Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as award number HTA NIHR130177. The contractual start date was in January 2021. The draft manuscript began editorial review in July 2023 and was accepted for publication in November 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Gray et al. This work was produced by Gray et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Gray et al.
Chapter 1 Introduction
Background
Children and adolescents with learning disabilities are at increased risk of developing mental health problems, including anxiety, compared to their typically developing peers. 1,2 The estimated prevalence of specific phobia in children and adolescents with learning disabilities ranges from 1.9 to 17.5%. 2–4 In contrast, estimates of phobias in children in the general population range from 5 to 9%. 5 In direct comparison studies, children and adolescents with learning disabilities are at least twice as likely to experience specific phobia than their typically developing peers. 2
In typically developing populations, specific phobias usually first present in childhood and are associated with an increased risk of developing lifetime psychiatric disorders, particularly anxiety disorders. 6,7 Despite high rates of specific phobia in children and adolescents with learning disabilities, rates of treatment are low. In one study, only 2.4% of children with learning disabilities and a specific phobia had received treatment for their phobia. 3
Building the Right Support outlines the plan for England to develop better community-based services for people with learning disabilities with mental health difficulties. 8 The service model specifies that all individuals with learning disabilities and/or autism should be offered both mainstream and specialist NHS healthcare services as needed, including mental health treatments. While there are well-developed, evidence-based interventions for the general population, such an evidence base is lacking for children and adolescents with moderate to severe learning disabilities. Our recent review of mental health treatments for people with severe learning disabilities failed to find good evidence for any psychological treatment for anxiety, including specific phobia. 9 Despite significant need, there is a lack of research evidence to guide treatment for children with learning disabilities and specific phobia.
Specific phobias have a significant impact on children and families, resulting in considerable impairment. For example, phobias associated with medical procedures can result in the need for anaesthesia or sedation for routine procedures and check-ups, blood/injury/injection phobias make vaccinations and blood tests difficult and can compromise health care, and dog phobias can result in risky behaviour when dogs are encountered in the community. 10
Only a minority of children and adolescents with learning disabilities and significant mental health difficulties are likely to receive mental health services. 11,12 However, costs are high due to the overall need for more services, and increase when young people also have behaviour and emotional problems. 13–15 Effective early interventions and mental health supports have the potential to reduce longer-term care costs. 13,14
The needs of children and adolescents with learning disabilities have been identified as a research priority and a priority service area by NHS England. 16,17 Psychological interventions for mental health problems in children with learning disabilities have been identified as a top 10 research priority. 18 NHS England19 has also highlighted that research must reduce health inequalities among patients, which is of direct relevance to individuals with moderate to severe learning disabilities who face a double inequality (existing health inequalities coupled with a lack of evidence about how to reduce these).
There is evidence to support the use of cognitive behavioural therapy (CBT) and graded exposure to treat specific phobias in typically developing children and children with autism without learning disabilities. 20–23 These interventions focus on both cognitive and behavioural strategies; require good verbal communication, abstract thinking and affect labelling skills; and, in the case of internet-delivered interventions, require independent learning skills. Depending on associated impairments, individuals with learning disabilities may present with significant communication difficulties, including difficulties in articulation and phonology affecting speech intelligibility; morphosyntax affecting sequencing of ideas in utterance; lexicon affecting vocabulary and understanding for meaning; and discourse and pragmatics affecting social use and function of communication. 24,25 The high prevalence of motor and sensory differences also needs to be taken into account. 26,27 As such, existing interventions focusing on both cognitive and behavioural strategies are typically not appropriate or fully accessible for children and adolescents with moderate to severe learning disabilities.
Although National Institute for Health and Care Excellence (NICE) guidance recommends guided exposure for the treatment of specific phobia in people with learning disabilities, NICE found very little high-quality evidence about interventions for mental health problems in children with learning disabilities,28 resulting in a call for more research evidence. Our group has recently completed a systematic review of interventions for mental health problems for children and adults who have severe learning disabilities (including those who are autistic). 9 Very few studies met the eligibility criteria for inclusion, and those evaluating psychological therapies made use of minimal-quality single-case experimental designs – with a resulting poor current evidence base.
Rationale for the current study
The research literature on the treatment of specific phobia consists largely of single-case design studies and small non-controlled trials to treat dog phobia. 10,29–31 There is a clear need for the development and evaluation of interventions for children with moderate to severe learning disabilities and a broad range of specific phobias.
Aims and objectives
This research aimed to develop, and evaluate the feasibility of, an exposure-based intervention for specific phobia in children and adolescents with moderate to severe learning disabilities. This work was undertaken in two phases: (1a) intervention development and (1b) description of treatment as usual (TAU); and (2) evaluation of the feasibility of the proposed intervention.
Phase 1a: intervention development
The objectives were to:
-
establish an Intervention Development Group (IDG), and using coproduction over a series of meetings, develop an intervention for specific phobia for use with children and adolescents who have moderate to severe learning disabilities and a range of specific phobias, with or without autism
-
develop a treatment fidelity checklist to be used alongside the intervention manual
-
appraise and consider several candidate outcome measures of anxiety-related symptoms, and secondary outcomes, and make a recommendation for use within phase 2.
Phase 1b: description of treatment as usual
The objective was to describe the current standard treatment provided for children and adolescents with moderate to severe learning disabilities and specific phobia within the UK.
Phase 2: feasibility study
The objectives were to:
-
explore recruitment pathways
-
evaluate the manualised intervention to determine the acceptability and feasibility for all stakeholders, including children and young people, carers and therapists
-
review the appropriateness of proposed measures of anxiety-related symptomatology, and secondary outcomes, for use within a larger study
-
describe factors that challenge or facilitate the implementation of the intervention (e.g. comorbid behaviour problems, other mental health problems, community resources to support exposure)
-
determine the feasibility and acceptability of consent and associated processes
-
determine the acceptability of randomisation in a future trial
-
describe the parameters of a future study to examine the effectiveness of exposure-based therapy to treat phobias in this population.
Chapter 2 Intervention development
Theoretical framework
Phobias are generally considered to be learned fears, acquired through direct conditioning, vicarious conditioning (fear learned by observing the fear of others) or the transmission of information and/or instructions. 32,33 Fear usually builds up gradually, rather than being the sole consequence of a single traumatic event, and typically develops as a result of repeated frightening experiences and/or through social learning. 34 Behavioural treatment of fears stems largely from the work of Wolpe on systematic desensitisation. 35 It is based on the hypothesis that the fear is learned, and can therefore be unlearned and replaced with more adaptive reactions to the fear stimulus. This is achieved through exposure to the feared object that is graded (gradual). By reversing the desire to escape, withdraw or avoid the phobic stimulus, the person learns that the situation is not dangerous. Graded exposure, combined with positive reinforcement, therefore breaks the cycle of fear and avoidance that maintains the fear symptoms. 34
Cognitive behavioural therapy and graded exposure is the intervention of choice for specific phobia. 36 It is effective in treating specific phobias in typically developing children and adolescents. 37,38 There is evidence to support the use of CBT and graded exposure to treat specific phobias in autistic children without learning disabilities. 20–23 However, these interventions focus on both cognitive and behavioural strategies; require good verbal communication, abstract thinking and affective labelling skills; and, in the case of internet-delivered interventions, require independent learning skills. As such, these interventions are not appropriate or accessible for children and adolescents with moderate to severe learning disabilities.
Although NICE guidance recommends guided exposure for the intervention of specific phobia in people with learning disabilities,28 research in this area is sparse. The research literature on the intervention of specific phobia consists largely of single-case design studies and small non-controlled trials to treat dog phobia. 10,29–31
Co-applicant Williams developed an exposure-based intervention for children with severe learning disabilities and limited communication skills, and through a series of case studies demonstrated successful intervention delivery and outcomes. 10,29 This intervention, which is already designed to accommodate the necessary augmented communication strategies, as well as addressing behavioural, repetitive and sensory difficulties often experienced by this population, informed the development of the first draft manual for the SPIRIT intervention. Together with the IDG, this manual and accompanying materials were then reviewed and revised (phase 1a).
Methods
Recruitment
The IDG comprised six key stakeholders: a representative from the Foundation for People with Learning Disabilities (our PPI partner), two parents of children with learning disabilities and specific phobias, and three clinicians with experience of working with children and young people with learning disabilities and anxiety. Seven members of the research team had a background in psychology; other members had clinical backgrounds in child psychiatry and speech and language therapy. Members of the IDG were recruited by the Foundation for People with Learning Disabilities (PPI partner) and through the clinical networks of the research team.
Design
The IDG worked collaboratively over a series of five meetings over 2 months. Meetings were scheduled every 2 weeks, with the exception of the last two meetings which were 1 week apart. All meetings were online. The aims of the IDG were to:
-
define the needs and problems that are to be addressed for children and adolescents with moderate to severe learning disabilities and specific phobia
-
define the intervention objectives, with reference to likely barriers
-
review and revise proposed manualised intervention
-
develop a logic model
-
develop a fidelity checklist, based on approaches that have been successful in our recent learning disabilities trials within UK NHS settings39
-
advise on recruitment pathways
-
establish how to measure outcomes
-
consider the challenges/barriers to our evaluation plan, including likely solutions.
A draft intervention manual, materials, logic model, therapist training outline and the fidelity checklists were developed prior to the first IDG meeting (see Chapter 3). Three of the five IDG meetings focused on the intervention manual and corresponding materials, one on the fidelity checklists, logic model and therapist training, and one on outcome measures. Table 1 shows a detailed schedule of the IDG meetings.
| Meeting 1 |
|
| Meeting 2 |
|
| Meeting 3 |
|
| Meeting 4 |
|
| Meeting 5 |
|
The materials for each meeting were provided to all members at least 1 week prior to the meeting. Feedback was sought at each meeting, and following reflection, subsequent refinements were made to the manual, logic model, materials and the fidelity checklists by the research team that were then presented to the IDG at the next meeting for discussion. Any disagreements were discussed until consensus was reached. All changes and subsequent actions were recorded in a Microsoft Excel® (Microsoft Corporation, Redmond, WA, USA) spreadsheet which was shared with the IDG for approval. Feedback was also sought on a range of candidate outcome measures. The IDG were invited to make the final recommendation as to which outcome measures should be used within phase 2 of the study.
Results
Objective 1: SPIRIT intervention development
To develop the initial draft of the SPIRIT intervention manual, we drew on co-applicant Williams’s intervention for dog phobia in adolescents with severe learning disabilities and little to no speech. 10,29
The SPIRIT intervention was designed by the research team to be developmentally appropriate for use with both children and adolescents with moderate to severe learning disabilities, and with phobias related to any specific stimulus, as defined by the DSM-5 (animal, natural environment, blood-injection-injury, situational, other). 40 The intervention also included extended support for communication difficulties. A number of materials were developed to accompany the therapist intervention manual, together with a workbook for parents/carers.
The intervention is parent-mediated, with initial parent skills training and therapist support. The SPIRIT intervention consisted of two parts: (1) two parent/carer skills training group workshops (two half-days); and (2) weekly therapist support sessions with individual parents/carers over 8 weeks.
Following feedback from the IDG, revisions were made to the intervention manual and materials. See Chapter 3 for a detailed description of the SPIRIT intervention and accompanying materials.
Tables 2–8 summarise changes proposed to the intervention manual and materials by the IDG and how they were addressed.
| IDG feedback/suggestions | Action |
|---|---|
| General feedback | |
| Offer parents/carers a choice regarding when they would like to attend the skills training workshop and provide flexibility with timing. | We will consult with parents/carers within the treatment group and find a mutually convenient time. |
| Include regular monthly reviews with the therapist. | Parents/carers will have weekly support sessions with the therapist for 8 weeks following the initial training. |
| Simplify the language in the therapist intervention manual. | We have used vocabulary known to clinicians/therapists working in learning disabilities services. Where applicable we have added definitions in text boxes. |
| Add more definitions to the intervention manual. | Completed. |
| Add real-life examples. | Real-life examples added. More will be added after the study is finished based on experiences/feedback of the participating families and therapists. |
| Recheck the manual for spelling. | Completed. |
| Define vocabulary in tables or thought bubbles. | Completed. |
| Add a page of key terms. | We have added text boxes with definitions throughout the manual. |
| Restructure the manual: 1. general introduction to the problem; 2. the guiding framework/logic model; 3. the intervention itself that operationalises the aspects of the logic model; 4. All supporting concepts and session materials. | Completed. |
| IDG feedback/suggestions | Action |
|---|---|
| Restructure the manual: 1. general introduction to the problem; 2. the guiding framework/logic model; 3. the intervention itself that operationalises the aspects of the logic model; 4. All supporting concepts and session materials. | Completed. |
| Develop a resource bank including materials written in simple language, video materials, images and practical examples. | Completed. |
| Add a section on potential harms resulting from the intervention. | This information is included in the participant information sheet. We considered including this in the manual as well, but we decided it was best suited to the participant information sheet. However, discussion of all potential issues related to the intervention was added to the therapist training workshop. |
| Add a section on how likely it is that a behaviourist approach is going to work for an autistic person. | Explained in the section on theoretical background of the intervention. |
| Add the page explaining the role of the introduction and the theoretical section. | Completed. |
| Add a clear general framework/logic model that is informing the intervention and helping therapists make sense of the approach. | Completed. |
| Develop a script with practical suggestions on relaxation. | Adaptations to the relaxation strategies are included in the session on relaxation and in the parent workbook. This also includes consideration that for some young people traditional relaxation exercises might not be helpful and other strategies should be considered. |
| Emphasise the importance of rapport building and trust building. | Completed. |
| Emphasise the importance of a person-centred approach. | Completed. |
| IDG feedback/suggestions | Action |
|---|---|
| Support the section on reinforcement with practical examples. | Completed. |
| Explain the concepts of differential reinforcement of other behaviour, differential reinforcement of incompatible behaviour, and differential reinforcement of alternative behaviour in more depth and support them with practical examples. | Completed. |
| Rephrase the section on reinforcement effectiveness. | Completed. |
| Consider moving the toolkit to the appendix or add more explanation in the ‘How to use the manual’ section. | Was considered, but decided the toolkit should be part of the main body of the manual to ensure therapists read it. Added additional explanation on how the toolkit fits with the rest of the manual to the ‘How to use the manual’ section. |
| Delete section on active support. | Completed. |
| IDG feedback/suggestions | Action |
|---|---|
| Add more explanation and examples. | Completed. |
| Develop additional training handout with more information on each point covered in the ‘Considerations for working with young people with moderate to severe intellectual disabilities and their parents’ section. | Completed. |
| Rephrase good practice guidelines so that it is expressed as ‘do this’ or ‘do that’ rather than ‘It is important that’. | Was considered; however, felt this wording not appropriate. Revised to further emphasise the importance of the good practice guidance. |
| Specify ‘preferences and needs’. | Completed. |
| Add that it is important that the staff working with the young person know how to use the person’s communication aids effectively. | Completed. |
| Add that it is important to establish how the person communicates ‘stop’, ‘no’, ‘enough’ and requests a break. | Completed. |
| Add that it is important to ensure communication is adapted to the needs of the individual. | Completed. |
| To rephrase ‘keeping well’. | Reviewed and discussed; however, decision made by the IDG to retain this phrase. |
| IDG feedback/suggestions | Action |
|---|---|
| Consider how to communicate the content of the training to parents/carers who are not attending, especially if parents are separated. | Information added. |
| Consider when to introduce the rationale of the intervention (exposure but also indirect work with parents) and how to highlight it in the manual. | The rationale is first introduced in the ‘Intervention structure and rationale’ section and then further discussed in ‘Introduction to exposure therapy’. We have added a brief rationale for upskilling parents/carers in the ‘Introduction’ section. |
| Consider how to address potential anxiety of parents/carers. | Relevant information added. |
| Provide more rationale for upskilling parents/carers rather than doing direct work. | Completed. |
| Consider how to address potential concerns of parents/carers about their role in the treatment (e.g. confidence). Provide space for parents/carers to discuss this together at the beginning of the training and consider any barriers. | Discussed in the ‘Considerations for working with parents’ section. Parents were asked how they feel about their role in the intervention during the introduction section and had ample opportunities to discuss this further in small groups during the remainder of the workshop. |
| Highlight working together to improve family life. | Completed. |
| Add that exposure as a gradual approach is for everybody, not only the child. | Completed. |
| Rethink wording such as ‘neurotypical’ or ‘comorbid’. | As the intervention manual is intended for clinicians, concluded wording is appropriate. Wording not used in the parent/carer materials. |
| Consider adding a content warning to the video on different types of specific phobias. | Completed. |
| Perhaps the video could be a homework task for those who feel comfortable watching it. | Considered; however, decision was made to keep it as an activity completed during the workshop as facilitates discussion if parents/carers have just watched the video. A content warning was added, and parents/carers were asked to watch it on their own devices. |
| Perhaps ask people to watch the video on their own device, instead of showing it to the whole group. | Completed. |
| Consider other ways of illustrating the discussion on types of phobias and their impact for parents/carers who do not want to watch the video. | Parents/carers who do not want to watch the video are encouraged to reflect on situations when they felt afraid. The aim of this activity is to illustrate the impact of the specific phobia on their child and not only on family unit. |
| Rethink phrase ‘faulty thinking’. | Phasing changed. |
| Define specific phobia more clearly – clarify how this differs from being frightened/anxious about something or because of sensory needs or situations where an element of being afraid is ‘expected’. | Completed. |
| Rethink examples of different types of specific phobias (e.g. not animal-related, environmental, dental). | Completed. |
| Consider including a topographical definition of each type of specific phobia. Define what it looks like from a parent/carer point of view. | This is covered in the ‘Symptoms of specific phobia in young people with learning disabilities’ section. |
| Consider adding a clip of parent/carer talking about the impact of specific phobia on their child and family or a case study. | Considered, but not possible due to time and budgetary restrictions. To be considered for future work with the intervention. Parents/carers had opportunities to discuss the impact of their child’s phobia in small groups throughout the workshops. |
| Rethink materials used in the intervention manual and parent workbook to be more inclusive. | Completed. |
| Emphasise the flight concept in anxiety problems. | Completed. |
| Add how to communicate the training content to the parent/carer not attending the training. | Information added. |
| Consider how to communicate content of the training to the school the young person is attending, grandparents and break carers. Talking to parents/carers about who needs to know about the intervention. | Information added to the manual. Created a document called ‘Information Sheet for Other Carers’ that can be passed on to carers, other family members or school. |
| Rethink title of the ‘Motivation’ section (e.g. ‘Reinforcement’). | Name of the section changed to ‘Reinforcement’. Added a section called ‘How phobias develop’. |
| Make the link between reinforcement and preference assessment clearer. | Completed. |
| Emphasise that the exposure plan will be gradual and achievable for the young person so there will be opportunities to use reinforcement. | Completed. |
| Emphasise that the intervention focuses on gradual approximations to the target – so that there is always reinforcement available. | Completed. |
| Mention slow and fast triggers. | Completed. |
| Include a section on the child avoiding an anxiety-provoking event or engaging in other behaviours to reduce anxiety. | Completed. |
| Make distinction between reinforcement and bribery/reward clear. | Completed. |
| Rethink placement of group activity 5. | Considered different placements of this activity, but concluded the current placement works best for the flow of this section. |
| More time might be needed to introduce the preference assessment. | Added an additional 15 minutes to be spent on the ‘Reinforcement’ and ‘How phobias develop’ sections. Changed group activity 6 from practice in pairs to demonstration by the therapist to save time and be helpful to the parents/carers overall. |
| Add an example of the completed preference assessment in the parent workbook. | Completed. |
| Add a text box at the end of the preference assessment form which allows parents/carers to say anything else they would like to mention about their child’s phobia which has not been covered; that is, things which do not fit into the previous questions. It may give a fuller picture or allow them to express their concerns. | Completed. |
| Think about putting each type of reinforcement in the box or presenting it differently so the distinction is clearer. | Completed. |
| Rethink word ‘contrived’. | Wording changed. |
| Emphasise in the manual how parents/carers are supported and what happens if they feel they cannot continue with the intervention. | This is included in the ‘Introduction’, ‘Intervention structure and rationale’ and ‘Implementation plan’ sections. |
| Consider changing ‘reinforcement strategy’ to ‘reinforcement plan’. | Wording changed. |
| Change word ‘aversive’. | Wording changed. |
| Rethink flow of parent handout on reinforcement. | Completed. |
| Consider giving space for the parents/carers to state for what phobia they are collecting data on the ABC chart. | Completed. |
| Mention in aims of activity 7 child’s existing relaxation strategies. | Completed. |
| Add blowing bubbles, fidget things and sensory items as alternatives to standard relaxation exercises. | Already included in the adaptation section. |
| For parents/carers who have smartwatches – it might be worth asking them to track change in heart rate during activity 7. | Information added. |
| Consider introducing grounding in some form. | Information added. |
| Parent workbook – people with literacy difficulties find it much harder to read text in capitals, and lower case tends to be easiest to read. | Text reformatted. |
| Possibly have a video of a person doing the relaxation exercises for parents/carers to access. | Parents/carers were trying the exercises themselves during the workshop, so did not feel the video was needed. Provided a video on grounding as an option. |
| Add visuals for relaxation. | All visuals needed for relaxation exercises are provided in the image bank that comes with the intervention manual. |
| Consider different visuals so children are using visuals they are familiar with. | Used visuals from ‘Easy on the I’ for consistency. Therapists advised to use different visuals if there was a format the child was already familiar with. |
| Look into resources included in the PELICAN pack. (PELICAN resource from Foundation for People with Learning Disabilities41). | Added a hand massage as per the PELICAN materials as alternative to standard relaxation strategies. |
| Add video on visual schedules. | Completed. |
| Some children might only tolerate visual schedule for the morning or the afternoon rather than the whole day. | Revised this section so the visual schedule will be used during exposure tasks only. |
| IDG feedback/suggestions | Action |
|---|---|
| It might be helpful to talk about the fact that exposure therapy may seem a bit strange, but it does work. Ask people how they have overcome their own fears. | Completed. |
| Rethink name of ‘fear ladder’. | Changed to ‘exposure steps’. |
| Possibly consider a different analogy for the exposure steps. Maybe a mountain, thermometer or a horizontal progress to emphasise that steps should not be getting more scary. Possibly providing parents/carers with a few different analogies/templates to choose from. | Completed. |
| Maybe add an example of success of using exposure therapy to give parents/carers some hope. | After the feasibility study is finished, we will draw on information and learnings to develop case examples to include in future SPIRIT work. |
| Add information about the experience of feeling anxiety being also important. | Completed. |
| Emphasise that intervention is done at child’s pace. | Completed. |
| Sitting in the chair might not be appropriate for everybody for completing exposure steps. ‘Position themselves in a way which is comfortable for them’ is better phrasing. | Completed. |
| Emphasise that parents/carers will be working on the steps at slow pace and adding more steps once started. | Completed. |
| Consider adding some strategies parents/carers can use if they feel anxious themselves about any steps or feel like giving up. Just noticing such feelings may be enough. This may be a potential ‘barrier’ in applying the therapy for parents/carers. Some messages about looking after themselves, but also looking out for their own response. | Information added. |
| Add a picture or image on headings of the parent workbook. | Considered this, but the handout looked too busy with additional visuals. We have incorporated plenty of visuals for the parents/carers throughout all intervention materials. |
| Theoretically you do not need to tolerate exposure steps calmly to master them; you only need to be less anxious than before. | Phasing revised. |
| Change ‘fear evoking’ to ‘frightening’. | Completed. |
| Add to activity 12 that parents/carers should include steps that the child can currently tolerate as the first step. | Completed. |
| Mention that the fear ladder will evolve during the intervention and does not need to be perfect from the beginning. | Completed. |
| Add tips on how to break down the exposure steps. | Completed. |
| Consider suggesting online app to help parents/carers organise exposure steps. | Considered this, but did not find an app that was freely available and appropriately structured for the SPIRIT intervention. |
| Consider Post-It® type of board that parents/carers can move things on. | Created a template of a visual schedule that can be used as a fear ladder. |
| It would be helpful to highlight that for different children, different steps might be needed. Parents’/carers’ expertise will be crucial in designing the fear ladder. | Completed. |
| Add more information on practical issues around exposure to the handout on the fear ladder; for example, completing steps at the dentist. | Completed. |
| Possibly consider adding information about when to review the ladder and break down the steps. | The fear ladder is reviewed every week as part of the weekly support sessions. Information on breaking down exposure steps is in the ‘Troubleshooting’ section. |
| Consider changing ‘reaching mastery’ to ‘reaches goals’. | In the context of behavioural treatment, reaching goals is not a synonym for reaching mastery. As this is in a manual for professionals, the expression is considered appropriate. |
| If exposure needs access to specialist situations, for example dogs or dentist, then daily practice will not be possible. | More information added. |
| Consider asking parents/carers to let their child’s school know that their child has a dog phobia, so dogs are not brought to the school when the child is present. | Developed an information sheet for parents to use with school and in other relevant settings. |
| Add examples of organisations that can help with access to dogs: Pets as Therapy, Guide Dogs, Pets as Therapists. | Information added. |
| Consider adding a ‘partially successful try’ rating to the data sheet. | Completed. |
| On the data sheet – write the first step initially, then add the next step when the previous one is mastered in case you need to make amendments. | Information added. |
| Consider having two sample data sheets – one with all steps completed and one with just one step. | Completed. |
| Emphasise that the data sheet should be shared with the therapist during the weekly check-ins. | Completed. |
| Add to the troubleshooting section about checking how much time is spent on talking about exposure without doing it. | Completed. |
| A section is needed on parents/carers who have problems with anxiety themselves. | Discussed in the ‘Considerations for working with parents’ section. |
| Create a separate troubleshooting handout for parents/carers. Acknowledge that parents will already have some troubleshooting strategies they use regularly with their children, so this is an add-on. | Completed. |
| Add suggestion for the therapists to check when the best time is during the day to do exposure with parents/carers. | Completed. |
| Suggest using the same reinforcement scheme as that used at the child’s school. | Completed. |
| Consider if relaxation is being overemphasised. Could we reword this to techniques to cope with stress? Or ‘Relaxation and calming?’ | Reviewed, but concluded not appropriate in the context of exposure therapy. |
| Add more relaxation adaptations. | Completed. |
| Add suggestions on what to do if parents are struggling to get started. | Completed. |
| Consider adding some guidance for therapists and parents/carers about their avoidance as they are fearful of their child’s reaction and how to support parents. | Discussed in the ‘Considerations for working with parents’ section. |
| IDG feedback/suggestions | Action |
|---|---|
| Add review of the data sheet to the session outline. | Completed. |
| Build in more celebration of success and achievements, perhaps by having a document to record it every week. | Completed. |
| Therapist reminding parents/carers how brave their children are to work on exposure. | Completed. |
| Add congratulations for getting this far to the last support sessions. | Completed. |
| The Keeping Well plan should be available to parents/carers as a hard copy and Word document. | Completed. |
| Building more celebration of success and achievements, especially in the therapist handbook. | Completed. |
The cultural appropriateness of the parent workbook was discussed during consultation with a parent of ethnic minority background. The parent was sent the workbook to review, and met with the Study Manager (SM) and Research Assistant (RA) to discuss. The parent felt that the content did not need any adaptations; the sole suggested change was to include more diversity in the pictures used for parent-facing materials.
Logic model and therapist training
A draft logic model was presented to the IDG. Table 9 summarises proposed changes and actions.
| IDG feedback/suggestions | Action |
|---|---|
| Mechanisms should include antecedent interventions. | Added. |
| Define longer-term outcomes (sustained/further reduction in fear). | Added. |
| Specify short, medium and long term; for example, 4 weeks, 8 weeks and 6 months. | Considered; concluded that appropriate to define specific timelines. |
| It might be misinterpreted that children and young people themselves understand that they are at increased risk of developing anxiety. | This point has been rephrased to improve clarity. |
| Specify that anxiety might be incorrectly seen as part of a learning disability. Consider adding in brackets diagnostic overshadowing. | Added. |
| Add more about autism symptomatology without directly referring to autism. Consider adding more about specific difficulties that children and parents/carers might have, their impact on intervention and how to troubleshoot that (social difficulties, rigidity/preference for sameness/neophobia) to the intervention manual. | Added. |
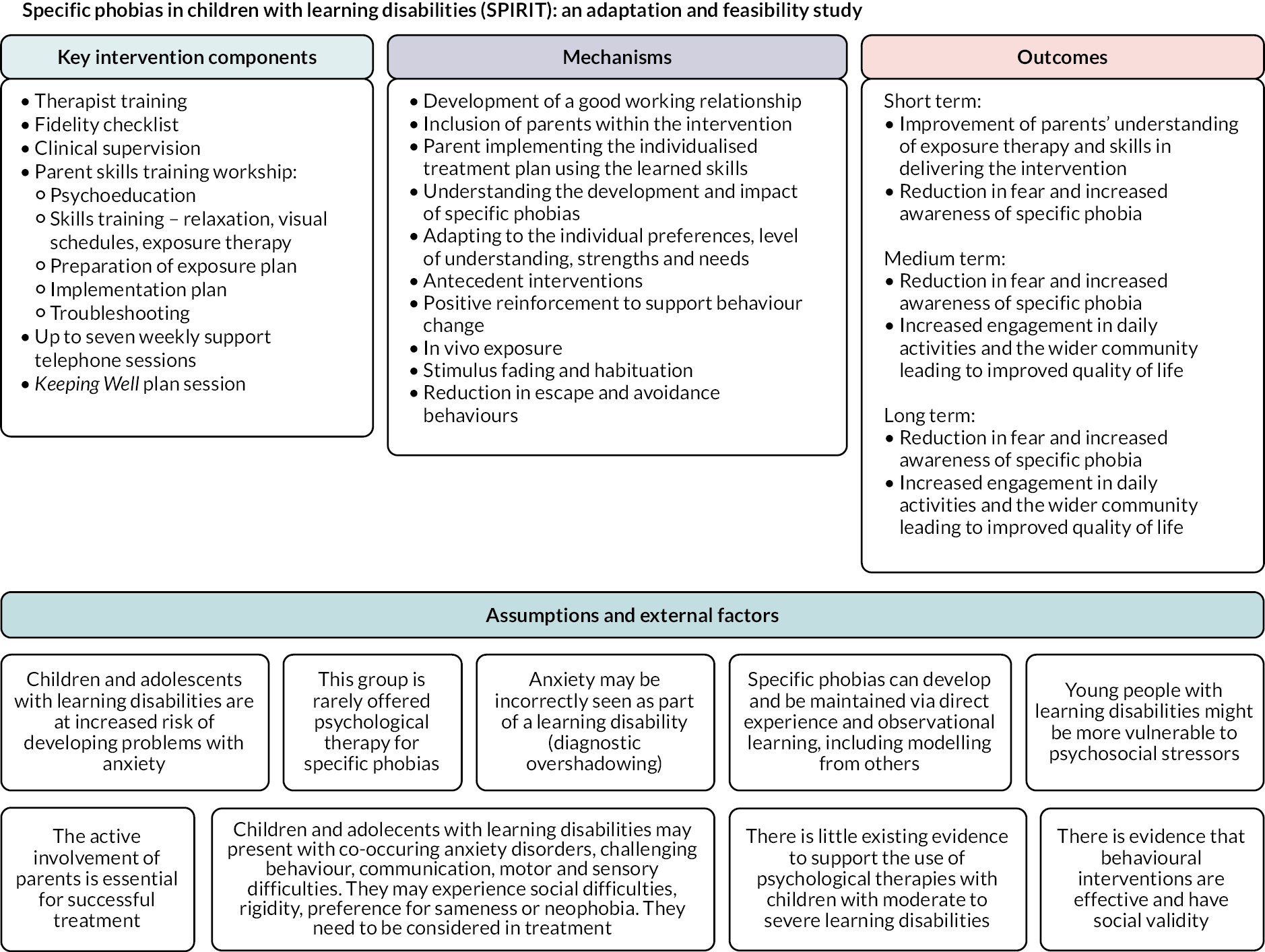
See Figure 1 for the finalised logic model.
FIGURE 1.
