Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 15/38/04. The contractual start date was in July 2016. The draft report began editorial review in April 2021 and was accepted for publication in September 2021. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2022 Wright et al. This work was produced by Wright et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: http://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 Wright et al.
Chapter 1 Introduction
Parts of this chapter have been reproduced from Wright et al. 1 © 2022 The Authors. Journal of Child Psychology and Psychiatry published by John Wiley & Sons Ltd on behalf of Association for Child and Adolescent Mental Health. This is an open access article under the terms of the Creative Commons Attribution License, which permits use, distribution and reproduction in any medium, provided the original work is properly cited. The text below includes minor additions and formatting changes to the original text.
Parts of this chapter have been reproduced from Wang et al. 2 Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data. The text below includes minor additions and formatting changes to the original text.
Background and rationale
A specific phobia is an intense, enduring fear of an identifiable object or situation (e.g. dogs, heights or injections) that leads to anxiety, distress and avoidance,3 and is one of the most common mental health difficulties. 4 It is estimated that between 5% and 10% of children and young people (CYP) have a specific phobia that is severe enough to affect their everyday functioning,5 and that the average duration of their phobia is 20 years. 6 Specific phobias are, therefore, common in the population, are persistent over time and can have significant impacts on health and well-being. For example, specific phobias are associated with poorer health-related quality of life (HRQoL),7 considerable academic difficulties8 and distress and interference with day-to-day activities,9 and may predict a range of future mental health difficulties. 10,11 Consequently, it is important that CYP have access to effective treatments for specific phobias so that both the immediate and the possible future impacts can be mitigated. However, the proportion of CYP with phobias who receive treatment for phobia is small, at around 10%,6 and those who do seek treatment are likely to meet barriers and challenges to accessing timely, evidence-based support. 12–15
Current treatment approaches for specific phobia
Interventions based on the principles of cognitive–behavioural therapy (CBT) remain the dominant model of delivery of therapy for specific phobias in the Children and Young People’s Improving Access to Psychological Therapies (CYP-IAPT) programme. 16,17 Indeed, CBT for specific phobias and for wider anxiety difficulties is effective and has a robust evidence base. 18–20 For example, Hudson et al. 21 reported that CBT in children with specific phobias resulted in significant reductions in clinician-rated phobia severity, as well as in both parent-reported and child-reported severity, and a significant increase in specific phobia diagnosis remission at follow-up. However, there are limitations to the provision of CBT. For example, face-to-face CBT is time-consuming22,23 and requires specially trained therapists,24,25 and, therefore, is often offered at high cost and with limited availability. 26,27 Furthermore, CBT is often offered over multiple sessions that can take many weeks and months to complete. Given that this requires CYP to be out of school, or the family to travel to receive therapy over many weeks and months, therapy provision can become a burden,28 which might contribute to the relatively high drop-out rate in CBT for CYP. 29,30 There is a need for brief, evidenced-based alternative treatments that can be offered in a more time- and cost-efficient manner for CYP living with specific phobias, as well as their families, and the clinical services providing care. One such option, with the potential to offer a brief and clinically effective treatment, is one-session treatment (OST).
One-session treatment: a brief and effective treatment for specific phobia
One-session treatment typically involves a combination of treatment techniques, including exposure, participant modelling, reinforcement, cognitive restructuring and skills training. At the core of OST is gradual exposure to the phobic stimulus, a process directed by the therapist using behavioural experiments. 31 Indeed, OST shares many of the same principles as CBT; however, unlike CBT, OST does not require an extensive treatment period. Instead, OST takes place over two sessions: (1) an initial assessment and planning session lasting around 1 hour and (2) one treatment session involving multiple graduated exposures lasting up to 3 hours, a procedure that has been shown to be clinically efficacious in CYP. 32–35 For example, in one of the largest randomised controlled trials (RCTs) of OST to date, conducted in the USA and Sweden, Ollendick et al. 33 randomised 196 CYP (aged 7–16 years) to one of three groups: (1) an OST group, (2) an education support group and (3) a waiting list control group. The authors reported that OST demonstrated superiority over both the education support group and the waiting list control group in terms of clinician-rated phobia severity, percentage of participants who were diagnosis free, and child ratings of anxiety and treatment satisfaction as reported by the children and their parents post intervention and at a 6-month follow-up point. OST, therefore, could offer a tool that can be used to reduce demands on therapist time, reduce the associated costs, prevent therapeutic drift and ultimately help CYP to recover more quickly from phobia.
Opportunities for advancement
Cognitive–behavioural therapy is the gold standard treatment for specific phobia and represents the dominant model of treatment provision; however, CBT is time-consuming and costly and has limited availability. Although the evidence base to date suggests that OST is a clinically efficacious treatment for phobia, there remain several areas of uncertainty that the present research aims to address. First, extant literature has tended to focus on the efficacy of OST, that is examining the performance of OST under more ‘ideal’ circumstances or in settings that do not reflect the ‘real world’. 36 For example, previous trials have tended to exclude participants based on specific characteristics that might influence treatment outcome if OST were to be implemented in clinical services, such as the presence of comorbid mental health difficulties,33 concurrent treatment for other difficulties33 or a diagnosis of autism spectrum disorder (ASD). 37 Consequently, it is unclear how well OST would perform in a more ‘real-world’ setting, such as Child and Adolescent Mental Health Services (CAMHS), where therapists are not always able to exclude CYP from therapy based on characteristics that might make treatment delivery more difficult (e.g. psychiatric comorbidity). 38,39 Second, to our knowledge, OST has not been compared with routinely delivered CBT with exposure (i.e. the gold standard treatment) in a RCT. Consequently, how OST performs against a much more active treatment, such as CBT, is unclear. Finally, although the consolidated, brief format of OST lends itself to being a more cost-effective tool than multisession CBT, to our knowledge, no study has performed an economic analysis to quantify any (potential) savings. Consequently, the cost-effectiveness of OST relative to CBT is unclear.
Research question, aims and objectives
The present research aims to address the gaps described above by conducting a pragmatic RCT of OST compared with multisession CBT for specific phobias experienced by CYP aged 7–16 years. Specifically, the primary aim of ASPECT (Alleviating Specific Phobias Experienced by Children Trial) is to investigate the non-inferiority of OST compared with multisession CBT for treating specific phobias experienced by CYP at a 6-month follow-up point. Non-inferiority would be demonstrated if OST was shown to produce similar, or improved, effects on the target specific phobia, as assessed using an in vivo exposure assessment tool: the Behavioural Avoidance Task (BAT) (i.e. the primary outcome). 40 In addition to the primary aims of ASPECT, several secondary aims are proposed. First, we aim to examine the cost-effectiveness of OST relative to CBT, with the resulting hypothesis being that OST will demonstrate superior cost-effectiveness relative to CBT. Second, the present research aims to investigate not only the effect of OST compared with CBT on the specific phobia itself, but also the impact on a wide range of associated outcomes, including broader mental health, quality of life (QoL), and school and social life. Finally, the present research aims to qualitatively investigate the acceptability of OST to the CYP receiving it, to their parents/guardians and to the clinicians administering OST. In conclusion, we believe that the present research has the potential to provide strong, high-quality evidence from which to base recommendations on not only the clinical effectiveness and cost-effectiveness of OST in real-world clinical settings, but also the perceived acceptability and feasibility of OST to CYP, their guardians and the clinicians responsible for providing care.
Chapter 2 Methods
Some text in this chapter has been reproduced from Wright et al. 41 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Parts of this chapter have been reproduced from Wright et al. 1 © 2022 The Authors. Journal of Child Psychology and Psychiatry published by John Wiley & Sons Ltd on behalf of Association for Child and Adolescent Mental Health. This is an open access article under the terms of the Creative Commons Attribution License, which permits use, distribution and reproduction in any medium, provided the original work is properly cited. The text below includes minor additions and formatting changes to the original text.
Parts of this chapter have been reproduced from Hayward et al. 42 © 2022 Hayward et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. The text below includes minor additions and formatting changes to the original text.
Parts of this chapter have been reproduced from Wang et al. 2 Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data. The text below includes minor additions and formatting changes to the original text.
Main trial methods
This report is concordant with the 2010 Consolidated Standards of Reporting Trials (CONSORT) statement. 43
Trial design
The study was a two-arm, pragmatic, multicentre, non-inferiority RCT with an internal pilot to compare the clinical effectiveness of OST with that of multisession CBT. An economic evaluation of both OST and CBT and a qualitative investigation of the perceptions and acceptability of OST were nested within the study.
Important changes to methods after trial commencement
ASPECT received Health Research Authority and Research Ethics Committee (REC) approval from the North East – York Ethics Research Committee (17/NE/0012) in February 2017, with recruitment commencing on 30 June 2017. A series of amendments were submitted in response to observations made during the recruitment period. Several amendments resulted in changes to the protocol (see Appendix 1, Table 29), with all substantial amendments presented in Table 1. The trial protocol was published in BMJ Open in August 2018. 41
| Amendment number: date | Details | Protocol version number |
|---|---|---|
| 1: July 2017 | Approval was sought to display a poster in NHS trust locations to supplement recruitment | v1: as original approval |
| 2: November 2017 | Approval was sought to recruit from participant identification centres to increase recruitment | Not required |
| 3: January 2018 |
As the qualitative interviews (see Qualitative methods) were due at least 6 months post baseline, obtaining additional consent was deemed necessary for individuals to make an informed choice about participation Additional trial promotion methods were added to the study protocol. These included using social media accounts to promote the trial to internal staff and potential participants, the use of local media to promote the trial to stakeholders and the use of a recruitment poster displayed in NHS trust locations (linked with substantial amendment 1) Two study documents were amended: a school letter sent to head teachers to inform them of the study and request their participation (see School recruitment) was shortened to enhance readability, and the parent/guardian consent form was amended to explicitly state that therapy sessions might be recorded |
Now protocol v4: 8 January 2018a |
| 4: July 2018 | Permission was sought to provide those participating in qualitative interviews with an additional £10 voucher as a thank you for their time | Not required |
| 5: December 2019 | An additional case report form was added to the study. This collected information pertaining to additional diagnoses of ASD, attention deficit hyperactivity disorder and learning disabilities that participants may have had and any additional phobia treatments they had received, alongside trial treatment | Now protocol v5: 2 December 2019 |
Participants and eligibility criteria
Inclusion criteria
Participants were CYP aged between 7 and 16 years experiencing a specific phobia, as defined by the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-V), criteria. These criteria are:
-
Marked and out-of-proportion fear of a specific object or situation.
-
Exposure provokes immediate anxiety.
-
The phobic situation(s) is avoided where possible.
-
The avoidance or distress interferes with the person’s routine or functioning (e.g. learning, sleep and social activities).
-
Present for ≥ 6 months.
Participant eligibility was first assessed by research assistants using a telephone screening tool (see Report Supplementary Material 1) developed by the research team and completed with the CYP’s parent/guardian. The tool was based on the Anxiety Disorder Interview Schedule (ADIS) and comprised five ‘yes’ or ‘no’ questions mapping directly onto the DSM-V, criteria for specific phobia. Parents/guardians needed to answer ‘yes’ to all questions to be considered eligible and, if they did, were invited to attend a face-to-face interview with the research assistant. At the interview, eligibility was further confirmed, with both the CYP and their parent/guardian completing the relevant versions of the ADIS (see Secondary outcome measures) to confirm that all five DSM-V criteria were met.
Exclusion criteria
Exclusions (pre randomisation) and withdrawals (post randomisation) were considered on a case-by-case basis. Reasons for exclusion or withdrawal were:
-
Exposure to the stimulus had the potential to be unsafe or cause harm (e.g. stimulus could not be safely produced or simulated).
-
A clinician decided, when referring or delivering treatment, that exposure therapy would not be the best first-line or best-available treatment option for the CYP (e.g. they had other needs that could make the therapy unsuitable, such as psychosis, severe learning disability, suicidality and severe conduct disorder).
Research settings
The sponsor, Leeds and York Partnership NHS Foundation Trust (LYPFT), in collaboration with the University of Sheffield Clinical Trials Research Unit (CTRU), coordinated the study nationally. Participants were identified through two main routes: (1) health-care and social care pathways and (2) schools.
Health-care and social care pathway recruitment
Given the trial’s pragmatic nature, recruitment took place within the services in which specific phobias were most likely to be seen. This included 12 NHS trusts comprising 26 CAMHS, three third-sector/voluntary services and one university-based CYP’s well-being service.
For the most part, participants were identified by therapists within these services at a range of different points within the care pathway, including at first contact with the services, during initial meetings with therapists to discuss needs, when on waiting lists to access support and following allocation to a therapist to receive therapy. Participants may have accessed the service specifically for their phobia, or were seeking support for a comorbidity and their specific phobia was identified.
Potentially eligible participants were given information about the study and an expression of interest form. The parents/guardians of interested participants were asked to return this form to the research team either directly or via a clinician. The research assistant then contacted the parent/guardian, discussed the study in detail and completed the initial telephone assessment (see Participants and eligibility criteria). If deemed eligible, a baseline visit was arranged.
During study recruitment, it became apparent that some CYP with specific phobias did not meet CAMHS acceptance criteria and were, therefore, unable to access the trial. To address this, a training clinic was set up by the study sponsor in one locality (York). This was staffed by clinicians who volunteered their time to offer therapeutic interventions. CAMHS clinicians referred CYP to the training clinic, and these clinics operated the same recruitment processes as those outlined above.
School recruitment
With previous experience recruiting from schools,44,45 the research team had established links to education services. Initially, a database of schools was compiled for each area linked to the study with the intention of identifying participants via an invitation pack posted out to families. However, this recruitment method proved unsuccessful, with few schools responding and many of those who did being unable/unwilling to distribute recruitment packs. Focus was, therefore, placed on recruiting via newly emerged school-based mental health and well-being services (see Chapter 3). A single school-based service took part, with schools within the service sent study information and invited to participate. When a school agreed, school nurses and the well-being service clinicians identified potential participants and gave them study information. Aligning to recruitment in CAMHS, the parents/guardians of interested participants were asked to return an expression of interest form to the research team either directly or via their school. Research assistants then contacted the family to discuss the study, ascertain eligibility and arrange a baseline visit.
Outcome measures
During ASPECT, outcome measures were completed by CYP and their parent/guardian. The assessments and their timings are presented in Table 2.
| Measure | Time points completed | Delivery method | Completed by |
|---|---|---|---|
| Screening checklist | Screening | Telephone interview | Parent/guardian |
| Demographics | Screening | Telephone interview | Parent/guardian |
| Baseline | Face to face | Parent/guardian | |
| Baseline | Face to face | Participant | |
| BAT | Baseline | Face to face | Participant |
| 6 months after randomisation | Face to face | Participant | |
| ADIS-P | Baseline | Face to face | Parent/guardian |
| 6 months after randomisation | Face to face | Parent/guardian | |
| ADIS-C | Baseline | Face to face | Participant |
| 6 months after randomisation | Face to face | Participant | |
| CAIS-P | Baseline | Face to face | Parent/guardian |
| 6 months after randomisation | Face to face | Parent/guardian | |
| CAIS-C | Baseline | Face to face | Participant |
| 6 months after randomisation | Face to face | Participant | |
| RCADS-P | Baseline | Face to face | Parent/guardian |
| 6 months after randomisation | Face to face | Parent/guardian | |
| RCADS-C | Baseline | Face to face | Participant |
| 6 months after randomisation | Face to face | Participant | |
| Goal-based outcome | Baseline | Face to face | Participant |
| 6 months after randomisation | Face to face | Participant | |
| CHU-9D | Baseline | Face to face | Participant |
| 6 months after randomisation | Face to face | Participant | |
| EQ-5D-Y | Baseline | Face to face | Participant |
| 6 months after randomisation | Face to face | Participant | |
| Resource use | Baseline | Face to face | Parent/guardian |
| 6 months after randomisation | Face to face | Parent/guardian | |
| Therapist logs | Ongoing over intervention | N/A | Therapist/clinician |
| OST integrity scale | Ongoing over intervention | N/A | Clinical supervisor |
| CBT fidelity scale | Ongoing over intervention | N/A | Clinical supervisor |
Data collection methods: children and young people and parents/guardians
Children and young people and their parents/guardians completed several outcome measures with a trained research assistant at baseline, following consent but before randomisation, and at 6 months post randomisation. These meetings were held where the intervention delivery was due to take place/had taken place or at a mutually convenient location. Where follow-up assessments were due for completion during the COVID-19 pandemic (see Chapter 3), information was collected remotely via telephone or video conferencing. Administering the ADIS over the telephone has been examined elsewhere and has demonstrated good to excellent agreement with in-person delivery. 46 At baseline, demographic information (e.g. age, sex and ethnicity) was collected. As part of a subgroup analysis, CYP were also asked whether or not they had a treatment preference prior to randomisation, but this did not affect therapy allocation. On some occasions, particularly when younger participants were involved, the collection of measures was completed over two meetings. The following measures were completed at baseline and repeated at 6 months’ follow-up.
Primary outcome measure
Behavioural Avoidance Task
The BAT33 (Dr T Davis III, Louisiana State University, 2017, personal communication) is a widely used behavioural outcome measure for assessing phobias in children9,34,40 and is specific enough to distinguish between multiple phobias. BAT completion involved gradually exposing participants to their phobic stimulus over 10 predefined steps that increased in difficulty each time. For example, CYP with a dog phobia would start at step zero, which would involve standing outside a room in which there was a dog. Subsequent steps would involve moving closer to the dog, with step 10 (the final step) involving stroking the dog for a specified period of time. The number of steps taken, determined by the research assistant, was the main unit of measurement; a smaller number of steps indicated a higher severity of phobia. The BAT also includes a measure of subjective units of distress (SUDS) whereby participants indicated their level of fear both at the start of the BAT and at the last step completed, ranging from 0 (no fear at all) to 8 (very, very much fear).
Secondary outcome measures
Anxiety Disorder Interview Schedule
The ADIS47 is a semistructured interview and a routinely used diagnostic tool in CYP phobia research. 48 The specific phobia subsection of the ADIS was used to assess full eligibility by obtaining information relating to the presence and type of specific phobias alongside the level of associated fear, avoidance and interference with daily life. During ADIS completion, both parents and CYP used rating scales ranging from 0 (not at all) to 8 (very, very much) to provide information about the level of fear and interference resulting from the specific phobia. Following guidance from the Trial Steering Committee (TSC), the research assistant selected the highest interference score between those provided by the parent and child or young person and used this to determine a composite clinical severity rating (CSR). Where a composite CSR score was ≥ 4, a child or young person was deemed eligible for study entry.
Child Anxiety Impact Scale
The Child Anxiety Impact Scale (CAIS)49 is a 27-item parent and child self-report questionnaire that is designed to measure anxiety-related functional impairment across three subdomains: school activities, social life and home/family life. 50 Participants used a four-point scale ranging from 0 (not at all) to 3 (very much) to describe their agreement with each statement. Both the parent and the child versions of the CAIS were completed.
The Revised Children’s Anxiety and Depression Scale
The Revised Children’s Anxiety and Depression Scale (RCADS)51 is a 47-item, self-report scale that is used to capture mental health information relating to CYP across six subdomains: separation anxiety disorder, social phobia, generalised anxiety disorder, panic disorder, obsessive–compulsive disorder and major depressive disorder. Participants used a four-point scale ranging from 0 (never) to 3 (always) to describe the frequency with which several statements related to them. Both the parent and the child versions of the RCADS were completed.
Goal-based outcome measure
A goal-based outcome measure, based on recent guidelines,52 was used to compare how far a child or young person felt that they had moved towards attaining specific goals set prior to treatment. At baseline, CYP set three goals, with progress towards meeting these assessed at the 6-month follow-up using an 11-point scale ranging from 0 (goal not met) to 10 (goal reached). For a dog phobia, goals may have included being able to stroke a dog, feed a dog or visit a place where a dog might be present.
EuroQol-5 Dimensions Youth version
The EuroQol-5 Dimensions Youth version (EQ-5D-Y)53 measures QoL in CYP on five dimensions (mobility, self-care, usual activities, pain/discomfort and anxiety/depression). Individuals classify their health relative to these dimensions using a three-point scale (1, no problems; 2, some problems; 3, a lot of problems). A visual analogue scale is used by participants to indicate their overall health status from 0 (worst imaginable state) to 100 (best imaginable state). The EQ-5D-Y can provide utility values for cost–utility analysis. The EQ-5D-Y was completed by the CYP only.
Child Health Utility 9D
The Child Health Utility 9D (CHU-9D),54 a child-completed, nine-item questionnaire, measures HRQoL for CYP. Participants describe their feelings in relation to several constructs (worried, sad, pain, tired, annoyed, schoolwork/homework, sleep, daily routine and activities) by selecting one of five sentences. The CHU-9D also provides utility values, allowing the calculation of quality-adjusted life-years (QALYs) for use in cost–utility analysis.
Resource use
Tailored questionnaires were used to collect resource utilisation information for CYP with specific phobias and for delivering interventions. The questionnaires were specifically designed for ASPECT and were based on previous studies focusing on CYP and CYP with mental health issues. 55–57 The questionnaire for service use was completed by the parent/guardian whereas the resource use questionnaire for intervention delivery was completed by the trial research team.
Outcome measures: scoring and interpretation
The ADIS CSR was scored on a scale of 0 to 8, with high scores suggesting the phobia is more disturbing for the child/young person. The CAIS score was calculated by summing scores for each question if no more than three items were missing, and ranges from 0 to 81, with higher scores representing greater impact on psychological function. RCADS domain scores were calculated if no more than two items in that domain were missing by summing the relevant question scores. RCADS total anxiety was calculated by summing contributing domain scores if all were available. RCADS total anxiety ranges from 0 to 111, with higher scores representing more anxiety symptoms. Value sets for the EuroQol-5 Dimensions, three-level version,58 were used to score the ED-5D-Y; the score ranges from –0.594 to 1 (0 means death, 1 is full health and a negative score is a state worse than death). The CHU-9D utility score was calculated by assigning utility values to each response and then summing these values59 if all questions were completed. The CHU-9D utility score ranges from 0.33 to 1, where higher scores represent greater HRQoL. Any missing items on any outcome measure were imputed with the mean of completed items for that scale.
Interventions
Following completion of all baseline measures, participants were randomised to either the intervention group (OST) or the control group receiving usual care (CBT). In all centres, usual care was multisession CBT (no sites were routinely offering OST). Most interventions were delivered in the location at which the CYP had been identified for study inclusion. For the research clinic, suitable spaces in the participant’s locality were identified and used for intervention delivery. As this was a pragmatic trial, the presence or absence of the parent/carer in the session was a clinical decision based on the age and needs of the child and the assessment of the parent/carer–child dyad, and was not considered a confound for analysis given that two previous studies found no clear signal of difference with or without a parent. 34,37
One-session treatment
One-session treatment uses many of the same techniques as CBT (e.g. exposure, participant modelling, reinforcement, cognitive restructuring and skills training). However, instead of being delivered over weekly 1-hour sessions, it takes a more condensed and intensive approach, with delivery comprising two sessions: an initial 1-hour functional assessment followed by a separate treatment session (lasting up to 3 hours) with graduated exposure.
The functional assessment session aims to assess maintaining factors for the phobia, collect information about the CYP’s catastrophic thoughts and generate a fear hierarchy. This session is also used to develop an understanding of the onset and course of the phobia as well as to build a rapport between the clinician, CYP and their parents. The session concludes with focus placed on the treatment rationale and a discussion about what will happen during the subsequent 3-hour exposure session. The therapist reiterates to the CYP that nothing will happen without their permission and, as all therapy tasks are graded, they will not move on to the next one until they have agreed to do so.
The aim of the exposure session is for the CYP to gradually confront and remain in each feared situation on the hierarchy until their anxiety and fear subsides by at least 50%. Participant modelling helps the CYP to approach their feared stimulus slowly and gradually through the therapist first discussing and then demonstrating how to interact with the object/situation and supporting the CYP to do so (an example of participant modelling for dog phobia is the therapist stroking the dog, the child placing their hand on the therapist’s shoulder, then on the therapist’s arm, then over the therapist’s hand, then stroking the dog themselves). Exposure tasks can be used to actively elicit, challenge and test catastrophic thoughts and beliefs associated with the feared object or situation. The CYP are encouraged to maintain their gains from the session by practising self-directed exposure tasks at home (e.g. refraining from avoiding/escaping the feared object/situation and trying to expose themselves to their feared stimulus daily). The main treatment session requires considerable organisation of materials for sequential exposure experiments (e.g. two or three different dogs over the 3-hour session).
Cognitive–behavioural therapy-based interventions
Cognitive–behavioural therapy uses cognitive and behavioural techniques to support people to change unhelpful behaviours and thought patterns that may occur in response to situations. Interventions based on the principles of CBT are the most common model of therapy delivery for specific phobias and are supported by a robust evidence base. 16–20,60,61 CBT for specific phobias aims to help CYP to:
-
recognise anxious feelings and bodily reactions to anxiety
-
gradually confront feared situations until anxiety subsides
-
capture and challenge anxious or scary thoughts when faced with a phobic situation or object, helping to adjust unhelpful or incorrect beliefs
-
develop coping strategies and use anxiety management techniques, especially if distress and physical symptoms become overwhelming and the CYP cannot stay in the feared situation for the purposes of therapy.
Cognitive–behavioural therapy-based interventions for phobias are typically delivered in weekly hour-long sessions comprising the usual practices of building a fear hierarchy, exposure and cognitive restructuring. Each session has a specific objective for the CYP to achieve, supplemented by homework tasks between sessions. Therapists providing CBT as part of ASPECT were asked to deliver their service’s usual CBT multisession treatment approach. There is currently no recommended number of CBT sessions for specific phobias; however, CYP would usually receive 6–12 sessions.
Therapist training
ASPECT therapists received OST training in a 1-day workshop (see Chapter 3, Intervention training and delivery). Some senior practitioners also attended a ‘train the trainer’ session that enabled them to train other therapists in the delivery of OST at their site. Although OST delivery followed a treatment protocol used in previous research,62 CBT delivery did not. However, a manual, co-written by several study principal investigators with extensive experience of delivering CBT to CYP was developed to support therapists.
Study therapists and data collection
All therapists involved in ASPECT were asked to provide some basic information about their professional experience (role, grade, organisation, years of experience and qualifications) before delivering any study treatments. Therapist preference between OST and CBT was also ascertained prior to randomisation. As part of the fidelity (see Assessment of fidelity) and economic evaluations (see Health economic methods) conducted, all therapists were asked to keep a log of the sessions that they delivered (see Chapter 4, Cognitive–behavioural therapy and one-session treatment intervention summaries; see also Table 7). Information was collected pertaining to session number, duration and frequency alongside the strategies employed, the resources required and the number of individuals in attendance at therapy sessions (i.e. whether or not a parent attended). Therapists were also asked to report all contact they had with study participants, any adverse events (AEs) (see Chapter 4, Safety and harms; see Table 16) and any instances where participants withdrew from treatment.
Assessment of fidelity
Therapists were asked to audio-record all treatment sessions, where possible, following informed consent from the CYP and their parents/guardians. To ensure that CBT principles were delivered in both treatment arms, five expert clinical members of the ASPECT team independently rated a random sample of the therapy session recordings (CBT and/or OST). Allocation of session recordings was determined using a randomising formula in Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA). Prior to assessment, the clinicians each assessed the same two session recordings (one CBT and one OST) for comparison to ensure inter-rater reliability. Recorded sessions were scored using the criteria in the session recording forms and one of the following measures relative to the treatment delivered.
The Cognitive Behaviour Therapy Scale for Children and Young People
The Cognitive Behaviour Therapy Scale for Children and Young People (CBTS-CYP)63 is a measure used with CYP to assess fidelity to CBT delivery that is based on the Cognitive Therapy Scale – Revised (CTS-R),64 which is the most widely used tool for measuring CBT competence with adults. Like the CTS-R, the CBTS-CYP utilises a 7-point Likert scale to assess competence over 14 items relating to the use of goals and assessments, behavioural technique use, cognitive technique use and the ability to facilitate self-discovery and child engagement. Scores range from 0 (incompetent) to 6 (expert) and there are two pass criteria: no single item is scored lower than 2 and the total score exceeds 50%. The measure has demonstrated high face validity, internal reliability and robust convergent validity with the CTS-R. 63
The One-Session Treatment Rating Scale
To assess the fidelity to the principles of OST delivery the One-Session Treatment Rating Scale, developed in a previous RCT of OST with CYP,37 was employed. A scale of 0 (not at all) to 6 (excellent) is used to indicate how well a therapist delivering OST adheres to the core principles of the approach over 13 items. Item examples include the extent to which the therapist ‘created a good and therapeutic relationship with the child’ and how well they ‘guided the child in the exposure procedure’. We used the same pass and fail criteria as for the CBT competence assessment (i.e. no single item is scored less than 2 and the total score exceeds 50%).
Fidelity was classified using established criteria to describe the extent of observed fidelity of delivery;65 if < 50% of intended content is delivered, this is classified as ‘low’ fidelity, 51–79% as ‘moderate’ fidelity and 80–100% as ‘high’ fidelity.
Sample size calculations
To our knowledge, no systematic review had examined the effect of CBT on specific phobias as measured using the BAT in CYP. Consequently, the assumptions for the proposed sample size and non-inferiority margin were based on two separate Cochrane reviews66,67 investigating the effects of psychotherapy for those experiencing anxiety. Wolitzky-Taylor et al. 66 conducted a review on studies that used both behavioural measures and self-report questionnaires on adults with specific phobias and reported an overall large effect size of d = 0.81. However, as the treatment may have a different effect on children, the review by Reynolds et al. 67 was also examined. This review was conducted on studies of children with specific phobias but used self-report questionnaires rather than the BAT. This review also reported a large effect size (d = 0.85) for multisession CBT.
As prior meta-analyses suggest that a standardised mean difference of around 0.8 on the BAT is clinically important, the non-inferiority margin was set to be half of this, at 0.4. 68 Assuming a correlation of 0.5 between baseline and final BAT measures, 200 participants (100 per arm) would have been required to have 90% power with a 2.5% one-sided significance level to demonstrate non-inferiority of OST compared with CBT. It was assumed that therapy would be delivered by therapists who would each see approximately 15 patients and therefore a weak therapist effect [intraclass correlation coefficient (ICC) = 0.01] was expected. This clustering was anticipated to result in a design effect of 1.14, which increased the number of participants required per arm to 114. We further assumed a 20% dropout rate, concluding that 286 (143 per arm) would need to be recruited to demonstrate non-inferiority of OST to CBT.
Sample size recalculation
In April 2019, a 7-month extension was requested from the funders in response to lower than expected recruitment, and the sample size was recalculated. As of 27 March 2019, data completeness on the primary end point was 64/88 (72.7%), which translated to a dropout rate of 27.3% (95% CI 18.3% to 37.8%). Based on this and the original timelines, this would have resulted in about 136 (68 per group) participants with 6-month primary outcome data.
We observed a correlation of 0.7 between baseline and 6-month primary outcome measures. We also observed that a therapist was expected to treat five CYP (instead of 15). If the original assumption made about the ICC (of 0.01) was accurate, then the design effect was 1.04 (instead of the planned 1.14). Given these observations, had ASPECT been extended to recruit the original sample size of 286 participants (143 per group), it would have had a power of 97.7% (0.7 correlation, 27.3% dropout rate, five CYP per therapist). Based on a conservative correlation of 0.6, observed dropout rate of 27.3%, each therapist treating an average of five CYP and an ICC of 0.01, a total of 246 participants (123 per group) was required to preserve a power of ≈ 90% for a one-sided 2.5% test with a standardised non-inferiority margin of 0.4. This resulted in 178 participants (89 per group) with primary outcome data for analysis. The decision to recalculate the sample size was presented to and supported by the TSC and the Data Monitoring and Ethics Committee (DMEC).
Stop/go criteria
The internal pilot embedded within ASPECT was due to last for 9 months before it was determined if the trial would need to be terminated against stop/go criteria. In response to delays in setting up some recruitment sites and in conjunction with TSC recommendations, this assessment was postponed by 4 months and was moved from March 2018 to July 2018. However, the original stop/go criteria targets for March 2018 were retained.
The stop/go criteria were based on the feasibility of both recruitment and retention alongside safety outcomes. Based on an anticipated recruitment rate of 12 participants per month, the overall stopping criteria of 75% of the target (n = 81) and 70% retention for those eligible for a 6-month follow-up (n = 25) were set. The safety of the trial was also reviewed by the DMEC.
Randomisation
The randomisation of eligible participants was conducted remotely through a secure web-based system developed by Sheffield CTRU. The randomisation sequence was generated prior to the start of the study by the trial statistician. Participants were randomised 1 : 1 to receive either OST or CBT. Randomisation was stratified according to both age (7–11 vs. 12–16 years) and phobia symptom severity [ADIS clinician’s severity rating (CSR) mild/moderate (scoring 4/5) vs. severe (scoring 6/7/8)] and restricted using randomly permuted blocks of size 4 and 6.
Parent/guardians and the designated therapist were informed of treatment allocation by an unblinded member of the research team. A letter was also sent to the participant’s general practitioner (GP) to inform them of study involvement and treatment allocation.
Allocation concealment and blinding
To reduce sources of bias, the research assistants responsible for conducting baseline and follow-up assessments remained blind to treatment allocation until the completion of all 6-month follow-up measures. Thus, the research assistants were not involved in the allocation procedure, had no involvement in organising therapy sessions and had only limited access to the study database. Furthermore, participants, their parents and therapists were explicitly reminded not to disclose their treatment allocation to the research assistant. All study tasks requiring knowledge of randomisation (e.g. organising therapies) were completed by unblinded members of the research team.
In the event that a research assistant who was responsible for collecting 6-month follow-up data was unblinded, arrangements were made for a different outcome assessor where possible. Information was collected pertaining to the unblinding incident; research assistants were asked about the suspected allocation, date, source and method of unblinding.
The trial statisticians and health economists were blind to treatment allocation while the trial was ongoing. To maintain blinding, the reports presented to the TSC and Trial Management Group (TMG) did not report treatment allocations.
Analysis populations
The intention-to-treat (ITT) population included all consented and randomised participants according to the randomised treatment assignment with complete primary outcome data. This excludes participants who withdrew before randomisation and includes participants who were found to be ineligible post randomisation. 69 The per-protocol (PP) population is a subset of ITT who receive their intervention in accordance with the protocol.
In ASPECT, participants in the OST group were defined as PP if, by the 6-month follow-up, they had attended:
-
one assessment session
-
one main exposure session
-
an optional extra session.
And all of the following had taken place during the therapy:
-
an assessment
-
establishment of a fear hierarchy
-
exposure.
Any participant who attended more than the maximum three sessions outlined above, before their 6-month follow-up occurred, was not classed as PP.
A participant in the CBT group was defined as PP if they had:
-
attended at least four CBT sessions.
If a participant was still undergoing therapy at the time of their 6-month follow-up assessment, only sessions conducted before the follow-up counted towards the PP assessment. An extended ITT population was used for participants who had secondary but not primary outcome data (owing to the COVID-19 pandemic) in the secondary outcome analysis.
Owing to the non-inferiority research question, the main analysis on the primary outcome (BAT score at 6 months post randomisation) was prespecified to be PP with sensitivity analysis on the ITT population. 68,70 We required both the PP and the ITT analyses to demonstrate statistically significant evidence of non-inferiority to declare that the treatment was non-inferior. If the results of the analysis were discrepant (e.g. the ITT rejected the null of inferiority but the PP analysis did not, or vice versa) then the conflicting results from both analyses would be reported, highlighting the inconclusive nature of the results.
Statistical methods
General considerations
All statistical analyses were performed in Stata® version 16 (StataCorp LP, College Station, TX, USA) statistical software. A comprehensive statistical analysis plan was developed while the statistician was blinded to treatment allocation. Data were reported and presented in accordance with the revised CONSORT statement43 and the non-inferiority trials CONSORT extension. 70
Analyses were conducted on the primary outcome (BAT score at 6 months) using all analysis sets (ITT, PP and sensitivity analysis). For all secondary outcomes, the analysis was reported on the ITT population unless there were important differences between results based on the ITT and PP sets. As a guideline, any difference in treatment effect, between ITT and PP populations, of more than 0.1 standard deviation (SD) on any inventory was assessed further.
Data completeness
A CONSORT flow diagram was used to display data completeness and participant throughput from first contact to final follow-up.
Baseline characteristics
The baseline characteristics, assessments and QoL data for participants and parents/guardians were summarised and assessed for comparability between the treatment groups. No statistical significance testing was conducted to test imbalances between the treatment groups but any noted differences are reported descriptively.
Primary outcome analysis
The primary outcome (BAT score at 6 months) was compared between groups using mixed-effects linear regression with robust standard errors and exchangeable correlation to allow for the clustering of outcomes within therapist. The mixed-effects regression was adjusted for baseline BAT score, site and stratifying variables (age and baseline phobia severity) as fixed effects. The null hypothesis of inferiority would have been rejected if the lower limit of the two-sided 95% confidence interval (CI) for the standardised difference was wholly below 0.4 (the range of clinical non-inferiority). The standardised difference was calculated using Hedges’ correction factor and the CI was calculated using the true standard error. 71 The standardised non-inferiority limit of 0.4 was back-transformed to the raw scale using pooled SD from baseline data for analyses presented on the raw scale.
Sensitivity analysis
The following pre-planned sensitivity analyses were undertaken on the primary outcome and displayed alongside the ITT and PP analyses.
To truly implement ITT analysis, multiple imputation was used to include all patients who were consented and randomised, including those with missing BAT outcome data. Participants’ baseline characteristics were summarised and compared between participants with and participants without 6-month primary outcome data. Multiple imputation imputed missing outcome data using chained equations (regression) with 100 imputations using baseline BAT score, age, ethnicity, treatment preference, ADIS CSR, sex and site, and 6-month CAIS, RCADS total anxiety and EQ-5D-Y as covariates in the imputation equation, and excluding treatment group. The model described in the primary outcome analysis was applied to the multiply imputed data.
A sensitivity analysis on the primary outcome was conducted (excluding participants with data collected more than 4 weeks pre and 6 weeks post the 6-month follow-up date).
Further analysis of outcomes in relation to OST and CBT compliance consisted of complier-average causal effect (CACE) analysis72 using a two-stage least squares regression (excluding clustering adjustment) but including site and baseline covariates (age, phobia severity, EQ-5D-Y and BAT). The endogenous variable (treatment receipt) was regressed on the instrumental variable (random treatment allocation) and baseline covariates, generating a prediction of the endogenous variable. The primary analysis model was then fitted after replacing treatment with this prediction. CACE analysis was conducted for both CBT and OST. Compliance was defined using the PP definition for each group (see Analysis populations). Exploratory descriptive analysis compared compliers and non-compliers with respect to baseline data.
Secondary outcomes analysis
Secondary continuous outcomes were analysed using a mixed-effects regression model as for the primary outcome, including the baseline measurement of the respective outcome as a covariate. Secondary binary outcomes were analysed using a mixed-effects logistic regression model adjusted for age, site, phobia severity and therapist as the random effect.
Subgroup analyses
Pre-planned subgroup analyses were undertaken and regarded as exploratory. The following subgroups were investigated:
-
BAT stimulus set-up (simulated vs. real stimuli)
-
participant treatment preference (OST vs. CBT vs. no preference)
-
therapist treatment preference (OST vs. CBT vs. no preference)
-
phobia type [animal vs. vomit vs. blood injection injury (BII) vs. other].
The subgroup analysis used mixed-effects linear regression with BAT scores at 6 months as the response. The model included the main effects of treatment and subgroup and an interaction term between subgroup and was adjusted for covariates as in the primary analysis model. The evidence for treatment effect varying between subgroup was investigated using a statistical test for interaction between the randomised intervention group and the subgroup.
The impact of site and therapist on treatment difference was also investigated using the same methods. Sites were included in a subgroup analysis if at least five participants per group had primary outcome data for that site. The following therapist characteristics were analysed as subgroups:
-
setting (CAMHS vs. not CAMHS)
-
years of experience (0–2 vs. 3–10 vs. ≥ 11 years).
Additional pre-planned sensitivity analyses
To investigate the impact of differing time between the last session of treatment and the 6-month outcomes being collected in the two treatment groups, the following sensitivity analyses were conducted:
-
including a covariate of days between last session (prior to the 6-month outcome) and the 6-month outcome date in the primary analysis model
-
including the above covariate and an interaction term between treatment and the number of days between the last session and the 6-month outcome data being taken.
To investigate the moderating effect of baseline anxiety and depression, the primary analysis was repeated with a covariate of baseline RCADS and an interaction term of RCADS and treatment group. This was performed for RCADS child major depression domain and RCADS total anxiety score.
Safety and harms analysis
Adverse events and serious adverse events (SAEs) were summarised and assessed for similarity between treatment groups. Safety data were reported on an ITT basis for randomised participants only.
Patient and public involvement
Patient and public representatives were actively involved at all stages of this research. The original research was developed in consultation with the phobia charity ‘Triumph Over Phobia’ with their development manager named as a co-applicant. This co-applicant was also part of the TMG and provided advice throughout study completion.
In the development phase of ASPECT, the York Youth Council (a group of approximately 15 people aged 11–18 years who work to make a positive difference to young people living in York) were consulted. In addition to commenting on the study documentation, detailed feedback was received from the Youth Council regarding the methodology and the potential impact of the study in the community. This feedback was incorporated to ensure that the study methods and documentation were suitable for the target population
One member of the independent TSC was an individual with lived experience of phobia and provided advice regarding study oversight throughout trial implementation.
A patient and public involvement (PPI) group meeting was held after completion of the qualitative analysis. It was attended by an individual with lived experience of phobia, a therapist who had delivered OST for ASPECT and TB, with the aim of providing a sensibility check for the qualitative findings. The group were consulted on whether or not they felt that the main points and quotations selected were reasonable, and their recommendations were considered.
Health economic methods
Background
To investigate the cost-effectiveness of OST compared with CBT in CYP with specific phobias, an economic evaluation taking the form of a within-trial cost–utility analysis from the UK NHS and Personal Social Services (PSS) perspective was conducted.
Effectiveness
Effectiveness for the health economic analysis was measured using the EQ-5D-Y (see Secondary outcome measures) and the CHU-9D (see Secondary outcome measures) instruments. The measured utilities at baseline and follow-up were further joined through time, and the area under the curve approach was used to calculate QALYs for further cost–utility analyses. 73
Resource use and costs
All the resource use incurred during the 6-month follow-up was considered, including both intervention and all-cause service use required by CYP with specific phobias.
The resources required to train the professionals and to deliver the interventions were measured by the time spent by professionals as well as other resources used (including second therapist and phobic stimulus acquisition, e.g. animal hire). The relevant training and intervention delivery information was collected using the tailored questionnaire (see Secondary outcome measures) completed by the study team and therapists, respectively.
Children and young people’s service use included parent-reported use of primary and secondary health care, as well as social care. Other additional therapies and services received in either group during the trial period were recorded. Data on productivity loss due to absenteeism from work to care for the CYP were also collected. All resource use data were collected using tailored resource utilisation questionnaires (see Secondary outcome measures) completed by parents/guardians.
All the service use data were further multiplied by corresponding unit cost to arrive at a total cost in each arm using the bottom-up costing approach. Unit costs of health and social service use were obtained from the UK national database of National Cost Collection (previously called Reference Costs)74 and the Unit Costs of Health and Social Care report produced by the Personal Social Services Research Unit (PSSRU). 75 Unit costs of medication were based on the most recent version of the Prescription Cost Analysis – England. 76 Parental productivity costs were valued according to national average wage rates.
Economic analysis
The within-trial cost–utility analysis from a UK NHS and PSS perspective was conducted in line with National Institute for Health and Care Excellence (NICE)77 recommendations to compare costs and QALYs of OST and CBT interventions for CYP with specific phobias. Costs were measured using tailored service use questionnaires, and health outcomes (QALYs) were measured using the EQ-5D-Y. Discounting was not applied because of the short-term nature of the trial.
The primary analysis was based on a UK NHS and PSS perspective to calculate the incremental cost-effectiveness ratio (ICER), which was then compared with the national willingness-to-pay threshold of £20,000–30,000 per QALY gained to assess the cost-effectiveness of the OST intervention following the NICE recommendations. 77 A set of sensitivity analyses were conducted to account for the uncertainty.
Descriptive analysis
Total costs, including intervention and service utilisation costs, and QALYs were compared between the OST and the CBT groups using appropriate descriptive analyses
Handling missing data
Missing data existed in both service use and health outcome data. For service use, data were deemed as missing when all questions under a particular section were left blank. If one of these questions was answered, the others were assumed to be zero. For EQ-5D-Y, the whole section was considered missing if any of the five questions were not answered. The identified missing data were further imputed using Rubin’s multiple imputation method. 78
Regression analysis and bootstrapping
Regression models were used to compare mean costs and QALYs based on an ITT approach. The regression analyses were controlled for baseline differences in utility,79 cost, age, sex, site, phobia type and ADIS highest CSR score at baseline. The model specifications followed the approach recommended by Glick et al. ,80 which considers the distribution of the dependent variable as well as any correlation between the cost and the QALY outcomes. The ICER was then calculated based on the regression coefficients on intervention, as they represented the difference in mean cost and mean QALYs between the two groups. To take uncertainty into consideration, a non-parametric bootstrap resampling method on the basis of 5000 iterations was used to produce CIs for the ICERs. This was done because of the likely skewness in the distribution of regression residuals,81 and the number of 5000 iterations was chosen because it was considered to be sufficient to generate robust estimates of standard errors82 and is widely used in trial-based cost-effectiveness analyses for mental illness. 83–85
The bootstrapped results were presented in the conventional form of a cost-effectiveness plane and a cost-effectiveness acceptability curve (CEAC). The uncertainty based on the outcomes of the 5000 bootstrap iterations was represented graphically on the cost-effectiveness plane. The CEAC presented the probability of the intervention being cost-effective over a range of willingness-to-pay thresholds per QALY. 86
Sensitivity analysis
The following sensitivity analyses were conducted to test assumptions made in the primary analysis:
-
the impact of missing data, considered using the data from the complete case
-
the impact of the COVID-19 pandemic, considered using the data from those who received at least one intervention within the follow-up period
-
the impact of using CHU-9D instead of EQ-5D-Y to measure QALYs
-
the impact of taking a societal perspective, considered including parental productivity costs to account for the economic impact outside the NHS/PSS perspective
-
the impact of outcome measurement, considered using the phobia-specific measure of BAT score instead of a utility-based measure
-
the impact of OST training costs, considered excluding the one-off OST training costs to account for the economic impact once the OST is rolled out.
Qualitative methods
Introduction
Alongside examining the clinical effectiveness and cost-effectiveness of OST relative to quantitative outcomes, it was also important to examine its feasibility and acceptability from the perspectives of multiple stakeholders. Through obtaining a greater understanding from those receiving the treatment, their parents/guardians and those delivering OST, it was hoped that additional information to aid the interpretation of quantitative trial results would be gained. Furthermore, this information could be used to facilitate intervention refinement and, should OST show non-inferiority to CBT, optimise its implementation into service and clinical practice.
Aims and objectives
The ASPECT process evaluation aimed to establish the acceptability of OST to the CYP participating in the trial, their parents/guardians and the therapists administering OST.
Methods
Recruitment and sampling
Interviews were conducted with three participant groups: (1) CYP who had received OST, (2) parents/guardians of CYP receiving OST and (3) therapists delivering OST. Maximum variation sampling ensured a spread of participant characteristics, including age, sex, geographical location and phobia type. The final sample size was determined by data saturation (i.e. the point where no new themes, ideas and/or concepts emerge from the interviews). Based on previous nested qualitative research examining patient acceptability with brief psychological interventions,87 it was estimated that a maximum of 25–30 parent, 25–30 CYP and 15 therapist interviews would be required.
Children and young people who had received OST, their parents/guardians and therapists who had delivered OST during the trial were eligible to attend an interview if they provided consent to do so. Eligible participants were invited to take part via telephone or e-mail.
Interviewers
Interviews were conducted by research assistants working on ASPECT (JL, HE, AB, EH, JH and AS). Participants may have been familiar with interviewers from meeting during data collection visits, but did not know the interviewers personally. Five interviewers were female and one was male. All had Bachelor of Science (BSc) qualifications. All interviewers had previous experience of working with CYP, parents/guardians and clinicians, and were trained prior to the interviews being conducted. Interviewers did not have any access to emerging trial findings.
Interview timings and settings
All interviews with CYP and their parents/guardians were conducted after participants had completed the final outcome measures at the 6-month follow-up point. Interviews with therapists took place as soon as their involvement in the trial was complete. Parent interviews and interviews with older children (≥ 13 years) were conducted face to face or by telephone, depending on participant preference. Interviews with younger children (≤ 12 years) were all conducted face to face. Face-to-face interviews were conducted at mutually convenient locations, generally in participant’s homes or treatment settings. Interviews with CYP and parents/guardians were completed separately. There were some occasions where the parents/guardians were present during CYP’s interviews, but in these instances parents were instructed not to speak during the interview.
Therapist interviews were due to take place in clinic settings or by telephone. However, at the point when these interviews could convene, government restrictions in response to the COVID-19 pandemic were in place and therefore all therapist interviews were conducted by telephone.
Obtaining informed consent
Initially, at the baseline assessment, CYP and their parent/guardian were asked to provide informed consent to be approached for interview as part of the qualitative phase. Where consent to be approached had been given and the CYP had received OST, they and their parent/guardian were asked again if they would like to participate in a qualitative interview at the end of their 6-month follow-up visit. The parent/guardian and the CYP were given information outlining the qualitative research and had the opportunity to discuss this in more detail with the research assistant, who explained the study procedures and answered any questions. Informed consent was taken in person and in writing using age-specific consent forms. Parents/guardians were asked to provide separate consent for both themselves and the CYP to be interviewed. CYP were asked to provide assent to participate with parental consent required alongside.
For therapist interviews, consent was sought using an ethically approved form available in paper and electronic formats.
Interview content and structure
All interviews were semistructured and based on topic guides developed by the research team (see Appendix 2). These guides were endorsed by York Youth Council, whose members checked them and provided useful feedback on how they could be improved. Interviews with parents/guardians focused on phobia experiences, personal and family impact, perceived treatment need, treatment expectations, and treatment engagement and acceptability (e.g. content, delivery mode, format, setting and facilitation). Interviews with CYP focused on the same topics, adapted for age and developmental maturity. Face-to-face interviews with younger participants drew on the principles of ‘draw and write’ techniques, whereby they were offered an opportunity to draw a picture relating to their experiences as a prompt to initiate more in-depth discussion. 88,89 CYP interviews lasted up to 30 minutes and parent/guardian interviews lasted up to 60 minutes.
Therapist interviews lasted up to 60 minutes and focused on their experiences and views of delivering OST, barriers to and enablers of its implementation and roll-out, the individual, team and organisational-level supports required and the perceived suitability of OST for the identified client group.
All interviews were conducted by study research assistants who received training on the methodologies used in the interviews.
Data analysis
All interviews were digitally recorded using an encrypted digital recorder and transcribed verbatim with participant consent. No notes were taken during the interviews. Analysis followed a qualitative framework approach,90 a widely used method of analysing primary qualitative data pertaining to health-care practices with policy relevance. 91 Framework analysis permits both deductive and inductive coding, enabling potentially important themes or concepts that have been identified a priori to be combined with additional themes emerging de novo. A priori themes were determined by the literature and through discussion with the ASPECT team. Data coding was undertaken independently by trained researchers.
Five coders met regularly (fortnightly) to develop a shared coding manual and to ensure that all emerging codes remained grounded in the original data. NVivo version 12 (QSR International, Warrington, UK) software supported the coding of the transcripts, and an Excel spreadsheet was developed that incorporated preliminary framework themes as column headings and the demographic information related to participants who provided data under each theme. As the constant comparison of new data occurred and the coding team’s understandings of the themes under consideration developed, the framework was amended and reshaped to enable the introduction of new codes and/or the deletion of redundant, similar or otherwise compromised codes. In this way, a final framework was achieved that was considered representative of the entire data set. Data from each stakeholder group (CYP, parents/guardians and therapists) were coded separately. The final coding manuals, with example entries, were presented to the TMG and TSC to confirm validity, coherence and conceptual relevance. Co-applicant PB supervised the qualitative study and analysis.
Owing to ethics limitations, participants were not recontacted to discuss their transcripts, or study findings. Instead, coding trees and interim analyses were reviewed and discussed with a PPI panel.
Ethics considerations
Prior to the qualitative study, several ethical and practical issues were considered, with plans made to address them if required. If a participant became distressed during an interview, the researchers were well briefed about what to do, and had access to a specific protocol to follow [see www.journalslibrary.nihr.ac.uk/programmes/hta/153804/#/documentation (accessed 10 January 2022)]. Possible responses included encouraging the participant to take a break from answering questions, reiterating to participants that they did not have to answer anything that they did not want to and offering the participant the opportunity to stop the interview.
During the interviews there was the potential that the researchers could have become upset from listening to potentially distressing experiences. Regular contact between team members ensured the opportunity to seek support where necessary. A team approach to risk management was adopted and any concerns were communicated to the qualitative lead (PB) in the first instance.
Given that interviews could be conducted in participants’ homes, the trial sponsor’s lone worker policy was followed during all interviews to ensure the safety of research staff. Furthermore, any researcher conducting interviews in a participant’s home adhered to a ‘buddy system’, which ensured that their whereabouts were known to other team members who could inform the relevant people/authorities if contact with the researcher was lost.
Chapter 3 Challenges to the implementation and delivery of ASPECT
Parts of this chapter have been reproduced from Tindall et al. 92 © 2022 Tindall, Scott, Biggs, Hayward, Wilson, Cooper, Hargate, Wright and Gega. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms. The text below includes minor additions and formatting changes to the original text.
This section of the report provides a narrative summary of the challenges faced in implementing and delivering ASPECT. We describe the key challenges the study team faced (along with our approach to mitigation), including problems with (1) site set-up, (2) participant identification and recruitment, (3) data collection, (4) intervention training and delivery, and (5) COVID-19.
Setting up recruiting sites
Commissioning and service delivery restructuring
Recruitment to ASPECT coincided with the reorganisation of CAMHS by NHS clinical commissioning groups in response to the government papers Future in Mind93 and the Child Mental Health Green Paper. 94 In parallel, there were also large reductions in local authority and NHS child mental health service funding, which occurred against a backdrop of large increases in child mental health referral rates across England. Consequently, many CAMHS underwent significant restructuring alongside a reduction in staff. Moreover, in some cases CAMHS that the trial team had set up to recruit and deliver treatment disbanded completely, or merged with other NHS trusts, further complicating trial implementation.
This restructuring lead to widespread service reprioritisation of the types of mental health difficulties experienced by CYP so that already limited) resources could be available to CYP who needed it the most. This often meant that specific phobias were deemed lower priority, with many CAMHS ceasing to provide usual phobia support (i.e. CBT). In some areas specific phobia cases were passed to school-based services that were still under development within the care pathway, and unable to offer multisession CBT as required by the ASPECT protocol. Furthermore, in some CAMHS where treatments for specific phobias were still delivered, mental health problem severity thresholds for service acceptance were often set at high levels, with many accepting CYP with a specific phobia only if they had a mental health comorbidity severe enough to reach this threshold. These commissioning and service delivery changes led to challenges, both in terms of trial set up and intervention delivery; for example, given that specific phobias were given lower priority, and often referred to other school-based services, gaps in service provision emerged and there were far fewer participants with phobias available to be recruited than was initially planned.
Solutions: adding new recruiting sites
The ASPECT team implemented a number of strategies to mitigate the impact of commissioning and service delivery changes on recruitment and intervention delivery. The most impactful strategy was to substantially increase the number of recruiting sites from the five that had been originally planned to 12 NHS trusts. Over the course of the trial, study recruitment was conducted in 14 geographical regions across England encompassing 12 NHS trusts comprising 26 CAMHS, three third-sector/voluntary services, one university-based CYP’s well-being service and a research clinic.
From 2017 to mid-2019, the ASPECT team approached approximately 77 NHS trusts to expand the number of recruiting sites, managing to open an additional nine geographical locations (12% of the total approached). This meant that 68 potential sites (88%) that we approached were unable to open to recruitment (Figure 1 illustrates a breakdown of reasons). Initially, our approach to identifying viable ASPECT sites involved preliminary discussions with NHS research and development (R&D) teams, senior clinicians and service managers, who determined whether or not services had sufficient specific phobia referrals and the resources to be part of the study. We found that any of these people could, individually or collectively, act as facilitators of or barriers to the establishment of a site. We learnt that involving all of these individuals at an early stage allowed us to work with these complex systems more effectively. We also learnt that adapting our approach to directly include the therapists involved in delivering low-intensity therapies allowed us to learn additional information about service referrals, capacity and resources.
FIGURE 1.
A flow chart describing attempts to add additional recruiting sites to ASPECT. PI, principal investigator.
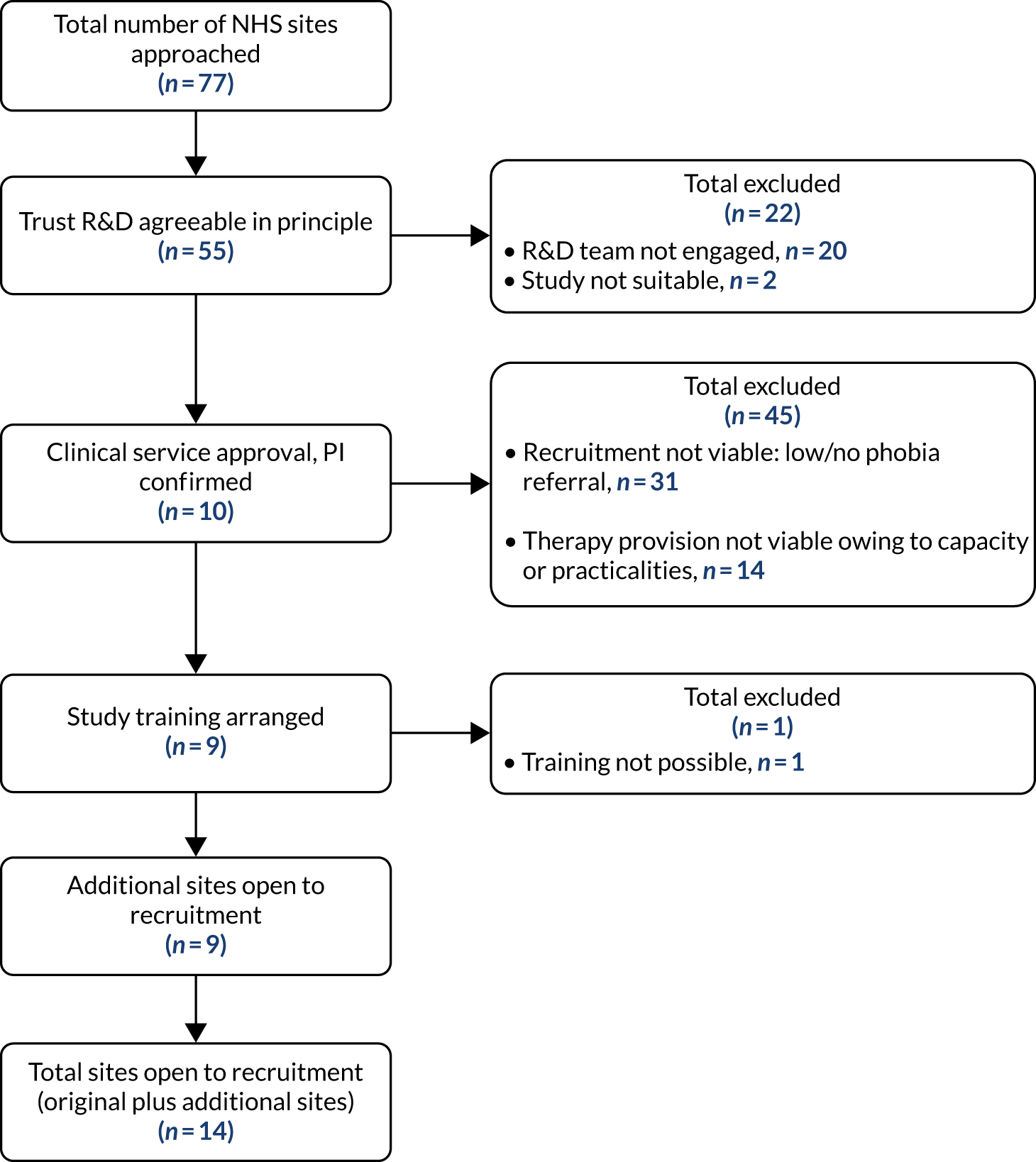
Solutions: facilitating local commissioner–provider discussions about care pathway provision
As discussed in one locality, there was a clear gap in provision of phobia treatment in the care pathway, as commissioners had not specified who would treat CYP with phobia. The research team engaged with local commissioners and providers and over time this issue was resolved.
