Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 14/170/01. The contractual start date was in March 2016. The draft report began editorial review in November 2018 and was accepted for publication in April 2019. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2021. This work was produced by Creswell et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2021 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Social anxiety disorder (SAD) is characterised by a persistent and disproportionate fear of social situations. It is the third most frequent of all mental health disorders, with a lifetime prevalence of up to 13%. 1,2 The age at onset is typically during adolescence (median 13 years),3,4 with most people developing the condition before they reach their twenties. Indeed, studies that have focused on young people between the ages of 11 and 17 years have estimated that 0.7% and 10.9%5 of young people meet diagnostic criteria at SAD at any one point in time, with European studies (in Germany and Finland) identifying prevalence rates between 1.4% and 3.2%. 6–8
Social anxiety disorder is differentiated from normal shyness by the marked disability and interference caused in day-to-day life. For example, among adults it often has a negative impact on social relationships (e.g. friendships,9 marriages and children8) and is associated with more days off work,10 receipt of state benefits11 and more outpatient medical visits than the general population. 12 SAD is also associated with an increased risk of other mental health problems, including other anxiety and mood disorders, substance abuse and psychosis,2,13,14 and has the lowest natural recovery rate of all anxiety disorders. 15 Several of the handicaps that result from having the condition in adolescence (e.g. missed opportunities for social learning and poor educational achievement)16 cannot be overcome by treatment when the person reaches adulthood. These factors highlight the need for effective treatment for SAD in adolescence.
Currently, the most commonly delivered treatment approach for adolescents with SAD is a generic cognitive–behavioural therapy (CBT) anxiety programme that is used across a range of anxiety disorders. Unfortunately, in recent studies, young people with SAD have had significantly poorer outcomes than those with other anxiety disorders (e.g. for 7- to 17-year-olds, remission rates of 40.6% for SAD vs. 72% for other anxiety disorders). 17 However, among adults, a focused form of cognitive therapy for SAD (CT-SAD), which targets key psychological mechanisms that are known to maintain the disorder,18 achieves much higher recovery rates of up to 84% in randomised controlled trials (RCTs). 19–21 Among adults, it has also been shown to be superior (in terms of clinical effectiveness and cost-effectiveness) to traditional group CBT, guided CBT self-help, exposure therapy, interpersonal psychotherapy, psychodynamic psychotherapy and medication (selective serotonin reuptake inhibitors),22,23 and is recommended by the National Institute for Health and Care Excellence (NICE) as a first-line intervention for SAD in adults. 24
There is recent evidence that the same psychological mechanisms maintain SAD in adults and adolescents. 25–28 Therefore, adapting CT-SAD so that it is suitable for use with adolescents may significantly enhance treatment efficacy. NICE guidance also highlights that treatment for SAD in adolescents should address the need to create treatment supporting environments, by working with parents, teachers and/or peers as appropriate. 24
A recent case series in which cognitive therapy for SAD was adapted for use with adolescents (CT-SAD-A) reported excellent outcomes. 29 All adolescents (n = 5; 11–17 years) had severe SAD and achieved excellent outcomes after receiving CT-SAD-A, with overall reductions in social anxiety symptoms that were greater than the average reductions achieved with adults. Of note, all the adolescents were free of their primary diagnosis of SAD as well as comorbid mental health diagnoses post treatment. Promising findings have also come from a RCT which compared individual cognitive therapy to group CBT and an attentional control. 30 The individual cognitive therapy condition was associated with significantly greater reductions in symptoms and impairment than group CBT and the attentional control, which did not differ from each other. Notably, the cognitive therapy programme applied within this trial included a number of important departures from the Clark and Wells’ approach,31 including a focus on psychoeducation and developing a generic formulation for anxiety maintenance over the first four sessions. Nonetheless, given this evidence, it seems possible that CT-SAD-A may improve treatment outcomes for adolescents with SAD over the generic forms of CBT that are often applied. As SAD presents a risk for ongoing mental health problems, impaired educational performance, restricted employment and productivity, and increased medical needs, the successful development of a highly effective treatment for adolescent SAD also has the potential to bring direct benefits to the NHS and child and adolescent mental health services (CAMHS), as well as adult mental health services and society more broadly, by disrupting this negative trajectory.
Objective 1
This study initially set out to determine the feasibility of a RCT in routine NHS CAMHS to compare CT-SAD-A with the C.A.T. Project (a CBT programme that has been developed for adolescents with a range of anxiety disorders and that is already in use in CAMHS) for adolescents with SAD. Specifically, our aims were to train NHS CAMHS therapists to deliver the adapted treatment and assess therapist competency and young people’s outcomes; identify appropriate clinical outcome and economic measures for a subsequent definitive trial; and examine whether or not a definitive trial can be conducted on the basis of a feasibility trial that would:
-
explore the acceptability of the treatments and trial procedures
-
establish likely recruitment rates
-
establish the likely rate of treatment drop out
-
establish likely retention to research assessments post treatment and (in a subset of participants) at 3-month follow-up
-
establish if adapted CT-SAD-A can be delivered so that it is clearly distinct from the C.A.T. Project, with high levels of fidelity by practitioners and credibility with patients in both arms;
-
conduct exploratory analyses of possible outcomes for the two treatments, including changes in social anxiety symptoms and diagnostic status, depression, social functioning, school attendance, concentration in class, quality of life, health-care resource use and other outcomes identified through patient and public involvement (PPI)
-
describe negative impacts of the treatments and the trial procedures (to patients, their parents and therapists).
Objective 2
Unfortunately, during the training phase of the study, it became clear that the proposed trial would not be feasible within routine CAMHS (see Chapter 4) and, on the basis of liaison with the Study Steering Committee (SSC) and the National Institute for Health Research (NIHR), the study aims were adapted to examine the training in and delivery of CT-SAD-A in routine NHS CAMHS, in terms of therapists’ ability to deliver CT-SAD-A, young people’s outcomes, and the experiences of both participating families (young people and their parents/carers) and the therapists involved (both therapists delivering the treatment and their service managers) within a CAMHS setting. Specifically, the aims were to:
-
train NHS CAMHS therapists to deliver the adapted treatment and assess therapist competency (an independent rater is currently rating therapist competency, and these outcomes will be reported in a later publication) and young people’s outcomes
-
estimate the cost of delivering CT-SAD-A within an NHS CAMHS setting
-
understand the experience of receiving CT-SAD-A and participating in a research study within a CAMHS setting among young people and their parents
-
understand the experience of CAMHS therapists receiving training in and delivering CT-SAD-A and their experience of being part of a research study
-
understand the experiences of the CAMHS service managers in relation to supporting the training and delivery of CT-SAD-A and the accompanying research procedures within their services.
Chapter 2 Methods
Participants
Participating therapists were identified within the participating NHS trusts on the basis of meeting the following inclusion criteria:
-
currently in clinical practice within participating CAMHS
-
willing to be randomly allocated to deliver either (1) the C.A.T. project, or (2) CT-SAD-A, and to receive training and supervision for the allocated treatment approach
-
have at least 2 years’ experience of using CBT as their main treatment approach, receiving regular CBT supervision during this time
-
a minimum of 2 years working clinically with children and young people
-
have treated at least two adolescent/adult social anxiety disorder cases and 10 anxiety cases using CBT.
Young people were referred to CAMHS in the participating trusts through usual routes (e.g. by general practitioners, school nurses) for treatment of anxiety or mood disorders. Adolescents and their parents completed the NICE screening questions24 (see Appendix 1) and the Revised Children’s Anxiety and Depression Scale (RCADS) to identify potential SAD within a routine CAMHS assessment. Where adolescents ‘screened positive’, they were invited to take part in the research. An initial assessment included a structured diagnostic interview with the young person and carer [Anxiety Disorders Interview Schedule for Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, child and parent version (ADIS-C/P)]32 to establish whether or not the young person met the following criteria:
Inclusion criteria
-
Young people (aged 11–17.5 years at intake) whose primary presenting disorder was a Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), diagnosis of SAD.
-
If young people had been prescribed psychotropic medication, the dosage must have been stable for 2 months.
Exclusion criteria
-
Young people who had previously received CBT for SAD were excluded if they had received more than four sessions in which key procedures of CT-SAD-A had been used (i.e. video feedback, attention training, memory work and multiple behavioural experiments).
-
Young people with established autistic spectrum disorders [or suspected on the basis of Social Cognitions Questionnaire (SCQ)18; see Measures], learning disabilities, suicidal intent or recurrent self-harm (i.e. comorbid conditions that are likely to interfere with treatment delivery).
-
Young people with a primary presenting disorder other than SAD.
The managers/clinical leads who were involved in managing the participating therapists on a day-to-day basis were invited to take part in qualitative interviews.
Procedures
Ethics review
The study was approved by the NHS South Central – Oxford B Research Ethics Committee (REC reference: 16/SC/0315) and the University of Reading Research Ethics Committee (UREC 16/43).
Therapist training
CAMHS therapists were provided with a detailed treatment manual ahead of the training. They were also given a memory stick loaded with short video clips demonstrating many of the key steps in CT-SAD-A. Finally, they received a pack containing all worksheets needed to support CT-SAD-A. The training materials that were used in this study are freely available here: https://oxcadatresources.com.
Participating therapists completed a training programme comprising an initial 2-day workshop, focusing on the CT-SAD-A model and the key procedures involved in the first stage of therapy. Therapists were offered 6 months of weekly case supervision via Skype™ (Microsoft Corporation, Redmond, WA, USA) or telephone and a further 1-day workshop, which covered the key procedures used later in the therapy in more detail.
Supervision sessions involved a review of questionnaire measures, a detailed discussion of the previous treatment session, a discussion of any problems that had arisen and step-by-step planning for the next session. Videotaped treatment sessions were discussed on a regular basis in the supervision sessions.
Intervention: cognitive therapy for social anxiety disorder in adolescents
All young people received CT-SAD-A. Treatment was delivered in the CAMHS clinic in which the therapists usually worked, with behavioural experiments conducted in different environments, as required (e.g. in a shopping centre or a café). This therapy is based on Clark and Wells’ model of the maintenance of the disorder. 31 The treatment programme consists of 14 weekly sessions, each lasting 90 minutes, plus 2-monthly booster sessions and focuses on changing social anxiety-related beliefs and behaviours, with a particular emphasis on the four maintenance processes specified in the model. 31 These are (1) increased self-focused attention and observation (self-consciousness) and an associated decrease in observation of other people and their responses, (2) use of internal information (feelings and images) to make excessively negative inferences about how one appears to others, (3) use of overt and covert safety behaviours that prevent patients from discovering that their fears are unrealistic and interfere with the initiation and flow of social interactions, and (d) pre- and post-event processing (e.g. anticipatory worry and rumination). Given this, CT-SAD-A involves a number of components:33 (1) the development of a personalised cognitive model including the patient’s negative thoughts, self-images, focus of attention, safety behaviours and anxiety symptoms; (2) an experiential exercise to demonstrate the adverse effects of self-focused attention and safety behaviours; (3) video (and still photograph) feedback to correct negative self-imagery; (4) training in externally focused attention; (5) behavioural experiments to test patients’ negative beliefs by dropping safety behaviours and focusing attention externally on social situations and by also purposefully displaying feared behaviours or signs of anxiety (decatastrophising); (5) surveys to discover other people’s views of feared outcomes; (6) memory work (discrimination training and memory rescripting) to reduce the impact of social trauma experiences. The components of CT-SAD-A were well received by the adolescents in the case series. 29
Key adaptations were made to CT-SAD for working specifically with adolescents on the basis of previous experience from a development case series. 29 These were as follows: (1) working with peer victimisation (which is likely to involve school liaison) and (2) working with parents/carers. The degree of parental involvement varied from case to case. Typically, parents are involved at the start of treatment to learn about social anxiety and cognitive therapy and at the end of therapy to learn about their child’s relapse prevention plan and their role in supporting their child to stay well. Some parents will bring their child to sessions and will help to ensure that they complete their weekly measures. In some cases, therapists may speak with parents individually to identify and work with parental social beliefs that may interfere with their child’s progress in therapy. As described in Chapter 3, our PPI co-applicant and young people with relevant lived experience also gave feedback on their experiences of treatment, the treatment manual and the reviewed treatment materials to ensure it was appropriate and acceptable for adolescents with SAD.
Measures
Young people and their primary caregivers completed measures (1) prior to treatment, (2) at each treatment session, both to guide treatment and so that data from the last weekly session that was attended could be used to assess outcomes at the end of treatment, and (3) after the last booster session (1.16–4.63 months after the final weekly session). These time points will be referred to as ‘pre’, ‘sessional’ and ‘follow-up’, respectively, in the descriptions below. Each participant (young people, parents, therapists and service managers) who took part in the qualitative interviews was compensated for their time (£20 each).
Initial screening measures
The screening questions proposed in the NICE guideline on the identification, assessment and treatment of SAD24 were used to screen participants for social anxiety symptoms in the absence of any validated brief screening measures. The young person and their parents/carers were asked whether or not the young person gets scared about doing things with other people, whether or not they find it difficult to do things when others are watching and whether or not they ever feel they cannot do these things or try to avoid them (see Appendix 1).
The Social Communication Questionnaire (SComQ) was used to identify young people with an undiagnosed autism spectrum disorder (ASD). This is a 40-item, parent-report measure based on the Autism Diagnostic Interview Revised. It requires a ‘yes/no’ response to 19 items assessing behaviours occurring at any time throughout the young person’s life and 21 items assessing behaviours between the ages of 4 and 5 years. The questionnaire consists of three subscales: reciprocal social interaction (13 items), communication (8 items) and repetitive, restrictive behaviours and interests (RRBI) (6 items). A score above the cut-off point of 15 indicates a possible diagnosis of ASD. Therefore, young people scoring ≥ 15 were excluded from the study.
Outcome measures
The young person self-report version of the Liebowitz Social Anxiety Scale for Children and Adolescents (LSAS-CA-SR)34 was administered to assess the adolescents’ self-reported social anxiety symptom severity (at all time points: pre, sessional and follow-up). The LSAS-CA includes 24 items, rated on a scale from ‘none’ (0) to ‘severe’ (3), to assess fear and avoidance of social interaction and performance (range 0–144). The LSAS-CA has well-established psychometric properties when administered to children and young people from 7 to 18 years of age. 35 Reliable improvement in the LSAS-CA-SR is defined as a drop of 16.13 points, calculated using internal consistency data over the course of treatment. 35
Symptoms of broader anxiety disorders and depression were assessed using the Revised Children’s Anxiety and Depression Scale (RCADS),36 which is routinely collected within CAMHS as part of the Children and Young People’s Improving Access to Psychological Therapies programme (CYP IAPT) initiative. The RCADS is a 47-item child report scale that assesses symptoms of separation anxiety disorder, SAD, generalised anxiety disorder (GAD), panic disorder, obsessive compulsive disorder and major depressive disorder (MDD). Responders rate how often each item applies on a scale of 0 (‘never’) to 3 (‘always’). T-scores can be calculated according to a child’s age and sex. The RCADS has been shown to have robust psychometric properties in children and young people from 7 to 18 years of age. 37 We focused on the social anxiety subscale and the depression and GAD subscales, as these are the most common co-occurring difficulties. The RCADS was administered at all time points (pre, sessional and follow-up).
The Anxiety Disorders Interview Schedule – child and parent report (ADIS-C/P)38 is a structured diagnostic interview used to determine whether or not the young person meets diagnostic criteria for SAD and other comorbid anxiety, mood and behavioural disorders and to establish clinical severity ratings (CSR) for each disorder. The ADIS-C/P was administered to young people and their parents by research assistants (psychology graduates) trained to a high level of inter-rater reliability through observation, role play and ongoing supervision. All diagnostic interviews were discussed with an independent experienced therapist, who also assigned diagnoses and ratings. Agreement (kappa/intraclass correlation) was > 0.85 for diagnoses and CSRs across all anxiety disorders and for SAD specifically. The ADIS-C/P was used at two time points: pre and follow-up.
Concentration in class scale – young person report was used to measure the young person’s self-reported concentration in class, administered at all time points (pre, sessional and follow-up). This is a single-item self-report scale on which the young person indicates from 0 (‘not at all’) to 100 (‘totally’) how well they have been able to concentrate on what the teacher is saying and what they have been learning in class in the preceding week. This scale has been used in the recent (2016) pilot work by DC/EL, and respondents have found it to be a relevant indicator of change. 29
The CYP IAPT goals progress scale is a simple 10-point rating scale on which a young person rates the extent to which they have made progress towards their therapy goals. This scale is routinely used in both participating NHS trusts as part of the CYP IAPT initiative, and it was also administered at every therapy session (sessional time point).
Social functioning was examined using an 18 item self-report measure of social participation and social satisfaction, developed by Alden and Taylor39 for use with adults with SAD. Respondents indicate on a seven-point scale how often they have engaged in different social activities and how satisfied they have felt with their relationships with different types of people. This scale has been used in the recent pilot work by DC/EL, and young people have found it to be a relevant indicator of change. 29 It was administered at pre and follow-up and also as a mid-treatment measure at session 7.
The Outcome Rating Scale (ORS)40 comprises four simple rating scales on which the young person/parent rates how they (or their son/daughter) have been feeling over the last week (individually, interpersonally, socially and overall). This scale is routinely used in both participating NHS trusts, as part of the CYP IAPT initiative, and was administered at all time points (pre, sessional and follow-up).
Measures of treatment mechanisms
Social cognitions and attitudes were measured using the SCQ18 and the Social Attitudes Questionnaire (SAQ),18 both of which were adapted for children and adolescents. The SCQ is a 22-item questionnaire assessing SAD-related negative automatic thoughts. Each thought is rated twice. First, the respondent rates the frequency with which the thought occurred in the last week when he/she was ‘nervous or frightened’. The frequency rating scale is as follows: 1 = ’thought never occurs’, 2 = ’thought rarely occurs’, 3 = ’thought occurs during half of the times when I am anxious’, 4 = ’thought usually occurs’, 5 = ’thought always occurs when I am anxious’. Second, the respondent rates the extent to which the thought was considered to be true. The belief rating scale runs from 0 = ’I do not believe this thought’ to 100 = ’I am completely convinced this thought is true’. The SCQ has high internal consistency and discriminant validity in adults. 18 It was adapted for use with children and adolescents on the basis of PPI consultation, in that the wording was amended to be more developmentally appropriate in seven items, and a further seven items were added (specifically: ‘I will embarrass myself’; ‘People will be angry with me’; ‘I will wet myself/have diarrhoea’; ‘I will get picked on/teased’; ‘I will look stupid’; ‘I will be forced to do things I don’t want to do’; ‘People will laugh at me’). The SCQ was administered at all time points (pre, sessional and follow-up).
The SAQ is a 50-item scale that assesses beliefs that are thought to make an individual vulnerable to SAD. The beliefs were intended to fit into three broad categories: ‘excessively high performance standards’, ‘conditional beliefs’ and ‘unconditional beliefs’. However, item selection was based more on clinical experience than on an attempt to sample each category in a comprehensive manner. Each item is rated on a scale that ranges from 1 to 7: 1 = ’totally agree’, 2 = ‘agree very much’, 3 = ’agree slightly’, 4 = ’neutral’, 5 = ’disagree slightly’, 6 = ’disagree very much’, 7 = ’totally disagree’. Respondents are asked to choose the rating that ‘Best describes how you think’. The SAQ has high internal consistency and discriminant validity in adults. 18 For children and adolescents, two further items were included (‘If I make a mistake in a social situation people will laugh at me or be angry with me’; ‘If people see I am anxious I will be forced to do things I don’t want to do’) and the language was changed to be more developmentally appropriate on the basis of PPI consultation. The SAQ was administered at pre and follow-up and also as a mid-treatment measure at session 7.
Safety behaviours associated with SAD were measured using the Social Behaviours Questionnaire (SBQ)18 – adapted for children and adolescents. The SBQ is a 28-item scale assessing the use of social phobia-related safety behaviours when respondents are anxious or in a social situation. Each behaviour is rated on a four-point scale ranging from 0 to 3: 0 = ’never’, 1 = ’sometimes’, 2 = ’often’ and 3 = ’always’. The SBQ has good psychometrics properties in adults. 18 It was adapted for use with children and adolescents through the addition of four further questions (‘Wear clothes so I blend in’; ‘Seek reassurance from my friends and family’; Get other people to speak for me or do things for me’; ‘Have an excuse or ‘get out’ of planned activities’) and through changes to the wording in four other items, to be more developmentally appropriate on the basis of PPI consultation. The SBQ was administered at pre assessment and follow-up and also as a mid-treatment measure at session 7.
The final versions of the SCQ, SAQ and SBQ that were adapted for use with adolescents can be found at https://oxcadatresources.com (accessed 7 February 2019).
Participant acceptability rating
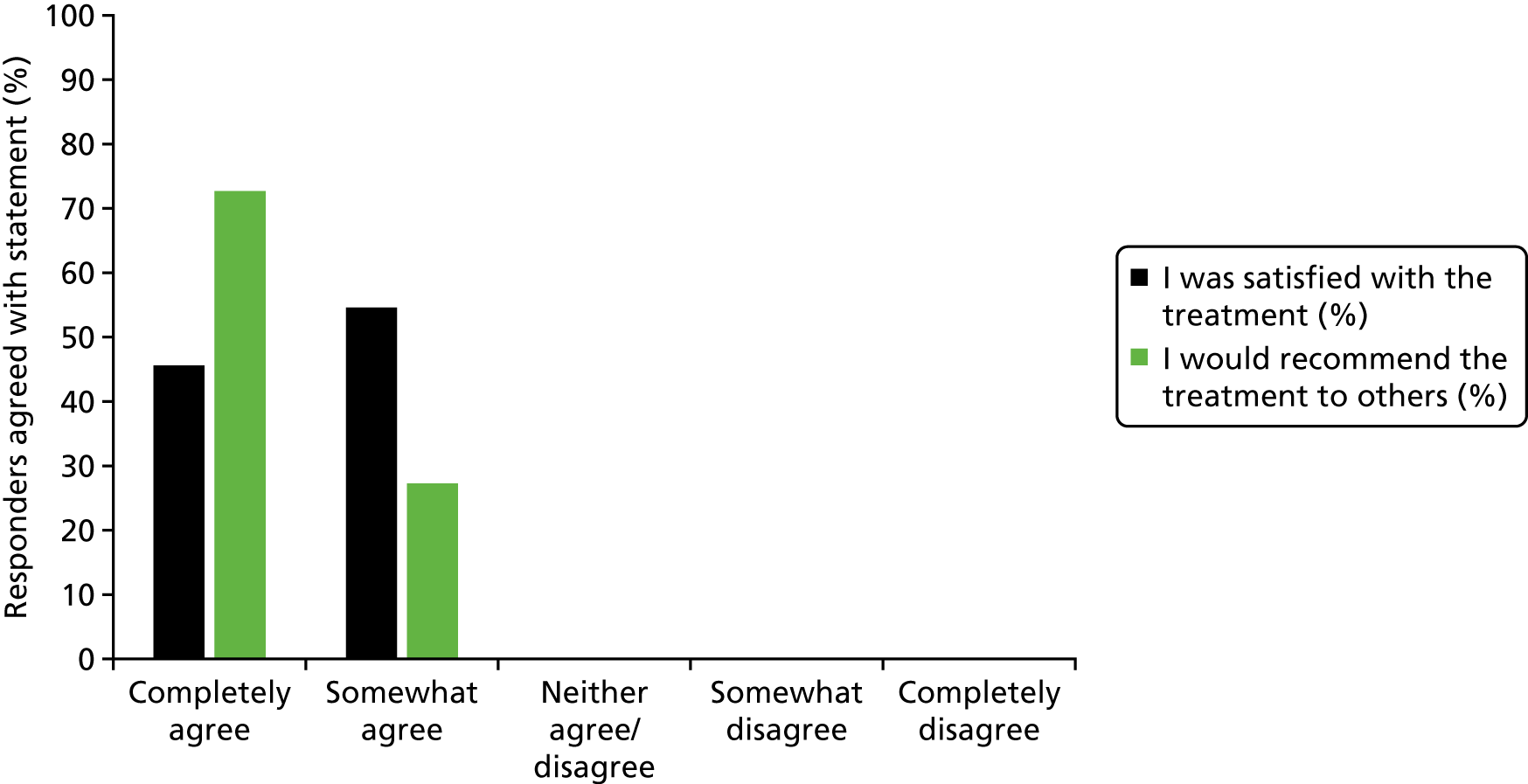
At the end of treatment (follow-up), participants rated how acceptable they found the treatment. 41 Young people were specifically asked to report on the extent to which they agreed with the two statements ‘I was satisfied with the treatment’ and ‘I would recommend the treatment to others’ on a five-point scale from ‘completely agree’ to ‘completely disagree’. They also had the opportunity to complete a free-text box to comment on the treatment.
Other adolescent self-report measures
Patient Health Questionnaire-9 (PHQ-9) is a nine-item measure assessing the presence of the main symptoms of major depression on a four-point scale from 0 (not at all) to 3 (nearly every day) over the last 2 weeks. This is followed by one item asking young people to rate how difficult these problems have made it for them to work, take care of things at home or get along with other people on a four-point scale from ‘not at all difficult’ to ‘extremely difficult’. This measure is widely used and has robust psychometric properties when used with young people. 42 This measure was added (after the study had started) to ensure that suicidal ideation was routinely monitored within sessions. Because the data were incomplete and the measure was included (at pre and follow-up time points) for clinical management purposes, we have not included this as an outcome measure.
Health economic records
Clinician’s logs were designed to capture the amount of health-care resources (i.e. qualified staff time) necessary to implement the CT-SAD-A treatment within a CAMHS setting. They were completed by both supervisors and therapists who recorded, as applicable, the amount of time spent in activities related to the CT-SAD-A treatment, including training, supervision, preparation and delivery (i.e. contact with client) of the CT-SAD-A treatment. Data recorded in the clinician’s logs were used to calculate the total mean amount of qualified staff time used by the NHS per adolescent treated. Results were stratified by type of staff time use (i.e. time spent in training, supervision, preparation and delivery of the CT-SAD-A treatment).
Qualitative interviews
Interviews were conducted with young people, parents, therapists and their managers/clinical leads to explore their experiences of the intervention and the research study. The approach and design of the qualitative work is described in full in Chapter 7.
Chapter 3 Patient and public involvement
We have described PPI in line with the GRIPP2-SF reporting checklist. 43 We have also provided specific examples of PPI activity to illustrate our adherence with the NIHR INVOLVE National Standards for Public Involvement (Table 1). 44
| Standard number and title | Example of what we did to meet the standard |
|---|---|
| Standard 1: inclusive opportunities |
|
| Standard 2: working together |
|
| Standard 3: support and learning |
|
| Standard 4: communications |
|
| Standard 5: impact |
|
| Standard 6: governance |
|
Aim
To collaboratively involve patients as research partners at all stages of the project.
