Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 16/78/04. The contractual start date was in May 2018. The draft report began editorial review in November 2020 and was accepted for publication in May 2021. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2023 Jones et al. This work was produced by Jones et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2023 Jones et al.
Chapter 1 Introduction and background context
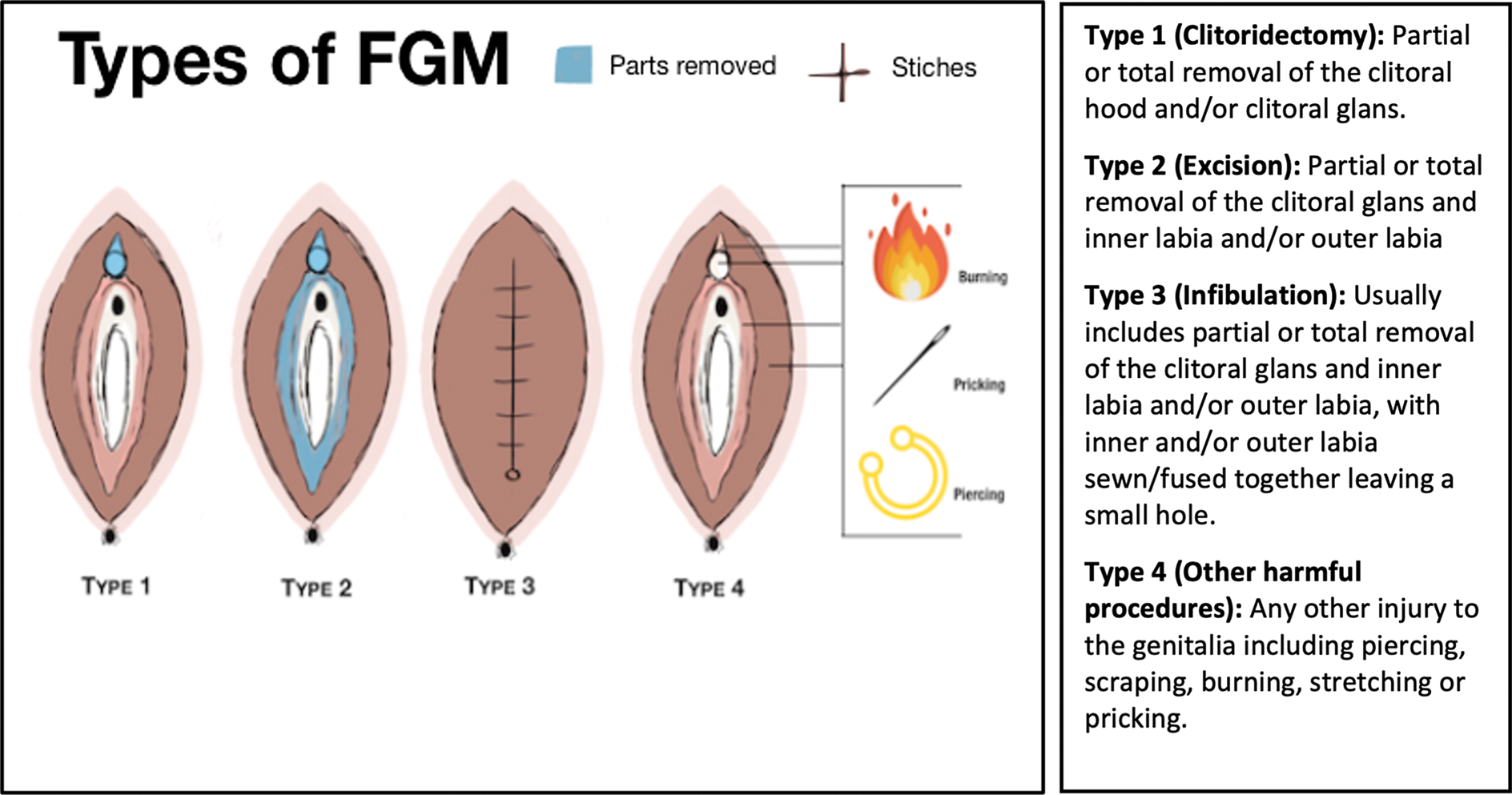
Defining female genital mutilation
Female genital mutilation (FGM) involves the partial or total removal of or any other injury to the female genitalia for non-medical reasons. 1 Since 1997, FGM has been classified into four distinct types (types 1–4; Figure 1), ratified by a joint statement from the World Health Organization (WHO), the United Nations Children’s Fund (UNICEF) and the United Nations Population Fund (formerly the United Nations Fund for Population Activities; UNFPA). 4 The FGM typology has since been strengthened by the inclusion of a further seven subtypes to capture variations of the practice. 4,5 Generally, the extent of tissue removed increases from type 1 to type 3, with type 3 (infibulation) being the most extensive and often requiring surgical intervention (deinfibulation). 6 Nevertheless, there may still be some difficulty with classification of FGM since traditional cutters who perform the practice do so based on the culture of the community rather than conforming to a specific typology. 7
Although the WHO definitions are most widely used when describing FGM typology, further definitions have emerged from a social and political perspective that may reflect the impact of FGM on the survivor and their family. For example, FGM is a violation of the human rights of women and girls,8 a form of child abuse9 and a severe form of violence against women and girls (VAWG). 10,11 The practice is deeply entrenched in gender inequalities and discrimination. 12,13 The term female genital mutilation and the acronym FGM emerged following an ethnographic study14 presented to the WHO in 1979. Although the term was conceived by an outsider of the practice and the report was deemed to be demeaning to communities that believed FGM to be an important part of cultural heritage (see the Glossary for explanations of the terms used and justification of their choice in this report),15 the WHO ratified the use of the term given that it clearly describes the harmfulness of the act, makes it clear that it is a violation of human rights and differentiates it from male circumcision. 1 Although there has been some controversy surrounding the use of the term FGM,16 it is the most widely known term to describe cultural, non-medical alteration of the female genitalia and will therefore be used throughout this report. However, it is important to recognise that FGM is a dynamic practice, with ongoing and context specific changes to the practice globally. 17 FGM has been, and continues to be, a divisive issue between activists and academics, reflecting a wide range of discourses around and worldviews on the practice. 17
Global prevalence of FGM
The origins of FGM remain obscure; however, it is likely that FGM has been performed for millennia, and there is some evidence that it has been practised in Egypt since as early as the fifth century BC. 18 In 2020, UNICEF published a report highlighting that FGM is now practised across 31 (predominantly African) countries;19 however, Cappa et al. 20 have found evidence of the practice in as many as 50 countries, including Eastern Europe, Latin America, South-East Asia and the Middle East. Although it can be problematic to accurately estimate the prevalence of FGM because of the lack of representative data, an estimated 200 million women and girls have experienced FGM, which equates to approximately 5% of the global female population. 21 Approximately 1 in 10 of these women and girls will have experienced type 3 FGM. 12 An estimated 3 million women and girls are at risk of FGM each year, with most being cut aged < 15 years. 13 Without sustained and effective measures to eradicate FGM, it is anticipated that, given the projected rise in the global population over the next 15 years, the number of women and girls who experience FGM will also increase. 19,22 The eradication of FGM by 2030 is a Sustainable Development Goal 5 target. 23 To meet this target, UNICEF has posited that, even in the countries where the prevalence of FGM is reducing, progress would need to be at least 10 times higher than the current rate. 19 In some countries where the practice was historically almost universal (e.g. Egypt and The Sudan), there is some evidence of a reduction in prevalence; however, in other countries (e.g. Somalia and Guinea) there has been little, if any, change in the prevalence of FGM over the last 30 years. 19
UK prevalence of FGM
In 2015, a report using census data estimated that, on the basis of the country of their birth, 137,000 women and girls with FGM were permanent residents in England and Wales in 2011. 24 A further study, again using 2011 census data, reported that 178,781 women and girls aged > 10 years with FGM were resident in the United Kingdom (UK) at that time. 25 Although it remains challenging to accurately estimate the prevalence of FGM in the diaspora living in the UK,26,27 MacFarlane and Dorkenoo’s24 research highlighted that women and girls with FGM lived in every local authority in England and Wales.
To better inform FGM prevalence estimates and to support service-planning and provision in England,28 NHS Digital has attempted to collect FGM-related data from English NHS acute trusts, mental health trusts and general practices using the Female Genital Mutilation Enhanced Data set (FGMED) since 2015. 29 Between 2015 and 2019, 40,030 health-care attendances related to FGM and 20,470 previously unidentified cases of FGM in England were recorded via the FGMED. 26 A report published in early 2020 showed that between April 2019 and March 2020 there were a total of 11,895 attendances where FGM was identified: 6590 of these attendances were recorded as individual attendances. 30 A total of 88% (n = 5815) of these survivors were of child-bearing age (aged 18–40 years), with only 0.5% (n = 35) of survivors being aged < 18 years. 30 FGM type was known/recorded in 60% (n = 3965) of individual women and girls. Of the women and girls that had a known FGM type, 21% (n = 825) were reported as having type 3; 2% (n = 90) had a history of type 3 (that is, they had type 3 but have since been deinfibulated); and 1.5% (n = 60) were type 3 where reinfibulation had been identified. 30
However, Karlsen et al. 26,27 argue that these data should be interpreted with caution given, for example, that only a minority of general practices (≈ 2%) and not all NHS trusts (≈ 62%) have submitted data to the FGMED since it was initiated. Moreover, these data are reliant on FGM survivors accessing health and social care services, and they do not take into account FGM survivors who have not accessed health care. In addition, census data do not account for FGM survivors who have entered the UK as asylum seekers or those who have entered the UK illegally. Hence, FGM prevalence estimates in the UK may be significantly higher than the current statistics suggest.
Reasons why FGM is practised
To provide some context to the views around FGM, it is useful to explore the rationale for the practice. Since the mid-twentieth century, a number of reasons have been reported in the literature, and these vary between affected communities and cultures. 1,13 Six core themes or reasons for FGM have been identified: sociological, tradition and cultural; socioeconomic; psychosocial; hygiene, aesthetic and femininity; marriageability; and religious reasons. 1,12 Burrage31 reports that religion, culture and tradition are the most commonly cited reasons for the practice. In Western society, some have argued that there is no religious connotation or mandate for practising FGM,32 but evidence suggests that there is a strong belief in a religious rationale among some communities that perpetuate the practice. 33
Although culture and tradition are dominant reasons given for the practice of FGM, the cultural connotations are widely regarded as being under the control of women. For example, in a qualitative study exploring Egyptian men’s views of FGM, it was reported that men considered FGM to be the responsibility of mothers and grandmothers, but both men and women believed that FGM prevented women becoming ‘oversexed’, thus affecting marital stability. 34
Nevertheless, FGM has been described as an important cultural practice that has endured the colonial period and signifies the transition from childhood to adulthood. 35 In parallel, anti-FGM campaigns have been described as constructs of colonialism, with African nations labelled as a ‘land of torture’ whereas the West is described as the lands of ‘freedom and liberty’. 36 Therefore, while the knowledge and understanding of FGM in Western society appears to be polarised from FGM-practising communities, which are predominantly in the East, there is further evidence of polarisation within and between affected communities. However, we do recognise that there may be pockets of Westernisation in some of the countries that practise FGM.
Consequences of FGM
The WHO suggests that all women and girls are likely to report physical and/or psychological consequences as a result of their FGM. 1 There are no physical health benefits, and women and girls with more extensive forms of FGM, such as type 3, report more severe complications. 6,37 The physical health impacts of FGM are wide-ranging, and the large number of consequences identified in the literature can be subdivided into immediate, short- and long-term consequences. 1 Immediately and shortly after FGM, women and girls are typically at risk of more than one health complication. 38 Immediate complications include severe pain; haemorrhage and haemorrhagic shock; acute urine retention; urinary, vaginal and uterine infections; septicaemia; trauma to adjacent tissues; transmission of blood-borne viruses [e.g. human immunodeficiency virus (HIV)]; fracture of bones from being held down; and, potentially, even death. 1,3,38–40 Shorter-term complications include delayed wound healing, scarring/keloid formation, pelvic infection, epidermoid cysts/abscesses and/or neuroma. 1,3,39,40 Longer-term impacts include reproductive tract infections, haematocolpos (impaired flow of menstrual blood), dysmenorrhoea (painful menstruation), dysuria (painful and difficult urination), dyspareunia (difficult or painful sexual intercourse), morbidity and mortality during pregnancy and childbirth, pelvic inflammatory disease/infertility, increased risk of HIV transmission or death. 1,39–45 Pregnant survivors are also at increased obstetric risks, including of prolonged and difficult labour, perineal tearing, episiotomy, instrumental delivery, caesarean section, post-partum haemorrhage and a longer maternal hospital stay. 1,6,41,42,45 Babies who are born to women who have undergone FGM also have an increased risk of stillbirth, early neonatal death and needing to be resuscitated at birth. 1
The consequences of FGM are broader than just physical health impacts, with evidence that FGM can have psychological, psychosexual, social and economic impacts for survivors and their communities. 6,39,40,42,46–52 Although there is less evidence for this than for the physical health outcomes of FGM, a recent systematic review has shown an association between FGM and adverse mental health outcomes. 37 For example, survivors are at an increased risk of developing conditions such as low self-esteem, anxiety and post-traumatic stress disorder (PTSD), compared with women who have not experienced FGM. 51,52
Compared with women without FGM, survivors report impaired sexual function, including experiencing pain during sex, problems becoming stimulated and low sexual desire and satisfaction. 51,52 There is a significant economic burden of FGM at the individual, societal and governmental levels. 53 In 2020, the WHO estimated that the global annual financial cost for health care for survivors was US$1.4B. 54 If the practice of FGM is not abandoned, then these costs could increase by 50% by 2050. 54 In 2016, the annual cost of NHS care for FGM survivors in the UK was estimated at £100M. 55 Given the increasing migration of the FGM diaspora to the UK, this cost is likely to escalate going forward.
Deinfibulation for type 3 FGM survivors
Type 3 FGM (infibulation) involves the most extensive tissue removal from the female genitalia and has the most significant physical health impact. 12 Generally, type 3 FGM is carried out in the east of Africa and is most prevalent in Somalia, The Sudan and Djibouti. 12,22 Deinfibulation is a procedure to surgically release the narrowed vaginal introitus in women and girls with type 3 FGM. 56 The WHO has reported56 that deinfibulation is associated with improved health and well-being, as well as allowing sexual intercourse and childbirth. However, currently, there is only limited direct evidence to support this statement. For example, a recent systematic review reported no evidence that deinfibulation improved urological complications. 57 There is, however, stronger observational evidence, albeit of very low quality, to suggest that deinfibulation is associated with improved gynaecological and obstetric outcomes. 58 Deinfibulated women were at a significantly lower risk of undergoing a caesarean section [odds ratio (OR) 0.19, 95% confidence interval (CI) 0.09 to 0.39; two studies] and post-partum haemorrhage (OR 0.31, 95% CI 0.12 to 0.83; one study) than those women with type 3 FGM without deinfibulation. 58 Compared with women without FGM, deinfibulated women were at a similar risk of episiotomy (OR 0.79, 95% CI 0.61 to 1.02; two studies), caesarean delivery (OR 0.60, 95% CI 0.33 to 1.10; one study), vaginal lacerations (OR 0.80, 95% CI 0.39 to 1.65; one study), post-partum haemorrhage (OR 2.52, 95% CI 0.49 to 13.07; one study) and volume of blood loss at vaginal delivery (ml) [mean difference (MD) 9.50, 95% CI –15.47 to 34.47; one study]. They also had similar length of second stage of labour (hours) (MD –0.18, 95% CI –2.47 to 2.10; two studies) and length of hospital stay (days) (MD –0.30, 95% CI –0.69 to 0.09; one study). 58
Evidence around preferences for timing of deinfibulation for type 3 FGM survivors
The development of evidence-based care to improve outcomes for FGM survivors, in particular regarding the optimal or preferred timing of deinfibulation, has been limited to date, with expert opinion and low-quality evidence typically informing recommendations. 1,39,56,58–60
Two recently published qualitative evidence syntheses have explored survivors’ experiences of accessing and receiving FGM health care61 and the factors that influence provision of FGM health care from the perspective of health-care professionals (HCPs). 62 These reviews61,62 and the associated full study report63 explored experiences, communication, timing and outcomes of deinfibulation. In line with preventative health care, the review62 highlighted that HCPs identified ‘compelling’ reasons for antenatal deinfibulation, such as the availability of outpatient care and local anaesthetic, the assurance of professionals who were competent and confident in the deinfibulation procedure and the potential for reduced costs through the avoidance of associated emergencies during intrapartum care. 62 However, much of this evidence was weak, and preventative health care such as antenatal deinfibulation was outside the cultural norms of FGM survivors. 62 HCPs reported that they believed that FGM survivors preferred labour deinfibulation so that they experienced only one procedure, but there was limited evidence to support this interpretation. In addition, the review highlighted that, despite participating in training, HCPs were anxious about deinfibulation, an anxiety that was rooted in a lack of awareness and understanding of the procedure itself. Evidence also suggested that there were inconsistent practices around deinfibulation, guidelines lacked consistency and HCPs were influenced by cultural stereotypes, which reflected cultural dissonance and ethnocentric views.
In the review exploring survivors’ views,61 there were strong cultural imperatives to avoid deinfibulation prior to marriage and pregnancy. A survivor’s family (prior to marriage) and her husband (after marriage) were particularly influential in decision-making around deinfibulation, with evidence to suggest that some women felt the need to seek permission to undergo the procedure outside childbirth. The majority of studies included in the review reported that survivors preferred intrapartum deinfibulation to avoid undergoing two procedures. However, there was evidence that women could ‘be persuaded’ towards the HCPs preferred option of antenatal deinfibulation following discussion and where there was a ‘trusted’ relationship between the survivor and the HCP. Overall, the review61 highlighted that women with type 3 FGM would benefit from more discussion, information and advice throughout their life, as well as both prior to and after deinfibulation.
Current guidance on the timing of deinfibulation for type 3 FGM survivors
Deinfibulation can be undertaken at any point during a survivor’s life; however, the main times suggested in the literature are ‘outside of or during pregnancy’. 1,59 There is considerable variation between and within clinical guidance around the optimal time for deinfibulation. 60,63 For example, the Royal College of Obstetricians and Gynaecologists (RCOG) guidelines9 recommend that deinfibulation should be offered prior to pregnancy and preferably before first sexual intercourse. However, these guidelines also state that deinfibulation can be performed antenatally, in the first stage of labour, at the time of delivery or during a caesarean section. The Royal College of Nursing (RCN) FGM guidance64 does not provide a clear indication on the optimal timing of deinfibulation, with one statement indicating that the procedure is best performed when the woman is not pregnant and another statement suggesting that deinfibulation is best undertaken before or at least during the second trimester of pregnancy. The WHO guidelines on the management of FGM56 recommend either antepartum or intrapartum deinfibulation, with the caveat of a suggestion that timing should be based on wider contextual factors, including patient preference, access to health-care facilities, place of delivery and the skill level of the HCP. In addition to a lack of consensus about when deinfibulation should be performed, there is also debate about whether or not timing affects outcomes, with some studies suggesting that obstetric risks increase the later that deinfibulation is undertaken. 65,66 However, these findings were not substantiated in a systemic review of low-quality observational evidence comparing childbirth outcomes between antepartum and intrapartum deinfibulation. 59
In 2016, the Department for Education and the Department of Health and Social Care in collaboration with the Home Office issued Multi-Agency Statutory Guidance on Female Genital Mutilation for those working in England and Wales. 67 The multiagency guidance has three key functions: to provide (1) information on FGM, (2) strategic guidance on FGM and (3) advice and support to front-line professionals. 67 Interestingly, other than a definition, deinfibulation is not discussed within this guidance.
Legal aspects of FGM
The practice of FGM is illegal in at least 59 countries, including the UK. 12 FGM has been illegal in the UK since 1985 as a result of the Prohibition of Female Circumcision Act 1985. 68 The 1985 Act was replaced in England, Wales and Northern Ireland in 2003 by the Female Genital Mutilation Act 200369 and in Scotland in 2005 by the Prohibition of Female Genital Mutilation (Scotland) Act 2005. 70 In 2015, Section 70(1) of the Serious Crime Act 201571 amended section 4 of the Female Genital Mutilation Act 2003 in England, Wales and Northern Ireland. In 2020, Scotland introduced the Female Genital Mutilation (Protection and Guidance) (Scotland) Act 2020,72 which amended and added to the Prohibition of Female Genital Mutilation (Scotland) Act 2005. Despite increasing legal frameworks and growing political support to end FGM, FGM remains a global issue with little enforcement of legislation, even in countries such as the UK. For example, despite being illegal in the UK for > 35 years, as of October 2020, only five people have been prosecuted for FGM-related offences, with only one leading to a conviction. 73,74
Legislation around FGM has strong associations with practice guidelines, both clinical and social. For example, the RCOG published guidelines with the clinical remit of managing FGM survivors’ care. 9 Although the guideline encompasses clinical care, there are specific recommendations that relate to the legal implications of FGM. 9 As such, when RCOG guidance on FGM informs or benchmarks local clinical guidance on FGM, there is a possibility that the recommendations relating to legal implications are transferred into local guidelines. This has the potential to lead to the discussions between HCPs and survivors being overly focused or framed around the legal aspects of FGM, rather than on the provision of respectful, person-centred and culturally appropriate care. 63
Education and training for health-care professionals around FGM
The care provided to FGM survivors depends on the knowledge and awareness of HCPs, the foundation of which is derived from health-care education. An online FGM educational programme has been developed by NHS Health Education England, in partnership with key stakeholders, and is available for free to NHS health and social care professionals. 75 Other professionals are able to gain access to FGM training using the eIntegrity platform76 or through a Home Office learning package. 77 The Health Education England training covers topics including (1) communication skills, (2) legal and safeguarding issues, (3) management of FGM with children and young women, (4) management with women during pregnancy and (5) psychological impact. 75 This training recommends that deinfibulation should take place around the twentieth week of pregnancy. However, there is no current evidence to substantiate this, with recommendations for the timing of deinfibulation in clinical guidance being based on clinician opinion only. 1,9,64 Although the Health Education England training package is aimed at HCPs, the Home Office training is aimed at a multiagency audience. 77 Nevertheless, there are similar notions throughout the Home Office training; for instance, there is a strong victimisation of survivors depicted, with the word ‘victim’ being used on several occasions in audio excerpts. There is a parallel with the Health Education England training package in that there is a lack of the survivor’s voice inherent in the training. Furthermore, negative ‘power’ words are used; for instance, there is a statement that points out that professionals should ‘not fear being branded racist or discriminatory’. The wider evidence base suggests that HCPs would benefit from additional training in relation to FGM and, in particular, deinfibulation;63 however, the current training packages lack the voices of survivors, are not based on best evidence and potentially victimise those from FGM-affected communities.
FGM service provision
Services for FGM survivors across the UK still appear to be sporadic and suboptimal. 62 The Foundation for Women’s Health Research and Development (FORWARD) has identified 21 clinics that currently provide services specifically for FGM survivors. 78 Yet the majority of these services are attached to NHS maternity services and they are concentrated in inner-city NHS trusts. As a result, many women may not access these services or be aware of their existence until pregnancy. In an attempt to alleviate this issue, in 2019, NHS England commissioned eight community clinics for FGM survivors. The clinics accept referrals from general practitioners (GPs) and other HCPs, as well as FGM survivors’ self-referrals and walk-in appointments. 79 However, this service provision is concentrated in the Greater London area, with only three clinics currently serving the rest of England.
Study justification
FGM remains a significant global health concern that is an important health-care challenge in the UK as a result of the increase in the diaspora from countries where FGM is practised. 22 The NHS will be required to provide culturally acceptable and safe evidence-based care to growing numbers of FGM survivors. There is evidence to suggest that current care provided to FGM survivors may be not culturally sensitive or appropriate. 63
Current estimates of the prevalence of FGM in the UK diaspora potentially underestimate the true burden of FGM given the sensitive nature of disclosure, a perceived lack of clinical and cultural competence among HCPs, language barriers and the often limited engagement of FGM survivors with health-care services. 63 This lack of engagement with FGM services is likely to reflect a complex picture, including the fact that there may be an absence of FGM service provision in some areas of the UK and, where there is provision, services may be disjointed and invisible to survivors.
Type 3 FGM is associated with significant health, psychological, sexual and economic consequences that have an impact on girls, women and men. 1 The WHO has suggested that deinfibulation is beneficial for the health and well-being of girls and women and that it reduces the risk of negative outcomes in childbirth. 56 Currently, however, there is no clear preference for the timing of deinfibulation for type 3 FGM survivors. 56,59,60,63 Recommendations for future FGM research suggest that ‘there is an urgent need for well-designed research to inform evidence-based guidelines, and to improve the health care of women and girls with FGM’. 60 In addition, there is a specific need to focus on exploring preferences for the timing of deinfibulation, involving a diverse range of FGM survivors, men and HCPs, across multiple centres. 60,63,80 At present, there is a lack of robust qualitative evidence of UK-based deinfibulation experiences from the perspective of FGM survivors, HCPs and, in particular, men.
Health services in the UK have increasingly sought to develop patient-centred care. 81 Qualitative research actively seeking a diversity of experiences from those who are recipients of care can provide richer insights to direct quality improvement. 82 Barker82 argues that methodologically robust qualitative research has an ‘increasingly important role to play’ in health service design and delivery, and when a diversity of patients’ voices are heard, the benefits can be gained by all stakeholders.
Research aims and objectives
The overarching aim of the FGM Sister Study was to explore and understand the views of FGM survivors, men and HCPs on the timing of deinfibulation and how NHS services can best be delivered to meet the needs of FGM survivors and their families. This overarching aim was addressed through two work packages (WPs).
Work package 1
The aim of WP1 was to qualitatively explore and understand the timing preferences for deinfibulation and how NHS FGM services could be improved for type 3 FGM survivors (WP1a), men (WP1b) and HCPs (WP1c). This was achieved through the following objectives:
-
to explore knowledge, awareness and understanding of FGM and deinfibulation (WP1a, b and c)
-
to elicit views on preferences for the timing of deinfibulation and the rationale for these views (WPs 1a, b and c)
-
to explore perspectives on the decision-making process around deinfibulation (WPs 1a and b)
-
to explore knowledge, awareness and experiences of FGM services and support (WPs 1a, b and c)
-
to understand the enablers of, motivators of and barriers to FGM care-seeking behaviours (WP1s a and b)
-
to explore how HCPs describe, explain and reason about their care provision for FGM survivors and their families (WP1c)
-
to understand how FGM care provision could be improved to best meet the needs of FGM survivors, their families and HCPs who support them in their local context (WPs 1a, b and c).
Work package 2
The aim of WP2 was to use established techniques to synthesise the qualitative research findings, inform best practice and policy recommendations around the timing of deinfibulation and FGM care provision, and identify future actions. This was achieved through the following objectives:
-
to explore views and reflections on the trustworthiness of our interpretation of the data and the conclusions drawn (WPs 2a and b)
-
to establish if there is a consensus on the optimal timing of deinfibulation (WPs 2a and b)
-
to identify the key recommendations to inform NHS FGM care provision (WPs 2a and b)
-
to explore the facilitators of and barriers to implementation of changes to NHS FGM care provision (WP2b)
-
to explore views on the requirements for future FGM research (e.g. randomised trials) (WP2b).
Structure of the report
Chapter 2 presents the methodology and methods, including the theoretical foundation of the study; the conceptual framework used to underpin the methods, sampling, data collection and analysis; and ethics considerations. Changes to the protocol are also documented in Chapter 2. Chapter 3 presents the thematic results interpreted from the synthesised and analysed data. Chapter 4 presents the interpreted roots and manifestations of silences. Chapter 5 presents the address of silences, discussion of the interpreted results situated within the context of the wider literature, discussion of the robustness of the results, the limitations of the research and findings and makes recommendations for further research, as well as implications and recommendations for health-care provision as a result of this study. Chapter 6 presents the conclusions of the study.
Chapter 2 Methodology and methods
Introduction
This chapter presents an overview of the methodology and methods of the study. The study protocol has been published83 and the study was prospectively registered as International Standard Registered Clinical/soCial sTudy Number (ISRCTN) 14710507. 84 This study has been reported against the Standards for Reporting Qualitative Research (SRQR) guidelines. 85 As highlighted in Chapter 1, the aim of the FGM Sister Study was to explore and understand the views of FGM survivors, men and HCPs on the timing of deinfibulation and how NHS services can best be delivered to meet the needs of FGM survivors and their families. This overarching aim was addressed through two WPs. WP1 was undertaken by the research team and WP2 was a collaboration between the research team and our charity partner – the National FGM Centre (Ilford, UK).
Study design and underpinning framework
The methods of this qualitative study were structured around the Sound of Silence framework (SSF). 86 The SSF is underpinned by broader theoretical approaches that accept that reality (or truth) is not objective; rather, the social world is influenced by people in a particular society at a particular point in time. 87 Truth is influenced by subjective individual and group interpretations of events and experiences, and the social and personal contexts in which these occur. 86 The SSF is aligned with philosophical approaches, including feminist, ethnic and criticalist viewpoints that recognise that interpretations of lived experiences, for example through qualitative research, are subjective and inherently influenced by particular social and political viewpoints. 86
‘Silences’ define areas of research and experiences that are little researched or understood or are unheard,86,88 and are useful for researching sensitive issues and/or the health-care needs and perspectives of marginalised populations. 86 Within the context of this study, although FGM is a contemporary issue that has increasingly become the subject of political and media interest, it remains a sensitive issue prevalent among marginalised populations and one that is under-researched. The nature of this study, namely working with potentially marginalised groups on a sensitive issue, needed to be accounted for in our methodology and methods. Using an appropriate framework was important to ensure that the perspectives of such marginalised groups were respected and at the forefront of the research, and that the needs of such marginalised groups were identified in relation to their requirements.
Sound of Silence framework
Next is a brief overview of the salient features of the five stages outlined in the SSF86 and how the FGM Sister Study aligned with each stage. This is supplemented by Figure 2, which provides a schematic overview of the SSF.
FIGURE 2.
The Sound of Silence Framework (adapted from Serrant-Green86). Serrant-Green L, Journal of Research and Nursing 16(4), pp. 347–60, copyright © 2011 by SAGE Publications. Reprinted by permission of SAGE Publications.

Sound of Silence framework stage 1: working in silences
Stage 1 provided the context for the research through a critical review of the existing literature on FGM. Stage 1 aims to ascertain preliminary answers to some initial key questions, including what is currently known, what is evident, whether or not silence already exists by exploring what appears to be unreported and how things currently are in relation to knowledge and practice. This stage is important for helping to expose the real world in which the research will take place,86 which facilitates contextual understanding and a basis for the research. This stage (see Chapter 1) has already helped shape the research study and the published protocol. 83
Sound of Silence framework stage 2: hearing silences
Stage 2 identified the silences inherent in conducting the research study, by researcher A at time X and with marginalised group/individual B. This was an important step in ensuring that the researchers were aware of what they as individuals brought to the research, for instance their preconceived ideas and biases at a particular place/time. The researchers were the primary vehicle through which silences were heard86 and so they had to be open to and reflexive in identifying and exploring silences related to their role in the research. This stage, therefore, recognised that different researchers may hear different silences and participants may identify/experience different silences. This stage outlined the methodological importance of reflexivity, whereby the researcher is reflexive with respect to reporting on and exploring participants’ or listeners’ identification of screaming silences.
Sound of Silence framework stage 3: voicing silences
Stage 3 explored the data that were collected from the participants to attempt to identify ‘silences’ in the context and from the perspectives of survivors, family (e.g. the partners of survivors) and care providers (e.g. HCPs). Importantly, this stage involved ‘transferring power to the participants, thus ensuring that their experiences [and preferences] count as valuable and ensuring their voices [are] not further silenced’. 89
Sound of Silence framework stage 4: working with silences
Stage 4 aimed to ensure that the aims and objectives of the research had been met, and facilitated a critical reflection on the contribution of the research by looking at how the researcher and collective voices have had an impact on the research. It sought to develop recommendations across a number of relevant domains, including informing clinical practice.
Sound of Silence framework stage 5: planning for silences
This stage sought to develop recommendations for future research, explore the implications of the findings and offer mechanisms for planning for and alleviating current and future silences.
Study setting
Survivors live in every local authority in England and Wales,24 so the study was undertaken across multiple regions, settings and services in the UK. However, census and NHS data suggest that larger populations of FGM survivors generally reside in inner-city areas. 24,90 For example, the following regions have some of the highest prevalence rates of FGM survivors: London (21.0 per 1000 people), Birmingham (12.4 per 1000) and Manchester (16.2 per 1000). 24 Moreover, Birmingham and Manchester have large FGM diaspora from countries that almost universally practise type 3 FGM, and practitioners anecdotally reported that London has a more transient FGM population: survivors were more likely to be type 3 and present in labour/at the point of delivery, without previously having accessed care. Therefore, these three regions offered a range of potentially different realities to explore and we purposively sought to recruit survivors and men in these locations. Given the significant variation in FGM service provision, we sought to identify HCPs and wider stakeholders from diverse regions and settings (including those with high and low prevalence) across the UK.
Eligibility
Work packages 1 and 2
WP1a and WP2a used the same inclusion and exclusion criteria. The inclusion criteria for these WPs were FGM survivors who were:
-
aged ≥ 18 years
-
resident in the UK
-
able to speak fluent English, Somali, Arabic and/or French
-
willing and able to provide voluntary informed consent (written, electronically completed or verbal).
The exclusion criterion was:
-
FGM survivors who experienced psychological distress related to FGM that prevented them from consenting and/or participating in the study.
For WP1b, the inclusion criteria were male participants who:
-
were aged ≥ 18 years
-
were resident in the UK
-
were able to speak fluent English, Somali, Arabic and/or French
-
were willing and able to provide voluntary informed consent (written, electronically completed or verbal)
-
had a partner/spouse or family member who had experienced FGM.
Recruitment for WP1b included snowballing from WP1a, so there was one exclusion criterion for this cohort:
-
Partner/spouse does not consent to their participation (if identified through a WP1a participant).
WP1c comprised HCPs who were providing care to FGM survivors and their families or who had provided care within the last 5 years. As such, the inclusion criteria were being:
-
aged ≥ 18 years
-
able to speak fluent English
-
willing and able to provide voluntary informed consent (written, electronically completed or verbal)
-
a HCP (including, but not limited to, GPs, practice nurses, midwives, obstetrics and gynaecology clinicians, genitourinary clinicians and sexual health specialists) who was currently or recently (within the last 5 years) involved in the delivery of care to FGM survivors and their families in the UK.
There were no exclusion criteria for this cohort.
WP2b comprised stakeholders in FGM care and the delivery of services. The inclusion criteria for this group were being:
-
aged ≥ 18 years
-
able to speak fluent English
-
willing and able to provide voluntary informed consent (written, electronically completed or verbal)
-
a key FGM stakeholder, such as HCPs (see WP1c inclusion criteria), policy-makers, FGM-specialist researchers/academics, health economists, commissioners and representatives from third-sector organisations (e.g. charity and advocacy groups), who was currently or recently (within the last 5 years) involved in the planning and delivery of care to FGM survivors and their families in the UK.
There were no exclusion criteria for this cohort.
Sampling and recruitment
There were four core target cohorts of participants (survivors, men, HCPs and FGM stakeholders). The following section presents the methods used for the sampling and recruitment of each of these core participant groups.
Work package 1a sampling
The sample of women targeted for this study were FGM survivors resident in the UK. Although the focus of the study pertains to type 3 FGM survivors, during consultation it was acknowledged by patient and public involvement (PPI) representatives and specialist FGM clinicians that FGM typology is usually diagnosed during health-care episodes, particularly maternity care episodes. Women who were recruited through non-NHS organisations may not be aware of FGM typology; hence, survivors who had experienced types of FGM other than type 3 were not specifically excluded. Pregnant and non-pregnant women were purposively sampled91 to give a broad range of experiences and views on service provision. This sample was inclusive of women who had (1) not had a deinfibulation procedure, (2) a deinfibulation procedure for health and/or personal reasons, (3) a deinfibulation procedure antenatally and (4) a deinfibulation procedure during labour or at the point of birth. To maximise the diversity of the sample,92 women from a range of locations, ages, education levels and FGM-affected communities were included.
Work package 1a recruitment
There was significant discussion and consultation with the study team’s specialist clinicians and PPI survivor group regarding advertising the study for recruitment. Evidence suggests that women from hard-to-reach communities, such as FGM-affected communities, may not relate to language used in recruitment, mistrust the research process and/or believe that the research will not be beneficial to their community, as well as that it could potentially cause harm. 93 Therefore, recruitment was primarily through trusted networks and advocates, such as midwives who facilitated FGM-specialist clinics and community support workers. This was supplemented with discrete advertising in clinics, community settings, social media and through culturally sensitive snowballing. 94 A range of advertising material was developed with support from our PPI survivor group to provide study information and aid recruitment, with participant information leaflets (PILs) containing more detailed information (see www.journalslibrary.nihr.ac.uk/programmes/hta/167804/#/documentation; accessed 25 August 2021). We trained potential recruiters (e.g. at site initiation visits) to approach survivors to participate in the study. Survivors were approached, in the first instance, by a member of their usual care team or by a trusted advocate in community organisations. Advocates briefly screened survivors for eligibility and introduced the study. Survivors who responded positively to study participation were then asked to complete and sign a contact detail form that gave permission for us to contact them to discuss the study further. A researcher then contacted the survivor (supported by an interpreter, as needed) to check her eligibility, discuss the study further, answer any questions she might have and arrange a mutually convenient time and location for the interview. At the end of the interview women were asked if their male partner and other survivors that they knew would wish to participate in the study. When survivors responded positively, our contact details were provided and the men/other survivors were asked to contact us directly.
Work package 1b sampling and recruitment
The sample of men targeted for this study were predominantly identified through their female partners who took part in WP1a, as well as community and third-sector organisations and social media.