SPIRIT intervention logic model.
A draft therapist training plan was presented to the IDG. Table 10 summarises proposed changes and actions.
| IDG feedback/suggestions | Action |
|---|---|
| Training in the intervention might possibly include the behavioural section before the intervention detail. The ‘order’ of training basically might be different to the logical order of the manual itself. | Considered, but concluded important to introduce the intervention before working on specific concepts. |
| Role-plays could work well in breakout rooms if the task is manageable and designed for online format. | Option of role play added. |
| It would be helpful if trainers were role-playing. | Considered; however, parent skills training workshop may be delivered by one trainer so role play may not be possible. Added videos of different techniques instead. |
| Provide longer breaks. | Duration of breaks changed to 15 minutes. |
| Invite parents/carers to the training and ask for their contribution. | Considered; however, not possible to implement due to budgetary restrictions. We will consider inviting parents/carers for future training sessions or making videos with parents to be shown during the training. |
| Add video interview footage of a parent/carer talking about their child’s anxiety and specific phobias. | Considered; however, not possible due to time and budgetary restrictions. Will consider this for future evaluation work. |
| The first part of the toolkit of behavioural strategies is longer than needed but the second part is too short. | First part shortened to 45 minutes and second part extended to 75 minutes. |
| Add a section on possible trauma that parents/carers may experience coping with some extreme phobias their child has. Also, some parents might be hurt physically in managing certain behaviour. | Section on impact added. If indicated, this section will be developed further based on feedback from parents/carers taking part in the study. |
| Give therapists some places they can refer parents/carers for extra support if needed. This should be also added to the intervention manual to ensure that therapists appreciate and recognise that signposting to additional resources and supports may be needed. | Therapists directed to provide signposting information relevant to their service/region. |
| Add trainer-level troubleshooting around what happens if parents/carers are not able to do exposure tasks, cannot fit it in the schedule or are worried into the intervention manual and the training outline. | Information added. |
See Chapter 3 for a detailed description of the therapist training.
Objective 2: develop an intervention fidelity checklist
A fidelity checklist was developed for the SPIRIT intervention, based on checklists used in a previous study. 39 It included seven main sections:
-
general workshop/session preparations
-
coverage of workshop/session plan
-
understanding and accessibility
-
interpersonal effectiveness
-
engaging participants
-
workshop/session content
-
comments.
Checklists were developed for each of the workshops and each of the eight support sessions. Therapists were asked to reflect on the workshop or session and indicate whether they had fulfilled the aims by checking ‘yes’ or ‘no’. See Report Supplementary Material 7 for a sample fidelity checklist and Chapter 3 for a detailed description.
Draft fidelity checklists were prepared and presented to the IDG meeting. Following feedback from the IDG, revisions were made. Table 11 summarises changes proposed by the IDG and how they were addressed.
| IDG feedback/suggestions | Action |
|---|---|
| Add a statement on the top of the checklist that when scoring these items, it is important to think of majority of parents/carers, rather than all. | Statement added. |
| It might be hard to judge impact on parents/carers if the checklist is self-reported – feedback from parents would be needed. | Considered; however, it was felt parents already have sufficient intervention tasks to complete each week. Their experience of the intervention and working with their therapist will be captured during post- intervention interviews. |
| Self-reflection tool needs more work; consider adding a reflection box. | Notes section added to the bottom of each document. |
| Reflection might be difficult for some people – some cross-referencing with parent feedback would be helpful. | Considered; however, it was felt parents already have sufficient intervention tasks to complete each week. Their experience of the intervention and working with their therapist will be captured during post-intervention interviews. |
| Add a section where therapists can reflect on what worked well and what could be better. | Notes section added on the bottom of the document. |
| Therapists should be rating concepts rather than behaviours. | Reviewed and implemented for parts of the checklists; however, concluded it was not appropriate for sections directly relating to session objectives. |
| It might be easier to admit that the criterion was only ‘partially met’ rather than just selecting ‘no’. | Considered; however, concluded a broader scale would not be appropriate for this checklist. Feedback will be sought from the therapists on the fidelity checklist and potential revisions to be made for a future study. |
| The child Improving Access to Psychological Therapies measures include some form of patient-reported session-by-session recording. The Dagnan Confidence Scale42 might also be helpful. | Different checklists were considered. |
| Feedback about parents’ experience is vital. | Considered; however, it was felt parents already have sufficient intervention tasks to complete each week. Their experience of the intervention and working with their therapist will be captured during post-intervention interviews. |
| It might be helpful to think about the role of clinical supervision here. | Considered, but felt it would not be appropriate to include this on the fidelity checklist. This checklist is intended to be used for this specific study, rather than intended for clinical supervision. |
Objective 3: appraise and consider several candidate outcome measures of anxiety-related symptoms, and secondary outcomes, and make a recommendation for use within phase 2
A range of potential outcome measures were considered, including parent/carer questionnaires, interviews, behavioural measures and physiological measures. These included:
Eligibility assessment
Specific phobia
Emotional and behavioural difficulties
Physiological measures
-
Apple Watch® (Apple, Inc., Cupertino, CA, USA)
-
Fitbit® watch (Fitbit, Inc., San Francisco, CA, USA)
The IDG was presented with detailed information about the measures, including content/purpose of measure, format, age range, time needed to complete and psychometric properties. They were also given access to all potential outcome measures apart from smartwatches. Following a discussion, the IDG made recommendations about outcome measures to use in phase 2 of the project. Table 12 summarises IDG feedback and actions on the measures reviewed.
| Measure | IDG feedback/suggestions | Action |
|---|---|---|
| Eligibility | ||
| ADIS44 | IDG recommends using this measure. | Measure included in eligibility assessment. |
| Diagnostic checklist for anxiety based on DM-ID-243 | IDG recommends using this measure. | Measure included in eligibility assessment. |
| VABS-345 | IDG recommends using this measure. | Measure included in eligibility assessment. |
| Specific phobia | ||
| Severity Measure for Specific Phobia – Child Age 11–17.46 SPIRIT adaptation for people with little or no language: caregiver version | Add section for additional comments. | Added. |
| Rephrase question 10. | Question rephased. | |
| Consider families that avoid certain situations so might not have had contact with feared stimuli in the last 7 days. An additional text box could be a good solution, so parents/carers can add further details. | Text box added. | |
| Consider how parents/carers can report on children’s emotional states and bodily states that are not easily observable (e.g. racing heart). Consider phrasing such as ‘It looks like your child might be experiencing . . .’ or ‘Did they seem to have . . .’. | Questions rephrased. | |
| Consider how to capture what children communicate. | Text box added. | |
| Add a section on the top of the checklist to ask parents/carers how their child behaves when in the presence of feared stimuli. | This information would be captured by another measure. | |
| Children might not be engaging in avoidance because their families are avoiding situations where they might be exposed to feared stimuli, so they do not have a chance to escape the situation. | Text box added so parents/carers can mention this information. | |
| IDG recommends using this measure with recommended revisions. | Measure added to the baseline and follow-up assessment. | |
| Emotional and behavioural difficulties | ||
| SDQ: Impact supplement.47 SPIRIT adaptation | Consider changing the rating scale. | Only three questions were used from the questionnaire, and therefore felt the scale was appropriate. |
| Question on ‘do the difficulties that upset or distress your child’ seems redundant. | Question deleted. | |
| Add a question about the difficulties getting worse or escalating in the last 12 months. | This information would be captured by another measure. | |
| Add a question on avoidance and level of stress. | This information would be captured by another measure. | |
| Obsessive–compulsive disorder materials might be helpful to capture this information. | Reviewed these but felt the questionnaire captured the necessary information. | |
| The measure could be helpful to assess broad issues and is easy to complete. However, it is not as useful to detect change or capture more specific information. | Feedback noted. | |
| Possibly the scale could be changed to 2 weeks to capture potential change. | Questions referring to specific timescale were not used. | |
| Consider how to capture the effort families put into avoiding specific situations/items. | This information captured by another measure. | |
| Think about further dividing the ‘home life’ and ‘leisure’ categories. | We considered this but decided to proceed with the question in its current form and ask parents/carers for feedback. | |
| Make it clear that the difficulties are in relation to specific phobia. | Clarification provided to parents/carers. | |
| Possibly agree on four most important areas with the parent/carer at the beginning and track change in relation to those. Goal attainment scaling might be helpful to look at. | Reviewed and decided on three main questions that the IDG preferred. | |
| Look at goal-based outcomes measure where individual goals are scored on 0–10 scale to estimate how close parents/carers feel to goal. | Reviewed, but felt not appropriate for this questionnaire. | |
| IDG recommends using this measure with recommended revisions. | Measure added to the baseline and follow-up assessment. | |
| ABC-C48 | IDG does not recommend using this measure due to its length and vocabulary used. | Measure not used. |
| DASH-II49 | IDG does not recommend using this measure due to its length. | Measure not used. |
| DBC2: Parent Form50 | •Good feedback from clinicians but not clear what parents/carers think about it. •Contains preferred language in relation to disability. •IDG recommends using this measure. |
Measure added to the baseline and follow-up assessment. |
| BPI for Individuals with Intellectual Disabilities – Short Form51 | •Good feedback from clinicians and parents/carers. •IDG recommends using this measure. |
Measure added to the baseline and follow-up assessment. |
| Physiological measures | ||
| General feedback on using smartwatches to record heart rate | •There is a risk that the watch becomes associated as a cue that exposure is coming if it is only used for the exposure – would need to be worn more regularly. •A colourful watch might be better tolerated by children. |
Feedback noted; however, it might not be possible for children to wear the watch outside of intervention time due to battery life and risk of damage. |
| Apple Watch | Some watches might be distracting, especially Apple Watch. | Apple Watch excluded. |
| Fitbit watch | •One of the clinicians had experience using Fitbits in research – many devices were lost, damaged or ran out of battery. The solution could be to only use them during exposure tasks. •Most children tolerated the Fitbit. •Could enquire about a discount or donation from Amazon or Fitbit. •Concluded testing the Fitbit was the best option. |
Feedback noted; the watch will be used only during intervention time. |
Chapter 3 SPIRIT intervention description
Description and structure of the intervention
The SPIRIT intervention has been specifically created to meet the needs of children and young people with moderate to severe learning disabilities and specific phobias. It is a parent-mediated approach which uses graded exposure paired with strategies such as reinforcement, visual schedules and communication training to ensure it is accessible to young people with moderate to severe learning disabilities.
With the use of augmentative and alternative communication strategies, visual schedules, and consideration of unusual fears, restricted and repetitive behaviours and sensory aversions, this intervention is also appropriate for autistic young people with moderate to severe learning disabilities. Further specific adaptations for autistic children address difficulties with discourse and pragmatics, understanding and inference. Difficulties with discourse and pragmatics were managed through the use of concrete vocabulary/lexical items (avoidance of abstract concepts and metaphors) and simplified morphosyntax (sequencing of ideas in utterance).
The intervention consists of two half-day parent skills training workshops and eight support sessions (in-person, online or by telephone) with the therapist. Each of the workshops lasts for 4 hours and focuses on specific phobias, behaviour change and graded exposure. Workshops are led by at least two trained therapists and can be delivered online or face to face. Table 13 shows the structure of the workshops.
| Stage | Main focus | Key activities/focus points |
|---|---|---|
| PARENT SKILLS TRAINING WORKSHOP | DAY 1 | |
| Introductions (20 minutes) |
|
|
| Psychoeducation | ||
| Introduction to specific phobias (30 minutes) |
|
|
| How phobias develop (15 minutes) |
|
|
| Intervention overview (10 minutes) |
|
|
| Introduction to exposure therapy (15 minutes) |
|
|
| Skills training | ||
| Reinforcement (50 minutes) |
|
|
| Introduction to the visual schedule (20 minutes) |
|
|
| DAY 2 | ||
| Day 2 check-in (10 minutes) |
|
|
| Introduction to relaxation (40 minutes) |
|
|
| Building the exposure plan | ||
| Building exposure steps (40 minutes) |
|
|
| How to work through exposure steps (20 minutes) |
|
|
| Next steps and troubleshooting | ||
| Exposure plan (20 minutes) |
|
|
| Role of the parent/carer and the therapist (10 minutes) |
|
|
| Troubleshooting (35 minutes) |
|
|
The workshops are designed for groups of up to six parents/carers; however, final group sizes were determined by recruitment at the participating site. The small-group format is advantageous as it provides parents/carers with shared learning experiences in a supportive and safe environment, and direct support is provided by other parents/carers who have had similar experiences. It is also efficient to teach principles and skills involved in the SPIRIT intervention in a group format before providing more tailored, individual support.
Following the two workshops, parents/carers are supported by therapists during weekly support sessions (telephone or online), each lasting approximately 30 minutes, for up to 8 weeks. Therapists are advised to allow for 30 minutes to prepare and write notes after the support session. Whenever possible, the support sessions are led by the same therapist each week. These sessions are designed to check on the well-being of the child and parents/carers, monitor progress, address questions, problem-solve and help to plan the week ahead. Prior to the support session, parents/carers are asked to send a photo of the data sheet to the therapist or share it during the session. Table 14 shows the structure and content of the weekly support sessions.
| Weekly support sessions | |
|---|---|
| Support session 1 (30 minutes) |
|
| Support session 2 (30 minutes) |
|
| Support session 3 (30 minutes) |
|
| Support session 4 (30 minutes) |
|
| Support session 5 (30 minutes) |
|
| Support session 6 (30 minutes) |
|
| Support session 7 (30 minutes) |
|
| Support session 8 (30 minutes) |
|
Both parents/carers are encouraged to attend the workshops and support session. However, if one parent/carer is not available, they can familiarise themselves with the intervention using the parent workbook. See the Materials section for more details on the content of the parent workbook.
Key components
Exposure therapy
Exposure therapy is an integral component of the SPIRIT programme. It is an intervention method that involves gradually exposing the young person to the feared stimulus and pairing it with relaxation techniques. It involves three main steps:
-
teaching deep breathing and relaxation strategies
-
building exposure steps, which are a list of situations, places or things connected to the young person’s feared stimulus ranging from least distressing to most distressing
-
gradually exposing the young person to the steps included in the exposure steps while practising relaxation strategies.
This approach helps the young person to build their tolerance of the feared object or situation at a pace that they are comfortable with. The experience of feeling anxious is an important component of exposure therapy, as children learn how to manage this feeling. The aim is to reduce the young person’s fearful response and help them learn that the feared object or situation may not be as dangerous as they believe. In exposure therapy, regular practice is key. Ideally the young person should work on exposure each day, even if they practise a step only once.
Parents/carers are guided to identify exposure steps during the workshops using the form described in the Materials section. Exposure steps are reviewed during the support sessions and broken down further if needed. Parents/carers are encouraged to include things the child can already tolerate as the first few steps.
Relaxation
Relaxation strategies help to reduce tension in the body and reduce anxiety. When the child experiences feelings of anxiety or fear, their muscles tighten, and it can be difficult for them to feel calm. By introducing relaxation, tension in the body is reduced, which helps them feel calmer. Relaxation strategies are used when the child is feeling anxious or overwhelmed, as well as during exposure tasks. Some examples of relaxation strategies include deep breathing and muscle relaxation.
During the workshops, parents/carers are taught breathing exercises that involve taking a deep breath through the nose, counting to five and exhaling through the mouth while counting to seven. This exercise is repeated five times. For muscle relaxation, parents/carers are asked to inhale through the nose and clench their hands. The breath is held for 5 seconds and released as the hands are relaxed. This exercise is repeated with different body parts – shoulders, back, face, stomach and feet. Parents/carers are also taught how to do a hand massage in case they need to help the child relax when quiet space is not available.
During the workshops, the therapist spends some time discussing children’s existing relaxation strategies with parents/carers, such as sensory play or self-stimulatory behaviours, and identifying new strategies that could be tried. Parents/carers are also guided to explore possible adaptations of traditional relaxation strategies (e.g. deep breathing and muscle relaxation) to meet the needs of their child. This can include:
-
reduced verbal language in instructions
-
reduced number of body areas targeted for muscle relaxation
-
teaching body parts before moving on to the muscle relaxation
-
using modelling to demonstrate the exercises
-
using example and non-example procedure – modelling a ‘relaxed’ and ‘not relaxed’ pose and asking the child to only copy the relaxed pose
-
incorporating child-friendly scenarios and favourite objects or stories into the exercises; for example, bubbles or feathers
-
using physical prompting to teach the child the exercises
-
introducing a visual cue or signal, for example picture card(s), to signal relaxation
-
incorporating relaxation aids like a stress ball, therapeutic putty, dimmed lights or relaxing music.
Reinforcement
Reinforcement is a consequence which follows a behaviour and increases the likelihood the behaviour will occur again in the future. In the SPIRIT intervention, reinforcement is used to teach new skills, such as requesting a break and relaxation, and after completing the exposure tasks. To identify the young person’s reinforcers, parents/carers are asked to complete a preference assessment before starting exposure. A preference assessment is a systematic process that allows the parent/carer to identify six things the young person likes the most. To complete the preference assessment, parents/carers use the ‘What I like and enjoy’ form, which is described in more detail in the Materials section. Parents/carers are asked to review identified reinforcers frequently and redo the preference assessment if needed.
Generalisation and maintenance
Another component of the SPIRIT intervention is generalisation and maintenance. Generalisation is an ability to perform a behaviour learned in one context in a different context. While neurotypical individuals often generalise behaviours themselves by observing others and through indirect learning, people with learning disabilities may need help with generalisation. Therefore, working on the generalisation of acquired behaviours/skills in a systematic and structured way is an essential (and crucial) part of a successful behaviour change. This includes teaching and practising new behaviours:
-
in different environments
-
with different people
-
with varying instructions
-
using different materials.
In terms of ensuring that behaviour change is maintained, a variety of strategies are incorporated, such as:
-
focusing on behaviours that are meaningful to the young person
-
teaching until mastery
-
providing opportunities to practise new behaviours
-
adjusting the level of reinforcement.
Strategies to encourage generalisation and maintenance of new behaviours are incorporated into the intervention. During the last support session, the therapist makes a plan with the parent/carer to support continued work on generalisation and maintenance.
Communication
It was anticipated that a number of young people using the SPIRIT intervention would have communication support needs. Therefore, the intervention includes a number of augmented communication strategies such as visual aids and a visual schedule. These supports were reviewed and expanded by co-applicant Bunning (speech and language therapist), drawing on aided (e.g. using graphics and objects) and unaided (e.g. using manual signs and gestures) options from established augmentative and alternative communication methods. 52
Intervention procedures
Order of intervention activities
The skills training workshops provide parents/carers with an opportunity to learn about specific phobias and all components of the SPIRIT intervention. After both workshops, parents/carers should have:
-
an understanding of how the intervention works, their responsibilities and support available
-
an understanding of their child’s specific phobia – their triggers, behaviours associated with being afraid, and tolerance levels of items or situations related to their specific phobia
-
an understanding of how to teach new skills using modelling and prompting
-
completed the preference assessment
-
completed a relaxation plan and developed an understanding of how to adapt the relaxation strategies
-
an understanding of how to prepare and use the visual schedule
-
an understanding of how to monitor their child’s well-being and how to use the rating scale
-
a complete list of exposure steps
-
an understanding of how to collect monitoring data and work though the exposure steps
-
knowledge of what to do when challenges arise.
After the workshops, parents/carers are asked to work on introducing relaxation, the visual schedule and the rating scale to their child. This work forms the focus of the first support session. After that, parents/carers introduce the first exposure step and start working though the remaining steps. It is important that parents/carers do not start working on exposure before they identify how the child relaxes and ensure that they can request a break or communicate that they want to stop.
Work on exposure continues until the seventh support session, where ending the SPIRIT intervention support sessions is discussed. Parents/carers are asked to reflect on the intervention and the progress so far. During the last support session, the therapist prepares a plan with the parent/carer to support further exposure work if needed and for maintenance and generalisation. This is contained within the Keeping Well plan (see Materials section for more details). We anticipate that 8 weeks might not be enough to complete all exposure steps for some young people. The idea of the SPIRIT intervention is that parents/carers will develop sufficient expertise to continue with the exposure once support from the therapist ends.
We recognise that many young people will have more than one specific phobia. However, for the purposes of the intervention, parents/carers are asked to focus on one phobia at a time. Once the intervention finishes, parents/carers should have sufficient expertise to apply the same procedures to their child’s other phobias.
Implementation of the exposure steps
Parents/carers should have the complete list of exposure steps after attending both workshops; however, the steps should be reviewed during the support sessions and amended if needed. Parents/carers are asked to work on one step at a time and not skip steps. They start with a step that is the least fear-evoking for the young person and initially expose them for a short period of time. The duration is extended in the subsequent steps. Initially, the child should be reinforced for attempting the exposure steps (e.g. by praising them).
Depending on the nature of the relaxation strategies selected, the child should be encouraged to focus on relaxation during the exposure or immediately before and after (if it is not possible to implement them at the same time).
The visual schedule should be prepared and reviewed with the young person before working on exposure (for more information, see the Materials section).
The next exposure step is introduced only when the young person reaches the mastery criterion: three successfully (independently) completed attempts in a row. If the young person is consistently struggling to complete the same step for over a week, the therapist discusses revising the exposure steps with the parent/carer.
Data collection
Parents/carers are asked to collect data after each attempt at the exposure step to help with monitoring progress and making decisions about moving to the next step. Parents/carers learn how to use the data sheet (for more details, see the Materials section) during the workshops. They are asked to record each attempt of an exposure step as correct (completed without help), partially correct (completed with some help) or incorrect (not completed).
Parents/carers are asked to share their data sheet with the therapist during each support session.
Materials
All materials for parents/carers are put together in one folder. The folder was assembled by the research team and posted to parents/carers prior to the first workshop.
Intervention manual
The intervention manual, parent workbook and all materials were developed together with the IDG.
The therapist intervention manual includes both background and a step-by-step guide to treatment for specific phobias for children with moderate to severe learning disabilities. The manual provides therapists with detailed plans for the workshops and the support sessions, as well as general guidelines on working with parents/carers and children with learning disabilities.
Parent workbook
The parent workbook contains eight sections and covers the key information presented during the workshops:
-
introduction to specific phobias
-
introduction to exposure therapy
-
reinforcement
-
visual schedule
-
relaxation
-
exposure steps
-
key points to remember
-
troubleshooting.
The workbook was designed to be accessible and clear for parents/carers to follow. The idea is that parents/carers can refer to the workbook while working on the intervention and can share it with coparents and other carers.
Assessment for parents
Prior to the first workshop, parents/carers are sent the ‘Assessment for parents’ along with the instructions for completion. This assessment asks questions about their child, including what they are like in different environments, and their phobia. Parents/carers are asked to complete the document ahead of time and send it back to the therapist a week before the parent workshop. The assessment helps parents/carers to start thinking about their child’s phobia in preparation for the workshops and also provides the therapist with information to individualise the content of the intervention for each parent/child.
About my child’s phobia
‘About my child’s phobia’ is a worksheet that parents/carers complete during the second workshop. The worksheet summarises information about their child’s phobia, including triggers and associated behaviours, so they can easily refer to it while working on exposure.
My child’s story
Parents/carers are sent the ‘My child’s story’ worksheet prior to the intervention starting and are asked to complete it with their child if possible. The worksheet covers information about their child’s strengths and interests, and their phobia. Parents/carers are asked to use the worksheet to introduce their child to the group during the first workshop.
Rating scale
The rating scale is a tool used by parents/carers to monitor their child’s mood and level of discomfort during exposure work. It can help parents/carers identify when their child is becoming distressed. The rating scale consists of three options: good, OK and bad. These options are accompanied by a corresponding hand signal and colour (green, amber and red).
Relaxation routine
During the second workshop, parents/carers are asked to write down what relaxation strategies they are planning to try with their child, and potential adaptations. This document is updated once the child’s relaxation routine is decided.
Visual schedule
The visual schedule is a visual representation of activities planned for the child. It allows the young person to know what will be happening and provides an opportunity to manage transitions in a more controlled manner. For some children, it might be helpful to use the additional ‘now/next’ board which is embedded in the visual schedule. It helps the young person know what is happening at that moment and what is happening next.
Parents/carers are asked to prepare the visual schedule every time they work on exposure. It is suggested that the young person is involved in this process as much as possible.
What I like and enjoy
The ‘What I like and enjoy’ form guides parents/carers though the preference assessment process. Parents/carers are first asked to identify six potential reinforcers. Then they pair them together to see which ones are preferred by the child. Later, they create a reinforcer ranking which is used during exposure work.
Exposure steps
‘Exposure steps’ is a list of situations, places or things connected to a child’s specific phobia, arranged from least feared or distressing to most feared or distressing. Parents/carers are given a choice of an exposure steps template that they find most suitable. Some of the options include a ladder, stairs and a horizontal or vertical schedule.
Data sheet
The data sheet is used to record progress with the exposure steps. Parents/carers are asked to use it each time they work on exposure to record how the attempt went. They can put a tick on the data sheet to indicate a successful try (completed independently), a dash for a partially successful try (when the young person needed help to complete the step) or a cross for an unsuccessful try (when the young person did not complete the step).
Information sheet for other carers
To help with sharing information about the intervention with the child’s other carers and school, we created the ‘Information sheet for other carers’. This document summarises information about specific phobias and the SPIRIT intervention to help with consistency.
Exposure summary
When preparing for the end of the intervention, parents/carers are asked to complete the exposure summary. The worksheet asks them to reflect on the progress with the intervention: what went well, the impact on the child and their family, and barriers that they overcame. The worksheet helps parents/carers prepare for continued exposure work after the therapist’s support ends.
Keeping Well plan
During the last intervention session, the therapist creates a Keeping Well plan with the parent/carer to help with exposure work after the support ends. This summarises short- and long-term goals and ways in which they will be achieved, as well as strategies to ensure maintenance and generalisation of skills learned.
Therapists and therapist training
The intervention is delivered by a trained therapist, who could be a nurse, clinical psychologist, assistant psychologist, allied health professional or other suitably qualified health professional with experience of working with young people with learning disabilities and their families. Therapists were trained by the Chief Investigator and the SM. Supervision was provided by the clinical supervisors at the therapists’ workplace.
All therapists were required to take part in a one-and-a-half-day training course on the delivery of the intervention. Table 15 lists the content of the therapist training. The training included a mixture of PowerPoint® presentation, whole-group discussions and work in small groups. Training was delivered online by the research team. For small groups of therapists, it is possible to complete the training in 1 day.
| Training day | Focus | Activity |
|---|---|---|
| Day 1 | Introduction to the SPIRIT intervention | Welcome and introductions |
| Intervention overview | ||
| How to use the intervention manual | ||
| Intervention structure | ||
| Good practice guidelines | ||
| Background and rationale | ||
| Key concepts and strategies | ||
| Additional strategies | ||
| Considerations for working with young people with moderate to severe learning disabilities and their parents | ||
| Sample parent workshop schedule | ||
| Parent skills training workshop day 1 | Introductions | |
| Introductions to specific phobia | ||
| How phobias develop | ||
| Intervention overview | ||
| Introduction to exposure therapy | ||
| Reinforcement | ||
| Introduction to the visual schedule | ||
| Parent skills training workshop day 2 | Day 2 check-in | |
| Introduction to relaxation | ||
| Day 2 | Building exposure steps | |
| How to work through exposure steps | ||
| Exposure plan | ||
| Role of the parent and the therapist | ||
| Troubleshooting | ||
| Weekly support sessions | ||
| Fidelity checklists |
Therapists received regular supervision as per their existing supervision arrangements; this was at least monthly. Supervisors were given the opportunity to attend the SPIRIT training and received a copy of the intervention manual. The research team was in regular contact with the therapists to check on progress and offer support.
Adherence
Therapist adherence to the intervention manual was measured with fidelity ratings (number of completed session components) after the parent/carer skills training workshop and after each support session.
Patient adherence was defined as attendance of intervention sessions. To meet the adherence criterion, parents/carers needed to attend both workshops and at least 80% of the weekly support sessions, taking into account, for example, holidays and illness.
Fidelity checklist
Therapists completed a self-report fidelity checklist at the end of each parent workshop and after each support session to record intervention adherence. Items on the checklist are organised into seven sections:
-
general workshop/session preparations
-
coverage of workshop/session plan
-
understanding and accessibility
-
interpersonal effectiveness
-
engaging participants
-
workshop content
-
further comments.
Therapists were asked to reflect on all session aims and indicate whether they were completed by circling ‘Yes’ or ‘No’ on the checklist. Supervisors were encouraged to review the fidelity checklist with their supervisees.
Chapter 4 Treatment as usual survey
Objective
To describe the current standard treatment provided for children and adolescents with moderate to severe learning disabilities and specific phobia within the UK, we conducted two surveys. The parent survey was designed for parents/carers of children aged 5–15 years who identified their child as having moderate to severe learning disabilities and a specific phobia. The professional survey was designed for health and care professionals working in services that provide care to children and young people with moderate to severe learning disabilities and specific phobias. The surveys aimed to characterise the treatments and supports (i.e. TAU) children and young people are receiving for their specific phobias, from the perspective of parents and professionals.
Methods
Participant recruitment
Parent survey
Participants were parents/carers of children aged 5–15 years, living in the UK, who identified their child as having moderate to severe learning disabilities and a specific phobia. Families that were not offered any treatment/support options by health services were still eligible and were encouraged to participate in the survey.
The invitation to participate in the survey was disseminated via our existing Midlands and wider UK networks of schools, support groups and charities. The Foundation for People with Learning Disabilities (PPI partner) also promoted the survey among its members. As part of the recruitment process, we sent an e-mail invitation to special schools across the UK and organisations providing support for children and young people with additional support needs and their families (e.g. Mencap, Down’s Syndrome Association, National Autistic Society). This included information about the survey for the organisation and for the parents/carers, as well as the link to the survey. Information about the survey was also available in the public domain (Twitter and University of Warwick departmental website) as well as being shared in the Cerebra 1000 Families Study and Affinity Hub newsletters.
Professional survey
Participants were health and social care professionals working in services providing care to children aged 5–15 years with moderate to severe learning disabilities. Participants were recruited via the Child and Adolescent Intellectual Disability Psychiatry Network in the UK, the Research in Developmental Neuropsychiatry (RADiANT) consortium of NHS providers and the study’s coinvestigators. E-mail invitations were sent to NHS Trusts and special schools in England. This included information about the survey for the organisation and a link to the survey. Information about the survey was also available in the public domain (University of Warwick departmental website) as well as being shared in the Affinity Hub newsletter.
The survey asked participants to describe the treatment(s) for specific phobias that their service offers to children and adolescents with moderate to severe learning disabilities. Professionals whose service does not offer any treatments for specific phobias were still encouraged to complete the survey.
Consent
The participants had a choice to complete the survey online on Qualtrics® (Qualtrics, Provo, UT, USA) or as an interview with a member of the research team [via Microsoft Teams® (Microsoft Corporation, Redmond, WA, USA) or over the telephone]. For participants completing the survey online, the participant information sheet and participant consent form were embedded in Qualtrics. Participants who opted for an interview were e-mailed the participant information sheet and participant consent form ahead of time and asked to sign it electronically. Participants had to provide their consent before accessing the survey. All parents completed the survey online.
The parent and professional survey data were collected between June 2021 and January 2022.
Withdrawals
Participants had the right to withdraw their consent at any time. Withdrawals were recorded.
No participants withdrew their consent or their data from either of the surveys.
Survey questions
Parent survey
Survey questions were developed based on the Template for Intervention Description and Replication (TIDieR) checklist. 53 This checklist is used to provide a description of an intervention. There were two types of questions. The closed questions provided the participants with several response options along with a text box to add a description if the option ‘Other’ was chosen. For open-ended questions, participants were able to provide their response in a text field. Initial questions were about the nature of the specific phobia and whether support or treatment was offered (this could include psychological treatments, medication or any other treatment). Parents/carers who indicated their child was offered treatment or support were asked about: the type of support or treatment offered; by whom, how and where the treatment was delivered; materials used; name and dose of medication (if applicable); and any modifications made to the treatment to meet the needs of the young person. The parents/carers were also asked about the number, frequency and duration of treatment sessions. At the end of the survey, the participants were asked whether their child was offered any additional treatment for their specific phobia, apart from the one they had already described. If yes, the parents/carers were asked to answer the same set of questions but in relation to the additional treatment option. Parents/carers who indicated their child was not offered any treatment or support for the specific phobia were redirected to the end screen. For more information about the survey questions, see Report Supplementary Material 1.
