Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 15/170/02. The contractual start date was in March 2017. The draft report began editorial review in July 2020 and was accepted for publication in December 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research, or similar, and contains language which may offend some readers.
Permissions
Copyright statement
Copyright © 2021 Gidlow et al. This work was produced by Gidlow et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2021 Gidlow et al.
Chapter 1 Introduction and background
Parts of this chapter have been reproduced with permission from Gidlow et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Cardiovascular disease and NHS Health Check
Cardiovascular disease (CVD) accounts for over one-quarter of UK deaths and costs the NHS around £9B annually. 2 Given that CVD mortality has decreased in the UK (68% reduction between 1980 and 2013), the number of people living with CVD remains large. 3 Therefore, prevention, for which the NHS Health Check (NHSHC) programme plays an important part, remains a priority. 4,5 NHSHC aims to assess the CVD risk of adults in England aged 40–74 years who are not known to have certain cardiovascular-related diseases. 6 It is the largest CVD risk identification and management programme of its kind globally. NHSHCs have been linked to some increases in the detection of risk factors and chronic disease, and in statin prescriptions,7,8 but there are gaps in the evidence for long-term benefits for CVD risk, morbidity and mortality,9–14 and mixed predictions of future benefit from microsimulation studies. 15,16
Health check consultations typically take place in primary care with a health-care assistant (HCA) or practice nurse (PN), and comprise (1) assessing patients’ CVD risk and (2) communicating CVD risk, which should inform (3) the discussion of CVD risk management through lifestyle, or subsequent medical appointments or referrals. Public Health England (PHE)’s best practice guidance17 specifies that those attending a health check ‘must be told their BMI, cholesterol level, blood pressure and AUDIT score as well as their cardiovascular risk score’ (p. 14; contains public sector information licensed under the Open Government Licence v2.0.). However, this guidance document primarily focuses on legal requirements for local authorities delivering health checks, processes for risk assessment and clinical pathways. The associated competence framework for practitioners who deliver health checks, both the version available at the time of data collection18 and the updated version,19 are more explicit in the role of CVD risk communication and expectations of practitioners. They make clear that it is important that practitioners understand CVD risk information and are able to communicate it so that patients understand, and the need to involve patients in strategies to manage their risk (Box 1).
The use of a risk engine together with clinical judgement and observations/discussions during the assessment, to calculate the individual’s risk of developing cardiovascular disease. Thereafter, understanding the results that must be communicated to them.
Communication of risk
All healthcare professionals involved with delivering the NHS Health Check should be trained in communicating the risk score and results to the client. It is important to understand that sharing information about risk with people may not necessarily motivate them to change.
Therefore, the use of behaviour change methods, such as motivational interviewing techniques, should engage clients in person-centred conversations about their own reasons for change.
Risk should be communicated in everyday, jargon free language, so the client understands their level of risk. Advice should be tailored to the client’s values and beliefs for better health outcomes, and the impact of the wider social determinates of health should also be considered.
Brief intervention/signposting/referral
These competences enable the effective and appropriate signposting of clients to the range of locally available interventions in a supportive manner. It requires more than a simple communication of information; the person signposting must be able to engage the client in the choice and communicate in a manner that will maximise the potential that the client will take up the agreed action and sustain it.
Some material has been reproduced from Public Health England,20 which contains public sector information licensed under the Open Government License v2.0 (www.nationalarchives.gov.uk/doc/open-government-licence/version/2/).
Despite a growing body of evidence on NHSHC, little is known at present about the nature or content of health check consultations. What we know about what takes place in the consultations is limited to qualitative data from retrospective interviews with patients and practitioners, who are asked to recall and reflect on their experiences. 21 Although these data have value, they do not present a complete understanding of the dynamics and interactions that may influence the outcomes of a health check.
Cardiovascular disease risk communication
Practitioner–patient interactions are complex,22 and communicating risk is challenging. 23 For health checks to promote health-protective behaviours that reduce CVD risk, risk information must be effectively communicated and understood, such that the patient leaves the consultation with the knowledge and intention to act.
A review of 70 risk-scoring methods concluded that there is no single ‘correct’ approach. The appropriate method depends on individual preferences and understanding, which differs with education, numeracy and personality traits, such as optimism. 24 The emotional response to the communication of risk, how and by whom the information is conveyed, presentation of risk and the influence on health behaviour, differs greatly between patients. 25–28 Poor communication of risk can cause patients anxiety and reduce their confidence in health professionals who use risk communication techniques. 29 However, if risk communication is delivered effectively, it can enhance knowledge, aid decision-making about treatment, empower and create autonomy. 30 Wells et al. 31 assessed whether or not an electronic CVD risk visualisation tool facilitated explanation of CVD risk to primary care patients. They found that watching a video about the communication of risk increased associated practitioner confidence and understanding, which led to greater efficiency. Researchers who interviewed general practitioners (GPs) indicated that the GPs vary their strategy for communicating CVD risk depending on factors such as patient’s perception of risk, motivation and anxiety, and recommended that clinicians should have alternative ways to explain absolute risk to improve how the metrics were used in practice. 32
Cardiovascular disease risk communication in health checks
For CVD risk assessment in NHSHC, QRISK® (QRISK®2 and, more recently, QRISK®3) is the mandated CVD risk calculator. 17,33 QRISK provides a percentage risk of a CVD event in the next 10 years, and this must be communicated to patients for the health check to be considered ‘complete’. It is integrated within the general practice electronic medical record software, so can be calculated from pre-populated and new data. The score is then saved directly to the patient’s record. However, there are limitations to the QRISK score and how it is used. First, 10-year risk estimates, such as those presented by QRISK, have been criticised for being heavily influenced by age and sex, thereby underestimating risk in younger adults and women, and not accounting for risk from other diseases as effectively as long-term (lifetime) estimates. 34,35 Second, qualitative studies indicate limited practitioner and patient understanding of percentage CVD risk. 21 Practitioners report difficulties in explaining percentage CVD risk. 26,36–38 In turn, patients attending health checks have been unable to recall being provided with a risk score or have found it confusing. 21
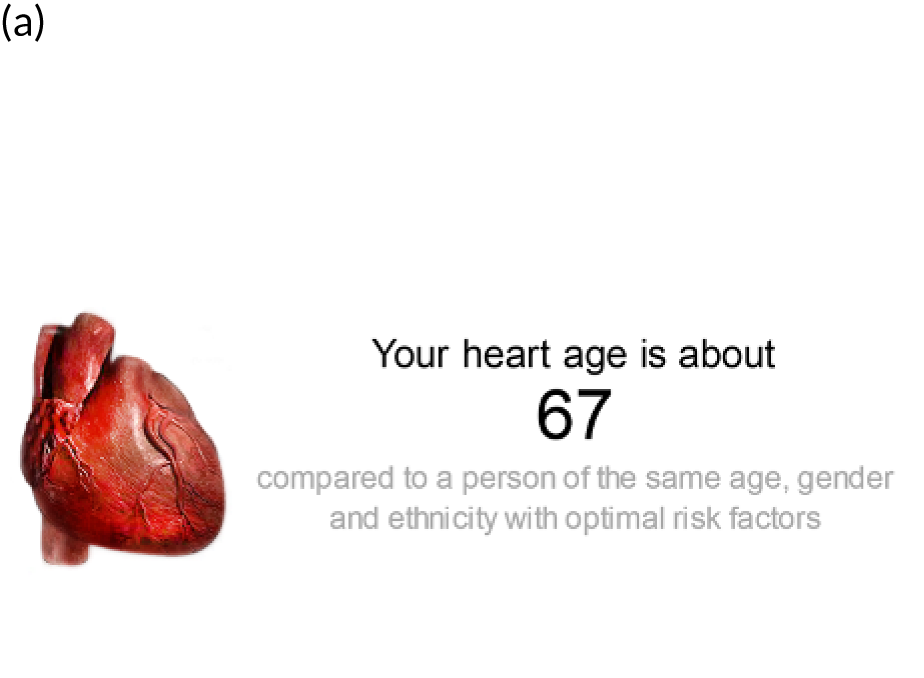
In 2014, the Joint British Societies (JBS) launched the JBS3 risk calculator. JBS3 has a primary focus on lifetime risk,34 which can address some of the limitations of short-term risk estimates and identify raised CVD risk that would not be picked up through conventional 10-year risk estimates. 39 JBS3 has a range of features (Figure 1):
-
Heart age. This is the estimated age of someone of the same sex and ethnicity, and with the same annual risk of an event, but with all other risk factors at ‘optimal’ levels (see Figure 1a); for example, an individual with a heart age of 67 years has the same CVD risk at someone aged 67 years, of the same sex and ethnic group, who has optimal levels of risk factors. Those with an ‘old’ heart age should be motivated towards risk-reducing behaviours to bring their heart age back to their real chronological age. There is evidence that heart age is more easily communicated to, and understood and recalled by, patients. 41,42 A recent review concluded that randomised controlled trials testing the effects of CVD risk communication using heart age have reported improvements in some risk factors (cholesterol and blood pressure) and intentions to improve lifestyle compared with usual care or alternative risk scores. 43
-
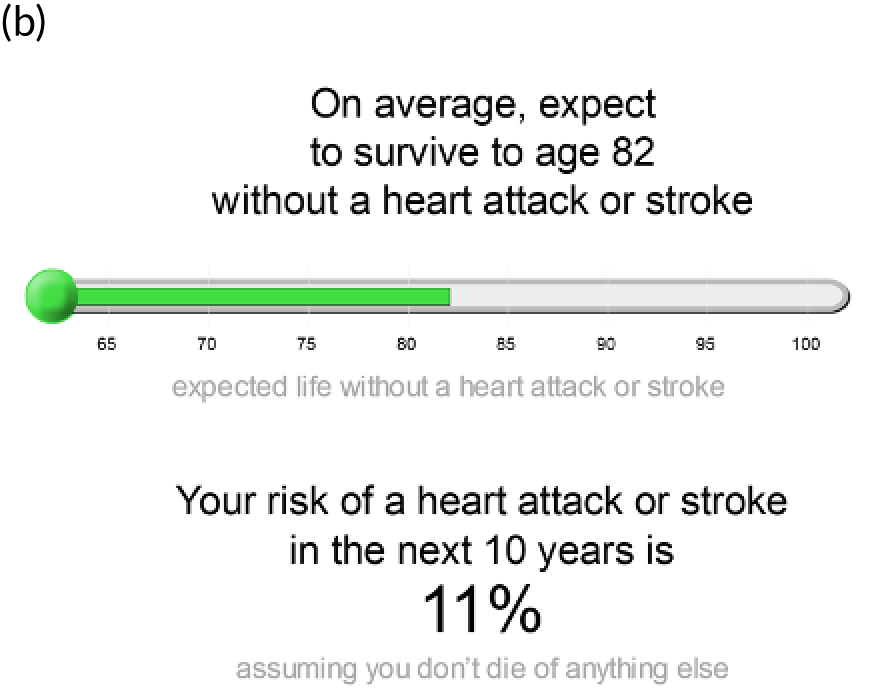
Event-free survival. This is the age by which an individual might expect, based on their current risk profile, to sustain their first CVD event. This is presented on a visual analogue scale that indicates the average expected age of a cardiac event for an individual (based on demographic and risk factor profile; see Figure 1b).
-
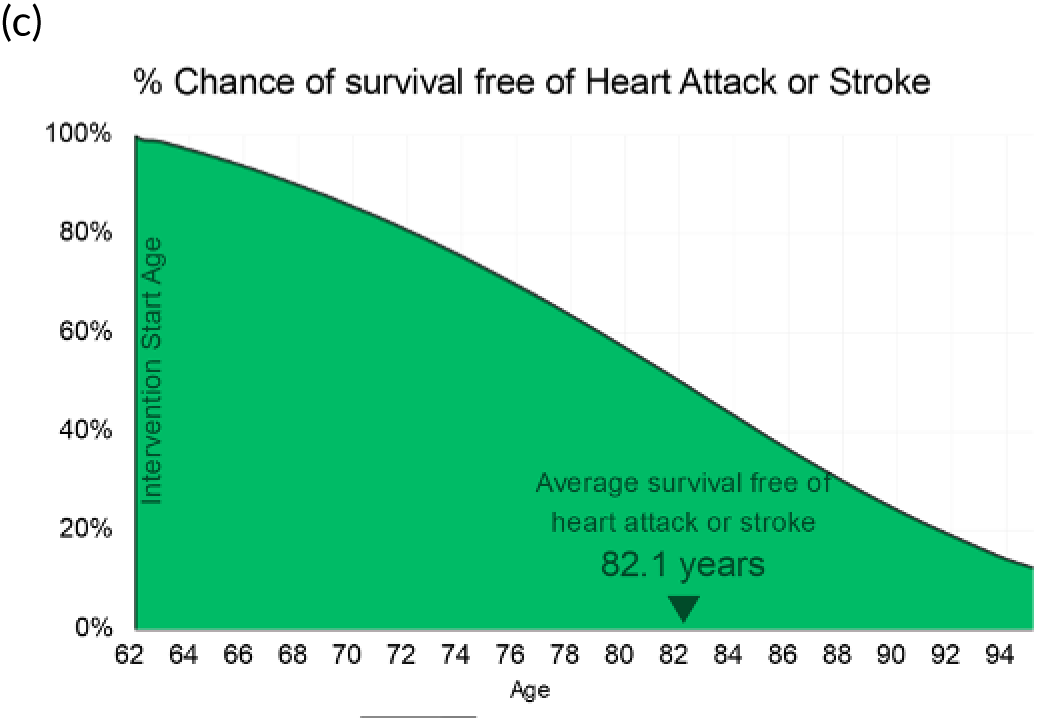
Percentage chance of survival free of heart attack or stroke, by age. This is presented as a survival curve, showing the reduction in the percentage chance of being free of heart attack or stroke as age increases (see Figure 1c).
-
A range of visual displays. Lifetime risk scores are presented using a range of images, including icon array or Cates’ plots, an image of a heart for heart age, visual analogue scales and a survival curve. This variety aims to accommodate a range of preferences23 and can be preferable for promoting risk-reducing behaviour. 44
-
Risk score manipulation. Risk factors can be modified (e.g. altering smoking status or reducing blood pressure or cholesterol level) to show the beneficial effect of effective intervention on risk scores (see Figure 1d). This ability to interact with graphics has the potential benefit of engaging the individual with the information and promoting their understanding and retention. 23,45
FIGURE 1.
Example JBS3 outputs. (a) Heart age; (b) event-free survival age; (c) percentage change of survival free of CVD event; (d) risk score manipulation (showing the effect on event-free survival of reducing blood pressure and cholesterol). Source: JBS3 risk Calculator 201440 [reproduced with permission from British Cardiovascular Society for the prevention of CVD, personal communication, 2020 (Copyright© UoC/BCS. All rights reserved)].

Collectively, these attributes of JBS3 might accommodate a range of patients and facilitate practitioner communication that allows patients to understand and retain their CVD risk, and perhaps foster intentions towards risk-reducing behaviour. 23,31 Yet, to our knowledge, a comparison of the relative benefits JBS3 and QRISK2 for communicating CVD risk in health checks has not been undertaken.
The most effective way to address CVD risk during health checks is to involve the patient in a discussion of their risk and allow them to identify strategies that they could adopt to manage that risk. This is preferable to a didactic consultation, in which practitioners are providers of information and patients are the passive recipients. Studies of clinician–patient interactions have identified that short, clinician-dominated (or ‘paternalistic’) consultations are less patient centred and are linked with low patient and clinician satisfaction,46–49 which, in turn, have been linked with poorer patient outcomes, such as poor adherence to clinical recommendations and failure to adopt health-promoting behaviour. 50 As noted in the competence framework (see Box 1), CVD risk management should be negotiated through a mutual exchange between practitioner and patient (i.e. a person-centred approach) that places the individual at the centre of their own care, service or treatment, as part of a shared decision-making process. 51 At present, there is no evidence regarding the practitioner–patient balance during health checks, particularly the extent to which patients are engaged in discussion of their CVD risk and its management.
Patient outcomes from health checks will depend on patients’ actions, and the support and interventions available to them following their consultation (e.g. referral to effective lifestyle support programmes or appropriate specialist referrals). There is evidence that patient outcomes from primary care consultations are influenced by patients’ experience; hence, there is a need to understand more about the dynamics of the health check event. If delivery of the health check consultation does not create a positive experience for patients, their engagement with and effectiveness of the subsequent risk management actions could be undermined. To optimise the efficacy of health checks in laying the foundations for the management of identified risks, a better understanding of what is already occurring during health check consultations and identification of areas requiring improvement are necessary.
In summary, the NHSHC programme aims to assess CVD risk and prompt patients and practitioners to undertake risk management behaviours. At present, there is insufficient knowledge about how they are conducted, the nature and adequacy of CVD risk communication, and the potential benefit of using alternative CVD risk calculators, such as JBS3. Knowing which approach best delivers the information that patients need to foster intentions for risk-reducing behaviour (or actual behaviour change) could inform decisions about practitioner training and resource allocation.
Research objectives
RIsk COmmunication in NHS Health Check (RICO) was a qualitative study and quantitative process evaluation that aimed to explore practitioner and patient perceptions and understanding of CVD risk when using the JBS3 lifetime risk calculator or the QRISK2 10-year risk calculator, the associated advice or treatment offered by the practitioner and the response of the patient.
Specific study objectives were to:
-
explore how practitioners use QRISK2 and JBS3 to communicate CVD risk during the consultation
-
explore how patients respond to the risk information
-
explore how QRISK2 and JBS3 promote patient and practitioner understanding and perception of CVD risk
-
explore patient intentions with respect to health-protective behaviours
-
explore mechanisms by which intentions for health-protective behaviours are elicited
-
make recommendations regarding use of QRISK2 or JBS3 during health checks.
Theoretical basis
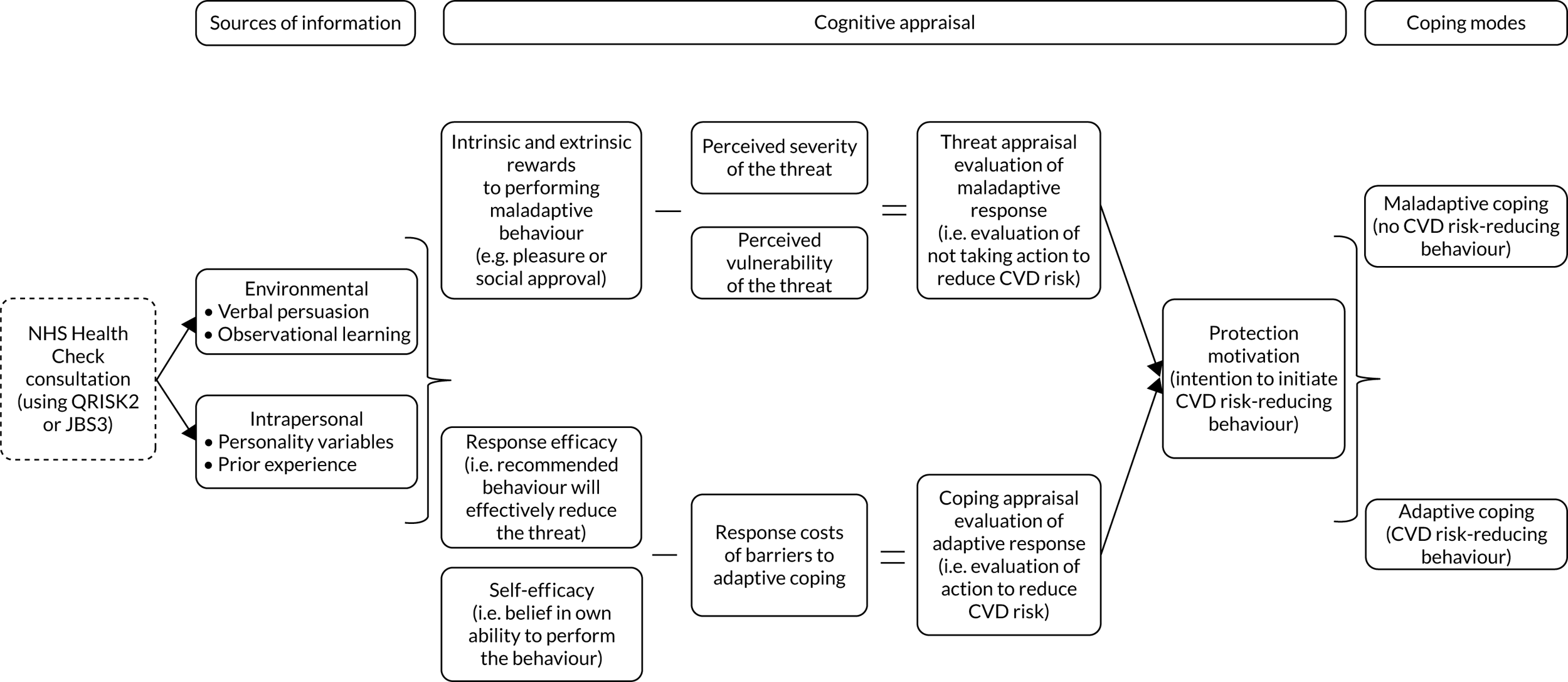
Given the complexity of practitioner–patient interactions52,53 and the translation of risk information into health-protective behaviour,54 we used a theoretical framework based on the revised protection motivation theory (PMT). 55 In PMT, ‘protection motivation’ refers to the intention to undertake health-protective behaviour resulting from the cognitive appraisals (or internal assessments). CVD risk communication could be a key source of information feeding into such appraisals (Figure 2).
Protection motivation theory is informed by fear-driven models, which recognise that behaviour change can be prompted by fear-inducing communications that motivate action to reduce the perceived threat (or risk). 54,56 However, protection motivation is influenced by two cognitive appraisals: appraisals of the threat (risk of CVD) and coping (consequences of undertaking positive behaviour change). Threat appraisal evaluates maladaptive responses (i.e. not initiating positive behaviours in response to recognising an elevated CVD risk). This considers the source of the threat (i.e. practitioner/health check), intrinsic rewards (e.g. enjoyment associated with health risk behaviour) and extrinsic rewards (e.g. social approval), and the perception of the threat (i.e. perceived severity and personal vulnerability). Coping appraisal evaluates the adaptive response to cope with the threat (i.e. CVD risk), and considers the likelihood that positive behaviour change (adaptive response) will reduce the patient’s risk (response efficacy), the patient’s own ability to make the necessary changes (self-efficacy), and the burdens of, or barriers to, making the change (response costs). 54,55,57,58 Threat and coping appraisals are influenced by both environmental aspects (e.g. persuasive communication and observational learning) and intrapersonal variables [e.g. personality and feedback from prior experience of both positive (adaptive) and negative (maladaptive) behaviours]. 54 In the context of this study, PMT emphasises the key role of practitioners in providing information on CVD risk (severity and vulnerability) and incorporating a patient’s beliefs, priorities and experiences into strategies to reduce this risk so that patients feel they can achieve adaptive behaviours55 and subsequent health outcomes.
Protection motivation theory is particularly pertinent to the study of the relative merits of different CVD risk calculators and the mechanisms by which they might promote positive behaviour change for several reasons. First, it was initially developed to examine intention to adopt behaviours relating to disease prevention. 59 Second, it does not assume rationality in behaviour choices,54,60 that is people will undertake unhealthy behaviours because they serve other purposes, for example enjoyment or social integration. Third, its components have been associated with (intention for) behaviour change in relevant contexts (e.g. smoking cessation and exercise). 55,57 Finally, it provides an understanding of why attitudes and behaviour can change when people are confronted with threats (i.e. the mechanisms). 54
Chapter 2 Methodology
Parts of this chapter have been reproduced with permission from Gidlow et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Design and setting
This qualitative study, with quantitative process evaluation, was undertaken in 12 general practices in the West Midlands of England that were already delivering NHSHCs. Six practice pairs, which were approximately matched on level of deprivation,61 were randomly assigned to one of two groups: the QRISK2 (usual practice) group, in which practitioners continue to use QRISK2 to communicate CVD risk, or the JBS3 (intervention) group, in which practitioners use the JBS3 CVD risk calculator to communicate CVD risk following brief introductory training about the platform. Participating practices were asked to video-record NHSHCs using the allocated CVD risk calculator until 20 useable consultations were recorded. Data collection took place from January 2017 to February 2019 and comprised (1) video-recording NHSHC consultations; (2) post-consultation video-stimulated recall (VSR) interviews with patients within 4 weeks of their health check, using excerpts from recorded health checks to facilitate recall and reflection; (3) VSR interviews with practitioners after their final recorded health check; and (4) patient medical record reviews 12 weeks post health check to determine subsequent action (e.g. GP appointment, lifestyle referrals, lifestyle referral and statin prescription).
Sample
General practices
General practices were recruited if they met the following criteria:
-
were delivering NHSHCs
-
were already using the QRISK2 percentage risk score during health checks
-
were already delivering (or were willing to deliver) health checks in specific clinics to facilitate data collection
-
had signed up to the ‘incentive scheme’ implemented by the Clinical Research Network (CRN) to ensure that the practice is ‘research ready’
-
were willing to participate.
Postcodes were used to stratify general practices into the bottom or top 50% based on national deprivation rankings,62 as a proxy for the typical socioeconomic status of the local population (Table 1).
| Age (years) | Sex (n) | |
|---|---|---|
| Female | Male | |
| 40–54 | 4 (3 white British/1 ethnic minority) | 4 (3 white British/1 ethnic minority) |
| 55–64 | 3 (2 white British/1 ethnic minority) | 3 (2 white British/1 ethnic minority) |
| 65–74 | 3 (2 white British/1 ethnic minority) | 3 (2 white British/1 ethnic minority) |
Patients
The patient population were those eligible for NHSHCs based on national criteria. These criteria excluded people who:
-
were outside the target age range of 40–74 years
-
had existing diagnoses for certain cardiovascular-related chronic conditions
-
were taking statins
-
had attended an NHSHC in the last 5 years
-
were known to be at high risk of CVD (i.e. had a 10-year CVD risk score of ≥ 20%). 17
Practitioners
Participating practitioners were health-care professionals who usually delivered health checks in participating practices and who were willing to participate (usually one or two PNs or HCAs per practice).
Recruitment
Practice sampling
The CRN facilitated practice sampling. Briefly, this involved an initial e-mail inviting expressions of interest, followed up with telephone calls and subsequent practice visits. Practice participation was incentivised through financial reimbursement of service support costs and additional remuneration for completing all parts of the study. Following practice-level consent, practice pairs that were matched on level of deprivation (bottom vs. top 50% of national deprivation rankings), were randomly assigned to the QRISK2 or the JBS3 group using a random number generator in Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA). After randomisation, the research team completed initiation meetings at practices to provide further information and basic training for staff involved.
Patient and practitioner sampling
There were three levels of patient sampling:
-
Total sample (target, n = 240) – to achieve the 144 recorded consultations suitable for qualitative analysis (12 recorded consultations per practice allowing for non-attendances and consultations with no/minimal discussion of CVD risk), the aim was that health check clinics were recorded until 20 recordings per practice (240 total) were complete. In each practice, the patient database was searched to identify eligible patients, who were then stratified by age, sex and ethnicity to ensure that there was representation from different demographic groups (see Table 1).
Invitation letters, information sheets and consent forms were sent out to eligible patients (up to 400 per practice depending on the size of the eligible cohort), asking them to contact the CRN for more information or to arrange their video-recorded health check. Those who did not respond were contacted by telephone by the general practice staff.
-
Qualitative analysis (target, n = 144) – video-recordings were quantitatively coded soon after the health check to identify those for qualitative analysis (target of 12 video-recordings per practice) and VSR interview (target of four VSR interviews per practice). Where risk was not discussed by patient or practitioner, the patient’s data were not used for either.
-
VSR interviews (target, n = 48) – VSR interviews were conducted with patients (target, n = 24 VSR interviews per group) sampled from the 144 recorded health checks. The aim was to stratify by sex, age and CVD risk (Table 2), although issues with recruitment meant that this could not be strictly adhered to and, in some under-recruiting practices, all those who consented were asked to take part.
| Age (years) | CVD riska (n) | |
|---|---|---|
| Low (< 10%) | Medium–high (≥ 10%) | |
| 40–54 | 2 males/2 females | 2 males/2 females |
| 55–64 | 2 males /2 females | 2 males/2 females |
| 65–74 | 2 males/2 females | 2 males/2 females |
The target of 144 recorded consultations (12 per practice) was comparable to other studies using audio-recordings of similar consultations to explore CVD risk communication in patients with psoriasis (e.g. n = 130 in 10 practices),63 while the targets of 48 patient VSR interviews and 18 practitioner VSR interviews were in alignment with the number of interviews carried out in other VSR studies (n = 9–39). 52,64
All practitioners who delivered the video-recorded health check were asked to participate in VSR interviews.
Groups
General practices were randomly assigned to one of two groups:
-
QRISK2 group (usual practice) – practitioners delivered health checks using the QRISK2 risk calculator as per usual practice.
-
JBS3 group (intervention) – practitioners delivered health checks using the JBS3 risk calculator. 40 An introductory session with practitioners established the minimum requirements to use:
-
the first two output screens, which show heart age and healthy years (event-free survival age)
-
risk score manipulation to show the effects of intervention through modifying one of those risk factors (e.g. lowering blood pressure, smoking cessation) (see Figure 1).
-
Practitioners were also asked to practise using JBS3 in at least two health checks prior to the video-recorded clinics and could seek further clarification from the research team should they wish. During these introductory sessions, practitioners were provided with a verbal explanation of the tool, given written materials to support data entry and given a digital versatile disc (DVD) and link to an online training video (www.youtube.com/watch?v=idecGzlwIc4%26feature=youtu.be; accessed June 2021), which was also played to them during the introductory session. As a requirement of the NHSHC programme, patients in the JBS3 group were also told their QRISK2 10-year risk.
Data collection procedures
Video-recorded health checks
Digital camcorders were positioned in health check clinic rooms to provide an audio-visual record of consultations. Informed by patient and public involvement (PPI) and pilot work, cameras were positioned to capture both the patient and the practitioner, but prioritising the view of the patient. Video-recordings were screened soon after the health check. If there was no discussion of CVD risk, this was noted and the file retained. In the case of consultations that involved discussion of CVD risk and were eligible for qualitative analysis, the audio-recording was separated from the visual recording [using Adobe® Premiere Pro (Adobe Systems Incorporated, San Jose, CA, USA)] for transcription and qualitative analysis.
Semistructured video-stimulated recall interviews with patients and practitioners
Semistructured one-to-one VSR interviews with patients were conducted at the patients’ home or their general practice (depending on patient preference) within 4 weeks of their health check. VSR interviews with practitioners were conducted at the general practice within 2 weeks of their final recorded health check. No others (i.e. non-participants) were present in the room during interviews. After each clinic, the recorded heath checks were watched to identify sections of the consultation to use in VSR interviews that related to discussion of the CVD risk score, modification of the risk score (in the JBS3 group) and practitioner advice, recommendations and interventions. During their VSR interviews, practitioners were shown excerpts of video consultations with some of their patients who had subsequently been selected for VSR interview. Semistructured VSR interviews followed a pre-piloted process and topic guide, with variation depending on whether the patient/practitioner was in the QRISK2 group or the JBS3 group. All VSR interviews were audio-recorded and transcribed verbatim for analysis.
Patient medical record review
Data from the 12 weeks following the health check were extracted from patient medical records. Data were processed by the principal investigator (CJG), with verification by a GP co-investigator (EC), to identify any relevant recorded activity or prescriptions that occurred as a result of the health check. Classifications were data driven, as detailed in Appendix 1, Tables 11 and 12. Where possible, these were based on Read codes/terms, but also included uncoded additional text.
Patient and public involvement
Patient and public involvement activities informed study development and were used throughout. There were three PPI strategies. First, we engaged with Patient Participation Groups (PPGs) by attending meetings at three general practices on two occasions to gather opinion on the study concept and overall design and, subsequently, the methods and protocols. This initial engagement had an impact through validating the study as being important and the acceptability of video-recording methods, while making important links for ongoing PPI. One PPG facilitated the completion of four mock health checks (with the PN and four PPG members) to allow testing of protocols including camera placement, video-recording quality, participant consent and debrief processes, development of the quantitative and qualitative coding frameworks, post processing of the video for VSR excerpts and development of the VSR topic guide and protocols. This had an important impact on all of our data collection processes, and the mock health check data allowed development of coding processes. Second, two patient representatives sat on the Programme Advisory Board, which was important to ensure that the patient voice was considered at the level of project management, as well as at the operational and process levels. Third, a virtual study patient group was established using a closed Facebook (Facebook, Inc., Menlo Park, CA, USA; www.facebook.com) group. This novel approach had an impact throughout data collection by allowing engagement with a large number of patients and members of the public (membership reached over 270), who provided rapid feedback that further informed study processes (e.g. consent forms, participant information sheets, camera placement) and how we responded to problems with recruitment.
Data processing and analysis
Qualitative and quantitative data were analysed to inform the quantitative process evaluation, qualitative outcomes and case studies. The processes are summarised by data source.
Qualitative data: recorded health check consultations
Qualitative data were analysed using deductive thematic analysis,65 following the six-stage process described by Braun and Clarke66 (Table 3). A coding template was developed around PMT. 56 Use of this framework (see Figure 2) was considered appropriate to investigate the use of the two CVD risk assessment tools given the complexity of patient–practitioner interactions52,53 and the translation of risk information into health-protective behaviour. 54
| Phase | Summary |
|---|---|
| 1. Familiarisation | Analysis started with a period of familiarisation involving watching and re-watching the video-recorded consultation (or listening to audio-records in the cases of interviews), noting initial thoughts in the transcript |
| 2. Initial coding | For deductive analysis, codes from the PMT template were applied to the transcript independently by two researchers (where possible); for inductive analysis, codes were generated based on interesting features and recurrent patterns in the data. For both inductive and deductive analysis, the researchers checked their own codes, before discussion to verify and agree final codes |
| 3. Searching for themes | Agreed codes were collated into potential themes, gathering all data relevant to each potential theme |
| 4. Reviewing themes | Constant comparison was used to check themes by revisiting data to ensure that they were representative |
| 5. Defining and naming themes | Ongoing analysis was used to refine the specifics of each theme, and the overall story, generating clear definitions and names for each theme |
| 6. Reporting | Illustrative extracts were selected to include in a narrative that tells the overall story |
Each transcript was uploaded to NVivo version 12 (QSR International, Warrington, UK) qualitative data analysis software. 67 This allowed the interpretation of how QRISK2 and JBS3 were used to communicate risk in the context of PMT components (e.g. verbal persuasion, influencing patient prior beliefs and priorities, and how patients respond, which will reflect the nature of their appraisal within the consultation).
Initially, 14 transcripts were inductively coded independently by Lisa Cowap and Victoria Riley. This was to check the application of PMT to health check consultations and agree coding between the researchers. Following inductive coding, 13 new codes were added to the framework (e.g. medical history, clarification of results). The final version of the coding template, including examples for each code from health check consultations, is provided in Appendices 3 and 4. The remaining 114 transcripts were individually coded by Lisa Cowap and Victoria Riley; 2 out of every 20 transcripts were independently dual coded to check their reliability using kappa coefficients for each node in the PMT framework. Reliability ranged from 0.48 to 0.71 over the five reliability checks conducted, indicating fair to good reliability. 68 Data saturation was considered to have been reached at the point of completion of coding.
Subsequent analysis of codes was led by Sophia Fedorowicz (qualitative researcher and doctoral student, Staffordshire University) (supported by SG, CJG, NE and VR) to identify codes for key elements of the PMT model, splitting health checks into two groups (QRISK2 and JBS3). Specific parts of transcripts that illustrated the practitioner communicating CVD risk to the patient, and the patient responses, were identified. These related to cognitive appraisal (threat appraisal and coping appraisal) and coping modes (adaptive and maladaptive).
Qualitative data: semistructured video-stimulated recall interviews with patients and practitioners
Patient VSR interview transcripts were analysed using inductive thematic analysis, with codes and themes generated from data based on individual reflections, perceptions and experiences. In the case of patient VSR interviews, line-by-line coding and preliminary theme development were undertaken by Lisa Cowap. Themes were discussed with Victoria Riley and Sarah Grogan, before reviewing and agreeing final themes.