Methods
-
An expert by experience (GS) was a co-investigator on the project and, as such, had a leadership role at all stages of the project, including the following:GS represented PPI views at the study management group to ensure that:In addition, GS attended all SSC meetings to express his own views and to also ensure that the young person member of the SSC was able to fully contribute. GS was involved in drafting the patient information sheets, the qualitative topic guide and theme development within the qualitative analysis. GS also co-wrote this PPI section of the final report and contributed to drafting all other sections.
-
Development of the research question – the study was a NIHR commissioned call, so the research questions were prespecified; however, they were based on one of the research recommendations of the 2013 NICE guideline on the identification, assessment and treatment of SAD. 24 GS was a patient representative on this NICE guideline and, as such, contributed to the development of research recommendations.
-
Development of the application – as an applicant, GS contributed to the development of all aspects of the application, in particular how to use PPI effectively throughout the study. Examples of specific proposals that came from his involvement include the following: (1) GS would jointly facilitate PPI panel meetings, bringing benefits from his personal and professional experience; (2) online materials would be produced for patients and the public about SAD in adolescence and its treatment (this aspect of the work was discontinued, as we did not progress to the trial).
-
Conduct of the study – as a co-applicant and member of the study management group, GS oversaw all aspects of the study.
-
the adapted treatment was appropriate and acceptable for adolescents with SAD
-
the clinical outcome and health economic measures that are meaningful to patients and carers were determined
-
recruitment and retention of trial participants were maximised by keeping participants’ needs in mind
-
patients’ experiences of the adapted treatment and the trial procedures were considered appropriately
-
dissemination to potential patients was delivered effectively.
-
-
A young person who had received treatment for SAD within CAMHS was a member of the SSC. She attended SSC meetings and, as such, contributed to decisions made about all aspects of the study. She also consulted on the drafting of the qualitative topic guide.
-
A group of four young people who had received CT-SAD-A within a pilot phase of work consulted on their experience of treatment, the adaptation of measures, and the development of the therapist manual and materials for young people. GS provided oversight of and input into this PPI work.
-
The Anxiety and Depression in Young People Research Advisors Group (AnDY RAG) at the University of Reading comprises young people who have had experience of anxiety and/or depression and parents/carers. They consulted on the drafting of all patient information sheets and the qualitative topic guide.
Results
The broad approach to PPI meant that patients’ views and experiences were incorporated at all stages of the study. Particular examples of how the study changed because of PPI are listed below; however, it is important to emphasise that these are a set of discrete examples that do not do justice to the overall influence of PPI input throughout the study.
-
After the initial SSC meeting, GS proposed changes to the structure of the agenda to ensure that PPI input was a standing item so that if the PPI member of the SSC had not felt able to participate at particular points in the discussion she would always have sufficient opportunities to express her views. We have maintained this agenda structure in all subsequent SSC meetings, for this study and others.
-
GS encouraged the inclusion of a general goals measure, with the aim of measuring the relevance of treatment to patients’ lives in their own terms, rather than through the use of clinical measures focused on specific elements of the cognitive model of social anxiety or specific symptoms.
-
A number of changes were made to the questionnaires measuring psychological mechanisms targeted in the treatment (the SCQ, SBQ and SAQ) on the basis of feedback from young people with SAD who had experience of the measures as part of treatment, AnDY RAG and the community population. Their feedback led to changes that made the language more developmentally appropriate (e.g. on the cognition measure ‘I am inadequate’ changed to ‘I am not good enough’) and the addition of items relevant to young people with SAD (e.g. on the measure of safety behaviours, ‘Seek reassurance from my friends and family’).
-
A number of changes were made to how CT-SAD-A treatment materials were formatted, worded and administered, based on feedback from young people who had had experience of it. Young people also reported generally preferring to complete worksheets by hand rather than using technology, as they found this helped them remember key points. A number of edits were made to paper worksheets to address issues raised by the group.
-
Young people and parents/carers in the AnDY RAG provided feedback on all patient information sheets. They made a large number of suggestions to change wording and formatting to clarify the aims and procedures of the study. Parents particularly emphasised the importance of providing greater clarity regarding the fact that the study was taking place alongside ‘usual NHS care’ and that participants would continue to be CAMHS patients. This was a particular concern for many families who had had experience of long waits and ‘battles’ to get seen within CAMHS. Young people also highlighted the importance of the information sheets having an ‘NHS-look’ about them so that they did not raise concerns that researchers were ‘experimenting on’ them. Changes were made to the wording and the design of the leaflet to show that it was fully integrated within NHS CAMHS and to address the other issues raised by the group.
-
The qualitative topic guide was developed with PPI input to take into account particular difficulties that young people with SAD may have interacting with an unfamiliar researcher in an interview setting. Emphasis was put on the use of visual materials, to increase clarity and remove demands for eye contact with the researcher, and on the importance of ensuring a clear message that there were no ‘wrong answers’ throughout. A number of specific items were also suggested, including questions relating to the impact of the treatment on the young person’s relationship with their parent(s). Notably, GS also highlighted areas in which further PPI input from young people was not needed, that is, regarding whether or not young people should be consulted about key terminology used within treatment, as this was not relevant to the experience or success of the treatment.
-
PPI input was used in the qualitative analysis to ensure that patients’ feedback on their experience of treatment was not inadvertently misunderstood.
A further outcome that is important to note is that the PPI representative on the SSC wrote to the principal investigator (PI) at the end of the study to express her thanks for having had the opportunity to participate. She stated not only that it had been an interesting experience that had helped her with her university applications, but that she also felt that it had played an important role in her recovery from SAD. This was in line with GS’s previous experience on the NICE Guideline Development Group in which he had the opportunity to contribute to a daunting social situation (large group, academic demands), but in which there was a supportive environment and his anxiety was acknowledged and accepted.
Discussion and conclusions
The PPI in this study was very effective and influenced important aspects of the study, as highlighted above. This might have been related to several factors. First, the PPI co-investigator had received training in relevant research methods and had extensive experience of representing patients’ views through his previous experience on a NICE Guideline Development Group. Second, the PPI member of the SSC also had experience of contributing to research through previous involvement in the AnDY RAG. Third, the researchers were experienced at involving patient partners in their research, for example through facilitation of the AnDY RAG for over 2 years as well as involving PPI representatives in specific studies.
GS was involved from the beginning of the study, allowing him to help shape the study from the start and ensure that the right procedures for PPI were in place. Successful involvement of patients in this study was also facilitated by pre-existing relationships between some of the PPI representatives and members of the research team, the collaborative approach taken by the team, funding to finance PPI time, and a supportive attitude of PPI involvement from the SSC.
Some limitations should also be noted. Because the PPI co-investigator role was a part-time (low % full time-equivalent) role, GS had to accommodate the role around his main occupation. He managed this very effectively, attending meetings in person on most occasions and, when necessary, remotely, for example by telephone or Skype. However, it was not possible to time the AnDY RAG meetings and the meetings with four young people who had experience of CT-SAD-A at times when the relevant researchers, young people and GS were available within the time frame needed to keep the study on track. Going forward, having more substantial PPI roles might help enable the flexible timing required to make full use of PPI co-investigators. A further limitation was that, because of often tight time frames, on occasion papers for meetings were sent to PPI members quite close to the time of the meetings. More time would have been useful to allow PPI members to understand the materials and ask questions about relevant terminology, which was necessary to be able to fully understand and digest the documents and prepare PPI feedback. Finally, though it is not particular to this study, despite their sometimes extensive relevant experience (such as GS’s involvement with the NICE Guideline Development), PPI participants may have only been involved in PPI with certain teams, which means that they may not have always been able to identify and be involved in how to use PPI input creatively and as far as possible. A specifically designed training course in PPI input and research methodology may be a useful resource to help address this challenge in which PPI representatives can become aware of a range of different examples of how successful PPI can be achieved.
Reflections/critical perspective
The PPI in the study was embedded as far as possible at every level.
A strength of the study was the combination of dedicated expert PPI, who knew the project well through close involvement, and the observations and contributions from the young person PPI representative on the SSC, the young people who had previously received CT-SAD-A, and the AnDY RAG who had a more distanced take on the study and was thus able to make unique contributions.
Patient and public involvement members also fed back that they felt supported and listened to, and that their feedback was treated as important and valuable at all times. This was especially important owing to the nature of SAD, and it enabled them to contribute effectively.
Future studies would benefit from costing more substantial PPI time to allow greater flexibility, consistent provision of papers, etc. at least 2 weeks ahead of all meetings and dedicated training to help PPI co-applicants in leading the development of creative and effective mechanisms to get the most out of PPI contributions.
Chapter 4 Results 1: feasibility in routine child and adolescent mental health services – recruiting and retaining therapists and young people
Recruiting and retaining therapists
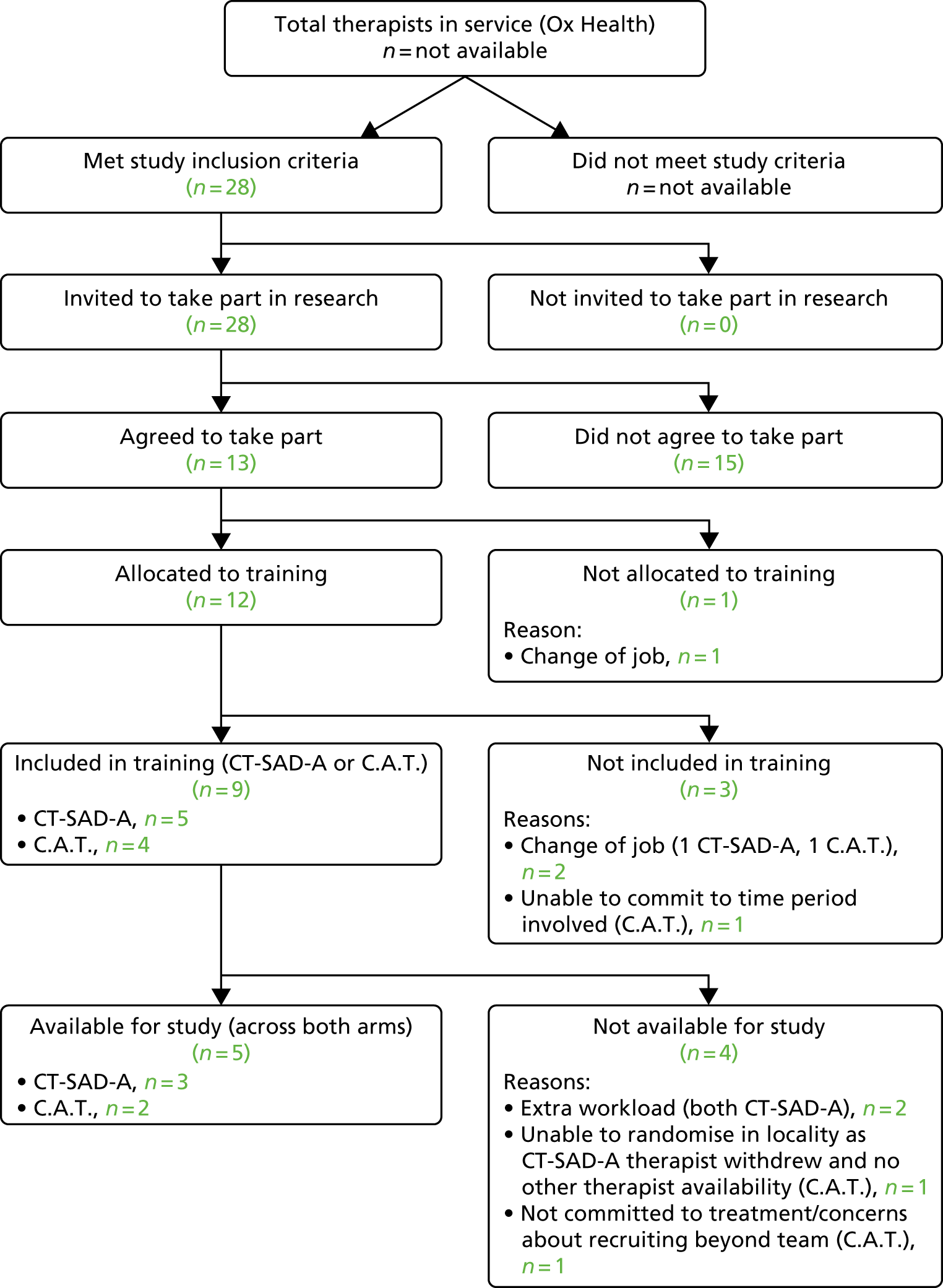
The initial protocol included a feasibility RCT to compare CT-SAD-A with a CBT programme that can be applied across different types of anxiety disorders and is commonly used in child and adolescent mental health settings (‘The C.A.T. Project’). 45 To ensure that we had enough trained therapists to deliver treatment within each arm (n = 3), we set out to identify 10–12 therapists to allow for a potential loss of trained therapists. In line with our plans, we initially identified 12 CAMHS therapists within the participating services who met our study inclusion criteria and who were willing to take part. Within the early stages of the study, five therapists withdrew from the project (Figures 1 and 2) after being allocated to training but prior to attending the workshop, the ‘not included in training’ box. This meant that we had to engage therapists from additional CAMHS teams within the participating NHS trusts and ensure that there would be therapist representation across both study arms in each of the five teams (as therapists were not able to work across teams). In total, 20 therapists were recruited to the study and 19 were allocated to treatment arms. In total, 10 of those therapists withdrew from the study (including the five therapists mentioned above) and one went on maternity leave towards the end of the training phase. In addition, one therapist resigned from her NHS role but agreed to continue to participate in the study. Figures 1 and 2 show therapist recruitment and retention to the study, and also reasons for therapist withdrawal. The final distribution of therapists across clinical teams is shown in Table 2, with their core professional training detailed in Table 3. As can be seen, in many locations there was only one therapist trained in each of the two therapies, which left the study extremely vulnerable to any further therapist loss.
FIGURE 1.
Therapist recruitment and retention to the study (Berkshire Healthcare NHS Foundation Trust). BHFT, Berkshire Healthcare NHS Foundation Trust.

FIGURE 2.
Therapist recruitment and retention to the study (Oxford Health NHS Foundation Trust). Ox Health, Oxford Health NHS Foundation Trust.
| NHS trust | Attended training workshops | Available for study (and completed training cases for CT-SAD-A) | ||
|---|---|---|---|---|
| CT-SAD-A | C.A.T. Project | CT-SAD-A | C.A.T. Project | |
| Oxford Health NHS Foundation Trust | ||||
| Team 1 | 2 | 1 | 2 | 1a |
| Team 2 | 1 | 1 | 1 | 1a |
| Team 3 | 1 | 1 | ||
| Team 4 | 1 | 1 | ||
| Berkshire Healthcare NHS Foundation Trust | ||||
| Team 1 | 2 (+ 1 on maternity leave) | 2 | 2 (+ 1) | 1a |
| Core professional training | Number of years since qualification (at consent) | |
|---|---|---|
| CT-SAD-A therapists | Clinical psychologist | 18 |
| Clinical psychologist | 1 | |
| Clinical psychologist | 5 | |
| Social worker | 5 | |
| Social worker/CYP IAPT | 4/same year | |
| CBT therapist (via IAPT CBT adult mental health training) | 2 | |
| C.A.T. therapists | Clinical psychologist | 1 |
| Clinical psychologist | 21 | |
| Clinical psychologist | 5 |
Owing to high service demand and staff vacancies in all participating CAMHS teams, all service managers placed restrictions on the amount of time (and, hence, the number of trial cases) that the participating therapists could spend on the study (meaning only one or two patient contacts per week were possible). Although we secured excess treatment costs (ETC) to reimburse teams for the additional therapist time taken by the trial, this was of limited help to them, as they all had unfilled vacancies and so there was no scope to backfill existing staff (particularly as ETCs are paid in arrears). As a result, with the therapists available, we would have been able to recruit a maximum of n = 26 (13 per arm), rather than n = 48 as initially planned to test the feasibility of a RCT. This was likely to be an optimistic figure based on therapists being able to seamlessly pick up new trial patients immediately after completing therapy with a previous patient. Although there was one further therapist in Berkshire Healthcare NHS Foundation Trust (BHFT) who was available and willing to take part in the study, none of the sites across Oxford Health NHS Foundation Trust (OxHealth) was able to provide additional therapists due to the high demand on services and there being a number of unfilled vacancies/staff on maternity leave across all sites. Given this, it was not possible to secure sufficient CAMHS therapist time to be able to run the feasibility trial within the participating NHS trusts.
Recruiting and retaining young people with social anxiety disorder
We found that some of the participating CAMHS teams identified few young people with a primary SAD, as activity was increasingly dominated by risk management. Given this, some of the participating sites struggled to identify suitable participants for the trial, recruitment of training cases was slow, and therapists were not always able to work at their full allocated capacity. For example, between July and December 2017, only one training case was recruited on a site in which there were three therapists participating in the study. To overcome this, we had to reach out beyond the services to identify suitable training cases (e.g. to neighbouring services and to local schools’ hubs). However, this created challenges for services who were already struggling to meet the existing demand.
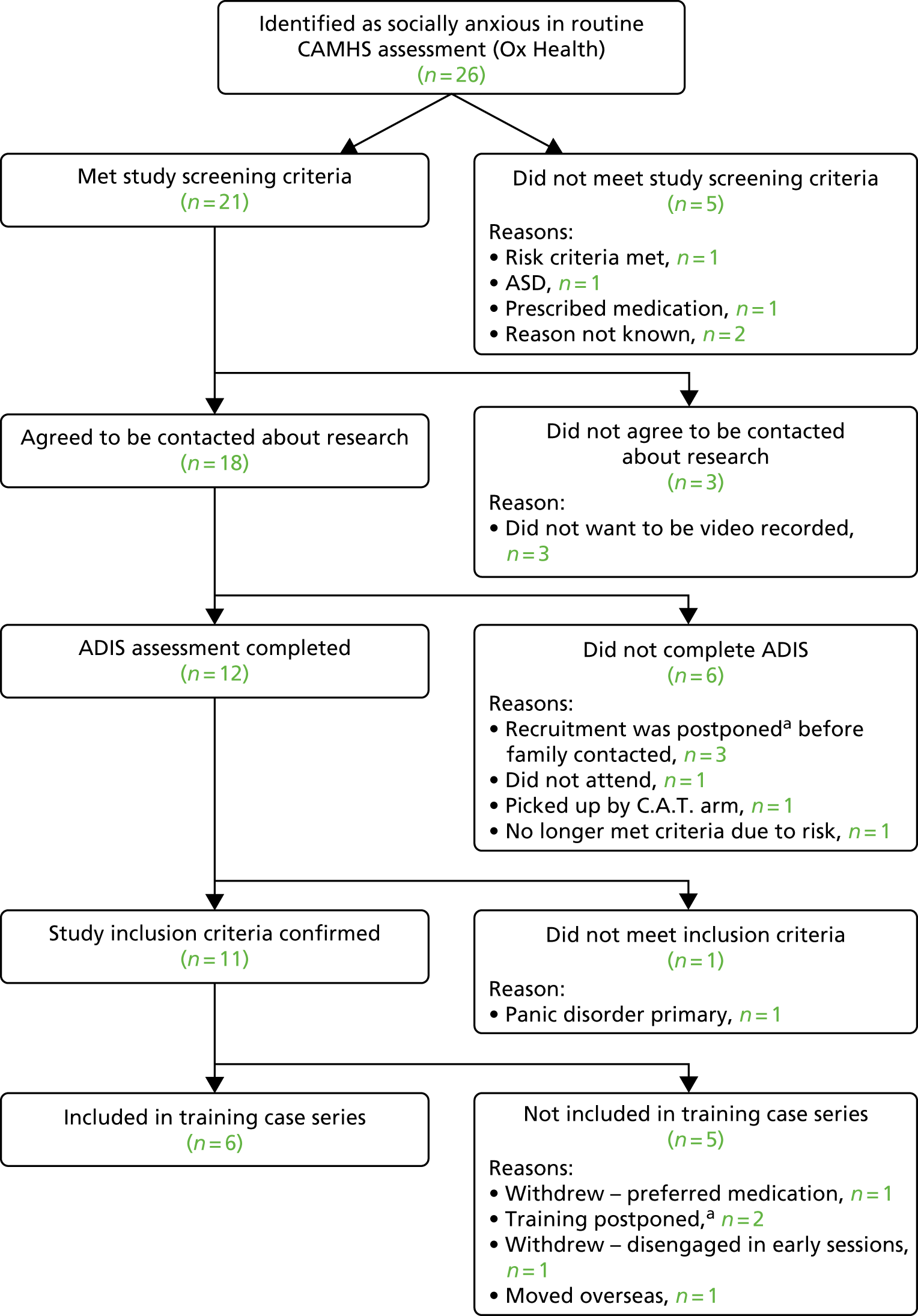
Figures 3 and 4 show patient participant recruitment and retention to the study. Of those young people identified as potentially eligible for the study, less than one-quarter ended up participating in the training series for a broad range of reasons. Notably, when potential participants were assessed and confirmed as eligible for the study, uptake and retention was high. In total, 26 out of 35 (74%) young people who were contacted by the research team participated in the study, 12 out of 14 (86%) were retained throughout treatment and 11 of these 12 (92%) completed the follow-up assessment.
FIGURE 3.
Patient recruitment and retention to the CT-SAD-A training phase (Berkshire Healthcare NHS Foundation Trust). a, Training was postponed from September 2016 to June 2017 while the primary supervisor was on maternity leave.

FIGURE 4.
Patient recruitment and retention to the CT-SAD-A training phase (Oxford Health NHS Foundation Trust). a, Training was postponed from September 2016 to June 2017 while the primary supervisor was on maternity leave.
Action taken
In response to the difficulties that we experienced with recruiting and retaining CAMHS therapists and identifying eligible young people within CAMHS, we considered extending recruitment to other NHS trusts. However, after extensive consultation with representatives from a range of CAMHS teams, it was clear that this was not going to be possible, because (1) a substantial increase in costs would be required to be able to conduct the required diagnostic assessments across a wider geographical area and/or (2) other NHS CAMHS teams reported having similar problems with staffing (i.e. unfilled posts and a rapid turnover of staff) and caseloads that were increasingly dominated by high levels of risk. As a result of the difficulties with therapist retention and participant identification, we concluded that the feasibility question that we set out to address had been answered and that the proposed RCT would not be feasible in the current CAMHS context. Given this, we felt that it was not a responsible use of NIHR funds to proceed to the RCT phase of the study. To maximise the learning from the work and investment that had taken place, we proposed the following next steps:
-
We would complete CT-SAD-A treatment and post-treatment assessments with all the training cases to report on an extended case series of application of the novel treatment (CT-SAD-A) in routine CAMHS (including costs of treatment delivery).
-
We would move forward qualitative work that had been planned alongside the RCT phase of the original proposal to learn about young people and parents’ experiences of receiving this novel treatment within a CAMHS setting to inform future work about how best to deliver specialist psychological treatments in CAMHS.
-
We would extend the proposed qualitative work to include therapists and service managers to learn from their experiences of (1) delivering CT-SAD-A within routine CAMHS and (2) participating in psychological therapies research in routine CAMHS, to learn both about the application of specialist psychological treatments in CAMHS and about what needs to happen to enable CAMHS to participate in research.
This proposal was agreed by the SSC and the NIHR HTA programme. The following chapters report on the outcomes of the revised programme of work.
Chapter 5 Results 2: training case series – clinical outcomes
Patient and therapy characteristics
The 10 females and two males included in the case series had an average age of 15.17 years (SD 1.80 years; range 12–17 years). The sample was predominantly white British (10/12), which was representative of the participating trust areas. None of the patients reported being prescribed psychotropic medication.
