Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 16/153/14. The contractual start date was in May 2018. The draft report began editorial review in July 2020 and was accepted for publication in October 2020. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Dedication
This report is dedicated to Deano, one of the SHARPS participants, who sadly died on 10 November 2020. Deano will be remembered for his humour, his strength and his love for his dog, Bailey. He will be missed by many.
Permissions
Copyright statement
Copyright © 2022 Parkes et al. This work was produced by Parkes et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2022 Parkes et al.
Chapter 1 Introduction and background
Parts of this report are reproduced or adapted from Parkes et al. 1 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Parts of this report are reproduced or adapted from Parkes et al. 2 This is an Open Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt and build upon this work, for commercial use, provided the original work is properly cited. See: http://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
This chapter introduces the background and rationale for the research, as well as the research questions as aims.
Response to commissioned call
This report presents the findings from a National Institute for Health Research (NIHR)-funded study that was conducted between May 2018 and May 2020. The study was developed in response to a Health Technology Assessment programme call in April 2017. The study explored the feasibility and acceptability of developing and implementing a peer-delivered, relational intervention to individuals experiencing homelessness and problem substance use. The team was commissioned to develop an ‘intervention’. The team considers the Peer Navigator (PN) intervention to be a ‘complex intervention’, using the Medical Research Council’s terminology,3 as the intervention comprised several interacting components. When the term ‘intervention’ is used in this report, it is intended to have this meaning.
Homelessness and substance use in context
Homelessness is a complex issue that often involves deep social exclusion. It is a term that includes the intersections of experiences of homelessness, substance use, institutional care and ‘street culture’ activities, such as begging and street drinking, along with other challenges. 4 ‘Homelessness’ encompasses a broad range of insecure living circumstances. 5 The European Typology of Homelessness and Housing Exclusion (ETHOS) classifies the living situations that constitute homelessness or housing exclusion as rooflessness, houselessness, insecure housing and inadequate housing. 6 Indicative estimates suggest that 307,000 people in the UK,7 550,000 in the USA8 and 235,000 in Canada9 experience homelessness at any one point. Although estimates are captured differently, rates of homelessness in these countries have been increasing, and may represent a global trend.
Homelessness can be viewed as being caused by ‘individualistic’ or ‘structural’ conditions, with different explanations favoured by different countries, and also by different stakeholders in countries. 10,11 Poverty and socioeconomic disadvantage; traumatic childhood, adolescent and adulthood experiences; interactions with the criminal justice system including imprisonment; and experience of institutional care are central to the causes of homelessness. 10,12,13 Homelessness may be understood as being both created and exacerbated by systemic changes in housing and social systems, combined with situational factors that make those with the least power and resources more vulnerable to becoming homeless. 12
People experiencing homelessness are vulnerable to ‘tri-morbidity’: the experience of poor mental health, poor physical health and problem substance use. 14 People who are homeless often report significantly worse physical and mental health than the general population;5,15–17 they are also four times more likely to die prematurely and seven times more likely to die as a result of drug use than the general population. 18 The use of alcohol and drugs is often a factor contributing to someone becoming homeless, and substance use can increase as a way of coping with homelessness. 19 There are also subpopulations of individuals experiencing homelessness who experience distinct and compounding health challenges. These groups include (but are not limited to) women;20 people who are engaged in sex work;21,22 young people;23 older people;24,25 individuals who identify as lesbian, gay, bisexual, transgender, queer or + (which includes any individual who feels that they do not fit into these categories, including intersex and asexual individuals) (LGBTQ+);26 individuals with experience of the criminal justice system;27 individuals who are veterans;27 and individuals who are refugees or asylum seekers, or have no recourse to public funds. 28
Despite many people who are homeless in the UK being registered with a general practitioner (GP), a significant number report that they are not receiving help with health problems. 28 Typically, they do not access health-care services until a crisis emerges, using accident and emergency (A&E) services rather than primary care. 14,29–31 Inpatients who are homeless also have high rates of emergency re-admission and A&E visits after discharge. 32 These trends can be costly to health-care funders. 14,33 Furthermore, when people who are homeless do access mainstream health care or substance use services, their needs are generally not well met. They often experience stigma and negative attitudes from staff, and service inflexiblity. 29,30,34–36 Such negative experiences can perpetuate through a person’s life,37 thereby shaping long-term attitudes towards mainstream health care, even as an individual’s life stabilises. 38 Collaborative working between health care and housing services is therefore essential;39 correspondingly, interventions to improve the health of people who are homeless have received increased attention over the previous decade. 4 Several systematic reviews have examined the effectiveness of interventions to improve health and substance use outcomes for those who are homeless, with findings indicating that having primary care services tailored to those experiencing homelessness,40,41 case management16,42,43 and provision of housing42 can be effective in improving mental and physical health and assisting with addressing problem substance use.
In terms of problem substance use, treatment approaches have traditionally been divided into those aimed at helping people to stop using alcohol and drugs, with abstinence being the goal, and those taking a harm reduction approach first and foremost, whereby the goal is to minimise harms associated with consumption. 44 More recently, there has been a move away from dichotomising these approaches. Despite recognition of commonalities between approaches, questions have been raised regarding whether or not abstinence-focused interventions are appropriate for people with very complex health and substance use needs,40 such as people who are homeless. Although abstinence-based interventions can be effective for some, they rely on people who are homeless having consistent access to services and resources, which cannot be guaranteed. Unstable living conditions can mean that treatment appointments are missed and that plans and regimes are challenging to maintain. 29 For most people experiencing homelessness who use alcohol and drugs, abstinence is unlikely to be achieved in the short term, so approaches that reduce harms associated with use are required. 44–46 It has therefore been recommended that harm reduction approaches be specifically employed to prevent harms related to substance use, with abstinence-based treatment available as an option. 25,45,47
Although there is no universal definition of harm reduction, harm reduction aims to support people ‘where they are at’, whereby substance use is met with a non-judgemental response. 48 Intervention is therefore concerned with preventing substance-related harms, rather than seeking particular goals. 49 This can facilitate greater autonomy because importance is placed on people exercising choice to set their own goals, rather than being forced to reduce use/become abstinent. 49–51 Harm reduction services can also, importantly, act as a ‘gateway’ to other services, including health and housing services, and specialised substance use treatment. 51,52 For those who are homeless, there is a need for a wide range of approaches and services to reduce risks associated with substance use, including the provision of the following: alcohol through managed alcohol programmes; overdose awareness training and naloxone; safer supplies; heroin-assisted treatment; drug consumption rooms; assertive outreach services; and non-abstinence-based housing. 48,53
In harm reduction services, the building of trusting relationships with staff is key, as is the importance of service user-directed goals, and being accepted as a person. 47,50 The participation of people who use drugs and/or alcohol (peers) in service delivery is an essential element of harm reduction services and one of its key principles. 48,54,55 Services that are accessible, with staff who are good listeners and have caring, non-judgemental attitudes, can facilitate engagement with a range of population groups that can be reluctant to engage with mainstream services. 56,57 What is essential is that people should be treated as human beings of worth,47,49 which is not necessarily what people experience when they access services. 58,59 Specifically, regarding those experiencing homelessness, the development of trusting, consistent and reliable relationships is also essential to facilitate access to services. 47,51,60–63 Although the experience of homelessness and problem substance use can be highly stigmatising, these experiences do not necessarily dominate individuals’ sense of self, as they attempt to hold on to their dignity and self-worth, and succeed in doing so. 64
Neale and Stevenson65 interviewed people who were homeless with problem substance use living in hostels in England to examine the nature and extent of their social and recovery capital. Participants viewed supportive relationships with professionals as critical to their well-being and future outcomes. Hostel staff were noted as being caring and responsive to needs, and protecting people. 65 Developing good relationships between health-care professionals and those who are homeless has also been found to be especially important for engagement with services, particularly when supporting individuals with substance use/other health problems. 40,66 Mills et al. 34 interviewed staff working in homelessness primary care services in the UK and found that development of trusting relationships and listening well to people were crucial to engagement. Importantly, when people who were homeless developed good relationships with health-care professionals, they would bring friends with them, thus extending reach. 34 Pauly67 has also highlighted the importance of trusting relationships as essential to access primary care in Canada. This literature shares commonalities with research on effective approaches for those experiencing homelessness and mental health problems, highlighting the importance of flexible services, good relationships with professionals, care based on mutual communication and advocacy, practical support, and having workers with lived experience. 68 Services viewed as unhelpful included those where staff were viewed as judgemental, lacking compassion and ‘clinically detached’, and used medical models of care. Refusing to give support because of continued substance use also featured. 41,68
Homelessness settings in the UK are increasingly employing an approach called psychologically informed environments (PIEs) to develop services for people with complex histories to enable such services to help individuals move on from homelessness and achieve a better quality of life. 69 The explicitly relational focus, working actively with a person’s experiences of trauma and ensuing emotional impact, lies at the core of PIEs. 69,70 The coping strategies that people develop to survive, including use of substances, are understood in this context. PIEs aim to help people make changes to behaviours on their own terms using supportive relationships. 70 PIEs as a concept is continually developing, but the most recent version (2.0) identifies five key areas: (1) developing greater psychological awareness of the needs of service users; (2) valuing training and support for all staff, volunteers and service users; (3) fostering a culture of learning and enquiry, which considers evaluation and improvement; (4) enabling ‘spaces of opportunity’ that seek to view the environment from service users’ perspectives; and (5) fine-tuning the rules, roles and responsiveness of the service, which focuses on managing and improving relationships. 71 Services implementing a PIE approach may, for example, change their reception areas to make them feel safer/more inviting, provide staff with opportunities for reflective practice, and review evictions protocols to allow for greater flexibility when there is an issue of compliance. PIEs aim to give benefit to service users and service staff/organisations. For example, reflective practice offers service staff dedicated time and space to process the emotions stemming from their work and, in turn, to reduce burnout and increase compassion. 72 Despite increasing implementation in practice,73,74 there is limited research exploring the effects and experiences of PIEs from a range of perspectives. 70
Individuals with lived experience make hugely important contributions to interventions in the housing/homelessness and health-care fields. Peer support refers to a process whereby individuals with lived experience of a particular phenomenon provide support to others by explicitly viewing situations through the lens of personal experience and actively drawing from that personal experience and experiential knowledge. 75–77 Peer support can be both informal, via friends and acquaintances, and formal, whereby support is provided in a structured way. 78 Peer Support Workers have been most commonly employed in mental health settings, where peer support was first formalised. 75 Peers can improve outcomes for those using services, particularly in terms of giving hope and facilitating empowerment and self-esteem. 79,80
In terms of substance use, peers are involved in harm reduction and recovery services in a range of ways, including provision of advice on safer injecting;5,81 management of safe injecting sites; needle and syringe exchange and outreach programmes;82–86 provision of information about drug quality;87 provision of take-home naloxone;5,88 facilitation of managed alcohol programmes;89 and advocacy across a range of political and public arenas. 90–92 In their systematic review, Marshall et al. 93 identified 36 different roles of peers in harm reduction initiatives, highlighting the diversity of involvement. The involvement of peers in these services is considered to be highly beneficial in terms of facilitating engagement with services;92,94 increasing access to, and engagement with, health/social care services and specialist substance use treatment;83,95 supporting adherence to antiretroviral therapy;83 and reducing drug-related deaths5 through the development of trusting relationships. 24,94,96–98 Peer-delivered interventions have also been found to be effective, compared with traditional outreach interventions, in reducing the risks associated with injecting drugs. 95,99 Those who use drugs/alcohol are willing and able to access peer-delivered services,100 and the peers offering services themselves report a range of benefits. 93
Peer support roles have also been developed and supported in homelessness settings in the UK (e.g. Groundswell) and, although rigorous or full evaluation is sparse, it is increasing. 101 O’Campo et al. 66 examined the literature on community-based services for people who were homeless and experiencing mental health and substance use problems and found that, in one programme, peer support staff were particularly effective in developing good relationships with service users. Research indicates that peer workers can benefit from their role in terms of increased confidence and self-esteem, and as a way of reintegrating into the community,96,102 and that such work can help peers maintain their own recovery. 103 More broadly, challenges associated with implementation of peer support include lack of boundaries, power imbalances, stress, unclear/poorly defined roles, tensions over professionalism, and responding to challenging behaviours,79,96,101,104–108 as well as the unique challenge of continually navigating the dual identities of ‘peer’ and ‘professional’. 109 Effective training, supportive and reflective supervision and management, clear role descriptions and acceptable pay are all important in proactively addressing such challenges. 79,94,96,110–112
Peers have also been involved in research in the fields of substance use and homelessness at different stages of the research process, including design, data collection and analysis,93 and literature is increasing as practice evolves and expands. 113 Peer research has been argued to be ethically imperative, particularly in areas of social exclusion and potential objectification. 114 Terry and Cardwell115 describe how peer research is based on an assumption that shared experiences generate understanding and empathy. This is believed to enhance the quality of the research overall. Accessible role models can help to challenge stigmatising views of people who use substances and are homeless. 101 Common features of positive and meaningful peer involvement in research include comprehensive and ongoing training, compensation for time, and continuing support and mentorship. 116
These challenges in both service/practice and research have been highlighted in a recent ‘state of the art’ systematic review75 conducted by some members of the team that reviewed literature on peer support at the intersection of homelessness and problem substance use. Taken together, these studies highlight the importance of particular components of harm reduction that can contribute to engaging positively with people who are marginalised in mainstream health, social and housing services. The critical component to both good engagement and subsequent progress on self-identified life goals seems to be facilitation of trusting, supportive relationships in which practical elements of support are also provided, such as access to primary health care and housing options. Non-judgemental attitudes are noted to be vital in engaging people with complex needs in health care, including those with problem alcohol and drug use who are experiencing, or at risk of, homelessness. The Supporting Harm Reduction through Peer Support (SHARPS) study aimed to add to this body of knowledge by combining some of the most effective components of harm reduction, PIEs and peer delivery.
Overview of study
The SHARPS study was a feasibility and acceptability study of a relational, peer-delivered intervention to support people who are homeless and experiencing problem substance use to address a range of health and social issues on their own terms. The study aimed to examine whether or not it is feasible and acceptable to deliver a peer-to-peer intervention (by PNs), based on PIEs, that provides practical and emotional support for people experiencing homelessness and problem substance use in non-NHS third-sector housing settings.
Informed by the evidence outlined previously, the research questions were as follows:
-
Is a peer-delivered, relational harm reduction approach accessible and acceptable to, and feasible for, people who are homeless with problem substance use in non-NHS settings?
-
If so, what adaptations, if any, would be required to facilitate adoption in wider NHS and social care statutory services?
-
What outcome measures are most relevant and suitable to assess the effect of this intervention in a full randomised controlled trial (RCT)?
-
Are participants and staff/service settings involved in the intervention willing to be randomised?
-
On the basis of study findings, is a full RCT merited to test the effectiveness of the intervention?
Objectives
This study aimed to:
-
develop and implement a non-randomised, peer-delivered, relational intervention, drawing on principles of PIEs, that aims to reduce harms and improve health/well-being, quality of life and social functioning for people who are homeless with problem substance use
-
conduct a concurrent process evaluation, in preparation for a potential RCT, to assess all procedures for their acceptability, and analyse important intervention requirements such as fidelity, rate of recruitment and retention of participants, appropriate sample size and potential follow-up rates, the ‘fit’ with chosen settings and target population, availability and quality of data, and suitability of outcome measures.
Study structure
Phase 1 (months 1–3) addressed objectives 1 and 2:
-
develop an intervention using co-production methods for use in community outreach/hostel settings
-
create a manual to guide the intervention and an associated staff training manual.
Phase 2 (months 4–21) involved a study that delivered the co-produced intervention in six third-sector intervention sites and addressed the following objectives:
-
test the feasibility of recruiting to the intervention and measure the rate of recruitment/attrition to determine appropriate sample size and follow-up rates for a full RCT
-
deliver a non-randomised, peer-delivered, relational intervention based on principles of PIEs, with integral holistic health checks (conducted by researchers) based on already identified outcome measures
-
assess the acceptability and feasibility of all procedures in the intervention using normalisation process theory (NPT), including staff and participant perceptions of its value, strengths and challenges
-
assess the acceptability of the holistic health checks/outcome measures, to determine the best way to measure outcomes for this particular intervention and population in a future RCT
-
assess fidelity, adherence to the manual, ‘fit’ to context, data availability and quality, and potential for wider adoption to NHS/statutory health and social care services.
Phase 3 (months 18–24) involved the analysis and write-up of all study findings to address our research objectives, focusing on evaluating the factors needed to deliver the intervention at scale.
Intervention: key components
-
A relational intervention, drawing on the principles of PIEs, that aims to reduce harms and improve health/well-being, quality of life and social functioning for people who are homeless with problem substance use.
-
Delivered by four PNs with lived experience of homelessness and/or problem substance use.
-
Delivered in three outreach services in Scotland and three residential services in England.
-
Maximum 12 months in duration (shorter in one setting).
Chapter 2 Intervention
This chapter sets out the key partnerships involved in the SHARPS study and its governance, and provides an overview of the intervention, including its development, the process evaluation and its underpinning framework.
Study team and governance
The team was led by Professor Tessa Parkes and comprised academics from the University of Stirling (CM, HC, MF, IA; and RF), the University of Aberdeen (GM) and the University of Victoria in Canada (BP). The team also comprised non-academic partners from NHS Lothian (JB and AB) and the Scottish Drugs Forum (SDF) (DL and JW). Tessa Parkes, Catriona Matheson, Hannah Carver, Maria Fotopoulou and Rebecca Foster are based in, or affiliated with, the Salvation Army Centre for Addiction Services and Research (SACASR) at the University of Stirling, which receives external funding from The Salvation Army (TSA). Rebecca Foster was the recruited study research fellow. SACASR academics have full academic freedom, but TSA partnership enables collaborative working; the SHARPS study fitted neatly with the ethos and work of TSA in homelessness and problem substance use, and aligned with the research experience and expertise of SACASR academics. TSA was the study’s key third-sector partner, alongside Streetwork (part of Simon Community Scotland) and the Cyrenians (latterly, Change Grow Live).
The study was independently overseen by a Study Steering Group (SSG). A patient and public involvement (PPI) group was also established, comprising individuals with lived experience of homelessness and/or problem substance use, to act as a quality assurance group for the study. Both of these were convened specifically for the SHARPS study for its duration. The PPI group preferred to be named the ‘Experts by Experience’ (EbyE) group; a detailed discussion of PPI is provided in Chapter 7.
The study was managed day to day by a project management team comprising Tessa Parkes, Catriona Matheson, Hannah Carver and Rebecca Foster.
Theoretical/conceptual framework
Normalisation process theory provided a framework for the intervention and process evaluation, being well-placed to support both. 117 NPT is particularly suited to evaluating complex health interventions, and is increasingly used in this sphere,118 by providing a means of understanding and improving the way in which interventions are implemented. 119 There are four components to NPT: coherence, cognitive participation, collective action and reflexive monitoring. 120 Coherence refers to the process of understanding that individuals/organisations go through to either endorse or prevent an intervention from being embedded into practice; cognitive participation involves enrolling and engaging individuals in the new practice; collective action is the work that individuals/organisations do to embed the new intervention into practice; and reflexive monitoring refers to formal and informal appraisal of the new practice. 119,120 As Murray et al. 117 outline, NPT recognises that health care is collective and requires a range of interactions from different actors, and it provides a framework to help understand how these interactions shape each other and also how they can be optimised. NPT fitted neatly with the complex nature of the SHARPS study and guided the development and implementation of the intervention, as well as the process evaluation.
Peer Navigators
Recruitment
Four part-time (30 hours per week for 18 months) posts were advertised by the lead partner agency, TSA, which employed the PNs. Posts were advertised on TSA’s vacancies web page and the SDF mailing list. As an essential criterion for the role, the PNs were required to have lived experience of homelessness and/or problem substance use. Other requirements included knowledge of the issues commonly faced by those experiencing homelessness and/or problem substance use, experience of working with individuals in these circumstances, genuine compassion for working with those in need, and excellent relational and interpersonal skills.
The PNs were recruited by the Chief Investigator (TP), Jason Wallace and a TSA service manager from each intervention setting, via an application form and interview. Four PNs were successfully recruited. Two PNs were recruited for the Edinburgh and West Lothian settings (see Settings: intervention and standard care), and one was recruited for the Bradford setting. No PNs were recruited from the local Liverpool area, as none of the shortlisted candidates attended the interview. One of the shortlisted candidates for the Bradford setting was offered the role for the Liverpool setting and accepted, with an agreement to be based in Liverpool for part of the working week, with travel and accommodation arranged and paid for by the study.
All appointed PNs underwent a Disclosure and Barring Service/Protecting Vulnerable Groups (PVG) check. The PNs were paid at TSA’s Specialist Support Worker salary scale and afforded the same terms and conditions as other staff in the organisation, including the right to continuing professional development. In its homelessness services, TSA employs a range of staff, including Assistant Support Workers, Support Workers and Specialist Support Workers. Specialist Support Workers carry additional responsibility and have enhanced knowledge/expertise in their area of specialism, for example problem substance use. The PNs started in June 2018; one PN left the role early in January 2019 and three PNs finished in December 2019. All secured further employment before finishing post.
Onboarding, training and support
The PNs received a comprehensive induction and advanced ‘front-loaded’ training in the first 4 months of their posts (June–October 2018). They also received training updates throughout the study, identifying training opportunities of particular interest/use, for example advanced motivational interviewing. ‘Core’ training encompassed areas related to the intervention, the relevance of trauma to substance use behaviour, professional boundaries, naloxone ‘train the trainer’, and therapeutic relationships and PIEs. The PNs also received training and induction to the study, including on recruitment and relevant ethics issues, such as assessing eligibility and obtaining informed consent. A training manual was produced and subsequently refined. Fidelity and adherence to the intervention manual and core components of the intervention were assessed in the interviews with PNs and are discussed in Chapter 6. Fidelity concerns the degree to which an intervention is delivered as it is intended. Adherence is defined in this study as the extent to which the PNs followed the intervention guide. These are related concepts. Although the intervention was ‘manualised’, the study team envisaged and understood that each PN would bring their own experiences and individuality to the intervention, and to their relationships with participants. The feasibility design allowed a diversity of approach to be well explored and reflected on, which is described in Chapters 4–6.
The PNs received regular one-to-one (face-to-face/telephone) clinical supervision with a consultant clinical psychologist with expertise in working with the participant group and supporting staff (AB). A WhatsApp (Facebook, Inc., Menlo Park, CA, USA) group was created for the PNs; Jason Wallace was also in this group to offer support/advice when required. The PNs were supported on a day-to-day basis by their service managers, Tessa Parkes and the project management team. They were provided with work mobile phones and Chromebook personal computers (Google Inc., Mountain View, CA, USA).
Intervention development
Phase 1 involved development of the bespoke intervention, with associated manual and staff training guidance. The intended purpose of the manual was to provide the PNs with necessary information to carry out their roles, with detailed information about particular concepts/approaches, health and social issues affecting participants, study information, the intervention itself, and key contacts and local information.
An ‘intervention development day’ was held in month 2 (June 2018) to discuss the key components of the intervention and how these would be implemented. At this meeting, there was consensus that the manual should be referred to as a ‘guide’. Following this full-day meeting, the project management team developed draft versions of the intervention and training guidance for circulation to all parties.
The intervention and intervention guide were co-produced by experts in homelessness, inclusion, health, and PIEs and relational interventions; representatives from homelessness and third-sector organisations; people who have experienced homelessness and/or problem substance use; and relevant health/medical professionals, following INVOLVE guidance. 121 The project management team led the writing of the guide and sought and received reviews from the following key individuals/groups: the wider co-investigator team; the SSG; the EbyE group; study PNs; TSA service and regional managers; service and regional managers from partner organisations (Streetwork and the Cyrenians); and other practitioners with relevant expertise, for example in the implementation of PIEs in practice.
Feedback was provided at face-to-face meetings and via e-mail. Some reviews were light touch or focused on specific sections, whereas others were more in-depth or cross-cutting. The guide was finalised in September 2018 and entitled ‘Peer Navigators – Navigating People towards Health’. Hard copies were given to the PNs and service managers, the chairperson of the SSG and TSA leaders.
As part of their induction and training, the PNs were also asked to develop their own ‘local directories’, which were inserted into their guide. The exercise of compiling the directories helped familiarise the PNs to the areas in which they were working, which were generally fairly new or unknown. The PNs were supported in the development of these directories by the project management team.
After the guide was finalised, and shortly before they began to recruit their participants, the PNs were asked to read the full guide and Tessa Parkes had an individual follow-up telephone call to ensure that they were familiar with the guide’s content, to help ensure fidelity and adherence. The project management team developed a ‘guide insert’ for the substantial change to the quantitative data collection (see Chapter 3, Alterations to quantitative data collection). The intervention organically evolved; some changes and adaptations occurred, but none was major and no additional guide inserts were developed.
Overview of intervention
The key feature of the intervention was the relationship between the PN and their participants, with the aim of developing relationships that were positive, trusting and non-judgemental. Trust is a broad term and concept. As informed by the literature described in Chapter 1, as well as the literature on therapeutic relationships,122 we defined a ‘trusting relationship’ as a relationship in which the participants had a belief that their PN was working in their best interests, felt that they could rely on their PN, and felt able to make disclosures to their PN and generally felt safe with them.
When participants were recruited to the intervention, the PNs worked with each individual to identify unique support needs. This enabled the PN to, for example, make referrals, support participants to attend appointments (e.g. GP, dentist), and support participants to build relationships with new services including drug/alcohol services. The PNs provided emotional support to participants in a range of ways, including spending time with them and listening to their stories and the challenges they were experiencing. Two PNs also facilitated weekly biopsychosocial groups in a service, which were available to all service users and staff, and often included some of their participants.
As part of the proposal development work, EbyE advisers were consulted by Jason Wallace; the importance of practical financial support to attend appointments was highlighted. To provide participants with such support, the PNs had access to a fund in their services. Up to £10,000 was available and was split equally among the services, which translated as £2500 per PN. This was primarily used to pay for travel and food/hot drinks, but the PNs were also able to draw from this to buy or pay for useful ‘extras’, including clothes, stamps, essential telephone calls, essentials while participants were in prison, emergency electricity and gas power, and household appliances to help maintain new tenancies. A guidance document was shared to advise the PNs and service staff on spend [see the guidance document on the project web page: www.journalslibrary.nihr.ac.uk/programmes/hta/1615314/#/documentation (accessed 2 December 2020)].
Participants received the intervention for up to 12 months (2–12 months, depending on the setting). They were not withdrawn by PNs or the study team on the basis of either continued problem substance use or abstinence. Towards the end of the intervention, the PNs had conversations with participants to identify a ‘winding-down’ strategy that would ensure that their support needs were met in the run up to the end of the intervention, as well as afterwards when they were no longer working with their PN.
The experiences of the intervention from all perspectives (participants, PNs and staff in services) are described in detail in Chapter 5. The case studies prepared by the PNs and the project management team also offer insights into the nature and breadth of support the PNs provided (see Appendix 2).
Settings: intervention and standard care
Three homeless outreach services in Lothian, Scotland, and three Lifehouses (TSA hostels) in Liverpool and Bradford, England, were chosen for the implementation of this intervention. The team developed this partnership with TSA (as introduced in Study team and governance) and developed new partnerships with other leading third-sector organisations.
All hosting services were non-profit, third-sector housing organisations. Three homeless outreach services in Lothian, Scotland, and three TSA hostels in England were selected as intervention settings. Two PNs were based in settings in Scotland, and two PNs were based in settings in England. In the Scottish settings, the two PNs had a base in a TSA setting (Niddry Street), but each also worked in another setting managed by different third-sector providers: Streetwork (Edinburgh) and Cyrenians (West Lothian). The decision to include both outreach and residential services enabled exploration of different models of working and consideration of potential fit. One PN was based in Liverpool and worked across two TSA Lifehouses. Another PN was based in a Lifehouse in Bradford (see Intervention settings).
To enable the study to assess differences between intervention and non-intervention care pathways, we identified two standard care settings (an outreach service in Scotland and a Lifehouse in England) that were similar to the intervention sites (e.g. third sector/type of funding/types of staff roles, numbers in place/aims of service). Whether or not the settings were completely comparable was explored in the process evaluation. As non-statutory, third-sector services developed to meet the needs of specific populations, it is highly unlikely that any two services are completely comparable, which applies to all settings.
In the two standard care sites, the same health check measures were conducted with a sample of residents/service users to assess any particular population differences and the feasibility and acceptability of use of these measures among these participants, which were conducted with a researcher, without a PN present to offer any support if needed. We also undertook non-participant observation in both intervention and standard care sites to document similarities and differences. Interrogating the role of context was key to our understanding of how the intervention works, most specifically in terms of the role of each of the services in hosting the PNs and the study, and particular facilitators of and barriers to the intervention.
All chosen settings catered for individuals who are vulnerable and disadvantaged, with a particular focus on those experiencing homelessness and problem substance use. All offered a range of support based on their areas of expertise, and the needs of their service users/residents; this responsive support means that the level/nature of support offered by each setting continually evolved.
Intervention settings
-
Streetwork, Edinburgh, Scotland (Simon Community Scotland): outreach service.
-
Niddry Street Wellbeing Centre, Edinburgh, Scotland (TSA): outreach service.
-
Pre-Sync 27 Recovery Hub, Bathgate, West Lothian (Cyrenians); managed by Change Grow Live from April 2019: outreach service.
-
The Orchard Day Shelter and Lifehouse, Bradford, England (TSA): residential service.
-
Darbyshire House/Ann Fowler House, Liverpool, England (TSA): residential services.
Standard care settings
-
Greenock Floating Support Service, Greenock, Scotland (TSA): outreach service.
-
Charter Row Lifehouse, Sheffield, England (TSA): residential service.
Process evaluation data collection
The process evaluation was informed by NPT119 and involved mixed-methods data collection. Academic researchers (RF and HC) collected all qualitative and quantitative data, except for interviews with intervention participants, which were conducted by SDF peer researchers (see Chapter 3).
Qualitative data collection involved the following:
-
intervention participants who undertook interviews in wave 1 of peer research interviews (n = 24)
-
intervention participants who undertook interviews in wave 2 of peer research interviews (n = 10)
-
participants who withdrew from the study and completed a short ‘exit’ questionnaire (n = 1)
-
PNs (n = 4), at three or four time points (15 interviews in total)
-
service staff in the intervention settings (n = 12)
-
service staff in the standard care settings (n = 4)
-
intervention participant case studies (n = 6)
-
observations in intervention settings (n = 6)
-
observations in standard care settings (n = 2).
Quantitative data collection consisted of:
-
intervention participants who completed wave 1 of the health check (n = 45)
-
intervention participants who completed wave 2 of the health check (n = 30)
-
standard care participants who completed the health check (n = 6).
Reflexive monitoring: process evaluation
The PNs were invited to complete reflective diaries to capture their personal reflections on the role and challenges experienced (see Chapter 3). Following NPT, and, specifically, the reflexive monitoring component in NPT, the project management team took detailed reflective notes for the full study duration encompassing personal views, experiences and feelings, alongside notes from conversations, meetings and interactions. These insights, alongside the formal data collection, are collectively drawn from in Chapter 6.
Outcome measures: health check
The questionnaires were chosen by the project management team, in consultation with TSA researchers and Atlas (Atlas, Cambridge, UK) developers. Atlas is TSA’s client management system. Questionnaire 1 was developed by the team, and was intended to capture key demographic information about the participants; the team was informed by discussions with the SSG chairperson on multimorbidity,123 as well as previous work by Catriona Matheson on older drug users24 and by Bernie Pauly on managed alcohol programmes. 47 Questionnaires 2–6 are validated questionnaires. The project management team made minor amendments to questionnaire 3 [the Maudsley Addiction Profile (MAP)] to make it more suitable for the study population, including adding a question on overdose and asking about use of other drugs not included [e.g. novel psychoactive substances (NPSs), such as synthetic cannabinoids (‘spice’)] in section A. There was also the addition of a follow-up question on residence, which asked specifically for how many days participants had lived at their current residence (section D). These adjustments mean that data from the study version of the MAP could not be fully compared with MAP data from similar populations. However, the decision was made to maximise the usefulness of this particular questionnaire for this group.
Questionnaires 2–6 are publicly available. The Substance Use Recovery Evaluator (SURE)124 and the Consultation and Relational Empathy (CARE) Measure125 require approval for use from the owners, which was obtained for both. The SURE and the CARE Measure are designed as self-completion questionnaires. The other measures can be completed by an individual or by a researcher on their behalf. The questionnaires were administered with participants as two ‘holistic’ or ‘whole-person’ health checks, one in the earlier stage of the intervention (November 2018–May 2019) and one at a later stage of the intervention (August–November 2019). Therefore, these questionnaires had a dual purpose of providing the study’s quantitative data and providing the PNs with information about participant health/circumstances:
-
Measure 1 – this questionnaire encompassed questions on sociodemographic characteristics, housing status/quality, general health status, education, medication use and future service use.
-
Measure 2 – the Patient Health Questionnaire-9 items (PHQ-9), a 9-item tool covering symptoms of depression, and the Generalised Anxiety Disorder-7 (GAD-7) anxiety and depression scale, a 7-item tool covering symptoms of anxiety. 126,127
-
Measure 3 – the MAP, measuring substance use. 128 The MAP is a 36-item tool covering substance use (type/frequency/method), overdose, treatment, injecting and sexual behaviour, physical and psychological health, social functioning, relationships and illegal activities.
-
Measure 4 –the SURE,124 a 26-item tool covering drinking and drug use, self-care, relationships, material resources, outlook on life and the importance of each of these items to respondents.
-
Measure 5 – RAND Corporation Short Form survey-36 items (RAND SF-36),129 a 36-item tool covering physical and emotional health status, the effect of health on daily activities and social activities, and experiences of pain.
-
Measure 6 – the CARE Measure,125 10-item tool assessing empathy in the context of a relationship, to measure the relationship between a participant and their PN.
The list of outcomes and corresponding measures can be found in Table 1.
| Characteristic/outcome | Measure |
|---|---|
| Demographics, living/housing circumstances | Measure 1 |
| Drug and alcohol use | Measure 3 (MAP) and measure 4 (SURE) |
| Mental health | Measure 1, measure 2 (PHQ-9 and GAD-7) and measure 3 (MAP) |
| Physical health | Measure 3 (MAP) and Measure 5 (RAND SF-36) |
| Perceptions/experiences of relationship with PN | Measure 6 (CARE Measure) |
Eligibility criteria for intervention participants
To take part in the intervention, participants had to be:
-
aged ≥ 18 years
-
homeless or at risk of becoming homeless
-
using drugs and/or alcohol in a way that has a negative impact on their lives (self-identification)
-
able to provide informed consent.
Participants were required to fulfil all inclusion criteria to take part. To capture all forms of precarious housing situations, this study adopted broad definitions of ‘homelessness’ and ‘at risk of homelessness’, as informed by the ETHOS framework. 6 ‘Problem substance use’ was defined as use of drugs and/or alcohol that has a negative impact on an individual’s life. The level and nature of this negative impact varied between individuals; the study was not prescriptive on this. Most participants were experiencing problem substance use that was severe and had a substantial impact on their daily lives. The self-assessment required individuals to recognise that their substance use was affecting their lives in a detrimental way. If an individual did not recognise this, the intervention was not offered (i.e. participant did not receive a participant information sheet), as it was not considered to be appropriate for that individual at that stage. Recruitment and retention are discussed in Chapter 4.
Approvals obtained
The University of Stirling’s NHS, Invasive or Clinical Research (NICR) ethics committee provided ethics approval in April 2018 (NICR 17/18 Paper 35). The ethics subgroup of the Research Coordinating Council of TSA provided ethics approval in June 2018. Four subsequent submissions were made and approved to both committees for approval for protocol changes; the dates are recorded in the trial registry.
Changes to protocol
The final version of the protocol is version 1.6. All changes made to the protocol are set out in Appendix 1, with the majority of changes being minor. The substantive changes involved one PN leaving post early, and a change to quantitative data collection. The latter is discussed in Chapter 3, and the PN’s resignation is discussed in the following section.
Peer Navigator resignation
The Liverpool-based PN resigned from post in November 2018 and left in January 2019, 11 months earlier than the end of their contract, for a combination of personal and professional reasons. The study team, in consultation with TSA and the SSG, did not feel that it was ethical or practical to re-recruit a PN for this vacant post for the remainder of the study period for a number of reasons. The Liverpool-based participants had consented to work with a specific PN with whom they had developed a relationship. The PNs each received a comprehensive 4-month induction: the time taken to recruit and re-offer this would not have been compatible with the tight study time scales. In addition, we had a commitment and responsibility to the other PNs and intervention participants, which meant that the study could not be paused. Taking all considerations into account, the PN offered a shortened 2- to 2.5-month intervention to their participants (n = 9) who were still involved, until mid-January 2019, when they finished in post. The decision was made to cap the case load at nine participants (rather than 15) to maximise the support available to these participants. The PN provided participants with the option to leave the intervention or stay under the shorter intervention terms; all chose the latter. At the end of the intervention, all nine participants were supported to access other support and services and also supported by staff in the Lifehouse.
The health check measures were conducted once with these participants before the PN finished (n = 5). A sample of these participants were interviewed in wave 1 of the peer research interviews (n = 3). Owing to the capped case load, we envisaged that these participants would still benefit from a shortened, but slightly more intensive, version of the intervention. The implications of this are considered in Chapter 6.
Chapter 3 Methods
As part of the feasibility study, we conducted a concurrent process evaluation employing a mixed-methods approach and informed by NPT. 119 The qualitative component involved conducting semistructured interviews with intervention participants, PNs and staff in intervention and standard care settings, alongside conducting non-participant observations in all intervention and standard care settings, collecting intervention participant case studies and reflective diaries kept by the PNs. The quantitative component involved collecting key quantitative data from participants via a range of measures at two time points. As mentioned in Chapter 2, academic researchers (RF and HC) conducted all interviews and observations, except for interviews with intervention participants, which were conducted by SDF peer researchers. Academic researchers (RF and HC) also conducted all quantitative data collection.
Part 1: qualitative data collection
Qualitative interviews with staff and Peer Navigators
The purpose of undertaking interviews with staff and PNs was to explore experiences of, and views on, the intervention from these perspectives, as well as to assess any changes in perceptions and practice over the course of the intervention. The purpose of interviewing members of staff from the standard care settings was to explore views on the potential fit of the PN intervention to these settings [see the interview topic guides on the project web page: www.journalslibrary.nihr.ac.uk/programmes/hta/1615314/#/documentation (accessed 2 December 2020)].
Peer Navigator interviews
When the PN role was advertised, applicants were made aware that an essential criterion for the role would be a willingness to participate in research interviews. The PNs were reminded of this when they were formally offered their positions; all appointed PNs were comfortable with this arrangement.
The intention had been to interview the PNs at three time points over the course of the intervention. Given the additional data collection of the case studies, a fourth interview was conducted with three PNs, who were consulted on this in advance of seeking ethics approval for this change. This additional interview was shorter and focused primarily on the collection of the case studies.
The first interviews took place in the induction/intervention development phase (June–July 2018). The second interviews took place in the middle of the intervention: November 2018 for the PN who left early and April 2019 for the others. The additional third interview took place in June 2019. The final interview for the PN who left early took place in January 2019, and in November 2019 for the others, nearing the end of the full intervention. In this way, the evolving experience of the intervention was captured. Two interviews took place via telephone; the rest were face to face in the intervention settings.
Staff interviews
Twelve members of staff in intervention settings and four members of staff in standard care settings were interviewed. A range of roles were represented in the interview sample, including Assistant Support Worker, Specialist Support Worker and service manager/service lead (or equivalent roles if organisations adopted different terminology). Members of staff had varied professional experience and different backgrounds, both within and beyond health and social care and housing/homelessness. Both male and female members of staff were interviewed and a broad age range was included in the sample.
The intention was to interview two members of staff across the six intervention settings to ensure, as much as possible, an equal representation of views across the intervention sites. We were unable to interview two members of staff in the Liverpool settings, as invitations to interview were not responded to; however, two out of the four originally allocated for the Liverpool settings were still conducted. The decision was made to substitute these interviews with an additional interview with a member of staff from two other intervention settings. All interviews were face to face.
Peer Navigator reflective diaries
The PNs kept reflective diaries from the start of their time in post until the end to capture their views, experiences and feelings. The decision to ask the PNs to complete diaries was in response to proposal reviewer feedback that suggested that diary-keeping could serve as a useful outlet, particularly at times of challenge. The study team shared this view, and also felt that insights shared in these diaries could constitute useful qualitative data. Although these data do not form part of our formal qualitative data collection, and are not discussed in Chapter 5, they were analysed and key themes are drawn from them in Chapter 6 to contextualise the findings.
Approach
Given the data collection and sharing dimension of the diary-keeping, a participant information sheet and consent form were created. It was emphasised to the PNs that completing these reflective diaries was a voluntary exercise. All agreed to keep diaries and to share entries with the project management team. The PNs were invited to complete entries in their preferred format and complete these as frequently as they wished: if they did complete diary entries, this took place during work time. Two PNs typed up reflections in Microsoft Word (Microsoft Corporation, Redmond, WA, USA) documents, and another two audio-recorded reflections on their mobile phones, which were then transcribed. It was emphasised to the PNs that they could choose what they shared; for example, they could complete a full entry and share only an excerpt from it. The PNs shared their entries in full. A template with some suggested bullet points was created to help facilitate diary-keeping [see the template on the project web page: www.journalslibrary.nihr.ac.uk/programmes/hta/1615314/#/documentation (accessed 2 December 2020)].
Observations
Semistructured, non-participant observations were conducted in all sites to gain an understanding of the culture and context of the settings, staffing levels, client group, activities provided, and fit of the intervention. Observations were also conducted in the standard care settings to provide comparison data. Forty-two hours of observation time was split across all intervention and standard care settings, meaning that ≈ 5 hours of observation were conducted at each setting.
Observations were conducted between June 2018 and June 2019. The observations in the standard care settings were prioritised and took place in the summer of 2018. Observations in the intervention settings required the PNs to be fully inducted and formally working with their participants. Intervention observations took place from October 2018 (start of the intervention) to June 2019.
