Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 15/162/02. The contractual start date was in June 2017. The draft report began editorial review in June 2022 and was accepted for publication in November 2022. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2024 Ondruskova et al. This work was produced by Ondruskova et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Ondruskova et al.
Chapter 1 Introduction
The Diagnostic and Statistical Manual of Mental Disorders1 describes developmental disabilities as intellectual disabilities, communication disorders, autism spectrum disorder (ASD) and motor disorders. Intellectual disability is a lifelong condition impairing an individual’s intellectual and adaptive functioning, affecting approximately 1.2 million children, young people and adults in England. 1,2 Children with developmental disabilities are approximately three to four times more likely to develop internalising and externalising behaviour problems compared to their non-disabled peers. 3,4 Figures from recent studies in England show that over 40,000 children with intellectual disabilities display behaviour that challenges, otherwise referred to as ‘challenging behaviour’. 5 Although the figures vary due to different methodologies used in the studies, the estimates show that between 10% and 45% of children with intellectual disabilities display behaviours that challenge. 6–11
The Royal College of Psychiatrists12 define behaviours that challenge as behaviours of such an intensity, frequency or duration; they threaten the quality of life and/or the physical safety of the individual or others and are likely to lead to responses that are restrictive, aversive or result in exclusion. These behaviours include self-injury, aggression, destructiveness and stereotypical behaviours, and are described as dangerous and interfere with participation in preschool, educational or adult services and often require special interventions. 1 Behaviours that challenge are reported to be more severe with a higher likelihood of long-standing presentation in children with intellectual disabilities and comorbid ASD, compared to children with intellectual disabilities only. 1,13,14 Multiple factors have been identified as vulnerabilities or risk factors of these behaviours, including underlying sensory problems, genetic syndromes, a higher degree of disability and a lack of communication skills. 4,9,15,16 The behaviours may only appear in specific environments and may be used to create sensory stimulation or to communicate the need for a carer’s attention or help. Poor understanding of behaviours that challenge can lead to the exacerbation and maintenance of such behaviour, and also to poor psychological outcomes in carers. 17 Indeed, a recent study found that early behaviour problems in children with intellectual disabilities were related to increased parenting stress levels and greater child behavioural problems during later childhood. 18
Parents or primary carers of children with intellectual disabilities play a key role in their child’s daily support and usually throughout their lifespan. Parents perform complex care tasks, respond to their child’s needs, manage behaviours that challenge and advocate for services and support for their child. These tasks are demanding and can lead to high levels of stress for the whole family. 18,19 In addition to daily tasks, parents may experience high distress from observing their child self-harming or can experience injuries from their child’s aggressive behaviours. For example, some parents report having bruises from being repeatedly kicked or punched and in some cases even need emergency hospital care. 19 As such, this group is vulnerable and at increased risk of a variety of negative psychological and physical health outcomes compared to the general population. 20,21 Interventions that aim to help parents effectively manage behaviours that challenge can lead to positive outcomes for both children and their parents and to create a more stable family environment. A common approach for children without intellectual or developmental disabilities is an early intervention delivered in groups to families, with children as young as 18 months. 22 Early intervention is recommended as it reduces early-onset child behaviour problems while it also increases parent efficacy in managing the child’s behaviours. 23 Parents learn new ways to manage behaviours that challenge which they can generalise to other areas of life, through positive parenting techniques (e.g. such as descriptive praise, reward charts, clear instructions) and contingency management strategies (e.g. exclusionary timeout, non-exclusionary timeout, logical consequences). 24,25 Many of those interventions, known as parenting programmes, are provided in group settings. The group format allows for the creation of valuable social networks between parents in similar situations, provides space for parents to share ideas, normalises the challenges they face at home and can reduce perceived isolation. 26,27 However, families with children with developmental delays and/or comorbid conditions may find these universal interventions inaccessible or unsuitable for their child’s needs or specific behaviours. Thus, it is essential to tailor universal parenting programmes to fit the needs of the families of children with more complex behaviours.
Several factors need to be considered when developing behaviour-management programmes for families with children with developmental disabilities to ensure they fit their needs. Qualitative research can inform us about what parents of disabled children are looking for from these interventions. For instance, parenting programmes that offer more specific information and education about coping with the child’s disability are seen as more relevant. 26 In a study by McIntyre,28 modifications to a universal parenting programme, the Incredible Years Parent Training, facilitated access and retention by adding content on functional assessment of behaviour problems in children with developmental disabilities. Furthermore, families with children with intellectual disabilities require high flexibility from parenting programmes because of the high likelihood of last-minute cancellations due to child behaviours or unexpected crisis moments. 29 If flexibility is not offered, parents may perceive these programmes as a burden adding to their daily stress levels. 30 The ability of the services to increase flexibility and adapt intervention delivery can facilitate access to families with children with intellectual disabilities. 31 Examples of reasonable adjustments for this population have been reported and include delivery of the programme in easily accessible locations (e.g. local community centres) or remotely, offering multiple times and dates for sessions, and offering catch-up sessions. 29,32,33 Another factor considered to be important is providing on-call support for parents (e.g. by regular practitioner−parent contact). 29 As such, early intervention is essential and needs to be delivered according to the child’s needs to ensure relevance and positive outcomes.
One of the most widely available parenting programmes to support parents of children with intellectual and socio-emotional disabilities and with sufficient evidence for efficacy is the Level 4 Stepping Stones Triple P (SSTP). SSTP is an adaptation of the Triple P Positive Parenting Programme (see www.triplep.uk.net/uken/home/) and was developed for families with children with intellectual disabilities who display behaviours that challenge. This programme combines psycho-educational and behavioural components and is designed for parents of children aged 2–8 years.
Stepping Stones Triple P aims to improve parental confidence and skills by promoting a positive parent–child relationship. The theoretical basis of this intervention is embedded in the social learning model, which emphasises the bidirectional and reciprocal nature of the parent–child interactions that surround behaviours that challenge. 34 The intervention encourages parents to develop skills to use in everyday situations, such as during mealtimes, bathing or dressing, rather than through artificial training scenarios. As such, SSTP aims to teach parents positive child management skills contrary to coercive parenting strategies.
Studies have shown that SSTP is effective, acceptable to parents, reduces problem behaviours and improves parenting styles. 25,35–38 While available to be delivered in the UK, it has yet to be tested in a randomised controlled trial. Following a research recommendation of the National Institute of Health and Care Excellence (NICE guideline 11),39 which recognised the paucity of available interventions for children with more severe intellectual or developmental delay, a randomised controlled trial to evaluate the SSTP in the UK was conducted. The current study provides a clinical and cost evaluation of SSTP to address behaviours that challenge in preschool children with intellectual disabilities (EPICC-ID). 40 The trial’s main objective was to assess whether SSTP reduces behaviours that challenge displayed by children with moderate and severe intellectual disabilities aged 3–5 years (30–59 months) when assessed at a 12-month follow-up.
Study aims and objectives
The study aimed to evaluate the clinical and cost-effectiveness of level 4 SSTP designed to reduce behaviours that challenge in preschool children with moderate to severe intellectual disability. The primary objective was to undertake a pragmatic randomised controlled trial to evaluate level 4 group SSTP in addition to treatment as usual (TAU). The secondary objective was to undertake an economic evaluation to assess the cost-effectiveness of the intervention compared to TAU.
Research questions
-
Does the addition of level 4 SSTP to TAU reduce behaviours that challenge displayed by children with moderate to severe intellectual disabilities aged 30–59 months at 12 months post randomisation compared to TAU alone?
-
Does SSTP reduce behaviours that challenge at 12 months post randomisation in blind-rated observations and caregiver/teacher questionnaire measures?
-
Is SSTP more cost-effective compared to TAU?
Chapter 2 Method
Some text in this chapter has been reproduced from Farris et al. 40 This is an Open Access article distributed following the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Trial design and setting
Study design
A parallel two-armed pragmatic multisite single-blind randomised control trial (RCT) was conducted with blinding of outcome assessors. A process evaluation was also included utilising parent and service manager qualitative interviews to enhance understanding of the appropriateness and feasibility of the intervention. The study was planned and implemented following the Consolidated Standards of Reporting Trials (CONSORT) extension to compare the cost-effectiveness of the combination of SSTP plus TAU, versus TAU alone in reducing behaviours that challenge at 12 months post randomisation. The trial design is summarised in Figure 1.
FIGURE 1.
The CONSORT flow diagram for the EPICC-ID RCT.

Randomisation
Participants were randomised into the intervention arm using the 3 : 2 ratio (SSTP vs. TAU) using randomly permuted blocks of different block sizes and stratification by site and the level of intellectual disability (moderate and severe). Eligible participants were allocated online to the next available treatment code in the relevant randomisation list. All randomisation and data management were provided by an internet-based site called Sealed Envelope.
Allocation concealment and implementation
At the end of the baseline assessment, the researchers entered the results on a web-based case report form (CRF) form. Parents and therapists were informed about the allocation status and arranged the commencing of the group sessions. Researchers were based in a different location from the staff involved in the delivery of the level 4 SSTP. Therapists were not involved in any treatment of the families that were allocated to TAU.
Blinding
Since parents and therapists were aware of the treatment allocation, it was not possible to ensure a completely blind trial. All research assistants who were collecting the data remained blinded to treatment allocation throughout the study. Parents were reminded not to disclose any information about their treatment allocation to the research assistant during assessments.
The researcher entered the results of all study assessments on web-based electronic case report forms (eCRFs). They did not have access to eCRFs that may pose a risk of unblinding them [e.g. Child and Adolescent Service Use Schedule (CA-SUS) at 4 and 12 months, Client Satisfaction Questionnaire, serious adverse event (SAE) form]. During coronavirus disease 2019 (COVID-19), CA-SUS forms were collected remotely, and the question relating to parenting groups was omitted and collected later.
The lead study statistician remained blinded to arm allocation throughout and the subsidiary trial statistician attended the Data Safety and Monitoring Board (DSMB) meetings. The lead statistician attended the Trial Management Group (TMG) and Trial Steering Committee (TSC) meetings during the study.
Outcomes
Primary outcome
Child Behaviour Checklist (CBCL)41
The primary outcome was parent-reported child’s behaviours that challenge at 12 months post randomisation. The severity of behaviours that challenge was measured by the preschool version of the CBCL. The CBCL is widely used in clinical trials and epidemiological studies assessing children with intellectual disabilities. 42,43 This version of the CBCL is used for children aged 1½–5 years. It measures behaviour on a 3-point Likert scale (0 – not true; 1 – somewhat/sometimes true; 2 – very/often true) over a period of 2 months. The 99 items measure emotional and behavioural problems. Respondents are also asked to provide more details for certain items and are asked open-ended questions at the end to describe the child’s illnesses and disabilities as well as their biggest concerns about the child and what the child does best. Items are grouped into seven subscales: (1) Emotionally Reactive, (2) Anxious/Depressed, (3) Somatic Complaints, (4) Withdrawn, (5) Sleep Problems, (6) Attention Problems and (7) Aggressive Behaviour. Subscale scores can also be grouped into two broader categories, Internalising Behaviours (problems that occur mainly within oneself) and Externalising Behaviours (involves conflicts with other people and their expectations for the child). The total raw score for each subscale is computed by summing the scores of 1 and 2 for all items of that subscale. A scoring algorithm is used to determine a T-score for the internalising and externalising behaviours and an overall T-score for the child’s Total Problem Behaviours. Children with a T-score of 60–63 are in the borderline clinical range and a T-score of 64 and above indicates clinically significant difficulties. A participant is excluded from the analysis if 8 or more items are missing. See Achenbach and Rescorla41 for validity studies.
Secondary outcomes
Revised Family Observation Schedule (FOS-RIII)
Direct observations were carried out by researchers using the FOS-RIII, a measure of parent–child interaction. 44 This measure is commonly used in studies that investigate SSTP. Parents are asked to interact with their child while being filmed for 20 minutes carrying out various activities that reflect tasks that likely happen in their daily life at home. Overall, there are four 5-minute tasks: (1) child’s free play; (2) a structured block task; (3) parent and child in the same room but each involved in separate activities; and (4) cleaning up after play. The FOS-RIII codes 10-second segments and computes four scores that indicate positive and negative child behaviours, and positive and negative parent behaviours (see Table 1 for further details). A senior developmental psychologist scored the video observations. The FOS-RIII has demonstrated reliability and discriminant validity and is sensitive to the effects of behavioural interventions. 45
| Child behaviours | ||
|---|---|---|
| Parent behaviours | ||
| Positive | Engaged activity | Any interval with no negative behaviours and with no intelligible verbalisation or vocalisation |
| Appropriate verbal activity | Any interval with no negative behaviours and in which intelligible speech/verbalisation/vocalisation occurs | |
| Affection | Any verbal or non-verbal affection directed towards the parent | |
| Negative | Non-compliance | When a child does not follow an instruction given by a parent or another adult |
| Complaint | Any instance of whining, crying, screaming, shouting, grizzling, intelligible vocal protests or displays of temper | |
| Physical negative | Any actual or threatened physical attack on an object or another person | |
| Interrupt | Child interrupts when parent is talking, in an intrusive, loud, annoying, abrupt or disruptive way | |
| Oppositional | Any inappropriate behaviour that cannot be categorised into any other negative behaviour category | |
| Positive | Praise | Any praise comment directed to the child about a specific behaviour or child characteristic |
| Positive physical contact | Parent initiated or parent maintained (e.g. hug, kiss) | |
| Positive instruction | Direct or indirect verbal commands that are used to initiate change in the child’s behaviour, with no anger, sarcasm or harsh tone | |
| Positive social attention | Any verbal or non-verbal attention not scored in other categories (e.g. look up to monitor child) and not aversive | |
| Affection | Any affectionate words or affectionate physical contact | |
| Negative | Negative physical contact | Contact that could cause pain or discomfort |
| Negative instruction | Direct or indirect commands in a harsh, angry, abrupt or annoyed tone of voice | |
| Negative social attention | Comments in unpleasant, sarcastic or abrupt voice tone or criticism of child | |
Child Behaviour Checklist Caregiver−Teacher Report Form (C-TRF)
We measured caregiver-reported child behaviour to allow additional perspective on the child’s behaviour outside of the home setting. 46 This measure was completed by caregivers other than parents (e.g. teachers, teaching assistants, grandparents). Teachers were asked questions about child’s behaviours that can be observed in a school setting, such as defiance, hyperactivity, destructiveness or social skill deficits. The behaviours are divided into two subscales, internalising and externalising problems. The preschool C-TRF measure is associated with other measures of child behaviour problems (see Achenbach and Rescorla46 for review of validity studies).
Caregiving Problem Checklist – difficult child behaviour
Frequency of the child’s behaviours that challenge during care-giving tasks was measured on a 7-point Likert scale ranging from 1 (never) to 7 (always). 47 The behaviour is assessed in seven care-giving areas, such as direct care, in-home therapy tasks, involvement in leisure activities and other. The total score is the sum of all items, whereby higher scores indicate a higher frequency of problematic behaviour.
General Health Questionnaire (GHQ-12)
Parent psychiatric morbidity was measured by the commonly used 12-item GHQ measure, following the recommendations by the Department of Health to include such measures in this type of study. The questionnaire assesses the severity of a mental problem over the past few weeks on a 4-point scale (from 0 to 3). The total score is the sum of all items. Validity studies report high internal consistency values (from α = 0.79 to 0.91). 48,49
Questionnaire on Resources and Stress (QRS-F short form)
This measure is used to assess parental stress in caregivers of children that are chronically ill or have intellectual disabilities. 50 It is a 31-item questionnaire with ‘Yes’ or ‘No’ response options.
Parenting Sense of Competence Scale (PSOC)
Parents rated their perceived competence in the areas of satisfaction and efficacy as a parent. 51 The measure comprises 17 items that are rated on a 6-point scale ranging from 6 (strongly disagree) to 1 (strongly agree). Studies report good internal consistency for this scale (α = 0.8)52
Child and Adolescent Service Use Schedule (CA-SUS)
A child’s health and social care service use was measured on a modified version of the CA-SUS form. 53 The CA-SUS collects information on the child’s use of a range of services for the 4 or 6 months preceding assessment. The form contains questions on contacts with primary and secondary healthcare services, social services, voluntary organisations and medication use.
Pediatric Quality of Life (PedsQLTM)
Health-related quality of life (HRQoL) was measured using the PedsQL™ covering four domains, including Physical, Emotional, Social and School Functioning. 54 The current study uses this measure to derive the quality-adjusted life years (QALYs) for the health economic evaluation. Validity and reliability studies show high internal consistency values (α = 0.9). 55
Euro-Qol-5D (EQ-5D)
Health-related quality of life in the parent/other caregiver was assessed using a self-completed EQ-5D questionnaire. 56 These data will be used in the economic evaluation.
Other measures
Mullen Scales of Early Learning
The Mullen Scales of Early Learning was used to measure a child’s level of disability at baseline. 57 It is a developmentally integrated system that assesses language, motor skills and perceptual abilities. This assessment was only used during face-to-face assessments.
Case report form (CRF)
Parent’s and child’s sociodemographic and clinical information about comorbidities were collected using the CRF.
Client Satisfaction Questionnaire
Parent intervention acceptability was measured using the Client Satisfaction Questionnaire. 23 This allowed parents to provide feedback about the intervention during the 4-month follow-up by commenting on their satisfaction with and experience of SSTP. This questionnaire was specifically created for use in research investigating SSTP and has high internal consistency (α = 0.92).
Schedule of assessment visits
Table 2 presents the schedule of assessment visits and measures used during each visit throughout the study.
| Visit number | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| Tasks | Screening | Baselinea | 4-month follow-up | 12-month follow-up |
| Allowed deviation window | N/A | ± 4 weeks | ± 4 weeks | ± 4 weeks |
| Informed consent (screening) | x | |||
| Assessment of eligibility criteria | x | x | ||
| ABAS (< 69) | x | |||
| Research assessments minimum 1 week, maximum 4 weeks after screening | ||||
| Informed consent (research) | x | |||
| Mullen Scales of Early Learning | x | |||
| CRF | x | |||
| Preschool CBCL | x | x | x | |
| Parent–child observation and FOS-RIII | x | x | x | |
| C-TRF | x | x | x | |
| GHQ-12 | x | x | x | |
| QRS-F short form | x | x | x | |
| Caregiving Problem Checklist | x | x | x | |
| PSOC | x | x | x | |
| CA-SUS | x | x | x | |
| Client Satisfaction Questionnaire | x | |||
| Peds-QL | x | x | x | |
| EQ-5D | x | x | x | |
Participants
Sample size
The original sample size calculation required a sample of 258 children in an allocation ratio of 3 : 2 (155 vs. 103) to detect a low to a moderate (standardised) effect size of 0.40 for the primary outcome CBCL at 12 months at the 5% significance level with 90% power; the equivalent to detecting a clinically important difference of 8 points, assuming a standard deviation (SD) of 20. This was calculated as follows: A standard calculation based on analysis of covariance (ANCOVA) leads to a sample size of 99 children per arm, assuming a correlation of 0.5 between baseline and follow-up measurements. An equivalent calculation (same power) based on an allocation ratio of 1.15 : 1 gives group sizes of 107 and 93. Increasing the SSTP arm (only) to allow for therapist clustering leads to 139 children in the SSTP arm, assuming an intraclass correlation of 0.05 and an average therapist group size of 7 (design effect = 1.3). An adjustment for the anticipated dropout of 10% leads to 155 children in the SSTP group and 103 in the control group.
Eligibility criteria
The inclusion criteria for the study were as follows:
-
parents aged 18 years or over;
-
child aged 30–59 months at identification;
-
child had a moderate to severe intellectual disability, measured by parent-reported Adaptive Behaviour Assessment Schedule (ABAS) General Adaptive Functioning score between 40 and 69;
-
reported child’s behaviours that challenge over a 6-month period prior to the study, but no less than 2 months;
-
obtain a written consent by parent/caregiver.
Exclusion criteria
Participants were not included in the study if:
-
child had a mild, profound or no intellectual disability on parent-reported ABAS form;
-
parent/carer had insufficient English language skills to complete the study questionnaires;
-
another sibling was taking part in the study.
Recruitment
Participants were recruited from various community services including Participant Identification Centres (PIC) in four main areas in England: Blackpool (and surrounding areas; Site 1), North London (Site 2), South London (Site 3) and Newcastle (and surrounding areas; Site 4). The services included National Health Services (NHS) settings (e.g. Child Development Teams), Child and Adolescent Mental Health Services (CAMHS), education (e.g. nursery, preschool) and third sector (e.g. caregiver groups). Health or social care professionals identified eligible participants through new referrals or existing cases. Children were assessed for developmental delay through the Healthy Child Programme, which aims to identify families that require further support with their children, and children aged 0–5 years who are at risk of ‘poor outcomes’. Flyers were put up at local parent groups, nurseries, special schools and general practitioners (GPs) to promote the study among families. We followed a multisource referral strategy facilitated by the clinical research networks, our national, clinical and third-sector contacts and social media. We opened five PIC adjacent to Site 4, three PIC sites adjacent to Site 2 and two PIC sites adjacent to Site 3 to reach our planned recruitment target at the sites. Several recruitment difficulties were addressed throughout the study. This included parents declining or not being eligible to take part in the study due to various reasons, such as time commitments, child-care issues, health problems, language barriers or parents not thinking that child has an intellectual disability or behaviours that challenge. Table 3 presents the overview of recruitment at each study site.
| Site | EOIs received | Participants randomised | EOI to randomisation rate (%) | 4-month follow-ups completed (%) | 12-month follow-ups completed (%) |
|---|---|---|---|---|---|
| Site 1 | 91 | 64 | 70 | 61/64 (95) | 55/64 (86) |
| Site 2 | 212 | 56 | 26 | 45/56 (80) | 44/56 (79) |
| Site 3 | 181 | 74 | 41 | 66/74 (89) | 61/74 (82) |
| Site 4 | 99 | 67 | 68 | 57/67 (85) | 53/67 (79) |
| Total | 583 | 261 | 229/261 (88) | 213/261 (82) |
Allocation arms
Intervention arm
SSTP is part of Triple P (Positive Parenting Program), a psycho-educational parenting and family intervention developed for families who have children with behavioural or emotional problems. 58 SSTP was adapted specifically for parents of children with intellectual disabilities. This trial provided the SSTP level 4 manualised course, which offers six group sessions and three individual telephone or face-to-face contacts with the parent over a period of 9 weeks. Each group session lasted approximately 2.5 hours and individual sessions took about 30 minutes. The combination of group and individual sessions allowed parents to share experiences and build on skills gained while providing personalised support. The group sessions aimed to educate and actively train parents in skills and behaviour management. The individual consultations aimed to facilitate independent problem-solving and allowed parents to pick strategies most relevant to their child’s difficulties. All parents also received a course book that covered topics from each session. Those who missed a session were contacted by the therapist to discuss their progress and were encouraged to attend the next sessions. The group sessions were delivered in person until March 2020. Afterwards, all group sessions were delivered online via Zoom or Microsoft Teams. Table 4 provides the outline of the SSTP sessions.
| Group sessions | |
|---|---|
| Telephone sessions | |
| Session 1 | Positive Parenting |
| Session 2 | Promoting Children’s Development |
| Session 3 | Teaching New skills and Behaviours |
| Session 4 | Managing Misbehaviour and Parenting Routines |
| Session 5 | Planning Ahead |
| Session 6 | Implementing Parenting Routines 1 |
| Session 7 | Implementing Parenting Routines 2 |
| Session 8 | Implementing Parenting Routines 3 |
| Session 9 | Program Close |
Treatment as usual arm
Treatment as usual was available to participants in both arms of the trial. Parents allocated to both arms also received a list of national resources and the Contact charity’s guide for managing behaviours that challenge with recommendations about social and health care support. We identified a variety of services and support offered to families with children with intellectual disabilities and autism in each of the study’s local areas. This included individual help from speech and language therapists, occupational therapists, child psychotherapists, clinical psychologists, child psychiatrists and family therapists. There were numerous children’s centres offering support with parenting advice, local child-care options and access to specialist services for families and their children with intellectual disabilities and parenting classes (e.g. Camden MOSAIC centre in Site 2; SLAM Child and Family Service in Site 3, etc.). Parenting programmes were available in each of the study local areas (N = 3 in Site1; N = 8 in Site 2; N = 9 in Site 3; N = 9 in Site 4). For example, the Early Bird parenting programme was available in all four study areas. This is a 3-month programme for parents providing general information about autism and advice about looking after children with autism. It combines group training sessions for parents with individual home visits where video feedback is used to help parents apply what they have learnt with their child. Parenting programmes that focus on conduct problems in children without an intellectual disability were also available, such as The Incredible Years (Site 2, Site 3 and Site 4), The Family Links Course (Site 2) and Triple P (Site 3). Other support included third-sector organisations, which provided wide-ranging help through workshops, home visits, child care, information and advice and time-limited interventions. Most of the available programmes focused on autism awareness and general information for parents about autism or intellectual disabilities, providing limited advice on parenting strategies and techniques for addressing behaviours that challenge displayed by disabled children.
Process evaluation
A process evaluation is an essential part of a trial that reviews the implementation of an intervention and supports the interpretation of trial results and outcomes. 59 We conducted a process evaluation using a mixed-methods approach, including exploring the views and experiences of participants in the study, looking at contextual components and monitoring the intervention fidelity, dose and reach.
Treatment fidelity
To assess treatment adherence, therapists completed a session checklist after each session and other paperwork detailing the content covered in sessions. To assess the therapists’ competence in delivering SSTP, we videotaped all group sessions and 10% were rated by an independent assessor and specialist in delivering SSTP.
Study procedures and assessments
Participant identification
The study population was parents of preschool children with moderate to severe intellectual disability, who were concerned about their child’s behaviour living in the community in the four study sites. We excluded children with mild intellectual disabilities, as they are likely to access other interventions more suitable for their needs. Similarly, children with profound intellectual disabilities were excluded as they were unlikely to be able to follow the observation tasks and the psychometric assessments. Eligible participants were identified by local community paediatric or CAMHS teams through new referrals or existing cases. Members of the clinical teams screened and reviewed identifiable personal information of potential participants. Parents who were approached by a member of clinical staff or a clinical study officer were given a description of the study, the study Patient Information Sheet and an Expression of Interest form to complete. Those who were eligible and interested in taking part completed the ‘Expression of Interest’ form, which was passed to the researchers, who then contacted the parents for further screening.
Screening process
The eligibility of each participant was confirmed during the screening assessment with a member of the research team. During the screening, the parent rated the child’s level of functional abilities on the ABAS form. Children who had a General Adaptive Functioning score between 40 and 69 were considered to have moderate to severe intellectual disability, and thus were eligible to participate. Parents also had to confirm that their child displayed behaviours that challenge continually over the 2 months prior to the screening assessment. If the result of the screening assessment indicated the child’s adaptive functioning to be outside of our inclusion criteria, parents were given the reason for non-inclusion, were thanked for their cooperation and time, and no further contact was made with the family. Those who were eligible after the screening assessment were contacted to schedule the baseline assessment. Following this, the participants were randomised into the intervention arm (SSTP plus TAU) or TAU.
Informed consent procedure
Informed consent was taken in two stages. First, the person who had parental responsibility for the child completed the consent form at the beginning of the screening assessment prior to completing the ABAS form. Second, if the child was eligible, the family was invited to enter the study and complete the consent form prior to their randomisation. Parents were given a minimum of 24 hours to decide whether they wanted to enter the study and were given contact details of the research assistant to ask further questions. For both stages, parents provided written or audio-recorded verbal informed consent. The right to withdraw at any time without giving a reason or affecting further treatment was explained to each participant. Each participant was given a copy of their informed consent form, and the signed original was retained at the study site.
The researchers were inducted into the study procedures about obtaining informed consent and completed the online Good Clinical Practice (GCP) course.
For the process evaluation, parents signed a consent form and were provided with a copy to keep if interviews were done in person. For telephone interviews, the consent process was audio-recorded and stored securely in Data Safe Haven (DSH), a secure online platform to store confidential data at University College London (UCL).
Participant safety
Reports of SAEs were collected by the trial manager who reported the information via the eCRF within 24 hours of becoming aware of the event. SAE was defined as any event that:
-
resulted in the death of the participant;
-
was life-threatening;
-
required hospitalisation or prolonged existing hospitalisation;
-
resulted in persistent or significant disability or incapacity;
-
consisted of a congenital anomaly or birth defect;
-
was otherwise considered medically significant by the investigator.
