Notes
Article history
The research reported in this issue of the journal was commissioned and funded by the Evidence Synthesis Programme on behalf of NICE as award number NIHR135520. The protocol was agreed in June 2022. The assessment report began editorial review in July 2022 and was accepted for publication in November 2022. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ manuscript and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this manuscript.
Permissions
Copyright statement
Copyright © 2024 Westwood et al. This work was produced by Westwood et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Westwood et al.
Chapter 1 Objective
The overall aim of this project was to provide a comprehensive summary of all available evidence that may be relevant to the potential implementation of KardiaMobile six-lead (6L), in the context of QT interval-based cardiac risk assessment for service users who require antipsychotic medication.
The assessment of KardiaMobile 6L as a triage step means that patients with QT prolongation, identified by KardiaMobile 6L, would be followed up using 12-lead electrocardiogram (ECG). Full cost-effectiveness analysis should, therefore, compare KardiaMobile 6L, followed by 12-lead ECG in patients in whom QT prolongation is identified, to 12-lead ECG in all patients (i.e. no triage step), or no ECG (in situations where 12-lead ECG is not available or is refused).
We defined a series of research questions that would need to be addressed, to support a full assessment of the clinical effectiveness and cost-effectiveness of using KardiaMobile 6L for the initial assessment (triage) of QT interval-based cardiac risk in service users prior to the initiation of antipsychotic medications which are associated with an established risk of QT interval prolongation, and for monitoring QT interval-based cardiac risk once medication has been established:
-
What is the accuracy/technical performance of KardiaMobile 6L, where prolonged corrected QT interval (QTc), determined by 12-lead ECG (the reference standard method) is the target condition?
-
What are the clinical effects (on cardiac and psychiatric outcomes) of using KardiaMobile 6L for the initial assessment (triage) of QT interval-based cardiac risk in service users taking antipsychotic medications that are associated with QT prolongation, both for baseline assessment before initiating medication and for ongoing monitoring, compared to 12-lead ECG in all patients (no triage step) or no ECG?
-
What are the effects of using KardiaMobile 6L on service user acceptability/satisfaction and on training and workflow issues?
-
What are the costs, from a UK NHS and Personal Social Services (PSS) perspective, of using KardiaMobile 6L for the initial assessment (triage) of QT interval-based cardiac risk in service users taking antipsychotic medications that are associated with QT prolongation?
-
What existing, published cost-effectiveness studies are available about QT interval assessment for service users who require antipsychotic medication?
Given the anticipated limitations of the evidence base, this early value assessment (EVA) used a broader scope to consider whether the KardiaMobile 6L device triage has the potential to provide an effective and safe alternative to 12-lead ECG for initial assessment and monitoring of the risk of cardiac problems in people taking antipsychotic medications. The assessment included evidence about secondary outcomes, which are not sufficient to inform decision-making about routine use in UK NHS clinical practice, in the absence of higher-level outcomes data (evidence about the clinical efficacy and safety of the device). These outcomes have been included to inform consideration of the potential benefits of implementing the KardiaMobile 6L device, as specified in the scope, and hence to indicate whether further research to establish clinical efficacy and safety is warranted. The available evidence has been summarised, with consideration of its relevance to the above research questions, and a detailed description of evidence gaps where further research is needed is provided. This assessment does not include cost-effectiveness modelling, because the evidence currently available is not sufficient to support this.
Chapter 2 Background and definition of the decision problem(s)
Population
The primary indication for this assessment is the use of the KardiaMobile 6L ECG device for the assessment of QT interval-based cardiac risk in service users prior to the initiation of antipsychotic medications, which are associated with an established risk of QTc prolongation, and for monitoring QT interval-based cardiac risk once medication has been established. The National Institute for Health and Care Excellence (NICE) Clinical Guidelines CG178 and CG185 on the prevention and management of psychosis and schizophrenia in adults1 and the assessment and management of bipolar disorder2 recommend that a person should be offered an ECG before starting antipsychotic medication if:
-
specified in the drug’s summary of product characteristics or
-
a physical examination has identified specific cardiovascular risk or
-
there is a family history of cardiovascular disease, sudden collapse or other cardiovascular risk factors such as arrhythmia or
-
the service user is being admitted as an inpatient.
A guideline from the NHS Northern England clinical network3 states that a baseline ECG should be done for all people starting antipsychotic medication. Published recommendations, from Leeds Teaching Hospitals NHS Trust,4 provide an algorithm for what clinicians should do when considering prescribing QT-prolonging medication. This algorithm includes the recommendations for the use of baseline and monitoring ECG, suggesting that when initiating drugs with a high risk of QTc prolongation, ECG should be done at baseline, and may be repeated once the drug reaches therapeutic levels (four to five half-lives). 4 If the service user is taking other QTc prolonging medication, or has risk factors for QTc prolongation, then regular ECG monitoring is recommended. An ECG is also recommended after dose changes. 4 The British Heart Rhythm Society clinical practice guidelines on the management of patients developing QTc prolongation on antipsychotic medication recommend that QTc is measured using either lead II or V5. 5 This guideline also notes that studies have indicated that antipsychotics are associated with a rate of sudden cardiac death that is two to three times higher than that of the general population (approximately 15 per 10,000 years of drug exposure), but that this is substantially lower than the mortality risk associated with uncontrolled psychosis. 5
This assessment considers the potential clinical effectiveness of using KardiaMobile 6L for the triage of QT interval-based cardiac risk in service users prior to the initiation of antipsychotic medications, which are associated with an established risk of QTc prolongation, and for monitoring QT interval-based cardiac risk once medication has been established. The assessment of KardiaMobile 6L as a triage step means that patients with QTc prolongation, identified by KardiaMobile 6L, would be followed up using 12-lead ECG; this would be the case both for both assessment prior to the initiation of antipsychotic medications and for monitoring QT interval-based cardiac risk once medication has been established. There may be additional circumstances where follow-up 12-lead ECG is required, for example where the KardiaMobile 6L readout is considered to be of insufficient quality for clinical decision-making.
Presentations for which antipsychotic medications, associated with a risk of QT prolongation, may be prescribed
Psychosis and schizophrenia
Psychosis (sometimes referred to as psychotic episodes or experiences) is a mental health condition that causes people to see or interpret things differently to other people. The main manifestations of psychosis are hallucinations and delusions. Psychotic disorders, based on the World Health Organization (WHO) International Classification of Diseases (ICD) chapter on Mental and Behavioural Disorders Diagnostic Criteria for Research (ICD-10),6 comprise two main types: schizophrenia and affective psychosis (psychosis in the context of severe mood disturbance such as depression or mania). Antipsychotic medications may be variously given, in service users with these conditions, to treat acute episodes and/or as part of long-term management. 1 The NHS Digital, Mental Health and Wellbeing in England: Adult Psychiatric Morbidity Survey 20147 reported the overall prevalence of psychotic disorders as 0.4% in 2007 and 0.7% in 20147 and noted that there were no significant differences in the rate between men and women. This survey used interviews with a sample of the household population, 7500 people aged 16 or over, including those who do not access services. 7 Although the observed rate was highest in those aged 35–44, associations with age were not statistically significant for the year 2014. 7 However, psychotic disorders were associated with ethnic group with rates found to be higher in black men (3.2%) than men from other ethnic groups; rates of psychotic disorder did not vary significantly between ethnic groups among women. 7 Socioeconomic factors were also reported to be strongly linked with psychotic disorder, with psychotic disorder being more common in those who are economically inactive. 7 Overall, four-fifths of people identified with psychotic disorder were reported to be in receipt of treatment, and approximately 76% were currently taking psychotropic medications. 7
Bipolar disorder
Bipolar disorder is a mental health condition in which a person experiences episodes of mania and episodes of depressed mood which can last for several weeks or months. 2 The peak age of onset is 15–25 years, and there is often a substantial delay between onset and first contact with mental health services. 2 Approximately 1 in every 50 adults will have bipolar disorder at some point in their life. 2 The NHS Digital, Mental Health and Wellbeing in England: Adult Psychiatric Morbidity Survey 20147 used a 15-item Mood Disorder Questionnaire to screen for bipolar disorder, with a positive screen requiring endorsement of at least seven lifetime manic/hypomanic symptoms, as well as several co-occurring symptoms, together with moderate or serious functional impairment; a positive screen indicated the likely presence of bipolar disorder and that fuller assessment would be warranted. Overall, 2.0% of the NHS Digital, Mental Health and Wellbeing in England population screened positive for bipolar disorder; rates were similar in men and women and a positive screen was more common in younger age groups (3.4% of 16–24-year-olds) and in economically inactive participants. 7 Approximately 39% of those screening positive for bipolar disorder were currently receiving some form of psychotropic medication. 7
Treatment-resistant depression
Based on the NICE definition of people with treatment-resistant depression, as those who have not responded to two antidepressants,8 approximately 2.7 million people in the UK have treatment-resistant depression (between 10% and 30% of people with depression). 9 If a person has depression that does not respond well to initial treatment with antidepressants, concomitant antipsychotic medication such as aripiprazole, olanzapine, quetiapine or risperidone may be used to augment treatment. 9 Decisions to use antipsychotics in this manner should be made with care, given that some antidepressants can also prolong the QTc. 9
Dementia
People with dementia may experience severe agitation, aggression or psychotic symptoms. According to the NICE guideline on dementia,10 assessment, management and support for people living with dementia and their carers, antipsychotic medications may be offered for people with these symptoms if they are at risk of harming themselves or others, or if they are experiencing agitation, hallucinations or delusions that are causing them severe distress. Apart from risperidone and haloperidol, this is generally an off-label use of antipsychotics. 11 NICE also recommends conducting a structured assessment to explore possible reasons for the distress before considering antipsychotic medication. It is recommended to use the lowest effective dose for the shortest possible time, and to reassess the person at least every 6 weeks to check whether ongoing medication is still required.
Intervention technology
People taking antipsychotic medications, which are associated with an established risk of QTc prolongation, may need to be screened for QTc prolongation before initiation of treatment and monitored for the development of QTc prolongation if treatment is ongoing.
Current practice is to use 12-lead ECG devices in primary or secondary care centres. An ECG is a test to measure heart rhythm and electrical activity. Electrodes in contact with the skin detect the electrical signals produced by the heart as it beats. Multiple views of the heart can be recorded by placing electrodes at different places on the body. These different views are referred to as ECG leads and are displayed as separate traces on the output. 12 A conventional ECG records 12 leads using 10 electrodes, which are split into 6 limb leads which view the heart in a vertical plane and 6 precordial leads which view the heart in a horizontal plane.
Twelve-lead ECG devices require the service user to partially undress, and the healthcare practitioner needs to use conductive gel to create contact between the service user’s skin and the electrodes. Some people may find these requirements distressing or unacceptably intrusive. Some portable ECG devices offer a less intrusive way to take ECG measurements that require less undressing (limb only electrodes) and may eliminate the need for conductive gel and may therefore be more acceptable to patients.
Some people needing ECG assessments may find travel or attendance at healthcare centres for appointments difficult. Portable ECG devices are easily transported, so they can be used by community healthcare practitioners in home visits. Use of the devices could increase the likelihood that people will have an ECG done regularly and may result in more cardiac irregularities being identified. Additionally, these devices have the potential to reduce costs and time associated with ECG monitoring by reducing the number of appointments in hospitals or general practitioner (GP) surgeries and could release capacity for 12-lead ECG use for other indications.
KardiaMobile six-lead (AliveCor)
The KardiaMobile 6L is a portable 6L ECG device that is manufactured by AliveCor. It uses three electrodes to record a person’s ECG and wirelessly transmits the data to a compatible smartphone or tablet via Bluetooth. The Kardia application allows the ECG data to be converted into a portable document format (PDF). This can then be sent via e-mail to physicians. User data are stored on a General Data Protection Regulation (GDPR)-compliant cloud-based system hosted in Frankfurt, Germany. The device is powered by a single-coin-cell battery.
There are two electrodes on the top of the device for use with the left and right hands, and one on the bottom of the device for use with the bare skin of the left knee or inside of ankle. The service user is usually seated for the test. In single-channel mode, the KardiaMobile 6L can record a lead-I ECG. In two-channel mode, it can record a 6L ECG.
The company has stated that healthcare professionals can be trained quickly by following the instructions for use and instructions from within the application, but training by company representatives can be supplied if required.
The company has further stated that the device provides an instant algorithmic analysis of a person’s heart rhythm upon completion of the ECG recording. This indicates normal sinus rhythm, atrial fibrillation, bradycardia, tachycardia or an unclassified result for both single-lead and 6L ECGs. Currently, QTc must be calculated by the user; however, the company is developing software to allow automated QTc analysis.
In a pilot programme, the results of the test were shared with a cardiologist or other appropriate clinician for analysis, and then sent to the service user’s clinical team with any abnormalities highlighted. 13 A 12-lead ECG may be required in cases where the outcome of the 6L device is unclear, or if other heart conditions such as ischaemia or left ventricular hypertrophy are suspected. 14
The KardiaMobile 6L has not been tested for and is not intended for paediatric use. The company states that significant body fat, body hair or very dry skin can interfere with the electrodes.
Pacemakers (and pacemakers that are also defibrillators) affect ECG devices, in that they generate sharply abnormal cardiac electrical activity, when they are active (pacing); this results in pacemaker ‘spikes’, which are readily recognisable by a human reader, but which may cause problems for automated interpretation. The manufacturer’s instructions for use, for KardiaMobile 6L, include the statement ‘DO NOT use with a cardiac pacemaker, ICDs, or other implanted electronic devices’.
Target condition
Some antipsychotic medications are associated with prolonged ventricular repolarisation, potentially giving rise to QT prolongation. This can sometimes lead to arrhythmias such as polymorphic ventricular tachycardia (including torsades de pointes), which can cause hypotension, with dizziness, fainting and convulsions, and can progress to ventricular fibrillation and sudden cardiac death. 15
The target condition, with respect to assessing the accuracy of KardiaMobile 6L, is QTc prolongation. It is important to note that the term QTc, which means corrected QT interval, is often used for QT interval, given that the QT interval needs to be corrected for heart rate. Definitions of abnormal QTc vary. The diagnostic thresholds for short QT syndrome and long QT syndrome, specified in the European Society of Cardiology 2015 guidelines for the management of patients with ventricular arrhythmias and prevention of sudden cardiac death,16 are QTc ≤ 340 and ≥ 480 ms (or > 500 ms in asymptomatic patients with no family history), respectively. British Heart Rhythm Society clinical practice guidelines on the management of patients developing QT prolongation on antipsychotic medication5 state that a QTc is considered normal if below 440 ms for men, or below 470 ms for women. The ECG should be repeated annually if a normal QTc is detected. If an abnormal QTc of more than 500 ms is detected, the guideline recommends immediate cessation of the suspected drug and urgent referral to a cardiologist. If the abnormal QTc is < 500 ms, it is advised to decrease the dose of antipsychotic or consider switching to an alternative drug with a lower risk of increased QTc. The Maudsley Prescribing Guidelines advise not to use QTc-prolonging drugs if QTc is more than 460 ms and the patient has had an unexplained syncopal episode. 17 If the QTc is between 480 and 499 ms, it is advised to consider alternative therapy or monitor QTc monthly, to correct electrolyte imbalances, and to consider referral to cardiology. If the QTc is more than 500 ms or has increased by more than 60 ms, the QT-prolonging drug should be discontinued, and the service user referred to cardiology. Khatib et al. 4 recommend that, if a significant change in QTc is observed (increase > 50 ms or absolute value more than 500 ms), dose reduction or drug cessation should be considered. Although cardiologists may be consulted in the case of uncertain ECGs, the authors note that the decision on dose change lies with the prescriber. This assessment will consider any reported definition of abnormal QTc.
QTc prolongation is, however, an interim outcome. This assessment will also consider the effects of implementing KardiaMobile 6L on the rates of adverse clinical outcomes, both cardiac and psychiatric.
Care pathway
Risk assessment
The National Clinical Audit of Psychosis recommended that people with psychotic disorders are assessed for risk of cardiovascular disease at least annually, using the Q-Risk tool. 18 The choice of antipsychotic medication, the starting dose and/or the increase in frequency of monitoring should then be influenced by the presence of any cardiovascular disease history, as well as other factors such as poor nutrition or liver disease. 15 Identification of any cardiovascular risk factors should also prompt a more detailed cardiac assessment including an ECG, which should be examined for evidence of ischaemic heart disease, left ventricular hypertrophy and repolarisation abnormalities. It should be noted that assessments of general cardiac health fall outside the scope of this assessment; this assessment focused on the use of ECG to assess QT interval-based cardiac risk.
Management/treatment
During scoping discussions, clinical experts advised that changes to antipsychotic medication following detection of prolonged QTc are made following an assessment of the relative risk and benefit of treating the psychiatric condition versus cardiac side effects. Some experts noted that the risk of cardiac complications is often considered lower than the risks of psychotic symptoms if antipsychotics are not given.
This assessment provides a systematic review of the evidence about the accuracy of KardiaMobile 6L, as an initial testing (triage) method for the detection of QTc prolongation, in service users prior to the initiation of antipsychotic medications, which are associated with an established risk of QT interval prolongation, and for monitoring QT interval-based cardiac risk once medication has been established. QTc prolongation is an interim outcome and this assessment, therefore, also considered evidence about effects of implementing KardiaMobile 6L on the rates of adverse clinical outcomes, both cardiac and psychiatric.
This assessment also considered any reported information on testing uptake and acceptability or patient satisfaction outcomes, and other intermediate outcomes (e.g. ease of use, number of 12-lead ECG requests, number of cardiology referrals/requests for cardiology interpretation, test failure rates, change to clinical decision, time to antipsychotic use) reported in studies of relevant populations.
This assessment aimed to provide a comprehensive summary of all available evidence that may be relevant to the potential implementation of KardiaMobile 6L, in the context of QT interval-based cardiac risk assessment for service users who require antipsychotic medication. It was anticipated that currently available evidence would not be sufficient to inform assessment of the efficacy and safety of KardiaMobile 6L, in people taking antipsychotic medications, and to support full cost-effectiveness modelling. The assessment, therefore, focused on whether the KardiaMobile 6L device has the potential to offer advantages over the use of 12-lead ECG for initial assessment and monitoring of QT interval-based cardiac risk in people taking antipsychotic medications, such that further research to establish clinical efficacy and safety is warranted. To this end, the assessment used a broad scope and included secondary outcomes, which are not sufficient to inform decision-making about routine use in UK NHS clinical practice, in the absence of higher-level outcomes data (evidence about the clinical efficacy and safety of the device). These outcomes were included to inform consideration of the potential benefits of implementing the KardiaMobile 6L device, as specified in the scope, and hence to indicate whether further research to establish clinical efficacy and safety is warranted. This assessment does not include cost-effectiveness modelling, because the evidence currently available is not sufficient to support this.
Chapter 3 Systematic review methods
Systematic review methods followed the principles outlined in the Centre for Reviews and Dissemination (CRD) guidance for undertaking reviews in health care,19 the NICE guide to methods of technology appraisal20 and the Cochrane Handbook for Diagnostic Test Accuracy Reviews. 21
This report contains reference to confidential information provided as part of the NICE Diagnostic Assessment process. This information has been removed from the report and the results, discussions and conclusions of the report do not include the confidential information. These sections are clearly marked in the report.
Search strategy
Search strategies were undertaken to identify studies evaluating KardiaMobile 6L (as described in Table 1), as recommended in the CRD guidance for undertaking reviews in health care19 and the Cochrane Handbook for Diagnostic Test Accuracy Reviews. 21
| Question | (1) What is the accuracy/technical performance of KardiaMobile 6L, where the target condition is QTc prolongation, determined by standard 12-lead ECG (the reference standard method)? | (2) What are the clinical effects of using KardiaMobile 6L, compared with 12-lead ECG or no ECG, on clinical outcomes (cardiac and psychiatric)? | (3) What are the effects of using KardiaMobile 6L on service user acceptability/satisfaction and on training and workflow issues? | (4) What are the costs, from a UK NHS and PSS perspective, of using KardiaMobile 6L for the initial assessment (triage) of QT interval-based cardiac risk in service users taking antipsychotic medications that are associated with QT prolongation?a | (5) What existing, published cost-effectiveness studies are available about QT interval assessment for service users who require antipsychotic medication? |
| Participants | Any populationb | People starting or maintained on antipsychotic medications that are associated with QT prolongation, in whom an ECG assessment of QT-based cardiac risk is indicated. | People starting or maintained on antipsychotic medications that are associated with QT prolongation, in whom an ECG assessment of QT-based cardiac risk is indicated (service user acceptability/satisfaction). Healthcare professionals or others delivering ECG assessment of QT-based cardiac risk, in settings applicable to the above population (training and workflow).b |
Any UK population.b | People starting or maintained on antipsychotic medications that are associated with QT prolongation, in whom an ECG assessment of QT-based cardiac risk is indicated. |
| Setting | Any setting | ||||
| Interventions (index test) | KardiaMobile 6L | Any ECG device | |||
| Comparators | None | 12-lead ECG or no ECG | 12-lead ECG or no comparator | Any other ECG device or no ECG | |
| Reference standard | 12-lead ECG | NA | |||
| Outcomes | Diagnostic accuracy (the numbers of TP, FN, FP and TN test results), where the target condition is QTc prolongation, determined by 12-lead ECG. Secondary outcomes:c concordance (of QTc or QT determined by KardiaMobile 6L with that determined by 12-lead ECG), test failure rates and reasons for failure. |
Cardiac outcomes (arrhythmias, sudden cardiac death), psychiatric outcomes, hospitalisations (cardiac or psychiatric), referrals to mental health crisis teams, other adverse effects of antipsychotic medication, HRQoL. Secondary outcomesc: change to treatment decision, time from decision to prescribe to treatment. |
Secondary outcomes:c measures of service user preference (e.g. rates of refusal or missed appointments), number of 12-lead ECGs required, number of cardiology referrals/requests for cardiology interpretation, appointment length (including time to take ECG and time for general care of the service user), ease of use (for service users and healthcare professionals), including training requirements, cleaning of the device between uses and time to obtain ECG. | Secondary outcomes:c costs related to use of devices (including purchase costs, software subscriptions and consumable costs), costs related to doing the tests (including staff time for travel, and time for testing and interpretation), cost of training (including operating ECG devices and interpreting ECG outputs), cost of treatment (including treatment of any cardiac or psychiatric conditions), cost of missed appointments. | QALYs |
| Study design | Diagnostic cohort studies or observational, non-inferiority/equivalence studies for concordance. | RCTs, CCTs or observational before and after (implementation) studies. | RCTs, CCTs and comparative or non-comparative observational studies. | Studies reporting a full economic analysis. | |
Candidate search terms were identified from target references, browsing database thesauri (e.g. MEDLINE MeSH and Embase EMTREE) and existing reviews identified during the initial scoping searches. Strategy development involved an iterative approach, testing candidate text and indexing terms across a sample of bibliographic databases, aiming to reach a satisfactory balance of sensitivity and specificity. Search strategies were developed specifically for each database and the keywords and thesaurus terms were adapted according to the configuration of each database.
The following databases were searched for relevant studies from inception to April/May 2022:
-
MEDLINE (Ovid): 1946 to 25 April 2022.
-
MEDLINE In-Process Citations (Ovid): 1946 to 25 April 2022.
-
MEDLINE Daily Update (Ovid): 1946 to 25 April 2022.
-
MEDLINE Epub Ahead of Print (Ovid): 1946 to 25 April 2022.
-
EMBASE (Ovid): 1974 to 25 April 2022.
-
PubMed-not-MEDLINE (Ovid):1946 to 17 May 2022.
-
PubMed (NLM) (Internet): up to 18 May 2022.
-
Cochrane Database of Systematic Reviews (CDSR) (Wiley): up to April 2022/Iss 4.
-
Cochrane Central Register of Controlled Trials (CENTRAL) (Wiley): up to March 2022/Iss 3.
-
Database of Abstracts of Reviews of Effects (DARE) (Internet) (www.crd.york.ac.uk/CRDWeb/): up to March 2015.
-
Health Technology Assessment (HTA) database (Internet) (www.crd.york.ac.uk/CRDWeb/): up to March 2018.
-
Cumulative Index to Nursing and Allied Health Literature (CINAHL) (EBSCO): 1881 to 27 April 2022.
-
PsycINFO (Ovid): 1806 to April 2022/Wk 3.
-
Kleijnen Systematic Reviews Ltd (KSR Ltd) Evidence (https://ksrevidence.com/): up to 26 April 2022.
-
Epistemonikos (Internet) (www.epistemonikos.org/): up to 27 April 2022.
-
International Network of Agencies for Health Technology Assessment (INAHTA) database Publication (Internet) (www.inahta.org/hta-database/): up to 27 April 2022.
-
National Institute for Health and Care Research (NIHR) Health Technology Assessment Programme (Internet) (www.nihr.ac.uk/): up to 27 April 2022.
-
International Prospective Register of Systematic Reviews (PROSPERO) (Internet) (www.crd.york.ac.uk/prospero/): up to 26 April 2022.
-
International Platform of Registered Systematic Review and Meta-analysis Protocols (Internet) (https://inplasy.com/): up to 27 April 2022.
-
Latin American and Caribbean Health Sciences Literature (LILACS) (Internet) (http://regional.bvsalud.org/php/index.php?lang=en): up to 28 April 2022.
-
Directory of Open Access Journals (DOAJ) (https://doaj.org/): up to 25 May 2022.
-
European Heart Journal – Digital health (https://academic.oup.com/ehjdh/): up to 19 May 2022.
Completed and ongoing trials were identified by searching the following resources:
-
National Institutes of Health (NIH) ClinicalTrials.gov (Internet) (www.clinicaltrials.gov/): up to 27 April 2022.
-
EU Clinical Trials Register (Internet) (www.clinicaltrialsregister.eu/ctr-search/search): up to 27 April 2022.
-
World Health Organization International Clinical Trials Registry Platform (WHO ICTRP) (Internet) (www.who.int/ictrp/en/): up to 28 April 2022.
-
ScanMedicine (Internet) (https://scanmedicine.com/): up to 27 April 2022.
To identify conference proceedings, searches in EMBASE were not restricted to exclude conference abstracts. In addition, a search was undertaken of the following conference proceedings resource:
-
Northern Light Life Sciences Conference Abstracts (Ovid): 2010–2/Week 16.
An additional search of the medRxiv PrePrint server was undertaken. All results retrieved from this resource were treated with due caution, as these are preliminary reports of work that have not undergone peer review.
-
medRxiv (Internet) (www.medrxiv.org): up to 27 April 2022.
No restrictions on language, publication status or date were applied. Searches included generic and other product names for the device where appropriate.
All search strategies are presented in Appendix 1.
The main EMBASE strategy for each search was independently peer reviewed by a second Information Specialist based on the Canadian Agency for Drugs and Technologies in Health (CADTH) Peer Review checklist. 22 References in retrieved articles were checked for additional studies to identify any additional relevant papers not retrieved by the searches and clinical experts were consulted to identify ongoing or unpublished studies.