Professional survey
Questions for the professional survey were developed based on the TIDieR checklist53 and covered the same content. Initially, professionals were asked if their service offered any treatment or intervention for specific phobias to children with moderate to severe learning disabilities (this could include psychological treatments, medication or any other treatment). If the professional indicated that their service offered treatment for specific phobia, they were asked a series of questions about the nature of the treatment and how it is delivered. At the end of the survey, participants were asked whether their service offered any additional treatment for specific phobia, apart from the one they already described. If yes, the professionals were asked to answer the same set of questions but in relation to the additional treatment option. For more information about the questions, see Report Supplementary Material 2.
Analysis
We used a mixed-methods design to analyse the data from both surveys by combining quantitative and qualitative methods. We summarised the number of responses to the closed questions and conducted qualitative content analysis of the open-ended responses. Initially, a set of codes was developed by one coder by grouping responses to the open-ended questions that shared the same meaning. If the response contained more than one concept, separate codes were generated. The codes represented the parents’ and professionals’ descriptions of the treatment offered for specific phobias. They were sorted into themes that were determined by each open-ended question (see Appendices 1 and 2 for themes, codes and extracts demonstrating themes).
Two researchers independently coded 10% of the open-ended responses. The inter-rater reliability agreement was 92% (12/13) for the parent survey and 95% (19/20) for the professional survey. Once reliability in coding was established, one researcher independently coded the remaining 90% of the open-ended responses. The other researcher then reviewed the coding, and any disagreements were discussed and consensus reached.
Participant characteristics
Parent survey
Fifty-two parents/carers of children aged 5–15 years with moderate to severe learning disabilities and specific phobias who live in the UK responded to the survey. Fifty participants chose to complete the survey online. Two participants requested to complete the survey in a form of an interview. Only one online interview was completed as the other participant did not provide the contact details needed to arrange the meeting, resulting in 51 responses in total. Thirty-two participants indicated that services supporting their child were in England, six in Northern Ireland and two in Wales.
Professional survey
Twenty-five health and social care professionals working in services providing care to children aged 5–15 years with moderate to severe learning disabilities responded to the survey. This included twenty-two health and care professionals, one allied health professional and two other learning disability professionals. Twenty-four participants chose to complete the survey online. One online interview was conducted. Twenty-two professionals provided a name of the service within which they worked. The services included twenty-one health and care services and one school. Nineteen participants categorised their service as community based, two as a combination of community and inpatient and one as school based. Twenty-two participants provided information on the country in which their service was located: England (n = 21) and Wales (n = 1).
Results
Parent survey
Types of specific phobia
Forty-eight parents/carers provided a description of their child’s specific phobia or phobias. The participants were able to describe more than one specific phobia. Overall, 85 types of specific phobia were mentioned which were grouped into the categories used in DSM-5. 40 The types of specific phobia mentioned were: animal (n = 15); situational (n = 15); blood, injection and injury (n = 10); environmental (n = 8); and other (e.g. food, showers) (n = 37).
Services/professionals
Forty participants provided information on services/professionals that supported their child. The participants were able to add more than one service/professional. The sources of support described by the participants were: health and care professionals (n = 38); allied health professionals (n = 37); school (31); other support teams (e.g. social worker) (n = 3); and none (n = 1). Overall, 110 services/professionals were mentioned. Of note, 28% of the treatments offered were school based.
Treatments
Of the 41 participants who responded to the question asking whether their child was offered any support or treatment for their specific phobia, 30 (73.2%) indicated that they were not offered any support or treatment; the remaining 11 participants (26.8%) indicated their child was offered support or treatment for their specific phobias. Out of those eleven participants, two were offered more than one treatment.
Of the 11 who indicated they were offered treatment, 9 provided further information. Overall, 10 treatment options were mentioned; these were grouped into: medication (n = 5; 50%), exposure therapy (n = 3; 30%), sensory integration (n = 1; 10%) and counselling (n = 1, 10%).
Five participants reported being offered medication for their child’s specific phobias: fluoxetine (n = 2), laxatives (n = 1), melatonin (n = 1) and one did not provide the name of the medication.
Three participants indicated their child was offered exposure therapy as a treatment for their specific phobia.
One parent/carer indicated their child was offered sensory integration as treatment for their specific phobias (change in routine, heights). They were provided with treatment materials in the form of handouts. The participant stated that the treatment was designed by an occupational therapist who trained school staff to deliver it. The treatment sessions were face to face, and the occupational therapist and school staff were present during the sessions. The participant indicated that the treatment included more than 24 sessions that were scheduled twice daily, for 15–30 minutes.
One participant indicated that their child was offered counselling as treatment for their specific phobia. However, they did not provide any information about this treatment apart from stating that they did not receive any materials.
Descriptions of treatment components by participants included desensitisation (n = 2), gradual exposure to dogs using images (n = 1), support (n = 1), play (n = 1), psychoeducation for parent (n = 1) and positive behaviour support (PBS).
Two parent/carers reported receiving treatment materials, with one specifying that pictures and a worry tree were used.
Three participants stated that the treatment was provided by a medical doctor who was not a psychiatrist, one by a psychiatrist and one by a nurse. Participants also mentioned that other professionals were present during the sessions: nurse (n = 1), and paediatrician and nurse (n = 1). Four participants indicated the treatment was delivered face to face, with two specifying the setting as community paediatrician centre (n = 1) and hospital (n = 1).
Three participants indicated the treatment consisted of one to six appointments, while one participant had more than twenty-four appointments. Two participants described the frequency of appointments as once a month (n = 1) and one-off (n = 1). Four participants provided information on the duration of the appointments: < 15 minutes (n = 1), 15–30 minutes (n = 1), 30 minutes to 1 hour (n = 1) and more than 1 hour (n = 1).
One participant indicated that the treatment was provided by a healthcare assistant and the remaining two by a psychologist. Participants also mentioned that other professionals were present during the sessions: play therapist (n = 1), psychologist (n = 1) and nurse and psychologist (n = 1). The treatment was delivered face to face for two families, with one specifying the setting as home and school, and online for the remaining participant.
All three participants specified the number of sessions as between one and six. They indicated the frequency and duration of the sessions as once a week for 15–30 minutes (n = 1), once a month for about 1 hour (n = 1) and once a week for < 15 minutes (n = 1).
None of the participants indicated that they were aware of any adaptations made to the treatment to meet their child’s needs. Three responses were excluded from the analysis as they were not relevant to the question asked.
See Report Supplementary Material 3 for all codes categorised according to type of treatment described by each participant.
Professional survey
Treatments
Twenty-five health and social care professionals working in services providing care to children aged 5–15 years with moderate to severe learning disabilities responded to the survey. Ten participants (45.5%) stated that their service did not offer any treatment or intervention for specific phobias.
Out of 25 participants, 22 (88%) responded to the question about what treatment/intervention their service offered for specific phobias in children and young people with moderate to severe learning disabilities. Twelve participants (54.5%) indicated that their service offered treatment or intervention. Of these 12 participants, 4 stated that the service offered more than one treatment. The participants were able to add more than one treatment option. Overall, 21 types of treatment were mentioned. The treatment types were: exposure therapy (n = 7), CBT (n = 4), medication (n = 4), systemic intervention (n = 2), primary care support (n = 2), acceptance and commitment therapy (ACT) (n = 1), psychoeducation and behavioural therapy (n = 1).
Exposure therapy
Seven participants indicated that their service offered exposure therapy as a treatment or intervention for specific phobias. The participants’ responses to the rationale for using exposure therapy were that it is evidence based (n = 3), it can be individualised (n = 3), the parent/carer involvement (n = 3), it is recommended by NICE (n = 1), it is a concrete way of working with phobias (n = 1) and increased confidence of the young person (n = 1).
Key elements of exposure therapy mentioned by the participants were: graded exposure (n = 3), relaxation (n = 2), fear hierarchy (n = 2), individualised assessment (n = 2), support from the parent/carer (n = 1), regular review of treatment progress (n = 1), exposure to a feared stimulus (n = 1), praise (n = 1), modelling (n = 1), parent/carer involvement (n = 2), skills teaching (n = 1), planning sessions (n = 1), family history (n = 1), exploring feelings (n = 1), monitoring person’s engagement (n = 1), involvement of family and care staff (n = 1), problem formulation (n = 1), psychoeducation (n = 1) and treatment toolkit (n = 1).
Additional key procedures, activities and processes were described by four participants and involved: collaboration with other specialists (n = 1), pictures (n = 1), videos (n = 1), clinician or family engagement (n = 1), social stories (n = 1) and explaining treatment to everyone involved (n = 1). The treatment materials used by professionals in exposure therapy were: exposure record forms (n = 4), materials individualised for the young person (n = 3), visuals (n = 2), pictures (n = 2), videos (n = 2), leaflets for parents (n = 1), photos (n = 1), sounds (n = 1), visiting the place (n = 1), rating scales (n = 1), anxiety coping plan (n = 1), instructions clearly communicated (n = 1), information sheets (n = 1), dental materials (n = 1) and social stories (n = 1).
The treatment was provided by a psychologist (n = 6), nurse (n = 5), healthcare assistant (n = 2), mediated by parent or support care (n = 3), speech and language therapist (n = 1), any team member (n = 1), support worker (n = 1), dental team (n = 1) and trainee clinical psychologist (n = 1).
During the sessions, different professionals were present: professional delivering the treatment (n = 3), school staff (n = 2), clinical psychologist (n = 2), assistant psychologist (n = 1), case manager (n = 1), dental therapist (n = 1), dental nurse (n = 1), dentist (n = 1) and teacher (n = 1). Other people present were: parents/carers (n = 4), young person and parent/carer (n = 1) and family (n = 1).
Six participants stated that the treatment was provided face to face and one through combined contact methods (face to face, virtual or over the telephone). Four participants specified the face-to-face setting: home (n = 3), clinic (n = 3), school (n = 2), short-break service (n = 1) and individualised to the treatment (n = 1). Three services offered the treatment online and one over the telephone.
Six participants specified the number of treatment sessions: 1–6 (n = 1), 1–12 (n = 2), 12–24 (n = 2) and variable (n = 1). The sessions took place once a week (n = 4), once a fortnight (n = 1), once a month (n = 1) or with variable frequency (n = 1). Six participants responded that the sessions lasted 30 minutes to 1 hour, and one more than 1 hour.
Five participants stated that their service monitored whether the treatment was implemented as planned. This was done through: reviews (n = 2), supervision (n = 2), outcome measures (n = 3), consultation with parents (n = 1) and videos (n = 1).
All seven participants indicated that the treatment involved adaptations to meet the needs of the young person. The situations leading to adaptations were specified by five participants. These situations were: treatment not being adapted to the young person (n = 2), treatment being too challenging for the young person (n = 2), the needs of the young person (n = 2), family not understanding the treatment (n = 1), the level of learning disability (n = 1), language difficulties (n = 1), cognitive difficulties (n = 1) and additional diagnoses (n = 1).
Treatment adaptations to exposure therapy mentioned by participants were: parent/carer involvement (n = 4); adapting materials (n = 4); adapting session number, duration or frequency (n = 2); including the young person in decision-making (n = 1); repetitions (n = 1); adapting language (n = 1); recording sessions (n = 1); being aware of acquiescence (n = 1); simplification (n = 1); behavioural approach (n = 1); skills teaching (n = 1); increased number of breaks (n = 1); use of incentives (n = 1); inclusion of creative activities (n = 1); and adjusting expectations (n = 1).
Cognitive behavioural therapy
Four participants indicated their service offered CBT as treatment for specific phobia. The participants specified the rationale for using this treatment as: the treatment can be individualised (n = 3), it is evidence based (n = 2), parent/carer involvement (n = 1) and it is recommended by NICE (n = 1). Key elements of the treatment as described by the responders were: graded exposure (n = 2), working with thought patterns (n = 1), behavioural experiments (n = 1), activity scheduling (n = 1), parent/carer involvement (n = 1), kindness and compassion (n = 1), information adapted to the young person’s needs (n = 1), control for the young person (n = 1), sense of safety and support (n = 1), praise (n = 1), modelling (n = 1), skills teaching (n = 1), problem formulation (n = 1), psychoeducation (n = 1), individualised assessment (n = 1) and a treatment toolkit (n = 1).
Additional key procedures were indicated by one participant: individualising (n = 1) and providing extra training for staff (n = 1). Treatment materials used with CBT were: individualised for the young person (n = 2), exposure recording forms (n = 2), thought diaries (n = 1), charts (n = 1), rating scales (n = 1), goal-setting forms (n = 1), anxiety coping plan (n = 1), visuals (n = 1) and information sheets (n = 1).
All four participants stated the CBT was provided by a psychologist.
Three participants indicated that the treatment was provided face to face and one through combined contact methods (face to face, virtual or over the telephone). Two specified the setting as home, two as community clinic, one as school, one as clinic and one as hospital. Two services offered the treatment online and one over the telephone.
Different people were present during the treatment sessions. They included a psychologist (n = 2), clinical psychologist (n = 2), parents/carers (n = 3), professional delivering the treatment (n = 1), assistant psychologist (n = 1), phlebotomist (n = 1), nurse (n = 1) and doctor (n = 1).
The participants estimated the number of treatment sessions as 6–12 (n = 2) or 12–24 (n = 2), and the frequency as once a week (n = 3) or once a fortnight (n = 1). They also indicated that the sessions lasted 30 minutes to 1 hour (n = 4).
Three services monitored the treatment implementation. This was facilitated by supervision (n = 2), patient measures (n = 1), reviews (n = 1) and outcome measures (n = 1). All four participants indicated that the CBT involved adaptations to meet the needs of the young person.
Reasons for adapting CBT were that the CBT was too challenging for the young person (n = 2), CBT was not adapted to the young person (n = 1), difficulties with consent and understanding (n = 1), family does not understand the treatment (n = 1), level of learning disability (n = 1), language difficulties (n = 1), cognitive difficulties (n = 1) and additional diagnoses. See Table 21 for descriptions of the adaptations.
| Site | Recruitment | Site-identified potential participants | Enrolled in study |
|---|---|---|---|
| Cambridgeshire Community Services NHS Trust | External recruitment and case list | 22 | 3 |
| Dorset Health Care University NHS Trust | Case list only | 10 | 1 |
| Avon and Wiltshire Mental Health Partnership NHS Trust | Case list only | 15 | 2 |
| Norfolk Community Health and Care NHS Trust | External recruitment and case list | 38 | 6 |
| Hertfordshire Community NHS Trust | Case list only | 8 | 3 |
| Total | 93 | 15 |
Adaptations to CBT were: parent/carer involvement (n = 3), adapting materials (n = 2); repetitions (n = 1); adapting language (n = 1); recording sessions (n = 1); being aware of acquiescence (n = 1); adapting session number, duration or frequency (n = 1); simplification (n = 1); behavioural approach (n = 1); skills teaching (n = 1); adaptations dependent on young person’s needs (n = 1); increased number of breaks (n = 1); use of incentives (n = 1); and inclusion of creative activities (n = 1).
Medication
Four participants indicated that their service offered medication as a treatment for specific phobias. The rationale for using this treatment was: pharmacological relief of anxiety (n = 2), evidence based (n = 2) and it helps the person engage in psychological therapies (n = 1).
Two participants provided information about key elements of the treatment, which were: medication (n = 1), psychiatric supervision (n = 1), assessment (n = 1), diagnosis (n = 1) and prescribing (n = 1).
An additional key procedure was mentioned by one participant. This was assessment of the family’s ability to support the use of medication.
Four participants specified the materials used with the treatment, which were: easy-read information (n = 1), information leaflets (n = 1), materials individualised for the young person, medication (n = 1) and leaflets for the young person (n = 1).
All four participants reported that a psychiatrist provided the treatment. One participant mentioned that a nurse was also involved.
Three participants indicated that the treatment was provided face to face (n = 3). The specific settings were: clinic (n = 2), community outpatient unit (n = 1) and school (n = 1). Two participants mentioned that the treatment was delivered online, one over the telephone and one using combined contact methods (face to face or virtual).
Professionals present at the appointments were: psychiatrist (n = 4), nurse (n = 2) and care co-ordinator (n = 1). Other people also present during the sessions were: parents/carers (n = 3), school staff (n = 1), support staff (n = 1), nurse (n = 1) and professional involved with the family (n = 1).
The estimated number of appointments was 6–12 (n = 2), 1–6 (n = 1) or 12–24 (n = 1). The participants indicated that the appointments took place once a month (n = 4) and lasted for 30 minutes to 1 hour (n = 3) or 15–30 minutes (n = 1).
Three participants stated that their service monitored treatment implementation, with two specifying ways of monitoring treatment implementation as reviews (n = 1), feedback from parents (n = 1), outcome measures (n = 1) and reports from other professionals (n = 1).
Three participants indicated that the treatment involved adaptations to meet the needs of the young person, with sensory issues (n = 1) and visits to the clinic being too challenging for the young person (n = 1) as situations leading to the adaptation of the treatment. Adaptations to the treatment involving medication included: easy-read information (n = 1), support from occupational therapist (n = 1), increasing acceptability of the medication (n = 1), school observation (n = 1) and a virtual session (n = 1),
Systemic intervention
Two participants said that their service offered systemic intervention for specific phobias. They described the rationale for using the treatment as: it is easily individualised (n = 1) and that difficulties with phobia can arise within families (n = 1).
The responses describing key elements of the treatment were: exploring narratives within the family (n = 1), identifying the family’s strengths (n = 1), information adapted to the young person’s needs (n = 1), control for the young person (n = 1), sense of safety and support (n = 1), kindness and compassion (n = 1).
Additional key procedures were described by one participant: individualising and providing extra training for staff.
One participant stated that no treatment materials were used.
Both participants reported that the treatment was provided by a psychologist, with one adding that it could also be provided by a play specialist. Professionals present at the sessions were: psychologist (n = 2), other professionals supporting the young person (n = 1) and carer (n = 1). Other people also present during the sessions were: the young person and family/carers (n = 1), phlebotomist (n = 1), nurse (n = 1) and doctor (n = 1).
The treatment was delivered face to face (n = 2). The participants specified the setting as: home (n = 2), community clinic (n = 1), hospital (n = 1) and community centre (n = 1). One service also provided the treatment online.
One participant stated that the treatment involved 6–12 sessions, and one 12–24 sessions. The sessions lasted 30 minutes to 1 hour (n = 2) and took place once a fortnight (n = 1) and once a week (n = 1).
One service monitored treatment implementation by using patient measures. Two participants indicated that the treatment involved adaptations to meet the needs of the young person. The reasons for adaptation of the systemic intervention were: the treatment was not adapted to the young person’s needs (n = 1), the treatment was too challenging for the young person (n = 1) and difficulties with consent and understanding (n = 1). The adaptations to systemic interventions were: parent/carer involvement (n = 1), adapting materials (n = 1), repetitions (n = 1), adapting language (n = 1), recording sessions (n = 1), being aware of acquiescence (n = 1) and adaptations dependent on the young person’s needs (n = 1).
Primary care support
Two participants stated that their service offered primary care support for specific phobias. One participant provided information on the rationale of using the treatment as being part of primary care. One participant also mentioned that the key element of the treatment was referral to secondary care.
One participant indicated that the treatment was provided at the general practitioner surgery by a medical doctor as well as a nurse. Professionals present at the sessions were the general practitioner and a nurse. The participant estimated the number of treatment sessions as one to six. The sessions took place once a month and lasted < 15 minutes.
One participant indicated that the treatment involved adaptations made to meet the needs of the young person.
Acceptance and commitment therapy
One participant stated that their service offered ACT as a treatment for specific phobias. The rationale for using this treatment was that it can be individualised.
Key elements of the treatment described by the participant were: information adapted to the young person’s needs, control for the young person, sense of safety and support, and kindness and compassion.
Additional key procedures, activities and processes used within the treatment were individualising and providing extra training for staff.
The participant indicated that a psychologist and play specialist provided the treatment. A psychologist, carer, phlebotomist, doctor and nurse were also present at the sessions. The treatment was provided face to face at home or in the community clinic or hospital. It included 6–12 weekly sessions, which lasted 30 minutes to 1 hour.
The service used patient measures to monitor treatment implementation. The participant described the reasons for adapting the treatment as: the treatment being too challenging for the young person, and difficulties with consent and understanding. Treatment adaptations depended on the young person’s needs.
Psychoeducation and behavioural therapy
One participant mentioned psychoeducation and behavioural therapy as a treatment for specific phobias offered by their service. The rationale for using the treatment was that the treatment can be individualised. Additional elements of the treatment were described as flexibility. The materials associated with the treatments were pictures and modelling roles.
The participant stated that the treatment was provided by a psychologist and a nurse. The sessions were face to face, at home or in the clinic. The young person and their parent/carer attended the sessions. The treatment consisted of more than 24 fortnightly sessions which lasted 15–30 minutes.
The service used reviews to monitor whether the treatment was implemented as planned. Psychosocial factors were considered when deciding on adaptations to the treatment. The participant indicated that treatment adaptations involved support from the school.
The service in which the participant worked offered more than one treatment for specific phobias.
Three responses were excluded from the analysis as they were not relevant to the question asked.
See Report Supplementary Material 4 for codes emerging from the professional survey data set.
Summary
In total, 52 parents agreed to participate in the TAU survey, with 51 providing information. The majority of the participants were from England (n = 32), with six parents from Northern Ireland and two from Wales. Overall, 73% (30/41) of parents reported that they were not offered any treatment for their child’s specific phobia. Of those who were offered treatment (n = 11), 10 different treatments were mentioned. Of these, 50% were medication, 30% exposure therapy, 10% counselling and 10% sensory integration therapy. The majority of the treatments provided were in community-based health and social care settings, although 28% were school based.
Twenty-five practitioners completed the TAU survey, with the majority (n = 21) stating they were from England and one from Wales. The majority worked in health and care services (n = 22), and one was based in a school. Just over half (54%; n = 12) indicated that their service offered treatment for specific phobia. Of these 12, 50% (n = 6) offered exposure therapy, with other therapies offered including CBT, medication, ACT, primary care support, systemic intervention and psychoeducation.
Chapter 5 Intervention feasibility study
Using the intervention developed in phase 1 of the study (see Chapters 2 and 3), we completed a feasibility study to model the intervention and determine its acceptability and feasibility for stakeholders, including service users, parents/carers and clinicians, as per the Medical Research Council (MRC) framework for the development of complex interventions. 54
Methods
Design
This phase of the study was a single-arm, non-randomised feasibility study, with participants receiving the adapted intervention developed in phase 1a (see Chapters 2 and 3). We recruited 15 children and young people, and their parental caregivers, who received the intervention in conjunction with other treatments they were receiving at the time through the NHS. Children currently receiving treatment for specific phobia or psychological intervention for other anxiety disorders were not eligible to participate.
Children and young people were assessed at three time points:
-
eligibility assessment
-
baseline assessment within 4 weeks before commencement of the intervention
-
follow-up assessment within 4 weeks of completing the intervention.
At the completion of the intervention, parents/carers were invited to participate in an interview, as were the therapists.
Ethics
The study received a favourable ethical opinion from the NHS Research Ethics Committee (REC) and received Health Research Authority (HRA) approval prior to any research activities taking place. All amendments to the protocol were submitted and approved by the ethics committee. See Report Supplementary Material 5 for the NHS REC approval and Report Supplementary Material 6 for the HRA approval.
Site recruitment
This single-arm, non-randomised feasibility study took place within the NHS – either specialist learning disabilities services or mainstream Child and Adolescent Mental Health Services (CAMHS) in England.
Before the study commenced, two sites confirmed that they wanted to be involved in the feasibility study. However, due to capacity issues both declined to be involved after the study opened, with one site withdrawing after three therapists had completed training in the intervention. The National Institute for Health and Care Research (NIHR) Clinical Research Network supported with promoting the study among the NHS Trusts in England. We also utilised contacts of co-applicant Langdon at the RADiANT consortium to identify potential sites.
A total of 22 NHS services were approached about being involved in the SPIRIT study. Five NHS services across England agreed to be our recruitment and delivery sites: Cambridgeshire Community Services NHS Trust, Dorset Health Care University NHS Trust, Norfolk Community Health and Care NHS Trust, Avon and Wiltshire Mental Health Partnership NHS Trust and the Hertfordshire Community NHS Trust. The learning disability team leads at each site determined which therapists in their team should undertake training and deliver the intervention.
The majority of sites that were approached declined involvement on the basis of capacity. During site recruitment, COVID-19-related pressures on the NHS services impacted the capacity of sites to be involved in the study. For example, a significant number of staff members from research and development (R&D) teams were redeployed to provide service support elsewhere in the Trust (e.g. for COVID-19 vaccinations). Many clinical staff members were also redeployed or were on long-term sick leave due to COVID-19. Another reason for declining to participate, other than capacity, is related to concerns about the lack of research experience among the learning disabilities staff who would be delivering the intervention, and lack of capacity to support them appropriately. Many of the sites declined to be involved due to the tight time frame of this phase of the study. Several sites stopped engaging after initially expressing interest in being involved in the study. Of the sites that declined to be involved, several voiced their interest in participating in a larger trial or future research.
Participant recruitment
We used a multipoint recruitment strategy, including NHS services, special schools and parent support groups, to maximise recruitment. Information about the study was placed within the public domain on the study’s website (CEDAR, University of Warwick) and the website of the Foundation for People with Learning Disabilities. However, only two of the sites agreed to accept participants who were not already part of their service; that is, participants who were living in the service region but were not already on their caseload. The remaining three sites recruited from within their service.
Parents and their children and therapists were invited to participate in the post-intervention interviews. We interviewed the first people to respond.
Sample size
The sample target was up to 20 parents/carers of children with moderate to severe learning disabilities and specific phobias. As this was a feasibility study, and the purpose was to provide estimates of key parameters for a future pilot trial rather than to power the study to detect statistically significant differences, a formal a priori power calculation was not conducted. 55 We aimed to interview at least one parent/carer per site and their child.
We aimed to recruit at least two therapists per site to deliver the intervention and interview at least one therapist from each site.
Eligibility criteria
Participants were eligible to take part in the study if they met all the following inclusion criteria and none of the exclusion criteria applied.
Inclusion criteria:
-
aged 5–15 years
-
existing diagnosis of moderate to severe learning disabilities, confirmed at eligibility assessment
-
suspected/diagnosed specific phobia (DSM-5), confirmed at eligibility assessment
-
parent/carer able to participate in the intervention.
Exclusion criteria:
-
currently receiving another psychological therapy for anxiety
-
eligibility assessment indicates anxiety behaviours are likely associated with a physical health condition (e.g. dental problems)
-
no consent obtained to take part in the research.
Screening
Screening of potentially eligible participants was conducted by clinicians with routine access to personally identifiable information (e.g. nursing staff working within community teams for people with learning disabilities). This screening took place only within the NHS and involved a search of patient records or a discussion with clinician teams. The personally identifiable information required for screening was diagnosis, which was taken from clinical records: specifically, a diagnosis of moderate to severe learning disabilities and information to suggest that the person has problems with specific phobia and whether they were already receiving psychological therapy.
Clinicians then shared information about the study with likely eligible participants. Interested parents/carers contacted the study team through two routes:
-
Parents/carers told clinicians that they wanted their contact details passed to the study team when asked. The study team received the details from clinicians and then contacted the parents/carers.
-
Parents/carers contacted the study team directly using the contact information they were provided.
Participants who were identified via schools or support/charitable organisations, and those who wanted to self-refer, contacted the study team directly using contact information they saw on the study’s websites or within adverts (e.g. information within newsletters or e-mails sent to parents/carers via their child’s school).
All potential participants were contacted by the SM or the RA to arrange a discussion about the study, either by telephone or online. All of these discussions with potential participants were carried out by the SM or Chief Investigator. During the discussion, the study was explained in detail, including the consent process and eligibility criteria, and parents/carers were able to ask any questions about the study and what was involved. If the parents/carers were interested in being involved and after this discussion it seemed they may be eligible, they were sent the participant information sheet and consent form.
Consent
Participants in the feasibility study were parents/carers of children with learning disabilities and specific phobias. Parents/carers were sent the participant information sheet and consent form prior to the screening/recruitment interview and were given sufficient time to read the information. The study was explained in detail during the interview, and any questions were answered. If the parent/carer was interested in taking part, informed consent was obtained. As screening interviews were completed over the telephone, parents/carers provided verbal consent during the conversation. A hard copy of the participant information sheet and consent form was then posted to the participant for signature. Parents/carers were provided with a prepaid return label in order to return the signed consent form to the research team.
Participants who agreed to take part in post-intervention interviews were asked to sign a separate consent form and return it to the research team.
Therapists who delivered the intervention were offered an opportunity to take part in a post-intervention interview and therefore become research participants. If they agreed to take part, the interview and consent processes were explained in detail and a hard copy of the therapist information sheet was posted to them for signature.
Eligibility assessment
After written consent was received from the parent/carer, the SM completed an eligibility assessment online (Microsoft Teams) or by telephone. This included the completion of the domain-level version of the VABS45 as an index of severity of intellectual disability. The VABS Adaptive Behavior Composite score was used to confirm a moderate to severe learning disability (a standard score below 55).
The eligibility assessment included the administration of the Specific Phobia section of the ADIS44 with the parent/caregiver. Information from this interview was used to complete a learning disabilities-sensitive DSM-5 diagnostic checklist based on the DM-ID-2. 43 The SM confirmed eligibility with the Chief Investigator. If eligible, the RA or SM arranged completion of baseline measures. If any concerns were raised during the eligibility assessment (i.e. the family were in crisis), the site Principal Investigator was contacted and asked to signpost the family to appropriate local support.
The research team took responsibility for determining eligibility. A site screening log of all ineligible and eligible but not consented/not approached parents/carers was kept at each site to monitor accrual. Logs did not contain identifiable information. A study screening log was kept by the study team who completed the definitive eligibility assessment.
Lost to follow-up
Participants were recorded as lost to follow-up if either of the following criteria were met:
-
no response to three attempts to schedule an appointment for either assessment or intervention, where at least one of these attempts was sending a letter to their home asking them to contact the research team
-
failure to attend at least three scheduled and consecutive appointments for either assessment or intervention, and no response to a letter sent to their home asking them to contact the research team following the third scheduled and consecutive appointment.
Withdrawals
Participants had the right to withdraw consent for participation in the study at any time. The participants’ care was not affected at any time by declining to participate or withdrawing from the study.
If a participant initially provided consent but subsequently withdrew from the feasibility study, a clear distinction was made as to what aspect of the study the participant was withdrawing from. These aspects could have been:
-
withdrawal of baseline data collected
-
withdrawal from the intervention only
-
withdrawal from future follow-up assessments
-
withdrawal of consent to all of the above.
Participants who consented and subsequently withdrew completed the study withdrawal form, or the withdrawal form was completed on the participant’s behalf by the study team member based on information provided by the participant and therapist.
Participant timeline
The steps in the pathway for the feasibility study were as follows:
-
All participants who consented to participate in the study completed an eligibility assessment with research staff to ensure they met the inclusion criteria for the study (parent/guardian consent, child assent).
-
Following baseline assessment, participants who met the eligibility criteria received the intervention (plus TAU).
-
Participants were assessed using the study outcome measures within 4 weeks of completion of the intervention.
-
A subsample of participants (parents/carers) and the therapists were invited to take part in semistructured interviews following completion of the intervention to further assess acceptability, their experience of the intervention, the study pathway, procedures, consent and associated factors in order to provide a description of the factors that facilitate or challenge the implementation of the intervention.
-
A subsample of young people (up to five, predominantly with moderate learning disabilities) who received the intervention were invited to take part in an interview to explore their experience of the intervention and their outcomes.