As shown in Table 4, seven patients received the planned 14 weekly therapy sessions, two patients received 10 weekly sessions and three patients received 11 sessions, 12 sessions, and 17 sessions, respectively. Four patients received the planned two booster sessions, one received three boosters, two received one booster and the remaining five did not receive a booster session. The follow-up assessment was carried out, on average, 2.88 months (SD 1.15 months, range 1.16–4.63 months) after the final weekly therapy session. Outcomes are presented graphically for each case below.
| ID | Young person’s sex | Young person’s age (years) at initial assessment | No. of weekly sessions | No. of booster sessions | Diagnostic profile of young person at initial assessment (diagnosis yes/no and CSR) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SAD | Specific phobia 1 | Specific phobia 2 | Panic disorder without agoraphobia | GAD | PTSD | Dysthymia | MDD | |||||||||||||
| 1 | Female | 16 | 14 | 2 | Yes | 6 | No | – | No | – | No | – | Yes | 4 | No | – | No | – | No | – |
| 2 | Male | 17 | 14 | 2 | Yes | 6 | Yes | 4 | No | – | Yes | 5 | Yes | 4 | No | – | No | – | No | – |
| 3 | Female | 12 | 14 | 3 | Yes | 7 | No | – | No | – | No | – | No | – | No | – | No | – | Yes | 6 |
| 4 | Female | 15 | 14 | 2 | Yes | 6 | No | – | No | – | No | – | Yes | 5 | No | – | No | – | No | – |
| 5 | Female | 17 | 14 | 1 | Yes | 7 | Yes | 4 | No | – | No | – | Yes | 6 | No | – | Yes | 6 | No | – |
| 6 | Female | 13 | 14 | 2 | Yes | 4 | No | – | No | – | No | – | No | – | No | – | No | – | No | – |
| 7 | Male | 13 | 10 | 1 | Yes | 5 | No | – | No | – | No | – | Yes | 4 | No | – | No | – | No | – |
| 8 | Female | 17 | 12 | 0 | Yes | 7 | No | – | No | – | No | – | Yes | 5 | No | – | No | – | No | – |
| 9 | Female | 15 | 11 | 0 | Yes | 5 | No | – | No | – | No | – | No | – | No | – | No | – | No | – |
| 10 | Female | 17 | 14 | 0 | Yes | 7 | Yes | 6 | No | – | No | – | Yes | 5 | Yes | 6 | No | – | Yes | 5 |
| 11a | Female | 14 | 10 | 0 | Yes | 7 | No | – | No | – | No | – | Yes | 5 | No | – | No | – | No | – |
| 12 | Female | 16 | 17 | 0 | Yes | 7 | Yes | 5 | Yes | 5 | No | – | No | – | No | – | No | – | No | – |
Patient outcomes
The mean and median pre-treatment and follow-up data are presented in Table 5. Given the small sample size and the non-normal distribution of a number of the variables, pre-treatment and follow-up comparisons were made with non-parametric Wilcoxon signed-rank tests. The z-statistic is presented in Table 5, with associated p-values and effect size estimates (r).
| Measure | n | Time point | Wilcoxon | p | r a | |||
|---|---|---|---|---|---|---|---|---|
| Pre treatment | Follow-up | |||||||
| Mean (SD) | Median (Q1, Q3) | Mean (SD) | Median (Q1, Q3) | Test statistic | ||||
| LSAS-CA-SR | 12 |
97.41 (26.02) |
100.09 (79.50, 119.50) |
36.18 (38.31) |
24.50 (3.50, 75.25) |
z = –3.06 | 0.002* | 0.62 |
| RCADS social anxiety T-score | 12 |
74.26 (21.93) |
70.29 (59.46, 78.19) |
44.00 (15.58) |
41.89 (30.61, 55.13) |
z = –2.93 | 0.003* | 0.60 |
| ADIS-C/P SAD CSR score | 11 |
6.09 (1.04) |
6.50 (5.00, 7.00) |
2.45 (3.11) |
0.00 (0.00, 5.00) |
z = –2.21 | 0.021* | 0.47 |
| RCADS depression T-score | 11 |
68.46 (16.84) |
67.17 (55.93, 85.91) |
47.35 (15.18) |
44.70 (37.96, 62.67) |
z = –2.94 | 0.003* | 0.63 |
| RCADS GAD T-score | 11 |
57.46 (9.18) |
56.77 (51.37, 64.49) |
38.04 (8.07) |
37.56 (29.81, 46.28) |
z = –3.02 | 0.003* | 0.64 |
| Parent RCADS social anxiety T-score | 11 |
76.57 (14.45) |
81.16 (60.23, 90.30) |
58.00 (15.37) |
52.97 (46.31, 72.03) |
z = –2.80 | 0.005* | 0.60 |
| Parent RCADS depression T-score | 11 |
75.34 (18.68) |
81.08 (54.15, 86.80) |
60.21 (18.23) |
59.32 (48.22, 69.21) |
z = –2.05 | 0.041* | 0.44 |
| Parent RCADS GAD T-score | 11 |
66.76 (13.62) |
81.08 (54.15, 86.80) |
50.84 (11.15) |
45.17 (42.28, 64.21) |
z = –2.49 | 0.013* | 0.53 |
| Social participation | 12 | 39.58 (15.46) |
41.50 (24.00, 51.75) |
60.35 (19.38) |
59.00 (42.50, 80.75) |
z = –2.90 | 0.004* | 0.59 |
| Social satisfaction | 12 | 14.83 (4.97) |
14.50 (10.50, 19.75) |
18.75 (6.69) |
20.50 (10.75, 24.75) |
z = –1.96 | 0.050 | 0.40 |
| Concentration | 12 |
53.33 (24.71) |
55.00 (35.00, 73.75) |
64.17 (28.73) |
65.00 (42.50, 91.25) |
z = –1.49 | 0.137 | 0.30 |
| ORS – individual | 12 |
39.05 (36.91) |
32.50 (3.16, 76.00) |
49.33 (38.65) |
46.50 (7.00, 90.75) |
z = –0.89 | 0.374 | 0.18 |
| ORS – interpersonal | 12 |
40.61 (38.75) |
22.15 (6.24, 84.50) |
55.55 (39.07) |
70.00 (8.13, 90.25) |
z = –0.86 | 0.388 | 0.18 |
| ORS – social | 12 |
24.55 (28.37) |
10.65 (1.90, 45.75) |
46.83 (42.19) |
48.00 (3.15, 93.25) |
z = –1.73 | 0.084 | 0.35 |
| ORS – overall | 12 |
28.14 (28.21) |
23.00 (3.98, 43.78) |
50.85 (39.43) |
50.00 (7.38, 94.50) |
z = –1.96 | 0.050 | 0.40 |
| CYP IAPT goal 1 | 7 |
1.57 (7.71) |
1 (1, 2) |
7.71 (1.98) |
8 (7, 9) |
z = –2.38 | 0.018* | 0.64 |
| SCQ – belief | 12 |
61.91 (23.18) |
68.69 (46.29, 81.17) |
13.61 (20.32) |
3.55 (1.46, 26.93) |
z = –3.06 | 0.002* | 0.62 |
| SBQ | 12 |
1.63 (0.50) |
1.71 (1.29, 1.96) |
0.64 (0.59) |
0.45 (0.24, 0.79) |
z = –2.85 | 0.004* | 0.58 |
| SAQ | 12 |
4.46 (1.22) |
4.84 (3.13, 4.99) |
2.86 (0.93) |
2.89 (2.50, 3.69) |
z = –2.67 | 0.008* | –0.55 |
Social anxiety symptom scales
Liebowitz Social Anxiety Scale for Children and Adolescents: self-report version
The Wilcoxon paired rank-sum test revealed a significant difference in LSAS-CA-SR scores from pre treatment to follow-up, with a large effect size. Scores dropped on average 66.80% over time, ranging from 3% to 100% (Figure 5). Ten participants, 83% of the sample, made a reliable improvement in their LSAS-CA-SR scores. Nine participants made a reliable and clinically significant improvement, based on a pre-treatment to follow-up change of at least 2 SDs from the original mean (a drop of 48.75 points).
FIGURE 5.
Individual patient LSAS-CA-SR scores at the following measurement points: pre assessment, mid-treatment, at the end of weekly sessions and at the follow-up assessment.

Revised Child Anxiety and Depression Scale: social anxiety subscale
RCADS social anxiety T-scores showed a significant and large decrease over the course of treatment. Before treatment, eight patients were on the borderline or in the clinical range based on their age and sex (T-score of > 65), whereas only one patient remained in the clinical range at follow-up (Figure 6).
FIGURE 6.
Individual patient RCADS social anxiety T-scores at the following measurement points: pre assessment, mid-treatment, at the end of weekly sessions and at the follow-up assessment.

Diagnostic profile
Table 6 shows the presence of diagnoses measured using the ADIS-C/P pre treatment and at follow-up for each participant. CSRs for SAD diagnosis at both time points are given in Table 5. CSRs for all other diagnoses are shown in Figure 7. Follow-up diagnostic data were missing for ID 11 and, therefore, they are not included in the following discussion (i.e. N = 11 for below).
| Time point | Social anxiety | GAD | Specific phobia | Panic disorder without agoraphobia | Depression | PTSD |
|---|---|---|---|---|---|---|
| Pre (n) | 11 | 7 | 5 | 1 | 3 | 1 |
| Follow-up (n) | 4 | 1 | 2 | 0 | 4 | 1 |
FIGURE 7.
The ADIS CSR pre treatment and at follow-up scores. Scores of ≥ 4 indicate a positive diagnosis. a, Follow-up ADIS data missing for ID 11.
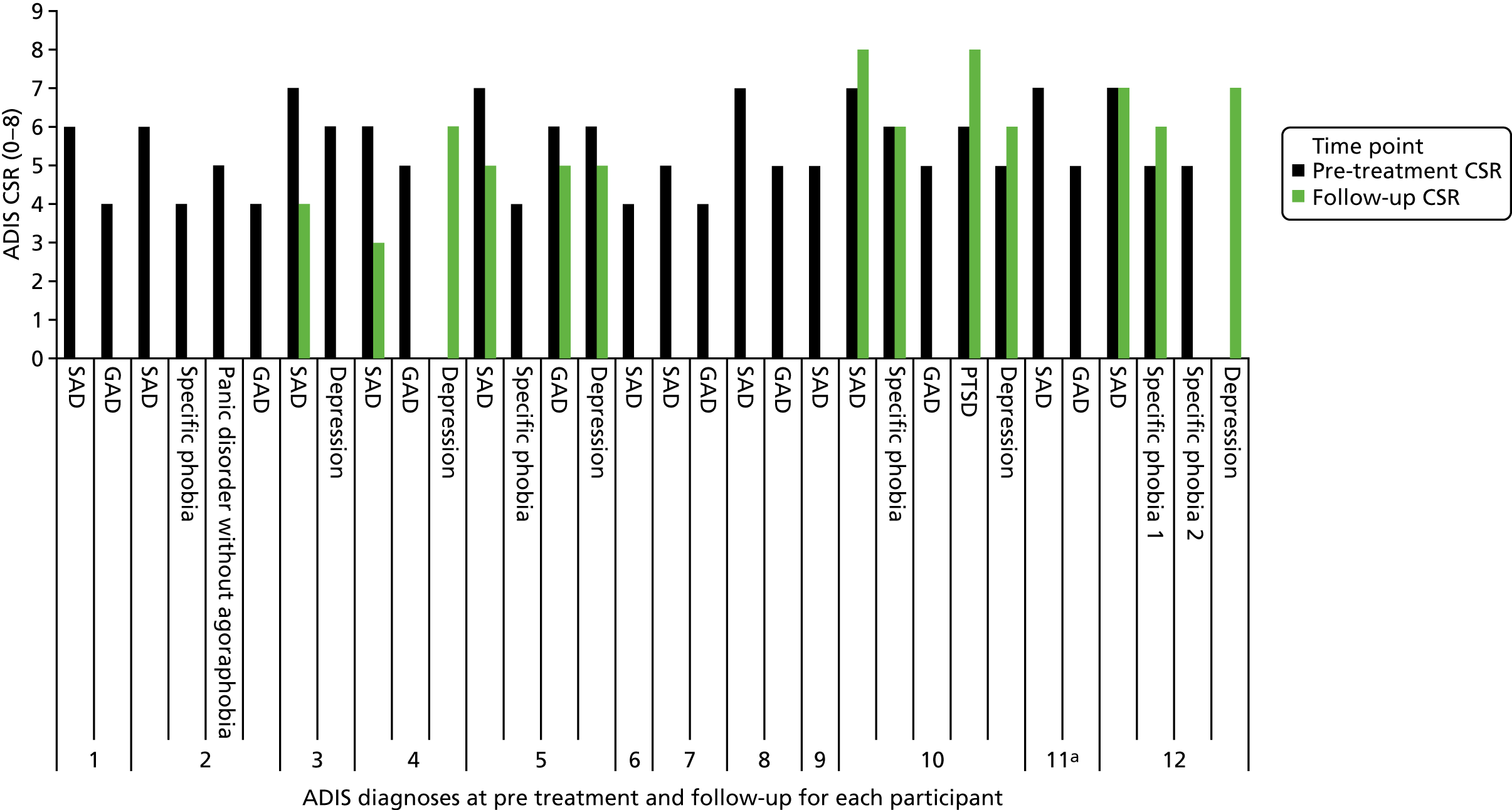
At pre treatment, all patients had a diagnosis of SAD. Only two patients had no comorbid diagnoses; GAD was present in eight patients and depression (either MDD or dysthymia) was present in three young people. There were five diagnoses of specific phobia pre treatment across four patients, with one patient diagnosed with two specific phobias. One patient had a diagnosis of post-traumatic stress disorder (PTSD) and one had a diagnosis of panic disorder. (This is detailed in Table 4. )
At follow-up, seven patients (63.64%) had lost their primary diagnosis of SAD. These same seven patients are also those patients who fell below the LSAS-CA-SR clinical cut-off at follow-up. Six patients lost their diagnosis of GAD, and three diagnoses of specific phobia were lost (one patient had two phobias at pre treatment and lost one of these at follow-up).
The number of depressive disorders in the sample increased from three to four by follow-up. Of the four patients who retained their diagnosis of SAD at follow-up, one had lost their diagnosis of depression, two had retained their diagnosis of depression and one had acquired a new diagnosis of depression. One patient lost their diagnosis of SAD, but had become depressed at follow-up.
Related clinical outcomes
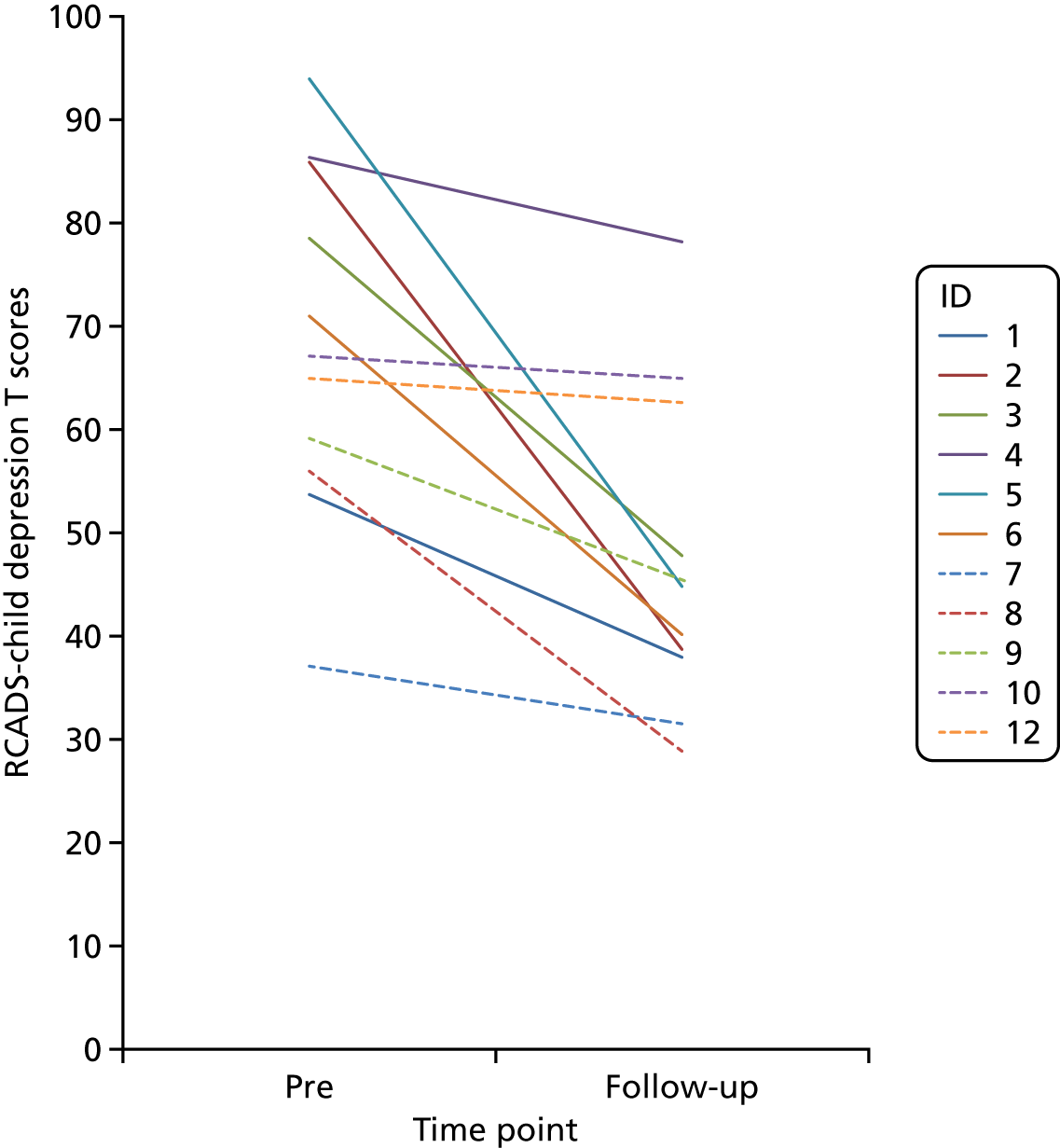
Revised Child Anxiety and Depression Scale depression scores
There was a large and significant drop in RCADS depression subscale scores over time (Figure 8). For nine patients, depression scores were below the suggested threshold (T < 65) at follow-up. ID 4 continued to show elevated symptoms of depression at follow-up and also developed a new diagnosis of depression over the course of treatment (see ADIS data in Table 6) while losing their SAD diagnosis.
FIGURE 8.
Individual patient RCADS depression T-scores at pre assessment and at the follow-up assessment.
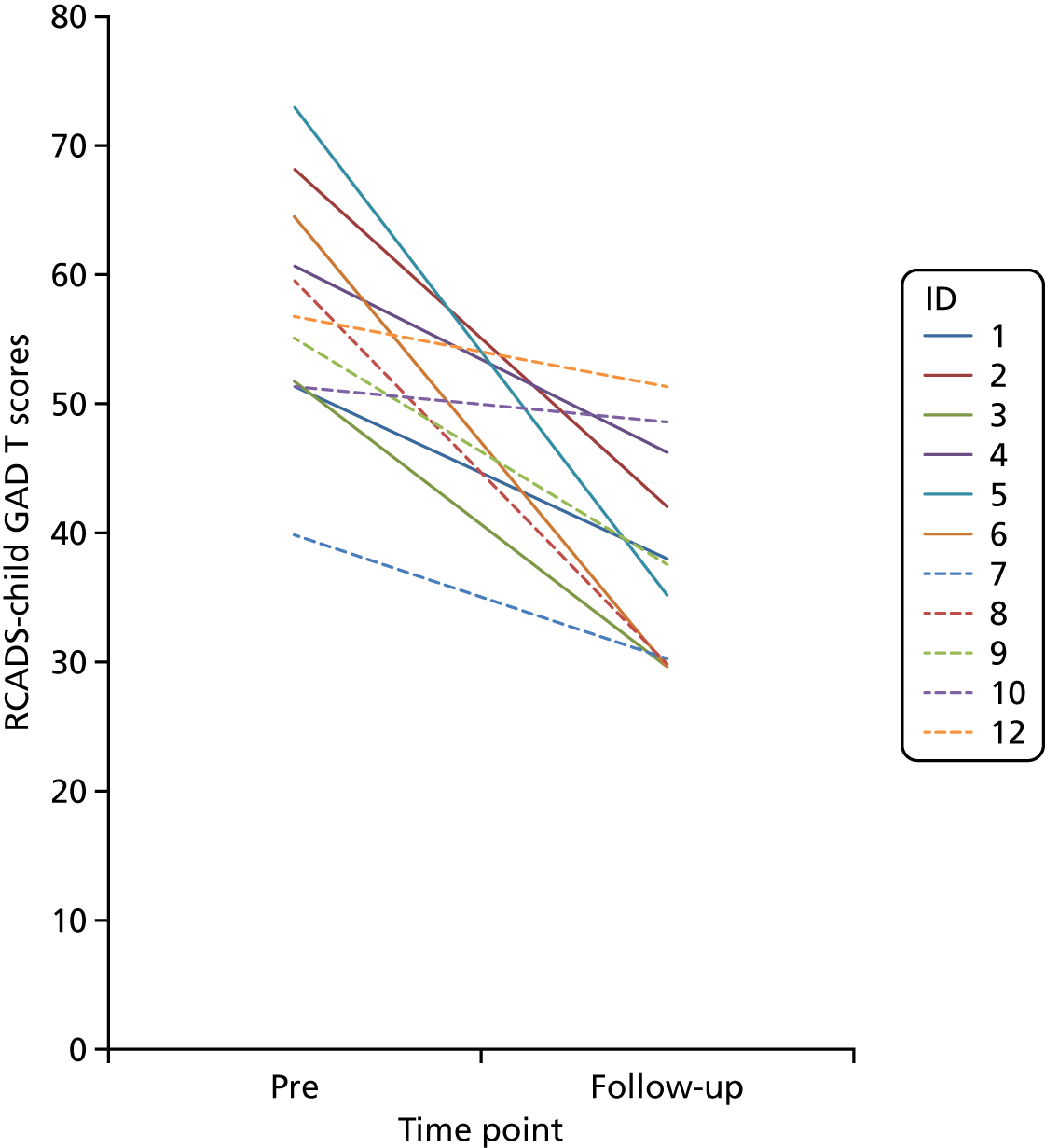
Revised Child Anxiety and Depression Scale generalised anxiety disorder scores
There was a large and significant drop in GAD scores over the course of treatment, with all patients scoring below threshold at follow-up (Figure 9).
FIGURE 9.
Individual patient RCADS GAD T-scores at pre assessment and at the follow-up assessment.
Parent-reported Revised Child Anxiety and Depression Scale
For the group as a whole (n = 11), parent ratings on the social anxiety, depression and GAD subscales of the parent RCADS were initially elevated (see Table 5) and reduced significantly by follow-up. Individual data for RCADS social anxiety subscale T-scores are presented in Figure 10. This indicates that all parents except ID 12 rated their child as making at least some improvement in their social anxiety symptoms.
FIGURE 10.
Parent RCADS social anxiety subscale T-scores pre treatment and at follow-up.

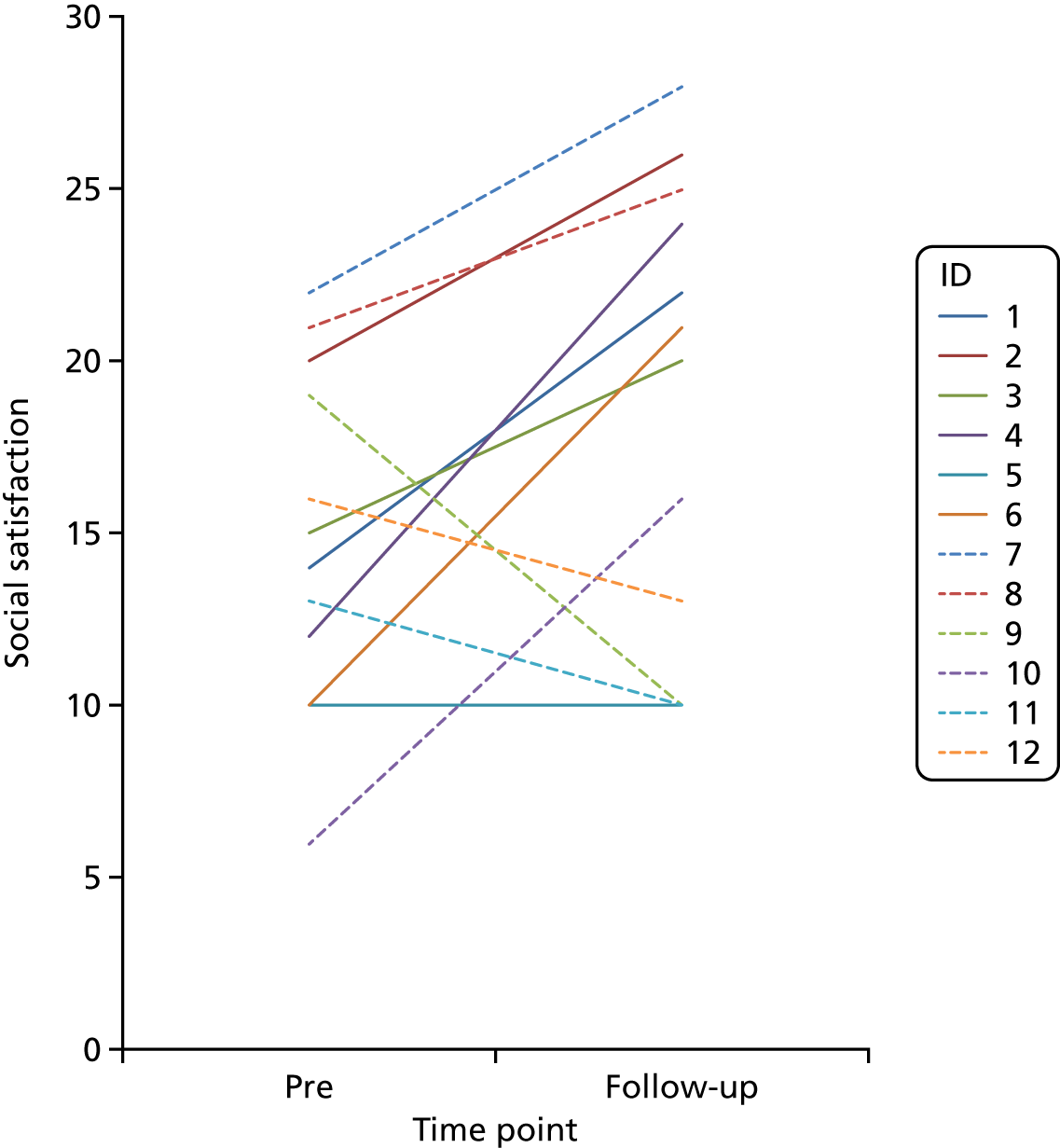
Social participation and satisfaction
The group as a whole showed large and significant improvements in their social participation (Figure 11). There was an improvement at trend level in ratings of social satisfaction for the group as a whole (Figure 12).
FIGURE 11.
Individual patient social participation scores at pre assessment and at the follow-up assessments.

FIGURE 12.
Individual patient social satisfaction scores at pre assessment and at the follow-up assessments.
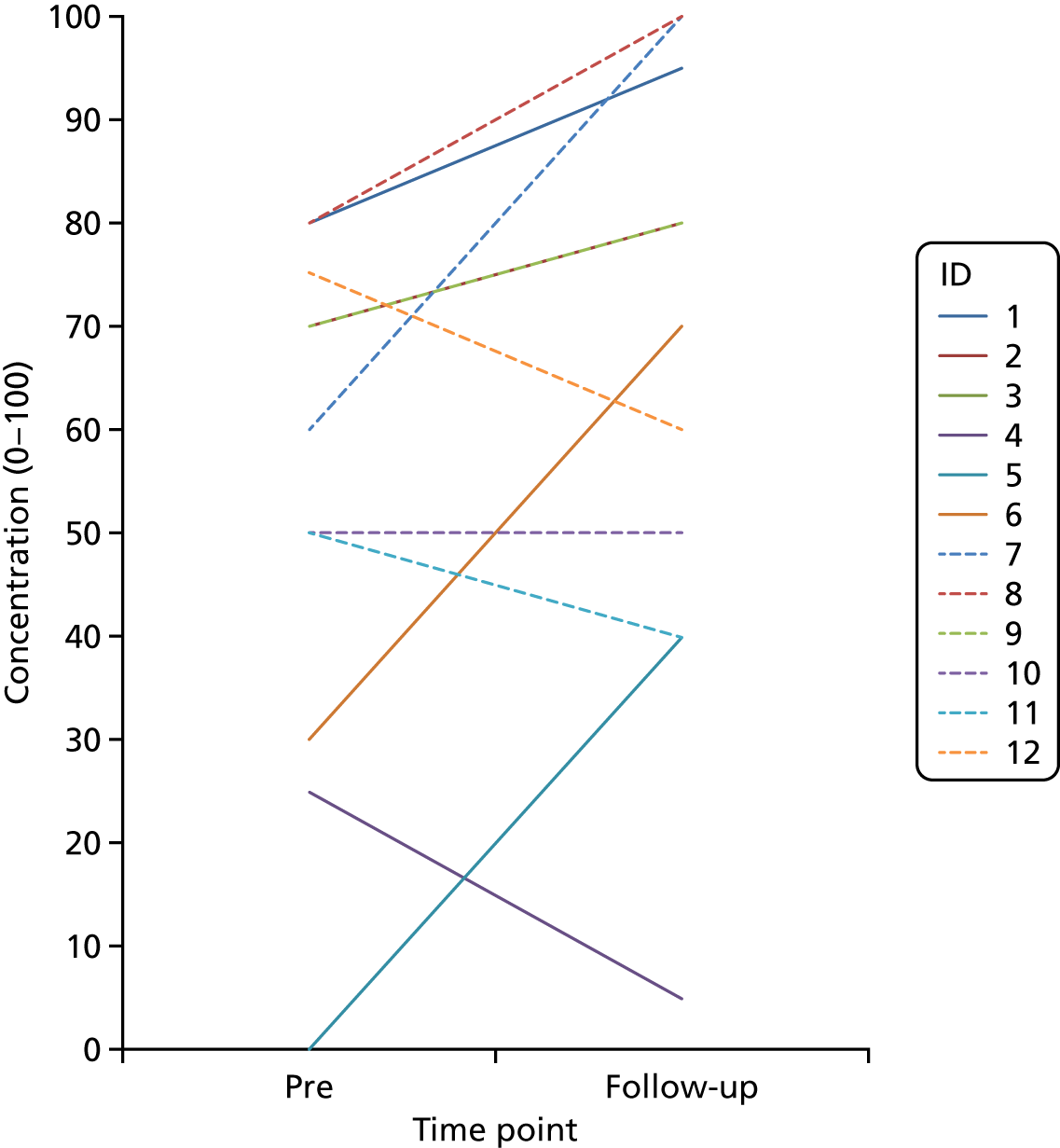
Concentration in class
The group as a whole showed a small to medium improvement in self-reported classroom concentration from pre treatment to follow-up, although this was non-significant. As shown in Figure 13, four young people showed either no change (ID 10) or a deterioration in their concentration (IDs 4, 11 and 12). Patients ID 10, 11 and 12 are those young people who did not show a clinically significant improvement on the LSAS-CA-SR and, while ID 4 lost their diagnosis of SAD, they developed a new diagnosis of depression during treatment.
