Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as award number NIHR128128. The contractual start date was in January 2020. The draft manuscript began editorial review in November 2022 and was accepted for publication in September 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Hughes et al. This work was produced by Hughes et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Hughes et al.
Chapter 1 Introduction
Co-occurring serious mental health problems and alcohol/drug use
The focus of the realist evaluation co-occurring (RECO) study is on people who have severe and enduring mental illness (SMI). This group is likely to require support and treatment from secondary mental health services such as inpatient mental health units and/or community mental health services for at least some of their lives, and approximately 30–50% of them have a coexisting alcohol/drug condition. 1,2 SMI includes individuals with psychotic disorders such as schizophrenia, paranoid psychosis, schizoaffective disorders, bipolar affective disorders, and long-term and severe depression. It is also recognised that many people (70–80%) who seek help for drug and alcohol conditions also experience co-occurring mental health problems such as depression, anxiety and personality disorders. However, serious mental health issues are less commonly seen in addictions services with 16–21%3 also having a SMI. 4
Co-occurring severe mental health and alcohol/drug conditions (COSMHAD) are associated with significant negative impacts on health and social outcomes including increased risk of suicide and self-harm,5 violence perpetration and victimisation,6,7 contact with the criminal justice system and forensic mental health,8 and higher overall service costs (as a result of more frequent and longer admissions to hospital) than those with single diagnoses,9 comorbid physical health problems10 and social problems including homelessness. 11 These issues are further compounded by comorbidities going untreated, with a UK study12 observing that over a third of drug users with a comorbid psychiatric disorder received no treatment for their mental health.
Co-occurring severe mental health and alcohol/drug conditions interventions
There is currently very limited evidence to inform the treatment of COSMHAD. The evidence to date comprises evaluations of psychosocial interventions,13,14 integrated treatment models15 and evaluations of workforce training. 16 There remains a lack of definitive evidence to inform how service models and treatments could improve health and other outcomes for this population. One of the challenges of undertaking research with individuals receiving care for COSMHAD is that they are a heterogeneous group. Individuals can differ greatly both in terms of the type of mental health problem(s) and the type and severity of alcohol and/or drug use. Furthermore, those receiving care for COSMHAD often present with a number of other diverse and complex needs, particularly around housing and employment. Research studies often exclude those who are currently mentally unwell (particularly those with SMI) and/or those who face barriers to participation such as homelessness. Consequently, the already limited evidence from the COSMHAD literature is further weakened by the findings potentially representing a very limited subsection of this population.
Co-occurring severe mental health and alcohol/drug conditions policy in the United Kingdom
Co-occurring mental health and alcohol/drug use (encompassing all mental health conditions, not just serious and enduring), which was previously referred to as ‘dual diagnosis’, has received a significant amount of attention from policy-makers. In 2000, the All Party Parliamentary Drugs Misuse Group published a short report outlining the challenges posed. This included people ‘falling between the gaps’ and consequently not receiving support for their mental health or substance use due to the narrow focus and differing philosophies of treatment organisations.
In 2002, the Department of Health published the Dual Diagnosis Good Practice Guide17 which set out the requirements for the treatment of co-occurring mental health and substance use. Central to this guide was the concept of ‘mainstreaming’. This approach advocates that the workforce in relevant services should have the appropriate training and capabilities to offer treatment that addresses and integrates both mental health and substance use issues. Mainstreaming requires clinical leadership roles to offer training and support to implement this at a local level. It was further recommended that care for this group should be integrated, with key agencies working together to develop agreed care pathways to ensure that people get the right help, in the right place, at the right time. However, 5 years after this guidance was released, there was still significant national variation in the provision of care, with 40% of local implementation teams failing to implement an agreed ‘dual diagnosis’ strategy and less than half having assessed the training needs of staff. 18
In 2011, the National Institute for Health and Care Excellence (NICE) published clinical guidance on the management of psychosis and substance misuse, to better support the provision of care for COSMHAD. 19 This was followed in 2016 by broader NICE guidance on COSMHAD treatment in community health and social care services, informed by a systematic review of research evidence as well as expert opinion. 19 More recently, Public Health England (PHE) released refreshed policy guidance. 20 This broadly reflects the original principles of mainstreaming (i.e. it’s ‘everyone’s job’, with ‘no wrong door’ for people trying to access help); however, it also broadens its remit to consider the wider health and social care sector including the third sector providers of substance use treatment, and the growth of volunteers and peer support. This broader remit reflects the core elements of the NHS Long Term Plan (LTP) and Community Mental Health Framework (CMHF),21 with the ambitions of these underpinning the unprecedented transformation currently happening within health and social care. Within this, there is a focus on working with multimorbidity, reflected in, for example, the definition of SMI used in the CMHF including multimorbidities such as substance use. Indeed, the CMHF states that ‘In this Framework, close working between professionals in local communities is intended to eliminate exclusions based on a person’s diagnosis or level of complexity’ (p. 5), with complexity noted as being influenced by multiple factors including ‘co-occurring drug and alcohol-use disorders’ (p. 20). Such transformation focuses on a move to integrated working and a focus on addressing health inequalities across the whole system with the creation of 42 Integrated Care Systems (ICSs) in England. Within ICSs sit Integrated Care Boards (ICBs) which have taken on the commissioning responsibilities throughout England, formalised legally by the new Health and Social Care Act that came into force in July 2022. Alongside this, ‘From Harm to Hope’, the 10-year drugs plan,22 was published in December 2021, which reflects commitment to implementing Dame Carol Black’s key recommendations,23 by ‘ensuring better integration of services – making sure that people’s physical and mental health needs are addressed to reduce harm and support recovery’ (p. 8).
Policy in the devolved nations has also called for improvements in the delivery of care for people with COSMHAD. ICSs have been in place in Scotland and Wales since their respective devolutions, with 31 health and social care partnerships across Scotland and 7 regional partnership boards across Wales. In Northern Ireland, substance use policy24 cross-references with mental health strategy and specifically calls for improvements in the delivery of integrated care for people with COSMHAD and specifies the ambition for expert leader posts to be created in every area to ensure that this happens. The Scottish mental health strategy 2017–2725 identifies specifically that people with COSMHAD fall through gaps in services and integration. It sets out that authorities should work jointly to address these gaps in order to provide holistic care. Mental health is briefly mentioned in the Scottish Alcohol and Drug Treatment strategy26 and calls for more integrated work treatment and suicide prevention. The Wales Substance Use Delivery plan 2019–2227 calls for improvements in joint working and mentions co-occurring mental illness as an area for development, particularly that no one should be excluded from mental health services because of a concurrent substance use issue.
However, despite the sustained development of policy related to COSMHAD across the UK, there remains a lack of operational and granular detail as to how to achieve ‘better integration of care’ and ‘prevent people falling through [the] gaps’. There is uncertainty about how care should be delivered, under what contexts it works (or does not work) and whether a range of approaches, rather than a single approach, is required to meet the needs of such a diverse group.
Study aims and outcomes
The aim of this study was to use a realist approach28 to understand COSMHAD treatment models by investigating what works for whom, why, and in what circumstances.
Structure of report
The report is divided into five chapters: Chapter 1 covers the background and aims. Chapter 2 covers the design and procedures for the three work packages (WPs), Chapter 3 covers WP2 mapping and audit findings and Chapter 4 covers the development of initial programme theories (IPTs) (realist synthesis of evidence) and the refinement of the PTs using data from the case study evaluation. Chapter 5 discusses the findings, strengths, limitations and implications for policy, research and practice.
Chapter 2 Design and methods
Overall study design
In order to address the aims of the study, the project was divided into three complementary WPs. The literature mapping and realist synthesis in WP1 provided valuable insights into existing treatment models and practices for COSMHAD, allowing us to develop and refine an overarching PT (explanatory framework) of what works, for who, in which circumstances and why. In WP2 a national mapping exercise and audit identified COSMHAD care provision in the UK, and gathered detail regarding how services function in practice, further refining the PTs developed in WP1 by elucidating the contexts in which COSMHAD treatment is intended to operate. Finally, in WP3, case studies were used to further test and refine the PTs in different models of COSMHAD care using data from people who work in those services and people who use those services (and carers). It is important to note that although the research is described in three distinct phases, the process of conducting realist research is iterative rather than linear, cycling between literature searching and data collection, with constant refinement of, adjudication between, and evidencing of emerging PTs.
Work package 1: developing programme theories
Justification for choice of realist synthesis framework
Realist approaches attend to the ways that interventions (or programmes) may have different effects for different people, depending on the context. An intervention or service for people with COSMHAD is considered to provide resources that alters the context, triggering a change in the reasoning of intervention participants, leading to a particular outcome, that is context + mechanism = outcomes (or CMOs). CMOs are used as explanatory formulae (otherwise referred to as realist PTs), which are then ‘tested’ either through literature (synthesis) or empirical data (evaluation) and refined as the project progresses. They, in effect, postulate potential causal pathways between interventions and impacts. Thus, use of a realist approach was intended to help expose the multiple resources delivered as part of services for COSMHAD, the ways these were employed with different people and how they generated different outcomes. Furthermore, with any service or intervention, implementation can lead to the programme being interpreted and/or utilised differently, with possible impact on outcome. Realist methodologies aid the development of a broader picture of how such combinations of context and underlying causal mechanisms can improve or impair programme fidelity and efficacy. 29 Realist synthesis methods provide valuable insights into ‘literature ideals’ and develop and refine PT(s) of what works, for who and in which circumstances.
Research questions
The research questions identified for the realist synthesis were:
-
What does the existing literature suggest ‘works’ (demonstrated by engagement and other health outcomes) in terms of COSMHAD, for whom and in which circumstances?
-
What are the current range and types of service systems that currently operate in the UK that aim to improve engagement and health outcomes for people with COSMHAD?
-
What are the specific contexts and mechanisms that make COSMHAD models successful (or not), for whom and in which circumstances?
To inform our understanding of the current range and types of service systems, we used a literature mapping approach to map the types of services/models that exist for people with COSMHAD in the UK. From this, a typology of service provision models was developed which was used to further focus the realist synthesis questions and inform the analysis of the national mapping study (WP2).
Methods for literature mapping
Seven health, social sciences and educational databases (Medline, Cochrane, EMBASE, Web of Science, CINAHL, PsycInfo and HMIC) were searched in March 2020. A comprehensive search strategy was developed using a combination of free text and controlled vocabulary terms and adapted for each database. Search terms were drawn from five categories relating to SMI, substance use, co-occurrence, service integration and delivery of health service-related terms. A full search strategy is included in Appendix 1 (see Tables 9 and 10). Database searches were supplemented by searching grey literature, websites related to mental health and substance use, and by checking the reference lists of retrieved articles and COSMHAD-related policy documents.
The searches identified 5099 articles which went through a two-stage title and abstract screening process by two reviewers (JH, TA) using the Covidence (Melbourne, VIC, Australia) review management software. Any conflicts were resolved through discussions with a third reviewer (LJ). In stage 1, an initial corpus of 817 articles focusing on co-occurring SMI and substance use service provision and use was identified. In stage 2, the number of articles was subsequently reduced to 414 which met the screening objectives for the literature mapping.
Studies were included in the literature mapping if they described services for people with COSMHAD aged 18 years and over. We excluded services which specifically integrated COSMHAD with addressing additional conditions/needs (such as HIV or violence/aggression) and those delivered in population specific specialist settings (such as veteran services, prison services and services for homeless populations). Empirical studies, reviews and service description focused articles in practice-based journals were eligible. Full text articles were screened by one researcher and 20% were double-screened by a second researcher (LJ). Due to a wide variety of literature and the contextual differences in delivering COSMHAD services in high-income countries, the decision was made to focus on UK-based studies. These papers were deemed most relevant to the wider aims of the study and best placed to develop a framework for the service mapping exercise.
Formal quality assessment of the articles included in the literature mapping was not undertaken. We used a structured approach to data extraction based on the four domains of the Effective Organisation and Practice of Care (EPOC) taxonomy developed by Cochrane (2015).
Methods for realist synthesis
Our protocol for the realist synthesis was prospectively registered with PROSPERO (CRD42020168667). In phase 1, we developed and verified potential PTs from the published literature and with stakeholders. In phase 2, we conducted a systematic search of the relevant literature, supplemented by further purposive explorations for evidence, underpinning each PT component. The review followed the five stages identified by Pawson:1 (1) identifying the review question, (2) search for studies, (3) quality appraisal, (4) extract the data and (5) synthesising the data and disseminating the findings.
Identification of programme theory
A classic realist synthesis begins with the identification of opinions and commentaries as a source of PTs for which evidence is then sought. 5 We therefore began by analysing policy documents and articles describing COSHMAD services in practice in the UK. We also held one 2-hour workshop with clinicians, policy-makers, managers and academic experts (n = 14) to gather their views on what worked for COSMHAD services in the UK, for who and in which circumstances. We also attempted to engage with individuals who had experience of COSMHAD; however, the coronavirus disease 2019 (COVID-19) pandemic and lockdown restrictions meant that this was not possible in the early stages of the realist synthesis.
The findings from the literature, key policy documents and the workshop were triangulated to develop a sketch of the COSMHAD programme (Figure 1) and 16 draft PTs. This was achieved by extracting if/then statements from the literature, workshop transcript and key policy documents (including from NICE and PHE) which were then grouped. Key concepts that were important to the programme (‘engagement’ and ‘integration’) were explored and defined from the relevant literature. The 16 draft PTs and an initial programme sketch (see Initial programme theories) were reviewed and refined by the entire project team (n = 9). By combining service descriptions from the practice literature and views of stakeholders, we were able to identify underpinning mechanisms by which different programme components achieve their outcomes, as perceived by those actively involved in designing and implementing COSMHAD services. The 16 draft initial PTs are shown below.
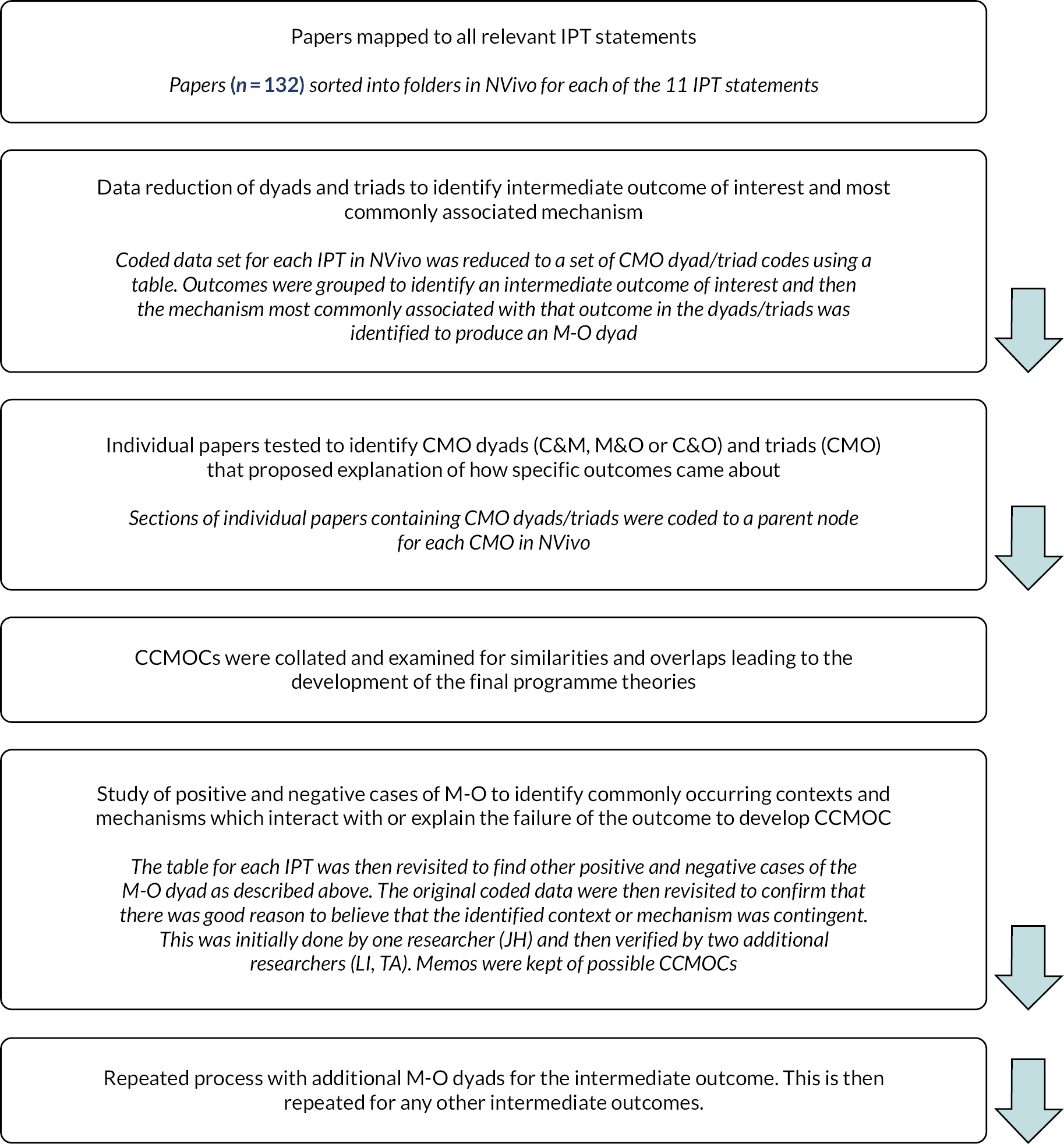
FIGURE 1.
Summary of the data extraction and analysis process for the realist synthesis.
-
‘Everyone’s business’: Recognising that COSMHAD is the responsibility of everyone who comes into contact with these service users will increase their access to mental health and substance use support and reduce exclusion due to crisis or intoxication.
-
Positive attitudes: A shared, empathetic and non-judgemental attitude towards individuals with COSMHAD across all services can reduce stigma, improve engagement and prevent premature discharge from services.
-
Collaboration: Strong and consistent management which promotes understanding of COSMHAD and the benefits of collaboration facilitates collaborative working between services to support multiple and complex needs.
-
Workforce education: Continuous education (from undergraduate/pre-registration onwards) which incorporates the biopsychosocial approach to individuals with COSMHAD will assist staff to deal with the complexities faced by these service users and appropriately employ behaviour change strategies.
-
Workforce support and development: Comprehensive workforce development which includes dual diagnosis training and ongoing supervision and skills development (e.g. shadowing, work-based learning and multiagency meetings) ensures that staff have the right values and skills to assess and respond to the needs of individuals with COSMHAD.
-
Leadership: COSMHAD opinion leaders are needed at the practitioner, operational management and strategies management levels to ensure that the needs of people with COSMHAD are met by driving forward new/modified practices.
-
Care pathways: A formalised collaborative pathway of care with ‘buy-in’ from all key agencies and opportunities for practitioners to meet with each other (e.g. through network) will ensure all teams, services and specialisms have good relationships to collaboratively respond to individuals’ needs.
-
Strategic senior level commitment: Senior managers/commissioners must believe it is right for them to be involved and accountable for COSMHAD service development by putting in place strategic frameworks to improve access to services and reduce health inequalities.
-
Sustaining practice: Continuous training and supervision is needed to sustain COSMHAD service models and allow staff to stay involved in practice.
-
Networks: Multiagency groups or networks for practitioners can increase their awareness of other services and improve service delivery (e.g. through improved referrals and reduced waiting times).
-
Mental health as lead agency for care: Mental health service care co-ordinators should take the lead in developing a care plan and co-ordinating services which will improve people with COSMHAD’s access and engagement with services, response to care, recovery and longer-term outcomes.
-
Commissioning: Strategic commitment to reconcile differing funding and commissioning arrangements is needed to develop an effective, collaborative COSMHAD pathway.
-
Evaluation impact of staff training: Evaluation measures need to be put in place to determine the impact of staff training on outcomes for service users.
-
Evaluation outcomes: Evidence-based quality improvement measures are needed to evaluate the impact of COSMHAD services and capture learning across services.
-
Recruitment and retention: Processes are needed to ensure that staff with the requisite COSMHAD skills, knowledge and values are recruited and retained in services to deliver better care.
Identifying formal theory to inform the initial programme theories
The process of identifying formal theories which assisted in explaining our PTs6 took place iteratively throughout the realist synthesis, mainly over two phases. Searches for theory to help inform the development of the IPTs, described in this section, and searching for theory to inform and develop the final PTs, took place during the data analysis phase.
Following the project team review of the if/then statements, we began working to refine these theories into context–mechanism–outcome (CMO) statements. In some realist synthesis, the intervention under investigation has well-defined boundaries and outcomes and the PT is explicitly stated. However, COSMHAD service models are complex, large scale and ‘messy’,7 requiring transformation and organisational culture change within publicly funded services. 8 As our early work developing draft PTs identified, COSMHAD programmes in the UK were often not a well-defined intervention, rather they were often a set of ideas which had been tried, and not always in a systematic or uniform way. We therefore undertook a purposive search of theories and frameworks that covered the various aspects of the COSMHAD service model. We developed an initial shortlist of 16 substantive theories (at the middle range)30 from the field of COSMHAD, other realist work looking at similar service transformation, and our own expertise in public health, psychology and other relevant fields.
The shortlisted theories were appraised according to the following criteria developed from Shearn et al.’s31 guidance for complex interventions: (1) the level in the social system (offering explanation at the micro, meso or macro level); (2) their fit with our research aim of explaining how COSMHAD services work, for who and in which circumstances; (3) their simplicity in inspiring theory generation; and (4) their compatibility with the realist notion of articulating causation. Four theories were selected which best fitted the criteria and helped explain various aspects of the PTs. Normalisation process theory (NPT)9 was used as an overall framework to inform the generation of the final PTs, with the four sense-making, relational, operational and appraisal domains used to organise the PTs. Three additional theories were used to help refine specific PTs, namely: the Health and Stigma Framework10 (PT 2), the Framework for Action in Interprofessional Education and Collaborative Practice11 (PT 3) and the Integrated Commissioning for Better Outcomes Framework12 (PT 10). The use of these theories expanded the team’s thinking around specific aspects of the PTs. For example, use of NPT allowed us to consider the relationship between the sense-making, relational, operational and appraisal work required of stakeholders when working to co-ordinate care for people with COSMHAD.
Finalisation of the initial programme theories
Eleven IPTs were developed, which included context, mechanism (including resource and response) and outcome. These PTs were reviewed and refined through consultation with the entire project team. Following development, we searched for empirical evidence to test and refine the IPTs. The decision was made to use the initial corpus of 817 articles identified in the literature mapping as the preliminary starting point for the realist synthesis. This is because, as recommended by Booth et al.,32 the initial search terms had been developed in consultation with the project team who represented a range of stakeholder perspectives and the literature identified through structured searches had been supplemented by literature provided by stakeholders and sampled purposively. These 817 articles provided us with an initial, exhaustive search of examples of service provision which we considered an ‘initial sampling frame of empirical papers’13 (p. 151). However, it is recognised that realist searching is an iterative process, with search criteria often emerging as theories are proposed, tested and refined. We therefore took an iterative approach to literature searching, with additional articles being identified and included through CLUSTER searching to identify sibling studies, citation tracking and named and complementary theory searches as the review progressed. 13
The 817 full texts were screened against criteria made up of the 11 PTs. Articles were selected for inclusion when they provided causal insights into the PTs by: (1) reporting on integration of services for people with COSMHAD; (2) describing features and functions of the integrated service architecture relevant to the PT; and (3) providing data on the outcomes of this integration. All texts were screened by the lead researcher (JH) with two researchers independently screening (TA, LJ) 10% of these articles. The three reviewers met regularly throughout the screening process to discuss their decisions and any disagreements were resolved through discussion. This discussion process was also used to identify potential studies and authors for CLUSTER searching and citation tracking, with additional purposive searches undertaken as a result. In total, 172 articles were selected for inclusion in the realist synthesis.
Quality appraisal
Realist synthesis approaches do not follow more rigid, traditional approaches to quality appraisal. The nature of the data collected by realist reviews is not always necessarily of the ‘highest quality’ in the traditional sense (i.e. they will be of variable trustworthiness). The aim of realist methods is not to arrive at the ‘final truth’ regarding the research topic. 33 Rather, realist reviewers recognise that we can only get as close as possible to a complete understanding. Realists assemble imperfect data into plausible and coherent arguments, but others may disagree with their claims. Quality appraisal in this review therefore considered each article on the basis of whether it was good enough to provide some evidence that would contribute to the synthesis. This was based on two grounds: (1) assessment of relevance and richness and (2) assessment of rigour. In the case of this review, relevance and richness were assessed as to whether the study helped to explain how context shapes the mechanisms through which UK service models for COSMHAD work, for whom, how and in which circumstances. Studies were considered as relevant where they met one of the three inclusion criteria described above and thus relevance was applied to both the topic (COSMHAD) and the PT. 34 Richness was discussed between the researchers, in terms of conceptual richness (conceptual and theoretical development) and thickness (the amount of detail provided). 35 Consideration of the study rigour took into account the plausibility and coherence of the method used to generate data and the limitations of the methods used. However, the decision to include a study in the synthesis was not restricted to a study level, pre-formulated checklist of methodological rigour. The rigour of each fragment of evidence was balanced with its relevance and the extent to which it assisted in explaining the relevant PT. Thus, assessments of a particular piece of evidence (i.e. the trustworthiness of the source) were considered alongside the overall coherence and plausibility of the PT. 36 Assessments of rigour are therefore commented on throughout the findings, at the evidence and theory level.
Data extraction and synthesis
Following this screening process, the articles were re-read and mapped to each of the IPT statements using a data extraction form. This revealed 132 articles that provided causal insights into one or more of the IPT statements. The selected articles were then imported into NVivo (version 12) (QSR International, Warrington, UK), which allowed for an organised and transparent audit trail of decisions related to the data analysis, using the linked memo function. 14 Source folders were created for each IPT and articles were uploaded to each folder based on the mapping exercise. In NVivo, parent nodes were created for each IPT and selected articles coded independently to each IPT. 14 Rather than separately coding the data from the articles into context, mechanism and outcome for each IPT statement, we attempted to identify CMO configurations directly from the literature as either dyads (context–mechanism/mechanism–outcome/context–outcome) or triads (CMO). 15 Following the identification of individual dyads and triads, we followed the process of data reduction described by Byng et al. 37 Firstly, we developed a reduced data set for each IPT by creating a table containing all lower-level codes for CMO dyads and triads. We were then able to group the outcomes (which usually had the least codes) and identify an intermediate outcome of interest for the IPT. We then reviewed the data table to identify the mechanism most associated with this outcome to create a mechanism–outcome (M-O) dyad. We then searched our coded data for positive and negative cases of the M-O to identify consistently occurring contexts and additional mechanisms which interacted or could explain the failure of the outcome which were used to produce ‘conjectured context–mechanism–outcome configurations’ (CCMOC). The CCMOC was checked against the original literature for face validity and the process was then repeated with each additional mechanism associated with the outcome and then any other intermediate outcomes for the IPT. The full process is described in Figure 1.
The process of mapping, extracting and coding data for each CMO dyad/triad was undertaken by one researcher (JH) through reading and re-reading of the data. Using a realist context–mechanism–outcome configurations lens for each outcome identified, the analysis sought to understand what contexts had fired the mechanism and underpinning common mechanisms between studies. After coding possible CMO dyads and triads, the researcher consolidated the data using tables and revisited the literature to develop the possible CCMOCs. The first stage of analysis was read and discussed with two additional researchers (LJ, TA) to ensure reliability and validity and the CCMOCs were refined following these discussions. The CCMO statements were then reviewed, refined and finalised in discussion with the realist methods lead for the project (SD).
Summary of literature mapping
A total of 23 papers met the inclusion criteria, which described 19 UK COSMHAD service models. Service models described in multiple publications were combined into a single entry on the data extraction form. Nine of the studies were delivered by mental health trusts in either community or inpatient settings, four by substance use services (three in the community and one specialist ward), and six studies involved collaboration between multiple service settings either through networks or liaison with specialist workers.
Models of service provision fell into three broad categories: (1) multidisciplinary COSMHAD groups or networks to establish provider relationships and co-ordinate care pathways; (2) placement of specialist COSMHAD link workers within existing mental health or substance use teams; and (3) specialist COSMHAD liaison workers working with mental health and substance use teams from a separate specialist COSMHAD team. These three categories are indicated in the first column of the Table 1, with the allocated colours indicating elements specific to that model.
| How and when care is delivered | |||
| Co-ordination of care among different providers | Multidisciplinary network groups establish provider relationships and co-ordinate pathways | Specialist COSMHAD link workers placed within existing teams | Specialist dual diagnosis liaison workers in a COSMHAD team |
| Group vs. individual interventions | Incorporating COSMHAD into existing provision of combined individual and group interventions. Majority draw on Cognitive Behavioural Therapy and Motivational Interviewing approaches | ||
| Triage | Inclusion of COSMHAD measures into existing assessments | Joint assessment or assessment by COSMHAD worker after referral | |
| Where care is provided and changes to the healthcare environment | |||
| Environment | Within existing service environment | ||
| Outreach | Minimal engagement with assertive outreach teams in majority of models (exception COMPASS) despite recognition of high dual diagnosis prevalence and benefits of proactive engagement | ||
| Site of service delivery | Site of usual provision | Mental health or substance use teams. Majority placed in mental health teams | Additional team providing separate or integrated care |
| Site of organisation | Model coverage usually by geographical area – majority defined by catchment of NHS Mental Health trust (small number by substance use service) | ||
| Who provides care and how the healthcare workforce is managed | |||
| Role expansion or task shifting | All staff have increased awareness of dual diagnosis and are able to co-ordinate care for these service users | Staff specialising in COSMHAD lead on raising awareness and facilitating co-ordinated care for team in
|
Staff specialising in COSMHAD provide time-limited service to raise awareness and support teams in delivering integrated care |
| Pre-licensure education | Range of experience and education among membership provides new perspectives | Challenging to find balance between mental health and substance use expertise, and between level of education and amount of experience in practice | |
| Co-ordination of care and management of the care process | |||
| Care pathways | Establishing and formalising collaborative care pathways for individuals with COSMHAD. Stepwise approach based on the US Integrated Treatment Model (detection, engagement, motivation, active treatment and relapse prevention) | ||
| Case management | Case management remains responsibility of service user’s existing case manager with time-limited specialist joint working, consultation and assessment to assist with this | Case management largely remains responsibility of case manager with support, but in some services the specialist may take over case management in cases with severe complexities or chaotic engagement | |
| Communication between providers | Communication should be transparent and built on mutual trusting relationships. This can be achieved formally through documentation at service and service user level, and informally through multidisciplinary attendance at groups and networks | ||
| Continuity of care, discharge planning and referrals | Discharge and continuity of care should be a key part of joint care plans | ||
| Shared care and decision-making | Shared care and decision-making between mental health and substance use teams (and wider services). Shared care protocols and documentation of care in care plans and referral letters is important | Shared care and decision-making between link/liaison worker and service user’s case manager. Link worker often brokers shared care arrangements with other services | |
| Funding | |||
| Funding | Majority of models operated on no dedicated funding or single source of funding (e.g. from local budgets or research funding) | ||
| Governance arrangements | |||
| Governance arrangements |
|
||
| Implementation strategies | |||
| Organisational culture | Integration means COSMHAD is the responsibility of all staff who encounter these service users. Address:
|
||
| Communities of practice | Formalised to varying degrees but involve groups of practitioners who work with people with COSMHAD meeting regularly for case discussion, sharing experiences and practice, peer support, local supervision and facilitating joint working. Learning then fed back to organisations | ||
| Clinical practice guidance | Resources such as manuals, service directories and local practice guidelines can support link workers and network members to deliver key principles of COSMHAD in their services | ||
| Interprofessional education | Two levels of training identified:
|
||
| Local opinion leaders | Two types of local opinion leader required:
|
||
| Managerial and clinical supervision | Link/liaison workers provide supervision to colleagues to assist them to work with people with COSMHAD but also require supervision from COSMHAD specialists to prevent them becoming isolated in their roles | ||
Work package 2: national mapping and audit of services
Work package 2a: national mapping procedure
The aim of WP2 was to identify the location and types of provision of service models for COSMHAD across the UK. This comprises a general mapping exercise then an audit form for those identified.
For the mapping process, requests for information were sent to organisations across the UK who were likely to be responsible for providing or commissioning COSMHAD care. This included every NHS mental health trust and local authority in the UK, as well as all clinical commissioning groups (CCGs; now recognised to have transitioned to ICBs) and devolved nation equivalents including health and social care NHS trusts and local commissioning groups in Northern Ireland, and health boards in Wales and Scotland. We also contacted Public Health England, the Northern Ireland Department of Health, Public Health Reform Scotland, Health Protection Scotland, Scottish Association for Mental Health, Inspire Wellbeing, Turning Point and Mind. We adopted a broad definition of COSMHAD care to include services. At this stage, our definition of what was included as a service or provision was sufficiently broad to be inclusive, but specific enough to meet the aims of the study in (1) explicitly containing elements of provision for people who meet our inclusion criteria and/or (2) having a written service level agreement or guidance describing what is offered and to whom in relation to COSMHAD.
Requests were sent in the first round by email, and in the second round using Freedom of Information (FOI) requests, asking for the following information (a complete version of the request sent can be seen in Report Supplementary Material 1):
-
Details of the approach/treatment pathway for COSMHAD treatment that the contacted organisation commissioned or was commissioned to provide – particularly whether it was commissioned specifically for COSMHAD.
-
Details of any other COSMHAD services that organisations were aware of operating in their region.
-
The name and contact details of the local COSMHAD/dual diagnosis lead.
The first wave of information requests was sent in March 2020, with a second wave sent in October 2020. The COVID-19 pandemic severely reduced the capacity of many organisations to engage fully with our requests. A third wave of requests was planned to be sent early in 2021; however, with a new national lockdown beginning in January 2021, it was decided that this third wave of requests would have been of limited utility.
Work package 2b: service audit/survey
To gain a deeper understanding of how COSMHAD services across the UK are commissioned and operate, a more detailed service audit was developed with input from the RECO team members, individuals with lived experience, and those involved in commissioning and delivering COSMHAD care. It included closed and open-ended questions on commissioning, provider, models of care and available treatments, managing joint working between mental health and drug and alcohol treatment, and staffing resource health economic data such as staff numbers and resource use (see Report Supplementary Material 2 for full questionnaire).
The RECO group reviewed the mapping data and identified 16 services that had at least one person employed as part of their local response to COSMHAD, and they were invited to complete the audit.
Potential services were first approached by e-mail, describing the RECO project as a whole and the rationale for collecting service provision information, and asking to be put in contact with an individual within the service best situated to provide the necessary information. Once contact was made with this individual, a link to the survey was sent along with instructions of how to complete the survey, including the option to complete the survey over the phone. Participants choosing to complete the survey online were given 2 weeks to complete and return the survey and were contacted by the study team if the survey had not been returned after this time. If a returned survey did not include sufficient detail, respondents were contacted to ask if they would be willing to be contacted by phone to collect missing details. Participants choosing to complete the survey over the phone were made aware of specific questions that may require preparation on their part (e.g. staff numbers dedicated to COSMHAD care) and a date was organised for the survey to be completed. Data from the online survey were downloaded into Statistical Package for Social Science to analyse multiple response sets and descriptive analysis.
Case study procedures
Site selection and setting
A set of six case study sites were chosen from those that completed the online audit. The services were grouped as follows based on the information they provided:
-
specialist worker plus link workers (lead and link)
-
consultancy model (consultancy)
-
network model (network).
From the responses, we chose case studies that represented all three types of models (three lead and link, one consultancy and two network). We also ensured that we included at least one service from a devolved nation. Case studies were specifically defined as the primary COSMHAD service (the mental health service provider) and the relevant partnering agencies. All case studies were complex in that they described a social complex service, but also because substance use treatment services did not neatly configure geographically with the mental health providers.
Staff recruitment
Staff were invited to participate if they worked in mental health and substance use services in the case study locality, including those in dedicated COSMHAD roles. Each case study had a link clinician through which the research team communicated. Initial e-mails were sent to COSMHAD care personnel in each of the six study sites, with individuals wishing to take part contacting the study team directly.
The researcher (JH) liaised with the link clinicians to book dates for staff focus groups at convenient times and undertook all focus groups and interviews for consistency. Each focus group was also co-facilitated by two RECO researchers (EH, AC, EG). Typically, two staff focus groups were required for each site, with relatively small participant numbers in each one to allow space for each person to discuss and contribute. Quotes from service providers in the narrative are indicated using the label SP.
Service user and carer recruitment
The target was to recruit 12 service users and 6 carers at each site. Service user inclusion criteria were broad and inclusive: people with a SMI (including psychosis, bipolar affective disorder, schizophrenia, severe depression, personality disorders) who had accessed local mental health and/or substance use services.
Co-occurring severe mental health and alcohol/drug conditions service users and carers were first approached by staff at case study sites who provided them with details of the study. Posters advertising the study were also placed in treatment centres. Those interested in taking part could contact the study team directly or elect for the treatment centre staff to pass their contact details on to the study team. All participants completed an online consent form prior to taking part in the focus groups, and mobile phone data vouchers were made available to allow access to the study.
The original intention was to conduct the interviews face to face, but due to the COVID-19 pandemic, there was a need to move data collection to an online format. Realist interviews are quite different to qualitative interviews; rather than taking a constructivist approach which aims to elicit participant narratives, the primary aim of realist interviews is the development, refinement and consolidation of PTs, depending on what stage of the research cycle the interviews are being conducted. 38 In the context of the RECO study, the interviews were intended primarily to facilitate the refinement and consolidation of the PTs developed through the earlier WPs. This entailed asking considered and purposeful questions to elicit specific information regarding PTs, including directly presenting interviewees with PTs in a conversational style, to spark discussion about how well they matched participants’ experiences.
A convenient date and time for the data collection were arranged and an invite to the Microsoft Teams meeting circulated. A topic guide was formulated to guide the focus groups, underpinned by the PTs from the realist review. However, with the constant iteration between testing and refinement of PT, the topics addressed at each focus group were highly dynamic. At the start of each session, participants were asked to respect the confidentiality of the focus group discussion. If during the session a participant became distressed, there was an option for one of the facilitators to meet them in a virtual break-out room. All service user and carer participants were offered an optional debrief call after the focus group. Participants were informed prior to the session that their name would be visible during the focus group, but all data would be anonymised for analysis. All service user and carer participants received a £10 gift voucher to thank them for their time.
The online interviews and focus groups were recorded and auto-transcribed in Microsoft Teams. Quotes from service users and their carers are indicated in the narrative using the label P. Carers are indicated in the quote label.
Costing case study sites
While there was not the scope or remit within this study to undertake an economic evaluation of the services, we costed the case study sites from an NHS perspective following a mix of top-down and bottom-up costing approaches. A generic costing pro forma was developed from the data identified in the service audit (WP2). This included costing categories on staffing resource (direct and indirect), costs directly related to intervention delivery, intervention-related costs, training, equipment and overheads related to delivery or maintaining the service. The costing pro forma was sent to the service leads in each of the six case study sites and followed up via e-mail. Where required, a Teams call was arranged to assist with completion. Where available, actual costs were obtained directly from the case study sites, otherwise NHS pay scales were used. Cost data were entered into Excel and total per annum costs over the financial year 2021–2 were estimated for each site. Recommendations for future health economic research are articulated in the discussion.
Ethics and governance
This study could be considered ‘low risk’ as the main data collection methods were qualitative interviews with staff, people with lived experience and their carers. However, this service user group is deemed by the nature of their mental health and co-occurring substance use to be a ‘vulnerable group’. The main ethical consideration was the potential for the interviews to be upsetting by asking people about their experiences of help-seeking (some of which may have occurred during times of crisis). The other consideration was that someone could disclose information about risk to self and/or others. NHS ethics and HRA approval were obtained on 17 June 2021 (Surrey Research Ethics Committee RE21/LO/0384 IRAS 277924).
Ethics amendments
Five amendments were approved, but most of these were minor administrative changes that did not affect any participants or the design:
-
Amendment one – extend the data collection period to 31 July 2022 (due to COVID delays).
-
Amendments two and three – adding additional sites.
-
Amendment four – changing name of NIHR to National Institute for Health and Social Care Research on the study documents.
-
Amendment five – to add the option to undertake data collection in person as well as online. This was added towards the end of the data collection period in June 2022 as COVID-19 restrictions had lifted and there was an opportunity to meet with a carer group.