An observation pro forma was developed to guide these observations [see the pro forma on the project web page: www.journalslibrary.nihr.ac.uk/programmes/hta/1615314/#/documentation (accessed 2 December 2020)]. The key prompts were ‘environment’, ‘social interactions’ and ‘activities’, and a number of subprompts were contained within these. Researchers took posters to all settings [see the observations poster on the project web page: www.journalslibrary.nihr.ac.uk/programmes/hta/1615314/#/documentation (accessed 2 December 2020)] to inform staff and service users/residents about the observations when they were taking place, but they also spent time introducing themselves and the study to service users/residents and staff. Researchers observed communal areas only. Researchers recorded the observations on-site using a notepad and pen; fieldnotes were later typed up, along with any additional reflections.
Case studies
The Salvation Army regularly use case studies to demonstrate its work in clear and accessible ways, and case studies are regular features of TSA briefings, reports and business cases. The study team also felt that case studies could be effective in outlining the range and depth of practical and emotional support PNs provided to their participants, alongside other data collection. After consulting with the PNs and their service managers, the project management team made the decision to develop six case studies with the PNs and a small sample of their participants.
Approach
A researcher (RF) led the collection of these case studies. The PNs were asked to each identify two participants. The decision on which participant(s) to approach was the PNs, but each spoke with Rebecca Foster and their service manager, and the following points were considered:
-
availability of the participant
-
‘distance travelled’ from the start of the relationship to now, and how this presented an opportunity to emphasise this progress to the participant
-
relationship between the PN and the participant, including changes over time
-
type of support the PN offered.
Rebecca Foster asked the PNs to approach two participants to be involved in the case studies, but also to have two ‘in reserve’: all participants approached agreed to be involved and separately provided informed consent. A template was prepared and sent in advance for the PNs to help prepare and to ensure consistency of content. The PNs shared these stories in interviews with Rebecca Foster, which were audio-recorded and transcribed. Rebecca Foster removed/edited identifying details and edited these transcripts to one or two pages to cover the key aspects. Rebecca Foster met the PNs face to face for the PN to review their case studies; each PN made minor edits for accuracy.
Rebecca Foster then met with the pairings of participants and PNs face to face; meetings took place either in the intervention setting or in a participant’s residence, depending on where the participant felt comfortable. Rebecca Foster and the PNs strongly encouraged participants to make changes if they wished to; none did and Rebecca Foster and the PNs were satisfied that participants were content.
Participants chose their own pseudonym, which some seemed to particularly enjoy doing. Rebecca Foster made minor proofreading edits to the case studies; the case studies are presented in Appendix 2. As the case studies were collected as part of interviews with the PNs, these have been analysed alongside other sources of data; the themes arising, along with excerpts, are presented in Chapter 5, and reflected on further in Chapter 6.
Qualitative interviews with intervention participants: peer research
Background and rationale
Peer researchers with lived experience of problem substance use interviewed a sample of intervention participants at one or two time points over the course of the intervention. The aim of the interviews was to examine participant experiences of being involved, focusing on the acceptability of the intervention in their lives and to their circumstances. The purpose of the second wave of interviews was to capture any change, in both an individual’s circumstances and in their relationship with their PN.
In addition, the intention was for peer researchers to interview participants if they withdrew from the study, to understand the underlying reasons for this decision (protocol version 1.0). However, the team decided that this would not be practical, both from the perspective of arranging the data collection and from the perspective of participants who may be experiencing additional challenges, perhaps underlying the decision to withdraw. Instead, we offered participants who withdrew the opportunity to complete an ‘exit’ questionnaire [see the questionnaire on the project web page: www.journalslibrary.nihr.ac.uk/programmes/hta/1615314/#/documentation (accessed 2 December 2020)].
Peer researcher role
The peer researchers who participated in this study were recruited as volunteers for the peer researcher programme organised by the SDF. They received a generic SDF induction and specific training on research, including questionnaire design and interviewing techniques. Peer researchers all undergo a PVG check prior to starting to volunteer. The peer researchers volunteer on research projects in their local area for approximately 1 day per week. They are supported by the SDF’s local user involvement officer and have regular ‘meet-ups’ with other volunteers. The peer researchers can also undertake other training offered by the SDF and other development opportunities.
Peer researchers in study
Eight SDF peer researchers were recruited to the study from this wider pool of peer researchers. Although some of these peer researchers also had experienced homelessness and aspects of severe and multiple disadvantage,10 the only requirements to be a peer researcher for the SHARPS study was that they had lived experience of problem substance use and were committed to supporting the study. Each peer researcher’s experiences with substances were unique, and each was at a different stage of their journey. The peer researchers also had varied research experience. Recruitment was informal and via one of the SDF’s user involvement officers. Academic researchers did not meet the peer researchers until the training session or on the data collection days.
The SDF convene two peer research groups in different areas of Scotland. The project management team did not have a preference regarding which group the peer researchers were from, as the budget was sufficient to allow for travel from either location. This flexibility made it easier for the user involvement officer to gender-balance the pairings or ‘threes’ of peer researchers who were involved in each data collection session. This was important given that the study included women participants, with gendered needs and experiences and, traditionally, with less visibility in services. 20,130 There was an attempt for the pool of researchers to be as consistent as possible, but the changing circumstances of people’s lives made this difficult. Some of the peer researchers did more than one session (some multiple sessions), but others did only one.
Onboarding and training of peer researchers
An academic researcher (HC) led a training session in January 2019 with two peer researchers who undertook the Liverpool data collection session. This involved giving a detailed introduction to the study and reviewing all participant materials, and the topic guide [see the topic guide on the project web page: www.journalslibrary.nihr.ac.uk/programmes/hta/1615314/#/documentation (accessed 2 December 2020)]. This also involved practising using the topic guide and the audio-recorders. Hannah Carver gave a presentation and all peer researchers were given a SHARPS study information booklet specifically designed for them, either at this training session or on site. This booklet introduced the SHARPS study and explained the important role of peer research within it. At the January training session, the peer researchers present reviewed the topic guide (which had previously been reviewed by the EbyE group and amended following the group’s feedback) and minor amendments were made. The participant topic guide was therefore strengthened from receiving two separate reviews by people with relevant lived experience.
The user involvement officer refreshed the training in advance of the sessions and academic researchers were available to provide additional information on the study and to answer any questions.
Participant recruitment
At recruitment to the intervention, participants were informed about another associated data collection element of the study prior to providing informed consent to participate: two semistructured qualitative interviews. This information was conveyed in a participant information sheet for the intervention itself (see Chapter 4 for an overview of intervention participant recruitment and the participant information sheet). The PNs reminded participants about this opportunity once the intervention was under way.
Academic researchers worked with the PNs to identify participants interested in taking part, taking account of inclusion criteria. For example, researchers asked the PNs to encourage some of their women participants to take part in these interviews, to ensure gendered experiences were captured. However, given the challenging circumstances experienced by many participants, a pragmatic approach was also adopted: the opportunity to take part in the peer research was made available to all participants so that no participant was denied this opportunity.
Participant interviews: waves 1 and 2
Wave 1 took place in the different settings between January and March 2019. Interviews were conducted with 24 intervention participants in wave 1. Wave 2 took place in the different settings between August and September 2019. The interviews were not re-attempted in the Liverpool site, given the shortened intervention there. Interviews were conducted with 10 participants in wave 2, out of a potential total of 21, taking out the participants who received the shortened intervention. The reasons for not being able to re-interview the participants were varied and included being in custody, being physically or mentally unwell, securing employment incompatible with scheduled interview times, or participants having less contact with PNs at the time of wave 2.
Data collection approach
Although the interviews were intended to be mid-length (20–40 minutes), most were shorter than this: on average, ≈15 minutes. The peer researchers were responsible for explaining the participant information sheet to participants, answering any questions prospective participants may have had, and gaining written informed consent from participants via a consent form. The PNs sometimes also reviewed the participant information sheet with participants in advance as they gave them more information about this opportunity, but this was not done on all occasions.
For all of the peer research data collection periods, the user involvement officer and an academic researcher were present, along with the PNs who supported their participants to attend. All of the services had private spaces in which to conduct the interviews, although access to these spaces was often limited, so they were pre-booked. After a peer researcher completed an interview, they handed over the consent form and audio-recording to an academic researcher, who then immediately uploaded the recording to their secure laptops and deleted the recording from the audio-recorder.
Reimbursement: peer researchers and participants
The SDF pays travel expenses for peer researcher volunteers, but does not reimburse them for their time, given that it is a voluntary role. The study budget covered travel, accommodation and subsistence expenses. The peer researchers were also given a £20 voucher per day to acknowledge their contribution to the SHARPS study, and this included their participation in meetings, interviews and in the analysis. Interview participants received a £10 voucher as a ‘thank-you’ for taking part in an interview. They received another £10 voucher if they completed a second interview.
The vouchers paid to both participants and the peer researchers were One4All® vouchers (The Gift Voucher Shop Ltd, Hemel Hempstead, UK), which can be used in store and online in a range of shops, excluding supermarkets. The monetary value was considered very carefully, as we did not wish to unduly persuade both groups to be involved in the study in these capacities, but we wanted to demonstrate that we valued individuals’ contributions. We hope that this balance was struck appropriately, but we also know that these tensions are recognised and discussions in the field are ongoing. 131
Debrief
The SDF peer researchers were sent thank-you cards after each wave of data collection. The intention was to involve the peer researchers in the analysis of a sample of the wave 1 interviews prior to wave 2 (see Appendix 1 for protocol changes). This meeting was cancelled owing to lack of peer researcher availability; instead, the EbyE group reviewed transcripts. The team still wanted to get the peer researchers’ perspectives on these interviews, so the decision was made to hold a meeting after both waves were complete, and to combine this with a general debrief/wrapping-up. A study researcher (RF) led this meeting, supported by the user involvement officer (in December 2019).
Qualitative data analysis
The framework method132 was used for the management and analysis of all qualitative data because of its ability to support the analysis of the six different settings as cases and because it allows straightforward within-case and between-case comparison. The framework method involves five stages: (1) familiarisation, whereby the transcripts are read multiple times; (2) identifying a thematic framework whereby the researchers recognise emerging themes in the data set; (3) indexing, which involves identifying data that correspond to a theme; (4) charting, in which the specific pieces of data are arranged in tables according to themes; and (5) mapping and interpretation, involving analysis of key characteristics in the tables and providing an interpretation of the data set. All stages were closely followed.
All qualitative data were analysed with the support of the computer software package NVivo version 12 (QSR International, Warrington, UK), with some manual coding of staff interviews piloting the approach. The staff interviews from all settings were analysed together, and the views and experiences from intervention and standard care settings compared. The interviews from all PNs were analysed together. The peer researcher interviews were analysed together (waves 1 and 2 were combined). As we collected data at different time points with both PNs and participants, the data analysis sought to specifically explore whether or not, and how, perceptions of the intervention, and of its challenges and benefits, changed over time. Data analysis was iterative throughout phases 1 and 2 of the study, supported by the use of NPT119 to identify contextual influences on the implementation of the intervention across the different settings. The application of NPT to the analysis is discussed in Chapter 5.
In addition to their other roles as outlined (see Chapters 4 and 5 for detailed accounts of EbyE group role), the EbyE group and study peer researchers were invited to participate in the data analysis and interpretation, supported by the study team. This acted as a form of ‘member checking’ to enhance the validity and trustworthiness of the findings. 133 At face-to-face meetings, these individuals were provided with an anonymised selection of interview transcripts and asked to provide their interpretations of the themes arising and their significance. These were then discussed in the meeting. Although the analysis at these meetings was very light touch, the themes raised were consistent with the themes identified by the academic researchers, enabling a consensus to be built on the themes from the data from these varied perspectives. 134
Part 2: quantitative data collection – holistic/‘whole-person’ health check
Introduction
As well as the qualitative data, a key part of the process evaluation involved the collection of quantitative data from participants via six questionnaires. As noted in Chapter 2, the completion of these questionnaires had a dual purpose of providing information about the health and circumstances of participants to the PNs and providing quantitative data for the study. Participants were asked to complete these questionnaires at two time points over the course of the intervention: once towards the beginning and the second towards the end. These were the ‘outcome measures’ for the study and were colloquially referred to by the PNs and researchers as ‘doing the measures’, as reflected in some of the interviews. Participants consented to undertake these measures as part of the consent process for participating in the intervention. A sample of service users/residents in the standard care settings were also asked to complete the quantitative measures (n = 6).
As well as providing key quantitative data, the purpose of conducting these measures was to assess the acceptability and feasibility of the data collection, and the selected measures (see Chapter 6). The purpose of undertaking these questionnaires with a sample of standard care service users/residents was to assess the acceptability and feasibility of conducting these with individuals who were not working with a PN, as well as to provide an indication of the comparability of the populations. Standard care participants took part in a short follow-up feedback exercise (of 5 minutes) with the researcher to share their views on the measures and the process.
Alterations to quantitative data collection
The original proposal was for the PNs to complete the questionnaires with each of their participants. This was intended to take place over a 2-week period at the beginning of the intervention, and then repeated towards the end. The information provided from the quantitative measures had a dual purpose, given that it informed participant support plans.
The intention was that the PNs would complete questionnaires 1–5 with the participants in a relational way using TSA’s Atlas client management system on their Chromebooks. The participants would be able to see the questions and their responses on the screen. As informed by the accompanying guidance for the CARE Measure, questionnaire 6 would be completed separately and by the participants themselves, with the aim of encouraging honest feedback on their relationship with their PN.
The Salvation Army Atlas developers created a bespoke version of Atlas for the SHARPS study, with measures uploaded. An Atlas expert delivered training to the PNs, the project management team and the Scottish TSA service managers. The training provided a detailed description of how to use Atlas and a half day was spent practising the questionnaires using Atlas before the PNs practised further themselves.
Unfortunately, the use of Atlas raised significant and unexpected intellectual property and General Data Protection Regulation (GDPR)135 concerns. GDPR came into force at the very start of this project (25 May 2018); this change created some challenges related to data sharing that were not foreseen or addressed in the original protocol or subsequent contractual agreements. Despite a commitment by all involved, these concerns were ultimately unresolvable. To protect this aspect of data collection, as well as the study overall, and after consultation with others, including the SSG and NIHR, the study team made the decision to change the approach from the PNs collecting the data to academic researchers (RF and HC) collecting the data. The timing of these issues overlapped with the start of the intervention and the recruitment period. Recruitment was paused for 3 weeks (5–26 November 2018) while these issues were ongoing.
As mentioned previously, when participants consented to take part in the study, they also consented to undertake the health checks as part of their involvement. These participants were provided with a revised participant information sheet by their PN that detailed that researchers would do the health checks [see the participant information sheet on the project web page: www.journalslibrary.nihr.ac.uk/programmes/hta/1615314/#/documentation (accessed 2 December 2020)]. If existing participants did not agree to do the health checks with a researcher, they were still able to continue to receive the intervention. All participants were content with the change and were re-consented to the intervention.
New participants were provided with this revised participant information sheet as a matter of course [see the participant information sheet on the project web page: www.journalslibrary.nihr.ac.uk/programmes/hta/1615314/#/documentation (accessed 2 December 2020)] and were required to consent to the holistic health checks with researchers, as part of the intervention. Therefore, to take part in the intervention, new participants needed to agree to conduct the health check as before, but this time with a researcher rather than a PN.
Data collection process: waves 1 and 2
The outcome measures were attempted twice for all participants who conducted the first set of measures. The exception was for the participants based in the Liverpool sites, who received a shortened intervention. It was not possible within the limited time frame to conduct these twice.
Wave 1 took place between October 2018 and May 2019. Wave 2 took place between August and November 2019. These measures were conducted as chronologically as possible, with the participants who completed wave 1 early on prioritised for completing wave 2 at the beginning of this wave. Another consideration was when participants were recruited. No participant could receive more than a 12-month intervention. This meant that those who consented to the intervention close to when it began were also prioritised, even if they undertook the wave 1 questionnaires at a later stage. Finally, there was a pragmatic element to conducting questionnaires with participants who were available and willing at a particular time, irrespective of either of these study-specific considerations, given the population group.
Approach
Academic researchers conducted the paper-based questionnaires with participants face to face, with the PN present in the room. The PN’s presence was intended to make the participants feel as comfortable as possible and afforded PNs the important opportunity to hear more about a participant’s health and other experiences, perhaps information they did not yet have or may have been unlikely to acquire if they did not directly ask. Furthermore, participants had often already shared information about their life and experiences with their PN. Sometimes participants then asked the PNs for help with some answers, for instance about their convictions (measure 1) or about how long they had stayed in their current place of residence for (measure 3: the MAP).
Although the PNs were in the room, sometimes they did not sit next to the researcher and the participant. Rather, they sat away from them and worked on other tasks on their Chromebooks. Some PNs felt that it was less intense for participants if they were in the room but working on their Chromebooks, while still listening. Others saw an opportunity to closely listen and observe how the participant interacted with the researcher and their overall mood.
The measures were completed in the order listed earlier in this section; this order appeared to be the most logical, and involved starting and ending the session with less intrusive or ‘easier to answer’ questions.
Location
The measures were conducted in a private room in the intervention services. These included staff offices and meeting rooms. There was a commitment by both the PNs and the researchers to ensure that participants felt as comfortable as possible when completing the measures. For example, the PNs arranged these, at times, to take account of participants’ substance withdrawals or other appointments, and the PNs and researchers provided snacks, typically at participants’ requests or of their choosing. If this was not in the service that they used, the PN and the researcher visited the participant in an alternative place, often in their supported accommodation.
During the course of the intervention, a number of participants became imprisoned. Most were released during the course of the intervention; sometimes they had more than one spell in prison during the intervention. One participant was in prison for both waves 1 and 2, so the measures were conducted there. Three participants became imprisoned around the timing of the wave 2 measures, so these measures were conducted in the prison visiting suites. Measures were conducted in three Scottish prisons. Owing to the practicalities of timing prison visits with Bradford study visits, the decision was made not to attempt to conduct the measures with the participant who was imprisoned near the Bradford Lifehouse. The measures were completed in single sittings and took between 30 minutes and 2 hours for researchers to complete all six questionnaires with a participant.
Standard care participants
An academic researcher (RF) completed the questionnaires with the six standard care residents/service users who completed the questionnaires. Rebecca Foster approached these in the same way as with the intervention participants, and participants seemed to be comfortable. A Support Worker was present during the Sheffield data collection (n = 3) but, owing to a lack of staffing, a Support Worker was not present in the Greenock sessions (n = 3). However, in Greenock, the door was left open, and the service manager checked in more than once to ensure that the participant was comfortable. No other members of staff or service users were in the building at the time, which afforded privacy.
Quantitative data analysis
The team entered anonymised data into an IBM SPSS version 23 (IBM Corporation, Armonk, NY, USA) database and checked 10% of entries to ensure accuracy. Data were analysed descriptively using frequency and per cent for binary and categorical data. Continuous data were described using a five-number summary (minimum, 25th centile, median, 75th centile, maximum). In Chapter 4, the means and standard deviations are reported, as well as the correlations between wave 1 and wave 2 data, to help other researchers plan studies using these outcomes. Tables report data on wave 1 responders, and then report wave 2 responders’ data for waves 1 and 2. The data are broken down this way to allow the judgement of potential differences between those who did and those who did not respond at wave 2. Change scores and confidence intervals (CIs) describe continuous data difference between waves 1 and 2. These have been summarised visually using before-and-after plots. The data were analysed using Stata® 15 (StataCorp LP, College Station, TX, USA).
Chapter 4 Recruitment, retention and findings from the quantitative data collection
This chapter presents key recruitment and retention information, as well as findings from the quantitative data collection.
Recruitment strategy
Recruitment to the intervention was an ongoing process and involved combining two trial recruitment strategies, as identified by Thoma et al. ,136 whereby participants were recruited continuously until the desired sample size was achieved, and participants were recruited until a fixed date was reached.
Recruitment was intensive in the first 2 months (October and November 2018), until a desired sample size of 60–70 participants was reached, which equated to approximately 19 individuals per PN (n = 10 for the PN who left post early). Recruitment was open until mid-April 2019, to enable participants to be replaced by new participants as people withdrew. This aimed to maximise the potential of the intervention and followed the approach of Ferguson and Xie’s137 feasibility study.
As each setting had considerably more individuals accessing the service who could potentially have met the inclusion criteria than the sample size of 60–70, we did not foresee any challenges associated with recruitment within the time frame. The decision to employ two recruitment strategies concurrently, however, afforded some contingency to this process.
Participant recruitment and flow
The flow of participants through each stage of the study is shown in the Consolidated Standards of Reporting Trials (CONSORT) flow diagram (Figure 1).
FIGURE 1.
The CONSORT flow diagram. a, Not offered owing to duration of intervention.
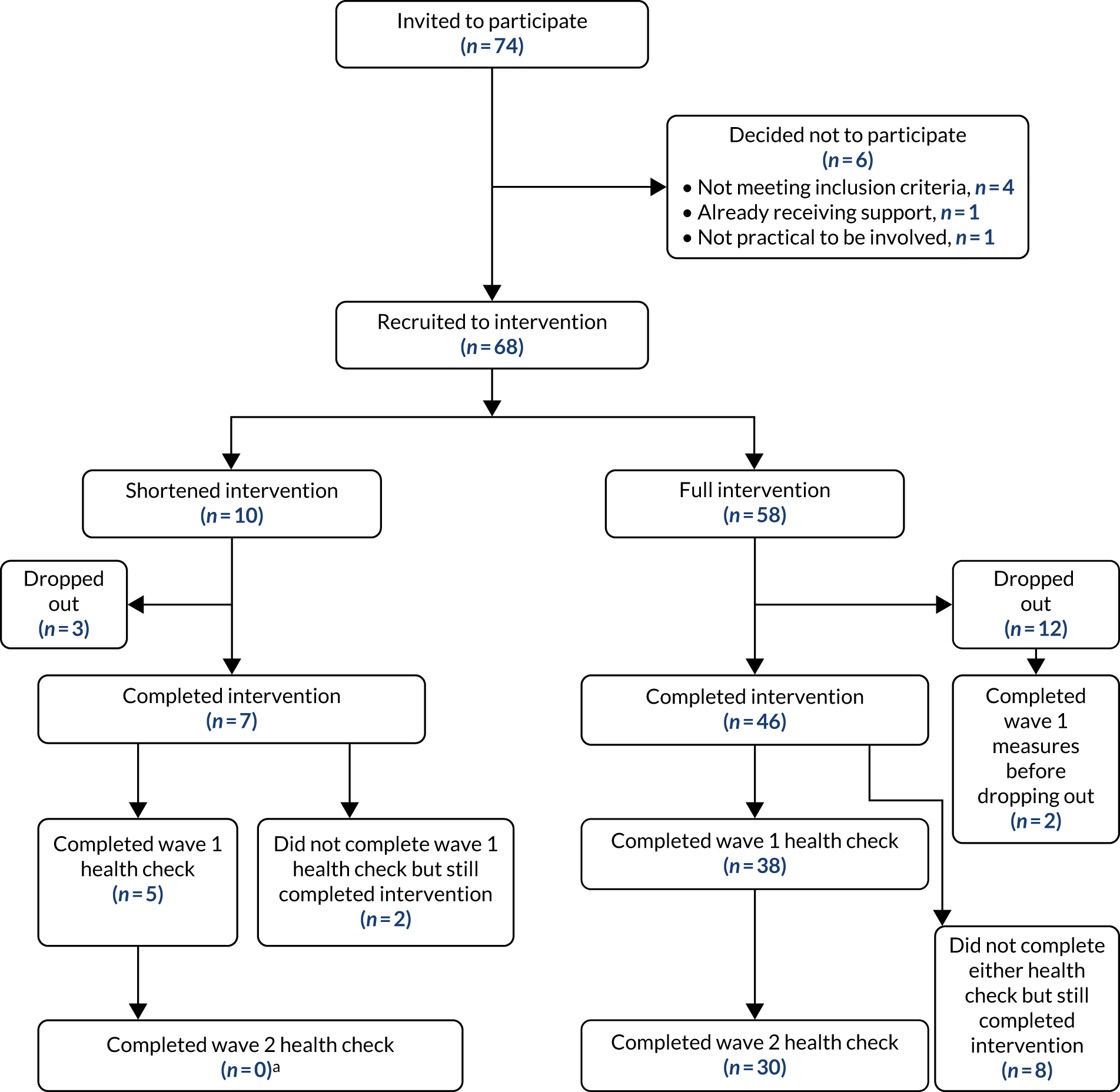
Recruitment approach
The PNs identified participants through the service in which they worked, from the outreach activities they engaged in and from other referral points such as health-care professionals and agencies in their local environments. Fourteen participants were recruited via outreach (20%). Informed by the findings of Mills et al. ,34 the PNs were permitted to accept word-of-mouth referrals from other participants, provided that potential participants met the inclusion criteria, were recruited properly, and there was case load space. Following the ethos of the study, a key aspect of recruitment involved the PNs developing trusting relationships with participants in advance of, or at the same time as, recruitment. The experience of recruitment from the perspectives of participants, staff and PNs is discussed in Chapter 5.
To determine the eligibility of each participant (see Chapter 1 for inclusion criteria), a collaborative process took place between a PN and their service manager, with input from the project management team. All identified eligible intervention participants who were approached by the PNs were provided with a participant information sheet . They were then asked to provide written informed consent after 1 week (allowing a ‘cooling-off’ period) if they wished to take part.
Seventy-four individuals were invited to take part in the study; 68 (92%) were recruited. Of the six individuals who were invited to take part but were not recruited, four did not meet the inclusion criteria (after a fuller discussion of requirements), one was receiving sufficient support from elsewhere, and one was due to move area, making participation unfeasible.
Engagement and dropouts
The anticipated dropout number over the course of the study was nine; the actual dropout number was 15. Twelve participants withdrew from the full intervention and three withdrew from the shortened intervention. If a participant expressed that they no longer wished to be involved in the study, this was treated as a dropout. If a participant did not engage with their PN for > 3 weeks while recruitment was open, and despite repeated attempts at contact (and using different forms, including calls, e-mails and texts), the participant was assumed to have withdrawn from the study and was also treated as a dropout. The aim was to balance a commitment to these participants, and to enable them to have some distance if they needed to, while also offering the intervention to as many interested/eligible individuals (within the parameters of case load) to maximise the potential of the intervention. If a participant later re-connected with their PN, after their ‘place’ was re-filled, the participant would have been able to re-join; however, this did not occur.
Participants generally engaged well throughout the intervention, with some participants engaging on a more intermittent basis. This is likely to have been because of the participant-focused nature of the intervention, whereby the pace was able to be directed by the participant (see Chapter 5). At the conclusion of the full intervention, the three PNs were asked to record the engagement patterns for each participant. Approximately 40% engaged consistently, and 60% engaged in a more intermittent manner.
Participants who withdrew from the study were invited to complete a short ‘exit’ questionnaire [see the questionnaire on the project web page: www.journalslibrary.nihr.ac.uk/programmes/hta/1615314/#/documentation (accessed 2 December 2020)] to share their views/experiences of the intervention, which was administered by the service manager, completed in private, and returned to the study team in a sealed envelope. Only one questionnaire was returned (out of 15). The PNs shared their understandings of the reasons for dropout for each participant via a separate form; the reasons were varied and multiple, including participants experiencing exacerbated mental health problems, moving away from the area, not engaging well, and moving on and becoming more stable.
No dropouts happened after the recruitment window closed in April 2019. This meant that 46 participants completed the full version of the intervention when it closed in November 2019. This is partly attributed to the adoption of a flexible approach, which enabled participants to re-connect after a period of reduced contact, and which is a contrast to the approach implemented during the recruitment period. The rationale for this decision, which was discussed in-depth among the project management team, was that it was very important to the study team that no ‘doors were closed’ for the participants, given how likely this was to have happened for them in the past through non-attendance at/participation with services. The team understood the potential of doing harm by taking decisions that fitted the needs of professional or service systems, rather than the needs of the vulnerable people using services. 41 The intervention was designed to be based on a trusting relationship; therefore, the team decided that ‘the door’ needed to be kept open once recruitment was complete.
Both these adopted approaches were intended to maximise potential in the different ways that were required at the different stages. In summary, 46 participants completed the full intervention, and seven participants completed the shortened intervention.
Quantitative outcome measures sample
Full intervention
Forty of the 58 participants who started the full intervention completed the wave 1 health check and 30 completed the wave 2 health check. Eight participants who completed the full intervention did not complete either the wave 1 or the wave 2 health check. Ten participants dropped out from the full intervention and did not complete any health check. Two participants dropped out from the full intervention and completed the wave 1 health check before withdrawing. On average, participants completed wave 2 measures within 6–8 months of completion of wave 1 measures.
Shortened intervention
Of the 10 participants who received the shortened intervention, five participants completed the wave 1 health check. A wave 2 health check was not offered to these participants because they received a shortened intervention, and it was not feasible to conduct the wave 2 health check within the time scales. Two participants who completed this intervention did not complete the health check. Three participants did not complete the health check because they withdrew from the study.
Missing data
Although either one or two health checks were conducted with the majority of the intervention participants, 10 individuals in total completed the intervention but did not complete a health check (n = 2 for the shortened intervention and n = 8 for full intervention). The reasons for not completing these were varied and included experiencing particularly poor mental health and having a particularly chaotic lifestyle; for the data collection in the England settings, the dates were fixed, meaning that sometimes these simply did not fit with a participant’s circumstances on these set days (see qualitative data on collection of measures in Chapter 5). The non-completion of measures means that we do not have quantitative data for these participants. If it had been possible for the measures to have been collected by the PNs themselves, as originally planned in the study protocol, we anticipate that all participants would have provided wave 1 measures at entry to the intervention. We also anticipate that more of the wave 2 measures would have been completed than were possible in this study. The implications of this for a future study are discussed in Chapter 6. The baseline data from all participants (n = 45; i.e. the full and shortened intervention) from the wave 1 health check were analysed together.
Standard care participants
As part of the feasibility and acceptability assessment of both the questionnaires and the approach to data collection, a sample (n = 6) of service users/residents from the two standard care settings undertook a health check with a study researcher (RF) on one occasion. These were selected on the basis of availability and willingness. Some key demographic characteristics of the standard care participants are presented in Table 2. Although there are obvious limitations with comparing these groups, particularly in the light of sample size, their characteristics were broadly similar to those of the intervention participants.
| Variable | Whole cohort (N = 45) | Both waves (N = 30) | Standard care (N = 6) |
|---|---|---|---|
| Age (years), mean (SD) | 38.6 (8.7) | 38.2 (8.0) | 44 |
| Male, n (%) | 35 (78) | 25 (83) | 6 |
| Marital status, n (%) | |||
| Single | 37 (82) | 24 (80) | 6 |
| Divorced | 3 (7) | 2 (7) | |
| In relationship | 4 (9) | 3 (10) | |
| Widowed | 1 (2) | 1 (3) | |
| White ethnicity, n (%) | 43 (96) | 28 (93) | 5 |
| Education, n (%) | |||
| Primary | 1 (2) | ||
| Secondary | 23 (51) | 18 (60) | 5 |
| College/diploma | 16 (36) | 9 (30) | 1 |
| University | 1 (2) | 1 (3) | |
| Postgraduate | 1 (2) | 1 (3) | |
| Other | 2 (4) | 1 (3) | |
| Missing | 1 (2) | ||
| Numeracy, reading and writing: self-reported as have no difficulties, n (%) | |||
| Numbers | 38 (84) | 26 (87) | 5 |
| Reading | 37 (82) | 25 (83) | 3 |
| Writing | 38 (84) | 26 (87) | 2 |
| Self-identified as having a disability, n (%) | 30 (67) | 18 (60) | 3 |
| Learning | 1 (2) | 1 | |
| Long term | 10 (22) | 5 (17) | |
| Mental health | 24 (53) | 15 (50) | 3 |
| Mobility | 8 (18) | 6 (20) | |
Sample characteristics
This section reports the demographic, health characteristics and living circumstances of the intervention participants at baseline (wave 1). Of the 45 participants, 35 (78%) were male. The average age was 39 years. The majority (96%) of participants described their ethnicity as ‘white’. Participants were asked about their ‘highest’ education level: this varied from primary to postgraduate level. The most frequently reported ‘highest’ education levels were secondary school (51%) and college (36%). The majority did not report experiencing difficulties with numbers (84%), reading (82%) or writing (84%). Thirty participants (67%) self-identified as having a disability, including mobility problems, sensory impairment, learning disability, developmental disability, mental health problems and long-term conditions.
Forty participants (89%) had been convicted of a criminal offence at some point in their lives. Of these, the highest proportion (15/40, 38%) had > 20 convictions, and 36 participants (36/40, 90%) had experience of being in prison. Three participants (7%) had served in the armed forces. Twenty participants (44%) had been in residential or foster care. Participants’ housing circumstances varied and included rough sleeping, sleeping temporarily with friends/family, living in a bed and breakfast (B&B), supported accommodation, a hostel and in their own home. The highest proportion (31%) were living in supported accommodation, as shown in Table 3.
| Variable | Whole cohort (N = 45) | Both waves (N = 29) | Standard care (N = 6) |
|---|---|---|---|
| Ever in armed forces, n (%) | 3 (7) | 3 (10) | 0 |
| Ever in residential or foster care, n (%) | 20 (44) | 14 (47) | 2 |
| Where currently sleeping, n (%) | |||
| Rough | 2 (4) | 2 (7) | |
| Hostel | 12 (27) | 3 (10) | 1 |
| Supported accommodation | 14 (31) | 11 (37) | 2 |
| B&B | 2 (4) | 2 (7) | |
| Temporary/friends/family | 2 (4) | 2 (7) | |
| Own home | 9 (20) | 6 (20) | 3 |
| Other | 4 (9) | 4 (13) | |
| Quality of current accommodation, median (25th centile, 75th centile) | 7 (5, 8) | 7 (5, 8) | |
| Ever convicted of a crime, n (%) | 40 (89) | 28 (93) | 3 |
| Number of convictions, n (%) | |||
| 1–5 | 10 (22) | 8 (27) | 1/3 |
| 6–10 | 8 (18) | 4 (13) | |
| 11–15 | 4 (9) | 2 (7) | |
| 16–20 | 3 (7) | 2 (7) | |
| > 20 | 15 (33) | 12 (40) | 2/3 |
| Ever been in prison, n (%) | 36 (80) | 25 (83) | |
| Years in prison | |||
| Median | 2.5 | 3 | |
| 25th centile, 75th centile | 0.6, 7 | 0.8, 7 | |
| Minimum, maximum | 0.04, 25 | 0.08, 14 | |
Health status
Participants were asked to rate their health in the previous 6 months. The highest proportion (40%) described their health as being ‘fair’, as shown in Table 4. Many participants (82%) reported taking prescribed medications; 31% reported taking medications that were not prescribed by a doctor but were instead obtained from other sources (e.g. community pharmacy, a friend or a street purchase). Almost all participants (96%) had been in hospital as an inpatient at some point in their life. Thirty-five participants (78%) reported having ever thought about self-harm or suicide, 20% in the previous month.
| Health status and medication use | Whole cohort (N = 45), n (%) | Both waves (N = 30), n (%) |
|---|---|---|
| Self-rated health in previous 6 months | ||
| Very good | ||
| Good | 4 (9) | 4 (13) |
| Fair | 18 (40) | 10 (33) |
| Bad | 15 (33) | 10 (33) |
| Very bad | 7 (16) | 6 (20) |
| Missing | 1 (2) | |
| Taking prescribed medication | 37 (82) | 25 (83) |
| Taking non-prescribed medication | 14 (31) | 12 (40) |
| Reason for taking non-prescribed medication | ||
| Physical health | 3 (7) | 3 (10) |
| Mental health | 5 (11) | 4 (13) |
| Both | 6 (13) | 5 (17) |
| Source of non-prescribed medication | ||
| Friend | 6 (13) | 5 (17) |
| Pharmacy | 2 (4) | 2 (7) |
| Relative | 2 (4) | 2 (7) |
| Street | 7 (16) | 6 (20) |
| Other | 2 (4) | 2 (7) |
| Taking prescribed medication for a drug or alcohol problem | 28 (62) | 17 (59) |
| Ever spent time as hospital inpatient | 43 (96) | 29 (100) |
| Ever thought about self-harm or suicide | 35 (78) | 21 (72) |
| When were last thoughts about | ||
| In the previous day | 5 (11) | 2 (7) |
| In the previous week | 5 (11) | 2 (7) |
| In the previous month | 9 (20) | 8 (28) |
| In the previous year | 9 (20) | 4 (14) |
| > 1 year ago | 7 (16) | 4 (14) |
| Ever acted on thoughts | ||
| No | 10 (22) | 9 (31) |
| Yes | 21 (47) | 12 (41) |
| Prefer not to say | 5 (11) | 4 (14) |
Participants reported experiencing a wide range of physical and mental health issues, both diagnosed and undiagnosed, as shown in Table 5. Many [n = 36 (80%)] reported that they had been diagnosed with anxiety, 37 (82%) had been diagnosed with depression, and 21 (47%) had been diagnosed with other mental health problems. Relatively common physical health problems included back problems, asthma, dental problems and chronic pain. All 45 participants reported at least one diagnosed health condition. The median number reported was 5 (25th, 75th centiles: 4, 8). Twelve participants reported an undiagnosed condition (see Table 5). Participants’ self-rated health varied, as shown in Figure 2. The range and frequency of participants’ physical health complaints and psychological health issues are shown in Figures 3 and 4 (both waves).
| Health condition | Whole cohort (N = 44), n (%) | Both waves (N = 30), n (%) | Wave 2 (N = 30), n (%) |
|---|---|---|---|
| Diagnosed health conditions | |||
| Angina | 3 (7) | 2 (7) | 2 (7) |
| Anxiety | 36 (80) | 22 (73) | 22 (73) |
| Arthritis | 9 (20) | 8 (27) | 6 (20) |
| Asthma | 13 (29) | 7 (23) | 6 (20) |
| BBV | 7 (16) | 6 (20) | 10 (33) |
| Back | 17 (38) | 14 (47) | 13 (43) |
| Bronchitis | 4 (9) | 2 (7) | 2 (7) |
| COPD | 9 (20) | 3 (10) | 2 (7) |
| Cancer | 4 (9) | 3 (10) | 2 (7) |
| Chronic pain | 15 (33) | 13 (43) | 11 (37) |
| Constipation | 7 (16) | 5 (17) | 6 (20) |
| Dental | 22 (49) | 18 (60) | 15 (50) |
| Depression | 37 (82) | 24 (80) | 26 (87) |
| Diabetes | 4 (9) | 3 (10) | 2 (7) |
| Diarrhoea | 3 (7) | 2 (7) | 3 (10) |
| Eczema | 5 (11) | 3 (10) | 4 (13) |
| Foot | 10 (22) | 8 (27) | 4 (13) |
| HBP | 9 (20) | 4 (13) | 4 (13) |
| Heart failure | 1 (2) | ||
| Heartburn | 6 (13) | 3 (10) | 7 (23) |
| Kidney | 3 (7) | 2 (7) | 3 (10) |
| Liver disease | 5 (11) | 4 (14) | 1 (3) |
| Migraine | 4 (9) | 2 (7) | 4 (13) |
| Other physical condition | 13 (29) | 8 (27) | 10 (33) |
| Other mental health conditiona | 21 (47) | 13 (43) | 14 (47) |
| Stroke | 1 (2) | ||
| Thyroid | 1 (2) | 1 (3) | 2 (7) |
| Undiagnosed health conditions | |||
| Angina | 1 (2) | 1 (3) | |
| Anxiety | 1 (3) | ||
| Asthma | 2 (4) | 1 (3) | |
| Back | 2 (4) | 1 (3) | 1 (3) |
| Bronchitis | 1 (2) | 1 (3) | |
| COPD | 1 (2) | 1 (3) | |
| Cancer | 1 (2) | 1 (3) | 1 (3) |
| Chronic Pain | 1 (1) | 1 (3) | |
| Dental | 1 (3) | ||
| Diabetes | 3 (7) | 2 (7) | 1 (3) |
| Diarrhoea | 1 (2) | 1 (3) | |
| Eczema | 1 (2) | 1 (3) | |
| Foot | 1 (2) | 1 (3) | 1 (3) |
| HBP | 1 (3) | ||
| Heart failure | 1 (2) | 1 (3) | |
| Heartburn | 5 (11) | 3 (10) | 1 (3) |
| Liver disease | 2 (4) | 1 (3) | |
| Migraine | 3 (7) | 1 (3) | |
| Other physical condition | 1 (2) | 1 (3) | |
| Other mental health conditiona | 1 (2) | 1 (3) | |
| Stroke | 1 (1) | 1 (2) | 1 (3) |
| Thyroid | 1 (2) | ||
FIGURE 2.
Tab plot of self-rated health in the previous 6 months at wave 2 against wave 1 (numbers are frequencies; N = 30 participants with data at both time points).
