Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 15/103/03. The contractual start date was in April 2017. The draft report began editorial review in May 2019 and was accepted for publication in December 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
Copyright © 2021 Cook et al. This work was produced by Cook et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2021 The authors
Chapter 1 Background
This report describes the methods and results of the Patch Augmented Rotator Cuff Surgery (PARCS) feasibility study, which assessed the acceptability and feasibility of conducting a randomised controlled trial (RCT) of the clinical effectiveness and cost-effectiveness of patch-augmented rotator cuff repair (RCR). This study was commissioned and funded by the National Institute for Health Research Health Technology Assessment (HTA) programme. 1
Rotator cuff tears
Shoulder pain is a common problem in the general population and is responsible for prolonged periods of disability, loss of productivity, absence from work and an inability to carry out household activities. It has been estimated that 2.4% of UK general practitioner (GP) consultations are for shoulder complaints. 2 Shoulder pain is frequently caused by problems with the tendons and muscles that surround and stabilise the shoulder joint, known as the rotator cuff. They account for up to 70% of shoulder pain problems and constitute the third most prevalent musculoskeletal disorder, after lower back and neck pain. 3 A common and debilitating rotator cuff problem is a rotator cuff tendon tear, which is found in approximately 25% of people aged ≥ 70 years. Symptoms include pain, weakness, lack of shoulder mobility and sleep disturbance.
Rotator cuff tears refer to a structural failure in the rotator cuff, most commonly involving the supraspinatus (Figure 1). It is estimated that the overall prevalence of tears is 34% and that risk increases significantly with age. 5
FIGURE 1.
Anatomical diagram of the shoulder joint showing rotator cuff tear in the supraspinatus. Reproduced from Acute Rotator Cuff Tears, Craig R, Holt T, Rees R, Vol. 359, p. j5366, 2017,4 with permission from BMJ Publishing Group Ltd.

Conservative management for rotator cuff tears
Initial management of rotator cuff tears is conservative and includes rest with simple pain management with paracetamol and non-steroidal anti-inflammatory drugs. Physiotherapy combined with advice for home exercises is often included in the package of care. If symptoms persist, patients are usually offered an injection of a corticosteroid into the space between the acromion process of the shoulder blade and the humerus (see Figure 1). 6 An ongoing HTA-funded trial, Getting it Right: Addressing Shoulder Pain (GRASP),7 is aiming to improve conservative treatment for rotator cuff disorders by evaluating the effects of progressive exercise versus best practice advice, with and without subacromial corticosteroid injection, in people with a rotator cuff disorder treated in primary care.
Some patients with rotator cuff tears have few, if any, symptoms. A combination of conservative management approaches may allow the inflammation to settle, undamaged muscles to adapt and good function to be restored.
However, there are limitations to conservative treatments. Approximately 40% of patients will continue to experience pain despite conservative management. There is also emerging evidence suggesting that multiple injections may increase the chance of a rotator cuff tear occurring, leading to long-term harm. 8,9
Surgery for rotator cuff repair
Generally, if symptoms of severe pain and lack of function continue to disrupt daily activities, despite conservative treatment for a minimum of 3 months, surgery is considered for the patient. Around 9000 RCRs were performed per year in the NHS in England from 2000 to 2010, at a cost of around £2600 per operation (£23M per year), and this number would appear to be growing. 2,10
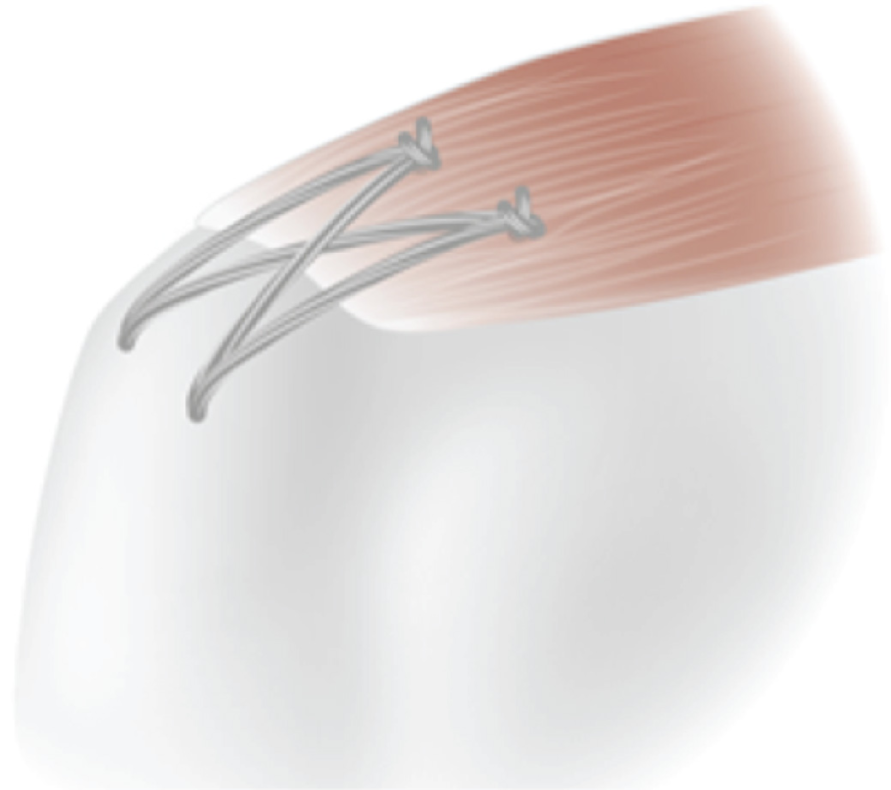
Surgical repair of the rotator cuff seeks to re-attach the tendon to the bone, allow the tear to heal and improve patient outcomes (Figure 2). The form of the repair depends on the nature of the tear and which tendons are involved. If the tendon is not able to be fully restored to its original position, a partial repair is often conducted to help encourage further healing.
FIGURE 2.
Surgically repaired rotator cuff (supraspinatus) tear. Reproduced with permission (Carr Group, Botnar Research Centre, University of Oxford, 2020, personal communication).
There is substantial variation in surgical practice. This can include the type of surgery (open or arthroscopic), the surgical techniques used (e.g. the use of anchors and type of suture) and the type and duration of conservative treatment before surgery. 11 A review of surgical management of rotator cuff tears published by Dunn et al. 11 in 2005 surveyed members of the American Academy of Orthopaedic Surgeons. At the time, 15% preferred arthroscopic surgery, but this is likely to have grown since.
Rotator cuff surgery can have mixed outcomes for patients, with failure rates between 25% and 50% within 12 months. 12–14 The UK Rotator Cuff Surgery trial (UKUFF)2 revealed a 40% failure rate of surgical repairs in a wide range of settings using different surgical techniques in the NHS. RCR surgery is expensive, invasive and inconvenient to patients, and reoperation is sometimes necessary.
Although there are different views about the key drivers of patient outcomes, a number of factors are consistently related to poor outcomes, particularly increasing age and tear size. 15 Repairs also commonly fail because of poor tissue and bone quality or inadequate fixing of the tendon to the bone, allowing the two to pull away.
A healed repair results in the best clinical and patient-reported outcomes. As a result, a number of surgical approaches have tried to improve RCR; unfortunately, these have been unsuccessful. 2,14,16,17 For example, the UKUFF trial found that minimally invasive (arthroscopic) surgery had no benefit over open surgery. 18
A Cochrane review,16 published in 2008, identified only two RCTs that evaluated surgery for a rotator cuff tear;19,20 both were judged to be susceptible to bias. An updated systematic search performed in 2014 to set the UKUFF trial findings in context revealed five more trials comparing two surgical interventions. 19–24 These RCTs were single-centre trials and were relatively small, with between 73 and 114 participants per trial and a mean participant age of around 60 years. They included participants with full-thickness rotator cuff tears and small and medium rotator cuff tears. 20–25 The studies mainly compared surgical approaches with arthroscopic, mini-open and open repair, with or without acromioplasty or subacromial decompression. 21–24 One study19 evaluated a minor variation in the suture used and not the surgical technique.
Attention has recently focused on improving the biology of the torn tendon at the time of surgery and for the critical 8-week period after surgery when effective healing is needed. 21
Patch-augmented rotator cuff surgery
A promising area for further advancement in rotator cuff surgery is the use of a patch to provide a support structure or ‘scaffold’ for the repair. The aim is to improve the fixing of the tendon to the bone and, thus, tendon healing. 26,27 A patch can be defined as an implantable human, synthetic or animal material that is used with the aim of improving tissue healing and/or patient outcome via some form of mechanical support. These implants are also referred to as an extracellular or acellular matrix (when made from human or animal cells) or as a graft (e.g. an allograft, autograft or xenograft, depending on the source material used to produce the patch). Some preclinical studies suggest that augmentation patches may have value in reducing the rate of repair failure and in improving patient outcomes. 28–31
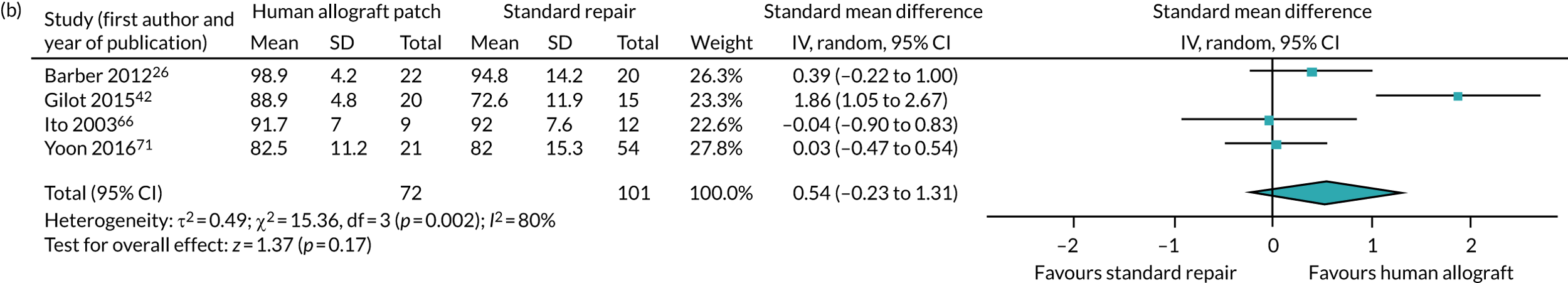
A patch can be used for one of two surgical indications (Figure 3). The patch can be surgically sutured on top of the tendon-to-bone repair, a technique known as ‘on-lay’, to strengthen the repair and aid tendon healing. 32 Some authors refer to this as ‘augmentation’, although the use of terminology to date has been far from consistent. Terminology such as reinforcement, bridging, reconstruction and interposition has been used, as well as augmentation. 27
FIGURE 3.
Surgical RCR augmented with a patch using the on-lay surgical approach. Reproduced with permission (Carr Group, Botnar Research Centre, University of Oxford, 2020, personal communication).

Alternatively, a patch can be sutured into the exposed area following a partial repair, known as ‘bridging’, to provide a scaffold for the regeneration of the tendon. 33 In this report we use the terms on-lay and bridging to refer to the two surgical approaches, and augmentation is used as an inclusive term for either approach. There are variations in how these approaches are carried out, such as the fixation approach and equipment used.
Patches have been made using different materials (human/animal heart, skin or intestine tissue and completely synthetic materials) and processes (e.g. woven or mesh), as well as in different sizes. 27,29 They can be designed to be absorbable, avoiding the possibility of later surgical removal. Patches differ in how they respond to tendon tissue and their mechanical properties. 28 Some have been designed specifically or can be tailored in size and shape for specific uses in rotator cuff surgery (‘on-lay’ or ‘bridging’), whereas others were initially developed for other soft-tissue contexts.
At the time of developing this study, > 20 patches (see Chapters 2 and 3) have received regulatory approval for use in surgical repair of the rotator cuff in the USA and/or by an EU-notified body. 34 A number of centres in the UK were using patches in RCR for private and/or NHS patients at the time of study set-up. Patches currently in use in the UK reflect different materials and original purposes. One example is the GRAFTJACKET (Wright Medical Group, Memphis, TN, USA); made from human cadaver dermis, originally developed for RCR, it is available in different sizes and thicknesses. Another is LARS™ ligament (Corin, Gloucestershire, UK), which is a completely synthetic material originally developed for anterior cruciate ligament reconstructions and is available in various versions, including specifically for RCR. A final example is Permicol™ (Warsaw, IN, USA), which is made from pig dermis and originally developed for hernia repair. Later, a version for rotator cuff was produced called the Zimmer® collagen repair patch (Zimmer, Warsaw, IN, USA)]. The use of a patch to augment rotator cuff surgery appears to be increasing.
The use of patches has not been without negative impact. One patch [Restore Orthobiologic Implant™ (DePuy Orthopaedics, Warsaw, IN, USA)] was withdrawn from the market following a clinical study that identified a severe autoimmune response. 35 In addition to safety concerns, the use of a patch, if not effective, is a waste of precious resources in terms of staff, time and the cost of the implant.
Recent advances in patches include the development of electrospun materials and exploration of the concurrent use of growth factors. 32 Electrospun materials have a structure that closely resembles the surrounding tissue; they provide biological cues to encourage cell growth and tissue healing. The aim of these and other biomimetic materials is to avoid adverse immunological responses. 35 Augmenting surgical repair with a patch may also enable the repair of tears that are currently considered irreparable. 26,33,35,36
The need for research
The pressing need to improve surgical options for RCRs and to improve outcomes for patients has been demonstrated. 37 The James Lind Alliance Priority Setting Partnership for Surgery for Common Shoulder Problems brought together patients, carers and clinicians to identify the ongoing important treatment uncertainties related to shoulder surgery. 38 Four of the top 10 uncertainties for common shoulder problems concerned rotator cuff tears. 38
At the time of inception of the PARCS study, only a handful of small, single-centre, predominantly North America-based, comparative studies had been carried out for a subset of the available patches, with mixed findings. Three relevant reviews had been carried out. The first review was a literature review of preclinical and clinical studies on candidate patches for use in rotator cuff surgery. 34 The review considered clinical and preclinical studies on > 20 available patches that can be used for rotator cuff surgery, including the Restore Orthobiologic Implant, which had been withdrawn from the market because of safety concerns. 29,30 It identified a variety of studies, but little clinical or comparative evidence. The second and third reviews were both recently published systematic reviews of clinical studies [identified through a search of the PROSPERO online registry and the Centre for Reviews and Dissemination (CRD) database], assessing patch-augmented rotator cuff surgery. 27,39 They collectively identified 16 clinical studies, of which only two were RCTs and two were observational comparative studies. 26,35,40,41 These four comparative studies assessed only four patches and one of these, a retrospective study, compared only two patches. 40 Two of the studies assessed the Restore Orthobiologic Implant. 35,41
In addition to the above reviews, there are a further three published comparative studies evaluating ‘irreparable’ rotator cuff tears: a RCT evaluating an autograft (self-donor) and two observational comparative studies assessing different biological patches. 33,42,43 During the conduct of the PARCS study, a third systematic review was published that included additional studies (although not all of the previous studies identified in the previous systematic reviews). 44
Study design
At the time of conduct, to our knowledge no comprehensive systematic review or health technology assessment of patch-augmented surgery for RCR had been performed. It is not clear whether or not patch use improves outcomes for patients following RCR. To establish certainty for patients in the UK, this needs to be evaluated in a large multicentre RCT that is relevant to the NHS setting. Existing studies in this clinical area have shown that a RCT of this kind is possible. For example, the UKUFF trial has demonstrated that a rotator cuff RCT can be conducted. 18 It offers valuable learning about recruiting patients undergoing rotator cuff surgery with regard to the timing and nature of the approach.
However, there remained uncertainty about how a RCT should be designed to evaluate patch augmentation specifically. Major uncertainties related to patch augmentation trial design include the patient population, which patches should be evaluated, the intervention and control groups, the associated surgical technique and the acceptability of such a trial to stakeholders, particularly patients and surgeons. Surgical trials are generally difficult to conduct owing to varied patient pathways throughout the NHS, surgical equipoise being difficult to establish and portray, and patients’ reservations about being recruited. 45–47 These uncertainties and difficulties are compounded by the sporadic introduction of the use of patches into the NHS and the variety of patches available.
It became apparent that a feasibility study would be necessary to address all of these concerns. However, an unnecessarily long feasibility study could miss the optimal timing for evaluating this innovation in a surgical trial, as stated in Buxton’s law:48 ‘It’s always too early for a rigorous evaluation until suddenly it’s unfortunately too late’. A multistage mixed-methods research study was used to address the uncertainties related to the conduct of a RCT of patch-augmented rotator cuff surgery. 1 The aim and objectives of the study are described in the following section. The methods and findings of the six stages of research that are part of the PARCS feasibility study are described in Chapters 2–5.
Aim and objectives
The aim of the PARCS study was to determine the design of a future definitive RCT assessing the clinical effectiveness and cost-effectiveness of a patch to augment surgical repair of the rotator cuff that is both acceptable to stakeholders and feasible. 1
The approach built on work by the Idea, Development, Exploration, Assessment, Long-term Follow-up (IDEAL) collaboration for evaluating surgical innovation and devices on early evaluations and RCTs. 49,50 Methodology was adapted from that for achieving expert consensus in guideline and core outcome sets for trials. 51–53 This feasibility study used a mixed-methods approach to assess current evidence and practice, and to achieve consensus on the optimal randomised trial design. 1
The study objectives were to:
-
review existing evidence to identify candidate patches for use in a RCT and the evidence relating to their clinical use
-
ascertain current NHS clinical practice relating to the use of patches to augment RCR
-
explore the acceptability of the proposed trial to patients, surgeons and other stakeholders
-
assess the feasibility of a trial of patch-augmented RCR
-
achieve consensus on the key elements of the design of a definitive RCT to assess the use of patches to augment RCR
-
confirm the scope of the health economic evaluation required in the trial to appropriately assess the cost-effectiveness
-
identify areas for further research related to PARCS.
Chapter 2 Systematic review
Introduction
It is critical to review the current evidence when designing a future RCT. Systematic reviews are a useful tool for this because they identify, collate and summarise results from individual studies, which makes the existing evidence easier to evaluate. Having a systematic review as the first stage in a mixed-methods feasibility study gives a foundation from which to generate new evidence.
It was particularly important to provide a systematic review of the clinical evidence (including non-comparative observational studies) on the use of patches in RCR. The growing number of available patches (made from different materials and originally for different purposes), mixed clinical and preclinical results and recent concerns over safety, including adverse immunological responses, had generated a clouded and uncertain landscape. 54
The aim of this systematic review was to identify and critically appraise those studies reporting on the clinical effectiveness and safety of patch-augmented surgical repair in adults with rotator cuff tears. 1 The key objectives of the systematic review were to:
-
undertake evidence synthesis using systematic review methodologies, including meta-analysis, to evaluate the relative effectiveness of patch-augmented RCR
-
undertake a review of safety/adverse events associated with all identified patches
-
identify the most clinically effective and safe candidate patches, as well as other key parameters that can inform a future definitive RCT.
Methods
Protocol and registration
Evidence synthesis was carried out in accordance with the recommendations of the Cochrane Handbook for Systematic Reviews55 and the Centre for Reviews and Dissemination (CRD) guidance for undertaking reviews in health care, and was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). 55–57 The review protocol and search strategy has been previously been registered and published in full. 58
Search strategy
A previous Cochrane systematic review had carried out a comprehensive search prior to April 2006. 16 Based on this search we searched the following databases between April 2006 and February 2017 (and updated our search in August 2018): EMBASE, MEDLINE, the Cochrane Library, incorporating Central Register of Controlled Trials (CENTRAL), Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effects (DARE), the HTA database and the NHS Economic Evaluation Database (NHS EED). In addition, the reference lists of all identified articles and reviews were checked for relevant articles. 17,27,39,44,59 The search strategy was initially developed for EMBASE (see Appendix 1) and has previously been published. 58 Our strategy was subsequently modified for use in MEDLINE and the Cochrane Library databases.
Inclusion and exclusion criteria
Population
The review incorporated studies of adult patients (aged ≥ 18 years) who required surgical repair of a rotator cuff tear. No restrictions were applied to tear type (partial or full thickness), size (small through to massive), tendon involvement (supraspinatus, infraspinatus, teres minor or subscapularis), primary or recurrent tears, or the presence of medical comorbidities. For the purpose of this review, small (< 1 cm), medium (1 cm to < 3 cm) and large (3 cm to 5 cm) tears were classified according to the DeOrio and Cofield classification. 60 Because of the large number of classification systems available, tears were also considered massive if they met one of the following criteria: (1) measured > 5 cm in the anteroposterior dimension, (2) involved two or more tendons61 or (3) were described as being massive by the study authors. 60,61
Interventions
All studies in which at least one treatment arm included the use of patches to augment rotator cuff surgery were included. A patch was defined as an implantable human, synthetic or animal material that is used with the aim of improving tissue healing and/or patient outcome via some form of mechanical support. Patch types were grouped into xenograft, allograft, autograft or synthetic. There was no restriction placed on the type of surgery received or the experience of the surgeon. The type of patch surgery was classified as either ‘on-lay’ or ‘bridging’ in accordance with previously reported definitions. 27 We excluded studies that investigated the use of sutures or anchors in isolation and studies that investigated drug therapy or physiotherapy, except when used as a comparator group or in addition to patch augmentation.
Comparators
No restriction was placed on the type or number of control groups.
Outcomes
The primary outcomes of interest in this review were:
-
shoulder-specific function and pain – measured using a previously validated scale
-
shoulder pain – measured using validated tools, such as the visual analogue scale (VAS) or non-validated scales
-
health-related quality of life (HRQoL) – measured using Short Form questionnaire-36 items (SF-36), EuroQol-5 Dimensions (EQ-5D) or other assessment measures
-
patch-related adverse events.
Secondary outcomes of interest were recurrence of rotator cuff tear (re-tear), radiological assessment of postoperative rotator cuff integrity, revision rates of the surgery, time to surgical revision and patient satisfaction.
Study types
We considered all relevant RCTs and observational studies (comparative and single group) that included at least five patients. No language restrictions were applied. In vitro studies, animal studies, review articles, editorials and studies involving five or fewer patients were excluded.
Study selection
Two authors (MB and NSN) independently screened all of the titles and abstracts identified from the search strategy. Full reports for all relevant studies identified were then reviewed and assessed against the eligibility criteria. A third independent reviewer (GG) was available to resolve any disagreements regarding study inclusion. Reasons for exclusion are detailed in the PRISMA flow diagram (Figure 4).
FIGURE 4.
The PRISMA flow chart of study selection. PRP, platelet-rich plasma; SR, systematic review.

Data extraction
Two authors (MB and NSN) extracted the following data from all eligible studies: general study information (authors, publication year and study location), study population (sample size, age, sex and tear size), study characteristics (study design, inclusion/exclusion criteria, duration of clinical and radiological follow-up, surgical technique and patch characteristics), all primary and secondary outcomes for each study and adverse events or complications. Each reviewer independently checked the results of the data extraction process.
Risk-of-bias assessment
The risk of bias was independently assessed by two authors (MB and NSN) and discrepancies were discussed with a third reviewer (GG), allowing resolution based on unanimous decision. RCTs were assessed using the risk-of-bias tool (2011 update) provided by the Cochrane Collaboration. 55 Each domain was rated as having a ‘low’, ‘high’ or ‘unclear’ risk of bias before the study was assessed as a whole. Observational comparative studies were assessed using the Risk Of Bias In Non-randomized Studies – of Interventions (ROBINS–I) tool. 62 The risk of bias for each domain was judged as low, moderate, serious, critical or no information, followed by an overall judgement of bias based around the judgements from each individual domain. Single-arm studies were not formally assessed for risk of bias.
Data analysis
Identified studies were grouped (RCTs, observational comparative and non-comparative) and a narrative summary of results was reported in accordance with the standards set out in the PRISMA checklist. 20 Data from all available studies were utilised in the quantification of complications. All studies that compared the outcomes of RCR with graft augmentation with standard RCR were considered for meta-analysis. A meta-analysis was conducted only for outcomes consistently reported across studies and reported using Review Manager version 5.3 (RevMan, the Cochrane Collaboration, The Nordic Cochrane Centre, Copenhagen, Denmark). Regardless of the observed statistical heterogeneity, we conducted an analysis for each patch type (xenograft, allograft, autograft or synthetic) when each type was represented by at least two comparative studies. Given the known controversy surrounding xenograft isolated from small intestinal submucosa (SIS), the analysis for xenografts was further divided into SIS-derived and non-SIS. There were insufficient study numbers to permit further subdivision based on graft configuration (on-lay or bridging). Complications (including patch-related adverse events) were grouped together given how they were reported across the included studies. They were not formally meta-analysed and only crudely summarised as overall numbers for augmentation and non-augmentation groups across all variations in patches and non-patches and reported events.
Statistical analysis
For dichotomous parameters included in the meta-analysis, the risk ratio (RR) with 95% confidence interval (CI) was calculated for each graft type. For continuous variables, such as shoulder-specific functional outcome scores, the effect was reported as the mean difference with 95% CI. Owing to the significant heterogeneity in the specific functional shoulder scores utilised between studies, a meta-analysis was conducted using the most frequently used score across all studies at final follow-up. In each patch type, if no single functional outcome score was consistently used, scores were combined and a standard mean difference was reported with 95% CI. Studies in which no standard deviation was calculable, or in which only subcomponents of functional outcome scores were reported, were reported only descriptively. Heterogeneity was characterised by use of the I2-statistic and a random-effect analysis used to incorporate heterogeneity among studies.
Patient involvement
Patient representatives were full members of the PARCS Study Steering Committee and provided critical feedback on the study protocol. 1
Results
Study selection
The search strategy identified 939 articles, of which 56 were duplicates (see Figure 4). A total of 883 abstracts were reviewed in detail, with 44 appearing to meet inclusion criteria. After full-text review, 27 articles were excluded based on the following criteria: included an abstract only (n = 3), treatment was a platelet-rich plasma-derived matrix lacking the structural properties of patch augmentation (n = 4), RCR did not involve any form of augmentation (n = 9) and the article was a duplicate (n = 4). A further 28 articles were identified from existing systematic reviews, which generated a total of 52 studies for inclusion. No economic evaluations of patch-augmented rotator cuff surgery were identified.
Study characteristics
Comparative studies
Four RCTs and 11 observational comparative studies involving 896 patients were identified. Most comparative studies assessed a single patch against standard repair, with some studies having up to three treatment arms. 40,63,64 Across all the comparative studies a total of 12 different patches were utilised. Study population sizes ranged from 30 to 89 patients (age range 29–82 years) for RCTs and from 21 to 152 patients (age range 36–83 years) for observational comparative studies, with a predominance of male participants across all studies. Only two studies included the full spectrum of full-thickness tear sizes, with most studies instead restricting recruitment to large or massive tears of the supraspinatus and infraspinatus. Other eligibility criteria were highly heterogeneous; however, the exclusion of patients with significant glenohumeral osteoarthritis (OA) (n = 10) emerged as a common theme (Table 1 and see Appendix 2, Table 19).
| Study (first author and year of publication) | Patch type | Group | Surgical approach | Surgical patch technique | Tear size | Patient demographics | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Xenograft | Human | Synthetic | Age at surgery (years), mean (range or ± SD) | Sex, n male (%) | |||||||||
| Dermal | Intestinal | Other | Allografta | Autograft | Resorbable | Non-resorbable | |||||||
| Randomised comparative studies | |||||||||||||
| Barber 201226 | ✓ | GRAFTJACKET | Arthroscopic | On-lay | Small to massiveb | 56 (43–69) | 18 (82) | ||||||
| Control | Small to largeb | 56 (34–72) | 13 (65) | ||||||||||
| Bryant 201665 | ✓ | cRestore® | Open | On-lay | Small to massiveb | 55 (29–40) | 29 (85) | ||||||
| Control | Small to massiveb | 58 (40–81) | 22 (79) | ||||||||||
| Iannotti 200635 | ✓ | cRestore® | Open | On-lay | Large to massiveb | 58 (NR) | 11 (73) | ||||||
| Control | Large to massiveb | 57 (NR) | 12 (80) | ||||||||||
| Leuzinger 201663 | ✓ | GRAFTJACKET | Arthroscopic | Massived | 66 (51–81) | 20 (71) | |||||||
| ✓ | eArtelon® | On-lay | Massived | 68 (52–79) | 23 (22) | ||||||||
| ✓ | cRestore® | Massived | 68 (50–82) | 20 (69) | |||||||||
| Non-randomised comparative studies | |||||||||||||
| Ciampi 201440 | ✓ | Repol Angimeshf | Open | On-lay | Massived | 66 (57–77) | 41 (79) | ||||||
| ✓g | hTUTOPATCH® | Massived | 66 (58–76) | 38 (78) | |||||||||
| Control | Massived | 67 (58–77) | 35 (69) | ||||||||||
| Gilot 201542 | ✓ | iArthroflex® | Arthroscopic | On-lay | Large to massiveb | 58 (± 6.2) | 8 (60) | ||||||
| Control | Large to massiveb | 62 (± 4.6) | 7 (47) | ||||||||||
| Ito 200366 | ✓ | Fascia lata | Open | Bridging | Large to massiveb | 63 (49–70) | 6 (67) | ||||||
| Control | Large to massiveb | 52 (36–66) | 10 (83) | ||||||||||
| Jeon 201767 | ✓ | Biceps (long-head) | Arthroscopic | Bridging | Mediumb | 62 (46–82) | 14 (45) | ||||||
| Control | Medium to largeb | 63 (46–82) | 16 (48) | ||||||||||
| Maillot 201864 | ✓ | jConexa™ | Open | On-lay | Medium to massiveb | 56 (46–63) | 5 (45) | ||||||
| Standard repair | Arthroscopic | Medium to massiveb | 58 (45–71) | 5 (42) | |||||||||
| Debridement | Arthroscopic | Medium to massiveb | 60 (54–76) | 3 (33) | |||||||||
| Mori 201333 | ✓ | Fascia lata | Arthroscopic | Bridging | Medium to massiveb | 65 (± 8.9) | 17 (71) | ||||||
| Control | Medium to massiveb | 65 (± 9.2) | 10 (42) | ||||||||||
| Mori 201568 | ✓ | Fascia lata + grade 1–2 atrophy | Arthroscopic | Bridging | Large to massiveb | 65 (± 9.0) | 18 (69) | ||||||
| ✓ | Fascia lata + grade 3–4 atrophy | Large to massiveb | 67 (± 6.2) | 11 (58) | |||||||||
| Tempelaere 201769 | ✓ | Quadriceps tendon | Open | Bridging | Massivek | NR | 18 (78) | ||||||
| Control | Arthroscopic | Massivek | NR | 15 (56) | |||||||||
| Vitali 201543 | ✓ | ✓ | Repol Angimesh + biceps (long-head) | Open | Bridging | Massived | 66 (55–78) | 15 (25) | |||||
| Control | Massived | 67 (56–77) | 18 (30) | ||||||||||
| Walton 200741 | ✓ | cRestore® | Open | On-lay | Large to massivel | 60 (± 3.5) | 10 (67) | ||||||
| Control | Large to massivel | 59 (± 3.1) | 11 (69) | ||||||||||
| Yoon 201671 | ✓ | mAllocover™ | Arthroscopic | Bridging | Large to massiveb | 64 (± 8.7) | 9 (43) | ||||||
| Control | Large to massiveb | 62 (± 6.7) | 26 (48) | ||||||||||
| Non-comparative studies | |||||||||||||
| Agrawal 201272 | ✓ | nAllopatch HD™ | Arthroscopic | On-lay | Large to massiveb | 54 (47–69) | 10 (71) | ||||||
| Audenaert 200673 | ✓ | oMERSILENE® | Open | Bridging | Massived | 67 (51–80) | 23 (56) | ||||||
| Badhe 200874 | ✓ | Zimmer collagen repair patch | Open | Bridging | Massiveb,d | 66 (46–80) | 5 (50) | ||||||
| Bektaser 201075 | ✓ | Coracoacromial ligamentq | Open | On-lay | Medium to massiveb | 54.3 (39–66) | 4 (9) | ||||||
| Bond 200876 | ✓ | GRAFTJACKET | Arthroscopic | Bridging | Massiveb,d | 54 (39–74) | 13 (81) | ||||||
| Burkhead 200777 | ✓ | GRAFTJACKET | Open | On-lay | Massived | 56 (NR) | 12 (71) | ||||||
| Cho 201478 | ✓ | rPermacol™ | Open | On-lay | Massiveb,d | 53 (45–57) | 3 (60) | ||||||
| Consigliere 201779 | ✓ | DX reinforcement matrixs | Arthroscopic | On-lay | Large to massived | 74 (65–82) | 6 (40) | ||||||
| Encalada-Diaz 201180 | ✓ | Polycarbonate polyurethane patcht | Open | On-lay | Small to largeb | 56 (44–65) | 0 | ||||||
| Flury 201281 | ✓ | GRAFTJACKET or Arthroflex | Arthroscopic | On-lay | Medium to largeb | 57 (50–68) | 5 (63) | ||||||
| Giannotti 201482 | ✓ | Zimmer collagen repair patch | Open | Mixed | Massivel | 66 (50–80) | 4 (44) | ||||||
| Gupta 201283 | ✓ | GRAFTJACKET | Open | Bridging | Massivel | 63 (45–83) | 12 (50) | ||||||
| Gupta 201384 | ✓ | Conexa | Open | Bridging | Massived | 60 (45–77) | 12 (46) | ||||||
| Hirooka 200285 | ✓ | GORE-TEX® PTFEu | Open | Bridging | Small to massiveb | 62 (44–75) | 20 (74) | ||||||
| Lederman 201686 | ✓ | Conexa | Open | On-lay | Largeb | 56 (40–69) | NR | ||||||
| Lenart 201587 | ✓ | X-repairv | Open | On-lay | Massived | 57 (42–68) | 9 (69) | ||||||
| Malcarney 200554 | ✓ | cRestore® | Open | Mixed | NR | NR | NR | ||||||
| Marberry 201388 | ✓ | Artelon | Open | On-lay | Massived | 65 (45–76) | 5 (29) | ||||||
| Metcalf 200289 | ✓ | cRestore® | Open | On-lay | Massivel | NR | NR | ||||||
| Modi 201390 | ✓ | GRAFTJACKET | Open | Bridging | Large to massiveb | 62 (47–72) | 41 (67) | ||||||
| Moore 200691 | ✓w | Cadaveric allograft | Open | Bridging | Massived | 59 (34–81) | 23 (72) | ||||||
| Nada 201092 | ✓ | Dacronx | Arthroscopic | Bridging | Massiveb,d | 66 (55–85) | 14 (67) | ||||||
| Neumann 201793 | ✓ | Conexa | Open | Bridging | Massiveb,d | 62 (38–82) | 21 (35) | ||||||
| Petrie 201394 | ✓ | yLARS™ | Open | Bridging | Massivel | 67 (NR) | 21 (70) | ||||||
| Petri 201695 | ✓ | Arthroflex | Open | On-lay | Large to massivel | 57 (26–68) | 11 (85) | ||||||
| Petriccioli 201396 | ✓ | zSportMesh™ | Open | On-lay | Subscapularis tears | 61 (51–68) | 8 (80) | ||||||
| Phipatanakul 200997 | ✓ | cRestore® | Open | On-lay | Massivel | 48 (31–62) | 9 (82) | ||||||
| Proctor 201498 | ✓ | X-Repair | Arthroscopic | On-lay | Massived | 66 (52–89) | NR | ||||||
| Rhee 200899 | ✓ | Biceps (long-head) | Mixed | Bridging | Massiveb,d | 61 (46–79) | 11 (35) | ||||||
| Rotini 2011100 | ✓ | Acellular human dermal matrix | Mixed | On-lay | Large to massivel | 48 (37–55) | 5 (100) | ||||||
| Sano 2010101 | ✓ | Biceps (long-head) | Open | Bridging | Massived | 64 (48–79) | 12 (86) | ||||||
| Scheibel 2007102 | ✓ | Periosteum | Open | On-lay | NR | 59 (44–71) | 16 (70) | ||||||
| Schlegel 2018103 | ✓ | Collagen sheeth | Arthroscopic | On-lay | N/A: partial thickness | 54 (34–75) | 19 (58) | ||||||
| Sclamberg 2004104 | ✓ | cRestore® | Open | Mixed | Large to massiveb | 67 (52–79) | 7 (64) | ||||||
| Sears 2015105 | ✓ | GRAFTJACKET | Arthroscopic | On-lay | |||||||||
| ✓ | Tissuemendaa | NR | 50 (37–70) | NR | |||||||||
| ✓ | Conexa | ||||||||||||
| Venouziou 2013106 | ✓ | GRAFTJACKET | Open | Bridging | Massivel | 54 (33–64) | 9 (64) | ||||||
| Wong 201032 | ✓ | GRAFTJACKET | Arthroscopic | Bridging | Massivel | 53 (39–67) | 36 (80) | ||||||
The RCTs employed various time points for data collection. One RCT collected data preoperatively and at 6 weeks, 3, 6, 12 and 24 months postoperatively. Another RCT collected data at 12 and 24 months, and a third at 14 months. 26,35,65 In terms of health-related quality-of-life outcomes, the SF-36 was collected in two RCTs and one comparative study. 35,42,65
Non-comparative studies
A total of 37 observational single-group studies involving 700 patients were identified. The study populations ranged from 5 to 61 patients (age range 26–89 years), with the majority (n = 28) recruiting patients with large or massive full-thickness tears only. Petriccioli et al. 96 was the only study to have reported on the use of patch augmentation in the treatment of isolated subscapularis tears, whereas Schlegel et al. 103 recruited patients with partial-thickness supraspinatus tears only.