Work packages 1a and 1b for speakers of other languages
Because English is not the first language in the regions where FGM is predominantly practised, potential participants may not have been fluent English speakers. Language diversity and inclusion was one of the primary considerations during the preliminary study design stage. UNICEF has identified > 30 countries where FGM is highly prevalent,22 with potentially > 1500 languages spoken across these countries. 95 It was identified that Arabic and Somali are the most widely spoken languages in these countries; however, because of historical colonisation, English and French are also widely spoken. 96 In addition, we sought the advice of the specialist clinicians in each of the three main recruiting regions to ascertain if Arabic, English, French and Somali are common languages of the survivors that they see in practice to ensure that these were the most appropriate languages to use. All participant-facing documents were available in Arabic, English, French and Somali. These were developed in English and then forward- and back-translated by native speakers of each language. The focus was on cross-cultural and conceptual translation, rather than linguistic or literal equivalence,97 to ensure that appropriate terminology and phrasing were used, and to facilitate fluency of the text in the translated versions.
Work package 1c sampling
Health-care professionals were purposively recruited from a diverse range of groups, including GPs, midwives, obstetricians and gynaecologists, genitourinary clinicians and sexual health specialists. Allied health professionals (i.e. physiotherapists, psychotherapists and psychologists) who met inclusion criteria were also recruited.
Work package 1c recruitment
Multiple recruitment pathways were employed as the target population for WP1c was UK-wide and dependent on the profession of HCPs. For example, NHS maternity units were contacted to invite midwives, obstetricians and gynaecologists to participate, whereas general practice surgeries were contacted with the view of inviting GPs and practice nurses to take part. Depending on the commissioning stream of FGM services, these were contacted either through NHS maternity services or directly (if they were stand-alone services); some of these maternity services were contacted through our personal networks. The study was also advertised on social media platforms, including Twitter (Twitter, Inc., San Francisco, CA, USA; URL www.twitter.com) and Facebook (Facebook, Inc., Menlo Park, CA, USA; URL www.facebook.com), as well as contacting professional bodies such as the Royal College of Midwives (RCM) and the RCOG to advertise the study on our behalf. To obtain a wide range of views and experiences of providing care for FGM survivors, recruitment took place in both high- and low-prevalence areas. Snowballing from potential HCP participants was also used,94 particularly in FGM services where other allied health professionals were involved in the provision of care to survivors as part of holistic care delivery. HCPs were asked to contact us directly if they were interested in taking part. Following contact, they were screened for eligibility, provided with further study information, given time to answer questions and then a mutually convenient time and location for the interview was arranged.
Work package 2a sampling and recruitment
FGM survivors who took part in WP1a and had expressed an interest in participating in WP2a were contacted by the research team. Recruitment was further supplemented through the same pathways as identified for WP1a and with support from our charity partners at the National FGM Centre, who advertised the study through their networks, community support workers and snowballing through trusted advocates in their community outreach groups. Potential participants were provided with information about the study and were able to liaise with us and the National FGM Centre team, as needed, ahead of the events.
Work package 2b sampling and recruitment
We recontacted each HCP who participated in WP1c and had responded positively to participating in WP2b. This was supplemented using the same pathways as described for WP1c. Other key stakeholders (see Eligibility) were identified through our and the National FGM Centre networks and collaborators, advertising on social media and snowballing. 94 Potential participants were provided with information about the study and were able to liaise with us and the National FGM Centre team, as needed, ahead of the event.
Consent
The method of consent for WP1a and WP1b was a two-stage process that commenced with the potential participant providing their consent for the research team to establish contact (for copies of consent forms, see www.journalslibrary.nihr.ac.uk/programmes/hta/167804/#/documentation; accessed 25 August 2021). Their contact details were passed to the research team through a live telephone conversation and recorded directly in the secure study database. We then attempted to contact each potential participant using their preferred method. When contact was not established on initial telephone call or there was no response within approximately 1 week, where permission had been given, alternative mechanisms of contact were attempted using an interpreter as necessary. Alternative contact mechanisms, up to a maximum of three attempts, and associated dates were documented in the secure study database. If, after three contact attempts, contact was not established in any form then a failed contact was documented.
In some cases, more than three attempted contacts were made when contact was deemed to have failed, but the potential participant contacted the study team after three contacts expressing their wish to participate.
On successful contact with a favourable response from the potential participant, the contacting member of the study team discussed the study in detail and provided options for voluntary informed consent to participate in the study. The options included:
-
consent form posted to the participant by postal mail, signed with wet ink and returned to the study team using a provided stamped addressed envelope
-
consent form posted to the participant by postal mail or sent by e-mail, printed and signed with wet ink, electronically scanned and sent to the research team by e-mail
-
consent form posted to the participant by postal mail or sent by e-mail, printed and signed with wet ink, photographed and sent back to the research team by e-mail
-
consent form posted to the participant by postal mail or sent by e-mail and completed at the time of face-to-face interview with a member of the research team
-
consent form sent by e-mail, completed electronically by the participant and e-mailed back to the study team
-
consent form posted to the participant by postal mail or sent by e-mail, completed verbally and recorded at the commencement of audio-recording of the interview during telephone interviews.
The last two methods of consent were added to mitigate against poor recruitment. The target population for this study was considered to be hard to reach and the consent process appeared to be a contributory factor to the disengagement of potential participants. Following discussion with the study management group (SMG) and the Study Steering Group (SSG), a substantial amendment to the protocol was incorporated to provide some flexibility in the consent process (FGM Sister Study Protocol v2.0). Although written informed consent was sought wherever possible, this flexibility resulted in improved engagement and increased recruitment. This was the only substantial amendment to the protocol during the course of the study.
The purpose of the informed consent was to gain permission for agreement to participate in the study, to collect demographic data in a background questionnaire (for copies of the background questionnaires, see www.journalslibrary.nihr.ac.uk/programmes/hta/167804/#/documentation; accessed 25 August 2021) and to audio-record the dialogue of the interview discussion (or event). At commencement of audio-recording of the data collection episode, all participants were asked to reconfirm their consent to participate. When verbal consent was gained, the audio-recording was started and each statement from the consent form was read out by the interviewing member of the research team. If a participant did not consent to any of the statements, the interview was terminated. Consent forms were available in all languages and verbal consent at the start of the interview was supported by an interpreter as necessary.
The consent processes for the other WPs were the same, aside from the fact that there was no consent to contact form. All participants were reassured that participation in the study was voluntary and that they were free to withdraw up to 2 weeks after the data collection event without providing a reason.
Anticipated sample sizes
Work package 1
We sought to recruit up to a total of 110 participants:
-
up to 50 women who are FGM survivors
-
up to 10 male partners
-
up to 50 HCPs.
Work package 2
We sought to recruit up to a total of 60 participants:
-
20–25 FGM survivors for the community engagement event
-
30–35 stakeholders for the national stakeholder event.
However, numbers remained flexible, and the adequacy of the final sample size was carefully monitored during the research process to ensure that the overall sample and associated data had sufficient information power to develop new knowledge in relation to the research questions. 98
Data collection
Work package 1
Data collection and analysis was undertaken in stage 3, ‘Voicing Silences’, of the SSF and was informed by stage 1, ‘Working in Silences’. Semistructured interviews were used as the data collection method during WP1, as these have been identified as one of the most appropriate methods for facilitating an in-depth exploration of participants’ experiences that may involve sensitive and traumatic events. 99 Following PPI feedback, we added focus groups to the protocol (prior to receiving ethics permission, thus this was not a substantial amendment) as an alternative method of data collection, but none of the participants expressed a preference for discussing their experiences as part of a group.
Each interview was conducted by a trained qualitative researcher who was independent of the participant. Two researchers conducted the majority of the interviews, with support from four others. Professional interpreters, who we had trained, supported data collection where necessary. Discussion guides (for copies of the discussion guides, see www.journalslibrary.nihr.ac.uk/programmes/hta/167804/#/documentation; accessed 25 August 2021), informed by the aims and objectives of the study, our critical review of the literature and discussion with our PPI group, were used to help guide WP1 interviews. Discussion guides were developed iteratively based on interviewer field notes and reflections and regular discussion across the research team. Interview audio files were transcribed by a specialist external transcription company.
Work package 2
Work package 2 consisted of two community engagement events and one national stakeholder event. Staff from the National FGM Centre facilitated the community engagement events and the national stakeholder event was hosted by the National FGM Centre, but facilitated by five members of the research team. At the beginning of each event, a brief overview of the study was presented to the group. Discussions focused on the credibility of our interpretation of the data and the findings of WP1, and whether or not it was possible to establish consensus regarding findings and conclusions.
The way the events were run differed slightly between WP2a and WP2b because of the number of participants. We initially planned to run one community event only; however, as a result of small numbers in the first event, a second event using the same facilitator was undertaken. For the community events, given the small numbers, the discussions were facilitated as a whole group. However, WP2b consisted of a larger number of participants and so the group was divided into four smaller ‘table’ groups that considered the homogeneity and inclusivity100 to create a safe space where participants felt empowered to share their views and question the views of others. The results of the smaller group discussions were then shared as part of the facilitated whole group discussion to establish whether preferences for deinfibulation and recommendations for service improvement were ratified, refuted and/or challenged to inform policy, practice and education. Small and whole group discussions were audio-recorded and the audio files were transcribed by a specialist external transcription company.
Development of the discussion guides for work package 2
The discussion guides (for copies of the discussion guides, see www.journalslibrary.nihr.ac.uk/programmes/hta/167804/#/documentation; accessed 25 August 2021) for WP2 were derived from the interpretation of findings from WP1, as the purpose of WP2 was to ratify, refute and/or challenge the initial findings. As such, the discussion guides used in WP2 differed slightly from those used in WP1. However, the focus remained the same: experiences of care and preferences for deinfibulation.
In parallel with the discussion guides, various quotations were selected from the data collected in WP1 to explore the credibility of the research team’s interpretation of the data. This method was also used in WP2a and WP2b. However, as the data collection tool was constructed from the initial findings, there were occasional subtle differences in the responses from event participants compared with the responses in WP1, albeit there were different stakeholders present in WP2b. Although these differences were categorised as ‘new data’, they did not generate new subthemes and/or overarching themes/silences. Instead, the new data supported the interpretation of subthemes and, subsequently, the overarching themes and silences (see Analysis).
Use of interpreters
During the planning stage of the study, it was acknowledged that there was a potential need for interpreters to facilitate communication between the participant and researcher to support recruitment and data collection through interviews. FGM is not openly discussed among the communities101 and, therefore, lay or peer interpretation was not appropriate. The PPI survivor group advised against the use of community members and/or peers of potential participants for interpretation; they explained that the potential stigma attached to FGM within the community may discourage participation and/or affect the information provided by the participant, as well as the accuracy of interpretation. As such, professional interpreters were employed to provide real-time interpretation during the recruitment, consent and interview processes. We trained interpreters on FGM, study processes (including taking consent) and how the interviews needed to be interpreted with a focus on conceptual equivalence, rather than word-for-word or literal translation. 97
Analysis
The framework method and alignment justification
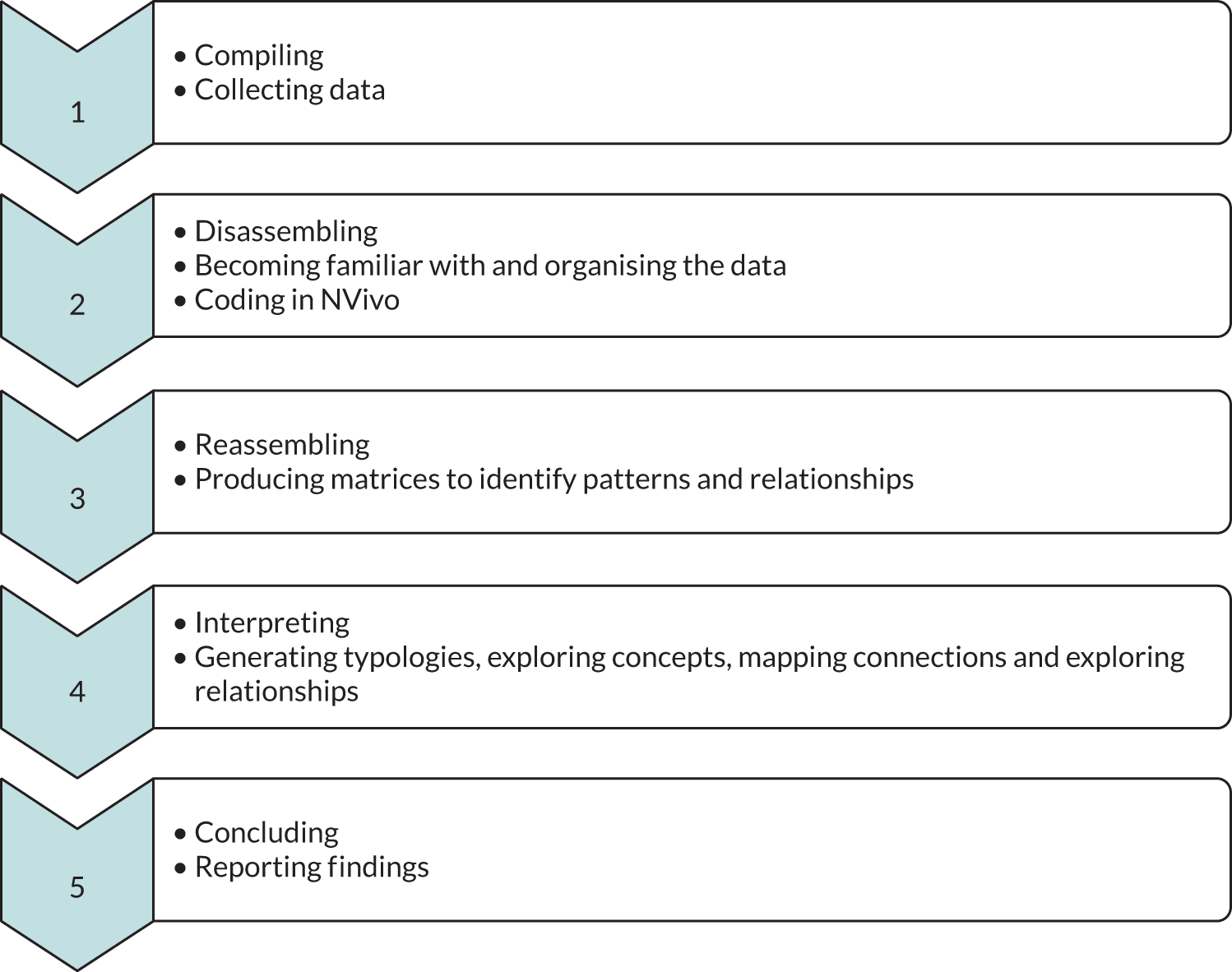
The framework method (FM) is a ‘systematic and flexible approach’ to qualitative analysis in multidisciplinary research, including applied health research. 102 The FM requires researchers to take a staged approach to research to facilitate the collection, interpretation and analysis of data. Although the FM is usually understood as a seven-stage method,102 more recent methodologists have refined the number of stages. 103 We have used the five-stage FM outlined by Castleberry and Nolen (Figure 3). 103
FIGURE 3.
Five-step model of the framework method (informed by Castleberry and Nolen103). Reprinted from Currents in Pharmacy Teaching and Learning, Vol. 10, Castleberry A and Nolen A, Thematic analysis of qualitative research data: is it as easy as it sounds? pp. 807–15, (2018) with permission from Elsevier. Coding in step 2 was performed using NVivo software, version 12 (QSR International, Warrington, UK).
The alignment of the SSF and the FM in a hybrid framework method (HFM) is important, as the framework utilised during research must (1) clearly answer the ‘what’ question,104 namely ‘what is the purpose of the study?’ and (2) provide adequate and project-relevant philosophical underpinnings for the research study. 105 However, the FM on its own does not provide (1) or (2); the FM provides a method for the management and analysis of qualitative data only. 102 In short, the FM requires supplementation, with a framework that addresses (1) and (2). We utilised the robustness of the FM and its effectiveness in multidisciplinary research by transposing the core features of the method onto the SSF, as this is appropriate to the research questions, the marginalised participants and the sensitive topics that we engaged with as part of the research.
The hybrid framework method: aligning the framework method and the Sound of Silence framework
Figures 4 and 5 provide outlines and descriptions of our HFM. The HFM is not in itself a discrete method, but rather a placeholder term used to describe and contain the alignment of the FM and the SSF. The HFM is divided into three categories: pre analysis, analysis and post analysis. This categorisation places the process of analysis at the heart of the method. Further details of stage alignment can be found in Appendix 1.
FIGURE 4.
The HFM.
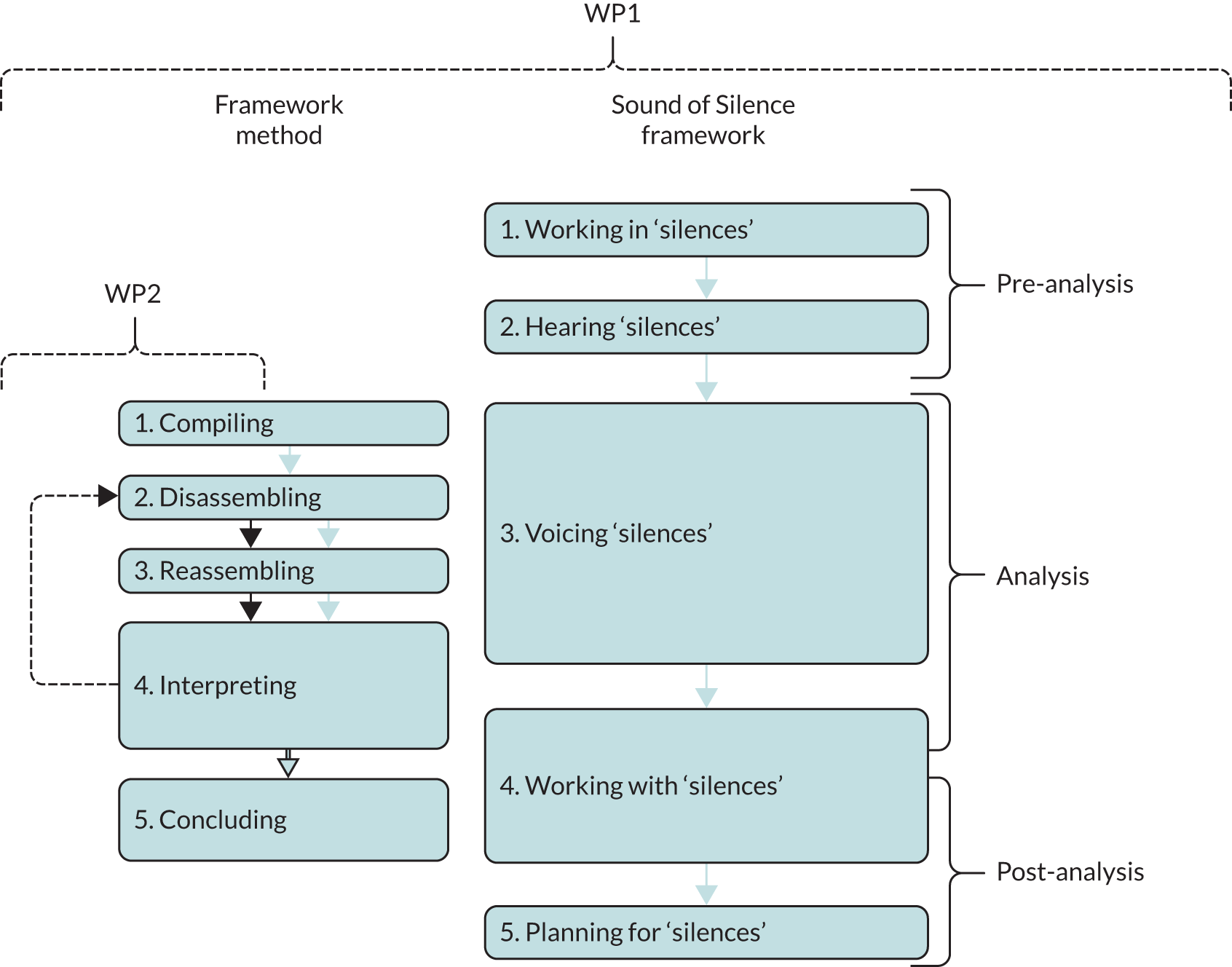
FIGURE 5.
Alignment of the HFM with the FM and SSF.

It is important to note that the results chapters (see Chapters 3 and 4) will present overarching themes and silences; there is, in many cases, an intrinsic relationship and cross-over between the themes and silences, although these are interpreted through different theoretical lenses.
Description of quotations used in Chapters 3 and 4
As a qualitative study, the participants’ voices were the cornerstone to the interpreted findings. Quotations used in Chapters 3 and 4 have not been edited to improve the narrative flow and are presented verbatim to ensure that the voices of participants were captured. It was important to capture the voices of the participants to ensure that these were not further silenced as a result of the research, analysis or interpretation. The quotations selected for Chapters 3 and 4 were identified across each of the participant cohorts to reflect our interpretations of the data. This also included deviant cases to ensure that a balanced view was presented.
Quality assurance of interpretation, transcription and translation
It was important to assure the quality of the interpretation and subsequent transcription of interviews undertaken in languages other than English. Therefore, we randomly selected one interview (which was in Arabic) and had the professional interpretation company transcribe and translate the whole interview into English, including what was said by the researcher, interpreter and participant. This provided us with an opportunity to check what had been asked by the researcher and whether or not the interpreter presented the core concepts correctly to the participant (conceptual equivalent interpretation). We were also able to check how the interpreter had presented concepts from the participant back to the researcher. In general, the conceptual equivalence was good. However, we did provide feedback to the interpreters regarding ensuring that they did not summarise what the participant had said in the feedback to the researcher, but that they interpreted all that had been said, and that they provided more regular interpretation, rather than waiting until a large amount of information had been discussed, as this could potentially lead to reduced recall accuracy.
Furthermore, we randomly selected four audio files (two Arabic and two Somali) and identified a 5-minute window in each where the researcher had asked about preferences for deinfibulation. These sections were transcribed and translated by the interpretation company and checked for conceptual equivalence. This process ensured confidence in interpretation and ensured that the voices of participants were not lost during interpretation. We therefore made the decision for the remaining interviews supported by an interpreter that only the English parts of the discussion would be transcribed.
Ethics considerations
The study was sponsored by the University of Birmingham (17-188). It has received a favourable opinion from the North West Greater Manchester East Research Ethics Committee (18/NW/0498) and approval from the Health Research Authority (HRA).
Assessment and management of risk
A detailed risk register was developed and maintained to assess risk(s) and implement actions to mitigate against or reduce risk(s). Risks were rated as red (high), amber (medium) or green (low) based on the likelihood that the risk would occur and the potential impact of the risk on the study. The register was reviewed on a monthly basis by the research team as risks (actual and potential) and the associated rating changed throughout the study period. The risk register was a rolling agenda item for the SMG and SSG meetings. Risks were categorised into three main sections:
-
general (e.g. staffing, ethics/governance approvals, subcontracting, COVID-19, resource constraints, time constraints, engagement of recruiters and stakeholders)
-
participant (e.g. identification, diversity of sample, recruitment, sensitivity of discussions, distress, eligibility, disclose of potential harm/illegal activity, language, availability for interview/events, location of interview/events)
-
researcher (e.g. sensitivity of discussions, distress, disclosure of harm, safeguarding, location and timing of data collection).
Managing distress and safety of the participants and the research team
FGM is a sensitive topic and discussions of FGM may cause distress during interviews with survivors or men. During data collection, the welfare of participants was of paramount importance and was placed ahead of the knowledge gained for the study. To mitigate against any potential or actual distress, a study-specific distress pathway was developed and embedded into the study protocol, aligned with the guidance from Draucker et al. 106 During data collection, when emotionally distressing aspects of the interview/community event occurred, these were dealt with in a sensitive manner and participants were encouraged to seek support from services specific to FGM survivors. Contact details of such services were provided in the PILs.
There was also potential for the research team to be exposed to highly distressing and sensitive information during data collection, including hearing and discussing the participants’ particularly challenging experiences. There was provision for debriefing sessions to support the research team if difficult and/or challenging circumstances arose. All members of the research team had access to senior members of the team to discuss concerns and decisions made in relation to the study.
Researchers also facilitated interviews in participants’ homes and in other ‘safe spaces’ (as defined by the participant). In these circumstances, the researcher was in participants’ homes or other spaces alone. Although it was possible that some participants would be non-English-speaking, interpreters were used to assist with telephone interviews only. The research team operated a ‘buddy system’, whereby another member of the research team was contacted at an agreed time by the researcher conducting the interview on arrival at the participant’s home and then contacted again following departure from the participant’s home. This was in line with the University of Birmingham’s Lone Worker Policy.
Safeguarding and legal aspects of FGM
FGM has been illegal in the UK since 1985. It is an offence under the Female Genital Mutilation Act 200369 to (1) perform FGM in the UK or take a girl abroad to be subjected to FGM, (2) assist in the carrying out of FGM in the UK or abroad, (3) assist, from the UK, a non-UK person to carry out FGM outside the UK on a UK national/permanent UK resident and (4) for someone in the UK to ‘aid, abet, counsel or procure’ FGM outside the UK (contains public sector information licensed under the Open Government Licence v3.0). The Serious Crimes Act 201571 (1) provides ‘anonymity for victims of female genital mutilation’, (2) created a new offence of failure to protect a girl from FGM, (3) introduced ‘FGM protection orders’ and (4) introduced a mandatory reporting duty requiring regulated health and social care professionals and teachers to report known cases of FGM in girls aged < 18 years to the police (contains public sector information licensed under the Open Government Licence v3.0).
As some members of the research team were regulated HCPs, it was felt that the team had a duty of care to all participants to follow the mandatory reporting guidance that was published by NHS England. 107 Therefore, all members of the team were trained on mandatory recording and reporting procedures, with the remit of implementing appropriate action following a disclosure during data collection. 107 As a research team, we made a conscious choice for our safeguarding protocol to align with mandatory reporting guidance, meaning that if there was disclosure of serious risk of harm, then we would need to break research confidentiality.
We understand that in some contexts it may be possible to truly maintain confidentiality for research participants, but we did not feel that this was the case when there was potential for disclosure of illegal activity and there was mandatory reporting legislation in place. A completely confidential safeguarding protocol within a FGM research study would fail to recognise that FGM is illegal. The reality of this means that if, for example, a woman was to disclose during a research interview that they were planning to have their daughter cut that the research team would do nothing, even though we knew that that child might be at serious risk and as a result might undergo a life-changing event that we could have potentially prevented. As well as considering this both morally and ethically inappropriate, many of the research team hold professional qualifications bound by codes of professional conduct. Within the participant information sheet and the consent form, it was made clear to potential participants that we would maintain their confidentiality unless they disclosed something that the research team thought put them or others at risk. Therefore, participants were aware of this prior to taking part.
During the study, there was one disclosure from a participant that was judged to require mandatory reporting. With the participant’s knowledge, this was reported to the police by the researcher to whom the disclosure was made. The disclosure was investigated, with no further action taken.
Reflexivity
Aligned with good practice in qualitative research, and as highlighted in stage 2 of the SSF, it was important that the research team were aware of how their worldview, preconceived ideas and biases may have influenced the study. In particular, it was important for the team to be reflexive with regard to exploring, identifying and interpreting silences related to their role in the research. Six researchers were involved in interview data collection (i.e. ED, BC, FCS, JC, LJ and LA). Two researchers (i.e. ED and BC) conducted the majority of the interviews. Of the six researchers, five were female and one was male. Two researchers were midwives, one was a philosopher and qualitative researcher and three were applied qualitative health researchers. Five were from non-FGM-affected communities and one was from a county with a history of practising FGM (predominantly type 2). We had a range of ontological views or worldviews. Two researchers (i.e. ED and BC) led the analysis, supported by Laura Jones. The wider research team, including Kate Jolly and Julie Taylor, provided investigator triangulation of the analysis and interpretation. The range of worldviews and lenses through which the data were interpreted provided triangulation and validation of findings. However, all but one of the research team were outsiders to the practice. Therefore, we were particularly mindful to ensure that we recognised that we may hold Western societal views of the practice, and discussed and reflected on this throughout the process.
Study support and management
Patient and public involvement: FGM Sister Study survivor group
In alignment with the SSF,86 active and sustained PPI involvement was central to the delivery of this study. Our approach to patient involvement was aligned with the six UK Standards for Public Involvement108; throughout this section, text in brackets represents the standards (e.g. support and learning, communication) relevant to each aspect of PPI involvement. We initially had a PPI co-applicant who supported the development of the protocol, but was unable to continue in this role after the study started owing to wider commitments.
A collaborative FGM Sister Study survivor group was established through contacts of one of the clinical co-applicants (AB). The survivor group consisted of four members who were type 3 FGM survivors, three of whom had undergone deinfibulation in the UK (inclusive opportunities, working together, communications). Laura Jones (on one occasion supported by ED) met with members of the FGM Sister Study survivor group on five separate occasions during the study. Members were supported to participate where needed (e.g. meeting at times and locations that suited them) and any paperwork was sent in advance in an agreed individual format [e.g. by WhatsApp (Facebook, Inc., Menlo Park, CA, USA), e-mail, post] (support and learning, communications).
The survivor groups have provided input to the study, including the design of the logo, the cohorts of participants that it was important to target, recruitment pathways, appropriate language to use around FGM, development of discussion guides and participant-facing materials, identification of solutions when difficulties were encountered (e.g. low recruitment), support of the early interpretation of data, planning for WP2 and the dissemination pathways (opportunities, working together, communications, impact). A summary of the discussions was written to document how the input of the survivor group had shaped the research and was sent to survivors when they requested this, which was not always the case; rather, some preferred that we discussed what was talked about at the previous meeting at the start of the subsequent meeting (impact, governance). We used a survivors’ WhatsApp group to facilitate regular ad hoc contact, rapid feedback on queries and group cohesiveness. Survivor group members were compensated for their input, in line with INVOLVE guidance. 109 Contributions from survivors have been documented and acknowledged (impact) and we have undertaken monitoring and evaluation of survivor involvement in the research, including what has worked well and what we could have changed (impact, governance).
Study management group
The SMG was chaired by the principal investigator (PI) and included all co-applicants and University of Birmingham research staff. The PI and research and study co-ordination staff were responsible for the day-to-day delivery of the study. The wider SMG met with the core research team to discuss all aspects of the study on seven occasions during the study, with additional ad hoc discussions as necessary. The PI met with the research team roughly every 2 weeks throughout the study.
Study Steering Group
The SSG consisted of eight members, comprising women’s health researchers, FGM academics, FGM-specialist clinicians, a FGM survivor and FGM third-sector organisation representatives (see Acknowledgements). The SSG provided independent oversight and overall supervision of the study and met with the PI, members of the SMG and the research team on four occasions during the study, with additional ad hoc discussions between the PI and the chairperson as necessary.
Final study sample and participant characteristics
This section provides a summary of the final study samples for each WP, including participant characteristics, the pathways to recruitment and a breakdown of the language and types of interviews conducted. Data were collected between September 2018 and October 2019 for WP1, in November and December 2019 for WP2a and in January 2020 for WP2b. The total sample was 101 participants for WP1 and 40 participants for WP2; therefore, the total sample size for the study was 141 participants. There was constant monitoring and reflection on sample size adequacy throughout the data collection period. A judgement about sample adequacy and information power was made across the whole cohort and by group. The overall sample and associated data had sufficient information power and adequacy to develop new knowledge in relation to the research question. There was also sample size adequacy for survivor and HCP groups, but not for men.
Work package 1a
A total of 44 survivors participated in interviews in WP1a. Table 1 provides an overview of the WP1a sample, highlighting that the majority of participants were recruited in London, were of Somali origin, were married, were aged < 40 years, reported having type 3 FGM and had been deinfibulated.
| Characteristic | Number of survivors interviewed (%) (n = 44) |
|---|---|
| Region | |
| Birmingham | 13 (30) |
| London | 29 (66) |
| Manchester | 2 (5) |
| Country of origin | |
| Eritrea | 1 (2) |
| Guinea | 5 (11) |
| Sierra Leone | 1 (2) |
| Somalia | 27 (61) |
| The Gambia | 5 (11) |
| The Sudan | 5 (11) |
| Faith/religion | |
| Muslim | 43 (98) |
| Not specified | 1 (2) |
| First language | |
| Arabic | 6 (14) |
| English | 2 (5) |
| French | 1 (2) |
| Fula/Fulani | 6 (14) |
| Jorla | 1 (2) |
| Mandinka | 3 (7) |
| Somali | 25 (57) |
| Preferred language | |
| Arabic | 6 (14) |
| English | 29 (66) |
| Somali | 9 (20) |
| Relationship status | |
| Married/civil partnership | 32 (73) |
| Partner | 4 (9) |
| Separated | 4 (9) |
| Single | 4 (9) |
| Age (years) | |
| 18–24 | 7 (16) |
| 25–29 | 14 (32) |
| 30–34 | 11 (25) |
| 35–39 | 8 (18) |
| 40–44 | 2 (5) |
| 45–49 | 1 (2) |
| 50–54 | 1 (2) |
| Employment status | |
| Homemaker | 11 (25) |
| Employed full time | 10 (23) |
| Employed part time | 10 (23) |
| Student | 7 (16) |
| Looking for work | 2 (5) |
| Unemployed | 1 (2) |
| Other | 3 (7) |
| Region of origin | |
| East Africa | 28 (64) |
| North Africa | 4 (9) |
| South Africa | 1 (2) |
| West Africa | 11 (25) |
| Type of FGM | |
| 1 | 3 (7) |
| 2 | 7 (16) |
| 3 | 22 (50) |
| Other | 1 (2) |
| Unsure | 11 (25) |
| Deinfibulated | |
| Yes | 31 (70) |
| No | 10 (23) |
| Unsure | 3 (7) |
| Number of children | |
| 0 | 13 (30) |
| 1 | 8 (18) |
| 2 | 5 (11) |
| 3 | 8 (18) |
| ≥ 4 | 8 (18) |
| Not specified | 2 (5) |
Work package 1b
A total of 13 men participated in interviews in WP2b. Table 2 provides an overview of the WP1b sample, showing that the majority were recruited in Birmingham, from The Gambia, aged 35–49 years, employed, and unsure or did not specify the type of FGM that their partner/spouse had experienced.
| Characteristic | Number interviewed (%) (n = 13) |
|---|---|
| Region | |
| Birmingham | 8 (62) |
| London | 4 (31) |
| Manchester | 1 (8) |
| Country of origin | |
| Guinea | 2 (15) |
| Mali | 1 (8) |
| Somalia | 3 (23) |
| The Gambia | 4 (31) |
| The Sudan | 3 (23) |
| Faith/religion | |
| Islam | 3 (23) |
| Muslim | 9 (69) |
| None | 1 (8) |
| First language | |
| Arabic | 3 (23) |
| French | 3 (23) |
| Mandinka | 4 (31) |
| Somali | 3 (23) |
| Preferred language | |
| Arabic | 3 (23) |
| English | 10 (77) |
| Relationship status | |
| Married/civil partnership | 11 (85) |
| Partner | 2 (15) |
| Age (years) | |
| 25–29 | 2 (15) |
| 30–34 | 1 (8) |
| 35–39 | 4 (31) |
| 40–44 | 4 (31) |
| 45–49 | 1 (8) |
| 50–54 | 1 (8) |
| Employment status | |
| Employed full time | 5 (38) |
| Employed part time | 3 (23) |
| Student | 1 (8) |
| Looking for work | 4 (31) |
| Region of origin | |
| East Africa | 3 (23) |
| North Africa | 3 (23) |
| West Africa | 7 (54) |
| Type of FGM partner/spouse experienced | |
| 1 | 1 (8) |
| 2 | 2 (15) |
| 3 | 3 (23) |
| 4 | 1 (8) |
| Unsure | 2 (15) |
| Not specified | 4 (31) |
| Has partner/spouse been deinfibulated? | |
| Yes | 4 (31) |
| No | 4 (31) |
| Unsure | 2 (15) |
| Not specified | 3 (23) |
| Number of children | |
| 0 | 3 (23) |
| 1 | 5 (38) |
| 2 | 2 (15) |
| 3 | 2 (15) |
| ≥ 4 | 1 (8) |
Work package 1c
A total of 44 HCPs were interviewed in WP1a. Table 3 provides an overview of the WP1c sample, showing that the majority were female, British European, aged ≥ 35 years and midwives. Participants were working across the UK, mainly in settings with a high prevalence of FGM.
| Characteristics | Number interviewed (%) (n = 44) |
|---|---|
| Gender | |
| Male | 3 (7) |
| Female | 41 (93) |
| Age (years) | |
| 18–24 | 1 (2) |
| 25–29 | 2 (5) |
| 30–34 | 3 (7) |
| 35–39 | 7 (16) |
| 40–44 | 4 (9) |
| 45–49 | 10 (23) |
| 50–54 | 11 (25) |
| 55–59 | 4 (9) |
| ≥ 60 | 2 (5) |
| Ethnicity | |
| British European | 22 (50) |
| Irish European | 4 (9) |
| East European | 1 (2) |
| South European | 1 (2) |
| West European | 1 (2) |
| East African | 3 (7) |
| South African (black) | 1 (2) |
| Middle Eastern | 1 (2) |
| Indian | 3 (7) |
| Pakistani | 1 (2) |
| Chinese | 1 (2) |
| South-East Asian | 1 (2) |
| Caribbean | 4 (9) |
| Profession | |
| GP | 3 (7) |
| Health visitor | 2 (5) |
| Hospital doctor | 13 (30) |
| Midwife | 20 (45) |
| Physiotherapist | 1 (2) |
| Practice nurse | 1 (2) |
| Psychologist/psychological therapist | 4 (9) |
| Region of UK where they work | |
| East Midlands | 2 (5) |
| London | 9 (20) |
| North East | 9 (20) |
| North West | 3 (7) |
| Scotland | 2 (5) |
| South West | 5 (11) |
| Wales | 3 (7) |
| West Midlands | 11 (25) |
| Care for FGM survivors | |
| Daily | 2 (5) |
| Weekly | 15 (34) |
| Monthly | 17 (39) |
| Three or four times per year | 5 (11) |
| One or two times per year | 1 (2) |
| Other | 4 (9) |
| Area prevalence | |
| High | 33 (75) |
| Low | 10 (23) |
| Unsure | 1 (2) |
Work package 1 referral pathways
Table 4 presents a summary of the different referral pathways and conversion rates for each of the WP1 cohorts. In WP1a, we received 107 survivor referrals; of these, 41% were then interviewed. A total of 75% of the participants interviewed were referred from NHS trusts. For men in WP1b, we received 20 referrals, with 65% being interviewed. A total of 62% of referrals came from charity/the third-sector or SSG networks. In WP1c, we had 197 referrals or direct contacts with the research team, of whom 51% were interviewed; 50% of these referrals came through NHS trusts.