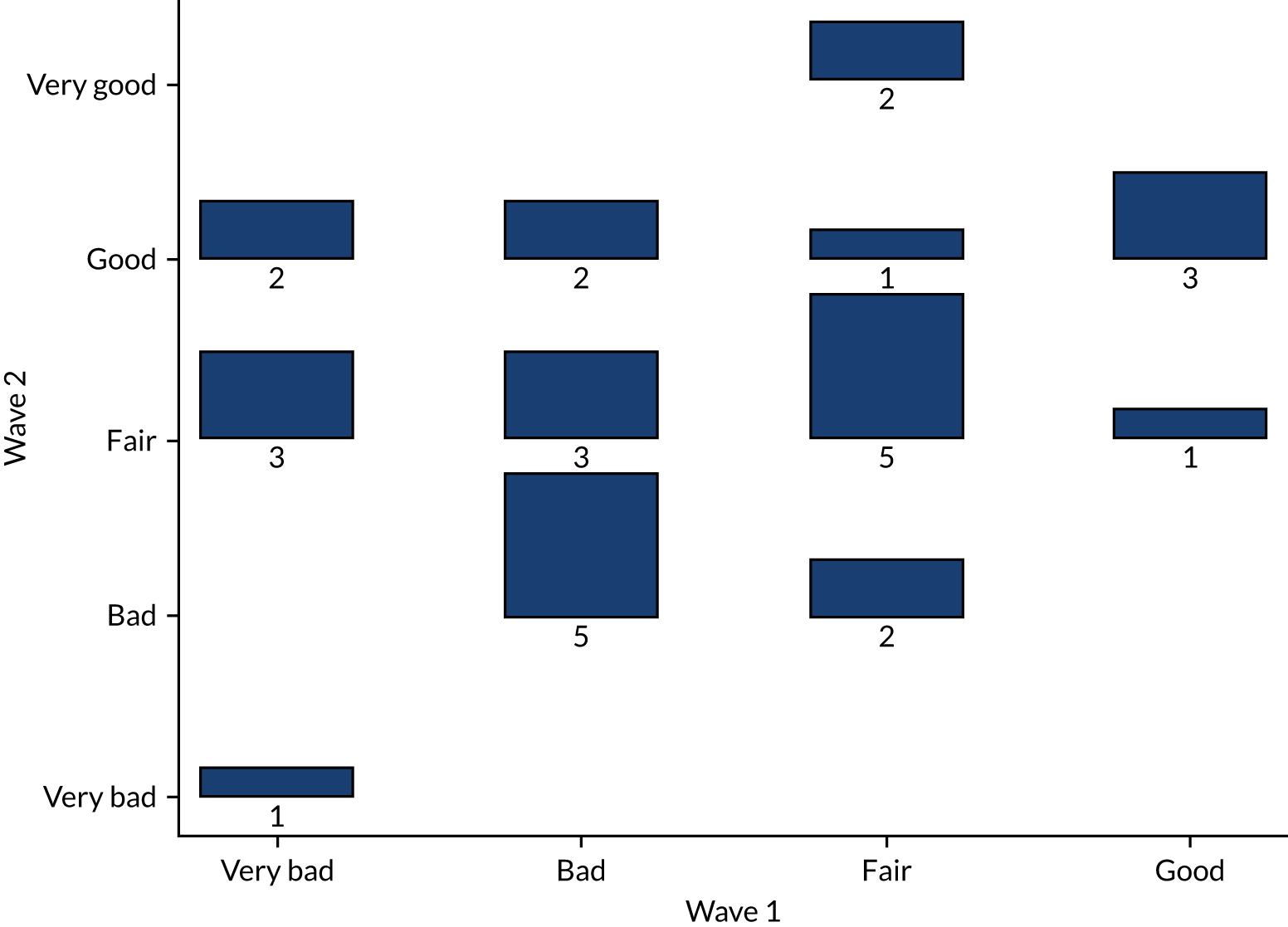
FIGURE 3.
The MAP: physical health problems. (a) Appetite; (b) tiredness; (c) nausea; (d) stomach pain; (e) breathing; (f) chest pain; (g) joint/bone pain; (h) muscle pain; (i) numbness; and (j) tremors. B/L, baseline; F/U, follow-up.
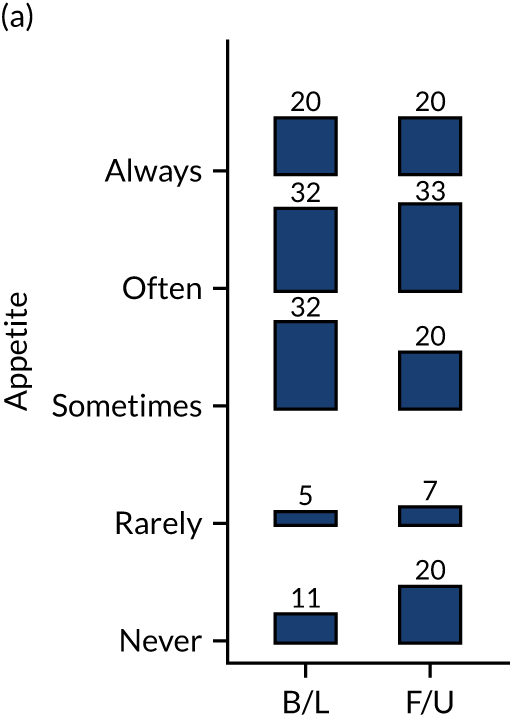
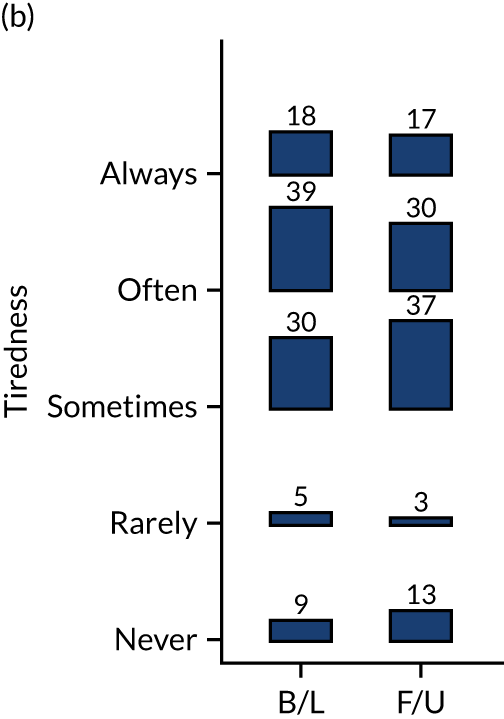
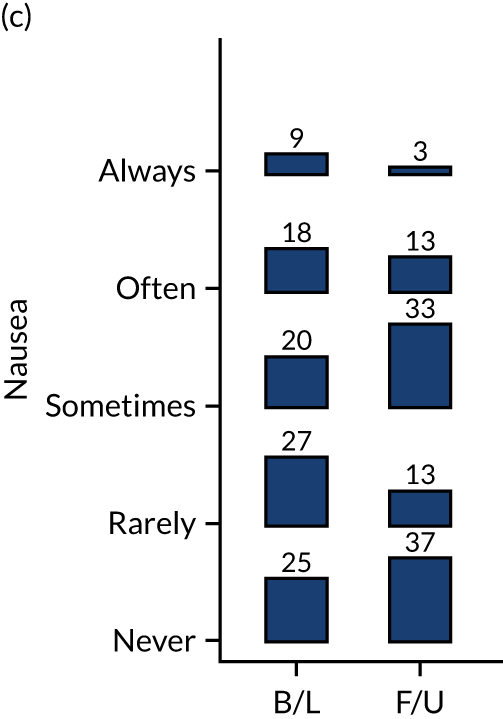
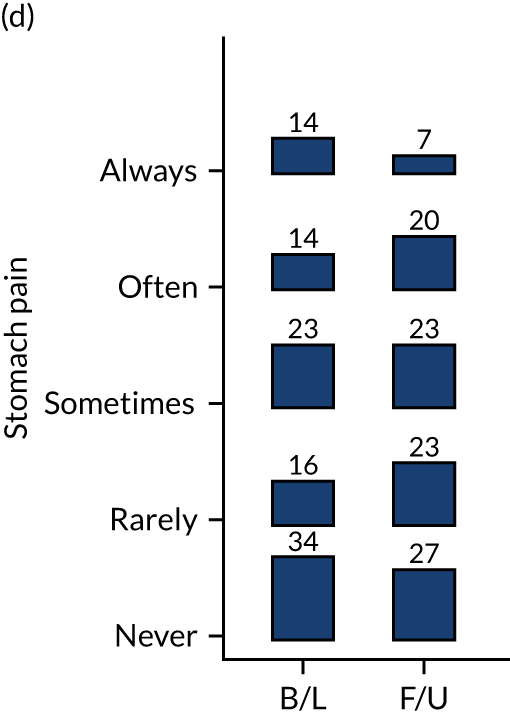
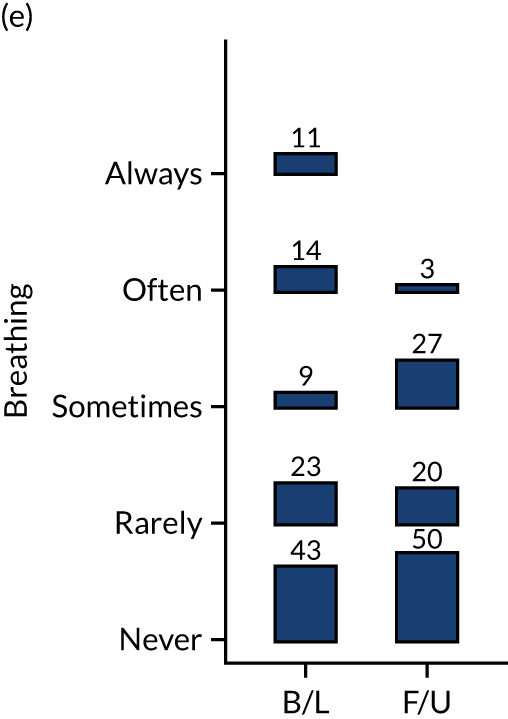
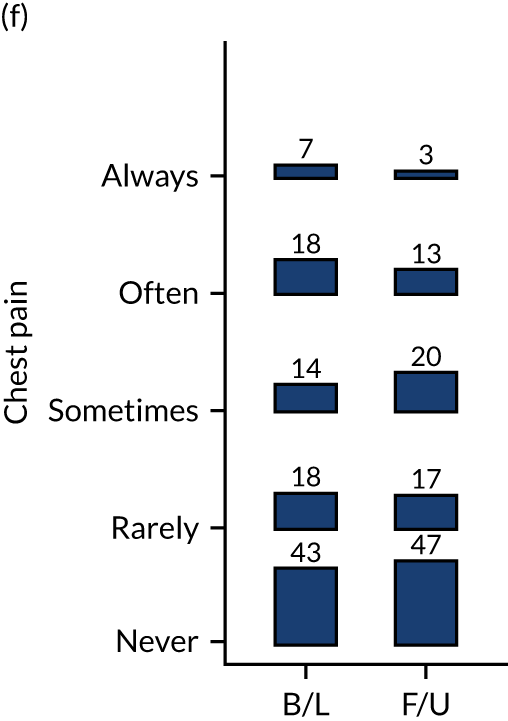
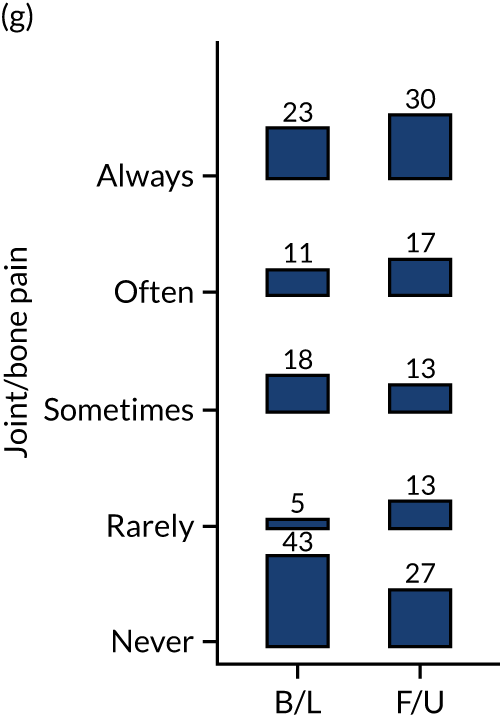
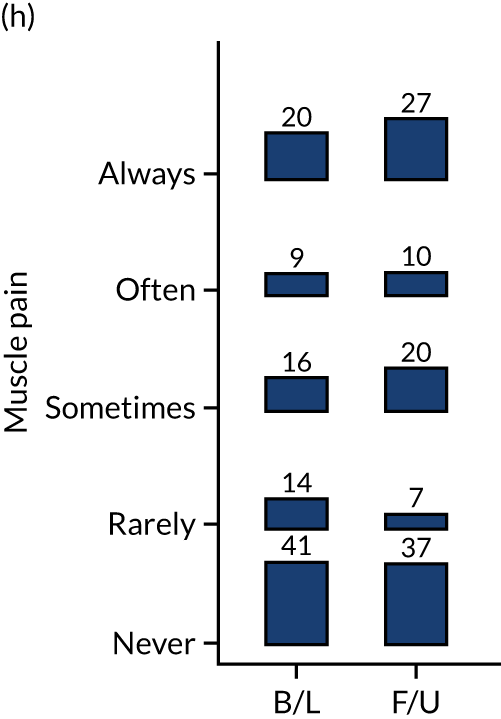
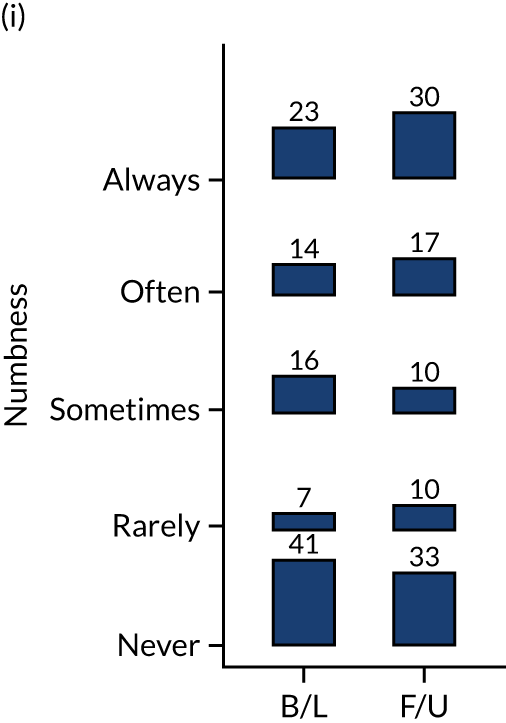
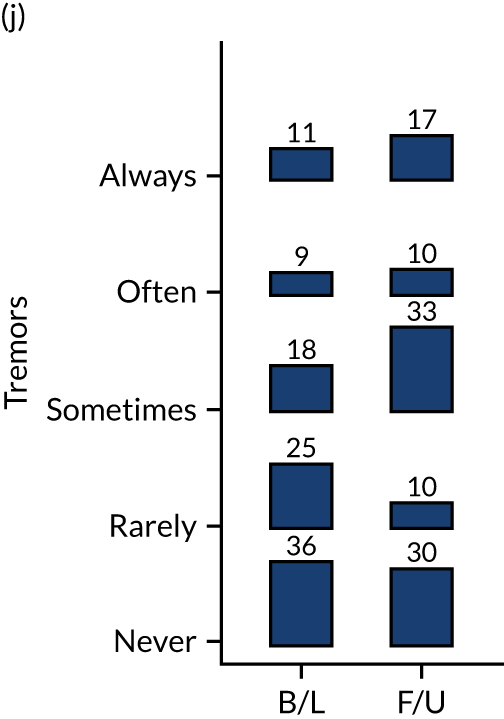
FIGURE 4.
The MAP: psychological health problems. (a) Nervous; (b) terror/panic; (c) hopeless; (d) worthless; (e) no interest; and (f) lonely. B/L, baseline; F/U, follow-up.
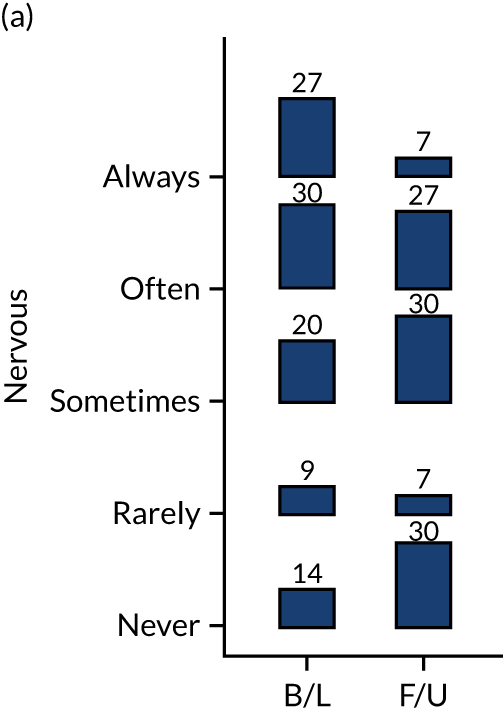
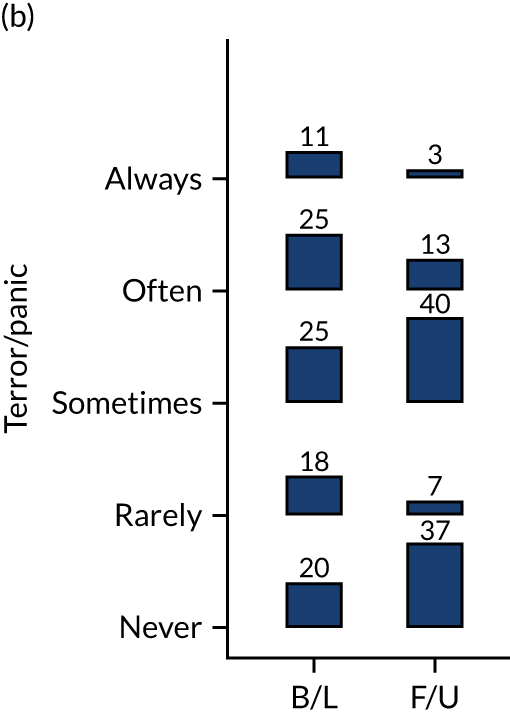
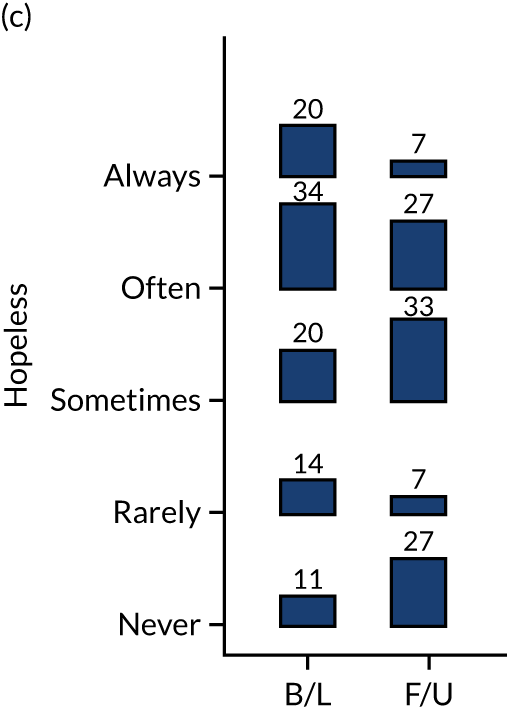
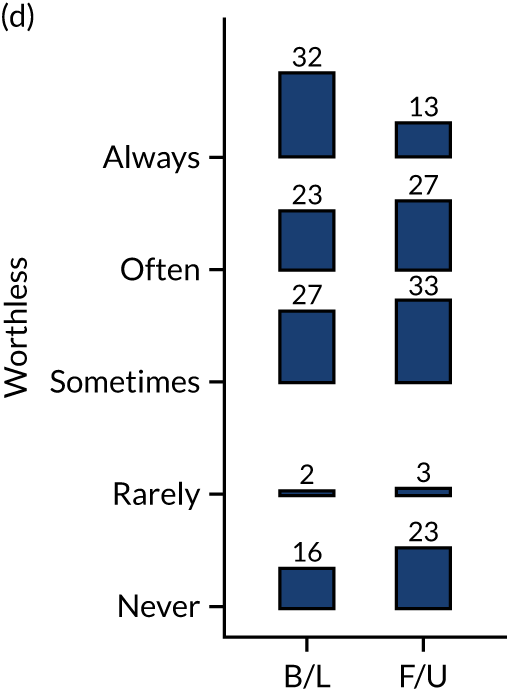
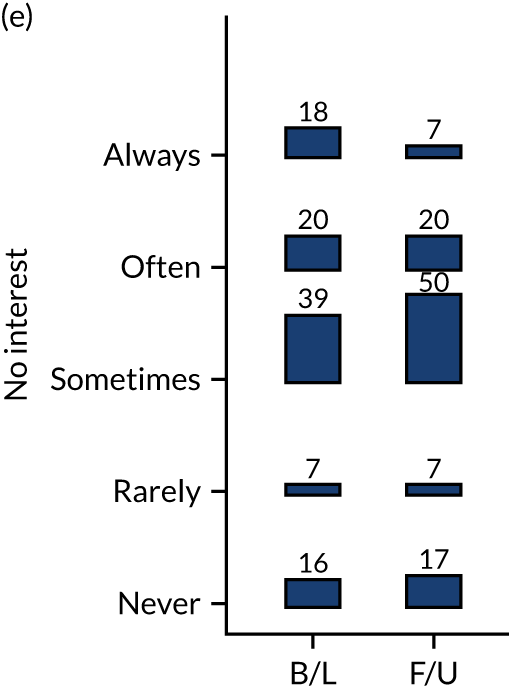
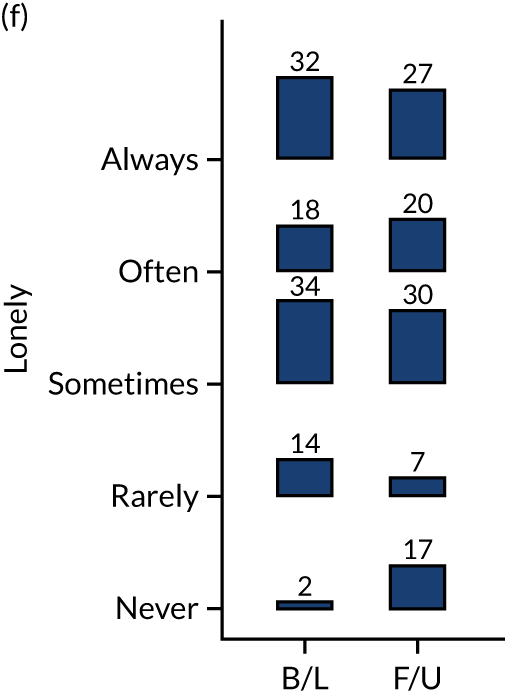
Participants were asked about the kinds of support/services that they would be interested in accessing in the future. Participants expressed an interest in receiving support in a range of pre-identified areas (e.g. employability, fitness, housing, detoxification). The highest proportion (84%) expressed a desire for support with welfare/benefits, as shown in Table 6.
| Service | Whole cohort (N = 45), n (%) | Both waves (N = 29), n (%) |
|---|---|---|
| Community activities | 20 (44) | 14 (47) |
| Community drug service | 26 (58) | 17 (57) |
| Counselling | 28 (62) | 18 (60) |
| Detoxification | 23 (51) | 15 (50) |
| Employability | 23 (51) | 16 (57) |
| Fitness | 21 (47) | 14 (47) |
| General health support | 27 (60) | 16 (53) |
| Hepatitis C treatment | 7 (16) | 6 (20) |
| Housing (of any kind)a | 34 (76) | 22 (73) |
| Independent living advice | 28 (62) | 17 (57) |
| Legal advice | 13 (29) | 8 (27) |
| Mental health support | 37 (82) | 23 (77) |
| Residential rehabilitation | 16 (36) | 11 (37) |
| Substitute treatment | 30 (67) | 20 (67) |
| Welfare and benefits | 38 (84) | 25 (83) |
| Wound management | 8 (18) | 6 (20) |
Substance use
Maudsley Addiction Profile
The MAP collected detailed information on the type, frequency of use and route of administration of drugs used in the past month. At wave 1 measurement, 43 out of 45 (96%) participants reported using at least one substance. The median number of substances used was 5 (25th, 75th centiles: 3, 5). Table 7 summarises the most commonly reported substances, and the self-reported number of days of use in the previous 30 days. At wave 1, a range of drugs, including alcohol, were used. The most frequently used substances were opioids [n = 25 (57%), oral use], heroin [n = 22 (50%), by injection and smoking/chasing] and crack cocaine [n = 23 (52%), mostly smoking/chasing, some injecting]. Sizeable proportions of participants also reported using alcohol [n = 21 (48%), orally], cannabis [n = 19 (43%), smoked], gabapentinoids [n = 15 (34%), predominantly orally] and benzodiazepines [n = 13 (30%), orally]. Participants’ experiences of overdose, drug treatment, service use history, opioid substitution therapy (OST) (also known as opioid substitution treatment) and injecting drug use behaviour are shown in Tables 8 and 9.
| Substance use | Whole cohort (N = 44) | Both waves (N = 30) | Wave 2 (N = 30) |
|---|---|---|---|
| Alcohol, n (%) | 21 (48) | 16 (53) | 15 (50) |
| Days of use, median (25th, 75th centile) | 12 (2, 30) | 19 (2, 30) | 5 (1, 30) |
| Heroin, n (%) | 22 (50) | 15 (50) | 9 (30) |
| Injecting (n) | 9 | 5 | 6 |
| Smoking (n) | 13 | 10 | 3 |
| Days of use, median (25th, 75th centile) | 13 (2, 30) | 6 (1, 30) | 2 (1, 3) |
| Cocaine (crack), n (%) | 23 (52) | 15 (50) | 11 (37) |
| Injecting (n) | 17 | 12 | 8 |
| Smoking (n) | 5 | 2 | 2 |
| Days of use, median (25th, 75th centile) | 13 (2, 30) | 11 (1, 21) | 2 (1, 8) |
| Opioids, n (%) | 25 (57) | 17 (57) | 23 (77) |
| Orally (n) | 22 | 14 | 22 |
| Sniffing (n) | 1 | ||
| Days of use, median (25th, 75th centile) | 30 (30, 30) | 30 (30, 30) | 30 (30, 30) |
| Benzodiazepines, n (%) | 13 (30) | 9 (30) | 7 (23) |
| Days of use, median (25th, 75th centile) | 30 (4, 30) | 30 (4, 30) | 30 (4, 30) |
| Gabapentinoids, n (%) | 15 (34) | 11 (37) | 7 (23) |
| Orally (n) | 14 | 9 | 6 |
| Snorting/sniffing (n) | 1 | 1 | 1 |
| Days of use, median (25th, 75th centile) | 3 (2, 30) | 10 (2, 30) | 2 (2, 30) |
| Cannabis, n (%) | 19 (43) | 13 (43) | 13 (43) |
| Smoking (n) | 19 | 13 | 13 |
| Days of use, median (25th, 75th centile) | 15 (2, 27) | 15 (14, 30) | 30 (30, 30) |
| Overdose, drug treatment and service use history | Whole cohort (N = 44) | Both waves (N = 30) | Wave 2 (N = 30) |
|---|---|---|---|
| Overdose history | |||
| Drug overdose in the previous month, n (%) | 2 (5) | 2 (7) | 0 (0) |
| How many (n) | |||
| 2 | 1 | 1 | – |
| 20 | 1 | 1 | – |
| If yes, previously overdosed? (n) | 1 | 1 | NA |
| If no overdoses in previous month, number of previous overdoses, n (%) | 42 | 28 | 30 |
| 0 | 16 (38) | 9 (32) | 10 (33) |
| 1 | 22 (53) | 18 (64) | 20 (67) |
| Missing | 4 (10) | 1 (4) | |
| Drug treatment | |||
| Ever in drug treatment, n (%) | 32 (73) | 22 (73) | 24 (80) |
| Number of times in drug treatment | 42 | 32 | 24 |
| Median [Q1, Q3] (minimum, maximum) | 2.5 [1, 5] (1, 10) | 2.5 [1, 5] (1, 7) | 2 [1, 4] (1, 7) |
| Length of time in treatment most recently (months) | n = 28 | n = 20 | n = 21 |
| Median [Q1, Q3] (minimum, maximum) | 11 [5, 54] (0, 288) | 12 [6, 23] (1, 288) | 12 [6, 24] (0, 300) |
| Service use, n (%) | |||
| Needle exchange | 28 (64) | 18 (60) | 20 (67) |
| Specialist OST | 25 (57) | 17 (57) | 18 (60) |
| GP-based OST | 16 (36) | 11 (37) | 14 (47) |
| Inpatient detoxification | 6 (14) | 6 (17) | 5 (17) |
| Residential rehabilitation | 7 (16) | 6 (20) | 7 (23) |
| Counselling | 12 (27) | 8 (27) | 16 (53) |
| Employment support | 9 (20) | 5 (17) | 6 (20) |
| Housing support | 18 (41) | 11 (37) | 19 (63) |
| Support group | 14 (32) | 11 (37) | 12 (40) |
| Other | 3 (7) | 3 (10) | 0 (0) |
| OST and injecting drug use behaviour | Whole cohort (N = 44) | Both waves (N = 30) | Wave 2 (N = 30) |
|---|---|---|---|
| Current OST, n (%) | 25 (57) | 17 (57) | 20 (67) |
| Current methadone patients | |||
| Years on methadone | n = 23 | n = 16 | n = 17 |
| Mediana [Q1, Q3] (minimum, maximum) | 2 [0, 5] (0, 27) | 1 [0, 2] (0, 27) | 1 [0, 3] (0, 27) |
| Current dose (ml) | n = 23 | n = 15 | |
| Median [Q1, Q3] (minimum, maximum) | 70 [50, 100] (30, 130) | 78 [50, 98] (30, 130) | 60 [45, 90] (30, 130) |
| Current buprenorphine patients | |||
| Years on buprenorphine | n = 3 | n = 2 | n = 3 |
| Median (minimum, maximum) | 1 (1, 2) | 1 (1, 1) | 0 (0, 1) |
| Injected in the previous month, n/N (%) | 16/44 (36) | 10/30 (33) | 2/30 (7) |
| If yes, how on many days did they inject | n = 10 | n = 5 | n = 1 |
| Median [Q1, Q3] (minimum, maximum) | 1.5 [1, 30] (1, 30) | 1 [1, 3] (1, 30) | 30 |
Other less frequently used substances were amphetamines [n = 2 (5%), one oral and one sniff user, both reporting using 1 day in the previous 30] and NPSs [n = 4 (9%), two reported smoking them, one reported taking them orally; three said that they used 1 day in the previous 30, and one reported using every day in the previous 30], and one person reported taking alprazolam.
At follow-up, there were changes in patterns of substance use. Of the 15 (both waves) that were taking heroin at wave 1, 10 had stopped by wave 2, but four participants who were not taking heroin at wave 1 had started by wave 2. ‘Opioid use’ (which includes all opioid drugs, i.e. prescribed and illicit) increased from 57% (both waves) at baseline to 77%: all those who were taking opioids in wave 1 continued to use them and six individuals started taking opioids between completion of wave 1 and wave 2. Sixteen reported being on OST at both waves; nine reported not being on OST at both waves; four started OST between wave 1 and wave 2, and one stopped.
Crack cocaine use had fallen to 37% (n = 11), as had gabapentinoid use [n = 7 (23%)]. Alcohol consumption and cannabis use remained relatively consistent (see Table 7). Of the 30 participants with data at both waves, four (13%) increased the number of substances they were taking by at least one, nine (30%) reported no change and 17 (57%) reduced the number of substances by at least one.
At baseline, two participants had experienced overdose in the previous month. At follow-up, no participants reported an overdose in the month preceding their completion of wave 2 measures. Previous experience of at least one overdose was 58% at baseline (see Table 8).
Substance Use Recovery Evaluator
In the SURE, a higher score or increase indicates that a person’s recovery is progressing well; this also applies to the individual domains. 124
In the SURE, there was an overall improvement in the total score between baseline and follow-up, as shown in Tables 10 and 11. At wave 1, the mean SURE score was 41.8 [standard deviation (SD) 8.3]. Of those who provided baseline data only, the mean score was 41.9 (SD 6.9); of those who provided data at both time points, the mean score was 41.8 (SD 9.2).
| Outcome | Whole cohort scores (N = 44) | Both waves cohort scores (N = 30) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Minimum | 25th centile | Median | 75th centile | Maximum | Minimum | 25th centile | Median | 75th centile | Maximum | |
| Substance use | 6 | 10 | 12 | 14 | 18 | 6 | 9 | 12 | 14 | 18 |
| Self-care | 3 | 6 | 7 | 8 | 9 | 5 | 5 | 7 | 11 | 14 |
| Relationships | 3 | 3 | 4 | 6 | 8 | 6 | 8 | 11 | 12 | 12 |
| Material resources | 5 | 8.5 | 11 | 12 | 12 | 3 | 5 | 7 | 8 | 9 |
| Outlook | 5 | 5.5 | 7 | 9.5 | 14 | 3 | 3 | 4 | 6 | 8 |
| Total | 28 | 35 | 41.5 | 48 | 60 | 28 | 34 | 39.5 | 48 | 60 |
| SURE factor | Time point | Scores | ||||
|---|---|---|---|---|---|---|
| Minimum | 25th centile | Median | 75th centile | Maximum | ||
| Substance use | Wave 1 | 6 | 9 | 12 | 14 | 18 |
| Wave 2 | 6 | 10 | 14 | 16 | 18 | |
| Self-care | Wave 1 | 5 | 5 | 7 | 11 | 14 |
| Wave 2 | 5 | 6 | 9 | 12 | 15 | |
| Relationships | Wave 1 | 6 | 8 | 11 | 12 | 12 |
| Wave 2 | 4 | 9 | 10 | 12 | 12 | |
| Material resources | Wave 1 | 3 | 5 | 7 | 8 | 9 |
| Wave 2 | 3 | 6 | 7 | 9 | 9 | |
| Outlook | Wave 1 | 3 | 3 | 4 | 6 | 8 |
| Wave 2 | 3 | 3 | 5 | 8 | 9 | |
| Total | Wave 1 | 28 | 34 | 39.5 | 48 | 60 |
| Wave 2 | 26 | 36 | 46.5 | 54 | 63 | |
The correlation between baseline and follow-up for those who provided data at both time points was 0.60 (95% CI 0.30 to 0.79). The mean follow-up SURE score was 44.4 (SD 10.7); the difference increase from baseline was 3.0 (95% CI –0.4 to 6.5).
There was a wide distribution in scores across domains at both time points and, for a small sample such as this, it is important not to over interpret findings (see Table 10) (Figure 5).
FIGURE 5.
The SURE scores at wave 1 and wave 2 for the 30 participants who completed the SURE at both waves. (a) Substance use; (b) self-care; (c) relationship; (d) material resources; (e) outlook; (f) SURE total score. Dark lines show improvement; light lines show deterioration.
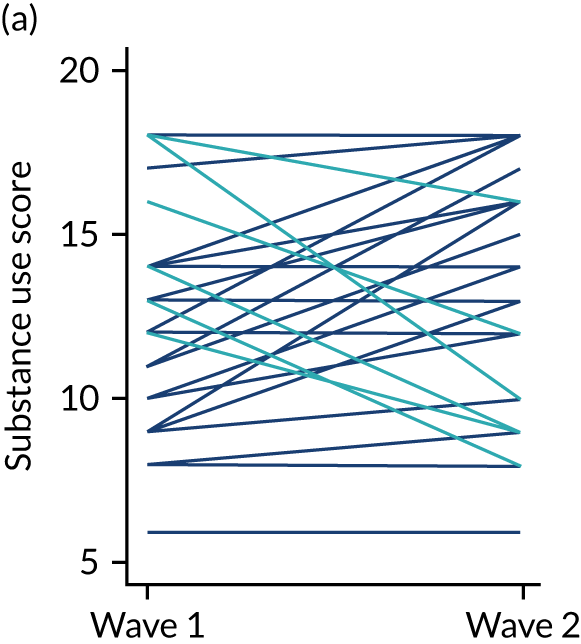
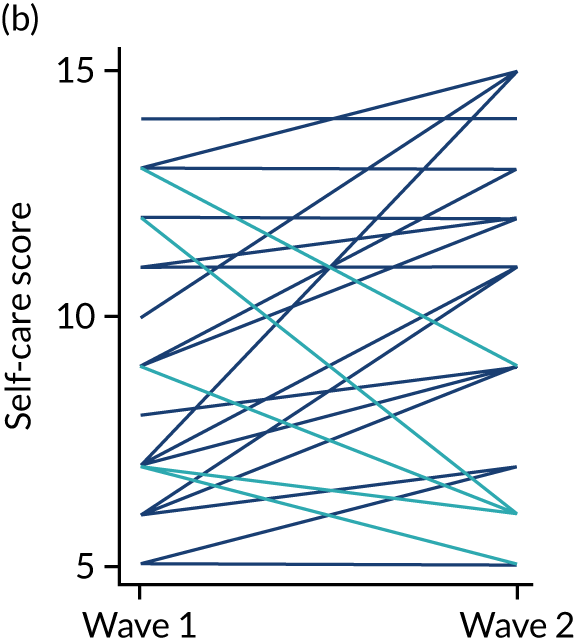
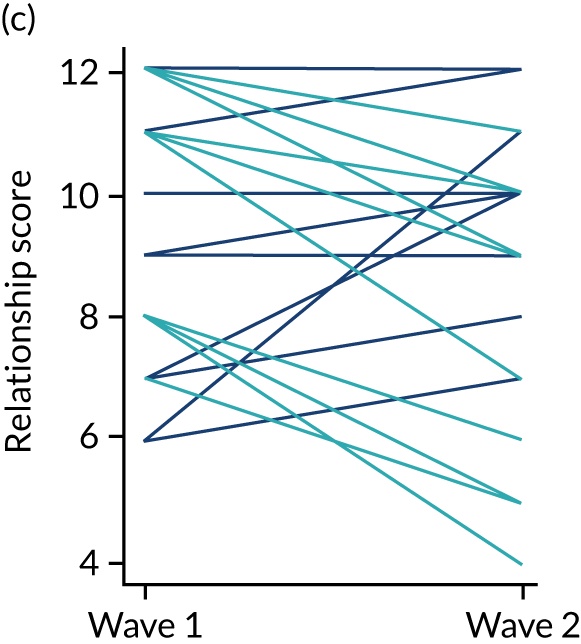
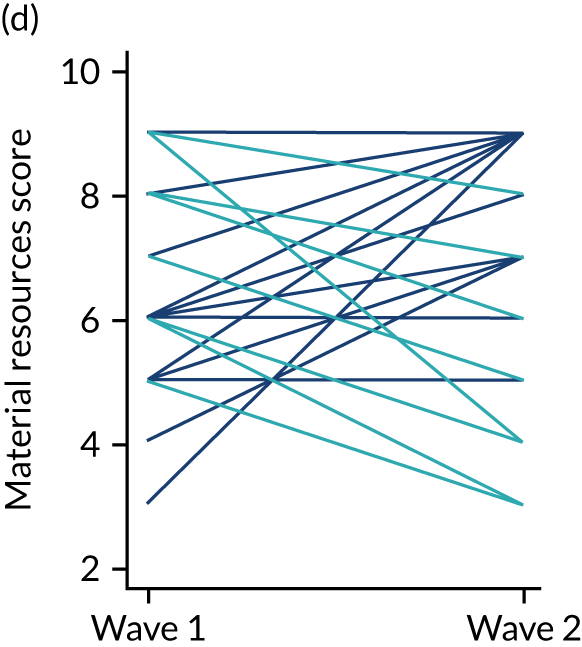
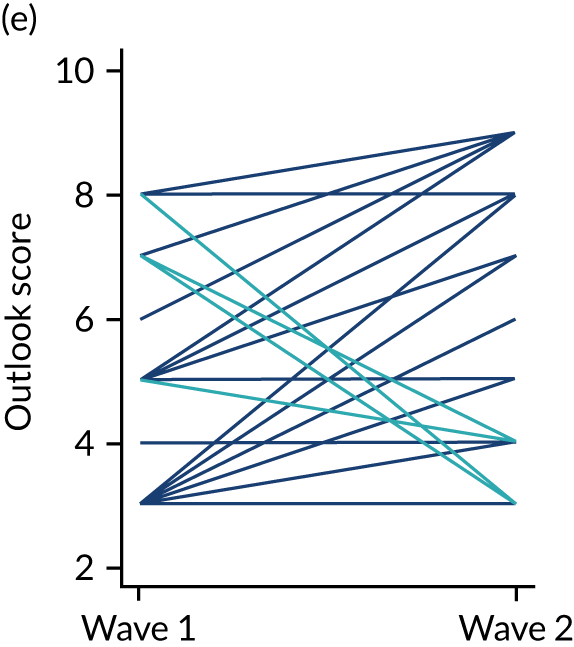
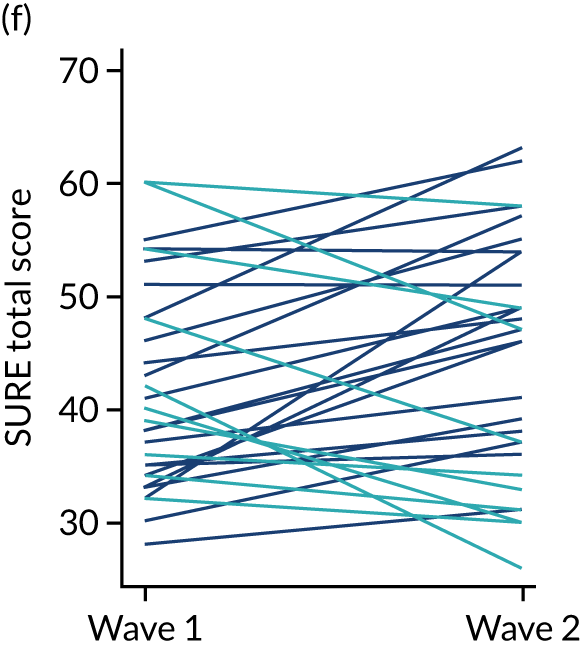
Overall health
Health status was assessed via measure 1, measure 5 (RAND SF-36) and subsections of the MAP; mental health was additionally captured via the PHQ-9 and GAD-7.
Physical health was assessed via an overall assessment of health, as well as through specific questions on a list of diagnosed and undiagnosed health conditions. For the overall assessment, a higher proportion of participants reported that their health was ‘fair’, ‘good’ or ‘very good’ at follow-up (22/30, 73%) than at baseline (15/30, 50%). There were small changes across a number of conditions (see Table 5); the largest increase (17%) was in the diagnosis of a blood-borne virus (n = 3 cases). This may reflect the PNs’ roles in encouraging testing.