None of the identified studies carried out a formal economics evaluation of patch use for rotator cuff surgery. Adverse events and their associated procedures were captured in all RCTs. Only one RCT reported information about patients’ capacity to return to work, as well as capacity to continue their recreational activities and medication utilisation at 6 weeks, 3 months and 6 months post surgery. 65
Surgical characteristics
Comparative studies
Across all the comparative studies, a total of 12 different patches were utilised. Decellularised xenograft patches were the most commonly investigated (n = 6; Restore, n = 4). Surgical techniques could be classified as fully arthroscopic (46%, n = 7), open (40%, n = 6) or a mixture of both (13%, n = 2). The method of patch utilisation was split fairly evenly between the categories of ‘on-lay’ (53%, n = 8) or ‘bridging’ (47%, n = 7).
Non-comparative studies
A full spectrum of patch materials [human allograft (32%, n = 12), human autograft (11%, n = 4), xenograft dermal (22%, n = 8), xenograft intestinal (11%, n = 4) and synthetic (24%, n = 9)] and surgical techniques were reported [on-lay (51%, n = 19), bridging (41%, n = 15) and mixed (8%, n = 3)].
Shoulder pain and function
Comparative studies
Eight different outcome scores were used to assess shoulder function (see Appendix 2, Table 19). The Constant Scale (60%), American Shoulder and Elbow Surgeons (ASES) (47%) and the University of California, Los Angeles (UCLA), Shoulder Scale (33%) scores were the most commonly reported, with most studies reporting multiple functional scores.
Among RCTs, only one study found a statistically meaningful improvement in ASES and Constant scores, but not the UCLA scale, following implantation of an allograft patch (see Appendix 2, Table 20). 26 The two RCTs investigating decellularised porcine small intestine submucosa (Restore)35,65 failed to demonstrate an improvement in patient-reported outcomes at 1- and 2-year follow-up, whereas the study by Leuzinger et al. 63 undertook only intragroup comparisons between preoperative and post-operative Constant scores, reporting similar improvements following implantation of an allograft, xenograft or synthetic patch.
Only three non-randomised comparative studies reported a significant improvement in functional shoulder scores for synthetic, human allograft and fascia lata autografts. 33,40,42 The remaining studies found no significant improvement, whereas the studies by Ito and Morioka66 and Vitali et al. 43 did not undertake intergroup comparisons.
Non-comparative studies
Of the non-comparative observational studies, 35 collected patient-reported outcome scores, with 25 reporting a statistically significant temporal improvement (see Appendix 2, Table 20).
Re-tear (including radiological assessments)
The integrity of the surgical repair was assessed by all RCTs and seven observational comparative studies, with a re-tear rate ranging from 10% to 73% following patch implantation and from 18% to 65% following a standard RCR (see Appendix 2, Table 21). Magnetic resonance imaging (MRI) was the commonest imaging modality (62%) utilised to diagnose recurrent tears, with a magnetic resonance arthrogram utilised in a further 23% of studies. The majority of studies undertook postoperative imaging after 1–2 years; however, there was considerable heterogeneity existing in the radiological classification of re-tears, and four studies did not provide any details. Definitions of re-tears could be broadly categorised into two themes: the presence of any tear or the presence of tears greater than the residual intraoperative defects. Five studies also attempted to subcategorise recurrent tears into ‘partial’ or ‘complete’. For example, the study by Iannotti et al. 35 described a third ‘partially healed’ group, which was defined as a smaller rotator cuff lesion than that observed during preoperative imaging.
Although the RCT investigating human allograft (GRAFTJACKET) demonstrated a significantly lower failure rate in the augmentation arm, neither of the RCTs investigating the xenograft patch Restore found any reduction in re-tear rate. 26,35,65 In conflict with these findings, a multipatch comparative study found no difference in failure rate between three different patches: xenograft (Restore), human allograft (GRAFTJACKET) or synthetic (Artelon). 30 Among the observational comparative studies, significantly lower rates of re-tears were reported after augmentation with synthetic (Repol Angimesh), autograft (fascia lata) or allograft patches (Arthroflex and Allocover), whereas no improvement in re-tears was observed following augmentation with a long head of biceps tendon autograft or for the Restore patch. 33,39–43,67,71
Non-comparative studies
Re-tear rate was assessed by 31 non-comparative studies, with a wide range of re-tear rates reported for each graft type [human allograft (0–25%, n = 7), human autograft (7–100%, n = 4), xenograft dermal (0–63%, n = 8), xenograft intestinal (8–90%, n = 4) and synthetic (7–62%, n = 8)].
Shoulder pain
Comparative studies
Only two studies (Gilot et al. ,42 Athroflex; Mori et al. ,33 fascia lata) reported a significant reduction in pain when compared with standard repair (see Appendix 2, Table 22). The remaining nine studies either did not provide intergroup comparisons (n = 3) or found no significant difference in pain scores between treatment arms (n = 6). Interestingly, the study by Walton et al. ,41 which utilised a ‘mean activity pain score’, found an increase in pain for the first 3 months following implantation of the Restore patch, which subsequently normalised by 6 months.
Non-comparative studies
In contrast to the comparative studies, of the 24 non-comparative observational studies reported pain scores, 22 reported a significant temporal improvement following augmented RCR.
Health-related quality of life
Comparative studies
Only three comparative trials reported the use of either the Short Form questionnaire-12 items (SF-12) or the SF-36 scores (see Appendix 2, Table 23). When compared with standard repair, two RCTs investigating porcine SIS xenograft (Restore) found no difference in the physical or mental components of the SF-36. 35,65 Conversely, an observational comparative study using human allograft (Athroflex) reported a significant improvement in both of these components at 6 months and 2 years postoperatively. 42
Non-comparative studies
Three non-comparative studies reported significant improvements in SF-12 scores at final follow-up (32–36 months postoperatively). Conversely, the study by Encalada-Diaz et al. 80 found no improvement in the physical or mental components of the SF-12 at 12 months, following implantation of a synthetic rotator cuff patch.
Patch-related adverse events
A total of 43 studies provided data on complications, of which 21 studies reported the occurrence of complications in a total of 73 patients. The more commonly reported events across the studies included superficial and deep infections, and inflammatory response. Other reported complications were shoulder bursitis, biceps rupture, fibrosis, unexplained fever, shoulder manipulation, wound erythema, shoulder stiffness, persistent pain, skin reaction, biceps deformity, ossification, cardiac event and possible inflammatory response. One study,69 which used a quadriceps autograft-based patch, reported knee-related problems and nerve injury.
Other secondary outcomes
No data on other secondary outcomes of interest were reported.
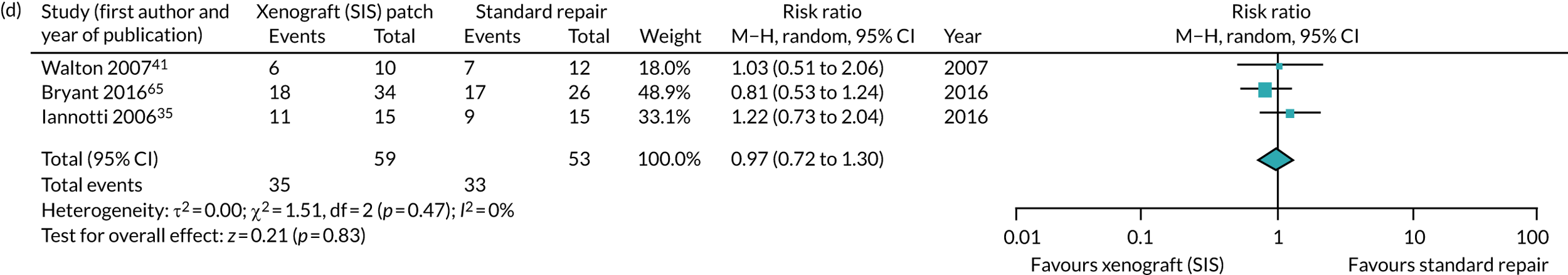
Meta-analysis
Shoulder pain and function scores
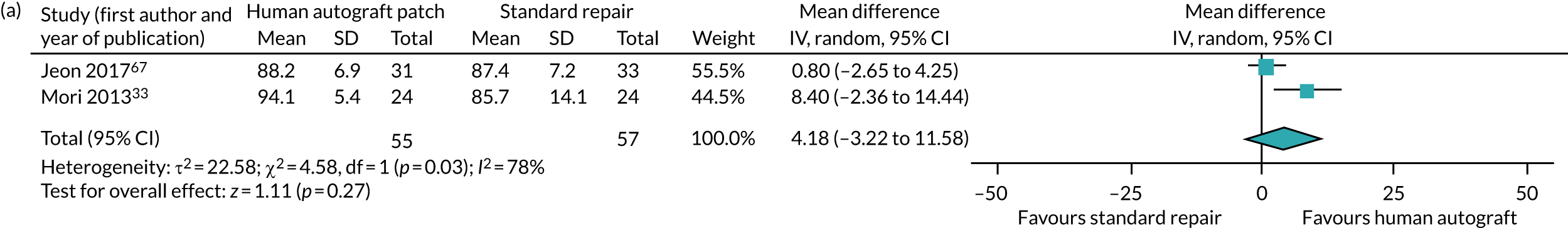
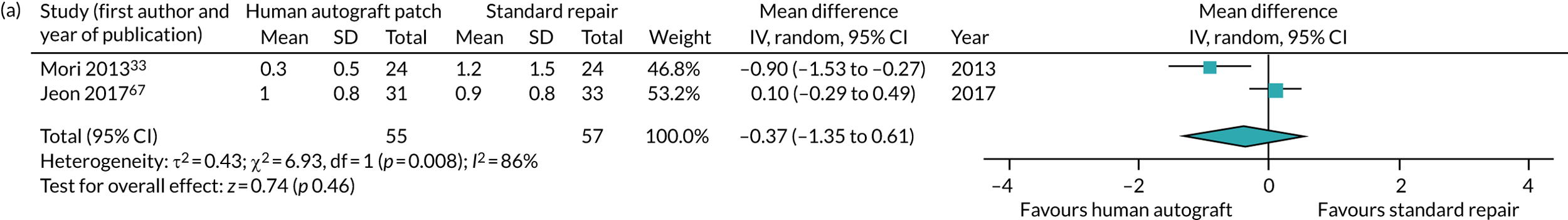
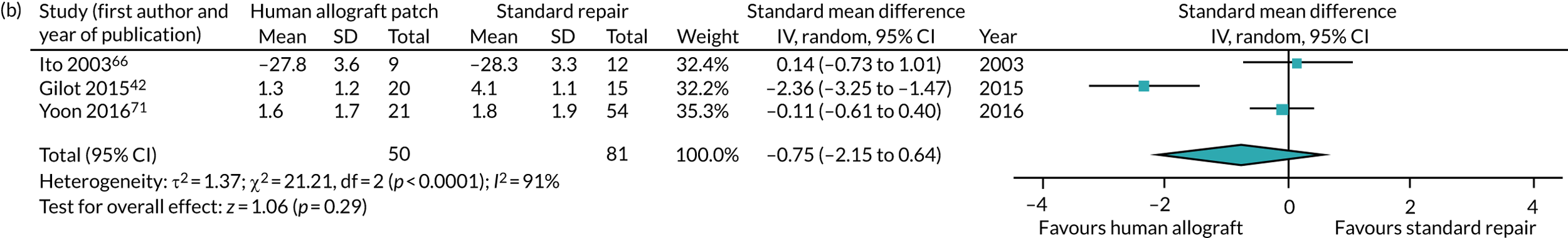
Of the 15 comparative studies, nine (eight observational and one RCT) provided sufficient data on post-operative functional outcome scores to be included in the meta-analysis (Figure 5). A 10-point improvement on the UCLA scale was observed for synthetic patches at 36 months postoperatively (mean difference 9.81, 95% CI 9.10 to 10.51; I2 = 0%) but not in the ASES score of studies of autografts (mean difference 4.18, 95% CI –3.22 to 11.58; I2 = 78%). Studies of allografts or xenografts derived from dermis or pericardium (non-SIS) used differing measures. No difference was found when the allograft studies were combined (standardised mean difference 0.54, 95% CI –0.23 to 1.31; I2 = 80%). There did not appear to be a difference between the sole RCT26 in this meta-analysis and the other studies. For studies of xenografts versus surgery, there was also no evidence of a difference (standardised mean difference –0.05, 95% CI –0.41 to 0.30; I2 = 0%, respectively). Insufficient data were available for xenografts derived from intestinal submucosa (SIS).
FIGURE 5.
Forest plot comparing shoulder-specific pain and function outcome scores at final follow-up between (a) autograph patches and standard repair; (b) allograft patches and standard repair; (c) allograft patches and standard repair (observational studies only); (d) xenografts (non-small intestine submucosa) and standard repair; and (e) synthetic patches and standard repair.
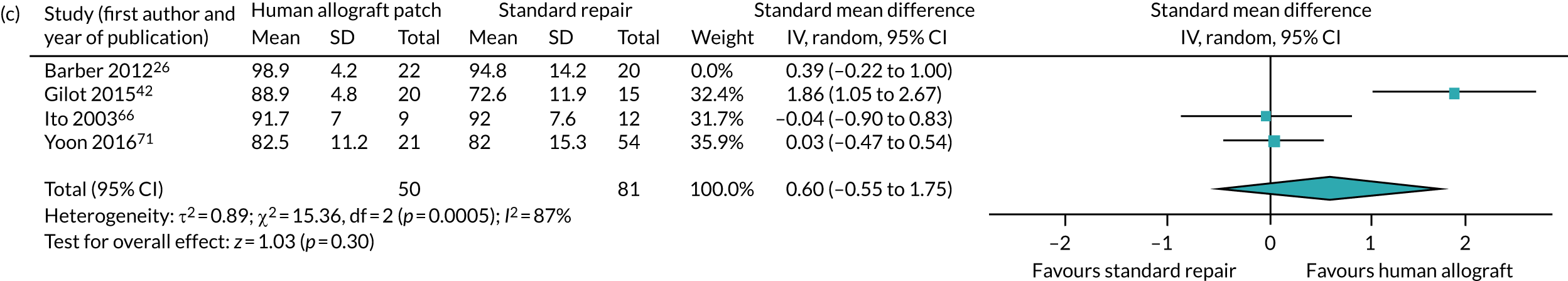
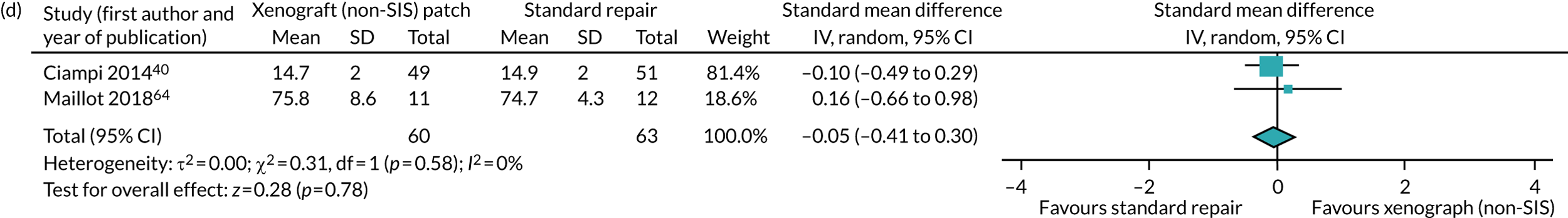

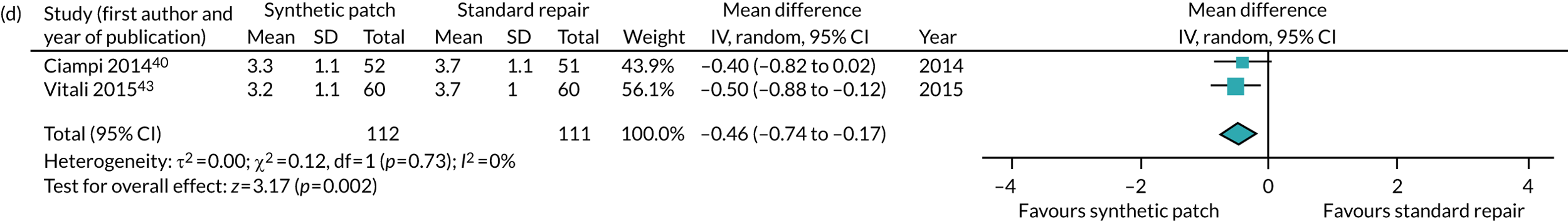
Shoulder pain
Eight observational comparative studies had sufficient data for a meta-analysis of postoperative pain (Figure 6). A small, probably non-clinically significant107 improvement in postoperative pain was observed for synthetic patches only (mean difference –0.46, 95% CI –0.74 to –0.17; I2 = 0%). For studies of non-SIS xenografts, there was no evidence of a difference in postoperative pain scores (standardised mean difference 0.26, 95% CI –0.16 to 0.68; I2 = 16%). There was substantial statistical heterogeneity between the studies of both autograft and allograft patches (mean difference –0.37, 95% CI –1.35 to 0.61, I2 = 86%; and standardised mean difference –0.75, 95% CI –2.15 to 0.64, I2 = 91%, respectively). Insufficient data were reported for a meta-analysis of shoulder pain following augmentation with xenograft patches derived from SIS.
FIGURE 6.
Forest plot comparing shoulder pain at final follow-up between (a) autograft patches and standard repair; (b) allograft patches and standard repair; (c) xenografts (non-small intestine submucosa) and standard repair; and (d) synthetic patches and standard repair.

Health-related quality of life
Only three comparative studies (two RCTs and one observational study) provided data on HRQoL, but there were insufficient data available to meta-analyse. 35,42,65
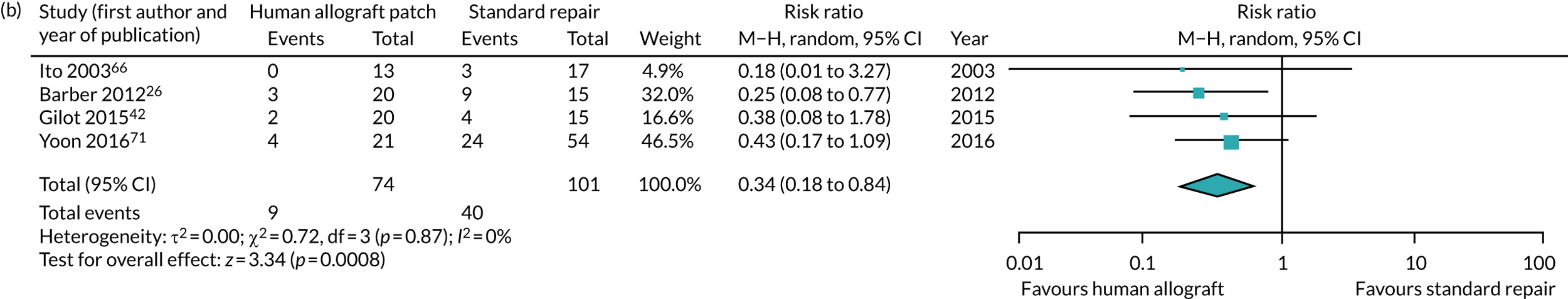
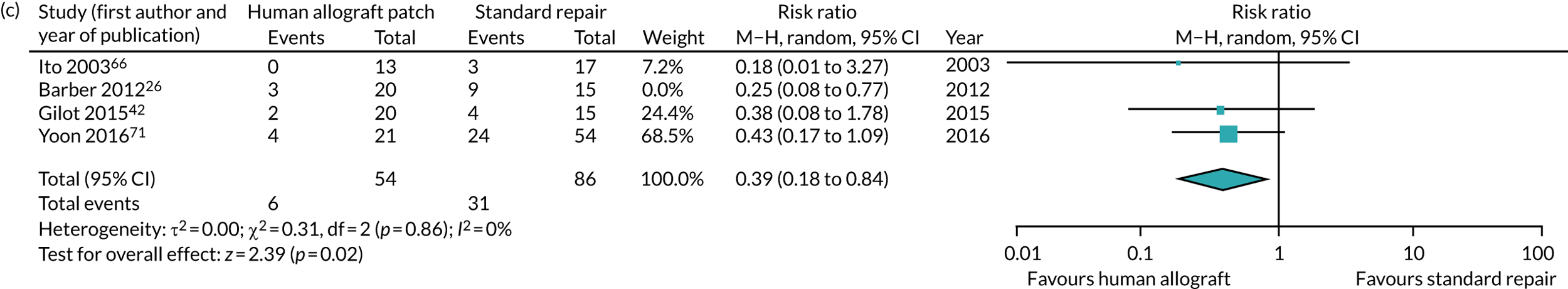
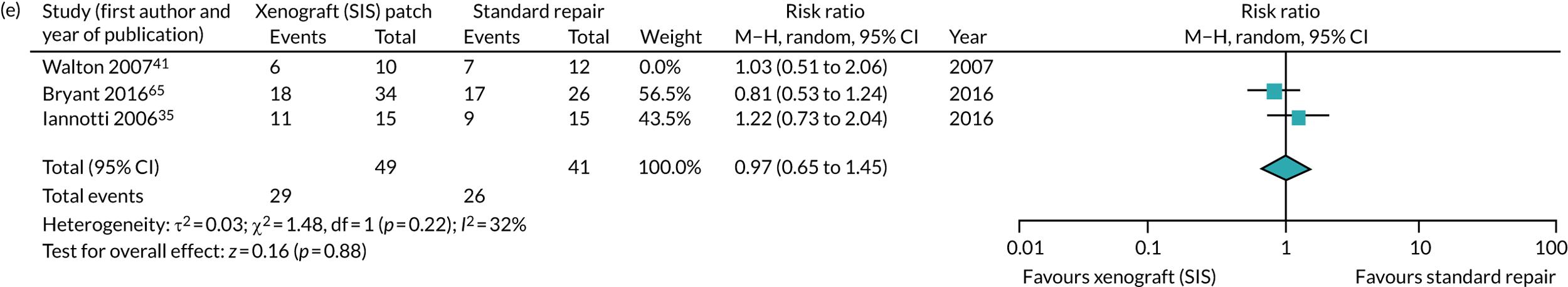
Surgical re-tear rate
In total, 11 comparative studies (four RCTs and seven observational studies) could be included in a meta-analysis for re-tear rate (Figure 7). A significantly lower re-tear rate was seen for an allograft patch (RR 0.34, 95% CI 0.18 to 0.64; I2 = 0%). The one RCT evaluating an allograft26 appears to have a consistent finding with the three observational studies. There was evidence from two observational studies for a lower re-tear rate with synthetic patches (RR 0.40, 95% CI 0.25 to 0.64; I2 = 0%). 41 There was no evidence of a difference for autografts (RR 0.69, 95% CI 0.40 to 1.18; I2 = 0%), based on two observational studies, or SIS-derived xenografts (RR 0.97, 95% CI 0.72 to 1.30; I2 = 0%), based on two RCTs and one observational study (the meta-analysis of only the two RCTs had similar findings). Insufficient data were available for non-SIS derived xenografts to meta-analyse.
FIGURE 7.
Forest plot comparing re-tear rates at final follow-up between (a) autograft patches and standard repair; (b) allograft patches and standard repair; (c) allograft patches and standard repair (observational studies only); (d) xenografts (small intestine submucosa) and standard repair; (e) xenografts (small intestinal patches) and standard repair (RCTs only); and (f) synthetic patches and standard repair. M–H, Mantel–Haenszel.


Complications (including patch-related adverse events)
A total of 43 studies provided data on complications, of which 21 studies reported the occurrence of 77 complications in a total population of 1381 patients undergoing any form of augmentative surgery and 372 patients receiving a standard rotator cuff repair. The overall crude complications rates were 4.8% for patients undergoing any form of patch augmentation and 1.9% following non-augmentative surgery. However, by excluding five studies in the augmentation group that had particularly high rates of complications (20–74%, following quadriceps tendon, Restore patch or humeral periosteal-augmented repair35,41,69,97,102), the overall rate of complications following patch augmentation was 2.9%. An inflammatory response was recorded in fifteen patients (see Appendix 2, Table 21). The majority of these events (n = 11) occurred in patients who received a SIS xenograft (Restore) patch but with reactions also reported after implantation of bovine-derived, irradiated, decellularized human allograft and synthetic patches. Excluding all adverse events concerning the Restore patch, which has been withdrawn from the marketplace, the crude complication rate for patches in potential clinical use was 2.3%.
Risk of bias
Assessment of bias was conducted for all RCTs and comparative studies (Tables 2 and 3). Only the study by Bryant et al. 65 was at a low risk of bias, with the remaining RCTs assessed as having an unclear risk. These findings are based on a lack of study methodology detail, in particular surrounding blinding of patients and outcome assessors. All observational comparative studies had a serious risk of bias, which centred around the potential for confounding, bias in patient selection and outcome measurement.
| Study (first author and year of publication) | Type of bias | Overall assessment | ||||||
|---|---|---|---|---|---|---|---|---|
| Random sequence generation | Allocation concealment | Blinding of participants and personnel | Blinding of outcome assessors | Incomplete outcome data | Selective reporting | Other sources of bias | ||
| Barber 201226 | Unclear | High | Unclear | Unclear | Unclear | Low | Higha | Unclear |
| Byrant 201665 | Low | Low | Low | Low | Low | Low | Low | Low |
| Iannotti 200635 | Low | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
| Leuzinger 201663 | Unclear | Unclear | Unclear | Unclear | Low | High | Low | Unclear |
| Study (first author and year of publication) | Type of bias | Overall assessment | ||||||
|---|---|---|---|---|---|---|---|---|
| Bias due to confounding | Bias in participant selection | Bias in classification of interventions | Bias due to deviation from intended interventions | Bias due to missing data | Bias in measurement of outcomes | Bias in selection of the reported results | ||
| Ciampi 201440 | Serious | Moderate | Low | Low | No information | Serious | No information | Serious |
| Gilot 201542 | Serious | Serious | Low | Low | Serious | Serious | Serious | Serious |
| Ito 200366 | Serious | Serious | Moderate | No information | No information | Serious | Moderate | Serious |
| Jeon 201767 | Moderate | Serious | Moderate | No information | No information | Serious | Moderate | Serious |
| Maillot 201864 | Moderate | Serious | Low | No information | Low | Serious | Serious | Serious |
| Mori 201333 | Serious | Serious | Low | Low | Serious | Serious | Serious | Serious |
| Mori 201568 | Serious | Serious | Moderate | Low | Moderate | Serious | Serious | Serious |
| Tempelaere 201769 | Serious | Serious | Moderate | No information | Serious | Serious | Moderate | Serious |
| Vitali 201543 | Serious | Serious | Low | No information | Serious | Serious | Serious | Serious |
| Walton 200741 | Moderate | Serious | Low | No information | Serious | Serious | Low | Serious |
| Yoon 201671 | Serious | Serious | Low | No information | Serious | Serious | Serious | Serious |
Discussion
The use of medical implants has recently come under increasing scrutiny. Surgical repair of the rotator cuff with patch augmentation has been proposed as a method of improving rates of tendon healing and patient outcomes. To the best of our knowledge, this systematic review is the largest and most comprehensive systematic appraisal of the clinical effectiveness and safety of such implants to date. Overall, the current evidence is not sufficiently robust to determine the effectiveness of patch-augmented RCR compared with standard repair alone. Interestingly, the consistently observed improvement in functional scores and pain observed in non-comparative observational studies was often not reflected when the same patch was tested in a controlled fashion, reinforcing the importance of well-designed clinical trials in the assessment of novel health technologies.
Although our meta-analysis suggests a small improvement in pain and shoulder function for synthetic patches and a moderate reduction in re-tear rate for synthetic and human allograft patches, study bias and heterogeneity mean that these results must be interpreted very cautiously. Furthermore, it is unclear if the observed 10-point improvement in UCLA score for the synthetic patches is clinically meaningful. To date, the minimal clinically important difference for the UCLA score following RCR has not been established. 108 However, a threshold of 30 UCLA points at 2 years has been proposed as an absolute cut-off point signifying treatment success for RCR. 109 In the studies investigating synthetic polypropylene patches, augmentation failed to meet this threshold. 40,43 Similarly, the small 0.46-point reduction in VAS pain scores is unlikely to be clinically meaningful. 107
Across 43 studies with a combined safety population of 1753 participants, complications rates were similar between augmented repairs (2.3%) and standard repairs (1.9%), with specific safety concerns associated with certain patches (Restore) or techniques (such as quadriceps allograft, humeral periosteal allograft). 37,38,45,69,102
Most studies reported on the use of patch augmentation for large to massive tears in patients aged 50–70 years. This demographic is similar to that reported by British shoulder surgeons (see Chapter 3), in which only 10% of respondents would consider augmentation for small and medium-sized tears. Only four studies were identified that included patients with small or medium-sized tears and none assessed the effect of tear size on outcome. It is interesting to note that small tears in patients aged 80 years are predicted to have a similar chance of repair failure as massive tears in patients aged 50 years. 15 It is, therefore, unclear why a dichotomy between small to medium and large to massive tears has emerged. Rather than viewing the degree of structural incompetence as the primary indication for patch augmentation, we would instead encourage a biological perspective, applying augmentation to cases in which tendon healing is the most impaired.
Interestingly, radiological findings seemed to closely echo patient-reported outcome measures (PROMs). Three studies35,65,67 found no significant improvement in either PROMs or rate of re-tear, whereas a further five studies26,33,40,42,68 reported significant improvements in both functional outcome scores and radiologically defined repair failure. This lends support to the notion that repair success is intimately linked with symptom resolution. Indeed, a subgroup analysis by Iannotti et al. 35 identified a significant association between tendon healing and postoperative improvements in the PENN score and SF-36 physical component. Similar findings have previously been reported by the UKUFF study,2 in which those with healed repairs had a better Oxford Shoulder Score (OSS) than patients with re-tears but with the worst results among those with an irreparable tear.
The systematic literature review lacked evidence of economic evaluation of patch use for rotator cuff surgery. The few RCTs that were found evaluated the clinical effectiveness rather than the cost or cost-effectiveness of patch use. However, the studies considered and collected resource utilisation related to the complications following a rotator cuff surgery and medication use, which can both be transformed into monetised units and, hence, considered as a further cost of the surgery. Evidence of the methods of patient data collection was revealed in one study. 65 The SF-36 was the preferred instrument of capturing HRQoL in the population under consideration. From a societal point of view, rotator cuff surgery is expected to have an impact on patients’ capacity to return to their daily activities following a rotator cuff operation. The return to daily activities, as well as capacity to return to work, was captured in a study by Bryant et al. 65
Strengths and limitations of the study
Strengths of this review include a priori published protocol,58 a comprehensive search strategy, inclusion of non-English language articles, duplicate assessment of eligibility, a risk-of-bias assessment and data extraction. Nonetheless, there remain several limitations to the current review, which are mainly a reflection of the quality of the published primary research available. Only four RCTs have been published, of which two relate to a product (Restore) that has now been withdrawn from market because of safety concerns. 26 In addition, substantial heterogeneity between studies was observed, with the majority of studies also judged to have a high risk of bias, which seriously limited our ability to draw firm recommendations. An exhaustive exploration of the heterogeneity has not been undertaken and indeed such an analysis was not declared a priori in our protocol paper. 58 However, separating studies by patch type did influence the degree of heterogeneity and we would, therefore, recommend that patch type should be considered in the design of future reviews.