FIGURE 13.
Self-reported concentration in class at pre assessment and at the follow-up assessment.
Outcome rating scales
Although no significant improvements were detected on the ORS, a small effect (at trend level) was observed on the overall scale and social scale. The overall and social subscale ratings for each individual at pre treatment and follow-up are shown in Figures 14 and 15.
FIGURE 14.
Individual patient ORS: overall subscale scores at pre assessment and follow-up.

FIGURE 15.
Individual patient ORS: social subscale scores at pre assessment and follow-up.

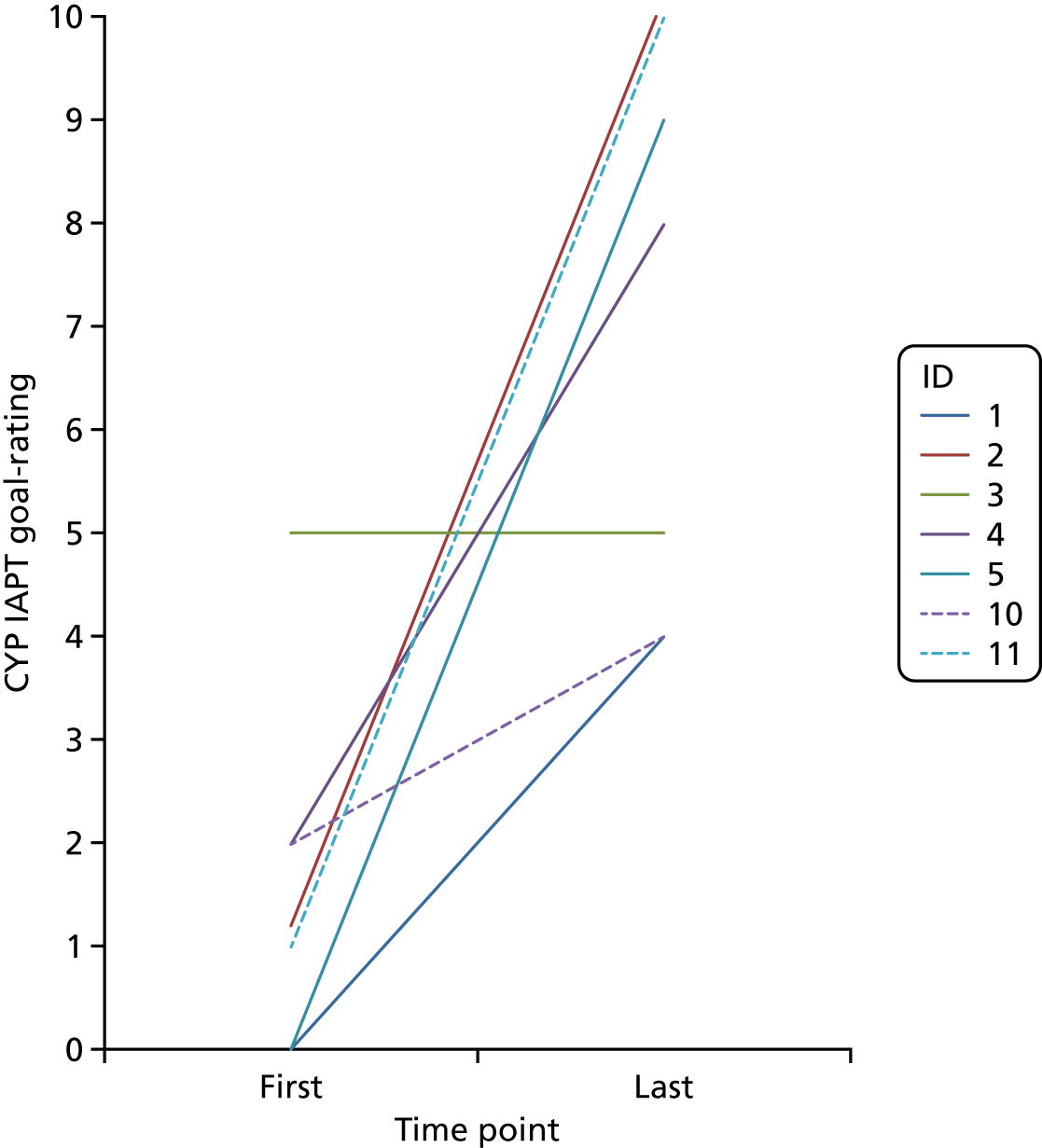
Children and Young People’s Improving Access to Psychological Therapies programme goal-rating
Therapists were expected to ask patients to identify their key goals and rate the extent to which they had reached those goals from 0–10 every session. There was wide variability in the collection and recording of these data, with data from two time points available for only 8 out of 12 participants. For one of these participants, there were only two time points at weeks 6 and 7, so these data have not been presented, as they do not accurately reflect initial and final progress. Data for the remaining seven patients’ primary goal are presented in Figure 16. Initial goals data were collected between sessions 1 and 3 for these participants. The last time this was collected was between sessions 8 and 14. Six patients rated themselves as closer to attaining their main goal at the last assessment point, while the remaining patient’s rating was the same at both the initial and final assessment points, although it did increase at points during the treatment.
FIGURE 16.
Individual patient data for first and last available CYP IAPT goal-ratings made by patients for their primary goal in therapy.
Psychological process measures
Social Cognitions Questionnaire
Social Cognitions Questionnaire – belief
All patients reported some reduction in ratings of belief in their social cognitions, and the group as a whole showed a large and significant reduction in belief ratings on the SCQ (Figure 17). For all but three patients, these reductions were substantial (belief rating reduced by 88–100%). The same nine patients who showed these large reductions in the SCQ also showed a clinically significant improvement on the LSAS-CA-SR, as indexed by a drop of 48.75 points on the scale.
FIGURE 17.
Individual patient SCQ mean belief scores at pre assessment and at the follow-up assessment.

Social Behaviour Questionnaire
All but three patients reported substantial reductions in their use of safety behaviours at follow-up, as indexed by scores of 0.55 or below on the SBQ (range 0–3) (Figure 18). The same nine patients who showed large reductions in the SBQ also showed a clinically significant improvement on the LSAS-CA-SR, as indexed by a drop of 48.75 points on the scale.
FIGURE 18.
Individual patient SBQ scores at pre assessment at the follow-up assessment.

Social Attitudes Questionnaire
For the group as a whole, there was a large and significant reduction in negative social attitudes (mean SAQ) from pre treatment to follow-up (Figure 19). Only one patient (ID 10) showed a strengthening of their negative social attitudes, and they also retained their SAD diagnosis at follow-up.
FIGURE 19.
Individual patient mean SAQ scores at pre assessment and at the follow-up assessment.

Treatment acceptability
Eleven young people completed the treatment acceptability scale at the follow-up assessment. All of them somewhat or completely agreed with the statements ‘I was satisfied with the treatment’ and ‘I would recommend the treatment to others’ (Figure 20).
FIGURE 20.
Treatment acceptability.
Chapter 6 Results 3: costs of treatment delivery in routine child and adolescent mental health services
Aim
The aim of the economic analysis was to estimate the cost of training therapists to deliver CT-SAD-A as well as the cost per adolescent treated from the perspective of the NHS.
Methods
Clinician’s logs (see Chapter 2, Health economics records) were completed by both supervisors and therapists. Data recorded in the logs were used to calculate the cost of training therapists to deliver CT-SAD-A and the mean total amount and cost of qualified staff time used by the NHS per adolescent treated. Results were stratified by type of staff (i.e. supervisor and therapist) time use (i.e. time spent in training, supervision, preparation and delivery of CT-SAD-A). Time spent by supervisors training and supervising therapists, as well as time spent by the therapists being trained and supervised, were attributed pro-rata to each patient treated. For each study participant, all components of treatment costs, stratified by category of resource use, were computed by multiplying units of resource use by their unit costs. Values were expressed in 2016/17 UK GBP (£). Unit costs used and their sources are summarised in Table 7. Results were reported in terms of total amount of qualified staff time and associated cost for training and supervision as well as in terms of mean values of qualified staff time and associated cost per patient treated, with variability around the mean measured by SDs. Percentage of missing values were reported. As missing data occurred exclusively on the time spent on face-to-face therapist contact with the young person and were highly deterministic (i.e. readily identifiable and standardised given observed practice), a conditional imputation method was conducted whereby missing data were estimated as an average of known durations for that patient. For patients for whom all information was missing, the average duration across all patients was used. Analyses were conducted using Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA), and Stata® statistical software, release 15 (StataCorp LP, College Station, TX, USA).
| Item | Cost | Source | Notes |
|---|---|---|---|
| Clinicians – therapists | £42/hour | Curtis and Burns47 | Table 12.647 – generic single-disciplinary CAMHS team |
| Clinicians – supervisors | £62/hour | Curtis and Burns47 |
Table 947 – scientific and professional staff Cost per working hour for community-based scientific and professional staff, band 8a |
Results
Data completeness
Supervisor-completed economic logs, which included information on time spent by supervisors and therapists in workshops and weekly case supervision practice, had a 100% completion rate. Therapist-completed economic logs, which included time spent in delivering CT-SAD-A to patients and associated activities (e.g. preparation time), had rates of missing values that ranged from 50% to 67% for various treatment sessions across all patients. No data were recorded for any of the treatment sessions throughout the whole treatment programme for 4 out of the 12 patients.
Qualified supervisors’ and therapists’ time and costs
Three supervisors provided training and supervision to therapists during the training phase of the study. Day-long (7 hours) workshop training was usually delivered by two supervisors. Five day-long workshops were conducted during the duration of the study, because new therapists had to be recruited partway through the project. Weekly case supervision was generally led by only one supervisor who was occasionally helped by a second supervisor for part of the session. Sixty-two weeks of active case supervision were reported during the study. The time between case supervision weeks could be longer than a temporal week. Case supervision sessions were intended to be delivered to groups of four therapists at a time but, because new therapists were recruited at different times throughout the programme, multiple supervision sessions were delivered to a less than optimal number of therapists, and, on several occasions, a one-to-one case supervision session had to be offered. The mean number of therapists attending weekly supervision sessions was 2.8 (SD 1.27).
Table 8 shows that, during the whole training phase of the study, supervisors spent overall 4740 minutes (around 79 hours) on preparation and delivery of all of the training workshops, which would cost the NHS £4898. The mean time and cost per workshop were 948 minutes (SD 50.20 minutes) and £980 (SD £51.87), respectively. For the whole case supervision, supervisors spent overall 8621 minutes (around 144 hours) on preparation and delivery of all of the case supervision. As supervisors reported overall preparation and delivery time per week of active supervision (even if more than one supervision session may have occurred in a week), the mean time and cost of qualified supervisor time per supervision week were 139 minutes (SD 71 minutes) and £144 (SD £74), respectively.
| Activity | Total timea (minutes) | Total costa (£) | Time (minutes), meanb (SD) | Cost (£), mean a (SD) |
|---|---|---|---|---|
| Training workshops | ||||
| Preparation | 540 | 558 | 108 (50.20) | 111.6 (51.87) |
| Delivery | 4200 | 4340 | 840 (0.00) | 868 (0.00) |
| Total | 4740 | 4898 | 948 (50.20) | 979.6 (51.87) |
| Total timec (minutes) | Total costc (£) | Time (minutes), meand (SD) | Cost (£), meand (SD) | |
| Case supervision | ||||
| Preparation | 2350 | 2428 | 37.90 (20.60) | 39.17 (21.28) |
| Delivery | 6271 | 6480 | 101.15 (54.20) | 104.52 (56.00) |
| Total | 8621 | 8908 | 139.05 (71.25) | 143.68 (73.63) |
Table 9 reports the mean time and cost of supervisor input per therapist attending each workshop and case supervision week. Results are stratified by time used for preparation and time used for delivery. Supervisors devoted on average 278 minutes (SD 157 minutes) (around 4.6 hours) to each therapist during the workshop training phase, which would cost the NHS £287 (SD £162) per therapist. The large cost was due to the long duration of each workshop (7 hours per day) and the relatively small number of therapists attending each workshop (two to six therapists per workshop day). The amount of qualified supervisor time per therapist was, on average, 50 minutes (SD 14 minutes) throughout the duration of the case supervision of the programme. The associated cost to the NHS would be £51.5 (SD £14.6) per therapist.
| Activity | Time (minutes), meana (SD) | Cost (£), meana (SD) |
|---|---|---|
| Training workshops | ||
| Preparation | 26 (5.48) | 26.87 (5.66) |
| Delivery | 252 (153.36) | 260.4 (158.47) |
| Total | 278 (157.07) | 287.27 (162.30) |
| Time (minutes), meanb (SD) | Cost (£), meanb (SD) | |
| Case supervision | ||
| Preparation | 13.7 (6.71) | 14.18 (6.93) |
| Delivery | 36.12 (9.91) | 37.32 (10.24) |
| Total | 49.84 (14.09) | 51.50 (14.56) |
There were five full-day workshops; the mean number of therapists participating in each workshop was 4.4, the number of weeks of active supervision was 62, and the average number of therapists participating in each supervision week was 2.8.
To have an estimate of the overall cost to the NHS of training therapists to deliver CT-SAD-A, the amount of therapist time spent being trained and the associated cost needed to be estimated. Overall, 9240 minutes (around 154 hours) of therapists’ time was spent on workshop training (five full-day workshops to train a total of eight therapists), which would equate to a total cost to the NHS of £6468. Each therapist spent on average 420 minutes (SD 0 minutes) (7 hours) at each workshop for an NHS cost per workshop attended by a therapist equal to £294 (SD £0).
Table 10 presents descriptive statistics referring to therapists’ time and cost of participating in the weekly case supervision phase of their training. A total of 62 case supervision weeks were recorded, as often weekly case supervision occurred with more than one therapist. On average, each therapist participated in 24 (SD 12) case supervision sessions.
| Therapists | Number of supervision sessions attended | Total time (minutes) spent being supervised | Cost (£) of total time spent being supervised | Time (minutes) per supervision session attended, mean (SD) | Cost (£) per supervision session attended, mean (SD) |
|---|---|---|---|---|---|
| Therapist 1 | 32 | 2680 | 1876 | 83.75 (37.48) | 58.63 (26.24) |
| Therapist 2 | 38 | 2885 | 2019.50 | 75.92 (38.97) | 53.14 (27.28) |
| Therapist 3 | 29 | 2405 | 1683.50 | 82.93 (38.53) | 58.05 (26.97) |
| Therapist 4 | 34 | 2710 | 1897 | 79.71 (39.25) | 55.79 (27.48) |
| Therapist 5 | 3 | 480 | 336 | 160.00 (34.64) | 112.00 (24.25) |
| Therapist 6 | 19 | 750 | 525 | 39.47 (13.43) | 27.63 (9.40) |
| Therapist 7 | 16 | 630 | 441 | 39.38 (13.28) | 27.56 (9.29) |
|
All – mean (SD) |
24.43 (12.34) |
1791.43 (1107.48) |
1254 (775.23) |
73.33 (39.93) |
51.33 (27.95) |
Overall, 12,540 minutes (around 209 hours) of therapists’ time was spent on case supervision sessions, which would equate to a total cost to the NHS of £8778. Each therapist spent in total 1791 minutes (SD 1107 minutes) (around 30 hours) on the whole case supervision sessions, which would equate to a cost to the NHS of £1254 (SD £775) per therapist. Each therapist spent on average 73 minutes (SD 40 minutes) at each case supervision session; the average NHS cost for a therapist to attend a supervision session would equate to £51 (SD £28).
Qualified clinician time and cost per adolescent treated
Tables 11 and 12 summarise the mean qualified therapists’ time per patient for each of the 14 treatment sessions and the two booster sessions, stratified by type of activity associated with each session, as reported by therapists. Data were reported for only half, or less than half, of the patients. Data on the associated costs are reported in Tables 13 and 14.
| Type of contact | Mean duration (minutes) per therapy session | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Session 1 (n = 6) | Session 2 (n = 5) | Session 3 (n = 5) | Session 4 (n = 4) | Session 5 (n = 6) | Session 6 (n = 6) | Session 7 (n = 4) | Session 8 (n = 4) | |||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| CT-SAD-A: face to face (with young person only) | 78.33 | 8.16 | 85.00 | 8.66 | 86.00 | 6.52 | 90.00 | 0.00 | 55.00 | 44.16 | 80.83 | 11.58 | 85.00 | 7.07 | 85.00 | 10.00 |
| CT-SAD-A: face to face (with young person and parent) | 7.50 | 6.89 | 3.00 | 4.47 | 5.00 | 7.07 | 1.25 | 2.50 | 9.17 | 18.00 | 2.50 | 6.12 | 3.75 | 4.79 | 2.50 | 5.00 |
| CT-SAD-A: face to face (with parent only) | 12.50 | 10.84 | 1.00 | 2.24 | 0.00 | N/A | 4.75 | 9.50 | 15.00 | 36.74 | 0.00 | N/A | 1.25 | 2.50 | 2.50 | 5.00 |
| Associated administration (e.g. writing notes/report about client) | 40.00 | 20.00 | 24.00 | 25.10 | 32.00 | 16.43 | 32.50 | 18.93 | 26.67 | 17.22 | 28.33 | 16.93 | 37.50 | 15.00 | 32.50 | 20.62 |
| Time spent on individual preparation for the session | 61.67 | 16.02 | 48.00 | 16.43 | 60.00 | 36.74 | 45.00 | 17.32 | 37.50 | 12.55 | 35.00 | 13.78 | 40.00 | 33.67 | 30.00 | 21.60 |
| Other | 14.17 | 16.86 | 15.00 | 18.71 | 15.00 | 18.71 | 16.25 | 21.36 | 20.83 | 18.00 | 17.50 | 19.94 | 18.75 | 22.50 | 11.25 | 22.50 |
| Total | 214.17 | 24.17 | 176.00 | 18.51 | 198.00 | 21.39 | 189.75 | 17.90 | 164.17 | 33.08 | 164.17 | 20.84 | 186.25 | 33.01 | 163.75 | 35.91 |
| Type of contact | Mean duration (minutes) per therapy session | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Session 9 (n = 4) | Session 10 (n = 4) | Session 11 (n = 4) | Session 12 (n = 4) | Session 13 (n = 4) | Session 14 (n = 4) | Booster 1 (n = 2) | Booster 2 (n = 1) | |||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| CT-SAD-A: face to face (with young person only) | 83.75 | 7.50 | 86.25 | 7.50 | 83.75 | 7.50 | 83.75 | 7.50 | 82.50 | 9.57 | 81.25 | 10.31 | 82.50 | 10.61 | 90.00 | N/A |
| CT-SAD-A: face to face (with young person and parent) | 3.75 | 4.79 | 3.75 | 7.50 | 6.25 | 7.50 | 6.25 | 7.50 | 6.25 | 7.50 | 7.50 | 8.66 | 7.50 | 10.61 | 0.00 | N/A |
| CT-SAD-A: face to face (with parent only) | 2.50 | 5.00 | 0.00 | N/A | 0.00 | N/A | 1.25 | 2.50 | 15.00 | 30.00 | 0.00 | N/A | 0.00 | 0.00 | N/A | |
| Associated administration (e.g. writing notes/report about client) | 32.50 | 20.62 | 32.50 | 20.62 | 33.75 | 18.87 | 33.75 | 18.87 | 38.75 | 20.16 | 37.50 | 15.00 | 27.50 | 17.68 | 40.00 | N/A |
| Time spent on individual preparation for the session | 28.75 | 10.31 | 22.50 | 9.57 | 25.00 | 12.91 | 35.00 | 23.80 | 40.00 | 14.14 | 27.50 | 12.58 | 40.00 | 28.28 | 10.00 | N/A |
| Other | 11.25 | 22.50 | 11.25 | 22.50 | 11.25 | 22.50 | 11.25 | 22.50 | 10.00 | 20 | 15.00 | 19.15 | 15.00 | 21.21 | 0.00 | N/A |
| Total | 162.50 | 34.76 | 156.25 | 34.49 | 160.00 | 31.89 | 171.25 | 27.80 | 192.50 | 51.72 | 168.75 | 30.65 | 172.50 | 67.18 | 140.00 | N/A |
| Type of contact | Mean cost (£) per therapy session | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Session 1 (n = 6) | Session 2 (n = 5) | Session 3 (n = 5) | Session 4 (n = 4) | Session 5 (n = 6) | Session 6 (n = 6) | Session 7 (n = 4) | Session 8 (n = 4) | |||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| CT-SAD-A: face to face (with young person only) | 54.83 | 5.72 | 59.50 | 6.06 | 60.20 | 4.56 | 63.00 | 0.00 | 38.50 | 30.91 | 56.58 | 8.11 | 59.50 | 4.95 | 59.50 | 7.00 |
| CT-SAD-A: face to face (with young person and parent) | 5.25 | 4.82 | 2.10 | 3.13 | 3.50 | 4.95 | 0.88 | 1.75 | 6.42 | 12.60 | 1.75 | 4.29 | 2.63 | 3.35 | 1.75 | 3.50 |
| CT-SAD-A: face to face (with parent only) | 8.75 | 7.59 | 0.70 | 1.57 | 0.00 | N/A | 3.33 | 6.65 | 10.50 | 25.72 | 0.00 | N/A | 0.88 | 1.75 | 1.75 | 3.50 |
| Associated administration (e.g. writing notes/report about client) | 28.00 | 14.00 | 16.80 | 17.57 | 22.40 | 11.50 | 22.75 | 13.25 | 18.67 | 12.06 | 19.83 | 11.85 | 26.25 | 10.50 | 22.75 | 14.43 |
| Time spent on individual preparation for the session | 43.17 | 11.21 | 33.60 | 11.50 | 42.00 | 25.72 | 31.50 | 12.12 | 26.25 | 8.78 | 24.50 | 9.65 | 28.00 | 23.57 | 21.00 | 15.12 |
| Other | 9.92 | 11.80 | 10.50 | 13.10 | 10.50 | 13.10 | 11.38 | 14.95 | 14.58 | 12.60 | 12.25 | 13.96 | 13.13 | 15.75 | 7.88 | 15.75 |
| Total | 149.92 | 16.92 | 123.20 | 12.95 | 138.60 | 14.97 | 132.83 | 12.53 | 114.92 | 23.15 | 114.92 | 14.59 | 130.38 | 23.11 | 114.63 | 25.14 |
| Type of contact | Mean cost (£) per therapy session | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Session 9 (n = 4) | Session 10 (n = 4) | Session 11 (n = 4) | Session 12 (n = 4) | Session 13 (n = 4) | Session 14 (n = 4) | Booster 1 (n = 2) | Booster 2 (n = 1) | |||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| CT-SAD-A: face to face (with young person only) | 58.63 | 5.25 | 60.38 | 5.25 | 58.63 | 5.25 | 58.63 | 5.25 | 57.75 | 6.70 | 56.88 | 7.22 | 57.75 | 7.42 | 63.00 | N/A |
| CT-SAD-A: face to face (with young person and parent) | 2.63 | 3.35 | 2.63 | 5.25 | 4.38 | 5.25 | 4.38 | 5.25 | 4.38 | 5.25 | 5.25 | 6.06 | 5.25 | 7.42 | 0.00 | N/A |
| CT-SAD-A: face to face (with parent only) | 1.75 | 3.50 | 0.00 | N/A | 0.00 | N/A | 0.88 | 1.75 | 10.50 | 21.00 | 0.00 | N/A | 0.00 | N/A | 0.00 | N/A |
| Associated administration (e.g. writing notes/report about client) | 22.75 | 14.43 | 22.75 | 14.43 | 23.63 | 13.21 | 23.63 | 13.21 | 27.13 | 14.11 | 26.25 | 10.50 | 19.25 | 12.37 | 28.00 | N/A |
| Time spent on individual preparation for the session | 20.13 | 7.22 | 15.75 | 6.70 | 17.50 | 9.04 | 24.50 | 16.66 | 28.00 | 9.90 | 19.25 | 8.81 | 28.00 | 19.80 | 7.00 | N/A |
| Other | 7.88 | 15.75 | 7.88 | 15.75 | 7.88 | 15.75 | 7.88 | 15.75 | 7.00 | 14.00 | 10.50 | 13.40 | 10.50 | 14.85 | 0.00 | N/A |
| Total | 113.75 | 24.33 | 109.38 | 24.14 | 112.00 | 22.32 | 119.88 | 19.46 | 134.75 | 36.20 | 118.13 | 21.46 | 120.75 | 47.02 | 98.00 | N/A |
Based on the available data, the main cost driver across all sessions was the therapists’ face-to-face contact with the young person only, which amounted to a mean time of 81.02 minutes (SD 16.86 minutes) and would cost the NHS £56.71 (SD £11.80) per patient per session. Therapists also spent a considerable amount of time preparing for each treatment session; on average, 39 minutes (SD 21 minutes) per patient per session, which would cost the NHS £28 (SD £15). Therapists’ time spent on administrative tasks amounted on average across all treatment sessions to 33 minutes (SD 18 minutes), which would cost the NHS £22.91 (SD £12) per patient per session. The overall amount of time spent by therapists on each treatment session and associated activities was on average across all sessions equal to 177 minutes (SD 32 minutes), which would cost the NHS £124 (SD £22) per patient per session.
