Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 15/107/02. The contractual start date was in September 2016. The draft report began editorial review in October 2019 and was accepted for publication in June 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2021. This work was produced by Parsons et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2021 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Background and rationale for the research
The NHS is the biggest employer in the UK, with NHS England alone employing more than 1 million full-time equivalent staff. 1 As a whole, the NHS performs relatively poorly across many measures of staff health and well-being, with sickness absence rates that are 27% higher than the UK public sector average and 46% higher than the average for all sectors. 2 In 2009, Department of Health and Social Care research estimated that NHS trusts in England could save an average of £350,590 per year by reducing sickness absence. 3 Financial considerations aside, there is an important link between the positive well-being of staff and better patient care. 3
In Britain, common mental health disorders (CMDs), including depression and anxiety, are the main causes of sickness absence in the working population,4 and poor mental health is estimated to account for more than one-quarter of staff sickness absence in the NHS. 3,5 The full cost of CMDs in NHS staff is hard to quantify because, as well as direct financial impacts on the NHS, individual staff members and their families incur losses, and there is a financial cost to society as a whole. While the majority of staff who go on sick leave with CMDs will eventually return to work (RTW), 15% of staff on long-term sick leave with a CMD never RTW. 4 It is generally recognised that sickness absence caused by CMDs involves a complex myriad of factors; as well as the severity of the condition, occupational and personal issues play an important role. Therefore, an intervention to improve RTW following sickness absence because of a CMD needs to address the biopsychosocial causes of the absence.
A recent Cochrane review of workplace interventions to improve capacity for work in people on sick leave found that the quality of evidence about the clinical effectiveness and cost-effectiveness of workplace interventions for workers with CMDs was low. 6 If an intervention for NHS workers who are on sick leave with CMD could, in a way that was cost-effective, accelerate return to useful work and prevent sickness absence extending beyond 6 months, there could be major benefits for the affected worker, their colleagues, their employers and NHS patients.
Existing literature and interventional studies
Previous work has indicated that interventions to reduce time away from work due to CMDs are most likely to be effective if they are multifaceted. 7–10 Systematic reviews suggest that an intervention should include:
-
identification of obstacles to RTW11
-
work-focused cognitive–behavioural therapy (CBT)12
-
focused problem-solving13
-
optimisation of clinical treatment; goal-setting; and a step-wise, written RTW plan based on discussion between the participant and their manager14
-
both physical and mental health interventions15
-
consideration of workplace adjustments, including flexible working and graded RTW10,11
-
service co-ordination and communication of the RTW plan with other health-care professionals [general practitioners (GPs) in particular]. 16
Equally important is the maintenance of contact between the line manager and the sick-listed worker. 17 A comprehensive systematic literature search on RTW interventions specifically for workers with CMD produced similar results:9 it explored whether or not any of the interventions were specific to health-care, and found that most of the evidence concerned mixed groups of occupations and did not focus on a single sector.
Two important guidelines relevant to the management of workers on sick leave with CMDs have been published in the Netherlands and the UK. 8,18 The Dutch guideline8 is specific to CMDs. The National Institute for Health and Care Excellence (NICE) guideline on managing sickness absence18 applies to all types of illness, and its implementation needs to be tailored to specific conditions and the local context. A few studies have evaluated the use of the Dutch guidelines. A randomised controlled trial (RCT) comparing the implementation of the first edition (published in 2000) with care as usual (CAU)19 showed a decrease in the time to RTW among workers with minor stress disorders but not in those with other CMDs. Similarly, a follow-up RCT evaluating the effectiveness of the 2007 Dutch guideline in improving RTW of workers with CMD,20 which compared its use by appropriately trained occupational physicians with management by others who have not received such training, showed that occupational physician adherence to the guidelines did not result in an improved RTW (either time to full RTW or time to first RTW) for workers with a CMD. It is important to note, however, that in the Netherlands each employee is required to have a rehabilitation consultation with an occupational physician when they take sick leave beyond a specified period. This is not the case in the UK, where NHS staff who take sick leave would possibly not see an occupational health (OH) professional at all and, if they do, would most likely see an OH nurse. Therefore, although we took the evidence about the Dutch guideline into account in planning our study, we could not assume that the evidence would be generalisable to NHS workers.
A Norwegian RCT21 demonstrated that work-focused CBT combined with individual job support for those on sick leave with CMD led to increased work participation compared with CAU, especially in those who had been on sick leave for longer than 12 months. However, the trial was not set in a workplace and the results are unlikely to be transferable to the UK, particularly because the Norwegian National Insurance Scheme provides 100% coverage for income lost from CMDs. Thus, these results may not be generalisable to the UK.
Collaborative care interventions such as case management and interventions focused on work-orientated problem-solving have been widely adopted and adapted for specific health conditions and areas, including occupational rehabilitation. 22–26 In essence, case managers (who are often specially trained, allied health professionals) work collaboratively with patients to address their care and treatment needs, usually within a biopsychosocial framework. In the health-care context, the focus is specifically on the biopsychosocial assessment of needs; co-ordination and engagement of services and support; case review, and follow-up. At the time of the production of this report, an ongoing RCT in Sweden is evaluating a new, work-orientated, problem-solving intervention delivered in primary care by specially trained rehabilitation co-ordinators for employees on sick leave with a CMD for a minimum of 14 days and a maximum of 13 weeks. 22
The importance of combining workplace and clinical interventions is reinforced by the findings of a recent Cochrane review of interventions to improve RTW in people on sick leave with depression,12 and also by a systematic review of characteristics of interventions that facilitate RTW after sickness absence. 27 Although there have been few interventional studies in the UK, one investigation carried out at an NHS trust in England suggested that an intervention could be cost-effective if it was based on multidisciplinary case management delivered by trained OH case managers (mainly OH nurses). 24 Another, the EASY (Early Access to Support for You) study,28 based in a Scottish health board, also used case management. In both studies a biopsychosocial approach to assessment was a key component of the intervention.
Proposed timing of the intervention
The NICE guidelines advise that RTW interventions should be delivered between 2 and 6 weeks (and a maximum of 12 weeks) into a period of sickness absence. 18 Other publications recommend that the interventions to facilitate RTW following sickness absence should be delivered between 4 and 6 weeks after work cessation. 14,29,30 Previous UK studies of interventions for all causes of sickness absence have intervened after workers have been absent for 4 weeks24 or 1 day. 28 Smedley et al. ’s24 choice was based on evidence from Waddell14 on the pattern of RTW, albeit for all causes of absence or musculoskeletal disorders.
The EASY study intervention at day 1 was by telephone and was based on the management of sickness absence in ‘commercially successful companies’. 28 The recommendations from Waddell,14 Black and Frost,29 and NICE18 were based on data relating to all causes of sickness absence, with the premise that most workers who are on sick leave RTW within 4 weeks without intervention. In contrast, the Dutch guidelines on RTW after absence due to CMDs8 recommend that the intervention should take place 2 weeks into the absence, and ongoing trials of interventions to improve RTW after sickness absence due to CMDs are intervening at ‘about two weeks’31 and before 3 months of sick leave (Professor Gunnar Bergström, University of Gävle, 2017, personal communication).
In considering the timing of the intervention for our study, we looked at two sets of data from NHS workers on sick leave with CMDs. The NHS electronic staff record (ESR) system has a code (S10) for sickness absence due to anxiety/stress/depression and CMDs. We obtained all staff sickness absence data for code S10 at Guy’s and St Thomas’ NHS Foundation Trust for 2015 (which included three staff members whose sickness absence for CMDs commenced in 2014). The corresponding Kaplan–Meier curve showed that ≈ 30% of staff who were on sick leave with CMDs at Guy’s and St Thomas’ NHS Trust between 1 January and 30 November 2015 returned to work within 1 week (Figure 1). At the time of this research, at Guy’s and St Thomas’ NHS Foundation Trust, there was no policy for intervention until day 27 of sickness absence.
FIGURE 1.
Kaplan–Meier survival estimate.

These data suggest that ≈ 25% of the trust staff who were off sick with a CMD returned to work within 1 week of absence and that about half of trust staff were still absent after 3 weeks.
We also obtained data from NHS Digital (Table 1).
| Duration (days) of sickness absence | Incidents of sickness absencea (%) | Days absentb (%) |
|---|---|---|
| All sickness absence | ||
| < 7 | 62.56 | 5.97 |
| 7–28 | 18.47 | 11.38 |
| > 28 | 18.97 | 82.65 |
| Selected attendance reasonsc | ||
| < 7 | 21.23 | 1.10 |
| 7–28 | 30.86 | 9.28 |
| > 28 | 47.91 | 89.62 |
These data indicate that 21% of absences for CMDs lasted less than 7 consecutive days. If we deliver an intervention too early, we risk intervening unnecessarily for the ≈ 20% of workers who are likely to RTW within a few days, making it less likely that any benefits will be cost-effective. Moreover, evidence from studies about early interventions in workers who go on sick leave because of back pain indicated that very early intervention may obstruct recovery, owing, in part, to labelling and attention effects, which may encourage illness behaviour. 32 In the UK, absences of ≤ 1 week are self-certificated, and fit notes provided by a GP are unlikely to be practically available as a method of case ascertainment in a hospital employment setting until the second week of absence at the earliest. Beyond 8 days, the curve outlined in Figure 1 becomes less steep. Moreover, a fit note with a written cause of absence should become available by day 8 of absence. Therefore, delivery of our intervention as soon as possible after 8 days seemed a suitable and pragmatic choice, and aligns with the evidence and commissioning brief.
Patient and public involvement
Four patient and public involvement (PPI) representatives informed our application. A NHS human resources (HR) manager who has used an OH service for management of his own depression strongly welcomed the proposal and advised that it should be feasible to deliver in the NHS. In addition, following advice from a community interest group providing consultancy for NHS OH services, we also included NHS Employers and the NHS Health at Work Network on the panel of stakeholders. Our main patient representative has a CMD and works full time. She has been involved as a PPI representative for research studies at University College London. Our PPI representatives were involved in the development of the final protocol and commented on the plain English summary. In addition, our main (patient) PPI representative, who had a history of CMD, attended the stakeholder meeting and was involved in the development of the intervention and protocol. We also invited our main (patient) PPI representative to comment on the participation sheets, consent forms and questionnaires. At the end of the study, the PPI representatives helped us deliberate on the study findings, lessons learned and recommendations for future development work.
Data collection tools
In the feasibility study, we developed and tested the acceptability and feasibility of data collection tools that we proposed for use in a full trial. This allowed us to generate information that could be used to refine the design of the full trial at the same time. The measures of interest included clinical and occupational outcomes, and prognostic and cost-effectiveness indicators. The data were obtained largely through participant self-completed questionnaires and case report forms completed by case managers and field workers, and also included electronic data collected by the ESR system at each participating trust. ESR is in use across all NHS trusts and health boards, and has a specific code (S10) for sickness absence due to anxiety/stress/depression and mental health.
There is no consensus on the best tools for collecting data on relevant occupational outcomes. Indeed, recently published NICE guidelines33 specifically call for more research on how the clinical effectiveness and cost-effectiveness of workplace health policies and programmes can be measured. We chose tools that had been used successfully in other studies and were considered feasible for use in this study.
Clinical outcomes
Clinical improvement in CMDs, such as a decrease in the number or severity of symptoms, can be captured using a range of well-established assessment tools. In this feasibility study we used the Patient Health Questionnaire-9 items (PHQ-9) and Generalised Anxiety Disorder-7 (GAD-7) because they are brief and designed to be completed by the patient, changes in their score accurately reflect changes in symptoms of depression and anxiety, and they are free to use. 7,34 Furthermore, PHQ-9 is used by GPs and practitioners involved in the Improving Access to Psychological Therapies (IAPT) initiative, providing an opportunity to compare the outcomes of this study directly with routine care in non-NHS workers. In addition, we collected information on adherence to and change in use of medication.
Occupational outcomes
We measured time to full RTW (defined in this study as working the same days or hours per week as before sickness absence in an identical or equivalent role for at least 4 weeks) and time to partial RTW (defined as working any number of hours in any role) through the ESR and self-completion questionnaires. A study examining a multistakeholder perspective on the definition of RTW after sickness absence due to CMD found that definitions of RTW based on working days and hours may not accurately reflect the priorities of all stakeholders. 35 Therefore, we selected the most appropriate questions and discussed these with our PPI representatives, who approved the final version for our study.
A number of instruments have been developed to measure presenteeism and workability, such as the Work Ability Index (WAI)36 (to explore the effect of physical co-morbidity on work ability) and the Work and Social Adjustment Scale37 (to measure global functioning). Initially, it was our intention to use both of these measures of occupational outcomes to allow us to compare the results from the measures and to recommend one or both for use in a full trial. However, we reviewed the use of these in the research team and with our two external, international experts (Professor Carel Hulshof and Dr Karen Nieuwenhuijsen). The Work and Social Adjustment Scale contains only one item on work: ‘Because of my problem, my ability to work is impaired’ (score 1–8). We considered this unsuitable as a robust work ability outcome for this study. We then compared the WAI with the World Health Organization Disability Assessment Schedule 2.0 (WHODAS)38 at the suggestion of our international experts. Although the WAI is widely used in rheumatology medicine in assessing RTW, its validity has not been assessed in mental health. The WHODAS appears to have more face validity in mental health and work research because it has two specific items relating to areas that are important functional modalities and are frequently impaired in workers with CMDs. These are learning a new task and concentrating on something for > 10 minutes. Both of these impairments are known to be associated with CMDs. The WHODAS has been used in mental health studies on RTW. 39
Prognostic indicators
At baseline, we collected demographic data about personal characteristics such as age, sex, job, previous sickness absence and history of CMD and physical ill health. We enquired about expectations of full RTW and self-efficacy with regard to RTW because both of these indicators are strongly associated with RTW outcomes. 40,41 Self-efficacy with regard to RTW was measured by the Return-to-Work Self-Efficacy (RTW-SE) scale,42 a self-report tool that has shown promising reliability and prediction of actual RTW within 3 months.
Cost-effectiveness measures
To assess cost-effectiveness in a future trial, we collected data on the health and social care services that may be used more or less as a result of the intervention.
To this end, we used a short, self-completed version of the Client Service Receipt Inventory (CSRI). 43 The objective was to determine which services were used during study follow-up and how often. Although the questionnaire was relatively short, the list of services was deliberately comprehensive; this list can be reduced as a result of the feasibility study. A full trial will involve linking costs for treatment and control arms with clinical outcomes and also quality-adjusted life-years (QALYs). The most widely used measure for generating QALYs is the EuroQol-5 Dimensions (EQ-5D). 44 The EuroQol-5 Dimensions, five-level version (EQ-5D-5L), was used in the study, and the relationship between the utility weights derived from it and the clinical measures was explored. This indicated the appropriateness of the measure in a full study. Sensitivity of the utility weights to change in other measures was assessed using correlations and standardised mean responses. Costs of delivering the package of interventions, including OH nurse time, participant and manager time, and cost of training OH nurses in case management, were measured.
Other measures
In addition to the above, we collected information about rates of recruitment, adherence to the intervention in those allocated to receive it and the management of those allocated to CAU. In addition, we collected information on rates of follow-up, and participants’ referral to and uptake of IAPT services and the government’s Fit for Work service, in accordance with the funder’s commissioning brief.
Chapter 2 Trial design and methods
Research questions
The feasibility study was undertaken to address the following research questions:
-
What is the most up-to-date evidence about the efficacy and cost-effectiveness of interventions to improve RTW in workers who go on sick leave with a CMD?
-
What is the current practice of NHS OH departments in managing staff who go on sick leave with a CMD?
-
What form of intervention is most likely to be cost-effective in promoting RTW in NHS staff who go on sick leave with a CMD, and how can this be manualised (written as an instruction manual) to meet individual and organisational needs in different OH settings?
-
What data collection tools should be used to assess changes in clinical state and occupational functioning as a consequence of such an intervention?
-
How feasible and acceptable is it to train OH nurses as case managers? What is the impact of the training on skill acquisition during the study period? How much additional training would case managers need to achieve established competency targets and prevent decay in skills?
-
How feasible and acceptable would it be to deliver such an intervention in different NHS settings? What rate of uptake could be expected, and how good would the adherence by OH staff and study participants be? What would be the resource implications of the intervention?
-
If a trial were conducted to test such an intervention, how well would methods of recruitment and data collection work in practice? What rates of recruitment and follow-up would be expected? What would be the likelihood of ‘contamination’ if, within the same OH department, the intervention were delivered to some staff and not to others?
The study was a 37-month mixed-methods project with four complementary work packages (WPs) to address the aims and objectives:
-
WP1 – the aim was to gather evidence and information to develop a practical and acceptable evidence-informed intervention.
-
WP2 – the aim was to gather information to develop a pragmatic protocol to evaluate the feasibility of the intervention.
-
WP3 – the aim was to test the feasibility and acceptability of the intervention in the NHS and to assess for contamination if the main trial were to be a RCT at departmental level.
-
WP4 – the aim was to inform the preparation for a future multisite trial in the UK.
The project addressed two elements of the development and evaluation process (i.e. developing the evidence base and feasibility) of the Medical Research Council (MRC)’s Framework for Developing and Evaluating Complex Interventions. 45 WP1 took account of Process evaluation of complex interventions: Medical Research Council guidance. 46
We used both qualitative and quantitative measures to allow an initial evaluation of process at this feasibility stage, particularly of the impact of context (NHS employment setting). We included both quantitative measures and more detailed qualitative analysis, with an iterative loop that allowed the basic assessment and development of fidelity and reach of the intervention during this feasibility stage. We anticipated that, should the intervention prove to be feasible, further process evaluation, including further work on fidelity, dose and mechanisms of impact, would be built in at the full trial stage.
Ethics approval and research governance
This study fell under the category of ‘research limited to the involvement of NHS or social care staff recruited as research participants by virtue of their professional role’ and, therefore, did not require ethics approval under the Governance Arrangements for Research Ethics Committee (GAfREC). Notwithstanding, approval to conduct the study within the NHS was granted from the Health Research Authority (IRAS reference 209317).
Data collection and follow-up
Outcomes were assessed using a mix of qualitative and quantitative methods.
Quantitative data
We collected the same data on all participants and participating trusts. Data from all groups (to which participants were allocated) were used to answer questions about rates of recruitment and follow-up, as well as the acceptability and performance of methods to assess possible outcome measures. Data from group A (intervention arm) and group D (intervention arm) provided information about the acceptability and costs of the intervention, as well as rates of adherence to the intervention. Data from group B (CAU arm) and group C (CAU arm) provided information about the distribution of possible outcome measures in the absence of the intervention (which would help in power calculations for a subsequent trial). Comparison of the management of participants in groups B and C gave an indication of the potential for major contamination. The follow-up period was 6 months from recruitment.
Before recruitment started, sites were advised on how to collect sickness absence data from their trust’s ESR. We assisted participating OH departments in liaising with their HR departments to ensure that the HR departments accurately recorded fit notes reporting CMD with the correct code (S10) in the ESR system.
Data on sickness absence for a CMD were collected at 6 months after the participant entered the study using data coded as S10 on the participating centre’s ESR and by self-report questionnaire. Additionally, we collected data about the distribution of possible outcome measures, including change in anxiety/depression, health-related quality of life, change in antidepressant use and RTW during the 6-month study period. Full and partial RTW was measured by total days of sickness absence before RTW (whether partial or full RTW). We collected information about participants’ referral to and uptake of IAPT services and the government’s Fit for Work Service.
Questionnaires were completed by study participants at the time of entry to the study and at 3 and 6 months after entry to the study. All participants in both arms completed the same baseline and intermediate questionnaires; however, responses provided in the intermediate questionnaire determined which version of the final questionnaire was used. Version 1 was used for participants back at work in any capacity for more than 4 weeks at the 3-month time point. Version 2 was administered to participants on sick leave due to a CMD at the intermediate questionnaire (including those who had not returned to sustained work) and those who did not return the intermediate questionnaire.
Participants were invited to complete hard-copy questionnaire booklets, and pre-paid envelopes were provided to facilitate return to the central research team. A series of reminders were used to encourage return of the study questionnaires. Reminders were sent as follows: one reminder via e-mail, one reminder via telephone and, finally, a second copy of the questionnaire booklet sent to the participants’ preferred postal address. This reminder strategy was used successfully in another OH study47 and was adopted for use in this study. Contact details were collected with the baseline questionnaire so that the follow-up questionnaires (and reminders, if needed) could be sent.
We recorded reasons for non-participation, baseline characteristics of those eligible for inclusion, adherence to the intervention in those allocated to receive it and the management of those who were not allocated to receive the intervention. We also recorded any protocol violations, reasons for not completing the intervention and any adverse events. Costs of delivering the package of interventions, including OH nurse time, participant and manager time, and cost of training OH nurses in case management, were also measured.
At the sponsor site (Guy’s and St Thomas’ NHS Foundation Trust), as well as at another non-participating NHS trust where a co-investigator was employed, additional exploratory work was completed to better understand the factors affecting the identification and referral of staff who were on sick leave with a CMD. Where appropriate and with relevant permissions, this included reviewing information on existing management referrals made to the OH department.
Qualitative data
Qualitative data collection was undertaken using semistructured focus groups and one-to-one interviews, once the quantitative data collection was complete. The qualitative work explored views and experiences in relation to:
-
strategies for screening and recruiting study participants, and for promoting the study across trusts (including barriers and enablers)
-
motivation for taking part in the study
-
RTW processes
-
communication pathways established during the study
-
use of study documentation and resources (usefulness and acceptability)
-
case manager training workshop (content, delivery and acceptability)
-
delivery of the case management intervention (how it worked in practice)
-
recommendations to consider for a future full trial.
Most of the interviews were conducted locally at each of the participating sites. Individual telephone interviews were conducted for those unable to attend in person. Purposive sampling was used to invite participants to take part in the focus group and interviews. Pilot interviews were carried out to assess comprehension, relevance and appropriateness of the interview schedule. We conducted one or two focus group sessions at each participating site, with the exception of Royal Papworth Hospital NHS Foundation Trust, which decided to withdraw from the study soon after participant recruitment commenced and chose not to participate in the follow-up interviews.
The central research team provided the local field workers with wording to promote and advertise upcoming focus group sessions, and requested that they promulgate this information via appropriate communication channels. Those interested in taking part were asked to contact the central research team so that further details (date/time/location) could be provided. Study participants (sick-listed workers participating in the study) were individually invited by e-mail to take part in a one-to-one interview. All participants in the focus groups and individual interviews were sent a participant information sheet at least 1 week before sessions were held and were given a chance to ask any questions that they may have in a telephone call with a member of the central research team. Prior to the commencement of each session, participants were asked to complete a consent form. For telephone interviews, verbal consent was taken and recorded on a paper consent form. Sessions took place in a quiet location and typically lasted 60–90 minutes. Most focus groups were facilitated by two members of the central research team (GG and VP) and one-to-one interviews were facilitated by one member of the central research team. Sessions were recorded on a digital audio-recorder and transcribed verbatim shortly after each session by a fully skilled medical secretary contracted by Guy’s and St Thomas’ NHS Foundation Trust. Audio-recordings were retained after transcription and will be kept for 20 years. No identifiable information was included during the transcription process. Transcripts were stored electronically using password protection. All transcriptions were uploaded onto NVivo version 8 (QSR International, Warrington, UK) to facilitate data management and coding.
Statistical methods
For the purpose of the intention-to-treat analysis, participants were considered as entered into the study on completion of the baseline questionnaire.
Quantitative analysis
In keeping with the objectives of this feasibility study, no formal statistical analysis beyond simple descriptive presentation of results was undertaken.
Rates of recruitment were calculated from the numbers of eligible participants and those who agreed to participate in the study. Characteristics of eligible participants were recorded at baseline and were summarised through means, medians, standard deviations (SDs) and interquartile ranges (IQRs). Outcome variables, including anxiety/depression scores, health-related quality of life scores and use of antidepressants, were summarised separately for baseline and follow-up. RTW time (full, partial or modified) was summarised and we compared data on RTW from participants’ self-report with data provided by case managers.
For each possible outcome measure, the prevalence of missing data was quantified. We calculated the proportion of participants who completed the intervention and the proportion of completed data sets.
Qualitative analysis
The interview and focus group transcripts were analysed using a thematic analysis approach as a guide. 48 This was chosen as the most suitable method to use on the basis that it is not aligned to any pre-existing theoretical or epistemological framework, and is widely considered a flexible and useful research tool. The qualitative components for the study, including the questions used in the interview schedules, were developed with the realist perspective in mind because we were interested in understanding the experiences and views of those who took part in the study (participants, OH case managers, line managers and HR personnel) as described in their own accounts.
The aim of the thematic analysis at this stage was to identify important and meaningful patterns in the data and to provide insights to account for the experiences and views of those involved in the study. As outlined in the study protocol, we initially planned to follow a six-phase, structured approach:
-
transcription of all interviews by a professional transcriber
-
familiarisation with text and creation of an initial list of emerging themes
-
coding of transcriptions uploaded to NVivo, a qualitative software package that allows data to be annotated as codes and cross-referencing of these codes
-
categorisation and interpretation through additional coding phases and development of representative themes and theoretical concepts emerging from analytical induction and cross-checking with an additional researcher on the team
-
identification of thematic frameworks in additional discussions with the team, which focused on further refinement through constant comparison within and between codes to ensure that the framework reflected the data
-
linking of findings with existing or newly generated theoretical concepts and models to provide context and confirm the relevance and robustness of the key findings of the study.
However, for pragmatic reasons we decided to adopt the following approach to the qualitative analysis. We initially created separate thematic coding frames in NVivo for each of the three qualitative data collection groups (focus groups, case managers and study participants). The final coding frame for each group can be found in Appendix 1. Most insights were derived primarily from research areas of specific interest included as topics in the interview guide (deductive analysis). These included site set-up, study promotion, participant recruitment, delivery of the intervention, stakeholder engagement and communication, and case manager training. In this regard, the analysis stopped short of developing overarching themes and subthemes (or a thematic map) because our focus was on addressing each of the specific research questions and objectives. As recommended by Braun and Clarke,48 we used this analytical approach, which did not occur in a linear fashion but rather reflected a process of going back and forth between different phases. A brief description of activities undertaken is given below.
Familiarisation of the data
Transcripts were read and re-read by two study team members (GG and VP). Where necessary, audio-recordings were listened to again to correct any minor discrepancies in the transcriptions. Importantly, this familiarisation with the qualitative data was enhanced by the involvement of the two study team members as facilitators of the focus group and individual interviews. In addition, this provided the two study members with an opportunity to develop and agree on, in consultation with the qualitative expert on the study (Stephani Hatch), the thematic coding frame to be used for the data analysis.
Generating initial codes and making annotations
Transcripts were coded (by either GG or VP) into NVivo using the thematic coding frame. This process enabled the data to be organised in a systematic and structured manner, ensuring that important and meaningful segments of data were extracted and applied to relevant codes (areas of interest), which allowed for additional codes (and nodes) to be created as new and emerging insights were revealed. Free-text annotations were also recorded next to relevant data extracts, allowing us to record our own interpretations of their significance during this phase.
Searching for themes
Once all transcripts had been coded into NVivo, the two researchers independently reviewed the collated extracts that had been coded to each code and deliberated on their significance and meaning (including the relationship between different codes) with the research questions and objectives in mind, until broad descriptions of the relevant codes were described in detail and supported by relevant verbatim quotations.
Rigour and trustworthiness
Several strategies were used during the study to demonstrate rigour and trustworthiness that were in keeping with fundamental principles of qualitative methods and analysis, for example collecting data using a variety of methods, constructing an audit trial to describe the approach used (including during the thematic analysis phase) and a peer review process to validate and question the analytic linkage being made between the data, coding framework and emerging insights.
A distress protocol was developed. The research team members who conducted the individual and focus group sessions were qualified health-care professionals and had experience providing counselling support. This allowed us to provide immediate support, if necessary, as well as providing the participant with information about local services and resources. In addition, the interviewers were supported by co-investigators with extensive clinical experience in occupational medicine and occupational psychiatry. We took a number of different measures to prevent and minimise upset; for example, participants were given the option to skip questions if they did not wish to provide an answer. Participants were also informed during the consent stages that they were free to withdraw from the study at any stage without giving a reason.
A further in-depth systematic thematic analysis exploring the broader myriad of issues (e.g. organisational, personal and cultural) relating to the provision of OH support for NHS staff with a CMD is proposed to be undertaken at a later time, with the emerging themes and subthemes published subsequently. At the time of writing this report, we have already progressed with a second independent rater, who was not involved in the formulation of the thematic coding frame and has not carried out any coding using the thematic coding frame, and who is now conducting an independent analysis of three random transcripts, one transcript from each study group. The purpose of this exercise is to compare and contrast relevant patterns in terms of insights that were identified by the two independent assessment approaches.
Economic analysis
Background
Establishing whether or not health-care resources are used in a way that represents value for money is necessary in a resource-constrained system. A full trial of this intervention would include a cost-effectiveness analysis in which health-care costs (including those of the intervention itself) would be combined with outcomes. This feasibility study explored the measurement of service use and health-related quality of life.
Aims and objectives
The objectives of the health economic component of the feasibility study were to (1) examine the feasibility of collecting service use data with the CSRI,43 (2) examine feasibility of collecting EQ-5D-5L data,49 (3) assess the appropriateness of the EQ-5D-5L in this population and (4) estimate intervention costs. Because this was a feasibility study, we did not focus on the costs of health services but rather their use, and we did not conduct a cost-effectiveness analysis. This would need to be done in a full trial.
Methods
The CSRI was developed in the 1980s and is a schedule commonly used to measure the use of services over a defined period. It is usually adapted for each study. We identified key services that we thought may be used by participants and asked participants at baseline and follow-up whether or not they had used these in the previous 3 months. We also asked for information on how many contacts were made. In the feasibility study we were particularly interested in the number of contacts made and what services were used.
The EQ-5D-5L is used to measure health-related quality of life. It consists of five dimensions (mobility, self-care, usual activities, pain/discomfort and anxiety/depression). Each of these receives a score of 1 (no problem in that area) to 5 (extreme problems). The EQ-5D-5L is used to generate QALYs by attaching weights anchored at 1 (full health) and 0 (death) to the health states that can be derived from the EQ-5D-5L. Scores < 0 are also possible for states considered worse than death.
Intervention costs were calculated based on the cost of training time, materials and therapy time. This information was recorded centrally by the research team.
Chapter 3 Work package 1
To inform intervention development and delivery in WP2 and WP3, we gathered relevant evidence through a systematic review of the literature and established CAU. In addition, we developed the intervention and data collection tools through an iterative process. Specific details are outlined in this chapter.
Systematic review of the literature
The systematic review of the literature concerned research question 1: what is the most up-to-date evidence available on the efficacy and cost-effectiveness of interventions to improve RTW in workers who go on sick leave with a CMD?
Study design
This was a systematic review of the literature.