Data management
The chief investigator (EH) at the University of Leeds (study sponsor) was the data controller. All RECO data were stored in University of Leeds RECO study Teams site and only the research group had access. Raw data in the form of transcripts were also stored securely at Liverpool John Moores University and analysed in NVivo, before being uploaded to the RECO Teams folder at the University of Leeds. All transcripts were anonymised, and we have removed identifiable information so that individuals cannot be identified. Personal data (such as participant names and contact details used for the purposes of arranging focus groups and interviews) were destroyed after data collection was completed. As well as being used to support the current research, data that have been anonymised may also be used to help with relevant future research and/or training, and this may be shared anonymously with other researchers (subject to relevant research governance processes such as confidentiality and data access agreements). Anonymised data may also be made available indefinitely on a public database so that when research is published, it is clear to everyone what the research process was. When we use anonymised data in this way, the participant will not be identifiable. Anonymised research data will be stored for 10 years and then destroyed in accordance with the University of Leeds’ research data policy.
Public and patient involvement
The proposal ideas were discussed with a group of people with lived experience of mental illness and substance use and they told us how difficult it could be to access services with this type of comorbidity. We had a co-investigator (CW) who has lived experience of SMI and is an author of the report. We engaged with people with lived experience during stakeholder consultation for the development of PTs for the realist synthesis, and also in the development of the protocol for the ethics application. They informed us not to combine data collection with staff and service users in one group, because they felt that service users may feel uncomfortable being honest about their experiences in front of service providers. They also advised on how best to promote participation and ways to make people feel safe during and after the interviews and focus groups. This included having an option for a debrief chat after the event. The PTs were also sense-checked with people with lived experience in a meeting following the analysis. We would have liked to have done much more patient and public involvement (PPI) work, but the COVID-19 pandemic impacted on peoples’ capacity to be involved and online methods did not suit everyone.
Chapter 3 National mapping data and audit
National mapping
Requests were sent to a total of 793 individual organisations between March and October 2020. A total of 311 responses were received, 230 from the first wave of requests and 81 from the second. Of these responses, 188 provided information about services and 42 responded to confirm that this information was not held, that the organisation was not responsible for commissioning or providing COSMHAD care, or that they were unable to deal with our request at that time. Table 2 shows the response rates from each of the organisations contacted.
| Organisation | 1st wave | 2nd wave | ||
|---|---|---|---|---|
| Contacted (n) | Responded (n) | Contacted (n) | Responded (n) | |
| Local Authorities | 435 | 75 | 337 | 37 |
| NHS Mental Health Trusts | 57 | 30 | 23 | 6 |
| CCGs | 177 | 48 | 120 | 25 |
| Care Quality Commission and Devolved Nation Equivalents | 5 | 5 | ||
| Health Boards Wales | 7 | 4 | 7 | 2 |
| Health Boards Scotland | 14 | 60 | 9 | 2 |
| Health and Social Care Partnerships Scotland | 31 | 3 | ||
| Alcohol and Drug Partnerships Scotland | 31 | 1 | ||
| Health and Social Care Trusts Northern Ireland | 5 | 0 | 5 | 5 |
| Local Commissioning Groups Northern Ireland | 5 | 2 | 5 | 0 |
| PHE | 1 | 1 | ||
| NI Department of Health | 1 | 1 | ||
| Public Health Reform Scotland | 1 | 1 | ||
| Scottish Association for Mental Health | 1 | 1 | ||
| Third Sector Drug and Alcohol Treatment Providers | 16 | 2 | ||
| Total | 725 | 230 | 568 | 81 |
Of the 311 responses received, 190 provided sufficient information about the approach to COSMHAD treatment to be categorised. Overall, just under half of the services that responded had a specific COSMHAD service (Table 3).
| Total number of responses | Specific COSMHAD service N (%) | No specific COSMHAD service N (%) | Unclear N (%) | |
|---|---|---|---|---|
| Total | 190 | 88 (46) | 78 (41) | 24 (13) |
| England | 156 | 73 (47) | 68 (44) | 15 (10) |
| Wales | 8 | 6 (75) | 0 | 2 (25) |
| Scotland | 18 | 5 (28) | 7 (39) | 7 (39) |
| NI | 5 | 4 (80) | 2 (40) | 0 |
Sixty-two per cent of responding services reported providing ‘integrated treatment’, with just over half of these not being specifically commissioned COSMHAD services. In England, integrated services were indicated more than twice as frequently than in the other devolved nations (Table 4).
| Number of responses | Integrated treatment N (%) |
Unclear N (%) | Oher N (%) | Integrated but no specific commissioned COSMHAD service N (%) | |
|---|---|---|---|---|---|
| Total | 190 | 117 (62) | 47 (25) | 66 (35) | 64 (34) |
| England | 156 | 108 (69) | 32 (21) | 46 (29) | 62 (40) |
| Wales | 8 | 2 (25) | 4 (50) | 5 (63) | 0 |
| Scotland | 18 | 6 (33) | 11 (61) | 11 (61) | 2 (11) |
| NI | 5 | 1 (20) | 0 | 4 (80) | 0 |
Service audit
From the mapping responses, areas that had some specifically commissioned service and personnel were selected to receive the audit. Audit responses were returned from 19 respondents representing 16 services. Multiple returns from the same organisation were merged and deleted when cleaning the data.
Most services were commissioned by local authorities (44%) [or via local authorities through PHE (19%)] (63% in total), with only 31% indicating that they were commissioned by the CCG, and even fewer were jointly commissioned. Conversely, services indicated that provision and delivery was primarily through NHS mental health services (50%), followed by substance use services (38%) and joint services (6%). This suggests that the burden for funding of dual diagnosis services falls disproportionately on local government. The majority of services were categorised as lead and link worker (31%). Most services offered a broad range of interventions and modes of delivery, with only two services reporting that they delivered one intervention using only one mode. This result reflects the size of these services. Interventions tended to be delivered one-to-one (81%) and over the phone (69%), likely the reflecting the complexity of cases.
Case study sites
Summary descriptions and costs at each case study site
The six case study sites are described from the information they provided in the audit (Table 5).
| Site | Service model category | Service remit | Service inclusion criteria | Training and supervision | Annual costs (£) |
|---|---|---|---|---|---|
| A | Network | Specialist secondary mental health service provider. No lead clinician in post; link workers are in situ and engage with the dual diagnosis working party | No exclusion criteria if person experiencing a SMI | Clinical supervision and review cases with staff in a group setting | 72,906 |
| B | Consultancy | To support secondary mental health services to deliver integrated treatment for people with dual diagnosis. Nurse practitioners offer assessments and interventions as required but the primary role is to support care co-ordinators with training and supervision to deliver the interventions themselves | A diagnosis of severe mental illness and problematic substance use | Mandatory e-learning package for all staff; 1–2 days training for ward staff; 3 days training for assertive outreach teams. Formal and informal supervision is offered | 444,267 |
| C | Lead and link | We advise on cases and offer training. We encourage mainstreaming and provide staff with support but ideally there will be an integrated approach. There is a consultant nurse lead and champion network across the city | Specialist dual diagnosis training provided to all mental health and substance use treatment services across the city | 111,164 | |
| D | Lead and link | To engage mental health clients with substance use with local treatment services. To begin this engagement process from inpatient admission | All staff have access to dual diagnosis training that is delivered in modules covering all aspects of substance use – offered online and face to face | 167,962 | |
| E | Lead and link | We adopt the dual diagnosis champion model in acute adult inpatient wards and community mental health settings | Training at postgraduate certificate in dual diagnosis or master’s in substance use. Supervision is offered formally and informally to the local champions via clinical lead | 83,070 | |
| F | Lead and link | Delivery of integrated treatment model whereby most service users with mental illness and substance use will have both needs met at the same time, in one setting by one team | A service user who is displaying a severity of mental illness that cannot be managed in primary care or presenting a risk to staff and/or themselves/others as a consequence of mental health symptoms | E-learning for all. Emphasis on experiential learning and ongoing practice development sessions to help embed learning into practice. Tailored learning and support for teams and shadowing opportunities to work alongside dual diagnosis experts. Quarterly dual diagnosis leads development days | 2,394,537 |
Recruitment at case study sites
We recruited a total of 58 staff. Table 6 provides details of the numbers and roles of the staff who participated in the study.
| Staff role | Case study site | ||||||
|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | Total | |
| Mental Health Inpatient | 4 | 1 | 5 | 4 | 14 | ||
| Community Mental Health | 4 | 1 | 1 | 6 | |||
| Community Drug and Alcohol | 5 | 3 | 1 | 9 | |||
| Community Drug and Alcohol (NHS) | 5 | 1 | 6 | ||||
| Early Intervention in Psychosis | 1 | 2 | 3 | ||||
| Dual Diagnosis Team | 4 | 2 | 1 | 2 | 9 | ||
| Assertive Outreach | 2 | 3 | 5 | ||||
| Homeless Team | 4 | 1 | 5 | ||||
| Adult Social Care | 1 | 1 | |||||
| Total | 11 | 6 | 16 | 10 | 6 | 9 | 58 |
| Mental Health Staff Nurse | 1 | 3 | 4 | ||||
| Drug and Alcohol Nurse | 3 | 1 | 4 | ||||
| Community Psychiatry Nurse | 3 | 4 | 7 | ||||
| Psychiatry Registrar | 1 | 1 | 1 | 3 | |||
| Doctor (Addictions) | 1 | 1 | |||||
| Consultant Psychiatrist | 1 | 4 | 1 | 4 | 10 | ||
| Ward Manager/Matron | 1 | 1 | 1 | 3 | |||
| Clinical Service Lead | 1 | 1 | |||||
| Social Worker | 2 | 2 | |||||
| Dual Diagnosis Lead (Nurse Consultant or equivalent) | 1 | 1 | 1 | 3 | 6 | ||
| Drug and Alcohol Recovery Worker | 4 | 2 | 6 | ||||
| Drug and Alcohol Assessment Worker | 1 | 1 | |||||
| Well-Being Practitioner | 3 | 3 | |||||
| Team Manager | 2 | 1 | 3 | ||||
| Mental health Advisor | 1 | 1 | |||||
| Occupational Therapist | 1 | 1 | |||||
| Training Lead | 1 | 1 | 2 | ||||
| Total | 11 | 6 | 16 | 10 | 6 | 9 | 58 |
In addition, we were able to recruit 25 service users and 12 carers (Table 7). There were challenges to recruiting service users and carers. This covered the period of early 2022 to summer 2022 when restrictions were still in place due to the Omicron surge of winter 2021–2. Initial ethics approval was for online focus groups (due to the requirement for social distancing and stay at home orders), but this method of data collection was not popular with participants who were not always familiar with and in some cases (e.g. those in hostel accommodation) did not have access to sufficient technology. We did offer data vouchers to compensate for the cost of data use on smart phones, but many potential participants were not comfortable with using MS Teams. Only 6 of 25 service user interviews were completed online with 19 participants preferring to speak over the phone. This required an ethics amendment which delayed data collection. Similarly, only 2 carers chose to undertake the data collection online with the remaining 12 taking place over the phone or face to face. In the last 2 months of the project, we were given approval via an amendment to NHS ethics to collect data face to face (which had not been permitted during the pandemic). We undertook a successful carer focus group at Site B in a non-NHS community venue. At this point, there was not sufficient time within the project timescales to get the R&D approval needed from each site to undertake research face to face and so we were limited to non-NHS venues. Many service users mentioned that the groups they had previously attended during the pandemic (e.g. in substance use services) were still not running face to face following the pandemic, and these would have been valuable contact points from which we could have promoted the study. A small number of service users did engage well with online groups [four of the participants who chose to participate online came from a successful online substance use and mental health support group for LGBTQ+ (lesbian, gay, bisexual, transgender and queer) people] but they were not popular with all service users or available at all case study sites (e.g. site E). We did attempt to incorporate our data collection into existing online groups at mental health and substance use services (e.g. at site D) but this was not successful due to groups taking place on a secure online portal which created access, data governance and storage issues. Recruitment was done through staff working in services (such as the COSMHAD leads and focus group participants). Many were still working in an extremely pressured post-pandemic environment alongside high demand for services which limited the time staff had for discussing the RECO study with potential participants. Given these significant challenges, the recruitment to the study is to be recognised as a real positive despite not meeting original targets.
| Case study site | Number of service users | Number of carers | Total |
|---|---|---|---|
| A | 6 | 3 | 9 |
| B | 3 | 9 | 12 |
| C | 10 | 1 | 11 |
| D | 0 | 0 | 0 |
| E | 4 | 0 | 4 |
| F | 2 | 0 | 2 |
| Total | 25 | 13 | 38 |
Chapter 4 Identifying and refining programme theories
Initial programme theories
Throughout the realist synthesis, substantive theory was used to further understand and refine on the PTs, in line with RAMESES guidelines. 29
Eleven IPTs were developed, which included Context, Mechanism (including resource and response) and Outcome. These PTs were reviewed and refined through consultation with the entire project team (n = 9) through written comments on drafts, and two meetings at which the PTs were presented and discussed in detail. The first meeting took place when the PTs were first developed and the second reviewed the finalised statements following testing in the literature. These final PTs are summarised in Table 8. A full and detailed description of each PT generated in the realist synthesis can be found in Report Supplementary Material 1.
| PT 1: first contact and assessment (‘It’s everyone’s business’) | If staff across all first contact services for people with COSMHAD accept that it is part of their role to work with this group, and that it is their responsibility to assess and refer these service users into suitable treatment (context), then individuals will have a more satisfying and structured first contact with services (mechanism – resource). People with COSMHAD will have less difficulties in entering appropriate services thus leading to increased optimism, confidence and willingness to engage in treatment (mechanism – response). This will lead to earlier identification of COSMHAD and more appropriate referrals and service access for service users, resulting in longer retention, reduced access at times of crisis (proximal outcomes) and more opportunity to progress towards recovery and stable lives (distal outcome) |
| PT 2: staff attitudes | Successful collaboration between mental health and substance use services requires non-judgemental staff attitudes towards people with COSMHAD and a desire to reconcile political, structural and philosophical differences between services (context). A team-wide response to training is needed to address staff beliefs and attitudes supported by clear policies and procedures to shift service philosophy (mechanism – resource). A team-based training approach leads to increased feelings of ownership and involvement among staff who will become less sceptical and more invested as they see people with COSMHAD responding positively to interventions (mechanism – response). This will result in enhanced staff empathy and better therapeutic relationships with service users which are more likely to be transferred across the organisation (outcome) |
| PT 3: encouraging collaborative case management | Collaborative case management between services for people with COSMHAD requires both formal co-ordination (top-down processes and network models) and informal collaboration (willingness to work together) (context). Clear, non-conflicting care co-ordination protocols and referral pathways with time for collaboration built into staff schedules (mechanism – resource) will help staff feel more supported in their roles and gives them permission to build trusting relationships with other service providers while taking a pre-emptive, preventative and whole person approach (mechanism – response). This will lead to an improved organisational system for people with COSMHAD with improved consistency of care and a more service user focused approach across the continuum of care (outcome) |
| PT 4: continuous exposure from undergraduate level | Staff are often ill-prepared to treat people with COSMHAD due to a lack of teaching on addictions as part of the biopsychosocial model and supervised exposure on undergraduate/postgraduate curricula. Even where staff have been trained in particular skills (e.g. motivational interviewing), they do not always make use of these skills in practice (context). An immersion model of training should begin at undergraduate clinical rotation and be maintained through core competencies for professional development and progression (mechanism – resource). This continuous supervision of practice will align educational targets to real time problems, foster communication between health professionals and allow staff to learn from practice and experience (mechanism – response). This emphasis on professional growth in practice will increase staff retention, decrease burnout and improve empathy for the daily experiences of service users (outcome) |
| PT 5: continuous workforce development | If service leaders appreciate the need for continuous and comprehensive workforce development (context) by combining didactic training to address knowledge and experiential training to practise skills (mechanism – resource) then staff will internalise compassionate, integrated values, skills and confidence to assess and respond to the needs of individuals with co-occurring disorders (mechanism – response). This will lead to a better therapeutic relationship between service users and health professionals leading to improved engagement and motivation to change (outcome) |
| PT 6: opinion leaders | Dedicated, respected leaders with the authority to implement integrated treatment are needed at all levels of the organisation (from commissioning through to team leaders) to communicate a shared vision of co-occurring disorders, prioritise implementation and make and disseminate administrative and policy changes (context). These leaders will sustain awareness and expectations surrounding co-occurring disorders (mechanism – resource) leading to an organisational climate where staff feel enthusiastic, motivated and supported to implement new practices in their work (mechanism – response). As a result, individuals with co-occurring disorders can engage with consistent, appropriate support for their condition (outcome) |
| PT 7: formalised networking opportunities | Formalised, structured and sustained opportunities for practitioners working with people with COSMHAD to meet, communicate and build relationships and take action (e.g. through a network) (context) will lead to increased awareness of other services’ collective contributions, opportunities for peer support and a multidisciplinary ethos (mechanism – resource). This will increase staff motivation, confidence and commitment to work collaboratively when treating people with COSMHAD (mechanism – response) leading to improved care co-ordination and better provision of stage appropriate interventions including more immediate referrals, assessments and care planning (intermediary outcome). Co-ordinated and welcoming services will make patients with co-occurring disorders feel more comfortable and engage in a more sustained way (outcome) |
| PT 8: co-ordinated care pathways | Committed and accountable leaders from NHS, local authorities and other partner organisations (context) should support, design and consistently advance a collaborative co-ordinated care pathway which uses organisational policies, functional procedures and defined outcomes to allow mental health, substance use and other relevant service providers to support each other in providing care for individuals with co-occurring disorders (mechanism – resource). This co-ordinated pathway will lead to increased collaboration between providers through shared goals and formalised relationships to deliver care (mechanism – response), giving staff a wider perspective on service users’ situations as they journey through care and reassurance to collaboratively work with service users in new ways (intermediary outcome). Service users receiving the accessible, comprehensive, continuous and non-contradictory interventions and services co-ordinated through the care pathway will experience more consistent and appropriate goal setting from health professionals which will rouse and maintain their motivation to work towards their goals and remain engaged in treatment (outcome) |
| PT 9: mental health led services | A high prevalence of people with COSMHAD within mental health services suggests their needs should be addressed in a mental health service setting with additional joint working from other services as needed (context). Having mental health clinicians responsible for care planning (mechanism – resource) means clinicians will increase their skills and competencies in using empirically supported treatment with measurable outcomes for COSMHAD (mechanism – response). By addressing the relationship between substance use and mental health simultaneously, service users will experience a more consistent and flexible approach to symptom reduction with tailored, non-conflicting goals (outcome) |
| PT 10: evaluation and quality improvement | Leadership across all involved services need to develop and establish accountability (context) in order for meaningful evaluation and quality improvement measures to be put into place to evaluate the structure, process and outcomes of integration and training interventions on service delivery for co-occurring disorders (mechanism – resource). This will ensure that commissioners, service managers and practitioners feel the work they do is valued (mechanism – response) and continue to make incremental progress in improving services by building on existing strengths and identifying priorities leading to better insights into the quality of care (outcome) |
| PT 11: recruiting and retaining talented staff | Service commissioners from both mental health and substance use services need to work jointly (context) to commit financial resources and organisational workforce policies (mechanism – resource 1) to ensure staff with the requisite skills, knowledge and values for treating people with COSMHAD are recruited and retained into services through appropriate selection, supervision and professional development (mechanism – resource 2). This will ensure that skilled staff feel encouraged, secure and legitimised in their posts (mechanism – response) leading to more effective, better quality and undisrupted therapeutic relationships with service users (outcome) |
Finalisation of the programme theories
The aim of the RECO study was to develop, test and refine a set of PTs that identified and described the contexts and associated mechanisms by which engagement and other health outcomes are achieved in service systems for COSMHAD, and for whom these are most effective.
This next section will address how the evidence from the real-world case studies supported the PTs generated from the realist synthesis. The realist review has been accepted for publication at the time of preparing the report. 39 Each PT will be discussed in light of the evidence from the staff, service user and carer perspective and a summary provided at the end of the chapter.
Refined programme theory 1: first contact and assessment (‘It’s everyone’s business’)
Summary of evidence
The concept of ‘everyone’s business’ comes from the position that a significant number of people who use mental health and substance use services have co-occurring disorders and therefore need to be equipped to engage people in treatment and attend to their multiple needs. This PT (Figure 2) describes how this concept can actually be operationalised. A key contextual factor facilitating successful engagement (especially on initial contact) is that staff should recognise that working with COSMHAD is a part of their job. Adams3 describes how ‘professional ambivalence towards comorbidity [context] … may influence the assessment process and subsequent interactions [mechanism–resource]’ (p. 102) and several studies have highlighted the importance of using assessment protocols and screening tools to help the clinician formulate a thorough picture of the client’s life circumstances. 40–44 This in turn allows the clinician to develop a richer understanding of the person’s situation, which promotes compassion. This was also supported by the case study data with staff emphasising the importance of a flexible and non-judgemental approach, that it’s ‘everyone’s business’ and a needs-led holistic approach can be effective in identifying the right care and treatment.
FIGURE 2.
Refined PT 1: first contact and assessment (‘It’s everyone’s business’).
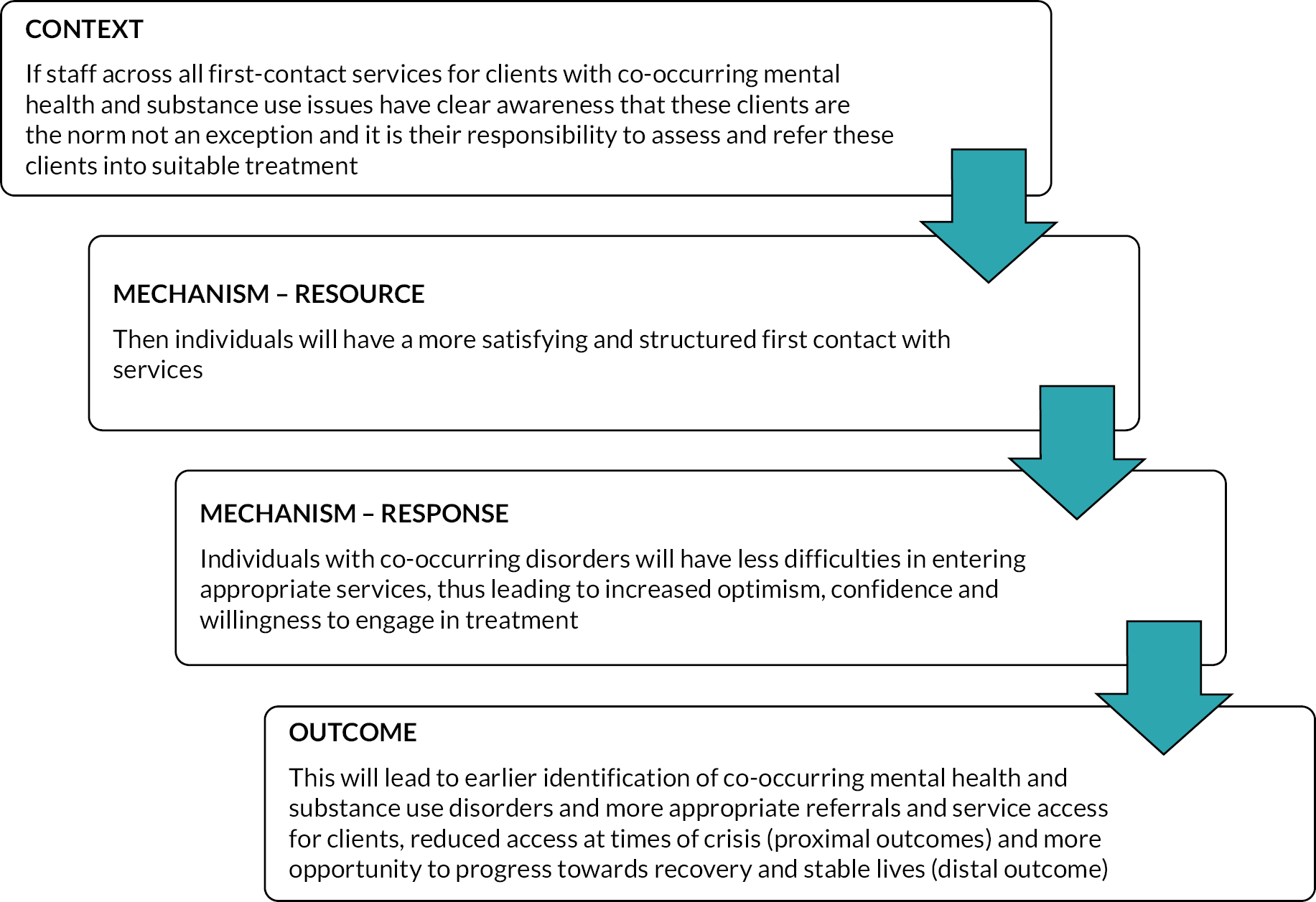
Across all sites, staff demonstrated awareness of their responsibility to assess and identify treatment for people with co-occurring disorders. Staff emphasised the importance of ‘responsiveness and flexibility’ (SP22, Case Study C) and described their approach as being ‘friendly, non-judgemental, just listening to them’ (SP92, Case Study B) and having this responsible and flexible context for first contact would lead to people with a co-occurring disorder feeling less judged and more likely to engage with services (mechanism – response) (Figure 3).
FIGURE 3.
Programme theory 1 context to mechanism.
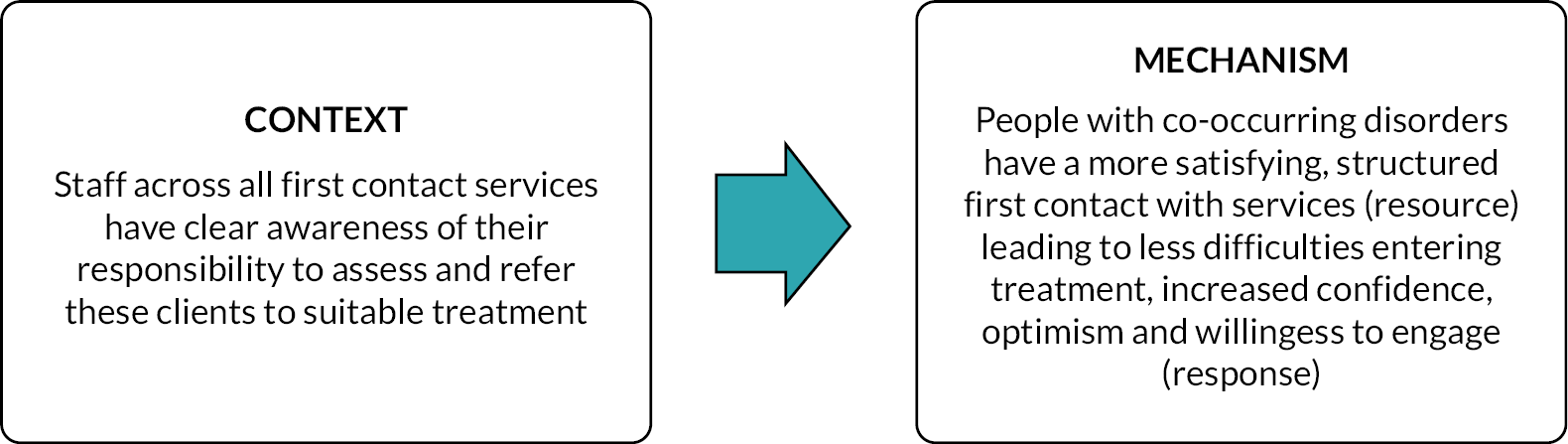
I would like them to be met at where they’re at and for us not to focus on what is wrong with you, but what’s happened to you as a first encounter … They’re not going to feel judged, are they? For a start. So, you’re optimising engagement. And I think it’s important for us not to come with our own personal, professional, organizational agendas.
SP10, Case Study C
Staff also demonstrated their awareness of national dual diagnosis guidance and policy: ‘You want to implement the principles of everybody’s business and no wrong door’ (SP52, Case Study F). There was a sense from some services that the high prevalence of co-occurring disorders had led to acceptance of these principles. However, this context varied between different mental health services, with Assertive Outreach, Early Intervention (EI) and Improving Access to Psychological Therapies (IAPT) (now known as NHS Talking Therapies) services viewed as being more proactive when compared with community and inpatient mental health services. When ‘no wrong door’ context was present within services, staff participants described health professionals feeling empowered to address clients’ needs (mechanism – resource) leading to reduced exclusion and stigmatisation of people with COSMHAD who feel reassured that they will have ongoing support for their mental health and substance use from knowledgeable staff (mechanism – response).
… another way of thinking about it is that the existing pathway, the treatment as usual pathway is for dual presentation because that’s the norm … And then it’s almost like unusual if you come into an EI team without substance use … the EI model of care has to work for people with this presentation, ’cause it’s most people.
SP37, Case Study A
However, service user and carer data suggested that challenges in accessing help still remained. Many service users discussed being unable to access mental health support until they had halted their drug or alcohol use, or they were unable to access drug or alcohol rehabilitation programmes while taking medication for their mental health conditions (context). Participants felt there was little awareness or appreciation of COSMHAD among services making their initial assessments (mechanism – resource) and described this scenario like ‘chicken and egg’ [P29, (Carer) Case Study B; P38, (Carer) Case Study A; P6, Case Study C], where services had stipulated that ‘we can’t fix both things. We have to do one or the other’ (P6, Case Study C). However, participants reported that in their experience, their mental health conditions and substance use were strongly related to each other. For example, substance use was described as a coping mechanism:
to self-medicate. You know to try and block out thoughts and feelings that you know that I was having.
P8, Case Study E
Service users and carers suggested that first response services (e.g. A&E or the police) were often the only way to receive any kind of support in a crisis (mechanism – resource). A number of carers discussed how they had often called the police as a last resort because they feared for their loved one’s safety and were at a loss as to where to receive support. In some cases, carers reported that they had been advised to call 999 by their local mental health crisis team (mechanism – response). Service users described being caught in a cycle of representing at times of crisis in an attempt to get support for their mental health with discharge often resulting in further suicide attempts or relapse of their drug/alcohol problems (outcome).
For service users, this separation of their mental health and substance use by services was frustrating. Some felt despondent about not being able to access mental health support until they had stopped their substance use (mechanism – response). These participants described themselves as having ‘fell through the cracks for many years’ (P8, Case Study E), ‘been in limbo’ [P28, (Carer) Case Study A] or ‘all the doors closed for him and it was blamed on … his drug using’ [P28, (Carer) Case Study A], which reduced their motivation to work towards their goals and could lead to relapse (outcomes).
The prevailing context for assessment was the importance of a relationship between the health professional and the person with a co-occurring disorder (mechanism – response). Key to this relationship was the client feeling ‘comfortable enough to just sit and be assessed and be happy to meet again’ (SP61, Case Study F) and ‘get to the point where they’re actually able to engage in therapy’ (SP51, Case Study D). However, it was also recognised that it was not always possible to build this relationship within a single, initial assessment and that
[I]t depends on their motivation at that specific time. It might be that when you initially see them that they don’t want any support, they’re not ready to make any kind of change. But then three months down the line, it might be a different kettle of fish.
SP91, Case Study B
This demonstrates the importance of a positive experience which could yield a positive outcome (engagement) in the future. Where a positive relationship exists (context), people with co-occurring disorders feel supported and hopeful and so are more willing and able to engage with services (mechanism – response).
Better for them to build a relationship rather than being ping-ponged around and inevitably falling through the gaps and having to restart again and fail and not … have any faith in services … this is part of why we’re trying to transform our community services so that people aren’t being pinged around between different services. So, they, you know, they stay put and you, you’re with them through the whole journey …
SP50, Case Study D
A trauma-informed approach was also emphasised as a way of engendering hope and engagement (mechanism – response). Experience of trauma can impact on engagement with statutory services and when a positive relationship is lacking (context), existing service structures can replicate people’s experiences (and in some ways be re-traumatising) and reinforce feelings of hopelessness and disengagement.
[P]eople start to get passed around … it’s that idea. Oh, here’s some risk that I can’t deal with. I don’t know what to do with that or I can’t deal with that. So, what I’m gonna do is send you to someone else now, I can’t help thinking that in some way, what we start to replicate is … that they were removed from their families of origin for a reason. They would possibly be removed from other services who said they’d keep themselves and help them because they were unmanageable and then here, we are again potentially replicating those, those relationships […], and so we’re undermining their basic … view of themselves … We’re replicating it and reinforcing a negative scheme.
SP38, Case Study A
Additional context
Additional contextual factors that negatively impacted first contact with services included operational processes that hindered engagement including telephone-only first assessments, limited follow-up before discharge, service remit which explicitly excluded clients due to their co-occurring substance use or severity of their mental health condition, overly long and repetitive assessment pro formas (due to services not being able to share care records) and a lack of clear point of contact following assessment.
Staff expressed frustration at ‘having to work in a system that maybe isn’t best placed to offer the service that you’re hoping to offer’ (SP5, Case Study A). They felt that this led to a fragmented experience of services for clients, disengagement and a lack of hope (mechanism – response).
… everybody has to cover their personal, professional, organizational, litigious liability thing with endless risk assessments … That assurance work would probably be much more limited if there was a much more joined up IT governance system across GP Services primary acute drug mental health services … if you could read it and say is there anything changed to this? As opposed to could you talk all about your childhood again or you know, blah, blah blah? I think that that would be quite a big difference.
SP38, Case Study A
Following assessment, people with COSMHAD were often referred to services that did not meet all their needs and were expected to engage with a ‘one-size-fits-all approach’ to treatment. As a result, clients could become despondent and disengage or fall into the gaps between services, often resulting in exacerbation of both their substance use and mental health problems (and leading to further crisis-led service use).
It’s very much a one size fits all, isn’t it? … you’re gonna get filtered out … if you don’t engage or you don’t fit into any mental health … So you get despondent. Drop out and then go back again because … mental health won’t pick him up until they stop drinking. And it’s like, well, they can’t stop drinking because … it’s such a vicious circle […] we’re seeing people die, aren’t we because nothing ever gets really addressed?
SP30, Case Study A
By that time, he is 18 … it’s really, really hard to actually get any help. The only way we could get help was to continuously ring the police to come and take him out of the house because he smashed the house. Until, finally, there was a psychiatric trauma analysis … and [son’s name] found himself in the [hospital name] at the [psychiatric intensive care unit] and from then a more supportive network was built around him. But from the word go it’s been horrendous just trying to access help in the 1st place. That’s the biggest, biggest problem.
P36, (Carer) Case Study B
Staff participants emphasised the importance of engagement with service users at first contact (mechanism – resource) and, if this was achieved, it could result in improved access to services (outcome) (Figure 4). However, this outcome required staff to support people with a co-occurring disorder to reach a level of stability where they felt able to access and attend services (outcome) (see Figure 4).
FIGURE 4.
Programme theory 1 mechanism and outcome.
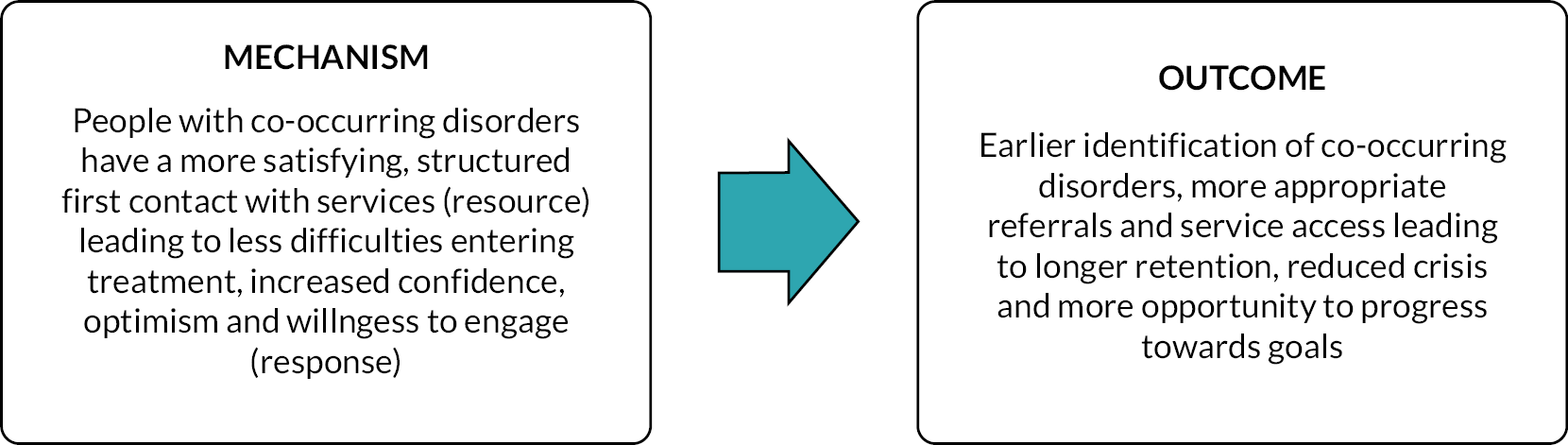
It makes a massive difference to our service users because they are being followed up in both camps and if we don’t do that in partnership working, it’s really difficult to get good outcomes for our service users … Yes. I think we have better outcomes if that happens because we see often if those two don’t go hand in hand, people become like frequent flyers, they come back through the same services, but not always jointly – separately. So we see more admissions, we see more, on the inpatient side, more mental health admissions. We also see on the physical health side, people are turning up more in A&E they are attending more with their general practitioner (GP). So if we can do that joint working together, those frequent admissions and attending places reduces as well.
SP41, Case Study D
Carers described feeling fearful, angry and frustrated that they were unable to access mental health support for their loved ones (mechanism – response). They felt that substance use services were ‘not equipped to deal with someone who has a mental health problem’ [P28, (Carer) Case Study A] and that more education was needed for staff around COSMHAD (mechanism – resource).
Obtaining a diagnosis could mean access to specific services; however, diagnostic labels could also represent a barrier (e.g. if that diagnosis was an exclusion criterion for a service). Many individuals had received multiple diagnoses over time, and this could lead to confusion over which service should be providing care, whereas it was suggested that taking a needs-led approach could lead clients to receiving a more integrated and trauma-informed approach to care.
Does diagnostic uncertainty broaden our thinking and help us integrate under that trauma-informed kind of framework rather than thinking you’ve got this disorder and that disorder and diagnostic labels are everything … then they’re problematic use is a behaviour alongside a bunch of other behaviours that we can think about. I think that’s what I was trying to say at the beginning. That sometimes that notion of dual disorder, I don’t know it I can’t quite get my head to think about it properly. But anyway, yeah, I think that the diagnostic uncertainty incomes could be quite helpful in integrating.
SP37, Case Study A
Overall, the literature from the realist synthesis and data from the staff interviews and client and carer focus groups suggested that an open door and flexible policy was essential for successful COSMHAD services. COSMHAD needed to be on the agenda for all staff wherever they worked to enhance first contact success and improve the engagement of service users.
Refined programme theory 2: attitudes
Summary of evidence
In the literature, there was a range of attitudes identified towards COSMHAD among healthcare professionals, and this also varied across professional group and work experience. 3 For staff in mental health services, attitudes were influenced by exposure within undergraduate and continuing professional development training. 45–47 Staff with positive attitudes were often interested in working with COSMHAD clients, expressed non-punitive beliefs about substance use, had a commitment to generate and maintain therapeutic relationships, and demonstrated pragmatic, flexible and individually tailored approaches3,47–55 (Figure 5).
FIGURE 5.
Refined PT 2: attitudes.
