Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as award number NIHR129804. The contractual start date was in January 2021. The draft manuscript began editorial review in August 2023 and was accepted for publication in February 2024. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Langdon et al. This work was produced by Langdon et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Langdon et al.
Chapter 1 Introduction
Within our report, we recognise that “learning” and “intellectual” disabilities are both used to refer to the same group of people in different parts of the world. In the United Kingdom, we tend to use learning disabilities. We have intentionally used intellectual disabilities in our title, while we have used learning disabilities throughout our report.
Background
There is evidence that ‘talking’ psychological therapies are likely effective for autistic people without learning disabilities and those with mild learning disabilities,1–3 but there is a lack of evidence that these interventions are effective for those with both autism and moderate to severe learning disabilities. 4 While there is substantial evidence that cognitive behavioural therapy is an effective intervention for anxiety disorders in adults,5 the inclusion of cognitive methods within behaviour therapy has been questioned, as there is evidence that these methods do not improve intervention outcomes,6–8 including outcomes following intervention for anxiety disorders. 9–12 There is evidence that behavioural interventions and, specifically, exposure therapy may work just as well as cognitive therapy for many anxiety disorders. 13–15 Considering the difficulties that autistic people with learning disabilities experience with communication, psychological therapies which focus upon behavioural interventions, such as exposure therapy, may be advantageous because of a potential reduced reliance upon verbal communication.
Rosen et al. 16 completed a systematic review of behavioural interventions used for anxiety disorders with autistic people with moderate or severe learning disabilities. Their review included seven studies involving children, adolescents and adults. None of the included studies were randomised control trials; instead, they made use of single-case experimental designs. Within the review, a variety of behavioural interventions with adaptations, such as the inclusion of parents or carers within therapy, were successfully modelled, which included: systematic desensitisation and the use of fear hierarchies,17–19 video modelling and mastery techniques,19 stimulus fading,20 positive reinforcement to support behaviour change19–22 and exposure techniques. 20–23 These studies suggested that behavioural interventions have the potential to be beneficial for anxiety amongst those with autism and moderate to severe learning disabilities. Additionally, we completed a systematic review of interventions for mental health problems for children and adults who have severe learning disabilities (including those with autism). 4 Very few studies met the eligibility criteria for inclusion, and those that evaluated psychological therapies made use of minimal-quality single-case experimental designs, with a resulting poor current evidence base, indicating that better modelling and feasibility studies are initially needed to inform the decision as to whether to proceed to larger studies.
It is clear that autistic people are at increased risk of developing mental health problems, including anxiety disorders, relative to their neurotypical peers. 24–27 Those with autism often present with atypical reactions to sensory stimuli as well as restricted and repetitive interests which are associated with anxiety, including an insistence on sameness and routine. 28,29 Approximately 32–43% of those with autism also have symptoms of anxiety,30,31 while members of our research team have identified that up to 14.3% will have a diagnosis of an anxiety disorder by the age of 27, compared with only 7.1% of the general population. 32 Adapted talking psychological therapies can be used to treat anxiety disorders with autistic people,2,33 and similar interventions can be used with people who have mild learning disabilities. 1,3,34 However, as already mentioned, the evidence to support their use with people who have autism and moderate to severe learning disabilities is sparse. 3
A variety of factors have been associated with the development of emotional disorders in autistic children, adolescents, and adults. It is important that these factors are considered and incorporated within intervention programmes for autistic people, and include:
-
difficulties with social functioning,35 and social skills difficulties,36,37 including social motivation38 and communication39
-
difficulties with friendship quality40 and lack of social support41,42
-
difficulties with the development and use of coping strategies35
-
seeing oneself as dissimilar from others45
-
autistic traits42
-
lack of flexibility and associated executive function difficulties, associated with anxiety47,48
-
difficulties with meta-cognition, associated with depression47
-
restricted and repetitive behaviours,28,49,50 including an insistence on sameness28,29,51–54
-
level of general intellectual functioning,55–58 which has not been consistently associated with emotional disorders in some studies59
-
sensory issues, including atypical sensory over-responsivity and avoidance of sensory input28,29,53,60,61
-
intolerance of uncertainty,28,62–65 which has been shown to mediate the relationship between sensory issues and anxiety, as well as anxiety and insistence on sameness66 and
-
alexithymia. 64
Autistic people with moderate to severe learning disabilities who have anxiety disorders have a high level of need, and this has been recognised by the NHS. In 2015,67 Building the Right Support was published, which was a national plan for England to develop community services for people with learning disabilities and/or autism in an attempt to reduce the need for psychiatric hospital admission. As part of this new national service model for people with learning disabilities and/or autism, all individuals should be offered both mainstream and specialist NHS health care, including mental health interventions, as needed. While there are well-developed evidence-based psychological therapies for the general population, such an evidence base does not exist for autistic people and those with moderate to severe learning disabilities. The results of our systematic review of interventions for mental health problems in individuals with severe learning disabilities, including those who have autism, showed no robust evidence for any psychological interventions for anxiety. 4 Thus, autistic individuals with moderate to severe learning disabilities face an evidence inequity whereby there is a lack of research to guide intervention despite significant levels of need. However, the National Institute for Health and Care Excellence does recommend psychological interventions, including relaxation training and exposure therapy, for adults with either autism or learning disabilities who have mental health problems. 68–70
Lifetime care costs for one person with autism and learning disabilities have been estimated at £1.5 million,71 while the literature about the economic benefits of healthcare interventions for autistic people with learning disabilities is scarce. Developing mental health interventions for autistic people was previously identified as the number one priority by stakeholders, including autistic people and their families, in the James Lind Alliance priority-setting exercise (www.jla.nihr.ac.uk/news/answering-the-questions-from-people-with-autism-their-families-and-health-professionals/7681). NHS England have identified autism and learning disabilities as a 10 Year Plan clinical priority for the NHS, while the need to eliminate any potential discrimination against those with a protected characteristic, as defined within the Equality Act, 2010, has been recognised by NHS England72 within their previously published research plan for the NHS. This has also included a recommendation that research must reduce health inequalities amongst patients, which is directly relevant to autistic people with moderate to severe learning disabilities who face a double inequality (existing health inequalities coupled with a lack of evidence about how best to reduce these).
However, developing and testing interventions for this population are associated with several challenges, and feasibility studies are needed to effectively model these challenges and develop effective solutions. First, individuals with autism and learning disabilities have significant communication difficulties. Second, there is an increased prevalence of behaviours that challenge (e.g. aggression, self-injurious behaviour) amongst this population,73,74 which may not be recognised as associated with a mental health problem,75,76 especially in those with more severe learning disabilities,77 but needs to be considered in the context of intervention for anxiety. Third, those with autism present with restricted and repetitive behaviours,28,49,50 an insistence on sameness,28,29,51–54 sensory over-responsivity and avoidance of sensory input,28,29,53,60,61 and rumination,41,46 amongst other difficulties42 which need to be considered within intervention. Fourth, a large proportion of this population are unlikely to have capacity to provide informed consent to take part in research. As such, the provisions of the Mental Capacity Act, 2005, in England and Wales must be followed. Fifth, the measurement of anxiety symptomatology within the context of a future clinical trial requires consideration, including the appropriateness of patient-reported outcome measures in this population and similar proxy-rated outcome measures.
Considering measurement, we previously completed a systematic review of measurement tools for mental health problems with people who have severe or profound learning disabilities, including those who have autism. 78 The measures deemed to be the most robust overall in terms of available data were both broad-based psychopathology tools: the Aberrant Behaviour Checklist (ABC-2)79 and the Diagnostic Assessment for the Severely Handicapped Scale-II (DASH-II). 80 Specific data on the measurement of anxiety in this population were limited. Thus, some work is required to determine the most appropriate measures to use within a clinical trial of behaviour therapy for anxiety in people with autism and moderate to severe learning disabilities.
Taking the aforementioned issues together, the current project aimed to adapt and model a manualised intervention for the intervention of anxiety disorders amongst autistic people who have moderate to severe learning disabilities within a feasibility study. We worked with carers, clinicians, and autistic people to adapt an existing intervention programme,81–83 complete a survey of intervention within existing services to characterise treatment-as-usual (TAU), and complete a feasibility study to model the intervention. This project comprised two phases: Phase 1: Intervention Adaptation and Description of Treatment-as-Usual, and Phase 2: a Feasibility Study.
Rationale for the current study
A large number of autistic people with learning disabilities have problems with anxiety and have a high level of need. However, a previous systematic review4 and a recent systematic review incorporating meta-analysis3 found no robust evidence for any psychological intervention approaches for anxiety for adults who have severe learning disabilities (including those who are autistic). To meet the needs of autistic adults with moderate to severe learning disabilities, therapies for anxiety need to be adapted to meet need and successfully modelled before future larger trials can take place to generate evidence about the efficacy.
Aims and objectives
To adapt an existing intervention for use with autistic adults who have moderate to severe learning disabilities and anxiety, investigate the feasibility of implementing the intervention, and characterise TAU by completing a national survey of services.
Phase 1a: intervention adaptation
Our objectives were:
-
to establish an intervention adaptation group (IAG) and, over a series of meetings, adapt an existing intervention used within a previous clinical trial to treat anxiety symptoms in autistic adults81–83 for use with people who also have moderate to severe learning disabilities
-
to develop an intervention fidelity checklist that can be used alongside the intervention manual
-
to appraise and consider several candidate outcome measures of anxiety-related symptoms and social care and make a recommendation for use within Phase 2
-
to develop an intervention logic model.
Phase 1b: description of treatment-as-usual
Our objective was:
-
to complete a national survey of existing interventions for autistic adults with anxiety disorders who have moderate to severe learning disabilities.
Phase 2: feasibility study
Our objectives were:
-
to model the manualised intervention to determine the acceptability and feasibility for all stakeholders, including patients, carers and clinicians, and adjust as required
-
to judge the appropriateness, including response rates, of our measures of anxiety-related symptomatology for use within a larger study
-
to examine the feasibility and acceptability of consent and associated processes
-
to describe factors that facilitate or challenge the implementation of our intervention.
Chapter 2 Phase 1a: intervention adaptation
Methods
Recruitment
We established an IAG of eight stakeholders. This included an autistic collaborator who chaired the meeting, a representative from the National Autistic Society (NAS) [our patient and public involvement (PPI) partner], a sibling of an autistic person with severe learning disability, and five clinicians with experience of working with autistic adults with learning disabilities including those who had additional caring roles. Members of the research team also attended and had a background in clinical psychology or speech and language therapy.
Design
We made use of methods drawn from action research84 by focusing upon collaboration and reflection with practitioners and patient and public involvement and engagement members in order to improve the intervention, logic model and fidelity checklist, and make decisions about candidate outcome measures. This happened over five meetings that lasted at least 2 hours over a 2-month period. Meetings were scheduled every 2 weeks, with the exception of the last two meetings, which were 1 week apart. All meetings were online and were recorded.
The aims of the IAG based upon our Phase 1a aims and objectives were to: (1) define the needs and problems that are to be addressed for autistic people with moderate to severe learning disabilities, (2) define the intervention objectives, with reference to the likely barriers, (3) adapt the existing manualised intervention and associated materials, (4) collaboratively develop the fidelity checklist with the researchers, (5) consider candidate primary and secondary outcome measures, including measures of social care, making a recommendation for use within the feasibility study (Phase 2), (6) consider any additional methods to identify users of the intervention and further development of implementation protocols as needed and (7) give further consideration of any challenges or barriers to our evaluation plan, including likely solutions.
Before the first IAG meeting, we prepared an initial draft of the intervention manual, intervention materials, logic model, therapist training outline and the fidelity checklist. Three of the five meetings focused on the intervention manual and corresponding materials, one on the fidelity checklist, logic model and therapist training, and one on outcome measures. Table 1 details the schedule of the IAG meetings.
| Meeting 1 |
|
| Meeting 2 |
|
| Meeting 3 |
|
| Meeting 4 |
|
| Meeting 5 |
|
Prior to each meeting, documents were circulated to participants. An agenda was set and discussion and reflection were encouraged amongst participants until consensus was reached for each decision. Any disagreements were discussed until the group reached consensus and a recommendation was made. Feedback and reflections were sought from participants about changes and refinements to the manual, logic model, materials, and the fidelity checklist. These changes were then presented to the IAG at the next meeting to ensure that they were enacted as previously recommended and to encourage further reflection. All recommendations were recorded in an Excel spreadsheet, which was shared with the IAG for approval. Feedback was also sought on the range of candidate outcome measures, and several candidate measures were presented to the IAG, which included a review of the items, psychometric properties, and likely ease of use. The IAG were invited to make the final recommendation as to which outcome measures should be used within Phase 2.
Results
Objectives
Objective 1: the adaptation of an existing intervention for anxiety
To develop the initial draft of the intervention manual, we used an existing intervention for anxiety symptoms in autistic adults. 81–83 Importantly, this intervention was developed explicitly for autistic people who did not have learning disability, and was previously evaluated.
In developing our initial draft of the intervention manual, we focused upon the following modules from our previously developed intervention manual: (1) relaxation training, (2) building fear hierarchies, (3) exposure therapy and systematic desensitisation and (4) behavioural experiments. A description of each of these modules and their associated content is found within Table 2.
| Module | Content |
|---|---|
| Relaxation | Participants are taught about the relationship between relaxation and anxiety. A variety of relaxation techniques are taught and practised, ranging from Jacobson85 muscle relaxation to breathing exercises. Participants are encouraged to try different methods and choose one they consider the most beneficial. Participants are encouraged to practise relaxation out of session and assigned associated homework and record forms. Participants are asked to record the frequency and length of time they took to practise each relaxation episode, along with the associated type, and their emotional state. |
| Building fear hierarchies | Collaboratively, participants work with the therapist to break down anxiety-provoking situations into a number of different components, ranking them from least to most fearful. Multiple fears and associated fear hierarchies can be chosen. The role of safety-seeking behaviours and avoidance is explained and discussed. |
| Exposure therapy and systematic desensitisation | These concepts are explained and the importance of using relaxation techniques while undertaking exposure therapy is discussed. Participants work through their hierarchy of fears, considering each step and how to apply relaxation strategies during exposure work. Initially, exposure techniques using imagery-based methods are used where participants begin with the least fearful step within their fear hierarchy and make use of relaxation techniques. This is repeated, leading to a reduction in anxiety. Participants are asked to practise these skills outside of the session. |
| Introduction to behavioural experiments | Participants review their out-of-session skills practice using their fear hierarchies, and the paradoxical role of safety-seeking and avoidance behaviours is further discussed and considered. In vivo exposure work is introduced, discussed and planned collaboratively with the participants and therapist. Participants are asked to continue to practise imagined exposure and relaxation techniques. |
| Behaviour experiments | Over a series of sessions, the planned in vivo exposure work is carried out based upon the previously created fear hierarchy, working from the least to the most feared situation. Participants are asked to continue to practise these techniques outside of the formal session throughout the week using their fear hierarchies and relaxation techniques. |
The intervention was initially adapted by the research team to be accessible to people with moderate to severe learning disabilities and presented to the IAG over a series of meetings for further adaptation. Our manualised intervention involved 12 sessions that focused upon: (1) building rapport and providing psychoeducation about anxiety, autism and learning disabilities to both carers and autistic people, (2) relaxation training and (3) the development of individualised exposure therapy leading to recommendations for maintenance and generalisation. We made use of a blend of sessions that involved both the carer and the autistic person with a learning disability, as well as carer-only sessions. Carer and participant handbooks were also developed for use during the intervention.
Following feedback from the IAG, a series of changes were made to the intervention manual and materials. See Chapter 3 for detailed description of the intervention and accompanying materials, including the logic model. Table 3 summarises changes proposed to the intervention manual and intervention materials by the IAG and how they were addressed.
| Feedback/suggestions | Action |
|---|---|
| General feedback | |
| To include explanation of safeguarding and the capacity to consent more overtly in the materials. | Completed |
| To replace ‘have’ with ‘may face’ when talking about challenges. | Completed |
| Check spelling throughout the intervention manual. | Completed |
| To consider producing easy-read versions of a future research paper. | To be actioned in the future following the completion of the project. |
| Introduction and intervention structure | |
| To add a section providing additional introduction and further information within the theoretical section. | Completed |
| To ensure the language on theoretical background and introduction is understandable to all staff. | Completed |
| To explain ‘operationalisation’. | Completed |
| To add real-life examples or case studies. | We added more case examples throughout, which could be further strengthened following the completion of Phase 2. |
| To break down the sentence: ‘The behavioural therapist is interested in behavioural contingencies (…)’ and to delete the phrase ‘young person’. | Completed |
| To add a paragraph about identifying a key carer or carers to participate in the intervention. This might be raised with a manager. | Completed |
| Key concepts and strategies | |
| To expand the text box under ‘Antecedent’ in the figure explaining Antecedent-Behaviour-Consequence (ABC). | Completed |
| To rephrase section on effectiveness of reinforcement. | Completed |
| To replace the word ‘satiation’ with another word or provide definition. | Completed |
| To further explain differential reinforcement – DRO, DRI and DrA. | Completed |
| To replace the term ‘attention’ with another term. | Completed |
| To consider how the idea of a ‘break allowance’ would be introduced to clinicians/carers delivering the intervention and how much training on implementing it there will be. | Completed |
| To move the behavioural toolkit section to the appendix or to add more explanation in the ‘How to use the manual’ section. | Completed |
| Delete active support from the manual. | Completed |
| Considerations on care and good practice guidelines | |
| To add more explanation and examples to the section on ‘What to consider when planning care’. | Completed |
| To specify ‘person’s preferences and needs’ in the good practice guidelines. | Completed |
| To add a further explanation about ensuring communication is adapted to the needs of the individual. | Completed |
| Use directive text within the good practice guidelines for therapists. | Changes were made to emphasise the importance of following good practice guidance. |
| To consider obtaining feedback on rapport-building after the study, including exploring whether the initial sessions were sufficient. | This was noted and we included questions about this within our post-intervention interviews with the therapist, carer, and participant when possible. |
| To emphasise the importance of responding to the person’s capacity to understand information and their communication ability. | Completed |
| To include phrases: ‘being conscious of infantilising’, ‘respectful’, ‘person-centred’. | Completed |
| To remove the term ‘age-appropriate’. | Completed |
| To emphasise the importance of treating the person as an adult and talking to and looking at them. | Completed |
| To emphasise the importance of using the same words and tone of voice when prompting. | Completed |
| To add that it is important that the staff working with the person know how to use the person’s communication aids effectively. | Completed |
| To add that it is important to establish how the person communicates ‘stop’, ‘no’, ‘enough’ and requests a break. | Completed |
| Sessions 1–12 | |
| To define vocabulary in tables or thought bubbles across all sections. | Completed |
| To re-structure the manual: (1) General introduction to the problem, (2) The guiding framework/Logic Model, (3) The intervention itself that operationalises the aspects of the Logic Model, (4) All supporting concepts and session materials. | Completed |
| To add a section on potential harms resulting from the intervention. | This information was included in the participant information and included in our training provided to therapists. |
| To add a section on how likely it is that a behavioural approach is going to work for an autistic person. | This was included within our theoretical background section. |
| To replace ‘Velcro’ with ‘loop sided fasteners (e.g. Velcro)’. | Completed |
| To simplify language. | Completed |
| To change 1.5 hours to 90 minutes. | Completed |
| To replace ‘communication aids’ with ‘augmented communication’. | Completed |
| To ask the carer to take photos of the person taking part in the activities they enjoy which could be included in the preference assessment. | Completed |
| To include instructions on the Preference Assessment form. | Completed |
| To replace ‘faulty thinking’ with ‘distorted thoughts’/‘unworkable beliefs’/‘unhelpful thinking’. | Completed |
| To define ‘regular intervals’. | Completed |
| Add description of the ABC chart to the intervention manual. | Completed |
| Emphasise consent when working on exposure and using touch with relaxation. | Completed |
| To replace ‘fear hierarchy’ with ‘fear ladder’. | Completed |
| To replace ‘systematic desensitisation’ with ‘gradual exposure’. | Completed |
| To include recommended frequency for practising exposure outside of the session. Daily if possible. | Completed |
| To add a reminder for the person that they cannot be anxious and relaxed at the same time. | Completed |
| Person and carer handbooks | |
| To change wording in the section on carer’s role. | Completed |
| To consider adding taste and temperature to the list of sensory sensitivities. | Completed |
| To make sure person-first language is used consistently throughout the manual and materials when talking about autistic people. | Completed |
| To add information about alexithymia to the Carer’s Handbook. | Completed |
| To add ‘butterflies in the stomach’ when explaining how anxiety can feel in the Person’s Handbook. | Completed |
| To remove acronyms from Person’s Handbook. | Completed |
| The words ‘anxiety’ and ‘worry’ are being used interchangeably but are arguably separate. Ensure consistency in the handbooks. | Completed |
| To emphasise consent when working on exposure and using touch with relaxation in the Carer’s Handbook. | Completed |
| To add examples that are not phobia-related to the section on Fear Ladders. | Completed |
| To consider asking the carer to take pictures of the person completing steps of the fear ladder to be included as visual representation. | We added that suggestion to the intervention manual and created a Fear Ladder template for visuals. |
| It would be worth looking at the literature on video (self) modelling and replicate some of these ideas in this context. I would hope that the person and carers could video anyway as long as the video is not passed on to anyone else. | We have added this suggestion to the intervention manual; however, questions were raised about whether this would be very time-consuming and it was not included as a core element of the intervention. |
| To replace ‘systematic desensitisation’ with ‘gradual exposure’. | Completed |
| To replace the ‘fear evoking’ phrase for one more appropriate for carers and people with LD. | Completed |
| Materials | |
| To add more space for notes in the Interview for carers. | Completed |
| To change some of the wording in the section in the Interview for carers. | Completed |
| To add a question about sensory triggers to the Interview for carers. | Completed |
| To consider adding a session countdown so the person can tick off each session as it is completed. | Completed |
A further description of our intervention can be found within Chapter 3. Our draft logic model and therapist training plan were also presented to the IAG. Table 4 summarises proposed changes and actions. Our logic model and therapist training are detailed further within Chapter 3, Figure 2.
| Feedback/suggestions | Action |
|---|---|
| Logic model | |
| To change some of the wording to improve understanding. | Completed |
| To add a point about harm and adverse reactions. | We decided that this was more suited for inclusion within the main body of the intervention manual where it was covered in detail. |
| To add a point about ‘Praxis difficulties’. | Completed |
| To add more information about restrictive and repetitive behaviours. | We decided that this should be included within the intervention manual where it was covered in detail. |
| Therapist training | |
| To change the structure to avoid starting with the most difficult concepts, for example, (1) Introduction, (2) Rationale for intervention, (3) Structure of the intervention, and (4) Toolkit of behavioural strategies. | Completed |
| To consider using visuals in PowerPoint presentations, worksheets and activities using different sensory resources. | Completed |
| To consider developing a jam board or a poster with definitions that trainees can refer to if needed. | We developed and included handouts. |
| To include 5-minute mindfulness/relaxation practice during the training. | Completed |
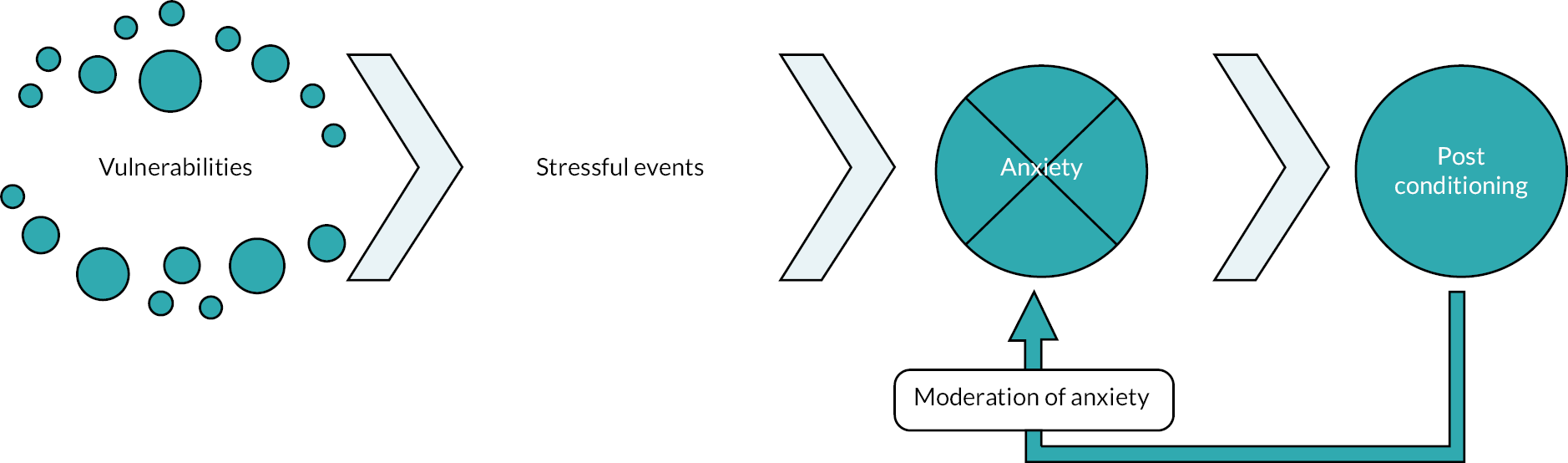
FIGURE 1.
Theory of change: as depicted, contemporary learning theory postulates that anxiety disorders develop as a consequence of direct and vicarious learning experiences which are affected by a variety of factors including pre-existing vulnerabilities, the predictability and controllability of stressful events, and temporal proximity to stressful events. Additional factors, such as sensory sensitivity, learning disability, restricted and repetitive behaviours, and lack of flexibility are markedly relevant for those with autism and moderate to severe learning disability. Further, the experience of anxiety is moderated by events that occur post-learning; for example, the nature and degree of avoidance behaviours, generalisation of anxiety, and additional stimuli which inflate or decrease anxiety, and directly inform interventions, such as exposure therapy.
Objective 2: intervention fidelity checklist
Our fidelity checklist was adapted from that used by Jahoda et al. 86 Eight sections were included as follows:
-
general session preparations
-
coverage of session plan
-
understanding and accessibility
-
interpersonal effectiveness
-
engaging participants
-
session content
-
inter-session tasks
-
further comments.
There were separate checklists for each of the 12 intervention sessions. Therapists were asked to reflect on the sessions and indicate if they have fulfilled the aims by circling yes or no on the checklist. See Appendix 3 for a sample fidelity checklist and Chapter 3 for a detailed description. Our draft fidelity checklist for each of our 12 sessions was prepared and presented to our IAG for discussion. The group accepted the checklist without suggesting any further changes and recommended that it should be used within Phase 2.
Objective 3: appraise and consider several candidate outcome measures of anxiety-related symptoms, and secondary outcomes, and make a recommendation for use within Phase 2
A broad range of potential measures were considered, including parent/carer questionnaires, behavioural measures, and physiological measures. These were initially selected by the research team and included:
Eligibility
Outcome measures
-
a draft version of the Clinical Anxiety Screen for people with Severe to Profound Intellectual Disability (CIASP-ID)90
-
Autism Spectrum Disorders – Assessment Battery for Intellectually Disabled Adults91
-
Aberrant Behaviour Checklist – Community92
-
DASH-II93
-
Developmental Behaviour Checklist-2 Adult (DBC2-A)94
-
the Behaviour Problems Inventory for Individuals with Intellectual Disabilities – Short Form95
-
the Index of Community Involvement96
-
Psychopathology in Autism Checklist (PAC)97
-
Anxiety, Depression and Mood Scale (ADAMS)98
-
Psychological Therapies Outcome Scale – Intellectual Disabilities 2nd Edition (PTOS-II). 99
The IAG was presented with detailed information about each instrument including format, intended age range, time needed to complete, and psychometric properties. Following a discussion, the IAG made recommendations about outcome measures that should be used in Phase 2 of the project. Table 5 summarises the IAG feedback on presented measures.
| Measure | Feedback/suggestions | Action |
|---|---|---|
| Eligibility | ||
| Diagnostic checklist for anxiety based on Diagnostic Manual – Intellectual Disability-2 (National Association for the Dually Diagnosed, 2016) | IAG recommended using this measure | Measure added to the eligibility case report form (CRF) |
| Vineland Adaptive Behaviour Scales – Third Edition (Sparrow et al., 2016) | IAG recommended using this measure | Measure added to the eligibility CRF |
| Social Responsiveness Scale 2 (Constantino et al., 2003) | IAG recommended using this measure | Measure added to the eligibility CRF |
| Outcome measures | ||
| CIASP-ID | Measure did not consider unexpected changes in person’s life | Not used |
| The group was not sure about validity of this measure | ||
| The group suggested this measure is more helpful for clinical practice rather than research | ||
| The measure was too long to be used repeatedly | ||
| The group did not recommend using this measure | ||
| DBC2-A | The group had questions about how change would be captured considering limited scale | Measure included in the baseline and follow-up CRF |
| The group was unsure if the measure captured communication well | ||
| There was limited evidence around using this measure with adults | ||
| Language was deficit-focused which might not be perceived well by some carers | ||
| The group agreed to include this measure as it is a measure of emotional and behavioural problems suitable for use with this population, noting the limitations | ||
| Autism Spectrum Disorders – Behaviour Problems for Adults | Language was deficit-focused which might not be perceived well by some carers | Not used |
| The group suggested the measure would take too long to complete | ||
| Communication domain was useful and the rating scale was seen as good | ||
| Some wording not helpful, especially for parents | ||
| The group did not recommend using this measure | ||
| Aberrant Behaviour Checklist (ABC-2) | The group felt that some of the language used in this measure was problematic, especially around stimming and special interests | Not used |
| Some people might have relevant conditions but not officially diagnosed which led to questions about the use of this measure | ||
| The group did not recommend using this measure | ||
| The Behaviour Problems Inventory for Individuals with Intellectual Disabilities – Short Form | The measure was user-friendly | Measure included in the baseline and follow-up CRF |
| Used by clinicians in the group and generally accepted | ||
| The group recommended using this measure | ||
| PAC | The rating scale was seen as helpful because you rate whether the person has improved, not changed or worsened | Measure included in the baseline and follow-up CRF |
| The group liked that this measure was short | ||
| Some items might be difficult to score for people with severe communication problems | ||
| The group recommended using this measure | ||
| DASH-II | The group felt that this measure was very deficit-focused | Not used |
| The group felt that this measure can be difficult to complete and was not user friendly | ||
| It might be difficult for carers to remember details about behaviours across so many items | ||
| The group did not recommend using this measure | ||
| ADAMS | It can be used for people regardless of disability and communication needs | Not used |
| Measure would focus on shorter time frame than 6 months | ||
| Questions were raised about carer’s objectivity rating a behaviour as problematic | ||
| Families might have higher threshold so the severity rating might not be accurate | ||
| Group felt that the items are accessible | ||
| Item about fatigue and weight was considered problematic | ||
| The group did not recommend using this measure | ||
| PTOS-II | This was the only measure that can be also completed by the person with learning disabilities | Not used |
| The informant version relies a lot on knowing how the person feels | ||
| Items were considered to be not specific | ||
| The group did not recommend using this measure | ||
| The Index of Community Involvement (Raynes, 1994) | IAG recommends using this measure as seen as short and easy to complete | Measure included in the baseline and follow-up CRF |
Summary
Within Phase 1a, we aimed to adapt an existing intervention for use with autistic adults with moderate to severe learning disabilities who have anxiety, develop a fidelity checklist, select candidate outcome measures for use with Phase 2, and develop an intervention logic model. Collaboratively, with our IAG using methods adapted from action research incorporating methods to develop consensus, a variety of changes were made to our intervention manual, a series of candidate outcome measures were selected, and our logic model was refined. No changes were recommended to the fidelity checklist. Our intervention and associated logic model are further considered within the next chapter.
Chapter 3 Intervention description
Within this chapter, a description of the theoretical framework informing the intervention is provided along with a thorough description of the intervention and associated logic model. Material found within this chapter is reproduced from the protocol for this study which we authored (see: www.fundingawards.nihr.ac.uk/award/NIHR129804).
Theoretical framework
Contemporary learning theories provide a robust explanation of both the aetiology and intervention of anxiety disorders, through the process of direct and vicarious learning experiences. Integral to these theories is not only the process by which anxiety is learnt (i.e. classical, operant and vicarious conditioning), but also the important role of vulnerabilities to anxiety, such as previous vicarious conditioning, individual genetic differences, previous and future life experience, cultural and familial transmission of fears, controllability, behavioural inhibition, interoceptive conditioning (i.e. internal states becoming a ‘trigger’ for anxiety), and exteroceptive conditioning (i.e. external stimuli becoming a ‘trigger’ for anxiety). 100–104 These factors impact upon the experience of stressful events, which are further moderated by the predictability and perceived controllability of events, and previous direct and vicarious learning experiences. Both interoceptive (e.g. sensory input) and exteroceptive (e.g. external stimuli) conditioned stimuli can moderate stress, leading to an increase or decrease in anxiety and the quality of associated anxiety, including the intensity of any conditioned association. Events that occur post-conditioning moderate anxiety further, and these can include unconditioned stimulus inflation (factors that promote anxiety), and derived relationship responding and stimulus generalisation (where related stimuli become conditioned due to their relationship with other conditioned stimuli). Further, multiple excitatory stimuli occurring within close proximity can lead to summation effects, further increasing anxiety. Other post-conditioning events serve to moderate anxiety through their inhibitory effects, such as safety-seeking behaviours and avoidance, which paradoxically maintain anxiety.
These learning processes will lead to the development of an anxiety disorder in some individuals, as depicted in Figure 1, which was adapted from Mineka and Zinbarg100 to incorporate additional factors relevant to autistic people and those with learning disabilities (e.g. sensory over-responsivity; lack of flexibility; restricted interests; cognitive ability, communication difficulties). Clinical interventions must reflect theory, and, primarily, these interventions are based upon psychological formulations using these models to inform individualised exposure techniques to successfully treat the symptoms of anxiety, making use of strategies, such as systematic desensitisation and fear hierarchies, leading to habituation or, in other words, a reduction in experienced anxiety over time.
There is some evidence drawn from single-case experimental designs that interventions based upon learning theory using exposure-based interventions and associated strategies may be effective for those with autism and learning disabilities. 16 Exposure-based interventions have been shown to be effective for a range of anxiety disorders amongst those without autism and/or learning disabilities including specific phobias, obsessive-compulsive disorder, panic disorder, agoraphobia, and post-traumatic stress disorder. 5,105 The exclusion of cognitive strategies, which are delivered using verbal communication within ‘talking’ therapy, and a reliance upon exposure-based techniques have been shown to be associated with no reduction in therapy effect size. 5,6,8 Considering this, psychological interventions which are not entirely delivered using verbal communication are likely to be advantageous when used with autistic adults with moderate to severe learning disabilities because it is not possible for many individuals to engage effectively within ‘talking’ psychological therapy due to their difficulties with verbal communication and processing. As a consequence, the delivery of appropriately adapted behavioural interventions for anxiety amongst autistic adults with moderate to severe learning disabilities may be advantageous.
Description and structure of the intervention
The BEAMS-ID intervention was specifically created to meet the needs of autistic adults with moderate to severe learning disabilities. It was further developed collaboratively with the IAG, composed of autistic people, therapists, carers and researchers experienced in working with autistic adults with moderate to severe learning disabilities (see Chapter 2 for more details). Parts of the intervention were originally developed and tested with autistic adults without learning disabilities,82 and then systematically adapted for use with autistic adults with learning disabilities collaboratively with our IAG drawing upon their theoretical and clinical knowledge and personal experiences of providing care to this group.
There are a number of potential challenges that were considered when delivering psychological interventions for anxiety to this group. These include different ways of communicating, behaviours that challenge, problems with recognising mental health issues, restricted or repetitive behaviours, and sensory differences, such as over-responsivity or avoidance of some types of sensory input, amongst others. Keeping these challenges in mind, we collaboratively adapted the intervention to meet the needs of autistic people with moderate to severe learning disabilities. These adaptations included:
-
involving carers or family members in the delivery of intervention
-
focusing on using methods that are less reliant upon verbal communication, including graded exposure, which involves gradually exposing someone to the feared object or situation in a progressive and safe way that is not overwhelming and is coupled with relaxation and reinforcement
-
using a person-centred approach – it is clearly recognised that many with moderate to severe learning disabilities communicate their needs well, while others require support, and this needs to be well understood by the therapist and incorporated into the intervention; this involves working with carers and others to help the therapist understand the needs of the person as an individual and tailor the delivery to their needs
-
performing a preference and functional assessment, and a thorough exploration of the nature of anxiety, avoidance, accommodation, and sensory issues to develop a psychological formulation; and
-
using adapted ways of communicating, such as visual schedules and easier to read materials.
The intervention consisted of 12 sessions that were up to 90 minutes long usually delivered on weekly basis. Three sessions were attended only by the carer to enable the therapist to develop a good understanding of the needs of the participants and to socialise the carer into the intervention. The remaining nine sessions were attended by the autistic person with learning disability and their carer. The intervention focused upon providing relaxation training, leading to the implementation of carefully planned graded exposure associated with delivery of reinforcement. Refer to Table 6 which details the structure of the BEAMS-ID intervention.
| Session | Main focus | Key activities/focus points |
|---|---|---|
| 1 | Psychoeducation on behaviour change CARER-ONLY SESSION |
|
| 2 | Building rapport |
|
| 3 | Psychoeducation on anxiety, autism and learning disability |
|
| 4 | Relaxation training |
|
| 5 | Design of individualised Intervention Plan CARER-ONLY SESSION |
|
| 6 | Building Fear Ladders CARER-ONLY SESSION |
|
| 7 | Graded exposure |
|
| 8 | Graded exposure |
|
| 9 | Graded exposure |
|
| 10 | Graded exposure |
|
| 11 | Wrap up |
|
| 12 | Wrap up |
|
Each session plan was composed of three core elements – objectives, materials and session activities/content. Each session started with an introduction during which the therapist planned the session with the person and their carer using a visual schedule. Session activities usually included a mixture of psychoeducation and practical tasks. Some sessions also included instructions for inter-session tasks that the carer was asked to support outside of the sessions. Sessions ended with a wrap-up, during which the therapist summarised the covered content and reminded the person and their carer of their next session.
To help carers and individuals understand and engage with intervention, they were provided with a variety of resources that were used by the therapist collaboratively with the individual and the carer. This included a Carer’s Handbook which focused upon psychoeducation about anxiety, relaxation, graded exposure, and the principles of behaviour change, including their role within the intervention. A Person’s Handbook with a focus upon explaining autism, learning disability, anxiety, and the intervention, including relaxation was also included and shared. See the Materials section for more details.
Logic model
Collaboratively with our IAG, we developed an intervention logic model, based upon our theoretical framework (Figure 2).
Key components
Considering the specialised nature of our intervention, key intervention components included staff training and ongoing supervision. Additional key components included the development of high-quality relationships with the autistic person with a learning disability and their carer, along with the provision of psychoeducation, a good understanding of the autistic person with a learning disability and their needs including any sensory sensitivities, and the development and provision of an individualised intervention plan using relaxation training and exposure therapy paired with reinforcement.
Carers
One of the key components to our intervention is carer engagement. Carers have a markedly important role in the delivery of the intervention because: (1) they know the person well and understand how the person communicates, (2) they have a role in helping to build the psychological formulation and collect data to inform this formulation, (3) they assist with helping to arrange and attend sessions, (4) they need to learn and practice new skills together with the person outside of the session to help promote learning and generalisation and (5) they communicate with other carers who are involved in delivering care to ensure they understand the intervention and are able to assist with inter-session tasks as needed.