Further additional literature searches were performed with the aim of identifying any published economic evaluations of ECG assessment of QT interval-based cardiac risk in service users prior to the initiation of antipsychotic medications or for monitoring QT interval-based cardiac risk once medication has been established. This review was not restricted by ECG device, as model structures used to evaluate the cost effectiveness of 12-lead ECG are likely to be relevant to future evaluations of KardiaMobile 6L or other mobile devices. A methodological study design filter to identify cost and economic studies was included in those in databases that are not health economic specific. The following databases and resources were searched to identify economic evaluations:
-
MEDLINE (Ovid): 1946 to 26 April 2022.
-
MEDLINE In-Process Citations (Ovid): 1946 to 26 April 2022.
-
MEDLINE Daily Update (Ovid): 1946 to 26 April 2022.
-
MEDLINE Epub Ahead of Print (Ovid): 1946 to 26 April 2022.
-
EMBASE (Ovid): 1974 to 26 April 2022.
-
NHS Economic Evaluation Database (NHS EED) (CRD): up to March 2015.
-
CEA Registry (Internet) (www.cearegistry.org): up to 28 April 2022.
-
Research Papers in Economics (RePEc) (Internet) (http://repec.org/): up to 28 April 2022.
All search strategies are presented in Appendix 1.
Inclusion and exclusion criteria
Separate inclusion criteria were developed for each research question. These are summarised in Table 1.
Inclusion screening and data extraction
Two reviewers [Marie Westwood (MW) and Pawel Posadzki (PP)] independently screened the titles and abstracts of all reports identified by the searches and any discrepancies were resolved by discussion. Full copies of all studies deemed potentially relevant, after discussion, were obtained and two reviewers (MW and PP) independently assessed these for inclusion; any disagreements were resolved by discussion.
Where available, data were extracted on the following: study design/details, participant characteristics (demographic characteristics, presenting symptoms/diagnosis, other cardiac risk factors, antipsychotic medication being initiated or which is the indication for monitoring, etc.), details of the implementation of KardiaMobile 6L (protocol for use, definition of abnormal QTc used, method of reporting output, experience and training of healthcare professionals administering the ECG and of those interpreting the output, etc.), application (baseline screening or monitoring), details of reference standard (12-lead ECG) including where and by whom this was performed and interpreted, measures of test accuracy (e.g. sensitivity and specificity) and test technical performance outcome measures (e.g. failure rate and reasons for test failure, concordance), cardiac outcomes (arrhythmias, sudden cardiac death), psychiatric outcomes, hospitalisations (cardiac or psychiatric), other adverse effects of antipsychotic medication, health-related quality of life (HRQoL), changes to treatment decision, number of 12-lead ECGs required, time from decision to prescribe to treatment, measures of service user preference (e.g. rates of refusal or missed appointments) and workflow and training outcomes (e.g. number of cardiology referrals/requests for cardiology interpretation, appointment length, training requirements). Data were extracted by one reviewer (MW) and checked by a second reviewer (PP); any disagreements were resolved by discussion.
The assessment also included scoping searches to identify cost studies KardiaMobile 6L likely to be of relevance to the UK setting (research question 4) and cost-effectiveness studies about ECG QT interval assessment for service users who require antipsychotic medication; a full systematic review of cost studies and cost-effectiveness studies was outside the scope of this assessment.
Quality assessment
There is no published, validated tool for the assessment of the methodological quality of technical validation studies of diagnostic technologies; the methodological quality of these studies, therefore, assessed using the relevant components of QUADAS-2. 23 No formal quality assessment was applied to the other study types (case series) included in this report, because the size and design of these studies render formal quality assessment inappropriate and because they have not substantially informed the aims of this EVA. We did not consider formal assessment of methodological quality or risk of bias to be appropriate for non-research study pilot project reports; however, our report includes a qualitative summary of the key issues, with respect to the reliability of the information provided by these reports to address the aims of this EVA (see Study quality). The results of all quality assessment processes have been used for descriptive purposes to provide an evaluation of the overall quality of the included studies and to provide a transparent method of recommendation for design of any future studies. Quality assessment was undertaken by one reviewer (MW) and checked by a second reviewer (PP); any disagreements were resolved by discussion.
The results of the quality assessments are summarised and presented in tables (see Study quality) and QUADAS-2 assessments are presented in full in Appendix 2.
Methods of analysis/synthesis
Meta-analysis was considered inappropriate, due to the small number of included studies and wide variation in study design, study populations and outcomes reported; we therefore employed a narrative synthesis. The results section of this report is structured by research question. A detailed commentary on the major methodological problems or biases that affected the studies is also provided, together with a description of how this may have affected the individual study results and the relevance or otherwise of these studies to the decision problem specified. The evidence gaps identified have been used to inform recommendations for future research.
Chapter 4 Systematic review results
The literature searches of bibliographic databases conducted for this EVA systematic review, including additional scoping searches conducted to identify costs and cost-effectiveness studies, identified 8505 unique references. After initial screening of titles and abstracts, 28 references24–50 were considered to be potentially relevant and ordered for full paper screening; of these 10 publications,26,31,34,37,39–43 relating to six studies, were included in the review. A further three publications, one provided by NICE/Specialist Committee Members (SCMs)14 and two provided by the manufacturer of KardiaMobile 6L, AliveCor,51,52 were assessed and included in the review. These publications related to two additional studies and were all published in a journal, European Heart Journal – Digital Health, which is not yet indexed in the bibliographic databases searched. All other potentially relevant studies cited in documents supplied by the test manufacturer, AliveCor, had already been identified by bibliographic database searches. Finally, two unpublished project reports of pilots of KardiaMobile 6L, conducted at Tees Esk and Wear Valleys (TEWV) NHS Foundation Trust53 and Cumbria, Northumberland, Tyne and Wear (CNTW) NHS Foundation Trust,54 and provided through NICE, were included in the review. Figure 1 shows the flow of studies through the review process. Appendix 3 provides details, with reasons for exclusion, of all publications excluded at the full paper screening stage.
FIGURE 1.
Flow of studies through the review process.

In addition to the studies included in this report, our searches of trial registries identified five potentially relevant ongoing studies; details of these studies and their current status are provided in Appendix 4.
Overview of included studies
Based on the searches and inclusion screening described above, 13 publications,14,26,31,34,37,39–43,51,52 relating to 8 studies, and 2 additional unpublished reports,53,54 were included in this review; the results section of this report cites studies using the primary publication only.
All eight14,26,31,37,41,42,51,52 of the included studies were published, in full, in peer-reviewed journals.
All eight of the included published studies were technical validation studies14,31,37,41,51 or case series,26,42,52 reporting some, very limited information relevant to research question 1, ‘What is the accuracy/technical performance of KardiaMobile 6L, where the target condition is QTc prolongation, determined by standard 12-lead ECG (the reference standard method)?’ One study37 reported data (time to register an ECG) relevant to research question 3, ‘What are the effects of using KardiaMobile 6L on service user acceptability/satisfaction and on training and workflow issues?’ Although it did not meet the inclusion criteria for this question, because it was not conducted in service users requiring antipsychotic medication, data from this study have been included in the results for research question 3, for completeness. 37
The two unpublished pilot project reports provided some information relevant to research question 3, as well as some information on UK-relevant costs. 53,54
We did not identify any studies which specifically addressed research question 2, ‘What are the clinical effects of using KardiaMobile 6L, compared with 12-lead ECG or no ECG, on clinical outcomes (cardiac and psychiatric)?’ Both the unpublished pilot project reports provided small amounts of information for the survey question, to healthcare professionals, ‘Did the use of the AliveCor KardiaMobile 6L device change the clinical outcome for your patient?’53,54 Finally, we did not identify any cost-effectiveness studies about ECG QT interval assessment for service users who require antipsychotic medication (research question 5).
Four of the eight published studies included in this report were conducted in Europe: two were conducted in the UK,14,42 one in Poland51 and one in Spain. 37 The remaining four studies were conducted in the USA26,31,52 and in Australia. 41
Only four14,26,31,41 of the included published studies provided any information about funding and, of these, two indicated support from AliveCor;26,31 details of all reported funding sources are provided in Table 2.
| Study ID | Study details | Objective | Does the study include people starting or maintained on antipsychotic medications that are associated with QT prolongation, in whom an ECG assessment of QT-based cardiac risk is indicated? | Study design and outcome(s) extracted |
|---|---|---|---|---|
| Azram 2021 (EVALECG Cardio)14 | Prospective study of 1015 cardiology inpatients and outpatients Full paper Single centre, tertiary care cardiology Country: UK Funded by: NR; two authors received funding from Biosense Webster |
To compare the diagnostic ability of the KardiaMobile 6L against the 12-lead ECG. | No | Observational technical validation study. Mean difference for QT and QTc measurements between KardiaMobile 6L ECG and 12-lead ECG, proportion of leads in which QT/QTc measurements could be performed, AUC for detection of abnormal QT interval. |
| Frisch 202126 | Prospective study of four COVID-19–positive inpatients, requiring ECG monitoring Full paper Single centre, university hospital Country: USA Funded by: Editing, manuscript review, formatting, reference checks and submission preparation were provided by Peloton Advantage, LLC, an OPEN Health company, and funded by AliveCor. Demonstration devices for this project were provided by AliveCor. |
To assess the feasibility of recording using KardiaMobile 6L, along with a tablet application (KardiaStation; AliveCor) in inpatients needing intermittent ECG monitoring, and to document the ease of use of contactless ECG recordings and to compare contactless ECG recordings from the KardiaMobile 6L with standard ECG recordings. | No | Case series QT and QTc intervals, per patient and per device. |
| Kleiman 202131 | Prospective study of 705 patients referred to a genetic heart rhythm clinic Full paper Single centre, tertiary care cardiology Country: USA Funded by: The research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors; however, one of the authors was an employee of AliveCor. |
To compare recordings from the KardiaMobile 6L device to ECGs collected with standard 12-lead ECG devices. | No | Observational technical validation study. Absolute values and mean and median difference for QT and QTcFa measurements between KardiaMobile 6L ECG and 12-lead ECG, and categorical difference data. |
| Krzowski 202151 | Prospective study of 98 cardiology patients Full paper Single centre, university hospital Country: Poland Funded by: NR |
To evaluate the usability of portable ECG recorders [KardiaMobile 6L (KM) and Istel (IS) HR-2000] by comparing rhythm and basic ECG parameters (PQ, RR and QT intervals, duration of QRS complexes, etc.) obtained with KM/IS to standard 12-lead ECG tracings. | No | Observational technical validation study. Mean QT measurements for KardiaMobile 6L ECG and 12-lead ECG. |
| Minguito-Carazo 202137 | Prospective study of 182 patients hospitalised with COVID-19 (within patient comparison of KardiaMobile 6L and 12-lead ECG was only undertaken for a consecutive cohort of 45 healthy patients) Full paper Single centre, university hospital cardiology department Country: Spain Funded by: NR |
To evaluate the feasibility of QTc monitoring with KardiaMobile 6L in COVID-19 patients receiving QTc-interfering therapies. | No | Observational technical validation study. Absolute values and mean difference for QTc measurements between KardiaMobile 6L ECG and 12-lead ECG, number of unreadable ECGs, and mean time taken to register ECG. |
| Orchard 202141 | Prospective study of 30 healthy athletes Full paper Single centre, university hospital Country: Australia Funded by: Authors were supported by an Australian Government Research Training Program scholarship and a NHMRC Practitioner Fellowship |
To examine and compare the level of similarity between resting 6L and 12-lead readings in athletes with a view to building evidence for the utility of the 6L-ECG as a practical and accurate clinical tool in athletic populations. | No | Observational technical validation study. Absolute values and mean difference for QT and QTc measurements between KardiaMobile 6L ECG and 12-lead ECG. |
| Puranik 202242 | Prospective study of 13 patients with multidrug-resistant tuberculosis and non-tuberculous mycobacterium infections Full paper Single centre, university hospital Country: UK Funded by: NR |
Not stated | No | Pilot study. Mean percentage difference and correlation coefficient between automated 12-lead readings and manually calculated KardiaMobile readings, for QTc (concordance). |
| Shah 202152 | Prospective study of three patients undergoing antiarrhythmic drug loading at home, during COVID-19 social distancing Full paper Single centre, university hospital Country: USA Funded by: NR |
To test the hypothesis that existing digital health technologies and virtual communication platforms could provide EM and support medically guided AAD loading for patients with symptomatic tachyarrhythmia in the ambulatory setting, while reducing physical contact between patient and healthcare system. | No | Pilot study. Absolute values and difference in QTc, per patient, pre and post loading, using KardiaMobile 6L and 12-lead ECG (concordance). |
| Tees and Esk and Wear Valleys NHS Foundation Trust 202153 | (confidential information has been removed) | (confidential information has been removed) | (confidential information has been removed) | (confidential information has been removed) |
| Cumbria, Northumberland, Tyne and Wear NHS Foundation Trust 202154 | Roll out project, during which 51 ECGs were completed using KardiaMobile 6L (6 April 2021 to 31 August 2021), by an unclear number of healthcare professionals Unpublished pilot project report Country: UK Funded by: NHSX, AHSN NENC |
Not a research study | Yes | Retrospective survey of healthcare professionals and service users. Numbers of cardiology referrals/12-lead ECGs required, comparison of time estimated mean time taken per ECG with KardiaMobile 6L compared to 12-lead ECG (staff estimates), comparison of estimated costs, qualitative data on service user and healthcare professional preferences, and changes to service user care. |
Initially, the project was to:
|
||||
protocol and policies
|
Both the two unpublished project reports related to an initial pilot53 and subsequent extended pilot project54 conducted in the UK NHS and funded by National Health Service user experience (NHSX), via the Academic Health Science Network North East and North Cumbria (AHSN NENC).
It is important to note that both these project reports relate to work undertaken as part of a wider AHSN pilot, they were not formal research projects and were not intended to be used in wider evaluations of KardiaMobile 6L for use in the NHS.
Further details of the characteristics of study participants and details of the conduct of the index test (KardiaMobile 6L) and reference standard/comparator (12-lead ECG) are provided in Tables 4 and 6.
Study quality
Assessment of the methodological quality of included technical validation studies, based on QUADAS-2, indicated low or unclear risk of bias in all domains, for all studies. However, it should be noted that none of these studies was a diagnostic test accuracy study (the study type for which QUADAS-2 is intended to be used), in that none of them reported data about the ability of the index test (KardiaMobile 6L) to determine the presence or absence of a clinical condition or intermediate outcome (e.g. QTc prolongation at a clinically relevant threshold), as defined by the reference standard method (12-lead ECG).
Applicability to the decision problem under consideration was the major issue for all the published studies included in this EVA report. Concerns regarding the applicability of these studies were high for both relevant domains (population and index test).
Concerns regarding the applicability of study populations were high, for all studies, because no study was conducted in the population of interest for this EVA, that is service users requiring antipsychotic medication.
Concerns regarding the applicability of the index test were high because, in all studies, all ECGs were interpreted by cardiologists and in three14,41,51 of the five studies assessed interpretation was undertaken by multiple readers. Measures of agreement with cardiologist-interpreted 12-lead ECG, where KardiaMobile 6L ECG results have been generated by multiple/expert readers, are unlikely to be reproducible by single non-cardiologist healthcare professionals, in real-world settings.
The results of the QUADAS-2 assessment are summarised in Table 3 and the full assessments are provided in Appendix 2.
| Study ID | Risk of bias | Applicability concerns | ||||
|---|---|---|---|---|---|---|
| Patient selection | Index test | Reference standard | Flow and timing | Study population | Index test | |
| Azram 202114 | ☺ | ☺ | ☺ | ? | ☹ | ☹ |
| Kleiman 202131 | ? | ☺ | ☺ | ☺ | ☹ | ☹ |
| Krzowski 202151 | ? | ☺ | ☺ | ☺ | ☹ | ☹ |
| Minguito-Carazo 202137 | ? | ? | ? | ? | ☹ | ☹ |
| Orchard 202141 | ? | ? | ? | ☺ | ☹ | ☹ |
Two unpublished project reports have been included in this EVA report. 53,54 These reports concern real-world piloting of KardiaMobile 6L in two NHS Foundation Trusts (TEWV and CNTW), which was undertaken under considerable operational pressures during the COVID-19 pandemic. These reports do not describe formal research projects with a priori research objectives and methods designed to address these objectives; therefore, we did not consider formal assessment of methodological quality or risk of bias to be appropriate. The following text provides a qualitative summary of the key issues, with respect to the reliability of the information provided by these reports to address the aims of this EVA.
However, it is important to note that these reports concern pilot projects which were not designed to be used in wider evaluations of KardiaMobile 6L for use in the NHS, such as the current EVA.
Potential sampling bias
The two pilots involved the distribution of (confidential information has been removed)53 and 4054 KardiaMobile 6L devices across multiple locations (confidential information has been removed), there is a potential for bias in survey responses arising from inclusion of staff who may have an a priori positive view on the potential usefulness of KardiaMobile 6L devices.
Issues relating to the reporting of numbers and outcome measures
Both unpublished pilot project reports included sections on (confidential information has been removed). 53,54 Where detail was provided (in addition to the yes/no response), this indicated that all changes reported were primarily in relation to service user care, with only one response making a subjective link to clinical outcome: ‘Able to start antipsychotic medication quicker than usual, as patient would have had a delay in getting a regular ECG done, therefore able to begin treatment almost straightaway resulting in early resolution of psychotic symptoms, and early recovery’. 54
The CNTW end of project report indicated that 51 ECGs had been recorded, using KardiaMobile 6L devices during the pilot period. 54 However, the number 51 was recorded as the denominator for data taken from the survey of staff members who had used the KardiaMobile 6L devices. 54 Taken together with further information from an additional survey, which stated that (as of 30 September 2021) a total of 59 ECGs had been recorded using the KardiaMobile 6L devices and 16 staff indicated that they had used the devices,54 this would indicate that the 51 survey responses included multiple responses per staff member. While this would have been appropriate for questions (e.g. change to clinical outcome) relating to per patient outcomes, it raises the potential problem of double counting with respect per staff member outcomes (e.g. staff preferences for KardiaMobile 6L or 12-lead ECG). 53,54
(confidential information has been removed)
Potential bias in survey questions
The two unpublished pilot project reports did not include full copies of the survey instruments used to collect information from staff and service users;53,54 Word versions of the CNTW online surveys have been provided separately (see Appendix 5). From the questions that were presented, there was some indication that the choice of questions/wording may have introduced bias in favour of KardiaMobile 6L. 54 For example, rather than being asked their views about using KardiaMobile 6L with equal weight being given to advantages and disadvantages, staff were asked about ‘benefits’ and ‘least helpful aspects’. 54 Similarly, when staff and service users were asked about their preferences (KardiaMobile 6L vs. 12-lead ECG), the supplementary questions used to inform preferences all focused on aspects of the ECG examination likely to favour the KardiaMobile device (ease of use, time savings, dignity and privacy, intrusiveness, comfort); no questions about clinical utility/reliability for decision-making were reported. 54 It was unclear whether staff or service users were ever asked to consider, for example the extent to which a ‘normal’ ECG reading, by each method, could reliably indicate ‘safety’ to proceed with antipsychotic treatment.
Provision of information to staff members and service users using KardiaMobile six-lead and completing the survey
The CNTW end of project summary report included links to online information and training materials that were provided to staff as part of the pilot. 54 Service users were given a choice of whether to have KardiaMobile 6L or 12-lead ECG and were directed to the AliveCor website for information about the device (verbal communication from Jonathan Richardson of CNTW to MW on 16 June 2022). When evaluating a new method of testing, such as KardiaMobile 6L, as part of a research project, the properties and intended use of the new method should be explained to study participants (staff and patients), for example that this is an initial test and any problems identified will be followed up with further testing and, importantly, what are the implications of a negative/normal test result (e.g. if 100 patients were tested using the KardiaMobile 6L, X would have a negative/normal test result and Y of these would actually have a problem that would have been identified using 12-lead ECG). Based on the findings of our systematic review, the implications of a negative/normal test result could not have been provided, because no information about the clinical diagnostic accuracy of KardiaMobile 6L has been identified (for any population). However, it could therefore be argued that, if these data have not been collected before future observational before-and-after implementation research studies, participants should be advised (using appropriate methods of explanation) that the clinical accuracy of the device, and hence the risk of obtaining false reassurance from a negative/normal result, is unknown.
Collection of workflow information through staff survey
Information about the average number of ECGs undertaken per month and average time taken to complete an ECG examination (both KardiaMobile 6L and 12-lead ECG) was taken from a retrospective survey of staff. 54 It may be possible to obtain more reliable information about the number of ECGs currently undertaken per month from NHS Trust records or from observational studies (see Uncertainties). Information about the mean time taken to complete an ECG examination, by each method, should be obtained by direct measurement (either in the context of research studies or real-world observations). In addition, there is a potential for bias in the estimates of average time taken to complete an ECG examination, in that only those staff who had chosen to use the KardiaMobile 6L device, during the pilot period, were asked to provide information about the average time taken to complete an examination (for both KardiaMobile 6L and 12-lead ECG). 54
Estimation of costs
Both unpublished pilot project reports included estimates of cost per ECG and projected annual costs, for both KardiaMobile 6L and 12-lead ECG, as well as estimates of the projected annual cost savings associated with the introduction of KardiaMobile 6L. 53,54 The methods used to obtain cost estimates, from the TEWV NHS Foundation Trust pilot, were not fully explained. 53 (confidential information has been removed) Importantly, the estimates presented for the KardiaMobile 6L testing pathway did not include the costs of subsequent 12-lead ECGs (whether required for follow-up of an abnormal finding or because of failure to obtain an adequate reading using KardiaMobile 6L), which were reported as being required at a rate of 60%. 54 Finally, acquisition costs were included for both devices;54 it is not clear whether this was appropriate as, if current practice is to attempt a 12-lead ECG in all cases, then sufficient 12-lead ECG devices should already be available to support this.
What is the accuracy/technical performance of KardiaMobile six-lead, where the target condition is QTc prolongation, determined by standard 12-lead electrocardiogram (the reference standard method)?
All eight of the published studies included in this report were either technical validation studies14,31,37,41,51 or case series,26,42,52 reporting some, very limited, information about the agreement between QT interval (corrected and/or uncorrected) measured by KardiaMobile 6L and QT interval (corrected and/or uncorrected) measured by standard 12-lead ECG. Details of study populations, ECG methods and interpretation are provided in Table 4 and the results of these studies are summarised in Table 5.