Training clinic
In the context of these discussions with commissioners and providers in this locality, it was agreed that complicated phobias (with comorbid conditions) would be treated by CAMHS and uncomplicated phobias would be treated by school-based workers funded by commissioners through the local authority. The latter clinical team indicated that they had not received recent CBT training for phobia. We, therefore, facilitated this and for a brief time two local CAMHS clinicians (with CAMHS trainees) worked with school-based workers who came through a training clinic that was termed the ‘research clinic’. This was a temporary arrangement to re-establish healthy care pathways and was successful. At the end of the study the care pathways in this area were working well.
Variation in the structure of services and phobia care pathways
As part of the Future in Mind93 paper, emphasis was placed on the notion of embedding a ‘single point of access’ (SPA) within local areas to allow all CAMHS mental health referrals to be processed via one system. This integrated approach aims to streamline referral criteria across a variety of services but was not always implemented successfully in some areas. Some localities had a SPA for each separate service and so were interpreting national guidance differently. The main challenge that arose in this context was that the care pathways for CYP with specific phobias were not always clearly defined across localities and varied widely between the study sites with multiple services (e.g. NHS CAMHS, voluntary agencies, school-based services and local authority-funded services). In some localities, CYP with specific phobias were routinely seen in CAMHS, whereas in others these individual cases were treated by new school-based services. Where CAMHS sites did routinely see phobia cases, variations were evident in the thresholds for service entry, the pathways to treatment and the length of time waiting for an initial assessment appointment.
Solutions to care pathway variation challenges
Owing to the variation in care pathways and service delivery, a ‘one size fits all’ approach to trial implementation could not be taken. A key strategy employed by the ASPECT team was to tailor the implementation of the trial to the specific structure of the clinical service. Over time, we learnt that the most effective way to engage with services was to involve all levels of the service hierarchy early on, including service and SPA managers, therapists, administration teams and the local R&D teams. This approach allowed us to identify the possible barriers to trial implementation from all perspectives within the service, and to work collaboratively with services to implement solutions that would facilitate the trial’s success. For example, one common barrier for clinical services was waiting list times to see a therapist, with these often exceeding the trial period of 6 months (a wait that was much longer than was expected when the trial was initially planned). This meant that if the trial team were to consent a participant, it was unlikely that the participant would have received any therapy before their final follow-up session. This is because the follow-up period was triggered at the point of randomisation rather than the start of therapy, an approach adopted to reduce bias created by variable rates. To address this, we worked with the clinical services to take a flexible recruitment approach, whereby CYP with phobias referred to the SPAs were recruited to the trial at the point when they were at the top of the waiting list, rather than at the point of referral. This process meant that clinical services could take part in the trial without long waiting times blocking recruitment; however, this was a resource-heavy process in that participants needed to be monitored on waiting lists by the clinical service with liaison with the trial team. To avoid placing additional pressure on services, this approach was flexible with services able to decide whether or not they adopted.
A second strategy that facilitated recruitment at clinical services was to ensure that clinicians and managers working in the SPAs were knowledgeable on the trial, and how it worked in each service. Those with greater ASPECT knowledge and ‘buy-in’ to the trial generally knew which pathways to place CYP with phobias onto, as well as the therapists who were ASPECT trained, and who to talk to in the trial team to ensure that waiting times were managed. In areas where this was not the case, the research team needed to take a more active role in reminding clinicians about the study and eligibility criteria to ensure that the study was routinely being offered. At times, this meant that specific phobias were not identified until an initial assessment appointment took place following a child or young person entering the service with a comorbidity.
Excess treatment costs
Excess treatment costs were applied for from Clinical Research Network funding streams and secured for many of the participating NHS trusts, enabling them to deliver OST as part of ASPECT. Overall, 11 Clinical Commissioning Groups committed to providing funding for ASPECT across Yorkshire and the Humber. However, mid-way through the recruitment period, in summer 2018, the National Institute for Health and Care Research amended the rules under which excess treatment costs could be claimed. As a result, NHS trusts needed to exceed a threshold based on their total expenditure before they could claim excess treatment costs. For many of the participating trusts, this threshold could not be reached. Under the new rules, trusts were informed that they had to use their own funds up to that threshold but many, because of financial difficulty, indicated that they were unable to do this. This had a direct impact on ASPECT, as it resulted in reduced access to additional funding during a period when clinical time was under considerable pressure.
Participant identification and recruitment
Originally, ASPECT was to adopt two methods of participant recruitment, the first from health-care and social care pathways in England (e.g. CAMHS or third-sector/voluntary organisations). The second involved identifying CYP through schools, checking that they met the eligibility criteria (including diagnosis of a phobia) and signposting them to the local treatment service. With regard to health-care and social care pathways, we have already detailed the clinical commissioning changes, variation in care pathways and difficulties with clinical service eligibility thresholds that substantially affected participant identification and recruitment earlier in the chapter. However, our intention to identify participants through schools (by posting invitation packs to families) also experienced significant challenges. First, owing to the structural changes to CAMHS described in Commissioning and service delivery restructuring, many services that were trained to deliver the trial treatments were overwhelmed with long waiting lists and limited resources. Therefore, many of our clinical services were reluctant to agree to speculative participant identification in schools, as it could further stretch already limited resources. Second, in those regions where CAMHS were happy for the trial team to contact schools, we had difficulties engaging both primary and secondary schools to take part. In total, after agreement with local clinical teams, the ASPECT team wrote to 121 schools across North East and North Cumbria, Hull and York; however, only a small proportion of schools replied despite follow-up, and fewer still were able to send out recruitment packs to families. Consequently, this strategy did not appear to be an efficient use of time to support recruitment to ASPECT. Finally, given that in many instances CAMHS were unable to accept speculative school referrals, we attempted to understand whether or not school-based mental health services themselves could recruit and deliver the trial treatments; however, only one school-based mental health service was able to commit the time and experience to deliver ASPECT treatments.
Collecting participant data
There were a number of logistical difficulties identified when embedding ASPECT in several sites specifically relating to the exposure included in both the baseline assessments and treatment deliveries. During completion of the BAT at baseline and the 6-month follow-up, and as part of exposure during therapy delivery, CYP had to come into close proximity to their phobic stimulus. Given that the majority of these procedures occurred in clinical services, careful consideration had to be given to ensuring that these could be conducted safely and that suitable spaces were available. Planning for animal and BII-type exposures was particularly resource heavy; for example, with BII phobias additional staff were required, including those trained in venepuncture, who demonstrated procedures as well as first-aiders who needed to be on call in the event that any child or young person experienced a vasovagal response. Animal-type exposures also required an additional member of staff to meet and greet animal handlers while the ASPECT researcher was completing data collection with families. It was also imperative for ASPECT researchers to brief and debrief staff who assisted with BAT assessments, and increased logistical planning was required to ensure that CYP did not come into contact with the stimulus until the BAT assessment. Additional staff were required for assessments with younger CYP to stay with the child during parent and child ADIS interviews, as responses to this were collected separately. Data collection required two separate rooms: one for the ASPECT researcher to collect baseline/follow-up measures and another to complete the BAT assessment. It was important for rooms to be close together and in a quiet location to ensure that the BAT assessment could be completed as sensitively as possible in the event that CYP became distressed. This presented some challenges in some CAMHS settings, as therapy rooms were already in high demand.
The research team worked flexibly, and alongside clinicians, to ensure that the requirements of the study could be completed, for example in the procurement of appropriate stimuli. Where a phobic stimulus was something that had the potential to cause harm (e.g. an animal), precautions were taken to ensure that the activities were completed safely. The research team also liaised closely with sites to ensure that any phobic stimulus could be brought to a site safely and within insurance remits. Where possible, additional suitable spaces to deliver baseline measures and therapy were identified.
Intervention training and delivery
Intervention training challenges
Training in the delivery of OST and the study procedures was provided to clinicians across all sites involved in ASPECT. The original intention had been to provide basic OST training to all designated trial therapists as well as providing advanced training to a separate more experienced group at each site, so that they could train other therapists within their respective localities. This approach aimed to mitigate the effects of staff turnover, while reducing the training burden on the central team; however, this proved unsuccessful, with those trained often leaving services, not having the capacity to train others or not feeling confident to deliver training. Consequently, clinical members of the central team provided training throughout the study, creating a need to direct resources towards this. This problem was compounded further, as the ASPECT team expanded the number of study sites almost threefold to meet recruitment demands. For example, originally, approximately 50 clinicians were trained to deliver OST; however, this figure increased to 170 by the end of the study. Many of these clinicians did not then go on to provide therapies for the study because of changes with contracts, capacity and availability. Furthermore, although some clinicians were enthusiastic to deliver therapies but unable to deliver them within the trial, others regarded the training as an opportunity for skill enhancement or curriculum vitae building, and not for future treatment delivery for ASPECT.
At times, limited planning of patient throughput resulted in significant delays between clinicians receiving training and them delivering therapy for the first time. As a result, some clinicians did not feel sufficiently confident to deliver the therapies and refresher training sessions were delivered in these instances. To address this issue, later sessions asked attendees to identify a potential phobia case ahead of the training. This not only ensured that clinicians had cases ready soon after completing their training but also assisted with training delivery, with real case examples used to guide the techniques learnt.
Intervention delivery challenges
ASPECT also faced several challenges with intervention delivery throughout the study. As described earlier in this chapter, in many CAMHS teams CYP experiencing mental health difficulties with more severe implications than specific phobias were often deemed higher priority in the context of limited resources. Therefore, in some situations, treatment priority had to be given to those with more severe comorbidities rather than focusing on phobia in the first instance. This resulted in some CYP not receiving phobia treatment until the conclusion of an additional therapy for a more severe comorbidity. This problem was compounded further in that the majority of CYP reporting specific phobias within CAMHS also report a primary comorbidity (e.g. anxiety, depression or eating disorders). Where this was prioritised for therapy, it meant that some CYP did not complete their phobia therapy before their 6-month follow-up measures were due for completion. It was left to clinicians to make appropriate decisions about the order of treatment. In other situations, the delivery of the study interventions needed to be carried out with care (e.g. where a child had a generalised anxiety as well) to accommodate the comorbidity (although the fundamental components of phobia treatment remained as described in training), with many clinicians being considerably experienced in doing this.
In addition, at times, individuals tasked with seeing these cases had limited experience of delivering phobia treatments; therefore, additional training, supervision and guidance were required in the delivery of both treatment arms. At times, the structure of services also impeded the delivery of treatment. Some clinicians, in particular those in school-based services, reported having maximum appointment times of 1 hour to see CYP; therefore, delivering therapy to those randomised to receive OST and requiring a session lasting up to 3 hours was difficult. In these instances, therapists often had to arrange OST sessions alongside holidays to be able to allocate enough time to the treatment sessions. In several instances a problem arose where a SPA clinician identified a child or young person as having a phobia and placed them on the waiting list only for the treating clinician to withdraw them from the study having decided either that a different course of treatment was more appropriate or that the child or young person did not have a phobia.
Staffing
Throughout ASPECT, there was a high turnover of staff in many of the services involved. Many sites identified their trainee psychologists or well-being practitioners as being best placed to deliver the study interventions. It was often felt that these individuals had the capacity to see trial participants, and accepting and treating phobia cases was deemed to provide good experience for professional development. However, many of these individuals were based in services for only a limited period and could, therefore, provide treatment to only a small number of individuals before their placements ended. This was particularly problematic in instances where CYP reached the top of the waiting list and were allocated to a clinician whose placement was nearly complete.
Dealing with COVID-19
In 2020, the COVID-19 global pandemic was announced, with a national lockdown commencing in England on 23 March 2020. Although recruitment to ASPECT had been completed in January 2020, a significant number of CYP were awaiting therapy, receiving therapy or due to complete their 6-month follow-up assessments when government restrictions were put in place. In response to the pandemic, immediate changes were implemented to ASPECT, with impacts on both treatment delivery and the completion of research-related activities.
All follow-up appointments after 23 March 2020 were conducted remotely, either by video conferencing or by telephone depending on participant resources and preference. Although the majority of follow-up measures could be completed this way, completion of the primary outcome measure (the BAT), which could not be administered remotely, had to be postponed until face-to-face contact could be resumed. However, we were unable to resume face-to-face contact by the end of the 6-month follow-up period in August 2020 and, therefore, a proportion of BATs (n = 48) could not be collected at the end of the trial. This equated to 24.4% of those completing a 6-month follow-up (21.6% randomised to CBT and 27% randomised to OST).
As ASPECT was a pragmatic trial, services were informed that therapy delivery during the time of the pandemic was to be based on individual policies and procedures. All services included in ASPECT reported that they had paused therapy delivery while government restrictions were in place. This significantly affected study timelines with many CYP reaching the time for their 6-month follow-up prior to receiving or completing therapy. When treatment deliveries recommenced, adaptations had to be made and therapies delivered remotely. While several clinicians were able to make suitable adaptations to the delivery of CBT, this was not the case for OST; many CYP allocated to OST had their remaining treatment paused.
Chapter 4 Results
Parts of this chapter have been reproduced from Wright et al. 1 © 2022 The Authors. Journal of Child Psychology and Psychiatry published by John Wiley & Sons Ltd on behalf of Association for Child and Adolescent Mental Health. This is an open access article under the terms of the Creative Commons Attribution License, which permits use, distribution and reproduction in any medium, provided the original work is properly cited. The text below includes minor additions and formatting changes to the original text.
Parts of this chapter have been reproduced from Hayward et al. 42 © 2022 Hayward et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. The text below includes minor additions and formatting changes to the original text.
Parts of this chapter have been reproduced from Wang et al. 2 Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data. The text below includes minor additions and formatting changes to the original text.
Main trial results
Internal pilot (stop/go assessment)
In July 2018, the Health Technology Assessment programme considered the performance of ASPECT against the stop/go criteria for the internal pilot (see Chapter 2, Stop/go criteria); to summarise:
-
The trial had recruited 82 participants across sites (target, n = 81).
-
Sixteen participants had provided data at a final 6-month follow-up point. This equated to 80% of those eligible for the 6-month follow-up, which exceeded the specified target of 70%.
-
The DMEC had no concerns regarding trial safety and was supportive of its continuation.
Having successfully met the stop/go criteria, the trial was allowed to progress to the full definitive trial.
Recruitment
Participant recruitment commenced on 30 June 2017. The original recruitment period was due to run for 24 months and be based within five NHS trusts. However, lower than expected recruitment resulted in the period being extended by 7 months, with recruitment continuing until 31 January 2020, at which point the revised target (see Chapter 2, Sample size recalculation) had been exceeded. Alongside this, the number of recruitment sites was increased from the original five to 12 NHS trusts, encompassing 26 CAMHS sites, three third-sector voluntary services and one university-based CYP well-being service. The trial’s follow-up period ran from December 2017 to August 2020.
Participant flow
Figure 2 shows the CONSORT flow of participants through the trial. In total, 274 participants consented and six withdrew prior to randomisation. Two hundred and sixty-eight participants were randomised, of whom 197 (74%) had some 6-month follow-up data and 149 (56%) had primary outcome data. The number of participants recruited exceeded our revised target of 246. More participants were retained at 6 months than our target (197, compared with a target of 178); however, because of the COVID-19 pandemic, in the last 5 months of the trial follow-up period participants had 6-month follow-up data collected remotely and were not able to complete the primary outcome. Table 3 displays reasons for withdrawal in the case of the 71 participants who withdrew post randomisation.
FIGURE 2.
The CONSORT flow diagram showing participant flow. DNA, did not attend. Reproduced with permission from Wright et al. 1 © 2022 The Authors. Journal of Child Psychology and Psychiatry published by John Wiley & Sons Ltd on behalf of Association for Child and Adolescent Mental Health. This is an open access article under the terms of the Creative Commons Attribution License, which permits use, distribution and reproduction in any medium, provided the original work is properly cited. The figure includes minor additions and formatting changes to the original figure.
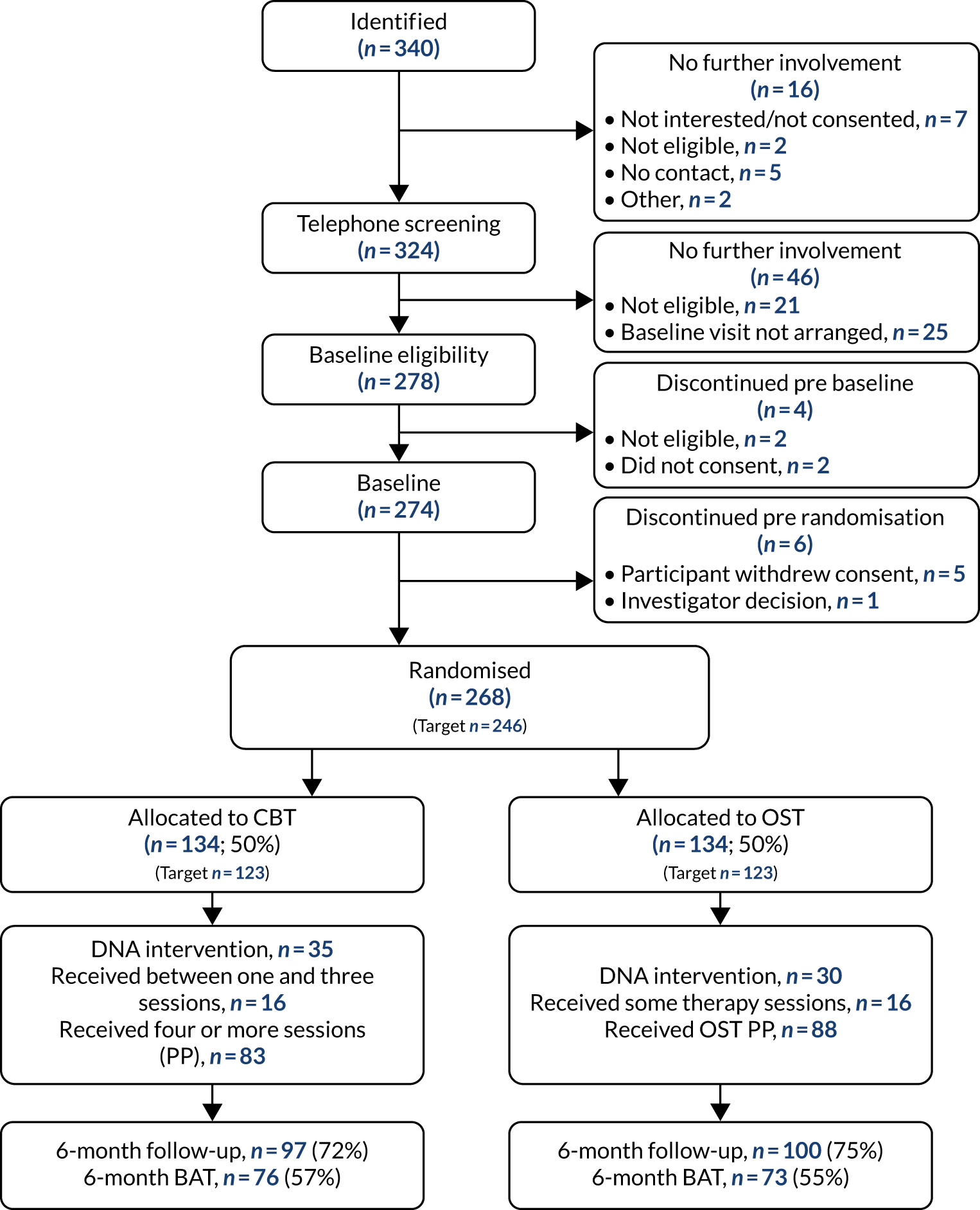
| Reasons for post-randomisation withdrawal | CBT group (n) | OST group (n) |
|---|---|---|
| Participant withdrew consent | 11 | 15 |
| Participant lost to follow-up | 20 | 16 |
| Investigator decision | 6 | 3 |
Baseline characteristics
The characteristics of the randomised participants are given in Table 4 and are well balanced between the groups. Thirteen sites comprising 12 NHS trusts (including 26 CAMHS sites and three affiliated voluntary agency services) and one university-based CYP’s well-being service recruited to the study, contributing between 1 and 78 participants per site. There were more girls (62%) than boys and participants were generally white British (96%). The average age of participants was 12 years. Almost half (47%) of the participants had no treatment preference and slightly more participants had a treatment preference for CBT than for OST (29% vs. 24%). The baseline characteristics of the parents/carers of all randomised participants are given in Table 5; they were more likely to be female (90%) and almost all (97%) were the parents of the participants.
| Characteristic | CBT group (N = 134) | OST group (N = 134) | All (N = 268) |
|---|---|---|---|
| Age | |||
| n (%) | 134 (100) | 134 (100) | 268 (100) |
| Mean (years) (SD) | 11.8 (2.6) | 11.8 (2.6) | 11.8 (2.6) |
| Median (years) (IQR) | 12.0 (10.0–14.0) | 12.0 (10.0–14.0) | 12.0 (10.0–14.0) |
| Site, n (%) | |||
| Humber | 10 (7) | 9 (7) | 19 (7) |
| Tees, Esk and Wear | 39 (29) | 39 (29) | 78 (29) |
| South West Yorkshire | 9 (7) | 5 (4) | 14 (5) |
| Norfolk and Suffolk | 21 (16) | 35 (26) | 56 (21) |
| Northumberland | 14 (10) | 10 (7) | 24 (9) |
| South Tyneside | 17 (13) | 18 (13) | 35 (13) |
| Leeds | 1 (1) | 0 (0) | 1 (0) |
| RDaSH | 10 (7) | 5 (4) | 15 (6) |
| Exeter | 1 (1) | 1 (1) | 2 (1) |
| Dorset | 5 (4) | 6 (4) | 11 (4) |
| Cumbria | 1 (1) | 1 (1) | 2 (1) |
| County Durham | 1 (1) | 3 (2) | 4 (1) |
| Dudley and Walsall | 5 (4) | 2 (1) | 7 (3) |
| Sex, n (%) | |||
| Male | 53 (40) | 48 (36) | 101 (38) |
| Female | 81 (60) | 86 (64) | 167 (62) |
| Ethnicity, n (%) | |||
| English/Welsh/Scottish/Northern Irish/British | 129 (96) | 127 (95) | 256 (96) |
| Irish | 0 (0) | 1 (1) | 1 (0) |
| Any other white background | 0 (0) | 1 (1) | 1 (0) |
| Pakistani | 1 (1) | 2 (1) | 3 (1) |
| White or black Caribbean | 1 (1) | 0 (0) | 1 (0) |
| White or black African | 2 (1) | 0 (0) | 2 (1) |
| White and Asian | 0 (0) | 2 (1) | 2 (1) |
| Any other mixed/multiple ethnic background | 0 (0) | 1 (1) | 1 (0) |
| Prefer not to say | 1 (1) | 0 (0) | 1 (0) |
| School attender, n (%) | |||
| No | 8 (6) | 5 (4) | 13 (5) |
| Yes | 126 (94) | 129 (96) | 255 (95) |
| Treatment preference, n (%) | |||
| CBT | 35 (26) | 43 (32) | 78 (29) |
| OST | 35 (26) | 30 (22) | 65 (24) |
| No preference | 64 (48) | 61 (46) | 125 (47) |
| Taking part in another study, n (%) | |||
| No | 132 (99) | 130 (97) | 262 (98) |
| Yes: phobia/anxiety | 2 (1) | 4 (3) | 6 (2) |
| Number of adults in household, n (%) | |||
| 1 | 18 (13) | 25 (19) | 43 (16) |
| 2 | 100 (75) | 101 (75) | 201 (75) |
| 3 | 13 (10) | 6 (4) | 19 (7) |
| 4 | 2 (1) | 2 (1) | 4 (1) |
| Number of children in household, n (%) | |||
| 1 | 37 (28) | 36 (27) | 73 (27) |
| 2 | 65 (49) | 68 (51) | 133 (50) |
| 3 | 28 (21) | 21 (16) | 49 (18) |
| 4 | 2 (1) | 8 (6) | 10 (4) |
| 5 | 2 (1) | 0 (0) | 2 (1) |
| Characteristic | CBT group (N = 134) | OST group (N = 134) | All (N = 268) |
|---|---|---|---|
| Age | |||
| n (%) | 132 (99) | 133 (99) | 265 (99) |
| Mean (years) (SD) | 41.3 (6.4) | 42.9 (7.2) | 42.1 (6.9) |
| Median (years) (IQR) | 42.0 (37.0–46.0) | 43.0 (37.0–48.0) | 42.0 (37.0–47.0) |
| Sex, n (%) | |||
| Male | 15 (11) | 12 (9) | 27 (10) |
| Female | 119 (89) | 122 (91) | 241 (90) |
| Ethnicity, n (%) | |||
| English/Welsh/Scottish/Northern Irish/British | 127 (95) | 126 (94) | 253 (94) |
| Irish | 1 (1) | 0 (0) | 1 (0) |
| Any other white background | 4 (3) | 4 (3) | 8 (3) |
| Pakistani | 1 (1) | 2 (1) | 3 (1) |
| White and Asian | 0 (0) | 1 (1) | 1 (0) |
| Any other mixed/multiple ethnic background | 1 (1) | 0 (0) | 1 (0) |
| Prefer not to say | 0 (0) | 1 (1) | 1 (0) |
| Highest qualification, n (%) | |||
| Primary or less | 0 (0) | 2 (1) | 2 (1) |
| Secondary | 24 (18) | 39 (29) | 63 (24) |
| Higher (e.g. university or college) | 80 (60) | 66 (49) | 146 (54) |
| Other qualifications | 27 (20) | 25 (19) | 52 (19) |
| Employment status, n (%) | |||
| Employed full time | 39 (29) | 38 (28) | 77 (29) |
| Employed part time | 52 (39) | 50 (37) | 102 (38) |
| Self-employed | 17 (13) | 13 (10) | 30 (11) |
| Currently unable to work owing to poor health | 6 (4) | 7 (5) | 13 (5) |
| Unemployed | 10 (7) | 12 (9) | 22 (8) |
| Retired | 0 (0) | 2 (1) | 2 (1) |
| Studying/student | 1 (1) | 6 (4) | 7 (3) |
| Other | 9 (7) | 5 (4) | 14 (5) |
| Relationship to child, n (%) | |||
| Parent | 129 (96) | 131 (98) | 260 (97) |
| Other relative/legal guardian | 5 (4) | 3 (2) | 8 (3) |
| Marital status, n (%) | |||
| Married/civil partnership: cohabiting | 83 (62) | 89 (66) | 172 (64) |
| Married/civil partnership: separated | 2 (1) | 4 (3) | 6 (2) |
| Single: living in a couple | 21 (16) | 11 (8) | 32 (12) |
| Single: not living in a couple | 14 (10) | 11 (8) | 25 (9) |
| Divorced: cohabiting | 3 (2) | 5 (4) | 8 (3) |
| Divorced: separated | 5 (4) | 6 (4) | 11 (4) |
| Widowed | 1 (1) | 1 (1) | 2 (1) |
| Prefer not to say | 0 (0) | 1 (1) | 1 (0) |
| Partner’s employment status, n (%) | |||
| Employed full time | 68 (51) | 70 (52) | 138 (51) |
| Employed part time | 13 (10) | 8 (6) | 21 (8) |
| Self-employed | 14 (10) | 18 (13) | 32 (12) |
| Currently unable to work owing to poor health | 5 (4) | 1 (1) | 6 (2) |
| Unemployed | 4 (3) | 3 (2) | 7 (3) |
| Retired | 2 (1) | 2 (1) | 4 (1) |
| Other | 1 (1) | 3 (2) | 4 (1) |
| Parent concerned about child or young person’s psychological or emotional health, n (%) | |||
| Yes | 67 (50) | 90 (67) | 157 (59) |
| No | 67 (50) | 44 (33) | 111 (41) |
| Child sought help for psychological or emotional problem in last 6 months, n (%) | |||
| Yes | 62 (46) | 65 (49) | 127 (47) |
| No | 72 (54) | 69 (51) | 141 (53) |
The baseline assessments and patient-reported outcome measures (PROMs) for the participants are given in Table 6. The measures were generally well matched across the treatment groups, and the majority of participants scored either 7 or 8 on the ADIS {median [interquartile range (IQR)]: 8 [7–8]}, meaning that they were assessed as having a severe phobia. The median number of steps completed on the BAT at baseline was three, over half of the CYP completed either 0 or all 10 steps (IQR 0–10) and the mean BAT score was slightly higher in the OST group than in the CBT group. Baseline characteristics and assessments are presented by missing data status (missing or complete primary outcome data at the 6-month follow-up) in Appendix 10, Tables 49 and 50. The characteristics were similar between participants with and participants without missing data; baseline anxiety measures (CAIS and RCADS) were slightly higher in participants with missing 6-month primary outcome data.
| Assessment/PROM | CBT group (N = 134) | OST group (N = 134) | All (N = 268) |
|---|---|---|---|
| Principal phobia (ADIS), n (%) | |||
| Spiders | 5 (4) | 6 (4) | 11 (4) |
| Dogs | 30 (22) | 26 (19) | 56 (21) |
| Bees/insects | 5 (4) | 6 (4) | 11 (4) |
| Other animals | 1 (1) | 1 (1) | 2 (1) |
| Heights | 1 (1) | 2 (1) | 3 (1) |
| Darkness | 2 (1) | 0 (0) | 2 (1) |
| Getting injections | 23 (17) | 23 (17) | 46 (17) |
| Having blood tests | 7 (5) | 8 (6) | 15 (6) |
| Seeing blood from a cut or scrape | 1 (1) | 5 (4) | 6 (2) |
| Lifts or small enclosed places | 0 (0) | 2 (1) | 2 (1) |
| Doctors/dentists | 1 (1) | 2 (1) | 3 (1) |
| Vomiting | 41 (31) | 36 (27) | 77 (29) |
| Costumed characters | 5 (4) | 1 (1) | 6 (2) |
| Choking | 0 (0) | 4 (3) | 4 (1) |
| Food/eating | 3 (2) | 5 (4) | 8 (3) |
| Other | 9 (7) | 7 (5) | 16 (6) |
| ADIS CSR | |||
| n (%) | 134 (100) | 134 (100) | 268 (100) |
| Mean score (SD) | 7.5 (0.9) | 7.6 (0.9) | 7.5 (0.9) |
| Median score (IQR) | 8.0 (7.0–8.0) | 8.0 (7.0–8.0) | 8.0 (7.0–8.0) |
| Number of BAT steps | |||
| n (%) | 134 (100) | 133 (99) | 267 (100) |
| Mean (SD) | 4.1 (4.2) | 4.8 (4.2) | 4.4 (4.2) |
| Median (IQR) | 2.0 (0.0–9.0) | 4.0 (0.0–10.0) | 3.0 (0.0–10.0) |
| Change in SUDS score | |||
| n (%) | 121 (90) | 120 (90) | 241 (90) |
| Mean (SD) | –0.3 (2.3) | –0.1 (1.9) | –0.2 (2.1) |
| Median (IQR) | 0.0 (–1.0–0.0) | 0.0 (–1.0–1.0) | 0.0 (–1.0–1.0) |
| CAIS child score | |||
| n (%) | 130 (97) | 133 (99) | 263 (98) |
| Mean (SD) | 17.8 (13.6) | 18.1 (14.1) | 17.9 (13.8) |
| Median (IQR) | 15.0 (8.0–24.0) | 14.0 (7.0–26.0) | 15.0 (7.0–25.0) |
| CAIS parent score | |||
| n (%) | 127 (95) | 129 (96) | 256 (96) |
| Mean (SD) | 20.2 (16.3) | 21.9 (16.7) | 21.1 (16.5) |
| Median (IQR) | 16.0 (6.0–30.0) | 17.0 (8.0–33.0) | 16.0 (8.0–32.0) |
| CHU-9D score | |||
| n (%) | 133 (99) | 132 (99) | 265 (99) |
| Mean (SD) | 0.9 (0.1) | 0.8 (0.1) | 0.9 (0.1) |
| Median (IQR) | 0.9 (0.8–0.9) | 0.9 (0.8–0.9) | 0.9 (0.8–0.9) |
| EQ-5D-Y score | |||
| n (%) | 134 (100) | 133 (99) | 267 (100) |
| Mean (SD) | 0.741 (0.276) | 0.748 (0.258) | 0.745 (0.266) |
| Median (IQR) | 0.812 (0.656–1.000) | 0.812 (0.689–0.883) | 0.812 (0.689–1.000) |
| EQ-5D VAS score | |||
| n (%) | 134 (100) | 133 (99) | 267 (100) |
| Mean (SD) | 79.1 (19.6) | 77.7 (18.6) | 78.4 (19.1) |
| Median (IQR) | 85.0 (70.0–95.0) | 80.0 (65.0–95.0) | 80.0 (70.0–95.0) |
| Goal-based outcome score: goal 1 | |||
| n (%) | 134 (100) | 134 (100) | 268 (100) |
| Mean (SD) | 1.7 (2.0) | 1.9 (1.9) | 1.8 (2.0) |
| Median (IQR) | 1.0 (0.0–3.0) | 1.5 (0.0–3.0) | 1.0 (0.0–3.0) |
| Goal-based outcome score: goal 2 | |||
| n (%) | 127 (95) | 129 (96) | 256 (96) |
| Mean (SD) | 1.9 (2.1) | 2.1 (1.9) | 2.0 (2.0) |
| Median (IQR) | 1.0 (0.0–3.0) | 2.0 (0.0–4.0) | 2.0 (0.0–3.5) |
| Goal-based outcome score: goal 3 | |||
| n (%) | 89 (66) | 92 (69) | 181 (68) |
| Mean (SD) | 2.0 (2.0) | 1.9 (1.8) | 1.9 (1.9) |
| Median (IQR) | 1.0 (0.0–3.0) | 2.0 (0.0–3.0) | 2.0 (0.0–3.0) |
| RCADS child social phobia score | |||
| n (%) | 134 (100) | 133 (99) | 267 (100) |
| Mean (SD) | 8.8 (6.1) | 9.7 (6.5) | 9.2 (6.3) |
| Median (IQR) | 9.0 (4.0–12.0) | 9.0 (5.0–14.0) | 9.0 (4.0–13.0) |
| RCADS child panic disorder score | |||
| n (%) | 134 (100) | 133 (99) | 267 (100) |
| Mean (SD) | 6.6 (5.4) | 7.8 (6.7) | 7.2 (6.1) |
| Median (IQR) | 6.0 (2.0–10.0) | 6.0 (3.0–11.0) | 6.0 (2.0–10.0) |
| RCADS child depression score | |||
| n (%) | 134 (100) | 133 (99) | 267 (100) |
| Mean (SD) | 7.8 (5.6) | 8.3 (5.7) | 8.0 (5.7) |
| Median (IQR) | 7.0 (3.0–11.0) | 7.0 (4.0–12.0) | 7.0 (4.0–11.0) |
| RCADS child separation anxiety score | |||
| n (%) | 134 (100) | 133 (99) | 267 (100) |
| Mean (SD) | 5.8 (4.7) | 6.0 (4.4) | 5.9 (4.5) |
| Median (IQR) | 5.0 (2.0–9.0) | 5.0 (2.0–9.0) | 5.0 (2.0–9.0) |
| RCADS child generalised anxiety score | |||
| n (%) | 134 (100) | 133 (99) | 267 (100) |
| Mean (SD) | 6.4 (4.2) | 7.1 (4.4) | 6.7 (4.3) |
| Median (IQR) | 6.0 (3.0–9.0) | 7.0 (4.0–10.0) | 6.0 (3.0–9.0) |
| RCADS child obsessive–compulsive score | |||
| n (%) | 134 (100) | 133 (99) | 267 (100) |
| Mean (SD) | 4.4 (3.8) | 5.0 (4.2) | 4.7 (4.0) |
| Median (IQR) | 4.0 (1.0–7.0) | 4.0 (2.0–7.0) | 4.0 (2.0–7.0) |
| RCADS child total anxiety score | |||
| n (%) | 134 (100) | 133 (99) | 267 (100) |
| Mean (SD) | 32.0 (19.1) | 35.6 (21.8) | 33.8 (20.5) |
| Median (IQR) | 28.5 (16.0–47.0) | 31.0 (19.0–52.0) | 30.0 (17.0–49.0) |
| RCADS parent social phobia score | |||
| n (%) | 134 (100) | 134 (100) | 268 (100) |
| Mean (SD) | 9.6 (5.8) | 11.4 (5.8) | 10.5 (5.9) |
| Median (IQR) | 9.0 (5.0–13.0) | 11.0 (7.0–15.0) | 10.0 (6.0–14.0) |
| RCADS parent panic disorder score | |||
| n (%) | 133 (99) | 134 (100) | 267 (100) |
| Mean (SD) | 6.1 (5.0) | 7.7 (5.9) | 6.9 (5.5) |
| Median (IQR) | 5.0 (2.0–8.0) | 6.0 (3.0–10.0) | 5.0 (3.0–10.0) |
| RCADS parent depression score | |||
| n (%) | 134 (100) | 134 (100) | 268 (100) |
| Mean (SD) | 8.0 (5.5) | 8.8 (5.8) | 8.4 (5.6) |
| Median (IQR) | 7.0 (4.0–11.0) | 8.0 (5.0–13.0) | 7.5 (4.0–12.0) |
| RCADS parent separation anxiety score | |||
| n (%) | 134 (100) | 134 (100) | 268 (100) |
| Mean (SD) | 6.4 (4.9) | 7.3 (5.2) | 6.9 (5.1) |
| Median (IQR) | 5.0 (2.0–10.0) | 6.0 (3.0–12.0) | 6.0 (3.0–10.0) |
| RCADS parent generalised anxiety score | |||
| n (%) | 133 (99) | 134 (100) | 267 (100) |
| Mean (SD) | 6.8 (4.3) | 7.7 (4.5) | 7.2 (4.4) |
| Median (IQR) | 6.0 (3.0–10.0) | 7.0 (4.0–11.0) | 7.0 (4.0–10.0) |
| RCADS parent obsessive–compulsive score | |||
| n (%) | 132 (99) | 134 (100) | 266 (99) |
| Mean (SD) | 3.6 (3.8) | 3.9 (3.1) | 3.7 (3.5) |
| Median (IQR) | 2.0 (0.5–6.0) | 3.0 (2.0–6.0) | 3.0 (1.0–6.0) |
| RCADS parent total anxiety score | |||
| n (%) | 132 (99) | 134 (100) | 266 (99) |
| Mean (SD) | 32.4 (19.1) | 37.9 (20.3) | 35.2 (19.9) |
| Median (IQR) | 29.0 (17.5–45.0) | 35.0 (23.0–51.0) | 32.0 (19.0–50.0) |
Cognitive–behavioural therapy and one-session treatment intervention summaries
Table 7 shows a summary of the CBT and OST interventions. Excluding participants who received no treatment, participants in the CBT group received an average of 6.1 hours of treatment over 5.9 sessions; excluding sessions that occurred after the 6-month follow-up, this reduces to an average of 5.4 hours of treatment. Participants in the OST group had an average of 2.2 sessions conducted over 3.8 hours. For the OST group, 63% received treatment PP, 6% were deemed as having too much treatment (either too long or too many sessions; see Chapter 2, Analysis populations, for the OST PP definition) and 31% did not attend any treatment sessions. Our estimates, based on service closure dates and our multisource data information system (PROSPECT), suggest that COVID affected six (14%) participants’ treatment; three received between one and three sessions of CBT, and three received no treatment sessions. For the CBT group, 57% received treatment PP (at least four sessions), 16% received between one and three sessions and 27% did not receive treatment (Figure 3). Our estimates, based on service closure dates and PROSPECT, suggest that for the approximately 14% (n = 3) of those in the CBT group who received between one and three sessions, this was a direct result of COVID-19, alongside 8% (n = 3) who received no treatment sessions. These figures are likely to be underestimates, as some clinicians did not provide this information.
| Characteristic | CBT group (N = 134) | OST group (N = 134) | All (N = 268) |
|---|---|---|---|
| Number of sessions recorded before 6-month visit | |||
| n (%) | 134 (100) | 134 (100) | 268 (100) |
| Mean (SD) | 4.3 (3.7) | 1.6 (1.2) | 3.0 (3.1) |
| Median (IQR) | 4.0 (0.0–7.0) | 2.0 (1.0–2.0) | 2.0 (0.0–4.0) |
| Total duration of treatment (hours): before 6 months | |||
| n (%) | 98 (73) | 102 (76) | 200 (75) |
| Mean (SD) | 5.4 (3.0) | 3.8 (1.2) | 4.6 (2.5) |
| Median (IQR) | 5.7 (3.2–7.0) | 4.0 (3.4–4.3) | 4.0 (3.3–5.9) |
| Number of sessions recorded | |||
| n (%) | 134 (100) | 134 (100) | 268 (100) |
| Mean (SD) | 4.9 (4.1) | 1.7 (1.3) | 3.3 (3.5) |
| Median (IQR) | 5.0 (0.0–7.0) | 2.0 (1.0–2.0) | 2.0 (1.0–5.0) |
| Total duration of treatment (hours): all | |||
| n (%) | 98 (73) | 102 (76) | 200 (75) |
| Mean (SD) | 6.1 (3.3) | 3.8 (1.2) | 4.9 (2.7) |
| Median (IQR) | 6.0 (3.9–7.9) | 4.0 (3.5–4.5) | 4.2 (3.5–6.0) |
| Number of sessions (excluding DNAs) | |||
| n (%) | 98 (73) | 102 (76) | 200 (75) |
| Mean (SD) | 5.9 (3.1) | 2.2 (0.9) | 4.0 (2.9) |
| Median (IQR) | 6.0 (4.0–7.0) | 2.0 (2.0–2.0) | 2.0 (2.0–6.0) |
| Treatment received: OST, n (%) | |||
| PP | 0 (0) | 85 (63) | 85 (32) |
| Too much treatment | 0 (0) | 8 (6) | 8 (3) |
| Did not attend treatment | 0 (0) | 41 (31) | 41 (15) |
| Treatment received: CBT, n (%) | |||
| PP | 77 (57) | 0 (0) | 77 (29) |
| 1–3 sessions | 21 (16) | 0 (0) | 21 (8) |
| No sessions | 36 (27) | 0 (0) | 36 (13) |
| Type of withdrawal, n (%) | |||
| Patient request | 16 (12) | 14 (10) | 30 (11) |
| Clinician decision | 21 (16) | 7 (5) | 28 (10) |
| COVID-19 | 2 (1) | 1 (1) | 3 (1) |
| Other | 3 (2) | 2 (1) | 5 (2) |
| Patients’ reasons for requesting withdrawal, n (%) | |||
| Not interested | 1 (1) | 1 (1) | 2 (1) |
| Lack of time | 3 (2) | 0 (0) | 3 (1) |
| Not happy with randomisation | 2 (1) | 3 (2) | 5 (2) |
| Too fearful of intervention | 3 (2) | 3 (2) | 6 (2) |
| Feeling better | 1 (1) | 1 (1) | 2 (1) |
| Already receiving support | 0 (0) | 2 (1) | 2 (1) |
| Other | 4 (3) | 2 (1) | 6 (2) |
| No reason given | 2 (1) | 2 (1) | 4 (1) |
| Receiving additional treatment for phobia, n (%) | |||
| No | 16 (12) | 26 (19) | 42 (16) |
| Yes | 1 (1) | 2 (1) | 3 (1) |
| Strategies used,a n (%) | |||
| Establishing a fear hierarchy | 87 (88.8) | 93 (100.0) | 180 (94.2) |
| Assessment and monitoring | 91 (92.9) | 93 (100.0) | 184 (96.3) |
| Goal-setting (and review of goals) | 89 (90.8) | 86 (92.5) | 175 (91.6) |
| Formulation | 84 (85.7) | 72 (77.4) | 156 (81.7) |
| Psychoeducation | 87 (88.8) | 88 (94.6) | 175 (91.6) |
| Cognitive restructuring | 63 (64.3) | 66 (71.0) | 129 (67.5) |
| Problem-solving | 49 (50.0) | 44 (47.3) | 93 (48.7) |
| Modelling | 58 (59.2) | 67 (72.0) | 125 (65.4) |
| Anxiety management/relaxation | 64 (65.3) | 52 (55.9) | 116 (60.7) |
| Relapse prevention | 49 (50.0) | 57 (61.3) | 106 (55.5) |
| General chat | 69 (70.4) | 70 (75.3) | 139 (72.8) |
| Homework setting and checking | 82 (83.7) | 47 (50.5) | 129 (67.5) |
| Exposure/behavioural experiments | 77 (78.6) | 91 (97.8) | 168 (88.0) |
FIGURE 3.
Number of treatment sessions attended before the 6-month follow-up by treatment group. (a) CBT; and (b) OST.
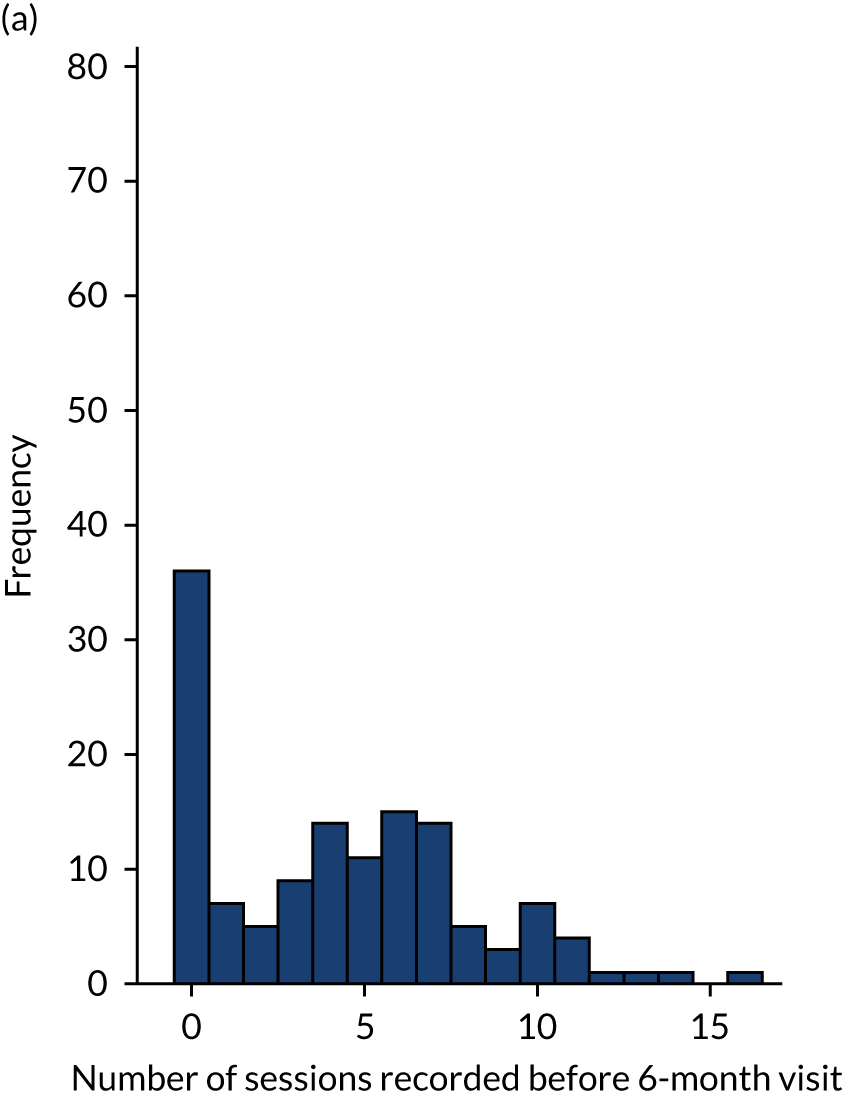
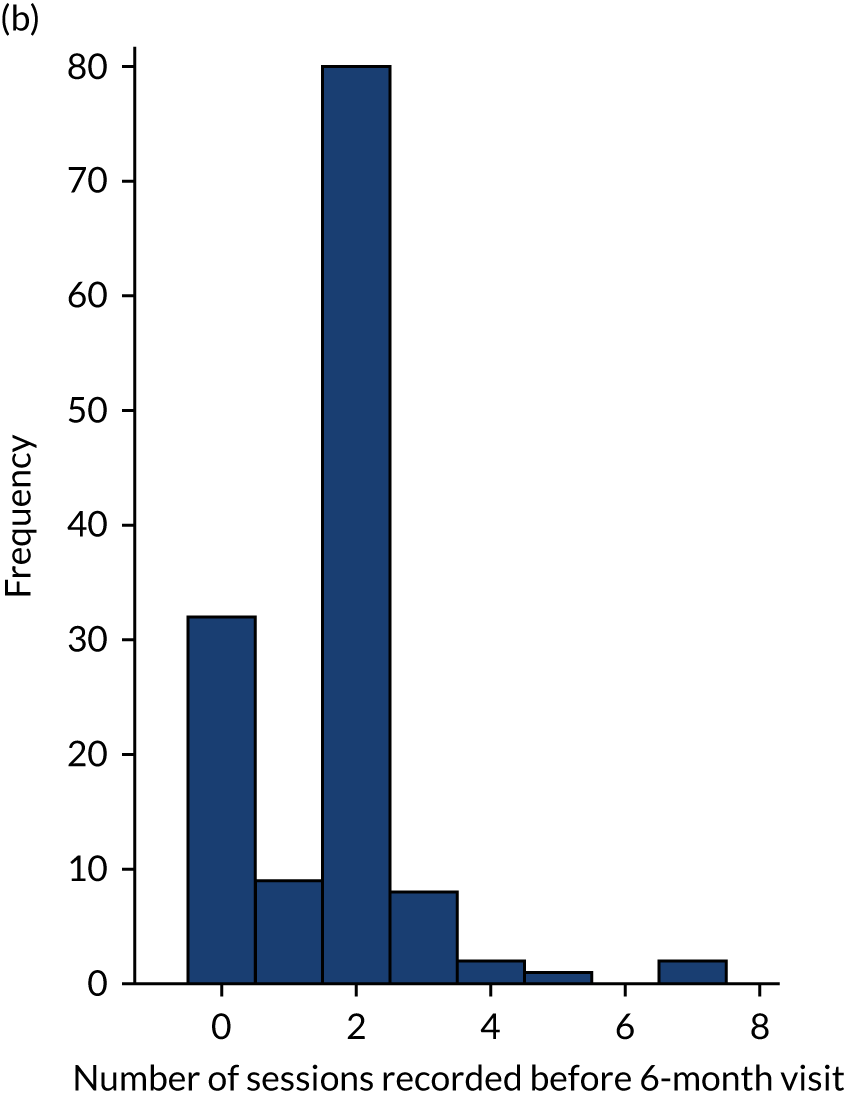
Characteristics of the per-protocol population
There was little evidence of differences in baseline site, child and parent/carer demographics, and child measures between compliance groups, based on within-group multinomial logistic regression (see Chapter 2, Statistical methods). Only the EQ-5D-Y was found to be associated with compliance in the CBT group; it was highest for those who received treatment PP (mean 0.787) and lowest for those who did not attend any sessions (mean 0.661). EQ-5D-Y and ADIS composite scores were associated with compliance in the OST group; ADIS composite scores were higher in the PP group and ‘too much treatment’ group than in the group that received no treatment (means of 7.69, 7.75 and 7.24, respectively). For OST, EQ-5D-Y scores were lowest in the ‘did not attend’ (DNA) group.
Therapist summaries
Table 8 shows the characteristics of the 85 therapists who delivered CBT and OST. Similar numbers of therapists expressed a preference for OST (35%) as expressed a preference for CBT (29%). Most therapists worked in CAMHS (85%) and there was a varied range of roles and qualifications.
| Characteristic | Summary (N = 85) |
|---|---|
| Number of years experiencea | |
| Number of therapists | 53 |
| Mean (SD) | 8 (8) |
| Median (IQR) | 5 (2–12) |
| Minimum, maximum | 0, 32 |
| Treatment preference, n (%) | |
| No preference | 17 (35) |
| CBT | 14 (29) |
| OST | 17 (35) |
| Organisation, n (%) | |
| CAMHS | 45 (85) |
| Local education authority (school-based service) | 4 (8) |
| Third-sector voluntary agency | 2 (4) |
| University-based CYP’s well-being service | 2 (4) |
| Role, n (%) | |
| Assistant/trainee psychologist | 6 (9) |
| Cognitive–behavioural therapist | 6 (9) |
| Clinical psychologist | 9 (14) |
| Counsellor | 2 (3) |
| Medical doctor | 2 (3) |
| Nurse | 3 (5) |
| Other | 14 (22) |
| Psychiatrist | 1 (2) |
| Trainee cognitive–behavioural therapist | 3 (5) |
| Well-being practitioner (CAMHS based) | 12 (19) |
| Well-being practitioner (school based) | 6 (9) |
| Qualification, n (%) | |
| GBC | 3 (4) |
| BACP | 2 (2) |
| BPS DClinPsy | 8 (9) |
| BABCP psychotherapist accreditation | 9 (11) |
| BABCP trainer accreditation | 3 (4) |
| BABCP-accredited well-being practitioner | 2 (2) |
| BABCP-accredited supervisor | 3 (4) |
| MBBS | 3 (4) |
| MRCPsych | 2 (2) |
| Counselling diploma | 2 (2) |
| Diploma in CBT | 17 (20) |
| Certificate in CBT | 8 (9) |
| CYP-IAPT | 17 (20) |
| PGCE | 2 (2) |
| Other associate degree | 3 (4) |
| Other bachelor’s degree | 11 (13) |
| Other graduate diploma | 9 (11) |
| Other master’s degree | 3 (4) |
| Other doctorate | 1 (1) |
Primary outcome analysis
The distribution of BAT steps shown in Figure 4 is similar for ITT and PP populations and a larger number of participants achieved 10 steps at 6 months than at baseline in both treatment groups; the majority of participants improved or achieved the same number of steps, even if not receiving treatment (Figure 5). The mean improvement is shown in Figure 6; a marginally larger improvement is seen for the PP group in both treatment groups.
FIGURE 4.
Behavioural Avoidance Task last steps by treatment group, time point and analysis population. (a) ITT, baseline (n = 149); (b) ITT, 6 months (n = 149); (c) PP, baseline (n = 149); and (d) PP, 6 months (n = 113).
