Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 15/106/04. The contractual start date was in January 2017. The draft report began editorial review in June 2021 and was accepted for publication in March 2022. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
Copyright © 2022 Randell et al. This work was produced by Randell et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 Randell et al.
Chapter 1 Introduction
Prevalence and impact of autism
The prevalence of autism in UK primary school-aged children is approximately 1–2%1 and the effects of autism are well documented, including increased incidence of mental health disorders, most commonly anxiety. Approximately 40–90% of children with a diagnosis of autism spectrum disorder (ASD) also meet the criteria for at least one anxiety disorder. 2,3 The impacts on family life are significant. Parents report higher levels of stress4 and loss of earnings,5 and the lifetime cost to the UK economy of supporting an autistic individual is estimated at £0.92–1.5M. 5 Relationship difficulties, particularly at school, are also commonly reported. Children with autism are significantly more likely than neurotypical peers to experience bullying6 and tend to have fewer friendships. 7
Prevalence and impact of sensory processing difficulties in autism
Difficulty in processing sensory information and, in particular, extreme sensitivity or insensitivity to sensory input from the environment is common in autism,8 with prevalence estimates of 90–95%. 9–11 Such difficulties may exacerbate social communication deficits and increase the frequency of restrictive and repetitive behaviour, and may occur because of impaired regulation of central nervous system arousal. 12 Hyper-reactivity, reflecting the autonomic nervous system ‘fight or flight’ response, may result in behaviours such as aggression, hypervigilance or withdrawal (owing to poor tolerance of noise, touch, smell or movement), or additional ‘safe space’ needs. Hyporeactivity, in contrast, is characterised by reduced awareness of sensory stimuli within the environment. 13 Impaired sensory processing may also result in poor motor control, affecting participation in daily life.
Sensory modulation difficulties (i.e. difficulty recognising and/or integrating sensory information) in children with autism probably pose substantial burden to children and families, limiting participation in leisure activities,14,15 and are linked to problems with activities of daily living, such as eating, sleeping, dressing, toileting and personal hygiene. 16 Such difficulties represent a long-term challenge for health services in terms of treating potential consequences, such as behaviours that challenge and mental health disorders. Awareness and management of sensory difficulties in mainstream educational settings is also likely to affect peer relationships and educational outcomes. The potential pathway of effect is unconfirmed [i.e. the mechanism(s) by which sensory difficulties affect key outcomes], but it is plausible that reducing sensory processing difficulties (SPDs) could lead to improvements across behavioural, social and educational domains.
Therapeutic approaches to treating sensory difficulties
The National Institute for Health and Care Excellence (NICE) guidelines on the management and support of children and young people with autism17 highlight parental perceptions of unmet need for occupational therapy (OT) input to address sensory and functional difficulties as part of the wider supportive network spanning education, health and social care. However, despite this clear unmet need, there is insufficient evidence to recommend any single therapeutic approach for SPDs. The NICE Guideline Development Group recommended further research to establish whether or not sensory integration therapy (SIT) improves SPDs in children and young people with autism across a range of contexts.
The primary goal of OT intervention is to enable participation in activities of everyday life18 by supporting people to engage in the occupations they need, want or are expected to do,19 considering their engagement and performance within relevant environments. 20 OT intervention for children with autism and SPDs is set within this context. There is a range of approaches used to achieve occupational goals, some of which focus on addressing underlying impairment (i.e. a ‘bottom-up’ approach21) and others on adapting the activity or environment for the individual to achieve these goals (i.e. a ‘top-down’ approach22). Both approaches aim to improve occupational engagement, participation and performance, with the distinction that ‘bottom-up’ approaches address underlying SPDs to improve activities of daily living, whereas ‘top-down’ approaches focus on environmental support to accommodate sensory difficulties. These ‘top-down’ approaches include the use of sensory strategies that are not intended to address underlying neurological factors but focus, instead, on adapting the task or environment to accommodate the individual’s sensory needs, or on more targeted support (e.g. helping the child to use self-regulation to manage their sensory needs). ‘Bottom-up’ treatment approaches include Ayres Sensory Integration® (ASI) therapy, which is a play-based intervention providing sensory–motor engagement in meaningful activities while adhering to fidelity principles,23 and sensory-based interventions, which are adult-directed application of sensory input to effect change in behaviour linked to sensory modulation difficulties. These interventions are intended to influence how the child integrates sensory information to facilitate the development of adaptive responses in everyday life.
Sensory-based interventions are usually adult-directed sensory stimulation strategies applied to the child (i.e. without their active engagement) or made available to the child for regulation of their reactivity within the home or school environment. Sensory-based interventions typically focus on a single or narrow range of sensory modalities or techniques (e.g. use of weighted blankets, pressure vests, brushing and sitting on a ball). Adaptations to family routines and the environment may be suggested. Although some studies report positive effects of this approach, for example by coaching children and families to adapt routines and activities,24 effectiveness evidence for functional performance is limited, particularly if strategies are not individualised to the child. 13 However, sensory-based interventions, as well as sensory strategies and environmental adaptations, are currently reported by many professionals and carers as the most common form of ‘usual care’ in a UK setting. Treatment that meets the fidelity requirements for SIT (in terms of content and dose) is not often reported within the UK context, although evidence suggests that parents’/carers’ preference is for this more intensive type of intervention (see Chapter 2).
Sensory-based interventions
Case-Smith et al. 13 systematically reviewed evidence (from 2000 to 2012) of sensory-based interventions and SIT for children with autism and SPDs. Nineteen studies were included in the review, including 14 studies of sensory-based interventions. Sensory-based interventions were defined as those that were based on individual assessment of the child’s sensory needs and functional performance, included explicit self-regulation goals and associated behavioural outcomes, and required the child to actively participate. Few positive effects were reported for studies evaluating sensory-based interventions. 13 Thirteen of 14 studies eligible for review were multiple baseline single-case evaluations of weighted vests, therapy balls and different types of vestibular stimulation (e.g. swinging and bouncing). One study25 found a positive effect for weighted vests on attention. There was limited evidence to support the use of therapy balls to increase sitting behaviours. 26,27 A further study28 demonstrated a positive effect of a sensory diet (e.g. brushing, swinging and jumping) on self-regulation behaviours. Only one study29 was a randomised controlled trial (RCT) (n = 30) of a ‘sensory diet’ protocol (i.e. exposure to a variety of different sensory experiences and practice of specific activities), which found positive effects in terms of a reduction in sensory difficulties overall, but did not assess fidelity or blind outcome assessors. The intervention also included several behavioural techniques (e.g. modelling, prompting and cueing) and, therefore, it is not possible to isolate the effects of sensory-based approaches. 13 In summary, evidence to support the use of sensory-based interventions is limited in scope, methodology and generalisability.
Sensory integration therapy
Sensory integration therapy is a clinic-based approach that focuses on the therapist–child relationship and uses play-based sensory motor activities to address sensory–motor factors specific to the child to improve their ability to process and integrate sensation. 30 To distinguish SIT from other sensory-based interventions, a set of fidelity principles to guide delivery was developed and registered as ASI. 31,32 A fidelity measure has also been developed for use in research. 23 These principles ensure that underlying sensory–motor difficulties affecting activities of daily living are addressed through presenting a range of sensory opportunities and active engagement of the child in sensory–motor play at the ‘just-right’ level of challenge, within the context of a collaborative therapist–child relationship. Studies meeting ASI fidelity principles have been shown to lead to improvement in client-oriented goals,33,34 but research is limited and, in some cases, interventions are poorly defined. 13 Case-Smith et al. 13 identified five studies specifically examining SIT, of which only two33,34 were RCTs. SIT was described in these studies as ‘ . . . clinic-based interventions that use sensory-rich, child-directed activities to improve a child’s adaptive responses to sensory experiences’. 13
Both RCTs33,34 included in the review13 demonstrated positive effects of SIT on the Goal Attainment Scale (GAS). There were, however, methodological issues with both trials, including small sample sizes [i.e. no formal sample size calculation and use of convenience samples (n = 3733 and n = 3234)], lack of long-term follow-up33,34 and limited description of usual care. 34 There are also well-documented methodological problems (with validity and reliability) related to the use of GAS as an outcome measure in clinical trials,35,36 particularly in paediatric contexts. 37 However, more recent research indicates that GAS may be a promising approach to measuring effectiveness of psychosocial interventions in autism and some recommendations for optimising reliability, including the use of a standardised approach to writing GAS goals, have been made. 38 Nonetheless, uncertainty remains about the use of GAS as an objective outcome measure in the context of a clinical trial, despite the appeal of an individualised approach to measurement of what could be considered an individualised form of therapy.
The three remaining studies assessing the efficacy of SIT reported positive effects on behavioural outcomes linked to sensory difficulties, although it is difficult to draw meaningful conclusions given the use of non-randomised designs, very small sample sizes and insufficient descriptions of outcome measures. 13 More recent systematic reviews39,40 did not identify any additional RCTs, but reported positive effects on several functional, developmental40,41 and play outcomes39,42 in two small non-randomised pilot studies (n = 842 and n = 2041) in which SIT was delivered with adequate fidelity.
Current evidence gaps and research priorities
The current evidence base to support use of SIT for children with autism is of low quality and insufficient to recommend treatment. 17 Significant methodological issues are evident from studies conducted to date, including poorly described interventions that are unlikely to meet fidelity standards. Even in randomised studies with good fidelity of intervention delivery, of which several systematic reviews13,39,40 have identified only two (i.e. Pfeiffer et al. 33 and Schaaf et al. 34), intervention protocols were variable in terms of dose and delivery period (e.g. 18 45-minute sessions delivered over 6 weeks in the Pfeiffer et al. 33 RCT and 30 sessions delivered three times per week for 10 weeks in the Schaaf et al. 34 RCT). Conclusions from all studies to date are limited by small convenience samples, poorly described comparators or definitions of what constitutes ‘usual care’ and a lack of long-term follow-up. The latter may be particularly important, given the focus of SIT on attention and learning rather than repetition of specific behaviours. Post-intervention treatment effects may be less specific, and we do not yet know whether or not SIT demonstrates sustained effects. 13
There is also uncertainty around appropriate intervention targets and associated outcome measurement, given the focus of previous trials on goal attainment as the primary outcome of interest and associated psychometric challenges. Furthermore, aside from considerable variation in the intervention protocols, SIT is resource intensive and would require significant investment to be rolled out as a potential treatment option within the NHS. It is critical, therefore, to evaluate both the clinical effectiveness and the cost-effectiveness of SIT for children with autism and SPDs across a range of key outcomes, and to determine whether or not any effects are sustained in the longer term.
The SenITA trial
The main aims of the SenITA (SENsory Integration Therapy for sensory processing difficulties in children with Autism spectrum disorder) trial (see Chapter 3 for methods) were to (1) describe usual care in trial regions and clearly differentiate this from the proposed intervention (see Chapter 2); and (2) evaluate the clinical effectiveness of manualised ASI therapy (see Chapter 5) in a two-arm RCT for SPDs in young children with autism. The intervention was evaluated in terms of the impact on behavioural problems and adaptive skills, socialisation, carer stress and quality of life (see Chapter 6), and in terms of cost-effectiveness (see Chapter 7).
Participants with a range of autism and sensory symptom severity, as well as functional and cognitive ability, were recruited from NHS, educational and third-sector settings. The primary outcome time point was 6 months post randomisation, and was reassessed at 12 months to determine whether or not any observed effects were maintained in the longer term. An internal pilot (see Chapter 4) examined whether or not the intervention differed significantly in content or intensity from usual care and assessed recruitment and retention. Contamination, adherence and fidelity of intervention delivery were measured as part of the process evaluation (see Chapter 8). Experiences of the intervention and usual care were also explored via semistructured interviews with carers and therapists (see Chapter 9).
Chapter 2 Usual care for children with autism and sensory processing difficulties
Aim
Prior to delivering SIT to trial participants, it was important to describe the scope of usual care for children with autism and SPDs (as per the commissioning brief). This would ensure that the therapy offered to the intervention group was clearly different from any treatment offered to the usual-care group. We aimed to explore the role of OT in the management and support of primary school-aged children (i.e. children aged 4–11 years) with autism and associated SPDs living in the UK. We wanted to know how carers and children with autism and SPDs accessed OT services, the nature of any assessments and whether or not specific interventions and/or support were received along the clinical pathway. In addition, we wanted to establish the most common behaviour or occupational performance issues and the profile of associated interventions used for children with autism and SPDs.
Methods
Recruitment and sampling
We were interested in the views of carers and the approaches used by occupational therapists. We chose a mixed-methods approach. Both carers and occupational therapists completed online questionnaires and, to build a more detailed picture of OT support provided, we also carried out qualitative focus groups and subsequent telephone interviews with occupational therapists.
Carer participants
An online questionnaire was distributed to carers of children with autism and SPDs aged 4–11 years and in mainstream education. The questionnaire was made available via the National Autistic Society (NAS) website, local NAS groups, social media [Facebook (Meta Platforms, Inc., Menlo Park, CA, USA; www.facebook.com) and Twitter (Twitter, Inc., San Francisco, CA, USA; www.twitter.com)], flyers at public events and through the Royal College of Occupational Therapists specialist section on children, young people and their families.
Occupational therapist participants
Online questionnaires
An online questionnaire was distributed to occupational therapists working with, or who had previously worked with, children with autism and SPDs aged 4–11 years and in mainstream education. The questionnaire was first distributed via the Welsh children’s OT network, the occupational advisory forum in Wales and the head of the children’s OT service in Cornwall. Occupational therapists from only the original trial recruitment areas (i.e. Wales and Cornwall) were asked to complete the questionnaire in this first phase and information was also collected on willingness to participate in focus groups/interviews. The questionnaire was then more widely distributed across the UK through the Royal College of Occupational Therapists.
Qualitative data collection
Occupational therapists were sampled from those who had participated in the first phase of the online survey from South Wales and Cornwall, working in the NHS and local authorities. Two focus groups and six telephone interviews were conducted with occupational therapists currently working, or having previously worked, with children with autism and SPDs aged 4–11 years and in mainstream education. Focus groups were conducted in Wales (group 1 had two participants and group 2 had three participants). Six occupational therapists in Wales and Cornwall were unable to take part in the focus groups and, therefore, were interviewed via telephone. Recruitment took place in February 2017, with the aim of carrying out focus groups before trial recruitment began.
Data collection
Online questionnaire to carers and occupational therapists
Online questionnaire data were collected using the Bristol Online Survey. Participants were presented with the purpose of the questionnaire and a data protection statement. Participants who agreed with the statements continued with the remainder of the questionnaire and participants who did not consent were automatically routed to a thank you screen. Both questionnaires consisted of a mixture of multiple choice and free-text questions. It was optional for participants to provide personal information to enable the research team to contact them directly. Respondents were asked about the nature and severity of common difficulties for children with autism. The carer questionnaire was separated into six different sections of (1) location (i.e. where the carer lived and where their child receive care), (2) child behaviours (carers were asked about 12 aspects of their child’s behaviour and how problematic each of these was for their child), (3) therapy (carers were asked whether or not their child had received therapy in the last 6 months that addressed any behaviours listed in the previous questions), (4) information received (carers were asked whether or not any teams/organisations identified in the previous section provided advice or materials), (5) intervention received (carers were asked whether their child had ever received or was currently receiving support from an occupational therapist and the extent of this) and (6) further information (carers were asked whether or not they would be interested in being contacted to take part in an interview or a focus group).
Data were merged following completion of all questionnaire phases. Questions to occupational therapists were split into two broad sections: (1) their role in the work setting and (2) their specific experience with this population. Occupational therapists were asked about their qualifications and years of experience; how many children with autism they saw; the type of assessments they completed and the type and extent of therapy delivered, including theoretical underpinnings for therapy to address SPDs; the type of occupational performance issues they associated with SPDs; the type of support and advice they offered children with autism and their families; and whether or not they would be interested in being contacted to take part in an interview or a focus group.
Focus groups, interview procedure and topic guide
Focus groups and interviews were carried out in English and audio-recorded. Verbal informed consent was obtained. Interviews were semistructured and consisted of five broad topic sections, beginning with an ‘ice breaker’ that allowed participants to introduce themselves, describe where they worked and describe the type of service provided. This ‘ice breaker’ was then followed by questions on usual practice regarding assessment of SPDs in a child with autism; advice and support given to children and carers of children with autism; background training in SPDs; and opinion of SIT. The interview topic guide was initially based on the questionnaire topics, but with further prompts and allowing for flexibility guided by participant responses. The guide was further adapted after the first focus group to shape ongoing data collection. The same topic guide was adapted for telephone interviews. Focus groups were conducted face to face, facilitated by an independent qualitative researcher with an additional note-taker/co-facilitator present. All telephone interviews were carried out following the focus groups by a second qualitative researcher, after having listened to audio-recordings of focus groups for familiarisation of the topic. All focus groups and interviews were transcribed verbatim for analysis and anonymised.
Ethics approval and data management
All activities adhered to the Research Governance Framework for Health and Social Care. Ethics approval was granted by a Health Research Authority Research Ethics Committee. All respondents consented to participate in questionnaires, interviews or focus groups.
Analyses
Online questionnaires
Descriptive analyses were used in the form of frequency tables for the quantitative data, and included summaries of the geographical area of respondents, nature of reported difficulties and contact with services, and information on OT assessment and treatment received. Free-text comments within questionnaires provided context and additional explanation for some responses. Examples have been included to give meaning and carers’ lived experience of services received. Free-text comments within questionnaires completed by occupational therapists were incorporated into the thematic analysis of focus group and interview data.
Focus groups and interviews
Transcripts were analysed using thematic analysis. This involved data familiarisation, generating initial themes, and searching, reviewing and defining themes. 43 The first two steps were carried out as a team by two experienced qualitative researchers and two members of the research team who were experienced occupational therapists. The final analyses were undertaken by the lead qualitative researcher.
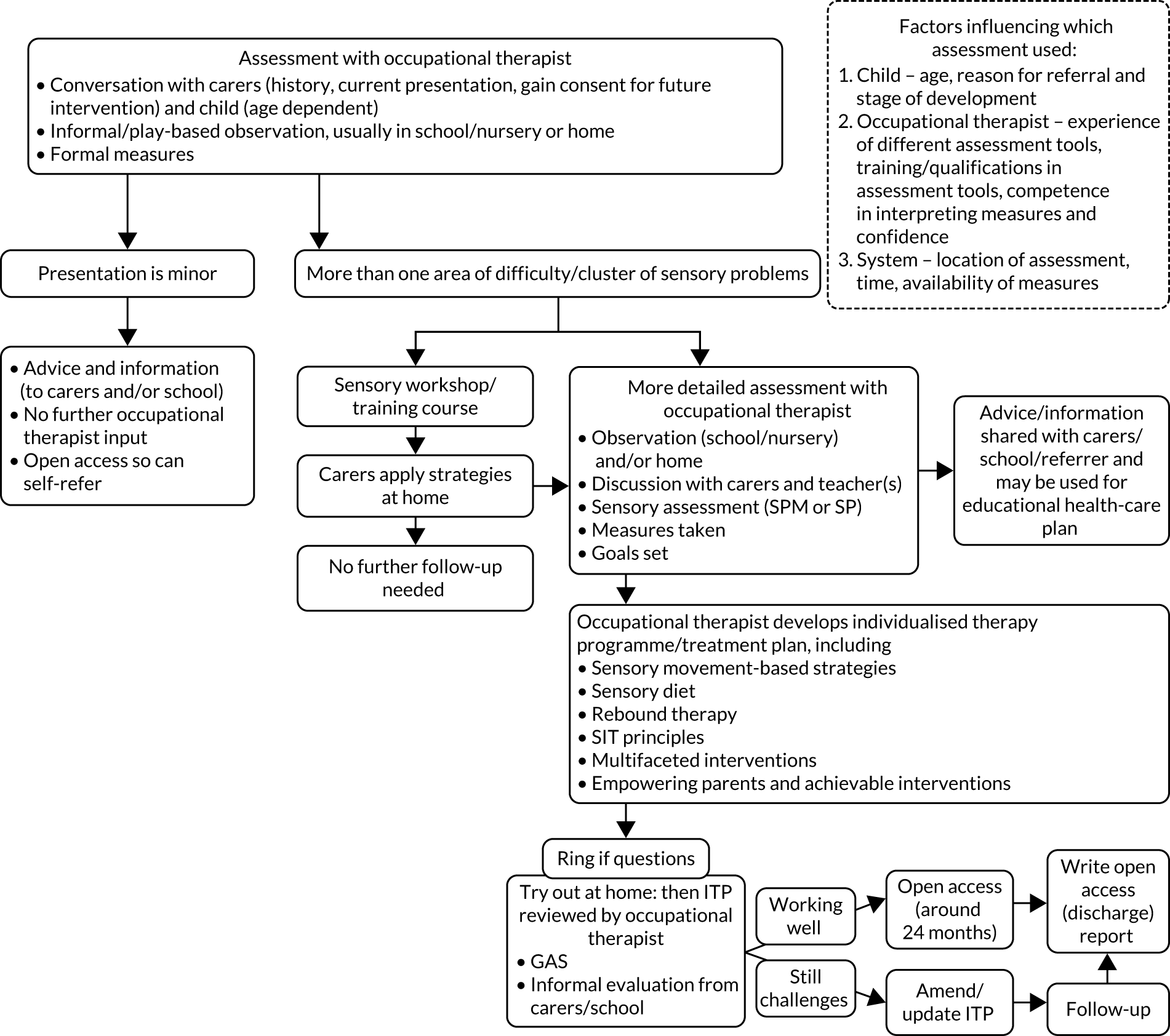
We carried out a thematic analysis using deductive methods to identify themes reflecting reality as reported across the whole data set. We initially coded data within six overarching themes (i.e. referral, initial assessment, initial management, further assessment, treatment plan/intervention, feedback and future plans) relating to the different phases of OT support for children with autism and SPDs. In addition, we used an inductive thematic approach to identify occupational therapists’ views, experiences and challenges relating to these processes, moving towards a more contextualist approach and ensuring that subthemes, which had not been pre-empted and initiated from occupational therapists themselves, were identified. These subthemes were factors influencing decisions around which assessment occupational therapists used (at child, OT and system level), factors influencing the location of assessment, the multifaceted nature of interventions, empowering others, and making interventions achievable for parents and schools. This analysis was then integrated with the results of the questionnaires. While interpreting the qualitative data we produced a visual map of the different phases of management of children with autism and SPDs (Figure 1). We developed this map this in a phased way, starting with one account in an interview and building on this with each new transcript, revising and incorporating as we progressed. In this way, data were constantly compared and contrasted. Developments in the analytic process were recorded through researcher memos and version control of the visual maps. The first transcript was discussed in detail and themes developed by a group of qualitative researchers and occupational therapists. Themes were then applied to the next transcript and discussed again. The research team were encouraged to reflect on their own professional role in asking and interpreting interview questions.
FIGURE 1.
Routes of support described by occupational therapists. ITP, individualised therapy programme/treatment plan; SP, sensory processing; SPM, Sensory Processing Measure.
Results
Carers’ views of usual occupational therapy for children with autism and sensory processing difficulties
A total of 159 carers responded to the questionnaire. Most (n = 149, 93.7%) carers were mothers. We received six (3.8%) responses from fathers, two from grandmothers (1.3%), one from a kinship carer (0.6%) and one from an educational visitor (0.6%). The spread of respondents across geographical regions is shown in Table 1. Thirty-two (20.1%) respondents were from Wales, 115 (72.3%) were from England, 11 (6.9%) were from Scotland and one (0.6%) was listed as ‘other’ (location not specified).
| Geographic area by country | n (%) | University health board/region | n (%) |
|---|---|---|---|
| Wales | 32 (20.1) | Aneurin Bevan University Health Board | 7 (4.4) |
| Cardiff and Vale University Health Board | 15 (9.4) | ||
| Cwm Taf University Health Board | 4 (2.5) | ||
| Hywel Dda | 4 (2.5) | ||
| Swansea Bay University Health Board | 1 (0.6) | ||
| Wales other | 1 (0.6) | ||
| England | 115 (72.3) | Buckinghamshire | 1 (0.6) |
| Cornwall | 11 (26.4) | ||
| Dorset | 2 (1.3) | ||
| England other | 101 (63.5) | ||
| Scotland | 11 (6.9) | Scotland | 11 (6.9) |
| Other | 1 (0.6) | Other | 1 (0.6) |
Nature of reported difficulties
The most frequently reported difficulties were difficulties with relationships and communication (84.3%) and difficulty making friends/joining in/playing with others (83.6%), followed by refusal to carry out daily activities (73.6%) and outbursts without any obvious reason (73.6%). A total of 77.3% carers reported at least moderate difficulty with sensory hyper-reactivity and 49.6% of participants reported at least moderate hyporeactivity. Being overactive and having repetitive behaviour that interrupts activity were reported by 64.8% of carers. Other difficulties encountered included sleeping difficulties (59%), poor co-ordination (56%), poor performance in school (54.1%) and feeding difficulties (39.6%). Less common difficulties included anxiety (n = 8, 5%), hyperacusis (n = 2, 1%), hypermobility (n = 2, 1%), poor concentration (n = 2, 1) and violent behaviour (n = 2, 1%).
Carers’ views on contact with services
A total of 119 (74.8%) carers reported some contact with services [e.g. children’s centres (health service) and local authorities (social care services)] in relation to difficulties in the last 6 months. Professionals seen within these organisations included occupational therapists (NHS and private), speech and language therapists, paediatricians, psychologists (clinical and educational), dieticians and specialist teachers. However, 40 (25.2%) carers reported that they had received no therapy/support in relation to their child’s difficulties in the same period. Further detail regarding contact with services is given in Table 2.
| Service | Contact, n (%) |
|---|---|
| Children’s centre (health service provision) |
|
| Special school |
|
| Local authority (social care provision) |
|
| CAMHS |
|
| Specialist autism team |
|
Ninety (56.5%) carers received information and advice on how to manage their child’s difficulties, such as anxiety, behavioural and sensory difficulties. Although 68 (42.8%) carers received specific advice on sensory information from services, a further 46 (28.9%) carers would have liked more information on these aspects of their child’s difficulties. Where advice and information on sensory issues had been given, this was most commonly by OT services. However, sometimes other NHS and third-sector organisations provided similar information. Information was typically in leaflet form and included information on sensory processing, exercises/programmes to do at home, social stories and contact information/websites for parent courses.
Carers’ views on occupational therapy assessments and treatment
Seventy (44.0%) carers had not received any input from OT services. Those who had received input (n = 89, 56.0%) generally received input in the form of assessment and observation plus advice. Assessment was most frequently through a carer questionnaire and observation of play. A few carers reported more formal testing of co-ordination skills. If direct intervention was offered, then this was typically for a limited block of therapy (e.g. four to eight sessions). Of the carers (89/159) who had received input from OT services, 64 (40.3%) were not currently in contact with an occupational therapist. Of the 44 carers who had seen an occupational therapist in the last 6 months, 10 had received more than five sessions in that period. In terms of length of overall contact with OT services, the majority of carers were discharged within a 6-month period (n = 76, 85%).
Of those carers who had ever received OT input, 15 (16.8%) reported that they had received weekly input and most visits were clinic based (n = 57, 35.8%), with intervention varying from sensory based (not SIT), parent-directed programmes, functional skills training, sensory diets and behavioural programmes. Most carers (n = 58, 36.5%) stated that the intervention that they received focused on sensory modulation. Fewer carers (n = 22, 13.8%) received intervention for both sensory modulation and dyspraxia, and an even smaller number of carers (n = 9, 5.7%) received intervention for dyspraxia alone. Forty-three (27.0%) carers reported that the intervention focused on other aspects, such as anger management, behavioural difficulties, speech and sleep. Carers were asked further details about specific interventions that their child received in terms of whether or not they felt that the therapy helped their child, how satisfied they were with the intervention received and whether or not they would recommend any changes to intervention delivery.
Sensory integration therapy
Five (3.1%) carers had accessed OT privately and had received, or were in receipt of, SIT at least once per week. All five carers felt that SIT had helped their child and reported high satisfaction with the intervention. However, all five carers also felt that longer-term therapy (i.e. more than six sessions) would be beneficial and/or that it should be available on the NHS.
Other interventions received
The intervention most often received by carers was adaptation to the home or school environment (n = 115, 72.3%), and 88 (76.5%) carers thought that adaptations helped their child and 83 (77%) carers were satisfied with the adaptations. Other interventions included sensory diets (n = 54, 34%), behavioural interventions (n = 42, 26.4%), parent-directed programmes (n = 45, 28.3%), functional skills training (n = 25, 15.7%) and sensory-based interventions (n = 24, 15.1%). Fewer carers (n = 16, 10.1%) received advice on desensitisation strategies. Generally, more respondents were satisfied with sensory diets (n = 40, 77%), desensitisation strategies (n = 12, 75%) and parent-directed programmes (n = 28, 65%) than behavioural interventions (n = 19, 51%). When asked whether or not interventions helped their child, carers felt that desensitisation strategies (n = 12, 75%), sensory-based intervention (n = 16, 66.7%) and functional skills training (n = 16, 64%) definitely helped their child. Carers were less certain about sensory diets (n = 28, 51.9%), parent-directed programmes (n = 20, 44.4%) and behavioural intervention (n = 15, 35.7%). When asked whether or not there was any aspect of the interventions/advice received that they would wish to change, carers commonly said that they would have liked additional input and direct support for their child, rather than just advice. Some carers noted that they would have liked more access to OT and speech and language therapy (SLT) support through the NHS. Several carers specifically requested training and support into schools to manage sensory difficulties (n = 11), as they felt that the school was not able to carry out the sensory support required. Some carers would have liked more specific advice for their child, including follow-up and monitoring visits, rather than generic information that was not personalised:
I would love for this intervention to be available as more than a one-off appointment with me as a parent. I would love to be able to access sensory support/therapy for my children on a regular basis.
Carer 66
Specific advice from a qualified OT [occupational therapist] specialising in sensory difficulties not just a parent googling what to try – trial and error as totally without support from NHS.
Carer 9
Make it available to everyone via the NHS. NHS input was limited and generalised, we had excellent input from a private OT [occupational therapist].
Carer 155
NAS website and research online; family and friends particularly those with children who have autism; colleagues at work.
Carer 145
Detailed responses of the interventions received by families are provided in Table 3.
| Strategy/intervention | Intervention received, n (%) |
|---|---|
| SIT at least once per week |
|
| Sensory-based interventions |
|
| Desensitisation strategies |
|
| Parent-directed programmes |
|
| Sensory diets |
|
| Behavioural intervention |
|
| Environmental adaptation |
|
| Functional skills training |
|
Finally, when asked what types of intervention would be the most useful, the most common carer responses were additional support for social communication (n = 16), desensitisation and other sensory issues (n = 15), support for managing behaviour, including aggression, anger and anxiety (n = 14), and specific SIT (n = 12). A significant number of carers reported having to source support via independently accessed behaviour training (n = 81, 50.9%) and regular contact with support groups (n = 87, 54.7%), and 81 respondents (50.9%) received informal support from family and friends:
Sensory integration therapy for social and behaviour skills.
Carer 5
More help with socialising with his peers so that he does not become socially isolated.
Carer 25
Help with controlling/managing violent outbursts.
Carer 47
Intervention specifically aimed at sensory issues in school.
Carer 68
Someone to work with my child teaching them about their sensory differences and how to manage them whilst exploring what works/doesn’t and teaching them coping techniques at their own pace.
Carer 77
Occupational therapist views of usual care
Questionnaire responses by occupational therapists
The questionnaire was completed by 79 occupational therapists. In phase 1, 38 questionnaires were completed by occupational therapists working in trial recruitment areas (i.e. Wales and Cornwall). In phase 2, 41 questionnaires were completed, including by occupational therapists in England and Scotland. Occupational therapists were generally very experienced: 53 (67.1%) occupational therapists reported having at least 10 years’ post-qualification experience and only 10 (12.7%) reported having < 5 years’ post-qualification experience. Eighteen (22.8%) occupational therapists reported postgraduate qualifications, with 11 (13.9%) specifically in sensory integration. Almost all (n = 77, 97.5%) occupational therapists reported seeing one or more children with autism and SPDs in the last 6 months, with 15 occupational therapists (15.2%) seeing more than 10 children each. However, only 11 (13.9%) occupational therapists were based within a specialist autism service. The settings in which children were seen included children’s centres, special and mainstream schools, local authority settings, Child and Adolescent Mental Health Services (CAMHS) and the child’s home. Most occupational therapists saw children referred for one to five contacts/sessions (n = 39, 49.4%), with only three (3.8%) occupational therapists seeing children for between 10 and 20 contacts/sessions. The frequency of contact was very varied, with the most common frequencies being weekly (27.8%), monthly (19%) or twice per month (17.7%). Most occupational therapists maintained contact with families for 3 months (n = 26, 32.9%) or 6 months (n = 20, 25.3%) prior to discharge.
Focus groups and interviews with occupational therapists
Two focus groups and six semistructured telephone interviews were conducted following the online survey, representing the views of 11 occupational therapists working in South Wales, Mid-Wales and Cornwall. Respondents described themselves as occupational therapists, paediatric occupational therapists and occupational therapist senior practitioners, and had experience of working in autism assessment units, core services, in the community, within the NHS, in social services and in the local authority. This section integrates occupational therapists’ views on usual care gathered from questionnaires, focus groups and interviews. Illustrative quotes are provided.
Nature of reported difficulties and referral
Survey responses indicated that the most common problems seen by occupational therapists included poor performance in school (n = 61, 77.2%), poor co-ordination and motor planning (n = 57, 72.2%), and refusal to carry out typical daily activities, sleep and outbursts without understandable reason (n = 56, 70.9%). Sixty-seven (84.8%) respondents felt that sensory hyper-reactivity hindered children’s engagement in activities, with 50 (63.3%) respondents reporting that hyporeactivity could be a factor hindering engagement. In focus groups/interviews, occupational therapists reported that referral may be via health professionals [e.g. general practitioners (GPs), paediatricians and professionals in SLT and mental health services], other services (e.g. integrated services for children with additional needs, education services and social services) or via carer self-referral. Referral criteria varied slightly, but required a child to demonstrate functional difficulties and SPDs, rather than behavioural and emotional problems alone, and did not necessarily require a diagnosis. One occupational therapist stated that they did not have clear written criteria setting out what they would and would not accept. Occupational therapists described that a triage meeting would take place at which occupational therapists and colleagues determined the appropriateness of a referral. Occupational therapists describe using clinical reasoning and professional experience to consider the information:
So it’s difficult to say whether people meet criteria because our criteria is still, it’s not always clear; it’s a little bit woolly but I think that’s quite historically common for OT that the criteria for a service for OT is generally quite woolly because we do cover such a wide remit.
Interviewee 4
Yes, there are a few of us here that are trained in using SIPT [Sensory Integration and Praxis Test], so sometimes we will do that for the children that are more highly functioning ASD, and that’s quite good because it gives us a really good profile on what their skills are, and their things to work on.
Interviewee 5
Theoretical framework underpinning decision-making
Most OT survey respondents reported that clinical reasoning within the referral, assessment and intervention process involved using OT theory as a guide (n = 76, 96.2%), with 55 (69.6%) respondents supporting this with sensory integration theory (27 respondents specifically referred to ASI). Other approaches included neurodevelopmental (n = 47, 59.5%), applied behavioural analysis (n = 29, 36.7%) and social approach (n = 8, 10.1%).
Assessment process
Most OT survey respondents reported using informal or structured clinical observations within the home, school or clinic setting (n = 68, 86%). In the focus groups/interviews, occupational therapists also talked about the value of observing informal activity. One occupational therapist compared informal and formal clinical observations and the different ways of thinking required for occupational therapists to process information. Occupational therapists also talked about sensory play as a way to practically demonstrate the challenges that the child and carer(s) face.
Occupational therapists reported that this observation was carried out alongside interviews/questionnaires and a developmental history with carers (n = 45, 57%), teachers (n = 22, 27.9%) and the child (n = 12, 15.1%). In addition, 33 (41%) survey respondents reported using a specific OT assessment of functional daily life skills. Forty-five (57%) respondents reported using a specific measure to assess SPDs [e.g. Sensory Profile 224 and the Sensory Processing Measure™ (SPM)44]. Fewer (n = 15, 19%) survey respondents reported using measures to assess motor difficulties (e.g. Movement Assessment Battery for Children-2 and Bruininks–Oseretsky Test of Motor Proficiency-245).
Occupational therapists also mentioned other measures [e.g. the Peabody Developmental Motor Scales,46 clinical observations assessment,47 the Canadian Occupational Performance Measure48 (COPM), Movement Assessment Battery for Children,49 The Roll Evaluation of Activities of Life Occupational Therapy assessment,50 Beery Visual Motor Integration51 and Kate Malcomess’ Care Aims Framework52]. Occupational therapists in the diagnostic assessment team and one other core service reported that they might use the Autism Diagnostic Observation Schedule (ADOS)53 or specific SLT assessments. Some occupational therapists used the Sensory Integration and Praxis Test54 (SIPT) in case studies if they had undertaken training in sensory integration (but did not then use this therapy in usual care), whereas others said that they did not have access to SIPT equipment. Only one occupational therapist said that they used the SIPT routinely.
In focus groups/interviews, occupational therapists reported that they talk with carers and schools/nurseries to set goals. Older children will discuss goals too. Occupational therapists described instruments used to support goal-setting [e.g. the Perceived Efficacy in Goal Setting Approach,55,56 Child Occupation Self-Assessment,57 SMART (Specific, Measurable, Achievable, Relevant, Time bound) goals58 and Kate Malcomess’ Care Aims Framework52]. However, one occupational therapist explained that they do not always have to use formal assessment/goals if sufficient information is gained through observation or is offered by the carer or child.
In focus groups/interviews, occupational therapists talked of assessment as an ongoing process. In deciding which assessment to use, occupational therapists considered different factors relating to three areas, that is, the (1) child, (2) occupational therapist and (3) wider system. At the level of the child, assessment choice depended on their age, stage of development, concentration level and reason for referral. At the occupational therapist level, assessment depended on their experience, training/qualifications in different tools, competence in interpreting measures, and personal confidence and preference. Finally, at the system level, assessment depended on location, time available, waiting list pressures, availability of measures and the focus for that service. The location of assessment also depended on several factors. Occupational therapists reported that location of observation was selected to limit distress to the child while determining the problem with greatest impact. The age of the child may also influence the setting for observation.
Again, reason for referral was also considered. Some occupational therapists said that they would see the child in their usual environment where difficulties presented and/or in another environment with carers (e.g. school/nursery). One occupational therapist also explained that the child would usually come to the children’s centre, as there was equipment there that could be tried out. If the child was to receive the intervention, then they would often be seen on several occasions in different locations. The location of assessment was also influenced by the ability of the carer to visit the clinic owing to, for example, socioeconomic status or learning difficulties:
Well I think in the battery of assessments that you have, and the observations that you can do it very much depends on the child because a lot of the children with autism they would get freaked out with maybe doing standardised assessments and you can’t, you have to do it by observation and play then. You’re very much guided when you meet the child on the day really . . .
Participant 1, focus group 1
. . . so we use a sensory profile, but it’s again down to the individual therapist, it’s not something that we necessarily do for everyone every time. We use just clinical observations and observing them in their home environment and their school environment, so that’s our main, I would say that’s our main first contact is just clinical obs [observations] and chatting to the parents and seeing how they are and then we may decide to use a sensory profile if we need to get a clearer picture.
Interviewee 4
If the child is going to be put in distress through coming to a new environment and a strange environment, and would be distressed in that setting, then you’re not going to get the best thing from that child, so that would influence my clinical decision of where I carried that out.
Interviewee 3
Advice and interventions
Frequency strategies described by OT survey respondents are detailed in Tables 4 and 5.
| Therapist advice to carers | n (%) |
|---|---|
| Information on the senses | 66 (83.5) |
| Introducing new/adapted sensations | 32 (40.5) |
| Sensory diet | 48 (60.8) |
| Advice to improve response | 41 (51.9) |
| Physical environment | 69 (87.3) |
| Social environment | 51 (64.6) |
| Other | 16 (20.3) |
| Intervention for children/families | n (%) |
|---|---|
| Sensory based | 42 (53.2) |
| Desensitisation | 32 (40.5) |
| Parent directed | 38 (48.1) |
| Education | 56 (70.9) |
| Sensory diets | 58 (73.4) |
| Behavioural | 29 (36.7) |
| Adaptations (physical and social) | 62 (78.5) |
| SIT | 5 (6.3) |
We then used interview and focus group data to understand the different phases of OT support and interventions for children (see Figure 1).
Presentation assessed as minor after initial assessment with occupational therapist
In focus groups/interviews, occupational therapists reported that if presentation was ‘minor’ then the carer/child would receive advice and information, but no further input. The carer/child may be provided with website addresses, handouts and signposting to other services. In addition, the carer/child would usually have the option to self-refer later if needed.
Sensory carer groups
Occupational therapists reported (in focus groups/interviews) that for more than one area of difficulty and/or a cluster of sensory problems, carers may be invited to attend a parent group (e.g. a one-off workshop or course of around three sessions). These sessions often consisted of an interactive element involving peer support (e.g. where carers shared difficulties and solutions) and professional support (e.g. providing theory and professional advice). A group with multiple sessions allows carers time to identify triggers/concerns, discuss and try out strategies, and then return to evaluate effectiveness of these strategies. Occupational therapists suggested that these groups give carers a foundation knowledge about sensory processing and help them to understand their child’s individual needs.
Sensory movement-based strategies, sensory diet and rebound therapy
Survey respondents reported that the most common intervention offered was advice on adaptation to the environment to accommodate sensory needs (n = 62, 78.5%) and activities for a sensory diet (n = 58, 73.4%).
Occupational therapists reported (in focus groups/interviews) that, based on observation, assessment and goal-setting, they would develop an individualised therapy programme/treatment plan with carers and the school/nursery. This would often involve multiple sessions (around four to six). A wide range of strategies might be drawn on and a plan provided for an individual child to try at home or at school/nursery. These strategies might include sensory movement-based strategies (e.g. vestibular and proprioceptive activities, such as heavy muscle work, yoga-type movement, peanut roll, scooter board, lycra blanket, soft play and sensory-weighted equipment) and may also include deep touch pressure, massage and brushing for alerting and desensitising, calming strategies and mindfulness, and swimming. Some equipment might be used for assessment/observations and treatment, for example therapy rooms with a smartboard, Wii Fit (Nintendo Co., Ltd, Kyoto, Japan), weighted blankets, supportive chairs or trampolines (interview 1). Another occupational therapist (interviewee 3) mentioned that they had a loan system for sensory items (e.g. weighted products, dance mats, vibrating items, seating and lap pad). Carers might have delivered strategies themselves or a technician/occupational therapist would offer a demonstration. One occupational therapist reported that they also offered groups that families can link into, such as bike skills groups, gymnastics and social skills groups.
Occupational therapists might also advise group interventions (e.g. The Alert Programme and Sequential Oral Sensory approach) or multidisciplinary team working/referral to other services [e.g. a portage worker, a specialist health visitor, a neurodevelopmental team, NAS, Barnardos (London, UK), primary mental health, a specialist autism service in the school, Autism Puzzles (Cardiff, UK) and a disability sports officer]. Occupational therapists also spoke of linking and contributing to transdisciplinary groups, including Next Steps, Early Bird, Early Bird Plus and Cygnets.
Sensory integration therapy
Five (6.3%) survey respondents reported delivering SIT. However, most (n = 55, 69.6%) respondents reported using sensory integration theory to inform practice and 19 (24.1%) respondents had undertaken postgraduate sensory integration training equivalent to ≥ 50 hours (i.e. the minimum requirement for trial therapists). Most interventions used were targeted at sensory modulation and/or dyspraxia (n = 44, 55.7%). Similarly, most occupational therapists reported that they either were not able to use ASI therapy in its pure form because of time or space, or did not use it at all. Occupational therapists who had received training in SIT said that they try to consider its principles, but expressed frustration that they could not carry it out. Only one occupational therapist reported using SIT ‘as much as possible’ for specific children, including using swings and climbing frames, wobble cushions, scooter boards and scooter board ramps, weighted balls and a range of wet and dry tactile exploration items (e.g. texture mats, textured balls, textured quoits, vibration balls, vibrating snakes and cushions), as well as trampettes that could be used at home:
We have a very positive response to it. And the number of parents that say oh if only we had known this. So yeah, it’s a very positive way of meeting a lot of people’s needs. And it also saves the therapist’s time, because otherwise what we feel is that those parents that then seek further intervention, they have a baseline of knowledge. And we all know what that level of knowledge is, so that we can start working at that higher level rather than having to cover the same groundwork individually with each child.
Interviewee 2
We don’t provide it, we don’t have any funding to provide that type of sensory equipment, but we do have access to them to be able to trial them for a 2-week period. After the trial we then make a decision whether we suggest that for the parents or the schools, or nursery or wherever that child is, to purchase that piece of equipment. But we don’t have funding to provide that.
Interviewee 3
In the house, and in the centre, we use a lot of suspended type equipment, so we’ve got things like T-bars, we have platform swings, and we have bolster swings. We have climbing frames, tyre swings, all that type of stuff.
Interviewee 5
Multifaceted interventions
Occupational therapists tended to describe the interventions that they offered as varied and multifaceted. Some occupational therapists highlighted the non-standardised nature of developing and delivering interventions. However, occupational therapists described using an evidence base, their clinical experience and the needs of the individual child to guide intervention/strategies.
Empowering parents and achievable interventions
Many occupational therapists (in focus groups/interviews) felt that an important part of intervention delivery was the carer’s motivation to engage with the intervention, as well as their ability and confidence to deliver the intervention. An important part of the occupational therapist’s role was empowering carers to continue the intervention. Occupational therapists reported that barriers to carers implementing strategies included the carer’s understanding of their child, other family commitments and child engagement. Occupational therapists reported that the effectiveness of interventions was also dependent on teachers’ ability to deliver the intervention. Therefore, occupational therapists stressed the need to make the intervention achievable and manageable at home and/or school:
In isolation it means nothing. You can carry out 30-odd sessions, but once that intervention finished it’s finished, unless the parent and the child . . . For me, the powerful bit is carrying that over into the child’s everyday life so it continues.
Participant 2, focus group 2
So I think for me it feels like it’s empowering others to do this work and then to understand what it is to provide it every day for the child feels more normal than going to a clinic setting all the time. Less medical. Nobody wants to be going somewhere . . . Children have got lives to live themselves and fun to have.
Participant 2, focus group 2
Evaluating the intervention plan, reports and open access
Occupational therapists (in focus groups/interviews) reported that after strategies had been tried at home and/or at school/nursery for several weeks the plan was reviewed, often using the GAS,35 an evaluation questionnaire and/or informal evaluation from carers or the school.
Discussion
Representativeness of views
The views reflected within our data were collated from survey responses from occupational therapists and carers in Wales, England and Scotland, and from interviews/focus groups conducted with occupational therapists in South Wales and Cornwall. The purpose was to determine how carers and children with autism and SPDs access OT services, the assessment process and what interventions and/or support are commonly provided. Determining the nature of usual care within trial areas and the wider UK context would ensure that our comparator was sufficiently different from SIT delivered in the intervention arm of the trial.
Theoretical approaches to intervention
Survey responses indicated that occupational therapists utilised OT theory to guide assessment and intervention. This core philosophy values human participation in meaningful occupations59 and this is reflected in the criteria that occupational therapists use to choose whether or not to accept a referral for assessment. Within the broader scope of theoretical approaches, sensory integration theory was reported as the most common approach to help to understand and manage SPDs. This is consistent with findings from Kadar et al. ,60 who found that 72.7% of occupational therapists used a sensory integration frame of reference. Likewise, Brown et al. 61 reported that sensory integration and client-centred practice models were most commonly used in a survey of Canadian paediatric occupational therapists.
Accessing services and the referral process
Although services differ, there appeared to be a common trend across the regions surveyed. From both quantitative and qualitative data, it was clear that most children were seen for initial assessment only if they met specific referral criteria, particularly with regard to SPDs affecting daily functional activities. Many services would not accept a referral unless there were clear occupational performance difficulties in self-care, play or school-related activities. It is likely that this more focused approach has been driven by increasing waiting lists for access to OT,62 ensuring that only the most appropriate children received therapy. There have also been government drivers to ensure that children are seen within 14 weeks of referral (e.g. the NHS Wales Delivery Framework and Reporting Guidance 2019–202063). From the carers’ perspective, understanding of what OT services could offer their child was less clear cut. Carers wanted support for their child’s social interaction, help with dealing with aggressive outbursts/frustration, help with understanding autism and help with siblings. Fewer carers listed functional skills, such as toileting, feeding, dressing and sleeping, as behavioural issues seemed to have a greater impact on quality of life. Respondents were, therefore, frustrated because they felt that they could not always access the service that they perceived would help them and their child, and expressed disappointment that services were not always offered by the NHS.
Assessment process
Both occupational therapists and carers reported that initial assessment included observations, interviewing the caregiver, questionnaires and, sometimes, more formal assessments. Observations of the child’s behaviour and performance were typically within the clinic setting and, to a lesser extent, within the school or home environment. Standardised assessments were not used routinely. Although most therapists reported using a sensory integrative approach, only very few reported using the SIPT to formally identify the nature of the sensory integration difficulty.
Some settings used structured goal-setting with carers to establish the child’s needs. There has been a consistent drive in recent years to develop family-centred practice, with services working in partnership to address concerns and goals. 64 From this survey, it appears that some carer concerns were addressed and that most were satisfied with the advice given, but many would have liked more input. After initial assessment, most services generated a report with advice on strategies for managing SPDs in everyday life. For some parents, contact with services ended at this point or they were referred to a workshop/training group. For others, additional OT support was received with further discussion and advice, the offer of loan of suitable equipment to support their child’s needs or some sessions of one-to-one intervention.
Intervention
Therapists appeared to have a two-pronged approach: (1) giving strategies and advice to support carers to manage their child’s SPDs to improve self-regulation, and (2) attempting to address SPDs directly with the aim of remediation of the dysfunction and underlying nervous system. 65
Strategies and advice to manage sensory processing difficulties
Both occupational therapists and carers concurred that strategies and advice were most commonly provided. Occupational therapists used a range of strategies, from advice including environmental adaptations, sensory diets and desensitisation strategies, which may take the form of generic advice, to more personalised advice following individual sessions. According to carers, the sensory-based interventions, sensory diets and parent-directed programmes helped in over 65% of the children receiving them. However, carers still felt that this was not enough and wanted ongoing support. Carers also wanted better transfer of advice and strategies into the school setting, more personalised intervention and further follow-up as the child developed. In terms of transfer of knowledge and to run an efficient service, several therapy services offered parent/carer groups with general information about sensory processing. Although carers found this useful, they also wanted more specific application to their own child’s difficulties.
Direct intervention
Carers and some occupational therapists expressed frustration that direct hands-on therapy was not always possible because of resource constraints. Carers particularly felt that they were missing out on intervention and that they had to seek support privately. Respondents whose children had received SIT were extremely satisfied and all felt that it had helped their child. Very few therapists in the NHS reported using SIT meeting fidelity criteria,23 but some were using sensory-based interventions, applying theory and principles of sensory integration and delivered less intensively for shorter periods. These interventions included activities applied to the child to improve behaviour associated with modulation disorders,13 such as massage, brushing, wearing a weighted vest or sitting on a gym ball.
Summary
Sensory-based difficulties are commonly reported in this population, and there is a clearly expressed demand from carers for additional contact and support from OT services. Current provision of usual care and most services offered focus on delivering sensory strategies and advice. This may be in the form of generic written information that is web based or a bespoke leaflet, or through parent groups or one-to-one consultation with carers. Some direct therapy may be offered using a sensory integration approach, but this usually comprised fewer than 10 sessions. Intensive treatment offered by a therapist with SIT training is available within the private sector and so is inaccessible for many carers.