Key questions:
-
Which workplace-based interventions are effective in improving RTW outcomes for workers with a CMD?
-
What are the key elements of effective interventions?
-
Are any interventions specific to the health-care sector?
-
Are any interventions specific to the UK?
Methods
Inclusion and exclusion criteria
-
The inclusion criteria focused on interventions based in the workplace that have RTW or work absence as outcomes.
-
We excluded papers in which the results were not presented separately for workers with CMDs or a specified subset of CMDs.
Search strategy
A comprehensive systematic review by Pomaki et al. 9 on RTW/stay-at-work interventions for workers with CMDs included studies up to November 2009. We extended that review to cover the 7-year period from 1 November 2009 to the end of September 2016.
Search terms
We combined three groups of terms (‘worker’, ‘mental health’, ‘intervention’) using an AND strategy. We restricted our search to English-language papers because papers in other languages are less likely to be relevant to the UK health-care service setting. We searched for systematic reviews, meta-analyses and primary quantitative and qualitative studies in five electronic databases [MEDLINE, EMBASE, Cumulative Index to Nursing and Allied Health Literature (CINAHL), PsycINFO and the Cochrane Database of Systematic Reviews]. The electronic database searches were supplemented by including the results of two relevant active reviews that had been identified on the International Prospective Register of Systematic Reviews (PROSPERO) (an international database of prospectively registered systematic reviews in health and social care, welfare, public health, education, crime, justice and international development where there is a health-related outcome):
-
Lyssenko L, Hahn C, Kleindienst N, Bohus M, Ostermann M, Vonderlin R. A Systematic Review of Mindfulness-Based Interventions in Occupational Settings. PROSPERO 2015: CRD42015019282. 50
-
Fishta A, Weikert B, Wegewitz U. Return-to-Work (RTW) Interventions for Employees with Mental Disorders: An Overview of Systematic Reviews. PROSPERO 2015: CRD42015023496. 51
At the time of the production of this report, both reviews were ongoing (to be completed).
To inform the systematic review of the published scientific literature, two guideline documents relevant to the management of workers on sick leave also informed the intervention development phase: (1) the Dutch national guideline,8 which is specific to CMDs, and (2) the NICE guideline on managing sickness absence. 18 The existing literature suggested that an intervention should include identification of obstacles to RTW,11,52 work-focused CBT,12 focused problem-solving,13 a focus on participant engagement and motivational interviewing (MI) techniques, optimisation of clinical treatment, goal-setting, written RTW plans based on discussion between the participant and their manager,14 consideration of workplace adjustments including flexible working and graded RTW, regular review and communication of the RTW plan with other health-care professionals, in particular GPs who are treating participants,11,16 along with maintenance of contact between the line manager and the sick-listed worker. 17
Data extraction and appraisal
A data extraction template was developed, focusing on the population to which the intervention was delivered, the setting of the intervention, the components of the intervention, economic costs, outcome measures and effect sizes. We appraised the papers and guidelines, taking into account the methodological quality of each paper, biases and confounders, and the direction of bias and size of effect of interventions. For RCTs we used the Cochrane risk of bias tool to assess the methodological quality of the trial. 53 Two reviewers appraised all papers independently. Where agreement was not obtained, papers were referred to a third reviewer. A meta-analysis was not conducted because of the high degree of heterogeneity of the included studies.
Outputs
We reported the systematic review based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. 54
Results
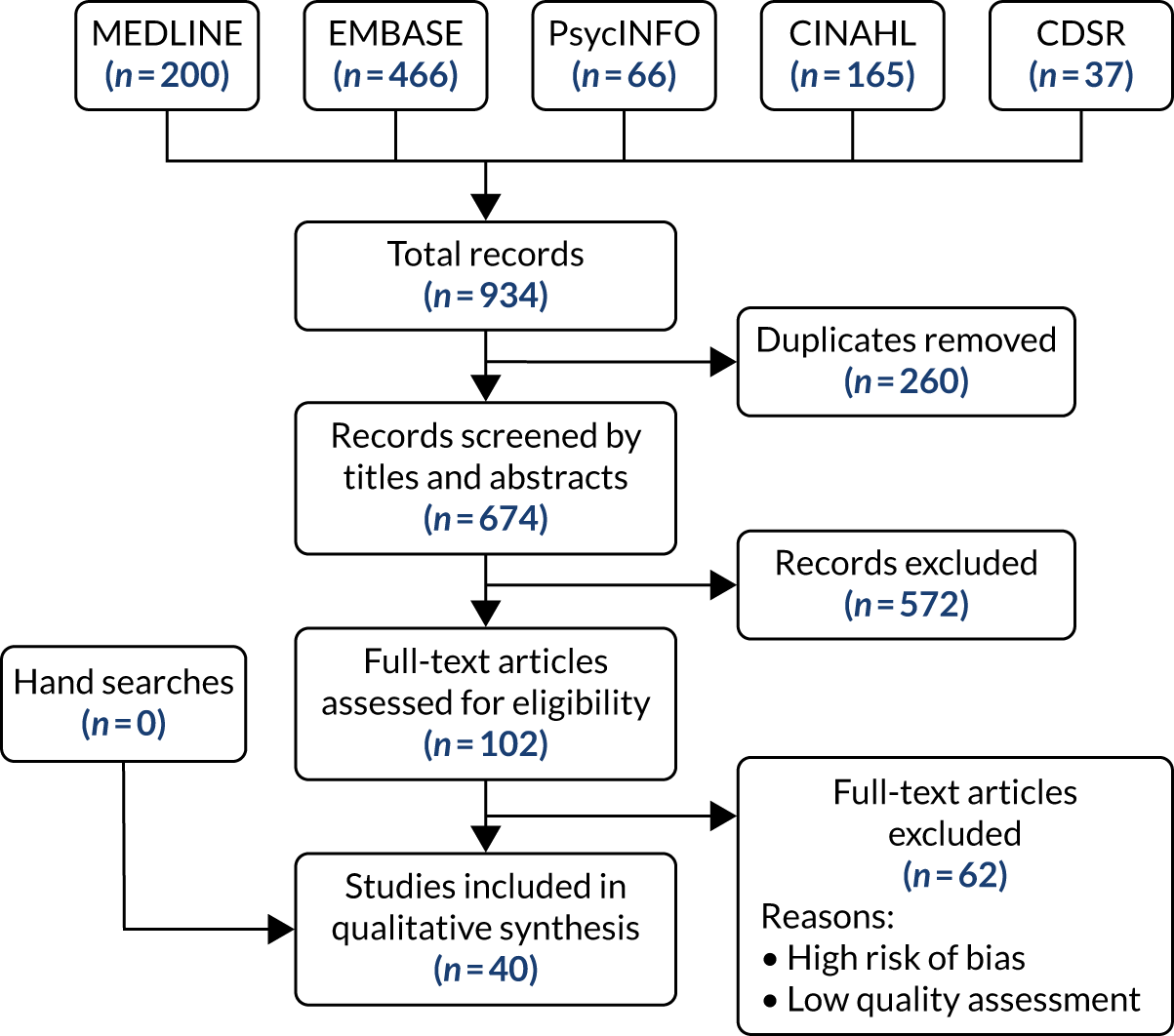
A total of 934 articles were retrieved from five databases (Figure 2). In total, 40 articles were included for qualitative synthesis and are listed in Table 2. Our search was sensitive because it included all CMDs. The majority of the 572 records excluded at the title/abstract stage were excluded because of studies not presenting results on CMDs.
FIGURE 2.
The PRISMA flow diagram of included studies. CDSR, Cochrane Database of Systematic Reviews.
| Number | Article |
|---|---|
| 1 | Netterstrom et al.55 |
| 2 | Bhui et al.56 |
| 3 | van der Feltz-Cornelis et al.57 |
| 4 | Cowls and Galloway58 |
| 5 | De Zeeuw et al.59 |
| 6 | Sahlin et al.60 |
| 7 | Eklund et al.61 |
| 8 | Evans-Lacko et al.62 |
| 9 | Falkenberg et al.63 |
| 10 | Grossi and Santell64 |
| 11 | Haraguchi et al.65 |
| 12 | Hees et al.66 |
| 13 | Hees et al.67 |
| 14 | Arends et al.68 |
| 15 | Jansson et al.69 |
| 16 | Joosen et al.70 |
| 17 | Joyce et al.71 |
| 18 | Reid et al.72 |
| 19 | Kroger et al.73 |
| 20 | Lagerveld et al.42 |
| 21 | Lagerveld et al.74 |
| 22 | Lemieux et al.75 |
| 23 | van Vilsteren et al.6 |
| 24 | Mackenzie et al.76 |
| 25 | Martin et al.77 |
| 26 | Nieuwenhuijsen et al.12 |
| 27 | Noordik et al.78 |
| 28 | Noordik et al.79 |
| 29 | Noordik et al.80 |
| 30 | Pomaki et al.81 |
| 31 | Rebergen et al.19 |
| 32 | Rebergen et al.82 |
| 33 | Reme et al.21 |
| 34 | Van Oostrom et al.83 |
| 35 | Van Oostrom et al.84 |
| 36 | Shippee et al.85 |
| 37 | Simpson et al.86 |
| 38 | Vlasveld et al.87 |
| 39 | Volker et al.88 |
| 40 | Hees et al.89 |
The following were key findings and recommendations from the systematic review and informed the development of the case management intervention; they relate to questions 1 (which workplace-based interventions are effective in improving RTW outcomes for workers with a CMD?) and 2 (what are the key elements of effective interventions?):
-
We found strong evidence suggesting that workplace-focused interventions significantly reduce the time until partial RTW, and low-quality evidence that they do not significantly reduce time to full RTW compared with no treatment.
-
The systematic review included four economic evaluations: two workplace-focused interventions were found to be cost saving from the perspective of the employer60,71 and two studies showed no economic benefit compared with CAU. 21,80
-
A review of qualitative studies58,69,78,86 that focused on the RTW process found that, from the employee perspective, the following considerations were prominent: (1) concerns about reduced working capacities, (2) difficulty setting limits in demanding work situations, (3) a sense of responsibility and a fear of being a burden to an employer, (4) recognition of exhaustion and (5) the need to control cognitions and behaviour such as perfectionism. An interesting finding was that most workers were able to describe solutions; however, few workers expressed an intention to implement or utilise the solutions in the workplace, with the exception being structural adaptations of work demands.
-
Several studies have demonstrated that a number of baseline characteristics appear predictive of a longer duration of sickness or poor RTW outcomes. These include a low level of education, a history of sickness absence, low self-esteem, low social functioning, older age and negative expectation regarding RTW.
-
Evidence suggests that different stakeholders have different perspectives regarding barriers to RTW. For example, employers tend to underestimate the importance of the work environment, whereas health-care professionals emphasise remaining at work, maintaining contact with employers and support in the work environment as important.
-
We found strong evidence that interventions should be based in the workplace and should involve problem-solving and an element of work-focused behavioural therapy.
For question 3, we found no interventions specific to the health-care sector.
For question 4, we found no interventions specific to the UK.
Collectively, the literature review suggested that our new intervention should include:
-
identifying obstacles to RTW11
-
work-focused CBT12
-
focused problem-solving13
-
focus on participant engagement and MI techniques, optimisation of clinical treatment, promoting sleep hygiene, goal-setting, written RTW plans based on discussion between participants and their manager14
-
workplace adjustments including flexible working and graded RTW, regular reviews, and communication of the RTW plan with other health-care professionals, in particular GPs who are treating participants11,16
-
maintenance of contact between the line manager and the sick-listed worker. 17
Discussion
The systematic review exercise was undertaken as an extension of the earlier review by Pomaki et al. ,81 and provided an important opportunity to incorporate updated information and learnings from the literature when developing our new case management intervention. We confirmed that interventions to improve RTW following sick leave with a CMD should be based in the workplace and based on work-focused behavioural changes. Although we undertook a comprehensive literature review, a more recent systematic review and meta-analysis52 exploring predictors of RTW for people on sick leave with CMDs was not completed during this present study, and so the findings and recommendations of this could not be taken into consideration when developing our case management intervention. 90–94 Another, concurrent review94 suggests that future interventions designed to facilitate RTW for people with CMD should attempt to ameliorate high workload issues. Our systematic review enabled us to identify key components of our proposed intervention.
Survey of care as usual
The survey of CAU concerned research question 2: what is the current practice of NHS OH departments in managing staff who go on sick leave with a CMD?
The published article relating to the survey of CAU95 can be found elsewhere.
Study design
This was a cross-sectional survey of OH departments providing OH services to NHS trusts and health boards.
Methods
We identified OH departments providing OH services to NHS trusts and health boards from two lists. Specifically, 122 providers of NHS OH services were identified from the NHS Health at Work Network and four providers were identified from the Commercial Occupational Health Providers Association. These 126 providers were invited to complete the survey of CAU.
We designed a 12-item electronic questionnaire that enquired about how OH providers currently manage NHS staff who go on sick leave with a CMD. We included questions on the type(s) of trust to which they provide OH services, who delivers the intervention, the nature of the intervention, how the line manager is involved, whether or not the workers have rapid access to mental health assessments or treatment (including CBT), and whether or not a worker’s treating health-care professional is involved.
The questionnaire was piloted among the 35 OH departments taking part in the SCIN (Skin Care Intervention in Nurses) trial. 96 We confirmed that nine OH departments were willing to take part in the feasibility study and use electronic OH data collection systems that would enable us to collect the data required for this study. We included OH departments that provide a service to acute and mental health trusts. NHS staff working in ambulance trusts have the highest sickness absence rates of all health-care workers, and the organisational structure of ambulance trusts is very different from that of acute trusts. In the light of this, we were keen to include an ambulance trust in our feasibility study. Because only one of the 35 centres we contacted provided OH care to an ambulance trust, we contacted one of the largest ambulance trusts in England (West Midlands Ambulance Service University NHS Foundation Trust). This trust completed the questionnaire and confirmed its willingness to participate in the feasibility study. Accordingly, we selected six NHS OH providers to take part in the feasibility study, with one as a reserve. The reserve site was intended to be opened if one of the existing sites withdrew at a very early stage during the study. Although Papworth Hospital NHS Foundation Trust subsequently withdrew from the study, it was not feasible because of time constraints to train an additional case manager from the reserve site.
Data analysis
We used descriptive statistics to summarise the patterns of management of CMDs.
Outputs
The information we collected gave us a picture of usual management of NHS staff who go on sick leave with a CMD.
Results
A total of 49 out of 126 (39%) OH providers who were invited to complete the survey responded. We found that the majority (98%) of respondents reported that they had an organisational policy specifically relating to the management of sickness absence that also included triggers for referral for staff on sick leave with a CMD. In 63% of cases, referrals by line managers of sick-listed staff with a CMD to OH occurred between 8 and 28 days after commencement of sickness absence. A total of 10 respondents (20%) accepted referrals on the first day of absence and one respondent accepted referrals as soon as a fit note was received. Timely access to assessment by a psychiatrist or therapist was available to 82% of respondents, whereas early access to treatment by a mental health professional, through online CBT or via a counselling or employee assistance programme service, was available to 88% of respondents. Table 3 details the usual clinical aspects covered during the first consultation.
| Element | Never/sometimes, n (%) | Often/always, n (%) | Do not know, n (%) |
|---|---|---|---|
| Exploration of typical symptoms of CMD | 0 (0) | 49 (100) | 0 (0) |
| Administration of standardised questionnaires | 20 (41) | 29 (59) | 0 (0) |
| Assessment of medication | 1 (2) | 48 (98) | 0 (0) |
| Assessment of non-pharmacological treatment | 4 (8) | 44 (90) | 1 (2) |
| Assessment of drug and alcohol misuse | 4 (8) | 45 (92) | 0 (0) |
| Assessment of risk to self (i.e. suicide and self-harm) | 3 (6) | 45 (92) | 1 (2) |
| Assessment of risk to colleagues and patients | 4 (8) | 45 (92) | 0 (0) |
| Assessment of support needs | 1 (2) | 48 (98) | 0 (0) |
| Signposting to support services (e.g. EAP) | 2 (4) | 46 (94) | 1 (2) |
| Identifying workplace barriers to RTW | 0 (0) | 49 (100) | 0 (0) |
| Identifying non-workplace barriers to RTW | 2 (4) | 47 (96) | 0 (0) |
| Problem-solving and goal-setting for RTW | 5 (10) | 43 (88) | 1 (2) |
| Consideration of workplace adjustments | 1 (2) | 48 (98) | 0 (0) |
| RTW planning with staff member and their manager | 4 (8) | 44 (90) | 1 (2) |
| Case management | 19 (39) | 29 (60) | 1 (2) |
| Arranging regular, timed reviews | 18 (37) | 31 (63) | 0 (0) |
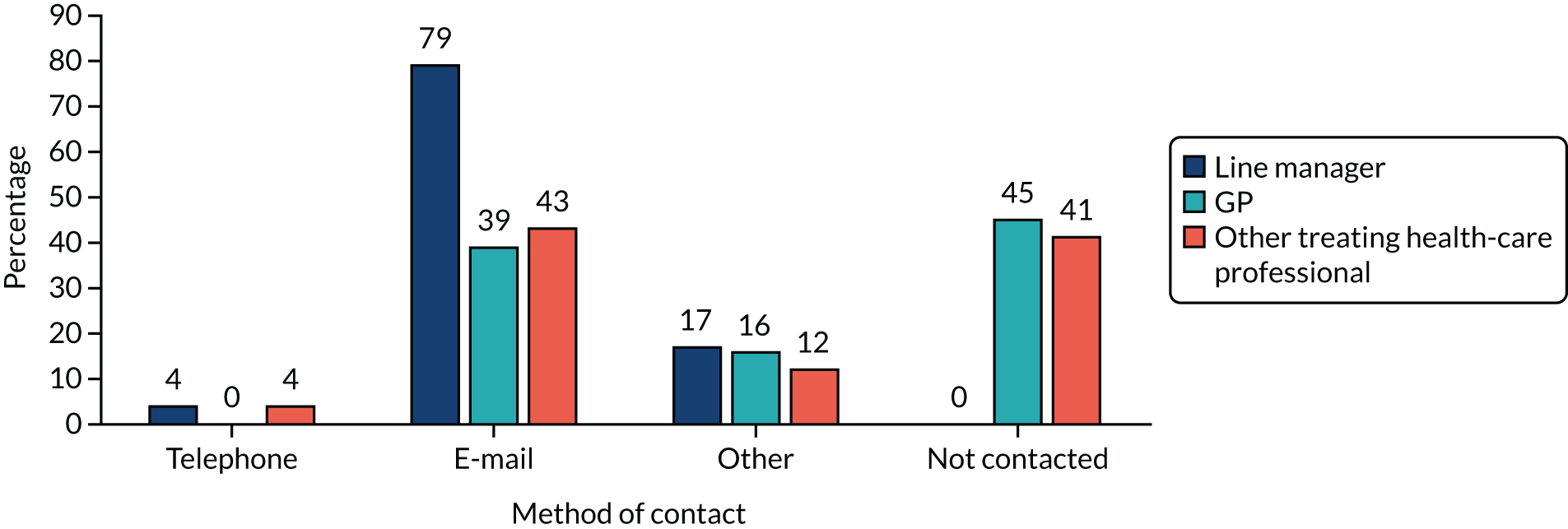
A key finding from the survey of CAU is that a large proportion of OH providers either do not deliver or only sometimes deliver a case management approach or regular, timed reviews (38.8% and 36.7%, respectively) for sick-listed workers with a CMD. Moreover, of those who reported that they do provide a form of case management or regular timed reviews, specific details with regard to the nature of both features were unknown. Forty-five OH providers (92% of responders) reported that a qualified OH professional, usually an OH nurse, undertook the first consultation. Seventeen (35%) OH providers always used face-to-face appointments for first consultations, while 22 (45%) OH providers used face-to-face consultations more than half of the time. The remainder predominantly used telephone consultations. All respondents provided contact and support for line managers of staff referred for CMDs. The most frequent advice provided was to maintain contact with sick-listed staff (86%). Most (80%) OH providers provided training for managers to better support staff with CMDs. The survey also found that some level of support or advice is provided by OH providers to line managers of NHS workers on sick leave with a CMD. Contact with the staff member’s GP or mental health professional was less consistent, and when this occurred contact was most commonly made by e-mail (Figure 3).
FIGURE 3.
Methods of contact initiated between OH providers and other stakeholders.
Discussion
This was the first national survey to report on current OH management practices for NHS staff with a CMD. This survey found noteworthy variation in the elements comprising the first OH consultation for NHS workers who are on sick leave with a CMD, particularly with regard to the time between the commencement of sick leave (in response to a CMD) and initial OH consultation. Our survey of CAU capitalised on one of the stated outputs of the SCIN trial: ‘to establish a network of NHS OH departments which would be in a good position to deliver future studies’. 96 Because only 39% of OH providers participated in the survey, an important limitation was the potential impact of non-response bias. Therefore, it is reasonable to argue that OH providers that are able to deliver superior OH services may have been more motivated to respond to the survey and, therefore, the results from this survey may not reflect routine OH management practices for sick-listed staff with a CMD. With regard to the variation in the method of conducting first consultation (i.e. telephone vs. face-to-face), these differences could be due to variation in OH service delivery (e.g. in-house OH service vs. external, contracted OH service). The findings from the survey highlight a need to promote the standardised adoption of early case management practices in the provision of OH services, which may facilitate the early and sustained RTW for NHS staff with a CMD. Embedding a standardised approach to the management of NHS staff with a CMD will also enable future widespread evaluation of OH services.
Chapter 4 Work package 2
Development and refinement of the intervention
The development and refinement of the intervention concerned research question 3: what form of intervention is most likely to be cost-effective in promoting RTW in NHS staff who go on sick leave with a CMD, and how can this be manualised (written as an instruction manual) to meet individual and organisational needs in different OH settings?
Study design
This was a two-stage, iterative consultation based on methodology that the chief investigator (Ira Madan) and co-investigator (Julia Smedley) have used in the development of national evidence-based guidelines. 97 This section describes the various stages used during the intervention development phase.
Stage 1: mapping of evidence from the literature and expert feedback
Methods
In April 2017, we conducted a 1-day mapping meeting, with seven members of the multidisciplinary research team (IM, JS, MM, MH, DJ, VP and our work/patient representatives) each contributing their expertise from their respective professional disciplines, including occupational medicine, occupational psychiatry, psychology and general practice. The objectives of the mapping meeting were threefold:
-
To discuss and deliberate on the evidence and learnings derived from the systematic review, taking into account participants’ professional expertise and knowledge.
-
To consider its relevance in relation to the scope and intention of the proposed intervention.
-
To map the relevant aspects of the evidence onto the preliminary case management intervention and to develop additional therapeutic resources (sleep hygiene leaflet and RTW resource booklets) that would underpin the intervention. This process was further refined with additional features added to the intervention. A step-wise flow diagram was created describing the key components of the intervention.
When developing the work-directed case management intervention for this feasibility study, care was taken to interpret the evidence in the context of its relevance to NHS staff and the NHS work environment. The definition of case management adopted for this study was that of Hutt et al. ,98 who propose that case management is a process typically comprising core stages such as patient assessment and planning, co-ordination of services and support and reviewing care. The core components of case management approaches commonly comprise case identification, assessment, care planning, care co-ordination (which can include medical management, self-care support, advocacy and negotiation, psychological support, monitoring and review) and case closure or discharge, with the option of providing time-limited case reviews where clinically necessary. We also recognised that the steps involved are non-linear and repeat reviews or further assessments may be required, as previously highlighted by Ross et al. 99
An iterative approach was adopted for intervention development. A particular focus when developing the intervention was the question: What form of intervention is most likely to be cost-effective in promoting RTW in NHS staff who go on sick leave with a CMD, and how can this be manualised (written as an instruction manual) to meet individual and organisational needs in different OH settings? The formulation of the provisional intervention model took account of the volume, quality and consistency of the evidence. Well-conducted studies with negative findings and studies that report significant associations were given appropriate weight. Where possible, we looked at the size of the effect of the intervention and considered the applicability of each intervention to our target population.
Output
The output was a provisional evidence-based model of a complex intervention to improve RTW among NHS staff on sick leave with a CMD. This was represented in the form of a flow chart.
Stage 2: stakeholder workshop
Methods
In May 2017, a 1-day multidisciplinary stakeholder workshop was held with participation from key stakeholder groups. The group comprised two OH nurses and an OH matron delivering OH services in the NHS setting, an NHS HR representative, representatives from the NHS Health at Work Network and NHS Employers, a representative from a health-care union (UNISON, London, UK) and our PPI representatives. The session was also attended by members of the research team (including an OH physician, GP collaborator, psychiatrist collaborator and post-doctoral research fellows) and was facilitated by the chief investigator. The purpose of the follow-up multidisciplinary stakeholder meeting was to deliberate on the proposed preliminary case management intervention, with a particular focus on the timing of each component of the intervention (referral to OH provision of first and subsequent appointments), referral pathways into the study, signposting follow-up services, the procedure for delivering each component of the intervention, agreement on the role and responsibility of each worker (line manager, HR and OH staff), and deciding on appropriate supplementary resources to make available to sick-listed workers and their line managers. In the stakeholder session, we also considered the optimal methods and screening tools for identifying and screening potentially eligible participants. In this feasibility study, we included in the study questionnaires Whooley questions100 and the PHQ-9 and GAD-7 to screen for depression and anxiety as recommended by NICE. 7 The aims of the workshop were to:
-
refine the map of the intervention, timelines, responsibilities, referral routes and checks and balances for each component of the intervention
-
encourage understanding, buy-in and ownership of the intervention for some of the staff who operated the system.
Outputs
-
A manualised model of the intervention, which we considered would be acceptable and feasible to its intended participants, for testing in the feasibility study.
-
A procedure for recruitment and selection of participants to enter the feasibility study.
In addition to the stakeholder workshop, the chief investigator and study co-ordinator met with two international experts from the Netherlands (Karen Nieuwenhuijsen and Carel Hulshof) in 2018 to review the proposed intervention model and seek their experience- and evidence-based advice so that further refinements to the intervention could be made.
Results
The preliminary case management intervention was developed using the iterative process (i.e. using results from the systematic review of the evidence on RTW and mental health, and mapping of the evidence onto the preliminary intervention) and was subsequently delivered in the feasibility study. As far as practicable, this is presented in keeping with the Template for Intervention Description and Replication (TIDieR) reporting requirements101 (Figure 4).
FIGURE 4.
Manualised model of the intervention (including recruitment and CAU pathways). PIS, participant information sheet.

The intervention was based on a case management approach delivered by an OH nurse (case manager) trained in a CBT-based approach to problem-solving in the context of CMDs. The assessment of the worker on sick leave followed a biopsychosocial approach and the focus of the intervention was on the present (forward looking): the case manager encouraged and facilitated active engagement with the sick-listed workers rather than providing passive instruction. The intervention included identification of barriers to RTW; problem-solving by the participant and manager, as recommended by Arends et al. 13 and Waddell et al. ;11 work-focused CBT [via online programmes, e.g. the HeadGear smartphone application (app) (version 1.1.27, Black Dog Institute, University of New South Wales, Sydney, NSW, Australia), or face-to-face therapy, depending on local access] as recommended by Nieuwenhuijsen et al. ;12 two evidence-informed leaflets on RTW (one for managers and and one for employees); optimisation of clinical treatment, goal-setting, peer-support networking, a written RTW plan based on discussion between the participants and their manager, and workplace adjustments including flexible working and graded RTW in discussion with the participant’s manager, as recommended by Waddell et al. ;11 maintenance of contact between the line manager and the sick-listed worker as recommended by Nieuwenhuijsen et al. ;17 communication of the RTW plan with the treating health-care professionals, including the participant’s GP; regular timed reviews as recommended by Stern and Madan16 and Waddell et al. ;11 and referral to an occupational physician or secondary services, if required. The intervention was delivered on receipt of a fit note (or management/self-referral to OH) or soon after. Consultations between case managers and sick-listed staff occurred in person, although there was the option for case managers to maintain contact by telephone, if necessary.
We used evidence from the systematic review to develop a bespoke information leaflet for managers on how to communicate with the sick-listed employee. The leaflet would be given to the line manager by the case manager. The line manager had the option to ask the case manager for additional practical advice on how to initiate supportive communication with a sick-listed employee who has a CMD. The evidence from the systematic review also informed the design of a bespoke sleep hygiene leaflet, especially for NHS workers with a CMD, as well as a My Action Plan (MAP) template to record actions employees would take to tackle their identified problems.
Discussion
The stakeholder group played a vital role in developing the intervention and ensuring that it would be acceptable to participants (employees), case managers, line managers and employers, which is in keeping with recommendations published in guidelines on developing and evaluating complex interventions. 45 Based on participants’ advice, we refined the pathways and processes of the intervention to maximise the chances of its success.
Based on the findings from this feasibility study, the preliminary manualised case management intervention was modified and finalised (see Figure 4).
Development of data collection tools
The development of data collection tools concerned research question 4: what data collection tools should be used to assess changes in clinical state and occupational functioning as a consequence of such an intervention?
Method
We developed a series of data collection tools that included self-report participant questionnaires and site-level case report forms that were completed by field workers (case managers and independent assessors). The study questionnaires were shared and discussed with our PPI representatives to obtain their views on comprehension and acceptability, particularly on the appropriate questions to measure RTW outcomes that are important for workers. We did not undertake reliability analysis on the data collection tools; instead, the research team made a decision about their suitability based on a review of the completeness of the data collected at the end of the study coupled with feedback on acceptability from our PPI representatives, participants, case manager and local field workers. This allowed us to assess whether or not the proposed data collection tools would be of sufficient scope to reliably report on each of the outcome measures.
Output
The output was a series of data collection tools for use in the feasibility study, including suitable questionnaires.