| Referral pathway | Survivors (N = 44) | Men (N = 13) | HCPs (N = 44) | Total sample (N = 101) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Referrals, n | Interviewed, n (% of referrals) | Pathway, percentage of total interviews | Referrals, n | Interviewed, n (% of referrals) | Pathway, percentage of total interviews | Referrals, n | Interviewed, n (% of referrals) | Pathway, percentage of total interviews | Referrals, n | Interviewed, n (% of referrals) | Pathway, percentage of total interviews | |
| NHS trusts | 94 | 33 (35) | 75 | 12 | 5 (42) | 38 | 21 | 12 (57) | 27 | 127 | 50 (39) | 50 |
| Charity/ third sector | 6 | 5 (83) | 11 | 4 | 4 (100) | 31 | 0 | 0 (0) | 0 | 10 | 9 (90) | 9 |
| SSG contacts/personal networks | 7 | 6 (86) | 14 | 4 | 4 (100) | 31 | 19 | 13 (68) | 30 | 30 | 23 (77) | 23 |
| Self-referral | 0 | 0 (N/A) | 0 | 0 | 0 (N/A) | 0 | 13 | 11 (85) | 25 | 13 | 11 (85) | 11 |
| Snowballing | 0 | 0 (N/A) | 0 | 0 | 0 (N/A) | 0 | 17 | 8 (47) | 18 | 17 | 8 (47) | 8 |
| Total | 107 | 44 (41) | 20 | 13 (65) | 70 | 44 (63) | 197 | 101 (51) | ||||
Work package 1 type and language of interviews
Table 5 presents a summary of the different types of interviews (face to face vs. telephone), whether or not an interpreter was involved and, if so, the language in which the interview was undertaken. A total of 68% of interviews were by telephone, with 55% of survivors, 46% of men and 89% of HCPs. A total of 16 interviews were supported by an interpreter; of these, 56% were conducted in Arabic.
| Interview characteristics | Number of participants (%) | |||
|---|---|---|---|---|
| Survivors (n= 44) | Men (n = 13) | HCPs (n = 44) | Total (n = 101) | |
| Type | ||||
| Face to face | 7 (16) | 4 (31) | 5 (11) | 16 (16) |
| Face to face with telephone interpreter | 1 (2) | 0 (0) | 0 (0) | 1 (1) |
| Telephone | 24 (55) | 6 (46) | 39 (89) | 69 (68) |
| Telephone with interpreter | 12 (27) | 3 (23) | 0 (0) | 15 (15) |
| Language | ||||
| English | 31 (71) | 10 (77) | 44 (100) | 85 (84) |
| Somali | 7 (16) | 0 (0) | 0 (0) | 7 (7) |
| Arabic | 6 (14) | 3 (23) | 0 (0) | 9 (9) |
Work package 2a
Work package 2a consisted of two events: one in London (four participants) and one in a city in the West Midlands (six participants). Table 6 provides a summary of the characteristics of the survivors who took part in WP2a.
| Characteristic | Number of participants (%) (n = 10) |
|---|---|
| Community event characteristics | |
| Location | |
| London | 4 (40) |
| City in the West Midlands | 6 (60) |
| Participant characteristics | |
| Country of birth | |
| Eritrea | 1 (10) |
| Saudi Arabia | 1 (10) |
| Somalia | 4 (40) |
| The Sudan | 3 (30) |
| Zambia | 1 (10) |
| Citizenship | |
| British | 4 (40) |
| Dutch | 3 (30) |
| Norwegian | 1 (10) |
| Missing | 2 (20) |
| Relationship status | |
| Married/civil partnership | 6 (60) |
| Partner | 2 (20) |
| Separated | 1 (10) |
| Single | 1 (10) |
| Age (years) | |
| 18–24 | 1 (10) |
| 30–34 | 3 (30) |
| 35–39 | 2 (20) |
| 40–44 | 2 (20) |
| 45–49 | 1 (10) |
| 50–54 | 1 (10) |
| Employment status | |
| Employed full time | 1 (10) |
| Employed part time | 4 (40) |
| Student | 1 (10) |
| Unemployed | 4 (40) |
| Housing status | |
| Renting | 9 (90) |
| Living with family/friends | 1 (10) |
| Faith/religion | |
| Christian | 1 (10) |
| Muslim | 8 (80) |
| Orthodox Christian | 1 (1) |
| Region of origin | |
| East Africa | 5 (50) |
| North Africa | 4 (40) |
| South Africa | 1 (10) |
| Experienced FGM | |
| Yes | 8 (80) |
| Unsure | 2 (20) |
| Type of FGM | |
| 1 | 2 (20) |
| 2 | 1 (10) |
| 3 | 3 (30) |
| 4 | 1 (10) |
| Unsure | 3 (30) |
| Deinfibulated | |
| Yes | 3 (30) |
| No | 0 (0) |
| Unsure | 2 (20) |
| N/A | 5 (50) |
| Number of children | |
| 0 | 2 (20) |
| 2 | 2 (20) |
| 3 | 2 (20) |
| ≥ 4 | 4 (40) |
Work package 2b
A total of 131 stakeholders were approached to participate in the national stakeholder event and, of these, a total of 30 stakeholders participated. Table 7 provides a summary of the characteristics of these participants.
| Participant characteristics | Number of participants (%) (n = 30) |
|---|---|
| Age (years) | |
| 18–29 | 4 (13) |
| 30–39 | 8 (27) |
| 40–49 | 8 (27) |
| 50–59 | 7 (23) |
| ≥ 60 | 3 (10) |
| Ethnic origin | |
| British European | 13 (43) |
| Caribbean | 1 (3) |
| East African | 5 (17) |
| East European | 1 (3) |
| Indian | 1 (3) |
| Middle Eastern | 2 (7) |
| North African | 1 (3) |
| Pakistan | 1 (3) |
| South European | 1 (3) |
| South Pacific | 1 (3) |
| West African | 2 (7) |
| Not specified | 1 (3) |
| Professional group | |
| Medical | 4 (13) |
| Charity/third-sector organisation | 9 (30) |
| Medical/academic | 1 (3) |
| Midwifery | 8 (27) |
| Police | 2 (7) |
| Policy-maker | 3 (10) |
| Safeguarding | 1 (3) |
| Social care | 2 (7) |
| Region of the UK participant works in | |
| East Midlands | 2 (7) |
| East England | 1 (3) |
| London | 10 (33) |
| Nationwide | 8 (27) |
| North West England | 1 (3) |
| South East England | 1 (3) |
| West Midlands | 5 (17) |
| Not specified | 2 (7) |
| Reported FGM prevalence in region where participant works | |
| High | 18 (60) |
| Low | 4 (13) |
| Unsure | 8 (27) |
Chapter 3 Results: themes
Introduction
This chapter presents the results for the six overarching themes interpreted across WP1a, WP1b and WP1c (hereafter referred to as WP1). Each of the six themes was intersected with three cross-cutting themes, the results of which are interwoven within the presentation of each theme. Figure 6 provides an overview of the themes and cross-cutting themes and how they align; and Figure 7 provides an illustrated summary of the thematic results to orientate the reader at the start of the chapter. See Appendix 2 for a full overview of how the subthemes, overarching themes, cross-cutting themes and silences (see Chapter 4) have been aligned. The purpose of WP2a and WP2b (hereafter referred to as WP2) was to test and ratify the findings from WP1. WP2 data were used to confirm and/or challenge the findings from WP1 and identify any new lines of enquiry or interpretations of the data that might have gone unnoticed at the time. A summary of the relevant WP2 data is presented at the end of each theme.
FIGURE 6.
Overview of themes.
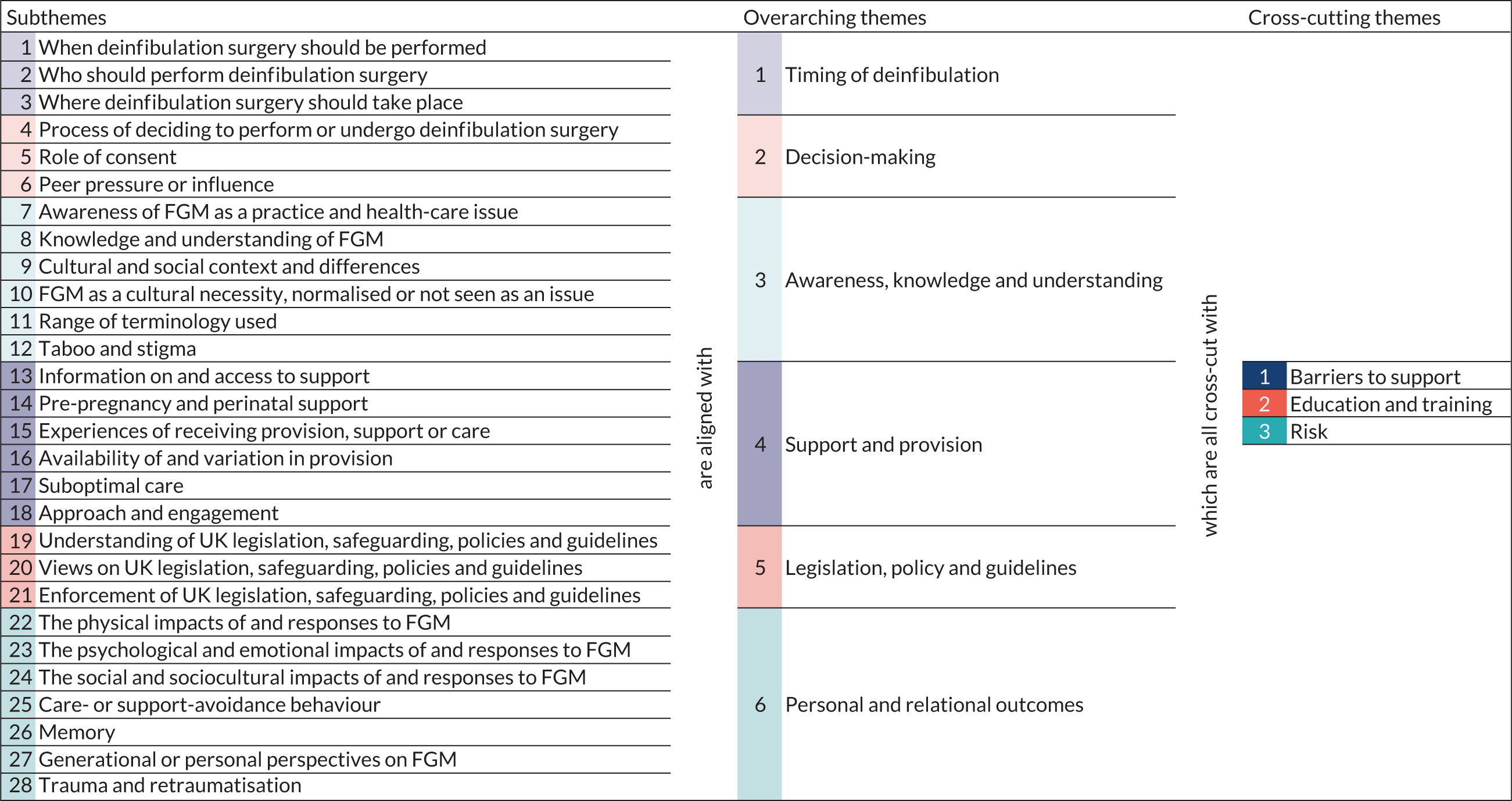
FIGURE 7.
Illustrated summary of themes. Reproduced with permission from Laura Brodrick [Think Big Picture (www.thinkbigpicture.co.uk; accessed 9 August 2021)]. This is an Open Access image distributed in accordance with the terms of the Creative Commons Attribution Non-Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for non-commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by-nc/4.0/.

Preferences for deinfibulation
Preferences for when deinfibulation should take place
Participants were asked when in a survivor’s journey deinfibulation should occur, if at all. Only one participant expressed the view that deinfibulation should not occur: ‘I don’t think . . . this is not the best time now. It [deinfibulation] shouldn’t be done at all, it shouldn’t be practised’ (Man 18). Importantly, preferences were not always mutually exclusive, with some participants across all three cohorts not expressing a singular preference. Some participants, particularly HCPs, offered multiple preferences or caveated their initial preference. Many HCPs said that survivors should decide when deinfibulation should occur; as it is the survivor who undergoes the surgery, it should ultimately be her choice:
In the second trimester it’s ideal timing unless [the] women decides that it’s better to have it done at delivery or even in the first stage of labour, it can be done [during the] first stage of labour, [or during the] second stage of labour, depending on the situation and [the survivor’s] preferences really.
HCP 37
When the preferences of all three WP1 cohorts were combined as a single data set, participants expressed an overall preference for antenatal deinfibulation. However, there were nuanced variations in preferences between cohorts. Survivors’ preferences were, overall, an almost equal split between antenatal deinfibulation and deinfibulation taking place before marriage. HCPs preferred antenatal deinfibulation to any other deinfibulation point; there was no clear consensus among men. Survivors and HCPs who expressed a preference for antenatal deinfibulation provided similar reasons for this preference, including allowing time for them to heal from their surgery before delivery:
If I can do it again I think I probably would have had it done before at 20 weeks when it was offered to me and healed from that, because it would have made my labour experience a more happier one, but I remember being in labour and just being in total pain and shock of how much I suffered to the point where I thought I was going to die. So I think my advice to other new mothers would be that have it done sooner, heal from that, and then labour will be much easier and safer really.
Survivor 54
Other survivors explained that they preferred antenatal deinfibulation because it was performed in a controlled environment and by an appropriate HCP, meaning that potential complications were minimised and infection could be controlled. Participants explained that antenatal deinfibulation was a ‘planned’ procedure and, therefore, occurs in a ‘controlled’ environment, which was ratified by WP2 data:
We would prefer her to have it done antenatally just so that we know that we’ve got a consultant there that experiences doing deinfibulation rather than doing it in labour [. . .] we would try and say to have it done antenatally, you’re going to have better outcomes if you do.
HCP 5
Health-care professionals’ overall preference for antenatal deinfibulation also generally reflects current deinfibulation guidance: ‘I think they are looking to doing it in the second trimester, which I think that’s with the RCOG guidelines as well, I think they suggest a second trimester is the better time to do it in’ (HCP 21). This was in contrast to intrapartum deinfibulation, which, depending on the situation and when a survivor presents, was sometimes viewed as an ‘emergency’ procedure:
An anterior episiotomy [deinfibulation] would be done in an emergency situation i.e. so a woman was coming in about to have a baby and that’s when they do the cut at that point so the women can deliver the baby and the episiotomy goes, so it’s a cut that goes upwards to open up the tissue that’s been close together due to the FGM. But I would think that deinfibulation would be a planned procedure where it’s a bit more carefully done how they open the tissue . . .
HCP 21
Aligned with survivors’ views, there was a prevalent nuance within the discussions of HCPs around how to conceptualise deinfibulation. Many HCPs regarded antenatal deinfibulation as a planned procedure and regarded intrapartum deinfibulation as an emergency procedure, further highlighting and reinforcing the prevailing HCP view that antenatal deinfibulation is preferable because it was planned and could be planned for. Survivors and men did not explicitly make a distinction between emergency and planned procedures, although they did indirectly refer to it:
The reason being is so you’re not going to be rushed, and they are not going to . . . maybe my experience was that was the case, midwife was rushing, maybe the doctor was rushing, maybe she doesn’t know what she was doing, she was cutting, cutting, and just leaving, didn’t take time, and the baby was . . . I was in labour for a long time when I was still closed so they can do it early. So I think during the pregnancy is the best thing.
Survivor 11
This links into discussions around deinfibulation and anterior episiotomy procedures, with the former strongly aligned to the concept of antenatal deinfibulation and, therefore, being a planned procedure and the latter being synonymous with intrapartum deinfibulation. The narrative around ‘emergency’ and ‘planned’ deinfibulation procedures was a contributory factor to both HCPs and survivors describing their reasons for preferring deinfibulation to take place antenatally. A planned antenatal deinfibulation was also linked with the perception that the ‘right person’ would usually be available to perform the procedure, in contrast to intrapartum deinfibulation, for example, where the availability of a suitable HCP might not be guaranteed. This also brings with it the benefit of potentially minimising complications arising from deinfibulation.
The benefit of a survivor having the time to physically and psychologically ‘heal’ from deinfibulation before labour was also discussed. Survivors and HCPs highlighted both the physical and psychological benefits of survivors healing from deinfibulation before labour. This was in contrast to one survivor’s comments about preferring ‘one cut, one pain’ (Survivor 32). Survivors expressed how antenatal deinfibulation might, would have or did afford them a ‘happier’ or ‘more relaxed’ labour.
Men’s preferences varied and there was no clear preference for one deinfibulation point. Of the men who articulated their thoughts, three expressed a preference for deinfibulation to take place as soon as possible, two for antenatal deinfibulation and two intrapartum deinfibulation. However, no man indicated that their partner (the survivor) should be the decision-maker regarding her own deinfibulation, including the decision of if or when she should be deinfibulated.
[Deinfibulation should be done] as soon as possible, because to me the more you leave it the more it becomes part of you.
Man 10
I think before because she need healing as well and they said before she will be 30 weeks you have to do it, and now she[‘s] 26/25 [weeks].
Man 20
Given the complexities and nuances of the preferences for when deinfibulation should take place and the challenges in reaching consensus within and between cohorts, we further explored these data to try to simplify the potential recommendations regarding time points that can be made for future service provision. The deinfibulation time points that emerged organically in interviews included:
-
before marriage
-
before first sexual intercourse
-
before pregnancy
-
antenatal
-
intrapartum
-
as soon as possible
-
up to the survivor.
Exploring these data further, it became apparent that participants’ reflections on preferences for being deinfibulated before marriage, before (first) sexual intercourse and/or before pregnancy could be interpreted as a single deinfibulation time point of pre pregnancy. This allowed us to explore preferences for three core deinfibulation time points of (1) pre pregnancy, (2) antenatal and (3) intrapartum, in addition to the caveated responses of (4) as soon as possible and (5) survivor’s choice, which were influenced by and dependent on the time point at which the survivor accessed services and the services available locally.
When exploring the preferences across WP1 for the three core deinfibulation time points, the overall preference shifts from antenatal to pre pregnancy. It also shifts the overall preferences for the individual cohorts of survivors and men. Survivors expressed a strong overall preference for pre-pregnancy deinfibulation:
Before pregnancy, before I have intercourse, before even I get married, I had it, so even when I get married it was easy process for me. I didn’t struggle because when you get married you will struggle.
Survivor 16
Before any of it, because how are you . . . what life are you going to have, how difficult is it going to be to even enjoy time with your husband? Because you are going to be in constant pain, pain, pain, it’s not worth it.
Survivor 47
It was interpreted that men’s preference for deinfibulation was that deinfibulation being performed as soon as possible was equally preferable to pre-pregnancy deinfibulation. The rationale for this was that pre-pregnancy deinfibulation enables sexual intercourse and mitigates or prevents painful (for survivors) or unpleasurable (for men) sexual intercourse:
It would be better if it was before the marriage or during the first days of marriage [. . .] after the deinfibulation we were able to have really enjoyable experience of sexual intercourse, not seeing her suffer like before.
Man 8
After when I [was] reopen[ed], it’s a relief, I am like other people, I fine, I can have sex.
Survivor 83
In summary, although the data do not support a universal, whole-cohort consensus on the timing of deinfibulation surgery, there were clearer preferences within each of the three cohorts, with survivors’ preferences tending to align with pre-pregnancy deinfibulation and HCPs’ preferences tending to align with antenatal deinfibulation. There was no clear consensus among men, but many suggested that deinfibulation should be carried out as soon as possible.
The WP2 data were largely confirmatory of the WP1 results. Community participants agreed that deinfibulation should (ideally) take place prior to pregnancy, giving the same reasons as participants in WP1. However, they also discussed how deinfibulation before marriage could (and often had) resulted in marital problems if the survivor was ‘opened’ prior to her marriage. Nevertheless, community participants also suggested that this prevailing view was changing and that the new narrative seeks to enable pre-pregnancy (i.e. pre-marriage) deinfibulation. Stakeholder participants further ratified the WP1 finding that deinfibulation should take place pre pregnancy, but they recognised that this might not be possible because of a lack of provision in some localities. However, like many HCPs in WP1, stakeholder participants often caveated their preferences with the view that it was ultimately the survivor’s choice. This was further clarified as, although the decision should ultimately be the survivor’s, the suitability of the survivor’s choice was largely dependent on whether or not their preference was safe to enact.
Preferences for who should perform deinfibulation
Participants were asked which ‘person’ should perform deinfibulation rather than which (health-care) ‘professional’ should perform deinfibulation to prevent influencing a preference for a HCP. Although questions were asked in a way that enabled participants to respond in a non-limiting way, all participants discussed their responses in relation to HCPs performing deinfibulation. Participants expressed a preference for any suitable HCP: hospital doctors (of all grades), midwives, specialist midwives and GPs.
None of the participants expressed a preference for non-HCPs to perform deinfibulation, although survivors did describe how deinfibulation outside the UK was often undertaken by non-HCPs, including by husbands as part of the consummation of a marriage. Although these ‘spousal deinfibulations’ described by participants diverge from the surgical operations that are undertaken in the UK and may not satisfy some criteria for being considered a deinfibulation procedure, the end result is similar or the same: infibulated women are ‘opened’. Many survivors and men described how an infibulated survivor can be ‘opened’ by their husband through forceful penetrative sex:
I think opening procedure is difficult, both for the men and women, so there’s some men, especially in the south of Somalia they think they have to open [their partner/wife] themselves, but they would open with difficult[y]. . . [causing] distress, depression, psychological problems, [and] damage of the [penis] [. . .] They open the size of this space with difficult[y], but [. . .] what he can open is a little.
Man 3
Most participants across all cohorts in WP1 reported that any suitably trained, knowledgeable, experienced or qualified HCP (hereafter referred to as ‘any suitable HCP’) should perform deinfibulation:
Someone with the appropriate skills, expertise and setting. I think it could be a GP in a community clinic, I think it could be a midwife, I think it could be an obstetrician or gynaecologist, but I think the important thing is not who they are, but that they have the support around them and the appropriate setting and the appropriate skills.
HCP 27
Participants described what they thought constituted a suitable HCP in various ways, including someone who fulfils one or more of the following criteria:
-
Trained – ‘As long as someone was trained to do it and experienced enough to do it, I was fine for anyone to do it’ (Survivor 71).
-
Knowledgeable – ‘Knowledgeable health-care professionals, whoever those health-care professionals are knowledgeable, so they understand what FGM is and what options there are, so knowledge would be the best one’ (HCP 15).
-
Experienced – ‘[It must be] someone that has experience in the FGM type[s] [. . .] [and] are professional and they know what they are doing’ (Survivor 82).
-
Qualified – ‘Whoever is qualified to do it’ (Man 13).
-
Specialist – ‘The person that can do the procedure [. . .] is the person that specialises in FGM’ (Survivor 87).
Participants thought that the person performing the deinfibulation procedure should not be limited to one type of HCP, as to do so could compromise a survivor’s care. Rather, the experience, expertise, knowledge and skillset of a HCP was more important than their title, position or typical clinical remit:
From my personal experience, it was great having my midwife do it, but I am sure under different circumstances, where you are not in labour, a doctor could have just done the job, it’s not she could have, or even a nurse. I just think it depends on experience and the qualification that person has.
Survivor 54
Participants used this narrative to explain their reasons for preferring any suitable HCP; explanations included the view that HCPs were more likely to be able to perform deinfibulation than a non-suitable counterpart and to be knowledgeable of potential issues and complications that might arise during or as a result of the deinfibulation procedure. This was particularly important to survivors who explained that it should be ‘somebody with huge expertise that could manage the complications and recognise the individual needs of the women’ (Survivor 27).
Where participants did specify a preference for a particular type of HCP, men and HCPs preferred a hospital doctor – equating hospital doctors with being the most suitable HCP, and thus largely echoing the reasons provided by participants who preferred any suitable HCP, as outlined in the previous paragraphs:
[It should be] a qualified doctor, in most cases I would even use surgeon, because they know what they are doing, they know where [to] touch, they know where to separate, they do the inspection, they do the case studies, they do the experiment, they know what would [. . .] and would not cause harm.
Man 10
By contrast, survivors preferred a midwife – considering them to be the most personable HCP and the HCP most able to provide a continuity of care:
A specialist midwife did it for me, she is a specialist midwife who always does it for all the ladies that need to be done, and she was brilliant. She was the best midwife ever [. . .] because she has experience of childbirth, she works with women, then women will feel more comfortable with people who study women, and then it’s women’s health, because they will be more related to them.
Survivor 9
Health-care professionals also stated that continuity of care was important for providing effective care to survivors:
[I]t is the midwives [that] build up the relationship with the woman, it’s about maintaining that relationship, that relationship that builds trust, that enables the woman to feel more relaxed and comfortable, and start to maybe talk about other safeguarding things she’s not actually disclosed to us or other concerns. So for me it’s very much about continuity, and continuity is key because I really believe that empowers the woman and empowers the relationship.
HCP 52
Very few HCPs expressed a preference for a midwife. This may be because of a divide between HCPs who thought that deinfibulation was a difficult/specialist procedure and should therefore be performed by senior/specialist HCPs (in this context equating to a hospital doctor), and those who thought that it was a relatively simple/easy procedure and so any trained HCP could perform the operation:
If we had proper training, maybe it could be a midwifery sphere, but I think, technically, I suppose, it is a form of surgery so it really should be a doctor that does that . . .
HCP 16
I don’t think you need an obstetrician to do it unless this woman has some complex concerns that sometimes you have diabetics, hypertensive, but most women are low risk in terms of they have got no other concerns the midwife can do it . . .
HCP 67
The divide between the two contrasting views cannot be consistently explained by the data. It was not clear why some HCPs thought that deinfibulation was a simple/easy procedure, but others, even when they were from the same clinical background, believed that it was a difficult/specialist procedure. However, the limits of the knowledge and experience of some HCPs ultimately installed a barrier to effective support. Some HCPs reported that they were not able to or did not feel comfortable performing deinfibulation themselves and it was not always possible to guarantee that a ‘suitable’ HCP would be available.
A small but consistent proportion of participants expressed a preference for a female HCP to perform deinfibulation. These gender preferences were usually in addition to other preferences (i.e. what kind of HCP should perform deinfibulation), but some participants offered gender preferences in lieu of any other preference regarding the person performing deinfibulation. However, of those that did express this preference, participants articulated their preference in strong terms: survivors not only said that they ‘liked the fact that [they] knew there was a woman that was doing it and this was her background’ (Survivor 2), they also stated that ‘[y]ou have to be a woman [to perform deinfibulation]’ (Survivor 60); it not only makes them ‘feel comfortable’ (Survivor 80), but, as one HCP articulated, ‘because [of] their culture they don’t want a man to see them in that way [. . .] it’s such an intimate part of your body that they might not be very comfortable with having a man to do that’ (HCP 24).
In summary, there was a clear preference across all three cohorts for any suitable HCP to undertake deinfibulation. The next most common preference across the cohort was for a hospital doctor; many of the reasons provided for this choice echoed the reasons provided by participants who articulated a preference for any suitable HCP. The underlying salient reason governing participants’ preferences regarding who should perform deinfibulation was primarily the experience, expertise, knowledge and skillset of a HCP, rather than a HCP’s job title or typical clinical remit. However, understanding what exactly constitutes a ‘suitable’ HCP and the extent to which a ‘suitable’ HCP needs to be trained, knowledgeable, experienced and/or qualified is open to interpretation and debate.
Community participants corroborated the main findings from WP1 regarding who should perform deinfibulation. They suggested that any HCP considered to be a specialist in the practice of deinfibulation should perform deinfibulation. What constitutes a suitable HCP was primarily aligned with a HCP’s clinical specialism. There was no clear gender preference; however, some community participants expressed a preference for female professionals to perform deinfibulation, but caveated this with the opinion that whoever was available and had specialist knowledge of deinfibulation should ultimately perform the surgery. The take-home message from the stakeholder event was that participants largely agreed and corroborated the WP1 finding that any suitable HCP could perform deinfibulation, with the suggestion that such a HCP should not carry a title of ‘nurse’, ‘midwife’, etc., but rather ‘FGM specialist’. Participants also ratified that the person performing deinfibulations should be an appropriately trained specialist. In addition, stakeholder participants suggested that an accredited, competency-based training programme that HCPs could undertake within their scope of practice should be developed and embedded into education and training pathways.
Preferences for where deinfibulation should take place
Participants were asked in what environment or setting or at what place or venue deinfibulation should be performed. Participants across all cohorts in WP1 expressed a clear preference for deinfibulation to be performed in hospitals. When exploring preferences by cohort, the majority of survivors and HCPs and all men said that deinfibulation should be performed in hospitals. Survivors and men believed that hospitals were ‘sterile’, ‘clean’ and ‘safe’ environments. The view that sterile and clean environments were ‘safe’ was often a natural next step in many survivors’ discussions and accompanied the view that deinfibulation needs to be performed in such an environment.
To understand why the hospital was the preferred place for deinfibulation, the triad (sterile—clean—safe) reason for the preference for hospital deinfibulation warrants further exploration. The safety element of this triad is partially explained by reference to the sterility and cleanliness of the hospital environment. Some survivors also discussed the relative safety of UK hospitals compared with some of the reportedly ‘unhygienic’ clinics in which they gave birth in their country of origin, or compared with the non-clinical and unsanitary environment in which they underwent FGM.
In addition to this, survivors explained that they perceived hospitals to be safe insofar as they are staffed by suitable HCPs. One of the salient reasons for the collective preference for hospital deinfibulation across all three cohorts was that the hospital setting enabled any complication or emergency resulting from deinfibulation to be dealt with quickly and efficiently:
I think hospital [is the] best place [. . .] [so that] they will deal with [any] emergency immediately.
Man 13
The reason participants expressed a preference for deinfibulation to take place in a hospital was closely related to participants’ reasons for preferring any suitable HCP to perform deinfibulation. There was a general underlying requirement to be able to prevent, mitigate and deal with any potential medical issues or problems linked to or arising from deinfibulation:
In hospital, because it’s the best place to do [deinfibulations] in hospital, because [in case] something is happening with you [. . .] [or] your baby, like maybe you will getting bleeding sometime, and when you are in hospital you are in exactly the place [to get help so] that you [do] not [need to] worry about it.
Survivor 88
Survivors in particular stated that it would be unlikely that they would be stigmatised for attending hospital and that this was an important factor, as they were worried about their community ‘discovering’ that they had been deinfibulated for fear of stigmatisation, judgement and isolation. Therefore, survivors believed that attending a hospital for FGM consultations and related surgery (i.e. deinfibulation) provided a level of anonymity that was unavailable in other settings and this further justified the preference for hospitals over other settings. This was particularly important for women who were having intercourse or seeking deinfibulation outside marriage because they may have been perceived as being promiscuous, unclean or otherwise deviating from a perceived cultural norm by their community:
In my opinion, a girl that is not married yet, there is that shame that if she goes and gets the opening [deinfibulation surgery] ends up saying ‘oh you’ve been with somebody else before’, so there’s that shame that to avoid being terrified that she is not a virgin, and I have even seen some girls that experience heavy period pains due to this, but when it’s suggested to them to do the opening ‘How can I? When I get married later the man will think that I have been with somebody else before because the man expects you to be . . . to not be opened, basically’.
Survivor 15
The reason provided by survivors for preferring hospitals for deinfibulation comprised two equally-weighted parts: a physical health reason and a well-being reason. The physical health reason concerned potential health complications and the ability to prevent, mitigate and address them in a clinical environment with appropriate clinicians at the ready; the well-being reason expressed concerns with preventing potential fallout in their own community because of cultural/community stigma associated with deinfibulation, particularly outside marriage, and thereby alleviating social and psychosocial issues, including fear of isolation, loneliness and ostracisation.
Health-care professionals thought that deinfibulation should be seen as a medical procedure and, therefore, should be performed in hospitals; undertaking deinfibulations in hospital was also seen as an effective method of infection control and ensuring sterility:
[So] from a medical perspective [. . .] I see a lot of perineal infection in my work and sterility in this kind of thing, particularly in pregnancy, is really important.
HCP 42
Further to this, HCPs highlighted that ‘it’s important this [deinfibulation] is seen as a medical procedure by the women to help them deal with what’s happening’ (HCP 42). This was also required to differentiate deinfibulation from the non-medical procedure of FGM, the often automatic intrapartum deinfibulation during labour in a survivor’s country of origin and cases of husbands ‘opening’ their wife during sexual intercourse. Setting deinfibulation surgery apart from a survivor’s other FGM-related experiences and procedures can be a mechanism of positive mental change and facilitate emotional and psychological recovery.
A small number of participants specified a place other than a hospital or did not express a preference for where deinfibulation should take place. For example, one survivor thought that the best place to be deinfibulated was in one’s own home:
By women, a female doctor or a specialist, and also to be at the hospital or at home [. . .] if women are given a choice to have the procedure at home [. . .] they will feel comfortable and not too many people involved knowing about the issue.
Survivor 32
Other divergent responses included two survivors and seven HCPs who thought that deinfibulation should be performed in a general practice surgery or in the community:
I think GP, because everybody go to GP always wherever you had need to go to GP [. . .] somebody [you] know very well, can talk to them [. . .] special GP first because people go to them first, they don’t go to the hospital.
Survivor 60
I could see it happening in a [general] practice with interested GPs because then the woman would be going to a place that she’s familiar with.
HCP 23
By contrast, other participants outlined why deinfibulations should not take place in general practice surgeries, including that doing so might be ‘dangerous’ and that it would be easier in a hospital:
[H]ospitals, they have the space, or have a place for that, exactly. It’s not easy to do that in the GP [general practice], because GPs [general practices] are small, just maybe have something dangerous for the mothers.
Survivor 10
The overall finding was that there was a whole-cohort preference for deinfibulation to take place in hospital because of the triad reason that hospitals are sterile, clean and safe environments. Community participants unanimously ratified the finding from WP1 that deinfibulation should be performed in hospital, citing that safety during the deinfibulation procedure was of the utmost importance and that this can be provided in a hospital setting. However, stakeholder participants did express that although there was an understanding of the safety fears regarding performing a deinfibulation procedure outside hospital, and so agreed that the hospital was likely the best place for deinfibulation, the deinfibulation procedure might be comparable to episiotomy during a homebirth, giving credence to the view that deinfibulation could take place in community settings. Therefore, participants partly ratified and partly challenged the findings on where deinfibulation should take place. This appeared to depend on the complexity of the case and so the location of deinfibulation should be decided with a personalised approach and as part of a personalised care pathway. For instance, survivors with other risk factors, such as bleeding disorders, should undergo deinfibulation in hospital. However, survivors with no known risk factors should be offered deinfibulation in community settings when safety permits. There was consensus across stakeholders that survivors should ideally be offered a choice as to where their deinfibulation takes place.
Choice and decision-making around FGM and deinfibulation
The presence or lack of choice and the process of decision-making were discussed at various points during interviews with participants, especially with survivors and HCPs. Discussions usually commenced with a survivor articulating their perception of the level of choice they had in their own experience of FGM; experiences were mixed, with some survivors explaining that they were forced to undergo FGM, ‘I don’t remember much, but I do remember being forced to it’ (Survivor 30), but other survivors saying that they asked to undergo FGM, willingly participated and looked forward to the event:
We were really taken care of like prince and princesses at the beginning, at least until we started healing [. . .] Yes, it was a happy time.
Survivor 18
Survivor’s experiences of being aware that they were to undergo FGM were equally varied; some were fully aware that they were going to undergo FGM, whereas others did not know until they were being cut, with some deceived into attending an event during which they were cut:
I was too young when they cutting me, I don’t remember, and I was maybe under 5 or 7 or 8 [years], because I don’t know when they happened.
Survivor 63
When the interview turned to the participants’ experiences and views of deinfibulation, choice and decision-making were framed in relation to the extent to which and how survivors made choices about their own deinfibulation, and the extent to which and how they engaged in the decision-making process. The main finding was that there was precarious decision-making related to deinfibulation. There was substantial variation in how participants, within and between cohorts, described their decision-making processes related to deciding to undergo or perform deinfibulation surgery. The key and determining factors that affected decision-making were related to the information provided or required to make a decision, who was involved in the decision-making process and who ultimately made the decision to perform deinfibulation or to be deinfibulated.
Participants described being involved in a number of types of decision-making, the variety of people involved in decision-making and the extent to which they and others influenced or guided the decision-making process and ultimate deinfibulation decisions. Types of decision-making included intramarital or with their partner; survivor only; survivor–HCP (at different stages and with various HCPs); involving family, friends or peers in their community; and a range of other processes.