All reports of SAEs were reviewed by the Chief Investigators (CI) or Principal Investigators (PI) within 2 days of receiving the report and the review outcome was recorded in the eCRF. Each SAE was assessed to determine if the event was related to the intervention (e.g. resulted from the administration of the research procedures or SSTP) and if the event was unexpected (e.g. the type of event was not listed in the protocol as an expected occurrence).
Serious adverse events that were related and unexpected would have been reported to the Research Ethics Committee (REC) that approved the trial, and to the PRIMENT Clinical Trials Unit using the SAE report form within 15 days of the CI becoming aware of the event. These would also have been reported to the Joint Research Office at UCL.
Data management
Data collection methods and handling
Data management in this study complied with the UK Data Protection Act 1998, PRIMENT Standard Operating Procedures (SOPs) and GCP. Researchers uploaded and stored all data into DSH, which is a secure system for storing sensitive information. Audio and video recordings were uploaded to the system, and researchers deleted all other versions of the data from digital machines where they were originally recorded.
The investigator was responsible for ensuring the accuracy of all data entered in the CRFs. Data verification checks were completed on 100% of CBCLs (primary outcome measure), and 10% of all secondary outcome measures. The original application stipulated that 5% of all secondary outcome measures would be checked, but due to researcher turnover, it was deemed necessary to carry out a higher percentage of checks for quality assurance in three study sites (Site 2, 3 and 4), where 10% checks were carried out. All study staff were also reminded of the importance of careful data entry to minimise errors.
Confidentiality
All personal data collected about the participant was managed following the PRIMENT SOP for Managing Personal Data. Each participant was given a unique identification number at randomisation. The participant’s initials, date of birth and unique randomisation number were used for identification. All other personal or identifiable information about the participants was stored separately and securely in the UCL DSH system. The CRFs did not contain identifiable information. We used a delegation log to track personnel responsible for data management.
Trial database
All data from the participants were entered into an online clinical data management system called Sealed Envelope. PRIMENT approved the quality management, software development and security of this system. The original paper forms of outcome measures were stored in secured locked cabinets in the office at each trial site. PRIMENT SOP Database Lock, Unlock and Closure was followed at the end of the trial.
Data entry
Baseline data for 261 randomised participants from all four sites were entered into the Sealed Envelope database. The primary outcome measure (CBCL) was available in the database for 261 participants and the CRFs for Source Data Verification (SDV) checking were available for all participants.
Four-month follow-up data for 229 participants from four sites have been entered into the database. The primary outcome measure was available for 223 participants.
Ethics
Approval
Approval for the study was given by the London – Camden and Kings Cross REC (reference: 17/LO/0659).
Substantial amendments
Ethics and Health Research Authority (HRA) approval for the study was given on 19 May 2017. Overall, there were six substantial amendments approved by the REC as well as nine non-substantial amendments to the study protocol.
-
Substantial amendment 1: added participant recruitment via third-sector organisations, such as ‘Contact’ (co-applicant) and added PIC sites to the study.
-
Substantial amendment 2: extended the screening and baseline visit window from 2 to 4 weeks, approved giving the brochure and list of resources to all participants in both arms of the trial.
-
Substantial amendment 3: included minor updates to the participant information sheets and the study poster, created treatment allocation letters for the participants and created a letter for clinicians, teachers or third-sector organisations to send the study information sheet and expression of interest form to potential participants.
-
Substantial amendment 4: added an independent reviewer to code the video interviews, included the possibility of verbal consent and the possibility of conducting qualitative interviews for process evaluation over the phone, and added sections of the transparency wording from the HRA website in line with the new General Data Protection Regulation (GDPR), added intervention survey, created a letter for parents from the intervention group that did not attend any of the sessions, provided minor amendments to information sheets, consent forms and topic guide for interviewing service managers.
-
Substantial amendment 5: approval to invite parents not taking part in the study to attend the SSTP groups to ensure viable group sizes, created a ‘Thank you’ card for parents to boost attendance at follow-up assessments, added a minor update to the information sheet.
-
Substantial amendment 6: approved use of external transcription service to transcribe recorded audio files and to include some participants from the TAU group in qualitative interviews, including information regarding the 10-month costed extension approved by the study funders.
Deviations from the study protocol
There were 37 protocol deviations at 4 sites. Most of these deviations concerned baseline or follow-up assessments being completed outside of the assessment window as specified in the protocol. The assessment window between screening and baseline was extended to 4 weeks as part of substantial amendment 2. Other deviations included issues with the consent forms (e.g. a participant signed a consent form with the wrong site logo). These consent forms were corrected, or the correct forms were completed retrospectively. Protocol deviations relating to the COVID-19 pandemic are described later in the report under the heading ‘COVID-19 Adaptations’.
Impact of the COVID-19 pandemic
The COVID-19 pandemic had a substantial impact on the study. Three non-substantial amendments (7, 8 and 9) were drafted to enable study changes to ensure participant and researcher safety and adherence to social distancing government regulations. These amendments allowed researchers to complete all assessments over the telephone and for the therapy to be conducted remotely. These amendments also included the addition of a COVID-19 parent survey to assess the impact of the pandemic on families (see Report Supplementary Material 1). Parents from the Parent Advisory Group (PAG) provided their views at the start of the pandemic, stating the situation was very stressful and families may need time to settle and find a routine before they can allocate time to the study.
We also discussed how to mitigate risks imposed on the conduct of the trial regarding the safety of participants and researchers, treatment delivery and adherence, data quality and completion, and statistical considerations with the Clinical Trials Unit and the Trial Oversight Committee.
Recruitment during the COVID-19 pandemic
In total, 51 out of 261 families in the trial were randomised on or after 16 March 2020. The non-substantial amendments also simplified the process for Clinical Study Officers to pass on expressions of interest to the study team and updated the study protocol to reflect all changes. Study recruitment was halted between 18 March 2020 and 18 May 2020, and the timescale for re-opening was determined independently by each site. Sites reopened gradually between May and August 2020. Study follow-ups continued throughout this period, although child−parent observations and cognitive neuropsychological assessments (i.e. Mullen Scales of Early Learning)57 that required face-to-face contact were omitted from the study, as we were unable to find alternative ways to conduct the assessments (max n = 51). Wet signatures for logs were replaced with online signatures, and verbal recorded consent was obtained rather than written consent.
Observing government guidance on the spread of COVID-19 led to the study team working remotely. Before the pandemic, the CA-SUS forms at 4 and 12 months were completed by parents during visits and then handed to the Trial Manager for data entry. As this was no longer possible, research assistants completed the CA-SUS assessment over the phone but did not ask questions about attendance at parenting groups that would unblind them. These data were collected once the participant had completed the final follow-up. Moreover, the issues associated with the pandemic caused further difficulties with completing the study assessments with participants. For example, some parents found it challenging to find the time to complete all questionnaires over the phone, therefore many only completed the primary outcome measure (CBCL). Since all work, appointments, therapies and school responsibilities became remote, many assessments were re-scheduled and this increased the number of missing assessments and those completed outside of the assessment window.
The restrictions from the COVID-19 pandemic caused difficulties with obtaining the secondary outcome measure (C-TRF), which was meant to be completed by the child’s teacher. Most of the schools were closed and many parents did not have other relatives or people who would know their child’s behaviours well enough to complete this measure.
Parents from the PAG reflected on their own experiences during the pandemic, including big routine changes, which could affect the availability of parents to complete assessments. In particular, single parents may not have had the time to dedicate to the study. One parent reflected that during the pandemic situation, it was difficult to make phone calls without interruptions, but as the situation progressed, the family started to settle into a routine and this increased their capacity to take phone calls and allocate time to more responsibilities. They said this may also be similar for other parents. Another parent from the PAG noted that many of these families may not have education health care plans yet, which was allowing children to continue attending school during lockdowns. For those without a plan, routines are being disrupted, which may have been extremely difficult for both children and their families. Overall, the COVID-19 pandemic brought challenges not only to the delivery of SSTP and other services in TAU but also to the daily lives of every individual. This likely resulted in a deterioration in children’s behaviour patterns, increased parental stress and poorer parental ability to manage behaviours. These disruptions likely challenged many parents’ ability to comply with study directives.
Treatment as usual during the COVID-19 pandemic
Treatment as usual could not have been delivered in the conventional way as most of the services available in local areas were interrupted or completely suspended from March 2020. As such, families that were recruited in this study from this time had little to no help or support available to them.
During the qualitative interviews conducted for the process evaluation, parents shared their views about the COVID-19 pandemic and the national lockdowns. They described this time as extremely challenging as the children’s challenging behaviours worsened due to lack of routine and limited access to school. Parents were trying to balance working from home and caring for their child with no additional support from services or school. As such, parents felt even more abandoned during the times when they felt the most need to be supported.
The behaviour during the three months of lockdown took its toll. It escalated to where it was, like, unmanageable most days. Um, but there wasn’t a lot we could do about that.
One of the biggest challenges I’ve ever had to face is being in three months lockdown with a child with needs … It was really, really unfair to do I think, what they done originally, was said children who have EHCP plans would be taken care of. We’d be taken into consideration, the needs, and it wasn’t.
Stepping Stones Triple P delivery during the COVID-19 pandemic
From March 2020, the intervention was adapted to follow the COVID-19 safety precautions and regulations. At the start of the pandemic, no online version of SSTP was available from the Triple P group. The therapists continued with the same session plans and content that was delivered before the COVID-19 pandemic and delivered this remotely. The final group combined participants from all sites to ensure a sufficient group size. The Triple P held a panel discussion on remote delivery in practice on 21 July 2020. This was attended by the Trial Manager. The Triple P developers granted permission for us to share the advice provided in this session, including:
-
Using video conferencing software, which allows for better participation than the telephone as parents can see the therapist when skills are being demonstrated.
-
Allowing space for discussing progress and being able to problem-solve technical challenges.
-
Acknowledging the stressors parents are facing and normalising the feelings they are experiencing. Offer hope that with the plans and strategies to be discussed, they will feel more confident in how to tackle this new normal, reduce stress and enjoy their parent–child interaction.
-
Maintain contact with fellow Triple P practitioners, including Peer-Assisted Supervision and Support (PASS) sessions, to support each other in learning this new format and maintain fidelity.
-
For parents with children at home, consider proposing that parents use a Planned Activities Routine to occupy the children so parents can participate fully in the session.
-
Consider sending parents text reminders of their upcoming session.
-
Resources can be available to pick up from an office (if open) or mailed to families.
-
Consider planning how to use behavioural rehearsal based on your chosen delivery format (on videoconference platforms, it can be done as usual).
-
When parents or practitioners are stressed or anxious, it may be more difficult to come up with ideas. Practitioners may need to think about giving more examples or offering more specific prompts sooner if they realise that parents are struggling with idea generation.
-
Provide an opportunity for informal communication between parents before or after the sessions.
-
Show DVDs by sharing your screen or demonstrate live the strategies. The DVD could also be played in the background, sharing the audio only (additional commentary may be required), or therapists should read the relevant section of the Positive Parenting Booklet.
-
Consider if the parent has safe activities for the children while they are taking part in the intervention.
-
Content can be fully delivered remotely, and the process/strategies should not change.
Data on attendance at parenting groups were collected once the participant has completed the study. Forms were sent to the Trial Manager for data entry.
Statistical analysis plan
Unmasking of the data and analysis was initiated after the last participant had completed their 12-month follow-up. All relevant data had been entered, checked and locked, and the analysis plan had been finalised and approved (see Report Supplementary Material 2 for the full Statistical Analysis Plan). Before the analysis was conducted, data were checked for quality. Incomplete or inconsistent data included missing data, data outside the expected range and other inconsistencies between variables (e.g. on the dates the questionnaires were completed). Any inconsistencies that were found were checked with the researchers, corrected and documented by the trial statistician. The primary analysis was performed independently by two statisticians (CQ and GA) to ensure its accuracy. For the primary analysis, we analysed participants with outcome data (CBCL) at 12 months according to their original assigned groups. The secondary analyses were carried out by one statistician (CQ) and checked by the lead statistician (GA). All the statistical analyses were performed using Stata version 15 (or above) and R version 3.5.0 (or above).
Assessment of baseline characteristics
Summary measures for the baseline characteristics of each group are presented as mean and SDs for continuous, symmetric variables, medians and interquartile ranges (IQR) for continuous, skewed variables and frequencies and percentages for categorical variables. We compared baseline characteristics visually to assess whether the balance had been achieved. Any notable imbalances prompted additional adjusted analyses (see later).
Adherence to allocated programme and attrition
Some loss to follow-up was expected over 12 months. The proportion of participants missing was summarised for each outcome measure, in each arm, and at each time point. Potential bias due to missing data was initially investigated by comparing the baseline characteristics of the trial participants who have (analysable) primary outcome data to those who do not, using descriptive comparisons, t-tests, chi-squared tests and Fisher’s exact tests as appropriate. Reasons for withdrawal from the programme were summarised. Participants’ adherence with SSTP is defined as attendance to most of the planned group and individual sessions, that is participation in at least 4 (out of 6) group sessions and 2 (out of 3) individual sessions. Participants who engaged with SSTP were compared descriptively with those who did not in terms of their baseline characteristics.
Analysis of primary outcome
The primary outcome is the CBCL total score at 12 months. The primary analysis used mixed models to perform an individual-level analysis and followed Roberts and Roberts60 in adjusting for therapist clustering in the intervention arm only (random coefficient model). This model also adjusted for baseline total CBCL score and randomisation stratification factors (centre, level of intellectual disability) using fixed effects. This was a complete case analysis. The only ‘imputation’ performed was done by following guidance from the CBCL scoring manual. That is, missing values for CBCL were scored as zero unless more than eight items were missing, in which case the participant was excluded. The presentation of all findings is in accordance with the latest CONSORT statement. The model assumes that the residuals are normally distributed and homoscedastic, which was checked using residual plots (e.g. normal Q−Q plots). Where substantial departures from normality occurred, a transformation of the outcome variable was considered.
Analysis of the secondary and other outcomes
In addition to the analysis of the total CBCL score, we analysed the internal and external scores separately using the same approach. In addition, analyses were performed for each of the secondary outcomes. Continuous outcomes were analysed using the same approach as that described for the primary outcome. For binary outcomes, we used analogous logistic mixed models,61 although without adjustment for baseline outcome scores. All analyses of secondary and other outcomes should be considered supportive analyses. Missing values in the outcomes were handled, where possible, using guidance from the corresponding manual.
Sensitivity analysis
The following additional sensitivity analyses were performed. We repeated the primary analysis with additional adjustments to see if any notable baseline imbalances were encountered (due to chance or missing data). We used a mixed model to analyse both the 4- and 12-month CBCL outcomes simultaneously. We repeated the primary analysis after imputing outcome data using multiple imputations using chained equations. Specifically, we imputed component items of the CBCL score (i.e. not the total score) using item information from the baseline, 4- and 12-month CBCL scores and other variables (as appropriate). Missing baseline data were imputed using single imputation methods where multiple imputation was not successful. Per-protocol and complier-average causal effect (CACE) analyses were performed as participant adherence was relatively low.
Coronavirus disease 2019 considerations and additional analyses
The following analyses were carried out to explore the effect of the COVID-19 pandemic on the trial findings. The baseline characteristics of children and parents were summarised by randomised group before and after 16 March 2020. In addition, adherence to the programme, attrition and adverse events were summarised before and after this time point. We performed a subgroup analysis to investigate whether the intervention effect differed depending on whether recruitment was before or after 16 March 2020. This was achieved using the primary analysis model with additional indicator and interaction terms. Finally, we considered whether the effect of the intervention depended on the size of session groups. Separate analyses considered: (1) the overall group size and (2) the average group size in sessions attended. These analyses were achieved using the primary analysis model with additional indicator and interaction terms. Similar health economics analyses were performed to assess whether the cost of the intervention was affected when intervention sessions were moved online. We also assessed whether the COVID-19 pandemic had an impact on children and carers’ mental health and HRQoL during this period.
Health economics analysis
The economic evaluation aimed to assess the cost-effectiveness of delivering the level 4 SSTP intervention from the NHS, personal social services (PSS) and parents’/caregivers’ perspectives (please see Report Supplementary Material 3 for the full Health Economics Analysis Plan).
Valuation of economic outcomes
The primary economic outcome measure was the QALYs derived from utility scores obtained using the PedsQL™ General Core Scales (GCS). Mapped EQ-5D-Y utility scores algorithm62 provided an empirical basis for estimating health utilities. For parents/caregivers utility scores were derived from responses to the EuroQol-5 Dimensions, five-level version (EQ-5D-5L) using valuations obtained from an English population. 63 These were used to form QALYs over the 12-month period, adjusting for any imbalances in baseline scores. 64 Measurements have been recorded at baseline, 4 and 12 months.
Valuation of resource use
Study records of the number of therapists attending training sessions were used to track resources used in the delivery of the training programmes including trainee and trainer time (and preparation time), travel costs, attendance incentives and course materials to calculate the fixed cost of training. For the intervention delivery, we recorded the number of sessions delivered, the time each therapist spent with a family, and also any materials provided to parents/caregivers.
For the NHS and PSS analysis, data were collected on the use of health services in primary and community care, investigations and prescribed medication, hospital admission and outpatient attendance, ambulance use and social care. Data on health and social care resource use were collected at baseline (for the past 6 months), 4 months (for the past 4 months) and 12 months (for the past 6 months) post intervention.
For the analysis from the parent/caregiver perspective, we additionally collected data on out-of-pocket expenses. Expenditure on private use of treatments and therapies was captured in the CA-SUS.
Health and social care resource use was costed using unit costs from the most recent Unit Costs of Health and Social Care published by the Personal Social Services Research Unit (PSSRU)65 and NHS reference costs. The costs of medications were estimated from the British National Formulary. The cost of each resource item was calculated by multiplying the number of resource units used by the unit cost. The total cost for each participant was estimated as the sum of the cost of resource use items consumed. The primary analysis included only health and social care data collected as part of the trial and hence covered only 10 months of the trial (missing months 4–6). We have projected costs from 4- and 12-month follow-ups to estimate the 12-month health and social care resource use as part of sensitivity analyses. All costs are reported in 2019–20 Great British pounds. No discounts were applied, as trial follow-up did not exceed 12 months.
The overall economic evaluation
All analyses were conducted using intention-to-treat (ITT) principles, comparing the two groups as randomised and including all participants in the analysis. Analyses were compliant with the accepted economic evaluation methods. 66
-
Cost-effectiveness analysis: mean incremental cost from the NHS and PSS perspective per change in CBCL. Incremental cost-effectiveness ratios (ICER) were reported, and uncertainty was explored using cost-effectiveness acceptability curves (CEACs). 67,68
-
Exploratory analysis of quality of life using PedsQL™ to predict utility scores. The mean cost per participant for the intervention and TAU was reported by type of service use. We calculated the mean cost per QALY using the mapped EQ-5D-Y. Mean QALY per participant was calculated as the area under the curve for the duration of the trial, adjusting for baseline values.
Cost−benefit analysis of the impact on the parents/caregivers: Responses to EQ-5D-5L were used to calculate QALYs in a standard format and valued as willingness to pay (WTP) for a QALY gained. We calculated the mean cost (including out-of-pocket expenditure) per QALYs. Mean QALY per participant was calculated as the area under the curve for the duration of the trial, adjusting for baseline values.
Missing data
Missing data were explored to determine any patterns, extent and association with participant characteristics. The primary analysis included all participants using multiple imputation to predict missing costs and outcomes. 69
Analysis of relative costs and outcomes
Cost and QALY data were combined to calculate an ICER. Uncertainty in the point estimate of the cost per QALY was quantified using bootstrapping methods to calculate confidence intervals around the ICER.
The results of the non-parametric bootstrap are presented on a cost-effectiveness plane (CEP). CEACs, showing the percentage of cases where the intervention is cost-effective, over a range of values of WTP for a QALY gained, were constructed using the bootstrap data from a range of values of WTP for a QALY gained for each different costing perspective and for the different methods of calculating QALYs. The probability that the intervention is cost-effective compared to TAU at a WTP for a QALY gained of £20,000 and £30,000, and £13,000 as a measure of opportunity cost were reported. 70
Sensitivity analyses
One-way sensitivity analyses were used to judge the potential impact of sources of uncertainty:
-
complete case analysis;
-
given that training costs may differ between the trial and implementation of the intervention due to learning or being delivered to a larger patient group, we tested the impact of varying training costs (particularly because of larger patient numbers per staff member trained) on the mean incremental cost per QALY gained.
Chapter 3 Patient and public involvement
Patient and public involvement (PPI) in this trial was defined as research carried out with members of the public at every stage of the project. 71 This included helping to identify research priorities, forming an advisory group, reviewing study documentation, problem-solving challenges and supporting dissemination strategies. This level of involvement is similar to other comparable trials within this population. 72
Ms Una Summerson, the Head of Policy and Public Affairs for the charity Contact, is one of the study’s co-applicants. Ms Summerson was involved with study design, recruitment strategies, documentation review and study dissemination. The research team produced a newsletter twice a year to provide study updates. This was shared with study participants and local investigators.
Parents of children with intellectual disabilities and behaviours that challenge were recruited from the Camden Special Needs Forum (CSNF) to assist in the development of the study proposal. Eight parents were originally invited to form the PAG. These parents were recruited through a national charity called Contact and meetings were facilitated by the Head of Policy and Public Affairs at Contact (Una Summerson). Three parent members regularly attended a meeting every 3 months to assist in overseeing the trial, discussing study progress and helping with materials. These parents were all mothers and were each based at different trial sites. After the first seven PAG meetings, it was agreed that from September 2019 onwards, the PAG meetings would be merged with the TMG meetings, and so, all PAG members were invited to attend every subsequent TMG meeting. Altogether, parents attended seven PAG meetings and 19 combined TMG and PAG meetings. The TMG meetings were held every month until January 2021 and it was then decided that meetings would be held every 2 months. All meetings were held face to face before March 2020. Due to the COVID-19 pandemic, all meetings after this time were held online via MS Teams.
Parents from the PAG group worked alongside researchers on tasks to oversee the successful running of the project. Parents were involved in the following tasks:
Study design
Parents from the CSNF helped us to develop the study proposal. The PI met with six parents for a discussion about the study and another five parents were contacted to provide views about the study application. Some of these parents continued to be involved once funding for the study was received. Parents felt there was a real need for the study and were complementary of the behavioural approach which they saw as a critical ingredient. ‘If we had the right strategies to use earlier, I could of gone back to work and the school wouldn’t be ringing me all the time’. We discussed the number and type of assessments, randomisation and the lay summary, and asked about any issues they considered as challenging. They said that research would be helpful even for the control group as it allows time to think about the child and their needs and has a positive impact on both groups. The parents we consulted with argued that there would be short and medium term benefits from providing the resource and even suggested a summary of the research assessment to be shared with the parent who took part in the study. They were also interested in potentially adding to collection of data on other variables that may be associated with challenging behaviour including food items.
We held two face-to-face meetings with CSNF parents from diverse ethnic backgrounds on 13 January 2016 (for the outline) and 19 April 2016 for the main application. We also had extensive e-mail correspondence and discussions with the CSNF group leaders and with our co-applicants Contact regarding the best way to involve parents. This helped to formalise a plan for the PAG group and its role throughout the study.
The PAG members assisted in training the research assistants (a topic mentioned was how to talk to the parents without the latter feeling blamed), examining the study parent information materials and consent forms, assisting with drawing up topic guides and in the process evaluation, attending TMG meetings, helping to format feedback to parents and interpreting and disseminating the findings.
Feedback on newsletters and study documents
Parents made suggestions on how to make the study documentation more accessible and comprehensible for families, including comments on study posters, information sheets, etc. For example, feedback was provided on the study poster, and it was suggested that pictures of children with various disabilities be included to make it more welcoming to families who have children with less common disabilities.
Improvements to recruitment strategies
The PAG proposed many strategies to support recruitment and overcome challenges that arose over the course of the study. At the beginning of the study, parents suggested the trial be promoted in parent forums and that the study poster be given to parents at meetings of local parent groups. This led to parents from London sites being invited to attend a parent meet and greet morning where two parents from the PAG group talked about the study. Parents were provided with study information and expression of interest forms at this meeting and were asked to share the information with other parents. This helped to increase recruitment rates at the London sites.
Towards the end of the study, we experienced challenges reaching parents for the 12-month follow-up assessments. The PAG members suggested we provide e-mails or a newsletter to explain the importance of the study and what will happen with the results and outcomes of the research. The idea with this was to try and increase parents’ motivation to complete the final study follow-up. This information was included as part of the study’s Christmas newsletter.
Problem-solving challenges
To improve attendance at the SSTP group meetings, it was suggested to offer an incentive to parents, such as providing food or snacks at the intervention group each week. This was appraised by parents who attended the groups and who said the hospitality during sessions created a welcoming atmosphere.
Providing lived-experience perspectives and insight throughout the course of the study
Parents taking part in the study often expressed their gratitude to research assistants for the opportunity to be a part of the study and to be able to talk to someone who is interested in hearing about their child. The parents from the PAG agreed and shared personal experiences of feeling that often parents only get little time to speak about their child and being appreciative of the time they get to talk to a professional.
The parents also discussed the need for and utility of group interventions. It was discussed that usually, the main carer receives all the training, and this may leave the other parent or another carer feeling helpless. It would relieve the pressure and burden if all the family could receive the training/intervention. As a result of these discussions, we enabled additional caregivers to attend intervention sessions.
Publication and involvement with research outputs
The PAG were involved in reviewing the full study report and dissemination plan. The parents have also provided commentaries and reflections that have been included in our study publications. The PAG provided the following commentary for the qualitative study results (publication being drafted for submission):
Intellectual disabilities occur in all racial, ethnic, and socioeconomic group/ lifestyles. Although its specific causes are still unknown, we do know one thing, the rate is increasing. Treatments and interventions are offered in brick and mortar centres, community providers, and by in-home therapists; derived from parent’s enticement of therapies that promise to do everything. Unfortunately, parents only escape from the confusing unforgiving treatment’s business is the NHS, which often through little fault of its own is stalled by unavoidable hurdles. The services are not efficient, and it often feels like parents know more than the professionals and are constantly teaching them rather than professionals providing support to parents. This makes parents lose trust and faith in the system. So, where does our support come from? The described points in this paper are concise and relevant, however parent’s feeling of loneliness and exclusion also come from the overwhelming and confusing online information overload, which can take years to declutter, to select the credible resources and build supportive and convenient entourage. An arduous job for parents, specially under time pressure to find and implement necessary early intervention for the child.
The behaviour during the three months of lockdown took its toll. It escalated to where it was, like, unmanageable most days. But there wasn’t a lot we could do about that.’ This quote highlights the striking reality that postcode often defines the level of lockdown discomfort and opportunities. Actually, all parents want is a consistent professional proficient support that is able to comprehensively listen to them and work collaboratively toward a better life quality for the child. The quotes in the paper were about appreciating talking, listening, understanding, talking through, and sharing ideas, opinions, and techniques. The caring role is a very lonely journey that parents shouldn’t have to take alone.
One parent from the PAG commented on their involvement with a publication of a case study:
I was part of the BMJ article writing a case study and doing a podcast. I believe having real parents on the panel helped the project understand real life problems that we face as families daily, including why we can’t always make appointments at last minute and as much as we need/want the support offered, just the situation we can find ourselves in can be so chaotic that we can’t always take part every time.
The three parents described their involvement with the study and experience of being part of the PAG:
Parent 1
As a parent of two children with additional needs that have very challenging behaviour, I was so excited to be part of this project to give the voices of parents who had genuine lived experience. I also had the benefit of being part of a large network, had opportunity to ask direct questions and got feedback from others. We were included in every part of the project. The information we gave as parents was always respected and included and we felt very much a part of the team. The professionals on the trial always listened to our opinions and genuinely wanted the support that we gave on the parent panel. I would definitely love to be part of any future projects like this and the whole team at UCL and NHS England treated us with respect and as a colleague with experience rather than just having to have us there as part of guidelines for the project. I found the face to face meetings beneficial as we all felt part of a wider team and network and they weren’t as daunting as online meetings. I think having face-to-face meetings before the COVID-19 pandemic resulted in better working when we had no alternatives than working online as relationships had already been formed. I am extremely proud of this project and how they altered as much as possible to meet the COVID-19 requirements. I hope that it results in helping families struggling with their children and would have benefitted from it when my children were that age.