Physical health status was measured via the MAP questionnaire. Figure 3 displays findings. There was a shift towards less frequent experience of breathing problems and fewer problems with poor appetite. However, there was a shift towards more frequent experience of muscle pain, numbness and tremors.
Mental health improved, as measured by the PHQ-9, GAD-7 and the psychological health questions in the MAP. The PHQ-9, GAD-7 and the combined score of these [Patient Health Questionnaire Anxiety and Depression Scale (PHQ-ADS)]138 demonstrated a reduction in the severity of self-reported depression and anxiety for many, although other participants’ mental health deteriorated (Table 12 and Figure 6).
| Outcome | Wave 1 for whole cohort (N = 44) | Wave 1 for both waves cohort (N = 30) | Wave 2 (N = 30) |
|---|---|---|---|
| GAD-7 | |||
| Mean (SD) | 14.7 (6.1) | 14.3 (6.3) | 11.7 (6.9) |
| Mean differencea (95% CI) | –2.6 (–5.4 to 0.2) | ||
| PHQ-9 | |||
| Mean (SD) | 15.5 (7.3) | 14.2 (7.3) | 13.6 (6.5) |
| Mean differencea (95% CI) | –0.6 (–1.3 to 2.2) | ||
| PHQ-ADS | |||
| Mean (SD) | 30.2 (12.6) | 28.4 (11.9) | 25.3 (11.7) |
| Mean differencea (95% CI) | –3.1 (–7.8 to 1.7) | ||
FIGURE 6.
Scores at wave 1 and wave 2 for (a) GAD-7; (b) PHQ-9; and (c) PHQ-ADS. Dark lines show improvement; light lines show deterioration.
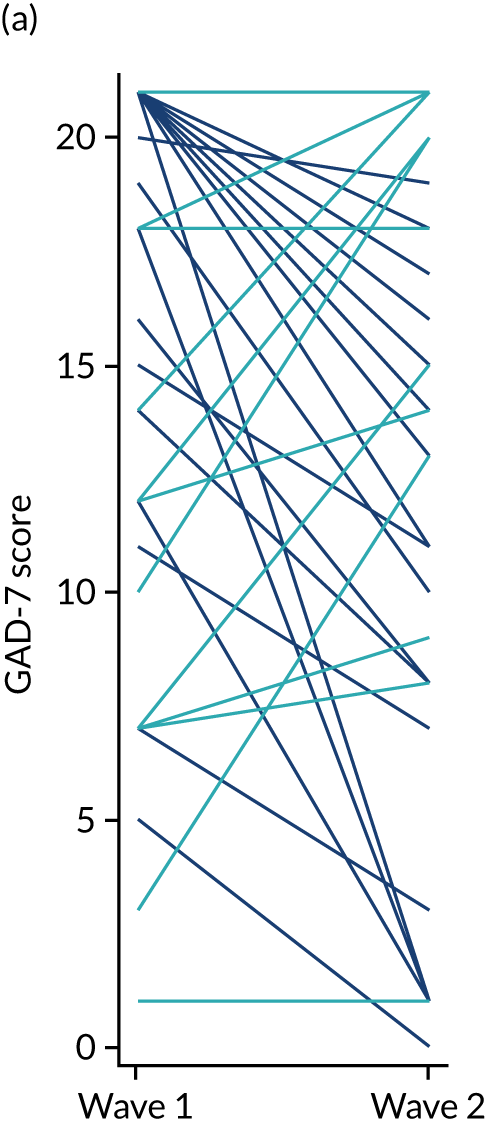
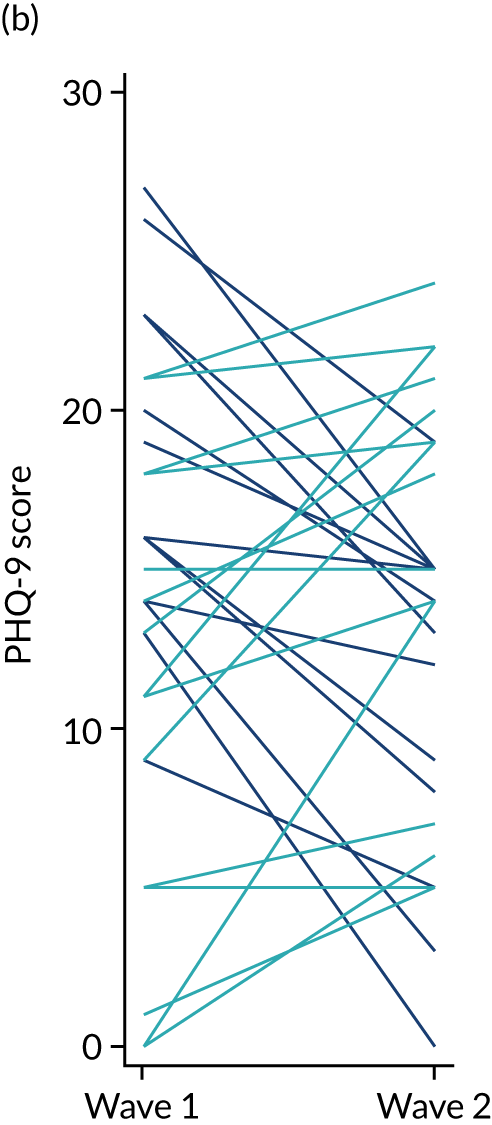
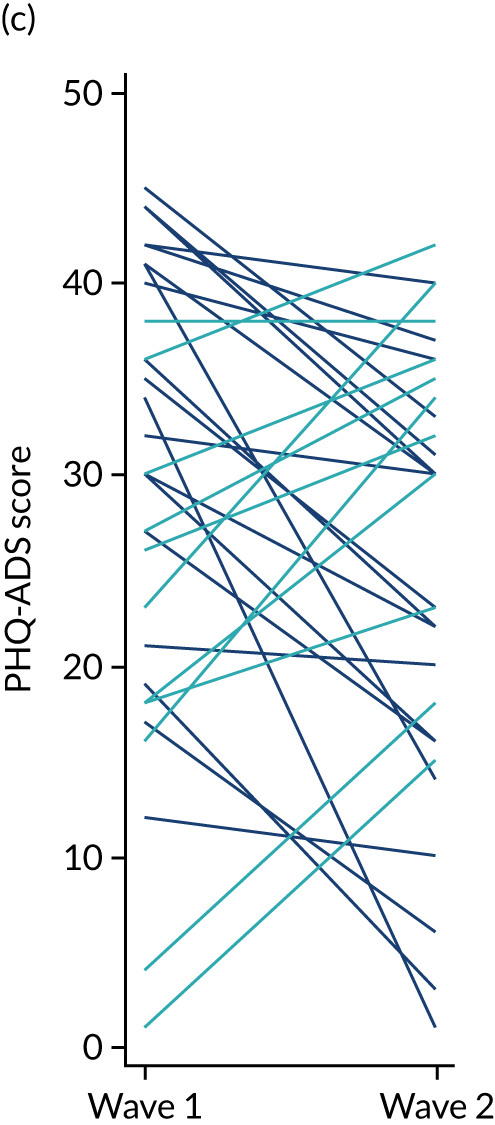
In the MAP, there was a positive shift in most domains towards less frequent experience of feeling nervous, hopeless, terror, worthlessness and a lack of interest. There was a less marked decrease in the proportion reporting feeling lonely (see Figure 4).
For the PHQ-9, a score of 0–5 represents mild depression, 6–10 represents moderate depression, 11–15 represents moderately severe depression and 16–20 represents severe depression. For GAD-7 anxiety severity, a score of 0–5 represents mild anxiety, 6–10 represents moderate anxiety; 11–15 represents moderately severe anxiety and 15–21 represents severe anxiety. The PHQ-ADS is the combined score of these. 138 The higher the number, the more severe the depression and/or anxiety. Participants’ scores and changes to them between waves 1 and 2 are shown in Table 12 and Figure 6.
The correlation between baseline and follow-up for those who provided PHQ-9 data at both time points was 0.46 (95% CI 0.11 to 0.71): mean wave 1 score 14.2 (SD 7.3), mean wave 2 score 13.6 (SD 6.5), difference –0.6 (95% CI –0.3 to 2.2). The correlation between baseline and follow-up for those who provided GAD-7 data at both time points was 0.38 (95% CI 0.01 to 0.65): mean wave 1 score 14.3 (SD 6.3), mean wave 2 score 11.7 (SD 6.9), difference –2.6 (95% CI –5.4 to 0.2). The correlation between baseline and follow-up for those who provided PHQ-ADS data at both time points was 0.43 (95% CI 0.07 to 0.7): mean wave 1 score 28.4 (SD 11.9), mean wave 2 score 25.3 (SD 11.7), difference –3.2 (95% CI –7.8 to 1.7).
Health risk behaviours were measured by self-reporting of injecting, sharing injecting equipment, and unprotected penetrative sex. There was a marked reduction in injecting behaviour: 36% (n = 16) reported injecting in the previous month at baseline (whole cohort), whereas 7% (n = 2) reported injecting in the previous month at follow-up (see Table 9). Regarding sharing equipment, 77% (n = 10/13) always used a new needle/syringe at baseline and two out of two always used a new needle/syringe at follow-up.
Regarding sexual risk, there was a reduction in the reported number of partners and instances of unprotected penetrative sex. At baseline, 32% (n = 14) of participants reported having had penetrative sex in the previous month, including unprotected sex, with either one (79%) or two (7%) partners on a median of 15 occasions. At follow-up, 27% (n = 8) reported penetrative sex in the previous month; this was unprotected with just one partner on a median of seven occasions.
RAND Corporation Short Form survey-36 items
All domains in the RAND SF-36 are scored so that a higher score relates to a better health state; the lowest and highest possible scores are 0 and 100, respectively. 139 Table 13 shows that, at wave 1, participants experienced limitations due to their physical health and emotional problems, with median scores of 12.5 and 0 (whole cohort), which are low. Their general health was also very poor. There was a general improvement in some domains for those reporting RAND SF-36 scores at wave 2 (Table 14). However, as is evident from Figure 7, there was considerable variation in the scores reported at both waves (and the change between points).
| Dimension | Whole cohort scores (N = 44) | Both waves cohort scores (N = 29) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Minimum | 25th centile | Median | 75th centile | Maximum | Minimum | 25th centile | Median | 75th centile | Maximum | |
| Physical function | 0 | 42.5 | 70 | 95 | 100 | 0 | 35 | 72.5 | 95 | 100 |
| Physical limitation | 0 | 0 | 12.5 | 100 | 100 | 0 | 0 | 25 | 100 | 100 |
| Emotional limitation | 0 | 0 | 0 | 33.3 | 100 | 0 | 0 | 0 | 33.3 | 100 |
| Energy | 0 | 15 | 32.5 | 45 | 100 | 0 | 15 | 27.5 | 55 | 100 |
| Emotional well-being | 0 | 24 | 36 | 52 | 88 | 8 | 24 | 42 | 56 | 88 |
| Social function | 0 | 12.5 | 25 | 50 | 100 | 0 | 12.5 | 37.5 | 50 | 100 |
| Pain | 0 | 22.5 | 45 | 70 | 100 | 0 | 20 | 32.5 | 67.5 | 100 |
| General health | 0 | 25 | 35 | 52.5 | 85 | 0 | 25 | 37.5 | 55 | 85 |
| Dimension | Time point | Scores | ||||
|---|---|---|---|---|---|---|
| Minimum | 25th centile | Median | 75th centile | Maximum | ||
| Physical function | Wave 1 | 0 | 35 | 72.5 | 95 | 100 |
| Wave 2 | 15 | 50 | 80 | 90 | 100 | |
| Role limitation: physical | Wave 1 | 0 | 0 | 25 | 100 | 100 |
| Wave 2 | 0 | 0 | 25 | 100 | 100 | |
| Role limitation: emotional | Wave 1 | 0 | 0 | 0 | 33.3 | 100 |
| Wave 2 | 0 | 0 | 0 | 66.7 | 100 | |
| Energy | Wave 1 | 0 | 15 | 27.5 | 55 | 100 |
| Wave 2 | 5 | 35 | 40 | 70 | 95 | |
| Emotional well-being | Wave 1 | 8 | 24 | 42 | 56 | 88 |
| Wave 2 | 4 | 40 | 48 | 76 | 96 | |
| Social function | Wave 1 | 0 | 12.5 | 37.5 | 50 | 100 |
| Wave 2 | 0 | 25 | 37.5 | 62.5 | 100 | |
| Pain | Wave 1 | 0 | 20 | 32.5 | 67.5 | 100 |
| Wave 2 | 0 | 32.5 | 45 | 80 | 100 | |
| General health | Wave 1 | 0 | 25 | 37.5 | 55 | 85 |
| Wave 2 | 5 | 25 | 40 | 50 | 95 | |
FIGURE 7.
Before-and-after plot for the eight dimensions of the RAND SF-36. (a) Physical function; (b) role limitation: physical; (c) role limitation: emotional; (d) energy fatigue; (e) emotional well-being; (f) social function; (g) pain; (h) general health. Dark lines show improvement; light lines show deterioration.

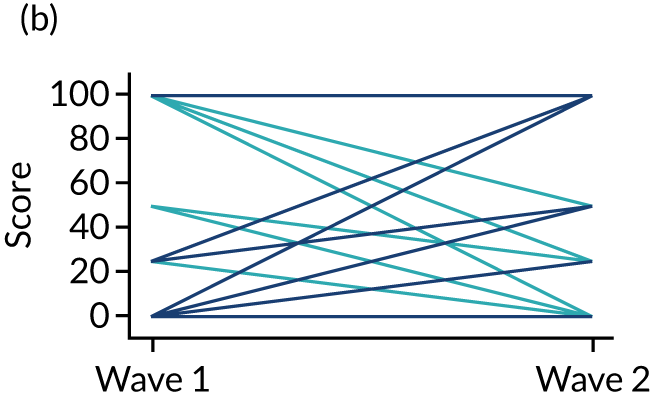
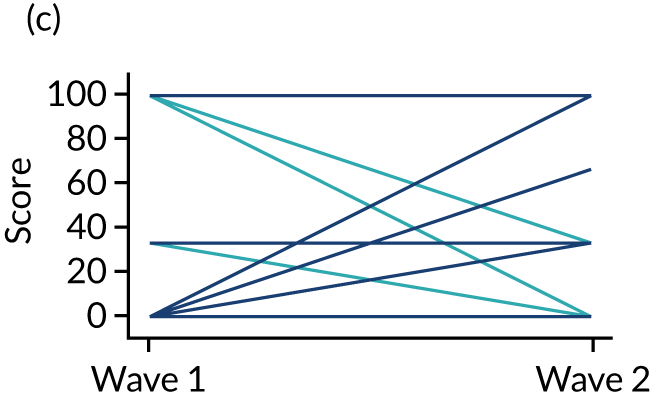
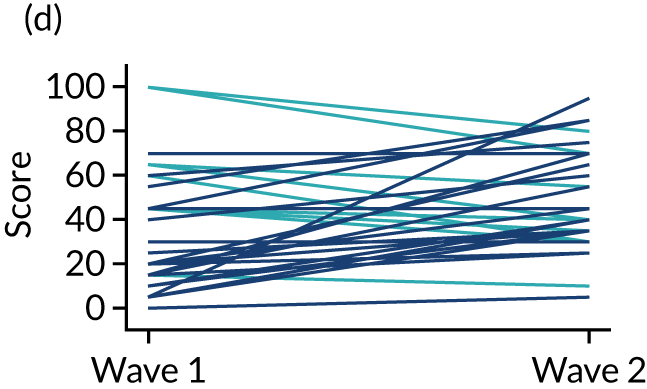
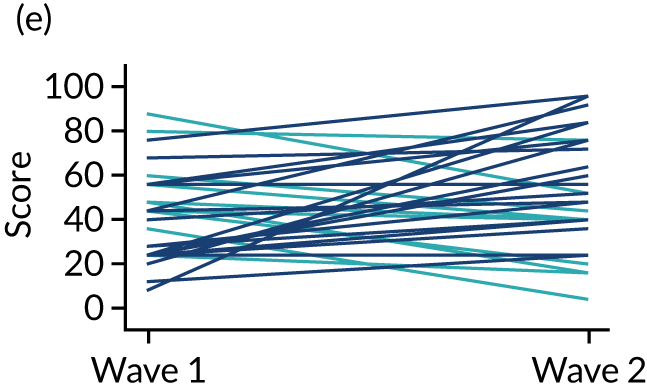
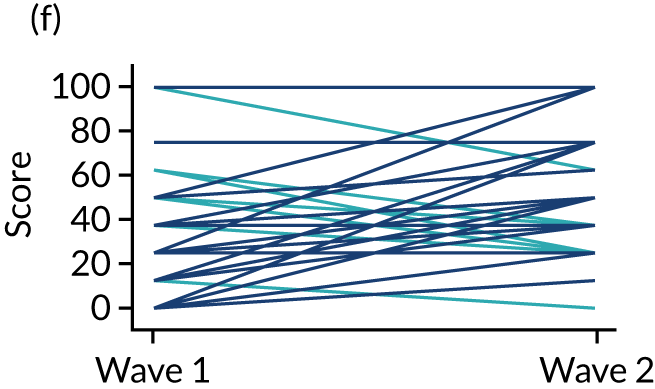
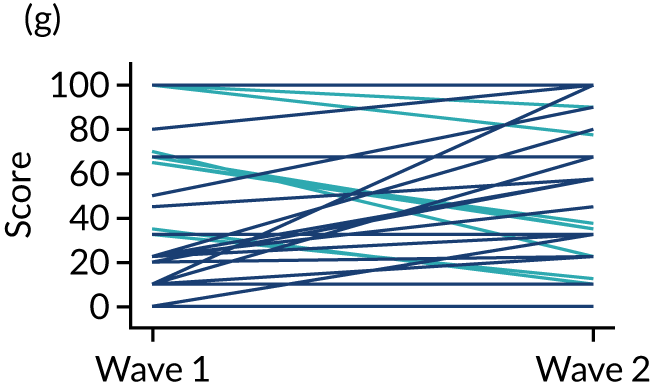
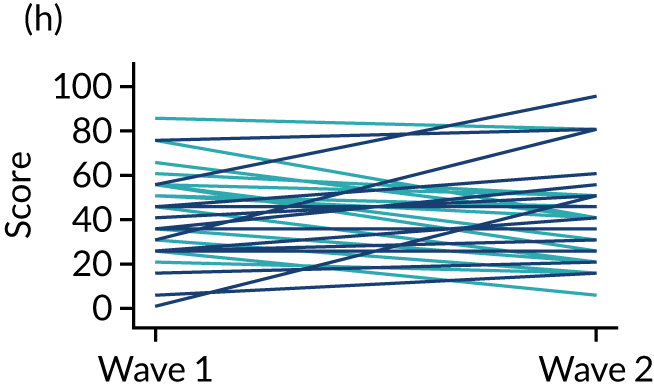
Relationship with Peer Navigator (Consultation and Relational Empathy Measure)
The scoring system for each item in the CARE Measure is ‘poor’ = 1, ‘fair’ = 2, ‘good’ = 3, ‘very good’ = 4 and ‘excellent’ = 5. All 10 items are then added, giving a maximum possible score of 50, and a minimum of 10. 125 The rating of the care provider (in this case, the PN) was good at wave 1 and increased further across all domains. The positive shift was particularly noticeable for ‘really listening’, ‘interested in me as a whole person’ and ‘explains clearly’, with 83%, 87% and 83%, respectively, rating this as excellent at follow-up, as shown in Table 15.
| CARE Measure domains | Wave 1, n (%) | Wave 2 (N = 30), n (%) | |
|---|---|---|---|
| Whole cohort (N = 44) | Both waves (N = 30) | ||
| Making you feel at ease | |||
| Good | 4 (9) | 3 (10) | 2 (7) |
| Very good | 11 (25) | 5 (17) | 5 (17) |
| Excellent | 28 (64) | 21 (70) | 23 (77) |
| Missing | 1 (2) | 1 (3) | |
| Letting you tell your ‘story’ | |||
| Good | 4 (9) | 4 (13) | 2 (7) |
| Very good | 9 (20) | 4 (13) | 8 (27) |
| Excellent | 29 (66) | 20 (67) | 20 (67) |
| Missing | 2 (5) | 2 (7) | |
| Really listening | |||
| Good | 5 (11) | 5 (17) | 2 (7) |
| Very good | 8 (18) | 4 (13) | 3 (10) |
| Excellent | 29 (66) | 20 (67) | 25 (83) |
| Missing | 2 (5) | 1 (3) | |
| Being interested in you as a whole person | |||
| Good | 3 (7) | 3 (10) | 2 (7) |
| Very good | 9 (20) | 6 (20) | 2 (7) |
| Excellent | 30 (68) | 20 (67) | 26 (87) |
| Missing | 2 (5) | 1 (3) | |
| Fully understanding your concerns | |||
| Good | 4 (9) | 4 (13) | 2 (7) |
| Very good | 9 (20) | 3 (10) | 6 (20) |
| Excellent | 29 (66) | 21 (70) | 21 (70) |
| Missing | 2 (5) | 2 (7) | 1 (3) |
| Showing care and compassion | |||
| Good | 5 (11) | 4 (13) | 2 (7) |
| Very good | 9 (20) | 5 (17) | 5 (17) |
| Excellent | 28 (64) | 20 (67) | 23 (77) |
| Missing | 2 (5) | 1 (3) | |
| Being positive | |||
| Good | 4 (9) | 4 (13) | 3 (10) |
| Very good | 9 (20) | 5 (17) | 5 (17) |
| Excellent | 29 (66) | 20 (67) | 21 (70) |
| Missing | 2 (5) | 1 (3) | 1 (3) |
| Explaining things clearly | |||
| Good | 5 (11) | 5 (17) | 2 (7) |
| Very good | 11 (25) | 5 (17) | 3 (10) |
| Excellent | 27 (61) | 19 (63) | 25 (83) |
| Missing | 1 (2) | 1 (3) | |
| Helping you to take control | |||
| Good | 6 (14) | 5 (17) | 2 (7) |
| Very good | 8 (18) | 5 (17) | 4 (13) |
| Excellent | 27 (61) | 18 (60) | 23 (77) |
| Missing | 3 (7) | 2 (7) | 1 (3) |
| Making a plan of action with you | |||
| Good | 4 (9) | 4 (13) | 3 (10) |
| Very good | 7 (16) | 3 (10) | 4 (13) |
| Excellent | 29 (66) | 21 (70) | 22 (73) |
| Missing | 4 (9) | 2 (7) | 1 (3) |
The CARE Measure includes a box at the end for respondents to provide additional comments. Twenty participants in wave 1 and 13 participants in wave 2 shared feedback in this way. Participants were very positive about their experiences; some representative comments are shared here (verbatim, with gender anonymised):
Best worker here, goes out of their way. Happy to help, does what they say they will. Good bloke/lass. Like them. Trust them.
Been amazing from the start, has helped me improve my life massively, and always gave me great support.
I wouldn’t be as far as I was if it wasn’t for their caring help.
They have helped me a lot and wouldn’t want any more help. They sort everything out, good worker.
I’ve found their attitude to be awesome, full of politeness, understanding my needs. They prompted me in an approach that was decent, different and made me see other perspectives.
I’ll miss them ☹.
Chapter summary
The findings from the quantitative data collection demonstrate that, in addition to the experience of substance use problems and housing instability, participants experienced a range of physical and mental health issues, both diagnosed and undiagnosed. Participants had experienced very high levels of interaction with the criminal justice system, and a substantial proportion had been in local authority care as children. The challenging circumstances experienced by these participants, both at the time of the measures and previously, resonate with the literature discussed in Chapter 1 and indicate that the study succeeded in recruiting individuals with extremely complex and challenging lives.
As noted, there are obvious limitations in drawing conclusions from the small sample sizes at both baseline and follow-up. With these caveats in mind, between baseline and follow-up, there were noticeable increases in prescriptions for OST and reductions in crack cocaine and gabapentanoid use, although cannabis and alcohol use remained fairly constant. There was a notable reduction in injecting behaviour and no overdoses during the intervention period. There were overall improvements to participants’ physical and mental health, with some improvements and some deteriorations for specific complaints or conditions. There were marked improvements in participants’ assessments of their health status. The relationship with the Peer Navigator was measured as excellent at baseline and follow-up. Given the profound challenges experienced by study participants, any improvement to their health or circumstances, however minor, is noteworthy.
Chapter 5 Findings from the qualitative data collection
Chapter introduction
This chapter presents and discusses findings from the study’s qualitative data collection, which was analysed using NPT as a guiding framework. As outlined in Chapter 2, the four constructs of NPT are ‘coherence’, ‘cognitive participation’, ‘collective action’ and ‘reflexive monitoring’. The analysis explored how individuals and groups understood, adopted or perceived the intervention; how those receiving it engaged; how the PNs made sense of their role; and other contextual factors affecting delivery. Unique insights provided by the different aspects of qualitative data collection are also shared. As a reminder, academic researchers (RF and HC) conducted all qualitative data collection, except for the interviews with the intervention participants, which were conducted by SDF peer researchers.
Non-participant observation
Researchers observed the environment, social interactions and practices in each of the settings to better understand the context and dynamics of these. This offered some, albeit limited, insight into, for example, cognitive participation (the extent to which people ‘bought in’ to the intervention) and collective action (how well the intervention was able to align with existing group practices). The observations in the standard care settings enabled comparison between these and the intervention settings, and were guided by an observation pro forma [see the observation pro forma on the project web page: www.journalslibrary.nihr.ac.uk/programmes/hta/1615314/#/documentation (accessed 2 December 2020)].
Setting responses to researchers
Across both intervention and standard care settings, the research team was generally warmly welcomed by service managers, the staff team and those using the services, as illustrated by the following fieldnote excerpt from a standard care setting:
[Staff] were all very friendly and welcoming to me. They were interested in the study and why I was there. They seemed supportive of the study and rationale, answered my questions and told me a lot about the service and their jobs, often unprompted.
In contrast, in one intervention setting, staff were less welcoming of researchers:
The woman asked us to sign in and informed me (a bit abruptly) that we were not allowed to go into the canteen because it was breakfast time. After the comment from the woman at reception, I didn’t feel that we could sit and wait in the canteen.
In another intervention setting, the PN seemed surprised at the welcome the researcher received:
[PN] said s/he would introduce me [to staff and service users], which surprised me a little. It was a nice idea, but I also thought I would be fine to introduce myself alongside them, and I was happy to do this . . . [PN] and I had a conversation later – s/he revealed how surprised s/he was that people were so welcoming to me and keen to chat when I arrived. S/he is still finding that some are a little suspicious (or at least unsure) of him/her.
Although these are small examples, they raise questions regarding contextual integration, which are explored below. As discussed in Chapter 3, researchers quietly observed interactions in communal areas, which some service users/residents queried:
I chatted to residents much more than planned, mainly because it felt too awkward to do ‘straight’ non-participant observation, e.g. at one point, when I was sitting in the corner of the canteen making some notes, the guys who I had been speaking to called me over, saying I didn’t need to sit in the corner! It was said in a playful way but got the point across all the same.
Study researchers generally integrated well into the settings during these observation periods. This seemed to relate to the willingness of both the researchers and service users/residents to have these informal conversations:
Some of the service users immediately started chatting to me and wanted to know more about me and the study (in a friendly way), before I had even had the chance to take my coat off! Around 7/8 were there, congregated around the table.
Overview of settings
In all settings, researchers observed positive interactions between members of staff and service users/residents. Staff greeted service users/residents by name and interactions tended to be friendly and relaxed. Members of staff often asked how they were getting on and generally showed an interest in the lives of service users. All settings were busy, with two settings being particularly busy, partly attributed to their location and the high demand for services in these areas, as well as their drop-in nature. These settings tended to be hectic or even chaotic, which was commented on by service staff as relating to service users typically experiencing significant challenges and sometimes also being under the influence of alcohol and/or drugs. Although another setting was also a drop-in centre, it was more recovery oriented, with service users being discouraged from attending if under the influence of alcohol and/or drugs out of respect for others trying to be abstinent. Those using this setting also tended to have more stable circumstances.
One of the standard care settings was a drop-in service, but those accessing the service were generally accessing it at specific times for group sessions or one-to-one appointments. Although the service supports those experiencing problem substance use, it receives referrals from the local authority to support individuals with a range of physical and mental health challenges not limited to, or necessarily including, problem substance use. Although all settings had a staff-controlled entrance, the residential settings (intervention and standard care) had additional security features, which contributed to a more institutional atmosphere, including use of staff handsets, glass panelling at reception desks to separate staff and residents, and demarcated staff areas including staff rooms, toilets and kitchens.
Conversations with standard care staff and service users/residents about the intervention
Conversations with staff and service users were unplanned, informal and unobtrusive, and often took place while sharing a hot drink. Conversations with staff and service users in the standard care settings suggested support for the intervention:
The member of staff said that she could see the PN model working with some of her clients that she doesn’t feel she can get any further with. She also mentioned the limited time and resources she has to support clients herself.
Service users were receptive . . . they were very supportive of the peer support aspect e.g. that peers were more likely to ‘get it’ and develop a connection.
One service user expressed that the value of peer support was that PNs were less likely to be worried about saying the ‘right thing’, and more likely to engage in ‘straight talking’. Similarly, a staff member reflected that the value of lived experience is not necessarily in the person having experienced the same issue/challenge but, rather, lived experience fosters a depth of empathy and conveys hope: ‘He’s done it, he’s managed it’. Indeed, lived experience as a conduit or catalyst to a deeper, more intuitive form of empathy was a powerful theme that came through the data sets. Recognition of the value of lived experience was shared by service users and staff in the standard care settings through recognition of the unique benefits of lived experience, despite not hosting a PN in their services.
Existing group practices and fit
Some of the settings were found to be particularly conducive to warm, friendly interactions between staff and service users, chatting with residents in communal areas and playing pool. One intervention setting simply had a table in a shared space as a reception desk, prompting informal interactions as people entered the building, and a sense of shared endeavour and community between staff and service users. Residential settings, both intervention and standard care, were more closed environments. These prompted, or necessitated, practices that created greater social distance between those working and those using the service, and contributed to more institutional atmospheres:
[Setting] is a pretty big building, perhaps reflected by the fact that the staff each check out a radio when they arrive for a shift and use this to communicate with each other during the day.
It felt slightly rabbit warren-like with lots of doors with staff swipe-card access only.
Staff in the reception area control access to and from the building. There’s CCTV [closed-circuit television] throughout and various screens in the reception area for staff to observe who’s waiting to get in the building, as well as through glass panels.
Despite the layout and practices of these settings, relationships between staff and service users appeared to be positive.
Summary
Although there are obvious limitations with conducting only 45 hours of observation across all settings, these observations revealed areas of similarity and differences across the settings. These data, alongside other qualitative data, provide in-depth insights into the environment, atmosphere and dynamics of settings. Although some had physical environments that created clear demarcation between staff and residents/service users, positive interactions and friendly exchanges were observed.
The conversations that took place in the standard care settings highlighted that service users and members of staff were very receptive to the intervention, and observations suggested that standard care settings were broadly comparable to intervention settings.
The insights from these fieldnotes alongside other forms of qualitative data suggest that the more institutional features associated with residential settings can add to the challenge of hosting a PN because these are more likely to jar with the informality and fluidity of the PN role. However, the attitudes and behaviours of staff and service users in the setting, such as a willingness to interact informally, can help to circumvent these challenges.
Peer researcher interviews with participants (waves 1 and 2)
As detailed in Chapter 3, interviews with a sample of intervention participants were conducted by SDF peer researchers. This section presents the findings of each wave of interviews separately. For anonymisation purposes, interviews from both the shortened and the full intervention were analysed together, and the themes were consistent across these.
Coherence and cognitive participation: the factors that supported participants to ‘buy in’ to the Peer Navigator’s support
A key focus of NPT is to identify the extent to which people understood the purpose or meaningfulness of the intervention, and were engaged in it, examining the factors that acted as barriers to, or promoted, engagement. The findings suggest that the clear visibility of PNs in services helped to reduce barriers to engagement because potential participants were able to observe them and their practice and engage in ‘small talk’ prior to becoming formally involved:
In here, s/he was talking to someone but s/he was always dead friendly and obviously s/he took me on to help.
This was experienced as meaningful because it helped to build trust and establish an informal relationship before commitment was required. Many participants felt that they had not been listened to in the past, and had negative past experiences of support, making lack of trust a significant barrier that had to be overcome. This familiarity with the PNs, and the fact that the PNs always acknowledged and welcomed them, conveyed respect and value, leading to participants reaching out, rather than the other way around:
I remember seeing them over there the first few times and s/he told me what it was all about . . . We started chatting and I asked ‘could you be my Support Worker?’ because I seen him/her helping out other people.
The social norms of the settings were particularly conducive to this because initial contact often happened over coffee or in shared eating spaces, common to all settings, providing an informality to pre-support encounters. Conversations were often not centred on problem substance use, which helped to communicate respect and positive regard for the person:
S/he was willing to talk to me just in general, just have a conversation, [compared with] when you go to the doctors, it’s just like . . . ‘where have you been, what have you been smoking, what have you been [doing]?’.
Although some participants expressed that members of staff in their current accommodation/drop-in service were supportive, others reported feeling ‘unseen’ by staff, being acutely aware of how busy they were. A PN’s continued visibility in the setting was understood by service users as meaning that they had more time to spend with them, making the PN a ‘go-to’ person in times of crisis, or when urgent support was needed:
It was so good because s/he’s so understanding and keeps you right. Sometimes there are days where I struggle and I come in here and get help straight away.
Many participants expressed a feeling of being seen, heard and understood by the PNs, particularly because, once a relationship had formed, the PNs could identify what was not being said and check in on difficult days. The practice of reaching out and checking in, particularly if someone had not been seen for a few days, was viewed as important, with many participants feeling that it conveyed genuine, authentic care:
S/he will help you to relax before you even talk, even when you are not having a meeting, if s/he sees you s/he will stop and talk with you . . . where I’ve been to two other places and they don’t even notice you. All they want to know is when you have the appointments, you go in and, that’s it, you get back out. But s/he does put himself/herself out there totally.
Initially, a few participants expressed feeling anxious that the PN might report conversations to the service manager, and being worried about the consequences of such disclosures; with time, this fear lessened.
Positive changes
Participants reported a number of positive outcomes that seemed to help them to continue to value, and ‘buy into’, the intervention. These outcomes included greater access to, and engagement with, health care, support services and housing support. The support offered by the PNs was viewed as the key factor that led to these positive outcomes. Attending appointments with participants was a meaningful, important practice because it was understood by participants to convey ‘you are not alone in this’. This helped to overcome stigma when accessing services, with many feeling empowered to advocate for their own needs as a result of the ‘steadying’ presence of a PN who had ‘been there’. This also appeared to offer hope and courage to overcome the difficulties involved in accessing services to meet wider needs:
That’s how it’s helped me because now, since I’ve been working with [PN C], I’ve started literally thinking, ‘no I am not going to ask them to do it, I’ve got to do it myself’.
This empowerment often laid the foundations for developing independence. Although some participants attributed this progress to their engagement with PNs, there was also recognition that the PNs would encourage them to absorb such progress as due to their own actions:
Most of my progress has been because of [PN B] . . . S/he would say it was because of me . . . because s/he doesn’t want to take credit for it. But it is, I wouldn’t have engaged the way I have if it hadn’t been for [PN B]. S/he motivates you and gets you thinking positive.
Participant perspectives: collective action
There was some evidence that the intervention was not entirely cohesive with the social norms of all services. Some participants noted that PNs had not been given adequate working spaces, attributing this to a power imbalance between staff and the PN. Many pointed out that privacy was required, but not always available:
S/he’s still coming into the room . . . and other people walk in, it were like a cubby hole . . . it wasn’t even an office.
Another participant indicated that the PN was not allowed access to the setting’s information technology equipment, which meant that it was difficult to help participants to bid for houses or make welfare applications, both key components of the support being offered. Many expressed frustration about this and attributed the lack of resources available to the PN to a lack of trust in their professional status. This raises questions about whether or not PNs experienced stigma relating to staff knowledge about their histories, or whether or not there was uncertainty about their roles, with many participants stating that the PNs were undervalued:
[PN D] should be a bigger part of the team. [PN D] is very underestimated. People will shout at him/her and give him/her grief and stuff and s/he does not deserve that. All s/he does is try to help people, and some people don’t appreciate it.
Some participants suggested that this sense of division was deliberate, suggesting that the PNs may not have been accepted by all members of staff:
Yeah, they try and make it hard for him/her, do you know what I mean? They don’t know what a hard day is.
Those who felt this way often expressed that the PN was more available and doing more for them than the other staff members in the setting, suggesting that the tension may have been present in the setting before the intervention and may have transferred to the PN as a proxy for ongoing conflict. It appeared that there was a coalescence, a togetherness, that existed, drawing PNs and participants to one side and staff to the other, in a type of ‘them and us’ social structure:
I shouldn’t really say this but s/he’s having a bit of trouble with the staff here . . . they don’t want to help you, do you know what I mean? Not at all.
Although conflicts did not feature in all settings, and were not referenced in all participant accounts, these emerged in some of the interviews, as well as in the reflective diaries and in the conversations between the PNs and project management team, suggesting elements of stigma and disempowerment existing for the PNs to actively manage as part of this intervention. In study interviews, the participants themselves also shared their own experiences of being stigmatised because of their problem drug use and life circumstances. Despite experiencing these challenges in intervention settings, each PN was able to build strong relationships of support with participants. It is not clear from these accounts why the tensions emerged; for example, it is unclear if these tensions were due to a lack of clarity about the role that could have been addressed more effectively prior to the start of the intervention, or if these tensions were inherent, given the stigma still associated with the lived experience of problem substance use and/or homelessness. This will be returned to in Chapter 6.
Development of trusting relationships
The relationships between PNs and participants were individual and formed gradually over several recognisable stages, beginning with small talk and informal contact, which built familiarity. Familiarity served as a relational foundation, allowing an offer of support to be made and accepted comfortably. Early in the relationship, support took the form of practical assistance with forms, attending appointments, and reminders on where to be and when. Reliability in practical arrangements acted as an initial step to building trust. Awareness of a PN’s lived experience helped to strengthen this trust, leading to reciprocal openness. Once non-judgemental, empathetic support had been provided consistently, relationships developed further whereby ‘straight talking’ was both tolerated and celebrated.
Practical support as a foundation for a therapeutic relationship
The practical support offered by PNs took a range of forms, closely reflecting the unique needs of participants. Some participants indicated that they required support to attend appointments, in many cases not because of a lack of capacity to engage, but because they had experienced significant stigma in services in the past. The support offered during appointments included advocacy, whereby a PN helped to overcome stigma by being a symbol that change was possible, while also being a well-trained, articulate professional, as one participant explained:
When [visiting a] doctor . . . they see drug addict and then they don’t want to know.
At the same time, some participants expressed that the PNs helped to reduce the anxiety involved in attending appointments by using a combination of empathy and humour:
To be honest s/he’s made it a lot easier for me to get to appointments, like at the hospital . . . I was getting down on it, no wanting to go because I remember, like, last year, it was just like a big long journey on the bus, ken [know] like being on your own and that, but we go through and have a laugh.
Using reassurance and connection to offset anxiety in emotionally challenging situations is often referred to as ‘emotional containment’, whereby the relationship and empathetic responses offered help to ‘contain’ emotions, holding them, diffusing them and reflecting them back in a diffused way, thereby building resilience and acting as a buffer to external stress. 140
Some participants also found the welfare/benefits system difficult to navigate, leading to situations where many had given up applying for support. Others noted the stress involved in attending welfare/benefits appointments; in these situations, the PN used practical skills to reduce stress and ensure more positive outcomes:
Aye, my PIP [Personal Independence Payment] and ESA [Employment and Support Allowance]. I was around the bend with them mate, but s/he took me, there is a boy in [city/town] who does all the PIP forms so [PN B] came with me to that appointment, met me at the train station, came and sat with me and all that. And spoke to the woman because I cannae, to be honest.
Often, emotional support was provided on journeys to and from appointments. One of the most valued aspects of the support was enabling participants to stay connected with other services, with PNs providing reminders about appointments on the same day and meeting them beforehand to ensure that participants were not late. One participant described how they needed a haircut and their PN had accompanied them, which enabled them to feel better about attending another important appointment. Participants seemed to experience this as solidarity:
It were a godsend really because there was someone there who would fight for us.
Finally, the practical support provided by the PNs also included some financial support, with PNs drawing from their ‘participant support monies’ fund (see Chapter 2). Participants expressed gratitude for this support.
Reliability and trust
The reliability of the PNs helped participants trust their PN. This strengthened the relationship and led to increasing openness and honesty over time:
S/he’s the best worker in this place, without a shadow of a doubt, s/he has bent over backward to do stuff for me, whereas other workers will say, like my actual Support Worker will just, I don’t know, they talk a good talk, but when it comes to it, they just let you down time after time after time.
As the preceding quotation illustrates, reliability was found to have two components: first, that the PN was consistent with arrangements and did not let the participant down, and, second, that the PN was flexible and able to support a wide range of needs. This also relates to role tensions with other members of staff, particularly Support Workers, discussed below.
Reliability was understood as a way of PNs showing that participants mattered. The trust of participants was not easily gained; it had to be earned. To gain this trust, the PNs had to demonstrate time and time again their availability, approachability, consistency and reliability. When a trusting relationship was established, it fostered openness and honesty.
Lived experience, empathy and pace
Participants’ awareness that the PNs had lived experience helped to reduce barriers to trust, enabling participants to be more comfortable sharing difficulties, including honesty about drugs, alcohol and risk of relapse:
I can be honest, open and tell him/her exactly how it is.
I get a lot of support, a lot of talk, like if I feel that I am going to relapse, I can go and talk because s/he’s been there in the past.
Once trust developed, many participants noted the value of the PN’s ability to give honest advice and engage in ‘straight talking’:
S/he wouldn’t beat about the bush. S/he wouldn’t say’ ‘oh come here poor little lad/lass’. S/he’d sort your head out, in a good way.
S/he told me straight . . . ‘listen if you are happy with your lifestyle, live with it; if you are not, do something about it’.