Survivors expressed different decision-making processes regarding the input and influence of their male partner, family and community. Survivors sometimes involved their male partner: ‘We discussed afterwards the issue with my husband and we discussed all the benefits that we will gain after the procedure’ (Survivor 6), but men were often excluded from decision-making or played a background role only:
He wasn’t involved in any discussion, and at one point she told him to leave the room, which I am sure that’s the protocol, I don’t know, and regards to my family they’re all aware.
Survivor 4
Men were sometimes excluded from the decision-making by the survivor, but men also self-excluded; sometimes, both occurred and this was when intramarital decision-making was completely silent. Men did not discuss the consent procedure with HCPs or the survivors. Lack of engagement from men, either by self-excluding (men often expressed that FGM-related issues are ‘a woman’s issue’) or by being excluded by their partner or a HCP, was identified as a barrier to effective communication and decision-making.
Some HCPs admitted that they often left men out of the discussions relating to decision-making and did not engage with the men who attended with survivors; sometimes this was because men did not attend appointments with survivors, but, when they did attend or engage, HCPs acknowledged that they did not always involve men or consider the impact that the FGM or deinfibulation had or would have on men:
I have never been involved in the decision, I believe she herself takes that decision together with the midwife in attendance.
Man 17
Health-care professionals often excluded men from decision-making, including those men who attended with the survivor, or they did not consider men to play a role:
[W]ith regards to my husband, he was all very bewildered, so she [the HCP] didn’t address my husband, she just said to him, she said, ‘After deinfibulation no sex for 4 weeks, OK?’ So she did look at him, that’s his only role, and then that was it, that’s all she said to him [. . .] he wasn’t involved in any discussion, and at one point she told him to leave the room, which I am sure that’s the protocol.
Survivor 4
I don’t think I’ve ever instigated a conversation about FGM with a husband on his own, just because it hasn’t ever been appropriate, well, I don’t recall that it’s been appropriate or relevant. I do think involving men in the dialogue is hugely helpful and important and really valuable, and I’ve certainly seen couples come together.
HCP 27
When it came to identifying who ultimately made the decisions, most survivors agreed, although sometimes contradictorily, that the decision to be deinfibulated was ultimately their choice, with most feeling as though they had made an informed decision:
I didn’t mind the midwife to be honest; she was very professional, she was very compassionate, she was very. . . wasn’t making decisions for me, she was listening to what I wanted and when I wanted it.
Survivor 54
However, survivors’ decisions were often informed by discussions with or advice provided by HCPs:
[W]hen I was first month pregnant, the midwife asked me, the first time you see them they ask you in the interview have you had it, and I said yes, and she said, ‘Are you happy for us to undo it?’ and it was difficult to answer that question. She was, ‘We’re only doing it for you because later on when you are giving birth there could be other complications, more painful’. She really made me understand, in a way, where it might be painful and dramatic now, but compared to the ones where you are giving birth, it’s going to be harder. And then I said to her, ‘OK I will try’ [. . .] [T]he midwife told me that if you are going to be in labour, it’s going to be hard for the vagina to open because it’s filled already, and then it’s going to be much painful, it’s going to be traumatic, and it could also cause death, she said. I understood and of course . . . then she was for you and the baby could be a risk for both of you, and when she made me understand and told me about it I said, yeah, I would be more than happy to go through it.
Survivor 9
Yet the ways that HCPs gained the knowledge on which their advice was based – and indeed the veracity, suitability and appropriateness, etc., of that knowledge and the subsequent information/advice – varied and were therefore interpreted as being suboptimal. There was a lack of consistency in the information provided and advice given to survivors by HCPs. To compound the issue, HCPs were often guided by their own experiences, misremembered information or were not able to provide details from guidance/guidelines or by previous outdated, historic or low-quality training. This was identified as being problematic because of a lack of clarity concerning the extent to which the advice of HCPs was based on or involved unbiased, factual and objective information. In this regard, the approach of HCPs may have led to subjective or biased opinion to form part of their medical advice. It was often difficult to isolate the personal opinions of HCPs and their medical advice as the two were often inseparably intertwined.
However, most HCPs, although offering their own clinical advice/preference, expressed or in some cases caveated their responses with the fact that it was ultimately the survivor’s choice:
In the second trimester is [the] ideal timing, unless [the] women decide[s] that it’s better to have it done at delivery or even in the first stage of labour, it can be done first stage of labour, second stage of labour, depending on the situation and preferences [of the survivor] really.
HCP 37
Indeed, there appeared to be some circularity in decision-making and uncertainty around who ultimately makes the decision to be deinfibulated (for further details, see Figure 8). Although HCPs reported that it was ultimately the survivor’s choice, some survivors reported feeling pressured or heavily influenced by HCPs:
[The HCP] was very unhappy with me when I decided to have it on the day instead of before. [. . .] [I]f I wasn’t, let’s say, a hard-headed person myself I think she could have easily persuaded me [. . .] she was very adamant that I have it done before, another doctor might not necessarily . . . she said you might not get a consultant, you might get a registrar who doesn’t know what he or she is doing, it would have to be right before the pushing stage, and you will have to wait for them. She just gave me a horror story and, I don’t know, I just said ‘I don’t want to deal with my pregnancy and this’, and I just said I didn’t want it [. . .] There was a point where I said ‘it’s my choice as the patient’ and I think she eventually backed down when I reminded her it was my choice.
Survivor 4
This was not an isolated case. As well as reporting feeling pressured by HCPs, survivors also reported feeling uncomfortable when engaging in decision-making with HCPs. For example, some felt that HCPs were patronising when providing information and that HCPs were unable to consider decision-making from the survivor’s point of view, as well as other reports of suboptimal survivor–HCP interactions around decision-making. The approach of HCPs when engaging with survivors and their male partners was also described, on occasion, as being inappropriate, offensive or intimidating. These findings are further explored in FGM support and provision and Awareness, knowledge and understanding of FGM and related procedures. Some HCPs also reported engaging in behaviour or discussions that we interpreted as being biased, leading or judgemental; acting in a way that could potentially be perceived as influencing; or pressuring survivors into making a certain decision. Although it is impossible to comment on the intentions of HCPs, in most cases, it was clear from the tone and other content of the interview that these HCPs did not engage with survivors in this way to apply pressure. This highlights both a silence rooted in education and knowledge (see Chapter 4) and a need to improve the ways in which HCPs interact with survivors through education and training.
However, it is important to note that, although some survivors spoke of feeling pressured or influenced by HCPs, others spoke positively of their interactions with HCPs and of shared decision-making with HCPs:
[The HCP] was so welcoming and she would assure you, she would say . . . this is what she said, ‘Don’t be scared, I know what you have been through, I have seen a lot of girls in your situation, so don’t be scared of us, feel free, go toilet, wash yourself, when you are ready you just come’. So she makes you welcome, accepted in the state that you are in, and reassure you that everything would be fine [. . .] [I]t was a calming situation for me hearing that I don’t have only this problem and there’s people who have worse than this, and worse than what you have happen to them. [. . .] [T]he fact that she was experienced and came across a lot of people and a lot of cases, it was like oh, yeah, you can rely on her. She basically knows what she is talking about, she knows what she is doing.
Survivor 47
Survivors reported other external influence, including from their male partner, family, friends and/or the community. Survivors also reported abstract influences, including adhering to cultural and community expectations and norms and abiding by and/or respecting religious doctrine or otherwise being truthful to their faith (as they perceived it). In other words, although family, friends and community members do not often take an active role in a survivor’s decision-making (e.g. family or friends do not explicitly converse with survivors about their deinfibulation options), they do play an important background role in a survivor’s decision-making. Peer pressure or pressure to conform to their community or cultural norms was identified by survivors as pervasive:
When I have done my reverse, reopen, and spoke to her [my mum] about it she’s like, ‘It’s okay, whatever’, didn’t really want to talk about it. [. . .] I don’t know, I say to her I’m going to do it, and she was like, ‘Oh yeah whatever, it’s up to you, you’re the grown up’.
Survivor 76
So some communities might be more accepting [of deinfibulation] to understand it more, whereas some communities might look down on some of the participants.
Survivor 54
[S]ome partners don’t want the women to expose themselves to other community members for them to know [. . .] there is one girl we tried to use as the face of our organisation [. . .] but the husband didn’t want her to go through that exposure, because he didn’t want the community to know what his wife has gone through.
Survivor 6
Survivors’ reported being worried about how they would be perceived by their community, family or peers. However, this did not seem to prevent survivors from deciding on a course of action that would be viewed as wrong by those groups (e.g. electing to undergo deinfibulation without reinfibulation), demonstrating that although family, partners, peers and the community played a role in their decision-making process (often manifesting as fear or other troubling feelings), these considerations or influences did not ultimately prevent survivors from deciding to be deinfibulated. They did, however, influence a survivor’s preferences for the timing of deinfibulation, who should perform the surgery and where it should be performed (see Preferences for deinfibulation).
The challenges to and complexity of decision-making were compounded when considering the presence and role of consent, for example HCPs ensuring that survivors provided voluntary, informed consent to be deinfibulated. The role of consent, particularly in relation to deinfibulation procedures, was mixed and depended on factors such as the time that deinfibulation was performed and how the procedure was framed by a HCP. For instance, HCPs described requiring written informed consent for deinfibulation procedures that were performed during the antenatal period and sometimes requiring this for ‘planned’ intrapartum deinfibulations. In contrast, only verbal consent was typically sought for ‘emergency’ or ‘unplanned’ intrapartum deinfibulations.
Health-care professionals discussed a perceived difference between deinfibulation and anterior episiotomy, with the former aligned with the concept of deinfibulation taking place antenatally and, therefore, being a planned procedure, and the latter being largely synonymous with intrapartum deinfibulation. However, the two were described as being clinically and procedurally identical as procedures to ‘open’ an infibulated (type 3) survivor:
[D]einfibulation, from what my understanding is, is more of a planned procedure before they’re in labour, whereas an anterior epis[iotomy], I know they did used to do them and they were, if it was known FGM and they had a care plan, sometimes the care plan would, say, assume the midwife to look after this woman for an anterior epis[iotomy] or a doctor to be present at birth to perform an anterior episiotomy [...] an anterior episiotomy would be done in an emergency situation.
HCP 21
Well, deinfibulation, that can be done at any point, can’t it? So an anterior episiotomy would be during child birth, but deinfibulation that can be done at any point for a woman that has disclosed it.
HCP 24
The only defining difference between some HCPs’ understandings of deinfibulation and anterior episiotomy was that the latter was solely an emergency intrapartum procedure. There appeared to be some confusion around the notion of and what constitutes a planned deinfibulation and an emergency deinfibulation, the kind of consent required for each procedure and how the related terminology can be overlaid against or substituted for terminology related to deinfibulation. This distinction brought with it differences in how the procedures were both consented and recorded by HCPs. HCPs’ understanding of the concept of, distinction between and narrative around planned/elective versus emergency procedures in the context of FGM was identified as a barrier to enabling survivors to make an informed choice and potentially had an impact on their decision-making. This, combined with some misunderstandings around and inconsistent use of this terminology, thereby installed a barrier to care as well.
In some cases, it seemed as though anterior episiotomy was used to circumvent some barriers to consent; however, a woman in labour had to provide oral consent for an episiotomy, with many HCPs saying the same would be required if an anterior episiotomy was required. Some HCPs suggested that it would be easier to obtain consent for an anterior episiotomy than for an intrapartum deinfibulation:
We will do in the best interest type of thing that if she is bleeding all over the place and there are tears everywhere then we have to just cut through the scar tissue. But, to be fair, then that is in the best interest, we will ask for her consent, obviously she is in labour, she is conscious.
HCP 43
I suppose, if you’re doing an elective procedure like you would any procedure, wouldn’t you? So if you’re doing it antenatally it’s like doing episiotomy almost, you don’t do a written consent for it.
HCP 50
That said, many HCPs reported that strict consent procedures were always followed and that the survivor’s wishes would always be respected, irrespective of the impact. There are also some related issues surrounding whether or not survivors were provided with enough and the right sort of information and advice from HCPs to provide voluntary informed consent. There was sometimes an absence of consent, including HCPs not seeking appropriate/informed consent, HCPs not ensuring that appropriate consent was provided or avoiding the consent process and survivors avoiding or not being engaged in the consent process.
Figure 8 shows the possible and often nuanced influences on decision-making related to a survivor’s decision to be deinfibulated. From the discussions with participants across all three WP1 cohorts, it was clear that the same key decision-stages were present for many survivors when trying to make a decision, but that there was no single decision-making route. The decision-making process for a survivor was unique to that survivor. The uniqueness of a survivor’s decision-making process was manifest in and the process itself was influenced by a number of factors. These included the survivor’s own individual preferences informed by their own personal experiences and worldview, etc.; the information and advice provided by the available HCP with whom the survivor discussed deinfibulation or with whom they jointly deliberated; and the information and advice provided by specialist or senior HCPs with whom the available HCP liaised or to whom the survivor was referred. A HCP might provide information or advice that the survivor then utilises to help them reach an informed decision and/or the HCP might caveat their information/advice with the view that, despite their advice, the decision to be deinfibulated ultimately rested with the survivor.
FIGURE 8.
Influences on decision-making for deinfibulation. Arrows represent the flow of influence: conditional (single-headed) arrows represent the restricted flow of influence from one source of influence to another; biconditional (dual-headed) arrows represent how the two connected influences can interact with each other – influence can flow between connected sources of influence on decision-making. Solid lines/arrows indicate necessary influences and dashed lines/arrows indicate optional, non-necessary or contingent influences on decision-making. Each group of influence is colour co-ordinated to highlight the ways in which the main subjects of influence (i.e. HCPs) interact with other influences.

There were also global and individual influences: a survivor could be influenced by their male partner, family, friends, the community, culture and faith/religion; survivors and HCPs were influenced by their experience, knowledge and personal preferences; and all could be influenced by local, national and international policies and guidelines, and by education and training. Figure 8 depicts a circularity of influence and portrays the often off-loaded burden of decision-making. These HCPs were often heavily influenced by their own experience, knowledge and personal preferences, and these were guided by the HCPs’ awareness and knowledge of guidelines and by their own (historic and current) education and training. During HCP–survivor interactions related to decision-making, there was, therefore, an inherent risk in the power-dynamic, which requires reflection to avoid the risk of undue influence or pressure.
The overall findings were that participants identified many routes to and influences on decision-making related to deinfibulation. There was complexity around decision-making, including who was or should be involved in decision-making; the role of HCPs in decision-making, and the type and quality of information and advice they provide to survivors; and, ultimately, who makes the relevant decision. The apparent circularity in decision-making makes the process opaque. Equally, there were issues surrounding how and the extent to which a survivor consented to deinfibulation.
Community participants ratified the findings from WP1. They stated that the decision for deinfibulation should be the survivor’s choice and that a survivor’s husband/partner very often played little to no role in the decision-making process. Reasons for this echoed those from WP1 in that men distanced themselves from FGM and related issues and that survivors may consciously decide to exclude men from decision-making. However, community participants also explained that part of their role as a wife was to educate their husband/partner about FGM and, in particular, the rationale for deinfibulation.
Stakeholder participants largely ratified the findings from WP1 by agreeing that the decision-making process for deinfibulation should be governed by the survivor, who should have the power to make their own decisions. There appeared to be some caution regarding the husband/partner’s involvement in decision-making; stakeholder participants were concerned that, given too much influence or if not properly managed, the husband/partner might unduly influence, direct or even force the survivor to act in a certain way or make a certain decision. They did not frame this as a potential domestic violence issue, but rather as displaying caution regarding how husbands/partners should be involved in the decision-making process; how much influence they should have compared with the influence they possibly do have based on the traditional, cultural gender roles prevalent in some practising communities; and how to mitigate any possible coercion. However, although not directly ratifying the findings from WP1 regarding the role of HCPs in the decision-making process, there was some discussion regarding the influence of HCPs. Generally, this appeared to reflect HCPs’ advice and the questions asked by HCPs that sometimes shaped decision-making. There was also a general reluctance to discuss consent and the topic/issue of consent did not arise organically during discussions of decision-making.
Awareness, knowledge and understanding of FGM and related procedures
Participants both within and between WP1 cohorts had varying levels of awareness, knowledge and understanding of FGM and related procedures, including deinfibulation. Some of the most salient areas of awareness, knowledge and understanding included the prevalence of FGM, the types of and variation in FGM, the reasons or motivations for FGM, misconceptions or misunderstandings of FGM, the practice of FGM globally and/or in specific regional or cultural contexts and FGM as a health-care issue.
Overall, suboptimal awareness, knowledge and understanding of FGM was present across all three cohorts. These deficits were sometimes minor, for instance participants not being aware of or incorrectly categorising the types of FGM, although no HCP discussed or identified the different subtypes of FGM:
A type 1 is where they maybe just the clitoris is removed but the opening is fine, so that is basically type 1 is just removing just a part of the clitoris. Type 2 is removing part or all of the clitoris or a bit of the surrounding labia, and [type] 3 is more of the labia minora removed and some say [types] 3 and 4 is labia majora stitched together . . .
HCP 43
Other participants exhibited limited awareness, knowledge and understanding to the extent that they could not express, even in simple terms, what FGM was:
FGM is just cutting I think, female system . . .
Man 18
Could you explain to me what happens during an FGM procedure if you know?
No, I don’t even know, apologies . . .
FGM is basically is go through cutting down below basically, that’s what FGM stands for I think . . .
Survivor 16
Some HCPs noted that they were often surprised that ‘some women don’t know whether or not it’s happened to them’ (HCP 28). However, the impact of suboptimal or limited awareness, knowledge and understanding arguably varied according to the type of participant. Survivors and their male partners expressed limited awareness, knowledge and understanding in relation to the type of FGM experienced and the related health outcomes or impacts. This was especially noticeable for male partners, whose understanding of negative outcomes of FGM, except for the impact of FGM on sexual functioning or pleasure, was limited:
During her life, she did not experience any other health issues, her period was regular and everything, although she struggled [with sex] during her first days of marriage . . .
Man 49
For survivors, a lack of awareness, knowledge and understanding sometimes had an impact on their ability to fully engage in conversations about FGM and their care with HCPs, thereby limiting clinically important discussions and potentially limiting their ability to engage in informed decision-making. For instance, without having awareness, knowledge and understanding of the potential risks of deinfibulation, of what would be involved or of their options, it was difficult to state that such survivors engaged in informed decision-making and, therefore, they might not have provided informed consent.
Survivors’ awareness, knowledge and understanding of culturally and personally relevant information related to FGM was, naturally, high. Survivors were able to clearly articulate the reasons for FGM, its prevalence and to detail their own and others’ experiences. Survivors and men discussed different experiences of FGM and their awareness of it, mostly related to both national and cultural differences and variations in practice. Survivors and men stated that there were often cultural, regional and community variations and dissonance in the practice of FGM, with many participants making a clear distinction between how those ‘in the city’ and those ‘in the country[side]’ perform FGM – the implication was that the latter were more ‘barbaric’ or traditional in their approach (Survivor 4), and that those were the communities in which infibulations were performed. This had an impact on the reasons participants provided for why FGM took place and the personal and societal motivation to undergo FGM:
There’s people in the city that see it as barbaric, and in the countryside it’s the norm, so it is our locality as well, where you live [. . .] I don’t want to say people in the countryside are less educated, but they are less aware; there is not much awareness in the countryside. So I was born in the countryside so they saw that as a good thing, and if a girl didn’t have FGM then she is considered an outsider, and you got to a certain age and you didn’t have FGM then it was ‘she’s not good enough’ . . .
Survivor 4
Some HCPs were only able to explain FGM with reference to the amount of tissue removed, did not know the different types of FGM, or were unaware of or did not understand the relevant FGM guidelines or legislation:
I think the most severe is probably type 3 that we see, but, no, I think everything else gets classified as type 4 . . .
HCP 39
There is type 1, 2 and 3; I remember NICE [National Institute for Health and Care Excellence] says that 4. I know that type 1 is one that’s not too bad, now you’ve got me [. . .] I know type 3 is remove everything . . .
HCP 45
What was perhaps most salient was the fact that some survivors had experiences of HCPs not knowing what FGM was therefore being unable to appropriately identify, monitor or refer FGM survivors and provide appropriate care or support:
[M]y GP at the time, he didn’t know that I have FGM; he would examine me to see what was wrong but there was no mention of the FGM, he didn’t know that I had it, or maybe he knew, but he didn’t say, didn’t mention. He said to me that ‘I can’t see anything wrong with you’ [. . .] there was no reference to the FGM at all . . .
Survivor 95
She remembers going into birth and doctors gathering around her because they didn’t know what was going on, it was quite a shock to them, and they didn’t know how to do an opening, so they just . . . they didn’t know how to do any FGM opening, so they just cut her . . .
Survivor 82
Some HCPs also expressed limited awareness, knowledge and understanding of the association between culture and FGM. For example, they were unaware of the cultural nuances of FGM, including a prevalent misunderstanding about the role and influence of religion on the practice of FGM. Survivors and men stated that their HCPs had a general misunderstanding or misconception about the role and influence of religion (specifically Islam) or personal faith on people’s understanding of FGM – they often expressed that religion/faith played little to no role in the decision to have FGM:
There is a misconception or just an idea that has been passed on from generation to generation believing that, practising FGM on the woman, it’s part of a religious requirement, which is wrong, completely wrong . . .
Man 16
FGM is something that is in culture, not in religion or anything . . .
Survivor 11
However, some HCPs did have a good understanding of and were, in some cases, able to explain some of the reasons and motivations for FGM – many of which aligned with the reasons and motivations identified by survivors, such as purity, cleanliness, preventing promiscuity, etc. There was also good awareness, knowledge and understanding of potential and nuanced issues in FGM, with a number of HCPs discussing issues around how type 4 FGM was defined and understood, and how type 4 FGM was approached with regard to recording, reporting and clinical procedures.
Participants identified and discussed a number of stigmas, and stigmatisation was a recurring theme across all three cohorts, but with different foci. Stigma permeated many aspects of survivors’ and men’s lives: FGM was consistently identified as a taboo topic, being heavily stigmatised and/or just not spoken about. Survivors discussed stigma in relation to the referral pathways into FGM care, the knowledge of HCPs and wider agencies and the environment in which FGM services were provided; for example, FGM care usually taking place in maternity departments, where a survivor’s presence was equated to them being pregnant.
Men discussed stigma in relation to more general, underlying stigma within practising communities; in particular, the issue of cultural insensitivity was a predominant stigma, especially in relation to ‘Western’ versus ‘non-Western’ views on or related to FGM. Men and survivors thought that people from non-affected countries were generally judgemental, intolerant and did not understand the practice of FGM nor their position as a survivor or partner of a survivor:
It is the perception people had, the way they, how do I say it? You feel less of a woman talking about it. Because they know that a part of your female organism has been cut, so people have opinion about that.
Survivor 69
In some cases, this stigma made its way into clinical settings and affected how HCPs interacted with survivors and their partners and/or the provision of care. Some survivors discussed how they had received culturally insensitive care from HCPs:
When I was in labour with my first child, the midwife who was there, I remember them saying to me . . . she tried to examine me and she said ‘I can’t examine here, what is this?’ And then the other said ‘She was from Africa, I can’t tell, some people have this kind of thing’. She tried to . . . she said ‘Oh my God, how can she get pregnant like this?’ And I remember them having a conversation over me . . .
Survivor 11
Some survivors reported that HCPs not being culturally aware or culturally sensitive of the issue of FGM, or not being sufficiently informed or experienced to provide information or advice about FGM, was a barrier to their care. Generally, HCPs reported gaps in or a lack of FGM-related training for HCPs and/or a lack of relevant FGM continued professional development (CPD) opportunities, which we interpreted as partly contributing to or leading to suboptimal awareness, knowledge and understanding of FGM. Moreover, without the appropriate knowledge, there was a potential risk of some HCPs providing advice that might not meet the needs of the survivor/man or providing advice that did not fully respect or acknowledge the personal or cultural needs of the survivor. From a clinical perspective, suboptimal awareness, knowledge and understanding might have an impact on a HCP’s ability to provide the right care at the right time.
The overall findings were, therefore, that there was some evidence of suboptimal awareness, knowledge and understanding across all three cohorts. Limited awareness, knowledge and understanding presented and manifested in different ways, sometimes with potentially important and clinically salient impacts related to decision-making, consent, engaging in FGM discussions and providing appropriate and culturally sensitive care.
Although awareness, knowledge and understanding were discussed by community participants, there appeared to be a different perspective of need in terms of addressing perceived deficits. Participants suggested that communities, rather than HCPs, should be the target of education. Community participants suggested that community members should disseminate knowledge and educate their peers, the wider community and the general public on FGM, the health impacts of FGM and FGM-related health options, including deinfibulation options. However, there was also discussion of the need for HCPs in primary care to receive more education on FGM to better understand the needs of survivors and have greater knowledge and awareness of other agencies to which survivors could be signposted for support outside the NHS.
Stakeholder participants partially ratified the findings in WP1, but they also challenged some of the findings. WP2b focused on the cultural understanding of FGM rather than the lack of clinical knowledge and the practicalities voiced by survivors and men. This seemed to reflect the findings from WP1c, in which HCPs reported a lack of cultural understanding and knowledge. However, there were concerns raised regarding the dilution of knowledge, which suggests a belief that comprehensive knowledge should be ‘ring-fenced’ to FGM specialists. This view was challenged by other participants in the stakeholder event who felt strongly that all front-line HCPs should have comprehensive FGM knowledge. This appeared to be related to cultural knowledge rather than clinical procedural knowledge.
FGM support and provision
The type, level, accessibility and appropriateness of FGM support and provision featured heavily in discussions across all three cohorts. Survivors primarily discussed the spatiotemporal accessibility of FGM services. There was a need for services to be accessible and the view that accessibility was lacking in many areas underpinned much of the discussion around current FGM support and provision, and how this acted as a barrier to care. Participants highlighted differences and variations in FGM services and provision across the UK (and internationally). This made it difficult for survivors, especially those who moved around the UK, to know exactly what support was available to them. For example, there was evidence that some survivors had given up trying to contact the NHS directly to ascertain what support was available and instead took to using the Google (Google Inc., Mountain View, CA, USA) search engine to discover services:
So, yeah, it was difficult not to openly discuss with someone or even have a solution; that’s why I just thought ‘OK, the internet will help, just go Google’, and that’s how I came across [FGM services].
Survivor 76
Services were sometimes inaccessible to survivors and their families because of geographical restrictions (e.g. a service or support being available to residents of a certain region only) or because survivors were otherwise unavailable to the support offered (e.g. being unable to travel to access support outside their local community). Even when similar services were available in two different locales, the pathways to accessing these services often looked different:
Signposting for health-care professionals I think is a big thing, so, again, like I said before, often women presenting at their initial pregnancy consultation one has never seen a health-care professional in this country or never really discuss it with their GP because they haven’t had multiple health problems or haven’t sought help for health problems. They have probably never really discussed it. [. . .] [There is] probably [a] lack of knowledge, so possibly they didn’t even know it exists, maybe, and also because until someone points it out often these women think this is a completely normal thing to have happened to them . . .
HCP 28
Men also acknowledged the variation in services, although they did not comment on identifying and accessing services and support, as this was largely left to their wife/partner. HCPs recognised that regional and national variation in support and provision could be problematic for survivors, but this was largely attributed to commissioning models and sometimes explained with reference to services adapting to need in high-prevalence areas. Lack of access to FGM services was recognised by all three cohorts and was identified by survivors as a barrier to receiving care.
As well as issues with spatiotemporal access to support, survivors identified the perceived cultural accessibility and suitability of provision and support as a barrier to appropriate care. The ways in which support was provided by some HCPs suggested that there was, at times, a lack of cultural awareness, knowledge and understanding relating to FGM. Some services appeared to have been established and to operate in a way that was insensitive to the cultural needs of survivors, and appeared to function in a way that enables stigma to be perpetuated in their community. This has the potential to place some survivors in a difficult position and/or to make them anxious about accessing these services. A further example of this was that survivors often did not know that there was FGM service provision, including deinfibulation, outside pregnancy. They highlighted the importance of transparent service provision and the need to improve access to support and provision.
This was most noticeable in the ways in which FGM services were predominantly, and in some cases exclusively, oriented around provision through maternity services. Some survivors who sought FGM services, including deinfibulation outside pregnancy and/or marriage, reported that they felt ‘forced’ to access care through these maternity services. This was perceived by some survivors as culturally insensitive because many of their cultural traditions and norms include the view that sex outside marriage is wrong. This view was supported by the comments of survivors and men who explained that one of the primary motivations for FGM was to prevent promiscuity and thereby ensure that a girl remains ‘pure’ for her future husband. Accessing maternity services for deinfibulation outside pregnancy and marriage could, some survivors suggested, reinforce stigma and create difficulties for them within their community:
If I get my FGM reversal done before I get married my husband will automatically say that I have been out doing things with other men, because that’s what we are told when we are younger.
Survivor 62
Participants identified various other deficiencies in current support and provision and called for more available, appropriate and effective pre-pregnancy, perinatal (specifically antenatal and intrapartum) and/or postnatal support and provision for FGM survivors and their families. They highlighted that this could be achieved by creating and implementing new provision, or improving, adapting or supplementing current provision. In particular, emotional, psychological, counselling or mental health support (before, during and after pregnancy) was identified as an important, but currently lacking, area of provision. Many participants reported that current services predominantly focused on physical health and well-being and that there was a gap in provision related to mental health and well-being for both survivors and their families. For example, mental health services to address trauma and traumatisation for survivors was specifically sought as a missing but key area of provision:
Everything is psychological, a lot of times psychological, even for me, for the first 3 or 4 years of my marriage I wasn’t happy, all I felt was pain, and I was like ‘when are you going to finish, when are you going to finish it, I am tired’ . . .
Survivor 78
When I went to my surgery [they said] ‘yes, we will fix the scars’, but it wasn’t a discussion of how does it does it affect your life for the last 10 years, how it affected your life. It was just like ‘why do you want it open? OK, it will be opened, this is what’s going to happen, done, go home, move on’, and that’s, for me, my personal experience. If someone is going through trauma and hardship and pain and infections and they will have a lot more to deal with, and I think they need someone to be able to tell all these things, someone to explain how it affected them, so yeah . . .
Survivor 76
Another area of missing provision, particularly identified by men, related to social and relationship support, including counselling. One of the intermarital impacts of FGM (discussed in Personal and relational outcomes related to FGM and deinfibulation) was the difficulties related to having sexual intercourse, a lack of pleasurable sex, low libido and other psychosexual and physical issues relating to sex, which can cause relationship issues and, ultimately, a breakdown of relationships. Some participants thought that more and better support for couples could have a positive impact on the well-being of survivors and men, and on their relationship:
[W]hen I’ve looked after women in labour or have participated in any care of women antenatally with FGM, they are very often nervous or scared or frightened of any physical examination or physical touch, and I think that would have a massive on their psychosexual relationships with their partners . . .
HCP 28
Although there are clear deficiencies in current FGM service provision, many survivors and men did not seek out or actively avoided accessing care. The reasons for this varied, but were, in general, linked to the approach of HCPs, availability of provision, uncertainty and, in some cases, a reluctance to engage in clinically relevant conversations because of concerns around stigma, cultural issues and being judged or not understood by HCPs. In some cases, participants did not engage in relevant discussions: men were often reluctant to discuss FGM with their wife/partner, some survivors chose to exclude their husband/partner from attending with them or from the decision-making, survivors often reported not asking relevant clinical or support-related questions when discussing their care with HCPs, and HCPs sometimes did not engage in relevant clinical or legislative discussions. In addition, some survivors were reluctant to talk about FGM, their own experiences or journey or the support/provision that they wanted or needed:
I think I’ve had it for so long I’m kind of getting used to it, so no I haven’t. I just cope with it.
Survivor 55
This was also sometimes exhibited in survivors and very often exhibited in men avoiding or not attending planned or appropriate/relevant clinical events, procedures or support. There was a general apathy from men around attending and supporting their wife/partner during consultations and other clinical events, and survivors sometimes expressed either not attending consultations or avoiding seeking care altogether:
To be honest, I have never thought of seeking any health-care help regarding the FGM thing because it’s something that I don’t really like talking about, do you get what I mean? Even though I get period pains here and there, but I will just use hot water bottle or maybe take some painkillers, and just that’s it really. But I have never ever sought any health-care support [. . .] sometimes my discharge has an odour smell and stuff like that, a foul smell. So I was actually quite worried about that, so I went to the GP at one point and they gave me some medication. I didn’t tell them anything about it, no one in my house knew about it, I didn’t even tell the GP that it could be because of an infection that I caught when I was on the FGM or anything like that, so I don’t want to talk about it . . .
Survivor 56
Although participants articulated a range of issues with current service provision, there was evidence of good practice, including positive interactions between survivors and HCPs. Although men spoke little about the support received, some did comment positively on the support their wife/partner received based on their discussions with their wife/partner. Survivors reported largely positive experiences of HCPs, including the caring approach of midwives, and that their approach and general demeanour were positive and made them feel at ease:
[S]he was lovely, she was very. . . I think she was specialised in FGM, and she was highly [. . .] informed of exactly what I had, what type I had and what the procedure was and how I was going to go about it.
Survivor 4
Some survivors and HCPs reported that increased continuity of care and support where there was a trusted relationship might be beneficial:
[T]he midwives build up the relationship with the woman, it’s about maintaining that relationship, that relationship that builds trust, that enables the woman to feel more relaxed and comfortable, and start to maybe talk about other safeguarding things she’s not actually disclosed to us or other concerns. So for me, it’s very much about continuity and continuity is key because I really believe that empowers the woman and empowers the relationship . . .
HCP 52
I think it’s ensuring that continuity of care because it’s such an intimate and difficult thing to have the same carer is really important, and that’s why maybe if community midwives could be more involved where you have a specialist who is not only there to provide the specialist clinic but that who can really champion understanding and training within trusts, because community midwives would be the ones having that first conversation, and that can really help aid that continuity too . . .
HCP 62
Survivors and men also discussed not being aware of and/or not accessing FGM support and services outside the NHS (albeit awareness of NHS provision was also limited). Aside from some identifying local community groups, participants expressed that they did not know about and/or did not access any voluntary and community sector FGM support. In addition, hardly any HCPs were able to specify what sort of community and voluntary sector support was available to survivors and their families both regionally and nationally. It was also clear that any current support and services both within and outside statutory provision were primarily for survivors, with men highlighting the sparsity of support for them:
I am sorry to say but it hurts me the fact that we do not have pretty much any support from the UK.
Man 6
Health-care professionals were also unable to identify any specific services or support for men within or outside the NHS.
Relatedly, survivors and men expressed that there was a lack of general awareness of FGM and related issues in the general population, potentially leading to further cultural divides, widening the cultural dissonance gap and further marginalising discourse between HCPs, survivors and men. Culturally sensitive posters, leaflets and awareness campaigns were identified by survivors and men as being necessary sources of information for making people aware of FGM and related issues, and also to make survivors and their families aware of available support and provision. Some suggested that such information needed to be accessible outside hospitals to ensure maximum accessibility:
But if there was leaflets at the GPs [general practices], or community centres, or where people normally often go, or even schools or college [. . .] if there was a leaflet at college when I walk in, I see it I will grab, maybe read it at home and then there’s information who I can contact, maybe more [. . .] So if there was a lot more availability I think that would have helped a lot . . .
Survivor 76
Many survivors and men thought that there needed to be more FGM support and services, especially in the community, and that services, including NHS support, would benefit from being co-led by or, at least, involving survivors. The idea of survivor-led support during FGM education was strong. Survivors thought that survivor engagement was ‘really beneficial because they went through the same experience’ (Survivor 6) and because ‘people will feel more comfortable talking to someone that they know or knowing that someone that they know is there [. . .] to reassure them there’s nothing wrong you talking about it’ (Survivor 12).
The overall findings were, therefore, that access to and awareness of FGM services varied substantially. There were mixed experiences of HCPs from survivors and men, with some reporting extremely positive experiences and others more negative experiences. There were some areas of need and gaps in service provision identified by all three cohorts, most notably mental health, well-being and counselling support.
Community participants ratified most of the findings from WP1 in relation to FGM support and provision, in particular around the need to receive and improve the emotional and psychological support offered and available to survivors. However, some participants did raise concerns around social services support, which appeared to be articulated as stigmatising. Mental health support was discussed by participants, who described a stigma around using the term ‘mental health’. For instance, some participants stated that ‘mental health concerns’ were sometimes linked to ‘witchcraft’ in their culture and community: someone with mental health problems could be branded as a ‘witch’ and perceived to be ‘possessed’ (community participants). As such, the community participants recommended that mental health support should be framed as trauma counselling to recognise the fact that trauma is an underlying cause of mental health problems and as a mechanism for reducing the stigma around seeking and receiving mental health support – this might, they suggested, increase the likelihood of survivors seeking mental health support. Indeed, participants ratified the WP1 finding that survivors needed both psychological and emotional support, although there was no mention of the psychological and emotional needs of or support provision for men.
Generally, stakeholder participants ratified the findings from WP1 in terms of more support mechanisms and services being needed by FGM survivors and their families. However, there appeared to be a focus on the community advising on the level and type of support. Although there was the notion of a ‘champion’ in each agency (e.g. police, education, social services) there seemed to be a challenge to this in terms of labelling FGM survivors as ‘other’ in polarisation to ‘normal’. Funding was discussed as a barrier to education for front-line HCPs, although this appeared to be specific to HCPs rather than multiagency workers.
FGM legislation, policy and guidelines
All cohorts were largely aware of the legalities around FGM in the UK, although some were able to articulate nuances better than others. The legal context surrounding FGM was discussed at length within interviews, along with the impacts of legislation, policy and guidelines on survivors, men and HCPs, as well as their interactions with each other. The following were the most salient and recurring areas of discussion:
-
issues related to FGM legislation; safeguarding; and local, national and international policies and guidelines
-
participants’ views on and understanding of UK FGM legislation, policy and guidelines
-
the experiences of survivors and their family when discussing the legal context of FGM with HCPs.