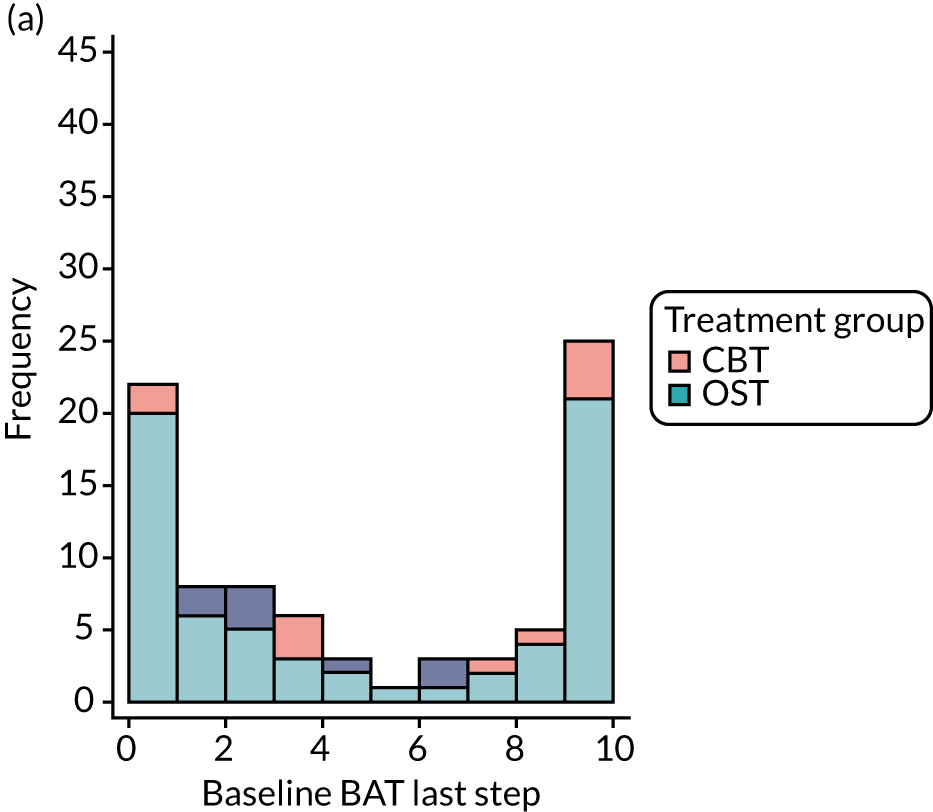
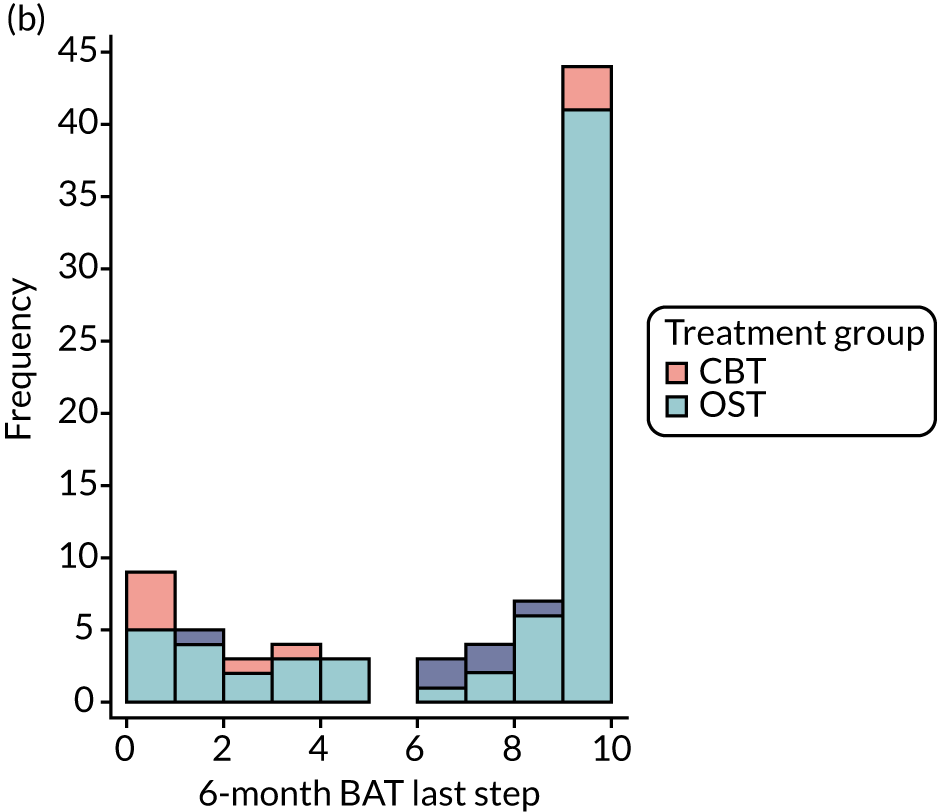
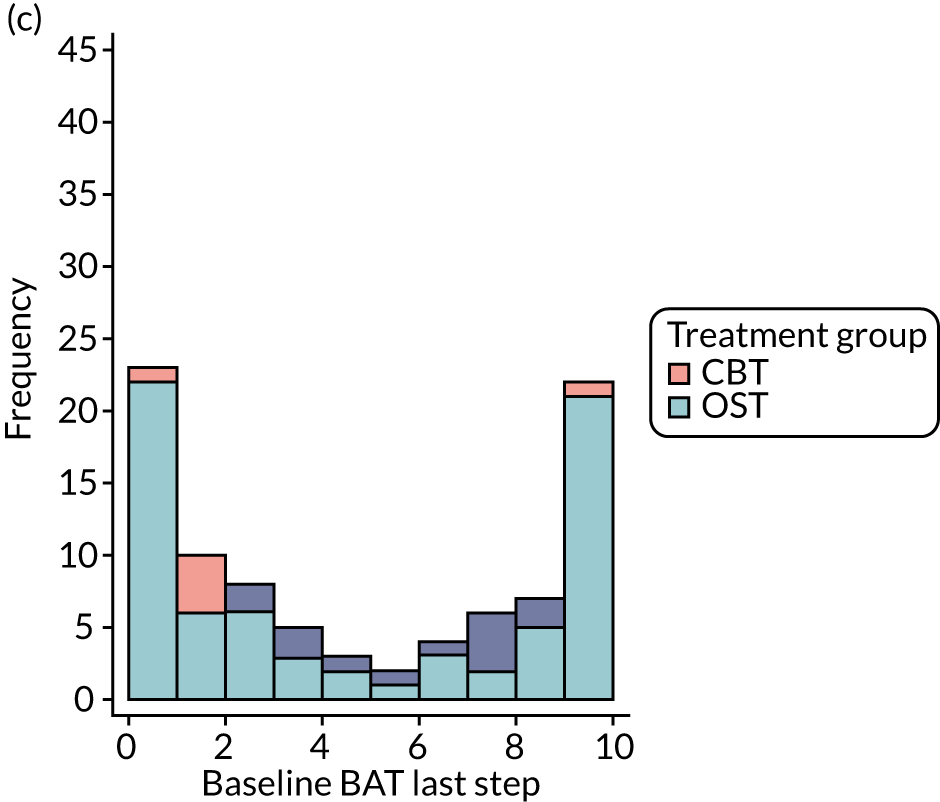
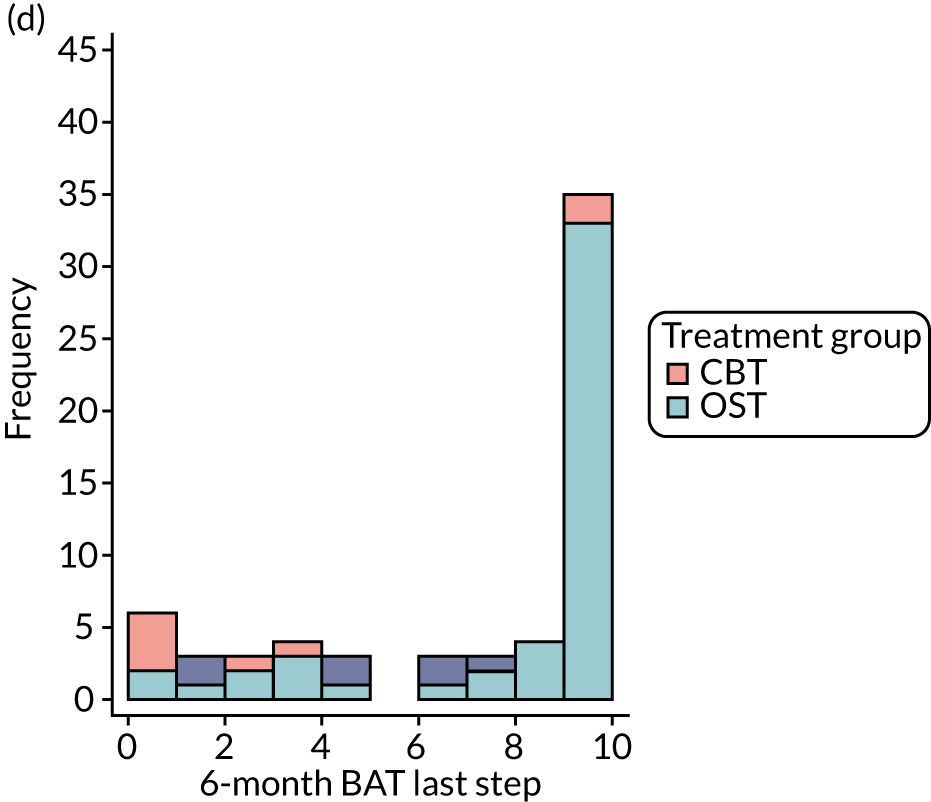
FIGURE 5.
Change in BAT last steps over time by treatment group and analysis population. (a) PP; and (b) ITT.
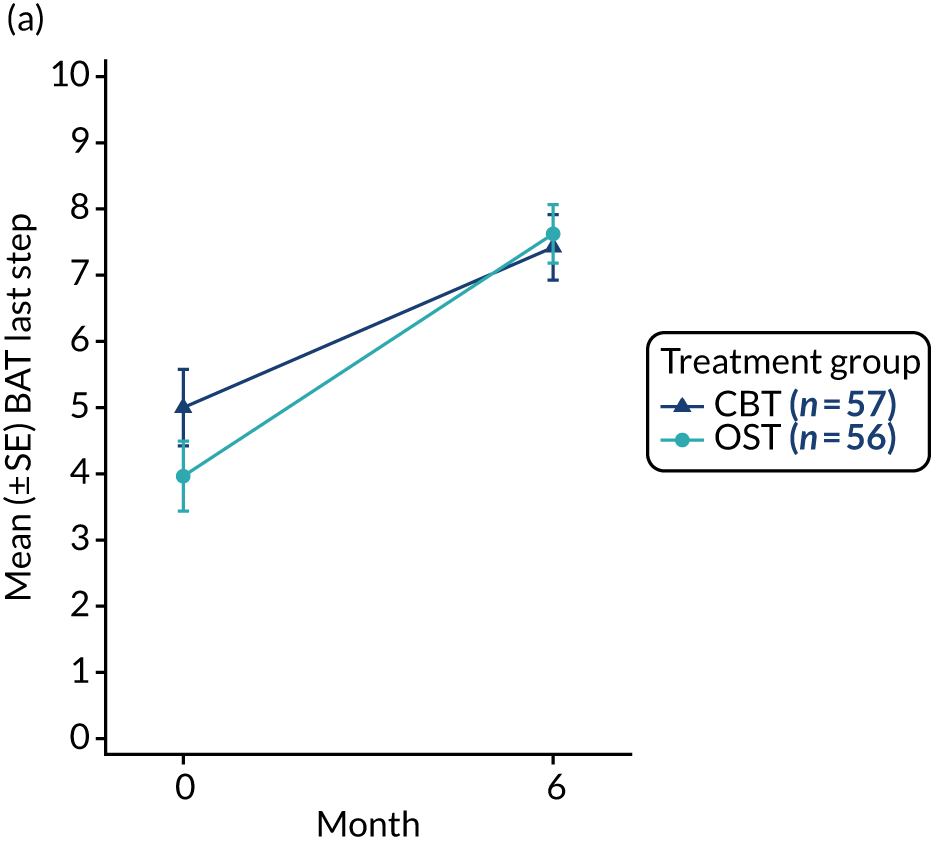
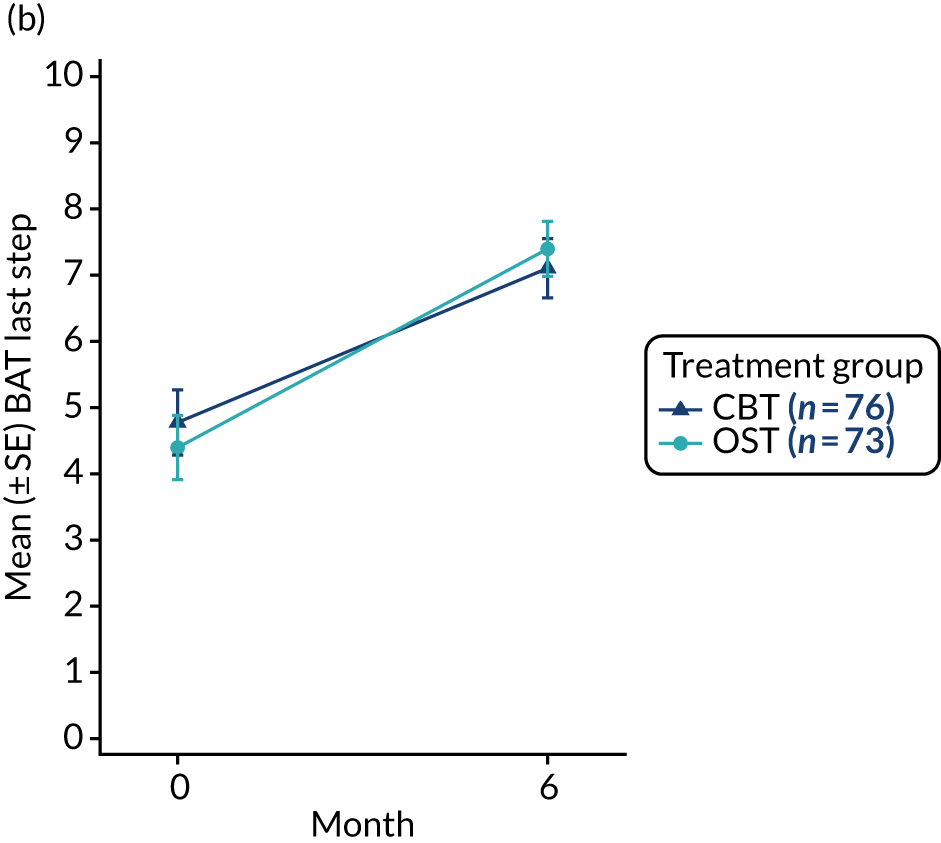
FIGURE 6.
Bubble plot of BAT last steps by treatment group for the ITT population. (a) CBT; and (b) OST. Reproduced with permission from Wright et al. 1 © 2022 The Authors. Journal of Child Psychology and Psychiatry published by John Wiley & Sons Ltd on behalf of Association for Child and Adolescent Mental Health. This is an open access article under the terms of the Creative Commons Attribution License, which permits use, distribution and reproduction in any medium, provided the original work is properly cited. The figure includes minor additions and formatting changes to the original figure.
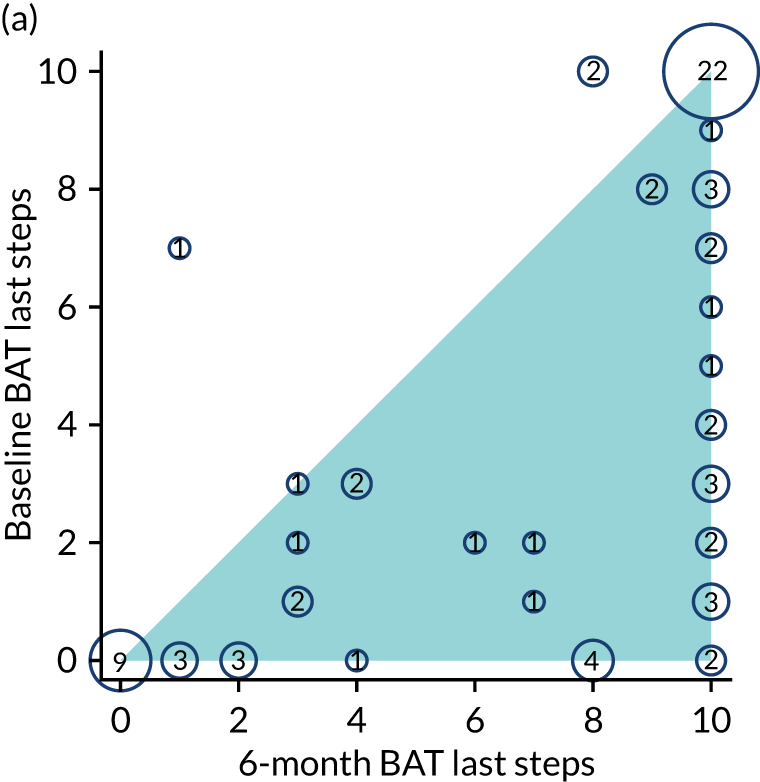
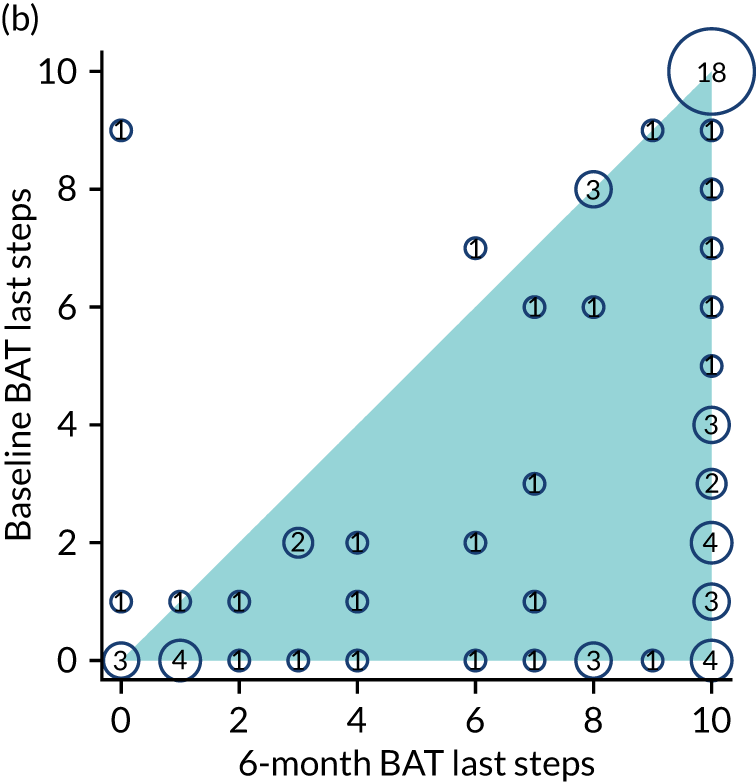
Among the participants completing the BAT at 6 months, the number of steps taken was similar across treatment groups. The mean BAT last steps at 6 months in the CBT group was 7.1 for ITT and 7.4 for PP; in the OST group it was 7.4 for ITT and 7.6 for PP (adjusted mean difference for CBT compared with OST –0.46, 95% CI –1.43 to 0.51 for ITT; mean difference –0.73, 95% CI –1.83 to 0.37 for PP) (Table 9). In each of these analyses the effect is larger for the PP group than the ITT group. On the standardised scale, 95% CIs for both ITT and PP were wholly below the standardised non-inferiority limit of 0.4 (Figure 7) and so there is evidence that OST is non-inferior to CBT.
| Outcome: BAT 6 months | Number of participants; mean (SD) | Raw scale,a mean difference (95% CI) | Standardised,b mean difference (95% CI) | |
|---|---|---|---|---|
| CBT group | OST group | |||
| ITT | 76; 7.1 (3.9) | 73; 7.4 (3.6) | –0.46 (–1.43 to 0.51) | –0.123 (–0.449 to 0.202) |
| PP | 57; 7.4 (3.7) | 56; 7.6 (3.3) | –0.73 (–1.83 to 0.37) | –0.204 (–0.579 to 0.171) |
| Excluding mistimed measurementsc | 61; 7.5 (3.7) | 68; 7.4 (3.6) | –0.13 (–1.27 to 1.00) | –0.037 (–0.389 to 0.315) |
| Multiple imputationd | 134; 6.9 (3.9) | 134; 7.5 (3.8) | –0.1 (–1.1 to 0.8) | |
| CACE: CBT PPe | –0.51 (–1.76 to 0.73) | |||
| CACE: OST PPe | –0.48 (–1.63 to 0.67) | |||
FIGURE 7.
Primary and sensitivity analyses of BAT steps between treatment groups on the standardised scale. Reproduced with permission from Wright et al. 1 © 2022 The Authors. Journal of Child Psychology and Psychiatry published by John Wiley & Sons Ltd on behalf of Association for Child and Adolescent Mental Health. This is an open access article under the terms of the Creative Commons Attribution License, which permits use, distribution and reproduction in any medium, provided the original work is properly cited. The figure includes minor additions and formatting changes to the original figure.
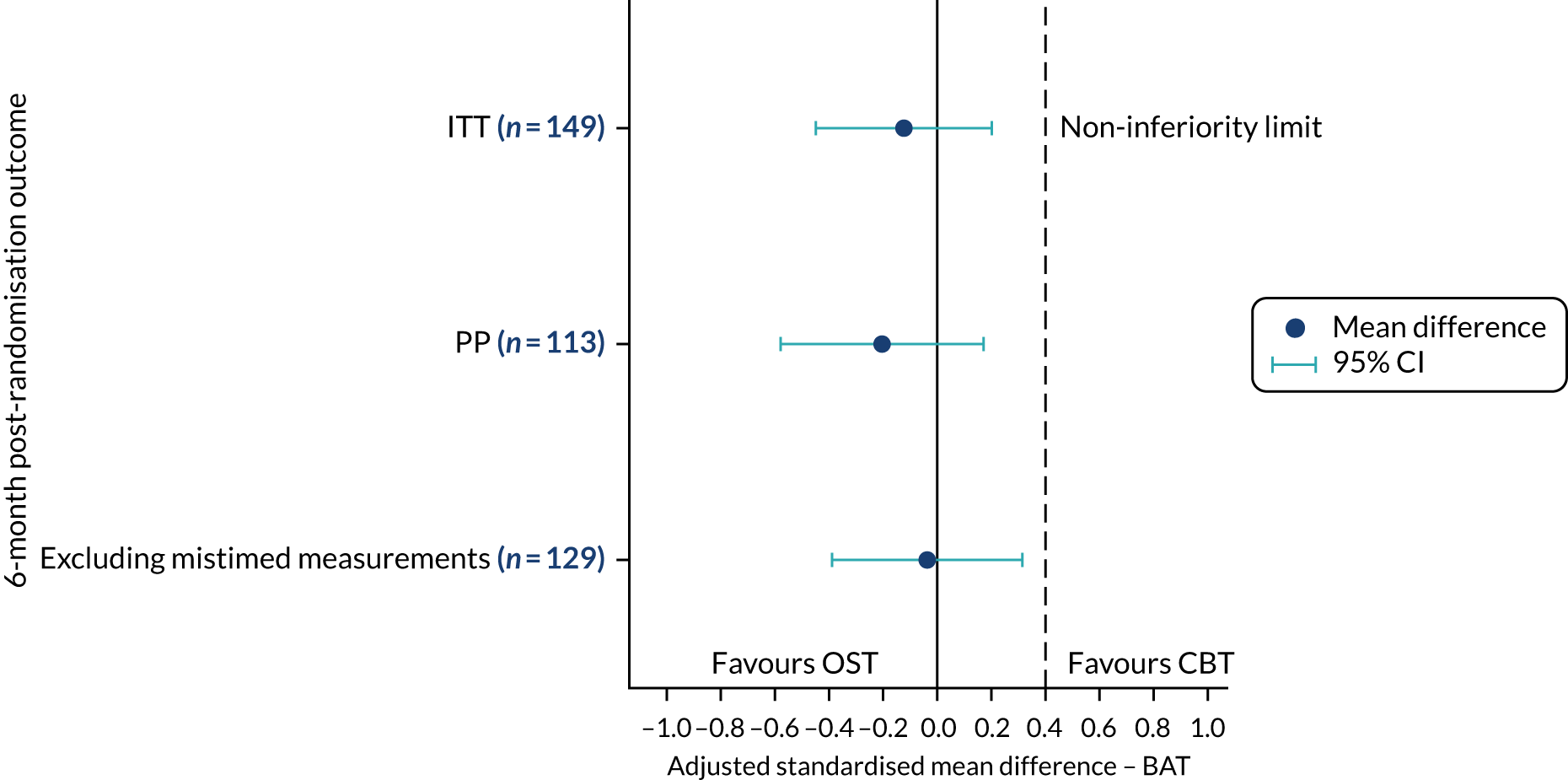
A number of sensitivity analyses were undertaken on the primary outcome (BAT last steps at 6 months) with regard to excluding mistimed measurements, multiple imputation for missing data and CACE analyses to explore treatment adherence. In all cases, the treatment difference remained similar and the CI was wholly below the non-inferiority limit (Figure 8). For mistimed measurements and multiple imputation, the treatment difference was closer to zero than the other analyses that were marginally in favour of OST.
FIGURE 8.
Primary and sensitivity analyses of BAT steps between treatment groups on the raw scale.
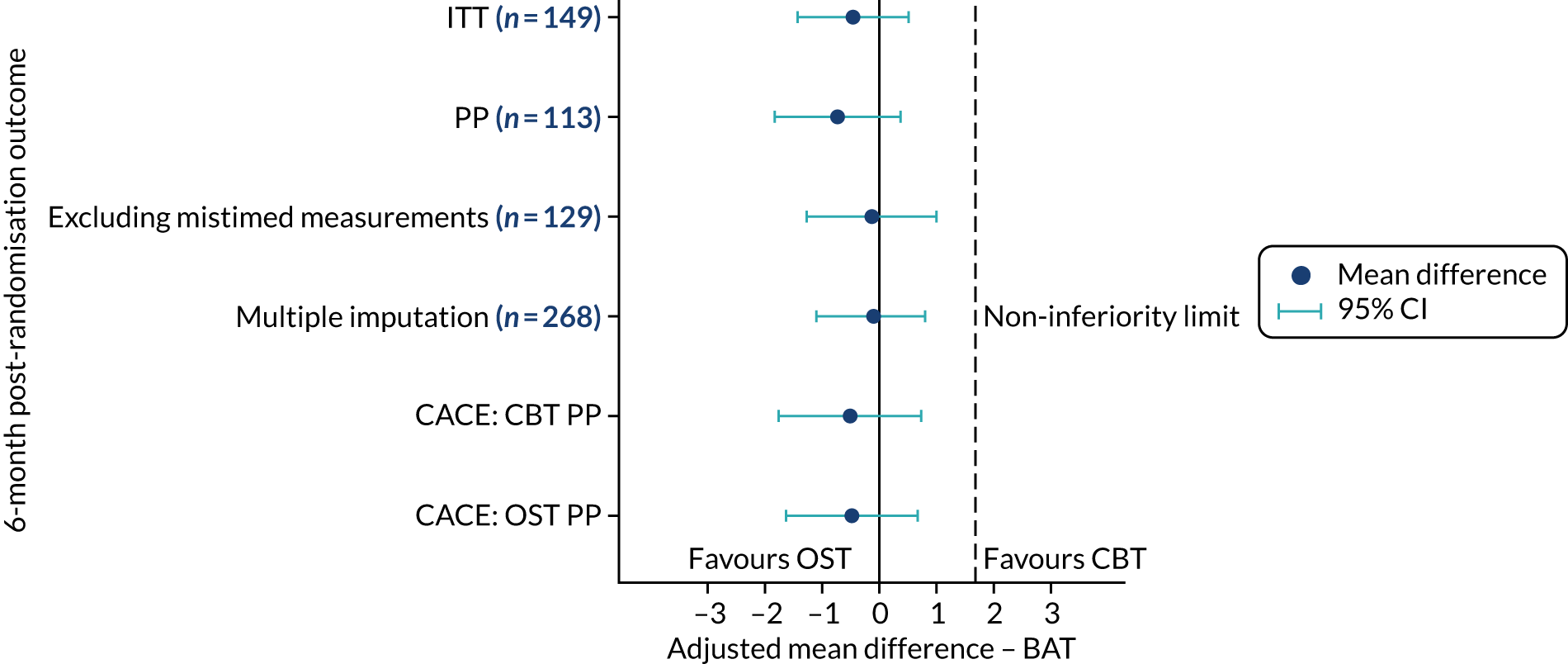
Secondary outcomes analysis
The comparison of secondary outcomes at 6 months is presented in Table 10. All treatment differences were small, with their corresponding CIs crossing zero, and hence were in keeping with the results for the primary outcome; the CBT and OST treatments appear comparable for the secondary outcomes. Some point estimates were slightly in favour of CBT and others were slightly in favour of OST; none were statistically significant.
| Outcome | Number of participants; mean (SD) | Adjusted mean differencea (95% CI) | |
|---|---|---|---|
| CBT group | OST group | ||
| SUDS before | 74; 3.8 (3.0) | 72; 3.7 (2.7) | 0 (–0.8 to 0.8) |
| SUDS change | 74; –0.8 (2.1) | 70; –0.5 (2.0) | –0.2 (–1.0 to 0.5) |
| ADIS CSR | 97; 5.1 (2.6) | 100; 4.9 (2.7) | 0.2 (–0.6 to 1.1) |
| CAIS child | 93; 12.0 (11.2) | 96; 14.5 (14.3) | –1.9 (–4.8 to 1.1) |
| CAIS parent | 92; 14.4 (14.5) | 92; 15.0 (15.8) | 1.9 (–1.1 to 4.9) |
| CHU-9D | 95; 0.89 (0.10) | 96; 0.87 (0.10) | 0.01 (–0.02 to 0.03) |
| EQ-5D-Y | 96; 0.81 (0.24) | 98; 0.82 (0.23) | 0 (–0.07 to 0.06) |
| EQ-5D-Y VAS | 96; 84.2 (16.3) | 98; 82.6 (17.1) | 1.3 (–2.8 to 5.3) |
| Goal-based outcome: goal 1 | 94; 6.4 (3.2) | 95; 5.8 (3.4) | 0.8 (–0.0 to 1.6) |
| Goal-based outcome: goal 2 | 91; 6.2 (3.5) | 94; 5.9 (3.2) | 0.3 (–0.6 to 1.3) |
| Goal-based outcome: goal 3 | 66; 6.5 (3.7) | 69; 6.1 (3.2) | 0.2 (–0.9 to 1.2) |
| RCADS child social phobia score | 96; 7.3 (5.8) | 97; 8.6 (6.0) | –0.3 (–1.4 to 0.8) |
| RCADS child panic disorder score | 96; 5.0 (4.7) | 97; 5.6 (5.2) | –0.3 (–1.4 to 0.8) |
| RCADS child depression score | 96; 5.8 (5.0) | 97; 7.0 (4.9) | –0.8 (–1.7 to 0.2) |
| RCADS child separation anxiety score | 96; 4.0 (4.3) | 96; 4.2 (4.0) | –0.2 (–1.1 to 0.7) |
| RCADS child generalised anxiety score | 96; 5.1 (3.9) | 97; 5.2 (4.1) | 0 (–0.8 to 0.8) |
| RCADS child obsessive–compulsive score | 96; 3.5 (3.6) | 97; 3.7 (3.9) | 0.3 (–0.5 to 1.0) |
| RCADS child total anxiety score | 96; 24.9 (19.0) | 96; 27.6 (19.8) | –0.5 (–4.4 to 3.4) |
| RCADS parent social phobia score | 96; 8.5 (5.9) | 97; 9.2 (5.6) | 0.7 (–0.4 to 1.8) |
| RCADS parent panic disorder score | 96; 4.5 (4.1) | 97; 5.3 (4.5) | 0.2 (–0.7 to 1.0) |
| RCADS parent depression score | 96; 6.1 (4.9) | 97; 6.3 (5.2) | 0.4 (–0.7 to 1.5) |
| RCADS parent separation anxiety score | 96; 5.1 (4.8) | 97; 5.6 (4.8) | –0.1 (–0.9 to 0.8) |
| RCADS parent generalised anxiety score | 96; 5.2 (3.8) | 97; 5.4 (3.8) | 0.4 (–0.3 to 1.2) |
| RCADS parent obsessive–compulsive score | 96; 2.5 (3.1) | 97; 2.9 (3.0) | 0 (–0.7 to 0.7) |
| RCADS parent total anxiety score | 96; 25.8 (18.1) | 97; 28.3 (18.4) | 1.5 (–2.0 to 5.0) |
The number of participants considered to still have specific phobia at 6 months (based on the ADIS CSR) is presented in Table 11; 73% of the ITT population were considered to still have a phobia diagnosis at 6 months, this was the same across treatment groups. Fewer PP participants had specific phobia at 6 months, slightly more in the CBT group than in the OST group (odds ratio 1.41, 95% CI 0.60 to 3.32).
| Outcome | Number of participants (%) | Adjusted ORa (95% CI) | |
|---|---|---|---|
| CBT group | OST group | ||
| Specific phobia (ADIS CSR ≥ 4) | |||
| ITT population | 71 (73) | 73 (73) | 0.96 (0.45 to 2.03) |
| PP population | 46 (68) | 49 (66) | 1.41 (0.60 to 3.32) |
Subgroup analysis
The potential moderating effects of four predefined subgroups were explored by including an interaction between treatment and subgroup in the mixed-effects regression model. Results of the subgroup analyses are presented in Table 12 and summarised in a forest plot in Figure 9. No reliable statistical evidence of subgroups effects or interactions were found between the treatment groups. The adjusted mean difference for treatment in BATs where the stimulus had to be simulated (for example BII) was similar to the BAT real stimuli, and both CIs were wholly below the non-inferiority limit. The adjusted mean difference appeared larger in favour of OST when the participant preferred OST and when the therapist preferred OST.
| Subgroup | Number of participants; mean (SD) BAT last steps at 6 months | Mean difference (95% CI) | Interaction coefficient (95% CI)a | p-value | ||
|---|---|---|---|---|---|---|
| CBT group | OST group | |||||
| BAT stimulus set-up | ||||||
| Real | 38; 6.6 (3.9) | 37; 7.2 (3.4) | –0.2 (–1.5 to 1.0) | 0.61 | ||
| Simulated | 38; 7.6 (3.9) | 36; 7.6 (3.8) | –0.7 (–2.2 to 0.7) | –0.5b (–2.4 to 1.4) | ||
| Treatment preference | ||||||
| CBT | 25; 7.3 (4.1) | 25; 6.9 (3.8) | 0 (–1.7 to 1.6) | 0.368 | ||
| OST | 12; 6.9 (4.3) | 14; 8.4 (2.8) | –1.6 (–3.4 to 0.2) | |||
| No preference | 39; 7.0 (3.8) | 34; 7.4 (3.7) | –0.4 (–1.8 to 1.0) | |||
| Therapist treatment preference | ||||||
| CBT | 12; 7.8 (3.5) | 8; 7.5 (3.9) | 0.7 (–1.5 to 2.9) | 0.448 | ||
| OST | 12; 7.7 (4.2) | 24; 7.9 (2.9) | –1.2 (–3.0 to 0.6) | |||
| No preference | 14; 6.4 (4.5) | 16; 6.8 (3.9) | –0.6 (–2.6 to 1.4) | |||
| Phobia type | ||||||
| Animal | 27; 7.1 (3.6) | 22; 6.5 (3.6) | –0.3 (–2.4 to 1.8) | 0.167 | ||
| Vomit | 20; 5.5 (4.3) | 14; 7.4 (3.7) | –2.5 (–4.7 to –0.2) | |||
| BII | 18; 9.9 (0.2) | 18; 8.6 (3.1) | 0.4 (–1.3 to 2.1) | |||
| Other | 11; 5.4 (4.7) | 19; 7.4 (3.7) | 0.3 (–2.9 to 3.5) | |||
FIGURE 9.
Mean 6-month BAT last steps score by subgroup and treatment group (n = 149).
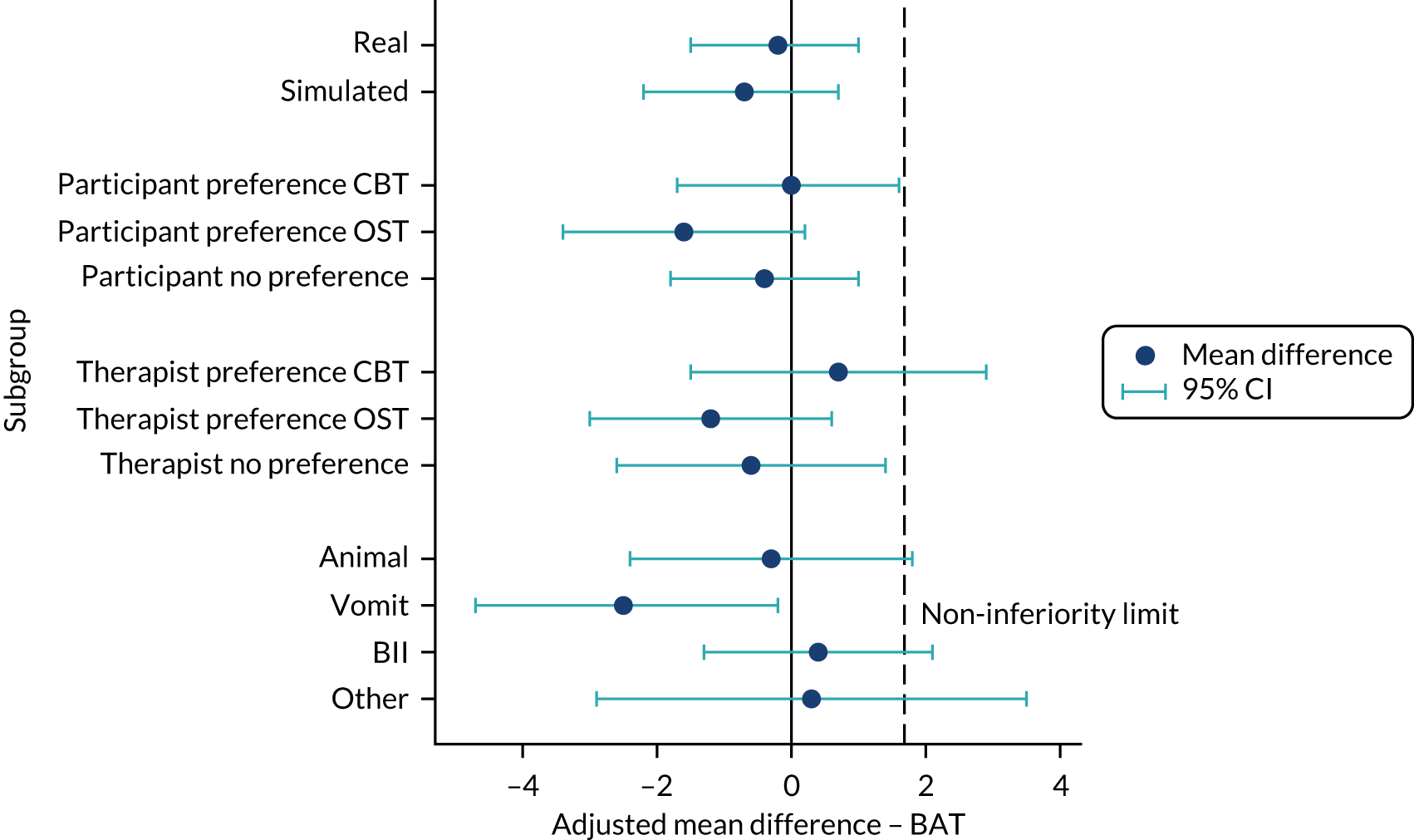
Assessment of post-treatment follow-up time in relation to outcome
The number of weeks between treatment finishing and outcome assessment was likely to be different between the treatment groups, as OST is completed in fewer sessions. Figure 10 compares the distribution of days between a participant’s last session and their outcome assessment. Thirty participants in the CBT group had recorded treatment sessions after outcomes were collected compared with three participants in the OST group. These show as negative values on the plot where the last session received was after the primary outcome measure. The second panel was capped at zero; therefore, if the last time was negative it was classed as zero. The rightmost panel shows the time from the last session received before the primary outcome measure. Adjusting for days between last session that occurred before 6 months’ follow-up in the PP analysis (so participants who had no sessions are excluded from the analysis) had minimal impact on the estimation of the difference in BAT scores between the treatment groups (changed the PP treatment difference to 0.67, 95% CI –0.60 to 1.95). Including an interaction between treatment and days between session and follow-up in the mixed-effects analysis was not statistically significant.
FIGURE 10.
Days between last session and follow-up by treatment group. (a) Days between last session and follow-up; (b) days between last session and follow-up, capped at 0; (c) days between last session and follow-up within 6 months. An outlying observation of –324 has been excluded from (a) for readability.
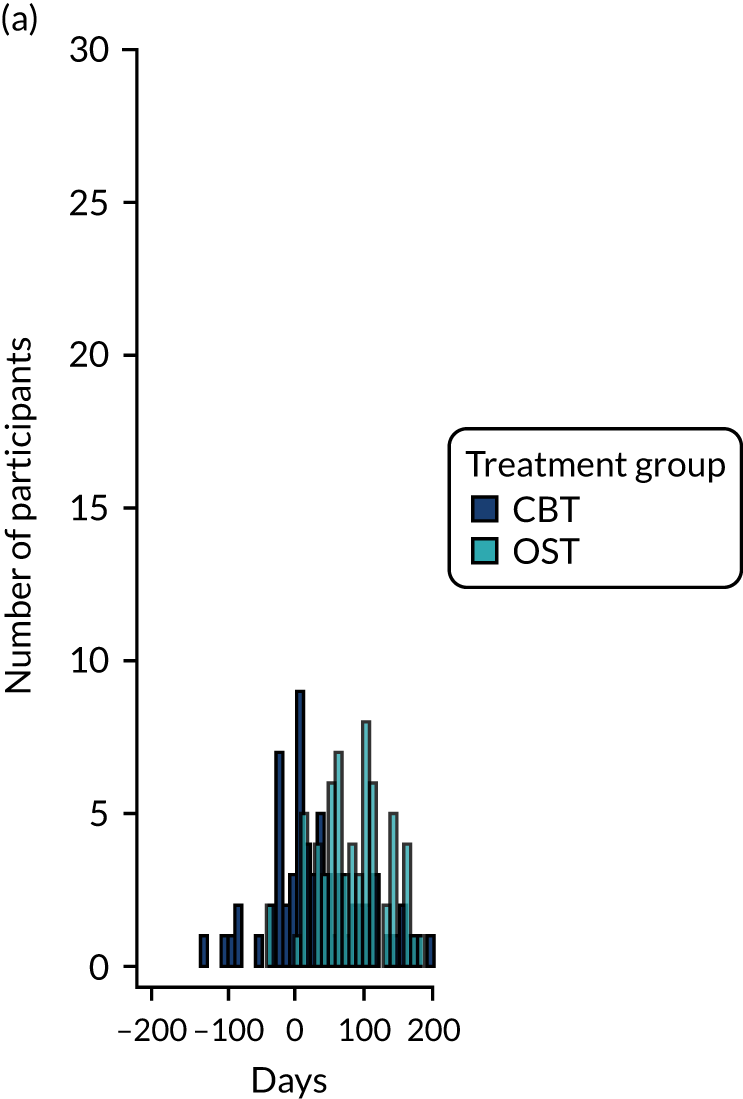
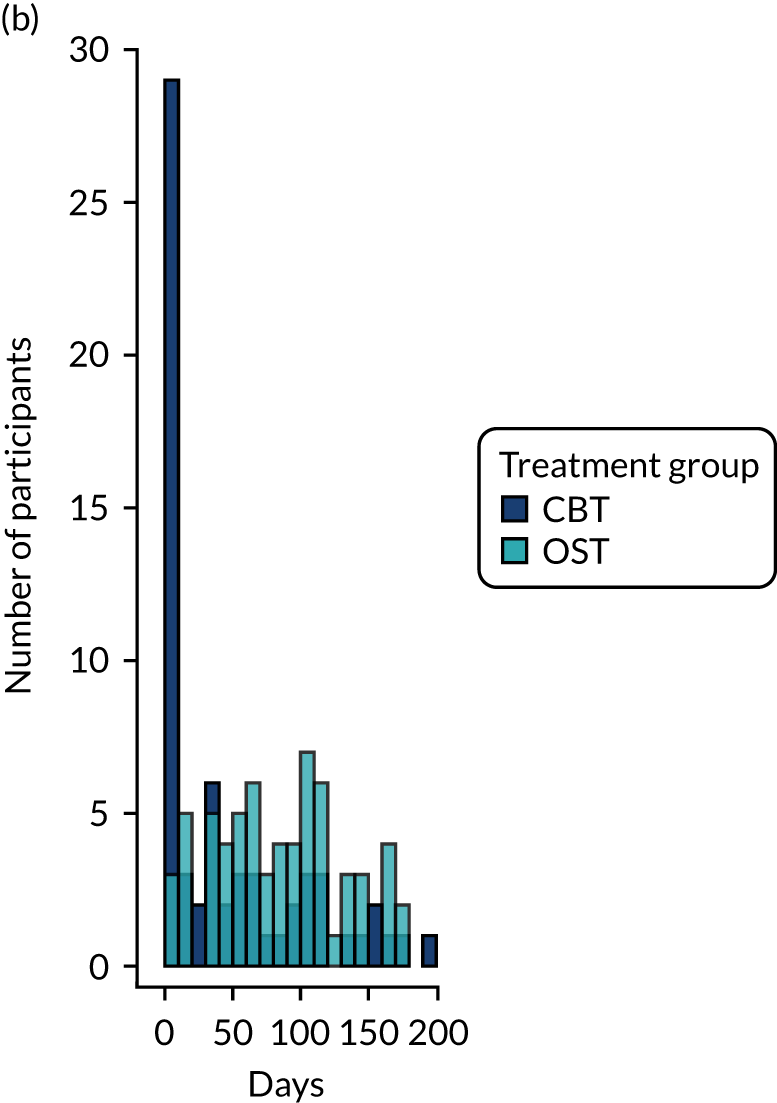
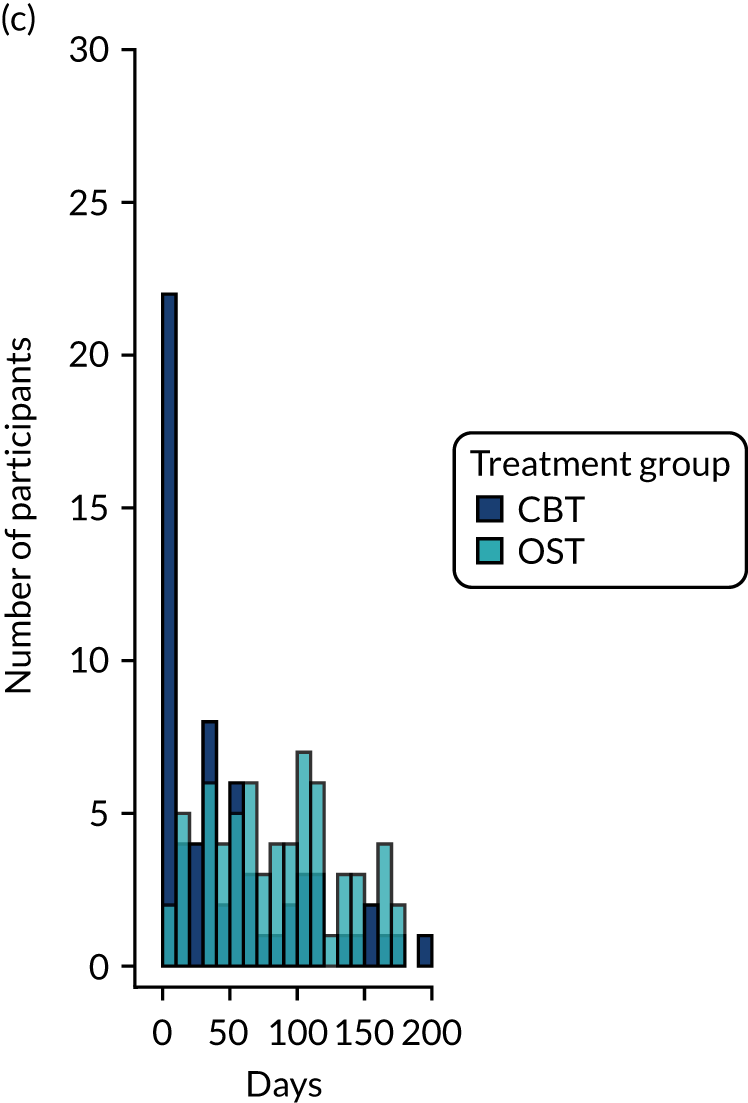
Baseline anxiety and depression
The potential moderating effect of baseline anxiety (measured by RCADS child total anxiety score) and depression (measured by RCADS child depression score) was explored. The primary analysis model was repeated with the addition of an interaction term between RCADS and treatment group; the coefficients for the interaction terms are given in Table 13. There was weak evidence of a negative relationship between RCADS total anxiety score and 6-month BAT last steps, which was more marked for the CBT group, as is shown in Figure 11.
| RCADS score | Interaction coefficienta (95% CI) | p-value |
|---|---|---|
| RCADS child depression score | –0.16 (–0.39 to 0.07) | 0.167 |
| RCADS child total anxiety score | –0.05 (–0.11 to 0.01) | 0.096 |
FIGURE 11.
Baseline anxiety and 6-month BAT last steps by treatment group. Best-fit lines for CBT and OST from linear regression.
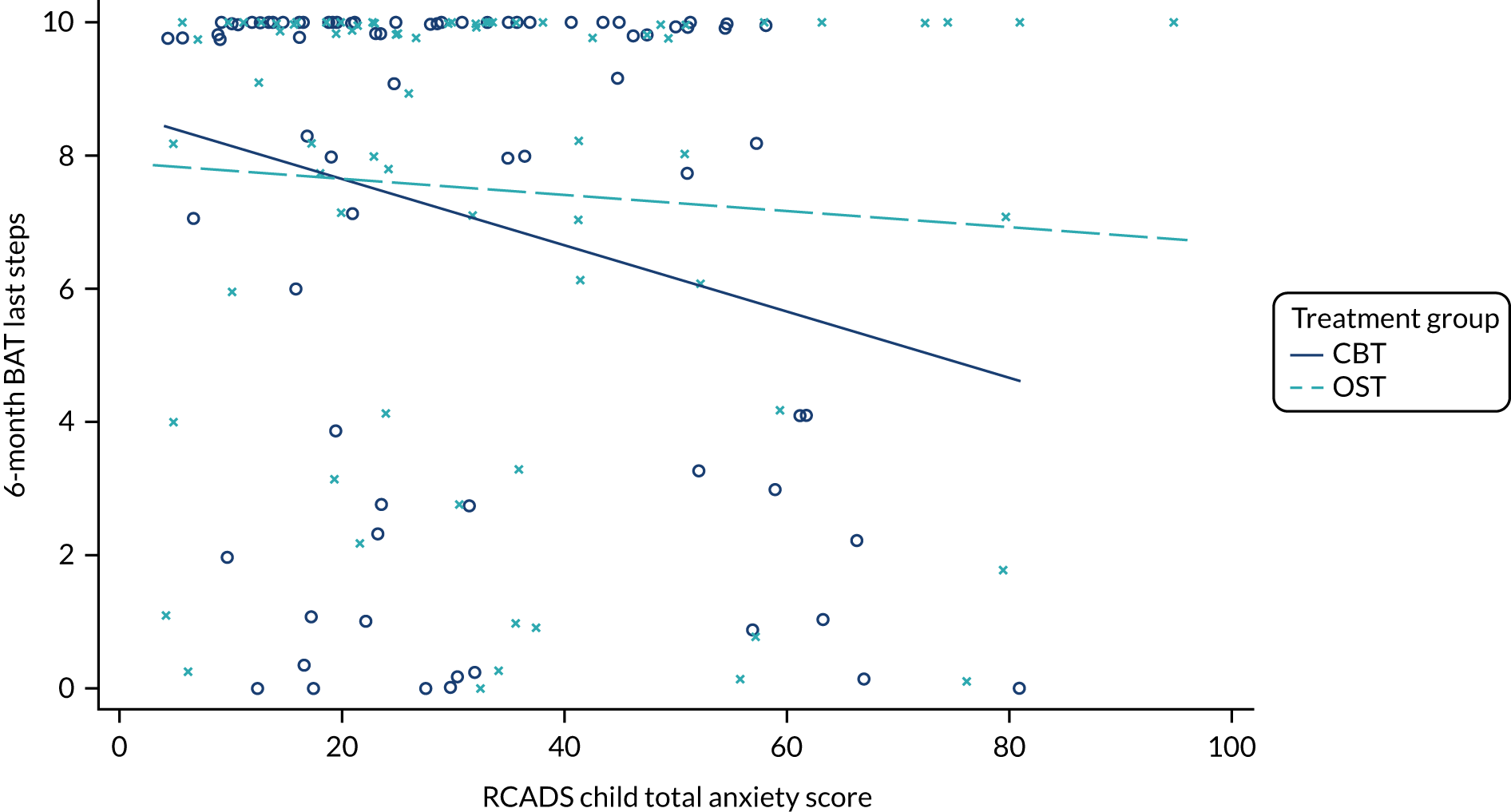
Impact of site and therapist
The impact of site on treatment difference is presented in Table 14 and Figure 12. Sites that had at least five participants per treatment group with outcome data were included in the analysis. The treatment difference across sites was broadly similar although based on small numbers at most sites.
| Site number | Number of participants; mean (SD) BAT last steps at 6 months | Adjusted mean difference (95% CI) | p-value | |
|---|---|---|---|---|
| CBT group | OST group | |||
| 1 | 8; 7.0 (4.0) | 6; 7.0 (3.8) | –0.9 (–3.2 to 1.4) | 0.689 |
| 2 | 22; 8.0 (3.3) | 21; 7.6 (3.4) | –0.2 (–1.6 to 1.1) | |
| 3 | 5; 2.6 (4.3) | 5; 6.6 (4.7) | –1.8 (–5.2 to 1.7) | |
| 4 | 11; 7.7 (3.9) | 11; 6.3 (4.5) | 0.3 (–3.1 to 3.6) | |
| 5 | 10; 7.1 (4.3) | 9; 8.4 (3.3) | –2 (–3.7 to –0.2) | |
| 6 | 13; 6.6 (4.0) | 11; 7.6 (2.5) | –0.9 (–2.5 to 0.7) | |
FIGURE 12.
Mean 6-month BAT last steps score by site.
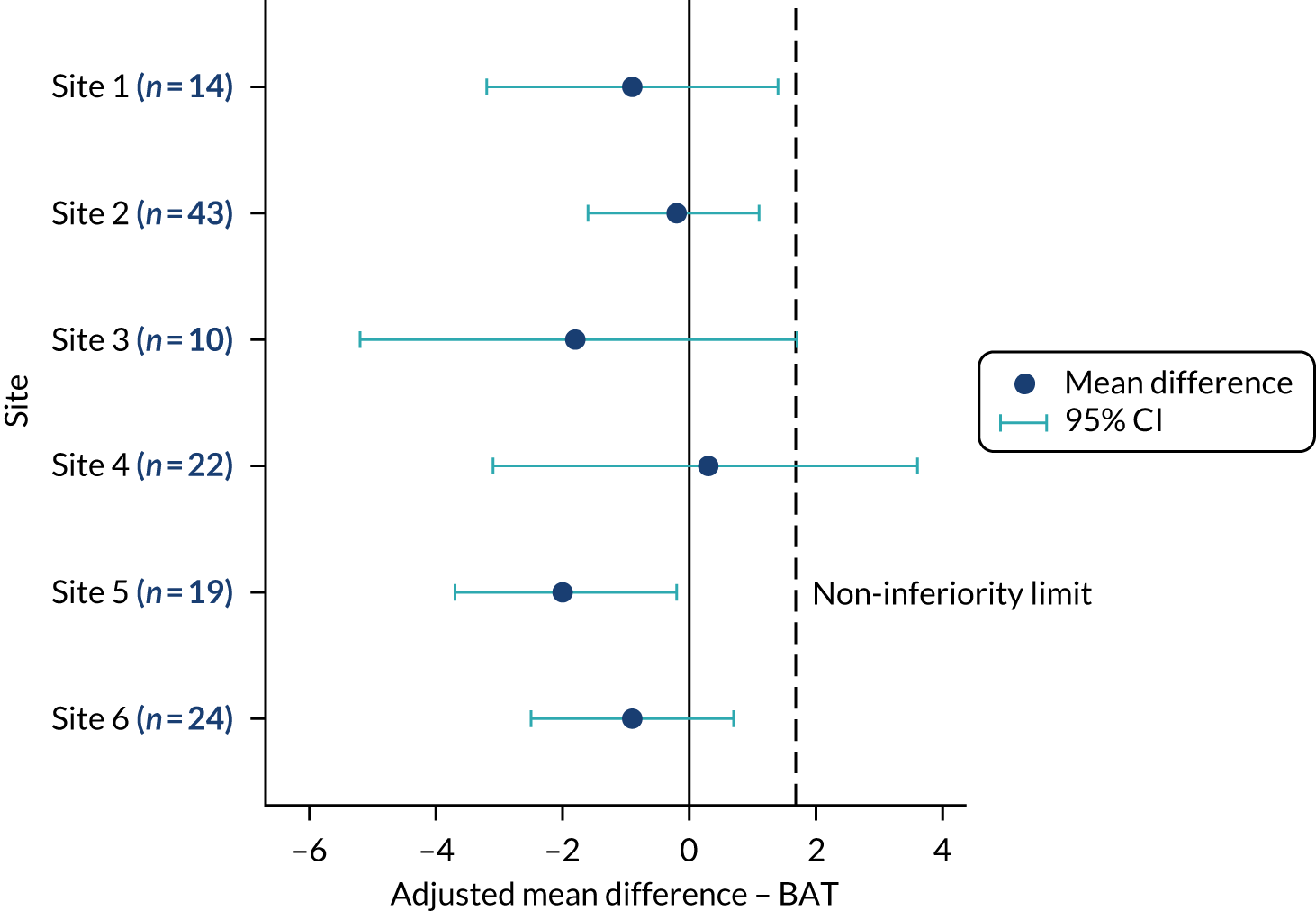
Therapists saw too few participants each on average to make meaningful comparisons (between 1 and 14 participants per therapist in the study). The ICC for the clustering effect of therapist in the primary analysis model reflected this (therapist ICC < 0.00001). The ICC was slightly increased when repeated on therapists who saw at least two participants (ICC < 0.001), indicating that there was little clustering within therapist. The therapist characteristics and their moderating effect on treatment are presented in Table 15 and Figure 13. There is some evidence that the number of years of experience delivering psychological interventions to CYP has a moderating effect on treatment difference (p = 0.019); for therapists with 0–2 years of experience, the mean treatment difference is in favour of CBT, and the two subgroups with more years of experience are increasingly in favour of OST.
| Subgroup | Number of participants; mean (SD) BAT last steps at 6 months | Adjusted mean difference (95% CI) | Interaction coefficient (95% CI) | p-value | |
|---|---|---|---|---|---|
| CBT group | OST group | ||||
| Setting | |||||
| CAMHS | 42; 7.3 (3.9) | 43; 7.4 (3.5) | –0.4 (–1.7 to 1.0) | 0.174 | |
| Not CAMHS | 9; 7.1 (4.5) | 12; 8.1 (3.2) | –2 (–3.9 to –0.0) | –1.6 (–3.9 to 0.7) | |
| Number of years of experiencea | |||||
| 0–2 | 8; 9.0 (2.8) | 14; 7.6 (3.9) | 1.9 (–0.4 to 4.1) | 0.019 | |
| 3–10 | 21; 7.6 (3.8) | 20; 7.6 (3.5) | –0.9 (–3.0 to 1.3) | ||
| ≥ 11 | 22; 6.3 (4.3) | 21; 7.5 (3.2) | –1.8 (–3.0 to –0.6) | ||
FIGURE 13.
Mean BAT last steps at 6 months by therapist subgroup.
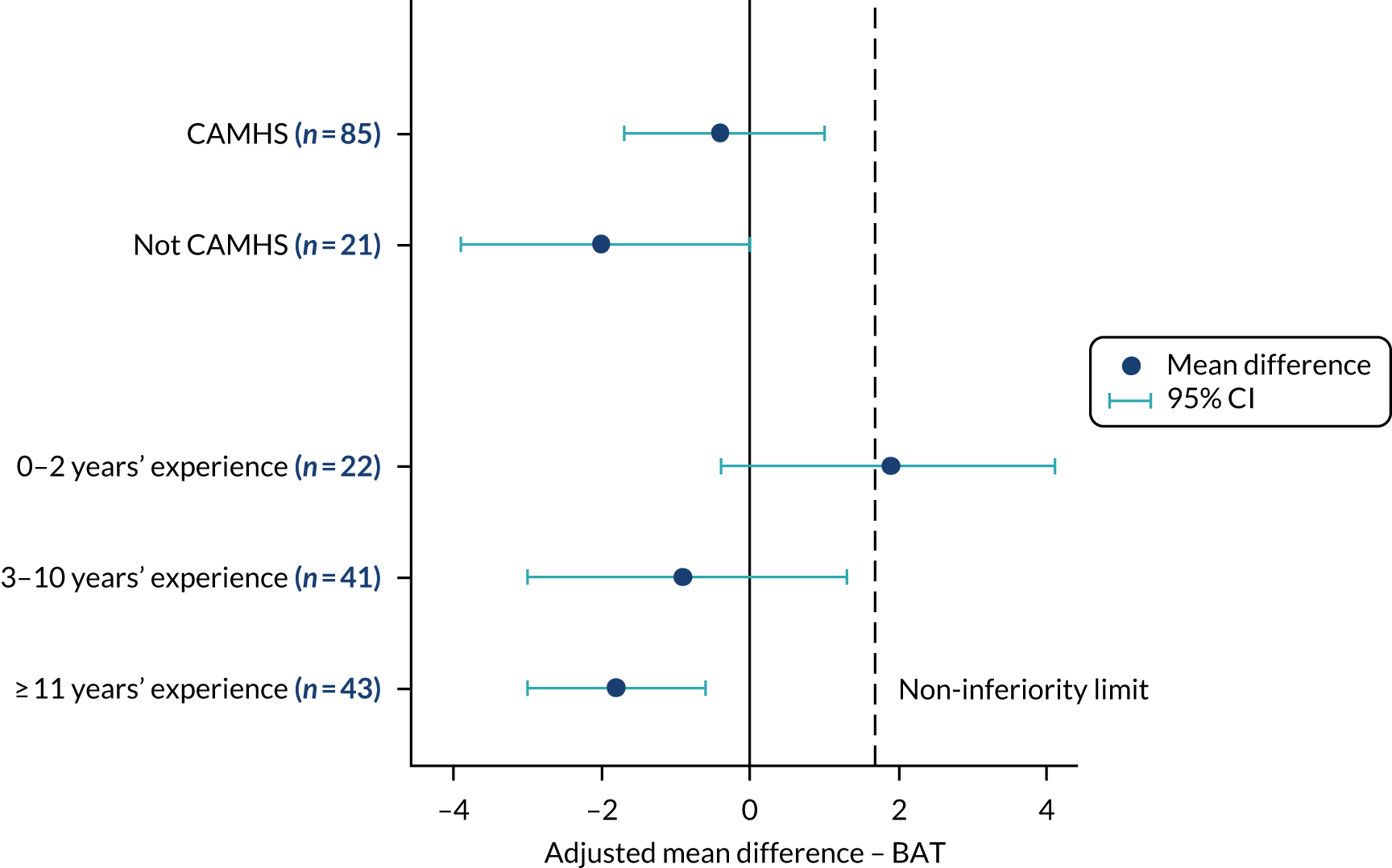
Unblinding
Researchers conducting the outcome assessments were blind to treatment group allocation. In cases where treatment group was revealed between baseline and the 6-month follow-up, a different researcher was sought to conduct the 6-month outcome assessment. In many therapy sites that were distant from the study coordinating centres in York and Sheffield, this was not always possible because of no available alternative research assistant. Overall, 14 unblinding incidents (over 13 participants) occurred for the CBT group and 20 incidents (over 16 participants) occured for the OST group. The majority were accidental (91%) via disclosure from the participant (38%) or therapist (26%). Summaries of the unblinding incidents are presented in Appendix 3, Table 30.