Exposure therapy
The intervention involved gradually exposing the person to the feared stimuli and pairing this with relaxation techniques. It involved three main steps:
-
teaching deep breathing and relaxation strategies
-
building a fear ladder (graded hierarchy of fears) which is a list of objects and/or situations related to the feared stimuli ranging from least distressing to most distressing and
-
gradually exposing the person to the steps included in the fear ladder while practising relaxation strategies.
This approach helped the person to build tolerance of the feared object or situation at a comfortable pace. The experience of feeling anxious is an important component of exposure therapy as the individual learns how to manage this feeling coupled with habituation. The aim was to reduce person’s fearful/anxious response and learn that feared objects or situations are not dangerous.
The Fear Ladder was developed in collaboration with the individual with learning disability and their carer to help promote engagement and avoid overwhelming the individual and their carer using the form described in the Materials section. The Fear Ladder was reviewed regularly and broken down further if needed.
Relaxation
Relaxation strategies reduce tension in the body and anxiety. When the individual experiences feelings of anxiety or fear, their muscles tighten, and it can be difficult for them to feel calm. By introducing relaxation, tension in the body reduces and promotes calmer feelings. Relaxation strategies were used when the person was feeling anxious or overwhelmed, as well as during exposure. Some examples of relaxation strategies included deep breathing and muscle relaxation.
During the sessions, the therapist spent time discussing existing relaxation strategies, which may be idiosyncratic, such as sensory activities or self-stimulatory behaviours, and whether the identification of new strategies could be helpful. If deemed appropriate, they were taught breathing exercises that involved taking a deep breath through the nose and exhaling through the mouth. Visual cards were used to support with this task. The therapist could also introduce muscle relaxation, which included clenching and relaxing muscle in different body parts – shoulders, back, hands, face, stomach and feet.
Some of the possible adaptations the therapist was able to consider to meet the needs of the person included:
-
reduced verbal language in instructions
-
reduced number of body areas targeted for muscle relaxation
-
teaching body parts before moving on to the muscle relaxation
-
using modelling to demonstrate the exercises
-
using the example and non-example procedure – modelling a relaxed and not relaxed pose and asking the person to only copy the relaxed pose
-
incorporating favourite objects or stories into the exercises. For example, bubbles or feathers
-
using physical prompting to teach the person the exercises
-
introducing of a visual cue or signal, for example picture card(s) to signal relaxation and
-
incorporating relaxation aids like a stress ball, therapeutic putty, dimmed lights, or relaxing music.
If the person was struggling to engage in deep breathing and muscle relaxation, different strategies were considered, such as the carer performing a hand massage, having a break in a quiet space, using fidgets and sensory equipment and so on.
Reinforcement
Reinforcement is a consequence which follows a behaviour and increases the likelihood the behaviour will occur again in the future. Reinforcement was used to teach new skills, such as requesting a break and relaxation, and after completing the exposure tasks during the intervention. To identify appropriate reinforcers, the therapist completed a preference assessment. A preference assessment is a systematic process that allows the therapist to identify six things the person likes the most. To complete the preference assessment, the therapist uses the Preference Assessment form, which is described in more detail in the Materials section. Identified reinforcers were reviewed frequently. If needed, the preference assessment was redone during the course of the intervention.
Generalisation and maintenance
Another component of the intervention was generalisation and maintenance. Generalisation is an ability to perform a behaviour learnt in one context in a different context. While neurotypical individuals often generalise behaviours themselves by observing others and through indirect learning, autistic people with learning disabilities may need help with generalisation. Therefore, working on the generalisation of acquired behaviours/skills in a systematic and structured way is an essential part of a successful behaviour change. This includes teaching and practising new behaviours:
-
in different environments
-
with different people
-
with varying instructions and
-
using different materials.
To ensure that behaviour change is maintained, a variety of strategies were incorporated, such as:
-
focusing on behaviours that are meaningful to the person
-
teaching until mastery (i.e. fluent in a skill)
-
providing opportunities to practise new behaviours and
-
adjusting the level of reinforcement.
Strategies to encourage generalisation and maintenance of new behaviours were incorporated into the intervention and discussed during the last session.
Communication
It was anticipated that all participants would have communication differences. Therefore, the intervention included a number of augmented communication strategies, such as visual aids and a visual schedule. These supports were reviewed and expanded on by a speech and language therapist, drawing on aided (e.g. using graphics and objects) and unaided (e.g. using manual sign and gesture) options from established augmentative and alternative communication methods (e.g. Signalong: www.signalong.org.uk; photosymbols: www.photosymbols.com; Talking Mats: www.talkingmats.com).
Intervention procedures
Order of intervention activities
The first session was a carer-only session focused upon explaining the intervention and included psychoeducation about anxiety while introducing aspects of functional analysis and behaviour change. The second session focused upon completing a preference assessment with the individual and their carer. This is a method that is used to help choose reinforcers that can be used during intervention to help support behaviour change. Session three focused upon psychoeducation about anxiety, routines, and sensory issues, along with teaching new concepts that are to be used later in the intervention. The fourth session focused upon teaching relaxation, while our fifth session was a carer-only session where the therapist worked collaboratively with the carer to help design an Individualised Intervention Plan for the next phase of therapy. This included developing strategies to help manage anxiety, including the use of reinforcement and relaxation. Sessions six and onwards were focused upon developing an individualised Fear Ladder and implementing graded exposure. This continued and within the penultimate session, ending was introduced, with a focus upon next steps. During the final session, strategies and goals for continuing beyond the end of therapy are developed collaboratively with the carer and the individual to encourage maintenance and further generalisation.
Fidelity and adherence
Fidelity to the intervention manual was measured with fidelity ratings (number of completed session components) after each session. This self-report measure was adapted from Jahoda et al. 34 Person and carer adherence was defined as attendance at intervention sessions. To meet the adherence criterion, the person and carer need to attend at least 80% sessions.
Materials
There were three sets of intervention materials developed:
-
materials for the therapist: intervention manual, Antecedent-Behaviour-Consequence (ABC) chart, fear ladder, fidelity checklists, preference assessment document, intervention plan document
-
materials for the carer: Carer handbook, ABC chart, assessment for carers, intervention plan, intervention summary
-
materials for the autistic person with learning disability: Person’s handbook, certificate of completion, rating scale, visual intervention schedule, intervention summary, visual schedule and associated materials.
Intervention manual
The Intervention manual was further developed with the help of the IAG. It included both the background and a step-by-step guide to the intervention of anxiety amongst autistic adults with moderate to severe learning disabilities. The manual provided the therapist with detailed plans for the intervention sessions, as well as general guidelines on working with autistic people with learning disabilities and their carers, which are summarised earlier within this report.
Person’s handbook
The Person’s handbook contained three sections and covered:
-
autism and learning disabilities
-
anxiety
-
relaxation.
Carer handbook
The Carer handbook contained seven sections and covered:
-
role of the carer
-
principles of behaviour and behaviour change
-
autism and learning disabilities
-
anxiety
-
relaxation
-
introduction to fear ladders
-
introduction to graded exposure.
Antecedent–Behaviour–Consequence chart
For the first five sessions, carers were asked to complete ABC charts in between the sessions every time the person with learning disabilities became anxious. The chart guided them through recording what happened immediately before the person became anxious, what they did when anxious, and what happened immediately after. The carer was asked to share completed charts with the therapist for the first five sessions to inform the intervention plan.
Assessment for carers
Prior to the start of the intervention, carers were sent the Assessment for carers along with the instructions for completion and asked to bring it to the first session. This assessment asked questions about the person they were caring for, including what they were like in different environments and their anxiety. Carers were asked to involve the autistic person with learning disability as much as possible in completing this document.
Certificate of completion
After the last session, the therapist was able to issue a Certificate of completion to the autistic person with learning disability to recognise their efforts and mark the end of intervention.
Fear ladder
A Fear ladder is a list of situations, places, or things connected to the person’s anxiety arranged from least feared or distressing to most feared or distressing. Autistic people with moderate to severe learning disabilities and their carers were given a choice of a Fear ladder template that they found most suitable. Some of the options included a ladder, stairs, and a horizontal or vertical schedule.
Fidelity checklist
Therapists used a self-report Fidelity checklist at the end of each session to record the extent to which the content was delivered according to the manual. Therapists were asked to reflect on the aims of each session and indicate if they were completed by circling ‘Yes’ or ‘No’ on the checklist. Supervisors were encouraged to review the Fidelity checklist with their supervisees.
Preference assessment
The Preference assessment form guided therapists though identifying a person’s preferred objects and/or actions. Together with the person and their carer, the therapist started by identifying six potential reinforcers. Then they paired them together to see which ones were preferred by the person. Later they created a reinforcer ranking, identifying preferred reinforcers, which were used during exposure work.
Rating scale
The Rating scale was used by carers to monitor a person’s mood and level of discomfort during exposure work. It helped carers identify when the person became distressed. The Rating scale consisted of three options – good, ok and bad. These options were accompanied by a corresponding hand signal and colour (green, amber and red).
Intervention plan
During the fifth session, the therapist and carer completed the Intervention plan. This document summarised the intervention strategies selected for the person and divided them into green (person’s anxiety is at their baseline), amber (person is becoming anxious) and red (person is anxious and distressed) strategies. This document was developed to allow for easy integration into an existing positive behavioural support plan.
Intervention sessions schedule
To help the person understand how they are progressing though intervention, the therapist was asked to use the Intervention session schedule. This was a visual schedule for the person that included all 12 sessions.
Intervention summary
While preparing for the end of the intervention, the person and their carer were asked to complete the Exposure summary. The worksheet asked them to reflect upon intervention progress – what were their goals, what they have achieved and what they still want to work on.
Visual schedule
The Visual schedule is a visual representation of activities planned for the person. It allowed the person to know what will be happening and provided an opportunity to manage transitions in a more controlled manner. For some autistic people with learning disabilities, it was considered helpful to use an additional ‘Now/Next’ board which was embedded in the Visual schedule. It helped the person know what is happening in that moment and what is happening next.
The Visual schedule was used during all intervention sessions and the carer was encouraged to also use it outside of the sessions.
Therapist training and supervision
The intervention was delivered by a trained therapist, who could be a nurse, clinical psychologist, assistant psychologist, medical doctor, allied health professional, or other suitably qualified health professional with experience of working with autistic people with learning disabilities and their carers.
All therapists were required to take part in a 2-day training course on the delivery of the intervention. Refer to Table 7 which depicts the content of the therapist training. The training included a mixture of PowerPoint presentations, whole group discussions and work in small groups. Training was delivered online by the research team and led by a consultant clinical psychologist, and training in the intervention lasted 1.5 days. The remaining half-day was used by participants to complete their training in good clinical practice (GCP).
| Training day | Activity |
|---|---|
| Day 1 | Welcome and introductions |
| Intervention structure | |
| Theoretical background and rationale | |
| Behavioural approaches to intervention of anxiety | |
| Key behavioural concepts and strategies | |
| Logic model | |
| Considerations for working with autistic adults with moderate to severe learning disabilities | |
| Sessions 1–2 (Intervention structure, Rapport building, Principles and behaviour and behaviour change, Anxiety disorders, ABC chart, Preference assessment) | |
| Sessions 3–5 (Psychoeducation on anxiety, autism and learning disability, Key vocabulary training, Relaxation techniques, Person’s key behaviours and strengths, Individualised Intervention Plan) | |
| Day 2 | Sessions 6–10 (Psychoeducation on Fear Ladders and Graded Exposure, Graded Exposure, Relaxation) |
| Sessions 11–12 (Graded Exposure, Intervention Summary) | |
| Troubleshooting | |
| Fidelity checklists |
Therapists received regular supervision as per their existing supervision arrangements; this was at least monthly. Supervisors were given an opportunity to attend the training and received a copy of the intervention manual. The research team remained in regular contact with the therapists to check on progress and offer support and supervision as required.
Summary
Anxiety disorders develop through a process of direct and vicarious learning experiences, and events that occur post-learning moderate the experience of anxiety. Not all autistic people with moderate to severe learning disabilities develop anxiety disorders, but this group presents with vulnerabilities that increase the probability of anxiety becoming problematic. These vulnerabilities include sensory sensitivities, information-processing difficulties, restricted and repetitive behaviours, and difficulties with flexibility, amongst others. Our intervention was developed with reference to this theoretical framework, and within our logic model we outlined the key intervention components and mechanisms that are considered to lead to a reduction in anxiety and increased community engagement.
Our intervention comprised 12 sessions which were delivered by trained therapists and developed in collaboration with our IAG. Carers attended all sessions, while some of the sessions involved only the carer. Our primary intervention strategies involved psychoeducation, relaxation training, and exposure therapy coupled with reinforcement. Our intervention was accompanied by a fidelity checklist which was also developed in collaboration with our IAG.
Chapter 4 Phase 1b: treatment-as-usual survey
Within this phase, data were collected to characterise interventions that were currently being delivered to autistic people with moderate to severe learning disabilities who have problems with anxiety.
Methods
Participants and recruitment
We recruited health and social care professionals working in services providing care to autistic adults aged 16 years and older with moderate to severe learning disabilities. We asked them to describe interventions for anxiety offered by their service to this population.
Participants were recruited via the Research in Developmental Neuropsychiatry (RADiANT; https://radiant.nhs.uk/) consortium of NHS providers. We also sent e-mail invitations directly to NHS Trust research and development (R&D) departments and charitable organisations which provide care to autistic adults with learning disabilities in the UK. This included information about the survey and an online link to the survey. Information about the survey was also available in the public domain on our website and information was further shared with e-mail distribution lists for professionals working with people with learning disabilities (e.g. British Psychological Society, Faculty for Intellectual Disabilities Listserv).
Ethical opinion
Our survey was granted a favourable ethical opinion by Wales Research Ethics Committee (REC) 6 and had associated NHS Health Research Authority Approval (Ref: 21/WA/0013).
Consent
The participants could choose to complete the survey online via Qualtrics (Qualtrics, Provo, UT, USA) or in the form of an interview with a member of the research team (via Microsoft Teams or over the telephone). For participants completing the survey online, the Participant Information Sheet (PIS) and Participant Consent Form were embedded in Qualtrics. Participants who opted for an interview were e-mailed the PIS and Participant Consent Form ahead of time and asked to sign it electronically. Participants provided consent to take part in the survey prior to accessing any survey questions.
Withdrawals
Participants had the right to withdraw their consent at any time. Withdrawals were recorded.
Survey questions
The questions for the survey were based upon the Template for Intervention Description and Replication (TIDieR) checklist. 106 Initially, participants were asked if their service offered any interventions for anxiety to autistic adults with moderate to severe learning disabilities (this could include psychological interventions, medication, or any other intervention). If participants indicated that their service offered interventions for anxiety, they were asked a series of questions about the nature of the intervention. See Appendix 1 for the questions included in the survey. At the end of the survey, participants were asked if their service offered any additional interventions for anxiety, apart from the one already described. If yes, participants were asked to answer the same set of questions but in relation to the additional intervention. This cycle repeated until the respondent indicated that their service offered no further interventions for anxiety.
Analysis
We summarised both the quantitative and qualitative data generated. The number of responses to the closed-end survey questions was counted and reported. Responses from the open-end questions were analysed using content analysis107 as our aim was to describe TAU. Initially, a set of codes was identified by one coder by grouping survey responses that shared the same meaning. If the response contained more than one concept, separate codes were generated for each concept. Codes were grouped into subthemes which represented the professional views on the intervention offered for anxiety to autistic adults with learning disabilities. The subthemes were sorted into themes that were determined by each survey question using the TIDieR checklist as an organisational framework.
Two observers independently coded 10% of the responses. The inter-rater reliability agreement was 93% (84 agreements and 6 disagreements). The final codes were discussed by the raters and consensus was reached.
Results
Sites and participant characteristics
Seventy-eight health and social care professionals working in services providing care to autistic adults aged 16 years and older with moderate to severe learning disabilities responded to the survey. Seventy-five participants chose to complete the survey online. One interview was conducted. Not all participants answered all the questions. For some questions, the total number of responses exceeded the number of participants who took part in this study because they could choose more than one answer.
Sixty-three participants provided information on the country in which their service was located: England (n = 59), Scotland (n = 3) and Wales (n = 1). Table 8 shows participants’ roles.
| Participant’s role | Number of responses |
|---|---|
| Nursing or care professional | 24 |
| Allied health professional | 14 |
| Psychology | 11 |
| Medical doctor | 10 |
| Dental professional | 7 |
| Leadership or management staff | 7 |
| Other | 6 |
| Behaviour specialist | 2 |
Sixty-two professionals provided the name of the service within which they worked. Table 9 shows types of services indicated by the participants.
| Type of the service | Number of responses |
|---|---|
| NHS Trust | 54 |
| Local authority service | 3 |
| Private service | 2 |
| Non-NHS community learning disabilities service | 2 |
| Learning disability charity | 1 |
Forty-one participants categorised their service as community-based, 15 as a combination of community and inpatient, 4 as inpatient and 2 as other types of services.
Objectives
Objective 1: complete a national survey of existing interventions for autistic adults with anxiety disorders who have moderate to severe learning disabilities
Sixty-four (out of 78) participants (82.1%) responded to the question asking if their service offered any intervention for anxiety to autistic adults with moderate to severe learning disabilities.
Fifty-nine participants (92.2%) indicated that their service offered a treatment or intervention for anxiety to this population. Five participants (7.8%) stated that their service did not offer any treatment or intervention for anxiety to autistic adults with learning disabilities.
Out of the 59 participants whose service offered the intervention, 21 stated they offered more than 1 type. Refer to Table 10 for the intervention types described in the survey. Participants were able to add more than one intervention option.
| Type of intervention | Number of responses |
|---|---|
| Psychological | 49 |
| Medication | 32 |
| Other (e.g. speech and language therapy, occupational therapy, music therapy) | 12 |
| Physical health support | 4 |
Psychological interventions
Forty-nine participants indicated that their service offered psychological intervention or intervention for anxiety to autistic adults with moderate to severe learning disabilities.
Table 11 summarises responses to the question on the rationale for using psychological intervention.
| Rational for using the intervention | Number of responses |
|---|---|
| Targets anxiety using proactive and reactive strategies | 39 |
| Person-centred | 16 |
| Improves quality of life | 13 |
| Collaborative working | 9 |
| Evidence-informed | 9 |
| Improves engagement in other important interventions | 7 |
| Develops a clinical formulation | 5 |
| Psychoeducation about anxiety or autism | 4 |
| Predictable and consistent | 3 |
| Complies with national guidance | 3 |
| Improved access to psychological intervention | 2 |
| Practical | 1 |
| Goal-oriented | 1 |
| Ethical | 1 |
| Supports staff well-being | 1 |
Refer to Table 12 for key procedures, activities and/or processes of the psychological intervention. A majority of participants indicated that the key procedure used as part of an intervention to treat anxiety was ‘psychological intervention’, which was non-specific. Only five participants indicated that their service offered exposure therapy as a key procedure or activity.
| Key procedures, activities and/or processes | Number of responses |
|---|---|
| Psychological intervention | 34 |
| Biopsychosocial assessment | 21 |
| Formulation | 15 |
| Liaison with other professionals | 12 |
| Skills training in autism and anxiety | 11 |
| Intervention planning and monitoring | 10 |
| Staff support or supervision | 6 |
| Functional analysis | 6 |
| Engagement with the patient | 5 |
| Graded exposure procedures | 5 |
| Reflective practice | 5 |
| Supporting communication | 4 |
| Observation | 4 |
| Carer engagement | 3 |
| As part of dental intervention procedures | 2 |
| Environmental adaptations | 2 |
| Mental Capacity Act procedures | 1 |
Participants were asked to describe materials used with the intervention. The most often mentioned were data collection materials (n = 40), information materials (n = 36) and an intervention plan (n = 14). Other materials included: psychoeducation materials (n = 9), communication tools (n = 8), anxiety-specific materials (n = 7) and intervention-specific and sensory aids (n = 5). The professionals also mentioned progress measurement materials (n = 2), informed consent materials (n = 2), training materials (n = 1) and exposure materials (n = 1).
The intervention setting was described as face-to-face by 39 participants. They specified that it included the person’s place of residence (n = 17), an NHS setting (n = 14), community (n = 6), day service (n = 5) and school (n = 1). A few participants mentioned that the intervention was delivered online (n = 3) and as a combination of face-to-face, online and over the phone as appropriate (n = 5).
Respondents were also asked to indicate who provided the treatment or intervention. Refer to Table 13 for details. The most frequently named professional group was psychologists, followed by nurses and occupational therapists.
| Person providing the intervention | Number. of responses |
|---|---|
| Psychologist | 36 |
| Nurse | 29 |
| Occupational therapist | 18 |
| Parent or support care-mediated intervention or intervention | 17 |
| Psychiatrist | 16 |
| Speech and language therapist | 15 |
| Healthcare assistant | 15 |
| Other | 14 |
| Social worker | 2 |
| Medical doctor who is not a psychiatrist | 1 |
Respondents mentioned other professional groups that were present at the sessions as shown in Table 14. The most frequent was nursing, followed by psychology, and allied health professionals.
| Professionals present at the sessions | Number of responses |
|---|---|
| Nursing or care professional | 46 |
| Psychology professional | 30 |
| Allied health professional | 27 |
| Medical doctor | 10 |
| Social care professional | 8 |
| Not specified health professional | 7 |
| Other professional | 5 |
| Teaching professional | 4 |
| Family or support care-mediated intervention or intervention | 4 |
| Dental professional | 3 |
| Health professions student | 3 |
We also asked who else might be present during the intervention. The most frequently named was family/carers (n = 49), person with learning disability (n = 20), advocate (n = 3), community (n = 3), friend (n = 1) and group session attendees (n = 1).
Respondents indicated the number, frequency and duration of the intervention sessions or contact. The frequency of sessions was reported as: 1–6 sessions (n = 22), 6 to 12 sessions (n = 11) more than 24 sessions (n = 11), and 12–24 sessions (n = 4). Sessions were reported as being delivered once a week (n = 16), variable (n = 9), once a fortnight (n = 8), once a month (n = 7), and more than once a week (n = 7). One participant mentioned that the intervention was one-off, and one did not provide details on the exact number. The sessions lasted 30 minutes to an hour (n = 26), more than 1 hour (n = 13) and 15–30 minutes (n = 6). Two professionals stated that the intervention sessions were ˂ 15 minutes long and one said they were about an hour.
Forty-two respondents indicated that their service monitored whether the intervention was implemented as planned and six indicated that this did not occur. Refer to Table 15 for more details about the methods used by services to monitor intervention implementation.
| Ways of monitoring the intervention implementation | Number of responses |
|---|---|
| Progress review | 13 |
| Outcome measures | 11 |
| Stakeholder feedback | 9 |
| Keeping records | 8 |
| Developing care plans | 8 |
| Supervision | 6 |
| Writing reports | 5 |
| Follow-up appointments | 2 |
| Reflective practice | 1 |
| Team discussion | 1 |
| Audit | 1 |
Forty-four participants indicated that they adapted the intervention depending upon patient needs. For information about situations leading to adaptations refer to Table 16. Four respondents stated that they did not adapt this intervention. The most frequent reason given for why the intervention was adapted was ‘communication needs’ following by the ‘degree of learning disability’.
| Situations leading to adapting the intervention | Number of responses |
|---|---|
| Communication needs | 20 |
| Degree of learning disability | 17 |
| Person’s needs | 13 |
| Systemic or environmental challenges | 10 |
| Autistic traits | 9 |
| Nature and degree of anxiety | 7 |
| Physical, health or mobility needs | 5 |
| Responsiveness to the intervention | 4 |
| Level of engagement | 3 |
| Behavioural needs | 3 |
| Person’s interests or preferences | 1 |
| Feedback from the person or carer | 1 |
| Carer or family understanding | 1 |
We asked participants to provide additional detail on the adaptations made to the interventions. Refer to Table 17 for more details on the adaptations. The most frequent was ‘communication support’ followed by ‘adjusting the session content or activities’ and ‘adjusting timing, duration, number, or frequency of sessions’.
| Intervention adaptations | Number of responses |
|---|---|
| Communication support | 37 |
| Adjusting session content or activities | 20 |
| Adjusting timing, duration, number or frequency of sessions | 14 |
| Involving carers in intervention and liaison with support networks | 14 |
| Environmental adaptations | 10 |
| Changing the setting | 8 |
| Liaison with other professionals | 8 |
| Consideration for person’s interests and preferences | 8 |
| Formulation-driven intervention plan | 5 |
| Psychoeducation | 5 |
| Assessment of needs | 3 |
| Increased practical support | 2 |
| MCA considerations | 1 |
Medication
Thirty-two participants stated that medication was an intervention offered for anxiety to autistic adults with moderate to severe learning disabilities.
Participants referred to the following aspects when describing the rationale for using this intervention type: targets anxiety using proactive and reactive strategies (n = 16), evidence-informed (n = 8), improves quality of life (QoL; n = 8), complies with national guidance (n = 4), improves engagement in other important interventions (n = 3), person-centred (n = 3), improves physical health (n = 3), supports staff well-being (n = 3) and reduces risk and risky behaviours (n = 1).
Key procedures, activities and/or processes of the intervention using medication involved intervention planning and monitoring (n = 18), psychological intervention (n = 18), biopsychosocial assessment (n = 16), formulation (n = 10), and liaison with other professionals (n = 6). Furthermore, three responses described Mental Capacity Act procedures, two mentioned the importance of engagement with the patient, two indicated that this was important as part of dental intervention procedures, one mentioned the importance of supporting communication, one mentioned skills training in autism and anxiety, and one mentioned the importance of observation.
The following intervention materials were used with medication: information materials (n = 45), data-collection materials (n = 20), communication tools (n = 4), intervention-specific and sensory aids (n = 2), psychoeducation materials (n = 1) and informed consent materials (n = 1).
Refer to Table 18 for information on who were involved with this intervention.
| Person providing the intervention | Number of responses |
|---|---|
| Psychiatrist | 30 |
| Nurse | 17 |
| Psychologist | 8 |
| Medical doctor who is not a psychiatrist | 7 |
| Healthcare assistant | 6 |
| Occupational therapist | 5 |
| Speech and language therapist | 5 |
| Parent or support care-mediated intervention or intervention | 5 |
| Other | 5 |
| Social worker | 1 |
The following professionals were said to be present when medication was prescribed: medical doctor (n = 24), nursing or care professional (n = 21), allied health professional (n = 11), psychology professional (n = 7), unspecified MDT or health professional (n = 4), dental professional (n = 3), health professions student (n = 3), social care professional (n = 1) and other professional (n = 1). Other people present were: family/carer (n = 37), person with learning disabilities (n = 10) and advocate (n = 4).
Twenty-five participants indicated that the intervention was provided face to face. Sixteen professionals specified that it took place in an NHS setting, eight stated it was in the community, six indicated the person’s home and five stated within a day service. Some services delivered the intervention online (n = 6), over the phone (n = 3) and using a combination of face to face, online and over the phone as appropriate (n = 4).
The number of intervention sessions or contacts offered for medication was: 1–6 (n = 18), 6–12 (n = 10) and more than 24 (n = 2). One participant mentioned the intervention involved 12–24 sessions or contacts.
These sessions or contacts took place once a fortnight (n = 8), once a month (n = 7), once a week (n = 4), and more than once a week (n = 3). Eleven participants indicated other frequencies of intervention sessions or contacts. They lasted 30 minutes to an hour (n = 22), 15–30 minutes (n = 6) and ˂ 15 minutes (n = 4).
Twenty-five participants stated that their service monitored if the intervention was implemented as planned. Refer to Table 19 for details on monitoring the intervention implementation. Seven professionals responded that there was no intervention implementation monitoring carried out within their service.
| Ways of monitoring the intervention implementation | Number of responses |
|---|---|
| Progress review | 9 |
| Stakeholder’s feedback | 6 |
| Developing care plans | 5 |
| Keeping records | 4 |
| Outcome measures | 4 |
| Writing reports | 4 |
| Medication or physical health monitoring | 2 |
| Audit | 1 |
| Follow-up appointments | 1 |
| Team discussion | 1 |
Thirty-two participants indicated that the intervention was adapted depending upon patient needs. Table 20 presents the situations which led to adapting the intervention. The most frequently cited reason for adapting the intervention was ‘communication needs’ followed by the ‘nature and degree of anxiety’ and ‘degree of learning disability’.
| Situations leading to adapting the intervention | Number of responses |
|---|---|
| Communication needs | 11 |
| Nature and degree of anxiety | 10 |
| Degree of learning disability | 9 |
| Responsiveness to the intervention | 6 |
| Person’s needs | 5 |
| Physical, health or mobility needs | 4 |
| Autistic traits | 3 |
| Behavioural needs | 3 |
| Systemic or environmental challenges | 2 |
| Person’s interests or preferences | 1 |
| Feedback from the person or carer | 1 |
Refer to Table 21 for details of implemented adaptations. The most frequently used adaptation was ‘communication support’ followed by ‘involving carers in intervention and liaison’ and ‘adjusting medication procedures’.
| Intervention adaptations | Number of responses |
|---|---|
| Communication support | 15 |
| Involving carers in intervention and liaison with support networks | 11 |
| Adjusting medication procedures | 8 |
| Adjusting timing, duration, number or frequency of sessions | 8 |
| Changing the setting | 4 |
| Liaison with other professionals | 4 |
| Environmental adaptations | 3 |
| Assessment of needs | 2 |
| Consideration for person’s interests and preferences | 1 |
| Adjusting session content or activities | 1 |
| Psychoeducation | 1 |
| MCA considerations | 1 |
Other interventions
We received 12 responses that mentioned other types of intervention for anxiety offered to autistic adults with moderate to severe learning disabilities. These included: speech and language therapy (n = 3), occupational therapy (n = 3), sensory strategies (n = 2), communication training (n = 1), increased support staff (n = 1) touch therapy (n = 1), and music therapy (n = 1). The rationale for using these interventions is presented in Table 22.
| Rationale for using the intervention | Number of responses |
|---|---|
| Person-centred | 5 |
| Targets anxiety using proactive and reactive strategies | 5 |
| Develops a clinical formulation | 4 |
| Improved access to psychological intervention | 4 |
| Improves quality of life | 3 |
| Collaborative working | 2 |
| Psychoeducation about anxiety or autism | 2 |
| Evidence-informed | 1 |
| Predictable and consistent | 1 |
| Improves engagement in other important interventions | 1 |
Key procedures, activities and/or processes involved: biopsychosocial assessment (n = 11), supporting communication (n = 5), liaison with other professionals (n = 4), environmental adaptations (n = 2), intervention planning and monitoring (n = 2), observation (n = 2), engagement with the patient (n = 2), psychological intervention (n = 2), formulation (n = 1), carer engagement (n = 1), Mental Capacity Act procedures (n = 1) and report writing (n = 1).
Materials used with the interventions were: communication tools (n = 18), data-collection materials (n = 6), intervention-specific and sensory aids (n = 5), information materials (n = 4), intervention plan (n = 1) and psychoeducation materials (n = 1).
The interventions were provided by an occupational therapist (n = 6), speech and language therapist (n = 5), nurse (n = 4) and other person (n = 4; e.g. music therapist). Two participants mentioned a psychologist as the person providing the intervention, one stated it was a psychiatrist, and one indicated that it was a healthcare assistant. One respondent mentioned that the intervention was mediated by a parent or support care.
The following professionals were present at the sessions: allied health professional (n = 11), nursing or care professional (n = 4), medical doctor (n = 2), health professions student (n = 2), psychology professional (n = 1), and other professional (n = 1). Family/carers (n = 15) and the person with learning disabilities (n = 4) were also present during the sessions.
The intervention was delivered face to face by 10 services, this included at the person’s place of residence (n = 5), day service (n = 3), NHS setting (n = 2) and community (n = 1). Using a combination of face-to-face, online and over the phone contact was mentioned by two participants.
The intervention included 1–6 sessions or contacts (n = 4), 6–12 (n = 3), 12– 24 (n = 3) and more than 24 sessions or contacts (n = 2). Intervention sessions were scheduled once a week (n = 4), once a fortnight (n = 3), once a month (n = 2), with variable frequency (n = 2), and more than once a week (n = 1). Seven participants indicated that the sessions lasted 30 minutes to an hour, four participants indicated 15–30 minutes, and one participant stated they lasted for more than 1 hour.
There were eight professionals whose service monitored if the intervention was implemented as planned. This was done by keeping records (n = 5), using outcome measures (n = 4), progress review (n = 2), stakeholder’s feedback (n = 1) and follow-up appointments (n = 1). Three participants stated that their service did not monitor the intervention implementation.
Twelve participants indicated that the intervention involved adaptations made depending on patient need. Refer to Table 23 for the situations leading to adapting the intervention. The most frequently cited situations leading to intervention adaptation were ‘degree of learning disability’ and ‘communication needs’. Table 24 detailed information about the nature of the adaptations made to interventions. The most frequent was ‘involving carers’, followed by ‘communication support’.
| Situations leading to adapting the intervention | Number of responses |
|---|---|
| Degree of learning disability | 8 |
| Communication needs | 5 |
| Responsiveness to the intervention | 4 |
| Person’s needs | 4 |
| Autistic traits | 3 |
| Nature and degree of anxiety | 3 |
| Systemic or environmental challenges | 1 |
| Intervention adaptations | Number of responses |
|---|---|
| Involving carers in intervention and liaison with support networks | 11 |
| Communication support | 9 |
| Adjusting timing, duration, number, or frequency of sessions | 6 |
| Environmental adaptations | 4 |
| Changing the setting | 2 |
| Adjusting session content or activities | 1 |
| Assessment of needs | 1 |
| Formulation-driven intervention plan | 1 |
Physical health support
Four participants indicated that their service offered physical health support as an intervention for anxiety amongst autistic adults with moderate to severe learning disabilities.
The rationale for using this intervention was described as: improves engagement in other important interventions (n = 4), reduces inequalities in health care (n = 2), complies with national guidance (n = 1), improves physical health (n = 1) and targets anxiety using proactive and reactive strategies (n = 1).
The responses on key procedures, activities and/or processes used with this intervention are presented in Table 25. The most frequent was ‘dental intervention procedures’ associated with dental anxiety.
| Key procedures, activities and/or processes | Number of responses |
|---|---|
| Dental intervention procedures | 5 |
| Psychological intervention | 4 |
| Engagement with the patient | 3 |
| Biopsychosocial assessment | 2 |
| Liaison with other professionals | 2 |
| Formulation | 2 |
| Supporting communication | 2 |
| MCA procedures | 1 |
| Intervention planning and monitoring | 1 |
| Carer engagement | 1 |
Materials used with this intervention were: information materials (n = 4), data-collection materials (n = 2), informed consent materials (n = 2), communication tools (n = 2), psychoeducation materials (n = 2), intervention-specific and sensory aids (n = 1) health information (n = 1), and intervention plan (n = 1).
The intervention was provided by a nurse (n = 3), medical doctor who is not a psychiatrist (n = 2) and other (n = 6; e.g. dentist). During the sessions, dental professionals (n = 7) and nursing or care professionals (n = 5) were present. The sessions were also attended by family/carer (n = 5) and the person with learning disabilities (n = 1).
Four participants stated that the intervention was provided face to face, with two specifying that it was in an NHS setting. Additionally, one service delivered the intervention online and one over the phone.
Three respondents indicated that the intervention consisted of one to six sessions or contacts. One stated that it involved 12–24 sessions or contacts. The frequency was variable, as indicated by three professionals. One response mentioned that the sessions were provided once a fortnight. Duration of the session was ˂ 15 minutes (n = 1), 15–30 minutes (n = 1), 30 minutes to an hour (n = 1), more than 1 hour (n = 1).
Three professionals indicated that their service monitored the intervention implementation. This was achieved by audits (n = 2) and writing reports (n = 1). One participant responded that the intervention implementation was not monitored.
All four participants stated that the intervention involved adaptations depending upon patient need. The situations that led to adaptations included nature and degree of anxiety (n = 2), communication needs (n = 1), physical, health or mobility needs (n = 1), the person’s interests or preferences (n = 1) and feedback from the person or carer (n = 1). The nature of the intervention adaptations is presented in Table 26. The most frequent was ‘communication support’.
| Intervention adaptations | Number of responses |
|---|---|
| Communication support | 5 |
| Adjusting timing, duration, number or frequency of sessions | 4 |
| Environmental adaptations | 3 |
| Reducing waiting time | 2 |
| Changing the setting | 2 |
| Assessment of needs | 2 |
| Involving carers in intervention and liaison with support networks | 1 |
| Liaison with other professionals | 1 |
See Appendix 2 for detailed responses received in the TAU survey.
Summary
We completed a survey of TAU for anxiety amongst autistic adults with moderate to severe learning disabilities and received 76 responses with the majority coming from the NHS in England. We have made an assumption that the responses provided are representative of the broader NHS, which is a potential weakness. Psychological interventions were used most often, followed by medication, and other interventions, including physical health support. Our findings indicated that while psychological interventions were the most frequently offered intervention for anxiety, graded exposure was infrequently offered. Participants indicated that they adapted interventions most frequently because of communication needs, the degree of learning disability, and the nature and degree of anxiety. Adaptations most frequently involved supporting communication, adjusting the content, timing, duration, number or frequency of sessions, and involving carers or adjusting medication procedures.
Chapter 5 Phase 2: feasibility study
Within Phase 2, we completed a feasibility study to model our intervention and generate sufficient data about parameters to inform the decision to proceed to a larger study. Our focus was upon determining the acceptability and feasibility of the intervention and research procedures for participants, carers, and clinicians. The objectives were: (1) to model the manualised intervention to determine the acceptability and feasibility for all stakeholders, including patients, carers, and clinicians, and adjust as required, (2) to judge the appropriateness, including response rates, of our measures of anxiety-related symptomatology for use within a larger study, (3) to examine the feasibility and acceptability of consent and associated processes and (4) to describe factors that facilitate or challenge the implementation of our intervention.
Methods
Design
This phase of the study was a single-arm non-randomised feasibility study of behavioural intervention plus TAU for the intervention of anxiety disorders amongst autistic people with moderate to severe learning disabilities. We used qualitative and quantitative research methods to help address key components of feasibility. Recruitment was open to participants with autism and moderate to severe learning disabilities who have anxiety disorders and their carers within five NHS Trusts within England. There were no changes to the methods following commencement of the feasibility study.
All participants were assessed at three time points using our candidate measures selected during Phase 1a: (1) eligibility screening, (2) baseline assessment within 4 weeks before commencement of the intervention and (3) follow-up assessment within 4 weeks after completing of the intervention. Additional components of feasibility (e.g. acceptability) were assessed using semistructured interviews and an associated qualitative analysis.
Site selection
This feasibility study took place within adult community learning disability services in the NHS in England. Our sites were: (1) Coventry and Warwickshire Partnership NHS Trust, (2) Herefordshire and Worcestershire Health and Care NHS Trust, (3) Mersey Care NHS Foundation Trust, (4) Solent NHS Trust and (5) Leicestershire Partnership NHS Trust.
Participant recruitment
We used a multi-point recruitment strategy, which primarily involved screening existing caseloads of NHS community learning disabilities teams for potentially eligible patients and sharing information about the study with those who were thought likely eligible. We also placed information about the study within the public domain, and directly contacted special schools and residential services for people with learning disabilities within the areas served by our NHS sites.
Sample size
As this was a feasibility study, and the purpose was to provide estimates of key parameters for a future larger study rather than to power the current study to detect statistically significant differences, a formal a priori power calculation was not conducted108 and the sample size was deemed sufficient. We aimed to recruit 30 autistic adults with moderate to severe learning disabilities as this sample size will provide reasonable precision around our estimates of parameters; for example, if 80% of participants complete the intervention, a sample size of 30 participants will allow us to calculate a 95% confidence interval (CI) around this estimate to within ± 14.5% (i.e. 65.5 to 94.5%). These data can be used to inform the design of any future larger study, provide adequate information about our candidate outcome measures, and allow us to try the intervention with important sub groups (i.e. moderate vs. severe learning disabilities) capturing the diversity of this population, much of which will be investigated using qualitative methods.