Finally, Table 15 reports the mean qualified clinician time and cost to the NHS of CT-SAD-A per adolescent treated, stratified by type of time use. Missing values in treatment sessions were handled as described in the Methods section, and clinicians’ training costs (workshops and weekly case supervision) were attributed pro-quota to each patient. Each adolescent treated required on average 5279 minutes (around 88 hours) of qualified clinicians’ time and would cost the NHS £4047 (SD £1003).
| Activity | Time (minutes) | Cost (£) | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| CT-SAD-A treatment (face to face) | 2658.15 | 511.98 | 1860.70 | 358.38 |
| Supervision (therapist) | 1005.00 | 496.12 | 703.50 | 347.28 |
| Supervisiona (supervisor) | 685.16 | 209.93 | 708.00 | 216.93 |
| Workshops (therapist) | 560.00 | 116.56 | 392.00 | 81.59 |
| Workshops (supervisor) | 370.67 | 77.15 | 383.02 | 79.72 |
| Total | 5278.98 | 1300.73 | 4047.22 | 1003.16 |
It has to be noted that, as therapists’ logs were not complete, we did not have any record of potential cancellation of sessions with the young person and, consequently, we could not account for the potential associated costs. To the best of our knowledge, this was not a recurrent event, but it is certainly a limitation of our results. However, on one occasion, one of the supervisors reported that the case supervision session with therapists was cancelled at the last minute because both therapists were unable to attend the supervision session. We did include the time that the supervisor had spent in preparing for that supervision session in our costs.
Finally, although in our analyses we focused on qualified clinician time and cost per adolescent treated, we acknowledge that other costs were incurred during the implementation of the treatment, such as costs of materials like memory sticks, binders, paper for information packs for therapists. All of those items were not accurately recorded in the clinicians’ logs and, therefore, were omitted from the analysis. Although every item of cost is important and should be included in any cost analysis and their omission is a limitation of our work, it is unlikely that those items would have represented key cost drivers.
Chapter 7 Qualitative interviews: approach, design, sample and analysis
Approach
We adopted an interpretative phenomenological analysis (IPA)48 approach to the qualitative component of the study. IPA is phenomenological and interpretive, as it is concerned with both understanding how people make sense of their experiences and acknowledging the role of the researcher in identifying patterns of meaning across experiential accounts. It has been used extensively to explore people’s experiences of psychotherapy and mental health services, including adult SAD. 49 It has also been used widely to explore families’ experiences of mental health issues.
Design
The qualitative component adopted a multiple perspective design,50 which incorporated the perspectives of young people, parents, therapists and managers. Each of these perspectives constitutes a homogeneous subsample. IPA has a commitment to an idiographic analysis, which means that a focus on ‘the particular’ is presented alongside and within the general themes that are typical of most qualitative methods. Constructing each subsample around a homogeneity of perspective means that important variations within each sample can be understood in terms of the participants’ differing perspectives on their experiences. In multiple perspective studies, the analysis of each sample is then combined to provide a broader and more fully contextualised view. This form of design is particularly effective for identifying conflicts and congruences between the experiences of different groups that are engaged with a shared phenomenon. For example, in this case each sample (young people, parents, professionals) had a perspective on the same form of treatment, but the perspective varied depending on whether one was receiving, supporting or delivering the intervention. As with most qualitative approaches, IPA does not aim to produce an objective, generalisable account; instead, the aim is to develop an interpretation that is credible and contextualised. That is, we set out to produce a plausible and transparent analysis of the patterns in our participants’ accounts.
Recruitment
The research team approached all families in which a young person had initiated CT-SAD (14 families), all therapists who were trained in CT-SAD (eight individuals) and all service managers responsible for a participating therapist (four individuals), to invite them to take part in the qualitative component of the research.
Sample
All of the young people, their parents/carers, therapists and their managers/clinical leads who had consented to the study were invited to participate. Six young people, six mothers, seven therapists and three managers consented to take part in the interviews.
Eight young people and their parents did not participate (one was still in treatment at the time of interviewing, one had moved abroad, two were uncontactable and four declined to take part). All the participating parents/carers were mothers. One therapist did not participate – this therapist had attended the training workshops but had not had any training cases and could not be contacted regarding participation in the qualitative component. Service managers/clinical leads were invited on the basis that they had service level responsibilities at their locations and were involved in the research at this level in some capacity. One manager did not participate as a result of a long-term absence from work. (Information about the participants are provided in Tables 16–19, with pseudonyms used as in the results section.)
| Pseudonym | Patient number, as used in the case series | Interview duration (minutes) | Diagnosis at post-treatment assessment | Months since end of treatment | Age (years) at interview |
|---|---|---|---|---|---|
| Jane | N/A | 23 | Post treatment not completed (young person completed only two sessions of cognitive therapy) | 21 | 15 |
| James | 7 | 17 | None | 21 | 15 |
| Julia | 4 | 20 | MDD | 8 | 16 |
| Jade | 6 | 26 | None | 5 | 14 |
| Jennifer | 8 | 29 | None | 1 | 18 |
| Jasmine | 12 | 20 | Social anxiety disorder, specific phobia of spiders, depression | 3 | 16 |
| Pseudonym | Interview duration (minutes) |
|---|---|
| Polly | 30 |
| Pippa | 13 |
| Phoebe | 29 |
| Paula | 36 |
| Patricia | 24 |
| Pamela | 44 |
| Pseudonym | Interview duration (minutes) | Background | Number of cases |
|---|---|---|---|
| Caroline | 41 | Clinical psychologist | 2 |
| Conner | 53 | Social worker | 3 (2 full) |
| Christopher | 21 | Social worker | 0 |
| Claire | 58 | Clinical psychologist | 2 (1 full) |
| Carol | 55 | Clinical psychologist | 3 (2 full) |
| Camilla | 45 | Social worker | 2 |
| Charlotte | 49 | CBT therapist (via adult IAPT) | 2 |
| Pseudonym | Interview duration (minutes) | Role |
|---|---|---|
| Margaret | 24 | Clinical team manager |
| Marian | 23 | Clinical lead |
| Monica | 21 | Head of psychological therapies |
Data collection and transformation
Interviews were conducted with individual participants (rather than in groups) so as to make interviews less daunting for young people with a history of SAD and for practical reasons (given the geographical spread of participants and the busy schedules of participating therapists and service managers). Indicative topic guides were used. Interviews were conducted by the trial assessors or a research fellow with qualitative expertise. They were all trained and supervised by a specialist in qualitative research (ML). Interviews with young people were devised to be engaging and sensitive to the interpersonal and communicative preferences of this population.
Interviews took place in person or over the telephone. All interviews were audio-recorded and transcribed in full and anonymised at the point of transcription.
Qualitative data analysis
Analysis involved detailed coding (to identify the experiences, claims and concerns of each participant), followed by the elaboration of emerging themes for each case. In keeping with a multiple perspective design, these themes were brought together at the level of each subsample group, before any form of between-sample synthesis was attempted. Coding for the three samples (young people, parents, professionals) was led by three different members of the research team (EB, SP, LT) with supervision and comparative coding provided by ML. The coding team worked together closely to compare both the organisation and the format of their work, and also the focus and plausibility of the codes themselves.
Credibility of the qualitative analysis was checked via analytic triangulation on two levels. First, in-depth triangulation was provided through supervision. This involved co-analysis of selected transcripts; use of reflexive practices in supervisory discussions; and audit checking for plausibility, coherence and comprehensiveness of analysis at each key stage of the process, with each subsample. The aim of this level was to maintain high standards of analysis.
Second, a broader triangulation exercise was conducted to check the appropriateness of the theme titles, the persuasiveness and plausibility of the overarching narrative, and the intelligibility of the overall structure. This involved a presentation of the draft analysis by the researchers conducting the qualitative analysis to both the SSC and the Study Management Group, which included the investigators, the PPI lead and the young person representatives with relevant lived experience, as well as independent therapists and researchers with relevant experience. These groups were invited to comment on the presentation and provide feedback on the sensitivity to the context, the rigour, transparency, coherence and utility of the analysis (after Yardley51). The aim of this level was to check that the analysis is meaningful, useful and accessible.
The final analytic structure is detailed and complex, and can be used as the basis for identifying cross-cutting themes within and across samples. In subsequent reporting for publication, we will take this approach, presenting our analyses in the thematic format that is typical of IPA work. For the purposes of this document, what is presented in the results is a more ‘concrete’ precis that presents information extracted from the case-level and sample-level summaries to address the stated research questions of the evaluation as directly as possible. For the most part, we present this preliminary analysis by focusing on each separate subsample. Subsequent reporting for publication will incorporate a more integrative analysis.
Chapter 8 Results 4: young people’s and parents’ experiences
Young people’s perspectives
On the basis of their interviews, young people generally appeared to find the intervention acceptable. The young people reported that the therapists were calm, friendly and understanding. For example, one young person commented: ‘[H]e was open [. . .] I could just talk for quite a long time and he wouldn’t like judge me or anything’ (James).
Varied motives and experiences
Before starting CT-SAD-A, the idea of therapy was framed as potentially difficult and challenging. Young people described a range of expectations – for example, some were sceptical and ‘didn’t really think it was going to work’ (Julia), or felt that it ‘wouldn’t be any different’ (Julia) from previous counselling experience; some expected that they would be ‘sat in a room talking the whole time’ (Jennifer), whereas others thought they were going ‘to talk about er, [their] problems’ and ‘learn some like, er, er, um techniques for them’ (James). One young person acknowledged that the only experience they had of treatment was ‘things on TV . . . and those are quite a distorted image, so [they] had no clue [what to expect]’ (Jade), and another expressed ‘hope’ that the therapy would bring about improvements to their independence and confidence.
In the pre-treatment assessments, young people described their desire to reduce their levels of social anxiety. However, in the research interviews, many of the young people reflected on their motivations for engaging in this treatment or via this context. For example, some young people commented that they felt motivated by being part of a research trial in which they would be helping others, while other young people were motivated by the idea of a more interactive therapy:
I felt good doing it, because I felt like I was helping people.
Jade
Um, yeah, i–it was kind of good to know that it was all going to research, it wasn’t just, like, going towards me or anything, it was kind of going towards like a bigger thing.
James
Instead of just like, you know, saying ‘ahh I think I can get over it’, just actually doing them umm, that umm, yeah and umm that seemed like quite a reasonable idea.
Julia
A challenging, helpful and active experience
The therapy itself was generally represented as challenging but helpful. Most young people were able to identify and reflect on features that were helpful. The pacing was felt to be appropriate, and the repetition, practice and ‘building on’ progress were valued. For example, here, Julia reflects on how the rehearsal of strategies meant that they were subsequently easy to access:
It’s been good, because it was so repetitive in the treatment that I like can, it’s like, something that just comes to me naturally now it’s not, it’s not such a hard thing to do.
Julia
Some therapists had involved parents more actively in some aspects of the therapy, and this was also largely experienced as helpful and positive by the young people who were interviewed. For example, a number of young people reported that their parents would attend parts of sessions, which ‘kind of help[ed], like, in that respect, because it meant my mum could help carry it on with me after’ (Julia), or support them outside of sessions:
She was very involved because she had to be the one to stop doing a lot of things for me.
Jennifer
Using measures to decide where to focus and to track progress
Many of the young people reported that they found the measures difficult and described them as ‘really thick, dense and . . . seem[ed] really, really daunting’ (Jade). Some described them as ‘tedious’ (Julia), and many reported that they took ‘quite a long time’ (Julia) to complete. Nonetheless, for many of the young people, the use of measures during the therapy was experienced as helpful, and some described how the measures ‘kind of just became part of the treatment’ (Jasmine). The measures were seen as helpful in two ways. First, the measures provided a focus for treatment (e.g. choice of a behavioural experiment), as illustrated here by Julia:
It meant that we could focus on specific things that were harder than others and I think that was quite useful because I don’t think–, if–, I don’t think, without the questionnaire, it would have been so obvious the things that needed to be worked on.
Julia
Second, the measures were perceived as helpful, because they allowed young people to see their progress represented visually:
It was quite useful cos you could see, you could compare the different things, what I’d done each week to see what I was progressing in and what I wasn’t.
Jasmine
Identifying active ingredients
In terms of therapeutic mechanisms, it was striking that the young people were consistently able to identify distinct features of the interventions that they could discuss knowledgeably, and evaluate in terms of their utility. This is not always the case in studies of therapeutic experience. Behavioural experiments were generally reported as one of the most useful and important features of the therapy (e.g. ‘I definitely think the ‘training my attention’ and the ‘behavioural experiments’ were, like, key for me’; Julia).
The young people recognised and appreciated the importance of the therapy as an active process of doing, rather than as just a space for talking and reflection. This is concisely illustrated here by Jade:
I would go and interact with people outside, which I didn’t like doing, but it was really, really helpful [pause] because [pause] just talking about it wouldn’t have been enough.
Jade
Note that Jade says, ‘which I didn’t like doing, but it was really, really helpful’. Behavioural experiments were a key component of this activity, and, interestingly, they were also often represented as the most challenging part of the therapy: they were seen as difficult to do but worth doing. We can see how the balance skews towards the positive in Jade’s repetition of ‘really, really’. This was typical of how the young people evaluated their involvement in behavioural experiments:
I hated doing it, I absolutely hated it . . . but that was probably my favourite bit because it did the most for me.
Jennifer
I was so scared to do that as well, but it was nice to know at the end, like, I could do it. So I would say that was helpful, it was difficult at the time, but it was necessary I think.
Jennifer
I just didn’t like doing the things because I felt uncomfortable, but I see the, the whole point that we did it was to challenge the way I thought, and it did.
Jade
The complex response here underlines the importance of including qualitative methods in studies of acceptability and mechanism. Had our interviews been responding to a rating scale here, we might have been detecting the affective content of the appraisal (‘I hate it’) and missing out on the evaluative reflection, which recognises the benefits (‘it was my favourite bit because it did the most for me’).
Other memorable features were the attention-training exercise, and the self-focused attention and safety behaviours experiential exercise (two conversations with different instructions for focus of attention and safety behaviours) and related video feedback. Young people were less clear about how and why these components had been helpful, in comparison with the strong endorsements around behavioural experiments and measures. For example, the experience of the two conversations appeared to be mixed. Some young people seemed to have engaged with the learning behind the experiment:
I was expecting there to be a big difference with the two videos, like umm you know look really awkward in the first one and there wasn’t that much of a difference, so it made me realise I don’t look as anxious to other people as I may think in my head.
Jennifer
Others seemed less clear about the learning behind the exercise:
I recognised the safety behaviours, it was easier to try and not do them and it was good to take them out and focus on them.
Jasmine
Learning from and with the therapist
The role of the therapist in establishing a collaborative relationship around these components seemed to be important to the young people. This is generally evident in the language used to report on these activities, which tended to highlight the collective voice:
We looked at my umm, behaviours and stuff that linked to it and then the things that I found the most umm, like, scary to do and then, after we went through them, we decided on things we could do that could like, get over them, and then we cos we were it’s quite easy to go to like shops and cafes and stuff and we just gradually built it up to things that I found the worst.
Julia
We’d figure out umm, what we could do umm, and then we can go and ask someone to if they know what the time is in the street and then we’d go and test it out umm, and then go back and reflect on it and see how it actually was how I felt.
Jennifer
It was also illustrated by examples of therapist modelling and engaging in activities:
[Therapist] would stutter, er, then we’d see their reaction, but erm, yeah, he, he showed me that there wasn’t, people didn’t really care, to be honest with you if you stuttered.
James
One young person expressed concerns about being able to apply what she had learned during therapy. She sometimes struggled to see the relevance of the activities to her wider experiences, for example, in one behavioural experiment she ‘had to go around and ask people for the time which [she didn’t] think [she’d] ever need to do again’. This may have been a consequence of not having fully engaged with the model underlying the intervention. As a result, this young person struggled to generalise the things she’d learned in these activities to situations that she found herself in outside treatment:
It was quite hard, I think. [Pause] because [pause] I do things there [pause] but I–, I had to know how to adapt it [pause] which was hard, yeah.
Jade
However, this young person also experienced depression, and aspects of her problems with low mood appeared to interfere with the focus on social anxiety. She was advised to apply things she had worked on in the sessions to her experience with mood, but she struggled to do this:
I did ask during the treatment, um, do you know how ki–, how I could get help for depression and they said oh, and [Therapist] said, um, ‘You can use the same techniques’ but I didn’t really know how.
Jade
For her, it ‘felt like the ending [of the treatment] was very very quick’ and that she ‘didn’t get much closure’ (Jade). For example, she described weekly sessions, followed by one 2-week gap and a final session after a further month (close to that described in the protocol), and felt that these sessions ‘tapered off really quickly’. There was a general sense that the young person had been left slightly ‘behind’ the pace of the therapy or outside the understanding of the therapist.
The other young people were generally confident that they could identify what they learned and apply it. The importance of practice (outside the sessions) seemed to underline this for most of the young people. For example, one young person noted that ‘remember[ing] all of the things [they’d] learned and then just keep going over it and over it’ helped after the sessions had ended, as ‘then it didn’t seem like such a difficult thing not having a session every week.’ (Julia). Some young people mentioned that the ‘experiment sheets’ were really helpful for this:
Yeah I got given like experiment sheets to fill out and do the same things in between like say on my lunch break, umm, go and buy something myself from the shops cos I would never do anything like that umm and then I’d have to fill out these sheets and then bring them back to my next session.
Jennifer
Of course, we might reasonably expect the young people to vary in terms of their preferences and motives for engaging in different aspects of the treatment, as they do here. The strong preferential consensus about the active focus of treatment is all the more striking against the background of variation with regard to other aspects of the experience. For the most part, the young people were also very positive about the consequences. Some reflected on the ‘recalibration’ of their worries:
Some really big things I still find quite daunting. I don’t know if I’ll be able to do that, but I think, I kind of have a lot of the tools to kind of try and build up my confidence and stuff, so I think that will be useful.
Jasmine
Young people were often able to identify areas of significant functional progress that were important to them, too. For example, here, James describes several improvements since engaging in the therapy:
I used to go to the support area, [. . .] for about 3 hours a day every school day. I haven’t been in about a year . . . I’d never put my hand up to answer questions, I wouldn’t really go to lessons that much, er, but now I kinda answer questions all the time and talk to people and all that. [. . .] Performing was a big problem as well, but I, I do music now.
James
To summarise, young people appeared to find some aspects of the intervention challenging, but they reflected on the benefits (especially the functional improvements) outstripping the costs. They found the approach taken by their therapists to be open and non-judgemental, and the therapeutic process to be active. They identified the use of measures and behavioural experiments as being particularly helpful.
Parents’ perspectives
On the basis of their interviews, parents generally appeared to find the intervention acceptable.
Keeping an open mind
The parents often shared ‘diffuse’ expectations about the therapy. They were unsure about what to expect, but they described their initial thoughts as hopeful or being ‘quite interested to see how it would [. . .] benefit’ their child. Experience of the problem and/or other interventions was framed as a ‘why not give it a try?’ opportunity by some parents:
No expectations, just; if it works, great, if it doesn’t, then, you know, at least we’re in the system and, um, we can get some help.
Pamela
It didn’t work so well with [the young person], but every child’s different, every child’s different, so yeah, give it a go, you’ve got nothing to lose.
Patricia
However, others were ‘really excited to be part of the study’, as they felt that there would be ‘a lot more audit, maybe, on [. . .] how the sessions were going’ (Phoebe) in comparison with experiences of standard services, prior to taking part in the study.
Noticing functional improvements
Parents were generally very positive about the impact of the intervention in terms of what the young person was now able to do. Some reported that it was ‘really helpful [. . .] very accommodating and [they] wish[ed] it was more available’ (Polly), or that the improvements that their child had made were ‘leaps and bounds very positive’ (Pippa). Parents noticed improvements in the young persons’ activities – particularly their engagement and involvement with friends, their autonomy and independence in communication, and their confidence in initiating activities outside the house. For example, one young person who had previously found it difficult to stay overnight at a youth event had, since the end of treatment, stayed at the event for an entire week and had further been selected to attend a 3-week event abroad:
He’d always liked the idea of going away for a weekend [. . .] but could never stay overnight [. . .] that was a big breakthrough for us, with him staying overnight [at event] [and now he’s] off [overseas] for three weeks next July.
Paula
These were incremental changes, which one parent described as ‘a very gradual process of, sort of, confidence’ (Pamela), and could not be pinpointed to a specific time in treatment. However, by the end of treatment, these improvements stood out as markedly different from the pre-treatment phase:
I don’t even know how to quantify how much better she is.
Polly
Parents reflected on the psychological changes that appeared to underpin these functional improvements. For example, one parent described their child’s ability to overcome difficult situations by shifting her focus of attention and drawing on learning from previous experiences:
When she went in for her theory test, you know, she was like, um, like she said ‘I took a deep breath, thought; right, I can do this, nothing is going to happen, it’s going to be fine’ and, you know, it’s those sort of things, like, that she, um, looks around her and her environment and takes it all in and knows that it’s, it’s OK.
Pippa
Appreciating the opportunity to be involved and informed
Parents appreciated the flexibility of the therapists. This was reflected in the flexibility of the session length, the appointment times, the information about the young person’s progress and the opportunity for involvement in the therapy. This last point was generally to do with understanding the therapy so that they could support and extend the young person’s progress outside the sessions. Some parents had a positive experience of feeling better equipped to support the young person outside sessions:
Lots of things that [. . .] she would tell me, I would um, the ideas of the stuff that I would try to, um, every time we went out, I would push her a little bit more to do little, little things and anything to help her along the way.
Pippa
Whereas, others felt more like they were ‘on the back burner’ and found it ‘a bit tough, not knowing what’s going on and just hoping that she was OK’. For example, Patricia felt less able to provide input between sessions because she was unaware of what was happening during sessions:
I think it would have been easier if maybe I kinda sat in on the first ones so I know what she was going through and then, if she wanted to talk about how it went, then I could say, you know, I could have had input because I knew, you know, that I had something to, to, yeah, base it on.
Patricia
There were varying degrees of involvement. For example, some parents felt that it was a ‘case of just keeping [them] in the loop and giving [them] a bit of evaluation of what is going on’, while others felt well informed but appreciated that the therapist was best placed to lead this:
We would have a little meeting for, sort of, 15–20 minutes and the things that [the young person] was willing to share, um, I was told about . . . I think, obviously [therapist] must have encouraged or made it part of the process to, to share those feelings with me, which of course is helpful.
Polly
Families varied in the extent to which they mobilised people around the young person. For example, Polly commented on having ‘lots of help’ throughout the therapy process and reported that she’d ‘talked to friends about it’ who had ‘listened, sympathetically’ (Polly). In contrast, Pamela chose not to involve others, reporting that it was ‘not the sort of thing [she] would tell [her] friends’, and that she ‘[hadn’t] really told [her] mum and dad the extent of it either’, because she thought ‘they’d be upset about it’, and the family ‘didn’t tell [the young person’s] little sister about it’, because they ‘didn’t feel she’d understand’.
Reflecting on relationships, roles and needs
Parents generally appreciated that the therapist was able to support the young person in ways that were not easily available to parents; they acknowledged that ‘it’s different when it comes from a parent somehow’ (Phoebe), but they wanted to be able to support the young person in ways that were consistent with what the young person was learning. There was an appetite for parental training, to provide this knowledge and to build confidence. For example, some parents found it ‘difficult to know what you should or shouldn’t be doing at home to help her and, um, or maybe what you’re doing that isn’t helping . . .’ (Pamela). Sometimes the therapist was appreciated, because they provided a new or different route for communicating with the young person.
Parents reflected on changes in their relationship with the young person. The time travelling to and from therapy was mentioned as a generally positive and shared experience by parents:
We would have that little bit of time in the car, just me and her, on the way, we’d chat about all sorts of stuff and I do, as [the young person] is a teenager, I don’t really get that time with her anymore, so actually it was quite nice, the sessions were quite nice in that respect . . .
Pamela
The sense that the problem was being addressed also provided relief from stress to the parents in some cases:
She’s not hitting rock bottom anymore . . . it does take the pressure off.
Patricia
However, others felt that they needed their own support:
I didn’t feel very supported as a parent, but I don’t know if that’s maybe something that I should have sought help for separately.
Pamela
Some parents also reflected on their own relationship with the therapist. In most cases, this was in the context of a contrast with the young people’s relationships with their therapist and the relative importance of these different relationships. For example, one parent reported that ‘[I]t’s not about me, it’s about him and, actually, he needs to be completely comfortable, um, with [the therapist] in order to maximise the benefits’ (Paula). Another mentioned that they were ‘solely focused on [the young person] and [they] didn’t really have the same relationship with [therapist] that she did’. (Pamela). However, another parent placed more importance on her relationship with the therapist and described the importance of the therapist giving the parent her own space to talk about her own concerns, reporting that ‘it kind of helped [her] to take some of the load off’ (Patricia).
The age of the young people’s siblings was varied, and siblings were not always involved in or informed about the problem. Some siblings were actively involved in supporting the young people; one parent speculated that ‘because [the young person’s sister]’s sort of observed how poorly he has been, she would just obviously recognise anything that would help him would be a good thing’ (Paula), and some siblings were reported to have found the young person’s reliance on their support difficult. Siblings sometimes had to ‘fill in the gaps’ in situations in which the young person’s social anxiety prevented them from doing something seemingly simple for themselves, such as asking for a table in a restaurant or going to the counter in a shop:
It’s been difficult throughout for her sister to understand . . . [the young person] couldn’t do it and her sister found that extremely frustrating.
Phoebe
Reflecting on the context of help-seeking
Parents did not express very strong views about the CAMHS context of the therapy. Parents did provide more discussion of this than the young people, but this was largely based on not knowing what to expect. One parent said that ‘not having dealt with any mental health service before . . . it was it’s all new and a bit scary’. (Pamela). The difficulty of accessing services was also a point of focus in some parents’ interviews. One parent described the referral process to CAMHS as ‘really lengthy’, and another felt that, had they not taken part in the trial, they ‘would have had to wait another year and [mum did not] know what would have happened’ (Polly). Others reported that their difficulty in accessing CAMHS lay in either themselves, or the young person’s school or college not knowing where to go for help:
I tried to get through to them at college when she was starting her apprenticeship, but I wasn’t getting much joy there.
Pippa
A number of the young people in the trial had a comorbid diagnosis of depression or experienced subclinical low mood. For some parents, the comorbid depression represented a barrier to engaging in the treatment:
Probably her underlying depression wasn’t you know, it wasn’t being treated at that time and I think that restricted her access to the CBT.
Phoebe
Others felt that, although the focus on social anxiety was helpful, there was some low mood left at the end of the treatment that was not then addressed:
I think, although it’s fixed the social anxiety, or helped with that, it hasn’t helped with her low mood . . .
Pamela
However, low mood was not a barrier for all of the young people who had mood problems at the start of therapy. For example, although one young person ‘was quite worried about it and thought, you know, “how’s this going to help me?”, because her mood was quite low as well’ (Pippa), her parent reported that this worry was not fulfilled, as she thought ‘it went very well . . . and, now, the end result, it was so worth it’ (Pippa).
Identifying active ingredients
Parents were able to identify features of the intervention that had struck them as important. These were generally framed in terms of their perceived helpfulness. As with the young people, the emphasis was often placed on the active components of treatment:
It’s very difficult to sit in a room for an hour and talk about yourself, I think, you know, to be able to go out and do those physical challenges, um, is probably a bit easier.
Phoebe
A number of parents commented on the fact that this approach was a better fit for the young person:
He felt that it was more around, it was more experiential and it was more, um, er, of a pragmatic, practical, um, treatment programme, rather than sitting and just talking about what he knew were issues . . . so, right from the outset, it felt different and, actually, never ever minded going.