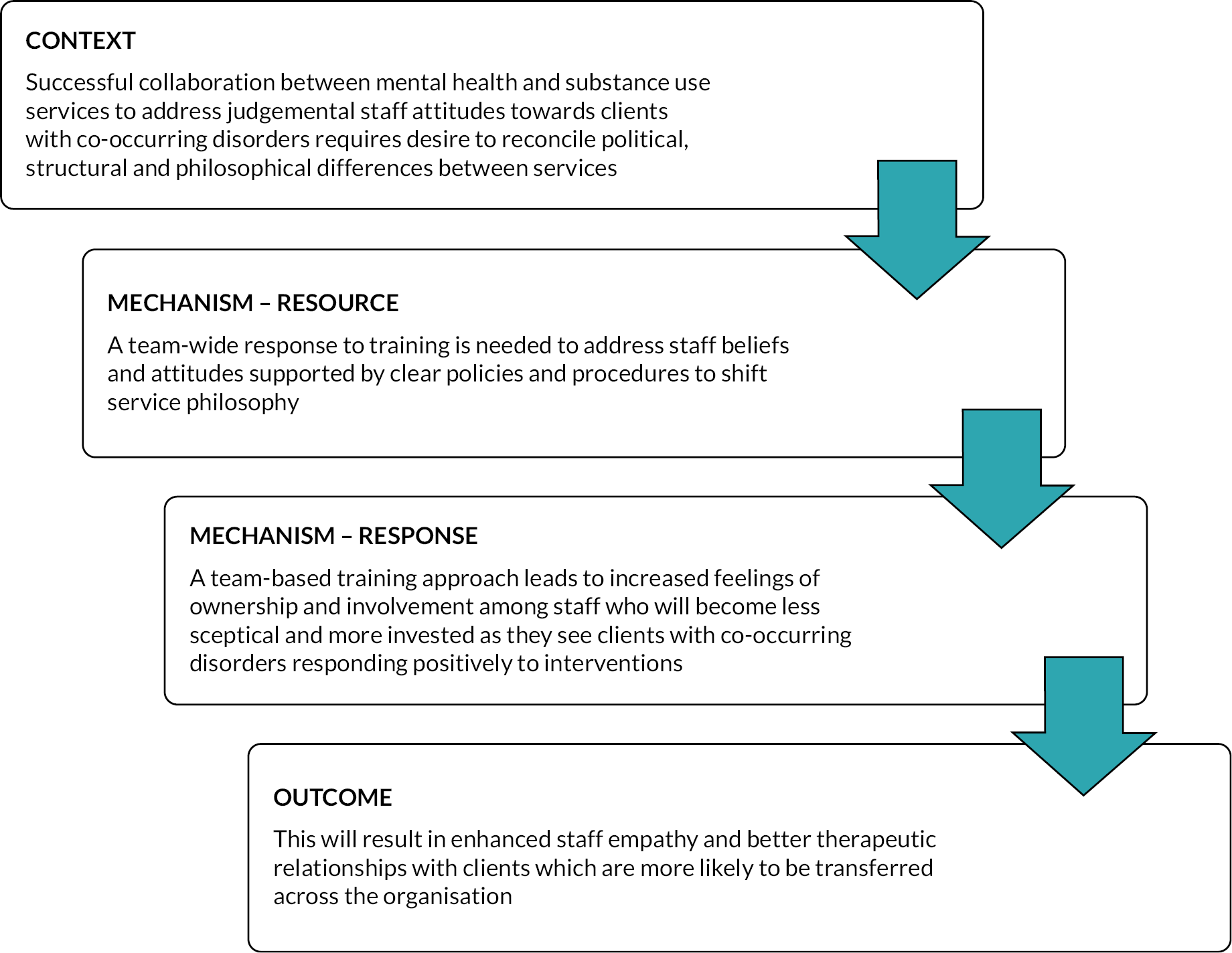
In the staff data, a wide range of staff attitudes were noted (context) which impacted on the way in which training and policy around staff attitudes (mechanism – resource) was implemented (Figure 6). Staff working within Case Study B (which had been operating for 16 years) reported an open approach towards clients with co-occurring disorders that focused on harm reduction and staff ‘not frowning on people, we’re trying to reduce the stress and triggers for use really and keep somebody well and out of hospital’ (SP92, Case Study B) (context). Staff in Assertive Outreach noted that the increasing numbers of people with COSMHAD within their service had been challenging (context) but that the support they received from the COSMHAD specialist team which included training and consultation-liaison (mechanism – resource) had helped them to develop the skills required to assist these clients in a non-judgemental manner (mechanism – response).
FIGURE 6.
Programme theory 2 context and mechanism.
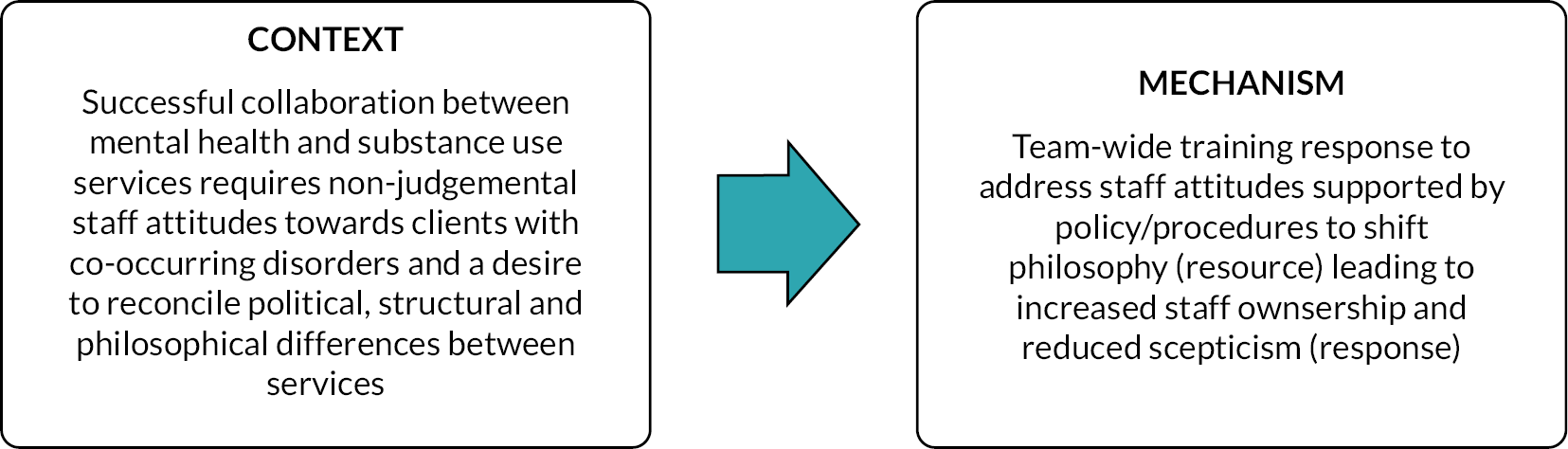
[W]e’ve had great support from the [name removed] team throughout … We’ve been really lucky to have had a worker working alongside us with our guys to try and look at the issues that come up and trying to build people to have the skills to deal with the issues around in the substances and not be judgmental or telling people ‘no … don’t do that’….
SP92, Case Study B
Service users and carers described several facets of positive staff attitudes, namely, trust, advocating for their clients’ needs, feeling listened to, and their level of experience. Service users and carers acknowledged that with individual staff members it ‘takes some time to trust somebody’ (P14, Case Study E) but that it was a key aspect of a positive relationship ‘for mental health patients not to feel threatened by mental health professionals. Because they don’t trust … And … when they trust, then half the job done’ [P21, (Carer) Case Study A]. A trusting relationship consisted of ‘openness … there’s no stigma, no judgement’ (P18, Case Study C) and showing ‘compassion, empathy and a bit of understanding’ (P25, Case Study A).
Where positive attitudes exist (context), service users felt that they were able to be open about their problems. There were more varied staff attitudes in other sites which were influenced by individual staff interest and organisational philosophy (context). This sometimes stemmed from philosophical approaches towards substances in mental health services (context):
[T]here’s a lot of emphasis, sometimes on medication, to the extent of almost omitting the psychological and the social approaches … I think that’s what feeds into sometimes attitude because there’s historically this thing was you couldn’t access psychological therapies if you were drinking [alcohol] or whatever.
SP65, Case Study F
Engagement with COSMHAD issues was often dependent on ‘an individual being interested’ and the existence of ‘little flagship teams’, and a broader cultural shift was required within organisations to ensure that all staff were supported and encouraged to work with these clients (mechanism – resource) which would lead to staff feeling enthusiastic, confident and supported to use the skills they have been trained in (mechanism – response). This was also confirmed by a participant from Case Study E, who described ‘group think’ within certain teams which impacted upon both current and new staff attitudes (context) and thus the effectiveness of training on co-occurring disorders (mechanism – resource).
There were examples where positive attitudes were not present and the reasons for this were connected to both a lack of organisational commitment and pressure on resources (context).
[S]taff are so busy. It’s also very hard to … do something consistently … I find that in our ward there’s always something that needs you know to be actioned or something that needs to be addressed … so it’s very hard to keep focus on it, and to keep the interest in it.
SP72, Case Study E
There was inconsistency in training coverage:
[I]t’s slightly pot luck about who will be in the room with that person on a given day … there are sometimes issues with staff recruitment and retention and some staff might not be as well informed or motivated to work with people with more dual diagnosis issues … whether it’s values or beliefs – can get in the way with engagement of someone … a sort of non-MI stance or just a lack of knowledge.
SP61, Case Study F
The impact of these positive attitudes being absent (context) led to a lack of joint working between mental health and substance use services leading to clients being left without access to services (mechanism – response).
[M]any people we support get the knock back from mental health services … and our clients have told us this … so, when we make referrals, we have to say how long somebody’s been abstinent for … and really, really labour that point and it’s hard sometimes what I want to write on a referral is this person is likely to be consuming less alcohol units than the person reading this referral. Because the judgment is felt so keenly from other professionals … the automatic assumption that any of their distress is automatically going to be put down to their substance use … and it needs to be addressed there and then otherwise they’re gonna relapse again.
SP16, Case Study C
… I joined the Community mental health teams as a CPN [community psychiatric nurse] and a team lead and I was kind of quite shocked and horrified, kind of the attitude was opposed towards people with drug and alcohol issues … They’re really, really busy, but there was great assessments going on by really qualified, really experienced members of staff. But the second a substance or alcohol misuse issue was kind of suggested or proposed or suspected all the other information would be lost in it would just be they need to refer themselves to [name of substance use service] … It was kind of like we can’t do anything for you until you’ve addressed this … that is something that’s just became maybe embedded, but it’s the attitude sort from the bottom up … I think is a real kind of issue because it’s almost like at anything else falls on deaf ears as soon as we hear drug or alcohol use is involved.
SP44, Case Study D
Four of the case study areas described offering formal training to address staff attitudes (Case Studies B, C, D, F) as well as boost skills. However, training in isolation of other initiatives is not sufficient. Staff participants in Case Study F proposed that if training was to have any longer-term impact on practice it must be accompanied with embedding positive attitudes into the structure and policy of teams as well as the wider organisation (mechanism – resource) (Figure 7). When this policy/procedural support was in place (mechanism – resource), staff ‘start feeling confident to do it and feeling they have permission to do it from the service or other disciplines sometimes’ (SP73, Case Study E) by ‘empowering other professionals to feel like there is something they can do and also to understand what success looks like’ (SP52, Case Study F). This is known as ‘role legitimacy’. The key to this is taking a team-wide approach as opposed to individual workers (mechanism – resource).
FIGURE 7.
Programme theory 2 mechanism and outcome.
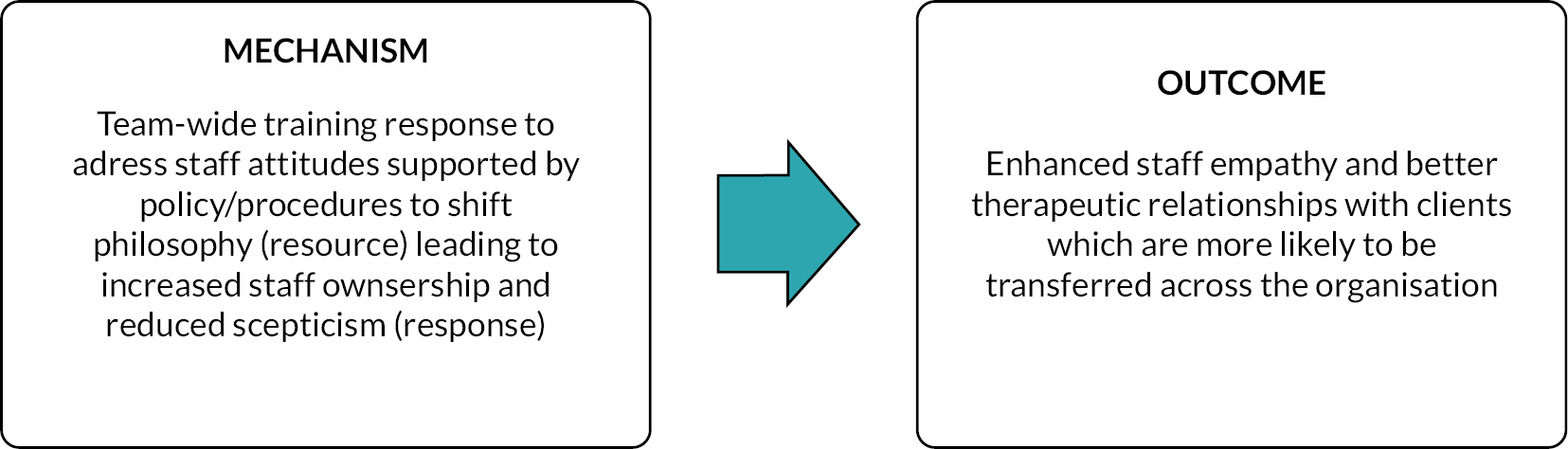
So you start teaching people on the course and … the language changes … that begins to change right there in the … seeing that change in how people are communicating about these issues and thinking about being flexible with some of the challenges, they’re also telling you that ‘oh, I feel much more able to talk to people about their substance use and no longer feel pressured to looking for solutions and now just have a chat with people and listen’. To them it’s easier … it’s not just about changing attitudes, but it’s about it creates a sense of confidence across the organisation about what you know, how to proceed and what needs to happen within and … ensuring that that is, you know we are embedding that and it’s ongoing, isn’t it? So, building this into the structure.
SP60, Case Study F
I think if individual practitioners are interested and feel confident and skilled and it’s on their radar, then they are much more likely to be more proactive with this. And I also think if they’ve got, if they’ve had good positive relation, working relationships with say staffing, turning point, that’s much more they’re much more than inclined to. Be more proactive with the people that they’re working with because they’ve already got those links.
SP52, Case Study F
Service user participants also emphasised the critical role of empathy, positive attitudes and better therapeutic relationships in creating a safe space where they feel able to open up about their feelings and issues:
[S]omebody that’s gonna be empathetic … when they come in … they took it kind of a step back … tell us what’s been going on. Tell us how you’re feeling … they let you get off your chest what you need to get off your chest … they then use that information to then open a dialogue with you. And I think that’s what you need is just someone who’s empathetic because, you know, when you are going through mental health issues or when you’re going through addictions, you know, your emotions are gonna be all over the place … Feel like they’re listening to what you’re saying. And that’s not to say that they’re gonna agree everything that you said because you know … You need to want to challenge you or to want to give you a bit of advice and to look at your reasoning and the way of thinking. You know, but you want someone who’s got a kind of way to be collaboratively make you feel safe … if you don’t feel safe, then you’re not really, really good at opening up.
P19, Case Study C
In addition, one person wanted to talk about the positive experience they had with the expert lead for COSMHAD, who they acknowledged had gone above and beyond their role to help, and in doing so had instilled hope in what was a bleak situation:
[H]e’s the one that is leading the dual diagnosis team from, you know […] and he is prodding and pushing in all of the right places behind the scenes and … he is doing that to prompt people from not just saying something in that meeting, but actually turning what they’re saying and what we talk about into reality. And that’s why I’m his biggest fan, by the way. I think he’s been fantastic … what the NHS really needs is about 100 of him … because you know my constant thing has been, it’s just there’s no joined up working … [dual diagnosis lead]’s come in and you know, join that working together for us, you know. And the unfortunate thing, [dual diagnosis lead]’s team isn’t a patient facing team, unfortunately, but they should be for me. And we’ve been very fortunate in so much that [he] has … been more customer facing than potentially he should be and he’s done that because he’s seen, you know, what desperate situation we’re in and you know, we power to his arm for that and credit to him for doing it … because I think then that just gives that assurances when things look so bleak.
P3, (Carer) Case Study C
Where training and policy was in place that promoted therapeutic optimism (mechanism – resource), staff described people with co-occurring disorder as being more engaged with treatment (outcome): ‘they’re not going to feel judged, are they? For a start. So, you’re optimising engagement. And I think it’s important for us not to come with our own personal, professional, organizational agendas’ (SP10, Case Study C). Staff participants described increased empathy among staff (outcome), this was achieved not simply by acquiring knowledge on co-occurring disorders but recognising that progress with co-occurring disorders is often small and incremental (mechanism – response) and having the confidence to listen to what the individual is telling them and respond reflexively to their needs.
Sometimes progress can be really slow contact with some service users and through no fault people can go, you know, back a few steps and that that you can take that personally as much as you don’t want to because you see as a failure in yourself to actually help somebody.
SP51, Case Study F
[I]t’s not coming with any, any preconceived ideas about what that person is going through? Because everybody is going to be having a different relationship with their drugs and their mental health. And I think sometimes if you go with too much, you can have the knowledge, but you have to go there with the premise that you haven’t got any knowledge almost, do you know what I mean? And well, you have got knowledge and that you understand what they’re going through, but I’m not that you’re going to make assumptions about what they’re going through because I think. I don’t know. I think I think from my point of view, I think that would be unhelpful if I had to be in a service where someone made assumptions about me and it wasn’t right.
SP11, Case Study C
Political, structural and philosophical differences were highlighted as obstructive to providing successful COSMHAD services throughout the realist synthesis and evaluation. These more macro contexts impacted on staff attitudes and subsequently therapeutic relationships with service users.
Refined programme theory 3: collaborative interdisciplinary/professional case management
Summary of evidence
Evidence from the realist synthesis demonstrated that when leaders implement (context) care protocols that clearly describe the co-ordination of care from initiation of care through to referral/discharge44,56–58 (mechanism – resource), this helped staff feel supported in their roles47 and enabled them to use their skills and knowledge (Figure 8). Furthermore, it provided permission for staff to take a more pre-emptive, preventative whole person approach to clients with COSMHAD59 (mechanism – response).
FIGURE 8.
Refined PT 3: collaborative interdisciplinary/professional case management.
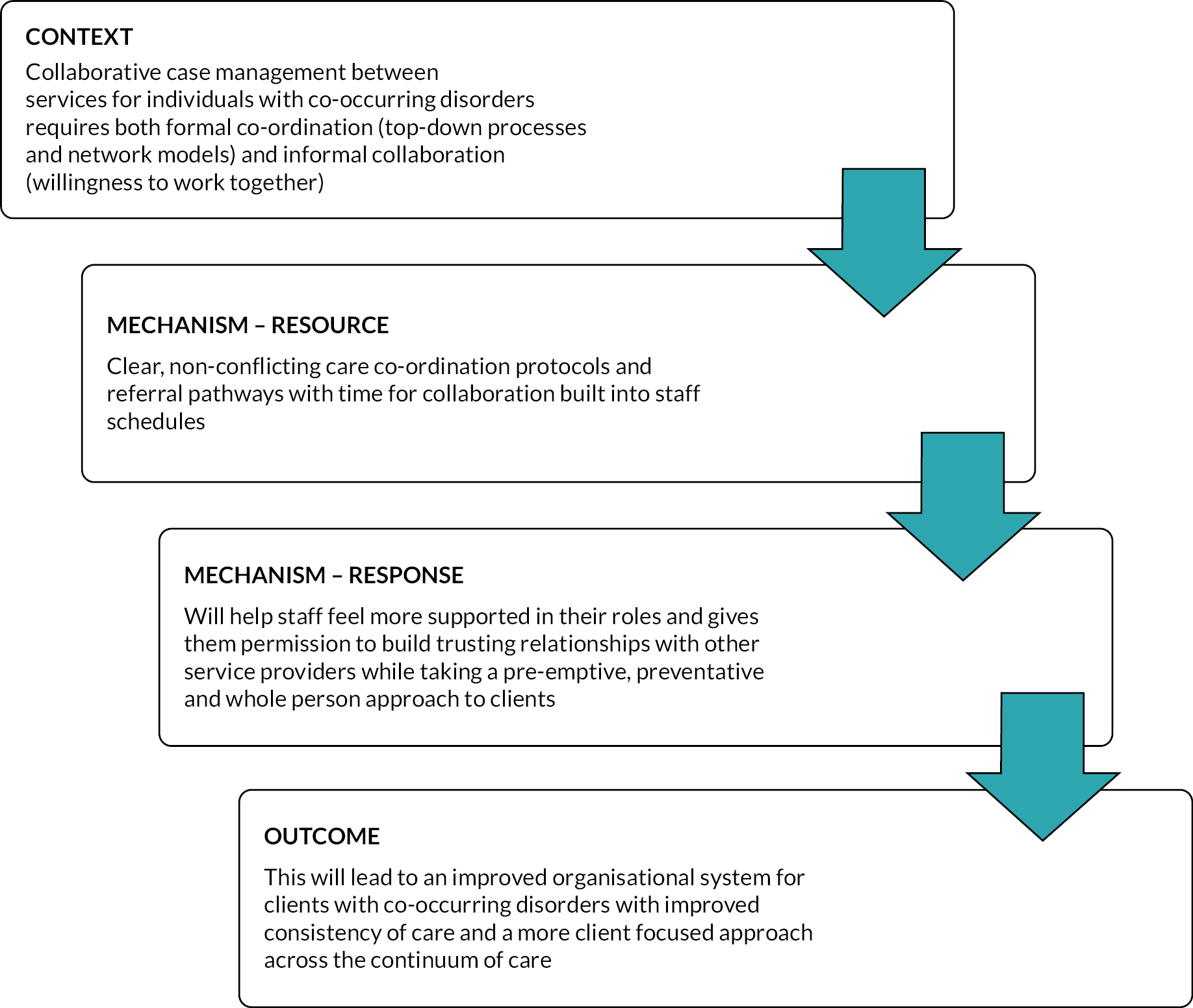
Staff data concurred with evidence from the realist synthesis which suggested that collaborative case management required both formal co-ordination and informal collaboration (context). They described several aspects of successful joint working including effective communication between teams, joint information technology (IT) systems (shared data) and joint care planning meetings (mechanism – resource) (Figure 9). Where these resources were in place staff felt that they had a good overview of service users’ care and were promptly alerted of any significant changes that could impact progress. Joint working was more successful when the staff already had an existing professional relationship with the other health professionals involved (context). This highlights the importance of having time for building those external relationships (mechanism – resource). When collaborative multiagency and interdisciplinary relationships were absent, it became harder to facilitate a service user accessing the right care. According to a substance use worker collaborative, they had to ‘advocate quite sort of strenuously for people to access psychological therapies’ (SP52, Case Study F).
FIGURE 9.
Programme theory 3 context and mechanism.
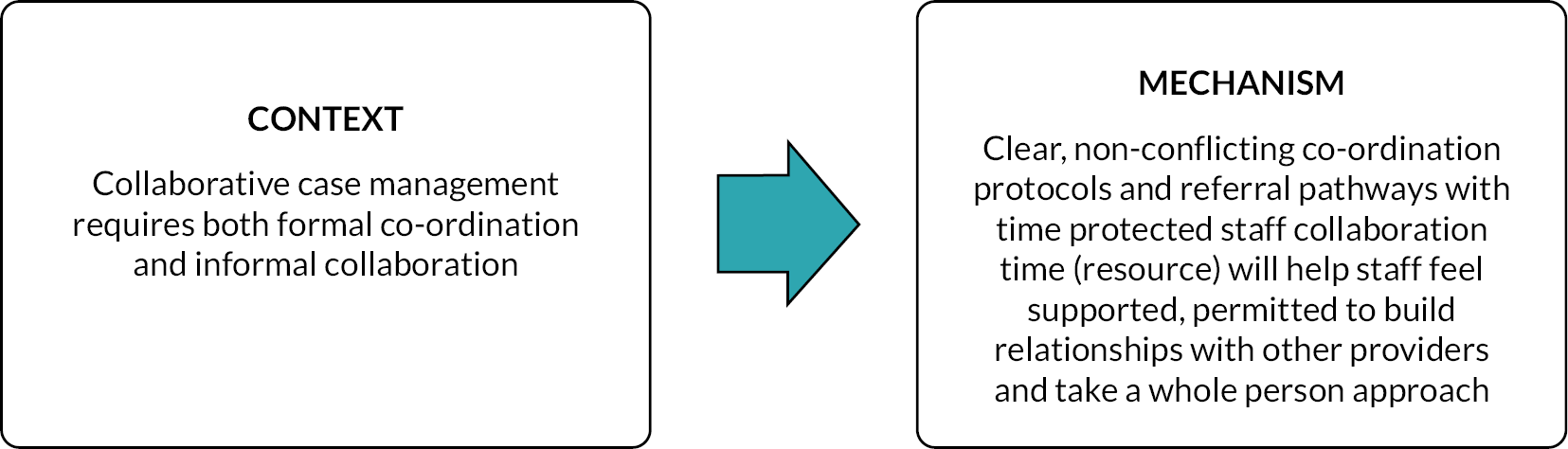
I think relationships with staff within other areas is key with this because you can actually do that joined up working much better if you’ve got those connections and you can actually sort of just pick up the phone and speak to somebody and say I’m not sure what to do with this person, you know? Can you help?
SP51, Case Study D
There is a need for organisational structures to support collaboration such as ‘just carving out some time to do that joint working, multi-agency working’ (SP66, Case Study F) (context). If collaboration wasn’t formalised through policy and protected time (mechanism – resource), there was a danger that all the responsibility for collaboration could fall to individual staff who were already overburdened by large caseloads (mechanism – response). In contrast, having structures for joint working (mechanism – resource) would allow staff to focus on building a trusting relationship with their clients that enabled them to successfully link them into other services (mechanism – response). Participants felt this collaborative way of working required a ‘cultural shift in an organisation that looks at a patient from the point of entry and says … we will work with substance use agencies from day one to manage this individual’ (context), which ‘demystifies it and takes if from being a separate thing to something that’s part of how people cope and manage’ (SP40, Case Study D).
… the structure of the service is very, very important … it’s about a whole model. It’s not just about picking out some people and saying they know stuff. You know I think the complete tragedy really that we have is we put everything on CMHT, any needs that we have in society around mental health or risk goes the doors of CMHTs and you know … that one care co-ordinator is meant to be an expert in, you know, care package commissioning, any type of mental health issue, anything based on, you know, anxiety and depression that’s affecting people’s functioning right up to extreme, you know, ends of mental illness and functioning. Now that is, that is not right to expect one person to know all that … We’re [homelessness service] able to have the contacts … that we’ve built up over time. We have contacts in substance misuse … So, we are able to react, and we know where to go to and we know who we need to get involved … whereas a CMHT cannot be like that at all, they cannot be really flexible and …all have a different approach for every single person because … People have caseloads of 40 like they have to just get on with their job.
SP2, Case Study C
The importance of the COSMHAD lead role in terms of fostering interprofessional relationships is supported by the case study data. Five of the six sites had some version of a COSMHAD lead role, and the remaining case study (A) had a vacant post. In addition, Case Study E and Case Study F had addictions psychologists employed within certain areas of their trusts, which made ‘joint working … probably on average easier’ (SP66, Case Study F). COSMHAD leads were described as leading on policy, training and strategy as well as supporting staff through joint meetings and case study discussion (mechanism – resource). One of the key things about the presence of such a role was that it ‘held [COSMHAD] in people’s minds and also possibly the organisations mind’ (SP37, Case Study A) and ‘keep it on the agenda and keep people thinking about issues within multidisciplinary team (MDT) meetings’ (SP61, Case Study F) (mechanism – response).
As well as working across their own organisation, the COSMHAD leads were key players in facilitating relationships with external organisations and this was helped by their oversight of the different service structures (mechanism – resource). If this lead role ‘was a senior position and … seemed to have some sort of organisational influence’ (SP47, Case Study A), it resulted in easier facilitation of collaboration (mechanism – response). However, several participants at Case Study C also felt that the personal qualities of the COSMHAD lead impacted upon their success in collaboration (context): ‘people who work with [COSMHAD lead] really get on with him, and maybe he brings the skills that he uses with service users to colleagues as well’ (SP4, Case Study C).
Finally, the participants thought that clarity of role as COSMHAD lead as well as for the link worker role was important especially in terms of protected time to focus specifically on COSMHAD issues otherwise other clinical priorities tended to take over: ‘whether that’s 50% of their role, whatever percentage that is, that has to be protected’ (SP51, Case Study D). Otherwise ‘the dual diagnosis practitioner has to sort of take it all on’ (SP52, Case Study F) or
they will get pulled into other stuff, … the link workers that we’ve had in place don’t get time to attend the meetings, that they don’t necessarily have the time to feed back that they try, you know, but that, falls at that hurdle.
SP51, Case Study D
I don’t like closing people, don’t like discharging them without going to every single effort. And if [dual diagnosis lead] can tell me who the Care coordinator is, and they might then ignore me. Probably not, because they’re being malicious because they’re stretched or whatever the reason, I don’t know. I can’t say what the reason is, but just ccing [dual diagnosis lead], just that alone has a really powerful effect and tends to generate a response.
SP13, Case Study C
Working collaboratively with other health professionals both informally and formally (context) brought a number of benefits including increased understanding of how other services worked, and increased effectiveness of communication between services regarding service user progress. Participants described how working together can reduce ‘duality … of thinking’ by allowing staff to bring together their differing expertise and pick up skills (mechanism – response) leading to ‘having really good conversations either for assessment or at different stages’ (SP37, Case Study A) (outcome) (Figure 10). Staff felt that working with those who had expertise in both mental health and substance use had the potential to reduce stigma and increase engagement (outcome). One participant describes a kind of ‘inreach’ approach where they were able to capitalise on the engagement in one service to gently introduce themselves and engage with the person rather than expect someone to attend another service to speak to an unknown professional.
FIGURE 10.
Programme theory 3 mechanism and outcome.
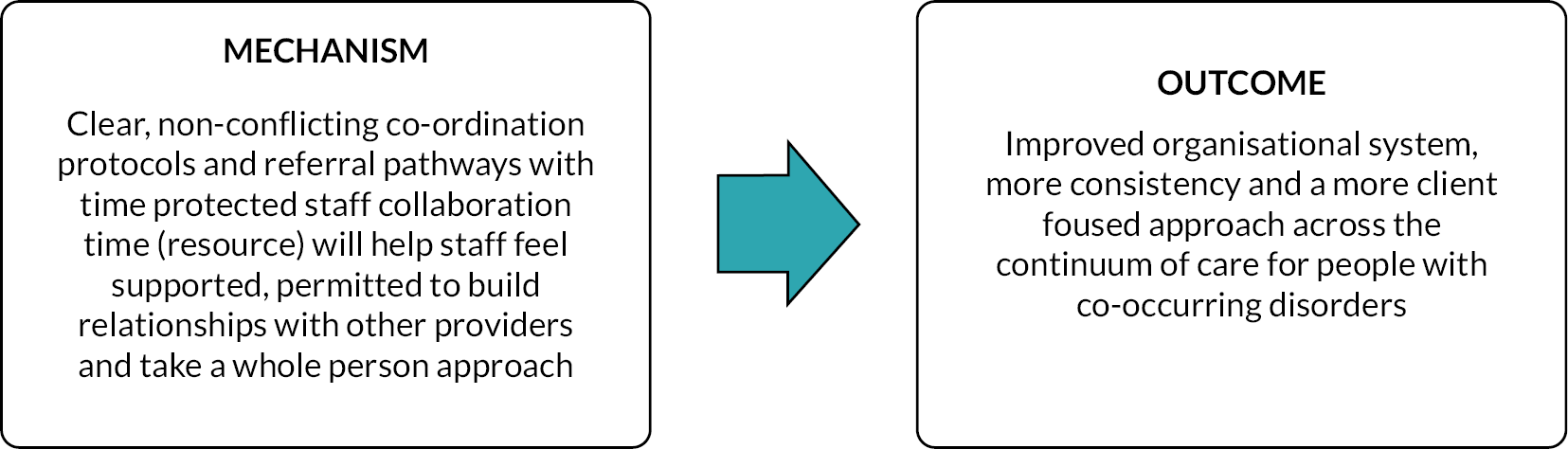
I can think back to times when I’ve not been able to engage with somebody, but the [substance use service] has been actively seeing them because there’s a reason for the person to engage with them and I’ve tagged along on, on, on a sort of like an appointment and said, you know, do you mind me being here? And that’s started that relationship which has been really useful. And just I think it’s also sort of really useful for staff because if you’ve got that sharing of information. And you develop that relationship with [substance use service] workers. You’re more likely to contact them, more likely to engage with them. And that actually gives you that level of confidence that you know what’s going on with somebody because there’s nothing worse than feeling that there’s a whole host of stuff going on with somebody and you’re not really privy to it and you don’t know what’s happening … and that feels risky and itself.
SP51, Case Study D
When staff were able to work collaboratively (mechanism – response) (mechanism – resource), it prevented service users from being passed between services (or falling through the gaps) and ensured a holistic approach to the treatment of their co-occurring disorders (outcome). Staff also agreed that a collaborative approach to care management (mechanism – resource) provided service users with consistency, which allowed them to develop trusting therapeutic relationships and engage with other services that they may require (outcome):
that one worker who has is in some ways been like one of the only secure attachments that they’ve had … they build up that trust with a service or a worker, to the point that they then trusting them to engage with the other services which would be specialist, a lot of our clients are really suspicious and not trusting.
SP6, Case Study C
I mean there have been times when I’ve had clients on my caseload and with certain mental health practitioners, we’ve done sort of joint work and that’s really worked well. But few and far between to be honest and that’s more about … having the time within my job to do all that networking with other people … And I think what happened is clients just get battered between drug services and adult mental health. It’s like chicken and egg, isn’t it? … And I think part of my frustration is even when I say it out loud it doesn’t make sense. But that’s the reality of the services … clients just get batted between one and the other … I know it comes down to resources but doesn’t even save any money. Never mind about what it costs the client, which … should be more important, but it doesn’t even save services money. You end up putting more money in and getting less positive outcomes for clients and it should be about the client.
SP24, Case Study A
Service users and carer participants reported a lack of perceived collaboration in services (mechanism – resource); communication between services often felt fragmented and inconsistent. Service users were often seen by multiple different staff members who did not seem to be fully aware of their case history. This meant that service users and carers had to repeat information to multiple health professionals. As a result, service users and carers felt they were not informed about their care or received conflicting and outdated information which left them feeling frustrated, confused and lacking in confidence in the care providers (mechanism – response). This led to a poor therapeutic relationship with health professionals and disengagement with services (outcome).
A bit too fragmented. They don’t have seemed to speak to each other. You know you hear so many times the communication breaks down between people and between services, between the mental health people between the police between the drug worker … you seem to find yourself saying the same thing over and over and over again to different members of the team. Because you lose your confidence that that that’s actually going to get passed on ….
P36, (Carer) Case Study B
The realist synthesis identified the importance of both top-down and bottom-up collaboration, to help staff feel supported to build collaborative relationships across services. This improved consistency of care for service users. However, service user and carer data highlighted that this is not currently the case in practice, with examples of disjoined working and miscommunications, leading to frustration, confusion and lack of confidence in the system. A lack of time and resources is cited as one of the reasons for this, but participants also recognise that resources are being used in trying to help but not being used in the most effective ways which leads to poor outcomes.
Refined programme theory 4: exposure to co-occurring severe mental health and alcohol/drug conditions in pre-registration education
Summary of evidence
Staff working in mental health services could be influenced by how much exposure they have to people with COSMHAD during their undergraduate training. 45–47 This includes being exposed to knowledge and skills in the theory aspect of the courses as well as by exposure to people with COSMHAD as part of clinical placements. Drugs and alcohol may be perceived as a ‘choice’ and not as a health and social problem deserving of help and compassion. Mental health service staff typically saw continued substance use that exacerbated mental health symptomatology as a sign of poor compliance and engagement. Often the focus for mental health service staff is abstinence (which is a requirement for inpatient settings), with limited attention given to the variety of available harm reduction strategies, possibly due to lack of skills and knowledge in this area. In addition, there are differences in the use of pharmacotherapies, ontological understandings of health, understandings of aetiology for COSMHAD, differing symptom classification frameworks and views on client autonomy that manifest themselves in how substance use and mental health services structure service delivery and set outcome expectations for treatment51,54,60 (Figure 11).
FIGURE 11.
Programme theory 4: exposure to COSMHAD pre-registration education.
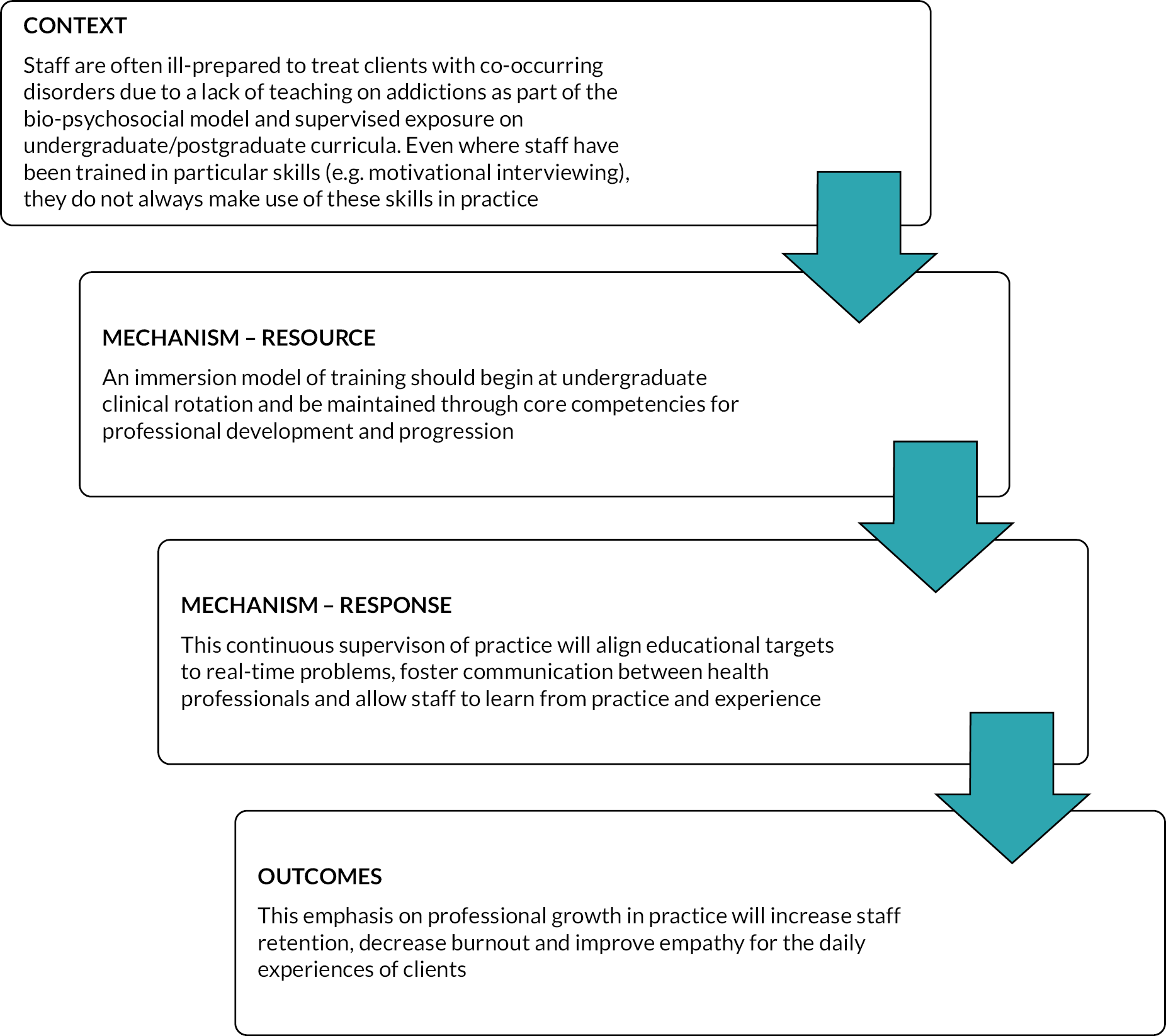
The realist synthesis identified that it was important that the workforce was exposed to issues related to COSMHAD during pre-registration training. However, in the case study data, there was little coverage of undergraduate and pre-registration training in the focus group discussions and, even after prompting by researchers, not much was elicited in relation to this PT. Thus, this PT was considered theoretically not rigorous.
Case Studies B, E and F briefly discussed training and shadowing arrangements for students and new intakes of staff which were felt to increase awareness of substance use and the harm reduction approach [‘so if we can [teach] our student nurses what the impacts of substances is in our guys. Then they need to be aware of how vulnerable they are as people in the community’ (SP88, Case Study B)] and procedural knowledge [‘training new intakes of students trying to skill them up to do assessments with patients on the wards and then knowing what to do with, you know, whether they need brief interventions, whether need more than that, linking in with specialist services’ (SP67, Case Study F)].
One participant argued against the traditional classroom-based training and suggested that working directly with people with co-occurring disorders could have a have a greater impact:
They’re just new shiny nurses [band 5] just finished their training and then they come to the service, they’ll go into a ward. They’re gonna learn more in the world than I’m going to be teaching them. So if the attitude on one ward is very much about, you know that’s not our problem … or you have a very energised, interested group of staff and dual diagnosis. And yeah, their mindset. So, it definitely comes down to the staff centres, their own experiences. I suppose if there was any training and it’s not just about the training as how does the ward manager incorporate that training into what’s going on in the ward.
SP83, Case Study E
The content and delivery of training for new trainees were very much controlled by external factors. For example, participants in Case Study F spoke about how a national project to increase addictions competencies in trainee psychiatrists (with two work-based assessments in addictions) had led to the development of a network of trainers, university-funded extra places in addictions for senior trainees, and the development of new training materials. In contrast, staff at Case Study B had been asked to deliver training to medical students at a local university but had been asked to halt the work by management within their organisation because there was no funding to support this work, not enough staff time to deliver it and no direct benefit from this work to the NHS trust.