| Study ID | Participants details n (%) | Details of index test (KardiaMobile 6L) | Details of comparator/reference standard (12-lead ECG) |
|---|---|---|---|
| Azram 2021 (EVALECG Cardio)14 |
Cardiology patients: 1015 Mean age ± SD (years): 62 ± 17 Male: 634 (62.4) Caucasian: 767 (75.6) South Asian: 62 (6.1) Black: 14 (1.4) Other: 172 (16.9) Diabetes: 193 (19) Hypertension: 385 (37.9) Previous coronary disease: 278 (27.4) History of arrhythmia: 258 (25.4) Known AF: 207 (20.4) Mean BMI ± SD: 28.6± 9 Outpatients: 613 (60.4) Inpatients: 402 (39.6) Indication for ECG Valve disease: 116 (11.4) Arrhythmia: 116 (11.4) Heart failure: 262 (25.8) Coronary disease: 478 (47.1) Inherited arrhythmia assessment: 110 (10.8) |
Device settings: Two handheld electrodes and a third electrode was placed on the left thigh (or the left ankle if this was not possible); maximum recording time programmed to 30 seconds; filter settings 0.05–40 Hz; sampling rate 300/s; sweep speed of 25 mm/s; amplitude of 1 mm/mV. Recording: Stored as a PDF on a mobile phone and then printed onto plain paper. Interpretation: Three experienced observers (one cardiologist and two cardiac physiologists) performed the ECG analysis independently of each other. Each ECG was analysed twice. |
Device and settings: MAC 550 (GE Healthcare, WI, USA); filter settings 0.05–100 Hz; sweep speed of 25 mm/s; amplitude of 1 mm/mV. Recording: Printed directly to ECG graph paper. Interpretation: Three experienced observers (one cardiologist and two cardiac physiologists) performed the ECG analysis independently of each other. Each ECG was analysed twice. |
| Frisch 202126 | Hospitalised COVID-19 patients, requiring ECG monitoring: 4 Age (years): 45, 48, 67, 96 Comorbidities: renal cancer (left nephrectomy and a renal transplant), hypertension, morbid obesity and sleep apnoea; none; advanced systolic heart failure and persistent atrial fibrillation; atrial fibrillation treated with anticoagulation therapy, mild aortic stenosis, dyslipidaemia, hypertension, chronic kidney disease and anaemia. Male: 3 (75) |
Device settings: NR Recording: Patients completed two recordings using the KardiaMobile 6L device with the healthcare provider outside the room. After a successful recording, the cardiologist let the patient know that the recording had been completed. Interpretation: QT/QTc interval analysis was requested through the KardiaPro account. Once requested, the QT/QTc interval analysis was performed by BioTelemetry, Inc. (Malvern, PA, USA), an independent third-party QTc measuring service. Within 1 hour, a cardiologist logged on to the KardiaPro website to review the mECG, the automatic interpretation, and the QT/QTc interval measurements reported by the third-party source. |
Device and settings: NR Recording: NR Interpretation: NR |
| Kleiman 202131 | Patients referred to a Genetic Heart Rhythm Clinic between April 2018 and February 2020: 705 (KardiaMobile 6L and 12-lead ECG results available for 685) Mean age ± SD (years): 28.7 ± 18.5 Male: 303 (43) Diagnoses after comprehensive cardiovascular evaluation LQTS: 343 (50) Normal: 146 (21) Hypertrophic cardiomyopathy: 36 (5.2) Arrhythmogenic cardiomyopathy: 23 (3.4) Idiopathic ventricular fibrillation: 14 (2.0) |
Device settings: Two handheld electrodes and a third electrode on the left leg; 2-minute recordings. Recording: Recordings taken by the patient. Using a smartphone-based application, the digital files containing the 6L recording were uploaded to a cloud-based server. ECGs from each subject were transferred digitally to a centralised ECG core laboratory, ERT and were uploaded into ERT’s validated data management system, EXPERT. IDMs were collected using computer-assisted calliper placements on three consecutive beats. Interpretation: ECGs were analysed by a cardiologist. |
Device and setting: GE Marquette 12-lead ECG device; patients in the supine position; filtered at 500 Hz. Recording: ECGs from each subject were transferred digitally to a centralised ECG core laboratory, ERT, and were uploaded into ERT’s validated data management system, EXPERT. IDMs were collected using computer-assisted calliper placements on three consecutive beats. Interpretation: ECGs were analysed by a cardiologist. |
| Krzowski 202151 | Consecutive inpatients in a tertiary care cardiology ward: 98 Mean age ± SD (years): 69 ± 12.9 Male: 62 (63) Smoking (current or former): 47 (48) Diabetes: 40 (40.8) Hypertension: 72 (73.4) Dyslipidaemia: 72 (73.4) Chronic kidney disease: 25 (25.5) Thyroid dysfunction: 19 (19.4) Asthma: 4 (4.1) COPD: 9 (9.2) Stable angina: 31(31.6) ACS (admission): 15 (15.3) Previous MI: 31 (31.6) Previous PCI/CABG: 41 (41.8) Heart failure: 55 (56.1) AF: 43 (43.9) CIED implanted: 34 (34.7) Pacemaker: 22 (22.4) |
Device settings: Two handheld electrodes and a third electrode on the left leg, no further details reported. Recording: Experienced technicians performed all recordings. Interpretation: All ECG recordings assessed by one of the two independent groups of experienced physicians. Every ECG was analysed by a younger cardiologist and checked by a senior physician; disagreements were resolved by discussion. |
Device and settings: No details reported. Recording: Experienced technicians performed all recordings. Interpretation: All ECG recordings assessed by one of the two independent groups of experienced physicians. Every ECG was analysed by a younger cardiologist and checked by a senior physician; disagreements were resolved by discussion. |
| Minguito-Carazo 202137 | Healthy (COVID-19 PCR negative) control patients: 45 Mean age ± SD (years): 63.7 ± 18.1 Male: 26 (56.8) No further details reported |
Device settings: The patient was told to sit and place the device on the bare skin of their left leg (at the knee or the ankle) holding his thumbs on the top of two electrodes for 30 seconds. Recording: The ECG output was wirelessly transmitted to and digitally uploaded by a dedicated app to a secure server. Interpretation: ECG records were reviewed and interpreted by at least one of two cardiologists. QTc interval was calculated using Bazett’s formula in leads II or V5 in the 12-lead ECG and in lead II when using the handheld 6L ECG. If these leads did not provide an accurate end of the T wave, I and aVL were preferably used as an alternative, although QTc measurement in any other lead was permitted. |
Device and settings: No details reported. Recording: No details reported. Interpretation: ECG records were reviewed and interpreted by at least one of two cardiologists. QTc interval was calculated using Bazett’s formula in leads II or V5 in the 12-lead ECG and in lead II when using the handheld 6L ECG. If these leads did not provide an accurate end of the T wave, I and aVL were preferably used as an alternative, although QTc measurement in any other lead was permitted. |
| Orchard 202141 | Healthy athletes with no existing cardiac diagnoses or family history of conditions associated with sudden cardiac death: 30 Mean age ± SD (years): 18.9 ± NR Male: 17 (57) No further details reported |
Device settings: 30 seconds recording while seated. Recording: No details reported. Interpretation: ECGs were analysed by four expert cardiologists; manual measurements were taken for QT interval using EPS digital callipers; QTc was calculated using Bazett’s formula. |
Device settings: Recorded supine. Recording: No details reported. Interpretation: ECGs were analysed by four expert cardiologists; manual measurements were taken for QT interval using EPS digital callipers; QTc was calculated using Bazett’s formula. |
| Puranik 202242 | Patients with multidrug-resistant tuberculosis or non-tuberculous mycobacterium, who were receiving cardiotoxic medications: 16 No further details reported |
Device settings: No details reported. Recording: No details reported. Interpretation: QTc calculations used the Bazett’s formula and manually calculated QT intervals from lead II of the KardiaMobile 6L device. Three clear areas of the KardiaMobile 6L device trace were randomly selected and used to estimate an average QT interval. |
Device and settings: Mortara ELI350; no further details reported. Recording: No details reported. Interpretation: QTc calculations used the Bazett’s formula. |
| Shah 202152 | Patients undergoing antiarrhythmic drug loading at home, during COVID-19 social distancing: 3 Participant 1: 35-year-old woman, hypertrophic cardiomyopathy, ejection fraction 35%, symptomatic paroxysmal AF Participant 2: 40-year-old man, alpha-actinin-2 deletion, history of ventricular fibrillation, sinus bradycardia and symptomatic paroxysmal AF Participant 3: 60-year-old man, hypertrophic cardiomyopathy, symptomatic ventricular tachycardia episodes refractory to sotalol |
Device settings: No details reported. Recording: No details reported. Interpretation: No details reported. |
Device and setting: No details reported. Recording: No details reported. Interpretation: No details reported. |
| Study ID | Number (%) of ECGs analysed, by KardiaMobile | Number (%) of ECGs analysed, by 12-lead | Mean or median QT interval, by KardiaMobile 6L (ms) | Mean or median QT interval, by 12-lead ECG (ms) | Difference/concordance measure | Other outcomes |
|---|---|---|---|---|---|---|
| Azram 2021 (EVALECG Cardio)14 | QT Lead I: NR (71.6) Lead II: NR (72.8) Lead III: NR (51.4) Lead AVR: NR (71.9) Lead AVL: NR (66.1) Lead AVF: NR (57.0) Longest: NR (75.9) QTca Lead I: NR (71.5) Lead II: NR (72.8) Lead III: NR (51.3) Lead AVR: NR (71.8) Lead AVL: NR (66.0) Lead AVF: NR (56.9) Longest: NR (75.9) |
QT Lead I: NR (67.9) Lead II: NR (76.6) Lead III: NR (55.4) Lead AVR: NR (68.6) Lead AVL: NR (58.2) Lead AVF: NR (61.5) Longest: NR (80.4) QTca Lead I: NR (67.9) Lead II: NR (76.6) Lead III: NR (55.4) Lead AVR: NR (68.6) Lead AVL: NR (58.2) Lead AVF: NR (61.5) Longest: NR (80.4) |
NR | NR | Mean difference (LLA, ULA) (ms), 12-lead vs. KardiaMobile 6L QT Lead I: 6.29 (−36.21, 48.79) Lead II: 7.03 (−31.80, 45.87) Lead III: 6.47 (−40.54, 53.48) Lead AVR: 7.06 (−34.46, 48.57) Lead AVL: 5.45 (−38.65, 49.56) Lead AVF: 8.49 (−36.59, 53.57) Longest QT interval: 11.6 (−28.79, 52.31) QTca Lead I: −0.27 (−55.48, 54.93) Lead II: 0.62 (−51.95, 53.19) Lead III: 1.15 (−55.05, 57.35) Lead AVR: −0.03 (−53.15, 53.10) Lead AVL: −2.02 (−57.65, 53.61) Lead AVF: 2.35 (−54.76, 59.46) Longest QTc interval: 5.71 (−47.42, 58.85) |
Proportion of patients where QTca analysis was possible (by lead) Lead I: 12-lead ECG 67.9%; KardiaMobile 6L 71.5% Lead II: 12-lead ECG 76.6%; KardiaMobile 6L 72.8% Lead III: 12-lead ECG 55.4%; KardiaMobile 6L 51.3% Lead AVR: 12-lead ECG 68.6%; KardiaMobile 6L 71.8% Lead AVL: 12-lead ECG 58.2%; KardiaMobile 6L 66.0% Lead AVF: 12-lead ECG 61.5%; KardiaMobile 6L 56.9% Longest QTca lead: 12-lead ECG 80.4%; KardiaMobile 6L 75.9% AUC AUC, where a normal QT interval was defined as 360–460 ms: QT > 70% (80% for the best lead); QTc > 60% (74% for the best lead). |
| Frisch 202126 | QT 7 (87.5) QTcb 7 (87.5) |
QT 8 (100) QTcb 8 (100) |
Mean ± SD QT 365 ± 25c QTcb 460 ± 30c |
Mean ± SD QT 366 ± 15c QTcb 464 ± 19c |
Mean difference (95% CI) (ms), 12-lead vs. KardiaMobile 6L QT 1.00 (−20.24 to 22.24)c QTcb 4.00 (−21.83 to 29.83)c |
All patients were able to record KardiaMobile 6L ECGs independently. |
| Kleiman 202131 | QT 671 (95.2) QTcFd 674 (95.6) |
QT 674 (95.6) QTcFd 674 (95.6) |
Mean ± SD QT 407.5 ± 49.14 QTcFd 428.5 ± 36.50 Median (minimum, maximum) QT 405 (490, 792) QTcFd 427 (327, 746) |
Mean ± SD QT 420.9 ± 51.87 QTcFd 431.0 ± 38.80 Median (minimum, maximum) QT 419 (306, 791) QTcFd 427 (316, 744) |
Mean difference (95% CI) (ms), 12-lead vs. KardiaMobile 6L QT 13.40 (8.00 to 18.80) QTcFd 2.50 (−1.52 to 6.52) Categorical breakdown of difference in QTcFd between 6L and 12-lead, n (%) Absolute difference < 10: 297(44.3) Absolute difference 10–19: 221 (32.9) Absolute difference 20–29: 69 (10.3) Absolute difference 30–39: 50 (7.5) Absolute difference 40–49: 19 (2.8) Absolute difference ≥ 50: 15 (2.2) |
Patients reported no difficulties in recording ECGs using the KardiaMobile 6L device. All 12-lead ECGs were of sufficient quality to allow IDM measurements and cardiologist interpretation, and only one of the 6L ECGs was unsuitable for IDM measurements (excessive artefact) but was adequate for cardiologist interpretation. |
| Krzowski 202151 | 97 (99) | 98 (100) | Mean ± SD QT 366 ± NR |
Mean ± SD QT 403 ± NR |
Not calculable | ECG quality ratings, n (%) KardiaMobile 6L Good: 70 (72) Acceptable: 22 (23) Poor: 5 (5) 12-lead ECG Good: 80 (82) Acceptable: 17 (17) Poor: 1 (1) |
| Minguito-Carazo 202137 | 45 (100) | 45 (100) | Mean ± SD QTca 409.1 ± 23.2 |
Mean ± SD QTca 411.8 ± 25.7 |
Mean difference (95% CI) (ms), 12-lead vs. KardiaMobile 6L QTca 2.7 (−7.7 to 23.2) |
For KardiaMobile 6L, QTc could be measured in lead II in most cases (90.9%) |
| Orchard 202141 | 30 (100) | 30 (100) | Mean ± SD QT 363 ± 28 QTca 391 ± 24 |
Mean ± SD QT 381 ± 26 QTca 401 ± 25 |
Mean difference (95% CI) (ms), 12-lead vs. KardiaMobile 6L QT 18.0 (4.33 to 31.67)c QTca 10.0 (−2.40 to 22.40)c |
None |
| Puranik 202242 | 13 (81.3) | 13 (81.3) | NR | NR | The mean percentage difference between the automated 12-lead and manually calculated KardiaMobile 6L readings was 3%. The largest percentage difference between the two readings was 12%. | In 12/13 cases (92%), KardiaMobile 6L underestimated the QTc in comparison to the corresponding 12-lead QTc readout. Pearson’s correlation coefficient = 0.43. |
| Shah 202152 | 3 (100) | 3 (100) | QTcb Pre-loading Participant 1: 423 Participant 2: 417 Participant 3: 430 Post-loading Participant 1: 430 Participant 2: 421 Participant 3: 451 |
QTcb Pre-loading Participant 1: 420 Participant 2: 419 Participant 3: 422 Post-loading Participant 1: 439 Participant 2: 415 Participant 3: 459 |
Difference (ms) QTc,b 12-lead vs. KardiaMobile 6L Pre-loading Participant 1: −3 Participant 2: 2 Participant 3: −8 Post-loading Participant 1: 9 Participant 2: −6 Participant 3: 8 |
Initially, participants described less than maximal (≤ 7/10) perceived ease using the KardiaMobile 6L; however, by study completion all reported the highest level of comfort with operating the device and transmitting ECGs. |
No study reported sufficient data to allow the calculation of measures of clinical diagnostic performance (e.g. sensitivity and specificity) for the target condition, that is QTc prolongation; hence, these studies cannot provide any indication of the proportion of patients, with QTc prolongation, who might be missed if KardiaMobile 6L were used for initial ECG assessment (triage). Where reported or calculable, the mean difference in QTc between devices (12-lead ECG vs. KardiaMobile 6L) was generally small (≤ 10 ms), see Table 5. However, one study, which reported data for 605 patients who had been referred to a genetic heart rhythm clinic, stated that the absolute difference in QTcF (correction method used, Fridericia or Framingham, not reported in the paper), measured by 12-lead ECG and KardiaMobile 6L, was ≥ 10 ms in 56% of participants and ≥ 40 ms in 5% of participants. 31 In general, the direction of the difference between the two methods indicated that KardiaMobile 6L underestimated the QTc in comparison to the corresponding 12-lead QTc readout. However, there was no information to indicate in how many (if any) patients this difference would have resulted in a change of clinical category.
With respect to failure rates, data were again very limited. One study reported a comparison, between KardiaMobile 6L and 12-lead ECG, with respect to the proportion of patients for whom each lead could be analysed (51% to 72% for KardiaMobile 6L and 55% to 77% for 12-lead ECG); the longest lead was usable for QTc in 80.4% of patients for 12-lead ECG and in 75.9% of patients for KardiaMobile 6L. 14 One further study reported that, for KardiaMobile 6L, QTc could be measured in lead II in most cases (90.9%). 37
As described in Study quality, above, all of the included technical validation studies have very limited applicability to the clinical setting specified for this EVA.
What are the clinical effects of using KardiaMobile six-lead, compared with 12-lead electrocardiogram or no electrocardiogram, on clinical outcomes (cardiac and psychiatric)?
We did not identify any studies which assessed the clinical effects of implementing KardiaMobile 6L ECG. All information in this section has been taken from unpublished project reports. 53,54
It is important to note that both these projects relate to work undertaken as part of a wider AHSN pilot, they were not formal research projects and were not intended to be used in wider evaluations of KardiaMobile 6L for use in the NHS.
Both the unpublished pilot project reports provided (confidential information has been removed)53,54 Responses were per staff member and not (as would be expected for change to clinical outcome) per patient.
The end of project summary report, from CNTW NHS Foundation Trust,54 reported responses to this question from six healthcare professionals; two responses indicated that the use of KardiaMobile 6L facilitated commencement of antipsychotic medication, two responses indicated that the KardiaMobile 6L result had been used to rule out heart abnormalities, and indicated that a 12-lead ECG was still needed. Only one of the six responses linked the change in care reported to clinical outcome: ‘Able to start antipsychotic medication quicker than usual, as patient would have had a delay in getting a regular ECG done, therefore able to begin treatment almost straightaway resulting in early resolution of psychotic symptoms, and early recovery’. 54 The number of ECGs/patients to which these observations applied was not clear.
(confidential information has been removed)
It should be noted that (with the exception of one response) all of the information, recorded in the two unpublished pilot project reports. 53,54 (confidential information has been removed)
What are the effects of using KardiaMobile six-lead on service user acceptability/satisfaction and on training and workflow issues?
One technical validation study37 reported a comparison of the time taken to record an ECG with KardiaMobile 6L versus 12-lead ECG, based on ECGs of 45 patients taken by both methods. The mean time taken to record a 12-lead ECG was slightly longer than that taken to record an ECG using KardiaMobile 6L {mean difference 2.1 [95% confidence interval (CI) 1.9 to 2.3] minutes}. Although it did not meet the inclusion criteria for this question, because it was not conducted in service users requiring antipsychotic medication, data from this study have been included in this section, for completeness. 37
The remaining information in this section has been taken from unpublished project reports. 53,54
It is important to note that both these project reports relate to work undertaken as part of a wider AHSN pilot, they were not formal research projects and were not intended to be used in wider evaluations of KardiaMobile 6L for use in the NHS.
Studies and project reports providing information on service user acceptability/satisfaction and on training and workflow issues are summarised in Tables 6 and 7.
| Study ID | Participants details n (%) | Details of index test (KardiaMobile 6L) | Details of comparator/reference standard (12-lead ECG) |
|---|---|---|---|
| Minguito-Carazo 202137 | Healthy (COVID-19 PCR negative) control patients: 45 Mean age ± SD (years): 63.7 ± 18.1 Male: 26 (56.8) No further details reported |
Device settings: The patient was told to sit and place the device on the bare skin of his left leg (at the knee or the ankle) holding his thumbs on the top of two electrodes for 30 seconds. Recording: The ECG output was wirelessly transmitted to and digitally uploaded by a dedicated application to a secure server. Interpretation: ECG records were reviewed and interpreted by at least one of two cardiologists. QTc interval was calculated using Bazett’s formula in leads II or V5 in the 12-lead ECG and in lead II when using the handheld 6L ECG. If these leads did not provide an accurate end of the T wave, I and aVL were preferably used as an alternative, although QTc measurement in any other lead was permitted. |
Device and settings: No details reported. Recording: No details reported. Interpretation: ECG records were reviewed and interpreted by at least one of two cardiologists. QTc interval was calculated using Bazett’s formula in leads II or V5 in the 12-lead ECG and in lead II when using the handheld 6L ECG. If these leads did not provide an accurate end of the T wave, I and aVL were preferably used as an alternative, although QTc measurement in any other lead was permitted. |
| Tees and Esk and Wear Valleys NHS Foundation Trust 202153 | (confidential information has been removed) | (confidential information has been removed) | (confidential information has been removed) |
| Cumbria, Northumberland, Tyne and Wear NHS Foundation Trust 202154 | Not explicitly stated, but appears to have been service users in whom ECG was indicated in relation to the use of antipsychotic medication 40 KardiaMobile 6L devices were distributed across four regional localities; the end of project report indicated that, of 50 ECGs carried out using KardiaMobile 6L, 34 were conducted in the community and 16 in inpatient settings. No details were provided about the service users who received ECG assessment using KardiaMobile 6L. |
Device settings: No details reported. Recording: No details were reported about the type of healthcare profession who recorded the ECG or their experience of recording ECGs. Interpretation: No details were reported about the type of health-care profession who interpreted the ECG results or their experience of interpreting ECGs. |
Device and settings: No details reported. Recording: No details reported. Interpretation: No details reported. |
| Study ID | Number (n) ECGs: healthcare professionals |
Time to record ECG, by KardiaMobile 6L | Time to record ECG, by 12-lead ECG | Difference |
|---|---|---|---|---|
| Minguito-Carazo 202137 | 45: NR | Mean ± SD (s) 93.3 ± 29.7 |
Mean ± SD (s) 217.8 ± 34.3 |
Mean difference (s) (95% CI) (s), 12-lead vs. KardiaMobile 6L: 124.5 (111.4 to 137.6)a |
| Tees and Esk and Wear Valleys NHS Foundation Trust 202153 | (confidential information has been removed) | (confidential information has been removed) | (confidential information has been removed) | (confidential information has been removed) |
| Cumbria, Northumberland, Tyne and Wear NHS Foundation Trust 202154 | Unclear: Unclear The end of project report stated that a total of 50 ECGs had been recorded using KardiaMobile 6L (as of 31 August 2021). However, n = 51 was also variously reported as the number of healthcare workers and the number of teams who had used the device |
Estimated mean, based on categorical data from a retrospective survey of healthcare professionals, who were asked ‘Approximately, and on average, how long would you spend with each patient when carrying out an ECG with KardiaMobile 6L?’ Excluding travel time: 8 minutes 28 seconds Including travel time: 23 minutes 35 seconds |
Estimated mean, based on categorical data from a retrospective survey of healthcare professionals, who were asked ‘Approximately, and on average, how long would you spend with each patient when carrying out a usual ECG?’ Excluding travel time: 24 minutes 28 seconds Including travel time: 44 minutes 40 seconds |
Average time saved, using KardiaMobile 6L: 19 minutes |
Both the unpublished pilot projects53,54 (confidential information has been removed) and 19 minutes, respectively); (confidential information has been removed). In the case of the CNTW report,54 the estimate of time saved was based on categorical information from a retrospective survey of those healthcare professionals who had used the KardiaMobile 6L device. In that survey, staff were asked, ‘Approximately, and on average, how long would you spend with each patient when carrying out a usual ECG?’ and ‘Approximately, and on average, how long have you spent with each patient when carrying out a ECG with the KardiaMobile 6L (app & device)?’ and response options were ‘less than 5 minutes’, ‘5–10 minutes’, ‘11–20 minutes’, ‘21–31 minutes’, ‘32+ minutes’ and ‘other’. 54 The estimate of average time taken was reported to have been based on the average of each time option available and frequency of reporting. 54 (confidential information has been removed)53
Both the unpublished pilot projects53,54 reported (confidential information has been removed). In the CNTW end of project report, 9 of the 16 healthcare professionals (56%), who stated that they had used the KardiaMobile 6L device, answered ‘yes’ to the question ‘Did the clinical situation require subsequent use of a 12-lead ECG after using the AliveCor KardiaMobile 6L device?’ As with the TEWV pilot, it was not clear as to how many ECGs/service users the reported requirement for an additional 12-lead ECG applied; specific reasons given for the additional 12-lead ECG requirement were poor readings (e.g. due to patient movement or inability to maintain contact with the electrodes) in four instances, requirement for more information or follow-up monitoring in three instances and an abnormal result in one instance. 54
Regarding the preferences/satisfaction of service users and healthcare professions, (confidential information has been removed). 53 The survey of healthcare professionals, reported in the CNTW end of project report,54 asked participants to indicate their preference for KardiaMobile 6L or 12-lead ECG with respect to five characteristics and to indicate an overall preference; 48/51 (94.1%) respondents indicated a preference for KardiaMobile 6L with respect to ease of use, 50/51 (98%) preferred KardiaMobile 6L for dignity and privacy, 44/51 (86.2%) indicated that they considered 12-lead ECG to be the more intrusive option, 49/51 (96%) indicated that they considered KardiaMobile 6L to be the more comfortable option, 40/51 (78.4%) indicated a preference for KardiaMobile 6L with respect to ease of sending information to the relevant professional, and 42/51 (82.3%) indicated an overall preference for KardiaMobile 6L. 54 A similar survey was reported for service users, 33 of whom provided responses; 32/33 (96.9%) indicated a preference for KardiaMobile 6L with respect to ease of use and dignity and privacy, 32/33 (96.9%) indicated that they considered 12-lead ECG to be the more intrusive option, all 33 (100%) indicated that they considered KardiaMobile 6L to be the more comfortable option, 31/33 (93.9%) indicated an overall preference for KardiaMobile 6L and 32/33 (96.9%) indicated that they would prefer KardiaMobile 6L for future monitoring. 54
What are the costs, from a UK NHS and PSS perspective, of using KardiaMobile six-lead for the initial assessment (triage) of QT interval-based cardiac risk in service users taking antipsychotic medications that are associated with QT prolongation?
We did not identify any studies that reported information about the costs of using KardiaMobile 6L for the initial assessment (triage) of QT interval-based cardiac risk in service users taking antipsychotic medications that are associated with QT prolongation, either from a UK NHS and PSS perspective or in non-UK settings. All information on costs, included in this report, was derived from the two unpublished pilot project reports from TEWV and CNTW NHS Foundation Trusts. 53,54
It is important to note that both these project reports relate to work undertaken as part of a wider AHSN pilot, they were not formal research projects and were not intended to be used in wider evaluations of KardiaMobile 6L for use in the NHS.
A presentation of the TEWV NHS Foundation Trust pilot55 (confidential information has been removed).
The end of project report from CNTW NHS Foundation Trust54 included details of the costs associated with local interpretation of ECGS (by a ‘doctor in training/CNTW member of staff’) or interpretation by a centralised service. The report concluded that KardiaMobile 6L ECG was associated with a reduction in cost of £2.37, for a Band 3 member of staff to take the ECG reading, compared to 12-lead ECG. Although not explicitly stated, this estimate appeared to be based on an average reduction in staff time needed to take the ECG reading calculated from staff estimates provided in a retrospective survey (see What are the effects of using KardiaMobile 6L on service user acceptability/satisfaction and on training and workflow issues?). The report also provided the following estimates of total annual costs for 204 ECGs (workload estimate based on 51 ECGs conducted during the 3-month pilot period):
-
KardiaMobile 6L = £1542.19 – based on ECG readings taken by a Band 3 staff member and local manual interpretation by a doctor in training/CNTW staff member, and including device costs (including iPad and licences).
-
Twelve-lead ECG = £4762.80 – based on ECG readings taken by a Band 3 staff member and local manual interpretation by a doctor in training/CNTW staff member, and including device costs (details not specified).
-
Twelve-lead ECG = £8779.56 – based on ECG readings taken by a Band 3 staff member and ECG being sent to a central location for immediate interpretation, and including device costs (details not specified).
Details of the comparative costs provided in the CNTW NHS Foundation Trust report54 are provided in Table 8. Based on these estimates, the expected annual cost saving associated with using KardiaMobile 6L would be between £3220.61 (based on ECGs, 6L and 12-lead were interpreted locally) and £7237.27 (based on all 6L ECGs being interpreted locally and all 12-lead ECGs being interpreted immediately, using the centralised service). However, these estimates do not include the costs of any 12-lead ECG which are required following an initial ECG reading using KardiaMobile 6L (whether for clinical follow-up of an abnormal result or due to failure to record an adequate ECG using KardiaMobile 6L). The survey of staff, included in the CNTW NHS Foundation Trust report,54 found that 60% of respondents reported still requiring a 12-lead ECG after initial use of KardiaMobile 6L. Based on the estimate of 204 ECGs performed per year, 122 12-lead ECGs would be required in addition to the initial ECGs using KardiaMobile. Estimated annual costs, after the introduction of KardiaMobile 6L, including the requirement for 12-lead ECG in 60% of cases have been added to Table 8 (entries in red text); these estimates include costs of reading and interpreting a KardiaMobile 6L ECG in all cases (n = 204), plus the costs of reading and interpreting a 12-lead ECG in 60% of cases (n = 122), plus the device acquisition costs for both KardiaMobile 6L and 12-lead ECG.
| ECG type | Cost/ECG reading (Band 3 staff member) | Cost/ECG interpretation (local by doctor in training/CNTW staff member) | Cost/ECG interpretation (centralised service, immediate interpretation) | Cost/ECG interpretation (centralised service, overnight interpretation) | Cost/ECG interpretation (centralised service, weekend interpretation) | Total annual cost for 204 ECGs | Device set-up costs | Total annual costs including device set-up |
|---|---|---|---|---|---|---|---|---|
| KardiaMobile 6L | £1.52 | £1.31 | NA | NA | NA | £577.32 | £964.87 | £1542.19 |
| KardiaMobile 6L + 12-lead ECG [applied to 122 (60%)a of ECGs] | £5.91 | £2.62 | £1272.72 | £4564.87 | £5837.59 | |||
| £5.91 | £1.31 | £21.00 | £3515.08 | £4564.87 | £8079.95 | |||
| £5.91 | £1.31 | £17.00 | £3027.08 | £4564.87 | £7591.95 | |||
| £5.91 | £1.31 | £14.00 | £2661.08 | £4564.87 | £7225.95 | |||
| 12-lead ECG | £4.39 | £1.31 | £1162.80 | £3600.00 | £4762.80 | |||
| £4.39 | £21.00 | £5179.56 | £3600.00 | £8779.56 | ||||
| £4.39 | £17.00 | £4363.56 | £3600.00 | £7963.56 | ||||
| £4.39 | £14.00 | £3751.56 | £3600.00 | £7351.56 | ||||
It should be noted that all of the estimates for cost savings, derived from the total costs indicated in the CNTW NHS Foundation Trust report,54 are substantially lower than the estimate for annual cost savings reported for the TEWV pilot. 55 Furthermore, when the costs of conducting additional 12-lead ECGs (at a rate of 60%) were taken into account, the figures in CNTW NHS Foundation Trust report54 indicate that introduction of KardiaMobile 6L could actually be associated with an increase in overall annual costs of £1074.79 61 (based on ECGs, 6L and 12-lead being interpreted locally) or a reduction in overall annual costs of between £125.61 and £699.61 (based on all 6L ECGs being interpreted locally and all 12-lead ECGs being interpreted centrally).
What existing, published cost-effectiveness studies are available about QT interval assessment for service users who require antipsychotic medication?