Safety and harms
The AEs and SAEs are summarised in Table 16. Four SAEs occurred during the course of the study, all were inpatient hospitalisation and were assessed by the relevant site principal investigator as unrelated to phobia treatment.
| AEs | Treatment group, n (%) | All (N = 268), n (%) | |
|---|---|---|---|
| CBT (N = 134) | OST (N = 134) | ||
| Participants who experienced ≥ 1 AE | 4 (3.0) | 5 (3.7) | 9 (3.4) |
| Number of AEs (including repeated events) | 5 | 5 | 10 |
| Participants who experienced ≥ 1 SAE | 2 (1.5) | 1 (0.7) | 3 (1.1) |
| Number of SAEs (including repeated events) | 3 | 1 | 4 |
| Occurred | |||
| Before randomisation | 1 (20.0) | 0 (0.0) | 1 (10.0) |
| After randomisation | 4 (80.0) | 5 (100.0) | 9 (90.0) |
| AE category | |||
| Fainting/light-headedness | 1 (20.0) | 1 (20.0) | 2 (20.0) |
| Needle injury/scratch | 1 (20.0) | 1 (20.0) | 2 (20.0) |
| Inpatient hospitalisation | 3 (60.0) | 1 (20.0) | 4 (40.0) |
| Other | 0 (0.0) | 2 (40.0) | 2 (20.0) |
| Severity | |||
| Inpatient hospitalisation | 3 (60.0) | 1 (20.0) | 4 (40.0) |
| Intensity | |||
| Moderate | 1 (20.0) | 1 (20.0) | 2 (20.0) |
| Severe | 2 (40.0) | 0 (0.0) | 2 (20.0) |
| Relationship to phobia treatment | |||
| Unrelated | 3 (60.0) | 1 (20.0) | 4 (40.0) |
Fidelity assessment results
The recording of sessions for the trial was much lower than expected, with 55 CBT sessions recorded (from 12 participants) and 15 OST sessions recorded (from 12 participants) out of a total of 889 sessions (from 203 participants). Of these sessions, 14 out of 55 of the CBT sessions were the first or second session and, therefore, were not included in the fidelity assessment (leaving 39 CBT sessions), and only 4 out of 15 of the OST sessions were exposure sessions; the CBT sessions were chosen randomly, and the four OST sessions were all reviewed and allocated randomly to the assessors.
The fidelity assessment of the audio-recordings was high in all recorded sessions; the average was 84.6% for OST and 76.9% for CBT, and ranged from 61.5% to 100% in both groups (see Appendix 4, Table 31). Multisession CBT may distribute therapeutic techniques across sessions and so any comparisons need to take this into consideration. Using established criteria from Borrelli et al. ,65 assessed sessions were classified as having either high fidelity (8/15 sessions) or moderate fidelity (7/15 sessions), with no sessions classified as having low fidelity.
The fidelity assessment of competence showed that none of the therapists scored lower than 2 for any of the competencies assessed in the session recording, and the total score was higher than 50% for all recorded sessions, which means that all sessions ‘passed’ using the Stallard et al. 63 pass criteria (see Appendix 5, Table 32). The average score for the OST assessed sessions was 56.5 (range 55–58) and for CBT it was 70.3 (range 55–83), indicating that the therapists in the CBT assessed sessions were more competent.
Health economic results
Introduction
The primary aim of the economic evaluation was to assess the cost-effectiveness of OST compared with CBT from the NHS and PSS perspective. An economic evaluation from the societal perspective was included in the sensitivity analysis, which included costs from the educational system, private out-of-pocket expenses and parental productivity costs reported in the trial.
Missing data
Availability of quality-of-life and cost data
A total of 340 CYP were recruited to the trial. After removing 72 ineligible CYP, 268 CYP with specific phobias were available for analysis (134 were allocated to OST and 134 to CBT). The complete case here refers to the CYP who completed EQ-5D-Y questionnaires and whose parents completed resource use questionnaires at any time point. Details of the QoL and cost data available at each data collection time point are shown in Table 17. As shown, QoL data (EQ-5D-Y) were fully available at any time point for 193 (72.0%) CYP, and cost data from the NHS and PSS perspective were available for 193 (72.0%) CYP. Overall, a total of 190 (70.9%) CYP had both EQ-5D-Y and resource use (from the NHS and PSS perspective) data at both collection time points. This sample constitutes the complete-case group, which is one of the two groups used for all the subsequent analyses. The second group (imputed-case or base-case group) is discussed in Multiple imputation.
| Type of data | Baseline (N = 268), n (%) | 6 months (N = 268), n (%) | Complete case (N = 268), n (%) |
|---|---|---|---|
| Cost data | |||
| Resource use data from the NHS and PSS perspective | 267 (99.6) | 194 (72.4) | 193 (72.0) |
| Resource use data from the societal perspective | 267 (99.6) | 194 (72.4) | 193 (72.0) |
| Health outcome data | |||
| EQ-5D-Y | 267 (99.6) | 194 (72.4) | 193 (72.0) |
| CHU-9D | 265 (98.9) | 191 (71.3) | 189 (70.5) |
| BAT score | 241 (89.9) | 144 (53.7) | 135 (50.4) |
| Economic evaluation | |||
| EQ-5D-Y and costs (NHS and PSS perspective) | 266 (99.3) | 192 (71.6) | 190 (70.9) |
| EQ-5D-Y and costs (societal perspective) | 266 (99.3) | 192 (71.6) | 190 (70.9) |
| CHU-9D and costs (NHS and PSS perspective) | 264 (98.5) | 189 (70.5) | 186 (69.4) |
| BAT and costs (NHS and PSS perspective) | 240 (89.6) | 141 (52.6) | 132 (49.3) |
Multiple imputation
To account for the data from the sample other than the complete-case group (29.1%), missing utility scores and costs were further imputed using multiple imputation via chained equations (assuming missing at random at each time point). The following variables were used in the imputation process to ensure best fit of the imputed results: trial arm, age, sex, site, underlying mental health conditions [ASD and attention deficit hyperactivity disorder (ADHD)], EQ-5D-Y utility scores and ADIS highest CSR scores at baseline. Given that it would be speculative to impute missing utility at baseline, one child or young person (0.4%) was excluded from the health economics study. The base-case (imputed) sample was 267 (133 allocated to OST and 134 allocated to CBT); this is the sample used for the primary cost-effectiveness analysis.
Baseline characteristics
The descriptive statistics of participating CYP characteristics and the additional predictors used in multiple imputation are presented in Table 18. Around one-third of the CYP in the OST and the CBT groups were male, and more than 50% of the CYP in both groups were of secondary school age (ranging from 11 to 16 years). Differences in the ADIS scores and EQ-5D-Y utility scores at baseline were marginal across arms and samples. Overall, the baseline characteristics are consistent across samples (base case and complete case) and with the main statistical analysis.
| Baseline characteristics | Base case (N = 267) | Complete case (N = 190) | ||
|---|---|---|---|---|
| OST group (N = 133) | CBT group (N = 134) | OST group (N = 94) | CBT group (N = 96) | |
| Male, n (%) | 47 (35.3) | 53 (39.6) | 34 (36.2) | 40 (41.7) |
| Age (years) | ||||
| 7–11, n (%) | 45 (33.8) | 39 (29.1) | 35 (37.2) | 30 (31.3) |
| 11–15, n (%) | 88 (66.2) | 95 (70.9) | 59 (62.8) | 66 (68.7) |
| Mean (SD) | 12.0 (2.6) | 11.9 (2.6) | 11.7 (2.6) | 11.7 (2.6) |
| Phobia type, n (%) | ||||
| Animals | 38 (28.5) | 41 (30.6) | 29 (30.9) | 34 (35.4) |
| BII | 36 (27.1) | 32 (23.9) | 21 (22.3) | 23 (24.0) |
| Vomit | 36 (27.1) | 41 (30.6) | 22 (23.4) | 25 (26.0) |
| Other | 23 (17.3) | 20 (14.9) | 22 (23.4) | 14 (14.6) |
| Mean (SD) ADIS CSR score | 7.6 (0.9) | 7.5 (0.9) | 7.6 (0.9) | 7.5 (0.9) |
| Mean (SD) EQ-5D-Y score | 0.84 (0.12) | 0.85 (0.12) | 0.85 (0.11) | 0.85 (0.13) |
| Site location, n (%) | ||||
| North West England | 70 (52.6) | 71 (53.0) | 58 (61.7) | 56 (58.3) |
| East of England | 35 (26.3) | 21 (15.7) | 17 (18.0) | 16 (16.7) |
| Yorkshire and Humber | 18 (13.5) | 30 (22.4) | 13 (13.8) | 18 (18.7) |
| South West England | 7 (5.3) | 6 (4.5) | 4 (4.3) | 4 (4.2) |
| West Midlands | 2 (1.5) | 5 (3.7) | 1 (1.1) | 2 (2.1) |
| North West England | 1 (0.8) | 1 (0.7) | 1 (1.1) | – |
Cost
Two types of costs were considered in this study: the cost of intervention (obtained from the therapists) and the cost of service use (self-reported by the parents/guardians). All costs were expressed in 2018–19 Great British pounds.
Unit costs
Individual-level resource use together with unit costs were used to calculate the total services cost for each child and young person with a specific phobia. Unit costs were obtained from published sources (i.e. Reference Costs 201874 and the unit costs of health-care and social care from the PSSRU 201875). Appendix 6, Tables 33–41, presents the summary of key unit costs used in the study.
Intervention costs
Intervention costs include both training and intervention delivery costs. The training cost information was obtained from our study team, and included both ‘train the trainers’ and ‘therapist training’ costs. The estimated training costs were allocated to each session and each child and young person who received the intervention. In relation to the intervention delivery costs, the information was obtained directly from the therapists using the self-reported questionnaires. Intervention sessions were costed on the basis of the salary of the therapists involved (for both preparation and session delivery) and the additional resources required. Table 19 shows the total and average costs of each component that were used to deliver the OST and CBT sessions. As shown, the main cost driver of training costs was trainer fees, whereas the main cost drivers of intervention delivery costs were the costs for intervention preparation and delivery and the costs for stimuli. On average, the estimated intervention costs for OST were £184.26 (£62.19 for training and £122.07 for intervention delivery) and for CBT were £58.59 (£0 for training and £58.59 for intervention delivery).
| Cost category | OST group (n = 134) | CBT group (n = 134) | ||
|---|---|---|---|---|
| Total cost (£) | Cost per session per CYP (£) | Total cost (£) | Cost per session per CYP (£) | |
| Training costs | ||||
| Train the trainers | ||||
| Venue | 140.00 | 1.47 | – | – |
| Refreshment costs | 335.00 | 1.45 | – | – |
| Consumable costs | 0.00 | 0.00 | – | – |
| Trainer’s travel costs | 6117.00 | 26.48 | – | – |
| Trainer fee | 1940.00 | 8.40 | – | – |
| Total | 8392.00 | 36.33 | – | – |
| Therapist training | ||||
| Venue | 160.00 | 0.69 | – | – |
| Refreshment costs | 732.40 | 3.17 | – | – |
| Consumable costs | 264.00 | 1.14 | – | – |
| Trainer’s travel costs | 317.20 | 1.37 | – | – |
| Trainer fee | 4500.00 | 19.48 | – | – |
| Total | 5973.60 | 25.86 | – | – |
| Intervention delivery costs | ||||
| Intervention (staff time) | ||||
| Therapy sessiona | 19,054.33 | 82.49 | 29,908.85 | 45.45 |
| Administration/preparationb | 5151.17 | 22.30 | 5507.37 | 8.40 |
| Additional resource | ||||
| Second therapist | 2037.00 | 8.82 | 550.67 | 0.84 |
| Assistant/nurse | 331.88 | 1.44 | 55.13 | 0.09 |
| Stimuli | 503.84 | 2.18 | 811.36 | 1.23 |
| Supervisionc | 1119.77 | 4.84 | 1717.01 | 2.61 |
| Total | 28,197.98 | 122.07 | 38,553.38 | 58.59 |
Service use and costs
Table 20 shows the summarised service use per CYP in each treatment group based on the complete cases only. The difference in service use between the OST and the CBT groups varies across items at two time points. At baseline, CYP in the OST group seemed to have used slightly more NHS services and incurred more private expenses and productivity than those in the CBT group. At the 6-month follow-up, resource use in both treatment groups decreased and such decreases were more prominent in the OST group than in the CBT group. The medication use for both treatment groups at baseline and the 6-month follow-up remained largely unchanged; the majority of medicines used were for conditions such as allergy, asthma, diabetes and mental health.
| Type of service | Unit | Mean (minimum, maximum) use at baseline | Mean (minimum, maximum) use at 6 months | ||
|---|---|---|---|---|---|
| OST group (n = 94) | CBT group (n = 96) | OST group (n = 94) | CBT group (n = 96) | ||
| NHS and PSS | |||||
| Community-based services | |||||
| CAMHS related | |||||
| Child psychiatrist | Appointment | 0.17 (0, 2) | 0.12 (0, 3) | 0.15 (0, 3) | 0.18 (0, 5) |
| Child psychotherapist | Appointment | 0.24 (0, 8) | 0.20 (0, 18) | 0.07 (0, 3) | 0.34 (0, 25) |
| Child psychologist | Appointment | 0.06 (0, 3) | 0.35 (0, 11) | 0.30 (0, 8) | 0.30 (0, 8) |
| Mental health nurse | Appointment | 1.91 (0, 24) | 1.03 (0, 9) | 1.97 (0, 27) | 3.09 (0, 24) |
| Family therapist | Appointment | – | 0.01 (0, 1) | 0.02 (0, 2) | – |
| Non-CAMHS related | |||||
| GP | Appointment | 1.65 (0, 20) | 1.17 (0, 10) | 0.55 (0, 10) | 0.73 (0, 8) |
| Nurse | Appointment | 1.30 (0, 11) | 1.50 (0, 12) | 0.17 (0, 3) | 0.39 (0, 12) |
| Community paediatrician | Appointment | 0.18 (0, 4) | 0.08 (0, 2) | 0.04 (0, 2) | 0.03 (0, 2) |
| Child development centre | Visit | 0.17 (0, 12) | 0.01 (0, 1) | 0.08 (0, 3) | 0.01 (0, 1) |
| Helpline/NHS Direct | Call | 0.05 (0, 2) | 0.05 (0, 1) | 0.06 (0, 3) | 0.04 (0, 2) |
| Walk-in centre | Visit | 0.13 (0, 2) | 0.11 (0, 2) | 0.10 (0, 3) | 0.10 (0, 3) |
| Social worker | Visit | 0.20 (0, 8) | 0.25 (0, 7) | 0.07 (0, 3) | 0.04 (0, 4) |
| Hospital-based services | |||||
| Emergency services | Visit | 0.17 (0, 2) | 0.09 (0, 2) | 0.12 (0, 2) | 0.07 (0, 2) |
| Inpatient admission | Admission | 0.04 (0, 2) | 0.03 (0, 2) | 0.02 (0, 1) | 0.04 (0, 2) |
| Outpatient visit | Attendance | 0.24 (0, 5) | 0.26 (0, 8) | 0.23 (0, 3) | 0.28 (0, 4) |
| Medication | |||||
| Mental health related | Type | 0.22 (0, 3) | 0.18 (0, 4) | 0.22 (0, 3) | 0.18 (0, 4) |
| Non-mental health related | Type | 0.48 (0, 7) | 0.38 (0, 8) | 0.48 (0, 7) | 0.38 (0, 8) |
| Education system related | |||||
| Educational psychologist | Appointment | 0.13 (0, 7) | 0.04 (0, 1) | 0.07 (0, 7) | 0.07 (0, 5) |
| Education welfare officer | Appointment | 0.06 (0, 3) | 0.32 (0, 20) | 0.17 (0, 10) | 0.05 (0, 2) |
| School nurse | Appointment | 0.20 (0, 5) | 0.67 (0, 20) | 0.13 (0, 11) | 0.01 (0, 1) |
| School counsellor | Appointment | 1.84 (0, 30) | 0.60 (0, 10) | 1.04 (0, 25) | 0.60 (0, 20) |
| Private expenses | |||||
| Self-paid treatment | Session | 0.44 (0, 24) | 0.19 (0, 10) | 0.04 (0, 2) | 0.02 (0, 2) |
| Travel for intervention | Hour | – | – | 1.85 (0, 7) | 5.31 (0, 16) |
| Productivity | |||||
| Parental productivity | Day | 2.73 (0, 63) | 1.15 (0, 19) | 0.89 (0, 10) | 0.82 (0, 12) |
| Productivity for intervention | Hour | – | – | 5.32 (0, 16) | 11.01 (0, 33) |
The total costs broken down by perspective, type of service and treatment group before and after imputation are presented in Table 21. As shown, the costs substantially varied from one child or young person to the other, as illustrated by the wide 95% CIs.
| Type of cost | Base case, cost (£) (95% CI) | Complete case, cost (£) (95% CI) | ||
|---|---|---|---|---|
| OST group (n = 133) | CBT group (n = 134) | OST group (n = 94) | CBT group (n = 96) | |
| NHS and PSS | 511.41 (348.69 to 674.13) | 544.00 (373.56 to 714.43) | 513.49 (351.10 to 675.89) | 549.05 (362.41 to 735.70) |
| Community-based services | ||||
| CAMHS related | 206.53 (133.49 to 279.57) | 280.43 (211.09 to 349.77) | 210.47 (138.33 to 282.61) | 277.34 (207.50 to 347.19) |
| Non-CAMHS related | 47.61 (30.83 to 64.39) | 43.65 (25.66 to 61.65) | 48.15 (30.36 to 65.94) | 44.83 (25.60 to 64.06) |
| Hospital-based services | 168.37 (36.05 to 300.69) | 129.57 (16.71 to 242.41) | 163.12 (35.05 to 291.18) | 135.77 (14.04 to 257.51) |
| Medications | ||||
| Mental health related | 26.29 (12.60 to 39.97) | 23.99 (3.61 to 44.36) | 24.80 (10.66 to 38.94) | 23.45 (2.38 to 44.52) |
| Non-mental health related | 74.65 (31.79 to 117.51) | 68.12 (7.58 to 128.67) | 66.95 (19.89 to 114.01) | 67.66 (–4.58 to 139.90) |
| Education system relateda | 25.87 (5.28 to 46.46) | 18.55 (1.64 to 35.47) | 28.77 (8.13 to 49.42) | 16.24 (2.97 to 29.51) |
| Private expenses | 26.18 (2.51 to 49.85) | 29.88 (12.96 to 46.80) | 24.30 (2.87 to 45.73) | 29.38 (11.90 to 46.85) |
| Productivity | 115.23 (73.65 to 156.81) | 136.13 (92.03 to 180.23) | 167.30 (123.24 to 211.37) | 213.56 (163.65 to 263.47) |
| Total costs | 678.69 (505.40 to 851.98) | 728.56 (549.15 to 907.98) | 733.88 (556.34 to 911.41) | 808.23 (610.74 to 1005.72) |
The total service costs to the NHS providers (before imputation) were £513.49 (95% CI £351.10 to £675.89) for the OST group compared with £549.05 (95% CI £362.41 to £735.70) for the CBT group. The average costs for health-care services were similar in the two groups, except the CAMHS costs. The average cost for the use of CAMHS-related services was marginally higher for the CYP with specific phobias in the CBT group (£210.47 in the OST group and £277.34 in the CBT group). Such a cost difference was likely to have been driven by one patient in the CBT group who reported 25 psychotherapist appointments over the past 6 months and, thus, incurred a high cost. Given that this value was entirely plausible, we kept it in the data set without any adjustment.
The average total cost for the use of education services (before imputation) was £28.77 (95% CI £8.13 to £49.42) in the OST group compared with £16.24 (95% CI £2.97 to £29.51) in the CBT group. As with the costs of CAMHS-related services, the higher average cost in the OST group was likely to have been driven by two high-cost patients, the first of whom received 10 education welfare officer visits and 11 school nurse visits over 6 months. Again, we kept these values in the analysis, as the scenarios were plausible.
Children and young people in the OST group also incurred lower average costs in private expenses and parental productivity losses than those in the CBT group. Overall, CYP in the OST group incurred lower average costs in both NHS/PSS and societal perspectives. This is observed in both the complete case and the base case. However, owing to the high-cost cases, the cost differences need to be interpreted with caution.
Quality of life
EuroQol-5 Dimensions Youth version
Table 22 shows the mean EQ-5D-Y (three-level) utility scores in the two treatment groups at each time point when scores were not imputed (complete case) and when scores were imputed (base case). It can be seen that in both treatment groups there was no significant change in EQ-5D-Y scores from baseline to 6 months. The fluctuations between baseline and 6 months were small in both the base case and the complete case. After calculation using the area under the curve approach (see Chapter 2, Effectiveness), it was found that OST produced similar mean QALYs (0.43 QALYs) to CBT. Further details for the responses in each domain can be found in Appendix 7, Tables 42 and 43.
| Time point | Base case, mean (95% CI) | Complete case, mean (95% CI) | ||
|---|---|---|---|---|
| OST group (n = 133) | CBT group (n = 134) | OST group (n = 97) | CBT group (n = 96) | |
| Baseline | 0.84 (0.82 to 0.86) | 0.85 (0.83 to 0.87) | 0.85 (0.83 to 0.88) | 0.85 (0.83 to 0.87) |
| 6 months | 0.88 (0.86 to 0.91) | 0.88 (0.86 to 0.90) | 0.88 (0.86 to 0.91) | 0.88 (0.85 to 0.90) |
| Total QALYs | 0.43 (0.42 to 0.44) | 0.43 (0.42 to 0.44) | 0.43 (0.42 to 0.44) | 0.43 (0.42 to 0.44) |
Child Health Utility 9D
The change in the mean CHU-9D scores between the two treatment groups at any time point is presented in Table 23. CYP in the CBT group had slightly higher utility scores at baseline than those in the OST group. As with the EQ-5D-Y results, the observed changes at the 6-month follow-up in either treatment group were marginal. Such marginal differences were observed in both the complete case and the base case. Consistent with EQ-5D-Y results, the OST produced similar mean QALYs (0.43 QALYs) to CBT. Further details for the responses in each domain can be found in Appendix 8, Tables 44 and 45.
| Time point | Base case, mean (95% CI) | Complete case, mean (95% CI) | ||
|---|---|---|---|---|
| OST group (n = 133) | CBT group (n = 134) | OST group (n = 95) | CBT group (n = 94) | |
| Baseline | 0.85 (0.83 to 0.87) | 0.86 (0.84 to 0.87) | 0.85 (0.83 to 0.87) | 0.86 (0.84 to 0.88) |
| 6 months | 0.87 (0.85 to 0.89) | 0.89 (0.87 to 0.91) | 0.87 (0.85 to 0.89) | 0.89 (0.87 to 0.91) |
| Total QALYs | 0.43 (0.42 to 0.44) | 0.43 (0.43 to 0.44) | 0.43 (0.42 to 0.44) | 0.44 (0.43 to 0.45) |
Behavioural Avoidance Task
The change in the mean BAT scores between the two treatment groups at any time point is presented in Table 24. CYP in the CBT group had slightly higher BAT scores than those in the OST group at baseline. The observed reductions at the 6-month follow-up in either treatment group were between two and three score points. Such differences were observed in both the complete case and the base case. In total, CBT reduced mean BAT scores slightly more (0.28 score points in base case and 0.32 score points in complete case) than OST. These represent incremental physical approaches to the feared stimulus (e.g. entering a room and approaching and stroking a dog for a person with a dog phobia). These all occur on 10-point scales, so a three-point difference is a clinically significant movement (e.g. when someone has not been able to enter the room scoring zero).
| Time point | Base case, mean (95% CI) | Complete case, mean (95% CI) | ||
|---|---|---|---|---|
| OST group (n = 133) | CBT group (n = 134) | OST group (n = 67) | CBT group (n = 69) | |
| Baseline | 5.68 (5.23 to 6.13) | 5.82 (5.35 to 6.28) | 5.67 (5.09 to 6.25) | 5.74 (5.14 to 6.34) |
| 6 months | 3.16 (2.47 to 3.86) | 3.07 (2.40 to 3.74) | 3.12 (2.45 to 3.78) | 2.87 (2.16 to 3.58) |
| Difference | –2.46 (–3.18 to –1.74) | –2.74 (–3.47 to –2.02) | –2.55 (–3.26 to –1.85) | –2.87 (–3.63 to –2.11) |
Economic analysis
Primary analysis
Table 25 shows the ICERs based on the base case for the primary analysis. Before any adjustments, on average, CYP with specific phobias receiving OST incurred £273.08 less costs than those receiving CBT from the NHS/PSS perspective, and maintained similar QALY improvements, as measured by EQ-5D-Y.
| Treatment group | Costs (£), mean (95% CI) | QALYs, mean (95% CI) | Incremental cost (95% CI) | Incremental QALYs (95% CI) | ICER |
|---|---|---|---|---|---|
| Before bootstrapping | |||||
| OST | 965.82 (785.76 to 1145.88) | 0.43 (0.42 to 0.44) | –261.9 | 0.000 | Dominant |
| CBT | 1227.72 (1016.71 to 1438.73) | 0.43 (0.43 to 0.44) | |||
| After bootstrapping | |||||
| OST | 956.59 (795.85 to 1131.23) | 0.43 (0.43 to 0.44) | –302.96 (–598.86 to –28.61) | 0.002 (–0.004 to 0.008) | Dominant |
| CBT | 1259.55 (1072.86 to 1487.56) | 0.43 (0.42 to 0.44) | – | – | – |
To account for the uncertainty and adjust for the imbalanced EQ-5D-Y utility scores and health-care costs at baseline, the estimates of incremental costs and the QALYs from regression were bootstrapped to simulate 5000 pairs of net cost and net outcomes, as recommended by NICE for health technology appraisals. 96 The regressions were controlled for age, sex, site, phobia type, EQ-5D-Y utility, health-care costs and ADIS CSR score at baseline. After bootstrapping, on average, CYP with specific phobias receiving OST incurred £302.96 (95% CI £28.61 to £598.86) less costs and gained 0.002 (95% CI 0.002 to 0.002) more QALYs than those receiving CBT. The calculated ICER was below the recommended threshold range specified for NICE decision-making in England and Wales (£20,000 to £30,000 per QALY gained), further confirming that OST is likely to be cost-saving.
Figure 14 shows the cost-effectiveness plane for OST compared with CBT based on 5000 bootstrapped estimates of incremental costs and incremental QALYs. The navy line represents the willingness-to-pay threshold of £20,000 per QALY gained. The simulated estimates were largely below the threshold line and sat in the fourth quadrant, suggesting that OST is likely to be cost-saving.
FIGURE 14.
Base-case cost-effectiveness plane of OST compared with CBT (outcome measure: QALY measured by EQ-5D-Y, NHS/PSS perspective). WTP, willingness to pay. Adapted with permission from Wang et al. 2 Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data. The figure includes minor additions and formatting changes to the original figure.
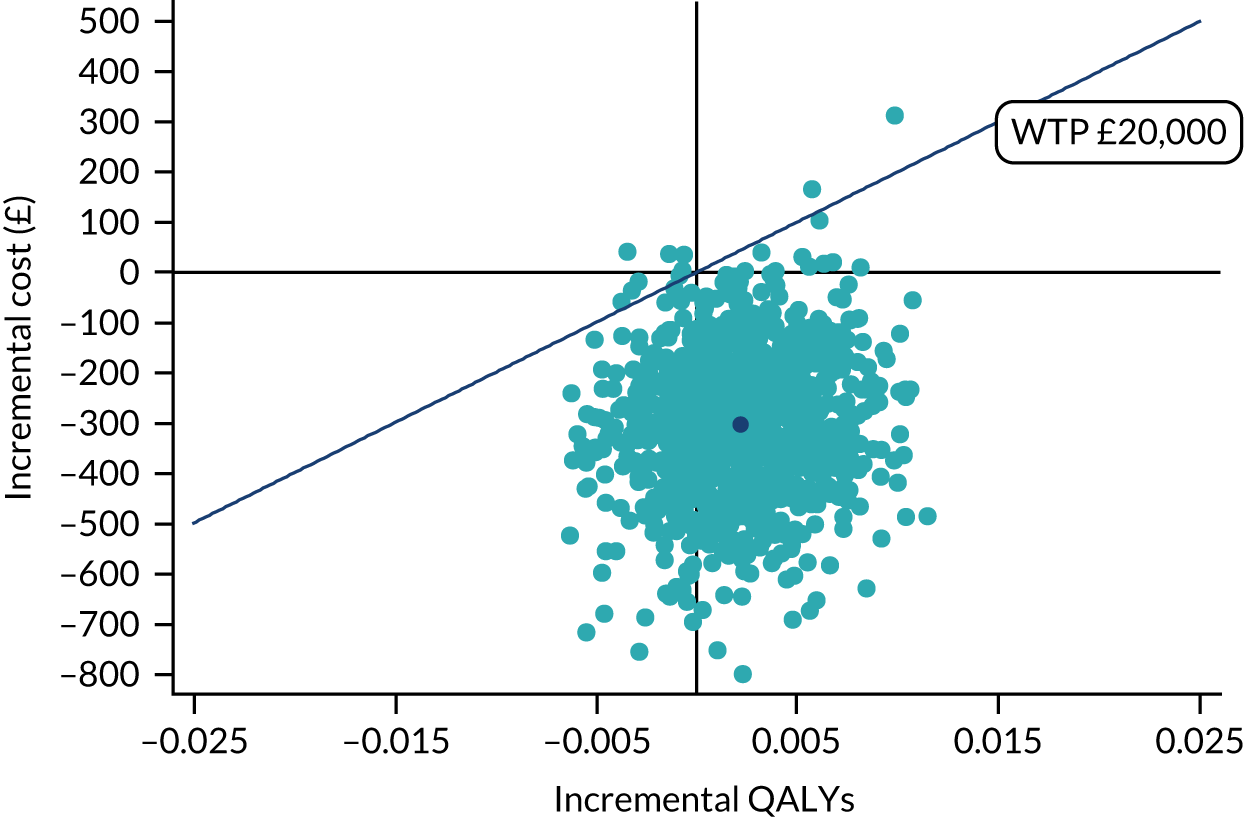
The CEAC of OST compared with CBT is presented in Figure 15. The probability of OST being cost-effective is 98% if decision-makers are willing to pay £20,000 for one QALY gained and 99% if they are willing to pay £30,000 per QALY gained.
FIGURE 15.
Base-case CEAC of OST compared with CBT (outcome measure: QALY measured by EQ-5D-Y, NHS/PSS perspective). WTP, willingness to pay. Adapted with permission from Wang et al. 2 Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data. The figure includes minor additions and formatting changes to the original figure.
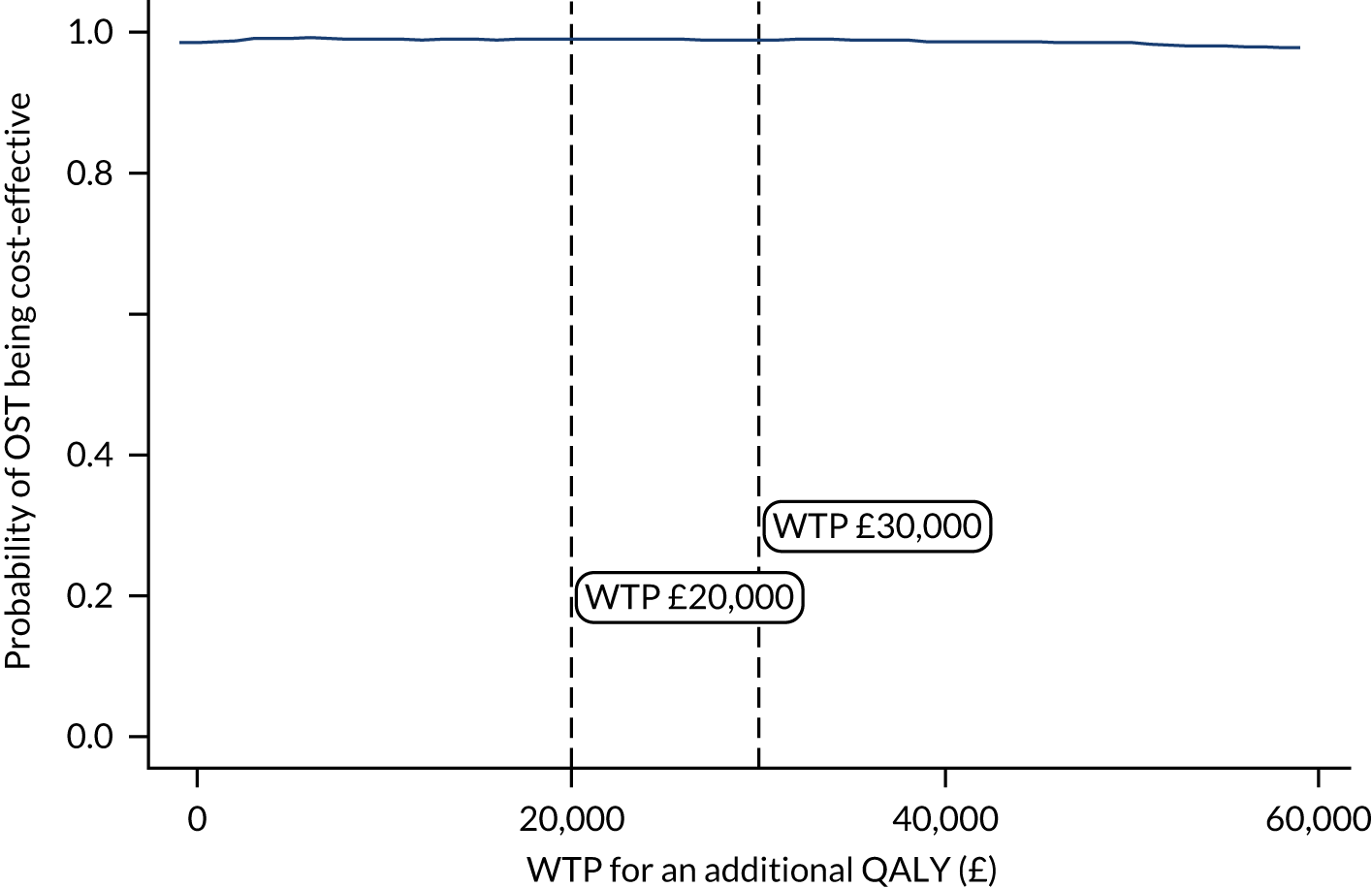
Sensitivity analyses
To account for uncertainty in the costs and QALY estimations, a set of sensitivity analyses were conducted (Table 26). The mean incremental cost and QALY estimates from the complete case were along the line of the base-case scenario, yielding a negative cost per QALY gained. The same was observed in the group that received at least one intervention session during the trial follow-up period. Those who did not receive any intervention sessions owing to the national lockdown caused by the COVID-19 pandemic were excluded from the analysis. Other sensitivity analyses using different cost perspectives and a different instrument (CHU-9D) to measure QALYs, and excluding one-off OST training costs, were also conducted. In the above-mentioned sensitivity analyses, the mean ICER pairs lay below the recommended NICE threshold (£20,000–30,000 per QALY gained) (see Table 26), and the majority of the bootstrapped estimates sat in the fourth quadrant and below the NICE threshold line (Figure 16), suggesting that OST is likely to be cost-saving and cost-effective. The cost-effectiveness of OST is supported by a range of sensitivity analyses; however, this is subject to the caveat that results are derived from a very small incremental change in the effectiveness parameter. When the measured health outcome was the BAT score, the calculated ICER was £1848.82 per BAT score. This means that, on average, the NHS needs to pay £1848.82 to decrease the BAT score by 1 point.
| OST vs. CBT | Incremental cost (£) (95% CI) | Incremental QALYs (95% CI) | ICER (£ per QALY gained) |
|---|---|---|---|
| Scenario 1: complete-case analysis from the NHS perspective | –31.10 (–154.21 to 88.14) | 0.001 (–0.002 to 0.005) | Dominant |
| Scenario 2: analysis on CYP who had at least one intervention from the NHS perspective | –298.40 (–599.68 to –23.90) | 0.002 (–0.005 to 0.009) | Dominant |
| Scenario 3: CUA (utility measured by CHU-9D) | –310.64 (–605.07 to –44.10) | 0.002 (–0.007 to 0.012) | Dominant |
| Scenario 4: CUA (cost from societal perspective) | –384.81 (–685.01 to –107.16) | 0.002 (–0.004 to 0.008) | Dominant |
| Scenario 5: CUA (outcomes measured by BAT scores) | –314.30 (–607.56 to –46.57) | –0.170 (–1.030 to 0.600) | 1848.82 |
| Scenario 6: CUA (excluding OST training costs) | –323.76 (–571.87 to –69.24) | 0.002 (–0.004 to 0.008) | Dominant |
FIGURE 16.
Sensitivity analysis: cost-effectiveness plans of OST compared with CBT. (a) scenario 1, NHS/PSS + EQ-5D-Y (complete case); (b) scenario 2, NHS/PSS + EQ-5D-Y (CYP had at least one intervention); (c) scenario 3, NHS/PSS + CHU-9D; (d) scenario 4, societal + EQ-5D-Y; (e) scenario 5, NHS/PSS + BAT scores and (f) scenario 6, NHS/PSS + EQ-5D-Y (excluding OST training cost). WTP, willingness to pay. Adapted with permission from Wang et al. 2 Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data. The figure includes minor additions and formatting changes to the original figure.
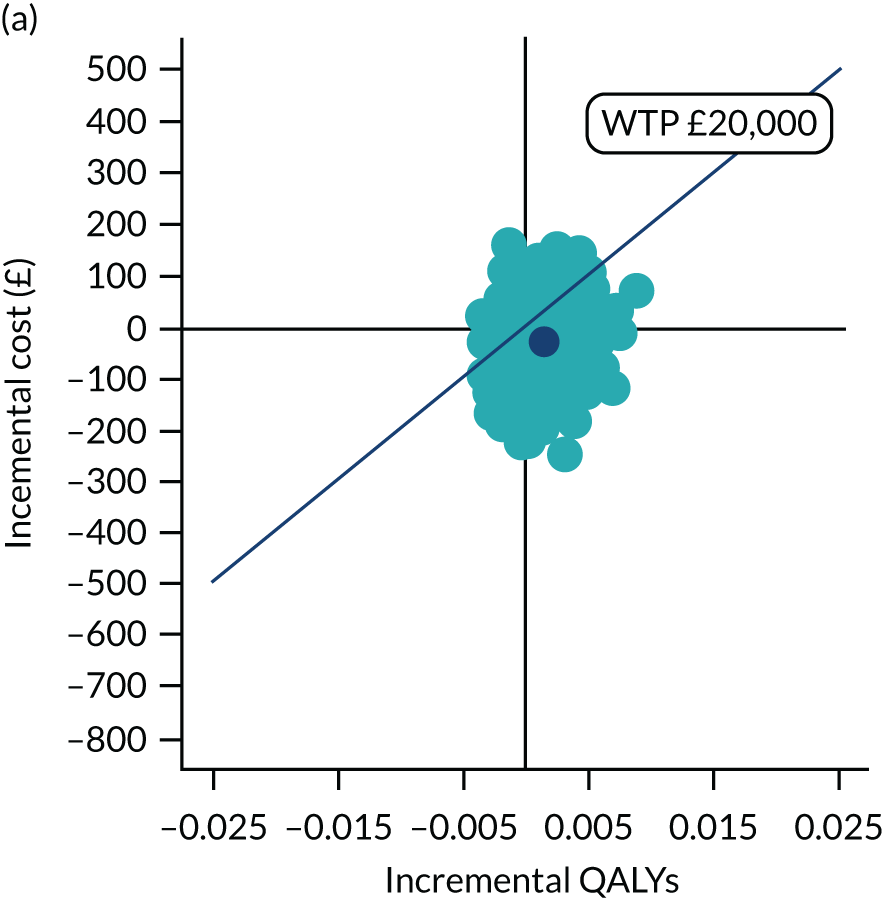
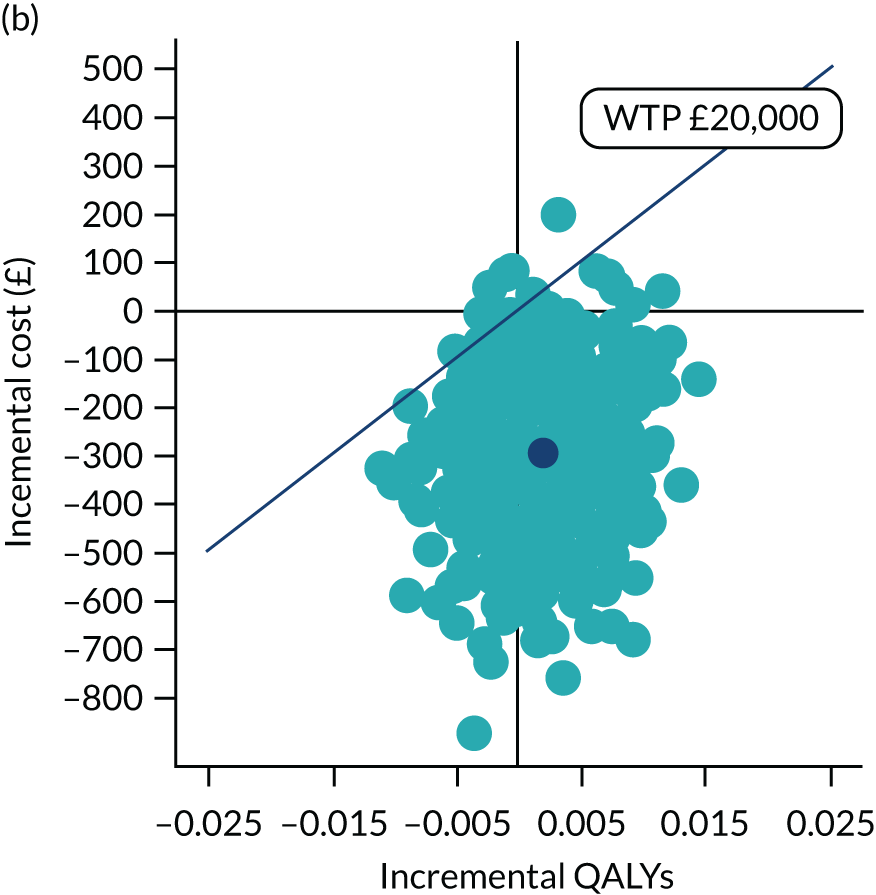
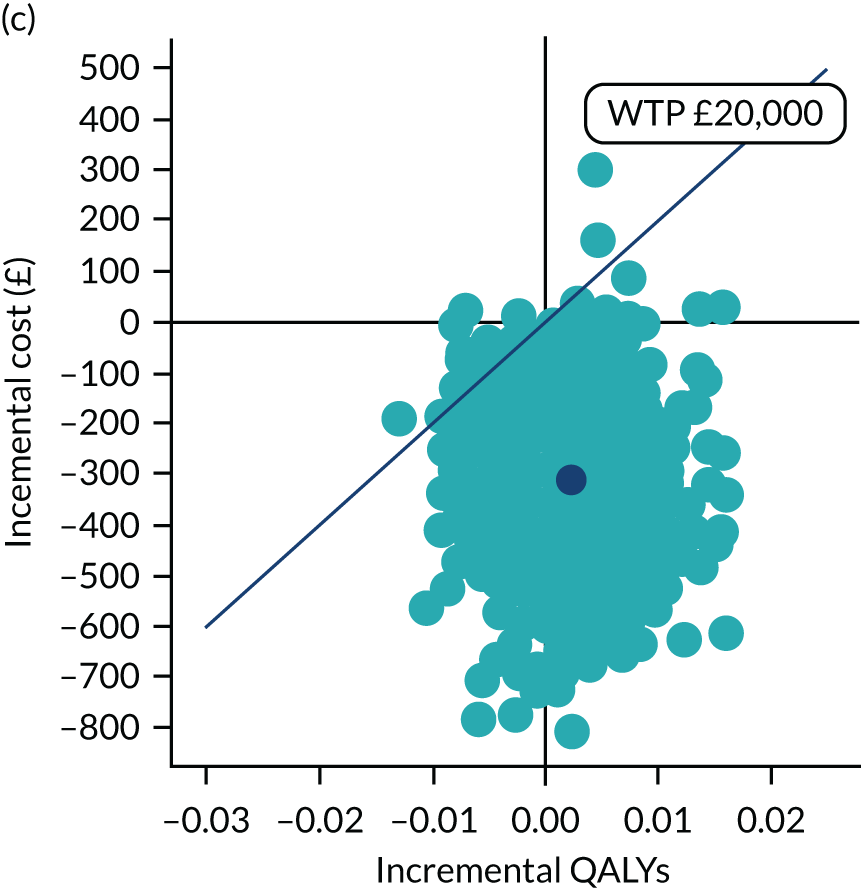
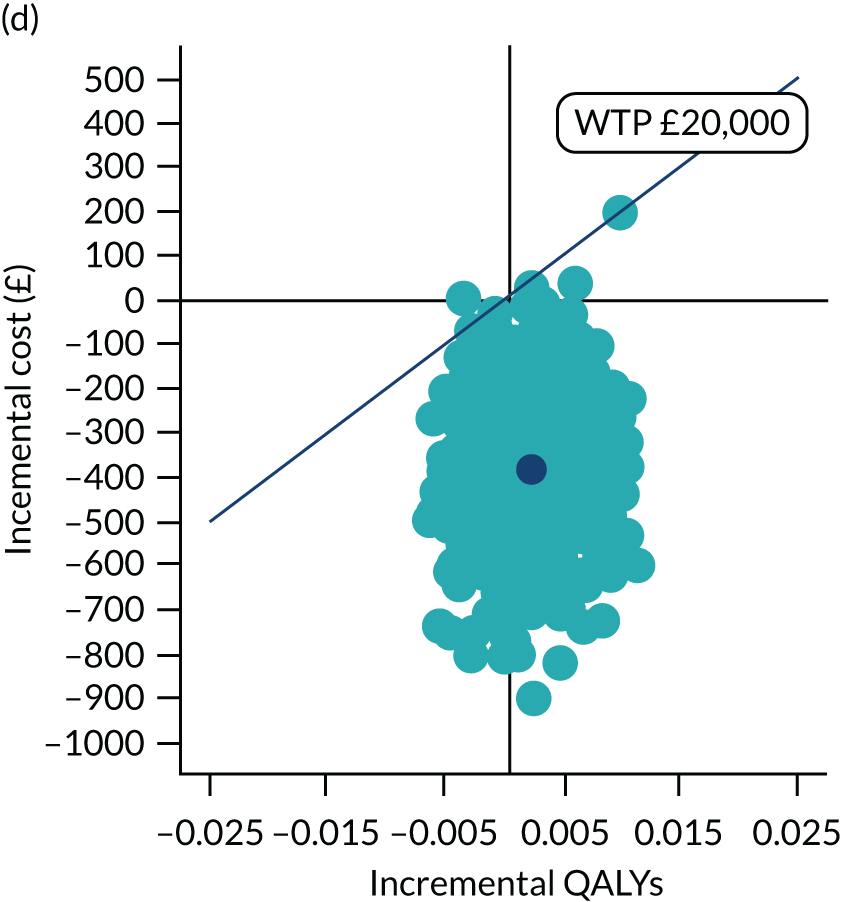
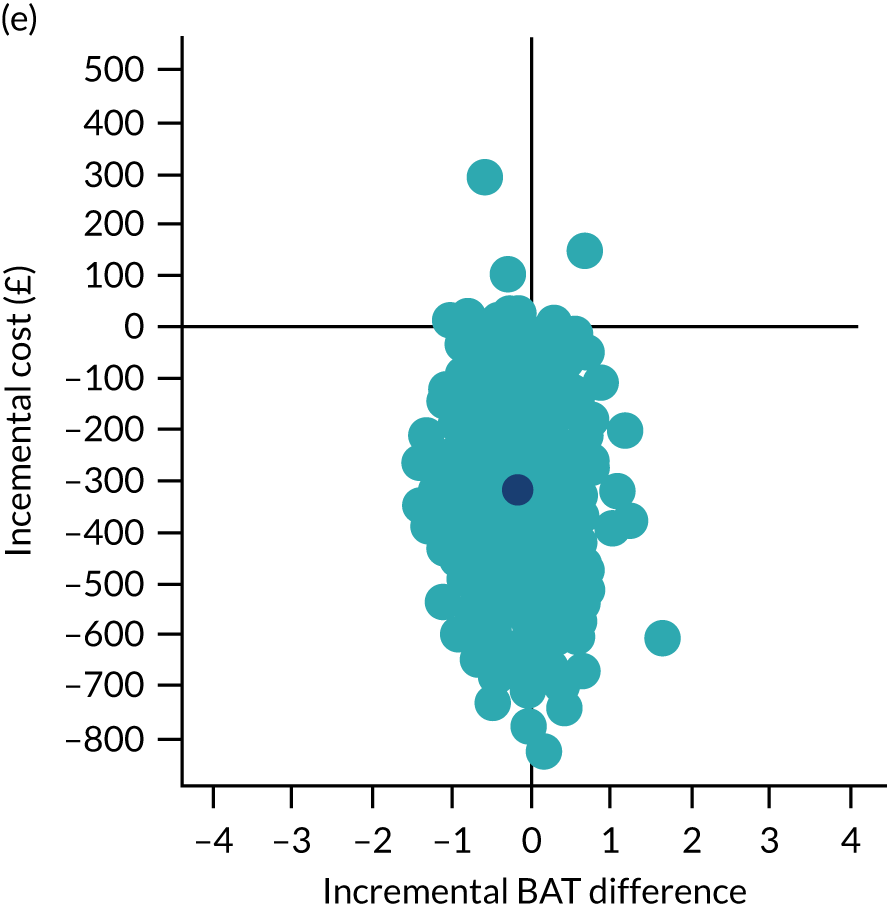
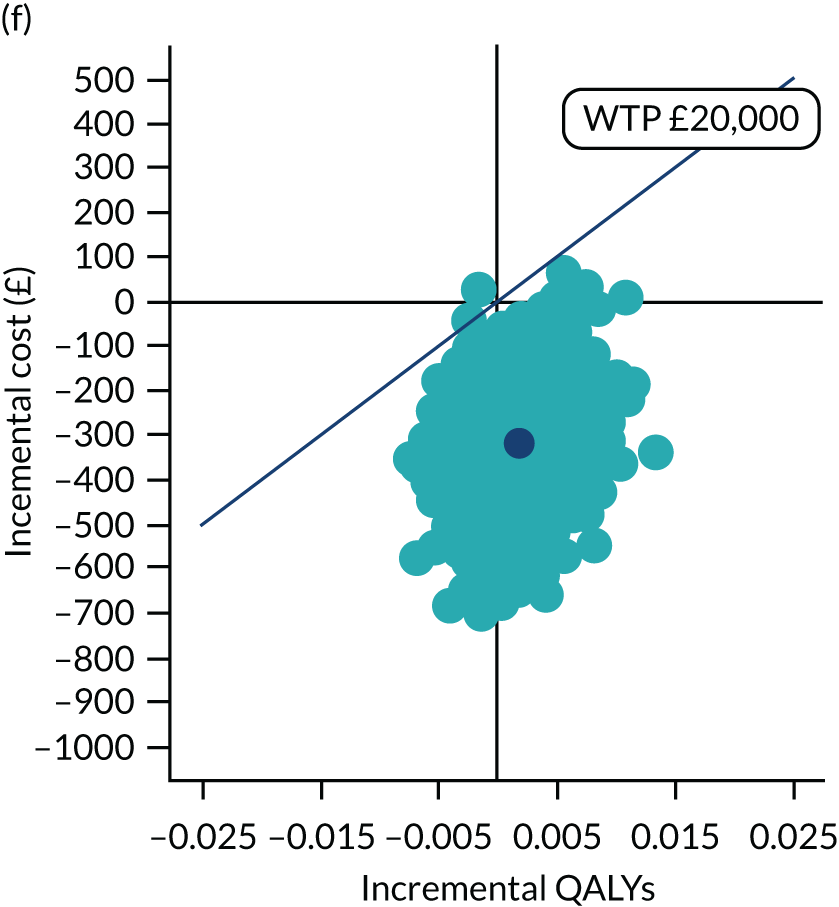
Summary
Compared with CBT, OST marginally decreased the service use costs and maintained similar QALY improvements. This is evident in both primary and sensitivity analyses, which considered costs derived from various perspectives and QALYs measured by different instruments.
Qualitative results: the feasibility and acceptability of one-session treatment
Intervention acceptability is a key priority in the development, implementation and evaluation of therapeutic initiatives. In applied health research, acceptability is typically defined as ‘a multi-faceted construct that reflects the extent to which people delivering or receiving a health-care intervention consider it to be appropriate, based on their anticipated or experienced cognitive and emotional responses to the intervention’. 97 Nesting qualitative research within RCTs is recommended to explore intervention acceptability fully.
Acceptability is generally perceived to have an important, although not exclusive, influence on treatment uptake, engagement and outcomes. In ASPECT, intervention uptake (i.e. the proportion of CYP receiving one or more sessions of their allocated treatment) was 69% and 73% for OST and CBT, respectively. Quantitative data reporting clinicians’ and families’ baseline treatment preferences are presented in Chapter 4, Baseline characteristics. Although informative, summary statistics can act only as proxy indicators of intervention acceptability and are limited in their ability to elucidate essential process learning.
Three qualitative studies were nested within ASPECT. The first two explored the acceptability of OST from the perspective of CYP who received it and their parents, and the third explored the feasibility and acceptability of delivering OST from the perspective of trial clinicians (see Chapter 2, Qualitative methods, for the methods for each of these studies).
Acceptability, when defined as a cognitive–emotional construct, has both prospective and retrospective components and can be influenced by cognitions or emotions occurring before, during and after intervention delivery. The extent to which these converge or diverge is ultimately an empirical question for the researcher.
Cognisant of this possibility, our findings are presented in line with the objectives of this study, namely to explore CYP, parent and clinician experiences prior to participation in ASPECT along with their experiences of OST delivery, and their subsequent reflections on intervention impact and acceptability. These objectives provided a basic, deductive framework for our analysis. Thorough descriptions of the inductive interpretive themes relevant to each objective are presented in turn, supported by direct quotations from the data. Participants are assigned a unique identifier rather than a name or pseudonym in the text, and relevant demographics are included for each. Additional data are included in the summary coding tables in Appendix 9, Tables 46–48.
Study 1: acceptability of one-session treatment to trial participants
The aim of the first study was to explore the acceptability of OST from the perspective of CYP participating in the trial.
Representativeness of the sample
All CYP who received OST and provided consent to be contacted for interview were eligible for inclusion (34 were approached and 27 participated). Baseline characteristics for the participating CYP are presented in Table 27. Data for the randomised ASPECT participants (n = 268) are provided for comparative purposes.
| Characteristic | Participant sample | ||
|---|---|---|---|
| Qualitative (N = 27) | OST group (N = 134) | Whole trial (N = 268) | |
| Age (years) | |||
| Mean (SD) | 11 (2.27) | 11.8 | 11.8 |
| Range | 7–16 | 7–16 | 7–16 |
| Sex (%) | |||
| Male | 33 | 36 | 38 |
| Female | 67 | 64 | 62 |
| Phobia category (%) | |||
| Animal | 44 | 28 | 30 |
| Vomit | 12 | 27 | 29 |
| BII | 30 | 27 | 25 |
| Other | 22 | 16 | 16 |
| Baseline treatment preference (%) | |||
| Conventional CBT | 30 | 34 | 34 |
| OST | 22 | 19 | 17 |
| No preference | 48 | 47 | 49 |
Children’s views
Children’s experiences of phobia prior to ASPECT
The qualitative analysis interpreted four themes from the data relating to CYP’s experiences of phobia prior to ASPECT. These themes highlighted (1) divergence and commonalities in child-led concepts of phobia, (2) widespread child and family burden, (3) a history of ineffective support and (4) a rising recognition of treatment need.
Divergence in CYP’s conceptualisations of phobia led to the delineation of two groups: those who attributed their difficulty to a discrete incident and those who had no clear memory of how or when their phobia emerged. Phobia was more readily rationalised as a logical response to a triggering stimulus in those who could pinpoint a seminal event:
I was at the beach when I was little and then my dad was trying to take a photo of me. And when my dad was trying to take a photo of me, a dog came up to me and knocked me over then licked me, so I kind of started with it like that.
CYP24, male, 7 years old, dog phobia
Common to all children was a desire to direct their energy towards conquering the functional challenges of phobia rather than to further their understanding of its origin or cause. A shared narrative among CYP endorsed a relatively simplistic, developmentally appropriate concept of phobia, in which an exaggerated fear response was conceived as an unwelcome entity that imposed unnecessary restrictions and generated feelings of sadness and shame:
I think that was kind of the main thing was that I was just getting quite embarrassed about not being to have it. Or going down and them all being – questioning me on why I’m not having it or feeling a bit like ‘oh why am I so afraid?’. You do just kind of question like ’cause I didn’t, you don’t really understand, make sense of it.
CYP5, female, 15 years old, needle phobia
The interviewed CYP described moderate to high levels of burden, affecting both the individual and their wider networks. A communal discourse delineated a growing sense of academic and peer exclusion, with access to specific classes or social events prohibited by phobias. Among older CYP, in particular, the avoidance of phobic stimuli had often led to the initiation of safety behaviours, with emotional reassurance derived from the long-term maintenance of self-imposed routines:
I refused to go places because of it, especially during the winter months when the bugs were going round. I wouldn’t leave the house because I’d be scared of catching something.