Results
A series of data collection forms (case report forms) were produced to record specific data relating to clinical, occupational, prognostic and cost-effectiveness measures. Data collection forms included participant self-completed questionnaires (i.e. previously validated tools including the PHQ-9, GAD-7, WHODAS, Work and Social Adjustment Scale, RTW-SE scale, CSRI and alcohol-use tools) and tools for the collection of site-level data by local field workers (including tools to record screening and recruitment activity, provision of CAU interactions, delivery of case management interventions, consultation time duration and sickness absence duration). The data collection tools used in this study are given in Table 4.
| Data collection tool | Completion by |
|---|---|
| Audit form | Independent assessor |
| CAU data collection form | Field worker |
| Checklist for case managers (intervention arm) | Field worker |
| Clinical form for initial consultation (form 1) | Field worker |
| Decliners questionnaire | Field worker |
| Eligibility form | Field worker |
| Monthly audit of fit notes received per department | Field worker |
| MAP | Study participant |
| Participant sickness record: ESR data | Field worker |
| Questionnaire A (baseline) | Study participant |
| Questionnaire B (3 months) | Study participant |
| Questionnaire C (6 months: control arm – has not returned to work) | Study participant |
| Questionnaire C (6 months: control arm – has returned to work) | Study participant |
| Questionnaire C (6 months: intervention arm – has not returned to work) | Study participant |
| Questionnaire C (6 months: intervention arm – has returned to work) | Study participant |
| Screening log: NHS workers | Field worker |
| Withdrawal form | Field worker |
| Withdrawal questionnaire | Study participant |
The site-level data collection tool capturing information on consultation time duration and number of follow-up consultations required was also suitable for use in the study. However, in relation to approaches for measuring time to RTW outcomes (partial or full), the results showed that there was poor agreement between the self-report and case manager feedback, and, unfortunately, this was consistent across the five possible outcomes (i.e. ‘RTW, any’, ‘RTW and stay continuously for > 4 weeks without any further sickness absence’, ‘returned to modified duties’, ‘returned to unmodified duties’, ‘returned to normal hours’). This observation reflects the accumulating evidence showing the inherent difficulty in reliably measuring RTW among sick-listed staff. 102
During the conduct of this study, researchers from the Netherlands undertook a project aimed at developing core outcome measures for sickness absence that can be used in research projects. In relation to measuring absenteeism (periods of sickness absence), the researchers recommended that recall of, at a maximum, 2 months could be collected by self-report from participants. Nevertheless, we found only modest consistency in the capacity of participants to accurately self-report ‘duration’ of recent episodes of sickness absence (i.e. during the study period) when these self-report data were compared with organisational sickness absence data (see Figure 9). Furthermore, we also found that not all participants were able to accurately recall each individual episode of sickness absence during the study period when we compared these self-report data with organisational data (although we also acknowledge that organisational sickness absence data are prone to inaccuracies). Collectively, this suggests that self-reported sickness absence is not a reliable measure to use alone.
A further complication with capturing RTW and sickness absence data from case managers and field workers during delivery of the case management intervention was the lack of access to trusts’ HR systems that record this information. In the light of these challenges, it is proposed that alternative, more reliable methods to capture RTW data are explored. One possible means would be to make use of short messaging service (SMS), sending texts to study participants on a regular basis (weekly/fortnightly) to request details of recent sickness absence periods. A notable advantage of this method is that it would help to minimise recall bias.
We also found that the site-level data collection tools (audit form and checklist form), as well as the participants’ study questionnaires, were reliable tools to measure intervention fidelity (uptake and adherence to individual components of the case management interventions). However, a notable shortcoming with the 6-month study questionnaire for participants in the intervention arm was that it did not capture important information on reasons for non-uptake of and non-adherence to the intervention. This additional source of information would have been helpful to gain a better understanding of the reasons why some participants chose not to engage with specific components of the intervention.
In terms of acceptability and feasibility regarding use of the data collection tools, various approaches were used by case managers and field workers to document and record study-specific data. Some found it more helpful to make initial handwritten notes during consultations rather than using the study’s data collection tools during clinic appointments. The benefits of this approach were that it allowed them to focus on the interaction with staff as this helped them to establish a therapeutic relationship with staff. Moreover, some case managers pointed out that an excessive amount of study documentation requiring completion by them and their participants could be considered an intrusive element in OH consultations, and others felt that the format of some of the data collection tools relating to RTW was not easy to follow or complete and they did not reflect the range of possible scenarios staff may present with. This is exacerbated further when OH clinic sessions are busy and when OH nurses are under pressure to keep within designated appointment times. Others found it difficult to remember to complete the case management form during OH consultations, which meant that important study data were missing at the end of the study. To mitigate some of these logistical issues, some of the field workers and case managers suggested linking the study’s data collection forms, specifically those relating to RTW, to existing electronic OH records to streamline the recording of this information, as this would also help to minimise any disruptions during the consultations. The use of an electronic tablet for field workers and participants to record study data was also proposed as a worthwhile alternative to paper records, although we have found in previous research, and in this present study, that implementation of a reminder strategy helped to optimise the return of paper questionnaires. 47 Moreover, the participants’ questionnaires were also considered by some case managers and participants to be too lengthy and the requirement to complete so many was considered an onerous burden. Furthermore, it was generally felt that clearer information was needed in terms of the purpose and timing of each questionnaire during the study period. It was also recommended that a useful strategy to optimise the response rate of study questionnaires in a future trial would be to administer these at the time that participants attend their follow-up review consultations, rather than relying on the postal delivery-and-return method, or to provide participants with the option of completing questionnaires online.
Discussion
The series of participant questionnaires used in the study were found to be of suitable scope to assess current (and changes in) clinical state relating to mental functioning (anxiety and depression indicators), workability/occupational functioning, RTW self-efficacy and health economic measures.
Agreement between periods of absence with a CMD as reported by participants and as extracted from ESRs was described graphically. Additionally, agreement between RTW patterns as reported by participants and in case-manager forms were described in cross-tabulations and assessed using the kappa statistic (see Figure 9).
Chapter 5 Work package 3
The study included a series of primary outcome measures that are reported in detail in Chapters 5 and 6. For ease of reference, Table 5 specifies where the data specific to each primary outcome measure can be found in the report.
| Primary outcome measure | Location in report and further details |
|---|---|
| 1.1. Rates of uptake among those eligible to participate | Figure 5, Tables 8, 9 and 11 |
| 1.2. Frequency and nature of protocol violations, assessed throughout the study period from file note data, feedback from sites and during the qualitative component (e.g. whether or not there were any difficulties in implementing the protocol) | What would be the likelihood of ‘contamination’ if, within the same trust, the intervention was delivered to some staff and not to others? (p. 59) and Protocol violations (p. 60) |
| 1.3. Completeness of data collection, assessed through a final report at the end of the study from the trial statistician detailing the extent of missing data | Missing data reported in each of the variables described throughout the report |
| 1.4. Average consultation times compared with CAU, assessed at the end of the study using the case management data and CAU collection forms | Table 19 |
| 1.5. Mean number of follow-ups per case, assessed at the end of the study using the case management data and CAU collection forms | Table 20 |
| 1.6. Extra line manager and human resources time per consultation compared with CAU, captured during qualitative data collection | pp. 59–69 |
| 1.7. Fidelity of the case manager training, assessed using the case management data collection form | Tables 6, 7 and 9 |
| 1.8. Adherence to the intervention in those allocated to receive it | Tables 9, 19, 21 |
| 2. Acceptability of the intervention, assessed during qualitative data collection | pp. 32–38 and 59–69 |
| 2.1. A summary of qualitative findings representing views on the intervention and its assessment expressed by participants, case managers, HR and line-managers. All qualitative data were transcribed and thematic analysis was undertaken. The findings of this will be outlined in the final study report | pp. 32–38 and 59–69 |
| 2.2. Reasons for not completing the intervention and any adverse effects, assessed throughout the study using the serious adverse events form, the withdrawal form, participant questionnaire parts C and D and qualitative interviews | Tables 9 and 21, p. 2 and pp. 59–69 |
| 3. Measurements of costs of delivering the package of interventions, including OH nurse time, participant and manager time, and cost of training OH nurses in case management. This was assessed using the CSRI to determine which services were used during the study follow-up and how often, along with the EQ-5D-5L as a measure of health-related quality of life to assist with this evaluation | Tables 22 and 23, and pp. 56–59 |
| 4. Manual development. This will be a two-stage process. Stage 1 (initial manual development) will be designed during the feasibility study period and stage 2 (finalisation of the manual) will be completed following data analysis and study completion | |
| 4.1. A complete specification of the intervention and standard operating procedures for different settings | Chapter 6, Finalisation of the manualised intervention and recommendations for the design of a randomised controlled trial, Results, Full instructions on how to deliver the case management intervention, pp. 71–74 and Figure 14 |
| 4.2. A manual for training the case managers | p. 72 (available on request from the corresponding author) |
| 5. Demographic data, including age, sex, job, previous sickness absence, and history of mental and physical ill health, assessed using the baseline questionnaire | Table 14 and p. 46 |
| 6. Expectations of full RTW and RTW self-efficacy, assessed using the RTW-SE scale at baseline and after 3 and 6 months | Table 15 and pp. 48–52 |
|
7. Common mental health disorders, assessed at baseline and after 3 and 6 months using: 7.1. PHQ-9 7.2. GAD-7 |
Table 16 and pp. 50–54 |
| 8. RTW, either full (working the same days or hours per week as before sickness absence in an identical or equivalent role for at least 4 weeks) or partial (working any number of hours in any role), determined from data collected from ESRs and self-report questionnaires at baseline and after 3 and 6 months | Table 18 and Figure 9. Note that these provide an agreement of absence period and RTW time between self-reports and other sources (ESRs for absence period and case manager forms for RTW patterns) |
| 9. Work ability, assessed using the WAI at baseline and after 3 and 6 months | A number of instruments have been developed to measure presenteeism and workability, such as the WAI36 (to explore the effect of physical comorbidity on work ability) and the Work and Social Adjustment Scale37 (to measure global functioning). Initially it was our intention to use both these measures of occupational outcomes to allow us to compare the results from the measures and to recommend one or both for use in a full trial. However, following discussion at a study management meeting, we decided that WHODAS would be better suited to this study and should be used instead |
Stage 1: case manager training
Case manager training concerned research question 5: how feasible and acceptable is it to train OH nurses as case managers? What is the impact of the training on skill acquisition during the study period? How much additional training would case managers need to achieve established competency targets and prevent decay in skills?
Training of OH case managers was an important component of the intervention.
Methods
We developed a 2-day bespoke training package and the workshop was held in London, UK, during September 2017. The workshop training comprised the following topic areas:
-
Background to the study.
-
Use of the study protocol, screening for eligibility and taking consent, completion of data collection tools, flow charts, use of the study pack, and safety issues.
-
Clinical assessment of CMD/risk assessment, and identifying and challenging unhelpful beliefs.
-
Problem-solving and promotion of engagement, theory and practice. The learning objectives for the problem-solving approach were as follows –
-
recognising engagement and disengagement
-
how to share information to empower the worker to set up their action plan
-
good-quality listening.
-
-
Use of clinical and case pro formas, writing RTW plans and improving RTW self-efficacy.
-
Communication – RTW leaflets; communication with GP, line manager and others; and access to CBT.
-
How to establish the peer network.
-
Suicide risk assessment, including a practical session.
-
Practical session – use of case management pro formas and roleplay.
-
-
Helping managers to stay in touch.
-
Seeking support and help – case manager network.
-
Knowledge assessment questionnaire – pre and post completion of the training.
-
Training evaluation feedback.
The small group size of up to six case managers (a maximum of two per intervention trust) allowed for in-depth training and discussion. We based our training on our experience of running case manager training days with an emphasis on problem-solving and the promotion of engagement (JS and RS),24 and on mental health training days for OH nurses (MH and IM). 103 Previously, we had shown that small-group training on mental health for OH nurses results in good knowledge transfer and use of knowledge in practice, as well as increased confidence and levels of satisfaction with the training. 104 The essential skill required of case managers is the capacity to create a supportive, empathic atmosphere in which they explore and make salient the client’s own reasons for returning to work, discuss their barriers to returning to work and support the client (when ready) to identify an acceptable pathway to change by facilitating structured personal goal-setting. This goal-setting element was orientated to increasing activities at home, gradually introducing and scaling up engagement with the employer, and phased RTW.
Therefore, training for case managers comprised a number of related elements that were integrated into the manual and training:
-
Clinical assessment of CMDs in the OH context, delivered by a consultant occupational physician and consultant psychiatrist. This component of the training covered an overview of CMDs (aetiology and prevalence); symptom and functional enquiry; mental state assessment; use of standardised questionnaires (e.g. GAD-7 and PHQ-9); principles of the optimal treatment of CMDs (counselling, talking therapies, drug treatment, and online CBT in conjunction with input from a therapist), and availability of treatments locally; addressing and overcoming barriers to work; problem-solving using a specified framework; RTW planning, including indications for phased hours, minimising shift work, exposure to stressors at work and work volume; and the management of relationships at work.
-
Problem-solving and MI. Case managers were taught to deliver problem-solving in the spirit of MI to promote participant engagement by Robert Shannon, who is experienced in teaching and delivering MI training in a variety of settings including chronic disease and OH case management.
-
A combination of workshop input and follow-up individualised supervision by way of regular teleconferences with case managers. The follow-up supervision sessions took place on three occasions, were between 30–60 minutes in duration and were largely unstructured in nature. These sessions provided an important opportunity for the newly trained case managers to report back on delivery of the intervention and any unforeseen issues that they may have encountered. In particular, these sessions were an opportunity for case managers to describe how they were approaching the participant screening and recruitment activities, the clinical assessments, and problem identification and problem-solving components of the intervention, and how they felt participants were engaging with the intervention. It was not deemed necessary to undertake additional roleplay exercises during the follow-up supervision sessions. We also incorporated a practical patient-actor/case manager roleplay session into the training workshop so that problem-identification, problem-solving and action-planning skills could be practised by all trained case managers.
-
CBT skills. Case managers were coached in basic CBT techniques. This was provided by a psychiatrist, but stopped short of conventional clinical CBT training, focusing instead on the use of CBT approaches (e.g. positive thought cycling) with a workplace focus, for example defusing negative thought cycling or rumination on problems in the workplace. We trained the case managers in risk assessment of serious self-harm and suicide in the study participants. We built an escalation procedure into the training, which took into account the case managers’ current local procedures.
-
Use of the study protocol and communications with line managers and GPs; setting up a peer-support network.
-
Safety issues – procedures for safeguarding vulnerable individuals, which were dovetailed with the local procedures at the case manager’s trust.
Evaluation
-
We evaluated the training by using the first three levels of the Kirkpatrick model of educational evaluation (learner satisfaction, learning outcomes and performance improvement),104 adapting the questionnaire we used in previous evaluation of mental health training for OH nurses. 103
-
We monitored the integrity of the case management delivery by conducting a case file-review audit exercise at the end of the study period. The purpose of this exercise was to assess the extent to which all components of the case management intervention were delivered. The case file review audit was undertaken at the end of the follow-up period by an independent non-case manager employed at the participating sites (see Table 9 for results).
Results
Overall, the results showed a sustained, gradual increase in knowledge across the subject area following participation in the training, although it was also noted that (‘correct’) knowledge in the pre-training assessment had diminished (for several questions) at the post-training evaluation for up to two case managers. Table 6 presents the overall increase/decrease in assessment scores for the group.
| Question | Correct answers (n/N) | Change | |
|---|---|---|---|
| Pre training | Post training | ||
| 1: The presence of prominent physical symptoms (such as pain and fatigue) in a depressed person means that they probably also have an underlying physical health problem | 5/6 | 4/6 | Decrease |
| 2: Discussing the topic of suicide will increase the risk of a patient harming themselves in the future | 6/6 | 6/6 | No change (all correct) |
| 3: Women are less likely than men to commit suicide | 6/6 | 4/6 | Decrease |
| 4: The majority of those who kill themselves have complained of psychological distress to their GP in the preceding month | 5/6 | 5/6 | No change |
| 5: In patients who have had one episode of major depression, 50–85% will go on to have a second episode | 5/6 | 3/6 | Decrease |
| 6: In panic disorder, the timing of panic attacks is usually unpredictable | 4/6 | 5/6 | Increase |
| 7: The likelihood of a worker returning to work after an episode of depression is strongly determined by the severity of their depression | 4/6 | 4/6 | No change |
| 8: The worker’s expectation of return to work is strongly predictive of when and if they will return to work | 6/6 | 6/6 | No change (all correct) |
| 9: The stages of problem-solving include – | |||
| a: setting a problem list | 2/6 | 4/6 | Increase |
| b: reviewing past successes and failures | 4/6 | 4/6 | No change |
| c: examining the patient–therapist relationship | 5/6 | 5/6 | No change |
| d: setting achievable goals | 5/6 | 5/6 | No change |
| e: defining problems precisely | 2/6 | 2/6 | No change |
| 10: Achievable goals in problem-solving should be – | |||
| a: chosen by the therapist | 6/6 | 5/6 | Decrease |
| b: achieved before the next treatment session | 6/6 | 5/6 | Decrease |
| c: achieved within a defined time span | 1/6 | 4/6 | Increase |
| d: related to problems chosen | 4/6 | 6/6 | Increase |
| e: linked to relationship difficulties | 6/6 | 6/6 | No change (all correct) |
| 11: Problem-solving treatment is a proven treatment for – | |||
| a: depressive disorders | 2/6 | 6/6 | Increase |
| b: simple phobias | 5/6 | 4/6 | Decrease |
| c: mania | 6/6 | 6/6 | No change (all correct) |
| d: adolescent depression | 6/6 | 6/6 | No change (all correct) |
| e: anxiety disorders in primary care | 1/6 | 3/6 | Increase |
| 12: Problem-solving treatment is most effective when – | |||
| a: combined with antidepressant medication | 2/6 | 1/5a | No change |
| b: delivered by community nurses | 6/6 | 5/5a | No change (all correct) |
| c: delivered over 10 sessions | 6/6 | 5/5a | No change (all correct) |
| d: patients have many psychosocial problems | 6/6 | 5/5a | No change (all correct) |
| e: patients have a chronic illness | 5/6 | 5/5a | No change (all correct) |
| 13: SMART goals are – | |||
| a: simple | 3/6 | 3/6 | No change |
| b: modest | 5/6 | 4/6 | Decrease |
| c: achievable | 4/6 | 6/6 | Increase |
| d: resisted | 5/6 | 5/6 | No change |
| e: timed | 2/6 | 5/6 | Increase |
Accordingly, future training of case managers will need to ensure that additional information is covered in the training with respect to the basic aetiology and epidemiology of CMDs and approaches to problem-solving in the context of CMD.
Overall, participants rated the training workshop very favourably in terms of acceptability, with most responding with ‘strongly agree’ to the following seven statements:
-
The objectives of the training were clearly defined.
-
Participation and interaction were encouraged.
-
The content was organised and easy to follow.
-
The materials distributed were helpful.
-
The trainers were knowledgeable about the training topics.
-
The trainers were well prepared.
-
The time allotted for the training was sufficient.
Additional feedback from case managers was captured on the post-training evaluation form and is summarised below (Table 7).
| Question | Response(s) |
|---|---|
| What did you like most about the training? | Common mental health disorders very interesting |
| Interesting to explore alternative ways | |
| Good to receive up to date information on anxiety/depression | |
| Enjoyed varied format, background theory followed by practical application, relaxed yet serious approach to subject, role plays very good | |
| Interactive sessions very good, knowledgeable presenters, well-paced | |
| Interactive, knowledgeable presenters, well-paced, varied format, relaxed yet serious approach, role plays very good | |
| Participation, working through the processes, session on suicide with Max, role-play was very good, thorough & enjoyable day, Max’s session particularly | |
| What aspects of the training could be improved? | More time for questions/answers with Max Henderson, role-play with actor should be brought forward in the agenda |
| Please share other comments or expand on previous responses here | Fantastic 2 days, great group, re-enforced good practice & development skills |
Table 8 provides an overview of the number of participants who contributed to the qualitative data collection. Table 9 provides an overview of adherence to the intervention.
| Trust | Participants (n) | Participants in focus group sessions (n) | Case managers (one-to-one interviews) (n) |
|---|---|---|---|
| Guy’s and St Thomas’ NHS Foundation Trust | 1 | 13 (HR, 1; management, 9; OH, 3) | 0 |
| Ipswich Hospital NHS Trust | 1 | 9 (HR, 3; management, 3; OH, 3) | 1 |
| University Hospitals of Leicester NHS Trust | 1 | 9 (HR, 1; management, 5; OH, 3) | 3 |
| Norfolk and Norwich University Hospitals NHS Foundation Trust | 2 | 8 (HR, 2; management, 3; OH, 3) | 2 |
| West Midlands Ambulance Service University NHS Foundation Trust | 0 | 9 (HR, 2; management, 4; research, 2; OH, 1) | 0 |
| Audit form statement | Response | n (%) |
|---|---|---|
| Evidence of problem-solving approach | Yes | 11 (100) |
| No | 0 (0) | |
| Identified problems and obstacles | Yes | 11 (100) |
| No | 0 (0) | |
| Solutions suggested/explored | Yes | 11 (100) |
| No | 0 (0) | |
| Written RTW plan | Yes | 11 (100) |
| No | 0 (0) | |
| Workplace adjustments or modifications taken place | Yes | 7 (64) |
| No | 3 (27) | |
| Missing | 1 (9) | |
| Evidence of engagement of peer support | Yes | 0 (0) |
| No | 11 (100) | |
| Sleep hygiene advice given | Yes | 11 (100) |
| No | 0 (0) | |
| Signposted to CBT or other therapies | Yes | 10 (91) |
| No | 1 (9) | |
| Pathway to CBT or other therapies | Workplace | 5 (45) |
| GP | 1 (9) | |
| IAPT | 1 (9) | |
| Online | 1 (9) | |
| Other | 1 (9) | |
| Workplace, other | 1 (9) | |
| Missing | 1 (9) | |
| Copy of the OH report sent to | Manager | 6 (55) |
| Manager/HR/GP | 4 (36) | |
| Manager/GP | 1 (9) | |
| Case conference between the OH professional and line manager taken place | Yes | 0 (0) |
| No | 11 (100) | |
| Workplace visit taken place | Yes | 0 (0) |
| No | 11 (100) |
The following analysis is based on qualitative data and represents the views of and feedback from case managers.
Overall, the case managers felt that the 2-day training workshop was well developed, covered a diverse range of relevant subject areas and was delivered by facilitators from key specialities (occupational medicine, occupational psychiatry and organisational psychology). Importantly, the case managers felt that the workshop supported them in developing new skills and competencies that were required for them to take on the new case manager role:
But it was good and the information that they gave you to be able to do the motivational interviewing and go through the case management and the problem-solving, I mean it was all well delivered and able to be lifted and taken back to my practice with no difficulties.
Case managers expressed the view that the skills they developed in the training enabled them to deliver an enhanced level of OH support during the study period; more specifically, it allowed them to shift the focus of their OH consultations away from information gathering only to an approach that actively sought to engage staff in a more participatory and therapeutic relationship. Participation in the training workshop was also recognised as a valuable opportunity for them to build on their own professional skills and capabilities, and allowed the case managers to use their new knowledge and skills in other areas of clinical practice:
We’re constantly short of time, short of clinic slots, short of staff, and whilst there is a place for telephone, I think we’ve gone totally virtually to telephone and I think the balance is not quite there and I don’t think I realised that until actually I came out of the lovely long face to face, where I had really good interaction with somebody. I felt as if I’d moved them along during the process of that assessment rather than just getting information from them, so it wasn’t just about gaining information, it was about gaining that information, putting some things into place, helping them to identify what they needed to do next, you know, identify some of their problems, talk to them about their action plan, and that they were leaving with something to go away with and do, and the first one just felt fabulous, it really did feel that I’ve made a real difference.
Prior clinical experience working in OH was considered a valuable quality to support case managers in taking on the new role. Those without significant OH clinical experience to draw on were therefore considered less likely to feel confident in facilitating discussions with clients in terms of problem-solving and action-planning. Moreover, incorporating their new skills and knowledge when delivering the case management intervention meant that some case managers felt suddenly less capable in their OH role than they had felt beforehand. Adopting a new style of working had initially slowed down their delivery of OH clinical practice and there was a consensus that proficiency in the application of their new case manager skills takes time to master. It was generally agreed that ongoing opportunities for case managers to use their new skills would help them to build the required competencies and confidence to deliver the case management intervention in the future. Several case managers reported accessing collegial support from other local case managers during the study, and these interactions were found to provide a useful opportunity for case managers to mentor each other as skills were developing:
[. . .] probably a little bit wooden, you have your own style of doing things and then when you’ve got to change that, I think it feels unnatural, probably not to the person that you are actually seeing, they probably don’t notice any difference but I guess I went from being able to do consultations almost on, not quite on autopilot because you are thinking about it, but in terms of the way you ask things to actually having to think about how I was phrasing every question, whether it was an open question or a reflected statement back and things like that.
We did support each other, yes, we talked about the cases afterwards, we’ve got quite a supportive team anyway and we’ve had to be over the last sort of few years, so we do discuss difficult clients and difficult cases, there’s always time at the end of the day to be able to do that and I’m [case manager’s] line manager so we often get together and have chats about things, but yes we certainly did support each other on this.
In terms of the timing for delivering the training, some case managers expressed concern that knowledge and skill development were likely to diminish if they were not used soon after training, and others felt that an opportunity for refresher training to underpin skills development would be practically beneficial and would help to prevent a decay in skills:
I think the actual sessions themselves were really good. I seem to remember there was a bit of a gap between doing the case management training and actually starting the recruitment onto the study, so actually by the time we started the recruitment process I probably did not feel as fresh as I could have done and I did have to go back several times through some of the slides and bits and pieces to re-get my head round some of the processes that we were supposed to be doing.
In particular, the assessment of CMDs and the suicide risk assessment components of the training were positively received and provided case managers with a useful opportunity to enhance their existing clinical knowledge and skills in this area or, for more novice OH case managers, acquire important foundation knowledge and new practical skills that they could then use when delivering the case management intervention. Most case managers were found to adopt a flexible yet holistic approach when assessing risk-related concerns (e.g. exploring suicide/self-harm and work-related issues). However, several case managers felt that the ‘assessment of risk’ predominantly related to a person’s capacity to perform their job role instead of suicide or self-harm:
I probably did feel more comfortable with asking the questions around suicide and deliberate self-harm and things like that than I have done previously.
The roleplay exercise was considered by some case managers to be a useful component in which to practice MI techniques during training; however, some felt that more time should be given for experiential learning so that new skills and techniques could be rehearsed in different scenarios. It was also noted that these practical roleplay sessions could make case managers feel anxious; they felt genuinely concerned that peers may negatively assess their capability to deliver the case management intervention effectively, preferring instead to incorporate new knowledge and to practise new skills and techniques in real-life situations:
There was one particular session, it was all really useful, it was one particular session where we did, normally I hate roleplay but we did a roleplay session and I found that really, I think that was towards the end of the [inaudible] once we’d had the basis of it, I found that really helpful in terms of applying it and that really made me sort of think about how you have to alter your perception of supporting people, so rather than advising people to do certain things, it was about turning it around and allowing people to come to their own decisions and conclusions, so I found that particular session very very useful from it all.
Generally, case managers had a preference for making use of the Microsoft PowerPoint® 15.0 (Microsoft Corporation, Redmond, WA, USA) slides that had been used during the training, as well as referring back to personal notes to familiarise themselves with the content post training, particularly with regard to the action planning and problem-solving components, and only a few case managers found it necessary to access the video-recordings of the workshop to support them in their new role:
[T]he slides were what was presented so that tended to be what I then reflected on, mentally relating back to the session.
Independent assessors at intervention/mixed intervention sites completed an audit form for 11 participants in the study. The purpose of this exercise was to assess delivery of each component of the case management intervention.
The OH case managers described the training workshop in positive terms and expressed the view that they had acquired the necessary new skills and competencies to deliver the case management intervention, particularly in relation to conducting a comprehensive clinical occupational history and mental state assessment, engaging and guiding participants in problem identification, problem-solving and action planning, as well as risk assessment. Post training, case managers provided useful feedback in terms of where refinements could be made to the content and method of delivery. This included the need to ensure that training provided additional information with respect to the basic aetiology and epidemiology of CMDs, and approaches to problem-solving that are specific to mental health symptomology. Moreover, the case management training workshop provided a valuable opportunity for the case managers to build on and enhance their existing clinical and interpersonal skills.
The independent audit of case notes found evidence that all participants in the intervention arm had engaged in the interactive problem identification and problem-solving components of the intervention and there was evidence that a formal RTW plan had been devised for all participants. All participants were provided with the sleep hygiene leaflet and the majority were signposted to follow-up counselling support provided either in the workplace or by an external provider. All line managers were given a copy of the formal OH report following delivery of the case management intervention. No participants were found to have engaged in local peer support, nor was there evidence that case conferencing (with line manager/sick-listed employee and case manager) or workplace visits had been required.
Discussion
Overall, we found that it was both feasible and acceptable to train experienced OH nurses as case managers. However, based on the workshop evaluation scores and qualitative feedback, it is important to carefully consider the prerequisite criteria when selecting OH nurses to be trained in delivering the intervention.
Prior OH experience was found to be a key attribute, since this provided a foundation on which newly trained case managers could learn and grow, coupled with benefits of having access to local collegial support from other trained case manager colleagues. A strength was the professionalism, enthusiasm and commitment of the case managers during their involvement in the study. Nevertheless, it is important to recognise that skill decay may occur relatively quickly if the new clinical skills and knowledge required to deliver the OH case management intervention are not applied in clinical practice soon after the training. This has important implications in terms of the timing of case manager training sessions, and the potential need to offer refresher training and to facilitate access to ongoing mentoring support as new skills are consolidated.
Stage 2: design and conduct of feasibility trial
Before a feasibility trial is mounted, we need to answer the following research questions:
-
Research question 6: how feasible and acceptable would it be to deliver such an intervention in different NHS settings? What rate of uptake could be expected, and how good would the adherence by OH staff and study participants be? What would be the resource implications of the intervention?
-
Research question 7: if a trial were conducted to test such an intervention, how well would methods of recruitment and data collection work in practice? What rates of recruitment and follow-up would be expected? What would be the likelihood of contamination if, within the same OH department, the intervention were delivered to some staff and not to others?
Study design
We hypothesised that the impact of an intervention to improve RTW in NHS staff who go on sick leave with a CMD would best be assessed through a cluster RCT in a variety of NHS trusts, provided that contamination could be avoided (i.e. delivery of the intervention did not inadvertently modify the management of controls). In population, intervention, comparator, outcomes (PICO) format, the design of the RCT that was envisaged can be summarised as follows:
-
Population – NHS staff in a variety of NHS trusts who have been on sick leave with a CMD for 7 or more consecutive days and less than 90 consecutive days.
-
Intervention – a complex intervention comprising various clinical and workplace provisions that, individually or in combination, are thought likely to be effective in this population (either from direct evidence or because they are known to be effective in other working populations or conditions).
-
Comparator – CAU (i.e. the provision of existing OH care as usual and support provided to NHS staff on sick leave with a CMD).
-
Outcomes – reduction in anxiety/depression; change in use of medication for CMDs; early, part, full and sustained RTW; change in health-related quality of life and well-being; relapse rates; and adverse events. We assessed the cost-effectiveness of the intervention both from a NHS and a societal perspective. In addition, the financial implications for employers were investigated.
To answer research questions 6 and 7, we recruited six OH departments from those that confirmed that they wished to participate in the study in response to an expression of interest correspondence sent to NHS trusts who participated in the SCIN trial, with one of the site’s being an ambulance trust. We selected NHS OH departments representative of the range of NHS trusts in the UK, providing OH services to a mixture of acute, mental health and ambulance trusts. All included trusts had electronic OH data capture systems, did not have case management in use at the time of the study and employed more than two OH nurses who advised on RTW in workers with CMD. One trust (Royal Papworth Hospital NHS Foundation Trust) withdrew from the study prior to the commencement of participant recruitment, citing OH staff storages.
