My quality of life is really low as I have no money, no transport and my mobility is severely affected. I don’t have much quality of life, sometimes I feel like I just want to go to sleep and never wake up. How desperate is that?
TAU
A further TAU participant reported:
I’m now looking for full time work which is proving difficult. Having not worked for 13 years hasn’t helped. At the moment I’m working 2 to 3 days a week as a forklift driver. The agency I’m with only found me this job which I started 3 weeks ago. Having now come off benefits is now a shock to the system. A wake-up call, more financial pressure.
TAU
The financial issues were also highlighted by an IPS participant:
I’m still waiting for court appeal to get back my benefits so do not have any income!
IPS
Role of health care in creating disability
An individual in the IPS arm reflected on their perceptions of the role of health care in their pain and disability:
I still struggle with the fact that for the best part of 3 years I struggled to cope with the pain and belief that I needed a total knee replacement when everything was cleared in February 2018 with an injection. These 3 years did an awful lot of damage to me psychologically – I ‘lost’ 3 years of my life to excruciating pain.
IPS
Health-care professionals, pain clinic recruiters and employment support workers
Six focus groups took place and included nine PCPs who were involved in recruiting to the pilot trial in primary care and one PCP in the community pain services who recruited for the InSTEP pilot. One-to-one qualitative interviews took place with both of the ESWs half-way through the pilot trial and again at the end, and the same process was carried out with the pain service OT.
Thematic analysis led to the following headings: recruitment (the process, barriers and facilitators); intervention [IPS for people with chronic pain, setting up the IPS intervention (multidisciplinary working, providing information about the programme, practicalities, training of the ESWs)]; IPS activities (gathering information from participants, roles within IPS, intervention and tools, outcomes and role of IPS); the TAU booklet as the control; and feedback to health-care professionals.
The PCPs who had completed searches using Read codes to find relevant participants described the difficulties resulting from the absence of a code for chronic pain:
There are so many different codes, you know, for pain and chronic pain.
PCP2
Primary care-based health-care professionals also reported the challenge when their records did not code employment status:
. . . in general practice we very rarely document if our patients are in work.
PCP6
. . . we don’t record employment status as a data point in our system. So we can’t search on it.
PCP7
A range of approaches were made by the primary care teams to refine the search strategies within their practice. As described above, practices used Read codes relating to diagnosis, referrals and medication to identify patients with chronic pain, and codes for fit notes and fitness to work certificates to identify patients who were unemployed. Within some practices, GPs and staff suggested individuals whom they were aware of:
I sent an e-mail round to the doctors to say . . . we’re doing this study, this is what it involves . . . have you any patients that you think that you think this might be suitable.
PCP1
Primary care-based health-care professionals described the frustration of these approaches:
. . . it took probably half a dozen times as we were finding other codes.
PCP2
The PCPs noted that often the search did not generate many results [‘we kept on saying to each other, didn’t we “there’s got to be more patients”’ (PCP2)] or found the results too generic and included patients who were not eligible [‘it generated too many people’ (PCP9)]. For some practices, the search strategy generated a long list and GPs were required to conduct an individual assessment on the search results:
Unfortunately there was a few bits of criteria we couldn’t necessarily do a search on, so that’s why we had to pass it to the GPs and they had to manually go through those lists and extract the patients that weren’t appropriate.
PCP4
Despite the difficulties described above, overall, PCPs felt that involvement with and recruitment for this pilot trial was simple. Once the list of potentially eligible patients was defined, the process of sending out the material was reported to be straightforward.
As described above, our recruitment strategy was widened to include recruitment in community pain clinics after the very slow start. The ESWs reported that this additional method of recruitment was helpful:
. . . they are continuously seeing people with chronic pain, so they’ve got . . . a continuous flow of patients coming through. So once they came on board, that’s definitely where it picked up. And I probably got the majority from them.
ESW
The pain clinic opportunistically recruited, with staff identifying potentially relevant patients and referring them into the study:
. . . if somebody turned up that they were unemployed and wanted to – were thinking of getting back to work, as a goal, then we talked about the scheme.
Pain clinic
This was made possible because employment is discussed at the pain clinic:
I think it’s kind of in their interest, part of what they do is to talk about work with their patients. So because it is already in the front of their mind, getting some extra help with their patients.
ESW
Interestingly, however, the pain OT pointed to some differences between the participants recruited through the two different routes. It was reported that those recruited via general practices were generally less disabled with fewer complexities than those referred from the pain team:
[People from] GP referrals, they were much less disabled than the pain team patients. So, you know, they were usually less complex and were – tended to manage themselves.
OT
The initial recruitment through general practices was felt by ESWs to be slow. They discussed that this was because of the difficulties of getting GPs on board with the study:
. . . people [practices] said ‘oh, you know, that was interesting’ and they would come back, and some of them did come back but then nothing came of that.
ESW
One PCP could see that the research aims might not be seen as that directly relevant to GPs:
. . . employment as much as it affects someone’s life isn’t massively health-care related.
PCP7
Primary care sites involved in recruitment also highlighted the difficulties in finding time for participation in any research projects:
Research does tend to have to go on the back burner if there’s stuff that is much more pressing. So there are very few times when there isn’t something more important. So research has to take second place.
PCP3
The primary care teams felt that the searches were not accurate or specific:
. . . the problem is that the search actually generated an awful lot of people who were not necessarily off sick for that reason, or they were on analgesics for different reasons, and I think there’s probably a reasonable coding issue.
PCP9
One site had a number of complaints from individuals because they had been sent information about the study when they did not meet the criteria. Patients telephoned to say they were in work or that the GP knew that they were retired:
It did take a lot of reception time, that obviously patients phoned, two or three of them needed to speak to me, because they wanted it escalated to a manager.
PCP6
There were a number of different individuals responsible for dealing with the searches at each site, this included research nurses, research administrators, data administrators, practice managers, nurse practitioners and GPs. Recruitment sites and the ESWs all highlighted the value of the study co-ordinator in recruitment, who had provided an in-depth brief of the trial and fielded questions before enrolment into the study:
I think when they spoke to [study co-ordinator] at the university, she had given them quite an in-depth brief about what the trials were.
ESW
The pain clinic also highlighted that the OT played an important role in successful recruitment from that setting, given her willingness and availability for answering questions from potential participants about the study:
. . . she was very much trying to be a conduit of information about the trial, about the interventions, and that the team generally referred to her rather than into the trial, and then she would refer into the trial . . . and she also acted as a conduit for communication with the employment advisors.
Pain clinic
In cases where the ESWs and study co-ordinator had in-depth conversations about the trial, primary care practices seemed more enthusiastic to be involved. ESWs felt that having PCPs recommend employment interventions would be very helpful in getting more people with health conditions to try IPS:
. . . they’ve got the advice from health professionals that this is [IPS], it’s positive steps ‘this is good for you, try it out, see what you can do to test your limitations’ I think that is definitely a massive help. Absolutely massive. Because they trust them, they trust health professionals.
ESW
The ESWs felt that participants had few questions about the trial, with a lot of information given to potential participants at recruitment:
I think the information that was given was good.
ESW
Primary care providers suggested that, if recruitment was to continue with the Read code searches, then an additional disclaimer should be added to the invitation letter to explain the reason for the letter and to apologise if patients did not meet inclusion criteria:
. . . just a paragraph to say that your records may not show whether you are employed or unemployed.