If there was something that I didn’t like in [PN B], I would feel secure enough to be able to say.
Such openness and honesty had a reciprocal quality, which was valued by participants and experienced as empowering.
‘S/he just gets it’
Another component of the intervention that was significantly valued by participants was that the PNs appeared to ‘just get it’, able to empathise without judgement:
What makes the difference is that s/he understands.
In most interviews, descriptions of ‘s/he just gets it’ linked to the fact that the PN had lived experience, had been there, and therefore understood:
When someone has been there, you feel you can open up.
S/he listens to my problems. I’ve told her/him things I’ve never told anyone in my life, do you know what I mean? Not even my Nan.
It feels like I’m not getting spoken down to. I hate people speaking down [to me].
When I first met him/her, I clicked with him/her straightaway, s/he’s been an ally to be honest, understands what we’ve been through.
S/he’s had his own life experiences, s/he’s had her/his own journey and whatever journey s/he’s been on in her/his life, it’s helping him/her to work in a more constructive manner. Nothing against the professionals that I’ve worked with in the past, but, due to the fact that s/he’s been there, I think that makes it so much easier to open up with. And s/he really does try to make you feel as comfortable and at ease as you could be.
And, on other occasions, shared experience, combined with a commitment to harm reduction and being non-judgemental, allowed the experience of unconditional acceptance:
[PN D] understands that, although I am a recovering alcoholic, I will sometimes still go out and have a drink when I am a bit low in morale and it doesn’t bother him/her. As long as I don’t show up absolutely wasted, s/he’s absolutely fine. S/he’s the best worker I’ve ever had in my life, and s/he’s such a lovely wo/man.
Relationships, therefore, began with practical support, reliability and consistency. With shared experience drawn on too, trust developed, establishing authenticity and acceptance, which, combined with humour, developed into unconditional positive regard and a therapeutic relationship.
Wave 2: pace, patience and respect
Follow-up interviews explored how the relationship evolved and how the intervention was experienced at a later stage. When these interviews were conducted, relationships had typically developed and were described by many participants as friendships:
Well you, sort of, you start thinking of them, like, as a friend.
Oh [PN D] is brilliant. [PN D] is like a mate, more than an actual worker.
For one participant who was working towards abstinence (their own goal), this was significant because many of their friends were still involved in active substance use, which caused this participant frustration. They valued the support of the PN as someone to turn to, to help manage related stress, an early indication that these roles might be useful for people in circumstances whereby social networks go through a period of transition and change:
Because most of the friends that I’ve got left they are all still . . . at it. Sometimes I feel like I can have a wee moan to [PN B] about them.
For most participants, the strength of the relationship continued to link to reliability and practical support, which offered, and seemed to tangibly demonstrate, genuine care and helped to maintain the therapeutic relationship:
S/he’s like a buddy . . . and s/he’s just likeable, eh, and I just think I’m lucky.
The seeds of change
Participants noted improvements in their access to a range of services and attributed this to the PNs attending appointments with them, which served to reduce barriers to engagement:
Aye, helping me, like, remembering me when I have got appointments and that, helping, s/he’s went to a couple of appointments with me, you know, it’s been good.
The presence of a supportive person helped to improve confidence and reduce anxieties:
Amazing, s/he is very good, I wouldn’t have went to some of my appointments if it wasn’t for [PN D].
Some participants indicated that they had not felt listened to when accessing health interventions in the past, so the advocacy role adopted by the PNs seemed to validate a participant’s health concerns to health professionals:
We’ve been to the doctors, and my CPN [community psychiatric nurse], and that’s about my back . . . [PN D] has gone to the interviews with me and, basically, I think it’s making a difference because they are starting to speak about specialists to see my back and before I was just fobbed off.
For many participants, attending appointments was a significant stepping stone to positive change:
Aye, well, I turn up for appointments and that now.
Turning up for appointments is all sort of linked . . . hospital appointments and things like that that I thought ‘it doesn’t matter’ and things like that have been detrimental to my health in the past.
All participants interviewed during the follow-up interviews reported positive change as a result of the PN intervention. For some, these changes related to harm reduction and substance use stability:
Because now I’ve got myself stable on a script and that.
I’ve cut down on my drug intake, but I’ve still had a couple of relapses.
I’ve got myself on a prescription now and stopped using because I am coming down on my methadone as well because I am going into rehab[ilitation].
For some of these participants, receiving substitute treatment, such as OST, made it easier to access residential rehabilitation services, suggesting that accessing some first-stage/lower-threshold services was an important first step in planning for future goals:
. . . helped me get off drugs and get onto a prescription and basically get into rehab[ilitation] to get off my prescription.
It is worth noting here, briefly, that the PNs were not explicitly encouraging participants to come off their OST prescriptions, but, if this was something an individual wanted, then they would support that, with appropriate harm reduction and other advice being provided. Although these tangible outcomes were discussed, many participants noted less tangible, tacit changes in their lives as a direct result of the intervention, including increased confidence and hope, which appeared to stem from the respect shown by the PNs, who acted as positive role models:
Like, s/he urges me to go and do what I’ve got to do, s/he was an alcoholic and on drugs at one point of his/her life, ken, but look at him/her, s/he’s got a partner now and a car, and a job, and s/he’s somebody to look up to basically, s/he’s a good role model.
Randomisation: findings in relation to support for a randomised controlled trial
In wave 2, participants were asked how they would feel about being part of a RCT. A follow-up question was asked about how they would feel about the research team having access to their health data for data linkage purposes, for example, in Scotland, using an individual’s Community Health Index (CHI) number to link data. Most were supportive of a RCT and did not see any issue with allowing data to be shared to help determine intervention effectiveness. However, some participants did not fully understand these questions, and this shaped their responses. This might have been easier to correct/address if the academic researchers had undertaken these interviews.
Those who did not fully understand what a RCT could mean for this type of intervention (specifically, settings/services would be randomised, rather than individuals, following a cluster trial methodology) expressed concern about the unfairness of some people being offered a PN and others not:
Aye, I don’t think, if somebody is wanting the service, they must need it for some reason, so no giving them that is kind of unfair, isn’t it?
Nonetheless, because many participants felt that the PN intervention was important, they saw the importance of systematically evaluating it:
That’s the only way you are going to be able to tell like, that doing it with somebody who has been through it will be better.
Most participants felt that randomisation could be acceptable, provided all those involved in the study fully understood what involvement entailed:
It’s a good idea, because you will be able to see how one side will get on without it, and one get on with it, and then you will be able to tell if people need a PN or not.
When participants were asked whether or not they thought that other people in their position would be amenable to having their data linked, nearly all participants stated that they could not speak for others. When participants were asked whether or not they thought that other people in their position would mind having their data analysed, nearly all participants replied that they could not speak for others. In general, there was support for a RCT (see Chapter 6).
Summary
The participant interviews indicate that, generally speaking, the PN intervention ‘fitted’ with the social norms of the intervention settings. The informal, shared spaces reduced barriers to initial engagement, creating familiarity, and led to a gradual ‘getting to know each other’ process that, in turn, enabled the building of trust. Participants were empowered to make up their own minds about becoming involved with the intervention, with many reaching out themselves to request the support. The relationships, which built gradually from repeated positive interactions, reliability and empathy, became an important factor in supporting cognitive participation in the intervention, and came through prominently in the wave 2 interviews. Many participants expressed feeling let down or stigmatised by other services, sometimes in their accommodation, indicating that the respect and authentic care demonstrated by PNs was fundamental to engagement.
Many participants reported that the intervention had been deeply meaningful and the source of positive change. The outcomes that were reported varied, but most centred on the fact that the participant was more engaged with wider support services and reported feeling more confident to access further support in the future. Many participants reflected having supported others in a similar position by making referrals to the PN intervention, seeing it as an important step towards recovery and self-determination. The PNs experienced disempowerment in some of the settings, although it was unclear whether this related to stigma or a lack of clarity about the role, or a combination of these and other factors, including workload pressures experienced within the service. This will be returned to in Chapter 6; these themes also emerged in the interviews with staff and PNs.
Interviews with staff
Twelve members of staff from intervention settings and four staff from standard care settings were interviewed. Views from the interviewed standard care staff are included in this section; these are noted as such where relevant, to avoid confusion. Findings are presented using the broad NPT domains (coherence, cognitive participation, collective action and reflexive monitoring).
Coherence and cognitive participation
Motivation and enthusiasm
Many members of staff, including service managers, expressed a view that the personality, skills and personal attributes of the PN were beneficial to the service as a whole:
S/he’s focused, s/he’s motivated, s/he’s a pleasure to have around.
Yes s/he’s been really good. S/he’s been really good to have around the place, of what I’ve seen, because obviously s/he’s been out on a lot of training. Which is good to have . . . someone that is really well trained.
This was perceived to be a result of a combination of personality, training and the experience gained from having lived experience of difficult times. Many interviewees tried to pinpoint which of these, specifically, resulted in the enthusiasm and determination that they witnessed:
Some of the stuff with [PN C’s] skills haven’t necessarily been taught, I think s/he’s a natural. In some areas, s/he’s an absolute natural.
It’s been that mix of ‘I’ve been there’, so it’s the experience side of what that means in terms of being able to build relationships with somebody. But also the training they’ve got. So there is that technical understanding of what might be happening with somebody that probably has enlightened them as to where they were when they were struggling, you know, and being able to reflect on that.
Many interviewees reflected that the PN appeared to be authentic and attuned to those around them.
Lived experience
A PN’s lived experience was obviously a central component of the intervention. Many of the staff interviewed discussed lived experience and how it contributed to the support that they witnessed:
I have always been a big advocate for peers. It gives you a good balance in the staff team. I can never say to somebody ‘I understand how you completely feel’. That’s where peers come into it.
Some had been sceptical at first, worried about how, where and when disclosures of personal experience would be made:
I wasn’t too sure at first how I would feel, knowing their background, and how different they would be about it . . . but they are so open about it and I don’t feel uncomfortable at all.
Those who expressed this view most commonly reflected that the intervention had surpassed their expectations and commented that personal disclosures were not necessarily made on all occasions. They also described a growing recognition that lived experience was about more than shared experience. Many staff and service managers praised the PNs’ ability to draw from their own lived experience as a source of empathy, knowledge and non-judgement, rather than drawing directly from the details of shared experiences:
The degree of compassion that s/he brought was really good, and I have found that very often in people with lived experience. It’s not even that they are more tolerant, it’s more that they understand that people aren’t really just trying to piss you off. They are not there just to give you a hard time. They are there because they are in a bad place. Having had that lived experience is an extra, it’s a bonus.
A senior member of staff praised the PN’s ability to use a deep well of compassion without overt personal disclosure, suggesting that managing boundaries was a valued part of a PN’s skill set:
I’m still unsure of [PN C’s] life story, so s/he’s never pushed, that I’m aware of. And even during these recovery groups, I’ve done a couple with her/him, s/he might have talked briefly about his/her time on a particular drug around the subject that we are looking at, but it’s never dominated the conversation.
For many, lived experience was important because it gave a deeper level of compassion and understanding, which reduced barriers and allowed connections to form between PNs and participants and others using the service. Although some interviewees recognised that they too could build excellent relationships with service users, they suggested that the PNs could do this work quicker, reducing the risk of individuals disengaging with services or relapsing:
Without a doubt relationship-building, a hundred per cent, and for me that is so important. The other stuff, I think you can learn, or can be encouraged to improve on, but I think hitting that relationship stuff . . . getting that connection. So for me it might take a bit longer to be able to get that connection with somebody. I do see that happening all the time. Constantly, you can see that connection happening much quicker than it potentially would for others.
Staff commented that the PNs had tenacity and determination to help their participants:
S/he’s very focused on the job in hand. And it appears to me that s/he goes over and above. You know, s/he is desperately trying to help the people that s/he is working with.
Finally, there was a sense that staff felt that having lived experience helped the PNs notice important details for those they were working with that could be overlooked by other staff:
There is a deeper understanding of the smaller detail that would have been missed by me and others because we’ve never been there.
Also, with them having lived experience of addictions and homelessness, they straight away knew where to take them, you know, like what service to refer them to. And I have the feeling, as well, for some service users they felt more comfortable maybe opening up with them. Feeling [they] maybe understood better . . . what support they might need, or why they would struggle to move on.
Relationships
Almost all interviewed staff members reflected that an important component of the intervention was the PNs’ ability to build therapeutic relationships with participants who often found it difficult to trust, mirroring comments made by service user participants:
[PN D] doesn’t go to anybody and start talking to them. They get drawn to [PN D], they’ve heard about him/her and they’ve seen how s/he works. S/he’s like a magnet.
Many interviewees found this particularly important, given the challenging circumstances of those the PNs tended to work with, and the description of ‘hard to reach’ that many of the participants had been given from other services:
They are working with, I hate the term . . . chaotic or ‘hard to reach’, because they are not but, you know, really vulnerable, complex . . . they are working with the right people that need support, without a doubt.
The above staff member went on to comment that, by being able to build meaningful relationships, the PNs had been able to engage with participants who had significant health issues and minimal or poor engagement with services. Several examples were offered whereby the relationship had been the platform that enabled individuals to access specialist health care and had initiated multiprofessional work. Therefore, although the services had found it difficult to meet the needs of these individuals, the PN’s ability to gradually build trust and attend appointments with participants had reduced the barriers to accessing services.
Bringing value to the staff team and wider organisation
Some staff members and service managers believed that the PNs brought a range of benefits to the team and service. In settings where Support Workers were not ‘floating’ or were more desk-based, the PNs’ flexibility enabled them to support service users in a variety of ways. This floating nature also enabled the PNs to continue to support participants if they moved on from the service, whereas Support Workers were no longer able to provide this:
It’s been great for us. Once [clients] move on, we don’t get to see them, so it was great to see the progression of one of my lads that [PN A] was looking after, and how he was getting along. S/he was able to go to the viewing of the flat with him. I think as a team member s/he fitted in well because s/he had those freedoms that we would love to do. It was better for us as staff because it was a more fulfilled role because we could see more action happening.
It fitted in quite well, in a sense, because we are restricted with paperwork and desk duties mainly.
The PN role of facilitating group work and supporting other individuals accessing their service (not only their participants) was also recognised. Their ability to undertake outreach, and engage more visibly with other services, was reported to have increased the profile of the organisation within professional networks:
They have then got introduced to the [specialist general practice] and the needle exchange. They have done that. They have built those relationships up. And it’s actually brought them to us, which we’ve not been able to do . . . made a big, big difference.
So that type of stuff [outreach work] has been really valuable. It’s that ability to respond really quickly, whereas if you are in a staffed centre, the staff can’t leave the centre to go elsewhere.
The intervention was praised by some service managers because, for them, it showed that the organisation was innovating and willing to try new approaches:
It’s raised the profile of the organisation because [the PNs] have been able to show that the organisation, which has been about for such a long time, is trying new things, it’s doing research.
In one setting, the PN’s knowledge about problem substance use and expertise in harm reduction was particularly valued:
I do hear lots of harm reduction conversations and lots of sharing experiences of really difficult times and how they have got through it . . . definitely hearing more harm reduction conversations.
Acceptability and fit
Many members of staff, but particularly those in leadership roles, expressed that the intervention was beneficial because the PNs were uniquely able to engage clients who had complex needs and, consequently, found it difficult to be supported within the confines of ‘traditional’ approaches:
The ones that they’ve either gravitated towards, or have gravitated to them, are the ones that are still really, really struggling with addiction and complex needs. It’s not been the ones that, you know, have been on a script for years and not touched anything else. That’s not who they’ve worked with.
So it’s been those really hardest to motivate guys. They’ve picked the guys that everyone else has avoided because they are hard work.
One service manager attributed this willingness and ability to engage with the most complex clients to the fact that the PNs were not tied to achieving set specific outcomes, affording them the flexibility required to conduct person-centred support. In one setting, a new staff team had formed at the same time that the intervention began. This led to additional benefits, because the PNs were able to allay any concerns or misunderstanding from the new members of staff, who were experienced in health and social care but had limited experience in working with the client group. The fact that staff were new to the setting was also noted to have been helpful because it meant that the PNs and staff began on an equal footing and were reciprocally supportive.
Collective action
Challenges: coherence, power and stigma
Despite a high level of cognitive participation (or buy-in) from service managers and staff in some settings, and a generally high level of understanding of the role and its purpose, the findings also suggest that, in some cases, the intervention was less well understood, and fitted less well, which shaped responses and actions by some members of staff. Findings suggest that a range of perspectives existed about peers, prior to the intervention taking place. Moreover, conceptual support for peers did not always translate to full understanding, buy-in and collective action. For example, in some settings, service managers and staff believed that peers, once recovered, could provide positive role models for clients. However, some interviewees saw this as a junior role, suggesting that the focus on the peer element of the intervention detracted from the fact that the PNs were all well trained and able to conduct specialist work (as reflected by their rate of pay):
I have always been an advocate for the service to have paid peers, or at least have a stepping-stone system so you would come in as a peer then you would get moved up to volunteering and then you’d get into a paid peer role. That’s where I’ve always wanted it to be. However, due to monetary issues, there never was enough money . . . to pay for peers.
For this member of staff, peers would be an initial stepping stone, coming somewhere above volunteering, but not on a par with formal support work. In another setting, the following interviewee struggled with definitions, offering some insight into the blurring of lines between peer and staff member:
S/he has that capability and shows everybody that s/he is a staff member, that s/he is not a peer. S/he is a peer in the sense that s/he has lived experience, so using maybe the actual name peer isn’t, it’s actually somebody with lived experience.
In some settings, there were strains and latent conflicts between the PNs and other staff that seemed related to the PNs being paid at the same rate as TSA Specialist Support Workers, in recognition of the fact that this role required a certain degree of specialism, and carried additional responsibility when compared with the Support Worker role (see Chapter 2). These strains and conflicts relate to the stigma that is still associated with having lived experience of problem drug or alcohol use, which seemed to make it difficult for some staff members to acknowledge the specialism and training built into the role, and that the PNs came to their roles with other wider experiences of employment. In exploring the potential fit of the intervention in their service, a member of staff in a standard care setting expressed that they would see the PN as accompanying a service user to meetings, but would not necessarily have their own ‘client list’, as this would be more akin to a Support Worker role.
In one of the host settings, there was overt recognition that the traditional Support Worker role was seen as more important than the PN role, leading to some tensions:
There is a thing, like a power imbalance, that comes when you are in some places, like being a Support Worker and what comes within that role.
A service manager expressed the view that, irrespective of how skilled, knowledgeable or trained the PN was, the relationship between them and some staff members would always be challenging because of an existing ‘them-and-us’ culture, with clear delineation between staff and service users:
It was no reflection on the person themselves, but I’ve seen it before as well, where people with lived experience often, it kind of challenges traditional services, you know, or there is often a ‘them and us’ type thing between the service providers and service users. When that gets blurred, people find it really challenging. They feel ‘less than’ because they have not got that experience.
These data show that role confusion and conflict, as reported in the wider literature on Peer Support Workers, were issues for this intervention; this will be returned to in Chapter 6.
The stigma of lived experience was also reflected in some of the interviews, although it was difficult to disentangle this from a wider lack of understanding of the intervention, including its complexity, and from the recognition of the tension, realised or otherwise, between members of staff with lived experience and those without. Overall, service managers tended to be more in favour of the intervention than other members of staff, including Support Workers. On some occasions, stigma was aligned with a ‘suspicion’ or concern about whether or not the role would cause the PNs to relapse and whether or not PNs could be trusted to maintain their recovery:
The lived experience is quite difficult. The suspicion around, you know, his/her past life and, it wasn’t that long ago I don’t think, and is s/he really clean. I’ve heard that said a few times, particularly at the beginning, not so much now, but at the beginning, ‘is s/he clean, I think s/he’s still using?’.
Nonetheless, in some cases it became apparent that the service manager’s support for lived experience and the PN intervention may have contributed to the power and suspicion dynamic. Staff were, for example, sometimes described as being ‘jealous’ of the role. On occasion, this related to lived experience and, on other occasions, it was thought to relate to the level of flexibility within the PN role, in contrast to their own:
Staff, I think they are suspicious of [PN C] because of his/her lived experience and probably jealous of his/her role. And because s/he can do stuff that they can’t and probably a misunderstanding of his/her role, you know. So I have had to say to staff: ‘S/he’s not a Support Worker . . . s/he’s a PN. S/he’s not expected to do the same as you are doing’. I’ve had that conversation.
One service manager expressed that, if all members of staff had been involved in the study at an earlier stage, some of these tensions might have been mitigated:
That is what we’ve learned. Staff would have felt perhaps more informed and been able to say right at the beginning ‘how would that work?’, and we could have thought about it a bit more, and thought about it together.
Perceptions of role crossover
Some of the power dynamics appeared to be embedded with staff perceptions of a crossover between the PN role and Support Worker role, despite the distinctiveness of the roles being simultaneously recognised. All participants based in the residential settings had a Support Worker; if they became involved in the intervention, they also had a PN. If participants moved on from the residential setting over the course of the intervention, they were supported by their PN only at this stage. Some interviewees commented on the tension that could ensue when dual support was offered:
The biggest problem has been in that crossover between Support Worker and what [PN A’s] role is. You get them saying ‘oh, well, I’ve got another Support Worker’ but they will kind of taunt the other residents. Or they will say ‘well, why haven’t I’? They get jealous, and envious that they think somebody else is getting something that they are not.
A more substantial frustration for some members of staff was that the PNs had the responsibility of supporting service users without the requirement to conduct structured assessments and other associated paperwork, giving them more time to spend working more informally:
[PN A] gets them treats and all that and they are all made up when they see [PN A], do you know what I mean? And s/he’s got that time to sit and talk to them, where sometimes we haven’t.
For some interviewees, there was the sense that the PN’s ability to spend time, or do more enjoyable activities, positioned the PN role against the Support Worker role:
Sometimes the staff can feel that we are a little bit like saying no and [PN C] is always the yes. It’s like ‘good cop, bad cop’.
Despite these frustrations, there was a recognition that having an opportunity to talk and connect was important:
Talking can be worth more than anything, just somebody that is genuinely interested in you. It’s worked from that point of view, but it also caused problems because [PN A] can’t work with everyone. Although, it doesn’t matter if you are on her/his case load or not, s/he would not say ‘no you can’t have a cup of tea because you are not on my case load’. S/he can end up with a circle of people and s/he might only be working with two of them.
The PN role disrupted the organisational structure in the residential settings where Support Workers had a particularly important role to play; this appeared to be felt most acutely in circumstances in which the PN had been able to give ‘perks’:
A couple of times the staff have felt a bit undermined because s/he’s gone off and done things, and they haven’t known about it . . . some of the things they haven’t agreed with. For example, s/he’s been giving out food parcels to people and, actually, part of their support plan is that actually they need to manage their money . . . and it’s caused a little bit of, if you are working with [PN C] you get these extra perks.
Another interviewee reflected that, because the Support Worker and the PN had the same aim of supporting service users, but a different approach to doing so, this could be challenging to both respond to and understand:
We start off from the same place, from the desire to help, to help people. When it comes to a certain point, we stop, and yet his/her role carries on. My staff will probably have to deal with 40 people on that day, whereas s/he will probably have to do two or three people. So I think we all start off with the same desire, this place of wanting to help people. We get to a point or a place where certain boundaries say we have to stop. And those boundaries might be around time, around appropriateness . . . I’m not sure about the appropriateness of whether we invested so much time into one group of people.
As the preceding quotation highlights, some interviewed staff members believed that resources should be shared among a greater number of service users and expressed reservations about the idea of focused, intensive support. In one setting, a senior member of staff expressed the view that service users would demand a great deal from the PNs, and that the relationship would be ‘needs’ based, rather than meaningful. This perspective contrasted with the views of most participants and, indeed, perspectives shared in other interviews. It has been included here, however, to demonstrate that beliefs about the client base and organisational culture are important factors to consider in terms of the acceptability and feasibility of the intervention. The level of cohesion thus appeared to be variable across the intervention settings, and among different members of staff within settings:
It’s very attractive, you know. My staff are working with 40-odd people and down there they have got a case load of 15, 16 people to carry that case load. You don’t have time to be going out every 5 minutes.
As will be noted again in Chapter 6, this also highlights the workload challenges that services, and staff within them, experience.
Many interviewed staff and service managers expressed that the intervention was broadly acceptable to the service and well received by service users, and that relationships among all staff, including the PNs, were generally positive. However, work was needed to clarify the roles, and additional preparatory work would be required should a further study be conducted, to allow a greater level of contextual integration:
The service users think it’s a great thing. I think some of the staff are maybe not convinced overall, just because they see some of the challenges, or the overlap. But having said that, they can see the value of what s/he is doing for the service users. I think it’s a clash of roles, not what [PN C] is doing. I guess it’s how we integrate it into the service.
In another setting, the service manager believed in the importance of the intervention and used their position to directly address resistance within the staff team:
I squashed that resistance. I just made the space for him/her, you know, and s/he could then get on. And I think there was a degree of acceptance about that from the members of staff. But . . . it’s absolutely nothing to do with your project and it’s nothing to do with [PN B’s] personality, it’s limitations within my staff team.
The preceding quotation implies that an apparent lack of fit could be attributed to existing issues within the staff team, perhaps strengthening the previous point that contextual integration could be improved with earlier, more proactive, engagement with the front-line staff team. Furthermore, the findings indicate that strong buy-in from service managers is important to enable PNs to be accepted by staff and supported in their roles.
Settings where some existing staff members had lived experience tended to have service managers who ‘bought in’ to the role of peer support, although reservation was still expressed in relation to some aspects of the intervention. These related to the level of training that the PNs received (which may relate to the lack of clarity surrounding the role), and their rate of pay. A standard care member of staff was supportive of employing peers and had extensive experience of supporting those with lived experience in their service. However, they also described a list of criteria and expectations that they would expect to be fulfilled before they could realistically comment on whether or not the PN intervention would be desired or feasible in their service.
Reflexive monitoring and reflections on study involvement
Beginnings: training period and settling into the role
Some interviewed staff reflected that the beginning of the study and intervention had been positive, whereas others voiced challenges. In particular, there were mixed views on the feasibility and acceptability of a 4-month training period at the start of the study, before the intervention began:
The idea of having a period before someone starts has made a big difference to them in terms of just their confidence and clarity of knowing what their job is, even though we are not quite sure what their job was, because this was all new. So it gave them that time to work through it all and think about it, and change their views about what they were going to do and how they were going to do it.
In the beginning, some staff expressed having felt apprehensive and unsure of what the new role would be:
When s/he initially came in here, I wasn’t sure of how the package would present itself, from my point of view I looked at him/her as another worker within this initial body to start with, because we were clear that s/he was going to take on a particular role.
This perspective was shared by a few service managers who had initially viewed the PN as an extra pair of hands who could be added to staff rotas. One service manager found the realisation that the PN would work relatively autonomously and independently challenging, leading to initial frustration:
When I do see him/her it’s like a flash and then s/he’s away again, ‘has such and such been here?’. ‘No, ‘I’ve not seen him/her, can I check?’ ‘Yes of course you can, on you go’, no problems after that.
Another service manager felt that they would have liked more control over the induction period, but was supportive of the intervention once the PN settled into their role:
So we wanted to instil the values that we have here, and we wanted him/her to be incorporated into that. But we also wanted him/her to sort of be able to go ‘right this is what I am doing.’ To give him/her that autonomy so that s/he could take her/his own direction. Not long after, it was quite a short period of time, s/he started to come to me, ‘can I do this, can I do that?’ And I was like ‘yes go for it’.
The training and induction period allowed the PNs to spend time in their services and engage with service users on an informal basis, without the pressure of (study) recruitment. Some members of staff found this period unsettling because they were unsure of the PN’s role:
The staff . . . I don’t know whether they were against it because of the [start] rather than the study, I felt like it was a bit sticky at the beginning.
I think that this has worked pretty well, I must admit, I think there were queries at the start in terms of that first 3 months, [that] was a long time for them.
For some service managers, the level of training provided at the start of the intervention was valuable, although concerns were expressed about the feasibility of offering this in a larger-scale study, including financial viability:
That’s a funny thing when you are used to people turning up and just getting on with the job. I’ve got two new workers who started on Monday and the expectation is that by Thursday they will be doing some of the tasks.
All the money for the training was great, but I don’t know how realistic that would be with other organisations, or if it was training massively outwith [the local area]. I also look for free training and then we’ve got the organisation’s training too.
Is that a true reflection of . . . the role? And would I be able to do that level of induction if I was going to take on a PN, would I be able to put in that level of training?
A further interviewed staff member also queried whether or not the PNs were able to internalise the level of training offered in this intensive period:
S/he’s had to take an awful lot on board very quickly. It’s been a massive, massive learning curve for him/her. I don’t know if the training has been too intensive because I am not sure how much of that you can absorb.
Recruitment
Some interviewees emphasised that participant recruitment was made easier by the fact that the PN had spent informal time in the setting before potential participants were invited to take part in the intervention:
S/he would just throw her/himself in the middle of the dining room, playing pool with them all and, you know, on their level and I think probably the lived experience kicked in with that.
For some interviewees, as mentioned previously, the ability to integrate organically into the setting was attributed to the PNs’ lived experiences. For others, it was attributed to simply having taken the time to be visible and become known:
S/he was really good at just being . . . when s/he first came here, you know, s/he would spend some time at the setting, s/he would get to know people. S/he spent some time in outreach with our outreach worker. A couple of times s/he went on the multiagency walk around, which was really helpful for meeting other agencies.
Although the PNs were recruiting participants for a sustained period, participants were being substituted as others withdrew. Sometimes, the numbers became difficult to keep track of, and the mid-April cut-off point added pressure. Although the PNs had a degree of autonomy and flexibility to recruit via the organic processes alluded to previously, they were supported in their decision-making by both the project management team and the service managers. For example, sometimes their service manager outlined their desire for the PN to work with service users whom they considered to be most in need, based on their level of risk:
From my point of view, working here as long as I have, I know quite a lot about people’s histories. I recognise a lot of the issues that are impacting on people, and what I wanted to do was immediately identify people that I felt, and the staff felt, were at risk and that was either drugs or alcohol. We would certainly point them out to [PN D].
Quantitative data collection
As staff were also affected by the change to the quantitative data collection, they were asked to share their experiences of this. A member of staff acknowledged the impact on the study team and PNs, and expressed their own reservations about the effectiveness of this approach, but reported that participants did not appear to be negatively affected:
Nobody has fed anything back to me. If there was an issue with it, I probably would know about it because if people are not happy, they are usually quite vocal and usually come and tell me. I also think people would withdraw, or they actually would not do it.
A further interviewee expressed that the honesty a participant had displayed during the health measures was actually an indication of their progress:
That was a bit of an eye-opener for them [PN] with [participant] when she was quite open with you. So it’s probably been really beneficial, in a way, you doing it.
Summary
The intervention was experienced as meaningful by staff, aligning with the experiences of others involved in the intervention. These include relationships, empathy, lived experience and multiprofessional networks. In some settings, the PNs were viewed as highly skilled, trained workers who made a valued contribution to the staff team, highlighting a high level of contextual integration. In other cases, particularly where there were pre-existing organisational norms and more social distance between service users and staff, the PNs appeared to occasionally be straddling an uncomfortable grey area whereby they were neither fully accepted as staff, nor viewed in the same way as service users. In these instances, lived experience was viewed suspiciously, with some staff members appearing to fear that they themselves were less valued because of a lack of lived experience, and others expressing concern that the PNs were not likely to be honest about being in recovery (e.g. hiding continued substance use).
The findings indicate that the intervention may have been viewed as more acceptable, particularly in residential settings, if all staff had been more involved in the planning process and had been brought on board the study at an earlier point. It should be noted that, although the latter half of this section has focused on areas of challenge, there were significant areas of buy-in, significant understanding of the role and its values, and a high level of praise for the intervention and the work of the PNs.
Interviews with Peer Navigators
Four interviews were carried out with the PNs at different time points in the study (three with the PN in Liverpool). This section also includes discussion of the findings from the case studies, which were captured through PN interviews (see Chapter 3).
Coherence and cognitive participation
Beginning the intervention: recruitment of participants
The PNs expressed that, at the start, it was valuable to be able to spend time with service users without the pressure to recruit them to the study immediately. Echoing the experiences of participants, this allowed time for the relationship to build informally:
I just did it [recruitment] over a period of time and the relationship was built over general conversation. [I’d be] walking around in the building, saying hello, introducing myself . . . inviting them for a cup of coffee.
However, because relationships took time to develop, and the PNs were committed to investing time in developing these, the lengthy recruitment window (October 2018–April 2019) was still experienced as somewhat pressured. In addition, the PNs re-recruited participants when spaces became available, which contributed to the workload (see Chapter 4).
The PNs reflected that it was sometimes challenging to accept that they could not work with everyone, both because of the restrictions of the eligibility criteria and their case load. A PN described a desire to work with those who were known to find it difficult to engage in alternative services:
There were people that were eligible, and I am finding that, the really difficult people, the people that aren’t engaging . . . I want to work with. And some of the staff are like ‘oh no, don’t bother’, like they’ve failed before.
This was a consistent theme across the data: the PNs tended to be drawn towards working with people who were generally viewed by existing staff as likely not to engage, echoing views from the staff interviews. Often, those working in the host services would caution the PNs about this, insisting that they may be wasting their time. The PNs tended to politely resist this advice, displaying a determination to recruit and work with exactly this ‘type’ of participant.
Flexibility of role
The pace of the support was considered to be an important factor that supported the cognitive participation or buy-in of those involved in the PN intervention. An ability to work at a participant’s pace, unencumbered by some of the demands and targets commonly required in social care, was seen as critically important, by allowing participants time to build trust in the PNs and engaging as much or as little as they felt able. The PNs expressed that they had more time available than a traditional Support Worker would:
As PNs, the main thing that we’ve got on our side is time. That is what separates me from a Support Worker is that it’s very much ‘we are in this together’ kind of relationship. We will do this. We will go and do that.
The ability to work at an individual’s pace was viewed as closely linked to respect for that person, something that supported the development of trusting relationships:
My aim’s to build a relationship with the clients that we are going to be working with. Getting on with them on a personal level and not having that little countdown clock on. You do your work with them and get a really nice relationship with them. Working through that with them, like, at their pace.
I wanted to allow him space to think and to keep the door and offer open. I knew it wasn’t going to shift when I wanted it to – it was almost just playing the waiting game and allowing that. There was a lot of learning in this for me as well – to just allow a process to run its course a bit really I think, and not try and meddle in it too much.
The PNs expressed that honesty could take a while to build too, and described the importance of not pushing for this until trust was established:
When we started off, contact was a bit sporadic. It took time to build trust. I feel like he was a little bit sceptical to start with. I think there was a patch of time where what was going on, and what was said was going on, were two totally different things. And it almost just played itself out. Some stuff kind of came up and sparked him to re-engage and potentially put a bit more effort in himself, and a bit more honesty.
In many cases, the PNs described a difference between participant accounts of substance use at the beginning with their accounts at a later stage. The PNs felt that accepting a person where they were at, allowing change and honesty to blossom slowly, was fundamentally important to the relationship. This also appeared to be linked to a commitment to harm reduction and participants feeling confident that the PNs were fully advocating this, rather than encouraging abstinence. Finally, the flexible pace of the relationship also enabled participants to direct the frequency of their engagement with the PN, for example taking a break for a period and then re-connecting. Overall, the case loads that each PN had were reported as high, but this flexibility of role allowed them to provide more or less intensive support to individuals as needed at any given time to manage this overall with their working weeks.
Holding space: sitting alongside people in their darkest moments
The PNs’ lived experience helped them in their role in myriad ways. The benefit was not necessarily about the shared experience itself. Rather, this experience allowed a deeper level of ‘knowing’ and an awareness of the right time to push people forward with ‘straight-talking advice’ and when to simply sit with people in their darkest moments, conveying the message that they need not face hard times alone. Lived experience acted as a conduit to an expression of empathy, respect and unconditional positive regard:
I know just from personal experience that it won’t be my job to go too deep with anyone because, whilst people are still in addiction, they are only superficially going to be able to deal with anything, they are literally just going to need a strong support. Just trying to, yeah, hold off the fear a little bit for them because that is what it was like for me initially. You need someone there to say ‘Am I alright? Am I going to be alright? Is this going to be alright?’ That was all I needed.
For the PNs, it was this ability to ‘hold space’, and quietly be there for someone while they got through one of the darkest, most frightening times in their life that was fundamental:
It’s almost like, it’s a bit like the counselling thing I guess, just managing silence, managing space, being OK to be uncomfortable, and to not rescue. Because that is how they will work through it, if every time you get upset everyone rushes to you to give you a hot cup of tea and a tissue and a big cuddle and tells you ‘there, there it’s going to be OK, you haven’t processed those feelings, they have been taken away from you. And I was told by one of the really good counsellors that you are robbing them, by doing that, you are actually robbing them of growth, because you don’t want to be uncomfortable, and who are you to not allow that person that bit of growth?
This highlighted a dual dimension to lived experience that the PNs appeared to intuitively be able to use: first, lived experience could break down barriers, creating trust, and, second, it helped to foster a conduit to emotionally attuned practice. Their lived experience created a level of empathy and intuition allowing the PNs to understand when to push and when to simply sit alongside participants, witnessing their pain, quietly using their presence to offer comfort and hope:
Companionship . . . not in the traditional sense of the word, but just that sharing space and time with someone. That’s the biggest thing I’ve ever got off any worker I’ve had. Just to sit and be, and to not need a solution, or be told ‘you’ve got to do this’. Just to sit for a minute. That’s how you get through to most people really. And then they start coming out of themselves a bit and whatever they may or may not want to talk about will just come around.
Linking with pace, this slower paced, emotionally attuned work was experienced as challenging by two PNs, who reported having to fight the urge to try to ‘fix the un-fixable’, in order to allow participants to express and feel pain in order to heal:
It’s a balance . . . just sitting around it sometimes is the hardest, most intense aspect of the job. Just sitting with someone who is obviously suffering quite a bit and just going ‘do you know what, I will sit with you while you feel like shit’.
These skills were viewed by the PNs as linked to a combination of training, skills, empathy and lived experience. When sharing a case study of one participant’s journey, a PN said:
Early on he was a bit fragile and the focus was on meeting up and getting him a cuppa. But that was probably some of the most meaningful work, and that probably laid the groundwork for him wanting to re-engage after that little bit of patchy time.
The values of respect, pace and a willingness to sit side by side in these difficult times when change did not feel possible constituted a framework for an equal partnership:
When participants say to me ‘I couldn’t have done this without you’, I say ‘well you can, we’ve worked together as a team, it’s been an equal partnership, I do what I can do for you and you do what you can do for you’.
Each PN chose one participant who would be used as a case study, to examine the effects of the intervention (see Chapter 3). It was in these reflections that the theme of pace came through most strongly, where links were made most visible between this respectful, slow start and significant positive progress in a participant’s life:
He was emphatically grateful for the support I gave him at the beginning. He said ‘no one else would have helped, that I’ve just been left here and if it wasn’t for you I would, I would be worried that I would still be here’. I’ve heard him pulling up others if they’ve been critical of groups that I run. He’s always been aware that a lot of the times I’ve been going above and beyond, and he definitely appreciates that.
The PNs spoke of their pride in participants’ achievements, showing genuine investment in their well-being:
He is much more settled now. He’s in a relationship. He’s looking a lot better. He’s put on quite a bit of weight. He’s drug-free. He enjoys attending the group session and always has a really good input to it. His confidence has improved quite a lot. And I get a sense that he’s thinking more about the future and where he might go next, as opposed to where he’s been and feeling stuck. This is just lovely to see.
Collective action
A distinct approach
This section outlines existing practices and how well the intervention aligned with these, noting a number of areas for further consideration. The PNs used a range of skills to respond to participants (participant-selected pseudonyms used in quotations); drawing from training and their lived experience, they were able to connect challenging behaviours to underlying trauma or other negative experiences:
I first heard about Charlie at the handover meeting at the service I work in. Charlie’s behaviour was mentioned: he’d had a bad weekend and some members of staff thought they should ask him to leave immediately because of this. In the meeting, I challenged this: we need to understand people’s behaviour, following the PIEs approach. I offered to sit down with Charlie and have a chat with him around his behaviour. I sat and spoke to him about his life, and how he ended up here, and all sorts of things for probably a good hour or two.
This approach often differed from the approach taken by staff in the settings. In the preceding excerpt, the PN explained that staff had found the participant’s behaviour problematic and he was on the cusp of being asked to leave. Yet, through the intervention, the PN’s skills and application of a PIE approach where tolerance and patience were shown, the participant was able to stay in the service and make positive changes to his life:
He is doing amazingly well, absolutely brilliantly. He’s not using drugs at all. No heroin, no crack, and he hasn’t done for 3 months, minus one slip-up. He is currently volunteering. He wants to go into a similar type of work to what I am doing, and he’s about to start a qualification.
In some settings, the difference in approach was noted to cause some tensions, raising questions over contextual integration and coherence with existing group practices. This theme was found to have three strands. First, it related to similarities and differences between Support Worker roles and the PNs. Second, it related to the approaches taken within contexts, specifically the extent to which the context embraced a harm reduction approach. Third, it related to perceptions of the PN’s role and training. The following quotation highlights that there was a sense that the PN’s role crossed over with existing Support Workers in some settings:
Every single person I am working with has got a Support Worker based in my service, so there were a lot of worries about treading on toes and duplicating work and stuff, which hasn’t really been the case. We are not duplicating work at all, but it’s just when everyone is working so closely together, there is a massive lack of communication.
This appeared to relate to clarity in terms of the role. The PN’s ability to tailor their intervention to meet the individual needs of participants meant that the role was difficult to define and communicate. The PNs expressed that they had often explained their role to staff, but it had not always been understood. The PNs were very clear on their own roles:
My role is to go on and improve the situation that they are in by, like, planting little seeds, but also doing all the networking I can be doing around housing, thinking of out the box for opportunities for them or getting them to appointments, accompanying them.