Chapter 3 Methods
Design
The SenITA trial was an individually randomised two-arm effectiveness trial that compared manualised SIT with usual care for children of primary school age with autism and SPDs. Randomisation was in a 1 : 1 ratio and was minimised by site, severity of SPDs (i.e. probable/definite) and sex of the child (i.e. male/female). The target was to recruit 138 children aged between 4 and 11 years in primary education. Children were recruited from a variety of sources, including CAMHS, OT services, paediatric clinics, support and/or social services and primary schools, and via self-referral. The intervention was delivered in OT clinics that were rated to ensure that they met full structural fidelity criteria for manualised SIT.
Children allocated to receive the intervention were provided with SIT in 26 1-hour sessions (Figure 2), that is face-to-face sessions twice per week for 10 weeks, tapering to twice per month for 2 months, and a telephone call once per month for 2 months. Where consent was provided, sessions were video-recorded, with a sample of recordings assessed for fidelity of delivery. 23 The comparator was usual care, which was defined as awaiting services or sensory-based intervention not meeting fidelity criteria for SIT (e.g. at least one face-to-face session per week).
FIGURE 2.
The SenITA trial participant flow diagram. APSI, Autism Parenting Stress Index; CarerQol, Carer Quality of Life; CSRI, Client Service Receipt Inventory; EQ-5D, EuroQol-5 Dimensions.
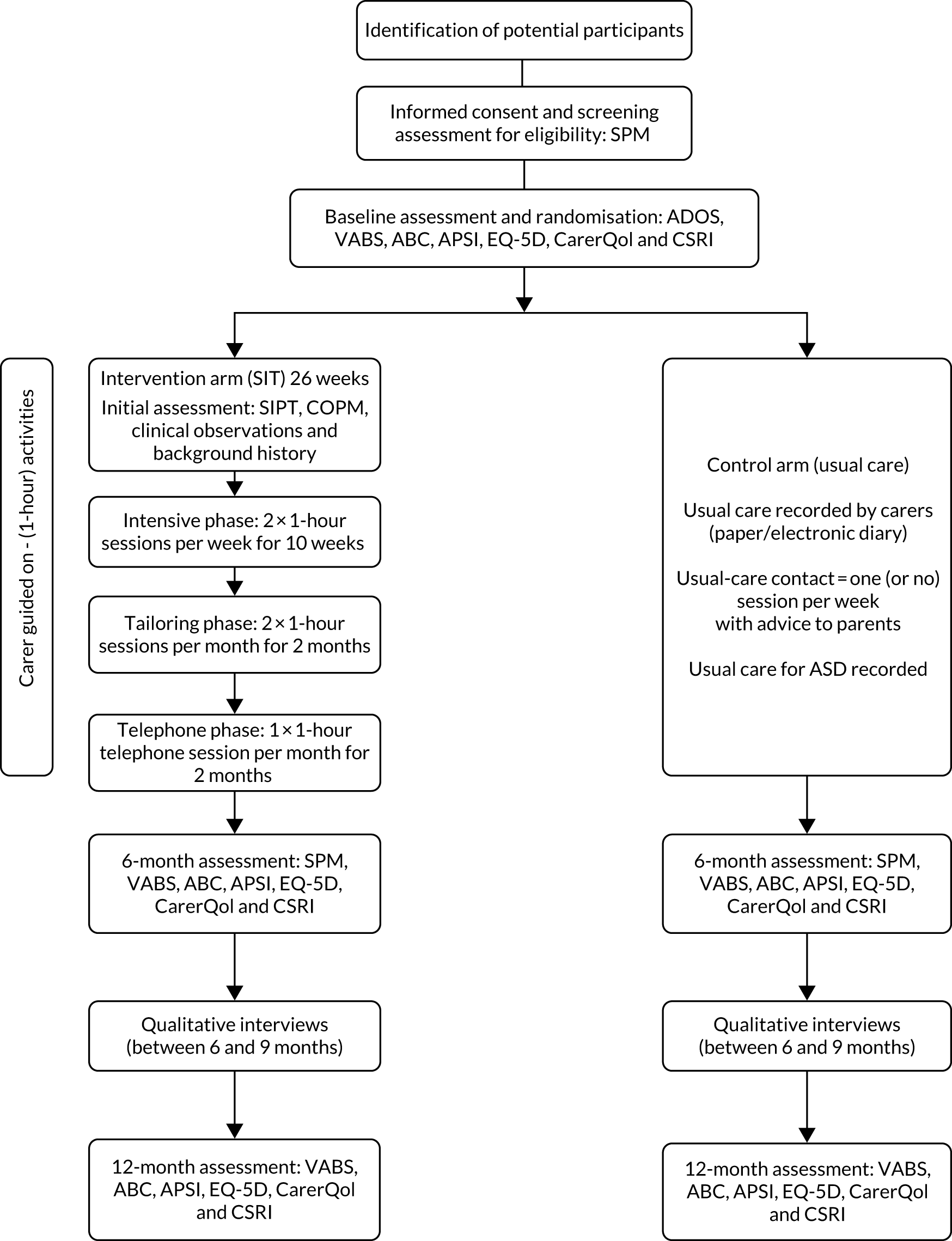
The trial also included an internal pilot (see Chapter 4) with progression criteria to assess recruitment and retention rates and whether or not usual care differed from expected provision.
Qualitative work included therapist and carer interviews to explore (1) the support experienced by families (outside the trial, i.e. usual care) and (2) the perceived impact and effectiveness of SIT for children with autism and SPDs. Interview and focus group data were double coded and analysed using a framework approach. 66 Ethics approval was granted by Wales Research Ethics Committee 3.
Objectives
The overarching objective was to answer the following research question: ‘what is the clinical effectiveness and cost-effectiveness of SIT for children with autism?’.
Primary objective
The primary objective was to determine the impact of SIT on irritability and agitation, as measured by the corresponding subscale of the Aberrant Behavior Checklist (ABC). 67
Secondary objectives
Secondary objectives were included to examine:
-
the effectiveness of SIT for additional behavioural difficulties (e.g. hyperactivity/non-compliance, lethargy/social withdrawal, stereotypic behaviour and inappropriate speech)
-
the impact of SIT on adaptive skills, functioning and socialisation
-
sensory processing scores post intervention (i.e. at 6 months) as a potential mediator of any association observed between SIT and the primary outcome at 12 months
-
age, severity of SPDs, adaptive behaviour, socialisation and comorbid conditions as potential moderators of any association between SIT and irritability/agitation, adaptive functioning (child) and carer stress
-
the impact of the intervention on carer stress and quality of life
-
cost-effectiveness (including direct intervention costs, costs of health, social care and education services, carer expenses and lost productivity costs)
-
fidelity, recruitment, acceptability, adherence, adverse effects and contamination in a process evaluation conducted alongside the main trial.
Site selection
Secondary care NHS and private OT treatment settings (where NHS capacity was insufficient to support the trial or no appropriate NHS treatment setting was available) across South Wales and South England were included as research sites. Sites evidenced that they met structural fidelity criteria for intervention delivery.
Participants
Inclusion criteria
Participants were eligible to take part if they:
-
had a diagnosis of autism (as documented on medical and/or educational records) or had probable or likely autism (defined as undergoing assessment within the local autism pathway)
-
were aged 4–11 years at the start of the trial
-
planned to remain in mainstream primary education until the primary outcome time point (i.e. 6 months post randomisation)
-
had definite or probable SPDs defined as (1) definite dysfunction on at least one sensory dimension (defined as all domains except social participation) and the total score on the SPM44 or (2) at least a probable dysfunction on two or more sensory dimensions and the total score
-
provided carer consent/child assent.
Exclusion criteria
Participants were excluded if they were:
-
currently undergoing or had previously undergone SIT
-
currently undergoing applied behaviour analysis therapy.
Recruitment process
Children were recruited from CAMHS, paediatrics, OT, schools and support or social services. Services sent carers of children referred into their service a letter informing them about the trial, as well as a participant information sheet (PIS) and details of how to express an interest in taking part. Details of the study were also posted on relevant websites (e.g. related charities’ websites) and via social media. A trial-specific website [URL: http://senitastudy.weebly.com (accessed 7 April 2022)] was also created as a place where individuals could get more information on the trial and could download information sheets. Carers were also able to self-refer into the study.
Informed consent
It was likely that potentially eligible children could have a range of impairments, including a degree of intellectual disability (ID). Provided that all inclusion criteria were met and exclusion criteria were not met, no child was excluded for this reason or for other comorbid conditions. In accordance with good clinical practice (GCP), written informed consent was taken from each child’s carer (i.e. their parent or legal guardian) and assent from children before any trial-related activities were undertaken. In signing the consent form, carers also consented to their participation in the trial (including completion of some outcome measures) and for the study team to contact the child’s school to ask for feedback on the child’s behaviour if necessary. Schools were also asked to complete the Aberrant Behavior Checklist – irritability (ABC-I) at the 6-month time point. Consent could be withdrawn by carers at any time. To complement the carers information sheet, age-appropriate information was presented to the child where appropriate and the views of children capable of expressing an opinion considered. Children deemed to have capacity and who were able to write were asked to sign an age-appropriate assent form.
Consent was sought from carers to video-record intervention sessions to assess fidelity of intervention delivery and for supervision feedback. Carers could also consent to video-recordings being used in future research or for training opportunities. In addition to intervention sessions, ADOS53 assessments were video-recorded to evaluate consistency among ADOS assessors. Refusal of consent to any video-recording did not affect the participants’ eligibility to otherwise take part in the trial. Carers received a copy of any consent form that they signed, with the original filed in the site file and a further copy held with participants’ clinical notes.
Once recruited to the trial, treating therapists remained free to give participants alternative treatment to that specified in the protocol if it was in the child’s best interest; however, the child would remain a participant in the trial for the purpose of follow-up and data analysis according to original treatment allocation. Further informed consent was taken from a small number of carers for participation in qualitative interviews. In compliance with Welsh-language requirements, the PIS, consent form and any other required participant documentation were available in Welsh. However, all outcome measures were available in English only, as none was validated in Welsh.
Risk assessment
A trial risk assessment was completed to assess:
-
known and potential risks and benefits to participants
-
the level of intervention risk compared with standard practice
-
how risks were to be minimised/managed.
The SenITA trial was categorised as low risk (i.e. no higher risk than standard medical care). This categorisation was used to inform the level and focus of monitoring activity undertaken during the trial.
Intervention
Sensory integration therapy
The intervention was delivered in regional clinics by OTs trained in SIT (typically NHS band 7) (see Chapter 5 for a description of the intervention). None of the therapists delivering the intervention delivered therapy to participants in the control arm. Fidelity of intervention delivery was assessed using the ASI intervention fidelity measure (see Chapter 8). 23
Comparator
To define usual care, scoping work in the form of a short survey, interviews and focus groups with therapists and carers was completed before the trial opened to recruitment (see Chapter 2). Carers also recorded usual care using a diary that was specifically designed for the trial. This could be completed either on paper or electronically. Usual care for autism was also recorded more generally, including any contact with NHS services (e.g. SLT, paediatrics and CAMHS). Therapists recorded usual care in accordance with local policy.
Outcomes
Screening and baseline measures
Screening measure
Sensory processing difficulties were assessed at screening using the SPM Home Form. 44 This version of the SPM provides eight standard scores: (1) social participation, (2) vision, (3) hearing, (4) touch, (5) body awareness (proprioception), (6) balance and motion (vestibular function), (7) planning and ideas (praxis), and (8) a total sensory symptoms score. Scores on each of these dimensions are classified as typical, some problems or definite dysfunction. To be eligible, participants’ SPD was defined as either (1) definite dysfunction on at least one sensory dimension (defined as all domains except social participation) and the total score or (2) at least probable dysfunction on two or more sensory dimensions and the total score. Participants scores on this measure were made available to treating SIT therapists to aid planning of intervention delivery.
Baseline-only measure
An ADOS assessment was completed at baseline to characterise the sample according to autism symptoms. Results of the ADOS were not shared with carers or therapists and it was not used as a diagnostic tool to determine eligibility. Members of the study team attended research reliability training for the ADOS and cascaded essential training to other members of the study team undertaking assessments. Reliability and consensus of administration and scoring was assessed as per the ADOS manual. A sample of video-recorded ADOS administrations were also used to facilitate assessment of reliability.
Primary outcome measure
The primary outcome was irritability/agitation at 6 months post randomisation, as measured by the corresponding ABC subscale (i.e. the community version ABC-I with 15 items67,68). The ABC-I was also measured at baseline and at 12 months post randomisation. The primary outcome comparison was based on carer ratings of ABC-I. However, teacher/teaching assistant ratings of ABC-I (assessed at 6 months post randomisation only for intervention and control arms) were also explored.
Secondary outcome measures
Problem behaviours
Other problem behaviours were measured at baseline and at 6 and 12 months using the remaining four ABC subscales: (1) lethargy/social withdrawal (16 items), (2) stereotypic behaviour (seven items), (3) hyperactivity/non-compliance (16 items) and (4) inappropriate speech (four items). Although moderate correlations between subscales are generally observed, researchers are advised not to use a total score, as construct validity is poor. 69 For all ABC subscales, items were rated on four-point Likert scales, ranging from 0 (not at all a problem) to 3 (the problem is severe in degree).
Adaptive behaviours, socialisation and functional change
Adaptive behaviours, socialisation and functional change were assessed at baseline and at 6 and 12 months using the parent/carer rating version of the Vineland Adaptive Behavior Scales, second edition (VABS II). 70 VABS II comprises four main domains: (1) communication (i.e. receptive, expressive and written), (2) daily living skills (i.e. personal, domestic and community), (3) socialisation (i.e. interpersonal relationships, play and leisure time, and coping skills) and (4) motor skills (i.e. gross and fine motor skills). Start points of each Vineland Adaptive Behavior Scales (VABS) subdomain vary depending on the child’s chronological age. Gross and fine motor skills are included in the composite score for younger children only (i.e. children aged 0–6 years).
Carer stress
Carer stress was assessed using the Autism Parenting Stress Index (APSI)71 at baseline and at 6 and 12 months. The APSI is a 13-item measure of parental stress, covering the social, physical and behavioural issues that characterise autism. Each item is scored according to five categories: (1) ‘not at all stressful’, (2) ‘sometimes creates stress’, (3) ‘often creates stress’, (4) ‘very stressful on a daily basis’ and (5) ‘so stressful that sometimes I/we feel we cannot cope’.
Quality of life
Carer quality of life was measured using two measures: (1) the EuroQol-5 Dimensions, five-level version (EQ-5D-5L),72 scale and (2) the Carer Quality of Life (CarerQol). 73 EuroQol-5 Dimensions (EQ-5D) is a health-related quality-of-life scale that is made up of five dimensions: (1) mobility, (2) self-care, (3) usual activities, (4) pain/discomfort and (5) anxiety/depression. The EQ-5D is assessed via single items with a five-category response option. These five dimensions are scored and combined into an index value using an algorithm. The EQ-5D is recommended for use in health technology assessments and includes a measure of general self-rated health on a vertical visual analogue scale with end points labelled ‘best imaginable health state’ and ‘worst imaginable health state’. The CarerQol instrument was used to measure and value the impact of providing informal care on carers. It combines a subjective burden measure that provides a comprehensive description of the caregiving situation using the Carer Quality of Life – 7 Dimensions (CarerQol-7D), with a valuation of informal care in terms of well-being [i.e. the Carer Quality of Life – visual analogue scale (CarerQol-VAS)]. 73 The CarerQol has been shown to be valid in populations of caregivers of children with autism. 74
Functional change
The COPM48 was used to measure functional change in the intervention arm only, as participants assigned to usual care were not routinely seen by services. High scores on the COPM indicate higher performance and satisfaction. If the average pre- and post-intervention difference was more than 2 points, this was regarded as clinically important.
Mediators
In addition to screening, SPM scores were assessed at 6 months to determine whether or not any effects of the intervention on the primary outcome at 12 months were mediated by severity of SPDs post intervention.
Cost-effectiveness outcomes
Staff and non-staff inputs directly associated with the intervention and usual care were recorded during the intervention period for each participant. Data were collected on services and support external to the intervention at baseline (covering the previous 6 months) and at 6 and 12 months post randomisation. The Client Service Receipt Inventory (CSRI)75 was adapted based on expert opinion for use in this study. It was used to collect service and support data for participants and data on health-care and social care services used by the child’s main carer, including out-of-pocket expenses incurred by the carer and time taken off work because of SPDs and autism difficulties experienced by the child they care for.
Randomisation
Using an online system, participants were randomly allocated to usual care or SIT in a 1 : 1 ratio. Randomisation utilised minimisation with a random component, which allocated participants to the group that caused the least imbalance. Minimisation included region (i.e. Wales or England), severity of SPD (i.e. SPM score) and sex of child.
Sample size
The initial aim was to recruit 216 participants in total (i.e. 108 participants allocated to usual care and 108 participants allocated to the intervention), which was based on 90% power at the 5% significance level to detect a standardised effect size of 0.5, allowing for 20% loss to follow-up.
The standardised effect size of 0.5 was arrived at by considering mean scores on the ABC-I found in the literature. Mean scores in control/untreated groups of between 12 and 24 were quoted, as well as standard deviations (SDs) of between 6 and 10. It is suggested that a 25% relative difference/effect size of between 0.4 and 1.0 represented a clinically meaningful difference on ABC subscales. We chose a conservative effect size of 0.5. The calculation was carried out using nQuery v3.0 (Statistical Solutions, Saugus, MA, USA).
However, following the internal pilot (see Chapter 4), an aim of which was to check assumptions used for the sample size calculation, a high correlation was found between baseline and 6-month ABC-I scores [0.86, 95% confidence interval (CI) 0.60 to 0.96]. Accounting for this result led to a revised sample size of 138 (usual care, n = 69; SIT intervention, n = 69) by applying a deflation factor. 76 This target assumed a correlation of 0.6, which was a conservative estimate to allow for the potential of a lower correlation at the end of the study, any therapist clustering and any reduction in retention as the study progressed. This target assumed that correlation was also consistent with previous RCTs77 in this field that used the ABC-I (which found correlations in ABC-I scores of 0.647 and 0.599 between baseline and 16 weeks post randomisation and between baseline and 10 months post randomisation, respectively).
Procedures
Trial oversight and patient and public involvement
The trial was conducted in accordance with Centre for Trials Research standard operating procedures. Oversight was provided by the Trial Management Group (including the investigators and directly employed trial staff), the Trial Steering Committee, the Data Monitoring and Ethics Committee and an advisory group of family carers. The advisory group, including the patient and public involvement co-investigator, provided feedback on study materials, recruitment and retention plans, and continue to advise on dissemination of results to stakeholders.
Staff training
Good clinical practice training was provided to staff carrying out trial-specific procedures (e.g. recruitment/consent, data collection and intervention delivery). Tailored training materials were created for all aspects of intervention delivery and data collection (see Intervention data collection). Principal investigators (PIs) and intervention therapists received an individualised session on delivering the intervention in accordance with the study protocol, following the detailed description in the intervention handbook (see Chapter 5). Therapists clearly marked participant consent on their clinical notes.
Sensory integration therapy sessions
Safeguarding procedures were in place for reporting or raising any concerns that arose during therapy sessions, and these procedures were detailed in the intervention handbook. It was the responsibility of each therapist to make participant’s session appointments. Future appointments were agreed at the child’s first assessment visit and recorded on an appointment card for carers to keep. The card held contact details for the therapist, including who was the first point of contact for carers and an emergency contact number. It was also the therapist’s responsibility to issue reminders of upcoming appointments and to reschedule appointments as necessary. If a participant could not attend a session as intended, up to two attempts could be made to reschedule within ± 3 days of the original appointment. If a session could not be rearranged to fit in that time frame, then it would be foregone.
For each session, therapists documented and video-recorded (where consent was given) the intervention delivered. Video-recordings were uploaded to password-protected secure OneDrive (Microsoft Corporation, Redmond, WA, USA) folders for fidelity analysis. Once uploaded, video-recordings were deleted from the recording device.
Assessment time points
Outcomes and follow-up time points (Table 6) were the same for both the intervention and the control group and were performed as close as possible to the required time point.
| Procedure | Visit | ||||
|---|---|---|---|---|---|
| Screening | Baseline | Treatment phase | Follow-up | ||
| 6 months | 12 months | ||||
| Informed consent | ✗ | ||||
| Demographics | ✗ | ||||
| Eligibility assessment: SPM | ✗ | ✗ | |||
| Randomisation | ✗ | ||||
| ABC | ✗ | ✗ | ✗ | ||
| ABC-I (teacher rated) | ✗ | ||||
| ADOS | ✗ | ||||
| APSI | ✗ | ✗ | ✗ | ||
| CarerQol | ✗ | ✗ | ✗ | ||
| CSRI | ✗ | ✗ | ✗ | ||
| Quality of life: EQ-5D | ✗ | ✗ | ✗ | ||
| VABS II | ✗ | ✗ | ✗ | ||
| COPM | ✗ (intervention group only) | ||||
| Delivery of intervention (including initial assessment) | ✗ | ||||
| Diary completion | ✗ | ||||
| SAEs | As necessary | ||||
| Withdrawals | As necessary | ||||
Data collection
A manual (Table 7) was created for research assistants carrying out any data collection. The document was created to ensure consistency of data collection from different research assistants and research network staff. Data were entered directly into the trial SQL (Structured Query Language) database via an online link, with the exception of the ADOS and VABS II, which were scored on paper first and then relevant total scores entered online.
| Section | Content |
|---|---|
| 1 | Introduction |
| 2 | Key aspects of study protocol:
|
| 3 | Informed consent |
| 4 | Study procedures:
|
| 5 | The SenITA data collection portal |
| 6 | Withdrawals |
| 7 | GCP |
| 8 | AE (safety) reporting |
| 9 | Monitoring and ethics |
| 10 | Key contacts |
The study team contacted carers to rearrange any missed follow-up data collection appointments as soon as possible. For those carers who were unable to attend appointments in person (or stay for the duration), there was the option to complete any remaining measures at home using a booklet that was to be returned to the study team. Those carers who were unable or unwilling to take the booklet home were given the option of answering key questions over the telephone. All individuals carrying out data collection (i.e. research assistants and clinical study officers from research networks) were appropriately qualified and completed relevant training. Clarification of any clinical questions relating to SIT that arose during appointments was deferred to the co-chief investigator.
Screening and baseline visit
There were two screening/baseline visits, which were split to reduce any burden on the child taking part. At the first meeting, the study team met with only the carer to discuss the study in detail and to take consent. Following consent, the carer completed the screening measure (i.e. the SPM) to confirm eligibility. If eligible, the carer was immediately asked to complete the baseline outcome measures (see Table 6). If not eligible, the carer was thanked for their interest and no further trial involvement took place. If the carer could not complete the baseline assessment immediately, then it was arranged for a convenient time.
The second meeting was held during the following week to complete an ADOS assessment (video-recorded where consent was given) with the child and to carry out randomisation. Carers in both arms were given access to a diary at this point to report health professional contacts and any home programmes or self-initiated activities for their child (Figure 3).
FIGURE 3.
Flow diagram of data collection procedures.
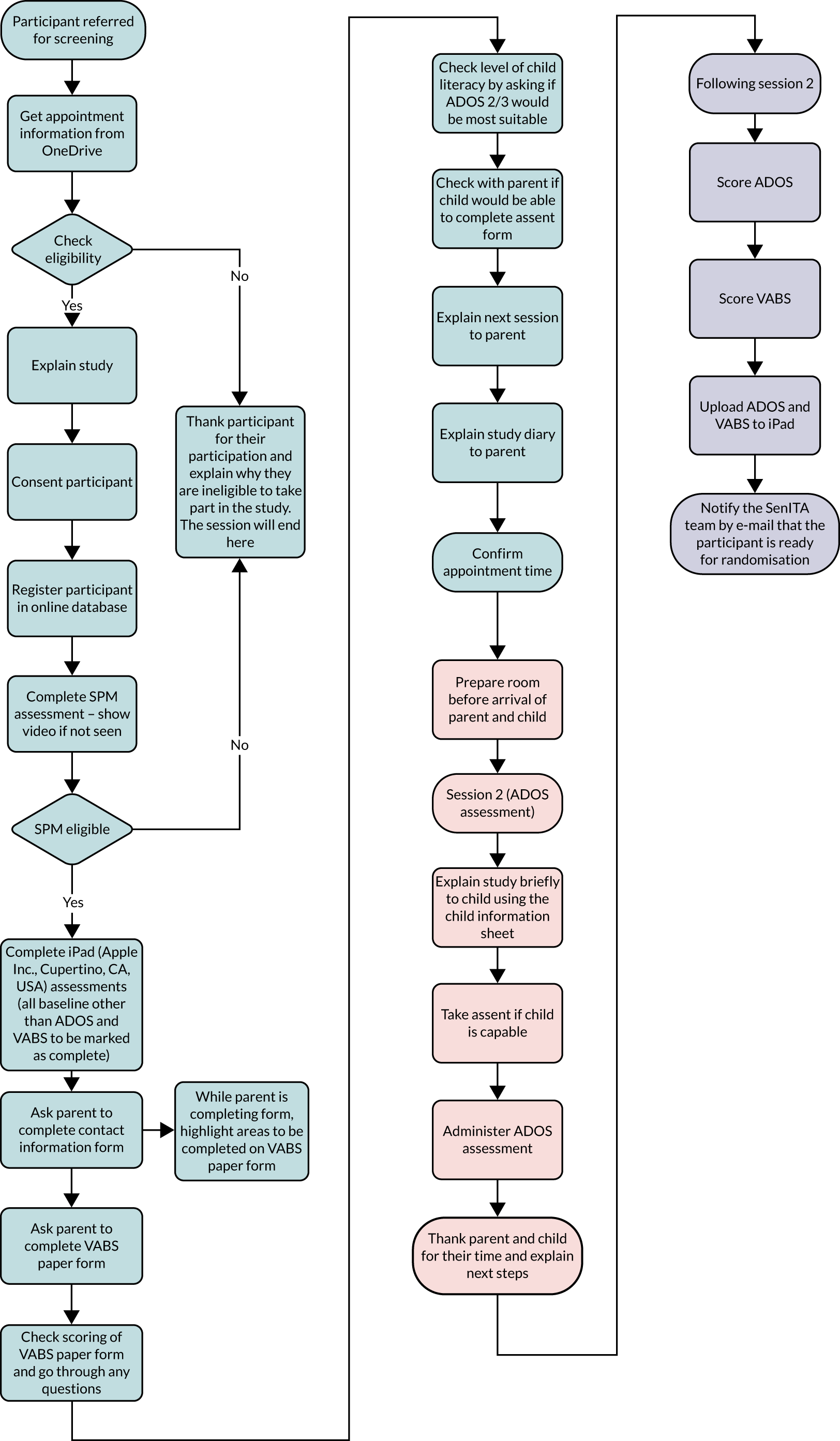
Follow-up data collection
Follow-up assessments for all participants were conducted 6 and 12 months after randomisation with a ± 4-week window. Reminders were sent out to participants/carers to complete the diaries using the text message service Esendex (Commify UK Ltd, Nottingham, UK). The text message system was also used to supplement data collection where necessary.
Intervention data collection
Therapists delivering the intervention were provided with written guidance in the form of a manual on how to collect and record all aspects of trial data (Table 8). The manual was very detailed and gave step-by-step instructions on using trial equipment, including screen shots and pictures to aid explanation. Each intervention therapist was given access to an iPad, which had been preloaded with links to the purpose-built trial SQL database and individual OneDrive accounts. Intervention therapists were also given access to a digital camera and tripod to record the intervention sessions.
| Section | Content |
|---|---|
| 1 | Introduction |
| 2 | Key aspects of study protocol:
|
| 3 | Intervention |
| 4 | Study procedures:
|
| 5 | GCP |
| 6 | AE (safety) reporting |
| 7 | Monitoring and ethics |
| 8 | Key contacts |
Once a participant had been randomised to receive the intervention, the next available therapist in their area was sent an e-mail to notify the therapist that a child had been allocated to them. The therapist then logged into their personal OneDrive space to pick up contact details for the participant and to arrange their first appointment. During the initial assessment, the therapist used their personal log-in details to access the secure trial database. The therapist completed online forms for the COPM48 and clinical observations. Therapists also completed the SIPT54 with each child. The SIPT was not available electronically and, therefore, therapists filled out a paper booklet with the child. To score the test, the booklet was sent to the trial team, who held the scoring software. To ensure that data were sent securely, therapists uploaded scans of each page of the booklet to their OneDrive account for the trial team to score. The SIPT report was then sent back to the therapist via OneDrive.
At the start of each intervention session, the therapist set up the camera and tripod to record the session. All recordings were transferred from the camera to the iPad and were uploaded to OneDrive. Recorded sessions could then be shared via OneDrive with relevant mentors and fidelity assessors, who were also given university-allocated single-use OneDrive log-in details. The manual included a flow diagram that each therapist could refer to (Figure 4).
FIGURE 4.
Flow diagram for therapist data collection. CTR, Centre for Trials Research.
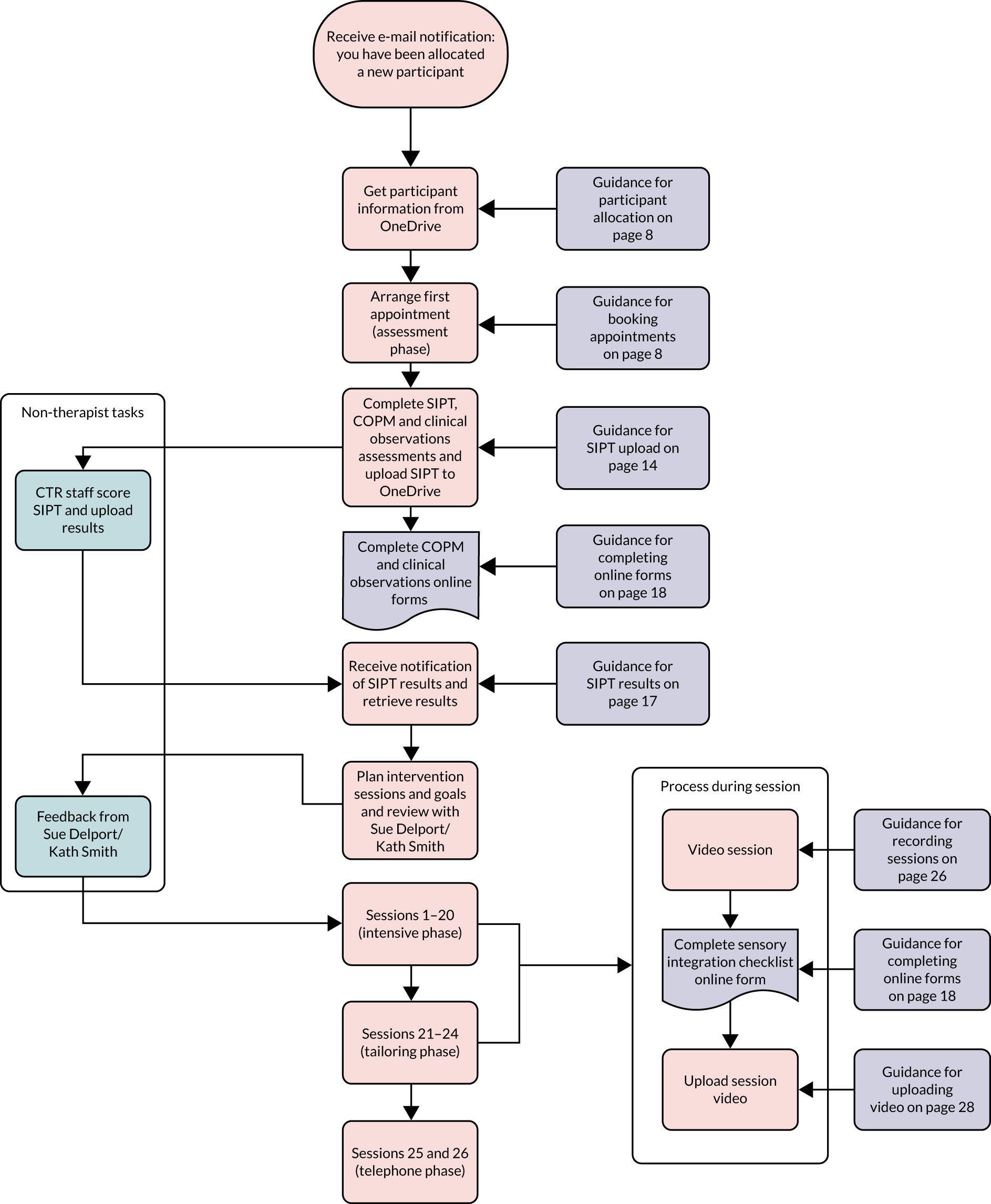
There were occasions when technology failed (e.g. when camera batteries ran out and when the camera failed to record), which led to some missing recordings. Intervention therapists received detailed training alongside the manual; however, there were several occasions where the trial team had to go out to site to help with technical issues. All data transfer and storage strictly adhered to GCP data handling and security specifications.
Qualitative data collection
Scoping focus groups with therapists
Prior to recruitment, focus groups and a small number of telephone interviews were held with clinicians providing treatment for SPDs to explore what was currently delivered/received as usual care in the health boards/trusts involved, and what, if any, difference existed in local provision and between regions (see Chapter 2 for full details). A small number of one-to-one telephone interviews were also held to supplement focus group data.
Interviews with carers and therapists (carried out during the trial)
Interviews took place either face to face or over the telephone. Interviews were audio-recorded and transcribed verbatim, with references to identifiable personal details, such as name, address and date of birth, removed (see Chapter 9 for full details).
Data management
Data collection was via a web-based SQL database. This secure encrypted system was accessed by username and password, complying with General Data Protection Regulations. 78 Back-up paper case report forms were available in the event that the web-based system was not accessible. A full data management plan was signed off prior to data collection.
Safety reporting
All serious adverse events (SAE) were reported immediately (and within 24 hours of knowledge of the event) to the study team by the PI at the participating site. The PI assessed each SAE to determine the causal relationship, which could not be downgraded by the chief investigator. The chief investigator then assessed expectedness of the event. There were no expected adverse events (AEs) or SAEs for the SenITA trial. Any planned treatments at the start of the study were not considered as AEs or SAEs.
Serious adverse events were reported from time of signature of informed consent, throughout the intervention period and then for a further month. All other AEs not classified as serious were not routinely collected, although none was reported.
Analyses
Analysis population
Participants were analysed based on the arm to which they were randomised. Main analyses were based on a modified intention-to-treat population, with those providing outcome data included in the analysis. A full intention-to-treat analysis set comprised all participants in the group to which they were randomised, with missing outcome data imputed using multiple imputation. This analysis set served as a sensitivity analysis to the primary outcome. Finally, a complier-average causal effect population comprised participants with outcome data in the group to which they were randomised, accounting for those who received the intervention as intended. This analysis set also served as a sensitivity analysis to the primary outcome.
Main analysis
The primary outcome analysis compared trial arms by fitting a linear regression to ABC-I scores at 6 months post randomisation, including a trial arm indicator (i.e. usual care/intervention), adjusting for baseline ABC-I, recruitment region (i.e. South Wales/South England region), severity of SPD (i.e. some problems/definite dysfunction) and sex of the child (i.e. male/female). We found no evidence of therapist clustering and, therefore, fitted single-level models only. Findings are reported as adjusted mean differences with associated 95% CIs and p-values.
Most secondary outcomes were analysed similarly. Teacher-assessed ABC-I was collected at 6 months only and, therefore, no baseline ABC-I adjustment was made for this analysis.
Subgroup analysis
We explored differential intervention effects on the ABC-I at the 6-month post-randomisation time point by age, severity of SPDs and comorbid conditions [i.e. attention deficit hyperactivity disorder (ADHD), ID or other neurodevelopmental/genetic conditions], site (n = 7), region (n = 2) and sex of the child. Our primary model was extended by including subgroup × trial arm interaction terms. These subgroup effects were also explored for APSI scores at 6 months post randomisation.
Sensitivity and exploratory analysis
Adjusting for missing data
Assuming that data were missing at random, given observed data, we used multiple imputation to investigate the potential influence of missing outcome data on the primary outcome. Specifically, we used Markov chain Monte Carlo procedures, assuming a multivariate normal distribution and fitting 25 imputations with an imputation model containing baseline ABC-I scores, region, sex and severity of SPD.
Adjusting for intervention receipt
We described the proportion of participants randomised to the intervention arm who initiated therapy using frequencies and percentages. Furthermore, we similarly described the proportion of participants randomised to SIT who received at least 13 SIT sessions during the intensive stage of the intervention and the absolute number of sessions received. Distinctions were made between intervention receipt that occurred prior to and following the primary outcome time point (i.e. 6 months post randomisation). Finally, we fitted instrumental variables regression models (estimated using two-stage least squares) to explore the relationship between intervention receipt and the primary outcome, while maintaining a comparison of groups as randomised. We considered the following three definitions of intervention receipt:
-
initiated intervention prior to 6-month follow-up (yes/no)
-
received at least 13 out of 20 sessions during the intensive stage of the intervention prior to 6-month follow-up (yes/no)
-
total number of sessions received prior to 6-month follow-up.
For the last definition, our model coefficients provided an estimate of intervention effectiveness per session received. Therefore, we multiplied coefficients by 26 to provide an estimate of the intervention effectiveness in those who received the intervention in its entirety.
Accounting for the COVID-19 pandemic
We conducted a series of sensitivity analyses to assess the impact of the COVID-19 pandemic on our findings:
-
We re-fitted our primary analysis for participants followed up during the pre-pandemic period (i.e. pre 23 March 2020).
-
We considered intervention effects in a hypothetical pandemic-free world, whereby any outcomes measured where intervention receipt (at least 13/20 intensive sessions attended prior to follow-up) was affected by the pandemic were set to missing and multiple imputation used to impute all missing values. The imputation model was similar to the original imputation model, with the addition of an indicator variable for whether the outcome was measured or should have been measured during the intrapandemic period.
-
We considered intervention effects in a world including a pandemic, where outcome data relating to participants who did not receive the intervention (as per our definition) were retained, and if the outcome was measured (or should have been measured) during the intrapandemic period was conditioned on in both imputation and analysis models.
Modelling outcomes over time
We fitted mixed linear regression models, accounting for the correlated nature of repeated observations within individuals (at 6 and 12 months post randomisation), to our primary and secondary outcome measures. Models adjusted for baseline measures and variables balanced on at randomisation.
Comparing agreement between teacher- and carer-rated ABC-I scores
We constructed Bland–Altman plots, calculated one-sample t-tests (on the difference in measures within participants) and calculated 95% limits of agreement to assess the agreement between teacher- and carer-rated ABC-I scores at 6 months.
Mediation analysis
We planned to conduct mediation analyses to explore whether or not any effect of the intervention on behavioural problems at 1 year (on all ABC subscales) was mediated through an effect on sensory sensitivities immediately post intervention.
Comparing Canadian Occupational Performance Measure scores pre and post intervention
We compared COPM scores collected at sessions 1 and 24 for participants in the intervention arm using paired t-tests.
Health economic analysis
The health economic analyses were carried out on an intention-to-treat basis. The main analyses compared cost and cost-effectiveness of SIT with usual care at the 6-month follow-up, and were conducted from an NHS and Personal Social Services (PSS) perspective. Secondary analyses adopted a societal perspective, adding education services, carer out-of-pocket expenses and lost productivity to NHS and PSS. The ABC-I at 6 months was used, in turn, as a measure of effectiveness in a series of cost-effectiveness analyses. The main cost-effectiveness measure was incremental cost per point improvement on the ABC-I (at 6 months).
Qualitative analysis
Qualitative data were analysed using thematic analysis43 to search across the data set to find repeated patterns of meaning and to identify key themes and subthemes. Double coding was carried out until consensus was reached. The qualitative component was designed using the principles of the Critical Appraisal Skills Programme qualitative checklist to ensure the quality of qualitative research. 79 Additional detail regarding qualitative methods is provided in Chapters 8 and 9.
Process evaluation
A process evaluation (see Chapters 8 and 9) was conducted to examine (1) recruitment, (2) retention, (3) fidelity, (4) acceptability, (5) adherence, (6) adverse effects and (7) contamination of intervention delivery within the trial. Recruitment rates/patterns, attendance and intervention fidelity were assessed quantitatively, whereas the acceptability of study processes and measures, intervention implementation and acceptability, and the role of contextual factors were examined through the qualitative interviews with therapists and carers.
Chapter 4 Internal pilot evaluation
As per the requirements of the commissioning brief, the design included an internal pilot with progression criteria. Assessments as to whether or not criteria were met and, subsequently, whether or not the trial should progress to a full effectiveness evaluation were made following recruitment of the first 40 participants. The methods and results for the pilot evaluation are presented in this chapter.
Aims and objectives
The aim of the internal pilot was to assess the feasibility of recruitment and retention, and to gauge the nature of usual care provided for SPDs (in the control arm). Specific objectives centred on providing early evidence of whether or not the study could be delivered in its entirety and covered the following elements.
Usual care
Usual care was expected to comprise use of sensory-based strategies not meeting fidelity criteria for SIT and no treatment at all in a significant proportion of cases (established via methods described in Chapter 2 and from carer diaries).
Recruitment of participants
Recruitment feasibility criteria would be met if at least 70% of those approached were eligible and at least 50% of those eligible were willing to be randomised.
Retention of participants at 6 months post randomisation
If dropout at the 6-month follow-up time point exceeded 20%, then we proposed to reassess the sample size calculation and associated implications for feasibility of recruitment.
Contamination (i.e. the extent to which participants allocated to the control arm received treatment/therapy similar to that in the intervention arm)
Carer-completed diaries were qualitatively assessed to determine whether or not usual care was sufficiently different from the intervention. Broadly defined, this criterion would be considered met if carers in the control arm did not receive any intervention meeting criteria for full SIT.
Adherence (i.e. receipt of intervention by participants allocated to the intervention arm)
An ‘effective’ dose for SIT has not yet been established. However, attending 13 of a possible 20 sessions delivered during the intensive intervention phase (two-thirds) was felt likely to indicate sufficient exposure, based on clinical experience and previous trials (see Chapter 5). 13,33,34,80
Fidelity of intervention delivery
A random sample of SIT sessions (lasting at least 15–20 minutes) delivered by individual therapists were evaluated using the fidelity measure. 23 To demonstrate adequate fidelity, therapists were expected to score least 80 out of 100 on the process fidelity measure for at least 80% of sessions rated. Each clinic was also assessed for suitability (of environment and equipment) prior to participant recruitment. 23
Sample size assumptions
To confirm the accuracy of the sample size calculation and other features of our proposed design, we obtained an estimate of the following: the proportion of participants providing primary outcome data, the SD of the ABC-I67 at the primary outcome time point (i.e. 6 months) in both trial arms, and the intracluster correlation coefficient (ICC) of therapists within participants for the ABC-I at the primary outcome time point (intervention arm only).
Adverse effects
We studied any adverse effects of study participation.
Outcomes
Primary outcome
The primary outcome for the internal pilot comprised those with prespecified progression criteria, as set out below.
Usual care
A key progression criterion was to demonstrate that the intervention and comparator were sufficiently different. To determine this we:
-
investigated pre-trial service provision in trial regions, as determined from interviews, focus groups and survey data from therapists and carers (see Chapter 2)
-
qualitatively assessed carer-completed diaries at the 6-month time point.
Recruitment
We calculated the number of children who were:
-
eligible (expressed as a proportion of those approached)
-
randomised (expressed as a proportion of those eligible).
Retention
We calculated the number of children with missing outcome data at 6 months post randomisation (expressed as a proportion of those who were randomised and had reached that time point).
Secondary outcomes
Secondary outcomes comprised outcomes without formal progression criteria (see Results: secondary outcomes).
Contamination
We calculated the number of children allocated to the control arm who received any intervention meeting criteria for full SIT (as per the fidelity checklist23) and/or more than one face-to-face session per week, and this is expressed as a proportion of those allocated to the control arm.
Adherence/acceptability
We calculated the number of children allocated to the intervention arm who received at least 13 out of 20 intervention sessions during the intensive phase (expressed as a proportion of those allocated to the intervention arm who had reached the less intensive phase) (see Chapter 5 for further intervention details).
Fidelity
The following fidelity measures were determined:
-
structural fidelity, that is the suitability of the clinic environment and equipment (scored as at least 85/110 on the structural fidelity checklist)
-
the number of therapists scoring at least 80 out of 100 on the process fidelity measure for at least 80% of sessions rated (expressed as a proportion of therapists who provide at least one video session).
Sample size assumptions
We calculated the:
-
SD of the primary outcome measure (i.e. carer-reported ABC-I at 6 months post randomisation)
-
correlation between baseline and 6-month post-randomisation carer-reported ABC-I scores.
Adverse effects
We calculated the number of:
-
children reporting at least one SAE (overall and by trial arm)
-
different SAEs reported (overall and by arm).
Progression criteria
Prespecified progression criteria are provided in Table 9.
| Objective | Outcome measure | Data source | Per cent required for determining progression |
|---|---|---|---|
| Recruitment | Number of people eligible (as a proportion of those approached) | Screening log | 70 |
| Number of people randomised (as a proportion of those eligible) | Screening and recruitment logs | 50 | |
| Retention | Number of people with missing outcome data at 6 months post randomisation (as a proportion of those who have been randomised and reached the time point) | Clinical database | 20 |
Methods
Statistical methods were descriptive in nature, with continuous data reported as means and SDs or as medians and interquartile ranges (IQRs), as appropriate, and categorical data reported as frequencies and proportions. Outcomes were estimated and reported alongside 95% CIs. Correlation coefficients were calculated (Pearson’s or Spearman’s, depending on distribution) and are presented with associated 95% CIs.
Qualitative methods employed to establish what was delivered and received as usual care in the trial regions (prior to the start of the SenITA trial) are described in Chapter 2. The aim of data collection was to gain a detailed understanding of the usual care provided by occupational therapists for children with autism and SPDs. This was not intended to be an exhaustive description or generalisable to all services in the UK.
Results: primary outcomes
Primary outcomes were those with specific progression criteria and are detailed below.
Usual care
A specific requirement of the commissioning brief for this trial was to demonstrate that the intervention was sufficiently different from usual care. At the point at which we reported on the pilot evaluation, that is after the first 40 participants were recruited, survey data had been received from 39 therapists and 131 carers with regard to their experiences of delivery and receipt of usual care. At this stage of the trial, we had also undertaken two face-to-face focus groups (group 1 had two participants and group 2 had three participants) and six (five individual and one shared) telephone interviews with therapists (n = 7) in trial regions only. The final survey results and a detailed qualitative exploration of usual care are provided in Chapter 2; however, characteristics of those who responded during the pilot evaluation period are given in Results: secondary outcomes, as is a brief summary of findings.
Therapist characteristics
A total of 39 therapists responded to the survey. Twenty-five therapists were from trial regions (Wales, n = 22; England, n = 3). Therapists were generally very experienced. In total, 24 out of the 39 (61.5%) therapists reported having at least 10 years’ post-qualification experience and only three (7.7%) reported having < 5 years’ experience. Most (37/39, 94.9%) therapists reported having seen one or more child with autism and SPDs in the last 6 months; however, only six (15.4%) therapists were based within a specialist autism/neurodevelopmental service.
Carer characteristics
A total of 131 carers responded to the survey. Most (124/131, 94.7%) carers were mothers. We received four (3.1%) responses from fathers, two from grandmothers (1.5%) and one from a kinship carer (0.8%). The spread of respondents across geographical regions is shown in Table 10.
| Health board/trust | n (%) |
|---|---|
| Aneurin Bevan University Health Board | 5 (3.8) |
| Cardiff and Vale University Health Board | 12 (9.2) |
| Cwm Taf University Health Board | 4 (3.1) |
| Cornwall Partnership Foundation NHS Trust | 2 (1.5) |
| Abertawe Bro Morgannwg University Health Board | 1 (0.8) |
| Wales other (non-trial regions) | 1 (0.8) |
| Dorset County Hospitals NHS Foundation Trust | 2 (1.5) |
| England other (non-trial regions) | 95 (72.5) |
| Scotland | 9 (6.9) |
| Total | 131 (100.0) |
Summary: assessment of usual care
Most of the contact that children with autism and SPDs and their families had with OT services was limited to assessment and advice, or provision of information around sensory strategies. Where interventions were delivered, these were sensory-based interventions, not meeting fidelity criteria for SIT, and were delivered less intensively and for shorter periods. Sensory-based difficulties were commonly reported in this population and there was clearly expressed demand from carer respondents for additional contact and support from OT services. Taken together, the findings of the surveys, focus groups and interviews indicated that the SenITA trial intervention was significantly different from usual care in trial regions, and across the UK more widely.
Recruitment
We planned to recruit participants from a wide variety of sources, namely via secondary care services (e.g. OT, paediatrics, CAMHS and specialist autism/neurodevelopmental services), schools, third-sector organisations and self-referral. We anticipated that most referrals would come from OT and/or specialist neurodevelopmental services. However, most expressions of interest came from third-sector organisations (e.g. local NAS support groups) and via self-referral. Reasons for this are likely to be complex, but might include, for example, the length of time from discharge from OT or specialist autism/neurodevelopmental services. Some specialist teams also expressed concerns about recruiting participants who were yet to receive a diagnosis (i.e. children were deemed eligible once they were on the local neurodevelopmental pathway provided that all other eligibility criteria were met; see Chapter 3 for inclusion criteria). In England, in particular, some OT services expressed concern that referring patients to the trial could have raised expectations of families in the area with regard to availability of interventional services, which they were not currently commissioned to deliver.
The number of people eligible at screening from expressions of interest received
Telephone screening
At the pilot evaluation analysis time point, expressions of interest had been received from 97 people. Following receipt of an expression of interest, the study team contacted each individual to carry out an initial telephone screening to confirm potential eligibility. Of the 97 people, 26 had yet to respond to a request for a telephone screening appointment, six were not interested following our response to their expression of interest and 14 were ineligible at referral.
Screening assessment
Following the telephone screening, 44 out of 97 potential participants who expressed an interest completed a screening assessment (with a further seven participants booked for assessment), of whom 42 were eligible (43.3%, 95% CI 33.9% to 53.2%).
The number of participants randomised from those eligible
Of the 42 people screened and eligible, we were able to randomise 40 (95.2%, 95% CI 84.2% to 98.7%), representing 41.2% (95% CI 32.0% to 51.2%) of the 97 people who initially expressed an interest. Those participants approached were defined as those who self-referred and those referred by secondary care services. Table 11 illustrates how recruitment figures compared with our progression criteria.
| Item | Expected n based on prespecified progression criteria | Achieved n |
|---|---|---|
| Number eligible | 68 (70% of those approached) | 42 (43.3% of those approached) |
| Number randomised | 34 (50% of those eligible) | 40 (95.2% of those eligible) |
Retention
The number of participants with missing outcome data at 6 months post randomisation
We received completed assessments from 13 participants of the 14 expected at the pilot evaluation time point (92.9%, 95% CI 68.5% to 98.7%). Table 12 illustrates how these data compared with progression criteria.
| Item | Expected n based on prespecified progression criteria | Achieved n |
|---|---|---|
| Number received | 11 (80% of those expected) | 13 (92.9% of those expected) |
Results: secondary outcomes
Secondary outcomes comprised those outcomes without formal progression criteria.
Contamination
We received 58 diaries and 107 SMS text messages (i.e. via the text service used to collect diary information; see Chapter 3 for a full description) from participants regarding their use of other services following randomisation. In the control arm, no participant indicated that they had received any intervention meeting criteria for SIT (i.e. according to fidelity criteria23 and/or face-to-face therapy more than once per week).
Adherence/acceptability
Of the 20 participants randomised to receive the intervention, eight participants were expected to have completed the intervention by the analysis time point, and we received attendance data for seven of these participants. All seven participants attended at least 13 of the 20 intensive sessions.
Fidelity
All trial clinics were assessed as having met structural fidelity criteria23 prior to opening for recruitment (see Chapter 8). Our outcome of interest was the number of therapists scoring at least 80 out of 100 on the process fidelity measure for at least 80% of sessions rated (expressed as a proportion of therapists who provide at least one video session). Fidelity scores were available for a total of 24 session recordings across six therapists. The mean fidelity score was 81.8 (SD 12.84). In total, 15 out of 24 (62.5%) sessions were scored at least 80 out of 100. The general impression score (measured via a single question that indicates whether or not the therapist intentionally applied ASI intervention theory and methods) was scored ‘no’ for one session only. The corresponding fidelity score for this session was 45 out of 100. All other sessions were scored ‘yes’. Complete fidelity ratings across all therapists are presented in Chapter 8.