Service users and carers were keenly aware of health professionals’ level of experiences, particularly key workers in substance use settings and care co-ordinators in mental health services. They felt that newly qualified staff were assigned their own caseloads too soon after registration and instead should be given time to shadow existing staff and gain experience of working with clients before working alone. They felt that inexperienced staff could not handle complex or crisis situations, had insufficient knowledge and did not build empathetic relationships with clients due to their lack of experience (mechanism – response).
The problem is with the mental health services … it’s the recruitment of the people who can actually do the job … so for getting a graduate in psychology degree … they need to have six months before they actually get into community … And very often they’re a lot more about the mental illness than the people.
P21, (Carer) Case Study A
… the intensive team came out to see her … who really were totally out of their depth, not their fault, but they were out of their depth, in that she was saying that people were trying to get her and … she’s gonna build a big fire … She was gonna throw herself on to. Something she wanted to do, and they had, they just stopped and looked at her like a rabbit in the headlights. They have no idea what to do … I think they didn’t have the experience or knowledge how to deal with the situation.
P21, (Carer) Case Study A
We have been allocated a key worker and I know that you should give everybody a chance, and what I’m going to say now I don’t mean it in a disrespectful way to them. However, they have allocated a very young person who is new to the service to [husband’s name] and I’m not alone in my thoughts that it should not have been the case with where [husband’s name] is and what’s gone on. It should have been someone with more experience and not somebody who’s literally three weeks ago started working in the service. And that’s horrible thing to say because people only get experienced by experience. However, you do have to take into account where people have been, what journey they’ve been on and where they are going and everything that’s happened. And you shouldn’t be putting … a fresh-faced graduate the job. That, you know, find no objections if that person is there to shadow – shouldn’t be the lead.
P3, (Carer) Case Study 3
Service users and carers described that when they encountered inexperienced staff who lacked basic knowledge, they also seemed to have a lack of empathy (mechanism – response) which made the service user feel uncomfortable and misunderstood, potentially leading to disengagement.
I was accessing their community care for the first time, actually … and the counsellor was there a bit, I’m not sure, that I was referred to didn’t have any … training on drug abuse whatsoever and they like, I was talking about some of the substances that I been using and they were pretty common […] but [they] didn’t know what I was talking about … didn’t have any knowledge of it, didn’t have any understanding of it. And instantly at that point when I realized that the person I was talking to didn’t understand my experience even from like an external perspective, yeah, I like just shut down then. I didn’t feel comfortable talking to you anymore. And I just thought blank it for the rest of the time until I could get discharged. Yeah. So I think like it’s really important for healthcare professionals to be tolerant and in their understanding not to necessarily have an encyclopaedic knowledge, but to like know a little bit about different classes of drugs like different effects that they might have, what kind of effect they might have on people’s mental health.
P17, Case Study C
In summary, while this theory was low in terms of rigour, partly as the focus of the study was not on pre-registration and we did not interview education providers, it was clear from a service user and carer perspective that a lack of confidence and knowledge on the part of a clinician could impact on how they express empathy and ability to engage.
Refined programme theory 5: continuous professional development
Summary of evidence
The realist synthesis61–67 indicated that when leaders valued the need for continuous workforce development (CPD) for COSMHAD (context) it was supported, and staff could be released from their routine responsibilities and supported to undertake such training. Traditional ‘classroom-based’ learning is important but insufficient to enact change unless accompanied by supervision and practice-based learning (mechanism resource). This can produce lasting changes in staff skills, values and confidence. 61–67 However, attitudinal shifts are less affected by training but can be improved when staff see that working in a different way (such as using motivational interviewing techniques) has a positive effect on service users59 (mechanism response) (Figure 12).
FIGURE 12.
Programme theory 5: continuous professional development.
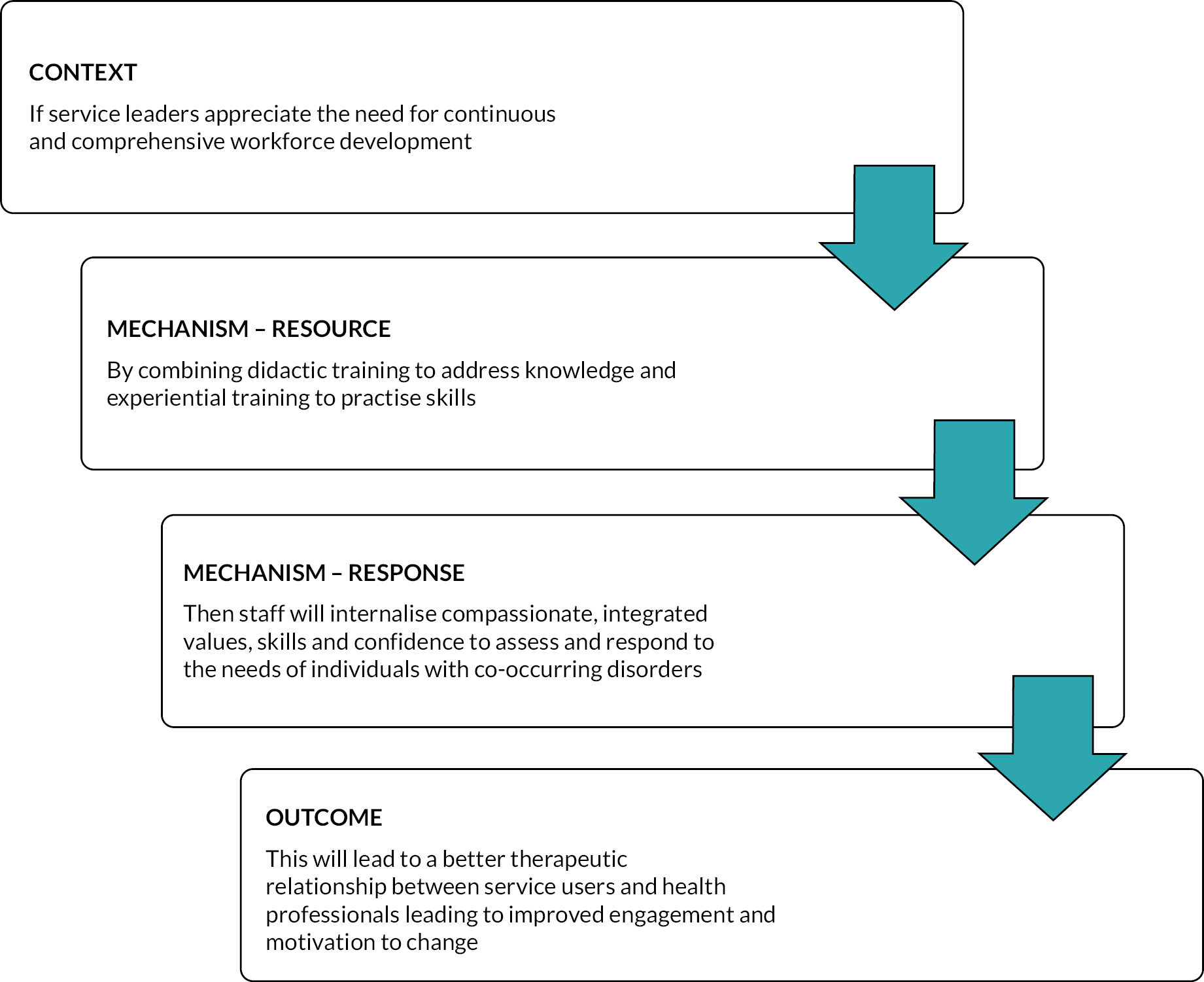
Some form of in-house ‘dual diagnosis’ training was offered in five of the six case studies and typically included a combination of mandatory training for all staff, supplemented by more flexible training and supervision opportunities which were guided by staff need, demand and local and national priorities (mechanism – resource) (Figure 13). This was typically delivered by a COSMHAD lead with support from staff in additional link worker or lead roles. In the one case study where training was not currently offered, this was due to a vacancy in the COSMHAD lead role.
FIGURE 13.
Programme theory 5 context and mechanism.
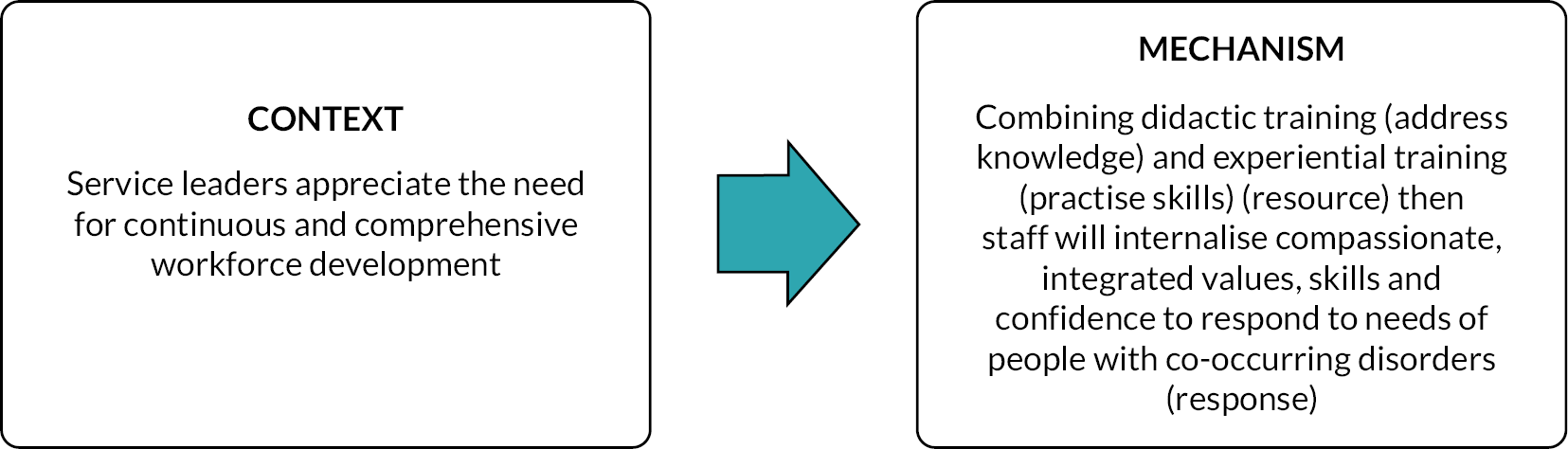
As in the realist synthesis, it was evident that the success of a training programme depended on organisational leadership recognising the need and ensuring that staff could attend (context). A participant from Case Study F highlighted that training programmes required a combination of ‘bottom-up and top-down support’ (SP60, Case Study F).
[O]ur leaders are very supportive of the development. You know, as much as they can be really and it’s crucial, you know. And cultural change is really quick when managers and more senior people are involved, isn’t it, because the opportunities are created for that to happen? … having the COSMHAD lead within services and at the base level, that still requires support of the team managers, you know giving them you know maybe time to come out for the development days and you know, maybe some ring-fencing some time once every week for them to do any work that they need to be doing to support their teams.
SP60, Case Study F
So having the space, having the time to think together as a team. So, it’s maybe about managers creating that space and that time and that ring-fenced, protected time where people, staff are supported to think collaboratively in terms of developing cultures, of compassionate understanding and skills.
SP20, Case Study C
Staff noted that where organisational commitment leadership context was absent, there was often over-reliance on individual interest: ‘if individual practitioners are interested and feel confident and skilled and it’s on their radar, then they are much more likely to be more proactive’ (SP50, Case Study D) and ‘start to train people and you get proper supervision in place and proper support, it’s a lot easier than to keep it on the agenda and you start to change the culture within the organization and within teams’ (SP50, Case Study D) but this will need wider organisation support.
Staff participants concurred with the synthesis that formal training was important (for increasing staff knowledge) but also needed to be combined with more experiential work-based development opportunities including regular supervision and team discussions to enable staff to embed new skills and knowledge into practice (mechanism – resource). As one participant summarised ‘your basic training is gonna provide some level of knowledge but if you don’t use it you lose it’ (SP15, Case Study C). When they had this opportunity to implement their knowledge on working with co-occurring disorders in a supported, supervised team environment then they would increase their confidence and skills to address the needs of people with co-occurring disorders and feel reassured and motivated to continue the work that they were doing (mechanism – response). If this was lacking, ‘it kind of goes off your radar if you don’t feel like you have your skill set to be able to deal with it’ (SP50, Case Study D).
[I]f I could have one of these guys [COSMHAD specialists] in my team at all time to come and join me lots of times with lots of people and having really good conversations either for assessment or at different stages to kind of check out or motivation or think about interventions or whatever, I think that would be really great. And I suspect that over time if we co-work enough, I would pick up some of your skills … You’d need a really sort of skilled practitioner in your team to really skill you up I think.
SP37, Case Study A
I think as well like just getting a bit of assurance. So for me, I’ve been running groups now since I started in November, never done anything like this before … and I’ve still not had anyone sitting in watching me in a group … and you know in the group lots of things happen and come up that I’ve not experienced before and it’s really difficult to know how to navigate … And just having someone be there, maybe even once a month and just say, yeah, I know you’re doing right. You handled that well, that kind of thing would be really great.
SP27, Case Study A
Being supported and supervised to practise their skills (mechanism – resource) was increasingly important in the current NHS climate, where factors including finances, time pressures, staff turnover and COVID-19 had reduced both the availability and uptake of formal training sessions (context). For example, a staff member working in mental health in Case Study C described how ‘we just have like a weekly CPD slot that we’ve, our consultant set up himself just because training is often lacking these days ’cause of funding and whatever else’ (SP15, Case Study C). As illustrated in the quotes from Case Studies D and E below, these time pressures were particularly felt in inpatient and community mental health where participation in training was limited due to large caseloads and competing priorities. The consequence of these pressures in Case Study D was that the training offered to staff had gradually been reduced by management.
I think also I mean obviously staff are so busy … It’s also very hard to and also to do something consistently is really hard because there’s always something else … I find that in our ward there’s always something that needs you know to be actioned or something that needs to be addressed … even in terms of quality improvement, there’s multiple things going on, so it’s very hard to keep the focus on it, and to keep the interest in … whenever you’ve got a high turnover or patients who all have different needs and different priorities I think that that makes it difficult to keep to keep running with it as well.
SP72, Case Study E
I think over the years it was longer. It was a whole day, then the trust said we didn’t have enough time. In the beginning we had linked workers and we did 10 days of training with them, and we’d have them out of the service. But what happened to us? We recently took on two band 6s that were going to work on dual diagnosis and they weren’t allowed to have the training … So then people don’t want to do the role because they’re not trained to do that. So, if you if you’re kind of given the label and then nobody supports you … here’s the training we’ll deliver and ‘Oh no. Can’t release. You’ve got too many patients. It’s not gonna happen’. And then it starts … why am I doing this job? … It needs to be funded to make it work. That’s the only thing that will make this work. I mean if I leave tomorrow, SP41 leaves tomorrow, this will collapse. There will be no service that will be here.
SP40, Case Study D
While staff recognised the contribution of austerity and national policy to this context, they still felt leadership played an important role (context): ‘they kind of prioritise other training before the dual diagnosis and that’s the realistic answer, isn’t it really’ (SP45, Case Study D) and without this prioritisation from management a culture shift could not be achieved. This is described by participant SP38 (Case Study A) as a barrier to staff developing compassionate values and confidence in their skills (mechanism – response):
[T]his hub and spoke thing became kind of the in vogue way of managing austerity … instead of having a team of people that hold expertise and an ability to respond to people, you have a hub of maybe 1 specialist, if you’re lucky, who kind of, you know, points at all the other people … so this issue of resources, investing in staff and investing in expertise that can be kind of available I think is a potential gap … and it’s a question about how you’re going to shift the culture into operating differently … takes a lot of tenacity, takes a lot of resilience. You’ve got to want to do it … you need people in motivated task force that’s valued.
SP38, Case Study A
Staff concurred that training and experience (mechanism – resource) led to increased confidence in their skills, increased compassion and empathy, and they were better able respond to the needs of individuals with co-occurring disorders (mechanism – response) leading to better therapeutic relationships and engagement (outcomes) (Figure 14). Communication and use of language was seen as really important. Participants described learning ‘the correct language, you’re having a deeper understanding of what they’re going through’ (SP14, Case Study C), ‘a problem-based learning approach … your learning is applicable to the people that that you work with’ (SP11, Case Study C). A COSMHAD lead who delivered training summarised this as:
FIGURE 14.
Programme theory 5 mechanism and outcome.
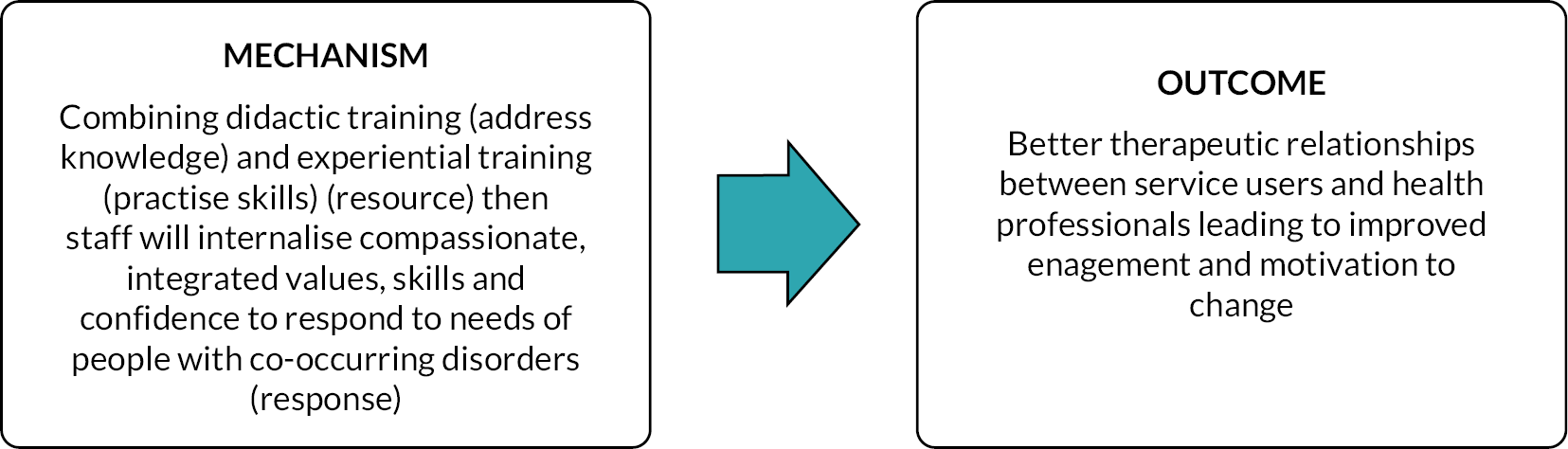
seeing that change in how people are communicating … and thinking about being flexible with some of the challenges, they’re also telling you … I feel much more able to talk to people about their substance use and no longer feel pressured to looking for solutions and now just have a chat with people and listen.
SP60, Case Study F
When staff were confident in their skills and knowledge (mechanism – response), they felt more able to have conversations with clients and be flexible in developing interventions for people with co-occurring disorders which in turn created better therapeutic relationships (outcome), whereas staff who lacked this confidence (mechanism – response) could shy away from these conversations with their clients (outcome).
Then you get into a situation where people are just scared to ask and you’re not able to start having a conversation with the service users because they always know more than you do. So if you haven’t got the vocabulary, if you don’t know what it is that you’re talking about, service users will pick that up straight away, and you’ve got no credibility … if you’ve got somebody who hasn’t got a clue what they’re talking about or comes with a particular set of opinions or preconceived opinions that aren’t particularly based on anything, I mean, you’re not, it’s not a respectful conversation, really.
SP12, Case Study C
To me, we all need to be confident to start that lower-level conversations … a lot of nurses are very scared of starting that conversation, ’cause they’re not sure where it’s going to go.
SP73, Case Study E
Key to this outcome is the combination of training along with supervised practice to help build skills and experience (mechanism – resource). With experience and knowledge regarding the nature of COSMHAD, staff learnt not to expect quick results and therefore become despondent when service users did not achieve this. Instead, staff become more empathetic towards people’s recovery and thus develop more flexible, tailored responses and better therapeutic relationships (outcomes).
[Y]ou get a lot of the staff thinking that they’ve engaged with somebody they’ve worked with somebody … the staff will say I gave him a lot of leaflets. He said he wanted to stop and he was off for three weeks and we were doing really well doing really well … And the next thing he’s back on the drink again and it’s almost as if it’s like a personal affront to them because he promised me he wasn’t … You’re getting staff concerned, but you’re getting staff frustrated and stuck as well … one of the ways when I start my training is to start and say give me the issues that you’re having with this cohort. Give me the problems. Give me the things that if you had a magic wand, you would fix. You never have to deal with again. And then you line it up against the symptoms of a substance use disorder under the DSM 5. And you’re saying that, oh, gosh … we’ve got the same thing. So, what you’re actually frustrated about as the symptoms of somebody not being well … They get that. But then what do they do? What do they do with that information? Now they have that. So yes, training is an issue there … And having the confidence to do … would come from the training support at work, good supervision, these things being picked up, understanding how this plays out, being able to talk to your colleagues about it, then everybody’s in the one path, you know, having that relationship with the carers … In terms of the staff, I think they do convey that, but … because our staff aren’t trained in them is so they wouldn’t be using that language.
SP83, Case Study E
Supervised practice is exemplified in the COSMHAD model delivered in Case Study B. In this model, staff receive training to deliver the interventions and then the consultant nurse from the specialist team works alongside them to implement into practice. This encourages staff ‘to try and do the work as well alongside her, which is right because we’ve all been trained in in it … So you know, although she’s a bit of the guide clinically, we try and look at our people’ (SP92, Case Study B). The intention of this model is ‘just to give to people that bit of confidence … it’s everyone’s responsibility … not just say oh, just refer to [specialist service name]. And so, people need that confidence to, you know, to be able to do some of the interventions themselves, really’ (SP84, Case Study B).
This balance between knowledge-based training and learning through experience (mechanism – resource) is summarised by SP11 (Case Study C) as becoming the ‘anti-expert’ – having the confidence, skills, knowledge of resources and flexibility to be able to respond (mechanism – response) to the needs of the person with co-occurring disorders in front of them in a way that best suits their needs (outcome).
I think the whole thing about learning so many facts about drugs, I don’t think it really helps my head because I can’t remember facts in a rote manner, but I think interventions in motivational interviewing and the work that [SP15’s] been doing, it’s been really useful because it’s a way of, of probably being an anti-expert and getting people to thinking a different way about their substances and to try and recognize the things as to why they use and why they don’t use rather than being an expert in you know the substances … And being the expert, I think it’s motivation interviewing I think is a bit like the anti-expert. You know the service user’s the expert you know you just ask the questions and it’s more of a formula rather than facts.
SP11, Case Study C
Service users’ and carers’ experiences echoed the PT in recognising that staff trained staff (mechanism – resource) who had confidence in their skills, experience of working with co-occurring disorders and compassion and empathy towards clients (mechanism – response) which lead to better therapeutic relationships with service users and carers (outcome). Service users recognised that lack of confidence in skills and lack of experience of working with people with COSMHAD wasn’t just an issue with new staff, but also in more experienced staff, hence the need for CPD (mechanism – resource).
… some people have worked in the Trust too long and … they kind of forget their role … sometimes how long they’ve been working there, I think they got a bit complacent …even, you know, the nursing staff can become just a bit hardened, really … people who [start] working at the support role level and then like work themselves up to maybe nursing and management or ward manager, when you get to that level you completely lose what you had when you was at the lower end because things are different – you got restraints, budgets and all that kind of thing.
P6, male, Case Study C
Service users and carers described how a lack of confidence and experience in providing care for people with co-occurring disorders (mechanism – response) could lead to poor communication between services; therefore health professionals were not passing on information to ensure that they got effective care (outcomes). Staff who had not been sufficiently trained (mechanism – resource) to be confident in their roles (mechanism – response) often delivered very ‘formulaic’ (P17, Case Study C) services where many of the conversations felt like ‘a box ticking exercise … it’s all very formal and paperwork’ (P13, Case Study C) rather than being more ‘holistic’ (P17, Case Study C), ‘build[ing] a rapport straight away’ (P13, Case Study C) and ‘being mindful because not everybody’s gonna be at the same stage’ (P6, Case Study C). Service users and carers observed that staff who were more confident in using a more tailored approach (mechanism – response) meant that service users were better informed about their care and involved in making choices about care for themselves (outcome). Such staff were infrequently encountered and often described as those who were seen to ‘go beyond the scope of their role’ (P17, Case Study C) when this should be ‘part of the job’ (mechanism – resource).
[I]f we get to the point where more people understand it’s functionality and where the care services are more holistic … I think that would make a big difference, at least in my experience. The good ones have been the ones that sort of go beyond the scope of their role, which they shouldn’t have to do, but the really, really good ones want to, and they do that. But ….
P17, Case Study C
Once service users and carers came into contact with staff who ‘go above and beyond’ [P3, (Carer) Case Study C], they described receiving more joined-up care, resolution of crisis situations and signposting to additional external support that they needed (outcomes). One carer described how a COSMHAD lead (in a non-patient facing role) had taken on their husband’s case (mechanism – response) and ensured that they received collaborative care (outcome) which they had not received from the community mental health team (CMHT). Another carer described how a newly appointed care co-ordinator intervened in an issue which had put her son in contact with the criminal justice system. They had previously sought support, but it was only because this individual staff member ‘really just came on side’ (mechanism – response) that they felt they got support from services (outcome).
… that one worker [trust name] … I think care co-ordinator … I don’t know who that man is, as far as I’m concerned … he wrote a letter … If he hadn’t written a letter and said that [son’s name] had been misdiagnosed, I believe that this lady’s son has been suffered with psychosis for quite a while and he has been misdiagnosed and has been battered backward and forward and I feel that this is a culmination of what happened. He is just as vulnerable … has not had the services … don’t know why he did that because, you know what, nobody else [at trust name] was prepared to do that … He looked through his notes … We had a couple of months with the early intervention, and he was [son’s] care co-ordinator. And he really just came on side, tried to look after [son], tried to look after the family.
P38, (Carer) Case Study A
Service users and carers felt that skilled staff (mechanism – resource) were those who had knowledge of mental health and substances, showed commitment to assisting those with co-occurring disorders and who communicated assertively and effectively with their service users (mechanism response). Service users often felt that they could not assertively communicate what they needed in terms of contacting services (e.g. in times of crisis) and engaging with treatment. They described how staff who communicated with them proactively were ‘like a safety net’ (P8, Case Study E) and supported them to remain engaged with treatment and work towards their goals even when they experienced setbacks (outcomes).
It’s like a safety net … if you’re failing and you reach out, you know, to somebody in the community mental health team and they say they’ll ring you back and you wait and you wait. And you don’t get that full call back. You’re unlikely to reach out again, you know, to try and access that help … but whenever you make that phone call and you do get speaking to somebody and, you know, you tell them that you need help … they get back to you … You’re more likely to reach out again … for me. Impulse is a big thing … but just being able to kind of reach out and say, you know, listen, I’m solo, this is what I feel like. Just knowing that there’s somebody professional there and that they’re going to get back to me can be enough to kinda take that impulse away.
P8, Case Study E
In line with the initial PT, service users and carers felt that when trained staff (mechanism – resource) had confidence in their skills, empathy towards clients and were sufficiently experienced (mechanism – response), then they developed better therapeutic relationships with clients (outcome). However, service users and carers suggested that staff like this were relatively rare in their own experiences, which highlights the need for continuous training and supervision to be integrated into services at a leadership level to ensure effective treatment for co-occurring disorders (context).
… but if it just makes them just treat somebody else. The child, lover, husband, daughter, son, Auntie, uncle, differently. In my heart it will be worth it to me because I can’t do anything else. Yeah, but if I can help somebody else, would they just have the milk of human kindness? Follow the policies and procedures they got because I don’t think that much really needs to change. They just need to follow the policies and procedures. Just follow them.
P38, (Carer) Case Study A
Refined programme theory 6: leadership
Summary of evidence
The SELFIE (Sustainable intEgrated chronic care modeLs for multi-morbidity: delivery, FInancing, and performancE) framework proposes that supportive leaders with clear accountability, visions and ambitions for integrating care are key to successful integration for multimorbidities. 68 The realist synthesis identified that leaders supporting the development of effective COSMHAD services (context) who took action to develop the listed policies, processes and procedures (mechanism – resources) led staff to feeling supported in taking a whole person approach (Figure 15).
FIGURE 15.
Refined PT6: leadership.
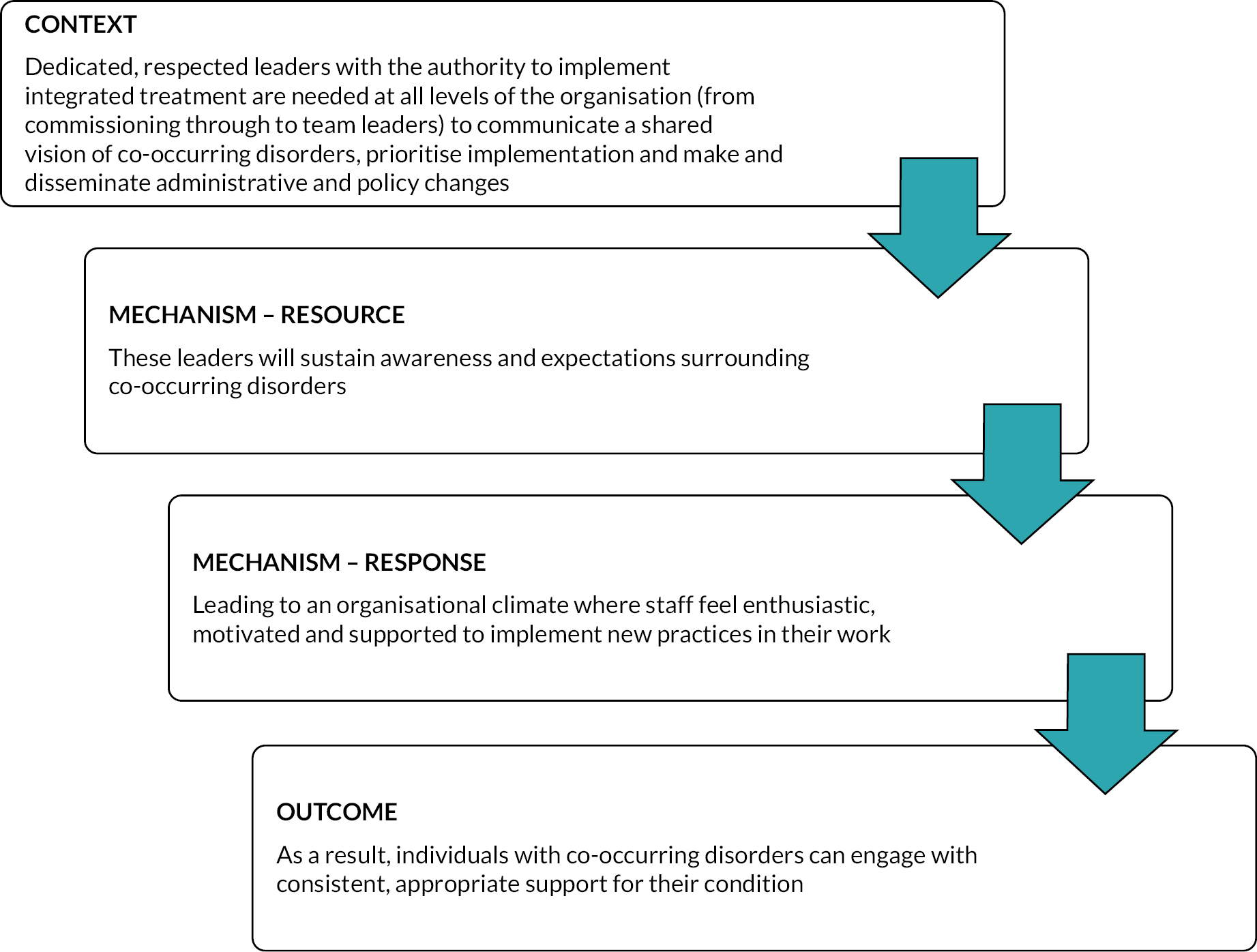
Staff participants in all six case study sites emphasised the importance of having visible leadership for co-occurring disorders (context) to advance the implementation of integrated treatment across their organisation. They identified that these leaders needed to exist at different levels of their organisation including at a senior, strategic level and operating at a more clinical management level.
Supportive and engaged senior leaders (context) were needed to keep co-occurring disorders on the organisational agenda (mechanism – resource) (Figure 16). Participants in Case Study F made several references to a supportive director who was active in promoting co-occurring disorders, but they were aware that this often depended upon the interests and priorities of the individual in a leadership role (context). A participant from Case Study E describes how senior managers need ‘clout to get things done’ (SP84, Case Study E), with this authority allowing them to get co-occurring disorders higher up on the organisational agenda and formalised through measures such as pathways and mandatory quality awards (mechanism – resource). These measures implemented by leaders were felt to emphasise the importance of co-occurring disorders to staff (mechanism – response), leading to better engagement with patients (outcome). In Case Study D, staff described support from leaders as ‘patchy’ and ‘not lead from the top down’, and without senior level leadership ‘it relies on clinicians doing it, if they choose to do so … unless you have a lead in every service at a senior level that says we must do this, it doesn’t happen’ (SP40, Case Study D).
FIGURE 16.
Programme theory 6 context and mechanism.
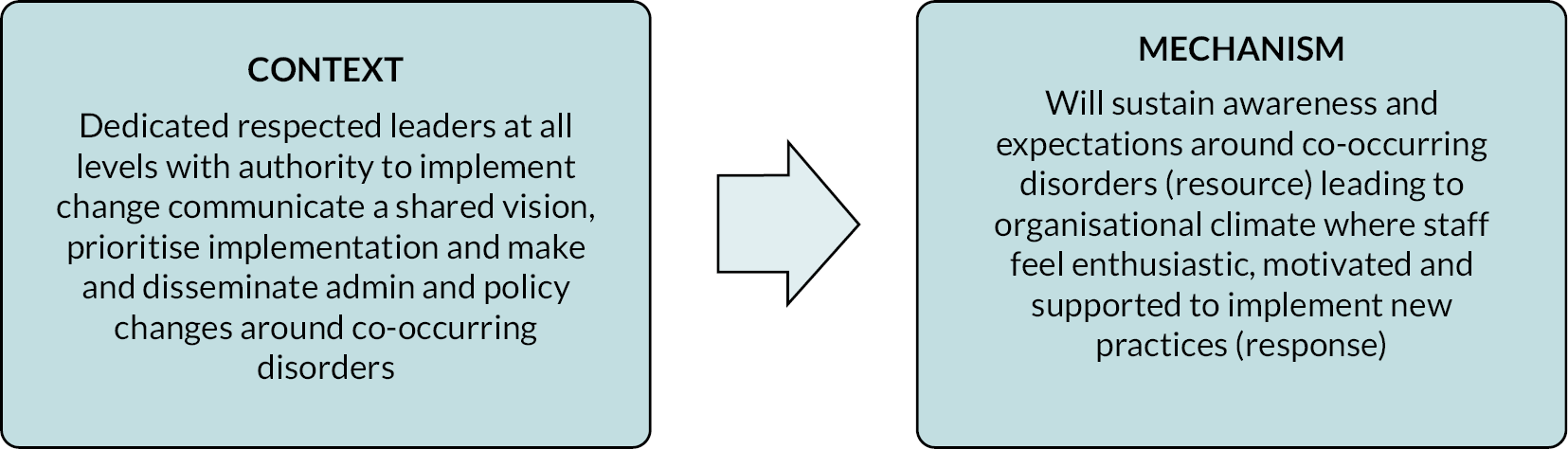
I have been in my post for about 6 years now and I’ve had different managers and not one of them has had any clout to get things done. I don’t have clout and I think there needs to be. It’s not that people are disinterested, it’s just that it’s not high enough in the agendas … and nobody is taking the lead or pushing at medical level, at psychology level, at clinical level … there’s nobody taking the lead and pushing for this. And yet, if you go and ask staff in the wards what’s your biggest worry, it’s these patients. If you ask staff in the emergency departments or the cardiac ward and the General Hospital, it’s these patients … but it’s not given priority at strategic level. It gets a couple of paragraphs in documents. … But in terms of dual diagnosis, something like that might be good where you have quality awards for it […] there’s that sense that this is important and therefore staff they’re forced to see how important is, they also see the benefits of that that we engage with patients that they stay with us, that they work with us better.
SP84, Case Study E
Senior leaders (context) were needed to achieve a
cultural shift in an organisation [mechanism – response] that looks at the patient from the point of entry and says ‘right, you have mental health and substance use issues’, we will work with substance use agencies from day one to manage this individual
and where ‘staff are using those skills that they … have been trained in with that client … because that’s the only way you’ll get change with individuals. If they’re constantly supported’ (SP40, Case Study E).
In contrast, staff felt that when senior managers did not have a sufficient understanding of people with co-occurring needs (context), they would create strategies, design services, and set outcome targets that were not feasible for staff and people with co-occurring disorders (mechanism – resource). This was described as creating additional pressures on both staff and service users leading to reduced staff motivation in their roles (mechanism – response) and reduced engagement with services (outcome).
I think that if the people at the top don’t know what their population group looks like and what their needs are … I think people need to have all of that knowledge in order for them to be able to actually strategise and put the right services in place … [for] people to be able to do their job, they need to be motivated. They need to have an interest in in what they do, because otherwise why would they turn up for it?
SP48, Case Study D
… the most difficult battles I’ve had have been with management who don’t understand co-occurring needs. It’s well, they do understand, but maybe not to the level or the acuity […] some managers you can come across and maybe they don’t have that understanding of trauma as well as you know co-occurring needs … [they’re] putting pressure on the caseworkers to maybe fit things into boxes or tick boxes … have you not got an outcome for that person yet? … But then when you look at the actual caseload of people, that’s never gonna be achieved, […] if you don’t have the right kind of goals and they’re unachievable then no one does well in that.
SP11, Case Study C
The other level of leadership that staff discussed frequently was the existence of (and resources for) dedicated clinical leaders for COSMHAD. These were typically positioned at a clinical management level and generally took responsibility for training, local strategy and provided specialist supervision (context). Four of the case studies had such COSMHAD lead roles who have an organisation-wide remit and these posts had been in existence for many years. Often these posts were held or created by people who had a long-standing interest in co-occurring disorders and had been ‘a sort of a pioneer for a long time’ (SP61, Case Study F). Staff described the key role played by the clinical leads were all ‘about relationships’ (SP10, Case Study C) which were developed by these individuals (mechanism – resource) which encouraged joint working from staff in other teams (mechanism – response) and increased accessibility for people with COSMHAD. Participants also described how these leads ‘let us know what was being discussed at a higher level … because it just doesn’t get communicated’ and responded to wider policy changes. As the quote below demonstrates, key to the success of these leads was someone who ‘leads by example’ (SP16, Case Study C) by putting the skills they taught to staff into action, and this helped staff feel motivated and supported to continue in their work and ‘stand a chance of making sure … support is in place’ (SP16, Case Study C) for service users.
However, it was clear that staff in these lead posts often felt it was challenging to maintain organisational commitment to co-occurring disorders without support from senior level leaders. There was also acknowledgement across all staff that because many of these posts had grown up from individual passion and interest to drive things forward (context), if these roles were taken away or individuals left the organisation then there would be no one to keep co-occurring disorders on the organisational agenda and ‘the whole system would fall apart’ (SP10, Case Study C) and ‘we will lose the drive for change’ (SP13, Case Study C). This was confirmed by staff in Case Study A, where the trust COSMHAD lead post was currently vacant and had been for some time (context), and staff described the support they were now lacking including someone to lead on co-occurring policy, strategy and training, assistance with case discussion and upskilling for team leads and the accessibility of ‘someone who people can just pick up the phone and call’ (SP28, Case Study A) (mechanism – resource). Participants described how when the post had been in place it ‘helped people to hold the work in mind in a more co-ordinated way … it held it in people’s minds and also possibly the organisation’s mind’ (SP37, Case Study A) (mechanism – response).
… what I reflect on a lot of the time and feel really concerned about is that I feel at times I’m an invisible voice in an organization. And although I’m quite vocal, but I actually represent these service users so I can see why they don’t get a service … you look at all these other services and will say, oh, we need … a hub service, we need an assertive outreach team – here’s your money. So, you’ve got the most complex need group of people with substance issue, some mental health issues, but actually you can’t have a penny. We just expect you to do it. So what happens is they’re difficult to engage, so they get brushed off.