In comparison with previous systematic reviews, we have included one additional RCT63 and three observational comparative studies representing 278 patients not otherwise identified. 27,44,59,63,66,67,71 Results from our meta-analysis are, in part, consistent with a previous analysis that found an overall reduction in re-tear rate and improved ASES scores following patch augmentation. 44 The substantial number of additional studies included in this current review provide greater precision and, although a subgroup analysis was not originally specified in our protocol, they have allowed us to hypothesise that patch type may have an effect on patient outcomes. The occurrence of adverse events with only certain patch types adds some credibility to this notion. Previous reviews of augmented RCR have, on the basis of a presumed effect on patient outcome, excluded studies based on the size of rotator cuff tear or surgical technique (on-lay or bridging). 27 It is possible that each technique reflects different patient cohorts; for example, the use of bridging scaffolds may represent larger, more chronic or even recurrent rotator cuff tears. However, we were unable to detect any overall difference in patient-reported outcomes, re-tear rate or pain scores between studies reporting on-lay or bridging techniques. It should be noted that differences in terminology makes comparison of these surgical techniques challenging; the terms ‘irreparable’, ‘bridging’, ‘interposition’ or ‘reconstruction’ were used interchangeably in a number of studies or to refer to the same approach. To help facilitate the future interrogation of the relationship between surgical technique and outcomes we would suggest that only the terms ‘on-lay’ (defined as repair augmentation) or ‘bridging’ (defined as repair reconstruction/augmentation) be utilised in accordance with previously published definitions. 27
There are a growing number of patches available for the augmentation of RCR. Despite the safety-related withdrawal of certain patches, as well as wider concerns surrounding medical device and mesh implantation, rigorous clinical evaluation of patch augmentation is lacking. 41,110 We were particularly concerned by the absence of publicly available research for several patches currently in clinical use [e.g. dCELL® (Tissue Regenix Group plc, Leeds, UK) and Leeds–Kuff™ (Neoligaments, Leeds, UK)]. Although some studies have indicated promise for specific patches, firm recommendations in terms of patch type or surgical technique cannot be made at present. There remains a need for well-designed comparative studies (preferably multicentre RCTs) that are capable of robustly evaluating the effectiveness and safety of multiple patch types. Furthermore, routine reporting of patch registry data could address the current lack of robust safety data for cuff-augmented RCR. 111
Chapter 3 Surveys
Introduction
When planning a RCT of patch use for rotator cuff tears, considering current practice alongside current evidence is critical. It is particularly important to understand practice in the setting in which a trial would be carried out. The constraints that potential investigators would have to work within are a key issue that will affect the conduct of a RCT. Two surveys were undertaken with surgeons to address these concerns, as stages 2 and 4 of this mixed-methods feasibility study. The first was a survey of the surgical membership of the British Elbow and Shoulder Society (BESS), also known as the BESS membership survey. The second was a survey of surgeons who had previously participated in large UK shoulder surgery trials, known as the surgeon triallist survey. 1
The aims of the surveys were to:
-
identify the current UK clinical practice of patch use
-
gather information on surgeon opinion of patch choice and patient suitability
-
explore the general attitude towards a RCT of patch-augmented RCR
-
explore the acceptability of proposed trial design elements to surgeons and to assess the feasibility of a RCT of patch-augmented RCR.
Methods
The surveys were developed and distributed using the Online Surveys tool (Jisc, Bristol, UK) (previously known as Bristol Online Surveys). Prior to finalising, each survey was reviewed and piloted internally among the study investigators and external individuals as appropriate.
Participant consent was implied by the completion and submission of the online survey. Information about the study and how the data would be collected and processed was explained in e-mail correspondence (invite and reminders) and at the start of the survey.
The response rate for the surveys was defined as the number of responding participants divided by the number of eligible people invited. Responses were summarised quantitatively or narratively as appropriate [using Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) (version 16.12) and GraphPad Prism (GraphPad Software Inc., CA, USA) (version 7.0)].
The methodology, findings and discussion for each survey are detailed separately below.
Stage 2: British Elbow and Shoulder Society membership survey
The BESS members are predominantly clinically active shoulder surgeons. The BESS office used the e-mail list to invite participants to complete the survey, avoiding the unnecessary sharing of personal data. Information about the PARCS study and a hyperlink to the survey was provided. There was no minimum number of responses required as the study was opportunistic in terms of sample size and was not driven by statistical testing.
The e-mail invitation was sent out in April 2017 and available to complete until the end of August 2017. Surgeon members of the BESS attending the annual meeting in June 2017 were also offered an opportunity to complete the survey at an exhibition stand. To assess respondent demographics, participants were asked about their grade (i.e. consultant, trainee or other) and place of work (i.e. district general hospital, university teaching hospital, private practice or other). To determine their familiarity with and experience of augmented RCR, participants were asked about their preferred surgical technique for RCR (predominantly open, predominantly arthroscopic or substantial amount of both open and arthroscopic repairs), whether or not they had previously used patch-augmented rotator cuff surgery (i.e. no, yes within 6 months or yes but not within 6 months) and the total number of augmented cuff repairs that they had undertaken. Further questions sought to determine the types of patch commonly in use and to investigate the factors influencing patch selection. Two separate free-text questions were posed: ‘Which patches have you used?’ and ‘Why did you use these specific patches?’. A final free-text box was provided to allow further comments about the choice of patch to be recorded.
To gather opinion on patient selection for augmented RCR, respondents were asked to consider discrete patient subgroups. Four different tear sizes (i.e. small, medium, large and massive) were combined with different four different ages (50, 60, 70 and 80 years) to produce 16 combinations. Participants were asked if they considered each patient combination appropriate for patch augmentation. An answer of ‘yes’, ‘no’ or ‘unsure’ could be provided for each scenario. A free-text box was also provided to capture further comments relating to patient suitability.
Respondents were then asked to consider participation in a future clinical trial in augmented RCR. Responders were asked if they would be interested in participating in a RCT of patch-augmented surgery (i.e. yes, no or maybe). Members were asked what factors could be addressed to encourage participation in a RCT.
The survey was piloted with four members of the shoulder and elbow surgical team who perform patch repair. The survey took approximately 10 minutes to complete.
Stage 4: surgeon triallist survey
The surgeon triallist survey was directed at surgeons who had taken part in previous large multicentre NHS shoulder trials and, therefore, the subset of surgeons who were most likely to participate in a RCT of patch-augmented rotator cuff surgery. Eligible participants were identified through a network of surgeon triallists who have participated in previous NHS-based shoulder surgical trials [i.e. Can Shoulder Arthroscopy Work (CSAW)?, UK Frozen Shoulder Trial (UKFroST) and UKUFF]. 18,112,113 They were invited to complete the survey by the PARCS project management group through a personalised e-mail or face-to-face invitation. The survey was open between June and August 2018. Non-responders received up to two e-mail reminders asking them to complete the survey.
The intention was to invite at least 30 research-active orthopaedic shoulder surgeons. This was considered large enough to meet the aim of this component of the project and ensured that a range of surgeons and centres were included. This would also be close to the number of surgeons needed to participate in a future trial of patch-augmented rotator cuff surgery.
The surgeon triallist survey was developed based on previous stages, including the systematic review, the above BESS membership survey and the stakeholder focus groups. Uncertainties related to the patient population, intervention, control and outcome (PICO) elements, and trial practicalities were incorporated into the survey design.
The survey started by asking if the triallists currently used a patch to augment a RCR on any of their patients. If they answered yes, the surgeons were then invited to respond to questions on how they typically used a patch (bridge, on-lay or other) and whether or not the state of the subscapularis affected their decision to use a patch. The next section included questions about a trial of patch-augmented rotator cuff surgery and which patients they would be willing to randomise. Other questions included what the comparator in a trial would be and more detail about patient characteristics, including tear size, age ranges, presence of atrophy, glenohumeral OA and cuff arthropathy. The survey also asked questions about logistical trial procedures, including the timing of randomisation, surgical repair technique, types of patch they would be willing to use, postoperative rehabilitation and length of patient follow-up.
The survey was reviewed and tested by members of the study team, including surgeons and trainees. The survey took approximately 15 minutes to complete. During the survey, participants were asked to register their interest in taking part in further stages of the PARCS study.
Results
Stage 2: British Elbow and Shoulder Society membership survey
A total of 550 medically qualified members of the BESS (of whom 481 were consultant orthopaedic surgeons) were invited to participate, with 105 (19%) responding. The respondents were mostly consultant surgeons (97%), with the majority working at district general hospitals (48%) (Table 4). Most participants (95%) worked within the NHS but with some reporting additional work within the private sector (32%).
| Category | n (%) (N = 105) |
|---|---|
| Training grade | |
| Consultant | 102 (97) |
| Other | 3 (3) |
| Place of work | |
| DGH | 50 (48) |
| Teaching hospital | 44 (42) |
| Mixed (DGH and teaching hospitals) | 6 (6) |
| Private hospital | 5 (5) |
Most respondents undertook arthroscopic RCRs (66%), with only a minority solely undertaking open repairs (14%) (Table 5). When asked whether or not they had ever used a patch to augment rotator cuff surgery, over half (58%) had done so. The majority of patch users had undertaken an augmented repair within the last 6 months (70%). The utilisation of patches among surgeons performing open repairs was slightly lower (40%) than for those reporting an arthroscopic (56%) or mixed open and arthroscopic practice (76%).
| Category | n (%) |
|---|---|
| Preferred repair technique (N = 105) | |
| Arthroscopic | 69 (66) |
| Open | 15 (14) |
| Open or arthroscopic | 21 (20) |
| Use of patch augmentation (N = 105) | |
| Yes: within 6 months | 43 (41) |
| Yes: not within 6 months | 18 (17) |
| No | 44 (42) |
| Number of patches implanted (N = 61) | |
| 1–5 | 32 (30) |
| 6–10 | 15 (14) |
| 11–15 | 0 (0) |
| 16–20 | 6 (6) |
| > 20 | 8 (8) |
A varied surgical experience was reported among those who had performed patch-augmented RCR. Most surgeons reported low use, with a median of five rotator cuff augmentation procedures performed; however, the maximum reported was 200 procedures.
Responses relating to the patch types used can be seen in Table 6. When asked about the patch types and products utilised during RCR, 13 different products were reported. Decellularised dermis accounted for 85% of the different patches used, and non-degradable synthetic meshes made up the remaining 15%. Human decellularised products were more frequently used, with only 13% of decellularised patches being porcine derived (the rest being human, except for one for which it was not clear what the source material was). All synthetic scaffolds that were reported were non-degradable and produced from a variety of polymers (i.e. polyester, polypropylene and polyurethane). Overall, GRAFTJACKET was the most commonly reported device (55%) with the Leeds-Kuff Patch (10%), Arthroflex (8%) and dCELL (8%) the next most common.
| Category | N (%) | n |
|---|---|---|
| Decellularised patches | ||
| Porcine derived | 10 (13) | |
| Arthrex DX reinforcement matrix | 1 | |
| Conexa reconstructive matrix | 5 | |
| Restore | 1 | |
| Zimmer collagen repair patch | 2 | |
| Manufacturer not specified | 1 | |
| Human derived | 56 (71) | |
| Arthroflex® | 6 | |
| dCELL | 6 | |
| GRAFTJACKET | 44 | |
| Type not specified | 1 (1) | 1 |
| Synthetic patches | 12 (15) | |
| Artelon | 2 | |
| Leeds–Kuff patch | 8 | |
| Vypro® | 1 | |
| Manufacturer not specified | 1 | |
Reported factors influencing patch selection are given in Table 7. The device’s perceived efficacy was an important theme, with clinical evidence (24%) and personal and peer experience (8% and 4%, respectively) cited as important determinants. Product characteristics formed another dominant theme, with patch usability, strength and material influencing selection. A product’s cost and availability within the local hospital was also important. In addition, the specific characteristics of a rotator cuff tear may also determine patch choice.
| Category | n (%) |
|---|---|
| Product efficacy (N = 29) | |
| Clinical evidence | 19 (24) |
| Personal experience | 6 (8) |
| Peer experience | 3 (4) |
| Regulatory approval | 1 (1) |
| Product characteristics (N = 18) | |
| Material type | 9 (11) |
| Strength | 5 (6) |
| Usability | 4 (5) |
| Product access (N = 17) | |
| Cost | 6 (8) |
| Local availability | 11 (14) |
| Tear characteristics (N = 15) | |
| Type of tear | 14 (18) |
| Tissue quality | 1 (1) |
Participants responded with their opinions on patient selection for a RCT of patch-augmented RCR (Figure 8). Responses for patients aged 50 or 60 years tended to be similar regarding patient suitability for receiving a patch. However, the effect of age on patient suitability was clearly influenced by tear size. Among older patients (aged 70 or 80 years) with small and medium-sized tears, a greater (although still relatively small) proportion of upper limb surgeons either would consider augmentation or were unsure (12–26%).
FIGURE 8.
The BESS membership survey responses relating to suitability on patient selection. Reproduced with permission from Baldwin et al. 114 © 2020 Baldwin et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited (https://creativecommons.org/licenses/by/4.0/). This includes minor additions and formatting changes to the original figure.

Conversely, the reverse trend was observed in large and massive tears, with a greater proportion of surgeons considering augmentation appropriate in the 50 or 60 years age groups (39–59%).
Overall, tear size seemed to be more important than age in assessing patient suitability. Just over half of respondents (range 19–59%) would use augmentation in large and massive tears, compared with ≤ 10% (range 3–11%) for small and medium-sized rotator cuff tears. However, it is worth noting that considerable uncertainty remains. Around one-fifth (range 19–27%) of respondents were unsure as to the role of augmentations in medium, large and massive tears.
Additional free-text comments were provided by 48 participants, with six dominant themes emerging (Table 8). Tear characteristics remained an important consideration during patch augmentation. As well as tear size, the degree of fatty atrophy, the intraoperative ability to mobilise the tendon and the tension of the repair were often mentioned as important factors during tear classification. Surgical assessment of tendon quality was reported as important by 17% of respondents. A lack of glenohumeral OA (13%) and the failure of a standard repair (27%) were provided as other important qualifiers during augmented repair consideration. For older patients (aged ≥ 70 years) with large tears, 10% of respondents justified avoiding augmented repair because of the perceived success of reverse shoulder arthroplasty.
| Category | n (%) (N = 48) |
|---|---|
| Tear characteristics | 28 (58) |
| Patient population | 17 (35) |
| Previous repair failure | 13 (27) |
| Tissue quality | 8 (17) |
| No OA | 6 (13) |
| Supportive evidence or experience | 5 (10) |
When asked if they would actively participate in a RCT of patch augmentation, half of the respondents confirmed an interest, with a further 22% undecided and the remainder not interested. Twelve respondents provided additional comments that explored barriers to participation. Further trial details were mentioned in almost half (46%) of comments and specific limits were placed on the inclusion/exclusion criteria by 23%, for example ‘no compulsion to use patch in small/medium tears’. A further 31% of comments listed concerns over the type of intervention or comparison that would be utilised. For example, ‘compared to balloon interposition’ or ‘comparing reverse [total shoulder arthroplasty] with patch repair’ were suggested.
Stage 4: surgeon triallist survey
Of the surgeons invited, 24 out of 31 (77%) completed the survey. All of the surgeons who responded had acted as the principal investigator for at least one of the UKUFF,2 CSAW112 and UKFroST113 trials.
Patch use was not as common in this population of surgeons as implied in the BESS membership survey (Table 9). Only 11 of the 24 surgeons (46%) regularly used patches. Nine (38%) do not currently use patches but would be willing to for the purpose of a trial and four do not use patches at all and would not consider using them in a trial setting. Responses from the four surgeons unwilling to use a patch in a trial have been excluded from the analysis. How the surgeons used a patch varied: six out of the 11 surgeons used patches as a bridge to fill a persistent defect after a standard repair and five used it as on-lay to reinforce a standard repair.
| Category | n (%) |
|---|---|
| Patch use to augment RCR (N = 24) | |
| Yes | 11 (46) |
| No, but I would be willing to for a trial of patch augmentation with suitable support | 9 (37) |
| No, and I would not be interested in being involved in a trial where I would have to carry out patch augmentation | 4 (17) |
| Typical use of patch (for those currently using a patch) (N = 11) | |
| Bridge | 6 (55) |
| On-lay | 5 (45) |
| Subscapularis state considered (N = 20)a | |
| Yes | 11 (55) |
| No | 9 (45) |
Among the 20 surgeons, there was a division of opinion related to the question on whether or not the state of the subscapularis muscle would affect their decision to use a patch, with 11 (55%) stating yes and 9 (45%) stating no. Comments related to these answers indicated that some surgeons would use a patch only if the subscapularis was intact or repairable, whereas others would make the decision based on other patient characteristics. Furthermore, some stated that they would never consider the state of the subscapularis when making a decision to use a patch.
Surgeons were asked to consider which patients they would be prepared to randomise in a number of given scenarios. The first scenario proposed a two-arm study, comparing RCR plus a patch with a cuff repair with no patch. The patient characteristics for consideration within this design included patients with medium, large or massive tears, patients having revision surgery, patients aged between 50 and 60 years, 60 and 70 years, 70 and 80 years and those aged ≥ 80 years. The second scenario proposed a three-arm study, comparing a standard RCR plus a specific patch (patch A) with a standard RCR plus a different patch (Patch B) versus a standard RCR with no patch. The same patient characteristic options were given as for the two-arm trial (Table 10). Surgeons had the option of indicating if they would not randomise any patients into either study.
| Category | Two-arm trial scenario, n (%) | Three-arm trial scenario, n (%) |
|---|---|---|
| N | 24 (100) | 24 (100) |
| Medium tear | 9 (37) | 9 (39) |
| Large tear | 17 (71) | 15 (65) |
| Massive tear | 15 (62) | 14 (61) |
| Revision surgery | 14 (58) | 14 (61) |
| 50–60 years | 19 (79) | 18 (78) |
| 60–70 years | 17 (71) | 16 (70) |
| 70–80 years | 9 (37) | 8 (35) |
| ≥ 80 years | 1 (4) | 1 (4) |
| Would not randomise any patients into such a study | 4 (17) | 4 (17) |
Large and massive tears were the most popular tear size group in both trial scenarios, with > 50% of surgeons opting for these patient groups to be included in a study. Revision surgery would also be considered within a trial patient population. Patients aged between 50 and 70 years make up the most common age range, with patients aged > 80 years being the less favoured to be included in a trial.
Further questions were asked about specific patient characteristics that surgeons felt should be excluded from a trial of patch-augmented RCR surgery. These included what degree of muscle atrophy would need to be present to consider exclusion. The grading of atrophy was based on the Goutallier Classification. 115 Surgeons were also asked to consider the degree of glenohumeral OA that would determine patient exclusion. This grading was based on the Kellgren–Lawrence Classification. 116,117 The presence of cuff arthropathy was also considered in this section of the survey.
Of the responses, 50% indicated the exclusion of patients with grade 3 and 4 atrophy (> 50% of fatty muscle atrophy). However, additional comments provided in this question implied that patients with a degree of atrophy could be included if other characteristics indicated patch use. Three of the responses indicated that atrophy was not an important consideration for patches (Table 11). Over half of the surgeons felt that patients with glenohumeral OA greater than grade 2 should be excluded from a trial of patch use. The presence of cuff arthropathy provided a definitive response as 86% of surgeons indicated that these patients should be excluded from a trial assessing patches in rotator cuff surgery. Additional comments suggested that surgeons would opt for a reverse total shoulder replacement procedure on patients with cuff arthropathy.
| Exclusion criteria category | n (%) |
|---|---|
| Degree of atrophy (N = 20) | |
| Grade 0 – normal muscle | 1 (5) |
| Grade 1 – some fatty streaks | 2 (10) |
| Grade 2 – < 50% fatty muscle atrophy | 0 (0) |
| Grade 3 – 50% fatty muscle atrophy | 1 (5) |
| Grade 4 – > 50% fatty muscle atrophy | 9 (45) |
| Not answered | 7 (35) |
| Degree of glenohumeral OA present (N = 20) | |
| Grade 0 – no radiographic evidence of OA | 2 (10) |
| Grade 1 – marginal osteophytes of doubtful importance | 1 (5) |
| Grade 2 – definite osteophytes | 7 (35) |
| Grade 3 – moderate joint space narrowing, subchondral sclerosis | 8 (40) |
| Grade 4 – severe joint space narrowing, cyst formation | 2 (10) |
| Presence of cuff arthropathy (N = 20) | |
| Yes | 17 (86) |
| No | 3 (14) |
Following on from patient characteristics that surgeons felt should be excluded from the trial, participants were asked questions related to the practical elements involved in designing a trial (Table 12). Surgeons were varied in their responses about the timing of randomisation: prior to the day of surgery was favoured by 35% and a further 40% opted for during the operation, once the shoulder pathology had been assessed. The remainder mostly favoured either in the anaesthetic room (5%) or at the start of the operation (15%). One surgeon (5%) suggested that randomisation should be completed at the time that patients are listed for surgery. There were practical reasons listed in the additional comments for wanting randomisation to be completed prior to the day of surgery. Most of the surgeons (85%) felt that an agreed standardised repair technique was optimal for a trial of this nature. However, they also indicated that uptake of this may be dependent on what the technique involves. Use of a specific brand of patch was supported by 75% of surgeons. There was 95% support to standardise postoperative rehabilitation in a trial. There was a fairly even split between opinions on the length of follow-up, with 50% of surgeons suggesting that 12 months would be sufficient and another 40% believing that 24 months would be more appropriate.
| Category | n (%) |
|---|---|
| Timing of randomisation | |
| Prior to the day of surgery (e.g. pre-surgery assessment) | 7 (35) |
| In the anaesthetic room | 1 (5) |
| In the operating room (at the start of the operation) | 3 (15) |
| In the operating room (once the shoulder pathology has been assessed) | 8 (40) |
| Other | 1 (5) |
| Standardised repair technique | |
| Use an agreed standardised repair technique | 17 (85) |
| I would not want to use a standardised repair technique, I prefer to use my own repair technique | 2 (10) |
| Not answered | 1 (5) |
| Use of a specific brand of patch | |
| Yes | 15 (75) |
| No | 4 (20) |
| Not answered | 1 (5) |
| Standardised postoperative rehabilitation regime | |
| Yes | 19 (95) |
| No | 0 |
| Not answered | 1 (5) |
| Length of follow-up to assess the outcome of the operation | |
| 6 months | 0 |
| 12 months | 10 (50) |
| 24 months | 8 (40) |
| Other | 1 (5) |
| Not answered | 1 (5) |
A few respondents stated that they were currently involved in or planning a study on patch augmentation.
Discussion
Two surveys were conducted with surgeons to inform the acceptability and feasibility of a RCT of patch-augmented rotator cuff surgery. The findings of the two surveys are discussed in turn below.
The BESS membership survey demonstrated a number of insights into surgeons’ use of and opinions around augmentation of RCRs. It also began to explore the acceptability of a RCT in this area.
Overall, 58% of surgeons had used patches, with 41% of all surgeons using these in the last 6 months. Although responders may not be fully representative of the wider surgical community, this survey suggests that a there was a substantial uptake of patch-augmented repair. The majority of surgeons had used the GRAFTJACKET device, which currently has the highest number of studies published to support its efficacy (see Chapter 2). This is consistent with the fact that the evidence base and product usability were cited as the most influential factors when choosing a device for augmented repair. However, there was a broad range of other patches (12 in total) currently in use. Reviews of the evidence have shown that, for many of these patches, there is very limited robust clinical data for surgeons to base their decisions on. There remains a clear need for more rigorous evaluation of current and future patches in a randomised trial. It would also appear to be a good time to undertake a RCT assessing the clinical effectiveness and cost-effectiveness of patch use, before use and acceptance of patches becomes so widespread as to become prohibitive. The difficulty in getting the timing right has been well articulated by Buxton’s law,48 whereby it is always too early for such an evaluation, until it is suddenly too late.
Many respondents commented that data on patch evidence and safety are needed. This is not surprising given the highly publicised adverse reactions of biomaterials, such as metal-on-metal hip replacements118 and vaginal mesh implants,119 as well as the adverse reactions resulting in the market withdrawal of the Restore patch. 35,54
There was a preference for arthroscopic interventions in those surveyed from university teaching hospitals and district general hospitals, which is in keeping with the general trends towards greater arthroscopic intervention. Surgeons who undertook RCR arthroscopically or reported a mixed open/arthroscopic practice were more likely to use patch augmentation, which might be reflective of a greater willingness among this cohort to adopt new technologies.
The survey also shed light on the relationship between tear size and use of an augmented RCR. Patches were more likely to be considered for use in large and massive, rather than small or medium, tears. The driving force behind this dichotomy remains unclear. It may be that large and massive tears are viewed among surgeons as requiring the most supportive healing environment. However, small tears in patients aged ≥ 80 years are predicted to have a similar chance of repair failure as massive tears in patients aged 50 years. Given that symptom resolution is linked with repair success, the use of patch augmentation with small to medium tears may gain traction in the future. 5
Involving surgeons in the early stages of trial design is integral to the participation and success of a trial. 120 The surgeon triallist survey allowed the surgical triallists to have an input into the trial question and protocol design. Involving them in this way allows the surgeon community to embrace research and provide evidence for their practices and for changing practices. 121 McCulloch et al. 122 state that surgeons tend to rush to learn new procedures or techniques, apparently not questioning the possible effects on patient care. The surgeons responding to this survey appeared more conservative, and their answers indicated that further exploration and discussion was required before ‘rushing’ forward to fully utilise patches in their practice. Furthermore, this perhaps is reflected in the surgeons’ positive response regarding potential participation in a RCT in the BESS membership survey, and through the proportion of triallist surgeons stating their willingness to conform to standard practice for a trial to provide clinically relevant evidence. Initially, half of the BESS respondents being willing to participate in a RCT may not seem an impressive number, particularly after considering the potential for responders being unrepresentative. However, the reality is that the number of surgeons who have been involved in a RCT of shoulder surgery in the past has been a very small proportion of the overall surgical community, making this number seem much better.
Patient characteristics and indications for surgery have not been well described in previous research of RCR. 123 Issues such as difficulties with daily function, failure of non-operative treatment, a history of night pain, age and tear size have been widely described as indications of repair failure. 2,15,123 Patients with a degree of muscle atrophy and with glenohumeral OA present have often not been included in previous studies looking at the integrity of RCR surgery. These characteristics are already perceived as an indication of failed surgical repair. 15,124
Responses to the triallist survey suggested that surgeons would be unwilling to augment RCRs on patients with the above characteristics in a two- or three-arm trial setting; however, there was some discrepancy among these answers. It could be that the range of responses reflect a misreading of the question, meaning that some participants answered with ‘patients to be included’ rather than ‘patients to be excluded’. If this was not the case, the surgeons’ answers could vary according to their assumption of tear size or repair technique. Perceived discrepancy was increased by some of the surgeons who ticked more than one response. In this case, the least amount of atrophy and OA selected as a response was reported in Table 11, under the assumption that any higher levels would also be excluded. Seven participants did not answer this question, indicating in the free-text box that this presentation is not important to them when deciding whether or not to use a patch. Not all surgeons use or refer to the Goutallier classifications,115,125 and a recent paper126 suggests that atrophy is reversible and, therefore, the classification may be seen irrelevant.
There was documented variation in how surgeons use a patch in RCR surgery. The technique of on-lay or bridging needs further exploration in a trial setting and may be determined by other factors. The systematic review conducted as part of this study suggests that the different techniques reflect different patient populations and characteristics, for example the use of bridging may be for larger or revision tears. This systematic review also highlighted the differences in the terminology and the meaning of the different techniques. How a patch is used and what patient population it will be used in will raise challenges when confirming the PICO elements of a trial. This will require further exploration in the later stages of this project.
The responses to the questions on practical aspects of trial design and set-up appeared to provide more cohesive results. However, there were still some conditions to full agreements. For some surgeons, the uptake of an agreed standardised repair technique would be dependent on the components involved. Surgeons generally undertake operations differently and have differing levels of skill that can influence the procedure, meaning that standardisation of any surgical intervention may prove challenging. 127 This is especially the case for any pragmatic trial in an NHS setting, and any standardisation would require monitoring, which may be difficult to conduct and report on.
The timing of randomisation showed great variation in surgeon perspective. Ideally, as some of the responses indicated, intervention should be conducted as soon after randomisation as possible. 128 However, the comments in the survey indicated the need to consider the availability of resources and time needed to conduct surgery involving patches when agreeing the point of randomisation. For example, it may be that the theatre team need more preparation if a patch is to be used and the procedure may take longer. This issue will need further exploration as the trial design emerges.
Strengths and limitations of the surveys
As with all survey-based data collection, there is potential for a response bias. In addition, the survey options potentially limit the generalisability of the findings of this survey. The achieved response rate to the BESS membership survey was low, but not dissimilar to that achieved in similar surveys of clinical professional groups. It is also consistent with responses to other surveys sent to the BESS surgical membership in the experience of the PARCS study team. BESS members, in particular those who are more likely to respond to this survey, are not necessarily representative of the wider upper-limb surgical community and may include more research-oriented surgeons. In this case, respondents may be more familiar with and supportive of patch use in RCR. Although steps were taken to ensure that there was anonymity, it is possible that respondents may have answered questions in a way that did not exactly reflect their personal beliefs. Few respondents were clearly not in favour of patch use. Moving forward, a wider range of upper-limb surgeons could be consulted to increase the robustness of studies such as this. The proportion who participated are probably more interested and perhaps more positive about the use of patches than the BESS surgical community as a whole.
The triallist survey sample was as expected (approximately 20 surgeons) and surgeons were invited personally, based on their previous experience in surgical trials. Their responses should not be taken as indicative of the surgical community as they were selected intentionally to be the subgroup of surgeons who would, in principle, be more likely to participate in a RCT. Furthermore, there may have been other research-active surgeons willing to participate but could not as they were unknown to the PARCS study team. This is a key limitation of the method. The survey was designed to be deliberately short and concise to keep surgeons engaged while also providing relevant data. Patient characteristics that indicate failure in standard RCR surgery could have been explored further in the surgeon triallist survey. Results suggest that surgeons would not be willing to conduct patch-augmented surgery on patients with muscle atrophy nor with glenohumeral OA present, yet it is unknown whether or not these patients would benefit from an augmented repair.
Conclusion
Despite the aforementioned limitations, there were a number of important findings from both of the surveys. It was clear that there are a substantial number of patches in clinical use across the NHS and that this includes patches of different types. Furthermore, a strong theme from the respondents was the lack of evidence to inform current practice, and the need for multicentre clinical trials. There was appetite to partake in a prospective RCT and emphasis that patches commonly used within the NHS (e.g. GRAFTJACKET) needed to be included. The general opinion was that more research is required to inform the use of patch augmentation, with a focus on assessing patient safety and efficacy. From the triallist survey, there was some agreement in the patient population and outcome timings, but what the final trial design incorporates remains uncertain. How a patch is used and at what point the decision is made to use one were also highlighted as questions requiring further exploration. The uncertainty around these aspects was taken forward into the consensus process.
Chapter 4 Focus groups
Introduction
Focus groups are widely used in health services research. They allow interactions between individuals, from which more information is generated than in individual interviews. 129 Focus groups enable participants to speak freely about their concerns and offer their views about the existing and proposed evaluation of a new approach to surgical treatment. 130,131 They are particularly useful for helping to identify issues that resonate with lay people and the public in matters of health care. 130,131
Using a set of focus groups, our aim was to access a broad range of stakeholder views and opinions on the acceptability of the use of patches in the augmentation of RCR and the trial design options that may be used to test them. Themes and issues identified from the BESS survey (see Chapter 3) helped to form topics for discussion. 1
Focus group members were recruited to separate focus groups, each reflecting the various key stakeholder groups:
-
patients/public with current or previous rotator cuff problems (carers were also invited)
-
two focus groups, each conducted in a different region of the UK (Thames Valley and South Tees)
-
-
regulatory body representatives, NHS managers, commissioners and other staff involved in surgical equipment procurement [e.g. members of research ethics committees and staff members from the local clinical research network (CRN) support service]
-
representatives from industry.
Group A was considered to be the key stakeholder group. However, the introduction of patches in the NHS has implications for industry, regulatory approvals and NHS costs; therefore, it was relevant to include the views and opinions of groups B and C in the study. 1
Where attending the same focus group was not practical, stakeholders were offered the possibility of individual or group interviews.
Methods
Potential participants were invited and recruited using various avenues according to the relevant stakeholder group(s).
Recruitment of patients and carers
Consultant orthopaedic surgeons (and PARCS investigators) based at the Nuffield Orthopaedic Centre in Oxford and the James Cook University Hospital in South Tees approached potential participants through their units. Patients had to meet the following inclusion criteria to be approached: willing and able to give informed consent for participation in the study; aged ≥ 18 years; have the ability to understand and communicate (read, speak, and write) in English at a level that permits effective interaction; and have active or previous shoulder problems involving the rotator cuff. Patients were invited regardless of whether or not they had undergone surgery, and their carers were also invited if available. At each site, a balance of men and women, and of patients and carers, was sought. A convenience sampling approach for recruitment was used from the Oxford-based patient clinics. At South Tees, potential participants were identified from (1) a list of patients who had previously registered interest to be involved in future patient and public involvement (PPI) activity as part of the pre-grant submission PPI evaluation conducted for the PARCS study, (2) a list of patients who received treatment for rotator cuff in the past 3 years within the unit and (3) a small number identified by prospective convenience sampling of patients attending the investigator surgeons’ outpatient clinic. Once identified, all participants were approached directly at their outpatient/physiotherapy appointments or via telephone by the PPI co-applicant at this site.
Those who responded positively and met the inclusion criteria were included in the PARCS study focus groups. Identification of potential participants continued until the target number of participants had been recruited (between four and eight participants per focus group).
Recruitment of other stakeholder groups
Representatives of regulatory bodies and industry were identified via local networks, approached and invited to participate directly. We also used snowballing as information was passed on to potential participants via professional acquaintances. 132
Focus groups
Ahead of the focus group session, potential participants were provided with a study information sheet specifically tailored to their stakeholder group, describing the aim of the focus group and what to expect. Each focus group lasted around 2 hours, with a break for refreshments. The cost of travel was reimbursed, and participants were offered a shopping voucher to the value of £25 as a token of appreciation. Each participant was asked to personally sign and date a consent form, of which they were given a copy.
During each focus group session, the aims of the PARCS study, and focus groups specifically, were briefly introduced. Participants were asked to consider a number of key issues, scenarios or vignettes. These included key items of information about the possible trial design options, such as the different kinds of patches available and their acceptability, the choice of comparative study arms, the most appropriate outcome measures, and the methods of data collection. The way in which this information was delivered was adapted according to participant group. For example, a more technical approach was used for the industry stakeholders. Participants were provided with the following definition of a patch: ‘an implantable human, synthetic or animal material which is used with the aim of improving tissue healing and patient outcome’.
We also asked focus group participants to provide some basic background information about themselves (i.e. sex, age, relevant experience and previous treatments). This information was anonymous. Participants were provided with a plain opaque envelope in which to place the completed ‘background information form’. They were asked to place this envelope into a box as they left.
The focus groups were facilitated by an appropriately trained member of the PARCS study team (NM). Discussions were audio-recorded and one or two observers (LK, JCC or CC) took notes to aid in the transcription of audio files and analysis. The resulting audio files and accompanying field notes were transcribed verbatim. Transcription was performed by an external transcription company. Any identifying information appearing in focus group transcripts was removed as soon as possible following transcription to minimise the risk of participant identification. The audio files and transcripts were encrypted for secure storage.
Analysis
The focus group transcripts were analysed by two members of the PARCS team (CC and JCC) using thematic analysis. 133 The following steps were followed:
-
Analysts familiarised themselves with the transcript.
-
One analyst (CC) initially coded the transcripts by hand, both deductively (guided by themes included in the focus group topic guides) and inductively (allowing unanticipated themes and subthemes to emerge). The first three transcripts were also independently coded by a second analyst (JCC). The codes were subsequently compared, discussed and agreed with the first analyst. The emphasis of the analysis was on the acceptability of the proposed trial and on factors that might influence such acceptability.
-
Analysts reviewed the coding and agreed a working thematic framework. This was applied to subsequent transcripts using QSR NVivo 10 software (QSR International, Warrington, UK) and evolved as analysis progressed. In accordance with the study design objectives, the themes were grouped into PICO elements, that is their relationship to patient population, intervention, control and/or outcome (including timing of measurements). The framework also included practical considerations to take forward.
The final thematic framework and its content were used to inform the questions posed in the triallist survey, which followed the focus groups (see Chapter 3).