We also recruited carers to take part in the study as they were asked to attend each of the intervention sessions and take part in post-intervention interviews about their experiences of taking part in both the intervention and the research. For some autistic adults with moderate to severe learning disabilities, we recruited more than one carer. Similarly, we also recruited trained therapists who delivered the intervention and invited them to take part in our post-intervention semistructured interviews about their experience of delivering the intervention and taking part in the research.
Eligibility criteria
Participants were eligible to take part in the study if they met all the following inclusion criteria and none of the exclusion criteria applied:
Inclusion criteria:
-
aged over 16 years old
-
diagnosis of autism confirmed by case note review
-
existing diagnosis of moderate to severe learning disabilities, confirmed at screening
-
existing diagnosis of an anxiety disorder confirmed or initially made at screening
-
carer or family member able to support participation in the intervention and
-
for those who do not have capacity, successful identification of a personal or nominated consultee who provided advice indicating that the person should take part in the project and would likely wish to take part in the study if they had capacity in accordance with the Mental Capacity Act, 2005.
Exclusion criteria:
-
currently receiving another psychological therapy for a mental health problem.
Screening
Screening of potentially eligible participants was conducted by clinicians with routine access to personally identifiable information (e.g. staff working within NHS community teams for autistic people with learning disabilities). This initial screening took place within the NHS and involved a search of patient records or a discussion with clinician teams. The information required for this initial search of potentially eligible participants was diagnosis, which was taken from clinical records, and specifically a diagnosis of autism and moderate to severe learning disabilities and information to suggest problems with anxiety. Clinicians also checked whether potential participants were currently receiving psychological therapy.
Information about the study was then shared with potential participants and their carers by sites. Interested participants and their carers contacted the study team through two routes:
-
Participant and their carer told clinicians that they wanted their contact details passed to the study team; the study team received the details from the clinician and then contacted the participant and/or carer; and
-
Participant and their carer contacted the study team directly using the contact information they were provided within our PIS.
Participants who were identified via special schools, residential placements, or those who wanted to self-refer, contacted the study team directly using contact information within the public domain.
All potential participants were contacted by a member of the research team to arrange a short screening/recruitment interview, either by telephone or online. All interviews were carried out by research staff. During the interview, the study was explained in detail, including the consent process and eligibility criteria.
Ethical opinion
This study was granted a favourable ethical opinion by Wales REC 6 and associated NHS Health Research Authority Approval (Ref: 21/WA/0013). Our Participant Information Sheet and Consent Form for people with learning disability can be found within Report Supplementary Material 1: Participant information sheet and consent form.
Consent
Participants in the feasibility study were autistic adults with moderate to severe learning disabilities and their carers. While the assumption was made that all participants would have capacity to make a decision as to whether they wish to take part in this study, it was anticipated that many participants would not have capacity to make a decision about whether they wished to take part in our research and the provisions within the Mental Capacity Act, 2005, were used.
If a participant was interested in the study, the person explaining the study and seeking informed consent was responsible for determining whether the potential participant had capacity to make a decision. To help participants with learning disabilities make the decision about their involvement in the study, we developed an adapted PIS. Additional aids to support communication and understanding were used as needed to meet the needs of individual participants in consultation with carers. If a participant was deemed to have capacity to consent and wanted to take part in the study, they were asked to sign the consent form. If a participant was judged to lack capacity to make a decision about participation, steps were taken to seek advice from either a personal or nominated consultee:
-
A personal consultee is known to the person and trusted with decisions about their welfare. A personal consultee is not paid to provide care. This could be a friend or family member, as well as an attorney or deputy appointed by the Court of Protection.
-
A nominated consultee is someone who may or may not be known to the person. It may be someone who provides paid carer or professional service (e.g. medical doctor). A nominated consultee cannot be involved in the study or employed by the sponsor.
We made use of Consultee Information Sheets that were approved by an NHS REC which provided information about the study and an explanation of their role. The process that we followed during this study is depicted in Figure 3. We asked consultees for advice about whether a person should be included in this research project, and their opinion about the views and feelings the person would have about participating in this research if they had capacity to make a decision. Throughout the duration of the intervention, therapists were responsible for continuously assessing whether a person who lacked capacity was communicating that they did not wish to take part in the study or the intervention procedures. The right of the participant or consultee to refuse to participate in the study without giving reasons was respected.
FIGURE 2.
Logic model – behavioural interventions to treat anxiety in adults with autism and moderate to severe learning disabilities.
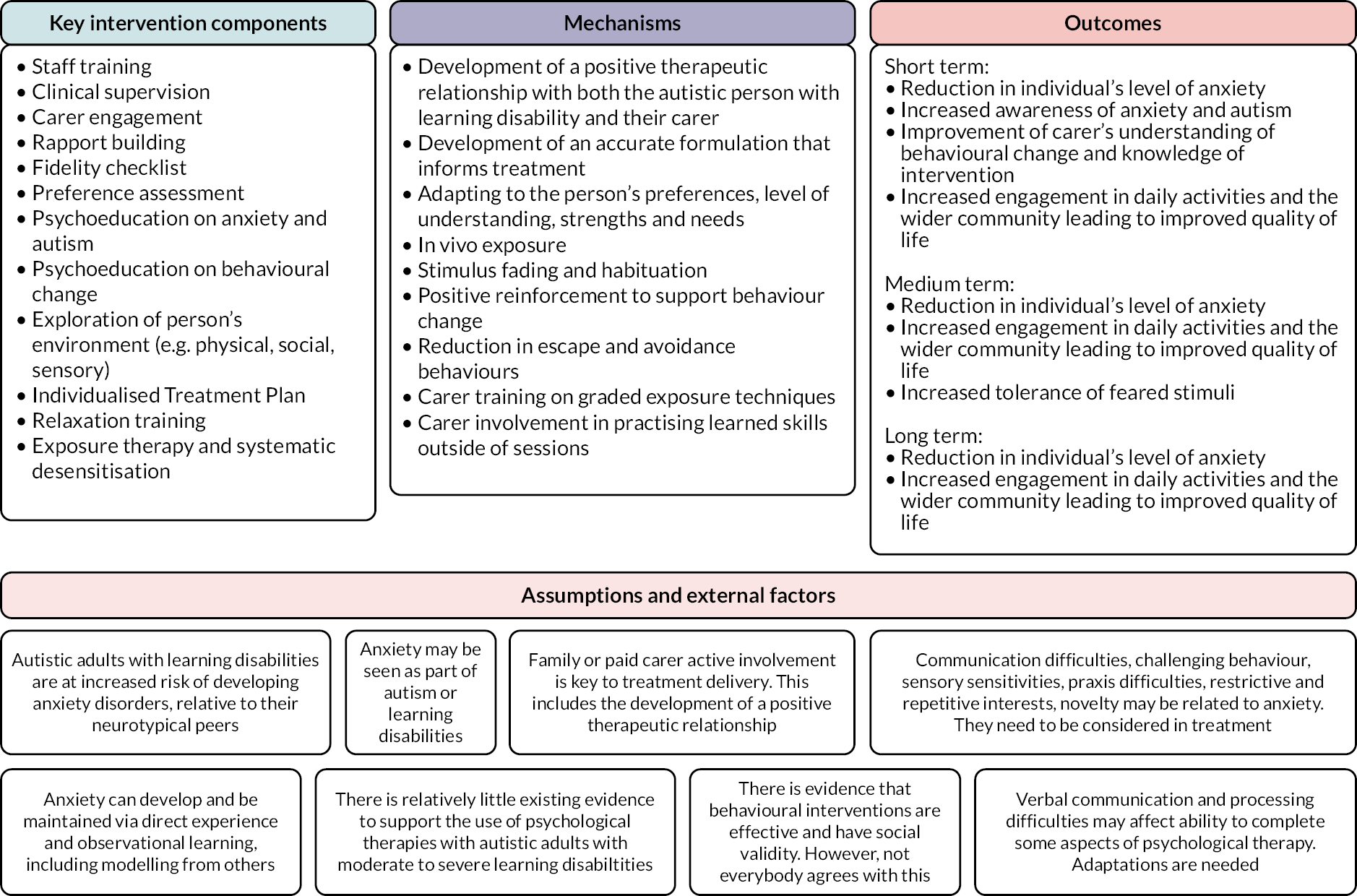
FIGURE 3.
Flow chart depicting decision process when a participant was thought to not have capacity to consent.
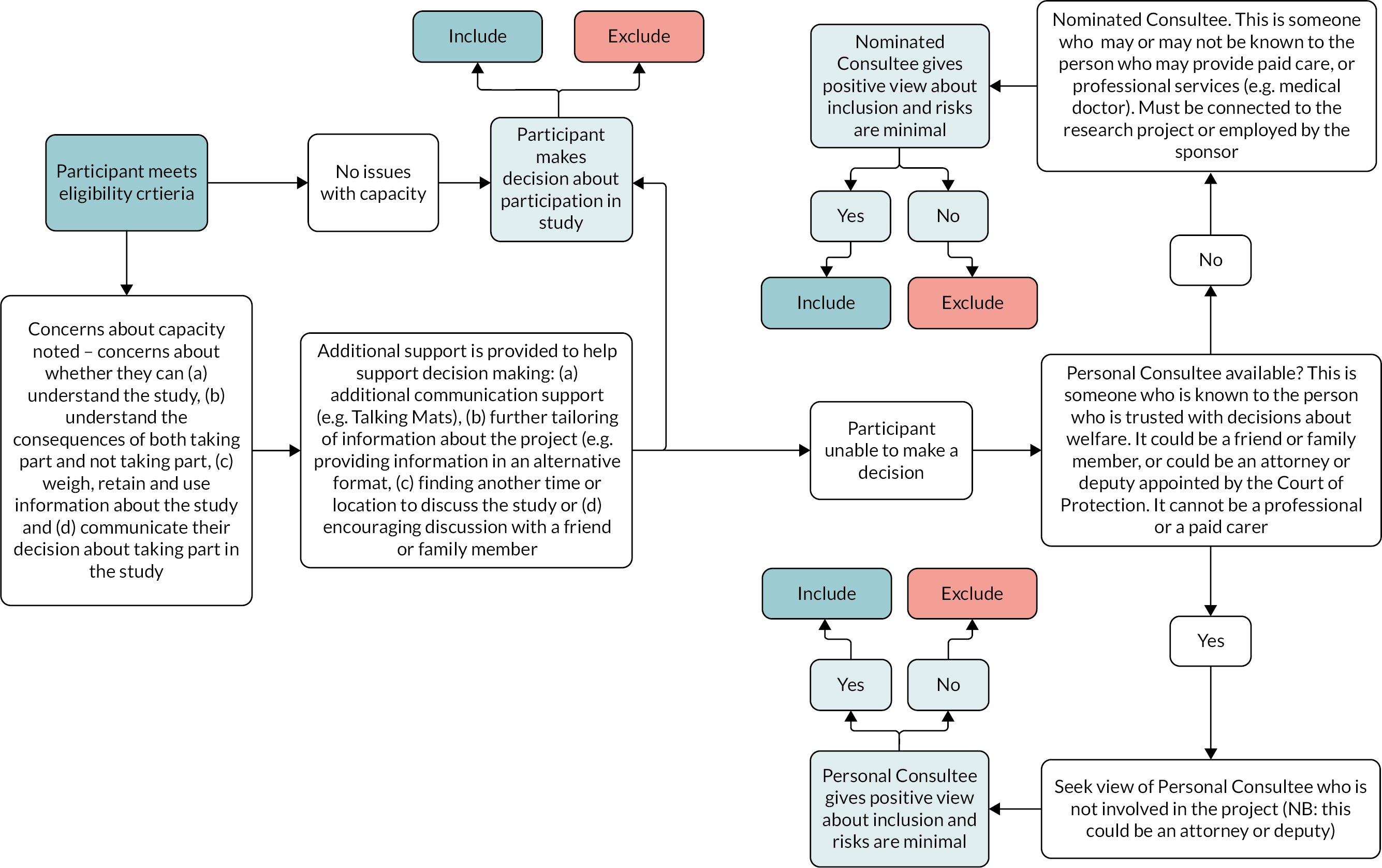
Carers of participants who decided to take part in the study were approached about their involvement. If interested, they were given a Carer Information Sheet and an associated consent form which they were asked to sign. Carers who lacked capacity to make a decision about whether they wished to take part in the study were not eligible to take part in this study.
Therapists who delivered the intervention were offered an opportunity to take part in a post-intervention interview and therefore became research participants. If they agreed to take part, the interview and consent process were explained in detail and a hard copy of the Therapist Information Sheet and consent form was posted to them for signature and return to the research team.
Eligibility screening
After written consent was received from a participant (or advice from the consultee that indicated that the person should be included in our research) and their carer, a member of the research team carried out eligibility screening over the phone or in person with carers. This included the completion of the domain-level version of the Vineland Adaptive Behaviour Scales 3109 to provide an estimate of the degree of learning disability to confirm they had moderate to severe learning disabilities (a standard score below 55). Carers also took part in a semistructured interview using a diagnostic checklist based on Diagnostic Manual – Intellectual Disability-2 (52) to confirm a diagnosis of an anxiety disorder. All participants had to have a diagnosis of autism prior to enrolment, but carers were asked to complete the Social Responsiveness Scale 2, Second Edition (SRS-2)89 to measure social difficulties associated with autism. Participants who met the eligibility criteria completed a baseline assessment with a member of the research team. The research team took responsibility for definitive screening to determine eligibility.
Lost to follow-up
Participants were recorded as lost to follow-up if the following criteria were met:
-
they did not respond to three attempts to schedule an appointment for either assessment or intervention, where at least one of these attempts was sending a letter to their home asking them to contact the research team or
-
they have not attended at least three scheduled and consecutive appointments for either assessment or intervention and have not responded to a letter sent to their home asking them to contact the research team following the third scheduled and consecutive appointment.
Withdrawals
Participants had the right to withdraw consent for participation in the study at any time. Participants and consultees were clear that care was not affected at any time by declining to participate or withdrawing from the study.
Participants were able to withdraw from taking part in the intervention while continuing to take part in the research study. Those who wished to withdraw from both the intervention and the research were asked to voluntarily complete a study Withdrawal form. This form could be completed on behalf of the participant by a member of the study team following a conversation with a participant or carer in consultation with the consultee and therapist.
If a participant who lacked capacity communicated in such a way as to suggest that they no longer wished to take part in the study, including the intervention, continuing participation was discontinued and the consultee was contacted for further advice, and withdrawal was discussed. This was also discussed with the carer. The reason for this was to make sure that the participant was likely communicating that they no longer wished to take part in the study rather than a different need (e.g. tooth pain) if there was uncertainty. Where a participant who lack capacity clearly indicated they no longer wished to take part in the study, they were withdrawn.
Participant timeline
The steps in the pathway for the feasibility study were as follows:
-
All participants who provided consent, or participants where a consultee, in accordance with the Mental Capacity Act, 2005, provided advice that the participant can be included, were screened by research staff to ensure eligibility criteria were met.
-
Participants who meet eligibility criteria completed the outcome measures within 4 weeks prior to starting intervention and assigned to receive the behavioural intervention plus TAU over 12 individual sessions (Table 27).
-
Following the completion of the intervention sessions, participants again completed the outcome measures within 4 weeks of completion of the intervention (see Table 27).
-
All of the outcome measures were completed by carers.
-
A subsample of participants (participants with learning disabilities and their carers) and the therapists were invited to take part in semistructured interviews following completion of the intervention to ascertain acceptability and the experience of the intervention and the research to create a description of factors that promote or challenge the implementation of the intervention and study procedures.
| Procedures | Number of visits | |||
|---|---|---|---|---|
| Screening | Baseline | Intervention phase | Follow-up | |
| Informed consent or advice from a consultee | 1 | |||
| Demographics | 1 | |||
| Medical history | 1 | |||
| Eligibility assessment | 1 | |||
| Delivery of intervention | 12 sessions | |||
| Fidelity | 12 (therapist completed) | |||
| Anxiety symptoms | 1 | 1 | ||
| Anxiety diagnostic checklist | 1 | 1 | ||
| Autism symptoms | 1 | 1 | ||
| Emotional and behavioural problems | 1 | 1 | ||
| Behaviours that challenge | 1 | 1 | ||
| Medication | 1 | 1 | ||
| Community involvement | 1 | 1 | ||
| Adverse event assessments (if required) | 1 | 1 | ||
| Semistructured interviews | 1 | |||
Refer to Table 27 for study time points.
Outcome measures
Participants were enrolled in the study for approximately 6 months. Participants were assessed at three times points: (1) screening, (2) baseline assessment within 4 weeks of commencement of the intervention and (3) follow-up assessments within 4 weeks of completion of the intervention. The choice of measures was decided in Phase 1a of the project (see Chapter 2 for more details).
The outcome measures were completed by the carers and were:
-
DBC2-A94
-
the Behaviour Problems Inventory for Individuals with Intellectual Disabilities – Short Form95
-
the Index of Community Involvement96
-
PAC. 97
Information about medication taken by the participant was also collected. No changes to the outcome measures were made during the feasibility study.
For participants who discontinued intervention, and wished to remain enrolled in the study, data were captured as per protocol. This meant that data were captured within the 4-week period following when the intervention would have been completed had the participant continued to take part in the intervention.
Post-intervention semistructured interviews
We conducted semistructured interviews to examine the views of participants, carers, and therapists about the intervention and research to address key feasibility questions. This information was integrated to create a description of factors that promote or challenge the implementation of the intervention with reference to our logic model and our research procedures.
The interview schedule for carers included 25 questions organised into 10 sections:
-
warm-up
-
acceptability of consent process
-
intervention accessibility and acceptability
-
helpful and unhelpful aspects, including barriers to change
-
the value of our adaptations
-
relationship with the therapist within the intervention
-
acceptability of outcome measures
-
acceptability of randomisation within future trial
-
effects of participation
-
closing questions.
The interview took up to an hour. It was conducted either online (via MS Teams), over the telephone or in person by members of the research team. All interviews were recorded and transcribed verbatim. See Appendix 4 for interview schedules for carers.
The interview schedule for therapists included 27 questions organised into the same sections as the carer interview. Interviews took up to an hour and were conducted online (via MS Teams) by members of the research team. All interviews were recorded and transcribed verbatim. See Appendix 5 for interview schedules for therapists.
We also completed interviews with autistic participants with learning disabilities to explore their experience of the intervention and taking part in our research study. We recognised that autistic participants with moderate to severe learning disabilities present with communication differences and some may not be able to take part in an interview that relies heavily on spoken language. We made use of Talking Mats, which is a structured approach to help people with communication difficulties to organise and express their views. Talking Mats have been used previously with this population. 110 The Talking Mats framework was developed at the University of Stirling and the intellectual property rights are owned by the University of Stirling and assigned to Talking Mats Ltd. Talking Mats is a registered trademark. The Symbols are © to Adam Murphy and assigned to Talking Mats Ltd. in perpetuity. All materials are the intellectual property of Talking Mats Ltd. and were copied or reproduced with permission. The term ‘Talking Mats®’ cannot be used commercially by other organisations. Training in Talking Mats must be delivered by an accredited trainer who holds a current licence with Talking Mats Ltd.
Members of the research team who were trained in using the Talking Mats guided the process with participants. The interview included 13 questions, all represented by assigned visuals. Participants were asked to tell us how they felt about various parts of the intervention by putting corresponding visuals in one of the three categories – like, unsure and do not like. For some participants, only two main categories of like and do not like were used to make the process more accessible. Interviews were conducted in the participant’s home or in clinic. See Appendix 6 for interview plan using Talking Mats. After the interview, the interviewer took a photograph of the completed mat and completed the Effectiveness Framework which guides through reflecting on different parts of the Talking Mats interview:
-
engagement
-
participant’s understanding
-
interviewer’s understanding of thinker’s views
-
participant’s communication
-
symmetry of communication
-
time frame and
-
participant satisfaction.
See Appendix 7 for the effectiveness framework form.
Analysis
Main analysis
The study is reported in accordance with the Consolidated Standards of Reporting Trials extension pilot and feasibility studies and recommendations for non-randomised pilot and feasibility studies. 111 A detailed statistical analysis plan was written and agreed by the study statistical advisor and an independent statistician prior to the analysis.
As this was a feasibility study, the analysis was descriptive in nature. Continuous data were reported as means and standard deviations (SD), and we additionally calculated the within-group effect size while recognising that this effect size is biased. Categorical data were reported as frequencies and proportions. Outcomes were estimated with their associated 95% CIs. No formal hypothesis testing took place. We also calculated and reported our accrual and attrition rate and the percentage of missing data across our outcome measures along with the number of sessions attended and session fidelity data.
Qualitative analysis
We used Framework analysis112 to analyse the data generated from our semistructured interviews with carers and therapists. Framework analysis is a pragmatic method which is advantageous within this context because it allows researchers to investigate key issues of interest, rather than analyse data for all emergent themes. We used framework analysis to examine the views of carers and therapists on several key areas, including: (1) the accessibility and acceptability of the intervention, (2) helpful and unhelpful aspects, including barriers to change, (3) the value of our adaptations, (4) relationships with professionals within the intervention, (5) acceptability of outcome measures and (6) acceptability of consent and associated processes, including randomisation in a future trial. We used Excel spreadsheets for data organisation and management.
Progression criteria
This study estimated key parameters for a future trial, which were used (1) to determine whether the funder advertises for a future trial and (2) to assist potential applicants in designing a future trial. The following criteria were used to determine the feasibility of a future trial within the following domains: (1) recruitment, (2) protocol adherence and (3) outcome data leading to three possible recommendations for trial progression. 113
Green
If all of the following criteria are met a recommendation that a pilot or internal pilot-full trial was considered warranted: (1) recruitment: (i) accrual rate is at least three patients per site per month on average and (ii) attrition rate is 30% or lower; (2) protocol adherence: (i) fidelity ratings indicate therapist adherence to the intervention of at least 70%, (ii) at least 70% of carers and clinicians report that the intervention and consent procedures were acceptable, (iii) participants received an average of 70% or more intervention sessions and (3) outcome data: (i) at least 70% of participants and carers complete outcome data at each time point, (ii) at least 75% of items within each outcome measure for each participant are complete and (iii) at least 70% of carers judge our outcome measures to be acceptable.
Amber
If green criteria were not met but the following criteria were met, then the research team examined the reasons for this, and carefully considered what remedial action could be taken to improve the likelihood that a larger trial should take place. For example, difficulties could have been related to a delay in research ethics or governance approvals or a longer than expected time to build relationships with referrers which could be managed effectively within a larger trial: (1) recruitment: (i) accrual rate is less than 3 but greater than 2 patients per site per month on average, or builds up to three per month in the latter months of recruitment and (ii) attrition rate is greater than 30% but less than 50%; (2) protocol adherence: (i) fidelity ratings indicate therapist adherence to the intervention is less than 70% but greater than 60%, (ii) less than 70% but greater than 55% of carers and clinicians report that the intervention and consent procedures were acceptable, (iii) participants received an average of less than 70% but greater than 55% or more intervention sessions; and (3) outcome data: (i) less than 70% but greater than 60% of participants and carers complete outcome data at each time point, (ii) less than 75% but greater than 60% of items within each outcome measure for each participant are complete, and (iii) less than 70% but greater than 65% of carers judge our outcome measures to be acceptable.
Red
If green or amber criteria are not met, and following a thorough review of the reasons for this, including consideration as to whether remedial action could be taken, a recommendation to proceed to a larger trial could not be made: (1) recruitment: (i) accrual rate is less than 2 patients per site per month on average and (ii) attrition rate is greater than 40%; (2) protocol adherence: (i) fidelity ratings indicate therapist adherence to the intervention is less than 50%, (ii) less than 55% of carers and clinicians report that the intervention, and consent procedures were acceptable, (iii) participants received an average of less than 55% or more intervention sessions and (iv) less than 60% of participants received their allocated intervention and (3) outcome data: (i) less than 50% of participants and carers complete outcome measures at each time point, (ii) less than 50% of items within each outcome measure for each participant are complete and (iii) less than 65% of carers judge our outcome measures to be acceptable.
Results
Participants
Autistic adults with moderate to severe learning disabilities
Thirty-four participants were referred for eligibility screening. Prior to eligibility screening, five were excluded due to declining to participate, not having a diagnosis of autism, or not responding to our attempts to contact them. Twenty-nine participants were assessed for eligibility, and one was excluded at this point due to not having a moderate or severe learning disability (Figure 4). This means that 82% of those who were referred for eligibility screening took part in the study. Twenty-two of 28 participants (79%) were judged not to have capacity to make a decision about taking part in this study. For these participants, on average, it took M = 4.21, SD = 1.80 [95% CI (3.09 to 5.33), minimum = 1.50, maximum = 8.00] weeks per participant to confirm consultee advice and enrol the participant.
FIGURE 4.
Participant flow diagram.
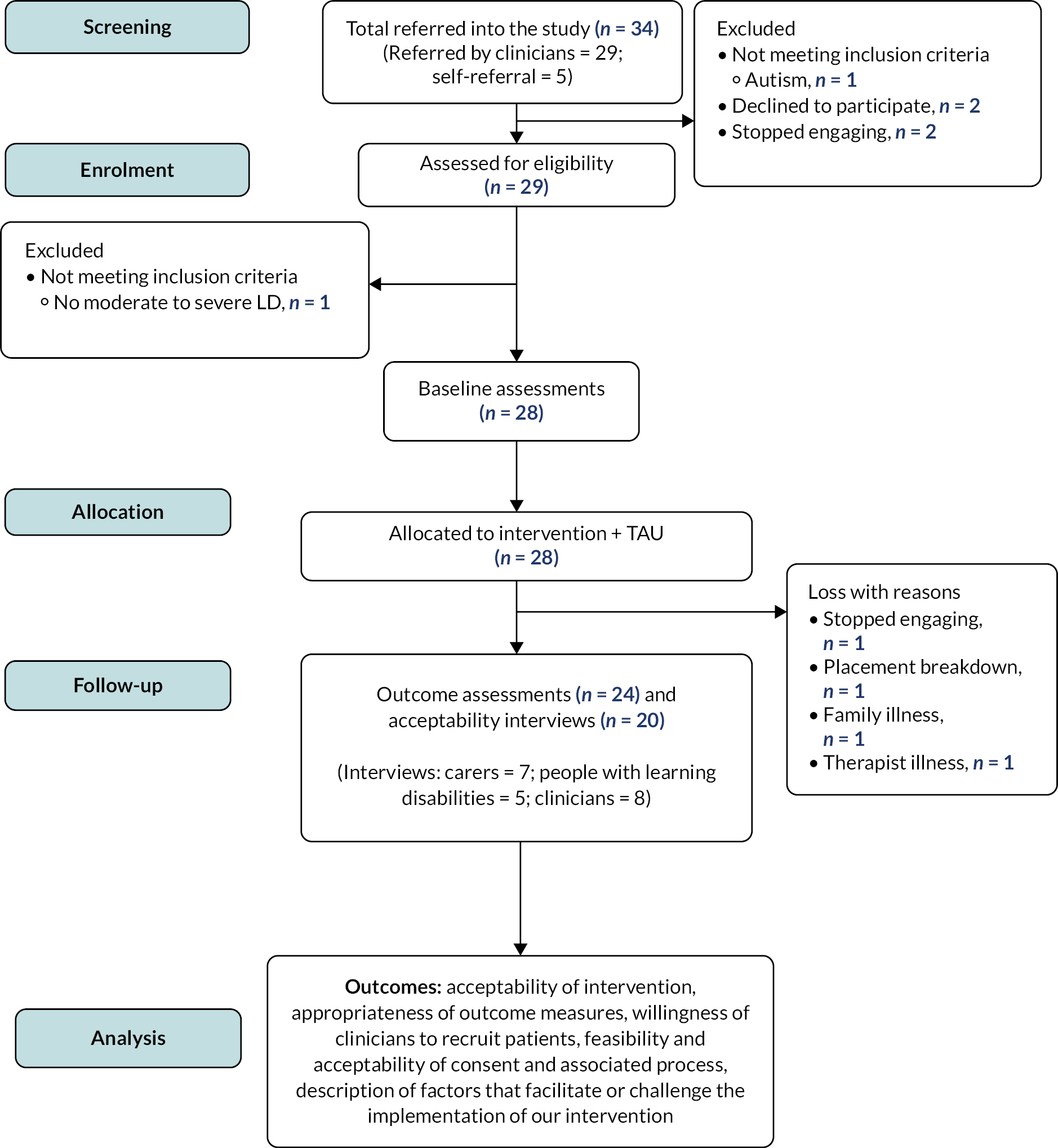
Twenty-eight participants with moderate to severe learning disabilities took part and were allocated to receive the intervention (see Figure 4). Their average age was M = 26.79, SD = 8.39 and 64.3% were male. Just under 79% were White British and 18% were from other backgrounds. Just under 54% had severe learning disabilities and just over 46% had moderate learning disabilities. The majority (71.4%) lived at home with their family (Table 28).
| N | % | |
|---|---|---|
| Ethnicity | ||
| White – British | 22 | 78.6 |
| Mixed – white and Asian | 2 | 7.1 |
| Asian or Asian British – Pakistani | 1 | 3.6 |
| Asian or Asian British – Indian | 1 | 3.6 |
| Black or Black British – African | 1 | 3.6 |
| Prefer not to say | 1 | 3.6 |
| Participant’s primary place of residence | ||
| Family home | 20 | 71.4 |
| Supported living | 5 | 17.9 |
| Residential placement | 2 | 7.1 |
| Degree of learning disability | ||
| Moderate | 13 | 46.4 |
| Severe | 15 | 53.6 |
| Medication | ||
| Antihistamines | 10 | 35.7 |
| Antidepressants | 10 | 35.7 |
| Antipsychotics | 8 | 28.6 |
| Constipation/stomach medication | 7 | 25 |
| Benzodiazepines | 6 | 21.4 |
| Antiepileptic | 5 | 17.9 |
| Vitamins/supplements | 5 | 17.9 |
| Contraceptive pill | 4 | 14.3 |
| Painkillers | 4 | 14.3 |
| Melatonin/sleeping tablet | 4 | 14.3 |
| Proton pump inhibitor | 4 | 14.3 |
| Other (including antidiabetic and thyroid treatments) | 12 | 42.9 |
In additional to a diagnosis of autism and learning disabilities, participants also had diagnoses of attention-deficit-hyperactivity disorder (3.6%), Tourette syndrome (3.6%), Down syndrome (3.6%), microcephaly (3.6%), and other conditions, such as hypothyroidism (3.6%), poor peripheral vision (3.6%) and skin conditions (7.2%). The majority (71.4%) were taking medication with the most frequently prescribed for medical conditions, such as diabetes, thyroid problems and allergies. The most frequently prescribed psychotropic medications were antidepressants, following by antipsychotics (see Table 28).
Four participants were lost at follow-up. There were four different reasons for this loss associated with each individual participant: (1) did not respond to our attempts to make contact, (2) placement breakdown, (3) illness within their family and (4) therapist illness (see Figure 4). This was an attrition rate of 14%.
Accrual
Our initial site opened to recruitment on 2 December 2021, followed by the second site on 17 December 2021. Additional sites were opened on 4 April 2021, 4 August 2022 and 6 September 2022. Recruitment closed on 30 September 2022 as planned and the study was open to recruitment for approximately 10 months.
Difficulties with recruitment were encountered, much of which was attributable to the COVID-19 pandemic. During December 2021, the Omicron variant was spreading within England and the government announced a series of measures to curtail its spread, which included compulsory wearing of facemasks and working from home where possible. This was preceded by two lockdowns and increasing pressure upon the NHS.
We were frequently in contact with our sites, who reported a series of other and pandemic-related challenges:
-
NHS clinicians were reluctant to get involved in research due to caseload pressures.
-
Sites had multiple unfilled staff vacancies.
-
Some trained therapists were lost at site due to redeployment due to the pandemic or an ending of their employment contract.
-
Sites noted that some participants were not eligible because they did not have a diagnosis of autism but met all remaining eligibility criteria. Clinicians expressed concern about this and suggested that all people with moderate to severe learning disabilities should be included, rather than just those with autism.
-
Two sites told us that clinicians were not willing to assist with capacity assessments and help gain participant consent because of increased work pressure.
-
Two sites raised concerns about gatekeeping by clinicians (e.g. withholding information about the study from participants who may be eligible).
-
Many participants needed home visits when delivering the intervention which added to workload and was resisted due to the pandemic.
-
Two sites were affected by the ransomware attack on Advanced, an Information Technology (IT) provider to the NHS responsible for electronic patient record systems. This caused challenges as screening caseloads for eligible participants was no longer possible.
-
Sites also cited challenges with delays because clinicians did not complete their GCP training in good time, and associated delays due to a lack of sufficient staffing within NHS R&D departments.
Keeping the aforementioned challenges in mind, our average monthly accrual rate overall was 2.80, 95% CI (1.86 to 4.05), participants, which is likely to be an underestimate of the likely accrual rate in a future study. The reason for this conclusion is that there were extraordinary circumstances that impacted this study and, specifically, a global pandemic coupled with associated challenges. We noted that during the final 3 months of the study, from July to September 2022, our average accrual rate increased to 6.33, 95% CI (3.81 to 9.89), participants per month.
Coventry and Warwickshire Partnership National Health Service Trust
This site opened on 2 December 2021, and there were challenges with recruitment. The site was open for 10 months, and we recruited eight participants. The first participant was recruited in April 2022. For the initial 7 months, the monthly accrual rate was 0.29 participants per month, and increased during the final 3 months to 2.00 per month.
Herefordshire and Worcestershire Health and Care National Health Service Trust
This site opened on 17 December 2021, and was open for 9 months. Five participants were recruited. During the initial 7 months, the monthly accrual rate was 0.29 participants per month, and increased to 1.5 per month during the last 3 months.
Mersey Care National Health Service Foundation Trust
This site opened in April 2022. Eleven participants were recruited. During the initial 3 months, the accrual rate was 1.33 participants per month, and during the last 3 months, this increased to 2.33 participants per month.
Leicestershire Partnership National Health Service Trust
This site opened on 4 August 2022, and a single participant was recruited. This site had a single trained therapist who was able to provide the intervention and, consequently, this impacted recruitment.
Solent National Health Service Trust
This site opened on 6 September 2023. Three participants were recruited during this month, achieving an accrual rate of three participants in ˂ 1 month.
It was noted that the accrual rate at the majority of sites improved during the summer of 2022. During the final 3 months of the study during this period, we recruited 19 participants, which is an accrual rate of 6.33 participants per month.
Carers
We recruited 37 carers who also took part in the study and supported autistic participants with moderate to severe learning disabilities. Nineteen carers were family members, while 18 were paid carers. We recruited more carers than the number of autistic participants with moderate to severe learning disabilities because we included paid carers, meaning that sometimes different carers were supporting participants when attending intervention sessions. Following the completion of the intervention, seven carers took part in our post-intervention interviews.
Therapists
We recruited and trained 40 therapists to deliver our intervention across our five NHS Trusts. Seven of these therapists (18%) did not complete their GCP training and therefore did not move forward to act as a therapist during this study even though they completed the mandatory intervention training. A further seven (18%) did not work as a therapist during the duration of this study. Therapists who did not deliver the intervention most frequently cited that they were too busy with their existing workload to take part in research or did not respond to further attempts to contact them. One therapist was re-deployed into another role due to NHS staffing difficulties associated with the COVID-19 pandemic and was not able to work as a therapist. Twenty-six therapists delivered the intervention to participants. The majority of therapists were registered psychologists (37%), followed by assistant psychologists (23%), nurses (20%), occupational therapists (7%), psychiatrists (7%), and trainee clinical psychologists (3%) and behaviour specialists (3%). Eight therapists (31%) took part in our post-intervention semistructured interviews (see Figure 4).