Parent 2
I was given the opportunity to join the parent advisory group for the EPICC-ID clinical trial as I was involved with various projects run by Contact – the Charity for families with disabled children. I did not know what to expect from the trial as I have never been involved with anything like this before. I knew that the trial was studying the impact of a particular intervention for children with intellectual disabilities who exhibited challenging behaviour. As this is something that affects myself and my family personally I felt very fortunate to have been asked to take part. I can honestly say I have learnt so much from the whole experience. From finer details such as defining exactly what challenging behaviour is, to the bigger picture of how National clinical trials actually work and the complexities of randomisation and blind controls. It was a steep learning curve but always a privilege to share time with so many brilliant, respected consultants working in the field of Child and Adolescent Psychiatry. Throughout the trial I gained a lot of confidence and was encouraged by the professionals to share views and opinions about the process and the Triple P intervention itself. I always felt my contributions were valued and it was amazing to be involved in the drafting of a journal for the BMJ. This is not something many people outside of medicine can say! I have seen how clinical trials – like EPICC-ID open doors to advancing prevention and improving lives. The team always made it clear that clinical trial volunteer participants like myself play an important part in the trial process and I would not hesitate to be involved with a parent advisory group again. I am very grateful to Contact, Professor Angela Hassiotis and all the team for inviting me to take part.
Parent 3
I really enjoyed being on the SSTP trial, from sitting on an advisory parent’s group to analysing data. Progressively, I’ve seen perquisite effort to adapt contextual factors to improve recruitment numbers and resilience to complications like COVID-19 pandemic. Thank you for asking me to be part of the trial, I would love to do it again. It’s very rewarding.
Trial Steering Committee patient representatives
The study TSC also included two independent PPI representatives. The committee met every 6 months (a total of nine meetings), and the PPI representatives attended these meetings and reviewed data reports produced for the Data and Safety Monitoring Board. Their roles included deciding on whether the trial should continue and approving strategies to improve recruitment or follow-up.
Dissemination
There are continued plans to involve members of our PAG in the dissemination of the study results. This includes the filming of a short accessible video to present the study results to the public and this will be shared through organisations such as Contact, Triple P and the Challenging Behaviour Foundation. The study findings will also be presented to public audiences at various events and will be shared to study participants via e-mail and social media channels.
Chapter 4 Results
Clinical effectiveness
Participant flow and retention
A total of 261 participants were enrolled in the trial and randomised. Of these participants, 155 were allocated to the SSTP intervention, and 106 were allocated to TAU. Figure 1 shows a CONSORT flow diagram summarising the flow of participants into the trial.
Baseline characteristics
Participant baseline characteristics were well balanced between the allocation arms. Table 5 and 6 present baseline characteristics of participating children and parents, respectively. We also explored potential differences in the baseline data per allocation arm for the participants with completed follow-up data at 12 months (N = 211). As there were no differences found, we only present the baseline characteristics of the whole sample. The participating children had a mean age of 3.7 years (SD = 1; IQR = 3.2–4.4), 75% were male and 57% were of white ethnicity. The participating parents were on average 34.4 years old at baseline (SD = 6.4, IQR = 30–39), and 62% were of white ethnicity.
| TAU (n = 106) |
SSTP (n = 155) |
Total (N = 261) |
|
|---|---|---|---|
| Mean (SD); median (IQR) | Mean (SD); median (IQR) | Mean (SD); median (IQR) | |
| Age (years) | |||
| 3.7 (0.9); | 3.8 (1.0); | 3.7 (1.0); | |
| 3.8 (3.2–4.3) | 3.9 (3.2–4.4) | 3.9 (3.2–4.4) | |
| Missing | 0 | 1 | 1 |
| n (%) | n (%) | N (%) | |
| Sex | |||
| Female | 29 (27.4) | 37 (23.9) | 66 (25) |
| Male | 77 (72.6) | 118 (76.1) | 195 (75) |
| Ethnicity | |||
| White | 62 (58.5) | 87 (56.1) | 149 (57) |
| Mixed | 10 (9.4) | 19 (12.3) | 29 (11) |
| Asian | 11 (10.4) | 17 (11.0) | 28 (11) |
| Black | 16 (15.1) | 25 (16.1) | 41 (16) |
| Other | 7 (6.6) | 7 (4.5) | 14 (5) |
| Severity of intellectual disability | |||
| Moderate | 101 (95.3) | 151 (97.4) | 252 (97) |
| Severe | 5 (4.7) | 4 (2.6) | 9 (3) |
| Site | |||
| Site 1 | 25 (23.6) | 39 (25.2) | 64 (25) |
| Site 2 | 22 (20.8) | 34 (21.9) | 56 (21) |
| Site 3 | 31 (29.2) | 43 (27.7) | 74 (28) |
| Site 4 | 28 (26.4) | 39 (25.2) | 67 (26) |
| ASD | |||
| Yes | 68 (64.2) | 90 (58.4) | 158 (61) |
| No | 38 (35.8) | 64 (41.6) | 102 (39) |
| Missing | 0 | 1 | 1 |
| Physical health | |||
| Yes | 61 (57.5) | 79 (51.0) | 140 (54) |
| No | 45 (42.5) | 76 (49.0) | 121 (46) |
| Mobility difficulties | |||
| Yes | 21 (34.4) | 31 (39.2) | 52 (37) |
| No | 40 (65.6) | 48 (60.8) | 88 (63) |
| Missing | 45 | 76 | 121 |
| Sensory impairments | |||
| Yes | 32 (52.5) | 41 (51.9) | 73 (52) |
| No | 29 (47.5) | 38 (48.1) | 67 (48) |
| Missing | 45 | 76 | 121 |
| Epilepsy | |||
| Yes | 6 (9.8) | 5 (6.3) | 11 (8) |
| No | 55 (90.2) | 74 (93.7) | 129 (92) |
| Missing | 45 | 76 | 121 |
| Constipation | |||
| Yes | 13 (21.3) | 26 (32.9) | 39 (28) |
| No | 48 (78.7) | 53 (67.1) | 101 (72) |
| Missing | 45 | 76 | 121 |
| Education, health or care plan | |||
| Yes | 36 (34.0) | 61 (39.4) | 97 (37) |
| No | 70 (66.0) | 94 (60.6) | 164 (63) |
The baseline demographic characteristics of the parents by allocation arm are presented in Table 6. The groups have been compared visually and appear similar except for living situation, employment and relationship status.
| TAU (n = 106) |
SSTP (n = 155) |
Total (N = 261) |
|
|---|---|---|---|
| Mean (SD); median (IQR) | Mean (SD); median (IQR) | Mean (SD); median (IQR) | |
| Age (years) | |||
| 34.8 (6.2); | 34.0 (6.6); | 34.4 (6.4); | |
| 35 (31–39) | 33 (29–38) | 34 (30–39) | |
| n (%) | n (%) | N (%) | |
| Respondent | |||
| Mother | 94 (88.7) | 143 (92.3) | 237 (90.8) |
| Father | 11 (10.4) | 10 (6.5) | 21 (8.1) |
| Other | 1 (0.9) | 2 (1.3) | 3 (1.2) |
| Ethnicity | |||
| White | 66 (62.3) | 95 (61.3) | 161 (62) |
| Mixed | 3 (2.8) | 6 (3.9) | 9 (3) |
| Asian | 12 (11.3) | 17 (11.0) | 29 (11) |
| Black | 18 (17.0) | 29 (18.7) | 47 (18) |
| Other | 7 (6.6) | 8 (5.2) | 15 (6) |
| Living situation | |||
| Owned property | 31 (29.2) | 29 (18.7) | 60 (23) |
| Rented property | 71 (67.0) | 123 (79.4) | 194 (74) |
| Other | 4 (3.8) | 3 (1.9) | 7 (3) |
| Employment status | |||
| Unemployed | 5 (4.7) | 11 (7.1) | 16 (6) |
| Part-time paid employment – < 30 hours/week | 31 (29.2) | 47 (30.3) | 78 (30) |
| Full-time paid employment | 14 (13.2) | 11 (7.1) | 25 (10) |
| In education | 1 (0.9) | 4 (2.6) | 5 (2) |
| Looking after home and family | 53 (50.0) | 77 (49.7) | 130 (50) |
| Other | 2 (1.9) | 5 (3.2) | 7 (3) |
| Relationship status | |||
| Single | 25 (23.6) | 52 (33.5) | 77 (30) |
| Married | 51 (48.1) | 60 (38.7) | 111 (43) |
| Separated | 4 (3.8) | 6 (3.9) | 10 (4) |
| Divorced | 4 (3.8) | 5 (3.2) | 9 (3) |
| Cohabitating | 22 (20.8) | 32 (20.6) | 54 (21) |
|
Main income
(can choose one or more) |
|||
| Salary/wage | 58 (54.7) | 82 (52.9) | 140 (54) |
| Family support | 11 (10.4) | 25 (16.1) | 36 (14) |
| State benefit | 91 (85.8) | 139 (89.7) | 230 (88) |
| Other | 4 (3.8) | 5 (3.2) | 9 (3) |
|
Benefit
(can choose one or more) |
|||
| Income support | 24 (26.4) | 40 (29.0) | 64 (28) |
| Housing benefit | 36 (39.6) | 68 (48.9) | 104 (45) |
| Job seeker allowance | 1 (1.1) | 3 (2.2) | 4 (2) |
| Child benefit | 67 (73.6) | 115 (82.7) | 182 (79) |
| Other | 78 (85.7) | 115 (83.3) | 193 (84) |
| Mental health problems | |||
| Yes | 32 (30.2) | 41 (26.5) | 73 (28) |
| No | 74 (69.8) | 114 (73.5) | 188 (72) |
| Alcohol or drug abuse | |||
| Yes | 0 (0) | 3 (1.9) | 3 (1) |
| No | 106 (100) | 152 (98.1) | 258 (99) |
| Family violence | |||
| Yes | 7 (6.6) | 11 (7.1) | 18 (7) |
| No | 99 (93.4) | 144 (92.9) | 243 (93) |
Analysis of the primary outcome
The primary outcome is the CBCL total score at 12 months. Table 7 provides a summary of the CBCL total scores, stratified by allocation arm at baseline, 4 and 12 months. Figure 2 displays the boxplots of CBCL total score at all time points, and it shows that the IQR is larger in TAU than SSTP at 4 months.
| Allocation arm | ||||
|---|---|---|---|---|
| TAU (n = 106) | SSTP (n = 155) | |||
| n | Mean (SD) | n | Mean (SD) | |
| Baseline | 105 | 93.3 (28.3) | 155 | 96.1 (24.8) |
| Month 4 | 92 | 91.6 (32.3) | 137 | 91.5 (28.9) |
| Month 12 | 83 | 91.0 (30.1) | 129 | 90.0 (31.2) |
FIGURE 2.
Boxplots of CBCL total score at baseline, 4 and 12 months by allocation arm.
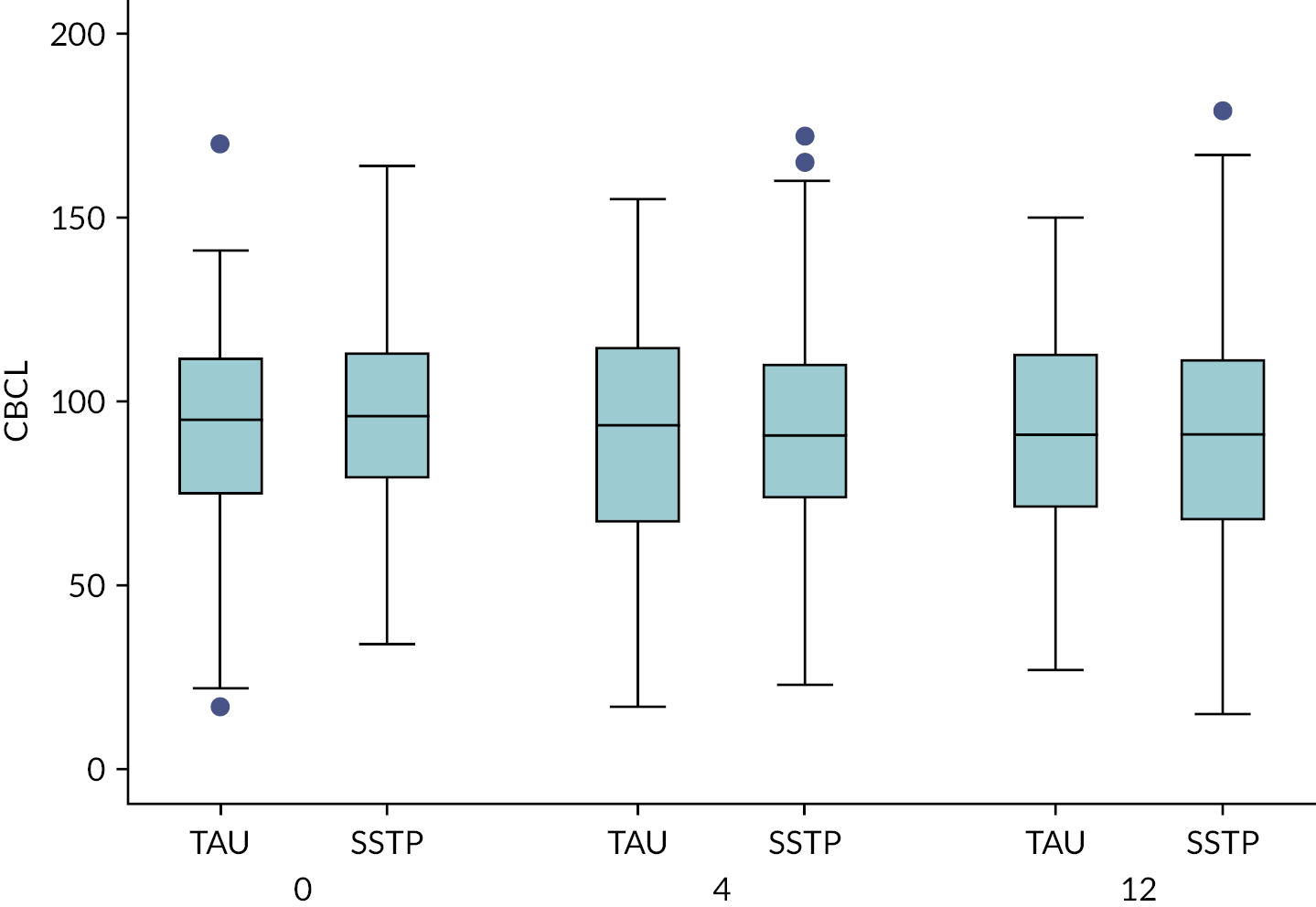
A linear mixed-effects model was fitted with CBCL total score at 12 months as the outcome variable, with fixed explanatory variables for (1) CBCL score at baseline, (2) centre, participant-level of intellectual disability indicator and (3) intervention group indicator (TAU = 0 and SSTP = 1). A random effect was included to account for clustering in the intervention arm and separate variance parameters estimated for the group-level error terms in the TAU and SSTP arms. This model included only those participants whose total CBCL scores were available at both baseline and 12-month follow-up.
The intervention reduced the CBCL score over 12 months by an average of 4.23 points (95% CI −9.99 to 1.53; p = 0.147). As such, there is no statistical evidence to suggest a difference in the CBCL total score at 12 months between the TAU and SSTP groups. The ICC was calculated as 0.04 in the SSTP arm. The model assumptions were checked and found to be appropriate.
The same linear mixed-effects model was fitted with CBCL total score at 4 months as the outcome variable. The intervention reduced the CBCL score over 4 months by an average point of 2.55 (95% CI −7.63 to 2.53; p = 0.322). As such, there is no statistical evidence to suggest a difference in the CBCL total score at 4 months between the TAU and SSTP groups. The model assumptions were checked and found to be appropriate.
The intervention effect estimate for the analysis of the primary outcome at 4 and 12 months is presented in Table 8.
| Difference | 95% CI | p-value | |
|---|---|---|---|
| CBCL (4 months) | |||
| SSTP vs. TAU | −2.55 | (−7.63 to 2.53) | 0.322 |
| CBCL (12 months) | |||
| SSTP vs. TAU | −4.23 | (−9.99 to 1.53) | 0.147 |
Analysis of the secondary outcomes
Table 9 provides a summary of the descriptive statistics for the secondary outcomes stratified by allocation arm, at baseline, 4 and 12 months, namely (1) C-TRF, (2) GHQ-12, (3) QRS-F, (4) Caregiving Problem Checklist and (5) PSOC.
| Measure | Assessment | Allocation arm | |||
|---|---|---|---|---|---|
| TAU (n = 106) | SSTP (n = 155) | ||||
| n | Mean (SD) | n | Mean (SD) | ||
| C-TRF | Baseline | 52 | 70.1 (28.3) | 90 | 69.6 (33.1) |
| 4 months | 46 | 69.1 (28.0) | 65 | 67.8 (33.1) | |
| 12 months | 33 | 59.4 (32.5) | 49 | 65.7 (28.6) | |
| GHQ-12 | Baseline | 104 | 14.8 (6.3) | 150 | 15.1 (6.4) |
| 4 months | 86 | 13.2 (5.9) | 131 | 13.1 (6.2) | |
| 12 months | 74 | 13.2 (6.6) | 114 | 13.2 (6.9) | |
| QRS-F | Baseline | 93 | 15.1 (3.8) | 141 | 16.0 (4.1) |
| 4 months | 77 | 15.8 (4.6) | 124 | 15.8 (4.2) | |
| 12 months | 69 | 15.2 (4.3) | 107 | 15.2 (4.0) | |
| Caregiving Problem Checklist | Baseline | 100 | 33.5 (8.8) | 144 | 34.1 (7.8) |
| 4 months | 85 | 32.8 (10.3) | 127 | 33.6 (7.7) | |
| 12 months | 70 | 31.6 (10.0) | 108 | 30.4 (9.7) | |
| PSOC | Baseline | 99 | 67.5 (11.2) | 143 | 69.4 (11.3) |
| 4 months | 82 | 70.0 (11.4) | 127 | 68.9 (10.8) | |
| 12 months | 71 | 72.0 (12.7) | 109 | 69.8 (9.9) | |
Other caregiver reported Child Behaviour Checklist caregiver−teacher report form at 4 and 12 months
A linear mixed-effects model was fitted with C-TRF total score at 4 months as the outcome variable. This model included only those participants for whom total C-TRF scores were available at baseline and 4-month follow-up. The intervention increased the C-TRF total score at 4 months by an average of 6.17 points (95% CI −7.05 to 19.38; p = 0.351). As such, there is no statistical evidence to suggest a difference in the C-TRF total score at 4 months between the TAU and SSTP groups. The model assumptions were checked and found to be appropriate. Similarly, a linear mixed-effects model was fitted with C-TRF total score at 12 months as the outcome variable. This model included only those participants for whom total C-TRF scores were available at both baseline and 12-month follow-up. The intervention increased the C-TRF score over 12 months by an average of 10.920 points (95% CI −4.07 to 25.91; p = 0.147). As such, there is no statistical evidence to suggest a difference in the C-TRF total score at month 12, between the TAU and SSTP groups. The intervention effect estimate is given in Table 10.
| Difference | 95% CI | p-value | |
|---|---|---|---|
| C-TRF (4 months) | |||
| SSTP vs. TAU | 6.17 | (−7.05 to 19.38) | 0.351 |
| C-TRF (12 months) | |||
| SSTP vs. TAU | 10.92 | (−4.07 to 25.91) | 0.147 |
General Health Questionnaire-12 at 4 and 12 months
A linear mixed-effects model was fitted with GHQ-12 total score at 4 months as the outcome variable. The intervention reduced the GHQ-12 score over 4 months by an average of 0.23 points (95% CI −1.75 to 1.29; p = 0.764). As such, there is no statistical evidence to suggest a difference in the GHQ-12 total score at 4 months between the TAU and SSTP groups. The model assumptions were checked and found to be appropriate. Similarly, a linear mixed-effects model was fitted with GHQ-12 total score at month 12 as the outcome variable. The intervention reduced the GHQ-12 score over 12 months by an average of 0.42 points (95% CI −2.37 to 1.52; p = 0.666). As such, there is no statistical evidence to suggest a difference in the GHQ-12 total score at month 12, between the TAU and SSTP groups. Again, the model assumptions were checked and found to be appropriate. The intervention effect estimate is given in Table 11.
| Difference | 95% CI | p-value | |
|---|---|---|---|
| GHQ-12 (4 months) | |||
| SSTP vs. TAU | −0.23 | (−1.75 to 1.29) | 0.764 |
| GHQ-12 (12 months) | |||
| SSTP vs. TAU | −0.42 | (−2.37 to 1.52) | 0.666 |
Questionnaire on Resources and Stress-short Form at 4 and 12 months
Similarly, a linear mixed-effects model was fitted with QRS-F total score at month 4 as the outcome variable. The intervention reduced the QRS-F score over 4 months by an average of 0.38 points (95% CI −1.40 to 0.63; p = 0.456). As such, there is no statistical evidence to suggest a difference in the QRS-F total score at month 4 between the TAU and SSTP groups. The model assumptions were checked and found to be appropriate. Similarly, a linear mixed-effects model was fitted with QRS-F total score at month 12 as the outcome variable, the intervention effect estimate is given in Table 11. The intervention increased the QRS-F score over 12 months by an average of 0.09 points (95% CI −1.02 to 1.20; p = 0.874). As such, there is no statistical evidence to suggest a difference in the QRS-F total score at month 12, between the TAU and SSTP groups. Again, the model assumptions were checked and found to be appropriate. The intervention effect estimate is given in Table 12.
| Difference | 95% CI | p-value | |
|---|---|---|---|
| QRS-F (4 months) | |||
| SSTP vs. TAU | −0.38 | (−1.40 to 0.63) | 0.456 |
| QRS-F (12 months) | |||
| SSTP vs. TAU | 0.09 | (−1.02 to 1.20) | 0.874 |
Caregiving Problem Checklist at 4 and 12 months
The same linear mixed-effects model was fitted with Caregiving Problem Checklist total score at 4 months as the outcome variable. The intervention increased the Caregiving Problem Checklist total score over 4 months by an average of 0.09 points (95% CI −2.08 to 2.25; p = 0.937). As such, there is no statistical evidence to suggest a difference in the Caregiving Problem Checklist total score at month 4, between the TAU and SSTP groups. The model assumptions were checked and found to be appropriate. Similarly, a linear mixed-effects model was fitted with Caregiving Problem Checklist total score at month 12 as the outcome variable. The intervention reduced the Caregiving Problem Checklist total score over 12 months by an average of 2.05 points (95% CI −4.72 to 0.61; p = 0.129). As such, there is no statistical evidence to suggest a difference in the Caregiving Problem Checklist total score at month 12, between the TAU and SSTP groups. Again, the model assumptions were checked and found to be appropriate. The intervention effect estimate is presented in Table 13.
| Difference | 95% CI | p-value | |
|---|---|---|---|
| Caregiving Problem Checklist (4 months) | |||
| SSTP vs. TAU | 0.09 | (−2.08 to 2.25) | 0.937 |
| Caregiving Problem Checklist (12 months) | |||
| SSTP vs. TAU | −2.05 | (−4.72 to 0.61) | 0.129 |
Parenting Sense of Competence Scale at 4 and 12 months
The same linear mixed-effects model was fitted with PSOC total score at month 4 as the outcome variable. The intervention reduced the PSOC score over 4 months by an average of 1.66 points (95% CI −4.14 to 0.81; p = 0.186). As such, there is no statistical evidence to suggest a difference in the PSOC total score at month 4, between the TAU and SSTP groups. The model assumptions were checked and found to be appropriate. Similarly, a linear mixed-effects model was fitted with PSOC total score at month 12 as the outcome variable. The intervention increased the PSOC score over 12 months by an average of 2.20 points (95% CI −5.29 to 0.88; p = 0.160). As such, there is no statistical evidence to suggest a difference in the PSOC total score at month 12, between the TAU and SSTP groups. Again, the model assumptions were checked and found to be appropriate. The intervention effect estimate is given in Table 14.
| Difference | 95% CI | p-value | |
|---|---|---|---|
| PSOC (4 months) | |||
| SSTP vs. TAU | –1.66 | (−4.14 to 0.81) | 0.186 |
| PSOC (12 months) | |||
| SSTP vs. TAU | −2.20 | (−5.29 to 0.88) | 0.160 |
Internalising and externalising domains of Child Behaviour Checklist at 4 and 12 months
Table 15 provides a summary of CBCL internalising and externalising scores, stratified by allocation arm, at baseline, 4 and 12 months.
| CBCL domain | Assessment | Allocation arm | |||
|---|---|---|---|---|---|
| TAU (n = 106) | SSTP (n = 155) | ||||
| n | Mean (SD) | n | Mean (SD) | ||
| Internalising | Baseline | 105 | 69.5 (8.7) | 155 | 70.0 (8.0) |
| 4 months | 92 | 68.9 (9.7) | 137 | 69.6 (8.3) | |
| 12 months | 83 | 69.5 (8.6) | 129 | 69.9 (9.6) | |
| Externalising | Baseline | 105 | 73.3 (11.9) | 155 | 74.5 (11.2) |
| 4 months | 92 | 72.5 (13.9) | 137 | 71.8 (12.4) | |
| 12 months | 83 | 70.7 (12.7) | 129 | 70.3 (13.2) | |
Two linear mixed-effects models were fitted with CBCL internalising score at 4 months and at 12 months as the outcome variable. The intervention reduced the CBCL internalising score over 4 months by an average of 0.32 points (95% CI −2.37 to 1.72; p = 0.756). As such, there is no statistical evidence to suggest a difference in the CBCL internalising score at 4 months, between the TAU and SSTP groups. The model assumptions were checked and found to be appropriate. The intervention increased the CBCL internalising score over 12 months by an average of 0.21 points (95% CI −2.12 to 2.54; p = 0.856). As such, there is no statistical evidence to suggest a difference in the CBCL internalising T-score at 12 months, between the TAU and SSTP groups. Again, the model assumptions were checked and found to be appropriate. The intervention effect estimate is given in Table 16.
| Difference | 95% CI | p-value | |
|---|---|---|---|
| CBCL internalising T-score (4 months) |
|||
| SSTP vs. TAU | −0.32 | (−2.37 to 1.72) | 0.756 |
| CBCL internalising T-score (12 months) |
|||
| SSTP vs. TAU | 0.21 | −2.12 to 2.54 | 0.856 |
Child Behaviour Checklist externalising score at 4 and 12 months
The same linear mixed-effects model was fitted with CBCL externalising score at 4 months as the outcome variable. The intervention reduced the CBCL externalising score over 4 months by an average of 1.21 points (95% CI −2.97 to 0.54; p = 0.174). As such, there is no statistical evidence to suggest a difference in the CBCL externalising score at 4 months, between the TAU and SSTP groups. The model assumptions were checked and found to be appropriate. Similarly, a linear mixed-effects model was fitted with CBCL externalising score at 12 months as the outcome variable. The intervention effect estimates of both models at 4 and 12 months are given in Table 17. The intervention reduced the CBCL externalising score over 12 months by an average of 1.59 points (95% CI −3.58 to 0.39; p = 0.114). As such, there is no statistical evidence to suggest a difference in the CBCL externalising score at 12 months, between the TAU and SSTP groups. Again, the model assumptions were checked and found to be appropriate.
| Difference | 95% CI | p-value | |
|---|---|---|---|
| CBCL externalising T-score (4 months) |
|||
| SSTP vs. TAU | −1.21 | (−2.97 to 0.54) | 0.174 |
| CBCL externalising T-score (12 months) |
|||
| SSTP vs. TAU | −1.59 | (−3.58 to 0.39) | 0.114 |
Parent–child interaction measured by the Revised Family Observation Schedule
Table 18 provides a summary of child per cent negative behaviour, indicated by the percentage of 30-second observation intervals where at least one (often more than one) of the negative behaviours had occurred (Non-compliance, Complaint, Physical Negative, Oppositional, Interrupt). Table 19 provides descriptive statistics for the total number of intervals that each child and parent behaviour was observed, at baseline, 4 and 12 months, respectively.