PCP8
There were a number of other recommendations about recruitment made by PCPs and pain clinic staff during the qualitative interviews, many of which were tested during the study. These included opportunistic recruiting in consultations, having ESWs present in the general practices, recruiting directly via leaflets and posters, follow-up reminders to patients, recruitment via patient groups, formally recruiting from the pain clinic and recruiting from the job centre.
Clients on the InSTEP programme wanted to RTW:
. . . work was important to them, that, you know, it really mattered to them for their values, and wanted to be back to doing something purposeful.
OT
. . . they want to go to work. They are at a stage with their conditions, where they realise it’s not about cure it’s about managing their condition.
ESW
However, the ESWs commented that, in general, the individuals recruited to the pilot trial were further away from being work-ready than those on similar programmes:
. . . they didn’t have to look for work due to their status, or, really, do any work related activity.
ESW
Although clients had motivation to RTW and had volunteered to be on the programme, some clients had unrealistic expectations about work and a considerable number of barriers to returning to work:
. . . it’s harder to kind of bring somebody who’s further away from work.
ESW
This made it a long and complex process for the ESWs to support patients, encouraging gradual RTW:
. . . what I’m trying to do all the time is build things slowly, because if you take one big leap at it you can do a lot more damage.
ESW
The main barrier to employment was clients’ health:
A lot of people can’t go back to the same jobs they were doing before. Or just purely because there aren’t reasonable adjustments that can be put in place for them due to their pain.
ESW
Clients had also stopped work because of the information they perceived that they had been given by healthcare professionals:
I’ve worked with a lot of people who’ve been told they probably can’t work again, in some form or another that’s a conclusion they’ve come to themselves, or they’ve interpreted something they’ve been told, in a different way.
ESW
The ESWs commented on the need for them to understand the fluctuating nature of clients’ conditions and how this might limit and impact on work:
If they are having a bad day or bad week with their pain for example, then they’ll tend to put off doing activities, which is understandable. So that has always been the main barrier.
ESW
Other barriers to returning to work that they described included clients’ confidence and fears, financial implications and personal circumstances:
. . . some of these people have kind of hit rock bottom in themselves.
ESW
The multidisciplinary nature of the IPS programme was positively described. The pain clinic and OT felt that being able to refer to the ESWs was a good opportunity and resource when discussing work with patients:
I think they [ESWs] were really good resources. They really had their fingers on the pulse of what was available, in both cities, for training and employment opportunities.
OT
Including both ESWs and OT in the team was seen as incredibly beneficial, with both describing that their collaboration was useful and of benefit to the IPS participants. ESWs felt that clients were more likely to open up to the OT, and the OT would also ask more health-related questions, which enabled the ESW to more fully understand the clients’ condition:
I think that is part of the buy-in for them, erm, the fact that they get a meeting with a specialist.
ESW
The OT felt that having the ESW present at the joint consultation enabled a joined-up conversation to be had. The multidisciplinary nature of the intervention also meant that there was an opportunity for communication with and feedback to clinicians, rather than a separate process:
I got to have a relationship with [the OT], an understanding of the kind of talk openly and freely with her and it was – it became less of two separate services and more like we work, we were together, we were both on the same team towards a common goal.
ESW
There were, however, some discrepancies in understanding the roles of the ESWs within a multidisciplinary health-care team, and this led to expectations being mismatched. ESWs were invited to pain clinic team meetings, but could not always attend because of their personal work schedules. This meant that the ESWs felt that they were outsiders to the pain clinic team and did not get involved, but rather acted as observers:
It was very beneficial to understand, the pain, and how the pain team works, and then I could talk to my clients about that as well. I think the only negative about that was that because I was just attending the meetings, not all of the patients were to do with me, very few, very few.
ESW
The pain clinic and OT also reported that they felt more could be done by the ESWs in communicating and getting involved with the team meetings, and discussion of recruited participants and their progress:
Once they were in . . . that was it, and you wonder what happens to the patients, and how the intervention is going.
Pain clinic
ESWs noted that clients arrived with questions about the IPS programme (which were not necessarily about the trial, as such questions had been answered by the study co-ordinator):
. . . they come with their own questions and then you sort of answer those, and some are very general and some are just because they’re in a different place and a bit nervous.
ESW
Questions included how the programme works and whether or not they were eligible for the programme (with thoughts that they were unable to work because of their condition). There was also some misunderstanding of what was expected by IPS participants, including assuming that the ESWs were responsible for finding a job and that the programme was not voluntary:
They came with a set of ideas that . . . what was the catch to it – to the programme, you know, what was I going to try and spring on someone to try and force them into work.
ESW
For the purposes of this pilot trial, the ESWs worked in two different cities and for different councils, which resulted in a different system for each programme. Location and accessibility was an issue highlighted by both ESWs. For example, one ESW did not have an office space to meet with clients, and so often met clients in a public space. He suggested that this might have had an impact on clients opening up:
. . . if we didn’t have the rooms it would be – it would have been really really difficult and I don’t think I would have really got to understand or know people that well.
ESW
Although this was not an issue for the other ESW, he noted that clients could not always get to the specified meeting location because of their health condition:
. . . the medical conditions would get in the way of, well not get in the way of – but stop some of the appointments. So, for every appointment we had . . . there may have had to have been one cancelled two or three times.
ESW
As the intervention is personalised to the client, the timings of meetings with the ESWs varied by client. Some clients met with ESWs weekly, or monthly with weekly contact (e.g. via telephone call or e-mails).
ESWs reported that there were differences between clients with chronic pain and clients on a broader employment programme:
. . . it was a massive sort of learning curve for me.
ESW
Owing to this, they felt that they needed education and knowledge specifically on chronic pain. For example, understanding the common causes of chronic pain, patients’ experience of chronic pain and how chronic pain presents, were all valuable sources of information:
. . . listening to the individuals, as to how they deal with things on a day to day basis, how they function to deal with whatever condition they’re dealing with, because it’s from that that you get that sort of essence of ability to move forward, you know, because they’ve become expert at managing, a lot of them, their condition.
ESW
Although ESWs did learn as they went, discussing conditions with individual patients, ESWs also learnt through the pain clinic and pain clinic resources. In addition, ESWs benefited from discussions with the OT, who helped them to understand pain from the clients’ perspective:
I think just educating for the employment advisors on, like, the importance of being realistic on what people can achieve, you know, while managing their pain.
OT
ESWs felt that they needed to really understand clients’ motivations for returning to work and also the barriers perceived by that individual. Although ESWs used their first meeting to discuss some of these, they reflected that it was really only after a couple of meetings, including the joint session with the OT, that they were able to identify all the issues:
Although within our meetings, our one-to-one meetings with the patient, erm I would ask a lot of questions and find out a lot from them, I think the OT goes into very specific, and then I can tailor my support as well.
ESW
Employment support workers would make sure they had built up a rapport with clients before they started discussing some of these points:
. . . the worst thing you can kind of ask them is ‘what’s your motivation’, because it just doesn’t happen that people . . . you’ve got to kind of get it out of people over time as you get to know them.
ESW
Employment support workers also felt that there was a lot of paperwork involved in the initial sessions with clients (e.g. research questionnaire, consent form and IPS assessment) and that sometimes clients felt overwhelmed:
I think it’s difficult at first the amount of paperwork.