Eligibility screening
As part of eligibility screening, carers completed a semistructured interview to confirm that participants met diagnostic criteria for one or more anxiety disorders (Table 29). Participants most frequently fulfilled diagnostic criteria for generalised anxiety disorder (60.7%), followed by specific phobia (57.1%), social anxiety (25%) and agoraphobia (21.4%). Carers also completed a measure of adaptive behaviour, the Vineland Adaptive Behaviour Scale – 3 Domain Level version, and a measure of social difficulties associated with autism, the Social Responsiveness Scale (SRS) (see Table 29). The average Adaptive Behaviour Composite score for participants enrolled in the study was M = 38.21, SD = 11.20, minimum = 20, maximum = 53, which was within the range of moderate to severe learning disabilities. The SRS Total score average was M = 121.76, SD = 20.33, minimum = 76, maximum = 149, which is in the range associated with the presence of autism, with all participants scoring above the cut-off of 75. The percentage of missing items across the subscales of each measure was very low and ranged from 0% to 0.42%.
| Measures | Eligibility | |||
|---|---|---|---|---|
| N | % items missing | M (SD) | 95% CI | |
| Vineland Adaptive Behaviour Scale-3, Standard Scores | ||||
| Communication | 28 | 0.18 | 35.04 (13.81) | (29.68 to 40.39) |
| Daily living skills | 28 | 0.27 | 32.54 (9.91) | (28.69 to 36.38) |
| Socialisation | 28 | 0.8 | 37.86 (11.26) | (33.49 to 42.22) |
| Adaptive behaviour composite | 28 | 0.42 | 38.21 (11.20) | (33.87 to 42.56) |
| SRS-2 | ||||
| Social awareness | 28 | 0 | 14.11 (3.47) | (12.76 to 15.45) |
| Social cognition | 28 | 0.3 | 23.39 (5.39) | (21.30 to 25.48) |
| Social motivation | 28 | 0 | 20.75 (7.15) | (17.98 to 23.52) |
| Social communication | 28 | 0 | 40.04 (8.22) | (36.85 to 43.22) |
| Restricted interests and repetitive behaviour | 28 | 0.3 | 24.46 (6.33) | (22.01 to 26.92) |
| SRS-R Total Score | 28 | 0.11 | 121.76 (20.33) | (113.37 to 130.15) |
| Anxiety diagnostic checklist | % Meeting diagnostic criteria | |||
| Specific phobia | 16 | 0 | 57.1 | |
| Separation anxiety | 2 | 0 | 7.1 | |
| Social anxiety | 7 | 0 | 25.0 | |
| Panic | 1 | 0 | 3.6 | |
| Agoraphobia | 6 | 0 | 21.4 | |
| Generalised anxiety | 17 | 0 | 60.7 | |
Intervention attendance and fidelity
Participants completed M = 9.64, SD = 3.65, minimum = 1, maximum = 12 sessions. On average, participants who started the intervention attended 80% of sessions. Therapists completed a fidelity checklist following the completion of each of the 12 sessions. The percentage of times each item was endorsed by all therapists for each session is found within Appendix 8. These data are summarised in Table 30 for each section of the fidelity checklist. The data indicated that the average number of total items endorsed within each section of the checklist ranged from 88.23 to 99.54.
| M percentage items endorsed (SD) | Median percentage items endorsed | |
|---|---|---|
| General session preparation | 92.41 (6.44) | 94.10 |
| Coverage of the session plan | 91.64 (7.17) | 94.10 |
| Understanding and accessibility | 98.80 (2.39) | 100.00 |
| Interpersonal effectiveness | 99.54 (1.45) | 100.00 |
| Engaging participants | 99.08 (2.58) | 100.00 |
| Session content | 88.23 (10.09) | 90.00 |
| Inter-session tasks | 87.82 (9.16) | 88.20 |
Outcome measures
All outcome data across all our measures are found within Table 31. The missing data rate across our candidate outcome measures was low at baseline, ranging from 0% to 2.38%, and low at follow-up, ranging from 0% to 1.56% of items. At follow-up, scores were lower (compared to baseline) on the DBC-2 Self-Absorbed subscale (d = 0.63, 95% CI 0.19 to 1.07), and the PAC Total score (d = 0.45, 95% CI 0.03 to 0.87) and the PAC Depression (d = 0.65, 95% CI 0.20 to 1.07) subscales. Further, the frequency of aggressive and destructive behaviour (d = 0.65, 95% CI 0.20 to 1.09) and stereotyped behaviour (d = 0.50, 95% CI 0.07 to 0.92) as measured by the BPI-SF was also lower. Considering the design of the current study, it must be clearly stated that changes on our outcome measures over time cannot be said to have been caused by the intervention; however, they are indicative of positive change over time following the completion of the intervention. No adverse or serious adverse events were observed.
| Measures | Baseline | Follow-up | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | % items missing | M (SD) | 95% CI | N | % items missing | M (SD) | 95% CI | d = | d 95% CI | |
| Developmental Behaviour Checklist-2 Adult | ||||||||||
| Total | 28 | 0.13 | 67.68 (22.63) | (58.90 to 76.45) | 24 | 0 | 57.38 (28.68) | (45.26 to 69.48) | 0.40 | –0.02 to 0.81 |
| Disruptive | 28 | 0.14 | 14.32 (8.82) | (10.9 to 17.74) | 24 | 0 | 12.58 (9.61) | (8.53 to 16.64) | 0.20 | –0.21 to 0.60 |
| Communication and Anxiety Disturbance | 28 | 0.36 | 14.71 (7.31) | (11.88 to 17.55) | 24 | 0 | 13.13 (7.23) | (10.7 to 16.18) | 0.29 | –0.12 to 0.70 |
| Self-absorbed | 28 | 0 | 16.14 (7.69) | (13.16 to 19.13) | 24 | 0 | 12.38 (7.12) | (9.37 to 15.38) | 0.63 | 0.19 to 1.1 |
| Depressive | 28 | 0.27 | 6.54 (3.40) | (5.22 to 7.86) | 24 | 0 | 4.96 (4.58) | (3.02 to 6.9) | 0.32 | –0.10 to 0.72 |
| Social relating | 28 | 0 | 9.93 (4.59) | (8.15 to 11.71) | 24 | 0 | 8.58 (4.52) | (6.67 to 10.49) | 0.42 | –0.01 to 0.83 |
| PAC | ||||||||||
| Total | 28 | 0.17 | 79.61 (15.94) | (73.43 to 85.79) | 24 | 0.5 | 73.54 (18.65) | (65.67 to 81.41) | 0.45 | 0.03 to 0.87 |
| General adjustment problems | 28 | 0.3 | 26.07 (6.23) | (23.66 to 28.49) | 24 | 0 | 24.71 (7.69) | (21.46 to 27.95) | 0.33 | –0.08 to 0.74 |
| Psychosis | 28 | 0 | 17.53 (41) | (15.95 to 19.12) | 24 | 0.42 | 15.67 (4.71) | (13.68 to 17.65) | 0.41 | –0.01 to 0.82 |
| OCD | 28 | 0 | 13 (3.81) | (11.52 to 14.48) | 24 | 1.19 | 12.17 (4.63) | (10.21 to 14.12) | 0.20 | –0.21 to 0.60 |
| Depression | 28 | 0 | 13.36 (4.17) | (11.74 to 14.98) | 24 | 0 | 11.67 (4) | (9.98 to 13.35) | 0.65 | 0.20 to 1.07 |
| Anxiety | 28 | 0.6 | 9.64 (2.83) | (8.55 to 10.74) | 24 | 1.39 | 9.33 (2.43) | (8.31 to 10.36) | 0.05 | –0.35 to 0.45 |
| Behaviour Problems Inventory Short Form | ||||||||||
| Self-injurious behaviour | ||||||||||
| Frequency | 28 | 0.45 | 3.68 (3.53) | (2.31 to 5.05) | 24 | 0.52 | 3.08 (2.83) | (1.89 to 4.28) | 0.14 | –0.26 to 0.54 |
| Severity | 28 | 0.45 | 4.43 (4.09) | (2.84 to 6.01) | 24 | 1.56 | 3.58 (3.49) | (2.11 to 5.06) | 0.20 | –0.20 to 0.61 |
| Aggressive-destructive behaviour | ||||||||||
| Frequency | 28 | 2.38 | 4.14 (4.19) | (2.52 to 5.77) | 24 | 0.83 | 2.21 (3.12) | (0.09 to 3.53) | 0.65 | 0.20 to 1.09 |
| Severity | 28 | 2.38 | 5.96 (4.85) | (4.08 to 7.84) | 24 | 0.42 | 4.71 (5.63) | (2.33 to 7.09) | 0.25 | –0.16 to 0.66 |
| Stereotyped behaviour | ||||||||||
| Frequency | 28 | 0.3 | 12.32 (9.74) | (8.54 to 16.1) | 24 | 0 | 8.83 (8.12) | (5.41 to 12.26) | 0.50 | 0.07 to 0.92 |
| Index of Community Involvement | ||||||||||
| Total | 28 | 0.22 | 45.9 (25.36) | (36.06 to 55.73) | 24 | 0.43 | 45.83 (20.93) | (37 to 54.67) | 0.01 | –0.39 to 0.41 |
| Domestic leisure | 28 | 0 | 18.54 (7.75) | (15.53 to 21.54) | 24 | 0 | 19.13 (6.39) | (16.43 to 21.82) | –0.10 | –0.50 to 0.31 |
| Social | 28 | 0.65 | 9.14 (7.15) | (6.37 to 11.92) | 24 | 1.14 | 9.42 (7.34) | (6.32 to 12.52) | –0.08 | –0.48 to 0.32 |
| Community | 28 | 0.12 | 18.21 (15.57) | (12.17 to 24.25) | 24 | 0.29 | 17.29 (12.42) | (12.05 to 22.54) | 0.15 | –0.25 to 0.55 |
Post-intervention interviews
Participants
Five autistic people with learning disabilities took part in a post-intervention interview using Talking Mats about the experience of taking part in this study and receiving the intervention. Ratings of using the effectiveness framework indicated that the participants were engaged and understood the issues being discussed (Table 32).
| Indicators | 4, always | 3, often | 2, 50/50 | 1, occasionally | 0, none |
|---|---|---|---|---|---|
| Engagement | 3 | 2 | |||
| Participant’s understanding issue for discussion | |||||
| Participant understands the activities aspect of the topic | 3 | 2 | |||
| Participant understands that the activities are about doing them BEAMS-ID intervention | 4 | 1 | |||
| Interviewer’s understanding of participant’s views | 4 | 1 | |||
| Participants – on track | 2 | 3 | |||
| Symmetry | 3 | 2 | |||
| Real time | 4 | 1 | |||
| Interviewer’s chill factor | 4 | 1 | |||
The results of the Talking Mats interviews are found within Table 33. It was noted that not all participants recognised the BEAMS-ID logo and one participant responded that they liked this, while another was unsure. The remaining participant did not give a response. Four participants indicated that they liked the participant information booklets that were used during the intervention, with a single participant responding that they were not sure. One person responded that they liked the break during the intervention, while another again responded that they were unsure, with the remaining not giving a response. Four responded that they liked their carer helping, and three responded that they liked coming to the sessions. One person responded that they did not like coming, while another responded that they were unsure. Four participants liked the Fear Ladder, with a single person responding that they were unsure. One person responded that they liked learning about or experiencing anxiety during the intervention, while four responded that they did not like this. Four responded that they liked making choices during the intervention. Three were content to meet new people as part of the intervention, while one responded that they were unsure. Four liked the rating scale used, including two others who liked the adapted rating scale using Mr Men characters. All five responded positively about the use of relaxation, and one responded that they liked talking about things that made them anxious, while the remainder did not. Finally, all five responded that they liked the use of the visual schedule as part of the intervention.
| Component | Liked (N) | Disliked (N) | Not sure (N) |
|---|---|---|---|
BEAMS-ID |
1 | 1 | |
Booklet |
4 | 1 | |
Break |
1 | 1 | |
Carer helping |
4 | ||
Coming to session |
3 | 1 | 1 |
Fear Ladder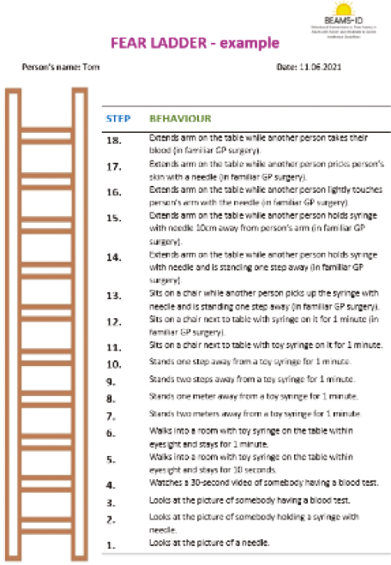 |
4 | 1 | |
Experiencing anxiety |
1 | 4 | |
Making choices |
4 | 1 | |
Meeting new people |
3 | 2 | |
Rating scale |
4 | ||
RC rating scale |
2 | ||
Relaxation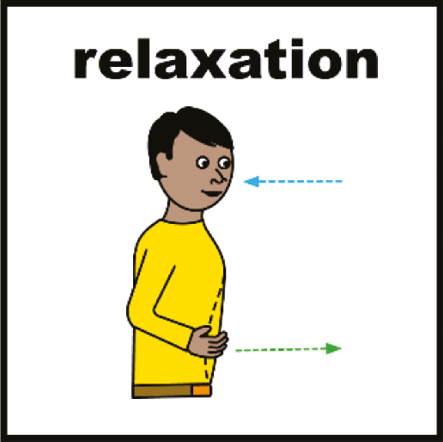 |
5 | ||
Talking about things that make me anxious |
1 | ||
Visual schedule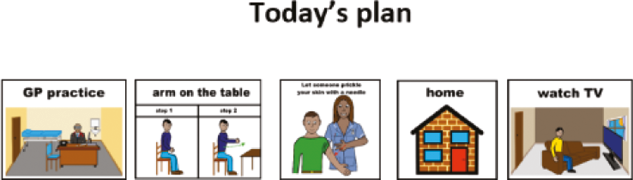 |
5 |
Carers
Eight carers took part in our interviews about participating in the research and the intervention. A summary of the results, including supportive quotes, is found with Tables 34–38.
| Theme | Subtheme | Example comment | Number of carers |
|---|---|---|---|
|
Straightforward | Yes, very straightforward. | 6 |
| Helpful | I thought it was very, very helpful and so did my colleague … We thought it was really helpful the book, it gave us an insight into what the course was going to bring. | 5 | |
| Clear | Yes. It was quite clear to me how it would work. | 1 | |
| Reference point | in fact, that we’ve still got them here and we still look through them every now and again. | 1 | |
| Unclear of duration | I don’t think I, from the booklet, I thought that it would be over a longer period. I got that it would be 12 sessions, but I thought the 12 sessions might have been over a 6 month period. | 1 | |
| Acceptable | Yeah, no problems. We had no problems. Yeah. | 1 | |
| Helpful to have researcher contact | I think we had some telephone calls with one of your researchers and that helped a lot. And it was a very open conversation. There was no time limit on it. And I think we were able to give a lot of advice. | 1 | |
| Benefit of therapist explanation | [practitioner] was really good at explaining it to [name of child]. He’d run through each question with her and then explain it, answer any questions and then ask her if she wanted to sign so I think that was quite an easy process. | 1 | |
|
Needs met | in every way it met [participant]’s needs. | 5 |
| Adapting to participant | By adapting to the needs of the individual I think we had more success. | 4 | |
| Positive outcomes | we had an outcome, a good positive outcome. Well, 2 actually because he had his blood test and then I took him on the Sunday to have his Covid vaccination – straight in and out, no messing, so very good. | 2 | |
| Needs not met | The carer felt the treatment didn’t meet persons needs as he is too complex.a | 1 | |
| Unsuitable | Carer didn’t feel the treatment was suitable or helpful for the person.a | 1 | |
| Accessible materials | (materials accessible to participant?) Yeah, absolutely. Yeah. | 1 | |
| Appropriate techniques | some of the techniques suggested to be used with patients with special needs are appropriate. | 1 | |
|
Recognising carers’ other commitments | [practitioner] realised that I was working as well and that was what was helpful as well. | 1 |
|
Repetitive questions | I think it is very obvious that the questions being asked twice in some cases in different areas as a cross check. But then once you realise that you think did I give the right answer. | 3 |
| Unrelatable questions | I think some of the questions didn’t relate to [YP name] as well. | 2 | |
| Difficulty answering | sometimes that can be quite hard because you’re thinking ‘yeah he does do that but he hasn’t done that for a while’ to try and give you an accurate description. | 2 | |
| Quantity | I think the only thing for me personally was the amount of paperwork and the amount of questions. | 2 | |
| Response display issues | You know when you’ve got 4 things to press and it tells you at the top and when you go scrolling through and think ‘oh I can’t quite remember’ so I had to keep going back up. | 1 | |
| Overthinking responses | Sometimes you can think too hard about the questions. | 1 | |
| Finding time | It’s just that sometimes the house can be so busy and obviously the mail comes in and we just sort of look at it when we can. | 1 | |
| Acceptable | ‘It was good.’ ‘It was fine.’ | 3 | |
| Easy | They were easy, I think. There were some good questions there. | 1 | |
| Carers coming to a consensus | It was interesting having two people myself and my wife taking part because on the scale of 1–5, shall we say, we weren’t far apart but we were just hovering between 2. So we came to consensus on that. | 1 | |
|
Reservations of participation | It depends how much time that would require and she enjoyed the sessions with [practitioner] but I was asking a lot of work to be having the time off and so that would be the side that I would struggle with. | 2 |
| Acceptable | No problem, absolutely no problem, because I think then we could work on what we didn’t get a chance. | 2 | |
| Dependant on the participant | I would if he can cope with it. It’s all for him. | 1 | |
| Helpful | So I think it would be immensely helpful if we could do it, let’s say, in a year or two years’ time as well to see what improvements we’ve made as well. | 1 | |
| Acceptable if BEAMS-ID offered after RCT | If the offer could be made if it is proved to be successful and if you are willing to, we can then try it. | 1 | |
| Unwilling to participate | No. I think I’m just too old now. I mean I did enjoy that course with [practitioner] but I’d not have the time, I’m sorry. | 1 | |
|
Open mindedness | I was just … to be honest, I was just open. Yes, I’ll give it a go. | 3 |
| Interested | I think I was quite interested to see what was the point of the study as well. | 2 | |
| Desire to learn more | I wanted to continue to learn more about Autism and how it related to [participant]. | 1 | |
| Desire to help others | So partly to help others and help expand the sphere of knowledge to help others in a practical way. | 1 | |
| Worth trying | I thought it was worth trying because obviously nothing helped before. | 1 |
| Theme | Subtheme | Example comment | Number of carers |
|---|---|---|---|
| 1. Attending therapy | Adaptable to participant’s needs | So we adapted the process to expose our daughter to this therapy for a smaller period, as we progressed and then let her get on with the rest of the activities during that day. | 4 |
| Therapist responding to participant’s needs | [practitioner] was always on time, because [participant] has got a really big thing, he’s got high functioning autism and one of it is that he lives by time … he always knocked on the door on the dot because he obviously got to know [participant] and knew that he had to be there at that time. | 3 | |
| Personalised approach | And for me, it’s helpful to have somebody come to the house, see our surroundings, see [YP name] and see what our background is. | 1 | |
| Initially daunting | And I think at first it was daunting. It was like what type of is it going to be? It was very down to Earth. I thought it was going to be very Academic. | 1 | |
| Session location | We didn’t just stay at the house. We actually went to, uh, booked a room at the local hospital as well to see how [YP name]. Because one of our problems was that [YP name] doesn’t like going out. | 1 | |
| Participant enjoyed sessions | I think she enjoyed them and looked forward to them so I don’t think anything could have been done differently. | 1 | |
| Informative for participant | The information was given about the treatment, about autism, about anxiety, how anxiety affects you and a lot of that was put in a text that [name of child] could understand so it was also good for her to know that she wasn’t the only person that had these issues and that there were people who would listen and help so it was a good positive experience. | 1 | |
| Positive experience | No I think she got on very well with Jo and the whole experience actually. I think it was good. | 1 | |
| Participant-led | So it was just [participant]-led really, it was whatever he wanted on the day. | 1 | |
| 2. Attending sessions | Acceptable | It was a good experience, I liked it, I enjoyed it actually. | 3 |
| Acceptable materials | I think the materials were fine. | 1 | |
| 1. Facilitators of change/positives of the intervention | Learning for carer | you learn about how to calm, how to actually not react and don’t push her so hard and understand don’t let the family decide how she is going to react to things. | 3 |
| Appropriate materials | (carers handbook) ‘Once you have got the examples of where … some of the things in here are very good’. | 2 | |
| Adaptability | we found it difficult to apply some of the structure, but if we’re allowed, as we did in this case, to have flexibility, I think the process is very good. | 2 | |
| Including participant’s interests | Obviously they’re all different so it’s finding out what calms them, what do they like and arranging their treatment for things that they can understand; maybe they’re characters, or a cuddly toy. | 1 | |
| Enlightening | I didn’t think he’d want to be involved at all so that was nice for me, that was enlightening. | 1 | |
| Practitioner contact | It’s enabled us to talk about it, and not to have to, you get different types of professionals and to actually ask questions as well, which I never would have done before I think yeah. So talking to somebody, going through that process of changes and saying it’s not just the autism, it’s the environment as well, and how we tackle it. | 1 | |
| Individualised | We really went through [participant’s] life. Like what he does, and what he doesn’t do as well, and what improvements can we do. | 1 | |
| Acceptable | It was brilliant. I liked it. I didn’t expect it to be so good. I am quite impressed with it. | 1 | |
| Therapist coming to participant | we changed from us going to the [location] in this case to the therapist coming to see [YP name] in her environment. I think that really helped if you can do that for the therapist to see on an ongoing basis the situation the young person lives in. | 1 | |
| 4. Barriers/issues/challenges of the intervention | Unforeseen circumstances | obviously it wasn’t a weekly thing because I think I was ill and then [practitioner] was on holiday, that was the only thing really | 2 |
| Access to phobic stimuli | we had to make do with a needle until we could get a nurse to come out and show him the proper one | 1 | |
| Issues of medication | We were going to try to get him to get his haircut at the Barber, but because of the medicines, there was no way we could do that. | 1 | |
| Adapting to suit participant | It seemed to me it was fitting something that is quite flexible, and more kind of nebulous thing into those structured way of working that didn’t at first didn’t quite fit, working around it and getting it to fit the situation. | 1 | |
| Quantity of information | (carers handbook) ‘It takes quite a lot to take it all on board’. | 1 | |
| Participant focus | (relaxation/adapting strategies) ‘It’s getting her to focus isn’t it, I think’. | 1 | |
| Use of fear ladder | But we did find this a little bit hard … That would be a bit more problematic to organise in a real world environment, on a spreadsheet or a suggestion list it sounds viable. | 1 | |
| Differing beliefs | The carer felt the treatment assumed that there was a reason behind person’s behaviours, but the carer felt that there wasn’t for this participant and that his behaviours are irrational. a | 1 | |
| Lack of participant involvement | They felt the treatment didn’t have enough questions for the person. a | 1 | |
| Challenges between therapist and carer | They mentioned the therapist said they didn’t think the treatment was suitable for the participant but didn’t give a reason despite the carer asking. a | 1 | |
| Not meeting goals | ‘it was just so unfortunate that he just wouldn’t have them vaccines’. | 1 | |
| Short-staffed | obviously we are a care home and sometimes we are a bit short of staff so there was I think a couple of occasions where my colleague couldn’t make it and I couldn’t make it. | 1 | |
| Time-consuming | it was a bit time-consuming at times, especially when we were having a really busy day or anything can happen, can’t it. | 1 | |
| Less suitable for participants without constant support | I did wonder if somebody else, maybe in a home and they just had carers popping in whether they would still get the same benefit that [name of participant] did because obviously at any point that [name of participant] was getting anxious, I was able to go ‘come on, do breathing’ and other people might not have that. | 1 |
| Theme | Subtheme | Example comment | Number of carers |
|---|---|---|---|
| 1. Number of sessions | Longer period | We could do with more time … So 12 weeks. I don’t think it was enough. I think maybe a couple of more months and then maybe we would see a much more difference. | 1 |
| Flexibility of duration | we had this intense 12 weeks or 12 to 16 weeks, maybe if you could have a little break and see whether or not the improvement that do one improvement have a break and then go back to it. | 1 | |
| Appropriate number and duration | I think it was the right amount of sessions. I think 12 over 12 weeks for [participant] it was enough. | 1 | |
| Shorter sessions | I did think they went on a bit too long in the beginning because it was like 2 hours of time … and we’d get maybe approaching an hour and I could see [participant] starting to lose interest. | 1 | |
| 2. Intervention | Observing participant in different environments | And maybe I should have suggested that [practitioner] could go and see him at the farm, to see just generally what he does and all that stuff … Because his behaviour does change. | 1 |
| Further adaptation | I think it would be difficult for [participant] to go through the process again to be truthful. Unless it was adapted. We could try adapted breathing techniques or something like that with an actor so somebody. | 1 | |
| More practitioner–participant one-to-one | The carer wanted the therapist to have more one-to-one time with the person and ask them why they do things they do. a | 1 | |
| No improvements required | I can’t say there was anything about the course that we didn’t like. | 1 | |
| Managing expectations of workload | maybe a bit more warning for that might have been welcome, but I think that’s more a case of I’m very busy and trying to fit everything in was hard. | 1 | |
| More information for carers | Maybe, to educate parents more, to be honest, because it all starts from us more than them, I think. The better we understand the better we can support them, I think. | 1 |
| Theme | Subtheme | Example comment | Number of carers |
|---|---|---|---|
| 1. Lessons learnt | Increased understanding of autism | I’ve never known anything about autism before she was diagnosed … I didn’t understand and I didn’t know how to deal with it to be honest. I think [practitioner] helped me understand a lot. | 2 |
| Improved responses | Sometimes where you had to record the ABC charts it did make you see things differently and you to react differently and actually to react better … it did actually make you better at dealing with situations. | 2 | |
| Consistency | Consistency. Just keep going back and getting him used … it’s all about being consistent and just keeping calm. | 1 | |
| Having resources to hand | keeping the visuals and the packs so it’s close and ready to hand and we do the relaxations. | 1 | |
| Working around the participant | if he didn’t want to listen that day just waiting for the opportunities when he’s open to listen. | 1 | |
| Finding solutions | And that’s what the study’s helped me to do, is look for a solution. | 1 | |
| To question | To question a bit more! | 1 | |
| Open-mindedness | to be a bit more open minded up, this is what’s going on and what do we do. | 1 | |
| Improved understanding of participant’s ability | I thought ‘I’m never gonna teach her this’ but after a couple of sessions and some patience [practitioner] was quite surprised when he came back and he could see how well she’d improved. | 1 | |
| Use of relaxation strategies | I think we both took out from the practising the relaxation the benefits of that and the muscle tension exercises … I think that was really, really good and I think we both got something out of that that we could keep forever. | 1 | |
| Keeping self-calm | I just have to remain calm. And I think that’s what I’m working on myself as well. Now, just to keep calm and not to worry as well. | 1 | |
| Self-reflection | I looked at my own behaviour as well. I do. I’ve realised now. I get anxious when I go out with [participant]. So that’s one thing I’m tackling at the moment. | 1 | |
| Increased understanding of participant’s anxiety | It was a cold day but [participant] hands were warm. After this event on the way back she held my hand and her hand was cold … So that is something we hadn’t noticed before. So just by concentrating on this it’s helped us to do this. | 1 | |
| 2. Impact and future intentions | Participant progress | What’s changed for me – I was gobsmacked that he actually had the blood test done on the 12th session. We didn’t think … and then I took him for his Covid and that was just, touch wood, really stress free … so for me that was very, very good. | 7 |
| Intention to continue with strategies | Keep using the things we have to use. I’ll definitely keep up with the relaxation techniques for him. | 4 | |
| Increased understanding | it helped [participant], but more helped me to understand how to react and how to interact with [participant] better. | 3 | |
| Increased confidence | I think definitely we’ve become more confident, me and [participant] have become more confident with the BEAMS study. | 3 | |
| Increased awareness | It’s like it’s raised awareness. So you notice things more, you don’t notice things if you’re not in that frame of mind. I think that is positive as well. When you are aware of what is happening for [participant]. | 2 | |
| Benefit of different perspectives | I do feel that the study has helped us immensely from that point of view as well. Just talking to somebody outside of the family and just getting their perspective as well. | 1 | |
| Improvements for family | So we’re doing little baby steps, I think, but it still is making improvement in our lives. | 1 | |
| Improved responses | I react better to her. I’ve noticed that actually If I don’t react and I just give it time her mood changes better quickly. Quicker. | 1 | |
| Alternative ways of thinking | And then also us thinking outside the box and saying to the doctor, why can’t you come to the house … And so, the doctor came to the house, no problems whatsoever. | 1 | |
| Intention to question more | I think we’ll definitely question things more. | 1 | |
| Improved participant communication | she is better at telling me when she gets to the point when she can’t cope with anything. When she wants to be left alone. Or the ones she doesn’t like. | 1 | |
| Desire for improved participant emotional regulation | My hopes are that she will start to control her temper better. | 1 | |
| No significant changes | (change for you and participant?) ‘Not really. It’s changed a little bit for [participant] around some of his behavioural issues but we’ve already had then so the answer to your question is no, not really’. | 1 | |
| Unable to achieve goal | I don’t know because I sort of got it into my head that that was [participant]s last sort of help to try and get him to have the vaccines and without that help from [practitioner] I just don’t think that will ever happen. | 1 | |
| Applying BEAMS strategies | the music/singing teacher … has started using some visual prompts to allow [participant] to express her mood … [music teacher] has also now lays out various booklets that [participant] is used to allow [participant] to choose the way the sessions will run … This has proved very successful and improved [participant]‘s engagement with the sessions … this is a direct consequence of applying some of the actions referred to in the BEAMS research project. | 1 | |
| Benefits of medication reduction | The reduction of Aripiprazole has in [participant]‘s case improved her presentation in terms of anxiety, engagement, ‘enjoyment of life’ (improved happiness, smiling etc.) and ability. | 1 |
| Theme | Subtheme | Example comment | Number of carers |
|---|---|---|---|
| 1. Experience of the therapeutic relationship | Positive rapport | [participant] had a really good rapport with [practitioner] which really helped as well, finding the right practitioner to suit. | 6 |
| Feeling supported | Yes, definitely … And I think it was very helpful as well to know that you’ve got somebody who you can, you know, you know that can come on Thursday and like, you say, this is what happened and what do we do from here? Yeah. | 6 | |
| Positive attributes | I think [practitioner] was absolutely brilliant. He was calm, he was considerate. | 4 | |
| Benefit of the right practitioner | So I think it’s good to have the right practitioner maybe as well which helps so yeah, I was quite surprised with how we went through and how we were feeling. | 1 | |
| Good communication | If we couldn’t make meetings we’d keep in contact. | 1 | |
| Benefit of having a professional to discuss with | It’s just nice to have somebody on the other side to talk to, a professional who and isn’t going to talk about medicines and isn’t going to talk behaviour, and just says what’s adaptable for your family at this time as well. | 1 | |
| 2. Ability to raise concerns and questions | Comfortable | Yes he was very easy to talk to and you never felt silly asking any questions. So very good. | 5 |
| Questions outside of research | I think it’s more about what was going on with the medicine. | 1 | |
| 3. Improving support | No improvements | No. I don’t think so. She did the best, I think. | 6 |
Research procedures: consent process and participant information booklets
Carers were positive about the process of gaining consent and the associated participant information booklets, which were considered ‘straightforward’ by 86% and ‘helpful’ or clear by 86%. One carer told us that they were unclear about the duration over which the intervention would take place. Two carers mentioned that it was helpful to have contact with either the research team or the therapist, who provided additional advice or information.
Research procedures: meeting participant and carer needs
Five carers (71%) shared the view that the research procedures meet the needs of autistic participants with moderate to severe learning disabilities, and four (57%) went on to discuss how adaptations helped with ensuring that need was met. Carers tended to shift to talking about the intervention when discussing whether the research procedures met participant need. One carer commented that participant need was not met due to their complexity and felt that aspects of the intervention were not suitable. However, others noted that the materials were accessible, and the techniques used were appropriate to meet needs and carer needs were met.
Research procedures: outcome measures
While 57% carers who were interviewed reported that the outcome measures were acceptable and easy to complete, others found some of the questions repetitive and had difficulty answering because some of the questions may not have related well to the participant. One carer suggested that they had difficulty with finding time to complete the outcome measures, while another suggested that responding to the questions prompted some overthinking of responses. This needs to be balanced against the finding that all carers completed all the measures, and the rate of missing data was low.
Research procedures: randomisation in a future trial
Carers were positive about randomisation within a future trial, but some expressed some reservations. One person commented that they were ‘too old’, while another commented that they would need to take time off work, while a further suggested that it would depend upon the needs of the participant at the time. While these were responses given to questions about randomisation, these carers tended to make reference to taking part in a further study rather than explicitly comment on whether randomisation was acceptable.
Research procedures: facilitators and barriers
Carers reported no barriers. In terms of facilitators, they reported approaching the research with an ‘open mind’ coupled with an ‘interest’ in understanding the study. Further, they spoke about a desire to help others and learn more, and considered the study ‘worth trying’.
Intervention: attending therapy and sessions
Cares were positive about attending therapy and the sessions. Multiple carers commented that the intervention was adapted to meet participants’ needs and that the therapists responded to participants’ needs. Three carers stated that attending therapy was acceptable. Others made comment that it was a positive experience, and the participant enjoyed the sessions, which were said to be informative. One carer commented that it was initially daunting but found the intervention to be ‘very down to earth’.
Intervention: facilitators
Carers spoke about a series of intervention facilitators, which included carer learning, the use of appropriate materials and making adaptations, such as including participant interests in the therapy process. The therapist and their approach were also considered to be a facilitator by carers; this included the opportunity to spend time with the therapist asking questions, and the therapist making adaptations to meet participant need.
Intervention: barriers
There were a series of practical issues that were raised by carers as potential intervention barriers. These included unforeseen circumstances (e.g. illness and holiday) and issues with paid-carer staffing levels. Carers also spoke about difficulties with access to appropriate materials, the quantity of information they were given, time-related issues, and issues with adapting therapy to meet needs, including engaging the participant more. One carer commented that making use of the Fear Ladder with one participant was challenging, while another commented that carers and the therapists may have differing beliefs about the causes of behaviour which may cause issues with the implementation of the intervention. Another carer mentioned that they wondered whether the intervention would be suitable for participants who do not have constant support due to the important role that carers had in the delivery of the intervention.
Intervention: improvements and revisions
One carer commented that they would have liked the intervention delivered over a longer period, while another carer commented that they would have liked shorter sessions. Another commented that the number and duration of the sessions were appropriate. This reflects the diversity of need amongst this population. One carer suggested that more information for carers would be helpful, while another commented that further adaptation to the breathing exercises might be helpful if they were to receive the intervention a second time. One carer commented that managing the expectations of the workload associated with the intervention was challenging, while another carer commented that no improvements were needed to the intervention.
Intervention: outcomes
Carers were positive about the outcomes associated with the intervention. They spoke about having an improved understanding of autism and anxiety, ability to respond to anxiety, consistency and access to resources. They also reported learning to question and be open-minded, while having an improved understanding of participants’ abilities, and an ability to use relaxation to help calm themselves. Considering impact, carers spoke about participants making positive progress, along with an increased understanding, awareness, and confidence in managing participant anxiety, and an improved understanding of participant communication. One carer mentioned that there had been no significant changes for the participant, and this same participant commented that they were unable to achieve their therapy goal. Another carer commented that taking part in the intervention was associated with a reduction in antipsychotic medication.
Intervention: therapeutic relationship
Carers were positive about the therapeutic relationship that they had with their therapist. Eighty-six per cent of carers commented that they had positive rapport with their therapist and stated that they felt supported. They mentioned the value of good communication, being able to raise concerns and ask questions, and positive therapist attributes, such as being calm and considerate. One carer commented that they felt that the participant did not make improvements, but thought that the therapist ‘… did the best, I think’.
Therapists
Eight therapists took part in our post-intervention semistructured interview. A group of therapists from one site also provided additional feedback via e-mail which was included within our analysis. The findings are summarised within Tables 39–43.