Paula
Parents were aware that young people found some of the active aspects of treatment difficult:
[Therapist] took her out and did practical things with her, which I thought was very good, much to [the young person’s], didn’t like it, but it it helped her, you know. She probably thought that was the worst things for her to do, but actually doing it, it proved to her that it worked.
Pippa
Others emphasised the importance of having someone to talk to in a non-judgemental environment:
I think just talking to someone, as I said, regardless really of what the therapy is, I think that she could, well I, I can’t discount [the treatment] obviously, but I, I honestly think, just the process of talking to somebody in a non-judgemental environment . . . was invaluable.
Polly
Accepting the need for measures
The parents sometimes found their own measures difficult to complete (e.g. Polly) because of not having the information they needed to answer some of the questions about their child’s feelings. For example:
I would read them and think ‘how am I supposed to know the answer to any of this?’. So it’s all guess work and that felt, felt like, a bit like cheating.
Polly
Especially, like, as a parent, whereas she might not have told me a lot of stuff, I found a lot of it quite difficult to answer because I just didn’t know.
Pamela
However, they accepted them as important, describing that they felt like ‘if it helps with the research, it’s got to be done’ (Pamela). Some parents found the measures to be unproblematic for the young people to fill out. For example, one parent reported that, because it was something that could be done in the ‘home environment’, it ‘didn’t involve much challenge, so that wasn’t a problem for [the young person]’ (Phoebe). Others commented on how repetitive they were:
We were filling in the same sort of forms over and over and over, which was explained and, you know, understandable, but I mean, it did seem to be fairly repetitive.
Polly
Others noted that the young people’s questionnaires were ‘helpful’, because ‘you actually get to see it, of how she was feeling at that time and whether her mood was low or high’ (Patricia), even if they sometimes also commented that the young people found them ‘very tedious’ or (in one case; Patricia) overwhelming to complete. Some parents commented that an electronic means of capturing the data would have been preferable for them and/or their children, as this would have been more convenient for the young people to fill in and would have taken the pressure off busy family life, since they would not have had to remember to take them to sessions. For example:
I hadn’t already got them in the car, or she’s forgotten to bring them with her, I can’t stop, it would make me late . . . but you could e-mail them if you’ve still got your phone with you, which 9 times out of 10, you’re gonna have.
Patricia
Measures were accepted as integral to participating in research, with one parent reporting that, ‘with that being part of the trial, [the young person] could, you know, that to him was, made logical sense that every so often you’d have to evaluate what he was doing’ (Paula).
Parents appeared to find participation in the research acceptable. For some, the research was a mechanism for receiving an intervention that otherwise might have been unavailable or that would have required a long wait:
We probably saw it as a way that we might get some help quicker.
Pamela
One of the parents was keen on the additional monitoring (of progress) and transparency (about progress) that research involves, compared with treatment as usual:
Prior to that, we hadn’t really felt that there’d been, certainly not, not, er, fed back to us that there hadn–, didn’t seem to have been that much reflection and, well – ‘are we actually progressing and has there been any developmental progress?’, those kinds of things we thought would be, um, a lot more part of the, the core of the study, really, so we were quite excited.
Phoebe
The motivations of parents also included the benefit of helping others (e.g. Paula, Pamela), which was important when previous experiences had been unhelpful. For example, one parent reported that, although their main motivation was that they ‘just wanted someone to help’ their child, ‘if it helps other people in the, in the long term, then that’s great’ (Pamela). Another parent reported that their child was initially reluctant to access treatment for their difficulties, stating ‘I don’t need to, I’m fine’, but that they were able to ‘discuss it with him around it being a research trial’ and were able to ‘bag it as something different, um, and he was more than happy to do that’ (Paula). Research was also framed as more inclusive than treatment as usual, with one parent explaining that ‘it possibly gave me an avenue to contribute more than treatment, um, which I wouldn’t normally, or I hadn’t previously been asked from my perspective what I thought, um, how I thought [the young person] was doing.’ (Phoebe).
To summarise, parents were aware that young people found some aspects of the intervention challenging, but they noticed and valued the benefits (especially the functional improvements). They found the approach taken by their therapists to be open and inclusive, and they noticed and appreciated that the therapeutic process was an active one. They accepted the need for measures. They reflected on some of the relational impacts of treatment, and some felt that they would have liked to have received support for themselves as well.
Chapter 9 Results 5: therapists’ and service manager/leads’ experiences
Child and adolescent mental health services therapists’ perspectives
Engaging and expert training
On the basis of their interviews, therapists generally appeared to find the training helpful. The therapists were very positive about the detail, format, focus and utility of the training (‘I think they were all great, I think there wasn’t one bad bit’; Caroline). The video clips illustrating particular treatment procedures were universally seen as ‘really, really useful’ (Carol).
The style of the training workshops was perceived to be very interactive, and therapists appreciated that the training was delivered by people who were acknowledged as experts in the field (e.g. ‘they are the bee’s knees’; Christopher). The appreciation of the trainers’ expertise and the interactive style of training was consistent. For example, Conner described how an advantage of ‘[B]eing trained by the person who, kind of, originated the protocol [was] that there was a much, kind of, closer knowledge of it’ (Conner). He went on to describe his appreciation of the blended teaching style, a point also made by Caroline:
Good mix of kind of didactic teaching and thinking together, some role plays, some getting out and doing behavioural experiments, experiencing them yourself, it was a really good mix I think.
Caroline
Challenging but supportive supervision
Therapists reflected on the ways in which supervision had been provided and how they had drawn on it. The use of supervision to support learning about and subsequently delivery of the treatment was largely positive. For example, Charlotte appreciated her supervisors’ ‘insightful comments’, and Carol reflected on how in supervision the ‘[A]dvice that you were given was massively helpful, so you really felt that you were developing your skills’.
Some aspects of this form of supervision were framed as ‘different’ from their usual or previous experiences of supervision. For example, focusing on therapy techniques in depth and using measures and videos to inform the session were indicative of distinctive attention to the treatment of a case (rather than as a forum for more general discussion of clinical issues). Generally, these differences were experienced as positive and constructive by our therapists, who noticed a shift towards ‘[F]ocusing very specifically on techniques and actual words so the minutiae . . .’ (Caroline). The videos, in particular, were an important learning mechanism for our therapists:
[Using videos is] much more powerful when you actually see the act– part of that session.
Christopher
We would watch videos in supervision, which was helpful, and then the feedback that came back was great, umm, going through the questionnaires was great. Yeah, I mean supervision was great.
Caroline
Supervision was thus framed as part of the wider learning opportunity provided by participation in the research and as being helpful in skill development and the growth of competence and confidence. This was one aspect of participation in the research that was attractive to the therapists:
I was kind of quite keen to umm, you know, see if there were things I could learn that might improve my practice.
Claire
Helps your professional development, checks that you’re doing the right thing.
Camilla
Therapists reflected that they had been motivated to participate in the research because of this opportunity to improve their skills. Learning from supervision was clearly understood as a component of this opportunity, as it provided clinical insights and informed the next steps in treatment planning. Here, Caroline and Claire both reflect on situations in which supervisory discussions helped them to plan their next sessions:
I guess I would always be keen for feedback on [when] I didn’t think I did that very well, how could I have changed that, how could I have done it, what would you have done in that situation, that kind of stuff. And then help planning behavioural experiments and umm, ones that would work practically, umm and then thinking about endings.
Caroline
I think supervision again was really, umm, necessary to help, ummhmm, you think about how you were going to umm structure the session and, and, and do the session.
Claire
Thus, we can see that supervision was framed partly as a mechanism for identifying what could have been done differently (areas for improvement) and partly as a mechanism for identifying what should be done next (treatment planning). Supervision in the project was often delivered with peers, rather than in a 1 : 1 format. Therapists generally liked the opportunity to learn from, and with, peers:
When it worked [with] the three of us, it worked brilliantly, and I preferred group supervision because of that richness.
Caroline
I think it’s useful to hear other people and how that is really, really key, especially if you’re struggling to do it all as well as you’d like to, you’re running out of time and you hear that they’re also doing that.
Camilla
Although therapists valued the ‘richness’ of learning alongside others and the benefits that came from their hearing about perspectives, some suggested that larger groups might have been preferable. Groups potentially offer the possibility of not always being in the spotlight, but that was not really provided in these smaller configurations. Charlotte reflected that:
It would have been nice if there was a couple more people, because it felt really intense with just two of us doing it.
Charlotte
However, one participant also felt that group supervision did not allow enough time to discuss their cases:
I would guess that I was just worried that I’d have enough time to discuss mine as well, but it was useful because you’re also hearing that somebody else is finding it difficult to fit it all in and practicalities of it as well.
Camilla
Thus, small groups would appear to have been a ‘best-fit’ compromise, striking a balance between the different preferences of the therapists. Some supervisees had not been able to meet their supervisor in person, and they felt that this would have been helpful: ‘it’s not the same as face to face to be honest’ (Christopher); ‘from a supervisee perspective and feeling, umm, kind of comfortable sharing your nightmare moments on video, it’s nice to have met somebody face to face’ (Caroline).
Less positive features of people’s experiences of supervision were generally related to one of two features. First, there were some early anxieties when they anticipated being on the receiving end of critical judgements about their competence. For example:
It was a bit nerve wracking and anxiety provoking when we first started . . . I thought supervision was done in a really, non-threatening way and I think, I think effort was put into that and I think it was appreciated.
Carol
I don’t think it made me seem like a particularly competent therapist at all.
Charlotte
As Charlotte’s quotation implies, these anxieties were not confined to the anticipation of scrutiny. Therapists also expressed some worries about the high standards that they wished to be able to meet and that they felt they would be measured against during supervision:
I found that quite difficult if I and, and that, that’s probably why one of the things I found it really difficult to do this and feel like I was doing it well which kind of like disappointed me and I always felt like ooo, I’m not doing this well.
Camilla
You’ve still got to deliver the video and stuff [yeah] and I think they put a lot of pressure on you to, to get it right.
Christopher
Second, therapists struggled with practical issues associated with access to supervision. This involved freeing up time, finding the time to prepare for supervision and making the technology work (‘I felt I needed to get this on camera’; Christopher). Freeing up time, and then protecting and using that time as planned, was a recurrent concern:
If I did particularly have a busy day if I had to split, you know if I’d had to slip something else in or I’d had to see like another family urgently or something umm and then it was on the back of the supervision session that was quite difficult.
Claire
[I needed to] have the questionnaires handed in, have the video uploaded, etc., all kinds of– and its weekly and it’s quite– and when you’re quite busy it’s hard to get it all ready.
Camilla
Issues with technology often compounded the sense of urgency and pressure that are captured in the accounts of Claire and Camilla above. Technological barriers included the ease and reliability of hardware and software, and the compatibility with people’s location and local systems:
It’s the technology, but, kind of, Skype was unreliable and that just made it kind of stressful, cos, when you’re kind of going into supervision and you got to spend 10 minutes trying to figure out how to actually get a clear line.
Conner
Every now and again where it would click off or something like that – yeah it was a pain yeah.
Christopher
These barriers were not insignificant: therapists expressed considerable frustration about technical problems and gave specific examples of the pressures on their time, such as ‘staying late trying to finish it all off’ (Claire) and arranging supervision on a non-work day (Caroline).
A useful and well-used manual
The manual (and training materials) were also appraised very positively:
I liked the way it was structured umm, and umm, having the manual there and everything so you knew exactly what you were doing.
Charlotte
The manual was really, obviously a brilliant resource.
Carol
Therapists used the materials in different ways. Some saw them as providing a grounding (‘I would have to go back to the manual if I was doing it again’; Camilla), and others saw them as a more integral part of growing their competence while delivering the intervention (‘I was constantly referring back to it’; Caroline). Alongside this, the use of video materials within the package was seen as particularly helpful. For example, Claire and Christopher both described how they used the videos to prepare for specific sessions, and how they had found this so useful that they hoped to be able to continue to incorporate the use of video materials into their future supervision.
There were a range of suggestions about additional materials that could be added to further enhance the resources. These included providing some form of checklist to help prepare for supervision (therapists felt that there was a lot to remember and bring) and including, in the training workshops, training in the use of all the equipment and software needed for recording and uploading sessions and accessing supervision. One therapist also suggested that it would be useful to have videos to show to the young people.
Developing competence
Therapists were confident that they understood that there was a ‘right way’ to deliver this intervention, but they were less confident that the work they were doing was always consistent with that. Some reported or described ways in which they experienced anxiety or pressure about meeting expectations. These examples were discussed in the context of therapists’ uncertainties about the degree of flexibility that was available to them. For example:
You kind of have to follow a very strict session pattern and it’s quite like clear instructions for each session.
Charlotte
I understand the need to get the research and to and to keep very purest in the research so that you can then perhaps go on and adapt some of the models.
Caroline
In applying their training, therapists appreciated the opportunity to focus on something specific (while framing this as a ‘luxury’ – ‘I think it was good, it felt like a luxury, actually’; Caroline) while also having the opportunity to develop their skills in ‘doing one thing really well.’ For example:
I quite liked it actually. I quite liked that you had a focus. Umm, and that was what you were working on and that you almost kind of didn’t get too distracted by anything else going on.
Claire
You’re just umm, doing social anxiety and you’re doing it slightly different, you’re getting umm, you’re using the formulation in a much more prominent way, right from the start.
Camilla
They looked forward to being able to take their new skills into their next roles, but, as we will see in the next section, they also worried about whether or not the flexibility required by ‘typical CAMHS’ work was at odds with doing so. The sense of developing both specific and transferable skills was common; however:
I think it has changed my practice a lot umm, not just with social anxiety, but I think with other treatments thinking about fidelity to the model umm behavioural experiments and how to develop a model umm, the attention training, the video feedback I think umm, not only in social anxiety cases where I feel a lot more confident and skilled in helping young people.
Claire
Identifying active ingredients
Therapists were able to identify features of the intervention that were particularly salient for their clinical work. These were generally framed in terms of helpfulness, but some features seemed to resonate more strongly than others. As with young people, behavioural experiments were singled out as a particularly important part of treatment. For example, they were ‘probably the most helpful’ aspect of the intervention (Camilla), ‘quite transformative’ (Conner) and ‘obviously a completely key part of it [that] the young people found [. . .] really helpful and were then able to go away and then put it into practice’ (Carol).
The requirement to ‘get’ out of the therapy room was generally incorporated well into the treatment sessions, even though therapists reported some practical barriers to this as ‘one of the biggest challenges’ of the trial (Claire), in terms of limitations of location and time to organise and complete the session within the session length. The benefits of the behavioural experiments were represented in terms of them being ‘more active’ than the therapists’ usual ways of working:
I was probably much more active than the CBT I was using before, I was probably much more passive [how do you mean?] Umm so right from the beginning you’re adding behavioural experiments [oh OK yeah] where I probably wouldn’t have done that before.
Claire
Another important feature was video feedback, which was described as ‘a very powerful part of the treatment’ (Claire), helping to ‘bring [. . .] alive the things we were talking about so that they could see it, rather than, just sit there and describe it’ (Conner).
Attention training was framed more ambiguously – therapists felt that it was difficult to implement and that the benefits were less tangible than for some of the other components. It was not ‘as helpful as some of the other techniques’ (Caroline), and therapists found it ‘hard to gauge how much a young person actually takes that on board’ (Conner). It could be difficult to implement too (Charlotte). One therapist did report more positively about attention training:
I always wondered how they were going to respond to this. Umm, just because it’s something that seems really different from the previous sessions and it sort of slowed, the pace has slowed down. Umm, but actually everyone seemed to engage well with it.
Carol
Affinity with the model
Some therapists appeared to endorse the model more confidently and consistently than others:
It is a great model, I love it, I love it from a theoretical and technical point of view, erm, I love its application and how much success you can get with it.
Conner
So, I would have been using Clark’s model anyway – social anxiety, but it was the, it was me applying it in the way that I think it was meant to be applied.
Carol
For others, it was one of the attractions of joining the trial, to be:
. . . trained in a model for social anxiety for young people. Umm, and then obviously being one of the therapists delivering the model.
Caroline
Some of this is reflected in variations in what therapists say about their confidence in the model, but much of it is illustrated more indirectly, through the way in which people talked about the model. For example, one therapist described the research as an opportunity to ‘tighten up’ (Caroline) on perceived inconsistencies in their CBT practice; another stated that ‘I kind of didn’t always really draw out the cognitive element of the learning enough. I think that was what supervision helped’ (Conner), and thus saw themselves as moving towards increasing consistency with the model:
[Developing] more of a sense of competence around was, of the cognitively driven element of that and targeting [pause] beliefs with behavioural experiments and selling that way of working to the young person.
Conner
By contrast, another therapist described sharing the young people’s doubts about engaging in some aspects of the activities or described times when they quickly abandoned a particular strategy because it did not appear to be working. Others expressed concerns about their grasp of some of the components (e.g. attention training, as we have seen). Some of these worries resurfaced in the desire for further confirmation that they were ‘doing it right’ or in requests for considerably more flexibility around complex cases: ‘the main thing is that it has to be a lot more flexible working with children’ (Charlotte).
Concerns about implementation
On the basis of their interviews, therapists generally appeared to find the delivery acceptable, but they expressed concerns about whether or not it was implementable within the current CAMHS context, which was consistently represented as ‘really complex’ (Charlotte). Their concerns included the views that CAMHS was too ‘stressful’ to support this form of intervention, and that intervention was too time-consuming. For example:
Perception would be that, even if the model had been proved to be more effective the actual deployment of that in everyday clinical CAMHS would [pause] be less likely.
Caroline
If you’re working in a, kind of [pause] a day-to-day CAMHS clinic as opposed to a research clinic, it’s more difficult, it’s more stressful, in my perception um, in terms of the, the kind of conflict with everything else.
Conner
When it’s taking more time, then maybe it looks on paper. In a context where you’re, you’re massively overstretched already.
Carol
In the examples above, note that Conner sees the stress arising from a perceived conflict between the intervention and ‘everything else’ in CAMHS. In the wider context of these discussions, it was evident that this conflict arose from different priorities (CAMHS was generally framed as having to prioritise responses to acute crises), and the requirement to adopt a responsive and flexible way of working to accommodate these demands. It is worth noting that Caroline (above) presents these conflicts as being so entrenched that, even if the evidence showed that the intervention was ‘more effective’ (than alternatives), she would still not be confident that it could be offered in CAMHS.
Therapists did recognise that social anxiety could have a significant impact and that CAMHS services needed to be able to offer effective interventions. For example, Carol said that it was ‘something that was needed’ and ‘the model’s great, I think the treatment is great’.
They were positive about the model, but worried that the majority of current CAMHS service users would present with more complex problems than the clients with whom they had worked during the research. For example:
I have massive admiration for it as a model and, and kind of think, y’know it would be, kind of, life changing for many young people that do have social anxiety, that there’s a kind of rub with um [pause] with the presentations that we see, I suppose.
Conner
The therapists were therefore keen to reflect on how much flexibility would be required to deliver the intervention with these service users and to work out how much flexibility would be consistent with adherence to the model. On the whole, they concluded that the model was not sufficiently flexible for CAMHS at present, but some of the barriers (time, technology) may be more easily addressed than others (structure, complexity).
An unexpected issue here was that therapists were concerned that the research effectively provided an intervention to a ‘less serious case,’ when time could have been devoted to addressing the needs of a young person whose situation was more pressing. For Caroline, this felt like an ethical dilemma, and she felt guilty about it:
[The] fact that I was only working with people who shouldn’t be in my team and there was a huge waiting list of CBT cases. So that guilt was quite big [. . .] I was working with people that I wouldn’t normally work with. I was giving them a lot of my time.
Caroline
‘Typical CAMHS’ cases were construed by all the therapists as more complex (usually meaning ‘with comorbidities’) and more acute. In some localities, cases were drawn from other CAMHS teams, or drawn up from tier 2 services to tier 3 (CAMHS) for the research, and so the concern was sometimes based on an accurate perception that the young people would not meet the threshold for the therapists’ usual service or were not typical of those who would. The comments from Camilla and Conner here are typical of the concerns that were raised by all therapists:
There is usually something that is comorbid with it so umm, although it was, it appeared effective on social anxiety, there is other stuff going on for some people.
Camilla
Most young people who come into CAMHS have multiple problems, some of which aren’t clear diagnosis er, kinda problems, but are more behavioural, or emotional, or kind of systemic in nature.
Conner
Thus, the therapists were concerned that the intervention might not be suitable for CAMHS as it is currently configured. We have already seen how this conflict was framed in terms of the tension between acute-complex and, by implication, chronic-simple presenting problems. The conflict was also evident in some very practical, structural features of the environment. CAMHS was configured to measure out time (clinical appointments, room bookings, etc.) in units of 1 hour. This meant that those therapists delivering the intervention carried reduced caseloads (‘Where’s that time coming from?’ Carol), owing to the ‘onerous [. . .] number of sessions [and] the length of the sessions, 90 minutes’ (Conner). This ‘threw’ the ‘diary structure’ (Conner).
Despite this, therapists generally appeared to find the research participation acceptable. In places, it was difficult to disentangle this from other elements of their experience:
I think it was clear, although I think it did, I think it did merge as well.
Claire
For example, workload issues were related to research and delivery of the therapy and were often presented as stressful to manage. It was stressful not only because of the ‘demands’ made on the therapist in terms of adhering to the therapeutic procedures (Conner), but also because of the requirements to complete the parallel research procedures (Claire). All therapists felt that they did not have sufficient time to meet these sets of demands. For example, preparation time was more extensive than for ‘normal working’, and the supervisory commitments were also more demanding. Efforts to provide the therapists with this time were undermined by the unpredictable nature of other routine work.
As we have seen above, there were also concerns about the time needed to manage the data extracted from measures, and the technological barriers to accessing supervision and making and uploading video recordings. The effect of trying to meet these ‘abnormal demands’ was generally reported as stressful for the therapists. Notably, the interviews were taken from the therapists after their training phase, rather than after the trial as planned. It would not, therefore, be surprising if, for example, preparation were to take longer, confidence were to be lower and anxiety about video in supervision were to be higher at this stage in the training.
Worrying about the number of measures
Concerns about the number of measures were related to both the intervention and the research. It was not always clear to therapists which measures were integral to the intervention and which were specific to its evaluation. For example, Claire described the ‘sheer number’ of measures as ‘overwhelming’ at the start. Here, Christopher describes his own initial concerns:
Oh my God this is what we’re gonna have to do every case, every client which is not true, but I don’t know if that was made explicit.
Christopher
Therapists also tended to frame their worries about the measures in terms of their perceptions of the young people’s experiences of completing the measures; they worried that the young people would find the measures boring or not helpful. Camilla, for example, felt that her clients were ‘a bit resistant to completing them’, because they found them to be ‘quite a chore’. Similarly, Carol felt that the young people found the measures to be ‘a bit of a pain.’ As we have seen, these concerns were not shared with us in the interviews with the young people.
There were also therapist concerns about the workload associated with managing the data, for example uploading the measures:
In real sort of you know day-to-day work, you haven’t got the capacity, no, that you can do the uploading and the interpreting and it’s err you know and if you’re doing four, five, six people a day you–you’re gonna struggle with that.
Christopher
Some measures were singled out as being particularly helpful in treatment. Most therapists preferred the anxiety-specific measures, which ‘felt much more relevant’ (Claire). The weekly measure of social cognitions (SCQ) was agreed as being one of the most useful, along with the less frequently used social behaviours measure (SBQ). The LSAS-CA-SR was talked about in terms of its use in treatment:
. . . kind of [to] do a comparison from week to week of what had changed and we’d pick things up.
Caroline
Some therapists did reflect on how they would make more use of the measures in their future work because of how useful they had been (e.g. Claire); others felt that the burden of including the measures was not acceptable to them because of the additional administrative load. It was evident that, for most of the therapists, the use of measures was one of the strongest distinctions from ‘normal working’.
In summary, the therapists were very positive about the training and the model. They found the process of developing competence through delivery and supervision challenging, but also constructive, acceptable and achievable. They framed the therapy as an active form of intervention and singled out behavioural experiments as a key component. Their confidence in other components of the therapy was more varied. They expressed concerns about the volume of measures involved and about the viability of delivering the therapy as part of routine CAMHS work. They identified features that they would incorporate into their future work, including the use of measures within treatment and the use of video in supervision.
Child and adolescent mental health services managers’/leads’ perspectives
On the basis of their interviews, managers generally appeared to support the idea of being involved in research (and one, who was specifically interested in the model, was ‘really excited’):
I was really keen to support the therapists, and the therapists were really enthusiastic and, and I thought from a CBT point of view it would be really good.
Monica
I was aware that the people who were allocated that condition were going off and getting this training and supervision which was quite excellent I was pleased that those skills were coming into the team and being developed.
Marian
Worrying about releasing staff time
Despite their support, they all expressed some concerns about being able to implement the intervention and research in the current CAMHS context (‘the reality was very, very tricky’; Marian). These concerns were generally framed in terms of the perceived pressure on staff, and specifically, the structural barriers to freeing up their time:
I did think it was going to put the staff members under pressure, if anyone piped up and said yes please, I’d like to be involved.
Margaret
There’s no way we could free them up for more than that time in the team, because they already had existing caseloads.
Monica
It was clear that some of these concerns pre-dated the managers’ agreement to be involved in the trial. The focus of their initial concerns was largely about the time needed by the therapists and the impact of protecting time for a specific client group (‘There is always a waiting list for CBT’; Margaret). At the outset, this took the form of uncertainties about what was involved and about what to expect. It was suggested that more explicit and precise information about the time needed at the outset would have been helpful. It was difficult for managers and therapists to anticipate what it is like to participate in research, and they emphasised the need for realistic information. For example:
[It’s important to be] really explicit up front because I suppose, we’ve learned from IAPT [Improving Access to Psychological Therapies] training, for example, that it’s often the amount of time people say is needed bears no resemblance to reality.
Monica
I don’t think it was ever set down clearly how much time the trial was supposed to take so my understanding is that was supposed to take half a day a week, but I think that wasn’t the same understanding as the people who were running the trial or the people who were involved in the trial who thought that they should just carve out as much time as it needs.
Marian
However, the managers’ worries about time appeared to expand as the process went on. This coloured the way in which they talked about every aspect of the project: the training phase (‘Oh my God this is much bigger than I ever anticipated’; Margaret), the therapists’ use of supervision, the research-specific aspects and the delivery of the therapy itself.
Freeing up staff to deliver the therapy and receive training and supervision was seen as a challenge, even when time was allocated for this (‘They had time allotted in their job plans for the trial and they were excited about the trial’; Marian). It was not always clear whether it was the managers or the therapists themselves who were responsible for negotiating (and working to) realistic job plans:
[Therapists should] make sure it’s actually job planned in before they embark on it, not after when they realise ‘oh my God I’ve, it’s a, I’m not able to do the job and the trial at the same time you know it’s too much’.
Margaret
I was really keen to umm, kind of, negotiate for therapists, a realistic amount of time to do it] in their job plans.