SP40, Case Study D
[T]here was a time when, you know when all the services went out of the NHS and everyone’s budget was being so squeezed and [former and current trust dual diagnosis leads] basically between them … kept dual diagnosis alive and they were passionate advocates for it and … because I think it’s well part both of their own personal commitment and their knowledge and skills and their networks with dual diagnosis. But I think they just negotiated for their time and budget.
SP66, Case Study F
[W]here it comes from the ground up, that’s brilliant and it works well, and managers don’t obstruct it, maybe don’t support it, but they don’t obstruct it. And it works brilliantly. But if one key member of staff leaves, that folds, it just collapses.
SP84, Case Study E
Staff described how, when they were working alongside their NHS organisation’s COSMHAD lead or specialist team (mechanism – resource), they felt reassured that they were taking the right approach towards working with service users and that they also became more confident to listen to people with COSMHAD and work in a way that was responsive to their needs (mechanism – response). This was described as ‘empowering other professionals to understand what success looks like … it’s just about having a conversation and forming that relationship and seeing where patient’s are at’ (SP52, Case Study F) and for service users, interacting with more empowered staff could end the ‘vicious cycle that they weren’t engaged with services because they don’t think they’re being listened to or particularly relevant’ (SP3, Case Study C) (Figure 17).
FIGURE 17.
Programme theory 6 mechanism and outcome.
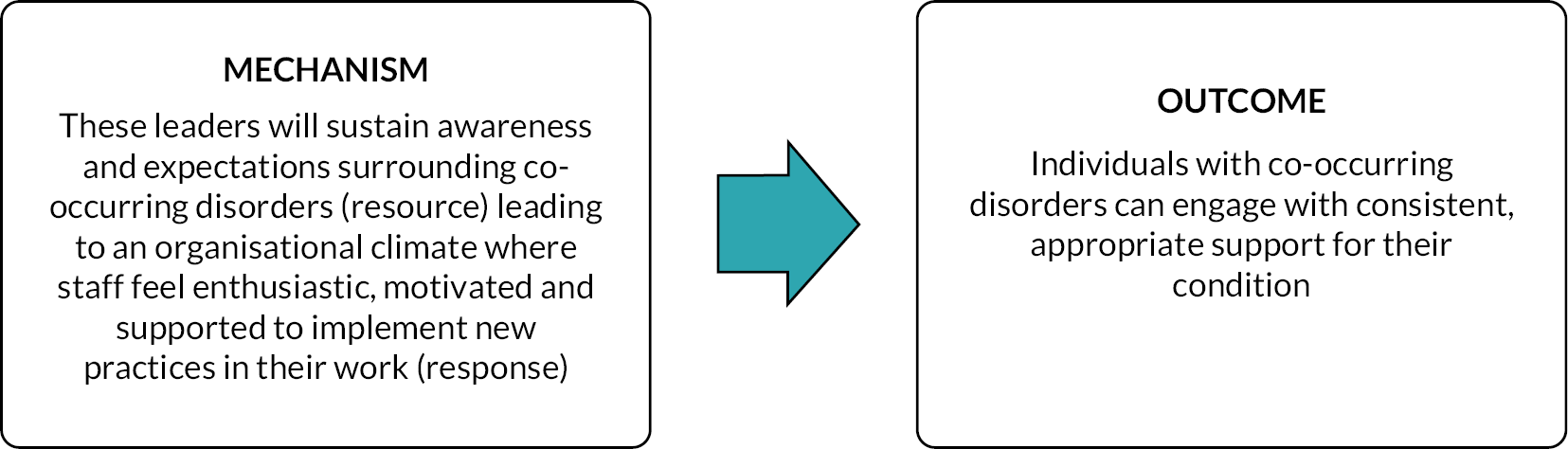
[W]e have got [dual diagnosis service name] worker that … will tend to be the person that we are drawn to, to discuss things. And we see her as a bit of our expert, although I know she likes us to try and do the work as well alongside her – which is right because we’ve all been trained in it. And I think we naturally just looked to her as our expert in that field, really … And I’m just getting the person involved, you know, because again, they’re the experts in what they’re doing and how they’re feeling and. So, you know, although she’s a bit of the guide clinically, we try and look at our people that are using really.
SP92, Case Study B
[A]nd [trust dual diagnosis lead] for example … is sort of my point of contact from the service to come along to sort safeguarding meetings and complex MDTs etc. And having that even if you know we’ve not got that specialist in that area engaging directly with the client, but to offer their advice and I suppose trying to as much as we can to manage that risk and when, when it happens for very complex cases, to be honest. So, I have had that recently, which was really, really helpful. And I think to offer reassurance that you are doing or you can or if there’s any other ideas to come forward about harm reduction that I wouldn’t usually think of in terms of, you know, substance use in particular. And so yeah, just having that sort of end-point to contact, it’s been really useful.
SP1, Case Study C
However, support was also needed from senior leaders in the organisation, and this support was required to help embed integrated care into routine practice. When this support was absent, there was too great a focus on key performance indicators (KPIs) over the needs of service users, and unclear structures to enable them to access the support needed from other teams. Under these circumstances, staff often had to advocate hard to get the support and resources service users needed and this often served to demotivate staff and make them despondent in their work (mechanism – response) which in turn demotivated service users (outcome).
That then becomes a little bit of a disjoint and the different services sort of battle against each other, and that doesn’t help because actually it’s not my client/your client. The client needs a service. We all look at them and through a different lens. So, there’s just work with the client. It’s not my statistic and I want to take that for my commissioner, but that’s what it comes down to. It’s like we all need to hit certain targets … the client has less, but we expect more from them and from a practitioner’s point of view you have to advocate quite hard for your client to get what they you shouldn’t need to advocate for. They should just get it and that can get you despondent let’s say that.
SP24, Case Study A
It’s quite difficult working in a system where that system is broken and where resources are less and where you can see the clients have less. You have to be really mindful of your motivation around the work you do. I’m really lucky I still really enjoy the client work and that’s what keeps me here. But to be honest it’s not an easy job and it’s not getting easier, and I don’t want to be negative too much about it. I’m just being realistic. The thing that keeps me here is I still like that connection with the clients. Well, my colleagues as well.
SP24, Case Study A
The service users and carers did not specifically mention leadership, not surprisingly as this aspect of their care would be invisible to them. However, they did mention that people in dedicated COSMHAD roles had gone the extra mile for them, and they appreciated this advocacy, compassion and commitment. The data indicated that the COSMHAD role was a lynchpin of good service, but they were stretched and given little resource to sustain their role. This led to service users having inappropriate support that was disjointed and not person-centred (e.g. KPI focused).
Refined programme theory 7: formalised networking opportunities
Summary of evidence
A critical aspect of integrated care is communication and effective relationships, both between colleagues in the same organisation as well as colleagues in external agencies. One way of creating and sustaining this is by providing formal opportunities to meet. By doing this, it allows for communication and relationships (context) that lead to networks that allow staff from different teams and services to work collaboratively (mechanism – resource) (Figure 18). The evidence from the realist synthesis suggests that these networks work best when they are formal, structured, sustained and responsive to the complexity and variety of needs experienced by people with COSMHAD. 69 There are numerous examples in the literature including steering committees,56,70 staff learning groups,71 communities of practice,72 collaborative case conferences73–75 and large multidisciplinary networks such as those in Leeds44 and Manchester. 76 Studies from both Europe and the USA found that these formalised networking opportunities for COSMHAD (context) led to opportunities for multidisciplinary peer support and ethos. 73,77–79
FIGURE 18.
Refined PT 7: formalised networking opportunities.
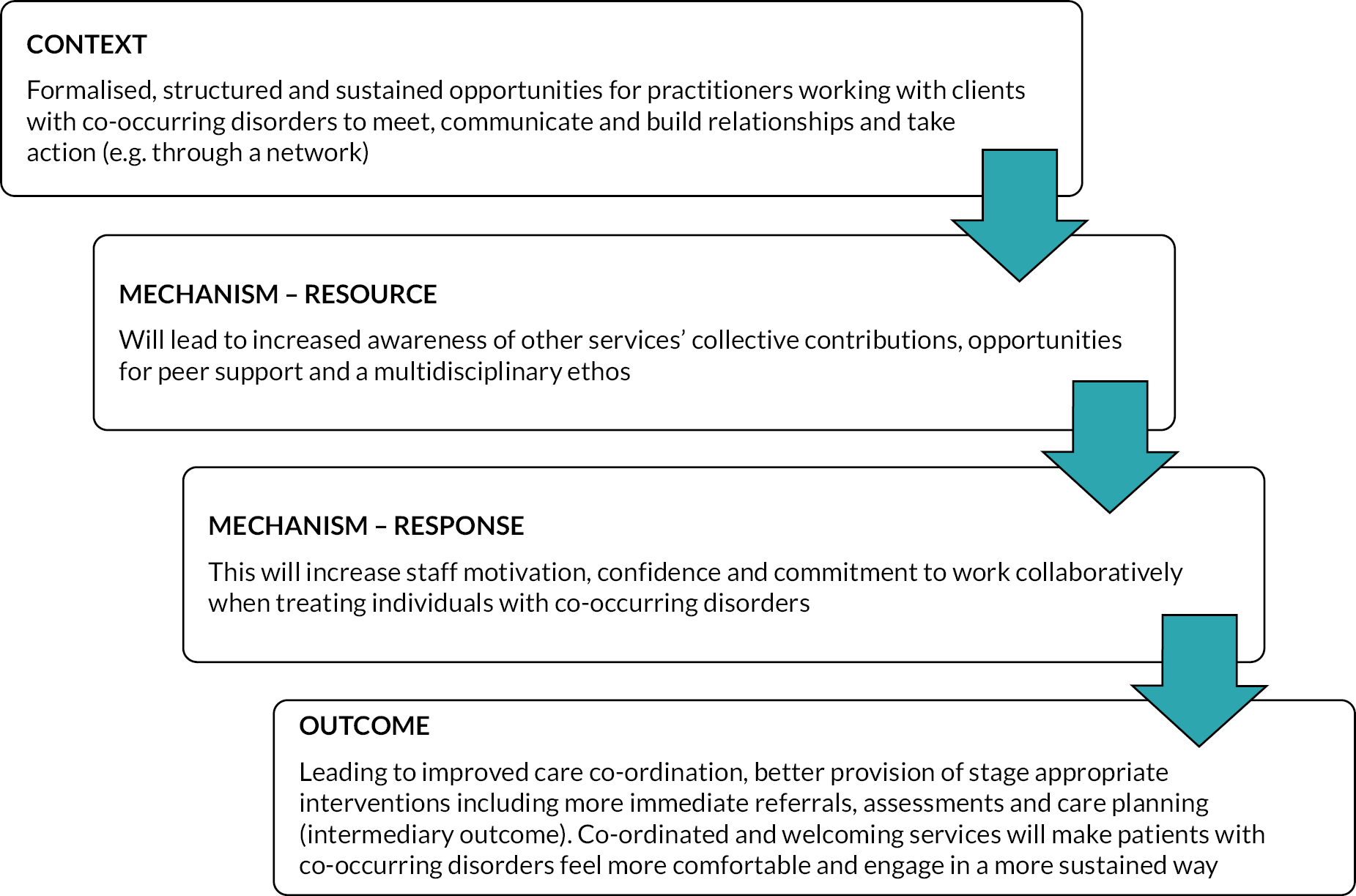
Co-occurring disorders networks existed across four (Case Studies C, D, E and F) of the six case study sites. In three sites (Case Studies D, E and F), there were networks which brought together designated COSMHAD champions or link workers who were positioned in different teams within the trust. Two case study areas (Case Studies C and F) also had more local level networks (at borough or local authority level) with multidisciplinary membership for case discussion (with Case Study D currently in the process of setting this up). Case Study C had a trust-wide network which was open to any professional within the geographical area who was working with people with co-occurring disorders. These networks provided multiple different functions including planning, training, information and resource sharing, dissemination of policy, case discussion, supervision and reflective practice. In line with the literature, the participants felt that these networks were most successful when they were formalised and sustained with support from management within each trust (context). Where this formal support was not present, it was challenging to maintain staff attendance and the networks had limited power to push forward the agenda of integrating care for COSMHAD (mechanism – response) (Figure 19).
FIGURE 19.
Programme theory 7 context and mechanism.
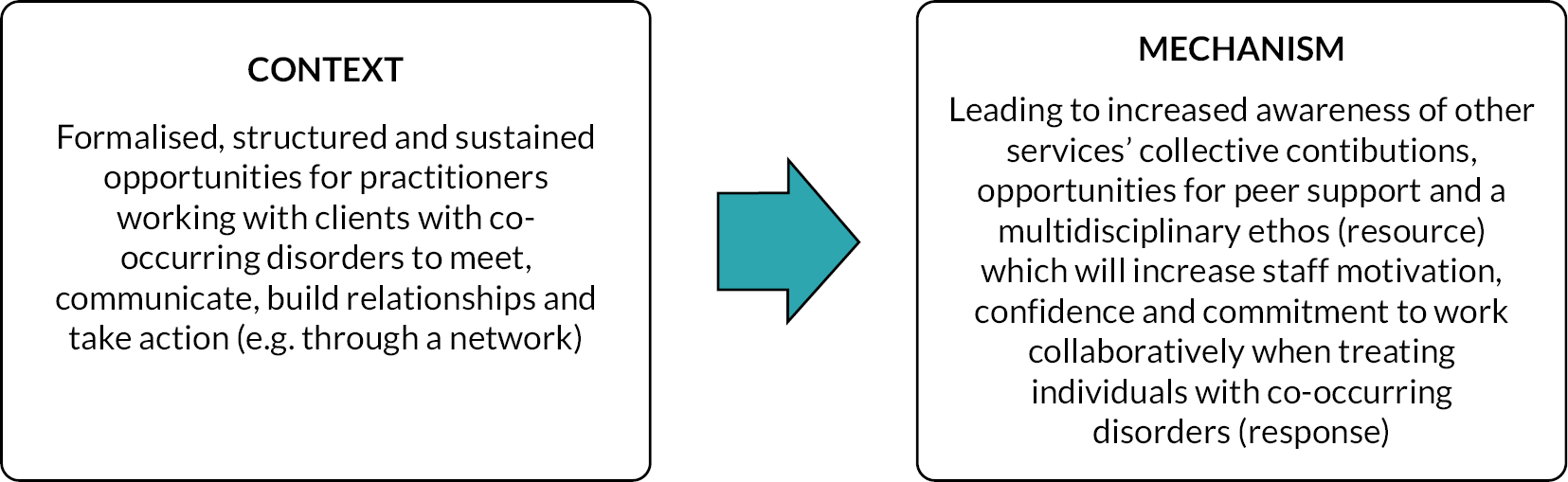
[O]ne of our difficulty is for them to find time to attend … the coordination of the ward managers to ask the staff to attend those training and so we are working with the ward managers as well to allow staff to attend those and encourage their staff and themselves as well to attend the said opportunities for any training or any conversations or forum that they can attend too.
SP57, Case Study F
Staff discussed several benefits of having these formal network opportunities (context) including bringing mental health and substance misuse services together (mechanism – resource) (see Figure 19): ‘and all those are different agencies and they’ve come together and that also helped it to be in peoples’ minds … reminding people what they do, how we work. So that would get filtered down the system’ (SP28, Case Study A) (mechanism – response). A key aspect of these networks was described as ‘forming an alliance’ (mechanism – resource) which led to ‘collaboration’ and ‘knowing how to navigate the system’ which was then viewed as spreading beyond those attending the network to colleagues within their teams: ‘so you can see how the collaboration and that knowledge and skills set and even the resources is spread so it can have a bigger impact, so you don’t necessarily need a bigger dual diagnosis team’ (SP10, Case Study C). Staff also felt that networks created the opportunities to raise awareness of co-occurring disorder policy (mechanism – resource) which could lead to more consistent policy implementation and thus more consistent care (mechanism – response).
Finally, staff also discussed how these networks gave them the opportunity for specialised supervision, case discussion with peers and reflective practice (mechanism – resource). This was often something they were lacking in relation to co-occurring disorders in their everyday roles, and that this provided them with emotional support, reassurance and confidence to continue pursuing effective care for people with co-occurring disorders (mechanism – response).
[T]he dual diagnosis network … that I go to, I find that that is more almost like reflective practice. For me anyway, I find that that really helps me emotionally with some you know dealing with challenging the system ’cause it is quite difficult to constantly challenge the system for your clients, so … as a way of cleansing myself.
SP2, Case Study C
I kind of see the Champions meetings as being a little bit like supervision and so although we might not discuss cases necessarily, it is about talking about … how things are on the ward or how are you managing with these new things … so I think that probably is the height of the sort of specific dual diagnosis supervision.
SP72, Case Study E
Staff described how the relationships built in these networks could lead to more collaborative working (mechanism – response) which would ensure staff had ‘a good overview of their [service user’s] care’ allowing them to ‘provide a good level of care’ (SP28, Case Study A) (outcome) (Figure 20). There was a sense that building a network amongst staff in different teams would mean staff were more likely to encounter a familiar face when co-ordinating care and have the support they needed in complex situations (mechanism – resource). As shown in the quotes below, there was a general sense that over time this could lead to more collaborative and consistent care for individuals with co-occurring disorders (outcome), but the challenges they experienced in developing and sustaining these networks in the short term (context) meant that they were uncertain if these long-term outcomes would be realised.
FIGURE 20.
Programme theory 7 mechanism and outcome.
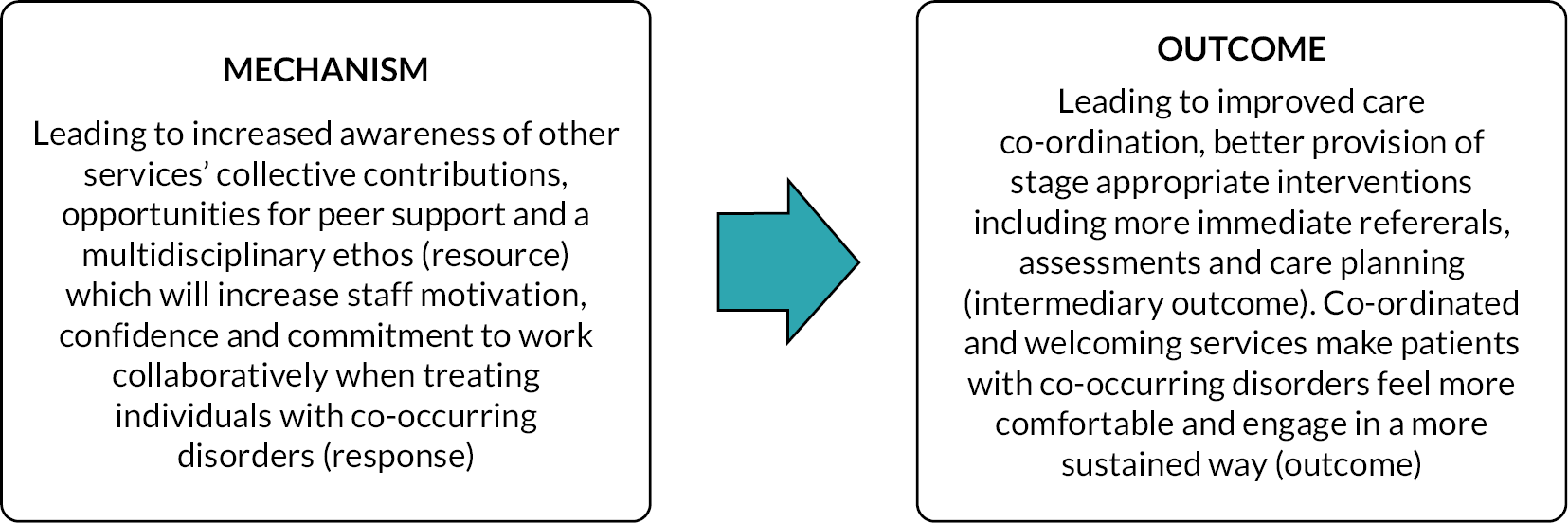
I suppose what they get out of it is the sense that they’re not on their own, there’s lots of them if they happen to be on a ward and they see one of their other champions that they’ve met at the meetings, there’s a connection there.
SP83, Case Study E
The networks largely functioned at a staff level offering opportunities for peer support and improved care co-ordination for individuals with co-occurring disorders, and so for this reason, it is perhaps unsurprising that there was little discussion of these networks within the service user and carer interviews. Only one carer had come into direct contact with these networks. As previously discussed, the COSMHAD lead at Case Study C had become involved in their husband’s case in order to facilitate a multidisciplinary working group to respond to their needs, but the carer acknowledged that this was outside of the staff member and group’s official role. P3 described how they felt the multiagency group had given them a voice and brought disjointed services together. This reduced the pressure they felt to be ‘constantly firefighting’ to co-ordinate care (outcome); however, they did also express some frustration at some members of the group ‘playing lip service to it rather than making a difference’ (context) and that it was the commitment of the COSMHAD lead that was making a difference to their husband’s care.
… we’ve had multi-agency meetings which have involved CMHT, [drug and alcohol service] and [recovery housing] … I think it’s giving me more of a voice … we’ve obviously got one of the Commissioners for mental health … her being on the call has meant that I can vent my frustrations … the biggest problem is that … the different services, don’t talk at the moment and it’s very, very disjointed. And so this has given an opportunity for the relevant services to all be in one place at one time, which … doesn’t happen otherwise … before it was constantly me, firefighting, picking up the phone, trying to speak to the right people, trying to, you know, getting one piece of information from one team, then getting a piece of information from one team and it was me that was acting as the conduit … […] I think the one person that’s made the biggest difference to us, to me, to our family, to [husband], has been [dual diagnosis lead].
P3, (Carer) Case Study C
However, what was not captured in the initial PT was the important role that formal peer networks and groups played in supporting service users and carers. The majority of service users accessed some sort of support group external to the NHS and they described how these groups were valuable in their recovery as they reassured them that others were experiencing the same things, reduced their isolation (mechanism – response), presented new strategies for approaching problems related to their mental health and substance use, and held them accountable to work towards their goals (outcomes).
… because you’re not on your own and people are experiencing what you’re doing to yourself … that is like reassuring for you.
P11, Case Study B
[F]rom the mental health side of things, it was absolutely beneficial in terms of reintegrating, feeling safe, feeling, trusted, feeling, able to talk openly, really openly and really honestly and feeling welcome, feeling valued, feeling like other people understand what you’re going through from the substance … you can get feedback and cross sharing and people talking about their experience or how they’ve been in a similar situation and how have they managed to navigate through it, whether it be positive or negative.
P6, Case Study C
However, participants were also clear that these kinds of external groups should not be seen as a replacement for one-to-one support with a therapist or key worker (context) and that these groups would not necessarily suit everyone depending on a range of factors including the stage in their recovery, treatment preferences and desired level of anonymity. For example, one participant described how being held accountable by an external group for their behaviours was not helpful at their current stage of recovery and instead created additional stress and pressure. Service users also acknowledged that it could take time ‘to find a group you feel comfortable in’ (P20, Case Study C). For example, a number of LGBT participants had sought out LGBT-specific groups because ‘you don’t have to like explain things or challenge things or explaining that sort of additional like mental effort and emotional labour to try and like challenge those things’ (P17, Case Study C) and ‘within the LGBT [community], the different drugs of choice like there’s a lot of people on crystal meth … if you’ve got a common understanding of where we’re coming from this community in terms of how society sees that, it just helps a little bit more’ (P20, Case Study C). Similarly, one participant described how she found the groups in a residential rehabilitation programme ‘a man heavy environment’ and so she set up a women’s group to allow women to ‘be vulnerable’ and discuss with other women.
And I think one-to-one support is important for couple of reasons. So for example the issue with a group setting is … they are useful because you’re getting more than one person’s opinion and you know there’s social aspects to it … but with one-to-one you can make me feel more comfortable talking about things that you couldn’t talk, and … to sort of focus on you and, you know, what’s going on with you and work through that … And … the lack of anonymity it is a problem, especially [with]… specific substances.
P16 Case Study C
Carers also described the benefits of having these kinds of external groups with other carers as they provided them with opportunities to learn more about their loved one’s addictions, to get time and support for themselves, and to talk openly about their situation and hear from others in this situation (outcome). In addition, some of these carer groups had taken on advocacy roles and were using them as a platform to feedback their service needs to the NHS and local authority.
[Y]ou go to these groups and you see other people who are just normal people and the same things happen to them and you hear their stories. And that’s exactly what’s happened to you … what they’re going through, and you realize, you know, you’re not alone. You can share experiences and, you know, you get affirmation that it’s not your fault … You also get practical advice and we can just support each other as well … and you become more empathetic … And yeah, it’s just mutual support and help.
P24, Case Study A
The synthesis and evaluation findings concur that formalised and structured opportunities for collaboration (such as COSMHAD networks) led to increased awareness of other networks, and peer support. However, the practicalities of attending these groups (e.g. cover for the ward) were often difficult and required senior level management prioritisation and buy-in. Carers and service users also highlighted the benefits they got from group peer support but were also clear in outlining that this should not be a replacement for one-to-one clinical support. Since the research focused on clinical services, additional programme theories to explain peer support groups, such as those that exist outside statutory services for service users and carers, were seen as out of scope, and therefore additional PTs were not developed.
Refined programme theory 8: care pathways
Summary of evidence
The evidence from the realist synthesis suggests that when committed and accountable leaders implement (context) care protocols that clearly describe the co-ordination of care from initiation of care through to referral/discharge44,56–58 (mechanism – resource), this helped staff feel supported in their roles47 and enabled them to use their skills and knowledge (Figure 21).
FIGURE 21.
Programme theory 8: care pathways.
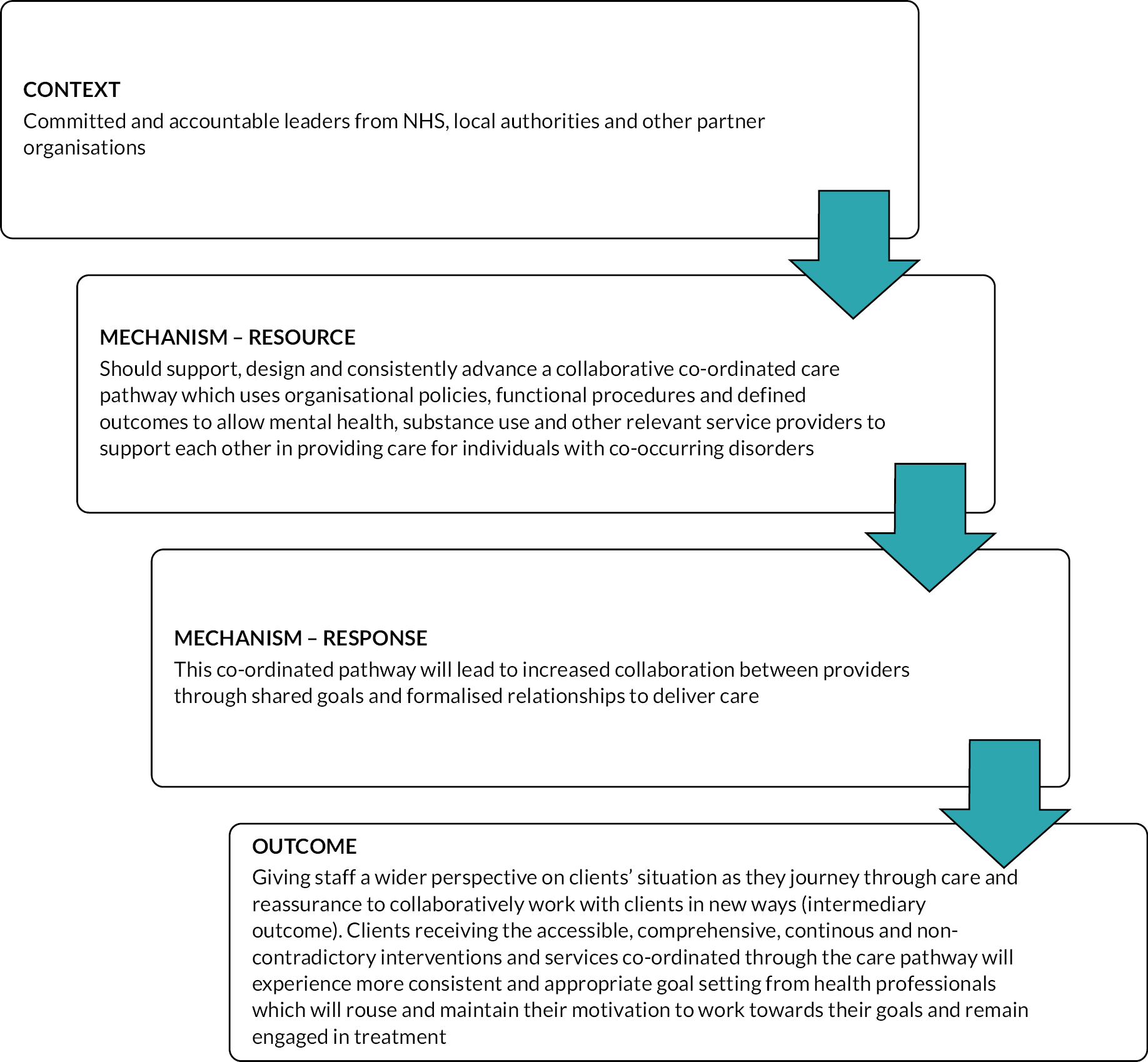
All six case study areas provided their COSMHAD policies as part of the research study, all of which included a diagram and description of their pathway for people with COSMHAD. However, except for the trust COSMHAD leads, awareness of these policies and pathways by the staff was quite low (context). This was because there was not a sufficient drive to promote their policies, and an acknowledgement that ‘it’s how those policies are actually then put into practice and made relevant is a difficult thing’ (SP3, Case Study C) (mechanism – resource) (Figure 22).
FIGURE 22.
Programme theory 8 context to mechanism.
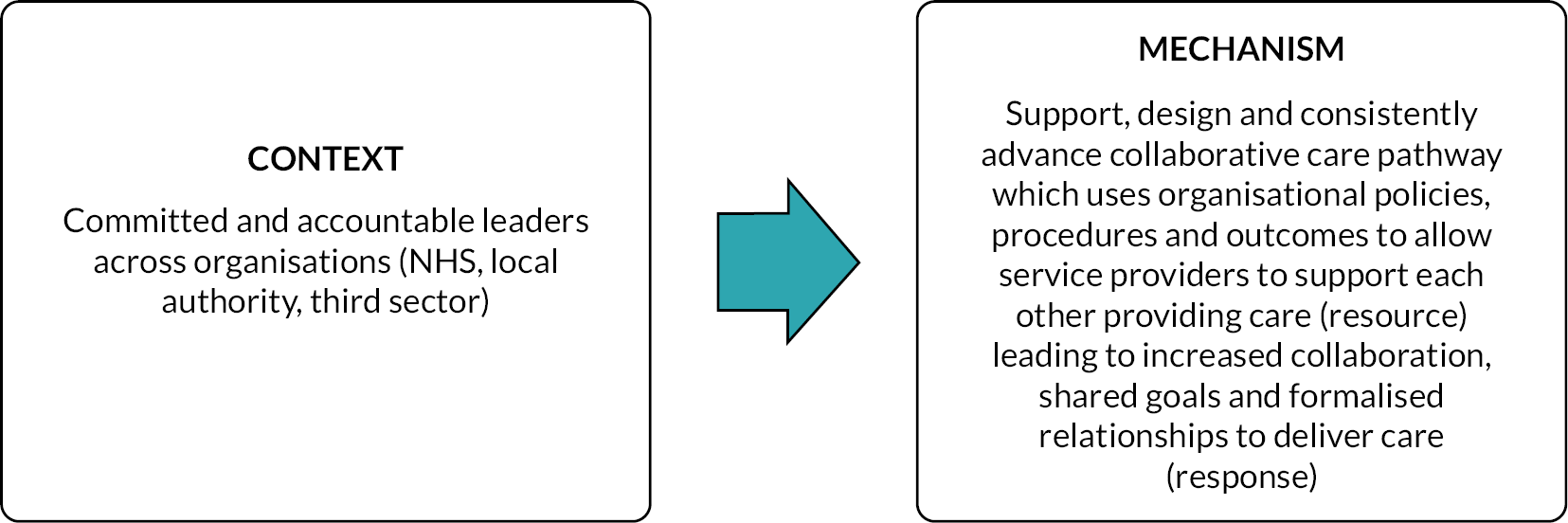
It wasn’t widely advertised, or published and the chap that wrote it left a couple of months after he did it. And what it lacks is a strategy, to follow it up, so at the moment it just feels like a document that sits there going this is what we should do. But there’s no kind of thought or plan of how it’s going to get done and what’s required to fulfil the policy so make of that what you will.
SP15, Case Study C
I mean, I think the pathways are quite clear and we’ve got policies and protocols in place and we’ve got a lot of staff if compared to other trusts, in terms of dual diagnosis. So I would say from my perspective that they’re they are clear but actually getting that message in across is the challenge.
SP67, Case Study F
The extent to which COSMHAD pathways were implemented within a trust (mechanism – resource) was felt to be dependent on funding, commissioning priorities and senior level support (context) (see Figure 22). As one participant described: ‘it depends on what the flavour of the month is as to what the push is’ (SP28, Case Study A) and ‘drugs and alcohol is a poor sister, mental health is another poor sister and dual diagnosis has been locked up in a shed at the back of the garden … dual diagnosis is definitely not going to the ball’ (SP38, Case Study A).
In contrast, ‘cultural change is really quick when managers and more senior people are involved’ (SP60, Case Study F). SP40 from Case Study D described how they had created ‘very clear pathways from start to finish’ and ‘every policy going’ but ‘none of it is followed … it just doesn’t happen’ ‘except where we force our way in’. SP40 felt the ‘biggest issue is that this is not a commissioned service’, ‘they don’t have anybody in every part of the organisation … committed to it’. This was linked to a lack of knowledge of co-occurring disorders among senior leadership: ‘I think people need to have all that knowledge in order for them to be able to actually strategize and put the right services in place’ (SP48, Case Study D). Participants in Case Study F similarly had developed multiple policies around COSMHAD and were in the process of ‘trying to put this all into one framework … the dual diagnosis pathway … it’s really us coming together and pulling all this thinking to one place so that we see where the gaps are’ (SP60, Case Study F). Much like Case Study E, staff were clear that ‘we don’t want this to be something sat on a shelf or in a file in the system and we try to build this into how we work naturally’, but they acknowledged that ‘there’s always hardly any new money in the system to create new posts and services. It’s quite often really about, you know, bending what we have to reduce this gap’ (SP60, Case Study F).
Researcher: But if the care pathway wasn’t there at all, what difference would that make at the moment?
SP40: I think it would lose the voice completely. So at least I’ve got something to battle people with. So I can say when it doesn’t work, I say, well, you were told to do this, this and this. So it is there to provide some safeguard. And it gives us something when we have inquiries or investigations to go to and say. But why didn’t you read this? And so I think it is necessary and I think it’s gaining more ownership of that and I think a lot of it will be when you have new starters that have or integrated into better practice.
SP40, Case Study D
In addition to these challenges in developing specialist pathways, staff felt that on some occasions existing pathways (mechanism resource) could hinder them from providing the support people with COSMHAD needed. Staff often felt constrained by the remit of their commissioned service meaning there was uncertainty about where responsibility to provide care (mechanism – response), thus limiting the care provided (outcome).
… because my contract ended with them and I came back to this team and then the manager was like we’re not commissioned for this anymore. We’re stopping it. And then it all stopped. And then they went back to being like, what do we do? We’ve got this knowledge that we can’t use anymore, but we’re not allowed to assess these people.
SP27, Case Study A
Staff described how accessing both mental health services and substance use services could be challenging for people with COSMHAD because often services present ‘one-size-fits-all’ which could lead to those who were not eligible becoming despondent and dropping out (mechanism – response). Clear pathways were therefore seen as beneficial in facilitating referrals between services (mechanism – resource), relieving the anxiety of having to access a new service (mechanism – response) and ensuring that they could move between services (as needs dictated) in a more co-ordinated manner (outcome) (Figure 23). Staff at Case Study D describe a project of active referral to ensure support for people who were not ready to access therapy or who had not followed through after assessment due to anxiety about taking the first step to access a service.
FIGURE 23.
Programme theory 8 mechanism and outcome.
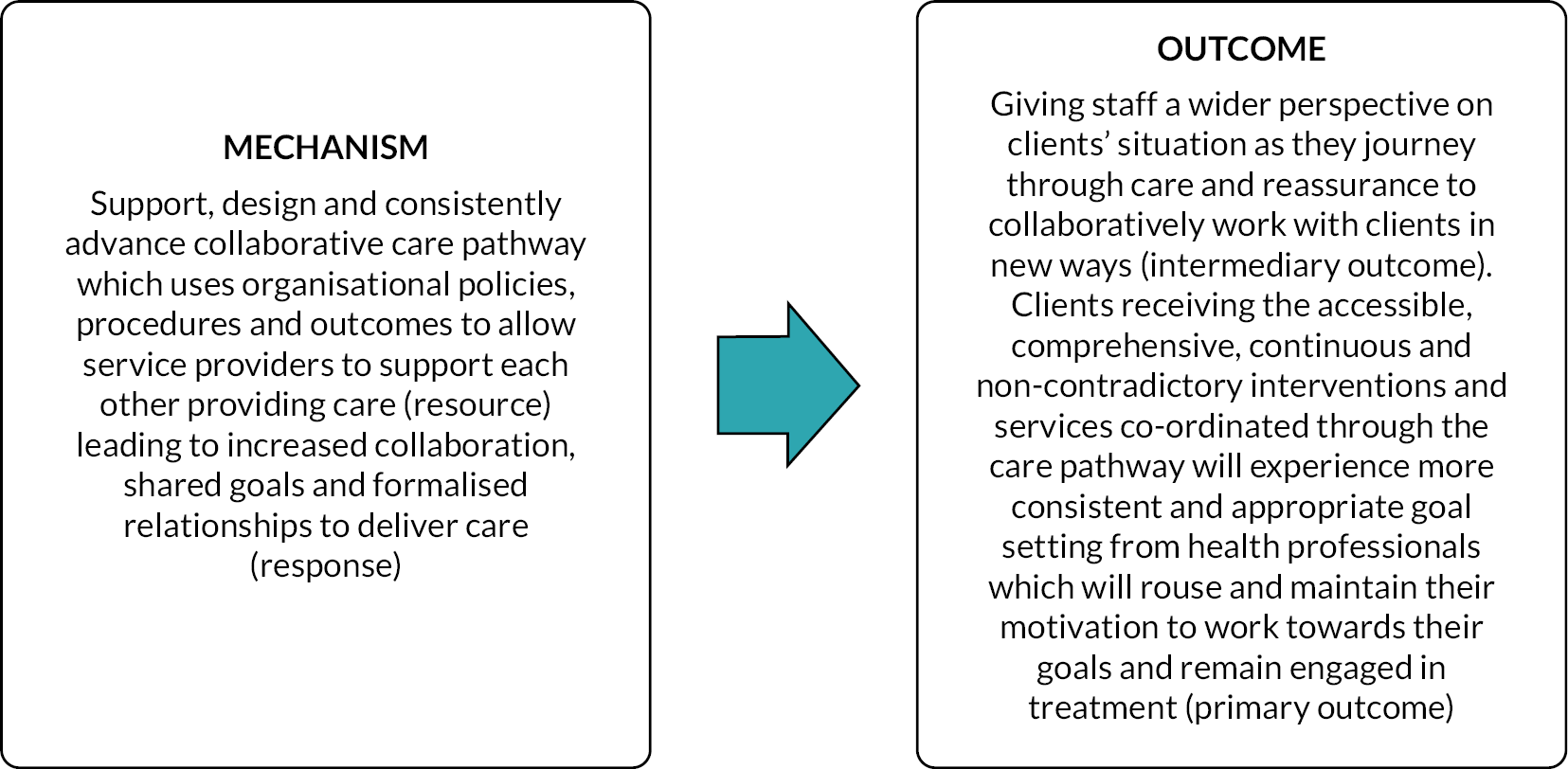
It’s very much a one size fits all, isn’t it? It’s like we go through the spot [substance use service] bit. Then you’re gonna get filtered out and various things. If you don’t engage or you don’t fit into any mental health that wanna know ’cause, he’s still drinking. So you get despondent. Drop out and then go back again.
SP30, Case Study A
Staff also discussed some barriers which could hinder the functioning of pathways (mechanism – resource) and thus prevent service users receiving comprehensive care which met their needs (outcome). This included not aligning with pre-existing KPIs within their services, risk assessment requirements and multiple IT systems which prevented the sharing of patient data. As each service required their own, data this meant that people had to repeatedly describe their often traumatic experiences to a range of health professionals. This could be avoided if there was better data-sharing infrastructure within a local area. Participants also discussed accountability and responsibility, highlighting that it was not always clear who was responsible for ensuring that service users received care at both a practitioner and an organisational level.