Table 16 shows the study time points.
| Procedures | Study time points | |||
|---|---|---|---|---|
| Eligibility | Baseline | Intervention phase | Follow-up | |
| Informed consent | X | |||
| Demographics | X | |||
| Medical history | X | |||
| Eligibility assessment, including completion of VABS-345 and confirmation of a diagnosis of specific phobia (symptom checklist) | X | |||
| Delivery of intervention | X | |||
| Fidelity | X (therapist completed) | |||
| Phobia symptom checklist | X | X | ||
| Severity measure for specific phobia | X | X | ||
| Impact of phobia measure | X | X | ||
| Specific phobia diagnosis | X | X | ||
| Emotional and behavioural problems | X | X | ||
| Challenging behaviour | X | X | ||
| Medication | X | X | ||
| AE assessments (if required) | X | X | ||
| Semistructured interviews | X | |||
Outcome measures
Participants were enrolled in the study for approximately 6 months. Participants were assessed at three time points: (1) eligibility, (2) baseline assessment within 4 weeks of commencement of the intervention and (3) follow-up assessments within 4 weeks of completion of the intervention. The choice of measures was decided in phase 1a of the project (see Chapter 2 for more details).
For participants who discontinued the intervention but wished to remain enrolled in the study, data were captured as per protocol. This meant that data were captured within the 4-week period following the time at which the intervention would have been completed had the participant continued to take part in the intervention.
The outcome measures were completed by the parent/carer and included:
Specific phobia severity
The Severity Measure for Specific Phobia – child age 11–17,46 SPIRIT adaptation for people with little or no language. This measure was completed by caregivers and consisted of 15 items. Items are rated on a five-point scale (0 = never; 1 = occasionally; 2 = half of the time; 3 = most of the time; and 4 = all of the time). The total raw score is calculated by summing the score on each item, with total scores ranging from 0 to 60. Higher scores indicate greater severity of specific phobia. The average total score is generated by dividing the raw total score by the number of items in the measure (i.e. 15); this score reduces the overall score to a 5-point scale, enabling assessment of specific phobia severity to be thought of in terms of none (0), mild (1), moderate (2), severe (3) or extreme (4).
Impact of specific phobia
The SDQ: Impact supplement47 was adapted to be used as a parent/carer-reported measure of the general impact of the specific phobia on the child and family. The adapted measure (Impact of Phobia measure) consisted of six questions, which are rated on a four-item scale: not at all, only a little, quite a lot and a great deal. The percentage of responses for each item is calculated.
Behaviour and emotional problems
The parent/carer report form of the DBC250 was used to assess child behaviour and emotional problems. The DBC2 consists of 95 items, which are rated on a three-point scale (0 = not true as far as you know, 1 = somewhat or sometimes true, 2 = very true or often true).
A Total Behaviour Problems Score (TBPS) is calculated by summing the responses on all 95 items, providing an overall measure of child behaviour and emotional problems, with higher scores indicating greater degree of behaviour and emotional problems. The maximum score for the TBPS is 190. The DBC2-P also provides subscale scores: Disruptive, Self-Absorbed, Communication Disturbance, Anxiety, and Social Relating. The Disruptive subscale describes behaviour that is challenging or disruptive, including aggressive and impulsive behaviours. The Disruptive subscale is composed of 27 items; the maximum score is 54. The Self-Absorbed subscale includes 29 items such as self-injurious behaviour, pica, aloof and excessive fascination with something; the highest possible score for this subscale is 58. Communication Disturbance includes behaviours related to unusual ways of speaking, such as echolalia, talking to self; this subscale contains 12 items, with a maximum score of 24. The Anxiety subscale consists of 12 items that are related to anxiety disorders including fears, nightmares, difficulties with separation, and distress in response to small environmental changes; the highest score possible for this subscale is 24. The final subscale, Social Relating, describes behaviours associated with social relating difficulties, including not showing affection, poor eye contact and unhappiness; this subscale is composed of 10 items and the maximum score is 20.
Behaviour problems
The BPI for Individuals with Intellectual Disabilities – Short Form51 was completed by parents/carers as a measure of self-injurious, aggressive/destructive and stereotyped behaviours. The short form of the BPI consists of 30 items, each assessing frequency and severity of behaviours.
The Self-Injurious Behavior scale measures behaviour that causes damage to oneself, such as head hitting. The Aggressive/Destructive Behavior scale includes behaviour that is directed towards others or property, such as biting others. The Stereotyped Behavior measures behaviours that are repetitive, voluntary acts that do not cause harm; for example, repetitive hand and/or finger movements. For the Self-Injurious and Aggressive/Destructive Behavior scales, frequency of occurrence is measured on a scale of 0–4 (0 = never/no problem, 1 = monthly, 2 = weekly, 3 = daily, 4 = hourly). Severity is then rated from mild (1), moderate (2) to severe (3). For the Stereotyped Behavior scale, the frequency of occurrence of behaviours that are present is recorded (monthly, weekly, daily, hourly). For Self-Injurious Behavior, the maximum score is 32 for frequency and 24 for severity. The maximum scores for Aggressive/Destructive Behaviour are 40 for frequency and 30 for severity. The maximum frequency score on the Stereotyped Behavior scale is 48.
Physiological measure (heart rate)
Child heart rate during exposure tasks was measured using a Fitbit. The practicality and feasibility of collecting heart rate data using a wearable device were assessed in the parent/carer post-intervention interviews.
Post-intervention interviews
After the intervention was completed, we conducted semistructured interviews to examine the views of parents/carers and therapists about the intervention to inform the study objectives. This information was integrated to create a description of factors that promote or challenge the implementation of the intervention with reference to the intervention logic model (Figure 1).
The interview schedule for parents/carers included 33 questions organised into 11 sections:
-
warm-up
-
acceptability of consent process
-
intervention accessibility and acceptability
-
helpful and unhelpful aspects, including barriers to change
-
the value of the adaptations
-
relationship with the therapist within the intervention
-
acceptability of outcome measures
-
acceptability of randomisation within future trial
-
acceptability of parent-mediated intervention model
-
effects of participation
-
closing questions.
The interview took up to 1 hour. It was conducted either online (via Microsoft Teams) or over the telephone by the SM or RA. All interviews were recorded and transcribed verbatim. See Report Supplementary Material 8 for the parent/carer interview schedule.
The interview schedule for therapists included 30 questions organised into the same sections as the parent/carer interview. Interviews took up to 1 hour and were conducted online (via Microsoft Teams) by the SM or RA. All interviews were recorded and transcribed verbatim. See Report Supplementary Material 9 for interview schedules for therapists.
An interview schedule using Talking Mats (Talking Mats Ltd, Stirling, UK) for young people with learning disabilities was developed to explore their experience of the intervention as delivered by their parents, and the outcomes for them. This is a structured approach to helping people with communication difficulties to organise and express their views. Talking Mats have been used previously with this population. 56 See Report Supplementary Material 10 for the interview plan using Talking Mats.
The SM approached parents/carers who agreed to participate in the post-intervention interviews to ask about also interviewing their child. However, parents/carers did not feel this was appropriate or accessible to their child as it referred to parent-mediated intervention, rather than an intervention delivered directly by a clinician. Parents felt that due to their communication difficulties they would not be able to sufficiently understand or discuss the intervention to treat their specific phobia, as implemented by their parent.
Analysis
As this was a feasibility study, the analysis is descriptive in nature. Continuous data are reported as means and standard deviations (SDs), or medians and interquartile ranges, as appropriate. Categorical data are reported as frequencies and proportions. Outcomes are estimated with their associated 95% confidence intervals (CIs). No formal hypothesis testing was undertaken.
The study is reported in accordance with the CONSORT extension for non-randomised pilot and feasibility studies. 57 A detailed statistical analysis plan was written and agreed by the study management team and the Study Steering Committee (SSC) independent statistician prior to analysis. The data cleaning, querying and analysis plans as well as the reporting templates were quality checked by coinvestigator Playle, a senior statistician within the Centre for Trials Research, Cardiff University.
Qualitative analysis
Framework analysis58 was used to analyse the data generated from the semistructured interviews with parents/carers and clinicians. Framework analysis is a pragmatic method which is advantageous within this context because it allows researchers to investigate key issues of interest, rather than analyse data for all emergent themes. Framework analysis was used to examine the views of parents/carers and professionals on several predefined key areas, including: (1) the accessibility and acceptability of the intervention; (2) helpful and unhelpful aspects, including barriers to change; (3) the value of intervention adaptations; (4) parent/carer relationships with professionals within the intervention; (5) acceptability of outcome measures; and (6) acceptability of consent and associated processes, including randomisation in a future trial. We used Excel spreadsheets for data organisation and management.
The location of source data is outlined in Table 17.
| Study data | Source data | |||||
|---|---|---|---|---|---|---|
| Qualtrics | CRF | Participant medical notes | SAE/AE form | Semistructured interviews | Therapist checklist and audio-recordings | |
| Phase 1b | ||||||
| Description of TAU (survey) | x | |||||
| Description of TAU (interviews/survey) | x | x | ||||
| Phase 2 | ||||||
| Diagnosis of moderate to severe learning disabilities and specific phobia | x | x | ||||
| Concurrent medications | x | x | ||||
| AEs | x | |||||
| Primary outcome | x | |||||
| Anxiety diagnostic checklist | x | |||||
| Phobia symptom checklist | x | |||||
| Severity measure for specific phobia | x | |||||
| Impact of phobia measure | x | |||||
| Specific phobia diagnosis | x | |||||
| Emotional and behavioural problems | x | |||||
| Challenging behaviour | x | |||||
| Data about acceptability and the experience of the intervention, the study pathway, and procedures, consent, outcome measures used, views about randomisation within a larger trial | x | |||||
| Fidelity | x | |||||
Progression criteria
The study aimed to estimate key parameters for a future trial that will be used to inform HTA decision-making with regard to advertising for a future trial and will assist researchers in developing proposals for a future trial. We proposed the following progression criteria with reference to several key indicators of success: (1) recruitment, (2) protocol adherence and (3) outcome data. These have been incorporated into three possible recommendations regarding feasibility of a larger trial. 59
Green
If all of the following criteria are met, the SSC will consider a recommendation that a larger trial is feasible:
-
Recruitment (1) Accrual rate is at least three patients per site per month on average; and (2) attrition rate is 30% or lower.
-
Protocol adherence (1) Fidelity ratings indicate therapist adherence to the intervention of at least 75%; (2) at least 70% of parents/carers and clinicians report that the intervention and consent procedures were acceptable; and (3) at least 90% of participants received the intervention.
-
Outcome data (1) At least 75% of participants complete outcome measures at each time point; (2) at least 75% of items across outcome measures for each participant are complete; and (3) at least 75% of parents/carers judge the outcome measures to be acceptable.
Amber
If any of the following criteria are met, then the research team will examine the reasons for this, carefully consider what remedial action can be taken to improve the likelihood that a larger trial is feasible, and provide this analysis to the SSC for consideration. For example, difficulties may be related to a delay in research ethics or governance approvals or a longer than expected time to build relationships with referrers which could be managed effectively within a larger trial:
-
Recruitment (1) Accrual rate is fewer than three but more than two patients per site per month on average, or in the later recruitment months the accrual rate reaches three per month; and (2) attrition rate is > 30% but < 50%.
-
Protocol adherence (1) Fidelity ratings indicate therapist adherence to the intervention is < 75% but > 60%; (2) < 70% but > 55% of parents/carers and clinicians report that the intervention and consent procedures were acceptable; and (3) < 90% but > 70% of participants received the intervention.
-
Outcome data (1) < 75% but > 60% of parents/carers complete outcome measures at each time point; (2) < 75% but > 60% of items across outcome measures for each participant are complete; and (3) < 75% but > 65% of parents/carers judge the outcome measures to be acceptable.
Red
If any of the following criteria are met, and following a thorough review of the reasons for this, including consideration as to whether remedial action could be taken, a recommendation to not proceed to a larger trial may be made by the SSC:
-
Recruitment (1) Accrual rate is fewer than two patients per site per month on average; and (2) attrition rate is > 40%.
-
Protocol adherence (1) Fidelity ratings indicate therapist adherence to the intervention is < 50%; (2) < 55% of parents/carers and clinicians report that the intervention and consent procedures were acceptable; and (3) < 60% of participants received the intervention.
-
Outcome data (1) < 50% of parents/carers complete outcome measures at each time point; (2) < 50% of items across outcome measures for each participant are complete; and (3) < 65% of parents/carers judge the outcome measures to be acceptable.
Participant characteristics
Parents/carers and young people
We recruited 15 parents/carers of children with moderate to severe learning disabilities and specific phobias. Fourteen parents/carers were female and one male. Intervention groups had between one and three participants. We initially planned to have up to six parents/carers in each of the groups; however, final group sizes were determined by recruitment at the participating sites.
Table 18 shows additional demographics of the young people.
| n = 15 | ||
|---|---|---|
| Age (years), mean (SD) | 11.38 (3.15) | |
| Sex (% male) | 53.3% | |
| n | % | |
| Ethnic background | ||
| White British | 12 | 80 |
| Asian or Asian British – Bangladeshi | 1 | 6.7 |
| Asian or Asian British – Indian | 1 | 6.7 |
| Mixed – White Asian | 1 | 6.7 |
| Additional diagnoses (parent report) | ||
| Autism | 10 | 66.67 |
| Down syndrome | 3 | 20 |
| Attention deficit hyperactivity disorder | 1 | 6.67 |
| Tourette syndrome | 1 | 6.67 |
| Other specified feeding and eating disordera | 2 | 13.33 |
| VABS standard scores | ||
| n (% missing) | Mean (SD) [95% CI] |
|
| Communication | 15 (0) | 46.73 (8.18) [42.20 to 51.26] |
| Daily living skills | 15 (0) | 45.87 (10.25) [40.19 to 51.54] |
| Socialisation | 15 (0) | 48.60 (4.17) [46.29 to 50.91] |
| Adaptive behaviour composite | 15 (0) | 50.8 (4.6) [48.25 to 53.35] |
Among young people with learning disabilities, 53.3% were male, and the mean age was 11.38 years (SD 3.15 years). The majority of the sample described themselves as White British. The primary place of residence for all children in this sample was the family home, and 86.7% of children attended a special school at the time of this study. The majority (53.3%) of children in the sample had not had any previous intervention for specific phobia; 26.7% of the children previously had behavioural therapy and 20% of children previously had another type of intervention such as acclimatisation sessions. Melatonin was the most prevalent medication reported (40.2%). Parents/carers also mentioned medication for allergies (20.1%), bowel issues (constipation) (26.8%) and asthma (6.7%). Additional medication included interventions for skin conditions (e.g. eczema), thyroid problems, diet and general health (i.e. vitamins). None of the children were taking medication for mental health or behaviour problems.
Young people’s adaptive behaviour scores on VABS-345 are presented in Table 18. In terms of degree of learning disabilities, all participants scored in the moderate range of impairment. Parents provided information on co-occurring diagnoses, with more than half of the sample having autism spectrum disorder (Table 18). Four parents (26.7%) described their child as having sensory processing difficulties.
Table 19 summarises the categorisation of specific phobias in the sample and the corresponding fear and interference rating on scales of 0 (not at all) to 8 (very, very much) from the ADIS. 44 Table 19 also details whether parents/carers described the child as avoiding the specific phobia. Parents/carers often reported that their child had multiple phobias, as shown by the number of participants per phobia category. In cases where the child had multiple phobias, the most severe phobia or the phobia causing the most disruption was chosen as the focus of the SPIRIT intervention. Fear ratings indicate that these stimuli cause substantial fear in the children and considerable disruption to the child’s life. Additionally, the avoidance percentages suggest that the majority of children in our sample had been actively avoiding the fear-inducing stimulus.
| Type | N | Fear rating (0–8) | Interference (0–8) | Avoidance | No/no response or ‘N/A’ (%) | ||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Yes (%) | |||
| Animal (e.g. dogs, spiders, birds) | 9 | 6.73 | 1.35 | 6.5 | 2.12 | 90.9 | 9.1 |
| Environmental (e.g. heights or storms) | 6 | 6.89 | 0.93 | 6.78 | 2.11 | 88.9 | 11.1 |
| Blood/injection/injury (e.g. blood test, COVID swab) | 8 | 6.74 | 1.51 | 6.30 | 2.51 | 91.7 | 8.3 |
| Other (e.g. balloons, costumed characters, loud noises) | 10 | 6.96 | 1.21 | 6.68 | 1.819 | 88.5 | 11.5 |
Therapists
A total of 18 therapists were recruited and trained to deliver the SPIRIT intervention, 10 of whom delivered the intervention. Most of the therapists recruited were assistant psychologists (n = 5) or clinical psychologists (n = 4). Other professions included psychological therapy practitioners (n = 2), learning disability nurses (n = 2), a high-intensity therapist, a learning disability CAMHS practitioner, a nurse therapist, a specialist practitioner and an occupational therapist. Five therapists signed consent forms to take part in post-intervention interviews, one from each of the NHS study sites.
Results
Recruitment pathways
Recruitment of sites
A total of 22 services were approached about being involved in the SPIRIT study, and 5 sites agreed to participate: Cambridgeshire Community Services NHS Trust, Dorset Health Care University NHS Trust, Norfolk Community Health and Care NHS Trust, Avon and Wiltshire Mental Health Partnership NHS Trust and Hertfordshire Community NHS Trust. Sites often declined to be involved on the basis of capacity, but some voiced their interest in a larger trial or future research.
The barriers to taking part in the study were staff capacity limitations and the tight timeline of the project. COVID-19 had a significant impact on the ability of sites to participate, and R&D teams also had reduced capacity due to COVID-19-related staff redeployment.
Five sites in total participated in the study: Cambridgeshire Community Services NHS Trust, Dorset Health Care University NHS Trust, Norfolk Community Health and Care NHS Trust, Avon and Wiltshire Mental Health Partnership NHS Trust and the Hertfordshire Community NHS Trust. Table 20 outlines the timeline for each site from training in the SPIRIT intervention to the delivery of the intervention.
| Site | Training | Opened to recruitment | Intervention started | Intervention completed |
|---|---|---|---|---|
| Cambridgeshire Community Services NHS Trust | 6 January and 7 February 2022 | 20 January 2022 | 18 May 2022 | 12 December 2022 |
| Dorset Health Care University NHS Trust | 6 and 7 January 2022 | 31 January 2022 | 26 May 2022 | 4 August 2022 |
| Avon and Wiltshire Mental Health Partnership NHS Trust | 28 January and 4 February 2022 | 9 February 2022 | 9 June 2022 | 12 December 2022 |
| Norfolk Community Health and Care NHS Trust | 26 and 27 January 2022 | 15 February 2022 | 18 May 2022 | 12 December 2022 |
| Hertfordshire Community NHS Trust | 23 August 2022 | 26 August 2022 | 10 October 2022 | 12 January 2023 |
Recruitment of participants
As outlined in Table 21, three of the sites recruited from case lists only. Two sites agreed to external recruitment. For both of these sites, the research team contacted local special schools and relevant support and advocacy organisations in the region to disseminate information about the study. In total, 93 potential participants were identified and contacted about the study; 47 of these were identified by NHS sites and 46 through external recruitment. The numbers at each site who consented to participate and met the eligibility criteria are shown in Table 21.
As shown in Figure 2, a total of 93 potential participants were either identified by sites and sent information about the study or contacted the research team through the external recruitment pathway.
FIGURE 2.
SPIRIT study CONSORT flow diagram.

A total of 15 families agreed to participate in the study and met eligibility criteria. One family withdrew from the study prior to baseline, due to not being available to attend the planned dates for the parent skills training workshops. Fourteen families completed baseline and commenced the intervention. Thirteen families completed the intervention. One family had to withdraw from the study due to a family bereavement that necessitated them going overseas for a period of time. They therefore did not complete the intervention and were not available for follow-up. The remaining 13 families completed treatment, and 12 completed follow-up assessments. One family did not respond to repeated contacts by the research and NHS site teams and was lost to follow-up. Seventy-two families were either not eligible, were not interested, or did not respond to contact by the research team. Reasons for not being eligible are summarised in the Figure 2 flow chart.
A total of 21 parents/carers consented to being involved in the study. Three withdrew as their child was no longer eligible due to their age, and two disengaged. Of these, 18 completed eligibility assessments, with eligibility confirmed for 15; the remaining 3 did not meet eligibility as they did not meet the study criteria for moderate to severe learning disabilities.
Recruitment challenges
In the post-intervention interviews, the practitioners were asked about the process of recruiting parents for the study and what challenges, if any, they encountered.
One site noted that the limited number of eligible children in the learning and disability teams was a barrier to successful recruitment and intervention delivery. Additionally, two sites highlighted that there was a limited availability of clinicians and that clinicians were reluctant to take part in research due to long waiting lists in their service. Two sites also noted that they had staff vacancies in their teams that had not been filled, impacting capacity. All sites noted that they received limited referrals for specific phobia unless other presenting issues warranted the referral, while one site added that specific phobia was not seen as urgent in services. In terms of understanding, two sites suggested there was limited understanding of specific phobia among clinical staff. Two sites also mentioned that parents have limited understanding of what learning disability is and sometimes are not fully aware of their child’s diagnosis. Three sites noted that their R&D teams were redeployed during the pandemic to help with vaccinations, reducing their capacity to conduct research.
Two sites suggested that learning disability is understood differently in special schools and in the NHS. This was predominantly around terminology, with schools using the broad phrase ‘learning difficulties’ rather than determining or describing a child as having a learning disability. They also mentioned that their engagement with special schools was limited. One site suggested that schools were not engaging in research in September 2022 due to pressure experienced in relation to the extra bank holiday and the Queen’s passing. Two sites reported they were unable to recruit in schools from July 2022. One site mentioned that they lost potentially eligible participants due to workshops being scheduled during summer holidays. Regarding engagement, all sites mentioned that there was reduced engagement with families during term breaks and summer holidays.
One site highlighted multiple reasons for delays, including the Royal Mail strike in August and September causing delays in receiving study documentation, the bank holiday for the Queen’s funeral resulting in cancellation of preplanned appointments about the study, and referrals being delayed due to participants and clinicians being on holiday (July, August and beginning of September).
The acceptability and feasibility of the manualised intervention for all stakeholders, including children and young people, carers and therapists
The post-intervention interviews asked parents (n = 5) and therapists (n = 5) about their views on the acceptability and feasibility of the intervention, the therapeutic relationship, and whether they had any suggestions for improvements or revisions to the SPIRIT intervention. Interviews also covered perceived impact of the intervention, and therapists were asked about their experiences of being involved in delivering the intervention.
Intervention feasibility and acceptability: parents/carers
All parents/carers (n = 5) had positive experience of attending the two initial workshops and found them helpful. One parent/carer mentioned that being able to talk with other parents during workshops was beneficial. Another parent/carer said that the small-group format of the workshops was advantageous.
The majority of parents/carers (n = 3) said that their therapist was supportive and helpful during the weekly support sessions. Three parents/carers also said that they had no issues attending the support sessions. Two parents/carers found reminders about the support sessions useful. One parent/carer found the support sessions were too frequent. Another parent/carer mentioned difficulties with fitting the support sessions in their family life. One parent/carer said they found support sessions easy to rearrange if needed.
The majority of parents/carers (n = 3) thought that the remote mode (online or over the telephone) of intervention delivery worked well as it saved them time. Two parents/carers mentioned they found the remote mode of delivery easier than face to face. Some parents/carers (n = 2) said that this was an appropriate way to deliver the intervention, while one found in-person sessions more appropriate.
Two parents/carers noted that their child made progress in their tolerance of feared stimuli but their intervention goal was not yet achieved. Two parents/carers said they would have preferred to receive support from the therapist for longer than 8 weeks. One parent/carer mentioned that therapists adapted the intervention well to meet the needs of their child. Another parent/carer felt that the intervention might be more suitable for older children.
A summary of parents’ experiences and views on the intervention is presented in Table 22.
| Theme | Subtheme | Example comment | Number of parents and carers |
|---|---|---|---|
| Experience of attending the two workshops | Positive experience and helpful | ‘with the workshops, we were all very sort of positive and very kind of “oh yeah this is gonna be really helpful.”’ | 5 |
| Benefit of discussing with other parents | ‘it’s always just nice to have other people to chat to that know where you’re coming from and you talk about things.’ | 1 | |
| Benefit of small group | ‘so I think that worked well and because our group was quite small (it was only three) there was always opportunity for people to speak and ask questions.’ | 1 | |
| Experience of attending the support sessions | Supportive/helpful therapist | ‘psychologists were always very supportive . . . if something had come up and I needed to postpone so they were flexible.’ | 3 |
| No issues attending | ‘Nothing would have stopped me.’ | 3 | |
| Reminders useful | ‘Just having the Teams link in the diary is helpful because the phone goes “bing”.’ | 2 | |
| Sessions too frequent | ‘Yeah it was a bit hit and miss . . . I actually found that every week was quite a lot.’ | 1 | |
| Difficulty of timing | ‘I don’t think there’s ever a perfect time that’s going to work when you’ve got your severely disabled child with you. But no, they were OK.’ | 1 | |
| Easy to rearrange | ‘I just had to rearrange a couple of times due to other appointments, but other than that, no it was fine.’ | 1 | |
| Acceptability of online/telephone format | Benefit of time | ‘It wasn’t a huge piece of your time so that worked well, I think.’ | 3 |
| Easier than face to face | ‘I think realistically that would probably be too difficult for the parents to all be involved.’ | 2 | |
| Appropriate format | ‘Yeah, I think through the phone is good, yeah.’ | 2 | |
| In-person more appropriate | ‘They were in person and sometimes they came to see me at home to see how he was getting on . . . it was right for me.’ | 1 | |
| Appropriateness of the intervention | Progress but goal not yet achieved | ‘We’re still not there yet . . . We’ve done really well and I think probably a lot of it is quite circumstantial . . . I’m really, really hoping that we get to the point.’ | 2 |
| More support required | ‘They did [meet needs] but when they stopped it would have helped to be carried on a bit longer.’ | 2 | |
| Adapting to meet child’s needs | ‘I think the ladies that delivered it came up with some really good sort of outside of the box suggestions of what we could do . . . things that he really enjoyed doing, a bit of role play and all that sort of stuff . . . I think it was all cleverly thought out.’ | 1 | |
| More appropriate for older children | ‘I don’t know if it has been or would be more effective for children that are slightly older, and although they’ve got learning disabilities they have a greater understanding and be able to engage more with them because it was very much I was leading it, and it would have been good if [name of child] could sort of be more involved and have a greater understanding of what was happening.’ | 1 |
Intervention feasibility and acceptability: therapists
A summary of therapists’ views on feasibility and acceptability of the intervention is presented in Table 23.
| Theme | Subtheme | Example comment | Number of therapists |
|---|---|---|---|
| Experience of delivering the two workshops | Successful delivery | ‘Workshop 1 went great.’ | 3 |
| Benefits of small group | ‘I think that we had a very small group, so I think it was easier for us to create a nice supportive, safe space.’ | 2 | |
| Benefits of peer support for parents | ‘Was also nice for local parents who have children with learning disabilities to come together and have open conversations about the difficulties they face – and potential to make contacts/friendships.’ | 2 | |
| Helpful structure and resources | ‘the fact the slides were ready and we could plan ahead and the visuals were ready and it was clearly outlined so we knew when we had to give a break and we could schedule it in other ways so that was really helpful.’ | 2 | |
| Helpful for parents | ‘I think it was a really helpful way to start them trying to do this focused intervention.’ | 1 | |
| Easy to deliver | ‘I think the workshops were very easy to deliver. I think everything was there in the materials, in the PowerPoint [presentation]. It just flowed quite easily, it was kind of . . . yeah, that was easy to deliver.’ | 1 | |
| Therapists supporting each other | ‘And if any one of us stumbled or had a brain fog, the other one would, someone would jump in and help.’ | 1 | |
| Enjoyable | ‘We really enjoyed facilitating the workshop.’ | 1 | |
| Overwhelming for parents | ‘A real theme throughout this workshop was parents being perhaps overwhelmed or worried about the amount expected of them to deliver the intervention – this was particularly in relation to getting things organised for exposure steps.’ | 1 | |
| Experience of delivering the support sessions | Helpful for parents | ‘I think parents found the support sessions really helpful. Having that check-in with someone.’ | 4 |
| Increased understanding of families | ‘it was good because I think throughout those support sessions I learnt a lot more about the child and about the parents as well.’ | 2 | |
| Enjoyable | ‘I really liked the weekly support.’ | 2 | |
| Benefits of troubleshooting | ‘Helpful to have . . . “troubleshooting” in the phone calls to discuss things that needed a bit more tweaking.’ | 2 | |
| Time-consuming | ‘I had initially left half hour aside for phone calls but actually was more likely an hour needed (to fill in paperwork from the study and write up notes).’ | 1 | |
| Seeing progress | ‘I really like working with the parents in helping them think through their child’s fears and seeing their confidence increase.’ | 1 | |
| Easy to individualise | ‘I could see how different both were and how much you adapted to each child . . . it was really unique to each of them.’ | 1 | |
| Confusing material location | ‘sometimes it was a bit confusing in which book or manual or treatment bit where things were in their folder or in different bits.’ | 1 | |
| Benefits for parents’ anxiety | ‘I think they really appreciated the weekly support sessions, someone to talk it through with and talk through their fears as well because one of the things that came up in sessions would be their well-being and how they’re struggling with it and you realise that parents have a lot of fears too . . . so they really benefited from it.’ | 1 | |
| Acceptability of online/telephone format | Preference for face to face | ‘I would like to have it face to face. Because what you miss out on virtual meetings is when you stop for a coffee break. It’s that in-between chitchat about people and their lives. And you get to know them a little bit better.’ | 4 |
| Online more appropriate | ‘Delivery was good. I think the support sessions worked well when it was online. I think it was easier for parents and for me to deliver it that way, it was just more convenient.’ | 3 | |
| Issues using technology | ‘She is not confident with technology and so asked for it to be a phone call rather than over video call. It was quite a difficult call due to the chaotic nature of the home . . . and also due to not being able to physically show Mum the resources that we were discussing which I think led to her feeling a bit confused and overwhelmed.’ | 2 | |
| Difficulty building rapport | ‘The person we were supporting struggled to do a video call which I think would have been OK but on the phone it didn’t feel that there was enough connection.’ | 2 | |
| Parents not prepared for calls | ‘people often using their phone, they’re not on a laptop . . . it meant that because she was always out of the house, she never had her SPIRIT materials in front of her.’ | 1 | |
| Acceptable and easy | ‘it was pretty easy, yeah.’ | 1 | |
| Benefit of privacy | ‘We could go through the data sheet verbally and it was often during the school day, so kids weren’t around, and they were able to have that confidential space.’ | 1 |
Most therapists (n = 3) described the workshops as successful. Two therapists highlighted the benefit of having the workshops in small groups, and two therapists said that having parents support one another was a positive experience of the workshops. Two therapists reported that the structure and resources provided for the workshops were helpful, and one therapist suggested that workshops were a helpful start for parents. Another therapist suggested that the workshops were easy to deliver, and one therapist described delivering the workshops as enjoyable, while another said that parents found the experience overwhelming.
In terms of support sessions, the majority (n = 4) of therapists said that these sessions were helpful for parents. Two therapists reported that they aided the understanding of families, and another two therapists said they enjoyed providing the sessions. The concept of troubleshooting was raised by two therapists, and they suggested this was a beneficial component of the support sessions. Another therapist said they saw progress through these sessions, while another therapist suggested that sessions were easy to individualise. One therapist proposed that these sessions had benefits for the parents’ anxiety. However, one therapist highlighted that these sessions were particularly time-consuming, and another reported that the location of the material was sometimes confusing.
Regarding the acceptability of online or telephone format, most therapists (n = 4) would have preferred a face-to-face format. However, it was recognised by three therapists that online was more appropriate. Two therapists reported that parents had encountered technology issues, and another two therapists highlighted the difficulty of building rapport over the telephone/online. Another therapist said that the format was acceptable and easy, and another highlighted that this way offered the benefit of privacy.