We did not identify any cost-effectiveness studies concerning QT interval assessment (by any ECG method), either prior to initiation of treatment or for monitoring during treatment, for service users who require antipsychotic medication.
Chapter 5 Discussion
Statement of principal findings
The evidence to inform this EVA of KardiaMobile 6L, for use in the context of QT interval-based cardiac risk assessment for service users who require antipsychotic medication, was extremely limited.
We did not identify any studies, which addressed any of the five research questions defined for this EVA, in the target population (service users who require antipsychotic medication).
All eight of the research studies identified were technical validation studies14,31,37,41,51 or case series,26,42,52 reporting some, very limited, information relevant to research question 1, ‘What is the accuracy/technical performance of KardiaMobile 6L, where the target condition is QTc prolongation, determined by standard 12-lead ECG (the reference standard method)?’ All of these studies were conducted in non-psychiatric populations (e.g. cardiac patients, COVID-19 patients), and all used cardiologists to interpret all ECGs and, in some instances, also applied optimised methods of interpreting ECGs (multiple reader assessment),14,41,51 such that the results obtained are unlikely to be reproducible by single non-cardiologist healthcare professionals, in real-world settings. Where reported or calculable, the mean difference in QTc between devices (12-lead ECG vs. KardiaMobile 6L), derived from these studies, was generally small (≤ 10 ms). However, the apparent direction of the difference between the two methods indicated that KardiaMobile 6L consistently underestimated the QTc in comparison to the corresponding 12-lead-derived value. Possible systematic underestimation of QTc may be a cause for concern, given that the intermediate outcome measure/target condition specified for this EVA was QT prolongation. However, it should be noted that none of the included studies provided any information to indicate in how many (if any) patients observed differences in measured QTc would have resulted in a change of clinical category.
All the information about the use of KardiaMobile 6L in the context of QT interval-based cardiac risk assessment for service users who require antipsychotic medication, included in this EVA report, was taken from two unpublished pilot project reports. 53,54 These reports describe real-world pilots of KardiaMobile 6L in two NHS foundation Trusts (TEWV and CNTW), which were funded by NHSX, via the AHSN NENC. They do not describe formal research projects and, as such, do not report a priori research objectives and methods designed to address these objectives. (confidential information has been removed)
It is important to note that both these project reports relate to work undertaken as part of a wider AHSN pilot, which was not intended to be used in wider evaluations of KardiaMobile 6L for use in the NHS.
The unpublished pilot project reports both (confidential information has been removed). 53,54 Where additional detail was provided in support of the yes/no response, most respondents indicated that they were reporting a change to service user care rather than a change to clinical outcome; only one respondent linked the change in care reported to clinical outcome: ‘Able to start antipsychotic medication quicker than usual, as patient would have had a delay in getting a regular ECG done, therefore able to begin treatment almost straightaway resulting in early resolution of psychotic symptoms, and early recovery’. 54
Both the unpublished pilot project reports53,54 (confidential information has been removed) and 19 minutes, respectively) (confidential information has been removed)53 and 9 of the 16 healthcare professionals (56%) in the CNTW NHS Foundation Trust end of project report,54 who had used the KardiaMobile 6L device, reported that a subsequent 12-lead ECG was required; it was not clear to how many ECGs/service users the reported requirement for an additional 12-lead ECG applied.
Regarding the preferences/satisfaction of service users and healthcare professions, (confidential information has been removed). 53 The results of the survey, reported in the CNTW NHS Foundation Trust end of project report,54 indicated that 42/51 (82%) staff respondents and 31/33 (94%) service user respondents had an overall preference for KardiaMobile 6L over 12-lead ECG. 54
A presentation of the TEWV NHS Foundation Trust pilot55 (confidential information has been removed). The CNTW NHS Foundation Trust end of project report54 estimated that the expected annual cost saving associated with using KardiaMobile 6L would be between £3220.61 and £7237.27. However, these estimates did not include the costs of any 12-lead ECG required following an initial ECG reading using KardiaMobile 6L (whether for clinical follow-up of an abnormal result or due to failure to record an adequate ECG using KardiaMobile 6L). The survey of staff, included in the CNTW NHS Foundation Trust end of project report,54 indicated 60% of respondents stated that a 12-lead ECG was still required after initial ECG using KardiaMobile 6L. Including the costs of any follow-up 12-lead ECG, at a rate of 60%, results in a maximum estimated annual cost saving of £699.61 and a possible annual cost increase of up to £1074.79 61 associated with using KardiaMobile 6L. It should be noted that the rate of 60% was reported per staff member/survey respondent and it was not clear as to how many ECGs/service users it applied. Hence, the cost savings for KardiaMobile 6L, reported in the unpublished pilot project reports,53,54 are likely to be overestimates (because they did not include the costs of any follow-up 12-lead ECGs required) and the corrected values that we have calculated are likely to underestimate potential savings (because they involved applying a rate of follow-up 12-lead ECGs that had been reported per staff member rather than per ECG).
Strengths and limitations of assessment
This report describes the results of a novel process which is being developed to provide EVA of new diagnostic technologies, where the evidence base is, as yet, underdeveloped. This process is intended to be applied where topic scoping has indicated that there is not sufficient evidence to inform a full Diagnostic Assessment Report and to support the development of a cost-effectiveness model(s). The use of an EVA approach acknowledges that there is currently not sufficient evidence to inform decision-making about routine use in UK NHS clinical practice. The aim of the process, as implemented in this assessment, was to assess whether a new diagnostic technology has shown sufficient evidence of potential advantage(s) over current practice to justify further research to inform full assessment of its clinical and cost effectiveness and inform decision-making, and to provide detailed recommendations about the research needed to inform such assessments.
The decision problem, for this assessment, was defined using the same process of scoping, expert and public consultation, and iterative drafting that would be used for a full Diagnostic Assessment; the decision problem, defined by this process, has informed our recommendations for research needed to inform a full Diagnostic Assessment (see Suggested research priorities). The inclusion criteria defined for this EVA (see Inclusion and exclusion criteria) were wider than would be indicated by the definition of the decision problem, for example studies conducted in populations other than that specified (service users requiring antipsychotic medications) were included. This wider approach to inclusion provided the potential to identify and summarise studies which, while not directly applicable to the decision problem, may inform assessment of the potential of the test to be an effective and cost-effective intervention. For example, if diagnostic accuracy studies had been identified which reported high sensitivity values for KardiaMobile 6L for the detection of QTc prolongation, when used by expert cardiologists in cardiology patients, this may have been considered sufficient indication of ‘good’ clinical diagnostic performance to justify further research to assess whether clinical diagnostic performance could be maintained when the device is used in context specified by the decision problem. Similarly, evidence indicating benefits for KardiaMobile 6L in relation to secondary outcome measures, such as service user acceptability/preference, time taken to conduct an ECG or costs, which are not sufficient to inform decision-making about routine use in UK NHS clinical practice (in the absence of higher-level outcomes data about the clinical efficacy and safety of the device), may be considered indicative of potential benefits, such that further research to assess clinical efficacy and safety is warranted.
Extensive literature searches were conducted in an attempt to maximise retrieval of relevant studies. These included electronic searches of a variety of bibliographic databases, as well as screening of clinical trials registers and conference abstracts to identify unpublished studies. Because of the known difficulties in identifying test accuracy studies using study design-related search terms,56 search strategies were developed to maximise sensitivity at the expense of reduced specificity. In order to be as inclusive as possible, we also conducted a search of the medRxiv, the preprint server, and asked clinical experts (SCMs for this topic) to provide details of any potentially relevant ongoing or unpublished studies, of which they were aware. Based on the submissions provided by the company (AliveCor) and clinical experts, we hand-searched the journal, European Heart Journal – Digital Health, which is not yet indexed in the bibliographic databases searched. Thus, large numbers of citations were identified and screened, relatively few of which met the inclusion criteria of the review.
The following text describes the key limitations of the evidence identified, with respect to informing the aims of an EVA.
All of the evidence identified in relation to research question 1, ‘What is the accuracy/technical performance of KardiaMobile 6L, where the target condition is QTc prolongation, determined by standard 12-lead ECG (the reference standard method)?’ was obtained from studies conducted in non-psychiatric populations (e.g. cardiac patients, COVID-19 patients), and concerned the technical validation of the KardiaMobile 6L device only. Studies reported measures of agreement, for QT interval (corrected and/or uncorrected), between KardiaMobile 6L and 12-lead ECG, but did not provide data to assess the sensitivity and specificity of the device for the detection of clinically relevant QTc prolongation (clinical diagnostic accuracy). It is therefore not known to what, if any, extent the levels of disagreement observed between the KardiaMobile 6L and 12-lead ECG would result in patients with clinically relevant QTc prolongation being missed if KardiaMobile 6L were used for additional assessment. In addition, the methods/personnel used to interpret ECGs, in the included technical validation studies,14,31,37,41,51 were such that the results obtained are unlikely to be reproducible in the real-world settings indicated by the decision problem.
All of the evidence, in relation to research questions 2–4, which concerns the use of KardiaMobile 6L in the population specified by the decision problem (service users who require antipsychotic medication), was derived from the results of surveys of staff and service users undertaken following pilots of the device in TEWV NHS Foundation Trust and CNTW NHS Foundation Trust. 53,54 The reported survey findings provided some indication that the KardiaMobile 6L device was preferred, by both staff and service users, over 12-lead ECG and may also be associated with reductions in the time taken to obtain an ECG and in costs of obtaining an ECG. However, it should be noted that these surveys were not undertaken as formal research projects with a priori research objectives and, as such, they were subject to a large number of substantial limitations, both in respect of the methods used (e.g. potential sampling bias, in that participants appear to have been included on the bases of their willingness to use KardiaMobile 6L, and potential question bias, in that some survey questions appear to have been phrased in a way which would be likely to favour KardiaMobile 6L) and the information collected (e.g. some per patient/ECG outcomes, such as change to clinical management, were collected per participating staff member, and some easily measurable outcomes, such as time taken to obtain an ECG, were estimated from staff opinion). These limitations are described more fully in Study quality of this report.
Uncertainties
Evidence to inform the aims of an early value assessment
With respect to test performance, we did not identify any evidence to support the technical validation of the KardiaMobile 6L device in the context specified by the decision problem, that is there were no studies which assessed the agreement between QT interval (corrected or uncorrected) determined using KardiaMobile 6L versus 12-lead ECG, when KardiaMobile 6L was used by the relevant healthcare professionals to assess service users who require antipsychotic medication. The methods/personnel used to interpret ECGs, in the included technical validation studies,14,31,37,41,51 were such that the results obtained are unlikely to be reproducible in the real-world settings indicated by the decision problem. In addition, no studies were identified which reported sufficient information to support estimation of measures of the clinical diagnostic performance of KardiaMobile 6L to identify the intermediate outcome/target condition QTc prolongation (in any population or setting). Hence, there is currently no information to inform estimates of the potential clinical sensitivity/rule-out reliability of the device (in any population or setting) and to assess whether evaluation in the specified population (service users who require antipsychotic medication) is warranted. Some included studies variously reported: limited information about the proportion of leads in which QT interval could be measured,14 subjective quality ratings,51 or that all patients were able to independently record an ECG using KardiaMobile 6L,26,31 (see Table 5). However, there were insufficient data to adequately assess the technical failure rates of KardiaMobile 6L when used to assess QT interval, particularly when used in the context of the assessment of service users who require antipsychotic medication. Qualitative staff survey information53,54 indicated that manual calculation of QTc and confidence about doing this was a key area of concern for staff and affected the willingness of some staff to use the device; this issue was emphasised, by CNTW project leads, as key for the potential implementation of the device (verbal communication from Jonathan Richardson, Stewart Little, Nicola Orkney of CNTW to MW on 16 June 2022).
The information provided in unpublished pilot project reports, under the heading (confidential information has been removed)53,54 was very limited, did not allow for the estimation of per patient outcomes, and mainly referred to changes in care rather than changes in clinical outcome. Neither of the two project reports included any information about baseline (pre-piloting of KardiaMobile 6L) rates of adverse cardiac outcomes (arrhythmias, sudden cardiac death) or psychiatric outcomes (e.g. symptom duration, inpatient admission, referral to the mental health crisis team), or any information about future plans to collect these data, for example after implementation of KardiaMobile 6L. 53,54 We did not identify any studies which reported information about the effects of using KardiaMobile 6L on the secondary clinical effectiveness outcome, time from decision to prescribe to treatment, and this outcome was not included in either of the two unpublished pilot project reports. 53,54
There was some evidence, from two unpublished pilot project reports,53,54 indicating benefits for KardiaMobile 6L in relation to secondary outcome measures, such as service user acceptability/preference, time taken to conduct an ECG and costs. This evidence may be considered as supportive of the need for further research to inform a full evaluation of the clinical and cost effectiveness of KardiaMobile 6L. However, it should be noted that the evidence provided in the two unpublished pilot project reports53,54 was methodologically weak and subject to substantial uncertainty; further details are provided in Study quality and Strengths and limitations of assessment of this report. The proportion of service users requiring antipsychotic medication, for whom ECG assessment of QT interval is clinically indicated, who accept an ECG and/or in whom and ECG is successfully completed, is also a potentially important secondary outcome measure. We consider assessment of this outcome measure to be important because, during scoping discussions with service users and clinical experts, and in survey results provided in the two unpublished pilot project reports,53,54 a preference for KardiaMobile 6L was indicated which was based on a perception that the device was less intrusive, easier to use and offered greater dignity and privacy than conventional 12-lead ECG. Given that these preferences form an important part of the value proposition for KardiaMobile 6L, it is important to understand the extent to which preferences expressed may translate into increased acceptance and completion of ECG examinations in practice. Unfortunately, this outcome measure was not assessed by any of the published or unpublished studies identified and included in this report. Nationally, the baseline rate of ECG recording in service users who require antipsychotic medication is unclear; the limited national audit data available on the monitoring of side effects of patients prescribed antipsychotics in the UK do not include ECG provision as one of the reported measures. 57 A recent article, submitted for publication and provided academic in confidence by one of the SCMs for this topic (GC), reported a 1-week service evaluation to investigate compliance with ECG monitoring on adult (> 18 years) psychiatric inpatient wards in the Yorkshire and Humber Region. 58 The study aimed to assess the proportion of service users who received an ECG, the average delay between admission and ECG completion and the common reasons for delay. 58 There were (confidential information has been removed) service users from (confidential information has been removed) wards caring for adults in (confidential information has been removed) different Trusts, who were included. Participating wards were working with (confidential information has been removed). The study found that (confidential information has been removed) (18%) of service users admitted during the study period did not receive an ECG at any point during their stay, and of those who did receive an ECG, (confidential information has been removed) experienced a delay of > 24 hours. 58 These proportions were higher for service users on antipsychotic medication (confidential information has been removed) and for service users on high-dose antipsychotics (confidential information has been removed). 58 Where a specific reason was given for non-completion of an ECG, the most common reported reasons were (confidential information has been removed), specifically, that the patient was (confidential information has been removed) in (confidential information has been removed) of instances. 58 Although falling outside the inclusion criteria for this EVA, because it did not report an evaluation of KardiaMobile 6L, this study provides a source of baseline data about ECG completion rates in a relevant population and important indication of the potential for improvement. 58
The estimates of the costs associated with KardiaMobile 6L and 12-lead ECG and the costs savings reported for KardiaMobile 6L, provided in the two unpublished project reports from pilots undertaken in UK NHS Foundation Trusts,53,54 are subject to high levels of uncertainty (further details are provided in What are the costs, from a UK NHS and PPS perspective, of using KardiaMobile 6L for the initial assessment (triage) of QT interval-based cardiac risk in service users taking antipsychotic medications that are associated with QT prolongation? and Statement of principal findings of this report). The possible relative annual Trust-wide costs of the two devices range from a cost increase of £1074.79 (ERG calculation) to (confidential information has been removed) associated with using KardiaMobile 6L.
Evidence to inform a full diagnostic assessment, including cost-effectiveness modelling
We did not identify any studies that reported data for the outcome measures needed to inform a full Diagnostic Assessment, including cost-effectiveness modelling. There were no data about the clinical diagnostic accuracy of KardiaMobile 6L for the detection of QTc prolongation in service users who require antipsychotic medication. In particular, there were no data to inform estimates of the clinical sensitivity/rule-out reliability of the device; if KardiaMobile 6L were used to triage for and rule-out QT prolongation, we do not know how many people with QTc prolongation may be missed.
We did not identify any studies, randomised controlled trials (RCTs), controlled clinical trials (CCTs), or observational before-and-after (implementation) studies that assessed the effects of using KardiaMobile 6L versus 12-lead ECG on cardiac or psychiatric outcomes, or measures of HRQoL. Neither of the two unpublished project reports, which described UK NHS pilots of KardiaMobile 6L, reported any information about future plans to collect clinical outcomes data, for example after implementation of KardiaMobile 6L. 53,54
The available evidence about the UK costs of KardiaMobile 6L compared to 12-lead ECG, in the context of QT interval-based cardiac risk assessment for service users who require antipsychotic medication, is highly uncertain. 53,54
Development of a cost-effectiveness model was outside the scope of this EVA and, hence, no additional targeted searches were undertaken to inform model parameters. Additional information needed to inform cost-effectiveness modelling could include: costs and utilities associated with relevant cardiac and psychiatric outcomes; effects of 12-lead ECG evaluation versus no ECG evaluation of QT interval, before prescribing antipsychotic medication, on cardiac and psychiatric outcomes; effects of 12-lead ECG evaluation versus no ECG, for monitoring QT interval in service users requiring ongoing antipsychotic medication, on cardiac and psychiatric outcomes; risk of adverse cardiac outcomes associated with QT prolongation in service users who are receiving antipsychotic medication; risk of adverse psychiatric outcomes in service users for whom antipsychotic medication is delayed, changed or discontinued consequent upon the conduct or findings of an ECG assessment.
Patient and public involvement
This study was secondary research with a short (8 weeks) project duration. These factors limit the opportunity for and potential contribution of patient and public involvement. However, patient representatives were included as members of the NICE specialist committee for the assessment. This means that patients were actively involved both in setting the scope for the assessment and in discussions of the evidence and its implications for decision-making.
Reporting equality, diversity and inclusion
This study was secondary research and followed a scope defined by NICE. The NICE scoping process includes consideration of equality and diversity issues. The following text describes the potential equality and diversity issues identified. 59
KardiaMobile 6L may not be suitable for use in people with upper limb amputations or missing fingers. The accuracy of readings taken using the devices may be adversely affected if a person has a skin condition causing irritation, inflammation or very dry skin. The devices may not perform correctly for people with a pacemaker or implantable defibrillator. Readings from people with tremors or difficulty sitting still may also be inaccurate.
Devices that use torso electrodes may need people with significant body hair to shave for adequate contact with the skin.
People may be uncomfortable with undressing for an ECG that requires torso electrodes for a variety of reasons, including:
-
culture or religion
-
having a different gender to the ECG operator
-
having a different gender identity to their birth sex
-
experiencing hyper-sensitivity, for example due to autism spectrum disorder
-
having a history of trauma or sexual abuse.
Service users should be asked to remove only clothing preventing access to the correct electrode positions. A chaperone may be requested for appointments using these devices. 60
People from minority ethnic backgrounds, particularly people of African and African-Caribbean family background living in the UK, are more likely than white British people to be diagnosed with schizophrenia. 61 They are also more likely to be detained, given medication against their will, or given higher doses.
Neurodivergent people (e.g. those with autism spectrum disorder) may be more likely to have antipsychotic medication than the general population. 62,63
Women typically have a longer QT interval than men and therefore may be more susceptible to the effects of QT-prolonging medication. Different QTc thresholds may be used for men and women. 5,16,64
Antipsychotic medication is likely to be given to people affected by postpartum psychosis. ECG testing may be appropriate for this population prior to initiation of treatment.
The KardiaMobile 6L instructions for use state that the device has not been tested for and is not intended for paediatric use; therefore the scope of this assessment has been restricted to adults.
Chapter 6 Conclusions
Implications for service provision
As anticipated during the scoping phase of this assessment and reflected in the decision to undertake an EVA, there is insufficient evidence to support a full Diagnostic Assessment evaluating the clinical effectiveness and cost-effectiveness of KardiaMobile 6L, in the context of QT interval-based cardiac risk assessment for service users who require antipsychotic medication.
The evidence to inform the aims of this EVA (i.e. to assess whether the device has the potential to be clinically effective and cost-effective) was also limited and it remains unclear whether KardiaMobile 6L has adequately demonstrated sufficient evidence of potential advantage(s) over current practice to justify further research to inform assessment of its clinical and cost effectiveness.
It is important to note that unpublished reports, used to inform the majority of the research questioned defined for this EVA, concern pilot projects which were not designed to be used in wider evaluations of KardiaMobile 6L for use in the NHS, such as the current EVA.
Suggested research priorities
The following additional studies may be useful, to adequately inform/reduce the uncertainty in EVA for this topic. These studies represent the first stage or work package in a programme of research and are only intended to inform consideration of the (confidential information has been removed) of KardiaMobile 6L to provide a clinically effective and cost-effective intervention.
-
Technical validation studies in the relevant population and setting – studies should be undertaken to establish whether QT interval, measured using KardiaMobile 6L, can reliably reproduce the QT interval measured using 12-lead ECG. These studies should be undertaken in representative populations of service users who require antipsychotic medication (including those in whom it would usually be difficult to obtain an adequate ECG). The ECGs should be taken, using both methods, in the same patients, and the ECG examinations should be undertaken by healthcare professionals who are representative of those who would be expected to undertake the examination in real-world clinical practice. In addition to measures of agreement for QT interval, such studies should record the technical failure rates, or proportion of ECGs judged to be inadequate for clinical decision-making, for both methods.
-
Assessment of the preferences of service users and healthcare professionals – a more reliable evaluation of preferences could be obtained from prospective survey studies, using survey instruments and methods designed with consideration to recognised sources of bias65,66 and established good practice for survey methods67 and reporting. 68
-
Comparison of time taken to complete an ECG examination using KardiaMobile 6L versus 12-lead ECG – an empirical comparison of the time taken to complete an ECG examination using KardiaMobile 6L versus 12-lead ECG should be undertaken. Time taken to complete ECG examinations should be measured in representative populations of service users who require antipsychotic medication (including those in whom it would usually be difficult to obtain an adequate ECG) and where ECG examinations are undertaken by healthcare professionals who are representative of those who would be expected to undertake the examination in real-world clinical practice. Measurements should include (1) actual ECG recording time and (2) staff travel time. A reliable comparison between KardiaMobile 6L versus 12-lead ECG could be achieved either by completing both examinations in all patients with the order of examination randomised (to control for possible effects of patient fatigue) or by randomising patients or locations to KardiaMobile 6L or 12-lead ECG. For designs where all participants do not receive ECG examination by both methods, studies should also record the success rate/rate of requirement for subsequent 12-lead ECG associated with KardiaMobile 6L.
-
Assessment of the effects of using KardiaMobile 6L on the up-take/acceptance of ECG by service users – before-and-after observational (implementation) studies of KardiaMobile 6L should assess the proportion of service users requiring antipsychotic medication, for whom ECG assessment of QT interval is clinically indicated, who accept an ECG and/or in whom an ECG is successfully completed. It may be that these data could be obtained from records associated with the two UK NHS pilots of KardiaMobile 6L described in this report,53,54 although it is unclear whether any baseline data (pre-piloting of KardiaMobile 6L) are available for the relevant NHS Foundation Trusts.
-
Assessment of the UK costs associated with KardiaMobile 6L versus 12-lead ECG – estimates of the relative costs of KardiaMobile 6L versus 12-lead ECG, when used as specified in the decision problem, should be calculated based on measured (rather than estimated) time to complete each examination, for the relevant healthcare professionals and should include all relevant costs for each diagnostic pathway (e.g. follow-up 12-lead ECG in the proportion of patients for whom this requirement has been recorded in real-world practice). It should be ascertained whether the per patient rate of follow-up 12-lead ECGs is obtainable from records associated with the two UK NHS pilots of KardiaMobile 6L described in this report. 53,54
If findings from the first stage, described above, were favourable for KardiaMobile 6L, the following studies could provide the additional data needed to inform a full Diagnostic Assessment, including cost-effectiveness modelling:
-
Diagnostic cohort studies evaluating the clinical accuracy of KardiaMobile 6L for the detection of QTc prolongation – these studies should evaluate the performance of KardiaMobile 6L, when used by healthcare professionals who are representative of those who would use the device in real-world clinical practice. Studies should be conducted in representative populations of service users who require antipsychotic medication (including those in whom it would usually be difficult to obtain an adequate ECG). It is important to evaluate the clinical accuracy of the device in the population specified by the decision problem because diagnostic accuracy may be affected the by underlying prevalence of the target condition and by other population characteristics, such as ability to remain still during the examination. Similarly, measures of accuracy obtained when the device is used by healthcare professionals with levels of expertise and experience which are not representative of real-world practice (e.g. interpretation by consensus of multiple cardiologists) may not be reproducible in the community of inpatient psychiatry settings relevant to the decision problem. Diagnostic cohort studies should also record the technical failure rates, or proportion of ECGs judged to be inadequate for clinical decision-making, for both methods.
-
Qualitative staff survey information53,54 indicated that manual calculation of QTc and confidence about doing this was a key area of concern for staff, and it affected the willingness of some staff to use the device; this issue was emphasised by CNTW project leads, as key for the potential implementation of the device (verbal communication from Jonathan Richardson, Stewart Little and Nicola Orkney of CNTW to MW on 16 June 2022). AliveCor have indicated (see Intervention technology) that it is their intention to develop an algorithm to support automatic calculation of QTc; it may therefore be considered appropriate to await the release of this algorithm and to evaluate the clinical diagnostic accuracy of the device in the context of its use.
-
Observational studies, evaluating the effects of implementing KardiaMobile 6L in relevant UK clinical settings, may also be of interest.
-
Before conducting observational before-and-after (implementation) studies or pilot studies of a new technology, it is important to ensure that the potential risks of implementing the technology in the relevant NHS setting have been adequately assessed. This is problematic for the example of KardiaMobile 6L for the assessment of QT interval in service users requiring antipsychotic medication because we have not been able to identify any data to estimate the clinical accuracy of the device for this target condition (in any population). The numbers of service users with QTc prolongation who might be missed, in a pilot or implementation study where KardiaMobile 6L was relied upon to rule out QTc prolongation, are, therefore, unknown. A possible approach to considering the potential relative risks (in terms of service users with QTc prolongation which is not detected) of implementing KardiaMobile 6L versus doing nothing may be to estimate the proportion of service users with QTc prolongation who are not being picked up by current practice, because, although recommended, 12-lead ECG is not always completed in practice. This number could be estimated from the product of the prevalence of QTc prolongation in the relevant population and the proportion of service users not currently receiving 12-lead ECG (unpublished study data described in Uncertainties). The proportion of service users with QTc prolongation who are not being picked up by current practice gives an indication of the minimum false-negative rate that KardiaMobile 6L would need to achieve in order for it to be a potential improvement over current practice.