CYP18, female, 16 years old, vomit phobia
Irrespective of age, most CYP described a growing reliance on behavioural adaptations that extended beyond their own social spheres to those of their family members. They described a heavy reliance on kin support for stimuli avoidance and acknowledged that, in this context, their immediate family absorbed a lot of the practical and emotional impact:
Well, I couldn’t watch certain TV [television] programmes. I couldn’t go into some shops. And they even appeared on websites too, which means, so it meant we had to be careful where we looked.
CYP10, female, 10 years old, puppet phobia
Consistent in CYP’s narratives was the notion that forced exposure by informal carers was unhelpful. Some CYP recounted specific incidents in which parents had deliberately introduced them to the stimuli without fully understanding the impact that this would have. Most CYP interpreted these attempts as well-meaning, although collusion and coercion on the part of family members was occasionally identified, engendering a sense of mistrust in those affected:
Well, my mum and dad tried to help me go under the high roofs of like the bits I was scared of, to try to overcome my fear of it. But it didn’t really work.
CYP27, male, 10 years old, high ceilings phobia
Children frequently alluded to a tendency for parents and peers to underestimate the severity of their phobia, precipitating a sense of cognitive dissonance (i.e. a misalignment with thoughts, beliefs and behaviour) in some participants. In older CYP in particular, awkwardness and embarrassment had emerged. Persistent minimisation of phobia led some to question the legitimacy of their condition and the credibility of their treatment need:
I had to go out school sometimes to go to the counselling things and then and they were a bit like ‘where are you going?’. I’m like ‘oh yeah I’ve got a phobia of needles’ and they’re like ‘why don’t you just have it? It isn’t that bad’, and then you kind of think, ‘am I just being dramatic?’. You kind of feel a bit bad about it. Yeah, yeah a bit kind of embarrassed I feel like I should be able to have this, why can’t I have this? It just doesn’t feel too great.
CYP5, female, 15 years old, needle phobia
Only a minority of CYP conceived their phobia as a diagnosable condition sufficient to warrant health service intervention. Previous support accessed by this subgroup of CYP included generalised anxiety management, hypnotherapy and play therapy, but each of these interventions had left them disappointed. CYP attributed their lack of effect to either a failure in problem recognition or the intervention content. Exposure and response prevention was regarded as a crucial element in phobia treatment and one that was lacking in non-specialist interventions. A shared discourse among CYP revealed a striking lack of awareness of phobia-specific treatment options:
No, ’cause I didn’t know it was available, so I didn’t even know it was a thing. So, I’d never gone to anyone. Even people I’d spoken to about it, I hadn’t even realised it was a thing.
CYP19, female, 16 years old, vomit phobia
Symptom minimisation served to both delay formal help-seeking and discourage onward referral. A small number noted that their phobia had been dismissed or downplayed by health-care professionals in the past, which they had found to be upsetting. Very few described physical or financial barriers to phobia treatment, most choosing to focus instead on attitudinal and emotional deterrents. Alongside professional and social attitudes, CYP described a wealth of internal barriers to treatment, including their own fears and anxieties about what formal treatment would involve:
I don’t think you want to go because of what you’re talking about and it’s a sensitive subject when you’re scared of it.
CYP20, female, 12 years old, needle phobia
CYP’s apprehension towards formalised phobia treatment contrasted sharply with their desire for effective intervention. Participants described an urgent and growing demand for symptom improvement, alluding to a potential turning point at which the anticipated benefits of treatment began to outweigh the costs. Adopting an ego-centric view, CYP were motivated to access treatment predominantly to ameliorate internal distress or to counter imminent health risks and offset risk behaviours:
For my meningitis injection, I could only get the polio and tetanus ones, and not the meningitis injection which is quite important. So, it was a pretty big and urgent matter to get, to sort it out.
CYP7, male, 15 years old, needle phobia
Well ever since I was little, I’ve been running into roads to avoid them. And it was, it was getting to the point where it probably needs sorting out, otherwise something dangerous could have happened.
CYP3, female, 16 years old, dog phobia
The optimal outcome of OST, from the CYP’s perspective, was a meaningful reduction in anxiety, with distal benefits for daily functioning and QoL. Although younger CYP tended towards expectations of a cure, older individuals were typically more cautious. Cognisant of the length of time that they had already lived with their phobia, older participants sought to moderate (rather than eliminate) their fear, dampening it down to a level more conducive to their daily routine:
Well I sort of like the idea of getting the phobia at least somewhat under control, ‘cause that genuinely that would take a massive hassle out of everyday life.
CYP7, male, 15 years old, needle phobia
Children and young people consistently expressed a hope that OST would work, but acknowledged that prior to the treatment they did not understand its primary mechanism of action. Some queried the extent to which an engrained phobia could be separated from the self, while others questioned how readily their stimuli could be replicated and how realistic this would be:
I sort of went in being like this isn’t going to help you know ’cause obviously they can’t get a really giddy dog because they can’t have one that you think might hurt you and whatnot.
CYP3, female, 15 years old, dog phobia
In some instances, CYP’s expectations were directly influenced by their previous treatment experiences. Those who were able to draw on prior experiences of CBT believed that OST would have a beneficial impact, while those with experiences of less-structured therapies were often more sceptical:
I knew from CBT very recently that it’s not just going to completely fix a problem and I wasn’t expecting that at all. But I was expecting it to sort of like ease the like impact it had on my life and be able to like give me methods to cope with it rather than just avoidance behaviours, ‘cause that isn’t really healthy and it gets in the way of things I want to do.
CYP19, female, 16 years old, needle phobia
I was just more like oh this probably gonna be like the play thing and probably it’s – probably is gonna go and do everything I’m probably not gonna have anything done from it but obviously I did.
CYP15, female, 12 years old, needle phobia
Common to all CYP’s narratives was the notion that deciding to engage in OST had been guided less by a guarantee of effectiveness and more by a lack of opportunity costs. Expectations of more efficient delivery under the OST model minimised the cognitive and emotional barriers that had historically prevented CYP from accessing treatment, leaving them with sufficient impetus to engage in this intervention:
I think going into the 3-hour sessions I was thinking like it’s going to be better than having to like do a session and then work and like – kind of in between that space like panic about it and just getting done.
CYP1, male, 10 years old, needle phobia
Children’s experiences of one-session treatment delivery
Three interpretative themes were derived from CYP’s accounts of their experiences of OST delivery within the trial. These themes identified three key elements critical to treatment acceptability: (1) session format, (2) expert facilitation and (3) partnership working.
Most CYP recognised and appreciated the stepped format of OST, accepting this as a largely suitable way to treat phobias. Specifically, graded exposure was viewed as an adaptable and secure way to challenge their fears and manage their anxiety responses:
I think because it’s so gradual you don’t ever feel so out of your comfort zone that it’s impossible. Because it’s just something you’ll have just done, it’s just like a tiny little step of what you’re about to do.
CYP3, female, 15 years old, dog phobia
Some commented on the length and intensity of the session, noting that the intervention left them feeling emotionally exhausted. These views did not appear to be age or phobia dependent however, clustering predominantly in CYP with additional learning needs (e.g. ASD). A strong counter-narrative identified session length as a beneficial feature of OST, advocating the continuity and efficiency of intervention delivery as a specific advantage of this treatment modality:
It was a lot and I did kind of get overwhelmed towards the end of it and I was like, I need to stop now ’cause it’s just too much.
CYP19, female, 16 years old, vomit phobia
If you were to go through the CBT, you’d be going back and forward and then there’s petrol and then there’s work and then there’s school. And all these things that need to be taken into consideration. But, with the one-session treatment, it’s half a day. You’re done.
CYP18, female, 16 years old, vomit phobia
Some children acknowledged that having a maximum of two sessions was less intrusive on their daily lives, minimising travel burden and opportunity costs and maximising their propensity for therapy engagement. Most, however, focused on emotional gains, closely aligning their in-session experiences with their original expectations of treatment. The condensed format of OST was appraised positively by most CYP, who appreciated not having to revisit previous sessions. A common view was that single-session therapy minimised the build-up of pre-treatment anxiety, thereby reducing their temptation to revert to safety behaviours or drop out of treatment completely. Although a direct comparison with other therapy models was not always possible, CYP hypothesised that the continuity of OST had increased the efficiency of their exposure, enabling them to capitalise on early progress and improve their outcomes:
Like you know because say if you didn’t enjoy this, then you got to go back for 12 other sessions or how long it was, it just seems a bit like you dread it a bit, and it doesn’t really be as effective.
CYP15, female, 12 years old, needle phobia
. . . it’s better to sit there for 3 hours and try and feel comfortable with the thing you don’t like than dread the week, the day of the week you have to go.
CYP25, female, 12 years old, dog phobia
Most CYP expressed positive views about the therapeutic environment, with their experiences particularly influenced by physical features of the clinical setting and, more frequently, the OST facilitators’ communication style. CYP consistently described the OST therapists as kind, friendly and relaxed, and perceived their gentle encouragement and non-judgemental attitudes as an important determinant of intervention success:
Even though there was the white colour scheme and the grey bland colour scheme, it still made me feel welcomed because of the rugs, the soft chairs, the nice people.
CYP21, male, 12 years old, needle phobia
I think she understood me, so she’d know when I was a bit like ‘no!’, and then she’d be able to encourage me when she thought I could do a bit more, so it’s the right balance.
CYP3, female, 15 years old, dog phobia
Therapist competency, as well as their confidence, was identified as a core ingredient of effective facilitation, placing OST firmly within the remit of a trained health professional’s role. Considerable value was placed on flexible, child-centred approaches, with different narratives highlighting the potential for individual therapist effects. Although a small number reported feeling rushed through their treatment, the majority described an intervention that was coherent and empowering, with progress determined at an appropriate pace:
It was definitely a well-thought-out, more like, well-designed intervention. And the actual like getting, having more control over it, meant it felt more like personalised and you were in control.
CYP7, male, 15 years old, needle phobia
High importance was placed on partnership working, with many CYP regarding the OST assessment session as an invaluable opportunity to meet their therapist and input directly into their treatment session. They reported deriving a breadth of benefits from collaborative treatment planning; one participant rationalised that it was easier to progress through treatment when the steps were known in advance and another suggested that the use of self-directed challenges maximised treatment relevance and meaning:
You feel like you’re more involved in the actual therapy, you don’t feel like it’s just been planned by someone else like for you. You feel like it’s more personalised to your own, like, fears and what and how far you actually want to go.
CYP7, male, 15 years old, needle phobia
Successful collaboration was predominantly defined in terms of a synergistic relationship established between the OST therapist and the child. Very few children expressed the need to have a parent or carer present, although, where this occurred, it was positively received, helping children to articulate their thoughts and providing reassurance:
I mean for yeah for me it was useful kind of having someone there ’cause of course I don’t know [therapist name] that well I don’t – didn’t know the nurse that well so having someone that I know really well as support is something really useful for me anyway.
CYP5, female, 15 years old, needle phobia
Children’s reflections on the impact and acceptability of one-session treatment
The qualitative analysis interpreted a final three themes from CYP’s post-therapy reflections. These themes were (1) children’s perceptions of treatment outcomes, (2) a potential role for participant suitability criteria and (3) possible modifications to treatment delivery.
CYP’s narratives revealed a tendency for pre-treatment expectations and post-therapy reflections to diverge. Those who reported feeling anxious before therapy recounted treatment experiences that were much more positive than they had anticipated, CYP’s appraisals of treatment outcomes were also largely positive, with many perceiving that they had either achieved or exceeded their intervention goals:
. . . it’s always worse in your head than it is when you’re actually going through it. And I was really nervous going in, but when I was actually having the treatment I was kind of like ‘Why was I scared? What was there to be scared of?’.
CYP18, female, 16 years old, vomit phobia
I had become so used to this life of living with phobias that I thought that that was what life is. And so when I was kind of like oh this isn’t what – I don’t know have to worry about everything like every single second of a day. It was kind of – it was a nice surprise you know. It was a nice surprise to not have to worry so much.
CYP16, female, 15 years old, vomit phobia
Overall, CYP reported feeling less anxious after OST. Valuing the realism of the stimuli that were encountered, they consistently praised the creativity and interactivity of OST and the learning opportunities embedded within OST. OST’s capacity to mimic real-world scenarios was frequently highlighted as an important element of the intervention, increasing CYP’s sense of self-efficacy and providing them with self-management skills:
Even when we came out afterwards there were some dogs on the street and, mum was amazed that I could just walk past them.
CYP3, female, 15 years old, dog phobia
In some instances, OST was reported to have had secondary benefits, having taught skills that were transferable to other developmental challenges and aspects of life. In particular, older CYP emphasised the ‘spillover’ effects of treatment, retrospectively identifying the positive effects of OST for both themselves and their network members:
I still get quite worked up about come quite distressed about my mocks because of my GCSEs [General Certificate of Secondary Education] and they’re stressful. But I was doing some breathing this morning as well kind of just going up on my way to school ’cause getting quite worked up and it is it was the kind of the same thing where I went, I was quite nervy, no before my exam, I went through my exam it wasn’t as bad as I thought it would be and then I’ve calmed myself down at that point so it yeah, useful things.
CYP5, female, 15 years old, needle phobia
Yeah, I feel a lot happier in myself as a person and around other people. And I think people feel more relaxed around me – like they don’t have to constantly be like – like worrying about what they say or anything.
CYP19, female, 16 years old, vomit phobia
Some children reported that the language used by the OST therapists had helped them to understand the origins of their phobia and enhanced their knowledge of physiological responses to phobic stimuli. Although not explicitly prioritised as one of their goals at therapy outset, CYP upheld this benefit as a valuable element of intervention delivery, acknowledging that it had played a central role in normalising their experience, reducing their embarrassment and nurturing a greater sense of internal control:
Because it helped me to understand why I was scared of them. It might sound weird but I never really knew why I was scared of them. So I was scared of them, up until now I didn’t know why.
CYP10, female, 10 years old, puppet phobia
A minority of CYP reported that OST had not enabled them to reach their treatment goals. Although disappointed, these individuals acknowledged that there were few opportunity costs to OST participation, accepting it as a helpful platform for additional intervention. Consequently, nearly all recommended OST an acceptable support mechanism for other CYP, albeit with the caveat that progress could not be guaranteed:
I’d explain how it worked for me, how my life has changed and just like, say like, yeah, ‘It’s helped me a lot. It might help you. You can always give it a go – there’s no harm in trying’, sort of thing. Obviously it might not work for everybody, but if there are people it could help and it could work for, that’s always a plus.
CYP19, female, 16 years old, vomit phobia
Reflecting on the potential variability in intervention outcomes, CYP highlighted a need for services to consider individual requirements when instigating a pathway of care. Older CYP expressed caution regarding the suitability of OST for younger individuals, although younger CYP themselves did not uphold this view. Developmental stage emerged as a stronger determinant of intervention acceptability than chronological age, with treatment engagement dependent on cognitive capacity and educational maturity:
I do think that like for teenaged years it definitely works. I don’t know with young children ‘cause I feel like 3 hours, they wouldn’t be able to like, they’d just get bored and start getting a bit like agitated, I feel like once you’re older you’re a bit more mature and you can actually like be in a room doing the therapy for multiple hours. It means you’re then, you’re more likely to actually gain something from it and not like just get fidgety and distracted.
CYP7, male, 15 years old, needle phobia
A shared discourse emphasised a need for OST participants to be able to maintain sufficient concentration for a prolonged appointment. One child expressed a preference for multiple shorter sessions of CBT, rationalising this in terms of their need to process information in shorter segments. Another, who lived with ADHD, suggested that his ability to engage in OST had most likely been affected by his capacity to focus:
After like an hour and a half to 2 hours I got really like ‘cause I’ve, with me having ADHD and only sitting like I get where he can’t sit for ages . . . and with us sitting there for a long time I get, I kept walking around the room so I just trying to distract myself.
CYP26, male, 10 years old, choking phobia
Children and young people’s acceptance of their phobia and the intensity of their fear were also raised in the context of suitability. Remaining open to the challenge of an exposure intervention and having sufficient resilience to cope with this over a sustained period were often highlighted as discrete prerequisites for OST:
I would only recommend it, if the person had kind of accepted their phobia and understood their phobia and felt ready to kind of deal with it. Obviously ’cause I feel like with the one-session treatment you have to be aware of how you’re feeling and you have to not be in denial about how you are.
CYP16, female, 15 years old, vomit phobia
Extrinsic influences, such as intervention context and timing, were also considered important, with life circumstances and family support emerging as two core features influencing treatment uptake and engagement:
It’s hard when you’ve got a lot going on in your life – it’s hard to focus your time and energy into overcoming the phobia because it does take a lot out of you. ’Cause all the energy you’d usually be using to worry about it you’re kind of having to force yourself to go ‘no, you’re OK – you don’t have to worry’, you’re having to kind of like actively think about it. So, it does take a lot, so I think it has to be at the right time.
CYP19, female, 16 years old, vomit phobia
If my mum wasn’t worried about me I probably wouldn’t of done anything to do with this. But you need the support from the people around you to actually be able to – [laughs] to almost shove you in it. Almost as much as, you’ve got to want to do it yourself. But you need someone like a bit of encouragement because it’s hard.
CYP3, female, 15 years old, dog phobia
Although session length was recognised as a defining feature of OST, this was also something that CYP often felt could be changed. Although a few CYP advocated for a longer session to accommodate more reticent individuals, the majority suggested that shortening the session, or at least providing a comfort break, could be advantageous:
I feel like a 10-minute break or something in the middle. An hour and a half or 2 hours or something then break in the middle and get a drink, or snack or stuff like that and then carry on.
CYP1, male, 10 years old, needle phobia
Some CYP also suggested that a follow-up session would improve their OST experience. This was typically to enable a practitioner to check on their progress or provide them with another supervised opportunity to consolidate their skills. In rare instances, the addition of a follow-up session was advocated as an opportunity for health service development and quality improvement:
. . . having a follow-up if it was about 2 or 3 weeks after just to kind of go through what I’ve been through, but not at the same length of time, not for 3 hours. But, just to kind of go back through it so you’ve still got it in your brain.
CYP18, female, 16 years old, vomit phobia
Because it would help him understand erm – maybe how erm – if they give him feedback then, then for his next person he could use that feedback.
CYP13, female, 10 years old, needle phobia
Summary of children’s views
Overall, CYP’s narratives upheld OST as a credible and engaging intervention that aligned with their treatment needs. CYP initially approached treatment with some trepidation, but confidence in their own ability to participate in the intervention increased with treatment experience. Qualitative data suggested that individuals perceived few opportunity costs to OST participation, although their own intrinsic readiness emerged as an important influence on treatment motivation. Improved information and orientation may have a role to play in ensuring that CYP are emotionally and cognitively prepared to receive OST.
Therapists’ competence, collaborative goal-setting and therapeutic rapport were identified as core features critical to the success of OST. Having a therapist who was knowledgeable, empathic and trustworthy was important to CYP. Most reported that OST had developed their understanding of their phobia and given them the skills to manage its symptomatic and functional effects. Transferable learning, in the form of improved anxiety management, was also reported by some.
The efficiency of single-session delivery was largely acknowledged to have a positive impact on therapeutic experience and outcome. However, CYP’s narratives raised an important issue around its universal suitability, suggesting that patient choice and personalisation should be retained as important features in referral pathways. Child-centred variables (e.g. developmental stage and additional needs) may best be considered in conjunction with family-centred variables (e.g. support availability) and phobia characteristics. Some additional modifications to OST delivery were advocated, specifically the addition of a follow-up session to improve individuals’ experiences of treatment closure and provide an opportunity for progress review.
Study 2: acceptability of one-session treatment to parents
Our second qualitative study aimed to explore the acceptability of OST from the perspective of the parents and caregivers of CYP who were allocated to receive OST.
Representativeness of the parent sample
All of the parents/guardians who were interviewed were female, were aged between 30 and 59 years and had CYP who had also participated in interviews. Characteristics of these CYP and their phobias are presented in Table 27.
Parents’ views
Akin to study 1, our findings for study 2 are laid out in line with the objectives of this work, namely to explore caregivers’ experiences of phobia prior to their participation in ASPECT, their experiences of OST delivery and their subsequent reflections on intervention impact and acceptability. These objectives provided a basic deductive framework for our analysis. Thorough descriptions of the inductive interpretive themes relevant to each objective are presented in turn, supported by direct quotations from the data. Participants are assigned a unique identifier in the text. Child age, sex and phobia type are provided. Additional data are included in the summary coding tables in Appendix 9, Tables 46–48.
Caregivers’ experiences of childhood phobias prior to ASPECT
The qualitative analysis interpreted four themes from the data relating to caregivers’ experiences prior to ASPECT. These themes highlighted (1) minimisation of childhood phobias, (2) suboptimal coping, (3) a rising need for intervention and (4) insecurity over treatment efficacy.
When reflecting on their understanding of phobia prior to ASPECT, parents’/guardians’ understanding of the severity and legitimacy of phobia varied. Many reported being dismissive of their children’s phobia initially, framing it as either a difficult developmental phase or a challenging and unnecessary behaviour:
We genuinely thought it would be something she’d just grow out of. And then as it came to a time for her to have vaccinations at school it became very apparent she wasn’t growing out of it.
P5, parent/guardian, 15-year-old girl, needle phobia
No, and it took a while for her to – to kind of talk about it. So it was coming across at the beginning that she just was being really difficult. Erm and – and so it took a bit of unpicking to finally get to the bottom of it.
P16, parent/guardian, 15-year-old girl, vomit phobia
Often parents alluded to a protracted period over which they felt that their child’s phobia had become engrained. Some were able to identify a specific time at which their child had been frightened by their phobic stimulus. These parents were more likely to rationalise their child’s behaviour and more likely to conceptualise it as a chronic yet coherent response:
I think it probably stemmed from when she was very small and we’d gone to see Disney on Ice [(an ice-skating show) The Walt Disney Company, Burbank, CA, USA] and then on the way back her friend projectile vomited in the car, which was obviously an enclosed space. And then it happened again with her sister, and then with her friend. So I think it stemmed from a very young age.
P19, parent/guardian, 16-year-old girl, vomit phobia
Few parents had sought professional help prior to the study. Specific phobias were commonly located outside lay constructs of mental health and were afforded less salience than other health issues, physical or mental, that their children encountered. This lack of recognition of phobia was typically compounded by a lack of awareness of viable treatment options, discouraging timely help-seeking and effective response:
I mean it didn’t even occur to me to go like to a doctor and ask for help. It hadn’t occurred to me at all, I think we were trying to manage it ourselves and I think it’s why it’s that – having that frustration and then realising actually it’s, it’s beyond what we thought.
P6, parent/guardian, 12-year-old girl, dog phobia
Everyone knows that CAMHS is there to support mental health, but you don’t consider a phobia to be part of the mental health.
P25, parent/guardian, 12-year-old girl, dog phobia
Occasionally, health services were held accountable for reinforcing a lack of parental action. A small number of caregivers who had tried to seek help alluded to both financial and attitudinal barriers to treatment access. These parents recognised NHS funding limitations for CYP’s mental health provision and a lack of validation of childhood phobias in primary care as two factors devaluing treatment need:
But I was also aware that the NHS don’t offer huge amount of support to kids as well. It’s not that they don’t want to, it’s just that there aren’t enough resources and I know that – that [child name]’s anxiety needs would not be huge compared to other kids. So I thought she would be at the bottom of a list and it wouldn’t really be a priority so I didn’t have huge expectations.
P17, parent/guardian, 8-year-old girl, dog phobia
I think once we went to the GP and regarding to her phobia but they said – they said they can’t really a do really anything because it’s something like most kids are afraid of and she will grow up out of it.
P9, parent/guardian, 9-year-old girl, insect phobia
Suboptimal recognition and help-seeking for childhood phobias meant that many families had become accustomed to challenging scenarios and behaviours. Accommodation was the most common coping strategy reported by the parents referred to OST, typically manifesting as either the intense negotiation or the complete avoidance of a phobia stimulus. Both forms of accommodation were purported to precipitate family stress. Tension was particularly evident in families living with health-related phobias (e.g. BII phobias), for which parents archetypally conceded to coercive rather than collaborative approaches. Irrespective of phobia type, conflict in parental responsibilities emerged, a shared parental narrative highlighting the guilt that caregivers incurred from trying to manage their children’s phobias:
It’s almost felt like it’s – they’re there to pin her arm down rather than to help her get over it. I think the more people get involved probably scarier it is, ’cause she is getting out of control, she’s pinned down and, you know, her arm’s pulled around my back and held in place so she can’t move and make it worse, but in her own mind that probably makes it a million times worse.
P12, parent/guardian, 10-year-old girl, needle phobia
Nearly all of the parents had witnessed their child’s phobic responses evolve and intensify, until such times that they could no longer uphold a developmental perspective. Parents described a rising need to alleviate the emotional burden of phobia on their children, identifying this as the primary reason that they had sought or accepted help. Most appeared motivated to reduce the anxiety that their children experienced when encountering a triggering stimulus. Occasionally, however, parents also verbalised an aspiration to ameliorate more chronic socioemotional effects. Some spoke of a desire to alleviate the shame and embarrassment that their children experienced, either to directly enhance their emotional well-being or to prevent social marginalisation by their peers:
I really wanted her to be able to find ways of managing anxiety, because she was upset by the fact that she’s scared of dogs.
P17, parent/guardian, 8-year-old girl, dog phobia
It’s quite crushing really like – I think he was worried his friends would pick on him.
P1, parent/guardian, 10-year-old boy, blood phobia
Additional drivers of help-seeking presented as parental concerns for childhood safety and physical health. Parents of CYP living with dog or insect phobias were often apprehensive that their children would flee into danger, while parents of children with blood or needle phobias were concerned that they would miss key vaccinations or subvert preventative health routines:
It’s distressing ’cause I don’t like to see him unhappy and then it creates that worry around – you know – there’s still a meningitis jab that he hasn’t had. So there’s that kind of worry, ’cause I’m sort of, trying to do the best for his health and that’s sort of a bit of a contradiction if he’s not had that vaccination isn’t it? So – and then the dental – the issue around the dental [the dentist] about making life much more complicated. ’Cause he had to have an operation under general anaesthetic which – you know, I don’t believe in unnecessary surgery, so that sort of goes against some values but at the same time we have to compromise sometimes because I couldn’t see what the other options were really.
P7, parent/guardian, 15-year-old boy, needle phobia
Parental reports of CYP’s avoidance behaviours were common across the data set. A subset of parents highlighted a need to improve community and educational integration where possible. More consistently, however, parents were motivated to enhance family functioning, frequently advocating a need to improve parent–child relationships, alleviate stress on other family members and establish positive shared experiences:
In terms of outcomes it would – it would just be nice that I know that she could pick up a book that there might be a picture somewhere in it and that might be The Muppets [(group of puppet characters) The Muppets Studio, Los Angeles, CA, USA] and then she would be quite happy and wouldn’t be so scared she’d run off.
P10, parent/guardian, 10-year-old girl, puppet phobia
Against a backdrop of improving family interaction, parents hoped that OST would improve their own understanding and management of phobia, and facilitate constructive communication with their child:
I was just hoping that I’d get some advice on how to deal with [child name]’s phobia. And you know – what to do when she did see a dog.
P25, parent/guardian, 12-year-old girl, dog phobia
I thought it would be a good opportunity for us to talk about things more openly. [Child name] is really good at talking about things openly anyway, so we had already had conversations around it. But I saw another opportunity to have that.
P7, parent/guardian, 15-year-old boy, needle phobia
Parents reported scepticism when their child was referred to OST. A strong group narrative portrayed a cautious stance towards intervention efficacy, with caregivers being keen to protect themselves and their children from disappointment. Some ensured that their families also retained realistic expectations, while others worked hard to conceal their cynicism from their child:
My impression was I’m concerned that this is not going to meet his needs. I didn’t – I didn’t discuss any of that with [child name] I made sure that he was very focused on you know. And I think [child name] had really big expectations of it as well of what it was going to be for him.
P8, parent/guardian, 9-year-old boy, insect phobia
I was quite realistic with it because I thought ‘You can’t cure it in 3 hours’. I understand the idea around it, but I was just hoping it would give him more confidence in how to deal with it. So, I was hoping that he would feel stronger . . . So, that’s what I wanted out of it, was coping mechanisms, but I didn’t have any – I didn’t want to set myself up and think ‘He’s gonna be absolutely fine when he walks out’ because that’s just upsetting for both of us. So I thought I’ll be practical and I’ll hope it gives him the tools he needs, but I didn’t think it would cure him.
P1, parent/guardian, 10-year-old boy, blood phobia
Notions of a curative treatment were often discarded by parents and replaced with more pragmatic expectations of self-management support. Some doubted whether or not a time-limited intervention could ameliorate an engrained phobia, while others worried that OST would not align with their child’s needs:
I wondered how effective it would be, because knowing how [child name] reacted when he, you even mention the word blood, never mind needles and having blood taken, it would just send him into a spiral. You know if he thought he was going anywhere near a doctors surgery and there’s anything to do – you couldn’t even say the word blood test. We had to say ‘BT’ and abbreviate it for him – for him to be comfortable. So I just didn’t know how effective it was gonna be.
P21, parent/guardian, 12-year-old boy, blood phobia
I thought it would help her, but from the other side I was a bit scared at how can you treat a phobia, especially the one she had, when it so common. And you are just like sort of – you are facing it every single day, because they are – obviously the flies everywhere. How can you treat it with just one session? So I was hoping it would help her, but I just – like I was in doubt [laughs] yeah that we might need some extra help after that.
P9, parent/guardian, 9-year-old girl, insect phobia
Parents’ experiences of one-session treatment delivery
Three interpretative themes were derived from parents’ accounts of OST delivery. These themes centred on (1) the strengths of OST facilitation, (2) potential adaptations to support treatment effects and (3) the impact of the treatment delivery protocol.
Overall, parents reported that their children’s experiences of OST had been positive. Participants partially attributed this success to the high degree of control that CYP were afforded over treatment, acknowledging that collaborative treatment planning and child-led progression had enabled their child to set a comfortable therapeutic pace:
For me I think [therapist name] reiterated that [child name] has control all the way through the session, you know. And I think that gave her the confidence to move forward knowing that – you know if she’s uncomfortable she could speak out.
P24, parent/guardian, 7-year-old girl, dog phobia
Most parents recognised the influential role that OST practitioners played in children’s treatment experiences. One parent suggested that the dialogue between the clinician and the child had sometimes come across as patronising, but more commonly caregivers commended the use of child-centred communication techniques. Emphasis was placed on the importance of clinicians making quick connections with OST participants; parents often upheld this as a crucial factor determining the quality of the therapeutic alliance and its outcome. For some families, the patience and consistency displayed by OST practitioners contrasted sharply with the reactive emotions expressed at home, providing a new and reassuring perspective for their child:
She had a really good understanding of children as well, she had a lovely manner with her, and she spoke in a language that [child name] understood, which put [child name] at ease as well.
P23, parent/guardian, 7-year-old girl, dog phobia
We lost our patience and maybe that patience from the therapist it helped her. That somebody really actually sat down with her and explained everything about it. And let her understand why she’s afraid and how to manage it.
P9, parent/guardian, 9-year-old girl, insect phobia
Parents acknowledged the benefits of having a skilled and knowledgeable therapist, recognising these as essential characteristics for optimal information transfer and the development of targeted, personalised treatment sessions. Equally salient, however, was the sense of objectivity that trained facilitators bestowed. OST practitioners were typically located outside parents’ and CYP’s social networks; the sense of independence and impartiality that this afforded was frequently recognised by parents as advantageous for therapeutic rapport:
Phobias are so specific to certain people; you need to understand the science and the right questions to ask somebody to get into the thing.
P12, parent/guardian, 10-year-old girl, needle phobia
I’ve tried to do what I can with him, but it’s very different when you’re emotionally involved. It needs to be somebody sometimes I think, you’ve gotta accept that sometimes you need somebody who’s outside, who’s a professional, who is gonna be able to just walk away from it at the end of the day.
P7, parent/guardian, 15-year-old boy, needle phobia
Parents recommended some ways that OST delivery could be improved. Many articulated the need for a follow-up session, often highlighting this as a valuable, but currently missed, opportunity for clinicians to review a child’s progress and sustain their self-management skills. A small number conceptualised the follow-up session as a potentially shorter, parent-centred communication, which would enable caregivers who had not observed the therapy to better understand the intervention and support their child’s learning:
I know that 3-hour session was a one treatment session, but maybe another something similar afterwards to see how she’s, [child name]’s progressed from where she was then to dealing with a dog again. So, yeah I just feel like there should be a little something just to see how she is with the dog again.
P3, parent/guardian, 15-year-old girl, dog phobia
Yeah, I think even if they’re given like you know a handout, or something like that to pass on. Yeah or – just like a follow-up phone call with like oh, this is you know, what we did, or you know, just some kind of follow-up information.
P14, parent/guardian, 7-year-old girl, dog phobia
Parental involvement in the intervention varied and appeared to be determined largely by clinician preference. Those who had been present during therapy reported gaining a deeper understanding of childhood phobias and believed that they had developed some specific skills to support their child’s progress. In this context, parental inclusion was perceived as an important therapeutic ingredient and a potential determinant of sustained treatment effect:
For me it was really useful to see the techniques and the skills that she was being given because then in my head I was thinking at this precise moment in time she’s never going to walk into a GP’s surgery on her own and have an injection by herself. And, you know, for me to go in and just try and gently remind her of those skills and the breathing and the relaxation techniques, and what have you, is really useful.
P5, parent/guardian, 15-year-old girl, needle phobia
Parents who were not able to observe OST confirmed this view. These individuals described their ideal of a shared appointment, noting that they would have welcomed additional guidance to help their child following treatment:
The organisation was a big thing ’cause, like I say – I feel like if I could have been there and known what strategies they put in place and you know, just the things that they did then I could have carried that on. Like you know, on the walk to school, or you know, that sort of thing.
P14, parent/guardian, 7-year-old girl, dog phobia
Limited access to transport, substantial travel distances and the available appointment times conflicting with family commitments were all cited as barriers that discouraged access to face-to-face treatment. Unique to OST, however, was the need to dedicate a continuous amount of time to therapy, which for some incurred significant opportunity costs:
You’ll have to take a bit of time off school, most kids won’t mind that. I suppose if – I work part time, so it wasn’t so much of an issue really for me, but perhaps some parents, if they work full time, it might be inconvenient to take their kids to some of them. But if it is an actual phobia, I would imagine it impacts on those families lives anyway. You know, if it’s significant enough to try and get help for it then, I would imagine you’re prepared to invest some time in it as well.
P13, parent/guardian, 12-year-old girl, insect phobia
Competing participant narratives emerged regarding the acceptability of the OST delivery format. Some upheld the single session as logistically more manageable, manifesting in less interruption to school and work commitments. Many were keen to minimise the emotional burden of treatment and construed the lone appointment as less intimidating and anxiety-provoking for their children. Intervention efficiency was also acknowledged; parents suggested that there was less repetition or potential for regression with continuous therapy and more opportunity to evidence early improvement. Some advocated that this continuity was critical to intervention engagement, positing that their child would have been substantially less motivated and unable to sustain exposure if they had been referred to weekly CBT sessions:
I’d say a lot of it was the time constraints. You know, that’s got to be the honest reason, is the time constraints for myself and trying to manage her school.
P12, parent/guardian, 10-year-old girl, needle phobia
She could really look back and just see how things had changed from before she went there and then when she’d left. Rather than it being something spread over so that she couldn’t so easy reflect on the difference.
P17, parent/guardian, 8-year-old girl, dog phobia
Concomitantly, OST delivery was acknowledged to have its limitations. Perceptions of therapeutic intensity sometimes confounded those of session length, with emotional exhaustion recognised as a specific treatment risk. Several parents alluded to the cognitive impact of the intervention on caregivers and CYP. Some reported that their children needed a day off school to accommodate its acute effects:
She had no energy to do anything. She had no motivation or anything. She were just kind of like slumped as though there was a lot on her shoulders. But then it would be ’cause it was intense.
P20, parent/guardian, 12-year-old girl, needle phobia
You’ve got to stop keeping them so long. ’Cause it’s exhausting for us and it’s exhausting for the child.
P21, parent/guardian, 12-year-old boy, needle phobia
A shared discourse highlighted the importance of service organisation, both within treatment sessions and across the care pathway. Coordination of resources and effective communication with families was often a challenge. Parents tended to rationalise delays in treatment access that were incurred while sourcing stimuli, but were less sympathetic to setbacks caused by workforce shortages or procedural constraints. Several parents recommended that the interval between treatment planning and delivery needed to be shorter, with some noting that they had struggled unnecessarily when this was prolonged:
[We] had like real problems with getting the session arranged. The lady that we were allocated to actually arrange it, she was – she only worked a couple of days a week and she said like the dog that they had worked on Monday and they didn’t have a venue on a Monday that allowed dogs and things. So, it took quite a long time to arrange, well, all of the summer to be honest with you. I think it was, it was the – she was definitely back at school in the September, possibly the October when we actually got the treatment arranged and I did feel that we only actually managed to get it arranged because I contacted [trial manager name] . . . it just seemed to drag on far too, too long. And then when – when it was arranged it was arranged for a day when I was at work and we only got a week’s notice as well, so I couldn’t put in a holiday request.
P14, parent/guardian, 7-year-old girl, dog phobia
Post-treatment reflections
The qualitative analysis interpreted two final themes from parents’ post-treatment reflections. These themes centred on (1) parents’ perceptions of treatment outcomes and (2) treatment suitability.
Parents generally felt that their children had benefited from OST. The most common benefits that parents reported for their children comprised increased knowledge and understanding of their phobia and their physiological responses to emotions; increased self-confidence; and reduced anxiety. Most described their children as feeling proud of what they had achieved in therapy and more self-efficacious following treatment, crediting this to the new knowledge and skills that they had acquired:
Her first thing she said when she came out was she was really proud of herself. So that was really nice.
P5, parent/guardian, 15-year-old girl, needle phobia
Yeah definitely, it’s made a big difference, just for example like walking to school, she will run off through the park, you know, ahead of us. Whereas you know you wouldn’t go through the park initially and then to begin with, you’d hold her hands, but now you’re just carefree aren’t you?
P24, parent/guardian, 7-year-old girl, dog phobia
Variation was apparent in the magnitude of effect that parents perceived. Although some parents reported marked improvements in their child’s behaviour, others reported a more moderate response. Typically, parents described partial progress, noting that, although some features of phobia were still present, their children were more likely to employ effective self-management strategies and less likely to engage in avoidant behaviours:
Well [child name] will still message me, she’ll still send me text messages if she’s feeling anxious about – Erm, because there’s been a lot of norovirus at the moment and a lot of children have been going off, schools have been closed and things so she has been quite anxious about catching that. So she will message me if, you know, a child’s been feeling unwell at college. Erm, but they’re so much shorter [laughs]. And, erm, I think she comes down a lot quicker. Her anxiety comes down so much quicker. And, and you can reason with her as well. And I don’t think, as far as I’m aware I don’t think she’s running out of rooms. You know, she’s managing to stay.
P19, parent/guardian, 16-year-old girl, vomit phobia
A small subset of parents described OST as a useful experience, but one that was ultimately disappointing in terms of the magnitude of effect that it conferred. Reflecting on the intervention, these parents indicated that that they might have entered therapy with high expectations that were not aligned with their child’s condition. Disenchantment largely, although not exclusively, clustered in parents of children with BII-type fears:
I just expected the result to be – that she’s over the phobia and she’d have a blood test or a needle any time. A bit presumptuous, really, and hoping and wishing, but that’s what I believed she would be like. And it clearly it wasn’t like that, ’cause even though she had the blood test, it took so much hard work from us and so much cooperation from the doctor, and for her to understand.
P20, parent/guardian, 12-year-old girl, needle phobia
One interviewee recounted a wholly negative experience of OST, reporting a marked decline in their child’s well-being post treatment. In this case, the parent’s treatment expectations appeared more measured, but a lack of demonstrable progress and the exacerbation of existing symptoms meant that disappointment nonetheless ensued:
The whole experience was not what I expected because I did expect to have a little improvement and it wasn’t it went totally the other way and that really shocked me, so I guess I was a bit shocked with the reaction.
P8, parent/guardian, 9-year-old boy, insect phobia
Variability in treatment outcomes precipitated a review of treatment suitability. Several parents questioned the universal applicability of OST, giving rise to a shared narrative that emphasised the importance of personalised care pathways and patient choice. The anxiety that children experienced between treatment allocation and onset was identified as one of the biggest challenges to intervention engagement by parents. Caregivers were consistent in articulating the optimal conditions for OST delivery, strongly emphasising a need to ensure that children were emotionally and cognitively ready for stimulus exposure:
If they’re already anxious about something, why would they want to put their self in that situation? You know, if someone’s scared of something, it takes some courage to go and actually face that fear and I think that’s what would probably stop most people. If they’re not gonna go there, it’s for that reason.
P12, parent/guardian, 10-year-old girl, needle phobia
I think they’ve got to be, in their own head, they’ve got to be ready. They’ve got to sort of think to themselves, ‘Right, I’m ready to do this now’. Because it’s them that has to do it at the end of the day. So, it’s – it’s pointless me saying ‘[child name] you’re doing this’. She has to do it for herself. So, I didn’t wanna push her into doing anything she didn’t want to do, it could have been too soon.
P3, parent/guardian, 15-year-old girl, dog phobia
Competing participant narratives considered whether chronological or developmental age should be used as an explicit criterion for participant referral. For some, chronological age was an acceptable marker of treatment capacity, but for others cognitive ability and individual needs took precedence:
I don’t imagine that we’d got, we would have got very far with a GP really when she was 7 or 8. Even if she’d had this therapy I don’t think she’d have been sort of really up for it, and now I’ve like, since she’s been about 9, like this last kind of year and a half, she’s really come on in a lot of, in a lot of ways just being able to cope with things.
P10, parent/guardian, 10-year-old girl, puppet phobia
Counter to a dominant discourse that emphasised the inherent efficiencies of OST, a minority of parents remained steadfast in believing that repeated treatment sessions were necessary to build an effective therapeutic alliance, expressing their preference for a more regular and intermittent approach. These parents typically cared for children with attention or information-processing deficits, acknowledging this as the primary reason why they felt that OST was unsuitable for their child:
I think it depends on the individual. For anybody with a phobia I think – it depends I suppose, on if the child’s got any additional needs or any other problems. They might find it too much in one 3-hour period. Might be a bit overwhelming.
P1, parent/guardian, 10-year-old boy, blood phobia
I do think the smaller sessions would have probably worked better for her overall. Like I say, just to build that confidence and you know, maybe like you know, just going into a room with a dog and you know, eventually like just like a slower approach I guess of all the different steps.
P14, parent/guardian, 7-year-old girl, dog phobia
The integration of multiple viewpoints nonetheless cautioned against adopting a fixed approach. Although one parent of a child with ADHD reported that they had found it difficult to sit for the duration of the OST session, another felt that it offered a more suitable format than CBT. For this reason, comorbidities were acknowledged to encompass a spectrum of need, with several parents emphasising the importance of clinicians and families working together to optimise treatment pathways and deliver child-centred care:
He was thrown in at the deep end to deal with such a lot for [child name]. But his sensory, his social, you know we understand [child name] and we understand his needs and these people OK, they’ve met him once before – to me I think you need to get to know the family and the child just a little bit more if you’re offering this session of what works for this child and this family. Because as you know autism is a massive spectrum and what works for one, might not work for the other.
P21, parent/guardian, 12-year-old boy, blood phobia
Summary of parents’ views
A tendency for parents to minimise and accommodate phobia commonly contributed to a delay in help-seeking, which has been reported elsewhere. 98 Phobias were often chronic and ingrained, and families sought help only when informal management became ineffective. Inadequate responses from health services contributed to symptom minimisation and limited treatment access. Historically, levels of service demand many not have equated to treatment need. Public health and education may have a role to play in facilitating access to timely, effective intervention.
Parents’ treatment goals aligned well with the remit and purpose of OST. Cautious perceptions of intervention efficacy at treatment referral may be ameliorated by enhancing parents’ understanding of the intervention and its underpinning evidence base.
Parents highlighted the critical role of clinicians’ competencies and rapport-building skills, as did CYP. Treatment planning and collaborative working were consistently highlighted as key components of OST in parents’ narratives. Enhanced follow-up and improved handover may benefit parents, facilitate home-based skills practice and contribute to the maintenance of treatment effects.
Parents perceived a range of treatment effects, highlighting a potentially important role for expectation management in treatment orientation. Patient choice in treatment mode should be retained, with an emphasis on shared decision-making at referral, aided by the provision of child suitability guidance. Reflections from parents highlighted some potential weakness in OST implementation. Intervention provision and coordination may benefit from greater standardisation and target-setting for treatment waiting times and communication.
Study 3: acceptability of one-session treatment to trial clinicians
The aim of the third study was to explore the acceptability of OST from the perspective of the clinicians delivering the intervention in the trial.
Representativeness of the sample
Seventy-seven clinicians were eligible to participate, of whom 16 expressed an interest and were subsequently interviewed. These individuals represented eight of the 13 sites that were open to recruit CYP to ASPECT. Table 28 summarises the characteristics of this sample. A comparison of 48 of the 77 practitioners who delivered interventions in ASPECT and disclosed their characteristics is provided.
| Characteristic | Clinician sample (%) | |
|---|---|---|
| Qualitative | Whole trial | |
| Years of experience delivering psychological interventions to children | ||
| ≤ 5 | 53 | 52 |
| 6–10 | 27 | 17 |
| 11–20 | 7 | 21 |
| ≥ 21 | 13 | 10 |
| Baseline treatment preference | ||
| Conventional CBT | 13 | 29.1 |
| OST | 60 | 35.4 |
| No preference | 27 | 35.4 |
Clinicians participating in the qualitative interviews held a variety of roles and worked in different services at different levels; the three most common roles of those who delivered OST in ASPECT (cognitive–behavioural therapist, CYP psychological well-being practitioner and CAMHS practitioner) were well represented in the qualitative study. The length of time spent delivering psychological interventions to CYP was also distributed similarly between the clinician sample in the acceptability study and the clinician sample in the trial.
Clinicians’ views
Clinicians’ views of one-session treatment at the outset of ASPECT
The qualitative analysis interpreted six themes from the data relating to clinicians’ views of OST at the outset of ASPECT. These themes explored (1) how OST aligned with professional roles, (2) clinicians’ perceptions of treatment demand, (3) clinicians’ motivations for trial participation, (4) the perceived effectiveness of OST, (5) perceptions of intervention feasibility and (6) the anticipated demand on OST practitioners.
Clinicians identified dichotomous drivers of their participation in ASPECT. For some, particularly those who routinely worked with CYP experiencing mild to moderate anxiety and depression, their professional role was the main motivator for intervention delivery. These individuals perceived OST to align readily with their existing skill set, viewing the intervention to be conceptually and logistically coherent with their current role:
[B]ecause the role of a children’s well-being practitioner does work with children that have mild to moderate anxiety or depression, I could see that being able to do one-session treatment as part of our skills set. Having one-session treatment there would be beneficial and that would fit in normally within our practices.
T1, psychological well-being practitioner, CAMHS
For others, participation had been determined predominantly by their capacity to absorb additional work. These individuals were typically clinicians within wider service remits, most notably clinical psychologists and psychiatrists, whose professional remit normally extended to more complex presentations. These individuals were consistent in perceiving OST as a research intervention, mismatched with their normal role.
Therapeutic orientation also appeared to influence the ease of fit between OST and individual practitioner roles. Many of the interviewed clinicians had worked with CBT models throughout their careers and highlighted clear synergies between their prior experience of these interventions and the delivery requirements of OST. This alignment was evident irrespective of whether or not CBT practitioners had treated specific phobias before, with parallels drawn between the strategies used by OST and the techniques used with other anxiety-related disorders:
Maybe about 65% of my caseload for intervention at any one time would be behavioural experiments for symptoms of social anxiety. And that is really, fundamentally is a phobia. It’s just not – you know, it’s just not really seen as one. So, it was kind of not really any different in as much as for symptoms of social anxiety we do use behavioural experiments where we would think about a situation somebody’s avoiding that’s maintaining their anxiety, like raising their hand in class, and elicit a cognition – the thing they’re thinking about happening.
T2, psychological well-being practitioner, university-based Improving Access to Psychological Therapies (IAPT) research clinic
A common narrative among clinicians was an apparent lack of demand for phobia-specific therapies. Prior to ASPECT, practitioners reported that referrals for phobias had been low, with few cases accepted by local services. Proactive practitioners had searched service caseloads at study commencement but yielded few exemplars. One clinician reported an average of only two phobia cases per year.
Cross-case comparison across the qualitative data set revealed some opacity in these views. Although some individuals perceived a lack of treatment demand, others presented a more nuanced view. Rather than being absent from service referrals, specific phobias were sometimes acknowledged to have been overlooked by teams whose remit and culture had evolved to address more complex diagnoses. In these instances, specific phobias were known to present alongside other difficulties, but were unlikely be identified as ‘core business’ or prioritised as a treatment goal for CYP:
So it was usually part of something that was going on so there’d be some family issue and that was, sometimes it wasn’t even touched. They would mention it at some point, and it wouldn’t even get touched upon. ’Cause the main presenting goal they wanted was erm something different to – to, to look at the relationship with their parents.
T3, senior counselling practitioner, third-sector/voluntary organisation based
Professional development emerged as the primary driver of trial participation among those interviewed. Clinicians who followed systemic practices were curious to see how OST might work, while those who routinely delivered CBT-based treatment expressed a desire to expand their existing skill set. Newly qualified practitioners reported that OST competencies integrated well with and complimented the core training that they had recently completed:
I think there was a little bit of trepidation initially. I think I was also – yeah I was quite excited to see how it would pan out. And I think I just thought, I think I just felt it’s going to be a really worthwhile challenge to take on really.
T4, psychiatrist, CAMHS
I guess at the time that I did the training for the one-session treatment, I just – I can’t remember exactly at what point it was. But, I was either in the middle of the training year or just finished it. So I was still kind of in the mode of learning new interventions for anxiety. So from that perspective, I was looking forward to having another, I guess, method of being able to do that.
T1, psychological well-being practitioner, CAMHS
Clinicians were largely complimentary about OST training, advocating that the management of a protracted treatment session demanded dedicated training provision beyond the acquisition of generic CBT-based skills. Sessions were upheld as a necessary and invaluable opportunity to educate therapists, strengthen OST buy-in, and address individual and team concerns. Some particularly enjoyed the practical examples nested within the training, and others felt that the training format and the range of resources offered to aid learning were comprehensive.
More rarely, clinicians expressed a need for additional training, suggesting that this should include the dissemination of example treatment plans and additional skills practice. Although some interviewees posited that training needs were likely to be individualised and offset by clinical experience, others advocated the utility of universal skill development and review:
I already felt quite confident with things like CBT and I’ve delivered in the past, so maybe didn’t feel like I needed lots of in-depth – and training. So it felt right, for me. Perhaps if I was at the beginning of my training or something like that, then I would’ve wanted a bit more.
T5, psychiatrist, CAMHS
I think training’s always really good as like – even if you are a skilled practitioner, I think to have somebody stand in a room and go through the protocol and you know it – it just sort of reminds you of – it’s an opportunity really to just think out loud and maybe some difficult cases. So I would say I probably could have done but actually it, it’s been better practice because of having the training.
T6, consultant clinical psychologist/core CAMHS clinical lead, CAMHS
One participant mentioned a substantial delay between training and treatment delivery, which challenged the retention of learning and negatively impacted their confidence to deliver OST. A broader, supporting discourse explored the value of ‘top-up’ training sessions, with some suggesting that knowledge refreshment would have helped them to maintain intervention fidelity and sustain enthusiasm as an OST treatment provider.
After completing their ASPECT training, most clinicians displayed a level of openness towards OST, drawing on a combination of evidence and tacit learning to enhance their confidence in its acceptability and effects. Irrespective of their professional role or baseline treatment preference, most hypothesised that OST would be effective for specific phobias, the main rationale being that there was a coherent link between theory and practice:
I think just looking at the intervention on a practical level I think it seems – yeah I suppose it feels like a common-sense approach. Yeah, I think I had confidence in it, in, certainly, alleviating some of the distress caused by the phobia.
T4, psychiatrist, CAMHS
I read one of the journal articles, one of the publications, and I thought ‘that sounds great’. And I had already heard about single session sort of treatments for adult phobias, sort of spider phobias and stuff like that, in a service I’d worked in before. And I’d heard that they can be really, really effective. And so I guess I may have – I may have come into it having, um, possibly having a belief that maybe sitting down and having the space and the opportunity to work up the hierarchy together, ensuring that a lot of the distractions in terms of seeking reassurance and things like that, that that could be quite carefully controlled. I had imagined that it might be more effective.
T2, psychological well-being practitioner, university-based IAPT research clinic
Despite this strong, communal enthusiasm for OST, several clinicians retained some core efficacy concerns. A common fear was that OST would enable CYP to overcome their anxiety in a supervised setting but that the intervention would ultimately lack transferability and sustainability in the real world. Some specifically questioned whether or not OST could offer sufficient support, suggesting that a single appointment might lack openings for generic psychoeducation and/or limit opportunities for CYP to consolidate their newly acquired skills:
It’s different to the traditional model of the kind of therapy that we provide which tends to be like weekly over a period of time, and in-between sessions that you’d expect there to be some kind of homework or more exposure work for the young person to carry out. Because I guess I worried that somebody might be able to overcome their anxiety in the room with me there with them, but then go out of the room and not be able to do that in in the wider world, really, when they got home.
T5, psychiatrist, CAMHS
I think with the CBT, um, we always tend to do an hour work psychoeducation and kind of mindfulness and teaching strategies and things. And it’s maybe a little bit broader. So, you’re teaching children sort of how their thinking impacts on their emotions and strategies and physical symptoms and the different ways and different ideas of managing that. And almost like a jigsaw, putting something together that works for them. So, specifically working on that phobia in one session – whether it would have the breadth and the longevity of impact that the CBT.
T7, school well-being worker, school based
Although a restricted number of treatment sessions was hypothesised to limit intervention scope, it was the qualitative aspects of OST delivery that participants posited to be more likely to emerge as important influences on treatment engagement and outcome.
Cognisant of the OST protocol, many clinicians reflected on the potential impact of a protracted session, often accepting this as a pragmatic method of increasing treatment access by reducing opportunity costs. OST was repeatedly presumed to require a shorter time commitment from CYP overall, with frequent conjecturing that this would reduce school absences alongside increasing children’s engagement with and motivation for treatment. For older CYP especially, the OST format was conceived to align well with patient expectations, offering a coherent, person-centred intervention that could deliver fast results. Single-session delivery was considered advantageous, in terms of both capitalising on early contact and avoiding external distractions, two core features that clinicians perceived might expedite and amplify treatment effects:
My excitement was in that kind of adolescent process there is a lot about, ‘I want it, I want it now’. I think if they can see a movement to get rid of it they – the kind of motivation for carrying on, if you can push enough forward, I think motivation for carrying on, because they want this contact with their friends, they want to be seen, they, you know, that kind of thing, egotistical kind of thing. That age range love quick, you know, they are into that quick change, ‘let’s move it and let’s move it fast, I’m you know I’m important’ all of those kinds of things I thought it would fit into. So I was excited even at the training stage.
T3, senior counselling practitioner, third-sector/voluntary organisation based
I thought it would be beneficial in, in terms of the saying ‘strike while the iron’s hot’. So if you’ve got a young person who is coming to the clinic ’cause they want to get over their phobia and they’re motivated actually sort of – I was thinking actually if you can use that motivation sort of whip up that motivation a bit more and then do that treatment in that one extended session then and keeping that energy going in the session, then my prediction was that that could be much more successful in terms of getting further up their hierarchy erm than if you did it over you know several months. And often over those several months something else can happen – so a family member might pass away or erm you’ve got exams come up or a holiday or illness or, and there’s all sorts of things that could come up.
T6, consultant clinical psychologist/core CAMHS clinical lead, CAMHS
Concern regarding the acceptability and feasibility of OST delivery was nonetheless strong. Evident in clinicians’ diffidence was an underlying concern that CYP would feel devalued and disenfranchised by the offer of one session, leading to a weaker therapeutic alliance and potential disengagement. Traditional notions of relationship-building and rapport seemed to be challenged by the OST model, with several clinicians expressing uncertainty as to whether or not sufficient trust could be established in a single session to ensure a meaningful outcome. A common pre-treatment belief was that shorter, more regular contact may be required to engage younger CYP and those living with neurodevelopmental disorders or dealing with mental health complexities or trauma:
I guess that was something I was –, I was maybe a bit unsure about. Because I suppose, when you’re doing the –, I suppose, when you’re delivering the low-intensity model over a number of weeks, you – you do get like more opportunity to build maybe rapport. Build a relationship which can, I feel, can have a lasting impact on you know, maintaining positive change. That kind of thing. So, I suppose in some respects, there was maybe a fear that that –, I think that – well an expectation that, therapeutic alliance might not be strong with OST.
T8, psychological well-being practitioner, CAMHS
I do have more anxieties about those young people who have got more comorbid presentations or some neurodevelopmental difficulties that actually, for those children, the children whose experienced significant trauma, who may really struggle to trust a therapist. That actually for those young people would it be as successful? And would – would you need more time for that engagement? Not necessarily the treatment session, but would you do more of an extended assessment to actually develop that young person’s trust in you as a therapist.
T5, consultant clinical psychologist/core CAMHS clinical lead, CAMHS
A core concern for clinicians was the amount of distress that OST would invoke in CYP and the high responsibility that they faced in managing these challenging emotions over time. The risk of overwhelming CYP in a single, uninterrupted treatment session was something that several clinicians admitted to feeling quite daunted by, owing to not only the potential effect that it could have on CYP, but also the effect it would have on them:
I think obviously you’re dealing with somebody who’s kind of very anxious and kind of you know it’s, it’s that kind of constantly trying to help them manage that and staying calm when it can be – you know quite distressing.
T9, clinical psychologist, CAMHS
Therefore, at treatment outset OST was often perceived as a potentially efficacious yet riskier model than traditional CBT. Single treatment appointments created the notion of a ‘one chance’ intervention and placed considerable weight on session planning and preparation. Clinicians contrasted this with the more intermittent approach of conventional CBT, which was perceived to offer greater opportunities to adjust and reflect on a treatment plan depending on how an individual responded. Some were unclear about how they would manage a stalled therapy appointment. Others were concerned about how easily families could access alternative provision should their own intervention prove unsuccessful. Individual narratives highlighted a lack of communally defined strategies for addressing poor treatment response or relapse:
There was just a bit of – I think a bit of misconception or a bit of confusion about the one-session treatment or CBT. The family were saying ‘What happens if the one-session treatment doesn’t work? What would happen then?’. The treatment is finished, so we would end treatment and be discharged.
T10, interpersonal therapist, CAMHS
Clinicians’ experiences of one-session treatment delivery
Three interpretative themes were derived from clinicians’ accounts of OST delivery. These themes explored (1) the work involved in delivering OST, (2) the value of parental involvement and (3) the logistical challenges encountered in intervention delivery.