We allocated the participating trusts to mixed intervention/CAU (groups A and B), CAU only (group C) and intervention only (group D) based on sampling groups, with the aim of achieving broad comparability between the types of trust (Table 10). Sites were not randomly allocated to a particular treatment arm during the study design; instead, for pragmatic reasons, this decision was made by the research team based on feedback from individual sites, such as whether or not they had the capacity to deliver the case management intervention. For instance, OH services at our NHS ambulance trust were delivered by an external OH provider and it was not deemed feasible to implement a new case management intervention or train external OH staff within the existing contractual arrangement.
| Site | Target number of participants, n (group) | |
|---|---|---|
| Intervention | CAU | |
| CAU | ||
| Guy’s and St Thomas’ NHS Foundation Trust | N/A | 14 (C) |
| West Midlands Ambulance Service University NHS Foundation Trust | N/A | 14 (C) |
| Mixed intervention/CAU | ||
| Ipswich Hospital NHS Trust | 7 (A) | 7 (B) |
| Norfolk and Norwich University Hospitals NHS Foundation Trust | 7 (A) | 7 (B) |
| University Hospitals Leicester NHS Trust | 7 (A) | 7 (B) |
| Intervention | ||
| Royal Papworth Hospital NHS Foundation Trust | 7 (D) | N/A |
Methods
Participants
Participants were staff with CMDs, with or without an associated physical disorder, who had been on sick leave for a period of more than 7 consecutive days (i.e. on receipt of fit note) and less than 90 consecutive days. We did not include staff with a psychotic disorder, bipolar disorder, substance abuse or dementia. Staff under formal investigation for misconduct or in the formal process of disciplinary action were excluded because these processes may have been an effect modifier.
Recruitment
We aimed to recruit 77 participants using a 1 : 1 ratio of intervention to CAU. We initially planned to determine if it was feasible to randomise at departmental-group level. Prior to the commencement of participant recruitment, sites were asked to review existing OH referral activity data and trust ESR data so that they could identify up to four departments with the largest number of management referrals to OH for staff on sick leave with a CMD, and to identify which departments at their trust had a high incidence of sickness absence for > 7 days due to a CMD. The purpose of this was to optimise participation and to assist sites in meeting their agreed recruitment target, as shown in Table 10. Field workers were asked to liaise with the management teams at each department during the study set-up stage so that line managers were aware of their trust’s participation in the study and to encourage line managers to initiate a referral to OH as soon as possible for staff who went on sick leave with a CMD. The decision to open up recruitment to all departments was later made in response to the small number of referrals to OH from the previously nominated departments.
Screening for eligibility
Participants were screened for eligibility at the time of sending a fit note to their line manager, at the time of referral to OH or during their first OH appointment. The recruitment period was March 2018 to September 2018 and the follow-up period took place from June 2018 to March 2019.
For pragmatic and operational reasons, several approaches were adopted across the participating sites with respect to the screening and consenting of eligible participants. For example, initially, field workers at Guy’s and St Thomas’ NHS Foundation Trust assessed prospective sick-listed workers for eligibility based solely on information provided on management referral forms sent to OH by local line managers. In some circumstances, information on the management referral forms was sufficiently detailed so that field workers were able to identify those sick-listed workers who were on sick leave with a CMD. Those participants were then sent a participant information sheet along with the details of their first OH appointment. However, feedback from some of the participating sites showed that information on the management referral forms was often insufficient or ambiguous, rendering it difficult for field workers to identify sick-listed workers who were on sick leave with a CMD. In these circumstances, it was found that workers on sick leave with a CMD were identified as eligible for entry into the study only during their first OH appointment. In response to this, it was decided to open up participant recruitment to all departments, and to provide field workers with the option of screening and consenting eligible participants during their first OH appointment. To ensure that all prospective sick-listed workers were aware of the study, a copy of the participant information sheet was sent out along with the appointment details. Those who wished to participate were asked to provide consent and were formally screened for eligibility for the study either on attendance at their first OH appointment or beforehand by telephone. Eligible participants who chose not to take part were invited to complete a brief decliner questionnaire that captured basic demographic details (age, sex, expected duration of current sick leave period, job type and rating of depression/anxiety indicators).
In response to the smaller than expected number of participants recruited into the study, we also provided sites with specific wording to further raise the profile of OH and their local OH departments’ involvement in the study. The decision on whether or not it was operationally or strategically appropriate to promulgate this information across each trust was left to participating sites. To further optimise the recruitment of participants, centres were also provided with the option of consenting participants who self-referred to OH for support. The duration of recruitment was 7 months.
At mixed intervention sites (intervention and control arm), field workers were asked to sequentially allocate participants to either the intervention or the control arm as they were recruited into the study.
Informed consent
At time of consent, participants were provided with an opportunity to read through the participant information sheet again and to ask any questions before consent for entry into the study was taken. Informed written consent was obtained from participants at the time that they were recruited into the study. Participants were provided with a copy of the consent forms and copies were also retained in the site file and OH records. All participants were provided with a GP information sheet so that their GPs were aware of their participation in the trial.
Sample size
With a sample size of 60, we estimated a participation rate of 80%, with a 95% confidence interval (CI) of 10%. We allowed for 77 participants to be recruited, so we were confident that we would have a high degree of precision in participation and completion rates. It is important to note that, on reviewing the preliminary study data once recruitment was under way, the independent statistician on the Study Steering Committee postulated that the initial target was likely to be too high and, therefore, could be revised down to a more achievable range. We anticipated that all OH departments that confirmed that they wished to take part would see > 20 staff who went on sick leave with CMDs in a 6-month period. Therefore, we considered that it would be feasible to recruit 14 participants at CAU and mixed intervention/CAU centres and seven participants at the intervention-only centre.
Outputs
-
An assessment of the feasibility and acceptability of the intervention to workers who go on sick leave with a CMD, line managers, OH departments and HR managers.
-
A manual for training case managers.
-
An assessment of the feasibility, acceptability and impact fidelity of the training in strengthening motivation and CBT-directed goal-setting skills.
Results
During the recruitment phase, 42 NHS workers were screened for eligibility. A total of 24 participants were consented to take part in the study and 18 NHS workers were not consented for various reasons (e.g. ineligible, declined). It is noteworthy that a proportion of sick-listed staff were already on a RTW plan at the time of their first OH appointment, although we did not collect any data on the duration of their sickness absence prior to their first OH appointment. A Consolidated Standards of Reporting Trials (CONSORT) flow diagram of the screening, recruitment and response rate to the study questionnaires is provided (Figure 5).
FIGURE 5.
The CONSORT flow diagram. a, Total number of staff on sick leave with a CMD during the study at participating sites (does not reflect the number of staff invited to take part or referred to their local OH department). One participant returned a questionnaire at 3 and 6 months but not at baseline.
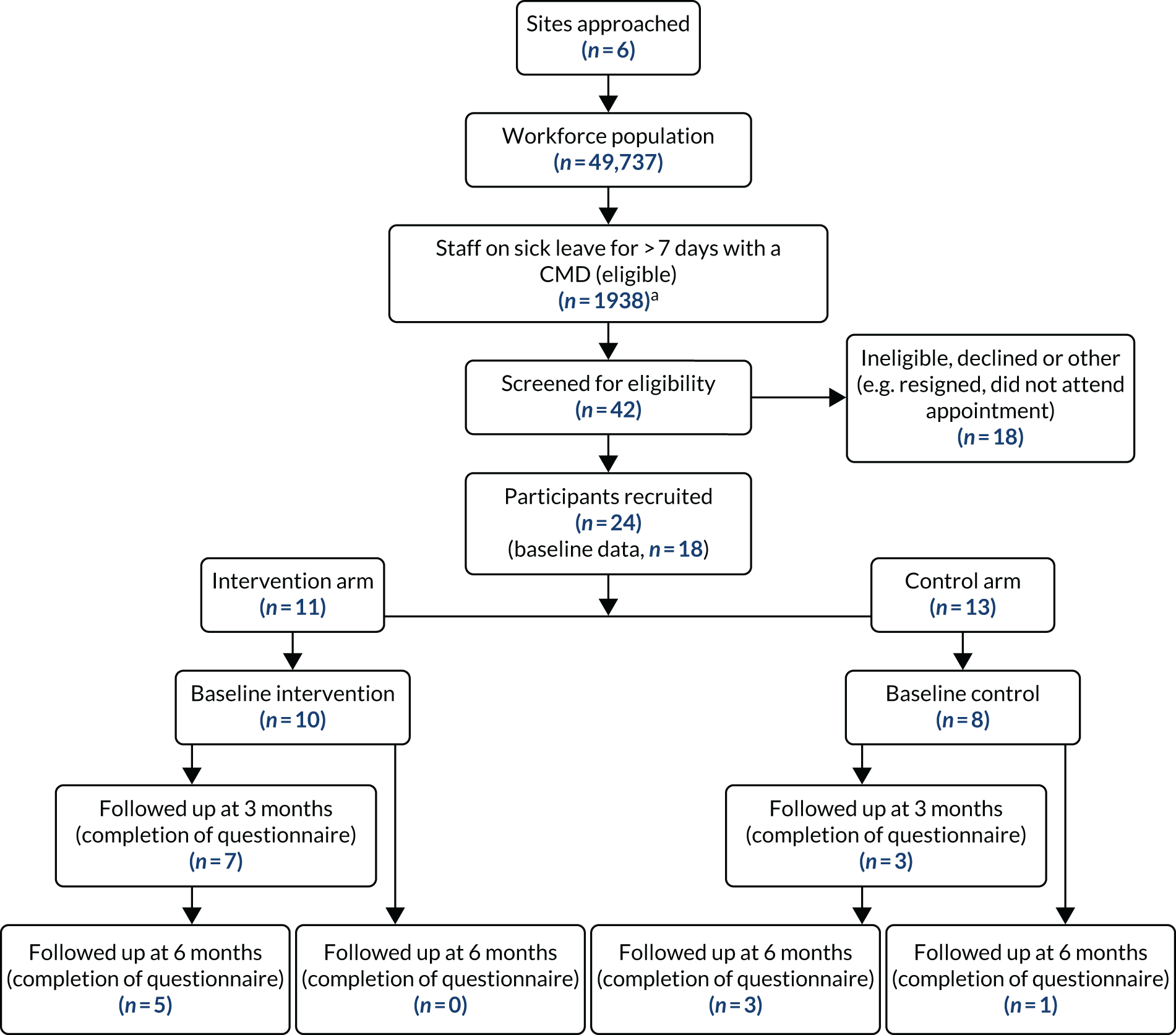
Table 11 presents the total workforce population size, (estimated) number of staff on sick leave with a CMD, number of sick-listed staff who were screened for eligibility and number of staff who were recruited to take part during the 7-month recruitment period, as well as the follow-up response rates to the study questionnaires, by site. We chose to collate the total size of workforce populations and the total number of staff sick-listed with a CMD during the study period because of the smaller than expected number of participants who were screened for eligibility during the study period and to ascertain how many potentially eligible participants were not referred to OH by their line managers during the study period.
| Site | Workforce size (as of April 2019) | Number of staff on sick leave with a CMD for 7 or more consecutive days during the study period | Number of staff who had multiple episodes of sick leave for 7 or more consecutive days during the study period | Number screened for eligibility | Number of participants recruited | Number of participants who returned baseline questionnaire | Number of participants followed up at 3 months (returned questionnaire) | Number of participants followed up at 6 months (returned questionnaire) |
|---|---|---|---|---|---|---|---|---|
| Guy’s and St Thomas’ NHS Foundation Trust | 16,641 | 296 | 62 | 11 | 3 | 2 | 0 | 0 |
| Ipswich Hospital NHS Trust | 4660 | 304 | 21 | 9 | 1 | 1 | 1 | 1 |
| University Hospitals of Leicester NHS Trust | 15,550 | 632 | 75 | 8 | 7 | 5 | 3 | 3 |
| Norfolk and Norwich University Hospitals NHS Foundation Trust | 7500 | 556 | 22 | 13 | 12 | 10 | 6 | 5 |
| West Midlands Ambulance Service University NHS Foundation Trust | 5386 | 150 | 5 | 2 | 1 | 0 | 1 | 1 |
In this study, we found that decisions on why referrals to OH were and were not made by line managers when staff were on sick leave with a CMD varied considerably. For example, we found that there was significant variation across participating sites in the organisational requirements (commonly referred to as ‘trigger points’), as outlined in sick leave policies, for when to initiate referrals to OH for staff who are on sick leave with a CMD. At one participating site (University Hospitals of Leicester NHS Trust), the policy recommends an early referral to OH for any staff who are on sick leave with stress- or anxiety-related conditions, and offers further guidance on what specific line management actions (e.g. contact employee in first week of absence, refer to OH, conduct stress risk assessment) should be taken in these situations. Similarly, at Guy’s and St Thomas’ NHS Foundation Trust, managers are encouraged to manage sickness absence at a local level in the first instance, with OH referrals to be made at 4 weeks of sickness absence. However, the OH service’s policy at Guy’s and St Thomas’ NHS Foundation Trust105 recommends that early OH referrals should be considered in situations where it is unclear if an employee is currently under the care of a health-care professional for their CMD. It is a requirement at West Midlands Ambulance Service University NHS Foundation Trust that staff who go on sick leave with a CMD are referred to OH on the first day of sickness absence. By contrast, other sites provide no policy recommendations specific to the management of CMD presentations or recommend that referrals to OH for any reason should be initiated only when staff have been absent from work for > 4 weeks or if managers observe a regular pattern in periods of sickness absence. With this backdrop, it is likely that requiring line managers to adhere to a different OH referral requirement for the purpose of this research (as stipulated in the study protocol), which is fundamentally incongruent with existing organisational policy requirements, may result in cognitive dissonance for them.
In spite of trigger points outlined in these policies for initiating referrals to OH, this study found that a substantial number of staff who were on sick leave with a CMD during the study period were not referred to OH by their line managers. This reflected similar observations in the previous CAMEOS (CAse Management to Enhance Occupational Support) trial. 23 Furthermore, we found that the proportion of sick-listed staff with a CMD who were referred to OH within 8–28 days was smaller than the proportion reported by the OH providers who participated in the survey of care as usual.
The research team deliberated on the lower than expected recruitment response rate in the context of the overall number of staff on sick leave with a CMD during the study period and concluded that there are several plausible explanations to account for this anomaly:
-
Sick-listed staff with a CMD may not have consented to being referred to OH by line managers (possibly owing to a fear of disclosing a CMD to their employer or because they did not want contact with the workplace during their sickness period).
-
Employees may not have felt ready to engage with the workplace or OH at a particular point in their sickness absence episode.
-
Line managers were adhering to existing organisational policy guidelines about the timing of when OH referrals should be made (i.e. preferring to wait until 4 weeks of sickness absence had passed).
-
Line managers felt confident and competent in managing the sickness absence locally (including the eventual RTW process) without the need for OH guidance.
-
Possible preferences to delay engagement with OH, the purpose being to seek OH validation once proposed RTW plans had been formulated and agreed between the sick-listed staff and their line manager.
-
Misconceptions and a lack of knowledge and awareness among line managers and staff of the role of OH and the support they are able to offer.
-
Negative past experiences involving OH discouraging engagement.
-
The widespread need, recognised by the Study Steering Committee, to raise the profile of OH across the NHS and improve managers’ OH referral practices.
In addition, this study found that there was a large proportion of cases where referrals to OH coincided with an employee’s imminent or actual RTW, rather than occurring earlier in the period of sickness absence. Unfortunately, the study did not capture the duration of sickness absence for staff who were already on a RTW plan at the time that OH referrals were made. Therefore, it was not possible to determine how many additional participants may have been previously eligible for entry into the study had they been referred to OH at an earlier time point, or whether or not intervening earlier in their episode of sickness absence may have facilitated an earlier RTW.
Moreover, many participating sites were known to offer a dedicated managers’ telephone advice line where managers could obtain initial OH advice on current employee-related matters, including discussions on whether or not a formal OH referral is necessary for an individual case. It is likely that these initial consultative interactions between line managers and OH may have mitigated the need for formal OH referrals to be made. Contrary to this, participants (line managers) in the focus group sessions conducted during the qualitative process evaluation often reported poor or no knowledge of the availability of the managers’ advice line service.
The study also found wide variation across participating sites in the method used for screening participants for entry into the study. For example, at some sites, the lead field worker (OH nurse) reviewed all OH management referral forms as they were received into the department and attempted to identify staff who were on sick leave with a CMD from the details provided by line managers. Those identified as meeting the inclusion criteria were sent a copy of the participant information sheet along with their OH appointment details. However, this was not found to be a wholly reliable approach for screening prospective participants because either ambiguous information was provided on the management referrals forms (e.g. CMD masked as a physical complaint such as back pain or fatigue) or the information described non-specific health reasons (e.g. broad psychosocial factors) as the reason for the sickness absence. In short, this method relied solely on the completeness of background case information provided by managers. This meant that there were occasions where eligible participants were assessed as eligible only during their first OH appointment. There were also several occasions where it was deemed inappropriate to proceed with taking participant consent just prior to the first OH appointment because of the emotional distress individuals were displaying when being approached by the field workers.
Table 12 presents OH referral data from the University Hospital Southampton NHS Foundation Trust (a non-participant recruiting site). We collated these data because we wanted to gain referral information from a trust with excellent data recording systems and that already had an early referral to OH system in place. Moreover, this NHS trust was the site of the pilot case management approach on which our intervention was based. 24 According to feedback from this site, in a 7-month period, 72 staff members on sick leave with a CMD at the time of referral to OH were likely to have been identified as eligible for entry into the study prior to their first OH appointment based on information recorded on management referral forms. Furthermore, there were five cases where it was not clear that the staff members were on sick leave with a CMD until they were first seen by an OH practitioner. In addition, 143 cases were referred with a CMD (confirmed at the first OH appointment) but were not on sick leave at the time of their first OH appointment [i.e. they had returned to work (of any form)].
| Number of referrals to OH for CMDa | Number of people with a CMD who were not on sick leave when seen in OH |
|---|---|
| 77 (OH referral forms were cross-checked: 72 cases had clear indication of CMD stated and 5 cases were not clear until the person was seen at first appointment) | 143 [non-severe CMD (eligible), n = 138; severe CMD (ineligible), n = 5] |
Data collection tools
We found that the data collection tools developed or adapted and administered during this study were fit for purpose, and completion rates for participants and field workers were high. We concluded that in a future feasibility trial we would use the self-report and ESR data collection methods to capture sickness absence data.
For the health economic data collection tools, a reduced version of the CSRI may be more appropriate.
Response rate to study questionnaires: sample and lost to follow-up
In summary, 18 out of 24 participants returned the baseline questionnaire. Among these, 10 (56%) participants returned the intermediate questionnaire (3 months after entry into the study) and 9 (50%) returned the final questionnaire (6 months after entry into the study). One participant returned both follow-up questionnaires without having returned a baseline questionnaire. The counts of participants by time of questionnaire and intervention arm are shown in Table 13. Several reminders were used to encourage participants to return completed questionnaires to optimise the response rate.
| Questionnaire(s) | Control arm | Intervention arm | Total |
|---|---|---|---|
| Baseline only | 4 | 3 | 7 |
| Baseline and 3 months | 0 | 2 | 2 |
| 3 and 6 months | 1 | 0 | 1 |
| Baseline and 6 months | 1 | 0 | 1 |
| Baseline and 3 and 6 months | 3 | 5 | 8 |
| All | 9 | 10 | 19 |
As shown in Table 14, 94% of participants were female, with a mean age of 43 years. In terms of main job role, the largest proportion of participants were categorised as nursing, midwifery and health visiting staff. On average, participants worked > 30 hours per week, and the majority reported working day shifts only. Feedback on consumption of alcohol and history and impact of CMDs is also detailed in Table 14.
| Baseline characteristic | n (%) |
|---|---|
| Total number of participants | 18 (100) |
| Age (years), mean (SD)/median (IQR) | 42.8 (12.9)/42 (34–55) |
| Female | 17 (94) |
| Main job role | |
| Administration and estate staff | 3 (17) |
| Health care assistants and other support staff | 3 (17) |
| Health-care scientists | 1 (6) |
| Nursing, midwifery and health visiting staff | 7 (39) |
| Nursing, midwifery and health visiting learners | 1 (6) |
| Other | 1 (6) |
| Scientific, therapeutic and technical staff | 2 (11) |
| Contracted hours, mean (SD)/median (IQR) | 31.5 (7.8)/36.8 (26–37.5) |
| Shifts, n (%) | |
| Day shifts only | 14 (78) |
| Day and night shifts | 4 (22) |
| Frequency of alcohol consumption, n (%) | |
| Never | 5 (28) |
| Less than monthly | 4 (22) |
| Monthly | 4 (22) |
| Weekly | 5 (28) |
| Daily | 0 (0) |
| Missing | 0 (0) |
| Previous CMD, n (%) | |
| No | 4 (22) |
| Yes | 14 (78) |
| Missing | 0 (0) |
| If yes, sickness absence due to CMD | |
| No | 6 (43) |
| Yes | 6 (43) |
| Missing | 2 (14) |
| Treatment for CMD | |
| No | 2 (15) |
| Yes | 11 (79) |
| Missing | 1 (7) |
| Health condition (other than CMD), n (%) | |
| No | 4 (22) |
| Yes | 14 (78) |
| Missing | 0 (0) |
| If yes, what? | |
| Respiratory | 4 (29) |
| Cardiac | 1 (7) |
| Musculoskeletal | 1 (7) |
| Neurological | 1 (7) |
| Other | 7 (50) |
| Missing | 0 (0) |
| If other, specify | |
| Gallstones/gall bladder removal | |
| Diabetic symptoms; diagnosed with diabetes in January 2018 | |
| Eyesight and hearing | |
| Gastrointestinal | |
| IBS; under investigation for IBD | |
| Sinusitis | |
| Bowel disease | |
| Sickness absence due to a health condition other than CMD | |
| No | 11 (61) |
| Yes | 4 (22) |
| Missing | 3 (17) |
The impact of CMDs on occupational functioning was assessed at baseline only. For those participants who reported previous episodes of sickness absence (for any health reason) in the previous 12 months and prior to this current episode, the median number of days on sick leave was 3.8. Seven (39%) participants reported that they expected that the duration of their sick leave would be < 4 weeks and the remaining 11 (61%) participants expected that the duration would be ≥ 4 weeks. Moreover, more than half of participants (59%) reported overall positive job satisfaction, and 12% of participants reported a level of dissatisfaction (Table 15).
| Variable | Results |
|---|---|
| Days of sickness absence in the past 12 months before this episode | |
| Mean (SD) | 7.8 (12.4) |
| Median (IQR) | 3.8 (1–9) |
| Range | 0–49 |
| Missing values | 2 |
| I expect to be back to work within the next few weeks, n (%) | |
| Strongly disagree | 0 (0) |
| Disagree | 1 (6) |
| Not sure | 8 (44) |
| Agree | 6 (33) |
| Strongly agree | 3 (17) |
| Expected duration (weeks) of sick leave in this episode of sickness absence, n (%) | |
| 1–3 | 7 (39) |
| 4–7 | 5 (28) |
| 8–11 | 3 (17) |
| 12–15 | 2 (11) |
| 16–25 | 1 (6) |
| 26–50 | 0 (0) |
| ≥ 1 year | 0 (0) |
| Job satisfaction, n (%) | |
| Extremely dissatisfied | 1 (6) |
| Very dissatisfied | 0 (0) |
| Moderately dissatisfied | 1 (6) |
| Not sure | 2 (11) |
| Moderately satisfied | 9 (50) |
| Very satisfied | 1 (6) |
| Extremely satisfied | 3 (3) |
| Missing | 1 (6) |
Figure 6 presents changes in participants’ perceived capacity to function in the workplace (workability). Higher scores indicate greater difficulty in each domain. Data are presented for the CAU and intervention arms. The results showed that participants were able to answer the relevant questions. The small numbers mean that it is difficult to draw reliable inferences from the results, but there appears to be a trend in the CAU arm to perceive reduced workability at 3 months compared with baseline. This trend is not apparent in the intervention arm.
FIGURE 6.
Self-report measures of participants’ capacity to function in the workplace across different domains. (a) CAU arm; and (b) intervention arm.


In some categories the numbers are very small, resulting in wide CIs.
Return-to-work self-efficacy was assessed at the three time points during the study (Figure 7), with higher scores indicating more positive perceptions of personal capabilities in relation to RTW self-efficacy. The results showed that the participants were able to answer the questions. While the numbers are small, there was a trend towards greater improvement in RTW self-efficacy at 3 months in the intervention arm compared with the CAU arm.
FIGURE 7.
Self-report measures of participants’ self-efficacy associated with RTW across different domains. (a) CAU arm; and (b) intervention arm.

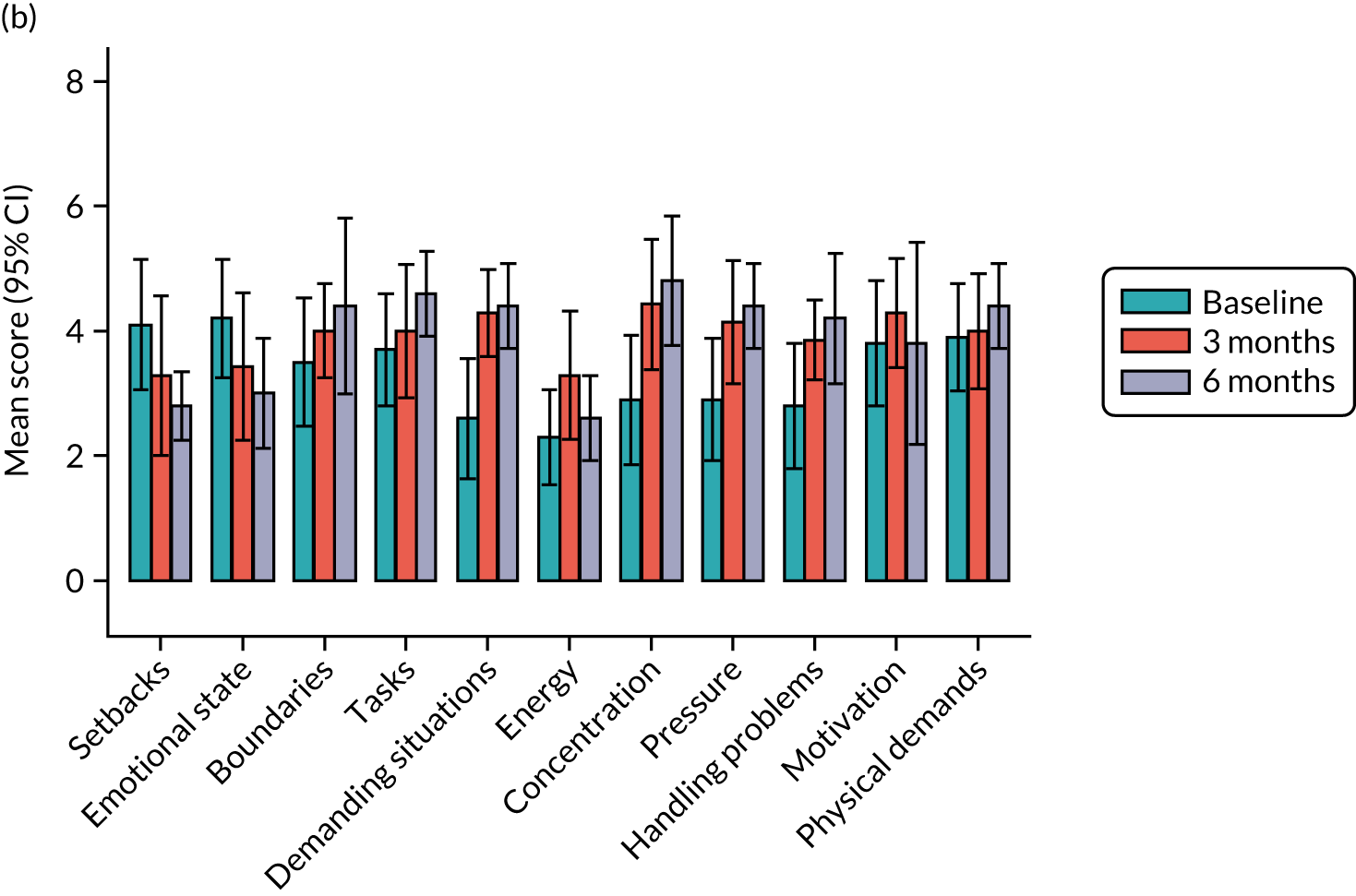
Several measures of self-efficacy were assessed, with higher scores indicating greater levels of self-efficacy. There was an improvement in most measures of self-efficacy for both the CAU and intervention arms. In those measures, improvement seemed more gradual in the CAU arm, from baseline to 3 months and 3 months to 6 months, while improvement in the intervention arm was stronger at 3 months following baseline and scores remained stable at the subsequent follow-up. A few measures of self-efficacy (coping with setbacks and emotional state) showed the opposite effect (i.e. lower scores over follow-up time; see Figure 7).
Perceptions of the availability of collegial support and access to supportive working environments remained relatively static across the six domains in both groups. Higher scores indicate more positive perceptions (Figure 8).
FIGURE 8.
Self-report measure of perception of workplace support across different domains. (a) CAU arm; and (b) intervention arm.