-
As is the case for diagnostic cohort studies, the way in which the technology is implemented is critical to the utility of observational, before-and-after implementation studies for UK decision-making. The populations assessed and the way in which the intervention (KardiaMobile 6L) is used and interpreted during the study period should reflect the way in which it will be used in real-world clinical practice; for example, healthcare professionals involved in the study should reflect the disciplines, training and experience of those expected to use KardiaMobile 6L in real-world clinical practice. The study design should also reflect the way in which KardiaMobile 6L is intended to be used for clinical decision-making; for example, if it is intended to be used as a triage test, patients in whom an abnormality is observed using KardiaMobile 6L should receive follow-up 12-lead ECG and those with a normal KardiaMobile 6L examination should receive no further investigations at that time, with all patients being followed up to assess outcomes. Observational comparative studies provide a lower level of evidence with respect to the effects of an intervention than RCTs. Where observational study designs are used to provide estimates of effect, it is therefore important to control, as far as possible, for potential confounding factors (factors other than the ECG method that may affect the outcome or outcomes being assessed), for example by matching participants in the intervention and comparator groups on key risk factors. It is also important that the care pathway remains unchanged, other than with respect to the implementation of KardiaMobile 6L. Studies of the effects of the implementation of KardiaMobile 6L should measure clinical outcomes (e.g. adverse cardiac outcomes, duration of psychotic episode) alongside intermediate outcomes such as the proportion of service users who accept an ECG and/or in whom an ECG is successfully completed and time to appropriate intervention, and should report outcomes for test-negative as well as test-positive patients (i.e. outcomes should be reported for all study participants irrespective of whether or not QTc prolongation was identified and/or confirmed by follow-up 12-lead ECG and irrespective of the care received subsequent to testing).
-
Cluster RCTs, where inpatient and outpatient centres prescribing antipsychotics are randomised to implement KardiaMobile 6L or to continue with current practice, would offer a more methodologically robust approach to evaluating the effects of implementation as defined above. Stratification may be required in order to ensure that all relevant types of centres (e.g. inpatients and outpatient settings, general adult psychiatry, older adult psychiatry, forensic psychiatry) are represented in both study arms. Studies of this type represent the definitive study design for this topic.
Acknowledgements
The views expressed in this report are those of the authors and not necessarily those of the NIHR Evidence Synthesis Programme. Any errors are the responsibility of the authors.
The authors would like to acknowledge the hard work of all members of the teams involved in the pilot projects conducted at CNTWNHS Foundation TEWV NHS Foundation Trust. We would particularly like to thank all of those involved for their generosity in sharing unpublished information about their work, to inform both this assessment and the development of the NIHR EVA process. The authors would also like to acknowledge the additional contributions of Dr Jonathan Richardson (Chief Clinical Information Officer and Consultant Old Age Psychiatrist), Ms Nicola Orkney (Project Manager, Informatics Customer Services) and Mr Stewart Little (Project Lead, Project Team, Informatics Department), of CNTW NHS Foundation Trust, in answering our questions and engaging in further discussion of their work. The authors like to thank all of the clinical specialist members of the NICE diagnostic appraisal committee for this topic for their assistance and expert input throughout this project, and Dr George Crowther (Consultant, Liaison Psychiatry for Older People. Leeds and York Partnership NHS Foundation Trust) for sharing a pre-publication manuscript. Finally, the authors would like to thank the lay members of the NICE Diagnostics Advisory Committee and Assessment Sub-group for providing input on the patients’ perspective at key stages of the assessment process.
All data requests should be submitted to the corresponding author for consideration.
Work on the production of a conceptual cost-effectiveness model for this topic is ongoing at the NICE Decision Support Unit, University of Sheffield (anticipated date of completion 13 February 2023). The results of this EVA, together with further discussions with the report’s authors (MW and NA) have contributed to the development of the conceptual cost-effectiveness model.
Contributions of authors
Marie Westwood (https://orcid.org/0000-0002-6257-0653) (Reviews Manager and Diagnostic Assessment Lead) planned and performed the systematic review and interpretation of evidence.
Nigel Armstrong (https://orcid.org/0000-0002-7443-4798) (Senior Health Economist) contributed to planning and interpretation of the systematic review.
Pawel Posadzki (https://orcid.org/0000-0002-5153-3654) (Reviews Manager) planned and performed the systematic review and interpretation of evidence.
Caro Noake (https://orcid.org/0000-0003-0329-4772) (Information Specialist) devised and performed the literature searches and provided information support to the project.
All parties were involved in drafting and/or commenting on the report.
Ethics statement
This report concerns secondary research, for which ethics approval is not required.
Data sharing
Requests for access to data should be addressed to the corresponding author.
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the HTA programme or the Department of Health and Social Care.
Disclaimers
This manuscript presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HTA programme or the Department of Health and Social Care.
References
- National Institute for Health and Care Excellence (NICE) . Psychosis and Schizophrenia in Adults: Prevention and Management 2014. www.nice.org.uk/guidance/cg178 (accessed 3 February 2022).
- National Institute for Health and Care Excellence (NICE) . Bipolar Disorder: Assessment and Management 2014. www.nice.org.uk/guidance/cg185 (accessed 3 February 2022).
- NHS Northern England . Guidelines for the Management of QTc: Prolongation in Adults Prescribed Antipsychotics 2017. www.england.nhs.uk/north/wp-content/uploads/sites/5/2018/12/QTc-flow-diagram-with-medications-final-Dec-17-A3-with-logos.pdf (accessed 3 February 2022).
- Khatib R, Sabir FRN, Omari C, Pepper C, Tayebjee MH. Managing drug-induced QT prolongation in clinical practice. Postgrad Med J 2021;97:452-8.
- Lambiase PD, de Bono JP, Schilling RJ, Lowe M, Turley A, Slade A, et al. British Heart Rhythm Society clinical practice guidelines on the management of patients developing QT prolongation on antipsychotic medication. Arrhythm Electrophysiol Rev 2019;8:161-5.
- World Health Organization . The ICD-10 Classification of Mental and Behavioural Disorders Clinical Descriptions and Diagnostic Guidelines n.d. www.who.int/publications/i/item/9241544228 (accessed 3 February 2022).
- Mental Health and Wellbeing in England: Adult Psychiatric Morbidity Survey 2014. Leeds: NHS Digital; 2016.
- National Institute for Health and Care Excellence (NICE) . Depression in Adults: Treatment and Management (Update) 2017. www.nice.org.uk/guidance/gid-cgwave0725/documents/html-content (accessed 8 February 2022).
- McLachlan G. Treatment resistant depression: what are the options?. BMJ 2018;363.
- National Institute for Health and Care Excellence (NICE) . Dementia: Assessment, Management and Support for People Living With Dementia and Their Carers 2018. www.nice.org.uk/guidance/ng97 (accessed 8 February 2022).
- National Institute for Health and Care Excellence (NICE) . NICE Key Therapeutic Topic 7. Antipsychotics in People Living With Dementia 2015. www.nice.org.uk/advice/ktt7 (accessed 8 February 2022).
- Sattar YCL. StatPearls. Treasure Island, FL: StatPearls Publishing; 2021.
- NHS England, The AHSN Network . Innovation Collaborative: Using Remote ECG Device Technology in the North East and Yorkshire. Part One: Planning and Implementation n.d. www.alivecor.co.uk/resource-hub/Case_Study_NE__Yorkshire_FINAL_FOR_PUBLICATION.pdf (accessed 8 February 22).
- Azram M, Ahmed N, Leese L, Brigham M, Bowes R, Wheatcroft SB, et al. Clinical validation and evaluation of a novel six-lead handheld electrocardiogram recorder compared to the 12-lead electrocardiogram in unselected cardiology patients (EVALECG Cardio). Eur Heart J Digit Health 2021;2:643-8.
- Royal College of Psychiatrists . Consensus Statement on High-Dose Antipsychotic Medication: College Report CR190 2014. www.rcpsych.ac.uk/docs/default-source/improving-care/better-mh-policy/college-reports/college-report-cr190.pdf?sfvrsn=54f5d9a2_11 (accessed 3 February 2022).
- Priori SG, Blomström-Lundqvist C, Mazzanti A, Blom N, Borggrefe M, Camm J, et al. ESC Scientific Document Group . 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: The Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC). Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Eur Heart J 2015;36:2793-867.
- Maudsley Prescribing Guidelines (MPG) n.d. www.maudsley-prescribing-guidelines.co.uk/ (accessed 23 June 2022).
- Royal College of Psychiatrists . National Clinical Audit of Psychosis: National Report for the Core Audit 2018 2018. www.rcpsych.ac.uk/docs/default-source/improving-care/ccqi/national-clinical-audits/ncap-library/ncap-national-report-for-core-audit-2018.pdf?sfvrsn=23c6a262_4 (accessed 8 February 2022).
- Centre for Reviews and Dissemination . Systematic Reviews: CRD’s Guidance for Undertaking Reviews in Health Care 2009. www.york.ac.uk/inst/crd/SysRev/!SSL!/WebHelp/SysRev3.htm (accessed 23 March 2011).
- National Institute for Health and Care Excellence (NICE) . Guide to the Methods of Technology Appraisal 2013 2013. www.nice.org.uk/process/pmg9/ (accessed 30 July 2019).
- Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy 2023. https://training.cochrane.org/handbook-diagnostic-test-accuracy/current (accessed July 2023).
- Canadian Agency for Drugs and Technologies in Health . PRESS – Peer Review of Electronic Search Strategies: 2015 Guideline Explanation and Elaboration (PRESS E&Amp;E) 2016. https://www.cadth.ca/press-peer-review-electronic-search-strategies (accessed 16 November 2020).
- Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al. QUADAS-2 Group . QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 2011;155:529-36.
- Abellas Sequeiros M, Lozano Granero C, Garcia Sebastian C, Franco Diez E, Hernandez Madrid A, Moreno Planas J, et al. Monitoring of QTc interval in patients with COVID-19. First experience with a portable EKG-recording device. Presented at Annual Congress of the European Heart Rhythm Association (EHRA 2021); 23–25 April 2021; Virtual. Europace 2021;23:iii566-7.
- Collins MC, Elliott EE, Stain NS, Malcolmson JM, Monkhouse CM. A review of hand-held Electrocardiogram (ECG) recording devices. Virtual. Eur J Cardiovasc Nurs 2021;20.
- Frisch DR, Frankel ES, Farzad DJ, Woo SH, Kubey AA. Initial experience in monitoring QT intervals using a six-lead contactless mobile electrocardiogram in an inpatient setting. J Innov Card Rhythm Manag 2021;12:4433-40.
- Giudicessi JR, Schram M, Bos JM, Galloway CD, Shreibati JB, Johnson PW, et al. Artificial intelligence-enabled assessment of the heart rate corrected QT interval using a mobile electrocardiogram device. Circulation 2021;143:1274-86.
- Hoehns JD, Witry M, Oelmann M, Froerichs R, Greenwood J, Nichols R, et al. Community pharmacist use of mobile ECG to inform drug therapy decision making for patients receiving QTc prolonging medications. Virtual. JACCP 2020;3.
- Hoehns JD, Witry M, Oelmann M, Frerichs R, Greenwood J, Nichols R, et al. Community pharmacist use of mobile ECG to inform drug therapy decision making for patients receiving QTc prolonging medications. JACCP 2021;4:793-800.
- Karacan M, Celik N, Gul EE, Akdeniz C, Tuzcu V. Validation of a smartphone-based electrocardiography in the screening of QT intervals in children. North Clin Istanbul 2019;6:48-52.
- Kleiman R, Darpo B, Brown R, Rudo T, Chamoun S, Albert DE, et al. Comparison of electrocardiograms (ECG) waveforms and centralized ECG measurements between a simple 6-lead mobile ECG device and a standard 12-lead ECG. Ann Noninvasive Electrocardiol 2021;26.
- Ko ATY, Chen LS, Pang IX, Ling HS, Wong TC, Sia TLL, et al. Smartphone electrocardiogram for QT interval monitoring in coronavirus disease 2019 (COVID-19) patients treated with hydroxychloroquine. Med J Malaysia 2021;76:125-30.
- Koltowski L, Balsam P, Glowczynska R, Rokicki JK, Peller M, Maksym J, et al. Kardia Mobile applicability in clinical practice: a comparison of Kardia Mobile and standard 12-lead electrocardiogram records in 100 consecutive patients of a tertiary cardiovascular care center. Cardiol J 2021;28:543-8.
- Krzowski B, Osak G, Skoczylas K, Zurawska N, Peller M, Zych A, et al. Kardia Mobile 6L and Istel HR 2000 applicability in clinical practice: a comparison of Kardia Mobile, Istel HR 2000 and standard 12 lead electrocardiogram records in 98 consecutive patients of a cardiovascular care center. Virtual. Kardiol Pol 2020;78.
- Liu HH, Ezekowitz MD, Columbo M, Khan O, Martin J, Spahr J, et al. Testing the feasibility of operationalizing a prospective, randomized trial with remote cardiac safety EKG monitoring during a pandemic. J Interv Card Electrophysiol 2022;63:345-56.
- Mercer B, Leese L, Ahmed N, Holden AV, Tayebjee MH. A simple adaptation of a handheld ECG recorder to obtain chest lead equivalents. J Electrocardiol 2020;63:54-6.
- Minguito-Carazo C, Echarte-Morales J, Benito-Gonzalez T, Del Castillo-Garcia S, Rodriguez-Santamarta M, Sanchez-Munoz E, et al. QT interval monitoring with handheld heart rhythm ECG device in COVID-19 patients. Glob Heart 2021;16.
- Noseworthy PA, Msee ZIA, Dugan J, Schram M, Giudicessi JR, Bos JM, et al. Assessment of drug-induced QT prolongation using an AI-ECG algorithm on a mobile 6-lead ECG platform. Presented at Heart Rhythm 2021. Heart Rhythm 2021;18:S432-3.
- Orchard J, Raju H, La Gerche A, Puranik R, Semsarian C. Comparison between a 6-lead smartphone ECG and 12-lead ECG in athletes. Virtual. Heart Lung Circ 2021;30.
- Orchard J, Orchard JW, Raju H, La Gerche A, Puranik R, Semsarian C. Validation of a 6-lead smartphone ECG against 12-lead ECG in athletes. Presented at ESC Preventive Cardiology 2021; 15–17 April 2021; Virtual. Eur J Prev Cardiol 2021;28.
- Orchard JJ, Orchard JW, Raju H, La Gerche A, Puranik R, Semsarian C. Comparison between a 6-lead smartphone ECG and 12-lead ECG in athletes. J Electrocardiol 2021;66:95-7.
- Puranik S, Harlow C, Martin L, Coleman M, Russell G, Park M, et al. Monitoring prolongation of QT interval in patients with multidrug-resistant tuberculosis and non-tuberculous mycobacterium using mobile health device AliveCor. J Clin Tuberc Other Mycobact Dis 2022;26.
- Puranik S, Harlow C, Park M, Martin L, Coleman M, Russell G, et al. Monitoring prolongation of QT interval in patients with multidrug-resistant tuberculosis and non-tuberculous mycobacterium using mobile health device alivecor [P159]. Virtual. Thorax 2020;76:A175-6.
- Rotella JA, Taylor DM, Wong A, Greene SL. Accuracy of QT interval measurement on electrocardiographs displayed on electronic ‘smart’ devices. Emerg Med Australas 2016;28:187-92.
- Singh M, Rao R, Gupta S. KardiaMobile for ECG monitoring and arrhythmia diagnosis. Am Fam Physician 2020;102:562-4.
- Stavrakis S, Garabelli PJ, Smith L, Albert D, Po SS. Clinical validation of a smartphone based, 6-lead ECG device. Presented at Resuscitation Science Symposium, ReSS; 11–13 November 2017; Anaheim, CA. Circulation 2017;136.
- Stavrakis S, Garabelli PJ, Smith L, Albert D, Po SS. Clinical Validation of a Smartphone Based, 6-Lead ECG Device n.d. www.abstractsonline.com/pp8/#!/4412/presentation/46943American (accessed 17 May 2022).
- Stavrakis S, Whyte S, Sample K, Barber R, Albert D, Po SS. Clinical validation of a novel, smartphone-based 12-lead ECG device. Presented at ACC 22; 2–4 April 2022; Washington, DC. J Am Coll Cardiol 2022;79.
- Titus-Lay E, Jaynes H, Tomaselli-Muensterman E, Walroth T, Ott CA, Williams G, et al. Comparison of QT interval measurements between a smartphone electrocardiogram and a 12-lead electrocardiogram in patients undergoing maintenance methadone therapy in a narcotic treatment center. Presented at American Heart Association Scientific Sessions, AHA; 16–18 November 2019; Philadelphia, PA. Circulation 2019;140.
- Titus-Lay E, Jaynes H, Tomaselli-Muensterman E, Walroth T, Ott CA, Williams G, et al. Comparison of QT Interval Measurements Between a Smartphone Electrocardiogram and a 12-Lead Electrocardiogram in Patients Undergoing Maintenance Methadone Therapy in a Narcotic Treatment Center 2019. www.abstractsonline.com/pp8/#!/7891/presentation/28401American (accessed 17 May 2022).
- Krzowski B, Skoczylas K, Osak G, Zurawska N, Peller M, Kołtowski L, et al. Kardia Mobile and ISTEL HR applicability in clinical practice: a comparison of Kardia Mobile, ISTEL HR, and standard 12-lead electrocardiogram records in 98 consecutive patients of a tertiary cardiovascular care centre. Eur Heart J Digit Health 2021;2:467-76.
- Shah RL, Kapoor R, Bonnett C, Ottoboni LK, Tacklind C, Tsiperfal A, et al. Antiarrhythmic drug loading at home using remote monitoring: a virtual feasibility study during COVID-19 social distancing. Eur Heart J Digit Health 2021;2:259-62.
- Tees, Esk and Wear Valleys NHS Foundation Trust . The TEES Remote ECG Pathway: Validation Exercise 2021.
- Cumbria, Northumberland, Tyne and Wear NHS Foundation Trust . AliveCor KardiaMobile 6L Device Project: End Project Summary Report 2021.
- Krishnan MS, Bennett L. Use of ECG device to monitor QT interval for patients on antipsychotic medication during COVID-19 pandemic: a real world evaluation 2020.
- Whiting P, Westwood M, Beynon R, Burke M, Sterne JA, Glanville J. Inclusion of methodological filters in searches for diagnostic test accuracy studies misses relevant studies. J Clin Epidemiol 2011;64:602-7.
- Barnes TRE, Bhatti SF, Adroer R, Paton C. Screening for the metabolic side effects of antipsychotic medication: findings of a 6-year quality improvement programme in the UK. BMJ Open 2015;5.
- Mumford J, Devlin E, Crowther G. Electrocardiogram (ECG) Monitoring on Adult Psychiatric Inpatients Wards [document provided by the author] 2022.
- National Institute for Health and Care Excellence (NICE) . KardiaMobile 6L for Measuring QT Interval in People Having Antipsychotic Medication: Final Scope 2022. www.nice.org.uk/guidance/hte10/documents/final-scope (accessed 15 March 2022).
- Campbell B, Richley D, Ross C, Eggett CJ. Clinical Guidelines by Consensus: Recording a Standard 12-Lead Electrocardiogram. An Approved Method by the Society for Cardiological Science and Technology (SCST) 2017. https://scst.org.uk/wp-content/uploads/2020/02/SCST_ECG_Recording_Guidelines_2017am.pdf (accessed 4 October 2022).
- British Psychological Society Division of Clinical Psychology . Understanding Psychosis and Schizophrenia: Why People Sometimes Hear Voices, Believe Things That Others Find Strange, or Appear Out of Touch With Reality, and What Can Help 2017. www.bps.org.uk/understanding-psychosis-and-schizophrenia (accessed 4 October 2022).
- Alfageh BH, Man KKC, Besag FMC, Alhawassi TM, Wong ICK, Brauer R. Psychotropic medication prescribing for neuropsychiatric comorbidities in individuals diagnosed with autism spectrum disorder (ASD) in the UK. J Autism Dev Disord 2020;50:625-33.
- Deb S, Nancarrow T, Limbu B, Sheehan R, Wilcock M, Branford D, et al. UK psychiatrists’ experience of withdrawal of antipsychotics prescribed for challenging behaviours in adults with intellectual disabilities and/or autism. BJPsych Open 2020;6.
- NHS Northern England Clinical Networks . Guidelines for the Management of QTc Prolongation in Adults Prescribed Antipsychotics 2017. www.england.nhs.uk/north/wp-content/uploads/sites/5/2018/12/QTc-flow-diagram-with-medications-final-Dec-17-A3-with-logos.pdf (accessed 4 October 2022).
- Choi BC, Pak AW. A catalog of biases in questionnaires. Prev Chronic Dis 2005;2.
- Ponto J. Understanding and evaluating survey research. J Adv Pract Oncol 2015;6:168-71.
- Lau F. Handbook of eHealth Evaluation: An Evidence-based Approach. Victoria, BC: University of Victoria; 2017.
- Sharma A, Minh Duc NT, Luu Lam Thang T, Nam NH, Ng SJ, Abbas KS, et al. A consensus-based Checklist for Reporting of Survey Studies (CROSS). J Gen Intern Med 2021;36:3179-87.
- Medical University of Lodz . Evaluation of Electrocardiography Performed with Mobile ECG Devices in Cardiac Patients and Healthy Volunteers. ClinicalTrials.Gov, NCT05206825 2022. https://clinicaltrials.gov/show/NCT05206825 (accessed 27 April 2022).
- University of Oklahoma . Clinical Validation of the AliveCor Kardia 12L and 6L Devices. ClinicalTrials.Gov, NCT05053243 2021. https://clinicaltrials.gov/show/NCT05053243 (accessed 28 April 2022).
- The Leeds Teaching Hospitals NHS Trust, Leeds and York Partnership NHS Foundation Trust . An Evaluation of the Safety and Clinical Utility of Handheld ECG Technology in Psychiatry. ClinicalTrials.Gov, NCT04227418 2021. https://clinicaltrials.gov/show/NCT04227418 (accessed 27 April 2022).
- The Leeds Teaching Hospitals NHS Trust . EVALECGcardio Study. ClinicalTrials.Gov, NCT04468477 2020. https://clinicaltrials.gov/show/NCT04468477 (accessed 28 April 2022).
- The Leeds Teaching Hospitals NHS Trust . VaLidation of the Simple Adaptation of the Kardia 6L ECG Recorder to Obtain Chest leAd EquivaLents: a Multi-centre International (LOCAL-ECG) Study; on Behalf of the Africa Heart Rhythm Association Investigators. ClinicalTrials.Gov, NCT05324111 2023. https://clinicaltrials.gov/show/NCT05324111 (accessed 27 April 2022).