A shared discourse among clinicians acknowledged OST delivery as tiring. The cognitive load experienced by OST facilitators appeared to be high, with multiple challenges inherent in managing both the emotional and the temporal elements of the session. The ability to plan and pace treatment in a manner that balanced assessment, engagement, psychoeducation and exposure was crucial. Multiple narratives upheld the early phases of therapeutic exposure as the main ‘bottleneck’ in intervention delivery: progressing too slowly risked wasting treatment time and limiting treatment effects. In this context, clinicians frequently noted that professional confidence was key. The critical importance of balancing power dynamics was articulated by multiple clinicians, who candidly acknowledged the effort that was required to integrate adult-led facilitation into a predominantly child-led treatment approach:
And I think it’s just that kind of been switched on constantly across that – you know that period and been really aware of do we need to alter the steps were making? You know we’ve kind of set this before but actually do we need to kind of make some smaller steps in between? So yeah I think it was – it was good but it definitely was. I remember been very tired afterwards.
T9, clinical psychologist, CAMHS
Clinicians often reported that their knowledge of a stimulus exerted an important procedural influence on the therapeutic outcomes. They frequently emphasised the need to prepare thoroughly before sessions, to acquire the expertise necessary to ensure that they could answer all of the CYP’s questions about a stimulus and to be able to model behaviour. Modelling behaviour was perceived to lend validity to the treatment and empower CYP to engage in exposure. In this context, practitioners emphasised the impact of their own self-efficacy and confidence on treatment efficacy; any doubt from the clinician was perceived to transfer to the CYP, which diluted the intervention potential:
I just think for the extended treatment session I think you just need to be super prepared beforehand and have everything there, everything ready and a real confidence in the approach as well. I think if you doubt it as a clinician that’s going to really come across to the young person or the parent. And children are you know – they’ve got these little antenna’s that they do pick up on any doubt in you as a therapist. Part of that was about ‘fake it ’til you make it’ belief in the model. You’ve really got to believe that this works and it and it does work.
T6, consultant clinical psychologist/core CAMHS clinical lead, CAMHS
A dominant narrative emphasised the value of establishing a strong therapeutic alliance, enriching the treatment experience with humour and enthusiasm. The importance of engaging and collaborating with CYP as equals was underscored in both intervention planning and delivery. Validating and normalising CYP’s feelings were perceived as crucial aspects of the clinician’s early role, eclipsed only by the importance of reviewing progress to ensure the sustainability of effects at the end of treatment:
To give them some validation and say how well they’d done to recognise you know – that they had a problem and they’d come and sorted it out. And we’ve come up with a plan and a way which to sort to manage that and then we can reflect back and see you know – those positive outcomes and actually you know. For someone at such a young age it’s a really valuable lesson or any problems they can come back in the future, with them and I think that’s a really, I think that’s a really nice message to give children, children of that, of that age really.
T4, psychiatrist, CAMHS
Views were mixed regarding the inclusion of parents, with a tendency for clinicians trained in systemic therapies to view parental involvement as more important than those who took a purist approach. Those who reflected on parental presence as a positive experience acknowledged that it was often helpful during the preparation and goal-setting phases of OST, particularly when working with younger CYP or those with whom they were still establishing rapport:
They can explain or clarify or you know – whereas you wouldn’t challenge a child that you didn’t know. Whereas the parent can say ‘Yeah, but remember the time that you . . .’, I don’t know ‘. . . were near a dog’ or whatever. They can come from a place where they know the child, or they can maybe challenge or offer additional information, which is really helpful.
T7, school well-being worker, school based
For younger CYP, parental presence was viewed as beneficial during OST to help the child to feel comfortable and maximise the continuity and magnitude of exposure. During treatment, parental involvement was optimised by ensuring that their role was clearly defined and that they were able to engage with and model positive behaviours with stimuli. Parental presence enabled clinicians to support caregivers in managing CYP’s anxiety and avoidance behaviours, a process that many clinicians perceived as fundamental to the facilitation of skills practice post intervention and the maintenance of therapeutic gains:
I’ve kind of said to Mum ‘She needs to keep practicing. You need to repeat it with another dog’ but because Mum wasn’t there, I had to almost explain all the stages and how we did it and everything to her. But Mum wasn’t able to for whatever reason. So, the gain or the progress wasn’t maintained.
T7, school well-being worker, school based
Therapists tended to be more supportive of therapeutic independence for older CYP, reflecting that caregiver absence provided greater opportunities for young people to develop their own self-management skills. This was considered particularly important in instances where caregiver anxiety was high or where parental involvement supported a safety behaviour. Although parental involvement often contributed a layer of complexity to treatment management, clinicians acknowledged that it was sometimes helpful to see how and where phobic behaviours had been maintained. Parental presence offered therapists an opportunity to strengthen parents’ understanding and appreciation of a child’s or young person’s perspective. It facilitated education at the family level, encouraging parents to identify moments of unintentional collusion or reflect on the emotional language that they used:
I did just mention you know about the some of the comments were a bit – I felt were a bit unhelpful. But mums sort of narrative about the initial incident where you know you could argue that the phobia began from and that kind of thing. But some of that narrative could do with sort of changing a little bit and we did have some conversations about that.
T11, clinical psychologist, CAMHS
Clinicians reflected on the logistical issues that arose when delivering OST, particularly the suitability of the treatment setting. For those whose role it was to support CYP across a large geographical area, the importance of families being able to access treatment at a central location was paramount. Travel burden for practitioners was also acknowledged:
I mean if a client didn’t have transport via a parent that might have been a bit of an issue. Just from our service in terms of me then having to put you know more business use on my car insurance and stuff like that to have etc. But clients that I had, their parents had transport, so we were just arranging to meet at a location and that just simplified it.
T12, primary care mental health worker, CAMHS
School-based professionals positively evaluated their experiences of meeting CYP in school settings, accepting that this offered a unique opportunity to reduce accessibility barriers and opportunity costs. A more dominant discourse, however, underscored the importance of having a neutral therapeutic space. OST was often posited to be more difficult than traditional CBT to deliver in an educational setting owing to challenges inherent in managing CYP’s distress and maintaining confidentiality over a protracted period of time. A minority of clinicians cautioned against school delivery, believing that this carried the risk of CYP establishing an association between a phobia and the classroom environment:
[We] don’t often have a therapeutic space. Some schools can provide that, but not all schools. So yeah I guess there was that kind of, if this all goes wrong, and this child’s really distressed, and we’re in the middle of a school and the parents are not around, and all them other things. I suppose there was a little bit of anxiety around how do we best manage that.
T13, school well-being worker, school based
Similar logistical challenges emerged in health-care settings. Therapists who were based in CAMHS settings reported constraints in securing therapeutic space, often highlighting a discrepancy between the 3-hour appointment times required for OST and the hourly room booking templates utilised by local administrative systems. Animal phobias were perceived as particularly difficult to accommodate, with additional permissions and space required to host live stimuli. Some clinicians highlighted practical challenges in ring fencing 3 hours of clinical time to facilitate OST and in securing the same dedication from third parties (e.g. dog handlers and community nurses), who were periodically needed to assist with exposure:
Other things that I found were, that make it more tricky, was dog phobia. OK sort of good to use a variation of dogs, it is, so say for example if you’ve got – if you’re using up to three dogs per 3-hour ASPECT session it, it worked wonderfully. But, where do you store the dogs? So what, what I’d – was fortunate enough to do was I was working on a Saturday when I did the OST for the dog phobias and I was fortunate enough to use different rooms within the CAMHS vicinity. So one room would have one dog in, another room would have another. Sort of which is how I got round but, in some services that might not be practical.
T8, psychological well-being practitioner, CAMHS
A shared narrative highlighted that a breadth of difficulties were encountered in obtaining and organising meaningful stimuli, with personalised treatment goals often necessitating substantial time investment to ensure that clinicians had sourced sufficient and appropriate resources. This time investment often compromised other elements of practice and was posited to be much longer and less manageable than traditional treatment preparation:
I found the, the intervention to be – I’ve enjoyed the sort of watching the progress of it. But I must admit I found the process of it to be quite stressful. Having to sort of juggle and arrange to get everything all into one place at one time. And that was probably one of the most sort of stressful parts of it. Whereas the CBT version of it was – although it was stressful getting the sort of the, the objects, it wasn’t working to a timetable in the exact same way.
T14, high-intensity CBT practitioner, CAMHS
Clinicians typically identified a service initiation phase during which the challenges of sourcing materials were amplified. Gradually, some clinicians established links with external providers and began to develop their own resources to draw on as they moved forward. Personal workarounds were common, but these relied heavily on the creativity of the individual or on proactive input from the ASPECT team. Therapists described a relatively high level of study support, encompassing both the provision of information and the physical and financial acquisition of treatment resources:
So, you know, there was some preparation, but it wasn’t impossible. But I think – I think just those initial ones, it sometimes took time to do that, you know. I think I put together a PowerPoint® [Microsoft Corporation, Redmond, WA, USA] and it was videos and recording and things. But had we kept doing that – I think it’s like anything. It’s when you start, or when you initially do something, you put more resource and time and energy into it. But had you kept doing it, you would just repeat.
T7, school well-being practitioner, school based
I found it really helpful like whenever I sort of e-mailed people to for resources of things like everybody sort of got back to me really quickly and gave me the things, or guided me to different resources, or passed different resources on to me. So that were all yeah kind of really, felt really supportive really.
T11, clinical psychologist, CAMHS
Post-treatment reflections
The qualitative analysis interpreted six themes from the clinician’s post-treatment reflections. These themes centred on (1) clinicians’ perceptions of treatment outcomes, (2) case suitability, (3) the impact of phobia type, (4) reflections on session format and length, (5) possible protocol adaptions and (6) OST sustainability.
Clinician’s post-treatment reflections were largely positive. Overall, therapists reported that they had enjoyed participating and for many the opportunity to observe CYP’s progress had been rewarding. OST was perceived to have both primary and secondary effects, with improvements in phobia reported alongside benefits to children’s family life, educational engagement and self-confidence. Clinical ‘spill over’ effects were also reported, with several clinicians reporting observable improvements in children’s comorbid presentations:
Not only has the treatment cured [child name]’s phobia – in inverted commas – but I believe it is largely responsible for [child name]’s overall improvement in his general confidence. He’s had a great year in school so far and he’s starting to shine, both teachers and family have commented on how much happier he seems.
T2, psychological well-being practitioner, university-based IAPT research clinic
Variability in clinician-reported effects was nonetheless apparent. In some cases, clinicians were surprised at how much progress had been made in one session, whereas others had been left disheartened. Drawing on this learning, some suggested that OST was the most effective for mild to moderate phobias. Others, however, took a more nuanced view. Expectation management emerged as a strong interpretative theme, with several advocating that the value of OST should be quantified through its capacity to deliver functional improvements rather than a clinical cure. In this context, OST was perceived to retain applicability across the severity spectrum, with clinicians assuming primary responsibility for the tailoring of meaningful and manageable goals:
Because there was another young person I saw that – actually didn’t even progress beyond the assessment appointment. It was kind of really severe – an impairing phobia. But it was never going to be realistic for that to have been cured in one session. But actually we could perhaps have set a, you know, a different goal that would’ve meant that the phobia was still around but more manageable.
T5, psychiatrist, CAMHS
Akin to CYP and parents, clinicians highlighted the need to consider an individual’s suitability for OST at referral based on an informal assessment of their treatment motivation, case complexity and needs. Consensus was that CYP needed to display sufficient intrinsic motivation to engage in the exposure work, although the potential impact of external motivators was also acknowledged. Where there was a time-sensitive reason for a child or young person to seek help (e.g. an upcoming school event or public health initiative), clinicians asserted that OST would most likely be preferable and advantageous for the child:
I think if there was – so say for example if we was against the clock like the patient was scared of needles but about to have an operation then in that sort of case then I would sort of strongly suggest they go down an OST-type route.
T14, high-intensity CBT practitioner, CAMHS
Having delivered OST, clinicians had no strong opinions regarding an optimal age range for treatment. Some retained their pre-treatment beliefs, suggesting that the length and intensity of treatment sessions could potentially challenge concentration in younger CYP and artificially limit its results. More frequently, however, clinicians reflected on the cognitive and behavioural demands of the intervention, confirming that the success of OST relied heavily on CYP’s capacity to concentrate and process information:
[O]bviously if we’re offering a one-session treatment, and you’ve got a spontaneous child with a lack of concentration, or a poor concentration span should I say, then actually it’s just going to make things a little harder.
T15, CBT practitioner/safe care lead, CAMHS
Contradictory to their expectations, clinicians had varied opinions on whether or not OST was suitable for CYP with additional needs. The impact of neurodevelopmental disorders in particular was difficult to predict. Cognitive rigidity, a defining characteristic of ASD, was conceived as both a driver of goal achievement during exposure and a potential barrier to therapeutic rapport. A shared narrative highlighted the need for additional preparatory time to be allocated to CYP living with these disorders, but the notion that neurodevelopmental criteria should dictate treatment access was largely rejected in favour of providing additional service support:
I suppose thinking about what – the scaffolding around them and actually whether there is something that can be done to sort of allow that person to engage with the support. I think if there’s that scaffolding, then I think either would be OK to do.
T8, psychological well-being practitioner, CAMHS
A dominant theme within the data set was the extent to which OST aligned with different phobia types. Clinicians revealed a level of uncertainty regarding the suitability of OST for BII- and vomit-induced fear. Key difficulties in these cases included both the practical challenges of coordinating exposure and the challenges inherent in replicating the physiological sensations or contextual influences necessary to trigger a fear response:
I guess with the needle phobia it’s a little bit different because although yes you can introduce them to the needles and have a little fake ‘ow’ etc., and some of that, . . . that just a little bit different [mm] to actually going into hospital and having that done so I think, yes, if you view all cases, apart from the needle therapy ones, I think, yeah, you’re satisfied that you’ve changed that [mm] and made a big difference just not quite as sure with the needle phobias really.
T4, psychiatrist, CAMHS
Multiple exposure sessions were considered more suitable for organising stimuli encounters across multiple settings and for securing timely access to BII- and vomit-related treatments. Clinicians reported that external permissions were often required to secure the commitment of allied health professionals, some of whom struggled to commit to a 3-hour therapy appointment in lieu of their own caseload. Exposure sessions were difficult to predict and collegial relationships were put at risk when OST appointments did not progress as planned:
I think in this case it was sort of having to locate and get a fake arm because I was doing needlestick phobia. Getting another member of staff who was a phlebotomist come in the session with me, so it was all these types of things that would in some ways it would make it a bit more tricky.
T14, high-intensity CBT practitioner, CAMHS
Repeat therapy appointments were advocated for both phobia types to address any delayed anxiety triggered by exposure to a potentially infectious stimulus. Clinicians accepted that the OST model did not offer this opportunity, noting that this posed a risk to CYP in the days following the treatment:
She was still really anxious after the OST ’cause she was waiting to get sick. So it was about how do you target that in a fear hierarchy in an OST? ’Cause it was you know – she didn’t have any rules about when it would happen. It was just she didn’t sleep for like a night and a day or something because she was so worried that she was going to get sick from it.
T1, psychological well-being practitioner, CAMHS
At study outset, many clinicians conceptualised OST as a ‘one chance’ intervention that placed considerable burden on a practitioner to achieve a positive outcome. Having delivered OST as part of ASPECT, several practitioners reflected on this concept, often reframing and refining their initial views.
A strong narrative within the data set revealed that, although it was perhaps logistically easier to implement conventional CBT, a single longer session of treatment arguably made more sense to clinicians from a theoretical point of view. Therapists largely felt that the therapeutic process of OST was clear and easy for families to understand. Most confirmed that the OST format was likely to maximise treatment engagement and outcome by removing educational attendance barriers, lessening pre-session fears and removing external distractions or treatment withdrawal temptations. Single-session delivery was also perceived to precipitate more efficient use of therapist and patient time, removing the need for between-session reviews and minimising the opportunities for the maintenance of safety behaviours:
I think it’s obviously more straightforward to just do treatment as usual, because it’s a similar setup to eight sessions for treatment of depression would be . . . but clinically, I just don’t feel as though, in the context of a phobia and exposure sort of stuff, I just don’t feel as though the week’s break is helpful. There could be you know – homework tasks in between sessional work stuff, but it’s very hard to know whether or not there were any maintaining behaviours going on, or any safety behaviours. And it’s, yeah – so I definitely think that, clinically, it’s a better fit to do the single-session treatment.
T2, psychological well-being practitioner, university-based IAPT research clinic
Some clinicians who had been concerned about session length at study outset described how treatment had progressed more quickly than they had expected, with CYP often capitalising on early success to progress further than they anticipated. Rather than being the inflexible treatment method that many clinicians had envisaged, OST was typically reframed as an adaptable model, with the additional time afforded by a longer session allowing CYP greater opportunities to move up and down their fear hierarchy in one continuous session. Thus, OST was perceived to enable more ‘side-stepping’ opportunities than conventional CBT, allowing CYP to repeat previous steps or vary them without losing treatment momentum:
The ability kind of in the moment to sort of move up and down that felt fitting for a young person you know. So you had the ability to do that, so you had that momentum you know whereby you could kind of move forward but equally you can kind of drop back in the moment if you felt that you needed to. Whereas of course in your separate sessions, you can do that but not in the same way that a one-session treatment allows.
T16, psychological well-being practitioner, CAMHS
Clinicians’ concerns regarding the constraints of the one session approach were most likely to be retained in instances where CYP had been unable to attain their treatment goals. Here, OST was at best considered a primer for further intervention and at worst a potentially disengaging experience for those who were left disappointed. A subset of clinicians supported protocol violations for more complex cases, having taken the personal decision to extend the intervention in these instances to ensure that treatment could be completed:
Kind of like what I was saying before, if there is complexities having that – that almost wiggle room to say actually we can do more.
T14, high-intensity CBT practitioner, CAMHS
Clinicians identified several amendments to OST procedures that they had implemented locally. Some had reconfigured assessment proformas to make them more individualised, while others had developed additional homework sheets and resources to support CYP post treatment. Occasionally, photographs and videos were used to document progress and disseminated to families to aid skills practice and maintenance. Larger adaptations were also evident. In some areas, therapists had set up supervision groups to assist with session-planning and case reflection.
Suggestions for future delivery enhancements clustered around three themes: (1) the allocation of dedicated time for psychoeducation and anxiety management during treatment, (2) a corresponding division within the planning session to accommodate this, and (3) follow-up sessions to review progress, promote skills consolidation and support relapse prevention. The first of these requires careful consideration given that relaxation and anxiety management are not part of OST as defined. The latter addition was specifically recommended to improve both the CYP’s and the clinician’s experiences of treatment end:
Erm I think we would find out how things have gone [hmm] erm and if things have maybe sort of regressed a bit [Yeah]. Then encourage them to think about what they need to do in order to build up again and overcome things. So I’d use it as a, as a way of being able to recap on the learning [hmm] that they did in the OST and the previous, in the appointment before that.
T8, psychological well-being practitioner, CAMHS
I think it would be having a chat with them seeing if there was anything that they needed to consolidate. Would there be – you know would they want to kind of be in that situation again and just practice. Would it just be a case of having a walk and seeing if we could encounter some kind of challenges and how they’d manage. But I suppose it would be very much what, what the value would be for that person really.
T9, clinical psychologist, CAMHS
Clinicians reported that their competence in completing exposure work had increased and that they felt confident in being able to complete similar work in the future. Delivering OST appeared to precipitate a range of professional effects, including increased understanding of phobia-specific therapies, the proliferation and enhancement of CBT skills within a team and an increased awareness and enthusiasm for early intervention in this population:
I think it’s given me another string to my bow really in terms of being able to sort of deliver specific phobia treatment. It’s a really encouraging confidence building thing when it comes to people managing anxiety in different ways. It’s a good way of demonstrating it. I also think it’s really improved my competence in terms of actually working with people to do like the exposure work as well. I think it’s really helped.
T8, children’s well-being practitioner, CAMHS
The notion that childhood phobias fell on or outside the periphery of CYP’s mental health services was a malleable one. A direct but unintended consequence of ASPECT was that services were prompted to recognise and address this deficit in care. Involvement in the research appeared to increase practitioners’ appreciation of the depth of impairment induced by specific phobias and in some instances instigated a service-level shift in referral acceptance rates. Attitudinal changes among staff were advocated to dispel tacit barriers to treatment access and promote local care pathways and behaviour change:
. . . it’s increased the services awareness and I think the difficulty for our service before, ’cause we’re a specialist CAMHS service, it was the belief that we didn’t treat phobias. So – but we do actually have a clinical pathway for phobias and we should be treating phobias, so what was great about the trial was that it raised – we have six community CAMHS teams and it raised their awareness that actually we should be accepting referrals for phobias. Yeah so it’s been great for our service in that regard that we’ve probably been accepting more phobias that have come through as a consequence of raising people’s awareness of the clinical pathway.
T6, consultant clinical psychologist/core CAMHS clinical lead, CAMHS
Clinician’s views on whether or not they themselves would continue to use OST in practice were mixed. For some, particularly those who were used to working systematically, CBT continued to be the treatment of choice. This decision was largely based on individuals’ perceptions that OST offered fewer opportunities to build a strong therapeutic alliance and client rapport:
I think I would continue to deliver the CBT one, but I don’t think I would continue with the one-session one as it is now. If it was more relationship led if you like and person centred in that way then I would probably be happier to do it. But that was the missing part for me, and I think that really, makes a huge difference in any therapeutic piece of work and relationship.
T13, school well-being practitioner, school based
Several organisational barriers to routine OST provision were identified. Clinicians reported that clinical and administrative procedures needed strengthening to ensure that phobia cases could be adequately tracked in referral systems. A dedicated, streamlined pathway for phobia treatment and resource allocation was perceived as essential to implementation success. Local service-level input was requested to ensure that adequate training, supervision and service support systems were established. Cross-pathway staffing was viewed as advantageous to promote team cohesion, enhance peer-to-peer learning and optimise team morale:
And actually the benefit that that then had for those practitioners who’ve then seen young people with say a simple phobia and they’ve got better, it’s boosted their motivation. So I think what it’s – what it’s now given us is something that we can go back to the managers and say actually this is you know, on lots of different levels, there’s a real incentive for actually having some presentation be seen much quicker. Even if there are only mild to moderate, it actually has a benefit for those clinicians in terms of their motivation and feeling like skilled therapists.
T6, consultant clinical psychologist/core CAMHS clinical lead, CAMHS
Summary of clinicians’ views
Overall, clinicians displayed a level of openness towards OST, accepting that it could reduce opportunity costs and increase treatment motivation and engagement for some CYP. The potential cognitive and emotional burden of treatment participation was acknowledged, as was the emotional and logistical demand that OST placed on therapists. Dedicated training for OST was upheld as important irrespective of professional role and experience. Some gaps in clinician’s understanding and preparation for OST delivery were evident; additional avenues for training expansion and tailoring are recommended.
Clinicians’ confidence in exposure treatment and their capacity to establish therapeutic rapport were perceived as critical process variables influencing treatment experience and success. Dual competencies in collaborative, child-centred working and effective time management were important. Clinicians displayed a level of openness towards third-party involvement in exposure therapy, although the greatest benefit of caregiver involvement was perceived to occur at OST assessment and treatment end.
Clinicians perceived OST to have utility in treating specific childhood phobias, although a diverse range of outcomes was acknowledged. Phobia type was perceived to impact on intervention feasibility and effects, with greater operational challenges present in vomit and BII phobias than other diagnostic categories. CYP readiness and developmental stage were also identified as potential influences on treatment suitability. Clinicians tended to support the development of intervention suitability guidance rather than the introduction of mandated eligibility criteria. The provision of additional treatment support may enhance OST accessibility.
One-session treatment implementation presented some organisational challenges. Greater resourcing and alignment with service administrative systems would probably support OST delivery in routine practice. Recognition and validation of the substantial time that clinicians spend preparing for OST would be advantageous.
Chapter 5 Discussion
Parts of this chapter have been reproduced from Wright et al. 1 © 2022 The Authors. Journal of Child Psychology and Psychiatry published by John Wiley & Sons Ltd on behalf of Association for Child and Adolescent Mental Health. This is an open access article under the terms of the Creative Commons Attribution License, which permits use, distribution and reproduction in any medium, provided the original work is properly cited. The text below includes minor additions and formatting changes to the original text.
Parts of this chapter have been reproduced from Hayward et al. 42 © 2022 Hayward et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. The text below includes minor additions and formatting changes to the original text.
Parts of this chapter have been reproduced from Wang et al. 2 Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data. The text below includes minor additions and formatting changes to the original text.
Summary of the main findings
Primary outcome
ASPECT sought to examine the non-inferiority of OST compared with routinely used CBT-based interventions for treating specific phobias in CYP in a multicentre study across England. The primary outcome measure was the BAT score at the 6-month follow-up, with a series of secondary measures completed alongside by both CYP and parents. The results demonstrated that using prospectively set non-inferiority limit OST is shown to be non-inferior in clinical effectiveness to multisession CBT. Where multiple imputation is used for missing values, this finding also applies. This signal pertains whether ITT or PP analysis is used. At the main outcome point, using the diagnostic measure (the ADIS), 27% of CYP are ‘no longer phobic’ using ITT analysis (same for OST and CBT) and 33% of CYP are ‘no longer phobic’ using PP analysis (34% in the OST group and 32% in the CBT group). In a review of the BAT outcome measure used with young people who have specific phobias, Castagna et al. 40 suggested that an average of 60% step completion (6 out of 10 steps) post treatment is an ‘expected’ outcome when reviewing multiple studies and, therefore, our finding of over 70% means that step completion in both treatment groups post treatment shows similar or slightly better treatment success rates in this patient group. These findings were similar to those reported by Ollendick et al. ,33 who found that those in the OST group achieved around 73% of BAT steps at the 6-month follow-up.
Secondary outcomes
Several secondary objectives were made a priori and were investigated by including an embedded health economic evaluation and qualitative interviews conducted with CYP, parents and clinicians. This work sought to examine:
-
Corroboration for the primary outcome.
All of the secondary outcome measures showed no differences between the two treatment groups. In particular, the other anxiety measures, including SUDS change scores, CAIS, goal-based outcome measures and RCADS anxiety scores, gave similar signals to the main outcome measure.
When sensitivity analyses were examined, vomit phobia was the only phobia found to respond better to OST than multisession CBT, although subgroup numbers would have been too small to explore this definitively.
-
The cost-effectiveness of OST compared with CBT and the relative impact of the interventions on CYP’s QoL, and school and social life.
Compared with CBT, OST marginally decreased the mean service use costs while maintaining similar QALY improvement. Compared with baseline, it was observed that both treatments decreased the resource use over time, but the cost difference (in either NHS/PSS or societal perspectives) between the two treatment groups at the 6-month follow-up was marginal. The cost differences were driven by higher treatment costs and CAMHS-related service costs in the CBT group. The higher average cost of CBT was caused by the low unit cost but high-frequency sessions involved, whereas the higher CAMHS costs are likely to have been caused by a few high (but plausible) values (see Chapter 4, Service use and costs). The cost saving of OST within the 6-month time frame is expected to have been larger if CYP in the CBT group did not pause or delay their sessions as a result of the COVID-19 pandemic. A similar trend was also observed in the QALY outcomes. Although both the EQ-5D-Y and the CHU-9D utilities showed improvements over time in both treatment groups, the difference in QALY improvements between the two treatment groups was negligible. After adjusting for the imbalanced utility and other characteristics at baseline, the increase in QALYs remains small (0.002 QALYs). Both our primary and our sensitivity analyses suggest that OST is likely to save cost and maintain similar QALYs as CBT.
The results of the health economic analysis demonstrated that, compared with CYP receiving CBT, on average, there is a £200–300 saving per person receiving OST. This is relatively small, but may be relevant for commissioners when considering resource utilisation if multiplied by the number of CYP with specific phobias in the UK.
-
-
The acceptability of OST from the perspectives of CYP, parents/guardians and clinicians.
The qualitative results show that the acceptability of and satisfaction with OST from the perspectives of CYP, parents/guardians and clinicians was good. When considering a range of acceptability parameters for OST, the core components that were consistently identified to influence treatment process and satisfaction were child readiness, therapist competency and collaboration. The main clinical challenges found in the study related to the flow of CYP through a complex health system, with many clinicians reporting that phobia was not deemed ‘core business’ by their managers. Implementation issues were also raised by clinicians, with emphasis on ensuring that adequate resources, time allocation, training and administrative support were in place to enable OST delivery, especially if rolling it out as a new therapeutic offering. It was felt that enhanced follow-up and improved handover may benefit parents, facilitate home-based skills practice and contribute to the maintenance of treatment effects.
Strengths and weaknesses
Strengths and weaknesses of the main trial
Strengths
Study aim and recruitment success
To the best of our knowledge, ASPECT was the first RCT to compare the clinical effectiveness and cost-effectiveness of OST with that of usual care (CBT) for CYP with specific phobias in England. It has been recommended that work be conducted to compare OST with multisession CBT in adults,99 which demonstrates the lack of evidence in the area and further justifies the importance of ASPECT. Although there were many difficulties in identifying CYP for study entry (as documented in Chapter 3), a sufficient number of CYP and their parent/guardians were recruited overall, demonstrating that it is possible to recruit to a study of this nature.
Widespread delivery of phobia treatments
Throughout the set-up and running of ASPECT, and as documented in more detail in Chapter 3, it became apparent that there was much variability in the services available for CYP with specific phobias across England. Although phobia treatments appear to be routinely delivered in some areas, other areas maintain high thresholds for service entry or do not offer such treatments at all. Through the completion of ASPECT, the importance of providing phobia treatments to CYP was widely disseminated to services across England. For this reason, many services started to identify and treat individuals with specific phobias who would otherwise have gone unnoticed. Furthermore, providing training to school-based services broadened the services available to CYP within this context.
Although ASPECT has now ended, it is hoped that a focus on delivering therapies for specific phobias will remain. As a result of the trial, approximately 170 clinicians have now received training in OST, which can continue to be delivered across services, as deemed appropriate. Anecdotal evidence from some of the participating services revealed that, despite not providing phobia treatment prior to ASPECT, provision of therapies for specific phobias is now being explored and expanded within services to ensure that treatment can be offered to CYP presenting with phobias. This was also evident in the findings obtained during the qualitative interviews with clinicians (see Chapter 4, Post-treatment reflections).
Pragmatic trial
Unlike other previous studies conducted in research settings,33,34,37,100 ASPECT was a pragmatic trial that allowed the effectiveness of OST and CBT to be compared in real-world usual clinical settings. Embedding the study in clinical teams was achieved without teams having to change their routine practice. This allowed us to compare OST against the usual delivery of CBT, which ensured a high level of ecological validity. Services using CBT were all following the usual practices of building a fear hierarchy, exposure and cognitive restructuring. Some services requested further information to ensure that their clinicians had clear guidelines and, for this reason, a CBT-as-usual guide was produced, which was co-written by several of the study principal investigators (BW and LG, 2018, personal communication) and used throughout the study.
Large number of UK centres
As discussed in Chapter 2, recruitment to ASPECT took place in the routine care pathways for phobia in CYP. This included 12 NHS trusts comprising 26 CAMHS sites, three third-sector/voluntary services and one university-based CYP well-being service in England. Recruiting from a diverse range of services allowed us to treat CYP in a variety of settings and positions in the care pathway.
Full range of phobia types included, unlike other studies
The design of ASPECT allowed CYP with a variety of phobias to take part in the research, with few exclusions. Providing that a child or young person could be in proximity with their phobic stimulus safely (either in reality or in simulation), they were able to enter the trial. As a result, across the sample, numerous phobias were identified that aligned to all of the subtypes described in the DSM-V criteria. All clinically presenting phobias were included, unlike some studies33 in which BII-type phobias were excluded.
Methodological strengths
ASPECT employed a number of methodological mechanisms to reduce bias. These included remote randomisation, blinding of researchers gathering outcome measures at all points, prospectively planned protocol and statistical analysis plans, and oversight of all procedures from both an independent TSC and a DMEC. The inclusion of the BAT alongside self-reported questionnaires allowed for a comprehensive and objective measure of phobia in CYP. We also measured treatment fidelity using both clinician reports and expert ratings of taped therapy sessions.
Weaknesses and challenges
Several challenges presented themselves to the study team and some weaknesses were apparent that affected both trial delivery and the overall results reported.
COVID-19
Most notable was the impact of the COVID-19 pandemic, which began in early 2020 and led to school closures, reduced service availability and changes to service delivery (e.g. from face to face to online). As documented in more detail in Chapter 3, several amendments were submitted to mitigate the impact of COVID-19 on this research trial, including remote data collection and remote therapy delivery where possible. However, despite these measures, the timing of the pandemic meant that recruitment to ASPECT remained unaffected, but therapy delivery for some CYP and the completion of the 6-month follow-up assessments were significantly impacted. Although only 4.5% (n = 3) of participants who withdrew from the trial cited COVID-19 as the reason, 37% (n = 98) of CYP completed their 6-month follow-up assessments having received no or incomplete treatment, some as a result of COVID-19 delays. Our estimates also suggest that approximately 17% (n = 7) of those in the OST group did not receive any treatment as a result of the pandemic, as well as 14% in the CBT group who received only one to three CBT sessions and 8% (n = 3) who received no sessions. Furthermore, measuring the primary outcome (the BAT) was not possible during periods in which social distancing restrictions and guidelines were in place because they prevented face-to-face contact with a researcher and/or exposure to a feared stimulus. This resulted in 48 (24.4%) CYP not completing this measure at follow-up (21.6% randomised to CBT and 27% randomised to OST). COVID-19 also may have affected treatment, such as continuing exposure work at home, because closing schools and reduced access to outside spaces may have reduced these opportunities.
Study withdrawals
In general, a large number of CYP withdraw from mental health treatment, with one meta-analysis reporting rates of between 25% and 75%. 29 In our study, 31% of participants in the OST group and 27% of participants in the CBT group had received no treatment sessions by the 6-month follow-up point, which are both at the lower end of the figures reported by de Haan et al. ’s29 review.
Large numbers of children in our study were withdrawn from phobia treatment by clinicians, which prompted us to look closely at reasons for this. First, inherent to phobia is an element of avoidance to the feared stimulus; however, treatment requires a child or young person to undergo exposure. This creates problems in two scenarios: first, where a parent/guardian is the motivation behind the treatment and the CYP is not motivated to engage, and, second, where the CYP is motivated but unable to overcome their fear to attend for treatment.
Given the pragmatic nature of ASPECT and its delivery in the real world, we expected some withdrawal of children by clinicians. Some of this was in response to the clinician not deeming the timing of the intervention to be right for the CYP (e.g. where a child had just entered foster care and was settling in). Similarly, at times, clinicians deemed that a child or young person with comorbidities needed assessment or treatment for a different condition before receiving phobia treatment (n = 4). This included young people with generalised anxiety disorder, post-traumatic stress disorder, generalised health anxiety and ASD. In some cases, the clinician believed that a more complex intervention was needed (n = 3), with two involving referrals to other trusts.
In two situations occurring in different sites, the clinician felt that the phobia was so severe that it would not be possible to treat it adequately using OST and, as a result, a child or young person who was allocated to OST received CBT as usual instead. Given that the clinicians had autonomy and were making decisions based on the best interests of the CYP, this made it important to consider the ITT analysis and the PP analysis together. This could be because some clinicians in a pragmatic trial involving large numbers of clinicians may not be in equipoise or because the child’s presentation may have changed. Indeed we had some instances in which the CYP had increased child mental health needs that had escalated since the initial assessment, perhaps related to long waiting times. One child or young person was referred to forensic CAMHS while they were on the phobia treatment waiting list. In another instance (not related to the phobia), a child or young person was admitted to hospital following a medication overdose.
Overall, 15 CYP had received a diagnosis for ASD or were currently awaiting an assessment (n = 4). Although we were able to treat those with ASD for phobia successfully, one of the clinicians described that the sensory fears of a young person with ASD were more related to this condition than to a phobia (as the initial clinical assessment had determined), and that they required an alternative therapeutic option for support.
Finally, on several occasions, triaging was completed by a clinician at the SPA of CAMHS and the assessment had recorded phobia as the main need for treatment; however, when they saw the clinician after waiting, the child was assessed as no longer having a phobia. It is not clear if these were spontaneous remissions or variations in clinician opinion. Previous research suggests that triage can rely on clinical experience to underpin decision-making rather than formal assessment tools. 101 Our finding that many CAMHS did not regard phobia as severe enough to treat in their service may lead us to speculate that CAMHS clinicians in SPA triage centres may have limited information on which to base decision-making or, in some instances, limited experience of phobia. It also has implications, as discussed in Chapter 4 (parents’ and CYP’s experiences), because CYP entering the study tended to, therefore, be at the more severe end of the phobia spectrum, with higher impacts and cormobidities. This is evidenced by the high ADIS scores at study entry.
Sample size and statistical power
As described above, the number of withdrawals (from both treatment and follow-up) and the impact of COVID-19 meant that a smaller number of participants had contributed primary outcome data than originally estimated. We exceeded our target of 136 participants with primary outcome data given that 149 participants contributed to the ITT primary analysis. However, fewer (113 participants) contributed to the PP analysis. Despite this, the CI for PP non-inferiority assessment was consistent with ITT and wholly below the non-inferiority threshold and, thus, provided sufficient evidence to declare non-inferiority.
Generalisability
Although recruitment to ASPECT was geographically diverse and conducted within a variety of different service settings, limited ethnic diversity was evident in the overall sample recruited. Of the 274 CYP recruited to the study, 95.5% described their ethnicity as white English, Welsh, Scottish, Northern Irish or British, alongside 94.4% of their parents/guardians. This is below that expected from some of our localities, which had higher rates of ethnic minority populations. This may be because some families in ethnic minority groups are less likely to access CAMHS because of stigma in their community,102 fear of joining research studies,103 or a perception that specialist services are not accessible to minority cultural groups or lack of awareness of services. 104,105 This may have also been compounded by a lack of awareness of treatment availability for specific phobias, as highlighted in the qualitative findings of the study.
Waiting times
Waiting times in CAMHS are currently long,106 which has been reported in a number of recent reports and papers. 107,108 This created problems in this study in that some CYP had not started treatment (OST, n = 11; CBT, n = 12) or had started but not completed treatment (OST, n = 7; CBT, n = 32) prior to their main outcome research measurement point. This gives good justification for the use of both ITT and PP analysis. We did not research the impact on waiting times in ASPECT, but it is possible that OST (mean number of sessions 1.7 when including those attending and not attending treatment) could reduce waiting times compared with CBT as usual (mean number of sessions 4.9). This is not a straightforward comparison because, although OST involved fewer sessions and less overall therapy time, it may require more planning per session, but this could ultimately equate to less planning time overall. OST may also require better diary management than CBT as usual. Future research would be necessary to prospectively examine these subtle differences.
Defining one-session treatment
Training for OST has become available in some of the training programmes for child mental health practitioners within the CYP-IAPT landscape109 in the three settings of low-intensity work, school-based provision and specialist CAMHS. There were relatively small departures from the PP definition of OST. For example, some services provided a third session after OST, which was primarily to fulfil the service requirements for a follow-up session to gather outcome measurements; this was the main reason for an increased average session number in the OST group (2.2 sessions, among those who attended treatment), with 6% of participants receiving more sessions, or longer treatment, than the OST PP definition. The mean time in hours for each treatment group (OST group, 3.8 hours; CBT group, 5.4 hours) reflects the way that clinical time is organised in each treatment (i.e. concentrated into fewer sessions in OST), as well as time pressures facing CAMHS clinicians.
Outcome measurement challenges
Several weaknesses were also identified pertaining to the data collection methods employed within ASPECT.
It became clear early in the study that scoring the ADIS was complex, given that the scores recorded independently by CYP and parent/guardians were sometimes very different. The CSR ratings from the ADIS used for analysis were scored by trained research assistants (the majority of whom were mainly psychology graduates). The ability of the ADIS to allow clinical discretion in reaching a final ‘consensus’ score between CYP and parent/guardian has been used by some studies. 33,37 A meeting of our clinical experts agreed that we should use the clear and strict process identified in a methodological paper by Evans et al. ,110 as recommended by the ADIS instrument authors. 111 This uses the higher of the scores given by CYP or parents/guardians, unless there is a strong reason to depart from this (e.g. clear evidence of unreliability of one score), in which case it is acceptable to apply judgement. Raters were trained in this difference in approach. The higher overall scores found in our study at baseline than those found by Ollendick et al. 33 may have been because of this approach and/or may have been related to the higher threshold of mental health problems to enter CAMHS found in this study.
Unblinded assessments occurred in very similar amounts in both groups of the study and were unlikely to create bias to the main results. The study team did everything that it could to mitigate these by providing alternative blinded research assistants where possible. Future studies could consider how to achieve this more effectively when there are very diverse geographical sites and limited numbers of research assistants.
The BAT assessments appeared to work well where the stimulus was real. However, as discussed previously, the BAT was more problematic where the stimulus was simulated. There were two types of simulation. One was where the feared object was manufactured/feigned but not real (e.g. vomit). The second was where the situation was feigned (e.g. where the CYP with needle phobia watch a fake arm used for medical training receiving the injection but know that they themselves will not receive that injection) or videoed (e.g. a storm watched on a video when the weather outside is good). Some international clinical colleagues use live injections in the BAT (Dr T Davis III, personal communication) but this is possible only in centres where this is readily available. Some CYP were able to reach all 10 steps of the BAT. These CYP are distributed approximately equally across treatment groups (n = 22 CYP in CBT; n = 18 CYP in OST). It became apparent early in ASPECT that many CYP with a BII phobia were able to successfully reach step 10 of the BAT at baseline (n = 39); this was 58% of those with a BII phobia. We believe this to be related to the inability to create a realistic simulated BAT for this phobia. Given that 25% of the overall study sample had a BII phobia, we explored this with sensitivity analyses and found that the treatment difference between OST and multisession CBT was in keeping with the difference for the main analysis, as it was also between real and simulated stimuli used in the BAT (see Table 12). Comparability with other child phobia studies needs to consider that some studies do not include BII phobia (e.g. Ollendick et al. 33). Difficulties simulating an actual blood draw/immunisation in therapies for adults with specific phobias have been described elsewhere (e.g. Hiermeier and Mofrad99).
Identification of subjects in complex systems
In some localities in which there was a SPA followed by referral into a service, there was a difference in opinion about whether or not a child required phobia treatment at that point. This was usually where the triaging SPA identified a child with a phobia and where a subsequent assessing clinician felt that treatment for a phobia at this point was not appropriate because of a comorbid mental health condition (e.g. depression or generalised anxiety). This could be both a weakness, as the child may have been randomised for treatment and then followed a different treatment path, or a strength, as it indicates that a child’s evolving mental health problems are given careful consideration to provide the most appropriate treatment. A total of 42.4% of those who withdrew from the trial did so in response to a therapist’s decision.
Strengths and weaknesses of the health economic analysis
To the best of our knowledge, this is the first study evaluating the cost-effectiveness of OST for CYP with specific phobias. The analyses account for the costs from a range of perspectives and the QALYs measured by different instruments. However, several weaknesses of the economic evaluation were apparent. First, and most importantly, cases that could not receive allocated interventions or where interventions were interrupted as a result of the COVID-19 pandemic were a concern. Although this could potentially introduce bias to our results, the sensitivity analysis for those who had interventions within the 6-month follow-up period showed that the results were largely the same as our primary analysis, thus supporting the robustness of the results. Sensitivity analyses imputing missing 6-month primary outcome data were consistent with the finding that OST was non-inferior from the primary analysis. Furthermore, the analysis of secondary outcomes (which included 48 participants who were unable to complete their primary outcome as a result of the COVID-19 pandemic but could complete secondary outcomes remotely) found the treatment groups to be similar, in keeping with the primary analysis results. Second, service use data were collected retrospectively and there may have been recall accuracy problems. However, this would not be likely to affect one group more than another. Hence, the study comparison results are likely to remain unchanged.
Finally, although the costs of DNA appointments to the NHS can be considerable,112 our study did not take these costs into account owing to the data constraints. This decision aligns with the NHS England’s 2020 national cost collection guidance for mental health, which advises that missed appointments/DNAs should not be included in the cost collection. 113
Strengths and weaknesses of the qualitative study
Our nested qualitative studies explored the feasibility and acceptability of OST from the perspective of the clinicians delivering the intervention, and the CYP allocated to receive the intervention and their parents/guardians. Synthesising the views of these different stakeholders provides a multidimensional insight into the acceptability of delivering OST. Our qualitative findings help to elucidate the intrinsic and extrinsic factors that may have influenced intervention delivery, engagement and outcomes, and, in doing so, help to contextualise the effect sizes observed in ASPECT’s quantitative analysis.
The sampling at baseline was close to the overall sex ratio. Our qualitative studies are subject to some limitations. We explored, in depth, families’ and clinicians’ views of OST but owing to resource constraints did not explore the acceptability of standardised CBT in the trial. Although many of our findings were shaped by the format of OST, we are unable to discriminate with certainty the aspects of acceptability that are unique to this intervention from those that may also apply to alternative forms of provision. The pre-treatment preferences of clinicians and participants were quantitatively measured at trial baseline but this information was not updated at follow-up; therefore, we are unable to compare stakeholders’ reflections of the two treatments at trial completion. Where we examined preferences, there was a trend in the expected direction of preference for both therapist and participant, but these were not statistically significant. Both the specific and the transferable facets of treatment acceptability are important for implementation and add value to future health service development and refinement.
The recruitment pools for our parent and CYP interviews were set by the number of individuals who (1) were randomised to OST and (2) consented at baseline to participate in our qualitative studies. Obtaining consent to be contacted about the qualitative study at baseline guaranteed that recruitment occurred independently of OST engagement or outcome, but additional steps could have been taken to ensure maximum variability in our interview samples with respect to engaging and non-engaging participants. All interviewees had consented to participate in a RCT comparing treatments for specific phobias and, for this reason, may be argued to have displayed a levels of openness towards psychological therapies that was atypical of the general population. Demonstrable compromises in QoL were evident in our data set at both the individual and the family levels. It is, therefore, possible that participants’ reflections on the acceptability of OST may have been inflated by these past experiences or by the cognitive–emotional barriers that they had previously encountered in identifying and accessing appropriate care.
Data saturation was agreed between the researchers contributing to qualitative data analysis and was achieved in both our parent and our CYP samples. We continued to recruit after reaching this group decision and completed an additional three interviews in each sample to confirm our beliefs. Many participants articulated positive aspects of OST and a common appreciation for its personalised, child-centred approach emerged across all of our data sets. At the same time, these views were challenged by a strong narrative proposing that child referral and suitability guidance may need to be revisited, suggesting that our sampling approach and data collection procedures were sensitive to a variety of participant experiences and nuances in the views obtained.
The sample of CYP recruited to our qualitative interview study compared favourably to our trial population with respect to age, sex and phobia type. The inclusion of children in the acceptability study was dependent on the consent of their parent but was not reliant on a parent/carer–child dyad taking part. Children were interviewed separately from their parents wherever possible to maximise the likelihood of obtaining child-centred insights and accounts.
Multiple researchers were involved in conducting interviews, most of whom had previously collected baseline and follow-up measures from families as part of ASPECT. Therefore, for some participants, relationships may already have been built, facilitating interview style and dialogue. However, a clear distinction between service delivery teams and trial outcome assessments is not always apparent to research participants, and it is equally possible that some families may have been reticent to express unfavourable views. The mix of opinions evident in our data set goes some way to negating this concern.
All interviews were conducted after OST had been completed and the trial’s primary outcome measure had been collected. This design maximised trial validity but left our qualitative data vulnerable to recall bias. Children’s accounts, as with parents’ and clinicians’ accounts, may be subconsciously influenced by a post hoc reconstruction of events. Flexible and creative methods were employed to enable and support data collection with younger children, but the accounts of older children were noticeably more detailed, facilitating a deeper latent analysis. Although this may have biased our interpretative themes towards the views of older and more articulate children, our cross data set synthesis helps to ensure that a holistic and robust account of OST acceptability has emerged.
The recruitment pool for our clinician interviews was set by the number of health professionals who were trained in OST and participated in ASPECT. It may be argued that these individuals could be more open to service development than their peers; however, the decision for clinicians to participate was determined at the site level, by managerial agreement, rather than by practitioner self-selection. It is possible that the clinicians who participated in our qualitative interviews displayed higher levels of cognitive or emotional investment in OST than those who were more reticent in coming forward. However, a broad range of experiences were collated and the recruitment of participants from different trial sites and service backgrounds maximised heterogeneity in professional roles, service contexts and views.
By employing a purposive sampling approach, we recruited clinicians who had delivered OST to at least one child in ASPECT. Very few of these individuals had prior experience of treating specific phobias in CYP. Their assessments of their confidence and skills in delivering OST may not be too dissimilar to their broader practice community.
We did not set an a priori threshold for intervention acceptability. Our three qualitative studies provide a valuable insight into practitioner, patient and family experiences and, for this reason, enable the identification of early implementation barriers to OST uptake and delivery. Our analyses benefited from data coding that was undertaken independently by six researchers. Our data interpretations were also discussed with three PPI representatives, optimising the rigour of our synthesis. We separately undertook intervention fidelity assessments (reported in Chapter 4), but did not obtain observational data on intervention delivery during ASPECT.
Strengths and weaknesses of the fidelity assessment
It is difficult to draw conclusions regarding the fidelity in the trial owing to the small number of recordings available for fidelity assessment. Those that were assessed had moderate/high fidelity and were competent in the delivery of the treatments.
The main limitation of the fidelity assessment was the number of recorded sessions available for review by the team. This was because of young people not consenting to the recording, therapists choosing not to record sessions and difficulties in recording active treatment sessions that were highly mobile (e.g. with dogs). High clinical staff turnover (reported in Chapter 3) also created problems with keeping track of the location of recording devices. It is possible that this limited number of recordings was not representative of the delivery of the two treatments within the trial owing to the Hawthorne effect. However, the self-reports for the recorded sessions tend to report using fewer strategies than the fidelity assessors, suggesting that therapists were not recording their ‘best’ sessions only. We did aim to record as many sessions as possible with participant consent; however, owing to the geographical spread, the number of teams and therapists involved in the delivery, and a global pandemic we were able to record and retrieve only a small number.
ASPECT in the context of extant literature
In the phobia treatment RCT conducted by Ollendick et al. ,33 49% of CYP were deemed phobia diagnosis free (as indicated by an ADIS CSR of < 4) in the OST treatment group at the similar time point of 6 months to our study. This apparent better recovery rate needs consideration. Their study and previous research in this area are different from our study in a number of key respects. First, Ollendick et al. 33 used a consensus diagnosis procedure in which the highest ADIS CSR was not necessarily taken (often the midway point between parent and child was taken), whereas our study used the highest score from parent or child. Second, Ollendick et al. 33 did not include BII phobias, which are a subtype of phobia that are difficult to treat. In ASPECT, 83.6% of CYP had one of three types of phobia: animal (29.9%), vomit (28.7%) and BII (25%). Higher rates of animal phobias have been reported in Ollendick et al. 33 (56%) than the rates found in ASPECT and other similar RCTs (e.g. Öst et al. ,34 50%; Flatt and King,114 43%). Although our rates have been comparable to some studies in relation to BII phobia (e.g. Öst et al. ,34 23%), these were excluded from Ollendick et al. 33 because they are regarded as complex to treat. The rates of vomit phobias were much higher in ASPECT than reported elsewhere (e.g. Ollendick et al.,33 1%). It should also be noted that many studies do not provide specific breakdowns of phobia types, instead grouping by subtype (e.g. situational); therefore, comparing rates of phobias, including BII or vomit, is difficult.
We had relatively few referrals for environmental phobia (e.g. storms) or dental phobias, although a number of isolated referrals were made for specific objects (e.g. buttons). Some of these carried high levels of impact (e.g. engaging in school activities in the context of a paper phobia). The large number of CYP with animal phobia is not surprising and these phobias were mainly dogs and spiders (both of which are very prevalent in society). Large numbers of BII phobias are also not unusual given CYP’s need for vaccination injections, particularly during our sample age range (e.g. human papillomavirus, MenACWY and three-in-one teenage booster), and for injections in the context of illness (e.g. blood tests and insulin in CYP diagnosed with diabetes mellitus). Vomit phobia has been relatively under-researched, but in most individuals the phobia starts before adulthood. 115 It can affect them in multiple ways, leading to leaving or avoiding school, avoiding being with children for fear that they might vomit or avoiding certain foods or situations for fear that they themselves might vomit. 115 These multifaceted impacts suggest that for some it can be a serious condition.
In addition, the study by Ollendick et al. 33 used the ADIS CSR consensus rating score after clinician discussion of the parent and child scores, whereas we used the suggested methodology of taking the highest of the parent and child scores (i.e. ‘composite score’, Evans et al. 110). Furthermore, our selection of recruits, mainly coming from CAMHS, meant that we had large numbers of children with severe, more complex anxiety disorders. This appears to be borne out by the finding that our pre-treatment ADIS phobic anxiety scores are higher than another large study in the USA that recruited through largely community mechanisms. 37
One important factor is that earlier studies have been conducted in highly controlled research contexts 33,37 using trained psychology graduate therapists. Our study was a pragmatic trial in the real world involving existing clinicians from various child mental health treatment centres across England. It has been suggested that findings in research clinics or contexts may show larger differences than later real-world trials, one aspect of the research–practice gap in mental health research. 116 This may be a factor here.
In summary, the finding that many CYP were still classified as having a specific phobia at follow-up (occurring in similar rates in both groups) may be related to a number of factors, including the COVID-19 pandemic affecting the study and causing treatment delays; the inclusion of phobias that are more difficult to treat; drawing largely from a CAMHS population in which CYP with phobias are more likely to have complex phobias or other cormobidities; a difference in the way that we measured phobia severity compared with other studies, which was more stringent; and the fact that the research in real-world services drew from clinicians with a range of backgrounds and skills (including trainees). Other factors may also have been at play.
Implications of ASPECT for future research
This study has shown that OST is as good as multisession CBT for CYP and that it is cost-saving. There are some challenges in organising therapy in busy services but it also carries some potential advantages, such as shorter treatment times.
A priority for future research would be to focus on whether some phobias respond better to OST or multisession CBT than others. For example, our subgroup analysis suggests that vomit phobia may respond better to OST than multisession CBT. Similarly, given some of the qualitative findings, it is possible that some phobias are less well suited to OST or that some CYP may do better with either OST or CBT (e.g. potentially based on age or comorbidities) and this could be explored in future research. On a similar note, there is some suggestion in the results that treatment response may be moderated by clinician experience, with more experienced clinicians associated with better OST outcomes. This would require further research because it may have implications for which therapies can be offered by different therapy teams (where the experience of clinicians may vary, for example, between school-based and clinical-based NHS child and adolescent mental health teams).
Further research would be helpful in identifying good outcome measures for phobia research and is also very important in clinical practice with CYP. The ADIS can be operationalised in different ways, as discussed above, and is influenced by the perspectives of raters. The BAT appears to be useful in animal phobias or those involving real exposure, but less useful in BII or other phobias for which the stimulus is simulated and ceiling effects appear.
Finally, given that a phobia is a life-long condition, more implementation science research could be conducted into how service delivery models and treatment options can enable more CYP to receive treatment and to improve the recovery rates. Any such research would need to be well integrated with commissioners and providers, and with strong PPI. The research has highlighted the need for future work in this area, particularly in developing quality standards and service specifications to develop training and care pathways for specific phobias in CYP.
Conclusions
We conclude that, in a UK context, OST for specific phobias in real-world current child mental health treatment centres is as clinically effective as the existing most common treatment of multisession CBT and is highly likely to be cost-saving. We also suggest that more work needs to be carried out in the development of service specifications, training and care pathways by commissioners and providers to ensure that treatments are readily available across the country for this treatable lifelong condition.
Acknowledgements
We gratefully acknowledge the hard work, support and advice from the following.
Day-to-day research activities, including participant screening, recruitment, data collection, and assisting with trial set-up and monitoring
Daniel Kelleher, Vanessa Moore and Saba Alam (Humber NHS Foundation Trust); Jules Beresford-Dent, Jamie Barrow, Megan Garside, Ellen Kingsley and Eleni Tsappis (Leeds & York Partnership NHS Foundation Trust); Joseph Horne (University of York); Daniel Beever (University of Sheffield Clinical Trials Unit); Kayte Russell, Zoe Inman, Michelle Hagon-Powley, Caroline Sheldon and Lauren Wright (Norfolk and Suffolk NHS Foundation Trust); Emily Clare (Northumberland, Tyne & Wear NHS Foundation Trust); Alix Smith (Rotherham, Doncaster & South Humber NHS Foundation Trust); Laura Daniells and Hollie Gay (University of Exeter Research Clinic); Brandon Bule, Rebecca Ledden and Stephanie Willshaw (Dorset Healthcare University NHS Foundation Trust); and Aurora Balalia, Amelia Parchment and Florentina Takacs (Dudley & Walsall NHS Foundation Trust).
Support on data management concerns
Chris Turtle, Tim Chater, Munya Dimairo (statistical cover for maternity leave) and Kirsty Pemberton (University of Sheffield Clinical Trials Unit).
Administrative and clerical support
Jessica Welburn, Elizabeth Skelton, Daniel Gottschalk and Heather Dakin (University of Sheffield); and Catherine Arthurson and Sharon Bird (Leeds & York Partnership NHS Foundation Trust).
Support on ethics and governance issues
Sinead Audsley (Leeds & York Partnership NHS Foundation Trust).
Patient and public involvement
Trilby Breckman (Triumph Over Phobia, Bath, UK), Olivia Lawler and York Youth Council.
We offer special thanks to the members of our two oversight committees.
Trial Steering Committee
Professor Cathy Creswell (Professor of Developmental Clinical Psychology, University of Reading), Professor Ian Norman (Professor of Mental Health, King’s College London), Dr Claire Henderson (Reader in Public Mental Health, King’s College London), Professor Dankmar Böhning (Professor of Statistics, University of Southampton) and Olivia Lawler (PPI representative).
Data Monitoring and Ethics Committee
Professor Chris Williams (Professor of Psychosocial Psychiatry, University of Glasgow), Professor Nigel Stallard (Professor of Medical Statistics, University of Warwick) and Dr Robbie Duschinsky (Senior University Lecturer, University of Cambridge).
The ASPECT research team
Trial Management Group
Professor Barry Wright (LYPFT/University of York), Professor Cindy Cooper (University of Sheffield Clinical Trials Unit), Dr Alex Scott (University of Sheffield Clinical Trials Unit), Lucy Tindall (LYPFT), Katie Biggs (University of Sheffield Clinical Trials Unit), Dr Dawn Teare (University of Sheffield), Dr Ellen Lee (University of Sheffield), Emily Hayward (LYPFT), Hannah Edwards (LYPFT), Jen Lomas (University of Sheffield Clinical Trials Unit), Amy Barr (University of Sheffield), Kiera Solaiman (University of Sheffield), Dr David Marshall (University of York), Professor Dean McMillan (University of York), Dr Shehzad Ali (Western University Canada/University of York), Han-I Wang (University of York), Dr Lina Gega (University of York), Joseph Horne (University of York), Rebecca Hargate (LYPFT), Dr Penny Bee (University of Manchester), Professor Karina Lovell (University of Manchester), Trilby Breckman (Triumph Over Phobia UK), Jon Wilson (Norfolk and Suffolk NHS Foundation Trust), Clare Elsdon (City of York Council), Chris Turtle (University of Sheffield) and Munya Dimairo (University of Sheffield).