| Theme | Subtheme | Example comment | Number of practitioners |
|---|---|---|---|
| 1. Suitability for the target population | Suitable | Yes definitely. It’s definitely worked. | 8 |
| More appropriate for specific phobia | And I think for a lot of the people that were finding it to be quite successful, it was more of the desensitisation to, um, to needles or different phobias. | 1 | |
| Not appropriate for all cases | I think maybe when the goals are a little bit more abstract. And maybe when there’s other factors that need addressing, first, it didn’t necessarily feel that appropriate. | 1 | |
| Helpful | I think for some people it’s really helpful. | 2 | |
| Challenges of working with this population | Because they all had moderate learning disability, their ability to cognitively to understand a lot of everything going on. They may not be that easy to, you know, enact if it was someone with mild learning disability, for example. | 1 | |
| 2. Engagement and understanding of carers | Understanding | the carer grasped the information very quickly. | 4 |
| Motivated | I had a particularly positive and motivated client and carer. Which really helped. | 3 | |
| Engaged | And they seemed to be really engaged and really wanting to be involved in the therapy | 3 | |
| Proactive | It was quite good in terms of him, the carer anyway, he was very proactive. He’d take a good initiative to do all the work. | 2 | |
| Enthusiastic | He was very enthusiastic. He was. In fact, he took a lot of the lead. | 2 | |
| Surpassing practitioner expectations | their response was much better than what I was expecting, they responded very positively. | 2 | |
| Challenging attitudes | And carers being, like, it doesn’t really affect her life. And obviously if people around you have got that attitude, and if this is the case. It’s very tricky to then sort of continue with the sessions in the way that they are structured according to the manual. | 1 | |
| Resistance to change | That we’re really resistant to changing the way they did things. Again, hearsay would be like, you know, we’ve always done it this way, this isn’t going to work. | 1 | |
| Reduction in engagement | So they maintained engagement throughout I would say, but I would say it dipped slightly … Probably somewhere in the middle, when it became more challenging for [participant] and I think it also became more challenging for them. | 1 | |
| Lack of comprehension | Dad struggled to use the ABC chart and again this would have taken a number of sessions to get him to use it as directed – he would write things down about what had happened but struggled to structure them as requested. Likewise with the rating scales. | 2 | |
| 3. Meeting needs of the patient | Benefited | Yeah, and she got some really positive outcomes and it worked really well for her. | 8 |
| Adapting to meet needs | So, we just adapted that. So, he held his nose when he breathed out of his mouth, covered his mouth when he breathed through his nose. | 7 | |
| Needs met | I believe it did meet the needs of participants, given how the treatment was delivered in a format that they could easily access and understand most of what was said to them. | 4 | |
| Appropriate intervention | Yes, it felt like the right intervention for this client. | 3 | |
| Achieved goal | She managed every step of her fear ladder and she was spontaneously using the strategies she got to day service and she continues to go to day service. So she’s going a day a week. Bearing in mind when we started, she wasn’t leaving the house at all. | 3 | |
| Independent development | And it just became quite organic, like it was just growing. You know, it didn’t need me to sort of say that it just, it was going to happen. They knew what to do. | 2 | |
| Positive experience | she just wanted to do more because she found it was straightforward and very rewarding, and was pleased with her progress, and she was excited to do more. | 2 | |
| Developed understanding | It answered a lot of the questions that [participant]] already had about her needs, about the nature of anxiety, mental health. | 2 | |
| Additional time | I did put a little bit of extra time into the sessions because she would want to sort of discuss her week a little bit … And I think she really valued that. | 1 | |
| Lack of investment | the investment to do something like graded exposure wasn’t there. | 1 | |
| Required a more person centred approach | I think her experience of that bit was maybe quite negative. Until we sort of restructured it to be a little bit more person centred. | 1 | |
| Strategies for future use | To try and integrate relaxation into the participants life – I think that that was helpful and something that can be taken forwards. | 1 | |
| Validation | And for somebody that you know would quite often reiterate that they felt like they weren’t listened to and that they were always in trouble and always blamed for things exploring those difficulties with a carer who could then be like, oh, that makes a bit more sense. I think was very validating for her. | 1 | |
| Needs not met | a lot of the more presenting needs were anxieties around physical health difficulties at the time, a lot of medication changes happening. And just, generally, very high anxiety, and dysregulated emotions, but not necessarily because of anything specific. | 1 | |
| Lack of understanding | I’m not sure really how much the client or the participant actually absorbed it. | 1 | |
| Positive engagement | He engaged really well with the preference assessment, that was really good. | 1 | |
| 4. Meeting needs of the carer | Helpful | Yeah, because Mum needed something clear. And I think the fact that it was structured, and she knew it was 12 weeks, gave her something solid to hold on to, like, okay, this might improve things, you know, in 12 weeks. So that was helpful for her. | 5 |
| Benefited | I think that it maybe gave her a footing, a sure footing, to be able to challenge [YP name], where perhaps she wasn’t challenging her before. And it does generate a sense of coping within the household, like not reaching out to others, not looking for medical interventions. | 4 | |
| Developed more understanding | And she’s since said to me, this has been really powerful because I understand things I never understood before and I’m able to support my daughter in a way that I couldn’t before. | 4 | |
| Valued | I think they appreciated some of the depth we were going into. The opportunity to discuss some of those specifics. They were really quite bought in at that point. | 3 | |
| Not meeting expectations | I think their expectation probably is not what BEAMS would be able to achieve for them. | 1 | |
| Participant progress | And this area of separation from parents has allowed her then to gain a bit more independence, which is kind of what the parents would have liked as well. | 1 | |
| Unable to determine | Very hard to say because I saw, pretty much, a different carer every week, to be honest. | 1 | |
| Worked well | worked well for the carer | 1 | |
| Supported | And I think, you know, they did feel really supported by the therapy by the intervention. | 1 | |
| Accessible and amenable | It’s very accessible and amenable to the people and their carers. | 1 | |
| Carer-led | And the psychoeducation bit became just a really healthy opportunity to just kind of ask around what she wanted to ask around and it wasn’t me leading it as much as anything. | 1 | |
| Intention to use strategies with other patients | He’s even talked about (and I don’t know if he’s necessarily allowed) but certainly some of the behavioural elements to take that forward, obviously with this chap as well but also for the other guys that are living in the house. | 1 | |
| 5. Appropriateness of materials | Appropriate | Yeah, yeah, they were appropriate so I didn’t need to make any changes. | 6 |
| Acceptable manual | I thought the manual was quite comprehensive and clear, I think, with what was required. | 4 | |
| Visual resources not appropriate for participant | I don’t know how much he really engaged in terms of the visuals. Didn’t really seem like he needed those, like it wasn’t obvious that he needed those. | 3 | |
| Participant unable to comprehend | That’s the bit I’m not sure it was pitched properly for him, given his level of ability. | 2 | |
| Appropriate for carers | They really liked the carers booklet. That was kind of given to them in small sections and they really appreciated that, that that booklet was divided up. | 2 | |
| Helpful | I think having sort of the carers handbook and those resources were really helpful. | 2 | |
| Resources not appropriate for participant | I used some of the like the ‘yes’ and the ‘no’. Although she didn’t use them. I tried to use them, but she didn’t like to choose, and I think that was just her. | 1 | |
| Creating additional resources | I made quite a lot of sort of … not really resources, but a lot of different symbols that just weren’t there, but that’s to be expected. | 1 | |
| Appropriate measures | I think what you’ve already used already were fine, yeah. | 1 | |
| Manual lacked information | sometimes, the actual manual itself didn’t provide enough resource or enough information there to adapt it to my patient. | 1 | |
| Helpful to have physical copies | And it was good to have them because they are time-consuming to create, aren’t they? | 1 | |
| Accessible | It was, yeah, but materials were accessible. | 1 | |
| Intervention summary less adapted | maybe that treatment summary was probably the less kind of adapted of the materials. | 1 | |
| 6. Acceptability of the intervention for practitioners | Need for experience with LD | following the steps is okay as long as it is a professional that understands learning disabilities. | 2 |
| Challenging | it did a lot of the time feel like I was hitting my head against a brick wall. | 1 | |
| Ease of delivery | But it was very easy to follow for someone like me who hasn’t delivered the intervention that much. | 1 | |
| Balance of instruction and professional judgement | It’s nice as a professional to have that balance between some instruction and, you know, some guidance and some parameters. But being allowed a little bit of that professional judgement to kind of bring those things in that you kind of know and that awareness of the individual. | 1 | |
| Benefit of person-centred approach | And there’s lots of that very person centred asking about what motivates people and things like that. So yeah, really enjoyed that. | 1 | |
| Clear structure | The structure of the project was very clear and organised. | 1 | |
| Practitioner commitment | In terms of time, BEAMS is a significant commitment for clinicians. Suggest that BEAMS trained clinicians take on only one BEAMS client if they are also to maintain their usual work. | 1 | |
| Worthwhile intervention | A feeling that this is a worthwhile intervention. | 1 | |
| Valuable experience | Appreciative of the opportunity to be involved in LD research – something we are really wanting to promote the importance of. | 1 | |
| 7. Using BEAMS-ID with future clients | Appropriate | I would be more than happy to deliver it again to those with anxiety problems because I think it works really well and in my experience it has. | 5 |
| Intention to share techniques/strategies | I’m even drawing on the materials from it now, you know with other clients. | 4 | |
| Useful if flexible and adaptable | And I just think realistically, when you’re working with learning disabilities and autism, the flexibility you need to apply is always going to make it really hard to follow research to a tee, but when it’s out there as a generalised intervention, or if it is and you can apply that sort of more clinical judgement to it and be more adaptable and flexible without affecting research fidelity, then that would be really helpful. | 2 | |
| Useful | I think the program itself might have been quite useful down the line. | 1 | |
| Dependent on need | Not general anxiety problems, no. I would say almost definitely not for that. | 1 | |
| Dependent on carer | Yes, without a doubt. I think the condition is that there’s a carer who’s reliable, engaged consistently and going to fully partake and understand what we’re doing. | 1 | |
| Extending training to other professionals | I wonder whether there would be scope to extend the project further, to include delivery of the BEAMS-ID training to healthcare professions, both NHS and private care homes, using the materials and knowledge within BEAMS-ID. | 1 | |
| Accessible | I could happily imagine some of the nurses doing this and it’s accessible the way it’s designed, is accessible, which is good. Yeah. | 1 | |
| 8. Acceptability of randomisation within a future trial | Beneficial | I think it probably would be helpful to know whether there is a tangible difference between the two. | 4 |
| Acceptable | I think ultimately, I have no issues with that. I think it would probably be worthwhile. | 3 | |
| Acceptable if shown to be beneficial | I think having very clear identification for the necessity of BEAMS, I think there’s 100% a place for it. But the random allocation would have to be based off of, you know, actually there is a really clear benefit of BEAMS in this situation. | 1 | |
| Requires clear eligibility criteria | I think that there’s such a benefit to some people. That yeah, you know, it should be quite positive. But having it being a really clear eligibility criteria I suppose. Would be sort of a key thing. | 1 | |
| Assumption it would not influence outcome | I think for my patient, I don’t want to say, but it may. I think it wouldn’t matter for her. | 1 | |
| Interesting to compare outcomes | It will be interesting to know, sort of, if the structure of BEAMS would have helped her develop something like, you know, and whether treatment-as-usual would have been any different. | 1 |
| Category | Theme | Example comment | Number of practitioners |
|---|---|---|---|
| 1. Therapist training | Helpful | the training was really helpful. | 5 |
| Opportunity to ask questions | The frequent opportunity to ask questions was really useful. | 4 | |
| Positive experience | Yeah, I remember it being quite a positive experience. | 4 | |
| Interactive | And it was quite interactive, which I enjoyed. | 3 | |
| Recapping | there’s a lot of overlap actually … between some of the concepts of themes and some of that graded exposure work that I’ve done previously. So it was really, it was kind of a recap in some ways. | 2 | |
| Furthering knowledge | it went probably a bit beyond what I’d done, in the previous piece of work that I’ve done. And so it was nice to kind of learn in a bit more detail. | 2 | |
| Sufficient | I think from my perspective, yes. I felt as though I kind of understood the core principles and yeah, I felt it was, it was enough. | 2 | |
| Benefit of prior experience | But given my psychology background, I think that really helped as well. And my kind of knowledge on learning disabilities and autism already, helped a lot. | 2 | |
| Collaborative | It felt like very collaborative training. | 2 | |
| Accommodating | And then we were able to sort of find a time that fit us, which was really considerate actually for us to do the training online. | 2 | |
| Benefit of knowing group | It was helpful because the people I trained with were people I knew. | 2 | |
| Lacked guidance on dealing with challenges | but not necessarily how to manoeuvre the barriers that were created because of the circumstances. | 1 | |
| Clarifying strategies | I think going over the understanding of different types of reinforcement, and clarifying that, was quite helpful. | 1 | |
| Too fast | although I had some knowledge of the treatment, but because I don’t do it a lot of it in my line of work, I thought perhaps some of it was a bit too quick, for me anyway. | 1 | |
| Solutions to challenges | But it was nice to actually have a few examples of what we might expect and what challenges we might face. And how then we could move forward and try and manage those challenges. So that was, I think, that was really helpful. | 1 | |
| Duration between training and study | The only thing was, it was just a little bit of a gap between that and then starting the study. | 1 | |
| Meeting needs to support engagement | the visual schedules and we looked at, we thought about people’s level of communication need. And how it can adapt to that and help them engage better with the intervention. | 1 | |
| Benefit of small group | And it was also nice that it was quite a small training group. Which always gives people more of an opportunity to kind of participate. | 1 | |
| Benefit of different perspectives | So we came at the training from a slightly different perspective. It was quite nice to hear | 1 | |
| Uncertainty of feeling prepared | I’m hesitating because I still felt that I didn’t fully grasp the treatment until I’d really thoroughly read the manual. And I don’t know whether that was about the training not preparing me, or whether that was about me not being ready for the training when it came. | 1 | |
| Engaging | Training was engaging. | 1 | |
| Well explained |
The rationale through different approaches in therapy were well explained.
The need to gather data and how data is being gathered was well explained. |
1 | |
| Over-prepares | I think actually, that the training probably (it’s not that it’s a bad thing), but it over prepares you because it tells you about everything that you might possibly need to know about using the treatment. | 1 | |
| Wider research initiative | So you felt like you were part of a much bigger picture and you know, going into deliver the therapy you could see how it fitted with the wider research initiative. | 1 | |
| Useful discussions | The thing that stands out for me most of all, I think was the journey into getting informed consent and the conversations we had back and forth about do we need to do anything else? | 1 | |
| 2. Therapist benefits/professional development | Enjoyable | I found it very enjoyable. | 7 |
| General learning | Yes, I feel knowledgeable about graded exposure and working directly with the individual as well as working indirectly with the carer. | 5 | |
| Beneficial | As well as being involved in research which for someone who aspires to go on to a clinical doctorate is a really positive thing, and something that I’ve been really kind of honoured to be a part of. | 3 | |
| Doing something different | the sessions were really good from my point of view because it’s not something I do regularly, so for me it’s something quite fresh and different to what I do. | 3 | |
| Implementing learned skills | the fact that our psychologist has now done the BEAMS study I think it would be really beneficial for us to work together and focus on more of a behavioural approach to anxiety because we’ve both seen that actually it really works. | 3 | |
| Reflection | And so I think it gave me cause for reflection on my practice and how I might still sometimes rush towards an outcome without necessarily considering all the basis to that. | 3 | |
| Seeing progress | just really, really enjoyed seeing them being able to get over something that is quite life limiting. | 2 | |
| Enlightening | it’s opening up our eyes to a few things that we’re gonna do differently. | 2 | |
| Positive experience | And so overall I found it really positive, and I got a lot out of it both from a kind of personal perspective, but also in terms of my training and my understanding of psychology in the LD population. | 1 |
| Category | Theme | Example comment | Number of practitioners |
|---|---|---|---|
| 1. Session timing and frequency | Longer sessions | I added time at the beginnings of sessions to allow for general discussion, which felt really important. I did have to add time at the end of sessions. | 7 |
| Appropriate frequency | in terms of frequency, I suppose, weekly was ideal. | 3 | |
| Appropriate length | Yeah, but in terms of the actual … length of sessions, I think, yeah, that was probably just about right. | 1 | |
| Session delays | Frequency, that’s very tricky, because things were constantly happening that meant sessions were delayed. | 1 | |
| Carer commitment | I think we found that it’s quite a commitment for her mom. It was quite a big commitment for [mum’s name]. I think that it got to the point where she was having to take time off work to do the sessions and it was a little bit more tricky. | 1 | |
| Sessions too long | When seeing clients, particularly those with LDs, and especially when seeing them within their own homes (as is often the case in community LD services), a 2 hour session is too long. | 1 | |
| 2. Experience of delivering the sessions | Positive experience | I had a really positive experience delivering the sessions. | 7 |
| Ease | And it went really straight forward, you know relatively, without any hiccups for me. | 3 | |
| Time-consuming | I had to generally add at least half an hour/to an hour to my BEAMS sessions, which meant that they would sort of take up a whole afternoon. Plus the resource preparation. | 1 | |
| Seeing progress | I kind of knew what the program looked like, but it still surprised me that we made so much progress. | 1 | |
| Enjoyable | I really enjoyed delivering the treatment. | 1 | |
| Useful structure | the carer only sessions were very cleverly strategically placed. I felt very useful. | 1 | |
| Slow-starting | so it was a bit of a mixture, it was off to a bit of a slow start. | 1 | |
| Bias in fidelity checklists | An element of bias in completing the sessions feedback forms when completing these ourselves – noticed wanting to ‘appear competent’ in the intervention. | 1 | |
| Supporting participant and carer | The last couple of sessions was just sort of being there with the client, supporting them, supporting the carer | 1 | |
| Low fidelity | So I think it was about Session 6 onwards, the fidelity was low with what was actually being asked from BEAMS. | 1 | |
| 3. Carer involvement in sessions | Positive involvement | he was really structured. He filled in all the ABCs every week for us, he was sending me photos in between each session of what they were doing. And e-mailing me constantly ‘we’ve just done this!’. | 6 |
| Mixed responses | Very mixed, very, very mixed. So some were really positive. Um, sort of really valued some of it. | 1 | |
| Carer inconsistencies | It’s very tricky because they weren’t consistent throughout the sessions. So maybe if it had been consistent, they’d have constantly been a little bit more invested. | 1 | |
| Valuable | And also having the space to think these things through and have that reflection, and think about some of the underlying reasons for things, and some of the more proactive strategies, we’re quite valuable. | 1 | |
| Keen to progress | But it felt like he was very keen just to get to … putting the fear ladder together and just doing the intervention. | 1 | |
| One-to-one follow-up | she would then be removed from the session and then the carer and me will then follow up with all the different triggers and everything that had gone on so that she wasn’t sort of hearing it and then getting distressed, because she does have a degree of understanding. | 1 | |
| Nervousness | But what she was most nervous about, you know, because the model itself, some of it fitted very easily and some of it was a less comfortable fit as well, I want to say. And it took longer for it to fit. | 1 | |
| Difficulty implementing relaxation | Dad also found these [relaxation work] ideas difficult and was not able to do this with me. | 1 | |
| 4. Facilitators of successful intervention | Structure | I think having sort of the structure of sessions there was quite nice. So even if the content within the sessions was a bit skewed, having that consistency of session structure made things a bit easier. | 6 |
| Resources and materials | I think the study guide was so easy to follow, it was well-written and I was able to just go ‘boom, boom, boom’ so it was good. | 5 | |
| Engaged carer | The carer, he was very proactive, very engaging and if he wasn’t so, I would have found it more difficult. | 3 | |
| Carer understanding | I was lucky enough for the carer to have a background in kind of supporting people with learning disabilities and autism … Which really helped that process and allowed me to kind of talk about things more quickly than I would have if the carer was kind of less informed about those concepts. | 3 | |
| Additional support | the three of us that were involved kind of gave each other some peer support. So that was quite helpful. | 3 | |
| Group supervision sessions | Because it’s great having the group supervisions they were really, really useful | 2 | |
| Participant-led | And I think some of that is because we let him sort of lead. So we very much followed his cue. | 2 | |
| Preference assessment | Just thinking about when we did the preference, I thought that was really useful for him. | 2 | |
| BEAMS strategies | I think elements of the reinforcement strategy is the specifically positive reinforcement was really helpful and that was utilised throughout my time doing the intervention with the individuals. | 2 | |
| Research team | The research team were easily accessible and extremely helpful throughout. | 2 | |
| Fidelity checklists | I suppose the fidelity checklists were … They were helpful as a little prompt … it’s a reminder that it’s expected that you would adhere to the treatment manual. | 2 | |
| Consistent carer | I did manage to get a consistent carer for a couple of sessions, which was really, really helpful. | 1 | |
| Intervention plan | Yeah, I think the treatment plan was a really helpful thing to do. I found that quite positive, I think the care staff found that quite validating because a lot of it was coming from them. | 1 | |
| Carers as the expert | So it is sort of positioning them as, you know, them [care staff] and the participant as you’re the expert here and you know, I’m not coming in as a researcher, you know, this is very much supposed to be you. And that was quite valuable. | 1 | |
| Time to explain processes | And when you had the chance to sit and walk someone through that process a bit more the response generally became quite positive. | 1 | |
| Physical environment | he tolerated the sessions very well … I think some of that might be to do with the way the house is set up and him having lots of physical space to move around. | 1 | |
| Support sessions | it was helpful to have the in-between sessions, support sessions. | 1 | |
| Research team completing measures | I think it’s good that you do the measurements rather than us … Because I think that really can put people on the back foot sometimes. When you first meet and you’re bombarding with measurements. | 1 | |
| Check-in format | The check-in format worked really well. | 1 | |
| Flexibility | whilst there were boundaries around it, so obviously had to be true to the manual. There was some flexibility. So you know if you need to do it slightly differently to get the person to engage | 1 | |
| Using clinical judgement | That it was okay to use my clinical judgement and that that was part of the process. | 1 | |
| Carer sessions | But it made an enormous difference to be able to step away from the direct therapy intervention and look at it more objectively and talk about it in terms of planning it and how it’s going to be executed with, her mum the carer, away from her directly. So that was very helpful. | 1 | |
| Not problem-focused | I think that was one of the good things there. It wasn’t problem focused. | 1 | |
| Timing of intervention | Christmas like lots of; social, family, fun things to do. Naturally occurring events became steps on the fear ladder. | 1 | |
| 5. Barriers/issues/challenges of intervention delivery | Difficulty with relaxation | things like breathing and progressive muscle relaxation for an LD demographic, particularly with moderate to severe LD, are really hard relaxation activities. | 6 |
| Participant characteristics/behaviour | One thing that I found hard was just the client was sometimes not always that engaging, I guess. And I guess that their attention span was short. | 5 | |
| Carer attitudes/beliefs | Two main carriers who were involved in the therapy …. They had quite different approaches. And that was very much on a behavioural level, so it did affect the therapy. | 3 | |
| Illness | Staff members were going off sick constantly. | 3 | |
| Motivation | And then really it became just trying to keep going and really just to not go backwards or not to stop, and to motivate them to keep persevering, even though we’d hit a sort of a stumbling block. | 3 | |
| Engagement | I think the minimal engagement at the beginning and even though I did try to sort of have a couple of engagement sessions. | 2 | |
| Different carers | And I found myself almost having to re explain what BEAMS was, once the intervention had started. Which was quite difficult because the buy-in then, wasn’t necessarily there, and the understanding wasn’t necessarily there. | 2 | |
| Implementing strategies | That became a bit tricky then because towards the end we didn’t follow that fear ladder concept, so yeah. | 2 | |
| Carer commitment | I think around how much his carers have going on and actually for them to be able to take something else on board. | 2 | |
| Time-consuming | And it became a really, really time-consuming venture. | 2 | |
| ABC charts not completed | The filling in of weekly ABC charts was also quite a challenge. It was difficult for carers to do that consistently on a weekly basis due to kind of other commitments they had and other responsibilities. | 2 | |
| Practitioner commitment | The requirements that had to be completed prior to the training were an added burden. | 2 | |
| Study constraints | That wasn’t because of BEAMS itself, it was the situation. It was the system. And the lack of flexibility that because it’s research. | 1 | |
| Lack of flexibility | And trying to follow a very structured manual felt quite tough. | 1 | |
| Preparing resources | if you’ve not thought about that ahead of time and prepared those things, or you know brought resources with you for that kind of thing, you might be left in a bit of a situation where you don’t really know what to do because it’s not in the manual. | 1 | |
| Lack of communication with carers | Having to sort of take accountability for that lack of clear communication at the beginning was quite difficult. | 1 | |
| Circumstances | It’s just circumstantially it was quite tricky to deliver. | 1 | |
| Logistics | So there was a challenge around actually the logistics of them getting out of the house with [participant] and managing him in public settings and their schedules and their work lives and their family commitments. | 1 | |
| Session interruptions | So Mum went away a couple of times. And I think [participant] wasn’t well. So we had a few sessions which were interrupted. | 1 | |
| Developing fear ladder | I think that we struggled a bit when it came to developing the fear ladder. | 1 | |
| Fitting content in sessions | the challenges were sometimes fitting all the material into one session. So sometimes I had to go over two. | 1 | |
| Implementing breaks | A lot of the time service users couldn’t kind of make that decision to have a break themselves. They’d need to be prompted or we would rely on carers noticing that they were disengaging, or myself noticing that they were disengaging. | 1 | |
| Carer understanding | slightly difficult was kind of the psychoeducation for the service users around anxiety, learning disabilities and autism. That was kind of well understood by one, but quite difficult for another one to kind of understand. | 1 | |
| Understanding carer comprehension | for myself to understand the level of their comprehension on these concepts. | 1 | |
| Carers keen to progress | carers kind of had the tendency to rush exposure and I had to remind them to kind of take it slowly. | 1 | |
| Issues with day services | And I suppose what was challenging is that sometimes the day services weren’t fully signed up to that … And then the activity that we planned to do couldn’t run for some reason, and things like that. | 1 | |
| Using new strategies | I’d never done a preference checklist before, not like that. So I really had to get my head round what that looked like. And then I think because the behavioural bit isn’t my bread and butter, I needed a bit of support to get my head round the reinforcers. | 1 | |
| Overcoming safety behaviours | But it’s just kind of those safety behaviours. They’re not necessarily referenced in the manual and you encounter them as you go through and you realise that somebody’s doing something that they might attribute their success to, which is not part of the treatment. | 1 | |
| Explaining definitions and presentations | Defining the different types of phobias and, like, different types of anxiety presentations and what keeps them going. And I think it felt that it was a bit labour involved, but it was very worthwhile. | 1 | |
| Involving other carers | Involving her dad, involving another carer, secondary career, was challenging … Her dad wasn’t very psychologically minded. He wasn’t particularly interested. | 1 | |
| Accessing materials | I just couldn’t get my network, so SharePoint was a bit tricky getting to it. | 1 | |
| Strategies or materials not appropriate | I think one of them was around writing down or drawing a picture of your emotions and that type of thing … he’s not very keen on painting, drawing that type of thing … he didn’t quite grasp the concept. | 1 | |
| Behaviours that challenge | From the start of the session, [participant] seemed distressed and this escalated throughout the session; started with distressed sounds and then started hitting herself and the wall … [as the intervention unfolded], no longer appeared distressed, that she was no longer screaming and shouting, and that her self-injurious behaviours had reduced to a less than weekly … you have observed that [participant] is smiling and laughing more with the care staff, and that her communication has improved in that she has been more assertive is telling others what she needs. | 1 | |
| Balance of feasibility and participant’s best interests | A real balance of trying to stick to the manual (in order to be true to feasibility study) whilst also working in the client’s best interests. | 1 | |
| Difficulty accessing services | Clinicians experienced some of difficulties implementing the intervention, e.g. have identified there are no services available to provide blood tests. | 1 | |
| Inappropriate session structure | Not all of the sessions were required for the client to achieve the goal, and it was not possible for all sessions to be used in exactly the way prescribed. | 1 | |
| Issues with conducting research within the NHS | It is exceedingly challenging within the current parameters of the NHS to meet the needs of university-based research. | 1 | |
| Implementing a different approach | Whilst evidence-based manualised approaches have their place, they are not something which qualified clinical psychologists would generally use. I found it difficult to follow a prescribed approach that was essentially what I would be doing anyway but had to alter my established practice to use. | 1 |
| Category | Summary point | Example comment | Number of practitioners |
|---|---|---|---|
| 1. Experience of the therapeutic relationship | Positive relationship | I developed a therapeutic relationship with [participant] and his carers. Which was quite a nice thing to be able to see patients regularly over a sustained period of time. | 3 |
| Difficulty building rapport | for my particular client it was difficult to build rapport and it was hard to then balance the needs of the person with the needs of the research and session agenda. | 2 | |
| Quickly developed | we were able to build that rapport up really quick. | 1 | |
| Positive indicators | And then we got lots of smiles, lots of giggles. | 1 | |
| Aided by preference assessment | But by doing the preference assessment and getting to know them really helped with them opening up and being able to express themselves. | 1 | |
| Benefit of the home environment | although I was in the family home it still felt okay but nice because then you could have that sort of like that little social chat. Professional social chat. | 1 | |
| Developed through programme | I sort of had to build it in. | 1 | |
| 2. Impact of structure on therapeutic relationship | Supported development | And having that time the length of time of the sessions and the regularity I think really helped to build a strong therapeutic relationship in a way in which we as psychiatrist don’t usually have that opportunity. | 4 |
| Helpful | Both participants really benefited from that structure. | 3 | |
| Adapting structure | it was adding in the time at the beginning and the end to sort of have those relationships and build that trust and that engagement alongside the session, but not necessarily in the session. | 2 | |
| Appropriate | I really had time to get to know him and really had time also to get to know the carers because they’re so fundamental to [participant] and he’s so dependent on them. | 2 |
| Category | Suggested improvement/revision | Example comment | Number of practitioners |
|---|---|---|---|
| 1. Number of sessions | More sessions | some were a little bit more content heavy and maybe they should have been done over 2 sessions. | 8 |
| Appropriate number | it worked fine in 12 sessions. And it was quite nice actually because rarely (I don’t know whether other professionals do this), but rarely do I start and go right, we’ve got 12 weeks together. | 3 | |
| Follow-up session | A follow-up with the client and carer would be helpful, to check they’re not exposing the client too much and still using the fear ladder appropriately, paired with the relaxation exercises. | 2 | |
| More flexibility | just a little bit more flexibility in terms of the content of the sessions, um how many sessions it’s over. | 2 | |
| Reduce session content | depending on the individual, you might want to split up some of the sessions, so you are delivering less in a session. | 1 | |
| More carer-only sessions | think perhaps having more time with the carer before the service user is involved in that second session. | 1 | |
| Initial meet-and-greet | I wonder whether having an additional session at the start, for an informal ‘meet and greet’ with both client and carer, before starting the BEAMS-ID work and before having any set agenda, would be useful to consider in the future. | 1 | |
| Visual formulation session | Maybe it would be nice to have that sort of visual formulation session. To bring it all together. | 1 | |
| 2. Intervention | Further resource adaptation including additional information | A feeling that the resources could be adapted further (e.g. language simplified further). ‘(manual) the actual manual itself didn’t provide enough resource or enough information there to adapt it to my patient’. Reviewing the ABC charts would benefit from more focus in the manual – more guidance about how to do this and what to do with this information. ‘So maybe in the manual it might be easier just to say, you know. Fine to adapt, or whatever is needed as well as long as it’s within the concepts of delivering BEAMS’. | 8 |
| BEAMS-ID supervision | Might be beneficial in the future for the research team to offer BEAMS supervision. | 2 | |
| Intervention takes time | Recognition that behavioural approaches take a huge amount of time and commitment. | 2 | |
| More contact with research team | Clinicians would have liked more contact with the research team – at times felt unsure about expectations and what feedback would be helpful. | 1 | |
| Involvement in information gathering | I wasn’t involved in a lot of the screening and in some of the pre intervention questionnaires and that information gathering. That part would have been really, really helpful. | 1 | |
| Mid-point check-in | mid treatment touchpoint would have been really helpful. | 1 | |
| Prior meeting/training with care team | I think if working with a care team, I think going in at the beginning and sort of delivering maybe some training, just brief training, or a brief overview of what it is, to our staff team as a whole. Would have made quite a big difference, particularly with time and sessions. | 1 | |
| Consistency with care team | I think had there been more consistency the potential for reinforcement to be introduced maybe would have gone a bit better. | 1 | |
| Slower training pace | maybe the (training) pace could have been a bit slower, I guess. | 1 | |
| Knowledge of fear | It may be helpful to know, have some degree of knowledge of potentially what would be their fear when they come into the study. | 1 | |
| Earlier introduction of concepts | And perhaps some of those earlier sessions, could have been devoted to making smaller rungs on the fear ladder. | 1 | |
| Intervention Supplementary Material 1 | That they might struggle with some of the kind of theoretical stuff, so whether a video, short video or a clip, or even a link, or something that they could be referred to, they could look at in their own time, might just demonstrate what we’re trying to do. | 1 | |
| Removal of visual material | And I don’t think that [visual materials] was something that my particular client really valued. So, if I was doing that independent of the study, I probably wouldn’t have used those. | 1 | |
| More relaxation techniques | being given more suggestions on relaxation techniques that work specifically. Particularly well with those with moderate to severe learning disabilities would be really helpful. | 1 | |
| More in-depth carer information | I think perhaps the resources for carers could be slightly more in-depth … carers did mention that they would benefit from that. | 1 | |
| Information about applying to different care teams | So the treatment plan applied to the service user as well as mum … I think there is sort of a nod to it in the manual, but whether there’s something more explicit about that. | 1 | |
| Information about the participant’s wider system | I thought it would be helpful in the manual to have that sort of explicit bit about there’s a wider system around the person. | 1 | |
| Less repetition | There were some things I thought maybe were a bit repetitive. So by the time we got to maybe session 10 and it obviously reminds you to go through the breathing exercises with the person. I didn’t think she needed that because she was using them quite spontaneously. | 1 | |
| Linking back to functional assessment | So the first session like, maybe there needs to be something about how you link it back to those sort of the functional assessment bits. | 1 | |
| Inclusion of safety behaviours and cognitive elements | I think maybe it felt a little simplistic, like perhaps overly simplistic at points like the fact they didn’t include the safety behaviours, didn’t include cognitive elements, and those arose. | 1 | |
| Clarity around assessment interview | I was confused about the assessment interview, in terms of who and when this should be completed … maybe more clarity around this would be helpful for future therapists. | 1 | |
| Interview assessment prior to session | It’s easier if carers to the interview assessment prior to the session. | 1 | |
| Discussion of preference pictures | If carer doesn’t take pictures of preferred activities for the preference assessment, it could be harder to complete. Perhaps including a quick conversation about this in Session 1 could be a good way forward, as therapist could prepare some visuals to bring. | 1 | |
| More space for explanation on fidelity checklists | The feedback form might benefit from more space to explain ‘why’ we put the answers we put. | 1 | |
| More options for feedback | It feels like the clinicians have lots more feedback that they haven’t been able to give. Unclear if this feedback is relevant to a feasibility study and how this feedback can be given, if helpful. | 1 | |
| Therapist skill | For some clients it would have been appropriate to involve the client in the development of the fear ladder. The skills of an experienced LD clinician are required to determine what is and isn’t appropriate. | 1 | |
| Include behavioural formulation model | A suggestion to include a behavioural formulation model in the manual. | 1 | |
| Work required before intervention | Certain things need to be in place before the intervention (e.g. basics such as meaningful activity, sleep routine and prior understanding of the person’s communication needs). | 1 | |
| Improve recruitment strategy | The recruitment stage seemed to take a long time – clients met with many different professionals. Recruitment away from the service set up expectations that the service may have been unable to fulfil. | 1 | |
| Additional clinician training | One recommendation of the research might be that clinicians (e.g. nurses) within community LD services are trained up in taking blood tests. | 1 | |
| 3. Additional measures | QoL | I guess it did you say you’ve got like a quality of life one haven’t you? … thought that would potentially be useful. | 2 |
| Meltdowns | probably incidents or meltdowns, something like that. | 1 | |
| Carer confidence | I think the carers’ confidence in supporting the person that they’re caring for would be really helpful. | 1 | |
| Goal attainment | like goal attainment scaling which I really like because you can adapt it so much to the individual. So that’s probably quite a nice outcome measure, I think. | 1 | |
| Participant self-esteem | there’s something about her and her development as an individual separately to the carer … I don’t know what the measure might be, but whether it is self-esteem. | 1 |
Acceptability and suitability of BEAMS-ID
Findings relating to the acceptability and suitability of BEAMS-ID are found within Table 39. Therapists were of the view that the intervention was suitable for autistic participants with moderate to severe learning disabilities, although one therapist commented that it may not be suitable for all cases, or may be more suitable for certain presentations. Another therapist mentioned that offering interventions to people with moderate learning disabilities is more challenging relative to those with mild learning disabilities.
Therapists were also positive about carer engagement, and commented that carers were motivated, engaged and enthusiastic. Two therapists who were interviewed commented that carer engagement surpassed initial expectations. Some of the therapists mentioned that resistance to change, a reduction in engagement, and a lack of comprehension were potential issues.
All of the therapists were positive about the intervention meeting the needs of the participant, and commented that the intervention met needs. Moreover, they all described positive outcomes for participants, and the value of the adaptations to meet participant needs. Some commented that additional time was needed, and in one case a lack of investment to complete graded exposure was described. Similarly, the majority of the therapists were of the view that the intervention met the needs of carers. The intervention was considered helpful and valued, and carers were seen to have benefited or said they felt supported. One therapist mentioned that the carers considered the possibility that the intervention would be helpful for other people who live within supported living. However, one therapist mentioned that the intervention may not have met expectations, or they were uncertain, and another indicated that they had difficulties due to having different carers turn up to each session.
The majority of therapists (75%) interviewed considered that the materials used during the intervention, including the manual itself, were appropriate and acceptable. Some of the therapists commented that some participants may not need the visual materials that were available, while others commented that they were unsure whether the participant had understood some of the materials. One therapist spoke about needing to create additional resources but considered that this is to be expected, and another indicated that more information about how to adapt the intervention was needed for their specific participant. They also commented that the materials were appropriate for carers. Therapists also commented that therapists needed to be experienced in working with people with learning disabilities when delivering the intervention, while others commented that the intervention was easy to follow, with a clear structure, which was worthwhile and valuable. One therapist indicated that the intervention was well balanced in providing instruction and encouraging clinicians to make decisions to meet participant need.
Therapists were also positive about using the intervention in the future and intended to carry on using the techniques that they have learnt. Another commented about the importance of ensuring the manual was flexible enough to meet participant need, and another commented on the importance of ensuring that carers are engaged. One therapist was of the view that using the intervention in the future would be dependent upon having carers available to support intervention delivery, which is a key included adaptation. Some spoke about using their learning with other people with learning disabilities and training other professionals in the delivery of the intervention. Therapists were also positive about the use of randomisation within a future trial (see Table 39).
Therapist training
Therapists were positive about the training they received in the intervention (see Table 40). Training was described as helpful, positive, engaging, interactive and well-explained, along with further positive findings. One therapist commented that the pace was too fast for them because they did not do a lot of this type of intervention work in their day-to-day practice. Considering benefits for therapists, including benefits for their own professional development, therapists were again positive, with 88% mentioning that the training was ‘enjoyable’. They reported that the experience helped promote learning and the implementation of skills. Some commented that taking part in training and delivering the intervention changed their practice and two therapists made comment about the value of helping participants make progress.
Intervention delivery
Therapists were interviewed about their experience of delivering the intervention (see Table 41). The majority of therapists (88%) reported that they needed additional time for each session but felt that the frequency of sessions was appropriate. However, not all shared this view, and one therapist commented that the sessions were too long, while another indicated the length was appropriate. These findings suggest that some revisions to the intervention manual are required to ensure that therapists are aware that they are able to adapt the length of sessions to meet participant needs. The majority (88%) were positive about the experience of delivering the sessions, which were said to be easy and enjoyable, but one commented that the sessions were time-consuming, and another reported that it was slow to get going. There was also a comment that self-reported fidelity may be associated with bias as it is completed by the therapist themselves, and another commented that fidelity may have dropped off for them part way through the intervention.
The majority (75%) reported that involvement of carers was positive, while others reported mixed responses or raised issues regarding lack of consistent carer support, or difficulties with implementing some aspects of the intervention (e.g. relaxation). Therapists noted that it was sometimes challenging to teach relaxation skills to people with moderate to severe learning disability.
Considering intervention facilitators, therapists said that the structure, resources and materials, and carer engagement and understanding, along with having a consistent carer attending sessions helped ensure success. Other facilitators were said to be supervision and support, along with adopting a participant-led approach. Specific aspects of the intervention were also regarded as facilitators, including the preference assessment, fidelity checklists, intervention plan, flexibility, carer sessions, and other specific aspects of the intervention (e.g. use of reinforcement, developing an intervention plan).
Considering intervention barriers, therapists thought that some difficulties with delivering specific components with specific individuals were challenging (e.g. 75% noted difficulties implementing relaxation). Carer attitudes or beliefs, carer understanding, difficulties communicating with carers, having different carers attend sessions, and carer commitment were also seen to be barriers. Therapists also reported some challenges with implementing some aspects of the intervention which linked to the specific needs of participants, including motivation and engagement, and difficulties with developing the fear ladder, covering all the material within a single session, or overcoming safety behaviours, behaviours that challenge, and accessing materials or resources. One therapist commented that one participant did not need all the sessions as prescribed to reach their goal. One clinical psychologist commented that it was challenging to meet the needs of university-based research within the NHS, and also commented that clinical psychologists do not generally use evidence-based manualised interventions; they further commented that the intervention was essentially what they would be using in their clinical practice but also commented that they had to change their clinical practice when using the intervention (see Table 42).
Therapeutic relationship
A summary of our findings about the experience of the therapeutic relationship from the viewpoint of the therapists is found within Table 42. Therapists reported that they experienced the therapeutic relationship as positive, but some commented that it was difficult to establish with some participants. One therapist commented that the preference assessment within the intervention helped, while another commented that it developed over time. They also commented that the structured nature of the intervention helped to encourage the development of a therapeutic relationship.
Suggested improvements or revisions
Therapists were asked to make recommendations about how the intervention could be revised and a summary of our findings is found in Table 43. All the therapists suggested that the addition of more sessions would be helpful, while at the same time a proportion of these therapists also made comment that the number of sessions was appropriate. They suggested a reduction in the amount of content, but also an increase through the addition of a follow-up session, coupled with more flexibility and more carer-only sessions. In terms of materials, they all suggested increased information to clarify how much adaptation can be made by therapists. While some suggested a reduction in content, others suggested increasing content, such as the inclusion of more material for carers, and more relaxation work. There were also some suggestions for greater input from the research team at various points during the research process. Therapists were also asked about their views on additional outcome measures that they may consider appropriate. They suggested a measure of QoL, and a measure that indexed ‘meltdowns’, as well as carer confidence, goal attainment, and self-esteem. There were comments acknowledging that some of these measures were already included.
Chapter 6 Discussion
Summary of findings
Phase 1a
Objective 1: adaptation of an existing intervention
We further adapted an existing intervention manual for use with autistic adults with moderate to severe learning disabilities within Phase 1a over five meetings with our IAG composed of carers and clinicians, led by an autistic person. Our resulting intervention manual comprised 12 sessions and a full description of the intervention is found within Chapter 3.
Objective 2: development of an intervention fidelity checklist
We adapted an existing fidelity checklist,34 which was accepted by our IAG without any revisions.
Objective 3: appraise and consider several candidate outcome measures of anxiety-related symptoms, and secondary outcomes, and make a recommendation for use within Phase 2
A series of candidate outcome measures were considered by the IAG, including detailed information about the format, intended age range, time needed to complete, and psychometric properties. The group recommended that a measure of behavioural and emotional problems,94 behaviours that challenge,95 anxiety and other psychopathology,97 and a measure of community engagement96 were used within Phase 2.
Objective 4: development of a logic model
The final objective for Phase 1a was the development of a logic model collaboratively with our IAG. This was successfully completed and is found in Figure 2.
Phase 1b
Objective 1: complete a national survey of existing interventions for autistic adults with anxiety disorders who have moderate to severe learning disabilities
A national survey of TAU was undertaken to describe interventions for anxiety amongst autistic adults with moderate to severe learning disabilities. The results indicated that psychological interventions were the most frequently used intervention. The key procedures and activities within psychological interventions were described in rather generic terms, and only 3% of responses indicated that exposure therapy was used. Respondents also indicated a variety of adaptations would be made to psychological interventions to meet participant needs, which included providing communication support, adjusting session content, timing and duration, and involving carers within sessions, amongst other adaptations.
The next most frequently mentioned intervention was medication. Other infrequently mentioned interventions included sensory strategies, communication training, increased staff support, touch therapy, music therapy, along with speech and language therapy and occupational therapy.
The most salient finding from our TAU survey was that exposure therapy, which is a key part of the BEAMS-ID intervention, was infrequently offered to autistic adults with moderate to severe learning disabilities who are anxious.
Phase 2
Objective 1: to model the manualised intervention to determine the acceptability and feasibility for all stakeholders, including patients, carers, and clinicians, and adjust as required
The findings indicated that the intervention was acceptable to all stakeholders, including autistic participants with moderate to severe learning disabilities. However, one carer commented that the intervention required further adaptation due to the complexity of the autistic person with moderate to severe learning disabilities. The results indicated that it was feasible to deliver this intervention to autistic participants with moderate to severe learning disabilities with support from carers. Adjustments to the intervention following the completion of this study were recommended which included: (1) reinforcing the importance of consistent carer engagement, understanding, and motivation, (2) further guidance on the timing, frequency and number of intervention sessions, (3) further guidance on the creation of bespoke intervention materials to meet participant need, (4) further guidance about teaching relaxation to people with learning disabilities, noting that it is challenging to teach relaxation to some people with moderate to severe learning disabilities, (5) increased guidance about the nature and degree of intervention adaptation to meet need and (6) formalising arrangements for supervision within the context of a future trial. This would most likely be group-based supervision led by members of the trial team and in addition to local supervision.
The intervention was successfully modelled with 28 autistic participants with moderate to severe learning disabilities. Participants attended, on average, 80% of the intervention sessions. Our fidelity ratings were successfully completed by therapists and scores ranged from 88.23 to 99.54 out of a maximum of 100.
Autistic participants with moderate to severe learning disabilities indicated that they liked the materials used during the intervention, including the use of the Fear Ladder, making choices, and some indicated that they liked some of the adaptations (e.g. carer attending, adapted rating scales, visual schedules). It was noted that a majority indicated that they did not like learning about anxiety.