Appendix 1 Literature search strategies
Clinical effectiveness searches
| Database | Date span | Hits retrieved |
|---|---|---|
| MEDLINE + Med in P | 1946 to 25 April 2022 | 3207 |
| EMBASE | 1974 to 25 April 2022 | 3816 |
| PubMed-not-MEDLINE | 1946 to 17 May 2022 | 180 |
| PubMed | up to 18 May 2022 | 728 |
| CDSR + CDSR P | up to April 2022/Iss 4 | 40 |
| CENTRAL | up to March 2022/Iss 3 | 390 |
| DARE | up to March 2015 | 2 |
| HTA (CRD) | up to March 2018 | 4 |
| CINAHL | 1881 to 27 April 2022 | 886 |
| PsycINFO | 1806 to April 2022/Wk 3 | 79 |
| KSR Evidence | up to 26 April 2022 | 41 |
| Epistemonikos | up to 27 April 2022 | 23 |
| INAHTA | up to 27 April 2022 | 30 |
| NIHR HTA | up to 27 April 2022 | 37 |
| PROSPERO | up to 26 April 2022 | 33 |
| INPLASY | up to 27 April 2022 | 1 |
| LILACS | up to 28 April 2022 | 430 |
| DOAJ | up to 25 May 2022 | 55 |
| European Heart Journal – Digital health | up to 22 May 2022 | 63 |
| ClinicalTrials.gov | up to 27 April 2022 | 291 |
| EUCTR | up to 27 April 2022 | 101 |
| WHO ICTRP | up to 28 April 2022 | 121 |
| ScanMedicine | up to 28 April 2022 | 259 |
| Northern Light | 2010–2/Wk 16 | 165 |
| MedRxiv | up to 27 April 2022 | 145 |
| Total | 11,127 |
MEDLINE (Ovid) and Epub Ahead of Print, In-Process, In-Data-Review and Other Non-Indexed Citations and Daily: 1946 to 25 April 2022
Searched 26.4.22
Six-lead ECGs or named KardiaMobile (NoA)
-
(portable or hand?held or 6?lead$ or lead?6 or leads?6 or six?lead or six?channel$ or 6?channel$ or 6l or 6?l).ti,ab,ot,hw. (48356)
-
exp Electrocardiography/ or (Electrocardiogram$ or electrocardiograph$ or ECG or ECGs or cardiogram$ or cardiograph$ or EKG or EKGs or electriccardiogram$).ti,ab,ot,hw. (272158)
-
1 and 2 (1151)
-
(KardiaMobile$ or Kardia$ or KardiaBand or KardiaPro or AliveCor$).ti,ab,ot,hw. (2291)
-
or/3–4 (3407)
-
exp animals/ not (exp animals/ and humans/) (4998919)
-
(letter or editorial or comment).pt. (2056043)
-
5 not (6 or 7) (3207)
EMBASE (Ovid): 1974 to 25 April 2022
Searched 26.4.22
-
(portable or hand?held or 6?lead$ or lead?6 or leads?6 or six?lead or six?channel$ or 6?channel$ or 6l or 6?l).ti,ab,ot,hw. (59823)
-
exp Electrocardiogram/ or exp electrocardiography/ or (Electrocardiogram$ or electrocardiograph$ or ECG or ECGs or cardiogram$ or cardiograph$ or EKG or EKGs or electriccardiogram$).ti,ab,ot,hw. (402153)
-
1 and 2 (1877)
-
(KardiaMobile$ or Kardia$ or KardiaBand or KardiaPro or AliveCor$).ti,ab,ot,hw. (2379)
-
or/3–4 (4172)
-
animal/ (1571378)
-
animal experiment/ (2802350)
-
(rat or rats or mouse or mice or murine or rodent or rodents or hamster or hamsters or pig or pigs or porcine or rabbit or rabbits or animal or animals or dogs or dog or cats or cow or bovine or sheep or ovine or monkey or monkeys).ti,ab,ot,hw. (7232812)
-
or/6–8 (7232812)
-
exp human/ (23537816)
-
human experiment/ (572513)
-
or/10–11 (23539828)
-
9 not (9 and 12) (5478029)
-
5 not 13 (4018)
-
(letter or editorial or note).pt. (2836000)
-
14 not 15 (3816)
MEDLINE (Ovid) PubMed-not-MEDLINE: 1946 to 17 May 2022
Searched 18.5.22
-
(portable or hand?held or 6?lead$ or lead?6 or leads?6 or six?lead or six?channel$ or 6?channel$ or 6l or 6?l).ti,ab,ot,hw. (9168)
-
exp Electrocardiography/ or (Electrocardiogram$ or electrocardiograph$ or ECG or ECGs or cardiogram$ or cardiograph$ or EKG or EKGs or electriccardiogram$).ti,ab,ot,hw. (10731)
-
1 and 2 (114)
-
(KardiaMobile$ or Kardia$ or KardiaBand or KardiaPro or AliveCor$).ti,ab,ot,hw. (78)
-
or/3–4 (186)
-
exp animals/ not (exp animals/ and humans/) (1)
-
(letter or editorial or comment).pt. (140866)
-
5 not (6 or 7) (180)
PubMed (NLM) (Internet): up to 18 May 2022
Searched 18.5.22
-
9 #7 and #8 728
-
8 (pubstatusaheadofprint OR publisher[sb] OR pubmednotmedline[sb]) 4,680,678
-
7 #5 or #6 9251
-
6 (KardiaMobile* or Kardia* or KardiaBand or KardiaPro or AliveCor*) 2706
-
5 #1 and #4 6598
-
4 #2 or #3 274,648
-
3 Electrocardiography [MeSH Terms] 213,442
-
2 (Electrocardiogram* or electrocardiograph* or ECG or ECGs or cardiogram* or cardiograph* or EKG or EKGs or electriccardiogram*) 274,648
-
1 (portable or hand-held or handheld or ‘6 lead*’ or ‘lead 6’ or ‘leads 6’ or ‘six lead’ or ‘six channel*’ or ‘6 channel*’ or 6l or ‘6 l’) 301,635
CDSR (Wiley): up to April 2022/Iss 4
CDSR Protocols (Wiley): up to April 2022/Iss 4
CENTRAL (Wiley): up to March 2022/Iss 3
Searched 26.4.22
-
(portable or hand?held or handheld or 6?lead* or lead?6 or leads?6 or six?lead or six?channel* or 6?channel* or 6l or 6?l) 6727
-
(Electrocardiogram* or electrocardiograph* or ECG or ECGs or cardiogram* or cardiograph* or EKG or EKGs or electriccardiogram*) 33251
-
MeSH descriptor: [Electrocardiography] explode all trees 8998
-
#2 or #3 33357
-
#1 and #4 266
-
(KardiaMobile* or Kardia* or KardiaBand or KardiaPro or AliveCor*) 176
-
#5 or #6 431
CDSR retrieved 38 records
CDSR Protocols retrieved 2 records
CENTRAL retrieved 390 records
DARE (CRD) (www.crd.york.ac.uk/CRDWeb/): up to March 2015
HTA (CRD) (www.crd.york.ac.uk/CRDWeb/): up to March 2018
Searched 26.4.22
-
(portable or hand held or handheld or 6 lead* or lead 6 or leads 6 or six lead or six channel* or 6 channel* or 6l or ‘6 l’) 197
-
MeSH DESCRIPTOR Electrocardiography, Ambulatory EXPLODE ALL TREES 34
-
(Electrocardiogram* or electrocardiograph* or ECG or ECGs or cardiogram* or cardiograph* or EKG or EKGs or electriccardiogram*) 669
-
#2 OR #3 669
-
#1 AND #4 8
-
((KardiaMobile* or Kardia* or KardiaBand or KardiaPro or AliveCor*)) 1
-
#5 OR #6 9
-
(#7) IN DARE 2
-
(#7) IN NHSEED 3
-
(#7) IN HTA 4
DARE retrieved 2 records
HTA retrieved 4 records
CINAHL (EBSCO): 1881 to 27 April 2022
Searched 27.4.22
Advanced search, All fields
-
S7 S5 OR S6 886
-
S6 (KardiaMobile* or Kardia* or KardiaBand or KardiaPro or AliveCor*) 224
-
S5 S1 AND S4 674
-
S4 S2 OR S3 59,015
-
S3 (Electrocardiogram* or electrocardiograph* or ECG or ECGs or cardiogram* or cardiograph* or EKG or EKGs or electriccardiogram*) 59,015
-
S2 MH Electrocardiography 43,849
-
S1 (portable or hand?held or handheld or 6?lead* or lead?6 or leads?6 or six?lead or six?channel* or 6?channel* or 6l or 6?l) 29,304
APA PsycINFO (Ovid): 1806 to April 2022/Wk 3
Searched 26.4.22
-
(portable or hand?held or 6?lead$ or lead?6 or leads?6 or six?lead or six?channel$ or 6?channel$ or 6l or 6?l).ti,ab,ot,hw. (4210)
-
exp Electrocardiography/ or (Electrocardiogram$ or electrocardiograph$ or ECG or ECGs or cardiogram$ or cardiograph$ or EKG or EKGs or electriccardiogram$).ti,ab,ot,hw. (5251)
-
1 and 2 (47)
-
(KardiaMobile$ or Kardia$ or KardiaBand or KardiaPro or AliveCor$).ti,ab,ot,hw. (34)
-
or/3–4 (79)
KSR Evidence (https://ksrevidence.com/): up to 26 April 2022
Searched 26.4.22
-
(portable or hand held or handheld or 6 lead* or lead 6 or leads 6 or six lead or six channel* or 6 channel* or 6l or ‘6 l’) in All text 3165 results
-
(Electrocardiogram* or electrocardiograph* or ECG or ECGs or cardiogram* or cardiograph* or EKG or EKGs or electriccardiogram*) in All text 684 results
-
#1 and #2 in All text 37 results
-
(KardiaMobile* or Kardia* or KardiaBand or KardiaPro or AliveCor*) in All text 6 results
-
#3 or #4 in All text 41 results
Epistemonikos (www.epistemonikos.org/): up to 27 April 2022
Searched 27.4.22
Advanced search limits: systematic review/no Cochrane reviews
| Keywords title and abstract | Hits |
|---|---|
| (title:((portable OR ‘hand held’ OR handheld OR ‘6 lead’ OR ‘6 leads’ OR ‘lead 6’ OR ‘leads 6’ OR ‘six lead’ OR ‘six leads’ OR ‘six channel’ OR ‘6 channels’ OR ‘6 channel’ OR 6l OR ‘6 l’)) OR abstract:((portable OR ‘hand held’ OR handheld OR ‘6 lead’ OR ‘6 leads’ OR ‘lead 6’ OR ‘leads 6’ OR ‘six lead’ OR ‘six leads’ OR ‘six channel’ OR ‘6 channels’ OR ‘6 channel’ OR 6l OR ‘6 l’))) AND (title:((Electrocardiogram* OR electrocardiograph* OR ECG OR ECGs OR cardiogram* OR cardiograph* OR EKG OR EKGs OR electriccardiogram*)) OR abstract:((Electrocardiogram* OR electrocardiograph* OR ECG OR ECGs OR cardiogram* OR cardiograph* OR EKG OR EKGs OR electriccardiogram*))) | 16 |
| (title:((KardiaMobile* OR Kardia* OR KardiaBand OR KardiaPro OR AliveCor*)) OR abstract:((KardiaMobile* OR Kardia* OR KardiaBand OR KardiaPro OR AliveCor*))) | 7 |
| Total | 23 |
INAHTA (www.inahta.org/hta-database/): up to 27 April 2022
Searched 27.4.22
Advanced search
| All fields | Hits |
|---|---|
| (‘Electrocardiography’[mhe] or (Electrocardiogram* or electrocardiograph* or ECG or ECGs or cardiogram* or cardiograph* or EKG or EKGs or electriccardiogram*)) AND ((portable or hand?held or handheld or 6?lead* or lead?6 or leads?6 or six?lead or six?channel* or 6?channel* or 6l or 6?l)) | 29 |
| KardiaMobile* OR Kardia* OR KardiaBand OR KardiaPro OR AliveCor* | 1 |
| Total | 30 |
NIHR HTA (www.journalslibrary.nihr.ac.uk/): up to 27 April 2022
Searched 27.4.22
| Search terms | Journal reports | Research projects |
|---|---|---|
| ECG | 6 | 24 |
| ECGs | 0/2 | 0/4 |
| Electrocardiogram | 1/3 | 3/11 |
| Electrocardiograph | 0/4 | 3/5 |
| Total | 7 | 30 |
NIHR HTA retrieved 37 records
PROSPERO (CRD): up to 26 April 2022
Searched 26.4.22
-
Electrocardiogram* or electrocardiograph* or ECG or ECGs or cardiogram* or cardiograph* or EKG or EKGs or electriccardiogram* 1007
-
MeSH DESCRIPTOR Electrocardiography EXPLODE ALL TREES 71
-
#1 OR #2 1022
-
portable or hand held or handheld or 6 lead* or lead 6 or leads 6 or six lead or six channel* or 6 channel* or 6l or ‘6 l’ 574
-
#3 AND #4 22
-
(KardiaMobile* or Kardia* or KardiaBand or KardiaPro or AliveCor*) 12
-
#5 OR #6 33
INPLASY (Internet) (https://inplasy.com/): up to 27 April 2022
Searched 27.4.22
| Keyword | Hits |
|---|---|
| (Electrocardiogram OR Electrocardiograms OR electrocardiograph OR electrocardiographs OR electrocardiography OR ECG OR ECGs OR cardiogram OR cardiograph OR EKG OR EKGs OR electriccardiogram) | 1 |
| (KardiaMobile OR KardiaBand OR KardiaPro OR AliveCor) | 0 |
| Total | 1 |
Literature in the Health Sciences in Latin America and the Caribbean (LILACS) (Internet) (http://regional.bvsalud.org/php/index.php?lang=en): up to 28 April 2022
Searched: 28.4.22
Limited LILACs only
((Electrocardiogram* or electrocardiograph* or ECG or ECGs or cardiogram* or cardiograph* or EKG or EKGs or electriccardiogram*) AND (portable or ‘hand held’ or handheld or ‘6 lead*’ or ‘lead 6’ or ‘leads 6’ or ‘six lead’ or ‘six channel*’ or ‘6 channel*’ or 6l or ‘6 l’)) OR ((KardiaMobile* or Kardia* or KardiaBand or KardiaPro or AliveCor*))
LILACS retrieved 430 records
DOAJ (https://doaj.org/): up to 25 May 2022
Searched 25.5.22
| Keywords | In title | In abstract |
|---|---|---|
| Kardia | 0 | 14 |
| KardiaMobile | 1 | 7 |
| AliveCor | 6 | 27 |
| Total | 7 | 48 |
DOAJ retrieved 55 hits
European Heart Journal – Digital health (https://academic.oup.com/ehjdh/): up to 19 May 2022
Searched 19.5.22
| Keywords | Hits |
|---|---|
| Kardia* | 20 |
| 6L | 6 |
| AliveCor* | 11 |
| ECG AND hand-held | 4 |
| ECG AND six | 24 |
| ECG AND 6 lead | 61*(Please note: would not display past page 1 of results only able to access first 20 results) |
| Electrocardiogram AND six | 26 |
| Total | 152 |
| Total after dedupe and missing results | 63 |
NIH ClinicalTrials.gov (Internet) (www.clinicaltrials.gov/): up to 27 April 2022
Searched 27.4.22
| Expert search | Hits |
|---|---|
| (portable OR handheld OR hand held OR ‘6 lead’ OR ‘6-lead’ OR ‘6 leads’ OR ‘lead 6’ OR ‘leads 6’ OR ‘six lead’ OR ‘six leads’ OR ‘six channel’ OR ‘six channels’ OR ‘6 channel’ OR ‘6 channels’ 6l OR ‘6 l’) AND (Electrocardiogram OR Electrocardiograms OR electrocardiograph OR electrocardiographs OR electrocardiography OR ECG OR ECGs OR cardiogram OR cardiograph OR EKG OR EKGs OR electriccardiogram) | 242 |
| (KardiaMobile OR KardiaBand OR KardiaPro OR AliveCor) | 49 |
| Total | 291 |
EU Clinical Trials Register (EUCTR) (Internet)
Searched 27.4.22
| Expert search | Hits |
|---|---|
| (portable OR handheld OR hand held OR ‘6 lead’ OR ‘6-lead’ OR ‘6 leads’ OR ‘lead 6’ OR ‘leads 6’ OR ‘six lead’ OR ‘six leads’ OR ‘six channel’ OR ‘six channels’ OR ‘6 channel’ OR ‘6 channels’ 6l OR ‘6 l’) AND (Electrocardiogram OR Electrocardiograms OR electrocardiograph OR electrocardiographs OR electrocardiography OR ECG OR ECGs OR cardiogram OR cardiograph OR EKG OR EKGs OR electriccardiogram) | 101 |
| (KardiaMobile OR KardiaBand OR KardiaPro OR AliveCor) | 0 |
| Total | 101 |
WHO ICTRP (www.who.int/ictrp/search/en/): up to 28 April 2022
Searched 28.4.22
Advanced search option
| Keywords | Hits |
|---|---|
| Title: (portable OR handheld OR hand held) AND (Electrocardiogram OR Electrocardiograms OR electrocardiograph OR electrocardiographs) | (3 record for) 3 trials found |
| Intervention: (portable OR handheld OR hand held) AND (Electrocardiogram OR Electrocardiograms OR electrocardiograph OR electrocardiographs) | (11 records for) 11 trials found |
| Title: (portable OR handheld OR hand held) AND (electrocardiography OR ECG OR ECGs OR cardiogram OR cardiograph OR EKG OR EKGs OR electriccardiogram) | (15 record for) 15 trials found |
| Intervention: (portable OR handheld OR hand held) AND (electrocardiography OR ECG OR ECGs OR cardiogram OR cardiograph OR EKG OR EKGs OR electriccardiogram) | (45 records for) 44 trials found |
| Title: (6 lead OR 6-lead OR 6 leads OR lead 6 OR leads 6 OR six lead OR six leads) AND (Electrocardiogram OR Electrocardiograms OR electrocardiograph OR electrocardiographs) | (1 record for) 1 trial found |
| Intervention: (6 lead OR 6-lead OR 6 leads OR lead 6 OR leads 6 OR six lead OR six leads) AND (Electrocardiogram OR Electrocardiograms OR electrocardiograph OR electrocardiographs) | (15 record for) 14 trials found |
| Title: (6 lead OR 6-lead OR 6 leads OR lead 6 OR leads 6 OR six lead OR six leads) AND (electrocardiography OR ECG OR ECGs OR cardiogram OR cardiograph OR EKG OR EKGs OR electriccardiogram) | (4 record for) 4 trials found |
| Intervention: (6 lead OR 6-lead OR 6 leads OR lead 6 OR leads 6 OR six lead OR six leads) AND (electrocardiography OR ECG OR ECGs OR cardiogram OR cardiograph OR EKG OR EKGs OR electriccardiogram) | (38 record for) 37 trials found |
| Title: (six channel OR six channels OR 6 channel OR 6 channels) AND (Electrocardiogram OR Electrocardiograms OR electrocardiograph OR electrocardiographs) | (0 record for) 0 trials found |
| Intervention: (six channel OR six channels OR 6 channel OR 6 channels) AND (Electrocardiogram OR Electrocardiograms OR electrocardiograph OR electrocardiographs) | (1 record for) 1 trial found |
| Title: KardiaMobile OR KardiaBand OR KardiaPro OR AliveCor | (4 records for) 4 trials found |
| Intervention: KardiaMobile OR KardiaBand OR KardiaPro OR AliveCor | (32 records for) 32 trials found |
| Total | 166 |
| Total after deduplication | 121 |
ScanMedicine (Internet) (https://scanmedicine.com/): up to 27 April 2022
Searched: 27.4.22
| Keywords | Hits |
|---|---|
| KardiaMobile* | Kardia* | KardiaBand | KardiaPro | AliveCor* | 108 |
| ECG + 6L | 7 |
| ECG + ‘6 lead’ | 13 |
| ECG + ‘hand held’ | 24 |
| ECG + portable | 70 |
| Electrocardiogram + portable | 22 |
| Electrocardiogram + ‘hand held’ | 12 |
| Electrocardiogram + ‘6 lead’ | 2 |
| Electrocardiogram + 6L | 1 |
| Total | 259 |
Northern Light Life Sciences Conference Abstracts (Ovid): 2010–2022/Wk 16
Searched 26.4.22
-
(portable or hand?held or 6?lead$ or lead?6 or leads?6 or six?lead or six?channel$ or 6?channel$ or 6l or 6?l).af. (3801)
-
(Electrocardiogram$ or electrocardiograph$ or ECG or ECGs or cardiogram$ or cardiograph$ or EKG or EKGs or electriccardiogram$).af. (9338)
-
1 and 2 (60)
-
(KardiaMobile$ or Kardia$ or KardiaBand or KardiaPro or AliveCor$).af. (109)
-
3 or 4 (165)
MedRxiv (Internet) (www.medrxiv.org): up to 27 April 2022
Searched 27.4.22
Advanced search
| Abstract or title (match any word) | Hits |
|---|---|
| ECG ECGs electrocardiograph electrocardiographs ECG ECGs cardiogram cardiograph EKG EKGs |
144 |
| KardiaMobile KardiaBand KardiaPro AliveCor |
1/3 |
| Total | 147 |
| Total without duplicates | 145 |
Cost effectiveness searches
| Database | Date Span | Hits retrieved |
|---|---|---|
| MEDLINE + Med in P | 1946 to 26 April 2022 | 28 |
| EMBASE | 1974 to 26 April 2022 | 257 |
| CEA Registry | up to 28 April 2022 | 44 |
| RePEc | up to 28 April 2022 | 125 |
| NHS EED | up to March 2005 | 1 |
| Total | 455 |
Antipsychotics + ECGs + Costs (No A)
MEDLINE (Ovid) and Epub Ahead of Print, In-Process, In-Data-Review & Other Non-Indexed Citations and Daily: 1946 to 26 April 2022
Searched 27.4.22
-
exp Electrocardiography/ or (Electrocardiogram$ or electrocardiograph$ or ECG or ECGs or cardiogram$ or cardiograph$ or EKG or EKGs or electriccardiogram$).ti,ab,ot,hw. (272187)
-
(KardiaMobile$ or Kardia$ or KardiaBand or KardiaPro or AliveCor$).ti,ab,ot,hw. (2293)
-
(CardioSecur or ‘Personal MedSystems GmbH’).ti,ab,ot,hw. (3)
-
(D-Heart or ‘D Heart’).ti,ab,ot,hw. (171)
-
(‘RhythmPad GP’ or CurAlive).ti,ab,ot,hw. (0)
-
or/1–5 (274143)
-
exp Antipsychotic Agents/ or (antipsycho$ or anti-psycho$ or neuroleptic$).ti,ab,ot. (149938)
-
((major or butyrophenone) adj3 (tranquiliz$ or tranquilis$)).ti,ab,ot. (211)
-
(pimozide or antalon or r 6238 or opiran or orap or pimocide or pimoride or pimozide or pizide or ‘2062−78−4’).ti,ab,ot,hw,rn. (2608)
-
(Amisulpride or aktiprol or amilia or aminosultopride or amiprid or amisan or amissulprida or amisulgen or amisulid or amisulpiride or amisulpisan or amisulprid or amisulprida or amisulpridlich or amisulpridum or amitrex or amsulgen or apd 421 or apd421 or aposuprid or aracalm or barhemsys or dan 2163 or dan2163 or deniban or isofredil or nodasic or pridosil or sertol or socian or solian or sulamid or sulpitac or ‘71675−85−9’ or ‘81342−13−4’).ti,ab,ot,hw,rn. (1414)
-
(Chlorpromazine or 2601 a or 4560 r p or aminasin or aminasine or aminazin or aminazine or ampliactil or amplictil or ancholactil or aspersinal or bellacina or cepezet or chlomazine or chlorpromazine or chlor pz or chloractil or chlorbromasin or chlordelazine or chlorderazin or chlormazine or chloropromazine or chlorpromanyl or chlorpromazine or chlorpromed or clonazine or clordelazin or clorpromaz or chlorpromazine or clozine or contomin or Duncan or elmarin or esmino or fenactil or hibanil or hibernal or hibernol or hl 3746 or hl 5746 or klorproman or klorpromazin or klorpromex or laractyl or largactil or largactyl or matcine or megaphen or megatil or ml 5746 or neomazine or neurazine or novomazina or phenethyl or plegomazin or plegomazine or proma or promacid or promactil or promapar or promazil or promexin or propaphen or propaphenin or prozil or prozin or psychozine or psynor or rp 4560 or sanopron or skf 2601 a or solidon or sonazine or taroctil or taroctyl or thor prom or thorazene or thorazine or torazina or vegetamin a or vegetamin b or winsumin or wintamine or wintermin or zuledin or ‘50−53−3’ or ‘69−09−0’).ti,ab,ot,hw,rn. (26942)
-
(Haloperidol or alased or aloperidin or aloperidine or ‘apo−haloperidol’ or avant or benison or brotopon or celenase or cereen or cerenace or cizoren or depidol or dores or dozic or duraperidol or einalon s or fortunan or govotil or haldol or halidol or ‘halo−p’ or halojust or halomed or haloneural or haloper or haloperil or haloperin or haloperitol or halopidol or halopol or halosten or haricon or ‘haridol−d’ or keselan or linton or ‘lodomer−2’ or mcn jr 1625 or mcn jr1625 or mixidol or novoperidol or nsc 170973 or nsc170973 or peluces or perida or peridol or peridor or r 1625 or r1625 or selezyme or seranace or serenace or serenase or serenelfi or siegoperidol or sigaperidol or ‘trancodol−10’ or ‘trancodol−5’ or ‘1511−16−6’ or ‘52−86−8’).ti,ab,ot,hw,rn. (28145)
-
Methotrimeprazine/ or (levomepromazine or ‘apo−methoprazine’ or bayer 1213 or cl 36467 or cl 39743 or cl36467 or cl39743 or hirnamin or l mepromazine or levium or levo mepromazine or levo promazine or levomeprazine or levopromazin or levopromazine or levoprome or levozin or mepromazine or methotrimeprazine or methotrimeprazine or methozane or milezin or minozinan or neozine or neuractil or neurocil or nirvan or nozinan or rp 7044 or rp7044 or sinogan or skf 5116 or skf5116 or tiscerin or tisercin or veractil or ‘1236−99−3’ or ‘60−99−1’ or ‘7104−38−3’).ti,ab,ot,hw,rn. (1090)
-
(quetiapine or alcreno or alzen or atrolak or biquelle or desiquet or ici 204636 or ici 204646 or ici204636 or ici204646 or ketileppt or ketilept or ketipinor or kvelux or kventiax or psicotric or quetex or quetiapine or quetiapine or seresano or seroquel or setinin or socalm or tienapine or tomel or xeroquel or ‘111974−72−2’).ti,ab,ot,hw,rn. (5629)
-
(aripiprazole or abilify or abilitat or opc 14597 or opc 31 or opc14597 or opc31 or ‘129722−12−9’).ti,ab,ot,hw,rn. (4776)
-
(Asenapine or org 5222 or org5222 or saphris or secuado or sycrest or ‘65576−45−6’ or ‘85650−56−2’).ti,ab,ot,hw,rn. (483)
-
(clozapine or alemoxan or azaleptin or clopine or clopsine or clozapine or clozaril or denzapine or dorval or dozapine or elcrit or fazaclo or hf 1854 or hf1854 or lapenax or leponex or lozapin or lozapine or sizopin or versacloz or zapen or zaponex or ‘5786−21−0’).ti,ab,ot,hw,rn. (13804)
-
(Flupentixol or flupenthixol or flupenthixole or emergil or fluanxol or flurentixol or fluxanxol or lc 44 or lc44 or n 7009 or n7009 or siplaril or siplarol or ‘2413−38−9’ or ‘2709−56−0’).ti,ab,ot,hw,rn. (1575)
-
(Loxapine or adasuve or ‘alxz 004’ or alxz004 or ‘az 004’ or az004 or cl 62,362 or cl 62362 or cl62,362 or cl62,362 or cloxazepin or cloxazepine or ‘int 0036’ or int0036 or loxapane or loxapin or loxitane or oxilapine or sum 3170 or sum3170 or ‘1977−10−2’ or ‘54810−23−0’).ti,ab,ot,hw,rn. (535)
-
(Prochlorperazine or 6140 rp or antinaus or bayer a 173 or bayer a173 or capazine or chlormeprazine or chlorpeazine or chlorperazine or compro or dicopal or emelent or klometil or kronocin or meterazine or metherazine or nautisol or nipodal or normalmin or pasotomin or prochlor or prochlorpemazine or prochlorperacine or prochlorperzine or prochlorpromazine or proclorperazine or rp 6140 or rp6140 or skf 4657 or skf4657 or tementil or temetil or ‘58−38−8’).ti,ab,ot,hw,rn. (1639)
-
(Olanzapine or anzatric or dopin tab or jolyon md or lanopin or lanzac or ly 170053 or ly170053 or meltolan or midax or olace or oladay or olan or olandus or olanex or olansek or olapin or olazax or oleanz or olexar or oltal or olzap or onza or ozapin md or psychozap or relprevv or zalasta or zelta or zypadhera or zyprex or zyprexa or zyprexav or ‘132539−06−1’).ti,ab,ot,hw,rn. (11522)
-
(Paliperidone or Invega or r 76477 or r76477 or ro 76477 or ro 92670 or ro76477 or ro92670 or trevicta or xeplion or ‘144598−75−4’ or ‘199739−10−1’).ti,ab,ot,hw,rn. (1605)
-