Co-applicants
Professor Cindy Cooper (University of Sheffield Clinical Trials Unit), Katie Biggs (University of Sheffield Clinical Trials Unit), Dr Dawn Teare (University of Sheffield), Dr David Marshall (University of York), Professor Dean McMillan (University of York), Dr Lina Gega (University of York), Dr Shehzad Ali (Western University Canada/University of York), Professor Simon Gilbody (University of York), Rebecca Hargate (LYPFT), Dr Penny Bee (University of Manchester), Professor Karina Lovell (University of Manchester), Dr Thompson Davis (Louisiana State University) and Trilby Breckman (Triumph Over Phobia UK).
Local principal investigators
Ravi Mahendra (Humber NHS Foundation Trust), Ollie O’Mara (Tees, Esk & Wear Valley Foundation Trust), Simon Eltringham (South West Yorkshire Partnership NHS Foundation Trust), Jon Wilson (Norfolk & Suffolk NHS Foundation Trust), Lina Gega (Northumberland, Tyne & Wear NHS Foundation Trust/South Tyneside and Sunderland NHS Foundation Trust), Katie Glazebrook (Leeds Community Healthcare Trust), Adrian Philipson (Rotherham, Doncaster & South Humber NHS Foundation Trust), Catherine Gallop (University of Exeter Research Clinic), Jennifer Murphy (Dorset Healthcare University NHS Foundation Trust), Deborah Vaughn (Cumbria Partnership NHS Foundation Trust), Dawn Egginton (County Durham and Darlington NHS Foundation Trust), and Arif Khan and Sita Ratner (Dudley & Walsall NHS Foundation Trust).
We would also like to extend our thanks to all of the CYP, parents/guardians and clinicians who were involved in ASPECT. Furthermore, we thank those who allowed the successful delivery of the trial through providing phobic stimuli for assessments and therapy sessions.
The views expressed in this report are those of the authors and not necessarily those of the National Institute for Health and Care Research Health Technology Assessment programme. Any errors are the responsibility of the authors.
Contributions of authors
Barry Wright (https://orcid.org/0000-0002-8692-6001) (Co-applicant/Chief Investigator) was involved in trial conception and design, delivered study intervention training, was involved in the analysis and interpretation of the data, contributed to the management and conduct of the trial, and produced the first draft of the report.
Lucy Tindall (https://orcid.org/0000-0002-7486-5037) (Trial Manager) contributed to the management and conduct of the trial and produced the first draft of the report.
Alexander J Scott (https://orcid.org/0000-0001-7426-7099) (Trial Manager) contributed to the management and conduct of the trial and produced the first draft of the report.
Ellen Lee (https://orcid.org/0000-0003-4529-7410) (Statistician) was involved in the analysis and interpretation of the data and produced the first draft of the report.
Katie Biggs (https://orcid.org/0000-0003-4468-7417) (Co-applicant/Assistant Director of CTRU) was involved in trial conception and design, was involved in the analysis and interpretation of the data, contributed to the management and conduct of the trial, and produced the first draft of the report.
Cindy Cooper (https://orcid.org/0000-0002-2995-5447) (Co-applicant/Director of CTRU) was involved in trial conception and design, was involved in the analysis and interpretation of the data, contributed to the management and conduct of the trial, and produced the first draft of the report.
Penny Bee (https://orcid.org/0000-0002-5600-0400) (Co-applicant) was involved in trial conception and design, was involved in the analysis and interpretation of the data, and produced the first draft of the report.
Han-I Wang (https://orcid.org/0000-0002-3521-993X) (Health Economist) was involved in the analysis and interpretation of the data, and produced the first draft of the report.
Lina Gega (https://orcid.org/0000-0003-2902-9256) (Co-applicant/Principal Investigator) was involved in trial conception and design, delivered study intervention training, and was involved in the analysis and interpretation of the data.
Emily Hayward (https://orcid.org/0000-0002-2413-0104) (Research Assistant) was involved in the acquisition, analysis and interpretation of the data, and produced the first draft of the report.
Kiera Solaiman (https://orcid.org/0000-0003-2244-5345) (Research Assistant) was involved in the acquisition, analysis and interpretation of the data, and produced the first draft of the report.
M Dawn Teare (https://orcid.org/0000-0003-3994-0051) (Co-applicant/Senior Statistician) was involved in trial conception and design, and was involved in the analysis and interpretation of the data.
Thompson Davis (https://orcid.org/0000-0002-5180-8822) (Co-applicant) was involved in trial conception and design, delivered study intervention training, and was involved in the analysis and interpretation of the data.
Karina Lovell (https://orcid.org/0000-0001-8821-895X) (Co-applicant) was involved in trial conception and design, and was involved in the analysis and interpretation of the data.
Jon Wilson (https://orcid.org/0000-0002-5279-6237) (Co-applicant/Principal Investigator) was involved in trial conception and design, and was involved in the analysis and interpretation of the data.
Dean McMillan (https://orcid.org/0000-0002-2901-8410) (Co-applicant) was involved in trial conception and design, and was involved in the analysis and interpretation of the data.
Amy Barr (https://orcid.org/0000-0002-7990-7451) (Research Assistant) was involved in the acquisition, analysis and interpretation of the data.
Hannah Edwards (https://orcid.org/0000-0002-0500-2123) (Research Assistant) was involved in the acquisition, analysis and interpretation of the data.
Jennifer Lomas (https://orcid.org/0000-0002-2446-7153) (Research Assistant) was involved in the acquisition, analysis and interpretation of the data.
Chris Turtle (https://orcid.org/0000-0003-3109-425X) (Data Specialist) was involved in the analysis and interpretation of the data, and contributed to the management and conduct of the trial.
Steve Parrott (https://orcid.org/0000-0002-0165-1150) (Senior Health Economist) was involved in the analysis and interpretation of data.
Catarina Teige (https://orcid.org/0000-0002-8958-6487) (Trial Manager) contributed to the management and conduct of the trial.
Tim Chater (https://orcid.org/0000-0002-1138-0147) (Data and Information Systems Manager) was involved in the analysis and interpretation of the data, and contributed to the management and conduct of the trial.
Rebecca Hargate (https://orcid.org/0000-0001-6532-2375) (Co-applicant) was involved in trial conception and design.
Shehzad Ali (https://orcid.org/0000-0002-8042-3630) (Co-applicant) was involved in trial conception and design.
Sarah Parkinson (https://orcid.org/0000-0003-3512-8509) (Research Assistant) was involved in the acquisition of data.
Simon Gilbody (https://orcid.org/0000-0002-8236-6983) (Co-applicant) was involved in trial conception and design.
David Marshall (https://orcid.org/0000-0001-5969-9539) (Co-applicant) was involved in trial conception and design.
All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Publications
Hayward E, Solaiman K, Bee P, Barr A, Edwards H, Lomas J, et al. One-session treatment for specific phobias: barriers, facilitators and acceptability as perceived by children & young people, parents, and clinicians. PLOS ONE 2022;17:e0274424.
Tindall L, Scott AJ, Biggs K, Hayward E, Wilson J, Cooper C, et al. The Alleviating Specific Phobias in Children Trial: challenges and solutions to implementing a randomised controlled trial in clinical services. Front Child Adolesc Psychiatry 2022; in press.
Wang HI, Wright B, Tindall L, Cooper C, Biggs K, Lee E, et al. Cost and effectiveness of one session treatment (OST) for children and young people with specific phobias compared to multi-session cognitive behavioural therapy (CBT): results from a randomised controlled trial. BMJ Psychiatry 2022;22:547.
Wright B, Tindall L, Scott AJ, Lee E, Cooper C, Bee P, et al. One session treatment (OST) is equivalent to multi-session cognitive behavioural therapy (CBT) in children with specific phobias (ASPECT): results from a national non-inferiority randomized controlled trial [published online ahead of print August 1 2022]. J Child Psychol Psychiatry 2022.
Data-sharing statement
Any requests for statistical code should be made to the corresponding author or the CTRU. The ASPECT management team will consider the sharing of data on a case-by-case basis in line with the ethics approval and patient information sheets. Any presented data do not contain any direct identifiers.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HTA programme or the Department of Health and Social Care.
References
- Wright B, Tindall L, Scott AJ, Lee E, Cooper C, Bee P, et al. One session treatment (OST) is equivalent to multi-session cognitive behavioural therapy (CBT) in children with specific phobias (ASPECT): results from a national non-inferiority randomized controlled trial [published online ahead of print August 1 2022]. J Child Psychol Psychiatry 2022. https://doi.org/10.1111/jcpp.13665.
- Wang HI, Wright B, Tindall L, Cooper C, Biggs K, Lee E, et al. Cost and effectiveness of one session treatment (OST) for children and young people with specific phobias compared to multi-session cognitive behavioural therapy (CBT): results from a randomised controlled trial. BMJ Psychiatry 2022;22. https://doi.org/10.1186/s12888-022-04192-8.
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition 2013. https://doi.org/10.1176/appi.books.9780890425596.
- Hofmann SG. Cognitive processes during fear acquisition and extinction in animals and humans: implications for exposure therapy of anxiety disorders. Clin Psychol Rev 2008;28:199-210. https://doi.org/10.1016/j.cpr.2007.04.009.
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 2005;62:593-602. https://doi.org/10.1001/archpsyc.62.6.593.
- Stinson FS, Dawson DA, Patricia Chou S, Smith S, Goldstein RB, June Ruan W, et al. The epidemiology of DSM-IV specific phobia in the USA: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol Med 2007;37:1047-59. https://doi.org/10.1017/S0033291707000086.
- Comer JS, Blanco C, Hasin DS, Liu SM, Grant BF, Turner JB, et al. Health-related quality of life across the anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). J Clin Psychiatry 2011;72:43-50. https://doi.org/10.4088/JCP.09m05094blu.
- Ialongo N, Edelsohn G, Werthamer-Larsson L, Crockett L, Kellam S. The significance of self-reported anxious symptoms in first grade children: prediction to anxious symptoms and adaptive functioning in fifth grade. J Child Psychol Psychiatry 1995;36:427-37. https://doi.org/10.1111/j.1469-7610.1995.tb01300.x.
- Ollendick TH, March JS. Phobic and Anxiety Disorders in Children and Adolescents: A Clinician’s Guide to Effective Psychosocial and Pharmacological Interventions. Oxford: Oxford University Press; 2004.
- Bittner A, Egger HL, Erkanli A, Jane Costello E, Foley DL, Angold A. What do childhood anxiety disorders predict?. J Child Psychol Psychiatry Allied Discip 2007;48:1174-83. https://doi.org/10.1111/j.1469-7610.2007.01812.x.
- Lieb R, Miché M, Gloster AT, Beesdo-Baum K, Meyer AH, Wittchen HU. Impact of specific phobia on the risk of onset of mental disorders: a 10-year prospective-longitudinal community study of adolescents and young adults. Depress Anxiety 2016;33:667-75. https://doi.org/10.1002/da.22487.
- Anderson JK, Howarth E, Vainre M, Jones PB, Humphrey A. A scoping literature review of service-level barriers for access and engagement with mental health services for children and young people. Child Youth Serv Rev 2017;77:164-76. https://doi.org/10.1016/j.childyouth.2017.04.017.
- Crenna-Jennings W, Hutchinson J. Access to Child and Adolescent Mental Health Services in 2019 2020. https://epi.org.uk/publications-and-research/access-to-child-and-adolescent-mental-health-services-in-2019/ (accessed 19 March 2021).
- Rocks S, Glogowska M, Stepney M, Tsiachristas A, Fazel M. Introducing a single point of access (SPA) to child and adolescent mental health services in England: a mixed-methods observational study. BMC Health Serv Res 2020;20. https://doi.org/10.1186/s12913-020-05463-4.
- Sayal K. Annotation: pathways to care for children with mental health problems. J Child Psychol Psychiatry 2006;47:649-59. https://doi.org/10.1111/j.1469-7610.2005.01543.x.
- Kendall PC, Robin JA, Hedtke KA, Suveg C, Flannery-Schroeder E, Gosch E. Considering CBT with anxious youth? Think exposures. Cogn Behav Pract 2005;12:136-48. https://doi.org/10.1016/S1077-7229(05)80048-3.
- Kendall PC, Hedtke KA. Cognitive-behavioral Therapy for Anxious Children: Therapist Manual. Ardmore, PA: Workbook Pub Inc.; 2006.
- Butler AC, Chapman JE, Forman EM, Beck AT. The empirical status of cognitive-behavioral therapy: a review of meta-analyses. Clin Psychol Rev 2006;26:17-31. https://doi.org/10.1016/j.cpr.2005.07.003.
- Davis TE, Ollendick TH. Empirically supported treatments for specific phobia in children: do efficacious treatments address the components of a phobic response?. Clin Psychol Sci Pract 2005;12:144-60. https://doi.org/10.1093/clipsy.bpi018.
- Hofmann SG, Asnaani A, Vonk IJ, Sawyer AT, Fang A. The efficacy of cognitive behavioral therapy: a review of meta-analyses. Cognit Ther Res 2012;36:427-40. https://doi.org/10.1007/s10608-012-9476-1.
- Hudson JL, Rapee RM, Lyneham HJ, McLellan LF, Wuthrich VM, Schniering CA. Comparing outcomes for children with different anxiety disorders following cognitive behavioural therapy. Behav Res Ther 2015;72:30-7. https://doi.org/10.1016/j.brat.2015.06.007.
- Aschim B, Lundevall S, Martinsen EW, Frich JC. General practitioners’ experiences using cognitive behavioural therapy in general practice: a qualitative study. Scand J Prim Health Care 2011;29:176-80. https://doi.org/10.3109/02813432.2011.595582.
- Wiebe E, Greiver M. Using cognitive behavioural therapy in practice: qualitative study of family physicians’ experiences. Can Fam Physician 2005;51:992-3.
- Stallard P, Udwin O, Goddard M, Hibbert S. The availability of cognitive behaviour therapy within specialist child and adolescent mental health services (CAMHS): a national survey. Behav Cogn Psychother 2007;35. https://doi.org/10.1017/S1352465807003724.
- van der Gaag M. The efficacy of CBT for severe mental illness and the challenge of dissemination in routine care. World Psychiatry 2014;13:257-8. https://doi.org/10.1002/wps.20162.
- Cavanagh K. Geographic inequity in the availability of cognitive behavioural therapy in England and Wales: a 10-year update. Behav Cogn Psychother 2014;42:497-501. https://doi.org/10.1017/S1352465813000568.
- Shapiro DA, Cavanagh K, Lomas H. Geographic inequity in the availability of cognitive behavioural therapy in England and Wales. Behav Cogn Psychother 2003;31. https://doi.org/10.1017/S1352465803002066.
- Ollendick TH, Ryan SM, Capriola-Hall NN, Austin KE, Fraire M. Have phobias, will travel: addressing one barrier to the delivery of an evidence-based treatment. Behav Ther 2018;49:594-603. https://doi.org/10.1016/j.beth.2017.11.003.
- de Haan AM, Boon AE, de Jong JT, Hoeve M, Vermeiren RR. A meta-analytic review on treatment dropout in child and adolescent outpatient mental health care. Clin Psychol Rev 2013;33:698-711. https://doi.org/10.1016/j.cpr.2013.04.005.
- Wergeland GJ, Fjermestad KW, Marin CE, Haugland BS, Silverman WK, Öst LG, et al. Predictors of dropout from community clinic child CBT for anxiety disorders. J Anxiety Disord 2015;31:1-10. https://doi.org/10.1016/j.janxdis.2015.01.004.
- Zlomke K, Davis TE. One-session treatment of specific phobias: a detailed description and review of treatment efficacy. Behav Ther 2008;39:207-23. https://doi.org/10.1016/j.beth.2007.07.003.
- Davis TE, Ollendick TH, Öst LG. One-session treatment of specific phobias in children: recent developments and a systematic review. Annu Rev Clin Psychol 2019;15:233-56. https://doi.org/10.1146/annurev-clinpsy-050718-095608.
- Ollendick TH, Ost LG, Reuterskiöld L, Costa N, Cederlund R, Sirbu C, et al. One-session treatment of specific phobias in youth: a randomized clinical trial in the United States and Sweden. J Consult Clin Psychol 2009;77:504-16. https://doi.org/10.1037/a0015158.
- Öst LG, Svensson L, Hellström K, Lindwall R. One-session treatment of specific phobias in youths: a randomized clinical trial. J Consult Clin Psychol 2001;69:814-24. https://doi.org/10.1037/0022-006X.69.5.814.
- Ryan SM, Strege MV, Oar EL, Ollendick TH. One session treatment for specific phobias in children: comorbid anxiety disorders and treatment outcome. J Behav Ther Exp Psychiatry 2017;54:128-34. https://doi.org/10.1016/j.jbtep.2016.07.011.
- Singal AG, Higgins PD, Waljee AK. A primer on effectiveness and efficacy trials. Clin Transl Gastroenterol 2014;5. https://doi.org/10.1038/ctg.2013.13.
- Ollendick TH, Halldorsdottir T, Fraire MG, Austin KE, Noguchi RJ, Lewis KM, et al. Specific phobias in youth: a randomized controlled trial comparing one-session treatment to a parent-augmented one-session treatment. Behav Ther 2015;46:141-55. https://doi.org/10.1016/j.beth.2014.09.004.
- Becker ES, Rinck M, Türke V, Kause P, Goodwin R, Neumer S, et al. Epidemiology of specific phobia subtypes: findings from the Dresden Mental Health Study. Eur Psychiatry 2007;22:69-74. https://doi.org/10.1016/j.eurpsy.2006.09.006.
- Kim SJ, Kim BN, Cho SC, Kim JW, Shin MS, Yoo HJ, et al. The prevalence of specific phobia and associated cormobid features in children and adolescents. J Anxiety Disord 2010;24:629-34. https://doi.org/10.1016/j.janxdis.2010.04.004.
- Castagna PJ, Davis TE, Lilly ME. The behavioral avoidance task with anxious youth: a review of procedures, properties, and criticisms. Clin Child Fam Psychol Rev 2017;20:162-84. https://doi.org/10.1007/s10567-016-0220-3.
- Wright BD, Cooper C, Scott AJ, Tindall L, Ali S, Bee P, et al. Clinical and cost-effectiveness of one-session treatment (OST) versus multisession cognitive-behavioural therapy (CBT) for specific phobias in children: protocol for a non-inferiority randomised controlled trial. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2018-025031.
- Hayward E, Solaiman K, Bee P, Barr A, Edwards H, Lomas J, et al. One-session treatment for specific phobias: barriers, facilitators and acceptability as perceived by children & young people, parents, and clinicians. PLOS ONE 2022;17. https://doi.org/10.1371/journal.pone.0274424.
- Schulz KF, Altman DG, Moher D. CONSORT Group . CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. Trials 2010;11. https://doi.org/10.1186/1745-6215-11-32.
- Wright B, Marshall D, Adamson J, Ainsworth H, Ali S, Allgar V, et al. Social Stories™ to alleviate challenging behaviour and social difficulties exhibited by children with autism spectrum disorder in mainstream schools: design of a manualised training toolkit and feasibility study for a cluster randomised controlled trial with nested qualitative and cost-effectiveness components. Health Technol Assess 2016;20. https://doi.org/10.3310/hta20060.
- Wright B, Marshall D, Collingridge Moore D, Ainsworth H, Hackney L, Adamson J, et al. Autism Spectrum Social Stories In Schools Trial (ASSSIST): study protocol for a feasibility randomised controlled trial analysing clinical and cost-effectiveness of Social Stories in mainstream schools. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2014-005952.
- Lyneham HJ, Rapee RM. Agreement between telephone and in-person delivery of a structured interview for anxiety disorders in children. J Am Acad Child Adolesc Psychiatry 2005;44:274-82. https://doi.org/10.1097/00004583-200503000-00012.
- Silverman WK, Albano AM. Anxiety Disorders Interview Schedule (ADIS-IV) Child and Parent Interview Schedules. Albany, NY: Greywind Publications; 1996.
- Silverman WK, Saavedra LM, Pina AA. Test-retest reliability of anxiety symptoms and diagnoses with the Anxiety Disorders Interview Schedule for DSM-IV: child and parent versions. J Am Acad Child Adolesc Psychiatry 2001;40:937-44. https://doi.org/10.1097/00004583-200108000-00016.
- Langley AK, Bergman RL, McCracken J, Piacentini JC. Impairment in childhood anxiety disorders: preliminary examination of the child anxiety impact scale-parent version. J Child Adolesc Psychopharmacol 2004;14:105-14. https://doi.org/10.1089/104454604773840544.
- Langley AK, Falk A, Peris T, Wiley JF, Kendall PC, Ginsburg G, et al. The child anxiety impact scale: examining parent- and child-reported impairment in child anxiety disorders. J Clin Child Adolesc Psychol 2014;43:579-91. https://doi.org/10.1080/15374416.2013.817311.
- Chorpita BF, Moffitt CE, Gray J. Psychometric properties of the Revised Child Anxiety and Depression Scale in a clinical sample. Behav Res Ther 2005;43:309-22. https://doi.org/10.1016/j.brat.2004.02.004.
- Law D, Jacob J. Goals and Goal Based Outcomes (GBOs). London: CAMHS Press; 2013.
- The EuroQol Group . EuroQol – a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199-208. https://doi.org/10.1016/0168-8510(90)90421-9.
- Stevens K, Ratcliffe J. Measuring and valuing health benefits for economic evaluation in adolescence: an assessment of the practicality and validity of the child health utility 9D in the Australian adolescent population. Value Health 2012;15:1092-9. https://doi.org/10.1016/j.jval.2012.07.011.
- Barrett B, Byford S, Chitsabesan P, Kenning C. Mental health provision for young offenders: service use and cost. Br J Psychiatry 2006;188:541-6. https://doi.org/10.1192/bjp.bp.105.010108.
- Marshall D, Wright B, Allgar V, Adamson J, Williams C, Ainsworth H, et al. Social Stories in mainstream schools for children with autism spectrum disorder: a feasibility randomised controlled trial. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2016-011748.
- Wright B, Tindall L, Littlewood E, Adamson J, Allgar V, Bennett S, et al. Computerised cognitive behaviour therapy for depression in adolescents: study protocol for a feasibility randomised controlled trial. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2014-006488.
- Dolan P. Modeling valuations for EuroQol health states. Med Care 1997;35:1095-108. https://doi.org/10.1097/00005650-199711000-00002.
- Stevens K. Valuation of the Child Health Utility 9D Index. PharmacoEconomics 2012;30:729-47. https://doi.org/10.2165/11599120-000000000-00000.
- Hofmann SG, Smits JA. Cognitive-behavioral therapy for adult anxiety disorders: a meta-analysis of randomized placebo-controlled trials. J Clin Psychiatry 2008;69:621-32. https://doi.org/10.4088/JCP.v69n0415.
- Davis TE, May A, Whiting SE. Evidence-based treatment of anxiety and phobia in children and adolescents: current status and effects on the emotional response. Clin Psychol Rev 2011;31:592-60. https://doi.org/10.1016/j.cpr.2011.01.001.
- Davis TE, Jenkins W, Rudy B, Davis TE, Ollendick TH, Öst LG. Intensive One-Session Treatment of Specific Phobias. New York, NY: Springer; 2012.
- Stallard P, Myles P, Branson A. The Cognitive Behaviour Therapy Scale for Children and Young People (CBTS-CYP): development and psychometric properties. Behav Cogn Psychother 2014;42:269-82. https://doi.org/10.1017/S135246581300115X.
- Blackburn IM, James IA, Milne DL, Baker C, Standart S, Garland A, et al. The revised cognitive therapy scale (CTS-R): psychometric properties. Behav Cogn Psychother 2001;29:431-46. https://doi.org/10.1017/S1352465801004040.
- Borrelli B. The assessment, monitoring, and enhancement of treatment fidelity in public health clinical trials. J Public Health Dent 2011;71:52-63. https://doi.org/10.1111/j.1752-7325.2011.00233.x.
- Wolitzky-Taylor KB, Horowitz JD, Powers MB, Telch MJ. Psychological approaches in the treatment of specific phobias: a meta-analysis. Clin Psychol Rev 2008;28:1021-37. https://doi.org/10.1016/j.cpr.2008.02.007.
- Reynolds S, Wilson C, Austin J, Hooper L. Effects of psychotherapy for anxiety in children and adolescents: a meta-analytic review. Clin Psychol Rev 2012;32:251-62. https://doi.org/10.1016/j.cpr.2012.01.005.
- Jones B, Jarvis P, Lewis JA, Ebbutt AF. Trials to assess equivalence: the importance of rigorous methods. BMJ 1996;313:36-9. https://doi.org/10.1136/bmj.313.7048.36.
- Altman DG. Practical Statistics for Medical Research. London: Chapman and Hall/CRC Press; 1991.
- Piaggio G, Elbourne DR, Pocock SJ, Evans SJ, Altman DG. CONSORT Group . Reporting of noninferiority and equivalence randomized trials: extension of the CONSORT 2010 statement. JAMA 2012;308:2594-604. https://doi.org/10.1001/jama.2012.87802.
- Goulet-Pelletier J-C, Cousineau D. A review of effect sizes and their confidence intervals, part I: the Cohen’s d family. Quant Methods Psychol 2018;14:242-65. https://doi.org/10.20982/tqmp.14.4.p242.
- Angrist JD, Imbens GW, Rubin DB. Identification of causal effects using instrumental variables. J Am Stat Assoc 1996;91:444-55. https://doi.org/10.1080/01621459.1996.10476902.
- Whitehead SJ, Ali S. Health outcomes in economic evaluation: the QALY and utilities. Br Med Bull 2010;96:5-21. https://doi.org/10.1093/bmb/ldq033.
- NHS Improvement . National Cost Collection 2018–2019 n.d. https://www.england.nhs.uk/publication/2018-19-national-cost-collection-data-publication/ (accessed January 2021).
- Curtis L, Burns A. Unit Costs of Health and Social Care 2018. Canterbury: PSSRU, University of Kent; 2018.
- NHS Digital . Prescription Cost Analysis – England, 2018 2018. https://digital.nhs.uk/data-and-information/publications/statistical/prescription-cost-analysis (accessed January 2021).
- National Institute for Health Care and Excellence (NICE) . Developing NICE Guidelines: The Manual 2020.
- Rubin DB. Statistical matching using file concatenation with adjusted weights and multiple imputations. J Bus Econ Stat 1986;4:87-94. https://doi.org/10.1080/07350015.1986.10509497.
- Manca A, Hawkins N, Sculpher MJ. Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ 2005;14:487-96. https://doi.org/10.1002/hec.944.
- Glick HA, Doshi JA, Sonnad SS, Polsky D. Economic Evaluation in Clinical Trials. Oxford: Oxford University Press; 2014.
- Hoch JS, Briggs AH, Willan AR. Something old, something new, something borrowed, something blue: a framework for the marriage of health econometrics and cost-effectiveness analysis. Health Econ 2002;11:415-30. https://doi.org/10.1002/hec.678.
- Briggs AH, Wonderling DE, Mooney CZ. Pulling cost-effectiveness analysis up by its bootstraps: a non-parametric approach to confidence interval estimation. Health Econ 1997;6:327-40. https://doi.org/10.1002/(SICI)1099-1050(199707)6:4<327::AID-HEC282>3.0.CO;2-W.
- Tyrer P, Salkovskis P, Tyrer H, Wang D, Crawford MJ, Dupont S, et al. Cognitive-behaviour therapy for health anxiety in medical patients (CHAMP): a randomised controlled trial with outcomes to 5 years. Health Technol Assess 2017;21. https://doi.org/10.3310/hta21500.
- Hedman E, Andersson E, Ljótsson B, Axelsson E, Lekander M. Cost effectiveness of internet-based cognitive behaviour therapy and behavioural stress management for severe health anxiety. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-009327.
- Lindsäter E, Axelsson E, Salomonsson S, Santoft F, Ljótsson B, Åkerstedt T, et al. Cost-effectiveness of therapist-guided internet-based cognitive behavioral therapy for stress-related disorders: secondary analysis of a randomized controlled trial. J Med Internet Res 2019;21. https://doi.org/10.2196/14675.
- Fenwick E, O’Brien BJ, Briggs A. Cost-effectiveness acceptability curves – facts, fallacies and frequently asked questions. Health Econ 2004;13:405-15. https://doi.org/10.1002/hec.903.
- Lovell K, Bower P, Gellatly J, Byford S, Bee P, McMillan D, et al. Clinical effectiveness, cost-effectiveness and acceptability of low-intensity interventions in the management of obsessive-compulsive disorder: the Obsessive-Compulsive Treatment Efficacy randomised controlled Trial (OCTET). Health Technol Assess 2017;21. https://doi.org/10.3310/hta21370.
- Angell C, Alexander J, Hunt JA. ‘Draw, write and tell’: a literature review and methodological development on the ‘draw and write’ research method. J Early Child Res 2015;13:17-28. https://doi.org/10.1177/1476718X14538592.
- McWhirter J. The draw and write technique as a versatile tool for researching children’s understanding of health and well-being. Int J Heal Promot Educ 2014;52:250-9. https://doi.org/10.1080/14635240.2014.912123.
- Ritchie J, Spencer L, Bryman A, Burgess R. Analyzing Qualitative Data. London: Routledge; 1994.
- Dixon-Woods M. Using framework-based synthesis for conducting reviews of qualitative studies. BMC Med 2011;9. https://doi.org/10.1186/1741-7015-9-39.
- Tindall L, Scott AJ, Biggs K, Hayward E, Wilson J, Cooper C, et al. The Alleviating Specific Phobias in Children Trial: challenges and solutions to implementing a randomised controlled trial in clinical services. Front Child Adolesc Psychiatry 2022.
- Department of Health and Social Care (DHSC) . Future in Mind: Promoting, Protecting and Improving Our Children and Young People’s Mental Health and Wellbeing 2015. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/414024/Childrens_Mental_Health.pdf (accessed 9 April 2021).
- Department of Health and Social Care and Department for Education . Transforming Children and Young People’s Mental Health Provision: A Green Paper 2017. www.gov.uk/government/consultations/transforming-children-and-young-peoples-mental-health-provision-a-green-paper (accessed 9 April 2021).
- Wiles N, Thomas L, Abel A, Barnes M, Carroll F, Ridgway N, et al. Clinical effectiveness and cost-effectiveness of cognitive behavioural therapy as an adjunct to pharmacotherapy for treatment-resistant depression in primary care: the CoBalT randomised controlled trial. Health Technol Assess 2014;18. https://doi.org/10.3310/hta18310.
- National Institute for Health and Care Excellence (NICE) . Guide to the Methods of Technology Appraisal 2013 2013. www.nice.org.uk/process/pmg9/chapter/foreword (accessed 22 March 2021).
- Sekhon M, Cartwright M, Francis JJ. Acceptability of healthcare interventions: an overview of reviews and development of a theoretical framework. BMC Health Serv Res 2017;17. https://doi.org/10.1186/s12913-017-2031-8.
- Thompson A, Issakidis C, Hunt C. Delay to seek treatment for anxiety and mood disorders in an Australian clinical sample. Behav Chang 2008;25. https://doi.org/10.1375/bech.25.2.71.
- Hiermeier UM, Mofrad L. Feasibility of one-session treatment for specific needle phobia in an adult IAPT service – a case series. Cogn Behav Ther 2020;13. https://doi.org/10.1017/S1754470X2000046X.
- Haukebø K, Skaret E, Ost LG, Raadal M, Berg E, Sundberg H, et al. One- vs. five-session treatment of dental phobia: a randomized controlled study. J Behav Ther Exp Psychiatry 2008;39:381-90. https://doi.org/10.1016/j.jbtep.2007.09.006.
- Sands N. An exploration of clinical decision making in mental health triage. Arch Psychiatr Nurs 2009;23:298-30. https://doi.org/10.1016/j.apnu.2008.08.002.
- Bradby H, Varyani M, Oglethorpe R, Raine W, White I, Helen M. British Asian families and the use of child and adolescent mental health services: a qualitative study of a hard to reach group. Soc Sci Med 2007;65:2413-24. https://doi.org/10.1016/j.socscimed.2007.07.025.
- Hussain-Gambles M, Atkin K, Leese B. Why ethnic minority groups are under-represented in clinical trials: a review of the literature. Health Soc Care Community 2004;12:382-8. https://doi.org/10.1111/j.1365-2524.2004.00507.x.
- Stein SM, Christie D, Shah R, Dabney J, Wolpert M. Attitudes to and knowledge of CAMHS: differences between Pakistani and White British mothers. Child Adolesc Ment Health 2003;8:29-33. https://doi.org/10.1111/1475-3588.00042.
- Young A, Ferguson-Coleman E, Wright B, Le Couteur A. Parental conceptualizations of autism and deafness in British deaf children. J Deaf Stud Deaf Educ 2019;24:280-8. https://doi.org/10.1093/deafed/enz002.
- NHS Benchmarking Network . 2019 Child and Adolescent Mental Health Services Project – Results Published 2019. www.nhsbenchmarking.nhs.uk/news/2019-child-and-adolescent-mental-health-services-project-results-published (accessed 8 April 2021).
- Smith J, Kyle RG, Daniel B, Hubbard G. Patterns of referral and waiting times for specialist Child and Adolescent Mental Health Services. Child Adolesc Ment Health 2018;23:41-9. https://doi.org/10.1111/camh.12207.
- Young Minds . New Figures on CAMHS Waiting Times 2018. https://youngminds.org.uk/blog/new-figures-on-camhs-waiting-times/ (accessed 8 April 2021).
- Ludlow C, Hurn R, Lansdell S. A current review of the Children and Young People’s Improving Access to Psychological Therapies (CYP IAPT) program: perspectives on developing an accessible workforce. Adolesc Health Med Ther 2020;11:21-8. https://doi.org/10.2147/AHMT.S196492.
- Evans R, Thirlwall K, Cooper P, Creswell C. Using symptom and interference questionnaires to identify recovery among children with anxiety disorders. Psychol Assess 2017;29:835-43. https://doi.org/10.1037/pas0000375.
- Albano AM, Silverman WK. The Anxiety Disorders Interview Schedule for Children for DSM-IV: Child Version. San Antonio, TX: Psychological Corporation; 1996.
- NHS Digital . GP Appointments Data Published 2018. https://digital.nhs.uk/news-and-events/latest-news/gp-appointments-data-published (accessed 12 February 2021).
- NHS England . Approved Costing Guidance 2020 for Mental Health 2020. www.england.nhs.uk/approved-costing-guidance-2020/#approved-costing-guidance-collections (accessed 12 February 2021).
- Flatt N, King N. Brief psycho-social interventions in the treatment of specific childhood phobias: a controlled trial and a 1-year follow-up. Behav Chang 2010;27:130-53. https://doi.org/10.1375/bech.27.3.130.
- Keyes A, Gilpin HR, Veale D. Phenomenology, epidemiology, cormobidity and treatment of a specific phobia of vomiting: a systematic review of an understudied disorder. Clin Psychol Rev 2018;60:15-31. https://doi.org/10.1016/j.cpr.2017.12.002.
- Jensen PS, Foster M. Closing the research to practice gap in children’s mental health: structures, solutions, and strategies. Adm Policy Ment Health 2010;37:111-19. https://doi.org/10.1007/s10488-010-0286-z.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2015. Canterbury: PSSRU, University of Kent; 2015.
- UNISON . National Joint Council for Local Government Services. National Agreement on Pay and Conditions of Service 2018. www.unison.org.uk/content/uploads/2018/07/NJC-Green-Book-18.pdf (accessed 10 January 2022).
- Office for National Statistics . Employee Earnings in the UK: 2018 2018. https://www.ons.gov.uk/employmentandlabourmarket/peopleinwork/earningsandworkinghours/bulletins/annualsurveyofhoursandearnings/2018 (accessed January 2021).
- Low Pay Commission . The Minimum Wage in 2018. Low Pay Commission Analysis 2018. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/695810/The_minimum_wage_in_2018_-_LPC_analysis.pdf (accessed January 2021).
Appendix 1 Changes to the protocol
| Changes to protocol | Date | Approved by |
|---|---|---|
| Protocol v2; 19 January 2017 was approved following several changes suggested by the REC. These changes included replacing the ADIS with a bespoke checklist for screening potential participants over the telephone, moving qualitative interviews for completion after the 6-month follow-up instead of before and providing more clarity in relation to exclusion criteria. Protocol v1 (14 December 2016) was, therefore, never approved by the REC | 10 February 2017 | North East – York Research Ethics Committee |
| Protocol v3; 21 April 2017 redefined the RCADS as one outcome measure, amended the wording of the exclusion criteria for clarity, made it clearer that the telephone screening checklist was based on the ADIS alongside revising the checklist wording, amended the procedure for monitoring and recording unblinding, removed references to the self-assessment tool for clinicians to complete and revised the procedure for fidelity checking to make it more practical | 5 May 2017 | North East – York Research Ethics Committee |
| Protocol v4; 8 January 2018 described the new consent process for taking part in a qualitative interview and added additional sources of trial promotion methods | 16 February 2018 | North East – York Research Ethics Committee |
| Protocol v5; 2 December 2019 described the completion of the new case report form to obtain information about additional diagnoses and treatments | 28 January 2020 | North East – York Research Ethics Committee |
Appendix 2 Qualitative interview topic guides
ASPECT qualitative interviews for participants: parents (exit and engager)
Introduction
-
Ensure that the patient has received and read the patient information sheet.
-
Recap the purpose of the ASPECT research, including the ethics review.
-
Explain the objective of the qualitative interview substudy.
-
Explain how the interviewee was selected.
-
Outline the content of the interview: it will not take longer than 60 minutes (parent) and if they want to stop for a break this will be OK.
-
Explain that if the interviewee does not want to answer a particular question then they should not feel under any pressure to do so.
-
Remind the interviewee that their answers will be confidential unless they disclose a risk to self or others.
-
Explain the purpose of digital recording and how the data will be anonymised and stored.
-
Emphasise that the mental health services that they receive will not be affected in any way.
-
Explain they will be sent a summary of findings when the study is completed.
-
Explain the consent process to the interviewee and ensure that they are still willing to take part.
-
Allow time for any other questions.
-
Take consent.
Phobia
-
Tell me about your child’s phobia and how it has affected their life (probe length and impact).
-
What has been the impact on your own life/your family’s life?
-
What help (if any) have you had in managing your difficulties (mental health services, GP, third sector, self-help books) (probe helpfulness/unhelpfulness).
Expectations
-
What were you broad expectations of treatment [probe not just the interventions we are delivering but more broadly, that is (1) what treatment they should get from the NHS and (2) what outcomes they might expect (e.g. help and support, helping them cope, major resolution of symptoms and complete cure)].
Preferences
-
When you first agreed to the study did you have a preference for the treatment you wanted to receive (probe reasons for preference)?
-
What were your expectations of the treatment you received (probe treatment in its own right, treatment that would help, just something to do and first impressions).
Engagement
-
What motivated you/stopped you from attending/engaging in treatment?
-
Could any of these things have been resolved?
-
What (if anything) might stop other children/families attending?
-
What type of family/child would this treatment most suit?
Intervention (engagers only)
-
What was your experience of the intervention like (probe whether or not it was helpful/unhelpful overall; was it easy/challenging; specific ways it helped/did not help with examples; was there anything missing)?
-
What was your child’s experience?
-
Do you think that you/your child experienced changes with the intervention (probe what had an impact; how did you change/not change; was this expected/not expected; the most important change)?
-
What do you think led to the changes you did/did not experience (probe how did the intervention work; how many sessions, mode of sessions face to face/telephone/mixed; was there anything important that happened outside treatment)?
-
What did you think about the health professional who supported you (probe any helpful/unhelpful aspects of their relationship; specific and non-specific factors)?
-
What was most helpful (if anything was): the person or the content of the intervention?
-
Is there anything that you think would make the intervention better (probe length of treatment, length of sessions, follow-up, etc.)?
Following the intervention (engagers only)
-
What did you do following the intervention (probe whether resolved or sought other treatment)?
-
How did your experience relate to your initial expectations (probe their decision-making about next steps)?
-
Would you recommend this treatment to others?
Ending
-
Thank participant for their time and information.
ASPECT qualitative interviews for health professionals
Introduction
-
Ensure the health professional has received and read the information sheet.
-
Recap the purpose of the ASPECT research, including the ethics review.
-
Explain the objective of the qualitative interview substudy.
-
Explain how the interviewee was selected.
-
Outline the content of the interview: it will not take longer than 60 minutes and if they want to stop for a break this will be OK.
-
Explain that if the interviewee does not want to answer a particular question then they should not feel under any pressure to do so.
-
Remind the interviewee that their answers will be confidential unless they disclose any evidence of malpractice, which may be reported to the relevant authority.
-
Explain purpose of digital recording and how the data will be anonymised and stored.
-
Emphasise that the mental health services that they work for will not be directly affected in any way but that the information supplied may help to improve patient services in future.
-
Explain that their views will remain confidential and not be passed on to other parties, including their employer.
-
Explain they will be sent a summary of findings when the study is completed.
-
Explain the consent process to the interviewee and ensure that they are still willing to take part.
-
Allow time for any other questions.
-
Take written consent (or confirm existing receipt of consent if conducting a telephone interview).
Phobia
-
What was your understanding of child phobia before beginning the trial (professional)?
-
Has the trial increased your awareness of children’s phobias (knowledge and understanding of treatment, etc.)?
-
Have you had any experience of treating phobias before (yes/no – if yes what in what setting? IAPT training? Public, private, third sector – what approach did you use – CBT or other)?
Expectations
-
What were your general expectations of delivering the OST/CBT treatment?
-
beneficial/non-beneficial intervention
-
interventions suitable/supportive enough
-
fit with services/professional support needs.
-
-
Did you have specific expectations about supervision and training for the trial?
-
How did these expectations differ from delivering treatment for other mental health problems/childhood anxiety disorders?
Preferences
-
When you first agreed to facilitate the study, did you have the chance to deliver CBT or OST? Did you have a preference for any one of these (probe reasons for preference – so why did you prefer this type of intervention?/past experiences with both – positive or negative)?
-
When children are allocated to this type of intervention, what if any would be your main reasons for accepting or not accepting them (probe type of treatment, workload commitment, service requirements/attitudes/personal preferences)?
Intervention
-
What was your opinion of the treatment you delivered (probe treatment in its own right, OST comparison with ‘full CBT’, first impressions)?
-
What did you think of the trial as a whole (standard of training, quality, structure and resources)?
-
What was your experience of delivering the intervention like (probe whether or not it was helpful/unhelpful overall; what did you find positive/negative about it; specific ways it helped/did not help with examples; was there anything missing)?
-
Were there any logistical issues/challenges experienced while delivering the intervention (accessibility/usability of information provided – workbook, work sheets – for you as the facilitator and for the patient)?
-
Personally, how effective do you think this intervention was?
-
What contributing factors led to the changes you experienced or did not experience (probe all sessions required, mode of sessions face to face/telephone/mixed, length of sessions – too long initially or too short; was there anything important that happened outside treatment)?
-
What did you think to the intervention manual/resources (probe thoughts on the manual – did they refer to it during sessions – what specifically they liked/disliked during and outside the sessions)?
-
Has delivering the (OST) intervention developed your clinical skills (probe how and in what way)?
-
Is there anything that you think would make the intervention better (probe length of treatment, length of sessions, follow-up, etc.)?
-
How easy was it to embed/integrate into your service (probe impact/logistical issues from practitioner level to team and service levels – if known)?
-
Given the choice, would you continue to deliver this treatment?
Ending
-
Thank the participant for their time and information.
ASPECT qualitative interviews for participants: child (exit and engager)
Introduction
-
Ensure that the child has received and read the children’s patient information sheet.
-
Explain the aim of the chat today.
-
Outline what the meeting will be like (drawing/chat); explain that it will not take longer than 30 minutes and if they want to stop this will be OK.
-
Explain that if the child does not want to answer a particular question then that is OK. Explain the purpose of digital recording and what happens to the recording that you make.
-
Emphasise that the people who they met for their treatment will not be affected in any way.
-
Explain that we will let all children in the study know what we find.
-
Ensure that they are still willing to take part.
-
Allow time for any other questions.
-
Take child and parent consent.
Phobia (use drawings where children choose)
-
Tell me a little about why you are here. What are you scared of/what did we see you about?
-
How has this affected you? What can you do/not do, how do you feel?
-
Who helps you the most? How?
-
Is there anyone else who can help/has helped? How?
-
What help (if any) have you had before (parents, friends, other people, health services) in managing your difficulties (mental health services, GP, third sector, self-help books) (probe helpfulness/unhelpfulness)?
Expectations
-
How much did you know/were you told before you met [clinician’s name]?
-
What did you think you were going to do when you came for help/saw [clinician’s name]?
-
Was it different from what you thought?
-
Did you look forward to coming? Why?
-
Could we have made things easier/better for you in any way? How?
-
Do you think other children would like to come? Why?
-
What type of family/child would like it the most?
Intervention (engagers only)
-
What did you do with [clinician’s name]? Probe whether or not it was helpful/unhelpful overall; was it easy/challenging; specific ways it helped/did not help with examples.
-
Do you think it has made a difference to you (probe what had an impact; how did you change/not change; was this expected/not expected; the most important change)?
-
What do you think led to the changes you have just told me about (probe how did the intervention work; was there anything important that happened outside treatment)?
-
Do you think the treatment was long enough? Would you like to have had more? How much more?
-
What did you think of [clinician’s name] who supported you (probe any helpful/unhelpful aspects of their relationship; specific and non-specific factors)?
-
Is there anything that you think would make the intervention better (probe length of treatment, length of sessions, follow-up, etc.)?
Ending
-
Thank the participant for their time and information.