Although the legislation, policy and guidelines were discussed, they were often brought up in discussion when less relevant or necessary. For example, some HCPs may have engaged in behaviours that were perceived as being unbalanced and with an unevenly weighted discussion of the law during health-care interactions. For these reasons, some survivors and men thought that health-care interactions were intimidating and culturally targeted:
To me, there is fear, that is the barrier here, because if you go to any GP they will ask ‘where did you have this, where did it happen, where did it occur’, etc., etc., and that link of communication if they come from other parts like Somalia, [The] Sudan etc., that person will not talk, simply because she might think ‘I am going to endanger [my children]’ . . .
Man 10
I don’t want to end up going to prison . . .
Man 7
Survivors and men reported that this extended to other areas too:
[T]he school made assumption, the GP made assumption, social services made assumption, so some of the police, especially with a child protection, made assumptions.
Man 3
Participants described frequent and sometimes repetitive discussions around legislation, policy and guidelines, especially between survivors and HCPs during consultations and other health-care interactions. Participants reported a disproportionate amount of time spent discussing these aspects, resulting in feelings of confusion, resentment and anger in survivors and men. Many HCPs themselves admitted that they engaged in frequent and repetitive discussions of the law during interactions with survivors and men because they perceived that this was a required element of care provision. The perception of survivors was that the disproportionate amount of time spent discussing the law with HCPs undermined or had an impact on their care and/or had a negative impact on their relationship with that HCP and/or other HCPs. It also made survivors less likely to engage in conversations with HCPs. The way that HCPs framed their discussions of the law with survivors seemed, in many cases, to be a ‘tick-box exercise’, particularly around safeguarding:
[T]here was that assumption that people thought I would take my children to Somalia and do it [. . .] [T]he health-care professionals, whenever they say you do know that this against the law, I tell them I know, I am against it as well . . .
Survivor 15
As soon as they see you with children, especially girls, there is this question that ‘are you going to do FGM for your children’, just because you had it done you have that question being asked, and then I don’t have a problem saying what I feel about it, but it’s like it’s not something that we will ever escape. Always there will be that question ‘are you going to do it to your child’, every health-care place you go they will ask you that question. [. . .] I understand the reason why they do this, but there is a point it becomes too much . . .
Survivor 47
Linked to earlier discussions of the benefits of continuity of care, it was suggested that receiving care from consistent, named HCPs might allow better, more appropriate engagement with survivors; that is, HCPs may not have or feel the need to discuss the law with survivors or ask them to repeat information they have previously provided to other HCPs. Many HCPs thought that such an approach might help to break down barriers within care provision:
[I]t’s important to build a rapport or a bond with this women who you’re going to perform this procedure on.
HCP 51
There were mixed opinions on the extent to which legislation acted as a deterrent to engaging in FGM and related illegal activities. Many survivors, men and HCPs thought that the legislation was strict enough and acted as a sufficient deterrent; they were able to specify the length of imprisonment and other legal repercussions for engaging in FGM activities in the UK. Others acknowledged this, but cited that very few people had been successfully prosecuted under FGM legislation as evidence that the enforcement of the law was not strict enough and, therefore, did not serve as a sufficient deterrent. Some survivors and men said that FGM legislation did not act as a sufficient deterrent, partly because the law would not be able to over-ride someone’s intention to continue a practice they saw as being normal or a part of their culture:
[I]t’s all very well for people to be like ‘it’s against the law, there will be a punishment for it’, but again people’s values, it’s like it’s not going to stop them . . .
Survivor 2
To complicate the matter, some survivors and men were not aware of some of the legislation around FGM related to safeguarding, and this misunderstanding or unawareness of relevant legislation or legal/statutory requirements was likely to undermine the legislation in and of itself.
Some survivors expressed fear in relation to the law and possible legal ramifications, which affected how and when they interacted with HCPs. This fear was prevalent in many interviews with survivors and men, often linking this fear to why they were cautious of their interactions with HCPs, entering into discussions and answering questions related to legislation. They were worried that this information could be used against them and this was a clear barrier to accessing care. Survivors said that discussing their FGM or revealing that they had FGM could have an impact on how they were perceived, and so they saw this as a risk associated with being a FGM survivor and discussing their FGM with others. A particular example of this perceived risk was survivors’ and men’s views that there was a perpetual risk of them being questioned, detained or punished in relation to them potentially subjecting their daughter(s) to FGM. They were worried about and even fearful of the risk of their children being taken into care or intervention by social services.
[T]he simple fact that if you tell people that you have gone through FGM the social services will jump on you, they will tell you ‘if you have a daughter will you get her to be circumcised for FGM to be done’, it’s really scary. If you want to open up for help, if you are looking for help and then the social services want to come through, your life it’s so stressful . . .
Survivor 94
It’s like, I feel like when the midwife ask[s] me about it and [she says] ‘we have to inform the social worker’, they are making [it seem like] [. . .] the things that happen to me I am [going to be] doing to my kids. Put [it on] your record, whatever you want, don’t make me [feel like] it’s my fault, it’s not my fault [. . .] don’t see me [like] I am a criminal, I am not a criminal, it wasn’t my choice . . .
Survivor 63
A sense of fear was also apparent within HCPs narratives. HCPs reported being cautious in their practice, as well as during their discussions with us as researchers. This was particularly true when talking about the law in relation to consent and reinfibulation. HCPs often referenced, discussed and, in one case, offered cautionary tales of HCPs who had been prosecuted, disciplined or stuck-off because of their actions. Many HCPs discussed risk to themselves in relation to their clinical and legal obligations to monitor and report FGM and safeguarding issues, and to avoid any potential perception of reinfibulation when suturing ‘anterior episiotomies’ or engaging in other surgical procedures. This worry of and risk of prosecution or losing their job was evident in some interviews.
In summary, survivors and men often reported that HCPs discussed or focused on the law too much and that this had an impact on their ability to trust or form a relationship with them or other HCPs. HCPs’ narratives supported this in many ways, with HCPs reporting that they were aware of legislation and that their interaction with survivors and men did frequently involve discussions related to legislation, policy and guidelines. There was an underlying sense of fear across all cohorts. For survivors and men, this was based on the potential consequences of making a disclosure around FGM; for HCPs, this was around the potential ramifications of failing to adhere to legislation.
Generally, community and stakeholder participants ratified the findings on legislation from WP1. However, new data were generated by stakeholders around the practice of genital piercing and the intricate and grey area of type 4 FGM and legislation. A group discussion took place regarding the legality of genital piercing and the age at which an individual should be permitted to undergo this. Stakeholder participants also ratified WP1 during discussions of the sensitivity and potential unintended consequences of continually discussing the legal implications for FGM with survivors and men.
Personal and relational outcomes related to FGM and deinfibulation
Survivors and men reported a variety of outcomes, both positive and negative, related to their experiences of FGM and NHS support, including deinfibulation. HCPs also provided a clinical perspective and outlined some of the outcomes they were either aware of or had encountered clinically. Participants across all three cohorts expressed various multifaceted and often interconnected individual, personal, social and familial outcomes. These included physical health; emotional, psychological and mental health; and psychosocial, psychosexual, sociocultural and other related outcomes.
Numerous problematic outcomes were reported related to a survivor’s FGM journey. These were associated with the act of FGM; dealing with the consequences; seeking and accepting related support and procedures to minimise, mitigate or otherwise attempt to alleviate negative health outcomes and create a more positive sense of well-being; and their personal relationships. All participants expressed deep emotional responses related to their own experience of FGM or their involvement with or proximity to those who have experienced FGM; in some cases, remembering and discussing these experiences demonstrably upset participants.
A number of physical health outcomes were identified by participants across the cohorts, for example itchiness, infection, death, menstruation problems, urinary problems (e.g. difficulty passing urine, urinary tract infections), intrapartum problems (e.g. pain during birth) and many more:
It’s having a lot of impact because it’s very hard on the young when they start for period, bleeding, and after when they are having the babies, they are facing all kinds of difficulties . . .
Survivor 80
I remember feeling a lot of pain when I was giving birth, periods are painful, intercourse is painful, and just hate it . . .
Survivor 64
Trauma and retraumatisation were recurring discussion points, specifically in relation to survivors experiencing/displaying anxiety, fear and, potentially, PTSD. HCPs reported that survivors would have or often do have PTSD, or are otherwise traumatised by their FGM:
I was sweating, I said ‘Can you put the fan on?’ Because the flashbacks and the memories is coming back, because that’s the only time where I ever opened my legs and then somebody is cutting me after what happened when I was 5 . . .
Survivor 9
[Y]ou’ve got the psychological impact, so often women are traumatised from the time where the procedure was undertaken, so they can suffer from flashbacks or certainly be affected by post-traumatic stress related as to how they felt at the time, what they went through at the time . . .
HCP 5
These issues often presented during pregnancy and, in particular, during the deinfibulation procedure. Survivors and HCPs discussed how medical birthing positions, specifically supine in lithotomy, triggered specific emotions, sensations and memories due to being in a similar position to when they experienced FGM. The very experience of childbirth was therefore expressed as a triggering event that, in some cases, caused survivors to become retraumatised:
Because it’s a very traumatic event happening to the younger girl, and when later on she becomes an adult and she comes to give birth and you expect her to be lying down, the same position as she was lying down probably some years back, and someone taking a knife, cutting her without any local anaesthetic, without any warning, and you have now professionals coming trying to do a similar thing but for a different outcome, you can understand the trauma and the flashbacks and the worry, the anxiety, and also how that even affects the baby being born . . .
Man 16
The trauma of the FGM procedure and an awareness of potential triggers made some survivors express wanting to forget or even not wanting to remember their FGM experiences. This, combined with the young age at which survivors had FGM, meant that many survivors had difficulty remembering or recalling their FGM experiences:
[S]he remembers being cut as a child but she can’t remember any details . . .
Survivor 28, via an interpreter
Discomfort and pain during sexual intercourse was commonly reported by survivors and men. Survivors spoke about how they ‘struggled during [the] first days of marriage’ (Survivor 49) because of the cultural and social expectation to have sexual intercourse regardless of their FGM. Both survivors and men reported experiencing pain and discomfort during sex, with this having an impact on them individually and as a couple:
[On our wedding night, my husband] was like, ‘OK can we try at least, we can we try it, and then if you feel pain we can stop it’. So then we tried it and it was really painful, the first time was really painful, I did not enjoy it at all, it was really painful, and I said ‘I can’t go through this’, I was crying, I was like ‘I can’t go through this, stop this’ . . .
Survivor 9
As a result, many survivors expressed how they now accepted pain as part of their life:
But [I] never enjoyed what is sex, always in pain. Hearing people talking about pleasure in your mind, you wonder what are they talking about, but as a woman sometimes you do lie to yourself like, oh yeah [. . .] [but] you are not really enjoying the sex. But as a woman it’s part of your life . . .
Survivor 13
Some survivors and men reported psychosexual problems and negative outcomes for their relationships. Both reported difficulties and breakdowns in their personal relationships, with the family and, particularly, within their marriage, as a result of FGM:
I want to get intercourse with my wife and I am trying my best and I am not getting anything, and she is here crying and she is pushing me, she is stopping me, why should I carry with the wife I am not having the sex with, for example [. . .] Your husband might end up send[ing] you home or leave you, and by the time you get all your needs it’s gone, and that break[s] the relationship . . .
Man 7
One survivor said that she had experienced continual breakdowns in relationships and domestic abuse because FGM had left her unable to derive sexual pleasure:
[M]y exes used to bully me saying ‘we are not going to marry you because you don’t have no feelings, you don’t have no . . . your feelings have been taken away, you don’t have no sexual desires’.
Survivor 9
One man explained that FGM had had a major impact on his life and heavily contributed to feelings of discontent and his subsequent divorce; he went as far as to say that men were also victims of FGM:
But you realise, at the end of the day, you are the first victim, you have got a wife, she is not responding for all levels, she is not taking care of you, the intercourse is difficult and she is traumatised whenever you try to speak to her about FGM, and you feel like what’s going on? I am left out, I have been misguided, everything I have been told about this FGM is nonsense and now I am here alone in the UK [. . .] OK I am done in this, please try to get another life, let me go . . .
Man 7
Men reported that sex was important to them and that the health of their marriage/relationship often depended on the health of their sex life. For some men, survivors not wanting or being able to engage in sex therefore affected their psychosexual well-being, but also how they perceived their relationship with their wife/partner. Survivors were also conscious of the potential impact of reduced sexual activity on their husband/partner and on the relationship; survivors were aware of a general expectation to engage in sexual intercourse and sexually gratify their husband/partner regardless of their own wants, and their comments reflected this.
Within their narratives, men did, at times, also express a deep care for their wife/partner, particularly their sexual and general health, but were often distant when it came to discussing FGM; in other words, many couples did not often discuss the impacts of FGM. Men’s discussions were, however, disproportionately focused on the impact FGM had on their sex life. Some men described infibulation as having the benefit of making sexual intercourse more pleasurable for them, as it made the vaginal orifice tighter, despite it demonstrably causing significant pain or displeasure for their wife/partner. One man stated that some men ‘don’t like the idea of deinfibulation itself [because] he wants his wife to be tight’ (Man 8). Some HCPs expressed that tightness could have psychological impacts too:
[S]he may feel that her husband is not enjoying that anymore because she’s now very open and not as tight as she was before.
HCP 5
Men often indirectly discussed risk in relation to sexual activity and causing pain to their partner during sexual intercourse. Although some men identified general health risks related to FGM (most often related to morbidity, and usually gained from their sister’s or friend’s experiences of FGM), many spoke about the potential risk of causing physical harm and pain to their infibulated wife/partner when having sexual intercourse. Some men also talked about the risk of them potentially being driven to engaging in adultery should their wife/partner refuse to engage in or be unable to derive pleasure from sexual activity because of experiencing pain or discomfort:
If you aren’t too strong it could lead you to cheat, to go and do something else, because the pleasure is not there. You will be making love to your wife and then all what will come from your wife, it’s ‘OK, take it easy’, and then all what will come from your wife is ‘I am dying’ . . .
Man 10
I have got someone in my community [. . .] the guy has got rid of his wife because she had a type FGM 3 I think, the one they got the things, and he was not happy sexually with his wife, all the time it was very painful. What he did, he said ‘I don’t want you anymore as a wife, I am going to get someone else’ . . .
Man 7
The impact of FGM on a couple’s sex life and relationship/marriage was often described as being quite profound. Some survivors even described feeling guilty about having FGM because of the impact it had on their relationship:
I felt a lot of guilt because I felt like I was holding back my marriage from going forward, especially because, at this point, it was about a year and a half in, and I just felt like I was burdening my husband, so in that sense I did feel a lot of guilt, and because he’s so nice about it as well it just made it worse as well . . .
Survivor 71
Additional mental health and psychological problems arising from or related to FGM were identified by survivors, including identity issues and/or acute existential crisis. For instance, some survivors discussed how they both looked and felt different from women who had not experienced FGM, and described not feeling or being ‘normal’:
[B]asically, I look different now than the normal people . . .
Survivor 6
It’s difficult because I don’t feel like a woman like everybody else . . .
Survivor 47
In contrast to the negative experiences articulated earlier in the chapter, some survivors reported that they had ‘not experienced major difficulties’ (Survivor 98) as a result of having FGM. When asked about whether FGM has had any impact, one survivor stated ‘no, except when I saw my midwife and [they] told me about it’ (Survivor 88). This suggested that FGM had not had an impact on the survivor until she was told that FGM was usually associated with negative outcomes. However, reports of FGM having no impact on survivors were rare; HCPs and men often said that FGM has had an impact on survivors, and very few survivors stated that they had not experienced any FGM-related problems, although some said that they got the impression from some survivors that the impact of FGM was low:
I have also had women insisting it hasn’t been or, I don’t know, women who have given me a sense that it hasn’t had a huge impact on them or not as much.
HCP 27
Participants also reported positive impacts after being deinfibulated. One survivor stated ‘I am so glad I had it done; I would say it’s one of the best things I’ve ever done in my lifetime’ (Survivor 62). Deinfibulation was reported to have had a positive impact on many survivors’ ability to engage in sexual intercourse; enabled them to menstruate and urinate properly, thus, potentially, reducing pain during menstruation and urination; and improving their general sense of well-being. Men also reported positive outcomes of deinfibulation:
[M]y period pain disappeared [after being deinfibulated], I was getting a lot of blood with period pain, my period pain disappeared and I was getting 4 days now, my period it has improved a lot. Intimacy has improved a lot, before it was so painful to start, everything was pain, pain, throughout, but every little bit I relaxed . . .
Survivor 78
I probably do feel a lot more comfortable [after deinfibulation] within myself and within my body and how I am, yeah, definitely . . .
Survivor 71
[Sex] was [a] very painful experience during the first days of marriage, because she has a little opening and we both struggle[d] and we were both in pain to have sexual intercourse, however I believe she is more painful than mine. I was able to tolerate the pain, but I know she struggled a lot until we managed to have sexual intercourse comfortably together [. . .] we were not able to have really comfortable positions or enjoying our sexual life until she had the procedure of deinfibulation during her pregnancy . . .
Man 8
Overall, there are numerous, multifaceted and inter-related personal and relational outcomes, with many participants discussing the physical and emotional impacts of FGM, but the most prevalent impacts seemed to be the psychological impacts of FGM and the impacts of FGM on their sexual health and relationships. In many cases, deinfibulation helped to mitigate, alleviate or remove these impacts.
Community participants ratified the findings from WP1 by agreeing that there are multiple, salient problematic outcomes associated with FGM. Participants agreed that FGM had resulted in multiple, frequent and often life-long physical, emotional and mental health problems. There was further discussion of relationship outcomes, particularly around men’s tolerance of survivors who felt unable to engage in sexual intercourse because of pain and lack of sensation. Stakeholder participants further ratified these findings by identifying many personal outcomes, most notably specific physical health problems, mental health problems (including PTSD and trauma) and psychological distress. One participant identified the psychosexual problems as being a particularly undesirable outcome. Stakeholder participants diverged from WP1 slightly in the potential sociocultural outcomes and implications of FGM for survivors and their families, including stigmatisation from those from a non-practising community/background and, potentially, from those from a practising background if they were deinfibulated.
In addition to the qualitative findings already reported, there were some further findings relating to survivors’ reported experience of FGM and survivors’ and men’s reported preferences for the timing of deinfibulation when compared across the quantitative (demographic questionnaire) and interview data sets. (An outline summary of these findings can be found in Appendix 3, Figures 11–14.)
Chapter 4 Results: silences
Introduction
This chapter presents the silences that were interpreted across the cohorts of data. In this study, silences existed in the void between cultural heritage, ideology and cross-cultural discourse. Although silence was defined as a general absence of voice and/or sound – and particularly an abstract absence of thought, knowledge and/or speech – in this study, silences were defined as the absence of a specific idea, particular information and/or distinct knowledge. Therefore, silence was termed a privation of knowledge or understanding of FGM, its implications and the choices and decisions made by survivors and/or HCPs. We have used the 'root of silence' to articulate the original or foundation of the silences interpreted within the data. These roots of silence cut across the overarching themes and cross-cutting themes. Silences manifested in different ways in each environment and/or relationship, which resulted in knowledge, understanding and opinions remaining silent. Silence related terms can be found in the Glossary. Figure 9 provides an overview of the silences and Figure 10 provides an illustrated summary to orientate the reader at the start of the chapter. See Appendix 2 for a complete overview of how the subthemes, overarching themes, cross-cutting themes and silences have been aligned.
FIGURE 9.
Overview of silences.
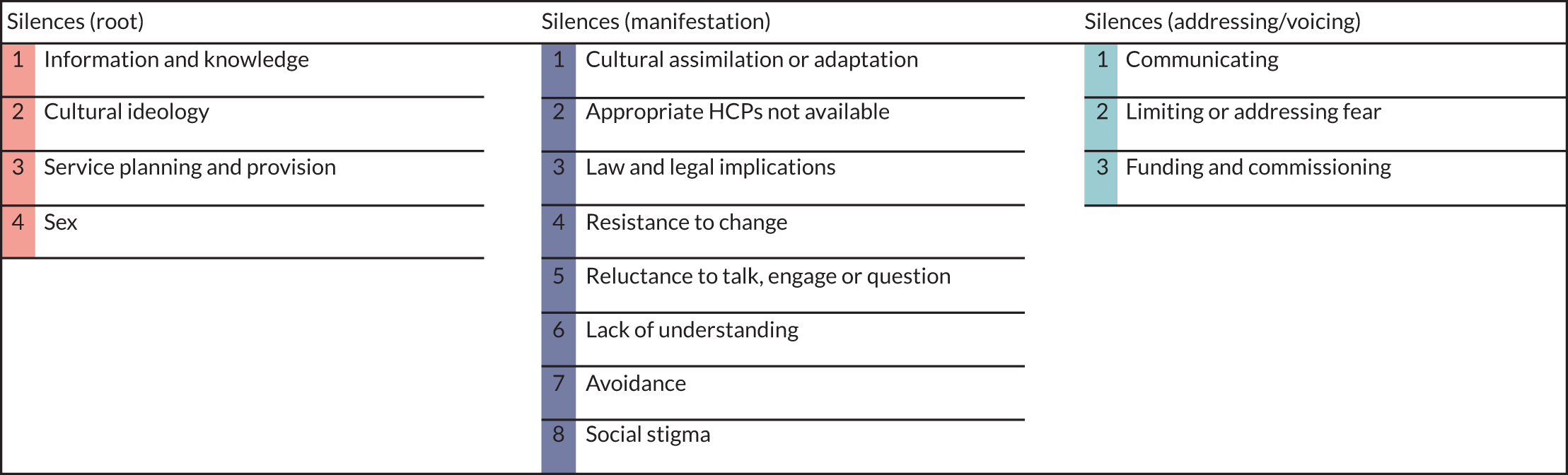
FIGURE 10.
Illustrated summary of the roots and manifestations of silence. Reproduced with permission from Laura Brodrick [Think Big Picture (www.thinkbigpicture.co.uk; accessed 9 August 2021)]. This is an Open Access image distributed in accordance with the terms of the Creative Commons Attribution Non-Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for non-commercial use, provided the original work is properly cited. See: https://creativecommons.org/licenses/by-nc/4.0/.

Silences heard
Four roots of silence were interpreted or heard across the data. These consisted of (1) information and knowledge, (2) cultural ideology, (3) service-planning and provision, and (4) sex. Although silences were heard across the interpreted themes, these silences manifested in different ways depending on the situation, environment, interpretation and the people engaged in these silences. Hence, the roots of silence that were heard are presented, with associated manifestations of silence used to illustrate how silence was embedded across all themes.
Information and knowledge
Awareness, knowledge and understanding was an overarching theme interpreted within the data. However, the way in which knowledge was created from information exposed a silence across the cohorts and themes. There appeared to be a distinction between ‘knowledge’ and ‘information’, with particular reference to HCPs’ knowledge and the dissemination of information to survivors and their families. Information was provided to HCPs through their trust’s clinical guidelines and education available on FGM, which were typically rooted in the legal implications of FGM, as well as child protection. This led to the foundation of their knowledge on FGM being influenced by legal and child protection procedures, rather than the expressed experiences of FGM survivors and/or meeting their needs. Information gathered by HCPs from FGM survivors during their provision of care was collated and interpreted using this foundational knowledge, which meant that the knowledge did not always encompass FGM survivors’ views, experiences or cultural reality. Hence, such information was potentially interpreted through the lens of Western society’s (see the Glossary) understanding and interpretation of FGM, with information from FGM survivors being at risk of misinterpretation and/or misrepresentation in the resultant knowledge disseminated by HCPs.
As a result, silence around information and knowledge was also rooted in FGM support and provision, but manifested in different ways. This was potentially due to interpreting information through a Western society lens in which cultural knowledge of FGM was limited or silent. For instance, some survivors and men felt that the questions around FGM posed to them by HCPs in different interactions were repetitive and that, at times, these questions or lines of enquiry were accusatory because of a focus on or questioning in relation to child health/protection. HCPs understood that these questions were potentially damaging to the relationship between them and the survivors and their families. However, at times, there was a lack of understanding from HCPs of the difficulties that some survivors and men faced when voluntarily (or involuntarily) assimilating into Western culture and society:
The problem is like, [for] me, sometimes I will tell people I have gone through FGM, the simple fact that if you tell people that you have gone through FGM the social services will jump on you, they will tell you ‘if you have a daughter, will you get her to be circumcised for FGM to be done?’. It’s really scary . . .
Survivor 94
Where there were issues with cultural adaptation and assimilation that related to information and knowledge, there appeared to be an avoidance of care by survivors and men, and care provision by some HCPs. A reluctance to talk and/or engage because of the way that information would be interpreted into knowledge appeared to be rooted in issues of child protection and perceived victimisation. This interpretation was ratified by the survivors’ collective voices in WP2:
We are suffering from, we need more understanding about the system, we need more help to the woman affected, not the woman who come with a big book [. . .] moving the women to the child in need, while the woman is in need of help, a single mam with no help, no family, no relatives, everyone is back home . . .
Community participant
However, this avoidance was cyclical, as misinterpretation of information led to difficulty for those attempting to culturally adapt and assimilate, resulting in further avoidance and a reluctance to engage. Nevertheless, the lack of information due to this reluctance perpetuated the lack of knowledge that was disseminated by HCPs as information to others. Consequently, this manifestation became cyclical and self-perpetuating. As such, there appeared to be a reluctance to ask questions, which appeared to manifest as fear: from the perspective of survivors and men, this was a fear of intervention from public services, such as child protection services, social care and the police; and from the perspective of HCPs there was a fear of cultural insensitivity:
I worry about the potential impact on the willingness of people to come forward and talk to us who I think it is some of the law I have no, but in terms of the . . . it’s just being mindful of potential unintended consequences of thinking if it ever impacted on how willing people are to come and talk to me.
HCP 27
Permeating all of the silences was a stigma surrounding FGM that was rooted in information and knowledge and was a screaming silence (see the Glossary) across all cohorts. The manifestation of stigma itself arose because of a belief that survivors were vulnerable, which itself created and perpetuated the narrative of vulnerability. For instance, HCPs generally described FGM as ‘taboo’ and ‘abuse’, which was rooted in the silence of information and knowledge, with a belief among some that the families of survivors required intervention from child protection services and/or social care. However, survivors and men described feeling stigmatised because of this perceived need for intervention, which then became cyclical and created feelings of wanting to avoid contact with HCPs and other services.
There were examples of where HCPs lacked cultural knowledge, meaning that their behaviours and the language they used when discussing or interacting with survivors and men from FGM-affected communities appeared to reflect an interpretation of the practice through a Western society lens. This lens may have led to ‘sensationalising’ the issue of FGM, with descriptions of survivors as ‘other’ compared with women who have not experienced FGM. The need to address this lack of cultural knowledge was ratified as part of WP2:
There’s something for me around non-sensationalising the issue, not turning it into this thing where you see a particular person from a particular community [. . .] you have made them the other, we’re talking about everyday people, everyday lives, that just happen to be affected by this one particular issue.
Stakeholder participant
This Western society lens also deemed the practice of FGM to be abuse or mutilation, and the women who had undergone FGM to be victims rather than survivors. Although some survivors internalised the victim narrative, this was not the case for all survivors. Still, all HCPs interpreted survivors as victims who had been or were silenced by their own culture:
The woman is not given a chance and she is not seeing in a way that she is a victim herself.
HCP 32
Along with the reluctance to talk, avoiding engaging and the associated stigma came a general resistance to change, with the associated shift in personal and cultural ideals. This suggests that HCPs were resistant to changing their perspective and approach to assimilate new information and adapt their knowledge, and that this resistance is reflected in current legislation69,71 and HCP guidance. 9,67,107,130–132 Yet, although there was a strong belief from HCPs that survivors were ‘victims’, there were differences in how HCPs thought that they should act on this belief. Some HCPs believed that all survivors should be referred to mental health services, whereas others believed it should be on a case-by-case basis, depending on the survivor’s needs. The perceived need to involve child protection services was also mixed; for instance, some felt that the referral itself was detrimental to the relationship between the HCPs and the survivor, with others reporting that it was ‘necessary’ to protect the woman and her baby.
It is important to recognise that HCPs’ knowledge was constructed over time. Their knowledge was partly based on information provided by survivors, so the extent and scope of assimilation and interpretation of knowledge depended on each HCP and the type of information provided by survivors. Equally, as explained earlier, information provided to HCPs was usually interpreted and assimilated through a Western society lens, which may have misaligned the information and thus contributed to HCPs misinterpreting or misrepresenting this in their construction and subsequent transmission of knowledge to others. An example of this is where HCPs believed that survivors had no wish to discuss their experiences because of stigma:
The women don’t want to talk about it. In general, the women are very ashamed about it, even if it was nothing that they did, they just consent to it.
HCP 14
This belief was in contrast to those of survivors, who often expressed that HCPs did not talk to them, that HCPs did not ask them about their experiences or that HCPs assumed that the subject was taboo. Although this was not a reality for all survivors, it was a reality for many.
Overall, given the silences interpreted above, it was not unexpected that HCPs reported was that only a small percentage of HCPs generally have the requisite skills and knowledge to provide survivors and their families with advice to support decision-making, and to perform deinfibulation procedures. For example, survivors expressed that any suitable HCP could provide this care, although men felt that doctors were best placed for this. However, when speaking to HCPs, many explained that there were few, and in some cases no, appropriate HCPs available to disseminate knowledge and/or information, no one available to interpret information to create knowledge and no one available to provide information derived from knowledge.
Cultural ideology
Health-care professionals’ cultural reality (see the Glossary) was rooted in their knowledge and education, which is likely to have been constructed in Western society’s medical and professional ideology. This was evident in discussions regarding the timing of deinfibulation, particularly around preferences for when deinfibulation should take place, which manifested in the way that services were provided and in HCPs expressed initial preference for antenatal deinfibulation, with the caveat that it is ultimately the survivor’s choice (see Chapter 3).
Some HCPs also described the presence of silence in their responses, which encompassed several of the themes. There were descriptions of vulnerability when discussing survivors and their families, but this was interspersed with deviant narratives, such as the requirement for child protection/safeguarding and social services involvement. This suggested a silence in the understanding of the impact and outcomes of survivors from the perspective of FGM-care experience. In parallel, HCPs recognised that there was a deficiency in services for psychological and mental health care; with some HCPs suggesting or stating that survivors may require mental health and/or psychological help. However, some survivors stated that FGM had not had an impact on their physical or mental health. Furthermore, although decision-making was conveyed in terms of HCPs being involved in shared decision-making with survivors and families, these comments were often caveated with the view that decision-making should ultimately rest with the survivor.
The same manifestation of service provision ideology was potentially rooted in cultural ideology in terms of where deinfibulation should take place, and this cut across several themes. Some survivors described their experiences of FGM in their childhood as a traumatic event that occurred in community settings: many had a lasting memory of bleeding, being in pain and crying/screaming. Some also described the death of family, friends and community members as a result of FGM. As such, the majority of survivors and all men suggested that the safest place for deinfibulation to take place was in a hospital setting, with access to HCPs, who would be able to help in a medical emergency, thus mitigating potential health risks.
Although many HCPs viewed deinfibulation as a specialist procedure, there were some who interpreted it in the same way as surgical incision performed at the time of childbirth to aid the birth process. This suggested a dominance of Western medical ideology, without an understanding of the nuances of the trauma that survivors might experience during the process or the trauma triggered by flashbacks. As such, it could be interpreted that silence manifested in the potential ideological perspectives of HCPs, who may view medicine through a Western societal lens and thus be focused on the task of deinfibulation, rather than considering the potential retraumatisation of the survivor. This silence was heard and ratified during WP2 when discussing the preference for who should perform deinfibulation procedures:
It’s not just any procedure, any surgery. You have to understand what actually happened, how it happened, and then there’s the trauma around it as well; the person needs to be able to speak to whoever the surgeon or the doctor is and have that confidence ‘oh, this person understands me, this person knows what I am talking about, where I am coming from, and they can go through the . . . just how I feel. I can’t go to any doctor’. Yes, if you have a broken arm, you can go to the doctor and you know what they are doing, but it’s a different procedure, very private, and there’s a lot of stigma around it.
Community participant
It is much more difficult to do an episiotomy and suture that than it is to do deinfibulation [. . .] Actually, for anyone who does deinfibulation, they will know particularly under local anaesthetic that is by far and away the absolute easiest part of the whole thing [. . .] for me, anyone who can wield safely a pair of scissors, a scalpel, local anaesthetic and suture could do a deinfibulation with the right training.
Stakeholder participant
This cut across the silence of information and knowledge, which manifested as the lack of appropriate HCPs who possess the requisite clinical and cultural knowledge. The silent aspects of the culture related to information on the experiences of FGM, the cultural guidance that perpetuates FGM, and the opinions of FGM from survivors and men whose cultural heritage has embedded FGM as a cultural norm. As such, there was overlap with the silence rooted in information and knowledge and cross-cultural discourse, particularly around mental health support for survivors that, from a cultural ideological perspective, manifested in stigma and taboo around mental health care. This was ratified during WP2:
It’s like they won’t allow themselves to feel anything like emotions and things like that, they just cut everything out just to stay strong for your children and because they are scared of the social workers and everything.
Community participant
This silence was further ratified during WP2, but there was also a challenge to the manner in which FGM was viewed and approached that suggested that survivors and their families might be at risk of being further silenced. Although this challenge was rooted in cultural ideology, it manifested in law and the legal implications of FGM:
We who haven’t had FGM think that we should be offering these people. We feel sorry that we are almost talking to them about the law, we feel sorry that we are almost saying ‘if you do this to your child you will be arrested by the police’. We feel so sorry that we are having to intervene, and I hear that so often that one of my biggest worries is what I have written to listen to the academics rather than all the people on the ground.
Stakeholder participant
There was further evidence of a cross-cultural silence that was rooted in all of the themes. For example, HCPs described a strong culturally driven rationale for FGM, which generally encompassed patriarchal explanations and nuances. However, there also appeared to be attempts at facilitating cultural assimilation (in terms of supporting voluntary assimilation into the culture of UK health care) that suggested that cultural sensitivity (as well as cultural heritage) were potentially silent in current FGM service provision. The responses during WP2 ratified this interpretation:
We talked a lot about health-care professionals, but we [also] talked about women. We ought to be helping them to understand what they can expect from the health service, and that not everyone is going to be able to understand.
Stakeholder participant
There were nuances of cultural dominance and deviance, particularly in the language used that depicted survivors and their families/communities as ‘other’. As highlighted earlier, this was strongly associated with the silence rooted in information and knowledge, which manifested through an absence of understanding, particularly in relation to survivors and men when accessing health care and their desire and ability to adapt and/or assimilate into the UK health-care culture. This strengthens the notion that FGM is viewed through a culturally ideological lens and was ratified during WP2:
It’s about empowerment and not seeing this group of people or these women as the other, as something sensational or something different.
Stakeholder participant
Service-planning and provision
There was silence in the provision of services that, as demonstrated earlier in the silences of information and knowledge, was, in addition to cultural ideology, provided from a Western society ideological perspective. For example, clinical guidance, which was benchmarked against national guidance and the cornerstone of service provision, recommended deinfibulation in the antenatal period. 9 However, this recommendation in national guidance is based on ‘expert opinion’ and reflects the opinions of those who have experience in providing such care, but not the perspective of survivors and their families. Yet the perpetuation of knowledge from a Western societal perspective appeared to manifest in a resistance to change; this was interpreted from the reluctance to use language other than mutilation to describe FGM. Although some survivors internalised the label of being mutilated and the subsequent label of victim, there were others who preferred to avoid using the term FGM, which might pose problems for the ‘labelling’ of services:
I didn’t understand what all that means because for me I looked normal, I didn’t see anything that is abnormal, and that’s because in my community we don’t talk about sexuality, you don’t get to see what other untouched, uncircumcised girls look like basically. So I thought that I was normal.
Survivor 95
Nevertheless, pathways of care were embedded in service provision and reflected the national pathway of care. However, there was an overlap between the planning and provision of services and knowledge, information and cultural ideology that can have an impact on the services that survivors and their families experience and can lead to being silenced. For example, there was a misalignment with the prioritisation of need within services, which were predominantly led from or by maternity services. As such, services were shaped around maternal health in terms of childbirth, with the aim of facilitating vaginal birth. In view of this, the interviewed HCPs may have predominantly preferred antenatal deinfibulation, with services specifically arranged to enable this. This seemed to lead to a belief that services for survivors (and their families) required maternity care input. The responses from WP2 ratified this silence as their discussion around service provision was in conjunction with maternity services:
There’s not going to be any [deinfibulation] options, I am sorry to say that, but I can actually from NHS there is not going to be any options, only because last few months maternity ward was full to the maximum and it was ladies who were getting to labour there was no bed, so that comes again, so maternity is usually full.
Community participant
Further credence was given to this silence through reference to cervical screening, which was discussed by participants throughout the data collection process. For instance, one survivor explained that she had profound difficulties with cervical screening and was therefore reluctant to attend any invitation for screening, resulting in her not attending in her adult life. She confirmed that this reluctance to engage was as a result of trauma experienced during the primary act of FGM, but also because of a lack of understanding of her trauma by HCPs. In parallel, a HCP described the reluctance of survivors to discuss cervical screening and that they rejected or ignored invitations to attend. This suggests a perpetuation and self-sustaining cycle of silence that manifests in avoidance, leading to a reluctance to engage and/or talk. This ultimately led to a lack of information and understanding among HCPs and resulted in silence. This cyclical silence was voiced, supported and ratified in WP2 in terms of providing support for survivors in a wider context than just within maternity care:
Ultimately her health needs are really important and if we can support that the benefit there isn’t just for her and her FGM, it’s for when she goes for her smear, that she will go for a smear, it’s that she will go for her diabetes check, and I think that positive . . . the opportunity to have a positive health experience has wider ramifications.