ESW
However, the ESWs used varied techniques to complete this paperwork, including splitting up the paperwork over two sessions or completing overlapping questions on the IPS assessment forms after the client had left. Clients also seemed not to expect some types of questions, such as mental health questions, which meant that the ESWs and OTs were required to explain the importance and relevance of the information:
People don’t expect, but chronic pain, is a whole life experience and mental health can exacerbate people’s pain and it’s quite common for people that have chronic pain to have depression and anxiety so I was just checking on that and to see if they were aware of the connections of that and, you know, if there was any risk there.
OT
However, the questions were seen as beneficial to the ESWs, identifying issues that they may not have previously discussed:
It forced us into an area where I thought ‘oh that’s interesting, I wouldn’t have picked up on that’ so the fact that the questionnaire actually flagged it up was useful.
ESW
The main role of the ESWs was described as providing face-to-face support to clients:
. . . talking about things they are interested in, finding out what they had done in the past, what their worries are, letting them air their thoughts.
ESW
This support included discussions around barriers, providing practical advice, reassuring clients, signposting to services and training, and discussing reasonable adjustments at work. When discussing the most useful aspect of the IPS, the OT commented:
I think about the reassurance, and you know, affirming that they are in the right place to be going back to work and the health benefits about going back to work, and I think probably having the support from the clinician and the employment advisor is that added extra layer of security to give them confidence.
OT
Another important feature was that ESWs also provided continued contact once clients were in employment or on placements.
The OT provided health-related information to clients, signposting to health-related services and discussed their health-related needs. The OT used a standardised holistic approach with all of the IPS participants, which would consider several factors:
. . . we would take a pain history, I would ask them about their mental health, their social support, returning to work, and then I would say with return to work please consider the following, and any recommendations I would make.
OT
The ESWs saw the OT as giving valuable advice:
. . . potential different types of work they might like to move in to, and then what she would think was suitable, if there was any suggestions she could make, onward referrals, techniques, tips, that maybe the patient hadn’t been told or thought of.
ESW
Goal-setting was frequently used by ESWs:
I suppose when we meet and set goals, setting lots of goals, forward plans with them, and then I suppose it’s when they can see the benefit of what they are doing, and the activity they are doing. And if they can see a benefit from it and are experiencing a benefit, and a good feeling from it, like if you get to do a course, or if you feel you are moving towards work and where you want to be, then it does change around eventually. People become a lot more work focused.
ESW
However, the goals needed to be flexible and ESWs felt that they often took longer to reach because of the fluctuating nature of the clients’ chronic pain condition:
. . . because there was then a time gap because the appointments had been cancelled, you may then have to go back to what you were doing before . . . so you know, for every one step forward there seemed to be sort of one step back sometimes.
ESW
Understanding how to pace the clients’ activities was felt to be important.
Employment support workers felt that building rapport was key to IPS being successful [. . . it’s all about sort of partnership working (ESW)], and this helped to reduce clients’ concerns and anxieties and build trust over the process:
I think there was a couple who had been on courses, employment type courses before, some of them had involvement with job centres which they felt was a very negative experience for them.
ESW
Individualised placement and support participants were all encouraged towards a work placement. ESWs felt that this was very beneficial for clients:
. . . because that helped somebody who had been out of work for a long time, helped them with the fear because that’s huge, the fear of going back to work and being in the workplace again, the financial side, the fact that I didn’t then sever my ties with them because I was still there, – I was still going and collecting their timesheets and making sure their wages were paid at the same time so I’m still a part of that.
ESW
Employment support workers also reported that in some cases they had provided training or signposted to relevant training opportunities, such as motivational sessions and mock interviews. ESWs would also work with clients on improving their curriculum vitae and spending time looking for work with them:
. . . for a lot of people the job market has changed, the way recruitment processes happen has changed, the way you apply, how interviews are conducted, so it would just be sort of getting people up to speed with that.
ESW
ESWs acknowledged that the ultimate goal of IPS was to get clients back to work, but for some individuals they had found that the process was about improving their readiness for work:
. . . there was always a goal, sort of, to get people into work but you clearly you could tell fairly quickly that some people were nearer and some people were further away from arriving at that final goal really . . . but it was important just to feel that they were moving forward, generally.
ESW
Employment support workers found that clients gained more confidence and knowledge over time. In their view, clients seemed more empowered, started to identify their own ideas for work and were moving in the direction of going to employment. Some clients had been referred to home assessment, community teams or signposted for appropriate training:
. . . the feedback has been very good, that the people who want to move towards work who have the health conditions are actually saying like they feel more focused, they feel they’ve got more confidence because they’ve been coming in to see me and take part in sessions and a couple of those people have actually gone into work.
ESW
The booklet was seen as a good control-group intervention to provide some support for patients:
. . . at least, actually, you were still giving them advice.
PCP9
Primary care providers identified that some patients may not read the booklet:
. . . in my experience, patients don’t read anything. As simple as that sounds, it is something that I’ve noticed working here. It’s not that people avoid reading things but on a subconscious level, people don’t tend to read the things that they are given.
PCP7
Primary care providers highlighted the good practice of having the study co-ordinator go through the booklet with the control group, but acknowledged that this might be difficult to do in a larger study or in a practice setting. Suggestions included regular sessions to go through the booklet [‘I think the way around with it is to do, like, a one to one or maybe even a group session so people might have the same thing’ (PCP1)] and also making the booklet widely available to patients:
I wondered actually for some patients they would just take it and use it, probably, and it probably gave them a better framework . . . there was a lot of good information in it, plus some stuff you could work on yourself.
Pain clinic
Primary care providers had no positive or negative feedback from clients about the trial or IPS itself:
I personally didn’t hear back from a single one of them.
PCP6
They discussed relying on the results of the trial to come out to see if there had been any benefit to their patients. The pain clinic also identified that it would be beneficial to have more feedback to and communication with the team of health-care professionals about how the clients were moving through the programme.
Employers who provided a work placement as part of the InSTEP pilot trial
Three individuals from two small and medium-sized enterprises (SMEs) who had hosted a work placement for a participant in the InSTEP pilot trial agreed to be interviewed informally about their experiences. The themes that emerged from these discussions covered motivation for providing a placement as an employer, benefits to the employer, role of the ESW and the importance of being able to select the individual to the post.
Motivation of the employer
All three employers expressed the importance to them of being involved with work placements, describing their involvement altruistically as ‘giving back to the community’ (employer B). Interestingly, one employer explained that the directors of the company were particularly keen and supportive of this InSTEP placement because a family relative also suffered a chronic pain condition.
Benefits to the employer of providing these work placements
One employer commented that it had proved easier to obtain an individual prepared to work part-time hours (which was what the company needed) through this mechanism than on the conventional job market ‘where most people want full time’ (employer B). An employer raised that they perceived that senior management had persuaded them to be involved in the programme on the basis that it was ‘free labour for 6 months’ (employer A), but that they did not view it as such; rather they were willing to give a person unemployed with a health condition a chance. They acknowledged that it was a leap of faith and an unknown quantity when they offered the placement, but stated that it had been well worth the gamble in their opinion and they ‘would not hesitate to offer future work placements if funding became available again. It was brilliant’ (employer A). They observed the job satisfaction experienced by the individuals (this company had placed two individuals through SJP). The employers appeared to be genuinely pleased to see their employee flourishing at work. They did not, however, consider that they had done anything out of the ordinary or special in terms of offering work placements.