Other sample size assumptions
Standard deviations for the ABC-I at 6 months post randomisation
The pooled SD for the ABC-I at 6 months was 11.78 (95% CI 8.45 to 19.45).
Correlation between ABC-I score at baseline and ABC-I score at 6 months
Based on 13 observations, the correlation between ABC-I score at baseline and ABC-I score at 6 months was 0.864 (95% CI 0.597 to 0.959).
Adverse effects
No adverse effects were reported.
Summary of progress against progression criteria
Our internal pilot findings are summarised in Table 13.
| Outcome | Projected | Attained | Comment |
|---|---|---|---|
| Usual care | N/A | N/A | Intervention is sufficiently different from usual care |
| Number of participants randomised | 78 | 40 | Lower than expected owing to difficulties opening sites and limited occupational therapist availability in Wales |
| Percentage of participants eligible from those approached | 70 | 43 | Lower than originally expected because of primary referral pathways being different from those expected |
| Percentage of participants randomised from those eligible | 50 | 95 | Higher than originally expected because of primary referral pathways being different from those expected |
| Percentage of participants randomised from those approached | 35 | 41 | Higher than originally expected |
| Percentage of participants with missing outcome data at 6 months post randomisation | 20 | 7 | High levels of retention from trial participants |
| Contamination (usual-care participants accessing full SIT) | N/A | 0 | No evidence of any contamination |
| Adherence (number of SIT participants receiving at least 13/20 intensive sessions) | N/A | 100 | High levels of intervention receipt |
| Fidelity (number of therapists scoring at least 80/100 for at least 80% of sessions rated) | N/A | Lower than expected. Assessing only 15–20 minutes of each session may have skewed this score, considering that the global impression score for 23/24 sessions reflected that the therapists intentionally applied ASI intervention |
Proposed modifications to design
Sample size implications
It would have been premature to use the SD and correlation estimates gathered at this time point to make alterations to the target sample size (as prespecified and described in Aims and objectives). Using a deflation factor of 1 – ρ2,76, Table 14 illustrates how the sample size could be reduced by accounting for this correlation (fixing all other assumptions).
| Correlation between baseline and follow-up ABC-I | Required sample size (n) |
|---|---|
| 0 | 216 |
| 0.1 | 214 |
| 0.2 | 207 |
| 0.3 | 197 |
| 0.4 | 181 |
| 0.5 | 162 |
| 0.6 | 138 |
| 0.7 | 110 |
| 0.8 | 78 |
| 0.9 | 41 |
| 1 | 0 |
At the request of the Health Technology Assessment programme and as advised by the Independent Data Monitoring and Ethics Committee, this correlation was revisited at two further time points: (1) when primary outcome time point data were available for 38 participants (correlation between baseline and 6-month ABC-I scores 0.806, 95% CI 0.654 to 0.895) and (2) when outcome data were available for 53 participants (correlation between baseline and 6-month ABC-I scores 0.69, 95% CI 0.52 to 0.80). This high level of correlation supported a reduction in the target sample size from 216 to 138 (a correlation of ≥ 0.6 indicates a sample size of ≤ 138 with 90% power).
Discussion
Formal progression criteria relating to recruitment and retention were met. Although the proportion of participants recruited via the various recruitment routes differed from that anticipated (i.e. there were more self-referrals and third-sector referrals) we did not encounter any difficulties in generating expressions of interest. Given the large number of self-referrals, the proportion of those eligible from initial expressions of interest was inevitably lower than anticipated. However, the proportion of those participants randomised from those eligible was much higher than originally estimated.
We clearly demonstrated that the intervention was significantly different from usual care within trial sites, and more widely within the NHS (see Chapter 2). Carer responses to the survey also suggested that there is significant need and demand for additional occupational intervention for sensory difficulties. There was no evidence of contamination, and all participants randomised to receive the intervention at this point had received our prespecified minimum number of intensive sessions.
In terms of fidelity, the measure used to assess this has six contextual elements and four sensory–motor factors addressing the child’s sensory–motor strengths and challenges (each element is rated on a scale of 1–4, with 4 being ‘certainly, the therapist intentionally used this strategy’, 3 being ‘probably’, 2 being ‘doubtful’ and 1 being ‘no, the therapist did not use this strategy’). We stated that an independent SIT-trained therapist would view 15–20 minutes of a session to determine fidelity. However, it is possible that some of the fidelity elements may not have been present in the video clip selected. This is particularly relevant when treating children with autism, as some of the elements of fidelity (e.g. ‘collaborates in activity choice’, ‘challenges praxis and organisation of behaviour’) may be particularly challenging to demonstrate without the assessor being privy to the goals and particular areas of difficulty of the child. Therefore, we refined the fidelity protocol to explicitly define how fidelity was recorded to ensure that it was reliable and consistent. This included using an additional assessor and checking inter-rater reliability (see Chapter 8). Continued mentoring, as well as peer support, was also in place to support fidelity adherence for treating therapists.
Chapter 5 Intervention
Overview: sensory integration therapy
Sensory integration therapy, as delivered in the SenITA trial, was consistent with manualised ASI and established fidelity criteria. 23,31,32 Participants allocated to the intervention arm received 26 1-hour sessions of therapy, delivered over 26 weeks [i.e. two sessions per week for 10 weeks (intensive phase), followed by two sessions per month for 8 weeks and then one telephone session per month for 8 weeks (tailoring phase)]. An ‘effective’ dose for SIT had not been established prior to the current trial. However, based on clinical experience and available evidence,13,33,34,80 attending 13 of a possible 20 sessions delivered during the intensive intervention phase (two-thirds) was felt likely to indicate sufficient exposure.
A detailed assessment of sensory processing deficit was undertaken by treating therapists (i.e. SIPT54), along with clinical observations post randomisation, to inform intervention planning (intervention arm only). This detailed assessment facilitated the development of a hypothesis for each child as to the nature of the underlying sensory difficulty affecting function. To further inform hypothesis development, therapists were given access to participants’ scores on the SPM44 (which was used as a screening tool to assess the level of SPD prior to enrolment in the trial; see Chapter 3). In addition to considering background history (assessed via completion of an Occupational Profile assessment with carers30), the COPM48 was conducted. This allowed the sensory–motor content of the SIT (i.e. proprioceptive, vestibular or tactile) to be individualised to meet the specific sensory needs hypothesised to underlie the functional goals of the participant. SIT uses the ‘just-right’ challenge for each child and therapy is adjusted to functional ability (as assessed by therapists using the tools and measures described above, prior to initiating treatment).
Carers were encouraged to observe or actively participate in sessions to facilitate engagement. Specific sensory–motor activities to support their child’s sensory integration, guided by clinical assessment, were discussed with carers to incorporate into family routines between sessions. Written guidelines were included where appropriate. Success of these strategies was discussed at subsequent sessions. A detailed intervention handbook was developed to guide therapists during intervention delivery and a summary of key content is presented in this chapter.
Therapists
The intervention was delivered by 16 occupational therapists (typically NHS band 7) in regional clinics. All therapists were trained in SIT with training meeting fidelity criteria (see Fidelity assessment tool). Clinics were in localities covered by five university health boards in South Wales (i.e. Cardiff and Vale, Aneurin Bevan, Cwm Taf Morgannwg, Swansea Bay and Hywel Dda) and two localities in South England (i.e. Cornwall and North Buckinghamshire) (eight sites in total). Intervention therapists were mentored prior to, and during, the trial by an independent sensory integration-trained therapist. Intervention therapists provided therapy to participants randomised to the intervention arm only (i.e. participants in the control arm who did have face-to-face contact with OT services were treated by different therapists). However, most families in the control arm were not receiving direct OT input. Where face-to-face therapy was provided as part of usual care, frequency of contact was typically less than once per week and the intervention received did not meet SIT fidelity criteria.
Fidelity assessment tool
Fidelity of intervention delivery was assessed using the ASI intervention fidelity measure,23 which included essential, structural and process fidelity elements. An independent fidelity assessor visited sites in South Wales and an experienced therapist visited sites in South England and scored each site for the essential element, according to level of therapist training/qualifications. Following this scoring, a structural fidelity assessment was carried out, for which a minimum score of 85 out of 110 for the following four areas was required: (1) safety of the environment; (2) assessment details and content of therapist-held records, including therapist–carer collaboration in relation to goals set during therapy; (3) physical space and equipment; and (4) communication with carers. In addition, the intervention sessions were measured for process fidelity to determine whether or not the therapist ensured physical safety; provided sensory opportunities; helped the child to maintain an appropriate level of alertness; challenged postural, ocular, oral or bilateral motor control; challenged praxis and behavioural organisation; collaborated in activity choice; tailored activity to provide appropriate challenge; ensured activities were successful; supported intrinsic motivation to play; and established therapeutic alliance. The scale demonstrates high content validity according to expert ratings and high reliability for process elements (total score ICC 0.99; Crohnbach’s α = 0.99). 23
Following provision of consent, face-to-face sessions were video-recorded. Fidelity of delivery was discussed with mentors through viewing video-recorded face-to-face sessions delivered to a participant for individual therapists early in the treatment series. A sample of recorded sessions in the intensive phase were also rated for fidelity by independent sensory integration-trained therapists who had successfully passed fidelity training (based on a randomly selected sample of the full sessions, of a minimum of 15–20 minutes in duration). Demonstration of adequate fidelity of intervention delivery was defined as scoring at least 80 out of 100 on the fidelity measure23 across at least 80% of sessions sampled (see Chapter 8 for fidelity outcome data).
Fidelity principles
The key ingredients of the intervention can be described as the contextual elements that detailed the interactive context between the therapist and the child, and the therapeutic alliance that occurred. These elements delineated the playful and supportive atmosphere in which the intervention took place and the strategies that ensured that the child’s motivation and interest were maintained through play, that is, the ‘just-right’ challenge. Next, the specific sensory–motor therapeutic activities that were individually tailored for each child were delineated. These activities were grouped into four areas:
-
sensory perception (with special emphasis on tactile, proprioceptive and vestibular systems)
-
postural and ocular control and bilateral integration
-
praxis
-
sensory reactivity (with particular emphasis on hyper-reactivity to tactile, vestibular, visual and auditory, and olfactory and gustatory sensation, and hyporeactivity to tactile, proprioceptive and vestibular sensation).
These elements were dynamic, that is they did not necessarily occur in sequential order, but were fluid and interacted with each other. The intervention involved systematic decision–making in the context of a safe, playful, collaborative and therapeutic environment that focused on the ‘just-right’ challenge and targeted the sensory and motor factors that facilitate skills and abilities needed for participation in daily activities. These specific therapeutic activities were designed based on initial and ongoing assessment data about the child and family, analysed in moment-to-moment interactions and interpreted though the lens of knowledge and skills of the therapist.
Initial assessment
The initial assessment for participants randomised to the intervention arm was carried out over two sessions, which were 1–2 hours in length and no more than 2 weeks apart. The assessment comprised the following.
Initial greeting and scene-setting
We began with an initial greeting, which involved scene-setting, a summary of the purpose of the study and the intervention, and checking consent for recording of sessions.
Clinical observations
Unstructured observations, including descriptive assessment of level of arousal, postural control, organisation of behaviour and motor planning ability, were carried out. In addition, a set of structured observations based on sensory integration principles, covering an assessment of performance/difficulties in proprioception, vestibular processing, motor planning and postural and ocular control, were carried out. Specific guidelines on administration, interpretation and scoring were written in the intervention handbook to ensure consistency between therapists.
The Sensory Integration and Praxis Test
The SIPT54 provides detailed information on the sensory processing and practice (i.e. motor planning) abilities that underlie learning and behaviour, and facilitates identification of specific areas of difficulty. There are 17 subtests that fall into four overlapping areas. The tests that are most closely associated with each of the areas are as follows:
-
motor-free visual perception (i.e. the ability to visually perceive and discriminate form and space without involving motor co-ordination), including –
-
space visualisation
-
figure-ground perception.
-
-
somatosensory perception (i.e. tactile, muscle and joint perception, encouraging the child to ‘feel’ rather than to ‘see’), including –
-
manual form perception
-
kinaesthesia
-
finger identification
-
graphesthesia
-
localisation of tactile stimuli.
-
-
praxis (i.e. the ability to motor plan in a range of ways), including –
-
design copying
-
postural praxis
-
bilateral motor control
-
praxis on verbal command
-
constructional praxis
-
motor accuracy
-
sequencing praxis
-
oral praxis.
-
-
sensorimotor (i.e. sensory integration at multiple levels), including –
-
standing/walking balance
-
postrotary nystagmus.
-
Occupational profile
The occupational profile questions were given to the carer to complete between assessment sessions. The occupational profile questions also included information about the child’s play preferences and strengths, their school, their medical and developmental history, and infant and current behavioural patterns. The therapist encouraged the carer to think of functional issues that were affecting their child’s performance for discussion at the next session.
Sensory Processing Measure
The SPM44 was used as a screening measure to ensure a minimum level of SPD as an inclusion criterion. The SPM provides eight standard scores for the following dimensions: (1) social participation, (2) vision, (3) hearing, (4) touch, (5) body awareness (proprioception), (6) balance and motion (vestibular function), (7) planning and ideas (praxis) and (8) a total sensory symptoms score. Scores on each of these dimensions were classified as typical, some problems or definite dysfunction. For the purposes of the SenITA trial, SPD was defined as either (1) a definite dysfunction on at least one sensory dimension (all domains except social participation) and the total score or (2) at least a probable dysfunction on two or more sensory dimensions and the total score. Treating therapists were able to access these scores to aid hypothesis development and delivery of the intervention.
Canadian Occupational Performance Measure
The COPM48 is an individualised measure designed to detect change in a child’s (and carer’s) self-perception of occupational performance over time. The COPM comprises the following four key steps.
Problem definition
Defining the problem involved identifying occupational performance and participation problems.
Rating the importance of the identified participation challenge
Once problems were identified, the participant was asked to rate each activity in terms of its importance in his or her life. Importance was rated on a 10-point scale. This process allowed the child and/or carer to set intervention priorities and facilitated goal-setting and intervention planning (note that the measure comprised pictorial rating scales and examples of childhood activities to facilitate completion by children).
Selecting the main problem areas to target for intervention
Using the information above, the participant (or carer) chose up to five problems that were the most pressing or important. If the child had capacity to be part of this process, the therapist chose areas that were relevant to both the carer and the child. These identified problems formed the basis for the intervention goals. An example script was provided to therapists for the COPM interview.
Contacting the carer to complete the Canadian Occupational Performance Measure rating of performance and satisfaction with performance
Following completion of all other assessments and initial mentor discussions, carers were asked to rate goals in terms of current performance and their satisfaction with this level of performance.
Interpretation of assessment
All assessment scores (i.e. SIPT, SPM and clinical observations) were interpreted using the ASI Assessment® Interpretation Tool©. The ASI Assessment Interpretation Tool is intended for use in conjunction with the instructional information provided in the clinician’s guide for implementing ASI30 and in specialised ASI training programmes (adapted for the SenITA trial by Kath Smith and SD).
Hypothesis development
Using the assessment data as indicated on the interpretation tool, therapists developed a hypothesis about which areas of dysfunction were particularly influencing the child’s performance and participation.
Goal development
Therapists were encouraged to use the FEAST (Functional, Expectation, Action, Specific condition, Timeline) model to assist in articulating the specific goals identified by the child/carer in the COPM. The functional element asks ‘why’ a goal is required (i.e. the area of occupation to be addressed, such as to dress himself/herself). The expectation element specifies ‘who’ (i.e. ‘X will . . . ’). The action element looks at ‘what’ is to be undertaken (e.g. ‘X will put his/her shirt and shorts on’). The specific condition element considers ‘how’ this will be carried out (e.g. with three verbal prompts once the clothes have been laid out). Finally, the timeline element considers ‘when’ this will be carried out (e.g. by the end of session 24).
Summary of strengths, participation challenges and goals
The child’s strengths were summarised from the occupational profile and discussion with the carer. Participation challenges were summarised from the occupational profile and carer discussion. Therapists then produced a summary of their interpretation of the assessment results. From the assessment results and hypothesis of underlying difficulties, the therapist selected specific SIPT items and clinical observations to reassess at the end of therapy (proximal outcomes), in addition to the child or carer re-rating their performance and satisfaction with their goals on the COPM (distal outcomes).
Mentoring
All therapists were assigned a mentor. Mentors were senior occupational therapists who were fully trained and experienced in the delivery of SIT (note that a separate pool of independent and sensory integration-trained therapists rated sessions for fidelity, as described in Chapter 5). Therapists discussed the first two sessions that they delivered with mentors to confirm their hypothesis and direction of therapy. Fidelity of delivery was discussed with mentors early in the series of treatment, once rapport between the child and the therapist was established, to support therapists. Mentoring sessions of approximately 1 hour in length were provided monthly (or more often within the first 2 months of the intervention delivery phase if the therapist requested this), tapering to once per month or at least once every 6 weeks thereafter. A Facebook (Meta Platforms, Inc., Menlo Park, CA, USA; www.facebook.com) group was also set up for treating therapists and mentors to join, should they wish; 17 members used this facility. This was a forum for therapists to support each other in the trial and to share ideas. The group was active throughout the trial, although not all participants contributed. In addition, all therapists had a joint training session (including fidelity training) at the start of the trial before recruitment of participants. This was followed by a 2-hour individual therapist training session to confirm the therapy protocol and explain the detail in the intervention handbook, followed by an additional training session on saving and uploading data. Further support was offered during the trial, including two face-to-face half-day events to share ideas, challenges and solutions.
Following assessment and interpretation, therapists were encouraged to contact their mentor. Mentors were given access to a shared folder that allowed therapists to share specific information with them, including SIPT scores (uploaded by the research team), interpretation summaries, assessment videos (where available) and the summary of participation strengths, challenges, goals and hypotheses. Mentors were also able to access SPM data and clinical observations as required. Therapists were given detailed guidance on how to share information with mentors, and discussed hypotheses and goals with them, allowing any changes to goals or hypotheses to be made at this stage, before contacting the carer to complete the COPM rating of performance and satisfaction.
Mentors were given a manual that detailed key elements of the study, therapist requirements and expected timelines for mentoring sessions. Although therapists were all trained in SIT, most therapists carried a varied caseload of children with a range of difficulties and, therefore, would typically use a range of treatment approaches. Therefore, a list of watch points/common errors was also provided to mentors, which included the following:
-
Therapists may need to break eclectic habits (as this was a research study of SIT and not a standard NHS intervention).
-
Therapists may find it difficult to swap from therapist- to child-directed play.
-
Therapists may not be used to treating for this many sessions. Therefore, therapists may be anxious by sessions 7 or 8 and may need support to continue to challenge their participant. Grading will become increasingly important and experience indicates that changes start to occur by about weeks 8–10 and, therefore, therapists are encouraged to keep going.
-
Therapists may need support to be playful, as this may not be the style of their traditional therapy.
-
Therapists may need reminders that they should not work only on modulation. Praxis may be quite markedly poor and overlooked with other concerns taking precedence.
-
Therapists should keep data and hypotheses in mind for each session.
Intervention session content
A brief outline of session content is given below.
Session 1
Key steps and activities were as follows:
-
Goals and hypotheses for underlying sensory–motor difficulties were checked prior to the session.
-
The room was set up with provisional equipment and toys that were in keeping with hypothesis from assessment data, considering strengths, challenges and needs.
-
The video camera was checked and switched on.
-
Carer and participant were greeted. The child was made comfortable with a simple explanation of the activities that they would be doing and how these games would help them.
-
The therapist used their professional and clinical reasoning to apply each of the ASI fidelity principles to ensure that the challenges were appropriate for the child’s age, ability levels and needs.
-
The carer was encouraged to participate in the session or to watch as they felt comfortable. The level of carer engagement was negotiated with the carer during the telephone call (see Fidelity assessment tool).
-
There was no set sequence, manner or format for incorporating all of the key principles and implementing tailored activities. However, the flow of the session could be divided into three phases of beginning, middle and end. Sessions lasted about 50–55 minutes, including 5–10 minutes to have a short discussion with the carer about activities or strategies to try at home. Advice sheets may have been given at this point, if appropriate.
Beginning of the session
At the first session, therapists had all information about the child from the assessment, including the hypothesis of underlying sensory motor difficulties. In addition, therapists had formulated a plan of activities that could help facilitate these areas. As the child arrived, the therapist was usually able to form an impression in the moment as to their mood and state. This initial impression paired with the knowledge of the child determined what happened at the beginning of the session. Given that therapeutic alliance and prioritisation of the context of play are so important, the tone set at the beginning of the session was key, as the child may have needed time to get organised and feel comfortable.
Middle of the session
The middle part of the session was generally when sensory–motor factors underlying the child’s main participation strengths and challenges were addressed. For example, if a child liked dinosaurs but had tactile perception difficulties, the therapist could hide dinosaurs in places that incorporated a tactile element. The full range of fidelity elements (see Fidelity assessment tool) needed to be considered throughout to ensure that that playful activities were utilised within the ‘just-right’ challenge level. Levels of adaptive responses (Table 15) were used when determining the ‘just-right’ challenge for sensory–motor activities and the level of functioning within the capacity of the child.
| Level | Adaptive response |
|---|---|
| 1 | Responds to passive stimuli |
| 2 | Holding on and staying put |
| 3 | Alternating contracting/relaxing muscle groups |
| 4 | Initiating an activity, but not completing it independently |
| 5 | Moving independently in a somewhat familiar pattern |
| 6 | Moving through the environment in an unfamiliar way |
| 7 | Performing complicated activities using unfamiliar movement |
The affordances of different pieces of equipment needed to be considered (e.g. a platform swing could be used in sitting in a linear direction, or prone lying and rotating, or even in an orbital arc while upright kneeling). The therapy required creative flexible thinking and clinical reasoning informed by the underpinning goals.
End of the session
At the end of the session, the therapist would help the child to be ready to transition out of the intervention setting. Some children who become very engaged in the fun and meaningful intervention activity may be sad to see the session finish and may protest fiercely; therefore the therapist would monitor the child’s state of arousal, activity level and emotional state to help the child be ready to leave. This could involve engaging the child in putting heavy therapy equipment away and helping them to be calm and organised while creating a natural sense of closure. Likewise, therapists would help children to orient to cues, such as a clock or last steps for completion of an activity. If a child was due to return (i.e. for future sessions) then therapists would talk about what might happen ‘next time’. Reflective questions for each session were completed.
Contact with school
On some occasions, it was appropriate to contact the school to get additional feedback on the child’s participation and to give verbal advice if there were sensory–motor challenges that needed to be addressed. This advice may include sensory–motor activities that had been effective within the intervention that could be applied within the school context (e.g. if the child calmed after using proprioceptive activities, the therapist may suggest that the teacher incorporates activities that demand muscle work, such as playing with weighted balls). Any contact with the school was recorded in the intervention notes.
Intervention sessions 2–20
Intervention sessions 2–20 continued as with session 1 above and included a review of any activities carried out since the last session with the carer.
Intervention sessions 21–23
After the twice-weekly intense phase of therapy, instead of sessions ceasing altogether, a tailoring phase of therapy sessions once per fortnight was delivered and continued with planning as previously detailed in Intervention session content, Session 1, Beginning of the session. This was designed to aid transition from therapist-directed intervention to carer-supported management of the child, and provided an opportunity to discuss any issues that arose to jointly think of solutions.
Intervention session 24
For session 24, the SIPT or clinical observation items identified as proximal outcome measures were reassessed. The COPM was re-administered to determine how the carer (and the child if they had capacity to do this) initially rated the five goals for performance and satisfaction with that performance. The therapist then explained to the participant that there would be two follow-up telephone calls to monitor progress and to problem-solve any issues that might arise. Strategies and advice for continuing the progress made during the face-to-face sessions were discussed.
Intervention session 25
Session 25 comprised a telephone call, which was carried out 1 month following the last intervention session. The purpose of the telephone call was to:
-
follow up on the child’s performance and behaviour in the past month
-
determine whether or not any advice and strategies previously given were successful
-
offer support and advice for any ongoing issues.
Possible prompt questions were provided to therapists to discuss with participants.
Intervention session 26
Session 26 was the same as session 25, but with the additional purpose of closure, as this was the final contact with the carer. The purpose of this telephone call was twofold. First, to follow up (as in the previous telephone call) and discuss any changes to behaviour and to determine whether or not any advice and strategies were carried out. Second, to consider the goals chosen at the beginning of therapy and informally discuss the progress of the child, and, finally, to thank the carer for their engagement in the process (prompt questions were provided to be used as needed).
A brief written summary of the intervention was provided to carers/schools if requested. The summary did not include the outcome of intervention, as this was not appropriate within the research trial; however, it did include the goals that were set prior to intervention, including the specific target areas that were concentrated on.
Information regarding fidelity of intervention delivery, participant adherence and therapist experience of therapy and of trial participation is provided in Chapter 8.
Chapter 6 Quantitative results
Recruitment and participant flow
Between August 2017 and June 2020, we screened 150 individuals, of whom 142 (94.7%) were eligible and consented. Of the 142 consented participants, 138 (97.2%) were randomised. Of those randomised, 107 (77.5%) provided data at 6 months post randomisation. Two participants withdrew from the study prior to this time point and 29 participants were lost to follow-up. Data were provided at 12 months post randomisation by 96 (69.6%) participants. There were no further withdrawals between 6 and 12 months, but 40 participants were lost to follow-up (Figure 5).
FIGURE 5.
A CONSORT (Consolidated Standards of Reporting Trials) flow diagram.
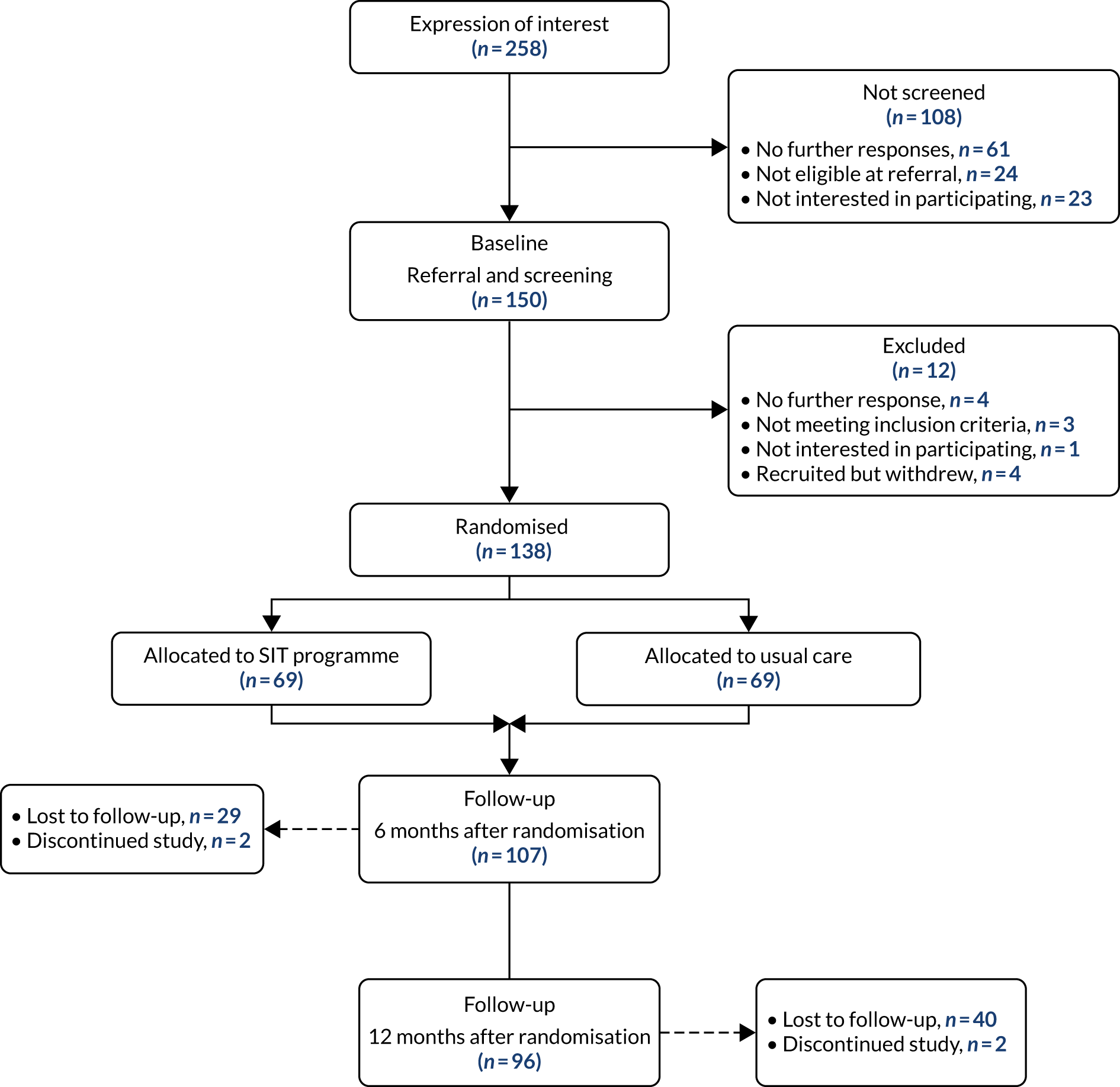
Baseline characteristics
Participant characteristics at baseline were reasonably well balanced between trial arms. Differences of note were present for the sex of child [i.e. male participants represented 57/69 (82.6%) control arm participants vs. 52/69 (75.4%) intervention arm participants], statement status [27/69 (39.1%) participants had a statement in the control arm vs. 32/69 (46.4%) participants in the intervention arm] and EuroQol visual analogue scale (EQ-VAS) [the control arm had a median EQ-VAS score of 80 (IQR 70–87) vs. a median EQ-VAS score of 75 (IQR 70–80) in the intervention arm].
Overall, participants had a mean age of 7.87 (SD 1.73) years, 99 out of 138 (71.7%) participants were recruited from South Wales and, based on their SPM results, 107 out of 138 (77.5%) had scores indicative of ‘definitive dysfunction’ (Table 16).
| Characteristic | Study arm | All participants (n = 138) | |
|---|---|---|---|
| Control (n = 69) | Intervention (n = 69) | ||
| Age (years), mean (SD) | 7.77 (1.76) | 7.97 (1.72) | 7.87 (1.73) |
| Sex of child, n (%) | |||
| Male | 57 (83) | 52 (75) | 109 (79) |
| Female | 12 (17) | 17 (25) | 29 (21) |
| Region, n (%) | |||
| South Wales | 51 (74) | 48 (70) | 99 (72) |
| South England | 18 (26) | 21 (30) | 39 (28) |
| Site, n (%) | |||
| Aneurin Bevan | 5 (7) | 7 (10) | 12 (9) |
| Cardiff and Vale | 24 (35) | 21 (30) | 45 (33) |
| Cornwalla | 11 (16) | 11 (16) | 22 (16) |
| Cwm Taf | 8 (12) | 6 (9) | 14 (10) |
| Hywel Dda | 10 (14) | 10 (14) | 20 (14) |
| Pace Centrea | 7 (10) | 10 (14) | 17 (12) |
| Swansea Bay | 4 (6) | 4 (6) | 8 (6) |
| Ethnicity,b n (%) | |||
| White British | 41 (84) | 50 (93) | 91 (88) |
| Asian/Asian British: Indian | 2 (4) | 0 (0) | 2 (2) |
| Mixed/multiple ethnic groups: white and black Caribbean | 2 (4) | 0 (0) | 2 (2) |
| Other | 4 (8) | 4 (7) | 8 (8) |
| Type of school attended, n (%) | |||
| Mainstream (full time) | 47 (70) | 55 (83) | 102 (77) |
| SRB (full time) | 4 (6) | 5 (8) | 9 (7) |
| Mainstream and SRB | 4 (6) | 3 (5) | 7 (5) |
| Special school (day) | 1 (1) | 0 (0) | 1 (1) |
| PRU | 1 (1) | 0 (0) | 1 (1) |
| Other | 10 (15) | 3 (5) | 13 (10) |
| Statement status, n (%) | |||
| Yes | 27 (39) | 32 (46) | 59 (43) |
| No | 39 (57) | 33 (48) | 72 (52) |
| Not sure | 3 (4) | 4 (6) | 7 (5) |
| Cormorbidity,c n (%) | |||
| Yes | 22 (45) | 28 (48) | 50 (47) |
| No | 27 (55) | 30 (52) | 57 (53) |
| Number of comorbidities if answered ‘yes’, n | |||
| 1 | 18 | 20 | 38 |
| 2 | 4 | 7 | 11 |
| 3 | 1 | 1 | |
| ADHD, n (%) | |||
| Yes | 10 (20) | 17 (29) | 27 (25) |
| No | 39 (80) | 41 (71) | 80 (75) |
| ID, n (%) | |||
| Yes | 4 (8) | 11 (19) | 15 (14) |
| No | 45 (92) | 47 (81) | 92 (86) |
| Other neurodevelopmental/genetic, n (%) | |||
| Yes | 12 (24) | 9 (16) | 21 (20) |
| No | 37 (76) | 49 (84) | 86 (80) |
| SPM, n (%) | |||
| Some problems | 16 (23) | 15 (22) | 31 (22) |
| Definite dysfunction | 53 (77) | 54 (78) | 107 (78) |
Autism Diagnostic Observation Schedule assessments were carried out at baseline to characterise the sample in terms of autism symptoms, but not as a diagnostic measure. A summary is presented in Table 17 for each assessment module spilt by arm. Data are presented for 135 out of 138 participants. It was not possible to obtain ADOS scores for three participants who were unable to engage with this aspect of the assessment process.
| Social effect | Module 3, n (%) | Module 2, n (%) | Module 1, n (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Control (N = 59) | Intervention (N = 57) | Total (N = 116) | Control (N = 5) | Intervention (N = 8) | Total (N = 13) | Control (N = 4) | Intervention (N = 2) | Total (N = 6) | |
| Communication | Three items: maximum score = 6 | Two items: maximum score = 4 | Three items: maximum score = 6 | ||||||
| Scored 2 on all items (100%) | 11 (18.6) | 6 (10.5) | 17 (14.7) | 2 (40) | 1 (12.5) | 3 (23.1) | 2 (50) | 2 (100) | 4 (66.7) |
| Scored 2 on 50–99% of items | 23 (38.9) | 27 (47.4) | 50 (43.1) | 2 (40) | 6 (75) | 8 (61.5) | 1 (25) | 0 (0) | 1 (16.7) |
| Scored 2 on < 50% of items | 25 (42.4) | 24 (42.1) | 49 (42.2) | 1 (20) | 1 (12.5) | 2 (15.4) | 1 (25) | 0 (0) | 1 (16.7) |
| Reciprocal social interaction | Seven items: maximum score = 14 | Eight items: maximum score = 16 | Eight items: maximum score = 16 | ||||||
| Scored 2 on all items (100%) | 2 (3.4) | 2 (3.5) | 4 (3.4) | 0 (0) | 2 (25) | 2 (15.4) | 0 (0) | 0 (0) | 0 (0) |
| Scored 2 on 50–99% of items | 25 (42.4) | 21 (36.8) | 46 (39.7) | 4 (80) | 3 (37.5) | 7 (53.8) | 2 (50) | 2 (100) | 4 (66.7) |
| Scored 2 on < 50% of items | 32 (54.2) | 34 (59.6) | 66 (56.9) | 1 (20) | 3 (37.5) | 4 (30.8) | 2 (50) | 0 (0) | 2 (33.3) |
| Restricted and repetitive behaviours | Four items: maximum score = 8 | Four items: maximum score = 8 | Four items: maximum score = 8 | ||||||
| Scored 2 on all items (100%) | 2 (3.4) | 1 (1.75) | 3 (2.6) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Scored 2 on 50–99% of items | 12 (20.3) | 7 (12.3) | 19 (16.4) | 3 (60) | 3 (37.5) | 6 (46.2) | 0 (0) | 1 (50) | 1 (16.7) |
| Scored 2 on < 50% of items | 45 (76.3) | 49 (85.9) | 94 (81) | 2 (40) | 5 (62.5) | 7 (53.8) | 3 | 1 (50) | 5 (83.3) |
Average scores on clinical measures at baseline were generally within the middle of the score range, with exceptions being for ABC lethargy/social withdrawal (lower end of the scale, indicating lower levels of lethargy/social withdrawal), ABC stereotypic behaviour (lower end of the scale, indicating lower levels of stereotypic behaviour) and EQ-5D (higher end of the scale, indicating higher levels of health utility and quality of life). However, the range of scores spanned most of the scale for all measures (see Tables 19 and 20).
Intervention receipt and fidelity
Initiation of sensory integration therapy
Of the 69 participants randomised to the intervention arm, 61 (88.4%) initiated SIT and 49 out of 57 (86.0%) initiated prior to their primary outcome follow-up. In those who initiated SIT, the median time from randomisation to initiation was 48 (IQR 32–85) days (Figure 6).
FIGURE 6.
Time from randomisation to initiation of SIT in days (for the 61 participants allocated to and initiating SIT). a, Figure includes 61 out of 69 participants who initiated SIT.
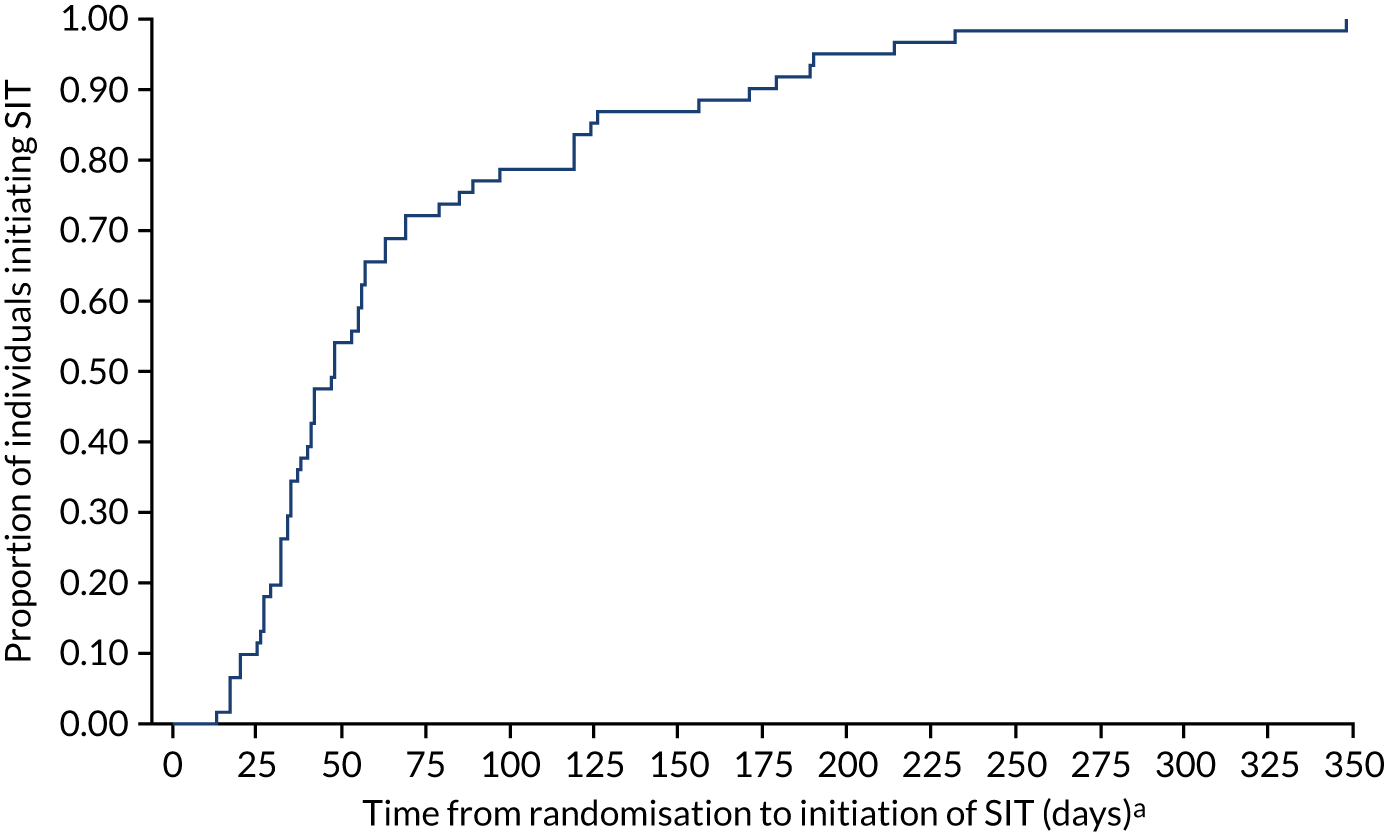
Implementation of sensory integration therapy
Overall, 54 (78.3%) participants allocated to the intervention arm received at least 13 SIT sessions during the intensive stage, with 38 out of 57 (66.7%) participants with primary outcome follow-up data receiving at least 13 SIT sessions during the intensive stage. The median number of SIT sessions received was 20 (IQR 16–21) and the median number of SIT sessions received prior to primary outcome follow-up (in those with primary outcome data) was 18 (IQR 10–21).
Receipt of SIT sessions varied considerably between participants. Figure 7 highlights different patterns of SIT session receipt for six participants, with Table 18 providing summary statistics for each participant. Participants A, B and C display typical patterns of participants who initiated SIT early (i.e. between 20 and 48 days post randomisation) and attended most of their sessions. Participant A received two SIT sessions after their primary outcome data were collected. Participant D initiated SIT late (i.e. at 119 days post randomisation) and shows a typical pattern of someone who attended most of their sessions, but received a substantial number of them after their primary outcome data were collected. Participant E displays a pattern of someone who started SIT but who stopped early on. Participant F is a participant who started SIT 348 days post randomisation and, therefore, all sessions received were after collection of their primary outcome data.
FIGURE 7.
Panel plot of session attendance for six different participants. (a) Participant A; (b) participant B; (c) participant C; (d) participant D; (e) participant E; and (f) participant F.
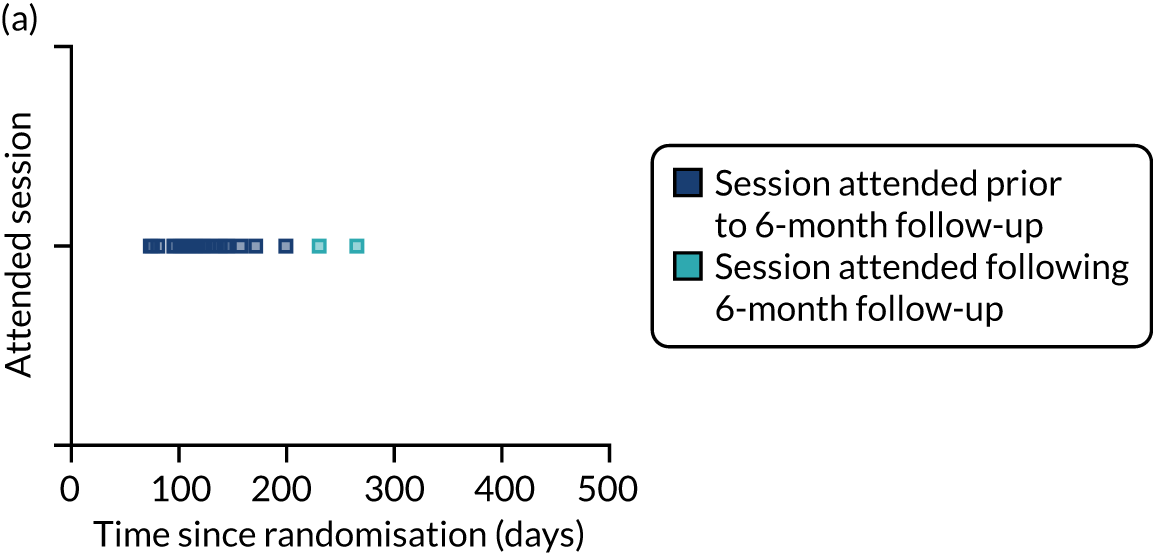
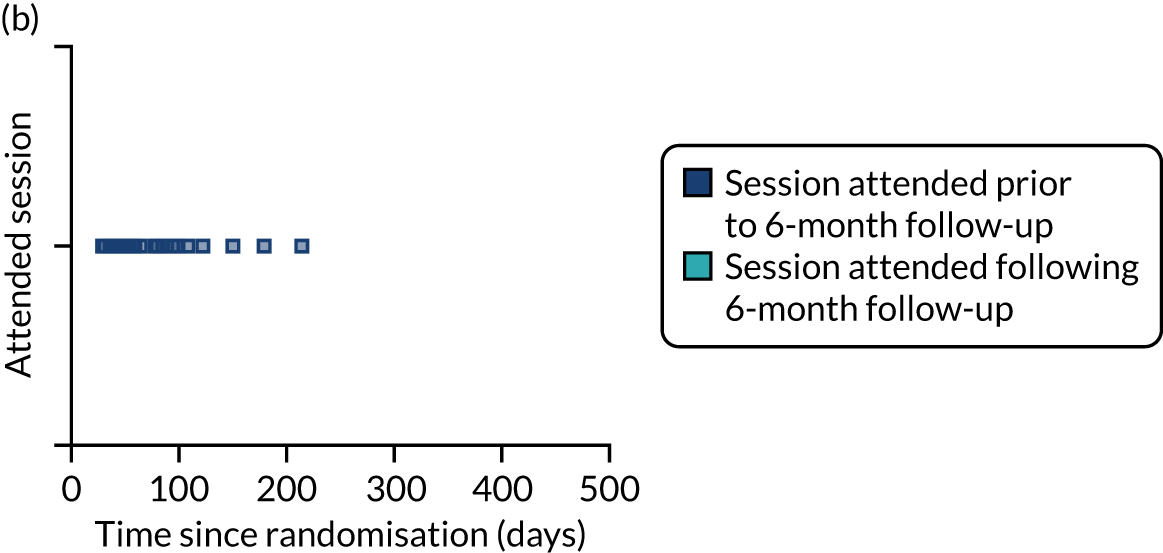
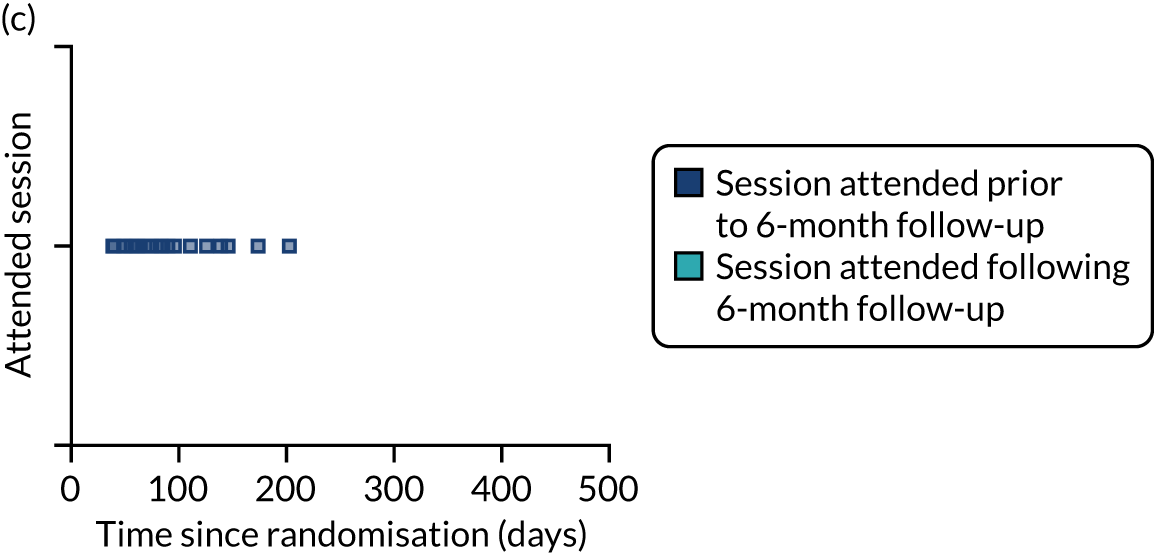
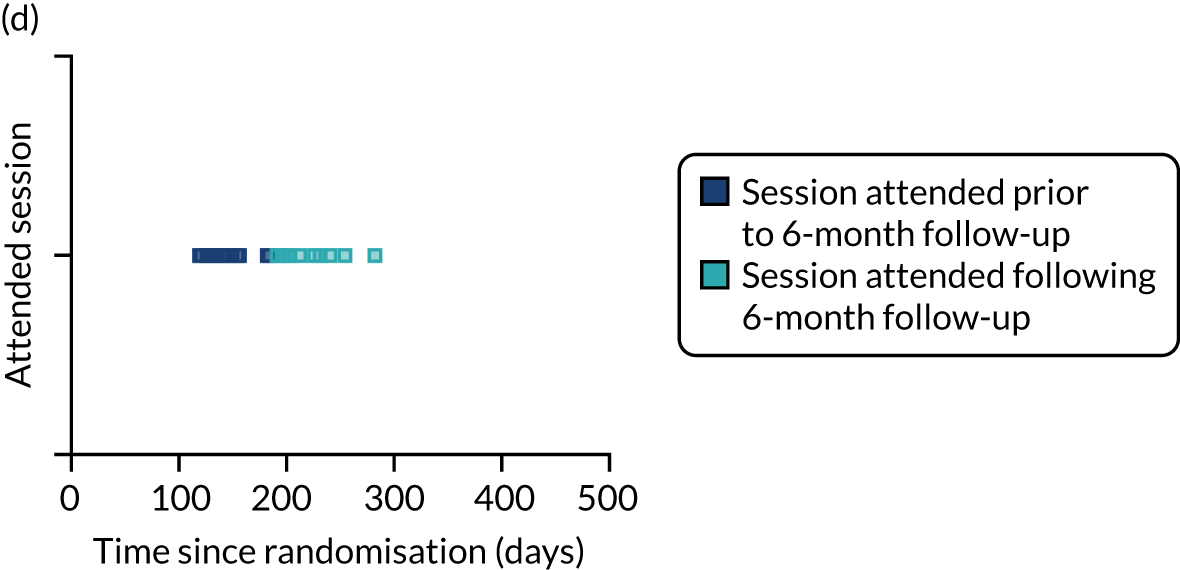
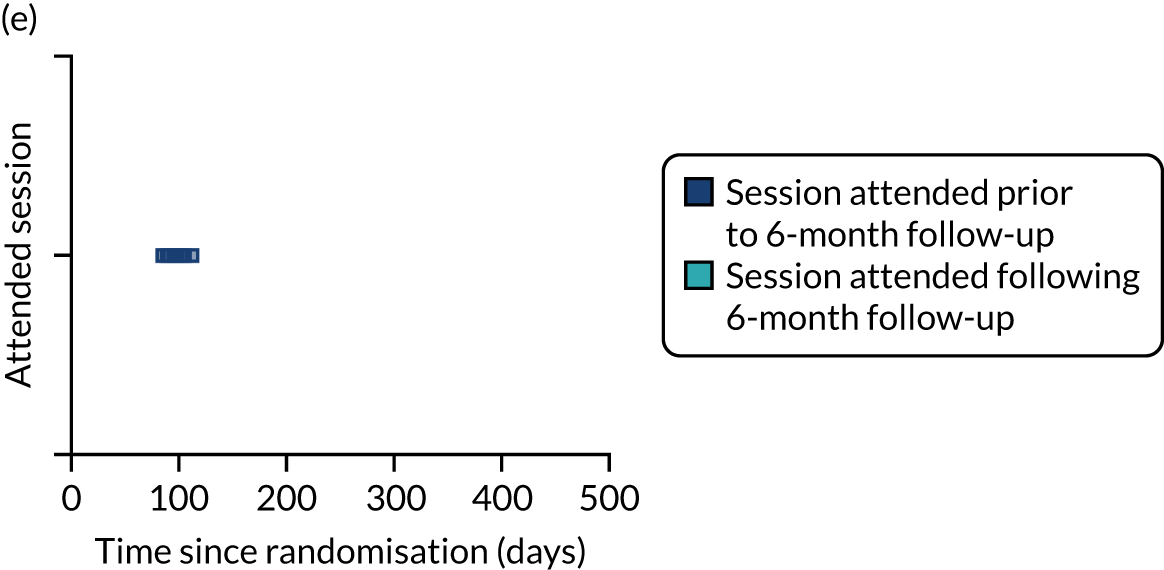
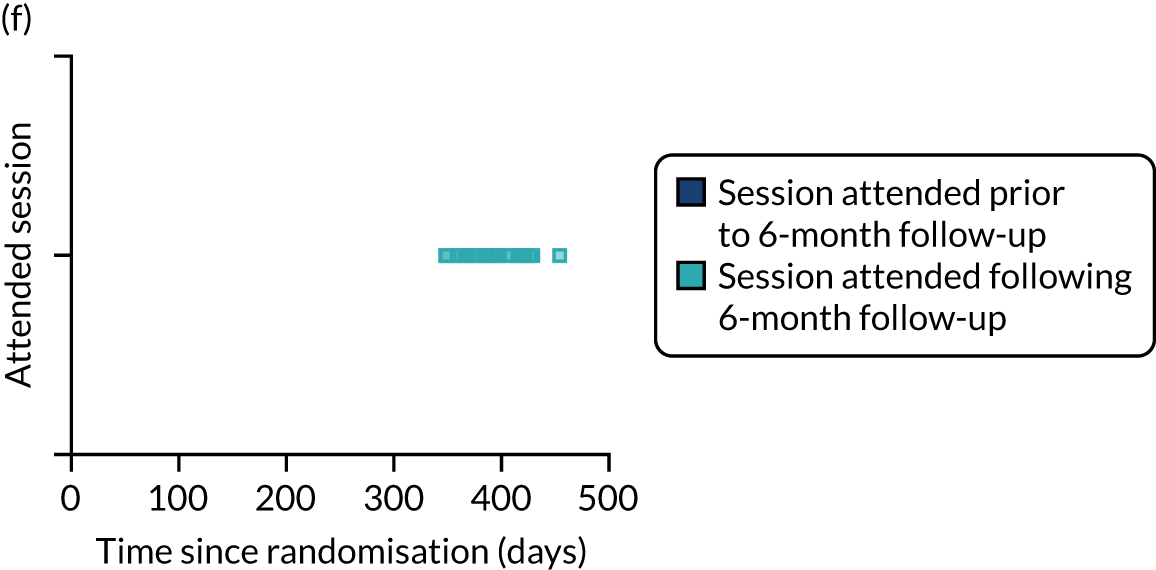
| Participant | Days from randomisation to initiation of SIT | Number of sessions attended in total | Number of sessions attended prior to 6-month follow-up |
|---|---|---|---|
| A | 48 | 22 | 20 |
| B | 29 | 21 | 21 |
| C | 20 | 19 | 19 |
| D | 119 | 23 | 13 |
| E | 85 | 8 | 8 |
| F | 348 | 21 | 0 |
Outcome variables are summarised in Tables 19 and 20 at baseline and at 6 and 12 months post randomisation. For the primary outcome (i.e. ABC-I), Figure 8 illustrates baseline and 6-month scores by study site.