Stakeholder participant
The silence in service provision was strongly associated with the variation of services in terms of geographical location, which manifested in the availability of appropriately trained and knowledgeable HCPs. Service-planning has historically been linked with statistical data collected by the NHS and other agencies. However, this relies heavily on HCPs’ and other agencies’ knowledge of FGM. As silence has already been interpreted in HCPs’ knowledge and understanding of FGM, it strongly suggests that such data are potentially unreliable. Furthermore, there was an assumption that survivors generally reside in inner-city areas, as these areas report the most populous communities of FGM diaspora. However, this might also reflect the knowledge and understanding of HCPs in these areas, who have greater access to education and training on FGM than HCPs in other areas. As such, appropriately trained and knowledgeable HCPs are sporadically located across the UK, which has an impact on service-planning and provision. This interpretation was supported by the findings of WP2:
I think the focus is always on inner cities and not necessarily on other areas. So, for example, I know that in [. . .] a big rural community they get quite a lot of unaccompanied asylum seekers, so children in are because they are unaccompanied asylum seekers being trafficked and maybe experienced FGM or various other things. But actually they are out in a big rural community.
Stakeholder participant
Hence, there appeared to be silence rooted in the planning and provision of services, which manifested in a lack of understanding and availability of appropriately trained and/or experienced HCPs. Yet this manifestation of silence was also rooted in information and knowledge when few HCPs were in possession of the knowledge required to provide such services from a culturally sensitive perspective. As such, there was no standardisation (or uniformity) of knowledge on FGM, which resulted in incomplete or partial knowledge of the needs of survivors and their families. This silence was ratified during WP2, which also highlighted a reluctance within the FGM HCPs community to share knowledge of good practice, particularly around deinfibulation:
An awful lot has been done over the last few years, hasn’t it? In this country people have made videos, people have made films, there’s been meetings, there’s been learning, education course [. . .] So we had the launch of the NHS England clinics and there’s loads of stuff and I don’t know [. . .] people who work with FGM, it feels very competitive [. . .] it feels to me like lots of people who work in FGM feel very protective of the way they work, feel very protective of their service [. . .] we don’t seem to be as good at sharing as we could be [. . .] I know it’s a difficult issue, but there must be other difficult issues that we have managed to do better on a national basis.
Stakeholder participant
Although this knowledge was concentrated in and around deinfibulation procedures, it did not encompass the psychological and psychosexual aspects of care that had an impact on the provision of services and the silence rooted in sex (presented in Sex). Therefore, although there was individualised care and choice, this was superseded by what was available, including the availability of HCPs with the requisite knowledge to provide such care. This also correlated with the changing opinions of survivors around the timing of deinfibulation. For instance, although some survivors initially suggested that intrapartum deinfibulation was preferable, there was evidence that their preferences could be changed once they had had contact with HCPs. Reasons for this change included communication around risk, which reflected the elements of risk within the national guidance1,9,67,107,130–132 and suggests that risk discussions might have an impact on the decisions made by survivors. Consequently, this suggested that survivor’s preferences may be silenced because of service provision and the need for HCPs to align survivors with a generalised and archetypal pathway of care. Therefore, although individualised care is advocated for in NHS policy and guidance,1,9,67,107,130–132 such individualisation does not appear to exist for survivors and it could be interpreted that care for survivors appeared to be totalised, as current service provision does not take into account their individual health-care needs.
Silence that was rooted in information and knowledge led to silence being interpreted in service provision, particularly in terms of information for consent and the process of obtaining consent for deinfibulation. In Chapter 3, it was demonstrated that HCPs’ interpretation of consent was based on the language used to describe deinfibulation, differentiating between emergency and planned procedures and the types of consent sought. It appeared that using the term deinfibulation alluded to a specialist procedure and, therefore, the use of anterior episiotomy was more in-line with procedures that midwives routinely perform. This suggested that the silence that manifested around the lack of appropriate HCPs extends to the terminology used to describe the deinfibulation procedure itself:
Deinfibulation, from what my understanding is, is more of a planned procedure before they’re in labour, whereas an anterior epis[iotomy], I know they did used to do them and they were if it was known FGM and they had a care plan, sometimes the care plan would say assume the midwife to look after this woman for an anterior epis[iotomy] or a doctor to be present at birth to perform an anterior episiotomy.
HCP 21
This interpretation of silence around the terminology used paralleled the availability of appropriate HCPs and echoed through all of the silences. For example, from a service-planning perspective, HCPs’ preferences mirrored the recommendations in the RCOG guidelines9 despite there being limited evidence to support these. These recommendations state that designated HCPs, such as a named obstetrician or midwife, should provide and lead FGM services for survivors. Notably, this does not refer to multiple specialists in one health-care institution. It is therefore unlikely that these designated HCPs would be available during the FGM survivor’s intrapartum episode of care, for example.
Nevertheless, as highlighted earlier, such guidance was based on the interpretation of needs by HCPs, rather the opinions of survivors, which suggests that there was a silence that manifested as a lack of understanding. Furthermore, it appears that survivors were involuntarily assimilated into maternity services by HCPs rather than by choice, and thus survivors’ reluctance to raise questions with HCPs manifests alongside HCPs’ resistance to change, ultimately resulting in the silence of survivors’ choices. This was ratified during WP2:
We seem to see a lot of women who would prefer to do it in labour, we seem to have to persuade people quite a lot if they are say 30 weeks or so, 30 or more, we will often have a discussion where the woman is saying ‘well I really would prefer to have this done in labour’, but our worry is that, on our labour ward anyway, she may well come in and find that there’s not a midwife or a doctor on duty who knows what to do, and so therefore we have seen women who have had caesarean sections for example because nobody has known what to do.
Stakeholder participant
The planning and provision of mental health care for survivors and their families was a silence that resonated throughout the data. During WP1, many survivors and men described varying impacts of FGM on their mental health that ranged from anxiety to PTSD. However, the term ‘mental health’ was notably absent in their descriptions. Although HCPs did describe mental health care, this was largely around psychological and trauma care. The term ‘mental health’ was silent (or silenced) among survivors. When addressing the provision of mental health care within WP2, this silence was voiced in terms of cultural ideological silence:
If they hear that they have got a mental health [problem] and go to that hospital, no one will trust her again [. . .] when they hear mental health they don’t think about emotions, they don’t think about depression, they don’t think about mental health straight away, they think that this person is possessed, that this person has jinns or something like that, they don’t really believe that drugs can do that or emotions, situations that you have been through [. . .] in our country the person get[s] a mental illness until they die.
Community participant
Sex
Sexual intimacy was integral to many issues that survivors and men described in relation to FGM, but it was also described as central to the rationale for performing and undergoing FGM. Sexual dysfunction was described by all three cohorts of WP1 and so sex did not appear, at first, to be a root of silence around FGM. However, through discussions that related to sex and intimacy, we interpreted a manifestation of silence that was ultimately rooted in sex. Survivors described sexual intercourse as painful and traumatic, but functional in terms of childbearing. Only a minority of survivors reported that sex was or should be enjoyable. The majority of survivors saw the role of sex and sexual relationships as a duty and a biological and cultural process of providing children, rather than as an activity that should be enjoyed or a method of expressing intimacy with their partner.
Although deinfibulation contributed to the functional aspect of sex, the majority of survivors explained that it did not alleviate their lack of fulfilment, enjoyment or pleasure. Some survivors referred to trauma and PTSD in relation to sexual intercourse despite having been deinfibulated, whereas other survivors expressed concern at their inability to fulfil their partner’s sexual needs. This led to the interpretation that survivors were self-silent around sexual intercourse, which manifested as avoiding discussion of sex and related issues with their partners and co-existed with the manifestation of stigma and taboo, particularly in terms of privacy, embarrassment and shyness. This silence was ratified in the responses from WP2:
Sex happens as well, so that is a trick[y] one; if you was together to have sex, it’s pain instead of pleasure [. . .] this matter is a taboo thing. You wouldn’t even want to speak about [it]. I don’t mind speaking about it, but that’s women that’s scared to say something because things like ‘what are people going to do, everyone else, how are they going to think about me’.
Community participant
When analysing the responses from men, in relation to the accounts of survivors (and the collective responses from WP2 community participants), this silence appeared to be more profound. Although men also described sexual dysfunction and pain during sexual intercourse, there was an appreciation of the impact on sexual pleasure for both men and their FGM survivor partners. Some men expressed deep concern for their partners regarding the effect that sexual intercourse had on their partner in terms of inflicting pain or trauma; however, there was no evidence in the data that men actively sought to discuss this with their partners because of the perception that survivors were too shy and/or embarrassed to discuss sex. This gave credence to the interpretation that discussions around sex were silent within relationships:
Culturally about sexual issue not woman . . . partners don’t discuss because of the culture, and shyness of the ladies, and also that is the issue.
Man 3
In contrast, some HCPs described FGM as patriarchal in nature, with some descriptions alluding to the practice being performed to improve the sexual enjoyment of male partners. Although sexual intercourse was discussed by male partners, it was in association with pain (for both men and survivors), as well as fear of causing psychological distress to their partners. Furthermore, many survivors explained that older women in their families controlled and often enforced the practice of FGM to prepare girls for marriage, as a method of retaining and proving their virginity and thereby upholding and promoting the honour and status of the family. This exposed a silence in the knowledge of HCPs, potentially due to silence around information and knowledge. Hence, it was interpreted that information around sexual dysfunction appeared to be either misinterpreted or misrepresented, despite the abstract nuance of patriarchy, and has led to an understanding of FGM being performed for male pleasure:
From a cultural aspect, this is something that women . . . their families, they want the children to have this done. It’s seen as a good thing, it’s seen that it makes women more fertile, it’s better for a husband, it’s better for them, it’s supposed to be hygienic, even though it’s the exact opposite of all those things.
HCP 21
However, this did not reflect all responses from HCPs. Some HCPs had insight that silence existed and was rooted in sex through discussions of the associated psychological issues that coexist with the pain experienced by survivors. Nevertheless, many HCPs commented on FGM being performed for male pleasure, which seemed to be divergent from some of the accounts provided by men:
I’ve seen people, well, men, who have been really distressed, and more men are distressed, I would say, than anything else. I don’t think it’s something they particularly agree with now either [. . .] I think it’s probably more women and the generation sort of thing. The partners get distressed, and especially the language that we use in the hospitals [. . .] sometimes I think they feel a little bit guilty, even though they have not instigated it themselves, I think they know that it’s predominantly done for males, so I don’t think they feel really guilty.
HCP 16
The silence rooted in sex was complex and overlapped with silence rooted in information and knowledge, the provision of services and cultural ideology. Sexual fulfilment and enjoyment existed as a silence in sexual relationships, but the knowledge of psychosexual issues remained silent because of the lack of information provided to and by survivors and men. However, it may also be the case that the information provided has been misinterpreted and/or misrepresented because information was viewed through a Western societal lens. It was notable that few psychologists/psychosexual professionals operated or offered services in relation to survivors and their partners, which gives further credence to this silence manifesting because of the unavailability of appropriately trained HCPs to interpret such information. The interpretation of this silence was ratified during WP2:
We don’t really know, and then there’s the thing about what you were saying about the psychosexual, see [. . .] there’s been a lot of focus on deinfibulation because I think we focus on, I’m going to say it again, sorry, but I think we focus on having babies; vaginas are there to put things in, get things out of. But, actually, there is an awful lot more to it than that, and I think we have got to be a lot more subtle about it than that. But psychosexual provision is more or less axed from the NHS anyway [. . .] we haven’t got anybody at our fingertips and that’s what I think we need a lot of in the service.
Stakeholder participant
Summary of silences
This chapter has presented the interpretation of silence across the cohorts of data. Although Chapter 3 presented the interpreted themes, silences coexist with the themes. Furthermore, it has been demonstrated that silences are rooted and have manifested throughout the interpreted themes in cross-cultural discourse, which may have led to a misinterpretation and misrepresentation of information. There was an apparent lack of appropriately trained/skilled HCPs to interpret information to create knowledge and thus disseminate information, and to provide care to FGM survivors and men. As a result, the voices of FGM survivors and men may have been silenced by cultural ideological interpretation that deems Western society and medical ideology to be dominant. Hence, services are planned and provided that often silence the experiences, perspectives and preferences of FGM survivors and their families. In addition, intermarital silence has been interpreted, particularly in relation to sexual intimacy. However, in contrast to other identified silences, this silence manifested because of stigma and taboo and FGM survivors’ self-silencing. Yet the same silence might manifest because of a lack of appropriate HCPs who are able to interpret the information received from FGM survivors and their partners around sexual dysfunction, provide support and disseminate these experiences as knowledge.
Chapter 5 Discussion, implications and recommendations
Introduction
Female genital mutilation remains a significant global health concern and is an important health-care challenge in destination countries such as the UK. 22 FGM survivors and their families may face complex challenges as part of their voluntary or involuntary adaption and assimilation to UK culture and, specifically, UK health-care culture. 110,111 These cross-cultural challenges can influence and have an impact on all those involved in the receipt, delivery and/or configuration of health-care services. 112,113 The NHS is increasingly required to provide evidence-based, culturally appropriate, competent and safe care to FGM survivors and their families; however, recent evidence suggests that current FGM care may be neither culturally sensitive nor appropriate. 63 This chapter presents a discussion of the main findings of and the silences interpreted within the FGM Sister Study with regard to survivors’, men’s and HCPs’ preferences for the timing of deinfibulation and their experiences of and views on current and future FGM support provision in the UK. These findings will be discussed within the context of the evidence base and we will explore ways in which these silences can be addressed or voiced to prevent survivors and their families from being silenced or further silenced. We will then present the strengths and limitations of the study, followed by a summary of the implications and recommendations for future policy, practice and research.
Summary of key findings and integration with the evidence base
Preferences for and decision-making around deinfibulation
One of the core aims of this study was to explore and understand the preferences of survivors, men and HCPs around deinfibulation, including when it should take place (timing), who should undertake the procedure and where deinfibulation should take place. It was difficult to reach an overarching consensus across groups on the optimal timing of deinfibulation. This was due to the nuanced variations in preferences of different stakeholders, preferences that were context specific and/or caveated around who was responsible for decision-making. There was, however, clearer consensus across groups on who should perform the procedure and where it should be undertaken.
Initial analysis suggested that the overall cohort preference was for antenatal deinfibulation. However, within individual groups or cohorts, HCPs expressed a preference for antenatal; there was no consensus for men, but many suggested as soon as possible; and there was an almost equal split of before marriage and antenatal for survivors. Further exploration of these nuanced data, including combining before marriage, before (first) sexual intercourse and before pregnancy into a singular time point of pre pregnancy, shifted the overall group preference to pre pregnancy. If all options were available and local service provision could facilitate it, then survivors expressed a clear preference for deinfibulation pre pregnancy and ideally prior to marriage. HCPs’ preference for antenatal deinfibulation remained. These nuanced discourses suggested that there is a need for deinfibulation provision to be made available across a woman’s life course to maximise her choices and support informed decision-making.
Deinfibulation can be undertaken at any time point during a survivor’s life; however, the evidence base around optimal timing is limited and ambiguous. 60 There are two main deinfibulation points presented in the evidence base, one suggesting that it should be carried out outside pregnancy and the other that it should be carried out during pregnancy. 1,59 Although there are two main time points suggested, there is considerable variation between and within clinical guidance about when deinfibulation should be undertaken. 59,60,63 For example, RCOG guidelines9 recommend that deinfibulation should be offered prior to pregnancy and, ideally, before first sexual intercourse, which aligns with the preferences of the survivors in our study. However, these guidelines also state that deinfibulation can be performed antenatally, aligned with our HCPs’ preferences, in the first stage of labour, at delivery or during a caesarean section. RCN FGM guidance64 includes two statements, one indicating that the procedure is best performed when not pregnant, again, aligning with survivor preferences, and another that deinfibulation is best undertaken before or at least within the second trimester of pregnancy, which aligns with the preferences of the HCPs in our study. The WHO guidelines on the management of FGM56 recommend either antepartum or intrapartum deinfibulation; however, these recommendations were caveated with the need to take into account wider contextual factors, such as patient preference, access to facilities and the skill level of the HCP performing the procedure. Aligned with this, although HCPs had a preference for antenatal deinfibulation, this was often caveated with it ultimately being the choice of the survivor.
The finding that survivors had a preference for deinfibulation pre pregnancy and, specifically, prior to marriage was contradictory to previous research that showed that this was ‘an unusual choice’ and that the majority of women have a preference for being deinfibulated in labour to avoid having to undergo two procedures. 61,63 A qualitative evidence synthesis reported that survivors’ preferences around deinfibulation were influenced by cultural norms of virginity and chastity, making it difficult for some women to seek deinfibulation outside marriage. 61 We did see the influence of the community and cultural norms to some extent within our data, but there was still a clear preference for pre-pregnancy deinfibulation. Many of the survivors who we spoke to who had undergone deinfibulation provided preferences for what they wished they had had or would have liked to have been offered when deciding to be deinfibulated. It is, however, important to reflect that a preference for a specific deinfibulation time point might be different from a decision to actually undergo deinfibulation at that time point. In addition, we know that current awareness, knowledge and understanding of service provision is limited within FGM-affected communities and so they may not be receiving the right information, at the right time, to make informed choices. 63 Our data suggest that there is a need for the provision of services and care pathways for non-pregnant survivors to facilitate choice, which aligns with recently published NHS England commissioning guidance. 114 Certain clinics, such as the Sunflower Clinic in London, do provide care for non-pregnant women with FGM and a recent case series review led to the development of the Acton model, a holistic woman-centred model of care, that was suggested to help facilitate access to deinfibulation and counselling. 115 However, this model of care was still midwife led, which can be culturally challenging for some survivors who are not married/pregnant and who may associate seeing a midwife with antenatal care. The Acton Model of care would benefit from further evaluation.
Decision-making around deinfibulation was complex, with multiple routes to and influences on the process, including at what time point the survivor presented to the NHS and what services were available to her. There was evidence of circularity in decision-making, with the HCP suggesting that it was ultimately the survivor’s choice, but the survivor also seeking guidance and advice from HCPs. The guidance and advice given in some cases appeared to be suboptimal, with survivors reporting feeling pressured or influenced by HCPs. This is supported by wider evidence that suggests that survivors can be persuaded by HCPs to change their preferences around when they would prefer to be deinfibulated;116,117 and that they often report a lack of choice, control and ability to voluntarily consent to intervention, particularly in maternity settings, leaving them feeling vulnerable and disempowered. 63 Overall, this may be indicative of an unequal power dynamic between HCPs and survivors, and thus current FGM services and care pathways may not be culturally safe. 118 There is a need to redress this power balance to facilitate shared decision-making. In addition to this, there is a need to improve the clinical FGM knowledge and cultural competence of HCPs working with survivors and there are likely unmet HCP training needs, as highlighted in other studies. 63,119–123
Health-care professionals and some survivors justified their preference for antenatal deinfibulation as it could be planned and undertaken in a controlled environment by a suitable HCP. There was also discussion of both the physical and the psychological benefits of survivors undergoing and healing from deinfibulation prior to labour. This was in contrast to perceptions around intrapartum deinfibulation, highlighting that this was seen as an emergency procedure, sometimes conflated with anterior episiotomy, and one where the presence of an appropriate HCP could not be guaranteed. Mitigating the potential risks of intrapartum deinfibulation by undertaking an elective planned procedure aligns with the wider literature that suggests that there are compelling reasons, in particular around safety and minimising risk, to undertake deinfibulation antenatally. 9,56,124,125
This evidence around perceived safety and the need to mitigate risk is also linked with the reported preferences and reasons for who should undertake deinfibulation and where it should take place within our study. There was agreement across all three cohorts that any suitable HCP could undertake deinfibulation surgery. Suitability was primarily guided by the experience, expertise, knowledge or skillset of a HCP, rather than their job title or typical clinical remit. Our stakeholder participants agreed that any appropriately trained HCP could perform deinfibulation, with the suggestion that such HCPs should not carry a title of nurse, midwife, etc., but rather should be a FGM specialist who had been appropriately trained. There was disagreement both within and between HCP groups as to whether deinfibulation was a specialist or non-specialist procedure, although this is likely to depend on the survivor’s clinical presentation. It was also highlighted that appropriately trained and knowledgeable HCPs were sporadically located across the UK. This highlights a clear gap in the current skills base of HCPs and an unmet training need within the FGM workforce that may limit service provision and choice for survivors around deinfibulation. An accredited competency-based training programme that HCPs could undertake within their scope of practice could be developed and embedded into education and training pathways.
There was consensus across all cohorts that deinfibulation should be undertaken in a hospital setting. The rationale for this was that deinfibulation should be seen as medical procedure; there would be other HCPs available if needed; and the hospital environment was perceived as sterile, clean and safe, thus mitigating potential risks should anything go wrong. The perception of safety is a key component of overall patient experience and satisfaction when undergoing surgery. 126,127 Hospital deinfibulation reportedly helped survivors to manage their physical and psychological well-being. This is a key aspect of culturally safe service provision given the need to manage and counsel women around deinfibulation, as there is potential that clinical interactions/interventions could lead to triggering, traumatisation or retraumatisation, which may then lead to survivors not engaging in subsequent care provision. 63,128 This aligns with the WHO’s advocation for providing survivors seeking deinfibulation with extensive counselling and support. 1 Recently published guidelines have sought to address the lack of literature, training and good practice guidance for working therapeutically with survivors, which are key to supporting future FGM service provision. 128 This preference for hospital deinfibulation challenges NHS England’s recent establishment of eight community-based FGM clinics that offer a range of support, including deinfibulation. Our findings suggest that survivors would not want to be deinfibulated in the community, as there was a perception that these settings were not culturally appropriate. Being seen in a community clinic can be stigmatising for survivors, whereas the hospital setting affords a level of anonymity. It is important to empower survivors to feel in control, feel physically and psychologically safe, and have trust in the HCPs and the system. There is a need for further evaluation of these community based clinics to understand if they are meeting the needs of survivors, in particular around deinfibulation.
Our study has provided novel insights that help to better understand the nuances and complexities around deinfibulation preferences and decision-making regarding when it should take place (timing), who should undertake the procedure and where deinfibulation should take place. Although we have not been able to provide a consensus across groups (there were, however, clear cohort-specific preferences) on the optimal timing for deinfibulation (as was the original aim), it is important to acknowledge from our learning that there might not actually be one deinfibulation point that is ideal for all stakeholders. The WHO argue that deinfibulation is associated with improved health and well-being56 and this was supported by survivors and some men in our study who reflected that deinfibulation helped to mitigate or alleviate some of the negative impacts associated with FGM, such as pain during intercourse. However, there is only limited low-quality quantitative evidence to suggest that deinfibulation is associated with improved gynaecological and obstetric outcomes,58 and no evidence that it is associated with improved urological outcomes. 57 Further to this, there is also debate about whether or not the timing of deinfibulation affects outcomes. Some studies have suggested that obstetric risk increases the later deinfibulation is performed,65,66 but a systematic review published in 2017 showed no evidence of a significant difference in obstetric outcomes between antenatal and intrapartum deinfibulation. 59 This is important as surgical risks and outcomes associated with deinfibulation should form part of the discussion between the survivor and the HCP(s) to support shared decision-making around when is the right time point for her to be deinfibulated. This requires further research to help support survivors to make fully informed decisions around deinfibulation.
Views on current and future FGM support provision in the UK
There has been a concerted multiagency effort around FGM support and service provision in the UK in recent years. This has included but is not limited to the introduction of stronger FGM legislation;71,72,129 development of policy and guidelines,67,130–132 including commissioning guidance;133 development of e-learning, training and resources for providers;75–77,132,134,135 and the establishment of the FGM-enhanced data set29 and information sharing systems. 136 The 2015 commissioning services guidance highlights that the benefits of dedicated high-quality care services for FGM survivors are considerable. 133 FGM commissioning guidance114,133 sets out the minimum that these services should offer to (1) meet the physical health needs of survivors, (2) meet the mental health needs of survivors and (3) safeguard women/girls and other children within family units. 133 Although there was evidence of good practice within our data, including positive interactions between survivors and HCPs, in particular with midwives, overall current FGM service provision remains suboptimal62 and, in some cases, did not meet the minimum service standards. 114,133 Most FGM services are not meeting the needs of survivors and their families – an issue that has been identified and articulated previously. 63,137 Further to this, and a novel finding of our research, was that current FGM services often silence the experiences, perspectives and preferences of survivors and their families.
The assertion that service provision, in general, remains suboptimal incorporated a range of issues and/or deficiencies. Survivors, men and HCPs reported that service provision was opaque and, at times, invisible or hidden. Our finding that survivors, men and many HCPs lacked knowledge and understanding of FGM and awareness of the availability of health services aligned with the findings of other similar studies138–140 and a recent review. 61 There was significant geographical variation in provision, with most services attached to NHS maternity services and concentrated in inner-city NHS trusts. Although commissioning will be linked to perceived needs locally, in reality, this means that many survivors and their families may not have local services that they can access, provision can be ‘hit and miss’61 and, even if there are local services, they may not be aware that they exist until pregnancy. This is likely to be an even bigger problem in areas with low FGM prevalence. 141 Even when pregnant, service provision and access varied, particularly regarding the time points deinfibulation was offered/available. This does not provide an inclusive approach to ensuring that the physical and mental health needs of survivors are met, as specified in commissioning guidance in England. 114,133 The opaqueness of service provision probably reflects a lack of nationally consistent care pathways, which needs to be addressed as part of future service development activities.
Previous studies61,63 have suggested that ‘there is a need communities to be more aware of FGM/C [female genital cutting]-related services and of potential interventions’; however, this places the burden on the communities themselves, but, in reality, this needs to work both ways. FGM-affected communities do have a responsibility and have suggested that they need to raise awareness of FGM and its consequences, with a view to reducing stigma about accessing care,61,142 but there is also a need to provide information about services to communities in a transparent and culturally sensitive way, and using a range of different media (e.g. leaflets, apps) and languages. Survivors and men told us that education in schools, national awareness campaigns and community events and training were needed. However, it is not currently known how best to share information and raise awareness of FGM and service provision, but there have been suggestions around the use of community advocates or champions. 61,63 Although we did not see this in our own data, FGM community champion models have been advocated, as they can be the voice of the community, drive change through trusting relationships and reach members of the community that cannot be reached through traditional methods. 143
Further to this, FGM-affected communities are keen to work in partnership with stakeholders to create change in future services and training. 144,145 This aligns with the findings from our study, which suggested that future NHS support and services should be developed with survivors where possible. The idea of survivor-led support during FGM education was strong. Genuine and sustained involvement of survivors and men will allow for the development of culturally sensitive and congruent clinical guidelines,145 and for the co-creation of learning and resources that can be shared between survivors, communities and professionals. 144 All of these are likely to improve FGM service provision and build trust between individuals, communities, HCPs and services. There is, however, a need to understand, through future research, how we can best facilitate partnership working between communities and stakeholders in relation to FGM service design and provision. 144
Underlying many of the perceived and reported issues around service provision was a lack of, misinterpreted or misrepresented information and knowledge. This manifested in a number of different ways for survivors, men and HCPs, and was the root of several silences. This was in addition to issues around a lack of awareness highlighted earlier for survivors and men. Much of these discussions focused on culture and cultural dissonance between survivors/men and their HCPs/health service. Health-care interactions are a shared environment within which facets of equality, diversity and culture intersect. 146 UK health-care services should be equitable, culturally sensitive, reactive and responsive to the diverse needs of service users; however, repeated reports have shown that many services are culturally inadequate and do not meet the needs of the increasingly diverse UK population. 147,148 Cultural competence and safety are particularly important within the context of FGM service delivery and configuration. 63 There were examples within our study of HCPs lacking cultural knowledge, meaning that their behaviour and the language that they used when discussing or interacting with survivors and men from FGM-affected communities appeared to reflect an interpretation of the practice through a Western society lens. This lens may have led to ‘sensationalising’ the issue of FGM, with descriptions of survivors as ‘other’. The ‘othering’ of minority groups in health care is an important and challenging problem, reflecting a deficit rather than a partnership model between the survivor and their HCP, which can further reinforce marginalisation and feelings of disempowerment. 63,149 Those who have experienced negative interactions within the health system and those who feel unwelcome, through a lack of cultural awareness and ‘othering’ from culturally incompetent HCPs, are less likely to seek appropriate care and re-engage with the health system in the future. 150 There was evidence of this incompetence and associated subsequent disengagement within our data. Cultural competency training of FGM providers is clearly needed to support them in caring for survivors and men with insight and understanding of their FGM-related cultural values and norms. However, recent evidence suggested that current cultural competency training in the UK needs to be reformed to meet the needs of our diverse population. 146,147 Cultural competency training by itself is also unlikely to address these issues within FGM service provision. Cultural competency and safety should be embedded, monitored and evaluated at individual, service, organisational and system levels. 151
One of the minimum standards of the FGM commissioning guidance is to meet the mental health needs of survivors. 133 The findings from our study and that of the wider literature63,128 suggest that services continue to fail to effectively recognise and support the psychological well-being of survivors and their families. This is particularly relevant to deinfibulation, as discussed earlier, but also to wider service provision, as any clinical interaction can be triggering for survivors. 120,121,152 There were interesting discussions within our data around the use of the term ‘mental health’ and the labelling of mental health services for FGM survivors, which may be culturally inappropriate as a result of the stigma associated with needing mental health support, compounded by the stigma of seeking care for their FGM. This is an important consideration in future service-planning. Linked with inadequate mental health care provision was the recognition that current services are not recognising and supporting the psychosexual, sexual health and intimate relationship needs of survivors and their partners. Although the sexual health and psychosexual consequences are well documented in the quantitative literature,1,51,52 there is far less discussion within the qualitative evidence base. 61 This is perhaps why we identified that sex was a silence within our data and that this silence is perpetuated within the wider evidence base. There is a need to better support survivors and their partners and this is particularly important given the silence between husband and wife, between whom sex was not discussed. Provision of psychosexual and sexual health support should be included as part of future service provision and further research is needed to more fully understand exactly what support is needed and at what time points.
Our participants highlighted that clinical interactions were disproportionately focused on the law and that they experienced frequent and, at times, repetitive discussions. These types of interactions, where HCPs lacked knowledge and information, led to anger, resentment and, at times, feelings that the discussions were victimising and or accusatory in nature (e.g. around child protection). This continued questioning and framing around the legal aspects of FGM led to some survivors and men avoiding health-care interactions and resulted in a loss of trust in their relationship with their HCPs and the wider system. It also led to some HCPs avoiding engaging with survivors because of concerns about being culturally insensitive and lacking knowledge on how to address legislative issues identified within the discussions. This is problematic as trust is key for building and maintaining health-care relationships. 153,154 The greater the trust between a survivor and their HCP, the better their overall satisfaction with treatment and quality of life. 155 Trust in HCPs and in the UK health-care system is likely to be even more important for survivors and men as they encounter UK health-care culture as migrants with potentially culturally sensitive FGM health-care needs. For trust to be established and maintained, there is a need for HCPs working with survivors and their families to be knowledgeable and to be able to communicate information in an appropriate and culturally sensitive way. We identified that improving communication was one of the ways to address the silences interpreted around knowledge and information. This would help to facilitate a more equal power dynamic and foster shared decision-making. 118 Both survivors and HCPs suggested that a continuity of carer model, including relationship and management continuity within FGM care pathways, may help to build trust, open communication and reduce the likelihood of having repeated discussions framed around the law. Continuity of care can help to empower women by allowing them to have control over their own care, supported by HCPs who are knowledgeable and confident to address women’s sociocultural needs. 156 Continuity of care models and personalised care plans are advocated in maternity settings157–159 and this may help to meet the needs of pregnant survivors. There is also a need for continuity of care and personalised care plans to be effectively integrated into FGM service delivery for survivors outside the maternity setting, such as through their GP. This requires further research and service development. Continuity of care is not referred to in the 2018 FGM commissioning guidance,114 although health-care pathways are presented for both pregnant and non-pregnant women. There is also a need to educate HCPs through training and guidelines to support them in improving their communication and understanding how to reach the right balance in terms of their legal responsibilities and providing equitable health care. 145
Linked with the avoidance of care and health-care interactions highlighted earlier, we interpreted a sense of fear running through the narratives of participants, including HCPs. This was a nuanced fear, rather than outright fear. For survivors and men, there were concerns about disclosing the fact that they came from FGM-affected communities within the UK health-care setting. These fears were rooted in concerns that disclosures, such as being deinfibulated, may get back to their community, which could lead to reprisals, exclusion and/or isolation. In addition, there were concerns that a disclosure to a HCP, particularly if they had a daughter(s), may lead to intervention from social services/the police and the perception that their children ‘might get taken away’. HCPs were fearful of cultural differences and being culturally insensitive or incompetent when interacting with survivors and men. They were also worried about being able to deliver care within the current statutory guidance on FGM. 67 There is a clear need to limit or address these fears as part of future FGM service provision.
These fears were likely rooted in deficits in awareness, knowledge and understanding across all participating groups and were also linked with shortfalls in communication skills. Survivors and, to some extent, men articulated that most HCPs lacked FGM-relevant clinical knowledge and cultural competence, which has been shown in other studies. 156 There was evidence within our study to suggest that many HCPs lacked the appropriate training and skills to adequately disseminate FGM information and provide appropriate care. As a result, the voices of survivors and men may have been silenced. The lack of skilled HCPs and wider deficits in knowledge resulted in potentially important and clinically salient impacts linked to decision-making, consent, engaging in discussions around FGM and, ultimately, the ability to provide appropriate care. This highlights further gaps in the current skills base of HCPs and potential unmet training needs within the FGM workforce.
As reported in Chapter 1, the current education and training resources75–77 available to UK professionals have multiple limitations, in particular the use of victim and victimisation terminology and the heavy focus on the legal aspects of FGM care. In 2018, FGM standards for training of HCPs160 were published, building on the existing safeguarding curriculum, which specify the clinical skills required by HCPs and what knowledge and understanding constitutes competence. Unfortunately, the focus on the law and victim terminology remains in these standards, and the need for awareness of the potential for cultural dissonance between provider and survivor is not mentioned. Aligned with our findings, this guidance160 makes it clear that all HCPs working in the NHS should have some knowledge of FGM, with a smaller number of HCPs needing specialist skills and training. The development of effective training, in collaboration with survivors, is needed to increase and support the maintenance of knowledge across all NHS staff, with further specialist training developed for the FGM-specific workforce. This training should encompass information on how to facilitate shared decision-making around deinfibulation, clinically relevant FGM knowledge, culturally competent communication, how to recognise and manage the psychological and sexual health needs of survivors, and how to engage men as part of care provision. As highlighted earlier in relation to deinfibulation, there is a need for competency-based education and training to increase the number of HCPs able to perform this procedure safely and competently. These FGM-specialist HCPs need to be trained across all settings, not just within maternity settings, which appears to be the case currently. HCPs within our study articulated that they would be willing to undertake deinfibulation with the right training and support. An increase in suitable HCPs across all settings is likely to improve the choices for survivors around deinfibulation.
The majority of HCPs within the study indicated that funding for FGM-specific services was inadequate. This was in parallel to suggestions by survivors and some men regarding the need to improve FGM services. Therefore, to address the issues in service provision and the additional training needs of the FGM workforces that we have highlighted, greater funding is needed. This would support the development and commissioning of new services to better meet the needs of survivors and their families, and so facilitate the roll out of consistent, accessible national FGM services.
Study strengths
Our study had many strengths. As far as the authors are aware, this is the largest cross-culture and cross-language qualitative exploration of survivors’, men’s and HCPs’ views around deinfibulation and NHS FGM service provision in the UK. A total of 141 diverse stakeholders participated, including 54 women and 13 men affected by FGM, in three languages. We have managed to successfully recruit marginalised populations and discuss the challenging and often unheard topic of FGM in depth.
Further to this, we have undertaken a rigorous and methodologically robust qualitative study. Through our reflexive practice, we have positioned ourselves within the research and have acknowledged the influences of our own views, context, experiences and roles in shaping the research and interpretation. 161 We used the SSF,86,88 which was aligned with our aim of researching the sensitive issue of FGM and the health-care needs of marginalised FGM-affected populations. We have used the SSF in two novel ways. First, we aligned the SSF with the FM103 to create a novel method – the HFM. Second, we have used the SSF to identify the roots and manifestation of silences and how these silences can be voiced and addressed.
We employed a range of different recruitment pathways to support recruitment of survivors and men through trusted advocates or gatekeepers. 162 Patient-facing materials were reviewed by our PPI group, as cultural insiders, to ensure cultural sensitivity. 163 To facilitate our cross-language research and inclusivity, patient-facing materials were available in a range of languages to ensure that we heard the voices of those unable to communicate in English. 163 Participants were offered a choice of data collection methods, types and locations to help build trust and rapport. 164 Survivors and men also received £20 compensation, which helped to promote the participation of diverse groups. 165
We trained specialist, qualified medical interpreters166 on FGM and how to appropriately support recruitment and data collection using conceptual equivalence methods. 167 Discussion guides were developed iteratively based on interviewer field notes and reflections, early analysis and regular discussion across the research team. Given the sensitive nature of the discussions and the potential for disclosures that might indicate risk of harm, we had distress and safeguarding pathways in place. The adequacy of the final sample size was carefully monitored during the research process to ensure that the overall sample and associated data had sufficient information power to develop new knowledge in relation to the research questions. 98 Further to this, we had multiple interviewers and analysts to support investigator triangulation and ensure that the data were viewed and interpreted through multiple lenses. 168
Study limitations
We have reflected on the potential limitations of the study. Of the six interviewers, only one could be perceived as a cultural insider;163 the rest of the interviewers and wider research team were cultural outsiders. Although not insiders, three team members (i.e. ED, AB, PL) were very experienced, having worked clinically with survivors and their families for an extended period. Three other team members (i.e. LJ, BC and ED) were highly experienced qualitative researchers who were able to apply their methodological knowledge and reflexivity to approach the data appropriately. There are potential benefits to being outsiders, as our PPI group highlighted that, given the Western stigma and taboo that surrounds FGM, talking to outsiders was perceived as safer than talking to insiders, who may have connections within their FGM community. However, they also said that being outsiders might make it more difficult for the research team to be culturally sensitive and that the research team might face culture shock during data collection and analysis. 169
Linked to this is the potential for power imbalances between outsider researchers and the participants. We were aware of and attentive to the potential power differential between the researchers and the participants in the research, in particular the survivors. Given the nature of semistructured interviews, we as researchers set the main agenda for the discussion and, therefore, this could be perceived as us holding the power. 170 To try to redress the power balance, we provided choice as to when, where and how the interviews took place; tried to build rapport with each participant prior to and at the start of the interview; actively listened during interviews, for example by reflecting back the language used by participants; and tried to conduct interviews in a participant-focused manner so that the discussions went in directions important to the participants.