[W]ho almost takes the responsibility for what happens. For me, putting them forward for a detox. The feedback I get back is, well, who supports them during this and who supports him afterwards and who supports them in the meantime leading up to it. So, who takes that responsibility of detoxing them? But it’s a mental health issue because … that’s why he’s using or whatever it is, just an ongoing circle and it is just so frustrating and disheartening. And that’s for me, as the professional never mind the client who I’m trying to go back through and let him keep them updated as to what’s happening, particularly for the one I’ve got in mind. I’ve got his daughter, bless her who’s always trying to figure out what’s going on and try and take that responsibility herself, you know, driving to appointments, do everything they can, but it just doesn’t work. We both for the mental health services and for me, one of us has to say that we can take that responsibility, but we’re not actually allowed to because of the policy and procedure of it. It’s just really difficult, obviously.
SP27, Case Study A
Service user and carer participants had limited perceptions that local care was integrated and co-ordinated. Service user participants described the services they received as ‘definitely not integrated … I think they’ve been entirely separate’ (P17, Case Study C). There were exceptions to this. Two service users from Case Study F were being treated by an integrated alcohol care team based at one of the city’s hospitals (mechanism – resource) and they described this as the first time their alcohol problems, physical and mental health had been considered in an integrated way. They reported that this had increased awareness of the comorbid nature of their conditions, improved mental health support, and a sense of relief that they had consistent, continuous support available (outcomes). Similarly, two carers (P24, Case Study A and P29, Case Study B) described how their adult children had recently been given places in residential programmes run by local charities (mechanism – resource) after being made homeless and being released from prison respectively. While both carers appreciated that this was not a long-term solution, there was a sense of relief in knowing that their loved ones had consistent and integrated support for all their needs (outcome). P29 (Case Study B) presented this in contrast to the ‘up and down and up and down’ of accessing support in the community.
[T]he difference between going to the integrated clinic, [name hospital removed]. I don’t know what will happen in the future, but … that ongoing support … eventually takes the pressure off … Because of the nature of it, it’s the first consultant ever that I’ll probably be going back there at least every six months or so. That’s the rest of my life. So that does take some of the pressure away … You know, it’s not all physical. It’s not all mental. I’ve got a combination of the two and the integrated clinic.
P3, Case Study F
Service users generally reported poor communication between services. They felt that they often had to repeat themselves and received information from different services that was incorrect or outdated (mechanism – resource). As a result, service users and carers reported losing confidence that information about care and referrals would be passed between services and thus lost confidence in the services themselves (mechanism – response). Service users and carers described having to frequently collate information and follow up care with various services themselves. This placed a significant burden on them (particularly when service users were struggling with their mental health symptoms) and they felt this would be reduced by having integrated and co-ordinated care (outcome).
A bit too fragmented. They don’t seem to speak to each other. You know, you hear so many times the communication breaks down between people and between services: between the mental health people, between the police between the drug worker and … even within the same team you seem to find yourself saying the same thing over and over and over again to different members of the team because you lose your confidence that that’s actually going to get passed on ….
P36, (Carer) Case Study B
Sometimes, I’m on the phone all day … because they’ll say you, you need to speak to this person. You speak to that person or you need to go to A&E if you feel suicidal … I don’t feel suicidal, I said, I just don’t feel great, I said this medicatio isn’t working. Oh well, I’m afraid I can’t deal with that. Shouldn't be done by psychology, try phoning psychiatry. The psychiatrist never called.
P15, Case Study C
… when I’m not feeling well, everything is exhausting … simple things like send an email or the phone or things that I guess that for most people seem simple … Those things are really hard and like if you’re struggling … The thought of picking up the phone is like people are gonna dread it. We’re not gonna do it. Like managing those kinds of things … get very difficult very quickly … it’s definitely something that I’ve struggled with especially like because there tends to be a lot of like admin … like the amount of forms to fill in … there are then many obstacles in your way to being able to access these services, not just so within forms, but while completing online application or making phone calls or a bunch of stuff that they’re very challenging problem to solve … if it’s challenging systemically, imagine how challenging it is for the individual.
P17, Case Study C
Where this communication was lacking (context), service users and carers described experiencing inappropriate referrals, immediate discharge from services and service users often falling in the gaps between services due to a lack of follow-up on their mental health from services (mechanism – response). Service users often felt that when they were discharged from mental health inpatient settings or reached the end of their allocated number of therapy sessions, they were left without any support. Some participants described losing faith in NHS mental health services and pursued private health care as an alternative. Among others, for whom private health care was not an option, this led to relapse and worsening of mental health symptoms (including suicide attempts) (outcomes). Participants attributed this failed communication (mechanism – resource) to a lack of individual staff members ‘to be the central point who co-ordinated care’ [P32, (Carer) Case Study B] and who were ‘willing to, you know, join the dots’ (P10, Case Study E) and ‘if these services were a little bit more holistic and focused on, like, what kind of health problems does someone have, what kind of identity does someone have, like in what ways are they marginalised’ (P17, Case Study C).
I’ve been referred to like [name of mental health service] and they said it was too complex. Didn’t really understand that. I went to psychologist, and they said there was no behavioural problems with me and he’s discharged me … I don’t understand why I didn’t have the psychologist do a bit more work with me and she literally did about four assessments and it was about like history and she said, oh no, there’s no behavioural issues. But we will be seeing you again, we will be referring you back. So GP … I had to go and refer back to the access team to go back to some you know psychology services to go to psychiatry to wait on the waiting list. So it’s just been … like … four years just to get this kind of level of service [for] dual diagnosis or, you know, and the trust and the drugs team and the doctors actually working together.
P15, Case Study C
It just made me kind of distrust the NHS really and think that this is this isn’t something that I can use that have to go private again, but luckily, I’m in a position to go private. Not everyone is, so I think it was more just a disappointment in the process of going through the NHS.
P20, Case Study C
Participants held almost universally favourable views around greater co-ordination of care pathways and services (mechanism – resource) and this was frequently described in terms of a ‘safety net’. The key characteristics of this safety net were having a key staff member within services who they knew they could contact in times of need and who would provide referral and access to services they needed (outcome). Another key defining characteristic of the ‘safety net’ was a service that would regularly and proactively contact them to ‘check in’. Service users felt this would be invaluable when they were experiencing poor mental health as it would reduce their isolation and reassure them that someone cared and was attentive to their needs (mechanism – response). As P17 described ‘your life can be chaotic and without much structure … it’s really important to manage things carefully, because just pull the rug out from someone, they can feel like all the other times in their life that they’ve had the rug pulled out from under them’. Participants felt this could prevent crisis and relapse and would be more cost effective than allowing them to fall into the gaps between services and relying on blue light and primary care referrals (outcome).
… like a quarterly review … just a quarterly check in where you know you get an appointment a couple of times a year … particularly when you’re really isolated, if that reassurance that someone cares enough to check in with you, and if you’re not OK, you have the opportunity to let them know and then like whatever it is that he is can be arranged on your behalf and by someone with the skills to do that, and its’s not placing all of your onus on the unwell person to do that for themselves.
P17, Case Study C
It’s picking up the phone and knowing that I can get hold of her care co-ordinator, I can actually get hold your care coordinator and speak to the psychologist. You know, if we need to do something now, for instance.
P21, (Carer) Case Study A
The realist synthesis and evaluation identified the importance of collaborative care pathways; however, the evaluation indicated that in practice often these pathways were not actively implemented, leading to lack of collaboration between organisations. This resulted in disjointed services for service users and carers. Co-ordination of COSMHAD care and communication with service users and carers was highlighted in the realist synthesis as important, but service user and carer interviews indicated consistently that co-ordination was lacking in services they had received. Service users made clear that it was important for services to reach out to them, instead of them trying to co-ordinate their own care, which was difficult when managing mental health and substance use issues.
Refined programme theory 9: mental health services as primarily responsible for those with serious mental illness and co-occurring substance use condition
Summary of evidence
Evidence from the synthesis reinforces the policy guidance that people with SMI who also have co-occurring substance use issues should have their needs met primarily by statutory mental health services. The rationale for this is the high prevalence of co-occurring disorders (context) within mental health services, and the need for integrated care planning for service users (mechanism – resource). Graham et al.,80 in their study of integrating COSMHAD services through the COMPASS liaison model in the UK, argue that this requires ‘integration of treatment both at the level of the clinician and service’ (p. 184) and will result in ‘a conceptual shift within the organisation and those working in it’81 (p. 586) with a single mainstream clinician being able to address the holistic needs of people with COSMHAD (mechanism – resource)80,81 (Figure 24).
FIGURE 24.
Refined PT 9: mental health as holding primary responsibility.
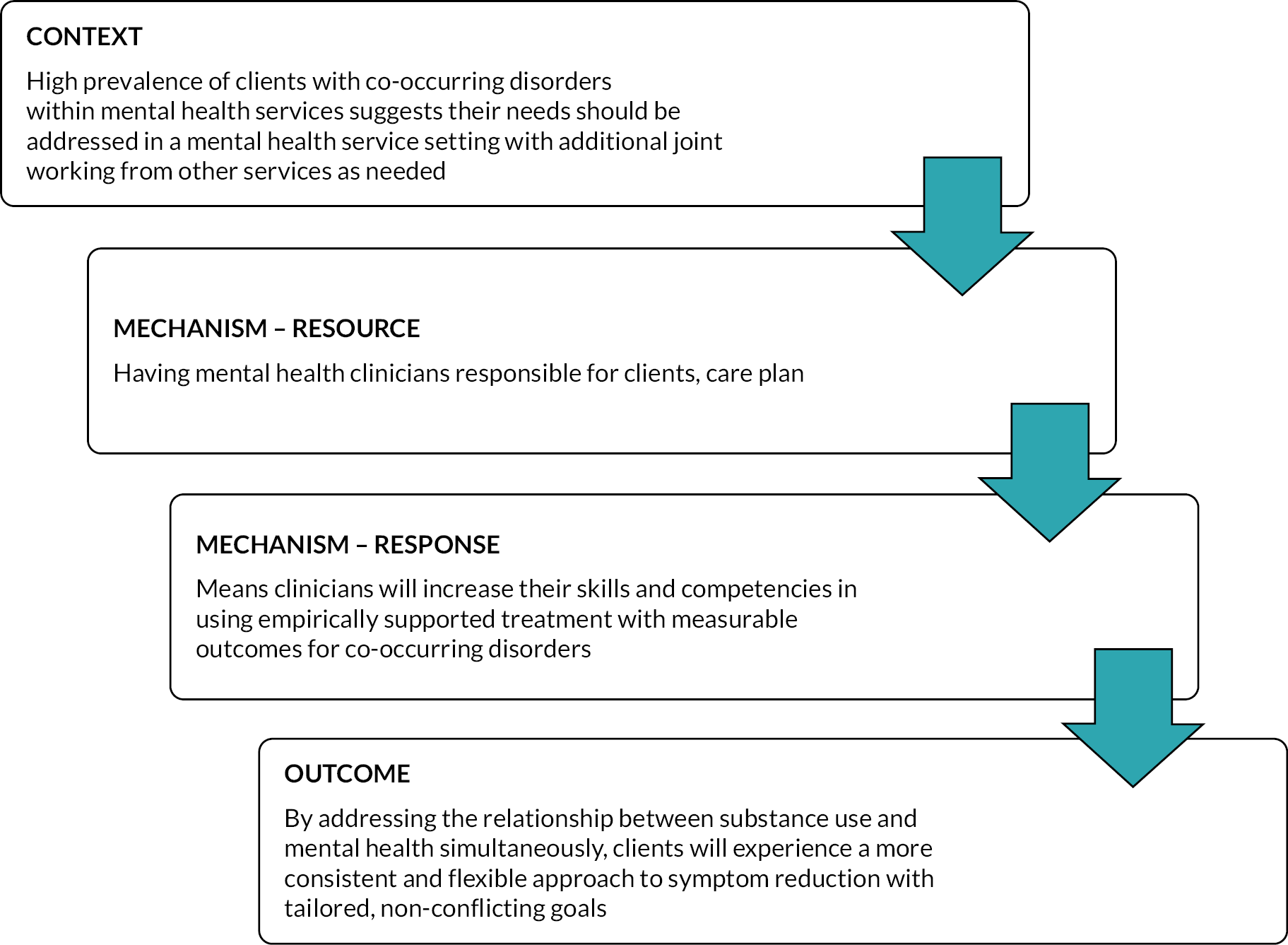
Staff participants recognised that there was a high prevalence of co-occurring disorders within mental health services (context) and that it was a core aspect of mental health care. As one participant stated, CMHTs were ‘recognising we’re dealing with it anyway. it’s a core part of … our patients are dual diagnosis’ (SP83, Case Study E). Some participants discussed the ‘siloed nature of healthcare and substance use specific services and … the difficulty with aligning those’ (SP20, Case Study C) and that this could be addressed in mental health services if ‘everybody should have a basic set of skills’ that could address both mental health and substance use (SP20, Case Study C) because ‘this is knowledge that everyone should have’ (SP28, Case Study D) to enable them to work with people with COSMHAD. Participants described how ‘more support in like the overall workforce’ (mechanism – resource) would lead to ‘having these competencies and skills and confidence to work with this group of people’ (mechanism – response) (Figure 25).
FIGURE 25.
Programme theory 9 context to mechanism.
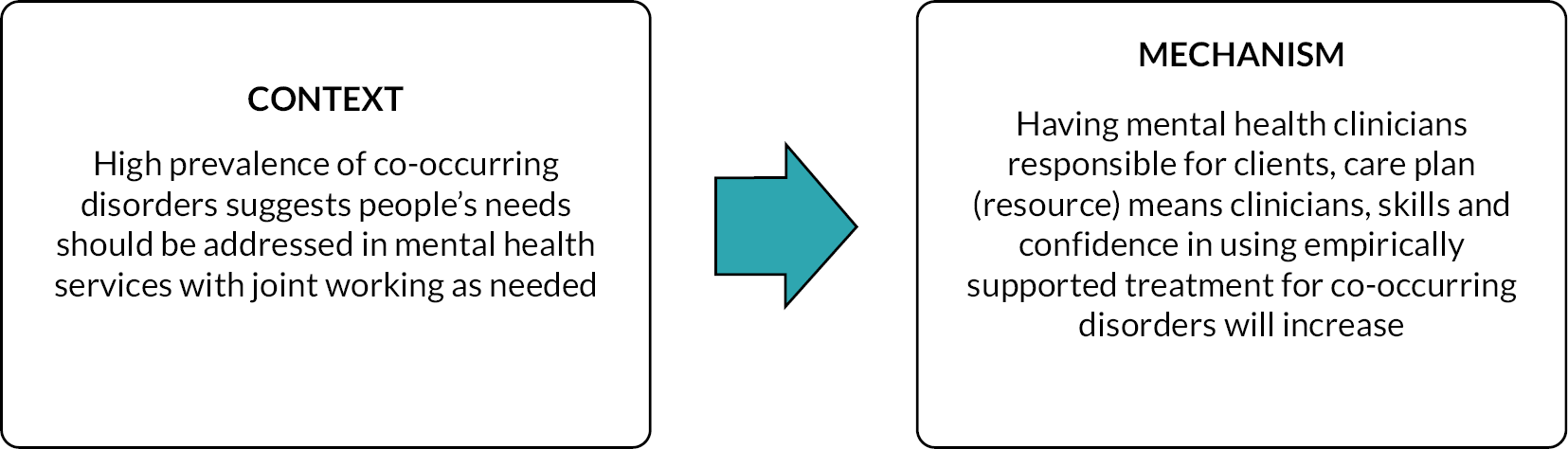
However, staff also identified additional contextual factors within mental health services which impacted upon their ability to be responsible for care planning (mechanism – resource). The term ‘mainstreaming’ which originated in early COSMHAD policy17 has not been operationalised and is therefore open to interpretation. It has been thought erroneously that mainstreaming placed all responsibility for someone with COSMHAD on the care co-ordinators (under care programme approach) in mental health. However, high caseloads and pressure in mental health services (context) made it challenging for them to ‘hold in [their] mind’ (SP29, Case Study D) the various needs of people with COSMHAD (mechanism – response). A care co-ordinator in a psychosis service described how she felt that she didn’t have sufficient time to provide effective support for substance use (mechanism – resource) on top of the immediate, complex needs of the service user, particularly when they were responsible for seeking out training and advancing their knowledge on COSMHAD themselves (context). Consequently, staff felt that they were unable to provide meaningful interventions to address COSMHAD leading to service users having unresolved needs or, in some cases, being discharged from services where they do not meet the assessment criteria to alleviate the pressure on case managers (outcome).
Well, if you’ve got 50 to 100 people on your caseload as a care co-ordinator and there’s a possibility that you can say if you don’t stop using this substance, I can’t do very much with your mental wellbeing, then you’re going to say that probably, you know, just from a position of managing.
SP37, Case Study A
So from my role as a care coordinator, I find that when sort of there is so much to remember and to learn and to do and we are coordinators of care rather than being able to do everything I suppose for an individual who often has very complex needs, one of those being substance use … I can do so much in terms of what I learned through sort of training or looking up things myself … There’s too much to remember … especially when you specialize in psychosis … and as part of that as we know, it is very much often trauma related, stressful housing, financial, you name it and obviously we always talk about substances and work on the risk of relapse if they continue to use … it’s so complex. So yeah, I don’t know really. I’d love to. But in reality, it’s hard just to do the basics at the moment to be honest with you, when you’ve got 25 plus clients, very complex, somebody is being in crisis of becoming homeless … to be able to engage sort of therapeutically meaningfully and without those basics, it’s very difficult to go ‘Now let’s talk about this’.
SP1, Case Study C
Staff emphasised that in their view the focus of mainstreaming should be on building relationships with service users (mechanism – resource) which meant that the service users and carers trusted that the care co-ordinator would be able to secure support from other agencies and teams as required (mechanism – response). Some staff described that training on COSMHAD in mental health services was insufficient to sustain practice in the long term, and that access to practice-based learning (including access to expert support from an expert clinical lead) was required. Therefore, the concept of mainstreaming requires workforce development opportunities as well as expert support and collaborative integration of local services. As SP15 describes, ‘knowing where the experts live and how to use them’ (context) would ensure more effective care planning in mental health for co-occurring disorders (mechanism – resource).
It is unfair to expect one worker to be, you know, specialist in every area and to be the one to, you know, provide all that knowledge and all those interventions to their client. I think you know it’s a lot of knowledge for somebody to take on and unfortunately in [city] there’s just not enough resources for a care co-ordinator to be able to do that … And that mainstreaming in that situation for me would be that they build up that trust with a service or a worker, to the point that they're trusting them to engage with the other services which would be specialist, a lot of our clients are really suspicious and not trusting. So I can agree to a certain extent that it’s helpful to have allocated workers. But if, you know, I really do feel for care co-ordinators in [name of city] who don’t have the time or resource is too.
SP6, Case Study C
Staff also felt that mainstreaming often lacked the organisational and wider structural support needed to make it happen (context); one participant described the concept as ‘a worthy aspiration that’s dressed up as a policy direction’ without sufficient organisational direction to train a generalist workforce in COSMHAD. This was felt to be hindered by the competitive commissioning structures which existed in many substance use and non-NHS services (context), and which acted as a barrier to collaborative working (mechanism – response). As a result, staff felt people with COSMHAD continued to fall into the gaps between services (mechanism – response) because there was no organisational directive in mental health for teams to take responsibility for their care.
And in terms of the mainstreaming, I think it’s a worthy aspiration that’s dressed up as a policy direction … So those committed individuals like us to actually try and work at the margins because the people that we’re talking about are at the margins. And they always have been. And it’s, there is not any kind of organizational direction to train the workforce to be kind of generalists in a sense.
SP12, Case Study C
[P]eople just don’t want the responsibility unless the client fits in a pigeonhole … I think it’s great to see all care coordination stuff. It makes absolute sense. But we’re not talking around common sense right now. We’re talking about … commissioning bids … there’s different organizations and sometimes we don’t all work together as one organization ’cause it’s like [name of substance use service] do this and [name of substance use service] do this … because the way the bidding’s done and everyone’s in competition with each other. But actually, I think the tension is the bid isn’t fit for purpose … But I think sometimes we don’t, as [name of overarching substance use service], we don’t see each other as one organization.
SP24, Case Study A
[T]hey’re hot potatoes as everybody in mental health thinks they should be with addictions and everybody in addictions … will say … They need to get back to mental health and vice versa. And then they end up with the crisis team and the crisis team will work very well with the mental health crisis. But then it’s off in the other directions … the community mental health teams are stretched and without new ways of working model staff leave and staff change in adopting new staff, et cetera, et cetera, all the other stuff that has to be done. And I think they would just see it as they don’t retain.
SP83, Case Study E
While wider contextual factors were highlighted as a challenge for mental health clinicians taking lead responsibility for people with COSMHAD care (mechanism – resource), they still agreed that this would lead to confidence in using empirically supported treatment for co-occurring disorders (mechanism – response) and a more consistent and tailored approach to symptom reduction with non-conflicting goals (outcome) (Figure 26). As one participant described ‘you got one person who’s care co-ordinating it. It makes absolute sense ’cause there’s a lot of care to co-ordinate and the client has a single point of contact. And someone has responsibility’ (SP24, Case Study A). Participants felt that having responsibility for co-ordination meant that they could be more responsive to their needs and be more consistent.
FIGURE 26.
Programme theory 9 mechanism to outcome.
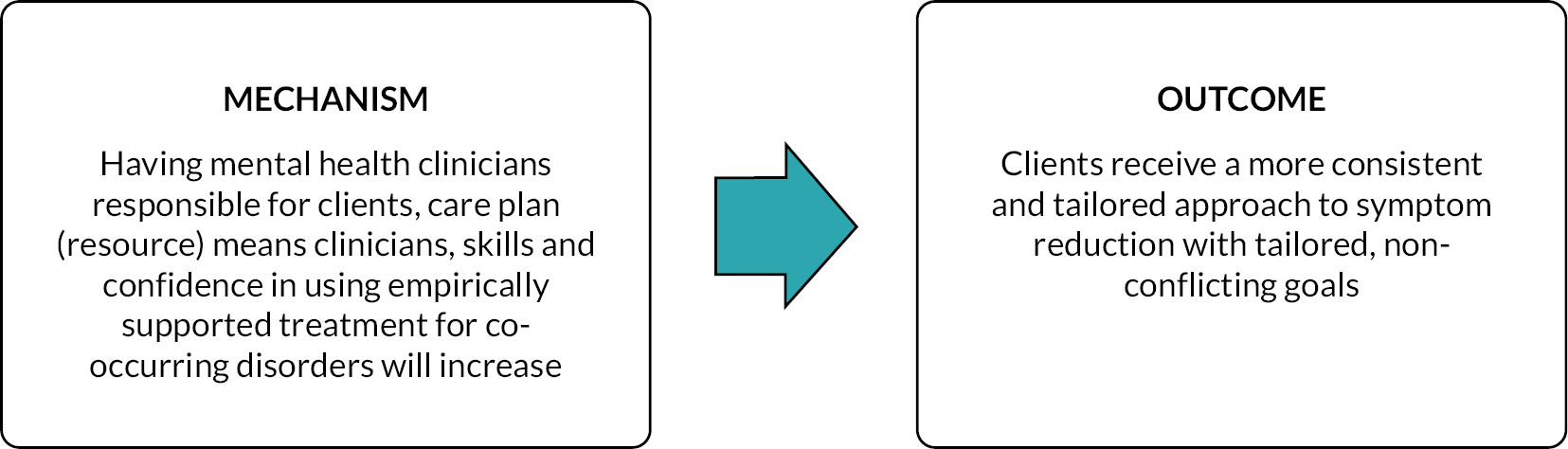
This sounds like it would be good for the client, know just in terms of consistency. You have one person who’s the point of contact, and especially in that mental health role and they can then go on and say if you might need support in these other areas and you can almost back them up. But I would imagine that be helpful. I don’t think that I don’t think we definitely don’t have that system, [city name].
SP27, Case Study A
Some noted the importance of taking a trauma-informed approach
[W]e have a duty to learn about trauma and that knowledge really has to be cascaded down and shared … How dare we try and do this job without being trauma-informed? We’re going to re-traumatise people, cause them more damage.
SP16, Case Study C
[S]ome of our service users, they don’t want to be seen by mental health and vice versa that ’cause they feel more comfortable either within substance misuse services or mental health. And it’s kind of working with what they present with. And then kind of getting a good working relationship and exploring things you know. How can we do things differently in order for you to, to get better outcomes and working together with the other services if necessary. But it’s where the service user presents and what they want to do I think is the most important thing. It’s a starting point.
SP41, Case Study D
Service users and carers valued consistent support from a skilled and empathetic member of staff who took responsibility for leading their care (mechanism – resource). They also acknowledged that staff in substance use services did not always have the expertise required to deal with mental health needs, and that having access to someone in mental health services meant they could access care for their mental health. However, waiting times were a key context which impeded this support. Service users in general reported significantly less difficulty accessing drug and alcohol services compared to accessing mental health support where they reported longer waiting times to gain access (context).
… He’s been waiting. He’s always had a CPN and he’s always been in a team … under early intervention then moved out to community about 3½ years ago … He was lucky to get the CPN, very lucky, even though we desperately just need one. But I pushed for a CPN and … he was given one. But she recognized he needed additional help, so he was put on a waiting list for the outreach team … and it’s taken two years … to get to the top of this list, and he’s had his first visit from the care team yesterday.
P36, (Carer) Case Study C
Service users and carers recognised the different philosophical stances in substance use and mental health services (context). They also acknowledged that quite often they had to have stopped using substances in order to access some mental health services which they felt was counterintuitive, especially when their substance use was exacerbated by poor mental health. This rejection from mental health services was interpreted by some as mental health services deliberately managing demand by turning away complex clients (mechanism – response).
Probably always had a mental health issue, but it’s always been about, you know, there is no mental health issue. It’s all drugs. But now it seems like … we’ve wasted all that very valuable time when he was younger and could have been helped … I think we’ve gotta stop, you know, blaming drugs for everything … I think even it’s fairly well accepted now even amongst … more forward-thinking mental health professionals. That addiction is a mental health issue.
P28, (Carer) Case Study A
I think it should be more integrated, but unfortunately the … thing I’m coming up against is that therapists don’t want to treat people who are using drugs, you know … they’ve got justification, which is, you know, if you are under the influence of something, you’re not accessing your emotions properly. But it’s ironic that it’s the therapy that is required to help with the drug use. So it’s kind of convoluted … But I guess that is the way the situation is at the moment … but I think that therapists exercise their preference in not having clients who are drug users rather than they can’t.
P18, Case Study C
Service users and carers also frequently referred to the multiple additional needs experienced by people with COSMHAD including additional physical and neurodevelopmental conditions, learning disability, trauma and housing needs. All of these issues could be better co-ordinated if mental health services were more holistic. Carers described how they felt that once their loved ones were placed in housing, they were often left without purpose or holistic support from mental health (mechanism – resource) which could lead to exacerbation of their mental health symptoms and relapse of their drug or alcohol problems (mechanism – response).
[I]t just needs to be more open-minded and … within the mental health services to offer support. You know, people are going through addiction … like we’re not, I know it’s [a] hard diagnosis, but there might be some sort of review to see what’s supposed to be put in place there and then. And even if it is only short term … If I’d have had that extra support, it might be a little bit better for me.
P19, Case Study C
In summary, practitioners concurred that in cases where the main concern was a SMI, it makes sense for those with mental health expertise to take the lead role. However, this is impacted by several complex contextual factors (e.g. overstretched workloads, resources). Service users also felt that mental health services did not want to engage with complex clients, when dealing with such pressures, and were frustrated that substance use was not being recognised as a part of mental health issues.
Refined programme theory 10: accountability and quality improvement
Summary of evidence
Meaningful quality metrics must be selected to collect data on clinical processes and health outcomes for populations with co-occurring SMI and substance use disorders. 56,82 Chichester et al. 83 found that getting departmental leadership buy-in was vital to ensure that quality improvement measures were implemented across all organisations and departments (context) and that once departmental leadership was aligned with the idea of COSMHAD being everyone’s business, ‘change flowed as if a dam had been opened’ and ‘co-occurring disorder requirements were inserted into every contract the department has with providers’. People with COSMHAD have complex and variable needs which require integration across multiple services83 and services can also experience practical challenges in tracking patient data across multiple software systems56,82,83 As Currie79 found in their work in Ohio, it is therefore important that quality improvement structures, processes and outcome measures (mechanism – resource) are built on realistic expectations from leaders across organisations, of the nature of the existing system, patient preferences and realistic expectations of incremental progress (Figure 27).
FIGURE 27.
Refined PT 10: accountability and quality improvement.
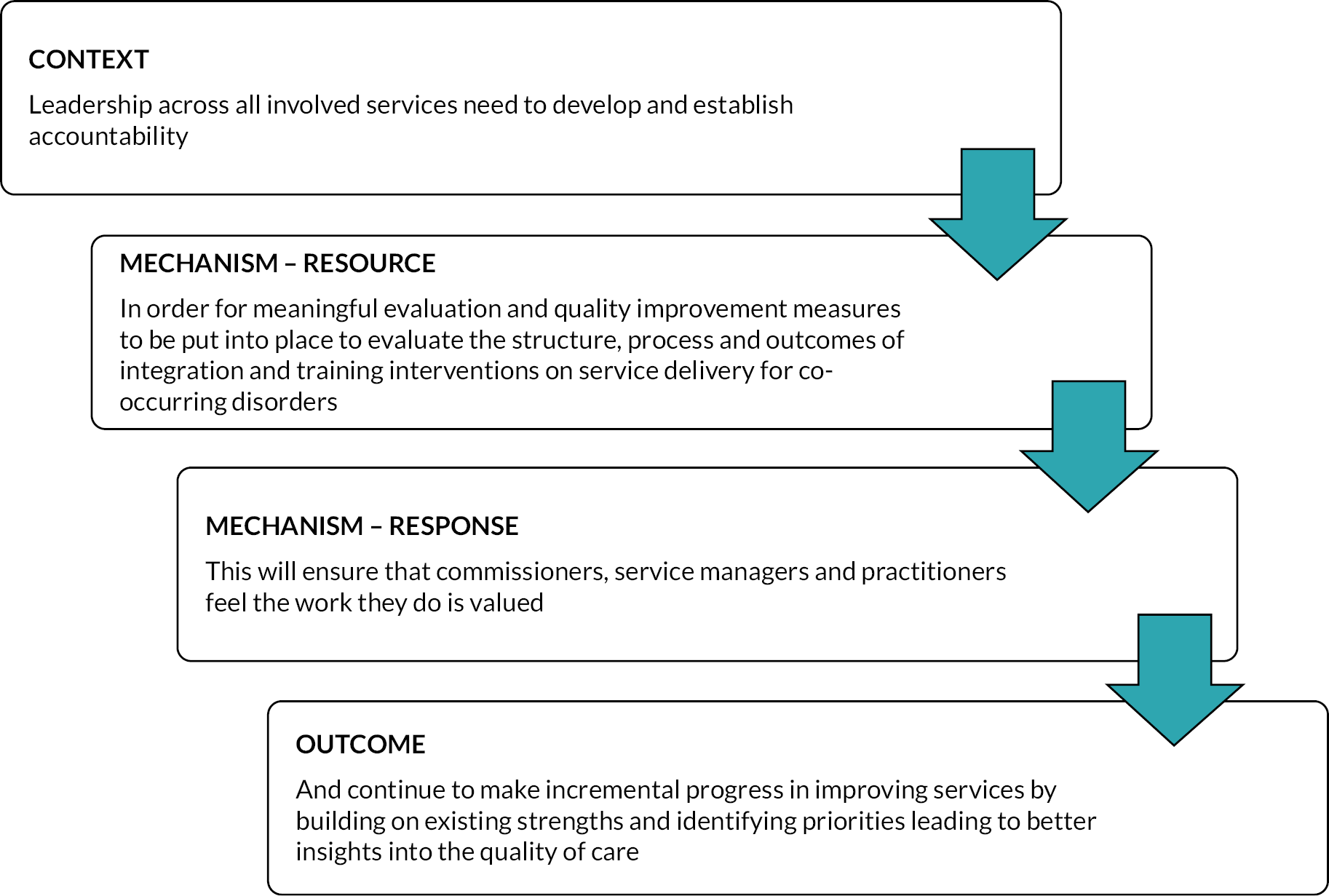
There was limited evidence within the case study data regarding evaluation of services and quality improvement projects. Staff mentioned a few examples of smaller quality improvement projects which had been undertaken in their trusts in relation to areas such as assessment, assessing training needs or evaluating training programmes. The staff focus groups confirmed the link between leaders being accountable (context) for meaningful quality improvement measures (mechanism – resource) and staff feeling that work they do is valued (mechanism – response) (Figure 28). If leaders introduced (context) mandated quality standard awards for COSMHAD (mechanism – resource), then these could help staff recognise the importance and value of the work (mechanism – response). This was seen as particularly important for staff working with people with COSMHAD, where improvements may be slower and more incremental when compared, for example, with working with someone with a single diagnosis with less complexity in a community mental health setting (outcome).
FIGURE 28.
Programme theory 10 context and mechanism.
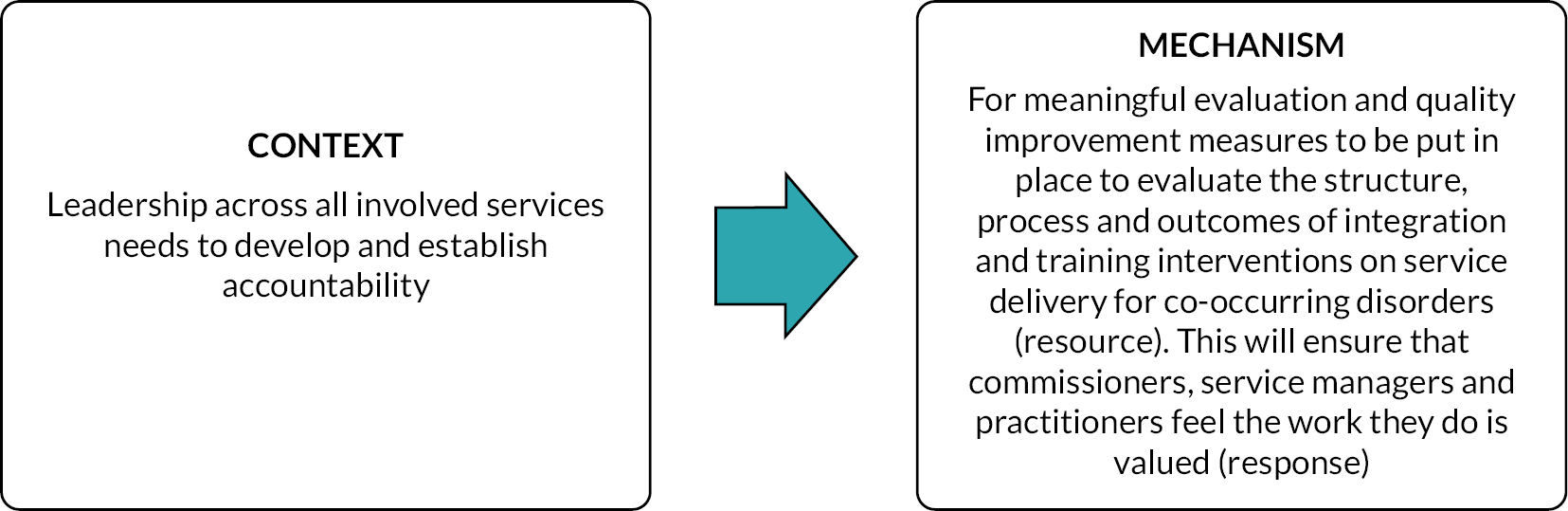
It was clear that when staff felt quality improvement and evaluation measures were perceived as more of a ‘tick box exercise’ (SP67, Case Study F) based on mandated organisational priorities rather related to service user needs, they were less likely to feel that the work they did was valued. It was felt that quality improvement measures only resulted in better quality services when staff could see the value of the mandated audit measures on their patients: ‘you don’t like it to just be a stick … you want people to do it because it is good clinical practice to do, not because … you have to because that ultimately ends up impacting on the quality’ (SP67, Case Study F). In addition, when audit and measurement work was done, staff wanted to feel that the results of these audits were used to implement recommendations which once again demonstrated the value of their work.
We’ve done audits across all services, so community services, what they’re offering, what the teams introduce, recommendations are made, and they’re never implemented ’cause they go back to the team leads to implement and nothing happens … we don’t get funded for it. So there doesn’t seem to be any real incentive to do it.
SP40, Case Study D
What do you do? What’s your plan once you’ve got this information from the patient, what do you do with it? And there’s gaps there in terms of what do we do, what staff trained and what does the trust want us to do? What’s their expectations? What’s the corporate plan for this?
SP83, Case Study E
The accountability of leadership (context) in selecting and implementing quality improvement measures was also seen to directly impact upon whether appropriate and trauma-informed outcomes were achieved, which improved the quality of care for people with COSMHAD (Figure 29). As one participant highlighted, these measures needed to reflect the incremental and individual outcomes that represented progress for each person with COSMHAD:
FIGURE 29.
Programme theory 10 mechanism and outcome.
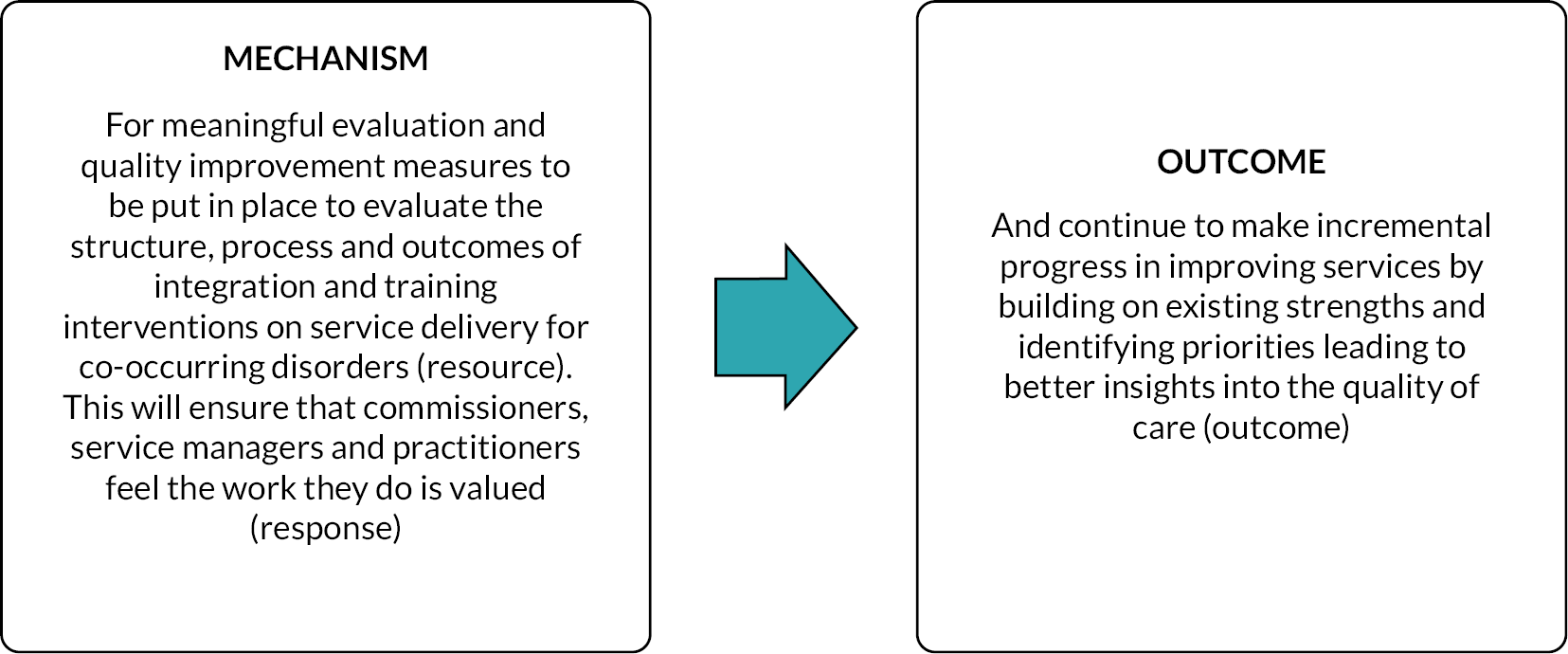
[T]he computers don’t run us. We should be running them. There should be a way of being able to capture the fact that, you know, it’s not the same type of treatment for everybody that there are certain cohorts that we have to have a different way of measuring their input and contacts and things. I mean, for some patients, it could be if they don’t come to the appointment it’s a good thing because you made an appointment with them and said that’s there, if you need it … it’s not just the fact that every contact is a success. It could be the fact that a patient felt well enough. They don’t need to come to see you that week and they’re gonna leave it another week … but we can’t account for that.