| Allocation arm | ||||
|---|---|---|---|---|
| TAU (n = 106) | SSTP (n = 155) | |||
| n | Mean (SD) | n | Mean (SD) | |
| Baseline | 77 | 32.6 (20.3) | 102 | 34.3 (21.1) |
| 4 months | 54 | 26.3 (17.7) | 75 | 28.3 (20.2) |
| 12 months | 35 | 26.9 (20.0) | 45 | 24.0 (18.2) |
| Allocation arm | ||||||
|---|---|---|---|---|---|---|
| TAU (n = 106) | SSTP (n = 155) | |||||
| n | Mean (SD) | Range | n | Mean (SD) | Range | |
| Child behaviours | ||||||
| Positive behaviours | ||||||
| Appropriate verbal activity | ||||||
| Baseline | 77 | 7.3 (8.8) | 0–33 | 102 | 9.1 (10.2) | 0–36 |
| 4 months | 54 | 9.6 (9.5) | 0–32 | 75 | 10.1 (10.7) | 0–36 |
| 12 months | 35 | 12.2 (11.1) | 0–29 | 45 | 12.6 (11.1) | 0–36 |
| Engaged activity | ||||||
| Baseline | 77 | 19.4 (9.1) | 1–39 | 102 | 17.0 (9.6) | 0–38 |
| 4 months | 54 | 19.8 (8.5) | 2–37 | 75 | 18.5 (9.0) | 0–37 |
| 12 months | 35 | 17.0 (12.3) | 1–40 | 45 | 17.3 (10.1) | 1–38 |
| Negative behaviours | ||||||
| Non-compliance | ||||||
| Baseline | 77 | 10.3 (6.4) | 0–28 | 102 | 10.5 (6.6) | 0–30 |
| 4 months | 54 | 8.0 (5.6) | 0–19 | 75 | 9.2 (7.3) | 0–32 |
| 12 months | 35 | 6.4 (5.5) | 0–23 | 45 | 6.2 (5.2) | 0–20 |
| Complaint | ||||||
| Baseline | 77 | 3.6 (5.4) | 0–29 | 102 | 4.3 (6.9) | 0–40 |
| 4 months | 54 | 2.9 (3.6) | 0–15 | 75 | 3.4 (5.4) | 0–28 |
| 12 months | 35 | 2.9 (3.9) | 0–16 | 45 | 1.9 (3.1) | 0–16 |
| Physical negative | ||||||
| Baseline | 77 | 1.2 (2.8) | 0–16 | 102 | 1.3 (2.4) | 0–13 |
| 4 months | 54 | 1.1 (2.3) | 0–9 | 75 | 0.9 (2.0) | 0–12 |
| 12 months | 35 | 1.3 (2.2) | 0–9 | 45 | 0.9 (2.1) | 0–12 |
| Oppositional | ||||||
| Baseline | 77 | 1.0 (1.7) | 0–6 | 102 | 1.2 (2.0) | 0–9 |
| 4 months | 54 | 0.9 (2.1) | 0–10 | 75 | 0.5 (1.3) | 0–7 |
| 12 months | 35 | 1.5 (2.7) | 0–12 | 45 | 0.8 (1.8) | 0–10 |
| Parent behaviours | ||||||
| Positive behaviours | ||||||
| Praise | ||||||
| Baseline | 77 | 5.7 (3.8) | 0–14 | 102 | 5.0 (3.9) | 0–21 |
| 4 months | 54 | 6.3 (3.7) | 0–19 | 75 | 6.5 (4.5) | 0–19 |
| 12 months | 35 | 7.5 (4.5) | 0–20 | 45 | 5.0 (4.6) | 0–18 |
| Contact positive | ||||||
| Baseline | 77 | 9.7 (7.4) | 0–29 | 102 | 8.8 (7.7) | 0–32 |
| 4 months | 54 | 8.6 (8.3) | 0–29 | 75 | 9.8 (8.4) | 0–38 |
| 12 months | 35 | 8.7 (8.3) | 0–30 | 45 | 7.7 (6.2) | 0–23 |
| Instruction | ||||||
| Baseline | 77 | 25.7 (6.0) | 10–38 | 102 | 25.3 (5.5) | 6–39 |
| 4 months | 54 | 24.3 (4.7) | 14–36 | 75 | 25.7 (4.3) | 14–37 |
| 12 months | 35 | 25.5 (5.0) | 14–36 | 45 | 23.6 (5.5) | 9–36 |
| Social attention | ||||||
| Baseline | 77 | 6.4 (4.8) | 0–23 | 102 | 6.9 (4.4) | 0–23 |
| 4 months | 54 | 7.3 (4.6) | 0–16 | 75 | 5.6 (3.8) | 0–19 |
| 12 months | 35 | 7.2 (4.8) | 0–16 | 45 | 7.2 (5.1) | 0–19 |
| Affection | ||||||
| Baseline | 77 | 8.8 (4.6) | 1–18 | 102 | 7.8 (4.7) | 0–21 |
| 4 months | 54 | 9.7 (4.9) | 1–25 | 75 | 9.8 (4.9) | 0–21 |
| 12 months | 35 | 11.1 (5.5) | 3–22 | 45 | 8.0 (5.9) | 1–26 |
| Negative behaviours | ||||||
| Contact negative | ||||||
| Baseline | 77 | 0.0 (0.3) | 0–2 | 102 | 0.1 (0.7) | 0–6 |
| 4 months | 54 | 0.0 (0.1) | 0–1 | 75 | 0.1 (0.7) | 0–5 |
| 12 months | 35 | 0.1 (0.3) | 0–2 | 45 | 0.1 (0.5) | 0–3 |
| Instruction negative | ||||||
| Baseline | 77 | 0.1 (0.6) | 0–5 | 102 | 0.3 (1.2) | 0–9 |
| 4 months | 54 | 0.1 (0.5) | 0–3 | 75 | 0.1 (0.4) | 0–2 |
| 12 months | 35 | 0.2 (0.6) | 0–3 | 45 | 0.0 (0.0) | 0–0 |
| Social attention negative | ||||||
| Baseline | 77 | 0.0 (0.0) | 0–0 | 102 | 0.0 (0.1) | 0–1 |
| 4 months | 54 | 0.0 (0.2) | 0–1 | 75 | 0.0 (0.1) | 0–1 |
| 12 months | 35 | 0.3 (1.9) | 0–11 | 45 | 0.0 (0.0) | 0–0 |
| Number of intervals | ||||||
| Baseline | 77 | 39.6 (1.9) | 26–40 | 102 | 39.8 (1.2) | 33–40 |
| 4 months | 54 | 39.9 (0.8) | 34–40 | 75 | 39.9 (0.7) | 35–40 |
| 12 months | 35 | 39.9 (0.3) | 38–40 | 45 | 39.2 (2.8) | 26–40 |
Mullen Scales of Early Learning
The summary statistics of child level of disability of cognitive functioning measured using the Mullen Scales of Early Learning is provided in Table 20.
| Allocation arm | ||||
|---|---|---|---|---|
| TAU (n = 106) | SSTP (n = 155) | |||
| n | Mean (SD) | n | Mean (SD) | |
| Cognitive T Score | 68 | 98.2 (30.5) | 99 | 97.4 (31.6) |
| Early Learning Composite Standard Score | 68 | 56.1 (11.7) | 98 | 55.6 (13.1) |
| Age equivalent scores | ||||
| Visual reception | 69 | 27.0 (11.3) | 99 | 26.1 (11.9) |
| Fine motor | 70 | 25.7 (10.2) | 101 | 26.5 (10.6) |
| Receptive language | 69 | 22.9 (10.7) | 99 | 23.7 (12.0) |
| Expressive language | 68 | 23.0 (11.2) | 101 | 23.3 (11.6) |
Client Satisfaction Questionnaire
Forty-nine participants from the SSTP group provided feedback at 4 months of their experience of the intervention, including ease of use, format and helpfulness. The total score of the questionnaire is 32. The average score from 49 participants is 27.6 points [SD = 3.0; median = 29 (18, 30)].
Adherence to allocated programme and attrition
Baseline characteristics by primary outcome completion
Whether the participants in the primary analysis were representative of those randomised was initially investigated by comparing the baseline characteristic of the trial participants who had complete primary outcome data to those who did not. Summaries of demographic and outcome variables at baseline, stratified by if the primary outcome is missing, are provided in Tables 21 and 22 for children and parents, respectively. p-values indicate that there is no evidence to suggest a difference between the two groups, except for increased rates of mental health problems in parents who dropped out of the study (40% vs. 25%).
| Missing in primary outcome | p-value | ||
|---|---|---|---|
| Yes (n = 50) |
No (n = 211) |
||
| Mean (SD) | Mean (SD) | ||
| Age (years) | 0.39 | ||
| 3.6 (1.0) | 3.8 (1.0) | ||
| n (%) | n (%) | p -value | |
| Sex | 0.39 | ||
| Female | 15 (30.0) | 51 (24.2) | |
| Male | 35 (70.0) | 160 (75.8) | |
| Ethnicity | 0.46 | ||
| White | 32 (64.0) | 117 (55.5) | |
| Mixed | 7 (14.0) | 22 (10.4) | |
| Asian | 3 (6.0) | 25 (11.8) | |
| Black | 5 (10.0) | 36 (17.1) | |
| Other | 3 (6.0) | 11 (5.2) | |
| Severity intellectual disability | 0.81 | ||
| Moderate | 48 (96.0) | 204 (96.7) | |
| Severe | 2 (4.0) | 7 (3.3) | |
| Site | 0.46 | ||
| Site 1 | 9 (18.0) | 55 (26.1) | |
| Site 2 | 14 (28.0) | 42 (19.9) | |
| Site 3 | 13 (26.0) | 61 (28.9) | |
| Site 4 | 14 (28.0) | 53 (25.1) | |
| ASD/other disorder | 0.60 | ||
| Yes | 32 (64.0) | 126 (60.0) | |
| No | 18 (36.0) | 84 (40.0) | |
| Missing | 0 | 1 | |
| Physical health problems | 0.32 | ||
| Yes | 30 (60.0) | 110 (52.1) | |
| No | 20 (40.0) | 101 (47.9) | |
| Mobility problems | 0.36 | ||
| Yes | 9 (30.0) | 43 (39.1) | |
| No | 21 (70.0) | 67 (60.9) | |
| Missing | 20 | 101 | |
| Sensory problems | 0.79 | ||
| Yes | 15 (50.0) | 58 (52.7) | |
| No | 15 (50.0) | 52 (47.3) | |
| Missing | 20 | 101 | |
| Epilepsy | 0.62 | ||
| Yes | 3 (10.0) | 8 (7.3) | |
| No | 27 (90.0) | 102 (92.7) | |
| Missing | 20 | 101 | |
| Constipation | 0.28 | ||
| Yes | 6 (20.0) | 33 (30.0) | |
| No | 24 (80.0) | 77 (70.0) | |
| Missing | 20 | 101 | |
| Education, health or care plan | 0.85 | ||
| Yes | 18 (36.0) | 79 (37.4) | |
| No | 32 (64.0) | 132 (62.6) | |
| Missing in primary outcome | p-value | ||
|---|---|---|---|
| Yes (n = 50) |
No (n = 211) |
||
| Mean (SD) | Mean (SD) | ||
| Age (years) | 0.17 | ||
| 33.2 (6.0) | 34.6 (6.5) | ||
| n (%) | n (%) | p -value | |
| Ethnicity | 0.60 | ||
| White | 34 (68.0) | 127 (60.2) | |
| Mixed | 2 (4.0) | 7 (3.3) | |
| Asian | 4 (8.0) | 25 (11.8) | |
| Black | 6 (12.0) | 41 (19.4) | |
| Other | 4 (8.0) | 11 (5.2) | |
| Living situation | 0.93 | ||
| Owned property | 12 (24.0) | 48 (22.7) | |
| Rented property | 37 (74.0) | 157 (74.4) | |
| Other | 1 (2.0) | 6 (2.8) | |
| Employment status | 0.13 | ||
| Unemployed | 4 (8.0) | 12 (5.7) | |
| Part-time paid employment – < 30 hours/week | 8 (16.0) | 70 (33.2) | |
| Full-time paid employment | 7 (14.0) | 18 (8.5) | |
| In education | 1 (2.0) | 4 (1.9) | |
| Looking after home and family | 30 (60.0) | 100 (47.4) | |
| Other | 0 (0) | 7 (3.3) | |
| Relationship status | 0.60 | ||
| Single | 15 (30.0) | 62 (29.4) | |
| Married | 21 (42.0) | 90 (42.7) | |
| Separated | 0 (0) | 10 (4.7) | |
| Divorced | 2 (4.0) | 7 (3.3) | |
| Cohabitating | 12 (24.0) | 42 (19.9) | |
|
Main income
(can choose one or more) |
|||
| Salary/wage | 25 (50.0) | 115 (54.5) | 0.57 |
| Family support | 7 (14.0) | 29 (13.7) | 0.96 |
| State benefit | 44 (88.0) | 186 (88.2) | 0.98 |
| Other | 2 (4.0) | 7 (3.3) | 0.81 |
|
Benefit
(can choose one or more) |
|||
| Income support | 12 (27.3) | 52 (28.1) | 0.91 |
| Housing benefit | 19 (43.2) | 85 (45.7) | 0.76 |
| Job seeker allowance | 0 (0) | 4 (2.2) | 1.00 |
| Child benefit | 31 (70.5) | 151 (81.2) | 0.12 |
| Other | 39 (88.6) | 154 (83.2) | 0.38 |
| Mental health problems | 0.04 | ||
| Yes | 20 (40.0) | 53 (25.1) | |
| No | 30 (60.0) | 158 (74.9) | |
| Alcohol or drug abuse | |||
| Yes | 1 (2.0) | 2 (0.9) | 0.47 |
| No | 49 (98.0) | 209 (99.1) | |
| Family violence | 0.73 | ||
| Yes | 4 (8.0) | 14 (6.6) | |
| No | 46 (92.0) | 197 (93.4) | |
Baseline demographic characteristics by adherence
Participants’ adherence is defined as attendance at the majority of the planned group and individual sessions, that is participation in at least 4 (out of 6) group sessions and 2 (out of 3) individual sessions. Of the 155 participants who were randomised to the SSTP arm, 50 participants were adhering to the SSTP intervention. Participants who were adhering to SSTP were compared descriptively with participants who did not adhere to the intervention in terms of their baseline characteristics and results are provided in Tables 23 and 24 for children and parents, respectively. p-values indicate there is a difference between the groups based on adherence in children’s mobility problems, parents’ living situation, relationship status and the receiving of state benefits.
| Adherence | p-value | ||
|---|---|---|---|
| No (n = 105) |
Yes (n = 50) |
||
| Mean (SD) | Mean (SD) | ||
| Age (years) | 0.26 | ||
| 3.7 (1.1) | 3.9 (0.9) | ||
| n (%) | n (%) | p -value | |
| Sex | 0.41 | ||
| Female | 23 (21.9) | 14 (28.0) | |
| Male | 82 (78.1) | 36 (72.0) | |
| Ethnicity | 0.70 | ||
| White | 56 (53.3) | 31 (62.0) | |
| Mixed | 15 (14.3) | 4 (8.0) | |
| Asian | 12 (11.4) | 5 (10.0) | |
| Black | 18 (17.1) | 7 (14.0) | |
| Other | 4 (3.8) | 3 (6.0) | |
| Severity intellectual disability | 0.61 | ||
| Moderate | 102 (97.1) | 49 (98.0) | |
| Severe | 3 (2.9) | 1 (2.0) | |
| Site | 0.16 | ||
| Site 1 | 22 (21.0) | 17 (34.0) | |
| Site 2 | 21 (20.0) | 13 (26.0) | |
| Site 3 | 32 (30.5) | 11 (22.0) | |
| Site 4 | 30 (28.6) | 9 (18.0) | |
| ASD/other disorder | 0.79 | ||
| Yes | 60 (57.7) | 30 (60.0) | |
| No | 44 (42.3) | 20 (40.0) | |
| Missing | 1 | 0 | |
| Physical health problems | 0.39 | ||
| Yes | 51 (48.6) | 28 (56.0) | |
| No | 54 (51.4) | 22 (44.0) | |
| Mobility problems | 0.05 | ||
| Yes | 24 (47.1) | 7 (25.0) | |
| No | 27 (52.9) | 21 (75.0) | |
| Missing | 54 | 22 | |
| Sensory problems | 0.25 | ||
| Yes | 24 (47.1) | 17 (60.7) | |
| No | 27 (52.9) | 11 (39.3) | |
| Missing | 54 | 22 | |
| Epilepsy | 0.05 | ||
| Yes | 1 (2.0) | 4 (14.3) | |
| No | 50 (98.0) | 24 (85.7) | |
| Missing | 54 | 22 | |
| Constipation | 0.69 | ||
| Yes | 16 (31.4) | 10 (35.7) | |
| No | 35 (68.6) | 18 (64.3) | |
| Missing | 54 | 22 | |
| Education, health or care plan | 0.64 | ||
| Yes | 40 (38.1) | 21 (42.0) | |
| No | 65 (61.9) | 29 (58.0) | |
| Adherence | p-value | ||
|---|---|---|---|
| No (n = 105) |
Yes (n = 50) |
||
| Mean (SD) | Mean (SD) | ||
| Age (years) | 0.66 | ||
| 33.9 (6.7) | 34.4 (6.4) | ||
| n (%) | n (%) | p -value | |
| Ethnicity | 0.74 | ||
| White | 63 (60.0) | 32 (64.0) | |
| Mixed | 3 (2.9) | 3 (6.0) | |
| Asian | 12 (11.4) | 5 (10.0) | |
| Black | 22 (21.0) | 7 (14.0) | |
| Other | 5 (4.8) | 3 (6.0) | |
| Living situation | 0.04 | ||
| Owned property | 14 (13.3) | 15 (30.0) | |
| Rented property | 89 (84.8) | 34 (68.0) | |
| Other | 2 (1.9) | 1 (2.0) | |
| Employment status | 0.32 | ||
| Unemployed | 8 (7.6) | 3 (6.0) | |
| Part-time paid employment – < 30 hours/week | 32 (30.5) | 15 (30.0) | |
| Full-time paid employment | 10 (9.5) | 1 (2.0) | |
| In education | 4 (3.8) | 0 (0) | |
| Looking after home and family | 48 (45.7) | 29 (58.0) | |
| Other | 3 (2.9) | 2 (4.0) | |
| Relationship status | 0.01 | ||
| Single | 43 (41.0) | 9 (18.0) | |
| Married | 34 (32.4) | 26 (52.0) | |
| Separated | 6 (5.7) | 0 (0) | |
| Divorced | 3 (2.9) | 2 (4.0) | |
| Cohabitating | 19 (18.1) | 13 (26.0) | |
|
Main income
(can choose one or more) |
|||
| Salary/wage | 56 (53.3) | 26 (52.0) | 0.88 |
| Family support | 14 (13.3) | 11 (22.0) | 0.17 |
| State benefit | 98 (93.3) | 41 (82.0) | 0.03 |
| Other | 5 (4.8) | 0 (0) | 0.18 |
|
Benefit
(can choose one or more) |
|||
| Income support | 30 (30.9) | 10 (24.4) | 0.44 |
| Housing benefit | 50 (51.0) | 18 (43.9) | 0.44 |
| Job seeker allowance | 2 (2.1) | 1 (2.4) | 1.00 |
| Child benefit | 82 (83.7) | 33 (80.5) | 0.65 |
| Other | 79 (81.4) | 36 (87.8) | 0.36 |
| Mental health problems | 0.39 | ||
| Yes | 30 (28.6) | 11 (22.0) | |
| No | 75 (71.4) | 39 (78.0) | |
| Alcohol or drug abuse | 0.55 | ||
| Yes | 3 (2.9) | 0 (0) | |
| No | 102 (97.1) | 50 (100) | |
| Family violence | 0.71 | ||
| Yes | 8 (7.6) | 3 (6.0) | |
| No | 97 (92.4) | 47 (94.0) | |
Per-protocol and CACE analyses were performed as the participant adherence to intervention was relatively low.
Per-protocol analysis
To account for non-adherence in the SSTP arm, a per-protocol analysis was calculated to measure the effect of the intervention on CBCL total score at 12 months, using a linear mixed regression. This analysis excludes non-adhering participants from SSTP and compares the adherence with the TAU group. The effect of the SSTP on CBCL total score at 12 months was estimated as −10.77 (95% CI −19.12 to −2.42). This implies there is a large difference to the previous conclusions concerning the effect of the SSTP intervention on CBCL total score at 12 months. The per-protocol analysis results are presented in Table 25.
| CBCL (12 months) | Difference | 95% CI | p-value |
|---|---|---|---|
| SSTP vs. TAU | −10.77 | (−19.12 to −2.42) | 0.014 |
Complier-average causal effect analysis
A CACE estimate was also calculated to measure the effect of the intervention on CBCL total score at 12 months, using a two-stage least squares approach. This analysis adjusts for non-adherence and maintains randomisation balance by comparing SSTP compliers with TAU participants who would have complied if randomised to SSTP. The effect of the SSTP intervention on CBCL total score at 12 months was estimated as −11.53 (95% CI −26.97 to 3.91). The treatment effect is similar to that from the per-protocol analysis, and the p-value tends to be similar to that from the primary (ITT) analysis. CACE analysis results are presented in Table 26.
| CBCL (12 months) | Difference | 95% CI | p-value |
|---|---|---|---|
| SSTP vs. TAU | −11.53 | (−26.97 to 3.91) | 0.143 |
Imputing Child Behaviour Checklist total score at baseline, 4 and 12 months
Fifty out of 261 participants were missing in the ITT analysis. Therefore, we imputed the primary outcome data using multiple imputation techniques based on chained equations. Specifically, we imputed the total score of the CBCL by two arms using information from the baseline (child age, child sex and baseline CBCL), 4- and 12-month CBCL total scores and other variables (site and level-LD). A total of 19 imputed data sets were created, as there are 19% missing values in the CBCL total at 12 months. Estimates from imputed data sets were combined using Rubin’s rule. The effect of the SSTP intervention on CBCL total score at 12 months was estimated as −4.85 (95% CI −10.24 to 0.54). The results of this analysis are presented in Table 27. The treatment effect is slightly larger than that of the primary analysis, and the p-value indicates that there is weak statistical evidence to suggest a difference in the CBCL total score at 12 months, between the TAU and SSTP groups.
| CBCL (12 months) | Difference | 95% CI | p-value |
|---|---|---|---|
| SSTP vs. TAU | −4.85 | (−10.24 to 0.54) | 0.078 |
Group size
Subgroup analysis based on group size
We also considered whether the intervention effect depends on the size of the session groups. Separate analyses were conducted for: (1) the overall group size; (2) the average group size in sessions attended. We note that these analyses feature post-randomisation variables (session size) and that groups are not balanced by randomisation. Hence these analyses should be regarded as exploratory.
The overall group sizes
The participants were assigned into the following four groups:
-
0 = TAU
-
1 = SSTP (not assigned to SSTP group)
-
2 = SSTP (assigned to SSTP group with at most five people)
-
3 = SSTP (assigned to SSTP group with more than five people).
The same linear mixed-effects model was fitted with CBCL total score at 12 months as the outcome variable. The estimates of the effect of the three intervention groups on CBCL total score at 12 months are given in Table 28.
| CBCL (12 months) | N | Difference | 95% CI | p-value |
|---|---|---|---|---|
| 1: SSTP vs. TAU | 20 | −0.80 | (−11.67 to 10.08) | 0.885 |
| 2: SSTP vs. TAU | 47 | −8.26 | (−16.20 to −0.33) | 0.041 |
| 3: SSTP vs. TAU | 62 | −2.08 | (−10.11 to 5.96) | 0.595 |
This exploratory analysis suggests that children allocated to smaller groups saw bigger reductions in CBCL scores (compared to TAU).
The average group size in sessions attended
The participants were again assigned into the following four groups:
-
0 = TAU
-
1 = SSTP (no group sessions)
-
2 = SSTP (average size 1–3)
-
3 = SSTP (average size > 3).
A linear mixed-effects model was fitted with CBCL total score at 12 months as the outcome variable. The estimates of the effect of the three intervention groups on CBCL total score at 12 months are given in Table 29.
| CBCL (12 months) | N | Difference | 95% CI | p-value |
|---|---|---|---|---|
| 1: SSTP vs. TAU | 48 | −0.93 | (−8.40 to 6.54) | 0.806 |
| 2: SSTP vs. TAU | 41 | −10.08 | (−18.04 to −2.12) | 0.014 |
| 3: SSTP vs. TAU | 40 | −1.79 | (−10.46 to 6.88) | 0.676 |
This exploratory analysis again suggests that parents of children allocated to smaller session groups saw bigger reductions in CBCL scores (compared to TAU).
Unblinding
There were 47 reported unblinding events. Most of the unblindings occurred in the process of scheduling assessments or during a follow-up visit. When unblinding occurred, another researcher from the same or different site completed the subsequent follow-up assessment when possible. Researchers obtained letters of access for other sites and were able to complete follow-ups for other researchers when needed. If researchers were unblinded during the 12-month follow-up, no further action was taken.
Coronavirus disease 2019 considerations
Baseline demographic characteristics before and after 16 March 2020
To study the effect of the COVID-19 pandemic on this trial, the baseline characteristics of children and parents were summarised in Tables 30 and 31 by allocation arm, before and after 16 March 2020.