Results
Focus group participants
A total of 24 people took part in the focus groups (Table 13). Thirteen participants were patients who had previously been treated in the NHS for their shoulder problem. Ten of the patients had undergone shoulder surgery. Five patients reported ongoing shoulder problems (of whom three had had surgery), whereas two reported that their problems had resolved (of whom one had had surgery). Two carers (partners) of patient representatives also participated.
| Variable | Patients and carers | Industry | NHS Research Ethics Committee members | CRN representatives |
|---|---|---|---|---|
| Attendees | 15 | 4 (from 3 companies) | 2 | 3 |
| Thames Valley region | 7 (2 carers) | 2 | 3 | |
| South Tees region | 8 | |||
| Sex | ||||
| Female | 4 | 1 | 1 | 3 |
| Male | 11 | 3 | 1 | 0 |
| Age (years) | ||||
| 46–55 | 2 | |||
| 56–65 | 6 | |||
| 66–75 | 7 | |||
Views on patient population for a trial assessing patches in rotator cuff repair surgery
Patients and regulatory body representatives were eager to discuss which characteristics patients would need to be present for the patch to be a treatment option:
To me it’s got to go on the size of the tear and how much discomfort they’re getting because you can’t treat everyone the same.
P504 – patient, South Tees
Would age be a big factor in this?
P505 – patient, South Tees
So, the surgery, the inclusion criteria, would you say that they’ve done everything possible, like physio?
P401 – regulatory representative, Ethics
Some patients felt that all patients having RCR surgery should be offered a patch:
. . . so you’re going to get . . . you’re getting a high percentage [of success] at the moment, 60% [success rate after standard RCR] as against 40% [re-tear rate after standard RCR], so you’ve already got that percentage of success so my argument is if you’ve got that surely anybody that’s prepared to take the trial should just go for the patch . . .
P101 – patient, Thames Valley
It seems silly, like you said, why aren’t they just using [patches] now, if they’re using [patches] elsewhere in the body . . .
P506 – patient, South Tees
Other participants felt that the patient population needed to be more specific. Industry representatives were strong in their opinion that, for a patch’s effectiveness to be assessed, confounding factors and certain patient characteristics should be excluded:
. . . in the end it’s a clinical decision and also the patient, patient age, bone quality, tissue quality, smoker or not, again . . . keep them out of the way. Steroid abusers need them out the way as well.
P203 – industry representative, company 2
To me it’s got to go on the size of the tear and how much discomfort they’re getting because you can’t treat everyone the same [each patient is different].
P504 – patient, South Tees
Patients’ reactions to being hypothetically offered a patch were generally positive, as they focused on the idea that patches augment repairs and, therefore, ‘can only be better’ (P101 – patient, Thames Valley). Patients had a risk-seeking approach to manage their pain:
Can I go on your list first to have it done, please? (Addressing Investigator 3)
P504 – patient, South Tees
I mean it’s not as if you’re having a heart transplant or anything like that which you would discuss, or cancer, it’s not is it, it’s something which is just . . . you’ve got pain there and you know there’s a relief, you can have an operation and the extra patches, yeah, let’s go for it.
P501 – patient, South Tees
So something different [like patches] might just assist it.
P103 – patient, Thames Valley
However, there were also some cautious questions from the patient groups about what happens to the patch after the operation:
Does that stay in then, that patch, or not?
P506 – patient, South Tees
Are the patches likely to break down in compound over a period of time?
P103 – carer, Thames Valley
There were no apparent negative views towards using a patch in rotator cuff surgery. However, some patients expressed a preference for human-derived patches. One patient was concerned about the safety of animal-derived patches:
I would probably steer to one that comes from human beings . . . probably not cows and pig due to CJD [Creutzfeldt–Jakob disease] . . . foot and mouth because we don’t really still understand those two diseases . . .
P102 – patient, Thames Valley
Views on potential interventions and controls in a trial assessing patches in rotator cuff repair surgery
Focus group participants had varying perspectives on what a trial intervention and control group should look like. The issue of randomisation was discussed, as were patch elements and types that may be used within a trial. These topics were then related to willingness, of both industry and patients, to participate in a trial.
Industry stakeholders had variable opinions on what a trial of patch use should look like. One recognised the need to provide an evidence base before progressing with patch development further:
I think [a patch A vs. patch B trial] is something a bit down the line isn’t it, I think really we need to know that this [patch] works in the first place before you start enhancing it.
P202 – industry representative, company 2
Other industry representatives felt that current surgical practices had evolved further than this and that current trends needed to be represented in any study design involving the use of patches in rotator cuff surgery:
If clinical practice is moving onto augmentation already for these sorts of cuff tears, the question in the industry is who’s got the best patch . . .
P203 – industry representative, company 2
I think [surgeons] would want to know which avenue to take as opposed to cuff versus patch as a broad thing, I think we’d want a little bit more than that, I think we’re at that position now.
P202 – industry representative, company 2
There was also discussion among the patients about whether or not there was a need for a RCT at all, given the known failure rate of standard repair and widespread use of the patches in other parts of the body:
. . . why you’re doing this research is basically because of the patches, so put the standard repair out of the window as far as I’m concerned and go right, we’re doing nothing but patches here, that’s all it’s about.
P501 – patient, South Tees
If the normal process [standard repair] was only available and there was nothing else then I’d probably go down that [trial participation] route but because of listening to the percentages [40% failure rate for standard repairs] I still don’t see the logic of having that [repair with no patch] as against the patch. Because you’ve moved on . . .
P101 – patient, Thames Valley
If you know the success rate of a patch on a certain [different] part of the body is 99% or whatever or 90% then you go, ‘yeah, we can safely use that one as a guide’.
P501 – patient, South Tees
In line with their initial risk-seeking reaction to being hypothetically offered a patch, some patients said that they would seek to participate in a trial, regardless of what treatment they would potentially receive:
I’d go into trial to get rid of the pain, regardless of what they were going to do, I just have to have something done.
P107 – patient, Thames Valley
Excerpt from South Tees patient focus group:
If [it] was thought I’d have 50 : 50 chance of getting the patch or whatever even to have the normal surgery, I’d go for it.
P506 – patient, South Tees
Yeah, so would I.
P504 – patient, South Tees
Because it’s something or nothing.
P506 – patient, South Tees
Yeah, yeah, you can’t lose.
P504 – patient, South Tees
However, consistent with their positive reaction to the idea of being offered a patch, patients who had experienced numerous rounds of conservative treatment tended to dislike the concept of randomisation and the consequential risk that they may not receive a patch:
. . . [if] people decide to go for the trial they’re not going to know which one they’ve had [patch or no patch]. I wouldn’t even go down that route . . . If I had the patch I’m quite prepared to go down that route, but I’m not prepared to go down the route of I don’t know what’s happening.
P101 – patient, Thames Valley
The CRN discussions highlighted the importance of considering existing patch use at participating trusts when determining the content of the trial arms:
So if you standardise and say you have to use, say, these five [patches] and that’s not what they’re using then there could be a sourcing issue.
P302 – regulatory representative, CRN
Whatever they use as part of standard care if they’re just using that and they’re just taking another one [patch] off the shelf it’ll go through [local trust approvals] a lot easier.
P303 – regulatory representative, CRN
The willingness of those in the industry to offer their products to a potential trial of patch augmentation was complex. Their involvement would depend on all the PICO elements that were proposed and what the definition of a patch was within the trial. The type of repair products used during the cuff repair was flagged up as an important element by one member of the industry focus group, in this case the anchors and tape (to anchor down the tendon) used in the operation:
There are just too many variables out of our control and potentially out of your control as in the ideal study, playing devil’s advocate, so the ideal study would be [surgeons] all have to use [company Z] anchors with tape ‘cause it’s best [general laughter] with their [company Z] artificial patch or [company Z] dermal graft and that’s the study, that’s easy.
P203 – industry representative, company 2
Manufacturing processes, rehabilitation guidelines and the purpose of a patch would also need to be considered for industry representatives to participate and willingly put forward their product to be assessed:
The way [patches are] kind of weaved and that kind of thing all affects its strength and how it works, how it then heals in the patient that kind of thing . . . so we probably wouldn’t want ours bunched in with [other patches in one treatment arm] . . .
P202 – industry representative, company 2
The industry group highlighted the importance of declaring conflicts of interest and of ensuring that there was transparency of involvement in any trial.
The regulatory body representatives also expressed some concerns about the components of a patch to be used within a trial and how these could exclude some communities within an otherwise eligible patient population.
Excerpt from regulatory representatives’ discussion:
That’s going to raise some practical difficulties though, because if you’re at a centre and they are using patches that have got animal products in, and then they have a patient consent to take part in a study, but then they don’t want one of those particular patches, will you, the study, then provide [non-animal derived] patches to that centre? . . . Or you exclude that patient.
P401 – regulatory representative, ethics
[Excluding those patients] can be difficult. For instance, we’ve had studies where they use a standardised fatty diet, which contains bacon, and they’ve actually excluded anyone who won’t eat bacon. . . . Our [ethics] committee did actually have an issue with that, because, obviously, that excludes all Jewish people and Muslim people. So, then we were saying, ‘Well, hang on, are you denying access to clinical trials for taking part in research to particular ethnic or religious groups?’ It’s just something that, if that’s the direction you’re going to go down, you just have to be prepared to have, to make, that argument.
P402 – regulatory representative, ethics
Views on the outcomes to explore in a trial assessing patches in rotator cuff repair surgery
Stakeholder opinions on outcomes of importance appeared to stem from their own experiences and knowledge about treatment and products. Patients highlighted that pain was the most important issue to address with treatment, regardless of what that treatment involved:
That’s the bottom line . . . that pain is the bottom line and that’s it.
P501 – patient, South Tees
If I didn’t have the pain that I’ve got but I had the restricted movement I could probably live with that, it’s living with the pain.
P506 – patient, South Tees
Certainly pain relief. I think that’s the main issue with all these things because how much pain you can tolerate . . .
P101 – patient, Thames Valley
Other outcomes that were important to patients included sleep and being able to perform everyday activities.
. . . my pain was different actually because it manifested itself at night, I couldn’t sleep.
P104 – patient, Thames Valley
No, I was the same, I didn’t sleep for about 6 months.
P107 – patient, Thames Valley
During the day, for some reason, it didn’t really irk me but at night it really was a problem.
P104 – patient, Thames Valley
Mine was . . . about 6 months I didn’t sleep. Because the pain was so bad.
P107 – patient, Thames Valley
You might be doing things around the house like women do and I know men do as well, and you think ‘oh, I’ll just go and do that because it’s all right’ and you do it and you think, ‘ooh, I shouldn’t have done that’, that sort of thing. It catches you off the cuff . . .
P102 – patient, Thames Valley
Patients, along with industry representatives, discussed the importance of preventing further surgery. With the current re-tear data in mind (40% re-tear rate following standard rotator cuff surgery), there was the feeling that treatment needed to be definitive and not used as a back-up if the initial repair failed:2
Safety seat belts, maybe it’s overkill but the patient wants one procedure not two. [In discussion about why a patch would be used.]
P203 – industry representative, company 2
I think [patches] should be used from the start.
P506 – patient, South Tees
If it goes again how many times can you actually have that repaired the ordinary way before you end up with so much scar tissue that it’s not going to happen at all? As against if you have the patch you’ve got a higher rate of success and you may not ever have to have it done again . . .
P101 – patient, Thames Valley
Outcome measurement was also discussed in some focus groups. Potential methods ranged from radiological imaging (‘you’re not going to get a second look’ – P203 industry representative) to patient-reported questionnaires, safety measurements and reporting of failure (i.e. further surgery). Regulatory stakeholders highlighted the importance of product safety monitoring and minimising the burden of follow-up for patients:
Keep the study as simple as possible, so that the burden on the patient is as little as it can be. So, things like biopsies, if that’s what you need to be able to answer your outcomes, then do the biopsies and explain it, but if you don’t need to do the biopsies to answer your question, then I would say consider them very carefully. Also, I don’t know if we addressed how painful they are. If you can do something that’s quick and painless, then that’s not really a burden to the patient. If the biopsies are going to be as painful as, like, a lumbar puncture, then make sure you’ve got a really, really good reason for doing it.
P402 – regulatory representative, ethics
So, the key thing I’ve got is about safety and monitoring, because whatever patch you do, or whatever CE [Conformité Européene] mark, how do they currently monitor whether it’s doing the job it’s meant to be? Obviously, there’s subjective [indicators], where you fill out questionnaires . . . but showing that the patch hasn’t moved or slipped, do you do imaging?
P401 – regulatory representative, ethics
Practical considerations when designing a trial assessing patches in rotator cuff repair surgery
Practical elements of trial design and trial set-up were discussed within the PICO themes above. Participants also suggested other considerations in trial design and set-up, including what information about patches and treatment should be presented to patients when informing them about the trial.
The patient and the regulatory focus groups raised questions about the type of information patients may seek about patches, how the patch is physically inserted into the shoulder and what other research is being carried out:
Have you actually tested the patches on anybody else yet or . . . ?
P101 – patient, Thames Valley
Are the patches likely to break down in compound over a period of time?
P104 – patient, Thames Valley
Is your research part of a worldwide programme or is it just part of [named academic institution]?
P102 – patient, Thames Valley
I think you could say that there’s different patches, and then tell them to speak to their doctor about which one they’re likely to get at their centre.
P402 – regulatory representative, ethics
Patients also raised some questions about the safety that would need to be considered when developing patient information. This included the permanency and ease of removal of a patch:
Does that stay in then, that patch, or not?
P506 – patient, South Tees
If you have the patch done and it really gives you hell afterwards is it easy enough to get out again?
P105 – patient, Thames Valley
Discussion
The focus groups highlighted many elements to consider in the design of a trial assessing patches in rotator cuff tear surgery. Stakeholders held differing views as to the patient population that would be suitable for such a trial. Those patients who had undergone numerous rounds of treatment for their rotator cuff felt that the patch should be readily available to all patients having RCR surgery. Although a patch-augmented approach to repair was also advocated by industry, they would be more selective about the patients who would receive a patch to demonstrate efficacy. This is indicative of industry trends in clinical research. 134,135 However, a narrow selection of patients may also be needed to support the use of a product for a particular patient population. This correlates with the claim from Suvarna136 that industry need to not focus on which product is best, but more on which patients will benefit more from the product. Industry involvement in a trial would need further discussion when a trial design has been finalised.
Views on intervention and control arms in a proposed trial also varied within stakeholder groups. Some emphasised the need to provide evidence for best practice and felt that the trial question should be ‘does a repair with a patch work better than a repair without a patch?’. Other stakeholders felt that a ‘no patch’ control arm was unnecessary and would not serve to advance treatment. However, this strategy would contradict the current drive to provide evidence for practice as early as possible. 128 Moving forward to compare a patch with another patch could be seen as unethical by stakeholders who believe that there first needs to be evidence of effectiveness of patch use in general. As evident in the systematic review conducted for this project (see Chapter 2), the evidence for any patch use in RCR surgery in itself is not yet sufficient to make clinical practice recommendations, even in fairly broad terms.
The chosen intervention and control arms, and the availability (or not) of a patch within usual care, would also seemingly affect patients’ willingness to participate and be randomised. In general, patients appeared very keen to receive a patch, believing that this should enhance repair. A recent survey of surgical trials in head and neck oncology revealed that the top two barriers to participant recruitment were ‘patients’ consent refusal because of expressed treatment preference’ and ‘patients’ consent refusal owing to aversion to randomisation’. 137 Our findings suggest that a RCT with a ‘no patch’ control, in a setting where patches are available as part of usual care, might struggle to recruit participants. This chimes with a qualitative study by Harrop et al. ,138 which found that patients primarily declined to participate in a surgical trial because they had preferences for a particular treatment arm (a new technology) and in usual practice could choose which surgical method they would be given. The authors concluded that for trials in which the ‘new technology’ is available to patients, there will probably be difficulties with recruitment. Research in this area by the QUINTET group suggests that patient preferences can be explored during recruitment, and need not always hinder recruitment. 139
Randomisation is a well-documented contentious issue when recruiting patients to clinical research. 140 Patients often do not recognise the need for randomisation and, therefore, decline to participate in trials. 139 In any trial, details need to be presented to potential patient participants in an unbiased manner. Patient preferences also need to be explored to assess what these are based on and to ensure that patients entering a trial understand what will happen and why. 139
Safety issues were discussed in all groups; however, these did not appear to be major concerns. The regulatory representatives advocated for the provision of full, appropriate patient information and safety monitoring. Patients, despite the recognition of recent media coverage on implants and an understanding of the risk involved in having a patch used in their shoulder, were overwhelmingly positive about patch use. 118,119 The basis of this preference seemed largely because of the severity of symptoms experienced and the hope that a patch would prevent the need for further treatment. Bower et al. 141 state that beliefs like this are based on ‘personal subjective expectancies’, when patients believe that they are particularly suited to an intervention that current evidence implies it may not be beneficial. Patients may also believe that procedures considered ‘new’ are more effective. 142
Strengths and limitations
This qualitative study enabled us to elicit and understand the views of a broad range of stakeholders, including patients with experience of shoulder problems in northern and southern England. This would not have been possible through the use of crude surveys. The focus group participants included a balanced mix of men and women, and the patients had varied experiences of shoulder surgery (no surgery, surgery without a patch and surgery with a patch). The participation of industry representatives was a strength of this study, providing an insight into product development and use that is not often available to people outside the clinical setting.
However, because of the time-limited nature of the focus groups, we were unable to explore some complex issues in more depth. For example, the circumstances under which patients would or would not be willing to take part in a RCT of patch-augmented surgery were touched on but were not exhaustively investigated. The study team acknowledge that this could be an issue and will review it further during the design of recruitment and training processes in a definitive trial. Participation in the focus groups depended on patients’ ability and willingness to travel to NHS sites outside routine appointments and on a weekday, potentially excluding those with daytime commitments or lacking transportation. It is possible that focus groups held at a community venue, at a weekend or in a different part of the UK may have resulted in a wider range of views being captured. The semistructured discussions with regulatory body representatives (CRN and ethics committee members) would have ideally included more participants. However, there were challenges in identifying appropriate people who were working in regulatory bodies, such as the Medicines and Healthcare products Regulatory Authority. The study team were also unable to organise a discussion with people who work in procurement in the NHS.
Conclusion
Overall, there was general support for patch use in RCR surgery from all stakeholders who participated in the focus groups. There was acknowledgement of the risk involved in receiving an implant such as the patch, and advocacy for product safety monitoring during the trial. However, there was some discrepancy among stakeholders about what the patient population, intervention and control arms of the trial should be. Patients may be unwilling to participate in a trial with a ‘no patch’ control arm if access to a patch is available within routine care. Improvement in pain and function and preventing further treatment were important outcomes identified in the focus groups. How and when these would be measured in a trial needs further exploration. The uncertainties and further questions that emerged from the focus groups were used to inform the surgeon triallist survey (see Chapter 3) that followed. These included (1) who should have a patch, and how are patches used by surgeons? and (2) what could a patch be compared with within a trial?
Chapter 5 Consensus process
Introduction
This chapter reports the methods and findings of stages 5 (Delphi study) and 6 (consensus meeting and finalising) of the PARCS feasibility study. These two stages were intentionally designed to complement and link with each other, with the Delphi study leading into the consensus meeting (Figure 9). 1 Details on the methodology and implementation of the two stages are given below.
FIGURE 9.
Interaction between the Delphi study and the consensus meeting.
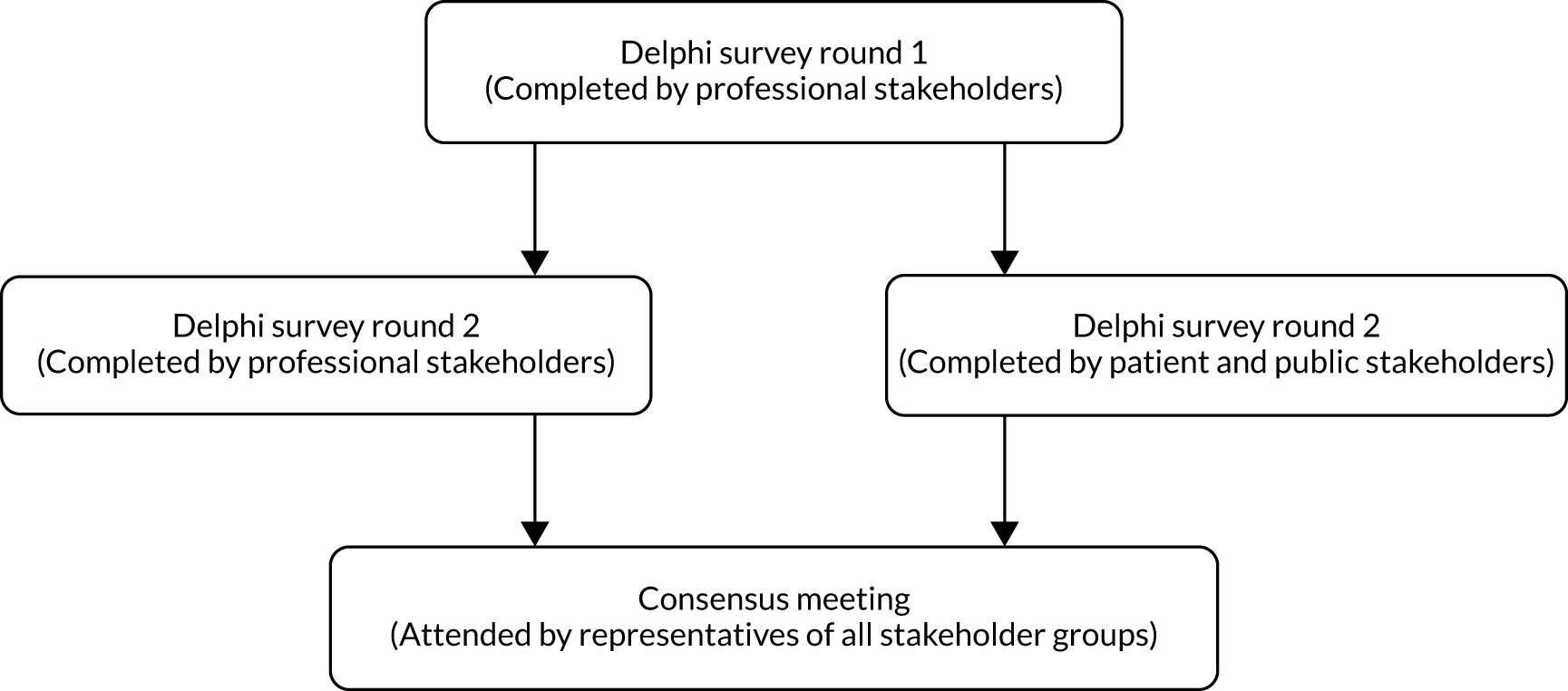
Methods
Stage 5: Delphi study
A Delphi study to develop a consensus on the best way to design a clinical trial of patch-augmented rotator cuff surgery was conducted. The Delphi method is a structured process of obtaining information from a group of experts using a series of related questionnaires, each one refined using respondents’ feedback from a previous version. 143 It is a well-known and increasingly common method used in the clinical setting to establish a consensus. 130,143,144 A multiple-stage online Delphi survey consisting of at least two but no more than three rounds was conducted. The surveys were developed and conducted online.
Participants involved in stages 2–4 of the PARCS study were invited to take part in stage 5, according to stakeholder group.
Given the nature of the study, there has been no formal sample size calculation, but around 50–80 responses were originally anticipated. 1 There are generally no accepted guidelines for the optimal sample size needed to achieve consensus in Delphi studies. 145 This sample size was based on previous experience of conducting this type of survey and anticipated attrition rates at each round. Substantial loss from the initial to the final round is not unusual. 144,146
All participants invited into the Delphi survey had been involved in earlier stages of the project. The Delphi study proposed different options for elements of RCT design. The aim of this was to help reach a degree of agreement to take forward to the final consensus meeting. Findings from stages 1–4 were used to determine the trial design elements to be included in the first round of the Delphi study.
Initially it was intended for all stakeholders to take part in both rounds. Based on feedback received from the patient representatives on the project team, the initial round was sent to the non-patient stakeholders only (i.e. surgeons, physiotherapists, industry and researchers). This was because of concern that the initial round would be too ambiguous and would be unfair to the individual to assess. Patients were involved in the second round only (a third round was not anticipated to be necessary once the initial round had been outlined). Two versions of the second-stage survey were used, one for patient and public stakeholders and one for professional stakeholders (e.g. surgeons and researchers). The patient and public version had a subset of the full set of questions that were most pertinent to this stakeholder group and were presented using more accessible language and avoiding, as far as possible, technical terminology.
An e-mail was sent to each participant containing a personalised link that enabled access for convenient survey completion. For a subset of potential participants’ paper copies were sent as per the participants’ preference, or a generic link was sent to a specific group of stakeholders.
During completion of the first round, survey participants were asked their stakeholder group and their place of work (professional stakeholders only). Data were extracted to Microsoft Excel and summarised for data analysis.
Participants were presented in the survey with proposed trial design elements (e.g. choice of two- or three-arm trial design, eligibility criteria for participation and information on the timing of the outcome data collection) and asked to score agreement with each using a 1–5 scale, where 1 represents complete disagreement and 5 represents complete agreement. A ‘do not know/not relevant’ option was provided as applicable. Participants were given the opportunity to comment further in free-text boxes. The aim was to allow the justification of any answers and the communication of new or proposed adjustments to the design elements. No new elements were suggested by participants in round 1 of the Delphi survey, although a number of the existing ones were revised.
For each section on the second round Delphi study, a summary of the findings from the previous round was offered. Participants then scored their agreement on each design element. The final set of proposals, areas of provisional consensus and remaining disagreement and uncertainty were then taken forward to the consensus meeting in stage 6 and used as the basis for discussion.
Where necessary, in both rounds of the Delphi survey non-responders received a maximum of two reminder messages. The final reminders contained a specific deadline for survey closure. 147 Each survey took approximately 15 minutes to complete. Scores (range 1–5) from each round were calculated as a percentage of the total responses. Consensus for a proposed design element was defined as > 70% of responses scoring the element 4 or 5, and no more than 15% of responses scoring the element one. Median and ranges were also produced for the scores. We explored similarities and differences across stakeholder groups. Textual responses were summarised narratively.
Stage 6: consensus meeting
Findings from stages 1–5 were fed into, and informed the structure of, a 2-day face-to-face consensus meeting. This meeting sought to agree on an acceptable and feasible trial design for a definitive RCT to assess the clinical effectiveness and cost-effectiveness of a patch to augment surgical RCR. A range of stakeholders were involved, including surgeons, triallists and patient and public representatives, who took part in stages 2–5 of the study. An independent academic surgeon was invited to chairperson the meeting. Participants were selected for invite based on their perspectives and experience to ensure that there was a variety or representation. For example, surgeons who do currently use patches to augment RCR were invited along with those who would be potentially willing to do so for a trial. To ensure that a robust decision was made, approximately 30 stakeholders were invited to participate. 1
Ahead of the consensus meeting, participants were sent a proposal of a trial scenario for consideration, based on the results from the Delphi study. Patient and public representatives were reimbursed for expenses and compensated for their time. 148 The meeting was structured to ensure that key areas of uncertainty and disagreement were reviewed and discussed. Consensus on key elements of the trial design was sought, namely patient eligibility, intervention and control definitions, surgeon requirements, outcomes and target difference. Previous stages informed draft guidance, options and recommendations for a RCT assessing patch-augmented rotator cuff surgery. A post-meeting report was drafted and circulated to participants for their review and comments. The report included details of the key design decisions made at the meeting with points for clarification.
Results
Stage 5: Delphi study
Twenty-nine out of the 43 (67%) individuals who were invited to take part in the Delphi study took part: 18 surgeons, two industry representatives, four physiotherapists, two medical researchers and three patient representatives. Table 14 gives a breakdown of the groups and the location of work for the participants. Round 1 had 23 responses and round 2 had 24, including three patient participants. Findings from the two rounds are presented in turn below.
| Category | n (%) |
|---|---|
| Stakeholder type | |
| Surgeons | 18 (62) |
| Physiotherapists | 4 (14) |
| Project team | 2 (7) |
| Industry | 2 (7) |
| Patients | 3 (10) |
| Place of work | |
| District general hospital | 5 (17) |
| Teaching hospital | 9 (31) |
| Other | 2 (7) |
| University | 1 (3) |
| Private hospital | 1 (3) |
| Commercial company | 2 (7) |
| District general hospital, private hospital | 2 (7) |
| District general hospital, teaching hospital, private hospital | 1 (3) |
| Teaching hospital, private hospital | 2 (7) |
| Teaching hospital, university | 1 (3) |
| N/A | 3 (10) |
Round 1
In the first round of the Delphi survey, non-patient stakeholders completed questions that covered their stakeholder group and place of work, in addition to asking about agreement related to patient eligibility, surgical approach, patch use, trial design and follow-up. Patient participants did not take part in this round. Findings from round 1 are summarised in Table 15, in which the nature of question is also given along with a breakdown by response.
| Proposal | Responses, n (%) | |||||
|---|---|---|---|---|---|---|
| Completely agree | Somewhat agree | Neutral | Somewhat disagree | Completely disagree | Do not know/not relevant to me | |
| Patient eligibility | ||||||
| No clinically significant OA present (e.g. patients with Kellgren–Lawrence Classifications grades 3 and 4 will be excluded) | 16 (70) | 4 (17) | 1 (4) | 0 (0) | 0 (0) | 2 (9) |
| < 50% muscle atrophy present (patients with ≥ 50% will be excluded) | 2 (9) | 9 (39) | 3 (13) | 5 (22) | 2 (9) | 2 (9) |
| Medium, large and massive tears (patients with small tears will be excluded) | 13 (57) | 8 (35) | 0 (0) | 1 (4) | 0 (0) | 1 (4) |
| Primary repairs only (patients with re-tears/revisions will be excluded) | 9 (39) | 6 (26) | 2 (9) | 3 (13) | 1 (4) | 2 (9) |
| Patients aged < 50 years | 8 (35) | 5 (22) | 3 (13) | 1 (4) | 5 (22) | 1 (4) |
| Patients aged 50–70 years | 16 (70) | 5 (22) | 1 (4) | 0 (0) | 1 (4) | 0 (0) |
| Patients aged > 70 years | 5 (22) | 3 (13) | 6 (26) | 5 (22) | 4 (17) | 0 (0) |
| Patients with other shoulder conditions, not just rotator cuff problems, that affect their muscles, joints, bones, tendons, etc. (e.g. OA) | 0 (0) | 2 (9) | 4 (17) | 3 (13) | 13 (57) | 1 (4) |
| Surgical approach | ||||||
| Use on-lay approach only, in which a patch overlies a successful primary repair | 5 (22) | 4 (17) | 4 (17) | 2 (9) | 2 (9) | 6 (26) |
| Use bridge approach only, used to fill a residual defect for tears that cannot be repaired at or near their anatomical insertion site | 5 (22) | 2 (9) | 1 (4) | 5 (22) | 4 (17) | 6 (26) |
| Depends on patient characteristics, allow the operating surgeon to vary the approach depending on the patient in front of them | 9 (39) | 1 (4) | 3 (13) | 3 (13) | 2 (9) | 5 (22) |
| Patch use | ||||||
| Patches made from animal products | 6 (26) | 3 (13) | 2 (9) | 5 (22) | 3 (13) | 4 (17) |
| Synthetic patches (e.g. made from plastic type of material) | 8 (35) | 3 (13) | 2 (9) | 2 (9) | 4 (17) | 4 (17) |
| Allograft patches (made from another human’s tissue) | 11 (48) | 6 (26) | 2 (9) | 0 (0) | 1 (4) | 3 (3) |
| Autograft patches (made from the patient’s own tissue) | 10 (43) | 2 (9) | 2 (9) | 1 (4) | 4 (17) | 4 (17) |
| Trial design | ||||||
| Randomised trial of standard repair with a patch vs. standard repair with no patch | 11 (48) | 6 (26) | 3 (13) | 2 (9) | 1 (4) | N/A |
| Randomised trial of standard repair with patch A vs. standard repair with patch B vs. standard repair alone | 7 (30) | 6 (26) | 4 (17) | 2 (9) | 4 (17) | N/A |
The level of agreement with the proposed eligibility criteria varied substantially. For example, the number in either complete or somewhat agreement ranged from 20 (87%) to 11 (48%) for the OA and the muscle atrophy criterion, respectively. Thirteen comments were made, all of which suggested possible modifications (some mutually exclusive of others). Neither the exclusion of OA nor the exclusion of other shoulder conditions was raised in these comments, suggesting that these were not the likely source of disagreement. Specific comments addressed age, although four of the five commenting on this noted uncertainty about the specific age limit that might be used. One respondent commented that they would not repair a ‘massive tear in over 70s’. Two commented on muscle atrophy, questioning its value as an eligibility criterion, and one surgeon noted that they always used a patch in a revision RCR operation.
When asked about the surgical approach when using a patch, there was general approval for on-lay use once the primary repair had been successfully completed (39% agreed vs. 18% disagreed). Use of bridging was supported less, with more disagreement than agreement (31% agreed vs. 39% disagreed). A substantial number stated that this topic was not relevant to them, of whom all except one were not surgeons (26%). Varying the approach in accordance with patient characteristics was mostly agreed with (43%), although there was still sizeable disagreement. Four additional comments addressed the different use of patches for on-lay versus bridging with reference to a completed repair. Three of these comments queried whether or not two separate studies would be needed or if stratification was necessary.
Participants were asked for their opinions patches of different types. There was 39% agreement for using animal products versus 35% disagreement. Synthetic, allograft and autograft patches had more support, with approximately ≥ 50% agreement and 26% less disagreement. Regarding the use of patches in a trial, there was similar level of agreement between using what was readily available in the NHS (10, 43%) and using only one specific type of patch (9, 39%). There was much less support for using only a specific patch within a trial (3, 9%). Three additional comments were received. Two of these noted concern about specific patch types (namely the safety of animal product-based patches and the practical challenge of autograft use). One comment noted a desire for consistency in patch use within a trial or a larger study for all issues to be explored. Another noted a desire for surgeons to use their usual patch.
Participants responded with a good level of agreement for a comparison of repair with a patch with standard repair with no patch (74%) and less, although reasonable, agreement for a three-arm trial that compared two types of patch with no patch (56% agreement). One respondent noted the potential value of a ‘no surgery’ group. When asked about the best time to measure outcomes, there was equal support for 12 and 24 months (10, 43%) as the primary assessment time point. There was much less support for 18 months (3, 9%). One participant noted a desire for MRI-based assessment to be the primary outcome.