Practitioner VSR interviews were line-by-line coded by Naomi J Ellis and Sarah Grogan (see Acknowledgements). Sian Calvert led theme development and was supported by Victoria Riley and Christopher J Gidlow, who reviewed and agreed the final themes.
Quantitative: content of health check consultations (process evaluation)
Recorded health checks were viewed by two authors (LC and VR) and the content of the consultations was characterised using a second-by-second coding framework developed specifically for this study. The framework comprised 36 items grouped into six categories: patient–practitioner communication, health check general (e.g. collecting and inputting data), risk dialogue (e.g. overall discussion of risk, 10-year risk reference, heart age, patient question on CVD risk), causal CVD risk factors (e.g. medical, lifestyle), risk management (lifestyle intervention or medical intervention) (see Appendix 2). This allowed derivation of aggregate indicators for each consultation to allow between-group comparisons of:
-
length of health check
-
time (absolute and proportion of consultation) discussing CVD risk, CVD risk factors (overall, lifestyle, medical) and risk management (lifestyle, medical)
-
practitioner–patient communication balance (proportion of health check time for which practitioners and patients spoke, ratio of practitioner to patient speaking time)
-
number and proportion of patients asking questions about CVD risk
-
use of heart age, healthy years (event-free survival age) and risk score manipulation (as fidelity check in the JBS3 group).
As noted in a previous paper,1 the coding process and framework development was iterative, using four mock health checks that were video-recorded as part of PPI. To reach consistency in approach, Naomi J Ellis and Lisa Cowap coded mock health checks by consensus. Victoria Riley then coded the same four consultations independently and intraclass correlation coefficients (ICCs) demonstrated excellent inter-rater reliability (ICCs from 0.968 to 0.995). Once data collection had started, health checks were coded by authors Lisa Cowap and Victoria Riley, with verification of 10% (2 out of every 20 independently coded) to mitigate the risk of coder drift. ICCs ranged from 0.992 to 0.999, indicating excellent inter-rater reliability.
Data on patient sex, age, ethnic background (classified as white British or ethnic minority) and lower-layer super output area (which was used to derive deprivation decile)62 were also extracted from patient medical records.
Following checks for normal distributions, QRISK2 and JBS3 groups were compared using key variables. To take into account the nature of the sampling, which was in clusters, 95% confidence intervals (CIs) were calculated; as usual, where the CIs of the two groups do not overlap then the groups can be considered to differ significantly. Data processing and analysis were performed in SPSS version 26 (IBM Corporation, Armonk, NY, USA).
Quantitative: patient medical record review (process evaluation)
Activities extracted from the patient medical records were classified as relating to further assessment of CVD risk (or QRISK), weight, blood pressure, cholesterol level, diabetes, other tests (e.g. liver function test, kidney function test, echocardiography), lifestyle, lifestyle referral and new diagnoses. Relevant medications that were prescribed following the health check were grouped as statin/lipid lowering, anticoagulants, cardiovascular or diabetes. The specific composition of each category is shown in Appendix 1, Tables 11 and 12.
Between-group comparisons were explored, but were somewhat limited by the relatively small number of patients with relevant recorded activity or prescriptions in their medical records.
Case studies
A subsample of 10 patients were selected for within-case analysis. Selection was on the basis of evidence of positive patient intentions and/or behaviours to reduce their CVD risk following the health check, and to provide coverage across general practices. The aim was to further explore apparent mechanisms by which the risk calculators may lead to changes in patient or practitioner behaviour. A data extraction template was created to bring together data from all sources (see Appendix 6, Table 13).
Quantitative data
-
Patient medical records: age, sex, ethnicity, deprivation level of home neighbourhood and 10-year CVD risk recorded in the health check, and relevant activities, diagnoses and prescriptions recorded in the 12 weeks following the health check.
-
Quantitative coding of health checks: total duration (in minutes), practitioner–patient communication balance (ratio of practitioner to patient minutes), practitioner speaking (as percentage of total health check), patient speaking (as percentage of total health check), no speaking (as percentage of total health check) and total minutes discussing CVD risk.
-
Non-verbal patient engagement: non-verbal communication during sections of the health checks in which CVD was discussed, was assessed independently by two researchers. As detailed in Appendix 6, a Likert scale was derived and piloted, informed by existing measures of non-verbal communication. Results for each case study patient are presented in Appendix 7.
Qualitative data
Transcripts of recorded health checks and VSR interviews with the patients and the corresponding practitioners were revisited, and excerpts were extracted to provide information on:
-
the patient (e.g. current lifestyle, awareness and perceptions of NHSHC)
-
the practitioner (e.g. role, experience, training)
-
how the NHSHC was conducted
-
the use, understanding and perceptions of QRISK2, heart age, event-free survival age and risk score manipulation
-
risk management (recommendations and subsequent intentions or action)
Christopher J Gidlow, Victoria Riley and Naomi J Ellis extracted all data and drafted case studies, with support from a GP co-investigator, Elizabeth Cottrell.
Sample size
A priori determination of sample sizes for qualitative research is a point of contention. 69,70 In the present study, it was necessary to estimate requirements for the patient VSR interviews and use this to inform the total number of recorded health checks required per practice. The target of 48 VSR patient interviews (24 per group, four per practice) was chosen to allow patient sampling stratified by sex, age and CVD risk (see Table 2), and to compare favourably with studies using VSR or audio-recordings of primary care consultations (ranging from 9 to 44). 63,64 These 48 recorded health checks were to be selected (with stratification) from 144 (72 per group, 12 per practice) recorded health checks that were subject to deductive qualitative analysis (i.e. 12 per practice was deemed sufficient to allow stratified sampling of four patients per practice). To obtain the 144 recorded health checks suitable for qualitative analysis, we aimed to record 240 health checks (120 per group, 20 per practice).
This oversampling aimed to serve two purposes. First, it would allow for exclusions owing to non-attendance, technical issues and health checks that contained little or no discussion of CVD risk. Second, a sample size calculation undertaken for the target between-group quantitative comparison estimated that 120 consultations per group, six clusters (practices) per group with a two-tailed probability and an alpha of 0.05, would provide statistical power of 0.8 to detect an effect size (r) of 0.24 (small to medium effect). The overall number of eligible practices from which the clusters were chosen was 625 (in the absence of a definitive estimate of how many West Midlands general practices conducted health checks, the total number of general practices in the region was used). 71
Chapter 3 Results 1: quantitative analysis of NHS Health Check consultations and medical record reviews (process evaluation)
Parts of this chapter have been reproduced with permission from Gidlow et al. 72 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
General practice characteristics
General practices were recruited in matched pairs, based on the level of deprivation [Index of Multiple Deprivation (IMD) deciles 1–5 vs. deciles 6–10],62 and randomly assigned to the QRISK2 group or the JBS3 group (Table 4). Practices were located across eight CCG areas in the West Midlands. Variation in practice size was not used for stratification. Many large modern practices are aggregations of smaller practices, such that the total list size is large but the operation of individual surgeries within them would be more aligned to ‘small’ practices. The proportion of ethnic minority patients averaged 13.5%, but this figure ranged from 1.5% to 63.7%.
| Practice ID | Practice characteristic | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| CVD risk calculator | Deprivation decilea (1 = most deprived; 10 = least deprived) | Practice size (nearest 1000) | Health check practitioners | Blood test procedures | NHSHC appointment time (minutes) | QOF achievementb (%) | Patients with positive experiencec (%) | Ethnic minorityd (%) | Number of patients recruited for the RICOe study | |
| 1 | JBS3f | 6 | 13,000 | 1 HCA, 1 PN | PoC | 30 | 98.4 | 96.2 | 2.0 | 12 |
| 2 | QRISK®2+f | 6 | 9000 | 1 HCA | PoC | 25 | 98.4 | 90.2 | 1.9 | 22 |
| 3 | QRISK2 | 1 | 4000 | 1 HCA | Prior | 20 | 78.1 | 88.9 | 31.6 | 14 |
| 4 | JBS3 | 4 | 45,000 | 1 HCA | PoC | 20 | 98.5 | 67.4 | 6.4 | 29 |
| 5 | JBS3 | 2 | 5000 | 1PN | Prior | 30 | 99.6 | 75.9 | 3.9 | 7 |
| 6 | QRISK2 | 9 | 4000 | 2 PN | Prior | 30 | 98.6 | 74.8 | 2.5 | 17 |
| 7 | JBS3f | 10 | 8000 | 1 HCA | PoC | 30 | 99.6 | 95.0 | 2.4 | 20 |
| 8 | JBS3 | 6 | 4000 | 1 HCA, 1 PN | Prior | 30 | 98.7 | 95.5 | 2.5 | 24 |
| 9 | QRISK2 | 4 | 7000 | 1 HCA | PoC | 30 | 82.4 | 95.3 | 16.5 | 5 |
| 10 | QRISK2 | 2 | 3000 | 1 PN | Prior | 15 | 100.0 | 85.8 | 26.6 | 3 |
| 11 | JBS3 | 2 | 5000 | 1 HCA | Prior | 25 | 99.4 | 49.9 | 63.7 | 8 |
| 12 | QRISK2+f | 6 | 8000 | 1 PN | PoC | 30 | 100.0 | 83.0 | 1.5 | 12 |
Half of the practices used point-of-care (PoC) testing to measure cholesterol levels during the health check and half required patients to have blood tests in advance. Four practices (two in each group) routinely used Informatica74 during health checks, an additional software embedded into the health check template that has some JBS functionalities, such as heart age and risk manipulation. The two practices (2 and 12) that were assigned to the QRISK2 group were asked to continue with their usual practice (i.e. QRISK2 plus Informatica). For those assigned to JBS3 (practices 1 and 7), JBS3 was used instead.
As proxies for practice quality, data from the Quality and Outcomes Framework (QOF) were retrieved for overall QOF achievement and patients reporting positive experiences. These showed some variation, with three practices scoring markedly lower on patient experience (practices 4, 6 and 11; two JBS3, one QRISK2).
There was marked variation in the success of patient recruitment. Each practice was asked to continue with recruitment until 20 useable recorded health checks had been completed. This was achieved in only four practices, but each practice exhausted its list of eligible patients. When recruitment was more successful, there was some over-recruitment of patients to boost the overall sample size. The varied success of recruitment across practices created an imbalance of patients across the QRISK2 and the JBS3 groups.
There was a trend towards practices in the most deprived 50% of areas (based on the IMD), on average, recruiting fewer patients and allocating shorter appointment slots to health checks than those in the least deprived 50% of areas (mean recruitment 11.0 ± 9.6 vs. 17.8 ± 5.1 patients; mean appointment allocation 23.3.0 ± 6.1 vs. 29.2 ± 2.0 minutes). This vindicated sampling of practices stratified by level of deprivation.
Practitioner characteristics
Practitioners (n = 15) all worked within primary care (nine HCAs, six PNs; Table 5) and all were female. Thirteen were classified as white British and two were of Asian British ethnic background. On average, the practitioners had been delivering health checks for 4.7 ± 2.4 years, ranging from 9 months to 9 years. Where training in health checks was reported (n = 9), it tended to be focused on general delivery and health check processes. Six practitioners had received no training.
| Practice | Practitioner characteristic | |||||||
|---|---|---|---|---|---|---|---|---|
| Risk calculator | PID | Role | Sex | Ethnicity | Time delivering NHSHCs | NHSHC training | Number of recorded NHSHCs | |
| 1 | JBS3 | 1.1 | PN | Female | WBRI | 9 years | No formal training | 7 |
| 1.2 | HCA | Female | WBR | 6 years | Generic training, PoC training | 5 | ||
| 2 | QRISK2 | 2.1 | HCA | Female | WBRI | 2.5 years | Generic training | 22 |
| 3 | QRISK2 | 3.1 | HCA | Female | WBRI | 2.5 years | No formal training (at time of study) | 14 |
| 4 | JBS3 | 4.1 | HCA | Female | EM | 2 years | No formal training | 29 |
| 5 | JBS3 | 5.1 | PN | Female | WBRI | 8 years | Generic training × 2 | 7 |
| 6 | QRISK2 | 6.1 | PN | Female | WBRI | 2 years | No formal training | 6 |
| 6.2 | PN | Female | WBRI | 6 years | Generic training, lifestyle advice and referrals | 11 | ||
| 7 | JBS3 | 7.1 | HCA | Female | WBRI | 5 years | Generic training, PoC training (could not recall details) | 20 |
| 8 | JBS3 | 8.1 | HCA | Female | WBRI | 5 years | Generic training | 11 |
| 8.2 | PN | Female | WBRI | 9 months | No formal training | 13 | ||
| 9 | QRISK2 | 9.1 | HCA | Female | WBRI | 6 years | Generic training (could not recall details) | 5 |
| 10 | QRISK2 | 10.1 | PN | Female | WBRI | 3 years | No formal training | 3 |
| 11 | JBS3 | 11.1 | HCA | Female | EM | 8 years | Generic training × 2 (8 and 1 years earlier) | 8 |
| 12 | QRISK2 | 12.1 | PN | Female | WBRI | 4 years | Generic training (4 years earlier) | 12 |
Patient characteristics
A total of 175 video-recorded health checks were completed, of which 173 were included in the analysis (QRISK, n = 73; JBS3, n = 100). Two were excluded because practitioner process error invalidated the consultation. The sample comprised approximately equivalent proportions of males and females (Table 6). The proportion of patients who were white British or from ethnic minorities was approximately representative of the general practice populations from which they were drawn (see Table 4). There was a spread of deprivation levels in both study groups, with a trend towards more participants from the JBS3 group residing in more deprived areas (but with a relatively small effect size; see Table 6). The average age was higher in the JBS3 group (mean 60.87 years, 95% CI 58.91 to 62.83 years) than in the QRISK2 group (mean 54.70 years, 95% CI 51.66 to 57.70 years), while 10-year CVD risk was slightly higher in the JBS3 group (mean 9.71, 95% CI 7.85 to 11.57) than in the QRISK2 group (mean 8.69, 95% CI 5.56 to 11.81).
| Characteristic | Total | Study group | Difference | ||||
|---|---|---|---|---|---|---|---|
| JBS3 | QRISK | ||||||
| n | % | n | % | n | % | r a | |
| Age (years) | |||||||
| 40–54 | 60 | 34.68 | 24 | 24.00 | 36 | 49.32 | 0.32 |
| 55–64 | 54 | 31.21 | 30 | 30.00 | 24 | 32.88 | |
| 65–74 | 59 | 34.10 | 46 | 46.00 | 13 | 17.81 | |
| Total | 173 | 100 | 73 | ||||
| Sex | |||||||
| Male | 86 | 49.71 | 49 | 49.00 | 37 | 50.68 | 0.05 |
| Female | 87 | 50.29 | 51 | 51.00 | 36 | 49.32 | |
| Total | 173 | 100 | 73 | ||||
| Ethnicity | |||||||
| White British | 144 | 83.24 | 81 | 81.00 | 63 | 86.30 | 0.07 |
| Ethnic minority | 29 | 16.76 | 19 | 19.00 | 10 | 13.70 | |
| Total | 173 | 100 | 73 | ||||
| Deprivation quintileb | |||||||
| 1 | 32 | 18.50 | 16 | 16.00 | 16 | 21.92 | 0.13 |
| 2 | 33 | 19.08 | 16 | 16.00 | 17 | 23.29 | |
| 3 | 37 | 21.39 | 22 | 22.00 | 15 | 20.55 | |
| 4 | 34 | 19.65 | 22 | 22.00 | 12 | 16.44 | |
| 5 | 37 | 21.39 | 24 | 24.00 | 13 | 17.81 | |
| Total | 173 | 100 | 73 | ||||
| CVD risk categoryc | |||||||
| Low | 104 | 60.12 | 57 | 57.00 | 47 | 64.38 | 0.06 |
| Medium–high | 67 | 38.73 | 41 | 41.00 | 26 | 35.62 | |
| Total | 171 | 98 | 73 | ||||
Headline findings from the process evaluation
-
Health check duration varied greatly, but most lasted < 20 minutes.
-
Health checks were often verbally dominated by practitioners.
-
There was little discussion of CVD risk overall (< 2 minutes per health check, on average).
-
Compared with health checks using QRISK2, in those using JBS3:
-
there was more discussion of CVD risk
-
consultations were less verbally dominated by practitioners
-
more patients asked questions about CVD risk.
-
-
At 12 weeks post health check, relevant follow-up activity was recorded for fewer than one-third of patients, < 9% had received prescriptions as a result and there were 10 new diagnoses. There were no corresponding statistical differences between the QRISK2 group and the JBS3 group.
Quantitatively coded health checks
Length of NHS Health Check consultations
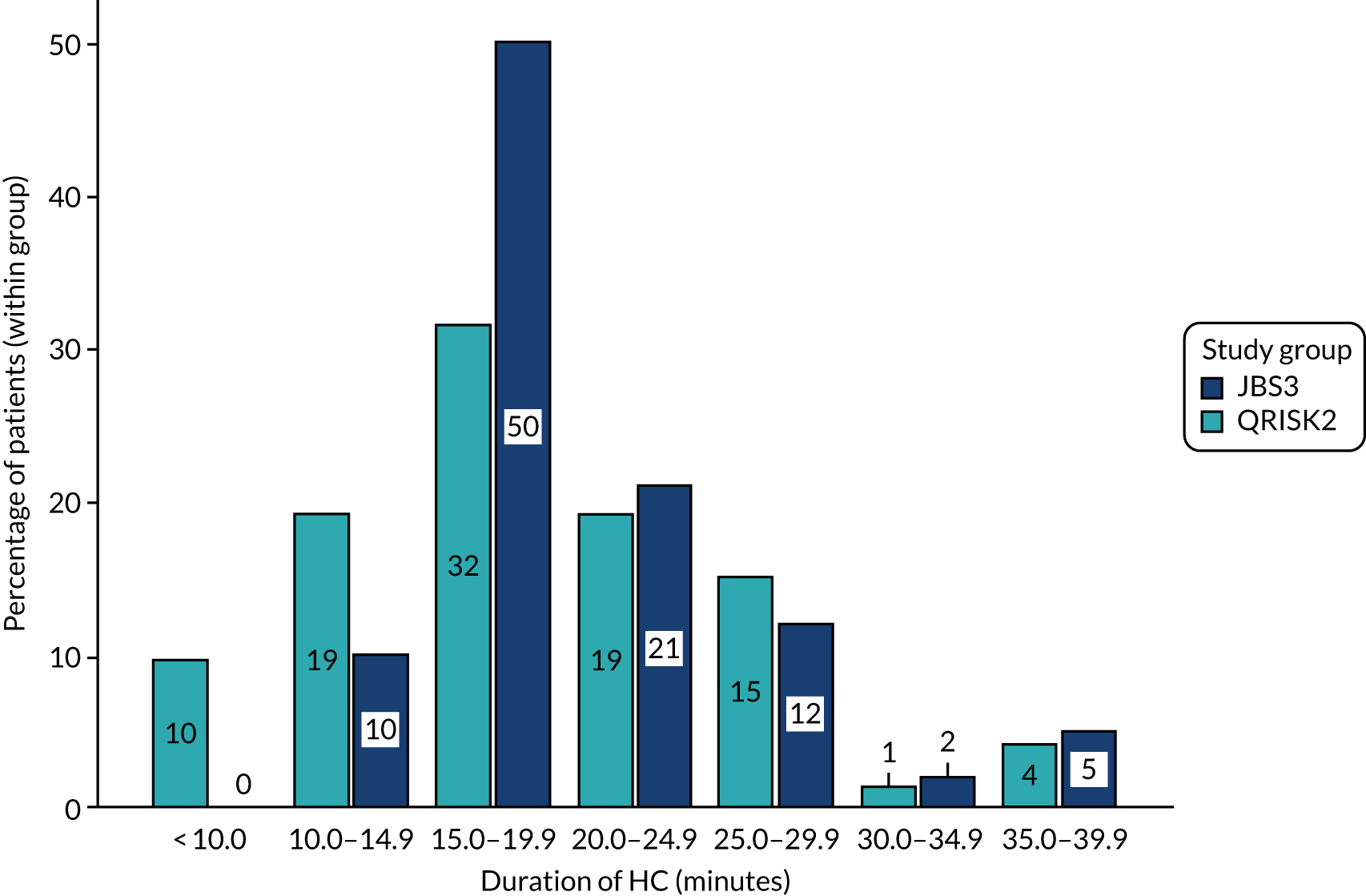
Table 7 summarises the characteristics of health check consultations by study group and overall. Consultation duration varied widely (range 6.8 to > 38 minutes), but the majority of consultations lasted between 15 and 20 minutes, with most consultations (60%) lasting < 20 minutes (Figure 3). Consultations were only slightly shorter, on average, in the QRISK2 group than in the JBS3 group (with a relatively small effect size of 0.13).
| Outcome | Total | Study group | Differencea (QRISK2 vs. JBS3) | ||||
|---|---|---|---|---|---|---|---|
| JBS3 | QRISK2 | ||||||
| Mean (95% CI) | SD | Mean (95% CI) | SD | Mean (95% CI) | SD | r | |
| Duration (minutes) | 20.06 (18.87 to 21.24) | 6.21 | 20.66 (18.89 to 22.42) | 5.65 | 19.24 (15.28 to 23.19) | 6.84 | 0.13 |
| Verbal dominance | |||||||
| Percentage of total time practitioner speaking | 50.07 (45.90 to 54.24) | 9.55 | 46.60 (41.36 to 51.84) | 8.79 | 54.82 (50.00 to 59.64) | 8.48 | 0.42 |
| Percentage of total time patient speaking | 23.37 (19.87 to 26.87) | 10.62 | 24.67 (20.47 to 28.87) | 10.53 | 21.6 (15.71 to 27.43) | 10.56 | 0.15 |
| Verbal dominance ratiob | 2.70 (2.23 to 3.19) | 1.50 | 2.35 (1.89 to 2.81) | 1.31 | 3.21 (2.44 to 3.97) | 1.62 | 0.27 |
| Percentage of total health check time | |||||||
| Discussing CVD risk | 9.06 (7.36 to 10.76) | 4.30 | 10.24 (8.01 to 12.48) | 4.07 | 7.44 (5.29 to 9.58) | 4.08 | –0.32 |
| Discussing risk factors | |||||||
| Total | 37.54 (32.92 to 42.17) | 12.96 | 35.33 (27.76 to 42.90) | 13.29 | 40.58 (36.20 to 44.96) | 11.91 | 0.22 |
| Medicalc | 21.34 (18.35 to 24.33) | 9.41 | 20.13 (15.33 to 24.94) | 9.38 | 22.98 (19.96 to 26.31) | 9.26 | 0.16 |
| Lifestyled | 16.11 (13.79 to 18.44) | 7.03 | 15.08 (11.87 to 18.30) | 6.49 | 17.52 (14.16 to 20.88) | 7.53 | 0.16 |
| Discussing risk management | |||||||
| Total | 19.64 (16.48 to 22.81) | 11.37 | 18.82 (13.92 to 23.73) | 11.12 | 20.77 (16.59 to 24.94) | 11.69 | 0.08 |
| Lifestyle | 16.59 (13.44 to 19.74) | 10.2 | 15.94 (11.27 to 20.62) | 10.04 | 17.48 (12.95 to 22.01) | 10.41 | 0.08 |
| Medicale | 63% | 58% | 69.9% | –0.12 | |||
FIGURE 3.
Duration of health check consultation by CVD risk calculator group.
Discussion of cardiovascular disease risk
Overall, < 10% (9.1% ± 4.3%) of consultation time was devoted to CVD risk discussion, which equated to 1.7 ± 0.83 minutes. A higher proportion of consultation time was spent discussing CVD risk when using JBS3 (equivalent to 2.1 ± 0.82 minutes) than when using QRISK2 (equivalent to 1.31 ± 0.63 minutes), with a medium effect size. Nearly all health checks in both groups included reference to the 10-year percentage CVD risk score (94% vs. 94.5%; r = 0.01). The proportion of patients asking questions about CVD risk was higher in the JBS3 group than in the QRISK2 group (32.0% vs. 12.3%; r = 0.23).
In the JBS3 group, nearly all health checks included discussion of heart age (100%) and event-free survival age (97%), and manipulation of the risk score(s) to show the potential effect of intervention on risk (92%). This showed fidelity to the requested minimum use of JBS3 outputs. Use of heart age and risk manipulation was also evident in 52.1% and 21.9% of QRISK2 consultations, respectively. This is a result of two general practices in the QRISK2 group using Informatica (a software addition that offers some JBS3 functionalities), and because heart age and risk manipulation are possible (but not main features) in QRISK2.
Discussion of cardiovascular disease risk factors and risk management
Over one-third of total health check time was spent discussing causal CVD risk factors. This was slightly higher in health checks using QRISK2 than in those using JBS3 (small to medium effect size), but with wide variation within groups (see Table 7).
Interventions to manage risk were discussed for approximately one-fifth of total consultation time and predominantly related to lifestyle rather than medical intervention, which was not discussed at all in over 30% of QRISK2-informed and 42% of JBS3-informed health checks (r = –0.12).
Verbal dominance
Practitioners spoke for just over half of the total time in QRISK2 consultations and just under half in JBS3 consultations (compared with ≈ 23% for patients) (Figure 4). There was an indication of higher practitioner verbal dominance in health checks using QRISK2 than in those using JBS3 (r = 0.27).
FIGURE 4.
Mean percentage of total health check time with speaking by practitioner or patient. Error bars: 95% CI.

Patient medical records: activity and prescriptions 12 weeks post health check
Fewer than one-third of all patients had resulting activity (30.1%) and 8.7% had prescriptions logged in their medical records in the 12 weeks following their health check. Figures 5 and 6 show the between-group comparisons. Chi-squared tests confirmed that there were no statistical differences between risk calculator groups (all had p-values > 0.05).
FIGURE 5.
Proportion of patients in each risk calculator group with relevant activity within 12 weeks of their health check. Data from all patients (n = 173).

FIGURE 6.
Proportion of patients in each risk calculator group with relevant prescriptions within 12 weeks of their health check. Data from all patients (n = 173).

The most common follow-up activities were related to blood pressure measurement or discussion (20.2%), followed by lifestyle discussion (9.8%), CVD risk assessment or discussion (9.2%) and cholesterol measurement or discussion (8.7%). Among the 173 patients, there were 10 new diagnoses (three pre-diabetes, three diabetes, two hypertension and two hyperlipidaemia).
Just 5% of all patients received prescriptions for lipid-lowering or cardiovascular medication, with 1% receiving prescriptions for anticoagulants or diabetes medication.
Figures 7 and 8 show that, as expected, the proportion of patients in whom relevant follow-up activity or prescriptions were recorded was higher among those at medium risk (with a QRISK2 score of 10–19.9%) or high risk of CVD (with a QRISK2 score of ≥ 20%) than among those at low risk (with a QRISK2 score of < 10%). Despite the relatively small numbers, differences between low- and medium-/high-risk groups reached significance for any medication (Fisher’s exact test, p = 0.028) and statin/lipid-lowering medication (Fisher’s exact test, p = 0.006), and for a number of relevant follow-up activities (Fisher’s exact tests: any activity, p = 0.004; weight related, p = 0.029; blood pressure related, p = 0.006; cholesterol related, p = 0.010; lifestyle referral, p = 0.022).
FIGURE 7.
Proportion of patients at low or medium/high risk of CVD with relevant activity within 12 weeks of their health check. Data from 171 patients (CVD risk missing for two patients in JBS3 group).
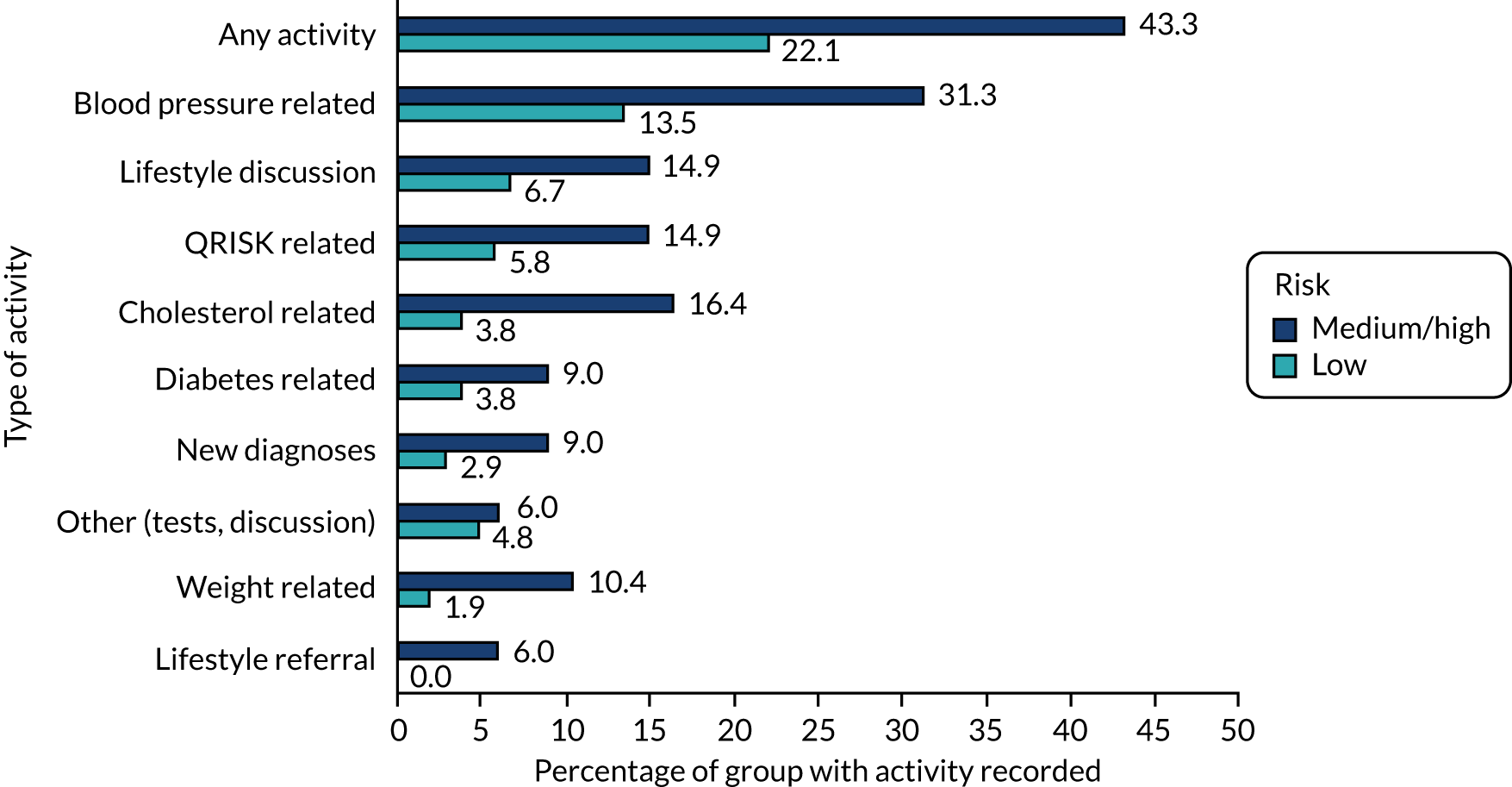
FIGURE 8.
Proportion of patients at low or medium/high risk of CVD with relevant prescriptions within 12 weeks of their health check. Data from 171 patients (CVD risk missing for two patients in JBS3 group).

Summary
Second-by-second quantitative coding of 173 video-recorded health checks (JBS3, n = 100; QRISK2, n = 73) and a review of patient medical records 12 weeks after their health check revealed a number of key findings.
-
Health check duration varied greatly (6.8–38.0 minutes), with most consultations lasting < 20 minutes. During this time, practitioners are expected to complete a range of clinical and administrative tasks, such as CVD risk assessment, involving measurement of (and data entry for) weight, blood pressure and, sometimes, cholesterol level through PoC testing; assessment of lifestyle (physical activity, alcohol, diet); explaining to patients their CVD risk score(s) and what it means; and patient-centred discussion of risk management to prompt risk-reducing behaviours.
-
There was evidence of practitioner verbal dominance because, on average, practitioners spoke for half of the total consultation time. This suggests more information provision than patient-centred, two-way interaction (see Chapter 4).
-
On average, CVD risk was discussed for < 2 minutes (9.1% ± 4.3% of the consultation time). Discussion of causal risk factors accounted for the largest proportion of total health check time.
-
There were indications that, compared with health checks using QRISK2, those using JBS3 involved more CVD risk discussion and were less verbally dominated by practitioners.
-
One in three patients (32%) in JBS3 consultations asked questions about their CVD risk, compared with one in eight patients (12%) in QRISK2 consultations, suggesting that there is better engagement with JBS3 than with QRISK2.
-
Fewer than one-third of all patients (30.1%) had relevant activity logged in their medical records in the 12 weeks following their health check, and just 8.7% received prescriptions as a result. Among the 173 patients, there were 10 new diagnoses. There was a trend for follow-up activities and prescriptions to be more frequent in patients at medium/high risk of CVD than among those at low risk, and for the number of prescriptions issued to be higher following health checks using QRISK2 than those using JBS3.
Chapter 4 Results 2: qualitative analysis of NHS Health Check consultations
Parts of this chapter have been reproduced with permission from Riley et al. 76 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Headline findings from deductive thematic analysis of recorded health checks
-
There was little discussion of CVD risk, particularly in health checks using QRISK2.
-
Practitioners often relayed the risk score without discussing the implications or risk management.
-
Patients offered minimal responses to the risk information (e.g. single-word acknowledgement).
-
Practitioners frequently missed cues from patients who were unclear about their risk score.
-
For QRISK2, it was unclear whether or not the patient understood 10-year percentage risk, or trusted its credibility or relevance.
-
JBS3’s visual presentations of risk and heart age appeared more impactful and better understood (than 10-year risk in QRISK2).
-
JBS3’s event-free survival age lifetime risk was often misunderstood (patients and practitioners).
-
JBS3 may provide more opportunities to initiate risk factor and management discussion than QRISK2.
-
Positive responses were more evident when practitioners checked patient understanding, made risk meaningful to the patient, and asked for patient feedback around the CVD risk score.
Participant characteristics
To define the sample for the qualitative analysis, a further 19 of the 173 recorded health checks (included in the quantitative analysis) were excluded for reasons including communication of projected (not actual) risk score (n = 7), no discussion of risk (n = 2), no communication of lifetime risk (n = 4), incorrect use of JBS3 (n = 4) and insufficient use of the English language (n = 2). Of the remaining sample (n = 154), 64 health checks included communication of CVD risk using QRISK2. Therefore, 64 health checks using JBS3 were identified, matched on patients’ sex, CVD risk score and ethnicity, giving a sample of 128 for analysis (Table 8).
| Characteristic | Total | Study group | ||||
|---|---|---|---|---|---|---|
| JBS3 | QRISK2 | |||||
| n | % | n | % | n | % | |
| Total | 128 | 64 | 64 | |||
| Sex | ||||||
| Female | 64 | 50.00 | 32 | 50.00 | 32 | 50.00 |
| Male | 64 | 50.00 | 32 | 50.00 | 32 | 50.00 |
| Age (years) | ||||||
| 40–54 | 55 | 42.97 | 21 | 32.81 | 34 | 53.13 |
| 55–64 | 37 | 28.91 | 20 | 31.25 | 17 | 26.56 |
| 65–74 | 36 | 28.13 | 23 | 35.94 | 13 | 20.31 |
| Ethnicity | ||||||
| White British | 114 | 89.06 | 56 | 87.50 | 58 | 90.63 |
| Ethnic minority | 14 | 10.94 | 8 | 12.50 | 6 | 9.38 |
| CVD risk categorya | ||||||
| Low | 86 | 67.19 | 43 | 67.19 | 43 | 67.19 |
| Medium–high | 42 | 32.81 | 21 | 32.81 | 21 | 32.81 |
The results of deductive thematic analysis demonstrate how practitioners communicated risk using either QRISK2 or JBS3, and patient responses, to explore similarities and differences between the two calculators. The analysis, therefore, focused on parts of the health checks in which CVD risk was discussed. As noted in Chapter 3, this accounted for < 10% of consultation time, on average, and most patients said little in response to CVD risk information. Therefore, where there was evidence of two-way dialogue around CVD risk, we present quotations that best illustrate risk communication and subsequent patient response. Each quotation is labelled to denote which risk calculator was used (using QRISK®2+ where Informatica was used), the consultation identifier, patient sex and age. Where dialogue is reported, ‘P’ denotes the patient’s contribution and ‘HP’ denotes the health professional’s contribution (i.e. the practitioner).