| Measure | Study arm | |||||
|---|---|---|---|---|---|---|
| Intervention | Control | |||||
| n | Mean (SD) | Range | n | Mean (SD) | Range | |
| ABC (higher scores reflect higher levels of behaviour/worse outcome) | ||||||
| ABC-I: range 0–45 | 69 | 21.20 (9.22) | 2–42 | 69 | 21.09 (9.64) | 1–42 |
| ABC-W: range 0–48 | 69 | 15.41 (7.64) | 3–41 | 69 | 13.67 (7.55) | 1–37 |
| ABC-S: range 0–21 | 69 | 7.55 (4.83) | 0–21 | 69 | 7.62 (5.07) | 0–21 |
| ABC-H: range 0–48 | 69 | 26.90 (9.70) | 5–45 | 69 | 27.49 (10.73) | 7–48 |
| ABC-IS: range 0–12 | 69 | 5.14 (2.85) | 0–12 | 69 | 5.38 (3.27) | 0–12 |
| VABS (standardised, mean 100) | ||||||
| Composite score | 57 | 65 (6.31) | 49–82 | 62 | 66 (5.21) | 54–84 |
| VABS domain | ||||||
| Communication | 66 | 72 (10.32) | 49–100 | 66 | 71 (6.61) | 59–95 |
| Daily living skills | 64 | 63 (6.57) | 46–79 | 65 | 63 (8.44) | 28–89 |
| Socialisation | 61 | 65 (7.75) | 51–85 | 63 | 65 (6.62) | 51–81 |
| APSI: range 0–65 (higher score indicates more stress) | 69 | 24.59 (10.03) | 3–48 | 69 | 24.43 (9.10) | 8–49 |
| EQ-5D-5L | ||||||
| EQ-VAS: range from 0 (worst health) to 100 (best health) | 69 | 75 (70–80)a | 20–100 | 69 | 80 (70–87)a | 9–100 |
| Index value: range from –0.28 to 1 (higher score indicates better health) | 69 | 0.77 (0.72–0.88)a | 0.15–1 | 69 | 0.84 (0.74–0.88)a | –0.27–1 |
| CarerQoL (higher score reflects better care situation) | ||||||
| CarerQol-7D: range 0–14 | 69 | 7.77 (2.43) | 3–13 | 69 | 8.09 (2.42) | 1–14 |
| CarerQol-VAS: range 0–10 | 69 | 6.63 (1.43) | 3–10 | 69 | 6.60 (1.74) | 2–10 |
| Measure | 6 months | 12 months | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | |||||||||
| n | Mean (SD) | Range | n | Mean (SD) | Range | n | Mean (SD) | Range | n | Mean (SD) | Range | |
| ABC (higher scores reflect higher levels of behaviour/worse outcome) | ||||||||||||
| ABC-I: range 0–45 | 57 | 18.54a (9.33) | 1–43 | 49 | 18.82a (10.48) | 1–39 | 52 | 17.69 (9.00) | 0–37 | 44 | 19.93 (11.19) | 1–43 |
| ABC-W: range 0–48 | 49 | 12.35 (8.09) | 2–34 | 36 | 11.61 (5.93) | 0–25 | 36 | 14 (7.75) | 1–31 | 24 | 12.71 (6.52) | 1–28 |
| ABC-S: range 0–21 | 49 | 5.71 (4.45) | 0–18 | 36 | 5.94 (4.60) | 0–17 | 36 | 6.31 (4.40) | 0–17 | 24 | 5.50 (3.97) | 0–16 |
| ABC-H: range 0–48 | 49 | 22.76 (9.42) | 8–41 | 36 | 24.58 (11.71) | 1–46 | 36 | 23.06 (10.59) | 5–45 | 24 | 25.46 (11.84) | 4–46 |
| ABC-IS: range 0–12 | 49 | 4.51 (2.80) | 0–12 | 36 | 4.81 (3.56) | 0–12 | 36 | 5.17 (2.80) | 1–12 | 24 | 5.25 (3.29) | 0–11 |
| ABC-I (teacher assessed): range 0–45 | 25 | 9.60 (10.06) | 0–35 | 19 | 10.48 (9.48) | 0–34 | Not measured | Not measured | ||||
| VABS (standardised, mean 100) | ||||||||||||
| Composite | 39 | 67 (6.52) | 44–85 | 31 | 67 (6.52) | 57–85 | 22 | 64 (5.59) | 55–78 | 14 | 65 (4.96) | 55–71 |
| Domain | ||||||||||||
| Communication | 42 | 73 (8.99) | 57–100 | 32 | 72 (7.08) | 61–85 | 24 | 70 (9.51) | 52–93 | 16 | 72 (7.67) | 59–87 |
| Daily living skills | 42 | 62 (8.06) | 27–75 | 32 | 64 (6.44) | 54–83 | 24 | 62 (5.75) | 48–73 | 15 | 62 (4.25) | 52–68 |
| Socialisation | 39 | 68 (6.87) | 51–85 | 31 | 68 (10.63) | 55–96 | 22 | 65 (7.28) | 51–78 | 16 | 64 (8.62) | 51–81 |
| APSI: range 0–65 (higher score indicates more stress) | 48 | 20.08 (8.11) | 4–37 | 35 | 20.14 (8.91) | 0–40 | 36 | 21.17 (8.76) | 8–42 | 24 | 20.88 (8.79) | 6–36 |
| EQ-5D-5L | ||||||||||||
| EQ-VAS: range from 0 (worst health) to 100 (best health) | 48 | 75 (70–80)b | 7–96 | 35 | 80 (75–85)b | 50–100 | 36 | 72.5 (60, 82.5) | 10–90 | 24 | 80 (65, 87.5) | 45–95 |
| Index value: range from –0.28 to 1 (higher values indicate better health) | 48 | 0.77 (0.74–0.88)b | 0.17–1 | 35 | 0.84 (0.73–0.88)b | 0.17–1 | 36 | 0.84 (0.71, 0.88) | –0.19–1 | 24 | 0.78 (0.69, 0.88) | 0.11–1 |
| CarerQoL (higher score reflects better care situation) | ||||||||||||
| CarerQol-7D: range 0–14 | 48 | 8.02 (2.43) | 3–12 | 35 | 8.31 (2.60) | 3–13 | 36 | 7.67 (2.57) | 2–12 | 24 | 7.63 (2.99) | 3–13 |
| CarerQol-VAS: range 0–10 | 48 | 6.71 (1.79) | 2–10 | 35 | 7.15 (1.24) | 5–9.3 | 36 | 6.60 (1.35) | 2–10 | 24 | 7.08 (1.14) | 5–9 |
FIGURE 8.
ABC-I scores at baseline and 6 months, by site. (a) Site 1, Aneurin Bevan; (b) site 2, Cardiff and Vale; (c) site 3, Cornwall; (d) site 4, Cwm Taf; (e) site 5, Hywel Dda; (f) site 6, Pace Centre; and (g) site 7, Swansea Bay.
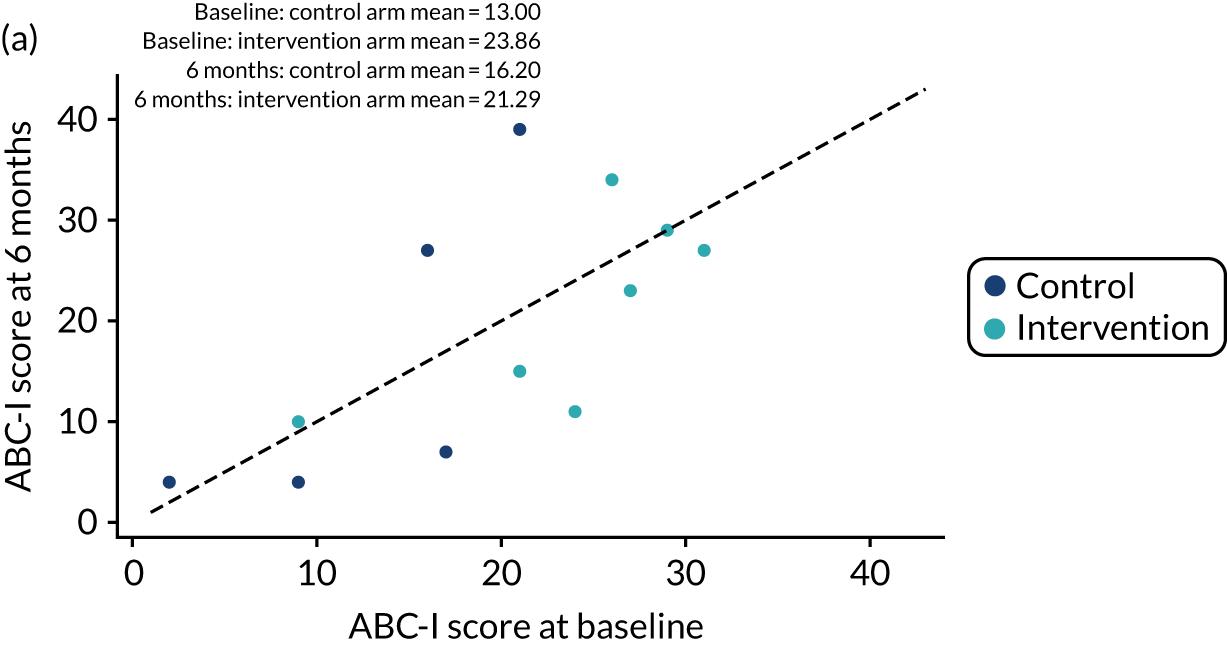
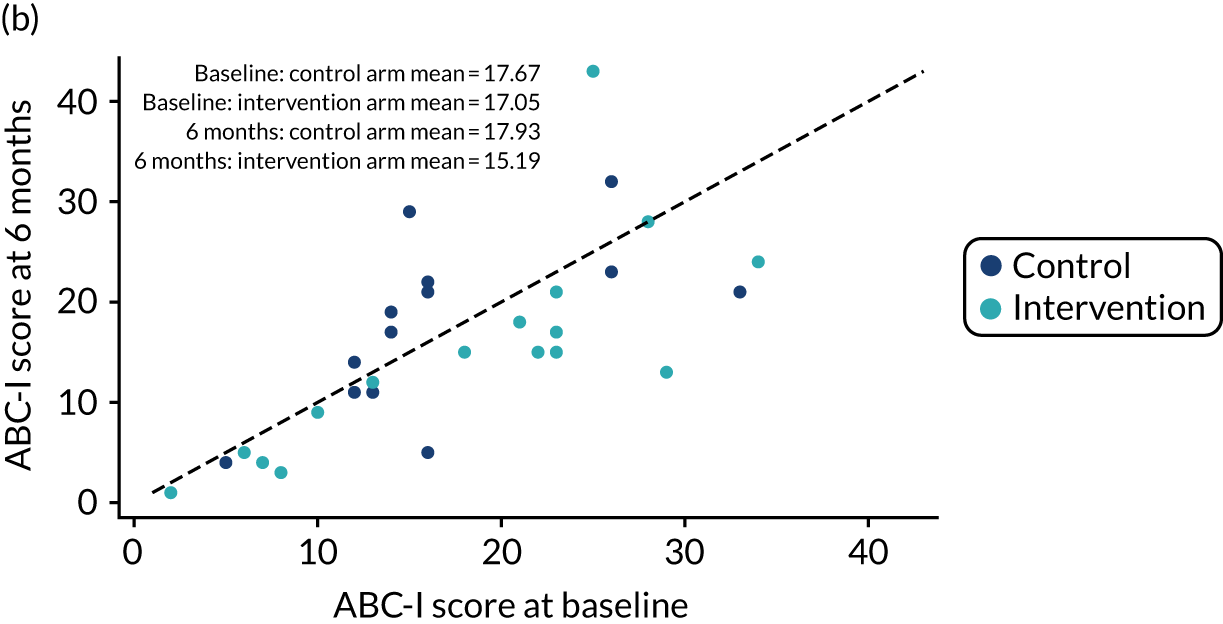
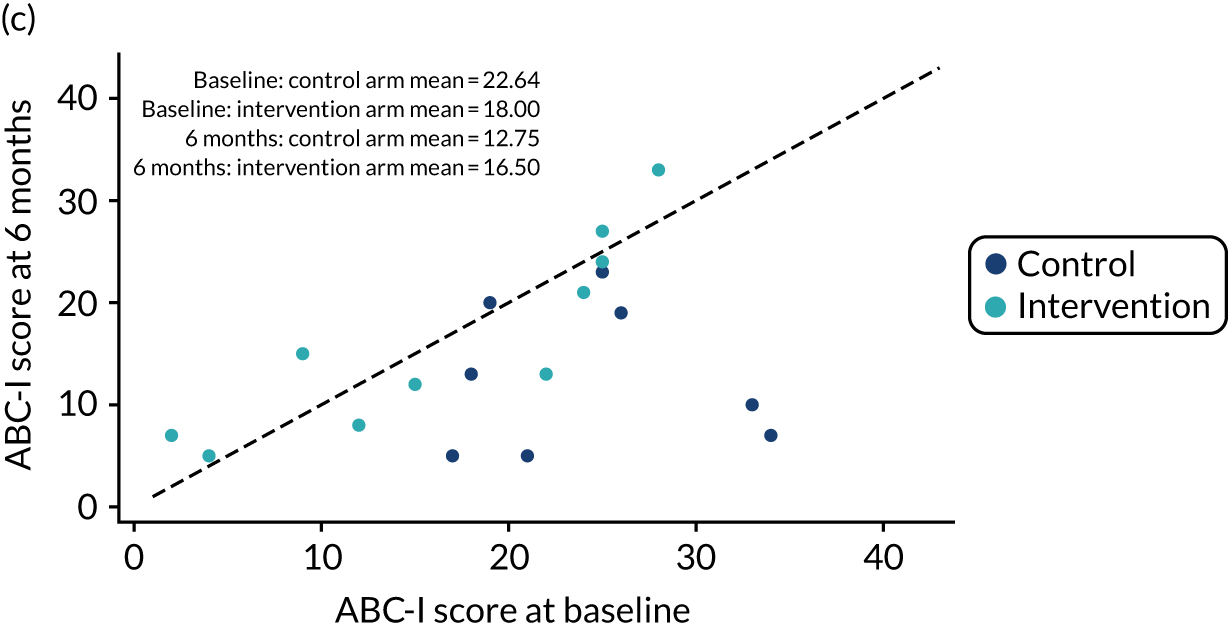
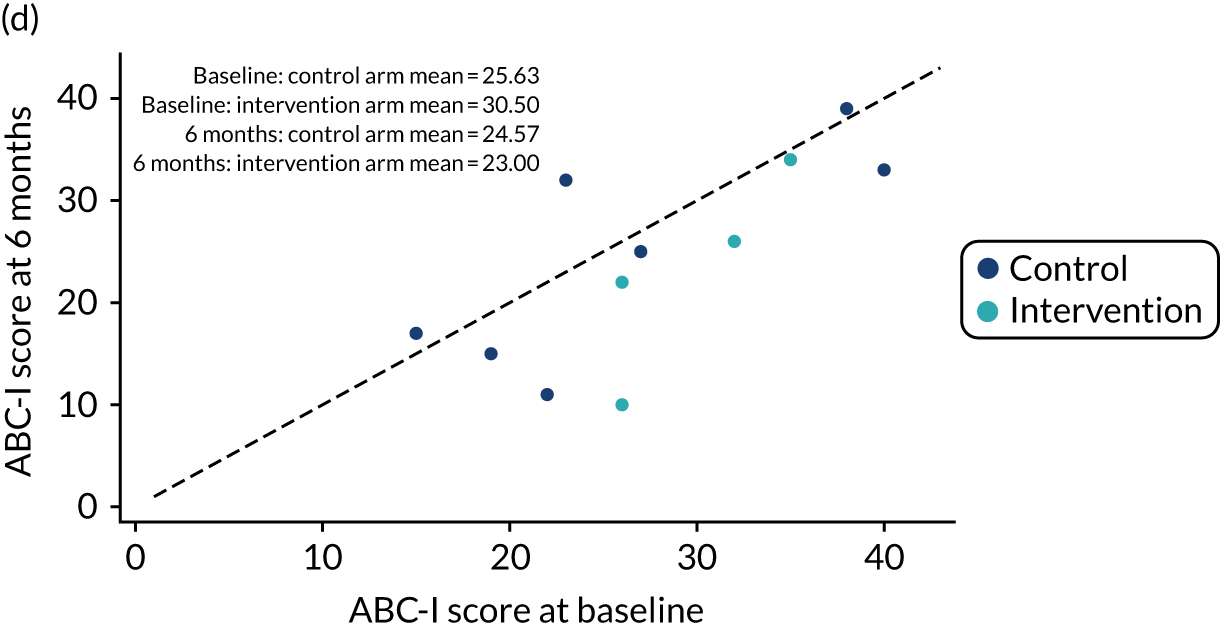
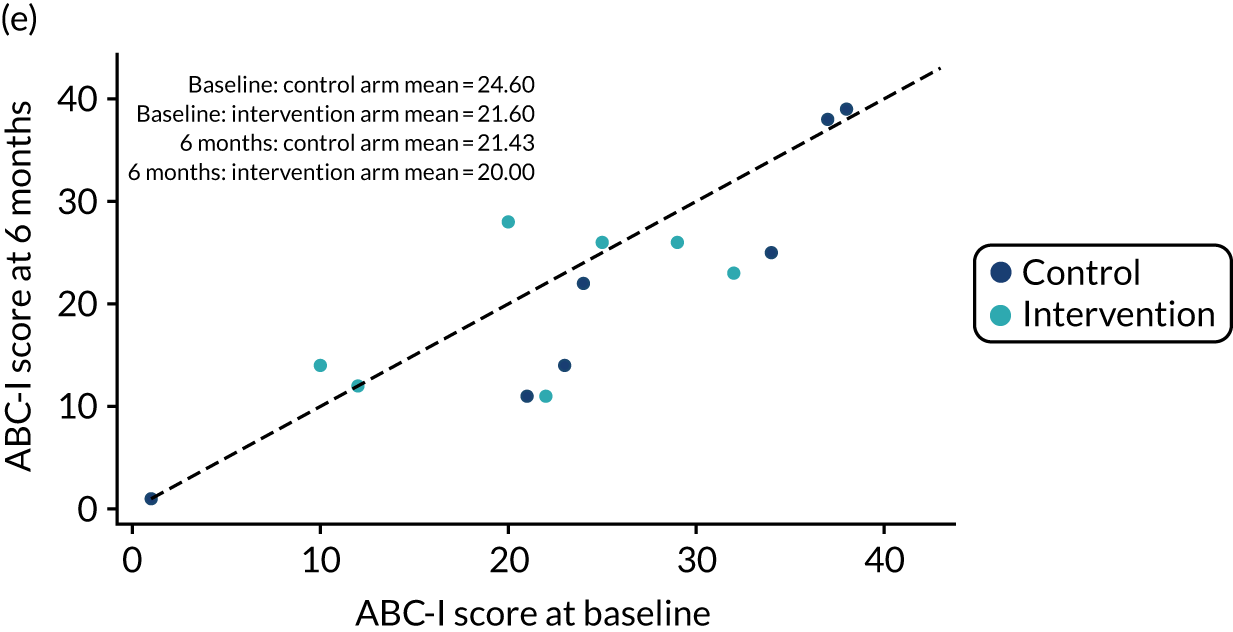
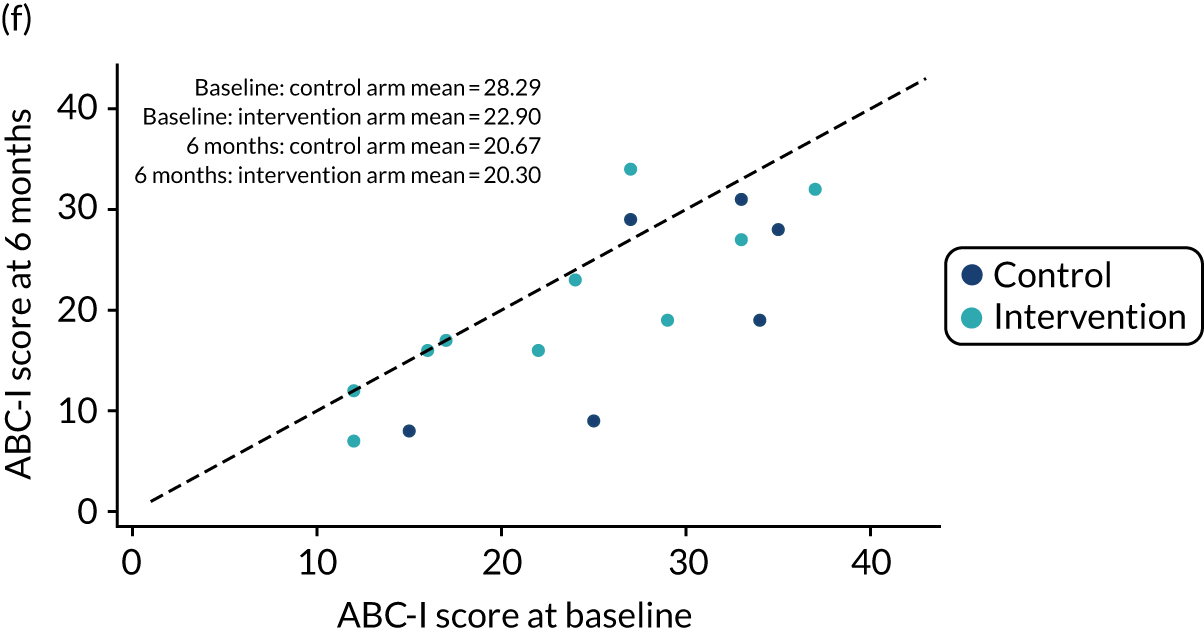
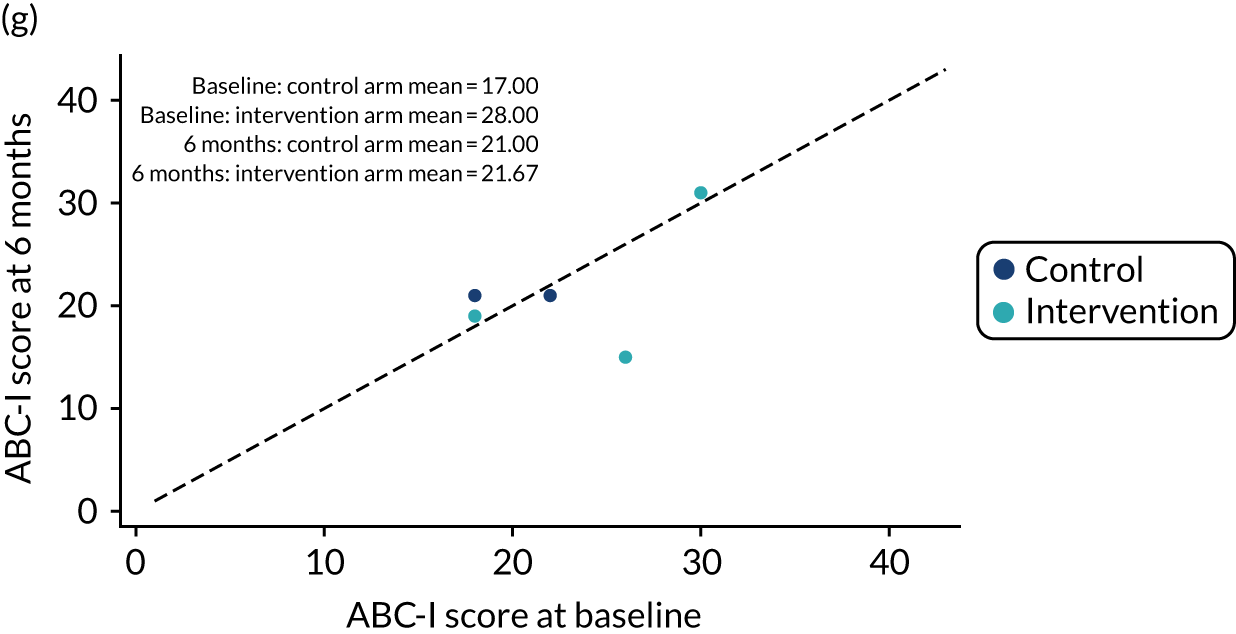
Our primary analysis included 106 participants. At 6 months post randomisation, the mean ABC-I score was 18.8 (SD 10.48) in the control arm and 18.5 (SD 9.33) in the intervention arm. The correlation between baseline and 6-month ABC-I score was 0.698 (95% CI 0.585 to 0.784). After adjusting for baseline ABC-I, sex of child, SPM category and region, the between-arm difference was 0.40 points higher in the intervention arm than in the control arm (95% CI –2.33 to 3.14; p = 0.77) (Table 21).
| Measure | n | Estimate | 95% CI | p-value |
|---|---|---|---|---|
| ABC score | ||||
| ABC-I | 106 | 0.40 | –2.33 to 3.14 | 0.77 |
| ABC-W | 85 | –0.45 | –2.73 to 1.84 | 0.70 |
| ABC-S | 85 | –0.22 | –1.60 to 1.16 | 0.75 |
| ABC-H | 85 | –0.19 | –3.32 to 2.95 | 0.91 |
| ABC-IS | 85 | –0.23 | –1.29 to 0.82 | 0.66 |
| VABS | ||||
| Composite | 63 | –0.17 | –2.74 to 2.40 | 0.90 |
| Communication | 72 | 1.02 | –1.54 to 3.59 | 0.42 |
| Daily living skills | 71 | –2.06 | –5.12 to 0.99 | 0.18 |
| Socialisation | 65 | –0.63 | –3.91 to 2.66 | 0.71 |
| APSI | 83 | 0.17 | –2.96 to 3.30 | 0.91 |
| EQ-5D-5L | ||||
| EQ-VAS | 83 | –4.18 | –10.73 to 2.37 | 0.21 |
| Index value | 83 | 0.01 | –0.06 to 0.08 | 0.71 |
| CarerQol | ||||
| CarerQol-7D | 83 | –0.07 | –0.93 to 0.79 | 0.87 |
| CarerQol-VAS | 83 | –0.38 | –0.98 to 0.20 | 0.19 |
Secondary analysis of primary outcome
Accounting for repeated measures over time, the between-arm difference was 0.61 points lower in the intervention arm than in the control arm (95% CI –3.13 to 1.92; p = 0.64). The conclusions drawn from our primary analysis were also unaffected by sensitivity analyses accounting for missing data (see Table 28), intervention receipt (see Table 28) or the COVID-19 pandemic (see Table 27).
At 12 months post randomisation, an ABC-I score was available for 96 participants. The mean ABC-I score was 19.9 (SD 11.19) in the control arm and 17.7 (SD 9.33) in the intervention arm. After adjusting for baseline ABC-I, sex of child, SPM category and region, the between-arm difference was 2.01 points lower in the intervention arm than in the control arm (95% CI –5.38 to 1.36; p = 0.24).
Secondary outcomes
Behavioural measures
At 6 months post randomisation, secondary outcomes relating to behaviour were available for 85 participants. There was no evidence of any differences between arms across the lethargy/social withdrawal, stereotypic behaviour, hyperactivity or inappropriate speech domains of the ABC (see Table 21).
At 12 months post randomisation, secondary outcomes relating to behaviour were available for 60 participants. Similarly, we found no evidence of any differences between arms across these measures (Table 22).
| Measure | n | Estimate | 95% CI | p-value |
|---|---|---|---|---|
| ABC score | ||||
| ABC-I | 96 | –2.01 | –5.38 to 1.36 | 0.24 |
| ABC-W | 60 | 0.78 | –2.49 to 4.04 | 0.64 |
| ABC-S | 60 | 0.08 | –1.86 to 2.03 | 0.93 |
| ABC-H | 60 | –1.46 | –6.09 to 3.17 | 0.52 |
| ABC-IS | 60 | 0.10 | –1.26 to 1.47 | 0.88 |
| VABS | ||||
| Composite | 32 | –0.90 | –4.01 to 2.21 | 0.56 |
| Communication | 39 | –5.69 | –9.87 to –1.51 | 0.009 |
| Daily living skills | 37 | –0.46 | –3.07 to 2.15 | 0.72 |
| Socialisation | 35 | 0.15 | –4.55 to 4.85 | 0.95 |
| APSI | 60 | 0.49 | –3.47 to 4.46 | 0.81 |
| EQ-5D-5L | ||||
| EQ-VAS | 60 | –5.29 | –14.03 to 3.45 | 0.23 |
| Index value | 60 | 0.03 | –0.07 to 0.13 | 0.60 |
| CarerQol | ||||
| CarerQol-7D | 60 | 0.16 | –1.03 to 1.35 | 0.79 |
| CarerQol-VAS | 60 | –0.31 | –0.92 to 0.31 | 0.32 |
Adaptive behaviour measures
The analysis of adaptive behaviour measures at 6 months included between 63 and 72 participants. For the composite measure and communication, socialisation and daily living skills domains, there was no evidence of any differences between arms (see Table 20). At 12 months, the communication domain score was 5.69 points lower in the intervention arm than in the control arm (95% CI –9.87 to –1.51; p = 0.009). There was no evidence of any differences between arms for the composite measure or other domains (see Table 20).
However, an error in administration of this measure for the majority of participants meant that we had introduced an artificial ceiling effect and scores were potentially less sensitive to change. Start points of each subdomain depend on the child’s chronological age, and age ranges are given as indicators of where performance might be expected to lie. Indicative upper limits are not intended to be used as cut-off points during administration, but were, for most participants, potentially limiting the magnitude of change that could be observed. It is uncertain whether or not this error masked any differences between arms with regard to adaptive behaviour domains. However, given the absence of any marginal effects (excepting a negative effect on communication at 12 months, which may also be reflective of multiple testing) and an absence of effect across other outcomes, this is perhaps unlikely.
Parenting stress
At 6 months, APSI scores were available for 83 participants. We found no evidence of between-arm differences for this measure. Similarly, we found no evidence of between-arm differences at 12 months.
Health utility and quality of life
At 6 months, EQ-5D and CarerQoL scores were available for 83 participants. Similar to other outcomes, we found no evidence of any differences between arms with regard to health utility, generic health-related quality of life or carer quality of life (see Table 20). Similarly, we found no evidence of between-arm differences at 12 months (see Table 20).
Teacher-assessed Aberrant Behavior Checklist – irritability
The mean of the difference between carer- and teacher-assessed ABC-I at 6 months was 10.28 (SD 14.48), with a 95% limit of agreement of –18.12 to 38.68. There was strong evidence of difference between the two measures (p < 0.001), indicating that, on average, carer-assessed ABC-I scores were higher (Figure 9).
FIGURE 9.
Carer- and teacher-assessed ABC-I. Mean difference of 10.28; 95% limits of agreement of –18.12 to 38.68.
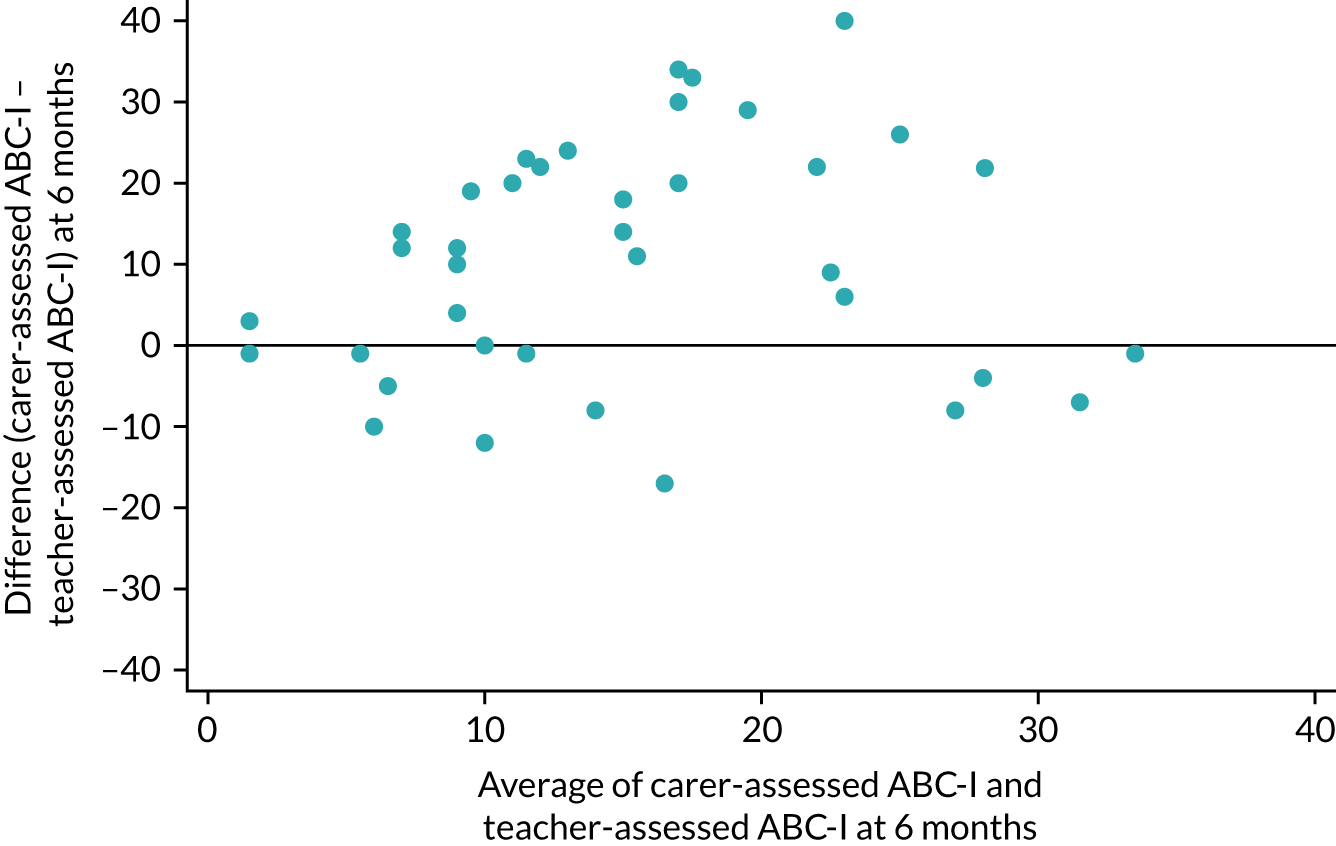
Canadian Occupational Performance Measure
Carer-rated goal performance and satisfaction were available for 43 and 42 participants, respectively. There was strong evidence of an increase in score between session 1 and session 24 for both measures (p < 0.001 for both). The mean change in score was 2.75 (95% CI 2.14 to 3.37) for carer-rated performance and the mean change in score was 3.34 (95% CI 2.63 to 4.40) for carer-rated satisfaction. Child-rated outcomes were available for between 10 and 12 participants. There was evidence of an increase in score for both performance and satisfaction (p = 0.01 for both) (Table 23).
| COPM | n | Session 1, mean (SD) | Session 24, mean (SD) | Difference (session 24 – session 1) | p-value | |
|---|---|---|---|---|---|---|
| Mean (SD) | 95% CI | |||||
| Carer rated | ||||||
| Performance | 43 | 3.29 (1.46) | 6.04 (1.51) | 2.75 (1.99) | 2.14 to 3.37 | < 0.001 |
| Satisfaction | 42 | 3.09 (1.54) | 6.43 (1.75) | 3.34 (2.27) | 2.63 to 4.04 | < 0.001 |
| Child rated | ||||||
| Performance | 12 | 4.30 (2.00) | 6.78 (1.44) | 2.48 (2.75) | 0.73 to 4.22 | 0.01 |
| Satisfaction | 10 | 3.89 (1.95) | 6.23 (0.94) | 2.34 (2.27) | 0.72 to 3.96 | 0.01 |
Subgroup analysis
Subgroup effects for the Aberrant Behavior Checklist – irritability
We found evidence of a differential effect of SIT on the ABC-I at 6 months by region (intervention arm × South England region interaction = 9.77, 95% CI 4.04 to 15.49; p = 0.001), indicating higher levels of irritability in the South England intervention arm at 6 months.
There was some evidence suggesting that there was also a differential effect of SIT on the ABC-I at 6 months by sex of child (intervention arm × female = 6.42, 95% CI 0.00 to 12.85; p = 0.050), with the intervention being less effective in girls than in boys.
There was also some evidence to suggest that the intervention was more effective in those with ADHD (intervention arm × ADHD present = –6.77, 95% CI –13.55 to –0.01; p = 0.050). We found no evidence of a differential effect of SIT on the ABC-I at 6 months by SPM range or general comorbidity, or by ID and other neurodevelopmental or genetic condition specifically (Table 24).
| Subgroup analysis | Variable | Estimate | 95% CI | p-value |
|---|---|---|---|---|
| Region (reference group = South Wales) | SIT main effect | –2.62 | –5.77 to 0.53 | 0.10 |
| S-WE region main effect | –8.42 | –12.72 to –4.12 | < 0.001 | |
| SIT × S-WE region interaction | 9.77 | 4.04 to 15.49 | 0.001 | |
| Age (continuous variable) | SIT main effect | –5.83 | –18.52 to 6.85 | 0.36 |
| Age main effect | –0.50 | –1.66 to 0.65 | 0.39 | |
| SIT × age interaction | 0.81 | –0.80 to 2.42 | 0.32 | |
| Sex (reference group = male) | SIT main effect | –1.08 | –4.16 to 2.00 | 0.49 |
| Female main effect | –1.96 | –6.79 to 2.87 | 0.42 | |
| SIT × female interaction | 6.42 | –0.00 to 12.85 | 0.05 | |
| SPM range (reference group = some problems) | SIT main effect | 1.82 | –4.17 to 7.81 | 0.55 |
| Definite dysfunction main effect | 0.75 | –4.63 to 6.13 | 0.78 | |
| SIT × definite dysfunction interaction | –1.79 | –8.54 to 4.96 | 0.60 | |
| Comorbiditya (reference group = no comorbidity) | SIT main effect | 0.73 | –3.39 to 4.84 | 0.73 |
| Comorbidity present main effect | 3.35 | –1.09 to 7.79 | 0.14 | |
| SIT × comorbidity present interaction | –1.08 | –6.92 to 4.75 | 0.71 | |
| ADHDa (reference group = no ADHD) | SIT main effect | 1.28 | –2.01 to 4.58 | 0.44 |
| ADHD present main effect | 7.91 | 2.48 to 13.34 | 0.01 | |
| SIT × ADHD present interaction | –6.77 | –13.55 to –0.01 | 0.05 | |
| IDa (reference group = no ID) | SIT main effect | –0.09 | –3.26 to 3.08 | 0.96 |
| ID present main effect | 3.88 | –3.37 to 11.13 | 0.29 | |
| SIT × ID present interaction | –1.03 | –10.10 to 8.05 | 0.82 | |
| Other neurodevelopmental or genetica (reference group = not present) | SIT main effect | –0.66 | –4.06 to 2.73 | 0.70 |
| Neurodevelopmental/genetic present main effect | –0.87 | –5.83 to 4.09 | 0.73 | |
| SIT × neurodevelopmental/genetic present interaction | 3.29 | –4.05 to 10.64 | 0.38 |
| Subgroup analysis | Variable | Estimate | 95% CI | p-value |
|---|---|---|---|---|
| Region (reference group = South Wales) | SIT main effect | –2.25 | –6.05 to 1.56 | 0.24 |
| S-WE region main effect | –4.02 | –9.30 to 1.26 | 0.13 | |
| SIT × S-WE region interaction | 7.01 | 0.45 to 13.56 | 0.04 | |
| Age (continuous variable) | SIT main effect | 9.69 | –4.79 to 24.18 | 0.19 |
| Age main effect | 0.65 | –0.73 to 2.03 | 0.35 | |
| SIT × age interaction | –1.24 | –3.08 to 0.60 | 0.18 | |
| Sex (reference group = male) | SIT main effect | 0.03 | –3.46 to 3.52 | 0.99 |
| Female main effect | 0.66 | –5.34 to 6.66 | 0.83 | |
| SIT × female interaction | 0.73 | –7.24 to 8.70 | 0.86 | |
| SPM range (reference group = some problems) | SIT main effect | 2.73 | –3.58 to 9.04 | 0.39 |
| Definite dysfunction main effect | 1.21 | –4.58 to 7.00 | 0.68 | |
| SIT × definite dysfunction interaction | –3.40 | –10.67 to 3.87 | 0.36 | |
| Comorbiditya (reference group = no comorbidity) | SIT main effect | 1.31 | –3.45 to 6.08 | 0.58 |
| Comorbidity present main effect | 3.65 | –1.69 to 8.99 | 0.18 | |
| SIT × comorbidity present interaction | –4.02 | –10.78 to 2.74 | 0.24 | |
| ADHDa (reference group = no ADHD) | SIT main effect | –0.19 | –4.08 to 3.69 | 0.92 |
| ADHD present main effect | 2.14 | –4.35 to 8.62 | 0.51 | |
| SIT × ADHD present interaction | –2.83 | –10.78 to 5.13 | 0.48 | |
| IDa (reference group = no ID) | SIT main effect | –1.45 | –4.93 to 2.03 | 0.41 |
| ID present main effect | 0.58 | –9.43 to 10.59 | 0.91 | |
| SIT × ID present interaction | 5.25 | –6.88 to 17.39 | 0.39 | |
| Other neurodevelopmental or genetica (reference group = not present) | SIT main effect | 1.28 | –2.44 to 4.99 | 0.50 |
| Neurodevelopmental/genetic present main effect | 5.78 | 0.19 to 11.37 | 0.04 | |
| SIT × neurodevelopmental/genetic present interaction | –9.53 | –18.08 to –0.98 | 0.03 |
Subgroup effects for the Autism Parenting Stress Index
Similarly, we found some evidence of a differential effect of SIT on carer stress (using the APSI) at 6 months by region (intervention arm × South England region interaction = 7.01, 95% CI 0.45 to 13.56; p = 0.04) (Table 25). There was also some evidence to suggest that there was a differential effect of SIT on APSI at 6 months by the presence of other neurodevelopmental or genetic conditions (intervention arm × neurodevelopmental/genetic condition present = –9.53, 95% CI –18.08 to –0.98; p = 0.030).
We found no evidence of a differential effect of SIT on the ABC-I at 6 months by sex of child, SPM range or general comorbidity, or by ID and ADHD specifically (see Table 24).
Additional sensitivity analyses
Accounting for intervention receipt
Figures 10–12 highlight that scores on the ABC-I at 6 months were generally lower (i.e. better) in those who initiated and received SIT than in those who received usual care.
FIGURE 10.
Distribution of ABC-I scores at 6 months in those who did and did not initiate SIT.
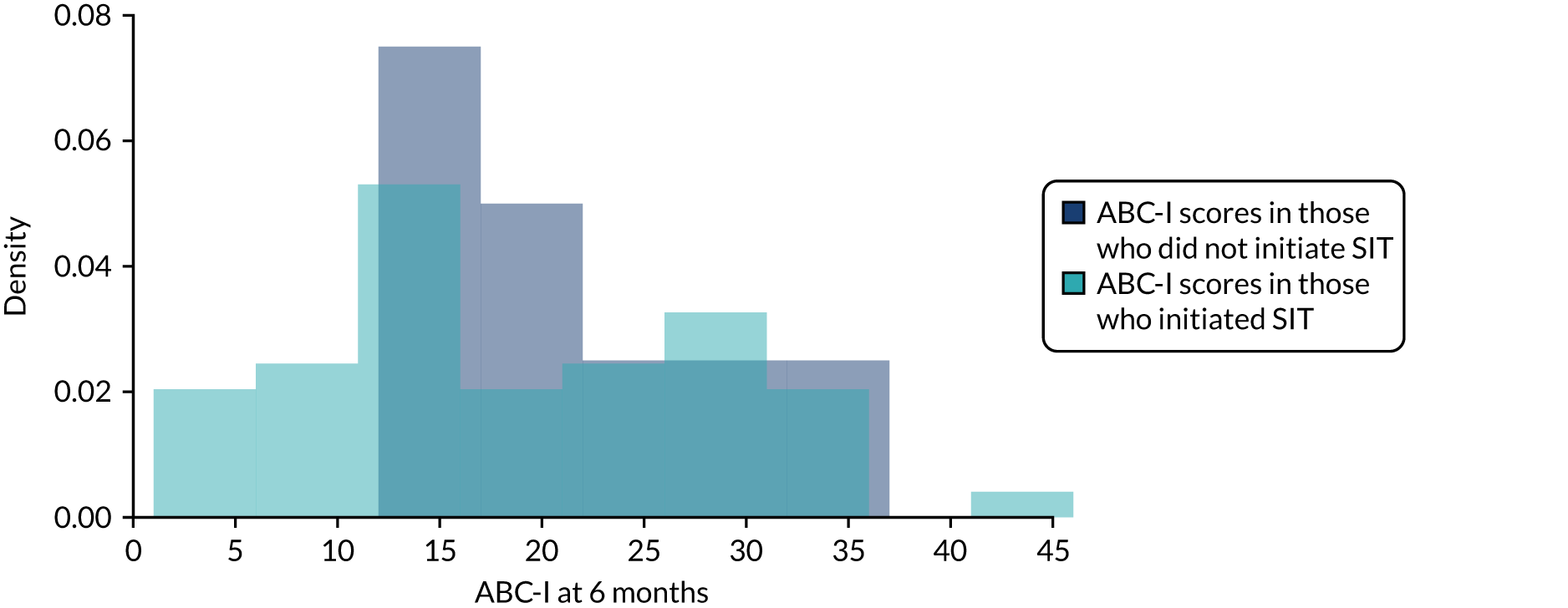
FIGURE 11.
Distribution of ABC-I scores at 6 months in those who did and did not receive at least 13 SIT sessions during the intensive phase.
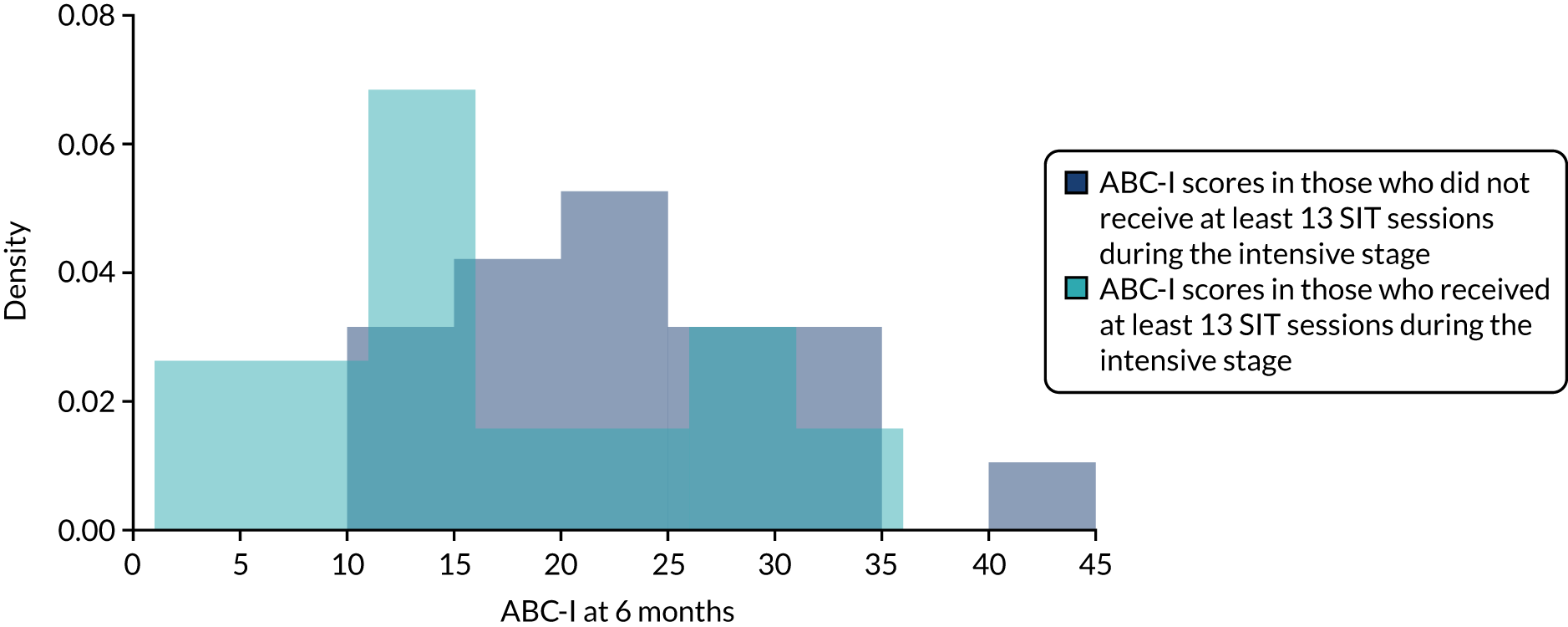
FIGURE 12.