Round 2
In the second round of the Delphi survey, 21 non-patient stakeholder participants completed questions related to patient eligibility, timing of randomisation, patch use and trial design. Three patient participants completed a tailored survey that covered patch types to be used, trial design, timing of randomisation, blinding of participants and follow-up regimes. Findings from the combined second round are summarised in Table 16, in which each question is given, along with a breakdown by response.
| Proposal | Responses, n (%) | |||||
|---|---|---|---|---|---|---|
| Completely agree | Somewhat agree | Neutral | Somewhat disagree | Completely disagree | No opiniona | |
| Non-PPI participants | ||||||
| Patient eligibility | ||||||
| Adults with a rotator cuff tear suitable for primary repair with or without a patch should be included in the RCT. Within this population it was indicated the following should be excluded: small or partial tears, patients unfit for surgery, patients with clinically significant OA, patients with > 50% muscle atrophy and patients needing revision surgery | 7 (33) | 4 (19) | 2 (10) | 5 (24) | 3 (14) | 0 (0) |
| Timing of randomisation | ||||||
| Randomisation will take place in theatre after the primary repair has taken place. At this point the surgeon will know which technique is needed for the repair and this can be used to stratify the patients | 11 (52) | 7 (33) | 2 (10) | 1 (5) | 0 (0) | 0 (0) |
| Patch use | ||||||
| Using an ‘off-the-shelf’ patch as part of the RCT. The patches used must fall into the subtypes synthetic, animal product, allograft or autograft. A non-animal patch should be available in case of surgeon or patient preference | 9 (43) | 8 (38) | 2 (10) | 0 (0) | 1 (5) | 1 (5) |
| Trial design | ||||||
| What do you think about a two-arm RCT comparing RCR augmented with an ‘off-the-shelf’ patch with repair without a patch? | 13 (62) | 5 (24) | 0 (0) | 2 (10) | 1 (5) | 0 (0) |
| Answers from the first round of the survey suggested that both 12 months and 24 months are appropriate time points to measure key outcomes. It was also indicated that both imaging and PROMs would be valuable. Therefore, the project team propose for imaging (specifically MRI) and PROMs to be collected at 12 and 24 months post randomisation as key outcomes for the study | 17 (81) | 2 (10) | 0 (0) | 1 (5) | 1 (5) | 0 (0) |
| PPI participants | ||||||
| Patches | ||||||
| Work for PARCS so far suggests that four types of patches are used in the NHS and there is not an overall preference for one type of patch compared with another. These types are synthetic patches, patches made from animal products, patches made from human (donor) tissue and patches made from your own tissue. All these patches are already used clinically in the NHS and have been approved as a safe implant to insert into the human body. Given that there is no clear evidence to support one type of patch over another, we would like to allow the different types of patches to be used in the study. This would reflect current practice in the NHS. In the study, a participant could then receive any of the different types. There would be an alternative to patches made from animal products (e.g. synthetic) for participants who do not want them. What do you think of all of the different types of patches being available for use in a study? The option of a non-animal-based patch would be available to all participants | 3 (100) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Trial design | ||||||
| Findings from the PARCS study so far suggest that a reasonable way to look at the use of patches in RCR surgery within a study is to compare the following two groups of patients: group 1 – this group would have their rotator cuff tear repaired without a patch; group 2 – this group would have their rotator cuff tear repaired with a patch. What do you think about comparing these two groups? | 3 (100) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Blinding | ||||||
| Often in studies, patients are ‘blinded’ to their randomised group. This term means that they do not know which group they are in when the study is running. This is done to get a more scientifically reliable result from the study. For PARCS, this means a participant would not know whether or not their shoulder was repaired with a patch, unless there was a significant safety issue that meant that they needed to know | 2 (67) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (33) |
| Timing of randomisation | ||||||
| As was explained at the focus group, patients in a study are given a treatment at random from those available. This is undertaken because it is the best way to fairly compare different treatments. All patients in the study will be allocated a treatment in this way. Whatever group participants are in, they will still be under the care of their doctor and followed up regularly. Randomisation can happen at any point between entering the study and receiving the treatment. Findings from the PARCS study so far suggest that the best time to randomise participants may be in the operating theatre. This would mean that, going into the operation, the participant would not know whether or not a patch would be used. The participant could expect to have their rotator cuff repaired, although this would depend on the nature of the shoulder problem, which can be more easily assessed during the operation. We would like to know whether or not patients would be comfortable with this idea. What do you think about participants being randomised in the operating theatre as described above? | 3 (100) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Follow-up | ||||||
| To find out whether or not using a patch helps to repair the rotator cuff tear, it would be useful to follow up participants for 24 months after entering the study. For example, they might be asked to complete a questionnaire at 6, 12 and 24 months about their shoulder symptoms and related care | 3 (100) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| What do you think about participants coming to hospital 24 months after joining the study for a study-specific visit? | 1 (33) | 0 (0) | 1 (33) | 0 (0) | 0 (0) | 1 (33) |
Just over 50% of the respondents agreed either completely or somewhat with the proposal for patient eligibility based on the responses from round 1. There was substantial disagreement from 38% of respondents. Thirteen provided specific comments related to their response, raising one or more specific topics. Six disagreed on the muscle atrophy criterion and five commented on the presence of OA. They were generally in favour of the presence of either as an exclusion criterion but suggested that a fuller definition was needed. Three participants noted that revision operations should be included; all three commented on how the size of tears would alter who would be operated on, and one noted concern about ‘too many confounding factors’.
There was very good agreement about randomising in theatre after the initial repair had taken place (86% agreement). Only one (5%) somewhat disagreed and commented with the justification that they would like to know before they start the repair whether or not a patch would be used. Two respondents noted that the randomisation process would need to be straightforward for in-theatre randomisation to work. All three PPI participants agreed with the proposal regarding patches.
Non-PPI participants agreed (81%) with using the patch that is available locally, with the caveat of making sure that a non-animal product patch was available. Only two were neutral (10%) and only one completely disagreed (5%). Five specifically confirmed this by noting a desire not to use an animal product patch. Four comments expressed a preference, to varying degrees, for more consistency in the patch type used or for this to be addressed in the design and analysis. All three PPI participants agreed with the proposal regarding patches.
Non-PPI respondents agreed (86%) with the proposed two-arm design. Only one (5%) completely disagreed and two somewhat disagreed (10%). One respondent queried whether or not a placebo comparison might be useful and another whether or not the proposal would give the required answer. One comment noted that a specific patch would be desirable in the trial design. All three patient respondents agreed with this proposal. Two out of three agreed that participants should be blinded whether or not they have received a patch, with the third being unsure. The non-PPI participants agreed (90%) with the proposed outcome follow-up strategy, with PROMs and imaging collected at 12 and 24 months. One respondent commented that imaging was less important to them. One respondent thought that 3 months would be a useful time point to collect some data and another indicated that imaging at only one time point would be sufficient. All three patient respondents were happy with the proposed questionnaire follow-up strategy and timing. There were mixed views among these respondents on a hospital visit at 24 months for the study (one agreed, one neutral and one unsure).
Stage 6: consensus meeting
The consensus meeting was held on 29 and 30 January 2019 in Oxford. A total of 22 individuals attended the meeting: representatives from industry (2), patients (2), surgeons (8), researchers (4), project team members (5), and an independent chairperson. Prior to the meeting, the agenda and a summary of a trial proposal using the round 2 Delphi survey were circulated. The proposal had only minor adjustments from the round 2 Delphi survey, with the explicit age restriction removed and imaging clarified to take place only at 12 months. In addition, a number of issues related to each component raised in the Delphi study were included in the proposal, highlighted for discussion in the meeting. Towards the end of the first day it became clear that the proposal trial design needed revision to address the varied use of patches and a revised proposal was presented at the beginning of the second day. The overall decision of the meeting was that a RCT of RCR with a patch was both acceptable and feasible. However, it was agreed that a single study or randomised comparison would not be able address all the key questions. The outline of two RCTs was agreed in principle at the meeting, as was the desire for a study to capture safety data for patch use irrespective of involvement in a trial (e.g. registry study). Following the meeting a summary of the proposal was circulated and agreed.
Study proposal
An outline of the agreed study proposal is given in Tables 17 and 18. Two areas for a RCT assessing the use of patches in rotator cuff surgery were identified. The first one assesses the use of a patch for patients with a completed RCR and the second relates patients with a partial RCR. Figure 10 illustrates the patient flow, along with patients who potentially could contribute data to a registry to inform on the safety of specific patches. The two randomised comparisons could potentially be within one more comprehensive trial or conducted separately.
| Element | Details |
|---|---|
| Patients | Include adults with full-thickness rotator cuff tears involving supraspinatus, with or without infraspinatus involvement, confirmed intraoperatively (no restriction on size) |
| Exclude no rotator cuff tear present, full-thickness tear involving subscapularis only and patients with glenohumeral OA | |
| Note: patients are consented prior to operation and are randomised only after eligibility confirmed | |
| Surgeon eligibility | Consultant shoulder surgeon |
| Surgical approach | RCR with double row, no restrictions on the use of anchors or suture material |
| Randomise patch use once RCR has been completed | |
| Bicep tenodesis or tenotomy at surgeon’s discretion | |
| Suitable patch | Types: allograft, synthetic or xenograft suitable for on-lay use |
| Note: need to be available within NHS and have no evidence of safety concerns | |
| Intervention and comparison groups | Intervention: RCR with on-lay use of patch |
| Control: RCR with no use of patch (standard RCR) | |
| Outcome/time frame | Key outcomes: patient-reported pain and function, MRI assessment of full-thickness tear |
| Follow-up time frame: 12 and 24 months |
| Element | Details |
|---|---|
| Patients | Include adults with full-thickness rotator cuff tears involving supraspinatus, with or without infraspinatus involvement, confirmed intraoperatively (no restriction on size) |
| Exclude no rotator cuff tear present, partial-thickness tears, full-thickness tears involving subscapularis only, and patients with glenohumeral OA | |
| Note: patients are consented prior to operation and are randomised only after eligibility confirmed | |
| Surgeon eligibility | Consultant shoulder surgeon |
| Surgical approach | RCR with double row, no restrictions on the use of anchors or suture material |
| Randomise patch use once RCR has been attempted but cannot be completed | |
| Bicep tenodesis or tenotomy at surgeon’s discretion | |
| Suitable patch | Types: allograft, synthetic or xenograft suitable for bridging use |
| Note: need to be available within NHS and have no evidence of safety concerns | |
| Intervention and comparison groups | Intervention: RCR with bridging of patch |
| Control: RCR with no use of patch (standard RCR) | |
| Outcome/time frame | Key outcomes: patient-reported pain and function, MRI assessment of full-thickness tear |
| Follow-up time frame: 12 and 24 months |
FIGURE 10.
Proposed study patient eligibility pathway.

Discussion
Together, there was agreement from the Delphi study and the face-to-face consensus meeting about the acceptability and feasibility of a RCT for evaluating the use of a patch when carrying out RCR. Findings from the previous stages of the PARCS feasibility study were built on in the two rounds of the Delphi survey with the rough outline of a potential trial. During the consensus meeting, it was clear that, although a trial could be conducted, it would need to respect two distinct uses of patches (on-lay and bridging). Accordingly, two separate trials could be envisaged; alternatively, one overall study that accounts for both uses and has two distinct random allocations could be developed.
Using differing methods and multiple rounds of approaches to build consensus is a key strength of this work. The consensus was also strengthened at the attempt to involve all stakeholder groups as much as possible in the consensus-building process. It was also informed by and built on the previous stages of the PARCS feasibility study. Although not without its limitations, this was a much more structured and systematic approach to considering the feasibility and design of a future study than is typically the case.
Limitations of the work include the self-selecting nature of the participants that may make them, particularly in terms of surgical practice, somewhat atypical. For example, the sample is likely to include more who use a patch than may be typical across surgical practice in the NHS. However, to an extent this is not concerning if they reflect more closely the pool of surgeons who would likely participate in a RCT. Indeed, it was a conscious aim to include these surgeons from the point of the triallist survey through to the consensus meeting. A number of surgeons participated following this structure. The Delphi study had fewer participants than initially had been hoped, which is a limitation as it increases the potential for unrepresentative findings or an absence of less common, but relevant, viewpoints. In particular, the number of patient participants was disappointing, despite the effort made to produce a specific questionnaire for them, and also despite approaching individuals who had shown interest in the study to date. We had only two rounds of the Delphi process, which would be considered a minimum by many, and the study did not reach agreement on one of the key (patient eligibility) design features at this point. More generally, our Delphi approach varied somewhat from the approach used in previous studies, given the more fluid nature of the study and the varied topics on which consensus was being sought. Other Delphi studies53 have tended to use very specific questions about inclusion of provided items or domains in all rounds.
Although the desire and feasibility of a trial were generally agreed, the specifics within the trial were debated. Of all the topics, patient eligibility was the most contentious, reflected as being the only component that did not meet the a priori criteria for ‘consensus’. The challenge is to maintain sufficiently broad inclusion criteria to allow as many as surgeons to participate as possible, without undermining the validity and relevance of the findings. However, it is worth noting that the eligibility criteria designate who can be included and, within that pool, the surgeon’s clinical decision-making (and both surgeon and patient equipoise) is still key to recruiting patients. The disagreement, although exhibited in the response to patient eligibility, seems to relate to the surgical approach as well. The consensus meeting proposal sought to deal with the most problematic aspects of this.
As with other areas where a medical device is used for a surgical operation (e.g. hip and knee replacement surgery) and where there are important variations in both the device’s use and the design, there is a tension between proposing a deliverable trial and carrying out the perfect study that addresses all key research questions. This was reflected in some of the responses to the Delphi survey where concern about the value of a study that allowed different types of patches when the main comparison was against no patch. Although focusing on the use of a specific patch in a specific way has a number of benefits, it runs great risk of not being generalisable. It also risks providing a potentially redundant finding, because of changes in the design of patches. For example, GRAFTJACKET is probably the current market leader in the UK for rotator cuff tear repairs, and has been available for 12-plus years, yet is purported to be about to undergo a revision of its design.
In summary, the findings of the PARCS feasibility study are that a RCT evaluating the use of a patch for rotator cuff surgery is both acceptable to stakeholders and feasible. An outline of the design (see Figure 10 and Tables 17 and 18) that such a study can take has been produced.
Chapter 6 Discussion
Summary of findings
This feasibility study has confirmed the need for a RCT of the clinical effectiveness and cost-effectiveness of patch-augmented RCR. It has demonstrated that this trial would be both acceptable to key stakeholders and feasible. Across the five stages of the feasibility study with stakeholder engagement, these groups demonstrated general support for further research on the use of patches, including the willingness to participate in a RCT. There were key challenges related to the implementation of such a trial, and decisions related to its conduct were identified and tackled. Given the variations in the patches and their current use, it is unlikely that a single study would be able to address all of the key research questions.
Strengths and limitations of the work
The main strength of the PARCS feasibility study was the use of multiple methods to engage with all potential stakeholders to address the aim and objectives of the study. The objectives were addressed as intended. However, there were a number of limitations to the work. Inevitably the success of engagement with the stakeholder groups varied, with the most limited input from industry representatives. The response rate of the BESS membership survey was low, even if consistent with other surveys sent to the society. Participation in the Delphi study was lower than originally hoped. It is difficult, therefore, to know how representative the findings are of each stakeholder groups’ views. However, there is confidence that those who participated, particularly the surgeons, would want to be involved in a trial.
Three studies that would progress the field were identified, including two RCTs. Ultimately, the value of the PARCS study will be confirmed only if a RCT assessing the use of a patch in the UK NHS setting is attempted and, if successful, how influential the study is for clinical practice.
Key issues related to conducting a randomised controlled trial
Patient eligibility
Patient eligibility provided the most disagreement in the study. A number of aspects were agreed on, such as the exclusion of patients with other shoulder problems and with clinically significant OA. There was a variety of specific exclusion criteria proposed by individual respondents, with a range of views on age, muscle atrophy, tear size and having a previous RCR. The relationship between patient eligibility and patch technique was noted by a number of participants. The final proposal reflects an inclusive approach whenever possible. The broad criteria were accepted, although the details were not fully resolved.
Types of patches
A variety of patches are available for clinical use, reflecting different materials, processes and designs. The systematic review (see Chapter 2) identified 28 different patches, defined as an implantable human, synthetic or animal material that is used with the aim of improving tissue healing and/or patient outcome via some form of mechanical support. Of these, 22 could be classed as a product, and six were a tissue graft from either the patient or (in one case) a cadaver. There was comparative evidence for only 12 different patches. The survey of the surgical BESS membership identified 13 different patches currently in use in the UK. Most are produced from decellularised human dermis, with the rest being made form porcine or synthetic materials. It is concerning that these two groups did not overlap fully, with at least two patches (dCELL and Leeds–Kuff) in current clinical use that have no clinical evidence identified. No single type of patch could be considered either to be dominant in terms of use or to have compelling evidence in its favour. There was some evidence for the support of allograft and synthetic patches to improve the re-tear rate and for synthetic patches to reduce pain. Mostly the evidence is non-existent, or too weak to draw even tentative conclusions.
With regard to running a large definitive trial, it was clear that the use of a specific patch would be unwarranted but a decision about which types of patch to allow within the study would be important. Any secondary evaluation of evidence, such as safety of the included patches, would be advantageous. Uncovering the need for preliminary safety evaluation of patches was unexpected in this study. The requirement for a non-animal patch in the trial design, particularly an alternative to a porcine based patch, was noted.
Surgical use of a patch
The surgical use of patches in rotator cuff surgery falls broadly into two groups. In an on-lay technique the patch is sutured on top of the tendon-to-bone repair, whereas in a bridging technique the patch is sutured into the exposed area following a partial repair. Although to some degree a partial repair can be anticipated in advance, this is not always the case, as the quality of the tissue is not entirely clear until the repair has been attempted.
The distinction between the two techniques was clear in some of the studies in the systematic review. This became increasingly apparent as surgeon stakeholders were engaged through stages 2–6. To reconcile the two techniques, two RCTs for patch use were proposed: one for on-lay use and one for bridging. Different patch types and designs may be thought to be better suited to each approach.
Beyond this, there was overall support for flexibility for surgeons to conduct patch-augmented RCR according to their personal practice. A standardised postoperative regime was supported by the surgeon triallists in stage 4.
Conducting a randomised controlled trial
Specific information related to how a RCT might be conducted was gained from the surgeon triallist survey, the Delphi study and the consensus meeting. The Delphi study and the consensus meeting showed most support for a two-arm trial of RCR with and without patch use. Although differences between patch types were noted by a number of participants as being of interest, the difference in how patches are used appeared to be a higher priority for evaluation. This is reflected in the research recommendations of the study.
Randomisation during the operation was most supported, once the RCR had been attempted. This has the benefit of confirming the presence and nature of a tear and knowing whether or not the repair could be completed.
Participants in the surgeon triallist survey, Delphi study and consensus meeting supported use of both a patient-reported pain and function measure and imaging as trial outcomes. There was support for a 24-month follow-up. The timing of assessments within this period indicate support for an ‘early’ assessment around 4 months, followed by further assessments at 12 and 24 months. It would not be necessary to have the same outcomes at every time point.
Economic evaluation considerations
A future definitive RCT of patch use should consider embedding an economic evaluation of the patches under investigation to assess their cost to the NHS as well as their benefits to patient HRQoL.
Little evidence was available to shape a RCT economic-based evaluation. Considerations about the types of data (e.g. inpatient/outpatient visits, medication), frequency and intensity of patient data collection (e.g. 1 and 4 months post surgery) as well as the means of data collection (e.g. paper/electronic forms) have to be made when designing a prospective RCT. Resource utilisation not related to the surgery, such as use of non-NHS care to deal with daily activities, as well as loss of income caused by surgery, are also recommended to be included in the patient data collection process. Although SF-36 was the only HRQoL measure to be captured in the current literature, a future economic evaluation should also administer the EQ-5D measure, which is recommended by NICE.
Further research priorities
As outlined in Chapter 5, there were four clear research questions that require evaluation. Proposed research studies to address these are as follows:
-
a RCT to assess the on-lay use of a patch in rotator cuff surgery once the surgical repair of the rotator cuff has been completed
-
a RCT to assess the bridging use of a patch where the surgical repair of the rotator cuff is partial
-
a registry or observational study to assess the safety of all patches available for clinical use
-
an economic evaluation of the use of patches in RCR preferably embedded within a RCT or as a standalone evaluation.
An outline of the proposed studies is given in Tables 17 and 18 and in Figure 10.
Acknowledgements
The authors would like to acknowledge all of the survey and focus group participants for their willingness to participate and giving up precious time for this. In addition, the authors are particularly very grateful to the patient representative attendee of the consensus meeting who gave up their time to take part and inform this key stage of the process.
Contributions of authors
Professor Jonathan A Cook (https://orcid.org/0000-0002-4156-6989) (Associate Professor, Chief Investigator) led the study design and funding application, provided overall oversight of the project, contributed to conduct of all stages and approved the report.
Dr Mathew Baldwin (https://orcid.org/0000-0002-8790-9975) (DPhil student) led the systematic review and BESS membership survey and contributed to the writing of the report.
Mrs Cushla Cooper (https://orcid.org/0000-0002-3790-3428) (Operational Lead) contributed to overall study design and conduct, and to the preparation and writing of the report.
Dr Navraj S Nagra (https://orcid.org/0000-0002-6899-4465) (DPhil Student) contributed to the design and conduct of the systematic review and reviewed the report.
Dr Joanna C Crocker (https://orcid.org/0000-0002-8223-0349) (Research Fellow) contributed to the design and conduct the focus groups and reviewed the report.
Mrs Molly Glaze (https://orcid.org/0000-0001-6529-6189) (Clinical Trial Manager) contributed to overall study conduct, prepared and reviewed the report.
Ms Gemma Greenall (https://orcid.org/0000-0002-2833-7217) (Clinical Trial Manager) contributed to the design and conduct of the systematic review and reviewed the report.
Professor Amar Rangan (https://orcid.org/0000-0002-5452-8578) (Professor of Orthopaedic Surgery) contributed to the study design, provided clinical input and reviewed the report.
Dr Lucksy Kottam (https://orcid.org/0000-0002-7976-2416) (Career Scientist) contributed to the study design and conduct of the focus groups and reviewed the report.
Professor Jonathan L Rees (https://orcid.org/0000-0003-1818-5800) (Professor of Orthopaedic Surgery and Musculoskeletal Science) contributed to the study design, provided clinical input and reviewed the report.
Mr Dair Farrar-Hockley (https://orcid.org/0000-0002-5034-1669) (Patient Representative) provided PPI input to the study design, conduct, and the report.
Mrs Naomi Merritt (https://orcid.org/0000-0002-3769-1998) (Clinical Trial Manager) contributed to overall study conduct and design and reviewed the report.
Professor Sally Hopewell (https://orcid.org/0000-0002-6881-6984) (Associate Professor) contributed to the study design and reviewed the report.
Professor David Beard (https://orcid.org/0000-0001-7884-6389) (Professor of Musculoskeletal and Surgical Science) contributed to the study design and reviewed the report.
Mr Michael Thomas (https://orcid.org/0000-0003-0870-4371) (Orthopaedic Consultant) provided clinical input and contributed to the overall conduct of the study.
Dr Melina Dritsaki (https://orcid.org/0000-0002-1673-3036) (Senior Health Economist) contributed to study design, provided health economic evaluation input and contributed to the writing of the report.
Professor Andrew J Carr (https://orcid.org/0000-0001-5940-1464) (Professor of Orthopaedics) contributed to study conception and design, provided clinical input and reviewed the report.
Publications
Cook JA, Merritt N, Rees JL, Crocker JC, Hopewell S, Dritsaki M, et al. Patch-augmented rotator cuff surgery (PARCS) study-protocol for a feasibility study. Pilot Feasibility Stud 2018;4:188.
Greenall G, Carr A, Beard D, Rees J, Rangan A, Merritt N, et al. Systematic review of the surgical management of rotator cuff repair with an augmentative patch: a feasibility study protocol. Syst Rev 2018;7:187.
Baldwin MJ, Nagra NS, Merritt N, Rees JL, Carr AJ, Rangan A, et al. The use of a patch to augment rotator cuff surgery – a survey of UK shoulder and elbow surgeons. PLOS ONE 2020;15:e0230235.
Baldwin M, Nagra NS, Greenall G, Carr AJ, Beard D, Rees J, Rangan A, Merritt N, Dritsaki M, Hopewell S, Cook JA. Use of patch augmentation for rotator cuff repair – a systematic review and meta-analysis. BMJ Open 2020;10:e039552.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care.
References
- Cook JA, Merritt N, Rees JL, Crocker JC, Hopewell S, Dritsaki M, et al. Patch-augmented rotator cuff surgery (PARCS) study-protocol for a feasibility study. Pilot Feasibility Stud 2018;4. https://doi.org/10.1186/s40814-018-0380-7.
- Carr A, Cooper C, Campbell MK, Rees J, Moser J, Beard DJ, et al. Effectiveness of open and arthroscopic rotator cuff repair (UKUFF): a randomised controlled trial. Bone Joint J 2017;99–B:107-15. https://doi.org/10.1302/0301-620X.99B1.BJJ-2016-0424.R1.
- Linsell L, Dawson J, Zondervan K, Rose P, Randall T, Fitzpatrick R, et al. Prevalence and incidence of adults consulting for shoulder conditions in UK primary care; patterns of diagnosis and referral. Rheumatology 2006;45:215-21. https://doi.org/10.1093/rheumatology/kei139.
- Craig R, Holt T, Rees JL. Acute rotator cuff tears. BMJ 2017;359. https://doi.org/10.1136/bmj.j5366.
- Goldberg BA, Smith K, Jackins S, Campbell B, Matsen FA. The magnitude and durability of functional improvement after total shoulder arthroplasty for degenerative joint disease. J Shoulder Elbow Surg 2001;10:464-9. https://doi.org/10.1067/mse.2001.117122.
- Buchbinder R, Green S, Youd JM. Corticosteroid injections for shoulder pain. Cochrane Database Syst Rev 2003;1. https://doi.org/10.1002/14651858.CD004016.
- Hopewell S, Keene DJ, Maia Schlüssel M, Dritsaki M, Dutton S, Carr A, et al. Clinical and cost-effectiveness of progressive exercise compared with best practice advice, with or without corticosteroid injection, for the treatment of rotator cuff disorders: protocol for a 2x2 factorial randomised controlled trial (the GRASP trial). BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-018004.
- Dean BJ, Franklin SL, Murphy RJ, Javaid MK, Carr AJ. Glucocorticoids induce specific ion-channel-mediated toxicity in human rotator cuff tendon: a mechanism underpinning the ultimately deleterious effect of steroid injection in tendinopathy?. Br J Sports Med 2014;48:1620-6. https://doi.org/10.1136/bjsports-2013-093178.
- Dean BJ, Lostis E, Oakley T, Rombach I, Morrey ME, Carr AJ. The risks and benefits of glucocorticoid treatment for tendinopathy: a systematic review of the effects of local glucocorticoid on tendon. Semin Arthritis Rheum 2014;43:570-6. https://doi.org/10.1016/j.semarthrit.2013.08.006.
- Judge A, Murphy RJ, Maxwell R, Arden NK, Carr AJ. Temporal trends and geographical variation in the use of subacromial decompression and rotator cuff repair of the shoulder in England. Bone Joint J 2014;96–B:70-4. https://doi.org/10.1302/0301-620X.96B1.32556.
- Dunn WR, Schackman BR, Walsh C, Lyman S, Jones EC, Warren RF, et al. Variation in orthopaedic surgeons’ perceptions about the indications for rotator cuff surgery. J Bone Joint Surg Am 2005;87:1978-84. https://doi.org/10.2106/00004623-200509000-00010.
- Kulkarni R, Gibson J, Brownson P, Thomas M, Rangan A, Carr AJ, et al. Subacromial shoulder pain. Shoulder Elbow 2015;7:135-43. https://doi.org/10.1177/1758573215576456.
- Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am 2004;86:219-24. https://doi.org/10.2106/00004623-200402000-00002.
- Matthews TJ, Hand GC, Rees JL, Athanasou NA, Carr AJ. Pathology of the torn rotator cuff tendon. Reduction in potential for repair as tear size increases. J Bone Joint Surg Br 2006;88:489-95. https://doi.org/10.1302/0301-620X.88B4.16845.
- Rashid MS, Cooper C, Cook J, Cooper D, Dakin SG, Snelling S, et al. Increasing age and tear size reduce rotator cuff repair healing rate at 1 year. Acta Orthop 2017;88:606-11. https://doi.org/10.1080/17453674.2017.1370844.
- Coghlan JA, Buchbinder R, Green S, Johnston RV, Bell SN. Surgery for rotator cuff disease. Cochrane Database Syst Rev 2008;1. https://doi.org/10.1002/14651858.CD005619.pub2.
- Papalia R, Franceschi F, Zampogna B, D’Adamio S, Maffulli N, Denaro V. Augmentation techniques for rotator cuff repair. Br Med Bull 2013;105:107-38. https://doi.org/10.1093/bmb/lds029.
- Carr AJ, Rees JL, Ramsay CR, Fitzpatrick R, Gray A, Moser J, et al. Protocol for the United Kingdom Rotator Cuff Study (UKUFF): a randomised controlled trial of open and arthroscopic rotator cuff repair. Bone Joint Res 2014;3:155-60. https://doi.org/10.1302/2046-3758.35.2000270.
- Boehm TD, Werner A, Radtke S, Mueller T, Kirschner S, Gohlke F. The effect of suture materials and techniques on the outcome of repair of the rotator cuff: a prospective, randomised study. J Bone Joint Surg Br 2005;87:819-23. https://doi.org/10.1302/0301-620X.87B6.15638.
- Gartsman GM, O’Connor DP. Arthroscopic rotator cuff repair with and without arthroscopic subacromial decompression: a prospective, randomized study of one-year outcomes. J Shoulder Elbow Surg 2004;13:424-6. https://doi.org/10.1016/j.jse.2004.02.006.
- Abrams GD, Gupta AK, Hussey KE, Tetteh ES, Karas V, Bach BR, et al. Arthroscopic repair of full-thickness rotator cuff tears with and without acromioplasty: randomized prospective trial with 2-year follow-up. Am J Sports Med 2014;42:1296-303. https://doi.org/10.1177/0363546514529091.
- van der Zwaal P, Thomassen BJ, Nieuwenhuijse MJ, Lindenburg R, Swen JW, van Arkel ER. Clinical outcome in all-arthroscopic versus mini-open rotator cuff repair in small to medium-sized tears: a randomized controlled trial in 100 patients with 1-year follow-up. Arthroscopy 2013;29:266-73. https://doi.org/10.1016/j.arthro.2012.08.022.
- MacDonald P, McRae S, Leiter J, Mascarenhas R, Lapner P. Arthroscopic rotator cuff repair with and without acromioplasty in the treatment of full-thickness rotator cuff tears: a multicenter, randomized controlled trial. J Bone Joint Surg Am 2011;93:1953-60. https://doi.org/10.2106/JBJS.K.00488.
- Mohtadi NG, Hollinshead RM, Sasyniuk TM, Fletcher JA, Chan DS, Li FX. A randomized clinical trial comparing open to arthroscopic acromioplasty with mini-open rotator cuff repair for full-thickness rotator cuff tears: disease-specific quality of life outcome at an average 2-year follow-up. Am J Sports Med 2008;36:1043-51. https://doi.org/10.1177/0363546508314409.
- MacDermid JC, Holtby R, Razmjou H, Bryant D. JOINTS Canada . All-arthroscopic versus mini-open repair of small or moderate-sized rotator cuff tears: a protocol for a randomized trial. BMC Musculoskelet Disord 2006;7. https://doi.org/10.1186/1471-2474-7-25.
- Barber FA, Burns JP, Deutsch A, Labbé MR, Litchfield RB. A prospective, randomized evaluation of acellular human dermal matrix augmentation for arthroscopic rotator cuff repair. Arthroscopy 2012;28:8-15. https://doi.org/10.1016/j.arthro.2011.06.038.
- Ferguson DP, Lewington MR, Smith TD, Wong IH. Graft utilization in the augmentation of large-to-massive rotator cuff repairs: a systematic review. Am J Sports Med 2016;44:2984-92. https://doi.org/10.1177/0363546515624463.
- Smith RD, Carr A, Dakin SG, Snelling SJ, Yapp C, Hakimi O. The response of tenocytes to commercial scaffolds used for rotator cuff repair. Eur Cell Mater 2016;31:107-18. https://doi.org/10.22203/eCM.v031a08.
- Baldwin M, Snelling S, Dakin S, Carr A. Augmenting endogenous repair of soft tissues with nanofibre scaffolds. J R Soc Interface 2018;15. https://doi.org/10.1098/rsif.2018.0019.
- Smith RDJ, Zargar N, Brown CP, Nagra NS, Dakin SG, Snelling SJB, et al. Characterizing the macro and micro mechanical properties of scaffolds for rotator cuff repair. J Shoulder Elbow Surg 2017;26:2038-46. https://doi.org/10.1016/j.jse.2017.06.035.
- Chaudhury S, Holland C, Thompson MS, Vollrath F, Carr AJ. Tensile and shear mechanical properties of rotator cuff repair patches. J Shoulder Elbow Surg 2012;21:1168-76. https://doi.org/10.1016/j.jse.2011.08.045.
- Wong I, Burns J, Snyder S. Arthroscopic GraftJacket repair of rotator cuff tears. J Shoulder Elbow Surg 2010;19:104-9. https://doi.org/10.1016/j.jse.2009.12.017.
- Mori D, Funakoshi N, Yamashita F. Arthroscopic surgery of irreparable large or massive rotator cuff tears with low-grade fatty degeneration of the infraspinatus: patch autograft procedure versus partial repair procedure. Arthroscopy 2013;29:1911-21. https://doi.org/10.1016/j.arthro.2013.08.032.
- Smith RDJ. Investigating the Role of Scaffolds for Rotator Cuff Repair 2016.
- Iannotti JP, Codsi MJ, Kwon YW, Derwin K, Ciccone J, Brems JJ. Porcine small intestine submucosa augmentation of surgical repair of chronic two-tendon rotator cuff tears. A randomized, controlled trial. J Bone Joint Surg Am 2006;88:1238-44. https://doi.org/10.2106/00004623-200606000-00010.
- Hakimi O, Murphy R, Stachewicz U, Hislop S, Carr AJ. An electrospun polydioxanone patch for the localisation of biological therapies during tendon repair. Eur Cell Mater 2012;24:344-57. https://doi.org/10.22203/eCM.v024a25.
- Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal?. J Bone Joint Surg Am 2005;87:1229-40. https://doi.org/10.2106/00004623-200506000-00007.
- Rangan A, Upadhaya S, Regan S, Toye F, Rees JL. Research priorities for shoulder surgery: results of the 2015 James Lind Alliance patient and clinician priority setting partnership. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-010412.
- Thangarajah T, Pendegrass CJ, Shahbazi S, Lambert S, Alexander S, Blunn GW. Augmentation of rotator cuff repair with soft tissue scaffolds. Orthop J Sports Med 2015;3. https://doi.org/10.1177/2325967115587495.
- Ciampi P, Scotti C, Nonis A, Vitali M, Di Serio C, Peretti GM, et al. The benefit of synthetic versus biological patch augmentation in the repair of posterosuperior massive rotator cuff tears: a 3-year follow-up study. Am J Sports Med 2014;42:1169-75. https://doi.org/10.1177/0363546514525592.
- Walton JR, Bowman NK, Khatib Y, Linklater J, Murrell GA. Restore orthobiologic implant: not recommended for augmentation of rotator cuff repairs. J Bone Joint Surg Am 2007;89:786-91. https://doi.org/10.2106/JBJS.F.00315.
- Gilot GJ, Alvarez-Pinzon AM, Barcksdale L, Westerdahl D, Krill M, Peck E. Outcome of large to massive rotator cuff tears repaired with and without extracellular matrix augmentation: a prospective comparative study. Arthroscopy 2015;31:1459-65. https://doi.org/10.1016/j.arthro.2015.02.032.
- Vitali M, Cusumano A, Pedretti A, Naim Rodriguez N, Fraschini G. Employment of synthetic patch with augmentation of the long head of the biceps tendon in irreparable lesions of the rotator cuff: our technique applied to 60 patients. Tech Hand Up Extrem Surg 2015;19:32-9. https://doi.org/10.1097/BTH.0000000000000072.