Theme 1: cognitive appraisal
Threat appraisal
Threat appraisal focuses on the source of a threat (CVD risk) and factors that increase or decrease the probability of maladaptive responses (i.e. behaviours that inhibit patients’ ability to adjust to the threat). This theme is central to the health check. It focuses on the discussion of risk as it relates to patients’ perceived severity of CVD risk, the consequences of CVD, the perceived vulnerability to future CVD, and the intrinsic and extrinsic rewards for not addressing CVD risk [i.e. perceived benefits of not acting to manage or reduce risk (maladaptive response)]. Threat appraisal was the most commonly identified element of the PMT model. It was observed in all health checks, although less frequently in those using JBS3 (coded 584 times; average 9 times per consultation) than those using QRISK2 (coded 634 times; average 10 times per consultation).
Patients, when presented with their 10-year risk, generally acknowledged it, but the extent of their understanding was often unclear. For example, one asked ‘Is that percentage of risk alright?’. Most often, the risk score was acknowledged with a single-word response, such as ‘yeah’ or ‘OK’, limiting practitioners’ ability to gauge the patient’s understanding and classification of response for this analysis. Heart age in JBS3 aided patient understanding of CVD risk, resulting in questions such as ‘. . . so really what can I do about that? I mean I know it is all estimated’. Such questions reflected a level of understanding of the score and intention towards risk-reducing behaviour. Several patients expressed surprise at their risk. The patient in the extract below appeared to question how the score was calculated because he perceived himself to be healthier than the outcome suggested, leading to some mistrust. They also made two references to being ‘fitter’ than the risk score indicated, which was not addressed by the practitioner:
I thought I was fitter than that though.
[Laughter] You are doing good exercises.
But I was fitter than that though . . .
OK, so the health years, so on average expect to survive is 80 for yourself without a heart attack or a stroke, yeah? And then your risk of a heart attack or stroke in the next 10 years is 15%, so you do need to look after yourself, because we would say that is a medium risk.
Yes.
So wouldn’t say it is too high or low, but a medium to high.
OK.
OK, and then that’s what it looks like so from now until there, that’s the last one the chance of surviving without a heart attack.
That’s estimated?
This is estimated, we don’t know what’s going to happen you might be even longer.
So about 94 I might snuff it?
JBS3, 11_028, male, 58
Because the practitioner appeared to ignore the patient’s surprise, continuing to focus on the process of the health check, the patient switched off briefly, until presented with his event-free survival age. Moreover, there was evidence of misunderstanding among some patients and practitioners who interpreted event-free survival age as estimated age of survival (i.e. age of death).
Practitioners provided little follow-up explanation of risk scores when using QRISK2 or JBS3:
Right, this is the screening I was telling you about. I will just print that out for you. So your risk of any heart disease is 15%.
Yeah, which is not very high.
It does increase with age. If it is above 10% we then pass it on for them to have a look at it and they will be able to decide when to have your next health check, which should be 3 years or 1 year. Obviously next time you come in any results you’ve got in the red tend to up your risk and they tend to up your heart age as well. So when you come in next time if your blood pressure is back down, and obviously it could be less so . . . Your heart age has come up as 66.
Well I am 66 this year.
Yes, yes, so it is quite near isn’t it? Yes. So, for example, if you were a smoker and that was in the red that would put your heart age at 75. So the only one we have got in the red really is that one cholesterol . . .
It’s only marginal though isn’t it?
QRISK2+, 2_016, male, 65
The patient quoted above was identified as medium–high risk, but the practitioner did not elaborate on the severity or implications, leaving the patient’s interpretation of his risk score as ‘not very high’. This was compounded when the patient received his heart age. The practitioner did not address the patient’s misinterpretation of the severity of his risk nor explain why his results were conflicting (i.e. percentage risk score is age and sex dependent, heart age is not), again perhaps focusing on the consultation process more than the patient. This led the patient to dismiss his elevated cholesterol as ‘only marginal’. The absence of active listening skills was recurrent across both groups, making it difficult to gauge patient understanding, and lends support to the apparent imbalance between patient and practitioner contributions (see Chapter 3).
There was evidence, albeit still limited, that patient engagement in conversations about the threat of CVD was greater in the JBS3 group, prompted by risk score manipulation (e.g. practitioners visually showed patients that a reduction in blood pressure could lower their heart age):
. . . so obviously your blood pressure is not too bad, that is fine where it is at 128, but your cholesterol, so ideally we like that to be below 5. So if you could get it below 5, so let’s put it down to 4.8, you can see that automatically that it brings your risk down to 1.8%.
Oh, I see, yes.
. . . improves your life expectancy slightly, and probably brings your heart age down a year. So it is just, you know, showing that it can and, obviously, the lower you can keep these factors that you influence, for longer, the better quality of life and life expectancy there is . . . your risk is going to increase slightly with age. So it is about trying to moderate those other factors.
So what impact does exercise have on that?
It has quite a significant impact on your cholesterol, it does help your cholesterol a lot. We know that it helps because that increases your good cholesterol, which can help increase the balance so, that can help with it as well.
So what’s the normal range that is seen for HDL cholesterol?
HDL can be anything from sort of 1.1 to about 2.5, you don’t get much over, I can’t say I have seen many, I have seen a few. But your cholesterol could be anything down to you know 3.5.
OK and really bad would be?
6 or 7s, so would be sort of . . .
Oh, OK – so 5.6 is yeah it is edging up, isn’t it?
JBS3, 7_020, male, 45
The patient evaluated the threat and sought information to facilitate their appraisal. Although positive, this exchange again demonstrated misunderstanding of CVD event-free survival age as expected survival age, this time on the part of the practitioner. The visual impact of demonstrating how CVD risk can be reduced through risk factor modification (e.g. cholesterol, smoking status) appeared to aid patient understanding and realistic threat appraisal. There were fewer examples of active engagement during discussion of the CVD risk score during QRISK2 consultations, which may be because of the inability to show risk factor modification when using the calculator.
Coping appraisal
Coping appraisal focuses on the coping responses available to the individual to deal with a health threat (i.e. evaluation of ways to reduce CVD risk). This included patients’ perceptions of self-efficacy to engage in adaptive coping, practitioners’ promotion of self-efficacy through individualisation, the perceived response efficacy of adaptive coping and the response cost of adaptive coping (see Figure 2). References to coping appraisal were more common in JBS3 (n = 60, 94%) than QRISK2 health checks (n = 55, 86%). The communication of risk in JBS3 consultations was not observed in the same way as in those using QRISK2; most such consultations focused on facilitators of adaptive coping (i.e. risk-reducing changes that patients could make):
Erm and then this gives you your healthy years outlook [event-free survival age]. So based on your current lifestyle your risk of a heart attack or a stroke in the next 10 years is coming out at 2.4%. We aim for people’s risk to be below 10% so that’s . . .
Yeah.
. . . absolutely fine and on average you expected to survive to an age of 84 without a heart attack or stroke, so brilliant. So as I say, your blood pressure pretty good as it is, you not going get that much lower.
No.
Diet-wise would you say you got a pretty good diet do you know the sorts of . . .
We sort of grow our own vegetables and fruit and stuff like that . . .
Yeah.
. . . so, erm, I mean we eat reasonably healthy.
JBS3, 7_044, female, 54
Following communication of the risk score, the practitioner moved on to ways that the patient could maintain a low risk through dietary behaviours. This suggested that, although practitioners (from both groups) spent little time talking about the CVD risk score, the additional risk information in JBS3 may have helped to facilitate more risk factor discussion between the patient and the practitioner (than if using QRISK2).
Discussions around response costs for adaptive coping (i.e. perceived costs associated with a recommended behaviour) related to the use of statins or blood pressure medication, and were only observed in seven JBS3 consultations (11%) and none of the QRISK2 consultations. Data are limited, but may offer some evidence to suggest that JBS3 was more likely than QRISK2 to promote discussion around adaptive coping:
Obviously we’ve tried them, and they haven’t agreed with you.
I tried the [medication name] statin.
Yeah, and there are other statins we can discuss and obviously benefits of those they can reduce your cholesterol obviously and we can reduce your risk of cardiovascular disease so it might be worth having a think about and if you want to just discuss that further or a different type of statin . . .
All they did was it affected my reflux and it made the reflux worse.
Yeah.
So.
Yeah.
I was on that and an aspirin – I did the aspirin first and then . . .
Yeah, but it was affecting you. I mean it might be worth a having another . . . err you know a think about whether you wanted to erm take that, because obviously it would lower your cholesterol, obviously add to a healthier heart erm and reduce that risk of cardiovascular disease, but then obviously we’ll not gonna push that onto you, err it is something you can talk to myself, one of the doctor’s once you have had time to think erm and they can advise or [name] the prescribing nurse, because they can prescribe, you know talk about you know what’s best, which statin would be best, and not all statins agree with everybody but there might be one out there that actually has a better erm compatibility with yourself OK?
Yeah.
How do you feel about what I have told you today?
I would consider it.
JBS3, 8_177, male, 71
Here, the patient’s prior engagement with statins as a response cost was discussed, leading to a re-evaluation of the medical intervention by the patient. However, rather than addressing the patient’s concern regarding their previous experience of statins, the practitioner appeared to interrupt them to repeat the benefits of statins. There were examples where the perceived cost of taking statins provided motivation to adopt risk-reducing lifestyle behaviours:
But well done!
I am pleased about that, yes.
That’s really good, no I am very pleased with you because that’s really good. And where you were at 10% just before, it is now 5%, so you have halved the risk in that time. So that’s really good. So it shows it can be done.
Yeah, yeah, and that’s what I would rather do than taking tablets.
Of course.
I would rather think, no I know what’s wrong, I will deal with it in time.
QRISK2+, 12_055, female, 64
However, opportunities to discuss facilitators of adaptive coping were sometimes missed by practitioners who communicated risk using QRISK2:
I look at your [total : HDL cholesterol] ratio and your ratio is good. But just to keep a little eye on it, maybe they will test it again in a year’s time. You probably won’t be due this Health Check, because your risk is only 3%, which is low. It will increase as you age, so your Health Check wouldn’t be due again for 5 years, but you could probably have your cholesterol done in about a year, with you know normal bloods taken out of your arm. Erm your heart age, because you got such results in the green, your heart age has come up less than your actual age, but that’s with the 2 years added on from being an ex-smoker.
So is it possible that I could get that even lower? If my cholesterol came down a lot.
Well we will have a look now, I will play about with it. So if you had never smoked at all, your heart age would be 45. If you were still smoking, it could be 51. So being an ex-smoker tends to add 2 years, so with your cholesterol, it could be brought down to 46.
Massively, yeah.
QRISK2+, 2_077, male, 48
The patient above attempted to understand how their risk could be reduced. The practitioner did not engage with this to encourage the risk-reducing behaviour or discuss ways to reduce cholesterol. Rather, they proceeded to talk about the impact of previous smoking status (which is unmodifiable) on CVD risk. Although references to coping appraisal were more common in JBS3 consultations, practitioners in both groups appeared to focus on the consultation process more than the patient.
Theme 2: coping modes
Maladaptive coping
Maladaptive coping is classified as the patient negatively engaging in risk management discussion and being dismissive of suggestions (e.g. the patient believes that they have a sufficiently healthy lifestyle and dismisses discussion about change). As noted, patient responses to risk information were often limited to a single word. Where context allowed, apparent lack of engagement and minimal verbal responses from patients were also interpreted as a maladaptive coping response if the risk information communicated by the practitioner did not provoke a response by the patient. Risk management interventions were classified as medical [appointment referral, medication (e.g. blood pressure or cholesterol lowering), re-testing and managing blood pressure or retesting cholesterol] or lifestyle (weight reduction and management, increasing physical activity, diet modification, smoking cessation and reducing alcohol consumption). Maladaptive coping was identified in 49 (77%) QRISK2 consultations (coded 139 times; average 2.8 times per consultation), compared with 40 (62.5%) JBS3 consultations (coded 110 times; average 2.8 times per consultation). The practitioner in the exchange below briefly communicates QRISK2 before moving on to heart age (using Informatica):
Yeah this is the screening I was telling you about. So, your risk is 9%.
Right.
Which is your key risk for you over the heart disease and diabetes and stroke risk.
And heart disease.
As you, as you age your risk does seem to increase, erm any results that you’ve got in the red tend to push up your heart age slightly.
Aha.
So if we can get the results out of the red and back into the green, that can reduce that one down.
Right, OK.
So, for example, being an ex-smoker actually puts 2 years onto your heart age there.
Yeah.
So would be its 66 and it would be 66 if you never smoked at all.
Right.
Erm, if you were still smoking it would be 73.
Oh my gosh!
Your heart age has come up as 71 – you are 66. Any results you have got in the red do tend to increase your heart age. It is just that one cholesterol one that was in the red.
QRISK2+, 2_001, female, 66
Sometimes, maladaptive responses to the 10-year percentage risk score could be shifted towards a more positive response through communication of heart age. The brief exchange prior to the communication of heart age (above) may have also suggested that the practitioner was less confident discussing QRISK2, a recurrent observation (see Chapter 6). If practitioners cannot clearly explain the meaning of a patient’s percentage risk score to confer understanding, subsequent discussion/actions regarding risk management may be undermined, and the link between CVD risk and lifestyle may be unclear.
Minimal engagement following communication of the risk score was also identified in JBS3 consultations:
OK. And your blood pressure being under 82 but that’s fine everything is OK with that. Now, on average what they’re saying is that your risk of a heart attack or stroke in the next 10 years is 15%, again, that is down to the fact that you smoke.
Hm.
OK.
[Sigh.]
And to expect to survive till the age of 78 without a heart attack or a stroke OK. And if we have a look at the next, this one, just reiterates its this, but if I changed it to . . . say if you didn’t smoke OK and we went to the next your heart age would then become equal with your age.
Hm hm.
And your risks in . . . of a heart attack or stroke in the next 10 years comes down to 9.6% and your actual survival to the age of 83 without a heart attack or a stroke OK and that reiterates it in that as well.
Hm hm.
OK so that’s the difference.
Hm hm.
Hm hm.
OK. Erm.
[Cough.]
So it gives you food for thought.
Hmm hmm. You haven’t told me anything I didn’t already know.
JBS3, 1_181, male, 65
The patient’s dismissal of discussion around smoking cessation may reflect the influence of environmental and social factors on their smoking behaviour (and related intentions), preventing a meaningful exchange. The practitioner did not encourage the patient to quit smoking or explore previous experience of attempted smoking cessation and, therefore, was unlikely to promote intentions to change behaviour. There is an added pressure of time during health check consultations. Appointment times allocated to health checks ranged from 15 to 30 minutes (see Table 4), during which time practitioners need to assess CVD risk, communicate the risk score(s) and discuss risk management. Adherence to the process of completing the health check may result in patients being passive recipients of information. As shown above (and throughout), the practitioner delivered the information presented on the screen without asking questions to check understanding or provide context. This prompted little response from the patient, which may be indicative of deference to the practitioner’s health knowledge, which would indicate a power imbalance.
Negative engagement in discussion of risk factor management was also evident following the suggestion of statin use:
What we do tend to say if you risk is above 10%, obviously I don’t know whether the doctors have ever discussed a statin with you?
I don’t see the point, I mean if I am going to live to 83, I am quite happy to live to 83.
So it’s just about being aware that we know that taking a statin can help reduce your overall risk, so it’s one that sort of we usually advise that . . .
If we do this next time and I don’t know, it was ’04 [last cholesterol check], and we are now in 2018, so what does that mean, it could be another 12 to 14 years [for the next health check]?
Well I do normally try and do these every 5 years, so yeah.
So yes, if it is hugely worse.
Yeah.
. . . in 5 years, I will consider it.
JBS3, 7_012, male, 70
Again, the patient misinterpreted event-free survival age and suggested that their risk was not severe enough to consider medical intervention in the short term, only if it was ‘hugely worse’ at the next health check. This was another example of a missed opportunity for the practitioner to question the patient’s understanding of their risk and potential false reassurance provided by the 10-year percentage risk score (which was 15%).
Adaptive coping
Adaptive coping focused on the patient’s positive engagement with discussion of interventions to manage CVD risk, apparently listening and engaging in the consultation and accepting what is being said/suggested. Adaptive coping was identified in 58 QRISK2 (91%) consultations (coded 310 times; average 5 times per consultation) and 55 JBS3 (86%) consultations (coded 328 times; average 6 times per consultation). The frequency of occurrences overall and per consultation was similar between the two groups for adaptive coping in medical interventions [39 QRISK2 (61%) consultations and coded 116 times (average 2.9 per consultation); 42 JBS3 (66%) consultations and coded 142 times (average 3.4 per consultation)] and lifestyle change [11 QRISK2 (17%) consultations and coded 15 times (average 1.4 per consultation); 20 JBS3 (31%) consultations and coded 32 times (average 1.6 per consultation)]. A number of patients showed intentions to change their behaviour as a result of their CVD risk:
So your ratio is 3.5. So this is the screening I was telling you about. So your risk is 3%. That will increase as you age.
Yeah.
And obviously if we can, perhaps with your smoking, it has pushed your heart age up to 48, and your age is 41. Because that is the only result you have got in the red. Because all your other results are really good, they are in the green.
They are really good, so I need to . . .
Yeah, so if you had never smoked at all, your heart age would be aged 40.
I think I need to do something about that don’t I?
QRISK2+, 2_122, male, 41
This was another example of how heart age changed the way that the patient responded to the information presented. Although a positive response was evident, the practitioner did not allow much time before moving on. By giving the patient time to confirm his understanding, the practitioner gave the patient the opportunity to increase his confidence in engaging in coping behaviours. Another example of positive engagement during the discussion of risk was identified from another practice:
OK that’s good. Err let’s see your key risk.
If I know what weight so I can just try to change my life.
Yeah, yeah, it would be good if you can cut down and, and lose a bit of the weight err what was it 13.8. So it’s only a little higher, it should ideally be below 10% is what we want so 13.8 is a bit high but it is because of, because of your weight. OK, you don’t smoke, you don’t drink alcohol, so that’ all good, but your waist is a bit big as well.
Yeah
Your waist is erm it’s 112, let’s have a look.
Around my tummy around here.
Yeah let’s have a look. So your waist is 44 inches.
And that’s this bit here.
QRISK2, 3_259, male, 57
The patient above engaged with the information presented about their risk and suggested a need for weight management, somewhat reinforced by the practitioner. However, the interaction was disjointed, possibly because the practitioner needed to complete all other elements of the health check and created a barrier for adaptive coping through not truly attending to what the patient was saying. Although scarce, a successful strategy for supporting adaptive coping used by one practitioner was to ask the patient to reflect on the risk information that they had received, prompting consideration of action needed:
So average survival free of heart attack or stroke is 84.1 years OK? So how do you feel about that?
Oh I will make more of an effort to lose some weight.
JBS3, 1_154, female, 70
The approach adopted by the practitioner encouraged the patient to express their immediate reaction to their CVD risk, which gave the patient an opportunity to evaluate their action and show intention to change their behaviour. This was a rare example of PMT in action, showing connection between the risk information and the patient’s intention to change her behaviour, helping to redress the power imbalance evident in most consultations across both groups. It also demonstrated the significant role that the practitioner plays in ensuring that risk communication is delivered effectively regardless of the risk calculator.
Summary
Deductive thematic analysis of the 128 video-recorded health checks highlighted a number of key findings:
-
Components of PMT coded most frequently in consultations using JBS3 (compared with QRISK2) included threat appraisal, facilitators of and response costs to adaptive coping. This suggests that JBS3 may provide more opportunities than QRISK2 to initiate discussion of risk factors and their management.
-
Lifetime risk communicated using JBS3’s event-free survival age was misunderstood by both patients and practitioners, who confused estimated age of survival free of a cardiovascular event with estimated age of survival.
-
Patients presented with a QRISK2 score acknowledged their risk level, but it was unclear whether or not they understood 10-year percentage risk (or trusted its credibility or relevance to them). Visual presentations of risk and heart age, such as those provided in JBS3, and those which are not typically communicated within standard practice systems (although they can be generated in QRISK2/3) appeared to be more impactful and better understood by patients than the QRISK2 score.
-
Regardless of the risk calculator used, and despite the recognised importance of risk communication in the health check best practice guidance17 and competence framework,19 there was little discussion of CVD risk. This was particularly marked in QRISK2 consultations. Often, practitioners simply relayed the risk score without discussing the implications of the risk for the patient or what they could do about it. Equally, most patients offered minimal responses to the risk information, which was often acknowledged with a single word.
There was an apparent absence of active listening by practitioners who frequently missed cues from patients who were unclear about their risk score. Positive outcomes were identified when practitioners checked patient understanding, relayed information in a way that was meaningful to the patient (e.g. heart age) and asked for patient feedback around the CVD risk score.
Chapter 5 Results 3: video-stimulated recall interviews – patients
Headline findings from inductive thematic analysis of video-stimulated recall patient interviews
-
Most patients reported some impact of attending their health check (through intentions or modest behaviour change).
-
Patients often did not understand CVD risk information, especially 10-year risk (QRISK2) and event-free survival age (JBS3).
-
JBS3’s heart age and risk score manipulation were liked by patients and can confer patient understanding and appraisal of the risk severity and vulnerability that the score conveys.
-
JBS3’s visual presentation and risk score manipulation were liked by most patients and made the important link between lifestyle change and overall CVD risk.
-
A CVD risk score alone is insufficient to enable patients to understand or recognise their personal risk.
-
Practitioners should check patients’ understanding of CVD risk, tailor the information and make clear the implications for their health.
Participant characteristics
As detailed in Chapter 2, patients were recruited for VSR interviews to give approximately equal numbers across risk calculator groups, sexes and age categories (Table 9). However, the subsample of patients who took part in VSR interviews, compared with the overall sample, included a higher proportion of patients with low CVD risk (70% vs. 60%) and a higher proportion of patients of white British ethnicity (90% vs. 83%).
| Characteristics | Total | Study group | ||||
|---|---|---|---|---|---|---|
| JBS3 | QRISK | |||||
| n | % | n | % | n | % | |
| Total | 40 | 21 | 19 | |||
| Age (years) | ||||||
| 40–54 | 14 | 35.00 | 6 | 28.57 | 8 | 42.11 |
| 55–64 | 14 | 35.00 | 7 | 33.33 | 7 | 36.84 |
| 65–74 | 12 | 30.00 | 8 | 38.10 | 4 | 21.05 |
| Sex | ||||||
| Male | 21 | 52.50 | 13 | 61.90 | 8 | 42.11 |
| Female | 19 | 47.50 | 8 | 38.10 | 11 | 57.89 |
| Ethnicity | ||||||
| White British | 36 | 90.00 | 18 | 85.71 | 18 | 94.74 |
| Ethnic minority | 4 | 10.00 | 3 | 14.29 | 1 | 5.26 |
| CVD risk categorya | ||||||
| Low | 28 | 70.00 | 13 | 61.90 | 15 | 78.95 |
| Medium–high | 12 | 30.00 | 8 | 38.10 | 4 | 21.05 |
Analysis of the data resulted in four main themes: (1) relief regarding CVD risk, (2) mixed levels of understanding, (3) positive impact of health checks and (4) importance of presentation style and content. These are discussed in turn using illustrative quotations, including some interviewer–patient exchanges. Quotations are labelled to show CVD risk calculator (QRISK2+ where Informatica was used), consultation identifier, patient sex and age. Where dialogue is reported, ‘I’ denotes the interviewer’s contribution and ‘P’ denotes the patient’s contribution.
Relieved about cardiovascular disease risk
In general, many patients felt relieved about their CVD risk, perceived their CVD risk to be low, and were unconcerned. For many patients, expectations of their CVD risk did not match up to the reality, especially for 10-year risk and heart age. It appeared that 10-year risk was often anticipated to be higher, and heart age anticipated to be lower. Yet there was also some consensus that, if CVD risk were higher, patients would be concerned and consider risk-reducing behaviour change.
Not concerned by cardiovascular disease risk
For most patients, perceptions were largely focused on a lack of concern, regardless of the way in which CVD risk information was delivered. One patient described how being told her 10-year risk ‘didn’t alarm me . . . I thought 6% wasn’t too bad at all really . . . I thought that was a pretty good, average’ (QRISK2+, 12_131, female, 57). Other patients described how they were ‘quite relaxed about that really’ (JBS3, 7_117, male, 49) after being told their heart age. A small number of patients spoke of their worries after finding out their CVD risk information. For example, on learning that his heart age was 6 years older than his chronological age, one patient explained: ‘that shocked me. No, it concerned me’ (JBS3, 7_105, male, 59).
Receiving CVD risk results also appeared to reassure patients, regardless of the way in which risk was presented. For example, one patient talked about the relief of being given a 10-year risk that she perceived to be low:
So saying to be 6.0 – well under 10, so yeah, yeah, yeah, it is reassuring. Which when she said it was under 10 that’s why I forgot the number, but I was just relieved.
QRISK2, 3_125, female, 56
This was also observed for heart age: ‘I was quite pleased because it came out with my heart age at being my age, so I thought phew [laughter]’ (JBS3, 4_263, female, 61).
It is possible that patients’ lack of concern about their level of CVD risk was related to a widespread perception in the sample of a low level of personal CVD risk (as 70% of the 128 were classified as low risk). However, this perception that personal CVD risk was ‘small’, ‘low’ or ‘quite low’ or ‘wasn’t that high’ was observed among patients with different levels of risk. For example, one patient whose 10-year risk was estimated at just 1% (which was heavily influenced by his relatively young age):
. . . so do you remember what you were told by the practitioner about your level of developing cardiovascular disease, or your risk?
I was very low 1% something like that.
QRISK2+, 12_064, male, 40
And another patient who had a 10-year risk just under the 10% threshold at which intervention might be recommended:
OK so she said that your risk of heart attack or stroke was 8.1%.
Yes so quite low.
JBS3, 8_162, female, 67
However, a patient considered at high risk (≥ 20%) described how they felt when informed of their 10-year risk score, indicating that even those with a high risk of developing CVD did not perceive or understand the severity of this information:
Err, well it didn’t really err, how can I put it, well err, err, well it . . . I thought about it but, 25% that’s yeah I thought well err most people walking round now are at, what is it 25%? . . . You know erm, I, I thought the odds were pretty good myself to be honest with you [laughter].
JBS3, 5_132, male, 74
Patients who were told that they had a low risk of CVD were understandably reassured (see Positive impact of Health Checks). However, there is evidence of false reassurance for those with a high risk of developing CVD who do not recognise the risk severity from the information provided or the related discussion. This can be linked to a lack of understanding (see Mixed levels of understanding), particularly surrounding the notion of percentage risk.
In addition, several patients commented on CVD risk being an estimate or a prediction, and this appeared to influence the perceived severity of threat to their health:
So getting your actual cholesterol result, so rather than having kind of your 10-year risk or your heart age, or your survival age, it would be your cholesterol . . . ?
Yeah very much so because that is the now, you know all those other things are projections.
OK, that’s interesting.
Like a forecast as such. This is the forecast, but that forecast is only determined by the here and now. If there is a lifestyle change tomorrow that information that was given yesterday is null and void to a degree.
JBS3, 4_080, male, 57
This appeared quite prominent in relation to event-free survival age, which this patient considered less credible than heart age:
Cause, yes that [lifetime risk] . . . I think I’d take that as a pinch of salt, to be honest . . . You can’t predict that . . . You know, that’s pretty ridiculous . . . I can listen to myself and think err . . . I’ve got a 51-year heart or you know . . . they’re gonna know that . . . But to predict how long I’m gonna, live really that’s errr . . . science fiction ain’t it really?
QRISK2, 9_087, male, 48
Patients viewing their CVD risk results as a prediction or estimate might facilitate beliefs that CVD risk can be reduced, in turn, enhancing self-efficacy towards positive behaviour change (see Facilitating change). However, for other patients this could be detrimental to the appraisal of their risk and lead to a fatalistic view, rather than considering their CVD risk as being in their control.
I would be more worried if cardiovascular disease risk was higher
Patients dismissed their CVD risk if they perceived it to be low (regardless of risk level). For example, one woman, whose heart age was 5 years older than her chronological age, said:
No I just thinking well it doesn’t bother me ’cos, 5 years OK 5 years, 5 years, but it’s not you know about 20 years, 20 years be thinking ‘Oh my God’, you know . . . horrified, but I think 5 years is not too bad and there’s things that I can work on to try and reduce that really so I wasn’t horrified by it, no.
QRISK2+, 12_131, female, 57
This suggests that this patient, because her heart age was similar to their actual age, regarded the threat as not severe, and perceived that she had self-efficacy over the changes needed to reduce it. Similar thinking was observed in relation to 10-year risk. In the example below, the practitioner had suggested that a 10-year risk of 1.6% was slightly raised:
You tend to look at it and then tend to be kind of, I don’t know, kind of brush it away . . . although she said it was quite high, I think because I think it is such a low percent, it’s kind of not at the front of my mind and I am not concentrating on it.
QRISK2, 9_083, female, 39
Therefore, it appeared that patients’ perceptions of the severity of their CVD risk and vulnerability to it are important in fostering intentions towards risk-reducing behaviour (in line with PMT).
It was common for patients to explain that, if their CVD risk had been higher (whether this was higher 10-year risk, older heart age, or older event-free survival age), they would have been more concerned, and this would have been more likely to prompt change. For example, one patient believed that if he had been given a 10-year risk that was double his current risk (15%), it would have prompted more concern and increased steps to lower it:
You know, I mean if you’d said to me it was 30% . . .
Hm.
. . . a risk . . .
Yeah.
. . . obviously I’d be concerned about it.
Yeah, cos it would have been high . . .
High, it’d be double really, and higher, and obviously I’d have to take erm . . . or listened more, or look at taking steps, to . . .
Hm.
. . . to rectify it or do something about it.
JBS3, 11_028, male, 58
Similarly, patients frequently noted, that if their heart age had been a lot higher than their actual age, it would have been perceived as a more severe threat, prompting behavioural action (in this example, heart age was 51 years vs. chronological age of 55 years):
If it [heart age] had of been a lot higher then I would have thought ‘oh I will definitely go and get a bike and I will go swimming as well’ [laughs].
QRISK2+, 12_083, female, 55
This suggests that an increased understanding surrounding CVD risk level is required for patients to appraise how their individual risk may affect them. If patients do not perceive their CVD risk as a threat, then they are perhaps less likely to make positive behaviour changes and follow practitioner recommendations.
Feedback on cardiovascular disease risk was unexpected
Throughout patient accounts, it became apparent that there were mismatches between expectation and reality of CVD risk. Some patients expected to be told that their overall CVD risk was higher than it was based on known risk factors:
I thought they [10-year risk] were going to be higher, because of saying with my blood pressure and the cholesterol, and so I thought ‘oh I am in trouble here’, yeah and I thought . . . I really did think it was going to be high.
QRISK2, 3_125, female, 56
This was particularly true for 10-year risk. One patient, for example, explains that he was expecting the score to be higher than it was, despite it placing him in a medium–high risk category: ‘I think it was a case of [name] understood that I understood the 17% . . . As I say, I expected it to be higher but thankfully it wasn’t’ (QRISK2 +, 2_084, male, 64).
Many patients had expectations of their heart age that did not match the estimates from the health check and expected a low heart age based on a perception of being in relatively good health:
That is a bit of a surprise really for that, because I don’t feel that you know, and I don’t know I still feel quite energetic and still play you know the sports I do, I am never tired, or feeling like I can’t go on any . . . you know, in fact I do the complete opposite. Yeah, if I feel oh right I am feeling a little bit – like if I am playing badminton for example, I can always push and push and push yeah, to you know go a little bit harder and that so you know I was a bit shocked at that to tell the truth. Not shocked, as in disappointed, but I thought you know . . .
You thought it would be lower rather than higher.
Lower than that yeah, because I don’t feel like I physically can’t do anything.
JBS3, 4_311, male, 57
This suggests that patient awareness or perceptions of their own health status are important. If a patient perceives themselves to be physically fit, they may underestimate their personal level of CVD risk, which might be elevated. This could stem from a lack of understanding of the CVD risk score itself and the information on which it is based, which is important if patients are to understand how lifestyle changes can be used to manage and reduce their risk.
Theme summary
It is likely to be insufficient to provide patients with their 10-year risk, or a heart age, in the absence of supporting information. Putting these results into context or presenting them in a different way to ensure that the severity of patient’s risk is understood is important to engage patients in discussion to address misunderstandings or misperceptions about what the score means, why it might be higher/lower than expected and the implications for their health.
Mixed levels of understanding
Perceived understanding of CVD risk varied. Some patients thought that they understood the information provided to them, but others felt confused, particularly in relation to percentage 10-year risk. In addition, there was confusion around the concept of event-free survival age. Providing context around CVD risk appeared important to facilitate understanding.
Understanding versus lack of understanding
Throughout patient accounts, there was a distinct division between patients who seemed to understand the CVD risk information provided and those who did not. This was particularly true for 10-year risk and event-free survival age and, to a lesser extent, heart age. Some patients demonstrated a level of understanding of percentage 10-year risk (albeit with some confusion):
Yeah, OK, and do you know erm . . . kind of do you understand what [practitioner] meant when she gave you that percentage score?
Yeah that you’ve got 6% risk of, of getting heart disease in life really yeah, out of 100 people you know 1 in 6.
QRISK2+, 12_131, female, 57
For other patients, gaps in knowledge and understanding of the score were observed. Some could not recall what their score meant. For example, one patient struggled to ‘remember what the significance of 9.5 was’ (JBS3, 4_233, female, 69), when talking about her 10-year risk. Other patients found it difficult to put the percentage score into context in terms of a ‘good’ and ‘bad’ outcome. This was evident across all risk categories (low, medium and high). For example, a patient with a relatively low percentage demonstrated confusion about her 3% 10-year risk:
It depends, like I said, what it actually means. If 3% is not good, then obviously that information wasn’t useful to me, because I have gone away thinking that’s fantastic. Even though I am a bit sceptical, erm but if you are saying 3% actually is good, then yeah it was accurate what she was saying to me. But it almost seems as if, because she did say like slightly higher, I think if 3% is a high risk of you know heart disease, then 3% is not good, because 3% makes you think it’s good, because 3 out of 100 is good.
QRISK2, 9_295, female, 51
This lack of clarity was also observed where risk was higher:
I can’t quite understand what like 25% is, what’s, what’s good and what’s bad with 25%?
JBS3, 5_132, male, 74
This suggests that, regardless of the actual score, patients may find it difficult to understand the implications and severity of a 10-year risk. Despite misunderstanding, some described their experience of being told 10-year risk positively: ‘I thought that bit of it was very good indeed, obviously I didn’t recall it, but I did think that was good how that was explained and showed’ (JBS3, 4_080, male, 57). Yet the potential benefit of such positive perceptions is likely to be undermined by the lack of recall or understanding of CVD risk information.
Lack of understanding was also common for JBS3 event-free survival age. Instead of viewing lifetime risk as the expected age of survival free from CVD events, some patients interpreted this as predicted age of survival. This appeared to be the case not only for patients who were given this lifetime risk estimate during the health check, but also for QRISK2 patients when asked their opinion on this alternative way of presenting CVD risk:
So this would be your age to expect to live to without a heart attack, or a stroke . . .
Hm.
. . . and then after that age, your risk would increase significantly.
Hm hm.
So it is not necessarily kind of when you are dying.
When you are expected to live to? Hm. Hm. Well you see now, what’s interesting about that, because now that I have read that, I have realised what it says . . .
Hm.
. . . but initially, what I thought, and I think that’s probably what a lot of people would think. Initially you read it quickly and it looks like it is saying that we expect you to live until this age.
OK, so life expectancy.
And when you see that, then you cut off from what that’s saying . . .
Right OK.
. . . so I think that’s . . . because that is exactly what I have just done.
Yeah
I have just dismissed that bit there, and only read to there, on average expect to survive to 73.