Box plot of ABC-I scores at 6 months for those who received differing levels of SIT.
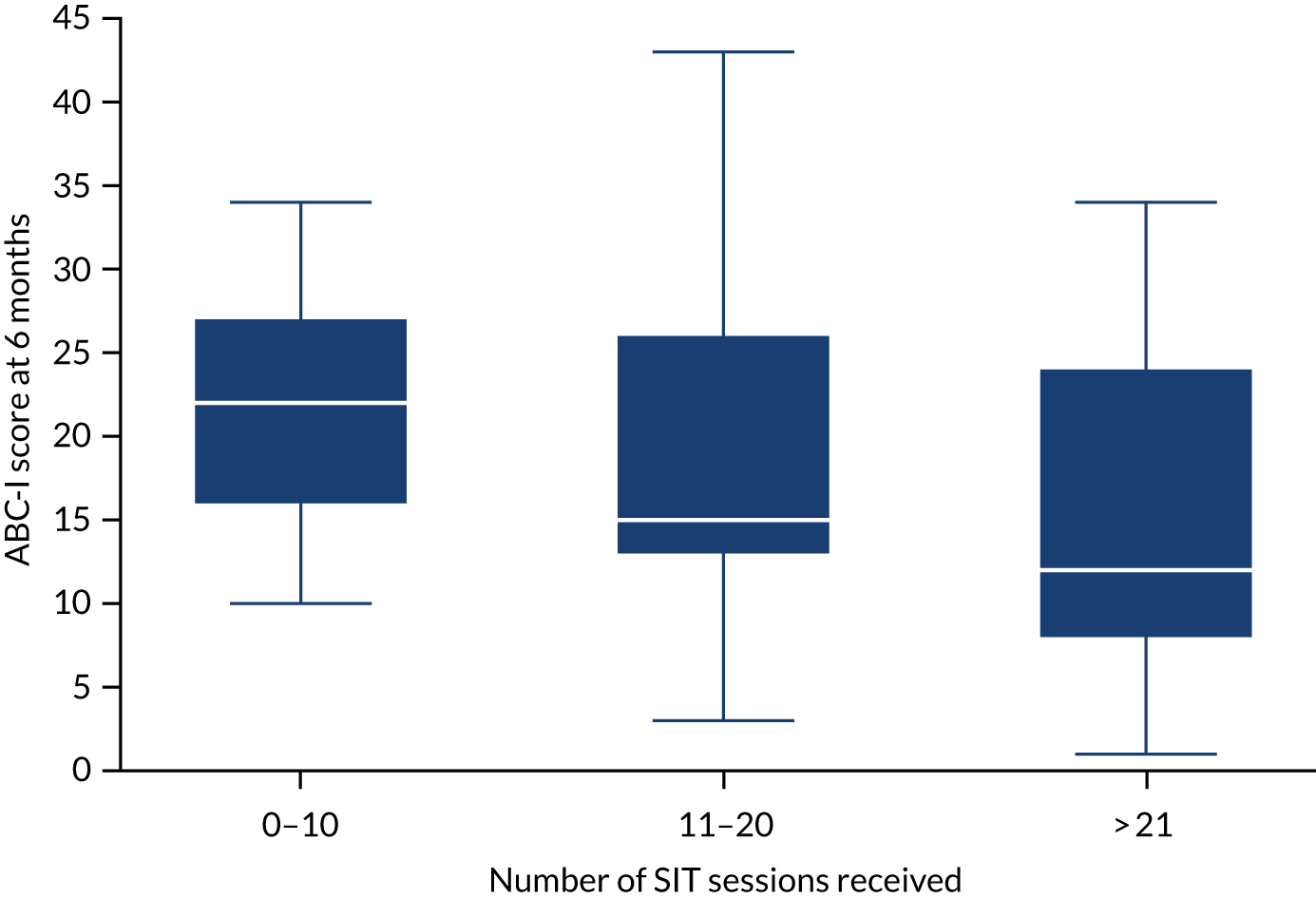
Table 26 provides results from the sensitivity analyses accounting for receipt of SIT. Although the point estimates change slightly, the conclusions drawn from the primary analysis remain unaltered.
| Analysis | n | Estimate | 95% CI |
|---|---|---|---|
| Primary (MITT) | 106 | 0.40 | –2.33 to 3.14 |
| Accounting for those who had not initiated SIT by 6 months | 106 | 0.46 | –2.56 to 3.48 |
| Accounting for the number of sessions attended by 6 months (per session) | 106 | 0.03 | –0.15 to 0.20 |
| Accounting for the number of sessions attended by 6 months (all sessions, i.e. row above multiplied by 26) | 106 | 0.69 | –3.82 to 5.19 |
| Accounting for those who did not attend at least 13 sessions during the intensive phase | 106 | 0.60 | –3.31 to 4.50 |
Impact of the COVID-19 pandemic
Changes of underlying event rates and/or treatment effects may change
Primary outcome data were collected for 11 participants during the intrapandemic period.
Although exclusion of those participants with primary outcome data available during the intrapandemic period led to an increase in our point estimate (i.e. between-arm adjusted mean difference of the ABC-I at 6 months), the CI remained wide and the conclusions drawn on our primary analysis remain unaltered (Table 27). Baseline to 6-month follow-up ABC-I correlation was slightly higher following exclusion of participants who provided 6-month data during the intrapandemic period. Figure 13 illustrates differences in ABC-I scores at 6 months by arm and by time period.
| Analysis | n | Estimate | 95% CI | p-value | ABC-I correlation between baseline and 6 months (95% CI) |
|---|---|---|---|---|---|
| Original primary analysis | 106 | 0.40 | –2.33 to 3.14 | 0.770 | 0.698 (0.585 to 0.784) |
| Primary analysis on participants followed up pre pandemic | 95 | 0.50 | –2.40 to 3.39 | 0.733 | 0.712 (0.596 to 0.799) |
FIGURE 13.
Box plots of ABC-I scores at 6 months by arm and by time period.
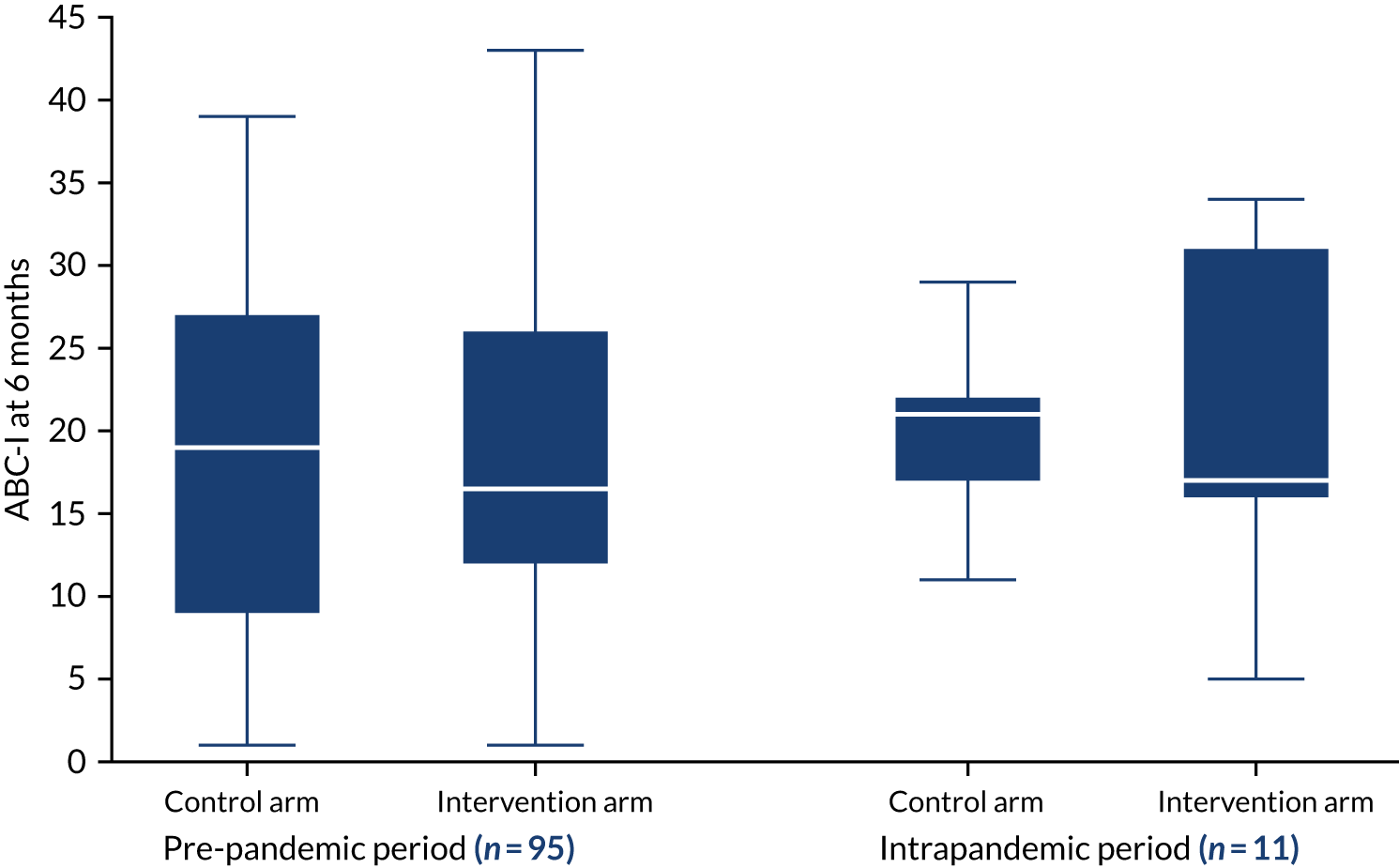
Missing outcome data
Primary outcome data were available for 106 out of 138 participants, with 30 out of 32 missing responses expected during the pre-pandemic period.
Intervention receipt
In total, 57 participants allocated to the intervention arm provided primary outcome data. Of these 57 participants, 38 received at least 13 out of 20 intensive intervention sessions, but 19 did not. Pandemic-related reasons were indicated for 11 out of 19 participants who did not receive an adequate level of SIT.
Impact of COVID-19 pandemic on trial findings
Table 28 shows that the findings in our primary analysis were insensitive to missing data and intervention receipt that was affected by the COVID-19 pandemic.
| Analysis | n | Estimate | 95% CI | p-value |
|---|---|---|---|---|
| Original primary analysis (MITT) | 106 | 0.40 | –2.33 to 3.14 | 0.770 |
| Original full ITT analysis with multiple imputation | 138 | 0.45 | –2.36 to 3.27 | 0.751 |
| Primary analysis on participants followed up pre pandemic | 95 | 0.50 | –2.40 to 3.39 | 0.733 |
| Pandemic-free world estimand | 138 | –0.20 | –3.30 to 2.90 | 0.896 |
| World including pandemic estimand | 138 | 0.40 | –2.30 to 3.10 | 0.770 |
Adverse events
There were no SAEs during the trial. One AE was reported to the trial team by a therapist as a SAE; however, it was clear that this event did not meet the criteria of ‘serious’ as laid out in the reporting guidance.
Chapter 7 Health economics
Introduction and methods
The aim of the economic evaluation was to compare the cost-effectiveness of SIT with that of usual care. The main evaluation took an NHS/PSS perspective81 and covered use of all hospital, community health and social services. A secondary analysis explored the sensitivity of the results using a broader societal perspective (including NHS/PSS costs, education costs, carer expenses and lost productivity). The primary economic analysis was an available-case analysis for cost and cost-effectiveness at 6-month follow-up of SIT compared with usual care, with outcome expressed as irritability/agitation (i.e. ABC-I). ABC-I data were collected at baseline and at 6 and 12 months post randomisation. All unit costs were for the financial year 2020/21 and updated where necessary. 82
Identification of resources
We collected resource use in the following cost-related profiles:
-
autism-related intervention (child)
-
autism-related carer programme
-
education services
-
use of NHS/PSS (child) –
-
GP
-
practice nurse
-
speech and language therapist
-
community paediatrician
-
CAMHS psychiatrist
-
clinical psychologist
-
counsellor/psychotherapist
-
behaviour support team
-
social worker
-
respite carer
-
outreach/family support worker.
-
-
hospital care services (child) –
-
inpatient admission (mental health and physical health)
-
accident and emergency attendances (requiring/not requiring hospital stay)
-
other (e.g. occupational therapist, physiotherapist, dentist, dietitian, optician and alternative therapies).
-
-
police and youth justice system (child)
-
use of NHS/PSS (carer) –
-
GP
-
practice nurse
-
counsellor
-
self-help/support group
-
alternative therapist
-
telephone helpline
-
hospital outpatient clinic
-
inpatient admission (mental health and physical health)
-
accident and emergency attendances (requiring/not requiring hospital stay).
-
-
out-of-pocket expenses (carer)
-
productivity costs (carer)
-
half-days off work (main carer) owing to participant’s condition.
-
Measure of resources
Intervention delivery
The intervention arm received 24 face-to-face and two telephone sessions, which were used as the basis for calculation of intervention costs.
Usual care
Data on usual-care services and support were recorded using the CSRI,75 and were adapted to reflect the type of data collected and to record service use that would facilitate cost estimation. Usual care involved contact with OT, autism-specific services and any other NHS services.
NHS/Personal Social Services
Information about the use of services by participants and carers was collected from carers at baseline and at 6- and 12-month follow-up, covering a retrospective 6-month period. Carers were asked to record contact with various services and professionals (for themselves and their child). At each time point, service use since the previous assessment was recorded.
Productivity losses
Data regarding the number of half-days taken off work by the main carer to provide support were collected (last 6 months).
Valuation of resources
All resources were costed by applying a unit cost (GBP) for the financial year 2020–21. Total resource use was calculated for each participant.
Sensory integration therapy sessions
The unit cost of an occupational therapist was derived using established unit costing principles. 83 Therapists were NHS band 7 and national insurance, superannuation contributions and overheads were added to the average salary. We used protocol-driven information on intervention sessions. A total of 24 sessions were delivered face to face and two were conducted over the telephone. All sessions lasted approximately 1 hour. To derive the cost of the intervention, we multiplied occupational therapist time spent delivering the intervention by the unit cost of an occupational therapist. The total cost of intervention delivery over 6 months was £1538.16 (Table 29), which is equivalent to a monthly cost of £256.36 per person.
NHS/Personal Social Services
For all health-care and social care service use data, including voluntary sector, nationally applicable unit costs were attached at 2020–21 prices, or at the most recent price level on which costs were available, to reflect long-run marginal opportunity costs from available public sources. Costs older than the chosen financial year were inflated using the NHS Cost Inflation Index. 82
Costs per unit of measurement for each NHS/PSS service type were taken from the Personal Social Services Research Unit Costs of Health and Social Care compendium. 82 NHS reference costs84 were used for inpatient and outpatient attendances and community-based services. Unit costs not obtained from these sources were estimated directly based on salary of the professional delivering a service, plus employer on-costs, overheads, costs of supervision and equipment/consumables.
Productivity costs
Productivity losses were calculated by multiplying time taken off work by carer’s wage rate. We calculated the hourly rate for each carer by dividing their gross annual income by the number of weeks per year and weekly working hours reported. We then multiplied rate per hour by number of hours in the half-days off work reported at follow-up assessments (Table 30).
| Service (unit) | Cost (£) | Source |
|---|---|---|
| Autism-related therapies | ||
| Early intensive applied behaviour analysis (minute) | 0.37 | Rodgers et al.85 |
| Social skills programme (hour) | 25.00 | Blooming Tree86 |
| Parent-mediated communication programme (minute) | 1.90 | Byford et al.,87 inflated to 2020/21 prices82 |
| Behaviour management training (day) | 75.00 | Child Autism UK88 |
| Alternative and augmentative systems (day) | 200.00 | Ace Centre89 |
| Parent nurture programme (hour) | 95.00 | Connect to Autism90 |
| ASD awareness (hour) | 23.00 | Dulwich Prep London91 |
| Cygnet/one-to-one classes with Bernardo’s (session) | 185.00 | Stuttard et al.,92 inflated to 2020/21 prices82 |
| Education-based services | ||
| Individual tuition at home (hour) | 60.00 | Tutorful93 |
| One-to-one support in school (hour) | 8.89 | Payscale94 |
| Group support in school (hour) | 11.64 | Education Endowment Foundation95 |
| School nurse (hour) | 49.20 | Prospects,96 Curtis and Burns,82 inflated to 2020/21 prices |
| Educational psychologist (minute) | 0.99 | Prospects,96 Curtis and Burns,82 inflated to 2020/21 prices |
| School counsellor (minute) | 0.82 | Prospects,96 PSSRU 2020, inflated to 2020/21 prices |
| SEN co-ordinator (minute) | 0.61 | Prospects,96 Curtis and Burns,82 inflated to 2020/21 prices |
| Autism specialist teacher (minute) | 0.61 | Prospects,96 Curtis and Burns,82 inflated to 2020/21 prices |
| Autism champion (minute) | 0.53 | Curtis and Burns,82 inflated to 2020/21 prices |
| Community-based services | ||
| GP visit (minute) | 4.35 | Curtis and Burns,82 inflated to 2020/21 prices |
| Practice nurse (minute) | 0.71 | Curtis and Burns,82 inflated to 2020/21 prices |
| CAMHS (minute) | 0.82 | Curtis and Burns,82 inflated to 2020/21 prices |
| Occupational therapist (minute) | 0.83 | Curtis and Burns,82 inflated to 2020/21 prices |
| Speech and language therapist (minute) | 0.69 | Curtis and Burns,82 inflated to 2020/21 prices |
| CAMHS psychiatrist (minute) | 2.67 | Curtis,97 inflated to 2020/21 prices |
| Clinical psychologist (minute) | 2.59 | Curtis,97 inflated to 2020/21 prices |
| Counsellor/psychotherapist (minute) | 1.65 | Curtis and Burns,82 inflated to 2020/21 prices |
| Behaviour support team (minute) | 1.01 | Netten and Curtis,98 inflated to 2020/21 prices |
| Social worker (minute) | 1.30 | Curtis and Burns,82 inflated to 2020/21 prices |
| Outreach worker (minute) | 0.43 | Curtis and Burns,82 inflated to 2020/21 prices |
| Dietitian (minute) | 1.60 | Curtis and Burns,99 inflated to 2020/21 prices |
| Radiographer (minute) | 0.88 | Curtis and Burns,82 inflated to 2020/21 prices |
| Physiotherapist (minute) | 0.84 | Curtis and Burns,82 inflated to 2020/21 prices |
| Endocrine consultant (minute) | 2.00 | Curtis and Burns,82 inflated to 2020/21 prices |
| Helpline (minute) | 0.82 | The National Archives,100 inflated to 2020/21 prices |
| Integrated Community Mental Health Teams (minute) | 0.78 | Curtis and Burns,101 inflated to 2020/21 prices |
| Primary mental health worker (minute) | 0.77 | Curtis and Burns,99 inflated to 2020/21 prices |
| Continence nurse (minute) | 1.38 | Curtis and Burns,99 inflated to 2020/21 prices |
| Counsellor (hour) | 55.54 | Slade et al.,102 inflated to 2020/21 prices |
| Community paediatrician (contact) | 157.00 | Curtis and Burns,82 inflated to 2020/21 prices |
| Respite care (session) | 100.00 | NHS103 |
| Paediatric consultant (contact) | 241.70 | Curtis and Burns,82 inflated to 2020/21 prices |
| Optician (contact) | 33.30 | Curtis and Burns,104 inflated to 2020/21 prices |
| Dentist (contact) | 135.90 | Curtis and Burns,82 inflated to 2020/21 prices |
| Audiologist (contact) | 107.80 | Curtis and Burns,82 inflated to 2020/21 prices |
| CBT therapist (session) | 106.00 | Curtis and Burns,82 inflated to 2020/21 prices |
| Hydrotherapy (session) | 80.00 | The Canine Fitness Centre105 |
| Chiropractor (session) | 55.00 | NHS106 |
| Art therapy (session) | 18.50 | Uttley et al.107 |
| Hospital-based care | ||
| Inpatient admission: physical health (bed-days) | 3440.16 | Department of Health and Social Care,84 inflated to 2020/21 prices |
| Accident and emergency: not admitted (attendance) | 145.21 | Department of Health and Social Care,84 inflated to 2020/21 prices |
| Accident and emergency: admitted (attendance) | 174.46 | Department of Health and Social Care,84 inflated to 2020/21 prices |
| Hospital outpatient clinic (appointments) | 206.85 | Department of Health and Social Care,84 inflated to 2020/21 prices |
| Day hospital (attendance) | 785.61 | Department of Health and Social Care,84 inflated to 2020/21 prices |
Data analysis
Resource use was reported as means by arm and as a percentage of the arm having at least one contact. Differences in service use between arms (i.e. baseline, 6-month follow-up and 12-month follow-up) were reported descriptively. All relevant data on service use and support were checked for missing values and values outside an acceptable range. Missing data were imputed using multiple imputation.
Service and support use
Differences in the number of participants using each type of service and the mean number of contacts were compared between arms at baseline, 6 months and 12 months. Resource use patterns are presented descriptively, given that the economic evaluation was focused on NHS/PSS and societal costs and cost-effectiveness and to avoid multiple testing.
Analysis of costs
The health economic analysis was an available-case analysis. Costs were calculated using data on the type, number and length of contacts. Mean costs were analysed using regression analysis and bootstrapping. We analysed differences between arms in health-care (i.e. NHS/PSS) or societal costs in secondary analyses at 6 months by regressing the total cost on treatment allocation, baseline ABC-I, recruitment region, severity of SPDs, sex of child and baseline costs. To mitigate effects of data skewness, non-parametric bootstrapping methods were used to estimate 95% CIs for mean costs with 10,000 resamples. No discounting was needed, as we assessed cost over periods of < 1 year.
Cost-effectiveness analysis
Cost-effectiveness analyses were conducted from an NHS/PSS perspective and a wider societal perspective. The primary economic analysis focused on cost-effectiveness of SIT compared with usual care, assessed in terms of cost per point improvement in carer-reported ABC-I. The incremental cost-effectiveness ratio (ICER) was calculated as the difference in mean costs divided by difference in mean ABC-I. 108
Cost-effectiveness acceptability curves (CEACs) were plotted to locate findings in their wider decision-making context. Non-parametric bootstrapping from cost and effectiveness data generated a joint distribution of incremental mean costs and effects for comparators to explore the probability that each is the optimal choice, subject to a range of maximum values (i.e. a ceiling ratio) that a decision-maker might be willing to pay for an additional point improvement in ABC-I. Each CEAC was derived using a net benefit approach. Monetary values of incremental effects and incremental costs for each case were combined, and net monetary benefit was derived as:
where λ is willingness to pay for a 1-point difference in ABC-I, and a and b denote SIT and usual care, respectively. We explored a range of willingness-to-pay values for each outcome.
Sensitivity analyses
An intention-to-treat analysis was carried out (with missing data imputed using multiple imputation) to explore the sensitivity of results using a broader societal perspective, including NHS/PSS costs, education service costs, carer expenses and lost productivity.
Results
Data completeness
At baseline, service use data were available for 138 participants (intervention, n = 69; usual care, n = 69). At 6-month follow-up, data were available for 60% of participants (intervention, n = 48; usual care, n = 35). At 12-month follow-up, 23 and 36 participants provided data in the control arm and intervention arm, respectively.
Resource use
The difference in service use between arms at baseline was broadly similar (Table 31). As shown in Table 32, at 6-month-follow-up, usual-care participants reported considerably higher contact with education services [mean 425.97 (SD 388.37) vs. mean 333.46 (SD 354.10)], slightly greater use of community-based health and social care services and more accident and emergency unit attendances (14.29% vs. 6.25%) than participants in the intervention arm. However, carers in the intervention arm spent, on average, more half-days off work [mean 18.19 (SD 37.22) days vs. mean 4.14 (SD 9.02) days]. At 12-month follow-up, modest but higher utilisation of health-care and social care resources was reported by families in the intervention arm across all categories (Table 33).
| Service use (unit) | Study arm | |||
|---|---|---|---|---|
| SIT (N = 69) | Usual care (N = 69) | |||
| n (%) using | Mean (SD) | n (%) using | Mean (SD) | |
| Child | ||||
| Autism intervention package (contact) | 3 (4.35) | 0.09 (0.54) | 6 (8.70) | 0.87 (5.01) |
| Service use by the child: education (contact) | 61 (88.41) | 332.59 (448.07) | 64 (92.75) | 302.51 (350.94) |
| Community-based health and social care | ||||
| GP (contact) | 29 (42.03) | 0.88 (1.81) | 26 (37.68) | 0.88 (1.57) |
| Paediatrician (contact) | 21 (30.43) | 0.33 (0.56) | 22 (31.88) | 0.44 (0.74) |
| SLT (contact) | 13 (18.84) | 0.61 (2.55) | 15 (21.74) | 0.44 (1.01) |
| Other community health-care services (contact) | 43 (62.31) | 4.00 (5.86) | 49 (71.01) | 4.32 (7.14) |
| Hospital-based health and social care | ||||
| Inpatient stay: physical health (bed-days) | 2 (2.90) | 0.04 (0.27) | 1 (1.45) | 0.02 (0.12) |
| Accident and emergency: not admitted (attendance) | 6 (8.70) | 0.22 (1.22) | 8 (11.59) | 0.22 (0.84) |
| Sibling | ||||
| Community-based health and social care | ||||
| Counsellor (contact) | 9 (13.04) | 1.29 (4.52) | 6 (8.70) | 0.36 (1.40) |
| Other community health-care services (contact) | 9 (13.04) | 0.54 (1.91) | 4 (5.80) | 0.65 (3.49) |
| Carer | ||||
| Autism-related training (minute) | 19 (27.54) | 2.09 (5.04) | 19 (27.54) | 1.25 (2.92) |
| Community-based health and social care | ||||
| GP (contact) | 29 (42.03) | 1.93 (5.23) | 22 (31.88) | 1.22 (2.34) |
| Other community health-care services (contact) | 25 (36.23) | 3.29 (8.92) | 21 (30.43) | 2.25 (5.08) |
| Hospital-based health and social care | ||||
| Inpatient stay: physical health (bed-days) | 0 (0.00) | 2 (2.90) | 0.04 (0.27) | |
| Accident and emergency: not admitted (attendance) | 2 (2.90) | 0.03 (0.17) | 3 (4.35) | 0.04 (0.21) |
| Accident and emergency: admitted (attendance) | 0 (0.00) | 2 (2.90) | 0.06 (0.38) | |
| Hospital outpatient clinic (appointments) | 7 (10.14) | 0.19 (0.67) | 7 (10.14) | 0.46 (1.88) |
| Out-of-pocket expensesa | 50 (72.46) | 38 (55.07) | ||
| Half-days off work | 29 (42.03) | 10.07 (23.27) | 26 (37.68) | 5.49 (24.27) |
| Service use (unit) | Study arm | |||
|---|---|---|---|---|
| SIT (N = 48) | Usual care (N = 35) | |||
| n (%) using | Mean (SD) | n (%) using | Mean (SD) | |
| Child | ||||
| Autism intervention package (contact) | 4 (8.33) | 0.08 (0.45) | 4 (11.43) | 1.69 (6.74) |
| Service use by the child: education (contact) | 41 (85.42) | 333.46 (354.10) | 32 (91.43) | 425.97 (388.37) |
| Community-based health and social care | ||||
| GP (contact) | 15 (31.25) | 0.92 (1.97) | 9 (25.71) | 0.66 (1.64) |
| Paediatrician (contact) | 13 (27.08) | 0.35 (0.64) | 13 (37.14) | 0.63 (1.03) |
| SLT (contact) | 7 (14.58) | 0.54 (1.97) | 9 (25.71) | 0.69 (1.35) |
| Other community health-care services (contact) | 32 (66.67) | 3.42 (4.94) | 27 (77.14) | 5.54 (7.15) |
| Hospital-based health and social care | ||||
| Accident and emergency: not admitted (attendance) | 3 (6.25) | 0.08 (0.35) | 5 (14.29) | 0.14 (0.36) |
| Sibling | ||||
| Community-based health and social care | ||||
| Counsellor (contact) | 7 (14.58) | 0.50 (1.46) | 2 (5.71) | 0.06 (0.34) |
| Other community health-care services (contact) | 2 (4.17) | 0.04 (0.29) | 4 (11.43) | 0.49 (2.08) |
| Carer | ||||
| Autism-related training (minute) | 9 (18.75) | 1.02 (2.48) | 9 (25.71) | 2.17 (6.98) |
| Community-based health and social care | ||||
| GP (contact) | 19 (39.58) | 1.38 (2.38) | 14 (40.00) | 1.03 (1.47) |
| Other community health-care services (contact) | 16 (33.33) | 1.27 (2.79) | 11 (31.43) | 1.49 (3.07) |
| Hospital-based health and social care | ||||
| Inpatient stay: physical health (bed-days) | 1 (2.08) | 0.08 (0.58) | 0 (0.00) | |
| Accident and emergency: admitted (attendance) | 1 (2.08) | 0.02 (0.14) | 0 (0.00) | |
| Hospital outpatient clinic (appointments) | 8 (16.67) | 0.31 (0.85) | 3 (8.57) | 0.26 (1.07) |
| Out-of-pocket expensesa | 34 (70.83) | 24 (68.57) | ||
| Half-days off work | 23 (47.92) | 18.19 (37.22) | 15 (42.86) | 4.14 (9.02) |
Caregiver-reported gross income and the mean annual income was £17,537.31 (SD $15,909.86) for SIT and £18,405.8 (SD £14,956.87) for usual care.
| Service use (unit) | Study arm | |||
|---|---|---|---|---|
| SIT (N = 36) | Usual care (N = 23) | |||
| n (%) using | Mean (SD) | n (%) using | Mean (SD) | |
| Child | ||||
| Autism intervention package (contact) | 4 (11.11) | 0.33 (2.00) | 3 (13.04) | 0.87 (2.94) |
| Service use by the child: education (contact) | 28 (77.78) | 368.64 (379.77) | 19 (82.61) | 356.78 (447.21) |
| Community-based health and social care | ||||
| GP (contact) | 10 (27.78) | 0.44 (0.88) | 4 (17.39) | 0.22 (0.52) |
| Paediatrician (contact) | 16 (44.44) | 0.69 (1.09) | 5 (21.74) | 0.22 (0.42) |
| SLT (contact) | 6 (16.67) | 0.64 (2.17) | 3 (13.04) | 0.39 (1.08) |
| Other community health-care services (contact) | 26 (72.22) | 6.19 (16.88) | 10 (43.48) | 2.65 (5.32) |
| Hospital-based health and social care | ||||
| Accident and emergency: not admitted (attendance) | 4 (11.11) | 0.11 (0.32) | 1 (4.35) | 0.04 (0.21) |
| Sibling | ||||
| Community-based health and social care | ||||
| Counsellor (contact) | 5 (13.89) | 2.39 (8.99) | 4 (17.39) | 0.65 (2.52) |
| Other community health-care services (contact) | 5 (13.89) | 0.83 (2.54) | 2 (8.70) | 1.30 (5.10) |
| Carer | ||||
| Autism-related training (minute) | 5 (13.89) | 0.42 (1.54) | 0 (0.00) | |
| Community-based health and social care | ||||
| GP (contact) | 14 (38.89) | 1.25 (2.31) | 6 (26.09) | 0.57 (1.04) |
| Other community health-care services (contact) | 12 (33.33) | 2.69 (7.32) | 8 (34.78) | 2.30 (5.99) |
| Hospital-based health and social care | ||||
| Inpatient stay: physical health (bed-days) | 2 (5.56) | 0.06 (0.23) | 0 (0.00) | |
| Accident and emergency: not admitted (attendance) | 2 (5.56) | 0.06 (0.23) | 0 (0.00) | |
| Accident and emergency: admitted (attendance) | 2 (5.56) | 0.06 (0.23) | 0 (0.00) | |
| Hospital outpatient clinic (appointments) | 1 (2.78) | 0.08 (0.50) | 3 (13.04) | 0.48 (1.41) |
| Out-of-pocket expensesa | 28 (77.78) | 16 (69.57) | ||
| Half-days off work | 13 (36.11) | 7.08 (18.16) | 5 (21.74) | 2.13 (5.22) |
Total costs
The total costs for the child, sibling and carers by sector and perspective were reported as adjusted mean differences with bias-corrected 95% CIs.
NHS/Personal Social Services perspective
At baseline, the main contributor to the total NHS/PSS cost was community-based care. Education-based services constituted the major proportion of societal cost (Table 34). From an NHS/PSS perspective, the mean total health-care and social care cost at 6 months (Table 35) was £1915.2 in the intervention arm and £554.42 in the control arm. The adjusted mean difference was statistically significant (£1325.1, 95% CI £1057.6 to £1592.6). When SIT costs were not included in the total NHS/PSS costs, NHS/PSS costs were significantly higher for usual care than for SIT at 6 months (mean –£177.38, 95% CI –£431.36 to £76.59).
| Cost | Study arm (£) | Unadjusted mean difference (95% CI) (£) | Adjusted mean difference (95% CI) (£)a,b | |
|---|---|---|---|---|
| SIT (n = 69), mean (SD) | Usual care (n = 69), mean (SD) | |||
| a. Child | ||||
| Autism intervention package | 1.46 (12.13) | 45.6 (321.11) | –44.14 (–120.64 to 32.36) | –42.64 (–114.22 to 28.93) |
| Community-based care | 426.99 (542.62) | 409.24 (622.14) | 17.76 (–178.77 to 214.29) | 23.37 (–168.60 to 215.35) |
| Hospital-based care | 181.14 (932.45) | 81.42 (427.93) | 99.71 (–144.54 to 343.97) | 95.59 (–149.59 to 340.78) |
| Total health and social care (child) | 609.59 (1112.9) | 536.26 (833.52) | 73.34 (–257.69 to 404.36) | 76.32 (–266.29 to 418.93) |
| b. Sibling | ||||
| NHS/PSS | 142.69 (452.48) | 52.17 (161.33) | 90.53 (–23.83 to 204.89) | 89.96 (–19.98 to 199.92) |
| c. Carer | ||||
| Autism-related training | 264.04 (806.26) | 199.11 (543.17) | 64.92 (–166.52 to 296.37) | 47.86 (–165.08 to 260.79) |
| Community-based care | 270.84 (784.84) | 214.85 (548.35) | 55.98 (–171.95 to 283.92) | 59.99 (–162.39 to 282.37) |
| Hospital-based care | 43.18 (142.74) | 207.02 (834.00) | –163.83 (–365.27 to 37.60) | –167.58 (–361.59 to 26.42) |
| d. Out-of-pocket expenses (caregiver) | 1016.1 (3632.2) | 234.43 (513.37) | 781.64 (–91.67 to 1654.9) | 804.14 (–132.81 to 1741.1) |
| e. Unpaid care | 478.33 (1354.2) | 436.39 (2859.9) | 41.94 (–711.40 to 795.29) | 25.38 (–761.14 to 811.89) |
| f. Education (child) | 3465.6 (4573.5) | 2982.7 (3336.8) | 482.81 (–864.98 to 1830.6) | 527.64 (–827.22 to 1882.5) |
| Total societal (a–f) | 6290.3 (6378.2) | 4862.9 (5019.7) | 1427.33 (–504.98 to 3359.6) | 1463.7 (–488.33 to 3415.7) |
| Cost | Study arm (£) | Unadjusted mean difference (95% CI) (£) | Adjusted mean difference (95% CI) (£)a,b | |
|---|---|---|---|---|
| SIT (n = 48), mean (SD) | Usual care (n = 35), mean (SD) | |||
| a. Intervention cost | 1538.16 (–) | |||
| b. Child | ||||
| Autism intervention package | 3.28 (17.43) | 46.56 (188.79) | –43.28 (–97.69 to 11.13) | –46.40 (–110.83 to 18.02) |
| Community-based care | 361.65 (449.41) | 487.11 (675.27) | –125.46 (–371.14 to 120.21) | –218.26 (–432.68 to –3.85) |
| Hospital-based care | 12.10 (50.42) | 20.74 (51.55) | –8.64 (–31.15 to 13.87) | –8.57 (–31.42 to 14.27) |
| Total health and social care | 377.04 (455.67) | 554.42 (706.16) | –177.38 (–431.36 to 76.59) | –213.07 (–484.49 to 58.37) |
| Total health and social care (a + b) | 1915.2 (455.67) | 554.42 (706.16) | 1360.8 (1106.8 to 1614.8) | 1325.1 (1057.6 to 1592.6) |
| c. Sibling | ||||
| NHS/PSS | 49.47 (144.32) | 15.88 (49.56) | 33.59 (–17.06 to 84.24) | 19.91 (–18.27 to 58.09) |
| d. Carer | ||||
| Autism-related training | 180.79 (548.03) | 145.67 (428.49) | 35.12 (–186.59 to 256.84) | 31.35 (–186.16 to 248.86) |
| Community-based care | 179.99 (300.10) | 118.26 (238.89) | 61.73 (–60.36 to 183.82) | 52.01 (–59.84 to 163.86) |
| Hospital-based care | 139.94 (570.36) | 53.19 (220.64) | 86.76 (–115.52 to 289.03) | 96.86 (–71.63 to 265.35) |
| e. Out-of-pocket expenses (caregiver) | 253.42 (782.64) | 137.66 (359.87) | 115.76 (–167.34 to 398.86) | 154.68 (–133.29 to 442.66) |
| f. Unpaid care | 749.49 (2176.88) | 72.66 (148.22) | 676.83 (–57.74 to 1411.4) | 77.34 (–233.47 to 388.16) |
| g. Education (child) | 3315.9 (3309.9) | 5321.2 (8518.5) | –2005.2 (–4688.7 to 678.17) | –2150.3 (–5373.2 to 1072.5) |
| Total societal without intervention (b–g) | 5246.1 (3727.1) | 6418.9 (8866.3) | –1172.8 (–4006.6 to 1660.9) | –1891.7 (–5022.1 to 1238.7) |
| Total societal with intervention (a–g) | 6784.2 (3727.1) | 6418.9 (8866.3) | 365.32 (–930.3 to 4737.3) | –353.57 (–3518.9 to 2811.7) |
Societal perspective
From a societal perspective, the mean total costs at baseline were £6290.30 and £4862.90 for SIT and usual care, respectively. The adjusted mean difference in costs of £1463.70 was not statistically significant (95% CI –£488.33 to £3415.70) (see Table 34). The mean total societal costs, including intervention at 6 months, were £6784.2 and £6418.9 for the intervention arm and control arm, respectively. The adjusted mean difference was not statistically significant (mean –£353.57, 95% CI –£3518.9 to £2811.7). When intervention costs were excluded, the mean total societal cost at 6 months was statistically higher for usual care than for SIT (mean –£1891.70, 95% CI –£5022.10 to £1238.70). Costs measured at 12 months were higher overall in the intervention arm, with an adjusted difference in total societal care cost of £1141.50 (95% CI £1333.4 to £3616.4); however, the adjusted mean difference was not statistically significant (Table 36).
| Cost | Study arm (£) | Unadjusted mean difference (95% CI) (£) | Adjusted mean difference (95% CI) (£)a,b | |
|---|---|---|---|---|
| SIT (n = 36), mean (SD) | Usual care (n = 23), mean (SD) | |||
| a. Intervention cost | 1538.16 (–) | |||
| b. Child | ||||
| Autism intervention package | 26.24 (120.47) | 0.73 (3.50) | 25.51 (–24.97 to 75.98) | 26.68 (–19.67 to 73.02) |
| Community-based care | 615.73 (1299) | 229.79 (443.26) | 385.93 (–177.73 to 949.60) | 288.38 (–94.13 to 670.89) |
| Hospital-based care | 16.13 (46.28) | 6.31 (30.28) | 9.82 (–12.02 to 31.66) | 12.19 (–5.54 to 29.92) |
| Total health and social care | 658.11 (1324.29) | 236.84 (454.70) | 421.27 (–153.62 to 996.15) | 403.02 (–93.74 to 899.78) |
| Total health and social care (a + b) | 2196.3 (1324.3) | 236.84 (454.70) | 1959.4 (1384.5 to 2534.3) | 1941.1 (1476.3 to 2406) |
| c. Sibling | ||||
| NHS/PSS | 273.08 (922.12) | 91.13 (273.20) | 181.94 (–214.81 to 578.69) | 103.03 (–247.77 to 453.82) |
| d. Carer | ||||
| Autism-related training | 5.89 (25.96) | 0.00 (–) | 5.89 (–4.97 to 16.77) | 6.75 (–3.71 to 17.22) |
| Community-based care | 208.43 (476.77) | 259.77 (754.44) | –51.34 (–371.73 to 269.05) | –75.43 (–424.1 to 273.25) |
| Hospital-based care | 226.12 (913.45) | 98.93 (291.66) | 127.19 (–267.49 to 521.87) | 182.40 (–216.71 to 581.51) |
| e. Out-of-pocket expenses (caregiver) | 92.92 (267.23) | 51.35 (87.11) | 41.56 (–74.04 to 157.18) | 18.92 (–53.1 to 90.94) |
| f. Unpaid care | 369.26 (859.86) | 159.91 (440.33) | 209.35 (–179.37 to 598.06) | 165.17 (–177.92 to 508.28) |
| g. Education (child) | 3587.6 (3596.5) | 3665.4 (4625.6) | –77.89 (–2229.39 to 2073.6) | –335.71 (–2241.6 to 1570.2) |
| Total societal without intervention (b–g) | 5421.4 (5153.2) | 4563.4 (5190.5) | 857.98 (–1904.3 to 3620.3) | –396.65 (–2870.8 to 2077.5) |
| Total societal with intervention (a–g) | 6959.5 (5153.2) | 4563.4 (5190.5) | 2396.1 (–366.1 to 5158.4) | 1141.5 (–1333.4 to 3616.4) |
Outcomes
Cost-effectiveness: 6-month follow-up
In terms of challenging behaviour, NHS/PSS costs were higher in the intervention arm than in the control arm and outcome showed no statistically significant difference, generating an ICER (i.e. the additional cost divided by the additional effects) of £3312.75 per 1-point improvement in the ABC-I score from the NHS/PSS perspective (Table 37). For the secondary analysis, we explored cost-effectiveness from a societal perspective and evaluated incremental cost per point improvement in ABC-I over the same period. It was not necessary to calculate ICERs, as there were no significant differences in costs and effects in the primary outcome. However, there is uncertainty around these results. A Bayesian decision-making approach was adopted, and available data on costs and effects were used to plot a CEAC. Non-parametric bootstrapping generated a joint distribution of incremental mean costs and effects for SIT compared with usual care to explore the probability of SIT being cost-effective subject to a range of values (λ) that a decision-maker might be willing to pay for an improvement in outcomes.
| Item | Health and social care perspective, mean (95% CI) | Societal perspective, mean (95% CI) | ||
|---|---|---|---|---|
| 6 months | 12 months | 6 months | 12 months | |
| Incremental cost | £1325.1 (£1057.6 to £1592.6) | £1941.1 (£1476.3 to £2406) | £1184.5 (–£1906.2 to £4275.4) | £1141.5 (–£1333.4 to £3616.4) |
| Points improvement in ABC-I | 0.40 (–2.37 to 3.17) | 2.01 (–5.37 to 1.35) | 0.40 (–2.37 to 3.17) | 2.01 (–5.37 to 1.35) |
| ICER: additional cost per additional point improvement in ABC-I | £3312.75 | £965.72 | Mean differences in costs and outcome did not reach statistical significance (5% level) | Mean differences in costs and outcome did not reach statistical significance (5% level) |
Figures 14 and 15 present scatterplots of the bootstrapped cost and effectiveness of SIT compared with usual care, from NHS/PSS and societal perspectives. Points in the scatterplot for the NHS/PSS perspective fall in the north-east and north-west quadrants of the cost-effectiveness plane, suggesting that SIT is more costly than usual care, with unclear conclusions regarding effectiveness. Points in the scatterplot for the societal perspective fall in all four quadrants of the cost-effectiveness plane.
FIGURE 14.
Bootstrapped mean differences in health and social care costs and effects (6-month ABC-I total score): cost-effectiveness plane – SIT vs. usual care (NHS/PSS perspective).
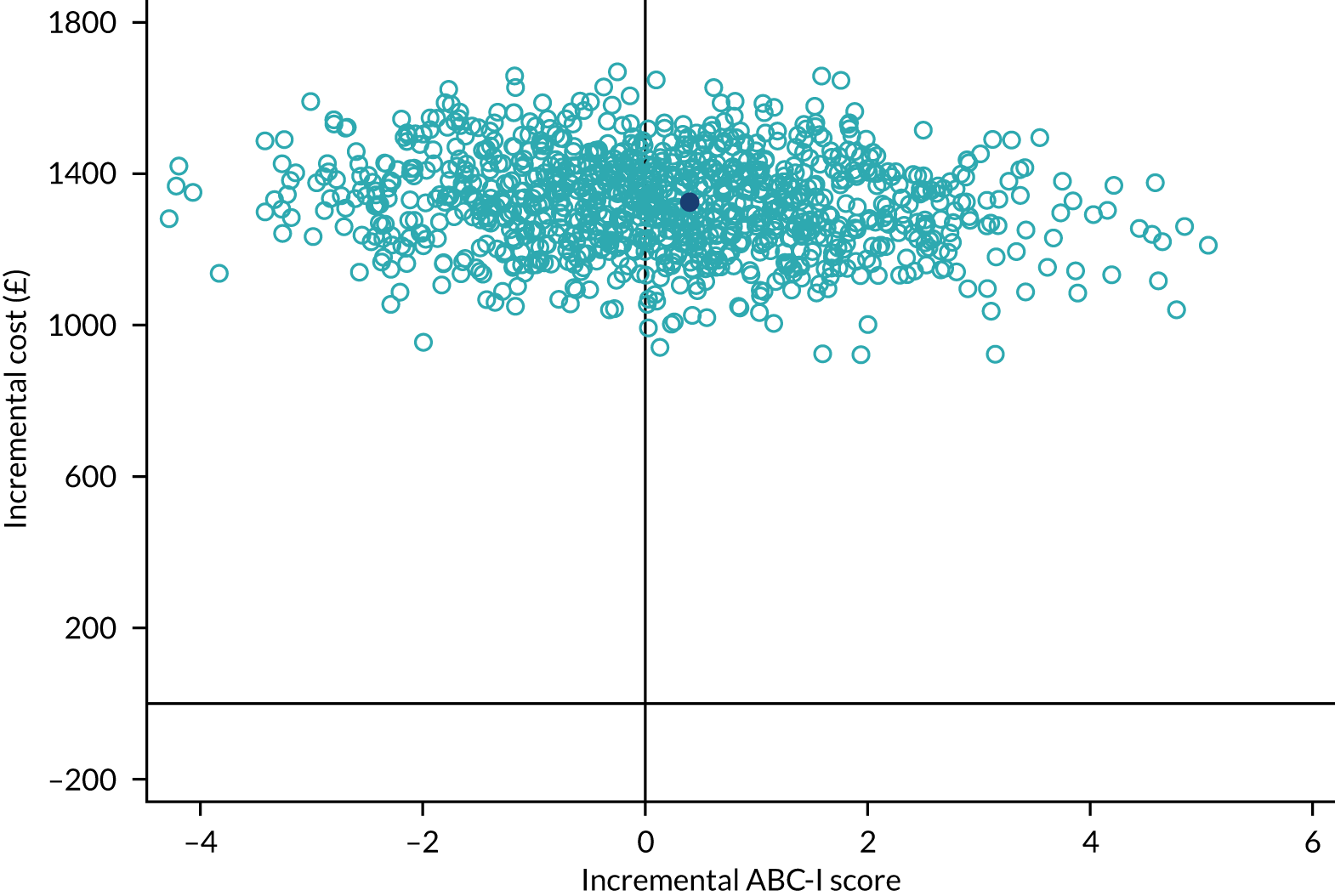
FIGURE 15.
Bootstrapped mean differences in societal costs and effects (6-month ABC-I total score): cost-effectiveness plane – SIT vs. usual care (societal perspective).
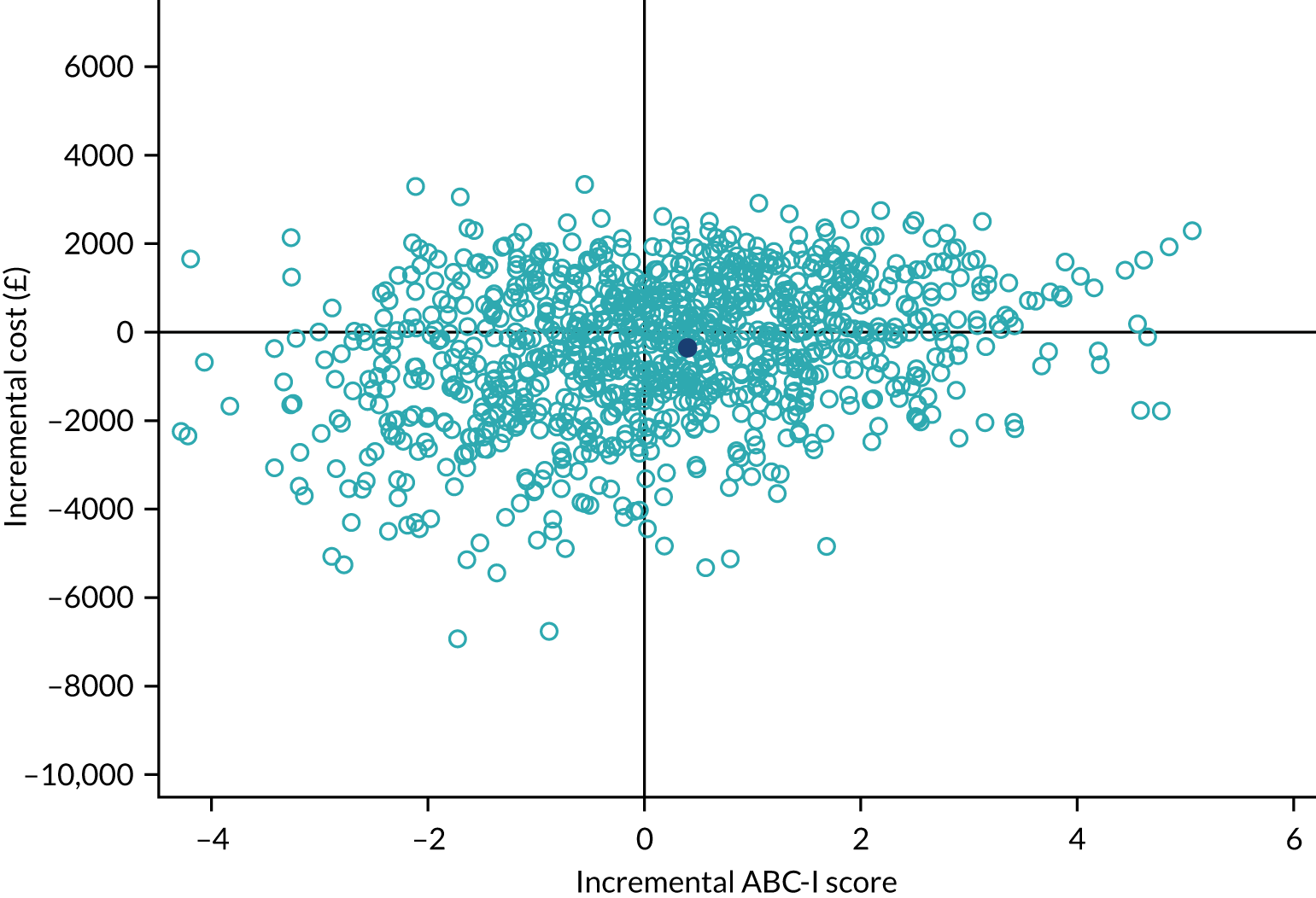
Statistical uncertainty around the ICER was explored using CEACs (Figures 16 and 17). Given the lack of suggested monetary thresholds for assessing cost-effectiveness using ABC-I, we assumed a willingness-to-pay threshold of £500. The probability that SIT is cost-effective from the NHS/PSS perspective was < 10% (see Figure 16). From the wider societal perspective (including education services, carers’ health-care use, out-of-pocket expenses and lost productivity, in addition to health and social care costs), the probability that SIT is cost-effective increased to just under 60% for a willingness-to-pay threshold of £500 (see Figure 17). At 6 months, the probability that SIT is cost-effectiveness rose from 10% under an NHS/PSS perspective to 60% under a societal perspective because of the higher cost of education in the control arm. Higher education costs offset costs in NHS/PSS and in other sectors, closing the gap in societal care costs at 6 months between arms (from £1360.80 under an NHS/PSS perspective to £356.32 under a societal perspective; see Table 35).