P83, Case Study F
In contrast, staff felt that if meaningful quality improvement measures were not put in place, then they could not help in the way that they needed: ‘I just don’t get that when you’ve got a kid in front of you struggling … Why would I wanna know what the PHQ-9 is? What I want to know is how can I help you?’ (SP38, Case Study A). If leaders were not accountable (context) for developing meaningful quality improvement measures (mechanism – resource), then it would hinder services’ ability to take a trauma-informed approach to care (outcome) (see Figure 29). The importance of compassionate leadership was noted organisationally to underpin trauma-informed care, with compassion suggested to promote psychological safety.
I mean the stuff that’s come into my consciousness over this last couple of months has been stuff like Karen Treisman and the Compassionate Mind Foundation, people who are starting to talk about leadership from a compassionate … really sort of out there looking at kind of what it’s like to work from an organizational point of view with people that are traumatized do you know what I mean? And the bottom line of it is … it seems to be a massive part of the job where any of any sort of substance misuse is kind of involved, whether it’s a little t or a big T it doesn’t matter, but kind of soaking all of that up and having some sort of acknowledgement at an organizational level again seems to be completely relevant, but completely missed and obscured by an obsession with data and figures.
SP38, Case Study A
There were no data on this PT from the service user and carer interviews.
Refined programme theory 11: staff recruitment and retention
There was some limited reference to recruiting and retaining people with the right skills and attitudes to deliver effective care for people with COSMHAD. This required joint working with commissioners and leaders of relevant organisations to commit resources for specialist posts as well as ensuring that the rest of the workforce were required to have the skills. This not only applied to recruitment but ongoing opportunities for professional development (including training and supervision). This in turn leads to more job satisfaction and reduction of burnout82 and a better-quality experience for the service user and carers52 (Figure 30).
FIGURE 30.
Refined PT 11: staff recruitment and retention.
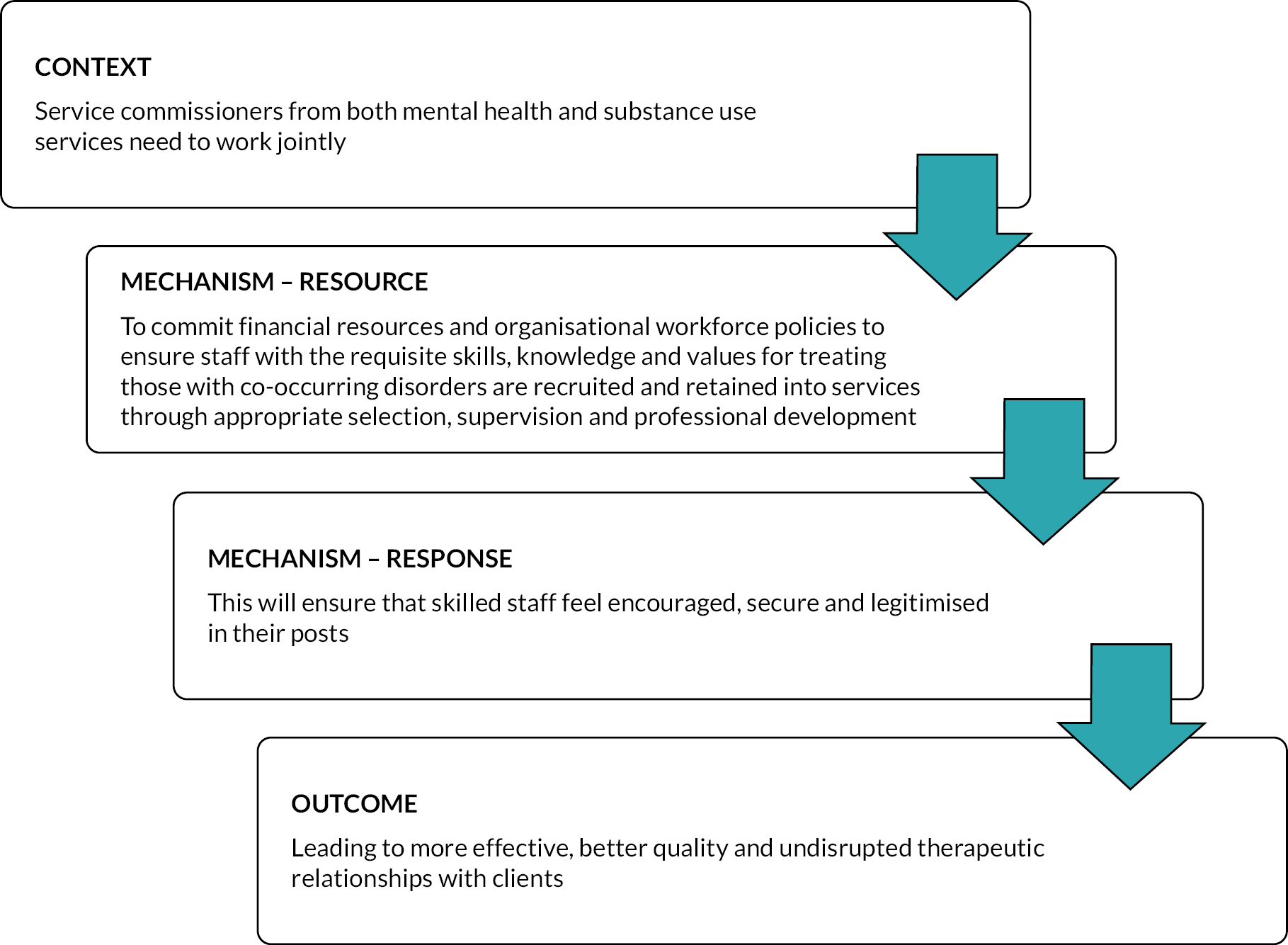
Staff recruitment and retention was less frequently discussed than some of the other PTs, potentially due to a lack of participation from senior management and commissioners in the research. However, staff broadly agreed with the evidence from the realist synthesis, recognising that when staff were not adequately prepared and supported with only minimal training offered (mechanism – resource), they faced significant challenges in meeting the needs of people with COSMHAD (mechanism – response). This was compounded by loss of experienced staff due to national mental health workforce retention issues (context). As a result, additional pressure was placed on both experienced and inexperienced staff who remained in services, leading to staff burnout and a workforce who do not feel valued (mechanism – response). It was suggested this also impacted upon service users, who may disengage with services as they perceive lack of contact as staff not wishing to see or treat them (outcome) (Figure 31).
FIGURE 31.
Programme theory 11 context and mechanism.
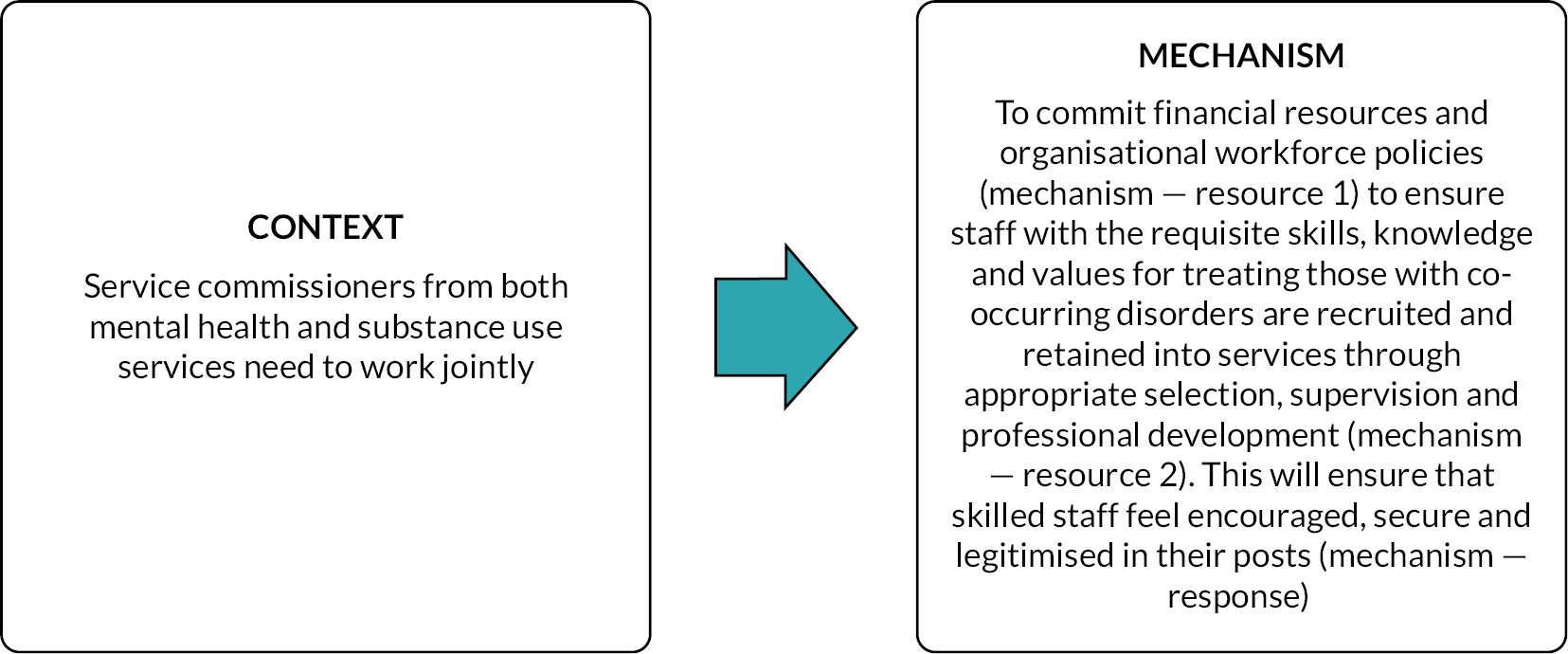
[O]ne of the things again I’ve noticed is that again this hub would then offer to like two or three days training to an organization. And certainly, that then allowed them to make referrals of quite complicated people with three days training in … And suddenly there’s a cut and to me what you know my experience of learning about mental health and learning about therapy and people and nursing and all sorts of bits and pieces drop … these people that are a wealth of knowledge. We’re losing them … we’re not holding on to them. We’re not keeping them you know and we losing roles I mean I think the drug services in [city name] if my memory serves they’re a quarter the size they were from 15 years ago … we are not ready to respond to the post COVID surge, you know, and so this issue of resources, investing in staff and investing in, expertise that can be kind of available I think is a potential gap that will have … knock-on effects … you’ve got young people being exposed to listening to trauma over and over again. Becoming vicariously traumatized. And leaving because they can’t deal with it because they’re going home and crying, you know, and upset and distressed, you know, I mean, even old timers … people are just getting fed up with being the one that people come to with all their troubles. So, they kind of get fed up and move on … they’re just really interesting dynamics and it’s a question about how you’re going to, shift the culture into operating differently … To work with someone that’s got a severe drug and alcohol problem and severe mental health problems takes a lot of tenacity, takes a lot of resilience. You’ve got to want to do it … because if you don’t want to do it, it’s all over you and people fear with that … I’m just gonna put my hand up and say I’ve come through, lived experience … and turning up to places where people don’t want to see you … There’s nothing more soul-destroying … you need people in a motivated task force that’s valued and that could offer a service.
SP38, Case Study A
Staff recognised that recruitment and retention was influenced by both national and organisational contextual factors, including a lack of training on substance use among psychiatrists and the wider mental health workforce. Staff acknowledged that the ‘mainstreaming’ ambition required a suitably capable workforce (context). However, they felt that mainstreaming could only work if there was sufficient investment in the existing workforce. Time-limited funding for pilot joint interventions for mental health and substance use in their services (mechanism – resource) resulted in staff feeling inspired to stay longer in their posts (mechanism – response) (see Figure 30) and improved outcomes for service users.
The whole ethos, it is all national policy and every time you go to any meeting or conference [they] will say, well, we need to co-work with other agencies … I’ve been in post 19 years, been saying it for 19 years. It doesn’t work in its entirety. It needs to be funded to make it work. That’s the only thing that will make this work.
SP40, Case Study D
I can give a great example of this because my post’s within [substance use agency]. Initially it was within my job description that I would provide support around mental health or more complex service users, but we weren’t being commissioned for that. But since September 2021, we’ve been given some funding from our mental health commissioners to work with more complex service users who do have mental health problems and substance misuse issues and that was a nine-month pilot which came to an end just recently at the end of March. But we’ve all we’ve already been given another year’s funding to continue this because there are good outcomes. So, it needs to be funded properly … there is good outcomes when it is funded properly, and it’s led well.
SP41, Case Study D
And one of the concerns that often comes up is that we are losing skills among general psychiatrists, because we don’t have as many addictions training posts as we used to do … when I when I trained, I could do a year in an addiction service and now … people don’t have those skills so … And I think it’s really difficult because the evidence base is very limited, isn’t it? So, when you’re trying to convince commissioners that something would be helpful, ideally we’d want to [be] evidence driven … So there are these like pockets of like really great services that we have and that we can potentially access but again they’re research funded … hopefully helpful for recruitment and retention as well because if you know we’ve, we’ve got the usual massive issue of band 6 nurse recruitment across the board. And I think if you know one of the things [trust name]’s trying to do or trying to help with career development and so being able to do these, these slightly more specialized, interesting, maybe research linked training posts that’s hopefully going to incentivize people to stay a bit longer and make their jobs bit more sustainable.
SP66, Case study F
Staff also considered organisational level context within their trusts which also impacted upon the recruitment and retention of skilled staff (mechanism – resource). Staff described how competency in both mental health and substance use was rarely included in staff job descriptions or a requirement for staff recruitment, with most of this drawn from their own experiences of either applying or interviewing candidates for band 6 and band 7 nursing posts (Case Studies A, C and E). Participants employed in substance use services recalled being asked about their ‘knowledge of local services … one of the essentials was having an understanding of the barriers that can prevent people from accessing the service … how mental health can get in the way of accessing treatment’ (SP16, Case Study C) and ‘a values-based interview … separate from the competency based’ (SP22, Case Study C). Participants felt that having staff within teams designated as COSMHAD leads was often seen as an alternative to hiring people with the requisite skills or providing sufficient training. However, staff identified several barriers which impacted on how legitimised, valued and enthusiastic these COSMHAD leads felt (mechanism – response). This included a lack of role definition, insufficient support to undertake these roles, a lack of protected time to undertake this work and insufficient monitoring of these roles during appraisals.
So what happens is you you’ll be hired as the mental health worker and then even in our team we have a list of lead roles and dual diagnosis one of them. So someone says ‘I’ll do that’ and then ‘what am I supposed to do?’ And they’re [managers] like, go to a meeting somewhere …. so how much you get out of that lead role is how much you put into it.
SP28, Case Study A
It’s everybody’s business …, everybody needs to have some degree of skill. But we need if we’re looking at those specific roles, they have to come from a position where you’ve got the staffing in those teams already because what happens is that those stuff get pulled into other generalist work if you like, and I hate that term generalist work, I think it’s all specialised, but I think it’s about making sure that you’ve got the staff in in place to be able to support that as a process or that you do something else and that’s whether that’s up skilling everybody.
SP51, Case Study D
I think they just negotiated with you know for time and budget because you know one of the things you were talking about assessment earlier is that … care coordinators, the number of things they have to do is just expanded enormously in recent years … dual diagnosis is just one of those things. So, making those roles more manageable … there’s still a lot in that role. And so, I think, yeah, the leadership probably helped in terms of prioritizing what people do with all those competing things that we told you are essential.
SP66, Case Study F
Service users and carers agreed with the evidence from the synthesis that when skilled staff were retained (mechanism – resource), the service users had better therapeutic relationships with staff (outcome). Service users also recognised that broader service level and national level issues impacted on retention, and also felt it was important that services were able to recruit staff with the right skills and experience to support people with COSMHAD. They also acknowledged that there is ‘a shortage of mental health practitioners in the NHS’ (P19, Case Study C) and that ‘it’s a numbers game’ (P18, Case Study C) (mechanism – resource) with staff shortages leading to existing staff being overstretched and unable to deliver the support and care needed (mechanism – response). As a result, carers described how they felt that they often had to fight hard to enable their loved ones to get the individual level staff support they felt they needed (mechanism – response), as illustrated in the quote below where a carer describes trying to secure community mental health support for her son.
[I]t’s just not enough like resources and money in the service … in terms of the staff, they’ve just not the time anymore … They need to employ more. But it’s not fair … you can see the exhaustion. I mean the staff, you know, they’re really understanding … you know, and they do what they can. But the staff nurses, you know, can I speak to you? And where that should be available to speak to you because they’re the qualified one … not about giving you the chance to kind of talk through things properly, yeah.
P13, Case Study B
How do I push the CPN? I became very mouthy and I became very good at writing letters and keeping on top of things, recording everything when he when he went, who should he see, what’s expected, what are you supposed to do, what are you going to do for months? Then you have to learn to fight. You really have to learn to fight. And in fact, he’s his previous psychiatrist. I mean, I became so noisy that she asked me to write foreward in her book, which I did. Because when your son or daughter loved one is diagnosed with a severe mental health disorder you have to.
P36, (Carer) Case Study B
Staff reported how challenging it was to develop and sustain an approach to COSMHAD when funding for such initiatives (and roles) was often short-term only (mechanism – resource; as described above). Initiatives were often halted at the end of funding periods which meant that staff skills developed during that period were not sustained or legitimised (mechanism – response). The removal of these initiatives was also perceived to place a greater burden on people with COSMHAD which could hinder engagement and the development of therapeutic relationships. A staff participant from Case Study A describes having a post which supported staff in delivering joint mental health and drug/alcohol assessments, but this was removed at the end of the dedicated funding period, meaning that people with COSMHAD were often required to have three separate assessments from mental health, drug and alcohol teams (outcome) (Figure 32). In Case Study F, service managers had tried to address this funding issue and deliberately ‘ensured that when we have funding for this post, we try and embed them within clinical teams’ (SP60, Case Study F). Having these dedicated, funded posts which were integrated within clinical teams (mechanism – resource) led to greater role legitimisation among both COSMHAD leads and all staff who were encountering people with COSMHAD (mechanism – response).
FIGURE 32.
Programme theory 11 mechanism and outcome.
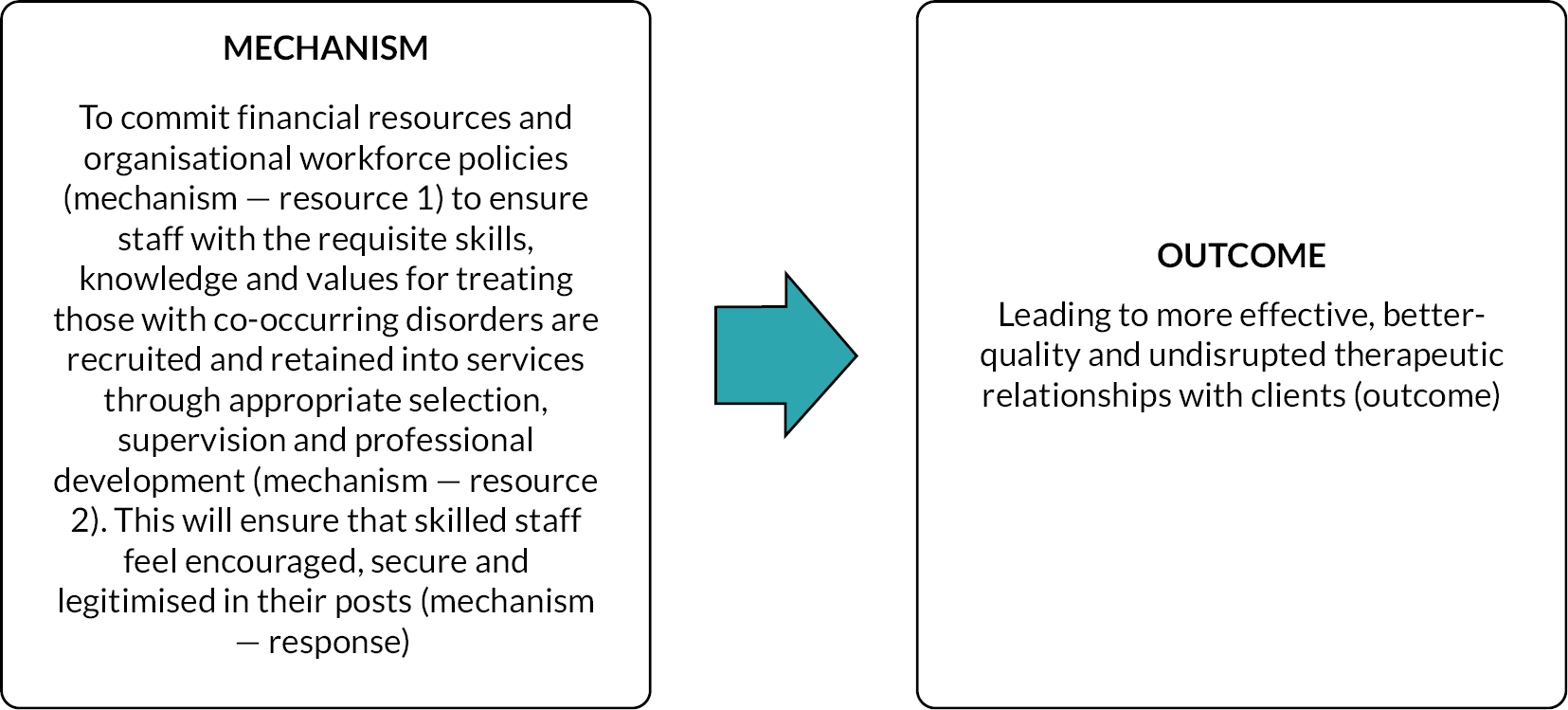
… it worked really well, but then because my contract ended with them, and I came back to this team and then the manager was like we’re not commissioned for this anymore. We’re stopping it. And then it all stopped. And then they went back to being like, what do we do? We’ve got this knowledge that we can’t use anymore, but we’re not allowed to assess these people … because we’re not commissioned to do this … it does feel a bit disjointed because you’ll have within the [hospital name], you’ll have mental health team, you’ll have drugs team and then alcohol team, whereas sometimes all three of them need to be together and they’re all going in for separate assessments … it can feel really difficult to actually address all three in one go because they can be really big things and you get a lot thrown at you. But then who wants 3 assessments in one day?
SP37, Case Study A
I think I think it should be the case that we need to mainstream this. It needs to be part of everybody’s competency package and the role of people who are dual diagnosis leads or practitioners should be to support others and just be a repository of reassurance, wisdom and knowledge. If that’s not too much of a burden, and that that feels much better, I think it feels it feels much more positive for the dual diagnosis practitioner, and I think it can allow people to feel really contained by them.
SP52, Case Study F
In contrast, where this funding was not available, staff often struggled to know what action to take within their roles. A staff member from Case Study E described how in her role supporting staff she felt ‘it’s not that the staff don’t connect with them or feel sorry for them. They just don’t know what to do’ (SP83, Case Study E) (mechanism – response). She linked this lack of clearly defined staff roles with a lack of flexibility which led to poorer outcomes including increased fatalities (outcomes). Dealing with such emotional impact led to staff burnout and poor retention (mechanism – response).
Patient had been discharged two weeks earlier and news had come through about the fatality. We think it was accidental. And I mean, it was as if a close relative … had just died. They were devastated … It was so intense. They were really, really upset about that. The consultant coming back from the inquest was just absolutely beside himself. You know, it’s not that they don’t get it. You know, they’re really, really heartbroken when their patients have a poor outcome. And that’s draining as well. You know, staff retention is a big thing at the minute. And so, I mean, I saw, felt and heard their pain that day. I mean, that’s just one out of how many and it was it was real, that was genuine, you know. It turned out I knew the girl as well. Didn’t realize at the time, but I did. So, I had my own version of it. When I went home that night.
SP83, Case Study E
Service users and carers described the impact that staff leaving (mechanism – resource) had on their therapeutic relationships and engagement with services. Service users described how it often took time for them to develop a good relationship with care co-ordinators and key workers (or equivalent roles) but that when that relationship was established, they felt a sense of trust towards the member of staff (outcome). They also often relied on these staff members to ensure that they got access to additional support particularly in times of urgent need (outcome). Consistency and continuity of staff (mechanism – resource) was vital to ensure that they were fully appraised of each person’s care and could provide empathetic support to both the service user and their family (mechanism – response).
Wonderful lady. I’m [name] was devastated [when she left] because over a year she’s built up, you know, I knew I could just give her a call on the mobile, you know, any time and arrange for helping you get help. I think [name] needs to see doctor around last year or so it was immediate.
P21, (Carer) Case Study A
I think consistency, for example … home-based treatment team, it’s different people come out every time … you’re told, you know, [name]’s gonna be [husbands name]’s key worker … but we’ve not seen him … so, yeah, continuity I think helps. And having a single point of contact helps … Home based treatment team are very good when you pick up the phone and they obviously have the notes readily available in front of them … they know who I am and they are fully aware of [husbands name]’s situation and I do think that that makes a difference. Rather than you having to get on the phone and explain over and over and over again to every single different person there is that continuity there where you know, people do seem to be aware of the case and where what’s happened and where things are up to.
P3, (Carer) Case Study C
Service users and carers also described how they found it very difficult when staff left their roles (mechanism – resource). They found it challenging to build relationships with new staff and they found that they often had to reappraise the new member of staff of their whole medical and care history, which was often an upsetting and tiring experience (outcome). Service users also described feeling fearful when a staff member left that they would no longer continue to receive the same standard of care, and several participants described how the member of staff who was leaving the service often had to pursue the issue repeatedly to ensure continuity of care (outcome).
[I]t was a different person every two days … from [husbands name]’s perspective, he feels like he’s got to dredge up all of that … each time he meets a new person, he’s gotta go through it all again, I have to go through it all again to make sure that they are up to speed with where they should be and what’s gone on in the past … it’s like reopening old wounds, you know … I’m a sales director, OK, if I deal with a customer, I ensure that the person that deals with that customer at the beginning is the person that takes them through their entire journey. If I kept on sending a different salesperson in each point of, you know, contact with that client, that client wouldn’t feel any affinity towards us as an organization, and they wouldn’t necessarily take our, you know, give us their business because they feel like they’ve been passed from pillar to post … that’s exactly where we feel now with the NHS, you know? … you only build trust by … becoming recognized to somebody … you can only build a relationship if you have an opportunity to build that relationship.
P3, (Carer) Case Study C
… they don’t have complete access to your history and your background, whereas you know my support worker does and my support worker is able to go directly to you know the higher-ups in the mental health community, mental health, and discuss any you know concerns and you know anything that I bring … that I need that extra bit of support. You know I can get appointments brought forward or you know medication reviews and you know all that kind of stuff.
P8, Case Study E
Staff recognised that recruitment and retention was influenced by both national and organisational contextual factors (e.g. lack of training on substance use among psychiatrists and the wider mental health workforce) and acknowledged that the ‘mainstreaming’ ambition of current national policy aimed to address this skills deficit. However, they felt that this national agenda could not succeed without sufficient funding to invest in the existing workforce. Where funding was provided, positive results were seen. They acknowledged that the wider organisational structure and climate impacted on whether skilled staff were retained and felt it was important that services first recruited staff with the correct skills and experience to support people with COSMHAD. They also highlighted that staff shortages lead to existing staff being overstretched and unable to deliver the support and care needed. Staff leaving services also had negative impacts on service users and carers, leading to a lack of continuity and consistency, and fear of having to repeat their trauma and build up a new relationship with another clinician.
Summary
From the realist synthesis a set of 11 PTs were finalised. Three broad contextual factors were identified across the 11 PTs – these were committed leadership across organisations involved in providing care for people with COSMHAD, a general acceptance that staff will be required to provide care for people with COSMHAD and structured networking and co-ordination across organisations to assist in integrating care. These contextual areas align well with the SELFIE framework developed by Leijten et al. 68 which was developed by a European consortium to contribute to the improvement of integrated, person-centred care for multimorbidity. The SELFIE framework groups concepts relating to integrated care for multimorbidity at the micro, meso and macro level, split across six components: service delivery, leadership and governance, workforce, financing, technologies and medical products. The three contextual areas identified in our overall PT align well with these first three domains: (1) service development (structured networking and co-ordination), (2) leadership and governance (committed leadership across organisations) and (3) workforce (co-occurring disorders are the expectation in services). The 11 PTs have been mapped to these concepts below (Figure 33).
FIGURE 33.
Programme theories mapped to components of the SELFIE framework.
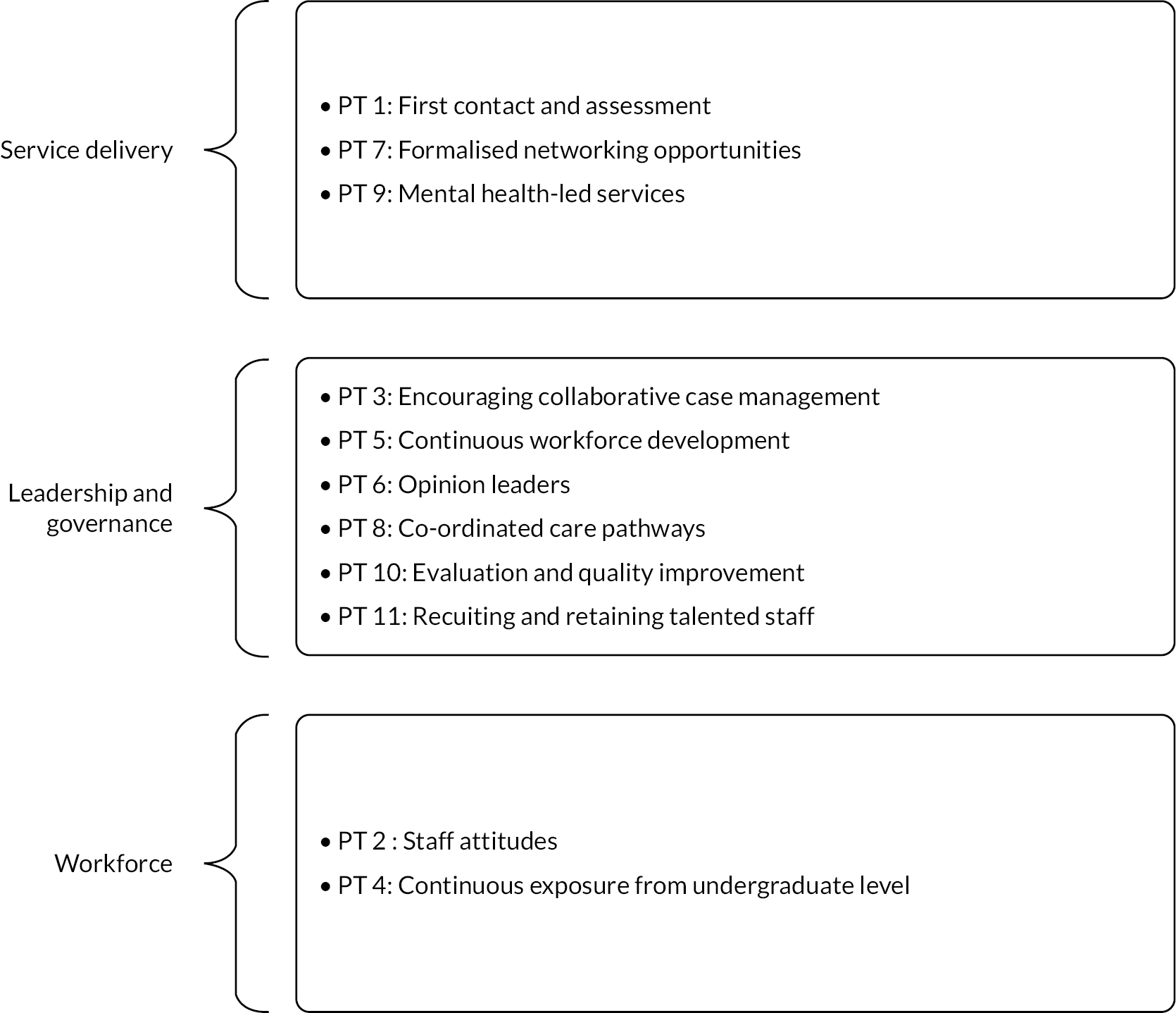
Figure 34 illustrates the contexts, mechanisms and outcomes and how the 11 PTs fit within this model.
FIGURE 34.
Adapted SELFIE. Model with RECO programme theories.
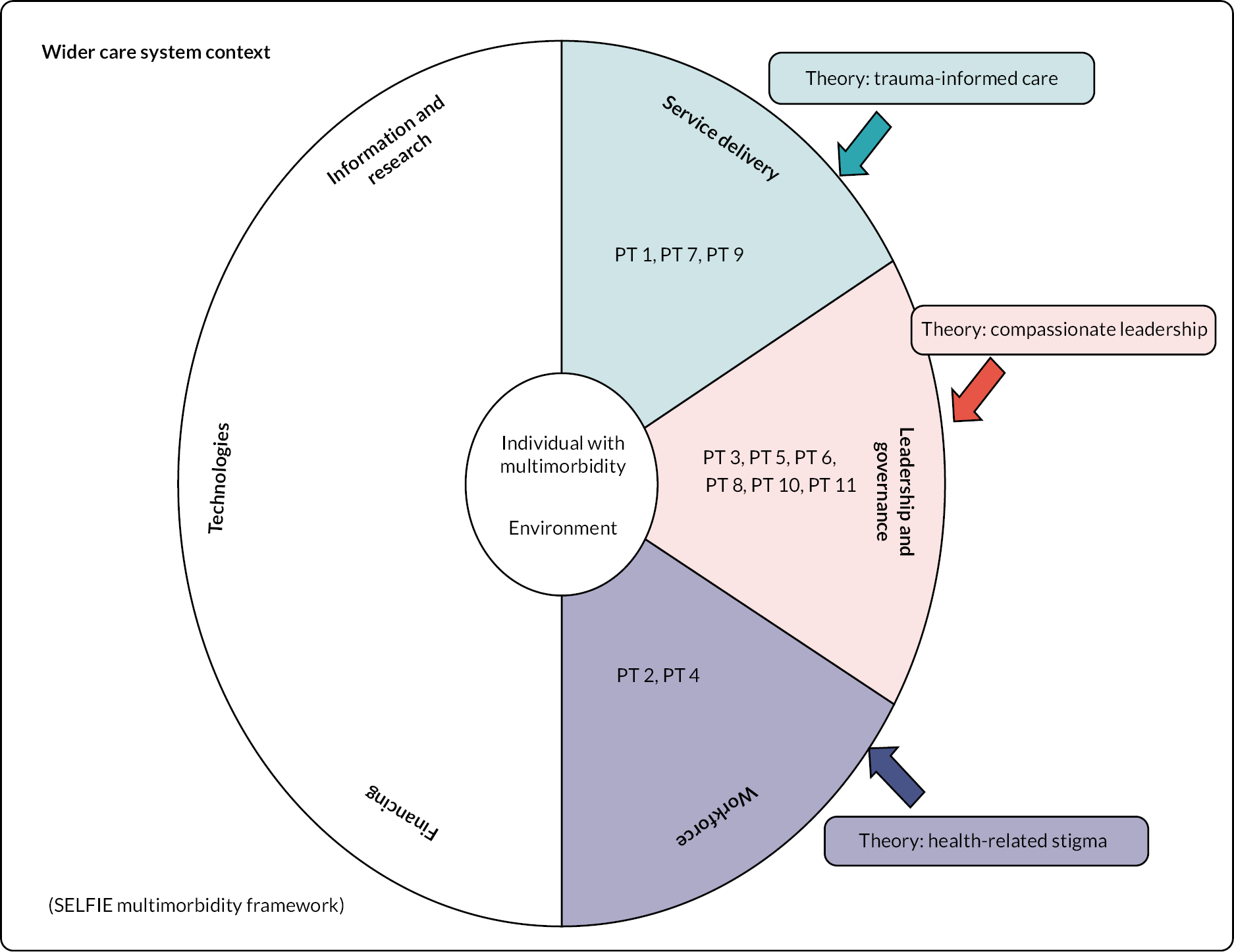
In sum, if there is commitment from leaders within organisations (at a local, regional and national level), as well as a general agreement that working with COSMHAD is a legitimate part of mental health and substance use services, and there are the opportunities to connect to other services and/or external agencies, then this fosters the contextual conditions that allow the mechanisms (resource and response) to work effectively in order to produce favourable outcomes for staff, service users and carers.
In a realist evaluation, the outcomes are not necessarily ‘hard outcomes’ such as reduction of symptoms or reduction in inpatient bed days. Rather, we have been able to identify a set of outcomes from the synthesis of literature and the case study analysis which have meaning for both staff and service users and their carers. One of the most important outcomes identified is engagement. This was something that both staff and service users discussed extensively. Service users clearly articulated the mechanisms that led to their engagement and much of this focused on how staff demonstrated positive attitudes including empathy and confidence in their own skills and knowledge. In addition, it was recognised that with a flexible and person-centred approach, service users were more likely to work towards their own goals. This in turn improved staff efficacy and reduced burnout. Ultimately, these outcomes alignto a more compassionate based, needs-led service that is trauma-informed.
While each PT has been discussed individually along with the evidence, it is important to acknowledge the interconnectedness of the system. Staff attitudes are linked to access to training and practice development opportunities which is in turn dependent on a commitment for staff to be released for such opportunities as well as having sufficiently skilled and experienced clinical leaders to be able to provide this. Service users and carers were most concerned by their experience of a sometimes confusing and fragmented care system, staffed by people who have needs in terms of skills and experience in managing complexity. However, we also learnt that if someone has some training and access to good-quality support and supervision, then this promotes better engagement for the service user who in turn is more likely to have their needs accurately identified and possibly met. This also increases job satisfaction and may contribute to a reduction in burnout and retention of staff. The importance of having a locally agreed care pathway and properly co-ordinated care was identified, and this is especially pertinent given that we found evidence that even in areas where a lot of work had gone into improving the care for COSMHAD, people were still falling through the gaps in services. This was particularly noted with the issue that people would be refused mental health care if not abstinent from drugs or alcohol, which is difficult if the person is using substances to cope with the mental health issues.
Chapter 5 Discussion, recommendations and conclusion
Approximately 30–40% of people with SMI have co-occurring alcohol and/or drug conditions. 1,2 This is associated with adverse outcomes such as relapse, higher crisis service use, physical health problems, homelessness, violence, victimisation and suicidality. NICE guidelines for psychosis and SMI, as well as policy guidance,21 have been produced to drive improvements in quality of care for this group; however, it remains unclear how to operationalise guidance. The NIHR Health Technology Assessment Programme commissioned research on behalf of the Department of Health and Social Care to examine and evaluate current service models for COSMHAD to make recommendations for policy, practice and research (RECO study). The RECO study took a realist approach28 to understand COSMHAD treatment models by investigating what works for who, why and in what circumstances. This was achieved by three WPs: WP1 undertook a realist synthesis of published literature, WP2 mapped and described the characteristics of current UK service models, and WP3 sought to test and refine the PTs generated in WP1 in six locations (case studies) that had some type of service model for COSMHAD. These were sampled from services identified in WP1. WP3 consisted of focus groups and interviews with a range of staff, service users and carers.
The research questions identified were:
-
What does the existing literature suggest ‘works’ (demonstrated by engagement and other health outcomes) in terms of COSMHAD, for whom, and in which circumstances?
-
What are the range and types of service systems that currently operate in the UK that aim to improve engagement and health outcomes for people with COSMHAD?
-
What are the specific contexts and mechanisms that make COSMHAD models successful (or not), for whom, and in which circumstances?