QRISK2, 9_295, female, 51
This was also the case for one patient on being informed of his event-free survival age in the health check, which was relatively close to his actual age. The confusion understandably caused a great deal of concern (until this was identified and resolved):
So did you, did it make you feel sort of what emotions was it sparking was it . . . ?
Erm deflated me a little bit.
Yeah.
Erm, because I’ve never, ever thought about it and err it was my fault, that, that was the bit I felt where it let itself down a little bit.
Yeah.
Erm, if she’d have said yeah, yeah we can guarantee, well not guarantee, but we can see you’ve got reasonable amount of having good health until you’re 80 you know 82.
Yeah.
And then things might deteriorate a little bit.
Yeah.
That would have been perfect I’d have . . .
Yeah.
But then as I say 82.7 mentioned and I thought to myself and I never, that was it, the end of the interview really, I think.
Yeah.
As I thought, then, then it gets in your, gets in your head then.
JBS3, 5_132, male, 74
Understanding of heart age was also mixed, but patients seemed to have a better understanding of this than on other risk scores, and the comparison with chronological age allowed patients to quickly appraise their individual risk as ‘good’ or ‘bad’:
Where it says ‘your heart age is’ and gives you a heart age, straight away you know whether that is good, or bad, because if your [chronological] heart age is lower than the reading [heart age estimate], then you know straight away that is not so good. Whereas if it is higher you know. So I think that one is a bit more clearer.
QRISK2, 9_295, female, 51
However, some patients found the concept of heart age challenging, and failed to understand the context or implications of a heart age different to their actual age:
. . . again it, it’s there was this lack of information you know, what do these numbers mean? . . . I can’t remember ever being told what the numbers actually mean . . . You know what is the, you’ve got a heart of a 72-year-old, or 73-year-old and you’re, you’re 62. What does that actually mean?
JBS3, 4_143, male, 62
Overall, lack of understanding was evident across all methods, especially QRISK2 and event-free survival age. This highlights the need for practitioners to check patient understanding during the consultation and, where necessary, tailor the information to the patient.
Importance of context
One way to improve understanding of CVD risk relates to the context in which the different risks are presented [i.e. the extent to which practitioners demonstrate the relevance to patients (its severity or their vulnerability to it)]. This was highlighted by some patients, who believed that the CVD risk information lacked context, making it difficult to understand or appreciate the severity:
. . . walked off and probably thought afterwards, I could have done with actually understanding is the heart age kind of thing, normal . . .
Hm.
. . . I was kind of thinking come out probably late 30s mid to late 30s something like that . . .
Yeah.
. . . but that’s without knowing anything about it . . .
Hm and was it useful to be told a heart age?
It’ it needs more context think . . .
Hm.
. . . on reflection as I walked away I don’t, didn’t really ask what that meant, it’s just stuck in me that it’s like hm . . . it’s not younger than me which, I imagined it should be.
QRISK2+, 12_064, male, 40
This idea was also discussed in relation to 10-year risk, in which additional context helped the patient to understand (in this example, as noted in Chapter 7, this quotation also reflected understanding conferred through a follow-up telephone call in which a specialised nurse practitioner provided further explanation):
Erm, and did you understand what she meant when she said a risk of 17%?
Erm, yes, I think . . . We did do kind of an analogy of you know like 100 people in a room – 17 can be expected . . . but you don’t know which of the 17 . . . which I thought was quite a nice graphic analogy to give you a visual picture.
Yes. Was that something that she showed you on a screen or was it . . . ?
No we just discussed it.
It was conversation?
Conversation, yes.
Brilliant. So that kind of helped you to put it into context a little bit about sort of the 17%?
Yes.
QRISK2+, 2_084, male, 64
Patients who were not given as much detail on the 10-year risk to put it into context appeared to have less understanding of the implications:
I think with the percentage unless you have been given the range it should be in for your age and for your, you know, capabilities, then it’s kind of a mismatch of information. I don’t know which to kind of . . . they are saying it’s high, but I think it’s quite low, but I don’t know what high is because I haven’t been given anything to compare it against.
QRISK2, 9_083, female, 39
Therefore, the context in which CVD risk information is communicated is important to aid understanding. Providing patients with more explanation on how to position their score relative to the population might facilitate understanding of the severity of their personal risk. One method of doing this is to provide some more information (e.g. use of analogies, relative risk) during the CVD risk discussion. Another method relates to the presentation of information, particularly given the positive perceptions of the ability to manipulate a patient’s CVD risk using JBS3 (see Importance of presentation).
Perceived changeability of cardiovascular disease risk
In addition to varied understanding of CVD risk in general, there were apparent differences in understanding of whether or not it could be changed by lifestyle factors. A small number of patients thought that it was fixed:
Yeah, you know, so err and having known the fact that my dad had a heart attack has increased my score . . . and she said herself on the video you can’t do anything about that. That’s just there you are there’s 10 points on the score.
QRISK2, 6_044, male, 61
In contrast, other patients talked about CVD risk as changeable: ‘Yeah, yeah, I remember thinking so I could do something about it’ (JBS3, 4_233, female, 69), or even acknowledged their own role in lowering the score: ‘But obviously it could come down, it could be better I guess if I change . . .’ (QRISK2 +, 2_001, female, 66). There was also an awareness that CVD risk could also increase over time, an important point for patients to understand from a prevention perspective:
. . . so, but again she did say that it wouldn’t stay the same it would change, so I do know that I, I do need to start looking after me self . . . a bit better.
QRISK2, 10_539, male, 51
The idea of CVD risk being a prediction or a ‘lottery’ was also evident in relation to discussion about the patient’s ability to make changes. This highlights an important separation between patient’s lifestyle or risk-reducing behaviours and what they see as a prediction of future disease risk, which might lack credibility:
Yeah, so was that information in particular helpful, or unhelpful, the 9%?
Oh!
To you?
To me it didn’t mean anything, because to me you know I can change my lifestyle and all that sort of thing, but at the end of the day it is a bit of a sort of like lottery really isn’t it? [Laughs].
Yeah, yeah, I think it is isn’t it really?
I would be quite happy if I had 9% chance of winning the lottery! [Laughing].
QRISK2+, 2_001, female, 66
This could be positive because of associations with change and adaptability, but negative in terms of fatalistic attitudes and not recognising CVD risk as the context or reason for making health-promoting changes.
Finally, despite the predominant belief that CVD risk (or risk factors) was modifiable, some patients lacked understanding about how to implement positive changes, for example to reduce cholesterol:
So it then led me to think ‘Well, where am I with it, can I do something about it?’. I don’t think I can do much more with my standard of living and exercise to be honest. So I think ‘well if there is an issue it might be genetic’, but I am now in the process of thinking ‘well you know what let’s get this tested again and see where we are’.
JBS3, 4_080, male, 57
Or in terms of lowering CVD risk itself:
But that part wasn’t . . . I am not clear about, erm I think at that point you are just . . . I am not sure actually, I am not sure how . . . right now so it’s 4.8% over the next 10 years, but I don’t know how you would lessen that.
JBS3, 4_263, female, 61
This makes clear the important link between clarity and understanding of CVD risk information, and patients’ perceptions (and subsequent intentions) regarding their ability to reduce risk through lifestyle changes.
Theme summary
Patients often do not understand CVD risk information (particularly 10-year risk and event-free survival age) and the implications of the scores. They are often unable to determine if their CVD risk is higher than that of others of the same age and, therefore, they may not be sufficiently motivated to change their behaviour. Patients would benefit from practitioners providing further information to make clear the relevance of their CVD risk. Visual presentation and risk score manipulation offer tools that can accommodate the range of patients, and also to make the important link between lifestyle change and overall CVD risk.
Positive impact of health checks
Despite some of the more problematic parts of the health check, there was evidence that attending had a positive impact on the majority of patients including increases in awareness, contemplation of behaviour change and positive intentions, as well as implementation of recommendations made by the practitioner (albeit with small changes). One aspect of the health check that seemed particularly positive was providing a heart age to patients.
Facilitating change (risk management)
The extent to which patients reported to have altered their intentions or behaviours as result of the health check varied. For some, the health check prompted them to contemplate behaviour change: ‘did make me think a bit more . . .’ (JBS3, 7_136, female, 53); ‘put it [CVD risk] on my mind’ (QRISK2 +, 12_083, female, 55). For some, it resulted in a positive change in attitude towards health: ‘Overall . . . I came out with the attitude I’ve got to be more health focused’ (JBS3, 7_105, male, 59). For others, it appeared to increase their awareness of lifestyle aspects that might need to be changed, and promoted contemplation to engage with this:
Erm . . . no, the good thing was like you know get your cholesterol checked I had that, had previously checked it was still little bit high, but I’d gone up again erm . . . so it’s made me think about changing my diet and . . . and erm . . . tweaking it a little bit here and there . . .
QRISK2+, 12_131, female, 57
Consequently, a number of patients had not made any changes based on the recommendations provided, but were considering change. Others had made positive changes to lifestyle and behaviour. Overall, the health check seemed to facilitate patients to ‘work on that [behaviour] a bit harder’ (JBS3, 4_311, male, 57). Positive changes in several health behaviours were seen, mostly those most discussed by practitioners (see Chapter 4), such as physical activity, healthy eating and blood pressure monitoring.
Many patients talked about increasing their levels of physical activity following the health check. Typical examples involved increasing walking ‘I’ve started to go out a few minutes earlier and walking up the hill [laughs] . . . it’s just a few minutes a day . . . might make a difference’ (QRISK2 +, 12_055, female, 65), or other home-based exercise:
I have, I mean like I have got my step machine . . . I have got a step machine that was in the garage, I have brought that inside, so I can do that while I am watching television.
How brilliant!
So like it does get me out of breath.
QRISK2, 9_202, female, 46
There were also several instances of dietary change. This could involve reducing intake of certain foods:
I’ve cut sugar down no end.
JBS3, 5_132, Male, 74
Brilliant. So has being told your level of cardiovascular risk, so either the percentage, the heart age, the survival age, has that affected you in any way at all, sort of you know how you are approaching kind of lifestyle and things like that?
Well, certainly, over diet really, over the cheese, because I was . . . she actually suggested cutting it down to a couple of times a week, which I have done already, so that definitely has had an impact.
JBS3, 4_263, female, 61
Others had substituted foods:
Do you mind me asking what change you made?
. . . erm . . . cut out some dairy . . . so I stopped using milk in porridge, and things like that and using water . . . got coconut milk as well, erm . . . and cut out bread . . . and erm . . . I’ve actually got a bit more, I’m not gonna go vegetarian, but I’ve gone a bit more vegetarian . . . I’m eating probably slightly less, but I’ve cut the crap out . . .
QRISK2+, 12_064, male, 40
When blood pressure was highlighted as a particular issue during the health check, some participants engaged in positive behaviour change related to further monitoring, either at the general practice or at home:
But the fact that I went out and ordered a small blood pressure monitor and one thing and another erm and presented my wife with those sheets and whatever. I’ve never done anything like that before.
JBS3, 7_105, male, 59
Despite the positive contemplation and actual behaviour change taking place, the changes made by patients were small: ‘I have not made any massive changes’ (JBS3, 7_105, male, 59). This could be explained by a number of the preceding themes, such as feeling reassured by their CVD risk, thinking CVD risk was low, considering behaviour change only if CVD risk is perceived to be high, believing that they were already doing the right thing, and perceived ability to change. For example, one patient talked about taking a ‘small step’ as a result of attending the health check:
And then erm, I forgot about the heart age, when she said about the heart age yeah. I just went back with the erm the life expectancy age. Erm, yeah so it has it, it gave me the momentum to do something, I know it’s only a small step but it’s a step.
JBS3, 5_185, male, 47
Overall, evidence related to contemplation of change and also the relatively modest changes made by many patients suggests that something else, in addition to what was included in the health check, may be needed to facilitate intentions for, and implementation of, more consistent and substantive behaviour change.
Impact of heart age
When asked about the CVD risk information they could remember, numerous patients could recall their heart age, more so than 10-year or event-free survival age. As a result, heart age seemed to stand out to patients as being more impactful:
I think, I think the thing that registered with me and that sort of really grabbed my attention, and I know I said this earlier, all I could see was that 65 on that screen.
Yeah.
And I couldn’t . . .
Yeah so the heart age really kind of . . .
. . . that was wallop.
Yeah.
Yeah. That heart age and I think perhaps I missed some of the, shall we say, the finer detail because I was focused on that.
Yeah.
I could see that 65 and I was thinking, bloody hell, I ain’t 65!
JBS3, 7_105, male, 59
Clearly, it would be problematic if patients, in trying to process heart age information, ‘switch off’ and are unable to engage with subsequent recommendations from the practitioner. However, given the lack of retention of 10-year risk (and confusion over event-free survival age), understanding the implications and retaining one of the metrics can be interpreted as a positive, as it could provide the context for a meaningful discussion of risk management.
The concept of heart age was also well received by patients in the QRISK2 group who were interviewed, who were shown alternative ways of presenting CVD risk information during their VSR interview:
Err I think that one has got the most positive impact really. Even if it wasn’t positive from point of view of your heart age, if it was higher than what your [chronological] heart age is. I think you would still straight away understand that more and know what you have got to do.
QRISK2, 9_295, female, 51
Heart age was perceived to increase understanding of CVD risk among patients in both the JBS3 group and the QRISK2 group:
But when it was very clearly written, you know so the model brings it up as your heart age, given the information that it has got, is 61 years and I thought ‘well that is so clear and understandable’, so I found that very helpful, because if it had been much higher, then that would have also been very understandable.
JBS3, 4_263, female, 61
In addition, heart age appeared more relatable and, perhaps, more credible. As reported earlier, one patient described event-free survival age as ‘science fiction’, but could believe the idea of heart age:
I can, I can listen to myself and think err . . . I’ve got a 51 year heart, or you know . . . they’re gonna know that . . .
QRISK2, 9_087, male, 48
This links in with the earlier idea that CVD risk is only a prediction. If heart age is perceived as more relatable and credible, patients may have an increased understanding of how their risk of developing CVD, be able to appraise its severity and their vulnerability to it and, therefore, be more likely to make behaviour changes to mitigate the risk. This was illustrated in the patients accounts around heart age prompting change as ‘it is that swift kick to say: “get out there and do something” ’ (QRISK2 +, 2_084, male, 64):
Don’t get me wrong, it was enough to make me say to my wife ‘I’ve got to do something about what I eat, and I’ve got to get more exercise and I’ve got to do this, and I’ve got to get that’, and I ordered a blood pressure monitor and all the other things. I even checked that the bathroom scales worked properly.
JBS3, 7_105, male, 59
The other methods of presenting CVD risk information (10-year risk, event-free survival age) were also commented on by patients in terms of their strengths, limitations, ability to increase understanding and also impact on behaviour change. However, conversations around heart age were much more common, and rarely in a negative context. Some patients were alarmed or even shocked to learn that their heart age was higher than their actual age and clearly did not expect to receive such information:
Well it made me, what she said is that this is the age group I would be . . . so obviously that’s alarming, because . . . it’s like adding another 10 years to your life. You know which you don’t want . . . you know you don’t mind erm . . . being at the level where you are at your age . . .
JBS3, 11_028, male, 58
Clearly, a CVD risk metric, such as heart age, that is understandable and impactful has the benefit of giving patients a better appreciation of their risk than does 10-year or event-free survival age.
Theme summary
There was evidence that attending a health check had a positive impact on many patients, but these often related to contemplating change or making relatively small changes to lifestyle. Heart age appeared to be preferred by patients, and beneficial for facilitating patients’ understanding and appraisal of CVD risk (compared with 10-year or event-free survival age).
Importance of presentation style and content
Throughout patient accounts there was evidence that the way in which CVD risk is presented can affect recall, understanding and attempts at risk-reducing behaviour change. Patients commented that it can be difficult to take in all of the information provided during a health check, particularly if this is communicated predominantly verbally. Potential ways of enhancing delivery of CVD risk communication include presenting the information visually and with visual demonstration (or manipulation) of how making positive changes to lifestyle factors (i.e. ‘interventions’ in JBS3) can reduce CVD risk. These two factors were perceived positively by patients, and are both related to functionality within the JBS3 calculator.
Difficult to absorb information
Patients frequently highlighted the difficulties in absorbing information presented in the health check and commented that they ‘Didn’t really sort of take in you know what the numbers were’ (QRISK2, 3_125, female, 56). They felt that the volume of information provided to them in a short space of time limited their capacity to retain and accurately recall it:
As I say, when you are in somewhere like that you can’t take on too much either can you really? Because it all becomes a bit muddled together.
JBS3, 4_263, female, 61
This appeared particularly problematic when exclusively presenting information verbally, which is common practice during a health check:
You know what I mean, you, you could take the time to look at it whereas, when, when it’s when it’s spoken to yer, it’s spoken then it’s gone.
QRISK2, 10_539, male, 51
This supports evidence for the benefit of presenting risk information visually. 23,77 Patients who feel overloaded with information that they cannot effectively process will be limited in the extent to which they understand their own personal CVD risk and appraise the implications.
Positive impact of presenting cardiovascular disease risk visually
One key feature of the JBS3 risk calculator, aside from the various risk metrics (10-year risk, heart age, event-free survival age), is the visual presentation of risk information. The interactive nature of the tool facilitates a more collaborative consultation between patient and health-care practitioner. It was often observed in the video-recorded health checks that practitioners would share their computer screen with patients to communicate CVD risk information (see Chapter 4).
Patients in the JBS3 group typically commented on the visual presentation of information, which was perceived positively and overcame some of the barriers related to verbal communication of information:
It was good that you could see the screen and how she actually . . . how she worked it out as well rather than somebody just telling you . . . I thought it was a good to see . . .
JBS3, 7_044, female, 54
There was also a common feeling that seeing information written on the screen, and the accompanying visuals, strengthened the message and aided recall (more than simply hearing it from the practitioner):
. . . because it was on the screen, I think that is such an aid to memory . . . you know it’s just that sort of interactive ability really to be able to see something, rather than just being told information. Because in any situation that is new to you, if there’s a lot of things going on and you are not sure what’s going on, you don’t hear . . . But if you see it, it is actually much, much clearer to you.
JBS3, 4_263, female, 61
Patients also reported that they took more notice of the information when presented graphically, and that the presentation influenced intentions to engage in positive behaviour change:
I certainly got the gist of what [practitioner] was saying and it’s quite graphic seeing it there on screen erm, you know heart age 65 and I’m, I’m not quite 60 so you’re thinking yeah I ought to do something about that and yeah the intention is there.
JBS3, 7_105, male, 59
This did not appear limited to one type of CVD risk information provided. Rather, visual presentation appeared to increase understanding and impact of 10-year risk (‘Yeah she did give me a percentage score, she did something on the computer that showed you erm what it was and that was quite good actually’; JBS3, 7_044, female, 54) and heart age (‘But the 65 was a big 65 on the screen’; JBS3, 7_105, male, 59) although was not commented on in terms of event-free survival age.
Positive perception of risk manipulation
The JBS3 calculator function that allows the practitioner to manipulate a patient’s CVD risk by altering modifiable risk factors was perceived positively by patients, with one describing it as ‘quite impressive really’ (JBS3, 8_162, female, 67):
Yes I think it helps, rather than somebody talking to you and saying, ‘well it’s like this, it’s like that’, but actually when you can see it and then by altering it, you know and saying, ‘if we put this information in you can see how . . . so if you were much heavier say, for example, or if you smoke, or if you do these sorts of things’, so I found that really helpful. Really clear and understandable from my point of view anyway.
JBS3, 4_263, female, 61
This also appeared to have more of an impact on patients, potentially increasing motivation to engage in behaviour change:
You can see the differences . . . not just somebody saying or if you do this, you can, you’d be better . . . or better off . . . shall we say, not better, better off, you know but if you can, if you can read it and you can, you can compare the two at the same time . . . You can, you can it, it has better more, more of an impact.
QRISK2, 10_539, male, 51
It was also evident that some patients had made positive lifestyle changes and followed practitioner recommendations based on their risk manipulation in JBS3:
Erm do you remember being shown how your risk might change, you kind of mentioned it a little bit earlier how she said if you reduce your cholesterol erm it could have an effect on your risk.
Yes she did yeah bring the percentages down and all this, all the above which is as I say I took on board . . . Which err you come out, I came out thinking well yes my lifestyle needs to change . . . because it’s an easy thing to slip into . . . I have made the effort and through that, through this meeting you know so it . . . the benefits are there it’s definitely done something for me . . . In as much as made me decide well ‘come on enough pull your finger out get on with this’, you’ve been told, you know.
JBS3, 4_394, male, 65
Theme summary
Patients are given a lot of information in health checks, which they can struggle to absorb and retain. There appeared to be benefits of visual presentation of CVD risk information and risk score manipulation within JBS3 to foster patient understanding of CVD risk and motivation to follow recommendations for behaviour change.
Summary
Data from VSR interviews with 40 patients regarding their perceptions and experiences of CVD risk communication as part of a health check (delivered using QRISK2 or JBS3), and their subsequent intentions or actions, highlighted six key findings:
-
Most patients reported that attending a health check had some impact, in terms of contemplating change or making small changes to lifestyle.
-
Patients often did not understand CVD risk information. This was true for all metrics, but particularly for 10-year risk. Event-free survival age was misinterpreted by some as estimated age of survival. Heart age and risk score manipulation were perceived positively by patients and can be used to confer patient understanding of the risk and allow appraisal of its severity and vulnerability (and, therefore, its personal relevance).
-
Providing patients with a CVD risk score alone is insufficient. Further information is needed to put the results into context, or the results should be presented in a different way, with further discussion to ensure that the severity of the risk is understood.
-
Visual presentation and risk score manipulation appealed to most patients, and also helped them to make the important link between lifestyle change and overall CVD risk.
-
Patients are given a lot of information in health checks, which they can struggle to absorb and retain. The visual presentation of CVD risk information and risk score manipulation offered by JBS3 fosters patient understanding of CVD risk and motivates patients to follow recommendations for behaviour change.
-
Building on findings from Chapter 4, the range of issues identified highlights the need for practitioners to check patient understanding during the consultation and, where necessary, tailor the information and address misunderstandings or misperceptions about what these risk scores mean, why they might be higher/lower than expected and the implications for their health.
Chapter 6 Results 4: video-stimulated recall interviews – practitioners
Parts of this chapter have been reproduced with permission from Gidlow et al. 75 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Headline findings from inductive thematic analysis of video-stimulated call practitioner interviews
-
QRISK2:
-
The 10-year risk score was used as a tool to guide clinical decisions, rather than for CVD risk communication.
-
Practitioners expressed confidence in delivering 10-year risk.
-
Practitioner understanding of 10-year risk often did not extend beyond applying thresholds for low, medium and high risk.
-
-
JBS3:
-
Practitioners perceived that patients were more responsive to heart age and the risk score manipulation.
-
There was a perception that patients liked the visual displays in JBS3.
-
Event-free survival age was misinterpreted by some practitioners.
-
-
Practitioners relied on patient reactions to gauge understanding and intentions.
-
Practitioner roles appear to be providers of information, rather than facilitators of change.
-
Risk management strategies focused on lifestyle advice, with limited referrals to lifestyle support programmes (a lack of follow-up regarding attendance or effectiveness).
-
Practitioner training is required to increase confidence and understanding in CVD risk communication.
Participant characteristics
Practitioner characteristics were presented in Chapter 3 (see Table 5).
Thematic analysis of data from the 15 practitioner (9 HCAs, 6 PNs) produced three main themes: (1) communicating CVD risk, (2) understanding of CVD risk and (3) risk management. These are discussed in turn using illustrative quotations. Each quotation is labelled to show the practitioner identifier, risk calculator used (QRISK2+ where Informatica was used), and their role (HCA or PN). Where dialogue is reported, ‘I’ denotes the interviewer contribution and ‘HP’ denotes the health professional (i.e. practitioner) contribution.
Communicating cardiovascular disease risk
The first theme discusses practitioners’ perceptions and confidence regarding use of the CVD risk scores and the extent to which they enabled risk communication. Four subthemes were identified: 10-year risk (QRISK2), event-free survival age (JBS3), heart age (JBS3) and risk score manipulation and visual displays (JBS3). Overall, 10 (out of the 15) practitioners liked JBS3, of those, nine were in the JBS3 group and, therefore, had direct experience of using it. The five practitioners who spoke positively about QRISK2 were mostly from the QRISK2 group, so lacked experience of JBS3 for comparison. Mixed views of QRISK2 were expressed by practitioners from both groups.
Ten-year percentage risk (QRISK2)
QRISK2 is presented as percentage 10-year risk, and an equivalent score is also presented in JBS3. Practitioners generally reported feeling confident in communicating to patients their estimated 10-year risk (QRISK2): ‘I think I’m OK, I think I’m confident . . . I think I deliver it well . . .’ (9.1, QRISK2, HCA); ‘Quite confident’ (11.1, JBS3, HCA); and ‘I feel fairly confident’ (6.1, QRISK2, PN).
However, there was reported variation in its application. Some practitioners stated that they tend to deliver the CVD risk information to all patients in the same way: ‘I’m like a robot. I think I say the same thing to every patient . . .’ (6.1, QRISK2, PN). This is problematic given the evidence supporting tailored risk communication to accommodate varying patient needs and understanding. 24 Other practitioners said that they adapted their delivery of 10-year risk, recognising that ‘the way in which it’s delivered can sometimes [be] more than the actual QRISK . . .’ (10.1, QRISK2, PN):
I try and explain it for the level of the person that is sitting there and adapt it.
6.2, QRISK2, PN
Despite the communication of QRISK2 (or QRISK3) being mandated in NHSHC,17 there was variation in whether or not practitioners chose to communicate 10-year risk during the health check:
[If] you think the patient perhaps is not going to pay any attention to you, they are not going to take it in, then no.
6.2, QRISK2, PN
I personally always do it . . . because the whole point of the health check is that you reach that number . . . the QRISK is below the percentage that you want and that you know, and that is fine.
1.1, JBS3, PN
Some practitioners suggested that the decision of whether or not to tell patients their 10-year CVD risk ‘very much depends on the patient’ (6.1, QRISK2, PN) and can be informed by patients’ age, level of understanding and engagement.
Other factors that appeared to influence the extent to which practitioners used 10-year risk included, first, the perceived usefulness. Through identifying patients with elevated risk (i.e. ≥ 10%), 10-year risk was seen to have value in guiding recommendations and clinical decision-making: ‘QRISK is more the sort the diagnosis and the referrals and things’ (2.1, QRISK2+, HCA). But it was generally not considered beneficial for the patient:
. . . giving them a percentage, doesn’t inspire them, doesn’t motivate them really . . .
1.2, JBS3, HCA
I suppose when you look at it and you have got that 10%, it is quite clear isn’t it? . . . Because you see it and you think about it ‘well they are going to need a statin’ . . . So it is quite clear cut then. I don’t always know how helpful it is to patients.
6.2, QRISK2, PN
Practitioners descriptions of the QRISK2 suggested that it was not used to facilitate discussion of CVD risk with patients: ‘A quick go-to tool. . . it’s OK. It’s all that we have’ (10.1, QRISK2, PN). In addition, although practitioners expressed confidence in communicating 10-year risk, there was evidence that their understanding of and confidence in explaining the score was, in fact, limited and that this prevented them from engaging patients in a discussion of their risk:
Several things are taken into account, so age, sex, their BMI [body mass index] . . . which does make it, to me, very complicated. . . to try and explain it to [patients] is the hardest.
12.1, QRISK2+, HCA
There was also a perception among practitioners that patients’ ability to understand risk information is limited, and as a result it is challenging for practitioners to communicate information in a way that patients will understand:
What I find difficult is sort of putting it in a way that the patient will actually understand . . .
10.1, QRISK2, PN
This has implications for practitioner training. There is clearly a need to improve practitioner competency in communicating CVD risk communication in a way that enables a meaningful discussion around risk management, in accordance with the competency framework. 19
Event-free survival age (JBS3)
Practitioners who used JBS3 discussed issues with communicating lifetime risk to patients. For some, this was new, and it became easier with experience: ‘. . . it is new for me, it is new for the patients and yeah it just got easier every clinic that I did’ (11.1, JBS3, HCA). But event-free survival age appeared to be ‘. . . the hardest one to try and communicate . . .’ (7.1, JBS3, HCA). This difficulty was two-fold. First, unlike 10-year risk, there are no thresholds for event-free survival age to identify patients as low, medium or high risk, and, therefore, no prompts to initiate discussion or action (e.g. risk > 10% would be followed up with further tests and discussions around statins):
. . . That’s there’s no benchmark to give that comparison to be like ‘right you can live till 84 and so-and-so live till 82’, so that one was harder . . .
7.1, JBS3, HCA
Second, as the above example illustrates, there was some confusion around the meaning of event-free survival age. Despite providing brief introductory training and a training video in the use of JBS3 and its outputs (see Chapter 2), some practitioners described lifetime risk in terms of expected age of survival (rather than CVD event-free survival). This is clearly an issue, resulting in the communication of incorrect or misleading information.
One practitioner also questioned whether event-free survival age would motivate a patient to make a change if the predicted age the patient is expected to live without a CVD event was high:
Again, because you have told them that they are going [to] live until they’re 82 without any heart attacks or strokes . . . Is that motivating them, or not motivating them? I would say not really motivating them.
Why?
Because . . . they are going get to 82 without anything happening to them.
1.2, JBS3, HCA
Overall, event-free survival age appeared problematic in terms of practitioner understanding and application. There was a perception that this kind of information could shock patients into changing their lifestyle to reduce long-term risk: ‘. . . if that’s telling them younger, than they’d expect it to be then that’s quite a shock tactic isn’t it . . .’ (9.1, QRISK2, HCA). But this did not reflect the majority view or experience.
Heart age (JBS3)
The heart age output from JBS3 was perceived positively. Practitioners expressed confidence in communicating heart age, ‘ ’cos it’s just the easier one to . . . sort of explain’ (8.2, JBS3, PN). Heart age has inherent benchmarking through comparison with chronological age, which overcomes a perceived limitation of event-free survival age: ‘. . . they know how old they are and then they are exactly . . . “oh it’s the same age as me”, so I think they understood that more’ (11.1, JBS3, HCA). Practitioners also suggested that patients liked and responded strongly to the ‘visual of heart age’:
. . . because it is an actual [heart] when you go onto that screen of heart age. The heart is there, you can’t escape that and then you have got your age right by it.
8.1, JBS3, HCA
. . . they liked the heart age . . . I don’t know whether it was because there was a picture of the heart . . .
8.2, JBS3, PN
It appeared that practitioners were using heart age as a motivational tool to highlight to patients the need to make lifestyle changes rather than simply a risk score metric to be relayed to patients, as was the case for 10-year risk.
Risk score manipulation and visual displays (JBS3)
The risk factor manipulation function and visual displays in JBS3 were discussed positively. Those using JBS3 reported that visual features provided an alternative method to deliver key messages to patients: ‘. . . [patients] have said it is quite nice to see visually, [as] opposed to me talking’ (8.1, JBS3, PN). Some practitioners perceived that patients were more engaged when presented with visual information, based on non-verbal cues:
Because, like I said, it is visualised. They are seeing, they actually are interested. They have come closer to me, their body language was good, they were looking at that, they did ask questions and they were happy, because I think it was visualised.
11.1, JBS3, HCA
The visual stimuli in JBS3 were thought to ‘make a far better impact’ by being ‘able to show them visually, rather than just verbally tell them’ (5.1, JBS3, PN), promoting interaction and discussion with patients:
So, this is the point [going through JBS3 outputs] then they [are] starting to ask questions, or looking like they [are] actually wanting to be here . . .
8.2, JBS3, PN
There was some conflicting evidence from the video-recorded health checks that most patients give limited responses when presented with risk information, even when JBS3 was used; often single-word acknowledgements, infrequent questions and scant non-verbal cues (see Chapters 4 and 7).
Theme summary
Ten-year risk is viewed as a guide for clinical decision-making, not for facilitating discussion of CVD risk, and the evidence suggests that practitioners lack the understanding and confidence to explain the score. Event-free survival age appeared problematic in terms of practitioner understanding and application; training would be needed before this type of metric was recommended for use in practice (in addition to general training in discussion of risk with a preventative focus). Heart age was favoured for being easier to explain and well-received by patients, who were thought to appreciate the visual presentation. Practitioners thought that patients responded well to the risk manipulation and visual displays in JBS3.
Understanding of cardiovascular disease risk
The second theme discusses practitioner understanding of CVD risk and potential factors that could influence perceived patient understanding, and has three subthemes: practitioner understanding, perceived patient understanding, and barriers to and facilitators of understanding.
Practitioner understanding
There was a strong link between practitioners’ understanding and communication of CVD risk. The majority described 10-year risk in a similar way, with reference to current lifestyle and risk factors:
. . . so the score that we are giving them is their risk of heart attack or stroke in the next 10 years, based on their . . . current lifestyle as it is as the moment, so it’s not sort of you know if their lifestyle changes or any risk . . .
7.1. JBS3, HCA
They also referred to the thresholds used to identify those with elevated risk: ‘So, we are looking at patients over the 10% mark, so their risk factors of developing strokes and heart disease is increased’ (6.2, QRISK2, HCA). Despite apparent confidence in communicating 10-year risk expressed by most, one practitioner doubted their understanding of what the score meant (and cited a preference for heart age):
I feel confident in the way that I give it . . . but then you are only reading off a piece of paper . . . I don’t feel that I understand . . . what the percentage is really . . . I prefer the heart age.
1.2, JBS3, HCA
Conversely, some felt that they understood the risk score, but questioned their ability to communicate it effectively:
Putting it into sentences which they can think well OK, or they might say, ‘well it just doesn’t make sense’ . . . I can probably babble sometimes and think, even I didn’t understand that.
12.1, QRISK2+, HCA
In some cases, watching the video-recordings of themselves delivering health checks (during the VSR interview) prompted practitioners to appraise their risk communication, with comments such as ‘It was just sort of abrupt wasn’t it? . . . There didn’t seem to be much of a consultation around it’ (1.2, JBS3, HCA) and ‘There is definitely room for improvement I can see myself there’ (6.1, QRISK2, PN).
Several practitioners acknowledged a need for additional training to improve risk communication with health check patients:
No, I think we do need more training in that.
1.1, JBS3, PN
We need more training to understand the risks better to deliver it to the patients.
1.2, JBS3, HCA
When asked about any training they had received, practitioners discussed this in terms of ‘can’t even really call it on-the-job training, can you, really?’ (1.1, JBS3, PN) and ‘. . . it’s been on how to use the [PoC testing] machine . . . rather than how to talk . . . and understand the risks’ (6.2, QRISK2, PN). The latter point offers support to findings from the video-recorded consultations (see Chapter 4), which suggested that the process often takes precedence over quality; the need to populate all parts of the NHSHC template might be at the expense of the quality of interaction.
Perceived patient understanding
It was suggested that patients who understand risk information are more likely to acknowledge their personal CVD risk and understand the options that could help them modify their risk factors: ‘Because if they understand that, they make changes to their lifestyle’ (4.1, JBS3, HCA). Perceived barriers to understanding the risk information conveyed within the health check, included patients’ level of education and possible ‘language barrier[s]’ (11.1, JBS3, HCA), but also a willingness to engage:
Why do you think some don’t understand [% risk score]?
Maybe poor education . . . maybe they do understand, but they don’t care . . . so they don’t want to know, they don’t want to discuss it . . .
3.1, QRISK2, HCA
Similar to findings from patient VSR interviews (see Chapter 5), there was also the suggestion that the consultation involved a lot of information for patients to process, which could contribute to lack of understanding and engagement:
. . . So, it’s alright giving them all the information [10-year risk], but whether they’ve taken any of it in . . .
8.2, JBS3, PN
Practitioners reported using patients’ verbal and non-verbal reaction to risk information to gauge understanding: ‘Nodding their head, so I think they all understood what I was trying to say’ (11.1, JBS3, HCA). They also appeared to recognise that this was limited: ‘It was based on their reactions, but you did wonder sometimes whether they actually fully understood’ (5.1, JBS3, PN). The challenge of using patient response to judge understanding was evident from analysis of video-recordings of their health check consultations, which rarely demonstrated clear patient responses, positive or negative (see Chapter 4). Here, there was a common feeling that even if patients ‘say they understand the percentage, some will, and some won’t’ (12.1, QRISK2 +, HCA) (i.e. that patients might not tell practitioners when they do not understand the CVD risk information presented):
Yes, they seemed to be [understanding % risk score], that’s the impression that I had got, and they didn’t say otherwise, but maybe they wouldn’t, I don’t know.