Monica
Some managers were more concerned than others about their ability to meet the requirements of the research (e.g. one felt ‘massively relieved’ when they heard the trial was closing). Concerns by this point had expanded to include the identification of appropriate cases, the impact of the work on therapists, the secondary impact on waiting lists and managers’ perceived lack of acceptability of the intervention to young people. For example, one manager expressed doubts about whether or not there were young people in CAMHS who were ‘suitable and motivated and ready for a very, very kind of disorder-specific intervention’ (Monica). Another expressed concerns about the acceptability of the measures for young people, stating that ‘it actually had an adverse effect on the child’s anxiety because of all the measures that were needing to be done’ (Margaret). The context and origins of these concerns were unclear.
Struggling to identify suitable cases
The identification of cases was perceived to be problematic, because (much as above, with the therapists), the availability of suitable cases was felt to be limited in Tier 3 CAMHS. For example, Monica described how it was ‘quite tricky’ to find cases that matched the study requirements. As a consequence, managers expressed concerns about ‘less serious’ cases ‘leapfrogging’ the waiting list. This was framed as an ethical issue:
It feels wrong, doesn’t it, if you’ve got these people phoning up and you’re saying I’m really sorry you’re waiting and they’re desperate to be seen umm, and then the other people are being seen quickly who don’t have the same severity of difficulties.
Marian
The availability of cases varied across sites. One of the managers interviewed did not report finding cases problematic, had a ‘readymade case load’ and felt that this ‘is a very relevant service for people to do this sort of trial in’.
Managing staff workloads
Managers shared their concerns about the impact of the work on the therapists’ other commitments. Margaret described how ‘it nearly sinks them’, and Monica worried about her staff’s capacity to cope with the workload but ‘didn’t feel that I could be asking on their behalf or saying “actually they need to stop doing it” ‘.
Managers were aware that therapists had to meet the standards required for participation in the research. They were represented as being under considerable pressure to perform:
They were worried about the demands on them.
Marian
It’s quite tough that I think.
Margaret
Technical problems were perceived as undermining therapists’ confidence – ‘you look rubbish in front of children and families’ (Margaret). Consequently, there was a call for more training around the practical issues associated with the treatment and research (such as recording and uploading videos). This call underlines the challenges of including technological components in the implementation of an intervention. The research team did provide support to the therapists (i.e. they provided step-by-step written guidance on how to use all the technology – including video cameras and Skype – and face-to-face support where needed), but it was still difficult for the therapists to manage these aspects of the trial in their day-to-day work.
In another example, the postponement of other commitments to accommodate supervision was framed as ‘cancellation’ of ‘core’ work:
People felt such obligation to be part of this treatment trial that they cancelled their prior clinical commitments which are a key part of their job.
Marian
Managers struggled to support the delivery of supervision, owing to the perceived pressure that therapists may have felt to meet the demands, in terms of both performance and expectations on their time, although one commented that they weren’t ‘. . . involved in any of that’ (Margaret). For example:
I think also the fact that the supervision was coming from such experts and the training was coming from experts made them feel umm, slightly more worried about how whether they couldn’t ‘you know’ meet the demands.
Marian
Extra stuff I suppose that hadn’t been factored in like umm, you know watching, watching videos or reading protocols or whatever, that, that they couldn’t fit into the half a day or whatever it was that we’d negotiated and I don’t think people were able, necessarily able or, or, or willing to kind of do it in their own time.
Monica
Concerns were also raised about the therapists’ perceived stretching of their usual professional boundaries to attend supervision (e.g. attending at times when they would not usually work) and whose responsibility it was to protect this:
. . . in a way it’s my, you know, who’s responsibility is it to say that that shouldn’t have happened?
Marian
Doubts were raised about whether or not the intervention was appropriate for CAMHS clients but not universally. Margaret, for example, reported that ‘I do not think we have a problem with that. We get lots of children with social anxiety’, while Monica expressed doubts about whether or not there were young people in CAMHS who were ‘suitable and motivated and ready for a very, very kind of disorder-specific intervention’ (Monica).
However, on the whole, the delivery of the therapy itself was not a huge concern for managers (‘People that had the treatment umm, got on well and they made a lot of progress’; Marian), except in the context of the impact on waiting lists (as above) and backfilling therapist time.
Problems with backfill
The limited utility of excess treatment costs meant that ‘there wasn’t anybody [else] to do the work’ that the therapist was not doing, because ‘you can’t actually do anything with little tiny bits of money’. This was a significant factor in the managers’ preoccupying concern with therapist’s time and capacity:
It wouldn’t have felt so difficult because all those people [. . .] who’d been waiting on the waiting list and then got triaged as not suitable for the trial could have had somebody else to see.
Marian
Managers expressed relief that the research was brought to a premature close, despite sharing in the disappointment of their therapists, who had ‘gained a lot in terms of the skills and supervision’ (Marian):
[I] felt really disappointed for the research team umm, and also for the clinicians I suppose on, because you know the clinicians had been really enthusiastic about it.
Monica
I thought ‘great, some of our patients who are really needy and risky can be seen now’.
Marian
To summarise, managers were sceptical about the viability of both the research and the intervention. They were concerned about the pressure on staff and used ‘time-as-a-limited-resource’ as the main means of framing this problem.
When we consider the combined perspectives across the two samples, it is notable that managers appear to overestimate the difficulty of therapists delivering the treatment. Therapists do notice the burden of the additional work, but they also accept and value the intervention and the opportunity to develop their skills. However, interestingly, they also mirror their managers in apparently overestimating the burden of the outcome measurement on the young people with whom they work.
Chapter 10 Adverse events
No adverse events were reported that resulted from the treatment that was delivered.
Three adverse events were reported that related to the research procedures. In all three cases, NHS therapists who were participating in the study e-mailed identifiable patient information to the research team’s university e-mail address. This was a breach of our data protection procedures.
To avoid this situation, we had informed therapists in person and in writing, as they joined the study, that they should not e-mail any identifiable patient information to non-NHS e-mail addresses, as these are not secure. Therapists signed an agreement to demonstrate that they had read, understood and agreed to this (and other relevant) procedures.
The following steps were taken when the protocol breaches occurred:
-
The research team immediately contacted the therapist to remind them that university e-mail addresses are not secure and not to send identifiable information.
-
The e-mail containing identifiable information was deleted.
-
The University Information Management and Policy Services were informed. They advised that, as the breach came from the NHS trust, NHS managers should be informed, and NHS procedures should be followed.
-
Managers of the relevant team were informed.
-
All participating therapists and managers were reminded of the study procedures with regard to data protection.
-
The SSC were informed.
Chapter 11 Discussion
This study was conducted in response to an NIHR Health Technology Assessment commissioned call to address the question of ‘How feasible is a study to investigate the clinical effectiveness and the cost-effectiveness of psychological therapy specific to adolescents with social anxiety disorder compared to generic psychological therapy within Child and Adolescent Mental Health Services (CAMHS)’. The proposed design was to (1) develop and manualise an appropriate intervention, and (2) evaluate the intervention within a pilot randomised controlled trial.
We produced a manual and training materials for NHS therapists to deliver an adapted form of CT-SAD-A (see https://oxcadatresources.com) and undertook a phase of work focused on training CAMHS therapists in this treatment approach. Unfortunately, during this phase of work, it became clear that the proposed feasibility trial would not be feasible because of high CAMHS staff turnover, an insufficient number of available therapists to participate, restrictions on the amount of time therapists had available (and hence study cases that could be seen) owing to high service demand and unfilled posts within participating services, and a lack of suitable young people reaching the services. Because of long waiting lists, a shift in the nature of referrals to cases associated with high risks and limited resources within teams, we were not able to identify potential study cases beyond the usual service referral routes. As a result of the difficulties with therapist retention and participant identification, we concluded that the proposed RCT would not be feasible in the current CAMHS context, but we have reported on the outcomes of the training case series, the cost of delivering CT-SAD-A within CAMHS, and the experience of participating young people, parents, therapists and managers. We will now discuss each of these parts of the study in turn.
Treatment of social anxiety disorder in adolescents within child and adolescent mental health services
The findings of the training case series provide preliminary evidence that good outcomes can be achieved from the delivery of CT-SAD-A in standard NHS CAMHS. Patients were predominantly routine referrals to CAMHS services, and all presented with a primary diagnosis of SAD and received cognitive therapy provided by CAMHS therapists as part of their training in this novel treatment. The majority had comorbid difficulties. The group as a whole demonstrated large and significant improvements in social anxiety symptoms (across a range of measures) as well as associated clinical outcomes, including symptoms of depression, generalised anxiety, social functioning and idiosyncratic appraisals of important areas in their lives. Substantial improvements in the psychological mechanisms that are proposed to drive change in this treatment (social beliefs and behaviours) were also reported, and treatment acceptability was high.
Outcomes in the training case series are broadly comparable with those reported in the first case series of the treatment undertaken by our group,29 for example a drop in the LSAS of 67% at follow-up here compared with 88% at follow-up in Leigh and Clark. 29 The mean change of 61 points on the LSAS reported here compares favourably with the figures reported for adult CT-SAD. For example, mean changes of 43 and 46 on the LSAS were reported by Clark et al. in two RCTs (200320 and 2006,19 respectively).
From visual inspection of the most detailed and commonly used specific measure of social anxiety symptoms within our battery (LSAS-CA-SR), it is clear that 9 out of the 12 patients reported considerable improvement in symptoms over the course of therapy. These nine participants reported an average reduction of 85% on the measure (vs. 13% for the other three patients), and also attained a clinically significant improvement. Seven of the nine patients lost their primary SAD diagnosis and the other two showed reductions on their ADIS CSR SAD rating (a reduction in CSR from 7 to 4 and from 7 to 5). All nine patients improved to below clinical thresholds on the social anxiety and GAD subscales of the measure that is typically used to measure anxiety/depression outcomes in CAMHS (RCADS). All but one fell to below the threshold on the depression subscale (although, notably, four met criteria for a depression diagnosis). These findings appear to compare favourably with outcomes of children and young people with SAD from trials of more general forms of CBT, for example Ginsburg et al. 17 reported recovery rates of 40% among children and young people with SAD who received 14 sessions of an individual CBT treatment that can be applied across a range of anxiety disorders.
Importantly, scores on measures of the psychological mechanisms that are targeted in CT-SAD-A [i.e. social cognitions and safety behaviours (SCQ, SBQ, and SAQ)] all reduced substantially over the course of therapy for the nine improvers, in contrast to the non-improvers. On the SCQ, the average reduction was 96% (range 89% to 100%) for the nine improvers vs. 32% (range 23% to 46%) for the three non-improvers; on the SBQ, it was 77% (range 68% to 100%) vs. 7% (range –3% to 25%); and, on the SAQ, it was 43% (range 2% to 75%) vs. –4% (range –48% to 22%).
Although we would not expect any treatment to be effective for all patients, it is interesting to consider why the three remaining patients responded considerably less to the therapy than the other nine. It does not appear to be a function of SAD severity. Possible explanations include factors relating to how the treatment was delivered. It may be that the particular therapists did not gain as much from the training as the others or had less time available, so had less time to prepare, were less able to conduct full length sessions 90 minutes) and were therefore less able to facilitate behavioural experiments in socially challenging situations outside the therapy room. Examination of different elements of therapist competence by rating therapist competence while blind to patient outcome will shed light on this hypothesis. For one of the non-responders, the presence of comorbid PTSD may have been associated with the lack of treatment success. Despite SAD appearing to meet criteria for ‘primacy’ at the initial assessment, it became clear during the treatment that PTSD warranted treatment in its own right and may have interfered with the ability of the young person to make the most of the treatment for SAD. Larger trials would provide the opportunity to examine potential predictors of response to treatment more systematically.
Strengths of the study included the thorough assessment and training procedures that were implemented within the CAMHS context. However, there are, of course, important limitations of the training case series, including the small homogeneous sample, which included only two males out of a total of 12 participants, and the uncontrolled design lacking a baseline assessment phase, which means we cannot rule out the possibility of symptom change as a result of the passage of time, or non-specific therapy effects – although the qualitative findings would suggest that this is not the case. We would suggest that it is unlikely that improvements are due to the passage of time, as the patients had all experienced symptoms for at least 6 months to qualify for a diagnosis, and in many cases social anxiety had been present for much longer, reflecting the long time it can take to travel through the standard CAMHS referral process. However, we cannot rule out potential non-specific therapeutic benefits of therapist contact and support, and, therefore, a controlled comparison is needed to test this alternative explanation. We also did not have the resources to conduct longer-term assessments to monitor young people’s outcomes over the subsequent months and years. Longer-term outcomes should certainly be included in any further systematic evaluation.
It should be noted that, while a strength of the study was the ‘real-world’ context in which it was conducted, in one of the participating CAMHS services, participants who may not have ordinarily met service entry threshold were included, which somewhat compromised the real-world validity. This context also meant that we were reliant on therapists to identify potentially suitable study participants. Services were provided with screening resources, but it was difficult to establish how reliably and effectively these were implemented. Furthermore, while we provided guidance on our definition of recurrent self-harm (to capture those young people with a level of self-harm that should be the focus of intervention in its own right to keep the young person safe), it is unclear the extent to which therapists adhered to this guidance and if young people may have been excluded unnecessarily. It is also important to note that these guidelines were based on clinical experience and consultation, and the circumstances in which targeted psychological interventions for anxiety disorders can be implemented in the context of self-harm have not been firmly established.
Notably, the patient outcomes described are for those treated during the CAMHS therapists’ training, and so it is possible that the outcomes reported may be an underestimation of the potential gains patients could experience, because we would expect therapists to achieve better outcomes as they gain more experience delivering the therapy. Future research would benefit from establishing the extent of and optimum modalities for delivering therapist training in CT-SAD-A to achieve optimal outcomes. Notwithstanding these issues, the findings highlight the potential benefit of delivering CT-SAD to adolescents.
Costs of delivering cognitive therapy for social anxiety disorder in adolescents in child and adolescent mental health services
The results of our economic analysis indicated that delivering CT-SAD-A in CAMHS, as delivered in this training series, would cost the NHS, on average, £4047 (SD £1003) per adolescent treated. To the best of our knowledge, this is the first detailed cost analysis of treatment for social anxiety specifically tailored to young people. NICE guidelines24 for SAD reported a lack of studies assessing cost and cost-effectiveness of treating children and young people with SAD. Our results, therefore, start filling this gap in the economic evidence for young people affected by SAD.
The estimated cost of delivering treatment (excluding training and supervision of therapists) was £1861 per young person treated within our study, which was admittedly based on a small sample size. Nevertheless, in a tentative comparison with treatments for adults, our cost compares favourably to the estimated cost of delivering Clark and Wells’ cognitive therapy for SAD per patient with adults (£2341). 23 Notably, where the relative cost-effectiveness of different psychological and pharmacological interventions for SAD (in adults) has been compared, individual psychological interventions (particularly Clark and Well’s cognitive therapy) have been found to be most cost-effective, in terms of the net monetary benefit at a willingness to pay threshold of £20,000 (in line with NICE guidance),24 despite the relatively high intervention costs. This appears to be due to the combination of high effectiveness and low relapse rates that ultimately bring both higher health benefits and lower health and personal social service costs. 23
However, our economic results need to be interpreted in light of some limitations. Although the response rate of supervisor-completed economic logs was 100% throughout the study duration, therapist-completed economics logs had rates of missing values that ranged from 50% to 67% for various treatment sessions across all patients, and imputation methods had to be used to handle missing data. Using mean imputation reduced sample variability, with the consequence that uncertainty around our cost estimates was underestimated. Therapists’ feedback on the economic logs indicated that the economic forms were easy to fill in, but therapists struggled more generally to carve out and then protect enough time to complete the forms requested by the study protocol. Economic logs were usually left until last and were therefore often left incomplete because of multiple pressures on the therapists’ scarce time.
It also has to be noted that the way in which the training phase was conducted was less than optimal, because new therapists were recruited at different times throughout the training programme. Consequently, two cohorts of therapists were trained separately, causing a duplication of supervisors’ time in the training phase, which led to inflated costs. In ‘real-world’ practice, a day-long workshop could be delivered to a much larger number of therapists (DC has conducted similar workshops with up to 250 therapists). As an example of the potential cost savings, if only 30 therapists attended a training workshop at once, the amount of supervisor time for a 7-hour workshop would amount to 28 minutes per therapist – which is about 10 times lower than the time that was found in the study, that is, 287 minutes – and would cost the NHS £29 per therapist (in the study the corresponding cost was £287). However, at this stage, these are only speculative estimates, which should be validated in future studies. Furthermore, it has to be noted that, given the difficulty encountered when implementing this new treatment in the study, the actual administrative costs to the NHS (e.g. expanding capacity, system changes, workload rearrangement, setting up new procedures), if the intervention were to be implemented in practice, would probably be relatively high at the beginning, which decision-makers would need to take into account when assessing the intervention. Finally, the lack of a control condition precludes any conclusions about cost-effectiveness in comparison with current usual practice.
Participant experiences
Young people, parents and therapists on the whole liked and valued the intervention. There were lots of concrete examples of positive change and positive experiences of the process. The active aspects of the intervention, and specifically the use of behavioural experiments, were consistently identified as having the most impact. Therapists and their managers found it difficult to implement the intervention within their CAMHS teams because of a range of competing pressures.
There were a number of areas in which the accounts drawn from different perspectives did not overlap. Where young people commented on the involvement of parents, they were positive about their individual experience of it, but involvement of parents was not something generally discussed by many of the young people. However, for parents, their concern about how to best support the young person was discussed consistently. In particular, they wanted to know more about the intervention so that they could provide support that was consistent with the work carried out during therapy. There was variation in parents’ experiences of this, apparently because the therapeutic dyads made different decisions about how much to involve parents.
The issue of the meaning and usefulness of measures was particularly contentious. Young people and parents were generally positive about the measures; even if they found them tedious, they were positive about their utility. By contrast, therapists and their managers appeared to be more sceptical. Some of these concerns were expressed in terms of time pressures and practicality, and they did not challenge utility directly. Others were based on projected inferences about their acceptability to young people; on the whole, the professionals’ concerns here were not borne out by the young people’s own accounts.
The challenging context of CAMHS (or specifically, ‘CAMHS as it is currently configured’) loomed large in the accounts of therapists and managers. For young people, CAMHS was not particularly significant: they did not talk about the intervention in ways that suggested awareness of the service context. For parents, CAMHS was relevant in terms of some of their prior difficulties with accessing support and an appreciation that the practicalities of treatment times in the trial were suited to family life. For therapists and managers, there were concerns that converged on the greater ‘complexity’ of typical CAMHS cases, the urgent needs of many of those cases, which were typically referred at times of crisis, the potential impact of research on the fairness of waiting lists, and the problem of resolving the practical issues associated with delivering this intervention within a system that has specific limitations around units of time and the resources allocated to a given client. The issue of ‘complexity’ may have been less meaningful for differentiating between ‘trial’ cases and ‘typical’ cases than the issue of urgency. Many of the training phase participants also had other comorbidities. Thus, CAMHS is often implicitly represented as a service for managing risk and crises, rather than a service for delivering treatments.
Therapists and managers also varied in terms of whether they thought that finding suitable cases was a problem or not, indicating variation in the sorts of young people who are able to successfully access CAMHS in different localities.
Managers expressed concerns about the pressure and expectations placed on their staff by participating in the research, owing to the demands on time and the level of scrutiny. Some of the therapists reflected on feeling this pressure, and others described working hard to meet expectations. The status of the trainers and supervisors was attractive in terms of motives to take part, but it also raised the stakes in terms of wanting to perform well. The concept of ‘good enough’ practice did not always filter through to the therapists. However, the therapists were generally very positive about their experience of training, supervision and subsequently delivering the therapy. They also reflected on the skills that they had added to their repertoire for future use. Overall, it seemed that there was some discrepancy between managers and their staff, in terms of the ‘burden’ of the trial work.
It was difficult for managers and therapists to anticipate what it is like to participate in research. For feasibility studies in which procedures are often being tried out for the first time, this presents a challenge; trials may benefit from the insights of ‘graduates’ of earlier stages of research. Concerns from therapists and managers about the implementation in the current CAMHS context appear to confirm that early closure of the trial was the correct decision.
It is important to reflect on the strengths and limitations of the qualitative work. The qualitative analysis was based on 22 interviews. This is a relatively large sample for an IPA study, although it is typical of the sample sizes found in multiple perspective designs. The construction of the sample supports the reflection on how different experiences might relate to one another, and this has proven useful (e.g. with regard to differing perspectives on measurement). The opportunity to triangulate the findings from the point of view of the three samples (young people, parents, professionals) was taken up many times during the analysis process, to make sense of ambiguities and uncertainties.
The sample includes all but one of the eligible therapists and all but one of the eligible managers. It includes 6 parent–child dyads from a possible 14, which is a good recruitment rate for a qualitative study; nevertheless, one potential weakness of our findings is that the experiences of the other eight dyads are not available to us.
Interviews were of varying length. Interviews with young people are often shorter than interviews with adults, and they were relatively short in this case too. However, in our study the interviews with parents were also quite brief. Despite this, the level of description and reflection in both of these sets of interviews was generally rich, and there was sufficient depth to support a detailed analysis. In particular, the steps that we took to support participants in reflecting on the details of therapy were notably successful, and we have been able to offer insights into which features the participants found helpful and why.
We have presented a preliminary analysis here, but this preliminary analysis was conducted by a collaborating team, rather than by a single analyst, and it has thus benefited from multiple opportunities for sense-checking. The analysis was overseen by a team member who does not deliver psychological therapies and who has been involved in the study of experiences of therapies across a range of modalities (e.g. cognitive, systemic, psychodynamic and art therapy). During the development of the analysis, the team received considerable insights from the wider study team and management group, including the experts by experience, at two large review meetings.
Chapter 12 Conclusions and recommendations
From our experience of working closely with young people and their parents/carers, NHS CAMHS therapists and their managers, a number of conclusions can be drawn, with implications for (1) the treatment of SAD in adolescents, (2) treatment delivery in CAMHS more broadly and (3) conducting research within CAMHS settings.
Implications for the treatment of social anxiety disorder in adolescents
Our preliminary findings suggest that therapists working in busy CAMHS settings can achieve good outcomes for routinely referred SAD patients, even while undergoing their training in the therapy, and our results point to the potential value of delivering the training more widely. Based on our small sample and working within the current CAMHS context, the cost of delivering CT-SAD-A appeared to be no more than the cost of delivering CT-SAD with adults and would be expected to bring greater economic advantages because of the earlier onset of benefits, including those potentially related to increased engagement in education. Given the promising clinical outcomes, it was a great shame that we experienced such substantial problems implementing the training and delivery of CT-SAD-A within participating CAMHS teams as a result of severe restrictions on their capacity. There were three particular challenges for CAMHS in implementing the training and intervention: (1) identifying patients for whom the treatment was appropriate; (2) retaining therapists for a long enough period within services to receive training and go on to deliver treatment; and (3) participating therapists being able to carve out sufficient time/flexibility to participate in training and supervision and to deliver core aspects of the treatment.
In relation to identifying patients for whom the treatment was appropriate, it is clearly essential that the treatment is offered only to those patients for whom it is intended and does not prevent young people from accessing a more appropriate treatment to meet different sets of needs. Through conducting this study, it became clear that the majority of young people were presenting to CAMHS with high levels of risk and that those young people who were experiencing psychological disorders, such as SAD, in the absence of risk were not reaching CAMHS. Notably, risk is typically much more time limited than SAD, which runs a chronic course,52 highlighting the need to address not just the presenting risk but also the underlying mental health problems. The difficulty that young people and families have accessing CAMHS has been well documented. 53 Initiatives have recently been launched to begin to address this, for example through School Mental Health teams. 54 It will be essential that these teams provide the means to identify and facilitate or provide psychological therapies for young people with primary SAD, given its chronicity,52 and particularly given the substantial impact SAD has on educational engagement and outcomes. 55
Given the high service demands and relatively low capacity within CAMHS, therapists and managers struggled to carve out and then protect the time needed to participate in training and deliver the treatment. Difficulties were compounded by a traditional diary system, which meant that delivering sessions for 90 minutes, for example, caused problems in the context of overstretched room booking systems, which allowed only 1 hour per week per patient. Young people and parents particularly emphasised the importance of the ‘active’ approach to treatment, in which the young person and the therapist would go out of the therapy room to test out the young person’s negative predictions in a relevant social context. However, this also presented challenges for therapists, as it required more time and preparation, for which they felt they did not have the capacity. Some of these difficulties may be overcome by making modifications to how treatment is delivered, for example using self-study modules in either booklet56 or online form57 so that face-to-face therapist contact can be reduced. These approaches have been found to be associated with similar outcomes of more intensive face-to-face modalities, while reducing therapy costs, when implemented with young people with other anxiety disorders. 58 They also bring the advantage of providing core content in a structured way, which may somewhat reduce the training needs for therapists and ensure high levels of treatment fidelity. Online treatments can also easily embed routine measures, to ensure that these are completed consistently. However, it is important to highlight that young people and therapists emphasised the importance of working together outside the therapy room to test out negative predictions, and it seems critical that future developments ensure that therapists have the opportunity to train in this aspect of the intervention. We would also argue against simply shortening treatments, as considerable gains were made between the middle and end of the treatment for many young people in the training case series. Furthermore, booster sessions were well used within the training case series, and appear to provide a safety net for young people and an opportunity to encourage them to continue to apply their learning from within the therapy sessions.
Broader implications for treatment delivery within child and adolescent mental health services
In this study, young people completed a number of measures both before and after treatment and prior to each session. Measure completion was high; for example, for our most thorough session-by-session measure of social anxiety (LSAS-C/A), 96% of all the sessional measures were collected. This is notable, as implementation of sessional measures within the CYP IAPT programme has been a challenge, with only 7–20% of cases having paired data (compared with 99%59 in adult IAPT services). Previous studies have identified a range of barriers including increased time demands on therapists and administrative staff, a lack of therapist training on how to integrate measures into practice, a lack of data management systems with which to record, review and audit the data, and a perceived lack of clinically useful information,60 for example if they did not include items to assess suicidal risk. 61
The qualitative interviews that were conducted within this study indicated that therapists recognised the value of sessional measures that accurately captured the problem and helped guide treatment, but they expressed worries about the measures’ acceptability to young people. Notably, in addition to the social anxiety and intervention process measures, we added a further depression measure to the one that is used within the CYP IAPT data set (RCADS) to ensure that we routinely asked about suicidal risk (via the PHQ-9). However, therapists were concerned that the young people found the measures burdensome and, as in previous reports,62 the therapists themselves struggled to make time to manage and interpret the questionnaire data between sessions. One manager was particularly concerned about the number of measures that were administered on a sessional basis, seeing this as overly burdensome for young people. However, while frequently commenting on the length and number of measures, the young people appeared to find them acceptable. They recognised that the measures needed to be comprehensive for and applicable to different young people. Young people particularly appreciated the value of sessional measures to help them track progress and to also guide the content of sessions. Indeed, for some young people, the use of measures to guide therapy stood out as a particularly important, positive component.