Carers were positive about the intervention and indicated that it met the needs of autistic participants along with their own needs. They also indicated that the intervention materials and adaptations were appropriate, along with the approach taken by therapists. One carer commented that the person they care for had needs that were too complex for the intervention. Carers were also positive about the outcomes following the completion of the intervention. They indicated that they had an improved understanding of autism and anxiety, and how to respond to anxiety, which are outcomes described within our logic model (Figure 2). Carers also noted that the therapeutic relationship with the therapists was valuable, which is seen as part of the mechanism of change, as described in our logic model (see Figure 2).
Therapists were of the view that the intervention was suitable for autistic participants with moderate to severe learning disabilities and met their needs. They were also of the view that the manual and associated materials were appropriate and acceptable. Therapists were positive about engaging carers within the intervention, which is again described in our logic model (see Figure 2), and thought that the intervention met carers’ needs. Therapists, in a similar way to carers, also indicated that the therapeutic relationship was valuable, but commented further that developing a positive therapeutic relationship was challenging in some cases. Therapists made a series of suggestions for the research team to consider, which included increasing or decreasing the number of sessions and the length of each session. They also suggested the inclusion of additional guidance about the nature of adaptations that can be made by therapists. These were addressed by the study team in subsequent revisions of the intervention manual.
Objective 2: to judge the appropriateness, including response rates, of our measures of anxiety-related symptomatology for use within a larger study
The percentage of missing data across the outcome measures was low and ranged from 0% to 2.38% (see Table 30). There were no issues with response rates, as all those who remained enrolled in the study completed the outcome measures across time. Our measures were completed by carers, and they commented that some individual items appeared repetitive, and some said they had difficulty answering some of the questions. Some noted some issues with completing them online, which was related to the way the questions were displayed upon their screen and can be easily addressed in the future. There was comment from one carer that they struggled to find the time to complete them, while 57% of those interviewed commented that the outcome measures were acceptable and easy to complete. In the context of a future trial, researchers should make attempts to lessen the number of outcome measures or make use of shorter measures.
Objective 3: to examine the feasibility and acceptability of consent and associated processes (e.g. use of the Mental Capacity Act)
Carers reported no marked difficulties with our PIS or consent processes, which were seen as clear, helpful, and straightforward. However, 79% of autistic participants with moderate to severe learning disabilities were judged not to have capacity to make a decision about taking part in this study. For these participants, on average, it took nearly 5 weeks to enrol them in the study to enable eligibility screening. The reason for this delay was predominantly the length of time taken to identify a consultee and seek their advice. While seeking consent from participants or advice from a consultee was acceptable and feasibile, the time taken to seek advice from a consultee would need to be considered when designing a randomised trial with a larger sample size.
Objective 4: to describe factors that facilitate or challenge the implementation of our intervention
Talking Mats was used to help give autistic participants with moderate to severe learning disabilities a voice. Participants indicated that they liked the information booklets that were used as part of the intervention, liked coming to the sessions, liked that their carer was involved, and liked the Fear Ladder, doing relaxation, and using the ratings scales and visual schedules, which are core parts of the intervention. A majority indicated that they did not like experiencing anxiety during the intervention but liked meeting new people.
Carers indicated that the key facilitators to the implementation of the intervention were: (1) the intervention was adapted to meet the needs of autistic people with moderate to severe learning disabilities, which included adopting a person-centred approach, (2) the experience of attending therapy was positive, informative, and enjoyable, and (3) the formation of a positive therapeutic relationship with the therapist. Some of the intervention barriers described by carers were related to circumstances not directly attributable to the intervention (e.g. illness, holidays, lack of staff), or were related to difficulties with accessing appropriate materials (e.g. challenges with accessing phlebotomy), difficulties with making use of the intervention with some individuals (e.g. difficulties with engaging some participants), the quantity of information, and the time taken to take part in the intervention. It is important to make sure that carers understand the commitment associated with taking part in this intervention and their role. There was one instance where differing therapist and carer beliefs about the function of behaviour was described as a barrier.
Therapists described the following key facilitators to the implementation of the intervention: (1) clear structure, (2) therapists who understand learning disabilities and are committed, (3) commitment from therapists, (4) carer understanding and engagement, (5) meeting carer needs, (6) making use of appropriate materials that are adapted, (7) high-quality therapist training and associated benefits for therapist professional development, (8) access to supervision, (9) a specific aspect of the intervention (e.g. fidelity checklists, preference assessments, reinforcement, carer-only sessions, positive therapeutic relationship) and (10) flexibility. Factors that had the potential to challenge the implementation of the intervention from the viewpoint of the therapists were: (1) difficulties implementing relaxation techniques which required further adaptation, (2) difficulties with participant engagement and motivation, (3) different carers attending sessions, (4) difficulties with implementing some aspects of the intervention with some participants (e.g. ABC charts not completed, or difficulties with the Fear Ladder), (5) too much session content, (6) therapists needing time to learn of new techniques, and (7) encountering behaviours that challenge.
Recruitment and retention
Recruitment into Phase 2 was challenging, and the issues encountered were attributable to attempting to recruit autistic participants with learning disabilities during a global pandemic. The aim was to recruit 30 autistic adults with moderate to severe learning disabilities. Thirty-four potential participants were referred into the study, and 85% (N = 29) were assessed for eligibility. Ninety-seven (N = 28) per cent of those assessed for eligibility were enrolled in the study and allocated to receive the intervention. These participants were recruited over 12 months. We were able to successfully recruit autistic participants with severe learning disabilities and recruited slightly more of this group than those with moderate learning disabilities. The accrual rate was 2.80 participants per month, which is likely to be an inaccurate estimate of the likely accrual rate in a larger study given that the study took place during the COVID-19 pandemic and was estimated using a small sample; there was evidence that our accrual rate increased over time. Our last site to join the study on 6 September 2022 recruited three participants in ˂ 1 month. Participant retention was judged to be positive, as the observed attrition rate was 14%. The reasons for participant loss in three cases were not associated with the intervention or research processes. In one case, the reason for loss was not clear as they did not respond to repeated attempts to make contact.
Feasibility and acceptability of study processes and outcome measures
Carers were positive about the consent process and our participant information booklets. They also indicated that our materials for autistic adults with moderate to severe learning disabilities were appropriately adapted to meet need. One carer commented that they would have appreciated more information about the duration of the intervention when the study was explained to them, and this can be addressed in the future. Carers reported no barriers associated with the study processes and willingness to take part and spoke about a desire to learn more and help others while being open-minded and interested. Randomisation in a future trial was judged to be acceptable to both carers and therapists. The most significant challenge was the amount of time it took to enrol participants who lacked capacity to make a decision about whether they wished to take part in this study; additional time would need to be incorporated within any future clinical trial considering that for those who lacked capacity, it took on average over 1 month to confirm consultee advice.
All those enrolled in the study completed all outcome measures at both baseline and follow-up. The percentage of missing items at baseline was low, and ranged from 0% to 2.38%, and was also low at follow-up, and ranged from 0% to 1.56%. While outcome measure completion was positive, carers did indicate that they found some of the items repetitive or unrelatable. One person commented that there were too many questions, and another said they had difficulties finding time to respond. However, another said they were acceptable, and another mentioned they were easy to complete. Considering implications for a future study, further attempts to thin the number of questions should be undertaken. One carer commented that they had difficulties with the display of items on their computer screen; the labels for the scale would disappear as they scrolled down through the items. This can be easily addressed to ensure that the labels remain on the screen.
There was change over time on our outcome measures in the desired direction which cannot be attributed to the intervention due to the design of this study. There were noted changes in emotional and behavioural problems, and behaviours that challenge. There is evidence of an association between anxiety and behaviours that challenge amongst people with learning disabilities114 and interventions to treat anxiety amongst this population would be expected to lead to a reduction in behaviours that challenge.
Feedback from sites
There were a series of challenges reported by sites during this study. The majority were related to the pandemic, insufficient staffing, and clinician workloads. However, additional challenges were encountered within two sites due to a national ransomware attack on electronic patient records which made screening for potentially eligible participants impossible, and this was beyond the control of the research team and our NHS sites.
Some sites raised concerns with the study team that clinicians may be gatekeeping by withholding information about the study from participants who may be eligible. This is of concern. One of the associated reasons for this was clinician workload, and within a future study it would be appropriate to seek further reassurance to ensure that therapists who are trained to deliver an intervention have capacity and support from their NHS line managers to contribute to the study.
Sites and the research team also noted that information about the study was not being shared with some participants with moderate to severe learning disabilities because a formal diagnosis of autism had not been previously completed; these individuals were eligible for and in receipt of services from NHS community learning disabilities support, but it was not possible to formally diagnosis autism to enable an eligibility assessment to take place. Some clinicians and sites expressed concern about this because the intervention has the potential to benefit all adults with moderate to severe learning disabilities who are anxious. Widening the eligibility criteria to all those with moderate to severe learning disabilities, including those with and without autism, may improve accrual rates in a future study.
Intervention training, adherence and fidelity
During Phase 2, 40 therapists were trained, and 35% (N = 14) did not go on to work as a therapist during the study. Seven therapists did not complete their GCP training, and a further seven did not go on to act as a therapist even though all requirements had been met. The most frequently cited reason was that therapists were too busy or simply did not respond to attempts to contact them despite repeated attempts by both the research team and local R&D teams. While some therapist loss may be attributable to the pandemic, and it is difficult to judge the likely magnitude in the future, the loss of trained therapists has implications for the feasibility of a future larger study in terms of costs and training time. In a future study, further assurance that trained therapists have capacity to deliver the intervention should be sought by the research team in collaboration with NHS R&D teams.
On average, participants attended 80% of sessions, suggesting good adherence. Therapists completed a fidelity checklist for each session, and the percentage of items endorsed ranged from 88.23 to 99.54, suggesting high fidelity.
Patient and public involvement
This study was developed in collaboration with the NAS. NAS were a partner working with us to develop our initial application for funding, which included writing and study design. They also helped to develop all our participant-facing materials and dissemination strategy, and attended the Study Management Group (SMG) and Study Management Committee (SSC), providing regular input throughout the duration of the study. Our partnership with NAS will continue as we embark upon our dissemination plan.
There was good PPI representation within our SSC, which was composed of family carers of autistic adults with moderate to severe learning disabilities, some of whom also had problems with anxiety. While there are challenges with included autistic adults with moderate to severe learning disabilities as PPI members, an autistic adult was a member of our SMG and our SSC.
The BEAMS-ID intervention was adapted for use with autistic adults with moderate to severe learning disabilities together with the IAG, which was chaired by an autistic person, leading to changes to the content of the intervention and the associated processes. This group comprised family carers and clinicians, and they worked collaboratively together with the research team. They also appraised our candidate outcome measures, making recommendations, reviewed our fidelity checklist, and provided feedback on our draft logic model. Our candidate outcome measures and fidelity checklist were tested within Phase 2. Considering a future larger study, in the absence of an IAG composed of PPI members, it would be important to include a PPI advisory group that met regularly throughout the project to ensure the voice of carers and autistic people have a genuine impact. Many family carers have caring responsibilities and arrangements would need to be made to ensure that carers are able to attend meetings.
Equality, diversity and inclusion
This research project involved autistic participants with moderate to severe learning disabilities and their carers. This group is often excluded from research, and, due to the nature of their disability, interventions need to be adapted. Autistic people with moderate to severe learning disabilities have a high level of need, but there is no robust evidence that psychological interventions are effective for treating anxiety with this population. 4 Autistic individuals with moderate to severe learning disabilities face an evidence inequity whereby there is a lack of research to guide interventions despite being more likely to develop anxiety disorders. The current project focused upon adapting an existing intervention further for use with this population.
The current project was a feasibility study designed to address needs by adapting and modelling an existing intervention. We had near equal representation of autistic participants with moderate or severe learning disabilities. Just under 54% of our participants had severe learning disabilities, and just over 46% had moderate learning disabilities, and the evidence we generated indicated that the intervention and associated research processes were feasible with those with moderate and severe learning disabilities. Just under one-fifth of our participant sample were from non-white backgrounds, suggesting that diversity in ethnicity was present amongst our participant population; this is slightly higher than the estimate of the non-white population within England and Wales. 115 To ensure that our intervention was likely to be acceptable, we refined our adaptations together with carers, autistic people, and clinicians.
We also made use of easier-to-read participant information and consent forms for autistic participants with moderate to severe learning disabilities. These were booklets which were smaller in size than standard-sized participant information leaflets. Our participant information booklet for autistic adults with learning disabilities is found within our Report Supplementary Material 1. These were developed with guidance from a speech and language therapist who was a member of the research team, with further input from NAS. We made use of visual materials taken from Easy on the I (www.learningdisabilityservice-leeds.nhs.uk/easy-on-the-i/). This is a free-to-use repository of visual images developed by Leeds and York Partnership NHS Foundation Trust for use with people with learning disabilities to promote and enable communication. These visual materials were also used throughout our intervention to improve accessibility.
Strengths and limitations of the research
The key strengths to this research project are:
-
The intervention used within this feasibility study was a previously developed anxiety intervention for use with autistic adults. This was adapted for use with autistic adults with moderate to severe learning disabilities in collaboration with autistic people, carers and clinicians. This group also selected the outcome measures, refined the intervention logic model, and reviewed the intervention fidelity checklists. PPI involvement in this study is a genuine strength. This increased the probability that the intervention would be acceptable to stakeholders, including autistic adults with learning disabilities which was reflected within our evaluation.
-
Within this feasibility study, a strength is that the focus was to model the intervention to determine its acceptability and make further refinements as required prior to completing a larger study. A series of interviews were undertaken with autistic adults with learning disabilities, carers, and clinicians as part of this process, ensuring that the views of all stakeholders were represented. It is a strength that the voice of autistic participants with moderate to severe learning disabilities was included.
-
Another strength is the inclusion of those with severe learning disabilities, who were well represented amongst our participant population, which helped to ensure that the intervention was successfully modelled with this group.
-
TAU was also described, and the findings indicated that exposure therapy for anxiety disorders is not frequently offered to autistic adults with moderate to severe learning disabilities within the NHS.
-
This project was completed during a global pandemic, which likely had a detrimental impact upon accrual. However, sufficient numbers of participants were recruited to allow us to model the intervention and research processes successfully, which is a clear strength.
The limitations to this research project are:
-
This project was completed during the time of a global pandemic which resulted in challenges beyond the control of the research team, clinicians, and NHS sites. This means that some of our parameter estimates (e.g. accrual rate) were calculated during a period when many routine services were being delivered differently within the NHS.
-
It should be noted that our sample size was small, and this was a single-group modelling study. For a study of this type, this was appropriate, as it provided the research team an opportunity to focus upon modelling the intervention and recommend future refinements. However, due to the design of the study, it was not possible to model randomisation, bearing in mind that this was considered within our carer and therapist interviews. A future pilot trial with randomisation would need to be completed to test this adequately before proceeding to a definitive trial.
-
The fidelity checklist was completed by therapists. Audio recording of sessions and fidelity ratings using these recordings by raters were not tested during this study. This would need to be incorporated within any future pilot trial.
-
Finally, our candidate outcome measures were all proxy-rated instruments completed by carers. The reason for this is that it is not possible for many adults with moderate to severe learning disabilities to complete self-report outcome measures. While this could be considered a weakness, it is the case that the chosen candidate outcome measures are standardised and have good validity.
Implications for the BEAMS-ID intervention
The findings indicated that the intervention was acceptable to autistic adults with moderate to severe learning disabilities, carers, and clinicians. However, our findings indicated that some revisions were required as follows:
-
Carers: there were some issues with different carers attending sessions, which was seen to have a detrimental impact upon communication and engagement within the intervention. Related to this, there were issues with carer engagement and motivation described in some cases. This was more of an issue for individuals who were supported by paid carers, rather than for those who were supported by family members, although some family members also experienced difficulties. The importance of consistent carer engagement, understanding and motivation needs to be strengthened within the intervention and within the carer materials.
-
Timing, frequency, and number of sessions: our findings indicated that there were some disparate views at times about the timing, frequency, and number of sessions. Some indicated that the number of sessions, timing and frequency were appropriate, while others indicated that fewer or more, shorter or longer, or more or less frequent sessions would have been helpful, often related to participant needs. Increased flexibility about the number of required sessions, along with their timing and frequency, is an appropriate adaptation. This would allow therapists, collaboratively with carers and participants, to adapt the timing, frequency, and number of sessions, ensuring that the intervention is delivered in a person-centred manner, while still delivering the core components of the intervention.
-
Intervention resources: there was evidence that the intervention resources were appropriate for participants, but this was not the case for all. Within the intervention, it is recommended that therapists make use of existing communication strategies and draw upon existing interests and materials to promote engagement. While the intervention included guidance on making further adaptations, including the development of bespoke materials to meet needs, this should be strengthened further within the intervention.
-
Relaxation sessions: therapists described some challenges with the delivery of relaxation sessions associated with working with people with learning disabilities. Increased guidance on how to deliver this aspect of the intervention to this population should be incorporated in the manual.
-
Adaptations: it was apparent that therapists were uncertain at times as to the nature and degree of adaptations that they could make to meet participant need while still delivering the core components of the intervention. The majority of the findings from therapists about suggested improvements to the intervention centred within this domain. Adapting the intervention to meet need is a core component of the intervention, and this was an interesting finding, suggesting that this needed strengthening within the manual and during therapist training. This should be incorporated within the revision.
-
Supervision: the supervision arrangements for therapists during this study were provided at site by experienced clinicians, while the research team provided ad hoc supervision and advice as required. This was not markedly problematic, but increased supervision from the research team was requested by some therapists. Formalising the arrangements for supervision in the delivery of the intervention within the context of a future pilot trial is recommended.
Progression criteria and potential for future trial
Our progression criteria are detailed in Table 44 and were considered by the SSC. It was noted that the accrual rate and carer acceptability of our outcome measures were graded ‘red’, while all other criteria were graded ‘green’. As already discussed, our accrual rate was most likely impacted by the global pandemic and is a likely underestimate of the accrual rate outside this context. It was noted that the last NHS site to enrol in this study towards the end of 2022 achieved an accrual rate of three participants in ˂ 1 month as the effects of the pandemic reduced. The view was that the accrual rate would probably be higher within a future trial taking place during a period when a global pandemic is not happening.
| Progression criterion | Progress | Number | Explanation |
|---|---|---|---|
| Recruitment: accrual rate is at least three patients per site per month on average | Red | CWPT: Initial 7-month rate: 0.29; final 3-month rate: 2.00 HWCT: Initial 7-month rate: 0.29; final 3-month rate: 1.5 Mersey: Initial 3-month rate: 1.33; final 3-month rate: 2.33 Leicestershire: 1 participant. Solent: last site to join the study and recruited 3 in ˂ 1 month. |
Recruitment was unduly affected by the pandemic. The accrual rate increased over time. Overall accrual rate collapsing across sites within the final 3 months was 6.33 per month. The average final 3-month site accrual rate was 2.21, which is ‘amber’. Target rate achieved by last site to join the study. |
| Attrition rate is 30% or lower | Green | 14% | Attrition appeared not to be related to the intervention or research processes. |
| Fidelity ratings indicate therapist adherence to the intervention of at least 70% | Green | 88.23–99.54% | – |
| At least 70% of carers and clinicians report that the intervention and consent procedures were acceptable | Green | 86% of carers considered the consent procedures acceptable. 88% of carers considered the intervention acceptable to meet need or considered the therapist responded to need. 100% of therapists considered the intervention was suitable or described benefits. |
It was noted that the Mental Capacity Act provisions lengthened the time taken to enrol a participant. |
| Participants received an average of 70% or more intervention sessions | Green | 80% | – |
| At least 70% of participants and carers complete outcome data at each time point | Green | 100% | – |
| At least 75% of items within each outcome measure for each participant are complete | Green | 97.62–100% | – |
| At least 70% of carers judge our outcome measures to be acceptable | Amber | Carers completed all the outcome measures. Rates of missing data were low. The majority were of the view that they were acceptable. However, some expressed some concerns about some of the questions. | Carers completed all the outcome measures. Rates of missing data were low. Their view was that some of the items within and across questionnaires seemed repetitive or they had difficulty answering. Some of this was probably associated with testing several measures within a feasibility study; this can be easily re-visited prior to a larger study. |
Considering outcome measures, carers commented that there were too many items, some had had difficulty responding, or they found some of the items repetitive. However, this must be balanced against the finding that all carers completed all the outcome measures, and the rate of missing data was low. It was advised that the research team should consider reducing the number of outcome measures in a future trial.
The SSC recommended that that the research should progress to a trial. A pilot trial with randomisation incorporating progression criteria towards a definitive randomised trial would be an appropriate next step.
Additional information
CRediT contribution statement
Peter E Langdon (https://orcid.org/0000-0002-7745-1825): Conceptualisation, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Visualisation, Writing – original draft, Writing – reviewing and editing.
Magdalena M Apanasionok (https://orcid.org/0000-0002-3861-3801): Data curation, Formal analysis, Investigation, Project administration, Resources, Supervision, Visualisation, Writing – original draft, Writing – reviewing and editing.
Emma Scripps (https://orcid.org/0000-0001-6140-2976): Data curation, Formal analysis, Investigation, Visualisation, Writing – original draft, Writing – reviewing and editing.
Karen Bunning (https://orcid.org/0000-0002-7396-9205): Conceptualisation, Funding acquisition, Methodology, Visualisation, Writing – reviewing and editing.
Malwina Filipczuk (https://orcid.org/0009-0001-5051-9842): Data curation, Formal analysis, Investigation, Resources, Visualisation, Writing – original draft, Writing – reviewing and editing.
David Gillespie (https://orcid.org/0000-0002-6934-2928): Conceptualisation, Funding acquisition, Methodology, Visualisation, Writing – reviewing and editing.
Richard P Hastings (https://orcid.org/0000-0002-0495-8270): Conceptualisation, Funding acquisition, Methodology, Visualisation, Writing – reviewing and editing.
Andrew Jahoda (https://orcid.org/0000-0002-3985-6098): Conceptualisation, Funding acquisition, Methodology, Resources, Visualisation, Writing – reviewing and editing.
Rachel McNamara (https://orcid.org/0000-0002-7280-1611): Conceptualisation, Funding acquisition, Methodology, Visualisation, Writing – reviewing and editing.
Dheeraj Rai (https://orcid.org/0000-0002-7239-3523): Conceptualisation, Funding acquisition, Methodology, Visualisation, Writing – reviewing and editing.
Kylie M Gray (https://orcid.org/0000-0001-6518-4240): Conceptualisation, Data curation, Formal analysis, Funding acquisition, Methodology, Project administration, Resources, Supervision, Visualisation, Writing – reviewing and editing.
Acknowledgements
We wish to sincerely thank all the autistic people who took part in our study and their carers who showed such enthusiasm and appreciation for the opportunity to take part in this study. We also wish to express our gratitude to the National Autistic Society and Robyn Steward (www.robynsteward.com).
We also wish to thank all the therapists who delivered the intervention and our principal investigators (PI):
-
Coventry and Warwickshire Partnership NHS Trust: Sarah Croom (PI), Cheryl Burbidge, Sophie Bates, Bethany Roberts, Sophie Hodges, Paula Kiley, Emily Fulton-Hamilton, Alexandra Gordon-Brown, Serena Hinze, Rachel Lee.
-
Herefordshire and Worcestershire Health and Care NHS Trust: Katherine Byron-Daniel (PI), Jodie Chippendale, Sarah Bravey, Natasha Tacy.
-
Leicestershire Partnership NHS Trust: Asit Biswas (PI), Amrita Dhanda.
-
Mersey Care NHS Foundation Trust: Alex Cookson (PI), Alastair Barrowcliff (PI), Claire Lloyd, Sarah Wastell, Bethany Bell, Andrew Tong, Charlotte Marshall, Linda Helsby, Lyndsey Miller, Dionne Broda, Liam Kingdon.
-
Solent NHS Trust: Lawrence Patterson (PI), Louise Hannant, Penny Vanderplank, Jo Ball.
We also wish to thank all the hard-working R&D staff within sites for persevering with this study during a global pandemic. We wish to thank Diana Smith and Alison Baker from the Centre for Research in Intellectual and Developmental Disabilities, University of Warwick, for providing administrative support.
Patient data statement
Using patient data is vital to improve health and care for everyone. There is huge potential to make better use of information from people’s patient records, to understand more about disease, develop new treatments, monitor safety, and plan NHS services. Patient data should be kept safe and secure, to protect everyone’s privacy, and it’s important that there are safeguards to make sure that they are stored and used responsibly. Everyone should be able to find out about how patient data are used. #datasaveslives. You can find out more about the background to this citation here: https://understandingpatientdata.org.uk/data-citation.
Data-sharing statement
All data requests should be submitted to the corresponding author for consideration. Access to anonymised data may be granted following review.
Ethics statement
This study was granted a favourable ethical opinion by Wales REC 6 and associated NHS Health Research Authority Approval (Ref: 21/WA/0013).
Information governance statement
Coventry and Warwickshire Partnership NHS Trust is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under the Data Protection legislation, Coventry and Warwickshire Partnership NHS Trust is the Data Controller, and you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our Data Protection Officer here www.covwarkpt.nhs.uk/privacy-notice-patients.
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/MWTQ5721.
Primary conflicts of interest: Kylie M Gray is a co-author of the manual for the Developmental Behavior Checklist (DBC2), published by Western Psychological Services. Royalties received from the sale of the DBC2 manual are donated to the funding of ongoing research in intellectual and developmental disabilities. David Gillespie was a National Institute for Health and Care Research (NIHR) Health Technology Assessment (HTA) Associate Board Member to 30 November 2020 and is a NIHR HTA Commissioning Committee Member from 1 September 2021 to 31 May 2025.
Publication
Langdon PE, Apanasionok MM, Scripps E, Barrowcliff A, Biswas A, Bunning K, et al. Behavioural interventions to treat anxiety in adults with autism and moderate to severe intellectual disabilities: The BEAMS-ID feasibility study. J Appl Res Intellect Disabil 2024;37(5):e13282. https://doi.org/10.1111/jar.13282
Disclaimers
This article presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HTA programme or the Department of Health and Social Care.
References
- Vereenooghe L, Langdon PE. Psychological therapies for people with intellectual disabilities: a systematic review and meta-analysis. Res Dev Disabil 2013;34:4085-102.
- Weston L, Hodgekins J, Langdon PE. Effectiveness of cognitive behavioural therapy with people who have autistic spectrum disorders: a systematic review and meta-analysis. Clin Psychol Rev 2016;49:41-54.
- Tapp K, Vereenooghe L, Hewitt O, Scripps E, Gray KM, Langdon PE. Psychological therapies for people with intellectual disabilities: an updated systematic review and meta-analysis. Compr Psychiatry 2023;122. https://doi.org/10.1016/j.comppsych.2023.152372.
- Vereenooghe L, Flynn S, Hastings RH, Adams D, Chauhan U, Cooper SA, et al. Interventions for mental health problems in children and adults with severe intellectual disabilities: a systematic review. BMJ Open 2018;8. https://doi.org/10.1136/bmjopen-2018-021911.
- Hofmann SG, Smits JA. Cognitive-behavioral therapy for adult anxiety disorders: a meta-analysis of randomized placebo-controlled trials. J Clin Psychiatry 2008;69:621-32.
- Sweet AA, Loizeaux AL. Behavioral and cognitive treatment methods: a critical comparative review. J Behav Ther Exp Psychiatry 1991;22:159-85.
- Hayes SC. Mindfulness and Acceptance: Expanding the Cognitive-Behavioral Tradition. New York: Guilford Press; 2004.
- Longmore RJ, Worrell M. Do we need to challenge thoughts in cognitive behavior therapy?. Clin Psychol Rev 2007;27:173-87.
- Borkovec T, Costello E. Efficacy of applied relaxation and cognitive-behavioral therapy in the treatment of generalized anxiety disorder. J Consult Clin Psychol 1993;61.
- Emmelkamp PM, Mersch PP, Vissia E, van der Helm M. Social phobia: a comparative evaluation of cognitive and behavioral interventions. Behav Res Ther 1985;23:365-9.
- Mattick RP, Peters L, Clarke JC. Exposure and cognitive restructuring for social phobia: a controlled study. Behav Ther 1989;20:3-23.
- Vogel PA, Stiles TC, Gotestam KG. Adding cognitive therapy elements to exposure therapy for obsessive compulsive disorder: a controlled study. Behav Cogn Psychother 2004;32:275-90.
- Norton PJ, Price EC. A meta-analytic review of adult cognitive-behavioral treatment outcome across the anxiety disorders. J Nerv Ment Dis 2007;195:521-31.
- Ougrin D. Efficacy of exposure versus cognitive therapy in anxiety disorders: systematic review and meta-analysis. BMC Psychiatry 2011;11.
- Podina IR, Visla A, Fodor LA, Fluckiger C. Is there a sleeper effect of exposure-based vs. cognitive-only intervention for anxiety disorders? A longitudinal multilevel meta-analysis. Clin Psychol Rev 2019;73. https://doi.org/10.1016/j.cpr.2019.101774.
- Rosen TE, Connell JE, Kerns CM. A review of behavioral interventions for anxiety‐related behaviors in lower‐functioning individuals with autism. Behav Interv 2016;31:120-43.
- Koegel RL, Openden D, Koegel LK. A systematic desensitization paradigm to treat hypersensitivity to auditory stimuli in children with autism in family contexts. Res Prac Pers Severe Dis 2004;29:122-34.
- Love SR, Matson JL, West D. Mothers as effective therapists for autistic children’s phobias. J Appl Behav Anal 1990;23:379-85.
- Luscre DM, Center DB. Procedures for reducing dental fear in children with autism. J Autism Dev Disord 1996;26:547-56.
- Shabani DB, Fisher WW. Stimulus fading and differential reinforcement for the treatment of needle phobia in a youth with autism. J Appl Behav Anal 2006;39:449-52.
- Schmidt JD, Luiselli JK, Rue H, Whalley K. Graduated exposure and positive reinforcement to overcome setting and activity avoidance in an adolescent with autism. Behav Modif 2013;37:128-42.
- Wolff JJ, Symons FJ. An evaluation of multi‐component exposure treatment of needle phobia in an adult with autism and intellectual disability. J Appl Res Intellect Disabil 2013;26:344-8.
- Allison G, Harrop C, Ellett L. Perception of peer group rank of individuals with early psychosis. Br J Clin Psychol 2013;52:1-11. https://doi.org/10.1111/j.2044-8260.2012.02041.x.
- Baird G, Simonoff E, Pickles A, Chandler S, Loucas T, Meldrum D, et al. Prevalence of disorders of the autism spectrum in a population cohort of children in South Thames: the Special Needs and Autism Project (SNAP). Lancet 2006;368:210-5.
- Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry 2008;47:921-9.
- Hofvander B, Delorme R, Chaste P, Nydén A, Wentz E, Ståhlberg O, et al. Psychiatric and psychosocial problems in adults with normal-intelligence autism spectrum disorders. BMC Psychiatry 2009;9.
- Joshi G, Wozniak J, Petty C, Martelon MK, Fried R, Bolfek A, et al. Psychiatric comorbidity and functioning in a clinically referred population of adults with autism spectrum disorders: a comparative study. J Autism Dev Disord 2013;43:1314-25.
- Wigham S, Rodgers J, South M, McConachie H, Freeston M. The interplay between sensory processing abnormalities, intolerance of uncertainty, anxiety and restricted and repetitive behaviours in autism spectrum disorder. J Autism Dev Disord 2015;45:943-52.
- Lidstone J, Uljarević M, Sullivan J, Rodgers J, McConachie H, Freeston M, et al. Relations among restricted and repetitive behaviors, anxiety and sensory features in children with autism spectrum disorders. Res Autism Spectr Disord 2014;8:82-9.
- Bakken TL, Helverschou SB, Eilertsen DE, Heggelund T, Myrbakk E, Martinsen H. Psychiatric disorders in adolescents and adults with autism and intellectual disability: a representative study in one county in Norway. Res Dev Disabil 2019;31:1669-77.
- Bradley E, Bolton PF, Bryson SE. Psychiatric comorbidity in persons with intellectual disability (ID) with and without autism. J Intellect Disabil Res 2004;48.
- Nimmo-Smith V, Heuvelman H, Dalman C, Lundberg M, Idring S, Carpenter P, et al. Anxiety disorders in adults with autism spectrum disorder: A population-based study. J Autism Dev Disord 2020;50:308-18.
- Linden A, Best L, Elise F, Roberts D, Branagan A, Tay YBE, et al. Benefits and harms of interventions to improve anxiety, depression, and other mental health outcomes for autistic people: a systematic review and network meta-analysis of randomised controlled trials. Autism 2023;27:7-30. https://doi.org/10.1177/13623613221117931.
- Jahoda A, Hastings R, Hatton C, Cooper SA, Dagnan D, Zhang R, et al. Comparison of behavioural activation with guided self-help for treatment of depression in adults with intellectual disabilities: a randomised controlled trial. Lancet Psychiatry 2017;4:909-19.
- Pouw LBC, Rieffe C, Stockmann L, Gadow KD. The link between emotion regulation, social functioning, and depression in boys with ASD. Res Autism Spectr Disord 2013;7:549-56. https://doi.org/10.1016/j.rasd.2013.01.002.
- Bellini S. Social skill deficits and anxiety in high-functioning adolescents with autism spectrum disorders. Focus Autism Other Dev Disabl 2004;19:78-86.
- Bellini S. The development of social anxiety in adolescents with autism spectrum disorders. Focus Autism Other Dev Disabl 2006;21:138-45.
- Factor RS, Condy EE, Farley JP, Scarpa A. Brief report: insistence on sameness, anxiety, and social motivation in children with autism spectrum disorder. J Autism Dev Disord 2016;46:2548-54. https://doi.org/10.1007/s10803-016-2781-x.
- Martinez-Gonzalez AE, Cervin M, Piqueras JA. Relationships between emotion regulation, social communication and repetitive behaviors in autism spectrum disorder. J Autism Dev Disord 2022;52:4519-27. https://doi.org/10.1007/s10803-021-05340-x.
- Whitehouse AJ, Durkin K, Jaquet E, Ziatas K. Friendship, loneliness and depression in adolescents with Asperger’s syndrome. J Adolesc 2009;32:309-22. https://doi.org/10.1016/j.adolescence.2008.03.004.
- Gotham K, Bishop SL, Brunwasser S, Lord C. Rumination and perceived impairment associated with depressive symptoms in a verbal adolescent-adult ASD sample. Autism Res 2014;7:381-91. https://doi.org/10.1002/aur.1377.
- Hedley D, Uljarevic M, Foley KR, Richdale A, Trollor J. Risk and protective factors underlying depression and suicidal ideation in autism spectrum disorder. Depress Anxiety 2018;35:648-57. https://doi.org/10.1002/da.22759.
- Hedley D, Uljarević M, Wilmot M, Richdale A, Dissanayake C. Understanding depression and thoughts of self-harm in autism: a potential mechanism involving loneliness. Res Autism Spectr Disord 2018;46:1-7. https://doi.org/10.1016/j.rasd.2017.11.003.
- Vickerstaff S, Heriot S, Wong M, Lopes A, Dossetor D. Intellectual ability, self-perceived social competence, and depressive symptomatology in children with high-functioning autistic spectrum disorders. J Autism Dev Disord 2007;37:1647-64.
- Hedley D, Young R. Social comparison processes and depressive symptoms in children and adolescents with Asperger syndrome. Autism 2006;10:139-53. https://doi.org/10.1177/1362361306062020.
- Crane L, Goddard L, Pring L. Autobiographical memory in adults with autism spectrum disorder: the role of depressed mood, rumination, working memory and theory of mind. Autism 2013;17:205-19. https://doi.org/10.1177/1362361311418690.
- Wallace GL, Kenworthy L, Pugliese CE, Popal HS, White EI, Brodsky E, et al. Real-world executive functions in adults with autism spectrum disorder: profiles of impairment and associations with adaptive functioning and co-morbid anxiety and depression. J Autism Dev Disord 2016;46:1071-83. https://doi.org/10.1007/s10803-015-2655-7.
- Hollocks MJ, Jones CR, Pickles A, Baird G, Happe F, Charman T, et al. The association between social cognition and executive functioning and symptoms of anxiety and depression in adolescents with autism spectrum disorders. Autism Res 2014;7:216-28. https://doi.org/10.1002/aur.1361.
- Spiker MA, Lin CE, Van Dyke M, Wood JJ. Restricted interests and anxiety in children with autism. Autism 2012;16:306-20. https://doi.org/10.1177/1362361311401763.
- Magiati I, Ong C, Lim XY, Tan JW, Ong AY, Patrycia F, et al. Anxiety symptoms in young people with autism spectrum disorder attending special schools: associations with gender, adaptive functioning and autism symptomatology. Autism 2016;20:306-20. https://doi.org/10.1177/1362361315577519.
- Gotham K, Bishop SL, Hus V, Huerta M, Lund S, Buja A, et al. Exploring the relationship between anxiety and insistence on sameness in autism spectrum disorders. Autism Res 2013;6:33-41. https://doi.org/10.1002/aur.1263.
- Rodgers J, Glod M, Connolly B, McConachie H. The relationship between anxiety and repetitive behaviours in autism spectrum disorder. J Autism Dev Disord 2012;42:2404-9. https://doi.org/10.1007/s10803-012-1531-y.
- Black KR, Stevenson RA, Segers M, Ncube BL, Sun SZ, Philipp-Muller A, et al. Linking anxiety and insistence on sameness in autistic children: the role of sensory hypersensitivity. J Autism Dev Disord 2017;47:2459-70. https://doi.org/10.1007/s10803-017-3161-x.
- Uljarevic M, Lane A, Kelly A, Leekam S. Sensory subtypes and anxiety in older children and adolescents with autism spectrum disorder. Autism Res 2016;9:1073-8. https://doi.org/10.1002/aur.1602.
- Mazurek MO, Kanne SM. Friendship and internalizing symptoms among children and adolescents with ASD. J Autism Dev Disord 2010;40:1512-20. https://doi.org/10.1007/s10803-010-1014-y.
- Weisbrot DM, Gadow KD, DeVincent CJ, Pomeroy J. The presentation of anxiety in children with pervasive developmental disorders. J Child Adolesc Psychopharmacol 2005;15:477-96.
- Niditch LA, Varela RE, Kamps JL, Hill T. Exploring the association between cognitive functioning and anxiety in children with autism spectrum disorders: the role of social understanding and aggression. J Clin Child Adolesc Psychol 2012;41:127-37. https://doi.org/10.1080/15374416.2012.651994.
- Dubin AH, Lieberman-Betz R, Michele Lease A. Investigation of individual factors associated with anxiety in youth with autism spectrum disorders. J Autism Dev Disord 2015;45:2947-60. https://doi.org/10.1007/s10803-015-2458-x.
- Moss P, Howlin P, Savage S, Bolton P, Rutter M. Self and informant reports of mental health difficulties among adults with autism findings from a long-term follow-up study. Autism 2015;19:832-41. https://doi.org/10.1177/1362361315585916.
- Green SA, Ben-Sasson A. Anxiety disorders and sensory over-responsivity in children with autism spectrum disorders: is there a causal relationship?. J Autism Dev Disord 2010;40:1495-504. https://doi.org/10.1007/s10803-010-1007-x.
- Green SA, Ben-Sasson A, Soto TW, Carter AS. Anxiety and sensory over-responsivity in toddlers with autism spectrum disorders: bidirectional effects across time. J Autism Dev Disord 2012;42:1112-9. https://doi.org/10.1007/s10803-011-1361-3.