6.2, QRISK2, PN
Moreover, there was little evidence that practitioners routinely explored patient understanding through asking them, which again confirms findings from video-recorded consultations that health checks tend to be practitioner dominated (see Chapter 4).
Heart age and risk manipulation functions of JBS3 were again discussed favourably. Heart age was considered easier for patients to understand (than 10-year percentage risk): ‘. . . they can get their head around that concept of their [heart] age a lot better than risk score . . .’ (7.1, JBS3, HCA). This could be due to the inherent comparison/benchmark for heart age. The visual demonstration of manipulating risk was thought to promote patient understanding; it provided a tool to help facilitate discussion of risk-reducing behaviours, not just a risk score. This was discussed in terms of showing patients the positive effects of their risk-reducing lifestyle choices; this is an example of gain framing (i.e. benefits of reducing risk), which has been linked with increased self-efficacy to prevent heart disease:78
No, I think they understand more, because then they have an idea how . . . what they need to do to change to find the results so . . . When you show them that if you bring your blood pressure down, your cholesterol down, your weight down . . . how that can affect the results . . . And they start to think about exercise and lifestyle . . . it’s like an eye opener to them . . .
4.1, JBS3, HCA
There was also a suggestion that this was used to present risk with a loss frame (i.e. consequences of high CVD risk), which might be more appropriate for those with a family history of CVD:78
So when I was increasing the blood pressure, or the cholesterol, or if they were a smoker, they actually saw the difference and then they were like, ‘no I won’t, and thank God I am not [a smoker]’, you know so it was a difference on them as well.
11.1, JBS3, HCA
Theme summary
Practitioners acknowledged gaps in their understanding or communication of 10-year risk, often relying on the thresholds (low, medium or high risk). There was recognition that understanding of CVD risk varied between patients, and a perception that heart age was understood more easily. Practitioners associated patient understanding with lifestyle changes. They relied on patient reactions to information to gauge understanding, rather than asking patients, although the VSR interviews did prompt a reflection that they should involve patients more.
Risk-management
The third theme discusses how practitioners reported encouraging patients to reduce their CVD risk and the associated barriers. This theme has two subthemes: promoting risk management and barriers to risk reduction.
Promoting risk management
Practitioners described some routine medical follow-up for patients with elevated CVD risk: ‘raised risk score over 10%, we’d always get them to come back have a complete workup of blood test done and book in to see a doctor’ (7.1, JBS3, HCA). Practitioners reported that, during the consultation, they try to promote risk management, primarily through educating and advising patients on how to modify lifestyle (i.e. improving diet, increasing exercise, reducing alcohol consumption) to lower cholesterol, blood pressure and body mass index:
I sometimes go into portion sizes and carbohydrates and things like that.
2.1, QRISK2+, HCA
Get a little bit more movement back and to get their heart pumping and use up some of the fats and calories that they are eating and storing.
12.1, QRISK2+, HCA
Alongside this, some practitioners said that they use written materials, which they felt helped patients to understand lifestyle and recommended changes: ‘. . . and then when we give that diet sheet, then they look at it and they read and they go “oh, yeah, this is where I am going wrong” ’ (11.1, JBS3, HCA).
Referral to services to support risk reduction, such as exercise referral, smoking cessation and weight management, were discussed. Some practitioners suggested that not all those referred to such services will attend, ‘they don’t very often like to take you up on them’ (12.1, QRISK2+, HCA), and, for those who do, attendance might not be sustained: ‘we have a big drop-out . . .’ (10.1, QRISK2, PN). Practitioners suggested that a variety of contributing factors could explain uptake and retention of intervention services, such as the cost of continued attendance (e.g. gym membership after period of subsidised exercise referral); the absence of local services; lack of time to attend (working or lack of childcare); or preferring to make lifestyle changes unaided: ‘Oh well I know what changes I need to make, I’ll go away and make them’ (7.1, JBS3, HCS).
There were a small number of reports by practitioners about patients making lifestyle adjustments following a health check:
I see patients in general around the practice . . . say 6 weeks later and somebody will catch me and say, ‘oh, I really took in what you said, I’ve made some changes and my diet’s changed and this that and the other’.
9.1, QRISK2, HCA
A lack of communication between the general practice and external services to which patients could be referred meant that practitioners were uncertain if patients attended such programmes and, therefore, how effective programmes were. Even when patients are referred to the GP following the health check, practitioners were sometimes unsure about subsequent actions and outcomes.
Barriers to risk reduction
Practitioners identified several patient factors related to environment and intrapersonal factors in the PMT (see Figure 2) that could be barriers to patients forming risk-reducing intentions or behaviours. Some practitioners inferred that patients’ culture and personal beliefs could be barriers to risk reduction. It was suggested that cultural beliefs may affect current lifestyle choices and patients may not recognise that current lifestyle choices pose a health risk: ‘Yeah, because if you do say to them, they just say, “oh, but we have parties, we have this that, and we have a lot of sweet food” ’ (4.1, JBS3, HCA). Further, personal health beliefs may affect intentions towards behaviour change. Practitioners suggested that patients who do not feel unwell may have less incentive to make a change: ‘You know think they’re fine they think they’re invincible and you know nothing wrong, ’cos they don’t feel poorly’ (9.1, QRISK2, HCA). Practitioners also indicated that some patients believe that their risk of ill health is related to family history, rather than their lifestyle:
Sometimes, no matter how much you say to patients ‘I think it’s your diet and lifestyle’, they are still adamant that, because their mum and dad have got it, that that’s why they have got it.
6.2, QRISK2, HCA
Moreover, some practitioners reported finding it difficult to refer patients to an intervention service because local lifestyle support services were no longer operating or were not considered to be effective:
So, they have taken the lifestyle programme off us haven’t they, so we can’t offer that any more.
6.1, QRISK2, HCA
In addition, some practitioners expressed a lack of confidence in intervention services’ ability to support patients to change, despite referring patients to such services: ‘I don’t think the Help to Quit is very useful’ (2.1, QRISK2+, HCA). This experience and perception could explain the relatively low number of referrals observed in patient medical records following health checks (see Chapter 3).
There was a common inference that patients’ willingness or apparent intentions to make risk-reducing changes was largely determined by their intrinsic motivation, that although practitioners could provide information, the impact that it had depended on patient motivation:
You can give them all the options in the world and then I think a lot of it is down to the patient and their motivation to change.
6.2, QRISK2 HCA
It just depends how important they think it is for themselves, erm we can only do what we can do here. Once they are out that door we don’t know, yeah, so hopefully some people do take the recommendations and do what they can do.
11.1, JBS3, HCA
In support of this idea that patients are recipients of information and advice, rather than active participants in a discussion of their risk and its management, one practitioner described how they might respond to a patient who does not understand CVD risk by moving on to risk factors and modification:
That they just might not have understood, like the complexity of how you explain the QRISK and that maybe where I would then adapt it, and maybe there are times when I might explain it, but not explain the QRISK and the percentage as much, like I did with those patients you know?
So how would you explain it with those types of patients then?
Just basically saying your risks of strokes and heart disease have increased . . . You have got a lot of risk factors, you know, we need to give you a statin to bring you down. I need you to stop smoking, I need you to eat better. You know and keep it a bit more basic.
6.2, QRISK2, PN
With this approach, the practitioner would be telling patients what to do, rather than engaging in patient-centred dialogue. This confirms the indications that many health check consultations are practitioner dominated (see Chapters 3 and 4) and do not include elements of motivational interviewing, as recommended in the best practice guidance. 17
Finally, even if patients appear to understand and respond positively to the risk information and advice in the consultation, there can be uncertainty about the sustainability of the changes implemented:
Well I think it will have quite a good impact. Whether it would be sustained is another thing, but initially it did seem as though ‘oh yeah I will do something about that’, but it is like human nature isn’t it with things . . .
5.1, JBS3, PN
Theme summary
Most practitioners described risk management as lifestyle advice, routine medical follow-up triggered by raised 10-year CVD risk (≥ 10%) or risk factors, and referral to support services (e.g. exercise referral). Lifestyle advice was the most common intervention, sometimes supplemented by written information. Perceived barriers to risk management included patients feeling healthy and, therefore, not recognising the need for risk management (risk severity or vulnerability), lack of patient motivation, and limitations of the services to which patients could be referred.
Summary
Analysis of data from VSR interviews with 15 health check practitioners regarding the perceptions and experiences of undertaking health checks using QRISK2 or JBS3 highlighted a number of findings.
-
Practitioners were relatively confident about their ability to deliver 10-year risk. However, this metric was largely used to identify patients with elevated risk, and to trigger routine medical follow-up if a certain threshold was exceeded. It was generally not seen as a tool to facilitate a discussion of CVD risk with patients, most likely because practitioners lacked understanding of 10-year risk and were not confident about explaining it to patients.
-
There was a perception that patients were more responsive to, and therefore more likely to display intentions for risk-reducing behaviours in response to, heart age and the risk score manipulation and that patients liked the visual displays in JBS3 (including the heart age image). The limitation of using patient reactions to gauge understanding and intentions and the lack of routine follow-up to know what happens post health check were acknowledged.
-
Event-free survival age was misunderstood by some practitioners, and the lack of thresholds to indicate when risk was ‘high’ (as with 10-year risk) and lack of inherent comparison (as with heart age vs. chronological age) limited its application.
-
Risk management strategies largely focused on lifestyle advice during the health check. Again, the role of practitioners appeared to be as providers of information, rather than as facilitators of change, the success of which was often discussed in terms of patients’ receptiveness to advice or motivation to change.
-
Referrals to lifestyle support programmes were discussed, but such programmes did not appear to be regarded as particularly well attended. The lack of follow-up to or communication between general practices and referral services limited practitioner knowledge regarding patient attendance or effectiveness of such services.
-
The need for training to increase practitioner confidence and understanding in CVD risk communication was evident and was recognised by practitioners.
Chapter 7 Results 5: case studies
Introduction
A subsample of 10 patients were selected for within-case analysis to further explore mechanisms by which the risk calculators may lead to changes in patient or practitioner behaviour. Selection was on the basis of evidence of positive intentions and/or behaviours to reduce CVD risk following the health check, to provide balance across QRISK2 and JBS3 groups, to cover a range of general practices and practitioners, and to provide a variety in the type of positive experiences.
Using patient pseudonyms, each case study is presented under the following subheadings:
-
Summary – a brief statement to illustrate how the health check led to positive patient intentions, behaviours or outcomes.
-
Patient – patient background such as family history, basic health or lifestyle information and general attitude towards the health check.
-
Practitioner – practitioner background in terms of their role, experience and training. All practitioners expressed positive perceptions of the NHSHC programme as a means of identifying unknown issues in patients who otherwise might not visit the practice. These perceptions are not included in case studies, but can be assumed for all.
-
The NHS Health Check – summary of the consultation, including duration, CVD risk communication and level of patient involvement, and any notable events or perceptions from patient or practitioner.
-
What worked well – summary of the reasons that appeared to explain why the patient demonstrated positive intentions or behaviours relevant to CVD risk reduction following their health check.
-
Areas to improve – parts of the consultation that could have been improved.
Two case studies from the QRISK2 group used Informatica and are labelled as QRISK2+.
Case study 1: Abbie (JBS3)
Summary
This case study describes Abbie, who was in relatively good health, with no clear CVD risk factors and who did not require any post-health check follow-up. CVD risk was communicated using heart age and risk manipulation prompted Abbie to make dietary changes to address her elevated cholesterol, which was identified in the health check.
Patient
Abbie is a 61-year-old white British female living in a relatively deprived area (IMD decile 2). She does not drink alcohol or smoke, walks at least 10,000 steps a day, and regularly undertakes gardening and housework. She has no family history of CVD and has lost 8 kg since her weight was last recorded (8 years previously). She feels that having this type of health check is important and expresses gratitude to the practitioner. Her total cholesterol is slightly elevated, but not enough to warrant follow-up.
Practitioner
This health check is delivered by a British Asian female HCA with 2 years’ experience of delivering health checks and who has received ‘on the job’ training (no formal training). The HCA is positive about NHSHCs in general and likes the JBS3 manipulation options. She feels confident in communicating the risk score as the ‘GP has explained it’ to her and thinks that, in general, patients understand the information presented to them.
The NHS Health Check
The health check is shorter than average (just over 17 minutes). However, the HCA talks for a smaller than average proportion of time (46.0%) and Abbie speaks a little more than average for the sample. Abbie’s QRISK2 score is calculated as 4.8% and her heart age is estimated as 61 (equal to her actual age).
What worked well
Abbie reacted positively to heart age:
I was pleased to hear that [heart age was 61] and encouraged really . . . I found the whole thing encouraging, it encourages me to make some changes and to look after myself, because I think that is my duty.
Abbie liked the visual element of heart age: ‘because it was on the screen, I think that is just such an aid to memory’ and ‘an understandable way of presenting it’. The HCA also recognised Abbie’s positive reactions. She felt that being able to show Abbie her heart age on screen had helped Abbie to understand the concept, and that it was helpful for the two of them to compare Abbie’s heart with her true age, to see whether it was ‘good or bad’.
During risk score manipulation, there was discussion around good and bad cholesterol, and how to reduce Abbie’s total cholesterol, which was elevated. Abbie and the HCA appeared to enter into a mutual discussion, which concluded with Abbie thanking the practitioner. Abbie later reflected:
I thought that was very well done actually, and because the nurse showed me . . . by changing some of the data . . . that was very clear and understandable to me, so I thought that was quite a good way of doing it.
This information was remembered by Abbie, who had implemented some changes: ‘[the practitioner] actually suggested cutting [cheese] down to a couple of times a week, which I have done already, so that definitely has had an impact’. Abbie said during her VSR interview that when ‘information was given to me in the recommendation . . . I have implemented that immediately’. The HCA also liked using the risk manipulation function within JBS3, describing it as an ‘eye opener’ for patients.
Areas to improve
Abbie highlighted the challenge for practitioners in reading patients’ reactions to CVD risk information, and the need to ask patients if they understand and tailor appropriately. Abbie could not remember her 10-year risk: ‘I am not sure I fully understood the importance of the cardiovascular part of it’. However, the HCA perception of Abbie’s response, when she watched the video clip of their consultation (‘they just nodded and quite calm’), and our ratings of engagement based on non-verbal cues identified Abbie as being generally positively engaged.
The HCA liked JBS3 and being able to ‘show [patients] on the screen, they can see what is going on’, but referred to event-free survival age risk as ‘a good way to show patients if you can control things, your life expectancy will increase’. This showed that the HCA misunderstood the score and, as a result, did not describe it clearly to Abbie during the health check: ‘So on average it’s [the system] picked inside 80–85 about a heart attack or stroke’.
In turn, Abbie did not understand or ask for clarification. Comparing it with heart age, she said she did not understand it ‘as clearly I don’t think . . . I don’t think I took it on board quite in the same way’. This lack of understanding was not obvious to the HCA, who attributed Abbie’s lack of reaction to the fact that she was reading the screen and taking in the information, rather than to a lack of understanding.
Risk score manipulation was performed using blood pressure, which was normal, rather than cholesterol, which was elevated. This highlighted the need for tailoring. Abbie left with unmet information needs. She was keen to learn more about how to implement a change, but did not follow-up:
Until you know what to do you can’t implement it and particularly over blood pressure. I would like to learn [more about] the blood pressure, but I don’t know how you go about doing that.
Had the HCA asked Abbie if she understood or required further clarification, this could easily have been addressed.
Case study 2: Barry (JBS3)
Summary
This case study describes Barry, a patient who presented with a number of CVD risk factors including increased alcohol consumption, poor diet and slightly elevated cholesterol. Barry was recommended to make a specific lifestyle change that he was already considering. Despite other elements of CVD risk communication being suboptimal, he made a positive change, demonstrating that the health check can serve as a prompt to initiate risk-reducing behaviour when patients are on the cusp of acting.
Patient
Barry is a 47-year-old white British male living in a deprived area (IMD decile 1) who drinks 40 units of alcohol per week, has never smoked and reports doing ‘a bit of running every now and again’. His diet is the main area of discussion, as he admits to eating ‘a whole pack of chocolate biscuits every single day’ and excessive consumption of dairy products. Barry has a family history of heart problems (maternal grandmother) and diabetes ‘runs in my family’.
Practitioner
This health check is delivered by a white British female PN who has 8 years’ experience of delivering health checks and had previously attended two NHSHC training courses with the last being ‘at least 2 years ago’. The PN felt that she did not ‘have any problems’ with communicating CVD risk to patients and preferred JBS3 over QRISK2 because ‘you can actually communicate far better, and it’s got visual . . . everything about it, the patient can actually understand it better than just me talking’.
The NHS Health Check
This health check lasts just over 22 minutes, approximately average for the JBS3 sample, but is relatively dominated by the practitioner, who speaks for 56% of consultation time, and Barry speaks for 18.4% of the time. Barry’s 10-year risk is 3.1%. Only total cholesterol was considered ‘a little bit high’, at 5.3 mmol/l (ideally < 5 mmol/l). Barry’s heart age was estimated at 54, which was 7 years older than his actual age, which the PN attributes to his family history and elevated cholesterol. Based on a discussion of lifestyle, the main recommendations are to reduce consumption of chocolate biscuits and increase fruit and vegetable intake.
What worked well
About 3 weeks post health check, Barry had implemented dietary changes and felt that this was sustainable. Although he had ‘wanted to reduce my biscuit intake anyway’, the health check ‘prompted’ this change, and he had not ‘eaten chocolate biscuits now for over a fortnight’. The discussion around alcohol had also moved Barry to consider moderating his alcohol, but he saw this as a next step. A blood test 3 weeks post health check showed that cholesterol had fallen to within the normal range and, after an appointment with Barry’s GP, no further action was taken.
Areas to improve
Barry said that he was ‘expecting more’ from the health check, ‘something more in depth’, with more tests.
Although the PN was confident in delivering 10-year CVD risk and believed that ‘the majority of them [patients]’ understand, when watching the video clips of her interview she ‘did wonder sometimes whether they [patients] actually fully understood’. Barry could not remember his 10-year risk when asked by the researcher, even when prompted with a video clip. Although he interpreted the score as ‘quite low’, he said that he ‘didn’t remember it no, I don’t understand it’.
In line with current findings from the VSR patient interviews (see Chapter 5), the PN felt that being told heart age would be shocking, but Barry did not react in this way. His interview demonstrated that he had not fully understood how this information had been derived. The consultation would have been improved by the PN picking up on the trigger of this apparently contradictory result (of old heart age, but low 10-year risk).
There was misinterpretation of the discussion of event-free survival age, from which Barry took away that he had survival age of 73 (rather than event-free survival). Barry’s response was to ‘live my life to the full’, but such misunderstandings could have significant negative consequences including a sense of futility in relation to lifestyle that negatively affects health behaviour. The practitioner’s VSR interview revealed that the PN had similarly misinterpreted this risk score.
Finally, the PN altered the blood pressure as an example of how making small changes can be effective, but this point was missed by Barry, who was confused by the different numbers being entered: ‘I thought my blood pressure was low?’.
Case study 3: Carl (JBS3)
Summary
This case study illustrates a patient, Carl, who presented with a number of CVD risk factors, and in whom presentation of heart age had a significant impact. This resulted in Carl making a number of small lifestyle changes following his health check.
Patient
Carl is a 59-year-old white British male who lives in a relatively affluent area (IMD decile 9). He reports rarely drinking and that he stopped cigarette smoking in 2015, after ‘40 odd years’. He does little exercise because of ‘spinal problems’ and had a paternal grandfather who ‘had a stroke . . . he was late 60s, 70s’. Carl reveals that his friends and family ‘think I’ve got type 2 diabetes’, which was one of the reasons for attending the health check.
Practitioner
This health check is delivered by a white British female HCA with 5 years’ experience of delivering health checks. She received training in health checks prior to delivering them, but this primarily focused on PoC testing, and she cannot otherwise recall the training content. The HCA is ‘quite happy communicating’ CVD risk to patients’ and ‘primarily do[es] it in the same way’ for all patients she sees. She prefers ‘JBS3 because it has got the heart age on it’.
The NHS Health Check
This health check lasts longer than average (> 27 minutes) and involves more patient speaking than most (32.9% of total time), and CVD risk is discussed for > 2 minutes. Carl’s QRISK2 is 11% (medium risk), described as ‘a little bit higher than we’d like it to be’, and his total cholesterol has ‘gone up a little bit’, to 4.9 mmol/l from 4.5 mmol/l (in 2016). It is suggested that Carl considers improving his good cholesterol. His blood pressure is ‘just sort of on the higher end of where we’d want it to be’ and his body mass index (BMI) is 28.4 kg/m2.
What worked well
Carl said the health check was ‘what I expected and I’m very happy, yeah’ and was ‘now more mindful of, of what I am or I’m not doing’.
The visual presentation of heart age had the most impact on Carl. He reported that it ‘shocked me, no it concerned me’, and made him think ‘yeah, I ought to do something about that’. He remembered ‘the picture on that screen, the 65 . . . being in the middle’ and ‘thinking bloody hell I ain’t 65’.
The HCA manipulated Carl’s information within JBS3 to illustrate that reducing his total cholesterol and increasing HDL cholesterol through simple changes to his diet and physical activity levels would reduce his CVD risk to 9.3% and lower his heart age to 62. The HCA thought ‘it’s really good having that option’ because ‘they can actually visually see the changes’. Carl did ‘remember that’, but had ‘already got the message’ by that point.
Carl found a diet sheet provided by the HCA ‘helpful’. He reported several positive behaviour- and health-related outcomes:
-
‘ordered a small blood pressure monitor’, which he admitted he had ‘never done anything like that before’
-
felt ‘more mindful’, and was trying to ‘do a bit more exercise’ and ‘now looking at certain foods’
-
had ‘been researching because of my concerns about diabetes’
-
diabetes was later diagnosed following a full blood check at 6 weeks post health check and Carl was prescribed metformin.
Areas to improve
Ten-year risk was not explained by the HCA and, subsequently, was not recalled or understood by Carl. On watching the corresponding video clip, he said that it ‘didn’t make a significant impact on me’. In the absence of an explanation from the HCA, Carl questioned ‘exactly how she arrived at that percentage’, only remembering that ‘they’d like me to be 10% or less and I’m only 11’.
The HCA did not understand and, therefore, miscommunicated event-free survival age: ‘currently you can sort of expect to survive the age of 79 based on your lifestyle factors’. The HCA found it ‘the hardest one to try and communicate’. In this health check, it did not create a serious issue as Carl reported that seemed ‘a long way off, you’re looking like 20 years in the future’ and recalled thinking ‘well that’s better than what my dad or what my grandparents had’.
Case study 4: Deborah (JBS3)
Summary
This case study presents Deborah, a patient in good health, for whom the health check provided reassurance. In this example, Deborah attended with a positive attitude to her health. She tried to lead a healthy lifestyle and was grateful of the health check as an opportunity for reassurance.
Patient
Deborah is a 63-year-old white British female living in a relatively affluent area (IMD decile 10) who has never smoked, reports modest alcohol consumption (‘7–10 units per week’), ‘excellent . . . varied diet, nice portion sizes’ and is a ‘Pilates teacher’ who teaches aerobics, and practises yoga for 2 hours each day. She has no known family history of CVD, but is aware of high cholesterol in the family (including herself).
Practitioner
The health check is delivered by a white British, female, newly qualified PN. She has 9 months’ experience of conducting health checks and has ‘had a lot of shadowing’, but no formal health check training. She felt confident ‘explaining what the QRISK is . . . yeah I’m fine with that’.
The NHS Health Check
This health check is relatively short (17 minutes), but includes > 3 minutes of CVD risk discussion, and Deborah speaks for > 28% of the health check (above average). Deborah’s 10-year risk is 4.7% and her heart age is 58 years. Total cholesterol is slightly elevated (5.8 mmol/l) but, in the context of LDL and HDL figures, her cholesterol level is described as ‘within normal range’.
What worked well
Overall, Deborah reported that the health check ‘was as I expected’ and that it was ‘good to actually have some reassurance that everything is OK’. She said, ‘I have always been interested in my health, so, erm, for me it’s a positive thing’ and was ‘grateful that [they] had the opportunity’ to have the health check.
Heart age was the CVD risk information that affected Deborah most positively: ‘when she told me that my heart age was 5 years less than my actual chronological age’ it served as ‘a positive reinforcement both for me and within my job’. The PN reported that heart age came ‘more naturally the more I used it’ and felt that patients ‘generally responded really well’.
The PN correctly described event-free survival age and, in turn, Deborah later interpreted it to mean that ‘I should be alright until I am in my 80s, yeah, before anything might start to develop . . .’. This emphasises the importance of practitioners having accurate knowledge of CVD risk scores in order to convey this to patients and mitigate against misinterpretation.
Using JBS3 had led to a change in practice. The PN suggested that they ‘much prefer using [JBS3]’ as they ‘think it gives the patients a better understanding’ and ‘still use it now’ following the conclusion of the study.
Areas to improve
First, information presented without a visual aid was forgotten. Deborah was unable to recall her 10-year risk and, when watching the corresponding video clip, reflected that she ‘understood’ it and ‘wasn’t confused at all’. The PN also thought that ‘they [patients] all understood fully the 10-year risk’, but that QRISK2 is ‘lacking . . . the visual aids’.
Second, event-free survival age was communicated accurately by the PN in the health check, perhaps as they read the information from the screen, during the VSR interview, their discussion of this risk score indicated some misunderstanding: ‘really good you know . . . [patients can think that] “I am going to survive to 82” ’.
Third, risk manipulation could have been better tailored to Deborah by showing potential CVD risk reductions through lowering cholesterol (which was raised), rather than how risk would increase should they start smoking. Deborah had never smoked and confirmed the irrelevance of this scenario: ‘would never happen’. In contrast, the PN thought that manipulating patients’ risk scores ‘had a positive effect’ and that patients ‘really responded to that’. This highlights a mismatch between practitioner perceptions of how patients received CVD risk information and the reality.
Fourth, there was some inaccuracy in how the PN relayed patient HbA1c information in relation to a result in the normal range, which ‘put a big red flag up in my head when I heard that’. Despite describing it as ‘up at the top end’, the PN did not engage in a discussion around this, but rather spoke about what would happen if it was in the pre-diabetes range. This resulted in Deborah deciding to ‘work on that although my solution to that is not to buy [sugar] and not have it in the house’. This could be an unnecessary burden resulting from inaccurate information.
Finally, Deborah was positive about the overall experience. However, her body language during CVD risk discussion was rated as either passive or slightly positively engaged. If picked up by the practitioner, this could have triggered a discussion to address some of the above issues with how CVD risk information was provided and received.
Case study 5: Eid (JBS3)
Summary
This case study presents, Eid, a patient with a generally healthy lifestyle in whom the health check identified mild hypertension. Although this prompted lifestyle changes, follow-up tests and an appointment, heart age was the only CVD risk information that he could recall and no lifestyle advice was offered.
Patient
Eid is a 58-year-old Asian British male who lives in a relatively deprived area (IMD decile 2). He has never smoked, does not drink alcohol and ‘play[s] a bit of sport’ including football and table tennis. Eid reports ‘eat[ing] a lot of fruit’ and has no known family history of CVD. He felt having a health check ‘would[n’t] do any harm’ as there is ‘nothing wrong with making sure everything is OK’.
Practitioner
The health check is conducted by an Asian British female HCA who has been delivering health checks ‘ever since the NHS programme started’ and received training ‘when it started’ and ‘. . . last year as well, and then it’s online as well’. The HCA feels ‘OK’ about communicating risk to patients and as ‘I know what I am saying, I am more confident and happy to speak to the patient’. She thought JBS3 was ‘really good, because it tells you the heart age, erm, it tells you the lifespan’ (reflecting a misunderstanding of event-free survival age observed among other practitioners). The HCA ‘enjoyed using it [JBS3]’, preferring it to QRISK2 ‘because it’s visualised, the patients you know they are seeing what their results are. It is not just more score’.
The NHS Health Check
The health check lasts just over 15 minutes. The HCA speaks for only 36% of the time, but Eid’s contribution is low (20%) and a relatively high proportion of the health check passes without either participant speaking. Eid’s 10-year risk of 15% is described as ‘medium’ and his heart age is estimated at 59, approximately 6 months older than his actual age. As Eid’s blood pressure is ‘high’, the HCA tells him that she will speak with the GP, who will ‘get back to you [Eid]’, and advises Eid that he is likely be called ‘in for a 24-hour blood pressure’ check.
What worked well
Overall, Eid felt that the health check was ‘helpful for me because, obviously, it gives me an idea of how things are’, as he rarely attended the surgery. Ultimately, the success of this health check was in identifying and following up the identified hypertension. Eid remembered that his blood pressure ‘was a bit on the high side’ and was ‘surprised’ as he had not ‘had any issues with it before’.
The most impactful element of CVD risk communication was heart age, with which Eid was ‘quite happy’ and found it ‘very useful to know’. The result ‘reassured what I already knew, that I was quite healthy’. The HCA suggested that patients ‘understood [heart age] a lot more . . . because obviously . . . they know how old they are’ and believed that the visual presentation was helpful (‘them seeing it, I think it’s a big difference’) compared with relaying the percentage risk score, as is usual practice.
Areas to improve
Eid did not recall the HCA telling him ‘what I needed to do’. Indeed, the HCA did not offer advice aside from clinical follow-up (re-test/GP appointment). Consequently, Eid had received ‘a few tips on what to do’ to reduce his blood pressure from his sister. Eid assumed that this was because the HCA ‘wouldn’t know until’ she had completed further blood pressure monitoring.
There were several issues with CVD risk communication. First, Eid had a medium–high 10-year risk, yet could not recall it, nor did he ‘put any importance on it’ (when reminded in his VSR interview) because he was ‘well within the percentage of being healthy’ and ‘thought the risk out of 100 was minimal’. The HCA reported using only the risk categories (‘high/medium and low’) because patients ‘don’t really understand the percentage of the number’. This seemed to be an assumption and was not checked by enquiring about Eid’s understanding or feelings.
Second, in the health check, the HCA communicated event-free survival age by saying ‘on average expect to survive is 80 for yourself without a heart attack or a stroke’. The HCA later discussed how this was a challenging screen and her communication suffered as a result: ‘telling them that your life expectation, it could be . . . I think I find it a bit hard’. This highlights a mismatch between what the HCA read from the screen in the consultations (which was correct) and her apparent understanding of this score as expected survival age. Moreover, the HCA thought that Eid ‘knew exactly what I was saying’ on watching the video clips. In contrast, Eid could not ‘recall it, I think she said . . . something about 80 something’, again misinterpreting event-free survival age as expected age of mortality: ‘I’ve got a few more years to live’.
Finally, Eid had never smoked and presented with mild hypertension. Yet, for risk manipulation in JBS3, the HCA showed how Eid’s risk would increase if he were a smoker. He appreciated being ‘reassured . . . that what I’m doing with my health is good and I’ve got to keep it going’, but a more relevant and tailored manipulation of risk would have been preferable.
Case study 6: Freddie (QRISK2+)
Summary
This case study describes Freddie, a male patient with a range of CVD risk factors, and a medium–high 10-year CVD risk. Freddie was aware of the need to change his lifestyle. He attended with an ‘open mind’, and received quick and multiple follow-ups after the health check. In this way, the health check served as a catalyst for change and Freddie subsequently made multiple positive lifestyle changes. Quickly, his efforts were rewarded with weight loss and a reduction in blood pressure.
Patient
Freddie is a 64-year-old white British male who lives in an area of approximately average affluence (IMD decile 6) and has not visited his GP for 13 years. He has no family history of CVD, but presents with a range of risk factors: BMI of 45 kg/m2 (morbidly obese category), moderate hypertension (167/90 mmHg) and very high alcohol consumption. His main reason for attending is to achieve weight loss, but he also has concerns about the physical effects of his alcohol intake. Freddie is positive about the health check, which he recognises as being about ‘prevention rather than cure’.
Practitioner
The health check is delivered by a female white British HCA with 2.5 years’ experience of delivering health checks and who has attended generic NHSHC training and shadowed a colleague. Despite positive perceptions of the programme, she feels that it ‘needs tweaking’, and thinks that the primary purpose of QRISK2 is to identify patients to refer to the GP, rather than to facilitate discussion around CVD risk.
The NHS Health Check
This general practice has access to Informatica, which offers some of the JBS3 functionalities, including heart age and risk score manipulation, which were used in this health check. At 27 minutes, this health check is considerably longer than most, and Freddie speaks more than the sample average (31% of total time). Freddie’s 10-year risk is 17% (approaching high risk, 20%), which he interprets as being ‘. . . lucky that’s quite low really – I was expecting it to be higher’. The HCA is disappointed with her delivery of 10-year risk information when watching the corresponding video clip (‘like a parrot’; ‘maybe I don’t do enough on that’).
What worked well
Freddie appeared engaged throughout the health check and spoke more than many other patients in the sample. He was ready to make changes, and the suggestions made by the HCA resonated with the issues of which he was already aware. This meant that Freddie was later able to recall parts of the health check conversation with the HCA (e.g. ‘wine has got sugars in them – sugars go to the wrong places’). This appeared to make Freddie receptive to suggestions and meant that the HCA did not need to convince him of the importance of CVD risk or lifestyle.
Freddie received a telephone consultation with a specialist nurse practitioner within ‘a couple of hours’ of his health check to reinforce the messages given (telephone reinforcement). This appeared to facilitate understanding and retention of 10-year risk, as he was able to recall ‘an analogy of you know like 100 people in a room – 17 can be expected . . .’ (words not used in his health check). A barrier to exercising was identified (could not afford gym membership), and the health check and subsequent telephone consultation led to a series of outcomes:
-
discussion of statins
-
exercise referral for 12 weeks of subsidised gym sessions at a local authority leisure centre
-
Freddie changed his diet and alcohol intake ‘. . . I have dropped all the things that I know I should not be eating and it seems to be having an effect . . . I seem to have dropped a few pounds . . . I have dropped the booze a lot – well totally for the minute, erm, which has helped me sleep a lot better’
-
reduction in blood pressure to the normal range.
Areas to improve
Freddie’s 10-year risk put him close to the high risk category, yet he did not recognise the risk severity.
Freddie could not recall being provided with heart age or the HCA manipulating risk scores, which contrasted with the HCA’s perceptions that ‘heart age is most effective’. Heart age is likely to have been forgotten because the follow-up telephone consultation focused on 10-year risk. There was scope to better tailor CVD risk discussion; for risk manipulation, the HCA showed how heart age would increase if Freddie were a smoker, yet he had never smoked and subsequently forgot his heart age. It would have been more appropriate to show changes in a risk factor more relevant to Freddie, such as reducing blood pressure through modifying alcohol and diet: ‘Well that just reaffirms my thinking about smoking and I did think, erm, the alcohol side might come into it’.
Case study 7: Grace (QRISK2)
Summary
This case study of Grace illustrates that, even when relatively short with minimal discussion of CVD risk, a health check can be valuable in identifying areas for change, if the patient is already actively trying to improve their health.
Patient
Grace is a 56-year-old white British female who lives in a relatively deprived area (IMD decile 2). Her parents died suddenly of heart failure in their 70s. She stopped smoking 14 months earlier, attends Slimming World® (Alfreton, UK), has not gained weight since her last visit to the GP, and reports moderate alcohol intake. Grace is engaged with, and has a positive view of, preventative health care (‘usually have the well-woman check’) and describes the health check as a way ‘to find out if there’s any underlying problems which you may have and it’s just really good to keep on top, because you feel fine but you don’t know what is going on inside’.
Practitioner
The health check is delivered by a white British female HCA with 2.5 years’ experience of delivering health checks. After participating in the recorded health checks, the HCA completed training in NHSHC, after which she concluded ‘I don’t think you should give these health checks unless you have had the training’.
The NHS Health Check
The Health Check lasts just 16 minutes and Grace speaks for only 10% of the total time. CVD risk is discussed for just over 40 seconds. During the health check, Grace’s 10-year risk is calculated at 6.9% (low). Slightly raised total cholesterol (6.1 mmol/l) and blood pressure are flagged as initial concerns.