We attempted to recruit survivors, men and HCPs through a variety of pathways to reach a diverse range of participants. However, the majority of survivors (75%) and HCPs (50%) were recruited through NHS trust maternity units. This meant that the majority of the survivors were accessing maternity services or were midwives (45%) working within hospital maternity services. This might have shaped views and preferences around antenatal deinfibulation as it is likely to reflect the direct experience of our participants. Ideally, we would have talked to more survivors outside maternity services, which has been identified as a research gap. 63 However, we were able to talk to younger women, with almost half (48%) of our survivors aged 18–29 years and, of these, 15% were aged 18–24 years. Hearing the voices of younger survivors has been identified as a research gap,63 but what ‘younger’ means remains unclear. Our stakeholder participants highlighted that there is a need to hear the voices and explore the experiences of adolescent girls aged < 18 years.
The other potential limitation of our survivor sample was linked to their difficulty in knowing what type of FGM they had experienced. This was not unexpected as many women do not know what type of FGM they have, if they are aware that they have FGM at all. For example, in England, the vast majority of survivors (≈ 80%) are identified via maternity services. 28 Therefore, it is not until they have been examined by a HCP and informed of what type of FGM they have experienced that they might be in a position to know their type and be able to share that with others. We had taken this into account when planning the study as there was no specific inclusion criterion for women to identify as a type 3 survivor, despite our aim being to elicit preferences around deinfibulation (surgery for infibulated/type 3 survivors). However, this meant that some of the survivors who were not type 3/had not been deinfibulated found it more challenging to explore their preferences for deinfibulation as the questions were hypothetical rather than experiential.
We may have also benefited from having greater diversity in the HCP sample, including more male HCPs and also including wider professionals groups involved in FGM care provision, such as social workers and school nurses. Recruiting men was particularly challenging and we had limited success with snowballing from survivors. Of the men recruited, 62% were identified through our contacts with voluntary/community organisations. We initially planned to recruit a smaller sample of men (n = 10) than survivors (n = 50) and HCPs (n = 50), as they were not the main focus of our study; however, evidence suggested that there was a need for further research with men,60 that they may perceive themselves as victims of the practice171–173 and that they may have a potentially important role to play in decision-making around deinfibulation. 63 We did succeed in interviewing 13 men; however, these data were relatively information poor in some areas, and so the sample potentially lacked adequacy for this type of exploratory study. 174 Similarly, we had initially planned to use independent synthesised member checking175 with a larger group of community participants in WP2a, but were able to recruit only 10 women across two events. We sought feedback as to why community members did not want to participate and this reflected issues with having to sign a consent form and the discussions being audio-recorded.
Implications and recommendations
The implications of the findings and subsequent discussion are presented in the following sections. The implications presented form an integration of the findings and discussion, and represent implications from this study as a whole, incorporating data synthesis across the data. Early implications and recommendations were identified and discussed as part of the stakeholder event. Although the implications have been integrated to avoid repetition, as many implications span the specific categories as presented in Chapters 3 and 4, the implications and recommendations will be aggregated but also categorised under two main relevant headings: those relevant to policy, practice and education, and those relevant to research.
Implications and recommendations for policy, practice and education
-
Deinfibulation service provision needs to be transparent in what is available and offer the procedure in hospital settings, by suitable professionals and at a range of time points, in particular pre pregnancy, to facilitate choice for survivors. Where possible, this should not be carried out in a maternity setting given the potential stigma for women seeking deinfibulation outside marriage/pregnancy. Survivors may also benefit from additional psychological support or counselling when considering and undergoing deinfibulation.
-
Care pathways for survivors outside maternity settings need to be evaluated and further developed in both high and low prevalence settings. Prototype service models should be formally tested using appropriate study designs.
-
Development and testing of effective training is needed to increase and support the generation and maintenance of FGM knowledge across all NHS staff, with further specialist training, including competency-based training around deinfibulation, developed for the FGM-specific workforce. This FGM-specific workforce needs to include all settings where FGM survivors may access/receive care and should not be limited to just maternity settings.
-
There are clear gaps and unmet training needs for HCPs, in particular around:
-
clinically relevant FGM knowledge
-
clinical knowledge and skills to undertake deinfibulation (for those undertaking this procedure)
-
cultural competence
-
open communication
-
legal aspects of FGM, including mandatory reporting and recording
-
balancing the legal responsibilities and providing equitable health care
-
supporting shared decision-making around deinfibulation
-
recognising and responding appropriately to the mental health, psychological and psychosexual needs of survivors and men
-
how to appropriately engage men.
-
-
The development of trust, a shared cultural understanding and open communication between survivor and HCPs are key to survivors feeling physically and psychologically safe when accessing services.
-
Interactions between survivors and HCPs should not be framed around the law/legal aspects of FGM; this should form a minor part of the discussion unless immediate risk concerns are identified.
-
Survivors and the wider FGM-affected community must be involved in future planning, commissioning and provision.
Recommendations for research
-
Undertake a comprehensive mapping exercise of UK FGM service provision at local, regional and national level. This should use a multi-informant and multisource methodology to explore structures, processes and outcomes.
-
Use rigorous qualitative research methods to explore the experiences and needs of girls (aged < 18 years), younger survivors (aged 18–24 years) and unmarried survivors, men and a wider range of professionals (e.g. social workers and school nurses) involved in the delivery of care.
-
Use rigorous qualitative research methods to explore the psychological and sexual health information and support needs of survivors and men at different time points throughout their life course (e.g. deinfibulation, marriage, first sexual intercourse, pregnancy, delivery).
-
Establish the training needs of professionals involved in the provision of FGM care and use these data to inform the development and testing of education packages.
-
Undertake primary data collection and/or analysis of pre-existing large data sets to better understand surgical risks and outcomes associated with deinfibulation at different time points.
-
Evaluate how best to facilitate partnership working between FGM-affected communities and stakeholders in relation to FGM service design and provision.
Chapter 6 Conclusions
The study has heard the voices of 141 survivors, men, HCPs and wider stakeholders to understand their preferences around deinfibulation and their views on current and future FGM services. As far as the authors are aware, this is the largest cross-language and cross-culture in depth qualitative exploration of deinfibulation and FGM care in the UK. Although other studies have explored views and experiences of deinfibulation, to the best of our knowledge, this is the first to do so in the UK context in such depth, with a broad range of stakeholders and in multiple languages. The findings from this study actively contribute robust in-depth qualitative evidence to support the improvement of current and future FGM service provision, in particular deinfibulation-related care.
We did hear examples of good practice and positive care interactions in relation to FGM service provision across the UK. However, despite the concerted multiagency effort around FGM support and service provision in the UK in recent years, our study has shown that, in general, current service provision remains suboptimal. Many services do not meet the minimum service requirements set out in commissioning guidance. In addition, we have shown that current FGM services often silence the experiences, perspectives and preferences of survivors and their families. Future FGM services need to carefully reflect the experiences and preferences of survivors, their families and FGM-affected communities to ensure that their voices are heard.
Deinfibulation service provision needs to be transparent in what is available and offer the procedure in hospital settings, by suitable professionals at a range of time points, in particular pre pregnancy, to facilitate choice for survivors. Survivors and the wider FGM-affected community should be involved in future planning, commissioning and provision to ensure that services are clinically and culturally appropriate. This will help to develop mutual trust between survivors, communities, providers and the health service. Local and national guidelines should be updated to better reflect the needs of survivors and to ensure consistency in provision of information and support.
Dissemination of findings
Activities undertaken to date
-
Publication of the study protocol. 83
-
Community and national stakeholder events where early findings were discussed.
-
Publication of a feature article in The Birmingham Brief176 to coincide with International Zero Tolerance of FGM day (February 2020).
-
FGM Sister Study Twitter #WeChat event hosted by #WeMidwives (October 2019); as of March 2020, Twitter analytics estimated the chat had a total reach of 1,100,313 users.
-
Abstracts submitted and accepted for presentation at the (1) British Maternal and Fetal Medicine Society Annual Conference 2020; (2) Faculty of Sexual and Reproductive RCOG Annual Scientific Meeting 2020 and (3) Nightingale2020 Conference (note that all presentations/conferences were subsequently cancelled as a result of COVID-19).
-
Publication of lay community and stakeholder reports based on findings from the events run as part of the study.
-
Development and dissemination through multiple pathways of illustrations of the main thematic results (see Figure 7) and silences interpreted within the study (see Figure 10).
-
Presentation of early study findings at Barnardo’s International Women’s Day Conference, London (March 2020).
-
Presentation of study outline at North West Central Social Care Conference, Birmingham (July 2019).
-
Publication of study findings in international peer-reviewed journals.
Knowledge translation and impact
-
We are currently considering establishing a task force, including participants from our PPI survivor group, community and stakeholder events, to support and co-ordinate the implementation of the recommendations from our research.
Acknowledgements
We would like to thank all of those who have shared their experiences, insights and time to support the FGM Sister Study. In particular, we would like to thank the members of the FGM survivor group, Hodan, Ayan, Hodo and one other (who did not wish to be identified), who have proved invaluable throughout the project.
Thanks to all of those who facilitated recruitment within the NHS and via third-sector organisations. We would like to specifically acknowledge our partnership with the National FGM Centre (part of Barnardo’s Children’s Charity) and the input of its staff, including Amat Saeed, Glenda Bonde, Leethen Bartholomew and Rohma Ullah. We would also like to thank two other National FGM Centre staff who supported data collection in the London community event.
We are also grateful to Lailah Alidu for her contributions in the early phases of the study and to Laura Brodrick, Graphic and Creative Facilitator at Think Big Picture, who created the illustrated thematic (Figure 7) and silences (Figure 10) summaries.
Acknowledgement of the Study Steering Group
We would like to thank each member of the SSG for their invaluable insight to and guidance of the successful completion of the FGM Sister Study:
-
Professor Charlotte Clarke (chairperson), Executive Dean Social Sciences and Health, Durham University, Durham, UK.
-
Ms Juliet Albert, Specialist FGM Midwife, Imperial College Healthcare NHS Trust, London, UK.
-
Mrs Sylla Mama Barry, FGM survivor representative.
-
Professor Hazel Barrett, Professor of Development Geography, Centre for Trust, Peace and Social Relations (CTPSR), Coventry University, Coventry, UK.
-
Dr Catrin Evans, Associate Professor/Director of Global Engagement, University of Nottingham, Nottingham, UK.
-
Ms Emma Mills, Consultant Midwife at Clinical Research and Innovation Centre, Aneurin Bevan University Health Board, Newport, UK.
-
Ms Toks Okeniyi, Head of UK Programmes and Operations, Forward UK, London, UK.
-
Ms Rachael Oluyemi, Coventry Haven FGM Co-ordinator, Coventry Haven Women’s Aid, Coventry, UK.
Contributions of authors
Laura Jones (https://orcid.org/0000-0002-4018-3855) (Senior Lecturer, Applied Health Research) was principal investigator and was involved in and responsible for all phases of the study.
Emma Danks (https://orcid.org/0000-0002-9166-1650) (Research Fellow) was involved in the design, recruitment, data collection, analysis, interpretation and reporting phases.
Benjamin Costello (https://orcid.org/0000-0003-4744-5659) (Research Fellow) was involved in the recruitment, data collection, analysis, interpretation and reporting phases.
Kate Jolly (https://orcid.org/0000-0002-6224-2115) (Professor, Public Health and Primary Care) was involved in the design, interpretation and reporting phases.
Fiona Cross-Sudworth (https://orcid.org/0000-0002-5223-1789) (Study Co-ordinator) was involved in the recruitment, data collection, interpretation and reporting phases.
Pallavi Latthe (https://orcid.org/0000-0003-0529-0409) (Consultant, Urogynaecology) was involved in the design, recruitment, interpretation and reporting phases.
Meg Fassam-Wright (https://orcid.org/0000-0002-1864-5291) (Interim Head, National FGM Centre) was involved in the design, recruitment, interpretation and reporting phases.
Joanne Clarke (https://orcid.org/0000-0003-2563-5451) (Study Co-ordinator) was involved in the recruitment, data collection, interpretation and reporting phases.
Alison Byrne (https://orcid.org/0000-0002-2366-0162) (FGM-Specialist Midwife) was involved in the design, recruitment, interpretation and reporting phases.
Julie Taylor (https://orcid.org/0000-0002-7259-0906) (Professor, Child Protection) was involved in the design, data collection, analysis, interpretation and reporting phases.
All authors made contributions to the conception and design, recruitment or data collection, as well as the analysis and interpretation of data. All were involved in the drafting of the report or revising it critically for important intellectual content, and all authors approved the final version to be published
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Patient data
This work uses data provided by patients and collected by the NHS as part of their care and support. Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that it is stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care.
References
- World Health Organization . Care of Girls and Women Living With Female Genital Mutilation: A Clinical Handbook 2018. www.who.int/reproductivehealth/publications/health-care-girls-women-living-with-FGM/en/ (accessed 1 May 2021).
- National FGM Centre . Female Genital Mutilation 2020. http://nationalfgmcentre.org.uk/fgm/ (accessed 11 May 2020).
- National FGM Centre . Potential Health Consequences of Female Genital Mutilation 2020. http://nationalfgmcentre.org.uk/wp-content/uploads/2019/02/FGM-and-Health-Consequences-Infographic-1.pdf (accessed 11 May 2020).
- World Health Organization . Female Genital Mutilation: A Joint WHO UNICEF UNFPA Statement 1997. http://apps.who.int/iris/bitstream/10665/41903/1/9241561866.pdf (accessed 20 April 2017).
- World Health Organization . Sexual and Reproductive Health: Classification of Female Genital Mutilation 2007 n.d. www.who.int/reproductivehealth/topics/fgm/overview/en/ (accessed 19 April 2017).
- Banks E, Meirik O, Farley T, Akande O, Bathija H, Ali M. WHO study group on female genital mutilation and obstetric outcome. Female genital mutilation and obstetric outcome: WHO collaborative prospective study in six African countries. Lancet 2006;367:1835-41. https://doi.org/10.1016/S0140-6736(06)68805-3.
- Almroth L, Almroth-Berggren V, Hassanein OM, El Hadi N, Al-Said SS, Hasan SS, et al. A community based study on the change of practice of female genital mutilation in a Sudanese village. Int J Gynaecol Obstet 2001;74:179-85. https://doi.org/10.1016/S0020-7292(01)00392-7.
- World Health Organization . Eliminating Female Genital Mutilation: An Interagency Statement (OHCHR, UNAIDS, UNDP, UNECA, UNESCO, UNFPA, UNHCR, UNICEF, UNIFEM, WHO) 2008 n.d. http://apps.who.int/iris/bitstream/10665/43839/1/9789241596442_eng.pdf (accessed 19 April 2017).
- Royal College of Obstetricians and Gynaecologists . Female Genital Mutilation and Its Management: Green-Top Guideline No. 53 2015 n.d. www.rcog.org.uk/globalassets/documents/guidelines/gtg-53-fgm.pdf (accessed 21 December 2016).
- Royal College of Midwives . Tackling FGM in the UK: Intercollegiate Recommendations for Identifying, Recording and Reporting 2013.
- United Nations Women . Female Genital Mutilation Cutting and Violence Against Women and Girls: Strengthening the Policy Linkages Between Different Forms of Violence 2017. www.unwomen.org/-/media/headquarters/attachments/sections/library/publications/2017/policy-note-female-genital-mutilation-cutting-and-violence-against-women-and-girls-en.pdf?la=en%26vs=905 (accessed 27 May 2020).
- United Nations Fund for Population Activities (UNFPA) . Female Genital Mutilation (FGM) Frequently Asked Questions 2015. https://doi.org/10.1002/9781118371923.ch2 (accessed 9 August 2021).
- World Health Organization . Female Genital Mutilation 2016. www.who.int/mediacentre/factsheets/fs241/en/ (accessed 21 December 2016).
- Hosken F. Genital and Sexual Mutilation of Females: The Hosken Report. Report on Ethnographical Observation Study 1979.
- Hay MJ. The Hosken report: genital and sexual mutilation of females (book review). Int J Afr Hist Stud 1981;14:52-6. https://doi.org/10.2307/217712.
- Public Policy Advisory Network on Female Genital Surgeries in Africa . Seven things to know about female genital surgeries in Africa. Hastings Cent Rep 2012;42:19-27. https://doi.org/10.1002/hast.81.
- Essen B, Mosselmans L. How to ensure policies and interventions rely on strong supporting facts to improve women’s health: the case of female genital cutting, using Rosling’s factfulness approach. Acta Obstet Gynecol Scand 2021;100:579-86. https://doi.org/10.1111/aogs.14059.
- 28TooMany . What Are the Origins and Reasons for FGM? 2013. www.28toomany.org/blog/what-are-the-origins-and-reasons-for-fgm-blog-by-28-too-manys-research-coordinator/#:~:text=Some%20researchers%20have%20traced%20the,British%20Museum%20dated%20163%20BC (accessed 7 February 2020).
- United Nations Children’s Fund (UNICEF) . Female Genital Mutilation: A New Generation Calls for Ending an Old Practice 2020.
- Cappa C, Van Baelen L, Leye E. The practice of female genital mutilation across the world: data availability and approaches to measurement. Glob Public Health 2019;14:1139-52. https://doi.org/10.1080/17441692.2019.1571091.
- Worldometer . Worldometer – Real Time World Statistics n.d. www.worldometers.info/ (accessed 24 May 2020).
- United Nations Children’s Fund (UNICEF) . Female Genital Mutilation Cutting: A Global Concern 2016.
- United Nations . Transforming Our World: The 2030 Agenda for Sustainable Development A RES 70 1 2015. https://sustainabledevelopment.un.org/content/documents/21252030%20Agenda%20for%20Sustainable%20Development%20web.pdf (accessed 11 May 2020).
- Macfarlane AJ, Dorkenoo E. Estimating the numbers of women and girls with female genital mutilation in England and Wales. J Epidemiol Community Health 2015;69. https://doi.org/10.1136/jech-2015-206256.117.
- Van Baelen L, Ortensi L, Leye E. Estimates of first-generation women and girls with female genital mutilation in the European Union, Norway and Switzerland. Eur J Contracept Reprod Health Care 2016;21:474-82. https://doi.org/10.1080/13625187.2016.1234597.
- Karlsen S, Howard J, Carever N, Mogilnicka M, Pantazis C. Available evidence suggests that prevalence and risk of female genital cutting/mutilation in the UK is much lower than widely presumed - policies based on exaggerated estimates are harmful to girls and women from affected communities. Int J Impot Res 2022.
- Karlsen S, Mogilnicka M, Carver N, Pantazis C. Female genital mutilation: empirical evidence supports concerns about statistics and safeguarding. BMJ 2019;364. https://doi.org/10.1136/bmj.l915.
- NHS Digital . Female Genital Mutilation Datasets 2020. https://digital.nhs.uk/data-and-information/clinical-audits-and-registries/female-genital-mutilation-datasets (accessed 18 May 2020).
- NHS Digital . SCCI2026: Female Genital Mutilation Enhanced Dataset 2018. https://digital.nhs.uk/data-and-information/information-standards/information-standards-and-data-collections-including-extractions/publications-and-notifications/standards-and-collections/scci2026-female-genital-mutilation-enhanced-dataset#current-release (accessed 18 May 2020).
- NHS Digital . Female Genital Mutilation: Annual Report – April 2019 to March 2020 (Experimental Statistics Report). Statical Data Report 2020.
- Burrage H. Eradicating Female Genital Mutilation: A UK Perspective. Burlington, VT: Ashgate Publishing; 2015.
- Burrage H. Female Genital Mutilation in Britain: The Scandal About to Break 2012. https://hilaryburrage.com/2012/06/07/female-genital-mutilation-fgm-in-britain-a-scandal-about-to-break/ (accessed 17 January 2022).
- Abdi MS. A Religious Oriented Approach to Addressing FGC Among the Somali Community of Wajir, Kenya. Washington, DC: Population Council, Frontiers in Reproductive Health; 2007.
- El-Mouelhy MT, Johansen REB, Ragab AR, Fahmy A. Men’s perspectives on the relationship between sexuality and female genital mutilation in Egypt. Sociol Stud 2013;3:104-13.
- Ahmadu FS, Shweder RA. Disputing the myth of the sexual dysfunction of circumcised women: an interview with Fuambai S. Ahmadu by Richard A. Shweder. Anthropol Today 2009;25:14-7. https://doi.org/10.1111/j.1467-8322.2009.00699.x.
- Njambi WN. Dualisms and female bodies in representations of African female circumcision: a feminist critique. Fem Theory 2004;5:281-303. https://doi.org/10.1177/1464700104040811.
- Abdalla SM, Galea S. Is female genital mutilation/cutting associated with adverse mental health consequences? A systematic review of the evidence. BMJ Glob Health 2019;4. https://doi.org/10.1136/bmjgh-2019-001553.
- Berg RC, Underland V. Immediate Health Consequences of Female Genital Mutilation/Cutting (FGM/C). NIPH Systematic Reviews: Executive Summaries. Oslo: Knowledge Centre for the Health Services at The Norwegian Institute of Public Health; 2014.
- Berg RC, Underland V, Odgaard-Jensen J, Fretheim A, Vist GE. Effects of female genital cutting on physical health outcomes: a systematic review and meta-analysis. BMJ Open 2014;4. https://doi.org/10.1136/bmjopen-2014-006316.
- Iavazzo C, Sardi TA, Gkegkes ID. Female genital mutilation and infections: a systematic review of the clinical evidence. Arch Gynecol Obstet 2013;287:1137-49. https://doi.org/10.1007/s00404-012-2708-5.
- Berg RC, Odgaard-Jensen J, Fretheim A, Underland V, Vist G. An updated systematic review and meta-analysis of the obstetric consequences of female genital mutilation/cutting. Obstet Gynecol Int 2014;2014. https://doi.org/10.1155/2014/542859.
- Berg RC, Underland V. The obstetric consequences of female genital mutilation/cutting: a systematic review and meta-analysis. Obstet Gynecol Int 2013;2013. https://doi.org/10.1155/2013/496564.
- Biglu MH, Farnam A, Abotalebi P, Biglu S, Ghavami M. Effect of female genital mutilation/cutting on sexual functions. Sex Reprod Healthc 2016;10:3-8. https://doi.org/10.1016/j.srhc.2016.07.002.
- Reisel D, Creighton SM. Long term health consequences of female genital mutilation (FGM). Maturitas 2015;80:48-51. https://doi.org/10.1016/j.maturitas.2014.10.009.
- Lurie JM, Weidman A, Huynh S, Delgado D, Easthausen I, Kaur G. Painful gynecologic and obstetric complications of female genital mutilation/cutting: a systematic review and meta-analysis. PLOS Med 2020;17. https://doi.org/10.1371/journal.pmed.1003088.
- Bishai D, Bonnenfant YT, Darwish M, Adam T, Bathija H, Johansen E, et al. Estimating the obstetric costs of female genital mutilation in six African countries. Bull World Health Organ 2010;88:281-8. https://doi.org/10.2471/BLT.09.64808.
- Knipscheer J, Vloeberghs E, van der Kwaak A, van den Muijsenbergh M. Mental health problems associated with female genital mutilation. BJPsych Bull 2015;39:273-7. https://doi.org/10.1192/pb.bp.114.047944.
- Mpinga EK, Macias A, Hasselgard-Rowe J, Kandala NB, Félicien TK, Verloo H, et al. Female genital mutilation: a systematic review of research on its economic and social impacts across four decades. Glob Health Action 2016;9. https://doi.org/10.3402/gha.v9.31489.
- Obermeyer CM. The consequences of female circumcision for health and sexuality: an update on the evidence. Cult Health Sex 2005;7:443-61. https://doi.org/10.1080/14789940500181495.
- Stein K, Hindin MJ, Chou D, Say L. Prioritizing and synthesizing evidence to improve the health care of girls and women living with female genital mutilation: an overview of the process. Int J Gynaecol Obstet 2017;136:3-12. https://doi.org/10.1002/ijgo.12050.
- Berg RC, Denison E, Fretheim A. Psychological, Social and Sexual Consequences of Female Genital Mutilation/Cutting (FGM/C): A Systematic Review of Quantitative Studies. NIPH Systematic Reviews. Oslo: Knowledge centre for the Health Services at The Norwegian Institute of Public Health; 2010.
- Buggio L, Facchin F, Chiappa L, Barbara G, Brambilla M, Vercellini P. Psychosexual consequences of female genital mutilation and the impact of reconstructive surgery: a narrative review. Health Equity 2019;3:36-4. https://doi.org/10.1089/heq.2018.0036.
- Refaei M, Aghababaei S, Pourreza A, Masoumi SZ. Socioeconomic and reproductive health outcomes of female genital mutilation. Arch Iran Med 2016;19:805-11.
- World Health Organization . The Economic Cost of Female Genital Mutilation 2020 n.d. www.who.int/news-room/detail/06-02-2020-economic-cost-of-female-genital-mutilation (accessed 18 May 2020).
- Hex N, Hanlon J, Wright D, Dale V, Bloor K. Estimating The Costs of Female Genital Mutilation Services to the NHS 2016 n.d. www.york.ac.uk/media/healthsciences/images/research/prepare/reportsandtheircoverimages/EstimatingCostsOfFGMServices.pdf (accessed 14 June 2019).
- World Health Organization . Guidelines on the Management of Health Complications from Female Genital Mutilation 2016. www.ncbi.nlm.nih.gov/books/NBK368491/ (accessed 1 May 2021).
- Effa E, Ojo O, Ihesie A, Meremikwu MM. Deinfibulation for treating urologic complications of type III female genital mutilation: a systematic review. Int J Gynaecol Obstet 2017;136:30-3. https://doi.org/10.1002/ijgo.12045.
- Okusanya BO, Oduwole O, Nwachuku N, Meremikwu MM. Deinfibulation for preventing or treating complications in women living with type III female genital mutilation: a systematic review and meta-analysis. Int J Gynaecol Obstet 2017;136:13-20. https://doi.org/10.1002/ijgo.12056.
- Esu E, Udo A, Okusanya BO, Agamse D, Meremikwu MM. Antepartum or intrapartum deinfibulation for childbirth in women with type III female genital mutilation: a systematic review and meta-analysis. Int J Gynaecol Obstet 2017;136:21-9. https://doi.org/10.1002/ijgo.12055.
- Abdulcadir J, Rodriguez MI, Say L. Research gaps in the care of women with female genital mutilation: an analysis. BJOG 2015;122:294-303. https://doi.org/10.1111/1471-0528.13217.
- Evans C, Tweheyo R, McGarry J, Eldridge J, Albert J, Nkoyo V, et al. Seeking culturally safe care: a qualitative systematic review of the healthcare experiences of women and girls who have undergone female genital mutilation/cutting. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2018-027452.
- Evans C, Tweheyo R, McGarry J, Eldridge J, Albert J, Nkoyo V, et al. Crossing cultural divides: a qualitative systematic review of factors influencing the provision of healthcare related to female genital mutilation from the perspective of health professionals. PLOS ONE 2019;14. https://doi.org/10.1371/journal.pone.0211829.
- Evans C, Tweheyo R, McGarry J, Eldridge J, Albert J, Nkoyo V, et al. Improving care for women and girls who have undergone female genital mutilation/cutting: qualitative systematic reviews. Health Serv Deliv Res 2019;7. https://doi.org/10.3310/hsdr07310.
- Royal College of Nursing . Female Genital Mutilation: An RCN Resource for Nursing and Midwifery Practice (Second Edition) 2015. www.rcn.org.uk/-/media/royal-college-of-nursing/documents/publications/2015/february/pub-004773.pdf (accessed 17 January 2022).
- Albert J, Bailey E, Duaso M. Does the timing of deinfibulation for women with type 3 female genital mutilation affect labour outcomes?. Br J Midwifery 2015;23:430-7. https://doi.org/10.12968/bjom.2015.23.6.430.
- Paliwal P, Ali S, Bradshaw S, Hughes A, Jolly K. Management of type III female genital mutilation in Birmingham, UK: a retrospective audit. Midwifery 2014;30:282-8. https://doi.org/10.1016/j.midw.2013.04.008.
- Department for Education, Department of Health and Social Care, Home Office . Multi-Agency Statutory Guidance on Female Genital Mutilation 2016. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/800306/6-1914-HO-Multi_Agency_Statutory_Guidance.pdf (accessed 1 June 2020).
- Great Britain . Prohibition of Female Circumcision Act 1985 1985. www.legislation.gov.uk/ukpga/1985/38/section/1?view=extent (accessed 1 June 2020).
- Great Britain . Female Genital Mutilation Act 2003 2003. www.legislation.gov.uk/ukpga/2003/31/contents (accessed 1 June 2020).
- Great Britain . Prohibition of Female Genital Mutilation (Scotland) Act 2005 2005. www.legislation.gov.uk/asp/2005/8/contents (accessed 1 June 2020).
- Great Britain . Serious Crime Act 2015 2015. www.legislation.gov.uk/ukpga/2015/9/pdfs/ukpga_20150009_en.pdf (accessed 1 June 2020).
- Great Britain . Female Genital Mutilation (Protection and Guidance) (Scotland) Act 2020 2020. www.legislation.gov.uk/asp/2020/9/contents/enacted (accessed 1 June 2020).
- Crown Prosecution Service . Mother First to Be Convicted of Female Genital Mutilation 2019. www.cps.gov.uk/london-north/news/mother-first-be-convicted-female-genital-mutilation (accessed 1 June 2020).
- Dyer C. FGM: Mother is first person in UK to be convicted of female genital mutilation. BMJ 2019;364. https://doi.org/10.1136/bmj.l546.
- NHS Health Education England . FGM E-Learning to Improve Awareness and Understanding of FGM 2020. www.e-lfh.org.uk/programmes/female-genital-mutilation/ (accessed 5 June 2020).
- eIntegrity healthcare e-learning . Female Genital Mutilation Awareness Training n.d. www.eintegrity.org/e-learning-healthcare-course/female-genital-mutilation.html (accessed 5 June 2020).
- Home Office . Female Genital Mutilation: Recognising and Preventing FGM 2016. www.virtual-college.co.uk/resources/free-courses/recognising-and-preventing-fgm (accessed 1 May 2021).
- FORWARD UK . Female Genital Mutilation Specialist Health Services in the UK 2019. www.forwarduk.org.uk/wp-content/uploads/2019/06/SPECIALIST-CLINICS-FGM-Clinic-Services-.pdf (accessed 14 September 2020).
- NHS . National FGM Support Clinics – Female Genital Mutilation (FGM) 2019. www.nhs.uk/conditions/female-genital-mutilation-fgm/national-fgm-support-clinics/ (accessed 24 May 2020).
- Smith H, Stein K. Surgical or medical interventions for female genital mutilation. Int J Gynaecol Obstet 2017;136:43-6. https://doi.org/10.1002/ijgo.12053.
- DiCicco-Bloom B. Ethical considerations for qualitative research. J Dent Educ 2000;64:616-18. https://doi.org/10.1002/j.0022-0337.2000.64.8.tb03368.x.
- Barker KL. How can qualitative research be utilised in the NHS when re-designing and commissioning services?. Br J Pain 2015;9:70-2. https://doi.org/10.1177/2049463714544553.
- Jones L, Danks E, Clarke J, Alidu L, Costello B, Jolly K, et al. Exploring the views of female genital mutilation survivors, their male partners and healthcare professionals on the timing of deinfibulation surgery and NHS FGM care provision (the FGM Sister Study): protocol for a qualitative study. BMJ Open 2019;9. https://doi.org/10.1136/bmjopen-2019-034140.
- ISRCTN Registry . FGM Sister Study: Exploring the Views of Female Genital Mutilation Cutting Survivors, Male Partners and Healthcare Professionals on the Timing of Re-Opening Surgery 2018. www.isrctn.com/ISRCTN14710507?q=%26filters=%26sort=%26offset=11%26totalResults=17335%26page=1%26pageSize=20%26searchType=basic-search (accessed 1 May 2021).
- O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med 2014;89:1245-51. https://doi.org/10.1097/ACM.0000000000000388.
- Serrant-Green L. The sound of ‘silence’: a framework for researching sensitive issues or marginalised perspectives in health. J Res Nurs 2011;16:347-60. https://doi.org/10.1177/1744987110387741.
- Williams M, May T. Introduction to the Philosophy of Social Research. London: UCL Press; 1996.
- Serrant-Green L. Black Caribbean Men, Sexual Health Decisions and Silences. Nottingham: University of Nottingham; 2004.
- French K. Review: The sound of ‘silence’: a framework for researching sensitive issues or marginalised perspectives in health. J Res Nurs 2011;16:361-2. https://doi.org/10.1177/1744987110387742.
- Knighton P. Female Genital Mutilation (FGM) Enhanced Dataset: Data Quality Statement on Experimental Statistics. NHS Statistical Data. London: NHS Digital; 2015.
- Patton MQ. Qualitative Research and Evaluation Methods. Thousand Oaks, CA: SAGE Publications Ltd; 2002.
- Silverman D. Doing Qualitative Research. Thousand Oaks, CA: SAGE Publications Ltd; 2005.
- Ellard-Gray A, Jeffrey NK, Choubak M, Crann SE. Finding the hidden participant: solutions for recruiting hidden, hard-to-reach, and vulnerable populations. Int J Qual Methods 2015;14. https://doi.org/10.1177/1609406915621420.
- Sadler GR, Lee H-C, Lim RS-H, Fullerton J. Recruitment of hard-to-reach population subgroups via adaptations of the snowball sampling strategy. Nurs Health Sci 2010;12:369-74. https://doi.org/10.1111/j.1442-2018.2010.00541.x.
- Sawe BE. How Many Languages Are Spoken in Africa? World Atlas 2018. www.worldatlas.com/articles/how-many-languages-are-spoken-in-africa.html (accessed 17 January 2022).
- Kroulek A. The Top Languages in Africa: A Guide to the Most Spoken Languages 2018. www.k-international.com/blog/most-spoken-african-languages/ (accessed 17 January 2022).
- World Health Organization . Process of Translation and Adaptation of Instruments 2020. www.who.int/substance_abuse/research_tools/translation/en/ (accessed 21 September 2020).
- Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res 2016;26:1753-60. https://doi.org/10.1177/1049732315617444.
- Palinkas LA. Qualitative and mixed methods in mental health services and implementation research. J Clin Child Adolesc Psychol 2014;43:851-61. https://doi.org/10.1080/15374416.2014.910791.
- Krueger RA, Casery MA. Focus Groups: A Practical Guide for Applied Research. Thousand Oaks, CA: SAGE Publications Ltd; 2015.
- Mulongo P, Hollins Martin C, McAndrew S. The psychological impact of Female Genital Mutilation/Cutting (FGM/C) on girls/women’s mental health: a narrative literature review. J Reprod Infant Psychol 2014;32:469-85. https://doi.org/10.1080/02646838.2014.949641.
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13. https://doi.org/10.1186/1471-2288-13-117.
- Castleberry A, Nolen A. Thematic analysis of qualitative research data: is it as easy as it sounds?. Curr Pharm Teach Learn 2018;10:807-15. https://doi.org/10.1016/j.cptl.2018.03.019.
- Crotty MJ. The Foundations of Social Research: Meaning and Perspective in the Research Process. London/Thousand Oaks, CA: SAGE Publications Ltd; 1998.
- Anfara VA, Mertz NT. Theoretical Frameworks in Qualitative Research. Thousand Oaks, CA: SAGE Publications Ltd; 2014.
- Draucker CB, Martsolf DS, Poole C. Developing distress protocols for research on sensitive topics. Arch Psychiatr Nurs 2009;23:343-50. https://doi.org/10.1016/j.apnu.2008.10.008.
- Department for Education, Home Office . Mandatory Reporting of Female Genital Mutilation – Procedural Information 2016 n.d. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/573782/FGM_Mandatory_Reporting_-_procedural_information_nov16_FINAL.pdf (accessed 2 June 2020).
- National Institute for Health Research . UK Standards for Public Involvement 2020. https://sites.google.com/nihr.ac.uk/pi-standards/standards?authuser=0 (accessed 24 July 2020).
- National Institute for Health Research . Policy on Payment of Fees and Expenses for Members of the Public Actively Involved With INVOLVE 2016. www.invo.org.uk/wp-content/uploads/2016/05/INVOLVE-internal-payment-policy-2016-final-1.pdf (accessed 25 July 2020).
- Norman K, Hemmings J, Husseain E, Otoo-Oyortey N. FGM Is Always With Us: Experiences, Perceptions and Beliefs of Women Affected by Female Genital Mutilation in London: Results from a PEER Study 2009. https://options.co.uk/sites/default/files/uk_2009_female_genital_mutilation.pdf (accessed 15 October 2020).
- Dixon-Woods M, Baker R, Charles K, Dawson J, Jerzembek G, Martin G, et al. Culture and behaviour in the English National Health Service: overview of lessons from a large multimethod study. BMJ Qual Saf 2014;23:106-15. https://doi.org/10.1136/bmjqs-2013-001947.
- Phillimore J, Klaas F, Padilla B, Hernandez-Plaza S, Rodrigues V. Adaptation of Health Services to Diversity: An Overview of Approaches. Birmingham: Institute for Research into Superdiversity, University of Birmingham; 2016.