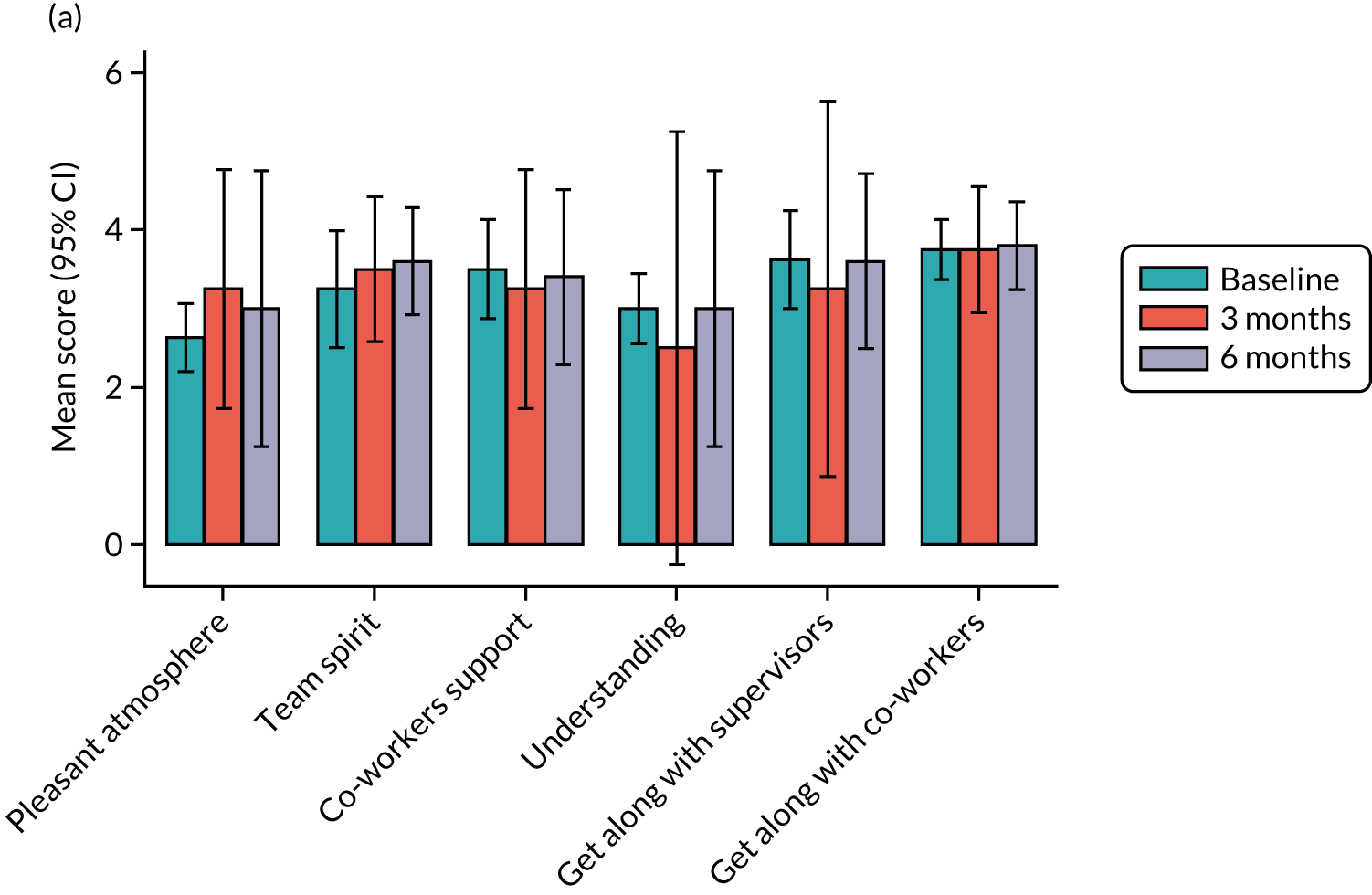
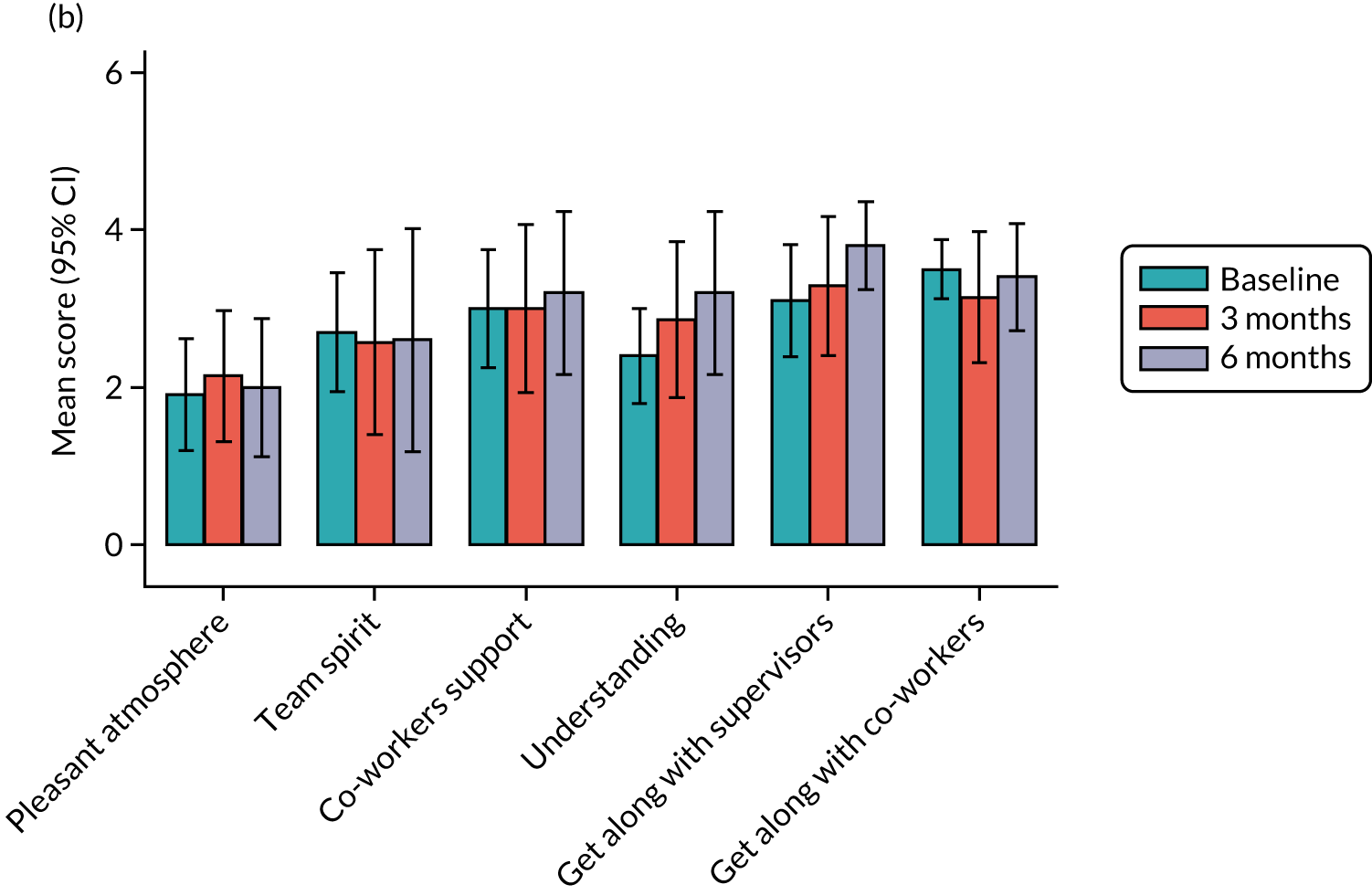
Distribution of outcome measures
Anxiety was assessed using the GAD-7. One participant did not answer one of the seven assessment tool questions at baseline and another did not answer one of the seven assessment tool questions at 6 months. Missing data were imputed as the mean value from the other six questions for those two participants. A score was generated from the seven questions for each of the three time points of the study (baseline and 3 and 6 months). A categorical variable of anxiety was generated using cut-points suggested by the NHS Data Model and Dictionary. 106
Depression was assessed using the PHQ-9. One participant did not answer one of the nine assessment tool questions at baseline and another did not answer one of the nine assessment tool questions at 6 months. Missing data were imputed as the mean value from the other eight questions for those two participants. A score was generated from the nine questions for each of the three time points of the study (baseline and 3 and 6 months). A categorical variable of depression was generated using cut-off points suggested by the NHS Data Model and Dictionary. 107
Differences in the continuous (anxiety and depression) scores from baseline to 3 and 6 months of follow-up were assessed using Wilcoxon matched-pairs signed-ranks tests, and differences in the scores between the two study arms were explored using Wilcoxon rank-sum tests.
Table 16 describes the distribution of outcome measures across the three time points of the study. Over half (77%) of participants reported moderately severe to severe anxiety at baseline. Moreover, there was a trend that this measure had improved marginally by 3 and 6 months. Similarly, over half (61%) of participants reported moderately severe to severe depression at the time of their entry into the study, with a similar trend for improvement at 3 and 6 months, with milder symptoms reported in the CAU arm at 6 months.
| Variable | Baseline (N = 18) | 3 months (N = 11) | 6 months | ||
|---|---|---|---|---|---|
| Total (N = 10) | CAU (N = 5) | Intervention (N = 5) | |||
| Anxiety (continuous score) | |||||
| Mean (SD) | 14.8 (4.4) | 6.6 (6.3) | 7.2 (6.7) | 8.0 (9.0) | 6.4 (4.3) |
| Median (IQR) | 15.5 (10.0–18.0) | 4.0 (3.0–9.0) | 6.5 (0.0–12.0) | 6.0 (0.0–12.8) | 7.0 (6.0–7.0) |
| Anxiety (grouped), n (%) | |||||
| Mild | 0 (0) | 6 (55) | 3 (30) | 1 (20) | 2 (40) |
| Moderate | 5 (28) | 3 (27) | 4 (40) | 3 (60) | 1 (20) |
| Moderately severe | 4 (22) | 1 (9) | 2 (20) | 1 (20) | 1 (20) |
| Severe | 9 (50) | 1 (9) | 1 (10) | 0 (0) | 1 (20) |
| Depression (continuous score) | |||||
| Mean (SD) | 16.4 (5.5) | 9.5 (8.3) | 9.5 (8.5) | 9.8 (12.0) | 9.2 (4.3) |
| Median (IQR) | 18.0 (12.4–21.0) | 9.0 (3.0–14.0) | 7.0 (4.0–14.0) | 4.0 (0–19.0) | 9.0 (5.0–13.0) |
| Depression (grouped), n (%) | |||||
| None | 1 (6) | 4 (36) | 3 (30) | 0 (0) | 3 (60) |
| Mild | 0 (0) | 2 (18) | 3 (30) | 3 (60) | 0 (0) |
| Moderate | 6 (33) | 3 (27) | 2 (20) | 2 (40) | 0 (0) |
| Moderately severe | 5 (28) | 0 (0) | 1 (10) | 0 (0) | 1 (20) |
| Severe | 6 (33) | 2 (18) | 1 (10) | 0 (0) | 1 (20) |
Baseline anxiety score was similar between the two arms of the feasibility study [CAU arm, median 15 (IQR 10–17) vs. intervention arm, median 14 (IQR 10–19); p-value for difference = 0.62]. Anxiety score was lower at 3 months (p-value for difference from baseline score = 0.005) and 6 months (p-value for difference from baseline score = 0.02), but the drop in the score was greater at 3 months. Reduction in anxiety score was more pronounced in the intervention arm at 3 months. However, at 6 months, the drop in anxiety score was similar between the two study groups.
As with the anxiety score, the depression score assessed at baseline was similar between the two arms [CAU arm, median 17.5 (IQR 11.5–22.0), vs. intervention arm, median 20.0 (IQR 13.0–21.0); p-value for difference = 0.9]. Depression score decreased at 3 months (p-value for difference from baseline score = 0.005) and decreased further at 6 months (p-value for difference from baseline score = 0.008). The depression score at 6 months was lower among those in the CAU arm than among those in the intervention arm. However, this difference was not statistically significant (p = 0.60).
Use of antidepressants was found to have increased slightly during the study period (Table 17).
| Number of antidepressants used | Time point, n (%) | |
|---|---|---|
| Baseline | 6 months | |
| 0 | 4 (22) | 2 (20) |
| 1 | 13 (72) | 6 (60) |
| 2 | 1 (6) | 1 (10) |
| 3 | 0 (0) | 1 (10) |
Among the 18 participants who returned baseline data, 11 completed the intermediate questionnaire. Among those who completed the intermediate questionnaire, nine (82%) reported returning to work. Among those who returned to work, seven (78%) continued at work for ≥ 4 weeks without further sickness absence. All participants who returned to work returned to modified duties/hours, with most participants subsequently returning to their normal duties (78%) and working hours (89%). Among those who returned to their normal duties/hours, most (63%) stayed at work in their normal duties/hours for > 4 weeks without further sickness absence.
Among the 18 participants who returned baseline data, five completed the 6-month follow-up questionnaire. Among those who completed the 6-month follow-up questionnaire, four (80%) reported that they had returned to work and all reported remaining at work for ≥ 4 consecutive weeks without further sickness absence. Most (3/4) returned to modified duties/hours, with two returning to normal duties and one returning to normal hours. Among the four participants who returned to work, two returned from modified duties/hours to normal duties/hours for > 4 weeks without further sickness absence.
Very few missing data were noted. However, associated dates for events were more poorly filled in. The outcomes relating to RTW (any RTW, RTW and continue for ≥ 4 weeks without any further sickness absence, return to modified duties, return to unmodified duties, return to normal hours, return to unmodified duties/normal hours and continue for ≥ 4 weeks without further sickness absence) were also reported by case managers. Table 18 shows the agreement between self-report and case manager forms for different RTW outcomes, with an indication of missing data. Overall, there was relatively poor agreement between the two data sources.
| Case manager forms data | Self-report data | κ | |||
|---|---|---|---|---|---|
| No | Yes | Missing | Total | ||
| Any RTW | |||||
| No | 1 | 2 | 0 | 3 | 0.313 |
| Yes | 0 | 7 | 0 | 7 | |
| Missing | 0 | 1 | 0 | 1 | |
| Total | 1 | 10 | 0 | 11 | |
| RTW and continue for ≥ 4 weeks without further sickness absence | |||||
| No | 1 | 3 | 0 | 4 | 0.015 |
| Yes | 0 | 4 | 2 | 6 | |
| Missing | 0 | 1 | 0 | 1 | |
| Total | 1 | 7 | 2 | 11 | |
| Return to modified duties | |||||
| No | 1 | 2 | 0 | 3 | 0.313 |
| Yes | 0 | 7 | 0 | 7 | |
| Missing | 0 | 1 | 0 | 1 | |
| Total | 1 | 10 | 0 | 11 | |
| Return to unmodified duties | |||||
| No | 1 | 3 | 1 | 5 | –0.013 |
| Yes | 1 | 3 | 0 | 4 | |
| Missing | 1 | 1 | 0 | 2 | |
| Total | 3 | 7 | 1 | 11 | |
| Return to normal hours | |||||
| No | 1 | 2 | 1 | 4 | 0.154 |
| Yes | 0 | 4 | 0 | 4 | |
| Missing | 1 | 2 | 0 | 3 | |
| Total | 2 | 8 | 1 | 11 | |
| Return to normal duties (unmodified duties/normal hours) for ≥ 4 weeks without further sickness absence | |||||
| No | 1 | 4 | 1 | 6 | –0.112 |
| Yes | 1 | 0 | 0 | 1 | |
| Missing | 1 | 2 | 1 | 4 | |
| Total | 3 | 6 | 2 | 11 | |
Comparison between self-reported time off and sick absence from records
Figure 9 shows the time periods of sickness absence for 10 study participants. Light blue lines represent periods of sickness absence reported by participants and dark blue lines represent periods of sickness absence calculated from dates recorded in their ESRs. For each of the 10 participants (pairs of lines) in the figure, the duration of sickness absence in weeks according to self-report and ESRs are shown. In most cases, there is very good agreement between the self-reported dates of sickness absence and dates of sickness absence extracted from ESRs. In a few cases it was observed that, using ESRs, it was possible to extract information on multiple spells of sickness absence.
FIGURE 9.
Line plot showing periods of sick leave with a CMD as reported by participants and as extracted from ESRs for 10 participants (corresponding to the 10 pairs of lines).
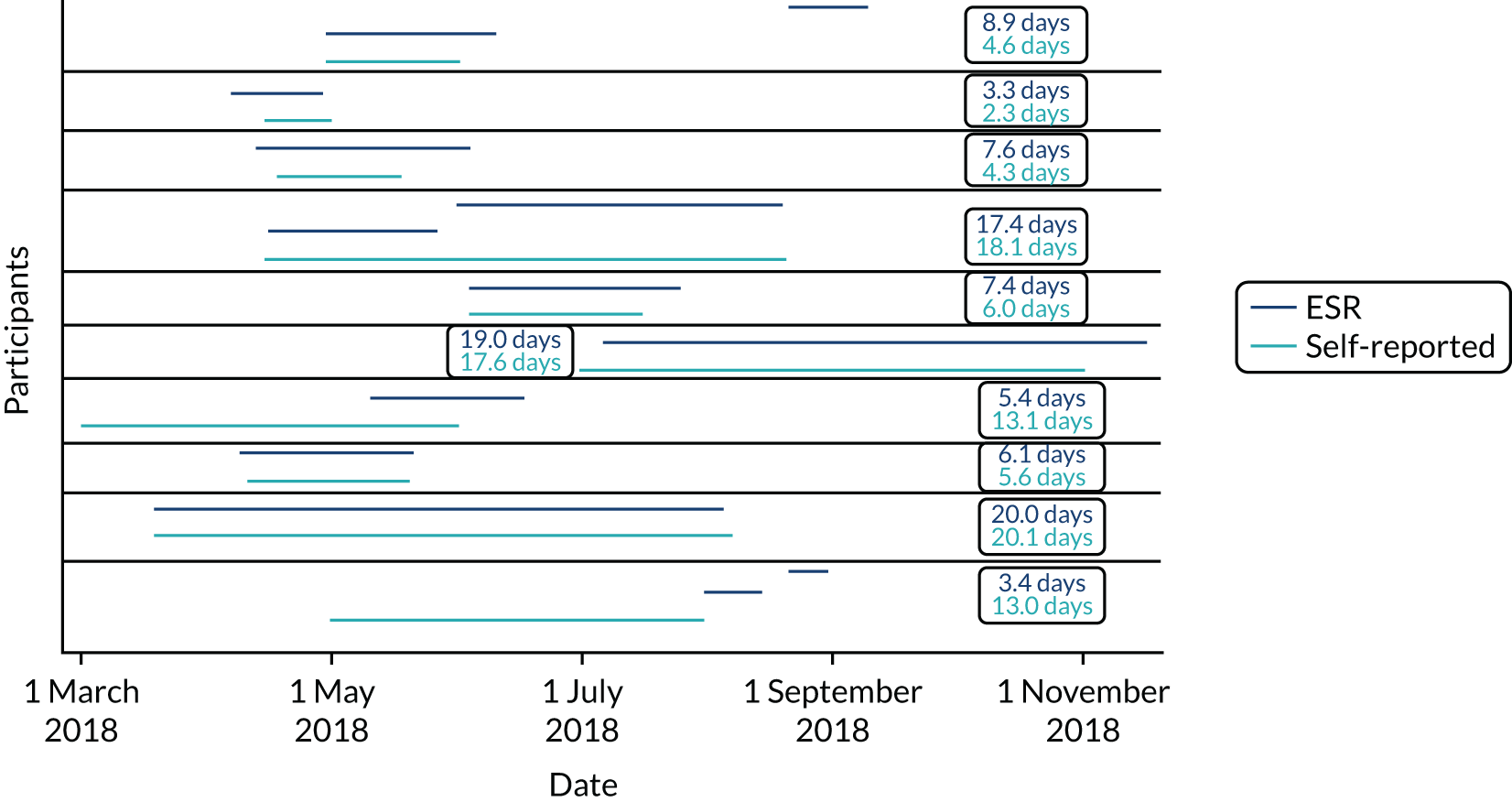
Table 19 presents data on consultation times and number of follow-ups. Among those in the case management group (n = 11), consultation time for at least one of the appointments was reported for 10 participants. Among these 10 participants, two had missing information on consultation time for the first appointment. Among those in the CAU arm (n = 12), consultation time for at least one of the appointments was reported for 11 participants. Among these, one participant had missing information on consultation time for the first appointment. Longer consultation times at first and subsequent appointments occurred for participants who received the case management intervention than for participants receiving CAU. Table 20 presents the number of follow-up appointment sessions per case. Those in the case management intervention had more appointments than those in the CAU arm.
| Variable | Intervention arm | CAU arm |
|---|---|---|
| All appointments | ||
| Participants, n | 10 | 11 |
| Consultation time (minutes) | ||
| Mean (SD) | 124.5 (44.7) | 69.1 (46.9) |
| Median (IQR) | 122.5 (90.0–165.0) | 60.0 (35.0–90.0) |
| Range | 45–190 | 20–181 |
| First appointment | ||
| Participants, n | 8 | 10 |
| Consultation time (minutes) | ||
| Mean (SD) | 85.0 (12.0) | 45.0 (14.7) |
| Median (IQR) | 90 (80–90) | 45 (35–60) |
| Range | 60–100 | 20–60 |
| Second and subsequent appointments | ||
| Participants, n | 8 | 5 |
| Consultation time (minutes) | ||
| Mean (SD) | 70.6 (28.2) | 62 (33.9) |
| Median (IQR) | 67.5 (45.0–90.0) | 45.0 (45.0–60.0) |
| Range | 40–120 | 39–121 |
| Number of follow-up appointments | Intervention arm | CAU arm |
|---|---|---|
| 1 | 3 | 7 |
| 2 | 2 | 2 |
| 3 | 4 | 3 |
| 4 | 1 | 0 |
| 6 | 1 | 0 |
Table 21 presents data from the 6-month questionnaire relating to self-reported uptake and acceptability of components of the case management intervention. Overall, the majority of participants who accessed and used the resources found them useful. Although the numbers are small, the RTW leaflet and the MAP were generally well received; there was less agreement about the usefulness of the other resources.
| Case manager has given or directed to . . . | Used, n (%) | Rate how useful you found these . . ., n |
|---|---|---|
| Sleep hygiene leaflet | No: 1 (20) | – |
| Yes: 4 (80) | Strongly disagree: 1 | |
| Disagree: 1 | ||
| Agree: 2 | ||
| RTW leaflet | No: 1 (20) | – |
| Yes: 4 (80) | Neither disagree nor agree: 1 | |
| Agree: 3 | ||
| HeadGear app | No: 3 (60) | – |
| Yes: 2 (40) | Neither disagree nor agree: 1 | |
| Agree: 1 | ||
| MAP | No: 3 (60) | – |
| Yes: 2 (40) | Agree: 2 | |
| Peer support | No: 3 (60) | – |
| Yes: 2 (40) | Strongly disagree: 1 | |
| Agree: 1 |
Health economics results
Client Service Receipt Inventory data were available for 18 participants at baseline and 10 participants at follow-up, with five participants from each arm (Table 22). The baseline data are considered as one group in the reporting of these results. At baseline, data on GP contacts were available for all participants. Data on the use of other services were available for 13 or 14 participants, depending on the service. At follow-up, data on GP contacts were available for all participants who completed the CSRI. Data on other services were available for more participants in the intervention arm than in the control arm. Data on other talking therapies in particular were missing for the control arm.
| Service | Baseline | Follow-up | ||
|---|---|---|---|---|
| Intervention arm | CAU arm | Intervention arm | CAU arm | |
| GP | 10 | 8 | 5 | 5 |
| Practice nurse | 8 | 4 | 5 | 4 |
| Psychiatrist | 8 | 5 | 5 | 3 |
| Other doctor | 8 | 8 | 4 | 3 |
| Counsellor | 9 | 5 | 5 | 3 |
| Psychologist | 8 | 5 | 5 | 3 |
| Social worker | 8 | 5 | 5 | 3 |
| Community mental health worker | 8 | 6 | 5 | 3 |
| Occupational therapist | 8 | 5 | 5 | 3 |
| IAPT | 8 | 6 | 5 | 3 |
| Other talking therapy | 8 | 5 | 5 | 2 |
| Online therapy | 8 | 5 | 5 | 3 |
| Fit for Work service | 8 | 5 | 5 | 3 |
Table 23 shows the number of participants using specific services. At baseline, all participants had GP contacts. Most other services were used by relatively few participants. None of the participants reported seeing psychologists or social workers. At follow-up, all participants reported having seen a GP. There were relatively high levels of use of counsellors and occupational therapists. However, a large number of services were not used.
| Service | Intervention arm | CAU arm | ||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | |||||
| Yes | No | Yes | No | Yes | No | Yes | No | |
| GP | 10 | 0 | 5 | 0 | 8 | 0 | 5 | 0 |
| Practice nurse | 2 | 6 | 0 | 5 | 1 | 3 | 2 | 2 |
| Psychiatrist | 1 | 7 | 0 | 5 | 0 | 5 | 0 | 3 |
| Other doctor | 1 | 7 | 1 | 3 | 1 | 5 | 0 | 3 |
| Counsellor | 3 | 6 | 4 | 1 | 1 | 4 | 3 | 0 |
| Psychologist | 0 | 8 | 0 | 5 | 0 | 5 | 0 | 3 |
| Social worker | 0 | 8 | 0 | 5 | 0 | 5 | 0 | 3 |
| Community mental health worker | 0 | 8 | 0 | 5 | 1 | 5 | 1 | 2 |
| Occupational therapist | 2 | 6 | 3 | 2 | 1 | 4 | 2 | 1 |
| IAPT | 0 | 8 | 0 | 5 | 1 | 5 | 0 | 3 |
| Other talking therapy | 0 | 8 | 0 | 5 | 1 | 4 | 0 | 2 |
| Online therapy | 1 | 7 | 1 | 4 | 0 | 5 | 0 | 3 |
| Fit for Work service | 0 | 8 | 0 | 5 | 1 | 4 | 1 | 2 |
Completion rates for the EQ-5D-5L were very good. All 18 participants provided scores at baseline and at follow-up; only the usual activities domain had a missing value (for the control arm).
Figures 10 and 11 present the distribution of EQ-5D-5L responses at baseline. For mobility and self-care, most participants reported ‘no problem’ and the only other response was ‘slight problem’. There were greater distributions of responses for the other three dimensions, although no participants reported having extreme problems.
FIGURE 10.
Distribution of EQ-5D-5L responses at baseline: intervention arm.

FIGURE 11.
Distribution of EQ-5D-5L responses at baseline: CAU arm.
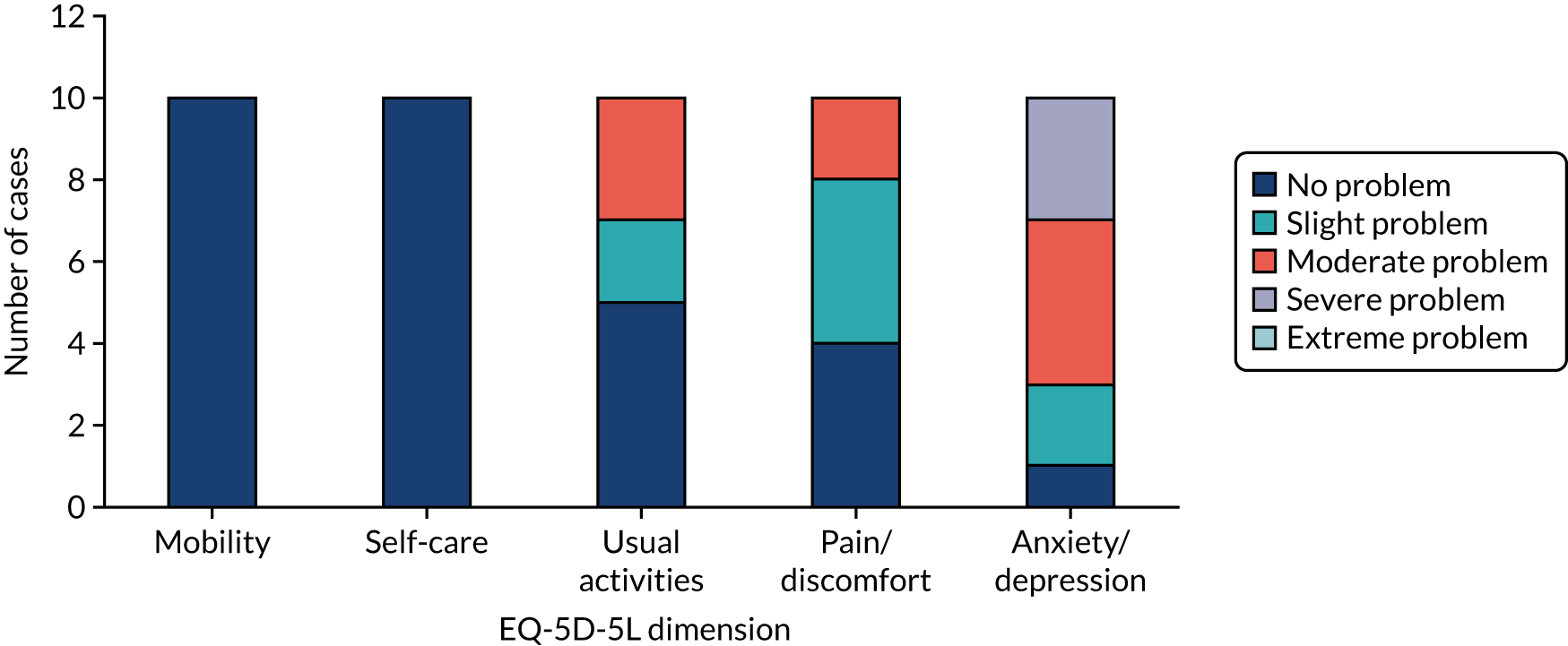
In Figure 12 we see that, for the intervention arm at follow-up, there is limited variation for mobility and self-care but a wider distribution for the other three dimensions. At follow-up, participants in the control arm reported ‘no problem’ or ‘slight problem’ for three dimensions (Figure 13). Usual activities showed most variation.
FIGURE 12.
Distribution of EQ-5D-5L data at follow-up: intervention arm.
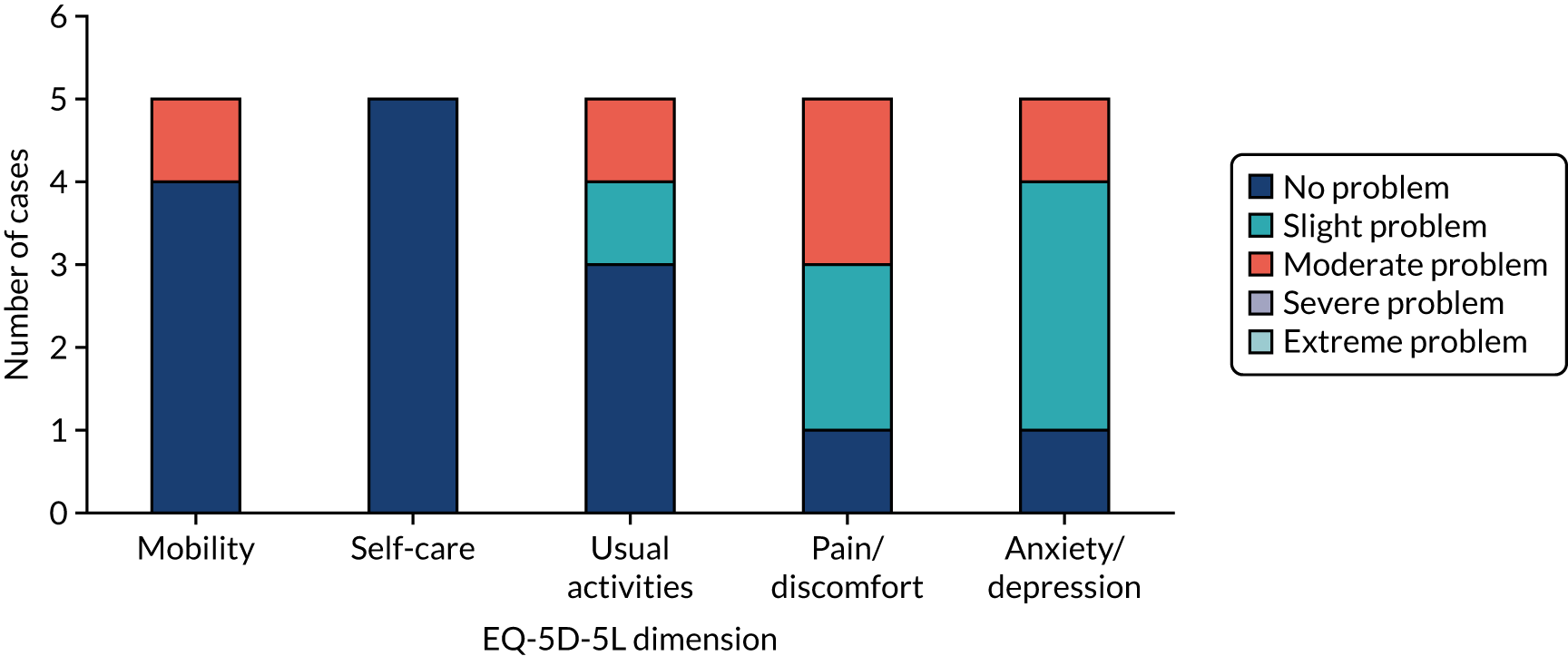
FIGURE 13.