Intervention acceptability and suitability: therapists
Therapists were asked about the acceptability and suitability of the SPIRIT intervention; Table 24 provides a summary of therapists’ views. Most therapists (n = 3) believed that SPIRIT is appropriate for the target population, and a further two therapists suggested that the intervention would also be acceptable for a wider population such as children with a mild degree of learning disabilities or communication difficulties. However, two therapists suggested that more adaptations were needed for the intervention to be appropriate for families who need extra support. Other observations included the view that the intervention is less appropriate for older children and in situations where children have severe mental health needs.
| Theme | Subtheme | Example comment | Number of therapists |
|---|---|---|---|
| Suitability for the target population | Appropriate for target population | ‘I really think it’s really helpful, because with the clinician brings the strategies and the tools, whereas the parent brings the expertise on their child. And so together they can make a really good plan. What works for that child.’ | 3 |
| Acceptable for wider population | ‘I think could work for a lot of people, even like children who haven’t got that kind of level of learning disability. I think it would be interesting to try it with . . . children with mild learning disabilities or those who are more kind of on that kind of borderline area as well. I think it’d be interesting to try out with children with other forms of extra needs like, communication needs, or like sensory needs . . . I think it’s got a lot of potential.’ | 2 | |
| More adaptations needed | ‘I think it is still useful for our parents but needs more adapting in order to fit for our population of families who need more support.’ | 2 | |
| Less appropriate for older children | ‘I think it works well for children . . . I’m wondering about the age . . . there was an adolescent . . . she was thoroughly aware of what Mum was helping her with. She had her own goals . . . So I think Mum was like, “oh, you haven’t talked enough about how I involve her in this study”. Whereas I think the other parents you know, they were making the decisions for their child’s best interests.’ | 1 | |
| More appropriate for less severe cases | ‘where things haven’t got so severe with the presentations and they’re needing that tertiary CAMHS service and things are more complex, I think it might be more effective at that level.’ | 1 | |
| Engagement and understanding of parents | Positive engagement | ‘I think both our families engaged really well, they were so on board so I think we were very lucky in that. They didn’t need any more prompting or anything to engage them better, they were just very, very engaged.’ | 6 |
| High expectations of parents | ‘The parents we were doing it with were quite overwhelmed with other children, other things going on with them and therefore it felt quite a battle for them to prioritise the session each week and to be doing the prepping.’ | 3 | |
| Lack of engagement | ‘frustration when you could hear that the parents weren’t fully engaged. And I thought that they’re missing some key elements.’ | 2 | |
| Issues completing data sheets | ‘The homework, you know the sheets that we had asked parents to fill in. In my experience, neither parent filled them in.’ | 2 | |
| Reduced motivation over time | ‘I do think that towards the end, people were getting a bit bored of it. Like there was a lot of energy for the first few weeks, I think that tailed off. But that possibly coincided with the summer holidays.’ | 1 | |
| Parents were the experts | ‘I think it was very clear that the parents in our group were real experts. They have so much knowledge of managing children with that level of extra need. It was quite humbling. And they were very good at saying straight away, “oh, that’s not going to work for my child.” They just knew.’ | 1 | |
| Parent determines outcome | ‘I think it’s about the parent being in the right place to do it.’ | 1 | |
| Good understanding | ‘parents have developed a good exposure plan.’ | 1 | |
| Difficult to contact | ‘second lady was really, really difficult to get a hold of. So it should have been eight weekly sessions, but it spanned over something like 11 or 12 weeks because I wasn’t able to get hold of her at the agreed time. So, it took a lot of my time to rearrange, to try and find a different time that would work.’ | 1 | |
| Meeting needs | Adaptations made to meet the needs | ‘I think invariably some things were adapted . . . the relaxation. Some people dropped it, or they weren’t doing it during the exposure. The reinforcers . . . I think people kind of ended up doing their own thing on that. I think we had to just be a bit flexible as therapists and kind of because we’d set it up as the parent was an expert in their child.’ | 4 |
| Child’s needs met | ‘I think it met their needs because obviously their fears were something that they really struggled with and they weren’t able to communicate . . . the fact that they are now overcoming their fears step by step, it’s making a difference in them.’ | 3 | |
| Parent’s needs met | ‘It certainly met both of my families’ needs.’ | 3 | |
| Useful | ‘I think it still definitely did have a benefit and I’m glad they’ve done it and it has been a useful intervention.’ | 2 | |
| Further support needed | ‘I think they were able to make some changes but I think it wasn’t sufficient for that family.’ | 2 | |
| Positive child reactions | ‘I think he enjoyed the sessions and I think it helped.’ | 1 | |
| Difficult to know if child’s needs have been met | ‘It’s difficult to answer that because we didn’t actually meet the young people and they weren’t the ones motivated for change.’ | 1 | |
| Suitable for less severe cases | ‘in terms of learning disabilities, I think they were quite moderate. So, I think a more able young person, who say, for instance, wanted to be able to be around dogs without running away. I think it would be very well targeted to them and be able to meet their needs.’ | 1 | |
| Dependent on parents | ‘To an extent, yes, it’s very dependent on the parents . . . I can think of one where they were very reliant on us as the therapists and gaining our advice each week, and despite trying to do that empowering process . . . I’m not sure if it met that parent’s needs.’ | 1 | |
| Appropriateness of materials | No changes made | ‘We didn’t adapt the workshop slides because they were really great, the ones you sent us.’ | 4 |
| Acceptable | ‘I found the materials easy to follow and the PowerPoint presentation was engaging.’ | 3 | |
| Useful point of reference | ‘They did refer to it a lot when they were struggling and I think they really liked the fact that they had a pack, so they had the resource and then the data sheets and then going through all of that in the training was very useful so I think it worked very well’. | 3 | |
| Difficulties with the rating scale | ‘[The rating scale] was quite tricky for parents and families and young people to grasp, and especially the level of learning disability really affected whether the young people could use the rating scale or not. And some parents just outright said they didn’t feel comfortable with kind of using that.’ | 1 | |
| Additional explanation needed | ‘should parents be creating a new visual stimulus for each step of the exposure ladder . . . For feedback, we felt that this needs further explanation in the manual.’ | 1 | |
| Adjustments made to the workshop materials | ‘I think the [PowerPoint presentations] we jigged around the order of some sections . . . so it made more sense in terms of the flow.’ | 1 | |
| Parent-mediated model | Parent–child relationship | ‘children are more willing to work with their parents because their parents are their safe space, they have an attachment to their parents and so rather than an outside person coming in, with parents they naturally have that (rapport) and they know their child . . . and they see them much more and so they can work on it more regularly and you can progress it better.’ | 3 |
| Parent empowerment | ‘I know there was a lot of like appreciative commenting in the workshops around. You’re the expert and your child, you know, trying to break down that hierarchy. And I know a lot of the parents really appreciated hearing that. And taking that lead.’ | 2 | |
| High expectations on parents | ‘I think that is quite a big ask for a lot of the parents we see who I think are just quite overwhelmed really in their caring role and have a lot of other demands on their time and things, that it felt quite overwhelming.’ | 2 | |
| Importance of parent motivation | ‘I think anything parent led tends to be more successful because they’re more easier to motivate for change. And it goes back to that motivation and why they want the change.’ | 1 | |
| Further adaptations needed | ‘I think it’s a really good idea but needs a bit more thinking about from the perspective of the parents and how it works in practice to have the best outcomes for the families.’ | 1 | |
| Importance of parent involvement | ‘I think it was vital. I couldn’t have just met with the child or young person, it wouldn’t work. They had all the expertise and the knowledge. They knew what would work for their child and what wouldn’t.’ | 1 | |
| Acceptable | ‘parents being involved, I think that is a really good way to go.’ | 1 | |
| Benefits for therapist | ‘there was a bit more confidence as a therapist because I know the parents know their child well and they can deliver it whereas I would not know the child as well.’ | 1 | |
| Long-term impact | ‘There was a huge amount that they’ve taken on from doing the treatment that then will have ongoing effects in terms of how they are able to support their young person, so I think that’s the real strength of the training package, really.’ | 1 | |
| SPIRIT intervention for future clients | Appropriate for wider distribution | ‘I think if it was available I would love to share it with our service and maybe provide them with training on that. It’s easily learnable; I think it would be good for staff to learn it and that package and that approach would be very beneficial for something like an intensive service like us and CAMHS . . . I think it’s very useful and if it was available I would love to share it.’ | 5 |
| Delivery through schools | ‘if it was available I would try and get schools to buy it in or us to deliver it through the schools to young people at an earlier level in their care journey.’ | 1 | |
| Further adaptation needed | ‘I think I might adapt it somewhat.’ | 1 |
In terms of the engagement and understanding of parents, all therapists (n = 6, including e-mail feedback) reported positive engagement of parents, and one therapist suggested parents had a good understanding of the intervention. However, three therapists highlighted that the programme placed high expectations on parents. Two therapists described a lack of engagement from parents, with one therapist mentioning a reduced sense of motivation from parents over time. The issue of parents not completing data sheets was raised by two therapists, and one reported difficulty with contacting a family.
Four therapists felt the adaptations made to the intervention met the needs of families, and three therapists reported that the child’s and parents’ needs were met through the intervention. The SPIRIT intervention was reported as useful by two therapists, but two suggested that further support was needed for families.
Regarding the appropriateness of materials, most therapists (n = 4) said that they did not make any changes to the materials provided, and three felt the materials were acceptable. The intervention materials were described as a useful point of reference by three of the therapists. One therapist reported that parents had difficulties using the rating scale, and another suggested that further explanation was needed for materials such as the visual schedule.
The therapists were also asked about their views on the parent-led intervention model. Three therapists highlighted the benefits of parent-mediated intervention, as the parent–child relationship can facilitate the delivery of the intervention. Two therapists mentioned that parent empowerment was an important feature of the intervention, and one therapist described the importance of parental involvement for this type of intervention. The long-term positive impact of the intervention for families was also mentioned by one therapist. When therapists were asked if they would use the intervention for future clients, all therapists (n = 5) reported that they felt the SPIRIT intervention was appropriate for wider distribution, and one therapist felt that it could be delivered through schools.
Therapeutic relationship: parents/carers
When asked about the relationship with their therapist, all parents/carers said they had positive interactions with them. Three parents/carers also mentioned that they felt supported by their therapists. All parents/carers felt comfortable asking questions and raising concerns with their therapist, and none felt that improvements were needed to the support offered by the therapists. One parent mentioned that they would have liked some help with accessing their child’s feared stimulus (dog). Table 25 summarises the views of parents/carers on their relationship with the therapists.
| Theme | Subtheme | Example comment | Number of parents and carers |
|---|---|---|---|
| Experience of the therapeutic relationship | Positive interactions with therapists | ‘It was good, really good. She was interested, enthusiastic, had good ideas and suggestions and allayed my fears when I had doubts about things.’ | 5 |
| Feeling supported by therapists | ‘Very much so, yeah, very much so. Really helpful and interested in . . . there was me and one other lady and they really listened and took on board what the phobia was and how we can go about it and thinking about step by step and everything so yeah, really good.’ | 3 | |
| Ability to raise concerns and questions | Comfortable raising concerns and questions | ‘Yeah definitely, yeah. There was loads of opportunities to ask questions and yeah, no judgement.’ | 5 |
| Improving support | No improvement to support required | ‘I think it was spot on really.’ | 5 |
| Support for accessing phobia | ‘Other than a ready route to dogs! If they could just come to the front door!’ | 1 |
Therapeutic relationship: therapists
Therapists were also asked about the experience of the therapist–parent therapeutic relationship, and Table 26 provides a summary of therapists’ responses. One therapist described the relationship positively, another therapist suggested that more time would have been beneficial for the therapeutic relationship, and one reported on the ease of developing a therapeutic relationship. When asked about how the structure and online delivery impacted the therapeutic relationship, two therapists said they would have preferred a face-to-face delivery, while one therapist suggested that the format worked well, and another felt that the online format was not a barrier to delivery. However, one therapist suggested that there was a lack of engagement as a consequence.
| Theme | Subtheme | Example comment | Number of therapists |
|---|---|---|---|
| Experience of the therapeutic relationship | Positive relationship | ‘well-being was a part of it and so naturally you do develop that good relationship . . . they feel like they can communicate with you better and that you are someone that they can get support from, for that and more actually.’ | 1 |
| More time would be beneficial | ‘More time would maybe have allowed a little bit more of a relationship to be built.’ | 1 | |
| Ease of developing relationship | ‘It comes naturally to me to build a relationship with parents . . . So I think kind of making it a safe space and active listening skills and all that, all that kind of stuff that’s just our day job really.’ | 1 | |
| Impact of structure and online delivery on therapeutic relationship | Preference for face to face | ‘I think that is the thing it misses in the face to face. The parents might click and gel with another parent. But then, you know, swap numbers and it’s always helpful to have another parent who’s going through a similar situation. But online your kind of barrier is the screen, and you don’t have that.’ | 2 |
| Worked well | ‘I think that worked well with the format we used.’ | 1 | |
| Online was not a barrier | ‘There was a lot of sharing and the online didn’t hinder that at all.’ | 1 | |
| Lack of engagement | ‘I don’t think she was engaged because the first workshop she was on the phone, and driving. So we were on the telephone while she was driving. I find that really off-putting.’ | 1 |
| Theme | Subtheme | Example comment | Number of parents and carers |
|---|---|---|---|
| Number of sessions | More support sessions | ‘I totally understand it’s a study but it didn’t feel long enough.’ ‘I got a bit stuck at the end because he was doing really well and it just sort of finished. He got stuck on one of the steps.’ |
4 |
| Additional check-ins after the study | ‘It felt like we should then have been handed over to a psychologist who could then supervise us through, even if it was only once a month or something, but just it felt like . . . it felt like being abandoned at the end.’ | 2 | |
| More flexibility of support sessions | ‘I would have preferred it like every other week . . . I would have gained a lot more from it because we would have had an opportunity to actually put into place what we were taught . . . and it would have gone on longer then as well.’ | 2 | |
| Additional group session | ‘I think it might be useful to have, say, a group session again maybe midway through the intervention just to sort of talk about how you’re getting on, it could be sort of again shared learning across with other participants, how they’re finding it.’ | 1 | |
| Intervention | Additional support in accessing feared stimulus | ‘if you could go somewhere, a phobia centre or something, and then it’s set up like something that would be helpful for children . . . and see the psychologist and play a fun game maybe that involves him interacting with his phobia in the form of a game so it would engage him and he’d want to do it, even if he got scared there would be enough in it that would make him want to go.’ | 2 |
| Managing expectations | ‘I think just thinking about how tiny the steps need to be and how long it will take.’ | 1 | |
| Access to online data sheets | ‘so if there was like an online thing that you could just log into and type up how you got on and then any observations, I think that would allow them to access it much more easily . . . yeah, a shared document on Teams would be good.’ | 1 | |
| Space for notes needed on the data sheet | ‘I suppose the charts that we had, where we were writing how we’d done with the intervention, it was just tick box with dates and it wasn’t very easy to kind of articulate or say anything around that, that would have been useful to understand why that had gone wrong, that step hadn’t worked that time or when steps were successful.’ | 1 | |
| Need for change of attitudes within services | ‘I just think it’s the work needs to be done on the other side now with the professionals. Even if they just took one thing away from it all and that is to give our young people processing time.’ | 1 | |
| Alternative relaxation strategies | ‘for the young people that really do have flight response and are very quick to reach it, the relaxation things need to be thought out a bit more of what kind of strategies you can use for that.’ | 1 | |
| Transferable medical documentation | ‘To make sure that for all medical appointments, they all have this health passport, they can all see the exposure steps ladder that you’re working on.’ | 1 |
Intervention improvements and revisions: parents/carers
When asked about revisions and improvements needed for the intervention, four parents/carers said they would have liked more support sessions. Another two parents/carers mentioned they would have liked an additional check-in with their therapist after the study finished. Two parents/carers would have benefited from increased flexibility with how the support sessions were organised, while one parent/carer mentioned they would have liked an additional group session.
Two parents/carers mentioned they would have liked more support with accessing their child’s feared stimulus (dog). One parent/carer mentioned that they would have liked to be told how small the exposure steps would need to be and how long it would take to complete the exposure steps plan before the intervention started. Another parent/carer said they would have liked to have access to online data sheets to improve communication with their therapist. Another parent/carer thought the relaxation strategies needed further development.
One parent/carer mentioned that there is a need for attitude change towards intervention for specific phobia in services. One parent/carer also mentioned that they would have liked to have transferable medical documentation (like a health passport) detailing their child’s phobia and intervention to take to medical appointments.
Table 27 gives a summary of parents’/carers’ suggestions for improvements.
Intervention improvements and revisions: therapists
Regarding suggested improvements or revisions to SPIRIT, three therapists reported that the number of workshops was appropriate, but four therapists suggested that more support sessions were required. However, it was mentioned by one therapist that more, but shorter workshops would have been more suitable. It was also highlighted by two therapists that more flexibility was required in the delivery format of the support sessions, and another two therapists suggested that the support sessions needed to be longer in duration.
One therapist suggested that more support was needed for parents after the workshops and before the support sessions. In terms of suggested improvements/revisions of the intervention, three therapists felt that more tailoring was required to meet the needs of parents, and a further three therapists proposed that involving the child’s school in the delivery of SPIRIT would be beneficial. Two therapists described the need to manage parents’ expectations of what their involvement would entail, and two suggested that it would be beneficial if they had the opportunity to have direct contact with the children. Another revision suggested by two therapists was having reduced or online documentation to speed up certain processes. Other suggested improvements included training more therapists to work collectively, including more specific scenarios in workshops and supporting access to the feared stimuli. Table 28 gives a summary of the improvements/revisions suggested by therapists.
| Theme | Subtheme | Example comment | Number of therapists |
|---|---|---|---|
| Number of sessions | More support sessions needed | ‘8 weeks is not long enough.’ | 4 |
| Number of workshops was appropriate | ‘I thought the workshop was fine, I think any more it would have been too onerous. There was a lot to cover, but I think the two half-days meant it was spaced out nicely, actually.’ | 3 | |
| More flexibility in delivering support sessions | ‘Maybe we should be guided by the families as to whether they needed that phone call that week.’ | 2 | |
| Longer support sessions needed | ‘30 minutes at times I thought were a bit too short because sometimes the parents had a lot they wanted to say, a lot of other issues they wanted to share with you . . . you have to at times speed them up a little bit or not dwell on it too much and progress.’ | 2 | |
| Shorter but more workshops | ‘I think there was a lot of information in each session, maybe particularly for the person we’re supporting, it felt like they were quite full after and for them it maybe would have been more helpful to break it down further and have four shorter sessions.’ | 1 | |
| More support after workshops | ‘I think going from the workshops to phone calls, that felt like it wasn’t really possible, to feel that, following the workshop, the parent wasn’t in a place to just start doing it and to have those phone calls. That felt difficult.’ | 1 | |
| Appropriate number of support sessions | ‘I think eight was a good number . . . I think eight was good to get them like really focused and dedicated on progressing as much as they could towards achieving the goal, which maybe if it was longer they would have lacked a little.’ | 1 | |
| Counting missed sessions | ‘When we can’t get hold of a family after agreeing a time, maybe this should count as one of their sessions unless the therapist is contacted beforehand? Lots of clinical time wasted chasing parents.’ | 1 | |
| Intervention | More tailoring needed to meet parents’ needs | ‘it might need to be adapted to meet those needs of parents who perhaps struggle more with communication and their understanding and their kind of resilience.’ | 3 |
| Involving child’s school in the delivery | ‘What about parents who are just too busy because they’ve kind of got other caring responsibilities, or perhaps, they have their own mental health needs, or physical health needs . . . could it be adapted for, like, professionals to deliver and professionals working in, like, residential settings? . . . Could it be delivered through special schools, through staff?’ | 3 | |
| Managing expectations | ‘just making it clear to parents when they sign up, the time commitment . . . It’s you’re going to need to make a serious commitment to making time to do exposure, like, every day.’ | 2 | |
| Having direct contact with children | ‘I think meeting or seeing the children or young person ourselves, I think that was a big omission . . . I wonder if that would have helped parents feel more secure in the advice that we were giving, and the support we were giving, if we knew a bit more about that young person.’ | 2 | |
| Online or reduced documentation | ‘I do wonder if just next time, like, if it could be online just to speed things up.’ | 2 | |
| No improvements needed | ‘I think it worked really well overall . . . I don’t really have any improvements to say about it because I think it worked really well . . . So I really don’t have any improvements, I think it’s really good.’ | 1 | |
| Multiple delivery models of the intervention | ‘I wonder if even the people who aren’t able to sign up for an intensive intervention like this, are there, like, management strategies? Are there, like, lower-level day-to-day things that they can be doing to at least prevent the phobia from escalating?’ | 1 | |
| Grouping parents more intentionally | ‘maybe once it’s rolled out in bigger groups, you can group it according to kind of their background knowledge.’ | 1 | |
| Training more therapists | ‘maybe even three.’ | 1 | |
| Including specific scenarios in workshops | ‘when they have these appointments that go badly, and it then puts them five steps back on their exposure that day. Like, how do parents tackle that?’ | 1 | |
| Alternative materials | ‘I think there needs to be a bit of other options if the rating scale doesn’t work. To, how to monitor the distress in the young person and how to know whether the exposure step is going too far.’ | 1 | |
| Including more visuals in materials | ‘the PowerPoint [presentation] could have done with a bit of work . . . it was just very simple. Kind of no visuals . . . for the parents with neurodiversity wasn’t very pleasing.’ | 1 | |
| In-person review of data sheets | ‘perhaps families would have completed the data collection sheets more if they were there in front of us rather than just showing them on the screen.’ | 1 | |
| Administrative support for parents | ‘parents may benefit from someone employed specifically to support with these practical issues and to be able to help arrange these sorts of resources.’ | 1 | |
| More initial assessment around anxiety needed | ‘My parent’s child actually arguably did not have a phobia but more generalised anxiety . . . hard to tell through the assessment though as Mum’s perception was that she definitely did have a phobia . . . maybe needed more assessment of anxiety in other settings etc. to understand it more.’ | 1 | |
| Supporting access to feared stimuli | ‘although the phobia needed to be something the family could work on, e.g. not having any access to dogs or injections etc. – maybe this is something the research team could look into before workshops had began and have a list of places the family could use.’ | 1 | |
| Clarifying therapist’s role | ‘A clearer message about the role of the therapist, e.g. should they be the ones making the visuals or is that down to the parents.’ | 1 | |
| Considering parents’ access to technology | ‘what if they don’t have access to a printer? Maybe finding apps as an alternative?’ | 1 |
Perceived impact of the SPIRIT intervention: parents
The majority of the parents/carers interviewed (n = 4) felt they learned skills to help their child, while two also mentioned they have better understanding of their child after participating in the study. One parent/carer reflected on the fact that they feel comfortable taking a step back when needed. Another parent/carer also mentioned they have better understanding of themselves as a consequence of participating in the study.
All of the parents/carers felt that their child made progress in their tolerance of the feared stimuli, and two parents/carers said they felt calmer as a result of the intervention. Another two parents/carers said they have been able to go to places previously avoided with their child. Some parents/carers (n = 2) said they feel hopeful about the future after taking part in the study. Two parents/carers said they feel confident in addressing their child’s other phobias. One parent/carer noted the positive impact of participating in the study on their family, while another said they intended to continue to implement the skills they had learned in the intervention.
The majority of the parents/carers (n = 3) said they learned appropriate and transferable skills as a consequence of participating in the study. Two parents/carers mentioned that their relationship with their child helped to introduce the intervention to their child. One parent/carer found participating in the study empowering, while another mentioned that it was a comfort to be able to deliver the intervention themselves rather than send their child to sessions with a clinician.
A summary of parents’ views on the impact of the intervention is presented in Table 29.
| Theme | Subtheme | Example comment | Number of parents and carers |
|---|---|---|---|
| Lessons learned | Learned skills to help the child | ‘so if he develops another phobia in the future I’ve got the skills now to go back and start again so yeah, I’m really glad I done it.’ | 4 |
| Improved understanding of the child | ‘I guess understanding a bit more about [name of child], how he’s feeling, why he’s feeling like that.’ | 2 | |
| Revisiting steps is not failure | ‘that it’s OK to go backwards . . . making it OK to go back before you can go forward again.’ | 1 | |
| Improved understanding of self | ‘Understanding how I feel about dogs.’ | 1 | |
| Impact and future intentions | Progress in phobia tolerance | ‘We have definitely come further along. It’s been very good since before and after putting all these strategies in place . . . She’s far more relaxed to be in that environment as well. We are winning.’ | 5 |
| Parents feeling calmer | ‘I feel less nervous when I see a pram approaching than I used to . . . I would go into fight or flight because I’d be expecting to be attacked so I’m staying calmer and I guess I give out a calmer vibe to her.’ | 2 | |
| Going places previously avoided | ‘we don’t categorically exclude places with dogs now.’ | 2 | |
| Hopeful about the future | ‘I think, you know, long term, one day she will not happily go and have her bloods done, but she’ll be able to tolerate it.’ | 2 | |
| Confident to address different phobias as needed | ‘if he develops anything else in the future, I’ve now got the skills to start again with something else so I think that’s a brilliant toolkit to have.’ | 2 | |
| Positive family impact | ‘Oh huge . . . Yeah, definitely.’ | 1 | |
| Intention to continue with the intervention | ‘we’re gonna try and get this therapy dog to do some interactions with him and . . . to just keep chipping away at it and then have a think about where we are and maybe try to step up our interventions and just try to keep on with it.’ | 1 | |
| Effects of parental involvement in the intervention | Learning appropriate and transferable skills | ‘So I think it’s transferring, getting those skills and being able to transfer them.’ | 3 |
| Parent–child relationship as a facilitator | ‘he has infinite trust in me so if anyone was gonna do it, it’s definitely gonna be me . . . the whole thing has just been helpful from start to finish; it’s been really helpful not just for this but for other things as well.’ | 2 | |
| Empowering | ‘for us as parent carers is, it was very empowering. It kind of reminded us that we, we know our child, the best out of everyone because we’re with them 24/7 and we can actually take control of this . . . So I think it was, it was very good in that sense, that we are the ones that can take the lead. You know, be firm, fair and assertive, basically.’ | 1 | |
| Comforting | ‘I wouldn’t have thought of sending him off somewhere knowing that he’d do something that would really upset him and not being there so I think it was really good to do that so you can sort of manage and know that he’s not getting too distressed.’ | 1 |
Therapists’ experiences of delivering the SPIRIT intervention
Table 30 provides a summary of the responses from the therapists regarding their experience of participating in the SPIRIT programme. Therapists described the training as helpful (n = 4), clear (n = 3), enjoyable (n = 2) and informative (n = 2). Benefits included general learning (n = 2), gaining information about the adaptation of CBT principles (n = 2), and the opportunity to reflect on therapeutic integrity, knowledge, and skills (n = 2). One therapist felt that involvement in the programme had increased their confidence in the use of graded exposure.
| Theme | Subtheme | Example comment | Number of therapists |
|---|---|---|---|
| Therapist training | Helpful | ‘the structure of both the training and then the package I think it really helpfully made sure you give enough attention to all the elements of the treatment.’ | 4 |
| Clear | ‘I found the training that was delivered online very clear.’ | 3 | |
| Enjoyable | ‘we loved the training.’ | 2 | |
| Informative | ‘we got a lot of information from it.’ | 2 | |
| Overwhelming | ‘I felt overwhelmed at times with the quantity of information.’ | 1 | |
| Sufficient | ‘I definitely think it was sufficient . . . I don’t think we needed any more training, but I’m assuming if you didn’t know PBS in the background it may be helpful to have a little bit more.’ | 1 | |
| Friendly atmosphere | ‘There was opportunity to ask questions and it was promoted in a friendly manner.’ | 1 | |
| Consolidation of knowledge and skills | ‘I really liked it . . . the training really helped consolidate my knowledge and give me more clarity, so really strengthened the skills I had which I’d gained from all over the place, the training.’ | 1 | |
| Therapist benefits/professional development | General learning | ‘I certainly learnt a lot from it . . . I really enjoyed the entire process; I learnt a lot from it.’ | 2 |
| Adapting CBT principles | ‘I learned a lot. I learned that, you know, the kind of principles of CBT for phobia treatment need a bit of a rethink with this population and that the parents have a lot of expertise.’ | 2 | |
| Therapeutic integrity, knowledge and skills | ‘I think for my professional development just reflecting on the importance of that level of detail to go into and kind of take the time to do things well and do them properly and the benefit of that.’ | 2 | |
| Increased confidence | ‘Definitely more confident about anything to do with graded exposure. I feel that I have a foundation knowledge on it.’ | 1 | |
| Enjoyable | ‘I really enjoyed it . . . And I really enjoyed having that contact with the families and seeing the progress or trying to do a lot of troubleshooting because that came up quite a lot.’ | 1 | |
| Helpful | ‘I don’t think there was anything completely new but I think just the level of detail to go into was really helpful.’ | 1 | |
| Generalisation of skills | ‘as therapists you learn more about your fears too! It’s a skill you can adapt to all areas of your life because I was able to think about my fears and how I can overcome them.’ | 1 |
Adherence: parent session attendance
Parent/carer attendance at the skills training workshops and the support sessions was recorded by the therapists. Overall, attendance was high.
Workshop attendance
All 14 parents/carers allocated to the intervention attended both of the skills training workshops (100% attendance).
Support sessions
One family withdrew from the study after the first support sessions, due to a family bereavement.
Of the remaining parents/carers, 11 completed 100% of the support sessions. One parent/carer attended 75% of the support sessions (six of eight sessions), as they felt that they had achieved their treatment goal in relation to their child’s phobia.
Fidelity of SPIRIT intervention delivery
Therapists completed a self-report fidelity checklist at the end of each parent workshop and after each support session to record fidelity of delivery of the intervention. Fidelity checklists for all of the sessions were delivered to each of the participants.
Items on the checklist were organised into seven sections:
-
general workshop/session preparations
-
coverage of workshop/session plan
-
understanding and accessibility
-
interpersonal effectiveness
-
engaging participants
-
workshop content
-
further comments.
Therapists were asked to reflect on all session aims and indicate whether they were completed by circling ‘Yes’ or ‘No’ on the checklist.
Workshops
The delivery percentages for each of the components for workshops 1 and 2 are detailed in Appendix 3. Overall, the self-reported ratings of delivery were very high for both workshops.
For workshop 1, 100% of the therapists responded ‘Yes’ to delivering 38 out of the 40 components in the checklist. The question concerning responding appropriately to interruptions (item 14) was answered ‘Yes’ by 80% of therapists. Therapists reported that it was a ‘challenge in keeping parent discussion specific to specific phobia’. The majority (80%) of therapists reported that they practised preparing visual schedules (item 39) during the workshop. It was reported that parents did not have the cut-out materials ready, so one therapist reported that they instead ‘talked through some examples on the screen and asked what they would pick and why’. The lowest ‘Yes’ response rate (70%) was for the use of the video (item 40) during workshop 1; however, this component was optional, and only used if needed. See Appendix 3.
For workshop 2 (see Appendix 3), all therapists reported completing all of the components for workshop 2.
Support sessions
The fidelity checklist percentages for sessions 1–8 are presented in Appendix 4.
Overall, the majority of the content of all sessions was delivered to a high degree of fidelity to the manual. There were some components where fidelity of delivery was inconsistent or low. Having materials prepared prior to each session (item 1) was not consistently completed for all sessions, with percentages ranging from 58 to 100% across the eight sessions.
The most challenging components related to data collection in monitoring the exposure steps. Receiving the data sheet from parents prior to or during the session (item 2) ranged in endorsement from 15 to 84%. Similarly, reviewing the data sheet (item 18) during the session was often not completed during the session.
Appropriateness of the measures of anxiety-related symptomatology, and secondary outcomes
Outcome measures
The objective in relation to the outcome measures was to assess the feasibility and acceptability of the measures, to inform future work. As this was a feasibility study, and not powered to detect statistically significant differences in outcomes, we did not compare the pre- and post-intervention data from the outcome measures.