- Bailey JR, Kim C, Alentorn-Geli E, Kirkendall DT, Ledbetter L, Taylor DC, et al. Rotator cuff matrix augmentation and interposition: a systematic review and meta-analysis. Am J Sports Med 2019;47:1496-506. https://doi.org/10.1177/0363546518774762.
- Young JM, Solomon MJ, Harrison JD, Salkeld G, Butow P. Measuring patient preference and surgeon choice. Surgery 2008;143:582-8. https://doi.org/10.1016/j.surg.2008.01.009.
- Wright JG, Katz JN, Losina E. Clinical trials in orthopaedics research. Part I. Cultural and practical barriers to randomized trials in orthopaedics. J Bone Joint Surg Am 2011;93. https://doi.org/10.2106/JBJS.J.00229.
- Rooshenas L, Elliott D, Wade J, Jepson M, Paramasivan S, Strong S, et al. Conveying equipoise during recruitment for clinical trials: qualitative synthesis of clinicians’ practices across six randomised controlled trials. PLOS Med 2016;13. https://doi.org/10.1371/journal.pmed.1002147.
- Buxton MJ, Drummond MF. Economic Appraisal of Health Technology in the European Community. Oxford: Oxford Medical Publications; 1987.
- Cook JA, McCulloch P, Blazeby JM, Beard DJ, Marinac-Dabic D, Sedrakyan A. IDEAL Group . IDEAL framework for surgical innovation 3: randomised controlled trials in the assessment stage and evaluations in the long term study stage. BMJ 2013;346. https://doi.org/10.1136/bmj.f2820.
- McCulloch P, Cook JA, Altman DG, Heneghan C, Diener MK. IDEAL Group . IDEAL framework for surgical innovation 1: the idea and development stages. BMJ 2013;346. https://doi.org/10.1136/bmj.f3012.
- Moher D, Schulz KF, Simera I, Altman DG. Guidance for developers of health research reporting guidelines. PLOS Med 2010;7. https://doi.org/10.1371/journal.pmed.1000217.
- Sinha IP, Smyth RL, Williamson PR. Using the Delphi technique to determine which outcomes to measure in clinical trials: recommendations for the future based on a systematic review of existing studies. PLOS Med 2011;8. https://doi.org/10.1371/journal.pmed.1000393.
- Williamson PR, Altman DG, Blazeby JM, Clarke M, Devane D, Gargon E, et al. Developing core outcome sets for clinical trials: issues to consider. Trials 2012;13. https://doi.org/10.1186/1745-6215-13-132.
- Malcarney HL, Bonar F, Murrell GA. Early inflammatory reaction after rotator cuff repair with a porcine small intestine submucosal implant: a report of 4 cases. Am J Sports Med 2005;33:907-11. https://doi.org/10.1177/0363546504271500.
- Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343. https://doi.org/10.1136/bmj.d5928.
- Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015;350. https://doi.org/10.1136/bmj.g7647.
- Centre for Reviews and Dissemination . Systematic Reviews – CRD’s Guidance for Undertaking Reviews in Healthcare 2009.
- Greenall G, Carr A, Beard D, Rees J, Rangan A, Merritt N, et al. Systematic review of the surgical management of rotator cuff repair with an augmentative patch: a feasibility study protocol. Syst Rev 2018;7. https://doi.org/10.1186/s13643-018-0851-1.
- Steinhaus ME, Makhni EC, Cole BJ, Romeo AA, Verma NN. Outcomes after patch use in rotator cuff repair. Arthroscopy 2016;32:1676-90. https://doi.org/10.1016/j.arthro.2016.02.009.
- DeOrio JK, Cofield RH. Results of a second attempt at surgical repair of a failed initial rotator-cuff repair. J Bone Joint Surg Am 1984;66:563-7. https://doi.org/10.2106/00004623-198466040-00011.
- Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am 2000;82:505-15. https://doi.org/10.2106/00004623-200004000-00006.
- Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;355. https://doi.org/10.1136/bmj.i4919.
- Leuzinger J, Sternberg C, Smolen D, Jakob R. Patch augmentation in rotator cuff repair surgery with elder patients. Z Orthop Unfall 2016;154:504-12. https://doi.org/10.1055/s-0042-106475.
- Maillot C, Harly E, Demezon H, Le Huec JC. Surgical repair of large-to-massive rotator cuff tears seems to be a better option than patch augmentation or débridement and biceps tenotomy: a prospective comparative study. J Shoulder Elbow Surg 2018;27:1545-52. https://doi.org/10.1016/j.jse.2018.05.023.
- Bryant D, Holtby R, Willits K, Litchfield R, Drosdowech D, Spouge A, et al. A randomized clinical trial to compare the effectiveness of rotator cuff repair with or without augmentation using porcine small intestine submucosa for patients with moderate to large rotator cuff tears: a pilot study. J Shoulder Elbow Surg 2016;25:1623-33. https://doi.org/10.1016/j.jse.2016.06.006.
- Ito J, Morioka T. Surgical treatment for large and massive tears of the rotator cuff. Int Orthop 2003;27:228-31. https://doi.org/10.1007/s00264-003-0459-4.
- Jeon YS, Lee J, Kim RG, Ko YW, Shin SJ. Does additional biceps augmentation improve rotator cuff healing and clinical outcomes in anterior l-shaped rotator cuff tears? Clinical comparisons with arthroscopic partial repair. Am J Sports Med 2017;45:2982-8. https://doi.org/10.1177/0363546517720198.
- Mori D, Funakoshi N, Yamashita F, Wakabayashi T. Effect of fatty degeneration of the infraspinatus on the efficacy of arthroscopic patch autograft procedure for large to massive rotator cuff tears. Am J Sports Med 2015;43:1108-17. https://doi.org/10.1177/0363546515569680.
- Tempelaere C, Desmoineaux P, Lespagnol F, Pierrart J, Beaufils P, Pujol N. Surgical repair of massive rotator cuff tendon tears: autologous quadriceps tendon graft versus arthroscopic repair. Orthop Traumatol Surg Res 2017;103:435-40. https://doi.org/10.1016/j.otsr.2016.12.020.
- Patte D. Classification of rotator cuff lesion. Clin Orthop Relat Res 1990;254:81-6. https://doi.org/10.1097/00003086-199005000-00012.
- Yoon JP, Chung SW, Kim JY, Lee BJ, Kim HS, Kim JE, et al. Outcomes of combined bone marrow stimulation and patch augmentation for massive rotator cuff tears. Am J Sports Med 2016;44:963-71. https://doi.org/10.1177/0363546515625044.
- Agrawal V. Healing rates for challenging rotator cuff tears utilizing an acellular human dermal reinforcement graft. Int J Shoulder Surg 2012;6:36-44. https://doi.org/10.4103/0973-6042.96992.
- Audenaert E, Van Nuffel J, Schepens A, Verhelst M, Verdonk R. Reconstruction of massive rotator cuff lesions with a synthetic interposition graft: a prospective study of 41 patients. Knee Surg Sports Traumatol Arthrosc 2006;14:360-4. https://doi.org/10.1007/s00167-005-0689-7.
- Badhe SP, Lawrence TM, Smith FD, Lunn PG. As assessment of porcine dermal xenograft as an augmentation graft in the treatment of extensive rotator cuff tears. J Shoulder Elbow Surg 2008;17:35S-39S. https://doi.org/10.1016/j.jse.2007.08.005.
- Bektaser B, Ocguder A, Solak S, Gonen E, Yalcin N, Kilicarslan. Free coracoacromial ligament graft for augmentation of massive rotator cuff tears treated with mini-open repair. Acta Orthop Traumatol Turc 2010;44:426-30. https://doi.org/10.3944/AOTT.2010.2423.
- Bond JL, Dopirak RM, Higgins J, Burns J, Snyder SJ. Arthroscopic replacement of massive, irreparable rotator cuff tears using a GraftJacket allograft: technique and preliminary results. Arthroscopy 2008;24:403-9.e.1. https://doi.org/10.1016/j.arthro.2007.07.033.
- Burkhead WZ, Schiffern SC, Krishnan SG. Use of graft jacket as an augmentation for massive rotator cuff tears. Semin Arthro 2007;18:11-8. https://doi.org/10.1053/j.sart.2006.11.017.
- Cho CH, Lee SM, Lee YK, Shin HK. Mini-open suture bridge repair with porcine dermal patch augmentation for massive rotator cuff tear: surgical technique and preliminary results. Clin Orthop Surg 2014;6:329-35. https://doi.org/10.4055/cios.2014.6.3.329.
- Consigliere P, Polyzois I, Sarkhel T, Gupta R, Levy O, Narvani AA. Preliminary results of a consecutive series of large & massive rotator cuff tears treated with arthroscopic rotator cuff repairs augmented with extracellular matrix. Arch Bone Jt Surg 2017;5:14-21.
- Encalada-Diaz I, Cole BJ, Macgillivray JD, Ruiz-Suarez M, Kercher JS, Friel NA, et al. Rotator cuff repair augmentation using a novel polycarbonate polyurethane patch: preliminary results at 12 months’ follow-up. J Shoulder Elbow Surg 2011;20:788-94. https://doi.org/10.1016/j.jse.2010.08.013.
- Flury M. Arthroscopic rotator cuff repair with patch augmentation. Oper Orthop Traumatol 2012;24:486-94. https://doi.org/10.1007/s00064-012-0158-7.
- Giannotti S, Ghilardi M, Dell’osso G, Magistrelli L, Bugelli G, Di Rollo F, et al. Study of the porcine dermal collagen repair patch in morpho-functional recovery of the rotator cuff after minimum follow-up of 2.5 years. Surg Technol Int 2014;24:348-52.
- Gupta AK, Hug K, Berkoff DJ, Boggess BR, Gavigan M, Malley PC, et al. Dermal tissue allograft for the repair of massive irreparable rotator cuff tears. Am J Sports Med 2012;40:141-7. https://doi.org/10.1177/0363546511422795.
- Gupta AK, Hug K, Boggess BR, Gavigan M, Toth AP. Massive or 2-tendon rotator cuff tears in active patients with minimal glenohumeral arthritis: clinical and radiographic outcomes of reconstruction using dermal tissue matrix xenograft. Am J Sports Med 2013;41:872-9. https://doi.org/10.1177/0363546512475204.
- Hirooka A, Yoneda M, Wakaitani S, Isaka Y, Hayashida K, Fukushima S, et al. Augmentation with a Gore-Tex patch for repair of large rotator cuff tears that cannot be sutured. J Orthop Sci 2002;7:451-6. https://doi.org/10.1007/s007760200078.
- Lederman ES, Toth AP, Nicholson GP, Nowinski RJ, Bal GK, Williams GR, et al. A prospective, multicenter study to evaluate clinical and radiographic outcomes in primary rotator cuff repair reinforced with a xenograft dermal matrix. J Shoulder Elbow Surg 2016;25:1961-70. https://doi.org/10.1016/j.jse.2016.02.029.
- Lenart BA, Martens KA, Kearns KA, Gillespie RJ, Zoga AC, Williams GR. Treatment of massive and recurrent rotator cuff tears augmented with a poly-l-lactide graft, a preliminary study. J Shoulder Elbow Surg 2015;24:915-21. https://doi.org/10.1016/j.jse.2014.09.044.
- Marberry TA. A synthetic reinforcement patch in repair of challenging two-tendon rotator cuff tears. Shoulder Elbow 2013;5:24-9. https://doi.org/10.1111/j.1758-5740.2012.00210.x.
- Metcalf MH, Savoie FH, Kellum B. Surgical technique for xenograft (SIS) augmentation of rotator-cuff repairs. Oper Tech Orthop 2002;12:204-8. https://doi.org/10.1053/otor.2002.36298.
- Modi A, Singh HP, Pandey R, Armstrong A. Management of irreparable rotator cuff tears with GraftJacket allograft as an interpositional graft. Shoulder Elbow 2013;5:188-94. https://doi.org/10.1111/sae.12021.
- Moore SR, Cain EL, Schwartz ML, Clancy WG. Allograft reconstruction for massive irreparable rotator cuff tears. Am J Sports Med 2006;34:392-6. https://doi.org/10.1177/0363546505281237.
- Nada AM, Debnath UK, Robinson DA, Jordan C. Treatment of massive rotator-cuff tears with a polyester ligament (Dacron) augmentation. J Bone Joint Surg 2010;92–B:1397-402. https://doi.org/10.1302/0301-620X.92B10.24299.
- Neumann JA, Zgonis MH, Rickert KD, Bradley KE, Kremen TJ, Boggess BR, et al. Interposition dermal matrix xenografts. Am J Sports Med 2017;45:1261-8. https://doi.org/10.1177/0363546516683945.
- Petrie MJ, Ismaiel AH. Treatment of massive rotator-cuff tears with a polyester ligament (LARS) patch. Acta Orthop Belg 2013;79:620-5.
- Petri M, Warth RJ, Horan MP, Greenspoon JA, Millett PJ. Outcomes after open revision repair of massive rotator cuff tears with biologic patch augmentation. Arthroscopy 2016;32:1752-60. https://doi.org/10.1016/j.arthro.2016.01.037.
- Petriccioli D, Bertone C, Marchi G, Mujahed I. Open repair of isolated traumatic subscapularis tendon tears with a synthetic soft tissue reinforcement. Musculoskelet Surg 2013;97:63-8. https://doi.org/10.1007/s12306-013-0260-5.
- Phipatanakul WP, Peterson SA. Porcine small intestine submucosa xenograft augmentation in repair of massive rotator cuff tears. Am J Orthopaedic 2009;38:572-5.
- Proctor CS. Long-term successful arthroscopic repair of large and massive rotator cuff tears with a functional and degradable reinforcement device. J Shoulder Elbow Surg 2014;23:1508-13. https://doi.org/10.1016/j.jse.2014.01.010.
- Rhee YG, Cho NS, Lim CT, Yi JW, Vishvanathan T. Bridging the gap in immobile massive rotator cuff tears. Augmentation using the tenotomized biceps. Am J Sports Med 2008;36:1511-18. https://doi.org/10.1177/0363546508316020.
- Rotini R, Marinelli A, Guerra E, Bettelli G, Castagna A, Fini M, et al. Human dermal matrix scaffold augmentation for large and massive rotator cuff repairs: preliminary clinical and MRI results at 1-year follow-up. Musculoskelet Surg 2011;95:S13-S23. https://doi.org/10.1007/s12306-011-0141-8.
- Sano H, Mineta M, Kita A, Itoi E. Tendon patch grafting using the long head of the biceps for irreparable massive rotator cuff tears. J Orthop Sci 2010;15:310-6. https://doi.org/10.1007/s00776-010-1453-5.
- Scheibel M, Brown A, Woertler K, Imhoff AB. Preliminary results after rotator cuff reconstruction augmented with an autologous periosteal flap. Knee Surg Sports Traumatol Arthrosc 2007;15:305-14. https://doi.org/10.1007/s00167-006-0173-z.
- Schlegel TF, Abrams JS, Bushnell BD, Brock JL, Ho CP. Radiologic and clinical evaluation of a bioabsorbable collagen implant to treat partial-thickness tears: a prospective multicenter study. J Shoulder Elbow Surg 2018;27:242-51. https://doi.org/10.1016/j.jse.2017.08.023.
- Sclamberg SG, Tibone JE, Itamura JM, Kasraeian S. Six-month magnetic resonance imaging follow-up of large and massive rotator cuff repairs reinforced with porcine small intestinal mucosa. J Shoulder Elbow Surg 2004;13:538-41. https://doi.org/10.1016/j.jse.2004.03.005.
- Sears BW, Choo A, Yu A, Greis A, Lazarus M. Clinical outcomes in patients undergoing revision rotator cuff repair with extracellular matrix augmentation. Orthopaedics 2015;38:e292-6. https://doi.org/10.3928/01477447-20150402-57.
- Venouziou AI, Kokkalis ZT, Sotereanos DG. Human dermal allograft interposition for the reconstruction of massive irreparable rotator cuff tears. Am J Orthop 2013;42:63-70.
- Tashjian RZ, Deloach J, Porucznik CA, Powell AP. Minimal clinically important differences (MCID) and patient acceptable symptomatic state (PASS) for visual analog scales (VAS) measuring pain in patients treated for rotator cuff disease. J Shoulder Elbow Surg 2009;18:927-32. https://doi.org/10.1016/j.jse.2009.03.021.
- Wylie JD, Beckmann JT, Granger E, Tashjian RZ. Functional outcomes assessment in shoulder surgery. World J Orthop 2014;5:623-33. https://doi.org/10.5312/wjo.v5.i5.623.
- Xu S, Chen JY, Lie HME, Hao Y, Lie DTT. Determination of threshold scores for treatment success after arthroscopic rotator cuff repair using Oxford, Constant, and University of California, Los Angeles shoulder scores. Arthroscopy 2019;35:304-11. https://doi.org/10.1016/j.arthro.2018.07.047.
- Berry MG, Stanek JJ. The PIP mammary prosthesis: a product recall study. J Plast Reconstr Aesthet Surg 2012;65:697-704. https://doi.org/10.1016/j.bjps.2012.02.019.
- Hirst A, Philippou Y, Blazeby J, Campbell B, Campbell M, Feinberg J, et al. No surgical innovation without evaluation: evolution and further development of the ideal framework and recommendations. Ann Surg 2019;269:211-20. https://doi.org/10.1097/SLA.0000000000002794.
- Beard D, Rees J, Rombach I, Cooper C, Cook J, Merritt N, et al. The CSAW Study (Can Shoulder Arthroscopy Work?) – a placebo-controlled surgical intervention trial assessing the clinical and cost effectiveness of arthroscopic subacromial decompression for shoulder pain: study protocol for a randomised controlled trial. Trials 2015;16. https://doi.org/10.1186/s13063-015-0725-y.
- Brealey S, Armstrong AL, Brooksbank A, Carr AJ, Charalambous CP, Cooper C, et al. United Kingdom Frozen Shoulder Trial (UK FROST), multi-centre, randomised, 12 month, parallel group, superiority study to compare the clinical and cost-effectiveness of early structured physiotherapy versus manipulation under anaesthesia versus arthroscopic capsular release for patients referred to secondary care with a primary frozen shoulder: study protocol for a randomised controlled trial. Trials 2017;18. https://doi.org/10.1186/s13063-017-2352-2.
- Baldwin MJ, Nagra NS, Merritt N, Rees JL, Carr AJ, Rangan A, et al. The use of a patch to augment rotator cuff surgery – a survey of UK shoulder and elbow surgeons. PLOS ONE 2020;15. https://doi.org/10.1371/journal.pone.0230235.
- Somerson JS, Hsu JE, Gorbaty JD, Gee AO. Classifications in brief: Goutallier classification of fatty infiltration of the rotator cuff musculature. Clin Orthop Relat Res 2016;474:1328-32. https://doi.org/10.1007/s11999-015-4630-1.
- Kohn MD, Sassoon AA, Fernando ND. Classifications in brief: Kellgren–Lawrence classification of osteoarthritis. Clin Orthop Relat Res 2016;474:1886-93. https://doi.org/10.1007/s11999-016-4732-4.
- Braun HJ, Gold GE. Diagnosis of osteoarthritis: imaging. Bone 2012;51:278-88. https://doi.org/10.1016/j.bone.2011.11.019.
- Heneghan C, Langton D, Thompson M. Ongoing problems with metal-on-metal hip implants. BMJ 2012;344. https://doi.org/10.1136/bmj.e1349.
- Heneghan CJ, Goldacre B, Onakpoya I, Aronson JK, Jefferson T, Pluddemann A, et al. Trials of transvaginal mesh devices for pelvic organ prolapse: a systematic database review of the US FDA approval process. BMJ Open 2017;7. https://doi.org/10.1136/bmjopen-2017-017125.
- Fletcher B, Gheorghe A, Moore D, Wilson S, Damery S. Improving the recruitment activity of clinicians in randomised controlled trials: a systematic review. BMJ Open 2012;2. https://doi.org/10.1136/bmjopen-2011-000496.
- Stirrat GM. Ethics and evidence based surgery. J Med Ethics 2004;30:160-5. https://doi.org/10.1136/jme.2003.007054.
- McCulloch P, Kaul A, Wagstaff GF, Wheatcroft J. Tolerance of uncertainty, extroversion, neuroticism and attitudes to randomized controlled trials among surgeons and physicians. Br J Surg 2005;92:1293-7. https://doi.org/10.1002/bjs.4930.
- Marx RG, Koulouvaris P, Chu SK, Levy BA. Indications for surgery in clinical outcome studies of rotator cuff repair. Clin Orthop Relat Res 2008;467:450-6. https://doi.org/10.1007/s11999-008-0585-9.
- Charousset C, Bellaïche L, Kalra K, Petrover D. Arthroscopic repair of full-thickness rotator cuff tears: is there tendon healing in patients aged 65 years or older?. Arthroscopy 2010;26:302-9. https://doi.org/10.1016/j.arthro.2009.08.027.
- Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res 1994;304:78-83. https://doi.org/10.1097/00003086-199407000-00014.
- Butt U, Rashid MS, Temperley D, Crank S, Birch A, Freemont AJ, et al. Muscle regeneration following repair of the rotator cuff. Bone Joint J 2016;98–B:1389-94. https://doi.org/10.1302/0301-620X.98B10.37231.
- Blencowe NS, Mills N, Cook JA, Donovan JL, Rogers CA, Whiting P, et al. Standardizing and monitoring the delivery of surgical interventions in randomized clinical trials. Br J Surg 2016;103:1377-84. https://doi.org/10.1002/bjs.10254.
- Cook JA. The challenges faced in the design, conduct and analysis of surgical randomised controlled trials. Trials 2009;10. https://doi.org/10.1186/1745-6215-10-9.
- Stewart DW, Shamdasani PN, Rook DW. Focus Groups Theory and Practice. Thousand Oaks, CA: SAGE Publications Ltd; 2007.
- Jones J, Hunter D. Consensus methods for medical and health services research. BMJ 1995;311:376-80. https://doi.org/10.1136/bmj.311.7001.376.
- Kitzinger J. Qualitative research. Introducing focus groups. BMJ 1995;311:299-302. https://doi.org/10.1136/bmj.311.7000.299.
- Braun V, Clarke V. Successful Qualitative Research: A Practical Guide for Beginners. London: SAGE Publications Ltd; 2013.
- Green J, Thorogood N, Green J, Thorogood N. Qualitative Methods for Health Research. London: SAGE Publications Ltd; 2014.
- Chopra SS. MSJAMA: Industry funding of clinical trials: benefit or bias?. JAMA 2003;290:113-14. https://doi.org/10.1001/jama.290.1.113.
- Laterre PF, François B. Strengths and limitations of industry vs. academic randomized controlled trials. Clin Microbiol Infect 2015;21:906-9. https://doi.org/10.1016/j.cmi.2015.07.004.
- Suvarna V. Investigator initiated trials (IITs). Perspect Clin Res 2012;3:119-21. https://doi.org/10.4103/2229-3485.103591.
- Kaur G, Hutchison I, Mehanna H, Williamson P, Shaw R, Tudur Smith C. Barriers to recruitment for surgical trials in head and neck oncology: a survey of trial investigators. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2013-002625.
- Harrop E, Kelly J, Griffiths G, Casbard A, Nelson A. Published on behalf of the BOLERO Trial Management Group (TMG). Why do patients decline surgical trials? Findings from a qualitative interview study embedded in the Cancer Research UK BOLERO trial (Bladder cancer: Open versus Lapararoscopic or RObotic cystectomy). Trials 2016;17. https://doi.org/10.1186/s13063-016-1173-z.
- Wade J, Donovan JL, Lane JA, Neal DE, Hamdy FC. It’s not just what you say, it’s also how you say it: opening the ‘black box’ of informed consent appointments in randomised controlled trials. Soc Sci Med 2009;68:2018-28. https://doi.org/10.1016/j.socscimed.2009.02.023.
- Mills EJ, Seely D, Rachlis B, Griffith L, Wu P, Wilson K, et al. Barriers to participation in clinical trials of cancer: a meta-analysis and systematic review of patient-reported factors. Lancet Oncol 2006;7:141-8. https://doi.org/10.1016/S1470-2045(06)70576-9.
- Bower P, King M, Nazareth I, Lampe F, Sibbald B. Patient preferences in randomised controlled trials: conceptual framework and implications for research. Soc Sci Med 2005;61:685-95. https://doi.org/10.1016/j.socscimed.2004.12.010.
- Wartolowska K, Judge A, Hopewell S, Collins GS, Dean BJ, Rombach I, et al. Use of placebo controls in the evaluation of surgery: systematic review. BMJ 2014;348. https://doi.org/10.1136/bmj.g3253.
- Murphy MK, Black NA, Lamping DL, McKee CM, Sanderson CF, Askham J, et al. Consensus development methods, and their use in clinical guideline development. Health Technol Assess 1998;2. https://doi.org/10.3310/hta2030.
- Cuthbertson BH, Campbell MK, MacLennan G, Duncan EM, Marshall AP, Wells EC, et al. Clinical stakeholders’ opinions on the use of selective decontamination of the digestive tract in critically ill patients in intensive care units: an international Delphi study. Crit Care 2013;17. https://doi.org/10.1186/cc13096.
- Kirkham JJ, Boers M, Tugwell P, Clarke M, Williamson PR. Outcome measures in rheumatoid arthritis randomised trials over the last 50 years. Trials 2013;14. https://doi.org/10.1186/1745-6215-14-324.
- Kearney A, Williamson P, Young B, Bagley H, Gamble C, Denegri S, et al. Priorities for methodological research on patient and public involvement in clinical trials: a modified Delphi process. Health Expect 2017;20:1401-10. https://doi.org/10.1111/hex.12583.
- Edwards PJ, Roberts I, Clarke MJ, Diguiseppi C, Wentz R, Kwan I, et al. Methods to increase response to postal and electronic questionnaires. Cochrane Database Syst Rev 2009;3. https://doi.org/10.1002/14651858.MR000008.pub4.
- NIHR . Involve n.d. www.invo.org.uk/ (accessed 12 December 2019).
- Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis 1957;16:494-502. https://doi.org/10.1136/ard.16.4.494.
- L’Insalata JC, Warren RF, Cohen SB, Altchek DW, Peterson MG. A self-administered questionnaire for assessment of symptoms and function of the shoulder. J Bone Joint Surg Am 1997;79:738-48. https://doi.org/10.2106/00004623-199705000-00014.
- Hayes K, Walton JR, Szomor ZR, Murrell GA. Reliability of five methods for assessing shoulder range of motion. Aust J Physiother 2001;47:289-94. https://doi.org/10.1016/S0004-9514(14)60274-9.
- Hamada K, Yamanaka K, Uchiyama Y, Mikasa T, Mikasa M. A radiographic classification of massive rotator cuff tear arthritis. Clin Orthop Relat Res 2011;469:2452-60. https://doi.org/10.1007/s11999-011-1896-9.
- Thomazeau H, Rolland Y, Lucas C, Duval JM, Langlais F. Atrophy of the supraspinatus belly. Assessment by MRI in 55 patients with rotator cuff pathology. Acta Orthop Scand 1996;67:264-8. https://doi.org/10.3109/17453679608994685.
- Sugaya H, Maeda K, Matsuki K, Moriishi J. Functional and structural outcome after arthroscopic full-thickness rotator cuff repair: single-row versus dual-row fixation. Arthroscopy 2005;21:1307-16. https://doi.org/10.1016/j.arthro.2005.08.011.