| Before 16 March 2020 | After 16 March 2020 | p-value | |||
|---|---|---|---|---|---|
| TAU (n = 87) |
SSTP (n = 123) |
TAU (n = 19) |
SSTP (n = 32) |
Before vs. After |
|
| Mean (SD), median (IQR) | Mean (SD), median (IQR) | Mean (SD), median (IQR) | Mean (SD), median (IQR) | ||
| Age (years) | 0.87 | ||||
| 3.7 (0.9) | 3.7 (1.1) | 3.8 (1.0) | 3.8 (0.9) | ||
| 3.9 (3.1–4.3) | 3.9 (3.2–4.5) | 3.8 (3.3–4.4) | 4.0 (3.1–4.3) | ||
| Missing | 0 | 1 | |||
| n (%) | n (%) | n (%) | n (%) | ||
| Sex | 0.27 | ||||
| Female | 21 (24.1) | 29 (23.6) | 11 (57.9) | 24 (75.0) | |
| Male | 66 (75.9) | 94 (76.4) | 8 (42.1) | 8 (25.0) | |
| Ethnicity | 0.27 | ||||
| White | 51 (58.6) | 76 (61.8) | 11 (57.9) | 11 (34.4) | |
| Mixed | 8 (9.2) | 14 (11.4) | 2 (10.5) | 5 (15.6) | |
| Asian | 11 (12.6) | 10 (8.1) | 0 (0) | 7 (21.9) | |
| Black | 12 (13.8) | 18 (14.6) | 4 (21.1) | 7 (21.9) | |
| Other | 5 (5.7) | 5 (4.1) | 2 (10.5) | 2 (6.3) | |
| Severity of intellectual disability | 0.52 | ||||
| Moderate | 82 (94.3) | 120 (97.6) | 19 (100) | 31 (96.9) | |
| Severe | 5 (5.7) | 3 (2.4) | 0 (0) | 1 (3.1) | |
| Site | < 0.01 | ||||
| Site 1 | 25 (28.7) | 39 (31.7) | 0 (0) | 0 (0) | |
| Site 2 | 17 (19.5) | 21 (17.1) | 5 (26.3) | 13 (40.6) | |
| Site 3 | 24 (27.6) | 32 (26.0) | 7 (36.8) | 11 (34.4) | |
| Site 4 | 21 (24.1) | 31 (25.2) | 7 (36.8) | 8 (25.0) | |
| ASD | 0.66 | ||||
| Yes | 55 (63.2) | 74 (60.2) | 13 (68.4) | 16 (51.6) | |
| No | 32 (36.8) | 49 (39.8) | 6 (31.6) | 15 (48.4) | |
| Missing | 0 | 0 | 0 | 1 | |
| Physical health | 0.67 | ||||
| Yes | 49 (56.3) | 65 (52.8) | 12 (63.2) | 14 (43.8) | |
| No | 38 (43.7) | 58 (47.2) | 7 (36.8) | 18 (56.3) | |
| Mobility difficulties | 0.88 | ||||
| Yes | 16 (32.7) | 26 (40.0) | 5 (41.7) | 5 (35.7) | |
| No | 33 (67.3) | 39 (60.0) | 7 (58.3) | 9 (64.3) | |
| Missing | 38 | 58 | 7 | 18 | |
| Sensory impairments | < 0.01 | ||||
| Yes | 23 (46.9) | 30 (46.2) | 9 (75.0) | 11 (78.6) | |
| No | 26 (53.1) | 35 (53.8) | 3 (25.0) | 3 (21.4) | |
| Missing | 38 | 58 | 7 | 18 | |
| Epilepsy | 0.40 | ||||
| Yes | 5 (10.2) | 5 (7.7) | 1 (8.3) | 0 (0) | |
| No | 44 (89.8) | 60 (92.3) | 11 (91.7) | 14 (100) | |
| Missing | 38 | 58 | 7 | 18 | |
| Constipation | 0.39 | ||||
| Yes | 9 (18.4) | 21 (32.3) | 4 (33.3) | 5 (35.7) | |
| No | 40 (81.6) | 44 (67.7) | 8 (66.7) | 9 (64.3) | |
| Missing | 38 | 58 | 7 | 18 | |
| Education, health or care plan | 0.51 | ||||
| Yes | 30 (34.5) | 46 (37.4) | 6 (31.6) | 15 (46.9) | |
| No | 57 (65.5) | 77 (62.6) | 13 (68.4) | 17 (53.1) | |
| Before 16 March 2020 | After 16 March 2020 | p-value | |||
|---|---|---|---|---|---|
| TAU (n = 87) |
SSTP (n = 123) |
TAU (n = 19) |
SSTP (n = 32) |
Before vs. After |
|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||
| Age (years) | 0.23 | ||||
| 34.6 (6.4) | 33.8 (6.4) | 35.7 (5.7) | 34.9 (7.3) | ||
| 34 (30–39) | 33 (29–38) | 35 (32–37) | 33.5 (29–41) | ||
| n (%) | n (%) | n (%) | n (%) | ||
| Ethnicity | 0.59 | ||||
| White | 52 (59.8) | 82 (66.7) | 14 (73.7) | 13 (40.6) | |
| Mixed | 3 (3.4) | 4 (3.3) | 0 (0) | 2 (6.3) | |
| Asian | 12 (13.8) | 10 (8.1) | 0 (0) | 7 (21.9) | |
| Black | 15 (17.2) | 22 (17.9) | 3 (15.8) | 7 (21.9) | |
| Other | 5 (5.7) | 5 (4.1) | 2 (10.5) | 3 (9.4) | |
| Living situation | 0.65 | ||||
| Owned property | 26 (29.9) | 25 (20.3) | 5 (26.3) | 4 (12.5) | |
| Rented property | 58 (66.7) | 96 (78.0) | 13 (68.4) | 27 (84.4) | |
| Other | 3 (3.4) | 2 (1.6) | 1 (5.3) | 1 (3.1) | |
| Employment status | 0.10 | ||||
| Unemployed | 3 (3.4) | 8 (6.5) | 2 (10.5) | 3 (9.4) | |
| Part-time paid employment – < 30 hours/week | 24 (27.6) | 39 (31.7) | 7 (36.8) | 8 (25.0) | |
| Full-time paid employment | 12 (13.8) | 4 (3.3) | 2 (10.5) | 7 (21.9) | |
| In education | 1 (1.1) | 4 (3.3) | 0 (0) | 0 (0) | |
| Looking after home and family | 45 (51.7) | 64 (52.0) | 8 (42.1) | 13 (40.6) | |
| Other | 2 (2.3) | 4 (3.3) | 0 (0) | 1 (3.1) | |
| Relationship status | 0.36 | ||||
| Single | 21 (24.1) | 42 (34.1) | 4 (21.1) | 10 (31.3) | |
| Married | 41 (47.1) | 42 (34.1) | 10 (52.6) | 18 (56.3) | |
| Separated | 3 (3.4) | 6 (4.9) | 1 (5.3) | 0 (0) | |
| Divorced | 3 (3.4) | 5 (4.1) | 1 (5.3) | 0 (0) | |
| Cohabitating | 19 (21.8) | 28 (22.8) | 3 (15.8) | 4 (12.5) | |
|
Main income
(can choose one or more) |
|||||
| Salary/wage | 46 (52.9) | 62 (50.4) | 12 (63.2) | 20 (62.5) | 0.19 |
| Family support | 10 (11.5) | 22 (17.9) | 1 (5.3) | 3 (9.4) | 0.16 |
| State benefit | 73 (83.9) | 113 (91.9) | 18 (94.7) | 26 (81.3) | 0.68 |
| Other | 3 (3.4) | 5 (4.1) | 1 (5.3) | 0 (0) | 0.50 |
|
Benefit
(can choose one or more) |
|||||
| Income support | 22 (30.1) | 35 (31.3) | 2 (11.1) | 5 (19.2) | 0.04 |
| Housing benefit | 32 (43.8) | 58 (51.3) | 4 (22.2) | 10 (38.5) | 0.04 |
| Job seeker allowance | 1 (1.4) | 2 (1.8) | 0 (0) | 1 (3.8) | 0.78 |
| Child benefit | 55 (75.3) | 95 (84.1) | 12 (66.7) | 20 (76.9) | 0.16 |
| Other | 62 (84.9) | 95 (84.8) | 16 (88.9) | 20 (76.9) | 0.66 |
| Mental health problems | 0.39 | ||||
| Yes | 28 (32.2) | 33 (26.8) | 4 (21.1) | 8 (25.0) | |
| No | 59 (67.8) | 90 (73.2) | 15 (78.9) | 24 (75.0) | |
| Alcohol or drug abuse | 0.39 | ||||
| Yes | 0 (0) | 3 (2.4) | 0 (0) | 0 (0) | |
| No | 87 (100) | 120 (97.6) | 19 (100) | 32 (100) | |
| Family violence | 0.18 | ||||
| Yes | 6 (6.9) | 7 (5.7) | 1 (5.3) | 4 (12.5) | |
| No | 81 (93.1) | 116 (94.3) | 18 (94.7) | 28 (87.5) | |
Adherence to the programme and attrition
The adherence to the programme and attrition are also summarised before and after 16 March 2020 in Table 32.
| Before 16 March 2020 | After 16 March 2020 | |||
|---|---|---|---|---|
| TAU (n = 87) (%) |
SSTP (n = 123) (%) |
TAU (n = 19) (%) |
SSTP (n = 32) (%) |
|
| Adherence | N/A | 40 (33) | N/A | 10 (31) |
|
Missing
primary outcome |
20 (23) | 21 (17) | 4 (21) | 5 (16) |
Subgroup analysis based on the coronavirus disease 2019 impact
We performed a subgroup analysis to investigate whether the intervention effect differed depending on whether recruitment was before or after 16 March 2020, using the primary mixed model with an interaction term. In this model, the mean difference of the effect of the SSTP intervention on CBCL total score at 12 months between those participants who were recruited before 16 March 2020 and those after 16 March 2020 were estimated as −7.12 and 7.61, respectively. The interaction p-value of 0.046 suggests the effect of SSTP was significantly different pre-pandemic compared to during the pandemic. In addition, the point estimates suggest the direction of effect may have reversed after the start of the pandemic, though the confidence interval for the ‘during’ estimate is wide due to small patient numbers. See Table 33 for further details.
| CBCL (12 months) | Period | Difference | 95% CI |
|---|---|---|---|
| SSTP vs. TAU | Before | −7.12 | (−13.44 to −0.81) |
| During | 7.61 | (−5.43 to 20.64) |
Serious adverse event reporting
Twenty SAEs were reported in total, with 12 in the SSTP arm and 8 in the TAU arm. Thirteen children were reported to have SAE incidents, with five from SSTP and eight from TAU; seven parents from the SSTP group reported SAEs. In the intervention arm, four children were admitted to hospital for illnesses such as tonsillitis and breathing problems. Two parents were also admitted to the hospital during the study for burns and other reasons. There was also one reported case of domestic abuse, two cases of child removal from the parent’s care and two cases of significant parent distress. One further parent reported persistent and significant disability. In the TAU arm, seven children were admitted to the hospital due to illnesses, such as ear or chest infections, or acute exacerbation of chronic conditions, including asthma. The final SAE was related to a child being removed from the parent’s care. None of these adverse events was deemed to be related to the intervention. All of these events were not side effects or outcomes of participation in the intervention.
Six SAEs were reported after 16 March 2020, with two parents and one child from the SSTP arm, and two children from the TAU arm.
Cost-effectiveness
Cost of training and delivery of Stepping Stones Triple P
In total, 11 therapists across the four services received training in delivering SSTP. The cost of the training was £26 per participant (Table 34). Details of the activities carried out by therapists were estimated at an average cost of £270 (see Report Supplementary Material 4). Training and delivery of the SSTP were estimated at a total average cost of £296 per study participant.
| Activity | Total cost |
|---|---|
| 1. Leaflet (postage) | £1827 |
| 2. Workshops | |
| I. SSTP – 3 days | £2107 |
| ll. Accreditation (30 minutes) | |
| III. SSTP trainer | |
| 3. Preparation for workshops (3 days × 0.5 hours) | £75 |
| Grand total | £4009 |
| Cost per participant (assuming 155 participants in intervention arm) | £26 |
Healthcare resource use costs
The participants accessed a wide range of health, education, social care and child-care services and attended a range of schools and child-care facilities (including nurseries, playgroups and childminders). Unit costs of health and social care and medication are presented in Report Supplementary Material 4 Tables S2 and S3. Descriptive statistics for resource use are reported in Report Supplementary Material 4 Table S4. Statistical tests were applied to cost differences. Health and social care and societal costs are reported in Table 35. Parental group costs were significantly higher for the SSTP arm (adjusted mean difference = £38.97, p = 0.013), whereas health visitor costs were significantly higher for the TAU arm (adjusted mean difference = £53.08, p = 0.001).
| SSTP | TAU | Adjusted* mean difference | p-value | 95% CI (lower limit) | 95% CI (upper limit) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | ||||||
| Hospital services costs | |||||||||||
| Inpatient stays | Baseline | 155 | 584 | 5005 | 106 | 336 | 1763 | ||||
| 4 months | 137 | 118 | 709 | 92 | 195 | 997 | |||||
| 12 months | 129 | 29 | 232 | 83 | 699 | 4842 | |||||
| Total cost | 124 | 844 | 5808 | 79 | 1413 | 6637 | −903.45 | 0.057 | −1833.80 | 26.90 | |
| Outpatient appointments | Baseline | 155 | 348 | 559 | 106 | 423 | 848 | ||||
| 4 months | 137 | 182 | 344 | 92 | 242 | 498 | |||||
| 12 months | 129 | 174 | 424 | 83 | 280 | 589 | |||||
| Total cost | 124 | 667 | 1018 | 79 | 995 | 1716 | −101.58 | 0.247 | −274.10 | 70.94 | |
| Accident and emergency attendances | Baseline | 155 | 72 | 168 | 106 | 117 | 292 | ||||
| 4 months | 137 | 41 | 119 | 92 | 61 | 141 | |||||
| 12 months | 129 | 49 | 251 | 83 | 64 | 210 | |||||
| Total cost | 124 | 171 | 464 | 79 | 254 | 567 | 8.07 | 0.842 | −71.60 | 87.74 | |
| Community services costs | |||||||||||
| GP | Baseline | 155 | 57 | 99 | 106 | 72 | 122 | ||||
| 4 months | 137 | 37 | 137 | 91 | 36 | 69 | |||||
| 12 months | 129 | 24 | 44 | 83 | 42 | 95 | |||||
| Total cost | 124 | 118 | 208 | 78 | 161 | 222 | −15.16 | 0.474 | −56.81 | 26.49 | |
| Practice nurse | Baseline | 155 | 12 | 35 | 106 | 16 | 40 | ||||
| 4 months | 137 | 9 | 42 | 92 | 5 | 17 | |||||
| 12 months | 129 | 5 | 15 | 83 | 10 | 30 | |||||
| Total cost | 124 | 26 | 72 | 79 | 33 | 62 | −1.60 | 0.785 | −13.16 | 9.96 | |
| Health visitor | Baseline | 155 | 72 | 160 | 106 | 60 | 117 | ||||
| 4 months | 137 | 24 | 92 | 92 | 46 | 107 | |||||
| 12 months | 129 | 8 | 29 | 83 | 24 | 74 | |||||
| Total cost | 124 | 97 | 209 | 79 | 133 | 205 | −53.08 | 0.001 | −85.37 | −20.79 | |
| Community paediatrician | Baseline | 155 | 250 | 350 | 106 | 227 | 285 | ||||
| 4 months | 137 | 108 | 192 | 91 | 119 | 238 | |||||
| 12 months | 129 | 94 | 185 | 83 | 147 | 309 | |||||
| Total cost | 124 | 480 | 559 | 78 | 506 | 545 | −72.84 | 0.139 | −169.54 | 23.85 | |
| Social worker | Baseline | 155 | 49 | 197 | 106 | 36 | 131 | ||||
| 4 months | 137 | 42 | 284 | 92 | 43 | 221 | |||||
| 12 months | 129 | 85 | 517 | 83 | 24 | 82 | |||||
| Total cost | 124 | 175 | 819 | 79 | 109 | 322 | 88.87 | 0.352 | −99.15 | 276.89 | |
| Educational psychologist | Baseline | 155 | 47 | 201 | 106 | 26 | 67 | ||||
| 4 months | 137 | 15 | 40 | 91 | 21 | 64 | |||||
| 12 months | 129 | 18 | 46 | 83 | 39 | 165 | |||||
| Total cost | 124 | 80 | 230 | 78 | 98 | 207 | −32.63 | 0.091 | −70.47 | 5.22 | |
| Special educational need co-ordinator/early years co-ordinator | Baseline | 155 | 38 | 105 | 106 | 33 | 98 | ||||
| 4 months | 137 | 22 | 124 | 91 | 13 | 27 | |||||
| 12 months | 129 | 17 | 62 | 83 | 17 | 46 | |||||
| Total cost | 124 | 81 | 187 | 78 | 61 | 112 | 13.98 | 0.430 | −20.89 | 48.85 | |
| Any parental group | Baseline | 155 | 34 | 91 | 106 | 16 | 67 | ||||
| 4 months | 137 | 51 | 89 | 92 | 13 | 50 | |||||
| 12 months | 128 | 17 | 51 | 83 | 13 | 66 | |||||
| Total cost | 123 | 100 | 129 | 79 | 47 | 120 | 38.97 | 0.013 | 8.48 | 69.47 | |
| Play therapist | Baseline | 155 | 26 | 183 | 106 | 15 | 89 | ||||
| 4 months | 137 | 8 | 48 | 92 | 13 | 67 | |||||
| 12 months | 129 | 1 | 7 | 83 | 13 | 73 | |||||
| Total cost | 124 | 33 | 197 | 79 | 43 | 163 | −22.20 | 0.087 | −47.65 | 3.25 | |
| Art/music/drama therapist | Baseline | 155 | 6 | 46 | 106 | 7 | 42 | ||||
| 4 months | 137 | 2 | 15 | 92 | 3 | 17 | |||||
| 12 months | 129 | 2 | 13 | 83 | 6 | 43 | |||||
| Total cost | 124 | 8 | 51 | 79 | 14 | 68 | −6.54 | 0.233 | −17.33 | 4.25 | |
| Occupational therapist | Baseline | 155 | 175 | 484 | 106 | 189 | 623 | ||||
| 4 months | 137 | 79 | 305 | 92 | 133 | 512 | |||||
| 12 months | 129 | 195 | 667 | 83 | 289 | 787 | |||||
| Total cost | 124 | 450 | 1352 | 79 | 673 | 1637 | −88.81 | 0.436 | −313.21 | 135.58 | |
| Speech and language therapist | Baseline | 155 | 407 | 729 | 106 | 459 | 924 | ||||
| 4 months | 137 | 235 | 556 | 92 | 302 | 806 | |||||
| 12 months | 129 | 363 | 1203 | 83 | 429 | 874 | |||||
| Total cost | 124 | 1008 | 1889 | 79 | 1272 | 2250 | −50.78 | 0.812 | −471.72 | 370.16 | |
| Physiotherapist | Baseline | 155 | 54 | 166 | 106 | 63 | 312 | ||||
| 4 months | 137 | 23 | 110 | 92 | 29 | 99 | |||||
| 12 months | 129 | 48 | 216 | 83 | 94 | 406 | |||||
| Total cost | 124 | 114 | 421 | 79 | 209 | 790 | −4.78 | 0.886 | −70.68 | 61.11 | |
| Dietician/nutritionist | Baseline | 155 | 16 | 56 | 106 | 34 | 142 | ||||
| 4 months | 137 | 11 | 38 | 92 | 13 | 47 | |||||
| 12 months | 129 | 6 | 35 | 83 | 5 | 22 | |||||
| Total cost | 124 | 27 | 73 | 79 | 59 | 181 | 0.93 | 0.912 | −15.49 | 17.34 | |
| Osteopath | Baseline | 155 | 0.3 | 3 | 106 | 2 | 12 | ||||
| 4 months | 137 | 0.3 | 3 | 92 | 0 | 0 | |||||
| 12 months | 129 | 0 | 0 | 83 | 0 | 4 | |||||
| Total cost | 124 | 0.3 | 4 | 79 | 3 | 16 | 0.31 | 0.554 | −0.72 | 1.34 | |
| Alternative therapies | Baseline | 154 | 0.6 | 7 | 104 | 23 | 168 | ||||
| 4 months | 134 | 0.4 | 4 | 88 | 119 | 1105 | |||||
| 12 months | 129 | 243 | 2679 | 80 | 5 | 40 | |||||
| Total cost | 121 | 254 | 2765 | 71 | 41 | 258 | 251.63 | 0.470 | −434.71 | 937.97 | |
| Equipment | Baseline | 155 | 113 | 674 | 106 | 70 | 268 | ||||
| 4 months | 137 | 100 | 666 | 92 | 36 | 206 | |||||
| 12 months | 129 | 33 | 173 | 83 | 34 | 129 | |||||
| Total cost | 124 | 284 | 1377 | 79 | 112 | 306 | 39.20 | 0.561 | −93.67 | 172.06 | |
| Prescriptions | Baseline | 155 | 61 | 148 | 106 | 96 | 413 | ||||
| 4 months | 137 | 38 | 98 | 92 | 46 | 148 | |||||
| 12 months | 129 | 54 | 144 | 83 | 106 | 381 | |||||
| Total cost | 124 | 154 | 302 | 79 | 268 | 992 | −13.27 | 0.564 | −58.57 | 32.04 | |
| Out-of-pocket expenditure | |||||||||||
| Equipment | Baseline | 155 | 801 | 8032 | 106 | 106 | 232 | ||||
| 4 months | 137 | 65 | 286 | 92 | 53 | 140 | |||||
| 12 months | 129 | 792 | 5584 | 83 | 261 | 1646 | |||||
| Total cost | 124 | 1006 | 5712 | 79 | 415 | 1698 | 497.23 | 0.468 | −851.42 | 1845.88 | |
| Supplements | Baseline | 155 | 17 | 30 | 106 | 16 | 33 | ||||
| 4 months | 137 | 11 | 26 | 92 | 13 | 64 | |||||
| 12 months | 129 | 17 | 36 | 83 | 10 | 28 | |||||
| Total cost | 124 | 48 | 63 | 79 | 41 | 99 | 1.28 | 0.878 | −15.15 | 17.71 | |
Quality-adjusted life-years
There were no significant differences between the SSTP and the TAU arms for QALYs (Table 36).
| SSTP | TAU | Adjusted* mean difference | p- value | 95% CI (lower limit) | 95% CI (upper limit) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | ||||||
| Child | Baseline | 140 | 0.637 | 0.145 | 98 | 0.615 | 0.157 | ||||
| 4 months | 119 | 0.643 | 0.174 | 80 | 0.626 | 0.154 | |||||
| 12 months | 109 | 0.641 | 0.155 | 70 | 0.613 | 0.152 | |||||
| QALYs | 89 | 0.653 | 0.138 | 59 | 0.609 | 0.140 | −0.002 | 0.930 | −0.038 | 0.035 | |
| Parent | Baseline | 152 | 0.799 | 0.189 | 106 | 0.799 | 0.211 | ||||
| 4 months | 130 | 0.810 | 0.216 | 86 | 0.811 | 0.180 | |||||
| 12 months | 116 | 0.827 | 0.203 | 75 | 0.826 | 0.194 | |||||
| QALYs | 108 | 0.820 | 0.171 | 67 | 0.823 | 0.148 | 0.007 | 0.718 | −0.032 | 0.046 | |
Overall economic evaluation
All economic analyses were carried out on an ITT basis using an analysis plan finalised prior to data analysis. Assuming the data are missing at random, multiple imputation by chained equations (MICE) was used to impute missing costs and utilities at 4 and 12 months. Thirty-five per cent of participants had missing data for at least one follow-up point, and hence 35 imputed data sets were created. Seemingly unrelated regression was used to account for the correlation between costs and outcomes, with adjustment for baseline costs, utilities, CBCL, site and level of intellectual disability. The results for total costs and QALYs are based on imputed data for calculating CEACs using bootstrapping and MICE for 100 draws of each of the 35 imputed data sets for 3500 replications in total.
The primary economic evaluation was a within-trial cost-effectiveness analysis at 12 months, covering 10 months of cost data, from a health and social care cost perspective with QALYs derived from health utility scores, obtained from the PedsQL™ GCS and mapped EQ-5D-Y utility scores algorithm to provide an empirical basis for estimating health utilities. Using imputed, bootstrapped, adjusted data, SSTP dominates TAU, with a mean cost saving of −£1057.88 per participant (95%CI −£3218.6 to −£46.67) and a mean QALY difference of 0.005 (95% CI −0.023 to 0.051). The CEP and CEAC are reported in Figures 3 and 4, respectively. There is an 89% probability that SSTP is cost-effective compared to TAU at a WTP for a QALY gained of £20,000 and £30,000. There is a 90% probability that SSTP is cost-effective compared to TAU at a WTP for a QALY gained of £13,000.
FIGURE 3.
Cost-effectiveness plane of SSTP compared to TAU from a health and social care cost perspective at 12 months, covering 10 months cost data.

FIGURE 4.
Cost-effectiveness acceptability curve of SSTP compared to TAU from a health and social care cost perspective at 12 months, covering 10 months of costs (results based on 3500 bootstraps of imputed data).
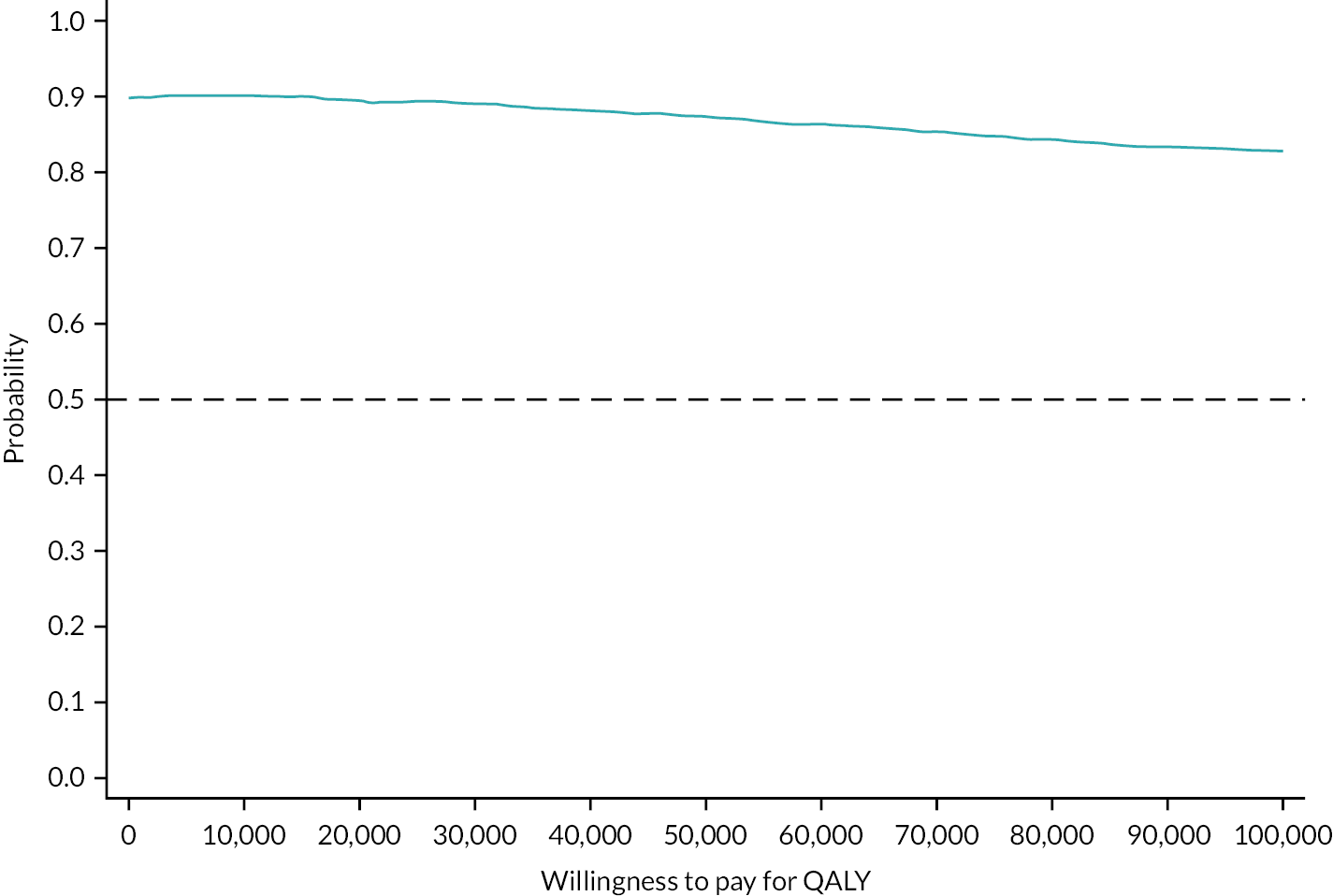
Secondary analyses
Societal costs include private service use and out-of-pocket expenses. We conducted cost-effectiveness analyses from the societal perspective with QALYs derived for children and parents/caregivers.
Analyses conducted with QALYs derived for children show that there is a mean cost difference of −£511.01 per participant (95% CI −£2378.17 to £1175.53) and a mean QALY difference of 0.006 (95% CI −0.023 to 0.050) between study arms. There is 70% probability that SSTP is cost-effective compared to TAU at a WTP for a QALY gained of £20,000 and 71% probability at a WTP for a QALY gained of £30,000. There is 69% probability that SSTP is cost-effective compared to TAU at a WTP for a QALY gained of £13,000 (Figure 5).
FIGURE 5.
Cost-effectiveness plane and CEACs of SSTP compared to TAU from a societal cost perspective with QALYs derived for children at 12 months, covering 10 months of costs.

Analyses conducted with QALYs derived for parents/caregivers show that there is a mean cost difference of −£984.87 per participant (95% CI −£2378.17 to £1175.53) and a mean QALY difference of 0.002 (95% CI −0.031 to 0.044) between the study arms. There is 78% probability that SSTP is cost-effective compared to TAU at a WTP for a QALY gained of £20,000, £30,000 and £13,000 (Figure 6).
FIGURE 6.
Cost-effectiveness plane and CEACs of SSTP compared to TAU from a societal cost perspective with QALYs derived for parents at 12 months, covering 10 months of costs.

Sensitivity analyses
We projected costs using linear regression from 4- and 12-month follow-ups to estimate the 12-month health and social care data to calculate cost-effectiveness from 200 participants with complete primary outcome and cost data. The mean cost difference for the imputed, bootstrapped, adjusted data was −£1133.79 per participant (95% CI −£3226.21 to −£78.51). The mean QALY difference was 0.004 (95% CI −0.023 to 0.050). There is an 88% probability that SSTP is cost-effective compared to TAU at a WTP for a QALY gained of £20,000, £30,000 and £13,000 (Figure 7).
FIGURE 7.
Cost-effectiveness plane and CEACs of SSTP compared to TAU from a health and social care cost perspective with projected costs to cover 12 months.
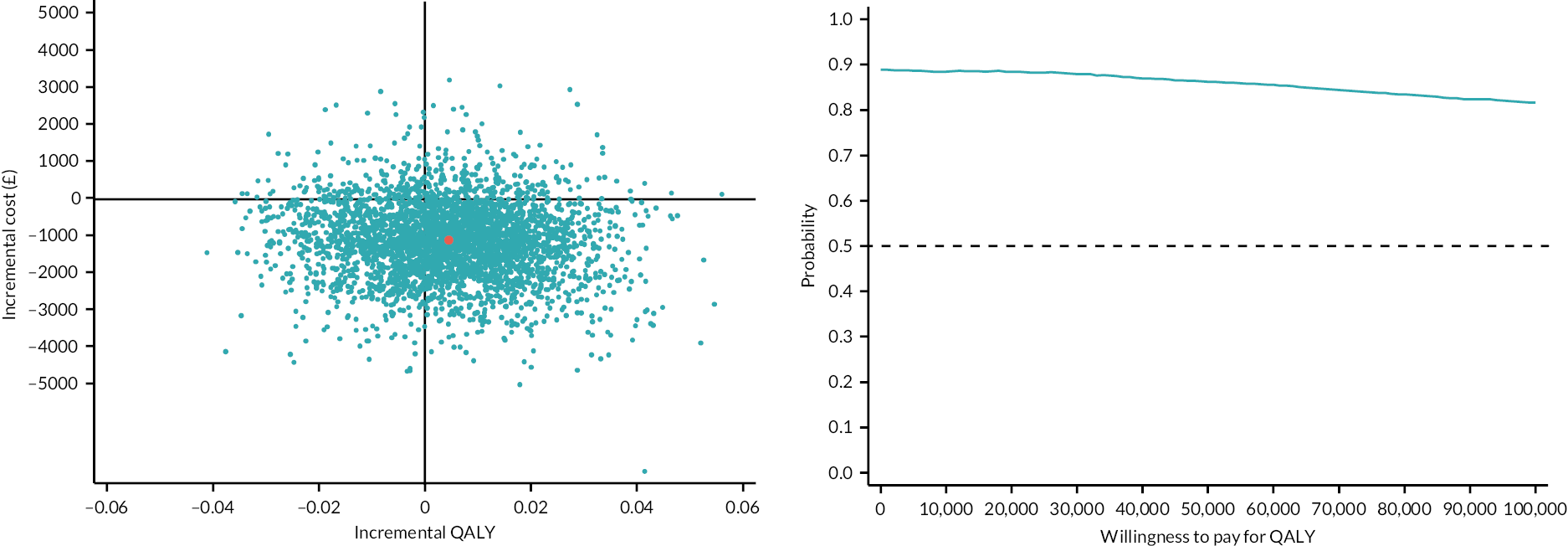
We tested the impact of varying training costs (particularly because of larger participant numbers per staff member trained) on the mean incremental cost per QALY gained. If all participants in the trial would have received the intervention, the cost of the training would have been reduced to £15 per participant. The mean cost difference for the imputed, bootstrapped, adjusted data was −£1068.88 per participant (95% CI −£3229.60 to −£57.67). The mean QALY difference was 0.005 (95% CI −0.023 to 0.050). There is an 89% probability that SSTP is cost-effective compared to TAU at a WTP for a QALY gained of £20,000 and £30,000 and a 90% probability at a WTP for a QALY gained of £13,000 (Figure 8).