FIGURE 16.
Health-care and social care costs and effects (6-month ABC-I scores): CEAC.
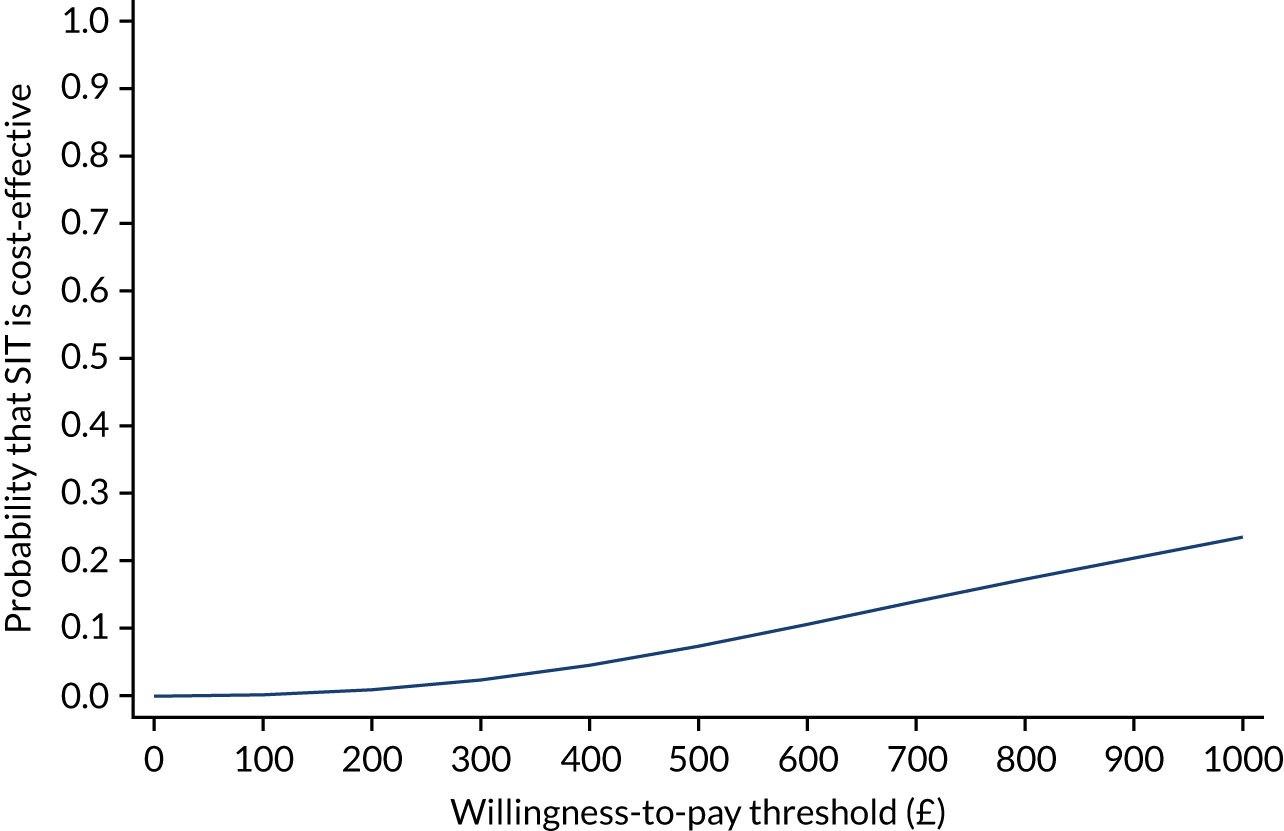
FIGURE 17.
Societal costs and effects (6-month ABC-I scores): CEAC.
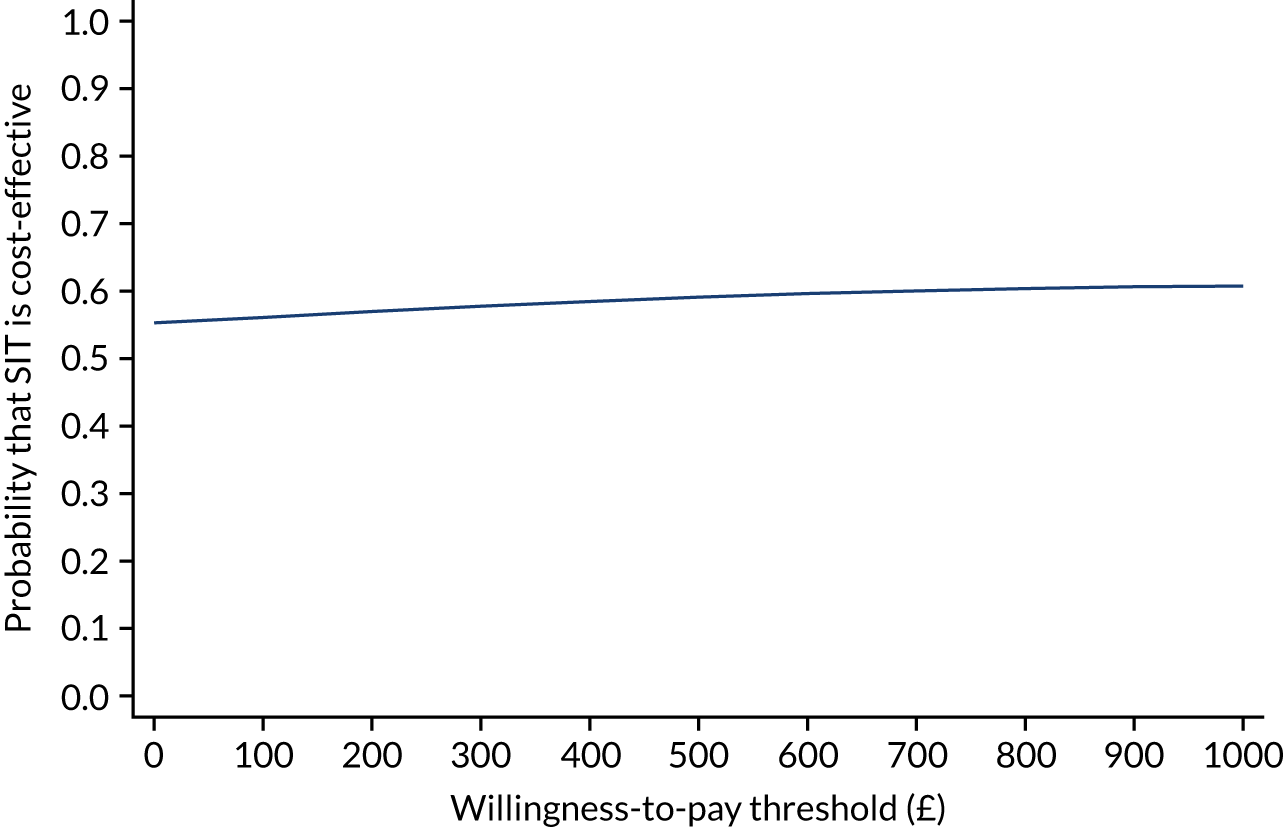
Cost-effectiveness: 12-month follow-up
At 12 months, it was not necessary to calculate the ICER, as there were no significant differences in costs and ABC-I scores under both the NHS/PSS and the societal perspectives (see Table 37). Figures 18 and 19 present scatterplots of the bootstrapped cost and effectiveness for SIT compared with usual care, from the NHS/PSS and societal perspectives at 12 months. Points in the scatterplot for the NHS/PSS perspective fall in the north-east and north-west quadrants of the cost-effectiveness plane, suggesting that SIT is more costly than usual care, with unclear conclusions regarding effectiveness. Points in the scatterplot for the societal perspective fall in all four quadrants of the cost-effectiveness plane, but are more concentrated in the north-east and north-west quadrants, suggesting that SIT is more costly than usual care, with unclear effectiveness.
FIGURE 18.
Bootstrapped mean differences in health-care and social care costs and effects (12-month ABC-I total score): cost-effectiveness plane – SIT vs. usual care (NHS/PSS perspective).
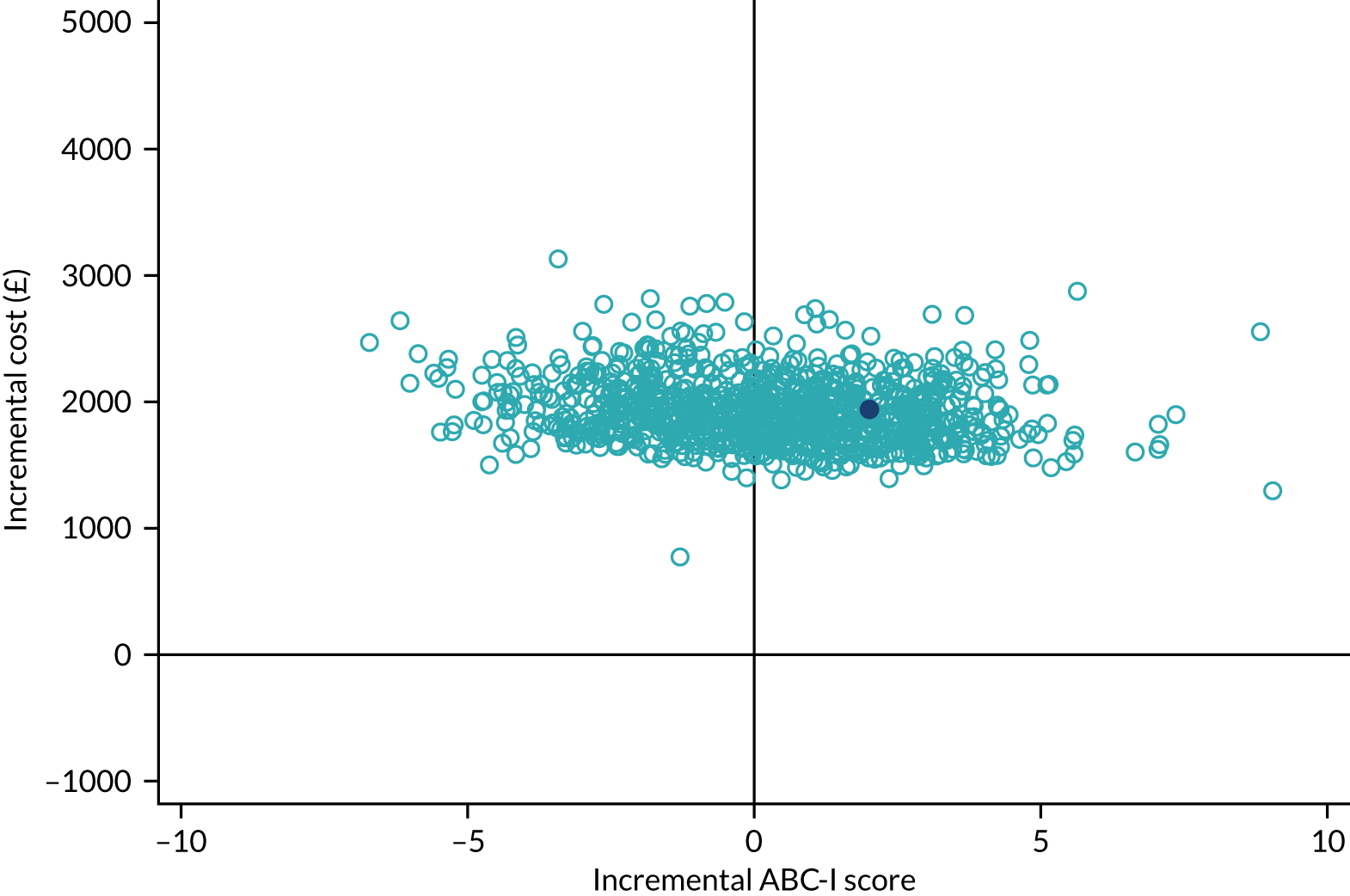
FIGURE 19.
Bootstrapped mean differences in societal costs and effects (ABC-I total score: 12-month complete-case analysis): cost-effectiveness plane – SIT vs. usual care (NHS/PSS perspective).
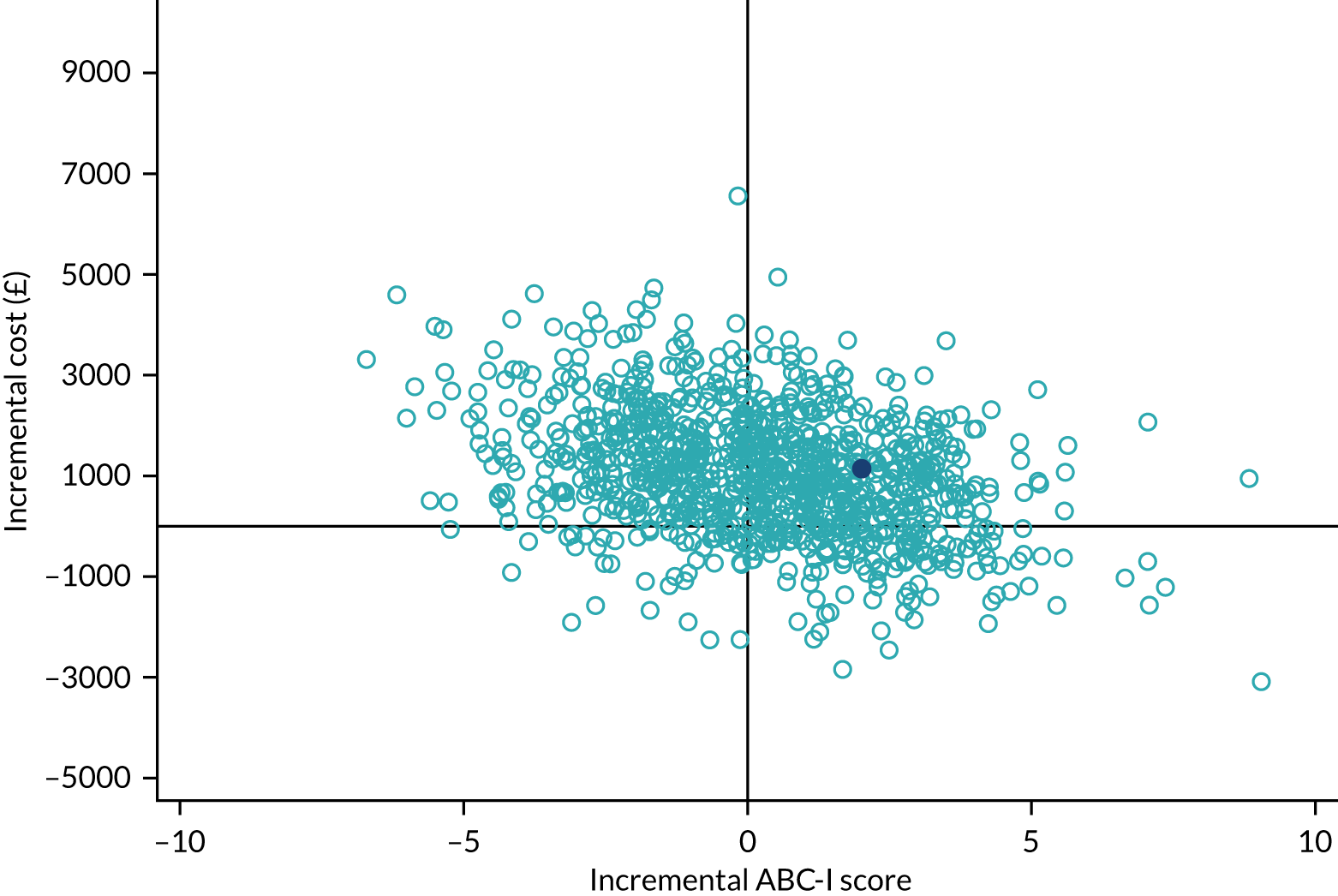
Cost-effectiveness acceptability curves for the 12-month follow-up showed similar results to the 6-month follow-up (Figures 20 and 21). The probability that SIT is cost-effective from the NHS/PSS perspective was < 10% (see Figure 20). From the wider societal perspective, the probability that SIT is cost-effective was just over 30% for a willingness-to-pay threshold of £500 (see Figure 21).
FIGURE 20.
NHS/PSS perspective (12-month ABC-I scores): CEAC.
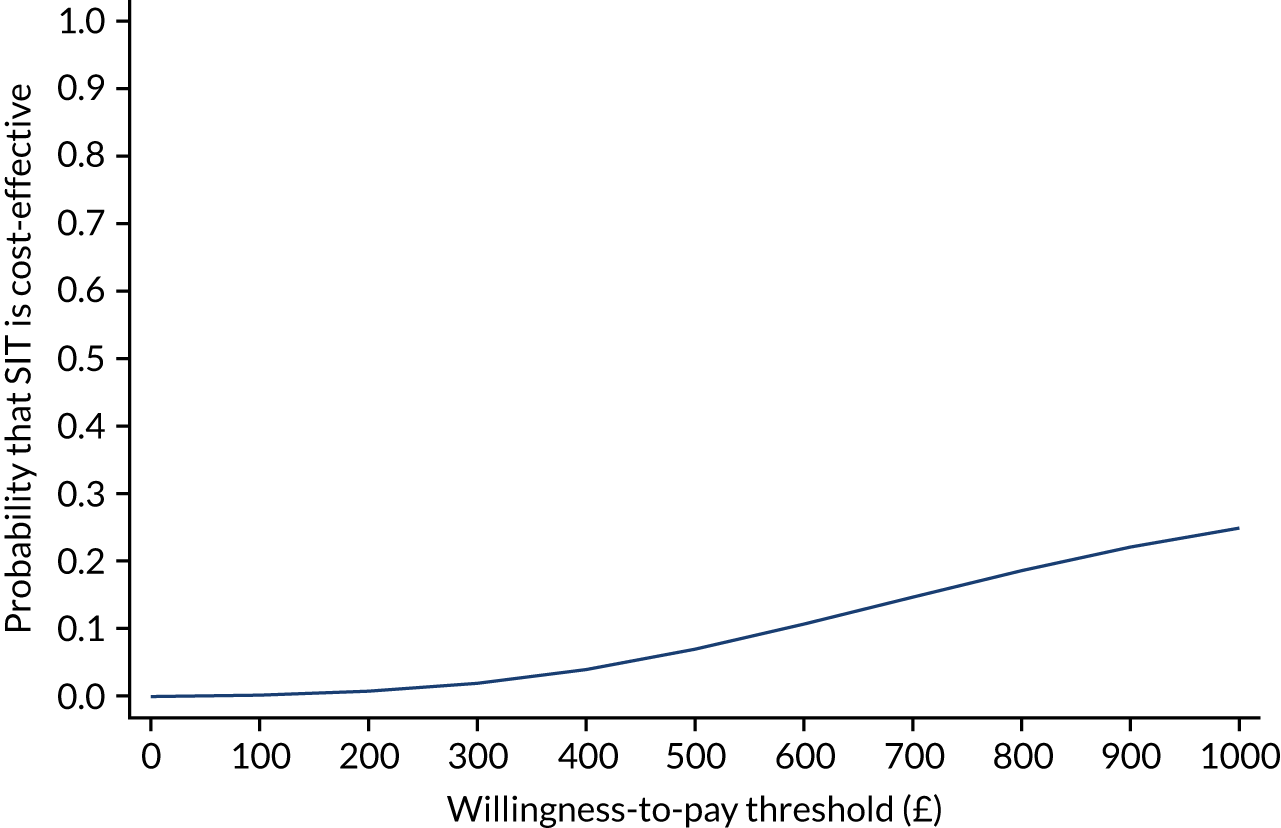
FIGURE 21.
Societal perspective (12-month ABC-I scores): CEAC.
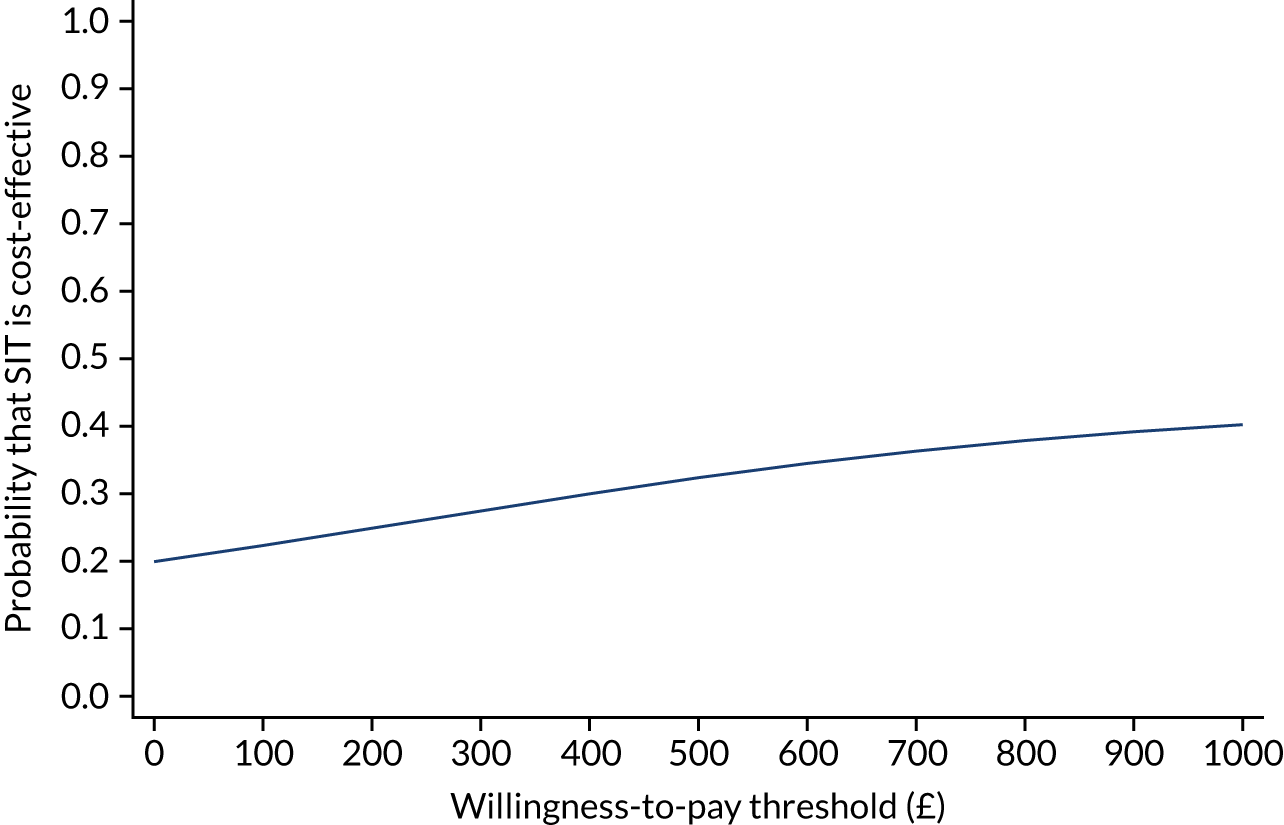
Impact of COVID-19
Follow-up resource use measures were collected via telephone, post and online. We expected minimal impact of COVID-19 on the proportion of participants providing information on resource use data and no meaningful difference between arms. However, we saw a reduction in overall service use owing to limited access. To explore potential impact on results, an intention-to-treat analysis was conducted (with missing data imputed assumed missing at random). We used multiple imputation using chained equations, fitting five imputations,109 assuming a predictive mean matching model with baseline ABC-I scores, baseline total cost, severity of SPDs, region and sex of child. We then performed a parametric bootstrap with the multiple imputed data set to obtain bias-corrected estimates of incremental cost and effect. The results did not alter conclusions drawn from the main analysis (Table 38). Total health and social care costs from an NHS/PSS perspective for 6 and 12 months were higher for SIT than for usual care. The adjusted mean differences between SIT and usual care for 6- and 12-month follow-up were statistically significant at 1317.2 (95% CI 1116.5 to 1517.9) and 2149.5 (95% CI 1807.8 to 2491.3), respectively. From a societal perspective, the adjusted mean difference between arms at 6 and 12 months suggests that SIT was more costly than usual care; however, the mean difference was not statistically significant (see Table 38). ICERs generated from an NHS/PSS perspective are shown in Table 39.
| Variable | Study arm | Unadjusted mean difference (95% CI) | Adjusted mean difference (95% CI)a,b | |
|---|---|---|---|---|
| SIT (n = 69), mean (SD) | Usual care (n = 69), mean (SD) | |||
| 6 months | ||||
| Total health-care and social care cost (£) | 1919.18 (66.03) | 563.03 (112.78) | 1356.15 (1087.58 to 1624.72) | 1317.2 (1116.5 to 1517.9) |
| Total societal cost (£) | 6799.9 (469.76) | 5691.87 (839.09) | 1108.1 (–836.03 to 3052.2) | 1016.2 (–776.33 to 2808.8) |
| Outcome: ABC-I | 18.29 (1.12) | 18.47 (1.47) | –0.18 (–3.94 to 3.59) | –0.38 (–3.59 to 3.52) |
| 12 months | ||||
| Total health-care and social care cost (£) | 2111.3 (146.63) | 245.49 (80.90) | 1865.8 (1519.5 to 2212.1) | 2149.5 (1807.8 to 2491.3) |
| Total societal cost (£) | 6585.3 (706.44) | 4906.2 (991.4) | 1679.1 (–1399.5 to 4757.7) | 1844.7 (–73.63 to 3763.0) |
| Outcome: ABC-I | 17.73 (1.36) | 19.44 (1.51) | –1.70 (–6.08 to 2.68) | –1.64 (–4.14 to 0.85) |
| Item | Health and social care perspective, mean (95% CI) | Societal perspective, mean (95% CI) | ||
|---|---|---|---|---|
| 6 months | 12 months | 6 months | 12 months | |
| Incremental costs | £1317.2 (£1116.5 to £1517.9) | £2149.5 (£1807.8 to £2491.3) | £1016.2 (–£776.33 to £2808.8) | £1844.7 (–£73.63 to £3763.0) |
| Points improvement in ABC-I score | 0.38 (–3.59 to 3.52) | 1.64 (–4.14 to 0.85) | 0.38 (–3.59 to 3.52) | 1.64 (–4.14 to 0.85) |
| ICER: additional cost per additional point improvement in the ABC-I scale | £3466.3 | £1310.7 | Mean differences in costs and outcome did not reach statistical significance (5% level) | Mean differences in costs and outcome did not reach statistical significance (5% level) |
Statistical uncertainty around the ICER was explored for imputed data using CEACs (Figures 22–25). Using a monetary threshold of £500, the probability that SIT is cost-effective, from the NHS/PSS perspective at 6-month follow-up, was just over 0.2% and increased to just over 30% for a willingness-to-pay threshold of £1000 (see Figure 22). From a wider societal perspective, the probability that the intervention is cost-effective was just over 20% (see Figure 23). CEACs for the 12-month follow-up concur with the conclusion that SIT has a low probability of cost-effectiveness from both the NHS/PSS and the societal perspectives (see Figures 24 and 25).
FIGURE 22.
Imputed data set: NHS/PSS perspective (6-month ABC-I scores) – CEAC.
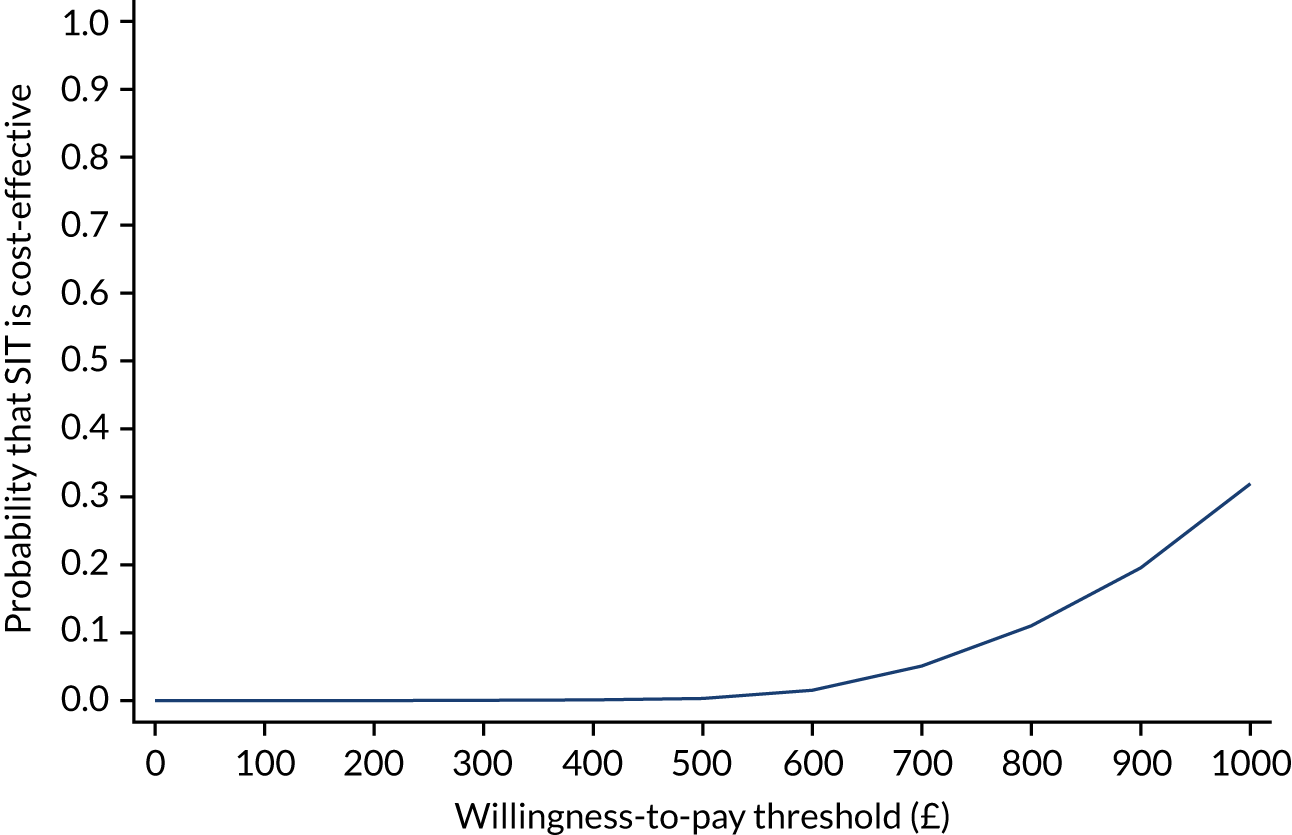
FIGURE 23.
Imputed data set: societal perspective (6-month ABC-I scores) – CEAC.
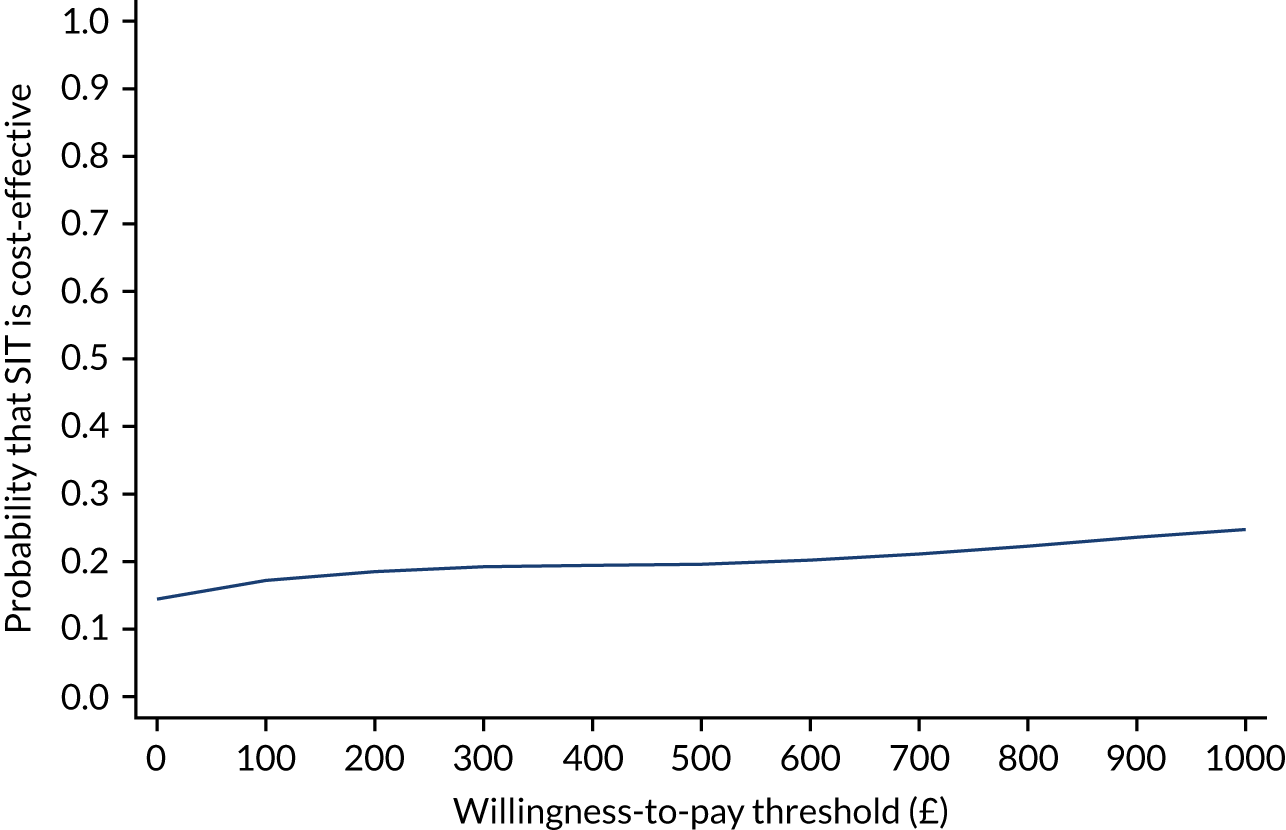
FIGURE 24.
Imputed data set: NHS/PSS perspective (12-month ABC-I scores) – CEAC.
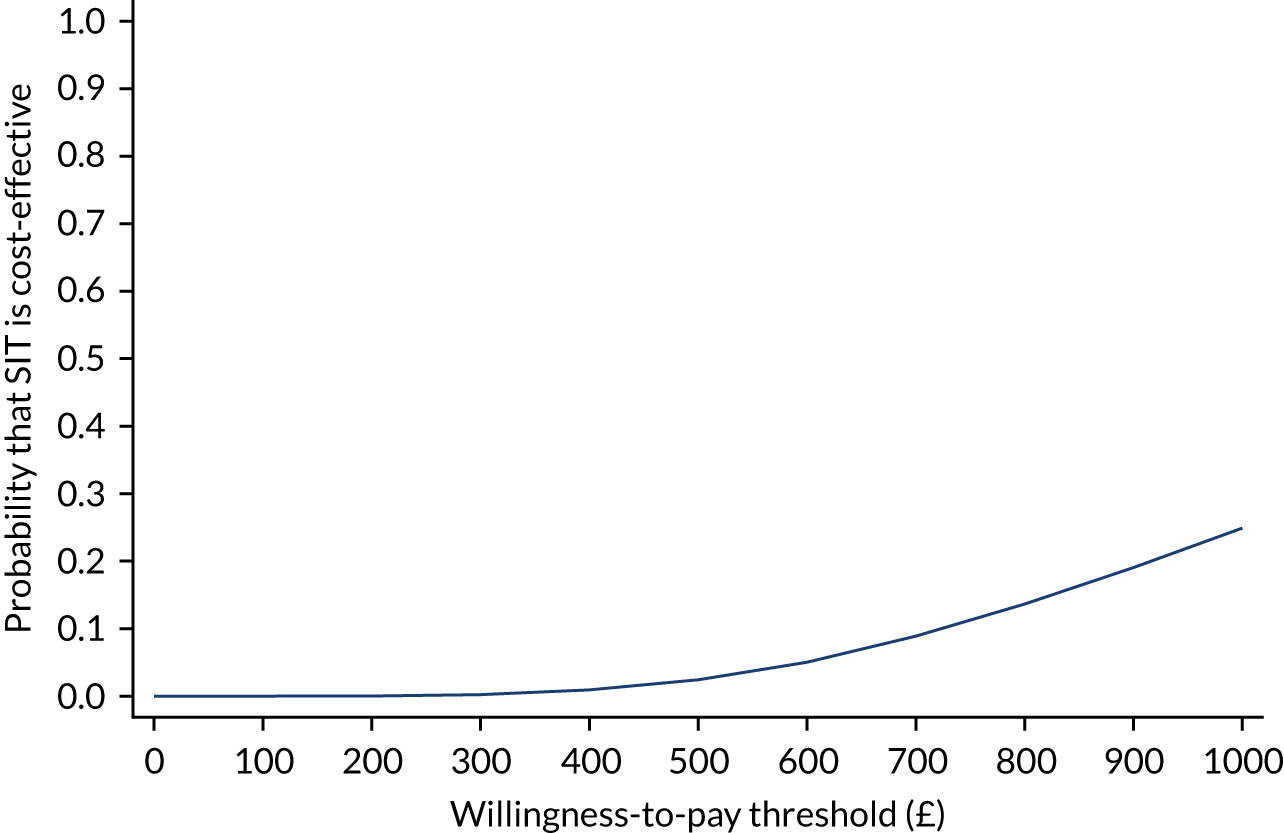
FIGURE 25.
Imputed data set: societal perspective (12-month ABC-I scores) – CEAC.
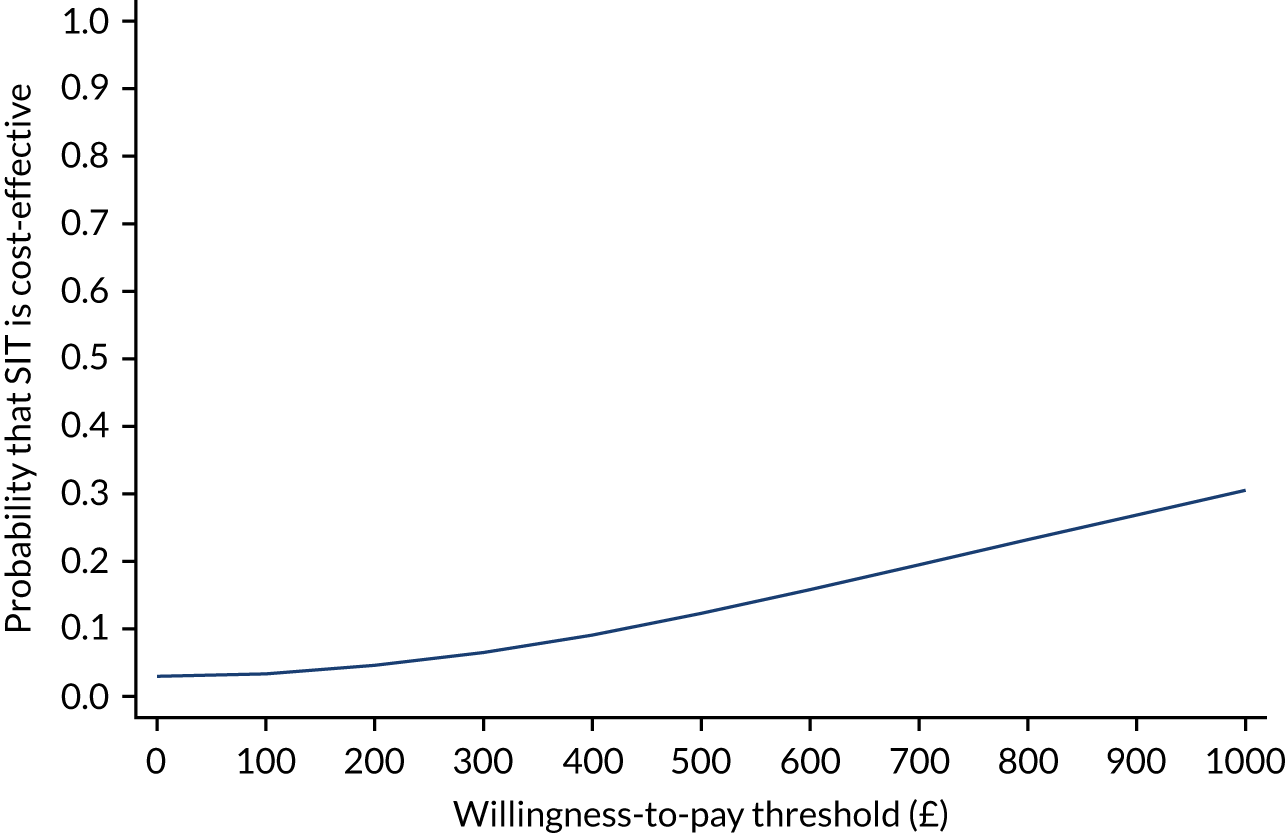
Summary
Delivery of SIT incurred significant additional costs. When intervention costs were not included in total NHS/PSS costs, NHS/PSS costs of care for usual care-only participants were significantly higher than for SIT participants. The mean difference in ABC-I scores between arms did not achieve statistical significance at 6 or 12 months, suggesting no additional clinical benefit of SIT. Economic evidence suggests that SIT has a low probability of being a cost-effective option compared with usual care.
Chapter 8 Process evaluation: recruitment, retention, fidelity and safety
The SenITA trial included a process evaluation that was conducted alongside the main trial. In accordance with Medical Research Council guidance, the process evaluation aimed to examine:110
-
recruitment of participants and therapists
-
retention
-
fidelity
-
acceptability
-
adherence
-
adverse effects
-
contamination.
These process evaluation components also formed part of the internal pilot (see Chapter 4). In addition, the process evaluation sought to explore contextual factors that might have an effect on the outcome of the intervention.
Methods and materials
Research design
The process evaluation employed a mixed-methods approach. Quantitative methods were used to assess recruitment rates/patterns, attendance and intervention fidelity. Qualitative interviews with therapists involved in intervention delivery and carers of children enrolled in the trial examined experiences of the trial recruitment process, the acceptability of trial processes and measures, intervention implementation and acceptability, and the role of contextual factors. Methods for collecting data as part of the process evaluation are described in the following sections. Table 40 summarises each set of data collected, the method of data collection and the objectives addressed.
| Data source | Process evaluation component | ||||||
|---|---|---|---|---|---|---|---|
| Recruitment | Participant retention | Intervention fidelity | Acceptability | Adherence | Adverse effects | Contamination in control arm | |
| Site delegation logs | ✓ | ||||||
| Screening and baseline questionnaire data | ✓ | ||||||
| Follow-up data at 6 and 12 months from the clinical database | ✓ | ||||||
| Video-recordings of intervention sessions | ✓ | ||||||
| Qualitative interviews with therapists | ✓ | ||||||
| Qualitative interviews with parents/carers | ✓ | ||||||
| Intervention attendance data | ✓ | ||||||
| SAE report form | ✓ | ||||||
| Participant diary | ✓ | ||||||
Quantitative data collection
Recruitment of participants and therapists
Baseline data were used to describe the characteristics of the recruited sample (e.g. age, degree of SPD and autism symptoms). The baseline data provide an indication of the trial ‘reach’, that is whether or not the intervention reaches the intended population. This is described here as the proportion of those eligible who were then recruited (see Chapter 10 for a discussion of sample representativeness).
The number of people eligible (expressed as the proportion of those approached) and randomised (expressed as the proportion of those eligible) were utilised within the process evaluation.
Sixteen therapists were recruited to deliver the intervention across eight sites/clinics.
Retention
The clinical database was used to capture retention data, that is the number of people with missing outcome data at 6 and 12 months post randomisation (as a proportion of those who had been randomised and reached the time point).
Fidelity of intervention delivery
Fidelity was assessed using the ASI intervention fidelity measure. 23 This measure includes assessment of both structural and process fidelity. The scale demonstrates high content validity according to expert ratings and high reliability for process elements (total score ICC 0.99; Crohnbach’s α = 0.99). 23 Independent raters were provided with a manual and training on how to score the sessions that they reviewed.
Structural fidelity is defined by:
-
the level of therapist training/qualifications, that is the occupational therapist providing the intervention is certified in sensory integration/SIPT (with a minimum of 50 education hours in sensory integration theory and practice)
-
supervision, that is the therapist has a history of mentorship, with an equivalent of 1 hour per month from an advanced therapist with 5 years’ experience of providing OT using ASI intervention for a period of 1 year
-
a score of 85 out of 110 across the following four areas – (1) safety of the environment; (2) detail and content of therapist-held records, including therapist–carer collaboration in relation to goals set during therapy; (3) physical space and equipment; and (4) communication with carers.
Process fidelity determines whether or not the therapist ensures physical safety; provides sensory opportunities; helps the child to maintain an appropriate level of alertness; challenges postural, ocular, oral or bilateral motor control; challenges praxis and behavioural organisation; collaborated in activity choice; tailors activity to provide appropriate challenge; ensures that activities were successful; supports intrinsic motivation to play; and establishes therapeutic alliance. This produces a process fidelity total score out of 100. Each rating reflects the rater’s global impression of whether or not a particular therapeutic strategy is an intentional part of the therapy being delivered within the observed sample of SIT. Therapist mentors considered initial assessment, goal-setting and delivery of the intervention for each therapist by reviewing and providing feedback on the first two video-recorded face-to-face sessions delivered to any participant.
Where consent was provided, face-to-face sessions were video-recorded. A sample of recorded sessions in the intensive phase were rated for process fidelity by at least one independent SIT-trained therapist (based on a randomly selected sample of the full session, of a minimum of 15–20 minutes in duration). To minimise bias through selecting ‘good’ sessions, the choice of which sessions to rate was made at random. To ensure that participants had both earlier and later sessions rated, the first session to be rated was randomly selected between session 6 and 12, and the second session was randomly selected between session 13 and 20. In the event that a session allocated for fidelity rating was not available (e.g. owing to the participant not attending), the next available session was rated. To ensure consistency of ratings, a selection of sessions were rated by multiple independent SIT-trained therapists. Demonstration of adequate fidelity of intervention delivery was defined as scoring ≥ 80 on the fidelity measure across at least 80% of sessions sampled.
Adherence
This was the level of intervention received by participants allocated to the intervention arm. An ‘effective’ dose for SIT has yet to be definitively established. However, attending 13 of a possible 20 sessions (i.e. two-thirds) delivered during the intensive intervention phase was felt likely to indicate sufficient exposure (based on clinical experience and available literature).
Adverse effects
Serious adverse events were reported from the time of signature of informed consent, throughout the treatment period up to, and including, 1 month after the participant received the intervention. A SAE is defined as any untoward medical occurrence in a participant who receives an intervention that was not necessarily caused by, or related to, that intervention (i.e. an AE) and that:
-
results in death
-
is life-threatening (as defined by GCP)
-
requires hospitalisation or prolongation of existing hospitalisation (as defined by GCP)
-
results in persistent or significant disability or incapacity
-
consists of a congenital anomaly or birth defect
-
is a medically important condition (as defined by GCP).
Adverse events that did not meet the criteria of serious were not systematically recorded and none was reported within the qualitative interviews.
Contamination
The potential for contamination, that is if participants recruited to the control arm received or sought therapy consistent with SIT or received enhanced/additional support from clinicians aware of their participation in the trial, is acknowledged. Therefore, there was an examination as to whether or not the usual care received differed in any way from the expected provision mapped out as a result of the scoping focus groups (see Chapter 2).
Qualitative data collection
Semistructured interviews were conducted with 30 carers of children and 13 therapists involved in intervention delivery (see Chapter 9 for full details of qualitative data collection methods). Carers were purposively sampled to ensure representation of intervention and usual care-only participants, trial region and a mix of child sex and age. All therapists involved in the trial were invited to take part in an interview.
Data analysis
Quantitative analysis
The approach taken to analyse quantitative data was described in a trial statistical analysis plan. Recruitment, retention, adherence and safety data are descriptive, and categorical data are presented using counts and percentages. Process fidelity ratings were completed in accordance with the categories described in the fidelity tool. 23 After viewing a short section of video from a session, raters gave a general impression of the intervention delivered by responding with ‘yes’ or ‘no’ to the statement ‘This intervention session is provided by a qualified therapist intentionally applying ASI intervention theory and methods’. Raters then scored each of the 10 process fidelity items according to whether or not the therapist demonstrated each item as a key therapeutic strategy in the session. Scores were from 1 to 4, representing:
-
No, I do not think the therapist intentionally uses this strategy.
-
Doubtful, I do not think the therapist intentionally uses this strategy.
-
Probably, I think the therapist intentionally uses this strategy.
-
Certainly, I think the therapist intentionally uses this strategy.
Scores were then calculated to give a total score (Table 41). If the general impression was that the session was delivered in accordance with ASI, then the expected total score would be ≥ 80%.
| Item | Multiply by | Calculated score |
|---|---|---|
| Number of certainly (4) ratings | 10 | |
| Number of probably (3) ratings | 7 | |
| Number of doubtful (2) ratings | 3 | |
| Number of no (1) ratings | 0 | |
| Total score | /100 |
Qualitative analysis
Interviews were audio-recorded, transcribed verbatim and anonymised. Interview transcripts were analysed thematically using a framework approach. 66 Two thematic frameworks were created (one for carer interviews and one for therapist interviews), drawing from the aims of the process evaluation and a review of transcripts. Data from carer and therapist interviews were coded separately in NVivo version 12 (QSR International, Warrington, UK). Thematic frameworks were discussed reflectively by the trial qualitative researchers, and a sample of interviews double coded. For the process evaluation, the viewpoints of carers and therapists have been collated and presented thematically (see Chapter 9 for full details of qualitative data analysis procedures).
Results
Recruitment of participants and therapists
The CONSORT (Consolidated Standards of Reporting Trials) flow diagram (see Figure 5) gives a detailed breakdown of recruitment. A total of 258 carers contacted the study team to express an interest in taking part. Of those 258 carers, 24 (9.3%) were not eligible at referral. A further 84 carers did not go any further for the following reasons:
-
no further response (n = 61)
-
not interested in participating (n = 23).
Screening appointments were held with 150 carers and children. Three children (2%) were screened as ineligible after not meeting inclusion criteria (other than SPD). Nine children did not progress for the following reasons:
-
no further response (n = 4)
-
not interested in participating (n = 1)
-
eligible and consented but then withdrew immediately (n = 4).
A total of 138 children were randomised into the trial (i.e. 92% of those screened and 53.5% of those who expressed an interest in taking part).
Participants were probably representative of the wider population of children in primary education with a diagnosis of autism presenting to services. The majority of participants were male (79%) and white British (88%) (see Chapter 6 for a description of baseline characteristics).
Recruitment of therapists to deliver the intervention occurred in stages as new health boards and clinic sites were opened. From August 2017, just one therapist was delivering the intervention to participants in South Wales (at a clinic in Cardiff University). By November 2017, a further five therapists across three South Wales university health boards (i.e. Hywel Dda University Health Board, Aneurin Bevan University Health Board and Cardiff and Vale University Health Board) started delivering the intervention. One occupational therapist was available to start in Cwm Taf University Health Board in February 2018, with another occupational therapist starting in May that year. A therapist at a private clinic in Cornwall started delivering the intervention in May 2018, with another therapist starting at the same clinic in July 2018. Given that each therapist could deliver the intervention to only one or two children at a time (given their NHS obligations), extra sites and therapists were recruited. In May 2019, a further therapist was recruited in Swansea Bay University Health Board, another therapist in Aneurin Bevan University Health Board and four were recruited at the Pace School in Buckinghamshire. Therapists’ capacity to see multiple children simultaneously depended on their working hours, leave and other commitments.