- Boulter C, Freeston M, South M, Rodgers J. Intolerance of uncertainty as a framework for understanding anxiety in children and adolescents with autism spectrum disorders. J Autism Dev Disord 2014;44:1391-402. https://doi.org/10.1007/s10803-013-2001-x.
- Neil L, Olsson NC, Pellicano E. The relationship between intolerance of uncertainty, sensory sensitivities, and anxiety in autistic and typically developing children. J Autism Dev Disord 2016;46:1962-73. https://doi.org/10.1007/s10803-016-2721-9.
- Maisel ME, Stephenson KG, South M, Rodgers J, Freeston MH, Gaigg SB. Modeling the cognitive mechanisms linking autism symptoms and anxiety in adults. J Abnorm Psychol 2016;125:692-703.
- Vasa RA, Kreiser NL, Keefer A, Singh V, Mostofsky SH. Relationships between autism spectrum disorder and intolerance of uncertainty. Autism Res 2018;11:636-44. https://doi.org/10.1002/aur.1916.
- Hwang YIJ, Arnold S, Srasuebkul P, Trollor J. Understanding anxiety in adults on the autism spectrum: an investigation of its relationship with intolerance of uncertainty, sensory sensitivities and repetitive behaviours. Autism 2019;24:411-22. https://doi.org/10.1177/1362361319868907.
- NHS England . Building the Right Support: A National Plan to Develop Community Services and Close Inpatient Facilities for People With a Learning Disability and Or Autism Who Display Behaviour That Challenges, Including Those With a Mental Health Condition 2015.
- National Institute for Health and Care Excellence . Autism: Recognition, Referral, Diagnosis and Management of Adults on the Autism Spectrum. NICE Clinical Guideline 2012.
- National Institute for Health and Care Excellence . Challenging Behaviour and Learning Disabilities: Prevention and Interventions for People With Learning Disabilities Whose Behaviour Challenges 2015.
- National Institute for Health and Care Excellence . Mental Health Problems in People With Learning Disabilities: Prevention, Assessment and Management 2016.
- Buescher AV, Cidav Z, Knapp M, Mandell DS. Costs of autism spectrum disorders in the United Kingdom and the United States. JAMA Pediatr 2014;168:721-8.
- NHS England . NHS Research Plan 2017.
- Holden B, Gitlesen JP. A total population study of challenging behaviour in the county of Hedmark, Norway: prevalence, and risk markers. Res Dev Disabil 2006;27:456-65.
- Cooper SA, Smiley E, Jackson A, Finlayson J, Allan L, Mantry D, et al. Adults with intellectual disabilities: prevalence, incidence and remission of aggressive behaviour and related factors. J Intellect Disabil Res 2009;53:217-32.
- Deb S, Thomas M, Bright C. Mental disorder in adults with intellectual disability. 1: prevalence of functional psychiatric illness among a community-based population aged between 16 and 64 years. J Intellect Disabil Res 2001;45:495-50.
- Deb S, Thomas M, Bright C. Mental disorder in adults with intellectual disability. 2: the rate of behaviour disorders among a community-based population aged between 16 and 64 years. J Intellect Disabil Res 2001;45:506-14.
- Painter J, Hastings R, Ingham B, Trevithick L, Roy A. Associations between mental health problems and challenging behavior in adults with intellectual disabilities: a test of the behavioral equivalents hypothesis. J Ment Health Res Intellect Disabil 2018;11:157-72.
- Flynn S, Vereenooghe L, Hastings RP, Adams D, Cooper SA, Gore N, et al. Measurement tools for mental health problems and mental well-being in people with severe or profound intellectual disabilities: a systematic review. Clin Psychol Rev 2017;57:32-44.
- Aman MG, Singh NN. Aberrant Behavior Checklist. East Aurora, NY: Slosson; 1986.
- Matson J. The Matson Evaluation of Social Skills for Individuals with Severe Retardation. Baton Rouge, LA: Scientific Publishers; 1995.
- Doble B, Langdon PE, Shepstone L, Murphy GH, Fowler D, Heavens D, et al. Economic evaluation alongside a randomized controlled crossover trial of modified group cognitive–behavioral therapy for anxiety compared to treatment-as-usual in adults with Asperger syndrome. MDM Policy Pract 2017;2. https://doi.org/10.1177/2381468317729353.
- Langdon PE, Murphy GH, Shepstone L, Wilson EC, Fowler D, Heavens D, et al. The people with Asperger syndrome and anxiety disorders (PAsSA) trial: a pilot multicentre single-blind randomised trial of group cognitive-behavioural therapy. BJPsych Open 2016;2:179-86.
- Langdon PE, Murphy GH, Wilson E, Shepstone L, Fowler D, Heavens D, et al. Asperger syndrome and anxiety disorders (PAsSA) treatment trial: a study protocol of a pilot, multicentre, single-blind, randomised crossover trial of group cognitive behavioural therapy. BMJ Open 2013;3.
- Greenwood DJ, Levin M. Introduction to Action Research: Social Research for Social Change. Thousand Oaks, CA: SAGE Publications Ltd; 2006.
- Jacobson E. The cultivation of physiological relaxation. Ann Intern Med 1943;19:965-72.
- Jahoda A, Hastings R, Hatton C, Cooper SA, McMeekin N, Dagnan D, et al. Behavioural activation versus guided self-help for depression in adults with learning disabilities: the BeatIt RCT. Health Technol Assess 2018;22:1-130.
- National Association for the Dually Diagnosed . Diagnostic Manual – Intellectual Disability: A Textbook of Diagnosis of Mental Disorders in Persons With Intellectual Disability 2016.
- Sparrow SS, Cicchetti DV, Saulnier CA. Vineland-3: Vineland Adaptive Behavior Scales. PsychCorp; 2016.
- Constantino JN, Davis SA, Todd RD, Schindler MK, Gross MM, Brophy SL, et al. Validation of a brief quantitative measure of autistic traits: comparison of the social responsiveness scale with the autism diagnostic interview-revised. J Autism Dev Disord 2003;33:427-33.
- Waite J. Clinical Anxiety Screen for People with Severe to Profound Intellectual Disability (Unpublished Instrument). Birmingham: Aston University; 2019.
- Matson J, Terlonge C, Gonzalez M. Autism Spectrum Disorders-Behavior Problems-Adult Version. Baton Rouge, LA: Disability Consultants, LLC; 2006.
- Aman M. Aberrant Behavior Checklist – Community. East Aurora, NY: Slosson Educational; 2017.
- Matson JL, Gardner WI, Coe DA, Sovner R. A scale for evaluating emotional disorders in severely and profoundly mentally retarded persons. Development of the Diagnostic Assessment for the Severely Handicapped (DASH) Scale. Br J Psychiat 1991;159:404-9.
- Gray K, Tonge B, Einfeld S, Gruber C, Klein A. (DBC2) Developmental Behaviour Checklist 2. WPB; 2018.
- Rojahn J, Rowe EW, Sharber AC, Hastings R, Matson JL, Didden R, et al. The Behavior Problems Inventory‐Short Form for individuals with intellectual disabilities: part I: development and provisional clinical reference data. J Intellect Disabil Res 2012;56:527-45.
- Raynes NV. The Cost and Quality of Community Residential Care: An Evaluation of the Services for Adults with Learning Disabilities. David Fulton; 1994.
- Helverschou SB, Bakken TL, Martinsen H. The Psychopathology in Autism Checklist (PAC): a pilot study. Res Autism Spectr Disord 2009;3:179-95.
- Esbensen AJ, Rojahn J, Aman MG, Ruedrich S. Reliability and validity of an assessment instrument for anxiety, depression, and mood among individuals with mental retardation. J Autism Dev Disord 2003;33:617-29.
- Vlissides N, Beail N, Jackson T, Williams K, Golding L. Development and psychometric properties of the Psychological Therapies Outcome Scale – Intellectual Disabilities (PTOS-ID). J Intellect Disabil Res 2017;61:549-59. https://doi.org/10.1111/jir.12361.
- Mineka S, Zinbarg R. A contemporary learning theory perspective on the etiology of anxiety disorders: it’s not what you thought it was. Am Psychol 2006;61:10-26. https://doi.org/10.1037/0003-066X.61.1.10.
- Dymond S, Roche B. A contemporary behavior analysis of anxiety and avoidance. Behav Anal 2009;32:7-27.
- Hofmann SG. Cognitive processes during fear acquisition and extinction in animals and humans: implications for exposure therapy of anxiety disorders. Clin Psychol Rev 2008;28:199-210. https://doi.org/10.1016/j.cpr.2007.04.009.
- Grupe DW, Nitschke JB. Uncertainty and anticipation in anxiety: an integrated neurobiological and psychological perspective. Nat Rev Neurosci 2013;14:488-501. https://doi.org/10.1038/nrn3524.
- Dunsmoor JE, Paz R. Fear generalization and anxiety: behavioral and neural mechanisms. Biol Psychiatry 2015;78:336-43. https://doi.org/10.1016/j.biopsych.2015.04.010.
- Deacon BJ, Abramowitz JS. Cognitive and behavioral treatments for anxiety disorders: a review of meta‐analytic findings. J Clin Psychol 2004;60:429-41.
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348.
- Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005;15:1277-88. https://doi.org/10.1177/1049732305276687.
- Arain M, Campbell MJ, Cooper CL, Lancaster GA. What is a pilot or feasibility study? A review of current practice and editorial policy. BMC Med Res Methodol 2010;10.
- Sparrow SS, Cicchetti DV, Saulnier CA. Vineland Adaptive Behavior Scales (Vineland-3). Minneapolis, MN: Pearson; 2016.
- Bradshaw J, Gore N, Darvell C. Supporting the direct involvement of students with disabilities in functional assessment through use of Talking Mats®. Tizard Learn Disabil Rev 2018;23:111-6.
- Lancaster GA, Thabane L. Guidelines for reporting non-randomised pilot and feasibility studies. Pilot Feasibility Stud 2019;5.
- Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013;13.
- Avery KN, Williamson PR, Gamble C, O’Connell Francischetto E, Metcalfe C, Davidson P, et al. Informing efficient randomised controlled trials: exploration of challenges in developing progression criteria for internal pilot studies. BMJ Open 2017;7.
- Pruijssers AC, van Meijel B, Maaskant M, Nijssen W, van Achterberg T. The relationship between challenging behaviour and anxiety in adults with intellectual disabilities: a literature review. J Intellect Disabil Res 2014;58:162-71. https://doi.org/10.1111/jir.12012.
- Office for National Statistics . Ethnic Group, England and Wales: Census 2021: The Ethnic Groups of Usual Residents and Household Ethnic Composition in England and Wales, Census 2021 Data 2022. www.ons.gov.uk/peoplepopulationandcommunity/culturalidentity/ethnicity/bulletins/ethnicgroupenglandandwales/census2021 (accessed 16 July 2023).
Appendix 1 Questions included in the treatment-as-usual survey
| Let us know how you want to complete the survey: online survey/interview. |
|---|
| Questions about you and the service within which you work. |
| What is your name? (optional) |
| What is your e-mail address? (optional) |
| What is the name of the service within which you work? Please tell us the name of your team and your organisation. |
| What country is your service in? |
| What region is your service in? |
| Is your service? Community-based/ Inpatient/Combination of community and inpatient/Other – please indicate below. |
| Questions about treatments or interventions. |
| Does your service offer treatments or interventions for anxiety to autistic adults with moderate to severe learning disabilities? This includes psychological treatments, medication and other interventions. |
| Provide name or phrase that describes the treatment or intervention your service offers to autistic adults with moderate to severe learning disabilities who have problems with anxiety. This includes psychological treatments, medication and other interventions. Provide name of one treatment or intervention. If describing the medication, please provide the drug class. You will have a chance to add more treatment or intervention options later. If describing the psychological treatment or intervention, please provide the name of the treatment or intervention (e.g. exposure and response prevention, cognitive therapy, psychodynamic psychotherapy). |
| Briefly outline the rationale for using this treatment or intervention for autistic adults with moderate to severe learning disabilities. We are asking you to tell us briefly about the treatment or intervention goal and rationale. Bullet points are fine. |
| Describe any key procedures, activities and/or processes used within this treatment or intervention. We are asking you to tell us briefly about the key or core components. Bullet points are fine. |
| What materials are used with this treatment or intervention? Include details of all materials used by those providing the treatment or intervention, including materials given to patients and carers, or those that might be used when training staff in the treatment or intervention (e.g. information leaflets, recording sheets, booklets or other materials). Bullet points are fine. |
Who provides the treatment or intervention?
|
| How is the treatment or intervention provided? |
Please select one.
Other (please describe below) |
| What professionals are present during the sessions? Please describe below all professionals present. |
| Is anyone else present during the sessions? |
| How many treatment or intervention sessions are offered? (If you are detailing treatment using medication, please estimate the number of contacts you would have with the patient specifically about medication.) |
Please select one.
|
| How frequent are the sessions or contacts? |
Please select one.
|
| How long is one session or contact? |
Please select one.
|
| Does your service monitor if the treatment or intervention was implemented as planned? |
Please select one.
|
| Are any adaptations to this treatment or intervention made depending on patient’s needs? |
Please select one.
|
| Can you briefly tell us about situations you may encounter with this population that would lead you to adapt treatment or intervention? Bullet points are fine. |
| What adaptations are made to this treatment or intervention (we are interested in any adaptations made to help meet the needs of autistic adults with moderate to severe intellectual disabilities)? Bullet points are fine. |
| Does your service offer any additional treatments or interventions for anxiety to autistic adults with moderate to severe learning disabilities? |
Please select one.
|
Appendix 2 Summary of the responses received to the treatment-as-usual survey
| Participant’s role | Number of responses | ||||||
|---|---|---|---|---|---|---|---|
| Nursing or care professional | 24 | ||||||
| Allied health professional | 14 | ||||||
| Psychology professional | 11 | ||||||
| Medical doctor | 10 | ||||||
| Dental professional | 7 | ||||||
| Leadership or management staff | 7 | ||||||
| Other | 6 | ||||||
| Behaviour specialist | 2 | ||||||
| No response | 3 | ||||||
| Treatment or intervention | Number of responses | ||||||
| Psychological | 49 | ||||||
| Medication | 32 | ||||||
| Other | 12 | ||||||
| Physical health support | 4 | ||||||
| Let us know how you want to complete the survey | |||||||
| Online survey | 75 | ||||||
| Interview | 2 One online interview was completed. The other participant did not respond to an email sent to arrange an interview. |
||||||
| No response | 1 | ||||||
| What is the name of the service within which you work? | |||||||
| Type of the service | Number of responses | ||||||
| NHS Trust | 54 | ||||||
| Council service | 3 | ||||||
| Private service | 2 | ||||||
| Learning disability charity | 1 | ||||||
| Other: Community LD (n = 2) |
2 | ||||||
| No response | 16 | ||||||
| What country is your service in? | |||||||
| Response | Number of responses | ||||||
| England | 59 | ||||||
| Scotland | 3 | ||||||
| Wales | 1 | ||||||
| No response | 15 | ||||||
| What region is your service in? | |||||||
| South West | 6 | ||||||
| East Anglia | 11 | ||||||
| West Midlands | 11 | ||||||
| Greater London | 2 | ||||||
| South East | 7 | ||||||
| Yorkshire and Humber | 8 | ||||||
| East Midlands | 5 | ||||||
| Scotland | 3 | ||||||
| Wales | 1 | ||||||
| No response | 24 | ||||||
| What kind of service or services are they? | |||||||
| Community-based | 41 | ||||||
| Combination of community and inpatient | 15 | ||||||
| Inpatient | 4 | ||||||
Other:
|
2 | ||||||
| No response | 16 | ||||||
| Does your service offer treatments or interventions for anxiety to autistic adults with moderate to severe learning disabilities? This includes psychological treatments, medication, and other interventions. | |||||||
| Yes | 59 | ||||||
| No | 5 | ||||||
| No response | 14 | ||||||
| Treatment or intervention offered by the service | |||||||
| Psychological | 49 | Medication | 32 | Physical health support | 4 | Other | 12 |
| Applied Behavioural Analysis/Positive Behavioural Support | 14 | Medication – not specified drug class | 11 | As part of a dental intervention | 3 | Speech and language therapy | 3 |
| Cognitive Behaviour Therapy | 11 | Selective serotonin reuptake inhibitors | 8 | Physical health support | 1 | Occupational therapy | 3 |
| Psychological intervention, psychoeducation, or counselling | 6 | Antipsychotics | 5 | Sensory strategies | 2 | ||
| Exposure therapy | 3 | Benzodiazepines | 3 | Communication training | 1 | ||
| Autism-specific strategies | 3 | Other anxiolytics | 2 | Increased support staff | 1 | ||
| Mindfulness | 2 | Other medication to promote sleep | 1 | Touch therapy | 1 | ||
| Behavioural therapy | 2 | Serotonin and noradrenaline reuptake inhibitors | 1 | Music therapy | 1 | ||
| Coping strategies and anxiety-reducing strategies | 2 | Other Class C drugs | 1 | ||||
| Systemic approach | 1 | ||||||
| Active support | 1 | ||||||
| Affinity therapy | 1 | ||||||
| Relaxation training | 1 | ||||||
| Family therapy | 1 | ||||||
| Supportive psychotherapy | 1 | ||||||
| Rationale for using the treatment | |||||||
| Psychological | Medication | Physical health support | Other | ||||
| Targets anxiety using proactive and reactive strategies | 39 | Targets anxiety using proactive and reactive strategies | 16 | Improves engagement in other important treatments | 4 | Person-centred | 5 |
| Person-centred | 16 | Evidence-informed | 8 | Reduces inequalities in health care | 2 | Targets anxiety using proactive and reactive strategies | 5 |
| Improves QoL | 13 | Improves QoL | 8 | Complies with national guidance | 1 | Develops a clinical formulation | 4 |
| Collaborative working | 9 | Complies with national guidance | 4 | Improves physical health | 1 | Improves access to psychological treatment | 4 |
| Evidence-informed | 9 | Improves engagement in other important treatments | 3 | Targets anxiety using proactive and reactive strategies | 1 | Improves quality of life | 3 |
| Improves engagement in other important treatments | 7 | Person-centred | 3 | Collaborative working | 2 | ||
| Develops a clinical formulation | 5 | Improves physical health | 3 | Psychoeducation about anxiety or autism | 2 | ||
| Psychoeducation about anxiety or autism | 4 | Supports staff well-being | 3 | Evidence-informed | 1 | ||
| Predictable and consistent | 3 | Reduces risk and risky behaviours | 1 | Predictable and consistent | 1 | ||
| Complies with national guidance | 3 | Improves engagement in other important treatments | 1 | ||||
| Improved access to psychological treatment | 2 | ||||||
| Practical | 1 | ||||||
| Goal-oriented | 1 | ||||||
| Ethical | 1 | ||||||
| Supports staff wellbeing | 1 | ||||||
| Key procedures, activities and/or processes | |||||||
| Psychological | Medication | Physical health support | Other | ||||
| Psychological treatment | 34 | Treatment planning and monitoring | 18 | Dental treatment procedures | 5 | Biopsychosocial assessment | 11 |
| Biopsychosocial assessment | 21 | Psychological treatment | 18 | Psychological treatment | 4 | Supporting communication | 5 |
| Formulation | 15 | Biopsychosocial assessment | 16 | Engagement with the patient | 3 | Liaison with other professionals | 4 |
| Liaison with other professionals | 12 | Formulation | 10 | Biopsychosocial assessment | 2 | Environmental adaptations | 2 |
| Skills training in autism and anxiety | 11 | Liaison with other professionals | 6 | Liaison with other professionals | 2 | Treatment planning and monitoring | 2 |
| Treatment planning and monitoring | 10 | MCA procedures | 3 | Formulation | 2 | Observation | 2 |
| Staff support or supervision | 6 | Engagement with the patient | 2 | Supporting communication | 2 | Engagement with the patient | 2 |
| Functional analysis | 6 | Dental treatment procedures | 2 | MCA procedures | 1 | Psychological treatment | 2 |
| Engagement with the patient | 5 | Supporting communication | 1 | Treatment planning and monitoring | 1 | Formulation | 1 |
| Graded exposure procedures | 5 | Skills training in autism and anxiety | 1 | Carer engagement | 1 | Carer engagement | 1 |
| Reflective practice | 5 | Observation | 1 | MCA procedures | 1 | ||
| Supporting communication | 4 | Report writing | 1 | ||||
| Observation | 4 | ||||||
| Carer engagement | 3 | ||||||
| Dental treatment procedures | 2 | ||||||
| Environmental adaptions | 2 | ||||||
| MCA procedures | 1 | ||||||
| Treatment materials | |||||||
| Psychological | Medication | Physical health support | Other | ||||
| Data-collection materials | 40 | Information materials | 45 | Information materials | 4 | Communication tools | 18 |
| Information materials | 36 | Data-collection materials | 20 | Data-collection materials | 2 | Data-collection materials | 6 |
| Treatment plan | 14 | Communication tools | 4 | Informed consent materials | 2 | Treatment-specific and sensory aids | 5 |
| Psychoeducation materials | 9 | Treatment-specific and sensory aids | 2 | Communication tools | 2 | Information materials | 4 |
| Communication tools | 8 | Psychoeducation materials | 1 | Psychoeducation materials | 2 | Treatment plan | 1 |
| Anxiety-specific materials | 7 | Informed consent materials | 1 | Treatment-specific and sensory aids | 1 | Psychoeducation materials | 1 |
| Treatment-specific and sensory aids | 5 | Health information | 1 | ||||
| Progress measurement materials | 2 | Treatment plan | 1 | ||||
| Informed consent materials | 2 | ||||||
| Training materials | 1 | ||||||
| Exposure materials | 1 | ||||||
| Person providing the treatment | |||||||
| Psychological | Medication | Physical health support | Other | ||||
| Psychologist | 36 | Psychiatrist | 30 | Other | 6 | Occupational therapist | 6 |
| Nurse | 29 | Nurse | 17 | Nurse | 3 | Speech and language therapist | 5 |
| Occupational therapist | 18 | Psychologist | 8 | Medical doctor who is not a psychiatrist | 2 | Other | 4 |
| Parent or support care-mediated treatment or intervention | 17 | Medical doctor who is not a psychiatrist | 7 | Nurse | 4 | ||
| Psychiatrist | 16 | Healthcare assistant | 6 | Psychologist | 2 | ||
| Speech and language therapist | 15 | Occupational therapist | 5 | Psychiatrist | 1 | ||
| Healthcare assistant | 15 | Speech and language therapist | 5 | Parent or support care-mediated treatment or intervention | 1 | ||
| Other | 14 | Parent or support care-mediated treatment or intervention | 5 | Healthcare assistant | 1 | ||
| Social worker | 2 | Other | 5 | ||||
| Medical doctor who is not a psychiatrist | 1 | Social worker | 1 | ||||
| Treatment setting | |||||||
| Psychological | Medication | Physical health support | Other | ||||
| Face to face | 39 | Face to face | 25 | Face to face | 4 | Face to face | 10 |
| Online | 3 | Online | 6 | Over the phone | 1 | Other – a combination of face to face, online and over the phone as appropriate | 2 |
| Other – a combination of face to face, online and over the phone as appropriate | 5 | Other – a combination of face to face, online and over the phone as appropriate | 4 | Online | 1 | ||
| Over the phone | 3 | ||||||
| Face to face treatment setting | |||||||
| Psychological | Medication | Physical health support | Other | ||||
| Person’s place of residence | 17 | NHS setting | 16 | NHS setting | 2 | Person’s place of residence | 5 |
| NHS setting | 14 | Community | 8 | Day service | 3 | ||
| Community | 6 | Person’s place of residence | 6 | NHS setting | 2 | ||
| Day service | 5 | Day service | 5 | Community | 1 | ||
| School | 1 | ||||||
| Professionals present at the sessions | |||||||
| Psychological | Medication | Physical health support | Other | ||||
| Nursing or care professional | 46 | Medical doctor | 24 | Dental professional | 7 | Allied health professional | 11 |
| Psychology professional | 30 | Nursing or care professional | 21 | Nursing or care professional | 5 | Nursing or care professional | 4 |
| Allied health professional | 27 | Allied health professional | 11 | Medical doctor | 2 | ||
| Medical doctor | 10 | Psychology professional | 7 | Health professions student | 2 | ||
| Social care professional | 8 | Not specified MDT or health professional | 4 | Psychology professional | 1 | ||
| Not specified MDT or health professional | 7 | Dental professional | 3 | Other professional | 1 | ||
| Other professional | 5 | Health professions student | 3 | ||||
| Teaching professional | 4 | Other professional | 1 | ||||
| Family or support care-mediated treatment or intervention | 4 | Social care professional | 1 | ||||
| Dental professional | 3 | ||||||
| Health professions student | 3 | ||||||
| Anyone else present at the sessions | |||||||
| Psychological | Medication | Physical health support | Other | ||||
| Family/carer | 49 | Family/carer | 37 | Family/carer | 5 | Family/carer | 15 |
| Person | 20 | Person | 10 | Person | 1 | Person | 4 |
| Advocate | 3 | Advocate | 4 | ||||
| Community | 3 | ||||||
| Friend | 1 | ||||||
| Group session attendees | 1 | ||||||
| Number of treatment sessions or contacts | |||||||
| Psychological | Medication | Physical health support | Other | ||||
| 1–6 | 22 | 1–6 | 18 | 1–6 | 3 | 1–6 | 4 |
| 6–12 | 11 | 6–12 | 10 | 12–24 | 1 | 6–12 | 3 |
| More than 24 | 11 | More than 24 | 2 | 12–24 | 3 | ||
| 12–24 | 4 | 12–24 | 1 | More than 24 | 2 | ||
| Frequency of treatment sessions or contacts | |||||||
| Psychological | Medication | Physical health support | Other | ||||
| Once a week | 16 | Once a fortnight | 8 | Other – variable | 3 | Once a week | 4 |
| Other – variable | 9 | Once a month | 7 | Once a fortnight | 1 | Once a fortnight | 3 |
| Once a fortnight | 8 | Once a week | 4 | Once a month | 2 | ||
| Once a month | 7 | Other – variable | 4 | Other – variable | 2 | ||
| More than once a week | 7 | More than once a week | 3 | More than once a week | 1 | ||
| Other – one-off | 1 | Other – 3–6 months | 3 | ||||
| Other – not specified | 1 | Other – 6–8 weeks | 2 | ||||
| Other – once a year | 1 | ||||||
| Other – not specified | 1 | ||||||
| Duration of treatment session or contact | |||||||
| Psychological | Medication | Physical health support | Other | ||||
| 30 minutes to an hour | 26 | 30 minutes to an hour | 22 | ˂ 15 minutes | 1 | 30 minutes to an hour | 7 |
| More than one hour | 13 | 15–30 minutes | 6 | 15–30 minutes | 1 | 15–30 minutes | 4 |
| 15 to 30 minutes | 6 | ˂ 15 minutes | 4 | 30 minutes to an hour | 1 | More than one hour | 1 |
| ˂ 15 minutes | 2 | More than one hour | 1 | ||||
| About an hour | 1 | ||||||
| Monitoring of treatment implementation | |||||||
| Psychological | Medication | Physical health support | Other | ||||
| Yes | 42 | Yes | 25 | Yes | 3 | Yes | 8 |
| No | 6 | No | 7 | No | 1 | No | 3 |
| Ways of monitoring the treatment implementation | |||||||
| Psychological | Medication | Physical health support | Other | ||||
| Progress review | 13 | Progress review | 9 | Audit | 2 | Keeping records | 5 |
| Outcome measures | 11 | Stakeholder’s feedback | 6 | Writing reports | 1 | Outcome measures | 4 |
| Stakeholder’s feedback | 9 | Developing care plans | 5 | Progress review | 2 | ||
| Keeping records | 8 | Keeping records | 4 | Stakeholder’s feedback | 1 | ||
| Developing care plans | 8 | Outcome measures | 4 | Follow-up appointments | 1 | ||
| Supervision | 6 | Writing reports | 4 | ||||
| Writing reports | 5 | Medication or physical health monitoring | 2 | ||||
| Follow-up appointments | 2 | Audit | 1 | ||||
| Reflective practice | 1 | Follow-up appointments | 1 | ||||
| Team discussion | 1 | Team discussion | 1 | ||||
| Audit | 1 | ||||||
| Are any adaptations to this treatment or intervention made depending on patient’s needs? | |||||||
| Psychological | Medication | Physical health support | Other | ||||
| Yes | 44 | Yes | 32 | Yes | 4 | Yes | 12 |
| No | 4 | ||||||
| Situations leading to adapting the treatment | |||||||
| Psychological | Medication | Physical health support | Other | ||||
| Communication needs | 20 | Communication needs | 11 | Nature and degree of anxiety | 2 | Degree of learning disability | 8 |
| Degree of learning disability | 17 | Nature and degree of anxiety | 10 | Communication needs | 1 | Communication needs | 5 |
| Person’s needs | 13 | Degree of learning disability | 9 | Physical, health or mobility needs | 1 | Responsiveness to the intervention | 4 |
| Systemic or environmental challenges | 10 | Responsiveness to the intervention | 6 | Person’s interests or preferences | 1 | Person’s needs | 4 |
| Autistic traits | 9 | Person’s needs | 5 | Feedback from the person or carer | 1 | Autistic traits | 3 |
| Nature and degree of anxiety | 7 | Physical, health or mobility needs | 4 | Nature and degree of anxiety | 3 | ||
| Physical, health or mobility needs | 5 | Autistic traits | 3 | Systemic or environmental challenges | 1 | ||
| Responsiveness to the intervention | 4 | Behavioural needs | 3 | ||||
| Level of engagement | 3 | Systemic or environmental challenges | 2 | ||||
| Behavioural needs | 3 | Person’s interests or preferences | 1 | ||||
| Person’s interests or preferences | 1 | Feedback from the person or carer | 1 | ||||
| Feedback from the person or carer | 1 | ||||||
| Carer or family understanding | 1 | ||||||
| Treatment adaptations | |||||||
| Psychological | Medication | Physical health support | Other | ||||
| Communication support | 37 | Communication support | 15 | Communication support | 5 | Involving carers in treatment and liaison with support networks | 11 |
| Adjusting session content or activities | 20 | Involving carers in treatment and liaison with support networks | 11 | Adjusting timing, duration, number, or frequency of sessions | 4 | Communication support | 9 |
| Adjusting timing, duration, number, or frequency of sessions | 14 | Adjusting medication procedures | 8 | Environmental adaptations | 3 | Adjusting timing, duration, number, or frequency of sessions | 6 |
| Involving carers in treatment and liaison with support networks | 14 | Adjusting timing, duration, number, or frequency of sessions | 8 | Reducing waiting time | 2 | Environmental adaptations | 4 |
| Environmental adaptations | 10 | Changing the setting | 4 | Changing the setting | 2 | Changing the setting | 2 |
| Changing the setting | 8 | Liaison with other professionals | 4 | Assessment of needs | 2 | Adjusting session content or activities | 1 |
| Liaison with other professionals | 8 | Environmental adaptations | 3 | Involving carers in treatment and liaison with support networks | 1 | Assessment of needs | 1 |
| Consideration for person’s interests and preferences | 8 | Assessment of needs | 2 | Liaison with other professionals | 1 | Formulation driven treatment plan | 1 |
| Formulation-driven treatment plan | 5 | Consideration for person’s interests and preferences | 1 | ||||
| Psychoeducation | 5 | Adjusting session content or activities | 1 | ||||
| Assessment of needs | 3 | Psychoeducation | 1 | ||||
| Increased practical support | 2 | MCA considerations | 1 | ||||
| MCA considerations | 1 | ||||||
Appendix 3 Sample fidelity checklist
Session 1 checklist
Even if the carer did not attend the session, please complete the section below:
Therapist’s initials: Date when completed:
Date of the session:
Name of the NHS Trust:
Herefordshire and Worcestershire Health and Care NHS Trust
Coventry and Warwickshire Partnership NHS Trust
Mersey Care NHS Foundation Trust
Leicestershire Partnership NHS Trust
Solent NHS Trust
Did the carer attend the session?
Yes
No
| General session preparations | Tick correct | |
|---|---|---|
|
YES | NO |
| Coverage of session plan | Tick correct | |
|
YES | NO |
|
YES | NO |
|
YES | NO |
|
YES | NO |
| Understanding and accessibility | Tick correct | |
|
YES | NO |
|
YES | NO |
|
YES | NO |
|
YES | NO |
| Interpersonal effectiveness | Tick correct | |
|
YES | NO |
|
YES | NO |
|
YES | NO |
| Engaging participants | Tick correct | |
|
YES | NO |
|
YES | NO |
|
YES | NO |
| Session content | Tick correct | |
|
YES | NO |
|
YES | NO |
|
YES | NO |
|
YES | NO |
|
YES | NO |
|
YES | NO |
|
YES | NO |
|
YES | NO |
|
YES | NO |
|
YES | NO |
|
YES | NO |
|
YES | NO |
|
YES | NO |
| Comments | ||
Signature of the Therapist:
This checklist was adapted from Jahoda et al., 2013.
Appendix 4 Carer interview schedule
BEAMS-ID interview schedule – carers
Target duration: 30 minutes
| Warm up |
| To start, please can you tell me a bit about yourself, and what led to you and [name of the person with LD] to taking part in the BEAMS-ID study? |
| Acceptability of consent processes |
| Before you and (name of the person with LD) started the BEAMS-ID treatment, what did you know or think about it? |
| What did you think about the booklet you received with information about the study? Was it helpful in understanding the study? |
| What did you think about the consent forms? Was the process of receiving and signing them straightforward? |
| Overall, what was your experience of joining this study? What did you think about how this was organised? Is there anything that you think we could be doing differently for people with learning disabilities and their carers in a future study? |
| Intervention accessibility and acceptability |
| What was your experience of attending the twelve treatment sessions as a carer? |
| How do you think [name of the person with LD] found the treatment sessions? Do you think anything could have been done differently to support them better? |
| Did anything help you and [name of the person with LD] to attend the BEAMS-ID sessions? Did anything stop you from attending them? |
| Were there any sessions that you couldn’t attend? What happened? |
| Helpful/unhelpful aspects, including barriers to change |
| What things do you think were good about the BEAMS-ID treatment for you and [name of the person with LD]? |
| Was there anything you didn’t like about the BEAMS-ID treatment, or that you would have liked to have been done differently? |
| The value of our adaptations |
| Do you think the treatment met [name of the person with LD]’s needs? |
| Do you think any further adaptations/changes are needed for the treatment to meet the needs of autistic people with learning disabilities and their carers? |
| Were the treatment materials accessible to the person you were supporting or easily adapted to meet their needs? Would you change anything in the treatment materials? |
| Relationships with therapists within intervention |
| What was your experience of working with the BEAMRS therapist? |
| Did you and [name of the person with LD] feel supported during the treatment? |
| Did you and [name of the person with LD] feel you were able to ask questions and raise concerns with your BEAMS-ID therapist? |
| Is there anything the therapist could have done differently to support both of you better? |
| Acceptability of outcome measures |
| Thinking back to when you completed the same set of questionnaires before and after the treatment, what was this experience like for you? |
| Acceptability of randomisation within a future trial |
| In future studies, some people with learning disabilities will receive the BEAMS-ID treatment in addition to the supports usually available, and some will continue with support options normally available in the NHS. Would you and [name of the person with LD] consider taking part in a study like that? |
| Effects of participation |
| What sort of things do you think that you learnt during the treatment sessions? |
| Do you think that anything has changed for you and [name of the person with LD] since you have completed the BEAMS-ID treatment? |
| Has the treatment made any difference to [name of the person with LD]’s life? |
| What do you think will happen in the future for [name of the person with LD] now that you have completed the BEAMS-ID treatment? |
| Closing questions |
| Is there anything else you think we should know? |
Appendix 5 Therapist interview schedule
Therapist interview schedule.
BEAMS-ID interview schedule – therapists
Target duration: 30 minutes
| Warm up |
| To start, please can you tell me a bit about your own background, experience and qualifications? |
| How did you hear about the BEAMS-ID study, and what made you want to work as a therapist on the study? |
| Training |
| Could you tell me about the BEAMS-ID training? |
| Do you think that the training prepared you well enough to deliver the treatment? |
| What, if any, elements of the BEAMS-ID training have helped you to support engagement with the participants you have been working with? |
| Intervention accessibility and acceptability |
| Can you tell me about your experience of delivering the twelve BEAMS-ID sessions? |
| How did participants respond to the BEAMS-ID sessions? |
| How did carers respond to the BEAMS-ID sessions? |
| Do you think the BEAMS-ID treatment is suitable for autistic adults with moderate to severe learning disabilities and their carers? |
| Did you enjoy delivering the BEAMS-ID treatment? |
| Helpful/unhelpful aspects, including barriers to change |
| Overall, how have the BEAMS-ID sessions gone with participants and their carers? What were the challenges, and what went well? |
| Could you give me an example of something you found easy in delivering the BEAMS-ID treatment? |
| Could you give me an example of something you found hard in delivering the BEAMS-ID treatment? |
| Was there anything you didn’t like about the BEAMS-ID treatment, or that you would have liked to have been done differently? Any suggestions for improvements? |
| What did you think about the number and frequency of the treatment sessions? |
| The value of our adaptations |
| Do you think the treatment met participants’ needs? If so, how? |
| Do you think the treatment met carers’ needs? If so, how? |
| Did you make any adjustments to the treatment to meet participant’s or carer’s needs? |
| Do you think any revisions are needed for the treatment to meet the needs of autistic people with learning disabilities and their carers? If so, what are they? |
| Were the treatment materials appropriate for participants and their carers? Did you need to make any changes to the materials? |
| Relationships with therapists within intervention |
| Do you feel the structure of the sessions enabled you to build a therapeutic relationship with the participant and their carer? If so, how? |
| Do you think any changes could be made to support participants and their carers to engage better with the BEAMS-ID treatment? |
| Outcome measures |
| Do you have any suggestions for outcome measures we could be using in future trials? |
| Acceptability of randomisation within a future trial |
| In future studies, some participants will be allocated to receive the BEAMS-ID treatment and some to continue with support options normally available in the NHS. How do you feel about this process? |
| Closing questions |
| Thinking about your professional development, did you experience any benefits from learning about and delivering the BEAMS-ID treatment? |
| If it was available, would you choose to use the BEAMS-ID treatment with future clients with anxiety problems? |
| Is there anything else you think we should know? |
Appendix 6 Interview framework for participants using Talking Mats
Talking Mats Interview Plan for BEAMS-ID participants
Target duration: 15 minutes
Talking Mats were used in this study as a communication tool for participants received the BEAMS-ID intervention. All interviews were conducted by a researcher who had been trained to use Talking Mats™.
A Talking Mat was used with all participants, irrespective of their communication abilities, to ensure that we are providing all participants with the same opportunity to express their thoughts and feelings. All Talking Mats contained three component parts: the Topic, Top Scale, and Options (see Figure 5).
FIGURE 5.
Example of a Talking Mat with labelled components.