FIGURE 8.
Cost-effectiveness plane and CEACs of SSTP compared to TAU from a health and social care cost perspective with reduced cost of intervention.

We conducted a sensitivity analysis using imputed, bootstrapped, adjusted data including therapist clustering in the intervention arm as a random effect. This model also adjusted for baseline CBCL score and randomisation stratification factors (centre, level of intellectual disability) using fixed effects. The mean t difference in cost is −£1158.85 per participant (95% CI −£1896.46 to −£421.24) and the mean QALY difference is 0.007 (95% CI −0.008 to 0.021).
Coronavirus disease 2019 pandemic considerations
We performed a subgroup analysis to investigate whether the effect of intervention on participants’ HRQoL differs depending on whether recruitment was before or after 16 March 2020 (start of lockdown), using the multilevel (mixed) model. The mean difference in the effect of the SSTP intervention on HRQoL in participants recruited before and after lockdown was estimated as 0.055 and −0.042, respectively, with a p-value of 0.119 which suggests that there is no interaction between the COVID-19 pandemic and the effect of the intervention on HRQoL (Table 37).
| Health utilities (12 months) |
Period | Difference | 95% CI |
|---|---|---|---|
| SSTP vs. TAU | Before | 0.055 | (−0.027 to 0.137) |
| After | −0.042 | (−0.173 to 0.088) |
Commentary
At 12 months, covering 10 months of costs, the intervention dominated TAU in that it cost £1058 less than TAU from a health and social care cost perspective with a positive mean point estimate for QALYs, although there was no significant QALY difference between trial arms. There is a high probability that SSTP is cost-effective compared to TAU for a range of WTP values for a QALY gained. The cost of training to deliver the SSTP intervention is relatively low for a psychological intervention at £26 per participant; this is also accompanied by a slight increase in QALYs, in the intervention arm compared with TAU, although not statistically significant. Nevertheless, this finding should be considered with caution as QALYs are a secondary trial outcome and PedsQL™ GCS and the mapped EQ-5D-Y utility scores algorithm were used to calculate QALYs. We were unable to include a generic outcome measure as there is no valid, preference-based measure for health state valuation in children under the age of 5 or children with intellectual disabilities.
In terms of service use, there were a few differences observed between the two arms. Parental group costs were significantly higher for the SSTP arm (adjusted mean difference = £38.97, p = 0.013), whereas health visitor costs were significantly higher for the TAU arm (adjusted mean difference = £53.08, p = 0.001). There was a statistically significant difference in total cost when analyses were conducted from the health and social care cost perspective. However, the results should be interpreted cautiously. Confidence intervals were wide due to substantial variation in several community services. The societal perspective only includes private service use and out-of-pocket expenses. Information on informal care and productivity losses however were not collected as part of the trial and hence the true wider societal cost will have been higher, with potentially greater differences between the two groups. Any future health economic evaluations in this area should continue to measure the impact on parents/carers by collecting all relevant information that might affect parents/careers to ensure a robust analysis.
In conclusion, the addition of the SSTP intervention to TAU for children aged between 3 and 5 years with intellectual disabilities did generate statistically significant cost savings alongside a positive mean point estimate in HRQoL compared to TAU; however, the improvements in HRQoL (QALYs) were not statistically significant.
Chapter 5 Process evaluation
Introduction
Stepping Stones Triple P can be defined as a complex intervention, meaning it includes a number of interacting components. 73 It can be challenging to evaluate whether complex interventions work and whether they are effective in practice. Process evaluations can be used to provide information on how an intervention may be replicated and assess factors that influence study outcomes and trial effects. 73,74 This can help to identify whether a lack of effect is linked to implementation shortcomings rather than the intervention itself and whether additional factors should be considered for the successful implementation of the intervention in the real world.
The process evaluation conducted in this trial was based on the revised Medical Research Council (MRC) guidance. 74 The framework incorporates several key functions that are essential to a process evaluation, including exploring implementation, mechanisms of impact, context and outcomes. The framework also recommends the development of a logic model to map out assumptions about how an intervention may work and includes several components, including inputs, processes, outputs and outcomes. 75
To explore how the intervention was implemented, we will present an evaluation of delivery challenges, treatment fidelity, adaptations, dose and reach. Looking at how the intervention brings about change and the context was explored using qualitative interviews with 18 participants across both trial arms and interviews with service managers and therapists. The interviews with service managers (n = 3) were used to explore implementation challenges with SSTP delivery and therapist views on group participation, retention, programme delivery and perceived impact of the intervention were captured during a therapist interview and through reviewing minutes from supervision notes.
Logic model
The logic model presented here (Figure 9) was adapted for the trial from the original Triple P model. Inputs include appropriate therapist training and supervision, ensuring access to resources, and fidelity assessments to check the quality of implementation relevant to the UK (England) context. The process and outputs predominantly focus on the therapists delivering the intervention as intended and the participants implementing the skills they learn outside of sessions. Anticipated outcomes include a reduction in behaviours that challenge, improvements in parental well-being and a reduction in service use.
FIGURE 9.
Logic model adapted for the EPICC-ID trial.

Implementation
Stepping Stones Triple P is a parenting intervention designed to support parents who have children with intellectual disabilities. Stepping Stones was adapted from the original Triple P programme for parents of typically developing children. It aims to help with parents’ concerns about their child’s behaviour and provide training for parenting skills to promote the child’s prosocial behaviour.
In the EPICC-ID study, SSTP was delivered in sessions consisting of a small number of parents and one to two therapists. Group sizes ranged from 1 to 8 (mean = 3.64, SD = 1.66). Each intervention group lasted for 9 weeks, including six face-to-face group sessions and three individual phone consultations with the therapists. Session breaks were included if sessions coincided with a school holiday. A total of 25 groups were run across the four sites [Site 1 (N = 6); Site 2 (N = 4); Site 3 (N = 7); Site 4 (N = 7); combined group from all sites (N = 1)]. The first group session commenced on 9 November 2017 and the last group started on 15 January 2021, with the last session being held on 12 March 2021. Therapy sessions at the London sites included participants from both North and South London due to the close geographical proximity of the sites. Due to the COVID-19 pandemic, all therapy sessions were moved online after March 2020. Five groups (out of the total 25) were delivered remotely [Site 2 (N = 1), Site 3 (N = 2), Site 4 (N = 1), combined group from all sites (N = 1)].
Delivery challenges
To understand the challenges of implementation of the SSTP intervention in healthcare settings, we interviewed three service managers. They were interviewed remotely during the first 9 months of the study as part of the internal pilot. The interviews discussed the recruitment and training of the therapists, any issues with delivery, and how they felt about facilitating the adoption of the intervention into their services. All interviews were audio-recorded, transcribed verbatim and entered into the NVivo® (2020) (QSR International, Warrington, UK) software for further analysis. The transcripts were read and coded by the research assistant who identified all important information that came up during the interviews.
The service managers discussed the perceived interest in a group parenting programme like SSTP and expressed concerns about whether parents would be interested in SSTP, specifically since their services already offered a variety of therapies, including Early Bird or the My Child Programme.
I was slightly concerned that we already offer quite a lot of interventions for families that meet the criteria anyway. So, I wasn’t sure about the difference between the intervention group and the control group. So that’s basically what my feeling about it was first, but I thought that if we can enhance anything then we would want to.
Service Manager 1
Despite this, service managers said they felt SSTP would be a valuable addition to their service, especially as it addresses behaviours that challenge displayed by young children. However, they also expressed concerns about costs and funding.
I thought this was going to be very helpful for families particularly coming through our child development team, which is often children aged nought to five with very complex needs. Behaviour is a very big issue and one that comes up from parents quite a lot. So, the idea of doing this enhanced Triple P seems like a very good thing to be able to offer them.
Service Manager 3
I would like to mainstream it and when that funding is coming to an end, so we have been thinking about we might mainstream the skills, but as with everything I really would struggle to fund it.
Service Manager 1
Running the sessions smoothly required careful preparation, including finding the right venue with appropriate equipment and setting up the room before sessions. Service managers described difficulties with finding a venue with a good location, size, equipment and parking facilities.
And that’s been tight in terms of getting rooms that are large enough to accommodate all of this that also provide the audio-visual facilities to play the videos, you know, which is what the therapy requires. So that’s caused a lot of challenges. We’ve eventually found the space, but parking isn’t great, and travelling is not great from here, you know, which is probably why we found the space. But no, eventually it worked out. But it has caused some challenges.
Service Manager 2
When providing SSTP in their service, managers emphasised the need to consider the timing of the sessions to ensure regular attendance by parents, who are often busy and cannot afford to spend long hours in group sessions.
My only concern would be that our experience of running groups and I think in particular with this research project is that it does take quite a lot of man hours to set up and run the groups. Also, some families that we work with really struggle to participate in the group setting so they would be my two caveats really …
Service Manager 1
Service managers also described difficulties with finding therapists to be trained in delivering SSTP. For example, service providers had to externally recruit a therapist to deliver three groups due to the limited availability of therapists in London and due to another therapist taking unexpected sick leave.
We had quite a lot of difficulty recruiting because we did have some people in the borough who are already trained, which we hoped we would be able to link with, but we actually weren’t able to do that because the service they were local authority employed and that service were not keen to give up their skills.
Service Manager 2
However, once recruited, service managers were happy with the skills and provision of the therapy.
The people that we did recruit, we were particular pleased that they both were embedded in our local specialist schools, so we thought would be a good link and also once they were trained that they maybe would be able to continue using those skills, so it’s all skill development.
Service Manager 1
Fidelity
The fidelity of the intervention was reviewed by an independent reviewer with experience delivering SSTP. A fidelity form was adapted from the i-Basis Intervention Fidelity rating scale (first developed for use in the Preschool Autism Communication Trial study). 76 This form balances the contribution between session content and delivery style. The therapists completed checklists from SSTP providers and attendance worksheets for every session.
The fidelity form includes:
-
general group procedures;
-
interpersonal effectiveness;
-
specific criteria for each session;
-
deviations from the manual;
-
video and sound.
Each section included items scored as ‘0’ for No, ‘1’ for Yes or N/A. These scores are summed to give a total fidelity score (max score = 10). A quality score is also given on a rating of 1–5 (poor–excellent). Sessions were video recorded and stored in the online platform, DSH.
Ten per cent of sessions were randomly selected from the total number of sessions, ensuring an even spread of site, group and session number. The selection was generated by the study statistician. This resulted in a total of 13 sessions being reviewed by an external reviewer (Maeve Darroux – SSTP deliverer at Brilliant Parents). Three out of the 10 sessions reviewed were delivered remotely. Fidelity scores ranged from 7 to 10 (M = 9.38, SD = 0.96). Eight sessions (62%) were scored as having the maximum score for fidelity. In terms of quality, two sessions were rated as 3 – adequate, with the remainder of the sessions being rated at 4 – good (N = 11).
Across the 13 sessions, therapists reported some deviations from the manual:
-
A practitioner referred to ‘quiet time’ being discussed before ‘logical consequences’ rather than after.
-
A practitioner demonstrated role play which the parent was not required to copy, but this was still described to be beneficial by the external reviewer.
-
Practitioner did not use a whiteboard or flip chart to support the strategies as recommended by Triple P. This occurred in three sessions, all at different sites. On one of the occasions, the whiteboard was not used because only one parent was present in the session.
-
Due to a small number of participants in one of the group sessions (N = 1), the therapist accommodated the attending parent’s preference to have an individual phone call session instead of a face-to-face session.
Therapist training and Stepping Stones Triple P delivery
Therapists were health professionals involved with assessing or treating children with behaviours that challenge. The trained therapists had the following professions: community social worker, specialist health visitor, assistant psychologist, specialist nurse, family and inclusion mentor and occupational therapist. The therapists were not involved in the routine care of study participants and were based at separate facilities from the researchers to avoid contamination and unblinding. We recruited 11 therapists to deliver SSTP: 2 therapists from Sites 1, 2 and 4, and four therapists from Site 3.
All therapists were trained in the Group Stepping Stones Training and Accreditation programme. This included three training days and a further half-day accreditation workshop after 6 weeks. SSTP requires a therapist to spend an average of 37.5 hours on each family receiving the intervention, including time spent on pre-session preparation, post-session reporting, fidelity checklist completion and supervision. The training was conducted by Dominic Weston, Deputy Head of Training (UK) and Implementation Consultant of Triple P UK and Ireland. Dominic Weston provided 28 hours of supervision to therapists. Triple P trainers observed therapist sessions to help build therapist competence to run the groups. Monthly supervision was provided to maintain and monitor therapist skills over time by a co-applicant trained in SSTP (seven times during the study duration). Each therapist took part in the supervision and had access to the wider Triple P network of practice, which provides ongoing advice about the programme delivery and a range of clinical resources. The learning objectives focus on maintaining behavioural change, using skills within a group learning environment, learning from peers in the group and sharing difficulties or achievements, providing support, considering if more intensive work is required, referring further if needed, and talking about risk and protective factors operating within families.
All groups were delivered by at least one therapist and six groups were delivered by two therapists.
Adaptations
The therapists discussed any adaptations they made to sessions during supervision meetings. These included:
-
Therapists agreed for parents to bring very young children if they struggled to find child care during the session time.
-
Parents were allowed to bring partners to the sessions, as this was the most common request at all sites.
-
To boost the number of people attending group sessions, we obtained ethical approval to include parents of children who had been screened for the study but were ineligible to take part due to not fulfilling the inclusion criteria.
-
As per protocol, therapists contacted parents who missed a session to remind them of the next scheduled meeting and asked parents to read the relevant chapter in the workbook. Due to the concerns about the impact of the missed session, therapists offered a catch-up session to explain the missed content. The catch-up sessions were helpful, but therapists had concerns about how many catch-up sessions could be provided as it interfered with their work schedules, was time-consuming, and was difficult to provide sufficient information about the session on the phone call.
Dose and reach
Participants were recruited through participating NHS healthcare services (including primary care), parent support groups and online multimedia channels through the charity Contact. This charity reaches 20% of families with disabled children each year. The majority of participants were recruited through Child Development Centres which provide the main point of access for assessment and diagnosis of children with developmental delay, and outpatient clinics provided by the CAMHS. It was not possible to keep a structured record of all patients approached due to the number of PIC and the number of clinicians supporting the project. However, expressions of interest were obtained from 583 patients. Data on the number of participants approached were available from a Site 3 PIC, and this provides an example of the proportions of people being approached that were then randomised into the intervention (Figure 10). A total of 79 participants were approached at Site 3 PIC and 54% of these expressed an interest in taking part in the study, with 17 people (22%) being randomised into the study. Based on these figures, we can approximate that the reach of the trial may have been around 1100–1300 people.
FIGURE 10.
An example of parents approached and reasons for exclusions from the Site 3 PIC.
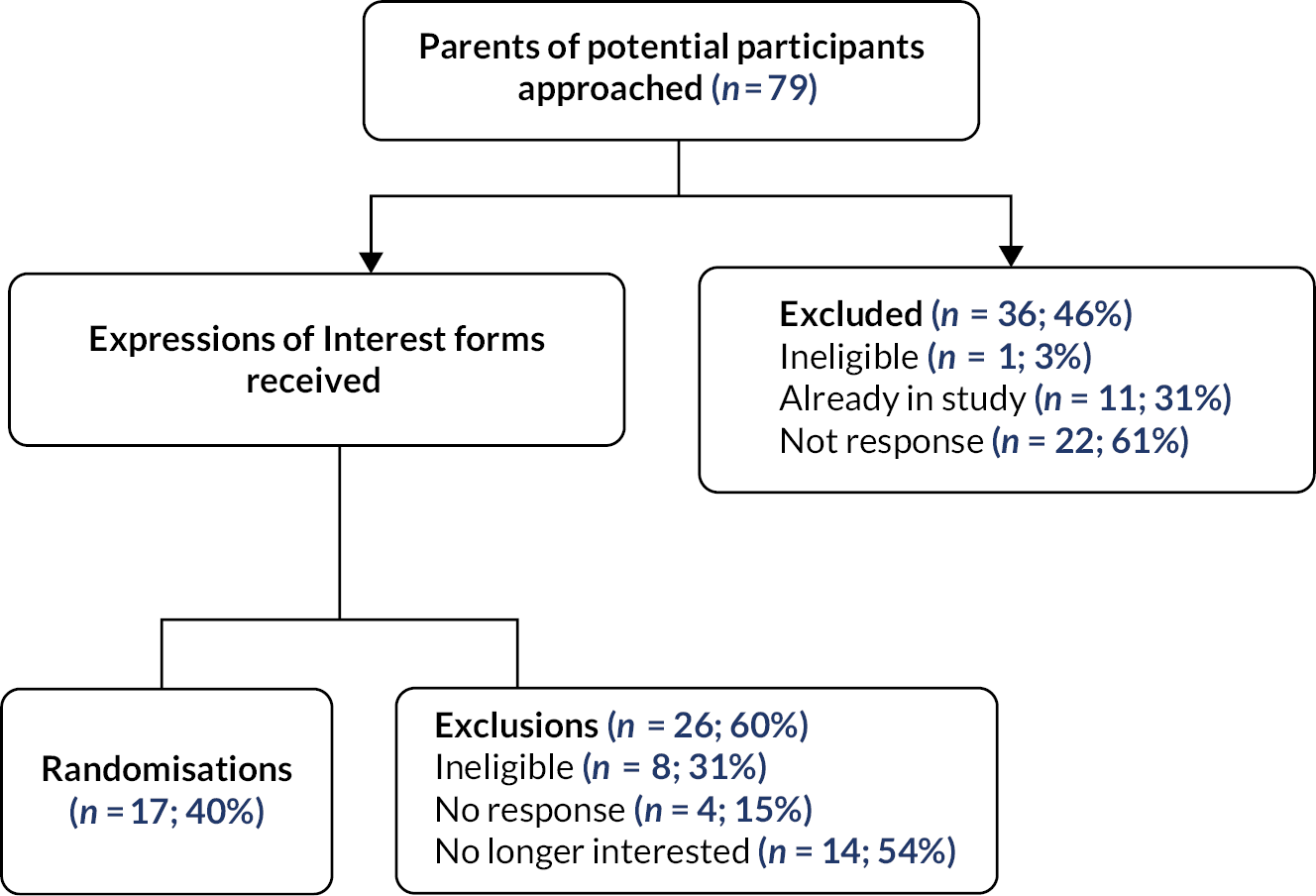
A total of 155 parents were invited to attend the SSTP group and 91 attended at least one session (59%). Sixty-four people did not attend any of the intervention sessions. The minimum acceptable dose of the intervention was stipulated to be four group sessions and two individual sessions. A total of 50 participants received this level of dosage (see Table 38 for the attendance breakdown by type of session).
| Number of individual sessions attended | |||||
|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | ||
| Number of group sessions attended | 0 | 64 | |||
| 1 | 8 | ||||
| 2 | 8 | 2 | 1 | ||
| 3 | 5 | 1 | 2 | 2 | |
| 4 | 3 | 6 | 3 | 4 | |
| 5 | 1 | 1 | 8 | 11 | |
| 6 | 0 | 1 | 7 | 17 | |
Therapists were asked to record reasons for non-attendance at sessions. Some reasons included the parent being in education, the child being unwell, lack of support with child care and clashes with other obligations or medical appointments (see Figure 11 for further details).
FIGURE 11.
Reasons for non-attendance reported by parents.
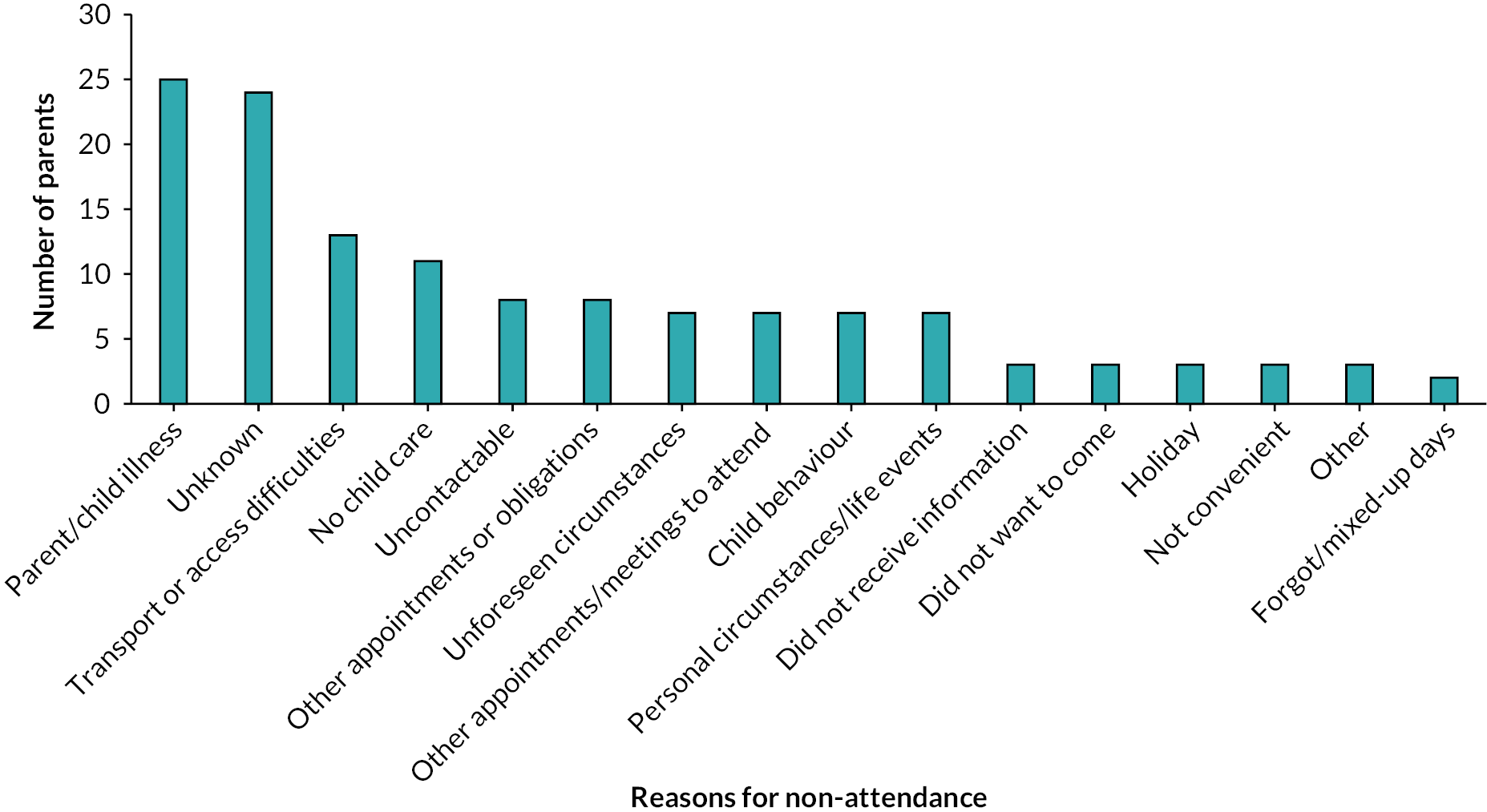
Mechanisms of impact
Stepping Stones Triple P is built on parents practising and giving feedback and thinking about what they have done well and what they can do differently. The intervention offers a variety of strategies and parents can choose which strategy they think will work for them. It was helpful to use concrete demonstrations for the parents, such as presenting examples of behavioural charts or videos that model specific situations. This made the content of the session more comprehensible and made parents feel that the goals of the session were more achievable. Some formats were seen as helpful. For example, the role-play format where parents are trying things out is unique. One of the therapists complimented the way information is presented: ‘It is really distilled down to the best takeaway messages and I think that is difficult to do and they have done it quite well. ’ Another important factor to improve the impact of the intervention is ‘to get to know the families before the start of the intervention to encourage attendance and build rapport’, as a therapist said. The intervention offered a variety of strategies, and the parent can choose which strategy they think will work for them. Some of the useful techniques that resulted in the child’s behaviour changes were distraction, planned activities, house rules and reward charts. Overall, the strategies provided in SSTP aimed to help children to improve their self-care skills.
Moreover, the group format of the SSTP created an opportunity for parents to meet others, normalise their struggles, learn from others’ experiences and made parents feel helpful to others by sharing their experiences.
Context
Parents and therapists described several contextual factors that affected the accessibility of the group sessions, namely, timing, group size, transport and setting. These are presented in further detail below.
Therapist views
Therapists noticed that the impact of the group depended highly on the parents’ abilities to comprehend and apply the skills presented:
I found the way the therapy is set up, to go through one session each week, is a lot of material and so the demand on the parent is quite large in terms of their ability to follow along, to understand and to be coached. It requires that both the person administering it has confidence in their coaching skills and that the parent is coachable. I think that some considerations didn’t go all the way to ensure participants are coachable.
Therapist 1, Interview
One therapist expressed the need for flexibility in offering more sessions depending on how quickly parents grasp the information being covered:
I would like to have more flexibility to gear the program to each particular group, i.e., to be able to add in an extra week if we weren’t getting through the sessions as quickly as we had hoped or to spend a bit more time on something or go back to something.
Therapist 1, Interview
One therapist expressed their thoughts on the length of sessions and potential need for splitting the sessions into shorter or more frequent sessions to be able to cover all material:
I could have easily used an extra day and could have broken down the 5 sessions into 6. The sessions are really long for everyone and that is definitely something to consider. By the end of running one, you are exhausted. You need to go through the material and watch the room to ensure everyone is engaged and be the cohesive glue for the group. Whoever is running it really needs experience in coaching. It is not an entry level experience programme and people really need coaching experience.
Therapist 1
Besides the struggles to find the best time for each parent in the group, the timing highly depended on the flexibility of the therapist, which was restricted by working hours:
One significant reason could be related to the timing of the groups, Site 1 has tried an evening group. One parent requested this, and it had to be early evening which didn’t suit everyone else. In most sites the therapists are only employed for 1 day and have other commitments so they cannot be flexible in offering differing days of the week.
Therapist supervision meeting
There were also concerns about parents with English as a second language and their understanding of the content.
Some of my personal experiences were that there were parents who had significant learning needs that meant they were not coachable and there were participants who struggled because English was not their first language. A lot of the material is explained clearly but I felt that some of the participants struggled due to their understanding of English.
Therapist 1, Interview
Several aspects of the SSTP therapy made it easier for parents to follow, even if their comprehension of the session was lower. For example, providing workbook exercises and a handbook that can be taken home were seen as helpful to keep parents on track. Moreover, the SSTP handouts are translated into five languages, which is useful for parents whose first language is not English.
When delivering the remote sessions, some parents found it difficult to log into MS Teams, and therapists found it challenging to not be able to see all participants when presenting slides. Zoom seemed to work better for therapists and allowed them to see more people on the screen. Session videos were shown by sharing the screen and the therapists acted out role plays with a second therapist remotely.