What worked well
This health check identified a rise in Grace’s cholesterol, which she attributed to less healthy dietary habits ‘creeping in’. Risk management discussion focused on this also; the interview data demonstrated that Grace was clear about her related goals:
I really am going to like get the cholesterol down that’s my main thing . . . So I am really, really saying right ‘no, we are not even having that in the house, we are not eating this, we are not having that any more,’ and we are definitely eating better . . .
Two in-clinic blood pressure measurements showed Grace’s blood pressure to be raised, but, at home readings were found to be normal, no further action was deemed to be necessary.
Areas to improve
The HCA spent very little time discussing 10-year risk:
I’m going to access your QRISK2 score, erm which is, which tells us your likelihood of contracting cardiovascular disease within the next 10 years . . . So it’s 6.85, which is still OK, it’s below 10.
Hmm.
So, erm so it’s not something that we really need to worry about, but getting your cholesterol down.
Grace could not recall her 10-year risk, only that it was ‘low’, and said she ‘just didn’t really absorb it . . . afterwards I thought “well she said it was under 10”, but what it was, I couldn’t quite put my finger on it’. Despite that, Grace was motivated to reduce her cholesterol. Encouraging Grace to maintain her good lifestyle while making small changes, particularly given her positive engagement with the health check, could prevent further decline.
Case study 8: Harry (QRISK2)
Summary
Harry presented with multiple CVD risk factors and the PN spent > 3 minutes explaining his CVD risk. This seemed to convince him of the need to go back on to a low-dose statin, despite initial reluctance. However, following the apparent success of his health check, Harry could not recall his 10-year CVD risk, remained reluctant to take statins and had no intention of changing his lifestyle.
Patient
Harry is a 61-year-old white British male, who lives in an area of approximately average affluence (IMD decile 5). He has a family history of heart attack (father) and has previously taken statins, but managed to come off them with the support of his GP. His blood sugars have been in the pre-diabetic range for 3 years, which is Harry’s motivation for attending the health check: ‘for the last couple of years the doctors been saying I am on the edge of becoming diabetic . . . that was the thing that was pushing me just to make sure I got the health check’. However, when asked if he had heard of the NHSHC he commented ‘Yes, but I wasn’t particularly bothered’.
Practitioner
The health check is delivered by a female white British, PN. She has 2 years’ experience of delivering health checks, but has not received formal training: ‘when I first started, I perhaps would have shadowed somebody doing them’. Despite feeling ‘fairly confident’ in communicating 10-year risk, she conceded that ‘all I have ever been told is anything over 10% needs to be started on a statin. Anything below 10% are fairly low risk, you know, and obviously yeah I discuss that with the patients, but other than that I don’t know a huge amount about that with the QRISK score at all’.
The NHS Health Check
The health check is one of the longest (> 37 minutes). Harry speaks for 29% of the total time, and CVD risk is discussed for > 3 minutes. During the health check, Harry’s 10-year risk is calculated as 14.2%, and blood results showed slightly elevated total cholesterol (5.4 mmol/l) and blood sugars in the pre-diabetes range. Blood pressure was normal. Both the PN’s assessment and our analysis of patient engagement from non-verbal cues of the video-recorded consultation suggested that Harry was positively engaged throughout the CVD risk discussion.
What worked well
The PN explained some factors from which Harry’s 10-year risk was calculated to highlight the need for him to consider going back on to a low dose statin as a means of lowering risk:
So this is your risk of getting heart disease in the next 10 years . . . that puts it to a calculation of your weight, your smoking, or lack of smoking . . . and your cholesterol, that sort of thing . . . it’s come out with a risk score of 14.2%. So ordinarily anything over 10% we would offer a cholesterol-lowering tablet . . . we would recommend that you start back on your statin.
The PN then went on to explain that Harry’s risk was above average for a man of his age:
. . . let me just go back on to that and I explain in a bit more detail. So like I say, erm ,this is coming out that your risk score is 14.2% the average 61-year-old male is 10.1%. So you’re slightly above the average . . .
After additional information was given, Harry appeared to recognise the severity of his CVD risk (‘I don’t like the fact . . . about the risk score’) and moved towards action:
So how do you feel about starting back on it?
I didn’t want to.
OK.
I will if that what it takes.
Harry showed confidence and positive engagement in requesting a discussion of his pre-diabetic status, which was his primary concern, and sought specific details: ‘What does that mean? Does it mean tablets, does it mean injections?’. This allowed the PN to explain and again highlight the importance of lifestyle (as well as medication) to prevent progression to diabetes.
Areas to improve
Harry could not recall his 10-year risk and reported that being shown the video clip ‘brought the disappointment back to me because I was expecting to be better than that’. However, ‘it didn’t make me feel any different . . . it hasn’t made me change my lifestyle at all’. He revealed that he had not yet picked up his statins, but ‘I still got my old ones which I had stopped taking. So I have been taking half of one of them every day’.
Harry’s description of the health check highlighted two issues that prevented more engagement with the PN’s recommendations. First, the PN’s explanation of his above average 10-year risk did not empower him:
Mainly to do with the fact that you got family history of cardiovascular disease . . . So although everything else is pretty good . . . we can’t help what you’re already predisposed to unfortunately, which is your dad.
This left Harry feeling like ‘there was nothing in there that I am not already doing. There was nothing to do’.
Second, a more tailored approach was needed. Harry expressed a desire for specific lifestyle guidance, as he left feeling that ‘without any clear direction, I haven’t got anything to change . . . the nurse said “keep walking the dogs, keep doing the exercise . . . just try and do healthy things, eat your greens and you know have your five a day”. . . do those things which I am doing anyway’. The lack of specific advice was acknowledged by the PN on watching the corresponding video clip of this health check:
I did notice when the diet one came up, I did just put a piece of paper in front of them, and I didn’t read it. So actually in hindsight, perhaps I should have said, ‘you shouldn’t eat this, you shouldn’t eat this, you shouldn’t eat this’ . . . in hindsight, I could have explained a little bit better. Like the statins, he wasn’t overly keen on taking the statins was he?
Finally, Harry thought that it would have been useful to have the opportunity to reflect and then ask further questions ‘In some kind of follow-up, even if it’s a week later on or whatever’. This confirms the potential role of telephone reinforcement.
Case study 9: Ian (QRISK2)
Summary
This case study describes Ian, a male who was very positive about the overall health check experience, the practitioner and the advice given, and had implemented some lifestyle changes. Ian had excessive alcohol intake and had made beneficial changes. The CVD risk discussion was brief and, ultimately, forgotten; however, in this case it did not matter.
Patient
Ian is a 48-year-old white British male who lives in a relatively affluent area (IMD decile 10) and is active through his job as a postman. He is an ex-smoker (of 4 years) and has been trying to improve his diet to manage his cholesterol, but reports excessive alcohol consumption (> 30 units per week). He has not heard of NHSHC.
Practitioner
This health check is delivered by a female white British HCA who has 6 years’ experience of delivering health checks and attended generic training several years earlier, but cannot remember the details. Although reporting confidence in communicating a 10-year risk, when asked about her understanding of the score, the HCA focuses only on the thresholds:
. . . anything over 10% is a higher risk, erm . . . so then other risk factors need to be taken in consideration like family history and things, erm . . . to see, like I say, if it’s worth going on a statin . . . those people are then would forward onto the doctor for further review or we’ve got a pharmacist.
The NHS Health Check
The health check lasts just under 19 minutes and Ian speaks for just 18% of the consultation. CVD risk is discussed for just over 1 minute. The HCA collects information on Ian’s lifestyle and offers advice before his 10-year risk is discussed. Ian’s 10-year risk is 4.5% (low risk), but he is noted to have a slightly elevated total–HDL cholesterol ratio and excessive alcohol intake. Discussions around dietary changes to manage cholesterol and reducing alcohol intake account for the majority of the health check.
What worked well
Ian thought it would be longer (‘I’d thought I’d been in there half an hour, at the most I were in there 10 minutes’), yet felt that the HCA ‘was excellent . . . she gave me some great advice’. The way in which the HCA communicated was clearly appropriate for him:
It weren’t sterile . . . we had a chat . . . it was like visiting a friend.
Ian’s alcohol consumption identified a risk of alcohol-related harm. The impact of the corresponding discussion was clear during Ian’s VSR interview: ‘I didn’t think it was a problem . . . and maybe it did become a problem’. Ian made immediate changes, ‘as soon as I talked to her I’d stopped drinking for a fortnight’. Although he had since had a drink, he had also made dietary changes to address the elevated cholesterol ratio through eating more fish (albeit tinned tuna, rather than the recommended oily fish) and vegetables: ‘I actually feel healthier’.
The health check ended with the HCA saying that ‘we are going to set some goals for you’, and Ian had responded. This was something the HCA specifically mentioned in her VSR: that she tends to set goals with the patient’s agreement:
I sometimes find if I ask the patient to set a goal they sort of sit there . . . they don’t really know what goals to set, so I do find that I do, sort of instigate . . . but they agree . . . It’s rare that I’ll instigate a goal and patients don’t agree with it.
In the light of the low 10-year risk, the HCA tried to emphasise the importance of prevention in general:
As we get older our percentage naturally goes up because we are older, so when we are a young age because that is a young age, that’s my age, so when we are of that age we have to look after yourselves and prevent, it’s all about preventative measures OK.
Areas to improve
When 10-year risk was conveyed, it was quickly given as a relative and then absolute percentage risk score, without much explanation or checking of Ian’s understanding:
OK, so, for your age group, the risk of developing heart disease in the next 10 years is 3.5%. Your risk is 4.5%, so it’s slightly up. Erm, is still a low risk percentage when no major concerns of that but we do need to say to you is that obviously you just need to make sure you keep active, which you are . . .
Communication of the risk score was brief, and Ian did not retain anything from the information given. During the interview he indicated that this information was not important to him and he had made changes without understanding this: ‘it don’t really bother me to be honest . . . don’t really register with me’.
The lifestyle goals could have been more tailored. They combined specific behavioural goals and general outcome goals, covering three lifestyle behaviours, and included an inappropriate exercise-related goal, which has not been implemented:
‘cos I’m a postman you see, so I was shocked when she says err, cos I walked 10–15 miles a day . . . with a big bag on me back and everything, and I was surprised when she said . . . ‘do you go home and do any gardening?’ . . . I just wanna go home and sit and chill.
Finally, Ian thought that it would have ‘helped turning the computer round and showing me the information . . . ’cos visual has always been better than audio for me for everything’.
Case study 10: Jessica (QRISK2+)
Summary
This case study describes the health check for a patient, Jessica, who had already made lifestyle changes following an ‘episode . . . they thought might have been a mini stroke’ 12 months prior (this was not confirmed as this would preclude her from NHSHC). Jessica’s engagement with, and positive experience of, the health check appeared to result from the reassurance that it provided around the success of steps she had already implemented.
Patient
Jessica is a 64-year-old white British female who lives in an area of approximately average affluence (IMD decile 5). She experienced an episode the previous year, which was initially suspected to be a ‘mini stroke’ (but was not confirmed). She was prescribed statins at that time, but ‘thought, “I don’t want to do this” ’ and consequently made dietary changes, reducing her cholesterol and successfully losing weight. She had not heard of NHSHC before and assumed it was a general health check, and wondered why it was focused on CVD: ‘why can’t you go into everything at the same time?’.
Practitioner
The health check is delivered by a white British, female HCA, who has 4 years’ experience of delivering health checks and received some training when she started, which she describes as: ‘slides and screen presentations . . . talked through it erm and then it was moving on to how to use the [point-of-care] machine . . . it was pretty straightforward really’.
The NHS Health Check
This health check lasts < 18 minutes, during which the HCA speaks for over 70% of the time. PoC testing confirms that Jessica has reduced her total cholesterol (from 6.7 mmol/l to 6.1 mmol/l) and total–HDL cholesterol ratio (from 3 to 2.8). CVD risk is discussed for about 1 minute, which shows a reduction from a measurement (recorded several years earlier): ‘you were at 10% just before, it is now 5%, so you have halved the risk in that time’. The HCA congratulates and encourages Jessica to keep going with changes she has made to lower her cholesterol and recommends that she increase her activity levels (as she is classified moderately inactive):
The one thing that will help you with that, is being a bit more physical, get doing something that is a little bit more cardiovascular, even if it’s upping your walking and doing it as a power walk, or doing hills, on an incline, it gets you out of breath.
What worked well
Overall, Jessica thought that the HCA was ‘very good’. At the start of the health check, the HCA made clear to the patient that it was ‘all to do with cardiovascular disease, so what we are looking for is how at risk you are of developing cardiovascular disease within the next 5 to 10 years’. This provided useful context for the subsequent discussion of risk factors and management.
Jessica appreciated feedback and reassurance regarding changes already made, and was pleased to see that ‘the work had been paying off’. She remembered clearly the main point to address and had made further small changes to her commute to work to incorporate moderate-intensity activity into their day: ‘I go to [work] on the school bus . . . it picks me up from outside the house, but I’ve started to go out a few minutes earlier and walking up the hill [laughs] . . . and meeting it up the hill [laughs] . . . it’s just a few minutes a day . . . might make a difference’.
She also appreciated the written report, as ‘you can’t take everything in straight away, so it’s nice to have that printout’ to ‘go back and have a look’.
Areas to improve
The 10-year risk score was mentioned briefly, but not explained. Jessica could partially recall the information as ‘. . . 5% over the next 5 years’. She had retained the correct percentage, but the timescale was incorrect (reflecting the HCA’s incorrect description, above) and she could not demonstrate a clear understanding of what it meant for her.
Summary
The 10 patient case studies confirmed many findings from Chapters 3–6 with several strong and inter-related themes. As noted in Chapters 3 and 4, CVD risk discussion was often brief. Therefore, these themes are not limited to CVD risk discussion, which might not have been sufficient or necessary for positive patient outcomes.
Patients attending already motivated to make changes
Health checks with patients who were already motivated to make lifestyle changes or, as in some cases, had started to implement changes had positive outcomes regardless of how CVD risk was communicated. These patients attended with a specific focus (e.g. behaviour change in mind), which provided the practitioner with an obvious focus to tailor risk management.
Cardiovascular disease risk communication
Explaining and checking patient understanding of cardiovascular disease risk
Even in these examples selected on the basis of positive patient intentions or outcomes, practitioners rarely explained what CVD risk meant for patients, or asked patients if they understood the information provided. Not knowing how the patient is receiving the information limits practitioners’ opportunities to tailor risk information.
Practitioner versus patient perceptions
The muted and minimal responses of most patients to risk information led practitioners to assume understanding (see Chapters 4 and 6); the case studies have highlighted that this was not necessarily correct. Assessing understanding from patient reactions to information can lead to a mismatch in perceptions (of practitioner and patient), which could be mitigated through asking patients (see Explaining and checking patient understanding of cardiovascular disease risk).
Tailoring of cardiovascular disease risk communication
This is an area of particular importance. Despite positive intentions and actions in some patients following the health check, there was little evidence of tailoring risk information or discussion to facilitate patient appraisal of their risk (severity or vulnerability), for example in CVD risk score manipulation. We observed practitioners demonstrating how non-smoking patients’ risk would increase if they started smoking, rather than showing them how they could reduce risk by manipulating a more relevant risk factor (e.g. lowering cholesterol identified as raised during the health check), which could facilitate a discussion around management through lifestyle.
Visual presentation of cardiovascular disease risk information
Case studies provided further confirmation that patients and practitioners appreciated the ability to see CVD risk outcomes presented on the screen. Patient heart age, in particular, was often (but not always) impactful and memorable, and, if used appropriately, the visual representation of risk reduction through modifying risk factors can be impactful.
Focus on modifiable risk factors
Focusing on non-modifiable risk factors, such as family history, which are outside the patient’s control, can promote fatalistic views and undermine potential for lifestyle change.
Preventative framing
Patients with low risk appreciated the reassurance provided by their health check and responded well to explicit discussion of prevention (i.e. changes in specific areas to maintain low risk, which will increase with age).
Written information
Patients liked having written information to take away and consider in their own time. This allowed time for reflection and to recall on CVD risk, which might raise questions that could be addressed through a follow-up call (see Post-health check telephone reinforcement).
Risk management
Tailoring and specificity of recommendations
This was most evident when patients arrived having already considered changes they wished to make (e.g. stop eating specific foods, reduce alcohol; see Patients attending already motivated to make changes). Case studies highlighted other examples in which patients were given recommendations to modify several behaviours, some of which did not resonate with the patient, who either forgot or dismissed them. As patients tend not to question the advice in the health check, this could be addressed through asking the patients (see Explaining and checking patient understanding of cardiovascular disease risk) and telephone reinforcement to confirm and revise agreed actions (see Post-health check telephone reinforcement).
Goal-setting
This was explicitly used in one case study, trying to get patients to agree to the practitioner recommendations. If these could be co-produced between practitioner and patient, with tailoring, more positive outcomes would be expected.
Post-health check telephone reinforcement
Telephoning patients soon after their health check seemed to have a range of benefits: allowing patients time to reflect on the health check discussion and identify questions or areas of uncertainty; further explaining CVD risk, answering questions and confirming patient understanding; confirming recommendations for risk management; and making specific plans where appropriate (e.g. referrals, follow-up appointments, further measurement).
Chapter 8 Discussion
In this chapter we present our main findings, compare our findings with other research around health checks, risk communication in general and specific CVD risk metrics (where available), present implications for practice and future research, and consider the strengths and limitations. Box 2 summarises the main lessons learned.
-
Consultations were verbally dominated by practitioners (nine HCAs and six PNs), often with little patient input or questions, particularly when using the QRISK2 10-year risk calculator.
-
Discussion of CVD risk in consultations was minimal (< 2 minutes or < 10% of consultation time on average), especially when using QRISK2, and was often information provision rather than a tailored two-way interaction in which patients could ask questions or discuss specific individual risk factors.
-
Practitioners rarely explained what CVD risk meant for patients or checked understanding. This limited opportunities to tailor risk information and to avoid misunderstandings.
-
QRISK2’s 10-year risk was commonly seen as a tool to identify those who required referral onto the GP/to discuss statins, rather than a tool to facilitate discussion of CVD risk and its management.
-
JBS3’s heart age was generally preferred (over 10-year and event-free survival age) by practitioners and patients.
-
JBS3’s event-free survival age information was delivered briefly, sometimes with a lack of clarity and accuracy, and was often misinterpreted.
-
JBS3’s visual representations of risk was valued by practitioners and patients.
-
JBS3’s risk score manipulation has potential and was generally perceived positively. However, it was sometimes limited by focusing on risk factors irrelevant to the patient (e.g. demonstrating the impact of smoking in a non-smoker) or because the patient was not clear about what was happening (e.g. why different blood pressure values were being entered).
-
Further practitioner training would be required to optimise use of lifetime risk and risk manipulation functions within JBS3.
-
Our data confirm that providing patients with a CVD risk score alone is insufficient to enable understanding.
-
With QRISK2, practitioners felt confident to deliver 10-year risk, but often did not understand it sufficiently to confidently engage patients in a discussion around what it meant for them (i.e. moving beyond application of low/medium/high risk thresholds).
-
JBS3’s heart age was the preferred CVD risk score overall. Practitioners and patients felt that they understood it and found it more impactful, and VSR interviews showed that patients could often recall their own heart age (more so than 10-year or event-free survival age).
-
JBS3’s CVD event-free survival age was misinterpreted by some practitioners and patients as expected survival age. The lack of thresholds (e.g. 10-year risk) or inherent comparison (e.g. heart age) made it difficult for practitioners and patients to interpret risk as low, medium or high.
-
JBS3 can be useful for offering a variety of delivery methods (risk score, visual representations, analogies, risk manipulation) to accommodate a range of patient preferences. But to make appropriate use would require that practitioners check patient understanding and tailor information.
-
JBS3’s visual presentation and risk score manipulation appealed to a range of patients who vary in preferences and understanding, and can make the important link between lifestyle change and overall CVD risk.
-
Practitioners’ reliance on patient reactions to gauge understanding of risk information was limited by the general lack of response from patients in health checks.
-
Patient VSR interviews identified positive changes in most patients following their health check, from increased patient awareness of lifestyle to implementation of specific recommended lifestyle changes.
-
Applying to PMT to analysis of practitioner–patient discussions during health checks (see Chapter 4) identified more evidence of cognitive appraisal in patients attending health checks delivered using JBS3 (than those using QRISK2); in particular, threat appraisal, facilitators of and response costs to adaptive coping.
-
Some patients identified JBS3’s heart age as a trigger for intentions to reduce their CVD risk.
-
Being able to understand heart age and recognise the personal relevance (more than other risk scores) seemed to allow patients to appraise the severity of the risk, their vulnerability to it and evaluate barriers to/facilitators of risk-reducing behaviour change.
-
In some health checks, discussions of patient lifestyle were not in the context of CVD risk; assessment of lifestyle and associated practitioner recommendations preceded CVD risk discussion.
-
The case study examples of health checks that led to risk-reducing intentions and behaviours were often patients already aware of the need to change, with intentions to change, or who had already started to implement changes.
-
Length of health check appointment allocated by practices ranged from 15 to 30 minutes, but actual duration of practitioner–patient interactions ranged from 6.8 to 38 minutes (60% of health checks lasted < 20 minutes).
-
Patients in both groups felt that they were given too much information within a short space of time, which limited their capacity to absorb or retain it. How time is apportioned within the health check should be revisited in terms of what practitioners are expected to achieve to ensure that adherence to process is not at the expense of opportunities for patient-centred discussion and shared decision-making.
-
Some patients expressed an appreciation of written information to take away and consider in their own time.
-
Telephone reinforcement shortly after the health check was successfully used to confirm patient understanding and (re-)confirm specific risk management actions.
-
There is a clear need for training to support practitioners, who reported having no formal training or having generic training that focused on health check processes (e.g. completing the template, operating the PoC testing machine).
Communicating and understanding cardiovascular disease risk using QRISK2 and JBS3 (objectives 1–3)
Table 10 summarises the relative merits of QRISK2 and JBS3 in health checks, which are discussed in turn, before considering themes common to health check in both groups.
| Main finding | QRISK2 | JBS3 | Comment |
|---|---|---|---|
| Overall CVD risk discussion | |||
| Amount of CVD risk discussion | – | + | JBS3 – more discussion of CVDa |
| Both groups – limited overalla | |||
| Patient engagement in discussion | – | + | JBS3 – health checks were less practitioner dominateda |
| JBS3 – more patients asked questionsa | |||
| = | = | Both groups – practitioners missed opportunities to engage patients in discussion of CVD risk and risk managementb | |
| Both groups – minimal responses to CVD risk information (e.g. single-word acknowledgement) in many patientsb | |||
| Risk score communication and understanding | |||
| 10-year risk | – | n/a | Seen as guide for clinical decisions, not tool to discuss CVD riskc |
| Practitioner understanding limited to applying thresholds to relay risk to patients as low/medium/highb,c | |||
| Patients often did not understand the score or its implicationsd | |||
| Event-free survival age | n/a | – | Misunderstood and incorrectly communicated by some practitionersb,c |
| Misunderstood by patientsb,d | |||
| Heart age | n/a | + | Liked by patientsd |
| Liked by practitionersc | |||
| Better perceived understanding and recall of informationb,c,d | |||
| More impactfulb,c,d | |||
| Some questioned the credibility of heart aged | |||
| Risk score manipulation | n/a | + | Liked by patientsd |
| Liked by practitionersc | |||
| Not used optimallyb | |||
| Risk factor discussion | |||
| Causal | + | – | QRISK2 – more discussion of causal risk factorsa |
| Risk management | – | + | JBS3 – more opportunities to initiate risk factor management discussionb |
QRISK2
Communicating CVD risk is central to the NHSHC,17,19 but formed a small part of consultations (< 2 minutes on average). When using QRISK2, practitioners often perceived 10-year risk as a way to identify patients for routine medical follow-up (if risk ≥ 10%), rather than to initiate discussion around patients’ risks and risk management. Consequently, they tended to relay the percentage 10-year risk score and whether it was low (< 10%), medium (10–19%) or high (≥ 20%), without expanding to make clear the relevance to the patient. Minimal patient responses to risk information, particularly for 10-year risk, with a single-word response (e.g. ‘yeah’, ‘OK’) made it difficult for practitioners to gauge patient understanding, which would then allow them to address misunderstandings or concerns. This is important given the evidence that engagement in primary care consultations is linked with patients’ understanding of the consultation and confidence, which has subsequent benefits for recall of information and adherence to recommended treatments. 79
Practitioners reported being confident in communicating 10-year risk, but mainly in application of thresholds (low/medium/high risk). Understanding and confidence to engage in a discussion with patients around what risk means for them was less evident. Perhaps as a result, patients often did not understand CVD risk information, particularly 10-year risk. Again, this is in line with evidence that practitioners who lack confidence are less likely to invite patient engagement in primary care consultations. 79 Our findings confirm the findings of qualitative studies, which have also indicated that practitioner and patient understanding of percentage CVD risk is limited,21 and that practitioners find it difficult to explain CVD risk,26,36–38 resulting in patients leaving health checks unable to recall or with limited understanding of their 10-year risk. 21
JBS3
Practitioners in the JBS3 group were free to use all features of JBS3. However, the minimum requirements in this study were that practitioners communicate heart age and event-free survival age (on the Healthy Years Screen), and manipulate at least one of these risk scores to demonstrate the effect of risk factor changes. QRISK2’s 10-year risk was also delivered as a requirement of the national programme.
Heart age
Practitioners showed patients the on-screen output for heart age, and this was generally preferred to other risk scores. Analysis of health checks and practitioner interviews revealed greater confidence with communicating heart age than with other risk metrics (10-year or event-free survival age). The finding that patients had better understanding and recollection of heart age (than of 10-year risk or event-free survival age) is consistent with the findings from studies of online heart age80 and heart age provided to NHSHC patients (in the form of a risk report). 41
Interview data suggested that the comparison inherent in the concept of heart age (chronological age compared with predicted heart age) allowed patients to quickly appraise whether or not to be concerned by their level of CVD risk. In turn, we observed more pronounced patient responses than for other risk scores – some were ‘shocked’, others were ‘pleased’ or ‘reassured’. Mixed responses depending on results are understandable and have been observed elsewhere. 41,81 Moreover, some patients questioned the credibility of heart age. There is evidence that heart age can prompt consideration of lifestyle change, regardless of the results (younger or older than chronological age) and its perceived credibility. 42,81 This was not necessarily supported by our data, which suggested a dismissal of heart age where it was not seen as credible. This would need further exploration. In any case, variation in preference is in line with the literature24 and highlights the importance of practitioners having different types of risk information (score, visual, analogies, risk manipulation), which they can tailor to patients’ needs and preferences.
In addition to the heart age score, the visual presentation of heart age appeared important for impact and recollection. QRISK2 and 3 also generate heart age, but do not offer a similar visual output. Such visual representations of risk were perceived favourably among our sample, and have been preferred for promoting risk-reducing behaviour. 44
Finally, it is important to be clear about the role of heart age as a form of lifetime risk. The 2014 JBS3 report34 stated that ‘lifetime risk measurement is an adjunct to the estimation of 10-year absolute risk levels. It is intended not primarily as a guide to decisions about drug initiation, but rather as a way of allowing an individual to understand the lifetime risk’. Heart age was not designed to guide clinical decisions,42,82 but our data support its use in health check as a means of promoting patient understanding of CVD risk and a useful prompt for patients to consider lifestyle changes. 42,81
Event-free survival age
Practitioners’ description of the average age to which patients could be expected to survive free from a CVD event was often unclear and sometimes incorrect, which illustrated a lack of understanding of event-free survival. There was evidence that this score was misinterpreted by some practitioners and patients as expected survival age (i.e. age of death). Sometimes the average event-free survival age was relayed to patients correctly during the health check through reading the score from the screen, but subsequent VSR interviews (in the same practitioner) revealed a lack of understanding.
There is a lack of evidence exploring this form of lifetime CVD risk score with which to compare our findings. It appeared from our data that the lack of thresholds (such as those in 10-year risk) or inherent comparison (such as that in heart age) made it difficult for practitioners and patients to interpret event-free survival age as low/medium/high or good/bad. In turn, this risk score generally did not engender much response from patients, who often could not remember it. The graphical representation of event-free survival age was in the form of a visual analogue scale (see Figure 1) with text showing the age. This was not the problem. Patients appeared able to read the result from the display, but often misinterpreted what the figures represented. To be more widely understood, practitioners need training to enable them to better explain event-free survival and communicate its significance unambiguously.
The use of, and response to event-free survival age underline the aforementioned importance of clarity of information such that patients understand and have the confidence to engage in consultations,79 which can then lead to a patient-centred experience. 83 Our data suggest that event-free survival age should not be recommended for use without specific and more substantive training than that provided to practitioners in the RICO study. We provided a verbal explanation during practice initiation visits, written materials and a short video tutorial on how to use JBS3, asked practitioners to practise using JBS3 in health checks in advance of data collection, and were available to answer practitioner questions throughout (in the practice during data collection or by telephone at any time). The decision not to include more intensive training was to allow us to understand how practitioners would use this tool if it were made available for use in NHSHC and has identified an obvious training need.
Cardiovascular disease risk score manipulation
Practitioners liked the risk score manipulation function in JBS3 and thought that it was impactful. Heart age was often the chosen metric for risk manipulation, reiterating practitioner preference for heart age. However, often, it was not used to its potential. The importance of user competence with interactive graphical displays of risk has been noted elsewhere. 23 In the RICO study, practitioners tended not to select the most appropriate risk factor to exemplify the potential risk-reducing benefits of intervention; for example, in non-smoking patients with raised cholesterol, practitioners defaulted to showing increases in risk if they did smoke, which lacked relevance to the patient. Therefore, despite the positive perceptions, it is likely that limited user competence undermined the potential impact of this function in JBS3.
Heart age and risk score manipulation were perceived positively by patients and, if used appropriately, can be used to confer patient understanding of the risk and its severity/relevance. Visual presentation and risk score manipulation offer tools that can accommodate the range of patients, and also to make the important link between lifestyle change and overall CVD risk.
Both groups
Regardless of CVD risk calculator, practitioners rarely asked if patients understood their risk. Patient questions about CVD risk were also rare, but more commonly observed in the JBS3 group (32.0% vs. 12.3%). CVD risk communication and the consultations overall were practitioner dominated, with patients speaking for less than one-quarter of health check time. Processes relating to measurement (CVD risk and lifestyle) and relaying information appeared to take precedence over creating dialogue with patients, who said little in the majority of health checks.
Practitioners usually relied on patient reactions to risk information to gauge understanding. This was limited by a general lack of response, which, unless followed up by the practitioner, can lead to patients failing to understand or recall their risk information. Even in the case studies of patients with positive intentions or outcomes, practitioners rarely explained what CVD risk meant for patients, or checked their understanding (but it mattered less for those patients who were already aware of their need for lifestyle changes, or were motivated to change). Not knowing how the patient is receiving the information limits practitioners’ opportunities to tailor risk information to instigate change.
In turn, there was a lack of tailoring in CVD risk information. Some practitioners admitted to delivering the same information to all patients, recognising that some would understand and some would not. Others said that they adapted the information to the patient. But as patients were not asked if they understood the information presented, there was little opportunity for such adaptation. This is an important limitation. There is no single ‘correct’ way to communicate risk. It depends on individual preferences and understanding, which differ with education, numeracy and personality traits, such as optimism. 24 Tailoring is therefore critical, but impossible unless practitioners know how patients receive the information.
Overall, patients in both groups were given too much information within a short space of time, some of which was irrelevant, limiting their capacity to absorb or retain it. Some expressed an appreciation of written information to take away and consider in their own time. Hawking et al. 41 interviewed patients who were given a personalised risk report to take away from their health check and found that this was mostly well received, often for reassurance, but with potential to motivate lifestyle and discussions and changes with family and friends.
As recognised in the NHSHC competence framework,19 our data confirm that providing patients with a CVD risk score alone is insufficient. There is a challenge for practitioners to facilitate understanding so that patients can appraise their CVD risk information in terms of the severity of the risk (patients with elevated risk recognise it) and the vulnerability to risk (patients not currently at high risk recognise the need for preventative action).
Intentions with respect to health-protective behaviours (objectives 4 and 5)
Patient VSR interviews identified positive changes in most patients including increased awareness or contemplation of risk-reducing behaviour, fostering of positive intentions or implementation of recommendations from the practitioner by making small lifestyle changes. This activity was largely self-reported by patients. Medical record data showed relevant follow-up activity in the 12 weeks post health check in 30% of all patients, most commonly related to blood pressure measurement or discussion (20.2%), followed by lifestyle discussion (9.8%), CVD risk assessment or discussion (9.2%) and cholesterol measurement or discussion (8.7%).
Deductive thematic analysis of verbatim speech during health checks (see Chapter 4) showed that, in consultations using JBS3, there was more evidence of threat appraisal, and facilitators of and response costs to adaptive coping than during consultations using QRISK2. This suggested that health checks using JBS3 could provide more opportunities to initiate risk factor and management discussion than those using QRISK2. The visual presentation (of heart age in particular) and risk manipulation tools in JBS3 did appeal to a range of patients and could help to make the important link between lifestyle change and overall CVD risk. As noted by others,81 some patients identified heart age as a trigger for intentions to reduce their CVD risk; it was understandable and personally relevant, which allowed consideration of lifestyle to reduce their risk, more so than 10-year or lifetime risk.
For risk manipulation, practitioners tended to use heart age to show how changing risk factors can affect the patient’s risk. In some cases, patients referred to this favourably. But as noted above, practitioners defaulting to demonstrating the impact of smoking, regardless of the patient risk factors and smoking status, is likely to limit the potential impact on risk-reducing behavioural intentions. Practitioners were advised that they could use this JBS3 function for preventative messages if patients were low risk; showing how a worsening of lifestyle could increase risk. But relevance to the patients should still be a central consideration of how this is performed.
As CVD risk generally was not explained in detail or discussed with patients, the subsequent or preceding discussion of behaviour change/lifestyle was often not contextualised in terms of reducing CVD risk nor tailored to their preferences or lifestyle. In some health checks, there was a clear separation – patient lifestyle was measured and discussed, with advice for changes, before CVD risk was relayed to patients and without confirming their understanding to make clear the implications (i.e. severity, vulnerability) and link to lifestyle [i.e. to foster discussion of how patients could manage their risk (see Figure 2)].
The most positive examples of health checks fostering risk-reducing intentions and behaviours were patients who were already aware of the need to change, had intentions to change, or had already started to implement changes. In these cases, it was not necessary for practitioners to foster the appraisal of severity of, or vulnerability to CVD risk, and the tailoring of risk management discussion and recommendations was effectively resolved by the patient in advance (e.g. they had identified specific changes, such as excluding certain foods or reducing alcohol consumption). These patients tended to be focused on a specific behaviour (often dietary change) or risk factor (e.g. cholesterol), rather than seeing these as a means of reducing overall CVD risk.
Implications for practice (objective 6)
The NHSHC programme is currently the largest CVD prevention initiative in England. It has come under scrutiny in the absence of evidence for long-term benefits for CVD risk, morbidity and mortality,9–14 but with some favourable predictions for avoidance of disease and premature mortality from a microsimulation study. 15 While an evidence-based review of NHSHC is ongoing5 and changes to the programme will probably follow, face-to-face consultations are necessary to deliver key elements of health check.
Our data gathered from a range of patients attending health checks in general practices that ranged in size and deprivation of the local area have identified a number of ways in which the programme could be improved. Several of the points below (see Table 10) make a case for use of JBS, or certain functions within it, to improve CVD risk communication in NHSHC. Specifically, use of heart age, visual presentations of risk and risk score manipulation appear more beneficial than QRISK2 10-year risk score for engaging patients in CVD risk discussion and conferring understanding of personal risk that might lead to risk-reducing intentions and actions. Other important areas for improvement are common to health checks conducted with either tool.
JBS3’s visual risk presentation and heart age
The visual presentations of risk, such as those in JBS3, are recommended for use in health check. In particular, the heart age output was widely liked and considered impactful. But having a range is useful to accommodate patient preference.
If applied appropriately, manipulation of CVD risk should also be considered as a way to demonstrate to patients the link between their behaviour (and any related recommendations) and their overall CVD risk, but this would need further practitioner training, and observation of application in practice, before effectiveness testing.