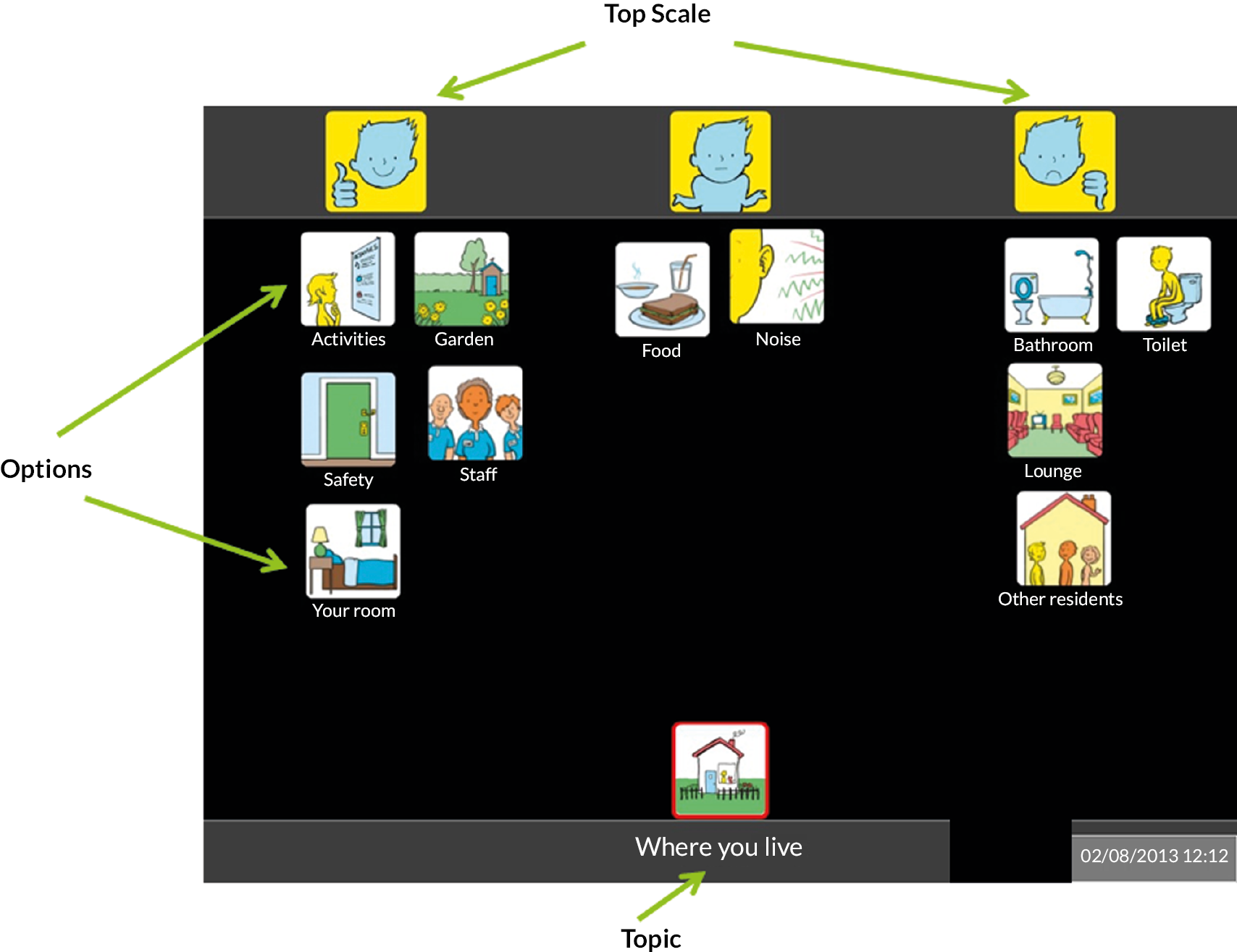
The Topic symbol represents the interview question and is a visual representation that can be drawn on throughout the interview should the participant go off topic. There is only one Topic per Talking Mat. In this study, the topic will be ‘How do you feel about the BEAMS-ID treatment?’
The Top Scale symbols are a three-point visual scale for the interviews, whereby the participant will be able to categorise their options. In this study, the top scale will represent ‘like’, ‘not sure’ and ‘I don’t like’. If some participants find it difficult to have a three-point top scale, this can be reduced to a two-point scale with only ‘like’ and ‘don’t like’.
The Options symbols represent the different responses related to the interview question. Participants will be given one symbol (or tile) at a time and asked to place it on the mat under the top scale symbol that represents their feelings about that option. Each option will be highlighted in turn and the participant will be asked the open question ‘How do you feel about … ?’ Only 10–15 options will be used within each Talking Mat. If it is possible to do so, the placing of the options symbols can lead to further conversation and questions about the option. In this study, the Options symbols will include: ‘coming to treatment sessions’, ‘the carer helping me’, ‘meeting new people’, ‘the therapist’, ‘talking about things that make me anxious’, ‘looking at pictures/booklet’, ‘learning about anxiety’, ‘relaxation’, ‘trying new things’, ‘making choices’, ‘using visual schedule’, and ‘talking about how I feel’. Options symbols will be taken from Easy on the I or we will use photographs. Participants will also have the option to add their own options symbols to the mat about other things that they liked/disliked about the BEAMS-ID treatment. Further to this, participants will be given the opportunity to review their mat and move the tiles to other top scale symbols if they have changed their mind.
OPTIONS (‘How do you feel about …?’):
-
Coming to treatment sessions
-
The carer helping me
-
Meeting new people
-
The therapist
-
Talking about things that make me anxious
-
Looking at pictures/booklet
-
Learning about anxiety
-
Relaxation
-
Fear Ladder
-
Making choices
-
Using visual schedule
-
Talking about how I feel (with photo of the Rating Scale)
Appendix 7 Effectiveness framework for interviews using Talking Mats
Effectiveness framework of functional communication
Engagement – the social closeness that is established in the interaction and maintained through rapport and joint attention.
Thinker’s understanding – based on verbal and non-verbal responses.
Listener’s understanding of thinker’s views – shown by non-verbal and verbal responses of listener.
Thinker – on track – the relevance of the thinker’s verbal and non-verbal responses to the topic being discussed.
Symmetry – the sense of equilibrium and balance that creates shared control in the interaction.
Real time – the extent to which the interaction happens within a typical time frame.
Listener – participant factor/satisfaction – the perspective of the listener about how easy it is to support and maintain the interaction.
| Effectiveness framework of functional communication | |||||
|---|---|---|---|---|---|
| Indicators | 4, Always | 3, Often | 2, 50/50 | 1, Occasionally | 0, None |
| Engagement | |||||
| Participant’s understanding issue for discussion: | |||||
| Participant understands the activities aspect of the topic | |||||
| Participant understands that the activities are about doing the BEAMS-ID treatment | |||||
| Interviewer’s understanding of participant’s views | |||||
| Participants – on track | |||||
| Symmetry | |||||
| Real time | |||||
| Interviewer’s chill factor | |||||
Appendix 8 Fidelity data for each therapy session
Fidelity checklist percentages for BEAMS Session 1
| Theme and question | Percentage of yes responses |
|---|---|
| Who was present at the session | |
| Was the carer present? | 100 |
| General session preparations | |
| 1. Gathered all resources listed in the materials section of the session plan. | 100 |
| Coverage of session plan | |
| 2. Agreed with the carer on the agenda for the session. | 100 |
| 3. Ensured that the carer clearly understood the purpose of the session. | 100 |
| 4. Session aims were fulfilled. | 91.7 |
| 5. Session was completed in 1.5 hours. | 79.2 |
| Understanding and accessibility | |
| 6. Adjusted the content and style of my own communication to help the carer’s understanding. | 95.8 |
| 7. Welcomed questions from the carer. | 100 |
| 8. Session was pitched at a level that was accessible to the carer. The carer remained engaged. | 100 |
| 9. Care was taken to pace the session at a rate that allowed the carer to keep up with what was happening. | 95.8 |
| Interpersonal effectiveness | |
| 10. Communicated with warmth, concern and understanding. | 100 |
| 11. In control of the session, communicated clearly without frequent hesitations/repetitions. | 100 |
| 12. Able to shift appropriately between listening and leading. | 95.8 |
| Engaging participants | |
| 13. Explained rationale and requirements for the different activities/elements of the session clearly. | 100 |
| 14. Did not criticise, disapprove, or ridicule the carer. | 91.3 |
| 15. Responded to seemingly irrelevant interruptions in an effective yet respectful manner. | 95.7 |
| Session content | |
| 16. Introduced myself and explained my role. | 100 |
| 17. Explained the structure of the treatment, including the frequency, duration, and number of sessions. | 100 |
| 18. Introduced the Carer’s Handbook. | 87 |
| 19. Introduced Graded Exposure and relaxation and explained their role in the treatment. | 87 |
| 20. Reviewed the Assessment Interview with the carer and asked additional questions about person’s circumstances if needed. | 87 |
| 21. Explored anxiety symptoms more likely to be observed in people with learning disabilities. | 82.6 |
| 22. Introduced Handout on principles of behaviour and behaviour change from the Carer’s Handbook. | 91.3 |
| 23. Explored how anxiety disorders are formed and maintained. | 82.6 |
| 24. Introduced the ABC chart and explained how to use it. | 91.3 |
| 25. Explained the inter-session task. | 91.3 |
| 26. Provided a 5-minute warning before the session ended. | 65.2 |
| 27. Summarised the session. | 91.3 |
| 28. Reminded the carer about the time of the next session and its focus. | 100 |
Fidelity checklist percentages for BEAMS Session 2
| Theme and question | Percentage of yes responses |
|---|---|
| Who was present at the session | |
| Person and carer | 70 |
| Person, carer and other | 30 |
| General session preparations | |
| 1. Gathered all resources listed in the materials section of the session plan. | 95.2 |
| 2. Ensured the person has their communication supports available (if needed). | 100 |
| 3. Agreed with the person and carer on frequency of breaks. | 90.5 |
| Coverage of session plan | |
| 4. Agreed with the person and carer on the agenda for the session and completed a Visual Schedule. | 85.7 |
| 5. Ensured that the person and carer clearly understood the purpose of the session. | 95.2 |
| 6. Session aims were fulfilled. | 85.7 |
| 7. Session was completed in 1.5 hours. | 95.2 |
| Understanding and accessibility | |
| 8. Adjusted the content and style of my own communication to help the carer and person’s understanding. | 95.2 |
| 9. Welcomed questions from the carer and the person. | 100 |
| 10. Session was pitched at a level that was accessible to the person and the carer. The person and the carer remained engaged. | 95.2 |
| 11. Care was taken to pace the session at a rate that allowed the person and the carer to keep up with what was happening. | 95.2 |
| Interpersonal effectiveness | |
| 12. Communicated with warmth, concern and caring. | 100 |
| 13. In control of the session, communicated clearly without frequent hesitations/repetitions. | 100 |
| 14. Able to shift appropriately between listening and leading. | 100 |
| Engaging participants | |
| 15. Explained rationale and requirements for the different activities/elements of the session clearly. | 100 |
| 16. Did not criticise, disapprove, or ridicule the person or the carer. | 100 |
| 17. Responded to seemingly irrelevant interruptions in an effective yet respectful manner. | 90 |
| Session content | |
| 18. Introduced myself to the person and explained my role. | 95 |
| 19. Reviewed ABC chart. | 60 |
| 20. Explained to the person the structure of the treatment, including the frequency, duration, and number of sessions. | 85 |
| 21. Explained to the person the role of the carer in the treatment. | 95 |
| 22. Built rapport with the person and explored their hobbies, interests, and preferences. | 95 |
| 23. Identified six items/activities/edibles that the person appears to prefer the most by talking to the person and the carer. | 85 |
| 24. Conducted a Preference Assessment. | 90 |
| 25. Introduced the Rating Scale and explained how to use it. | 80 |
| 26. Explored person’s and carer’s expectations of the treatment. | 85 |
| 27. Offered the person and the carer an opportunity to ask questions. | 100 |
| 28. Introduced the inter-session task. | 100 |
| 29. Provided a 5-minute warning before the session ended. | 70 |
| 30. Summarised the session. | 90 |
| 31. Reminded the person about the time of the next session and its focus. | 95 |
| Inter-session tasks | |
| 32. Reviewed previous week’s inter-session task (ABC chart). | 65 |
| 33. Encouraged carer to complete inter-session task. | 100 |
| 34. Asked carer if they anticipated any problems with inter-session task. | 100 |
Fidelity checklist percentages for BEAMS Session 3
| Theme and question | Percentage of yes responses |
|---|---|
| Who was present at the session | |
| Person | 4.8 |
| Carer | 4.8 |
| Person and carer | 57.1 |
| Person, carer and other | 28.6 |
| Other | 4.8 |
| General session preparations | |
| 1. Gathered all resources listed in the materials section of the session plan. | 95.5 |
| 2. Ensured the person has their communication supports available (if needed). | 100 |
| 3. Agreed with the person and carer on frequency of breaks. | 90.5 |
| Coverage of session plan | |
| 4. Agreed with the person and carer on the agenda for the session and completed a Visual Schedule. | 86.4 |
| 5. Ensured that the person and carer clearly understood the purpose of the session. | 95.5 |
| 6. Session aims were fulfilled. | 76.2 |
| 7. Session was completed in 1.5 hours. | 81.8 |
| Understanding and accessibility | |
| 8. Adjusted the content and style of my own communication to help the carer and person’s understanding. | 95.5 |
| 9. Welcomed questions from the carer and the person. | 100 |
| 10. Session was pitched at a level that was accessible to the person and the carer. The person and the carer remained engaged. | 90.9 |
| 11. Care was taken to pace the session at a rate that allowed the person and the carer to keep up with what was happening. | 100 |
| Interpersonal effectiveness | |
| 12. Communicated with warmth, concern and caring. | 100 |
| 13. In control of the session, communicated clearly without frequent hesitations/repetitions. | 95.5 |
| 14. Able to shift appropriately between listening and leading. | 100 |
| Engaging participants | |
| 15. Explained rationale and requirements for the different activities/elements of the session clearly. | 100 |
| 16. Did not criticise, disapprove, or ridicule the person or the carer. | 100 |
| 17. Responded to seemingly irrelevant interruptions in an effective yet respectful manner. | 100 |
| Session content | |
| 18. Reviewed ABC chart. | 76.2 |
| 19. Introduced Handout on anxiety for the person. | 100 |
| 20. Explored with the person what anxiety is and how it feels to them. | 90.5 |
| 21. Introduced concept of relaxation and how it feels to the person to be relaxed. | 85.7 |
| 22. Introduced Handout on autism and learning disability. | 90.5 |
| 23. Explored person’s traits and strengths and challenges related to autism and learning disability. | 90.5 |
| 24. Explored how person communicated distress, break and other important words and taught them if needed. | 95.2 |
| 25. Provided a 5-minute warning. | 76.2 |
| 26. Summarised the session. | 95.2 |
| 27. Reminded the person about the time of the next session and its focus. | 90.5 |
| Inter-session tasks | |
| 28. Reviewed previous week’s inter-session task (ABC chart). | 85.7 |
| 29. Encouraged carer to complete this week’s inter-session tasks (continue with ABC chart). | 100 |
| 30. Asked carer if they anticipated any problems with inter-session tasks. | 90.5 |
Fidelity checklist percentages for BEAMS Session 4
| Theme and question | Percentage of yes responses |
|---|---|
| Who was present at the session | |
| Person and carer | 83.3 |
| Person, carer and other | 16.7 |
| General session preparations | |
| 1. Gathered all resources listed in the materials section of the session plan. | 94.7 |
| 2. Ensured the person has their communication supports available. | 100 |
| 3. Agreed with the person and carer on frequency of breaks. | 89.5 |
| 4. Completed a Visual Schedule for the session. | 89.5 |
| Coverage of session plan | |
| 5. Agreed with the person and carer on the agenda for the session and completed a Visual Schedule. | 94.7 |
| 6. Ensured that the person and carer clearly understood the purpose of the session. | 94.7 |
| 7. Session aims were fulfilled. | 94.7 |
| 8. Session was completed in 1.5 hours. | 89.5 |
| Understanding and accessibility | |
| 9. Adjusted the content and style of my own communication to help the carer and person’s understanding. | 100 |
| 10. Welcomed questions from the carer and the person. | 100 |
| 11. Session was pitched at a level that was accessible to the person and the carer. The person and the carer remained engaged. | 100 |
| 12. Care was taken to pace the session at a rate that allowed the person and the carer to keep up with what was happening. | 100 |
| Interpersonal effectiveness | |
| 13. Communicated with warmth, concern and caring. | 100 |
| 14. In control of the session, communicated clearly without frequent hesitations/repetitions. | 100 |
| 15. Able to shift appropriately between listening and leading. | 100 |
| Engaging participants | |
| 16. Explained rationale and requirements for the different activities/elements of the session clearly. | 100 |
| 17. Did not criticise, disapprove, or ridicule the person or the carer. | 100 |
| 18. Responded to seemingly irrelevant interruptions in an effective yet respectful manner. | 100 |
| Session content | |
| 19. Reviewed the ABC chart. | 77.8 |
| 20. Introduced relaxation and explained how it can help with anxiety. | 100 |
| 21. Explained when to use relaxation techniques. | 100 |
| 22. Introduced deep breathing exercise and practised with the person. | 83.3 |
| 23. Introduced muscle relaxation exercise and practised with the person. | 88.9 |
| 24. Explored adaptations the person might need to benefit from relaxation techniques. | 94.4 |
| 25. Provided a 5-minute warning before the session ended. | 83.3 |
| 26. Summarised the session. | 88.9 |
| 27. Reminded the person about the time of the next session and its focus. | 83.3 |
| Inter-session tasks | |
| 28. Reviewed previous week’s inter-session task (ABC chart). | 83.3 |
| 29. Encouraged carer to complete inter-session task (continue with ABC chart). | 100 |
| 30. Asked carer if they anticipated any problems with inter-session task. | 88.9 |
Fidelity checklist percentages for BEAMS Session 5
| Theme and question | Percentage of yes responses |
|---|---|
| Who was present at the session | |
| Was the carer present? | 100 |
| General session preparations | |
| 1. Gathered all resources listed in the materials section of the session plan. | 100 |
| Coverage of session plan | |
| 2. Agreed with the carer on the agenda for the session. | 100 |
| 3. Ensured that the carer clearly understood the purpose of the session. | 100 |
| 4. Session aims were fulfilled. | 88.9 |
| 5. Session was completed in 1.5 hours. | 88.9 |
| Understanding and accessibility | |
| 6. Adjusted the content and style of my own communication to help the carer’s understanding. | 100 |
| 7. Welcomed questions from the carer. | 100 |
| 8. Session was pitched at a level that was accessible to the carer. The carer remained engaged. | 100 |
| 9. Care was taken to pace the session at a rate that allowed the carer to keep up with what was happening. | 100 |
| Interpersonal effectiveness | |
| 10. Communicated with warmth, concern and caring. | 100 |
| 11. In control of the session, communicated clearly without frequent hesitations/repetitions. | 94.4 |
| 12. Able to shift appropriately between listening and leading. | 100 |
| Engaging participants | |
| 13. Explained rationale and requirements for the different activities/elements of the session clearly. | 100 |
| 14. Did not criticise, disapprove, or ridicule the carer. | 100 |
| 15. Responded to seemingly irrelevant interruptions in an effective yet respectful manner. | 100 |
| Session content | |
| 16. Summarised the results from the Assessment Interview and ABC chart and discussed potential proactive strategies that can be implemented to help with person’s anxiety. | 94.1 |
| 17. Introduced the Treatment Plan and explained the difference between proactive and reactive strategies. | 100 |
| 18. Introduced strategies from green, amber, and red categories. | 94.1 |
| 19. Defined criteria for strategies from green, amber, and red categories based on person’s behaviours. | 94.1 |
| 20. Explored when to use strategies from green, amber, and red categories and how they can support the person. | 94.1 |
| 21. Summarised the session. | 100 |
| 22. Reminded the carer about the time of the next session and its focus. | 100 |
| Inter-session tasks | |
| 23. Reviewed previous week’s inter-session task (ABC chart). | 82.4 |
| 24. Encouraged carer to complete inter-session task (continue with ABC chart). | 94.1 |
| 25. Asked carer if they anticipated any problems with inter-session task. | 82.4 |
Fidelity checklist percentages for BEAMS Session 6
| Theme and question | Percentage of yes responses |
|---|---|
| Who was present at the session | |
| Was the carer present? | 100 |
| General session preparations | |
| 1. Gathered all resources listed in the materials section of the session plan. | 94.1 |
| Coverage of session plan | |
| 2. Agreed with the carer on the agenda for the session. | 100 |
| 3. Ensured that the carer clearly understood the purpose of the session. | 100 |
| 4. Session aims were fulfilled. | 94.1 |
| 5. Session was completed in 1.5 hours. | 94.1 |
| Understanding and accessibility | |
| 6. Adjusted the content and style of my own communication to help the carer’s understanding. | 100 |
| 7. Welcomed questions from the carer. | 100 |
| 8. Session was pitched at a level that was accessible to the carer. The carer remained engaged. | 100 |
| 9. Care was taken to pace the session at a rate that allowed the carer to keep up with what was happening. | 100 |
| Interpersonal effectiveness | |
| 10. Communicated with warmth, concern and caring. | 100 |
| 11. In control of the session, communicated clearly without frequent hesitations/repetitions. | 100 |
| 12. Able to shift appropriately between listening and leading. | 100 |
| Engaging participants | |
| 13. Explained rationale and requirements for the different activities/elements of the session clearly. | 100 |
| 14. Did not criticise, disapprove, or ridicule the carer. | 100 |
| 15. Responded to seemingly irrelevant interruptions in an effective yet respectful manner. | 100 |
| Session content | |
| 16. Reviewed ABC chart. | 76.5 |
| 17. Introduced Handout on Graded Exposure. | 88.2 |
| 18. Explained what Graded Exposure is. | 94.1 |
| 19. Explained how Graded Exposure can help with anxiety. | 94.1 |
| 20. Explained the difference between exposure and flooding. | 94.1 |
| 21. Introduced Handout on Fear Ladders. | 94.1 |
| 22. Introduced Fear Ladders. | 94.1 |
| 23. Explained how Fear Ladders are used in Graded Exposure. | 94.1 |
| 24. Provided an example of Fear Ladder. | 94.1 |
| 25. Explored anxiety-provoking situations for the person. | 100 |
| 26. Constructed a Fear Ladder with the carer. | 82.4 |
| 27. Explored barriers to doing Graded Exposure with the person. | 94.1 |
| 28. Reminded the carer about the importance of generalisation. | 82.4 |
| 29. Summarised the session. | 88.2 |
| 30. Reminded the person about the time of the next session and its focus. | 100 |
| Inter-session tasks | |
| 31. Reviewed previous week’s inter-session task (ABC chart). | 76.5 |
| 32. Encouraged carer to complete this week’s inter-session tasks (continue with ABC chart). | 94.1 |
| 33. Asked carer if they anticipated any problems with inter-session tasks. | 82.4 |
Fidelity checklist percentages for BEAMS Session 7
| Theme and question | Percentage of yes responses |
|---|---|
| Who was present at the session | |
| Carer | 5.6 |
| Person and carer | 72.2 |
| Person, carer and other | 22.2 |
| General session preparations | |
| 1. Gathered all resources listed in the materials section of the session plan. | 94.4 |
| 2. Ensured the person has their communication supports available (if needed). | 94.4 |
| 3. Agreed with the person and carer on frequency of breaks. | 94.4 |
| 4. Completed a Visual Schedule for the session. | 77.8 |
| Coverage of session plan | |
| 5. Agreed with the person and carer on the agenda for the session and completed a Visual Schedule. | 88.9 |
| 6. Ensured that the person and carer clearly understood the purpose of the session. | 100 |
| 7. Session aims were fulfilled. | 83.3 |
| 8. Session was completed in 1.5 hours. | 100 |
| Understanding and accessibility | |
| 9. Adjusted the content and style of my own communication to help the carer and person’s understanding. | 100 |
| 10. Welcomed questions from the carer and the person. | 100 |
| 11. Session was pitched at a level that was accessible to the person and the carer. The person and the carer remained engaged. | 94.4 |
| 12. Care was taken to pace the session at a rate that allowed the person and the carer to keep up with what was happening. | 100 |
| Interpersonal effectiveness | |
| 13. Communicated with warmth, concern and caring. | 100 |
| 14. In control of the session, communicated clearly without frequent hesitations/repetitions. | 100 |
| 15. Able to shift appropriately between listening and leading. | 100 |
| Engaging participants | |
| 16. Explained rationale and requirements for the different activities/elements of the session clearly. | 94.4 |
| 17. Did not criticise, disapprove, or ridicule the person or the carer. | 100 |
| 18. Responded to seemingly irrelevant interruptions in an effective yet respectful manner. | 100 |
| Session content | |
| 19. Reviewed the ABC chart. | 66.7 |
| 20. Did a 5-minute relaxation practice with the person and the carer. | 83.3 |
| 21. Reminded the person and carer why exposure to feared stimuli can help. | 94.4 |
| 22. Explained how Graded Exposure works. | 88.9 |
| 23. Practised working on the first step of the Fear Ladder. | 77.8 |
| 24. Provided a 5-minute warning before the session ended. | 72.2 |
| 25. Summarised the session. | 83.3 |
| 26. Reminded the person about the time of the next session and its focus. | 88.9 |
| Inter-session tasks | |
| 27. Reviewed previous week’s inter-session task (ABC chart). | 70.6 |
| 28. Encouraged carer to complete this week’s inter-session tasks (continue with ABC chart and practise Graded Exposure). | 100 |
| 29. Asked carer if they anticipated any problems with inter-session tasks. | 88.2 |
Fidelity checklist percentages for BEAMS Session 8
| Theme and question | Percentage of yes responses |
|---|---|
| Who was present at the session | |
| Person and carer | 82.4 |
| Person, carer and other | 17.7 |
| General session preparations | |
| 1. Gathered all resources listed in the materials section of the session plan. | 93.8 |
| 2. Ensured the person has their communication supports available (if needed). | 100 |
| 3. Agreed with the person and carer on frequency of breaks. | 87.5 |
| 4. Completed a Visual Schedule for the session. | 81.3 |
| Coverage of session plan | |
| 5. Agreed with the person and carer on the agenda for the session and completed a Visual Schedule. | 81.3 |
| 6. Ensured that the person and carer clearly understood the purpose of the session. | 93.8 |
| 7. Session aims were fulfilled. | 81.3 |
| 8. Session was completed in 1.5 hours. | 93.8 |
| Understanding and accessibility | |
| 9. Adjusted the content and style of my own communication to help the carer and person’s understanding. | 100 |
| 10. Welcomed questions from the carer and the person. | 100 |
| 11. Session was pitched at a level that was accessible to the person and the carer. The person and the carer remained engaged. | 100 |
| 12. Care was taken to pace the session at a rate that allowed the person and the carer to keep up with what was happening. | 100 |
| Interpersonal effectiveness | |
| 13. Communicated with warmth, concern and caring. | 100 |
| 14. In control of the session, communicated clearly without frequent hesitations/repetitions. | 100 |
| 15. Able to shift appropriately between listening and leading. | 100 |
| Engaging participants | |
| 16. Explained rationale and requirements for the different activities/elements of the session clearly. | 100 |
| 17. Did not criticise, disapprove, or ridicule the person or the carer. | 100 |
| 18. Responded to seemingly irrelevant interruptions in an effective yet respectful manner. | 100 |
| Session content | |
| 19. Reviewed the ABC chart. | 62.5 |
| 20. Did a 5-minute relaxation practice with the person and the carer. | 93.8 |
| 21. Checked on progress with Graded Exposure. | 81.3 |
| 22. Practised working on the next step of the Fear Ladder. | 62.5 |
| 23. Provided a 5-minute warning before the session ended. | 75 |
| 24. Summarised the session. | 81.3 |
| 25. Reminded the person about the time of the next session and its focus. | 93.8 |
| Inter-session tasks | |
| 26. Reviewed previous week’s inter-session task (ABC chart and Graded Exposure). | 75 |
| 27. Encouraged carer to complete inter-session task (continue with ABC chart and practise Graded Exposure). | 93.8 |
| 28. Asked carer if they anticipated any problems with inter-session task. | 87.5 |
Fidelity checklist percentages for BEAMS Session 9
| Theme and question | Percentage of yes responses |
|---|---|
| Who was present at the session | |
| Carer | 6.3 |
| Person and carer | 81.3 |
| Person, carer and other | 12.5 |
| General session preparations | |
| 1. Gathered all resources listed in the materials section of the session plan. | 100 |
| 2. Ensured the person has their communication supports available (if needed). | 100 |
| 3.Agreed with the person and carer on frequency of breaks. | 93.8 |
| 4. Completed a Visual Schedule for the session. | 75 |
| Coverage of session plan | |
| 5. Agreed with the person and carer on the agenda for the session and completed a Visual Schedule. | 81.3 |
| 6. Ensured that the person and carer clearly understood the purpose of the session. | 100 |
| 7. Session aims were fulfilled. | 87.5 |
| 8. Session was completed in 1.5 hours. | 93.8 |
| Understanding and accessibility | |
| 9. Adjusted the content and style of my own communication to help the carer and person’s understanding. | 100 |
| 10. Welcomed questions from the carer and the person. | 100 |
| 11. Session was pitched at a level that was accessible to the person and the carer. The person and the carer remained engaged. | 100 |
| 12. Care was taken to pace the session at a rate that allowed the person and the carer to keep up with what was happening. | 100 |
| Interpersonal effectiveness | |
| 13. Communicated with warmth, concern and caring. | 100 |
| 14. In control of the session, communicated clearly without frequent hesitations/repetitions. | 100 |
| 15. Able to shift appropriately between listening and leading. | 100 |
| Engaging participants | |
| 16. Explained rationale and requirements for the different activities/elements of the session clearly. | 100 |
| 17. Did not criticise, disapprove, or ridicule the person or the carer. | 100 |
| 18. Responded to seemingly irrelevant interruptions in an effective yet respectful manner. | 100 |
| Session content | |
| 19. Reviewed the ABC chart. | 68.8 |
| 20. Did a 5-minute relaxation practice with the person and the carer. | 81.3 |
| 21. Checked on progress with Graded Exposure. | 93.8 |
| 22. Practised working on the next step of the Fear Ladder. | 75 |
| 23. Provided a 5-minute warning before the session ended. | 81.3 |
| 24. Summarised the session. | 81.3 |
| 25. Reminded the person about the time of the next session and its focus. | 93.8 |
| Inter-session tasks | |
| 26. Reviewed previous week’s inter-session task (ABC chart and Graded Exposure). | 81.3 |
| 27. Encouraged carer to complete inter-session task (continue with ABC chart and practise Graded Exposure). | 93.8 |
| 28. Asked carer if they anticipated any problems with inter-session task. | 87.5 |
Fidelity checklist percentages for BEAMS Session 10
| Theme and question | Percentage of yes responses |
|---|---|
| Who was present at the session | |
| Carer | 5.9 |
| Person and carer | 82.4 |
| Person, carer and other | 11.8 |
| General session preparations | |
| 1. Gathered all resources listed in the materials section of the session plan. | 94.1 |
| 2. Ensured the person has their communication supports available (if needed). | 94.1 |
| 3. Agreed with the person and carer on frequency of breaks. | 94.1 |
| 4. Completed a Visual Schedule for the session. | 88.2 |
| Coverage of session plan | |
| 5. Agreed with the person and carer on the agenda for the session and completed a Visual Schedule. | 82.4 |
| 6. Ensured that the person and carer clearly understood the purpose of the session. | 100 |
| 7. Session aims were fulfilled. | 100 |
| 8. Session was completed in 1.5 hours. | 100 |
| Understanding and accessibility | |
| 9. Adjusted the content and style of my own communication to help the carer and person’s understanding. | 100 |
| 10. Welcomed questions from the carer and the person. | 100 |
| 11. Session was pitched at a level that was accessible to the person and the carer. The person and the carer remained engaged. | 94.1 |
| 12. Care was taken to pace the session at a rate that allowed the person and the carer to keep up with what was happening. | 100 |
| Interpersonal effectiveness | |
| 13. Communicated with warmth, concern and caring. | 100 |
| 14. In control of the session, communicated clearly without frequent hesitations/repetitions. | 100 |
| 15. Able to shift appropriately between listening and leading. | 100 |
| Engaging participants | |
| 16. Explained rationale and requirements for the different activities/elements of the session clearly. | 100 |
| 17. Did not criticise, disapprove, or ridicule the person or the carer. | 100 |
| 18. Responded to seemingly irrelevant interruptions in an effective yet respectful manner. | 100 |
| Session content | |
| 19. Reviewed the ABC chart. | 64.7 |
| 20. Did a 5-minute relaxation practice with the person and the carer. | 82.4 |
| 21. Checked on progress with Graded Exposure. | 82.4 |
| 22. Practised working on the next step of the Fear Ladder. | 58.8 |
| 23. Provided a 5-minute warning before the session ended. | 64.7 |
| 24. Summarised the session. | 94.1 |
| 25. Reminded the person about the time of the next session and its focus. | 88.2 |
| 26. Remind the person and carer that there are two sessions left. | 88.2 |
| Inter-session tasks | |
| 27. Reviewed previous week’s inter-session task (ABC chart and Graded Exposure). | 82.4 |
| 28. Encouraged carer to complete inter-session task (continue with ABC chart and practise Graded Exposure). | 88.2 |
| 29. Asked carer if they anticipated any problems with inter-session task. | 94.1 |
Fidelity checklist percentages for BEAMS Session 11
| Theme and question | Percentage of yes responses |
|---|---|
| Who was present at the session | |
| Person and carer | 86.7 |
| Person, carer and other | 13.3 |
| General session preparations | |
| 1. Gathered all resources listed in the materials section of the session plan. | 93.3 |
| 2. Ensured the person has their communication supports available (if needed). | 100 |
| 3. Agreed with the person and carer on frequency of breaks. | 86.7 |
| 4. Completed a Visual Schedule for the session. | 86.7 |
| Coverage of session plan | |
| 5. Agreed with the person and carer on the agenda for the session and completed a Visual Schedule. | 93.3 |
| 6. Ensured that the person and carer clearly understood the purpose of the session. | 100 |
| 7. Session aims were fulfilled. | 80 |
| 8. Session was completed in 1.5 hours. | 100 |
| Understanding and accessibility | |
| 9. Adjusted the content and style of my own communication to help the carer and person’s understanding. | 100 |
| 10. Welcomed questions from the carer and the person. | 100 |
| 11. Session was pitched at a level that was accessible to the person and the carer. The person and the carer remained engaged. | 100 |
| 12. Care was taken to pace the session at a rate that allowed the person and the carer to keep up with what was happening. | 100 |
| Interpersonal effectiveness | |
| 13. Communicated with warmth, concern and caring. | 100 |
| 14. In control of the session, communicated clearly without frequent hesitations/repetitions. | 100 |
| 15. Able to shift appropriately between listening and leading. | 100 |
| Engaging participants | |
| 16. Explained rationale and requirements for the different activities/elements of the session clearly. | 100 |
| 17. Did not criticise, disapprove, or ridicule the person or the carer. | 100 |
| 18. Responded to seemingly irrelevant interruptions in an effective yet respectful manner. | 100 |
| Session content | |
| 19. Reviewed the ABC chart. | 86.7 |
| 20. Did a 5-minute relaxation practice with the person and the carer. | 86.7 |
| 21. Checked on progress with Graded Exposure. | 86.7 |
| 22. Practised working on the next step of the Fear Ladder. | 66.7 |
| 23. Talked to the person and the carer about the treatment coming to an end. | 93.3 |
| 24. Introduced ‘Treatment summary’ and asked the carer to complete it for next session. | 86.7 |
| 25. Provided a 5-minute warning before the session ended. | 80 |
| 26. Summarised the session. | 86.7 |
| 27. Reminded the person about the time of the next session and its focus. | 100 |
| 28. Remind the person and carer that the next session is the last of this treatment. | 93.3 |
| Inter-session tasks | |
| 29. Reviewed previous week’s inter-session task (ABC chart and Graded Exposure). | 80 |
| 30. Encouraged carer to complete inter-session task (continue with Graded Exposure and complete ‘Treatment summary’). | 93.3 |
| 31. Asked carer if they anticipated any problems with inter-session task. | 100 |
Fidelity checklist percentages for BEAMS Session 12
| Theme and question | Percentage of yes responses |
|---|---|
| Who was present at the session | |
| Carer | 6.3 |
| Person and carer | 81.3 |
| Person, carer and other | 12.5 |
| General session preparations | |
| 1.Gathered all resources listed in the materials section of the session plan. | 100 |
| 2. Ensured the person has their communication supports available (if needed). | 100 |
| 3. Agreed with the person and carer on frequency of breaks. | 81.3 |
| 4. Completed a Visual Schedule for the session. | 72 |
| Coverage of session plan | |
| 5. Agreed with the person and carer on the agenda for the session and completed a Visual Schedule. | 81.3 |
| 6. Ensured that the person and carer clearly understood the purpose of the session. | 100 |
| 7. Session aims were fulfilled. | 93.8 |
| 8. Session was completed in 1.5 hours. | 93.8 |
| Understanding and accessibility | |
| 9. Adjusted the content and style of my own communication to help the carer and person’s understanding. | 100 |
| 10. Welcomed questions from the carer and the person. | 100 |
| 11. Session was pitched at a level that was accessible to the person and the carer. The person and the carer remained engaged. | 100 |
| 12. Care was taken to pace the session at a rate that allowed the person and the carer to keep up with what was happening. | 100 |
| Interpersonal effectiveness | |
| 13. Communicated with warmth, concern and caring. | 100 |
| 14. In control of the session, communicated clearly without frequent hesitations/repetitions. | 100 |
| 15. Able to shift appropriately between listening and leading. | 100 |
| Engaging participants | |
| 16. Explained rationale and requirements for the different activities/elements of the session clearly. | 100 |
| 17. Did not criticise, disapprove, or ridicule the person or the carer. | 100 |
| 18. Responded to seemingly irrelevant interruptions in an effective yet respectful manner. | 100 |
| Session content | |
| 19. Reminded the person and the carer that this was the last session. | 93.8 |
| 20. Reminded the person and the carer what anxiety is. | 93.8 |
| 21. Reminded the carer about the Treatment Plan and how to use it. | 93.8 |
| 22. Reminded the person and the carer about the importance of relaxation. | 93.8 |
| 23. Reminded the person and the carer about Fear Ladders and principles of Graded Exposure. | 87.5 |
| 24. Reviewed goals the person and carer identified in Session 2. | 87.5 |
| 25. Explored with the person and carer any possible changes to the Treatment Plan. | 93.8 |
| 26. Reminded the person and the carer about the importance of maintenance and generalisation. | 93.8 |
| 27. Identified maintenance goals and strategies. | 87.5 |
| 28. Identified generalisation goals and strategies. | 81.3 |
| 29. Provided a 5-minute warning before the session ended. | 81.3 |
| 30. Summarised the session. | 87.5 |
| 31. Did a relaxation exercise. | 75 |
| Inter-session tasks | |
| 32. Reviewed previous week’s inter-session task (‘Treatment summary’ and Graded Exposure). | 81.3 |
List of abbreviations
- ABC
- Antecedent-Behaviour-Consequence
- ADAMS
- Anxiety, Depression and Mood Scale
- CIASP-ID
- Clinical Anxiety Screen for people with Severe to Profound Intellectual Disability
- DASH-II
- Diagnostic Assessment for the Severely Handicapped Scale-II
- DBC2-A
- Developmental Behaviour Checklist-2 Adult
- GCP
- good clinical practice
- IAG
- intervention adaptation group
- NAS
- National Autistic Society
- PI
- principal investigator
- PIS
- Participant Information Sheet
- PAC
- Psychopathology in Autism Checklist
- PPIE
- patient and public involvement and engagement
- PTOS-II
- Psychological Therapies Outcome Scale - Intellectual Disabilities 2nd Edition
- QoL
- quality of life
- R&D
- research and development
- REC
- Research Ethics Committee
- SMG
- Study Management Group
- SRS
- Social Responsiveness Scale
- SRS-2
- Social Responsiveness Scale, Second Edition
- SSC
- Study Steering Committee
- TAU
- treatment-as-usual
- TIDieR
- Template for Intervention Description and Replication
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/MWTQ5721).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