Distribution of EQ-5D-5L data at follow-up: CAU arm.
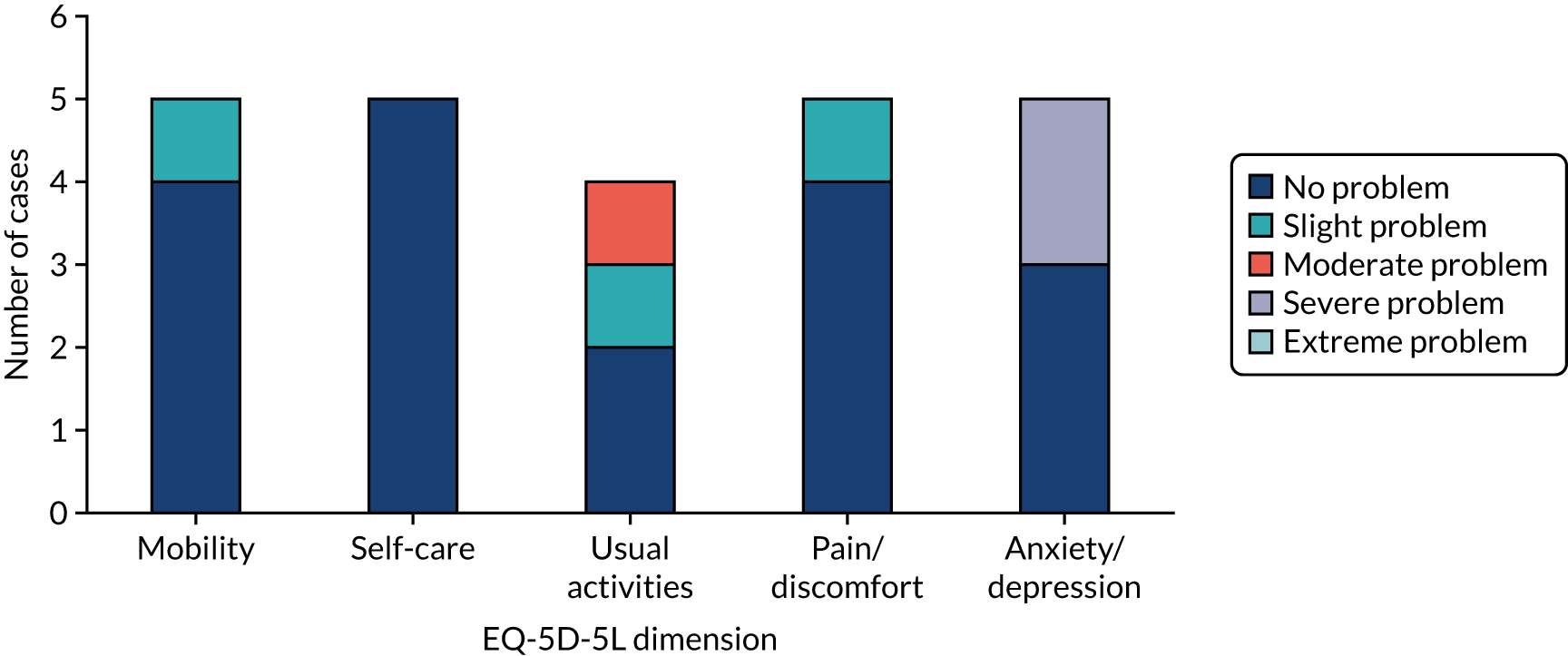
The mean EQ-5D-5L weights for the intervention arm were 0.786 (SD 0.133) at baseline, increasing to 0.836 (SD 0.109) at follow-up. For the CAU arm, the mean EQ-5D-5L weights were 0.649 (SD 0.155) at baseline and 0.870 (SD 0.166) at follow-up.
The intervention costs comprised £10,788 for training, £5025 for materials and £954 for therapy delivery. For the 11 recipients in the intervention arm, the therapy costs per person were £87.
In summary, this feasibility study has shown that the CSRI was reasonably well reported. However, it was apparent that most services were not used and, therefore, in a full trial a reduced version of the CSRI may be appropriate. The EQ-5D-5L was very well completed, but for some dimensions there was very little variation in responses. The intervention costs consisted of fixed elements for training and materials. It is unclear how these should best be apportioned, and they may be best considered as ‘sunk costs’ that do not recur. The costs of the therapy sessions per person were relatively low.
What would be the likelihood of contamination if, within the same trust, the intervention was delivered to some staff and not to others?
A number of case managers at intervention and mixed intervention sites expressed concern about the potential effects of contamination while delivering existing clinical OH services during the study period, and in response they had implemented several strategies to mitigate these risks (e.g. ensuring that study material was not accessible to any OH colleagues, and refraining from offering advice and suggestions to other non-trained OH colleagues on how clinical practice for sick-listed staff with a CMD could be enhanced based on the information and skills they had acquired during the case manager training workshop).
Moreover, mixed intervention sites posed particular challenges with regard to contamination, for example the logistical requirements when planning clinical sessions and providing follow-up consultations (i.e. ensuring study participants in the control arm are not inadvertently booked in to see trained case managers) and the need to ensure that case managers do not modify existing approaches to note-taking in OH records that could later be seen by non-trained OH colleagues. In addition, there were concerns that line managers in mixed intervention sites would have received some of the intervention if they referred a member of staff to the intervention arm and subsequently referred a member of staff to the control arm. We found one occasion where contamination was unavoidable because of an OH staffing issue.
Protocol violations
No protocol violations were recorded during the study. However, at one site an incorrect personal identification number (PIN) was recorded on two participant questionnaires (i.e. a PIN from the intervention arm was recorded instead of the correct PIN from the control arm). The central research team were notified by the site and it was agreed that the central research team would correct this on both questionnaires when they were returned in the post by the participants.
Qualitative results
We observed important issues relating to study promotion, OH referral, participant recruitment and data collection methods that would need to be carefully considered for a future trial.
Getting the message out: challenges in disseminating study information across trusts
Part of the difficulty with participant recruitment related to challenges in communicating information about the research to those who have line management and sickness absence management responsibilities. Moreover, the reliance on e-mail correspondence to promulgate study information across management networks was not viewed as the most effective method because some managers have limited access to emails or because of the sheer volume of e-mails that managers are expected to deal with on a daily basis, meaning that they potentially assign low priority to e-mails that are not considered directly relevant to current work issues. A lack of recognition of the value and benefits of health research in general, coupled with a lack of good communication to help raise the profile of health research (at least OH research) at an organisational level, were considered noteworthy barriers to the effective delivery of health research in the NHS environment. In some circumstances, study awareness among line managers occurred only after the OH referral had been processed by OH:
We tried to do it through our interface within meetings that we go to in the trust and then [name] kind of prepared some emails and we circulated that to quite a host of people, and there were a couple of groups that I noticed weren’t in the original e-mail trail and I just kept on copying it on, and yourself as well, and then I just forwarded it on as well just to try and get as many people aware of it as we possibly could.
Additional promotional strategies to raise the profile of the study were recommended. These included field workers regularly attending local management meetings to disseminate study information and to remind line managers to make early OH referrals, where necessary. It was felt that this would provide an important opportunity for current cases to be confidentially discussed between individual line managers and OH field workers. Working in a more collaborative manner with HR business partners was also acknowledged as a particularly worthwhile approach in facilitating the identification and targeting of prospective participants. It was also proposed that organisations could benefit from more robust tracking systems to monitor staff who have been on sick leave for long periods and to flag to managers those who may benefit from referral to OH:
I mean ideally that [study information] should have been filtered down through to our team because I [HR] was here and sit with managers in sort of sickness advisory meetings with staff. I think that would have been really helpful for them to have flagged it for managers, pushed it a bit more, ‘are you referring people through this?’, and kind of supported the work occupational health were doing, so, it’s a bit of a shame really.
Others suggested making use of other communication channels (e.g. intranet or payslips) for study promotion. Some recognised the importance of brokering executive-level buy-in and commitment as well as fostering their ongoing engagement and support to help facilitate study delivery:
[X] is executive director for the organisation and [X] is the executive director for workforce and then actually [X] can influence the board, so we try and really infiltrate the whole of the organisation from top to bottom in terms of the study. We didn’t put anything on [the intranet] I don’t think, and I really think that, as I’m talking to you, and actually everybody goes onto [the intranet] and that’s our trust sort of intranet site, and actually that was a real own goal, I can take blame for that, I didn’t think about that, but actually we should have had it on the intranet site, where managers got the referral, a big note in red to say . . . I don’t mean [name] and yourselves, I think we as a senior team for the trust’s occupational health service need to be much more methodical and brainstorming as to how we are going to make it real for the organisation, and maybe we left it too much to research.
Factors influencing decisions to refer sick-listed staff with a common mental health disorder to occupational health
A range of factors could influence managers’ decisions to refer sick-listed employees with a CMD to OH. Effectively engaging sick-listed staff in a collaborative decision-making process when initiating discussion relating to the need for an OH referral was thought to be paramount because this helps create a safe and supportive relationship. Engaging staff in the decision-making process allows them jointly to identify current issues and concerns and to agree on what type of support is required from OH:
We had a conversation, face to face. I had an understanding of her circumstance so I believe that it was important to send her to occupational health.
Importantly, staff themselves may consider it necessary to involve OH, and so may initiate discussions with their line manager regarding the need for an OH referral. Accordingly, decisions to involve OH were motivated by a desire to seek more specialist, work-focused advice and support, or when staff were keen to RTW earlier than planned.
Other factors influencing decisions to initiate an OH referral were when staff who had pre-existing or recurring CMDs that were thought to be affecting their capacity to perform their job role, or when previous attempts had been made to devise and implement an effective RTW plan at a local level:
. . . think if they’re not getting anywhere so they’re having meetings if they’re not managing to get them back to work and need a bit of further support and guidance that’s where occupational health may come into play.
Factors influencing decisions not to refer sick-listed staff with a common mental health disorder to occupational health
Multiple factors could influence the decision of managers to not refer staff to OH or, in some cases, to delay the referral process even though they were eligible for entry into the study. These include the severity of an employee’s current mental health condition at a particular time point or whether or not there was already ongoing, active involvement of other health-care professionals or support services. The involvement of other health-care professionals and support services seems to offer line managers and other stakeholders (e.g. HR and OH) a sense of reassurance that sick-listed staff were already receiving adequate care and support. Moreover, some staff may prefer to exercise a degree of autonomy over the timing of when OH engagement (e.g. referral) should take place and this appears to be closely linked to the severity of their condition at a particular point in the sickness absence episode:
. . . when I first raised it, she said well actually this is too early to be referred, I know I’m not going to be well enough to return until a future point but then we have referred her on so we have the advice.
. . . if they are in significant distress, for example if they’re under the care of a crisis team already or I suppose they’ve been admitted to a hospital, then clearly they can’t attend occupational health, but that’s again the manager and the HR’s discussion with that individual. If it’s going to be a detriment to that individual to go to the occupational health appointment, we would never do that.
In other circumstances, it was deemed more appropriate to delay or to coincide the OH referral with an employee’s imminent RTW journey, whereas others considered the engagement of OH to be more appropriate as the duration of sickness absence progresses and so did not consider it necessary to refer too early in the sickness absence period. In addition, some managers and OH staff felt that OH involvement may not be considered necessary, or indeed appropriate, for those who experience enduring CMDs or those in crisis who require more specialised psychiatric care. Some also felt that a lack of proactive management involvement could prevent timely referrals to OH being made:
. . . maybe psychiatric care or things like that at that time you tend not to cross the boundaries between the two.
I think they just hadn’t been managed, I think they’d just gone, people have just let it slide, this person has gone off five times and nothing was being done.
The practice of watchful waiting was considered a useful strategy when supporting staff during periods of sickness absence and, for some, this formed an important part of the stepwise approach when making decisions to engage OH. Manager discretion was also found to be an important factor when making decisions on whether or not to refer sick-listed staff to OH. In most cases, managers’ decisions not to refer were often in response to common life events where the effects on the staff member’s mental well-being were judged to be likely to resolve within a short time, or where grievance or disciplinary investigations were ongoing:
I had somebody that was off sick for about 4 weeks with stress because of a bereavement and she was seeing her GP and she was getting fit notes I think. I actually know her quite well, I didn’t even think to refer her to occupational health because I just thought she’d be . . . in the community, this is hopefully a self-limiting event.
In addition, manager discretion was linked to the extent to which managers felt confident managing employee health issues at a local level, regardless of whether or not their sick-listed staff would have met the study’s inclusion criteria.
Identifying, screening and consenting participants: what worked and what did not
We found no firm evidence to suggest that managers referred a sick-listed employee with a CMD to OH because they were required to do so as per the study requirements. Instead, at most sites the initial procedure to identify eligible participants involved the field worker scanning information on all OH referral forms as they were received, then making an initial assessment of a person’s potential eligibility for entry into the study based on the information provided. However, field workers often found that information recorded by line managers on OH referral forms could not be solely relied on to confidently assess a person’s potential eligibility for entry into the study because important background information (e.g. precise nature of the health condition or reason for sickness absence) was often unknown or missed:
We might have read between the lines that it was a mental health, potential mental health condition, but it didn’t spell it out with the words that you wanted, so often when we look at referrals, we use a bit of intuition . . . probably what a manager’s trying to say but actually not writing it down, which meant then we couldn’t necessarily include them because it wasn’t obvious that that’s why they were being referred.
In these circumstances, field workers needed to contact staff to gather further, clarifying information. This initial telephone contact was a useful approach to adopt at the screening phase because it also provided an opportunity for field workers to discuss the purpose of the study and to scope out an employee’s potential interest in taking part. Owing to the difficulties in identifying eligible participants from the OH referral forms, some sites sent the participant information sheet to all sick-listed staff who were offered an OH appointment with a case manager or field worker (at CAU sites), regardless of the nature of their health condition. This allowed field workers and case managers to conduct a proper assessment of eligibility at the time of the first OH appointment and proceed with taking participant consent:
Yes, any that we have thought would be part of the study I have contacted beforehand. I think the criteria is quite tight, so you kind of have to ring them to see whether they actually met that criteria and quite often they didn’t.
In addition, field workers needed to ensure that participants were fully able to understand study-related information that had been discussed with them over the telephone, particularly if prospective participants were too unwell at the time. However, making telephone contact with potential participants for the purpose of screening for eligibility was not always possible because of lack of employee engagement with the workplace in general; therefore, this was considered to be a further barrier to recruiting participants into the study. In addition, ineffective communication channels between line managers and OH were found to be a frustration for line managers. For some line managers, problems arose in terms of establishing initial contact with OH at the referral stage, and others were left feeling uncertain about the extent of OH involvement once the OH referral has been made:
If from the referral after a first look at it they might meet the criteria we had to look at their previous occupational health records to fulfil any known diagnosis or whether or not they were a current case. Then I would try to ring them because, to introduce them, ‘can I send you the information?’, but I’d want to try and ring first. A lot of the people weren’t answering the phones, I’d have to leave a message, that was sometimes problematic because then they’d call back it would be quite difficult to speak to them, but as I say, a lot of people weren’t answering the phones and some people didn’t come back to us at all despite several attempts, and then you have to stop stalking, but yes, and then if they made contact and you explained, it was only very few that got to that stage that they were willing to participate.
The study also revealed that there were delays in processing OH referrals that then prevented the timely identification of eligible participants after OH referrals had been made. In addition, the study revealed that a number of staff who were on sick leave with CMD were ineligible for entry into the study on the basis that they had already been on an extended period of sick leave at the time at which they were referred to OH. This created another missed opportunity to intervene earlier in the sickness absence period. However, in other cases, some referrals were found to be more proactive in nature and motivated by a desire to intervene at the earliest opportunity, ensuring that support was in place in a timely manner. Identifying and screening prospective participants during routine case meetings involving sick-listed staff, HR and line managers was found to be a useful method at one participating site:
HR and her manager met with her first as part of the welfare process and at that meeting we said would you be willing to participate and then telephone triage was done.
At some participating sites (non-ambulance trusts), once prospective participants were assessed as eligible for entry into the study, field workers reported successfully using the two methods for taking participant consent (verbal and in-person methods). However, the procedure and timing for when to take and record participants’ verbal consent was considered less straightforward than those for in-person consent taken at the time of the first OH appointment.
The process for screening and recruiting participants into the study was found to be a challenge at our participating ambulance trust on the basis that sick-listed staff were referred to the external OH provider within the first 24 hours of sickness absence, and so, within the first week of absence, staff could have already been seen by an OH practitioner before being screened for eligibility for the study. In addition, the ambulance trust had an internal OH nurse who managed the OH service contract and would not typically see staff herself. Furthermore, some focus group participants at this ambulance trust questioned the relevance of the research to their organisation because they have this proactive system of staff sickness management (albeit not modelled on a case management approach) already in place:
So the participant had to be captured between being seen by the line manager and HR and then them arriving at occupational health via our internal occupational health nurse who manages the contract but doesn’t see the participant directly . . . Both had to be lined up nicely for her to be able to interject these people, which is why from the beginning it was a bit of a challenge of squeezing our service into the format.
The extent to which it was ethically appropriate to take informed participant consent from sick-listed staff who were considered too unwell when attending their first OH appointment was highlighted as an area of particular concern in this study. For example, a number of field workers described occasions when it was felt that eligible participants may have lacked the emotional capacity to take part in the study owing to the extent of their CMD and, in these circumstances, field workers needed to exercise professional judgement when screening participants for entry into the study:
Yes, as I said before, for me, as soon as I saw this, the paperwork for this and the data collection, it was just . . . it’s too much.
Variation in organisational policy and practices relating to occupational health referral for sick-listed staff with a CMD
The study found noteworthy differences across participating sites in the organisational policies and practices relating to the timing of OH referrals, which contributed to differences in how soon sick-listed staff were referred to OH (e.g. referrals initiated on the first day of sickness absence at West Midlands Ambulance Service University NHS Foundation Trust versus referrals initiated after up to 4 weeks of sickness absence at other NHS trusts). In addition, at one participating site the sickness absence policy actively encouraged managers not to refer staff to OH too early, instead providing resources and guidance on how to manage cases at a local level in the first instance:
Because the trust absence policy is, tends to be people refer 4 weeks or longer, I was concerned as to how we would catch people at 7 days . . . We tend to often be more, slightly more reactive in reality than we really want to be.
We noted that West Midlands Ambulance Service University NHS Foundation Trust had been working on a unified and proactive approach to the management of staff who go off sick, with significant improvement in sickness absence rates as a result. However, unlike other participating sites, the front-line operational managers at West Midlands Ambulance Service University NHS Foundation Trust did not manage staff who were on sick leave with CMD; if any staff member is on sick leave with a CMD, this is automatically escalated to a senior manager who meets with a colleague from HR on a weekly basis to review cases (a practice that is in stark contrast to practices at other participating sites). Moreover, West Midlands Ambulance Service University NHS Foundation Trust had an early referral process to OH (on first day of absence) for any member of staff who reports a CMD. In addition, they ensured that regular contact was maintained with the staff member. The advantage of West Midlands Ambulance Service University NHS Foundation Trust using an external OH provider is that they had the capacity to initiate treatment sooner if they felt that it would help, and staff who require counselling are seen quickly by a ‘listening centre’:
Once the referral goes in, within 48 hours they get a telephone consultation back just like an initial I suppose exploratory . . . They’ve got specialist counsellors and obviously trained in different things . . . I think our average wait time is between 10 and 15 days for the first session . . . to actually take place face to face . . . whereas the NHS [achieves] 6 to 8 weeks if you’re lucky.
For some of the study participants, the case management intervention provided them with a valuable opportunity to discuss and work on issues and concerns in a supportive environment, and, as a result, this was considered a fundamentally positive aspect of their experience of taking part in the study. Several study participants felt that the professional experience of OH case managers was a particularly useful attribute because this allowed case managers to draw on their knowledge base and NHS experience when facilitating discussions on problem identification and problem-solving. Moreover, they were able to describe the therapeutic benefits that they experienced because they had engaged in problem-solving with OH case managers in a collaborative manner. This also encouraged them to adopt a structured approach to solving problems. In addition, longer consultation times with OH case managers were recognised as particularly valuable because they provided a safe space in which to discuss problems and deliberate on workable solutions. Furthermore, the case management intervention provided an opportunity for study participants and case managers to discuss and share life experiences, which could influence study participants to consider adopting new healthy behaviours. The sleep hygiene leaflet was considered by the study participants to be a useful resource to support them in their recovery.
The case management intervention was found to encourage more regular engagement and contact between case managers and staff than would otherwise occur, and this was thought to provide important therapeutic benefits for staff. From the case managers’ perspective, various components of the intervention were found to be particularly useful. These included the sleep hygiene leaflet (sleep hygiene was recognised by staff as an important contributing issue for them to focus on improving) and the managers’ resource booklet. The information booklet for managers on how to support staff with a CMD was considered (by case managers) to be highly practical and a useful resource for managers to refer to. Moreover, sending out this study material to managers was best administered in conjunction with other routine administrative tasks. In response to the question ‘What were the aspects that you found most helpful, do you think?’, we received the following responses:
Actually talking things through with somebody that was there to listen and not judge or compare, and I think they did that in a good way.
Yes, but yes, I mean that was my major problem and I just didn’t talk to anybody or have anybody to turn to, that I could talk to, and they did talk me through it and listen, you know, so I can only commend them for that.
[Case manager] said she was inspired and you could see that as she saw people, so the implications for us was there was longer appointment session, quite considerably longer, you know, it was a double appointment session that we allocated to these individuals, but seeing how [case manager A] and [case manager B] responded post those sessions, having had interaction without having the details, but you could just tell that they felt that they were adding value and an increased value into dealing with these individuals.
That varies depending on the cases that you’ve got but I did see them both I think five or six times each, but that seemed to help, they seemed to, they did seem to engage with that, and once I discharged them, they’ve not been back to see me, so I think that’s quite a good sign.
In addition, from the case managers’ perspective, access to and use of the HeadGear smartphone app was considered particularly helpful and deemed likely to have therapeutic benefits for study participants. However, in terms of accessibility, lack of time to actively engage in this resource and having to deal with unexpected technical difficulties were highlighted as potential barriers that would need to be overcome. Moreover, case managers described the MAP template as a useful tool for guiding discussions with study participants during OH consultations and to document outcomes with regard to problem identification and problem-solving. Furthermore, the participatory method of delivering the new case management intervention meant that staff appeared more motivated and engaged in their care, and this allowed consultations to take on a more staff-led focus:
I found the action plan really helpful and I found the actual identifying their problems and I used their problems and I worked with them with regards to how can you overcome that problem, what things need to happen and as part of their action plan, you know, we would maybe look at the problem as well within that as to what they needed.
Not wanting to guide and direct as much as you probably would usually rather than . . . so reaffirming what they’ve said and trying to get them to a solution themselves . . . initially just slightly awkward but as the conversations progressed, it did feel that it was worthwhile technique, so I did enjoy.
Several case managers, however, not only considered the problem-solving and action planning component difficult to master but also felt that it was not particularly helpful when guiding staff in discussion of issues. Moreover, one case manager questioned the usefulness of this action planning and problem-solving approach if participants lacked sufficient assertiveness qualities or even insight into their situation. This suggests that case managers may need to possess strong and flexible interpersonal skills/qualities themselves to engage and guide discussions in more challenging situations:
. . . may be difficult with an individual who’s naturally probably quite shy and not very assertive, so they’re just a couple of things that maybe, I wonder whether, thinking of the two people, and they were very interesting cases but they were quite confident and they engaged very well with it, I wonder whether it might have been different had there been . . . because people . . . naturally shy and don’t open up, so I wonder whether it would have been more challenging for me under those circumstances.
One case manager found it worthwhile to familiarise themselves with the study resources before consultations took place to provide participants with their own, personal perspective. While several case managers recognised the benefits of engaging GP and local mental health teams in care planning and RTW preparations, the engagement of other health-care professionals was found to vary from case to case. However, other components of the case management intervention, namely case conferencing or the availability of peer support, were not found to be used at participating sites. Moreover, it was also acknowledged that staff may find it difficult to engage in the new case management intervention because of the severity of their CMD, and so case managers needed to ensure that delivery of each component of the intervention was clinically justifiable and appropriately timed when offered:
I think the other thing is try not to overload people with too much. It’s a bit of a fine line sometimes, not overloading them too much with bits of paper and too much information and look at this, look at that, and look at, because again people can’t always take all that on board.
Although case managers were encouraged to adopt a flexible approach when considering the timing, frequency and mode (in-person or via telephone) of follow-up review consultations, we found that the 4–6 weekly intervals were generally considered ideal in this regard and were generally influenced by whether or not other support services were involved. However, in some circumstances, earlier and more frequent reviews were necessary, particularly when supporting participants with more severe CMDs or when monitoring a participant’s imminent RTW journey. Follow-up review consultations provided a useful opportunity to monitor participants’ progress and to modify existing action plans in response to changing circumstances.
The results also highlight the complex nature of RTW planning between case managers and staff, particularly in terms of how and by whom important decisions are made. They also highlight that a flexible and creative approach is generally needed when navigating this stage of the case management intervention. However, staff may not always be best placed to make autonomous decisions on the appropriateness of the timing of RTW. One participant felt that the OH support they had received as part of the study’s case management intervention was far superior to CAU. Notwithstanding, the study participants’ experience of the RTW journey was found to vary considerably and, for some, inappropriate timing of RTW coupled with poorly co-ordinated arrangements and differing expectations of how the RTW plan would work in practice had the potential to cause further distress during the recovery period. Moreover, facilitating discussions and making practical arrangements for phased RTW could be problematic if others are not fully cognisant of an employee’s job requirements or if specific RTW arrangements are not fully cascaded to specific line managers. In this regard, successful implementation of an employee’s RTW plan was more likely to succeed when senior management were engaged in the process and recognised as key agents to lead and promote a healthy workplace culture:
I remember distinctly going back one time thinking this will be it, I will be back to work in a few weeks’ time, and while that made me nervous, I thought, well that’s good, this means I am getting better with a step forward, but surprisingly they said ‘No, we don’t want to see you for another 6 weeks, you’re not better. This is the reason why’. And she explained it and she was right, and I think if I had gone back sooner I wouldn’t have been able to sustain my return.
Several case managers described making use of a new, pragmatic approach when producing written reports and other study resources when delivering the case management intervention. The purpose was to ensure that relevant health and work-related information was communicated in a succinct and practical manner that would be useful for managers to refer to when supporting participants to RTW. Some case managers also began communicating with staff members’ GPs, which was a new practice for them. One participant felt that the communication between themselves, their line manager and other colleagues during their period of sickness was a specific aspect of their care that was really valuable:
In terms of my reports going back, anything that falls over more than one page, I don’t think they’re going to read, or they’re not going to engage with, they’re not going to absorb, so I tend to try and keep my advice simple, bullet pointed, something that’s implementable, rather than fancy falutin sentences that they’ve got to interpret.
In terms of resource implications associated with delivering the intervention, it was identified that establishing clearly defined roles and responsibilities within OH teams with regards to local implementation of the study is paramount to study success. In this feasibility study, participating sites found it particularly difficult to raise the profile of the study across their entire workforce, which then directly affected the number of sick-listed staff who were screened for eligibility during the recruitment period. Several OH senior managers expressed genuine concerns that they would struggle to meet the increased demand for OH services if significantly more sick-listed staff with a CMD were suddenly referred for OH support. In addition, delivery of the new case management intervention affected existing OH service provision, and this meant that participating sites needed to establish new ways of working (notably offering longer appointment times) to accommodate delivery of the intervention. In the light of this, further reassurances about the requirement for increased resources to deliver a more time-consuming case management approach would also need to be carefully considered:
Initially I was quite anxious about that, how we would fit that in knowing that we were short on clinic times anyway and clinic slots, and really that was my main anxiety coming away from those days is how am I going to fit this in, how, you know, for both myself and [case manager]? Because we couldn’t fit it into normal clinics because we needed those clinic slots, so we had to do it in addition to . . . so it was really a case of blocking time in the diary to be able to accommodate.
Although evidence of the value of early OH referral was acknowledged, it was felt that this needed to be balanced against concerns over resources, operational impact and allowing managers to handle short-term absences at a local level. Moreover, when deliberating on the merits and methodology of a future trial, there are indicators that a lot of preparatory work would need to be undertaken if current organisational practice and policy with regards to the timing of OH referrals is vastly different from the study requirements. Participating sites may not see it as practical or realistic to initiate an organisation-wide change in OH referral practices and policy during a study period (such as referring all sick-listed staff at an earlier time point in the sickness absence period) to then revert to their previous practices at the end of the study.
Discussion
How feasible and acceptable would it be to deliver such an intervention in different NHS settings? What would be the resource implications of the intervention?
We found that the case management intervention could be reliably delivered as prescribed and, importantly, delivered alongside existing OH clinical services. However, this was reliant on participating sites having the capacity to accommodate longer OH consultation appointments for those who were receiving the intervention as well as having more timely OH referrals routes. In the present study, delivery of the case management intervention required longer consultations for the first appointment, followed by subsequent review appointments. This meant that some existing OH clinic sessions at intervention sites needed to be modified slightly during the study period so that longer consultation times could be accommodated.
The increase in financial costs required for OH services to deliver enhanced occupational support and case management was also observed in the earlier CAMEOS trial. 23 Notwithstanding the potential resource implications, there is a strong care to be made to NHS trusts’ executive boards that any potential increase in costs associated with providing extended OH consultation times could be offset if sick-listed staff are able to RTW sooner than they would have done otherwise.