Importance of flexibility
The employers acknowledged that the employees on these work placements tended to have more need for flexibility (e.g. more sick days), but perceived this as being straightforward to accommodate and that flexibility was shown by all colleagues in the organisation. Good communication regularly between the employee and their manager was considered essential. The employers also talked about the fluctuating nature of pain conditions and recognised that, once they had understood this, they were able to accommodate it. The employers suggested that involving everyone in the organisation in supporting their employee had been ‘good for the business’ (employer B) and they did not perceive any problems with relationships with other staff. They felt that the employees appreciated the support and flexibility (e.g. with working hours and tasks) that had allowed them to settle in. Employer A reported that a worker had been overwhelmed by the job initially, but with the support of the manager had been helped ‘to break the job down into manageable tasks’, which had enabled this worker to cope and, eventually, to compile a ‘how to’ booklet to help himself and other new recruits to perform the work effectively.
Need to match the individual to the work placement
The employers were not obliged to take anybody on through this placement scheme, but instead were able to interview applicants interested in working with them. In both cases, they felt that this was important for the success of the placement and that they would offer such placements only if they could make this selection. One employer explained that other candidates could not be offered a work placement with this SME (e.g. for communication issues and because of a physical disability that simply could not be accommodated in that employment). Another point of this interview valued by the employers was the chance to assess an individual’s motivation for the work. They drew a parallel with workers who had been sent via Job Centre Plus who were coming for an interview simply because they felt that they had no choice and did not want the job at all. Motivation to work was seen as pivotal to success of the work placement. It was the employer’s view that both recruits placed with them had demonstrated a keen enthusiasm and desire to work, which had led to them both being taken on rapidly after starting the placement. The managers identified this motivation as a necessity if the placements were to be successful.
Support of the employment support worker
Slightly different views were expressed about the ESW support. Interestingly, one employer had decided to recruit their work placement individual very quickly after they had started (i.e. within 4–6 weeks) and they found that the ESW support was then rather quickly withdrawn. In contrast, the other employer noted that their ongoing support and engagement throughout the placement had been helpful on issues such as benefits to both the employer and the employee (who had also ultimately been taken on by the organisation).
Benefits for health of being at work
All three interviewees reported that they were absolutely certain that the employment placement had benefited the health of their employee. In one case, the employer said that their employee had advised them that ‘he had come off all his pain medication within weeks’ (employer A). One commented that work gave ‘a sense of worth’ and kept the mind occupied (employer B). One commented that the employee had themselves expressed how much the work helps and had stated that they ‘look forward to coming to work’ (employer B).
Outputs
-
The WP provided a synthesis of the views of all stakeholders (i.e. participants, PCPs, ESWs, pain services and employers) about the pilot trial and IPS. Insight has been gained into the essential elements of IPS for chronic pain patients.
Discussion
The stakeholders were generally very positive about the InSTEP pilot trial. However, several challenges were encountered. First, recruitment through general practices, despite using a wide variety of approaches, proved inefficient and resource-intensive. Read code searches were easy to run but inefficient, as they yielded very large numbers of ineligible people and non-responders. The mailshot following a Read code search also created workload for the surgery and the potential for complaints, as a number of ineligible people wanted to assure their GP that they were employed or had retired. Hand-searching and opportunistic approaches were most efficient, but were resource-intensive and, in practice, the rate at which eligible patients were seen and recruited was slow. Recruitment through pain services appears effective and efficient, particularly when the pain team are integrated within the research, but the people recruited in this way might have been systematically different from those recruited in primary care, with more complex needs. This research highlights the need for a systematic way in which employment data can be linked to primary care data. Primary care recording of employment status could be initiated, but would be very difficult to keep updated. Our findings suggest that there needs to be system-level change that achieves integration or linkage of health-care and employment data if employment is ever going to be a feasible outcome for studies using primary care data.
Employment support workers enjoyed working with chronic pain patients, despite their complex needs, but they valued the additional training and the joint assessment with the pain OT. In practice, we had anticipated even greater integration of the pain and employment services than we achieved in the InSTEP pilot. This may be explained by the relatively small numbers involved and the slow speed of recruitment, but another barrier we identified was in the separation of health-care from employment services, both geographically and administratively. As above, our findings suggest that joint ways of working between the health and employment sectors are desperately needed if we are to make major strides in this area.
It was disappointing that so few participants were willing to agree to qualitative interviews after the InSTEP pilot. We did, however, receive some useful feedback from the analysis of comments made on the follow-up questionnaires. Taken together with our experiences throughout the research, we found that maintaining long-term engagement with this group of patients was perhaps more challenging than for some other groups of patients. This may reflect that, when the desired outcome of an intervention is employment, then this major lifestyle change can impact on participants’ ability to engage with research. However, it may also reflect that chronic pain is a long-term fluctuating and disabling condition than can have an impact on mental health, which also affects clients’ engagement with research.
Work package 6
Aim
Work package 6 aimed to bring together the shared learning from WPs 1–5 to manualise the IPS intervention for people unemployed for > 3 months with chronic pain.
Training for employment support workers about chronic pain
The ESWs, participants and pain team agreed that initial training about chronic pain was helpful for ESWs. Such training should aim to build confidence in the ESWs about talking to people about chronic pain, and provide a better understanding of the nature of chronic pain, and a better appreciation of the specific impacts on pain and quality of life, as well as workability. The specific content that all parties agreed was helpful could be covered in a didactic programme, but the parties felt that an interactive programme with case examples was particularly beneficial. The content should include the following:
-
What is chronic pain?
-
How does it present?
-
An explanation of pain medication and common side effects.
-
An explanation of the fluctuating nature of chronic pain.
-
An explanation of the relationship of chronic pain with fatigue, poor concentration and mental ill-health.
Existing e-learning packages may be helpful, with brief testing afterwards. 57
Summary of interventions for chronic pain recommended by the pain expert in the InSTEP pilot trial
A wide range of different pain interventions were recommended among the 22 InSTEP pilot trial participants (Table 15).
| Type of intervention | Subjects (n) |
|---|---|
| Medication tapering | 5 |
| Liaison with other teams (e.g. physiotherapy, orthopaedics, etc.) | 3 |
| Referral for rehabilitation through pain services | 6 |
| Referral to Immediate Access to Psychological Therapies | 6 |
| Referral to pain psychology | 2 |
| Psychoeducation on pain | 11 |
| Self-help manuala | 11 |
| Phased introduction to work | 13 |
| Work travel advice | 9 |
| Pacing activity during work | 14 |
| Restriction on duties | 9 |
| Ergonomic adjustments | 2 |
| Pain care after interview | 5 |
| Work-focused pain care after interview | 2 |
In most cases, several interventions were recommended. For the pilot trial, we chose a personalised approach to each individual, and the range and breadth of interventions prescribed would appear to suggest that this is the optimal approach. However, a standard advice and guidance package was developed that was suited to the needs of the majority of participants. This included:
-
psychoeducation on pain (recommending Understanding Pain in Less Than 5 Minutes, and What To Do About It!59)
-
a self-help manual about pain (e.g. a pain toolkit)
-
an advice package that covered:
-
a phased introduction to work
-
work travel
-
pacing activity during work
-
restriction on duties appropriate to personal needs
-
ergonomic adjustments.