A combination of confidence in their training, the support of the study team and their lived experience enabled the PNs to embrace an approach that many considered unique. All PNs described their roles as being distinct from traditional Support Worker roles, with some noting variation from the group norms and/or expectations of service managers or other staff in their settings:
It was difficult because [name of staff] wanted me to just be working with them around the drugs and alcohol. But obviously, when people are coming into me and you are doing a whole holistic thing around all the trauma they have suffered, you are not just sat there talking about drugs and alcohol, you are talking about sexual abuse, about them working on the streets, about all the different things. And I think this is where some of the other staff did have problems, and we did clash quite a few times because they didn’t understand my role.
All PNs described the importance of slowly building a therapeutic relationship, based on trust and mutual respect. Yet, once established, the individualised approach meant that the support they provided was highly varied:
Getting people on prescriptions, taking people to specialist wound clinics that there is no way they would have attended, or even been able to attend, which could have had dire consequences for them. Child protection stuff, adult protection stuff, basic food shopping, getting power on, homeless applications to get people in housing when they are rough-sleeping, specialist eating disorder clinics that people probably wouldn’t have referred themselves to, or been able to get to, mutual aid meetings, various hospital stuff, BBV [blood-borne virus] stuff, getting people started on hep[atitis] C treatment that probably wouldn’t have and were very shut down to the whole idea in the beginning. House clearances and new tenancies.
When describing the activities that formed their role, most PNs explained that they played a ‘bridging role’, helping participants to identify their needs and access services. Many stated that, without outreach services, or without support to attend, participants faced significant barriers:
I make an appointment with the mental health practitioner, we get in touch with him, we go and visit him in his house because he’s probably not reliable to be able to get down to the [setting] so we probably wouldn’t get to see him. We also take the nurse up with us to look at some of his wounds he’s got from where he’s been injecting. Then, because he’s had a lot of problems with his housing, I’ve had to speak to the management because they were threatening him with eviction, but it wasn’t a valid notice. So I got all the information from the housing officer and I could relay that back to them.
In the preceding quotation, the PN mentions that they arranged for a housing officer in place to help the participant going forward, suggesting that at least part of the PN role was to act as a co-ordinator, helping to advocate for participants, identifying their needs and facilitating engagement in services at a point when the person is not yet able to manage appointments without support.
The PNs discussed the financial budget available that could be accessed to help support participants, which they used in a variety of ways:
[When] they have moved into their own properties and have had absolutely nothing, it’s helped them set up. It’s basic things that you need to be able to move on, to be able to build successful lives, a fridge, a cooker, a washing machine. [Participant] had started working and they were having to wash their clothes in the bath, so having these funds has been really good to help them rebuild their lives again.
The PNs described situations in which participants, when housed in their own tenancies, had faced significant poverty, lacking food and electricity supply. The PNs were able to use their budgets to buy participants basics like electricity cards and food. In one case, a PN described helping a participant to see her daughter during supervised contact:
When she gets visiting rights, she only sees her daughter at certain times of the year and then she’s had no money to do no activities with her, so the travel to even get up to see her daughter [helps].
In the preceding case, this was described as a way of helping the participant to remain engaged in the intervention and hopeful of achieving recovery. Following a harm reduction approach was viewed in broad terms by the PNs: it was not limited to reducing harm associated with consumption, minimising poly-drug use, or using clean injecting equipment, along with other well-established harm reduction strategies. For them, harm reduction could include any activity, measure or change that had a positive impact, given that these types of change could lay the foundation for longer-term change and/or change more specifically focused on addressing problem substance use. One PN explained:
If you are talking about reducing a damaging behaviour, you are doing your job. If you are referring or taking someone to any service that could potentially do any of the above, then you are doing your job.
Each described reducing risk and harms as important to their role. Most talked about the steps towards positive change as being very different in each case. Having lived experience tended to act as a window, facilitating acceptance and understanding of the diverse nature of a journey towards recovery. Each described taking this at a participant’s pace, carefully gauging when to push, and when to simply accept where a person was at. Although some staff members, and service managers were supportive of this, the nature of the role was not understood, or accepted, by all:
. . . [staff] just find it hard to be able to build that relationship, and I think they find it difficult that I can do that, for people just to sit and be open and honest. And, don’t get me wrong, they are not always open and honest to me and I think some of the staff think I am a bit gullible sometimes.
The PNs’ willingness to accept that honesty would build with the relationship was sometimes described as being a source of tension, especially in circumstances in which the training that they had received was not known, or where the intricacies of the role were less clear:
This is what I’ve tried to explain to the staff, sit down and talk to them sometimes, and I’ve said ‘listen, my role is different from the support work that you are giving’, so it’s like, ‘there is nothing wrong with us all having different methods and different approaches about how we interact with people’.
The PNs described valuing the freedom that their roles offered:
I’d really struggle after doing this, just even for the really short time, to be really rigid with appointment times or closing people’s cases and stuff like that.
The PNs recognised that the principles and values underlining their approach did not always closely align with those of other members of staff:
The people that are the most resistant are the least trauma-informed, or they operate practice in a less psychologically informed way.
Part of it might be that [staff] see it as a threat, or they see it as a new-fangled thing, a new fad. But people don’t like to challenge what they already believe.
A further complication to contextual integration was that the PNs had a different approach to confidentiality to staff members in some of the contexts:
I’ve had discussions with [staff] and there have been quite a few that think that I make their role more difficult because they are all transparent with each other so they all understand what’s going on with each client. My participants can come and speak to me about things that then I won’t share with [these other members of staff] . . . [they] find that a bit difficult to get their heads around.
The issue of disclosure around drug use was partly related to tensions between harm reduction and abstinence-based approaches in residential settings. If a service encouraged some service users to be abstinent, for example, in order to live in a specific wing of the accommodation, staff considered it important for the PNs to report relapses as transgressions of the rules. In contrast, the PNs saw their roles as reducing health harms, which often meant not reporting minor use to staff, as long as the participant was safe and aware of harm reduction strategies. The following quotation highlights the position taken by the PNs:
I say to some of the people I am working with ‘listen, you don’t have to be abstinent to be in recovery, you can be in recovery from any single one of the traumas that you are going through, no matter what it is’. [I say] ‘if you are seeking support and you have made little steps to try and address the issues, then I am proud’.
These distinctions in the role and the approach taken meant that the PNs had an awareness that staff were often frustrated with them:
I explain that is my role, that it’s confidential what they [participants] come and talk to me about, so I can build that trusting relationship with them, so they can come and open up and talk about anything. I [try to explain] that it’s not me making their life difficult.
Sometimes these frustrations escalated into more visible tensions, raising questions over contextual integration and existing group practices. One PN described the following:
It can be a bit like a ridicule sometimes, like ‘oh, are you going out for a coffee with so and so again? Are you off to take him for something to eat again, or you are buying him this again?’ Do you know what I mean? Whereas they’re not, like, saying how I got three/four homeless people housing after 3 days.
As mentioned previously, the PN intervention was broadly welcomed, with positive reports coming from staff, management, participants and the PNs themselves. However, in other settings, where there was a lack of coherence with existing practices, a theme of in-group/out-group emerged:
I don’t think they see me totally as part of the team, they see me as a separate person.
I do just feel like a bit of an outsider.
This was not the case for all PNs, but the distinct nature of the role appeared to create frustrations and tensions between whether the PNs were team members or whether they belonged to a different group, linking with views expressed by staff:
I see myself as part of the team, but in a different role.
Where there was a distinction and a sense of in-group/out-group membership, it translated into a lack of trust in the PN, which, in turn, sometimes constrained their role:
My hands were constantly tied . . . every tiny thing that I wanted to do with someone, I’d have to run it by, like, three or four different people. And it’s like no one else had to do that. It just completely slowed everything down and made me feel like, you know, I wasn’t able to help anyone really because someone was going to come down on me about it.
On some occasions, there was a sense of hierarchy, whereby the PNs were required to justify their approach or decision-making to other members of staff. The PNs regularly sought guidance and leadership from their service manager and other senior members of staff in the services, and this was actively encouraged and supported by the study team. However, sometimes this was experienced in a less supportive way:
I got called into the office to explain why I’d questioned a certain member of staff. I am trying to say, ‘why am I not allowed to question another member of staff? I am not questioning the person to have an argument. I am questioning what they are actually saying and disagreeing with one of their comments about how we should maybe be doing things’.
These findings raise questions over cognitive participation and collective action, and suggest that the PN intervention may be more suited to settings where staff and practice more fully embody a harm reduction approach, given the inherent harm reduction element of the intervention. Furthermore, the findings highlight differences between the conceptual underpinnings of the PNs’ approach and the approaches of some of the existing staff in the intervention contexts. Furthermore, much of the tension between the role and the existing group processes was shown to relate to tensions between Support Worker roles and the PN role.
As the intervention progressed, the PNs became clearer on their role and its boundaries and distinctions. However, by this stage, there had often been a period of confusion and crossover, leading to ongoing mistrust of the role in some settings. The findings suggest that such tensions may be able to be overcome if care is taken to explore and try to mitigate these distinctions prior to the intervention being put in place. This has the potential to smooth out challenges, offering a platform for discussion that may be able to circumvent power dynamics and tension before they appear.
Reflexive monitoring and reflections on study involvement
Quantitative data collection
The PNs’ views on the change to the quantitative data collection appeared to evolve over time. The PNs expressed initial concern with the practicalities:
It’s going alright, just makes it logistically more difficult to organise. Potentially people could be a little more reluctant to do it, not only because they are having to arrange it at a set time or day or with some flexibility. But also just the prospect of them being someone that they are not that familiar with doing it. And the whole thing of having to get all three people together at the same time in the same place, rather than just be able to go: ‘Hi, you are here, do you fancy doing that now?’.
As also alluded to in the preceding quotation, the PNs were unsure if participants would be willing to complete measures with a researcher who they had never met, or only briefly met:
With all my clients I’ve got a relationship with them. Obviously, some of them I am really, really close with, and then others, you know, I am alright with. But, like, for [researcher] to come in blind, and I know that some of my participants are quite volatile, and, you know, they won’t have none of it.
Some of the PNs were disappointed with the change in approach and wanted to take on the responsibility of completing these measures as originally planned. There was a sense that this change undermined them a little, despite the change having no relationship to the abilities of the PNs. However, the PNs were pleasantly surprised at the levels of comfort participants tended to show when completing the measures with the researchers:
We did alright. People were open, people were honest, and whoever was about was willing to do them.
They felt that, by sitting in on the process, but not being the person asking the questions and recording the answers, they were afforded with the opportunity to learn more about their participant. They were able to do this in a less involved way, for example they could listen and reflect and did not immediately need to problem-solve. The PNs all emphasised the substantial amount of time they had to spend arranging the measures and supporting completion:
It was OK getting the people who were living at the [setting] because they were on-site to be able to just get them to be able to do the measures. It was a bit more complicated to get people who I was giving floating support to because they didn’t have phones, or I’d arrange a week before I’d left them a note this was happening in a week’s time and by probably the next day they’d forgotten about that.
To maximise the likelihood of a data collection session going ahead, the PNs sent reminder texts and WhatsApp messages, made calls and left voicemail messages. They arranged for taxis to pick up participants, or personally picked up participants via taxi, personal car or bus. The time taken to arrange and complete the measures appeared to depend on the type of host setting. The PNs noted that it took longer to arrange the measures with clients who were on ‘floating’ support, who lived in their own tenancies:
Because you are having to make the calls, arranging a time to go and pick them up and maybe having to go down in a taxi to get them and then they are not there. And then you might get a phone call saying ‘right I’m here now, so can you come down?’ So you are having to jump back in the taxi, go down pick them up to get them over there.
However, even if participants were in a more ‘fixed’ location (such as in a Lifehouse or prison), when all phone calls and messages were included, it still took a substantial amount of time to arrange the measures. The PNs estimated that the arrangements took an average of 2 hours. Consequently, the PNs expressed that it would have been easier if the measures had been done by them, as it would have reduced the amount of time spent making formal arrangements.
Support and training
When asked about their experiences of being part of a university study and working with the research team and partners, all PNs shared positive experiences:
I felt quite important, I felt like I was special, yeah because this is my first proper job that’s not just, like, menial. So yeah, getting on the train and having all that paid for, and the training stuff, felt nice, it felt good.
Being involved in co-producing the intervention, and working together with the academic team and other colleagues, was also highly valued by several PNs:
It was very well put together, especially the [intervention] development day, that was really, really special to be involved in. Yes, I’ve said before about how it flowed, and how everyone was . . . the right people were there and giving the right input, and it just flowed really well.
The PNs expressed feeling valued in academic settings, during intervention development days and training. The findings suggested that power had been managed mindfully throughout the study design stages, leading to positive experiences that helped to overcome initial anxieties:
It was walking into the day thinking ‘oh my God’. But it went swimmingly. It was nice that everyone was listening to everyone’s ideas no matter if you had been in research for 20 years or if you were brand new to the study. It’s like . . . everyone took on everyone else’s ideas, there was no hierarchy.
There was a feeling of collegiality whereby the PNs expressed surprise that, despite coming from different backgrounds, there was a shared aim and commitment to working together, supporting each other as equals:
All moving in the same direction, and from different directions. It’s quite easy for me, and I would imagine other people in my situation, to throw up barriers to that because I’ve got a different history.
Attending training and being able to attend and take part in conferences was highly valued by the PNs who felt that the training had helped them in their role, for example to better understand participant needs, and develop their confidence in carrying out their roles:
One of the best things I’ve taken from the job is the amount of stuff we got to do beforehand. Like, the conferences and getting to meet new people. If you’d just stepped into a Support Worker job role, or if you’d just stepped into a peer job, you wouldn’t have had the chance to meet half of them people and do half that training. It’s been so useful, and you can apply some of that to any job. It’s been amazing and it’s something I will talk about and use forever really.
The reach and remit of the project management team went beyond the academic setting, providing ongoing support to the PNs, in particular with respect to the working through of difficulties experienced in relation to their roles and working within existing practices in services, as described in detail above. The PNs reported feeling valued and supported, and always having someone to go to. This was particularly important given that many PNs reported being aware that ‘working on the front-line’ could present challenges to their own emotional well-being. The following PN reflected that they knew that aspects of the role could ‘trigger’ negativity, and that they needed to tend to self-care when required:
I am not invincible, and I am pretty solid in my recovery. There is some stuff that I should probably put a little bit more effort in, but I’ve been a little bit slack.
The PNs were generally aware of their own emotional needs and acknowledged that they had de-prioritised them at points. Although each pointed out that this was not as a result of the work, or workload, three of the PNs expressed worrying about their participants long after their day was finished. In this context, the ongoing service manager support and supervision were also very important to enable the PNs to carry out their roles and overcome challenges. Although the PNs sometimes found it difficult to book in their clinical supervision sessions because of conflicting diary appointments, they were highly valued, describing it as ‘A great addition . . . probably essential’ and ‘invaluable really’.
The PNs also used the clinical supervision sessions to talk about challenges they were experiencing in their personal lives and how these could affect their professional work. The recognition of the need for this layered support also demonstrates the resilience, emotional intelligence and self-awareness of the PNs.
Paired and lone working
As outlined in Chapter 2, two PNs shared an intervention setting. Although each worked with their own case load and also worked in their other settings, these PNs often worked closely together to facilitate group work and acted as a source of mutual support for each other, for example to run ideas by, or to exchange contact details or updates about local service provision. Occasionally, they were also able to ‘cover’ for each other and accompany participants to essential appointments when they experienced a clash or were on leave. Each of these PNs valued the support that they received from the other:
It’s like having an ally.
Especially with it being so new . . . we are quite a good support for each other.
They commented that they did not need this support all of the time, but knowing that the support was there was beneficial. They also recognised that they had shared similar experiences and recovery journeys, which were likely to have made this support more valuable. One PN who worked on their own in the setting reflected on their experience:
They [other PNs] can meet up and maybe have a discussion about what’s gone on with one of the participants . . . where, I think with myself [here], I’ve been a bit isolated.
A PN who shared a service reflected on how they would feel had they not shared a setting:
I am just thinking, like, it would be both, you’d get all the plaudits and you’d also get all the, you’d feel all the pressure.
When describing an ‘ideal’ arrangement, the PNs expressed that it would be beneficial to have another PN working in the local area, but not necessarily in the same building:
I think the ideal would be to at least have someone else doing the same role within the same locality, if not in the same building necessarily.
Therefore, the PNs felt that the paired working dimension was valuable and would be important to incorporate into the design of a future study, but that these pairs could be spread within the local area, rather than accommodated in the same service.
Harm reduction and abstinence: tensions and reconciliation
Each of the PNs had different experiences of problem substance use and different approaches to their personal recovery. At the beginning, some of the PNs struggled slightly with reconciling the harm reduction approach of the study with their belief in the value of abstinence-based approaches, despite being committed to practising harm reduction in their professional role:
From the job I was doing before, treatment, very in line with my recovery model . . . This is going to be very different. It’s going to be very different doing harm reduction.
I am certainly being brought around to the idea because, in the simplest terms, everyone’s journey, or most people’s journeys, begin with harm reduction.
Over the course of the study, and with the support of the study team, and as they had greater exposure to harm reduction in practice, the PNs fully embraced the harm reduction approach, as has been evidenced elsewhere in this chapter. The PNs also more fully understood harm reduction, recognising that harm reduction and abstinence-based approaches could work well together, and did not need to be seen in binary terms:
I saw a very sharp divide between recovery and harm reduction. I would love to be involved now in the sort of harm reduction stuff . . . and that’s not what I anticipated would be one of the outcomes.
I do think, through my own process, from when I first started, that I’ve arrived at a much more harm reduction-focused approach. And my attitude towards harm reduction, and what harm reduction is and what harm reduction isn’t, has changed a lot.
As discussed previously, the PNs also conceptualised harm reduction broadly and could see how their support, and the positive changes participants made, was a form of harm reduction, even if this was not specifically focused on addressing problem substance use. These themes are discussed further in Chapter 6. Finally, although the PNs sometimes reflected positively when participants had stopped using substances, for example in the case of Charlie described by PN C, and as described in the case study (see Appendix 2), this was because these were participants’ chosen goals.
Summary
The PNs felt that it was beneficial to spend time getting to know their participants prior to formal recruitment and valued the flexibility of the role, which enabled and encouraged this. The PNs found it challenging that they could not support all those with whom they interacted and described being drawn to those whom other members of staff felt were particularly chaotic, or avoided.
Drawing from their lived experience and training, as well as their own expert interpersonal skills, the PNs shared how they provided practical and emotional support to their participants. They shared experiences of resistance from other members of staff in their services, which they attributed to a range of factors including lack of clarity about the distinct PN role, role crossover and tensions between abstinence-based and harm reduction approaches.
The PNs felt included in the wider study team and partners, and felt well-supported by the project management team. They valued the training they had received, which they believed not only supported them in their current roles but also would support their future careers. The PNs felt that paired working was an important component of the study, and embraced and practised harm reduction every day in their roles, despite some acknowledged tensions with their own recovery.
Chapter 6 Discussion and conclusions
We have described the design and the implementation of the study, and the results from the quantitative and qualitative data collection. In this chapter, we pull together the key learning from the study and discuss the strengths and challenges. We take account of these in answering our research questions and determining intervention feasibility and acceptability. Although we draw primarily from findings from the formal qualitative data collection shared in Chapter 5, we also draw from the useful and important insights provided by the PNs via their reflective diaries and from our own detailed process evaluation notes and reflections, taken throughout the study, as noted in Chapter 2.
Strengths
Supporting individuals in a psychologically informed way
A key strength of the study was that individuals who are experiencing profound challenges, including problem substance use and homelessness most specifically, developed positive, trusting relationships with their PNs, who consistently followed a PIE approach, even when presented with challenges and practice that would not be considered to be psychologically informed. Alongside these challenges, the participants in this study typically had negative past experiences of professionals and services (as disclosed by them), which affected their ability to trust help-givers. The development of these relationships, irrespective of other benefits gained, is notable.
Participants reported being honest with their PN about what they were experiencing and how they were feeling and knew that they would receive honest advice and support in return. Participants reported being supported in ways that suited them, with support to address or work on what they wanted to address, at that particular time.
Participants reported achieving a number of positive outcomes during the course of the intervention, and valued the practical and emotional support provided by their PN to help them achieve these. In addition, they benefited from the PNs being able, and wanting, to spend time with them. Participants reported feeling that they were important and valued. Participants recruited to the intervention were, in the main, those who had been described as ‘chaotic’ and ‘hard to engage’ by other services or by staff in the intervention settings, people whom other professionals had experienced considerable difficulty in supporting. One-fifth of participants were recruited via the PNs’ proactive street outreach activities, testament to their ability to reach those who were not well connected with services.
This study contributes much-needed empirical evidence to the application and experience of the PIE approach, from varied perspectives. The PNs’ practising of a PIE approach was one of the most successful decisions made by the team and was an excellent fit.
Developing connections and networks
The SHARPS study was hosted in a range of residential and outreach settings, managed by different organisations and based in different areas of Scotland and England. Tessa Parkes and John Budd connected with key stakeholders in the areas, particularly in Edinburgh, in advance of the study starting, as well as during it, to help raise awareness of the study and to introduce the PNs when in post. The PNs were proactive in connecting participants with a wide range of services in their local areas, quickly became well-known and developed good working relationships with staff based in the services where they worked. For example, the Edinburgh-based PNs worked with the drug liaison nurses based in one of the city’s hospitals and received a number of referrals. The Bradford-based PN connected with Bevan Healthcare (Bradford, UK), a social enterprise providing health care to individuals experiencing homelessness or precarious housing and supported them in their street outreach work. All of the PNs attended multiagency meetings for a number of their participants on a regular basis. However, the value of their skills and experience was also recognised more generally, as they were invited to attend other meetings (e.g. board meetings for a city-wide inclusion health partnership) and events.
Findings clearly indicate that the study was successful in evidencing the benefits of a relational, peer-led, psychologically informed, harm reduction approach to a range of services across communities. It achieved this in large part as a result of the PNs making themselves visible, working hard and independently developing constructive and respectful working relationships with staff in these services.
Promoting peer work
The study involved the recruitment of four individuals with different life experiences, but common to all was their experience of problem substance use and/or homelessness. All individuals had different experiences of, and approaches to, recovery. All had unique skills, abilities and personalities. The PNs described their role as being challenging at times. They had to adjust to having a new and professional role, to living and working in new or unfamiliar areas, and to working with new organisations. The nature of the role was also challenging: working largely autonomously; having a different role to other, if not all, members of staff in a service; and working with a client group with a range of complex problems who often required urgent or very demanding support. Finally, the PNs spoke of being challenged as they navigated their dual identity of ‘peer’ and ‘professional’ and experienced resistance from other staff members. Their experiences as peers working in professional roles strongly resonates with the themes raised in wider literature,75 as set out in Chapter 1.
The PNs demonstrated exceptional resilience in adapting to the changes and challenges they experienced, and that manifested during the course of the study. All demonstrated high levels of self-awareness and knew when to seek additional support and what kind of support they needed at that time. Their own accounts clearly highlight their personal and professional development over the course of the study. They were supported to develop by the study team throughout, but also showed leadership in furthering their own development. All the PNs completed their roles having developed a wide range of new skills, acquired new experiences, and benefited from extensive and bespoke training that they could tailor to their needs and wants. All secured further employment in the health and social care sector and are currently enjoying their new roles and responsibilities.
The SHARPS study has demonstrated that, with appropriate support, peers can be employed in demanding professional roles, use their autonomy to make complex decisions in the support of vulnerable people, hold associated responsibilities for personalised budgets and case management, and perform a diversity of tasks and processes exceptionally well. The study has highlighted the importance of putting in place a range of support, offered by different individuals in different capacities (and including informal mentorship), to ensure that peers can excel in their work from a confident and reflective standpoint.
Working constructively with both harm reduction and abstinence support frameworks
Some of the PNs experienced an initial challenge in relation to working within a harm reduction framework. In addition to the interviews, these feelings were expressed by the PNs in our early conversations and captured in our project management team process evaluation notes. Jason Wallace supported the PNs to see how a harm reduction framework could fit alongside abstinence-based approaches. He provided a crucial mentorship role in the early months as the PNs were adjusting to their new roles, showing them how their own experience of abstinence-based recovery was important, but needed to be placed to one side to allow the participants they were working with to determine their own pathways and steps along the way.
The project management team also actively supported the PNs to balance their personal ‘what worked for me’ views with the focus of their roles, which was to allow the participants to direct the support they received, respecting their autonomy, choices and desired pace. This worked very well. Although the PNs knew that their experiences were important in forming their own skills in the job, there was a delicate balance to be struck between working from what was known to have worked for the self and close others, and the need to be focused completely on a participant’s own expressed needs at any given time. The PNs reflected on their journeys in this regard in our final debrief meeting. One explained how their views had changed substantially as a result of their work in the study. They had grown to understand the inherent value of a harm reduction approach and, indeed, had advocated for it strongly as the study progressed. Each PN observed how they had witnessed the considerable progress that their participants had made within a harm reduction framework, while also acknowledging that progress is not necessarily linear, and expectations must commonly be adjusted.
Zinberg’s141 theory of ‘drug, set and setting’ helps to interpret how and why the harm reduction/abstinence conflict seemed to wane over time in the SHARPS study. ‘Drug’ is used to refer, not simply to the pharmacological effects of the substance of choice, but, rather, its potency in the life of the individual, as, arguably, each substance has certain ‘hooks’ for certain people. 142,143 The term ‘setting’ is used to refer to the social, cultural and physical environment in which a person finds themselves. A person’s ‘set’ is their personal experience of the world, encapsulating beliefs about the self, beliefs about drug use, personal history, personality, motivations, as well as how they are feeling at the time of drug use. This can be divided into ‘long range’ and ‘immediate’, with the former being static factors such as personality and personal history, and the latter being factors such as emotions and psychological state. 144 Many participants, given their complex and challenging lives, would not have been ready to consider significant change. 44 Therefore, to respond to each participant’s ‘set’, PNs understood that longer-term aims needed to be paused. As mentioned in Chapter 1, those working in practice are able to manage this interplay, and abstinence and harm reduction can be seen as complementary approaches. 145 By responding to a participant’s ‘sets’, the PNs were able to support participants to reach a point where they were able to question their beliefs about drug use and their potential to effect change. The SHARPS study has evidenced how individuals navigate this terrain and, this contributes to more nuanced understandings of marrying harm reduction and abstinence for people who are experiencing homelessness and problem substance use, particularly for peers who themselves have survived and navigated life challenges similar to those of their clients.
Fidelity and adherence
As a reminder, fidelity concerns the degree to which an intervention is delivered as it is intended. Adherence is defined as the extent to which the PNs followed the intervention guide throughout the study. The PNs each delivered a relationship-based intervention that drew on the principles of PIEs and harm reduction. However, because the PNs provided individualised support to each participant as they were encouraged to do, the nature and form that this support took varied across participants. Moreover, each of the PNs had unique characteristics, backgrounds, identities, skills and personalities. These inexorably shaped the relationships they developed with the participants and the support they gave to their participants, as is documented elsewhere. 60
Given this, assessing the level of consistency of delivery across the host sites was a challenging research endeavour. Overall, we found that the ethos and values of the study remained consistent across all PN approaches. In the beginning, there was some anxiety caused by the ‘newness’ of the role, and the flexibility, in terms of how this would translate into practice. Specifically, the flexibility to work to a participant’s self-directed goals and work in whichever way helped to fulfil these could be seen as a limit to claims of study fidelity. Yet, it was fundamentally important to being able to connect with people in an individualised way, as eloquently articulated by the PNs in their interviews.
As one of the settings hosted two PNs, it enabled a comparison between their working practices. A member of staff reflected that each PN adopted a slightly different approach. They noted that while one PN worked in a more structured way and offered participants appointments (while being flexible), the other’s approach was more opportunity led, with a preference for a clearer diary to allow them to be responsive to issues and crises as they arose for participants. In this setting, the PNs’ different approaches were considered to balance each other out, creating perfect contextual integration. From the perspective of this interviewee, it was a combination of the PNs’ individual preferences and the needs of each participant that shaped the different working arrangements. Despite their different approaches, both demonstrated commitments to harm reduction, PIEs and the relational approach.
Adherence to the intervention guide
The PNs commented that the guide laid a foundation for their work, but, once they started to work with their participants, tailored support and care was needed. The PNs also described that the extensive training that they received (during induction/throughout the study), alongside other development opportunities, helped them to feel confident in their roles, and therefore less reliant on the information and advice in the guide. As mentioned previously, having other support systems in place, such as clinical supervision, from their service managers, and from each other, enabled the PNs to look after themselves. This meant, for example, that the self-care sections were less relied on in practice than they may otherwise have been.
The PNs also expressed that the demanding nature of their roles meant that they simply did not have time to regularly consult the guide. One also expressed that the physical size and weight of the guide meant that it was stored in their service office; had the guide been portable or digitised (e.g. contained in an application/website), it may have been consulted more ‘on the go’ and, consequently, consulted more often. This is a clear learning point for a guide format in any subsequent trial.
Although the project management team frequently signposted the PNs to the guide when they described a challenge they were facing (as well as providing emotional support to them at the time), the team did not routinely remind the PNs of the guide, nor did they ask them to read particular sections as a revision exercise. This may have played a part in this lack of consultation after the induction period. However, the team believed that the PNs used the guide as a ‘springboard’ to develop their expert practice and was still a necessary intervention support. As expressed by the PNs, it served as a useful and important foundation for their role and fulfilled its stated aims, but was consulted less after their induction period. In summary, the PNs adhered very closely to the principles and ethos contained in the guide and the SHARPS study has demonstrated that it is possible to manualise a complex, relationship-based intervention, provided there is consensus on the importance of flexibility to ensure person-centred and person-directed care. We reflect that standardisation is difficult to achieve in complex interventions and that a more nuanced understanding of standardisation is fitting when examining complex rather than simple interventions. As Hawe et al. 146 suggest, form can be adapted as necessary to suit the context and to maximise effectiveness, but the function and process should remain standardised.
Challenges
Quantitative data collection
We were required to change our approach to the quantitative data collection, as discussed in Chapter 3. Although some participants were slightly apprehensive about the prospect of completing these questionnaires with academic researchers rather than their PN, participants reported being placed at ease by the researchers and by having their PN present. The PNs were initially concerned that participants would not feel comfortable with completing the questionnaires with researchers and would, therefore, not complete them. They were reassured as more measures were successfully completed, and felt that their participants were comfortable during the process. However, they also expressed that arranging and undertaking the measures took a substantial amount of time.
The researchers felt that completing the measures with participants provided them with a unique, and privileged, insight into the lives and experiences of participants, and an opportunity to observe the positive and trusting relationships that had developed between the participants and the PNs. However, the process of arranging the measures could be time-consuming and frustrating, and completing the measures was sometimes challenging, emotional and draining. The major impact of this change in approach was on researcher time and overall study resources, which is raised again in Continuity of staffing and support for peers and Keeping the study on time and on budget.
Shortened intervention
As discussed in Chapter 2, the Liverpool-based PN left the post early and it was not appropriate or practical to re-recruit a PN for this setting. The PN offered a shortened 2- to 2.5-month intervention to their participants (n = 9) who were still involved, until mid-January 2019. The PN provided participants with the option to leave the intervention or to stay under the shorter intervention terms; all chose the latter. All were supported to access other support and services. Given that the measures were conducted only once with this group of participants (n = 5), it was not possible to compare the participants who received this version of the intervention with the other participants. Furthermore, although a sample of these participants were interviewed (n = 3), all interviews were anonymised and analysed together, and these were conducted only once.
Owing to the capped case load, we envisaged that these participants would still benefit from a shortened, but slightly more intensive, version of the intervention. The interview data demonstrate that there were no substantive differences in the support offered or benefits gained for this particular group of participants; the themes were common to all participant interviews. The absence of follow-up qualitative interviews and quantitative data collection makes drawing conclusions challenging. Our view is that the Liverpool-based participants benefited from being involved in the intervention, although they would have most likely benefited further had they received the full intervention as originally planned; however, these caveats are noted.
Continuity of staffing and support for peers
The study experienced a challenge regarding continuity of staffing, which manifested when one PN left post early. In terms of trying to mitigate risks to continuity, we put in place a comprehensive support system because, as informed by the literature outlined in Chapter 1, we fully understood the need for excellent and broad-ranging support of peers, including in orientation, training and ongoing informal support, to best facilitate their roles. As noted in Chapter 5, this package of support was very well received by the PNs, including by the PN who decided to leave the role early.
The project management team were highly attuned to power dynamics experienced by some of the PNs in some settings, and spent considerable time supporting the PNs in relation to this. They also offered general, day-to-day support through WhatsApp and text conversations, telephone calls and face-to-face meetings. Given the geographic constraints, the Liverpool- and Bradford-based PNs were supported more by telephone. We reflect that, although the support was still beneficial, greater face-to-face support would have been preferable for both PNs, particularly for the Liverpool-based PN. The presence of another PN in a nearby area would also have been beneficial in these cases, as discussed in Chapter 5.
The varied and extensive support provided by the PNs’ service managers, Adam Burley through clinical supervision; Jason Wallace through informal mentorship and support (as described earlier in this section); Tessa Parkes as joint line manager and lead mentor; and by Rebecca Foster and Hannah Carver as ‘go-to’ day-to-day support if needed, was central to ensuring that the PNs adhered to their role, and to ensure their overall well-being throughout. The amount of support provided needs to be fully considered when planning a next-stage study, in particular the need for this to be somewhat separated from the research team and provided by non-academic colleagues who have been identified to provide it. This is because it was a significant additional input for the academic researchers, in particular for Rebecca Foster.
Keeping the study on time and on budget
The change to the quantitative data collection meant that research team members (RF and HC) were required to collect data, rather than the PNs. Consequently, valuable time was spent that had not been work loaded or costed, putting the study potentially at risk of not meeting its projected timelines for tasks and deadlines. The unanticipated PN vacancy enabled us to re-profile the budget and bring in research assistance to support the qualitative data coding and analysis, and the quantitative data entry and analysis. This ensured that we could complete the study on time.
Ending the intervention
There were challenges for some of the participants and the PNs when the intervention concluded after 12 months. In the debrief support conversations and meetings, the PNs shared that it was emotionally difficult to end the intervention and relationship, and, to some participants, it seemed to come as a surprise, despite the parameters being clearly laid out at the beginning. The PNs described how some participants seemed ‘lost’. They also acknowledged the irony of a relational intervention where the relationship is advocated as key but is explicitly time-limited. However, they did understand the importance of the study being conducted to lay the foundation for a further trial.
Given the positive trusting relationships that we hoped would be developed, we anticipated that the end of the intervention would be challenging. This was raised and carefully considered at the intervention development stage and discussed in the intervention guide. As they supported participants to move forward, the PNs sensitively reminded them of the intervention’s close. All the PNs developed individual ‘wind-down’ plans for all participants and were supported by service managers and the project management team to complete these; a debrief sheet was also available to participants when they left the intervention, at whichever point [see the debrief on the project web page: www.journalslibrary.nihr.ac.uk/programmes/hta/1615314/#/documentation (accessed 2 December 2020)].
We are confident that participants were well-supported as the intervention came to a close, but acknowledge the discomfort and distress experienced, despite these measures. Our view is that the participants benefited overall from the support provided by this study. In addition, the positive relationships that have been developed may have been extremely reparative and provide a model for future positive relationships.
Addressing research questions
Overall assessment of feasibility and acceptability
The SHARPS study peer-delivered, relational harm reduction intervention, which was delivered in third-sector residential and outreach settings, was accessible and acceptable to, and feasible for, people who were homeless with problem substance use. Data were collected via interviews with participants, staff and the PNs, as well as through quantitative health check measures.
The quantitative health check measures allowed the study team to gain a nuanced and in-depth understanding of the population and their needs. Of those who participated, many identified as having a disability, had previously been convicted of criminal offences, had been in prison, and had been in local authority care as a child. Many felt that their physical health was fair or poor, and reported a range of physical and mental health problems. Participants also reported using a range of substances and had previously experienced substance use treatment episodes. These data highlight the complexity of participants’ lives, and the wide range of problems they experienced, suggesting that the PNs were able to engage with participants who met the study inclusion criteria for whom engagement with previous services had been problematic. Data also showed that participants were able to stay engaged with the intervention, with around 40% of participants consistently engaging with the PNs throughout the intervention and the remainder engaging in a more intermittent manner. The high levels of engagement by participants facing this level of challenge, and their ability to seek out the PNs when they required support, further highlights the feasibility of the approach. In a follow-on RCT, it would be important to record participant engagement more systematically and ask the PNs and participants about it in more detail.
Overall, the intervention was well received by participants, staff and service managers, although many reflected on both potential and real challenges. Challenges were experienced in terms of the logistics of the buildings (e.g. the lack of private spaces), raising questions about the feasibility of the intervention in a practical sense, and with the relationships with some other members of staff. For clarity, feasibility from the perspective of these key groups (participants, staff and the PNs) is outlined in the following sections.
Intervention participants
The intervention was perceived to be beneficial by the study participants, highlighting the acceptability, accessibility and feasibility of the approach. Key benefits were the reduction in harmful behaviours, positive service engagement and improvements in physical and mental health. The participants valued the therapeutic relationship they developed with the PN and the role of lived experience in fostering that.
Participants experienced a range of positive outcomes throughout the study, including changes and improvements in substance use, less injecting behaviour, accessing OST, and greater and more positive engagement with wider health and social care services. A key beneficial component for participants was the PNs’ lived experience of problem substance use and/or homelessness. Participants talked about the importance of developing trust at their own pace with the PNs, which led to therapeutic relationships developing. Lived experience was viewed as facilitating trust and honesty because the PNs could get closer to understanding a participant’s experiences without judgement.
Participants discussed the importance of having informal spaces where they could have conversations with the PNs over a game of pool or a cup of tea. Initial contact could also be very informal, without any pressure to engage, which facilitated access to, and engagement with, the intervention. The PNs were highly visible and accessible in their settings, allowing participants to get to know them over time. This visibility also meant that they were perceived as reliable and available to give practical and emotional support. Although these elements were perceived as beneficial, they also reflected on the PNs’ lack of private working spaces, which meant that they were more available than some staff who might be more office based. This was perceived by participants as being due to power imbalances between the PNs and other staff.
The PNs were perceived by participants as ‘different’ to other staff with whom they had previously worked, in part because of the flexibility of their role, but also in the way they interacted with them. The availability of practical support (such as attending appointments), sometimes enabled by drawing on financial support, was viewed as a significant additional benefit to the study. Such support helped participants to engage with services where they had had previous negative experiences.
Overall, participants described the PN intervention as acceptable, accessible and feasible. They developed therapeutic relationships with the PNs and were able to engage with other services, which, in turn, led to improved outcomes. They could be open and honest with the PNs in a way that was different from previous relationships with other non-peer staff. A limitation is that these views reflect the participants who participated in the interviews, who were more likely to be engaging positively at the time of interview; we were unable to speak to those who withdrew from the study.
Staff in intervention settings
Staff, including service managers, in the services in which the PNs were based generally felt that the intervention was acceptable, accessible and feasible because of the PNs’ lived experience, flexible role and visibility, and training and skills. Staff reflected on the personality, skills and personal attributes of the PNs as an asset, identifying their lived experience as significant. Many felt that this lived experience enabled them to be empathetic and compassionate, providing a deeper level of understanding of participants’ lives than those without such experience. They also noted that an additional benefit of the PNs’ lived experience was their ability to quickly build relationships with people. Although participants viewed the development of relationships as slow and gradual, staff viewed these as occurring very quickly: some described the PNs as like a ‘magnet’ for clients or as ‘naturals’. Staff reflected that the success of the PNs lay in the therapeutic relationships they built and sustained with participants. Some staff also felt that the PNs added value to the staff team, through the flexibility of their role, their additional time to work with participants and the increased visibility of the organisation among professional networks. Having staff on site with additional training and expertise to manage substance use crises, such as drug-related overdoses, was noted as an additional benefit in one of the sites. Staff also noted that the intervention was acceptable to participants.
In some settings, staff were less positive about the intervention, with concerns about the peer element of the role, tensions between this role and other staff roles, reservations surrounding PN pay and issues connected to wider stigma towards people with lived experience of substance use. Some staff expressed being unconvinced of the need to give such intensive support to the people whom the intervention was targeting. This highlights the need to provide more information to staff in service settings regarding why it is so important to provide such intensive support. To a certain extent, the study team believed that this was self-evident. Findings suggest that this was not necessarily the case, particularly in settings where staff had not had the benefit of training on PIEs, trauma-informed care, and common reasons why individuals end up experiencing homelessness and problem substance use.
Tensions were reported where the PNs were regarded with some degree of suspicion, and some members of staff felt jealous towards the PN, perhaps because of the flexibility of their roles and a misunderstanding of the work that they were undertaking with participants. Many of the difficulties seemed to arise from tensions specifically between the PN and Support Worker (or equivalent) roles. For example, the PNs were not expected to conduct the same assessments and associated paperwork as their colleagues, giving them more time to work directly with participants. This was particularly apparent at the beginning of the study. There were also issues around remuneration, with some members of staff expressing reservation at the comparably high rate of pay the PNs received. This sometimes connected to organisational structures where peers were associated with volunteering. Findings also indicated the presence of stigma towards histories of substance use that the PNs had to actively manage as part of their roles. Participants reported feeling an ‘in-group’ identification with the PNs that did not generally exist with other staff members, an experience echoed in the literature. 147,148 This will be important to address more proactively in a next-stage study; however, the study team also acknowledge that stigma is common in health, social care and homelessness settings, and is challenging to systemically eliminate in a study context. For some staff, the slow start to the intervention as a result of the training period was viewed as difficult to mainstream further into practice. There were initial concerns about participant recruitment and the whole-person health check/measures, although these did not come to fruition.
Overall, staff and service managers in the intervention settings were supportive of the peer-delivered, harm reduction approach, valuing the PNs and the benefits brought by their lived experience. The challenges experienced are important to consider when determining the feasibility of the intervention, as it appears to have been experienced differently by some staff members. This is something that can be proactively addressed in a next-stage RCT, through optimisation strategies. 149
Peer Navigators
The intervention was feasible and acceptable to the PNs because of the following key features: flexibility of the role; actively valuing their lived experience; extensive and varied training; and diverse, responsive and ‘layered’ support (different types of informal and formal support).