Appendix 3 Summaries of unblinding cases by treatment group
| Characteristic | Treatment group, n (%) | All (N = 34), n (%) | |
|---|---|---|---|
| CBT (N = 14) | OST (N = 20) | ||
| Total number of unblinding incidents | 14 (100) | 20 (100) | 34 (100) |
| Number of participants with an unblinding incident | 13 (93) | 16 (80) | 29 (85) |
| Source of unblinding | |||
| Participant | 4 (29) | 9 (45) | 13 (38) |
| Therapist | 5 (36) | 4 (20) | 9 (26) |
| Other | 5 (36) | 7 (35) | 12 (35) |
| Reason for unblinding | |||
| Accidental | 12 (86) | 19 (95) | 31 (91) |
| Other | 2 (14) | 1 (5) | 3 (9) |
| Method of unblinding | |||
| Face to face | 3 (21) | 5 (25) | 8 (24) |
| Telephone | 6 (43) | 9 (45) | 15 (44) |
| 4 (29) | 5 (25) | 9 (26) | |
| Other | 1 (7) | 1 (5) | 2 (6) |
| Suspected group | |||
| Definitely OST | 0 (0) | 15 (75) | 15 (44) |
| Probably OST | 0 (0) | 2 (10) | 2 (6) |
| Definitely CBT | 11 (79) | 2 (10) | 13 (38) |
| Probably CBT | 3 (21) | 1 (5) | 4 (12) |
| Correctly suspected group | |||
| No | 0 (0) | 3 (15) | 3 (9) |
| Yes | 14 (100) | 17 (85) | 31 (91) |
Appendix 4 Fidelity assessment of strategies used in the recorded sessions
| Treatment group | Participant ID | Strategies used in the session (n) | Percentage achieved | Fidelity classification |
|---|---|---|---|---|
| OST | 02–061 | 12 | 92.3 | High |
| OST | 02–069 | 8 | 61.5 | Moderate |
| OST | 06–037 | 13 | 100.0 | High |
| OST | 06–040 | 11 | 84.6 | High |
| CBT | 01–012 | 11 | 84.6 | High |
| CBT | 02–020 | 13 | 100.0 | High |
| CBT | 02–024 | 13 | 100.0 | High |
| CBT | 02–059 | 8 | 61.5 | Moderate |
| CBT | 06–009 | 12 | 92.3 | High |
| CBT | 06–015 | 9 | 69.2 | Moderate |
| CBT | 06–028 | 13 | 100.0 | High |
| CBT | 06–033 | 8 | 61.5 | Moderate |
| CBT | 06–038 | 8 | 61.5 | Moderate |
| CBT | 06–041 | 7 | 53.8 | Moderate |
| CBT | 06–043 | 7 | 53.8 | Moderate |
Appendix 5 Fidelity assessment of competence for the recorded sessions
| Treatment group | Participant ID | Total score | Average score | < 2 scored |
|---|---|---|---|---|
| OST | 02–061 | 58 | 4.5 | 0 |
| OST | 02–069 | 55 | 4.2 | 0 |
| OST | 06–037 | 57 | 4.4 | 0 |
| OST | 06–040 | 56 | 4.3 | 0 |
| CBT | 01–012 | 64 | 4.9 | 0 |
| CBT | 02–020 | 83 | 6.4 | 0 |
| CBT | 02–024 | 83 | 6.4 | 0 |
| CBT | 02–059 | 62 | 4.8 | 0 |
| CBT | 06–009 | 75 | 5.8 | 0 |
| CBT | 06–015 | 73 | 5.6 | 0 |
| CBT | 06–028 | 55 | 4.2 | 0 |
| CBT | 06–033 | 67 | 5.2 | 0 |
| CBT | 06–038 | 68 | 5.2 | 0 |
| CBT | 06–041 | 75 | 5.8 | 0 |
| CBT | 06–043 | 68 | 5.2 | 0 |
Appendix 6 Unit costs
| Item | Unit cost (£) | Source | ||
|---|---|---|---|---|
| At homea | At clinic/surgery | Via telephone/e-mail | ||
| GP | 44.12 | 37.40 | 37.70 | PSSRU 201875 (chapter 10.3, 10.4) |
| Community nurseb | 33.72 | 27.00 | 27.00 | PSSRU 201875 (chapter 6.1) |
| Community paediatrician | 44.12 | 37.40 | 37.70 | PSSRU 201875 (chapter 10.3, 10.4) |
| Child development centre | 20.72 | 14.00 | 14.00 | PSSRU 201875 (chapter 11.5) |
| NHS Direct | – | – | 6.00 | PSSRU 201875 (chapter 10.5) |
| NHS walk-in centre | – | 54.00 | – | PSSRU 2015117 (chapter 7.1) |
| Social services youth worker | 28.72 | 22.00 | 22.00 | PSSRU 201875 (chapter 11.2) |
| Social care workerb | 28.72 | 22.00 | 22.00 | PSSRU 201875 (chapter 11.2) |
| Helplinec | – | – | 6.00 | PSSRU 201875 (chapter 10.5) |
| Item | Unit cost (£) | Source |
|---|---|---|
| Child psychiatrist | 227.00 | Reference costs 2018/1974 (service code 711: Child and Adolescent Psychiatry) |
| Child psychotherapist | 91.00 | PSSRU 201875 (chapter 6.15) |
| Child psychologist or clinical psychologista | 212.00 | PSSRU 201875 (chapter 9) |
| Mental health nurse or CAMHS therapistb | 59.00 | PSSRU 201875 (chapter 10.1) |
| Family therapist | 31.00 | PSSRU 201875 (chapter 6.9) |
| Item | Unit cost (£) | Source |
|---|---|---|
| Accident and emergency | 133.00 | Reference costs 2018/1974 (service code: T01NA) |
| Urgent care centre | 53.00 | Reference costs 2018/1974 (service code: T04NA) |
| Outpatient visit | 148.00 | Reference costs 2018/1974 (national average) |
| Inpatient stay: knee fracture | 1604.00 | Reference costs 2018/1974 (HRG code: HE21G) |
| Inpatient stay: asthma | 1292.00 | Reference costs 2018/1974 (HRG code: PD12C) |
| Inpatient stay: suspected JIA | 1973.00 | Reference costs 2018/1974 (HRG code: PH34D) |
| Item | Chemical name | Dose | Unit cost (£ per quantity) | Source |
|---|---|---|---|---|
| Equasym XL_Cap 20 mg | Methylphenidate hydrochloride | 20-mg capsule (once daily) | 1.00 | PCA 201876 (0404000M0BCAEAQ) |
| Clenil Modulite_Inha 50 µg | Beclometasone dipropionate | 50 µg (two puffs daily) | 3.70 | PCA 201876 (0302000C0BPAABE) |
| Melatonin_Tab 2 mg | Melatonin | 2-mg tablet (once daily) | 1.69 | PCA 201876 (0401010ADAABKBK) |
| Fluoxetine HIC_Cap 20 mg | Fluoxetine hydrochloride | 20-mg capsule (once daily) | 0.02 | PCA 201876 (0403030E0AAAAAA) |
| Salbutamol_Inha 100 µg | Salbutamol | Two puffs of 100 µg inhaler (as required) | 1.57 | PCA 201876 (0301011R0AAAAAA) |
| Propranolo HIC_Tab 10 mg | Propranolol hydrochloride | 10-mg tablet (as required) | 0.07 | PCA 201876 (0204000R0AAAHAH) |
| Cetirizine HCl_Tab 10 mg | Cetirizine hydrochloride | 10-mg tablet (once daily) | 0.03 | PCA 201876 (0304010I0AAAAAA) |
| Movicol_Paed Pdr Sach | Macrogol 3350 | 6.9-g sachet (two sachets per day) | 0.15 | PCA 201876 (0106040M0BBAIAB) |
| Montelukast_Tab 10 mg | Montelukast | 10-mg tablet (once daily) | 0.04 | PCA 201876 (0303020G0AAABAB) |
| Calceos_Tab | Colecalciferol | 500-mg tablet (twice daily) | 0.06 | PCA 201876 (0906040G0BQAABW) |
| Item | Unit cost (£ per hour) | Sourcea |
|---|---|---|
| Educational psychologist | 23.20 | NJC Green Book 2018 (SCP 49)118 |
| Education welfare officer | 12.00 | NJC Green Book 2018 (SCP 25)118 |
| School or college nurse | 12.00 | NJC Green Book 2018 (SCP 25)118 |
| Item | Unit cost | Source |
|---|---|---|
| Privately paid mental health services | £360 per session | www.psychiatry-uk.com/fees/ (accessed January 2021) |
| Item | Unit cost | Source |
|---|---|---|
| Average weekly earnings of people in the UK | £522 per week | Office for National Statistics 2018119 |
Appendix 7 EuroQol-5 Dimensions Youth version responses by treatment group by data collection time point
| EQ-5D-Y dimension | Baseline, n (%) | 6 months, n (%) | ||||
|---|---|---|---|---|---|---|
| Level 1 | Level 2 | Level 3 | Level 1 | Level 2 | Level 3 | |
| Mobility | 87 (89.7) | 9 (9.3) | 1 (1.0) | 89 (91.8) | 7 (7.2) | 1 (1.0) |
| Self-care | 86 (88.7) | 7 (7.2) | 4 (4.1) | 87 (89.7) | 10 (10.3) | – |
| Usual activity | 63 (64.9) | 31 (32.0) | 3 (3.1) | 79 (81.4) | 16 (16.5) | 2 (2.1) |
| Pain/discomfort | 61 (62.9) | 36 (37.1) | – | 70 (72.2) | 24 (24.7) | 3 (3.1) |
| Anxiety/depression | 44 (45.4) | 43 (44.3) | 10 (10.3) | 55 (56.7) | 36 (37.1) | 6 (6.2) |
| EQ-5D-Y dimension | Baseline, n (%) | 6 months, n (%) | ||||
|---|---|---|---|---|---|---|
| Level 1 | Level 2 | Level 3 | Level 1 | Level 2 | Level 3 | |
| Mobility | 82 (85.5) | 13 (13.5) | 1 (1.0) | 86 (89.6) | 10 (10.4) | – |
| Self-care | 85 (88.5) | 11 (11.5) | – | 86 (89.6) | 10 (10.4) | – |
| Usual activity | 65 (67.7) | 27 (28.1) | 4 (4.2) | 76 (79.2) | 19 (19.8) | 1 (1.0) |
| Pain/discomfort | 61 (63.5) | 30 (31.3) | 5 (5.2) | 69 (71.9) | 25 (26.0) | 2 (2.1) |
| Anxiety/depression | 43 (44.8) | 47 (49.0) | 6 (6.2) | 49 (51.0) | 40 (41.7) | 7 (7.3) |
Appendix 8 Child Health Utility 9D responses by treatment group by data collection time point
| Response | Time point, n (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 6 months | |||||||||
| Level 1 | Level 2 | Level 3 | Level 4 | Level 5 | Level 1 | Level 2 | Level 3 | Level 4 | Level 5 | |
| Worried | 20 (44.4) | 16 (35.6) | 7 (15.6) | – | 2 (4.4) | 22 (48.9) | 12 (26.7) | 5 (11.1) | 3 (6.7) | 3 (6.7) |
| Sad | 32 (71.1) | 8 (17.8) | 2 (4.4) | 2 (4.4) | 1 (2.2) | 29 (64.4) | 6 (13.3) | 5 (11.1) | 4 (8.9) | 1 (2.2) |
| Annoyed | 27 (60.0) | 13 (28.9) | 4 (8.9) | – | 1 (2.2) | 27 (60.0) | 10 (22.2) | 5 (11.1) | – | 3 (6.7) |
| Tired | 9 (20.0) | 15 (33.3) | 8 (17.8) | 5 (11.1) | 8 (17.8) | 12 (26.7) | 13 (28.9) | 9 (20.0) | 5 (11.1) | 6 (13.3) |
| Pain | 28 (62.2) | 6 (13.3) | 6 (13.3) | 3 (6.7) | 2 (4.4) | 21 (46.7) | 11 (24.4) | 4 (8.9) | 2 (4.4) | 7 (15.6) |
| Sleep | 21 (46.7) | 12 (26.7) | 5 (11.1) | 3 (6.7) | 4 (8.9) | 20 (44.4) | 3 (6.7) | 7 (15.6) | 9 (20.0) | 6 (13.3) |
| Daily routine | 23 (51.1) | 12 (26.7) | 4 (8.9) | 3 (6.7) | 3 (6.7) | 19 (42.2) | 11 (24.4) | 7 (15.6) | 4 (8.9) | 4 (8.9) |
| Work | 27 (60.0) | 15 (33.3) | 2 (4.4) | 1 (2.2) | – | 23 (51.1) | 11 (24.4) | 7 (15.6) | 1 (2.2) | 3 (6.7) |
| Able to join activities | 23 (51.1) | 6 (13.3) | 10 (22.2) | 3 (6.7) | 3 (6.7) | 10 (22.2) | 14 (31.1) | 10 (22.2) | 9 (20.0) | 2 (4.4) |
| Response | Time point, n (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 6 months | |||||||||
| Level 1 | Level 2 | Level 3 | Level 4 | Level 5 | Level 1 | Level 2 | Level 3 | Level 4 | Level 5 | |
| Worried | 34 (66.7) | 8 (15.7) | 3 (5.9) | 2 (3.9) | 4 (7.8) | 33 (64.7) | 6 (11.8) | 7 (13.7) | 1 (2.0) | 4 (7.8) |
| Sad | 40 (78.4) | 5 (9.8) | 2 (3.9) | 1 (2.0) | 3 (5.9) | 37 (72.5) | 5 (9.8) | 5 (9.8) | 1 (2.0) | 3 (5.9) |
| Annoyed | 37 (72.5) | 7 (13.7) | 4 (7.8) | 2 (3.9) | 1 (2.0) | 34 (66.7) | 10 (19.6) | 5 (9.8) | – | 2 (3.9) |
| Tired | 14 (27.5) | 19 (37.3) | 5 (9.8) | 3 (5.9) | 10 (19.6) | 17 (33.3) | 19 (37.3) | 4 (7.8) | 7 (13.7) | 4 (7.8) |
| Pain | 33 (64.7) | 9 (17.6) | 3 (5.9) | 1 (2.0) | 5 (9.8) | 28 (54.9) | 9 (17.6) | 7 (13.7) | 3 (5.9) | 4 (7.8) |
| Sleep | 26 (51.0) | 10 (19.6) | 6 (11.8) | 3 (5.9) | 6 (11.8) | 23 (45.1) | 8 (15.7) | 8 (15.7) | 4 (7.8) | 8 (15.7) |
| Daily routine | 29 (56.9) | 8 (15.7) | 4 (7.8) | 4 (7.8) | 6 (11.8) | 24 (47.1) | 15 (29.4) | 7 (13.7) | 3 (5.9) | 2 (3.9) |
| Work | 34 (66.7) | 7 (13.7) | 6 (11.8) | 1 (2.0) | 3 (5.9) | 33 (64.7) | 10 (19.6) | 5 (9.8) | 3 (5.9) | – |
| Able to join activities | 30 (58.8) | 6 (11.8) | 5 (9.8) | 4 (7.8) | 6 (11.8) | 24 (47.1) | 8 (15.7) | 6 (11.8) | 8 (15.7) | 5 (9.8) |
Appendix 9 Summary coding tables
| Theme | Codes | Key messages and quotations |
|---|---|---|
| Child’s conceptualisation of phobia |
|
Children attributed the origin of their phobia either behaviourally or as a result of an external trigger/precipitating event. They also felt that phobias were not prioritised by others as a high priority in the health hierarchy:I had a lot of when I kind of mentioned cos I had to go out school sometimes to go to the counselling things and then and they were a bit like ‘where are you going?’. I’m like ‘oh yeah I’ve got a phobia of needles’ and they’re like ‘why don’t you just have it? it isn’t that bad’, and then you kind of think, ‘am I just being dramatic?’. You kind of feel a bit bad about it. Yeah, yeah a bit kind of embarrassed I feel like I should be able to have this, why can’t I have this? It just doesn’t feel too greatFemale, 15 years old, needle phobia |
| Motivation to seek help |
|
Children were motivated to seek help as a result of their phobia impacting their health, family functioning, school functioning and social functioning. They also described how they had not sought help previously because of their perception of phobias being at a lower level in the health hierarchy or had received ineffective support previously:Well ever since I was little, I’ve been running into roads to avoid them. And it was, it was getting to the point where it probably needs sorting out, otherwise something dangerous could have happenedFemale, 16 years old, dog phobiaNo, ’cause I didn’t know it was available, so I didn’t even know it was a thing. So, I’d never gone to anyone. Even people I’d spoken to about it, I hadn’t even realised it was a thingFemale, 16 years old, vomit phobia |
| Child and family coping |
|
Children described accommodation, avoidance and ignoring/delaying exposure as the most common ways they used to manage their phobia. They described how this had affected their relationship with their family and things not working when their parents tried to help them with their phobia:Well I couldn’t watch certain TV programmes. I couldn’t go into some shops. And they even appeared on websites too, which means, so it meant we had to be careful where we lookedFemale, 10 years old, puppet phobiaWell, my mum and dad tried to help me go under the high roofs of like the bits I was scared of, to try to overcome my fear of it. But it didn’t really workMale, 10 years old, high ceilings phobia |
| Goals of OST |
|
Children hoped that OST would help them to feel less anxious about their phobia and reduce the impact that it was having on their life:I looked forward to it in the sense that I really wanted to overcome the fear because it was getting to a point where it was completely starting to take over my lifeFemale, 16 years old, vomit phobia |
| Perceived efficacy |
|
Children often took a practical approach in their perception of how effective OST would be. They tended to view it as an opportunity to develop skills to reduce the impact it was having on their life:I was expecting it to sort of like ease the like impact it had on my life and be able to like give me methods to cope with it rather than just avoidance behaviours, ‘cause that isn’t really healthy and it gets in the way of things I want to doFemale, 16 years old, vomit phobia |
| Process |
|
Children whose parents had been present during the session felt that it benefited them because it helped them to feel more comfortable around new people. They also liked that they were able to be in control when designing the session and at each point during the exposure session:I mean for yeah for me it was useful kind of having someone there ’cause of course I don’t know [therapist name] that well I don’t – didn’t know the nurse that well so having someone that I know really well as support is something really useful for me anywayFemale, 15 years old, needle phobiaIt was definitely a well thought out, more like, well designed intervention. And the actual like getting, having more control over it, meant it felt more like personalised and you were in controlMale, 15 years old, needle phobiaChildren highlighted the importance of having a therapist who was empathetic and understanding during the process:They were understanding, they were patient, they were listening. They were very, very understanding of the situationMale, 12 years old, needle phobiaChildren highlighted the efficiency of OST in comparison to CBT:If you were to go through the CBT, you’d be going back and forward and then there’s petrol and then there’s work and then there’s school. And all these things that need to be taken into consideration. But, with the one-session treatment, it’s half a day. You’re doneFemale, 16 years old, vomit phobia |
| Child benefits |
|
Children reported a greater sense of understanding about their phobia and reduced anxiety, and this had helped to manage their phobia and improve their relationships with others:Because it helped me to understand why I was scared of them. It might sound weird but I never really knew why I was scared of them. So I was scared of them, up until now I didn’t know whyFemale, 10 years old, puppet phobiaYou get braver and braverMale, 7 years old, dog phobiaIt’s just made my life so much less stressful you know, like I don’t have to worry about so many thingsFemale, 15 years old, vomit phobiaYeah – I feel a lot happier in myself as a person and around other people. And I think people feel more relaxed around me – like they don’t have to constantly be like, like, worrying about what they say or anythingFemale, 16 years old, vomit phobia |
| Accessibility |
|
Children highlighted the importance of being in a place of acceptance of their phobia to be able to access and fully benefit from the treatment:I would only recommend it, if the person had kind of accepted their phobia and understood their phobia and felt ready to kind of deal with it, obviously (yeah) ’cause I feel like with the one-session treatment you have to be aware of how you’re feeling and you have to not be in denial about how you are, urm and yeah of course if I knew someone that was like thatFemale, 15 years old, vomit phobia |
| Suitability |
|
Children felt that it would be important to make sure OST was suitable, and the complexity of phobia, the presence of comorbidities and additional needs, and age would be factors in this owing to the intensity of the session:I suppose with dogs you get people who aren’t only afraid of dogs but pictures so if it’s like that when they can’t even see one, that might be a bit harder than like might be easier to take it a lot slowlyFemale, 15 years old, dog phobiaAfter like an hour and a half to 2 hours I got really like ’cos I’ve, with me having ADHD and only sitting like I get where he can’t sit for ages . . . and with us sitting there for a long time I get, I kept walking around the room so I just trying to distract myselfMale, 10 years old, choking phobiaFor some people it might again, the attention span thing cos I’m, I’m quite good at keeping my concentration sometimes urm like for this I can, my concentration will do it. So that wasn’t too bad but then for some people again like younger kids might be quite hard to retain itFemale, 15 years old, needle phobia |
| Post-therapy reflection |
|
Children felt that OST would be suitable for children with phobias and would cite their own experience when recommending it to others. They felt that it was important to manage expectations and view OST as a way to learn tools to manage their phobia as opposed to an overall cure. They described short-term and long-term effects on the phobia and being able to transfer this knowledge to other anxiety-provoking situations. They suggested that having a follow-up session would be helpful and a short break during the session to manage the intensity if needed:I think probably ones who were like me and really, really, really scared and then try to avoid things and then come and get a bit better at itFemale, 7 years old, dog phobiaSo yeah of course I would recommend it, because it worked for me and I’ve had so many people try and help me and have nothing work, so if this worked for me I feel like it would work for a lot of other people, because not a lot has worked for meFemale, 15 years old, vomit phobiaI just wouldn’t say my fear has gone, my fear of it is still the same but my control over that fear has got betterFemale, 15 years old, needle phobiaI still get quite worked up about come quite distressed about my mocks because of my GCSEs [General Certificate of Secondary Education] (yeah) and they’re stressful but I was doing some breathing this morning as well kind of just going up on my way to school cos getting quite worked up and it is it was the kind of the same thing where I went, I was quite nerv[ous], no before my exam, I went through my exam it wasn’t as bad as I thought it would be and then I’ve calmed myself down at that point so it yeah, useful thingsFemale, 15 years old, needle phobiaHaving a follow up if it was about 2 or 3 weeks after (yeah) just to kind of go through what I’ve been through, but not at the same length of time, not for 3 hours. But, just to kind of go back through it so you’ve still got it in your brain. Um. But, apart from that, I think everything was really goodFemale, 16 years old, vomit phobia |
| Theme | Codes | Key messages and quotations |
|---|---|---|
| Parent’s conceptualisation of phobia |
|
Parents attributed the origin of their child’s phobia behaviourally, as a result of health issues, and viewed phobias as low priority in the health hierarchy compared with other conditions:We genuinely thought it would be something she’d just grow out of and then as it came to a time for her to have vaccinations at school it became very apparent she wasn’t growing out of itParent/guardian, 15-year-old girl, needle phobiaThat’s when the incident with the dog first happened when she was – we were walking past a man with a dog that was very well known for not being a very nice dog and we were walking past. I grabbed hold of my other daughter, [sibling name], and [sibling name] grabbed hold of [child name]. But the dog just lunged for [child name] and it was a huge Akita-type dog and it went to bite her and just missed her by centimetres and from that day it just escalated. [Child name] fear was just, phobia, not fear, that was when it startedParent/guardian, 12-year-old girl, dog phobiaHe’s had all his vaccinations done and he was very ill as a child, because he got Strep B, when he was born and then he had Quinsy when he was 2. So I think that’s where the needle phobia came from, to be honest, he’s had all his vaccinations, but I think that’s due to because him being so young and not so aware. Obviously as he’s got older they get more of an opinion and they obviously can’t restrainParent/guardian, 12-year-old boy, needle phobiaI was also aware that the NHS don’t offer huge amount of support to kids as well, it’s not that they don’t want to, it’s just that there aren’t enough resources and I know that, that [child name] anxiety needs would not be huge compared to other kids and so I thought she would be at the bottom of a list and it wouldn’t really be a priority so I didn’t have huge expectationsParent/guardian, 8-year-old girl, dog phobia |
| Motivation to seek help |
|
Parents motivation to seek help focused on where the phobia affected their child’s health, family functioning, school functioning and social functioning. They described the challenges that they had faced in accessing timely support:I mean the in the street, if there was insects and it got to the point where I was worried for her safety because, I know she’s old enough not to run into the road, but she was almost kind of losing her mind, and it was a worry that she was going to progress to running into the road to get away from insectsParent/guardian, 12-year-old girl, insect phobia[Child name] has a needle phobia and it’s really affected her because obviously she suffers from a syndrome and therefore needs regular blood tests regarding her kidney function, plus other blood tests that need doing. She also needs like procedures doing, which obviously is dye injected in and stuff like that, so it’s all needlesParent/guardian, 12-year-old girl, needle phobiaAs I said it was just getting worse and worse, it was just getting to a point, it was just so hard it was just getting, every day was an argument just to get out the houseParent/guardian, 7-year-old boy, dog phobiaShe wasn’t wanting to go to school on the days they were even discussing the injection. She certainly didn’t want to be around when they were having themParent/guardian, 15-year-old girl, needle phobiaShe didn’t want to go to friends’ houses or family where there was dogs. So it was starting to really have an impact on, on all of usParent/guardian, 7-year-old girl, dog phobiaEveryone knows that CAMHS is there to support mental health, but you don’t consider a phobia to be part of the mental health. No one speaks about phobias, especially when it’s things like dogs because they just, people’s attitude towards [child name] was just, ‘Oh, it’s just a dog, it’s not gonna hurt you. Get on with it’ and, I don’t know, it’s just differentParent/guardian, 12-year-old girl, dog phobia |
| Parent and family coping |
|
Parents identified accommodation, ignoring/delaying exposure and minimising as the ways that they had coped with managing the phobia. They described the challenges and process of doing this as burdensome and this impacted the relationship and trust with their child:It became more extreme over recent years, like going, because we walk to school through the park, but then we had to stop doing that because she was screaming absolutely terrified and we had to avoid places like the beach and things like thatParent/guardian, 7-year-old girl, dog phobiaIt’s distressing ’cause I don’t like to see him unhappy and then it creates that worry around – you know – there’s still a meningitis jab that he hasn’t had. So there’s that kind of worry, ’cause I’m sort of, trying to do the best for his health and that’s sort of a bit of a contradiction if he’s not had that vaccination isn’t it? So – and then the dental – the issue around the dental about making life much more complicated. ’Cause he had to have an operation under general anaesthetic which – you know, I don’t believe in unnecessary surgery, so that sort of goes against some values but at the same time we have to compromise sometimes because I couldn’t see what the other options were reallyParent/guardian, 15-year-old boy, needle phobia |
| Goals of OST |
|
Parents hoped that their child receiving OST would help to reduce their child’s anxiety, support them in feeling more equipped to support their child with the phobia and improve their relationship with their child:I really wanted her to be able to find ways of managing anxiety, because she was upset by the fact that she’s scared of dogsParent/guardian, 8-year-old girl, dog phobiaI was just hoping that I’d get some advice on how to deal with [child name]’s phobiaParent/guardian, 12-year-old girl, dog phobiaJust to be able to do stuff instead of having to plan it and argue about itParent/guardian, 7-year-old boy, dog phobia |
| Perceived efficacy |
|
There were mixed views around whether or not they felt that OST would be effective. Some parents were sceptical about whether or not it would meet their child’s needs and often adopted a more cautious approach to protect them and their child from disappointment. Parents who believed that it would work cited their own understanding of phobia treatment and what they had seen in television programmes:I’ve seen things like the Speakmans [(British therapists who attempt to treat phobias on television) ITV Studios, London, UK] on TV [television], don’t know if you’ve heard of them? It’s on This Morning [(British daytime televsion show) ITV Studios, London, UK] on TV and they just do very quick sessions with people and just seem to have some really good resultsParent/guardian, 10-year-old girl, needle phobiaI thought it would help her, but from the other side I was a bit scared at how can you treat a phobia, especially the one she had, when it so common. And you are just like sort of – you are facing it every single day, because they are – obviously the flies everywhere. How can you treat it with just one session? So I was hoping it would help her, but I just – like I was in doubt [laughs] yeah that we might need some extra help after thatParent/guardian, 9-year-old girl, insect phobia |
| Process |
|
Parental involvement in the intervention varied from participant to participant, and appeared to be determined largely by clinician preference. Parents who had been present during therapy felt that it had helped them to understand more about their child’s phobia and how to support them. Parents who were not able to be present also confirmed this view:[Child name]’s got separation anxiety disorder, and for us we felt as though the study wasn’t handled very well that way, because all of a sudden it went from talking to you guys, sat in a room all together, he knew what was happening, to all of a sudden, then he had to go sit in a room for an hour and half away from us, while we sat in a waiting room. And what we was worried about is, that this anxiety of being separated away from us is now going to mask or totally knock off what he was there forParent/guardian, 12-year-old boy, needle phobiaI think it was useful us being there because when [child name] had that initial anxiety about each additional step, I think it was beneficial for her for us to be there to assist with her and just offer those kind of words of comfort which [therapist name] was doing. But knowing that we were there – it was useful having that input in that side of things as well, not only the design of it, but also being there to assist in supporting [child name]Parent/guardian, 7-year-old girl, dog phobiaParents liked the fact that their child was in control during the planning and exposure session. They also appreciated that the therapy took a more active and targeted approach instead of just talking:We felt that her wishes were completely respected at all times. And so there was no point during those injections did I feel that [child name] would have one against her will. You know there was never – it was made very clear to [child name] she could say no at any point. I mean obviously once the needle’s in then it’s too late but you know we understand the practicalities of that but you know up until that point and she could have said no and we felt 100% confident that [therapist name] would have stopped it. And I think that’s really important, I think to have that confidence in somebody, especially with the needle phobia because that element of control is super important I think. So yes it was great, it was really positiveParent/guardian, 15-year-old girl, needle phobiaIt was targeted to the actual problem in a practical way, which really works well with a young person. I think talking just seems, yeah talking it’s just I don’t know. It’s just not as effective as something that’s a real, practical, phobia. You know, you can see it, you can smell it, you can touch it, and you have the same sort of treatment. That it’s tactile rather than wordsParent/guardian, 15-year-old girl, vomit phobiaWhen you’re setting up the hierarchy, that was really interesting, ’cause that’s – I think that’s one of the benefits of this type of therapy, is it’s generated by the person themselves isn’t it? So it is something that is personal to them, which I think is one of the really good things about thisParent/guardian, 15-year-old boy, needle phobiaParents reported that having a skilled therapist who built a positive relationship with their child and adapted their language appropriately was beneficial:He worked quite closely with her. It wasn’t, sort of, a teacher–student relationship over a desk or anything. They were sat together. You know, so it was very much like a team. It was side by side, ‘We’re gonna do this together, come on, let’s do what we can do and let’s move on’. You know, ‘You’ve done really well there, great, let’s move on to the next step’ kind of thingParent/guardian, 10-year-old girl, needle phobiaParents/guardians reported that the single-session nature of OST would be beneficial because it would reduce interruption to school and work commitments:I think for me, it was the one-session treatment. The reason being with like [child name]’s medical issues, we’ve already missed quite a lot of school for appointments and time-off with illness and you know, various things and so to me like a 2-hour block out of school, or whatever was better than, I don’t know, 6 or 8 half hourParent/guardian, 7-year-old girl, dog phobia |
| Child benefits |
|
Parent/guardians reported that following OST children had an increased knowledge and education about their phobia, increased confidence and reduced anxiety:I think primarily [therapist name] explaining to [child name] what her reaction was with dogs and how she could understand that and cope with it. I think was really important because that was really helpful for [child name] because she’s bright, she’s articulate, she’s intelligent, she knows, she was able to understand the things that were explained to her by [therapist name], I think that really helpedParent/guardian, 7-year-old girl, dog phobiaI think confidence that [name] knows that, that she can push herself and that some things that cause her huge anxiety, that you don’t have to be as anxiety provoking. As soon as she thought they were gonna be – and actually can be strong, she can be brave. I think there’s that and that not everything’s gonna end up being a disaster, even things that are a bit scary, doesn’t actually end up being that scary and what it boils down to itParent/guardian, 8-year-old girl, dog phobia |
| Accessibility |
|
Parents/guardians identified physical barriers to accessing treatment, such as lack of transport and needing to take time out of school/work commitments. They also highlighted the emotional barriers and that this type of therapy may be overwhelming. This was particularly prevalent for children with additional needs and comorbidities:You’ll have to take a bit of time off school, most kids won’t mind that. I suppose if – I work part time, so it wasn’t so much of an issue really for me, but perhaps some parents, if they work full time, it might be inconvenient to take their kids to some of them. But if it is an actual phobia, I would imagine it impacts on those families lives anyway. You know, if it’s significant enough to try and get help for it then, I would imagine you’re prepared to invest some time in it as wellParent/guardian, 12-year-old girl, insect phobiaIf they’re already anxious about something, why would they want to put their self in that situation? You know, if someone’s scared of something, it takes some courage to go and actually face that fear and I think that’s what would probably stop most people. If they’re not gonna go there, it’s for that reasonParent/guardian, 10-year-old girl, needle phobiaI think it depends on the individual. For anybody with a phobia I think – it depends I suppose, on if the child’s got any additional needs or any other problems. They might find it too much in one 3-hour period. Might be a bit overwhelmingParent/guardian, 10-year-old boy, blood phobia |
| Suitability |
|
Parents of children with additional needs and comorbidities discussed their concerns around the suitability of OST for this population and that necessary adaptions that should be made:P:Yes, I hoped he would get the more extended sessions because I know what he’s like and a one hit wonder was not going to be enough for himI:So the cognitive behavioural therapy?P:Yes, yes because he – when we’re teaching him anything its repetitive works better for him. Like for instance even maths tables he’s been absolutely perfect with his tables, if you leave it for a little while and go back and revisit it a lot of its fallen out and we have to start again. So that seems to be how he learns, by a lot of repetition. So a one hit wonder to me it was a bit disappointing because I thought, well this isn’t going stick but that’s what I felt sureParent/guardian, 9-year-old boy, insect phobiaI think you need to get to know the family and the child just a little bit more if you’re offering this session of what works for this child and this family. Because as you know autism is a massive spectrum and what works for one, might not work for the otherParent/guardian, 12-year-old boy, blood phobia |
| Parent benefits |
|
Parents felt that they had experienced benefits in terms of an improved perception of their child’s behaviour, increased skills in being able to support them and an improvement in their child’s QoL:Because, I think it gives the child and the parent a clearer insight into exactly what’s wrong. And that 3-hour intensive session made me a lot more aware of how bad it was and what was actually going onParent/guardian, 10-year-old boy, blood phobiaGetting her to use the skills she’d learnt and I could tell how thrilled she was that she’d managed to do it. And the relief on her face when she realised she’d had it done and the relief when she realised it wasn’t as bad as she’d anticipated. And then when she had the second and then the third she was much, much, more relaxedParent/guardian, 15-year-old girl, needle phobiaI feel like I can at least support her now in that and I can say ‘Well, what if you just wait 10 minutes?’, she probably won’t pass out. Or, you know, if you can, you know, ‘[child name], what needle would you like?’. And give her that voice to say what she would like, ’cause sometimes with the best will in the world, they’ll rush in, they don’t have the chance to speak to a child. But they do tend to listen to parents. You know, so if you say ‘Right, just stop a minute, what needle are you using?’, You know, ‘What would you like [child name]?’ you know. It might just make that big difference that she feels like she’s got the control over itParent/guardian, 10-year-old girl, needle phobiaWe just get out more don’t we kid? We go out a lot more, we often walk to school which is nice and, like half term we’re gonna be getting out we’re gonna do things, go to country park and that. And that’s nice to get out and country park and things like that. We still have problems when dogs are off their leads, that’s the only time we do have a problem but if they’re on leads we just walk by now. But no it’s totally different, we can actually plan and do thingsParent/guardian, 7-year-old boy, dog phobia |
| Therapist role |
|
Parents described the importance of having a skilled and knowledgeable therapist who was external to the situation to deliver the intervention:I’ve tried to do what I can with him, but it’s very different when you’re emotionally involved. It needs to be somebody – sometimes I think, you’ve gotta accept that sometimes you need somebody who’s outside, who’s a professional, who is gonna be able to just walk away from it at the end of the dayParent/guardian, 15-year-old boy, needle phobia |
| Understanding phobia stimuli |
|
Parents highlighted the importance of having appropriate and realistic stimuli to benefit optimally from the therapy:She was very good and she kind of knew what things to do help her with it. So, the point, you know, at the end of it, pouring the sick into the toilet, just that horrible noise and even you said that was the worst bit. ’Cause that was very – ’cause that was almost like visually exactly what you’d – and the smellParent/guardian, 16-year-old girl, vomit phobia |
| Post-therapy reflection |
|
Parents felt that OST would work better with animal-type phobias but views were mixed from BII-type phobias. They also highlighted the importance of adaptions to be made for children with additional needs and comorbidities:Animal phobias I think definitely. Not sure about other phobiasParent/guardian, 12-year-old girl, dog phobiaIt’s not, it’s not a definite no. It just needs a little bit more work, that’s all. Like I said I think the study would work as it is, would work well for older neurotypical children. I think that the study would work, but for such as children with deeper roots, ASD, additional needs, there’s some more planning and preparation needs to be doneParent/guardian, 12-year-old boy, needle phobiaThe majority of parents who had taken a pragmatic approach in their expectations felt that these had been met:Really good. [Child name] doesn’t think so because she expected some switch to go off in her brain and she could just go and play with any dog that she saw, but she’s adjusting to the fact that it’s a gradual process and, you know, she’s come that far that she takes it for granted nowParent/guardian, 12-year-old girl, dog phobiaParents reported the short-term and long-term effects of OST on their child’s phobia:So, yeah, like I said before, we got super excited and had to go to the pub and have ice cream and cookie in a pub, obviously, where there’s dogs there. So, um, ’cause I just like, I was totally amazed about how well she had done. It was just amazingParent/guardian, 15-year-old girl, dog phobiaWell certainly sitting in the gardens with a fly on her foot, and she was even talking about it, it wasn’t as though she didn’t notice it, she did notice it was there, and she was talking about it, she wasn’t even wafting it out of the way, she was dealing with it quite well really. So that was quite impressive. And she sat, she did some gardening with me one day, and there was quite a few things around, and one of the plants must have been heavy with bees or something ’cause there was a lot of buzzing coming from it, and she didn’t hurtle inside, she probably avoided it a little bit, but she remained in the garden and continued with what she was doing, so that was quite impressive reallyParent/guardian, 12-year-old girl, insect phobiaParents made recommendations for how the therapy could be improved. The most prevalent was a brief follow-up session after the therapy had taken place:I think maybe I would have liked to – I know that 3-hour session was a one treatment session, but maybe another something similar afterwards to see how she’s, [child name]’s progressed from where she was then to dealing with a dog again. So, yeah I just feel like there should be a little something just to see how she is with the dog againParent/guardian, 15-year-old girl, dog phobiaSo, I think maybe after that long session, to show [child name] that she could be with a dog and do it, then maybe some specific sessions, for example at the beach, so, with [therapist name] at the beach and see how she reacts when a dog runs past. Or, at the park to follow up some more, kind of specific sessions because it was all very controlled and, and it was, it wasn’t really like real lifeParent/guardian, 7-year-old girl, dog phobiaParents highlighted the importance of service organisation during the treatment session and across care pathways for treatment to be offered in a timely and effective manner. Some described delays to therapy owing to coordination of treatment resources:We had like – we had like real problems with getting the session arranged. The lady that we were allocated to actually arrange it, she was – she only worked a couple of days a week and she said like the dog that they had worked on Monday and they didn’t have a venue on a Monday that allowed dogs and things. So, it took quite a long time to arrange, well, all of the summer to be honest with you. I think it was, it was the – she was definitely back at school in the September, possibly the October when we actually got the treatment arranged and I did feel that we only actually managed to get it arranged because I contacted [trial manager name] . . . it just seemed to drag on far too, too long. And then when – when it was arranged it was arranged for a day when I was at work and we only got a week’s notice as well, so I couldn’t put in a holiday requestParent/guardian, 7-year-old girl, dog phobia |
| Theme | Codes | Key messages and quotations |
|---|---|---|
| Therapist characteristics |
|
Roles were spoken about in context of ASPECT and how their skills/capacity would fit in with OST. Most clinicians were familiar with CBT, but not all had used it to treat phobias:I think that it could – I think that because the role of a children’s well-being practitioner does work with children that have mild to moderate anxiety or depression, I could see that being able to do one-session treatment as part of our skills set. Having one-session treatment there would be beneficial and that would fit in normally within our practicesPsychological well-being worker: CAMHS |
| Service-level perspectives |
|
Phobias were not seen regularly, as they were not prioritised (either by the service or on an individual level, where other presenting issues/goals were treated instead), or because of a lack of referrals (ASPECT debunked myth that phobias were not treated within the service):So it was usually part of something that was going on so there’d be some family issue and that was, sometimes it wasn’t even touched. They would mention it at some point, and it wouldn’t even get touched upon. ’Cause the main presenting goal they wanted was something different to, to, to – to look at the relationship with their parentsSenior counselling practitionerIt’s increased the services awareness and I think the difficulty for our service before, cos we’re a specialist CAHMS service, it was the belief that we didn’t treat phobias. So erm – but we do actually have a clinical pathway for phobias and we should be treating phobias. So what was great about the trial was that it raised – we have six community CAHMS teams and it raised their awareness that actually we should be accepting referrals for phobias. And yeah so it’s been great for our service in that regard that we’ve probably been accepting more phobias that have come through as a consequence of raising people’s awareness of the clinical pathwayConsultant clinical psychologist/core CAMHS clinical leadIt might sound simple when a GP sends a letter to say this young person’s got a fear of dogs and the person is reading that referral letter and thinks ‘oh it’s just a phobia’ and they bounce it back. But I think now clinicians are you know – recognise actually we should be taking those casesConsultant clinical psychologist/core CAMHS clinical lead |
| Perceived effectiveness of OST |
|
Most had positive view of the effectiveness of OST. It was more appealing to teenagers, less time commitment (clinicians and CYP) and easier for CYP to visualise results:My excitement was in that kind of adolescent process there is a lot about, ‘I want it, I want it now’. Erm are all important and all of those kinds of things and when you mix in that phobia that’s stopping some of that. I think if they can see a movement to get rid of it they, the, the kind of motivation for carrying on, if you can push enough forward. I think motivation for carrying on, because they want this contact with their friends, they want to be seen, they you know that kind of thing, egotistical kind of thing . . . that age range love quick, you know they are into that quick change, ‘let’s move it and lets move it fast, I’m you know I’m important’, all of those kinds of things I thought it would fit into. So I was excited even at the training stageSenior counselling practitionerThere were many concerns, including children’s lack of trust in the process, concerns about building a therapeutic relationship (especially in CYP with comorbidities), keeping CYP on task, being out of clinicians’ comfort zone and that CYP’s gains may not generalise in wider world:P:So, the idea of being able to turn it around kind of within that one session seemed huge really and sort of an apprehension around sort of knowing as to whether that can happen or not, and yeah, just sort of, nervous about how it would go, kind of, how the young people would respond to the idea that we were proposing they could overcome this in one sessionI:And did you – so you were concerned that the young people wouldn’t trust the one-session treatment? Is that fair to say?P:Yeah I suppose to some degree. I wouldn’t say that it was a huge concern for me but it was something that I sort of considered when saying I’m apprehensive, you know, how would the young person respond to this idea that you know we’re gonna get them in a room and were gonna spend 3 hours and do this or up to 3 hoursPsychological well-being worker, CAMHSErm, its th–, that, I guess that was something I was–, I was maybe a bit unsure about. Because I suppose, when you’re doing the–, I suppose, when you’re delivering the low-intensity model over a number of weeks, you– you do get like more opportunity to build maybe rapport, build a relationship. Which can, I feel can have a lasting impact on erm you know, maintaining positive change. That kind of thing. So, I suppose in some respects, there was maybe a fear that that–, I think that– well an expectation that, that– that therapeutic alliance might not be strong with OSTPsychological well-being worker, CAMHSErm, it’s different to the traditional model of the kind of therapy that we provide which tends to be like weekly over a period of time and in-between sessions that you’d expect there to be some kind of homework or more exposure work for the young person to carry out. Because I guess I worried that somebody might be able to overcome their anxiety in the room with me there with them, but then go out of the room and not be able to do that in in the wider world, really, when they got homePsychiatristHow much preparation would it take? All those things. I think it was more within our team, it was about the preparation – how do we get the resources where are we doing it, you know? Um how long? Because our usual way of working is to see a lot of children in a week. But from the information and guidance to school where one-session treatment you know for that big chunk of time and preparation, it was that kind of – the practicalities of how it would work. And especially, I think, with me and dogs, it was like ‘How am I gonna get a dog?’, where am I going to run the session, You know. Maybe I guess, because they say ‘Never work with children or animals’School well-being workerAnticipated that it would be more effective for certain phobia types (e.g. animal) than others (e.g. needle):I was thinking animal phobias. We could bring something into the actual room. And I’d had – I’ve had conversations with colleagues as well when they’ve kind of got a case or when I was involved in this, we’d have conversations about it and they spoke about their kind of experience with the phobias. And there was maybe animal ones are very specific (yeah, yeah). Use materials in the roomInterpersonal therapist |
| Motivating factors for clinicians |
|
Opportunity for new skills set: recently qualified clinicians were particularly keen: I was interested in experiencing it and seeing how that would look, because I’ve done CBT as normal, that might have been something that I already felt more comfortable with. OST was a new technique and a new type of treatment that I was actually interested in doing itInterpersonal therapistI guess at the time that I did the training for the one-session treatment, I just, I can’t remember exactly at what point it was. But, I was either in the middle of the training year or just finished it. So I was still kind of in the mode of learning new interventions for anxiety. So from that perspective, I was looking forward to having another, I guess, method of being able to do thatChildren’s well-being practitioner |
| OST training |
|
Training should be targeted at clinicians dependent on skills/experience/preference:I already felt quite confident with things like CBT (yeah) and I’ve delivered in the past, so maybe didn’t feel like I needed lots of in-depth (yeah) and, erm, training. So it felt right, for me (yeah). Perhaps if I was at the beginning of my training or something like that, then I would’ve wanted a bit more (yeah)PsychiatristTraining was mainly useful in learning how to plan, structure and manage OST:3 hours is very different from any other training I think you’ve had, you know personally that’s a long session and I think you’ve got to have planned, done your hierarchy really knowing what you’re gonna do at each stage, and that was – in the training we really got that. So I felt con, I think it could be a little overwhelming thinking of 3 hours with a client when they come in with their head down and not really prepared, you‘d think ‘blinking heck, 3 hours!?’ You know, you need to know, have a real good err kind of hold around what’s gonna happenSenior counselling practitionerOpportunity for top-up session would be useful – it is difficult to retain content from training if there is a large gap between treating first CYP with OST |
| Process |
|
Parent involvement can be positive (opportunity to educate them too, parent able to challenge child further), but their role must be clearly defined:They can explain or clarify or, you know, whereas you wouldn’t challenge a child that you didn’t know. Whereas the parent can say ‘Yeah, but remember the time that you . . .’ I don’t know ‘. . . were near a dog’ or whatever. They can come from a place where they know the child, or they can maybe challenge or offer additional information, which is really [h]elpfulSchool well-being workerParental involvement can be negative (safety behaviours); it can be useful to complete OST without the parent present:The parent was like wanting to give, like she went in the bag and got like a bottle of water to give to the child. So then I had to say oh sorry can you, because obviously that would interfere with the therapy because it could be seen as safety behaviourCBT practitionerClinicians like that it was collaborative process:But it was positive because they obviously were a part of it so it was a collaborative process. So, there was a lot of sort of times spent thinking about or or gauging how that young person wants that step by step to look like, how they want that session to look like and kind of focusing on them having sort of control around that to some degree. So I think that adds to kind of the positivity of it because they’re assessing their own goals you know and they’re setting, they they’ve got their own aspirations to what they want to seePsychological well-being practitionerValidation on recognition during session is important:To give them some validation and say how well they’d done to recognise, you know, that they had a problem and they’d come and sorted it out. And we’ve come up with a plan and a way which to sort o’ manage that and then we can reflect back and see, you know, those positive outcomes and actually, you know, for someone at such a young age it’s a really valuable lesson or any problems they can come back in the future, with them and I think that’s a really, I think that’s a really nice message to give children, children of that, of that age reallyPsychiatristClinicians valued the flexibility of OST (able to go at own pace, go backwards, go sideways):And also being able to you know work when we kind of built sort of a hierarchy or a step by step plan however you wanna kind of term it – the ability kind of in the moment to sort of move up and down that as felt fitting, for a young person. You know so you had the ability to do that so you had that momentum you know whereby you could kind of move forward but equally you can kind of drop back in the moment if you felt that you needed to. Whereas of course in your separate sessions, you can do that but not not in the same way that a one-session treatment allows. You know it’s a bit more staggered, which I think potentially could sort of stifle kind of progress could be made if you likePsychological well-being practitionerIntense session for clinician and CYP (CYP will be very anxious and quite distressed), may be useful to have additional therapist present to share load:I had an assistant psychologist in with me on that one and it were great, because whenever like my attention were dwindling, ’cause it is such a long time to focus, then she’d pick up, we were like a little tag team with itClinical psychologistNeedle and vomit phobias can be more difficult to treat:A little bit attribute of a child as well I suppose, there were no I think you know, I know there has been an examples of needle phobia done in the one-session treatment but I think maybe with him it was – yeah just a – I think he just found it incredibly difficult and needed some time in between to process each step he’d made and kind of just reflect on the positive progress he had madeClinical psychologistI think sometimes it can be quite useful for some patients it helps for them to sort of consolidate certain types of learning. Or, so say for example that the person you were seeing was nauseous, the nauseous feeling doesn’t just sort of sort of stay with them for just the sort of the session but they’ll carry that with them to the- maybe for a couple of hours afterwards. So, that would be for them then to also reflect on the fact that when they come back for the next session they will probably be able to say like well actually, I felt really uncomfortable but actually I wasn’t sick, and actually the, the, the saying something along the lines of actually I could find out I could push that symptom more. And, that’s good let’s give that a go again, whilst within the OST, you don’t really have the opportunity to push that symptom in the exact same way because a patient’s worked something out the same wayHigh-intensity CBT practitionerCompleting hierarchy in one session ensures that no safety behaviours happen in between exposure:I think it’s obviously more straightforward to just do treatment as usual, because it’s a similar setup to eight sessions for treatment of depression would be, and it’s just as-usual, isn’t it? Um, but clinically, I just don’t feel as though, in the context of a phobia and exposure sort of stuff, I just don’t feel as though the week’s break is helpful. There could be, you know, homework tasks in between sessional work stuff, but it’s very hard to know whether or not there were any maintaining behaviours going on, or any safety behaviours. And it’s, yeah – so I definitely think that, clinically, it’s a better fit to do the single-session treatmentPsychological well-being practitionerSome clinicians felt that add-ons were needed (e.g. a follow-up session, a child-friendly information sheet and an ongoing plan created for after session). Photos/videos taken during a session may be useful:I think different things. You know, like um, like a video clip, almost demonstrating um, I don’t know. I’m just sitting on the grass, but thinking maybe had we kind of videoed it and given the parent a recording so that, you know, if the child was having difficulties again, going like ‘This is what we did. This is how we did it’ breaking down the stages. I think that second parent who carried on the work I sent her, you know, the stages. And she asked. She proactively asked for kind of the video clips and the photos and, you know, we took pictures and things. And I think she then used those to continue it. Um. But that was that mum being proactive and assertive. So maybe just doing that – putting some kind of pack together ‘Here’s a clip. Here’s a picture of your child achieving their goals. These are the stages. These are the things you need to do’. You know. Really just breaking it down. ’Cause I sent – with the first mum, who didn’t carry it on – I sent her a lot of e-mails explaining what she needed to do to keep practicing. Yeah. Maybe just that, I would saySchool well-being worker |
| Planning/logistics |
|
School-based sessions are good because they minimise time out of school, but it may be difficult for CYP to return to their lessons straight after, and they are better if there is a clear therapeutic space:But the bad part of it was that they were in school, y’know being exposed to a phobia, a fear, and then, all be it I spent some time with them afterwards just having real general chats, y’know ‘what are you gonna do at the weekend?’, ‘what’s your next lesson?’, erm, y’know trying to kind of just get their anxiety right back down again, and almost distract their mind. They still then had to return to lesson after doing that, with like no contact with their parents or their carer or, no y’know that kind of . . . Yeah so that, y’know it almost feels like that does need to be done somewhere external. Y’know like you’d go to the doctors for that kind of thing, or you’d go to CAMHS for therapy, y’know. That sort of, because I suppose if it really didn’t go right, and you really struggled with it, then that’s gonna be another trigger, your school. You’re gonna associate school with vomit and then you’ve got an issue there so. All be it that wasn’t the caseSchool well-being workerBooking a room in CAMHS can be difficult, adequate space is needed (e.g. when treating dog phobia), booking time out in own diary for 3 hours can be difficult, it can be difficult to co-ordinate everything and it can be a struggle to get stimuli (needles, etc.):Other things that I found was, that make it more tricky, was dog phobia. OK, sort of good to use a variation of dogs, it is, so say for example if you’ve got – if you’re using up to three dogs per 3-hour ASPECT session it, it worked wonderfully. But, where do you store the dogs? So what, what I’d err was fortunate enough to do was I was working on a Saturday when I did the OST for the dog phobias and I was fortunate enough to use different rooms within the CAMS vicinity. So, so one room would have one dog in another room would have another. Sort of which is how I got round but, in some services that might not necessarily be practicalChildren’s well-being practitionerThe ASPECT research team provided support with planning and logistics; there would be implications if OST were to be delivered outside a research project:But for me, even though it was other logistics of finding the venue, the getting the dog and the child and the family. It’s more of that. But I felt like the guidance and support that we got was – you know, phenomenal, you know. It was just a phone call any issues we had, you were kind of there and sorting things. So you know, it felt really, really well supportedSchool well-being worker |
| Suitability of case | Child readiness
|
May be suited to older children (young children may struggle more with the long session, whereas teenagers are keen for quick improvement):I think it fits with the adolescence ‘I want to move, I want to change this’. Absolutely a time to change it because it’s hitting them at you know at a time they want to move away from their parents, move into their friendship groups. A lot of them were sticking to parents because they were so frightened of things (hmm hmm), so couldn’t move on, they were kind of trapped in this limbo bit where they wanted to go off with their friendsSenior counselling practitionerChildren’s cognitive development should be considered. Additional support (e.g. more psychoeducation or more time given to build relationship) could be put in place to help CYP who may struggle. OST may be preferable where there is a time-sensitive external reason for treatment:I think if there was – so say for example if we was against the clock, like the patient was scared of needles but about to have an operation, then in that sort of case then I would sort of strongly suggest they go down an OST type route. If as I mentioned before, in multiple complexities then probably going down the CBT type route when I’ve got that sort of time, we’ve got sort of time to explore, got the option to do a lot more between session work to get them to do different types of things tooHigh-intensity CBT practitionerIf comorbidities are present, they can make a case more complex (ASD, ADHD, other mental health issues, such as anxiety or trauma, adverse childhood experience or being ‘looked after’/in care). Rigid thinking in those with ASD may push CYP further, but it could be more difficult to shift thinking patterns. Some services do not treat these more complex phobia cases:I think y’know like children with autism, and I know that – I suppose, thinking about children who’ve previously experienced an adverse childhood experience, or a childhood trauma, looked after children . . . Y’know, it’s how does that impact on the feelings that they’re already trying to kind of cope with, manage, process if you like. I know that anxiety is quite prevalent in children with autism, so that’s already there in life, if you like. And then there’s that more specific anxiety and fear around the phobia. And it almost feels like that’s an extra layer for them? And likewise with children who’ve experienced trauma, they’re in that, y’know that hypervigilant mode all the time. And it’s hard and really, y’know, really overwhelming for them. And then you’re kind of adding that extra layer on top of thatSchool well-being workerP:Yeah. I wonder whether – you know, if there was comorbid with a young person who’d got autism, it might be more effective for them, I don’t knowI:Yeah? Why do you think that could be?P:Um. I suppose because maybe if their thinking ‘I’ve got to achieve this’ because of their rigid thoughts about you know, achieving this by the end of the session that they might really push themselves to work through it (yeah, definitely). There’s a time to achieve it byInterpersonal therapistIf we’re just thinking about specific ASD, ones, and for me with ASD, I think for me it was just considering how difficult it is for them to, y’know sometimes manage transitions from one thing into the next, and they need that preparation beforehand. Sometimes they like to know what’s happening next. Well obviously we should be explaining that, absolutely, in the one-session treatment. But I think that perhaps maybe the speed they move from one activity to the next might influence the treatment, I don’t knowCBT practitioner/safe care leadAs a service, we were actually – we were fairly brutal, to be honest. Um, we would carefully screen referrals and we would um, we would reject referrals prior to assessment sometimes. So, we would take a look at the presenting problems. So, for example, if the – if it straight up said that somebody had received a diagnosis of bipolar disorder in the past, we would say ‘OK, we’re a low intensity service offering mild to moderate stuff’ we would signpost as appropriate, because it’s a heartache for them, really, coming in and feeling heard and then being sent awayWell-being practitionerBecause as I said the severity of it and that came about as a result of her mother’s ill health and time in hospitals so you know when I said earlier about potentially there’s sort of, not always, what I’d constitute as trauma but potentially some form of you know you know experience that you know, significant experience that they’ve had that then so that one is one of those where potentially had they not got where we got, you know, she might’ve needed further work it may be that she would require further work at a later stage you know when you follow-up such as that I don’t knowPsychological well-being worker, CAMHSDistress levels should be considered:I:. . . when children are allocated to this type of intervention what if any would be your main reasons for accepting or not accepting them onto the intervention?P:I think it depends err, on, level of distress it would be, so say if the client came into the sort of the clinic room, highly distressed about the idea of within the certain amount of time that they’re gonna be doing X, Y and Z, (yeah) that may not be sort of feasible to do something like thatHigh-intensity CBT practitionerPhobia severity should be considered. Anything beyond mild to moderate phobia may not be suitable:Because there was another young person I saw that, erm, actually didn’t even progress beyond the assessment appointment. It was kind of really severe, an impairing phobia, but it was never gonna be realistic for that to have been cured in one session. But actually we could perhaps have set a, you know, a different goal that would’ve meant that the phobia was still around but more manageablePsychiatristNeedle phobias may not be suited to OST because they are difficult to treat in 3 hours owing to safety monitoring; it may be more useful to build up to having an injection after spending several sessions building it up to it and visiting alternative settings:Unfortunately, I don’t think it was very successful. On reflection, I think it was quite specific to needles. I do think the 3 hours – it didn’t work for either of them in the sense that they weren’t able to have the vaccinations. No, sorry, one of them wanted a vaccination, the other one just wanted to learn about them, I think. I know one – that was it, he wanted to watch someone have an injection done . . . I had contact with a vaccination nurse who was kind of asking about the treatment and I’d explained, you know, that they’d had the treatment – and they were kind of sharing their concern that they didn’t think that the one-session treatment worked cause they’ve had other young people and their personal thing was that actually when people have had CBT sessions that, you know, multiple sessions, that was much more effective in their experience of needle phobiasInterpersonal therapistMain point: vomit phobias may not be suited to OST because of fear of becoming sick in the days following treatment and clinicians are not able to expose CYP to the actual feeling of nausea:But she also had – so – and again when we’re talking about that core beliefs, there was – there was the vomit phobia which was bad for her, but her – her core belief was that it was gonna make her sick. So she was still really anxious after the OST ’cause she was waiting to get sick. So it was about how do you target that in a fear hierarch in an OST? ’Cause it – it – it was, you know, she didn’t have any rules about when it would happen, it was just she didn’t sleep for like a night and a day or something because she was so worried that she was gonna get sick from itPsychological well-being worker, CAMHSSuitability criteria would be useful:I think it’s having a sort of suitability criteria. That would be, more beneficial for the OST, but also kind of like what I was saying before, if there is complexities having that, that almost wiggle room to say actually, actually, we, we can do, more. We canHigh-intensity CBT practitioner |
| Post-therapy reflection |
Effectiveness of OSTEmbedding OST within clinical services (n.b. consider implementation issues of the study when writing this up)Clinician benefits Post-ASPECT treatment preferenceRecommendations for OST structureRecommendations for treatment delivery (potentially going to be dependent on clinician background)Change in perspective (how ASPECT changed knowledge or experience of services – in the context of their own services) Comparison with CBT |
Positive outcomes included improvements seen in other areas and improved confidence (during the session and after), and OST could be used as primer for further CBT, as it did not always completely cure the phobia:School well-being workerHigh-intensity CBT practitionerClinician-based success factors: clinician must be fully confident in OST, knowledgeable about the stimulus, model good behaviour, establish a good relationship with the CYP, over-the-top praise and step back at the right time:Consultant clinical psychologist/core CAMHS clinical leadParental presence can be success factor, but they must know when to step back. The child’s own motivation is key to success:Consultant clinical psychologist/core CAMHS clinical leadOST-based success factors: allows for quick progress and lots of immediate positive reinforcement, setting an ambitious but evenly spaced hierarchy leads to more success, OST allows for flexibility, momentum built quickly and enables fast progress:Well-being practitionerHigh-quality, realistic stimulus contributed to success:PsychiatristLimitations of OST: difficulty in being able to build a relationship with CYP remained a concern for some therapists after OST delivery; potential for a negative effect on the child if they do not complete:P:I:P:Clinical psychologistOST does have a place in some services: some felt that it was a good opportunity for cross-pathway working and reduced administrative burden on service (owing to less sessions). In response to ASPECT, a treatment team was set up in one service to see phobias:Consultant clinical psychologistConsultant clinical psychologistBarriers to offering OST in future include that it is challenging fitting phobia work into an already stretched service:PsychiatristHigh-intensity CBT practitionerThe therapists’ increased confidence and skills was a rewarding experience Mixed opinions on whether or not they would continue to deliver OST: some very enthusiastic about continuing to offer OST, one therapist did not want to owing to lack of relationship building:School well-being practitionerSome recommendations affect the definition of OST. Key recommendations for OST include adding a follow-up session, more time to focus on psychoeducation and sessions run by career mental health professionals as more likely to treat mild–moderate phobias:Children’s well-being practitioner |
Appendix 10 Baseline characteristics by missing data status
| Characteristic | Missing 6-month BAT, n (%) | Complete 6-month BAT, n (%) | ||||
|---|---|---|---|---|---|---|
| Treatment group | All (N = 119) | Treatment group | All (N = 149) | |||
| CBT (N = 58) | OST (N = 61) | CBT (N = 76) | OST (N = 73) | |||
| Site | ||||||
| Humber | 2 (3.4) | 3 (4.9) | 5 (4.2) | 8 (10.5) | 6 (8.2) | 14 (9.4) |
| Tees, Esk and Wear | 17 (29.3) | 18 (29.5) | 35 (29.4) | 22 (28.9) | 21 (28.8) | 43 (28.9) |
| South West Yorkshire | 4 (6.9) | 0 (0.0) | 4 (3.4) | 5 (6.6) | 5 (6.8) | 10 (6.7) |
| Norfolk and Suffolk | 10 (17.2) | 24 (39.3) | 34 (28.6) | 11 (14.5) | 11 (15.1) | 22 (14.8) |
| Northumberland | 4 (6.9) | 1 (1.6) | 5 (4.2) | 10 (13.2) | 9 (12.3) | 19 (12.8) |
| South Tyneside | 4 (6.9) | 7 (11.5) | 11 (9.2) | 13 (17.1) | 11 (15.1) | 24 (16.1) |
| Leeds | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (1.3) | 0 (0.0) | 1 (0.7) |
| RDaSH | 7 (12.1) | 1 (1.6) | 8 (6.7) | 3 (3.9) | 4 (5.5) | 7 (4.7) |
| Exeter | 1 (1.7) | 0 (0.0) | 1 (0.8) | 0 (0.0) | 1 (1.4) | 1 (0.7) |
| Dorset | 3 (5.2) | 3 (4.9) | 6 (5.0) | 2 (2.6) | 3 (4.1) | 5 (3.4) |
| Cumbria | 1 (1.7) | 0 (0.0) | 1 (0.8) | 0 (0.0) | 1 (1.4) | 1 (0.7) |
| County Durham | 0 (0.0) | 2 (3.3) | 2 (1.7) | 1 (1.3) | 1 (1.4) | 2 (1.3) |
| Dudley and Walsall | 5 (8.6) | 2 (3.3) | 7 (5.9) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Sex | ||||||
| Boy | 24 (41.4) | 20 (32.8) | 44 (37.0) | 29 (38.2) | 28 (38.4) | 57 (38.3) |
| Girl | 34 (58.6) | 41 (67.2) | 75 (63.0) | 47 (61.8) | 45 (61.6) | 92 (61.7) |
| Ethnicity | ||||||
| English/Welsh/Scottish/Northern Irish/British | 54 (93.1) | 56 (91.8) | 110 (92.4) | 75 (98.7) | 71 (97.3) | 146 (98.0) |
| Irish | 0 (0.0) | 1 (1.6) | 1 (0.8) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Any other white background | 0 (0.0) | 1 (1.6) | 1 (0.8) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Pakistani | 1 (1.7) | 2 (3.3) | 3 (2.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| White and black Caribbean | 1 (1.7) | 0 (0.0) | 1 (0.8) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| White and black African | 1 (1.7) | 0 (0.0) | 1 (0.8) | 1 (1.3) | 0 (0.0) | 1 (0.7) |
| White and Asian | 0 (0.0) | 1 (1.6) | 1 (0.8) | 0 (0.0) | 1 (1.4) | 1 (0.7) |
| Any other mixed/multiple ethnic background | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (1.4) | 1 (0.7) |
| Prefer not to say | 1 (1.7) | 0 (0.0) | 1 (0.8) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| School attender | ||||||
| No | 4 (6.9) | 2 (3.3) | 6 (5.0) | 4 (5.3) | 3 (4.1) | 7 (4.7) |
| Yes | 54 (93.1) | 59 (96.7) | 113 (95.0) | 72 (94.7) | 70 (95.9) | 142 (95.3) |
| Treatment preference | ||||||
| CBT | 10 (17.2) | 18 (29.5) | 28 (23.5) | 25 (32.9) | 25 (34.2) | 50 (33.6) |
| OST | 23 (39.7) | 16 (26.2) | 39 (32.8) | 12 (15.8) | 14 (19.2) | 26 (17.4) |
| No preference | 25 (43.1) | 27 (44.3) | 52 (43.7) | 39 (51.3) | 34 (46.6) | 73 (49.0) |
| Taking part in another study | ||||||
| No | 57 (98.3) | 60 (98.4) | 117 (98.3) | 75 (98.7) | 70 (95.9) | 145 (97.3) |
| Yes: phobia/anxiety | 1 (1.7) | 1 (1.6) | 2 (1.7) | 1 (1.3) | 3 (4.1) | 4 (2.7) |
| Number of adults in the household | ||||||
| 1 | 8 (13.8) | 18 (29.5) | 26 (21.8) | 10 (13.2) | 7 (9.6) | 17 (11.4) |
| 2 | 43 (74.1) | 41 (67.2) | 84 (70.6) | 57 (75.0) | 60 (82.2) | 117 (78.5) |
| 3 | 5 (8.6) | 2 (3.3) | 7 (5.9) | 8 (10.5) | 4 (5.5) | 12 (8.1) |
| 4 | 1 (1.7) | 0 (0.0) | 1 (0.8) | 1 (1.3) | 2 (2.7) | 3 (2.0) |
| Number of children in the household | ||||||
| 1 | 16 (27.6) | 17 (27.9) | 33 (27.7) | 21 (27.6) | 19 (26.0) | 40 (26.8) |
| 2 | 27 (46.6) | 28 (45.9) | 55 (46.2) | 38 (50.0) | 40 (54.8) | 78 (52.3) |
| 3 | 13 (22.4) | 8 (13.1) | 21 (17.6) | 15 (19.7) | 13 (17.8) | 28 (18.8) |
| 4 | 2 (3.4) | 7 (11.5) | 9 (7.6) | 0 (0.0) | 1 (1.4) | 1 (0.7) |
| 5 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (2.6) | 0 (0.0) | 2 (1.3) |
| Characteristic | Missing 6-month BAT, mean (SD) | Complete 6-month BAT, mean (SD) | ||||
|---|---|---|---|---|---|---|
| Treatment group | All (n = 119) | Treatment group | All (n = 149) | |||
| CBT (n = 58) | OST (n = 61) | CBT (n = 76) | OST (n = 73) | |||
| Child’s age | 12.2 (2.8) | 12.1 (2.7) | 12.2 (2.8) | 11.5 (2.5) | 11.6 (2.6) | 11.5 (2.5) |
| ADIS CSR | 7.6 (0.9) | 7.5 (0.9) | 7.5 (0.9) | 7.5 (1.0) | 7.6 (0.9) | 7.5 (0.9) |
| BAT steps | 3.1 (3.9) | 5.3 (4.3) | 4.2 (4.2) | 4.8 (4.3) | 4.4 (4.1) | 4.6 (4.2) |
| Change in SUDS | –0.5 (2.8) | 0.2 (1.5) | –0.2 (2.3) | –0.2 (1.9) | –0.3 (2.1) | –0.2 (2.0) |
| CAIS child | 20.1 (13.9) | 19.0 (15.5) | 19.5 (14.7) | 16.0 (13.2) | 17.3 (12.9) | 16.6 (13.0) |
| CAIS parent | 22.7 (16.4) | 24.7 (18.1) | 23.8 (17.2) | 18.3 (16.0) | 19.6 (15.2) | 18.9 (15.6) |
| CHU-9D | 0.8 (0.1) | 0.8 (0.1) | 0.8 (0.1) | 0.9 (0.1) | 0.9 (0.1) | 0.9 (0.1) |
| EQ-5D-Y | 0.71 (0.29) | 0.69 (0.28) | 0.70 (0.29) | 0.77 (0.26) | 0.80 (0.22) | 0.78 (0.24) |
| EQ-5D VAS | 75.9 (22.1) | 76.0 (20.1) | 76.0 (21.0) | 81.5 (17.2) | 79.1 (17.3) | 80.3 (17.2) |
| RCADS child total anxiety score | 33.4 (20.4) | 38.0 (22.4) | 35.7 (21.5) | 30.9 (18.1) | 33.5 (21.2) | 32.2 (19.7) |
| RCADS parent total anxiety score | 35.3 (20.1) | 41.3 (21.2) | 38.4 (20.8) | 30.2 (18.2) | 35.1 (19.1) | 32.6 (18.7) |
List of abbreviations
- ADHD
- attention deficit hyperactivity disorder
- ADIS
- Anxiety Disorder Interview Schedule
- AE
- adverse event
- ASD
- autism spectrum disorder
- ASPECT
- Alleviating Specific Phobias Experienced by Children Trial
- BAT
- Behavioural Avoidance Task
- BII
- blood injection injury
- CACE
- complier-average causal effect
- CAIS
- Child Anxiety Impact Scale
- CAMHS
- Child and Adolescent Mental Health Services
- CBT
- cognitive–behavioural therapy
- CBTS-CYP
- Cognitive Behaviour Therapy Scale for Children and Young People
- CEAC
- cost-effectiveness acceptability curve
- CHU-9D
- Child Health Utility 9D
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- CSR
- clinical severity rating
- CTRU
- Clinical Trials Research Unit
- CTS-R
- Cognitive Therapy Scale – Revised
- CYP
- children and young people
- CYP-IAPT
- Children and Young People’s Improving Access to Psychological Therapies
- DMEC
- Data Monitoring and Ethics Committee
- DNA
- did not attend
- DSM-V
- Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition
- EQ-5D-Y
- EuroQol-5 Dimensions Youth version
- GP
- general practitioner
- HRQoL
- health-related quality of life
- IAPT
- Improving Access to Psychological Therapies
- ICC
- intraclass correlation coefficient
- ICER
- incremental cost-effectiveness ratio
- ITT
- intention to treat
- LYPFT
- Leeds and York Partnership NHS Foundation Trust
- NICE
- National Institute for Health and Care Excellence
- OR
- odds ratio
- OST
- one-session treatment
- PP
- per protocol
- PPI
- patient and public involvement
- PROM
- patient-reported outcome measure
- PSS
- Personal Social Services
- PSSRU
- Personal Social Services Research Unit
- QALY
- quality-adjusted life-year
- QoL
- quality of life
- R&D
- research and development
- RCADS
- Revised Children’s Anxiety and Depression Scale
- RCT
- randomised controlled trial
- REC
- Research Ethics Committee
- SAE
- serious adverse event
- SD
- standard deviation
- SPA
- single point of access
- SUDS
- subjective units of distress
- TMG
- Trial Management Group
- TSC
- Trial Steering Committee
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/IBCT0609).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