Appendix 1 The EMBASE search strategy
| Searches | Results | |
|---|---|---|
| 1 | exp rotator cuff rupture/ | 5732 |
| 2 | exp rotator cuff injury/ | 8726 |
| 3 | exp tendon injury/ | 20,086 |
| 4 | (rotator cuff tear or rotator cuff rupture or rotator cuff injur* or supraspinatus tear or supraspinatus rupture or supraspinatus injur* or infraspinatus tear or infraspinatus rupture or infraspinatus injur* or subscapularis tear or subscapularis rupture or subscapularis injur* or tendon tear or tendon rupture or tendon injur* or shoulder pain or shoulder injur*).mp. | 38,603 |
| 5 | or/1-4 | 39,799 |
| 6 | exp tissue repair/ | 17,952 |
| 7 | exp shoulder surgery/ | 4863 |
| 8 | (tissue repair or shoulder surgery or augment*).mp. | 212,917 |
| 9 | exp tissue scaffold/ | 11,559 |
| 10 | exp extracellular matrix/ | 99,144 |
| 11 | exp bioprosthesis/ | 7140 |
| 12 | exp allograft/ | 40,591 |
| 13 | exp autograft/ | 13,831 |
| 14 | exp surgical mesh/ | 12,582 |
| 15 | exp acellular dermal matrix/ | 1282 |
| 16 | (tissue scaffold or extracellular matrix or bioprosthesis or allograft or autograft or surgical mesh or acellular dermal matrix or “GraftJacket” or “Zimmer Collagen Repair Patch” or “Permacol” or “TissueMend” or “BioBlanket” or “Conexa” or “AlloPatch” or “Shelhigh Encuff Patch” or “OrthADAPT” or “Restore” or “CuffPatch” or “Polytape” or “SportMesh” or “Arthelon” or “Gore-tex” or “BioFiber” or “STR Grafts” or “Lars Ligament” or “X-repair”).mp. | 321,825 |
| 17 | or/6-16 | 533,208 |
| 18 | 5 and 17 | 3914 |
| 19 | Clinical trial/ | 1,042,043 |
| 20 | Randomized controlled trial/ | 481,803 |
| 21 | Randomization/ | 84,993 |
| 22 | Single blind procedure/ | 29,844 |
| 23 | Double blind procedure/ | 141,452 |
| 24 | Crossover procedure/ | 55,396 |
| 25 | Placebo/ | 333,461 |
| 26 | Randomi?ed controlled trial$.tw. | 155,939 |
| 27 | Rct.tw. | 23,487 |
| 28 | Random allocation.tw. | 1668 |
| 29 | Randomly allocated.tw. | 27,352 |
| 30 | Allocated randomly.tw. | 2233 |
| 31 | (allocated adj2 random).tw. | 860 |
| 32 | Single blind$.tw. | 19,262 |
| 33 | Double blind$.tw. | 178,171 |
| 34 | ((treble or triple) adj blind$).tw. | 698 |
| 35 | Placebo$.tw. | 254,195 |
| 36 | Prospective study/ | 401,796 |
| 37 | Retrospective study/ | 538,437 |
| 38 | Longitudinal study/ | 109,396 |
| 39 | (Case control adj (study or studies)).tw. | 103,770 |
| 40 | (Cohort adj (study or studies)).tw. | 187,964 |
| 41 | or/19-40 | 2,619,904 |
| 42 | 18 and 41 | 794 |
| 43 | limit 42 to dd = 20060401-20170228 | 370 |
Appendix 2 Systematic review supplementary tables
| Study (first author and year of publication; location) | Design | Intervention | Stated eligibility criteria | Size | Follow-up | Outcomes | ||
|---|---|---|---|---|---|---|---|---|
| Recruiteda | Analysed | Primary | Secondary | |||||
| Randomised comparative studies | ||||||||
| Barber 2012;26 USA | RCT | GRAFTJACKET-augmented repair vs. no augmentation | Aged 18–75 years | NR | 42 | MRA at 12 or 24 months | Repair failure | Constant, UCLA, ASES |
| Large (> 3-cm wide and two tendon involvement) RC tears | Clinical evaluation at 6 and 12 months; annually thereafter | |||||||
| Primary RC repair | ||||||||
| Amenable to arthroscopic repair | ||||||||
| Good preoperative movement of contralateral arm | ||||||||
| Ability to perform postoperative exercises | ||||||||
| Ability to read and understand English for PROMs | ||||||||
| Willingness to participate in postoperative follow-up | ||||||||
| No massive (> 5 cm) or subscapularis tears | ||||||||
| No inflammatory disease, autoimmune disease, cancer, highly communicable disease or active infection | ||||||||
| Non-smokers only | ||||||||
| Bryant 2016;65 Canada | RCT | Restore-augmented repair vs. no augmentation | All patients scheduled for RC repair | 62 | 62 | MRA at 12 months | Repair failure | WORC, ASES, Constant, SST, SF-36 |
| Able to repair defect with a residual defect of ≤ 1 cm or < 1 cm of medialisation | ||||||||
| No other shoulder disease; grades II–IV SLAP lesion, Bankart lesion, Hill–Sachs lesion, ≥ grade 3 OAb | ||||||||
| No significant shoulder girdle paralysis | Clinic evaluation at 1.5, 3, 6, 12, 18 and 24 months | |||||||
| No systemic or active joint infection | ||||||||
| No major medical or psychiatric illness or developmental handicap | ||||||||
| No previous shoulder surgery (except acromioplasty or diagnostic arthroscopy) | ||||||||
| Ability to read and understand English | ||||||||
| Willingness to be assessed for 1 year after surgery | ||||||||
| Iannotti 2006;35 USA | RCT | Restore-augmented repair vs. no augmentation | Large or massive tears of supraspinatus and infraspinatus tendons on preoperative MRI | 32 | 30 | MRA at 12 months | Repair failure | PENN, SF-36 |
| Aged > 18 years | ||||||||
| Tear of ≥ 3 months’ duration | ||||||||
| Fully repairable tear – determined intraoperatively | Clinical scores, mean 14 months (range 12–26.5 months) | |||||||
| No prior shoulder surgery | ||||||||
| No glenohumeral arthritis, frozen shoulder or cervical spine disease | ||||||||
| Leuzinger 2016;63 Switzerland | RCT | GRAFTJACKET vs. Artelon vs. Restore | Primary or revision RC repair | 92 | 89 | MRI at 6 months | Repair failure, Constant, SSV | – |
| Stage > 2 fatty degeneration of supraspinatus according to Goutallier et al.115,125 | Clinical evaluation at 6 and 36 months | |||||||
| No history of glenohumeral OA | ||||||||
| Repairable tear not requiring bridging with a patch | ||||||||
| At least 3 years’ follow-up | ||||||||
| Non-randomised comparative studies | ||||||||
| Ciampi 2014;40 Italy | Comparative observational study | Repol Angimesh-augmented repair vs. TUTOPATCH-augmented repair vs. no augmentation | Preoperative MRI evidence of a full-thickness tear involving two tendons | N/A | 152 | US at 12 months | UCLA | VAS, repair failure |
| Postoperative residual retraction of 2 cm | ||||||||
| Stage 1 or 2 fatty degeneration according to Goutallier et al.115,125 | ||||||||
| Failure of 6-month non-operative management consisting of physical therapy and anti-inflammatory medications | ||||||||
| Duration of symptoms for at least 3 months | ||||||||
| No other shoulder pathology requiring additional procedures; grades II–IV SLAP lesion, Bankart lesion, biceps tenodesis | Clinical scores at 2 and 35 months | |||||||
| No glenohumeral OA, inflammatory arthritis or any rheumatic condition | ||||||||
| No cortisone injections within 12 weeks of surgery | ||||||||
| No contralateral shoulder injuries | ||||||||
| Gilot 2015;42 USA | Comparative observational study | Arthroflex-augmented repair vs. no augmentation | Patient is scheduled for primary RC repair | 40 | 35 | US and clinical score at 1.5, 3, 6, 12 and 24 months | Repair failure | SF-12, ASES, VAS, WORC, shoulder activity-level survey |
| Large to massive rotator cuff tear on MRI | ||||||||
| Aged 18–85 years | ||||||||
| Patient is willing and able to provide scores for the study | ||||||||
| No known allergy to the augmentation material | ||||||||
| No drug, solvent or alcohol addiction | ||||||||
| No bacteraemia, systemic or surgical site infection | ||||||||
| No pregnant or nursing patients | ||||||||
| No history of autoimmune disease | ||||||||
| No personal beliefs prohibiting use of grafts | ||||||||
| Ito 2003;66 Japan | Comparative observational study | Fascia lata allograft vs. no augmentation | Large or massive cuff tears on MRI or pneumoarthrography | 28 | 21 | Final follow-up (range 2–8 years) | Japanese Orthopaedic Association shoulder surgery score, ROM (degrees) | – |
| Pain and loss of function despite conservative therapy | ||||||||
| Jeon 2017;67 Republic of Korea | Comparative observational study | Long head of biceps vs. no augmentation | L-shaped rotator cuff tears | N/A | 64 | MRI at 6 months | ASES, Constant, VAS, strength (NR) | – |
| Minimum follow-up period of 2 years | US at 12 months | |||||||
| No revision surgery | Clinical evaluation at 3, 6 and 12 months and final follow-up (range 24–40 months) | |||||||
| No subscapularis tendon tears | ||||||||
| No glenohumeral OA or instability | ||||||||
| Maillot 2018;64 France | Comparative observational study | Conexa vs. standard repair vs. debridement only | Large to massive RC tear on MRI or CTA | 32 | 32 | Clinical evaluation at 3, 6, 12 and 24 months | Constant | VAS, ROM (degrees) |
| Failure of non-operative management consisting of a period of relative rest, non-steroidal anti-inflammatory medication, physiotherapy > 3 months and > 2 corticosteroids | ||||||||
| Functional impairment or unacceptable pain for a minimum of 3 months | ||||||||
| Stage 2 or 3 fatty degeneration according to Goutallier et al.115,125 | ||||||||
| No glenohumeral OA or prior ipsilateral shoulder surgery | ||||||||
| Mori 2013;33 Japan | Comparative observational study | Tensor fascia lata vs. no augmentation | Irreparable large or massive RC tear with pain and functional disability refractory to conservative treatment | N/A | 48 | MRI, NR | Repair failure | Constant, ASES, UCLA, VAS |
| Stage 3–4 fatty degeneration of supraspinatus and stage 1–2 degeneration of infraspinatus according to Goutallier et al.115,125 | ||||||||
| Intact teres minor tendon | ||||||||
| Availability of MRI to evaluate the integrity of the rotator cuff tendons and/or autografts preoperatively and postoperatively | ||||||||
| Minimum follow-up period of 24 months | ||||||||
| Absence of the drop-arm sign | Clinical evaluation at 6, 12 and 24 months | |||||||
| Absence of stage 3 or 4 fatty degeneration of infraspinatus | ||||||||
| Stage 1 or fatty degeneration of supraspinatus were excluded | ||||||||
| Absence of full-thickness subscapularis tendons | ||||||||
| No history of surgery, nerve palsy, glenohumeral OA, diabetes or symptom onset following motor vehicle accident | ||||||||
| Mori 2015;68 Japan | Comparative observational study | Tensor fascia lata and grade 1–2115,125 infraspinatus fatty atrophy vs. tensor fascia lata and grade 3–4115,125 infraspinatus fatty atrophy | Irreparable large to massive RC tear | N/A | 45 | MRI, NR | Repair failure | Constant, ASES, ROM |
| Pain and disability refractory to non-surgical treatment (oral anti-inflammatory medications, corticosteroid injections and physical therapy) | Clinical evaluation at 6, 12 and 24 months | |||||||
| Stage 3–4 fatty degeneration of supraspinatus according to Goutallier et al.115,125 | ||||||||
| Intact teres minor tendon | ||||||||
| < 75% fatty degeneration of infraspinatus | ||||||||
| Availability of MRI to evaluate the integrity of the rotator cuff tendons and/or autografts preoperatively and postoperatively | ||||||||
| Minimum follow-up period of 24 months | ||||||||
| Absence of the drop-arm sign | ||||||||
| No history of surgery, nerve palsy, glenohumeral OA, diabetes or symptom onset following motor vehicle accident | ||||||||
| No full subscapularis tears | ||||||||
| Tempelaere 2017;69 France | Comparative observational study | Quadriceps tendon vs. no augmentation | Massive RC tears | 80 | 50 | Final follow-up (range 12–116 months) | Constant, SSV, strength (kg) | – |
| Patients aged < 70 years | ||||||||
| Pain and loss of strength refractory to medical treatment (≥ 1 injection, rehabilitation session) | ||||||||
| No stage 3–4 fatty degeneration of supraspinatus or infraspinatus according to Goutallier et al.115,125 | ||||||||
| No history of ipsilateral shoulder surgery, dislocation, fracture, glenohumeral OA, diabetes or symptom onset following motor vehicle accident | ||||||||
| Vitali 2015;43 Italy | Comparative observational study | Repol Angimesh and long head of biceps-augmented repair vs. no augmentation | MRI evidence of a full-thickness tear involving two tendons | N/A | 120 | MRI at 12 months | UCLA | Repair failure, VAS, range of motion (degrees), strength (kg) |
| Stage 1 or 2 fatty degeneration according to Goutallier et al.115,125 | Clinical evaluation at 3 and 36 months | |||||||
| Patients with pain and a deficit in elevation, not responding to physiotherapy | ||||||||
| Intraoperative evidence of irreparable rotator cuff lesion | ||||||||
| Minimum follow-up of 3 years after surgery | ||||||||
| Active and motivated patients | ||||||||
| No other shoulder pathology requiring additional procedures: grades II–IV SLAP lesion, Bankart lesion, biceps tenodesis | ||||||||
| No glenohumeral OA, inflammatory arthritis or any rheumatic condition | ||||||||
| No cortisone injections within 12 weeks of surgery | ||||||||
| No contralateral shoulder injuries | ||||||||
| Walton 2007;41 Australia | Comparative observational study | Restore-augmented repair vs. no augmentation | Poor-quality tendon or a large to massive full-thickness tear of a tendon that could be attached to the greater tuberosity after appropriate mobilisation techniques | NR | 31 | MRI at 24 months | Repair failure, pain and function questionnaire,150 systematic shoulder examination,151 strength (N) | – |
| Intact subscapularis tendon | Clinical evaluation at 3, 6 and 24 months | |||||||
| Yoon 2016;71 Republic of Korea | Comparative observational study | Bone marrow stimulation and allocover-augmented repair vs. no augmentation | Massive RC tears | 87 | 75 | MRI at 12 months | VAS, UCLA, Constant, ASES, SST, repair failure | – |
| Persistent severe pain and disability | ||||||||
| Unresponsive to ≥ 6 months of non-operative treatment | ||||||||
| Repairable RC tears | ||||||||
| Minimum follow-up of 1 year after surgery | Clinical evaluation at 12 months and at the final follow-up (range 14–43 months) | |||||||
| No advanced glenohumeral OA (≥ stage 4, Hamada et al.152) | ||||||||
| No prior surgery to affect shoulder | ||||||||
| No contralateral shoulder lesions | ||||||||
| Non-comparative studies | ||||||||
| Agrawal 2012;72 USA | Non-comparative observational study | Allopatch HD | Primary RC tears ≥ 3 cm | N/A | 14 | MRI at 1–2 years |
Repair failure, Constant Flex SF |
– |
| Recurrent RC tears of any size | Clinical evaluation at 12 months | |||||||
| Arthroscopic repair undertaken | ||||||||
| Audenaert 2006;73 Belgium | Non-comparative observational study | MERSILENE | Primary massive full-thickness tears of two or more tendons, measuring > 4 cm in maximal diameter | 41 | 41 | US and clinical evaluation, mean 43 months (range 24–86 months) | Repair failure, Constant | – |
| Irreparable by simple suture | ||||||||
| Open repair undertaken | ||||||||
| Inability to elevate arm beyond 90° after 3 months, despite maximal conservative treatment | ||||||||
| Badhe 2008;74 UK | Non-comparative observational study | Zimmer collagen repair patch | MRI or US evidence of RC tears ≥ 5 cm involving both the supraspinatus and the infraspinatus tendons | 10 | 10 | MRI and US at ‘final follow-up’, mean 54 months (range 36–60 months) | Constant, repair failure | – |
| Refractory to a trial of non-operative management, including physiotherapy and steroid injections | Clinical evaluation at 12 months and ‘final follow-up’ | |||||||
| Bektaser 2010;75 Turkey | Non-comparative observational study | Coracoacromial ligament | (Eligibility criteria not explicitly stated) | N/A | 46 | Clinical evaluation at 1, 3 and 12 months (range NR) | Constant, acromiohumeral distance | – |
| Treated for a rotator cuff tear between 2003 and 2009 | ||||||||
| Bond 2008;76 USA | Non-comparative observational study | GRAFTJACKET | MRI evidence RC tears ≥ 5 cm and/or two tendon tears | N/A | 16 | MRI at 3 and 12 months | UCLA, Constant, SST, pain score, repair failure | – |
| Irreparable tears – determined at prior arthroscopy | Clinical evaluation at 3, 6 and 12 months and at the ‘final follow-up’, mean 26.7 months (range 12–38 months) | |||||||
| Burkhead 2007;77 USA | Non-comparative observational study | GRAFTJACKET | Massive (two or more tendons plus ≥ 5 cm) or recurrent RC tears | N/A | 17 | MRI/CTA and clinical evaluation, mean 14.4 months (range NR) | UCLA, pain, repair failure | – |
| Repairable tears only | ||||||||
| No active infection | ||||||||
| Cho 2014;78 Republic of Korea | Non-comparative observational study | Permacol | Posterosuperior massive RC tear (≥ 5 cm or two or more tendons), confirmed by MRI and arthroscopy | 5 | 5 | MRI at 6 months | VAS, UCLA, ASES, repair failure | – |
| Inability to reduce the residual cuff to the anatomic | Clinical evaluation at the ‘final follow-up’, mean 20.6 months (range 14–27 months) | |||||||
| Active individuals aged ≤ 60 years | ||||||||
| Unresponsive to > 3 months of non-operative treatment | ||||||||
| No prior shoulder surgery | ||||||||
| Able to comply with the postoperative rehabilitation programme | ||||||||
| Anterosuperior massive RC tears were excluded | ||||||||
| No irreparable RC tears – could be only partially repaired despite full mobilisation | ||||||||
| No superior humeral head migration | ||||||||
| No stage 3–4 fatty degeneration according to Goutallier et al.115,125 | ||||||||
| Consigliere 2017;79 UK | Non-comparative observational study | DX reinforcement matrix | Large (> 3 cm) and massive (more than two tendons) RC tears | 10 | 10 | Clinical evaluation at 3, 6 and 12 months | Constant, OSS, VAS | – |
| Repairable RC tears only | ||||||||
| Poor tissue quality only | ||||||||
| Patients will achievable objectives (pain relief and improved function) | ||||||||
| No evidence of cuff arthropathy | ||||||||
| No signs of glenohumeral OA | ||||||||
| No stage 4 fatty degeneration according to Goutallier et al.115,125 | ||||||||
| No active infections | ||||||||
| Encalada-Diaz 2011;80 Mexico | Non-comparative observational study | Polycarbonate polyurethane patch | Full-thickness tear of supraspinatus or infraspinatus tendon and intact subscapularis | 10 | 10 | MRI and US at 6 and 12 months | SST, VAS, ASES, UCLA, SF-12, repair failure | – |
| Clinical evaluation at 0.5, 1, 3, 6 and 12 months | ||||||||
| Flury 2012;81 Germany | Non-comparative observational study | GRAFTJACKET or Arthroflex | Symptomatic revision RC tear with poor-quality tendon (degeneration or delamination) | N/A | 8 | US or MRI at 6 months | Constant, OSS, SSV | – |
| Aged > 60 years with unfavourable comorbidities (massive rupture, diabetes, steroid therapy) | Clinical evaluation at 6 or 9 months | |||||||
| No irreparable RC tear | ||||||||
| Giannotti 2014;82 Italy | Non-comparative observational study | Zimmer collagen repair patch | (Eligibility criteria not explicitly stated) | N/A | 9 | US, MRI and clinical evaluation, mean 36 months (range 30–45 months) | Repair failure, ASES, Constant, strength (BMRC), electromyography | – |
| Massive RC tear with minimum follow-up of 30 months | ||||||||
| Gupta 2012;83 USA | Non-comparative observational study | GRAFTJACKET | Full-thickness RC tear with > 5-cm retraction on preoperative MRI | 24 | 24 | US, mean 36 months (range NR) | VAS, ASES, SF-12, ROM (degrees), strength (BMRC), repair failure | – |
| Unresponsive to > 6 months of non-operative treatment, including physiotherapy and non-steroidal anti-inflammatories | Clinical evaluation, mean 36 months (range 29–42 months) | |||||||
| Inability to reduce the residual cuff to the anatomic | ||||||||
| Ability to fully participate in the postoperative rehabilitation | ||||||||
| No glenohumeral OA and/or cuff tear arthropathy | ||||||||
| No stage 3–4 fatty degeneration according to Goutallier et al.115,125 | ||||||||
| No prior RCR | ||||||||
| Gupta 2013;84 USA | Non-comparative observational study | Conexa | Full-thickness RC tear with > 5-cm retraction and/or more than two tendons full-thickness RC tear visualised during arthroscopy | 26 patients, 27 shoulders | 26 patients, 27 shoulders | US and clinical evaluation, mean 32 months (range 24–40 months) | VAS, ASES, SF-12, ROM (degrees), strength (BMRC), repair failure | – |
| Unresponsive to > 6 months of non-operative treatment, including physiotherapy and non-steroidal anti-inflammatories | ||||||||
| Inability to reduce the residual cuff to the anatomic | ||||||||
| Ability to fully participate in the postoperative rehabilitation | ||||||||
| No glenohumeral OA and/or cuff tear arthropathy | ||||||||
| No stage 3–4 fatty degeneration according to Goutallier et al.115,125 | ||||||||
| Hirooka 2002;85 Japan | Non-comparative observational study | GORE-TEX-expanded PTFE patch | NR | 27 patients, 28 shoulders | 27 patients, 28 shoulders | Clinical evaluation, mean 44 months (range 24–72 months) | Japanese Orthopaedic Association shoulder surgery score, strength (kg) | – |
| Lederman 2016;86 USA | Non-comparative observational study | Conexa | Aged 40–70 years | 68 | 61 | MRI at 6 and 12 months | ASES, Constant, SST, repair failure | – |
| Repairable primary large (3–5 cm) RC tears | ||||||||
| ≥ 90° movement of the non-operative arm | ||||||||
| Able to perform postoperative exercises | ||||||||
| Able to return for all scheduled and required study visits | ||||||||
| No irreparable tears – inability to approximate the tendon to the tuberosity without tension | ||||||||
| No subscapularis tears | Clinical evaluation at 6, 12 and 24 months | |||||||
| No stage 3–4 fatty degenerationc | ||||||||
| No prior RC repair on the affected shoulder | ||||||||
| No patients with inflammatory disease, autoimmune disease, cancer, insulin-dependent diabetes, chronic steroid use, malnourishment, active infection, history of alcohol or drug abuse, significant mental illness, tobacco user within last 6 months or ASA class 4 or 5 | ||||||||
| Can walk without aids | ||||||||
| No known allergy to the augmentation material | ||||||||
| Lenart 2015;87 USA | Non-comparative observational study | X-repair | Massive RC tears (two or more tendons) repaired with X-repair patch | N/A | 13 | Clinical evaluation, mean 18 months (range 14.4–20.4 months) | ASES, PENN, SANE, repair failure | – |
| Primary or revision RC surgery | ||||||||
| No history of instability, moderate to severe glenohumeral OA or shoulder surgery within the follow-up period | ||||||||
| Malcarney 2005;54 Australia | Non-comparative observational study | Restore | A poor quality of deficient tendon | N/A | 25 | NR | Early complications | – |
| Five patients also met the criteria for a concurrent comparative trial (i.e. Walton et al., 200741) | ||||||||
| Marberry 2013;88 USA | Non-comparative observational study | Artelon | Large or massive RC tear diagnosed on MRI | 17 | 16 | MRI, NR | Constant, WORC, SF36, repair failure | – |
| Pain and insufficient muscle function for ≥ 3 months | Clinical evaluation at 3, 6 and 12 months | |||||||
| Reparable tendon of poor quality, determined at the time of surgery | ||||||||
| No evidence of active infection, significant OA in the shoulder, chronic dislocation or glenohumeral OA | ||||||||
| No systemic corticosteroids, chemotherapeutics or major medical conditions | ||||||||
| Metcalf 2002;89 USA | Non-comparative observational study | Restore | (Eligibility criteria not explicitly stated) | N/A | 12 | Clinical evaluation at 2 years | UCLA, SST, SF-36. ROM (degrees), strength (BMRC) | – |
| Massive RC tears (> 5 cm2) with retraction medial to glenoid | ||||||||
| Significant atrophy of supraspinatus and infraspinatus on preoperative MRI | ||||||||
| Modi 2013;90 UK | Non-comparative observational study | GRAFTJACKET | Irreparable large or massive RC tears (≥ 3 cm) | 61 | 61 | Clinical evaluation at 3, 6 and 12 months and yearly thereafter | OSS, VAS, ROM (degrees), strength (BMRC) | – |
| No history of inflammatory or autoimmune disease | ||||||||
| Patients undergoing RC repair after arthroplasty were excluded | ||||||||
| Moore 2006;91 USA | Non-comparative observational study | Cadaveric allograft | Irreparable, massive RC tears (two or more tendons) | N/A | 32 | MRI, mean 33.7 months (range 3–124 months) | Repair failure, UCLA | – |
| Clinical evaluation, mean 31.3 months (range 1–123 months) | ||||||||
| Nada 2010;92 UK | Non-comparative observational study | Dacron | Full-thickness massive RC tear (> 5 cm plus two or more tendons) on MRI | 21 | 21 | MRI and clinical evaluation, mean 36 months (range 30–46 months) | Constant, VAS, ROM(degrees), strength (BMRC), satisfaction | – |
| Pain and disability despite conservative treatment | ||||||||
| A functional deltoid muscle | ||||||||
| Primary or revision (three cases) RC repairs | ||||||||
| Compliance with postoperative rehabilitation | ||||||||
| No history of cuff tear arthropathy with stiffness or infection, or any neurological condition effecting the shoulder girdle | ||||||||
| Neumann 2017;93 USA | Non-comparative observational study | Conexa | Irreparable massive RC tear (> 5 cm) on MRI | 85 shoulders, 84 patients | 61 shoulders, 60 patients | US and clinical evaluation, mean 50.3 months (range 24–63 months) | Modified ASES, VAS, ROM(degrees), strength (BMRC) | – |
| Primary or revisions (eight cases) RC repairs | ||||||||
| Failure of 6 months non-operative management (non-steroidal anti-inflammatories and/or physical therapy) | ||||||||
| Able to participate in post-operative physical therapy | ||||||||
| No glenohumeral OA, cuff arthropathy, > 50% fatty infiltration of supraspinatus on MRI | ||||||||
| Petrie 2013;94 UK | Non-comparative observational study | LARS | Symptomatic massive RC clinically and radiologically | 53 shoulders, 50 patients | 31 shoulders, 28 patients | Clinical evaluation at 4 and 24 months | OSS | – |
| Stage 3–4 fatty degeneration according to Goutallier et al.115,125 | ||||||||
| Not amenable to primary arthroscopic repair | ||||||||
| No patients aged > 75 years with arthritis | ||||||||
| Petri 2016;95 USA | Non-comparative observational study | Arthroflex | Open revision of large to massive posterosuperior RC tears with biological augmentation | N/A | 13 | MRI, mean 9.9 months (range 0.3–26.3 months) | ASES, QuickDASH, SANE, SF-12, repair failure | – |
| Patients with concomitant SLAP tears, OA, biceps pathology or subscapularis tears were included | ||||||||
| No stage 3–4 fatty degeneration according to Goutallier et al.115,125 | Clinical evaluation, mean 30 months (range 24–48 months) | |||||||
| Patient who underwent primary-augmented repair, arthroscopic-augmented repair or revision of a prior augmented repair were excluded | ||||||||
| Petriccioli 2013;96 Italy | Non-comparative observational study | SportMesh™ | (Eligibility criteria not explicitly stated) | N/A | 10 | US and clinical evaluation, mean 23 months (range 12–34 months) | Constant, DASH, VAS, repair failure | – |
| Open repair of subscapularis tendon | ||||||||
| Phipatanakul 2009;97 USA | Non-comparative observational study | Restore | Rotator cuff tears that could not be advanced to the native footprint or to reinforce thin attritional tissues | 11 | 11 | MRA, mean 25 months (range 14–38 months) | UCLA, ASES, repair failure | – |
| Clinical evaluation, mean 26 months (range 14–38 months) | ||||||||
| Proctor 2014;98 USA | Non-comparative observational study | X-repair | Massive RC tears (two or more tendon tears) | 18 | 18 | US or MRI, NR | ASES, repair failure | – |
| Failure of non-operative treatment | Clinical evaluation at 3, 6 and 12 months and at the ‘final follow-up’, mean 42 months (range 35–47 months) | |||||||
| No evidence of adhesive capsulitis | ||||||||
| Rhee 2008;99 Republic of Korea | Non-comparative observational study | Long head of biceps | Massive (> 5 cm) RC tears at arthroscopy | N/A | 31 | MRI, NR | Constant, UCLA, SST, VAS, ROM (degrees), strength (kg) | – |
| No history of SLAP lesion, acromioclavicular arthritis requiring distal clavicle resection, glenohumeral OA or neural damage prior shoulder surgery | Clinical evaluation at 1.5, 3, 6 and 12 months and at the ‘final follow-up’, mean 32 months (range 24–67 months) | |||||||
| Rotini 2011;100 Italy | Non-comparative observational study | Acellular human dermal matrix | Aged < 55 years | N/A | 5 | MRI, NR | Repair failure, Constant | – |
| Healthy with high functional demands | ||||||||
| Large to massive tears61 | ||||||||
| Tendon retraction of < 3 according to Thomazeau et al.153 | ||||||||
| No stage 3–4 fatty degeneration according to Goutallier et al.115,125 | Clinical evaluation, mean NR (range 12–18 months) | |||||||
| ≥ 1-year follow-up | ||||||||
| No OA degeneration (even mild), frozen shoulder, symptomatic acromioclavicular arthritis, autoimmune connective tissue disease or allergy to penicillin or pork | ||||||||
| Able to engage with rehabilitation regimen | ||||||||
| Sano 2010;101 Japan | Non-comparative observational study | Long head of biceps | (Eligibility criteria not explicitly stated) | N/A | 14 | MRI and clinical evaluation, mean 28 months (range 48–79 months) | Repair failure, Japanese Orthopaedic Association shoulder surgery score | – |
| Irreparable massive RC tears (two or more tendons) with concomitant long head of biceps pathology | ||||||||
| > 12 months’ follow-up available | ||||||||
| Schlegel 2018;103 USA | Non-comparative observational study | Collagen sheet | Chronic, degenerative partial (≥ 25%) thickness tear of supraspinatus tendon | 33 | 33 | MRI and clinical evaluation at 3 months and 1 year | Repair failure, Constant, ASES | – |
| Aged ≥ 21 years | ||||||||
| Unresponsive to conservative therapy (analgesia, physiotherapy or injections) for > 3 months | ||||||||
| No patients with full-thickness tears, acute injuries, previous surgery on same shoulder, shoulder instability, chondromalacia (> grade 3), > grade 2 cuff muscle fatty infiltration, severe calcification, IDDM, Workers’ Compensation, smokers, hypersensitivity to bovine collagen, genetic collagen disease, autoimmune disease, immunodeficiency or chronic inflammatory disorders | ||||||||
| No oral steroid use for 2 months (or i.m. steroid use for 1 month) | ||||||||
| Scheibel 2007;102 Germany | Non-comparative observational study | Humeral periosteum | Degenerative symptomatic full-thickness supraspinatus tears | 20 | 20 | MRI at 12 months | Repair failure, Constant, SST | – |
| High functional demand | Clinical evaluation, mean 14.4 months (range 12–21 months) | |||||||
| Tendon retraction of < 3 according to Thomazeau et al.153 | ||||||||
| No stage 3–4 fatty degeneration according to Goutallier et al.115,125 | ||||||||
| No partial RC tears, traumatic history, prior surgery to affected shoulder or cuff tear arthropathy (acromiohumeral distance < 6 mm) | ||||||||
| Sclamberg 2004;104 USA | Non-comparative observational study | Restore | Symptomatic, atrophic, retracted large and massive (two or more tendon) RC tears on MRI and confirmed at surgery | N/A | 11 | MRI and clinical evaluation, mean, NR (range 6–10 months) | ASES, repair failure | – |
| Sears 2015;105 USA | Non-comparative observational study | GRAFTJACKET or Tissuemend or Conexa | (Eligibility criteria not explicitly stated) | 31 | 24 | MRI or US, mean 4.2 years (range, NR) | Repair failure, ASES, SANE | – |
| Full-thickness RCRs | Clinical evaluation, mean 4.2 years (range 30–112 months) | |||||||
| Revision surgery | ||||||||
| Venouziou 2013;106 USA | Non-comparative observational study | GRAFTJACKET | Massive (> 5 cm) RC tear | N/A | 14 | Clinical evaluation at 1.5, 3, 6 and 12 months and at the ‘final follow-up’, mean 30.2 months (range 18–52 months) | VAS, ASES, ROM (degrees), strength (BMRC) | – |
| Not capable of mobilisation | ||||||||
| ≥ 18 months’ follow-up was available | ||||||||
| Wong 2010;32 USA | Non-comparative observational study | GRAFTJACKET | (Eligibility criteria not explicitly stated) | N/A | 45 | Clinical evaluation, mean, NR (range 24–68 months) | UCLA, WORC, ASES | – |
| Large and massive RC tears | ||||||||
| Motivated, intelligent, younger patients with disabling pain but intact biceps tendons | ||||||||