Echoed by staff and participants, the flexibility of the role was important, particularly in terms of the time allowed for the PNs to develop relationships with participants. Case loads for the full intervention were experienced as high overall, but this flexibility of role allowed the PNs to provide more or less intensive support to individuals as needed at any given time to manage this. Their overt lived experience helped to facilitate these relationships, fostering a particular way of working that was perceived as unique in the chosen intervention context settings. The PNs were very proud of their role and the achievements of participants. They also identified role tensions with other staff and attributed these to a lack of understanding or clarity in the role.
The training they received throughout their role, particularly at the beginning, was vital in helping the PNs to develop in confidence, knowledge, skills and understanding. This ultimately influenced the acceptability, accessibility and feasibility of the approach, with the PNs highlighting the uniqueness of their role as a ‘selling point’ for participants. Their role was perceived as different from others, through their overt lived experience, the advocacy nature of what they provided, the provision of financial support and the importance of an explicitly harm reduction-focused approach, all of which appeared to meet the needs of participants at particular times. The PNs valued the time they were able to spend with participants as part of the recruitment process, but this, coupled with other challenges, meant that the recruitment period felt quite pressured for some. The PNs reflected on the challenges of delivering a harm reduction approach within more abstinence-oriented services, including compliance with the expectations for abstinence. In terms of feasibility, the intervention may be more suited to services that are more harm reduction oriented, to maximise ‘fit’, or to services that have been provided with a greater level of background information concerning the nature of the intervention and style of working. The PNs reflected that the approach was feasible to them, in that they could deliver a flexible, person-centred approach to a range of participants with varied needs. They reported feeling part of the study team and, to some extent and in some settings, part of the staff team in the services.
Overall, the PNs felt positive about their role and the impact they had on people’s lives. They also noted challenges in relation to fully embedding the role in practice. Finally, the co-production process facilitated engagement with the study team and allowed the PNs to look after their own well-being, which meant that they could carry out their roles successfully.
Application of normalisation process theory to the assessment of feasibility and acceptability
As detailed in Chapter 2, NPT was the underpinning framework for both the intervention and process evaluation. To briefly demonstrate how NPT enabled the overall assessment of feasibility and acceptability, we outline the four constructs and our application of these in Table 16.
| Construct | Application |
|---|---|
| Coherence | This related to the value placed on the PNs’ role by themselves and others, particularly participants and staff in intervention settings. To embrace the role, those involved needed to be clear about, and fully understand, the rationale for the intervention, as well as its core values (e.g. PIEs, harm reduction). The PNs benefited from a lengthy induction period that enabled them to understand their role and how it would fit within their service. Prior to the start of the study, service managers and organisational leaders were involved in a number of discussions about the role, and were involved throughout the study in key decisions and progress. All had a high level of understanding of the study and its values. Although service staff (e.g. Support Workers) were given information about the study, findings indicate that they would have benefited from receiving more information, at an earlier stage. This would have helped the intervention to have been better understood and valued by all and made it easier for the PNs to become better embedded in the settings at an earlier stage |
| Cognitive participation | To ensure that this intervention could be implemented effectively, support or ‘buy-in’ was required from a number of individuals in a range of organisations. Participants witnessed the PNs’ practice in their services, were quickly receptive to the PNs and were able to get to know them over time. Service managers helped the PNs to settle into their services and organisations, and supported them throughout the study through joint line management and informal support. Other members of staff supported the intervention within their own roles, for example the administration of the participant support monies fund, referring service users/residents to the PNs and signposting the PNs to local contacts. Participants, the PNs and staff in the intervention settings generally ‘bought in’ to the intervention, and became more supportive of the intervention as it developed. Greater understanding of the intervention would probably have facilitated greater buy-in |
| Collective action | To ensure that the intervention could be implemented, service staff made a number of adjustments to their work practice. For example, staff made workspaces available for the PNs as far as possible (although these were affected by the limited space in some of the services), and made introductions to other individuals/organisations to support the PNs in their roles. Over time, staff also adjusted to the different role that the PNs had, compared with themselves and others in their service, although this sometimes manifested as tensions, connected to a lack of understanding of the role and also, we believe, due to stigma towards people who have overt histories of problem substance use or addiction. The PNs also adjusted to the working practices of their setting and understood the importance of communication with all staff |
| Reflexive monitoring | The PNs, service managers and all service staff in the intervention settings continually appraised how the intervention was going in their services though informal communication, formal meetings and group reflective practice, in their staff teams and with the study team. The PNs’ role evolved during the course of the study. Each had their own ways of working, but they also made adjustments as needed to suit their individual participants and the context in which they worked. Interviews conducted with staff, participants and PNs over the course of the study, reflective diary-keeping and regular note-taking by the project management team ensured that the feasibility and acceptability of the intervention were being continually assessed and responded to by the study team, with adjustments being made as necessary. Examples are adding in the collection of case studies to capture the different types of support offered to participants and having regular conversations with the PNs about the importance of record-keeping |
Relevance and suitability of outcome measures to assess effectiveness of intervention in a randomised controlled trial
Overall assessment of outcome measures
Six measures were used in the health check (demographics, the PHQ-9/GAD-7, the MAP, the SURE, the RAND SF-36 and the CARE Measure). Of these, five were validated tools and one (measure 1) was a general demographic and health questionnaire compiled by the project management team. This was based on other measures used elsewhere, or in previous work by the team,24,47,123 and included health conditions and service use. Across the measures, there was some duplication, for example in coverage of mental and physical health conditions. Mental health was covered in the MAP, PHQ-9/GAD-7, RAND SF-36 and SURE. Because there was duplication, the total completion time was most likely too long for a single sitting, and the researchers and the PNs felt that some participants were frustrated at the length and repetitive nature of the questions. The standard care participants who were consulted for their views also commented on the repetitive nature of the questions. The time range for completion of all questionnaires was between 30 minutes and 2 hours. Researchers felt that 30 minutes was optimal, although this relied on participants answering the questions concisely and themselves wanting to complete the questionnaires fairly quickly. Therefore, it would be important for a RCT to involve fewer measures to avoid duplication and to reduce the time taken.
One measure, the RAND SF-36, was particularly unpopular. The American language and expressions made it less suitable for the UK context of the research. Some of the questions were not relevant to the client group or sensitive to their circumstances, for example references to the ability to undertake moderate activities such as ‘bowling or playing golf’. The researchers often had to repeat and explain questions. On this basis, we would strongly advise against the use of the RAND SF-36 to other researchers working with this client group. The EuroQol-5 Dimensions (EQ-5D) had been considered as the measure of quality of life, but it was not compatible with Atlas. In hindsight, the EQ-5D, which has been used previously with this client group,150 would have been a more suitable measure. It comprises five questions, all of which are quite generic and easy to understand.
Coverage of demographics, including housing and involvement with criminal justice, as well as mental health, drug use (as an assessment of risk-taking behaviour) and quality of life are very important measures. Demographics are important descriptors of the study group that allow comparison with other groups and the wider population. Mental health was generally poor at baseline. This improved, as assessed in the MAP and the PHQ-9/GAD-7.
Drug use was covered in detail in the MAP only. The SURE collects aggregated data on the number of days drugs (any) and alcohol are used. This does not allow for assessment of risk. Coverage of detailed drug use through the MAP section on drug use could be incorporated into the demographic questionnaire.
The CARE Measure recorded patient feedback on the PN. This measure was well received, quick to complete, and is recommended going forward. The quantitative data provided, alongside the qualitative data provided in its ‘free-text’ section, were validated by the qualitative data collected in the intervention participant interviews.
Completeness of data collection
Ten individuals did not want to complete the health check at all, despite completing the intervention (whether shortened or full). In a RCT, it would be essential for all to complete the baseline data collection to be entered in the trial. We have discussed the challenges of researchers undertaking the measures in Chapters 4 and 5.
Resource burden of data collection
A PN was present for all quantitative data collection, alongside the academic researcher who collected the data. Having PNs collect data, as was originally intended, would be ideal given the relational focus of the intervention. However, in a RCT, the control group would also require data collection to be undertaken. This is an important decision to be considered for a next-stage trial, given that there are risks and benefits for either PNs or academic researchers undertaking the measures in the intervention and control settings.
Summary
Some outcome measures were more suitable and easier to administer than others. Demographics, quality of life and health outcomes, in particular mental health and drug use, are important outcomes to include in a streamlined version of the outcome measures. These could be captured in an adapted demographic questionnaire that includes drug use from the MAP, the PHQ-9/GAD-7 (for mental health) and the SURE. The CARE Measure is also an important measure of PN support and interpersonal skills.
Qualitative data collection: availability and quality
As presented in Chapter 5, the qualitative data collected in the study were very rich and insightful. These data were essential for interrogating feasibility and acceptability from different perspectives. The academic researchers (RF and HC) were able to undertake the interviews and observations fairly easily, and data collection visits/trips were combined to reduce resource and cost.
The quality of the interviews conducted by the SDF peer researchers was also very good and there was some learning as the study developed. For example, on reviewing transcripts, the team recognised that there was a lack of prompting in early interviews, which we aimed to improve for wave 2, with some success. The organisation and co-ordination of both waves of interviews across multiple sites required considerable involvement from academic researchers, our SDF partners and the PNs. The costs and benefits of this approach would require more consideration in a RCT, and adaptations would probably be required, for example recruiting peer researchers from areas more local to the intervention settings to reduce time and cost.
Support for randomisation
Participants
In wave 2 of the peer research data collection, participants were asked how they would feel about being part of a RCT. A follow-up question was asked about how they would feel about the research team having access to their health data to link it to other outcomes, for example, in Scotland, using an individual’s CHI number. Only 10 participants undertook wave 2 interviews. Most participants were supportive of a RCT and did not see any issue with allowing data to be shared to help determine intervention effectiveness. However, some participants misunderstood these questions. We believe that this misunderstanding was due to a range of reasons: the questions were very long for the peer researchers to read out, making them hard to follow, the scenarios were inherently complex, and the peer researchers themselves had a limited understanding of a RCT, meaning that they were not able to clearly explain.
Those who did not fully understand what a RCT could mean for this type of intervention (specifically, settings/services would be randomised rather than individuals) expressed concern about the unfairness of some people being offered a PN and others not. Nonetheless, because many participants felt that the PN intervention was important, they could see the importance of evaluating it fully. Most participants felt that randomisation could be acceptable, as long as everyone in the study had the intervention fully explained to them.
When participants were asked whether or not they thought that other people in their position would mind having their data linked and analysed, nearly all participants stated that they could not speak for others. The confusion surrounding RCTs may have been minimised had academic researchers conducted these interviews instead.
Staff in services
As with the participant interviews, interviewed staff expressed broad support for running a RCT, but there was some confusion surrounding what a RCT would involve. Staff reiterated the value of the intervention and expressed support for any type of research that would strengthen the evidence base to enable further implementation. Again, concern was expressed around randomising individuals, although the researcher reassured them that it would be more likely that settings/services would be randomised, rather than individuals, following a cluster trial methodology. However, this also prompted a reservation that members of staff in the chosen settings/services could become invested when agreeing to take part in the overall study, and could therefore be disappointed if their service was not selected as an intervention setting. This is a more broadly recognised concern with cluster RCTs. 151
It was also expressed that the decision to support, or not support, a RCT was not their own and was, alternatively, the decision of someone more senior, demonstrating the considerations around organisational structure that may need to be worked around when developing and implementing a RCT. A member of staff also highlighted that a RCT would need to fit in with the service and other activity going on at that particular time, and the timing may not always be convenient.
Summary
Despite attempts to provide clarity, there was some confusion around what a RCT could or would involve, and this affected participant and staff member responses in the interviews. Those who had a better understanding tended to express support for conducting a RCT for the intervention; this was largely connected to a belief in the value and importance of the intervention. Members of staff and participants also highlighted some practical considerations to take account of in future trials.
Merit of a randomised controlled trial to test effectiveness
Intervention participants valued the support they received from their PN, and saw this support as offering something new and different from the kind of support they had received in the past, or to what they were currently receiving elsewhere. The development of trusting, supportive relationships between participants and PNs took time, given previous distrust of professional helpers, but was faster than for non-peer workers (according to staff members in the settings) and resulted in positive outcomes. The intervention enabled participants to be more or better engaged with wider support services, and to feel more confident to access support in future. Interviewed standard care staff expressed support for the intervention, including a willingness to host an intervention in principle. Although there were differences, and all settings are, of course, unique, the standard care settings and the service users/residents who used them were broadly comparable to the intervention settings and to those who used those, which suggests that the intervention could equally have been hosted in these settings.
A RCT would require a primary outcome measure to be defined. From the measures used and the change over time for those for whom there were two sets of data available, risk-taking behaviour, specifically, the number and frequency of illicit drugs used, would be a clear objective measure. Secondary outcomes of improvements in mental health and quality of life, service engagement, and therapeutic relationships would be feasible and appropriate. In summary, data are available from this study to aid a sample size calculation based on reduction in illicit drug use as a primary outcome measure, alongside other considerations. The dropout rate of 20% (12/58, full intervention length) will be taken into account, plus the figure of 30 out of 46 who completed wave 2 measures, when determining recruitment and sample size. The settings in a RCT would need to be sufficiently geographically dispersed to avoid contamination. For ethics reasons, settings, rather than individuals, would be randomised. The findings suggest that a RCT is merited to test the overall effectiveness, but also identify some changes that would be required to improve the intervention and to maximise effectiveness.
Adaptations required to facilitate adoption in wider NHS and social care statutory services
With some adaptations, the intervention could be adopted in wider NHS and social care statutory services, as well as other third-sector settings. Across all settings, the following considerations, actions and adaptations would be required:
-
securing staff buy-in from front-line staff, senior staff and staff from the wider organisation, through comprehensive and considerate preparatory work
-
ensuring that a private working area would be available to facilitate private support conversations and meetings
-
clearly defining the PN role and communicating this to all staff (linking with preparation)
-
remunerating PNs fairly for their specialist role, and attempting to secure consensus from all staff on this rate of pay (these would also need to be aligned with standard pay scales in statutory settings)
-
including a practical support monies fund, but making it easier to administer for both the PNs and staff
-
actively managing any stigma that manifests towards PNs and the role within services, given the presence of stigma in wider society towards those with lived experience.
Buy-in from staff would be required to ensure that the PNs are able to fully integrate into a service with minimal conflict. Training for all staff at the start of the intervention would help to minimise the risk of conflict. Training would encompass detailed information about the role, the intervention and the different approach taken by the PNs, compared with more conventional support work, as well as specific training on how the PNs would work within a harm reduction and PIEs framework. Clear distinctions between the role and other service roles, and a clear understanding of what it involves, would be essential. Service managers would also require training on how to manage the intervention in their services, as well as managing the unique staff dynamics that could emerge with the intervention. A key learning point from this study has been the importance of preparation by the study team, service managers and leads, as well as the wider hosting organisation, to maximise the likelihood of fit.
The working spaces available to the PNs would have to take into account the various aspects of their role, such as the need for confidentiality and privacy, and the use of formal and informal spaces, and the flexibility of the approach, with work being carried out in a range of places. We also recognise that these challenges experienced in the SHARPS study relating to working space are likely to be felt by staff across services. Importantly, and more broadly, we also recognise the challenge of working within the health and social care environment, including the necessity to continue to meet outcomes, but with constrained financial and staff resources. We also recognise the particular challenges of ‘key-working’ in residential settings. 72 These would need to be thoughtfully considered and responded to.
In addition, as well as having a clearly defined role, the PNs would have to receive a salary that is comparable to the salary of the PNs in the study. Wider implementation would have to ensure that there was consensus regarding payment, to ensure service buy-in and to minimise conflict. Relatedly, the practical support monies were shown to be both useful and valuable, but would need to be administered to minimise the burden on both PNs and service staff. The PNs suggested that easier access to the money could overcome these barriers, for example through a separate bank account or a prepaid debit card, as well as clearer guidance regarding what the money could be used for [enhancing the template that was provided – see template on the project web page: www.journalslibrary.nihr.ac.uk/programmes/hta/1615314/#/documentation (accessed 2 December 2020)]. The approach used in the SHARPS study placed a burden on administrative staff in services (e.g. to keep track of and reimburse expenses), which we would aim to minimise in a future study.
Finally, as discussed in Chapter 1, the stigma of having lived experience of problem substance use and homelessness continues to pervade society and, by extension, manifests in services. This would require active and ongoing management to ensure that the PNs were able to carry out their roles. Comprehensive training on the role and its rationale at the beginning would aim to minimise this stigma.
Specific setting types: NHS, other statutory settings and third-sector settings
In terms of NHS settings, homelessness general practices would be ideally suited to the intervention, as they provide health care to the target population. A&E settings would also be possible but would probably require further adaptation. A&E departments have been used for similar roles, such as Pathway’s Care Navigators152 and the Scottish Violence Reduction Unit’s Navigators. 153 The PNs would require a defined base, which may be external to A&E departments, to ensure adequate workspace to conduct meetings with participants.
In terms of other statutory settings, prisons would also be a feasible setting for the intervention, as many people who are released from prison become homeless or are at risk of homelessness154 and can be at increased risk of drug overdose. 155 The PNs supported a number of participants as they entered and left prison, and were able to provide valuable support. Statutory settings, with traditionally less experience of peer roles than in the third sector, are likely to require additional preparation to ensure that the rationale for the role, as well as its responsibilities, are clearly conveyed and understood. Finally, although all settings/sectors must fulfil key responsibilities to operate and deliver services, the organisation and function of statutory settings has unique/additional task requirements: the more fluid ‘task/outcome’ approach of the PN intervention has the potential to jar with this, necessitating careful and thoughtful preparation.
Finally, the intervention could be further implemented in additional third-sector organisations that work with the target population. The PNs experienced fewer challenges when they worked in services that were considered to be more ‘harm reduction-oriented’ than those that expected, or encouraged, abstinence from service users. Through the course of the study, the PNs became harm reduction experts, fully embodying a harm reduction approach,48 working in a compassionate, non-judgemental way that allowed them to meet participants where they were at. Therefore, third-sector services that more fully represent a harm reduction mindset would probably be better suited to the intervention than those that do not. This does not mean that the intervention would not work in more abstinence-based settings, but it would potentially require additional training of staff in services to maximise effectiveness. Again, the PNs would require workspaces that facilitated informal engagement, afforded privacy and were psychologically informed. To ensure a good fit between the context and the intervention, ideally, the staff in intervention settings should receive training and induction to the study and to the unique role of the PNs. The study team would ensure that these were conducted with sensitivity to roles, and the demands and pressures they are likely to experience.
Collectively, these provisions would help to maximise the effectiveness of the intervention. As required on setting up the study, Tessa Parkes consulted a member of the SSG who holds a senior commissioning role in the NHS (Susanne Millar) on the key findings of the study, to determine whether or not their view aligns with ours that these findings are applicable to mainstream NHS settings. This member affirmed the relevance of the study findings and this discussion helped in drafting the text in Adaptations required to facilitate adoption in wider NHS and social care statutory services and Specific setting types: NHS, other statutory settings and third-sector settings. More generally, as with any trial, optimisation is needed, but must be carefully balanced to ensure that the RCT is able to successfully test the intervention. 149 This will be considered in detail in the design of a future trial.
Recommendations for future research
We have established that a peer-delivered, relational harm reduction intervention is acceptable and accessible to, and feasible for, people experiencing homelessness and problem substance use. A full RCT is now required to assess its clinical effectiveness. On the basis of the evidence presented in this report, we would recommend a cluster RCT, stratified by setting, and using illicit drug use in previous month as the primary outcome. Given that the full RCT will be at a much larger scale, we propose an embedded pilot to test and refine recruitment and the data collection process.
Chapter 7 Reporting on patient and public involvement: involving those with lived experience
Introduction
We had different levels of PPI in this study. This section focuses on describing the involvement of the PPI group. We recognise that NIHR uses the term PPI and that this encompasses a range of individuals with a range of experiences, including patients within the NHS. However, in the context of our study, individuals expressed a preference for being referred to as individuals with lived experience, and as ‘experts by experience’ (EbyE). We have therefore used the term ‘EbyE’ whenever possible. The section is structured following the headings contained in Guidance for Reporting Involvement of Patients and the Public 2 (GRIPP2),156 which includes detail to allow the process to be replicated by other researchers.
Aim
Involving members of the public in research has the practical benefit of ensuring research quality and relevance. 121 The reasons for inclusion are more broadly informed by democratic principles relating to citizenship, accountability and transparency, particularly when research is publicly funded. 121 As this was a peer-delivered intervention, we believed that involving those with relevant lived experience throughout the study in various forms was essential and would improve the overall quality of the research. Alongside the central lived experience involvement in the PN intervention, the involvement of others with lived experience happened at different times throughout the study and involved a variety of approaches, individuals and activities. These were as follows: (1) the involvement of two individuals with lived experience on the SSG to ensure that their voice was heard throughout the independent oversight of the study, (2) individuals with lived experience participated in the intervention development, (3) an EbyE group comprising seven individuals with lived experience of homelessness and/or problem substance use provided quality assurance throughout the study and (4) the involvement of peer researchers who facilitated data collection and analysis. This section describes the EbyE group, given that the other elements have been covered in detail in other report sections. The EbyE group acted as a quality assurance group; it was assembled at the start of the study and closed shortly before the end.
The team closely followed the INVOLVE121 guidance throughout, and assessed the management of the EbyE group using the UK Standards for Public Involvement in Research. 157
Background
Prior to the study starting, the team invited individuals, through third-sector organisations, with lived experience of homelessness and/or problem substance use to be involved in a specially developed EbyE group for the study. Some individuals had experience of problem substance use, some had experience of homelessness, and others had experience of both, alongside other, often related, challenges such as poor mental health. Each person’s experiences were unique. The team recognised the contextual differences between and within the study sites in Scotland and England. To take account of this, it was hoped that two EbyE members, who lived in different parts of England, could offer insight into these differences if/when needed. The group comprised the following individuals, who have all provided consent to be named in this way:
-
Jason Wallace, co-investigator, SDF employee (chairperson).
-
Stan Burridge, Pathway, then Expert Focus (from June 2019).
-
Leslie Norris, Phoenix Futures – had to leave group in summer 2018 because of other commitments.
-
Tracy Polson, Turning Point Scotland – left in autumn 2019 as she had secured employment.
-
Philip Foley, Turning Point Scotland.
-
Joanne Denton, Sheffield Addiction Recovery Research Panel.
-
Alex Dunedin, Ragged University/Drugs Research Network Scotland.
Hannah Carver and Rebecca Foster worked with Jason Wallace throughout and provided leadership and practical and administrative support.
When the proposal for this study was peer reviewed, it was suggested that the EbyE group would benefit from a mix of ethnicity and involving those from LGBTQ+ communities. Despite attempts to recruit individuals who were non-white (or not from the UK), this was not possible. We also used our connections to recruit an individual who identified as being part of the LGBTQ+ community, but no one could commit to the study. Finally, we aimed to involve an individual with ‘living experience’ (actively using substances), but this was also not possible. Therefore, although we recognise that our group may not reflect experiences from these groups, the group did represent a wide range of experiences.
Methods
Introduction
The EbyE group met face to face four times, and by conference call twice, during the study. Each meeting was focused on a particular aspect of the study, although all meetings allowed time for general conversation, checking in and study updates. The team viewed this as important for ensuring that all members felt comfortable and valued. The face-to-face meetings were in Glasgow, were 4 hours long, and included lunch and comfort breaks. Lunch and refreshments were provided. Conference calls were scheduled for 1.5 hours.
Onboarding
At the first meeting, the group expressed reservations with the term ‘PPI’ and agreed that they would prefer to be called the ‘EbyE’ group. The team ensured that it was consistent with this terminology in all subsequent communication, including referencing the existence and work of the group to others. At the first meeting, the group agreed ‘ground rules’ for how the group and meetings would operate. These rules were generally concerned with ensuring that all members felt comfortable, welcome and respected. All members signed a confidentiality statement.
The meetings were chaired by Jason Wallace. The intention was to have a female member as the deputy chairperson, to make the leadership gender balanced. This opportunity was discussed at the first meeting, but none of the female members volunteered. It was not essential to have a deputy chairperson because the group was small and Jason Wallace was available to meet every time except once; on this occasion, Hannah Carver and Rebecca Foster co-chaired the meeting. Detailed notes were taken by Hannah Carver/Rebecca Foster at all meetings and reviewed by Jason Wallace before being sent round the group. The group was invited to flag any inaccuracies or omissions at that stage.
Communication
Jason Wallace received permission from all members to create a WhatsApp group to aid communication about meetings. Hannah Carver and Rebecca Foster communicated through this group, as well as via e-mail, to ensure that all members received the necessary information, in their preferred communication. Although the WhatsApp group was primarily used to communicate information about the meetings, sometimes members would initiate other conversations, as a way of catching up, or to share a news article of interest.
Reimbursement
Members were reimbursed for their time, in line with INVOLVE recommendations. 121 Members received travel expenses for attending meetings, including public transport or taxi fares provided at meetings (in cash), to ensure that no-one was out of pocket. Accommodation costs were covered if required, and meals and other incidental expenses were reimbursed (in cash) at meetings.
Key contributions of the Experts by Experience group
As mentioned, each meeting had a specific purpose, described in the following list. Some of the feedback offered in these meetings is also presented:
-
Meeting 1 (face to face) – May 2018.
Reviewing participant materials to ensure the use of straightforward lay language. The following materials were specifically reviewed:
-
participant information sheet – intervention participants
-
participant information sheet – interviews with intervention participants
-
participant information sheet – interviews with people who drop out
-
consent form – intervention participants.
-
-
Meeting 2 (conference call) – September 2018.
Reviewing a draft version of the intervention guide sent in advance of the meeting. The group were given the following questions to help focus their review:
-
Contents page – are we covering the right things?
-
How does it look – good balance between text and pictures? Spacing, readability, etc.?
-
Any particular sections you have looked at and thought we should make some changes to?
-
-
Meeting 3 (face to face) – December 2018.
Review of the topic guide for interviews with a sample of intervention participants by SDF peer researchers.
-
Meeting 4 (conference call) – April 2019. This call was cancelled because of a lack of availability.
-
Meeting 5 (face to face) – August 2019.
Review of a sample of interview transcripts to identify emerging themes. Five interview transcripts were discussed at the meeting.
-
Meeting 6 (conference call) – November 2019.
Discussion of a dissemination strategy for communicating study findings to individuals with lived experience.
-
Meeting 7 (face to face) – February 2020.
The intention for this meeting was to review the draft study report and other dissemination outputs; however, it was not possible to review these outputs as the report was not fully ready. Members were asked if they would be happy to stay in touch with the study team and support the study on an ad hoc basis, and on specific tasks only, and all were. One member inputted on the Plain English summary and some will be involved in the development of lay summaries and reimbursed for their time.
Study results and outcomes
The EbyE group’s input enriched the study and improved its overall quality; some of the feedback from a selection of the meetings is shared in the following sections to illustrate this. All of this feedback was/will be taken on board by the study team and implemented, when possible and appropriate.
Sample feedback from the group on intervention participant materials
-
Remove jargon and replace with more accessible terms (e.g. from ‘holistic’ to ‘whole person’, ‘transcript’ to ‘write-up’).
-
Alter/soften terminology and language to be more psychologically informed (e.g. from ‘chief investigator’ and ‘deputy chief investigator’ to ‘study lead’ and ‘deputy study lead’ to avoid triggering negative associations of interviews with police officers and Department for Work and Pensions representatives).
-
Simplify layout (e.g. add bullet points to break up large sections of text).
Sample feedback from the group on the draft intervention guide
The group was very positive about the guide overall in terms of design, layout and use of images. Group members said it was very comprehensive, covering a lot of important issues. However, members also offered a number of helpful improvements:
-
Add information about pain management and using other substances, such as prescription drugs to manage pain.
-
Add to the PN self-care section on sign/symptoms of burnout (e.g. taking out-of-hours calls, not taking a lunchbreak).
-
Add a note on effect of nutritional deficiencies and hormones on an individual’s health – in the physical health section or the section on women.
-
Add more information on bereavement as a risk factor for homelessness and also a challenging experience that can make health/other aspects of life more challenging.
-
Add glossary of key terms.
-
Ensure that all text, including text featured in or accompanying images, is easy to read.
Sample of feedback given by the group on the dissemination strategy for those with lived experience
-
Make a YouTube (YouTube, LLC, San Bruno, CA, USA) video or a podcast. Use simple language in all communication, an ‘ABC’, for example ‘this is what happened, these are the results, this is what they mean’. Do not solely rely on written outputs for sharing findings.
-
Make clear how the participants benefited – how did the study help them?
-
Do a press piece (e.g. Big Issue Scotland).
-
Produce report in A5 size, as this is easy for people to put in their pockets and carry.
Discussion and conclusions
At all meetings, members of the EbyE group provided constructive feedback. As well as these important contributions, the group also benefited from Stan Burridge supporting the SHARPS study in his capacity as EbyE lead at Pathway. For example, Stan Burridge helped the team to secure discounted places to present at its 2019 conference. This, alongside other funds, enabled Rebecca Foster, Wez Steele (PN) and Joanne Denton to attend.
The study team are very grateful for the work and commitment of the EbyE group to the SHARPS study. It was a privilege to work with the individual group members. It is important to emphasise that convening an EbyE group for a study like this is entirely worthwhile. Nonetheless, we also want to emphasise that facilitating an EbyE group that has meaningful involvement and impact requires commitment by the study team to take on the administration of this, as it is another formal group to manage. It also requires a commitment to provide ongoing informal support to ensure that all members feel valued, comfortable and welcome, as well as requiring a commitment to continuous evaluation. These are key components recently highlighted by Liabo et al. 158
Reflections and critical perspective
This section reflects on the process, from the perspectives of both the study team and the members of the EbyE group.
Discussion and reflections from the perspective of study team
Managing group dynamics
After each meeting, Rebecca Foster, Hannah Carver and Jason Wallace each made notes reflecting on how the meeting had gone. From their perspectives, the meetings went well and the group members appeared to feel comfortable to attend and share their views. Some work was needed to manage the dynamics and ensure that all members had an equal voice.
Changing circumstances of the Experts by Experience group and their implications
Two group members secured employment during the study. We decided not to replace them as we did not want a new member joining who did not have all of the background knowledge of the study, nor did we want to risk affecting the positive dynamic that had been fostered.
Stan Burridge was a member of both the EbyE group and the SSG. He was supported to give his time to these groups as part of his work time with Pathway, his employer, and did not receive any reimbursement for his participation. Stan Burridge became a freelance consultant for his own company in June 2019 and wanted to continue involvement in both the EbyE group and SSG. The study team also desired his continued involvement, so we reimbursed him for his time thereafter.
Ensuring that the group members felt comfortable, welcome and included
There was some anxiety about the first conference call. Hannah Carver and Rebecca Foster tried to alleviate this by giving clear instructions in advance. One member found the calls to be challenging, and so opted to provide feedback via e-mail instead. This member was reassured that this was completely fine, and the option was provided to all group members. There was consensus that the face-to-face meetings were preferable to conference calls. The research team acknowledged this and explained that only a set number of face-to-face meetings had been costed.
Supporting personal and professional development
The team was committed to offering other opportunities to the group, and to supporting group members with their personal and professional development. This included inviting them to attend relevant events and seminars and asking them to input on the team’s draft academic outputs for other projects, for which they were reimbursed.
Close of group and continuing involvement
At the final meeting, it was clear how much some members of the group valued being part of it. Some members vocalised that they were sad that the group was coming to an end. The team requested to stay in touch with the members on an individual basis if they wished and to offer opportunities to members as they arose. The team continues to be in touch with most of these members. The team has reflected that greater consideration should have been given to managing the ending of this group, in the same way that endings were managed for intervention participants.
Discussion and reflections from the perspective of the Experts by Experience group
At the final meeting, we invited members of the group to complete an anonymous feedback form. We allowed 30 minutes in the meeting to complete these. If the members could not attend the final meeting, they were invited to complete the form via e-mail (although this unfortunately meant anonymity could not be protected).
All feedback shared was positive. The members of the group reported that they enjoyed being involved in the study and feeling valued. They felt that the meetings had a clear purpose and that these were well communicated, the group dynamics well managed and the meeting durations were appropriate. All expressed a preference for face-to-face meetings rather than conference calls. Members felt that the communication between meetings was appropriate and supportive. Overall, members described the experience as very enjoyable and rewarding, with one member describing their involvement as ‘an honour’.
Acknowledgements
We would first like to acknowledge the intervention participants for taking part in this study and sharing their views and experiences on being involved. Second, we would like to thank our wonderful PNs, Josh Dumbrell, Rebecca Jones, Michael Roy and Wez Steele, for their compassion, commitment, vision for the project, honesty, integrity and hard work throughout.
The SHARPS study would not have been possible without the support and contribution of a wide range of individuals who offered their expertise and support at different stages of the study.
We would like to thank our SSG members, led by Professor Stewart Mercer: our supportive and wise chairperson, Professor Carol Emslie; Mr Stan Burridge; Professor Alex McConnachie; Dr Saket Priyadarshi; Professor Sarah Johnsen; Ms Rachel Beaton; Ms Susanne Millar; Mr Lee Ball; Dr Neil Hamlet, Dr Ruth McGovern and Dr Ruth Freeman; and Mr Jason Wallace and Professor Graeme MacLennan as study team representatives.
We would like to thank our TSA partners: Mitch Menagh, Malcolm Page, Susan Grant, Iain Wilson, Jeanette Lees, Steph Phillips, Andy Parkinson, Andrew McCall, Helen Murdoch, Laura Mitchell, Pam Knuckey, Nick Redmore, Tony Thornton, Gillian Coates, Amber Sylvester, Laura Logan and Sarah Lapido.
We would like to thank our Cyrenians/Change Grow Live partners: Tess Hamilton, John Arthur, Mike Wright and Amy Hutton.
We would like to thank our Streetwork/Simon Community Scotland partners: Rankin Barr, Jan Williamson, Cindy Pritchard and Hugh Hill.
We would like to thank our SDF partners and peer researchers who supported the data collection: Alex Murray, Emma Hamilton, Matthew McCue, Tammie Brown, Sylvia Fox and David Logan.
We would like to thank our EbyE group members: Joanne Denton, Philip Foley, Alex Dunedin, Stan Burridge, Tracy Polson and Leslie Norris.
We would like to thank the current and former members of our university team who supported the data entry and analysis: Ms Tracey Price, Mr Joe Schofield, Dr Mary Cobbett Ondiek, Ms Janette Clark, Dr Joanna Miler, Ms Wendy Masterton and Mr Marcus Cusack.
Finally, we would like to thank Renzo Cardozi and Jan Hay, who supported the study in valuable ways.
Contributions of authors
Professor Tessa Parkes (https://orcid.org/0000-0002-0409-3254) (Research Director of the SACASR) was Chief Investigator. She was responsible for the overall conception, design, data acquisition, and analysis and interpretation of findings at each phase of this research. She had overall responsibility for the PNs and jointly line managed them with their respective service managers. She is responsible for the overall content of this report.
Professor Catriona Matheson (https://orcid.org/0000-0002-7568-1125) (Professor of Substance Use) was Deputy Chief Investigator and co-applicant. She fully shared the overall conception of the study, development of the intervention and study design, oversaw the quantitative data collection and analysis, supported the Chief Investigator with decision-making throughout the study and shared the write-up of the report. She is also responsible for the overall content of this report.
Dr Hannah Carver (https://orcid.org/0000-0002-6846-2661) (Lecturer in Substance Use) was a co-applicant and shared in the conception of the intervention and study design. Together with Rebecca Foster and Tessa Parkes, she project managed the study and its budget; supported the original ethics submissions; liaised with staff in all settings; supported the EbyE group (alongside JW and RF); and supported many aspects of the data collection, analysis and report write-up.
Dr Rebecca Foster (https://orcid.org/0000-0002-8321-1801) (Research Fellow) was the recruited Research Fellow for the study and oversaw the day-to-day management of the study. She led the recruitment of participants, conducted or oversaw the data collection and analysis, supported the management of the EbyE group (with JW and HC), and supported the PNs during their time in post. She led a significant amount of the write-up of the report.
Dr John Budd (https://orcid.org/0000-0002-0988-782X) (Clinical Lecturer) was a co-applicant and was involved in the original conception of the intervention. By virtue of his clinical role, he provided valuable support to the Edinburgh-based PNs during their time in post through developing their networks and supporting their professional development. He supported decision-making throughout the study through attendance at meetings and e-mail correspondence.
Mr Dave Liddell (https://orcid.org/0000-0003-3019-2894) (Chief Executive Officer for the SDF) was a co-applicant and was involved in the original conception of the intervention. He was responsible for the quality of the research conducted by the peer researchers and facilitated access to important training for the PNs. He supported decision-making throughout the study through attendance at meetings and e-mail correspondence.
Mr Jason Wallace (https://orcid.org/0000-0002-3794-5118) (Senior Officer for Volunteering and Engagement, SDF) was a co-applicant, contributed to the development of the intervention, and led PPI on the initial proposal. He was a lived experience member of the SSG and led the EbyE group with Hannah Carver and Rebecca Foster. He delivered some of the training and provided essential informal support to the PNs. He supported decision-making throughout the study through attendance at meetings and e-mail correspondence.
Professor Bernie Pauly (https://orcid.org/0000-0002-4845-1383) (Professor of Nursing and Scientist) was a co-applicant. She advised on the development of the intervention, in particular the peer-delivered element of the work, and on the study design. She supported the project management team throughout the study on best practices in relation to the employment of peers. She supported decision-making throughout the study through attendance at meetings and e-mail correspondence.
Dr Maria Fotopoulou (https://orcid.org/0000-0001-5420-5632) (Lecturer in Criminology) was a co-applicant. She led the original ethics submission with Tessa Parkes and Hannah Carver, advised on the development of the intervention, and supported some elements of the qualitative data coding and analysis. She supported decision-making throughout the study through attendance at meetings and e-mail correspondence.
Dr Adam Burley (https://orcid.org/0000-0002-0631-0558) (Consultant Clinical Psychologist) was a co-applicant, supported the development of the intervention, and provided clinical supervision to each of the PNs. He supported decision-making throughout the study through attendance at meetings and e-mail correspondence.
Professor Isobel Anderson (https://orcid.org/0000-0001-8601-8049) (Professor in Housing Studies) was a co-applicant and advised on the development of the intervention. She also provided expertise in housing/homelessness policy and practice throughout the study. She supported decision-making throughout the study through attendance at meetings and e-mail correspondence.
Professor Graeme MacLennan (https://orcid.org/0000-0002-1039-5646) (Director of The Centre for Healthcare Randomised Trials) was a co-applicant. He provided trial expertise and advised on the quantitative data collection, approach, analysis and write-up, to inform the design of a future larger-scale study. He was a member of the SSG and supported decision-making throughout the study through attendance at meetings and e-mail correspondence.
All authors reviewed and revised the report critically for important intellectual content and gave final approval to this published version.
Publications
Parkes T, Matheson C, Carver H, Budd J, Liddell D, Wallace J, et al. Supporting Harm Reduction through Peer Support (SHARPS): testing the feasibility and acceptability of a peer-delivered, relational intervention for people with problem substance use who are homeless, to improve health outcomes, quality of life and social functioning and reduce harms: study protocol. Pilot Feasibility Stud 2019;5:64.
Parkes T, Matheson C, Carver H, Foster R, Budd J, Lidell D, et al. Assessing the feasibility, acceptability and accessibility of a peer-delivered intervention to reduce harm and improve the well-being of people who experience homelessness with problem substance use: the SHARPS study. Harm Reduct J 2022;19:10.
Data-sharing statement
Owing to the sample size, known geographical locations, and personal and organisational sensitivities, the qualitative and quantitative data sets will not be available for sharing. All requests for data should be sent to the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health and Social Care.
References
- Parkes T, Matheson C, Carver H, Budd J, Liddell D, Wallace J, et al. Supporting Harm Reduction through Peer Support (SHARPS): testing the feasibility and acceptability of a peer-delivered, relational intervention for people with problem substance use who are homeless, to improve health outcomes, quality of life and social functioning and reduce harms: study protocol. Pilot Feasibility Stud 2019;5. https://doi.org/10.1186/s40814-019-0447-0.
- Parkes T, Matheson C, Carver H, Foster R, Budd J, Lidell D, et al. Assessing the feasibility, acceptability and accessibility of a peer-delivered intervention to reduce harm and improve the well-being of people who experience homelessness with problem substance use: the SHARPS study. Harm Reduct J 2022;19. https://doi.org/10.1186/s12954-021-00582-5.
- Medical Research Council . Developing and Evaluating Complex Interventions: New Guidance 2019.
- Fitzpatrick S, Johnsen S, White M. Multiple exclusion homelessness in the UK: key patterns and intersections. Soc Policy Soc 2011;10:501-12. https://doi.org/10.1017/S147474641100025X.
- Wright NM, Tompkins CN. How can health services effectively meet the health needs of homeless people?. Br J Gen Pract 2006;56:286-93.
- European Federation of National Organisations Working with the Homeless (FEANTSA) . ETHOS: European Typology of Homelessness and Housing Exclusion 2017. www.feantsa.org/en/toolkit/2005/04/01/ethos-typology-on-homelessness-and-housing-exclusion (accessed 20 April 2020).
- Shelter . Far From Alone: Homelessness in Britain in 2017 2017.
- National Alliance to End Homelessness . State of Homelessness: 2020 Edition 2020. https://endhomelessness.org/homelessness-in-america/homelessness-statistics/state-of-homelessness-2020/ (accessed 24 June 2020).
- Gaetz S, Gulliver T, Richter T. The State of Homelessness in Canada in 2016. Toronto, ON: Canadian Observatory on Homelessness Press; 2016.
- Bramley G, Fitzpatrick S, Wood J, Sosenko F, Blenkinsopp J, Littlewood M, et al. Hard Edges Scotland: New Conversations about Severe and Multiple Disadvantage. London: Lankelly Chase Foundation; 2019.