Table 31 presents the means, SDs and 95% CIs for scores on the outcome measures completed by parents at baseline and post-intervention follow-up. The number of completed measures and the proportion (%) of missing items are reported for each measure, at each time point. All participants who participated in the intervention at baseline completed all of the measures, with no to very little missing data.
| Measures | N (% items missing) | Mean (SD) | 95% CI | N (% items missing) | Mean (SD) | 95% CI |
|---|---|---|---|---|---|---|
| Severity measure for specific phobia | ||||||
| Total raw score | 14 (0) | 36.21 (10.69) | 30.04 to 42.39 | 12 (0) | 22.75 (9.38) | 16.79 to 28.71 |
| Average total score | 14 (0) | 2.41 (0.72) | 2.00 to 2.83 | 12 (0) | 1.52 (0.63) | 1.12 to 1.91 |
| DBC2 | ||||||
| TBPS | 14 (0.07) | 77.64 (20.22) | 65.97 to 89.32 | 12 (0.09) | 70.75 (16.87) | 60.03 to 81.47 |
| Disruptive | 14 (0) | 21.57 (9.85) | 15.88 to 27.26 | 12 (0) | 20.08 (6.91) | 15.69 to 24.47 |
| Communication disturbance | 14 (0.07) | 10.79 (3.29) | 8.89 to 12.68 | 12 (0.09) | 9.75 (3.14) | 7.76 to 11.74 |
| Self-absorbed | 14 (0) | 24.92 (8.00) | 20.31 to 29.55 | 12 (0) | 23.17 (9.87) | 16.89 to 29. 44 |
| Anxiety | 14 (0) | 11.57 3.32 | 9.65 to 13.49 | 12 (0) | 9.58 (3.53) | 7.34 to 11.82 |
| Social relating | 14 (0) | 8.42 (3.46) | 6.43 to 10.43 | 12 (0) | 7.08 (2.81) | 5.3 to 8.87 |
| BPI short form | ||||||
| Self-injurious behaviour | ||||||
| Frequency | 14 (0) | 5 (4.66) | 2.31 to 7.69 | 12 (0) | 3.58 (3.5) | 1.36 to 5.81 |
| Severity | 14 (0) | 3.93 (3.93) | 1.66 to 6.2 | 12 (0) | 2.83 (2.55) | 1.21 to 4.46 |
| Aggressive-destructive behaviour | ||||||
| Frequency | 14 (0) | 7.71 (5.64) | 4.46 to 10.97 | 12 (0) | 9.75 (5.07) | 6.53 to 12.97 |
| Severity | 14 (2.14) | 6 (5.01) | 3.11 to 8.89 | 12 (0) | 7.75 (5.12) | 4.5 to 11 |
| Stereotyped behaviour | ||||||
| Frequency | 14 (0) | 16.07 (12.19) | 9.03 to 23.11 | 12 (0) | 14.83 (13.66) | 6.15 to 23.51 |
At baseline, there were no data missing from the Severity Measure for Specific Phobia. 46 There was a very small amount of missing data on the DBC2,50 with one person missing 1 item (out of a total of 95) at baseline. Similarly, there was a small amount of missing data on the BPI (short form),51 specifically for the severity rating scale of the Aggressive-Destructive Behavior subscale. One participant missed three items on this measure.
At post-intervention follow-up, there were a small number of data missing from the DBC2,50 with one person missing 1 item (out of a total of 95). There were no data missing from the Severity Measure for Specific Phobia46 or the short form of the BPI. 51
There were no missing data on the scores from the Impact of Phobia measure at baseline and post-intervention follow-up (Table 32).
| Baseline (percentage) | Post-intervention follow-up (percentage) | |||||||
|---|---|---|---|---|---|---|---|---|
| Not at all | Only a little | Quite a lot | A great deal | Not at all | Only a little | Quite a lot | A great deal | |
| Do your child’s difficulties upset or distress them? | 0 | 0 | 64.3 | 35.7 | 8.3 | 16.7 | 41.7 | 33.3 |
| Do your child’s difficulties interfere with their everyday life in the following areas? | ||||||||
| Home life | 7.1 | 21.4 | 50 | 21.4 | 8.3 | 41.7 | 41.7 | 8.3 |
| Friendship | 21.4 | 28.6 | 28.6 | 21.4 | 50 | 25 | 16.7 | 8.3 |
| Classroom learning | 28.6 | 21.4 | 21.4 | 28.6 | 58.3 | 8.3 | 16.7 | 16.7 |
| Leisure activities | 21.4 | 0 | 28.6 | 50 | 25 | 8.3 | 50 | 16.7 |
| Do your child’s difficulties put a burden on you or the family as a whole? | 0 | 0 | 57.1 | 42.9 | 0 | 16.7 | 58.3 | 25 |
Overall, the majority of the scores on the measures presented in Table 31 all showed decreases in symptoms from baseline to post-intervention follow-up, with the exception of the severity rating scale of the BPI Aggressive-Destructive Behavior subscale. 51 Improvements were also noted on the Impact of Phobia measure (Table 32), with scores suggesting a reduction in impact of the phobia on the child’s home life, friendships, classroom learning and leisure activities, and a reduction in burden on the family. As this was a feasibility study, not powered to detect statistically significant differences in outcome measure scores and with no comparator group, any changes in scores are unable to be interpreted.
Physiological measure (heart rate)
Three parents tested the feasibility and acceptability of having their child wear a Fitbit on their wrist, in order to be able to monitor heart rate both during exposure tasks and outside of exposure tasks. It was explained to parents that we were trying this out, and it was emphasised that there was no pressure to continue trying to use the Fitbit if their child became distressed. Therapists reported that this approach ‘reassured parents’, as there was initially ‘apprehension’ about their use when first introduced. In terms of the acceptability of the Fitbit, therapists reported differing experiences, with one young person described as tolerating the Fitbit; in contrast, another young person became ‘very, very distressed when wearing a Fitbit’ and use was discontinued. An issue raised by one therapist was that:
if the watch is only going on for the exposure work, which is causing a bit of distress, that’s then, you know, the young person is now associating the watch with doing exposure work and the distress, and parents were really conscious of that too. So we tried to kind of discourage that pairing.
One parent reported that their child has sensory difficulties so ‘she was not tolerating it at all’. Additionally, one parent reported the issue of ‘remembering to put it on’ and proposed that they could have pursued the use of the Fitbit as they believed it was a good idea, but also suggested that the Fitbit ‘didn’t show the heart monitor, you had to keep pressing the screen’. For the young person who could tolerate the Fitbit, use was inconsistent, but the parent found it helpful to visually see a difference in heart rate during the exposure therapy. In terms of the setup instructions provided, parents found them acceptable: ‘I’m not techie at all and I managed to do it all. So yeah, it was good.’
In terms of suggestions for future use, one therapist suggested that a different way of wearing the device is required and strategies are needed to increase a young person’s tolerance to increase the likelihood of Fitbit use being successful:
I think it was around the wrist is a bit of a tricky area for some of the young people . . . I’ve seen ones where you can wear them around your neck. Like some sort of other device or some way that you can build up the young person’s tolerance before kind of starting it together with exposure.
However, one parent highlighted that ‘if the child’s got sensory difficulties, you’re probably not going to win with it’.
Acceptability of outcome measures
Parents
The interviews (n = 5 parents/carers) asked questions about the acceptability of the measures they were asked to complete at baseline and follow-up. Two parents/carers reported that it was time-consuming but necessary. Two parents/carers mentioned that they preferred completing the measures online or over the telephone, rather than on paper copies. One parent/carer felt that the questions were unclear and another that the questions made them feel bad. One parent/carer felt the measures were straightforward and acceptable and another noted that it was quicker to complete the measures the second time (at follow-up). Table 33 provides a summary of parents’/carers’ responses about the outcome measures.
| Theme | Subtheme | Example comment | Number of parents/carers |
|---|---|---|---|
| Outcome measures | Time-consuming but acceptable | ‘took quite a lot of time, but then there’s not much you can do about that . . . So I think that was fairly . . . that was OK.’ | 2 |
| Preference for online/phone completion | ‘I’d rather do that [online] than postal ones, that’s for sure.’ | 2 | |
| Unclear questions | ‘Some of them were quite difficult to answer because I didn’t really know the answer.’ | 1 | |
| Negative perception of the questions | ‘With all things, when you start to think about your child’s disability it can make you feel a bit rubbish because you just think “oh my gosh, no he can’t do that” but that’s just par for the course with this.’ | 1 | |
| Straightforward/acceptable | ‘Yeah, that was fine. Yeah. Yeah, no worries.’ | 1 | |
| Familiarity with questions aided completion | ‘they seemed a bit briefer second time around but maybe that was just because I was familiar with some of the questions . . . and then you’re a bit more tuned in to think about various aspects so that was fine.’ | 1 |
Factors that facilitated or challenged the implementation of the SPIRIT intervention
Facilitators of and barriers to participating in the intervention: parents
When asked about positives of participating in the intervention, two parents/carers reflected on the progress their child made, while another (n = 2) mentioned that the intervention was interesting. Two parents/carers felt the intervention offered useful tools and strategies, while another parent/carer mentioned that the study was conducted well. One parent/carer reported increased confidence after completing the intervention, and one improved understanding of phobias.
When asked about barriers, issues and challenges of the intervention, one parent/carer mentioned that relaxation strategies did not work for her child. Two parents said they found it difficult to find time to work on the treatment, while one felt they needed more time for the treatment to make a difference for their child. One person mentioned being confused about the use of reinforcement, while another had issues with accessing their child’s feared stimulus (dog). One parent/carer mentioned difficulties with sharing data sheets with their therapist during the support session, and another mentioned it would have been helpful to have space for notes on the data sheet. One person mentioned difficulties with the child’s motivation to engage in treatment.
When asked about facilitators of and barriers to involvement, some parents/carers (n = 2) felt that there were no barriers to their participation and involvement in the treatment, while one parent/carer thought that there were logistical barriers. One parent/carer mentioned that they learned new strategies and techniques to support their child with their specific phobia. One parent/carer said they did not think the treatment is suitable for all parents, while another mentioned that it finished too quickly for them.
Table 34 gives a summary of parents’/carers’ views on barriers and facilitators.
| Theme | Subtheme | Example comment | Number of parents/carers |
|---|---|---|---|
| Positives of participation in the intervention | Progress made | ‘We’ve got to the stage where . . . she’s quite tolerant of this baby [shows toy baby]’ | 2 |
| Interesting | ‘I could see that it could work. There were some interesting things about it.’ | 2 | |
| Useful tools and strategies | ‘breathing techniques we’ve used quite a lot when he’s had a meltdown or . . . yeah, lots of good things came out of it.’ | 2 | |
| Conducted well | ‘I think it was done really well. Really well put together, no pressure because obviously it’s for SEND children and SEND parents are under a lot of pressure all the time so it was nice that it wasn’t “well, you’ve got to do this”.’ | 1 | |
| Increased confidence | ‘Just to give me the confidence to do the steps and teach me them.’ | 1 | |
| Improved understanding of phobias | ‘I understood a lot more about how I feel about dogs because I’m quite nervous about dogs as well and I guess just bringing it to the forefront of my mind I have to make sure that I’m very calm and just deal with them because he will follow my lead.’ | 1 | |
| Barriers/issues/challenges of the intervention | Strategy challenging | ‘The relaxation strategy has never really worked with her.’ | 1 |
| Difficulty with finding the time | ‘it was just hard to work it round everyday life, family life and the fact that you had to engineer situations with [name of child] so I think I maybe underanticipated the workload.’ | 2 | |
| More time needed to make a difference | ‘What I did feel was I wasn’t sure that the study had taken into account how teeny, tiny the steps need to be for kids with learning difficulties and the fact that it could take . . . a really long time to make a difference and I kind of felt that . . . we hadn’t got very far because it takes so long.’ | 1 | |
| Confusion about reinforcement | ‘I suppose I got somewhat confused between the definitions of incentive and reinforcement and reward because the only strong reinforcement to [name of child] would be food and not wanting to be giving her chocolate all the time.’ | 1 | |
| Support in accessing feared stimulus | ‘What would have been lovely is if we could have once a week me and [name of child] gone to somewhere that had dogs organised . . .. Trying to organise it was hard and not being a dog-lover myself it was a bit more difficult.’ | 1 | |
| Issues with sharing data sheet with therapists | ‘they couldn’t see, it was hard for them to see and also I had to e-mail them the document and stuff because it was on paper.’ | 1 | |
| Child motivation | ‘even if they do understand then spend a lot of time with the sequencing and the social stories to explain what we’re doing, why we’re doing it, it’s getting their motivation . . . because I guess with the autism as well you have that inflexibility where “he’s not” and that’s it.’ | 1 | |
| Facilitators and barriers of involvement | No barriers | ‘No, there were none.’ | 2 |
| Strategies and techniques learned | ‘everything that we got taught initially made it easier . . . those breathing techniques were amazing because I taught him to put his hand on my chest and listen to me do it and since then he often asks me now to do it, which is amazing.’ | 1 | |
| Logistical challenges | ‘I think it was just the time it took. Yeah, juggling work and kids and family life, so it was just the kind of logistics of it really.’ | 1 | |
| Not suitable for all parents | ‘it’s not going to suit all parents in the fact that you have to be quite assertive, because we’re obviously following a very structured process on our exposure ladder, and then you’ll go into the environment, and they might be skipping four or five stages of that ladder.’ | 1 |
Barriers to and facilitators of implementation and outcomes: therapists
When asked about the facilitators of successful intervention, two therapists said that the structure of the intervention was a facilitator, and one felt that the troubleshooting component was a facilitator. One therapist noted that placing parents as the experts on the child and their needs was important, while another suggested that including input from professionals facilitated engagement and good outcomes.
Therapists were also asked about any barriers, issues or challenges they experienced when delivering the intervention. Two therapists reported some difficulty implementing the relaxation strategies, and another two therapists felt that some elements of the programme were confusing. Family circumstances were noted as a challenge by two therapists. A further two therapists suggested that more support was needed with adaptations. Another challenge raised by one therapist was that parents would skip exposure steps, and another suggested it was difficult to complete the intervention in the time allocated for the study. Another issue highlighted by one therapist was gaining access to the feared stimulus (in this case a dog). One therapist also suggested that it was challenging to manage the negative experiences that families had had during exposure, while another therapist said that motivating parents was a challenge.
Table 35 gives a summary of therapists’ views on barriers to and facilitators of intervention success.
| Theme | Subtheme | Example comment | Number of therapists |
|---|---|---|---|
| Facilitators of successful intervention | Structure of the intervention | ‘SPIRIT was really useful because it had a structure of 30 minutes and . . . in the handbook on each of the weekly support sessions there is a clear outline of what the aim of the session is, what you need to focus on, what you need to ask and then there’s the general things that you need to be aware of . . . so that really helped me in terms of carrying out a therapy session which I never had before.’ | 2 |
| Troubleshooting | ‘And troubleshooting was very good because they had the freedom to be able to ask questions, think through, and us being attentive listeners was really good because then they could really just get their worries and their fears out and then we could really think through it with them.’ | 1 | |
| Parents as the experts | ‘you kind of set up the focus from the start on it being collaborative and that it was for the parent to deliver the intervention and them to be the expert in their child’s needs and to make those adaptations. I think that kind of helped because we weren’t kind of coming in and we weren’t positioning ourselves as experts.’ | 1 | |
| Input from professionals | ‘I think because we work in a service, that’s again, very similar. We already have that knowledge of what else we can offer.’ | 1 | |
| Goal-setting | ‘I think chatting to the parents during the workshop and having a rough plan of their goals. So you know the ladder and what I found helpful was where they want to start off with their own goal, and then we encourage them to have a middle goal as well.’ | 1 | |
| Having more than one trained therapist | ‘I think having two facilitators work really well because we got hit with a lot of illness, so I don’t think you could do it with just one person.’ | 1 | |
| Barriers/issues/challenges of intervention delivery | Difficulty with relaxation strategies | ‘The only thing I maybe struggled with a little bit was the breathing exercises and I think parents struggled a little bit with that, they were . . . parents needed more help and constant reminders and asking if they were doing it.’ | 2 |
| Some elements were confusing | ‘There was a section in the workbook that I didn’t understand and always fluffed it up when I was delivering.’ | 2 | |
| Family circumstances | ‘life events happening, illnesses . . . it meant that when the parent was trying to do the exposure task the child was having none of it.’ | 2 | |
| More support needed with adaptations | ‘coming up with exposure steps that the family could actually implement.’ | 2 | |
| Parents skipping exposure steps | ‘they [parents] wanted to progress so quickly that they skipped a few steps so you just have to guide them back.’ | 1 | |
| Difficult to finish the intervention in allocated time | ‘none of us approached the final fear, the last step and so thinking about how to leave them with that was hard because I think as a therapist myself, once you develop that relationship with parents and that particular client and their fear, you really want to help them achieve that final goal.’ | 1 | |
| Delay between training and intervention starting | ‘by the time we’d got the children that we were going to work with it took a while, so we had to refresh ourselves . . . that lag meant that we forgot a little bit but because the handbook was there meant we could really just refresh our memory.’ | 1 | |
| Difficulty answering parent questions | ‘all the questions that the parents were going to ask us . . . just after we did the first parent workshops because we were getting so many questions, and I thought, oh actually, oh, I don’t know.’ | 1 | |
| Access to feared stimulus | ‘actual access to a dog. Meant that we kind of got a bit stuck kind of using more spontaneous exposure.’ | 1 | |
| Varied knowledge in group | ‘I think it was difficult to balance those really different levels of knowledge on exposure within the same group.’ | 1 | |
| Managing negative experiences during exposure | ‘The impact that some negative experiences they had in those [medical] appointments was having on the exposure work. Parents feeling like they were taking millions of steps back and kind of having to work through that with parents. And I think that impacted a lot on exposure work and parents’ confidence in taking forward kind of SPIRIT principles.’ | 1 | |
| Motivating parents | ‘I found it quite hard to sometimes keep parents motivated, I guess. They were struggling to see the point of elements of the exposure . . . And a lot of parents voiced that they felt kind of guilty about implementing parts of SPIRIT and exposure. So we found that quite hard to navigate.’ | 1 | |
| Volume and navigating paperwork | ‘I think at times it felt like there was a lot of information in the parent workbooks and folders and the paperwork that wasn’t always super-easy to navigate and find the right relevant bits.’ | 1 | |
| Parent preconceptions | ‘They felt quite frustrated at, you know, trying exposure previously didn’t work, feeling quite let down, I guess by the NHS in general. And all those feelings kind of came forward during the SPIRIT workshop on the study. And the parent, had a very strong narrative around medication and when they found out that medication isn’t offered as part of SPIRIT that was a big let-down for them. The buy-in, I guess, wasn’t there as much at the beginning, but it was at the end, which I thought was really positive.’ | 1 |
Feasibility and acceptability of consent and associated processes
Parents
The majority of parents/carers (n = 4) felt that the consent process and participant information booklet were helpful and useful. Three parents/carers felt the format and content was acceptable. Two parents/carers mentioned that the consent process was easy. One parent/carer felt that their expectations were not managed fully in relation to the workload involved in the study. One parent/carer said they would have liked clearer instructions on how to complete the consent form. Another parent/carer recommended that other parents should read the information booklet a bit at a time to break the information down. One parent/carer mentioned they preferred to receive the information booklet and consent form by post, while another preferred online.
Table 36 provides a summary of parents’/carers’ responses on the consent process.
| Theme | Subtheme | Example comment | Number of parents/carers |
|---|---|---|---|
| Consent process and information booklet | Helpful/useful | ‘at the time I remember it being quite interesting and useful.’ | 4 |
| Acceptable | ‘That was fine, yes.’ | 3 | |
| Easy process | ‘I don’t remember there being anything onerous about it or it being any kind of problem. I think it was good, as far as I remember.’ | 2 | |
| Managing expectations | ‘I think I didn’t get from the early consent any information about the trial, quite how involved it would be and the logistics of it, how difficult that would be.’ | 1 | |
| Clearer instructions | ‘maybe just on the top of that make it big and bold that that’s what you’ve got to do rather than just tick.’ | 1 | |
| Breaking information down | ‘I think like I’d recommend other parents doing it to just do a little bit at a time rather than read the whole thing because I couldn’t take all of that in.’ | 1 | |
| Preference for postal consent | ‘I think sending it through the post is easiest because not everybody has got a printer and actually you read stuff from paper.’ | 1 | |
| Preference for online consent | ‘it’s just you’ve got to make a trip to the post box so maybe in the future if it takes off get an e-sign thing . . . yeah just to do it online rather than to keep posting back and forth all the time.’ | 1 |
Acceptability of randomisation in a future trial
Parents
When asked about participating in a study involving randomisation, the majority (n = 3) of parents/carers felt it was acceptable. Two parents expressed their reluctance to be involved in a trial with randomisation, due to the uncertainty around which condition they would be allocated to. One person said that participation in any study can be beneficial as even if they would be allocated to the control group, they would still receive some support from the NHS.
Table 37 gives a summary of parents’/carers’ views on randomisation.
| Theme | Subtheme | Example comment | Number of parents/carers |
|---|---|---|---|
| Randomisation | Acceptable | ‘I probably would if that was that eventually it was all gonna be dealt with then yeah.’ | 3 |
| Reluctance due to allocation | ‘So I don’t think I would sign up to anything that I knew wasn’t gonna definitely benefit [name of child] because that’s a lot of additional work for possibly something that’s not gonna work.’ | 2 | |
| Provides opportunity for support | ‘I suppose with any trial . . . actually even if we just get the NHS treatment only we’re getting some support to try and deal with this as opposed to nothing at all so I probably would still be happy for him to do that because you’d hope that you’d get in the intervention arm, but then at least you still get some kind of input and help with the problem.’ | 1 |
Therapists
Regarding randomisation within a future trial, three therapists suggested this would be acceptable if all children were then offered SPIRIT after the trial; two therapists described this potential trial as interesting and useful. However, one therapist felt that the SPIRIT intervention should be delivered to priority cases.
Table 38 gives a summary of therapists’ views on randomisation.
| Theme | Subtheme | Example comment | Number of therapists |
|---|---|---|---|
| Randomisation within a future trial | Acceptable if all offered the SPIRIT intervention after the trial | ‘as long as people are offered the option of then receiving the treatment later.’ | 3 |
| Interesting and useful | ‘I’d be interested to see the results. I think it’s the right way forward.’ | 2 | |
| Delivering to priority cases | ‘if it’s a big priority I think it should be provided to them.’ | 1 | |
| Alternative treatment | ‘I think the tricky part would be . . . would there be another treatment delivered instead potentially and would you be saying anything about what that could look like?’ | 1 |
Chapter 6 Discussion and conclusions
In this chapter, we first summarise and interpret the main findings of the research in relation to the primary objectives, then consider patient and public involvement (PPI) in the study, followed by a consideration of the strengths and limitations of the research and implications of the study findings for future research.
Summary and interpretation of findings
Phase 1a: intervention development
Objective 1: development of an intervention for specific phobia in children and adolescents with moderate to severe learning disabilities
In collaboration with the members of the IDG, we successfully developed a parent-mediated intervention for specific phobia for children and adolescents with moderate to severe learning disabilities. The intervention consisted of two parts: (1) parent/carer skills training group workshops (two half-days); and (2) weekly therapist support sessions with individual parents/carers over 8 weeks. A full description of the intervention is provided in Chapter 3.
Objective 2: development of a treatment fidelity checklist
A fidelity checklist was developed for the intervention, based on checklists used in a previous study. 39 The checklist was reviewed and discussed by the IDG, and subsequent revisions were made. See Chapter 3 for a description and Report Supplementary Material 7 for a sample fidelity checklist.
Objective 3: appraise and consider several candidate outcome measures of anxiety-related symptoms, and secondary outcomes, and make a recommendation for use within phase 2
A range of potential outcome measures were presented for the consideration of the IDG, together with information about the format, item content, intended age range, time needed to complete and psychometrics. Information was also presented on physiological (heart rate) measures. For the phase 2 eligibility assessment, the IDG recommended the use of a parent/carer interview on anxiety disorders (phobia section),44 a DSM-540 and DM-ID-243 informed checklist of symptoms of specific phobia, and a measure of adaptive behaviour. 45 For the phase 2 outcome measures, the IDG recommended the adaptation of a measure of the severity of specific phobia,46 making the items appropriate for children with little or no language; an adaptation of a measure of impact of a problem behaviour,47 adapted to refer to specific phobia; a measure of behaviour and emotional problems;50 and a measure of challenging behaviour. 51 All measures were parent/carer completed. The IDG also reviewed and decided on a smartwatch (Fitbit) as a measure of heart rate.
Objective 4: development of a logic model
The final objective for phase 1a was the development of a logic model collaboratively with the IDG. This was successfully completed (Figure 2).
Phase 1b: description of treatment as usual
Objective 1: describe the current standard treatment provided for children and adolescents with moderate to severe learning disabilities and specific phobia within the UK
A national survey of TAU was undertaken to describe interventions for specific phobia in children and adolescents with moderate to severe learning disabilities. Parents/carers of children and adolescents with specific phobia and moderate to severe learning disabilities were surveyed, as well as professionals working in services providing care to children and adolescents with moderate to severe learning disabilities.
A key finding from the survey was that a significant proportion of parents (73%) reported not being offered any treatment for their child’s specific phobia. Of those who did receive treatment for their child, a range of treatments were offered, with the most frequent being medication. Other treatments were psychological, and included exposure therapy, sensory integration therapy and counselling. While the majority of treatments provided were in community-based health and social care settings, 28% were school based.
Of the professionals who completed the TAU survey, the majority worked in health and care services (95%), and one was based in a school. Just over half (54%) indicated that their service offered treatment for specific phobia. Of these, 50% offered exposure therapy; other therapies were also offered, including CBT, medication, ACT, primary care support, systemic intervention and psychoeducation. With the exception of CBT, the other therapies did not include a graded exposure component.
A key finding from the TAU survey was that a significant proportion of children and adolescents with moderate to severe learning disabilities are not being offered treatment for specific phobia, and when they are, they are most often offered medication.
Phase 2: feasibility study
Objective 1: evaluate the manualised intervention to determine the acceptability and feasibility for all stakeholders, including children and young people, carers and therapists
Overall, parents felt the intervention helped them and their child; they felt they had learned skills to help their child and had a better understanding of their child and of themselves after participating in the intervention. A number also highlighted learning transferable skills they could use in the future. Parents and carers reported positive experiences of attending the two skills training workshops and found them helpful. They enjoyed the small-group format of the two workshops, particularly being able to talk with other parents. The majority of parents found the support of the therapist in the weekly sessions helpful. While the majority reported having no problems attending the support sessions, one parent felt they were too frequent. While one found it challenging to fit weekly sessions in with family life, others found it easy to reorganise the session times if needed. Some parents felt that they needed more than eight support sessions.
Parents found that the remote delivery of the intervention worked well, was time-efficient, and was easier than face to face. One parent preferred face-to-face sessions. Parents reported being able to develop a good working relationship with their therapist and felt supported by them. Overall, parents felt their child made progress in the management of their phobia and that the therapists and the intervention worked well to meet the needs of their child.
Most therapists described the skills workshops as successful and felt that the small-group format was beneficial for parents and facilitated support. The workshops were easy to deliver and the materials and resources were helpful. One therapist felt that the workshop was overwhelming for parents. Therapists reported finding the support sessions enjoyable to deliver and easy to individualise, and that they were helpful for parents, with some highlighting the troubleshooting and problem-solving aspect of the sessions as a key benefit.
Although therapists did acknowledge that the remote delivery was appropriate, the majority reported they would have preferred face-to-face delivery. Some noted the challenges of building rapport over the telephone/videoconferencing, and felt this impacted the therapeutic relationship.
Overall, the therapists found the intervention was appropriate for the target population, with some also noting that it would also be appropriate for children with mild learning disabilities and children with communication difficulties. The parents were engaged and had a good understanding of the intervention and how it worked. However, some therapists felt that the parent-mediated aspect of the intervention placed high expectations on parents, although this view was not expressed by the parents themselves. Parents reported feeling empowered and preferred delivering the intervention themselves, in particular being able to directly support their child when they were facing their feared stimulus. The majority of therapists felt that the parent-mediated aspect of the intervention was appropriate, important and empowered the parents, with the developed skills facilitating long-term positive impact.
Therapists found the intervention materials and resources useful, and the majority did not feel they needed to make any changes to these. Some felt that further explanation of the materials may be needed, for example the visual schedule and how to use the rating scale. One challenge was getting parents to complete the data sheet prior to the support session, something that was also reflected in the treatment fidelity ratings. Some therapists felt it would have been useful to meet the child themselves to gain a better understanding of them. Overall, it was felt that they would continue to use the intervention, with some noting that it may also be useful to be delivered in school settings.
In terms of ways to improve the intervention, parents felt more support sessions would be useful, and greater flexibility in terms of the delivery of the support sessions (e.g. not necessarily weekly). Therapists also suggested greater flexibility in delivery of the support sessions, including longer sessions. It was suggested that making the data sheets available online may facilitate completion. The inclusion of specific skills training scenarios in the workshops was suggested as a way of helping parents understand what to do when things do not go according to plan. A number of therapists suggested that the intervention may be able to be delivered through special schools.
Therapist training
The therapists reported finding the training in the intervention helpful, informative, clear, enjoyable and a good opportunity to reflect on their knowledge and skills. It was also noted that it increased their confidence in the use of graded exposure.
Fidelity of intervention delivery
Fidelity checklists were completed for all workshops and sessions delivered. Overall fidelity of delivery of the two workshops was very high at 80–100%.
In terms of the eight support sessions, overall, the majority of the content of all sessions was delivered to a high degree of fidelity to the manual. However, having materials prepared prior to each session was not consistently completed for all sessions, with percentages ranging from 58 to 100% across the eight sessions. The most challenging components related to data collection in monitoring the exposure steps. Receiving the data sheet from parents prior to or during the session ranged from 15 to 84%.
Adherence: parent attendance
One parent withdrew from the study prior to baseline, as they were not able to attend the workshops at the time scheduled by the site. Overall, parent attendance was high for those families who commenced the intervention, with 100% of parents (14/14) attending both of the skills training workshops. One family had to withdraw after completing the workshops due to a family bereavement that resulted in them having to go overseas for a period of time. One parent/carer attended 75% of the support sessions (six of eight sessions), as they felt that they had achieved their treatment goal in relation to their child’s phobia. The remaining 11 families attended 100% of the support sessions.
Objective 2: judge the appropriateness of the measures of anxiety-related symptomatology, and secondary outcomes, for use within a larger study
The study outcome measures were judged to be appropriate. With the exception of one parent, all measures were completed by parents/carers who remained in the study. The percentage of missing data on completed measures was extremely low, with the majority of measures completed fully at each time. Of those measures with missing data, this ranged from 0.07 to 2% which translated as one item on the DBC and three missing severity ratings on the BPI.
The proposed primary outcomes for the intervention were measures of the severity and impact of the specific phobia. As no measures were available that were appropriate for use with children and adolescents with moderate to severe learning disabilities, we adapted existing measures. These measures were able to be completed by parents, with no missing data. As these were adaptations of existing measures, further validation in a future study is needed.
Some found the measures straightforward, although time-consuming, to complete, but noted that it was important. It was noted that it was quicker to complete them the second time. The option of completing the measures through an interview with the trial manager or RA was appreciated and seen as preferable for some.
The use of the Fitbit as a measure of heart rate was challenging for some and it was not clear whether it was of any value in terms of monitoring physiological responses to exposure tasks. If physiological parameters were to be measured in a future study, exploring the use of different types of wearable devices would be warranted.
Objective 3: explore recruitment pathways
Recruitment of sites for phase 2 of this study was challenging, with the two original planned sites withdrawing from the study due to capacity issues. The study team discussed participation in the study with 22 sites in order to recruit 5. Sites often declined to be involved on the basis of staff capacity, but some voiced their interest in a larger trial or future research. Barriers to taking part in the study were COVID-19 related.