Therapists discussed the benefits and challenges of remote delivery of SSTP therapy. Some of the benefits included increased group sizes, the opportunity to be more flexible with timing and session length, and a greater possibility of additional caregivers joining sessions. Many parents preferred the convenience and flexibility of online delivery, which likely boosted attendance.
More parents have been able to attend, however some have been more distracted. Some of them have their child at home so there were situations where parents had to step away to manage something. I experienced better attendance and great opportunities by delivering remotely but this was balanced by distraction.
Therapist 1, Interview
Some challenges also included a limited opportunity for informal conversation between parents and therapists, which is important for building rapport and making parents more comfortable sharing with others. Therapists noticed fewer natural discussions, which meant they had to be more directive in their approach and invite people to comment. One way of tackling this was by using breakout rooms to encourage conversations between the parents without the therapist present.
Another challenge was internet and connectivity issues. Many people did not have unlimited data, and sometimes their broadband width was insufficient, making it hard to see their faces or resulting in crashes. This interrupted the flow of the session and wasted valuable time. Some parents commented that 2.5 hours spent online is a long time for many parents with young children at home.
Qualitative study
A subgroup of 18 parents from the four study sites participated in the qualitative interview study and were chosen at random. Nine of these parents had received SSTP, and nine parents were from the TAU group. Five interviews were conducted in person, and 13 interviews were conducted remotely. Separate topic guides were developed for participants from each trial arm to understand their experiences of the study and of the services they had received. Parents from the SSTP group were interviewed about their attendance at the SSTP sessions and their opinions on the impact of the group. Parents from the TAU group were asked about their experiences of usual treatment offered to their family and any experiences of previous group intervention participation. All interviews took 20–40 minutes. Following participation, each parent received a £15 voucher. All interviews were audio-recorded, transcribed verbatim by a professional company ‘Way with Words’ and were pseudo-anonymised. Data were entered into NVivo® (2020) with identifiable information removed. Based on the study timelines, there was a time difference of approximately 10 months between the two sets of interviews, and the TAU group was interviewed during the first wave of the COVID-19 pandemic.
The interviews were analysed using thematic analysis,77 involving the development of codes and themes driven by the data and grounded in participants’ experiences. The analysis process allowed us to work in a series of interconnected stages, moving back and forth across the data set until a coherent account of themes emerged for both trial groups. The first stage included identifying themes for each of the trial groups separately. After familiarisation with the data, two researchers (TO, KO) reviewed half of the transcripts to create an initial list of codes, followed by a discussion to create the provisional coding framework, which was extended and refined with the coding of subsequent transcripts. One researcher (TO) then coded all transcripts using the refined coding framework. All coding was inductive and data-driven, whereby equal attention was given to each data item. Once all interviews were analysed, the researcher (TO) re-read the transcripts to explore patterns and themes present in the coded data. The provisional coding matrix was discussed and was extended and refined with the coding of subsequent transcripts. Each code formed a potential category, and as the coding progressed, the code categories were grouped and formed initial themes. Final set of themes was developed and revised by the research team (TO, KO, AH, RR, HS), who identified themes that required merging or subdividing. The resulting themes were checked by the PAG group to ensure these reflected their experiences. The themes from the interviews were organised into three domains depending on the parent’s treatment group allocation (Table 39).
| TAU group |
|
| SSTP Group |
|
| All parents (both SSTP and TAU groups) |
|
1. Treatment as usual Group Results: ‘Need for intervention’
Parents in the TAU group described their experiences of receiving usual care that was locally offered to their children and described what they felt worked well and what did not work well.
1.1. Feeling of abandonment: ‘You are left to your own devices’
Parents described difficulties accessing support for their children. The support by the NHS depended on the family’s location, local signposting and the family’s motivation to fight for support. The support offered was viewed as insufficient to meet the children’s complex needs. While individual therapies (e.g. speech and language therapy, occupational therapy) were perceived as beneficial and specific to the child’s needs, they were deemed infrequent or too short-lived for parents to see improvements in the child’s behaviours:
… any progress would purely be because we’ve been doing it every single day with him.
Parent 1, TAU Group
As the following quote highlights, a lack of communication and signposting of the available services left parents feeling isolated and marginalised:
… there should be better signposting to parents, maybe at schools, maybe at GP surgeries, places that parents would go. Because you feel very alone when you have a child that has needs and you don’t know what to do as a parent, you don’t know what’s available, what services are available to you.
Parent 3, TAU Group
Most parents who were receiving usual care wanted further support and said they would welcome anything that could help their child, either with learning or managing behaviours:
I think it’s a very lonely experience having a child with special needs or with behavioural issues. They feel very marginalised and misunderstood, so I imagine parents just want all the help they can get. Especially with behavioural management …
Parent 2, TAU Group
1.2. The role of parents: ‘Constant battle’
Parents from the TAU arm reflected on their own role and felt their efforts were futile due to a lack of skills and limited understanding of their child’s behaviours. The lack of service provision left parents feeling overburdened and responsible for seeking and delivering most of the help for their child. Parents felt their child’s progress depended on their constant efforts to provide everyday support, which was often exhausting and time-consuming. Finding and receiving support was described as a battle:
Everything has been a battle, whether I’ve had to get a diagnosis, whether I’ve had to get speech therapy… Getting any sort of help has been a constant battle. Um, getting the HC [healthcare] plan in place, getting him into a specialist provision, everything is a battle. And it’s a really, really hard fight.
Parent 9, TAU Group
Parents felt supported when help was offered through schools, family and friends. Schools, particularly special needs schools, provided good signposting to professionals and therapies, and teaching assistants offered individual support, which benefited the child’s learning.
My (child) goes to a special needs school, so we managed this afterward. So, I felt like a lot of the pressure came off me at that point, to try and support her, to try and provide her with a range of therapies or input outside of school, now that it’s embedded in her school day.
Parent 2, TAU Group
Family and friends were described as a ‘sounding board’, providing emotional support to the parents, and allowing parents to have a break by offering child care. However, it was evident that this support was limited by a lack of skills and understanding of the complex behaviours of the child:
As my son gets older, it gets more difficult… to get parents or our parental support or grandparents support. You know, they just can’t handle it. And, he has epilepsy seizures, quite a big risk, and obviously you need more skill and confidence in dealing with that.
Parent 4, TAU Group
2. Stepping Stones Triple P Group Results: ‘Does the SSTP meet parents’ needs?’
Parents who received SSTP provided their reflections on which aspects of the intervention they found helpful.
2.1. Tools for managing the child’s behaviours
Parents from the SSTP group thought the therapy provided them with valuable techniques for managing their child’s behaviours. Parents were motivated to attend the sessions because they were ‘eager to learn’ how to help their children more effectively. Several parents appreciated the use of resources, such as watching the intervention videos, which made it easier to comprehend the content of each session and apply what they were taught in practice:
Especially the practical videos because that was very helpful to see again, how you did it in real life rather than just theoretically saying
Parent 14, SSTP Group
For instance, learning to anticipate and distract the child’s attention during a ‘meltdown’ was helpful:
We can deal with all sorts of different situations now. We see the tantrum coming and we sort of steer the attention to something else and it stops a lot of the meltdown
Parent 11, SSTP Group
Other useful techniques included planning activities and setting house rules using symbols or timetables, which made it easier for the child to comprehend what was expected of them and thus move from one activity to the next and reduce behaviours that challenge. Reward charts and stickers were seen to promote positive behaviours. Parents said they saw a positive change in the child’s behaviours, communication and manners:
The techniques that were learnt brought him out of himself, he makes a lot more eye contacts, he communicates a lot more in his own way, he’s a lot less demanding, he’s at the request stage
Parent 11, SSTP Group
2.2. Gaining confidence in the parenting role
Parents appraised SSTP sessions for boosting their confidence and said the sessions helped them to have a more open mind and adjust their parenting styles to be more suitable for their child’s needs. Parents felt like they understood and accepted their child’s behaviours more due to the course and learnt how their parenting behaviours could influence their child’s actions and responses.
You see things differently and don’t go back to the old way of thinking. You don’t look at it as naughty behaviour, but you know you should look for a reason behind it
Parent 14, SSTP Group
One parent described that:
The course opened my eyes to know what I can and can’t do with my child’ and that ‘autism got better explained to me
Parent 10, SSTP Group
2.3. Peer-to-peer support
Group intervention created an opportunity for parents to meet others in the same situation, learn from their experiences and share information. Parents reported being able to share issues they usually have no one else to talk with while receiving an empathetic response. This made people feel less marginalised and allowed them to form future networks. However, sometimes the differences in child’s difficulties meant that parents were less able to relate to each other and hence stay in touch.
It was nice to speak to people who understood what I was saying, and this is the first time I’ve met parents with the same situation
Parent 11, SSTP Group
Parents found the advice from others in the group extremely valuable, even comparing it to the advice given during the sessions by the therapist.
Group sessions were better than the one-to-one sessions because you have all the other parents’ experiences as well and that’s helpful, it’s almost as helpful as the advice given in the group because of being through it
Parent 18, SSTP Group
2.4. The role of the therapist
In general, parents held a positive opinion concerning the therapists, describing them as knowledgeable, professional and non-judgemental. Parents valued being able to receive feedback from the therapist who guided and supported them. Therapists made parents feel valued by ‘giving each person space to talk’ (Parent 14, SSTP Group).
She seems very knowledgeable, kind of somebody who knows as well, not just somebody who studied all the theory and is telling you what to do. Somebody who got a deeper understanding of how children’s minds work
Parent 14, SSTP Group
Despite SSTP being delivered in a group setting, many parents praised its individualised approach. Parents liked the additional phone calls with the therapist, which allowed them to talk about problems that came up at home and seek further advice:
Having a mix of that phone calls and that was actually really helpful. That would be a way of supporting people to talk through some of the issues that have come up that week or fortnight.
Parent 16, SSTP Group
The main issue with the individual support was that parents wanted more of it. Parents welcomed having more opportunities to speak to the professional and ask questions, or to have a one-to-one session with the professional and the child in the home setting:
I think it would be really helpful, maybe, if you swapped one of the telephone interviews if the person could come to your house and do a one-to-one session with your child. I think that would be really fantastic.
Parent 12, SSTP Group
While most of the parents had a positive experience with their therapist, one parent was critical of the therapist’s style of teaching and running the group.
They were constantly reading from the book, and it was kind of a little bit obvious. It didn’t give me an impression at the start like, do these people really know what the topic is or are they just reading the book
Parent 18, SSTP Group
3. Results from all parents (Stepping Stones Triple P and treatment as usual arms): ‘What are families looking for in a group intervention?’
The parents from both trial arms talked about their experience with group interventions, and their concerns and expectations if they were to be offered one.
3.1. Relevance of the group intervention
Parents reported being more likely to attend if the content of the sessions was relevant to them. Parents were hoping to learn more about practical help (e.g. toileting, hygiene, dressing), techniques for managing behaviours, strategies to help the child’s concentration and discover different learning methods that would be suitable for their child.
Several parents talked about the format of the groups, whereby having children present in the session was considered an asset, allowing parents to practice the tasks directly with their child under a specialist’s supervision:
It would be just someone else to observe your child and then, give you some ideas or things that they had tried. So then, rather than just describing what they do or how they behave, then somebody else can see it too. Then, might have an idea for you to try.
Parent 7, TAU Group
The majority of the parents stressed the importance of being in a group with parents who have children at the same developmental level to ensure that the content covered in the sessions was most relevant:
I think it’s not necessarily the same age. It is the same cognitive ability or the same disability. Obviously, autism is a spectrum and there’s another mum that her son is at the more extreme end of the spectrum, like my (child). So, we have quite a lot in common, even though her boy is 10. We can relate, based on disability.
Parent 7, TAU Group
A few parents suggested that having parents of children of older age would also be useful:
One of the mums who dropped out with an older child and at the same time at least you could see… where potentially you might be heading to or… you know like when you talk to a mum who says oh you know, the tantrums are fine now after they pass or whatever… three and a half, so at least you’ve got something to look forward to!
Parent 14, SSTP Group
These quotes highlight the usefulness of understanding what the future might look like for their child and the value of hearing from those with lived experience. Seeing others in a more difficult situation helped parents to realise that their own difficulties were manageable and to feel more appreciative of their situation:
All the other children had much more severe diagnoses, with more difficulties in daily life… which in a way made me happy, because always at home I kept telling my husband ‘I think we are lucky to have (child)…’.
Parent 15, SSTP Group
One parent with previous experience with group interventions valued techniques that boosted parental well-being, such as meditation or relaxation to improve parents’ self-care.
It is just as important to take care of myself as it is to take care of the children… I can’t care for him if I don’t care for me so that was a big focus like what are you doing for yourself, what support do you have in place for yourself and I think that was very useful
Parent 12, SSTP Group
Another factor seen to increase the relevance of the group sessions contributing to more efficient parenting was including the additional partner or another family member:
Because I think there’s nothing worse in the home than non-continuity. You’re doing one thing, one way and your husband’s doing it another way... It just causes yet more problems than it sometimes solves. I just think it would be really useful if they could attend some of the sessions, or at least, have some kind of input with it.
Parent 12, SSTP Group
3.2. Accessibility of the groups
Parents in both trial arms described four factors that affected the perceived accessibility of group interventions, namely, timing, group size, transport and setting (Table 40).
| Factor | Description | Quotes |
|---|---|---|
| Timing | Each family has a different preference for the timing of the group sessions (e.g. during school times or after work). Offering regular appointments would allow more flexibility for parents to choose when to attend. | ‘The only thing is I work full time and none of it happens out of working hours [laughs] … it’s generally in the middle of the day and I just can’t make those kinds of things, so I think that really makes it difficult for our family, you know’. (Parent 4, TAU Group) |
| Group size | Big groups offer better chance to network and find someone to relate to and learn from more parents. Small groups allow more space to talk and discuss child-specific difficulties. |
‘Generally, you can chat about whatever you want to chat about but there are some people that go there, that talk a lot and hijack it, sometimes. Then, you don’t really get a chance to say anything’. (Parent 7, TAU Group) ‘It was a small group we were able to go through things more quickly. But at the same time, if it was a bigger group, it would’ve been interesting to share more personal experiences’ (Parent 14, SSTP Group) ‘If it was a bigger group there would’ve been more opportunity to swap stories and stay in touch with’ (Parent 12, SSTP Group) |
| Transport | Choosing accessible locations would facilitate attendance. Offering travel reimbursement or providing free parking facilities would also reduce additional expenses for parents. | ‘It was our local walk-in centre, so it was a health clinic with all sorts of things, there was parking and stuff, so it was a nice place’ (Parent 11, SSTP Group) ‘It was £15 in a taxi to get there and I was thinking that even if my mum was able to drop us, it would’ve been a bit of a trek. If it had been more local to me that would’ve been better’ (Parent 17, SSTP Group) |
| Setting | A more relaxed setting creates an open atmosphere to share and bond with others. This can be boosted by hospitality, such as having tea and coffee before the session to allow parents to interact informally. | ‘I don’t know … whether if it would work in some less formal setting. I mean we were sitting behind a table and of course it was a video, but maybe somewhere where you can … just kind of … relax maybe more?’ (Parent 14, SSTP Group) ‘There was teas and coffees and biscuits, yes … Yes, I mean it’s really nice to have. Yes, particularly as it was in the morning, and we were all a bit tired. It made us laugh, about the coffee because we tend to have some coffee try to stay awake. So yeah, that was good’. (Parent 12, SSTP Group) |
Chapter 6 Discussion
Summary of main findings
For the primary outcome, using parent-reported child behaviours measured by the CBCL, we found evidence that a combined group and individual SSTP model reduces behaviours that challenge in preschool children with moderate to severe intellectual disability at 12 months post randomisation; however, this difference is not significant when compared to TAU. This pattern was also similar at 4 months. Additional analyses based on those who received at least four group sessions and two individual sessions indicated that the magnitude of change was greater and above the minimal clinically important difference of eight points on the CBCL, providing a clear signal that the intervention could be beneficial for those families. The T-scores which categorise the child’s behaviours into internalising and externalising scores show that the children appear to be within the clinically significant range for both internalising and externalising problems throughout the trial.
Regarding the secondary outcome of other caregiver-reported child behaviours, measured by the CBCL, we found that though not statistically significant, there was an increase in child behaviours at both 4 and 12 months. Although this appears to be counterintuitive given that parent-reported child behaviours decreased, behaviours that challenge are remitting-relapsing conditions and therefore, the finding may indicate a regression to the mean in either arm of the study. Further, there were substantially fewer completed C-TRF forms than expected and therefore, the result needs to be considered with caution.
In terms of clinical significance, it was surprising that parent-reported CBCL internalising and externalising scores placed the children in the clinical case range (> 64) in both study arms. In contrast, the other caregiver-reported CBCL internalising and externalising domains indicated a reduction in internalising and externalising behaviours in a borderline clinical case only in the TAU arm but not in the SSTP arm. However, as these results are based on returned questionnaires for a third of the sample, we advise caution in how the finding is to be interpreted. The children may display more severe behaviours in the home environment than when in structured settings such as schools. Also, a third of the research assessments occurred during the first and second lockdowns which may have influenced parental reporting. This may be reflected in our finding that the impact of the intervention was greater in those enrolled in the study pre-pandemic compared to after March 2020.
The researcher observed child–parent interaction, all of which occurred pre-pandemic, indicated that there was a sustained reduction in child negative behaviours at 12 months, as well as decreasing time during which those behaviours were observed, though parents in both arms of the trial displayed positive and negative behaviours for similar lengths of time.
We do not believe that the length of SSTP was unsuitable as it is considered a rather brief early intervention, but it is possible that these families have a greater need due to the severity of the child’s behaviour as well as multiple adversities. Therefore, the format of the intervention delivery might need to be tailored to families at greater risk. For example, there is an individual version of SSTP (level 5), but given the lack of evidence in the UK context of such interventions for children of this age group, we concluded that a hybrid version would be more appropriate for a wide range of clinical presentations.
The primary economic evaluation shows that SSTP is not only at least as effective as TAU but that there is a high probability that it is cost-effective compared to TAU, although the differences in service use cost between the trial arms were not significant. The cost of delivering training for the intervention was relatively low and was accompanied by slightly higher QALYs in the SSTP group compared to TAU. Both trial arms were similar in terms of service use, except for the total costs from the health and social care cost perspective. Overall, the pattern of service use costs and HRQoL were similar across groups.
In terms of service use, there was a statistically significant difference in total cost when analyses were conducted from the health and social care perspective. However, the results should be interpreted cautiously. Confidence intervals were wide due to substantial variation in services across the study sites. The inclusion of wider societal costs reduced the cost difference because of lower expenditure for specialist equipment or adaptations. The societal perspective only includes private service use and out-of-pocket expenses. Data on informal care and productivity losses were not collected.
At 10 months (as we collected data for the previous 6 months so missing the period between 4 and 6 months) the intervention dominated TAU in that it costs £1058 less than TAU from a health and social care cost-perspective with a positive, though non-significant, mean point estimate for QALYs. There is a high probability that SSTP is cost-effective compared to TAU for a range of cost-effectiveness thresholds for QALYs gained. Nevertheless, this finding should be considered with caution as QALYs are a secondary trial outcome and PedsQL™ GCS and the mapped EQ-5D-Y utility scores algorithm were used to calculate QALYs. We were unable to include a generic outcome measure as there is no valid, preference-based measure for health state evaluation in children under the age of 5 or children with intellectual disabilities.
The cost of training to deliver the SSTP intervention is relatively low for a psychological intervention at £26 per participant. It should be noted that intervention costs commonly reduce in the longer term, as therapists become more skilled, and service providers and commissioners benefit from both experience and economies of scale. All but one trial therapist were new to the SSTP intervention and were trained specifically to deliver SSTP for the trial. The SSTP developers suggest that a therapist requires 37.5 hours per participant, which may not be possible to reduce much further, even if more experienced therapists are employed. This should be considered in relation to any longer-term plans to invest in SSTP for this population with significant complex needs and comorbidity.
Overall, we did not find generalised symptom reduction with this intervention; however, there was a greater effect of the intervention when there was good adherence and during pre-pandemic with in-person groups. Further, SSTP is a feasible and inexpensive early intervention alternative to TAU and should be considered as part of the local offer for children with developmental delays at risk of displaying behaviours that challenge.
Findings in context
The study findings add novel data for younger children with intellectual disability and behaviours that challenge compared to a range of other clinical trials outside the UK that have found evidence for SSTP in mainly older children. 35,36 An Irish study with 84 families of children with developmental disabilities found significant improvements in parent-reported child behaviour and parental confidence, maintained after 5 months. 78 Similar results are echoed across other studies conducted in Australia, Canada and Germany, and with samples of children with ASD, genetic syndromes and intellectual disability. 38,79–81 A systematic review and meta-analysis found significant effects of SSTP on reducing child behaviours that challenge, with particularly robust results for level 4 SSTP37 (replicated in a more recent systematic review including 16 studies and 900 participants for children with significant morbidity). 25 We were unable to show such an effect in this trial.
The clinically important difference set in this study was eight points reduction for the primary outcome measure, the CBCL, based on a moderate standardised effect size of 0.4, which is in accord with the effect sizes reported in previous meta-analyses. It is possible that the minimal clinically significant difference may be lower for this population and the results could still be clinically important and useful. However, there is no such study yet available that has estimated the minimal clinically important difference in children with developmental disabilities and very small differences would require a significantly larger sample size that would make the conduct of the trial unachievable. A 4-point change would be a reduction from 2 to 0 in two items (e.g. cries a lot/avoids looking others in the eye/hits others) or a 1-point reduction in more items for example from 2 to 1 or 1 to 0 (very true to somewhat/sometimes true to not true).
Despite limited evidence for the primary analysis, the sensitivity analyses showed that the null result may be related to the low average dose of the intervention received; those receiving a sufficient dose (four out of six groups and two out of three individual sessions) did see positive effects above the pre-determined eight points. Of the 155 participants who were randomised to the SSTP arm, only 50 received the minimum acceptable dose of the intervention. The majority of previous SSTP trials have not reported challenges with uptake and intervention dosage, although, as noted above, these studies included slightly older children rather than those of preschool age. Surveillance including screening for the developmental delay is usually undertaken from the age of 9 months, but many children enrolled in the study had a suspected developmental delay though not yet having received a formal diagnosis. This can be a lengthy process with about one in four referrals to children’s mental health services not having received an appointment pre-pandemic after 3 months. 82 The process of seeking and obtaining a diagnosis and coming to terms with having a child with a disability can be a stressful and distressing time for parents. 83 The complexity of these parents’ lives may prevent them from being able to fulfil their commitment to attending weekly sessions even for moderate to severe behaviours that challenge. A UK-based trial for the Incredible Years parenting intervention also reported similar problems with attendance with parents of preschool children, with only half of parents attending more than 50% of sessions. 84 Child and family factors may influence attendance, for example we found that attenders in our trial were less likely than non-attenders to have children with mobility problems.
There was evidence to suggest SSTP was effective before the COVID-19 pandemic started, but not during the pandemic based on pre-specified subgroup analyses. There was a multitude of changes that occurred during this period, and it is not possible to pinpoint a single contributory factor that can account for these results. While some surveys reported improvements in children’s behaviour during lockdowns,85,86 we found that parents reported increased stress, deterioration in their own mental health and severe interruption of support from educational, social and healthcare services. 87,88 This may have impacted parents’ ability to engage successfully with the intervention during this time.
Families may have found it harder to engage during online delivery, particularly if their children were at home with them. Therapists reported that it was more challenging to build rapport and relationships with participants and this may have impacted engagement. Although there is evidence to suggest the utility of remote delivery of Triple P interventions,89–91 it may not be the best method of delivery for this specific population, who may gain more from the camaraderie and social support provided within group contexts.
Our economic evaluation indicates that SSTP is affordable and therefore, remains an option for children with intellectual disabilities whose parents cannot access or find universal parenting groups unsuitable.
Clinical implications
Stepping Stones Triple P appears to be a well-tolerated and possibly cost-neutral intervention, and it may be beneficial for children when parents are able to attend enough sessions. However, this trial indicates that many parents of preschool children with moderate to severe intellectual disabilities found it difficult to commit to the intervention at this stage in their child’s life. It is clear from other research on children without intellectual disabilities that such groups may experience low turnout reducing the justification for this use of often limited resources. However, the NICE guidelines have found enough evidence to state that parenting groups should be considered as a therapeutic option for those children and their families. 39 This is also supported by observations of the child−parent interaction during the trial that show a reduction in the display of negative behaviours in the child over 12 months. Parents are generally only offered one option of support with no alternative if that is not suitable. A more personalised and participatory approach is likely to be needed to ensure the intervention suits the needs of each family. Some may be able to benefit from group sessions, but others may require more intensive 1-1 support. We also believe that the extraordinary circumstances that were created due to the pandemic, including the pause of regular services, may in part be the reason behind the reversal of the direction of effect of SSTP compared to pre-pandemic.
Early intervention is endorsed as both preventing the display of behaviours that challenge and improving child outcomes in the medium to longer term. 92–94 However, interventions such as parent groups have the potential to be effective only if parents can engage in them successfully; therefore, incentives such as providing child care for other children, transport and other infrastructures are likely to be needed for programmes such as SSTP to ensure adequate implementation of delivery.
Remote delivery may go some way towards addressing some of the issues associated with in-person attendance but may not be suitable for all families and may be a particular problem for those who struggle to use technology, as well as more deprived families who experience digital poverty. 95 Still, some families may prefer the convenience and flexibility of remote delivery and with the move to a more online world in the post-pandemic era, services will need to reconsider their approach and potentially offer a choice in the modes of delivery to parents. The experience of telehealth during the pandemic may not be necessarily reflective of the host of facilitators and barriers that could operate during ‘normal’ times.
A further clinical challenge is the availability of trained therapists. In our trial, some left their posts midway through the study. We tried to overcome these issues by employing therapists outside the initial cohort of 8 and therapists delivering the intervention across sites where this was feasible, for example London sites. We boosted group numbers by inviting participants who were ineligible to enrol in the trial to join SSTP groups (e.g. where the child was older or had a mild intellectual disability).
Strengths and limitations
To our knowledge, this is the first pragmatic randomised controlled trial of an intervention to reduce behaviours that challenge displayed by preschool children with moderate to severe intellectual disability in the UK. The study also benefits from the first cost-effectiveness analysis of a complex early intervention in this population which makes it a significant contribution to the scientific literature and of benefit to commissioners of services and policymakers. There was also consistently high fidelity across therapists, indicating the intervention was delivered as intended. Participants were recruited and received the intervention via a range of local services including secondary paediatric care, and therefore, the findings have real-world relevance. Moreover, parents reported that they found SSTP helpful in boosting their confidence and improving their understanding of their child’s diagnoses and behaviours.
However, the study also has some limitations. The main threat to the trial validity is the lower-than-anticipated attendance to group and individual sessions. However, we are of the opinion that given the dearth of evidence regarding early intervention in this population, the findings uncover important challenges that must be addressed in the UK health and social care system in future research. As such, learning points can also be used by commissioners and services to identify ways in which they can support parents to attend such groups, including incentivisation (contributing to fares or child care expenses for families who qualify), appointing local champions, adopting behaviour change techniques which are all relevant to optimising implementation. 96 These proposals are further supported by the results of the per-protocol and CACE analyses which indicate that adherence is central to achieving the intervention effect, though they must be interpreted with caution given the limitations of the underlying methodological assumptions.
During the pandemic, all data collection became remote in order to comply with the public health restrictions; that prevented us from collecting data for some of the research assessments including baseline cognitive assessments and parent–child observations. It was also more difficult to identify other caregivers to complete the C-TRF as families were unable to meet and schools and nurseries were closed. Collecting the latter was also challenging even prior to the COVID-19 pandemic because researchers relied on parents to pass on the study information and did not have direct contact with these caregivers.
In summary, we have fully reported on all the potential impacts of the COVID-19 pandemic, including participant safety, intervention adherence, protocol compliance, data quality and completeness, study power and integrity. We have also reported on how we have mitigated some of those challenges where relevant. 97
Equality, diversity and inclusion
The study recruited its target sample size and retained study power (89.4%) despite a higher attrition rate than anticipated (20%). The sample was ethnically diverse, with 43% of participants from black, Asian, mixed or other backgrounds. These groups are often under-represented within research, and this study recruited a larger sample of people from ethnic backgrounds than is generally represented in the UK population (14%). 98
Patient and Public Involvement and Engagement
Five parents expressed interest in being members of the trial PAG but subsequently, two dropped out. Our PAG members advised us on how to optimise recruitment and problem-solve challenges that arose (e.g. those during COVID-19). They took part in the trial management meetings and took part in all the discussions about findings and interpretation as reported in Chapter 3. Parents reflected that their experiences of being involved with the EPICC-ID trial were very positive and felt their contributions were always valued. They also reported feeling proud of the project and that they had learnt a lot from their involvement. The paper reporting the survey of parent participants in the EPICC-ID trial, which includes a commentary from the PAG members, has already been cited 13 times and has 5440 views (as of 10 June 2022). 87 Finally, one of the parents (Mrs Rebecca Scurr) contributed the case vignette on a BMJ practice pointer article reviewing the management of a child with developmental disorders and subsequently took part in the BMJ Talk Medicine podcast alongside Absoud et al. 99
We experienced some challenges with meeting attendance for parent representatives on the TSC. Although there were two parent representatives, both were unavailable to attend 40% of the meetings.