These findings suggest that high levels of routine data completion can be achieved within CAMHS; however, for this to be facilitated, the measures need to be relevant and integrated with treatment for young people and therapists (and ultimately managers) to recognise their value. We had initially intended to use existing CAMHS data management systems to gather sessional measures electronically, but unfortunately participating services did not integrate these systems into their services and were reluctant for additional systems to have to be learned/used for this study. Efficient, reliable systems for sessional data capture are clearly needed, co-designed with CAMHS and young people and their parents to ensure that they meet their needs and are sufficiently flexible to include disorder/treatment relevant measures.
Implications for research in child and adolescent mental health services
This study set out to evaluate a novel psychological intervention within CAMHS settings, as required by the commissioned call. As it was a novel intervention, it was important to establish that the CAMHS therapists who were delivering the intervention were able to deliver it competently and with fidelity, and so we built a treatment training phase into the programme of work. Through this phase, it became clear that it would not be possible to run a trial that required participating therapists to have received training in the novel intervention and to have demonstrated competency in the treatment because of the high rates of staff turnover and restrictions on therapists’ time within the current CAMHS context. This was disappointing, as those therapists who participated in the training phase reflected on how valuable this had been, not just in delivering treatment within the study but also for their broader clinical work. It appeared that the training phase in this study provided an opportunity for therapists to discuss the same cases in detail and regularly throughout the treatment, with a particular focus on the specific disorder and psychological model. Indeed, for some therapists this felt like a ‘luxury’, which, despite its clear value, they felt would be difficult to sustain given their usual caseload.
An alternative approach would have been to offer therapists a very brief (e.g. 1–2 days) training session and then let them get on with treating young people in the trial. However, this treatment was new for the therapists and, if we had followed this approach, we would not have known whether or not we were actually testing the treatment as it should be delivered. A phase of supervised practice is a core part of clinical training (e.g. adult IAPT, clinical psychology, CYP IAPT) and training therapists for most RCTs, so it does not seem unreasonable. Indeed, it is considered essential in NHS England’s IAPT manual, which lays out detailed quality criteria for the delivery of NICE-recommended psychological treatments within the NHS. Notably, in CYP IAPT training, all training time is fully backfilled. In contrast, much of the time involved in training in a new intervention within a research study is considered to be a treatment or excess treatment cost, which means that participating NHS trusts have to either cover the costs themselves or wait for any ‘excess’ costs to be covered at the end of the financial year. For overstretched services that typically have unfilled therapist vacancies, the lack of upfront backfill provides unmanageable demands.
The allocation and management of costs incurred by NHS trusts also creates problems in delivering interventions that go above and beyond what services are currently able to deliver. We successfully secured excess treatment costs to support this study, and successfully applied for an increase in these when the full extent of the time required for therapists became clear from their completion of health economic logs. However, as noted above, overstretched services were unable to make use of the excess treatment costs when they needed them, because they were provided at the end of each financial year. Equally, where aspects of therapist time had been allocated as research costs (e.g. time to complete economic measures), services could not use these funds, as there were already unfilled vacancies within services, so there was no spare capacity to increase therapist availability. Therapists also reflected on how, even though they might have dedicated time for the research activities, this time would often get taken, because an urgent issue arose with a (non-research) case. It appears that, for services such as CAMHS to be able to participate and support research, the research needs to bring immediate financial/resource benefits, for example funding for dedicated research therapists who are able to accommodate the additional demands of taking part in research.
It was clear that, given the many demands that participating therapists and managers already faced in their services, it was important to try to fit within routine CAMHS ways of working wherever possible. Unfortunately, this presented huge challenges owing to issues such as restricted information technology within those settings. For example, many clinical settings had poor internet access, which created barriers to conducting clinical supervision remotely via the internet with an expert supervisor, uploading video recordings to NHS systems efficiently (with this taking up to 4 hours in some services) and being able to collect routine measures electronically in a way that therapists would be able to access them and use them within sessions.
As described in Chapter 3, this study benefited enormously from a dedicated PPI co-applicant, who was able to input into all aspects of the study, as well as a PPI member of the SSC and consultation with two groups of young people and carers (one who had received CT-SAD-A and one who had not). The PPI co-applicant observed that a greater amount of costed time would allow for greater flexibility in availability to contribute to the study, and that training that provides examples of good practice in PPI would enable the development of more creative PPI approaches going forward.
Summary and recommendations
Young people who received CT-SAD-A in routine CAMHS achieved good outcomes and were generally positive about the treatment approach. The cost of delivering CT-SAD-A compared favourably with the costs of delivering CT-SAD in adults and has potential to bring even greater economic benefits. Therapists valued the training and the treatment, but they struggled with implementing it within the current CAMHS context. Managers reinforced the difficulties in accommodating the treatment and broader research procedures within the current CAMHS context.
On the basis of these findings, we make the following recommendations for future research:
-
Consideration should be given to how to create therapeutic settings, in schools or elsewhere, that can predominantly focus on treating long-standing mental health problems, as opposed to dealing with crisis phases in an adolescent’s life.
-
Future research should consider how therapists can be best trained so they are competent to deliver CT-SAD-A and other specialised evidence-based psychological therapies.
-
A RCT of CT-SAD-A should be conducted within the most appropriate setting for the identification of suitable young people and where there is scope for the treatment to be delivered as intended.
-
Research funding should be made available to cover the full costs of efficacy trials for novel psychological treatments, prior to these being rolled out in routine care settings.
-
Full costs of research (including treatment costs) should be provided as part of the research grant to enable resource-limited services to participate.
-
Future studies would benefit from costing more substantial PPI time and providing access to dedicated training to help PPI co-applicants in leading on developing creative and effective PPI approaches.
Acknowledgements
We would like to express wholehearted thanks to the participating families, therapists, their service managers and clinical leads, and the R&D teams at the Oxford Health and Berkshire Healthcare NHS Foundation Trusts.
We are also extremely grateful to the independent members of the SSC [Roz Shafran (chairperson), Vicki Curry, Sam Cartwright-Hatton, Chris Foy and Ellie Hughes] and to our NIHR Programme Director, Lesley Dodd, for their advice and support throughout the study. We also thank Philip Kendall for his support with preparations to deliver the CAT project arm.
We would like to thank Laura Johnson, Frankie Glover, Rachel Evans, Helen Stockhill and Jessica Benyon for research support during the study, Ray Percy for diagnostic supervision, and Liz White for administrative support.
We acknowledge the support of the National Institute for Health Research Clinical Research Network (NIHR CRN).
Contributions of authors
Cathy Creswell (Professor of Developmental Clinical Psychology) was the chief investigator, oversaw all aspects of the study and was the lead author on report.
Eleanor Leigh (Clinical Research Fellow & Principal Clinical Psychologist) developed the CT-SAD-A manual and training programme, delivered CT-SAD-A training and supervision, analysed and drafted clinical outcomes and contributed to all aspects of the draft.
Michael Larkin (Reader in Psychology) oversaw all aspects of the qualitative components and contributed to all aspects of the draft.
Gareth Stephens (High-intensity Cognitive–Behavioural Therapist) oversaw all PPI and contributed to all aspects of the draft.
Mara Violato (Senior Researcher and Lecturer in Health Economics) oversaw and analysed all health economic components, and contributed to all aspects of the draft.
Emma Brooks (Clinical Research Assistant) contributed to data collection and management; qualitative analysis; and all aspects of the draft.
Samantha Pearcey (Clinical Research Assistant) contributed to protocol development; data collection and management; qualitative analysis; and all aspects of the draft.
Lucy Taylor (Clinical Trials Manager) oversaw and contributed to data collection and management, and contributed to qualitative analysis and all aspects of the draft.
Paul Stallard (Head of Psychological Therapies) was the local lead for Oxford Health NHS Foundation Trust. He was the lead for the C.A.T. project arm and contributed to all aspects of the draft.
Polly Waite (Associate Professor) was the local lead for Berkshire Healthcare NHS Foundation Trust. She contributed to all aspects of the draft.
Shirley Reynolds (Professor of Evidence Based Psychological Therapies) was the lead for linking to CYP IAPT programme/training delivery and contributed to all aspects of the draft.
Gordon Taylor (Professor in Medical Statistics) oversaw statistical aspects of the study and contributed to all aspects of the draft.
Emma Warnock-Parkes (Postdoctoral Research Associate) delivered CT-SAD-A training and supervision, and contributed to all aspects of the draft.
David M Clark (Professor and Chairperson of Experimental Psychology) oversaw all CT-SAD-A components of the study and contributed to all aspects of the draft.
Publications
Leigh E, Creswell C, Stallard P, Waite P, Violato M, Pearcey S, et al. Delivering cognitive therapy for adolescent social anxiety disorder in NHS CAMHS: a clinical and cost analysis [published online ahead of print]. Behav Cogn Psychother 2021.
Taylor L, Creswell C, Pearcey S, Brooks E, Leigh E, Stallard P, et al. Delivering cognitive therapy for adolescent social anxiety disorder in NHS CAMHS: a qualitative analysis of the experiences of young people, their parents and clinicians-in-training [published online ahead of print]. Behav Cogn Psychother 2021.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review and ethics approval.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, he HTA programme or the Department of Health and Social Care.
References
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 2005;62:593-602. https://doi.org/10.1001/archpsyc.62.6.593.
- Beesdo K, Bittner A, Pine DS, Stein MB, Höfler M, Lieb R, et al. Incidence of social anxiety disorder and the consistent risk for secondary depression in the first three decades of life. Arch Gen Psychiatry 2007;64:903-12. https://doi.org/10.1001/archpsyc.64.8.903.
- Magee W, Eaton W, Wittchen H. Agoraphobia, simple phobia, and social phobia in the National Comorbidity Survey. Year Bk Psychiatr Appl Ment Health 1997;1997.
- Wittchen HU, Fehm L. Epidemiology and natural course of social fears and social phobia. Acta Psychiatr Scand Suppl 2003;417:4-18. https://doi.org/10.1034/j.1600-0447.108.s417.1.x.
- Beesdo K, Knappe S, Pine DS. Anxiety and anxiety disorders in children and adolescents: developmental issues and implications for DSM-V. Psychiatr Clin North Am 2009;32:483-524. https://doi.org/10.1016/j.psc.2009.06.002.
- Essau CA, Conradt J, Petermann F. Frequency and comorbidity of social anxiety and social phobia in adolescents: results of a Bremen adolescent study. Fortschr Neurol Psychiatr 1998;66:524-30. https://doi.org/10.1055/s-2007-995294.
- Ranta K, Kaltiala-Heino R, Pelkonen M, Marttunen M. Associations between peer victimization, self-reported depression and social phobia among adolescents: the role of comorbidity. J Adolesc 2009;32:77-93. https://doi.org/10.1016/j.adolescence.2007.11.005.
- Wittchen HU, Fuetsch M, Sonntag H, Müller N, Liebowitz M. Disability and quality of life in pure and comorbid social phobia: findings from a controlled study. Eur Psychiatry 1999;14:118-31. https://doi.org/10.1016/S0924-9338(99)80729-9.
- Whisman MA, Sheldon CT, Goering P. Psychiatric disorders and dissatisfaction with social relationships: does type of relationship matter?. J Abnorm Psychol 2000;109:803-8. https://doi.org/10.1037//0021-843X.109.4.803.
- Stein MB, McQuaid JR, Laffaye C, McCahill ME. Social phobia in the primary care medical setting. J Fam Pract 1999;48:514-19.
- Patel A, Knapp M, Henderson J, Baldwin D. The economic consequences of social phobia. J Affect Disord 2002;68:221-33. https://doi.org/10.1016/S0165-0327(00)00323-2.
- Katzelnick DJ, Kobak KA, DeLeire T, Henk HJ, Greist JH, Davidson JR, et al. Impact of generalized social anxiety disorder in managed care. Am J Psychiatry 2001;158:1999-2007. https://doi.org/10.1176/appi.ajp.158.12.1999.
- Chartier MJ, Walker JR, Stein MB. Considering comorbidity in social phobia. Soc Psychiatry Psychiatr Epidemiol 2003;38:728-34. https://doi.org/10.1007/s00127-003-0720-6.
- Schutters SI, Dominguez MD, Knappe S, Lieb R, van Os J, Schruers KR, et al. The association between social phobia, social anxiety cognitions and paranoid symptoms. Acta Psychiatr Scand 2012;125:213-27. https://doi.org/10.1111/j.1600-0447.2011.01787.x.
- Bruce SE, Yonkers KA, Otto MW, Eisen JL, Weisberg RB, Pagano M, et al. Influence of psychiatric comorbidity on recovery and recurrence in generalized anxiety disorder, social phobia, and panic disorder: a 12-year prospective study. Am J Psychiatry 2005;162:1179-87. https://doi.org/10.1176/appi.ajp.162.6.1179.
- Katzelnick DJ, Greist JH. Social anxiety disorder: an unrecognized problem in primary care. J Clin Psychiatry 2001;62:11-5.
- Ginsburg GS, Kendall PC, Sakolsky D, Compton SN, Piacentini J, Albano AM, et al. Remission after acute treatment in children and adolescents with anxiety disorders: findings from the CAMS. J Consult Clin Psychol 2011;79:806-13. https://doi.org/10.1037/a0025933.
- Clark DM, Crozier WR, Alden LE. The Essential Handbook of Social Anxiety for Clinicians. New York, NY: John Wiley & Sons Ltd; 2005.
- Clark DM, Ehlers A, Hackmann A, McManus F, Fennell M, Grey N, et al. Cognitive therapy versus exposure and applied relaxation in social phobia: a randomized controlled trial. J Consult Clin Psychol 2006;74:568-78. https://doi.org/10.1037/0022-006X.74.3.568.
- Clark DM, Ehlers A, McManus F, Hackmann A, Fennell M, Campbell H, et al. Cognitive therapy versus fluoxetine in generalized social phobia: a randomized placebo-controlled trial. J Consult Clin Psychol 2003;71:1058-67. https://doi.org/10.1037/0022-006X.71.6.1058.
- Clark DM, Wild J, Grey N, Scott R, Liness S, Deale A, et al. Self-Study Enhances the Effects of Cognitive Therapy for Social Anxiety Disorder: A Randomized Controlled Trial 2012. www.isrctn.com/ISRCTN11178360?q=11178360 (accessed 7 February 2019).
- Mayo-Wilson E, Dias S, Mavranezouli I, Kew K, Clark DM, Ades AE, et al. Psychological and pharmacological interventions for social anxiety disorder in adults: a systematic review and network meta-analysis. Lancet Psychiatry 2014;1:368-76. https://doi.org/10.1016/S2215-0366(14)70329-3.
- Mavranezouli I, Mayo-Wilson E, Dias S, Kew K, Clark DM, Ades AE, et al. The cost effectiveness of psychological and pharmacological interventions for social anxiety disorder: a model-based economic analysis. PLOS ONE 2015;10. https://doi.org/10.1371/journal.pone.0140704.
- National Institute for Health and Care Excellence . Social Anxiety Disorder: Recognition, Assessment and Treatment 2013. www.nice.org.uk/guidance/cg159 (accessed 7 February 2019).
- Leigh E, Clark DM. Understanding social anxiety disorder in adolescents and improving treatment outcomes: applying the Cognitive Model of Clark and Wells (1995). Clin Child Fam Psychol Rev 2018;21:388-414. https://doi.org/10.1007/s10567-018-0258-5.
- Hodson KJ, McManus FV, Clark DM, Doll H. Can Clark and Wells’ (1995) cognitive model of social phobia be applied to young people?. Behav Cogn Psychother 2008;36:449-61. https://doi.org/10.1017/S1352465808004487.
- Parr CJ, Cartwright-Hatton S. Social anxiety in adolescents: the effect of video feedback on anxiety and the self-evaluation of performance. Clin Psychol Psychother 2009;16:46-54. https://doi.org/10.1002/cpp.599.
- Schreiber F, Höfling V, Stangier U, Bohn C, Steil R. A cognitive model of social phobia: applicability in a large adolescent sample. Int J Cogn Ther 2012;5:341-58. https://doi.org/10.1521/ijct.2012.5.3.341.
- Leigh E, Clark DM. Cognitive therapy for social anxiety disorder in adolescents: a development case series. Behav Cogn Psychother 2016;44:1-17. https://doi.org/10.1017/S1352465815000715.
- Ingul JM, Aune T, Nordahl HM. A randomized controlled trial of individual cognitive therapy, group cognitive behaviour therapy and attentional placebo for adolescent social phobia. Psychother Psychosom 2014;83:54-61. https://doi.org/10.1159/000354672.
- Clark DM, Wells A. A cognitive model of social phobia. Soc Phobia: Diagn Assess Treat 1995;41:00022-3.
- Silverman W, Albano A, Barlow D. Manual for the ADIS-IV-C/P. New York, NY: Psychological Corporation; 1996.
- Warnock-Parkes E, Wild J, Stott R, Grey N, Ehlers A, Clark DM. Seeing is believing: using video feedback in cognitive therapy for social anxiety disorder. Cogn Behav Pract 2017;24:245-55. https://doi.org/10.1016/j.cbpra.2016.03.007.
- Masia-Warner C, Klein R. The Liebowitz Social Anxiety Scale for Children and Adolescents (LSAS-CA) 1999.
- Masia-Warner C, Storch EA, Pincus DB, Klein RG, Heimberg RG, Liebowitz MR. The Liebowitz social anxiety scale for children and adolescents: an initial psychometric investigation. J Am Acad Child Adolesc Psychiatry 2003;42:1076-84. https://doi.org/10.1097/01.CHI.0000070249.24125.89.
- Chorpita BF, Yim L, Moffitt C, Umemoto LA, Francis SE. Assessment of symptoms of DSM-IV anxiety and depression in children: a revised child anxiety and depression scale. Behav Res Ther 2000;38:835-55. https://doi.org/10.1016/S0005-7967(99)00130-8.
- Chorpita BF, Moffitt CE, Gray J. Psychometric properties of the Revised Child Anxiety and Depression Scale in a clinical sample. Behav Res Ther 2005;43:309-22. https://doi.org/10.1016/j.brat.2004.02.004.
- Silverman WK, Nelles WB. The anxiety disorders interview schedule for children. J Am Acad Child Adolesc Psychiatry 1988;27:772-8. https://doi.org/10.1097/00004583-198811000-00019.
- Alden LE, Taylor CT. Relational treatment strategies increase social approach behaviors in patients with Generalized Social Anxiety Disorder. J Anxiety Disord 2011;25:309-18. https://doi.org/10.1016/j.janxdis.2010.10.003.
- Miller SD, Duncan BL. The Outcome and Session Rating Scales: Administration and Scoring Manual. Chicago, IL: Institute for the Study of Therapeutic Change; 2000.
- de Graaf LE, Gerhards SA, Arntz A, Riper H, Metsemakers JF, Evers SM, et al. Clinical effectiveness of online computerised cognitive–behavioural therapy without support for depression in primary care: randomised trial. Br J Psychiatry 2009;195:73-80. https://doi.org/10.1192/bjp.bp.108.054429.
- Allgaier AK, Pietsch K, Frühe B, Sigl-Glöckner J, Schulte-Körne G. Screening for depression in adolescents: validity of the patient health questionnaire in pediatric care. Depress Anxiety 2012;29:906-13. https://doi.org/10.1002/da.21971.
- Staniszewska S, Brett J, Simera I, Seers K, Mockford C, Goodlad S, et al. GRIPP2 reporting checklists: tools to improve reporting of patient and public involvement in research. Res Involv Engagem 2017;3. https://doi.org/10.1186/s40900-017-0062-2.
- National Institute for Health Research (NICE) . National Institute for Health Research National Standards for Public Involvement 2018. www.invo.org.uk/posttypepublication/national-standards-for-public-involvement/ (accessed 7 February 2019).
- Kendall PC, Choudhury M. The CAT Project: For the Cognitive–behavioral Treatment of Anxious Adolescents. Ardmore: Workbook Publishing; 2002.
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hoboken: Taylor & Francis; 1988.
- Curtis LA, Burns A. Unit Costs of Health and Social Care. Canterbury: Personal Social Services Research Unit (PSSRU), University of Kent; 2017.
- Smith JA, Flowers P, Larkin M, Smith JA, Flowers P, Larkin M. Interpretive Phenomenological Analysis: Theory, Method and Research. London: SAGE; 2009.
- McManus F, Peerbhoy D, Larkin M, Clark DM. Learning to change a way of being: an interpretative phenomenological perspective on cognitive therapy for social phobia. J Anxiety Disord 2010;24:581-9. https://doi.org/10.1016/j.janxdis.2010.03.018.
- Larkin M, Shaw S, Flowers P. Multi-perspectival designs and processes in interpretative phenomenological research. Qual Res Psychol 2019;16:182-98. https://doi.org/10.1080/14780887.2018.1540655.
- Yardley L. Dilemmas in qualitative health research. Psychol Health 2000;15:215-28. https://doi.org/10.1080/08870440008400302.
- Cairney J, McCabe L, Veldhuizen S, Corna LM, Streiner D, Herrmann N. Epidemiology of social phobia in later life. Am J Geriatr Psychiatry 2007;15:224-33. https://doi.org/10.1097/01.JGP.0000235702.77245.46.
- Reardon T, Harvey K, Baranowska M, O’Brien D, Smith L, Creswell C. What do parents perceive are the barriers and facilitators to accessing psychological treatment for mental health problems in children and adolescents? A systematic review of qualitative and quantitative studies. Eur Child Adolesc Psychiatry 2017;26:623-47. https://doi.org/10.1007/s00787-016-0930-6.
- Department of Health and Social Care . Transforming Children and Young People’s Mental Health Provision: A Green Paper 2017. www.gov.uk/government/consultations/transforming-children-and-young-peoples-mental-health-provision-a-green-paper (accessed 7 February 2019).
- Stein MB, Kean YM. Disability and quality of life in social phobia: epidemiologic findings. Am J Psychiatry 2000;157:1606-13. https://doi.org/10.1176/appi.ajp.157.10.1606.
- Clark DM, Salkovskis PM, Hackmann A, Wells A, Ludgate J, Gelder M. Brief cognitive therapy for panic disorder: a randomized controlled trial. J Consult Clin Psychol 1999;67:583-9. https://doi.org/10.1037/0022-006X.67.4.583.
- Hill C, Creswell C, Vigerland S, Nauta MH, March S, Donovan C, et al. Navigating the development and dissemination of internet cognitive behavioral therapy (iCBT) for anxiety disorders in children and young people: a consensus statement with recommendations from the #iCBTLorentz Workshop Group. Internet Interv 2018;12:1-10. https://doi.org/10.1016/j.invent.2018.02.002.
- Jolstedt M, Wahlund T, Lenhard F, Ljótsson B, Mataix-Cols D, Nord M, et al. Efficacy and cost-effectiveness of therapist-guided internet cognitive behavioural therapy for paediatric anxiety disorders: a single-centre, single-blind, randomised controlled trial. Lancet Child Adolesc Health 2018;2:792-801. https://doi.org/10.1016/S2352-4642(18)30275-X.
- Clark DM. Realizing the mass public benefit of evidence-based psychological therapies: the IAPT program. Annu Rev Clin Psychol 2018;14:159-83. https://doi.org/10.1146/annurev-clinpsy-050817-084833.
- Hall CL, Moldavsky M, Taylor J, Sayal K, Marriott M, Batty MJ, et al. Implementation of routine outcome measurement in child and adolescent mental health services in the United Kingdom: a critical perspective. Eur Child Adolesc Psychiatry 2014;23:239-42. https://doi.org/10.1007/s00787-013-0454-2.
- McCarthy-Hoffbauer I, Leach C, McKenzie I. Deliberate self harm in children and adolescents. Ment Health Learn Disabil Res Pract 2006;3:107-25. https://doi.org/10.5920/mhldrp.2006.32107.
- Johnston C, Gowers S. Routine outcome measurement: a survey of UK child and adolescent mental health services. Child Adolesc Ment Health 2005;10:133-9. https://doi.org/10.1111/j.1475-3588.2005.00357.x.
Appendix 1 The National Institute for Health and Care Excellence screen for social anxiety
As there is no brief screening measure available for social anxiety (and no data on specificity/sensitivity of subscales from RCADS/SCAS, etc.), the NICE screening questions were used, as detailed in Table 20.
| Sometimes people get very scared when they have to do things with other people, especially people they do not know. They might worry about doing things with other people watching. They might get scared that they will do something silly or that people will make fun of them. They might not want to do these things or, if they have to do them, they might get very upset or cross. | |
| Do you/does your child get scared about doing things with other people, like talking, eating, going to parties, or other things at school or with friends? | YES/NO |
| Do you/does your child find it difficult to do things when other people are watching, like playing sport, being in plays or concerts, asking or answering questions, reading aloud, or giving talks in class? | YES/NO |
| Do you/does your child ever feel that you/your child cannot do these things or try to get out of them? | YES/NO |
If a young person and/or parent respond YES to any of the items, proceed to ADIS-C/P.
Young people and parents will also be administered the RCADS as routine, so any young people that are above clinical cut-off points on the RCADS social anxiety scale who DO NOT screen positive on the above will also proceed to ADIS-C/P.
Glossary
- C.A.T. Project
- The adolescent version of ‘Coping Cat’, a cognitive–behavioural therapy programme that has been developed for a range of anxiety disorders.
List of abbreviations
- ADIS-C/P
- Anxiety Disorders Interview Schedule for Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, child and parent version
- AnDY RAG
- Anxiety and Depression in Young People Research Advisors Group
- ASD
- autism spectrum disorder
- BHFT
- Berkshire Healthcare NHS Foundation Trust
- CAMHS
- child and adolescent mental health services
- CBT
- cognitive–behavioural therapy
- CSR
- clinical severity rating
- CT-SAD
- cognitive therapy for social anxiety disorder in adults
- CT-SAD-A
- cognitive therapy for social anxiety disorder in adolescents
- CYP IAPT
- Children and Young People’s Improving Access to Psychological Therapies programme
- DSM-5
- Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition
- ETC
- excess treatment costs
- GAD
- generalised anxiety disorder
- IPA
- interpretative phenomenological analysis
- LSAS
- Liebowitz Social Anxiety Scale
- LSAS-CA-SR
- Liebowitz Social Anxiety Scale for Children and Adolescents, self-report version
- MDD
- major depressive disorder
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- ORS
- Outcome Rating Scale
- OxHealth
- Oxford Health NHS Foundation Trust
- PHQ-9
- Patient Health Questionnaire, 9 items
- PPI
- patient and public involvement
- PTSD
- post-traumatic stress disorder
- RCADS
- Revised Child Anxiety and Depression Scale (child/parent report)
- RCT
- randomised control trial
- RRBI
- repetitive, restrictive behaviours and interests
- SAD
- social anxiety disorder
- SAQ
- Social Attitudes Questionnaire
- SBQ
- Social Behaviours Questionnaire
- SComQ
- Social Communication Questionnaire
- SCQ
- Social Cognitions Questionnaire
- SSC
- Study Steering Committee