-
Integration of employment support within pain services
Participants, ESWs and pain services all pointed to the value of the integration of the IPS within the framework of health care for chronic pain. People with chronic pain gained more confidence about their capability to work with the support and encouragement of the health-care team, whom they perceived understood their condition best. ESWs valued the joint assessment with the pain team and reported a better understanding of the types of work for which their clients were suited by being present during this joint consultation. In practice, however, we encountered some difficulties achieving optimal integration within this small-scale and time-restricted pilot. First, even in this small trial, the two ESWs were employed by two different city councils with differently organised services. In addition, each area had a differently organised pain service. We were fortunate that only two ESWs and one specialist pain OT worked with all of the InSTEP pilot trial participants and that these three professionals were exceptional individuals who were enthusiastic about the research and keen to make it work. Even with this, however, the initial slow recruitment did not facilitate the relationship development and teamwork that was initiated by the training phase.
Second, the ESWs had a range of other clients within their city council roles and were accountable for their time. They, therefore, found it difficult to justify giving regular time to attend pain clinic meetings, which could have facilitated better teamwork, when such meetings involved only one or two of their shared clients. Moreover, in setting up this study, it was implicit in the integrated approach that participants could be referred seamlessly between the pain services and the ESWs (in both directions), but only 5 of 22 participants received any pain follow-up at all (two of whom received some work-focused support to manage pain at work). In addition, there is evidence from follow-up questionnaires that a number of people would have benefited from additional pain support. It seemed that the ESWs did not feel empowered enough (or did not know enough to judge when it could have been beneficial) to ask for additional support for their clients through the pain team, beyond the initial appointments. The trial management team would have also expected that the pain OT might have been more proactive in arranging planned follow-up of clients to establish how well they had understood and been able to comply with the advice given about pain management, and were surprised that this was not put into place on a more frequent basis. Again, it is unclear whether this was prevented by other clinical commitments, or if there had been an expectation that clients would ask for this or that ESWs would request it.
Manualisation of individualised placement and support
Figure 2 summarises the manualised approach to IPS for chronic pain patients, including initial training for ESWs and a joint consultation involving the ESWs and pain specialist to formulate a joined-up pain management plan. Integration of the IPS employment intervention with the pain services is recommended to maximise success; however, as we have found, this will need to be actively facilitated, which will involve the breaking of traditional barriers created by the usual separation of health-care services from employment services. Different models will need to be co-created, depending on the geography and organisation of services.
FIGURE 2.
Manualised individualised placement and support intervention. IAPT, Improving Access to Psychological Therapies.
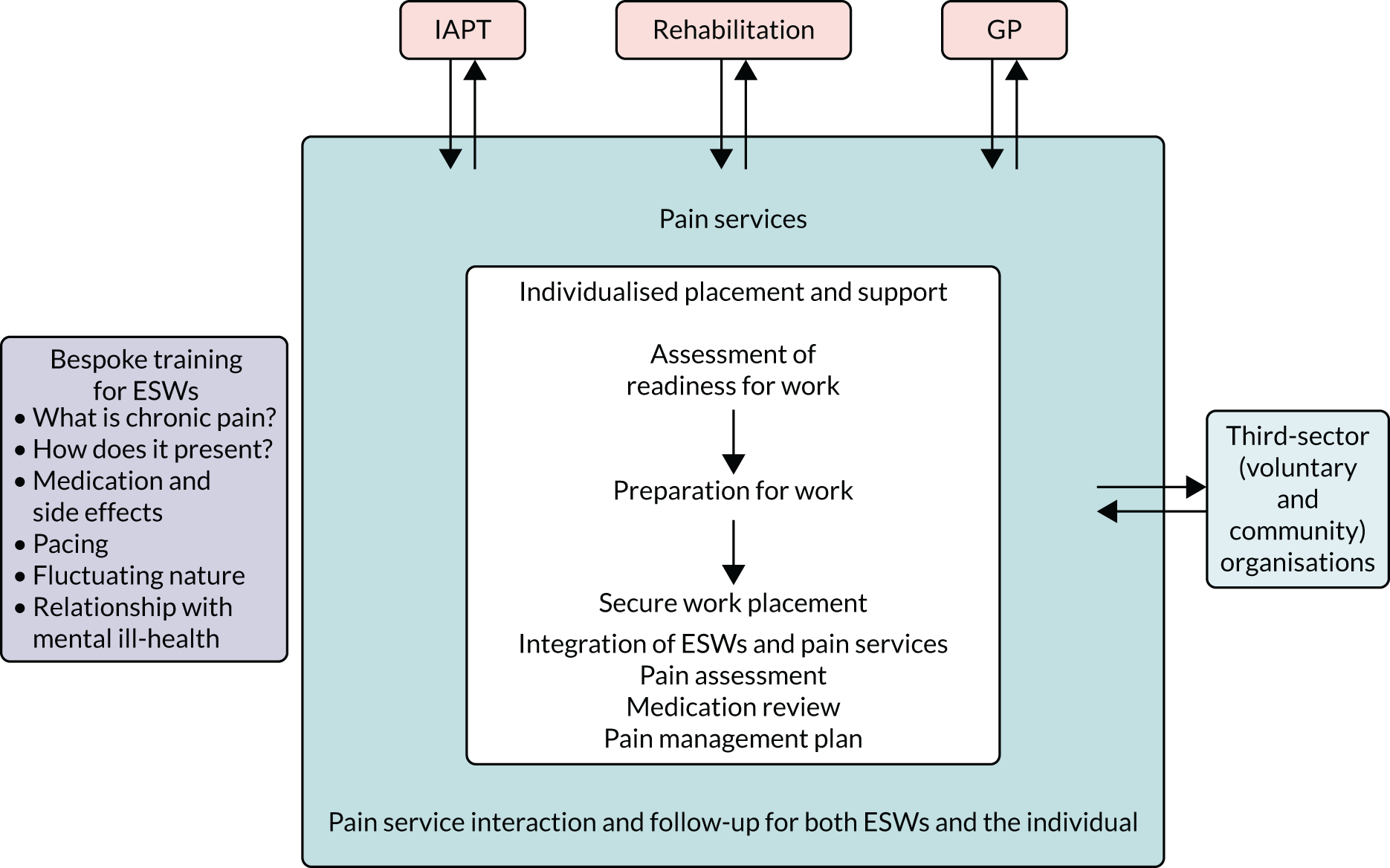
Chapter 3 Limitations of this research
The findings of our research need to be considered alongside a number of limitations. These will be described below.
Changes to protocol
For the most part, the research was carried out exactly as laid down in the full application and protocol. One proposed aim was to carry out analysis of the Knowledge and Attitudes Survey Regarding Pain among ESWs before and after they received training about pain and at the onset of WP 4. However, after further consideration during the study, it was decided that all IPS clients would have a joint appointment with both the ESW and the pain OT, at which all complex aspects of pain management would be discussed. Therefore, it became less of a requirement for the ESWs to develop the expertise that we had anticipated they might need. Our experience suggested that, to successfully roll out this sort of intervention in practice, this type of joint health-care practitioner/ESW appointment was efficient and improved communication between all parties, and it would be our recommendation that such a model would be optimal.
Recruitment
In WP 1, we aimed to obtain qualitative interviews with up to 10 clients who had been participants in the local IPS programme organised through the SJP. Ideally, these clients would also have had chronic pain conditions, but screening on the basis of the underlying health condition was impossible for reasons of confidentiality. Names and contact details of more than 10 suitable clients were made available to the study team, but these individuals (1) proved difficult to contact and (2) commonly did not attend agreed appointments. As a result, we collected all of the data available from all of the clients who did arrive for appointments (n = 9), but could not sample further to test whether or not data saturation had been reached. In WP 3, similarly, we hoped to sample all of the ESWs with involvement in the IPS programme in either city (n = 8); however, despite all but one of the ESWs agreeing to participate, practical difficulties arranging appointments again prevented sampling beyond five of the ESWs to test whether or not data saturation was obtained. Finally, in the qualitative work planned to be undertaken with study participants in WP 4, we were very disappointed that only 20% of participants consented to additional contact, among whom only half proved to be contactable and only one agreed to attend an interview with the qualitative researcher. Fortunately, we did successfully collect some qualitative ‘blank space’ answers from the follow-up questionnaires, but we point to this as a limitation of the current study.