(Risperidone or belivon or consta or dlp 114 or dlp114 or doria or eperon or jnj 410397 or jnj410397 or ‘ly 03004’ or ly03004 or neripros or noprenia or perseris or ‘r 064766’ or r 64766 or r064766 or r64766 or rbp 7000 or rbp7000 or relday or riperidon or risolept or rispen or risperdal or risperdalconsta lp or risperdaloro or risperidone or risperisphere or rispid or rispolept or rispolet or rispolux neo or rizodal or sequinan or tv 46000 or tv46000 or val 401 or val401 or zargus or zofredal or ‘zx 003’ or zx003 or ‘106266−06−2’).ti,ab,ot,hw,rn. (11085)
-
(Sulpiride or abilit or aiglonyl or arminol or dobren or dogmatil or dogmatyl or dolmatil or eglonyl or equilid or fk 880 or fk880 or isnamide or levair or levobren or levopraid or levosulpiride or meresa or miradol or neogama or sulfiride or sulpivert or sulpyride or synedil or vipral or ‘15676−16−1’).ti,ab,ot,hw,rn. (6394)
-
(brexpiprazole or opc 34712 or opc34712 or rexulti or rxulti or ‘913611−97−9’).ti,ab,ot,hw,rn. (271)
-
(Cariprazine or mp 214 or mp214 or reagila or rgh 188 or rgh188 or vraylar or ‘1083076−69−0’ or ‘839712−12−8’ or ‘955400−75−6’).ti,ab,ot,hw,rn. (313)
-
(Lurasidone or latuda or mk 3756 or mk3756 or sm 13496 or sm13496 or smp 13496 or smp13496 or ‘367514−87−2’ or ‘367514−88−3’).ti,ab,ot,hw,rn. (571)
-
(Trifluoroperazine or calmazine or eskazine or eskazinyl or espazine or fluoperazine or fluperin or flurazin or ‘iremo−pierol’ or jatroneural or leptazine or modalina or modiur or nerolet or nylipton or operzine or oxyperazine or psyrazine or skf 5019 or sporalon or stelazine or terfluzin or terfluzine or triflumed or trifluoperazide or trifluoperzine or trifluoroperazine or trifluorperacine or trifluorperazine or trifluperazine or triflurin or triftazin or triftazine or triftazinum or trinicalm or triozine or triphtazine or triphthasine or triphthazine or ‘117−89−5’ or ‘440−17−5’).ti,ab,ot,hw,rn. (375)
-
(Zuclopenthixol or cis clopenthixol or cisordinol or sedanxol or z clopenthixol or ‘53772−83−1’).ti,ab,ot,hw,rn. (342)
-
or/7–29 (173851)
-
economics/ (27450)
-
exp ‘costs and cost analysis’/ (257457)
-
economics, dental/ (1920)
-
exp ‘economics, hospital’/ (25558)
-
economics, medical/ (9195)
-
economics, nursing/ (4013)
-
economics, pharmaceutical/ (3063)
-
(economic$ or cost or costs or costly or costing or price or prices or pricing or pharmacoeconomic$).ti,ab. (938314)
-
(expenditure$ not energy).ti,ab. (34020)
-
(value adj1 money).ti,ab. (35)
-
budget$.ti,ab. (32959)
-
or/31–41 (1098733)
-
((energy or oxygen) adj cost).ti,ab. (4515)
-
(metabolic adj cost).ti,ab. (1599)
-
((energy or oxygen) adj expenditure).ti,ab. (27538)
-
or/43–45 (32619)
-
42 not 46 (1091218)
-
letter.pt. (1178093)
-
editorial.pt. (602942)
-
historical article.pt. (368305)
-
or/48–50 (2128461)
-
47 not 51 (1052283)
-
6 and 30 and 52 (28)
Costs filter:
Centre for Reviews and Dissemination. NHS EED Economics Filter: Medline (Ovid) Monthly Search. York: Centre for Reviews and Dissemination; 2010 [cited 28 September 2010]. URL: www.york.ac.uk/inst/crd/intertasc/nhs_eed_strategies.html
EMBASE (Ovid): 1974 to 26 April 2022
Searched 27.4.22
-
exp neuroleptic agent/ or exp atypical antipsychotic agent/ or (antipsycho$ or anti-psycho$ or neuroleptic$).ti,ab,ot. (288561)
-
((major or butyrophenone) adj3 (tranquiliz$ or tranquilis$)).ti,ab,ot. (268)
-
(pimozide or antalon or r 6238 or opiran or orap or pimocide or pimoride or pimozide or pizide or ‘2062−78−4’).ti,ab,ot,hw,rn. (8403)
-
(Amisulpride or aktiprol or amilia or aminosultopride or amiprid or amisan or amissulprida or amisulgen or amisulid or amisulpiride or amisulpisan or amisulprid or amisulprida or amisulpridlich or amisulpridum or amitrex or amsulgen or apd 421 or apd421 or aposuprid or aracalm or barhemsys or dan 2163 or dan2163 or deniban or isofredil or nodasic or pridosil or sertol or socian or solian or sulamid or sulpitac or ‘71675−85−9’ or ‘81342−13−4’).ti,ab,ot,hw,tn. (6303)
-
(Chlorpromazine or 2601 a or 4560 r p or aminasin or aminasine or aminazin or aminazine or ampliactil or amplictil or ancholactil or aspersinal or bellacina or cepezet or chlomazine or chlorpromazine or chlor pz or chloractil or chlorbromasin or chlordelazine or chlorderazin or chlormazine or chloropromazine or chlorpromanyl or chlorpromazine or chlorpromed or clonazine or clordelazin or clorpromaz or chlorpromazine or clozine or contomin or Duncan or elmarin or esmino or fenactil or hibanil or hibernal or hibernol or hl 3746 or hl 5746 or klorproman or klorpromazin or klorpromex or laractyl or largactil or largactyl or matcine or megaphen or megatil or ml 5746 or neomazine or neurazine or novomazina or phenethyl or plegomazin or plegomazine or proma or promacid or promactil or promapar or promazil or promexin or propaphen or propaphenin or prozil or prozin or psychozine or psynor or rp 4560 or sanopron or skf 2601 a or solidon or sonazine or taroctil or taroctyl or thor prom or thorazene or thorazine or torazina or vegetamin a or vegetamin b or winsumin or wintamine or wintermin or zuledin or ‘50−53−3’ or ‘69−09−0’).ti,ab,ot,hw,tn. (51556)
-
(Haloperidol or alased or aloperidin or aloperidine or ‘apo−haloperidol’ or avant or benison or brotopon or celenase or cereen or cerenace or cizoren or depidol or dores or dozic or duraperidol or einalon s or fortunan or govotil or haldol or halidol or ‘halo−p’ or halojust or halomed or haloneural or haloper or haloperil or haloperin or haloperitol or halopidol or halopol or halosten or haricon or ‘haridol−d’ or keselan or linton or ‘lodomer−2’ or mcn jr 1625 or mcn jr1625 or mixidol or novoperidol or nsc 170973 or nsc170973 or peluces or perida or peridol or peridor or r 1625 or r1625 or selezyme or seranace or serenace or serenase or serenelfi or siegoperidol or sigaperidol or ‘trancodol−10’ or ‘trancodol−5’ or ‘1511−16−6’ or ‘52−86−8’).ti,ab,ot,hw,tn. (66728)
-
(levomepromazine or ‘apo−methoprazine’ or bayer 1213 or cl 36467 or cl 39743 or cl36467 or cl39743 or hirnamin or l mepromazine or levium or levo mepromazine or levo promazine or levomeprazine or levopromazin or levopromazine or levoprome or levozin or mepromazine or methotrimeprazine or methotrimeprazine or methozane or milezin or minozinan or neozine or neuractil or neurocil or nirvan or nozinan or rp 7044 or rp7044 or sinogan or skf 5116 or skf5116 or tiscerin or tisercin or veractil or ‘1236−99−3’ or ‘60−99−1’ or ‘7104−38−3’).ti,ab,ot,hw,tn. (5687)
-
(quetiapine or alcreno or alzen or atrolak or biquelle or desiquet or ici 204636 or ici 204646 or ici204636 or ici204646 or ketileppt or ketilept or ketipinor or kvelux or kventiax or psicotric or quetex or quetiapine or quetiapine or seresano or seroquel or setinin or socalm or tienapine or tomel or xeroquel or ‘111974−72−2’).ti,ab,ot,hw,tn. (26546)
-
(aripiprazole or abilify or abilitat or opc 14597 or opc 31 or opc14597 or opc31 or ‘129722−12−9’).ti,ab,ot,hw,tn. (18025)
-
(Asenapine or org 5222 or org5222 or saphris or secuado or sycrest or ‘65576−45−6’ or ‘85650−56−2’).ti,ab,ot,hw,tn. (1802)
-
(clozapine or alemoxan or azaleptin or clopine or clopsine or clozapine or clozaril or denzapine or dorval or dozapine or elcrit or fazaclo or hf 1854 or hf1854 or lapenax or leponex or lozapin or lozapine or sizopin or versacloz or zapen or zaponex or ‘5786−21−0’).ti,ab,ot,hw,tn. (36526)
-
(Flupentixol or flupenthixol or flupenthixole or emergil or fluanxol or flurentixol or fluxanxol or lc 44 or lc44 or n 7009 or n7009 or siplaril or siplarol or ‘2413−38−9’ or ‘2709−56−0’).ti,ab,ot,hw,tn. (5896)
-
(Loxapine or adasuve or ‘alxz 004’ or alxz004 or ‘az 004’ or az004 or cl 62,362 or cl 62362 or cl62,362 or cl62362 or cloxazepin or cloxazepine or ‘int 0036’ or int0036 or loxapane or loxapin or loxitane or oxilapine or sum 3170 or sum3170 or ‘1977−10−2’ or ‘54810−23−0’).ti,ab,ot,hw,tn. (2834)
-
(Prochlorperazine or 6140 rp or antinaus or bayer a 173 or bayer a173 or capazine or chlormeprazine or chlorpeazine or chlorperazine or compro or dicopal or emelent or klometil or kronocin or meterazine or metherazine or nautisol or nipodal or normalmin or pasotomin or prochlor or prochlorpemazine or prochlorperacine or prochlorperzine or prochlorpromazine or proclorperazine or rp 6140 or rp6140 or skf 4657 or skf4657 or tementil or temetil or ‘58−38−8’).ti,ab,ot,hw,tn. (6771)
-
(Olanzapine or anzatric or dopin tab or jolyon md or lanopin or lanzac or ly 170053 or ly170053 or meltolan or midax or olace or oladay or olan or olandus or olanex or olansek or olapin or olazax or oleanz or olexar or oltal or olzap or onza or ozapin md or psychozap or relprevv or zalasta or zelta or zypadhera or zyprex or zyprexa or zyprexav or ‘132539−06−1’).ti,ab,ot,hw,tn. (40459)
-
(Paliperidone or Invega or r 76477 or r76477 or ro 76477 or ro 92670 or ro76477 or ro92670 or trevicta or xeplion or ‘144598−75−4’ or ‘199739−10−1’).ti,ab,ot,hw,tn. (5475)
-
(Risperidone or belivon or consta or dlp 114 or dlp114 or doria or eperon or jnj 410397 or jnj410397 or ‘ly 03004’ or ly03004 or neripros or noprenia or perseris or ‘r 064766’ or r 64766 or r064766 or r64766 or rbp 7000 or rbp7000 or relday or riperidon or risolept or rispen or risperdal or risperdalconsta lp or risperdaloro or risperidone or risperisphere or rispid or rispolept or rispolet or rispolux neo or rizodal or sequinan or tv 46000 or tv46000 or val 401 or val401 or zargus or zofredal or ‘zx 003’ or zx003 or ‘106266−06−2’).ti,ab,ot,hw,tn. (40396)
-
(Sulpiride or abilit or aiglonyl or arminol or dobren or dogmatil or dogmatyl or dolmatil or eglonyl or equilid or fk 880 or fk880 or isnamide or levair or levobren or levopraid or levosulpiride or meresa or miradol or neogama or sulfiride or sulpivert or sulpyride or synedil or vipral or ‘15676−16−1’).ti,ab,ot,hw,tn. (12967)
-
(brexpiprazole or opc 34712 or opc34712 or rexulti or rxulti or ‘913611−97−9’).ti,ab,ot,hw,tn. (715)
-
(Cariprazine or mp 214 or mp214 or reagila or rgh 188 or rgh188 or vraylar or ‘1083076−69−0’ or ‘839712−12−8’ or ‘955400−75−6’).ti,ab,ot,hw,tn. (827)
-
(Lurasidone or latuda or mk 3756 or mk3756 or sm 13496 or sm13496 or smp 13496 or smp13496 or ‘367514−87−2’ or ‘367514−88−3’).ti,ab,ot,hw,tn. (2094)
-
(Trifluoroperazine or calmazine or eskazine or eskazinyl or espazine or fluoperazine or fluperin or flurazin or ‘iremo−pierol’ or jatroneural or leptazine or modalina or modiur or nerolet or nylipton or operzine or oxyperazine or psyrazine or skf 5019 or sporalon or stelazine or terfluzin or terfluzine or triflumed or trifluoperazide or trifluoperzine or trifluoroperazine or trifluorperacine or trifluorperazine or trifluperazine or triflurin or triftazin or triftazine or triftazinum or trinicalm or triozine or triphtazine or triphthasine or triphthazine or ‘117−89−5’ or ‘440−17−5’).ti,ab,ot,hw,tn. (1055)
-
(Zuclopenthixol or cis clopenthixol or cisordinol or sedanxol or z clopenthixol or ‘53772−83−1’).ti,ab,ot,hw,tn. (2929)
-
or/1–23 (309037)
-
exp Electrocardiogram/ or exp electrocardiography/ or (Electrocardiogram$ or electrocardiograph$ or ECG or ECGs or cardiogram$ or cardiograph$ or EKG or EKGs or electriccardiogram$).ti,ab,ot,hw. (402165)
-
(KardiaMobile$ or Kardia$ or KardiaBand or KardiaPro or AliveCor$).ti,ab,ot,hw. (2379)
-
(CardioSecur or ‘Personal MedSystems GmbH’).ti,ab,ot,hw. (9)
-
(D-Heart or ‘D Heart’).ti,ab,ot,hw. (374)
-
(‘RhythmPad GP’ or CurAlive).ti,ab,ot,hw. (1)
-
or/25–29 (404178)
-
24 and 30 (6485)
-
health-economics/ (34200)
-
exp economic-evaluation/ (332620)
-
exp health-care-cost/ (317364)
-
exp pharmacoeconomics/ (217952)
-
or/32–35 (703617)
-
(econom$ or cost or costs or costly or costing or price or prices or pricing or pharmacoeconomic$).ti,ab. (1245105)
-
(expenditure$ not energy).ti,ab. (46018)
-
(value adj2 money).ti,ab. (2728)
-
budget$.ti,ab. (43331)
-
or/37–40 (1286035)
-
36 or 41 (1633007)
-
letter.pt. (1220949)
-
editorial.pt. (724072)
-
note.pt. (891248)
-
or/43–45 (2836269)
-
42 not 46 (1504929)
-
(metabolic adj cost).ti,ab. (1714)
-
((energy or oxygen) adj cost).ti,ab. (4764)
-
((energy or oxygen) adj expenditure).ti,ab. (34798)
-
or/48–50 (40110)
-
47 not 51 (1496696)
-
exp animal/ (28477822)
-
exp animal-experiment/ (2828547)
-
nonhuman/ (6869106)
-
(rat or rats or mouse or mice or hamster or hamsters or animal or animals or dog or dogs or cat or cats or bovine or sheep).ti,ab,sh. (6134952)
-
or/53–56 (30586996)
-
exp human/ (23540271)
-
exp human-experiment/ (573121)
-
58 or 59 (23542341)
-
57 not (57 and 60) (7045737)
-
52 not 61 (1357340)
-
31 and 62 (257)
Economics terms based on costs filter:
Centre for Reviews and Dissemination. Search Strategies: NHS EED EMBASE Using OvidSP (Economics Filter). York: Centre for Reviews and Dissemination; 2014 (accessed 2.6.14). URL: www.crd.york.ac.uk/crdweb/searchstrategies.asp#nhseedembase
NHS EED (CRD): up to March 2015
Searched 27.4.22
-
MeSH DESCRIPTOR Electrocardiography EXPLODE ALL TREES 303 Delete
-
((Electrocardiogram* or electrocardiograph* or ECG or ECGs or cardiogram* or cardiograph* or EKG or EKGs or electriccardiogram*)) 669 Delete
-
((KardiaMobile* or Kardia* or KardiaBand or KardiaPro or AliveCor*)) 1 Delete
-
((CardioSecur or ‘Personal MedSystems GmbH’)) 0 Delete
-
((D-Heart or ‘D Heart’)) 0 Delete
-
((‘RhythmPad GP’ or CurAlive)) 0 Delete
-
#1 OR #2 OR #3 OR #4 OR #5 OR #6 675 Delete
-
(#7) IN NHSEED 285 Delete
-
MeSH DESCRIPTOR Antipsychotic Agents EXPLODE ALL TREES 720 Delete
-
((antipsycho* or anti-psycho* or neuroleptic*)) IN NHSEED 188 Delete
-
((major or butyrophenone) adj3 (tranquiliz* or tranquilis*)) IN NHSEED 0 Delete
-
((pimozide or antalon or r 6238 or opiran or orap or pimocide or pimoride or pimozide or pizide or ‘2062?78?4’)) IN NHSEED 0 Delete
-
((Amisulpride or aktiprol or amilia or aminosultopride or amiprid or amisan or amissulprida or amisulgen or amisulid or amisulpiride or amisulpisan or amisulprid or amisulprida or amisulpridlich or amisulpridum or amitrex or amsulgen or apd 421 or apd421 or aposuprid or aracalm or barhemsys or dan 2163 or dan2163 or deniban or isofredil or nodasic or pridosil or sertol or socian or solian or sulamid or sulpitac or ‘71675?85?9’ or ‘81342?13?4’)) IN NHSEED 9 Delete
-
((Chlorpromazine or 2601 a or 4560 r p or aminasin or aminasine or aminazin or aminazine or ampliactil or amplictil or ancholactil or aspersinal or bellacina or cepezet or chlomazine or chlorpromazine or chlor pz or chloractil or chlorbromasin or chlordelazine or chlorderazin or chlormazine or chloropromazine or chlorpromanyl or chlorpromazine or chlorpromed or clonazine or clordelazin or clorpromaz or chlorpromazine or clozine or contomin or Duncan or elmarin or esmino or fenactil or hibanil or hibernal or hibernol or hl 3746 or hl 5746 or klorproman or klorpromazin or klorpromex or laractyl or largactil or largactyl or matcine or megaphen or megatil or ml 5746 or neomazine or neurazine or novomazina or phenethyl or plegomazin or plegomazine or proma or promacid or promactil or promapar or promazil or promexin or propaphen or propaphenin or prozil or prozin or psychozine or psynor or rp 4560 or sanopron or skf 2601 a or solidon or sonazine or taroctil or taroctyl or thor prom or thorazene or thorazine or torazina or vegetamin a or vegetamin b or winsumin or wintamine or wintermin or zuledin or ‘50?53?3’ or ‘69?09?0’)) IN NHSEED 40 Delete
-
((Haloperidol or alased or aloperidin or aloperidine or ‘apo?haloperidol’ or avant or benison or brotopon or celenase or cereen or cerenace or cizoren or depidol or dores or dozic or duraperidol or einalon s or fortunan or govotil or haldol or halidol or ‘halo?p’ or halojust or halomed or haloneural or haloper or haloperil or haloperin or haloperitol or halopidol or halopol or halosten or haricon or ‘haridol?d’ or keselan or linton or ‘lodomer?2’ or mcn jr 1625 or mcn jr1625 or mixidol or novoperidol or nsc 170973 or nsc170973 or peluces or perida or peridol or peridor or r 1625 or r1625 or selezyme or seranace or serenace or serenase or serenelfi or siegoperidol or sigaperidol or ‘trancodol?10’ or ‘trancodol?5’ or ‘1511?16?6’ or ‘52?86?8’)) IN NHSEED 57 Delete
-
((levomepromazine or ‘apo?methoprazine’ or bayer 1213 or cl 36467 or cl 39743 or cl36467 or cl39743 or hirnamin or l mepromazine or levium or levo mepromazine or levo promazine or levomeprazine or levopromazin or levopromazine or levoprome or levozin or mepromazine or methotrimeprazine or methotrimeprazine or methozane or milezin or minozinan or neozine or neuractil or neurocil or nirvan or nozinan or rp 7044 or rp7044 or sinogan or skf 5116 or skf5116 or tiscerin or tisercin or veractil or ‘1236?99?3’ or ‘60?99?1’ or ‘7104?38?3’)) IN NHSEED 2 Delete
-
MeSH DESCRIPTOR Methotrimeprazine EXPLODE ALL TREES 0 Delete
-
((quetiapine or alcreno or alzen or atrolak or biquelle or desiquet or ici 204636 or ici 204646 or ici204636 or ici204646 or ketileppt or ketilept or ketipinor or kvelux or kventiax or psicotric or quetex or quetiapine or quetiapine or seresano or seroquel or setinin or socalm or tienapine or tomel or xeroquel or ‘111974?72?2’)) IN NHSEED 40 Delete
-
((aripiprazole or abilify or abilitat or opc 14597 or opc 31 or opc14597 or opc31 or ‘129722?12?9’)) IN NHSEED 22 Delete
-
((Asenapine or org 5222 or org5222 or saphris or secuado or sycrest or ‘65576?45?6’ or ‘85650?56?2’)) IN NHSEED 2 Delete
-
((clozapine or alemoxan or azaleptin or clopine or clopsine or clozapine or clozaril or denzapine or dorval or dozapine or elcrit or fazaclo or hf 1854 or hf1854 or lapenax or leponex or lozapin or lozapine or sizopin or versacloz or zapen or zaponex or ‘5786?21?0’)) IN NHSEED 51 Delete
-
((Flupentixol or flupenthixol or flupenthixole or emergil or fluanxol or flurentixol or fluxanxol or lc 44 or lc44 or n 7009 or n7009 or siplaril or siplarol or ‘2413?38?9’ or ‘2709?56?0’)) IN NHSEED 5 Delete
-
((Loxapine or adasuve or ‘alxz 004’ or alxz004 or ‘az 004’ or az004 or cl 62,362 or cl 62,362 or cl62,362 or cl62,362 or cloxazepin or cloxazepine or ‘int 0036’ or int0036 or loxapane or loxapin or loxitane or oxilapine or sum 3170 or sum3170 or ‘1977?10?2’ or ‘54810?23?0’)) IN NHSEED 2 Delete
-
((Prochlorperazine or 6140 rp or antinaus or bayer a 173 or bayer a173 or capazine or chlormeprazine or chlorpeazine or chlorperazine or compro or dicopal or emelent or klometil or kronocin or meterazine or metherazine or nautisol or nipodal or normalmin or pasotomin or prochlor or prochlorpemazine or prochlorperacine or prochlorperzine or prochlorpromazine or proclorperazine or rp 6140 or rp6140 or skf 4657 or skf4657 or tementil or temetil or ‘58?38?8’)) 14 Delete
-
((Olanzapine or anzatric or dopin tab or jolyon md or lanopin or lanzac or ly 170053 or ly170053 or meltolan or midax or olace or oladay or olan or olandus or olanex or olansek or olapin or olazax or oleanz or olexar or oltal or olzap or onza or ozapin md or psychozap or relprevv or zalasta or zelta or zypadhera or zyprex or zyprexa or zyprexav or ‘132539?06?1’)) 269 Delete
-
((Paliperidone or Invega or r 76477 or r76477 or ro 76477 or ro 92670 or ro76477 or ro92670 or trevicta or xeplion or ‘144598?75?4’ or ‘199739?10?1’)) 33 Delete
-
((Risperidone or belivon or consta or dlp 114 or dlp114 or doria or eperon or jnj 410397 or jnj410397 or ‘ly 03004’ or ly03004 or neripros or noprenia or perseris or ‘r 064766’ or r 64766 or r064766 or r64766 or rbp 7000 or rbp7000 or relday or riperidon or risolept or rispen or risperdal or risperdalconsta lp or risperdaloro or risperidone or risperisphere or rispid or rispolept or rispolet or rispolux neo or rizodal or sequinan or tv 46000 or tv46000 or val 401 or val401 or zargus or zofredal or ‘zx 003’ or zx003 or ‘106266?06?2’)) 318 Delete
-
((Sulpiride or abilit or aiglonyl or arminol or dobren or dogmatil or dogmatyl or dolmatil or eglonyl or equilid or fk 880 or fk880 or isnamide or levair or levobren or levopraid or levosulpiride or meresa or miradol or neogama or sulfiride or sulpivert or sulpyride or synedil or vipral or ‘15676?16?1’)) 42 Delete
-
((brexpiprazole or opc 34712 or opc34712 or rexulti or rxulti or ‘913611?97?9’)) 0 Delete
-
((Lurasidone or latuda or mk 3756 or mk3756 or sm 13496 or sm13496 or smp 13496 or smp13496 or ‘367514?87?2’ or ‘367514?88?3’)) 12 Delete
-
((Trifluoroperazine or calmazine or eskazine or eskazinyl or espazine or fluoperazine or fluperin or flurazin or ‘iremo?pierol’ or jatroneural or leptazine or modalina or modiur or nerolet or nylipton or operzine or oxyperazine or psyrazine or skf 5019 or sporalon or stelazine or terfluzin or terfluzine or triflumed or trifluoperazide or trifluoperzine or trifluoroperazine or trifluorperacine or trifluorperazine or trifluperazine or triflurin or triftazin or triftazine or triftazinum or trinicalm or triozine or triphtazine or triphthasine or triphthazine or ‘117?89?5’ or ‘440?17?5’)) 0 Delete
-
((Zuclopenthixol or cis clopenthixol or cisordinol or sedanxol or z clopenthixol or ‘53772?83?1’)) 24 Delete
-
(#9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 or #30 or #31 or #32) 916 Delete
-
(#8 and #33) IN NHSEED 1 Delete
CEA Registry (www.cearegistry.org): up to 28 April 2022
Searched: 28.4.22
Keywords:
ECG OR ECGs OR Electrocardiogram OR electrocardiograph OR Electrocardiograms OR electrocardiographs OR electrocardiography
CEA retrieved 20 ratios
CEA retrieved 24 utilities
RePEc (Internet) (http://repec.org/): up to 28 April 2022
Searched 28.4.22
Searched via IDEAS database (https://ideas.repec.org/)
Keywords in title:
(Electrocardiogram | electrocardiograph | ECG | ECGs | EKG | EKGs | electriccardiogram)
IDEAS retrieved 125 records
Appendix 2 QUADAS-2 assessments
Study: Azram 202114
DOMAIN 1: PATIENT SELECTION
| A. RISK OF BIAS | |
| Prospective study of cardiology inpatients and outpatients. The only exclusion criteria were refusal or inability to provide informed consent | |
| Was a consecutive or random sample of patients enrolled? | Yes |
| Was a case-control design avoided? | NA |
| Did the study avoid inappropriate exclusions? | Yes |
| Could the selection of patients have introduced bias? | RISK: Low |
| B. APPLICABILITY | |
| The study was conducted in cardiology patients with a documented indication for ECG (no asymptomatic screening patients were included). The study did not include any patients where the indication for ECG was initiation of antipsychotic medication or monitoring during antipsychotic use. | |
| Do the included patients match the question? | Concerns: High |
DOMAIN 2: INDEX TEST(S)
| A. RISK OF BIAS | |
| 12-lead ECG was performed first, followed immediately by KardiaMobile 6L ECG. KardiaMobile ECG was performed, in triplicate, by a cardiologist and two cardiac physiologists. ECGs were anonymised and presented in random order for interpretation. | |
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes |
| If a threshold was used, was it pre-specified? | NA |
| Could the conduct or interpretation of the index test have introduced bias? | RISK: Low |
| B. APPLICABILITY | |
| Are there concerns that the index test, its conduct or interpretation differ from the review question? | Concerns: High |
DOMAIN 3: REFERENCE STANDARD/COMPARATOR
| A. RISK OF BIAS | |
| 12-lead ECG was performed first, followed immediately by KardiaMobile 6L ECG. 12-lead ECG was performed, in triplicate, by a cardiologist and two cardiac physiologists. ECGs were anonymised and presented in random order for interpretation. | |
| Is the reference standard likely to correctly classify the target condition? | Yes |
| Were the reference standard results interpreted without knowledge of the results of the index test? | Yes |
| Could the reference standard, its conduct, or its interpretation have introduced bias? | RISK: Low |
DOMAIN 4: FLOW AND TIMING
| A. RISK OF BIAS | |
| Analysis was not possible for all leads, for either ECG method; data were reported by lead rather than by patient | |
| Did all patients receive ECG both methods? | Yes |
| Was the time period between ECGs appropriate? | Yes |
| Were all patients included in the analysis? | Unclear |
| Could the patient flow have introduced bias? | RISK: Unclear |
Study: Kleiman 202131
DOMAIN 1: PATIENT SELECTION
| A. RISK OF BIAS | |
| Prospective study of patients referred to a genetic hearty rhythm clinic; unclear whether patients were recruited consecutively. No inclusion or exclusion criteria reported. | |
| Was a consecutive or random sample of patients enrolled? | Unclear |
| Was a case-control design avoided? | NA |
| Did the study avoid inappropriate exclusions? | Unclear |
| Could the selection of patients have introduced bias? | RISK: Unclear |
| B. APPLICABILITY | |
| The study was conducted in patients referred to a genetic hearty rhythm clinic. The study did not include any patients where the indication for ECG was initiation of antipsychotic medication or monitoring during antipsychotic use. | |
| Do the included patients match the question? | Concerns: High |
DOMAIN 2: INDEX TEST(S)
| A. RISK OF BIAS | |
| KardiaMobile 6L ECG was performed, by patients, in controlled conditions, and interpreted by cardiologists who were blinded to subject identifiers and details of the study. KardiaMobile 6L and 12-lead ECGs were evaluated in separate cohorts, using different subject identifiers, and in a randomised order. | |
| Were the index test results interpreted without knowledge results of the reference standard? | Yes |
| If a threshold was used, was it pre-specified? | NA |
| Could the conduct or interpretation of the index test have introduced bias? | RISK: Low |
| B. APPLICABILITY | |
| Are there concerns that the index test, its conduct or interpretation differ from the review question? | Concerns: High |
DOMAIN 3: REFERENCE STANDARD/COMPARATOR
| A. RISK OF BIAS | |
| 12-lead ECGs were interpreted by cardiologists who were blinded to subject identifiers and details of the study. KardiaMobile 6L and 12-lead ECGs were evaluated in separate cohorts, using different subject identifiers, and in a randomised order. | |
| Is the reference standard likely to correctly classify the target condition? | Yes |
| Were the reference standard results interpreted without knowledge of the results of the index test? | Yes |
| Could the reference standard, its conduct or its interpretation have introduced bias? | RISK: Low |
DOMAIN 4: FLOW AND TIMING
| A. RISK OF BIAS | |
| Eleven (1.6%) patients were excluded from the analysis because > 30 minutes had elapsed between KardiaMobile 6L and 12-lead ECG recordings. | |
| Did all patients receive ECG both methods? | Yes |
| Was the time period between ECGs appropriate? | Yes |
| Were all patients included in the analysis? | No |
| Could the patient flow have introduced bias? | RISK: Low |
Study: Krzowski 202151
DOMAIN 1: PATIENT SELECTION
| A. RISK OF BIAS | |
| Prospective study of consecutive patients on a tertiary care cardiology ward. No inclusion or exclusion criteria reported. | |
| Was a consecutive or random sample of patients enrolled? | Yes |
| Was a case-control design avoided? | NA |
| Did the study avoid inappropriate exclusions? | Unclear |
| Could the selection of patients have introduced bias? | RISK: Unclear |
| B. APPLICABILITY | |
| The study was conducted in tertiary care cardiology inpatients. The study did not include any patients where the indication for ECG was initiation of antipsychotic medication or monitoring during antipsychotic use. | |
| Do the included patients match the question? | Concerns: High |
DOMAIN 2: INDEX TEST(S)
| A. RISK OF BIAS | |
| KardiaMobile 6L ECG was performed by experienced technicians. All ECG recordings were assessed, blinded, by experienced clinicians. | |
| Were the index test results interpreted without knowledge results of the reference standard? | Yes |
| If a threshold was used, was it pre-specified? | NA |
| Could the conduct or interpretation of the index test have introduced bias? | RISK: Low |
| B. APPLICABILITY | |
| Are there concerns that the index test, its conduct or interpretation differ from the review question? | Concerns: High |
DOMAIN 3: REFERENCE STANDARD/COMPARATOR
| A. RISK OF BIAS | |
| 12-lead ECGs were performed by experienced technicians. All ECG recordings were assessed, blinded, by experienced clinicians. | |
| Is the reference standard likely to correctly classify the target condition? | Yes |
| Were the reference standard results interpreted without knowledge of the results of the index test? | Yes |
| Could the reference standard, its conduct or its interpretation have introduced bias? | RISK: Low |
DOMAIN 4: FLOW AND TIMING
| A. RISK OF BIAS | |
| One patient (1%) did not receive KardiaMobile 6L ECG, due to Parkinson’s disease-related tremor. KardiaMobile 6L and 12-lead ECG recordings were made consecutively | |
| Did all patients receive ECG both methods? | No |
| Was the time period between ECGs appropriate? | Yes |
| Were all patients included in the analysis? | No |
| Could the patient flow have introduced bias? | RISK: Low |
Study: Minguito-Carazo 202137
DOMAIN 1: PATIENT SELECTION
| A. RISK OF BIAS | |
| Healthy control patients from a study of COVID-19 patients. No selection criteria were reported | |
| Was a consecutive or random sample of patients enrolled? | Unclear |
| Was a case-control design avoided? | NA |
| Did the study avoid inappropriate exclusions? | Unclear |
| Could the selection of patients have introduced bias? | RISK: Unclear |
| B. APPLICABILITY | |
| The comparative data from this study were derived from healthy control patients. The study did not include any patients where the indication for ECG was initiation of antipsychotic medication or monitoring during antipsychotic use. | |
| Do the included patients match the question? | Concerns: High |
DOMAIN 2: INDEX TEST(S)
| A. RISK OF BIAS | |
| No details of who recorded the KardiaMobile 6L ECG were reported. All ECG recordings were reviewed by at least one cardiologist. It was not clear whether cardiologists interpreting KardiaMobile 6L ECG recordings had access to 12-lead ECG recordings. | |
| Were the index test results interpreted without knowledge results of the reference standard? | Unclear |
| If a threshold was used, was it pre-specified? | NA |
| Could the conduct or interpretation of the index test have introduced bias? | RISK: Unclear |
| B. APPLICABILITY | |
| Are there concerns that the index test, its conduct or interpretation differ from the review question? | Concerns: High |
DOMAIN 3: REFERENCE STANDARD/COMPARATOR
| A. RISK OF BIAS | |
| No information was reported regarding the conduct of 12-lead ECGs. All ECG recordings were reviewed by at least one cardiologist. It was not clear whether cardiologists interpreting 12-lead ECG recordings had access to KardiaMobile 6L ECG recordings. | |
| Is the reference standard likely to correctly classify the target condition? | Unclear |
| Were the reference standard results interpreted without knowledge of the results of the index test? | Unclear |
| Could the reference standard, its conduct or its interpretation have introduced bias? | RISK: Unclear |
DOMAIN 4: FLOW AND TIMING
| A. RISK OF BIAS | |
| All healthy control patients received ECG by both methods. | |
| Did all patients receive ECG both methods? | Yes |
| Was the time period between ECGs appropriate? | Unclear |
| Were all patients included in the analysis? | Yes |
| Could the patient flow have introduced bias? | RISK: Unclear |
Study: Orchard 202141
DOMAIN 1: PATIENT SELECTION
| A. RISK OF BIAS | |
| Healthy, asymptomatic athletes, with no existing cardiac diagnoses or family history of conditions associated with sudden cardiac death. No inclusion or exclusion criteria were reported. | |
| Was a consecutive or random sample of patients enrolled? | Unclear |
| Was a case-control design avoided? | NA |
| Did the study avoid inappropriate exclusions? | Unclear |
| Could the selection of patients have introduced bias? | RISK: Unclear |
| B. APPLICABILITY | |
| Study of healthy athletes. The study did not include any patients where the indication for ECG was initiation of antipsychotic medication or monitoring during antipsychotic use. | |
| Do the included patients match the question? | Concerns: High |
DOMAIN 2: INDEX TEST(S)
| A. RISK OF BIAS | |
| No details of who recorded the KardiaMobile 6L ECG were reported. All ECG recordings were reviewed by four expert cardiologists. It was not clear whether cardiologists interpreting KardiaMobile 6L ECG recordings had access to 12-lead ECG recordings. | |
| Were the index test results interpreted without knowledge results of the reference standard? | Unclear |
| If a threshold was used, was it pre-specified? | NA |
| Could the conduct or interpretation of the index test have introduced bias? | RISK: Unclear |
| B. APPLICABILITY | |
| Are there concerns that the index test, its conduct or interpretation differ from the review question? | Concerns: High |
DOMAIN 3: REFERENCE STANDARD/COMPARATOR
| A. RISK OF BIAS | |
| No information was reported regarding the conduct of 12-lead ECGs. All ECG recordings were reviewed by four expert cardiologists. It was not clear whether cardiologists interpreting 12-lead ECG recordings had access to KardiaMobile 6L ECG recordings. | |
| Is the reference standard likely to correctly classify the target condition? | Unclear |
| Were the reference standard results interpreted without knowledge of the results of the index test? | Unclear |
| Could the reference standard, its conduct or its interpretation have introduced bias? | RISK: Unclear |
DOMAIN 4: FLOW AND TIMING
| A. RISK OF BIAS | |
| All participants received ECG by both methods within 1 hour. | |
| Did all patients receive ECG both methods? | Yes |
| Was the time period between ECGs appropriate? | Yes |
| Were all patients included in the analysis? | Yes |
| Could the patient flow have introduced bias? | RISK: Low |
Appendix 3 Details of excluded studies with rationale
To be included in the review studies had to fulfil the following criteria:
-
Research question 1: ‘What is the accuracy/technical performance of KardiaMobile 6L, where the target condition is QTc prolongation, determined by standard 12-lead ECG (the reference standard method)?’
-
Population: Any
-
Setting: Any
-
Index test: KardiaMobile 6L
-
Comparator: None
-
Reference standard: 12-lead ECG
-
Outcomes: Diagnostic accuracy (the numbers of true-positive, false-negative, false-positive and true-negative test results), where the target condition is QT prolongation, determined by 12-lead ECG, concordance (of QT interval determined by KardiaMobile 6L with that determined by 12-lead ECG), test failure rates and reasons for failure
-
Study design: Diagnostic cohort studies or observational, non-inferiority/equivalence studies for concordance
-
Research question 2: ‘What are the clinical effects of using KardiaMobile 6L, compared with 12-lead ECG or no ECG, on clinical outcomes (cardiac and psychiatric)?’
-
Population: People starting or maintained on antipsychotic medications that are associated with QT prolongation, in whom an ECG assessment of QT-based cardiac risk is indicated
-
Setting: Any
-
Index test: KardiaMobile 6L
-
Comparator: 12-lead ECG or no ECG
-
Reference standard: Not applicable
-
Outcomes: Cardiac outcomes (arrhythmias, sudden cardiac death), psychiatric outcomes, hospitalisations (cardiac of psychiatric), referrals to mental health crisis teams, other adverse effects of antipsychotic medication, HRQoL, change to treatment decision, time from decision to prescribe to treatment
-
Study design: RCTs, CCTs or observational before-and-after (implementation) studies
-
Research question 3: ‘What are the effects of using KardiaMobile 6L on service user acceptability/satisfaction and on training and workflow issues?’
-
Population: People starting or maintained on antipsychotic medications that are associated with QT prolongation, in whom an ECG assessment of QT-based cardiac risk is indicated (service user acceptability/satisfaction)
-
OR
-
Healthcare professionals or others delivering ECG assessment of QT-based cardiac risk, in settings applicable to the above population (training and workflow)
-
-
Setting: Any
-
Index test: KardiaMobile 6L
-
Comparator: 12-lead ECG or no comparator
-
Reference standard: Not applicable
-
Outcomes: Measures of service user preference (e.g. rates of refusal or missed appointments), number of 12-lead ECGs required, number of cardiology referrals/requests for cardiology interpretation, appointment length (including time to take ECG and time for general care of the service user), ease of use (for service users and healthcare professionals), including training requirements, cleaning of the device between uses and time to obtain ECG
-
Study design: RCTs, CCTs and comparative or non-comparative observational studies
-
Research question 4: ‘What are the costs, from a UK NHS and PSS perspective, of using KardiaMobile 6L for the initial assessment (triage) of QT interval-based cardiac risk in service users taking antipsychotic medications that are associated with QT prolongation?’
-
Population: Any UK population
-
Setting: Any
-
Index test: KardiaMobile 6L
-
Comparator: 12-lead ECG or no comparator
-
Reference standard: Not applicable
-
Outcomes: Costs related to use of devices (including purchase costs, software subscriptions and consumable costs), costs related to doing the tests (including staff time for travel, and time for testing and interpretation), cost of training (including operating ECG devices and interpreting ECG outputs), cost of treatment (including treatment of any cardiac or psychiatric conditions), cost of missed appointments
-
Study design: RCTs, CCTs and comparative or non-comparative observational studies
-
Research question 5: ‘What existing, published cost-effectiveness studies are available about QT interval assessment for service users who require antipsychotic medication?’
-
Population: People starting or maintained on antipsychotic medications that are associated with QT prolongation, in whom an ECG assessment of QT-based cardiac risk is indicated
-
Setting: Any
-
Index test: Any ECG device
-
Comparator: Any other ECG device or no comparator
-
Reference standard: Not applicable
-
Outcomes: Quality-adjusted life-years
-
Study design: Studies reporting a full economic analysis
Table 9 summarises studies which were screened for inclusion based on full-text publication, but which failed to fulfil all inclusion criteria, for any research question.
| Study details | Research question | Study design | Population | Index test | Comparator | Reference standard | Outcome |
|---|---|---|---|---|---|---|---|
| Abellas Sequeiros 202124 | 1 | N | Y | Y | NA | N | N |
| 2 | Y | N | Y | NA | NA | N | |
| 3 | Y | N | Y | NA | NA | N | |
| 4 | Y | N | Y | NA | NA | N | |
| 5 | N | N | Y | NA | NA | N | |
| Collins 202125 | 1 | N | Review article abstract only, no data or references | ||||
| 2 | N | ||||||
| 3 | N | ||||||
| 4 | N | ||||||
| 5 | N | ||||||
| Giudicessi 202127 | 1 | N | Transcript of a podcast, no data | ||||
| 2 | N | ||||||
| 3 | N | ||||||
| 4 | N | ||||||
| 5 | N | ||||||
| Hoehns 202028 | 1 | N | Y | N | NA | N | N |
| 2 | Y | N | N | NA | NA | Y | |
| 3 | Y | N | N | NA | NA | Y | |
| 4 | Y | N | N | NA | NA | N | |
| 5 | N | N | N | NA | NA | N | |
| Hoehns 202129 | 1 | N | Y | N | NA | N | N |
| 2 | Y | N | N | NA | NA | Y | |
| 3 | Y | N | N | NA | NA | Y | |
| 4 | Y | N | N | NA | NA | N | |
| 5 | N | N | N | NA | NA | N | |
| Karacan 201930 | 1 | Y | Y | N | NA | Y | Y |
| 2 | Y | N | N | Y | NA | N | |
| 3 | Y | N | N | Y | NA | N | |
| 4 | Y | N | N | Y | NA | N | |
| 5 | N | N | N | NA | NA | N | |
| Ko 202132 | 1 | N | Y | N | NA | N | N |
| 2 | Y | N | N | NA | NA | Y | |
| 3 | Y | N | N | NA | NA | N | |
| 4 | Y | N | N | NA | NA | N | |
| 5 | N | N | N | NA | NA | N | |
| Koltowski 202133 | 1 | Y | Y | N | NA | Y | Y |
| 2 | Y | N | N | Y | NA | N | |
| 3 | Y | N | N | Y | NA | N | |
| 4 | Y | N | N | Y | NA | N | |
| 5 | N | N | N | NA | NA | N | |
| Liu 202235 | 1 | N | Y | Y | NA | N | N |
| 2 | Y | N | Y | N | NA | N | |
| 3 | Y | N | Y | N | NA | N | |
| 4 | Y | N | Y | N | NA | N | |
| 5 | N | N | Y | N | NA | N | |
| Mercer 202036 | 1 | Y | Y | N | NA | Y | Y |
| 2 | Y | N | N | Y | NA | N | |
| 3 | Y | N | N | Y | NA | N | |
| 4 | Y | Y | N | Y | NA | N | |
| 5 | N | N | N | NA | NA | N | |
| Noseworthy 202138 | 1 | Y | Y | Y | NA | Y | Y |
| 2 | Y | N | Y | Y | NA | N | |
| 3 | Y | N | Y | Y | NA | N | |
| 4 | Y | N | Y | Y | NA | N | |
| 5 | N | N | Y | NA | NA | N | |
| Rotella 201644 | 1 | N | Y | N | NA | Y | N |
| 2 | N | N | N | Y | NA | N | |
| 3 | N | N | N | Y | NA | N | |
| 4 | N | N | N | Y | NA | N | |
| 5 | N | N | N | NA | NA | N | |
| Singh 202045 | 1 | N | Review article | ||||
| 2 | N | ||||||
| 3 | N | ||||||
| 4 | N | ||||||
| 5 | N | ||||||
| Stavrakis 201746 | 1 | Y | Y | Y | NA | Y | N |
| 2 | Y | N | Y | Y | NA | N | |
| 3 | Y | N | Y | Y | NA | N | |
| 4 | Y | N | Y | Y | NA | N | |
| 5 | N | N | Y | NA | NA | N | |
| Stavrakis 201747 | 1 | Y | Y | Y | NA | Y | N |
| 2 | Y | N | Y | Y | NA | N | |
| 3 | Y | N | Y | Y | NA | N | |
| 4 | Y | N | Y | Y | NA | N | |
| 5 | N | N | Y | NA | NA | N | |
| Stavrakis 202248 | 1 | Y | Y | N | NA | Y | Y |
| 2 | Y | N | N | N | NA | N | |
| 3 | Y | N | N | N | NA | N | |
| 4 | Y | N | N | N | NA | N | |
| 5 | N | N | N | NA | NA | N | |
| Titus-Lay 201949 | 1 | Y | Y | N | NA | Y | Y |
| 2 | Y | N | N | Y | NA | N | |
| 3 | Y | N | N | Y | NA | N | |
| 4 | Y | N | N | Y | NA | N | |
| 5 | N | N | N | NA | NA | N | |
| Titus-Lay 201950 | 1 | Y | Y | N | NA | Y | Y |
| 2 | Y | N | N | Y | NA | N | |
| 3 | Y | N | N | Y | NA | N | |
| 4 | Y | N | N | Y | NA | N | |
| 5 | N | N | N | NA | NA | N | |
Appendix 4 Potentially relevant ongoing studies
-
Medical University of Lodz 2022 (NCT05206825) Evaluation of Electrocardiography Performed With Mobile ECG Devices in Cardiac Patients and Healthy Volunteers69 – status, ‘not yet recruiting’
-
University of Oklahoma 2021 (NCT05053243) Clinical Validation of the AliveCor Kardia 12L and 6L Devices70 – status, ‘active not recruiting’
-
Leeds Teaching Hospitals NHS Trust and Leeds & York Partnership NHS Foundation Trust 2021 (NCT04227418) An Evaluation of the Safety and Clinical Utility of Handheld ECG Technology in Psychiatry71 – status, up-date provided by a SCM (MT), ‘recruitment affected by COVID, unlikely to be completed’
-
Leeds Teaching Hospitals NHS Trust 2020 (NCT04468477) EVALECGcardio Study72 – status, up-date provided by a SCM (MT), ‘This has been published and has been included in one of your references. The paper is Azram et al.’14
-
Leeds Teaching Hospitals NHS Trust 2022 (NCT05324111) VaLidation of the Simple Adaptation of the Kardia 6L ECG Recorder to Obtain Chest leAd equivaLents: a Multi-centre International (LOCAL-ECG) Study; on Behalf of the Africa Heart Rhythm Association Investigators73 – status, up-date provided by a SCM (MT), ‘Recruitment has just started and will take some time so unlikely to report on time for this’
Appendix 5 Copies of staff surveys used in the CNTW pilot study
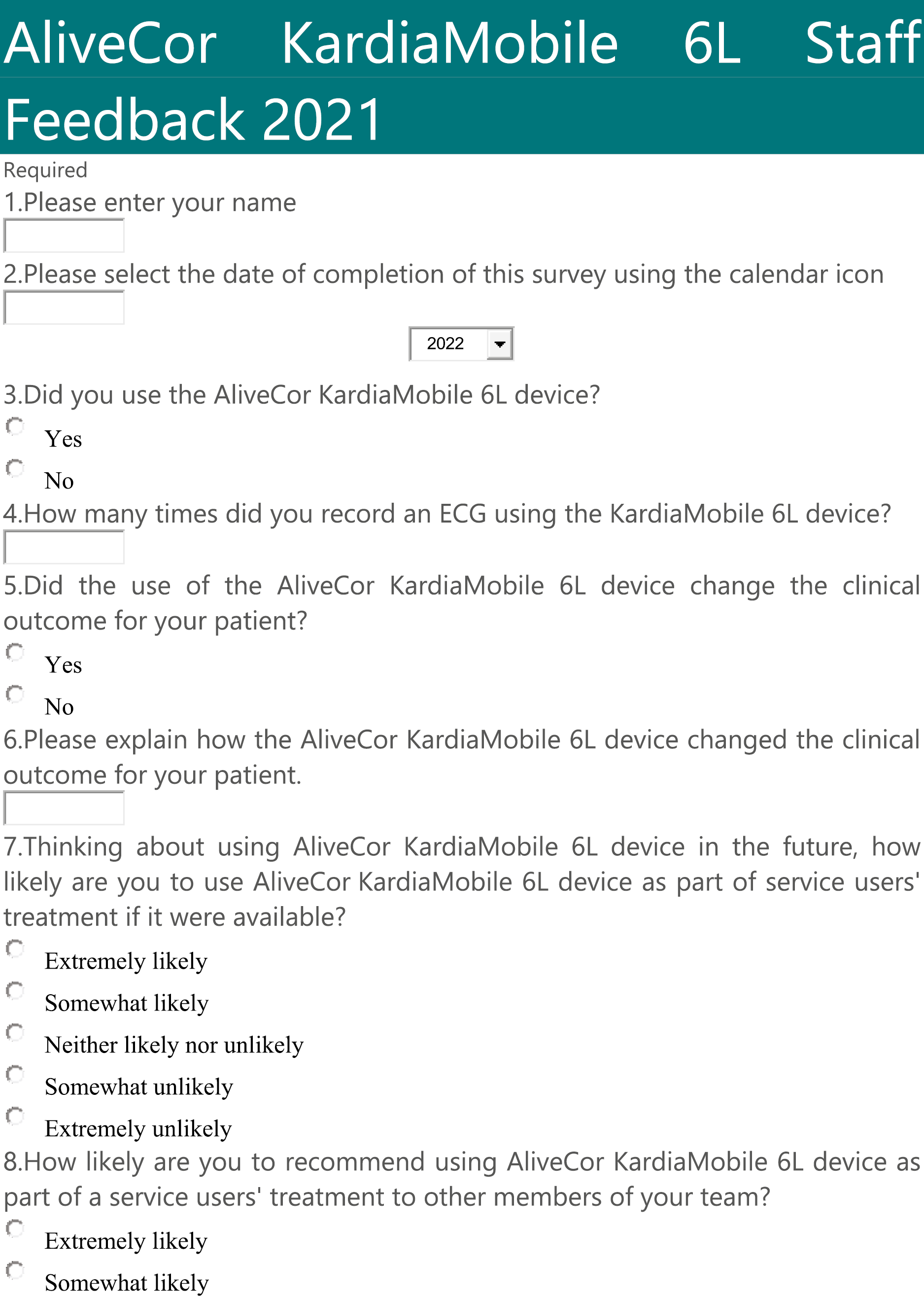
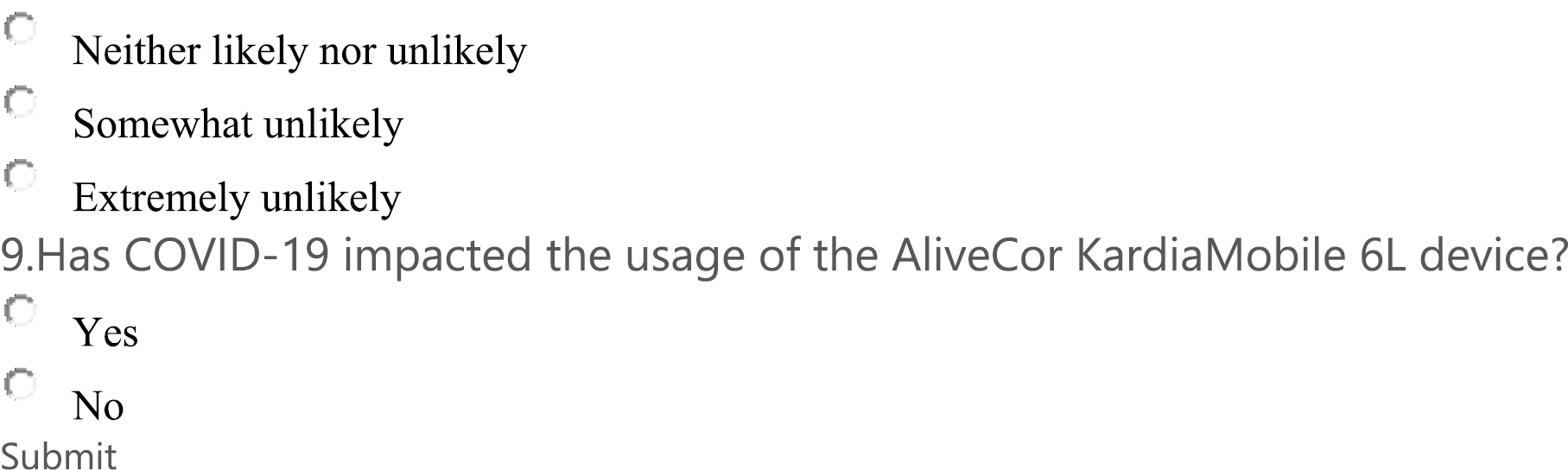




List of abbreviations
- 6L
- six-lead
- AHSN
- Academic Health Science Network
- CCT
- controlled clinical trial
- CDSR
- Cochrane Database of Systematic Reviews
- CENTRAL
- Cochrane Central Register of Controlled Trials
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CNTW
- Cumbria, Northumberland, Tyne and Wear
- COVID-19
- coronavirus disease 2019
- CRD
- Centre for Reviews and Dissemination
- DARE
- Database of Abstracts of Reviews of Effects
- DOAJ
- Directory of Open Access Journals
- ECG
- electrocardiogram
- EED
- Economic Evaluation Database
- EVA
- early value assessment
- HRQoL
- health-related quality of life
- HTA
- Health Technology Assessment
- ICD
- International Classification of Diseases
- ICTRP
- International Clinical Trials Registry Platform
- INAHTA
- International Network of Agencies for Health Technology Assessment
- KSR
- Kleijnen Systematic Reviews Ltd
- LILACS
- Latin American and Caribbean Health Sciences Literature
- NENC
- North East and North Cumbria
- NICE
- National Institute for Health and Care Excellence
- NIH
- National Institutes of Health
- NIHR
- National Institute for Health and Care Research
- portable document format
- PROSPERO
- International Prospective Register of Systematic Reviews
- PSS
- Personal Social Services
- QTc
- corrected QT interval
- RCT
- randomised controlled trial
- RePEc
- Research Papers in Economics
- SCMs
- Specialist Committee Members
- TEWV
- Tees Esk and Wear Valleys
- WHO
- World Health Organization
Notes
This monograph is based on the Diagnostic Assessment Report produced for NICE. The full report contained a considerable number of data that were deemed confidential. The full report was used by the Diagnostic Advisory Committee at NICE in their deliberations. The full report with each piece of confidential data removed and replaced by the statement ‘confidential information (or data) removed’ is available on the NICE website: www.nice.org.uk.
The present monograph presents as full a version of the report as is possible while retaining readability, but some sections, sentences, tables and figures have been removed. Readers should bear in mind that the discussion, conclusions and implications for practice and research are based on all the data considered in the original full NICE report.