Recruitment of participants was also challenging. Sites reported finding it challenging to identify potential participants from caseloads, as information on systems did not tend to record specific phobia as a primary problem. Information on the degree of learning disability was also sometimes not available. Three of the five sites were only able to recruit through current caseloads, while two sites were able to recruit externally, recruiting through local special schools and support/advocacy organisations in the region. In total, 93 potential participants were identified and contacted about the study; 47 of these were identified by NHS sites (caseloads) and 46 through external recruitment, highlighting the importance of being able to recruit from organisations outside of the NHS sites.
We aimed to recruit up to 20 parents/carers, with at least one per site. Due to COVID-19-related challenges, we recruited 15. As planned, we recruited at least two therapists per site to deliver the intervention and interviewed one therapist from each site. The original aim was to complete recruitment within 7 months; however, recruitment of 15 participants took 10 months (overall 1.5 per month). After having the original two sites withdrawn from the study, it took approximately 10 months to recruit five new sites.
Objective 4: determine the feasibility and acceptability of consent and associated processes
Parents/carers reported no difficulties with the participant information sheets and consent forms.
Objective 5: describe factors that facilitate or challenge the implementation of the intervention
For parents, logistical issues around finding time to do the tasks involved in the intervention seemed to be the biggest challenge. Other challenges included sharing the data sheets with the therapists and the need for further support with understanding reinforcement. Accessing the feared stimulus (e.g. dogs) was a challenge for some.
Therapists felt that the structure of the intervention and the troubleshooting component in particular facilitated the implementation of the intervention, and that placing parents as the experts on their child and their needs was a strength. Challenges included some difficulties with implementing the relaxation strategies, ensuring the exposure steps were sufficiently small and steps were not skipped, motivating parents, managing negative experiences during exposure and accessing a dog for exposure steps. A number felt that more support/time was needed.
Objective 6: determine the acceptability of randomisation in a future trial
The majority (60%) of parents felt that participating in a future trial with randomisation was acceptable; however, 40% were concerned they may not be able to access the intervention. Therapists felt that it would be acceptable if all children were able to be offered the intervention at the end of the trial.
Objective 7: describe the parameters of a future study to examine the effectiveness of exposure-based therapy to treat phobias in this population
The greatest challenge in this study was recruiting sites, and then participants. The challenges of recruiting sites were related to the COVID-19 pandemic. However, some of the challenges of recruiting participants were related to how information on patients is stored (limiting capacity to identify potential participants). The results of this study indicate that a future study (e.g. a pilot trial) would need to recruit a large number of NHS sites and allow for external recruitment (e.g. from schools and support/advocacy organisations).
The intervention itself was well received overall by parents/carers and therapists. A number of suggested adaptations can be taken into account to revise the intervention and the accompanying materials. A number of the challenges identified by the therapists can also be addressed in revisions to the therapist training workshop. These include, for example, building in some flexibility around the delivery of the support sessions, consideration of additional support sessions, offering delivery flexibility (remote and face-to-face delivery), revising materials around reinforcement, relaxation strategies, and exposure steps to provide more examples to improve understanding, and building case studies into the training workshops for therapists and into the skills training workshops for parents.
Study processes such as consent and the outcome measures used were well received. A future study would need to do further work on the validation of the specific phobia outcome measures.
Progression criteria
The phase 2 study progression criteria are detailed in Table 39 and were considered by the SSC. It was noted that the accrual rate was graded red, while all other criteria were graded green. As already discussed, our accrual rate was most likely impacted by the COVID-19 pandemic and is therefore likely an underestimate of the accrual rate outside of this context.
| Progression criterion | Progress | Number | Explanation |
|---|---|---|---|
| Recruitment | |||
| Accrual rate is at least three patients per site per month on average. | Red: not achieved overall | 1.5 per month per site overall | Recruitment was unduly affected by the pandemic. |
| Attrition rate is 30% or lower. | Green | 13% | Attrition was not thought to be related to the intervention or research processes. |
| Protocol adherence | |||
| Fidelity ratings indicate therapist adherence to the intervention of at least 75%. | Green | Average 93.8% | |
| At least 70% of carers and clinicians report that the intervention and consent procedures were acceptable. | Green | 80% of carers considered the consent procedures acceptable 100% of carers considered the intervention acceptable to meet need or considered the therapist responded to need 100% of therapists considered the intervention was suitable or described benefits |
|
| At least 90% of participants received the intervention. | Green | 93% | One had to withdraw. |
| Outcome data | |||
| At least 70% of participants and carers complete outcome data at each time point. | Green | 93% | – |
| At least 75% of items within each outcome measure for each participant are complete. | Green | 98–100% | – |
| At least 70% of carers judge our outcome measures to be acceptable. | Green | 80% | Comments were that some items were unclear. |
Patient and public involvement
Patient and public involvement during this project focused on two primary aspects of this study. First, a parent of a child with moderate to severe learning disabilities was an independent member of the SSC appointed by the funder. Payment was provided to the parent SSC member in addition to covering their expenses.
The IDG comprised six key stakeholders: a representative from the Foundation for People with Learning Disabilities (our PPI partner), two parents of children with learning disabilities and specific phobias, and three clinicians with experience of working with children and young people with learning disabilities and anxiety. The parents had active roles in all aspects of the IDG (see Chapter 2). The parents attended all IDG meetings and also had the opportunity to meet with the SM and the Chief Investigator after each IDG meeting to discuss any of the topics further, provide any additional feedback and reflect on the processes of the meeting. Working closely in this way with the members of the IDG (in particular the parent/carer members) ensured the intervention and intervention materials and resources were accessible and clear, and that study measures were acceptable and relevant in terms of purpose. Payment was provided to the parent IDG members in addition to covering their expenses. In the development of the parent materials for the phase 2 SPIRIT intervention, we also worked with a group of three parents from a range of ethnic minority backgrounds to review the cultural appropriateness of the intervention and associated materials. This work was done together with our PPI partner, the Foundation for People with Learning Disabilities.
The Foundation for People with Learning Disabilities also supported this study. They assisted with study paperwork, and invited parents/carers to review and provide feedback on our study paperwork for parents.
Equality, diversity and inclusion
In the phase 2 feasibility study, 80% of recruited parents/carers described themselves as being of White British ethnic background, and 20% described themselves as being of Asian/mixed White Asian background. According to the 2012 census, 81.7% of the total population of England and Wales is white. Thus, overall, the recruitment methods appeared to capture some diversity. Considering methods to increase ethnic diversity in the recruited sample in particular would be important for any future research, and some focused PPI work on this issue would be useful.
Strengths and limitations of the research
A particular strength of this research was the key role played by the members of the IDG, in particular the parents/carers who carefully reviewed and contributed to the development of the structure of the intervention and all materials, and the proposed study measures. The detailed post-intervention interview process was critical in understanding how the intervention was received and experienced by parents/carers as well as therapists. It helped to develop an understanding of the factors important to successful outcomes, as well as directly informing future revisions of the intervention.
Exploring the role of recruiting participants external to the NHS site caseloads was critical to the recruitment process. It was clear from this that any future study would need to include strategies to recruit from schools and other learning-disability-focused organisations.
The sample size for the intervention feasibility study was small; however, it was sufficient to address the study objectives. It was, however, not possible to interview the children and adolescents with moderate to severe learning disabilities whose parents participated in the intervention, primarily due to the degree of their communication difficulties.
The inclusion of a parent survey of TAU identified the need in the community for an intervention for specific phobia in children and adolescents with moderate to severe learning disabilities. The professional survey highlighted that exposure-based interventions for specific phobia in this population are not routinely provided. The results of the surveys are based on relatively small sample sizes. A larger study would be needed to determine a representative picture of service provision for specific phobia in the UK. A survey of necessary size and scope was beyond the means of the current study.
In the intervention feasibility study, the fidelity measure of delivery of components for each session was completed by the therapists who delivered the sessions. A future study should explore the acceptability and feasibility of alternate or supplementary methods of measured fidelity of treatment delivery.
There is the potential for a conflict of interest in having developed an intervention and found it feasible for a pilot or full trial. However, the progression criteria which determined the recommendation were defined prior to the commencement of the study, and agreed by the funder. The study was preregistered, and the outcomes were reviewed against the progression criteria by the independent SSC.
Recommendations for future research
Evaluating adaptations
A number of suggested adaptations can be taken into account to revise the intervention and the accompanying materials. The challenges identified by the therapists can also be addressed in revisions to the therapist training workshop. These include, for example: building in some flexibility around the delivery of the support sessions; consideration of additional support sessions; offering delivery flexibility (remote and face-to-face delivery); revising materials around reinforcement, relaxation strategies and exposure steps to provide more examples to improve understanding; and building case studies into the training workshops for therapists and into the skills training workshops for parents.
It was not possible to recruit young people with moderate to severe learning disabilities for the IDGs or for the post-intervention interviews. A future study could work together with parents and the PPI partner to develop appropriate methods to support this involvement.
Measures
A future study would need to do further work on the validation of the specific phobia outcome measures.
Randomisation
The majority (60%) of parents felt that participating in a future trial with randomisation was acceptable; however, 40% were concerned they may not be able to access the intervention. Therapists felt that it would be acceptable if all children were able to be offered the intervention at the end of the trial.
Recruitment
The results highlight the importance of being able to recruit from organisations outside of the NHS sites. A future study would need to recruit from schools and include promotion through learning-disability-focused organisations, as was undertaken in one of the study sites. PPI work could inform methods to increase diversity in a future study.
Monitoring physiological responses
The use of the Fitbit as a measure of heart rate was challenging for some, and it was not clear whether it was of any value in terms of monitoring physiological responses to exposure tasks. If physiological responses were to be measured in a future study, exploring the use of different types of wearable devices would be warranted.
Progression criteria and potential for future trial
The progression criteria are detailed in Table 39 and were considered by the SSC.
The SSC recommended that the research should progress to a trial. A pilot trial with randomisation incorporating progression criteria towards a definitive randomised trial would be an appropriate next step.
Additional information
CRediT contribution statement
Kylie M Gray (https://orcid.org/0000-0001-6518-4240): Conceptualisation, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Visualisation, Writing – original draft, Writing – reviewing and editing.
Magdalena M Apanasionok (https://orcid.org/0000-0002-3861-3801): Data curation, Formal analysis, Investigation, Project administration, Resources, Supervision, Visualisation, Writing – original draft, Writing – reviewing and editing.
Emma Scripps (https://orcid.org/0000-0001-6140-2976): Data curation, Formal analysis, Investigation, Writing – original draft, Writing – reviewing and editing.
Karen Bunning (https://orcid.org/0000-0002-7396-9205): Conceptualisation, Funding acquisition, Methodology, Visualisation, Writing – reviewing and editing.
Christine Burke (https://orcid.org/0000-0002-5562-8896): Conceptualisation, Funding acquisition, Methodology, Visualisation, Writing – reviewing and editing.
Malwina Filipczuk (https://orcid.org/0009-0001-5051-9842): Data curation, Formal analysis, Investigation, Resources, Visualisation, Writing – original draft, Writing – reviewing and editing.
Richard P Hastings (https://orcid.org/0000-0002-0495-8270): Conceptualisation, Funding acquisition, Methodology, Visualisation, Writing – reviewing and editing.
Ashley Liew (https://orcid.org/0000-0002-3825-225X): Conceptualisation, Funding acquisition, Methodology, Visualisation, Writing – reviewing and editing.
Rachel McNamara (https://orcid.org/0000-0002-7280-1611): Conceptualisation, Funding acquisition, Methodology, Visualisation, Writing – reviewing and editing.
Atiyya Nisar (https://orcid.org/0000-0002-1996-3603): Writing – reviewing and editing.
Rebecca Playle (https://orcid.org/0000-0002-2989-1092): Conceptualisation, Funding acquisition, Methodology, Visualisation, Writing – reviewing and editing.
Tim Williams (https://orcid.org/0000-0003-0072-3316): Conceptualisation, Funding acquisition, Methodology, Visualisation, Writing – reviewing and editing.
Peter E Langdon (https://orcid.org/0000-0002-7745-1825): Conceptualisation, Data curation, Formal analysis, Funding acquisition, Methodology, Project administration, Resources, Supervision, Visualisation, Writing – reviewing and editing.
Acknowledgements
We would like to thank all of the participants who took part in this feasibility study. Many thanks go to all members of the Study Steering Committee, the Study Management Group and the parents who contributed to the study through the Intervention Development Group. We also wish to thank all of the NHS sites who rose to the challenge of participating in the phase 2 study during a pandemic, including the research and development teams, the site Principal Investigators and the therapists who delivered the intervention. We also want to thank the Foundation for People with Learning Disabilities, particularly Christine Burke and David Mahon.
We also wish to thank Diana Smith and Alison Baker from the Centre for Research in Intellectual and Developmental Disabilities (CIDD) at the University of Warwick for providing essential support.
We would like to thank the Coventry and Warwickshire Partnership NHS Trust, who were the sponsors for this trial, in particular Marie McCauley from the research and development team.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Ethics statement
The research was reviewed by West Midlands – Edgbaston Research Ethics Committee and ethical approval was granted by NHS Health Research Authority on 12/07/2021 (reference number: 21/WM/0072).
Information governance statement
Coventry and Warwickshire Partnership NHS Trust is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679.
Under the Data Protection legislation, Coventry and Warwickshire Partnership NHS Trust is the Data Controller, and you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our Data Protection Officer here: www.covwarkpt.nhs.uk/privacy
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/LRWD7852.
Primary conflicts of interest: Kylie Gray is a coauthor of the manual for the Developmental Behavior Checklist (DBC2), published by Western Psychological Services. Royalties received from the sale of the DBC2 manual are donated to the funding of ongoing research in intellectual and developmental disabilities.
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HTA programme or the Department of Health and Social Care.
References
- Einfeld SL, Ellis LA, Emerson E. Comorbidity of intellectual disability and mental disorder in children and adolescents: a systematic review. J Intellect Dev Dis 2011;36:137-43. https://doi.org/10.1080/13668250.2011.572548.
- Emerson E, Hatton C. Mental health of children and adolescents with intellectual disabilities in Britain. Br J Psychiatry 2007;191:493-9.
- Dekker MC, Koot HM. DSM-IV disorders in children with borderline to moderate intellectual disability. I: prevalence and impact. J Am Acad Child Adolesc Psychiatry 2003;42:915-22.
- Emerson E. Prevalence of psychiatric disorders in children and adolescents with and without intellectual disability. J Intellect Disabil Res 2003;47:51-8.
- Ollendick T, King NJ, Muris P. Fears and phobias in children: phenomenology, epidemiology, and aetiology. Child Adolesc Ment Health 2002;7:98-106.
- Fichter M, Kohlboeck G, Quadflieg N, Wyschkon A, Esser G. From childhood to adult age: 18-year longitudinal results and prediction of the course of mental disorders in the community. Soc Psychiatry Psychiatr Epidemiol 2009;44:792-803.
- Stinson FS, Dawson DA, Chou SP, Smith S, Goldstein RB, Ruan WJ, et al. The epidemiology of DSM-IV specific phobia in the USA: results from the national epidemiologic survey on alcohol and related conditions. Psychol Med 2007;37:1047-59.
- Local Government Association, Association of Directors of Adult Social Services in England, NHS England . Building the Right Support: A National Plan to Develop Community Services and Close Inpatient Facilities for People With a Learning Disability and Or Autism Who Display Behaviour That Challenges, Including Those With a Mental Health Condition 2015.
- Vereenooghe L, Flynn S, Hastings RP, Adams D, Chauhan U, Cooper SA, et al. Interventions for mental health problems in children and adults with severe intellectual disabilities: a systematic review. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2018-021911.
- Williams TI, Lewis S, Marcham L, Palicka A. Treatment of dog phobia in young people with autism and severe intellectual disabilities: an extended case series. Contemp Behav Health Care 2018;3:1-5.
- Romeo R, Molosankwe I. Economic evidence in intellectual disabilities: a review. Curr Opin Psychiatry 2010;23:427-31.
- Toms G, Totsika V, Hastings RP, Healy H. Access to services by children with intellectual disability and mental health problems: population-based evidence from the UK. J Intellect Dev Disabil 2015;40:239-47.
- Buescher AV, Cidav Z, Knapp M, Mandell DS. Costs of autism spectrum disorders in the United Kingdom and the United States. JAMA Pediatr 2014;168:721-8.
- Einfeld SL, Ellis LA, Doran CM, Emerson E, Horstead SK, Madden RH, et al. Behavior problems increase costs of care of children with intellectual disabilities. J Ment Health Res Intellec Disabil 2010;3:202-9.
- Doran CM, Einfeld SL, Madden RH, Otim M, Horstead SK, Ellis LA, et al. How much does intellectual disability really cost?. J Intellect Dev Dis 2012;37:42-9.
- NHS England, National Institute for Health Research . NHS England’s Research Needs Assessment 2018. https://allcatsrgrey.org.uk/wp/download/commissioning/nhs-englands-research-needs-assessment-2018.pdf (accessed 24 April 2024).
- NHS England . The NHS Long Term Plan 2019. www.england.nhs.uk/publication/the-nhs-long-term-plan/ (accessed 24 April 2024).
- Morris C, Simkiss D, Busk M, Morris M, Allard A, Denness J, et al. Setting research priorities to improve the health of children and young people with neurodisability: a British Academy of Childhood Disability–James Lind Alliance Research Priority Setting Partnership. BMJ Open 2015;5. https://doi.org/10.1136/bmjopen-2014-006233.
- NHS England . NHS Research Plan 2017.
- Chalfant A, Rapee R, Carroll L. Treating anxiety disorders in children with high functioning autism spectrum disorders: a controlled trial. J Autism Dev Disord 2007;37:1842-57.
- Maskey M, Lowry J, Rodgers J, McConachie H, Parr JR. Reducing specific phobia/fear in young people with autism spectrum disorders (ASDs) through a virtual reality environment intervention. PLOS ONE 2014;9.
- Maskey M, Rodgers J, Grahame V, Glod M, Honey E, Kinnear J, et al. A randomised controlled feasibility trial of immersive virtual reality treatment with cognitive behaviour therapy for specific phobias in young people with Autism Spectrum Disorder. J Autism Dev Disord 2019;49:1912-27. https://doi.org/10.1007/s10803-018-3861-x.
- Vigerland S, Thulin U, Ljótsson B, Svirsky L, Öst LG, Lindefors N, et al. Internet-delivered CBT for children with specific phobia: a pilot study. Cogn Behav Ther 2013;42:303-14.
- McGregor KK, Berns AJ, Owen AJ, Michels SA, Duff D, Bahnsen AJ, et al. Associations between syntax and the lexicon among children with or without ASD and language impairment. J Autism Dev Disord 2012;42:35-47.
- Rice M, Warren S, Betz S. Language symptoms of developmental language disorders: an overview of autism, Down syndrome, specific language impairment, and Williams syndrome. Appl Psycholinguist 2004;26:7-27.
- Meuwese-Jongejeugd A, van Zanten B, Verschuure H, Eicchorn E, Koopman D, Bernsen R, et al. Prevalence of hearing loss in 1598 adults with an intellectual disability: cross-sectional population based study. Int J Audiol 2006;45:660-9.
- van Splunder J, Stilma JS, Bernsen RMD, Evenhuis HM. Prevalence of ocular diagnoses found on screening 1539 adults with intellectual disabilities. Ophthalmology 2004;111:1457-63.
- National Institute for Health and Care Excellence . Mental Health Problems in People With Learning Disabilities: Prevention, Assessment and Management 2016.
- Burton P, Palicka A, Williams TI. Treating specific phobias in young people with autism and severe learning difficulties. Cogn Behav Ther 2017;10.
- Chok JT, Demanche J, Kennedy A, Studer L. Utilizing physiological measures to facilitate phobia treatment with individuals with autism and intellectual disability: a case study. Behav Interv 2010;25:325-37.
- Newman C, Adams K. Dog gone good: Managing dog phobia in a teenage boy with a learning disability. Br J Learn Disabil 2004;32:35-8.
- Ollendick TH, King NJ. Origins of childhood fears: an evaluation of Rachman’s theory of fear acquisition. Behav Res Ther 1991;29:117-23. https://doi.org/10.1016/0005-7967(91)90039-6.
- Rachman S. The conditioning theory of fear acquisition: a critical examination. Behav Res Ther 1977;15:375-87.
- Butler G. Cognitive Behaviour Therapy for Psychiatric Problems. Oxford: Oxford University Press; 1989.
- Wolpe J. The systematic desensitization treatment of neuroses. J Nerv Ment Dis 1961;132:189-203.
- Eaton WW, Bienvenu OJ, Miloyan B. Specific phobias. Lancet Psychiatry 2018;5:678-86.
- Davis TE, May A, Whiting SE. Evidence-based treatment of anxiety and phobia in children and adolescents: current status and effects on the emotional response. Clin Psychol Rev 2011;31:592-60.
- Ollendick T, Ollendick TH, Ost LG, Reuterskiold L, Costa N, Cederlund R, et al. One-session treatment of specific phobias in youth: a randomized clinical trial in the United States and Sweden. J Consult Clin Psychol 2009;77:504-16.
- Jahoda A, Hastings R, Hatton C, Cooper S-A, Dagnan D, Zhang R, et al. Comparison of behavioural activation with guided self-help for treatment of depression in adults with intellectual disabilities: a randomised controlled trial. Lancet Psychiatry 2017;4:909-19.
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders (DSM-5) 2013.
- Foundation for People with Learning Disabilities . PELICAN: Promoting Emotional Literacy in Children With Additional Needs n.d. www.learningdisabilities.org.uk/learning-disabilities/our-work/employment-education/pelican (accessed 24 April 2024).
- Dagnan D, Masson J, Cavagin A, Thwaites R, Hatton C. The development of a measure of confidence in delivering therapy to people with intellectual disabilities. Clin Psychol Psychother 2015;22:392-8. https://doi.org/10.1002/cpp.1898.
- Diagnostic Manual – Intellectual Disability 2: A Textbook of Diagnosis of Mental Disorders in Persons with Intellectual Disability. Kingston, NY: National Association for the Dually Diagnosed; 2017.
- Silverman W, Albano A. Anxiety Disorders Interview Schedule. Oxford: Oxford University Press; 1996.
- Sparrow SS, Cicchetti DV, Saulnier CA. Vineland Adaptive Behavior Scales (Vineland-3). Minneapolis, MN: Pearson; 2016.
- Craske M, Wittchen U, Bogels S, Stein M, Andrews G, Lebeu R. Severity Measure for Specific Phobia – Child. Washington, DC: American Psychiatric Association; 2013.
- Goodman R. The extended version of the Strengths and Difficulties Questionnaire as a guide to child psychiatric caseness and consequent burden. J Child Psychol Psychiatry Allied Discip 1999;40:791-9.
- Aman MG, Singh NN. Aberrant Behavior Checklist. East Aurora, NY: Slosson; 1986.
- Matson J. Evaluation of Social Skills for Individuals with Severe Retardation. Los Angeles, CA: Scientific Publishers; 1995.
- Gray KM, Tonge B, Einfeld S, Gruber C, Klein A. Developmental Behavior Checklist (DBC2). Torrance, CA: Western Psychological Services; 2018.
- Rojahn J, Rowe E, Sharber A, Hastings R, Matson J, Didden R, et al. The behavior problems inventory‐short form for individuals with intellectual disabilities: part I: development and provisional clinical reference data. J Intellect Disabil Res 2012;56:527-45.
- Gevartera C, O’Reilly MF, Rojeslkia L, Sammarcoa N, Langb R, Lacionic G, et al. Comparisons of intervention components within augmentative and alternative communication systems for individuals with developmental disabilities: a review of the literature. Res Dev Disabil 2013;34:4404-14.
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions. BMJ 2014;348.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337:979-83.
- Arain M, Campbell MJ, Cooper CL, Lancaster GA. What is a pilot or feasibility study? A review of current practice and editorial policy. BMC Med Res Methodol 2010;10.
- Bradshaw J, Gore N, Darvell C. Supporting the direct involvement of students with disabilities in functional assessment through use of Talking Mats®. Tizard Learn Disabil Rev 2018;23:111-6.
- Lancaster GA, Thabane L. Guidelines for reporting non-randomised pilot and feasibility studies. Pilot Feasibility Stud 2019;5.
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13.
- Avery KN, Williamson PR, Gamble C, Francischetto EO, Metcalfe C, Davidson P, et al. Informing efficient randomised controlled trials: exploration of challenges in developing progression criteria for internal pilot studies. BMJ Open 2017;7.
Appendix 1 Treatment as usual professional survey themes and codes
| Question | Theme | Participant ID/row number | Code | Extract demonstrating theme |
|---|---|---|---|---|
| Provide name or phrase that describes the treatment or intervention your service offers to children with moderate to severe learning disabilities who have specific phobia. This includes psychological treatments, medication and other interventions. | Name of the treatment | Participant 1/row 2 | Exposure therapy | Systematic desensitisation. |
| Participant 2/row 3 | CBT | Adapted CBT. | ||
| Systemic intervention | Family/systemic intervention. | |||
| Exposure therapy | Graded exposure/relaxation strategies. | |||
| Medication | Medication – unsure what class. Would be medication to reduce anxiety. | |||
| Participant 7/row 8 | Systemic intervention | Support with procedural anxiety – psychological (systemic, behavioural, cognitive, ACT). | ||
| CBT | ||||
| ACT | ||||
| Participant 9/row 10 | Exposure therapy | Parent-led CBT, exposure based. | ||
| CBT | ||||
| Medication | Medication SSRI. | |||
| Participant 10/row 11 | Primary care support | Primary care support if needed, no specific interventions. | ||
| Participant 14/row 15 | Medication | SSRIs. | ||
| Psychoeducation and behavioural therapy | Psychoeducation and visual-aided behavioural therapy. | |||
| Participant 16/row 17 | Primary care support | Referral from primary care to community learning difficulties team. We may well support the family/pt and help with any medications issued by the team but would not be involved in specific therapy or initiating treatment ourselves for this issue. | ||
| Participant 18/row 19 | Acclimatisation | Acclimatisation. | ||
| Participant 22/row 23 | Exposure therapy | Desensitisation, graded exposure. | ||
| Participant 23/row 24 | Exposure therapy | We don’t have a specific name or pathway. I would say we use ‘desensitisation’ in the context of a PBS approach. | ||
| Participant 24/row 25 | Exposure therapy | Adapted CBT-based intervention – often mainly with parents – usually systematic desensitisation alongside psychoeducation and breathing/relaxation techniques. | ||
| CBT | ||||
| Medication | Medication. | |||
| No response | 4 | |||
| Briefly outline the rationale for using this treatment or intervention for children with moderate to severe learning disabilities? | Rationale for using the treatment | Participant 1/row 2 | Evidence based | Evidence based that it works with children. It is applicable to the young people and can be adapted so that it is clinically useful. It is very individualised, adapted to each person’s communication needs, understanding, how old they are. |
| Can be individualised | ||||
| Participant 2/row 3 | Recommended by NICE | Used more for those with more mild–moderate learning disabilities to support child/young person with their thinking and behavioural responses to the thing they have a phobia about. Adapted in line with recommendations from NICE. | ||
| Difficulties with phobia can arise within families | Patterns can evolve in families which contribute to difficulties with phobia arising; problems often not specific to an individual ‘pathology’; families/systems often another route to work through to support the child/young person. | |||
| Concrete way of working with phobias | Concrete/direct way of working with phobias, adapted in line with NICE recommendations. | |||
| Recommended by NICE | ||||
| Pharmacological relief of anxiety | Reduce anxiety with a view to supporting person to be able to access/engage with psychological therapies in situations where anxiety is so high that quality of life is so significantly impacted that a quicker-acting treatment is required while also engaging in psychological therapies. | |||
| Helps the person engage in psychological therapies | ||||
| Participant 7/row 8 | Can be individualised | We provide interventions to meet the CYP’s individual needs. | ||
| Can be individualised | We provide interventions to meet the CYP’s individual needs. | |||
| Can be individualised | We provide interventions to meet the CYP’s individual needs. | |||
| Participant 9/row 10 | Evidence based | Evidence base for intervention and suitability for use with children with learning disabilities. | ||
| Can be individualised | ||||
| Evidence based | Evidence base for intervention and suitability for use with children with learning disabilities. | |||
| Can be individualised | ||||
| Evidence based | Evidence base (often as adjunct to psychological therapy). | |||
| Participant 10/row 11 | Part of primary care | Part of primary care service. | ||
| Participant 14/row 15 | Pharmacological relief of anxiety | Pharmacological relief of anxiety. | ||
| Can be individualised | The need/severity of presentation. | |||
| Participant 18/row 19 | Increased confidence of the young person by familiarisation to the environment | To increase familiarisation to the dental environment, increase confidence and reduce generalised or dental-specific anxieties. | ||
| Participant 22/row 23 | Response excluded | We are a small team and isn’t something we offer as a stand-alone problem. Several patients have common phobias such as animals and needles. | ||
| Participant 23/row 24 | Parent/carer involvement | The children we see are referred for behaviour that challenges and are often also autistic. Typically, coming into a clinic environment for therapy is not feasible so we tend to work with parents/carers and support them to provide support. | ||
| Participant 24/row 25 | Evidence based | CBT is the evidence-based treatment for phobias for children and young people. We adapt it by working more with parents and using a lot more simplified and visual aids to work with children when we do. | ||
| Parent/carer involvement | ||||
| Can be individualised | ||||
| Evidence based | This would be prescribed by our psychiatrist based on the evidence base for this client group. | |||
| No response | 5 | |||
| What are the key elements that are essential to this treatment? | Key elements of the treatment | Participant 1/row 2 | Fear hierarchy | It is a construction of a hierarchy of events leading up to the most stressful being the event itself that they describe as being their phobia, breaking down to relatively manageable steps and working/encouraging parents to work from the bottom up, at the same time incorporating relaxation, whatever that looks like for the individual. It is paired with supporting parents so that they can be able to do that with their children and manage their own anxiety as the child inevitably gets anxious.