Therapists were not directly involved in trial recruitment but did refer potential participants to the trial team. Some therapists reported that they had difficulty identifying potentially eligible and willing children to take part, despite some being involved in publicising the trial through schools or presentations to professionals. One therapist thought that the trial criteria were too strict, particularly relating to age, as children either side of the age range may have benefited from the intervention.
Carers were asked during interviews where they had heard about the trial. A variety of sources was reported (Figure 26), most commonly via professional recommendation (note that one carer did not provide this information).
FIGURE 26.
How parents heard about the trial.
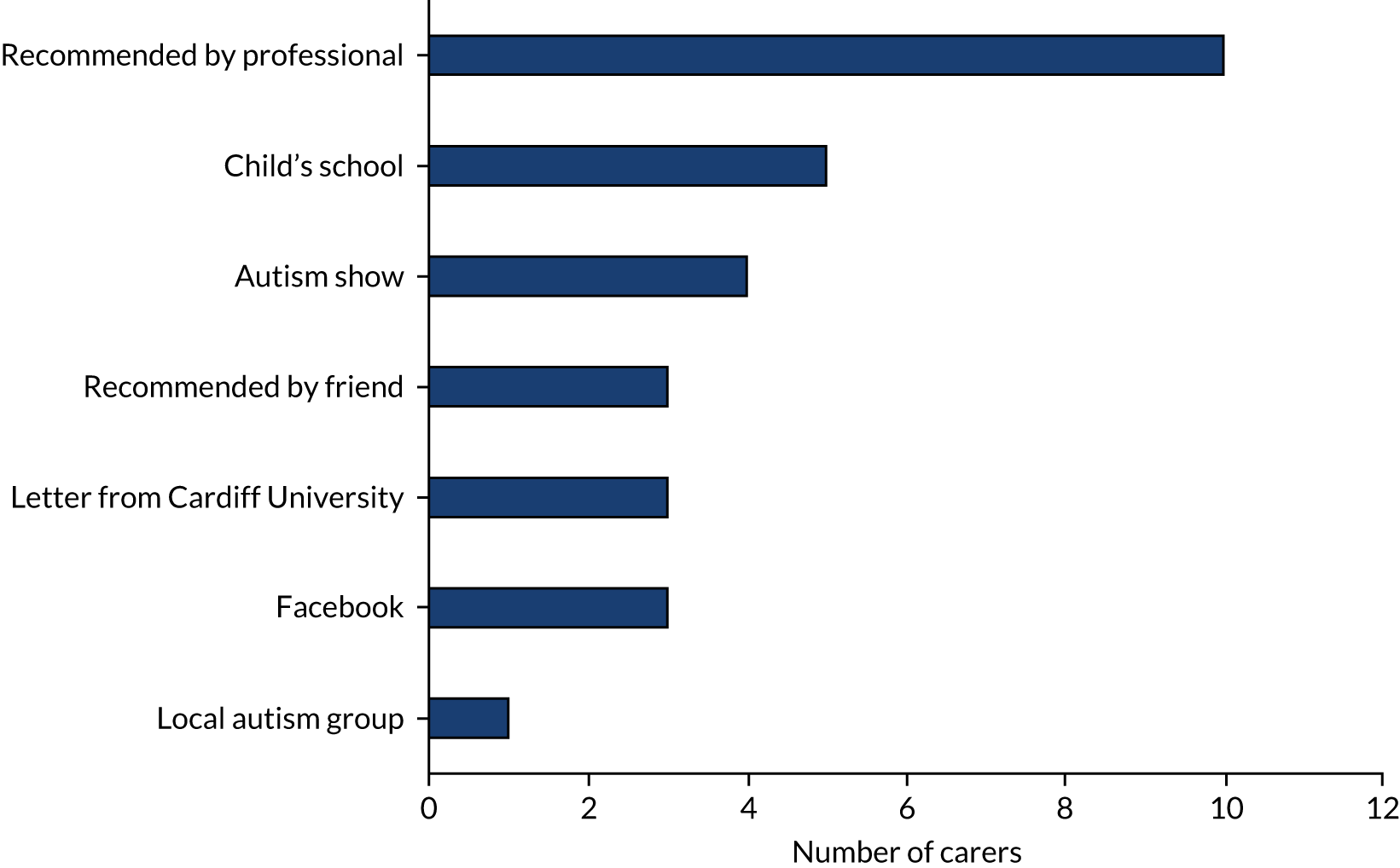
The main reasons that carers gave for taking part in the trial were that they hoped that their child would receive the intervention and that they wanted to improve support for children with autism and SPDs in the future. Some parents specifically wanted to pursue SIT for their child (having heard about it on courses, through their own research or via recommendations from friends), as they thought that it would be beneficial. It was often mentioned that carers and their child had received little or no support and, therefore, carers were happy to try anything that might help (carer interviews):
When we went in to [the trial it was] sort of like, not . . . a last resort, but like oh my God, something has got to help . . . I just think it’s really sad that there’s just nothing out there . . . and . . . maybe, maybe you know, in years to come, maybe this might be something that benefits everybody. So although it’s benefitting you, you’re also helping to benefit others.
P219, intervention arm
Most carers said that they had no concerns about their child taking part in the trial, although several worried that their child might be allocated to the control arm, meaning that they would not get the help that they needed. One carer was concerned that the intervention may not benefit their child, that is they would have ‘put him through’ appointments for nothing. Another carer was worried in case they were not allowed to stay with their child during appointments. One carer was concerned about anonymity owing to their profession, but was reassured when they were told that data would be labelled with participant numbers rather than names. Therapists did not report any concerns being expressed directly to them by carers.
Retention
Participant retention
The primary outcome time point was 6 months post randomisation, and these visits were all completed by 7 May 2020. Of 138 participants, 107 (77.5%) provided follow-up data at this time point. Twenty-nine participants were lost to follow-up and there were two withdrawals. Twelve-month follow-ups were completed on 17 December 2020. Of 138 participants, 96 (69.6%) provided data at this time point. Forty participants were lost to follow-up and there were no additional withdrawals.
Therapist retention
Of the 16 therapists delivering intervention, two were able to see only one child each before having to withdraw their involvement in the trial for personal reasons.
Fidelity of the intervention
Structural fidelity
Structural fidelity includes the level of therapist training/qualifications and supervision, coupled with achieving a score of 85 out of 110 across four areas (see Other areas).
Level of therapist training/qualifications
All SenITA trial therapists had completed postgraduate modules of ≥ 50 hours of face-to-face teaching, plus the hours to complete written assignments, and most therapists had completed two, three or four postgraduate modules.
Supervision
In the UK, there is no established SIT mentoring system. Therapists typically received mentoring of at least four sessions for completion of their postgraduate modules, followed by monthly mentoring sessions with an experienced occupational therapist. Therefore, we compensated by ensuring that mentoring occurred throughout their intervention sessions.
Other areas
Other areas included:
-
safety of the environment
-
detail and content of therapist-held records, including therapist–carer collaboration in relation to goals set during therapy
-
physical space and equipment
-
communication with carers.
Some clinics required additional equipment to be purchased to meet fidelity; however, all clinics met structural fidelity criteria prior to initiating therapy (all scores were > 85, with a range from 96 to 110).
Total fidelity scores
The outcome of interest for process fidelity was the number of therapists scoring at least 80 out of 100 on the process fidelity measure for at least 80% of sessions rated. Ninety-six sessions were rated, yielding 156 total fidelity scores from independent raters for 46 different intervention participants who were delivered SIT by 12 different therapists. The mean score across all 156 ratings was 90.1 (SD 13.1). Technical problems meant that recordings from four therapists were not available to be rated.
Multiple ratings
Four independent raters scored process fidelity for 96 sessions. All raters scored the same 17 sessions (17.7% where target had been between 15% and 20%) to assess the comparability of their ratings and were then allocated more sessions on an individual basis. The majority of sessions were scored by one rater (Table 42). Averages were taken where sessions were rated by more than one rater and, therefore, had multiple scores.
| Number of ratings | Total number of sessions (n = 96) | Percentage |
|---|---|---|
| 1 | 73 | 76 |
| 2 | 2 | 2 |
| 3 | 4 | 4 |
| 4 | 17 | 18 |
Fidelity threshold
The SIT delivered in the SenITA trial met fidelity, with 10 out of 12 therapists scoring, on average, at least 80 out of 100 on the process fidelity measure for at least 80% of each of their sessions. Two therapists (i.e. therapists 7 and 8) scored below this threshold (Tables 43 and 44). Rater 2 consistently scored both therapists lower than other raters for these sessions, which skewed the average. Both therapists had mentors to support them further and improved in delivering the intervention. It was noted that, although their clinic space met structural fidelity, it was also one that had limited flexibility.
| PID | Session | Average score | Rater 1 | Rater 2 | Rater 3 | Rater 4 | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Score from rater | GIS | Score from rater | GIS | Score from rater | GIS | Score from rater | GIS | |||
| 402 | 6 | 49.25 | 79 | 1 | 20 | 0 | 55 | ? | 43 | 0 |
| 402 | 7 | 76.0 | 76 | 1 | ||||||
| 402 | 13 | 85 | 85 | 1 | ||||||
| 402 | 15 | 77.75 | 79 | 1 | 47 | 0 | 100 | ? | 85 | 1 |
| 408 | 12 | 91 | 91 | 1 | ||||||
| 408 | 17 | 94 | 94 | 1 | ||||||
| 414 | 11 | 71.0 | 71 | 0 | ||||||
| 414 | 13 | 86 | 86 | 1 | ||||||
| PID | Session | Average score | Rater 1 | Rater 2 | Rater 3 | Rater 4 | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Score from rater | GIS | Score from rater | GIS | Score from rater | GIS | Score from rater | GIS | |||
| 403 | 7 | 95.5 | 97 | ? | 94 | 1 | ||||
| 403 | 13 | 75.75 | 76 | 1 | 36 | 0 | 100 | 1 | 91 | 1 |
| 411 | 6 | 64.0 | 64 | 0 | ||||||
| 411 | 19 | 53.0 | 53 | 0 | ||||||
Global Impression Score
Along with 156 process total fidelity scores from multiple raters, 144 (92.3%) participants achieved a Global Impression Score of 1 (i.e. ‘yes’), nine (5.8%) participants were scored as 0 (i.e. ‘no’) and three (1.9%) participants were missing this score. Even where total fidelity scores were < 80, Global Impression Score was mostly assessed as meeting sensory integration criteria.
Adaptations made by therapists
Therapists tailored intervention sessions to the needs of each child. Therapists had to adapt to working with children with autism, for example by providing more coaching/prompting and dealing with avoidance behaviour. In terms of specific changes made to trial processes, two therapists adapted the wording of the COPM to make it more child-friendly, one therapist asked for more time for discussions with parents and a second therapist conducted assessments in shorter blocks over a larger number of sessions.
Acceptability
Overall experiences of the trial
All carers agreed that if they were to go back in time, they would be happy to take part in the SenITA trial again. For some of those carers allocated to the control arm, this was because it would give them another chance to possibly receive the intervention. Carers in the intervention arm were very enthusiastic about the trial and said that they would ‘definitely’ participate again, as the intervention had helped their child:
Oh definitely yeah, definitely. Without a shadow of a doubt, like I’d love to take part again, I know I can’t . . . honestly definitely it was totally worth it, I’d recommend it 100%.
P304, intervention arm
Carers reported that members of the trial team who they encountered were friendly and understanding. Carers felt that the trial was explained very well and did not feel pressured to take part. The reminder text messages were useful and trial appointments were flexible. Some carers explained that just being selected to take part in the trial was positive, as they felt that their child’s difficulties had been acknowledged:
It’s been really good and [all the trial team have] been really kind and really understanding and really patient.
P514, intervention arm
However, some carers reported a lack of communication from the trial team. For example, one carer in the control arm reported that they had not been told which group their child was in and did not realise that their involvement in the trial had started until they got a reminder 4–5 months later to fill in the diary. Another carer had been allocated to the intervention arm, but their child had received no therapy after 6 months and they had not been told when it was going to start.
Trial information
Carers felt that they were given the right information about the trial before taking part and had the opportunity to ask questions. Some carers commented that there was plenty of information provided and, therefore, they knew exactly what would happen and what would be expected of them. Information was easily understood and well explained by trial staff. One carer felt that they had been given too much information, but another carer said that the information did not fully explain what would happen in the intervention sessions. Two carers had not immediately realised that they had been allocated to usual care, which caused some confusion. One carer appreciated that plenty of time was given to decide whether or not to participate and that consent was checked at several stages:
It’s been brilliant . . . I felt like I was always kept informed and really sort of, felt very much as though it was my choice, like I was never sort of bullied into it, like you’ve been offered this, it’s a golden opportunity, you should do it. It was never felt like that, it always felt like you know, you can stop this at any time . . . So I felt like the overall explanation of it and what was going to be involved, was explained really well.
P514, intervention arm
Most carers said that taking part in the trial had met expectations or (for those in the intervention arm) had been better than expected. The time commitment was mostly as anticipated. Two carers said that the trial had taken more of their time than they expected in terms of travelling to appointment sessions.
Trial appointments
Convenient and flexible appointment times were offered when possible. Some carers in the intervention arm mentioned having difficulty because all sessions were during school/working hours. In some cases, schools were happy for children to attend intervention sessions during school time, as they felt that it would benefit the child; however, other schools were less supportive. For example, one carer reported that their child’s school felt that the intervention was responsible for a deterioration in behaviour and, therefore, they had experienced issues with requesting time off school for trial appointments.
Although sessions were held in a convenient location for some carers, others found the trial to be a big commitment that was difficult to fit into their lives, mostly owing to travelling times. However, all carers were committed to attending appointments, as they felt that they were beneficial. Several parents mentioned parking issues at appointments. One parent said that they had been given no consistent time and date for sessions, and sometimes could not contact the therapist and, therefore, had been unsure of what was happening:
It’s an hour and a half to the session . . . an hour and a half home, and that was twice a week. So it was a big financial investment to, you know, fund the fuel alone, and then with my time . . . It was a massive investment in family life . . . I would pick him up at 12 o’clock on the dot. He’d have lunch in the car, and we’d just about get to [the session] for 1.30.
P112, intervention arm
Completing trial measures
Assessments
Two carers commented that assessments were a positive experience, as they were play based and the assessor had a good rapport with their child. One carer found that their child had already completed one of the tests and had remembered the answers, and so the results may not have accurately reflected his ability. One carer said that it would have been helpful to have been given a report of the test results, as this would have been useful for other professionals working with their child.
Several therapists found the SIPT demanding and difficult to conduct because of the length of the assessment and the avoidance behaviours displayed by children, which mean that it was not always fully achieved. One therapist was able to conduct the assessment jointly with a colleague, which was helpful. Another therapist had to ask carers to help. Several therapists conducted the assessment over two or more sessions, as they felt that it was too long for children to complete in one sitting. The following specific problems were reported by individual therapists:
-
Conducting the assessment at the end of the intervention was problematic, as children were disappointed that they would not be having a therapy session, particularly where the assessment was being conducted in the therapy room.
-
Starting with a standardised assessment before building rapport with the child and parents was unhelpful.
-
Some children would not engage with the copying exercises, as they had been told at school that it was wrong to copy and took this very literally and, therefore, the assessment may not have accurately reflected their ability.
Despite these issues, one therapist reported that assessments provided a useful starting point for planning the intervention.
Questionnaires
Carers found the questionnaires long, but relatively easy to complete. When carers did not understand how to interpret some of the questions, trial staff provided an explanation. Carers commented that a lot of questions seemed repetitive, with the same topic revisited several times with slightly different wording. Some questions were not appropriate for the age of the child, for example asking whether or not a 7-year-old took drugs. One carer found questions intrusive, for example those asking about their own personal relationships and mental health.
Some carers found the questionnaires and assessments useful, as they highlighted their child’s needs. Conversely, several carers found the questionnaires and assessments upsetting to complete, as they focused on all the things their child could not do:
It was . . . really long winded . . . mentally and physically exhausting . . . It’s like when you go and do a [Disability Living Allowance] application . . . you’ve got to take your child at their worst ever possible day and write it down . . . you want to spend your life . . . focusing on what your child can [do], despite their difficulties, not what they can’t do, and I think it is a bit depressing like that.
P609, intervention arm
Trial diary
Completing the trial diary was problematic for most carers. Some carers had difficulties logging on to fill in the diary online and, therefore, did not fully complete it. Other carers forgot to complete it regularly or did not have time to do so, and one carer commented that they did not seem to be able to go back to fill in previous weeks that they had missed. Several carers did not realise that they had to complete a diary. Some carers in the control arm felt that there was little incentive for diary completion, particularly where their child had received few appointments and, therefore, there was not much to fill in. Only a minority of carers completed the diary online with no issues.
Carers reported that it was useful having text reminders to complete the diary and found it much easier replying to the texts than completing the diary. One carer suggested that it would have been better if the information could all have been provided via text.
Data input
Therapists found filling in information after each session repetitive and ‘laborious’. One carer felt that it was a ‘tick-box exercise’ that was not helpful with planning future sessions, although others found it useful. Two therapists were not sure what to report under the different reflective headings and would have found it helpful to have more guidance.
Randomisation
Most carers had a good understanding of the purpose of randomisation. One carer had not initially realised that there would be two groups of children and thought that all would receive the intervention. Although all parents hoped that their child would be in the intervention arm, they appreciated the need for randomisation. Those carers allocated to the control arm were disappointed, but happy to continue their involvement in the trial. One carer suggested that the intervention could have been offered to usual-care children after the trial had been completed so that all children would have had the chance to benefit from it.
Trial information technology
Most therapists experienced information technology (IT) issues (summarised below) and found the technical aspects of the trial time-consuming. Several therapists found that they needed technical support and for some this was because they did not have previous experience of using an iPad. IT problems encountered by therapists included the following:
-
The camera had limited memory and could store only 60 minutes of footage and, therefore, videos often needed to be transferred onto the iPad, which was problematic. The 60-minute limit meant that conversations after the session with carers (which would have been useful to capture) were missed.
-
The camera battery sometimes ran out during the sessions.
-
Some mentors had difficulty accessing the session videos.
-
There was no internet at one clinic and so information could not be input or accessed directly, and data had to be uploaded offsite.
-
The connection between the camera and the iPad sometimes did not work.
-
Some iPads and cameras were shared between therapists, which caused difficulties with planning.
-
The internet connection at one clinic was unreliable and uploads had to be repeated.
One therapist identified that recording the sessions using a static camera on a tripod meant that, unless they had an assistant to move the camera around, parts of the sessions were not necessarily visible on the recording. Several therapists reported that they needed an extra person to manage the recording of sessions.
Support for therapists
Therapists generally felt supported by the trial team, reporting that they responded quickly to any problems raised. Most therapists found the data collection manual useful, clear and easy to follow. As mentioned above, some therapists needed additional technical support with the IT aspects of the trial.
Intervention delivery
What worked well?
Carers appreciated that the intervention was tailored to their child’s needs, abilities and interests. Carers commented that therapists had good ideas of how to make the sessions engaging, put a lot of thought into planning them and went out of their way to help. For example, therapists provided carers with ideas of activities to do at home and strategies to deal with particular situations:
The OT [occupational therapist] was absolutely amazing. Like if I needed any advice on anything I could do with the certain situations, she gave me a solution. Again she suggested books and different activities I could do and that as well.
P109, intervention arm
Therapists were very engaging and positive, and the equipment was varied; therefore, children enjoyed the intervention and were keen to go to the sessions. Carers were particularly positive about their child being able to have direct one-to-one therapy, which they felt had been lacking in usual care. Carers commented that this approach meant that their children fully engaged with the activities:
I didn’t expect to get so much out of it . . . or for [child] to enjoy it . . . I could hear from that room, sitting outside and she was laughing, and it was an actual, it wasn’t a put-on laugh that she does sometimes. So that was really nice just to hear her enjoying herself really, she was just so relaxed and comfortable, it was lovely.
P309, intervention arm
One carer appreciated that the therapist spent time at the end of each session to ensure that their child was calm when they left. One carer was pleased that their child had a certificate at the end of the sessions, as he had never received one before and so it meant a lot to him.
Therapists enjoyed being able to spend longer with one child than would be possible in usual care. This longer time enabled therapists to build a good relationship with children and carers. Most therapists appreciated the opportunity to provide SIT, as it was rewarding to be able to deliver sessions that children really enjoyed and engaged with. Several therapists mentioned that it was positive being able to provide a therapy that was child led:
It’s wonderful to be able to . . . really get to know the child and the parents really, really well . . . as part of my NHS [work], you’d be lucky if you saw a child once a week for a few weeks at a time.
T203
I think the fact that it’s child led makes it accessible, makes it engaging.
T206
What did not work well?
Most carers said that there were no negative aspects to the intervention or that the only downside was that it had to finish. Therapists found delivering the intervention intense and tiring. For example, it was difficult to think ahead all of the time while engaging with the child. It was also challenging to come up with new play ideas for a relatively long block of sessions, particularly because children tended to have limited imagination because of their autism. Some children had complex needs in addition to their autism diagnosis, for example pathological demand avoidance, which made it challenging to engage them in activities:
Thinking on your feet constantly . . . you’d have to think in terms of what, what equipment you can maybe adapt or change to make sure it’s just the right challenge so then they would achieve success in order for them to be motivated in your session . . . You’re constantly thinking about that. You’re constantly analysing. You’re constantly thinking ahead . . . it’s multitasking really.
T202
Some therapists found that they had insufficient time to engage with carers (e.g. some carers needed help to learn how to play with their child, and others needed support themselves or the chance to discuss issues arising). Therapists reported that in usual care they would typically have more time to talk to carers and were also able to go into the child’s school.
Some therapists identified that using a pure sensory integration approach was restrictive, as they felt that some goals could have been achieved more quickly via other more task-specific approaches.
Suggestions for improvement of the intervention
Several specific suggestions were made by individual carers who said that it would have been useful to have had:
-
a written report at the end of the intervention to pass onto their child’s school
-
information on where to buy sensory equipment
-
more suggestions of activities to do at home to help sustain their child’s progress
-
more time after the sessions ended to be able to contact the therapist so that they could ask for advice if things started to go wrong
-
more clarity of what to focus on at home each week.
Therapists suggested that more time to engage with carers or being able to visit the child’s school would have been helpful:
I think one of the things that . . . was tricky, because it didn’t feel like the circle had been closed really, was not being able to go into schools. I know we could speak to schools over the phone, but I think actually having someone from the school . . . coming on some of the sessions, or me to visit the school [would be useful] . . . because some of the issues were with school.
T210
Length of intervention
Around half of therapists felt that the intervention was too long in terms of number of sessions, as therapists struggled to come up with new ideas to fill all sessions and some children (particularly those who were more able) made no more progress in the last few sessions. Other therapists felt that it was the right number of sessions or that some children would have benefited from further sessions. Some carers also felt that it would have been helpful if sessions had carried on for longer. For example, one carer said that they were still seeing improvements when sessions finished and several carers found that changes were not sustained once the intervention had been completed:
For me, as a therapist, it can feel like you’re . . . treading water for those last four sessions in a way. But [with some children] I feel like they’re still making changes.
T211
Some therapists felt that having sessions twice per week was helpful in terms of consistency and building rapport and enabled changes to be made more quickly. However, one therapist suggested that this was too intense. Some therapists found that the transition to less-intensive sessions worked well where children were ready for it, and that it was helpful in providing a more gradual end to the intervention. However, other therapists found that it disrupted the flow and consistency of sessions and was a big change that could have been more gradual. Several carers agreed that the ending of regular sessions was too abrupt (e.g. going from two sessions per week to once per fortnight) and difficult for their child to cope with. One carer suggested that sessions could have been tapered down more gradually towards the end.
Most carers felt that they started to see changes in their child about halfway through the intervention sessions. Other carers said that they felt that there was a more gradual change throughout the intervention. Therapists agreed that changes seemed to occur around the halfway point.
Therapist time allocation
Therapists felt that there was insufficient time allocated for the delivery of the trial. Time allocation had been calculated based on length of each session, with additional time for intervention planning and the write up of sessions. Therapists’ time was covered by NHS excess treatment costs and, therefore, there had to be a standard time allocation for all. Excess treatment costs had been appropriately costed, yet most therapists reported that the trial had taken much more of their time than they had anticipated, which made their workload difficult to manage. Some therapists had had to work unpaid and one therapist found it stressful negotiating their time with their manager and the trial team. For example, the technical aspects (e.g. recording and uploading the sessions) took up a lot of time, sessions were time-consuming to plan and set up, and there was also administrative work, such as booking appointments and inputting data, which some felt had not been fully accounted for. There was also no time allocated for discussions with carers, which therapists felt would have been helpful. Some therapists found that assessments took longer than allocated. This all meant that some therapists had to complete trial-related work in their own time:
It was really difficult to manage kind of doing clinical research within the demands of . . . my NHS day job . . . that was probably one of the hardest things I would say, being able to manage the time that the study required, which was way above what I guess was ever anticipated or described to us.
T205
Goal-setting
Most carers found goal-setting straightforward, although some carers reported that, as there were multiple issues that they wanted to tackle, it was difficult to prioritise which to focus on. One carer found setting realistic goals difficult, as they were not sure how much their child would be able to achieve in 6 months. Another carer pointed out that, as they had become so used to their child’s difficulties in everyday life, it was difficult to identify what they needed to work on. Some children were able to set realistic goals for themselves; however, one child wanted to set goals based on what his peers were able to do, which he would have found difficult to achieve.
Therapists reported that carers needed prompting to set more specific goals that were functional, measurable and realistic, as they tended to come up with general objectives, such as wanting their child to be less aggressive. Children were mostly not able to be involved in goal-setting and, therefore, some therapists did this over the telephone with carers. In some cases, goals set by carers did not necessarily relate to what their child wanted to achieve. Some carers needed prompting to think of goals, and therapists reported that the COPM was useful in helping them think through their child’s difficulties.
Potential for the adoption of sensory integration therapy as usual care
All carers thought that SIT should be available as usual care because it had benefited their child and because of the lack of support available for children with autism and SPDs. All carers would ‘definitely’ recommend the intervention to others because it had helped their child, and some had already recommended it.
Most therapists felt that if there were sufficient resources, SIT (at the intensity offered during the trial) should be available as usual care for children where appropriate. Therapists saw that SIT made a big difference to some children and enjoyed being able to deliver one-to-one therapy tailored to the child:
I was absolutely staggered by the outcomes that we achieved.
T201
[SIT is] really much more targeted and . . . it really felt as though we were getting to the bottom of and really kind of problem-solving these . . . difficulties . . . with the child and with the family . . . I didn’t feel as though these children are going to need much more beyond this, whereas the usual care feels like, you kind of wonder when they’ll be back.
T210
However, some therapists felt that a sensory integration approach alongside other approaches would be more helpful in achieving children’s goals:
I think that sensory integration therapy is just a tool in the occupational therapy toolbox . . . I don’t think it’s the first port of call.
T212
If the intervention were to be adopted as usual care, therapists identified that considerably greater resources would be needed in terms of room capacity and funding for increased staff time and specialist training. Therapists suggested that research demonstrating the effectiveness of SIT would be needed to convince managers and funders that it should be implemented more widely. Therapists anticipated that waiting lists for therapy would increase because there would be great demand for it.
Adherence
Overall, 54 (78.3%) participants allocated to the intervention arm received at least 13 SIT sessions during the intensive stage. The median number of SIT sessions received was 20 (IQR 16–21). A full breakdown can be found in Chapter 6.
Adverse events
There were no SAEs during the trial. One AE was reported to the trial team by a therapist as a SAE; however, it was clear this did not meet the criteria of ‘serious’ as laid out in the reporting guidance.
Contamination
Changes during trial participation
Most carers reported that there had been no changes to the support that their child received during the trial period. However, one child allocated to usual care had received intervention consistent with SIT, one child started accessing support from local charities (after not meeting fidelity requirements of SIT), one child had started a specialist school and one child had received a statement of special educational needs. Six children had started new extracurricular activities (mainly sports) while participating in the trial.
Impact of the trial on therapists’ practice
Most therapists said that their approach to delivering usual care had not changed because of their involvement in the trial. For some therapists, this was because they did not have the time to implement any of the sensory integration approaches in their usual practice. Two therapists felt that they had increased their knowledge of sensory integration and one carer had shared some of what they had learnt with colleagues and carers.
Contextual factors
Carer understanding of sensory integration therapy
Although therapists found it easy to explain the trial to carers, explaining the intervention was more complex. Therapists felt that carers had a basic understanding of SIT, but that not all carers fully understood the approach, which affected the extent to which they engaged with the therapy (see Chapter 9 for further details).
Clinic space and equipment
The main facilitator to intervention delivery reported by therapists was having a good clinic space with a variety of equipment. Several therapists mentioned that it was useful having an assistant to help set up the room for each therapy session.
Therapists appreciated having a variety of equipment to work with, which was helpful for intervention delivery, as sessions could be adapted to challenge each child. However, sessions were time-consuming to plan because they were tailored to individual children and intervention sessions took longer to set up than usual-care sessions (typically 15–30 minutes to set up, with the same time required to put the equipment away). Some therapists had a dedicated therapy room that was partially set up, which enabled them to prepare for sessions more quickly, as only minor changes had to be made. However, other therapists had to set the room up from scratch each time, which was physically challenging, for example setting up heavy suspended equipment. Those therapists who had a technician to help them set up said that this was extremely helpful and, in some cases, necessary:
[You need] time . . . as well to think . . . what am I hoping to achieve in this session and how am I going to set the room up to achieve what I want to, so it’s all that mental thinking that you’re doing as well as just putting the equipment up.
T203
Changeovers could also be problematic, for example the room had to be cleaned between sessions if therapists used messy play.
Therapeutic relationship with the child
Carers commented that therapists put a lot of effort into engaging with their child and were able to develop a good rapport and working relationship, which enabled rapid improvements to be made:
She just loved all of it . . . because I think [the therapist] just worked really hard to get that, like that connection with her.
P219, intervention arm
Therapists agreed that being able to see one child over a number of sessions enabled them to build a good rapport. The fact that the intervention was enjoyable for children also helped with their therapeutic relationship:
It’s a therapy that I feel is great because the kids love to engage in it and feel empowered by it . . . when you’ve built up those relationships you get that ability to be able to push them a little bit, to challenge . . . their sensory systems that particularly need to be challenged . . . if you’ve got the child on your side then it feels like you can actually work with them and challenge them and move them forward.
T206
Support and training for therapists
Most therapists felt well supported to deliver the intervention. However, therapists identified that it would have been useful to have an extra member of staff to assist in therapy sessions, for example to help with the recording, provide technical support or assist with setting up and taking down the equipment. Some therapists did have this support, which was invaluable. One therapist found the videos of the sessions helpful to look back on, although this was carried out in their own time, but others said that they did not have time to do this.
In general, therapists found that intervention training was sufficient. The session to observe therapy and assess whether or not it met the fidelity measures was described by one therapist as particularly useful. Some therapists already delivered SIT as part of their usual practice and it was felt that those therapists who had not may have struggled. Some therapists felt that they were relative ‘novices’ in delivering SIT and one therapist reported feeling out of their depth and lacking knowledge for the more analytical aspects.
Mentorship was described as very helpful, with mentors providing advice and guidance to help with the planning of future sessions, including discussing specific issues experienced. However, one therapist did not receive mentorship and several therapists started mentorship sessions later than intended, for example not until after they had seen their first child as part of the trial. Some therapists experienced technical difficulties sharing session videos with their mentor. One therapist had useful support from a colleague who was experienced in SIT and another therapist said that it would have been useful if colleagues were delivering the therapy at the same time so that they could have discussed ideas.
Not all therapists used the trial Facebook group, some because they were not confident in using IT and others because they were not aware that there was one. For those therapists who did use it, they reported that the group was not very active. Therapists suggested that it would have been helpful to have group discussions with peers also delivering the intervention.
Conclusions
The process evaluation demonstrated that recruitment of participants and therapists and delivery of intervention all met required thresholds. Recruited participants were also probably representative of the population with autism presenting to services. Findings were consistent with those from the internal pilot in that recruitment criteria were met and there was little difficulty in generating expressions of interest. Participant recruitment into the study was, in part, tempered by therapist availability. Retention of participants was good, as was retention of therapists, although practicalities of juggling NHS caseloads with the trial meant that the overall trial recruitment period and, therefore, delivery of intervention was longer than initially anticipated.
Data show that structural and process fidelity were high. In cases where process fidelity was lower than anticipated, therapists were given extra support through mentoring. In these cases, it is possible that some fidelity elements may not have been present in the video clip selected or reflected poor agreement among raters.
Carers generally found trial processes acceptable and enjoyed being part of the trial. However, there were areas where adaptations could be made. Both therapists and carers reported that entering data online was not particularly easy. In the case of reporting diary data, carers generally struggled with this and often forgot or had difficulty using the online system. In their normal practice, therapists were used to taking hard-copy notes and, therefore, found an online system difficult to use during sessions. Therapists felt that there were numerous technical processes involved as part of their role in collecting data (e.g. setting up cameras, uploading data and finding WiFi), which added to their burden. However, therapists generally felt well supported by the trial team who were able to resolve queries in real time.
Overall, adherence to the intervention was high, although, on a practical level, carers sometimes found it difficult to fit the intensive phase of the intervention in with other events in their personal lives (e.g. school, holidays and leave from work). The intervention was safe, with no SAEs reported. There was minimal contamination in the control arm and families allocated to SIT did not report receipt of any other significant intervention or contact with services.
Chapter 9 Carer experiences of usual care, and carer and therapist experiences of the intervention
Methods
Overview
Semistructured interviews were carried out with a sample of carers and therapists who delivered the SIT intervention. Before taking part in an interview, carer participants were asked to complete a timeline of the support that they and their child had received, which was used to facilitate discussion of their experiences. The aims of the qualitative study were to explore the (1) support experiences of families (outside the SenITA trial, i.e. usual care) and (2) perceived impact and clinical effectiveness of the SIT intervention for children with autism and SPDs.
Participants
Interviews were conducted with 13 occupational therapists who delivered the SIT intervention and carers of 30 children enrolled in the SenITA trial (Table 45).
| Characteristic | n |
|---|---|
| Sex of child | |
| Male | 23 |
| Female | 7 |
| Child age group (years) | |
| 5–6 | 6 |
| 7–8 | 9 |
| 9–10 | 8 |
| 11 | 7 |
| Child ethnicity | |
| White British | 23 |
| Mixed ethnic background | 2 |
| White other | 2 |
| Not disclosed | 3 |
| Trial arm | |
| Intervention | 20 |
| Control | 10 |
| Trial region | |
| Wales | 20 |
| Cornwall | 6 |
| North Buckinghamshire | 4 |
Sampling and recruitment
For the carer interviews, participants were purposively sampled from the SenITA trial database, aiming for variation in terms of sex of child and age. Two-thirds of children in the interview study were recruited from the intervention arm to enable a more in-depth exploration of the perceived impact of the SIT intervention.
Carers were invited to take part in an interview once their child had reached the 6-month follow-up point of the SenITA trial. A qualitative researcher contacted carers by telephone or e-mail (in accordance with their stated contact preferences) to ask if they would consider taking part in an interview. Those carers who agreed were sent an information pack, which included a PIS, a template timeline with completion instructions and several coloured pens. Potential participants were re-contacted after approximately 1 week to check whether or not they would be willing to participate. Fifty carers were purposively sampled from the trial database and 30 agreed to participate, giving a response rate of 60%. Of the 20 carers who were sampled but did not participate, 15 could not be reached to discuss participation, three declined to take part as they had insufficient time and two said that they did not wish to take part in an interview, but did not give a reason.
All therapists (n = 16) who delivered the SIT intervention were e-mailed by the qualitative researcher to ask if they would be willing to participate in an interview once they had delivered all intervention sessions for at least one child as part of the trial. The e-mail included a participation information sheet with details of the interview study. Thirteen therapists agreed to take part in an interview and three could not be reached to discuss participation, giving a response rate of 81%.
Study materials
Separate sets of interview questions for carers and therapists were developed by qualitative researchers, with input from the SenITA Trial Management Group and parent/carer advisory group. Carer interview questions focused on experiences of the SIT intervention (for participants in the intervention arm only), if and how the intervention had affected their child’s behaviour and the implementation of activities or strategies suggested by the occupational therapist (for carers of children in the intervention group) and experiences of support for their child’s autism outside the SenITA trial (for all carers). Therapist interview questions focused on experiences of delivering the SIT intervention, perceptions of the impact of the intervention and the receptiveness of carers to suggestions of activities or strategies. Both sets of interview questions also covered carers’ and therapists’ experiences of trial processes (see Chapter 8 for related findings).
Before taking part in an interview, carers were asked to complete a template timeline of the support that they and their child had received. Carers were provided with timeline completion instructions that requested them to include any key events in their child’s life and the different forms of support experienced for their child.
Data collection
Interviews were conducted at a mutually convenient time and in accordance with participant preferences, that is either face to face at the participant’s home/workplace or over the telephone. Most therapist interviews took place over the telephone (n = 10), whereas most carer interviews were face to face (n = 19). Therapist interviews lasted between 27 and 58 minutes (mean 40.2 minutes, SD 10.6 minutes). Parent/carer interviews lasted between 12 and 86 minutes (mean 38.0 minutes, SD 17.6 minutes). With the consent of participants, all interviews were audio-recorded. Around half (n = 13) of carers completed the timeline template prior to the interview, whereas others said that they had insufficient time or had not remembered to do so. Following the interview, all carer participants were given a £10 shopping voucher to thank them for taking part.
Analysis
All interviews were transcribed verbatim and analysed using a framework approach66 by two qualitative researchers. First, transcripts were read in full and key themes were identified in accordance with the aims of the qualitative study. These key themes addressed both aspects of the study, that is the support experiences of families (carer interviews only) and the perceived effectiveness of SIT (interviews with therapists and carers of children in the intervention arm). Transcripts were then re-examined and emergent subthemes were identified within each main theme by the first qualitative researcher. After discussion with the second qualitative researcher, a thematic framework was developed and entered into NVivo. All interviews were then coded in NVivo by the first qualitative researcher, with 10% of transcripts coded by the second qualitative researcher to enhance reliability. Tables were created to summarise the experiences of each interview participant, corresponding to each theme and subtheme. The inclusion of illustrative quotes enabled the validity of findings to be reviewed. Both qualitative researchers met to discuss the identified themes and discussion continued until consensus was reached.
Results: part 1 – support experiences of families
Timelines completed by carers gave an overview of the support received by families. There was wide variation in experiences. However, in the early years of children’s lives, the involvement of professionals followed a similar pattern. Carers noted that they first became aware of signs that their child might be autistic at the age of 1 or 2 years, when the main professional point of contact was their health visitor. Early concerns were raised with the health visitor, but often dismissed. Professionals tended to notice children’s speech difficulties at an early stage, resulting in support from speech and language therapists and/or paediatricians. When children started formal education, this appeared to initiate additional support, for example from psychologists, occupational therapists and charitable organisations. However, in most cases, specialist autism support was not provided until children reached the later years of primary school. Some support provision – for example the EarlyBird programme (i.e. a specialist parental support programme) provided by NAS – could be accessed only when a child had been diagnosed with autism. After receiving a diagnosis, there was much greater variation in service provision and, aside from the EarlyBird programme, no clear pathway to support.
Three key themes were identified from interview transcripts and timelines, each with three emergent subthemes (Table 46). Each theme is discussed in the following sections, supported by participant quotes, which are labelled with participant identification numbers.
| Main theme | Subtheme |
|---|---|
| Support provision |
Variation in support received Support changes since diagnosis Carers’ learning and research |
| Usefulness of support |
Generic vs. specialist Statutory vs. voluntary Professionals vs. experts by experience |
| Unmet support needs |
Barriers to accessing support Gaps in support Limits in support |
Support provision
Variation in support received
The support received varied widely. Eight families had accessed between one and three forms of support, whereas nine families had received support from ≥ 10 professionals or organisations. No differences in support accessed were observed relating to the sex, age or location of the child. However, families living in Cornwall identified that there were limited services available locally. There was not a defined pathway to receiving support, which families accessed in a variety of ways, including as a result of parental networks and independent research and via school, medical professionals and charitable organisations. There was often a domino effect, with families being referred to one support organisation, which then referred them to a second form of support, and so on. One carer found that support seemed to be automatically provided once their child had received a diagnosis, but others had needed to proactively find support themselves:
[School] referred us to Team Around the Family, they came out, did an assessment . . . [that] led to CAMHS . . . they led us to OT . . . then we were passed on . . . to neurodevelopmental.
P15
I wasn’t hanging around waiting for stuff to happen . . . Once you have official diagnosis . . . you’re in the system and then suddenly everything kind of kicks in.
P6
I went off and did ASD parenting courses, as you do. And probably went into doing quite a lot of self-led learning and finding support groups for me and for the children . . . Everything we’ve done, we’ve done ourselves.
P23
Support changes since diagnosis
Once children received a diagnosis of autism, this enabled some to receive additional support. This additional support was most notable in school (e.g. the provision of a statement of special educational needs or a specialist school placement). However, some families accessed no additional support following diagnosis:
They just give you a book and . . . there we go, there’s nothing, there’s no therapy available or anything . . . I thought they’d be like, he’s diagnosed, here are some therapies you can access . . . The only thing the assessment changed is my peace of mind that it’s not me, it’s not my parenting . . . but that was the only [benefit] because we haven’t got access to anything extra really . . . it’s pointless, well it’s hard.
P13
Carers’ learning and research
Despite diagnosis not always resulting in additional support for families, carers identified that it empowered them to look for resources themselves and this had given them a greater understanding of their child (e.g. in relation to their behaviour and SPDs) and enhanced their ability to give them the support that they needed:
Some people say why would you want to put a label on it, it’s not about putting a label on her, but we didn’t know if we were doing things correctly . . . because obviously looking back now, some of the things that we were doing wasn’t helping, it was making things worse.
P16
Once their child had been diagnosed, many carers found local or online support groups and worked to increase their own knowledge of autism. However, their ability to do this depended on the networks and finance available to them. For example, some carers were able to pay for support, whereas others attended relevant courses through their own work in a similar field and some were able to gain advice from friends with specialist knowledge.
Usefulness of support
Generic versus specialist
Specialist support was viewed as being the most useful, whereas carers reported that more generic support tended not to address their child’s needs. For example, health visitors, who were often the initial source of support for carers and able to refer to specialist provision, were mainly described by carers as being dismissive of early concerns about autism. Likewise, carers identified that CAMHS and SLT appeared unable to deliver support that addressed the needs of their child. In contrast, carers viewed specialist support as being very useful, particularly parenting courses focused on autism and specialist OT advice, for example relating to their child’s SPDs:
I had concerns from quite a young age, but the health visitor I felt dismissed my concerns, because I was seeing lots of red flags and I think . . . they were thinking I was overanalysing.
P20
[CAMHS are] just . . . not equipped to deal with autism . . . she’s got severe, severe anxiety . . . but she’s not being treated for it because they don’t know how . . . We did a bit of work with one lady, after 4 weeks, she said ‘Oh I’m unable to help her . . . she just doesn’t understand it’ . . . Meanwhile . . . it’s getting a whole lot worse and having a massive impact on her life.
P8
I’ve been on loads and loads of [parenting] training . . . the only course I can honestly say that I did enjoy was the EarlyBird course. Now . . . that was a great help . . . more realistic . . . I really got on with the parents there, they were in the same situation as me and that’s what I wanted . . . it opened my eyes, I understand, understood a lot more.
P16
Statutory versus voluntary
Although statutory services (e.g. SLT and CAMHS) tended to be seen as unhelpful, carers reported that charitable organisations and local disability groups provided the most useful support, even when they were not specialist autism services. These forms of support helped to fill the identified gaps left by statutory services and were described as a vital source of help and advice. A key benefit of disability groups is that they enabled children to take part in activities (e.g. soft play, swimming and the cinema) that they usually experienced difficulties accessing. Carers noted that these groups provided a less pressured environment than they had encountered in mainstream activities:
[A local] charity helping disabled children [learn] through play . . . has been a lifeline . . . [The psychologist] is able to talk to him with the action figures, or with the Lego . . . they can talk about feelings through that, which is a great asset because . . . empathy was really hard for him. He really struggled.
P9
The National Autistic Society . . . they’re really good. We . . . meet up with other families every now and again so we go down to . . . an indoor play centre just down the road. Sometimes they rent it out for an evening . . . we also go to the cinema . . . where they do . . . dimmed lights which is good.
P2
Professionals versus experts by experience
As discussed previously, carers identified that professionals who they had come into contact with often did not have expertise in autism and, therefore, could not provide support that met the needs of their child. In some cases, professionals were described as ‘dismissive’ or ‘judgemental’. Conversely, contact (online or face to face) with other carers who were in a similar situation was valuable in allowing useful ideas or strategies to be shared and provided a non-judgemental form of support:
You see it time and time again, it’s schools being unsupportive. Professionals saying, ‘There’s absolutely nothing wrong’, even though it’s staring them in the face. It’s the parent, you know, the parental blame . . . your parenting skills.
P29
She was very negative . . . towards [our] parenting . . . And I actually spoke to CAMHS after all this and said, ‘I don’t want her coming back’, because . . . she made me, well she made us both feel like [we] haven’t done enough really.
P24
You know that somewhere [on the Facebook group] there’ll be . . . someone saying, yeah I hear what you’re saying, I’ve been there, I get it, you’re not the only one. And that can be a massive thing, because obviously being a parent of a child who’s got extra needs, it can feel quite lonely . . . and it’s nice to know that someone actually understands.
P29
Unmet support needs
Barriers to accessing support
Children’s difficulties being dismissed by professionals was a key barrier to support and resulted in delayed diagnosis, in a lack of support in school and in referrals for additional help being rejected. Several carers reported waiting years for their child’s autism diagnosis, despite noticing indicators of autism early on. In some cases, children (particularly girls) masked their difficulties when outside the home, which meant that signs of autism were sometimes missed by professionals. Schools were identified as important in providing support for some families. However, other carers reported that their child’s sensory needs were not recognised, understood or consistently met in the classroom:
I thought he was autistic for, you know, years now. But [school] weren’t bothered because he’s quite compliant and no trouble. You know they wouldn’t refer us to the Ed Psych [educational psychologist] because he’s not, his behaviours aren’t extreme or anything . . . they always refused to do anything really.
P13
He masks at school, he’s a complete masker at school . . . they love him, because he’s as good as gold. He’s never broken a rule in his life . . . he doesn’t present in the way people think is autistic. And I keep hearing, oh girls mask, girls mask, [but] boys do it too.
P23
At school he has a very strict rigid sensory timetable . . . six sensory breaks throughout the day . . . [but] when . . . he’s good for a couple of weeks . . . they slack on [it] . . . and then he’ll start to kick off. I’m like, ‘Well, are you doing all the sensory stuff?’. ’Oh no, because he’s been really good’.
P25
Gaps in support
A key gap in support was direct therapy for children, particularly OT addressing sensory issues. Some carers noted that most services they had encountered appeared to focus on support for carers rather than the child themselves, or that they were diagnostic rather than support services. Carers felt that it would be useful to have one ongoing point of contact to provide ad hoc advice in relation to issues arising and to signpost to relevant services. For several families, the main or only continuous support that they received was from their child’s school. Specifically, carers identified an important unmet need for mental health provision for children with autism. Some families had been unable to access CAMHS because of high referral thresholds (with children not eligible for help even where there were incidences of serious attempted self-harm), whereas others who did receive services found that provision was limited or not helpful:
[Support has been] more for us as parents, rather than [him].
P15
What I find now . . . if there’s an issue that crops up, because [three sources of support] have all finished, [I’ve] only really got the school to deal with now, so if I have an issue, I have got I suppose the Autistic Society . . . but I find I haven’t got anyone . . . like a professional I can actually ask . . . you know, what could I do to help this sort of situation?
P2
[We put in] another CAMHS referral because he started self-harming, putting things around his neck and that, but that got rejected.
P27
There’s no help . . . for these children at all . . . I think it took six referrals to CAMHS . . . she grabbed a knife, tried to chop her own head off . . . they weren’t really worried about it . . . how bad do things have to get before an intervention comes?
P8
Limits of support
Carers reported that the support their family received appeared to be time-limited or had stopped once their child had received a diagnosis. In cases where support had helped their child, children found the ending of services confusing and carers were frustrated. Limitations in funding or provision had meant that some families had experienced long waiting lists for support or were unable to afford the support that they felt their child needed. Carers living in Cornwall identified that local services were limited or non-existent and, therefore, some families were not provided with specialist support or had to travel long distances to access it:
I find the support have stopped . . . [the] occupational therapist has gone, it’s like everyone’s gone now. So we’ve got no support . . . [and] he’s still struggling every day.
P14
He’s had so many like different departments involved in his care . . . Now . . . it’s like right . . . we’ve helped you . . . we can’t do no more . . . so basically everybody’s signed him off. He’s confused because he now thinks that everyone’s just dropped him and doesn’t care.
P17
I’ve looked into private SI [SIT], but I can’t afford it, it’s stupidly expensive . . . it’s like £50-odd a session. I mean, I can’t afford that.
P13
We’ve been waiting about 8 months now for the next step [following diagnosis] and I don’t know when that’s going to be.
P1
It’s very hard in Cornwall to get onto any parenting course that’s in the evening, and [the courses are far away, so] I have to either catch the ferry . . . or drive the hour round trip, all around the coast . . . It’s not practical and it, it puts you off, you think . . . what’s the point, and . . . try and battle on.
P24
Results: part 2 – perceived impact of sensory integration therapy
Three key themes were identified from interview transcripts in relation to the perceived impact of SIT and within each key theme there were several emergent subthemes (Table 47). Each theme is discussed below and is supported by participant quotes. Quotes from carers are labelled with ‘P’, followed by their participant identification number. Quotes from therapists are labelled with ‘T’, followed by their participant identification number.
| Main theme | Subtheme |
|---|---|
| Effect on child |
Became calmer Developed skills Increased tolerance of everyday tasks Increased confidence and independence |
| Effect on school and family life |
Changed everyday life Learning for carers Strategies for home and school |
| Limitations |
Changes not always sustained Not always the best approach Outcomes dependent on parental engagement |
Effect on the child
Became calmer
Most carers identified that their child had become calmer following the intervention. For example, meltdowns and instances of aggressive behaviour reduced, and concentration in school improved. Some carers noted that their child remained calmer and more relaxed for several days after each intervention session. Carers reported that children had learnt coping skills and techniques, which they had been able to put into practice at home and at school. It was also identified by both carers and therapists that children became more self-aware and, therefore, they were better able to recognise their own feelings and sensory needs, enabling children to have more control over their behaviour:
[The sessions were] so good for him that . . . the rest of the day, well even the rest of the week . . . it made a big difference to him, his behaviour was better, he could concentrate more.
P109
He learnt pretty quickly from the beginning the techniques to calm himself down. And so that was really beneficial for him, to understand . . . what might make him feel better or what, what might make him feel worse.
P308
I think she was able to understand and recognise her own needs . . . that was a big . . . learning curve for her . . . understanding that when my body feels like this, this is what I need to do about it.
T210
That little bit of space in time, before the meltdown happens, she can actually say what she needs to avoid the meltdown . . . [She] is now aware of her body and what she needs to keep things under control.
P514
Developed skills
While receiving the intervention, children’s fine and gross motor skills improved. For example, children developed their ability to complete everyday tasks, such as getting washed and dressed, going to the toilet unaided and using a knife and fork. Improved physical skills enabled some children to access new activities, such as playing football, riding a bicycle and utilising a greater range of playground equipment, meaning that some were more able to join in with their peers. Children’s awareness of, and confidence in, their own body also improved, including through developments in co-ordination, balance, spatial awareness and motor planning, and this increased physical confidence and meant that some were more willing to attempt new activities:
One of the things that stood out for me . . . it might not seem like a big thing but for him it was . . . we went to a park and he just sat on the swing upright instead of prone, and he was able to do that with his friend, whereas before he would have just avoided it, because he wouldn’t have wanted to show his friend that he didn’t sit on the swing.