Randomisation
Unfortunately, one compromise that was required was for the proposed block randomisation throughout recruitment to the pilot trial to be stopped. Owing to the delays experienced with recruitment from primary care, our research timetable became compromised by the fact that IPS was available only until a fixed deadline, beyond which the SJP finished (i.e. the end of September 2019). Notably, the deadline had been voluntarily extended by the SJP team by 2 months, simply to enable our research to take place. However, in practice, when it was clear that we would need to alter our plans, the study team, in agreement with the TSC, obtained written informed consent for randomisation, but then allocated a group of consecutive participants to IPS until it was no longer available, and then recruited all subsequent participants to TAU. This could have resulted in a bias, particularly as we opened recruitment through pain services later in the study period when primary recruitment was clearly going to be ineffective. However, consideration of the allocations shows as follows:
-
Among the 13 participants recruited through pain services, nine received IPS and four received TAU.
-
Among the 37 participants recruited from primary care, 13 received IPS and 24 received TAU.
Therefore, if anything, the timing of the opening of pain clinic recruitment meant that participants recruited from this setting were more likely to receive IPS. Of course, we cannot rule out a bias in who ultimately received which allocation, but we feel that there was a good distribution of participants from both settings who received the active intervention. We have no reason to believe that participants recruited in the last 2 months were selectively different from those recruited up until that point.
Chapter 4 Conclusion and recommendations
Establishing the feasibility of the delivery of individualised placement and support within the NHS
The six WPs allowed us to explore the feasibility of performing a definitive RCT with the aim of establishing the clinical effectiveness and cost-effectiveness of IPS for improving quality of life among people unemployed for > 3 months with chronic pain. Overall, we have established that a trial such as this would not be possible if recruitment was through primary care in its current form. Our findings suggest that, unless accurate and up-to-date employment status information can be collected in primary care health records, or linkage can be established with employment records, research such as this relating to employment will be impracticable in primary care.
However, we have shown that it is feasible to recruit through community pain services and that, although these clients may differ (i.e. have more complex needs and have been unemployed for longer), we can identify people who wish to RTW, and who benefit from an integrated approach to their health care while developing the confidence and self-efficacy to RTW. Employers are willing to host such placements, particularly when they provide these placements on the basis of being able to select the individual suitable for their organisation. Undoubtedly, however, within the context of this study, work placements were facilitated by the city council paying a minimum part-time wage on behalf of employers for the first 6 months. Benefits counselling must be an integral part of ongoing support for employers and employees during the work placement.
Information about the acceptability, engagement and likely participation of patients and health-care providers in primary care in a future trial
Our research was carried out in the optimal circumstances:
-
The general practices and the PCPs who participated were enthusiastic and interested in the research.
-
Community pain services were integral to the research from the very beginning of the study (i.e. from the application stage).
-
IPS was being delivered locally, funded partly through the European Social Fund and partly through City Deals funds, and the managers of these services worked closely together with each other and the research team throughout.
Even given all of these ideal circumstances, we found challenges. For example, enthusiastic PCPs keen to recruit in primary care found it to be slow and resource-intensive.
Manualisation of individualised placement and support for individuals with chronic pain for a future definitive trial
The assessment of the fidelity of the IPS delivered suggested only a fair level of fidelity. We found several barriers preventing easy integration of pain and employment services. The input from our pain OT was more limited than expected, partly because of a lack of proactivity and partly because ESWs did not realise that they needed to ask for more input. Taken together, therefore, our findings hint that a great deal of change would be necessary if IPS was to become a pragmatic intervention to be made widely available in the context of primary care.
Development of outcome measures for a definitive trial
Despite the difficulties in undertaking the research and rolling out an IPS intervention in practice, health benefits were clearly seen by some participants and their employers within the InSTEP pilot study. Therefore, our data add to the growing body of data showing that employment is an important factor in health. Self-efficacy is an important measure of an individual’s perception of their ability to cope with different aspects of their life and work, something that can ultimately lead to independence, improved quality of life and diminished health-care costs.
It is imperative that health-care providers continue to grow their understanding of the potential importance of (good) work for health, and more closely integrate the health care that they are providing into the outcomes important to their patients, including ability to work and fiscal independence. One of the major barriers to this would appear to be our lack of a whole-systems approach to health and employment, and more consideration needs to be given to creating a better ability to link health and work data for the future.
Acknowledgements
We would like to thank all of the participants who generously gave their time to take part in the study. We acknowledge the hard work and efforts of the local field workers at the nine participating GP sites who assisted so generously with the study, especially Martina Brown (Research Nurse), Kat Hampson (Operations Manager), Irina Pockberger (Administrator), Kathy Chamberlain (Assistant Practice Manager), Philippa Larard-Young (Advanced Nurse Practitioner) and Kathryn Carey-Jones (Research GP). We are grateful to the members of the Study Steering Committee for their oversight and expertise: Professor Karen Walker-Bone, Dr Cathy Linaker, Dr Cathy Price, Dr Nick Maguire, Dr Simon Fraser, Mrs Kathryn Rankin, Mr Gareth Davies, Mrs Liz Crate, Mrs Ruth Nash and Ms Claire Buchan.
Our sincere gratitude is expressed to the TSC for their support and enthusiasm throughout this research: Professor Nicola Fear (chairperson), Dr Gwen Wynne-Jones, Dr Benjamin Ellis, Dr Dominic Aldington, Mr Gareth Jones (lay member), Dr Cathy Linaker and Professor Karen Walker-Bone.
We are very grateful to the employment teams of Southampton City Council and Portsmouth City Council and all those involved with the SJP, which enabled provision of IPS for this research. We would particularly like to acknowledge the generous support of Kathryn Rankin and Liz Crate and the support workers Stephen Hogan and Harry Tucker.
We thank Michelle Holmes and Sabina Stanesccu for their assistance in collection of the qualitative data and subsequent analysis for work packages 1–3. We are extremely grateful to Mrs Carol Stewart (Clinical Specialist OT) from the pain team at Solent NHS Trust for her expertise in the provision of specialist pain consultations with participants in the active arm of the pilot study.
We are grateful to the University of Southampton for their sponsorship of the trial and for providing support and guidance, as required, especially to the research and development unit for their research governance and financial management support.
Contributions of authors
Cathy Linaker (https://orcid.org/0000-0003-1091-9283) (Post-Doctoral Research Nurse) co-ordinated this research programme and was responsible for recruiting and supporting participating sites, delivered the TAU and conducted the follow-up data collection. She was involved in the data analysis, interpretation and drafting of the final report.
Simon Fraser (https://orcid.org/0000-0002-4172-4406) (Associate Professor in Public Health) brought the primary care and public health perspective to this research, including study design, set up with primary care colleagues, and analysis and interpretation.
Cathy Price (https://orcid.org/0000-0003-0111-9364) (Consultant in Pain Medicine and Clinical Director of Community Pain Services in Wessex) supervised the pain OT, assisted in engaging pain services in recruitment and brought her expertise throughout, including to the design of the study, the analysis and the write up of our findings.