|
| Parent/carer involvement | ||||
| Relaxation | ||||
| Support from the parent/carer | ||||
| Individualised assessment | ||||
| Regular review of treatment progress | ||||
| Participant 2/row 3 | Working with thought patterns | Identifying and working with thought patterns that contribute to development and maintenance of phobia, behavioural experiments, activity scheduling, etc. to challenge avoidance strategies. Involvement of family members/carers to support this. | ||
| Behavioural experiments | ||||
| Activity scheduling | ||||
| Parent/carer involvement | ||||
| Exploring narratives within the family | Engagement with family; exploring narratives and multiple perspectives in the family and system about the ‘problem’; working to support family to find their own strengths and solutions. | |||
| Identifying the family’s strengths | ||||
| Fear hierarchy | Graded exposure hierarchy approach, access to the thing the person has a phobia of, relaxation strategies being taught. | |||
| Exposure to a feared stimulus | ||||
| Relaxation | ||||
| Medication | Medication under supervision of psychiatry. | |||
| Psychiatric supervision | ||||
| Participant 7/row 8 | Kindness and compassion | Kindness, compassion, information given in a way that the young person can understand about the procedure, control for the young person and a sense of safety and support from the adults around them. | ||
| Information adapted to the young person’s needs | ||||
| Control for the young person | ||||
| Sense of safety and support | ||||
| Kindness and compassion | Kindness, compassion, information given in a way that the young person can understand about the procedure, control for the young person and a sense of safety and support from the adults around them. | |||
| Information adapted to the young person’s needs | ||||
| Control for the young person | ||||
| Sense of safety and support | ||||
| Kindness and compassion | Kindness, compassion, information given in a way that the young person can understand about the procedure, control for the young person and a sense of safety and support from the adults around them. | |||
| Information adapted to the young person’s needs | ||||
| Control for the young person | ||||
| Sense of safety and support | ||||
| Participant 9/row 10 | Praise | Praise for bravery, calm modelling, graded exposure, skills teaching of what to do if anxious. | ||
| Modelling | ||||
| Graded exposure | ||||
| Skills teaching | ||||
| Praise | Praise for bravery, calm modelling, graded exposure, skills teaching of what to do if anxious. | |||
| Modelling | ||||
| Graded exposure | ||||
| Skills teaching | ||||
| Not known | I don’t prescribe so I can’t comment. | |||
| Participant 10/row 11 | Referral to secondary care | Referral to secondary care if needed. | ||
| Participant 14/row 15 | Response excluded | Severity and level of impairments. | ||
| Response excluded | Acceptability. | |||
| Participant 18/row 19 | Parent/carer involvement | Parents understand the benefits and engaging with the sessions. | ||
| Participant 22/row 23 | Planning sessions | Regular sessions well planned. Graded exposure. Family history feelings and anxiety explored, monitoring patients’ engagement and willingness at each session, letting patient lead on time and sessions. | ||
| Graded exposure | ||||
| Family history | ||||
| Exploring feelings | ||||
| Monitoring person’s engagement | ||||
| Participant 23/row 24 | Involvement of family and care staff | Everyone (family, school, respite) being on board and understanding what is being done. | ||
| Participant 24/row 25 | Individualised assessment | Good assessment and understanding of the problem. Exposure in a systematic way, usually using a hierarchy or ladder. Identifying maintaining factors, safety behaviours and how others may play a role in this maintenance cycle. Psychoeducation for parents. Developing a toolkit of strategies (including breathing, relaxation, sensory strategies, etc.) to help the child relax. | ||
| Problem formulation | ||||
| Graded exposure | ||||
| Psychoeducation | ||||
| Treatment toolkit | ||||
| Assessment | Assessment, diagnosis and prescribing. | |||
| Diagnosis | ||||
| Prescribing | ||||
| No response | 5 | |||
| Can you briefly describe any additional key procedures, activities and/or processes used within this treatment or intervention. | Additional key procedures, activities and processes used within the treatment | Participant 1/row 2 | Collaboration with other specialists | Liaising with other services as well, such as Speech and Language Therapy to make sure that what we are using feels an appropriate format in which to present stuff. |
| Participant 7/row 8 | Individualising | We adjust the psychoeducation, communication style and intervention according to the YP’s needs. However, we would engage with more training for the staff team for a young person with additional needs. | ||
| Providing extra training for staff | ||||
| Individualising | We adjust the psychoeducation, communication style and intervention according to the YP’s needs. However, we would engage with more training for the staff team for a young person with additional needs. | |||
| Providing extra training for staff | ||||
| Individualising | We adjust the psychoeducation, communication style and intervention according to the YP’s needs. However, we would engage with more training for the staff team for a young person with additional needs. | |||
| Providing extra training for staff | ||||
| Participant 9/row 10 | Not known | I don’t prescribe so I can’t comment. | ||
| Participant 14/row 15 | Assessment of family’s ability to support use of medication | Assessment of the child and parental ability to support use of medication. | ||
| Flexibility | Flexibility. | |||
| Participant 18/row 19 | Social stories | Sometimes I use social stories to support the acclimatisation process and give the appointment structure. | ||
| Participant 22/row 23 | Pictures | Use of pictures and videos, clinician or family members’ engagement. | ||
| Videos | ||||
| Clinician and family engagement | ||||
| Participant 23/row 24 | Explaining treatment to everyone involved | Explaining it and breaking it down for everyone involved so the process is clear. Perhaps a meeting with all involved to agree/clarify the process. | ||
| Participant 24/row 25 | N/A | N/A | ||
| No response | 12 | |||
| What materials are used with this treatment or intervention? Please tell us of all materials used by those providing the treatment, including materials given to patients and carers, or those that might be used when training staff in the treatment (e.g. information leaflets, recording sheets, booklets or other materials). | Treatment materials | Participant 1/row 2 | Leaflets for parents | Psychoeducation leaflets for parents, some information provided to help them understand the process and what is going on so we can support them. Materials used with young people are very much depending on where they are at in terms of their abilities, like their understanding and communication – the materials are concrete, for example visual cards, pictures, photos, video clips, sounds, physically visiting the place relevant to the step of the hierarchy. There may be some recording forms to measure how it is going on with the hierarchy for parents to complete. |
| Individualised for the young person | ||||
| Visuals | ||||
| Pictures | ||||
| Photos | ||||
| Videos | ||||
| Sounds | ||||
| Visiting the place | ||||
| Exposure recording forms | ||||
| Participant 2/row 3 | Individualised for the young person | Variable depending on need but may include thought diaries/charts of some kind, rating scales to look at how phobia is changing, goal-setting forms, etc. | ||
| Thought diaries | ||||
| Charts | ||||
| Rating scales | ||||
| Goal-setting forms | ||||
| None | No specific materials. | |||
| Exposure recording forms | Possibly some graded exposure hierarchy worksheets, rating scales to rate anxiety levels as treatment progresses, etc. | |||
| Rating scales | ||||
| Medication | Medication. | |||
| Participant 7/row 8 | Response excluded | All our materials are designed to meet the needs of young people whatever their communication style or level of understanding. Any adaptations occur within the therapeutic relationship. Our service is not specifically for YP with a learning disability. | ||
| Response excluded | All our materials are designed to meet the needs of young people whatever their communication style or level of understanding. Any adaptations occur within the therapeutic relationship. Our service is not specifically for YP with a learning disability. | |||
| Response excluded | All our materials are designed to meet the needs of young people whatever their communication style or level of understanding. Any adaptations occur within the therapeutic relationship. Our service is not specifically for YP with a learning disability. | |||
| Participant 9/row 10 | Exposure recording forms | Exposure hierarchy, anxiety coping plan (e.g. social story). | ||
| Anxiety coping plan | ||||
| Exposure recording forms | Exposure hierarchy, anxiety coping plan (e.g. social story). | |||
| Anxiety coping plan | ||||
| Easy-read information | I don’t prescribe so I can’t comment. | |||
| I gather titration and monitoring may differ, but I am not aware of details as I don’t prescribe. We have easy-read information when needed. | ||||
| Participant 14/row 15 | Leaflets for the young person | Medication information leaflets relevant to children and adolescents with LD. | ||
| Individualised for the young person | ||||
| Pictures | Pictures and modelling roles. | |||
| Modelling roles | ||||
| Participant 18/row 19 | Social stories | Social story (‘in the dentist room’ Widgit sheet); dental materials to look at/‘play with’. | ||
| Dental materials | ||||
| Participant 22/row 23 | Videos | Videos, pictures, feelings and anxiety explored, monitoring patients’ engagement and willingness at each session, letting patient lead on time and sessions, all very individualised to the patient. | ||
| Pictures | ||||
| Individualised for the young person | ||||
| Participant 23/row 24 | Instructions clearly communicated | Tailor-made instructions – either e-mailed to parent and teacher or written up as part of a PBS plan. | ||
| Participant 24/row 25 | Information sheets | Information sheets about the key concepts used for psychoeducation, for example fight, flight, freeze, hot cross bun CBT formulation model. Individualised visual resources dependent on the level of functioning of the child. Visual hierarchies/exposure ladders. | ||
| Individualised for the young person | ||||
| Visuals | ||||
| Exposure recording forms | ||||
| Information leaflets | Information leaflets about medications, benefits and side effects. | |||
| No response | 6 |
Appendix 2 Treatment as usual parent survey themes and codes
| Question | Theme | Participant ID/row number | Code | Extract demonstrating theme |
|---|---|---|---|---|
| Provide name or phrase that describes the treatment your child was offered for their phobia/s. This includes psychological treatments and medication. | Name of the treatment | Participant 1/row 2 | Exposure therapy | Play therapist – desensitisation |
| Participant 18/row 19 | Exposure therapy | Visited young person, did assessment based on what Mum said, prepared report | ||
| Participant 26/row 27 | Exposure therapy | PBS – desensitisation | ||
| Participant 2/row 3 | Medication | Medication | ||
| Participant 10/row 11 | Medication | Medication – laxatives | ||
| Participant 25/row 26 | Medication | Medication | ||
| Participant 45/row 46 | Medication | Medication | ||
| Participant 16/row 17 | Medication | Medication for anxiety | ||
| Sensory integration | Sensory integration | |||
| Participant 40/row 41 | Counselling | Therapy/counselling | ||
| Briefly describe the treatment that was offered to your child for their phobia/s (e.g. what were the key elements). If your child was offered medication to manage their phobia/s then please state the name of the medication and dose if known. | Brief description of the treatment | Participant 1/row 2 | Support | Play therapist sent home and into school to offer support, play, desensitisation |
| Play | ||||
| Desensitisation | ||||
| Participant 10/row 11 | Laxatives | Laxatives to relieve the awful constipation | ||
| Participant 16/row 17 | Helping understand body and feelings | Understanding his body and feelings | ||
| Fluoxetine | Fluoxetine | |||
| Participant 2/row 3 | Fluoxetine | Fluoxetine – 10 mg | ||
| Participant 18/row 19 | Psychoeducation for parent | Introduce pictures of animals, gave a story book and gave Mum information how to do exposure therapy. Start at the bottom, looking at pictures then move to looking at dogs in community then stroking the dog | ||
| Gradual exposure to dogs using images first | ||||
| Participant 25/row 26 | Not known | I don’t know | ||
| Participant 26/row 27 | PBS | A course of support from a trained professional PBS – desensitisation | ||
| Desensitisation | ||||
| Participant 40/row 41 | Counselling | Counselling | ||
| Participant 45/row 46 | Melatonin | Melatonin – 2 ml before bed. To help calm anxieties to enable him to get to sleep |
Appendix 3 Fidelity checklist percentages for SPIRIT workshops
Fidelity checklist percentages for SPIRIT workshop 1 (n = 10)
| Theme and question | Percentage of ‘yes’ responses |
|---|---|
| General workshop preparations | |
| 1. Gathered all resources listed in the materials section of day 1 section of the manual. | 90 |
| 2. Agreed with the parents on frequency of breaks. | 100 |
| Coverage of workshop plan | |
| 3. Informed the parents about the plan for the day and estimated finish time. | 100 |
| 4. Ensured that the parents clearly understood the purpose of the workshop. | 100 |
| 5. Focus points for day 1 were covered and key activities were completed. | 100 |
| 6. Workshop finished on time. | 100 |
| Understanding and accessibility | |
| 7. Adjusted the content and style of my own communication to help the parents’ understanding. | 100 |
| 8. Welcomed questions from the parents. | 100 |
| Interpersonal effectiveness | |
| 9. Communicated with warmth, concern and understanding. | 100 |
| 10. In control of the workshop, communicated clearly without frequent hesitations/repetitions. | 100 |
| 11. Able to shift appropriately between listening and leading. | 100 |
| Engaging participants | |
| 12. Explained rationale and requirements for the different activities/elements of the workshop clearly. | 100 |
| 13. Did not criticise, disapprove or ridicule the parents. | 100 |
| 14. Responded to seemingly irrelevant interruptions in an effective yet respectful manner. | 80 |
| Workshop content | |
| 15. Introduced myself and explained my role. | 100 |
| 16. Asked parents to introduce themselves. | 100 |
| 17. Provided an overview of the training. | 100 |
| 18. Discussed parent–therapist working relationship. | 100 |
| 19. Asked parents to give 3-minute presentation about their child. | 100 |
| 20. Explained what specific phobias are. | 100 |
| 21. Explored key symptoms. | 100 |
| 22. Introduced characteristics of specific phobias in people with learning disabilities. | 100 |
| 23. Explained role of modelling in learning new behaviours. | 100 |
| 24. Explained how specific phobias are developed and maintained. | 100 |
| 25. Explored various triggers and how they might influence child’s behaviour. | 100 |
| 26. Introduced to SPIRIT treatment. | 100 |
| 27. Explained treatment goal and structure. | 100 |
| 28. Explored role of the parent and therapist. | 100 |
| 29. Introduced exposure steps. | 100 |
| 30. Introduced strategies used to support exposure therapy. | 100 |
| 31. Explained preparations needed before starting exposure therapy. | 100 |
| 32. Introduced reinforcement. | 100 |
| 33. Explained when reinforcement is the most effective. | 100 |
| 34. Explained the role of reinforcement in the treatment of specific phobia. | 100 |
| 35. Introduced preference assessment. | 100 |
| 36. Asked parents to complete a preference assessment before the next workshop. | 100 |
| 37. Introduced visual schedules. | 100 |
| 38. Explained how to use visual schedules. | 100 |
| 39. Practised preparing a visual schedule. | 80 |
| 40. Shared an optional video on visual schedules for the parents. | 70 |
Fidelity checklist percentages for SPIRIT workshop 2 (n = 8)
| Theme and question | Percentage of ‘yes’ responses |
|---|---|
| General workshop preparations | |
| 1. Gathered all resources listed in the materials section of day 2 section of the manual. | 100 |
| 2. Agreed with the parents on frequency of breaks. | 100 |
| Coverage of workshop plan | |
| 3. Informed the parents about the plan for the day and estimated finish time. | 100 |
| 4. Ensured that the parents clearly understood the purpose of the workshop. | 100 |
| 5. Focus points for day 2 were covered and key activities were completed. | 100 |
| 6. Workshop finished on time. | 100 |
| Understanding and accessibility | |
| 7. Adjusted the content and style of my own communication to help the parents’ understanding. | 100 |
| 8. Welcomed questions from the parents. | 100 |
| 9. Workshop was pitched at a level that was accessible to the parents. Parents remained engaged. | 100 |
| 10. Care was taken to pace the workshop at a rate that allowed the parents to keep up with what was happening. | 100 |
| Interpersonal effectiveness | |
| 11. Communicated with warmth, concern and understanding. | 100 |
| 12. In control of the workshop, communicated clearly without frequent hesitations/repetitions. | 100 |
| 13. Able to shift appropriately between listening and leading. | 100 |
| Engaging participants | |
| 14. Explained rationale and requirements for the different activities/elements of the workshop clearly. | 100 |
| 15. Did not criticise, disapprove or ridicule the parents. | 100 |
| 16. Responded to seemingly irrelevant interruptions in an effective yet respectful manner. | 100 |
| Workshop content | |
| 17. Checked in on parents’ progress with the preference assessment and engaged in troubleshooting if needed. | 100 |
| 18. Introduced relaxation. | 100 |
| 19. Explored possible adaptations to relaxation strategies. | 100 |
| 20. Asked parents to complete ‘About my child’s phobia’ document and introduced the exposure steps spreadsheets. | 100 |
| 21. Guided parents through completing the exposure steps spreadsheet of their choice. | 100 |
| 22. Explained how to use relaxation strategies in exposure therapy. | 100 |
| 23. Explained how to use visual schedule in exposure therapy. | 100 |
| 24. Explained how to use reinforcement in exposure therapy. | 100 |
| 25. Explained how to monitor child’s mood and level of discomfort. | 100 |
| 26. Guided parents through creating exposure plan folder. | 100 |
| 27. Explained how to collect data and monitor progress. | 100 |
| 28. Explained frequency of treatment sessions. | 100 |
| 29. Explained what parents should do after the workshop. | 100 |
| 30. Explored the role of the parent and the therapist. | 100 |
| 31. Explored potential difficulties/barriers the parents may encounter. | 100 |
| 32. Explored some of the potential solutions. | 100 |
| 33. Explained how to get support. | 100 |
Appendix 4 Fidelity checklist percentages for SPIRIT support sessions
Fidelity checklist percentages for SPIRIT support session 1 (n = 14)
| Theme and question | Percentage of ‘yes’ responses |
|---|---|
| General session preparations | |
| 1. Gathered all resources listed in the materials section. | 78.6 |
| 2. Gained access to the data sheet prior or during the session. | 28.6 |
| Coverage of session plan | |
| 3. Informed the parents about the plan for the session and estimated finish time. | 92.9 |
| 4. Ensured that the parents clearly understood the purpose of the session. | 92.9 |
| 5. Session aims were fulfilled. | 100 |
| 6. Session finished on time. | 78.6 |
| Understanding and accessibility | |
| 7. Adjusted the content and style of my own communication to help the parents’ understanding. | 100 |
| 8. Welcomed questions from the parents. | 100 |
| 9. Session was pitched at a level that was accessible to the parents. Parents remained engaged. | 100 |
| 10. Care was taken to pace the session at a rate that allowed the parents to keep up with what was happening. | 100 |
| Interpersonal effectiveness | |
| 11. Communicated with warmth, concern and understanding. | 100 |
| 12. In control of the session, communicated clearly without frequent hesitations/repetitions. | 100 |
| 13. Able to shift appropriately between listening and leading. | 100 |
| Engaging participants | |
| 14. Explained rationale and requirements for the different activities/elements of the session clearly. | 100 |
| 15. Did not criticise, disapprove or ridicule the parents. | 100 |
| 16. Responded to seemingly irrelevant interruptions in an effective yet respectful manner. | 100 |
| Session content | |
| 17. Checked on child’s and parents’ well-being. | 100 |
| 18. Checked on progress with relaxation and preference assessment. | 100 |
| 19. Engaged in troubleshooting with the parents. | 100 |
| 20. Set goals for upcoming week with the parents. | 100 |
| 21. Explored any potential barriers to starting with exposure and possible solutions. | 100 |
Fidelity checklist percentages for SPIRIT support session 2 (n = 13)
| Theme and question | Percentage of ‘yes’ responses |
|---|---|
| General session preparations | |
| 1. Gathered all resources listed in the materials section. | 84.6 |
| 2. Gained access to the data sheet prior or during the session. | 23.1 |
| Coverage of session plan | |
| 3. Informed the parents about the plan for the session and estimated finish time. | 76.9 |
| 4. Ensured that the parents clearly understood the purpose of the session. | 92.3 |
| 5. Session aims were fulfilled. | 92.3 |
| 6. Session finished on time. | 76.9 |
| Understanding and accessibility | |
| 7. Adjusted the content and style of my own communication to help the parents’ understanding. | 100 |
| 8. Welcomed questions from the parents. | 100 |
| 9. Session was pitched at a level that was accessible to the parents. Parents remained engaged. | 100 |
| 10. Care was taken to pace the session at a rate that allowed the parents to keep up with what was happening. | 100 |
| Interpersonal effectiveness | |
| 11. Communicated with warmth, concern and understanding. | 100 |
| 12. In control of the session, communicated clearly without frequent hesitations/repetitions. | 92.3 |
| 13. Able to shift appropriately between listening and leading. | 100 |
| Engaging participants | |
| 14. Explained rationale and requirements for the different activities/elements of the session clearly. | 100 |
| 15. Did not criticise, disapprove or ridicule the parents. | 100 |
| 16. Responded to seemingly irrelevant interruptions in an effective yet respectful manner. | 100 |
| Session content | |
| 17. Checked on child’s and parents’ well-being. | 100 |
| 18. Reviewed data sheet. | 46.2 |
| 19. Checked on progress with exposure tasks and relaxation. | 100 |
| 20. Checked that parents are using all secondary strategies – reinforcement, visual schedules, rating scale and relaxation. | 100 |
| 21. Engaged in troubleshooting with the parents. | 92.3 |
| 22. Set goals for upcoming week with the parents. | 100 |
| 23. Explored any potential barriers to continuing with exposure and possible solutions. | 92.3 |
Fidelity checklist percentages for SPIRIT support session 3 (n = 13)
| Theme and question | Percentage of ‘yes’ responses |
|---|---|
| General session preparations | |
| 1. Gathered all resources listed in the materials section. | 76.9 |
| 2. Gained access to the data sheet prior or during the session. | 46.2 |
| Coverage of session plan | |
| 3. Informed the parents about the plan for the session and estimated finish time. | 100 |
| 4. Ensured that the parents clearly understood the purpose of the session. | 92.3 |
| 5. Session aims were fulfilled. | 83.3 |
| 6. Session finished on time. | 83.3 |
| Understanding and accessibility | |
| 7. Adjusted the content and style of my own communication to help the parents’ understanding. | 100 |
| 8. Welcomed questions from the parents. | 100 |
| 9. Session was pitched at a level that was accessible to the parents. Parents remained engaged. | 100 |
| 10. Care was taken to pace the session at a rate that allowed the parents to keep up with what was happening. | 100 |
| Interpersonal effectiveness | |
| 11. Communicated with warmth, concern and understanding. | 100 |
| 12. In control of the session, communicated clearly without frequent hesitations/repetitions. | 100 |
| 13. Able to shift appropriately between listening and leading. | 100 |
| Engaging participants | |
| 14. Explained rationale and requirements for the different activities/elements of the session clearly. | 100 |
| 15. Did not criticise, disapprove or ridicule the parents. | 91.7 |
| 16. Responded to seemingly irrelevant interruptions in an effective yet respectful manner. | 100 |
| Session content | |
| 17. Checked on child’s and parents’ well-being. | 100 |
| 18. Reviewed data sheet. | 46.2 |
| 19. Checked on progress with exposure tasks and relaxation. | 100 |
| 20. Checked that parents are using all secondary strategies – reinforcement, visual schedules, rating scale and relaxation. | 100 |
| 21. Engaged in troubleshooting with the parents. | 92.3 |
| 22. Set goals for upcoming week with the parents. | 100 |
| 23. Explored any potential barriers to continuing with exposure and possible solutions. | 100 |
Fidelity checklist percentages for SPIRIT support session 4 (n = 13)
| Theme and question | Percentage of ‘yes’ responses |
|---|---|
| General session preparations | |
| 1. Gathered all resources listed in the materials section. | 84.6 |
| 2. Gained access to the data sheet prior or during the session. | 84.6 |
| Coverage of session plan | |
| 3. Informed the parents about the plan for the session and estimated finish time. | 100 |
| 4. Ensured that the parents clearly understood the purpose of the session. | 100 |
| 5. Session aims were fulfilled. | 100 |
| 6. Session finished on time. | 100 |
| Understanding and accessibility | |
| 7. Adjusted the content and style of my own communication to help the parents’ understanding. | 100 |
| 8. Welcomed questions from the parents. | 100 |
| 9. Session was pitched at a level that was accessible to the parents. Parents remained engaged. | 100 |
| 10. Care was taken to pace the session at a rate that allowed the parents to keep up with what was happening. | 100 |
| Interpersonal effectiveness | |
| 11. Communicated with warmth, concern and understanding | 100 |
| 12. In control of the session, communicated clearly without frequent hesitations/repetitions. | 100 |
| 13. Able to shift appropriately between listening and leading. | 100 |
| Engaging participants | |
| 14. Explained rationale and requirements for the different activities/elements of the session clearly. | 100 |
| 15. Did not criticise, disapprove or ridicule the parents. | 100 |
| 16. Responded to seemingly irrelevant interruptions in an effective yet respectful manner. | 100 |
| Session content | |
| 17. Checked on child’s and parents’ well-being. | 100 |
| 18. Reviewed data sheet. | 30.8 |
| 19. Checked on progress with exposure tasks and relaxation. | 92.3 |
| 20. Checked that parents are using all secondary strategies – reinforcement, visual schedules, rating scale and relaxation. | 92.3 |
| 21. Engaged in troubleshooting with the parents. | 92.3 |
| 22. Set goals for upcoming week with the parents. | 100 |
| 23. Explored any potential barriers to continuing with exposure and possible solutions. | 92.3 |
Fidelity checklist percentages for SPIRIT support session 5 (n = 13)
| Theme and question | Percentage of ‘yes’ responses |
|---|---|
| General session preparations | |
| 1. Gathered all resources listed in the materials section. | 100 |
| 2. Gained access to the data sheet prior or during the session. | 23.1 |
| Coverage of session plan | |
| 3. Informed the parents about the plan for the session and estimated finish time. | 92.3 |
| 4. Ensured that the parents clearly understood the purpose of the session. | 100 |
| 5. Session aims were fulfilled. | 92.3 |
| 6. Session finished on time. | 76.9 |
| Understanding and accessibility | |
| 7. Adjusted the content and style of my own communication to help the parents’ understanding. | 100 |
| 8. Welcomed questions from the parents. | 100 |
| 9. Session was pitched at a level that was accessible to the parents. Parents remained engaged. | 100 |
| 10. Care was taken to pace the session at a rate that allowed the parents to keep up with what was happening. | 100 |
| Interpersonal effectiveness | |
| 11. Communicated with warmth, concern and understanding. | 100 |
| 12. In control of the session, communicated clearly without frequent hesitations/repetitions. | 92.3 |
| 13. Able to shift appropriately between listening and leading. | 100 |
| Engaging participants | |
| 14. Explained rationale and requirements for the different activities/elements of the session clearly. | 100 |
| 15. Did not criticise, disapprove or ridicule the parents. | 84.6 |
| 16. Responded to seemingly irrelevant interruptions in an effective yet respectful manner. | 100 |
| Session content | |
| 17. Checked on child’s and parents’ well-being. | 100 |
| 18. Reviewed data sheet. | 38.5 |
| 19. Checked on progress with exposure tasks and relaxation. | 84.6 |
| 20. Checked that parents are using all secondary strategies – reinforcement, visual schedules, rating scale and relaxation. | 76.9 |
| 21. Engaged in troubleshooting with the parents. | 92.3 |
| 22. Set goals for upcoming week with the parents. | 92.3 |
| 23. Explored any potential barriers to continuing with exposure and possible solutions. | 100 |
Fidelity checklist percentages for SPIRIT support session 6 (n = 12)
| Theme and question | Percentage of ‘yes’ responses |
|---|---|
| General session preparations | |
| 1. Gathered all resources listed in the materials section. | 83.3 |
| 2. Gained access to the data sheet prior or during the session. | 25 |
| Coverage of session plan | |
| 3. Informed the parents about the plan for the session and estimated finish time. | 91.7 |
| 4. Ensured that the parents clearly understood the purpose of the session. | 91.7 |
| 5. Session aims were fulfilled. | 91.7 |
| 6. Session finished on time. | 91.7 |
| Understanding and accessibility | |
| 7. Adjusted the content and style of my own communication to help the parents’ understanding. | 100 |
| 8. Welcomed questions from the parents. | 100 |
| 9. Session was pitched at a level that was accessible to the parents. Parents remained engaged. | 100 |
| 10. Care was taken to pace the session at a rate that allowed the parents to keep up with what was happening. | 100 |
| Interpersonal effectiveness | |
| 11. Communicated with warmth, concern and understanding. | 100 |
| 12. In control of the session, communicated clearly without frequent hesitations/repetitions. | 100 |
| 13. Able to shift appropriately between listening and leading. | 100 |
| Engaging participants | |
| 14. Explained rationale and requirements for the different activities/elements of the session clearly. | 100 |
| 15. Did not criticise, disapprove or ridicule the parents. | 100 |
| 16. Responded to seemingly irrelevant interruptions in an effective yet respectful manner. | 100 |
| Session content | |
| 17. Checked on child’s and parents’ well-being. | 100 |
| 18. Reviewed data sheet. | 33.3 |
| 19. Checked on progress with exposure tasks and relaxation. | 91.7 |
| 20. Checked that parents are using all secondary strategies – reinforcement, visual schedules, rating scale and relaxation. | 100 |
| 21. Engaged in troubleshooting with the parents. | 91.7 |
| 22. Set goals for upcoming week with the parents. | 100 |
| 23. Explored any potential barriers to continuing with exposure and possible solutions. | 100 |
Fidelity checklist percentages for SPIRIT support session 7 (n = 12)
| Theme and question | Percentage of ‘yes’ responses |
|---|---|
| General session preparations | |
| 1. Gathered all resources listed in the materials section. | 58.3 |
| 2. Gained access to the data sheet prior or during the session. | 16.7 |
| Coverage of session plan | |
| 3. Informed the parents about the plan for the session and estimated finish time. | 100 |
| 4. Ensured that the parents clearly understood the purpose of the session. | 100 |
| 5. Session aims were fulfilled. | 91.7 |
| 6. Session finished on time. | 83.3 |
| Understanding and accessibility | |
| 7. Adjusted the content and style of my own communication to help the parents’ understanding. | 100 |
| 8. Welcomed questions from the parents. | 100 |
| 9. Session was pitched at a level that was accessible to the parents. Parents remained engaged. | 100 |
| 10. Care was taken to pace the session at a rate that allowed the parents to keep up with what was happening. | 100 |
| Interpersonal effectiveness | |
| 11. Communicated with warmth, concern and understanding. | 100 |
| 12. In control of the session, communicated clearly without frequent hesitations/repetitions. | 91.7 |
| 13. Able to shift appropriately between listening and leading. | 100 |
| Engaging participants | |
| 14. Explained rationale and requirements for the different activities/elements of the session clearly. | 100 |
| 15. Did not criticise, disapprove or ridicule the parents. | 100 |
| 16. Responded to seemingly irrelevant interruptions in an effective yet respectful manner. | 100 |
| Session content | |
| 17. Checked on child’s and parents’ well-being. | 100 |
| 18. Reviewed data sheet. | 25 |
| 19. Checked on progress with exposure tasks and relaxation. | 91.7 |
| 20. Checked that parents are using all secondary strategies – reinforcement, visual schedules, rating scale and relaxation. | 91.7 |
| 21. Engaged in troubleshooting with the parents. | 91.7 |
| 22. Set goals for upcoming week with the parents. | 100 |
| 23. Explored any potential barriers to continuing with exposure and possible solutions. | 100 |
| 24. Introduced ‘exposure summary’ and asked parents to complete it for next support session. | 83.3 |
Fidelity checklist percentages for SPIRIT support session 8 (n = 13)
| Theme and question | Percentage of ‘yes’ responses |
|---|---|
| General session preparations | |
| 1. Gathered all resources listed in the materials section. | 92.3 |
| 2. Gained access to the data sheet prior or during the session. | 15.4 |
| Coverage of session plan | |
| 3. Informed the parents about the plan for the session and estimated finish time. | 100 |
| 4. Ensured that the parents clearly understood the purpose of the session. | 100 |
| 5. Session aims were fulfilled. | 100 |
| 6. Session finished on time. | 84.6 |
| Understanding and accessibility | |
| 7. Adjusted the content and style of my own communication to help the parents’ understanding. | 100 |
| 8. Welcomed questions from the parents. | 100 |
| 9. Session was pitched at a level that was accessible to the parents. Parents remained engaged. | 100 |
| 10. Care was taken to pace the session at a rate that allowed the parents to keep up with what was happening. | 100 |
| Interpersonal effectiveness | |
| 11. Communicated with warmth, concern and understanding. | 100 |
| 12. In control of the session, communicated clearly without frequent hesitations/repetitions. | 100 |
| 13. Able to shift appropriately between listening and leading. | 92.3 |
| Engaging participants | |
| 14. Explained rationale and requirements for the different activities/elements of the session clearly. | 100 |
| 15. Did not criticise, disapprove or ridicule the parents. | 100 |
| 16. Responded to seemingly irrelevant interruptions in an effective yet respectful manner. | 92.3 |
| Session content | |
| 17. Reviewed the ‘exposure summary’ with the parent and encouraged them to reflect on their progress so far. | 76.9 |
| 18. Identified future goals with the parents. | 100 |
| 19. Completed a Keeping Well plan with the parents. | 100 |
List of abbreviations
- ABC-C
- Aberrant Behavior Checklist – Community
- ACT
- acceptance and commitment therapy
- ADIS
- Anxiety Disorders Interview Schedule
- AE
- adverse event
- BPI
- Behavior Problems Inventory
- CAMHS
- Child and Adolescent Mental Health Services
- CBT
- cognitive behavioural therapy
- CI
- confidence interval
- DASH-II
- Diagnostic Assessment for the Severely Handicapped Scale II
- DBC2
- Developmental Behavior Checklist 2
- DM-ID-2
- Diagnostic Manual – Intellectual Disability, 2nd edition
- HRA
- Health Research Authority
- HTA
- Health Technology Assessment
- IDG
- Intervention Development Group
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health and Care Research
- PBS
- positive behaviour support
- PPI
- patient and public involvement
- R&D
- research and development
- RA
- Research Assistant
- RADiANT
- Research in Developmental Neuropsychiatry
- REC
- Research Ethics Committee
- SD
- standard deviation
- SDQ
- Strengths and Difficulties Questionnaire
- SM
- Study Manager
- SSC
- Study Steering Committee
- TAU
- treatment as usual
- TIDieR
- Template for Intervention Description and Replication
- VABS
- Vineland Adaptive Behavior Scales
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/LRWD7852).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