We found that it would not be feasible to deliver the proposed intervention in NHS trusts where assertive OH involvement is initiated as care as usual, that is, on or around the first day of sickness absence, as was the case for one of our participating sites (West Midlands Ambulance Service University NHS Foundation Trust). Furthermore, we are unable to provide definitive advice on whether or not it would be feasible or even logistically practicable to deliver the intervention at NHS trusts where OH services are brokered from external OH providers.
What rate of uptake could be expected and how good would the adherence by occupational health staff and study participants be?
Overall, the results showed that there was good adherence by the OH case managers with regard to delivery of key components of the case management intervention. However, we found no evidence that case managers or participants felt that it was necessary to convene case conferences between the OH case managers, line managers and staff, or for participants to engage in local peer support, nor was there any evidence that workplace visits were required to facilitate the RTW of staff during the study period. Caution is warranted when drawing definitive conclusions from these results in terms of acceptability and adherence given the small number of participants who received the case management intervention.
If a trial were conducted to test such an intervention, how well would methods of recruitment and data collection work in practice?
The inclusion criteria were suitable for the intended population; however, important insights were gained about methods that were not found to be optimal for identifying potentially eligible participants. Lack of organisational awareness that the study was taking place at participating sites featured prominently in the qualitative process evaluation, and this was in spite of implementing a range of strategies for promoting the study among local management teams. On reflection, we recognise that the participating sites comprised vast workforce populations and that large numbers of NHS staff hold line management responsibilities that change daily, according to shift patterns. This made it impractical for the field workers to ensure that study promotion reached all levels of management. Other studies testing enhanced occupational support have used alternative methods to identify and target sick-listed staff, such as screening routine sickness absence reporting systems followed by direct mail invitations. 23 Although in Kenning et al. ’s study23 it was noted that identifying prospective participants via this method had generated a smaller than expected number of participants, the overall proportion of eligible sick-listed staff who were screened and consented into their study was larger than in the current study. Furthermore, it is envisaged that adopting a similar method in a future main study will vastly increase the number of prospective participants being screened for eligibility. This could be further supported by co-opting the support of a senior NHS executive who could help to launch and promote the research across each organisation and, if possible, draw on their own lived experience of dealing with a CMD and its impact on work.
What rates of recruitment and follow-up would be expected?
The method of recruitment used in this present study was not found to be an optimal approach, and so would not be recommended for future research. However, to assist with understanding the lower than expected recruitment rate in this present study, we also sourced OH activity data from a non-participating NHS OH provider (University Hospital Southampton NHS Foundation Trust). This site appeared to have had a much larger number of easily identifiable sick-listed staff with a CMD who were referred to OH, probably because of buy-in from senior management on the importance of early referral to OH that had led to a cultural change at line manager level. Nevertheless, our results suggest that it would be reasonable to expect that there would be a significant increase in the number of sick-listed staff who would be screened for eligibility (and potentially consented for entry into a study) if a more targeted and direct contact recruitment method were to be adopted.
Although, overall, we were satisfied with observed follow-up response rates in this study, we acknowledge that response rates may have been enhanced further if we had made use of electronic questionnaires to facilitate data collection and offered a financial incentive for completion. 108
Chapter 6 Work package 4
Finalisation of the manualised intervention and recommendations for the design of a randomised controlled trial
Method
We worked with our stakeholder group, including our PPI representatives, to review the information from the feasibility study and to determine whether or not a cluster RCT could be designed that was free from unacceptable contamination and avoidable logistical constraints. To inform finalisation of the manualised intervention and formulation of recommendations for design of a RCT, we reviewed the findings from the various qualitative, quantitative and economic analyses that were undertaken in this feasibility study. We paid particular attention to the response rate and likelihood of contamination to determine whether an individual or a cluster trial would be the more appropriate method for a definitive trial.
Proposed revised recruitment method
In Kenning et al. ’s study,23 potentially eligible staff who were on sick leave were identified by scanning organisations’ sickness absence reporting databases and sending out participant information sheets directly. A similar approach could be readily adopted for a future evaluation of our case management intervention while complying with current common law duty for confidentiality. Identification of prospective eligible study participants from the screening of routine records followed by sending study invitations is a method that has been used successfully in previous studies. 109,110 During data analysis, and at the time that this report was produced, the Guy’s and St Thomas’ NHS Foundation Trust Information Governance Committee (represented by the chief medical officer, the newly-appointed Caldicott guardian and others) was consulted and provided confirmation that the following method to identify and screen sick-listed staff with a CMD would be acceptable to implement:
-
HR colleagues will identify sick-listed staff with a CMD by searching the code S10 in ESRs.
-
HR will be responsible for sending out the participant information sheet to sick-listed staff with a CMD to inform them of the study and to opt in, should they wish to participate.
It is notable that we approached the former Caldicott Guardian at Guy’s and St Thomas’ NHS Foundation Trust in 2017 to explore the proposal of identifying sick-listed staff with a CMD for our study from ESR data and, at this time, we were advised that this approach would not be possible owing to data protection restrictions; more specifically, the OH department would not have authority to access these data for the purpose of identifying and approaching potentially eligible sick-listed staff for inclusion in a research study. In 2019, however, this method was presented to the Caldcott Guardian and Information Governance Committee with the suggestion that HR be responsible for sending out the participant information sheet directly to sick-listed staff. This revised method was approved for use in the future evaluation study on the basis that it did not contravene current data protection regulations. Unfortunately, we are unable to provide any reliable recruitment figure estimates using this alternative method without first undertaking further development work.
Outputs
-
Complete specification of the intervention package and potential staff and cost implications.
-
Recommendations for future development work and design for a main study.
Results
Finalisation of the manualised intervention
Figure 14 provides an overview of the final manualised case management intervention, taking into account the results from the feasibility study.
FIGURE 14.
Overview of the final manualised case management intervention.
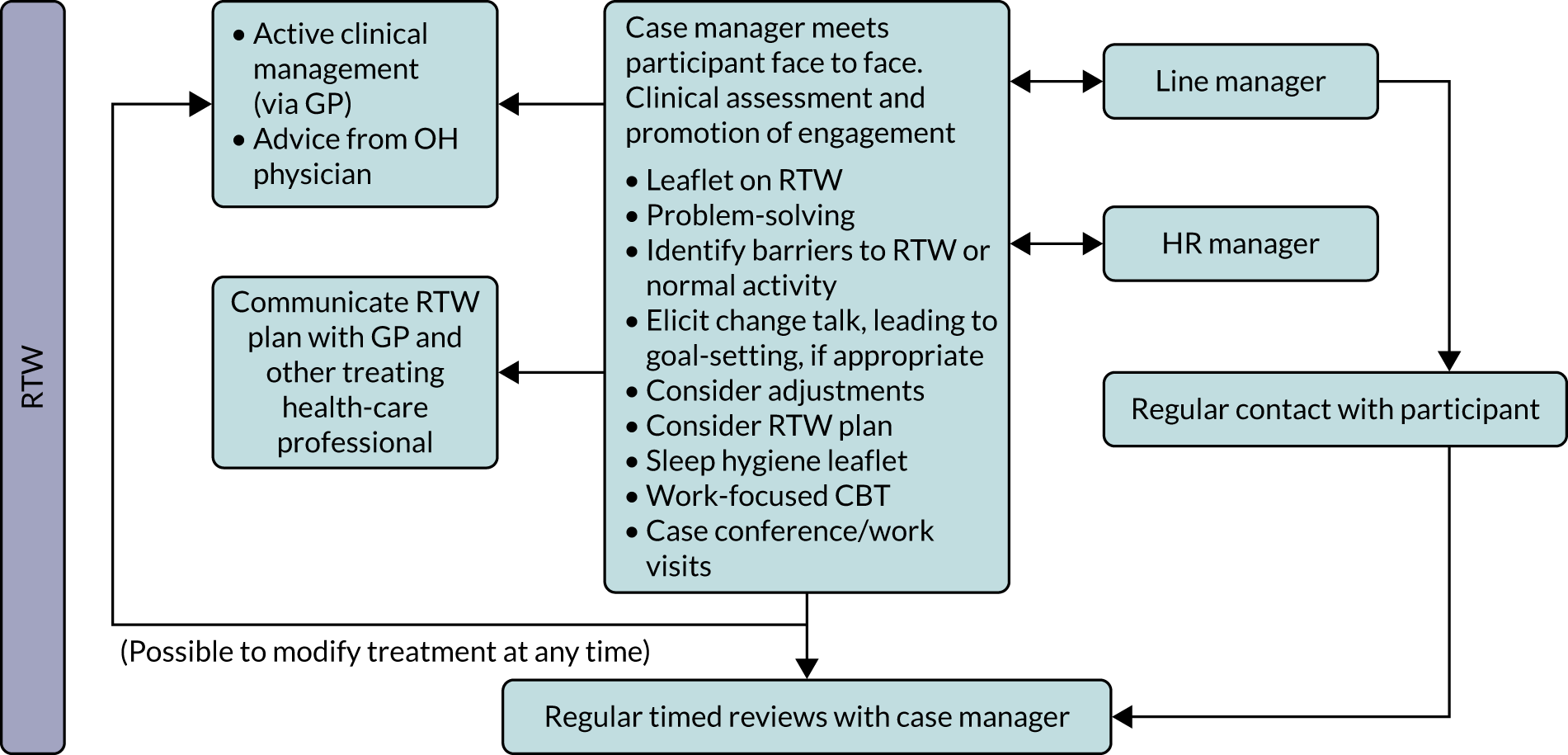
Full instructions on how to deliver the case management intervention
1. Worker seen by case manager within 5 working days of line manager receiving fit note with a reason for absence being a CMD
The worker should be seen within 2 weeks of going off sick. At this point, the case management intervention starts. At the first and subsequent OH appointments, the following activities are undertaken/revisited:
-
Case manager conducts a detailed assessment of the presenting problems. Clinical occupational history investigated and mental state examination conducted following standardised assessment pro forma (use clinical form 1 and retain in the OH record).
-
Case manager facilitates problem identification and problem-solving discussions using patient engagement and problem-solving techniques and skills (use case management form 2 and retain in the OH record). This component comprises the following seven stages:
-
Stage 1 – explain the rationale behind the treatment.
List symptoms; list problems; establish a link between symptoms and problems.
-
Stage 2 – problem definition.
Choose one particular problem from the list; define the problem.
-
Stage 3 – goal-setting.
Achievable within a short time frame; take into account their resources/barriers/obstacles; make the goal specific, measurable, achievable, relevant, timed (SMART); agree and write down the goal; aim to achieve it by the end of the next session.
-
Stage 4 – generate solutions.
Generate solutions for the set goal; brainstorm lots of solutions.
-
Stage 5 – choose preferred solution.
List the pros and cons for each potential solution; choose the one with the most benefit and least disadvantage.
-
Stage 6 – implement the solution.
Agree a clear set of steps (MAP) for next session.
-
Stage 7 – evaluate the outcome and reflect.
Discuss and assess progress against the action plan, which is done in cycles (revising the problem list, connection to symptoms, choosing a new problem or new subset of a problem and deciding on a preferred solution from a list of possible options, and forming a new action plan to achieve the preferred solution by next visit); each visit should bring the solutions nearer to RTW and a clear rehabilitation plan.
-
-
RTW plan (at earliest visit possible).
-
Self-guided structured activity (MAP) between sessions.
Discussions should cover or include the following:
-
Assessment of clinical need.
-
Overview of problem-solving rationale and principles (link symptoms to problems).
-
The case manager assisting the sick-listed worker to identify and define specific problems and obstacles to RTW, with a focus on workable goals/actions/solutions and prioritisation.
-
For example, what obstacles are preventing RTW? Of those, which can be changed/modified and which cannot? Prioritise the importance of obstacles in preventing RTW (e.g. on a scale of 1–10). Include domestic and non-work related issues. Encourage acceptance of issues that cannot change. Include activities of daily living and exercise. (Note: very early RTW might not be an attainable goal; instead, focus on more achievable goals that are likely to lead to eventual RTW (i.e. workers encouraged to see RTW as a ‘process’ and not an ‘event’).
-
-
Maintained focus on work outcomes based on CBT principles. 111,112
-
The worker recording a list of problems and an action plan on the MAP template.
-
Identification of and attempts to improve self-confidence in RTW (self-efficacy).
-
Setting of achievable homework activities.
-
Consideration of therapeutic RTW supported by adjustments/workplace visit.
-
Sleep hygiene leaflet.
-
Provide Returning to Work After Absence due to Mental Ill Health booklet (study-specific resource).
-
Download of the HeadGear smartphone app.
-
RTW plan for 2 weeks only, then review. (Make sure that all stakeholders know that the RTW plan is a minimum.)
2. Referral to other professionals
Case manager to refer the worker to other health-care professionals when red flag(s) present:
-
Referral to GP for active clinical management including medication review. Red flags for case manager referral to GP –
-
psychotic features
-
medication review
-
high risk of self-harm/harm to others
-
any major medical concern.
-
-
OH physician – red flags for referral:
-
final stages of sickness absence or not making progress towards RTW or ≥ 8 weeks of absence and not making progress towards RTW
-
worker reducing workload further (e.g. going part time again)
-
more complex cases (e.g. personality disorders).
-
3. Regular timed reviews: collaborative problem-solving
Case manager to meet the worker for a review 2–4 weeks after the initial appointment. These meetings are not about symptom recovery but functioning; they are supposed to be for setting and reviewing plans and progress. There is no prescribed number of reviews and the amount and frequency of appointments should be adjusted to individual needs. Once the worker has returned to work there will be one more review with the case manager, then an ‘open door’ policy.
4. Communication (line manager, HR and GP)
After the first appointment, the case manager sends a report to the line manager, HR and GP to keep all parties informed of the outcome of the first step of case management (and each subsequent consultation if there has been a change in the RTW plan). With the worker’s consent, case managers are encouraged to telephone the line manager of the worker (or meet them face to face) to inform them of the outcome of the first consultation and discuss possible communication between the line manager and the worker (communication from line managers could be perceived as putting pressure on the worker to go back to work quickly, so case managers should have detailed guidelines for line managers to emphasise what should be included in the communication, e.g. what support is available). Line managers provided with the resource booklet How to Support Employees Who Return to Work After Absence due to Mental Ill Health: A Guide for Line Managers (study-specific resource).
Letter to GP should be in hard copy and contain the following phrases to capture in their medical records: ‘RTW’ (Read code 13JP), ‘recommend phased RTW’ (Read code 9DIE) or ‘not fit for RTW’ (Read code 9D15.00).
5. Finalisation of the manualised intervention
Data from various sources (case note audits, participant questionnaires and feedback from the participant and case manager interviews) showed that the bespoke case management intervention developed and tested in this feasibility study was acceptable and feasible to deliver, provided sick-listed employers were referred to OH early enough. Results from the feasibility study were discussed at the co-applicants meeting on 12 June 2019. Overall, the group agreed that the case management intervention was fit for purpose but also agreed that the peer support component and the video-recording of the case manager training could be removed because of the lack of uptake. The final manualised intervention (including flow chart and full instructions) was presented and endorsed at the final Study Steering Committee meeting on 10 July 2019.
Chapter 7 Comparison with previous research
Although the aim of this study was to develop and test the feasibility of an intervention to improve RTW for sick-listed staff with a CMD, and to develop and test the feasibility of proposed study processes for use in the future trial, it is useful to make preliminary comparisons with previous studies in terms of study implementation and participant recruitment, as well as clinical, occupational and prognostic outcomes.
We observed notable similarities to Kenning et al. ’s23 pilot RCT trial of a new collaborative case management intervention with regard to the challenges we encountered with participant eligibility and recruitment. First, both studies experienced a screening and recruitment rate that was much lower than expected, in spite of the large number of potentially eligible staff who were on sick leave during the study period. This reflects previous literature, which has highlighted the inherent difficulties faced by researchers when recruiting participants into mental health trials. 113 Similarly, both studies also observed a large number of recently sick-listed staff who had already returned to work at the time that they were first seen by the local OH service and screened for entry into the study.
Previous studies (including a comprehensive systematic review and two national guidelines)7–9,11–17,52 have reported on the clinical effectiveness and cost-effectiveness of different forms of interventions to support RTW of sick-listed workers with a CMD. Although the purpose of the present feasibility study was not to assess the clinical effectiveness and cost-effectiveness of the new case management intervention in relation to RTW or clinical or prognostic outcome measures, the results showed that most components of the case management intervention were acceptable as well as feasible to deliver in the NHS environment (i.e. indicating reasonable intervention fidelity). In addition, unlike previous studies evaluating case management interventions based in OH and non-OH settings, which reported low (poor) levels of adherence to interventions by participants and case managers,87,114 the results from the present study showed solid uptake of engagement with and adherence to the intervention among the study participants and OH case managers.
A previous UK study24 found that case management is feasible and acceptable to deliver in a NHS setting. Furthermore, those who accessed individual components of the case management intervention found them useful. We are also aware of a number of other comparable studies testing work-focused interventions for support workers who experience mental ill health in returning to work,22,26 but the results of these studies were yet to be published when we were analysing our findings.
Harms
No harms were reported during the conduct of this study.
Strengths
There were a number of important strengths in relation to the study design, methodology and output:
-
A national survey of CAU and an updated systematic review.
We successfully completed a number of preparatory activities that helped us to finalise the proposed case management intervention. This included the first national survey of OH services in the NHS in relation to the provision of CAU for staff who are on sick leave with a CMD as well as a comprehensive updated systematic review of the scientific and academic literature.
-
Data collection from more than one source.
More than one source of data was used to enhance the richness and quality of the data, which helped to increase the internal reliability and creditability of the research findings. Moreover, use of qualitative methods and thematic analysis allowed us to gain, from different perspectives, important insights into the experiences of those who took part in the study as well as a greater understanding of the context in which the study was implemented. The qualitative interviews allowed what was important and meaningful to key stakeholders (e.g. participants, case managers, line managers, HR) to be given prominence, and provided an opportunity for them to describe real-life events and experiences as well as offering personal opinions. A selection of participants’ verbatim quotations were used to both support and underpin interpretations of the research data and to illustrate how experiences and meanings were expressed by the participants.
-
Expert and peer review.
Members of the Study Steering Committee, which included PPI representatives, were regularly consulted and contributed their academic and clinical knowledge and expertise throughout key stages of the study period. This included discussions about the feasibility of the proposed study design and methods for data collection and analysis as well as approaches to the implementation of the study in the NHS environment. Moreover, at the end of the study our expert members helped us to consider the meaning of the overall findings from the study and helped us to formulate suitable recommendations for further development work.
Weaknesses
A number of weaknesses were acknowledged:
-
Representativeness of the sample group –
-
The study participants had unique experiences and the issues that they were dealing with in relation to their CMD (including its impact on their capacity to work), so it is likely that the study sample group was not fully representative of all NHS staff who go on sick leave with a CMD. Moreover, it is possible that those who agreed to take part in the study may have been more motivated to do so because they had a greater level of interest in this area or because the severity of their condition was such that they felt that they had the capacity to participate. There were a number of participants who were invited to take part at the time of their referral to OH but who felt too unwell at that time to take part.
-
Similarly, many of the local issues and factors relating to the implementation of the study at each of the participating NHS sites may not be commonplace or relevant to other NHS sites.
-
Owing to the large proportion (61%) of OH providers who did not participate in the survey of CAU, the findings from this preparatory activity may not be representative of CAU in this area of OH clinical practice.
-
-
Aspects of the study design –
-
The major challenge and limitation with the study was the small number of sick-listed staff with a CMD who were screened and recruited into the study. This was in spite of the overall large number of staff who were on sick leave with a CMD during the study period and our best efforts to promote the study as widely as possible across management networks.
-
Owing to the restrictions the central research team had in accessing participants’ sensitive OH clinical notes, the study relied on the independent audit of clinical notes (using a checklist pro forma) by local colleagues who worked closely and alongside our case managers to determine the extent to which components of the case management intervention had been delivered as intended. Therefore, it is possible that local colleagues may have been biased when conducting these independent assessments, particularly if they were keen for their colleagues to be seen in a favourable way (i.e. adhering to the intervention delivery requirements). In addition, the structured checklist pro forma meant that we were not able to record any subtle but meaningful descriptive information about how each case manager engaged in and delivered the case management intervention (i.e. their individual styles and approaches). More specifically, the absence of observational work in this study meant that we were not able to observe the dynamics of case management in action. It is worth bearing in mind that this feasibility study was not intended to examine intervention fidelity per se, and so the inclusion of observational work as part of the process evaluation in future research will be recommended.
-
Participants in the individual and focus group sessions were required to reflect on their own experiences during the study period. This reflective activity required participants to, among other things, focus on their own involvement and actions during the study (e.g. in terms of approaches to screening and recruitment, study promotion and engagement with other stakeholders, and views on components of the case management intervention). Therefore, interviews relied on participants being able to recall complete and accurate accounts of their experiences, and their willingness to disclose this information to the researcher. Moreover, case managers may have felt hesitant about disclosing information that risked indicating poor knowledge of the study protocol and of their expected duties as case managers and field workers.
-
Given the relatively recent introduction of the case manager training workshop, coupled with the small number of participants taking part in the study at several intervention sites, it is likely that OH nurses who were trained in the case management intervention did not have enough opportunities in which to make use of their new clinical knowledge and case management skills. This is likely to have affected the quantity and quality of the experiences that they were able to reflect on during the interviews.
-
Chapter 8 Conclusions
This research successfully met its intended objectives, which were to update current evidence on the clinical effectiveness and cost-effectiveness of work-focused interventions targeting sick-listed staff with a CMD; to gain insight into the CAU offered by NHS-based OH departments across the UK with regard to the provision of mental health support; to develop a bespoke work-focused case management intervention and training workshop for OH case managers; to develop reliable data collection tools to measure a range of outcomes specific to CMD and sickness absence; and to test the developed data collection tools and other proposed study processes by conducting a feasibility study. However, in spite of these favourable study outcomes, the vast majority of NHS staff who were on sick leave with a CMD during the study period were not referred to their local OH department, despite attempts by the research team to ensure trust-wide study promotion. Unfortunately, this had a direct impact on the number of potentially eligible participants who were recruited for entry into the study. A new, targeted method to identify sick-listed staff with a CMD has been refined and it is now recommended that further development work is undertaken.
It became clear during the study that individual randomisation would not be possible in an effectiveness trial. There would be unavoidable contamination because line managers of intervention participants may also be line managers of control participants. Furthermore, for the intervention to be effective, policy changes would be required throughout a directorate in a trust or ideally throughout the entire trust. We have suggested possible study designs in Recommendations for future research.
Implications for practice
-
A case management intervention is acceptable and feasible to deliver in the NHS for the management of staff who are on sick leave with a CMD. However, the clinical effectiveness and cost-effectiveness of such an intervention has not yet been tested.
-
There is a need to improve manager OH referral practices across the NHS.
Recommendations for future research
Following deliberation of the results in the research team, and in consultation with our stakeholder group and international expert, the research group agreed that the following recommendations should be made to the funder. These were reviewed and endorsed by the Study Steering Committee on 10 July 2019.
As discussed in this chapter, we do not think that it would be possible to evaluate the effectiveness of the intervention through an individually randomised controlled trial without substantial contamination. Moreover, if the intervention were found to be clinically effective and cost-effective, it would require a policy change at trust level for it to be implemented. There is some evidence that the proposed intervention will do more good than harm and that the outcome (time to RTW) can be obtained by routinely collecting sickness absence data. The choice for an effectiveness study rests between a stepped-wedge design and a cluster RCT. For several reasons, we consider that the evaluation of the intervention would best be tested by a stepped-wedge design. 115,116 This pragmatic approach would allow us to test our new recruitment method in one trust as an internal pilot, with clear stop/go criteria, before rolling out the intervention to other trusts. A stepped-wedge design that incorporates this internal pilot would take account of temporal changes in sickness absence and cultural change during the study period.
The main barrier to any evaluation study is the low referral rate of workers sick-listed with a CMD to their OH service. Before proceeding to a full evaluation study, it is essential that a different system of recruitment be tested in an NHS trust.
The system of recruitment to be tested should be as follows:
-
HR review sickness absence records on a weekly basis to identify staff who are on sick leave with a CMD. HR send the participant information sheet to the sick-listed staff member. The participant information sheet encourages sick-listed staff to initiate self-referral to OH or to ask their line manager to refer them to OH.
-
The new recruitment strategy is tested at a single trust in a few selected directorates where there are known to be high rates of sickness absence with a CMD, because this will help to minimise the risk of overburdening OH with an increased number of new OH referrals during the study testing period.
-
If successful, the new recruitment strategy is extended to all directorates at that trust and the response is assessed.
-
A pre-specified minimum recruitment rate is applied as a stop/go criterion before the intervention is introduced and the recruitment methods are rolled out to other trusts as per the stepped-wedge approach.
Other trusts would be randomly assigned to implement the system of recruitment followed by the intervention sequentially as per a stepped-wedge design. We are aware that the recruitment method may work in one trust and not in another, so we would ensure stop/go criteria after implementation of the recruitment method at each trust.
Changes to the protocol (amendments)
Table 24 provides details of the various non-substantial and substantial amendments made to the study protocol to enhance study processes and procedures.
| Version number | Date | Amendments (explanation of changes) |
|---|---|---|
| 1.1 | 19 September 2016 | Adjusting ethics/Health Research Authority submission date and minor comments from Paul Grime |
| 1.2 | 27 September 2016 | Table relating to recruitment targets per site added to phase 3, p. 13 |
| 1.3 | 18 July 2017 |
|
| 1.4 | 06 September 2017 | Added two updated intervention flow charts (one for the control and one for the intervention arm) |
| 1.5 | 25 January 2018 | To allow for verbal consent to be taken over the telephone |
| 1.6 | 15 February 2018 |
|
| 1.7 | 29 June 2018 |
|
| 1.8 | 12 March 2019 | Adjusting study end date in section 9.0 (now mid-October 2019) |
Acknowledgements
We would like to take this opportunity to thank all of the participants who agreed to give up their valuable time to take part in this study. In addition, we acknowledge the commitment and hard work of the local field workers at participating sites who assisted with the study. We are grateful to members of the Study Steering Committee for their oversight and expertise: Dr Anne De Bono (Chair), Dr Ira Madan, Dr Vaughan Parsons, Dr Dorota Juszczyk, Professor Damien McElvenny, Ms Tracey West, Mr Andrew Walker, Associate Professor Karen Nieuwenhuijsen and Professor Ewan MacDonald.
We also extend our thanks and appreciation to Ms Jess Vlieland-Boddy (Assistant Research Manager) from the National Institute for Health Research (NIHR) for her ongoing support. A special thank you to Dr Gill Gilworth, who was seconded for a 9-month period from King’s College London to work on the study and who was chiefly responsible for leading the qualitative data collection and coding component of the study.
We also extend our appreciation to Guy’s and St Thomas’ NHS Foundation Trust, for their willingness to sponsor the trial and for providing ongoing practical support and guidance as required, and in particular to the Research and Development unit, for their research governance and financial management support, and the OH service, for hosting the research team.
Tracey West was one of the PPI representatives and she ensured that the sick-worker experientialperspective was included in the study.
Contributions of authors
Vaughan Parsons (https://orcid.org/0000-0003-0523-3770) (Research Manager and Research Fellow) was the research manager/research fellow and responsible for overseeing delivery of the study. He was responsible for recruiting and supporting participating sites, advising on local procedures for implementing the study processes and producing draft study documents. He was also involved in qualitative aspects of the study (facilitating several focus group sessions, coding the data and conducting the final qualitative data analysis), assisted with delivery of the case manager training and was responsible for drafting the final report.
Dorota Juszczyk (https://orcid.org/0000-0003-2187-8085) (Study Co-ordinator and Post Doctoral Researcher) was the study co-ordinator (part-period). She assisted with the preparatory work that was undertaken (i.e. the systematic review, survey of CAU and intervention development). She was responsible for supporting participating sites during the site set-up and participant recruitment period, and producing draft study documents and manuscripts.
Gill Gilworth (https://orcid.org/0000-0003-1408-8878) (Study Co-ordinator and Post Doctoral Researcher) was the study co-ordinator (part-period) and was responsible for delivery of the study. She was responsible for supporting participating sites, developing local procedures for implementing the study processes and producing draft study documents and manuscripts. She was also involved in qualitative aspects of the study (facilitating interviews and coding data).
Georgia Ntani (https://orcid.org/0000-0001-7481-6860) (Statistician) was responsible for the statistical aspects of design, analysis and interpretation of the quantitative aspects of the study.
Paul McCrone (https://orcid.org/0000-0001-7001-4502) (Health Economist) was responsible for the cost-effectiveness evaluation.
Stephani Hatch (https://orcid.org/0000-0001-9103-2427) (Professor of Sociology and Epidemiology)supervised the qualitative interviews and advised on the analysis and interpretation of the results.
Robert Shannon (https://orcid.org/0000-0002-1153-6754) (Chartered Psychologist) jointly facilitated the stakeholder meeting, assisted in training the case managers in engagement and MI, and assessed the fidelity of their training.
Max Henderson (https://orcid.org/0000-0002-1302-0284) (Professor and Consultant Liaison Psychiatrist) assisted in delivering the training of the case managers and advised on clinical psychiatry.
David Coggon (https://orcid.org/0000-0003-1930-3987) (Emeritus Professor of Occupational and Environmental Medicine) acted as a consultant, advising on study design, analysis and interpretation of results.
Mariam Molokhia (https://orcid.org/0000-0002-1989-7327) (Academic General Practitioner and Epidemiologist) advised on the role of and liaison with GPs in the study.
Julia Smedley (https://orcid.org/0000-0001-6464-3716) (Consultant Occupational Physician) assisted in the training of the case managers, particularly with regard to problem identification and problem-solving, and advised on OH software and mapping the evidence onto the proposed intervention.
Amanda Griffiths (https://orcid.org/0000-0003-1413-4328) (Professor of Occupational Health Psychology) assisted with the qualitative study.
Karen Walker-Bone (https://orcid.org/0000-0002-5992-1459) (Professor of Occupational Rheumatology) contributed her expertise in comorbidity with physical disorders. She has experience in clinical trials and the potential barriers to their success.
Ira Madan (https://orcid.org/0000-0003-2200-7329) (Consultant Occupational Physician and Reader) led and had overall responsibility for the management and delivery of the study, and was involved in all WPs. She acted as one of the reviewers on the systematic literature review, and assisted with developing and delivering the case manager training. She was responsible for writing the protocol and formulating the questionnaires and other case report forms, and finalised production of the final report.
Publication
See B, Juszczyk D, Parsons V, Smedley J, Gilworth G, Madan I. Managing common mental health disorders in healthcare workers. Occup Med (Lond) 2019;69:290–3.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care.
References
- Taylor R. Sustainability of the National Health Service as a Public Service Free at the Point of Need. London: House of Lords Library; 2015.