We produced plain English language newsletters twice per annum throughout the trial duration to inform participants and services about the study status. We are also planning to produce a short video of a parent testimonial and a videocast of the study findings.
The CONTACT co-applicant (Summerson) and a parent (to be confirmed) will run a joint workshop with Hassiotis at the in-person annual national conference of the British Association of Community Child Health in September 2022.
Conclusions and future directions
Overall, our study cannot draw definitive conclusions about the clinical and cost-effectiveness of SSTP as an intervention to address behaviours that challenge displayed by children with moderate to severe intellectual disabilities in the UK. However, there are clear indications the intervention can be beneficial under certain conditions, and this trial highlights the importance of sufficient dosage, and method of delivery, and highlights the difference in needs between families. Further research should investigate factors impacting parent engagement and delivery. Any future health economic evaluations on this topic and population should measure the impact of early onset behaviours that challenge on parents/carers by collecting all relevant information that might affect parents/carers to ensure that there exists robust evidence of the benefits of early intervention in reversing high care costs associated with behaviours that challenge over time. 100
Stepping Stones Triple P and other parenting interventions are complex interventions, and it is important that we consider their effect outside the conventional narrow parameters of statistical and clinical significance. As we have reported, the study faced several challenges including the impact of the pandemic. While we were unable to show that SSTP is superior to TAU, our work raises questions that must be considered and provide a wider perspective such as optimal implementation and personalisation of format and target population,101 especially given the heterogeneity of child behaviours and comorbidities. Children with intellectual disabilities are some of the most neglected population groups in terms of healthcare access and other inequalities. SSTP should be considered a worthwhile option for such children at risk and their families until firm recommendations can be made following updated meta-analyses that include emerging research.
Acknowledgements
Contributions of authors
Tamara Ondruskova (https://orcid.org/0000-0003-4904-8040) (Research Assistant, Psychology) was responsible for data collection and the write-up of the final study report.
Rachel Royston (https://orcid.org/0000-0002-9901-2284) (Clinical Trial Manager, Neurodevelopmental Disorders) conducted the day-to-day management of the trial and supported the write-up of the study report.
Michael Absoud (https://orcid.org/0000-0002-0577-1897) (Consultant, Paediatric Neurodisability) was a recruitment lead and supported the write-up for publication.
Gareth Ambler (https://orcid.org/0000-0002-5322-7327) (Associate Professor, Medical Statistics) oversaw the completion of the statistical analysis for the trial.
Chen Qu (https://orcid.org/0000-0001-8746-8105) (Research Associate, Statistical Science) conducted the statistical analyses for the trial and prepared the results for publication.
Jacqueline Barnes (https://orcid.org/0000-0001-5566-8997) (Emerita Professor of Psychology, Human Development) is an early intervention expert and supported all aspects of the process evaluation and the collection and coding of observational data.
Rachael Hunter (https://orcid.org/0000-0002-7447-8934) (Associate Professor, Health Economics) oversaw the completion of the health economics analysis.
Monica Panca (https://orcid.org/0000-0002-4031-6478) (Health Economist, Primary Care and Population Health) conducted the health economic analysis for the trial and prepared the results for publication.
Marinos Kyriakopoulos (https://orcid.org/0000-0002-4594-2646) (Consultant Psychiatrist, Child and Adolescent Psychiatry) was a patient and public involvement lead.
Kate Oulton (https://orcid.org/0000-0002-5778-3849) (Senior Research Fellow, Qualitative methodology and process evaluation) oversaw the interpretation, analysis and write-up of qualitative data for the process evaluation.
Eleni Paliokosta (https://orcid.org/0000-0003-4330-965X) (Child and Adolescent Psychiatrist, Neurodevelopmental Disorders) was one of the Principal Investigators and a recruitment lead for the North London site and contributed intellectual content to the report and other publications.
Aditya Sharma (https://orcid.org/0000-0003-4632-4521) (Clinical Academic Psychiatrist, Child and Adolescent Psychiatry) was one of the Principal Investigators and a recruitment lead for the Northeast England site and contributed intellectual content to the report and other publications.
Vicky Slonims (https://orcid.org/0000-0003-3339-2365) (Senior Speech and Language Therapist, Children’s Neuroscience) was a recruitment lead for the South London site, provided therapist supervision and supported with the development of a fidelity assessment for the process evaluation.
Una Summerson (https://orcid.org/0000-0001-5730-2147) (Head of Policy and Public Affairs, Disabled Children) co-ordinated patient and public involvement activities, facilitated PPI meetings for this study, and also read and commented on the final report.
Alastair Sutcliffe (https://orcid.org/0000-0001-8542-6155) (Consultant Paediatrician, Community Child Health) was a trialist and pathways lead and provided expertise on the running of the trial, also contributed to the funding application, trial conduct including promotion of the study. Contributed to the interpretation of findings and the report content.
Megan Thomas (https://orcid.org/0000-0002-4358-6166) (Associate Professor and Consultant, Paediatric Neurodisability) was one of the Principal Investigators and a recruitment lead for the Northwest England site and contributed intellectual content to the report and other publications.
Brindha Dhandapani (https://orcid.org/0000-0003-2032-6844) (Consultant Community Paediatrician) was a clinician at the Lewisham and Greenwich NHS Trust and recruited over 10 participants to the study. Authorship was used as an incentive to support recruitment.
Helen Leonard (https://orcid.org/0000-0003-4148-6281) (Consultant in Paediatric Neurodisability) was a clinician at the Newcastle Upon Tyne NHS Trust and recruited over 10 participants to the study. Authorship was used as an incentive to support recruitment.
Angela Hassiotis (https://orcid.org/0000-0002-9800-3909) (Professor and Honorary Consultant Psychiatrist) was the study chief investigator and was involved with all aspects and oversight of the trial. She reviewed and contributed to all iterations of the report.
Publications
Absoud M, Wake H, Ziriat M, Hassiotis A. Managing challenging behaviour in children with possible learning disability. BMJ 2019;365.
Farris O, Royston R, Absoud M, Ambler G, Barnes J, Hunter R, et al. Clinical and cost effectiveness of a parent mediated intervention to reduce challenging behaviour in pre-schoolers with moderate to severe intellectual disability (EPICC-ID) study protocol: a multi-centre, parallel-group randomised controlled trial. BMC Psychiatry 2020;20:1.
Paulauskaite L, Farris O, Spencer HM, EPICC-ID Group, Hassiotis A. My son can’t socially distance or wear a mask: how families of preschool children with severe developmental delays and challenging behavior experienced the COVID-19 pandemic. J Mental Health Res Intellect Disabil 2021;14:225–36.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Ethics statement
This research was conducted in accordance with the World Medical Association Declaration of Helsinki. The study was approved by the London-Camden and Kings Cross Research Ethics Committee on 19 May 2017 (reference: 17/LO/0659).
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HTA programme or the Department of Health and Social Care.
References
- Diagnostic and Statistical Manual of Mental Disorders: DSM-5. Washington, DC; 2013.
- Learning Disabilities and Behaviour That Challenges: Service Design and Delivery 2018. www.nice.org.uk/guidance/ng93 (accessed 14 June 2022).
- de Ruiter KP, Dekker MC, Verhulst FC, Koot HM. Developmental course of psychopathology in youths with and without intellectual disabilities. J Child Psychol Psychiatry Allied Discip 2007;48:498-507.
- McClintock K, Hall S, Oliver C. Risk Markers Associated With Challenging Behaviours in People With Intellectual Disabilities: A Meta-Analytic Study. J Intellect Disabil Res 2003;47:405-16.
- Emerson E, Blacher J, Einfeld S, Hatton C, Robertson J, Stancliffe RJ. Environmental risk factors associated with the persistence of conduct difficulties in children with intellectual disabilities and autistic spectrum disorders. Res Dev Disabil 2014;35:3508-17.
- Parmenter TR, Einfeld SL, Tonge BJ, Dempster JA. Behavioural and emotional problems in the classroom of children and adolescents with intellectual disability. J Intellect Dev Disabil 1998;23:71-7.
- Molteno G, Molteno CD, Finchilescu G, Dawes ARL. Behavioural and emotional problems in children with intellectual disability attending special schools in Cape Town, South Africa. J Intellect Disabil Res 2001;45:515-20.
- Emerson E, Kiernan C, Alborz A, Reeves D, Mason H, Swarbrick R, et al. The prevalence of challenging behaviors: a total population study. Res Dev Disabil 2001;22:77-93.
- Cooper SA, Smiley E, Jackson A, Finlayson J, Allan L, Mantry D, et al. Adults with intellectual disabilities: prevalence, incidence and remission of aggressive behaviour and related factors. J Intellect Disabil Res 2009;53:217-32.
- Lundqvist LO. Prevalence and risk markers of behavior problems among adults with intellectual disabilities: a total population study in Örebro County, Sweden. Res Dev Disabil 2013;34:1346-56.
- Davies L, Oliver C. The age related prevalence of aggression and self-injury in persons with an intellectual disability: a review. Res Dev Disabil 2013;34:764-75.
- Royal College of Psychiatrists . Challenging Behaviour: A Unified Approach. College Report CR144 2007.
- Rydzewska E, Hughes-McCormack LA, Gillberg C, Henderson A, Macintyre C, Rintoul J, et al. Prevalence of long-term health conditions in adults with autism: observational study of a whole country population. BMJ Open 2018;8.
- Farmer C, Butter E, Mazurek MO, Cowan C, Lainhart J, Cook EH, et al. Aggression in children with autism spectrum disorders and a clinic-referred comparison group. Autism 2015;19:281-91.
- Kiernan C, Kiernan D. Challenging Behaviour in Schools for Pupils With Severe Learning Difficulties. Ment Handicap Res 1994;7:177-201.
- Hastings R, Allen D, Baker P, Gore N, Hughes C, McGill P, et al. A conceptual framework for understanding why challenging behaviours occur in people with developmental disabilities. Int J Posit Behav Support 2013;3:5-13.
- Totsika V, Hastings RP, Emerson E, Hatton C. Early years parenting mediates early adversity effects on problem behaviors in intellectual disability. Child Dev 2020;91:e649-64.
- Woodman AC, Mawdsley HP, Hauser-Cram P. Parenting stress and child behavior problems within families of children with developmental disabilities: transactional relations across 15 years. Res Dev Disabil 2015;36:264-76.
- Griffith GM, Hastings RP. ‘He’s hard work, but he’s worth it’. The experience of caregivers of individuals with intellectual disabilities and challenging behaviour: a meta-synthesis of qualitative research. J Appl Res Intellect Disabil 2014;27:401-19.
- Gallagher S, Phillips AC, Oliver C, Carroll D. Predictors of psychological morbidity in parents of children with intellectual disabilities. J Pediatr Psychol 2008;33:1129-36.
- Most DE, Fidler DJ, LaForce-Booth C, Kelly J. Stress trajectories in mothers of young children with Down syndrome. J Intellect Disabil Res 2006;50:501-14.
- Ramchandani PG, O’Farrelly C, Babalis D, Bakermans-Kranenburg MJ, Byford S, Grimas ESR, et al. Preventing enduring behavioural problems in young children through early psychological intervention (Healthy Start, Happy Start): study protocol for a randomized controlled trial. Trials 2017;18:1-11.
- Roberts C, Mazzucchelli T, Studman L, Sanders MR. Behavioral family intervention for children with developmental disabilities and behavioral problems. J Clin Child Adolesc Psychol 2006;35:180-93.
- Sanders MR. Development, evaluation, and multinational dissemination of the Triple P – Positive Parenting Program. Annu Rev Clin Psychol 2012;8:345-79.
- Ruane A, Carr A, Moffat V, Finn T, Murphy A, O’Brien O, et al. A randomised controlled trial of the Group Stepping Stones Triple P training programme for parents of children with developmental disabilities. Clin Child Psychol Psychiatry 2019;24:728-53.
- Whittingham K, Sofronoff K, Sheffield J, Sanders MR. Stepping Stones Triple P: an RCT of a parenting program with parents of a child diagnosed with an autism spectrum disorder. J Abnorm Child Psychol 2009;37:469-80.
- Furlong M, McGilloway S. The incredible years parenting program in Ireland: a qualitative analysis of the experience of disadvantaged parents. Clin Child Psychol Psychiatry 2012;17:616-30.
- McIntyre LL. Adapting Webster-Stratton’s incredible years parent training for children with developmental delay: findings from a treatment group only study. J Intellect Disabil Res 2008;52:1176-92.
- Smith E, Koerting J, Latter S, Knowles MM, McCann DC, Thompson M, et al. Overcoming barriers to effective early parenting interventions for attention‐deficit hyperactivity disorder (ADHD): parent and practitioner views. Child Care Health Dev 2015;41:93-102.
- Koerting J, Smith E, Knowles MM, Latter S, Elsey H, McCann DC, et al. Barriers to, and facilitators of, parenting programmes for childhood behaviour problems: a qualitative synthesis of studies of parents’ and professionals’ perceptions. Eur Child Adolesc Psychiatry 2013;22:653-70.
- Sapiets SJ, Totsika V, Hastings RP. Factors influencing access to early intervention for families of children with developmental disabilities: a narrative review. J Appl Res Intellect Disabil 2021;34:695-711.
- Carr T, Lord C. A pilot study promoting participation of families with limited resources in early autism intervention. Res Autism Spectr Disord 2016;25:87-96.
- Hudson A, Cameron C, Matthews J. The wide-scale implementation of a support program for parents of children with an intellectual disability and difficult behaviour. J Intellect Dev Disabil 2008;33:117-26.
- Patterson GR. Antisocial Behavior in Children and Adolescents: A Developmental Analysis and Model for Intervention. Washington, DC; 2002.
- Whittingham K, Sofronoff K, Sheffield JK. Stepping Stones Triple P: a pilot study to evaluate acceptability of the program by parents of a child diagnosed with an autism spectrum disorder. Res Dev Disabil 2006;27:364-80.
- Roux G, Sofronoff K, Sanders M. A randomized controlled trial of group Stepping Stones Triple P: a mixed-disability trial. Fam Process 2013;52:411-24.
- Tellegen CL, Sanders MR. A randomized controlled trial evaluating a brief parenting program with children with autism spectrum disorders. J Consult Clin Psychol 2014;82:1193-200.
- Kasperzack D, Schrott B, Mingebach T, Becker K, Burghardt R, Kamp-Becker I. Effectiveness of the Stepping Stones Triple P group parenting program in reducing comorbid behavioral problems in children with autism. Autism 2020;24:423-36.
- National Institute for Health and Care Excellence (NICE) . Challenging Behaviour and Learning Disabilities: Prevention and Interventions for People With Learning Disabilities Whose Behaviour Challenges 2015. www.nice.org.uk/guidance/ng11 (accessed 14 June 2022).
- Farris O, Royston R, Absoud M, Ambler G, Barnes J, Hunter R, et al. Clinical and cost effectiveness of a parent mediated intervention to reduce challenging behaviour in pre-schoolers with moderate to severe intellectual disability (EPICC-ID) study protocol: a multi-centre, parallel-group randomised controlled trial. BMC Psychiatry 2020;20:1-11.
- Achenbach T, Rescorla LA. Achenbach System of Empirically Based Assessment. Retrieved from Mental Measurements Yearbook via EBSCOhost 2007.
- Dekker MC, Nunn R, Koot HM. Psychometric properties of the revised developmental behaviour checklist scales in Dutch children with intellectual disability. J Intellect Disabil Res 2002;46:61-75.
- Wallander JL, Dekker MC, Koot HM. Risk factors for psychopathology in children with intellectual disability: a prospective longitudinal population-based study. J Intellect Disabil Res 2006;50:259-68.
- Sanders MR, Waugh L, Tully L, Hynes K. The Revised Family Observation Schedule. Brisbane, QLD, Australia: Parenting and Family Support Centre; 1996.
- Sanders MR, Christensen AP. A comparison of the effects of child management and planned activities training in five parenting environments. J Abnorm Child Psychol 1985;13:101-17.
- Achenbach TM, Rescorla LA. Manual for the ASEBA Preschool Forms and Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2000.
- Plant KM, Sanders MR. Reducing problem behavior during care-giving in families of preschool-aged children with developmental disabilities. Res Dev Disabil 2007;28:362-85.
- Hankins M. The reliability of the twelve-item general health questionnaire (GHQ-12) under realistic assumptions. BMC Public Health 2008;8:1-7.
- Shevlin M, Adamson G. Alternative factor models and factorial invariance of the GHQ-12: a large sample analysis using confirmatory factor analysis. Psychol Assess 2005;17:231-6.
- Rousey A, Best S, Blacher J. Mothers’ and fathers’ perceptions of stress and coping with children who have severe disabilities. Am J Ment Retard 1992;97:99-110.
- Johnston C, Mash EJ. A measure of parenting satisfaction and efficacy. J Clin Child Psychol 1989;18:167-75.
- Ohan JL, Leung DW, Johnston C. The Parenting Sense of Competence Scale: Evidence of a Stable Factor Structure and Validity. Can J Behav Sci 2000;32.
- Byford S, Barrett B, Roberts C, Wilkinson P, Dubicka B, Kelvin RG, et al. Cost-effectiveness of selective serotonin reuptake inhibitors and routine specialist care with and without cognitive-behavioural therapy in adolescents with major depression. Br J Psychiatry 2007;191:521-7.
- Varni JW, Seid M, Rode CA. The PedsQLTM: measurement model for the pediatric quality of life inventory. Med Care 1999;37:126-39.
- Varni JW, Seid M, Kurtin PS. PedsQLTM 4.0: reliability and validity of the pediatric quality of life InventoryTM Version 4.0 generic core scales in healthy and patient populations. Med Care 2001;39:800-12.
- EuroQol Research Foundation . EQ-5D-5L User Guide 2019.
- Mullen E. Mullen Scales of Early Learning. MInnesota MN: AGS, Circle Pines; 1995.
- Sanders MR. Triple P-positive parenting program: towards an empirically validated multilevel parenting and family support strategy for the prevention of behavior and emotional problems in children. Clin Child Fam Psychol Rev 1999;2:71-90.
- Oakley A, Strange V, Bonell C, Allen E, Stephenson J. Process evaluation in randomised controlled trials of complex interventions. Br Med J 2006;332:413-6.
- Roberts C, Roberts SA. Design and Analysis of Clinical Trials With Clustering Effects Due to Treatment n.d. www.SCTjournal.com (accessed 14 June 2022).
- Roberts C, Batistatou E, Roberts SA. Design and analysis of trials with a partially nested design and a binary outcome measure. Stat Med 2016;35:1616-36.
- Khan KA, Petrou S, Rivero-Arias O, Walters SJ, Boyle SE. Mapping EQ-5D utility scores from the PedsQLTM generic core scales. PharmacoEcon 2014;32:693-706.
- Hernández Alava M, Pudney S, Wailoo A. Final report: estimating the relationship between EQ-5D-5L and EQ-5D-3L: results from an English Population Study. PharmacoEcon 2023;41:199-207.
- Manca A, Hawkins N, Sculpher MJ. Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ 2005;14:487-96.
- Curtis L, Burns A. Unit Costs of Health and Social Care. Canterbury: Personal Social Services Research Unit, University of Kent; 2017.
- National Institute for Health and Care Excellence (NICE) . The Manual Process and Methods. Health Technology Evaluations. NICE 2022. www.nice.org.uk/process/pmg36 (accessed 14 June 2022).
- Fenwick E, Byford S. A guide to cost-effectiveness acceptability curves. Br J Psychiatry 2005;187:106-8.
- Stinnett AA, Mullahy J. Net health benefits: a new framework for the analysis of uncertainty in cost-effectiveness analysis. Med Decis Making 2016;16:S68-80.
- Wimo A, Gustavsson A, Jonsson L, Winblad B, Hsu MA, Gannon B. Application of resource utilization in dementia (RUD) instrument in a global setting. Alzheimers Dement 2013;9:429-35.
- Claxton K, Martin S, Soares M, Rice N, Spackman E, Hinde S, et al. Methods for the estimation of the National Institute for Health and care excellence cost-effectiveness threshold. Health Technol Assess 2015;19:1-504.
- INVOLVE . Briefing Notes for Researchers: Involving the Public in NHS, Public Health and Social Care Research 2012.
- Hassiotis A, Poppe M, Strydom A, Vickerstaff V, Hall I, Crabtree J, et al. Positive behaviour support training for staff for treating challenging behaviour in people with intellectual disabilities: a cluster RCT. Health Technol Assess 2018;22:1-110.
- Craig P, Dieppe P, Macintyre S, Mitchie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337:979-83.
- Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350. https://doi.org/10.1136/bmj.h1258.
- Savaya R, Waysman M. The logic model: a tool for incorporating theory in development and evaluation of programs. Admin Soc Work 2005;29:85-103.
- Green J, Charman T, McConachie H, Aldred C, Slonims V, Howlin P, et al. PACT Consortium. Parent-mediated communication-focused treatment in children with autism (PACT): a randomised controlled trial. Lancet 2010;375:2152-60.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101.
- Ruane A, Carr A. Systematic review and meta-analysis of Stepping Stones Triple P for parents of children with disabilities. Fam Process 2019;58:232-46.
- Brian J, Tint A, Chiba Branson J, Pilkington M, Program D, Bloorview H. Effectiveness of Group Stepping Stones positive parenting program for children with autism spectrum disorder and disruptive behaviour: program evaluation from a large community implementation. JoDD J De Disabil 2021;26:1-9.
- Schrott B, Kasperzack D, Weber L, Becker K, Burghardt R, Kamp-Becker I. Effectiveness of the Stepping Stones Triple P group parenting program as an additional intervention in the treatment of autism spectrum disorders: effects on parenting variables. J Autism Dev Disord 2019;49:913-23.
- Sofronoff K, Jahnel D, Sanders M. Stepping Stones Triple P seminars for parents of a child with a disability: a randomized controlled trial. Res Dev Disabil 2011;32:2253-62.
- NHS Digital . Waiting Times for Children and Young People’s Mental Health Services 2018–2019 2019.
- Watson SL, Hayes SA, Radford-Paz E. International Review of Research in Developmental Disabilities. 2011.
- Morpeth L, Blower S, Tobin K, Taylor RS, Bywater T, Edwards RT, et al. The effectiveness of the Incredible Years pre-school parenting programme in the United Kingdom: a pragmatic randomised controlled trial. Child Care Pract 2017;23:141-61.
- Rogers G, Perez-Olivas G, Stenfert Kroese B, Patel V, Murphy G, Rose J, et al. The experiences of mothers of children and young people with intellectual disabilities during the first COVID-19 lockdown period. J Appl Res Intellect Disabil 2021;34:1421-30.
- Rose J, Willner P, Cooper V, Langdon PE, Murphy GH, Stenfert Kroese B. The effect on and experience of families with a member who has intellectual and developmental disabilities of the COVID-19 pandemic in the UK: developing an investigation. Int J Dev Disabil 2020;1.
- Paulauskaite L, Farris O, Spencer HM, Absoud M, Ambler G, Barnes J, et al. My son can’t socially distance or wear a mask: how families of preschool children with severe developmental delays and challenging behavior experienced the COVID-19 pandemic. J Mental Health Res Intellect Disabil 2021;14:225-36.
- Lee V, Albaum C, Tablon Modica P, Ahmad F, Gorter JW, Khanlou N, et al. The impact of COVID-19 on the mental health and wellbeing of caregivers of autistic children and youth: a scoping review. Autism Res 2021;14:2477-94.
- Hinton S, Sheffield J, Sanders MR, Sofronoff K. A randomized controlled trial of a telehealth parenting intervention: a mixed-disability trial. Res Dev Disabil 2017;65:74-85.
- Reese RJ, Slone NC, Soares N, Sprang R. Telehealth for underserved families: an evidence-based parenting program. Psychol Serv 2012;9:320-2.
- Reese RJ, Slone NC, Soares N, Sprang R. Using telepsychology to provide a group parenting program: a preliminary evaluation of effectiveness. Psychol Serv 2015;12:274-82.
- Gore N, Hastings R, Brady S. Early intervention for children with learning disabilities: making use of what we know. Tizard Learn Disabil Rev 2014;19:181-9.
- Roberts C, Mazzucchelli T, Taylor K, Reid R. Early intervention for behaviour problems in young children with developmental disabilities. Int J Disabil Dev Educ 2003;50:275-92.
- Cooper V, Emerson E, Glover G, Gore N, Hassiotis A, Hastings R, et al. Challenging Behaviour Foundation; 2014.
- Aref-Adib G, Hassiotis A. Frontline 2020: the new age for telemental health. Lancet Psychiatry 2021;8:3-4.
- Sanders MR, Mazzucchelli TG. Mechanisms of change in population-based parenting interventions for children and adolescents. J Clin Child Adolesc Psychol 2022;51:277-94.
- Meyer RD, Ratitch B, Wolbers M, Marchenko O, Quan H, Li D, et al. Statistical issues and recommendations for clinical trials conducted during the COVID-19 pandemic. Stat Biopharm Res 2020;12:399-411.
- Office for National Statistics . Ethnicity and National Identity in England and Wales 2011. https://www.ons.gov.uk/peoplepopulationandcommunity/culturalidentity/ethnicity/articles/ethnicityandnationalidentityinenglandandwales/2012-12-11 (accessed 14 June 2022).
- Absoud M, Wake H, Ziriat M, Hassiotis A. Managing challenging behaviour in children with possible learning disability. BMJ 2019;365. https://doi.org/10.1136/bmj.l1663.
- Einfeld SL, Ellis LA, Doran CM, Emerson E, Horstead SK, Madden RH, et al. Behavior problems increase costs of care of children with intellectual disabilities. J Mental Health Res Intellect Disabil 2010;3:202-9.
- Kennedy EMM, French L, Roberts C. Personalised interventions for subgroups of children with conduct problems. Cochrane Database Syst Rev 2017;2017. https://doi.org/10.1002/14651858.CD012746.
List of abbreviations
- ABAS
- Adaptive Behaviour Assessment System
- APA
- American Psychiatric Association
- ASD
- autism spectrum disorder
- CAMHS
- Child and Adolescent Mental Health Services
- CA-SUS
- Child and Adolescent Service Use Schedule
- CBCL
- Child Behaviour Checklist
- CEAC
- cost-effectiveness acceptability curve
- CEP
- cost-effectiveness plane
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- COVID-19
- coronavirus disease 2019
- CRF
- case report form
- CSNF
- Camden Special Needs Forum
- C-TRF
- Child Behaviour Checklist caregiver–teacher report forms
- DSH
- Data Safe Haven
- DSMB
- Data Safety and Monitoring Board
- DSM-5
- Diagnostic and Statistical Manual of Mental Disorders, 5th Edition American Psychiatric Association
- e-CRF
- electronic case report form
- EOI
- expression of interest
- EQ-5D
- EuroQoL Five Dimensions Scale
- FOS
- Revised Family Observation Schedule, FOS-RIII
- GCP
- Good Clinical Practice
- GCS
- General Core Scales
- GHQ-12
- General Health Questionnaire
- GP
- general practitioner
- HRA
- Health Research Authority
- ICER
- incremental cost-effectiveness ratio
- ID
- intellectual disability
- ITT
- intention to treat
- NHS
- National Health Service
- NICE
- National Institute of Health and Care Excellence
- PAG
- Parent Advisory Group
- PedsQLTM
- Pediatric Quality of Life
- PI
- principal investigator
- PSOC
- Parenting Sense of Competence Scale
- PSS
- personal social services
- PSSRU
- Personal Social Services Research Unit
- QALY
- quality-adjusted life-year
- QRS-F
- Questionnaire on Resources and Stress-short Form
- RCT
- randomised control trial
- REC
- Research Ethics Committee
- SAE
- serious adverse event
- SOP
- standard operating procedure
- SSTP
- Stepping Stones Triple P
- TAU
- treatment as usual
- TMG
- Trial Management Group
- TSC
- Trial Steering Committee
- UCL
- University College London
- WTP
- willingness to pay
Notes
Intervention materials and study questionnaires are available from the authors on request.
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/JKTY6144).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