| Functioning subscapularis muscle | ||||||||
| No glenohumeral OA, immunocompromised or heavy smokers | ||||||||
| Study (first author and year of publication) | Intervention | Shoulder-specific functional scores, mean (± SD or range) | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ASES | Constant | OSS | PENN | SST | UCLA | WORC | ||||||||||||||||
| Baseline | Intermediate | Finala | Baseline | Intermediate | Finala | Baseline | Intermediate | Finala | Baseline | Intermediate | Finala | Baseline | Intermediate | Finala | Baseline | Intermediate | Finala | Baseline | Intermediate | Finala | ||
| Randomised comparative studies | ||||||||||||||||||||||
| Barber 201226 | GRAFTJACKET | 48.5 (± NR) | 2 years: 98.9 (± 4.2) | 41.0 (± NR) | 2 years: 91.9 (± 9.2) | 13.3 (± NR) | 2 years: 28.2 (± 2.1) | |||||||||||||||
| Control | 46.0 (± NR) | 2 years: 94.8 (± 14.2) | 45.8 (± NR) | 2 years: 85.3 (± 11) | 15.9 (± NR) | 2 years: 28.3 (± 3.0) | ||||||||||||||||
| p = 0.035 | p = 0.008 | p = 0.43 | ||||||||||||||||||||
| Bryant 201665 | Restore | 52.2 (± 3.3) | 1 year: 83.3 (± 2.6) | 2 years: 84.6 (± 2.9) | 58.4 (± 3.9) | 1 year: 72.8 (± 3.0) | 2 years: 79.3 (± 3.5) | 47.2 (± 4.3) | 1 year: 78.5 (± 3.2) | 2 years: 78.5 (± 3.6) | 40.2 (± NR) | 1 year: 78.6 (± NR) | 2 years: 78.8 (± NR) | |||||||||
| Control | 54.6 (± 3.7) | 1 year: 84.8 (± 2.9) | 2 years: 87.9 (± 3.1) | 46.8 (± 4.2) | 1 year: 79.5 (± 3.1) | 2 years: 87.5 (± 3.7) | 40.7 (± 4.8) | 1 year: 82.1 (± 3.6) | 2 years: 85.4 (± 4.0) | 40.1 (± NR) | 1 year: 79.8 (± NR) | 2 years: 82.2 (± NR) | ||||||||||
| p = 0.69 | p = 0.44 | p = 0.14 | p = 0.13 | p = 0.48 | p = 0.21 | p = 0.73 | p = 0.46 | |||||||||||||||
| Iannotti 200635 | Restore | 42 (± NR) | 14 months: 83 (IQR 70–92) | |||||||||||||||||||
| Control | 34 (± NR) | 14 months: 91 (IQR 81–99) | ||||||||||||||||||||
| p = 0.07 | ||||||||||||||||||||||
| Leuzinger 201663 | GRAFTJACKET | 47.3 (± 7.3) | 6 months: 81.4 (± 11.4) | |||||||||||||||||||
| Artelon | 46.2 (± 9.6) | 6 months: 81.3 (± 11.1) | ||||||||||||||||||||
| Restore | 41.0 (± 9.6) | 6 months: 78.5 (± 12.3) | ||||||||||||||||||||
| p = NR | ||||||||||||||||||||||
| Non-randomised comparative studies | ||||||||||||||||||||||
| Ciampi 201440 | Repol Angimesh | 10.9 (± 1.5) | 2 months: 19.1 (± 2.0) | 36 months: 24.6 (± 3.2) | ||||||||||||||||||
| TUTOPATCH | 10.4 (± 1.2) | 2 months: 11.4 (± 1.5) | 36 months: 14.7 (± 2.0) | |||||||||||||||||||
| Control | 10.7 (± 1.1) | 2 months: 11.3 (± 1.5) | 36 months: 14.9 (± 2.0) | |||||||||||||||||||
| p < 0.001b | ||||||||||||||||||||||
| Gilot 201542 | Arthroflex | 63.8 (± 13.8) | 12 weeks: 60.6 (± 8.3) 24 weeks: 64.3 (± 7.8) | 96 weeks: 88.9 (± 4.8) | 54 (± 8) | 12 weeks: 52 (± 6) 24 weeks: 81 (± 12) | 96 weeks: 84 (± 4) | |||||||||||||||
| Control | 60.3 (± 9.5) | 12 weeks: 57.6 (± 8.8) 24 weeks: 60.4 (± 10.1) | 96 weeks: 72.6 (± 11.9) | 58 (± 5) | 12 weeks: 59 (± 8) 24 weeks: 64 (± 6) | 96 weeks: 66 (± 5) | ||||||||||||||||
| p = 0.59; p = 0.08 | p = 0.048 | p = 0.36; p = 0.05 | p = 0.04 | |||||||||||||||||||
| Ito 200366 | Fascia lata | |||||||||||||||||||||
| Control | ||||||||||||||||||||||
| Jeon 201767 | Biceps tendon | 52.8 (± 10.6) |
12 weeks: 60.1 (± 15.8) 24 weeks: 76.3 (± 10.6) |
29 months: 88.2 (± 6.9) | 43.2 (± 9.9) | 12 weeks: 54.9 (± 12.8) 24 weeks: 72.2 (± 12.8) | 29 months: 86.8 (± 6.2) | |||||||||||||||
| Control | 53.0 (± 11.8) | 12 weeks: 63.0 (± 10.2) 24 weeks: 75.7 (± 11.5) | 29 months: 87.4 (± 7.2) | 44.3 (± 11.3) |
12 weeks: 56.1 (± 10.8) 24 weeks: 71.6 (± 9.7) |
29 months: 84.0 (± 7.9) | ||||||||||||||||
| p = 0.901 | p = 0.742 | |||||||||||||||||||||
| Maillot 201864 | Conexa | 43.6 (± 11.0) | 12 weeks: 49.4 (± 14.1) 24 weeks: 59.0 (± 18.8) | 24 months: 75.8 (± 8.6) | ||||||||||||||||||
| Repair only | 45.7 (± 11.6) | 12 weeks: 52.4 (± 10.2) 24 weeks: 64.1 (± 8.5) | 24 months: 74.7 (± 4.3) | |||||||||||||||||||
| Debridement | 44.1 (± 11.6) | 12 weeks: 54.9 (± 10.0) 24 weeks: 62.2 (± 5.9) | 24 months: 64.2 (± 5.0) | |||||||||||||||||||
| p = 1.0c; p = 0.002d | ||||||||||||||||||||||
| Mori 201333 | Fascia lata | 40.8 (± 13.0) | 12 months: 84.9 (± 8.1) | 35 months: 94.1 (± 5.4) | 37.4 (± 8.1) | 12 months: 73.6 (± 6.6) | 35 months: 81.1 (± 5.7) | 14.3 (± 2.9) | 12 months: 28.6 (± 4.3) | 35 months: 32.6 (± 3.4) | ||||||||||||
| Control | 41.8 (± 11.3) | 12 months: 84.2 (± 19.7) | 35 months: 85.7 (± 14.1) | 36.3 (± 9.9) | 12 months: 72.9 (± 16.8) | 35 months: 69.9 (± 10.3) | 13.7 (± 3.1) | 12 months: 27.3 (± 6.1) | 35 months: 29.8 (± 5.3) | |||||||||||||
| p = 0.021 | p = 0.001 | p = 0.094 | ||||||||||||||||||||
| Mori 201568 | Fascia lata and grade 1–2 infraspinatus atrophy | 41.6 (± 13.0) | 41 months: 91.3 (± 6.7) | 38.7 (± 9.1) | 41 months: 78.4 (± 5.7) | |||||||||||||||||
| Fascia lata and grade 3–4 infraspinatus atrophy | 39.9 (± 9.9) | 67 months: 73.6 (± 10.1) | 40.7 (± 0.7) | 67 months: 63.9 (± 8.0) | ||||||||||||||||||
| p < 0.001 | p < 0.0001 | |||||||||||||||||||||
| Tempelaere 201769 | Quadriceps tendon | 42.9 (17–72) | 58 months: 67.5 (41–87) | |||||||||||||||||||
| Control | 45.7 (22–63) | 55 months: 72.1 (21–90) | ||||||||||||||||||||
| p = NS | ||||||||||||||||||||||
| Vitali 201543 | Repol Angimesh | 10.8 (± 1.4) | 3 months: 20.9 (± 1.3) | 36 months: 24.6 (± 3.3) | ||||||||||||||||||
| Control | 10.9 (± 1.2) | 3 months 11.3 (± 1.4) | 36 months: 14.7 (± 2.0) | |||||||||||||||||||
| p = unclear | ||||||||||||||||||||||
| Walton 200741 | Restore | |||||||||||||||||||||
| Control | ||||||||||||||||||||||
| Yoon 201671 | Allocover | 50.4 (± 15.3) | 1 year: 84.5 (± 12.2) | 2 years: 82.5 (± 11.2) | 56.3 (± 9.4) | 1 year: 79.0 (± 9.5) | 2 years: 78.3 (± 12.8) | 4.1 (± 2.3) | 1 year: 8.8 (± 2.9) | 2 years: 8.8 (± 2.9) | 23.0 (± 5.5) | 1 year: 29.5 (± 4.1) | 2 years: 29.5 (± 4.1) | |||||||||
| Control | 48.9 (± 16.0) | 1 year: 84.2 (± 13.1) | 2 years: 82.0 (± 15.3) | 53.6 (± 13.2) | 1 year: 80.0 (± 11.6) | 2 years: 75.7 (± 15.7) | 4.1 (± 2.6) | 1 year: 10.0 (± 2.7) | 2 years: 10.0 (± 2.7) | 23.7 (± 5.6) | 1 year: 29.8 (± 4.5) | 2 years: 29.8 (± 4.5) | ||||||||||
| p = 0.92 | p = 0.88 | p = 0.72 | p = 0.47 | p = 0.09 | p = 0.60 | p = 0.79 | p = 0.10 | |||||||||||||||
| Non-comparative studies | ||||||||||||||||||||||
| Agrawal 201272 | Allopatch | 49.7 (13–74) | 1 year: 81.1 (45–92) | |||||||||||||||||||
| p = 0.009 | ||||||||||||||||||||||
| Audenaert 200673 | MERSILENE | 25.7 (20–39) | 43 months: 72.1 (34–89) | |||||||||||||||||||
| p < 0.001 | ||||||||||||||||||||||
| Badhe 200874 | Zimmer collagen repair patch | 41.5 (13–78) | 1 year: 62.5 (50–97) | 4.5 years: 62.2 (50–80) | ||||||||||||||||||
| p = 0.0003 | p = NR | |||||||||||||||||||||
| Bektaser 201075 | Coracohumeral ligament | 45 (± NR) | 1 year: 80 (± NR) | |||||||||||||||||||
| p = NR | ||||||||||||||||||||||
| Bond 200876 | GRAFTJACKET | 53.8 (39–70) | 27 months: 84 (69–100) | 18.4 (11–25) | 27 months: 30.4 (22–35) | |||||||||||||||||
| p = 0.0001 | p = 0.0001 | |||||||||||||||||||||
| Burkhead 200777 | GRAFTJACKET | 9.06 (± NR) | 1.2 years: 26.12 (± NR) | |||||||||||||||||||
| p < 0.001 | ||||||||||||||||||||||
| Cho 201478 | Permacol | 39.4 (± NR) | 21 months: 86.4 (± NR) | 15.4 (± NR) | 21 months: 31.2 (± NR) | |||||||||||||||||
| p = 0.04 | p = 0.04 | |||||||||||||||||||||
| Consigliere 201779 | DX reinforcement matrix | 54 (± 4) | 3 months: 65 (± 12) | 7 months: 75 (± 11) | 30 (± 8) | 3 months: 38.7 (± 12.7) | 7 months: 47 (± 10) | |||||||||||||||
| p < 0.05 | p < 0.05 | p > 0.05 | p < 0.05 | |||||||||||||||||||
| Encalada-Diaz 201180 | Polycarbonate polyurethane patch | 44 (± NR) | 6 months: 61.3 (± NR) | 12 months: 73.3 (± NR) | 3.6 (± NR) | 6 months: 6.5 (± NR) | 12 months: 7.7 (± NR) | |||||||||||||||
| p = 0.008 | p < 0.001 | p = 0.02 | p = 0.004 | |||||||||||||||||||
| Flury 201281 | GRAFTJACKET or Artelon | 51 (29–74) | 6 months: 57 (43–71) | 21 (7–38) | 6 months: 38 (19–45) | |||||||||||||||||
| p > 0.05 | p < 0.05 | |||||||||||||||||||||
| Giannotti 201482 | Zimmer collagen repair patch | 38 (± NR) | 34 months: 79 (± NR) | 42 (± NR) | 34 months: 73 (± NR) | |||||||||||||||||
| p = NR | p = NR | |||||||||||||||||||||
| Gupta 201283 | GRAFTJACKET | 66.6 (± NR) | 3 years: 88.7 (± NR) | |||||||||||||||||||
| p = 0.0003 | ||||||||||||||||||||||
| Gupta 201384 | Conexa | 62.7 | 32 months: 91.8 (± 13.3) | |||||||||||||||||||
| p = 0.0007 | ||||||||||||||||||||||
| Hirooka 200285 | GORE-TEX PTFE | |||||||||||||||||||||
| Lederman 201686 | Conexa | 48.7 (± 20.2) | 1 year: 85.4 (± 18.4) | 2 years: 90.4 (± 15.3) | 45.4 (± 15.2) | 1 year: 68.7 (± 11.3) | 2 years: 71.7 (± 9.6) | 5.0 (± 2.6) | 1 year: 9.9 (± 2.7) | 2 years: 10.6 (± 2.2) | ||||||||||||
| p < 0.0001 | p < 0.0001 | p < 0.0001 | p < 0.0001 | p < 0.0001 | p < 0.0001 | |||||||||||||||||
| Lenart 201587 | X-repair | 32.8 (± 9.5) | 18 months: 74.2 (± 5.0) | 50.9 (± 4.2) | 18 months: 77.6 (± 5.3) | |||||||||||||||||
| p = 0.0001 | p < 0.005 | |||||||||||||||||||||
| Malcarney 200554 | Restore | |||||||||||||||||||||
| Marberry 201388 | Artelon | 17.1 (± 6.4) | 1 year: 67.1 (± 11.6) | 34 (± 18) | 1 year: 86 (± 12) | |||||||||||||||||
| p = 0.002 | p = 0.002 | |||||||||||||||||||||
| Metcalf 200289 | Restore | NR | NR | 9.3 (± NR) | 24 months: 19.9 (± NR) | |||||||||||||||||
| p = 0.01 | p = 0.01 | |||||||||||||||||||||
| Modi 201390 | GRAFTJACKET | 26 (8–40) | 1 year: 42 (21–48) | |||||||||||||||||||
| p = 0.001 | ||||||||||||||||||||||
| Moore 200691 | Cadaveric allograft | 12.1 (± NR) | 31 months: 26.1 (± NR) | |||||||||||||||||||
| p < 0.001 | ||||||||||||||||||||||
| Nada 201092 | Dacron | 46.7 (39–61) | 36 months: 84.5 (52–96) | |||||||||||||||||||
| p < 0.001 | ||||||||||||||||||||||
| Neumann 201793 | Conexa | NR | 50 months: 87.8 | |||||||||||||||||||
| p = NR | ||||||||||||||||||||||
| Petrie 201394 | LARS | 46.7 (± NR) | 3.3 years: 30.6 (± NR) | |||||||||||||||||||
| p < 0.0001 | ||||||||||||||||||||||
| Petri 201695 | Arthroflex | 64.5 (± 10.0) | 2.5 years: 86.0 (± 12.3) | |||||||||||||||||||
| p = 0.005 | ||||||||||||||||||||||
| Petriccioli 201396 | SportMesh | 47.0 (± NR) | 23 months: 69.0 (± NR) | |||||||||||||||||||
| p = NR | ||||||||||||||||||||||
| Phipatanakul 200997 | Restore | 36.3 (± NR) | 26 months: 71.8 (± NR) | 13.9 (± NR) | 26 months: 25.7 (± NR) | |||||||||||||||||
| p < 0.01 | p < 0.01 | |||||||||||||||||||||
| Proctor 201498 | X-Repair | 26 (± NR) | 3 months: 57 6 months: 68 12 months: 71 months | 42 months: 70 (± NR) | ||||||||||||||||||
| p < 0.05e | p < 0.05e | |||||||||||||||||||||
| Rhee 200899 | Biceps tendon | 48.4 (8–70) | 32 months: 81.8 (37–96) | 4.2 (1–8) | 32 months: 10.2 (8–12) | 12.5 (6–19) | 32 months: 31.1 (9–35) | |||||||||||||||
| p < 0.001 | p < 0.001 | |||||||||||||||||||||
| Rotini 2011100 | Acellular human dermal matrix | 64 (55–75) | > 1 year: 88 (77–95) | |||||||||||||||||||
| p = NR | ||||||||||||||||||||||
| Sano 2010101 | Biceps tendon | |||||||||||||||||||||
| Scheibel 2007102 | Periosteum | 51.8 (25–68) | 14 months: 80.9 (73–89) | 4.5 (1–8) | 14 months: 10.7 (8–12) | |||||||||||||||||
| p < 0.001 | p < 0.001 | |||||||||||||||||||||
| Schlegel 2018103 | Collagen sheet | 57.0 (± 3.2)f | 3 months: 73.9 (± 3.2) f | 1 year: 89.1 (± 2.8)f | 57.1 (± 2.8)f | 3 months: 62.3 (± 5.2)f | 1 year: 81.4 (± 2.2)f | |||||||||||||||
| p = 0.0001 | p < 0.0001 | p = 0.122 | p < 0.0001 | |||||||||||||||||||
| Sclamberg 2004104 | Restore | 60.3 (40–75) | > 6 months: 58.4 (30–95) | |||||||||||||||||||
| p = 0.70 | ||||||||||||||||||||||
| Sears 2015105 | GRAFTJACKET or Tissuemend or Conexa | 4.2 years: 67.2 (± 27.9) | ||||||||||||||||||||
| p = NR | ||||||||||||||||||||||
| Venouziou 2013106 | GRAFTJACKET | 23.8 (15–34) | 30 months: 72.3 (52–94) | |||||||||||||||||||
| p = 0.001 | ||||||||||||||||||||||
| Wong 201032 | GRAFTJACKET | NR | > 2 years: 84.1 (± NR) | 18.4 (± NR) | > 2 years: 27.5 (± NR) | NR | > 2 years: 75.2 (± NR) | |||||||||||||||
| p = NR | p < 0.001 | p = NR | ||||||||||||||||||||
| Study (first author and year of publication) | Intervention | Safety population (n) | Recurrence of rotator cuff tears | Reported? (yes/no) | Complications | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Definition | Imaging | Time of imaging, months (range) | Absolute risk of re-tear, % | p-value | Superficial infection, n (%) | Deep infection, n (%) | Inflammatory response, n (%) | Other, n (%) | |||||
| Randomised comparative studies | |||||||||||||
| Barber 201226 | GRAFTJACKET | 22 | Incomplete excursion of the repaired tendon to the greater tuberosity with gadolinium leakage | MRA | 14.5 (12–14) | 15 | < 0.01 | Yes | 0 (0) | 0 (0) | 0 (0) | Shoulder bursitis, 1 (5) | |
| Control | 20 | 60 | 2 (10) | 0 (0) | 0 (0) | Biceps rupture, 1 (5) | |||||||
| Post-traumatic fibrosis, 1 (5) | |||||||||||||
| Bryant 201665 | Restore | 34 | A > 5-mm increase in size of any immediate postoperative defect | MRA | 12 (NR) | 53 | 0.33 | Yes | 0 (0) | 1 (3) | 0 (0) | Biceps rupture, 1 (3) | |
| Unexplained fever, 2 (6) | |||||||||||||
| Control | 28 | 65 | 1 (4) | 0 (0) | 0 (0) | Shoulder manipulation, 1 (4) | |||||||
| Ianotti 200635 | Restore | 15 |
Not healed: tear size ≥ size on preoperative MRI Partially healed: smaller tear than preoperative MRI |
MRA | 12 (NR) | 73 | 0.11 | Yes | 0 (0) | 0 (0) | 2 (13) | Wound erythema, 1 (8) | |
| Control | 15 | 40 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |||||||
| Leuzinger 201663 | GRAFTJACKET | 29 | Complete integrity of the repair with no tendon retraction | MRI | 6 (NR) | 23 | 0.08 | Yes | 0 (0) | 0 (0) | 1 (3) | 0 (0) | |
| Artelon | 33 | 27 | 0 (0) | 0 (0) | 1 (3) | 0 (0) | |||||||
| Restore | 30 | 39 | 0 (0) | 0 (0) | 1 (3) | 0 (0) | |||||||
| Non-randomised comparative studies | |||||||||||||
| Ciampi 201440 | Repol Angimesh | 52 | NR | US | 12 (NR) | 17 | 0.001a | Yes | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| TUTOPATCH | 49 | 51 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |||||||
| Control | 51 | 41 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |||||||
| Gilot 201542 | Arthroflex | 20 | NR | US | 24 (NR) | 10 | 0.048 | Yes | 1 (5) | 0 (0) | 0 (0) | 0 (0) | |
| Control | 15 | 26 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |||||||
| Ito 200366 | Fascia lata | 30 | NR | MRI | NR | 0 | NR | Yes | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Control | 17 | 18 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |||||||
| Jeon 201767 | Biceps tendon | 31 | Complete tendon detachment from the footprint of the greater tuberosity or loss of continuity in the midsubstance portion | MRI | 6 (NR) | 32 | 0.55 | No | – | – | – | – | |
| Control | 33 | 39 | – | – | – | – | |||||||
| Maillot 201864 | Conexa | 11 | N/A | N/A | N/A | N/A | N/A | Yes | 0 (0) | 1 (9) | 0 (0) | Shoulder stiffness, 4 (4) | |
| Repair alone | 12 | 1 (8) | 0 (0) | 0 (0) | 0 (0) | ||||||||
| Debridement | 9 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | ||||||||
| Mori 201333 | Fascia lata | 24 | High signal intensity or tendon discontinuity on one or more T2-weighted images | MRI | NR | 21 | 0.015 | Yes | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Control | 24 | 42 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |||||||
| Mori 201568 | Fascia lata and grade 1–2 infraspinatus atrophy | 26 | High signal intensity or tendon discontinuity on one or more T2-weighted images (complete defect) or insufficient thickness (partial defect) | MRI | NR | 27 | < 0.001 | Yes | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Fascia lata and grade 3–4 infraspinatus atrophy | 19 | 89 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |||||||
| Tempelaere 201769 | Quadriceps tendon | 23 | N/A | N/A | N/A | N/A | N/A | Yes | 0 (0) | 0 (0) | 0 (0) | Knee pain, 12 (52) | |
| Patellar fracture, 2 (8) | |||||||||||||
| Quads tendon tear, 1 (4) | |||||||||||||
| Nerve injury, 1 (4) | |||||||||||||
| Knee stiffness, 1 (4) | |||||||||||||
| Control | 27 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | ||||||||
| Vitali 201543 | Repol Angimesh | 60 | NR | MRI | 12 (NR) | 15 | NR | Yes | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Control | 60 | 40 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |||||||
| Walton 200741 | Restore | 16 | Thickness of supraspinatus immediately medial to insertion. 0 mm if re-torn | MRI | 24 (NR) | 60 | NR | Yes | 0 (0) | 0 (0) | 4 (21) | 0 (0) | |
| Control | 16 | 58 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |||||||
| Yoon 201671 | Allocover | 21 | Sugaya classification grades 4 and 5 were considered re-tears154 | MRI | 12 (NR) | 19 | 0.036 | Yes | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Control | 54 | 46 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |||||||
| Non-comparative studies | |||||||||||||
| Agrawal 201272 | Allopatch | 14 | Sugaya classification grades 4 and 5154 | MRI | 16.8 (12–24) | 14 | N/A | Yes | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Audenaert 200673 | MERSILENE | 41 | NR | US | NR | 7 | N/A | No | – | – | – | – | |
| Badhe 200874 | Zimmer collagen repair patch | 10 | An identifiable gap between the greater tuberosity and the graft | US/MRI | 54 (36–60) | 20 | N/A | Yes | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Bektaser 201075 | Coracoacromial ligament | 46 | N/A | N/A | N/A | N/A | N/A | No | – | – | – | – | |
| Bond 200876 | GRAFTJACKET | 16 | NR | MRI | 12 (NR) | 19 | N/A | Yes | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Burkhead 200777 | GRAFTJACKET | 17 | NR | MRI/CTA | 14 (NR) | 25 | N/A | Yes | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Cho 201478 | Permacol | 5 | Fluid-equivalent signal or discontinuity of the rotator cuff in ≥ 1 T2-weighted images | MRI | 8 (6–12) | 20 | N/A | Yes | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Consigliere 201779 | DX reinforcement matrix | 10 | N/A | N/A | N/A | N/A | N/A | No | – | – | – | – | |
| Encalada-Diaz 201180 | Polycarbonate polyurethane patch | 10 | NR | MRI | 12 (NR) | 10 | N/A | Yes | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Flury 201281 | GRAFTJACKET or Arthroflex | 8 | NR | US/MRI | 6 (NR) | Full: 13 Partial: 25 | N/A | Yes | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Giannotti 201482 | Zimmer collagen repair patch | 9 | NR | US/MRI | 34 (30–45) | 0 | N/A | No | – | – | – | – | |
| Gupta 201283 | GRAFTJACKET | 24 | Not intact: a full-thickness defect at the graft–tendon or graft–humerus interface | US | 36 (NR) | Full: 0 | N/A | Yes | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Partially intact: a partial-thickness defect at the graft–tendon or graft–humerus interface | Partial: 26 | ||||||||||||
| Gupta 201384 | Conexa | 26 | As above (Gupta 201283) | US | 32 (24–40) | Full: 5 | N/A | Yes | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Partial: 22 | |||||||||||||
| Hirooka 200285 | GORE-TEX PTFE | 27 | NR | Arthrography | NR | 11 | N/A | Yes | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Lederman 201686 | Conexa | 61 | Complete: ≥ 80% of the size of the original tear in the sagittal plane | MRI | 12 (NR) | Full: 15 | N/A | Yes | 1 (2) | 0 (0) | 0 (0) | Superficial haematoma, 1 (2) | |
| Partial: tears between 1 cm and 80% of original size | Partial: 34 | ||||||||||||
| Lenart 201587 | X-Repair | 13 | NR | MRI | 18 (14–20) | 62 | N/A | No | – | – | – | – | |
| Malcarney 200554 | Restore | 25 | NR | Arthroscopy | NR | 16 | N/A | Yes | 0 (0) | 0 (0) | 4 (16) | 0 (0) | |
| Marberry 201388 | Artelon | 17 | NR | MRI | NR | 18 | N/A | Yes | 1 (6) | 1 (6) | 0 (0) | 0 (0) | |
| Metcalf 200289 | Restore | 12 | NR | MRI | NR | 8 | N/A | Yes | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Moore 200691 | Cadaveric allograft | 32 | NR | MRI | 34 (3–124) | 100 | N/A | Yes | 0 (0) | 1 (3) | 1 (3) | 0 (0) | |
| Modi 201390 | GRAFTJACKET | 61 | NR | MRI | 12 | Full: 0 | N/A | Yes | 0 (0) | 1 (2) | 0 (0) | Persistent pain, 1 (2) | |
| Partial: 17 | |||||||||||||
| Nada 201092 | Dacron | 21 | NR | MRI | 36 (30–46) | 19 | N/A | Yes | 0 (0) | 1 (5) | 0 (0) | 0 (0) | |
| Neumann 201793 | Conexa | 60 | Not intact: full-thickness defect at graft–tendon or graft–humerus interface | US | 50 (24–63) | Full: 5 | N/A | Yes | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Partial: less than full-thickness defect at graft–tendon or graft–humerus interface | Partial: 3 | ||||||||||||
| Petrie 201394 | LARS | 31 | N/A | N/A | N/A | N/A | N/A | Yes | 0 (0) | 0 (0) | 0 (0) | Persistent pain, 1 (3) | |
| Shoulder stiffness, 1 (3) | |||||||||||||
| Petri 201695 | Arthroflex | 12 | NR | MRI | 9.9 (0.3–26.3) | 17 | N/A | Yes | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Petriccioli 201396 | SportMesh | 10 | Bare area between the edge of subscapularis and the bicipital groove | US | 23 (12–34) | 10 | N/A | Yes | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Coexistence of fluid in the subacromial subdeltoid bursa and/or fluid in the long head of biceps sheath | |||||||||||||
| Phipatanakul 200997 | Restore | 11 | Partially intact: smaller tear than preoperative imaging. Otherwise not stated | MRA | 25 (14–38) | 50 | N/A | Yes | 1 (9) | 0 (0) | 0 (0) | Skin reaction, 3 (27) | |
| Proctor 201498 | X-Repair | 18 | NR | US/MRI | 12 | 17 | N/A | No | – | – | – | – | |
| Rhee 200899 | Biceps tendon | 31 | Fluid-equivalent signal or non-visualisation of supra-, infra- or subscapularis tendon in one or more T2-weighted images | MRI | NR | Full: 21 | N/A | Yes | 0 (0) | 0 (0) | 0 (0) | ‘Popeye’ biceps deformity, 2 (7) | |
| Partial: 14 | |||||||||||||
| Rotini 2011100 | Acellular human dermal matrix | 5 | NR | MRI | 12 | 20 | N/A | Yes | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Sano 2010101 | Biceps tendon | 14 | Sugaya classification > grade 4 were considered re-tears154 | MRI | 28 (12–51) | 7 | N/A | Yes | 0 (0) | 0 (0) | 0 (0) | ‘Popeye’ biceps deformity, 1 (7) | |
| Scheibel 2007102 | Periosteum | 20 | Fluid equivalent signal in the way of a tendon, discontinuity or retraction | MRI | 12 | 20 | N/A | Yes | 0 (0) | 1 (5) | 0 (0) | Ectopic ossification, 4 (20) | |
| Schlegel 2018103 | Collagen sheet | 33 | NR | MRI | 3 + 12 (NR) | N/A | N/A | Yes | 1 (3) | 0 (0) | 0 (0) | Persistent pain, 1 (3) | |
| Cardiac event, 1 (3) | |||||||||||||
| Possible inflammatory response, 1 (3) | |||||||||||||
| Sclamberg 2004104 | Restore | 11 | NR | MRI | (6–12) | 90 | N/A | No | – | – | – | – | |
| Sears 2015105 | ECM | 16 | NR | US/MRI | 50 (NR) | 63 | N/A | No | – | – | – | – | |
| Venouziou 2013106 | GRAFTJACKET | 14 | N/A | N/A | N/A | N/A | N/A | Yes | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Wong 201032 | GRAFTJACKET | 45 | N/A | N/A | N/A | N/A | N/A | Yes | 0 (0) | 1 (2) | 0 (0) | 0 (0) | |
| Study (first author and year of publication) | Intervention | Pain scores, mean (SD or range) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| VAS | Other pain scales | |||||||||||
| Baseline | Intermediate | p-value | Finala | p-value | Baseline | Intermediate | p-value | Finala | p-value | |||
| Randomised comparative studies | ||||||||||||
| Iannotti 200635 | Restore | 12.5b (± NR) | 14 months: 25b (± NR) | 0.18 | ||||||||
| Control | 12.0b (± NR) | 14 months: 29b (± NR) | ||||||||||
| Non-randomised comparative studies | ||||||||||||
| Ciampi 201440 | Repol Angimesh | 8.3 (± 1.0) | 2 months: 4.9 (± 0.9) | < 0.001c | 36 months: 3.3 (± 1.1) | < 0.001c | ||||||
| TUTOPATCH | 8.3 (± 1.1) | 2 months: 6.5 (± 1.0) | 0.01c | 36 months: 4.1 (± 1.0) | < 0.001c | |||||||
| Control | 8.2 (± 1.1) | 2 months: 7.0 (± 1.1) | < 0.001c | 36 months: 3.7 (± 1.1) | < 0.001c | |||||||
| Gilot 201542 | Arthroflex | 6.8 (± 1.6) | 12 weeks: 5.3 (± 1.6) |
12 weeks: 0.52 24 weeks: 0.04 |
96 weeks: 1.3 (± 1.2) | 0.013 | ||||||
| 24 weeks: 3.9 (± 1.6) | ||||||||||||
| Control | 6.9 (± 1.1) | 12 weeks: 5.8 (± 1.1) | 96 weeks: 4.1 (± 1.1) | |||||||||
| 24 weeks: 6.8 (± 1.1) | ||||||||||||
| Ito 200366 | Fascia lata | 10.0d (± 5.6) | 2.9 years: 27.8d (± 3.6) | < 0.01c | ||||||||
| Control | 9.2d (± 2.9) | 4.2 years: 28.3d (± 3.3) | < 0.005c | |||||||||
| Jeon 201767 | Biceps tendon | 5.1 (± 1.4) | 12 weeks: 3.7 (± 1.5) | NR | 29 months: 1.0 (± 0.8) | 0.892 | ||||||
| 24 weeks: 2.2 (± 1.4) | ||||||||||||
| Control | 5.2 (± 1.4) | 12 weeks: 3.9 (± 1.6) | NR | 29 months: 0.9 (± 0.8) | ||||||||
| 24 weeks: 2.1 (± 1.2) | ||||||||||||
| Maillot 201864 | Conexa | 7.1 (± 1.2) | 12 weeks: 3.5 (± 1.3) |
12 weeks: 1.0 24 weeks: 1.0 |
24 months: 0.6 (± 0.7) | 1.0e | ||||||
| 24 weeks: 1.9 (± 1.3) | ||||||||||||
| Repair only | 6.9 (± 1.2) |
12 weeks: 3.0 (± 1.9) 24 weeks: 1.6 (± 1.3) |
24 months: 0.7 (± 0.8) | |||||||||
| Debridement | 7.2 (± 0.8) |
12 weeks: 3.2 (± 1.2) 24 weeks: 1.4 (± 1.2) |
12 weeks: 1.0 24 weeks: 1.0 |
24 months: 1.0 (± 0.8) | 0.501e | |||||||
| Mori 201333 | Fascia lata | 7.0 (± 0.9) | 12 months: 1.2 (± 0.8) | NR | 35 months: 0.3 (± 0.6) | 0.028 | ||||||
| Control | 7.0 (± 1.0) | 12 months: 1.8 (± 1.7) | 35 months: 1.2 (± 1.5) | |||||||||
| Tempelaere 201769 | Quadriceps tendon | 5.5f (0–14) | 58 months: 11.9f (3–15) | NS | ||||||||
| Control | 7.6f (5–13) | 55 months: 12.6f (5–15) | ||||||||||
| Vitali 201543 | Repol Angimesh | 8.2 (± 1.1) | 3 months: 4.9 (± 0.9) | NR | 36 months: 3.2 (± 1.1) | Uncleard | ||||||
| Control | 8.4 (± 1.0) | 3 months: 6.9 (± 1.1) | 36 months: 3.7 (± 1.0) | |||||||||
| Walton 200741 | Restore | NR | 3 months:g 9.9 (± 1.6) | < 0.01 | NR | NR | ||||||
| Control | NR | 3 months:g 4.0 (± 1.3) | NR | |||||||||
| Yoon 201671 | Allocover | 6.0 (± 1.9) | 1 year: 1.5 (± 2.1) | 0.95 | 2 years: 1.6 (± 1.7) | 0.68 | ||||||
| Control | 6.1 (± 1.5) | 1 year: 1.6 (± 1.8) | 2 years: 1.8 (± 1.9) | |||||||||
| Non-comparative studies | ||||||||||||
| Agrawal 201272 | Allopatch | 7.7f (± NR) | 1 year: 13.6 (± NR) | 0.008 | ||||||||
| Audenaert 200673 | MERSILENE | 1.3f (± NR) | 43 months: 13.1f (± NR) | < 0.001 | ||||||||
| Badhe 200874 | Zimmer collagen repair patch | 6.8f (± NR) | 4.5 years: 14 (± NR) | 0.00003 | ||||||||
| Bond 200876 | GRAFTJACKET | 4.6b (± NR) | 26 months: 9.8 (± NR) | 0.0001 | ||||||||
| Cho 201478 | Permacol | 6.8 (± NR) | 21 months: 0.8 (± NR) | 0.041 | ||||||||
| Consigliere 201779 | DX reinforcement matrix | 7.0 (± 2) | 3 months: 0.8 (± 0.8) | < 0.05 | 6 months: 0.6 (± 0.8) | < 0.05 | ||||||
| Encalada-Diaz 201180 | Polycarbonate polyurethane patch | 5.7 (2–8) | 6 months: 3.8 (NR) | 0.009 | 12 months: 2.6 (0–4) | < 0.001 | ||||||
| Gupta 201283 | GRAFTJACKET | 5.4 (± NR) | 3 years: 0.9 (± NR) | 0.0002 | ||||||||
| Gupta 201384 | Conexa | 5.1 (± NR) | 32 months: 0.4 (± 1.0) | 0.002 | ||||||||
| Hirooka 200285 | GORE-TEX PTFE | 9.1d (± NR) | 44 months: 27.7d (± NR) | < 0.0001 | ||||||||
| Marberry 201388 | Artelon | 4.5f (± 2.9) | 1 year: 11.6f (± 3.3) | 0.002 | ||||||||
| Modi 201390 | GRAFTJACKET | 7.0 (4–10) | 3.6 years: 0.8 (0–5) | 0.001 | ||||||||
| Moore 200691 | Cadaveric allograft | 2.5h (± NR) | 31 months: 7.9h (± NR) | < 0.001 | ||||||||
| Nada 201092 | Dacron | 7.0 (5–8) | 36 months: 1.0 (0–2) | < 0.001 | ||||||||
| Neumann 201793 | Conexa | 4.0 (± 2.5) | 50 months: 1.0 (± 1.6) | < 0.001 | ||||||||
| Petrie 201394 | LARS | 7.7 (± NR) | 3.3 years: 4.4 (± NR) | < 0.0001 | ||||||||
| Petri 201695 | Arthroflex | 38.6i (± 8.6) | 2.5 years: 44.6i (± 10.6) | 0.506 | ||||||||
| Petriccioli 201396 | SportMesh | 7.9 (± 1.1) | 23 months: 2.0 (± 1.9) | NR | ||||||||
| Phipatanakul 200997 | Restore | 6.6 (± NR) | 26 months: 2.2 (± NR) | < 0.01 | ||||||||
| Rhee 200899 | Biceps tendon | At rest: 2.0 (0–7) | 32 months: 0.3 (0–5) | < 0.001 | ||||||||
| On exercise: 6.6 (3–10) | 32 months: 1.4 (0–10) | < 0.001 | ||||||||||
| Sano 2010101 | Biceps tendon | 13.1d (± 2.5) | 28 months: 22.9d (± 5.1) | 0.002 | ||||||||
| Scheibel 2007102 | Periosteum | 7.9f (6–12.5) | 14 months: 14.0f (12–15) | < 0.001 | ||||||||
| Schlegel 2018103 | Collagen sheet | 4.2i (± 0.4)j | 3 months: 1.5i (± 0.3)j | < 0.001 | 12 months: 0.6f (± 0.2)j | < 0.0001 | ||||||
| Venouziou 2013106 | GRAFTJACKET | 7.4 (4–9) | 30 months: 1.7 (0–5) | 0.001 | ||||||||
| Study (first author and year of publication) | Intervention | Quality-of-life outcome score, mean (SD or range) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SF-12 | SF-36 | ||||||||||||
| Baseline | Intermediate | p-value | Finala | p-value | Baseline | Intermediate | p-value | Finala | p-value | ||||
| Randomised comparative studies | |||||||||||||
| Bryant 201665 | Restore | PCS | 40.1 (± 1.3) | 1 year: 46.6 (± 1.4) |
PCS: 0.50 MCS: 0.52 |
1 year: 47.3 (± 1.6) |
PCS: 0.56 MCS: 0.83 |
||||||
| MCS | 48.8 (± 2.2) | 1 year: 55.7 (± 1.4) | 1 year: 55.0 (± 1.2) | ||||||||||
| Control | PCS | 40.5 (± 1.5) | 1 year: 48.1 (± 1.7) | 1 year: 48.7 (± 1.7) | |||||||||
| MCS | 52.8 (± 2.4) | 1 year: 54.3 (± 1.6) | 1 year: 55.0 (± 1.2) | ||||||||||
| Iannotti 200635 | Restore | PCS | 50.3 (± NR) | 14 months: NR | NS | ||||||||
| MCS | 56.3 (± NR) | 14 months: NR | |||||||||||
| Control | PCS | 51.8 (± NR) | 14 months: NR | ||||||||||
| MCS | 51.9 (± NR) | 14 months: NR | |||||||||||
| Non-randomised comparative studies | |||||||||||||
| Gilot 201542 | Arthroflex | PCS | 29.2 (± 6.4) | 12 weeks: 29.2 (± 5.1) |
12 weeks: 0.68 24 weeks: 0.05 |
96 weeks: 42.6 (± 10.8) |
PCS: 0.05 MCS: 0.04 |
||||||
| 24 weeks: 36.2 (± 4.4) | |||||||||||||
| MCS | 42.2 (± 12.1) | 12 weeks: 45.7 (± 10.8) |
12 weeks: 0.71 24 weeks: 0.06 |
96 weeks: 64.1 (± 9.3) | |||||||||
| 24 weeks: 47.3 (± 6.5) | |||||||||||||
| Control | PCS | 30.7 (± 6.0) | 12 weeks: 30.3 (± 5.7) | 96 weeks: 31.7 (± 9.5) | |||||||||
| 24 weeks: 30.4 (± 5.0) | |||||||||||||
| MCS | 43.1 (± 8.2) | 12 weeks: 47.1 (± 11.8) | 96 weeks: 42.9 (± 10.8) | ||||||||||
| 24 weeks: 41.1 (± 8.2) | |||||||||||||
| Non-comparative studies | |||||||||||||
| Encalada-Diaz 201180 | Polycarbonate polyurethane patch | PCS | 35.6 (± NR) | 6 months: 42.5 (±NR) | 0.03 | 12 months: 40.4 (± NR) | 0.13 | ||||||
| MCS | 45.4 (± NR) | 6 months: 53.1 (±NR) | 0.10 | 12 months: 51.1 (± NR) | 0.32 | ||||||||
| Gupta 201283 | GRAFTJACKET | 48.8 (± NR) | 3 years: 56.8 (± NR) | 0.03 | |||||||||
| Gupta 201384 | Conexa | 48.4 (± NR) | 32 months: 56.6 (± 6.1) | 0.04 | |||||||||
| Marberry 201388 | Artelon | NR | 1 year: ‘positive change for physical component’ | NR | |||||||||
| Petri 201695 | Arthroflex | PCS | 44.5 (± 8.9) | 2.8 years: 52.9 (± 5.7) | 0.005 | ||||||||
| MCS | NR | NR | NR | ||||||||||
List of abbreviations
- ASES
- American Shoulder and Elbow Surgeons
- BESS
- British Elbow and Shoulder Society
- CENTRAL
- Central Register of Controlled Trials
- CI
- confidence interval
- CRD
- Centre for Reviews and Dissemination
- CRN
- Clinical Research Network
- CSAW
- Can Shoulder Arthroscopy Work?
- DARE
- Database of Abstracts of Reviews of Effects
- EQ-5D
- EuroQol-5 Dimensions
- GP
- general practitioner
- HRQoL
- health-related quality of life
- HTA
- Health Technology Assessment
- MRI
- magnetic resonance imaging
- NHS EED
- NHS Economic Evaluation Database
- OA
- osteoarthritis
- OSS
- Oxford Shoulder Score
- PARCS
- Patch Augmented Rotator Cuff Surgery
- PICO
- patient, intervention, control, outcome
- PPI
- patient and public involvement
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PROM
- patient-reported outcome measure
- RCR
- rotator cuff repair
- RCT
- randomised controlled trial
- ROBINS–I
- Risk Of Bias In Non-randomized Studies – of Interventions
- RR
- risk ratio
- SF-12
- Short Form questionnaire-12 items
- SF-36
- Short Form questionnaire-36 items
- SIS
- small intestinal submucosa
- UCLA
- University of California, Los Angeles
- UKFroST
- UK Frozen Shoulder Trial
- UKUFF
- UK Rotator Cuff Surgery
- VAS
- visual analogue scale