Ask patients and tailor
When delivering CVD risk information, practitioners should ask patients about their understanding and how they feel about the information. Knowing how the information is being received would enable the practitioner to provide follow-up information or present risk in different ways to foster patient understanding and appraisal of risk and coping responses (i.e. risk management). This, in turn, can lead to risk-reducing intentions.
One practical approach to operationalise such a change would be for practitioners to record that they have checked patient understanding within the NHSHC template (within the practice system). However, adding to the already substantial list of administrative and clinical tasks could lead to this becoming another process for which there is insufficient time (see Time). Rather, this should be fundamental to the consultation approach, moving away from information provision, and towards shared decision-making. 51 We can consider this in terms of the characteristics of shared decision-making identified by Cipher et al. :83 (1) ‘accurate, objective and comprehensible information’ (i.e. CVD risk); (2) ‘a practitioner who is present and proficient in communication and able to individualise data to a particular situation’; and (3) that the ‘individual’s values, goals, informed preferences, and concerns are incorporated into the communications’. These recommendations identify the need for understandable and tailored CVD risk information and a practitioner who engages the patient in dialogue, which can then lead to discussion of risk management, as part of a two-way interaction.
Time
As discussed in Chapter 3, the time allocated to health checks and how that time is spent should be revisited in the context of what practitioners are expected to achieve.
Patients in our sample reported being provided with too much information, in too short a time. The length of appointments that practices allocated to health checks ranged from 15 to 30 minutes, yet the actual duration of practitioner–patient interaction ranged from 6.8 to 38 minutes (60% lasted < 20 minutes). Health check practitioners have a range of administrative and clinical tasks to complete within this appointment time: CVD risk assessment involving measurement of (and entry of data for) weight, blood pressure and, sometimes, cholesterol through PoC testing; lifestyle assessment (physical activity, alcohol, diet); explaining to patients their CVD risk score(s) and what it means; and patient-centred discussion of risk management to prompt risk-reducing behaviours.
Our data indicated that the health checks were process driven, rather than content focused, and some of the observed features of delivery reflected practitioners working through a series of administrative or clinical processes (e.g. interrupting the conversation, presenting information too quickly, or using inappropriate language). 84,85 Such behaviours reduce the likelihood that information will be understood and retained. 85 This suggests a need to revisit the health check to focus on content and the quality of interactions.
Consultations that involve shared decision-making take time. 85 NICE has endorsed ‘brief’ behaviour change interventions that take several minutes. The NHSHC practitioner competence framework19 refers to the ‘Brief intervention/signposting/referral’ part of the health check (i.e. risk management) as ‘more than a simple communication of information; the person signposting must be able to engage the client in the choice and communicate in a manner that will maximise the potential that the client will take up the agreed action and sustain’ (p. 23; contains public sector information licensed under the Open Government Licence v3.0). Therefore, even if the risk management discussion is brief, it should be delivered by practitioners with appropriate training, who are able to engage patients in designing their own risk management plan, thus tailoring it to patient needs. 86 However, NICE also recommends ‘extended brief interventions’, lasting ≥ 30 minutes, and potentially lasting several sessions;86 and motivational interviewing, which also features in the NHSHC competence framework, can require ≥ 15 minutes to be effective.
A short, practitioner-dominated health check might be sufficient when patients attend with motivation and ideas/actions about changes they need or want to make. If this appraisal has not taken place in advance, it is the role of, and challenge for, the practitioner to present CVD risk information that facilitates this patient appraisal, helping them towards risk-reducing intentions and behaviour. In this case, a short, practitioner-dominated health check in which CVD was risk neither well explained nor understood, is unlikely to be effective.
Therefore, our data suggest that:
-
some health checks appear too short to accommodate all health check tasks in a patient-centred manner
-
more time should be allocated to explaining CVD risk, allowing practitioners to check patient understanding and to tailor risk information using the appropriate tool for that patient
-
sufficient time should be allowed for practitioners and patients to co-produce a specific, relevant and meaningful risk management strategy.
This could be achieved through increasing the overall time available to health check or by reducing the number of administrative and clinical tasks required, and practitioners should be supported with appropriate training (see below).
Telephone reinforcement
Follow-up telephone calls to patients soon after the health check, by the practitioners who delivered the health check or other clinical staff with the required knowledge and skills, should confer a range of benefits:
-
patients have time to reflect on the health check and identify questions or areas of uncertainty
-
practitioners can provide further explanation of CVD risk, answer questions and reaffirm patient understanding
-
practitioners can confirm recommendations for risk management, making specific plans where appropriate (e.g. referrals, follow-up appointments, further measurement).
Such telephone reinforcement has been used in physical activity interventions to improve participant perceptions of the target behaviour87 and promote maintenance of that behaviour if used as part of an ongoing negotiated follow-up. 88 This has resource implications that are likely to be justified, but would need to be explored. For patients who do not require it, the call could be short and the resource implications modest. Others will need more time to revisit health check content and agree risk management.
Practitioner training
An overarching theme that cuts across all of the above implications for practice is the need to support practitioners (HCAs and PNs) with appropriate and specific training to ensure that practitioners know what they need to do in health checks, that they are confident and have the necessary knowledge and skills, and that they are supported with ongoing training to promote continued improvements in delivery. The Best Practice Guidance17 and practitioner competence framework19 set out high expectations. As the aim is to have consultations that are patient centred, for which shared decision-making has been described as the ‘pinnacle’,89 patients should be involved in the co-design of practitioner training. 90 Therefore, findings from this study highlight two training needs. First, there is a need for training to address the apparent knowledge deficit around different types of CVD risk. Here and elsewhere,21,91 it is clear that those delivering health checks either do not receive any training specific to conduct CVD risk measurement and how to communicate risk scores to patients or receive generic training that is focused on health check processes (e.g. completing the template, operating the PoC testing machine). Second, PNs and HCAs do not receive training in communication skills, such as those included in medical training. Our data have uncovered a previous ‘unknown unknown’ about a lack of communication skills in the context of real-world patient-centred risk communication and risk management discussion. The communication skills content of undergraduate and postgraduate nurse training and training of HCAs should, therefore, be evaluated in relation to this need.
Reflexivity
In qualitative research, it is important to consider the interpretive role of researchers in both data collection and analysis. 92 Willig93 notes that ‘Reflexivity is important in qualitative research because it encourages us to foreground, and reflect upon, the ways in which the person of the researchers is implicated in the research ad its findings’ (p. 18). Subsequently, the researchers engaged in reflexive practice throughout the study to ensure that they engaged with, and articulated, their positions as researchers and were aware of how their backgrounds, viewpoints, and experiences may have impacted on their interpretations of data. 94
All data collection and the majority of data analysis were conducted by two white female researchers: a qualified Health Psychologist and Lecturer in Health Psychology (LC; DPsych) and a Research Associate (VR; MSc). Lisa Cowap had wide-ranging prior research experience (e.g. children’s healthy eating, smoking), which included some research into uptake in NHSHC (in 2014). Victoria Riley had previous research experience in pregnancy and body image, and was completing a doctorate around NHSHC uptake and risk communication (including training practitioners to improve risk communication). Victoria Riley’s specific, relevant experience and knowledge could have meant that she approached the data collection and analysis differently to Lisa Cowap (who was less knowledgeable of NHSHC at the outset). However, prior knowledge of the programme was beneficial in overcoming the many challenges that arose during recruitment and data collection.
In relation to VSR interviews, both researchers had experience in relevant data collection methods (i.e. semistructured interviews, focus groups), interview techniques (i.e. face-to-face, telephone interviews) and qualitative methodologies (i.e. thematic analysis, grounded theory, interpretative phenomenological analysis), and with a variety of participant samples [i.e. children, students, adults (LC), adults, patients, practitioners, commissioners (VR); individuals from ethnically diverse backgrounds and various levels of social deprivation (LC and VR)]. In the RICO study, male and female participants were recruited from different localities across the West Midlands, resulting in a diverse sample from different socioeconomic and ethnic backgrounds, sometimes differing from the sex and background of the researchers, which may have influenced participant responses during data collection. 95 Barrett et al. 94 note the importance of challenging and articulating social and cultural influences and dynamics, and we reflected on how social context may have affected what participants shared with us. To maximise disclosure and to enable participants to feel as comfortable as possible, interviews were conducted in locations of the patients’ choosing (the general practice or their home), ensuring that they were comfortable and felt able to speak freely.
Data analysis was initially conducted by both researchers (both together and independently by LC following VR’s commencement of maternity leave) before verification by another member of the research team to check that themes were clear and comprehensive. 96 Two additional researchers and doctoral students, Sophia Fedorowicz (MSc) and Sian Calvert (MSc), were brought in to help with analysis of the deductively coded health checks and the VSR practitioner interviews, respectively. Both were young, white, female doctoral students without prior knowledge of the NHSHC programme who had substantial qualitative research experience in their respective areas of health psychology.
Finally, all themes were discussed and agreed over the telephone and over e-mail with other members of the multidisciplinary team of principal and co-investigators. This drew on a variety of backgrounds, including psychology, public health, health services research and general practice, to ensure that a range of perspectives on the data were taken into account to validate the themes throughout analysis.
Strengths and limitations
This study has 10 key strengths:
-
Video-recording of health checks provided the first objective account of health checks for detailed quantitative and qualitative analysis.
-
Data were collected across a diverse range of practices stratified by deprivation, with patient recruitment stratified by age, sex and ethnicity.
-
The comprehensive coding framework with excellent inter-rater reliability offers a methodological contribution for quantitatively describing health checks.
-
The sample sizes for the qualitative analyses were large (128 for deductive qualitative analysis of health checks, 40 for inductive thematic analysis of VSR patient interviews, 15 for inductive analysis of VSR practitioner interviews).
-
Deductive analysis of video-recorded health check was guided by the theoretically strong PMT framework, which was augmented through initial inductive coding.
-
VSR interviews were a novel way to allow participants to recall and reflect on the health checks, how they felt at that time, and their perceptions subsequently.
-
Case studies drew on six sources of data to explore in detail why some health checks appeared to lead to positive patient intentions or actions.
-
Our multifaceted PPI approach, including a virtual group that reached over 270 members of the public, allowed patient/public input on specific issues throughout at both operational and management levels.
-
Our multidisciplinary team of health psychologists, primary care researchers, applied health researchers and clinicians provided the necessary range of expertise.
-
Collecting data using a range of methods highlighted some strong, consistent findings on which to base recommendations.
A number of limitations were recognised:
-
Challenges with practice and patient recruitment meant that we did not achieve our target sample size of 240 (120 per group) and had an imbalance between groups. Changes to the recruitment processes requested by the Health Research Authority (HRA) resulted in a reliance on general practice teams (rather than CRN) to contact patients who did not respond to initial postal invitations. To mitigate the poor response, the size of initial mail-outs was increased and practice staff were offered support when telephoning potential participants, but this was unsuccessful in a number of practices that under-recruited. The poor response rate could have introduced bias through self-selection of patients who were not representative of the wider NHSHC patient population. A larger sample size might have identified more marked between-group differences through increasing the precision of our estimates for quantitative comparisons (i.e. narrowing CIs).
-
There was a between-group difference in mean age. Given the importance of age in determining 10-year risk scores, there was a potential that this age difference would create statistical differences in the CVD risk profiles of each group, but this was not evident.
-
Uptake of VSR interviews among patients did not permit stratification by age, sex and CVD risk as planned (see Table 2). In practices where overall recruitment was low, all patients who consented to VSR interviews were recruited. The resulting sample did, however, provide representation across age groups, males/females and CVD risk, but was less balanced than intended. For example, compared with the overall sample, there were smaller proportions of medium-high CVD risk patients and those from ethnic minority groups (see Table 9).
-
The lack of specific discussion around the risk scores and subsequent patient responses made it difficult to apply the PMT framework effectively (the framework required researchers to classify the response as positive or negative). Thus, a third ‘neutral’ classification was added to the framework and applied where appropriate. To mitigate the risk of misclassifying, the video-recordings could be consulted to determine the level of engagement, which might not be evident from transcripts alone.
-
Through observations of recorded health checks and VSR interviews, it is difficult to distinguish between patient understanding of the risk itself (i.e. what the score meant) and the risk in context (i.e. risk relative to others of similar age), and the ability of the information to motivate change (based on interview transcripts available). Related inferences were made from drawing on the multiple data sources.
-
After commencing data collection, we discovered that two QRISK2 practices used Informatica, an addition to practice software that has some of the JBS3 functionalities. The researchers were unaware of this addition and were not informed of its use throughout the numerous calls and practice visits during the recruitment and initiation stages with each practice. Use of QRISK2 + Informatica may have enhanced these consultations. To maintain the ecological validity of a ‘usual-care’ group, the 34 patients from these practices were retained and corresponding quotations were labelled to reflect use of Informatica in the reporting (‘QRISK2+’).
-
We cannot claim that our results are generalisable to the rest of England. However, through our stratified recruitment (where possible), we obtained a good balance of males and females, a good age range, representation across socioeconomic groups (based on deprivation) and proportions of white British and ethnic minority groups that were appropriate for the region.
-
It is possible that being video-recorded affected practitioner behaviour (Hawthorne effect). 97 To mitigate this, our PPI explored camera position to best capture patient response and minimise practitioner awareness of the camera. Practitioners in mock health checks reported forgetting about the camera during consultations. The Hawthorne effect tends to improve performance,97 which would mean that any effect would lead to an underestimate of challenges with health check delivery.
-
Most patient and practitioner VSR interviews were conducted in the general practices. It is possible that this context introduced some social desirability bias.
Implications for further research
Areas for further research include the following:
-
There is a clear need to explore specific practitioner competencies and patient needs to inform development of training, ideally co-designed with patients and practitioners. This could include a review of practitioner competencies covered in their basic training (e.g. undergraduate and postgraduate nursing), the fit with health check requirements and working with practitioners and patients to develop and test training.
-
Research should explore the reallocation of time during health checks, perhaps revisiting the processes currently mandated within consultations. As the national programme is under review, this could extend to exploring alternative types of consultations (e.g. online) in addition to evidence-based redesign of face-to-face health check consultations.
-
Qualitative methods and effectiveness trials could further explore use of heart age in health checks. Qualitative work could also be used to understand and help to overcome the challenges that practitioners clearly faced in understanding and communicating other lifetime risk metrics (e.g. event-free survival age), with quantitative assessment of benefits for patient outcomes.
-
Explore the benefits of telephone reinforcement of health checks in terms of patient understanding and retention of information, and subsequent intentions and implementation of recommendations. A health economic evaluation could be used to explore the benefits for patient outcomes versus the additional resource implications of making telephone calls.
Summary
Communication of CVD risk in health checks was brief, particularly in consultations supported by QRISK2. Patient understanding of, and responses to, CVD risk information were limited. Practitioners often missed opportunities to check patient understanding that could allow an appraisal of risk to encourage risk-reducing intentions and behaviour. Some aspects of JBS3 appeared to better promote opportunities to initiate discussion of risk factors and particularly their heart age, visual representation of risk and risk score manipulation, which were more easily understood and impactful than QRISK2. The apparent lack of effective CVD risk discussion in both groups resulted in misunderstandings, practitioner-dominated discussion and increased likelihood of a maladaptive coping response.
Data from the RICO study have brought to light some fundamental issues with delivery, regardless of which risk calculator was used. Addressing these issues could be expected to have considerable benefit for patient understanding of their CVD risk, the personal relevance of the information (vulnerability and severity), the link between overall risk and lifestyle, and what specific changes they could personally make to manage that risk.
Acknowledgements
We would like to thank all the participating general practices, practitioners and patients. We are grateful for the support of Clinical Research Network West Midlands, and all those who contributed to PPI activities, including the virtual PPI group who provided ongoing feedback on various aspects of study design, materials and data collection. We wish to thank the Programme Advisory Board for its oversight and support of the study. Thanks also go to Zoe Paskins for advising on VSR methods, and Sophia Fedorowicz and Sian Calvert for contributing to qualitative analysis.
Contributions of authors
Christopher J Gidlow (https://orcid.org/0000-0003-4990-4572) (Professor of Applied Health Research) led the grant application, and the conduct and reporting of all aspects of the study as principal investigator.
Naomi J Ellis (https://orcid.org/0000-0003-1909-4169) (Senior Lecturer in Physical Activity and Health) contributed to the grant application, protocol writing, led PPI and contributed to qualitative data analysis.
Lisa Cowap (https://orcid.org/0000-0002-8876-0260) (Lecturer in Psychology) co-ordinated day-to-day research activities in data collection and analysis, and contributed to reporting.
Victoria Riley (https://orcid.org/0000-0002-7981-0094) (Research Associate) undertook day-to-day research activities in data collection and analysis, and contributed to reporting.
Diane Crone (https://orcid.org/0000-0002-8798-2929) (Professor of Exercise and Health) contributed to the grant application, protocol writing and advised on qualitative analyses.
Elizabeth Cottrell (https://orcid.org/0000-0002-5757-1854) (GP and NIHR Academic Clinical Lecturer in Primary Care) contributed to the grant application, processing of patient medical records, development of case studies and advised on qualitative analyses.
Sarah Grogan (https://orcid.org/0000-0002-7510-765X) (Professor of Psychology Health and Wellbeing) contributed to the grant application, protocol writing and advised on all aspects of qualitative methods.
Ruth Chambers OBE (https://orcid.org/0000-0003-3980-7533) (GP and Director of Stoke-on-Trent Clinical Commissioning Group) contributed to the grant application and provided clinical input on all aspects of the study.
David Clark-Carter (https://orcid.org/0000-0002-1993-7050) (Professor of Psychological Research Methods) led statistical analysis of health checks and supervised all statistical analyses.
All authors contributed to the final report.
Publications
Gidlow CJ, Ellis NJ, Cowap L, Riley V, Crone D, Cottrell E, et al. A qualitative study of cardiovascular disease risk communication in NHS Health Check using different risk calculators: protocol for the RIsk COmmunication in NHS Health Check (RICO) study. BMC Fam Pract 2019;20:11.
Gidlow CJ, Ellis NJ, Cowap L, Riley VA, Crone D, Cottrell E, et al. Quantitative examination of video-recorded NHS Health Checks: comparison of the use of QRISK2 versus JBS3 cardiovascular risk calculators. BMJ Open 2020;10:e037790.
Riley V, Ellis NJ, Cowap L, Grogan S, Cottrell E, Crone D, et al. A qualitative exploration of two risk calculators using video-recorded NHS Health Check consultations. BMC Fam Pract 2020;21:250.
Gidlow CJ, Ellis NJ, Riley VA, Cowap L, Grogan S, Cottrell E, et al. Cardiovascular disease risk communication in NHS Health Checks: a qualitative video-stimulated recall interview study with practitioners. BJGP OPEN 2021;BJGPO.2021.0049.
Data-sharing statement
The data generated by this qualitative study are not suitable for sharing beyond that presented in this report. Most data are in the form of interview transcripts, which present ethics challenges regarding data-sharing for secondary analysis (e.g. threats to participant anonymity; unknown future use of data in relation to original participant consent and ethics approvals). 98 For more information please contact the corresponding author.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care.
References
- Gidlow CJ, Ellis NJ, Cowap L, Riley V, Crone D, Cottrell E, et al. A qualitative study of cardiovascular disease risk communication in NHS Health Check using different risk calculators: protocol for the RIsk COmmunication in NHS Health Check (RICO) study. BMC Fam Pract 2019;20. https://doi.org/10.1186/s12875-018-0897-0.
- Wilkins E, Wilson L, Wickramasinghe K, Bhatnagar P, Leal J, Luengo-Fernandez R, et al. European Cardiovascular Disease Statistics 2017. Brussels: European Heart Network; 2017.
- Bhatnagar P, Wickramasinghe K, Wilkins E, Townsend N. Trends in the epidemiology of cardiovascular disease in the UK. Heart 2016;102:1945-52. https://doi.org/10.1136/heartjnl-2016-309573.
- National Health Service . The NHS Long Term Plan 2019. www.longtermplan.nhs.uk/publication/nhs-long-term-plan/ (accessed 1 April 2020).
- Cabinet Office and Department of Health and Social Care (DHSC) . Advancing Our Health: Prevention in the 2020s – Consultation Document 2019.
- Department of Health and Social Care (DHSC) . Putting Prevention First. NHS Health Check: Vascular Risk Assessment and Management Best Practice Guidance 2009.
- Robson J, Dostal I, Sheikh A, Eldridge S, Madurasinghe V, Griffiths C, et al. The NHS Health Check in England: an evaluation of the first 4 years. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-008840.
- Forster AS, Burgess C, Dodhia H, Fuller F, Miller J, McDermott L, et al. Do health checks improve risk factor detection in primary care? Matched cohort study using electronic health records. J Public Health 2016;38:552-9. https://doi.org/10.1093/pubmed/fdv119.
- Soureti A, Hurling R, Murray P, van Mechelen W, Cobain M. Evaluation of a cardiovascular disease risk assessment tool for the promotion of healthier lifestyles. Eur J Cardiovasc Prev Rehabil 2010;17:519-23. https://doi.org/10.1097/HJR.0b013e328337ccd3.
- Gøtzsche PC, Jørgensen KJ, Krogsbøll LT. General health checks don’t work. BMJ 2014;348. https://doi.org/10.1136/bmj.g3680.
- Caley M, Chohan P, Hooper J, Wright N. The impact of NHS Health Checks on the prevalence of disease in general practices: a controlled study. Br J Gen Pract 2014;64:e516-21. https://doi.org/10.3399/bjgp14X681013.
- Si S, Moss JR, Sullivan TR, Newton SS, Stocks NP. Effectiveness of general practice-based health checks: a systematic review and meta-analysis. Br J Gen Pract 2014;64:e47-53. https://doi.org/10.3399/bjgp14X676456.
- Chang KC, Lee JT, Vamos EP, Soljak M, Johnston D, Khunti K, et al. Impact of the National Health Service Health Check on cardiovascular disease risk: a difference-in-differences matching analysis. CMAJ 2016;188:E228-38. https://doi.org/10.1503/cmaj.151201.
- Krogsbøll LT, Jørgensen KJ, Grønhøj Larsen C, Gøtzsche PC. General health checks in adults for reducing morbidity and mortality from disease: Cochrane systematic review and meta-analysis. BMJ 2012;345. https://doi.org/10.1136/bmj.e7191.
- Mytton OT, Jackson C, Steinacher A, Goodman A, Langenberg C, Griffin S, et al. The current and potential health benefits of the National Health Service Health Check cardiovascular disease prevention programme in England: a microsimulation study. PLOS Med 2018;15. https://doi.org/10.1371/journal.pmed.1002517.
- Kypridemos C, Allen K, Hickey GL, Guzman-Castillo M, Bandosz P, Buchan I, et al. Cardiovascular screening to reduce the burden from cardiovascular disease: microsimulation study to quantify policy options. BMJ 2016;353. https://doi.org/10.1136/bmj.i2793.
- Public Health England (PHE) . NHS Health Check Best Practice Guidance 2017.
- Public Health England (PHE) . NHS Health Check Competence Framework 2015.
- Public Health England (PHE) . NHS Health Check Competency Framework. Updated July 2020 2020.
- Public Health England . Draft South East Framework to Support COVID 19: Transition Planning for Multiple Exclusion Homelessness 2020.
- Usher-Smith J, Mant J, Martin A, Harte E, MacLure C, Meads C, et al. NHS Health Check Programme Rapid Evidence Synthesis. Cambridge: University of Cambridge; 2017.
- Asan O, Montague E. Using video-based observation research methods in primary care health encounters to evaluate complex interactions. Inform Prim Care 2014;21:161-70. https://doi.org/10.14236/jhi.v21i4.72.
- Spiegelhalter D, Pearson M, Short I. Visualizing uncertainty about the future. Science 2011;333:1393-400. https://doi.org/10.1126/science.1191181.
- Beswick A, Brindle P, Fahey T, Ebrahim S. A Systematic Review of Risk Scoring Methods and Clinical Decision Aids Used in the Primary Prevention of Coronary Heart Disease. (Supplement) [Internet]. London: Royal College of General Practitioners; 2008.
- Edwards A, Elwyn G, Covey J, Matthews E, Pill R. Presenting risk information – a review of the effects of “framing” and other manipulations on patient outcomes. J Health Commun 2001;6:61-82. https://doi.org/10.1080/10810730150501413.
- Gigerenzer G, Edwards A. Simple tools for understanding risks: from innumeracy to insight. BMJ 2003;327:741-4. https://doi.org/10.1136/bmj.327.7417.741.
- Gigerenzer G, Gaissmaier W, Kurz-Milcke E, Schwartz LM, Woloshin S. Helping doctors and patients make sense of health statistics. Psychol Sci Public Interest 2007;8:53-96. https://doi.org/10.1111/j.1539-6053.2008.00033.x.
- Goodyear-Smith F, Arroll B, Chan L, Jackson R, Wells S, Kenealy T. Patients prefer pictures to numbers to express cardiovascular benefit from treatment. Ann Fam Med 2008;6:213-17. https://doi.org/10.1370/afm.795.
- Thomson R, Edwards A, Grey J. Risk communication in the clinical consultation. Clinical Med (Lond) 2005;5:465-9. https://doi.org/10.7861/clinmedicine.5-5-465.
- Ahl AS, Acree JA, Gipson PS, McDowell RM, Miller L, McElvaine MD. Standardization of nomenclature for animal health risk analysis. Rev Sci Tech 1993;12:1045-53. https://doi.org/10.20506/rst.12.4.744.
- Wells S, Kerr A, Broadbent E, MacKenzie C, Cole K, McLachlan A. Does Your Heart Forecast help practitioner understanding and confidence with cardiovascular disease risk communication?. J Prim Health Care 2011;3:4-9. https://doi.org/10.1071/HC11004.
- Bonner C, Jansen J, McKinn S, Irwig L, Doust J, Glasziou P, et al. Communicating cardiovascular disease risk: an interview study of General Practitioners’ use of absolute risk within tailored communication strategies. BMC Fam Pract 2014;15. https://doi.org/10.1186/1471-2296-15-106.
- National Institute for Health and Care Excellence (NICE) . Cardiovascular Disease: Risk Assessment and Reduction, Including Lipid Modification. Clinical Guideline [CG181] 2015.
- JBS3 Board . Joint British Societies’ consensus recommendations for the prevention of cardiovascular disease (JBS3). Heart 2014;100:ii1-ii67. https://doi.org/10.1136/heartjnl-2014-305693.
- Karmali KN, Lloyd-Jones DM. Adding a life-course perspective to cardiovascular-risk communication. Nat Rev Cardiol 2013;10:111-15. https://doi.org/10.1038/nrcardio.2012.185.
- Gigerenzer G, Hoffrage U. How to improve Bayesian reasoning without instruction: frequency formats. Psychol Rev 1995;102:684-70. https://doi.org/10.1037/0033-295X.102.4.684.
- Hoffrage U, Gigerenzer G. Using natural frequencies to improve diagnostic inferences. Acad Med 1998;73:538-40. https://doi.org/10.1097/00001888-199805000-00024.
- Slovic P, Monahan J, MacGregor DG. Violence risk assessment and risk communication: the effects of using actual cases, providing instruction, and employing probability versus frequency formats. Law Hum Behav 2000;24:271-96. https://doi.org/10.1023/a:1005595519944.
- Johns I, Moschonas KE, Medina J, Ossei-Gerning N, Kassianos G, Halcox JP. Risk classification in primary prevention of CVD according to QRISK2 and JBS3 ‘heart age’, and prevalence of elevated high-sensitivity C reactive protein in the UK cohort of the EURIKA study. Open Heart 2018;5. https://doi.org/10.1136/openhrt-2018-000849.
- JBS3 Joint British Societies for the prevention of cardiovascular disease . Risk Calculator 2014. www.jbs3risk.com/pages/risk_calculator.htm (accessed 15 May 2019).
- Hawking MKD, Timmis A, Wilkins F, Potter JL, Robson J. Improving cardiovascular disease risk communication in NHS Health Checks: a qualitative study. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2018-026058.
- Bonner C, Bell K, Jansen J, Glasziou P, Irwig L, Doust J, et al. Should heart age calculators be used alongside absolute cardiovascular disease risk assessment?. BMC Cardiovasc Disord 2018;18. https://doi.org/10.1186/s12872-018-0760-1.
- Kulendrarajah B, Grey A, Nunan D. How effective are ‘age’ tools at changing patient behaviour? A rapid review. BMJ Evid Based Med 2020;25:1-2. https://doi.org/10.1136/bmjebm-2019-111244.
- Waldron CA, van der Weijden T, Ludt S, Gallacher J, Elwyn G. What are effective strategies to communicate cardiovascular risk information to patients? A systematic review. Patient Educ Couns 2011;82:169-81. https://doi.org/10.1016/j.pec.2010.04.014.
- Ancker JS, Weber EU, Kukafka R. Effects of game-like interactive graphics on risk perceptions and decisions. Med Decis Making 2011;31:130-42. https://doi.org/10.1177/0272989X10364847.
- Pawlikowska T, Zhang W, Griffiths F, van Dalen J, van der Vleuten C. Verbal and non-verbal behavior of doctors and patients in primary care consultations – how this relates to patient enablement. Patient Educ Couns 2012;86:70-6. https://doi.org/10.1016/j.pec.2011.04.019.
- Howie JG, Heaney DJ, Maxwell M. Measuring quality in general practice. Pilot study of a needs, process and outcome measure. Occas Pap R Coll Gen Pract 1997;75.
- Street RL, Makoul G, Arora NK, Epstein RM. How does communication heal? Pathways linking clinician-patient communication to health outcomes. Patient Educ Couns 2009;74:295-301. https://doi.org/10.1016/j.pec.2008.11.015.
- Roter DL, Stewart M, Putnam SM, Lipkin M, Stiles W, Inui TS. Communication patterns of primary care physicians. JAMA 1997;277:350-6. https://doi.org/10.1001/jama.1997.03540280088045.
- Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open 2013;3. https://doi.org/10.1136/bmjopen-2012-001570.
- NHS . Shared Decision Making 2019. www.england.nhs.uk/shared-decision-making/ (accessed 20 November 2019).
- Paskins Z, McHugh G, Hassell AB. Getting under the skin of the primary care consultation using video stimulated recall: a systematic review. BMC Med Res Methodol 2014;14. https://doi.org/10.1186/1471-2288-14-101.
- Henry SG, Fetters MD. Video elicitation interviews: a qualitative research method for investigating physician–patient interactions. Ann Fam Med 2012;10:118-25. https://doi.org/10.1370/afm.1339.
- Floyd DL, Prentice-Dunn S, Rogers RW. A meta-analysis of research on protection motivation theory. J Appl Soc Psychol 2000;30:407-29. https://doi.org/10.1111/j.1559-1816.2000.tb02323.x.
- Plotnikoff RC, Rhodes RE, Trinh L. Protection motivation theory and physical activity: a longitudinal test among a representative population sample of Canadian adults. J Health Psychol 2009;14:1119-34. https://doi.org/10.1177/1359105309342301.
- Conner M, Norman P. Predicting Health Behaviour: Research and Practice with Social Cognition Models. Maidenhead: Open University Press; 2015.
- Ritland R, Rodriguez L. The influence of antiobesity media content on intention to eat healthily and exercise: a test of the ordered protection motivation theory. J Obes 2014;2014. https://doi.org/10.1155/2014/954784.
- Armitage CJ, Sheeran P, Conner M, Arden MA. Stages of change or changes of stage? Predicting transitions in transtheoretical model stages in relation to healthy food choice. J Consult Clin Psychol 2004;72:491-9. https://doi.org/10.1037/0022-006X.72.3.491.
- Aguiar EJ, Morgan PJ, Collins CE, Plotnikoff RC, Callister R. Efficacy of interventions that include diet, aerobic and resistance training components for type 2 diabetes prevention: a systematic review with meta-analysis. Int J Behav Nutr Phys Act 2014;11. https://doi.org/10.1186/1479-5868-11-2.
- Munro S, Lewin S, Swart T, Volmink J. A review of health behaviour theories: how useful are these for developing interventions to promote long-term medication adherence for TB and HIV/AIDS?. BMC Public Health 2007;7. https://doi.org/10.1186/1471-2458-7-104.
- Department for Communities and Local Government (DCLG) . The English Indices of Deprivation 2010 2010.
- Department of Communities and Local Government (DCLG) . The English Indices of Deprivation 2015 Research Report 2015.
- Keyworth C, Nelson PA, Chew-Graham CA, Kane K, Pearce CJ, Griffiths CE, et al. Communicating cardiovascular disease risk to people with psoriasis: what techniques do practitioners use?. Int J Behav Med 2015;21:1-11.
- Paskins Z, Sanders T, Croft PR, Hassell AB. The identity crisis of osteoarthritis in general practice: a qualitative study using video-stimulated recall. Ann Fam Med 2015;13:537-44. https://doi.org/10.1370/afm.1866.
- Fereday J, Muir-Cochrane E. Demonstrating rigor using thematic analysis: a hybrid approach of inductive and deductive coding and theme development. Int J Qual Methods 2006;5:80-92. https://doi.org/10.1177/160940690600500107.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Edwards-Jones A. Qualitative data analysis with NVIVO. J Educ Teach 2014;40:193-5. https://doi.org/10.1080/02607476.2013.866724.
- Fleiss JL, Levin B, Paik MC, Fleiss JL, Levin B, Paik MC. Statistical Methods for Rates and Proportions. New York, NY: John Wiley & Sons Inc.; 2003.
- Sim J, Saunders B, Waterfield J, Kingstone T. Can sample size in qualitative research be determined a priori?. Int J Soc Res Methodol 2018;21:619-34. https://doi.org/10.1080/13645579.2018.1454643.
- Blaikie N. Confounding issues related to determining sample size in qualitative research. Int J Soc Res Methodol 2018;21:635-41. https://doi.org/10.1080/13645579.2018.1454644.
- NHS Digital . NHS Health Check Programme. Patients Recorded As Attending and Not Attending Financial Years: 2012–13 to 2017–18. Experimental Statistics 2019. https://digital.nhs.uk/data-and-information/publications/statistical/nhs-health-check-programme/2012-13-to-2017-18 (accessed 10 November 2019).
- Gidlow CJ, Ellis NJ, Cowap L, Riley VA, Crone D, Cottrell E, et al. Quantitative examination of video-recorded NHS Health Checks: comparison of the use of QRISK2 versus JBS3 cardiovascular risk calculators. BMJ Open 2020;10. https://doi.org/10.1136/bmjopen-2020-037790.
- Public Health England . National General Practice Profiles 2019. https://fingertips.phe.org.uk/profile/general-practice/data (accessed 1 May 2018).
- Informatica Systems . HealthChecks+ 2020. www.informatica-systems.co.uk/healthchecks/ (accessed 1 April 2020).
- Gidlow CJ, Ellis NJ, Riley VA, Cowap L, Grogan S, Cottrell E, et al. Cardiovascular disease risk communication in NHS Health Checks: a qualitative video-stimulated recall interview study with practitioners. BJGP OPEN 2021. https://doi.org/10.3399/BJGPO.2021.0049.
- Riley V, Ellis NJ, Cowap L, Grogan S, Cottrell E, Crone D, et al. A qualitative exploration of two risk calculators using video-recorded NHS Health Check consultations. BMC Fam Pract 2020;21. https://doi.org/10.1186/s12875-020-01315-6.
- Ancker JS, Senathirajah Y, Kukafka R, Starren JB. Design features of graphs in health risk communication: a systematic review. J Am Med Inform Assoc 2006;13:608-18. https://doi.org/10.1197/jamia.M2115.
- Scott LB, Curbow B. The effect of message frames and CVD risk factors on behavioral outcomes. Am J Health Behav 2006;30:582-97. https://doi.org/10.5555/ajhb.2006.30.6.582.
- Parsons S, Winterbottom A, Cross P, Redding D. The Quality of Patient Engagement and Involvement in Primary Care. London: The King’s Fund; 2010.
- Bonner C, Fajardo MA, Hui S, Stubbs R, Trevena L. Clinical Validity, Understandability, and Actionability of online cardiovascular disease risk calculators: systematic review. J Med Internet Res 2018;20. https://doi.org/10.2196/jmir.8538.