- Chartered Institute of Personnel Development (CIPD) . Absence Management 2013: Survey Report 2013.
- Department of Health and Social Care . NHS Health and Well-Being Review: Government Response 2009.
- Department of Work and Pensions, Department of Health and Social Care (DHSC) . Health in the Workplace – Patterns of Sickness Absence, Employer Support and Employment Retention 2019.
- Boorman S. NHS Health and Well-Being Review: Final Report – November 2009. 2009.
- van Vilsteren M, van Oostrom SH, de Vet HC, Franche RL, Boot CR, Anema JR. Workplace interventions to prevent work disability in workers on sick leave. Cochrane Database Syst Rev 2015;10. https://doi.org/10.1002/14651858.CD006955.pub3.
- National Institute for Health and Care Excellence (NICE) . Common Mental Health Disorders: Identification and Pathways to Care. 2011.
- van der Klink JJL, Ausems CMM, Beijderwellen BD, Blonk R, Bruinvels DJ, Dogger J, et al. [Guidelines for the Management of Mental Health Problems of Workers by Occupational Physicians.]. Utrecht: NVAB (Netherlands Society of Occupational Medicine); 2007.
- Pomaki G, Franche R, Khushrushahi N, Murray E, Lampinen T, Mah P. Best Practices for Return-to-Work Stay-at-Work Interventions for Workers With Mental Health Conditions: Final Report 2010.
- Cullen KL, Irvin E, Collie A, Clay F, Gensby U, Jennings PA, et al. Effectiveness of workplace interventions in return-to-work for musculoskeletal, pain-related and mental health conditions: an update of the evidence and messages for practitioners. J Occup Rehabil 2018;28:1-15. https://doi.org/10.1007/s10926-016-9690-x.
- Waddell G, Burton AK, Kendall NA. Vocational Rehabilitation – What Works, for Whom, and When? Report for the Vocational Rehabilitation Task Group 2008.
- Nieuwenhuijsen K, Faber B, Verbeek JH, Neumeyer-Gromen A, Hees HL, Verhoeven AC, et al. Interventions to improve return to work in depressed people. Cochrane Database Syst Rev 2014;12. https://doi.org/10.1002/14651858.CD006237.pub3.
- Arends I, Bruinvels DJ, Rebergen DS, Nieuwenhuijsen K, Madan I, Neumeyer-Gromen A, et al. Interventions to facilitate return to work in adults with adjustment disorders. Cochrane Database Syst Rev 2012;12. https://doi.org/10.1002/14651858.CD006389.pub2.
- Waddell G, Burton AK. Concepts of Rehabilitation for the Management of Common Health Problems. London: The Stationery Office; 2004.
- Wagner SL, Koehn C, White MI, Harder HG, Schultz IZ, Williams-Whitt K, et al. Mental Health interventions in the workplace and work outcomes: a best-evidence synthesis of systematic reviews. Int J Occup Environ Med 2016;7:1-14. https://doi.org/10.15171/ijoem.2016.607.
- Stern AF, Madan I. Optimal communication from occupational physicians to GPs: a cross-sectional survey. Br J Gen Prac 2012;62:e833-9. https://doi.org/10.3399/bjgp12X659312.
- Nieuwenhuijsen K, Verbeek JH, de Boer AG, Blonk RW, van Dijk FJ. Supervisory behaviour as a predictor of return to work in employees absent from work due to mental health problems. Occup Environ Med 2004;61:817-23. https://doi.org/10.1136/oem.2003.009688.
- National Institute for Health and Care Excellence (NICE) . Workplace Health: Long-Term Sickness Absence and Incapacity to Work 2009.
- Rebergen DS, Bruinvels DJ, Bezemer PD, van der Beek AJ, van Mechelen W. Guideline-based care of common mental disorders by occupational physicians (CO-OP study): a randomized controlled trial. J Occup Environ Med 2009;51:305-12. https://doi.org/10.1097/JOM.0b013e3181990d32.
- van Beurden KM, Brouwers EPM, Joosen MCW, de Boer MR, van Weeghel J, Terluin B, et al. Effectiveness of an intervention to enhance occupational physicians’ guideline adherence on sickness absence duration in workers with common mental disorders: a cluster-randomized controlled trial. J Occup Rehabil 2017;27:559-67. https://doi.org/10.1007/s10926-016-9682-x.
- Reme SE, Grasdal AL, Løvvik C, Lie SA. Øverland S. Work-focused cognitive-behavioural therapy and individual job support to increase work participation in common mental disorders: a randomised controlled multicentre trial. Occup Environ Med 2015;72:745-52. https://doi.org/10.1136/oemed-2014-102700.
- Björk Brämberg E, Holmgren K, Bültmann U, Gyllensten H, Hagberg J, Sandman L, et al. Increasing return-to-work among people on sick leave due to common mental disorders: design of a cluster-randomized controlled trial of a problem-solving intervention versus care-as-usual conducted in the Swedish primary health care system (PROSA). BMC Public Health 2018;18. https://doi.org/10.1186/s12889-018-5816-8.
- Kenning C, Lovell K, Hann M, Agius R, Bee P, Chew-Graham C, et al. Collaborative case management to aid return to work after long-term sickness absence: a pilot randomised controlled trial. Public Health Res 2018;6. https://doi.org/10.3310/phr06020.
- Smedley J, Harris EC, Cox V, Ntani G, Coggon D. Evaluation of a case management service to reduce sickness absence. Occup Med 2013;63:89-95. https://doi.org/10.1093/occmed/kqs223.
- Vlasveld MC, van der Feltz-Cornelis CM, Adèr HJ, Anema JR, Hoedeman R, van Mechelen W, et al. Collaborative care for major depressive disorder in an occupational healthcare setting. Br J Psychiatry 2012;200:510-11. https://doi.org/10.1192/bjp.bp.111.095687.
- Bergström G, Lohela-Karlsson M, Kwak L, Bodin L, Jensen I, Torgén M, et al. Preventing sickness absenteeism among employees with common mental disorders or stress-related symptoms at work: design of a cluster randomized controlled trial of a problem-solving based intervention versus care-as-usual conducted at the Occupational Health Services. BMC Public Health 2017;17. https://doi.org/10.1186/s12889-017-4329-1.
- Hoefsmit N, Houkes I, Nijhuis FJ. Intervention characteristics that facilitate return to work after sickness absence: a systematic literature review. J Occup Rehabil 2012;22:462-77. https://doi.org/10.1007/s10926-012-9359-z.
- Brown J, Mackay D, Demou E, Craig J, Frank J, Macdonald EB. The EASY (Early Access to Support for You) sickness absence service: a four-year evaluation of the impact on absenteeism. Scand J Work Environ Health 2015;41:204-15. https://doi.org/10.5271/sjweh.3480.
- Black C, Frost D. Health at Work: An Independent Review of Sickness Absence. London: The Stationery Office; 2011.
- Seymour L. Common Mental Health Problems at Work: What We Know About Successful Interventions: A Progress Review. London: Sainsbury Centre for Mental Health; 2010.
- van Beurden KM, Brouwers EP, Joosen MC, Terluin B, van der Klink JJ, van Weeghel J. Effectiveness of guideline-based care by occupational physicians on the return-to-work of workers with common mental disorders: design of a cluster-randomised controlled trial. BMC Public Health 2013;13. https://doi.org/10.1186/1471-2458-13-193.
- Staal JB. Low back pain, graded activity and return to work. Ann Intern Med 2003;140:77-84.
- National Institute for Health and Care Excellence (NICE) . Workplace Health: Management Practices 2015.
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16:606-13. https://doi.org/10.1046/j.1525-1497.2001.016009606.x.
- Hees HL, Nieuwenhuijsen K, Koeter MW, Bültmann U, Schene AH. Towards a new definition of return-to-work outcomes in common mental disorders from a multi-stakeholder perspective. PLOS ONE 2012;7. https://doi.org/10.1371/journal.pone.0039947.
- Ilmarinen J, Tuomi K. Work ability of aging workers. Scand J Work Environ Health 1992;18:8-10.
- Mundt JC, Marks IM, Shear MK, Greist JH. The Work and Social Adjustment Scale: a simple measure of impairment in functioning. Br J Psychiatry 2002;180:461-4. https://doi.org/10.1192/bjp.180.5.461.
- World Health Organization (WHO) . WHO Disability Assessment Schedule 2.0 (WHODAS 2.0) 2020. www.who.int/classifications/international-classification-of-functioning-disability-and-health/who-disability-assessment-schedule (accessed 23 November 2020).
- Lu SJ, Liou TH, Yen CF, Chang FH, Chen YL, Escorpizo R, et al. Determinants of employment outcome for the people with schizophrenia using the WHODAS 2.0. J Occup Rehabil 2019;29:375-83. https://doi.org/10.1007/s10926-018-9794-6.
- Nieuwenhuijsen K, Verbeek JH, de Boer AG, Blonk RW, van Dijk FJ. Predicting the duration of sickness absence for patients with common mental disorders in occupational health care. Scand J Work Environ Health 2006;32:67-74. https://doi.org/10.5271/sjweh.978.
- Nieuwenhuijsen K, Noordik E, van Dijk FJ, van der Klink JJ. Return to work perceptions and actual return to work in workers with common mental disorders. J Occup Rehabil 2013;23:290-9. https://doi.org/10.1007/s10926-012-9389-6.
- Lagerveld SE, Blonk RW, Brenninkmeijer V, Wijngaards-de Meij L, Schaufeli WB. Work-focused treatment of common mental disorders and return to work: a comparative outcome study. J Occup Health Psychol 2012;17:220-34. https://doi.org/10.1037/a0027049.
- Beecham J, Knapp M, Thornicroft G. Measuring Mental Health Needs. London: Gaskell; 2001.
- Group TE. EuroQol-a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199-208. https://doi.org/10.1016/0168-8510(90)90421-9.
- Medical Research Council (MRC) . Developing and Evaluating Complex Interventions: New Guidance 2008.
- Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350. https://doi.org/10.1136/bmj.h1258.
- Weston D, Parsons V, Ntani G, Rushton L, Madan I. Mixed contact methods to improve response to a postal questionnaire. Occup Med 2017;67:305-7. https://doi.org/10.1093/occmed/kqx032.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Herdman M, Gudex C, Lloyd A, Janssen MF, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727-36. https://doi.org/10.1007/s11136-011-9903-x.
- Lyssenko L, Hahn C, Kleindienst N, Bohus M, Ostermann M, Vonderlin R. A Systematic Review of Mindfulness-Based Interventions in Occupational Settings n.d. www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42015019282 (accessed 24 November 2020).
- Fishta A, Weikert B, Wegewitz U. Return-to-Work (RTW) Interventions for Employees With Mental Disorders: An Overview of Systematic Reviews n.d. www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42015023496 (accessed 24 November 2020).
- Mikkelsen MB, Rosholm M. Systematic review and meta-analysis of interventions aimed at enhancing return to work for sick-listed workers with common mental disorders, stress-related disorders, somatoform disorders and personality disorders. Occup Environ Med 2018;75:675-86. https://doi.org/10.1136/oemed-2018-105073.
- Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343. https://doi.org/10.1136/bmj.d5928.
- Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group . Preferred Reporting Items for Systematic reviews and Meta-Analyses: the PRISMA statement. Ann Intern Med 2009;151:264-9. https://doi.org/10.7326/0003-4819-151-4-200908180-00135.
- Netterstrom B, Eller NH, Borritz M. Prognostic factors of returning to work after sick leave due to work-related common mental disorders: a one-and three-year follow-up study. Biomed Res Int 2015;2015. https://doi.org/10.1155/2015/596572.
- Bhui KS, Dinos S, Stansfeld SA, White PD. A synthesis of the evidence for managing stress at work: A review of the reviews reporting on anxiety, depression, and absenteeism. J Environ Public Health 2012;2012. https://doi.org/10.1155/2012/515874.
- van der Feltz-Cornelis CM, Hoedeman R, de Jong FJ, Meeuwissen JAC, Drewes HW, van der Laan NC, et al. Faster return to work after psychiatric consultation for sicklisted employees with common mental disorders compared to care as usual. A randomized clinical trial. Neuropsychiatr Dis Treat 2010;6:375-85. https://doi.org/10.2147/NDT.S11832.
- Cowls J, Galloway E. Understanding how traumatic re-enactment impacts the workplace: assisting clients’ successful return to work. Work 2009;34:401-11. https://doi.org/10.3233/WOR-2009-0889.
- De Zeeuw ELEJ, Tak ECPM, Dusseldorp E, Hendriksen IJM. Workplace exercise intervention to prevent depression: a pilot randomized controlled trial. Mental Health Phys Activ 2010;3:72-7. https://doi.org/10.1016/j.mhpa.2010.09.002.
- Sahlin E, Ahlborg G, Tenenbaum A, Grahn P. Using Nature-based rehabilitation to restart a stalled process of rehabilitation in individuals with stress-related mental illness. Int J Environ Res Public Health 2015;12:1928-51. https://doi.org/10.3390/ijerph120201928.
- Eklund M, Wastberg BA, Erlandsson L. Work outcomes and their predictors in the redesigning daily occupations (ReDO) rehabilitation programme for women with stress-related disorders. Aust Occup Ther J 2013;60:85-92. https://doi.org/10.1111/1440-1630.12019.
- Evans-Lacko S, Koeser L, Knapp M, Longhitano C, Zohar J, Kuhn K. Evaluating the economic impact of screening and treatment for depression in the workplace. Eur Neuropsychopharmacol 2016;26:1004-13. https://doi.org/10.1016/j.euroneuro.2016.03.005.
- Falkenberg A, Nyfjäll M, Hellgren C. Social support at work and leisure time and its association with self-rated health and sickness absence. Work 2012;43:469-74. https://doi.org/10.3233/WOR-2012-1381.
- Grossi G, Santell B. Quasi-experimental evaluation of a stress management programme for female county and municipal employees on long-term sick leave due to work-related psychological complaints. J Rehabil Med 2009:41-38. https://doi.org/10.2340/16501977-0379.
- Haraguchi T, Yamanouchi N, Iyo M, Shimizu E. What factors do people with mental health problems consider important for return to work? A pilot study. Chiba Med J 2015;91:7-12.
- Hees HL, Koeter MWL, Schene AH. Longitudinal relationship between depressive symptoms and work outcomes in clinically treated patients with long-term sickness absence related to major depressive disorder. J Affect Dis 2013;148:272-77. https://doi.org/10.1016/j.jad.2012.12.007.
- Hees HL, Koeter MW, Schene AH. Predictors of long-term return to work and symptom remission in sick-listed patients with major depression. J Clin Psychiatry 2012;73:e1048-55. https://doi.org/10.4088/JCP.12m07699.
- Arends I, Bultmann U, Nielsen K, van Rhenen W, de Boer MR, van der Klink JJ. Process evaluation of a problem solving intervention to prevent recurrent sickness absence in workers with common mental disorders. Social Sci Med 2014;100:123-32. https://doi.org/10.1016/j.socscimed.2013.10.041.
- Jansson I, Perseius K, Gunnarsson AB, Björklund A. Work and everyday activities: experiences from two interventions addressing people with common mental disorders. Scan J Occupat Ther 2014;21:295-304. https://doi.org/10.3109/11038128.2014.894572.
- Joosen MCW, Brouwers EPM, Van Beurden KM, Terluin B, Ruotsalainen JH, Woo JM, et al. An international comparison of occupational health guidelines for the management of mental disorders and stress-related psychological symptoms. Occupat Environ Med 2015;72:313-22. https://doi.org/10.1136/oemed-2013-101626.
- Joyce S, Modini M, Christensen H, Mykletun A, Bryant R, Mitchell P, et al. Workplace interventions for common mental disorders: a systematic meta-review. Psychol Med 2015;46:683-97. https://doi.org/10.1017/S0033291715002408.
- Reid KJ, Aguilar KM, Thompson E, Miller RM. Value-based benefit design to improve medication adherence for employees with anxiety or depression. Am Health Drugs Benefit 2015;8:263-71.
- Kroger C, Bode K, Wunsch EM, Kliem S, Grocholewski A, Finger F. Work-related treatment for major depressive disorder and incapacity to work: preliminary findings of a controlled, matched study. J Occupat Health Psychol 2015;20:248-58. https://doi.org/10.1037/a0038341.
- Lagerveld SE, Bultmann U, Franche RL, van Dijk FJ, Vlasveld MC, van der Feltz-Cornelis CM, et al. Factors associated with work participation and work functioning in depressed workers: a systematic review. J Occupat Rehabil 2010;20:275-92. https://doi.org/10.1007/s10926-009-9224-x.
- Lemieux P, Durand M, Hong QN. Supervisors’ perception of the factors influencing the return to work of workers with common mental disorders. J Occupat Rehabil 2011;21:293-30. https://doi.org/10.1007/s10926-011-9316-2.
- Mackenzie A, Harvey S, Mewton L, Andrews G. Occupational impact of internet-delivered cognitive behaviour therapy for depression and anxiety: reanalysis of data from five Australian randomised controlled trials. Med J Aust 2014;201:417-9. https://doi.org/10.5694/mja14.00293.
- Martin M, Nielsen M, Petersen S, Jakobsen L, Rugulies R. Implementation of a coordinated and tailored return-to-work intervention for employees with mental health problems. J Occupat Rehabil 2012;22:427-36. https://doi.org/10.1007/s10926-011-9352-y.
- Noordik E, Nieuwenhuijsen K, Varekamp I, van der Klink JJ, van Dijk FJ. Exploring the return-to-work process for workers partially returned to work and partially on long-term sick leave due to common mental disorders: a qualitative study. Disabil Rehabil 2011;33:1625-35. https://doi.org/10.3109/09638288.2010.541547.
- Noordik E, van der Klink JJ, Geskus RB, de Boer MR, van Dijk FJ, Nieuwenhuijsen K. Effectiveness of an exposure-based return-to-work program for workers on sick leave due to common mental disorders: a cluster-randomized controlled trial. Scand J Work Environ Health 2013;39:144-54.
- Noordik E, van der Klink JJ, Klingen EF, Nieuwenhuijsen K, van Dijk FJ. Exposure-in-vivo containing interventions to improve work functioning of workers with anxiety disorder: a systematic review. BMC Public Health 2010;10. https://doi.org/10.1186/1471-2458-10-598.
- Pomaki G, Franche RL, Murray E, Khushrushahi N, Lampinen TM. Workplace-based work disability prevention interventions for workers with common mental health conditions: a review of the literature (structured abstract). J Occupat Rehabil 2012;22:182-95. https://doi.org/10.1007/s10926-011-9338-9.
- Rebergen D, Bruinvels D, van Tulder M, van der Beek A, van Mechelen W. Cost-effectiveness of guideline-based care for workers with mental health problems. J Occupat Environ Med 2009;51:313-22. https://doi.org/10.1097/JOM.0b013e3181990d8e.
- Van Oostrom SH, Van Mechelen W, Terluin B, De Vet HCW, Anema JR. A participatory workplace intervention for employees with distress and lost time: a feasibility evaluation within a randomized controlled trial. J Occupat Rehabil 2009;19:212-22. https://doi.org/10.1007/s10926-009-9170-7.
- Van Oostrom SH, Van Mechelen W, Terluin B, De Vet HCW, Knol DL, Anema JR. A workplace intervention for sick-listed employees with distress: results of a randomised controlled trial. Occup Environ Med 2010;67:596-602. https://doi.org/10.1136/oem.2009.050849.
- Shippee ND, Shah ND, Angstman KB, DeJesus RS, Wilkinson JM, Bruce SM, et al. Impact of collaborative care for depression on clinical, functional, and work outcomes: a practice-based evaluation. J Ambulatory Care 2013;36:13-2. https://doi.org/10.1097/JAC.0b013e318276dc10.
- Simpson G, Byrne P, Gabbay M, Rannard A. Understanding illness experiences of employees with common mental health disorders. Occupat Med 2015;65:367-72. https://doi.org/10.1093/occmed/kqv047.
- Vlasveld MC, Feltz-Cornelis CM, Adèr, HJ, Anema JR, Hoedeman R, Mechelen W, et al. Collaborative care for sick-listed workers with major depressive disorder: a randomised controlled trial from the netherlands depression initiative aimed at return to work and depressive symptoms. Occupat Environ Med 2013;70:223-30. https://doi.org/10.1136/oemed-2012-100793.
- Volker D, Zijlstra-Vlasveld MC, Anema JR, Beekman AT, Brouwers EP, Emons WH, et al. Effectiveness of a blended web-based intervention on return to work for sick-listed employees with common mental disorders: results of a cluster randomized controlled trial. J Med Internet Res 2015;17. https://doi.org/10.2196/jmir.4097.
- Hees HL, Vries G, Koeter MW, Schene AH. Adjuvant occupational therapy improves long-term depression recovery and return-to-work in good health in sick-listed employees with major depression: results of a randomised controlled trial. Occupat Environ Med 2013;70:252-60. https://doi.org/10.1136/oemed-2012-100789.
- Finnes A, Enebrink P, Ghaderi A, Dahl J, Nager A. Öst LG. Psychological treatments for return to work in individuals on sickness absence due to common mental disorders or musculoskeletal disorders: a systematic review and meta-analysis of randomized-controlled trials. Int Arch Occup Environ Health 2019;92:273-93. https://doi.org/10.1007/s00420-018-1380-x.
- Fisker J, Hellström L, Eplov L, Hjorthøj C, Mathiesen B, Mundy S. Predictors of Return to Work for People on Sick Leave due to Common Mental Disorders: A Systematic Review and Meta-analysis. York: Centre for Reviews and Dissemination, University of York; 2019.
- de Vries H, Fishta A, Weikert B, Rodriguez Sanchez A, Wegewitz U. Determinants of sickness absence and return to work among employees with common mental disorders: a scoping review. J Occup Rehabil 2018;28:393-417. https://doi.org/10.1007/s10926-017-9730-1.
- Salomonsson S, Hedman-Lagerlöf E, Öst LG. Sickness absence: a systematic review and meta-analysis of psychological treatments for individuals on sick leave due to common mental disorders. Psychol Med 2018;48:1954-65. https://doi.org/10.1017/S0033291718000065.
- Nigatu YT, Liu Y, Uppal M, McKinney S, Gillis K, Rao S, et al. Prognostic factors for return to work of employees with common mental disorders: a meta-analysis of cohort studies. Soc Psychiatry Psychiatr Epidemiol 2017;52:1205-15. https://doi.org/10.1007/s00127-017-1402-0.
- Madan I, Parsons V, Cookson B, English J, Lavender T, McCrone P, et al. A behavioural change package to prevent hand dermatitis in nurses working in the national health service (the SCIN trial): study protocol for a cluster randomised controlled trial. Trials 2016;17. https://doi.org/10.1186/s13063-016-1255-y.
- See B, Juszczyk D, Parsons V, Smedley J, Gilworth G, Madan I. Managing common mental health disorders in healthcare workers. Occup Med 2019;69:290-3. https://doi.org/10.1093/occmed/kqz068.
- Madan I, Paterson S, Harling K. Methodology for the development of NHS Plus evidence-based guidelines. Occup Med 2007;57:304-7. https://doi.org/10.1093/occmed/kqm073.
- Hutt R, Rosen R, McCauley J. Case Managing Long-term Conditions: What Impact Does It Have in the Treatment of Long-term Conditions. London: King’s Fund; 2004.
- Ross S, Goodwin N, Curry N. Case Management: What Is It and How It Can Best Be Implemented. London: King’s Fund; 2011.
- Whooley MA, Avins AL, Miranda J, Browner WS. Case-finding instruments for depression. Two questions are as good as many. J Gen Intern Med 1997;12:439-45. https://doi.org/10.1046/j.1525-1497.1997.00076.x.
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348. https://doi.org/10.1136/bmj.g1687.
- COMET (Core Outcome Measures in Effectiveness Trials) Initiative . Development of a Core Outcome Set for Work Participation (COS-WP) 2018. www.comet-initiative.org/studies/details/1195 (accessed 25 February 2020).
- Madan I, Henderson M, Hashtroudi A, Hope V, Harvey SB. Prospective evaluation of mental health training for occupational health practitioners. Occup Med 2013;63:217-23. https://doi.org/10.1093/occmed/kqt008.
- Kirkpatrick DL. Evaluating Training Programs: The Four Levels – Berrett-Koehler Organizational Performance Series. San Francisco, CA: Berrett-Koehler Publishers, Inc.; 1994.
- Guy’s and St Thomas’ NHS Foundation Trust . Your Occupational Health Service: A Managers Guide on Absence Management (Frequently Asked Questions) 2019.
- NHS Data Model and Dictionary . Generalised Anxiety Disorder Questionnaire 2019. https://patient.info/doctor/generalised-anxiety-disorder-assessment-gad-7 (accessed 5 January 2021).
- NHS Data Model and Dictionary . Patient Health Questionnaire-9 2019. https://patient.info/doctor/patient-health-questionnaire-phq-9 (accessed 5 January 2021).
- Edwards PJ, Roberts I, Clarke MJ, Diguiseppi C, Wentz R, Kwan I, et al. Methods to increase response to postal and electronic questionnaires. Cochrane Database Syst Rev 2009;3. https://doi.org/10.1002/14651858.MR000008.pub4.
- Coventry P, Lovell K, Dickens C, Bower P, Chew-Graham C, McElvenny D, et al. Integrated primary care for patients with mental and physical multimorbidity: cluster randomised controlled trial of collaborative care for patients with depression comorbid with diabetes or cardiovascular disease. BMJ 2015;350. https://doi.org/10.1136/bmj.h638.
- Gilbody S, Littlewood E, Hewitt C, Brierley G, Tharmanathan P, Araya R, et al. Computerised cognitive behaviour therapy (cCBT) as treatment for depression in primary care (REEACT trial): large scale pragmatic randomised controlled trial. BMJ 2015;351. https://doi.org/10.1136/bmj.h5627.
- National Institute for Health and Care Excellence (NICE) . Identifying and Assessing Common Mental Health Disorders 2016.
- van der Klink JJ, van Dijk FJ. Dutch practice guidelines for managing adjustment disorders in occupational and primary health care. Scand J Work Environ Health 2003;29:478-87. https://doi.org/10.5271/sjweh.756.
- Adams CE. Many more reasons behind difficulties in recruiting patients to randomized controlled trials in psychiatry. Epidemiol Psychiatr Sci 2013;22:321-3. https://doi.org/10.1017/S2045796013000267.
- Muntingh A, van der Feltz-Cornelis C, van Marwijk H, Spinhoven P, Assendelft W, de Waal M, et al. Effectiveness of collaborative stepped care for anxiety disorders in primary care: a pragmatic cluster randomised controlled trial. Psychother Psychosom 2014;83:37-44. https://doi.org/10.1159/000353682.
- de Hoop E, van der Tweel I, van der Graaf R, Moons KG, van Delden JJ, Reitsma JB, et al. The need to balance merits and limitations from different disciplines when considering the stepped wedge cluster randomized trial design. BMC Med Res Methodol 2015;15. https://doi.org/10.1186/s12874-015-0090-2.
- Hargreaves JR, Copas AJ, Beard E, Osrin D, Lewis JJ, Davey C, et al. Five questions to consider before conducting a stepped wedge trial. Trials 2015;16. https://doi.org/10.1186/s13063-015-0841-8.
- Black Dog Institute . Head Coach 2018. https://blackdoginstitute.org.au/research-projects/headcoach/ (accessed 15 December 2020).
Appendix 1 Coding frame
| Code | Node |
|---|---|
| Case manager | |
| Case manager delivery | Approaches to problem-solving and engagement |
| Components less competent or confident to deliver | |
| Components most competent or confident to deliver | |
| Frequency of appointments | |
| Key components during follow-up appointments | |
| Putting it into practice | |
| RTW planning and support | |
| Risk assessment and management | |
| Supporting material used | |
| Initial consultation | |
| Case manager training | General views |
| Less useful or helpful aspects | |
| Most useful and helpful aspects | |
| Online resources | |
| Study material and documents | |
| Suggestions for improving training | |
| Communication with others | |
| Identifying and screening new referrals | Barriers to screening and consenting |
| Overall impression | |
| Planning for a future trial | |
| Recruiting and consenting process | |
| Risk of contamination between trial arms | |
| Focus group | |
| Study set-up and delivery | Additional support or information to better manage employees on sick leave |
| Any aspects unclear | |
| Communication in relation to study set-up and delivery in the trust | |
| Setting up study in OH department | |
| Strategies to promote study across the trust | |
| Study resources | |
| Screening and identifying participants | Barriers to providing initial appointment within first 7 days |
| Consent procedures used at sites | |
| Early referral to OH | |
| Factors influencing decision not to refer to OH | |
| Factors influencing decision to refer | |
| Identifying participants | |
| Process used by OH to screen new referrals | |
| Staff who are unable or unwilling to engage with OH and/or HR | |
| Role of HR | |
| Most helpful | |
| Managers may need support too | |
| Factors to consider for main trial | |
| Communication with others | |
| Overall impression of the study | |
| Miscellaneous | |
| Study participants | |
| How was the study introduced | Feelings about participation in the study |
| Understanding of the study | |
| What interested them about taking part | Experience of study participants |
| Questionnaires and general feedback of study participants | |
| Experience of OH service | Changing attitudes of OH service |
| Management advice line | |
| More or less likely to use OH following this experience | |
| Most helpful parts (of OH support) | |
| Others resources and counselling | |
| Timing of referral to OH | |
| Changes to perspective and work–life balance | |
| Lines of communication (GP, OH, line managers, etc.) | |
| Other mental health support services (i.e. separate to OH department, such as services of a psychiatrist, mental health nurse) | |
| RTW process | |
| Taking time off work (for CMD) | |
| What could be done differently? Suggestions for us | |
List of abbreviations
- app
- application
- CAMEOS
- CAse Management to Enhance Occupational Support
- CAU
- care as usual
- CBT
- cognitive–behavioural therapy
- CI
- confidence interval
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CMD
- common mental health disorder
- CSRI
- Client Service Receipt Inventory
- EQ-5D
- EuroQol-5 Dimensions
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- ESR
- electronic staff record
- GAD-7
- Generalised Anxiety Disorder-7
- GP
- general practitioner
- HR
- human resources
- IAPT
- Improving Access to Psychological Therapies
- IQR
- interquartile range
- MAP
- My Action Plan
- MI
- motivational interviewing
- MRC
- Medical Research Council
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- OH
- occupational health
- PHQ-9
- Patient Health Questionnaire-9 items
- PICO
- population, intervention, comparator, outcomes
- PIN
- personal identification number
- PPI
- patient and public involvement
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PROSPERO
- International Prospective Register of Systematic Reviews
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- RTW
- return to work
- RTW-SE
- Return-to-Work Self-Efficacy
- SCIN
- Skin Care Intervention in Nurses
- SD
- standard deviation
- WAI
- Work Ability Index
- WHODAS 2.0
- World Health Organization Disability Assessment Schedule 2.0
- WP
- work package