- Szczepura A. Access to health care for ethnic minority populations. Postgrad Med J 2005;81:141-7. https://doi.org/10.1136/pgmj.2004.026237.
- NHS England . Commissioning Services to Meet the Needs of Women and Girls With FGM 2018. www.england.nhs.uk/wp-content/uploads/2018/04/commissioning-services-to-meet-the-needs-of-women-and-girls-with-fgm-1.pdf (accessed 9 August 2019).
- Albert J, Wells M. The Acton model: support for women with female genital mutilation. Br J Midwifery 2020;28:697-708. https://doi.org/10.12968/bjom.2020.28.10.697.
- Berggren V, Bergström S, Edberg AK. Being different and vulnerable: experiences of immigrant African women who have been circumcised and sought maternity care in Sweden. J Transcult Nurs 2006;17:50-7. https://doi.org/10.1177/1043659605281981.
- O’Brien O, Baldeh F, Hassan J, Baillie M. My Voice: Participatory Action Research Project With Men, Women and Young People on Female Genital Mutilation (FGM) in Scotland: (Phase 2) 2017. www.waverleycare.org/wp-content/uploads/2017/09/MyVoice-2017_web-Copy.pdf (accessed 2 October 2020).
- Browne AJ, Varcoe C, Smye V, Reimer-Kirkham S, Lynam MJ, Wong S. Cultural safety and the challenges of translating critically oriented knowledge in practice. Nurs Philos 2009;10:167-79. https://doi.org/10.1111/j.1466-769X.2009.00406.x.
- Abdulah DM, Dawson A, Sedo BA. The impact of health education on attitudes of parents and religious leaders towards female genital mutilation. BMJ Sex Reprod Health 2020;46:51-8. http://doi.org/10.1136/bmjsrh-2018-200211.
- Dawson A, Homer CS, Turkmani S, Black K, Varol N. A systematic review of doctors’ experiences and needs to support the care of women with female genital mutilation. Int J Gynaecol Obstet 2015;131:35-40. https://doi.org/10.1016/j.ijgo.2015.04.033.
- Dawson A, Turkmani S, Fray S, Nanayakkara S, Varol N, Homer C. Evidence to inform education, training and supportive work environments for midwives involved in the care of women with female genital mutilation: a review of global experience. Midwifery 2015;31:229-38. https://doi.org/10.1016/j.midw.2014.08.012.
- Turkmani S, Homer CSE, Dawson AJ. Understanding the experiences and needs of migrant women affected by female genital mutilation using maternity services in Australia. Int J Environ Res Public Health 2020;17. https://doi.org/10.3390/ijerph17051491.
- Oringanje CM, Okoro A, Nwankwo ON, Meremikwu MM. Providing information about the consequences of female genital mutilation to healthcare providers caring for women and girls living with female genital mutilation: a systematic review. Int J Gynaecol Obstet 2017;136:65-71. https://doi.org/10.1002/ijgo.12057.
- American College of Obstetricians and Gynecologists (ACOG) . Female Genital Cutting: Clinical Management of Circumcised Women 2007.
- Gayle C, Rymer J. Female genital mutilation and pregnancy: associated risks. Br J Nurs 2016;25:978-83. https://doi.org/10.12968/bjon.2016.25.17.978.
- Hamilton DK, Kong C, Hiratzka J, Contag AG, Ailon T, Line B, et al. Patient satisfaction after adult spinal deformity surgery does not strongly correlate with health-related quality of life scores, radiographic parameters, or occurrence of complications. Spine 2017;42:764-9. https://doi.org/10.1097/BRS.0000000000001921.
- Rathert C, May DR, Williams ES. Beyond service quality: the mediating role of patient safety perceptions in the patient experience-satisfaction relationship. Health Care Manage Rev 2011;36:359-68. https://doi.org/10.1097/HMR.0b013e318219cda1.
- Coho C, Parra Sepúlveda R, Husseain L, Laffy C. Female Genital Trauma: Guidelines for Working Therapeutically With Survivors of Female Genital Mutilation 2019. https://manorgardenscentre.org/resources/1924_Female_Genital_Trauma_Report_Web.pdf (accessed 2 October 2020).
- Department of Health and Social Care, NHS England . Female Genital Mutilation Prevention Programme: Requirements for NHS Staff 2014. www.nhs.uk/NHSEngland/AboutNHSservices/sexual-health-services/Documents/FGMstatementNHSCDec2014.pdf (accessed 5 June 2020).
- Department for Education . Statutory Guidance: Working Together to Safeguard Children 2019. www.gov.uk/government/publications/working-together-to-safeguard-children--2 (accessed 2 June 2020).
- Department of Health and Social Care . Female Genital Mutilation Risk and Safeguarding: Guidance for Professionals 2016. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/525390/FGM_safeguarding_report_A.pdf (accessed 4 June 2020).
- Department of Health and Social Care . FGM: Mandatory Reporting in Healthcare 2017. www.gov.uk/government/publications/fgm-mandatory-reporting-in-healthcare (accessed 1 June 2020).
- Department of Health and Social Care . Commissioning Services to Support Women and Girls With Female Genital Mutilation 2015. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/418549/2903842_DH_FGM_Commissioning_Accessible.pdf (accessed 24 May 2020).
- Reisel D, Creighton SM, Spicer J, Amadi O, Shakespeare J, Hodes D, et al. E-learning for Health: Female Genital Mutilation. E-Learning for Health 2016. www.e-lfh.org.uk/programmes/female-genital-mutilation/ (accessed 17 January 2022).
- Department of Health and Social Care . FGM: Video Resources for Healthcare Professionals 2016. www.gov.uk/government/publications/fgm-video-resources-for-healthcare-professionals (accessed 5th June 2020).
- NHS Digital . Female Genital Mutilation – Information Sharing 2020. https://digital.nhs.uk/services/female-genital-mutilation-information-sharing (accessed 2 June 2020).
- Creighton S, Hodes D. Chapter 3: Female Genital Mutilation. London: Department of Health and Social Care; 2015.
- Jones A. Working Psychologically with Female Genital Mutilation: An Exploration of the Views and Experiences of Women who have Experienced FGM and of Clinical Psychologists. London: University of East London; 2010.
- O’Brien O, Baldeh B, Sivapatham S, Brown E, O’May F. MY Voice: A Participatory Action Research Project With Men, Women and Young People on Female Genital Mutilation (FGM) in Scotland 2016. https://eresearch.qmu.ac.uk/bitstream/handle/20.500.12289/10580/10580.pdf?sequence=1%26isAllowed=y (accessed 20 October 2020).
- Safari F. A qualitative study of women’s lived experience after deinfibulation in the UK. Midwifery 2013;29:154-8. https://doi.org/10.1016/j.midw.2011.12.005.
- Norman K, Gegzabher SB, Otoo-Oyortey N. ‘Between Two Cultures’: A Rapid PEER Study Exploring Migrant Communities’ Views on Female Genital Mutilation in Essex and Norfolk, UK 2016. http://nationalfgmcentre.org.uk/wp-content/uploads/2015/12/Peer-Research-National-FGM-Centre.pdf (accessed 20 October 2020).
- Connelly E, Murray N, Baillot H, Howard N. Missing from the debate? A qualitative study exploring the role of communities within interventions to address female genital mutilation. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2017-021430.
- Khalifa S, Brown E. Communities Tackling FGM in the UK: Best Practice Guide: Tackling Female Genital Mutilation Initiative and Options Consultancy Services Limited 2016. www.bava.org.uk/wp-content/uploads/Communities-Tackling-FGM-Best-Practice-Guide.pdf (accessed 12 October 2020).
- Dixon S, Agha K, Ali F, El-Hindi L, Kelly B, Locock L, et al. Female genital mutilation in the UK – where are we, where do we go next? Involving communities in setting the research agenda. Res Involv Engagem 2018;4. https://doi.org/10.1186/s40900-018-0103-5.
- Vissandjée B, Denetto S, Migliardi P, Proctor J. Female Genital Cutting (FGC) and the ethics of care: community engagement and cultural sensitivity at the interface of migration experiences. BMC Int Health Hum Rights 2014;14. https://doi.org/10.1186/1472-698X-14-13.
- George R, Thornicroft G, Dogra N. Exploration of cultural competency training in UK healthcare settings: a critical interpretive review of the literature. Divers Equal Health Care 2015;12:104-15. https://doi.org/10.21767/2049-5471.100037.
- Gallagher RW, Polanin JR. A meta-analysis of educational interventions designed to enhance cultural competence in professional nurses and nursing students. Nurse Educ Today 2015;35:333-40. https://doi.org/10.1016/j.nedt.2014.10.021.
- Schouler-Ocak M, Graef-Calliess IT, Tarricone I, Qureshi A, Kastrump ME, Dinesh B. EPA guidelines on cultural competence training. Eur Psychiatry 2015;30:431-40. https://doi.org/10.1016/j.eurpsy.2015.01.012.
- Johnson JL, Bottorff JL, Browne AJ, Grewal S, Hilton BA, Clarke H. Othering and being othered in the context of health care services. Health Commun 2004;16:255-71. https://doi.org/10.1207/S15327027HC1602_7.
- Bowes A. South Asian women and health services: a study in Glasgow. New Community 1993;19:611-26. https://doi.org/10.1080/1369183X.1993.9976391.
- Brascoupe S, Waters C. Cultural safety: exploring the applicability of the concept of cultural safety to Aboriginal health and community wellness. J Aborig Health 2009;5:6-41.
- Moxey JM, Jones LL. A qualitative study exploring how Somali women exposed to female genital mutilation experience and perceive antenatal and intrapartum care in England. BMJ Open 2016;6. https://doi.org/10.1136/bmjopen-2015-009846.
- Murray B, McCrone S. An integrative review of promoting trust in the patient-primary care provider relationship. J Adv Nurs 2015;71:3-23. https://doi.org/10.1111/jan.12502.
- O’Donnell CA, Higgins M, Chauhan R, Mullen K. Asylum seekers’ expectations of and trust in general practice: a qualitative study. Br J Gen Pract 2008;58:e1-1. https://doi.org/10.3399/bjgp08X376104.
- Birkhäuer J, Gaab J, Kossowsky J, Hasler S, Krummenacher P, Werner C, et al. Trust in the health care professional and health outcome: a meta-analysis. PLOS ONE 2017;12. https://doi.org/10.1371/journal.pone.0170988.
- Turkmani S, Homer CSE, Dawson A. Maternity care experiences and health needs of migrant women from female genital mutilation-practicing countries in high-income contexts: a systematic review and meta-synthesis. Birth 2019;46:3-14. https://doi.org/10.1111/birt.12367.
- NHS England . National Maternity Review: Better Births: Improving Outcomes of Maternity Services in England – A Five Year Forward View for Maternity Care 2016. www.england.nhs.uk/wp-content/uploads/2016/02/national-maternity-review-report.pdf (accessed 10 October 2020).
- NHS England . Implementing Better Births: Continuity of Carer 2018. www.england.nhs.uk/mat-transformation/implementing-better-births/ (accessed 10 October 2020).
- Sandall J, Soltani H, Gates S, Shennan A, Devane D. Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database Syst Rev 2016;4. https://doi.org/10.1002/14651858.CD004667.pub5.
- NHS England . Female Genital Mutilation: Standards for Training Healthcare Professionals 2018. www.england.nhs.uk/wp-content/uploads/2018/04/fgm-standards-for-training-healthcare-professionals-1.pdf (accessed 20 October 2020).
- Green J, Thorogood N. Qualtiative Methods for Health Research. London: SAGE Publications Ltd; 2014.
- Eide P, Allen C. Recruiting transcultural qualitative research participants: a conceptual model. Int J Qual Methods 2005;4:44-56. https://doi.org/10.1177/160940690500400204.
- Knobf MT, Juarez G, Lee SY, Sun V, Sun Y, Haozous E. Challenges and strategies in recruitment of ethnically diverse populations for cancer nursing research. Oncol Nurs Forum 2007;34:1187-94. https://doi.org/10.1188/07.ONF.1187-1194.
- Renert H, Russell-Mayhew S, Arthur N. Recruiting ethnically diverse participants into qualitative health research: lessons learned. Qual Rep 2013;18:1-13.
- Yancey AK, Ortega AN, Kumanyika SK. Effective recruitment and retention of minority research participants. Annu Rev Public Health 2006;27:1-28. https://doi.org/10.1146/annurev.publhealth.27.021405.102113.
- Nasri NM, Nasri N, Talib MAA. Cross-language qualitative research studies dilemmas: a research review. Qual Res J 2020;21:15-28. https://doi.org/10.1108/QRJ-12-2019-0093.
- Williamson DL, Choi J, Charchuk M, Rempel GR, Pitre N, Breitkreuz R, et al. Interpreter-facilitated cross-language interviews: a research note. Qual Res 2011;11:381-94. https://doi.org/10.1177/1468794111404319.
- Carter N, Bryant-Lukosius D, DiCenso A, Blythe J, Neville AJ. The use of triangulation in qualitative research. Oncol Nurs Forum 2014;41:545-7. https://doi.org/10.1188/14.ONF.545-547.
- Bonner A, Tolhurst G. Insider–outsider perspectives of participant observation. Nurse Res 2002;9:7-19. https://doi.org/10.7748/nr2002.07.9.4.7.c6194.
- Saylor Academy . Sociological Inquiry: Qualitative and Quantitative Methods – Interviews: Qualitative and Quantitative Approaches 2012. https://saylordotorg.github.io/text_principles-of-sociological-inquiry-qualitative-and-quantitative-methods/s12-interviews-qualitative-and-qua.html (accessed 28 April 2021).
- Fahmy A, El-Mouelhy MT, Ragab AR. Female genital mutilation/cutting and issues of sexuality in Egypt. Reprod Health Matters 2010;18:181-90. https://doi.org/10.1016/S0968-8080(10)36535-9.
- Varol N, Turkmani S, Black K, Hall J, Dawson A. The role of men in abandonment of female genital mutilation: a systematic review. BMC Public Health 2015;15. https://doi.org/10.1186/s12889-015-2373-2.
- Almroth L, Almroth-Berggren V, Hassanein OM, Al-Said SS, Hasan SS, Lithell UB, et al. Male complications of female genital mutilation. Soc Sci Med 2001;53:1455-60. https://doi.org/10.1016/S0277-9536(00)00428-7.
- Vasileiou K, Barnett J, Thorpe S, Young T. Characterising and justifying sample size sufficiency in interview-based studies: systematic analysis of qualitative health research over a 15-year period. BMC Med Res Methodol 2018;18. https://doi.org/10.1186/s12874-018-0594-7.
- Birt L, Scott S, Cavers D, Campbell C, Walter F. Member checking: a tool to enhance trustworthiness or merely a nod to validation?. Qual Health Res 2016;26:1802-11. https://doi.org/10.1177/1049732316654870.
- Jones L, Costello B, Danks E, Cross-Sudworth F. Female Genital Mutilation (FGM): An Increasingly Important Healthcare Challenge in the UK. Birmingham: The Birmingham Brief; 2020.
- Yin RK. Qualitative Research from Start to Finish. New York: Guilford Press; 2015.
Appendix 1 The hybrid framework method stage alignment
The HFM is divided into three categories: pre analysis, analysis and post analysis. This categorisation places the process of analysis, specifically qualitative analysis, at the heart of the method. Pre-analysis stages across the SSF and approach (referring to the general/traditional research process) can be aligned. The first stage of this involves undertaking a literature review, which aligns with SSF stage 1 (working in ‘silences’) as the general aims at this stage in the research process are to understand the background to the topic/issue, furnish the research team with relevant and recent evidence, and identify and raise initial key questions related to the context of the study and topic/issue, and the inherent ‘silences’.
The second stage of the general/traditional research process is reflection and design, in which researchers reflect on the content of the first stage to produce a log of initial thoughts, inform the methodological approach of the study and define the research study itself. This aligns with SSF stage 2 (hearing ‘silences’), as researchers are encouraged to reflect on the context, background, current picture of issues and the landscape pertinent to the research topic/issue, thereby enabling researchers to ‘hear’ initial silences, further echoing the methodological importance of the researcher’s reflexivity. Although SSF stages 1 and 2 are essential methodological stages and underpin the analysis and process as a whole, they are primarily relevant to pre-analysis activities and so will not be discussed here. In addition, SSF stage 5 will not be discussed here as it is relevant to post-analysis activities only (e.g. making policy recommendations).
In the analysis category, the third stage of the general/traditional research process typically involves engaging in qualitative analysis, from data collection to analysing the data and then to presenting the findings. The research process typically undertaken at this stage can be aligned with both the FM and SSF.
This appendix focuses on this third stage by aligning the FM with SSF. SSF stage 3 aligns with the FM stages 1–3, and SSF stage 4 aligns with the FM stages 4 and 5. Although the headings of the HFM will match those of the FM presented in Chapter 2, the HFM stages encompass the alignment of the FM and the SSF, as described in Chapter 2. The headings of the FM stages 1–5 are used in the HFM to outline the suggested methodological approach. This should not be taken to suggest that the FM should take precedence over SSF nor that the FM stages themselves provide a more methodologically rich approach to analysis. Rather, the FM headings are employed as a mechanism for breaking down the larger and conceptually broader SSF stages 3 and 4, which enables a more focused and robust method for ensuring that each SSF stage captures some of the rigorous methodological elements salient in the FM. The following stages are therefore called the ‘HFM stages’ to differentiate them from the same headings in the ‘FM stages’.
The hybrid framework method stage 1: compiling
The FM stage 1 was aligned with (part of) SSF stage 3 and both of these primarily involve data collection. One of the ways in which the method of data collection reflects the SSF stage 3 aim is by ensuring that data are acquired by participant-focused, semistructured interviews (and discussion groups in WP2) that seek to locate ‘perceived silent voices’. This approach enables participants to provide a narrative and share their experience, journey, story, knowledge and/or expertise. Doing so ensures that power is transferred to the participant by ensuring that their reports and experiences are treated as authentic and valuable, thus further reflecting the antiessentialist underpinnings of the SSF.
Keeping a research journal on completed interviews (by the researcher conducting the interview) helped to create reference points that were then fed back to the team by providing a written record of key points arising from the interview. Receiving this information prior to the transcript facilitated the creation and/or initial corroboration of currently identified emergent themes (thereby enabling a continuation and progression of the analysis), enabled the effective identification of ‘silences’ during initial analysis in the HFM stage 2, and prevented further ‘silencing’. This research journal was also consulted throughout the analysis as a mechanism of triangulating emergent findings. Transcribing the interviews (and discussions groups in WP2) provided a record of data and facilitated the HFM stages 2–5.
The hybrid framework method stage 2: disassembling
The FM stage 2 was aligned with (part of) SSF stage 3 as both involve becoming familiar with and organising the data. The process of disassembling the data facilitated becoming familiar with it through listening to recordings, reading transcripts and revisiting the research journal – the combination of which was an important part of ensuring that the ‘silences’ were both heard and voiced. This disassembling enabled the data to be organised by creating ‘meaningful groupings’ through coding in NVivo. A process of coding that aligned with both the FM and the SSF was employed and the following steps were taken:
-
A preliminary codebook of nodes (analytical framework) based on the study aims, research questions and WPs (and accounting for participants) was developed (deductive approach).
-
Themes, concepts or ideas in the data that had connections with each other were identified.
-
The analytical framework was revised and refined based on meanings that were interpreted from the data to create hierarchical node structures (inductive approach, supplementing but not superseding the initial deductive approach).
-
The analytical framework was applied to other transcripts (continuing the inductive approach).
-
The analytical framework was updated, where appropriate (iterative procedure of the continued inductive approach).
The hybrid framework method stage 3: reassembling
The FM stage 2 was aligned with (part of) SSF stage 3 as, by producing matrices to identify patterns and relationships, the ‘charting’ of data into NVivo framework matrices allowed ‘silences’ to be exposed. The process of reassembling began by summarising transcripts (either in NVivo memos or in a separate summary document) and highlighting key quotations (using annotations in NVivo or in a separate document). These whole-transcript summaries served as an initial method of assembling the data in a way that sought to identify ‘silences’. A thematic matrix was then created in which cells were the intersection between cases and theme nodes to summarise the interpreted themes/nodes as defined in the analytical framework. These summaries and the style of summarising were compared across the research team to ensure consistency and to compare and triangulate interpreted themes and preliminary findings. These were ultimately used to facilitate the interpretation of the data in the next HFM stage.
The hybrid framework method stage 4: interpreting
The FM stage 4 was aligned with (part of) SSF stages 3 and 4 by emphasising the importance of a cyclical and iterative process of interpretation. Interpretation is a continual, iterative process that should aim to be complete, fair, accurate and representative, add value and be credible. 177 Doing so ensures that the identified ‘silences’ have been properly heard and solidifies the participant at the centre of the research, continuing to authenticate and value their experiences. It is in this stage that we sought to generate typologies, interrogate theoretical concepts, map connections and explore themes and relationships. During this, we sought to validate our interpretations and findings using two mechanisms: internal validation, whereby we discussed and tested interpreted findings against other data (triangulation) and corroborated the triangulated findings and discussed any inconsistencies; and external validation, whereby we ‘sense-checked’ interpretations, their analysis and emergent findings with experts by lived experience and other stakeholders. This external validation was achieved through SSG, SMG, and PPI involvement throughout the research study; and by hosting community engagement and national stakeholder events across WP1 and within WP2. This validation ensured that any misidentified or unidentified ‘silences’ were uncovered, corroborated the ‘silences’ identified and interpreted themes/findings. Doing so assured that participants and stakeholders were firmly placed at the centre of the research and reaffirmed the importance, authenticity and validity of their experiences.
Interpretation of the data was achieved in four phases by building on the phases outlined in the SSF: presenting the initial findings (phase 1, ‘researcher review’); incorporating stakeholder perspectives and creating a ‘silence dialogue’ to ‘ratify, refute, challenge or further contextualise the findings’ (phase 2, ‘participant review’); hearing from the ‘collective voices’ of the social networks of participants on the evidence (phase 3, ‘user voices’); and critically reflecting on the above and presenting the findings (phase 4, ‘researcher reflection’). 86 This systematic, interpretative and iterative process reflects the phases of analysis in SSF stage 3, which offers a cyclical process to minimise researcher biases and to draft, redraft based on input and reflect on the interpretations before concluding (and, indeed, offering this for further refinement/revision).
The hybrid framework method stage 5: concluding
The FM stage 5 was aligned with (part of) SSF stage 4 by ensuring that the findings of the research addressed the research aims/questions, part of which involved exposing and understanding ‘silences’. This stage provided a chance to reflect on the data and offer theoretical and pragmatic contributions. We assessed the final findings, as validated by the HFM stage 4, and compared them against the initial interpretations from the HFM stage 3. Determining whether the initial ‘silences’ remained the same or changed provided a platform for reflection and assisted us in assessing our own approach to the research. At this stage, we identified how the data and findings responded to and addressed the research questions and purpose of the research, ascertained and explored the emergent themes, and identified and discussed the ‘silences’.
Appendix 2 Overview and alignment of themes and silences

Appendix 3 Exploration of quantitative and qualitative data sets
Comparing participant responses across data sets
In addition to the qualitative findings presented in Chapter 3, there were some salient quantitative findings relating to survivors’ reported experience of FGM and survivors’ and men’s reported preferences for the timing of deinfibulation across data sets, namely the background questionnaire and interview responses. This appendix will outline these findings.
Comparing experiences of FGM and the timing of deinfibulation in questionnaire and interview responses
Participants’ responses in relation to the type of FGM experienced and timing of deinfibulation surgery were compared; their responses in their self-report questionnaires were compared with researchers’ (independently validated) interpretations of their responses to the same questions during their interview. When asked about when they (survivors) or their partner (male partners of FGM survivors) were deinfibulated (if at all), participants’ responses in both their questionnaire and during their interview were similar: 82% of survivors’ (n = 36) and 62% of men’s (n = 8) responses were identical. This shows that the majority of participants were consistent in reporting their own or their wife’s/partner’s type of FGM. However, when asked about their own (for survivors) or their wife’s/partner’s (for men) type of FGM, participants’ responses varied significantly across data sets: 41% of survivors (n = 18) and 46% of men (n = 6) did not report the same type of FGM across their questionnaire and interview. This shows that there was sufficient variation in responses to suggest that participants miscommunicated their experience of FGM in one or both data sets or they were sufficiently unclear or not sufficiently knowledgeable about FGM to provide consistent answers across data sets. This could be because of a misunderstanding or confusion regarding the types of FGM; a lack of clear or understandable information provided by HCPs; a potential deficit in providing and/or gaining effective, accessible or understandable information and/or knowledge; or difficulty understanding or answering the questionnaire. Figures 11 and 12 provide an overview of these findings.
FIGURE 11.
Agreement between type of FGM reported in background questionnaire and during interview. M, men; S, survivors.
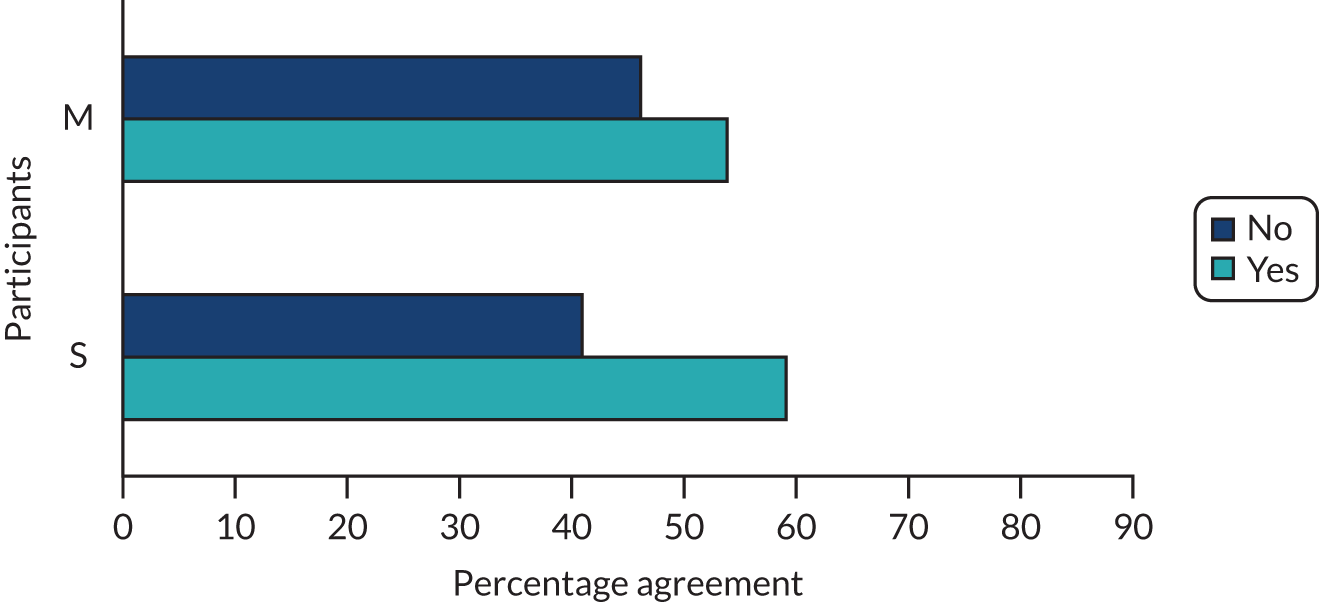
FIGURE 12.
Agreement between timing of deinfibulation reported in background questionnaire and during interview. M, men; S, survivors.

Comparing interview preferences for the timing of deinfibulation during interview with experiences of deinfibulation
During their interview, participants were asked for their preference on the timing of deinfibulation. Their responses (outlined and discussed in more detail in Chapter 3) were compared with participants’ responses in their background questionnaire and during their interview explaining when they (survivors) or their partner (men) were deinfibulated; this comparison was undertaken to assess the extent to which participants’ preferences for deinfibulation corresponded to their experience of deinfibulation surgery. Information pertaining to experiences of deinfibulation within both data sets (self-reported background questionnaires and interviews) was individually compared with participants’ preferences for the timing of deinfibulation to measure internal variation within these data and to assess concordance between experience and preference.
Results from both comparisons accorded with each other; in other words, there was accordance between the following two comparisons: (1) the participant’s preference for the timing of deinfibulation and when, according to their questionnaire, the participant (in the case of a survivor) or their partner (in the case of a survivor’s male partner) was deinfibulated; and (2) the participant’s preference for the timing of deinfibulation and when, according to their interview, the participant or their partner was deinfibulated.
Both questionnaire and interview data on the participant’s or their partner’s experience of deinfibulation surgery highlighted a disconnect between this experience and their preference for the timing of deinfibulation: in the participant questionnaire, 84% of survivors’ (n = 37) and 85% of men’s (n = 11) preferences diverged from their experience of deinfibulation; and in the participant interview, 80% of survivors’ (n = 35) and 62% of men’s (n = 8) preferences diverged from their experience of deinfibulation. In other words, according to both independent sets of data on the survivor’s or man’s experience of deinfibulation, their preference for the timing of deinfibulation was very often different from when they or their partner was deinfibulated.
Men’s responses on when their partner was deinfibulated diverged in both the participant questionnaire and the participant interview; this reinforces a general lack of engagement with FGM, which is often seen by men (and in many cultures in which FGM is practised) as ‘a women’s issue’:
When it comes to this FGM practice it’s like a common agreement, it’s a non-written rule that women deal with issues relating to women’s health.
Man 16
Figures 13 and 14 provide an overview of the findings of the participant questionnaire and the participant interview.
FIGURE 13.
Agreement between the time of deinfibulation reported in the participant questionnaire and preference for the timing of deinfibulation surgery. M, men; S, survivors.
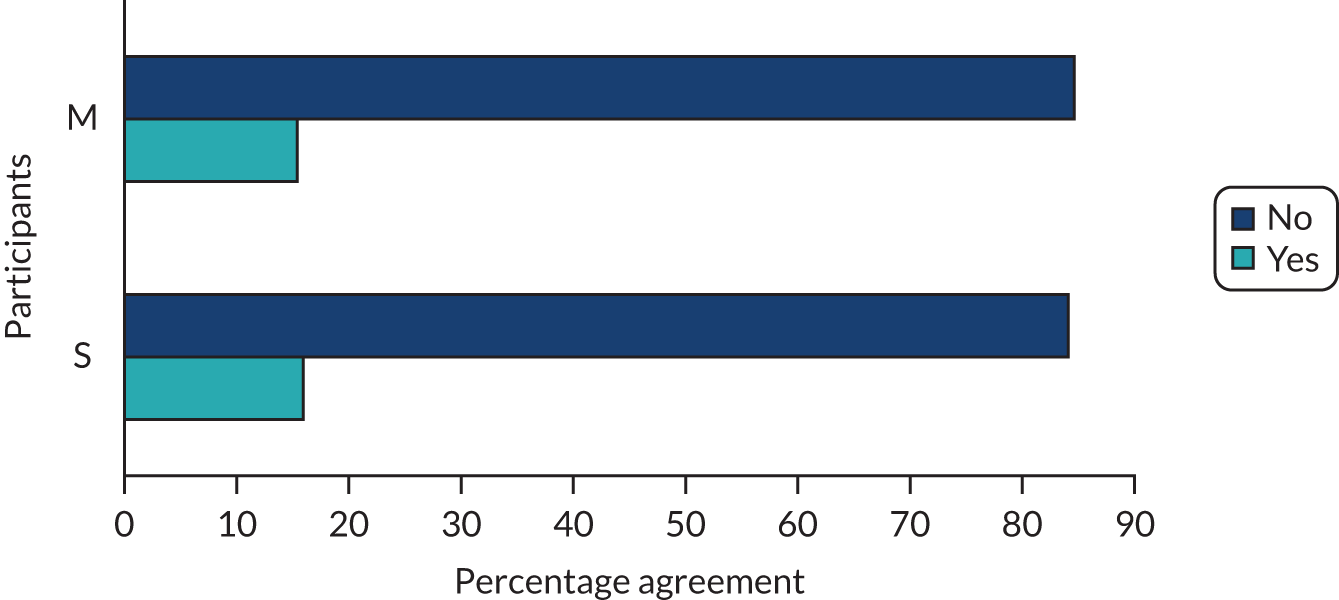
FIGURE 14.
Agreement between the time of deinfibulation reported during the participant interview and preference for the timing of deinfibulation surgery. M, men; S, survivors.

Glossary
- Addressing silences
- To address, limit, mitigate or prevent the root of silence and/or silences from manifesting. Addressing silences is synonymous with providing recommendations.
- Cultural adaptation
- The process and time it takes a person to integrate into a new culture and feel comfortable in it.
- Cultural assimilation
- The process by which a person’s or a group’s culture comes to resemble that of another group.
- Cultural heritage
- An expression of the ways of living developed by a community and passed on from generation to generation. This include customs, practices, places, objects, artistic expressions and values.
- Cultural ideology
- Cultural beliefs that justify particular social arrangements, including patterns of inequality.
- Cultural relativism
- Beliefs, customs and morality exist in relation to the particular culture from which they originate.
- Cultural schema
- Holds that human beings employ classification to understand members of other cultures and add new data to previously available categories.
- Cross-cultural (discourse)
- A historically transmitted, expressive system of communication practices, acts, events and styles, which are composed of specific symbols, symbolic forms, norms and their meanings.
- Deinfibulation
- A surgical procedure carried out to reopen the vaginal introitus of women living with type 3 female genital mutilation.
- Episiotomy
- A surgical incision of the perineum and the posterior vaginal wall, generally performed by a midwife or obstetrician. Usually performed during the second stage of labour to quickly enlarge the opening for the baby to pass through when there is potential or actual fetal compromise during birth.
- Ethnic absolutism
- A conceptual and political approach that views the differences between ethnic groups as fixed and absolute.
- Ethnocentrism
- The evaluation and interpretation of other cultures according to the knowledge and preconceptions originating in the standards and customs of one’s own culture.
- Individualised/individualisation
- The moral, political or social ideology that emphasises the worth of the individual. Individualism promotes the exercise of goals and desires and values independence and self-reliance. It advocates that the interests of the individual should hold precedence over the state or a social group, while opposing external interference on one’s own interests by society or institutions such as the government.
- Manifestation of silence
- The development of a silence or aspects within a silence. A conduit for the perpetuation of the silence.
- Marginalised (discourse)
- A discourse constructs the object of which it speaks. In terms of marginalised discourse, this relates to the production of power/knowledge and the categorisation of individuals, groups or social relations.
- Others-silencing (people)
- Silencing as a result of the action, inaction or omission of an individual (e.g. through speech) that directly or indirectly leads to/compels and/or coerces the silencing of another.
- Root of silence
- The foundation of the silence; often explains why the silence exists.
- Screaming silences
- Areas of research and experience that are, at best, under-researched and require more development or are, at worst, historically and/or politically undervalued, absent or invisible (also known as ‘silences’).
- Self-silencing
- An individual either choosing to be silent or feeling compelled to be or remain silent, particularly in relation to speaking and/or sharing information, knowledge or experience(s). This was evident across all cohorts. For instance, women and men might self-silence because of stigma, taboo, shyness, etc.; health-care professionals might self-silence because of a lack of knowledge/understanding or because of statutory/professional regulations.
- Service provision ideology
- The idea that services should be delivered in a specific way.
- Silence(s), silencing and silent
- Experiences and/or areas of research that are little understood, seldom researched or undervalued, and exist in marginalised and cross-cultural discourse. Silences exist in the void between the polarisation of cultural heritage and ideology. However, once identified, articulated and acted on, the ‘silence’ that was previously unheard becomes ‘voiced’. There are different variations of the term ‘silence’ with particular conceptual meanings. There are two main subconcepts of ‘silence’, namely ‘silencing’ and ‘silent’. The former is usually employed to reflect the action of silencing oneself or another, and the latter is used to reflect the state of being ‘silenced’. There are different variants of ‘silencing’ to better and more accurately reflect and conceptually refine the target of the silencing, that is who is being ‘silenced’.
- Survivor
- A girl or woman who has experienced any form of female genital mutilation. This term was defined by our patient and public involvement advisory group as their preferred language for the research and is therefore used throughout the report.
- System-silencing (societal)
- Broader silencing across a community, society or culture. In other words, the ways in which systems function that directly or indirectly silence through the way(s) in which they operate, provide support, deliver services, etc.
- Totalised/totalisation
- A Marxist/feminist concept that aligns with female genital mutilation and its interpretation.
- Universality
- The character or state of being universal; existence or prevalence everywhere. The relation, extension or applicability to all. A universal character or range of knowledge, interests, etc.
- Western medical ideology
- A philosophy related to an ethnocentric approach. Scientifically and medically proven processes are used to diagnose and treat an illness, disease or health condition, which is seen as something ‘going wrong’ with the body. Western medical ideology is closely aligned to western society ideology.
- Western society ideology
- The heritage of social norms, ethical values, traditional customs, belief systems, political systems, artefacts and technologies that originated in or are associated with Europe. The term also applies beyond Europe to countries and cultures whose histories are strongly connected to Europe by immigration, colonisation or influence.
List of abbreviations
- CI
- confidence interval
- FGM
- female genital mutilation
- FGMED
- female genital mutilation enhanced data set
- FM
- framework method
- GP
- general practitioner
- HCP
- health-care professional
- HFM
- hybrid framework method
- HIV
- human immunodeficiency virus
- MD
- mean difference
- OR
- odds ratio
- PI
- principal investigator
- PIL
- participant information leaflet
- PPI
- patient and public involvement
- PTSD
- post-traumatic stress disorder
- RCN
- Royal College of Nursing
- RCOG
- Royal College of Obstetricians and Gynaecologists
- SMG
- study management group
- SSF
- Sound of Silence framework
- SSG
- Study Steering Group
- UNICEF
- United Nations Children’s Fund
- WHO
- World Health Organization
- WP
- work package