- Bonner C, Jansen J, Newell BR, Irwig L, Glasziou P, Doust J, et al. I don’t believe it, but i’d better do something about it: patient experiences of online heart age risk calculators. J Med Internet Res 2014;16. https://doi.org/10.2196/jmir.3190.
- Bonner C, McKinn S, McCaffrey K, Glasziou P, Irwig L, Doust J, et al. Is the NHS ‘Heart Age Test’ too much medicine?. Br J Gen Pract 2019;69:560-1. https://doi.org/10.3399/bjgp19X706349.
- Cypher RL. Shared decision-making: a model for effective communication and patient satisfaction. J Perinat Neonatal Nurs 2019;33:285-7. https://doi.org/10.1097/JPN.0000000000000441.
- Singh Ospina N, Phillips KA, Rodriguez-Gutierrez R, Castaneda-Guarderas A, Gionfriddo MR, Branda ME, et al. Eliciting the patient’s agenda- secondary analysis of recorded clinical encounters. J Gen Intern Med 2019;34:36-40. https://doi.org/10.1007/s11606-018-4540-5.
- Pieterse AH, Stiggelbout AM, Montori VM. Shared decision making and the importance of time. JAMA 2019;322:25-6. https://doi.org/10.1001/jama.2019.3785.
- National Institute for Health and Care Excellence (NICE) . Public Health Draft Guidance: Behaviour Change 2017.
- Ory MG, Lee Smith M, Mier N, Wernicke MM. The science of sustaining health behavior change: the health maintenance consortium. Am J Health Behav 2010;34:647-59. https://doi.org/10.5993/AJHB.34.6.2.
- Desai PM, Hughes SL, Peters KE, Mermelstein RJ. Impact of telephone reinforcement and negotiated contracts on behavioral predictors of exercise maintenance in older adults with osteoarthritis. Am J Health Behav 2014;38:465-77. https://doi.org/10.5993/AJHB.38.3.15.
- Barry MJ, Edgman-Levitan S. Shared decision making – pinnacle of patient-centered care. N Engl J Med 2012;366:780-1. https://doi.org/10.1056/NEJMp1109283.
- Robert G, Cornwell J, Locock L, Purushotham A, Sturmey G, Gager M. Patients and staff as codesigners of healthcare services. BMJ 2015;350. https://doi.org/10.1136/bmj.g7714.
- Riley VA, Gidlow C, Ellis NJ, Povey RJ, Barnes O, Clark-Carter D. Improving cardiovascular disease risk communication in the UK national health service health check programme. Patient Educ Couns 2019;102:2016-23. https://doi.org/10.1016/j.pec.2019.05.014.
- Finlay L, Gough B. Reflexivity: A Practical Guide for Researchers in Health and Social Sciences. Oxford: Blackwell Publishing Ltd; 2003.
- Willig C. Introducing Qualitative Research in Psychology. Maidenhead: Open University Press; 2008.
- Barrett A, Kajamaa A, Johnston J. How to . . . be reflexive when conducting qualitative research. Clin Teach 2020;17:9-12. https://doi.org/10.1111/tct.13133.
- Willig C. Introducing Qualitative Research in Psychology. Maidenhead: Open University Press; 2013.
- King N, Cassell C, Symon G, Cassell C, Symon G. Essential Guide to Qualitative Methods in Organizational Research. Newbury Park, CA: SAGE Publications, Inc.; 2004.
- Yanes AF, McElroy LM, Abecassis ZA, Holl J, Woods D, Ladner DP. Observation for assessment of clinician performance: a narrative review. BMJ Qual Saf 2016;25:46-55. https://doi.org/10.1136/bmjqs-2015-004171.
- Chauvette A, Schick-Makaroff K, Molzahn AE. Open data in qualitative research. Int J Qual Methods 2019;18. https://doi.org/10.1177/1609406918823863.
- Ford S, Hall A, Ratcliffe D, Fallowfield L. The Medical Interaction Process System (MIPS): an instrument for analysing interviews of oncologists and patients with cancer. Soc Sci Med 2000;50:553-66. https://doi.org/10.1016/S0277-9536(99)00308-1.
- Schmidt Mast M. Dominance and gender in the physician-patient interaction. J Mens Health Gend 2004;1:354-8. https://doi.org/10.1016/j.jmhg.2004.10.013.
- Henry SG, Forman JH, Fetters MD. ‘How do you know what Aunt Martha looks like?’ A video elicitation study exploring tacit clues in doctor–patient interactions. J Eval Clin Pract 2011;17:933-9. https://doi.org/10.1111/j.1365-2753.2010.01628.x.
Appendix 1 Classification of activities and prescriptions from patient medical records
| Activity type | Codea | Term |
|---|---|---|
| QRISK (assessment, discussion, IHD prevention) | 38DP | QRISK2 cardiovascular disease 10-year risk score |
| 6C0 | Primary prevention of ischaemic heart disease | |
| Weight (measurement of weight, BMI, waist circumference; discussion of weight) | 22A | O/E – weight |
| 22K | Body mass index | |
| Blood pressure related (measurement, discussion) | 246 | O/E – blood pressure reading |
| 315B | Ambulatory blood pressure recording | |
| 662L | 24-hour blood pressure monitoring | |
| 242 | O/E – pulse rate | |
| 2431 | O/E – pulse rhythm regular | |
| Cholesterol related (tests for lipids, cholesterol) | 44lF | Serum cholesterol/HDL ratio |
| 44P | Serum cholesterol | |
| 44P5 | Serum HDL cholesterol level | |
| 44PL | Non-HDL cholesterol level | |
| 44Q | Serum triglycerides | |
| Diabetes related (tests, discussion) | 42W5 | HbA1c level – IFCC standardised |
| Other tests (kidney, liver, thyroid, ECG) | EMISNQAW1 | Test request: liver function test |
| 321 | ECG – general | |
| EMISNQAW1 | Test request: urea and electrolytes | |
| EMISNQAW1 | Test request: thyroid function test | |
| Lifestyle discussion (smoking, exercise, diet, alcohol, general lifestyle) | 8CAL | Smoking cessation advice |
| 137P | Cigarette smoker | |
| 137S | Ex-smoker | |
| 1371 | Never smoked tobacco | |
| 8CA4 | Patient advised regarding diet | |
| 8CA47 | Patient advised regarding low-cholesterol diet | |
| 66At | Diabetic dietary review | |
| 1F4 | Dietary calorie intake | |
| RF020 UHNM nutrition and dietetics V3 | ||
| 8CA5 | Patient advised regarding exercise | |
| 136 | Alcohol consumption | |
| 38D3 | Alcohol use disorders identification test | |
| 67H | Lifestyle counselling | |
| 67H9 | Education about lifestyle for risk of diabetes | |
| Lifestyle referral (smoking, exercise, diet, diabetes prevention) | 679m4 | Referral to NHS diabetes prevention programme |
| RF020 UHNM nutrition and dietetics V3 | ||
| 8H7q | Referral for exercise therapy | |
| New diagnoses | C10F | Type 2 diabetes mellitus |
| R102–1 | [D]Prediabetes | |
| C11y5 | Pre-diabetes | |
| G20 | Essential hypertension | |
| C324 | Hyperlipidaemia NOS | |
| C329 | Hypercholesterolaemia |
| Classification of medication | Medications included |
|---|---|
| Statin/lipid lowering | Atorvastatin, simvastatin, ezetimibe |
| Anticoagulant | Apixaban, rivaroxaban |
| Cardiovascular | Propranolol, ramipril, verapamil, amlodopine |
| Diabetes | Metformin, ivabradine |
Appendix 2 Coding framework data variables
| Category | Code | Code title |
|---|---|---|
| Patient–practitioner communication | PrDT | Practitioner dominated talk |
| PtDT | Patient dominated talk | |
| NT | No talking | |
| Health check general | I2HC | Introduction to health check |
| HCSUM | Health check summary | |
| C&ID | Collecting and inputting data | |
| TRG | Test result/recording given | |
| Risk dialogue | DoR | Discussion of risk |
| RSRef | Risk score reference | |
| HARef | Heart age reference | |
| SARef | Survival age free of cardiac event reference | |
| RSM | Risk score manipulation using either QRISK2 or JBS3 | |
| CVDRQ | Patient question about CVD risk | |
| CVD risk factors | FH-MHIS | Risk factor discussion – medical history |
| RF-FH | Risk factor discussion – family history | |
| RF-W | Risk factor discussion – weight | |
| RF-C | Risk factor discussion – cholesterol | |
| RF-BP | Risk factor discussion – blood pressure | |
| RF-D | Risk factor discussion – diabetes | |
| RF-MH&W | Risk factor discussion – mental health and well-being | |
| RF-PA | Risk factor discussion – physical activity/inactivity | |
| RF-DIET | Risk factor discussion – diet | |
| RF-A | Risk factor discussion – alcohol consumption | |
| RF-S | Risk factor discussion – smoking | |
| Lifestyle interventions | I-W | Intervention discussion – weight |
| I-C | Intervention discussion – cholesterol | |
| I-BP | Intervention discussion – blood pressure | |
| I-D | Intervention discussion – diabetes | |
| I-MW&W | Intervention discussion – mental health and well-being | |
| I-PA | Intervention discussion – physical activity | |
| I-DIET | Intervention discussion – diet | |
| I-A | Intervention discussion – alcohol | |
| IL-S | Intervention discussion – smoking | |
| Medical interventions | I-GP | Intervention discussion – GP appointment |
| I-PR | Intervention discussion – practitioner appointment (PN or HCA) | |
| I-M | Intervention discussion – medication | |
| Comments and recommendations |
Appendix 3 Coding table based on protection motivation theory for deductive thematic analysis
| Domains of PMT | Subdomains of PMT | Example codes |
|---|---|---|
| Sources of information | Environmental | Family history of CVD |
| Experience of family members with CVD (positive/negative/neutral) | ||
| Intrapersonal – personality variables | Biomedical risk factors | |
| Blood pressure | ||
| Cholesterol level | ||
| Diabetes | ||
| Weight and BMI | ||
| Waist circumference | ||
| Age | ||
| Sex | ||
| Lifestyle behavioural factors | ||
| Physical activity | ||
| Diet | ||
| Smoking status | ||
| Alcohol consumption | ||
| Taking of legal/illegal drugs | ||
| Psychosocial risk factors | ||
| Social support | ||
| Social isolation | ||
| Optimism | ||
| ‘Felt age’ | ||
| Health locus of control/fatalism | ||
| Mental health and well-being | ||
| Stress | ||
| Distress | ||
| Anxiety/depression | ||
| Intrapersonal – prior experience | Prior experience of CVD risk reduction (positive/negative/neutral experience) | |
| Use of statins | ||
| Smoking cessation | ||
| Attempts to reduce weight | ||
| Attempts to undertake physical activity | ||
| Attempts to modify diet | ||
| Cognitive appraisal | Threat appraisal | Discussion of risk |
| Perceived severity of CVD risk (high/low/neutral level of severity) | ||
| Consequences of CVD | ||
| Perceived vulnerability to future CVD/CVD-related events (high/low/neutral personal relevance) | ||
| Intrinsic and extrinsic rewards for not addressing CVD risk | ||
| Coping appraisal | Discussion of risk | |
| Self-efficacy to engage in adaptive coping | ||
| Promotion of self-efficacy through individualisation | ||
| Response efficacy of adaptive coping | ||
| Response cost of adaptive coping | ||
| Biomedical intervention/lifestyle intervention subcategories for each category and positive/negative/neutral subcategories | ||
| Coping modes | Adaptive coping | Biomedical intervention |
| GP appointment referral | ||
| Medications (for blood pressure/lipids) | ||
| Lifestyle intervention | ||
| Referral to lifestyle programmes? | ||
| Weight management | ||
| Increase physical activity | ||
| Diet related | ||
| Increase fruit and vegetable intake | ||
| Increase omega-3 fatty acid intake (e.g. fish) | ||
| Decrease fat intake | ||
| Decrease dietary cholesterol | ||
| Decrease sugar intake | ||
| Decrease alcohol intake | ||
| Decrease salt intake | ||
| Smoking cessation | ||
| Psychosocial intervention | ||
| Positively engaged with biomedical/lifestyle/psychosocial intervention discussion – apparently listening and engaged in the conversation; accepting of what is being said/suggested | ||
| Maladaptive coping | Negatively engaged with biomedical/lifestyle/psychosocial intervention discussion – apparently listening and engaged in the conversation, but dismissive of what is being said/suggested [already doing all I can (e.g. already feels that they are very active and eat well)]; not interested in making changes suggested (e.g. like smoking; hate physical activity) | |
| Passive/disengaged with biomedical/lifestyle/psychosocial intervention discussion – not engaged in the conversation (e.g. passively takes information, but no clear plans for further contact) |
Appendix 4 Coding table based on protection motivation theory for deductive thematic analysis – including example quotations
| Codes | Example quotation (if available) | ||
|---|---|---|---|
| Sources of information | Environmental | Family history of CVD and/or CVD-related factors | HP:Is there any family history, is there mum, dad, any brothers or sisters that were diagnosed with any form of blood pressure problems, strokes, heart problems, under the age of 60?P:No. Mum and dad are both 88, still living. They are now on heart sort of tablets and things though |
| Experience of family members with CVD and/or CVD-related factors (positive/negative/neutral) |
Positive experience No example available |
||
| Neutral experienceP:That’s alright. My Dad did suffer from high BP | |||
|
Negative experience No example available |
|||
|
Experience of GP The patient discusses motivating or demotivating factors for attending the Health Check in relation to their experiences of going to the GP and how they usually approach health care |
HP:So have you ever had your cholesterol and that done?P:No I’ve never no I’m one of the ones that tries to avoid the doctors at all costs so . . .HP:Thanks for coming inP:Oh no, I always say yes to these things [laughter] | ||
|
Environmental influences External influences that may have an impact on CVD risk factors (e.g. impact of work on exercise levels) |
P:Well I’m ex-army so a big part of my . . .HP:Yeah so you are used to itP:I joined the army when I was 15, so a big part of my life was in the armyHP:Ah oh yeah, the marching yeah | ||
|
Influence of significant others This category relates to discussion surrounding the positive or negative effect that significant others may have on their CVD risk factors or adaptive/maladaptive coping |
HP:And its that’s how you know how you feed your farmers up isn’t it?P:But you know he’s out in horrific weather, he needs good food | ||
| Intrapersonal personality variables | Biomedical risk factors | Evidence related to discussion of biomedical CVD risk factors | |
| Blood pressure | |||
| Cholesterol level | |||
| Diabetes | |||
| Weight and BMI | |||
| Waist circumference | |||
| Age | |||
| Sex | |||
| Urine | |||
| Pulse | |||
| Height | |||
| Lifestyle/behavioural factors | Evidence related to discussion of lifestyle/behavioural CVD risk factors | ||
| Physical activity | |||
| Diet | |||
| Smoking status | |||
| Alcohol consumption | |||
| Taking of legal/illegal drugs | |||
| Psychosocial risk factors | Evidence related to discussion of psychosocial CVD risk factors | ||
| Social support | |||
| Social isolation | |||
| Optimism | |||
| ‘Felt age’ | |||
| Feeling younger/older than chronological age | |||
| Health locus of control/fatalism | |||
| The belief that health outcomes are contingent on (a) personal behaviour (internal HLC), (b) other powerful people (powerful others HLC) and (c) forces such as fate or chance (chance HLC) | |||
| Mental health and well-being | Evidence related to discussion of mental health and well-being CVD risk factors | ||
| Stress | |||
| Distress | |||
| Anxiety/depression | |||
| Medical history | HP:Have you ever received treatment for blood pressure problems?P:Low blood pressure, not treatment for it, I have had a test for it, because it was very low at one time, but I think it goes up and down. I have just run a marathon not so long ago, so that might have had an effectP:Yeah, I’m due to have another one . . . I didn’t have cholesterol done I just had sugarHP:Your cholesterol’s in date actually it’s come up as blue on hereP:Oh has it what does that meanHP:Which means it was done last year, it was done in August last year | ||
| Patient discusses intrapersonal variables relating to their medical history (e.g. previous blood pressure measurements, previous weight measurements, etc.) This information would also be coded under the relevant medical risk factor | |||
| Intrapersonal prior experience | Prior experience of CVD risk reduction (positive/negative/neutral experience) | Positive experience (smoking cessation)P:And the only you know, and in fact I saw the Help to Quit nurse about 10 years ago when I stopped erm I mean she was . . . very, very unhealthy . . . she was . . . obeseHP:Oh rightP:But she was very good, very good | |
| Use of statins | |||
| Smoking cessation | |||
| Attempts to reduce or maintain weight | Negative experience (modifying/maintaining diet)P:Slimming World I could never accept | ||
| Attempts to undertake physical activity | |||
| Attempts to modify or maintain diet | |||
| Attempts to reduce or monitor alcohol consumption | Neutral experience (undertaking physical activity)HP:Yeah, so do you ever manage to go to the gym, or swimming, or any exercise classes?P:I used to go for the gym | ||
| Attempts to reduce blood pressure | |||
| Attempts to make or maintain lifestyle changes | |||
| Current experience | Current experience of CVD risk reduction (positive/negative/neutral experience) | Positive experience (alcohol consumption)P:Some people just pour it in, don’t they?HP:Aye they do, they do.P:I am aware, and if I think I have perhaps have had more than I should in the week, then I stop and don’t drink at all | |
| Use of statins | |||
| Smoking cessation | |||
| Attempts to reduce or maintain weight |
Negative experience (modifying/maintaining diet) No example available |
||
| Attempts to undertake physical activity | |||
| Attempts to modify or maintain diet | |||
| Attempts to reduce or monitor alcohol consumption | Neutral experience (modifying/maintaining diet)P:I think I probably eat more meat than vegHP:RightP:If in the whole scheme of thingsHP:YeahP:Which is something I’ve thought about lately | ||
| Attempts to reduce blood pressure | |||
| Attempts to make or maintain lifestyle changes | |||
| Cognitive appraisal | Threat appraisal | Perceived severity of CVD risk | Low severityHP:OK so your Heart Age is 68, how old are you at the moment?P:66HP:66, so it’s a couple of years olderP:How did you make that out? |
| The degree to which people think a particular condition is a severe risk – high/low/neutral level of severity, e.g.: | Neutral severityHP:Your Heart Age is 60 alright, ermP:But that’s what I am but I’m supposed, supposed to be better than I am is that what you’re saying?HP:Yeah because you’re very slimP:Yeah OK | ||
| ‘Bowel cancer is a serious illness’ | High severityHP:Right on average you should expect to survive until the age of 84 without a heart attack, or a strokeP:Oh my | ||
| ‘Oh 17% is not a very high number is it, so I’ll be fine’ | |||
| Consequences of CVD | No example available | ||
| Discussion about consequences of developing CVD, e.g.: | |||
| ‘I know developing CVD will reduce my quality of life’ | |||
| Perceived vulnerability to future CVD/CVD-related events | Low personal relevanceHP:OK so your Heart Age is 68, how old are you at the moment?P:66HP:66, so it’s a couple of years olderP:How did you make that out?HP:[Laugh] alright, because of the info of the stats that I have put in here | ||
| Perception of personal likelihood to develop a particular condition – high/low/neutral personal relevance |
Neutral personal relevance No example available |
||
| ‘How likely am I to develop CVD?’ |
High personal relevance No example available |
||
| ‘Does that mean I’m likely to have a heart attack?’ | |||
| Intrinsic (e.g. pleasure) and extrinsic (e.g. social approval) rewards for not addressing CVD risk | Extrinsic rewardsP:You see the thing is I’m trying to get my wife to stopHP:Oh she smokes as well?P:Yeah, but she won’t, she will not and she’s got COPDHP:Oh honestlyP:Yep, yep, yepHP:GoshP:YepHP:Oh yeah that’s very naughty isn’t it?P:Yep | ||
| ‘Being a curvaceous woman makes me happy so it doesn’t bother me that I am overweight’ | |||
| ‘I don’t want to give up smoking because my wife smokes too, it’s something we enjoy together’ | |||
| Neutral response to discussion of risk | HP:So, this is telling me today that your heart age is 71P:RightHP:A lot of that is to do with your smokingP:Hm | ||
| Patient responds in a neutral manner to the risk discussion. For example, the patient could respond with ‘hmm’, ‘right’, ‘OK’. Generally very short, one-word responses | |||
| Not enough information is present in the patient response to classify as either positively or negatively engaged in the discussion | |||
|
Consequences of CVD risk factors Split into two categories:Here the patient acknowledges or demonstrates awareness of the related health implications to engagement with an adaptive behaviour (e.g. undertaking physical activity).And:Here the patient acknowledges or demonstrates awareness of the related health implications to engagement with a maladaptive behaviour (e.g. smoking) |
Acceptance/awareness of health implications to engage/not engage in adaptive behaviourHP:OK and when you’re walking are you slow, steady or brisk would you say?P:BriskHP:Brisk. Which is brilliant because it’s put you down into that active categoryP:Gets the heart rate up, yeahHP:Yeah gets your heart rate upwards | ||
| Acceptance/awareness of health implications to engage/not engage related to maladaptive behaviourHP:So it gives you food for thoughtP:Hmm hmm. You haven’t told me anything I didn’t already knowHP:I know, I know, I know I didn’t . . .P:So yeah | |||
| Perceived severity of CVD risk factors | Low severityHP:I mean, you might find that when you are doing it at home your readings are absolutely fineP:They are what they are | ||
| Similar to perceived severity of CVD risk yet this category is related to patient-practitioner discussion of CVD risk factors specifically (e.g. cholesterol, blood pressure) |
Neutral severity No example available |
||
| High severityHP:Erm the other one in the red is that one cholesterol one which we were talking about thereP:Oh my God that’s well up isn’t it? | |||
| Clarification of results | HP:Your HDL, this figure, that’s your good cholesterol and we want to get this one higherP:Right so what is it, it’s on 1.5 at the moment?HP:Yeah 1.5 which is a good figure erm . . .P:So what what’s a good one?HP:Its above 1 that is that is a good figureP:Oh that’s a . . . yeah OK | ||
| Related to when a patient asked questions and sought clarification about their test results from the practitioner | |||
| Perceived vulnerability of CVD risk factors | Low personal relevance (in relation to smoking)P:I wouldn’t have thought that it would count nowHP:Well no because it seems a lot of time to regenerateP:Eighties, Nineties, 2000 – it is over thirty years agoNeutral personal relevance No example availableHigh personal relevanceHP:So let’s just have a look, we haven’t done a waist circumference it’s just. . . if you’d like me to do one I can do so we’ve got one for future reference?P:Yeah, we can do it but I’m sure it’s too big [laughter], no that’s fine I don’t mindHP:Are you happy with, yeah yeah, I’ll em, it’s not the most flattering because it’s just below your tummy button so I’m sorryP:OK you’ve got to find it first | ||
| Similar to perceived vulnerability to future CVD/CVD-related events yet this category is related to patient perceived vulnerability to related CVD risk factors specifically (e.g. cholesterol, blood pressure) | |||
| Perceived vulnerability to other medical conditions | P:I have gone through a bit of a stage last year thinking . . . I was going to die of everything you know, just eh oh God you get into that stage in life when you be oh really so | ||
| Similar to perceived vulnerability to future CVD/CVD-related events yet this category is related to patient perceived vulnerability to other medical conditions (e.g. cancer) | |||
| Perceived severity of other medical conditions |
Low severity No example available |
||
| Similar to perceived severity of CVD risk yet this category is related to patient perceived severity of other medical conditions (e.g. cancer). This is sometimes, but not always, in comparison with CVD |
Neutral severity No example available |
||
| High severityP:I’m going to. . . my massive fear factor is cancerHP:YeahP:Beyond beliefHP:Because you’ve got that within the . . .P:Mum’s died of it, all my aunties have died of it, my granny died on Mum’s side, well in fact to be honest they all did, but of an age we lost a lot in their 60s early 60sHP:Earlies, so that’s your fear factor as well isn’t it?P:That massively is yeah, yeah | |||
| Coping appraisal | Self-efficacy to engage in adaptive coping | No example available | |
| The belief that one is capable of performing the behaviour | |||
| ‘I am confident that I can change my diet’ | |||
| Response efficacy of adaptive coping | No example available | ||
| The recommended behaviour will be effective in reducing the threat | |||
| ‘Changing my diet would improve my health and lower my risk of CVD’ | |||
| Response cost of adaptive coping | (In relation to physical activity)HP:And you like physical exercise, don’t you? Do you ever cycle at all?P:Yes, in the summer. I am a bit of a fair-weather cyclist, so I do yeah | ||
| Barriers than inhibit the performance of the adaptive behaviour | |||
| ‘Healthy eating costs more money so it’s easier for me to stay as I am’ | |||
| Response cost of adaptive coping (previous coping) | P:Well up to a couple of years ago, I was doing some mountain ones, I don’t do it on the road anymore, because of my joints and things. But I do half-marathons yes | ||
| Similar to response cost of adaptive coping above yet this category relates to discussion of previous coping attempts, rather than current or future coping attempts | |||
| Facilitators of adaptive coping | P:I am a bit of a fitness . . .HP:Are you? OKP:If I don’t get my exercise I get all sort of ratty! | ||
| This relates to practitioner – patient discussion about any factors that may positively influence or facilitate engagement with adaptive coping | |||
| Coping Modes |
Adaptive coping Positively engaged with biomedical/lifestyle/psychosocial intervention discussion – apparently listening and engaged in the conversation; accepting of what is being said/suggested |
Biomedical intervention | (In relation to weight management):HP:So average survival free of heart attack or stroke is 84.1 years OK? So how do you feel about that?P:Oh I will make more of an effort to lose some weight(In relation to reducing blood pressure):P:So do I make the appointment todayHP:Yes to see me in a month’s time for your erm blood pressure checkP:OK |
| GP/PN/HCA appointment referral | |||
| Medications (for blood pressure/cholesterol) | |||
| Reducing blood pressure | |||
| Cholesterol re-test | |||
| Diabetes prevention | |||
| Lifestyle intervention | |||
| Referral to lifestyle programmes | |||
| Weight reduction and management | |||
| Increase physical activity | |||
| Lifestyle changes | |||
| Diet related | |||
| Increase fruit and vegetable intake | |||
| Increase omega-3 fatty acid intake (e.g. fish) | |||
| Decrease fat intake | |||
| Decrease dietary cholesterol | |||
| Decrease sugar intake | |||
| Decrease alcohol intake | |||
| Decrease salt intake | |||
| Decrease unhealthy snacking | |||
| Portion control | |||
| Smoking cessation | |||
| Alcohol consumption | |||
| Psychosocial intervention (e.g. referral to Healthy Mind) | |||
|
Maladaptive coping Negatively engaged with biomedical/lifestyle/psychosocial intervention discussion – apparently listening and engaged in the conversation, but dismissive of what is being said/suggested [already doing all I can (e.g. already feels that they are very active and eat well]; not interested in making changes suggested (e.g. like smoking; hate physical activity) Neutral response to biomedical/lifestyle/psychosocial intervention discussion – not engaged in the conversation (e.g. passively takes information, but no clear plans for further contact) |
Biomedical intervention |
Negative engaged (In relation to reducing alcohol consumption)P:HP:P:HP:(In relation to reducing blood pressure)HP:P:HP:P:Neutral response(In relation to blood pressure re-check)HP:P:HP:(In relation to smoking cessation)HP:P: |
|
| GP/PN/HCA appointment referral | |||
| Medications (for blood pressure/cholesterol) | |||
| Reducing blood pressure | |||
| Cholesterol re-test | |||
| Diabetes prevention | |||
| Lifestyle intervention | |||
| Referral to lifestyle programmes | |||
| Weight reduction and management | |||
| Increase physical activity | |||
| Lifestyle changes | |||
| Diet related | |||
| Increase fruit and vegetable intake | |||
| Increase omega-3 fatty acid intake (e.g. fish) | |||
| Decrease fat intake | |||
| Decrease dietary cholesterol | |||
| Decrease sugar intake | |||
| Decrease alcohol intake | |||
| Decrease salt intake | |||
| Decrease unhealthy snacking | |||
| Portion control | |||
| Smoking cessation | |||
| Alcohol consumption | |||
| Psychosocial intervention (e.g. referral to Healthy Mind) |
Appendix 5 Data extraction template for case study patients
| Patient information (medical records) | ||||||||
|---|---|---|---|---|---|---|---|---|
| PID | Gender (M = 1) | Age (at time of NHSHC) | Ethnicity (WBRI = 1) | 10-year risk | IMD decile (1 = most deprived) | Health Check duration (minutes) | Verbal dominance (Pr : Pt minutes) | |
| Health Check quantitative coding | ||||||||
| Practitioner speaking (as % of total HC) | Patient speaking (as % of total HC) | No speaking (as % of total HC) | Total minutes discussing CD risk | Activity in follow-up | Resulting diagnosis | Resulting prescription | ||
| Qualitative data | ||||||||
|
Background Patient |
Background Practitioner |
Overview of Health Check | QRISK®2 | Heart Age | Survival Age | Risk manipulation | Risk Management | |
| Recorded Health Check | ||||||||
| VSR patient interview | ||||||||
| VSR practitioner interview | ||||||||
Appendix 6 Analysis of patient engagement through non-verbal behaviours
For the case study participant, the purpose was to assess the level of engagement between practitioner and patient using cues from body language from video-recorded health checks. To categorise non-verbal behaviours (including some verbal cues) in sections of the health check involving discussion of CVD risk, non-verbal cues were categorised to reflect whether the patient was:
-
engaged (positive) – apparently listening and engaged in the conversation, accepting of what is being said/suggested
-
engaged (negative) – apparently listening and engaged in the discussion but dismissive of what is being said/suggested, not interested in making changes suggested
-
passive/disengaged – not engaged in the discussion, passively takes information.
Using non-verbal behaviour categorisation of patient and practitioner engagement used elsewhere,99–101 a list of non-verbal behaviours or cues were derived to allow classification into the above categories. Through piloting and revising, the Likert scale shown in Table 13 was applied to analyse non-verbal behaviour during CVD risk discussion.
For each case study participant, two researchers independently watched segments of the recorded health check in which CVD risk was discussed, and rated them using the Likert scale. The median of ratings for each segment were calculated, and range of these median values used to illustrate the approximate level of engagement.
| Passive | Negatively engaged | Positively engaged | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Very passive | A little passive | Very negative | A little negative | Slightly positive | Very positive | |||||||||||||||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | 25 | 26 | 27 |
| Passive: disengaged cues | Engaged: negative cues | Engaged: positive cues | ||||||||||||||||||||||||
| Negative body language – closed | Positive body language – open | Positive body language – open | ||||||||||||||||||||||||
| No eye contact, looking away (i.e. on the telephone) | Facing practitioner | Facing practitioner/giving eye contact | ||||||||||||||||||||||||
| Not responding to information | Limited chat from patient | Nodding/responding to information | ||||||||||||||||||||||||
| Refusing to answer questions | Little nodding/response | Talking lots to the practitioner | ||||||||||||||||||||||||
| Dismissive of comments or suggestions | Answering questions but with little expansion | Asking questions | ||||||||||||||||||||||||
| Shaking head/sighing | May smile at times | Smiling/laughing | ||||||||||||||||||||||||
For each case study participant, two researchers independently watched segments of the recorded health check in which CVD risk was discussed, and rated them using the Likert scale. The median of ratings for each segment was calculated, and the range of these median values used to illustrate the approximate level of engagement.
Appendix 7 Ratings of non-verbal engagement in case study patients (for each segment of health check in which cardiovascular disease risk was discussed)
| Pseudonym | Segment times | Assessor 1 | Assessor 2 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Start | Changea | Median | Start | Changea | Median | |||||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 1 | 2 | 3 | ||||||
| JBS3 | ||||||||||||||||
| Abbie | 12:22–13:35 | 9 | 26 | 27 | 25 | 24 | 26 | 24 | 23 | 24.5 | 10 | 27 | 24 | 25 | 24.5 | |
| 14:50–14:56 | 22 | 23 | 22.5 | 24 | 24 | |||||||||||
| 16:47–16:55 | 22 | 22 | 20 | 20 | ||||||||||||
| Barry | 11:16–11:34 | 3 | 6 | 13 | 10 | 8 | 9 | 9 | ||||||||
| 13:26–13:58 | 20 | 19 | 21 | 20 | 13 | 13 | ||||||||||
| 14:26–14:47 | 20 | 19 | 20 | 20 | 15 | 15 | ||||||||||
| 15:15–15:52 | 19 | 18 | 18.5 | 12 | 12 | |||||||||||
| 16:05–16:17 | 19 | 20 | 19.5 | 15 | 15 | |||||||||||
| 16:36–16:47 | 19 | 20 | 19.5 | 17 | 17 | |||||||||||
| 20:09–20:14 | 19 | 19 | 20 | 20 | ||||||||||||
| Carl | 01:31–01:35 | 24 | 24 | 19 | 19 | |||||||||||
| 17:44–19:08 | 25 | 22 | 23.5 | 20 | 20 | |||||||||||
| 19:17–19:45 | 22 | 22 | 20 | 20 | ||||||||||||
| 22:12–22:17 | 21 | 21 | 19 | 19 | ||||||||||||
| 22:39–22:45 | 22 | 22 | 18 | 18 | ||||||||||||
| Deborah | 13:49–16:38 | 17 | 19 | 20 | 19 | 18 | 17 | 18 | 19 | 21 | 19 | 9 | 9 | |||
| 16:51–16:59 | 21 | 21 | 11 | 11 | ||||||||||||
| Eid | 09:48–09:57 | 3 | 3 | 5 | 5 | |||||||||||
| 10:32–10:37 | 17 | 11 | 14 | 15 | 15 | |||||||||||
| 10:57–11:06 | 20 | 20 | 19 | 19 | ||||||||||||
| 11:23–12:38 | 19 | 18 | 21 | 18 | 22 | 21 | 19 | 20 | 19.5 | 19 | 20 | 19.5 | ||||
| 12:46–13:02 | 20 | 19 | 19.5 | 20 | 20 | |||||||||||
| QRISK2 | ||||||||||||||||
| Freddie | 18:10–18:24 | 25 | 25 | 25 | 25 | |||||||||||
| 22:54–23:53 | 25 | 26 | 25 | 26 | 25 | 25 | 24 | 24 | ||||||||
| Grace | 11:50–12:29 | 16 | 14 | 15 | 12 | 14.5 | 10 | 10 | ||||||||
| Harry | 07:44–08:15 | 22 | 20 | 21 | 22 | 22 | ||||||||||
| 08:51–09:38 | 20 | 21 | 20 | 21 | 22 | 21 | 22 | 22 | ||||||||
| 10:21–10:29 | 22 | 21 | 19 | 21 | 23 | 23 | ||||||||||
| Ian | 15:06–16:17 | 24 | 23 | 24 | 22 | 20 | 22 | 21 | 22 | 19 | 19 | |||||
| Jessica | 00:20–00:27 | 19 | 19 | 10 | 10 | |||||||||||
| 14:00–14:09 | 19 | 20 | 19.5 | 20 | 20 | |||||||||||
| 14:50–15:18 | 22 | 22 | 22 | 21 | 21.5 | |||||||||||
| 16:17–16:27 | 19 | 20 | 19.5 | 22 | 22 | |||||||||||
Glossary
- Informatica
- Software addition that offers some JBS3 functionalities.
- JBS3 risk calculator
- Lifetime cardiovascular disease risk calculator.
- Point-of-care testing
- Blood test during health check.
- QRISK®2
- Cardiovascular disease risk calculator for estimating the 10-year risk of having a cardiovascular event in people who do not already have heart disease.
- QRISK®2+
- Used to denote health checks in which QRISK2 and Informatica are used.
List of abbreviations
- BMI
- body mass index
- CI
- confidence interval
- CRN
- Clinical Research Network
- CVD
- cardiovascular disease
- GP
- general practitioner
- HCA
- health-care assistant
- ICC
- intraclass correlation coefficient
- IMD
- Index of Multiple Deprivation
- JBS
- Joint British Societies for cardiovascular disease prevention
- NHSHC
- NHS Health Check
- PHE
- Public Health England
- PMT
- protection motivation theory
- PN
- practice nurse
- PoC
- point of care
- PPG
- Patient Participation Group
- PPI
- patient and public involvement
- QOF
- Quality and Outcomes Framework
- RICO
- RIsk COmmunication in NHS Health Check
- VSR
- video-stimulated recall