P703
[One boy] loved football . . . and he was able to participate in playground football, having done this intervention . . . He just wasn’t able to do it, for various reasons, before . . . in the playtimes he would go to like a nurture class instead of going [outside].
T211
I feel that his confidence in his own body has increased. Before we would go to the park or something and he wouldn’t really explore the apparatus and stuff, but now he can, I can see that he’s got confidence to try things . . . I think he’s got more body awareness, and I think it’s just really increased his general confidence in himself and his ability of what his body can do.
P703
For one child her self-esteem had really increased and [her] willingness to try new things . . . she went on a school trip . . . [to] an activity centre . . . and her mum [said] . . . before she wouldn’t have attempted to go on any of the equipment. But, but this time she tried absolutely everything . . . it’s just giving her that kind of confidence about what she can do with her body.
T213
Increased tolerance of everyday tasks
Following the intervention, carers noticed that their child’s ability to tolerate everyday tasks, such as washing, nail cutting and hair brushing, had improved and this had meant fewer meltdowns and enabled some children to access activities that they had previously been unable to participate in (e.g. swimming). Notably, although one carer reported that their child’s tolerance of toothbrushing had increased, several identified that this was still an issue:
If you’ve got a child who is unable to tolerate water, and then . . . can’t go swimming, can’t access a splash park, [or] can’t tolerate wearing a helmet . . . [and then] can’t do those lovely early childhood occupations, like ride a scooter or a bike, then they’re missing out, aren’t they . . . The first child that I worked with . . . [learnt] to tolerate those things . . . [and] he was able to ride a scooter, which he’d never done . . . before because he wouldn’t wear a helmet.
T210
The toothbrushing was a complete failure. He still won’t do that at all.
P506
Increased confidence and independence
It was commonly identified by both carers and therapists that children’s confidence increased during the intervention. For example, carers reported that children were more willing to try new activities or foods and could cope more effectively with new situations and changes. Some children had begun to socialise more and, as their confidence increased and communication skills developed, they became more able to express their needs to others, which had enabled them to become more independent. For example, one carer reported that she was now more confident that her child – who had previously been looked after by family members only – would cope in holiday clubs:
Even [the therapist] saw a huge difference in him in the time that she’s been working with him, from a boy who didn’t feel that he had the confidence to do anything to all of a sudden just waltzing in, going off and doing his own thing.
P109
It’s really improved his confidence . . . he’s happy to go out in the community, he’s happy to try new things . . . he’s been less anxious . . . His parents have noticed a massive difference in his behaviour at home and he’s engaging in things that he never engaged in before, he’s doing things he’s never done before.
T207
Effect on family and school life
Changed everyday life
Some carers described the intervention as ‘life-changing’ for their child and the whole family. In some cases, this was because it was the first helpful form of support that they had been able to access. As children learnt new skills, had increased in independence and were better able to tolerate everyday tasks, their meltdowns reduced and daily routines became less problematic, resulting in less stress and improved quality of life for carers. Carers identified that children had improved their ability to cope with changes and new situations, meaning that they were more confident in going on family days out. Notably, several carers stated that now their child had received the intervention they could envisage them becoming independent in the future. For some children, teachers had also commented that their confidence, skills and general behaviour had improved. Carers too reported that children had increased in their ability to cope in the classroom:
Before the [intervention] I didn’t know what to do or where to go because he was struggling so much, but it seems to have made him settle down a lot . . . It’s literally changed his life but changed our life as well. You know, it’s only a short space of time but it has made so much difference to us . . . I am just completely in awe of the differences in him.
P109
Before the [intervention] I used to question whether he would ever be independent enough to live on his own. Whereas now I am starting to feel that maybe he would be OK.
P109
I’ve seen an improvement in [her] . . . and it’s not only me, it’s been school as well, they’ve noticed her behaviour has improved . . . she’s overall calmer and she can cope with situations better.
P514
Learning for carers
Carers reported that the intervention enabled them to understand their child better. For example, carers had increased their understanding of their child’s sensory needs, enabling them to make changes at home and at school. Understanding the reasons behind their child’s behaviour made some carers more confident and improved parent–child relationships, as they realised that some behaviours they had previously perceived as negative were because of their child’s sensory difficulties. As a result of this improved understanding, some carers became empowered to advocate for their child by, for example, ensuring that they were appropriately supported in school:
It’s helped us understand him a little bit more . . . I hadn’t appreciated . . . that he doesn’t like tilting his head backwards . . . and so we’re sort of working on ways . . . [to] try and help him . . . So that’s sort of been quite interesting, realising, learning about that for him.
P609
I think it was a huge step for mum in a way, whereas [before] she felt so helpless . . . what’s going on with my daughter and how can I help her, to the point of OK I can do this, that and the other . . . Definitely empowered her.
T206
We couldn’t really understand why she did certain things . . . what [the intervention] did was identify what she was doing and why . . . Just from learning why she does all the things she does . . . you just realise actually that she’s not being awkward, she’s not being selfish or stroppy, she has to do it that way to function and I think that’s the biggest thing we got from it, is maybe understanding her a little more.
P219
Strategies for home and school
Therapists had given carers strategies and ideas to try at home, which they mostly found effective. For example, advice to encourage children to be more physically active had helped to regulate their behaviour. Therapists had taught relaxation techniques to some older children, which had been used successfully at home and at school. Therapists had also provided ideas of sensory activities that carers could implement at home to address the needs of individual children, such as messy play or obstacle courses. Carers reported that suggestions of equipment to purchase were particularly helpful. For example, items such as a weighted blanket, which had helped their child to relax, and larger equipment such as swings or gym balls, which children could use to self-regulate. Some children had used suggested equipment, such as wobble cushions, in school, which had helped to improve their concentration. Therapists had also suggested strategies to help carers handle specific situations, such as giving children step-by-step instructions or providing sensory stimulation to children before carrying out certain tasks (e.g. hair brushing or nail cutting):
[The therapist] suggested an air cushion for him, for him to sit on in school and apparently it’s really good for concentration and stuff. So she lent us one to try and it worked really well.
P109
We noticed car doors are a big thing, he won’t open the car door if it’s wet, but . . . [now] we tend to give him a lot of pressure on his hands and things before he goes out, before he leaves the house. And then he’ll open the door, without even thinking about it. So it’s just little things like that.
P308
Limitations
Changes not always sustained
For some children, carers reported that changes in behaviour and tolerance of everyday tasks were sustained following the intervention. Some children had continued to make progress when carers carried out activities suggested by the therapist and as a result of greater support provision at school. However, some carers identified that their child’s behaviour had deteriorated after the intervention sessions finished, for example with increased meltdowns. Although some carers felt that their child would need therapy continuously, others suggested that lengthening the intervention could help to bring about more lasting changes:
He will still wear his helmet [and go in] his car seat . . . it’s really lasted, it’s really desensitised him to certain things, you know. I dread to think what he’d be like if we turn that back, oh God.
P304
I think it needs to be continuous input, [otherwise] it doesn’t really work . . . I don’t think it, it works and then you’re cured as such. You need to continue to do it . . . But I think it’s helped him, because we’ve got ideas at home that he can use.
P506
Not always the best approach
The therapist interviews did not include any questions relating to the perceived appropriateness of the intervention for children participating in the trial. However, a minority of therapists strongly felt that using pure SIT was restrictive. These therapists suggested that a flexible approach – whereby a range of techniques could be applied to tackle different therapy goals – would be more helpful, as SIT was not always the most efficient or appropriate way of achieving set outcomes. In particular, it was difficult to tackle issues such as problems with toothbrushing in the play environment, rather than in the context of the child’s home. Therapists also reported that using SIT to address functional skills necessitated a lot of input, as they were required to hypothesise how improvements in sensory integration could affect children’s skill performance, rather than working on improving the skills themselves:
Out of the three children [I saw] . . . if I hadn’t been part of the research, probably only one of those children I would have looked at using [SIT] for them. The other two children I would have used very different mechanisms to achieve the goals . . . in a much shorter . . . time . . . There was one about cutlery and I think if we [had] just looked at different adaptive cutlery, I think that they would have achieved that goal.
T205
You had to write your hypothesis . . . so for instance, when the child set bottom-wiping as a goal . . . my hypothesis was that because she had tactile issues and issues understanding where her body was in space . . . as she became more aware of her environment, was able to process tactile information more readily . . . she would have more success with bottom-wiping . . . It did work . . . But it’s an awful lot of input to give, to get to that.
T212
Outcomes dependent on carer engagement
Therapists identified that children’s progress was facilitated when carers were fully engaged with the intervention. Some carers were fully committed in terms of attendance, were interested in ideas suggested by the therapist and were keen to learn. Carers tried to suggest activities and strategies at home, and some purchased sensory equipment. However, where carers were less committed, their child’s progress was limited. For example, some carers did not ensure that their child attended intervention sessions regularly, did not implement suggestions at home or appeared not to be motivated to learn more about their child’s difficulties. Therapists noted that for therapy goals to be reached and changes to be sustained, it was important that activities from the sessions were continued at home.
Some families faced barriers to implementing the suggested activities at home. For example, some families did not have the time to engage in one-to-one activities with their child, as they had other children who also had additional needs, and some carers themselves had autism or sensory issues, which affected their ability to understand SIT and to engage in sensory play with their child. For instance, some carers did not realise the importance of play, did not understand how to play or had an aversion to messy play:
The first child that I worked with . . . alongside the [intervention] the parents have made sure they’ve been doing lots of [physical activity] with him outside, outside the sessions as well, and I’ve seen an absolutely massive difference in him, he’s like a different child.
T207
Some have been very . . . on board and open to any suggestions . . . others I think [have] not fully understood the commitment and found it quite hard and then that makes our life hard, because then we’re seeing changes but we’re not able to progress them . . . because their parents are not taking them on.
T208
She’d missed out on a lot of sensory experiences . . . And, you know her mum and dad did recognise that. So that was really interesting. And it was during some of the sessions where we used a lot of messy play and worked on her tactile system, you know you could see the parents were horrified . . . and they were able to recognise that they had some tactile issues themselves.
T201
It was a real challenge with the parents with autism to help them understand [the intervention] and I’m really not sure that they did.
T212
Summary
Support provision for families varied widely, and there was no clear pathway of support for children and families following autism diagnosis. In some cases, access to support was dependent on carers’ resources. Non-specialist services tended not to meet children’s needs. However, specialist provision was generally not accessed until the later years of primary school. Key barriers to support included professionals being dismissive of children’s needs, limited local service provision and lengthy waiting lists. Unmet support needs included a need for direct therapy for children, specialist mental health provision and ongoing information and advice for carers.
Following the SIT intervention, carers and therapists reported that children became calmer, developed their physical skills, were better able to tolerate everyday tasks and increased in confidence and independence, and this resulted in changes in day-to-day family and school life, making daily routines and changes being easier to manage. Carers developed a better understanding of their child and were able to implement strategies and activities suggested by the therapist. However, for some children, changes in behaviour were not sustained following the intervention. A minority of therapists felt that using SIT was not the right approach for all children who they provided therapy to. For example, functional skills, such as toothbrushing, may be better addressed in the context of the child’s home. It was also noted by therapists that therapy outcomes were dependent on the level of parental engagement in the intervention.
Chapter 10 Discussion
Overview
In this chapter, a summary of the results is presented, with interpretation of findings discussed in the context of previous research and the original commissioning brief for this study, which noted that, although SIT is sometimes delivered in the NHS, there is limited evidence to support effectiveness (as also stated in the NICE clinical guideline for children with autism17).
Summary and interpretation of findings
Recruitment and retention
The overall recruitment target (revised as per planned sensitivity analysis of sample size assumptions following the internal pilot) was met and 77.5% of randomised participants provided outcome data at the primary outcome time point. Loss to follow-up was slightly higher than the estimated 20%. However, given that all other assumptions relating to the sample size calculation were met, power to detect the target standardised effect size of 0.5 for the primary analysis remained at 90%. Longer-term (12-month) retention was lower at just under 70% (69.6%), although no between-arm difference was evident and this may reflect the complex life circumstances of the population (i.e. carers of young children with neurodisability who may also be working and caring for other children/family members).
Baseline characteristics and reach
Participants were well balanced across arms in terms of baseline characteristics. Most (79%) participants were male and white British (88%), reflecting those likely to have received an autism diagnosis. Autism is underdiagnosed in girls111 and ethnic minority boys112 for a variety of complex reasons, including stereotypical beliefs about presenting symptoms and perceived stigma. Most (71.7%) participants were recruited from South Wales and had a mean age of approximately 7 years and 10 months. Recruited participants showed significant sensory dysfunction. Eligibility criteria required at least probable dysfunction on two or more sensory dimensions of the SPM and the total score, or definite dysfunction on one dimension and total score. All potential participants screened met criteria, in line with available SPD prevalence estimates in autism,9–11 and 77.5% of participants had definite sensory dysfunction. A significant proportion of participants (25%) also had a diagnosis of ADHD.
Usual care and contamination
As detailed in Chapter 2, and confirmed during the internal pilot phase (see Chapter 4) and qualitative interviews with carers (see Chapter 9), usual care for young children with autism and SPDs is highly variable and, in many cases, comprises no formal OT intervention. Sensory-based difficulties are commonly reported and there is a clearly expressed demand from carers for services that specifically address sensory difficulties. Current NHS provision is generally focused on delivery of sensory strategies and advice (e.g. generic written information, bespoke leaflet, parent/carer groups and one-to-one consultations), although evidence to support the use of sensory strategies is limited (see Chapter 1). Some direct therapy may be offered using a sensory integration approach, but this does not generally meet fidelity criteria for SIT, in terms of both content and dose/frequency of contact. Where carers do access SIT, this is generally from private practitioners and, therefore, is inaccessible to most families. In terms of contamination, one trial participant allocated to the control arm received SIT, but sensitivity analysis suggests that this is unlikely to have influenced interpretation of results and no other evidence of sustained contact with OT services was reported. We found no evidence to suggest that families allocated to SIT were in receipt of significant OT intervention.
Fidelity and intervention receipt
Overall, SIT was delivered with good fidelity. All clinics were rated as achieving structural fidelity, meaning that the level of therapist training, documentation and the physical environment (including equipment) met the required standard for SIT. Ten out of 12 therapists met criteria for process fidelity consistently across sessions (i.e. ensured safety and established therapeutic alliance, and provided the appropriate level of challenge and sensory opportunity). It was not possible, however, to rate fidelity for all therapists (as no useable recordings were available for 4 out of 16 therapists). However, therapists did receive mentoring throughout intervention delivery, with a focus on aspects central to fidelity. Rater agreement was generally good, although lower average scores for two therapists may reflect poor inter-rater agreement, particularly where more than two ratings per session were available.
The pattern of intervention receipt was variable, although 78.3% of participants allocated to the intervention arm had received 13 out of 20 SIT sessions during the intensive delivery phase (defined as the target dose, of a possible 26 sessions overall). However, many participants received more than 13 sessions in total, with a median of 20 sessions received.
Acceptability
In terms of acceptability of trial procedures, most carers were very positive about their experience of taking part in the trial. A significant proportion of carers allocated to receive the intervention, however, reported some degree of difficulty or inconvenience in travelling to appointments, particularly given the frequency of contact. Outcome measures were also felt to be acceptable. Diary completion (detailing contact with other services) was poor, although the introduction of an automated text reminder service did increase response rates. Therapists reported a degree of difficulty with some trial processes and technology and were generally unfamiliar with the level of documentation required in clinical trials. In addition, most therapists reported difficulty in completing assessments and paperwork within the time estimated as per excess treatment costs.
Carers of children randomised to receive SIT reported high levels of satisfaction with the intervention, and many carers felt that it had been of significant benefit to their child and often to the wider family, in terms of facilitating activities it had not previously been possible to engage in. Carers and therapists tended to report that children were calmer, more independent and better able to tolerate everyday tasks following receipt of SIT. Carers also reported increased understanding of their child and felt able to implement strategies suggested by the therapist. However, perceived positive changes in behaviour were not necessarily sustained in all cases once therapy was complete.
Therapists’ experience of delivering SIT was also generally very positive. Many NHS therapists reported being unused to offering treatment so intensively and, although some therapists had found the experience challenging, felt that it had been professionally rewarding and was an approach that could offer benefit to some children. However, most therapists viewed SIT as part of a range of treatment options, the appropriate choice of which would depend on the child and their needs.
Behavioural outcomes
There was no evidence of a statistically significant difference between trial arms for the primary outcome, that is irritability/agitation, which is a measure of challenging behaviour (as assessed by the ABC-I67 at either 6 or 12 months). Parent-assessed ABC-I ratings at 6 months were, on average, higher than teacher ratings (where available). It is likely, however, that this indicates a true difference in behaviour and functioning in different settings, rather than a reporting bias on the part of either type of participant. Exploratory subgroup analyses suggest a differential effect of SIT on ABC-I at 6 months by sex of child, indicating that SIT was more effective for male participants. Subgroup analyses also indicate that the intervention was more effective in participants with a comorbid ADHD diagnosis. It is important to note, however, that even where statistically significant subgroup effects suggest clinically relevant change, that these analyses are hypothesis-generating only and may reflect multiple testing. We found no evidence of a differential effect of SIT on 6-month ABC-I scores by level of SPD, general comorbidity, ID or other neurodevelopmental or genetic condition. Likewise, no effect of SIT was observed for other ABC subscales (i.e. lethargy/social withdrawal, stereotypic behaviour, hyperactivity or inappropriate speech) at each time point.
Additional sensitivity analyses suggest that scores on the ABC-I at 6 months were generally better in those who initiated and received SIT. However, adjusting for the initiation of SIT did not alter the conclusions drawn based on the primary analysis (i.e. there was no evidence of a difference between the intervention arm and the control arm). Sensitivity analyses did not indicate any pandemic-related effects on outcome. No between-arm differences were observed at 6 or 12 months for adaptive behaviour, socialisation or daily living skills (using VABS domains). As detailed in Chapter 6, an error in administration of the VABS measure resulted in the introduction of an artificial ‘ceiling effect’ for these subdomains, meaning that it was less sensitive to change. A statistically significant between-arm difference was observed for the communication domain (indicating a negative intervention effect), although this is felt likely to reflect a combination of multiple testing, ceiling effects and an outlier in the control arm, rather than a clinically meaningful difference. Further sensitivity analyses would be unlikely to add to the interpretation of results, given that no other marginal effects were observed and the pattern of results was similar to that observed for all other outcome measures.
Parenting stress, quality of life and health utility
No between-arm differences were evident for parenting stress, quality of life or health utility. However, subgroup analyses suggest a differential effect of SIT on carer stress (using the APSI) at 6 months by region. A similar effect was observed for the presence of other neurodevelopmental or genetic conditions on carer stress, although this may indicate type I error.
Functional outcomes: occupational performance
There is strong evidence to suggest that carer-rated goal performance and satisfaction increased significantly with SIT exposure. This finding is in line with two previous trials of SIT,33,34 which reported significant effects for GAS. However, as detailed in Chapter 1, both trials were underpowered and did not assess maintenance of skills (i.e. did not include longer-term follow-up), and descriptions of comparators/usual care were limited. 33,34 It is possible that, given the individualised nature of SIT as an intervention, individualised goal-based outcome measures would be more sensitive to change. However, it is uncertain whether or not improvements in performance can be maintained in the longer term. Furthermore, data were available (COPM) for a subset of intervention participants only. It was not possible to collect these data from participants in the control arm, as participants in the control arm were not routinely seen by occupational therapists and not all intervention therapists recorded goals consistently.
Health economic analysis
Delivery of SIT incurred significant additional costs. When intervention costs were not included in total NHS/PSS costs, NHS/PSS costs of care for usual care-only participants were significantly higher than for SIT participants. The mean difference in ABC-I scores between arms did not achieve statistical significance at 6 or 12 months, suggesting no additional clinical benefit of SIT. Economic evidence suggests that SIT has a low probability of being a cost-effective option compared with usual care.
Summary
In summary, the SenITA trial was a robustly conducted evaluation of the clinical effectiveness and cost-effectiveness of SIT for behavioural, functional and quality-of-life outcomes. Targets for recruitment, retention and other key parameters used to estimate sample size were met, maintaining 90% power at the primary analysis time point. Usual care was significantly different from the intervention offered as part of the trial and was delivered with good fidelity and adherence. In addition, there is no evidence of significant contamination in the control arm or of those allocated to SIT receiving meaningful intervention via other routes. No adverse effects were reported. The population recruited are likely to be representative of young children with a diagnosis of autism and presenting to services, although this is distinct from being truly representative of the target population, given the well-documented underdiagnosis of autism in girls and minority ethnic children.
Trial procedures and outcome measures were acceptable to carers, and therapists generally found involvement in the trial to be a positive experience. However, many therapists reported issues with management of trial documentation and technology and many felt that the time allowed for assessment and recording clinical notes was insufficient. Carers in the intervention arm reported high levels of satisfaction and benefit of SIT, although no statistically significant quantitative change in carer stress was observed. Both carers and therapists tended to report improvements in well-being and daily functioning, although there is no evidence to suggest that these effects were maintained following the end of therapy. Therapists’ experience of delivering SIT was also generally positive, and most felt it to be an approach that could offer benefit to some children, depending on their needs.
There were, however, no statistically significant effects of SIT on any behavioural, functional, quality-of-life or well-being outcomes at either 6 or 12 months (with the exception of the VABS communication subdomain, as discussed above). Sensitivity analyses do suggest that scores on the ABC-I at 6 months were generally better in participants who received SIT and that intervention may work better for boys and participants with a comorbid ADHD diagnosis, although these were exploratory analyses and should not be overinterpreted. Carer-rated goal performance and satisfaction did increase significantly with SIT exposure. However, there is no evidence to suggest that improvements were maintained, and data were available for only a subset of intervention arm participants. Health economic evaluation also indicates that SIT is unlikely to represent a cost-effective treatment option when compared with usual care.
Strengths and limitations
Strengths
The key strength of the SenITA trial is that it was adequately powered to answer the key question in the original commissioning bid of ‘What is the effectiveness and cost-effectiveness of SIT for children with autism?’. Important outcomes, as detailed in the commissioning brief, were challenging behaviours, socialisation, engagement with activities and sensory sensitivities. Other potential outcomes listed included adherence to the therapy manual, process indicators, health-related quality of life, carer burden, adverse effects and cost-effectiveness. The trial was sufficiently powered to determine effectiveness of manualised SIT on the primary outcome, that is, a measure of challenging behaviour. The intervention was also delivered with good fidelity and adherence and was acceptable to both families and therapists; no adverse effects were reported. Inclusion of longer-term (12-month) outcome assessment is also a strength, as previous studies33,34 of SIT have assessed outcomes post intervention only (or at an equivalent time point in the comparator arm).
This trial has also made a significant contribution to knowledge around what is generally delivered as usual care to children with autism and SPDs. In addition, the trial has highlighted the gap between services generally available to families (e.g. advice, strategies to improve functional/daily living skills) and services that carers would most value (e.g. intervention to support behavioural problems).
Limitations
Although SIT was generally delivered with good fidelity and all therapists met the required minimum threshold for training and experience, most therapists in Wales were employed by the NHS and had little recent experience of delivering full-fidelity SIT within their NHS roles. In England, trial therapists were working privately, as we were unable to recruit sufficiently trained and experienced therapists in England for a variety of reasons, including a reluctance of therapists to offer therapy via participation in the trial that was not otherwise available and, therefore, setting a level of expectation among families that could not be sustained. Subsequently, therapists at English sites were more used to delivering SIT with this population and did not have to juggle the competing demands of local service targets. Therapists also reported that the time allowed for assessment and clinical reasoning was insufficient, particularly at initiation of therapy, meaning that the total costs of intervention would probably be higher than indicated in practice.
For a variety of pragmatic reasons, including therapist availability and workload, some participants allocated to receive SIT did not start intervention within the intended time frame and had, therefore, received a potentially lower dose of SIT by the primary outcome assessment time point. Sensitivity analyses, however, indicate that this is highly unlikely to have significantly affected any key findings. A further limitation is the artificial ceiling effect observed for domains of the VABS. Interpretation of the positive effect on carer-reported goal performance is also limited by the fact that not all intervention therapists reported this consistently and that it was not possible to measure this in the control arm, as participants were not generally in contact with services.
Conclusions and implications
The results of the SenITA trial indicate that SIT shows no clinical benefit across a range of outcomes (i.e. behavioural, functional, social, quality of life and well-being) over and above standard care for young children with autism and at least moderate SPDs. In addition, the results also indicate that SIT is not a cost-effective treatment option in this population. Several subgroup effects were observed, although these should be considered hypothesis-generating only and would require further exploration. Subgroup effects are, however, consistent with qualitative data, indicating that therapists felt that SIT could be of benefit to some, but not all, children with autism and sensory difficulties. It is likely that SIT is effective for individualised (carer-reported) performance goals; however, it is not known if this effect is observed over and above standard care and if improvements can be maintained following the end of treatment.
Acknowledgements
We would like to thank all of the children and parents/carers who took part in the SenITA trial. Many thanks go to all SenITA trial therapists, mentors and parents/carers who contributed to the study through the advisory group, and to all independent members of the Trial Steering Committee and Data Monitoring Committee. Thanks to Jacqui Thornton and Dunla Gallagher for their input to qualitative analysis of usual-care data (see Chapter 2) and to Kath Smith for input to the intervention handbook and therapist training. Thanks also to Jade Williams at the Centre for Trials Research for providing administrative support.
Contributions of authors
Elizabeth Randell (https://orcid.org/0000-0002-1606-3175) managed the trial, contributed to report writing and prepared the report for publication.
Melissa Wright (https://orcid.org/0000-0002-1011-4795) carried out the statistical analysis and wrote up the results for publication.
Sarah Milosevic (https://orcid.org/0000-0003-1973-8286) carried out interviews with carers and therapists, led the qualitative analysis and contributed to report writing.
David Gillespie (https://orcid.org/0000-0002-6934-2928) managed the statistical analysis and contributed to report writing.
Lucy Brookes-Howell (https://orcid.org/0000-0002-8263-7130) led the qualitative components of the trial and contributed to qualitative analysis and report writing.
Monica Busse-Morris (https://orcid.org/0000-0002-5331-5909) provided expertise in evaluation of therapeutic interventions and contributed to report writing.
Richard Hastings (https://orcid.org/0000-0002-0495-8270) provided expertise in research in children with autism and contributed to report writing.
Wakunyambo Maboshe (https://orcid.org/0000-0002-9195-0030) carried out data management.
Rhys Williams-Thomas (https://orcid.org/0000-0002-1779-3460) carried out trial and data management activities and collected quantitative data.
Laura Mills carried out quantitative data collection.
Renee Romeo (https://orcid.org/0000-0003-3871-9697) managed the health economics analysis and contributed to report writing.
Nahel Yaziji (https://orcid.org/0000-0002-2273-7957) carried out the health economics analysis.
Anne Marie McKigney provided clinical and research expertise in relation to children with autism.
Alka Ahuja (https://orcid.org/0000-0003-2658-2021) provided clinical and research expertise in relation to children with autism.
Gemma Warren led the patient and public involvement component of the trial.
Eleni Glarou (https://orcid.org/0000-0001-5666-2458) contributed to interpretation of therapeutic mechanisms and qualitative data.
Sue Delport (https://orcid.org/0000-0001-8065-5493) co-led the study, provided clinical expertise in relation to OT and the trial intervention, and contributed to report writing.
Rachel McNamara (https://orcid.org/0000-0002-7280-1611) co-led the study and contributed to report writing and preparation of the final report.
Data-sharing statement
All available data, study handbooks and the full trial protocol can be obtained by contacting the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HTA programme or the Department of Health and Social Care.
References
- Baron-Cohen S, Scott FJ, Allison C, Williams J, Bolton P, Matthews FE, et al. Prevalence of autism-spectrum conditions: UK school-based population study. Br J Psychiatry 2009;194:500-9. https://doi.org/10.1192/bjp.bp.108.059345.
- Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry 2008;47:921-9. https://doi.org/10.1097/CHI.0b013e318179964f.
- Ung D, Wood JJ, Ehrenreich-May J, Arnold EB, Fuji C, Renno P, et al. Clinical characteristics of high-functioning youth with autism spectrum disorder and anxiety. Neuropsychiatry 2013;3. https://doi.org/10.2217/npy.13.9.
- Hayes SA, Watson SL. The impact of parenting stress: a meta-analysis of studies comparing the experience of parenting stress in parents of children with and without autism spectrum disorder. J Autism Dev Disord 2013;43:629-42. https://doi.org/10.1007/s10803-012-1604-y.
- Buescher AV, Cidav Z, Knapp M, Mandell DS. Costs of autism spectrum disorders in the United Kingdom and the United States. JAMA Pediatr 2014;168:721-8. https://doi.org/10.1001/jamapediatrics.2014.210.
- Humphrey N, Hebron J. Bullying of children and adolescents with autism spectrum conditions: a ‘state of the field’ review. Int J Inclusive Educ 2015;19:845-62. https://doi.org/10.1080/13603116.2014.981602.
- Rowley E, Chandler S, Baird G, Simonoff E, Pickles A, Loucas T, et al. The experience of friendship, victimization and bullying in children with an autism spectrum disorder: associations with child characteristics and school placement. Res Autism Spectr Disord 2012;6:1126-34. https://doi.org/10.1016/j.rasd.2012.03.004.
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders 2013. https://doi.org/10.1176/appi.books.9780890425596.
- Chang YS, Owen JP, Desai SS, Hill SS, Arnett AB, Harris J, et al. Autism and sensory processing disorders: shared white matter disruption in sensory pathways but divergent connectivity in social-emotional pathways. PLOS ONE 2014;9. https://doi.org/10.1371/journal.pone.0103038.
- Leekam SR, Nieto C, Libby SJ, Wing L, Gould J. Describing the sensory abnormalities of children and adults with autism. J Autism Dev Disord 2007;37:894-910. https://doi.org/10.1007/s10803-006-0218-7.
- Tomchek SD, Dunn W. Sensory processing in children with and without autism: a comparative study using the short sensory profile. Am J Occup Ther 2007;61:190-20. https://doi.org/10.5014/ajot.61.2.190.
- Baranek GT. Efficacy of sensory and motor interventions for children with autism. J Autism Dev Disord 2002;32:397-422. https://doi.org/10.1023/a:1020541906063.
- Case-Smith J, Weaver LL, Fristad MA. A systematic review of sensory processing interventions for children with autism spectrum disorders. Autism 2015;19:133-48. https://doi.org/10.1177/1362361313517762.
- Hochhauser M, Engel-Yeger B. Sensory processing abilities and their relation to participation in leisure activities among children with high-functioning autism spectrum disorder (HFASD). Res Autism Spectr Disord 2010;4:746-54. https://doi.org/10.1016/j.rasd.2010.01.015.
- Ismael N, Lawson LM, Hartwell J. Relationship between sensory processing and participation in daily occupations for children with autism spectrum disorder: a systematic review of studies that used Dunn’s sensory processing framework. Am J Occup Ther 2018;72:7203205030p1-p9. https://doi.org/10.5014/ajot.2018.024075.
- Schaaf RC, Toth-Cohen S, Johnson SL, Outten G, Benevides TW. The everyday routines of families of children with autism: examining the impact of sensory processsing difficulties on the family. Autism 2011;15:373-89. https://doi.org/10.1177/1362361310386505.
- National Collaborating Centre for Mental Health . Autism: The NICE Guideline on the Management and Support of Children and Young People on the Autism Spectrum 2013.
- World Federation of Occupational Therapists . Definitions of Occupational Therapy From Member Organisations 2012. www.wfot.org/about/about-occupational-therapy (accessed 28 May 2021).
- Wilcock A, Hocking C. An Occupational Perspective of Health. Thorofare, NJ: Slack; 2015.
- Royal College of Occupational Therapists . RCOT Informed View: Sensory Integration and Sensory-Based Interventions 2021. www.rcot.co.uk/about-occupational-therapy/rcot-informed-views (accessed 28 May 2021).
- Trombly C. Anticipating the future: assessment of occupational function. Am J Occup Ther 1993;47:253-7. https://doi.org/10.5014/ajot.47.3.253.
- Rodger S, Vishram A. Mastering social and organization goals: strategy use by two children with Asperger syndrome during cognitive orientation to daily occupational performance. Phys Occup Ther Pediatr 2010;30:264-76. https://doi.org/10.3109/01942638.2010.500893.
- Parham LD, Roley SS, May-Benson TA, Koomar J, Brett-Green B, Burke JP, et al. Development of a fidelity measure for research on the effectiveness of the ayres sensory integration® intervention. Am J Occup Ther 2011;65:133-42. https://doi.org/10.5014/ajot.2011.000745.
- Dunn W, Cox J, Foster L, Mische-Lawson L, Tanquary J. Impact of a contextual intervention on child participation and parent competence among children with autism spectrum disorders: a pretest–posttest repeated-measures design. Am J Occup Ther 2012;66:520-8. https://doi.org/10.5014/ajot.2012.004119.
- Fertel-Daly D, Bedell G, Hinojosa J. Effects of a weighted vest on attention to task and self-stimulatory behaviors in preschoolers with pervasive developmental disorders. Am J Occup Ther 2001;55:629-40. https://doi.org/10.5014/ajot.55.6.629.
- Bagatell N, Mirigliani G, Patterson C, Reyes Y, Test L. Effectiveness of therapy ball chairs on classroom participation in children with autism spectrum disorders. Am J Occup Ther 2010;64:895-903. https://doi.org/10.5014/ajot.2010.09149.
- Schilling DL, Schwartz IS. Alternative seating for young children with autism spectrum disorder: effects on classroom behavior. J Autism Dev Disord 2004;34:423-32. https://doi.org/10.1023/b:jadd.0000037418.48587.f4.
- Van Rie GL, Heflin LJ. The effect of sensory activities on correct responding for children with autism spectrum disorders. Res Autism Spectr Disord 2009;3:783-96. https://doi.org/10.1016/j.rasd.2009.03.001.
- Fazlioğlu Y, Baran G. A sensory integration therapy program on sensory problems for children with autism. Percept Mot Skills 2008;106:415-22. https://doi.org/10.2466/pms.106.2.415-422.
- Schaaf RC, Mailloux Z. Clinician’s Guide for Implementing Ayres Sensory Integration®: Promoting Participation for Children with Autism. Bethesda, MD: American Occupational Therapy Association; 2015.
- Ayres A. Sensory Integration and Learning Disorders. Los Angeles, CA: Western Psychological Services; 1972.
- Ayres A. Sensory Integration and the Child. Los Angeles, CA: Western Psychological Services; 2005.
- Pfeiffer BA, Koenig K, Kinnealey M, Sheppard M, Henderson L. Effectiveness of sensory integration interventions in children with autism spectrum disorders: a pilot study. Am J Occup Ther 2011;65:76-85. https://doi.org/10.5014/ajot.2011.09205.
- Schaaf RC, Benevides T, Mailloux Z, Faller P, Hunt J, van Hooydonk E, et al. An intervention for sensory difficulties in children with autism: a randomized trial. J Autism Dev Disord 2014;44:1493-506. https://doi.org/10.1007/s10803-013-1983-8.
- Tennant A. Goal attainment scaling: current methodological challenges. Disabil Rehabil 2007;29:1583-8. https://doi.org/10.1080/09638280701618828.
- Krasny-Pacini A, Evans J, Sohlberg MM, Chevignard M. Proposed criteria for appraising goal attainment scales used as outcome measures in rehabilitation research. Arch Phys Med Rehabil 2016;97:157-70. https://doi.org/10.1016/j.apmr.2015.08.424.
- Steenbeek D, Ketelaar M, Galama K, Gorter JW. Goal attainment scaling in paediatric rehabilitation: a critical review of the literature. Dev Med Child Neurol 2007;49:550-6. https://doi.org/10.1111/j.1469-8749.2007.00550.x.
- Ruble L, McGrew JH, Toland MD. Goal attainment scaling as an outcome measure in randomized controlled trials of psychosocial interventions in autism. J Autism Dev Disord 2012;42:1974-83. https://doi.org/10.1007/s10803-012-1446-7.
- Schaaf RC, Dumont RL, Arbesman M, May-Benson TA. Efficacy of occupational therapy using Ayres Sensory Integration®: a systematic review. Am J Occup Ther 2018;72:7201190010p1-7201190010p10. https://doi.org/10.5014/ajot.2018.028431.
- Schoen SA, Lane SJ, Mailloux Z, May-Benson T, Parham LD, Smith Roley S, et al. A systematic review of ayres sensory integration intervention for children with autism. Autism Res 2019;12:6-19. https://doi.org/10.1002/aur.2046.
- Iwanaga R, Honda S, Nakane H, Tanaka K, Toeda H, Tanaka G. Pilot study: efficacy of sensory integration therapy for Japanese children with high-functioning autism spectrum disorder. Occup Ther Int 2014;21:4-11. https://doi.org/10.1002/oti.1357.
- Barker Dunbar S, Carr-Hertel J, Lieberman HA, Perez B, Ricks K. A pilot study comparison of sensory integration treatment and integrated preschool activities for children with autism. Internet J Allied Health Sci Pract 2012;10. https://doi.org/10.46743/1540-580X/2012.1407.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. https://doi.org/10.1191/1478088706qp063oa.
- Parham L, Ecker C, Miller Kuhaneck H, Henry D, Glennon T. SPM Sensory Processing Measure: Manual. Torrance, CA: Western Psychological Services; 2007.
- South M, Palilla J, Volmar FR. Encyclopedia of Autism Spectrum Disorders. New York, NY: Springer; 2021.
- Ulrich DA. Peabody developmental motor scales and activity cards. Adapt Phys Activ Q 2016;1. https://doi.org/10.1123/apaq.1.2.173.
- Blanche EI, Bodison S, Chang MC, Reinoso G. Development of the comprehensive observations of proprioception (COP): validity, reliability, and factor analysis. Am J Occup Ther 2012;66:691-8. https://doi.org/10.5014/ajot.2012.003608.
- Law M, Baptiste S, McColl M, Opzoomer A, Polatajko H, Pollock N. The Canadian occupational performance measure: an outcome measure for occupational therapy. Can J Occup Ther 1990;57:82-7. https://doi.org/10.1177/000841749005700207.
- Henderson ES, Sugden A, Barnett L. Movement Assessment Battery for Children – 2. London: Pearson Education; 2007.
- Roll K, Roll W. Assessment of Activities of Daily Living (ADLs) and Independent Activities of Daily Living (IADLs) in Children. London: Pearson Education; 2013.
- Beery K, Beery N. The Beery–Buktenica Developmental Test of Visual–Motor Integration (Beery VMI) with Supplemental Developmental Tests of Visual Perception and Motor Coordination and Stepping Stones Age Norms: Administration, Scoring and Teaching Manual. Minneapolis, MN: NCS Pearson; 2010.
- Care Aims Framework . Care Aims n.d. https://careaims.com (accessed 7 April 2022).
- Lord C, Rutter M, DiLavore P, Risi S, Gotham K, Bishop S. Autism Diagnostic Observation Schedule, (ADOS-2) Modules 1–4. Los Angeles, CA: Western Psychological Services; 2012.
- Ayres AJ. Sensory Integration and Praxis Tests: SIPT Manual. Los Angeles, CA: Western Psychological Services; 1989.
- Missiuna C, Pollock N. Perceived efficacy and goal setting in young children. Can J Occup Ther 2000;67:101-9. https://doi.org/10.1177/000841740006700303.
- Missiuna C, Pollock N, Law M, Walter S, Cavey N. Examination of the perceived efficacy and goal setting system (PEGS) with children with disabilities, their parents, and teachers. Am J Occup Ther 2006;60:204-14. https://doi.org/10.5014/ajot.60.2.204.
- Keller J, Kafkes A, Basu S, Federico J, Kielhofner G. The User’s Manual for Child Occupational Self-Assessment (COSA). Chicago, IL: Model of Human Occupation Clearing House; 2006.
- Rubin R. Will the real SMART goals please stand up. Ind Organ Psychol 2002;39. https://doi.org/10.1037/e576932011-003.
- Drolet MJ. The axiological ontology of occupational therapy: a philosophical analysis. Scand J Occup Ther 2014;21:2-10. https://doi.org/10.3109/11038128.2013.831118.
- Kadar M, McDonald R, Lentin P. Evidence-based practice in occupational therapy services for children with autism spectrum disorders in Victoria, Australia. Aust Occup Ther J 2012;59:284-93. https://doi.org/10.1111/j.1440-1630.2012.01015.x.
- Brown GT, Rodger S, Brown A, Roever C. A profile of Canadian pediatric occupational therapy practice. Occup Ther Health Care 2007;21:39-6. https://doi.org/10.1080/J003v21n04_03.
- Dunford C, Richards S. ‘Doubly Disadvantaged’: Report of a Survey on Waiting Lists and Waiting Times for Occupational Therapy Services for Children With Developmental Coordination Disorder 2003.
- NHS Wales . NHS Wales Delivery Framework and Reporting Guidance 2019–2020 2019.
- Rodger S, Kennedy-Behr A. Occupation-Centred Practice with Children: A Practical Guide for Occupational Therapists. Oxford: John Wiley & Sons; 2017.
- Royal College of Occupational Therapists . RCOT Informed View: Sensory Integration and Sensory-Based Interventions n.d. www.rcot.co.uk/about-occupational-therapy/rcot-informed-views (accessed 6 April 2022).
- Ritchie J, Spencer L, Bryman A, Burgess RG. Analyzing Qualitative Data. London: Routledge; 1994.
- Aman MG, Singh NN. Aberrant Behavior Checklist. New York, NY: Slosson Educational Publications; 1986.
- Aman MG. Aberrant Behavior Checklist: current identity and future developments. Clin Exp Pharmacol 2012;2. https://doi.org/10.4172/2161-1459.1000e114.
- Marshburn EC, Aman MG. Factor validity and norms for the aberrant behavior checklist in a community sample of children with mental retardation. J Autism Dev Disord 1992;22:357-73. https://doi.org/10.1007/BF01048240.
- Sparrow SS, Cicchetti DV, Balla DA, Newmark C. Major Psychological Assessment Instruments. Boston, MA: Allyn & Bacon; 1996.
- Silva LM, Schalock M. Autism Parenting Stress Index: initial psychometric evidence. J Autism Dev Disord 2012;42:566-74. https://doi.org/10.1007/s10803-011-1274-1.
- Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727-36. https://doi.org/10.1007/s11136-011-9903-x.
- Brouwer WB, van Exel NJ, van Gorp B, Redekop WK. The CarerQol instrument: a new instrument to measure care-related quality of life of informal caregivers for use in economic evaluations. Qual Life Res 2006;15:1005-21. https://doi.org/10.1007/s11136-005-5994-6.
- Hoefman R, Payakachat N, van Exel J, Kuhlthau K, Kovacs E, Pyne J, et al. Caring for a child with autism spectrum disorder and parents’ quality of life: application of the CarerQol. J Autism Dev Disord 2014;44:1933-45. https://doi.org/10.1007/s10803-014-2066-1.
- Beecham J, Knapp M, Thornicroft G, Brewin CR, Wing J. Measuring Mental Health Needs. London: Gaskell/Royal College of Psychiatrists; 1992.
- Borm GF, Fransen J, Lemmens WA. A simple sample size formula for analysis of covariance in randomized clinical trials. J Clin Epidemiol 2007;60:1234-8. https://doi.org/10.1016/j.jclinepi.2007.02.006.
- Willner P, Rose J, Jahoda A, Stenfert Kroese B, Felce D, MacMahon P, et al. A cluster randomised controlled trial of a manualised cognitive behavioural anger management intervention delivered by supervised lay therapists to people with intellectual disabilities. Health Technol Assess 2013;17. https://doi.org/10.3310/hta17210.
- Great Britain . General Data Protection Regulations 2016 2016.
- CASP UK . Critical Appraisal Skills Programme (CASP) Checklist: 10 Questions to Help You Make Sense of a Qualitative Research 2018.
- Schaaf RC, Benevides TW, Kelly D, Mailloux-Maggio Z. Occupational therapy and sensory integration for children with autism: a feasibility, safety, acceptability and fidelity study. Autism 2012;16:321-7. https://doi.org/10.1177/1362361311435157.
- National Institute for Health and Care Excellence (NICE) . Guide to the Methods of Technology Appraisal 2013 2013.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2020. Canterbury: PSSRU, University of Kent; 2020.
- Netten A, Knight J, Dennett J, Cooley R, Slight A. A Ready Reckoner for Staff Costs in the NHS. Canterbury: PSSRU, University of Kent; 1998.
- Department of Health and Social Care . NHS Reference Costs 2019 2019. www.england.nhs.uk/national-cost-collection/#ncc1819 (accessed 14 June 2021).
- Rodgers M, Marshall D, Simmonds M, Le Couteur A, Biswas M, Wright K, et al. Interventions based on early intensive applied behaviour analysis for autistic children: a systematic review and cost-effectiveness analysis. Health Technol Assess 2020;24. https://doi.org/10.3310/hta24350.
- Blooming Tree . Social Skills After School Club n.d. https://bloomingtree.co.uk/social-skills-after-school-club (accessed 20 April 2022).
- Byford S, Cary M, Barrett B, Aldred CR, Charman T, Howlin P, et al. Cost-effectiveness analysis of a communication-focused therapy for pre-school children with autism: results from a randomised controlled trial. BMC Psychiatry 2015;15. https://doi.org/10.1186/s12888-015-0700-x.
- Child Autism UK . Training Courses n.d. www.childautism.org.uk/for-families/training-courses/ (accessed 20 April 2022).
- Ace Centre n.d. https://acecentre.org.uk/event/aacunit1-2/ (accessed 20 April 2022).
- Connect to Autism . Fees for Diagnostic Assessment, Clinical Consultancy, Training n.d. https://connecttoautism.org/fees/ (accessed 20 April 2022).
- Dulwich Prep London . Dulwich Prep London Parent’s Nurturing Programme n.d. www.dulwichpreplondon.org/wp-content/uploads/2020/06/Parenting-Programme.pdf (accessed 20 April 2022).
- Stuttard L, Beresford B, Clarke S, Beecham J, Morris A. An evaluation of the Cygnet parenting support programme for parents of children with autism spectrum conditions. Res Autism Spectr Disord 2016;23:166-78. https://doi.org/10.1016/j.rasd.2015.12.004.
- Tutorful n.d. https://tutorful.co.uk/search/autism (accessed 20 April 2022).
- Payscale . Average Teaching Assistant (TA) Salary in United Kingdom n.d. www.payscale.com/research/UK/Job=Teaching_Assistant_(TA)/Salary (accessed 20 April 2022).
- Education Endowment Foundation . Small Group Tuition n.d. https://educationendowmentfoundation.org.uk/evidence-summaries/teaching-learning-toolkit/small-group-tuition/ (accessed 20 April 2022).
- Prospects n.d. https://prospects.ac.uk (accessed 20 April 2022).
- Curtis LA. Unit Costs of Health and Social Care 2014. Canterbury: PSSRU, University of Kent; 2014.
- Netten A, Curtis LA, Curtis LA, Netten A. Unit Costs of Health & Social Care 2005. Canterbury: PSSRU, University of Kent; 2005.
- Curtis L, Burns A. Unit Costs of Health and Social Care 2015. Canterbury: PSSRU, University of Kent; 2015.
- The National Archives . SET for Success. The Supply of People With Science, Technology, Engineering and Mathematics Skills n.d. https://webarchive.nationalarchives.gov.uk/ukgwa/+/http:/www.hm-treasury.gov.uk/d/robertsreview_introch1.pdf (accessed 26 April 2022).
- Curtis L, Burns A. Unit Costs of Health and Social Care 2016. Canterbury: PSSRU, University of Kent; 2016.
- Slade I, Hanson H, George A, Kohut K, Strydom A, Wordsworth S, et al. A cost analysis of a cancer genetic service model in the UK. J Community Genet 2016;7:185-94. https://doi.org/10.1007/s12687-016-0266-4.
- NHS . Carers’ Breaks and Respite Care n.d. www.nhs.uk/conditions/social-care-and-support-guide/support-and-benefits-for-carers/carer-breaks-and-respite-care/ (accessed 20 April 2022).
- Curtis L, Burns A. Unit Costs of Health and Social Care 2018. Canterbury: PSSRU, University of Kent; 2018.
- The Canine Fitness Centre . Treatment and Session Pricing n.d. www.thecaninefitnesscentre.co.uk/pricing/ (accessed 20 April 2022).
- NHS . Chiropractic n.d. www.nhs.uk/conditions/chiropractic/#:~:text=Most%20people%20who%20have%20chiropractic,to%20them%20for%20advice%20first (accessed 20 April 2022).
- Uttley L, Stevenson M, Scope A, Rawdin A, Sutton A. The clinical and cost effectiveness of group art therapy for people with non-psychotic mental health disorders: a systematic review and cost-effectiveness analysis. BMC Psychiatry 2015;15. https://doi.org/10.1186/s12888-015-0528-4.
- Knapp M, King D, Romeo R, Schehl B, Barber J, Griffin M, et al. Cost effectiveness of a manual based coping strategy programme in promoting the mental health of family carers of people with dementia (the START (STrAtegies for RelaTives) study): a pragmatic randomised controlled trial. BMJ 2013;347. https://doi.org/10.1136/bmj.f6342.
- van Buuren S, Brand JPL, Groothuis-Oudshoorn CGM, Rubin DB. Fully conditional specification in multivariate imputation. J Stat Comput Simul 2006;76:1049-64. https://doi.org/10.1080/10629360600810434.
- Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015;350. https://doi.org/10.1136/bmj.h1258.
- Ratto AB, Kenworthy L, Yerys BE, Bascom J, Wieckowski AT, White SW, et al. What about the girls? Sex-based differences in autistic traits and adaptive skills. J Autism Dev Disord 2018;48:1698-711. https://doi.org/10.1007/s10803-017-3413-9.
- Slade G. Diverse Perspectives: The Challenges for Families Affected by Autism from Black, Asian and Minority Ethnic Communities. London: National Autistic Society; 2014.
List of abbreviations
- ABC
- Aberrant Behavior Checklist
- ABC-I
- Aberrant Behavior Checklist – irritability
- ADHD
- attention deficit hyperactivity disorder
- ADOS
- Autism Diagnostic Observation Schedule
- AE
- adverse event
- APSI
- Autism Parenting Stress Index
- ASD
- autism spectrum disorder
- ASI
- Ayres Sensory Integration
- CAMHS
- Child and Adolescent Mental Health Services
- CarerQol
- Carer Quality of Life
- CarerQol-7D
- Carer Quality of Life – 7 Dimensions
- CarerQol-VAS
- Carer Quality of Life – visual analogue scale
- CEAC
- cost-effectiveness acceptability curve
- CI
- confidence interval
- COPM
- Canadian Occupational Performance Measure
- CSRI
- Client Service Receipt Inventory
- EQ-5D
- EuroQol-5 Dimensions
- EQ-5D-5L
- EuroQol-5 Dimensions, five-level version
- EQ-VAS
- EuroQol visual analogue scale
- GAS
- Goal Attainment Scale
- GCP
- good clinical practice
- GP
- general practitioner
- ICC
- intracluster correlation coefficient
- ICER
- incremental cost-effectiveness ratio
- ID
- intellectual disability
- IQR
- interquartile range
- IT
- information technology
- NAS
- National Autistic Society
- NICE
- National Institute for Health and Care Excellence
- OT
- occupational therapy
- PI
- principal investigator
- PIS
- participant information sheet
- PSS
- Personal Social Services
- RCT
- randomised controlled trial
- SAE
- serious adverse event
- SD
- standard deviation
- SenITA
- SENsory Integration Therapy for sensory processing difficulties in children with Autism spectrum disorder
- SIPT
- Sensory Integration and Praxis Test
- SIT
- sensory integration therapy
- SLT
- speech and language therapy
- SPD
- sensory processing difficulty
- SPM
- Sensory Processing Measure
- SQL
- Structured Query Language
- VABS
- Vineland Adaptive Behavior Scales
- VABS II
- Vineland Adaptive Behavior Scales, second edition