Range and types of services identified in the United Kingdom
The outcome of the UK mapping revealed few tangible examples of service models especially for COSMHAD. Obtaining data on the types and location of service models for people with COSMHAD in the UK was a challenging and time-consuming task. There is no centralised recording system at national or regional levels in England or the devolved nations. Much of the data obtained was as a result of ‘cold-calling’ commissioners, mental health and substance use providers and local authorities. From the responses to the national mapping, 793 services were contacted, 311 responded, and of these 181 provided information about local provision for COSMHAD. When the responses were reviewed most reported an ‘integrated care pathway’, however provided no other detail about models of care or dedicated staff teams to provide or support integrated care. Where it was indicated that a specific service was in place, we reviewed these responses and selected services that indicated that they had some resource in place (often resource related to specifically funded posts). These selected services were asked for more detail via an online form. Sixteen services responded to the audit and provided detailed information. These data were used to group the services into three types: ‘network’, ‘link and lead’ and ‘consultancy’. In terms of cost for the models, the main resource was staff dedicated time and/or posts specifically to deliver the COSMHAD services. There was a range of costs from the cheapest being the ‘network’ model. We did not have the scope to evaluate cost-effectiveness and value for money within this study. Across the three identified models there was much similarity in what they offered. While one team operated purely as a consultancy role (providing training, supervision and joint assessments), the other models also offered this approach. However, rather than have a dedicated team that was separate from the rest of the service delivery, the other models often had a lead clinician (most commonly a consultant nurse at band 8) as a leader with a network of link workers. In some cases, the link workers were volunteers and had no resource (protected time) for this role, and in some cases, the link workers were specifically employed to support the lead clinician in the COSMHAD role. Protected time was identified as an important resource. Without it, the link workers could not contribute to the COSMHAD work. The other important issue that was raised was the importance of stability of funding for COSMHAD roles. Short-term funding for roles that then disappeared after the funding ended was viewed as counterproductive especially when trying to sustain a long-term programme of improving care for those with COSMHAD. This fits with the factors suggested as important in the delivery of effective care for this client group in terms of ‘recognising that change can be slow especially when there are multiple needs at play, and taking a long-term view of progress’ (p. 34). 21 It is difficult to see how such a long-term view of progress for each client, and also in terms of service delivery, can be taken in the context of short-term funding and a lack of protected time for identified link workers.
The provision of integrated care across the entire health and social care system within England, including the leadership of this at all levels, is integral to achieving the ambitions of the LTP and CMHF. 21 During 2019 NHS England and NHS Improvement were tasked with identifying any required changes that would facilitate the achieving of these ambitions, with a key recommendation being transformation of the ‘system architecture of the NHS to increase co-ordination of services through the creation of integrated care systems’. ICSs throughout England draw together in partnership with commissioners and providers, local authorities and local partners to ‘plan, co-ordinate and commission health and care services’. Given the results of the RECO study, it is pivotal that consideration is given to the needs of individuals experiencing COSMHAD and their carers/representatives, especially given the prevalence and risk associated with being part of this client group. It is suggested that, given the experience of staff, service users and carers in relation to the gaps experienced between services, much can be learnt about good practice in the provision of integrated services. This would appear particularly important within the CMHF, given the definition of SMI utilised within the framework and the need to work holistically to meets the needs of individuals, including those using substances. The three explanatory areas of "workforce", "leadership" and "service delivery" identified in the RECO study are important in operationalising the holistic, integrated approach to meeting the needs of this (and other) client group as part of the CMHF.
Within this, integrated treatment, which at its core promotes and provides trauma-informed care, is key.
It is clear that the workforce is not equipped to deliver on the policy of ‘mainstreaming’ care for COSMHAD. This is due to structural issues (working in silos), poor attitudes towards those who use drugs and alcohol, and a lack of understanding of the nature of the relationship between substance use and mental illness. Stigma towards substance use is a significant barrier to care84 but can be addressed by advocating for the rights of stigmatised groups, education and close contact with the stigmatised group. NICE guidelines19 and other policy guidelines in the UK advocate the use of general therapeutic skills (empathy, reflection and unconditional positive regard) as well as more specific health behaviour change skills such as Brief Interventions and Motivational Interviewing,85 as well as cognitive–behavioural therapy. However, there is a lack of such clinical skills in the workforce especially with the disinvestment in CPD. It is also acknowledged that, in relation to psychosocial interventions, the most recent Cochrane review13 notes that there is no one specific recommended treatment approach for working with this client group in which to train staff. Dame Carol Black’s Review of Drugs report (England)23 identified that there was a lack of skilled people in the addictions services who can deliver psychosocial interventions and the caseload sizes need to be addressed to allow people time to spend with each person to be able to deliver effective care. In addition, Black23 calls for more pre-registration training for mental health nurses, social workers and doctors, as the current curricula offer limited input into substance use let alone COSMHAD. In some of the case studies, the clinical leads (and some of their link workers) were offering CPD style training in-house, but often lacked the resources to provide ongoing support and supervision to implement the new skills into practice. Training alone has been shown to have limited impact on service user outcomes.
In thinking about the needs of the workforce, the focus groups outlining a need for trauma-informed care would appear important. For staff to provide trauma-informed care, they need to work in a trauma-informed environment that resources them practically (e.g. training, support, supervision, resources, staffing) and psychologically (e.g. psychological safety, learning culture, compassionate and inclusive leadership, reflective practice) to work in a trauma-informed way. The Centre for Substance Abuse Treatment (USA)86 notes that an ‘organizational environment of care for the health, well-being, and safety of, as well as respect for, its staff will enhance the ability of counsellors to provide the best possible behavioural health service to clients’.
Leadership
One of the key findings was the importance of having a clinical expert leader – this works best when they are supported by a positive organisational culture that supports COSMHAD (senior managers and commissioning). This support equates to having designated time to be a broker; offer training and supervision; joint work and role modelling; and facilitate MDT discussions and local interest groups. In addition, most case studies operated a ‘link worker’ model which broadly speaking was key people in wards or community teams who had a special interest in COSMHAD and acted as a local link for the clinical specialist for communication. However, this role is challenging to do if there is no protected time and often usual work gets prioritised. The clinical leads often operate over a large service and partner agencies, and this means that without the support of link workers it is almost impossible to have significant impact. Many of the clinical leads had been in post for many years and were considered ‘pioneers’ by their colleagues. In one case study (Case Study A), the clinical lead had retired and not been replaced and this had meant that the COSMHAD initiatives lacked any leadership and were now at risk. The importance of a sustainable programme of work that is adequately resourced has already been raised.
The findings from the RECO study indicate the need for a shift in culture in leadership. The National Improvement and Leadership Development Board87 notes:
A healthcare organisation’s culture … shapes the behaviour of everyone in the organisation and directly affects the quality of care they provide … Leaders who model compassion, inclusion and dedication to improvement in all their interactions are the key to creating cultures of continuous improvement in health and care.
p. 20
The shift in culture to meet the needs of people with COSMHAD would appear incredibly timely given the transformation within the NHS and the wider health and social care system currently, in line with the ambitions of the LTP and CMHF. The LTP (2019)21 builds on the ambitions of Developing People Improving Care, to support the NHS in creating ‘inclusive and just cultures that leads to outstanding staff engagement and patient care’ (p. 89). The plan also highlighted that ‘Great quality care needs great leadership at all levels’ (p. 89), which reflects the need for compassionate clinical expert leaders for COSMHAD, and in addition, they need support form senior managers in the organisation.
Service delivery (care provision and pathways)
In this study, we have been able to operationalise the concepts of ‘mainstreaming’ (also known as ‘everyone’s business’); no wrong door; and integrated treatment as well as identify the contexts under which these mechanisms work to produce positive outcomes for staff, service users and carers. Mainstreaming has been poorly described and misinterpreted in practice. The RECO study found that the staff participants broadly agreed that COSMHAD was indeed their business, and this included staff from mental health, substance use, not just those in dedicated roles. However, for this to work there needs to be to a concerted and long-term programme of training and workforce development opportunities to ensure that a critical mass of staff have the requisite knowledge, attitudes and skills to meet the multiple needs of people with COSMHAD within an integrated treatment area. This is not a case of staff being expected to be experts, rather that they have an adequate base on which to operate and know how to get support from those with expertise or work jointly with other agencies. The challenge for mainstreaming is that this level of skills development is absent from pre-registration training, so all the workforce development initiatives happen post registration. Therefore, the system is constantly playing catch-up. However, addressing this will not only improve service user experience but also may play a role in reducing burnout and increase retention of staff. Staff who have been trained to work with COSMHAD feel more positive about this group and more self-efficacy in their work.
In addition to the role of individual workers, the wider care system needs to be better co-ordinated to ensure that gaps are identified and addressed, there is improved communication between agencies, and the system is flexible to meet the needs of the users as opposed to expecting people to fit into rigid service remits (particularly unhelpful is blanket rejections of people who are not abstinent from substance). The service users and carers talked at length about the importance of collaborative care pathways and the negative consequences for them when this is lacking. Many had experienced challenges in receiving care when they requested it, and that their substance use had been cited as an exclusion criterion for mental health services. This meant that people deteriorated until they were in a crisis (suicidal or at risk of violence) and this led to an emergency (and costly) response often involving the police, ambulance service and emergency departments. This is traumatic for the service users and carers, as well as the staff in the emergency services and crisis teams. When the policy of ‘no wrong door’ is implemented, this means that wherever people connect to services (whether mental health or substance use treatment agencies) they are supported while their needs are being assessed and a care plan constructed. Having clear and agreed roles and responsibilities across the agencies will support the ‘no wrong door’ approach.
When supporting someone with multiple needs it is important that someone is able to take a co-ordination or oversight role to ensure that care is being delivered and communicated as planned. If someone has a severe mental illness that requires secondary care, then it is important that they receive their primary care from mental health services (such as CMHT) but also recognising that other agencies may play an important role. Integrated care requires clarity of roles, willingness to work in a multidisciplinary way, and effective communication between agencies (including shared information systems). Local networks for COSMHAD have been identified as a useful mechanism to support integrated care in terms of fostering interagency relationships and shared learning opportunities. However, networks need leaders to organise and promote the networks, and often the local expert clinical lead performs this role. In addition, staff need to have protected time to attend the network meetings as well as other local CPD opportunities. Network meetings were highly valued by the staff in the RECO study and the biggest barrier to these was the time to access them.
In developing and improving care responses to COSMHAD, it is important to maximise the opportunities offered by the shift to integrated care, trauma-informed care, suicide prevention initiatives and initiatives that promote physical health in people with severe mental illness. Linking COSMHAD to these other initiatives will help to integrate COSMHAD issues and reduce the perception that this is just another novel initiative to be overlaid on an already overloaded health and social care system.
The RECO study has provided data on what are the key components for COSMHAD service models and this is presented as an adapted SELFIE model of integrated care for multimorbidity. 68 The areas in shade represent the areas where there is some evidence to support these components. The areas in white (information and research, technologies, and financing) are areas where we have limited data (which reflects the original aims of the study). In addition to our PTs, there were overarching theories relating to trauma-informed care, compassionate leadership and stigma. The wider care system context is also an important factor. The case study data were collected in a ‘post-pandemic’ period and mental health and other health and social services are facing significant challenges. Some of these challenges are as a consequence of the pandemic (staff sickness, staff left the service due to retirement or ill health) but also because demand is outstripping resource. There is a shortage of key staff including mental health nurses and psychiatrists and a surge in demand for mental health care. The consequence of short-staffing and increased referrals impacts on many aspects of the COSMHASD PTs including staff burnout leading to compassion fatigue, lack of time to access training and practice learning opportunities, higher caseloads (meaning less time to build relationships and deliver evidence-based interventions) and higher thresholds to access services, leading to more people with COSMHAD being excluded from services. Improving outcomes for people with COSMHAD (as well as other groups of people in need) requires an appropriate resourcing of mental health, substance use, social care and third sector agencies. 88
Strengths
This is the first realist evaluation of service models for people with COSMHAD using a robust methodology. This involved stakeholders and published literature to develop initial theories, which were refined during a realist synthesis and tested in six case studies which represented the three models of COSMHAD services identified. In addition to staff participants, people with lived experience and their carers participated in focus groups and interviews to ensure that we had all voices included. This was particularly important given that the service user voice was identified as distinctly lacking in the literature. In this evaluation, we have worked with people with lived experience and other stakeholders, including people in expert clinical leadership roles, throughout the process to ensure sense checking of findings and relevant steering of the project throughout. We have been able to operationalise concepts such as mainstreaming, no wrong door and integrated treatment in terms of the contexts and mechanisms that are required to deliver outcomes that have meaning to staff, as well as service users and their carers.
Limitations
The project was impacted by the COVID-19 pandemic which affected the responses to the mapping exercise and required a shift to online data collection methods for the case studies. It is possible that the mapping exercise did not identify some of the COSMHAD services. There was a target to undertake a number of focus groups and interviews with service users and carers in each case study site and these would have been face-to-face meetings. The recruitment targets for service users and carers were not met, despite the best efforts of the research team and our clinical colleagues. We do not know the exact reasons for this, but recruitment of underserved populations to research studies is challenging and it is likely that not being able to have a face-to-face presence impacted on recruitment. In addition, the online option may have been off-putting for some potential participants. However, sample size is less of a consideration in qualitative studies and the focus is on the lived experience. We were limited in the PPI input we had, despite several attempts to engage this group; we believe contact was also impacted by the COVID-19 pandemic. However, despite not having as much direct PPI as we had planned, we had lived experience involvement at every stage of the study from application development, stakeholder input into the realist synthesis, the protocol, and input into the analysis.
Equality, diversity and inclusion
The study was aimed at an underserved and marginalised group of people with severe mental illness with co-occurring substance use conditions. The study was planned before the COVID-19 pandemic, and we had intended to hold in-person and small focus groups with people with lived experience and their carers but we also recognised that to increase the diversity of voices, we would need to undertake a set of individual interviews using an flexible outreach model bringing the researcher to the places where people accessed care (such as hostels, substance use services, etc.) and in this way we could access people who would not normally attend a focus group. However, due to the pandemic and the restrictions on travel and requirement for social distancing, this was not possible to do.
We were able to offer vouchers for data to enable people to participate if this was a barrier. The research activities required extensive verbal communication, meaning that those without sufficient English skills were unable to take part. Future studies should include the provision of interpreters to enable those withoutspoken English to participate. We were able to include a diverse range of rural and urban case study sites including London, South West England, the Midlands and North West England as well as one from the devolved nations (Northern Ireland) which typically has less research involvement. In terms of the research team, CI is a female mental health nurse researcher and nurses are under-represented in NIHR. The co-applicants were made up of six females and three male academics. We have ensured that the Early Career Researchers that worked on the study are recognised for their work and have opportunities for their professional development. This has included methodological training opportunities and supervision. Harris was able to present the realist synthesis as a poster presentation at Lisbon Addictions Conference and was the first name author on the synthesis paper.
Recommendations for policy and practice
The RECO study aimed to examine the operationalisation of policy and guidance to identify the contexts and components of models of care that produce outcomes that are meaningful for staff, service users and carers, and make recommendations for further research.
-
At a macro contextual level, there needs to be closer integration of mental health and substance use policy at government level. This needs to be reflected at local commissioning level to ensure that local services are commissioned (in some cases, jointly commissioned) to meet the needs of people who span mental health and substance use services. Integrated care boards and partnerships should be able to plan local services that address the needs of this population.
-
Ensure that the issues of COSMHAD are included in the workforce development plans across mental health and substance use services in England and the devolved nations of the UK.
-
There is clear value in investment in the ‘expert leader’ role (such as consultant level nurses and allied health professionals) in driving the agenda for more integrated care and collaborative working with a range of agencies and disciplines. However, the people recruited to these roles require support from strategic leadership as well as support from a team of more junior colleagues who have protected time to undertake work as link workers or champions across a range of service settings.
-
Given the level of disparities and significant problems in accessing appropriate care which leads to adverse outcomes, COSMHAD should be seen as a top priority in mental healthcare services. We recommend that COSMHAD could and should be embedded as part of service improvement initiatives such as trauma-informed care, improving physical health disparities in mental health, and in suicide and violence prevention strategies.
-
Service users and carers should be included in the development of care pathways.
Recommendations for future research
The RECO study has highlighted further uncertainties that could be addressed through research. It was beyond the scope of RECO to evaluate the effectiveness (and cost-effectiveness) of the three COSMHAD models identified, especially when compared to areas where such models currently do not exist. We are more confident that we can identify the important components of COSMHAD integrated care, but less certain on the longer-term benefits. The trajectory of recovery for people with multiple needs is long-term and benefits of interventions may take years to translate into harder outcomes such as symptom reduction and reduction in service use. However, the RECO study identified a number of outcomes that have meaning and benefit for staff and service users including service satisfaction, engagement with services, job satisfaction and staff retention. There may be opportunities through data linkage to evaluate long-term outcomes without the challenge and burden of recruiting large numbers of people who are experiencing multiple challenges. Another area that was identified from the RECO study was the lack of pre-registration training related to substance use issues in nursing, allied health social care and medicine. There are uncertainties about what this training should include and who and where it should be delivered. For instance, this could be included in the content delivered by universities or integrated into practice placements. This has the potential to improve quality of care across other fields of health care, not just within the mental health sector.
Conclusions
People with co-occurring serious mental illness and co-occurring substance use (COSMHAD) are some of the most underserved populations, and they experience significant disparities in access to care and treatment. Many of the challenges faced by people with co-occurring serious mental illness and substance use are due to failings in the health and social care configurations. The RECO study identified less than 20 locations in the UK where there was a tangible investment in addressing this need. However, despite the lack of empirical evidence about what works for people with COSMHAD, there has been a consensus spanning 20 years about how services could be designed to best meet the needs of this underserved population. This requires joined-up and integrated care between mental health and substance use services (including workforce planning), as well as local leadership at strategic and operational levels. The three main components identified for potential success are: leadership, workforce development and service delivery (care provision and pathways). There is potential to make a significant difference to the outcomes for people with COSMHAD, but this requires a genuine commitment to integration from policy, to commissioning and practice. Further research is required to establish the clinical and cost-effectiveness of integrated care for COSMHAD.
Additional information
Contributions of authors
Elizabeth Hughes (https://orcid.org/0000-0002-4480-0806) (Professor of Substance Use Research) was the chief investigator, responsible for the overall management and delivery of the study, contributed to design, data collection, analysis and took responsibility for the report.
Jane Harris (https://orcid.org/0000-0001-6584-1642) (Research Fellow) was employed as research fellow and undertook realist review, recruitment and data collection, analysis and writing the report.
Tom Ainscough (https://orcid.org/0000-0001-5934-819X) (Research Fellow) was employed as research fellow and undertook realist review and mapping exercise in WP2.
Angela Bate (https://orcid.org/0000-0001-5277-4188) (Reader in Health Economics) was a co-investigator and provided realist health economic input into the report including calculation of resources in WP2 as well as contributing to the analysis and writing the report.
Alex Copello (https://orcid.org/0000-0003-3788-7197) (Professor of Addiction) was a co-investigator and provided input into the project management group, data collection in WP3, analysis and writing the report.
Sonia Dalkin (https://orcid.org/0000-0002-3266-5926) (Professor of Applied Health and Social Care Research) led on the realist methodology for all aspects of the study, project management group and was involved in design, analysis and writing the report.
Gail Gilchrist (https://orcid.org/0000-0002-5616-6283) (Professor in Addictions Healthcare Research) was a co-investigator, member of project management group and was involved in design, analysis and writing the report.
Emma Griffith (https://orcid.org/0000-0002-3973-4912) (Consultant Clinical Psychologist) was a co-investigator and provided input into the project management group, data collection in WP3, analysis and writing the report.
Lisa Jones (https://orcid.org/0000-0001-5136-5614) (Reader in Public Health) was a co-investigator and provided input into the project management group, led the realist review (WP1), as well as analysis and writing the report.
Michelle Maden (https://orcid.org/0000-0003-4419-6343) (Lecturer in Evidence Synthesis) was involved in designing the literature search strategy and undertaking the search in WP1 and contributed to the final report.
Luke Mitcheson (https://orcid.org/0000-0003-0107-0070) (Consultant Clinical Psychologist) was a co-investigator and provided input into the project management group, analysis and writing the report.
Harry Sumnall (https://orcid.org/0000-0002-7841-9245) (Professor in Substance Use) was a co-investigator and provided input into the project management group, data collection in WP3, analysis and writing the report.
Charlotte Walker (https://orcid.org/0000-0003-2244-350X) (Service User Researcher) was a co-investigator and a service user representative, provided input into the ethics application and protocol and provided input into the project management group, and contributed to the report.
Acknowledgements
We would like to thank Dilupa Samarakoon (Senior Research Fellow, Northumbria University) for her assistance in collating the cost data in the case study sites.
We would like to acknowledge Progress (national consortium of consultant nurses and other experts in co-occurring mental health and alcohol/drug conditions) who have provided stakeholder input for the development of the initial PTs, interpretation of data and refining report recommendations.
We are grateful to the people with lived experience who contributed their time to designing the study protocol and ethics paperwork.
We are grateful to all the services who provided us with information for the mapping exercise, the local staff who helped us recruit staff and service user participants and assisted us in setting up the focus groups.
We are indebted to the service users and carers who chose to share their experiences with us, and we hope that we communicate your experiences in order to effect change for the better.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to all anonymised data may be granted following review by the data controller [Hughes] and completion of a data-sharing agreement.
Ethics statement
NHS ethics and HRA approval were obtained on 17 June 2021 (Surrey Research Ethics Committee RE21/LO/0384 IRAS 277924).
Information governance statement
University of Leeds as the sponsor institution is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under the Data Protection legislation, University of Leeds is the Data Controller, and you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our Data Protection Officer here: https://ris.leeds.ac.uk/privacy-notice/.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/JTNT0476.
Primary conflicts of interest: Elizabeth Hughes declares research funding from NIHR HTA1343865; she has received expenses for speaking at Royal College of Psychiatrist Conference; she sits on NIHR Advanced Clinical Academic Fellowship Award funding panel; and she received honorarium for being a member of the management team for the Mental Health Network Research Scotland (Clinical Scientist Office, Scottish Government). Angela Bate declares research funding from NIHR Marie Curie and MRC and acted as an advisor NIHR PGFAR (RP-PG-0217-20004), TSC NIHR HSDR (NIHR16/177/03) SSC and NIHR PHR (NIHR129118) SSC. Alex Copello has research funding from NIHR RfPB 200477 and received royalties from a book on brief interventions for people with COSMHAD. Sonia Dalkin received grant income from NIHR HSDR 135102, HSDR 131016; she sits on advisory groups as an unpaid expert for NIHR 140416, 131623, EPOC, Yorkshire Cancer Research EPOC. Gail Gilchrist has grant income awarded from NIHR RP-PG-1214-20009, NIHR 129798, NIHR 16/117/03 RP-PG-0614-10016 and Nuffield Foundation. Emma Griffith has received royalties from a book on brief interventions for people with COSMHAD. Lisa Jones declares funding for NIHR project NIHR202988 and NIHR PRP 202988. Michelle Maden received grant income from NIHR 128842. Luke Mitcheson seconded 1 day a week as a clinical advisor to OHID/DHSC and receipt of funding from Indivior to run a multisite randomised control trial of depot buprenorphine. Harry Sumnall declares received personal payments for consultancy from AlphaSights and sits on the MIND foundation Scientific Advisory Group; he also declares funding from the NIHR-PRP (NIHR 202988). Charlotte Walker: none declared.
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HTA programme or the Department of Health and Social Care.
References
- Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, et al. Comorbidity of mental disorders with alcohol and other drug abuse: results from the Epidemiologic Catchment Area (ECA) study. JAMA 1990;264:2511-8.
- Menezes PR, Johnson S, Thornicroft G, Marshall J, Prosser D, Bebbington P, et al. Drug and alcohol problems among individuals with severe mental illness in south London. Br J Psychiatry 1996;168:612-9.
- Adams MW. Comorbidity of mental health and substance misuse problems: a review of workers’ reported attitudes and perceptions. J Psychiatr Ment Health Nurs 2008;15:101-8.
- McGovern MP, Xie H, Segal SR, Siembab L, Drake RE. Addiction treatment services and co-occurring disorders: prevalence estimates, treatment practices, and barriers. J Subst Abuse Treat 2006;31:267-75.
- Popovic D, Benabarre A, Crespo JM, Goikolea JM, Gonzalez-Pinto A, Gutierrez-Rojas L, et al. Risk factors for suicide in schizophrenia: systematic review and clinical recommendations. Acta Psychiatr Scand 2014;130:418-26.
- Fazel S, Buxrud P, Ruchkin V, Grann M. Homicide in discharged patients with schizophrenia and other psychoses: a national case-control study. Schizophr Res 2010;123:263-9.
- Witt K, van Dorn R, Fazel S. Risk factors for violence in psychosis: systematic review and meta-regression analysis of 110 studies. PLOS ONE 2013;8.
- Wright S, Gournay K, Glorney E, Thornicroft G. Dual diagnosis in the suburbs: prevalence, need, and in-patient service use. Soc Psychiatry Psychiatr Epidemiol 2000;35:297-304.
- McCrone P, Menezes PR, Johnson S, Scott H, Thornicroft G, Marshall J, et al. Service use and costs of people with dual diagnosis in South London. Acta Psychiatr Scand 2000;101:464-72.
- Robson D, Keen S, Mauro P. Physical health and dual diagnosis. Adv Dual Diagn 2008;1:27-32.
- Fazel S, Khosla V, Doll H, Geddes J. The prevalence of mental disorders among the homeless in western countries: systematic review and meta-regression analysis. PLOS Med 2008;5.
- Weaver T, Rutter D, Madden P, Ward J, Stimson G, Renton A. Results of a screening survey for co-morbid substance misuse amongst patients in treatment for psychotic disorders: prevalence and service needs in an inner London borough. Soc Psychiatry Psychiatr Epidemiol 2001;36:399-406.
- Hunt GE, Siegfried N, Morley K, Brooke-Sumner C, Cleary M. Psychosocial interventions for people with both severe mental illness and substance misuse. Cochrane Database Syst Rev 2019;12.
- Horsfall J, Cleary M, Hunt GE, Walter G. Psychosocial treatments for people with co-occurring severe mental illnesses and substance use disorders (dual diagnosis): a review of empirical evidence. Harv Rev Psychiatry 2009;17:24-3.
- Drake RE, Mercer-McFadden C, Mueser KT, McHugo GJ, Bond GR. Review of integrated mental health and substance abuse treatment for patients with dual disorders. Schizophr Bull 1998;24:589-608.
- Petrakis M, Robinson R, Myers K, Kroes S, O’Connor S. Dual diagnosis competencies: a systematic review of staff training literature. Addict Behav Rep 2018;7:53-7.
- Department of Health . Mental Health Policy Implementation Guide: Dual Diagnosis Good Practice Guide 2002.
- Care Services Improvement Programme . Mental Health NSF Autumn Assessment 2007 – Dual Diagnosis Themed Review 2008.
- National Institute for Health and Care Excellence (NICE) . Coexisting Severe Mental Illness and Substance Misuse: Community Health and Social Care Services 2016.
- Public Health England . Better Care for People With Co-Occurring Mental Health and Alcohol Drug Use Conditions – A Guide for Commissioners and Providers 2017.
- NHS England . Community Mental Health Framework 2019.
- Home Office . From Harm to Hope. A 10 Year Drugs Plan to Cut Crime and Save Lives 2022.
- Dame Carol Black . Review of Drugs Part Two: Prevention, Treatment, and Recovery 2021.
- Northern Ireland Department of Health . Preventing Harm, Empowering Recovery: A Strategic Framework to Tackle the Harm from Substance Use (2021–31) 2021.
- Population Health Directorate . Mental Health Strategy 2017–2022 2017.
- Population Health Directorate . Rights, Respect and Recovery. Alcohol and Drug Treatment Strategy 2018.
- Health and Social Services . Substance Misuse Delivery Plan 2019–2022 ‘Improving Lives for People and Communities Affected by Substance Misuse’ 2019.
- Pawson R, Tilley N. Realistic Evaluation. London: SAGE Publications Ltd; 1997.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist syntheses. BMC Med 2013;11.
- Wong G, Westhorp G, Greenhalgh J, Manzano A, Jagosh J, Greenhalgh T. Quality and reporting standards, resources, training materials and information for realist evaluation: the RAMESES II project. Health Serv Deliv Res 2017;5:1-108.
- Shearn K, Allmark P, Piercy H, Hirst J. Building Realist Program Theory for Large Complex and Messy Interventions. Int J Qual Methods 2017;16. https://doi.org/10.1177/1609406917741796.
- Booth A, Wright J, Briscoe S. Doing Realist Research. London: SAGE Publications Ltd; 2018.
- Pawson R. Evidence Based Policy. London: SAGE Publications Ltd; 2006.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist synthesis: an introduction. ESRC Res Methods Program 2004;2.
- Booth A, Harris J, Croot E, Springett J, Campbell F, Wilkins E. Towards a methodology for cluster searching to provide conceptual and contextual ‘richness’ for systematic reviews of complex interventions: case study (CLUSTER). BMC Med Res Methodol 2013;13.
- Monaghan M, Dalkin S, Emmell N, Greenhalgh J, Manzano A. Doing Realist Research. London: SAGE Publications Ltd; 2019.
- Byng R, Norman I, Redfern S. Using Realistic Evaluation to Evaluate a Practice-level Intervention to Improve Primary Healthcare for Patients with Long-term Mental Illness. Evaluation 2005;11:69-93. https://doi.org/10.1177/1356389005053198.
- Manzano A. The craft of interviewing in realist evaluation. Evaluation 2016;22:342-60.
- Harris J, Dalkin S, Jones L, Ainscough T, Maden M, Bate A, et al. Achieving integrated treatment: a realist synthesis of service models and systems for 2 co-existing serious mental health and substance use conditions. Lancet Psychiatry n.d.;108):632-43.
- Groenkjaer M, de Crespigny C, Liu D, Moss J, Cairney I, Lee D, et al. ‘The chicken or the egg’: barriers and facilitators to collaborative care for people with comorbidity in a metropolitan region of South Australia. Issues Ment Health Nurs 2017;38:18-24.
- Pinderup P, Thylstrup B, Hesse M. Critical review of dual diagnosis training for mental health professionals. Int J Ment Health Addict 2016;14:856-72.
- Kay-Lambkin FJ, Baker AL, Lewin TJ. The ‘co-morbidity roundabout’: a framework to guide assessment and intervention strategies and engineer change among people with co-morbid problems. Drug Alcohol Rev 2004;23:407-23.
- Minkoff K. Developing welcoming systems for individuals with co-occurring disorders: the role of the comprehensive continuous integrated system of care model. J Dual Diagn 2004;1:65-89.
- Bell R. A multi-agency evaluation of the Leeds Dual Diagnosis care co-ordination protocol. Adv Dual Diagn 2014;7:162-84.
- Mee-Lee D. Treatment planning for dual disorders. Psychiatr Rehabil Ski 2001;5:52-79.
- Renner JA, Quinones J, Wilson A. Training psychiatrists to diagnose and treat substance abuse disorders. Curr Psychiatry Rep 2005;7:352-9.
- Danda MC. Attitudes of health care professionals towards addictions clients accessing mental health services: what do we know and how can this be used to improve care?. J Ethics Mental Health 2012;7:1-5.
- Avery J, Dixon L, Adler D, Oslin D, Hackman A, First M, et al. Psychiatrists’ attitudes toward individuals with substance use disorders and serious mental illness. J Dual Diagn 2013;9:322-6.
- Graham HL. Coexisting severe mental health and substance use problems: developing integrated services in the UK. Psychiatric Bull 2004;27:183-6.
- Roberts BM, Maybery D. Dual diagnosis discourse in Victoria Australia: the responsiveness of mental health services. J Dual Diagn 2014;10:139-44.
- Canaway R, Merkes M. Barriers to comorbidity service delivery: the complexities of dual diagnosis and the need to agree on terminology and conceptual frameworks. Aust Health Rev 2010;34:262-8.
- Hind A, Manley D. Stamp Out Stigma campaign: challenging attitudes to support and build a recovery-orientated ethos in substance misuse, mental health and dual diagnosis services. Adv Dual Diagn 2010;3:23-5.
- Lawrence-Jones J. Dual diagnosis (drug/alcohol and mental health): service user experiences. Practice 2010;22:115-31.
- Sorsa M, Greacen T, Lehto J, Astedt-Kurki P. A qualitative study of barriers to care for people with co-occurring disorders. Arch Psychiatr Nurs 2017;31:399-406.
- Bjorkquist C, Hansen GV. Reducing service barriers to people with dual diagnosis in Norway. Cogent Soc Sci 2018;4.
- Annamalai A, Staeheli M, Cole RA, Steiner JL. Establishing an integrated health care clinic in a community mental health center: lessons learned. Psychiatr Q 2018;89:169-81.
- Davidson L, Evans AC, Achara-Abrahams I, White W. Beyond co-occurring disorders to behavioral health integration. Adv Dual Diagn 2014;7:185-93.
- Hodges CL, Paterson S, Taikato M, McGarrol S, Crome I, Baldacchino A. Substance Misuse Research Co-morbid Mental Health and Substance Misuse in Scotland. Edinburgh: Scottish Executive; 2006.
- Barnes L, Rudge T. Co-operation and co-morbidity: managing dual diagnosis in rural South Australia. Collegian 2003;10:25-8. https://doi.org/10.1016/s1322-7696(08)60051-7.
- Manley DS. What helps and what hinders recovery: narratives of service users and practitioners about dual diagnosis (co-existing mental health and substance misuse problems). PhD Thesis 2015. https://eprints.nottingham.ac.uk/30662 (accessed 19 August 2024).
- Louie E, Giannopoulos V, Baillie A, Uribe G, Byrne S, Deady M, et al. Translating evidence-based practice for managing comorbid substance use and mental illness using a multimodal training package. J Dual Diagn 2018;14:111-9.
- Drake RE, Bond GR. Implementing integrated mental health and substance abuse services. J Dual Diagn 2010;6:251-62.
- Devitt TS, Davis KE, Kinley M, Smyth J. The evolution of integrated dual disorders treatment at thresholds: lessons learned. Am J Psychiatr Rehabili 2009;12:93-107.
- Blakely TJ, Dziadosz GM. Creating an agency integrated treatment program for co-occurring disorders. Am J Psychiatr Rehabili 2007;10:1-18.
- Hepner KA, Hunter SB, Paddock SM, Zhou AJ, Watkins KE. Training addiction counselors to implement CBT for depression. Adm Policy Ment Health 2011;38:313-23.
- Graham HL. Implementing integrated treatment for co-existing substance use and severe mental health problems in assertive outreach teams: training issues. Drug Alcohol Rev 2004;23:463-70.
- Boyle P, Wieder B. Creating and sustaining integrated dual diagnosis treatment programs: some lessons learned in Ohio. J Dual Diagn 2007;3:103-10.
- Leijten FRM, Struckmann V, van Ginneken E, Czypionka T, Kraus M, Reiss M, et al. SELFIE Consortium . The SELFIE framework for integrated care for multi-morbidity: development and description. Health Policy 2018;122:12-2.
- Baldacchino A, Greacen T, Hodges CL, Charzynska K, Sorsa M, Saias T, et al. Nature, level and type of networking for individuals with dual diagnosis: a European perspective. Drugs Educ Prev Policy 2010;18:393-401.
- Barreira P, Espey B, Fishbein R, Moran D, Flannery Jr RB. Linking substance abuse and serious mental illness service delivery systems: initiating a statewide collaborative. J Behav Health Serv Res 2000;27:107-13.
- Barrett P, Roberts S. Enhancing dual diagnosis capacities in acute inpatient nurses: a practitioner-based action research project. Adv Dual Diagn 2010;3:24-31.
- Anderson S, Hennessy C, Cornes M, Manthorpe J. Developing inter-disciplinary and inter-agency networks: reflections on a ‘community of practice’ approach. Adv Dual Diagn 2013;6:132-44.
- Biegel DE, Kola LA, Ronis RJ, Boyle PE, Delos Reyes CM, Wieder B, et al. The Ohio substance abuse and mental illness coordinating center of excellence: implementation support for evidence-based practice. Res Soc Work Pract 2003;13:531-45.
- Clodfelter Jr RC, Albanese MJ, Baker G, Domoto K, Gui AL, Khantzian EJ. The MICA case conference program at Tewksbury Hospital, Massachusetts: an integrated treatment model. Am J Addict 2003;12:448-54.
- Swinden D, Barrett M. Developing a dual diagnosis role within mental health. Nurs Times 2008;104:26-7.
- Holland M. Substance use and mental health problems: meeting the challenge. Br J Nurs 1998;7:896-900.
- Engelhardt MA, Hills H, Monroe M. Comprehensive, continuous, integrated system of care development: Tampa-Hillsborough County, Florida. J Dual Diagn 2009;5:110-6.
- Bjorkquist C, Hansen GV. Coordination of services for dual diagnosis clients in the interface between specialist and community care. J Multidiscip Healthc 2018;11:233-43.
- Currie J. Review of dual diagnosis commissioning in the North West of England. Adv Dual Diagn 2011;4:135-40.
- Graham HL, Copello A, Birchwood M, Orford J, McGovern D, Georgiou G, et al. Service innovations: coexisting severe mental health and substance use problems: developing integrated services in the UK. Psych Bull 2003;27:183-6.
- Copello A, Graham H, Birchwood M. Evaluating substance misuse interventions in psychosis: the limitations of the RCT with ‘patient’ as the unit of analysis. J Ment Health 2001;10:585-7.
- Anastas T, Waddell EN, Howk S, Remiker M, Horton-Dunbar G, Fagnan LJ. Building behavioral health homes: clinician and staff perspectives on creating integrated care teams. J Behav Health Serv Res 2019;46:475-86.
- Chichester CS, Bepko C, Ogden J, Hornby H, McAuley K. Implementing an integrated system of care model in the state of Maine. J Dual Diagns 2009;5:436-46.
- Scottish Drug Deaths Taskforce . Changing Lives 2022.
- Graham HL, Copello A, Griffith E, Freemantle N, McCrone P, Clarke L, et al. Pilot randomised trial of a brief intervention for comorbid substance misuse in psychiatric in-patient settings. Acta Psychiatr Scand 2016;133:298-309.
- Center for Substance Abuse Treatment . Chapter 2, Building a Trauma-informed Workforce. Trauma-Informed Care in Behavioral Health Services 2014;57.
- National Improvement and Leadership Development Board . Developing People – Improving Care. A National Framework for Action on Improvement and Leadership Development in NHS-Funded Services 2010.
- NHS Confederation . Running Hot: The Impact of the Pandemic on Mental Health Services 2022.
Appendix 1 Search strategy
| Population | |
| SMI | Conditions that affect daily functioning and quality of life as well as requiring long-term support from services. Such as: |
| AND |
|
| Use of alcohol and/or drugs | Illegal drugs include heroin, cocaine, cannabis, cannabinoid receptor agonists and other novel psychoactive drugs as well as non-medical use of medicines and solvents |
| Intervention | |
A dual diagnosis:
|
|
| [PHE identify four service formats – integrated care, collaborative care, the care programme approach (CPA) and specialist dual diagnosis teams] | |
| English language High-income countries Adult populations (age 14 years and over according to PHE/NICE) |
| Search concepts | a. Broad terms | b. Specific/narrower terms |
|---|---|---|
|
‘mentala illa’ OR ‘mentala disordera’ OR ‘mentala diseasea’ OR ‘mental health’ OR psychiatric | schizoa OR psychotica OR psychosis OR psychoses OR bipolar OR majordepressive OR ‘major depressive’ |
|
(druga OR polydruga OR substancea OR alcohola OR tranquila OR chemicala OR narcotica OR opiata OR street druga OR solventa OR inhalanta OR psychotropica OR intoxicaa) AND (abusa OR usea OR misusa OR usina OR utiliza OR utilisa OR dependa OR addicta OR illegala OR illicita OR habita OR withdrawa OR behavia OR abstinencea OR abstaina OR rehaba OR intoxicaa OR non-prescria) | ((substance OR alcohol OR amphetamine OR cannabis OR opioid) AND (‘use disordera’ OR abusea OR dependena)) OR addicta |
|
co-occura OR co-morbida OR comorbida OR co-exista | ‘duala diagnosa’ |
|
(‘trauma informed’ OR ‘psychologically informed’ OR integrata OR mainstreama OR coordinata OR co-ordinata OR linka OR intersectorala OR multiagency OR multi-agency OR interagency OR inter-agency OR partnershipa) AND (system OR programa OR care OR servicea OR modela OR interventiona) | ‘Psychologically Informed Environmenta’ OR ‘Trauma Informed Care’ OR PIE OR TIC |
|
High Income Countries (not operationalised as filter, but identified through screening) | Great Britain OR United Kingdom OR England etca Ireland OR Eire OR Australiaa OR Canada OR (New Zealanda) OR (United States OR USA) OR (North Americaa) |
List of abbreviations
- CCG
- clinical commissioning group
- CCMOC
- conjectured context–mechanism–outcome configurations
- CMHT
- community mental health team
- CMO
- context–mechanism–outcome
- CMOC
- context–mechanism–outcome configurations
- COMHAD
- co-occurring mental health and alcohol/drug conditions
- CPD
- continuous workforce development
- EI
- Early Intervention (for Psychosis)
- IAPT
- Improving Access to Psychological Therapies
- IPT
- initial programme theory
- KPI
- key performance indicators
- MDT
- multidisciplinary team
- NICE
- National Institute for Health and Care Excellence
- PT
- programme theory
- RECO
- realist evaluation co-occurring (mental health and alcohol/drug conditions) – the study acronym
- SMI
- serious mental illness
- WP
- work package
Notes
-
Achieving Integrated Treatment: A realist synthesis of service models and systems for co-existing serious mental health and substance use conditions
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/JTNT0476).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