Nick Maguire (https://orcid.org/0000-0003-4295-8068) (Psychologist) brought the health psychology input to this project, including supervision of all the qualitative work, its analysis and write up.
Paul Little (https://orcid.org/0000-0003-3664-1873) (Professor of Primary Care) brought the primary care and public health perspective to this research, including study design, set up with primary care colleagues, and analysis and interpretation.
Ira Madan (https://orcid.org/0000-0003-2200-7329) (Reader in Occupational Medicine) provided academic occupational medicine expertise, drawing on their considerable clinical experience and a track record of occupational research, including clinical trials in workplace settings.
Rafael Pinedo-Villanueva (https://orcid.org/0000-0002-4723-5128) (Health Economist University of Oxford) provided support and advice about the health economic assessment of this research.
David Coggon (https://orcid.org/0000-0003-1930-3987) (Emeritus Professor of Occupational Medicine) provided academic occupational medicine expertise, drawing on their considerable clinical experience and a track record of occupational research, including clinical trials in workplace settings.
Cyrus Cooper (https://orcid.org/0000-0003-3510-0709) (Professor of Rheumatology) assisted with the evaluation of this complex intervention.
Georgia Ntani (https://orcid.org/0000-0001-7481-6860) (Senior Statistician) analysed the data presented in this report.
Karen Walker-Bone (https://orcid.org/0000-0002-5992-1459) (Professor of Occupational Rheumatology and Honorary Consultant Occupational Rheumatologist) was the principal investigator for this research, conceived the application, oversaw the delivery of each of the WPs and drafted the first few drafts of this report.
Data-sharing statement
Access to the study data is available from the corresponding author. Study data will be made available to other researchers on request, in accordance with ethics approval requirements and if judged to be appropriate by the co-authors.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care.
References
- Price C, Hoggart B, Olukoga O, Williams AC, de C, Bottle A. National Pain Audit Final Report 2010–2012 n.d. www.britishpainsociety.org/static/uploads/resources/files/members_articles_npa_2012_1.pdf (accessed 2 July 2020).
- Donaldson LJ. Pain: Breaking Through the Barrier. 150 Years of the Annual Report of the Chief Medical Officer: On the State of the Public Health 2008. http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/AnnualReports/DH_096206 (accessed 2 July 2020).
- Elliott AM, Smith BH, Penny KI, Smith WC, Chambers WA. The epidemiology of chronic pain in the community. Lancet 1999;354:1248-52. https://doi.org/10.1016/S0140-6736(99)03057-3.
- Bridges S. Health Survey for England – 2011, Health, Social Care and Lifestyles, Volume 1. Leeds: NHS Digital; 2012.
- British Society of Pain . A Report of the Pain Summit 2011 n.d. www.britishpainsociety.org/static/uploads/resources/files/members_articles_pain_summit_report.pdf (accessed 2 July 2020).
- Waddell G, Burton AK. Concepts of Rehabilitation for the Management of Common Health Problems. Norwich: The Stationery Office; 2004.
- Kposowa AJ. Unemployment and suicide: a cohort analysis of social factors predicting suicide in the US National Longitudinal Mortality Study. Psychol Med 2001;31:127-38. https://doi.org/10.1017/s0033291799002925.
- Nylen L, Voss M, Folderus B. Mortality among women and men relative to unemployment, part-time work, overtime work, and extra work: a study based on data from the Swedish twins register. Occup Environ Med 2001;58:52-7. https://doi.org/10.1136/oem.58.1.52.
- Mason V. The Prevalence of Back Pain in Great Britain. London: The Stationery Office; 1994.
- Black C. Working for a Healthier Tomorrow. London: The Stationery Office; 2008.
- Price C. Putting Pain on the Agenda: The Report of the First English Pain Summit n.d. www.policyconnect.org.uk/sites/site_pc/files/report/496/fieldreportdownload/cppc-puttingpainontheagenda.pdf (accessed 2 July 2020).
- British Society of Rehabilitation Medicine . Vocational Rehabilitation – The Way Forward: Report of a Working Party 2000.
- Bond GR, Peterson AE, Becker DR, Drake RE. Validation of the revised individual placement and support fidelity scale (IPS-25). Psychiatr Serv 2012;63:758-63. https://doi.org/10.1176/appi.ps.201100476.
- Marwaha S, Johnson S, Bebbington P, Stafford M, Angermeyer MC, Brugha T, et al. Rates and correlates of employment in people with schizophrenia in the UK, France and Germany. Br J Psychiatry 2007;191:30-7. https://doi.org/10.1192/bjp.bp.105.020982.
- Schneider J, Slade J, Secker J, Rinaldi M, Boyce M, Johnson R, et al. SESAMI study of employment support for people with severe mental health problems: 12-month outcomes. Health Soc Care Community 2009;17:151-8. https://doi.org/10.1111/j.1365-2524.2008.00810.x.
- Bond GR, Drake RE, Becker DR. Generalizability of the individual placement and support (IPS) model of supported employment outside the US. World Psychiatry 2012;11:32-9. https://doi.org/10.1016/j.wpsyc.2012.01.005.
- Drake RE. A brief history of the Individual Placement and Support model. Psychiatr Rehabil J 1998;22:3-7.
- Drake RE, Becker DR. The individual placement and support model of supported employment. Psychiatr Serv 1996;47:473-5. https://doi.org/10.1176/ps.47.5.473.
- Crowther RE, Marshall M, Bond GR, Huxley P. Helping people with severe mental illness to obtain work: systematic review. BMJ 2001;322:204-8. https://doi.org/10.1136/bmj.322.7280.204.
- Twamley EW, Jeste DV, Lehman AF. Vocational rehabilitation in schizophrenia and other psychotic disorders: a literature review and meta-analysis of randomised controlled trials. J Nerv Ment Dis 2003;191:515-23. https://doi.org/10.1097/01.nmd.0000082213.42509.69.
- Rinaldi M, Perkins R. Comparing employment outcomes for two vocational services: individual placement and support and non-integrated pre-vocational services in the UK. J Vocat Rehabil 2007;27:21-7.
- Bond GR, Becker DR, Drake RE, Vogler KM. A fidelity scale for the individual placement and support model of supported employment. Rehabil Couns Bull 1997;40:265-84.
- Burns T, Catty J, Becker T, Drake RE, Fioritti A, Knapp M, et al. The effectiveness of supported employment for people with severe mental illness: a randomised controlled trial. Lancet 2007;370:1146-52. https://doi.org/10.1016/S0140-6736(07)61516-5.
- Howard LM, Heslin M, Leese M, McCrone P, Rice C, Jarrett M, et al. Supported employment: randomised controlled trial. Br J Psychiatry 2010;196:404-11. https://doi.org/10.1192/bjp.bp.108.061465.
- Szplit K. Social Return on Investment (SROI) Forecast Analysis. Individual Placement and Support (IPS) for Period April 2010 to March 2011 2013. www.socialvalueuk.org/app/uploads/2016/03/IPS%20Forecast%20SROI%20Revised%20Feb%2013%20Assured.pdf (accessed 2 July 2020).
- Miller WR, Rollnick S. The effectiveness and ineffectiveness of complex behavioral interventions: impact of treatment fidelity. Contemp Clin Trials 2014;37:234-41. https://doi.org/10.1016/j.cct.2014.01.005.
- McCracken LM, Vowles KE. Acceptance and commitment therapy and mindfulness for chronic pain: model, process, and progress. Am Psychol 2014;69:178-87. https://doi.org/10.1037/a0035623.
- Bowling A. Research Methods in Health. Maidenhead: Open University Press; 2009.
- Wilkinson S, Joffe H, Yardley L, Marks DF, Yardley L. Research Methods for Clinical and Health Psychology. London: SAGE Publications Ltd; 2004.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Vaismoradi M, Turunen H, Bondas T. Content analysis and thematic analysis: implications for conducting a qualitative descriptive study. Nurs Health Sci 2013;15:398-405. https://doi.org/10.1111/nhs.12048.
- Taylor B, Taylor B, Francis K. Qualitative Research in the Health Sciences: Methodologies, Methods and Processes. Oxford: Taylor & Francis; 2013.
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349-57. https://doi.org/10.1093/intqhc/mzm042.
- Kitzinger J. The methodology of focus groups: the importance of interaction between research participants. Sociol Health Illn 1994;16:103-21. https://doi.org/10.1111/1467-9566.ep11347023.
- Chisholm J. The Read clinical classification. BMJ 1990;300. https://doi.org/10.1136/bmj.300.6732.1092.
- Mansfield KE, Sim J, Croft P, Jordan KP. Identifying patients with chronic widespread pain in primary care. Pain 2017;158:110-19. https://doi.org/10.1097/j.pain.0000000000000733.
- Eden D, Aviram A. Self-efficacy training to speed reemployment: helping people to help themselves. J Appl Psychol 1993;78. https://doi.org/10.1037/0021-9010.78.3.352.
- Wanberg CR. The individual experience of unemployment. Annu Rev Psychol 2012;63:369-96. https://doi.org/10.1146/annurev-psych-120710-100500.
- Norström F, Virtanen P, Hammarström A, Gustafsson PE, Janlert U. How does unemployment affect self-assessed health? A systematic review focusing on subgroup effects. BMC Public Health 2014;14. https://doi.org/10.1186/1471-2458-14-1310.
- Warr P, Jackson P. Adapting to the unemployed role: a longitudinal investigation. Soc Sci Med 1987;25:1219-24. https://doi.org/10.1016/0277-9536(87)90369-8.
- Creed PA. Improving the mental and physical health of unemployed people: why and how?. Med J Aust 1998;168:177-8. https://doi.org/10.5694/j.1326-5377.1998.tb126775.x.
- Audhoe SS, Hoving JL, Sluiter JK, Frings-Dresen MH. Vocational interventions for unemployed: effects on work participation and mental distress. A systematic review. J Occup Rehabil 2010;20:1-13. https://doi.org/10.1007/s10926-009-9223-y.
- Rødevand L, Ljosaa TM, Granan LP, Knutzen T, Jacobsen HB, Reme SE. A pilot study of the individual placement and support model for patients with chronic pain. BMC Musculoskelet Disord 2017;18. https://doi.org/10.1186/s12891-017-1908-3.
- Landmark T, Romundstad P, Dale O, Borchgrevink PC, Vatten L, Kaasa S. Chronic pain: one year prevalence and associated characteristics (the HUNT pain study). Scand J Pain 2013;4:182-7. https://doi.org/10.1016/j.sjpain.2013.07.022.
- Areberg C, Björkman T, Bejerholm U. Experiences of the individual placement and support approach in persons with severe mental illness. Scand J Caring Sci 2013;27:589-96. https://doi.org/10.1111/j.1471-6712.2012.01056.x.
- Brouwer S, Franche RL, Hogg-Johnson S, Lee H, Krause N, Shaw WS. Return-to-work self-efficacy: development and validation of a scale in claimants with musculoskeletal disorders. J Occup Rehabil 2011;21:244-58. https://doi.org/10.1007/s10926-010-9262-4.
- Black O, Sim MR, Collie A, Smith P. A return-to-work self-efficacy scale for workers with psychological or musculoskeletal work-related injuries. Qual Quant 2016;51:413-24. https://doi.org/10.1007/s11135-016-0312-7.
- Lagerveld SE, Brenninkmeijer V, Blonk RW, Twisk J, Schaufeli WB. Predictive value of work-related self-efficacy change on RTW for employees with common mental disorders. Occup Environ Med 2017;74:381-3. https://doi.org/10.1136/oemed-2016-104039.
- Black O, Keegel T, Sim MR, Collie A, Smith P. The effect of self-efficacy on return-to-work outcomes for workers with psychological or upper-body musculoskeletal injuries: a review of the literature. J Occup Rehabil 2018;28:16-27. https://doi.org/10.1007/s10926-017-9697-y.
- Black O, Sim MR, Collie A, Smith P. Early-claim modifiable factors associated with return-to-work self-efficacy among workers injured at work: are there differences between psychological and musculoskeletal injuries?. J Occup Environ Med 2017;59:e257-62. https://doi.org/10.1097/JOM.0000000000001172.
- Black O, Sim MR, Collie A, Smith P. Differences over time in the prognostic effect of return to work self-efficacy on a sustained return to work. J Occup Rehabil 2019;29:660-7. https://doi.org/10.1007/s10926-018-09824-z.
- Dworkin RH, Turk DC, Farrar JT, Haythornthwaite JA, Jensen MP, Katz NP, et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain 2005;113:9-19. https://doi.org/10.1016/j.pain.2004.09.012.
- Mendoza T, Mayne T, Rublee D, Cleeland C. Reliability and validity of a modified Brief Pain Inventory short form in patients with osteoarthritis. Eur J Pain 2006;10:353-61. https://doi.org/10.1016/j.ejpain.2005.06.002.
- Rosenberg M. Society and the Adolescent Self-Image. Princeton, NJ: Princeton University Press; 1965.
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16:606-13. https://doi.org/10.1046/j.1525-1497.2001.016009606.x.
- Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, et al. The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation. Health Qual Life Outcomes 2007;5. https://doi.org/10.1186/1477-7525-5-63.
- Health Education England . E-Learning for Health Pain Management Programme n.d. www.e-lfh.org.uk/programmes/pain-management/ (accessed 2 July 2020).
- Tasmanian Health Service . Understanding Persistent Pain: Turning Down the Volume on Persistent Pain 2014. http://outpatients.tas.gov.au/__data/assets/pdf_file/0003/172578/CSS_-_Physiotherapy_-_Understanding_Persistent_Pain_Booklet.pdf (accessed 2 July 2020).
- YouTube . Live Active. Understanding Pain in Less Than 5 Minutes, and What to Do About It! 2013. www.youtube.com/watch?v=C_3phB93rvI (accessed 2 July 2020).
List of abbreviations
- BPI
- Brief Pain Inventory
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- ESW
- employment support worker
- GP
- general practitioner
- InSTEP
- Individualised Support To Employment Participation
- IPS
- individualised placement and support
- IQR
- interquartile range
- OT
- occupational therapist
- PCP
- primary care-based health-care professional
- PHQ-9
- Patient Health Questionnaire-9 items
- PPI
- public and patient involvement
- RCT
- randomised controlled trial
- RTW
- return to work
- RTW-SE
- Return-to-Work Self-Efficacy Scale
- SJP
- Solent Jobs Programme
- SME
- small and medium-sized enterprise
- TAU
- treatment as usual
- TSC
- Trial Steering Committee
- WEMWBS
- Warwick–Edinburgh Mental Wellbeing Scale
- WP
- work package