- Canadian Observatory on Homelessness . Causes of Homelessness 2019. www.homelesshub.ca/about-homelessness/homelessness-101/causes-homelessness (accessed 16 June 2020).
- Bramley G, Fitzpatrick S. Homelessness in the UK: who is most at risk?. Hous Stud 2017;33:96-116. https://doi.org/10.1080/02673037.2017.1344957.
- McDonagh T. Tackling Homelessness and Exclusion: Understanding Complex Lives 2011. www.jrf.org.uk/sites/default/files/jrf/migrated/files/homelessness-exclusion-services-summary.pdf (accessed 27 August 2020).
- Hewett N, Halligan A. Homelessness is a healthcare issue. J R Soc Med 2010;103:306-7. https://doi.org/10.1258/jrsm.2010.10k028.
- Aldridge RW, Story A, Hwang SW, Nordentoft M, Luchenski SA, Hartwell G, et al. Morbidity and mortality in homeless individuals, prisoners, sex workers, and individuals with substance use disorders in high-income countries: a systematic review and meta-analysis. Lancet 2018;391:241-50. https://doi.org/10.1016/S0140-6736(17)31869-X.
- Hwang SW, Tolomiczenko G, Kouyoumdjian FG, Garner RE. Interventions to improve the health of the homeless: a systematic review. Am J Prev Med 2005;29:311-19. https://doi.org/10.1016/j.amepre.2005.06.017.
- Ijaz S, Jackson J, Thorley H, Porter K, Fleming C, Richards A, et al. Nutritional deficiencies in homeless persons with problematic drinking: a systematic review. Int J Equity Health 2017;16. https://doi.org/10.1186/s12939-017-0564-4.
- Morrison DS. Homelessness as an independent risk factor for mortality: results from a retrospective cohort study. Int J Epidemiol 2009;38:877-83. https://doi.org/10.1093/ije/dyp160.
- Thomas B. Homelessness: A Silent Killer – A Research Briefing on Mortality Amongst Homeless People 2011. www.crisis.org.uk/ending-homelessness/homelessness-knowledge-hub/health-and-wellbeing/homelessness-a-silent-killer-2011/ (accessed 27 August 2020).
- Reeve K. Women and homelessness: putting gender back on the agenda. People, Place Policy 2018;11:165-74. https://doi.org/10.3351/ppp.2017.8845235448.
- McGlennan C, D’Arcy R. Health needs of sex workers. InnovAiT 2013;6:636-42. https://doi.org/10.1093/invaitins100.
- Shelter . Off the Streets: Tackling Homelessness Among Female Street-Based Sex Workers 2004. https://england.shelter.org.uk/professional_resources/policy_and_research/policy_library/policy_library_folder/off_the_streets_tackling_homelessness_among_female_street-based_sex_workers (accessed 27 August 2020).
- Centre Point . More Than a Number: The Scale of Youth Homelessness in the UK 2017. https://centrepoint.org.uk/media/2396/more-than-a-number-the-scale-of-youth-homelessness.pdf (accessed 27 August 2020).
- Matheson C, Liddell D, Hamilton E, Wallace J. Older People With Drug Problems in Scotland. A Mixed Methods Study Exploring Health and Social Support Needs. Report to the Scottish Government 2017. www.sdf.org.uk/wp-content/uploads/2017/06/OPDP-mixed-methods-research-report-PDF.pdf (accessed 27 August 2020).
- Atkinson C. Service Responses for Older High-Risk Drug Users: A Literature Review 2016. www.sccjr.ac.uk/wp-content/uploads/2016/08/SCCJR-Report-062016.pdf (accessed 27 August 2020).
- Albert Kennedy Trust . LGBT Youth Homelessness: A UK National Scoping of Cause, Prevalence, Response and Outcome 2015. www.theproudtrust.org/wp-content/uploads/download-manager-files/AlbertKennedy_ResearchReport_Youth-Homelessness.pdf (accessed 27 August 2020).
- Advisory Council on the Misuse of Drugs . Drug-Related Harms in Homeless Populations and How They Can Be Reduced 2019. www.gov.uk/government/publications/acmd-report-drug-related-harms-in-homeless-populations (accessed 27 August 2020).
- Homeless Link . The Unhealthy State of Homelessness: Health Audit Results 2014 2014. www.homeless.org.uk/sites/default/files/site-attachments/The%20unhealthy%20state%20of%20homelessness%20FINAL.pdf (accessed 27 August 2020).
- Anderson I, Ytrehus S. Re-conceptualising approaches to meeting the health needs of homeless people. J Soc Policy 2012;41:551-68. https://doi.org/10.1017/S0047279412000220.
- Wise C, Phillips K. Hearing the silent voices: narratives of health care and homelessness. Issues Ment Health Nurs 2013;34:359-67. https://doi.org/10.3109/01612840.2012.757402.
- Queen AB, Lowrie R, Richardson J, Williamson AE. Multimorbidity, disadvantage, and patient engagement within a specialist homeless health service in the UK: an in-depth study of general practice data. BJGP Open 2017;1. https://doi.org/10.3399/bjgpopen17X100941.
- Lewer D, Menezes D, Cornes M, Blackburn R, Byng R, Clark M, et al. Hospital Readmissions Among People Experiencing Homelessness: A Cohort Study of Linked Hospitalisation and Mortality Data in England for 3,222 Homeless Inpatients 2019. https://ssrn.com/abstract=3475583 (accessed 7 January 2021).
- Zaretzky K, Flatau P, Spicer B, Conroy E, Burns L. What drives the high health care costs of the homeless?. Hous Stud 2017;32:931-47. https://doi.org/10.1080/02673037.2017.1280777.
- Mills ED, Burton CD, Matheson C. Engaging the citizenship of the homeless-a qualitative study of specialist primary care providers. Fam Pract 2015;32:462-7. https://doi.org/10.1093/fampra/cmv036.
- Pauly BB, McCall J, Browne AJ, Parker J, Mollison A. Toward cultural safety: nurse and patient perceptions of illicit substance use in a hospitalized setting. ANS Adv Nurs Sci 2015;38:121-35. https://doi.org/10.1097/ANS.0000000000000070.
- Rae BE, Rees S. The perceptions of homeless people regarding their healthcare needs and experiences of receiving health care. J Adv Nurs 2015;71:2096-107. https://doi.org/10.1111/jan.12675.
- O’Carroll A, Wainwright D. Making sense of street chaos: an ethnographic exploration of homeless people’s health service utilization. Int 2019;18. https://doi.org/10.1186/s12939-019-1002-6.
- Smith KG, Paudyal V, MacLure K, Forbes-McKay K, Buchanan C, Wilson L, et al. Relocating patients from a specialist homeless healthcare centre to general practices: a multi-perspective study. Br J Gen Pract 2018;68:e105-e113. https://doi.org/10.3399/bjgp18X694577.
- Wood L, Wood NJ, Vallesi S, Stafford A, Davies A, Cumming C. Hospital collaboration with a Housing First program to improve health outcomes for people experiencing homelessness. Hous Care Support 2019;22:27-39. https://doi.org/10.1108/HCS-09-2018-0023.
- Hwang SW, Burns T. Health interventions for people who are homeless. Lancet 2014;384:1541-7. https://doi.org/10.1016/S0140-6736(14)61133-8.
- Carver H, Ring N, Miler J, Parkes T. What constitutes effective problematic substance use treatment from the perspective of people who are homeless? A systematic review and meta-ethnography. Harm Reduct J 2020;17. https://doi.org/10.1186/s12954-020-0356-9.
- Fitzpatrick-Lewis D, Ganann R, Krishnaratne S, Ciliska D, Kouyoumdjian F, Hwang SW. Effectiveness of interventions to improve the health and housing status of homeless people: a rapid systematic review. BMC Public Health 2011;11. https://doi.org/10.1186/1471-2458-11-638.
- de Vet R, van Luijtelaar MJ, Brilleslijper-Kater SN, Vanderplasschen W, Beijersbergen MD, Wolf JR. Effectiveness of case management for homeless persons: a systematic review. Am J Public Health 2013;103:e13-26. https://doi.org/10.2105/AJPH.2013.301491.
- Pleace N. Effective Services for Substance Misuse and Homelessness in Scotland: Evidence from an International Review 2008. www.york.ac.uk/media/chp/documents/2008/substancemisuse.pdf (accessed 27 August 2020).
- National Institute for Health and Care Excellence . Alcohol Use Disorders: The NICE Guideline on the Diagnosis, Assessment and Management of Harmful Drinking and Alcohol Dependence n.d. www.nice.org.uk/guidance/cg115 (accessed 27 August 2020).
- Heather N, Raistrick D, Godfrey C. A Summary of the Review of the Effectiveness of Treatment for Alcohol Problems 2006. www.drugsandalcohol.ie/6178/1/3275-3458.pdf (accessed 27 August 2020).
- Pauly BB, Gray E, Perkin K, Chow C, Vallance K, Krysowaty B, et al. Finding safety: a pilot study of managed alcohol program participants’ perceptions of housing and quality of life. Harm Reduct J 2016;13. https://doi.org/10.1186/s12954-016-0102-5.
- Harm Reduction International . What Is Harm Reduction 2020. www.hri.global/what-is-harm-reduction (accessed 24 June 2020).
- Collins SE, Jones CB, Hoffmann G, Nelson LA, Hawes SM, Grazioli VS, et al. In their own words: content analysis of pathways to recovery among individuals with the lived experience of homelessness and alcohol use disorders. Int J Drug Policy 2016;27:89-96. https://doi.org/10.1016/j.drugpo.2015.08.003.
- Mancini MA, Linhorst DM, Broderick F, Bayliff S. Challenges to implementing the harm reduction approach. J Soc Work Pract Addict 2008;8:380-408. https://doi.org/10.1080/15332560802224576.
- Lee HS, Engstrom M, Petersen SR. Harm reduction and 12 steps: complementary, oppositional, or something in-between?. Subst Use Misuse 2011;46:1151-61. https://doi.org/10.3109/10826084.2010.548435.
- McNeil R, Small W. ‘Safer environment interventions’: a qualitative synthesis of the experiences and perceptions of people who inject drugs. Soc Sci Med 2014;106:151-8. https://doi.org/10.1016/j.socscimed.2014.01.051.
- Iversen L, Stevens A, Dale-Perera A. Reducing Opioid-Related Deaths in the UK: A Report of the Advisory Council on the Misuse of Drugs 2016.
- Collins SE, Clifasefi SL, Logan DE, Samples LS, Somers JM, Marlatt GA, et al. Harm Reduction: Pragmatic Strategies for Managing High-risk Behaviors. New York, NY: The Guilford Press; 2011.
- Pauly B, Wallace B, Pagan F, Phillips J, Wilson M, Hobbs H, et al. Impact of overdose prevention sites during a public health emergency in Victoria, Canada. PLOS One 2020;15. https://doi.org/10.1371/journal.pone.0229208.
- Hines L. The treatment views and recommendations of substance abusing women: a meta-synthesis. Qual Soc Work 2013;12:473-89. https://doi.org/10.1177/1473325011432776.
- Stead M, Parkes T, Nicoll A, Wilson S, Burgess C, Eadie D, et al. Delivery of alcohol brief interventions in community-based youth work settings: exploring feasibility and acceptability in a qualitative study. BMC Public Health 2017;17. https://doi.org/10.1186/s12889-017-4256-1.
- Neale J, Tompkins C, Sheard L. Barriers to accessing generic health and social care services: a qualitative study of injecting drug users. Health Soc Care Community 2008;16:147-54. https://doi.org/10.1111/j.1365-2524.2007.00739.x.
- van Boekel LC, Brouwers EP, van Weeghel J, Garretsen HF. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend 2013;131:23-35. https://doi.org/10.1016/j.drugalcdep.2013.02.018.
- Galbraith J. Homelessness workers negotiating the relationship between identity and practice: how gender, age and background influence worker-service user relationship. Hous 2019;37:198-213. https://doi.org/10.1080/14036096.2019.1584585.
- Johnsen S, Cuthill F, Blenkinsopp J. Qualitative Evaluation of Clinical Pharmacist Prescribing Input into the Care of People Experiencing Homelessness. Edinburgh: Institute for Social Policy, Housing and Equalities Research; 2019.
- McNeil R, Kerr T, Pauly B, Wood E, Small W. Advancing patient-centered care for structurally vulnerable drug-using populations: a qualitative study of the perspectives of people who use drugs regarding the potential integration of harm reduction interventions into hospitals. Addiction 2016;111:685-94. https://doi.org/10.1111/add.13214.
- Tiderington E, Stanhope V, Henwood BF. A qualitative analysis of case managers’ use of harm reduction in practice. J Subst Abuse Treat 2013;44:71-7. https://doi.org/10.1016/j.jsat.2012.03.007.
- Hoolachan J. Exploring the ‘spoiled’ and ‘celebrated’ identities of young and homeless drug users. Social Inclusion 2020;8:76-85. https://doi.org/10.17645/si.v8i1.2311.
- Neale J, Stevenson C. Social and recovery capital amongst homeless hostel residents who use drugs and alcohol. Int J Drug Policy 2015;26:475-83. https://doi.org/10.1016/j.drugpo.2014.09.012.
- O’Campo P, Kirst M, Schaefer-McDaniel N, Firestone M, Scott A, McShane K. Community-based services for homeless adults experiencing concurrent mental health and substance use disorders: a realist approach to synthesizing evidence. J Urban Health 2009;86:965-89. https://doi.org/10.1007/s11524-009-9392-1.
- Pauly B, Guirguis-Younger M, Hwang HS, McNeil R. Homelessness and Health in Canada. Ottawa, ON: University of Ottawa Press; 2014.
- Voronka J, Wise Harris D, Grant J, Komaroff J, Boyle D, Kennedy A. Un/helpful help and its discontents: peer researchers paying attention to street life narratives to inform social work policy and practice. Soc Work Ment Health 2014;12:249-79. https://doi.org/10.1080/15332985.2013.875504.
- Keats H, Maguire N, Johnson R, Cockersall P. Psychologically Informed Services for Homeless People: Good Practice Guide. London: Department for Communities and Local Government; 2012.
- Breedvelt J. Psychologically Informed Environments: A Literature Review 2016. www.mentalhealth.org.uk/sites/default/files/pies-literature-review.pdf (accessed 27 August 2020).
- PIElink . PIEs 2.0 2020. pielink.net/pies-2-0-the-up-dated-formulation/ (accessed 24 June 2020).
- Phipps C, Seager M, Murphy L, Barker C. Psychologically informed environments for homeless people: resident and staff experiences. Hous Care Support 2017;20:29-42. https://doi.org/10.1108/HCS-10-2016-0012.
- Jaman A. The Salvation Army youth and family services: a psychologically informed environment. Parity 2018;31.
- Ypeople . PIE n.d. www.ypeople.org.uk/about/resources/pie/ (accessed 24 June 2020).
- Miler JA, Carver H, Foster R, Parkes T. Provision of peer support at the intersection of homelessness and problem substance use services: a systematic ‘state of the art’ review. BMC Public Health 2020;20. https://doi.org/10.1186/s12889-020-8407-4.
- Byrne L, Wykes T. A role for lived experience mental health leadership in the age of Covid-19. J Ment Health 2020;29:243-6. https://doi.org/10.1080/09638237.2020.1766002.
- Gagne CA, Finch WL, Myrick KJ, Davis LM. Peer workers in the behavioral and integrated health workforce: opportunities and future directions. Am J Prev Med 2018;54:258-66. https://doi.org/10.1016/j.amepre.2018.03.010.
- Simpson A, Quigley J, Henry SJ, Hall C. Evaluating the selection, training, and support of peer support workers in the United Kingdom. J Psychosoc Nurs Ment Health Serv 2014;52:31-40. https://doi.org/10.3928/02793695-20131126-03.
- Repper J, Carter T. A review of the literature on peer support in mental health services. J Ment Health 2011;20:392-411. https://doi.org/10.3109/09638237.2011.583947.
- Johnson S, Lamb D, Marston L, Osborn D, Mason O, Henderson C, et al. Peer-supported self-management for people discharged from a mental health crisis team: a randomised controlled trial. Lancet 2018;392:409-18. https://doi.org/10.1016/S0140-6736(18)31470-3.
- Small W, Wood E, Tobin D, Rikley J, Lapushinsky D, Kerr T. The Injection Support Team: a peer-driven program to address unsafe injecting in a Canadian setting. Subst Use Misuse 2012;47:491-50. https://doi.org/10.3109/10826084.2012.644107.
- Bergamo S, Parisi G, Jarre P. Harm reduction in Italy: the experience of an unsanctioned supervised injection facility run by drug users. Drug Alcohol Today 2019;19:59-71. https://doi.org/10.1108/DAT-03-2018-0011.
- Deering KN, Kerr T, Tyndall MW, Montaner JS, Gibson K, Irons L, et al. A peer-led mobile outreach program and increased utilization of detoxification and residential drug treatment among female sex workers who use drugs in a Canadian setting. Drug Alcohol Depend 2011;113:46-54. https://doi.org/10.1016/j.drugalcdep.2010.07.007.
- Hayashi K, Wood E, Wiebe L, Qi J, Kerr T. An external evaluation of a peer-run outreach-based syringe exchange in Vancouver, Canada. Int J Drug Policy 2010;21:418-21. https://doi.org/10.1016/j.drugpo.2010.03.002.
- Kerr T, Oleson M, Tyndall MW, Montaner J, Wood E. A description of a peer-run supervised injection site for injection drug users. J Urban Health 2005;82:267-75. https://doi.org/10.1093/jurban/jti050.
- Bardwell G, Kerr T, Boyd J, McNeil R. Characterizing peer roles in an overdose crisis: preferences for peer workers in overdose response programs in emergency shelters. Drug Alcohol Depend 2018;190:6-8. https://doi.org/10.1016/j.drugalcdep.2018.05.023.
- Soukup-Baljak Y, Greer AM, Amlani A, Sampson O, Buxton JA. Drug quality assessment practices and communication of drug alerts among people who use drugs. Int J Drug Policy 2015;26:1251-7. https://doi.org/10.1016/j.drugpo.2015.06.006.
- Buchman DZ, Orkin AM, Strike C, Upshur REG. Overdose education and naloxone distribution programmes and the ethics of task shifting. Public Health Ethics 2018;11:151-64. https://doi.org/10.1093/phe/phy001.
- Pauly BB, Vallance K, Wettlaufer A, Chow C, Brown R, Evans J, et al. Community managed alcohol programs in Canada: overview of key dimensions and implementation. Drug Alcohol Rev 2018;37:132-9. https://doi.org/10.1111/dar.12681.
- Kerr T, Small W, Peeace W, Douglas D, Pierre A, Wood E. Harm reduction by a ‘user-run’ organization: a case study of the Vancouver Area Network of Drug Users (VANDU). Int J Drug Policy 2006;17:61-9. https://doi.org/10.1016/j.drugpo.2006.01.003.
- Ti L, Tzemis D, Buxton JA. Engaging people who use drugs in policy and program development: a review of the literature. Subst Abuse Treat Prev Policy 2012;7. https://doi.org/10.1186/1747-597X-7-47.
- McNeil R, Small W, Lampkin H, Shannon K, Kerr T. ‘People knew they could come here to get help’: an ethnographic study of assisted injection practices at a peer-run ‘unsanctioned’ supervised drug consumption room in a Canadian setting. AIDS Behav 2014;18:473-85. https://doi.org/10.1007/s10461-013-0540-y.
- Marshall Z, Dechman MK, Minichiello A, Alcock L, Harris GE. Peering into the literature: a systematic review of the roles of people who inject drugs in harm reduction initiatives. Drug Alcohol Depend 2015;151:1-14. https://doi.org/10.1016/j.drugalcdep.2015.03.002.
- Kennedy MC, Boyd J, Mayer S, Collins A, Kerr T, McNeil R. Peer worker involvement in low-threshold supervised consumption facilities in the context of an overdose epidemic in Vancouver, Canada. Soc Sci Med 2019;225:60-8. https://doi.org/10.1016/j.socscimed.2019.02.014.
- Broadhead RS, Heckathorn DD, Altice FL, van Hulst Y, Carbone M, Friedland GH, et al. Increasing drug users’ adherence to HIV treatment: results of a peer-driven intervention feasibility study. Soc Sci Med 2002;55:235-46. https://doi.org/10.1016/s0277-9536(01)00167-8.
- Walker G, Bryant W. Peer support in adult mental health services: a metasynthesis of qualitative findings. Psychiatr Rehabil J 2013;36:28-34. https://doi.org/10.1037/h0094744.
- Greer A, Buxton J, Group P. A Guide for Paying Peer Research Assistants: Challenges and Opportunities 2016. https://pacificaidsnetwork.org/files/2016/05/A-guide-for-paying-peer-research-assistants-challenges-and-opportunities.pdf (accessed 27 August 2020).
- Parkes T, MacAskill S, Brooks O, Jepson R, Atherton I, McGhee S, et al. Prison Health Needs Assessment for Alcohol Problems 2010. www.ohrn.nhs.uk/resource/policy/PrisonHealthNeedsAssessmentAlcohol.pdf (accessed 27 August 2020).
- Latkin CA, Sherman S, Knowlton A. HIV prevention among drug users: outcome of a network-oriented peer outreach intervention. Health Psychol 2003;22:332-9. https://doi.org/10.1037/0278-6133.22.4.332.
- Ti L, Hayashi K, Kaplan K, Suwannawong P, Wood E, Montaner J, et al. Willingness to access peer-delivered HIV testing and counseling among people who inject drugs in Bangkok, Thailand. J Community Health 2013;38:427-33. https://doi.org/10.1007/s10900-012-9635-z.
- Barker SL, Maguire N. Experts by experience: peer support and its use with the homeless. Community Ment Health J 2017;53:598-612. https://doi.org/10.1007/s10597-017-0102-2.
- Barker SL, Bishop FL, Bodley Scott E, Stopa LL, Maguire NJ. Developing a Model of Change Mechanisms within Intentional Unidirectional Peer Support (IUPS). Eur J Homelessness 2020;14:97-127.
- Jozaghi E, Reid AA. A case study of the transformative effect of peer injection drug users in the downtown eastside of Vancouver, Canada. Can J Criminol Crim Justice 2014;56:563-94. https://doi.org/10.3138/CJCCJ.2013.E30.
- Gillard S, Foster R, Gibson S, Goldsmith L, Marks J, White S. Describing a principles-based approach to developing and evaluating peer worker roles as peer support moves into mainstream mental health services. Ment Health Soc Incl 2017;21:133-43. https://doi.org/10.1108/MHSI-03-2017-0016.
- Jones M, Pietilä I. Alignments and differentiations: people with illness experiences seeking legitimate positions as health service developers and producers. Health 2020;24:223-40. https://doi.org/10.1177/1363459318800154.
- Eddie D, Hoffman L, Vilsaint C, Abry A, Bergman B, Hoeppner B, et al. Lived experience in new models of care for substance use disorder: a systematic review of peer recovery support services and recovery coaching. Front Psychol 2019;10. https://doi.org/10.3389/fpsyg.2019.01052.
- Gillard SG, Edwards C, Gibson SL, Owen K, Wright C. Introducing peer worker roles into UK mental health service teams: a qualitative analysis of the organisational benefits and challenges. BMC Health Serv Res 2013;13. https://doi.org/10.1186/1472-6963-13-188.
- Watson E. The growing pains of peer support. Ment Health Soc Incl 2017;21:129-32. https://doi.org/10.1108/MHSI-03-2017-0017.
- Voronka J. The mental health peer worker as informant: performing authenticity and the paradoxes of passing. Disabil Soc 2019;34:564-82. https://doi.org/10.1080/09687599.2018.1545113.
- Jacobson N, Trojanowski L, Dewa CS. What do peer support workers do? A job description. BMC Health Serv Res 2012;12. https://doi.org/10.1186/1472-6963-12-205.
- Barker SL, Maguire N, Bishop FL, Stopa L. Peer support critical elements and experiences in supporting the homeless: a qualitative study. J Community Appl Soc 2018;28:213-29. https://doi.org/10.1002/casp.2353.
- Pitt V, Lowe D, Hill S, Prictor M, Hetrick SE, Ryan R, et al. Consumer-providers of care for adult clients of statutory mental health services. Cochrane Database Syst Rev 2013;3. https://doi.org/10.1002/14651858.CD004807.pub2.
- Walker M, Beadman K, Griffin S, Beadman M, Treloar C. Involving peers in research: the UNSW community reference panel. Harm Reduct J 2019;16. https://doi.org/10.1186/s12954-019-0325-3.
- de Winter M, Noom M. Someone who treats you as an ordinary human being . . . Homeless youth examine the quality of professional care. Br J Soc Work 2003;33:325-38. https://doi.org/10.1093/bjsw/33.3.325.
- Terry L, Cardwell V. Refreshing Perspectives: Exploring the Application of Peer Research With Populations Facing Severe and Multiple Disadvantage 2016. www.revolving-doors.org.uk/file/1849/download?token=Yi0tjhmo (accessed 27 August 2020).
- Kaida A, Carter A, Nicholson V, Lemay J, O’Brien N, Greene S, et al. Hiring, training, and supporting peer research associates: operationalizing community-based research principles within epidemiological studies by, with, and for women living with HIV. Harm Reduct J 2019;16. https://doi.org/10.1186/s12954-019-0309-3.
- Murray E, Treweek S, Pope C, MacFarlane A, Ballini L, Dowrick C, et al. Normalisation process theory: a framework for developing, evaluating and implementing complex interventions. BMC Med 2010;8. https://doi.org/10.1186/1741-7015-8-63.
- McNaughton RJ, Steven A, Shucksmith J. Using normalization process theory as a practical tool across the life course of a qualitative research project. Qual Health Res 2020;30:217-27. https://doi.org/10.1177/1049732319863420.
- May C, Rapley T, Mair F, Treweek S, Murray E, Ballini L, et al. Normalization Process Theory On-Line Users’ Manual, Toolkit and NoMAD Instrument [Online] 2015. www.normalizationprocess.org/ (accessed 24 June 2020).
- McEvoy R, Ballini L, Maltoni S, O’Donnell CA, Mair FS, Macfarlane A. A qualitative systematic review of studies using the normalization process theory to research implementation processes. Implement Sci 2014;9. https://doi.org/10.1186/1748-5908-9-2.
- Hayes H, Buckland S, Tarpey M. Briefing Notes for Researchers: Public Involvement in NHS, Public Health and Social Care Research 2012. www.invo.org.uk/wp-content/uploads/2014/11/9938_INVOLVE_Briefing_Notes_WEB.pdf (accessed 27 August 2020).
- Laughton-Brown H. Psychodynamic contributions to counselling psychology practice. Couns Psychol Rev 2010;25:6-11.
- Mercer SW, Fitzpatrick B, Guthrie B, Fenwick E, Grieve E, Lawson K, et al. The CARE Plus study – a whole-system intervention to improve quality of life of primary care patients with multimorbidity in areas of high socioeconomic deprivation: exploratory cluster randomised controlled trial and cost-utility analysis. BMC Med 2016;14. https://doi.org/10.1186/s12916-016-0634-2.
- Neale J, Vitoratou S, Finch E, Lennon P, Mitcheson L, Panebianco D, et al. Development and validation of ‘SURE’: a patient reported outcome measure (prom) for recovery from drug and alcohol dependence. Drug Alcohol Depend 2016;165:159-67. https://doi.org/10.1016/j.drugalcdep.2016.06.006.
- Mercer SW. CARE Patient Feedback Measure 2004. www.gla.ac.uk/media/Media_65352_smxx.pdf (accessed 7 January 2021).
- Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006;166:1092-7. https://doi.org/10.1001/archinte.166.10.1092.
- Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr Ann 2002;32:509-15. https://doi.org/10.3928/0048-5713-20020901-06.
- Marsden J, Gossop M, Stewart D, Best D, Farrell M, Lehmann P, et al. The Maudsley Addiction Profile (MAP): a brief instrument for assessing treatment outcome. Addiction 1998;93:1857-67. https://doi.org/10.1046/j.1360-0443.1998.9312185711.x.
- RAND Healthcare . 36-Item Short Form Survey (SF-36) 2018. www.rand.org/health-care/surveys_tools/mos/36-item-short-form.html (accessed 27 August 2020).
- Milaney K, Williams N, Lockerbie SL, Dutton DJ, Hyshka E. Recognizing and responding to women experiencing homelessness with gendered and trauma-informed care. BMC Public Health 2020;20. https://doi.org/10.1186/s12889-020-8353-1.
- Neale J, Black L, Getty M, Horgan C, Lennon P, Lora C, et al. Paying participants in addictions research: is cash king?. J Subt Use 2017;22:1-3. https://doi.org/10.1080/14659891.2016.1259367.
- Ritchie J, Lewis J, McNaughton Nicholls C, Ormston R. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: SAGE Publications Ltd; 2013.
- Birt L, Scott S, Cavers D, Campbell C, Walter F. Member checking: a tool to enhance trustworthiness or merely a nod to validation?. Qual Health Res 2016;26:1802-11. https://doi.org/10.1177/1049732316654870.
- Sweeney A, Greenwood KE, Williams S, Wykes T, Rose DS. Hearing the voices of service user researchers in collaborative qualitative data analysis: the case for multiple coding. Health Expect 2013;16:e89-99. https://doi.org/10.1111/j.1369-7625.2012.00810.x.
- European Parliament, Council of the European Union . General Data Protection Regulation (GDPR) n.d. https://gdpr.eu/tag/gdpr/ (accessed 2 December 2020).
- Thoma A, Farrokhyar F, McKnight L, Bhandari M. How to optimize patient recruitment. Can J Surg 2010;53.
- Ferguson KM, Xie B. Feasibility study of the social enterprise intervention with homeless youth. Res Soc Work Pract 2008;18:5-19. https://doi.org/10.1177/1049731507303535.
- Kroenke K, Wu J, Yu Z, Bair M, Kean J, Stump T, et al. The Patient Health Questionnaire Anxiety and Depression Scale (PHQ-ADS): initial validation in three clinical trials. Psychosom Med 2016;78:716-27. https://doi.org/10.1097/PSY.0000000000000322.
- RAND Healthcare . 36-Item Short Form Survey (SF-36) Scoring Instructions n.d. www.rand.org/health-care/surveys_tools/mos/36-item-short-form/scoring.html (accessed 25 June 2020).
- Bion WR. Elements of Psycho-analysis. Oxford: Butterworth–Heinemann; 1963.
- Zinberg NE. Drug, Set, and Setting: The Basis for Controlled Intoxicant Use. New Haven, CT: Yale University Press; 1984.
- Warburton H, Turnbull PJ, Hough M. Occasional and Controlled Heroin Use: Not a Problem? 2005. www.jrf.org.uk/sites/default/files/jrf/migrated/files/1859354254.pdf (accessed 27 August 2020).
- Shewan D, Dalgarno P. Evidence for controlled heroin use? Low levels of negative health and social outcomes among non-treatment heroin users in Glasgow (Scotland). Br J Health Psychol 2005;10:33-48. https://doi.org/10.1348/135910704X14582.
- Hartogsohn I. Constructing drug effects: a history of set and setting. Drug Sci Policy Law 2017;3:1-17. https://doi.org/10.1177/2050324516683325.
- Lee HS, Zerai A. ‘Everyone deserves services no matter what’: defining success in harm-reduction-based substance user treatment. Subst Use Misuse 2010;45:2411-27. https://doi.org/10.3109/10826081003712060.
- Hawe P, Shiell A, Riley T. Complex interventions: how ‘out of control’ can a randomised controlled trial be?. Br Med J 2004;328. https://doi.org/10.1136/bmj.328.7455.1561.
- MacLellan J, Surey J, Abubakar I, Stagg HR, Mannell J. Using peer advocates to improve access to services among hard-to-reach populations with hepatitis C: a qualitative study of client and provider relationships. Harm Reduct J 2017;14. https://doi.org/10.1186/s12954-017-0202-x.
- Barker SL, Maguire N, Bishop FL, Stopa LL. Expert viewpoints of peer support for people experiencing homelessness: a Q sort study. Psychol Serv 2019;16:402-14. https://doi.org/10.1037/ser0000258.
- Mercer SW, O’Brien R, Fitzpatrick B, Higgins M, Guthrie B, Watt G, et al. The development and optimisation of a primary care-based whole system complex intervention (CARE Plus) for patients with multimorbidity living in areas of high socioeconomic deprivation. Chronic Illn 2016;12:165-81. https://doi.org/10.1177/1742395316644304.
- Sun S, Irestig R, Burström B, Beijer U, Burström K. Health-related quality of life (EQ-5D) among homeless persons compared to a general population sample in Stockholm County, 2006. Scand J Public Health 2012;40:115-25. https://doi.org/10.1177/1403494811435493.
- Jaffray M, Matheson C, Bond CM, Lee AJ, McLernon DJ, Johnstone A, et al. Does training in motivational interviewing for community pharmacists improve outcomes for methadone patients? A cluster randomised controlled trial. Int J Pharm Pract 2014;22:4-12. https://doi.org/10.1111/ijpp.12049.
- Pathway . What We Do, Teams n.d. www.pathway.org.uk/about-us/what-we-do/about-us-what-we-do-teams/ (accessed 30 June 2020).
- Scottish Violence Reduction Unit . Navigator n.d. www.svru.co.uk/navigator/ (accessed 25 June 2020).
- Cooper V. No Fixed Abode: The Implications for Homeless People in the Criminal Justice System 2013. https://howardleague.org/wp-content/uploads/2016/04/No-fixed-abode-report.pdf (accessed 27 August 2020).
- Merrall EL, Kariminia A, Binswanger IA, Hobbs MS, Farrell M, Marsden J, et al. Meta-analysis of drug-related deaths soon after release from prison. Addiction 2010;105:1545-54. https://doi.org/10.1111/j.1360-0443.2010.02990.x.
- Staniszewska S, Brett J, Simera I, Seers K, Mockford C, Goodlad S, et al. GRIPP2 reporting checklists: tools to improve reporting of patient and public involvement in research. BMJ 2017;358. https://doi.org/10.1136/bmj.j3453.
- UK Public Involvement Standards Development Partnership . UK Standards for Public Involvement in Research: Better Public Involvement for Better Health and Social Care Research 2019. https://sites.google.com/nihr.ac.uk/pi-standards/standards (accessed 27 August 2020).
- Liabo K, Boddy K, Bortoli S, Irvine J, Boult H, Fredlund M, et al. Public involvement in health research: what does ‘good’ look like in practice?. Res Involv Engagem 2020;6. https://doi.org/10.1186/s40900-020-0183-x.
Appendix 1 Changes to protocol
| Version number | Revision date | Previous revision date | Summary of changes |
|---|---|---|---|
| 1.0 | 25 April 2018 | ||
| 1.1 | 28 August 2018 | 25 April 2018 | Addition of Rebecca Foster’s (Research Fellow) details, updated health check measures, information about the health check, update to completion date of meta-ethnography, confirmation of the use of Atlas, Catriona Matheson added to project management team, confirmation of ethics approval |
| 1.2 | 1 November 2018 | 28 August 2018 | Changes to data collection approach for holistic health checks, change to recruitment of PNs, amended duration of interview with intervention participants |
| 1.3 | 3 December 2018 | 1 November 2018 | Changes to duration of intervention for Liverpool sites and sample, in the light of PN resignation; change in approach for participants who have dropped out (from interview with peer researcher to questionnaire); reduced number of participants for intervention interviews; change to standard care measures (from a manager or worker to researcher); updated reference list; updated study flow chart |
| 1.4 | 23 April 2019 | 3 December 2018 | Changes to staff position/role and additions to team; update on an organisational take-over; change to sample size for intervention participants and associated interviews (back to original sample size and following discussion with Research Manager on reporting practicalities); extension of recruitment period; alteration to peer research approach, including informed consent process |
| 1.5 | 4 June 2019 | 23 April 2019 | Changes to team – Miler replacing Patrick and update on Clark leaving the team; increase in the number of PN interviews and additional interview involving collection of case study data; change in approach to involving peer researchers and PPI group in qualitative analysis for practical reasons |
| 1.6 | 8 August 2019 | 4 June 2019 | Changes to team – addition of Price, Schofield and Cobbett Ondiek to study team and change in Burridge’s (SSG and PPI member) job; change in approach to involving peer researchers and PPI group in qualitative analysis for practical reasons – specifically, because of a lack of availability of peer researchers |
Appendix 2 Participant case studies (n = 6)
All names are participant-selected pseudonyms.
Charlie
I first heard about Charlie at the handover meeting at the service I work in. Charlie’s behaviour was mentioned – he’d had a bad weekend and some members of staff thought that they should ask him to leave immediately because of this.
In the meeting, I challenged this – we need to understand people’s behaviour, following the PIEs approach. I offered to sit down with Charlie and have a chat with him around his behaviour. I sat and spoke to him about his life and how he ended up here and all sorts of things for probably a good hour or two.
I started working with him more or less straightaway after this. I just said ‘I am always here if you want to talk about absolutely anything – just give me a shout and we will go and have a cup of coffee’. So I left that open to him, and after probably 3 or 4 days he just came and said ‘can I have a chat with you?’.
When I first started working with him, his issues included anxiety about moving into a new building and a new city. He had crack, heroin and alcohol addiction. At the beginning, I sat down and explained my background to him and all my own issues, so he knew he wasn’t getting judged on anything by me. I had that understanding of some of the stuff he was going through and where he was at, at the same time knowing his journey is different from mine.
Then we got his script sorted out and I supported him to keep working with another service. He had very little money as well, so at that time we were sorting food parcels and doing practical things.
We did a lot of sitting and talking. I was interested in finding out about his life, basically. He explained what had happened to him in his past, and then his drug issues came out later. I mentioned about introducing him to a community psychiatric nurse (CPN), which he was interested in – he then started working with them.
Our relationship is really good – we have lots of banter. We are both from a similar area – we chat about what life was like living there, we chat about football, we’ve chatted about everything basically.
It took him a while (probably a couple of months) for him to be able to come to me and say that he had ended up using drugs when he didn’t want to. My response to him (as with others) is ‘right, I really appreciate you coming to tell me that, because this is what it’s all about, being honest with each other so that we can help each other, working as that team to help each other’. So then it’s ‘what do we do next?’. Your most important move is your next one, you know what I mean, you’ve already done that, you’ve already used, so it’s what do we do next after that?
I’ve found Charlie really a pleasure to work with. Where he’s at now, he is doing amazingly well, absolutely brilliantly. He’s not using drugs at all – no heroin, no crack, and he hasn’t done for 3 months, minus one slip-up.
He is currently volunteering working with people who are in hospital. He wants to go into similar type of work to what I am doing and he’s about to start a qualification. I’ve been in touch with the volunteer co-ordinator in another service for when he has his qualification – other options for him to look into.
Charlie likes going camping and in the past he liked canoeing and being outdoors. So, at the end of the month, I am taking him and some others on a little camping trip, just for the night. We are going down to the river – we’re going to have a barbecue, do a bit of fishing and just have a nice chilled-out time – hopefully have a little swim too!
He’s still got his anxieties – this is why I’ve explained to him again about my past. I’ve explained how I had my anxieties when I came off certain drugs and when I went into this type of work. I told him that before, when it was coming around to my turn to speak in a team meeting, I’d have already rehearsed 20 or 30 times in my head the night before what I was going to say. Then when I spoke I’d feel myself going red and I’d be like sitting there thinking like ‘everyone can see me going red’. Then I say to him ‘listen, the more you learn and the more knowledge you get around things, then you are going to feel more comfortable, because you are then confident in your own ability to be able to do this’. So I say ‘just take your time’.
He’s doing really well. I am proud. When participants say to me ‘I couldn’t have done this without you’, I say ‘well you can, we’ve worked together as a team, it’s been an equal partnership, I do what I can do for you and you do what you can do for you’. I am very proud of what Charlie has gone on to achieve.
Charlie knows I’ve got that understanding – I’m not judging him around anything. He’s said to me ‘I just really appreciate all your support and what you’ve done and just being able to talk to you’.
William
I met William when he was volunteering and we were both sorting food for people in the service I work in. He asked about what job I was doing and I explained about the job and the study. We had a bit of time and then I just said to him ‘why don’t you come up and have a chat with me sometime?’.
He then came to see me. We had a chat for a good few hours. And then it just built slowly over the next few weeks. His issues were around his alcohol use – he told me that he’s had problems with alcohol for a lot a lot of years. He wouldn’t class himself as an alcoholic – he was more a binge drinker. But then he got to the point when he was drunk he was making the terrible decision of starting to smoke crack as well, and then at certain times he was offered heroin.
He had quite a lot going on in his personal life, with relationship issues and family members unwell. He was just trying to adjust to the situation really, and he had quite a bit of trouble with that.
I spent a lot of time sitting down and talking to him, speaking to him about his situation, letting him open up about things, and giving him some emotional support around all these things. It’s taken a bit of time, around 8 months, for William to start being properly honest with me about his using. I’d see him and wonder how he was doing and ask him, but he’d deny it. I just kept saying ‘listen mate, I am not judging you, I am not going to judge you, if you come and sit in the room with me and tell me you’ve used some crack and some alcohol, then I don’t judge you on that, why would I judge you, you know?’, so I had to keep getting that across to him.
We put in place a case so that he could move on from this service. He’s now living in his own place in an area he wanted to move to for a while. He’s happy in his new place and we managed to get him loads of furniture. We got him a little settee, a microwave, cutlery, units and a bed, so we got him all sorted out with that side of things. There’s still a couple more things that I am going to get for him. I’ve asked him to have a look on Freecycle [www.freecycle.org (accessed 30 November 2020)] too. He had to adjust to moving into this environment and now he’s having to adjust again to going back out into living in a totally different place.
He’s signed up now with another organisation to help him with his alcohol, just in case he needs it. He’s got his first appointment with them this week, so I’m going with him. I said ‘I think it’s important to get this put in place for you, just in case things escalate. So there is already that support put in place for you.’.
He’d been applying for jobs and he recently got accepted for one. He just needed to get a qualification for it (one more certificate). He explained this to me on the phone, so I told him I’d meet him the following week and said I’d pay for him to get the certificate done (out of study funds). I met him off the train, sorted out his fares, and accompanied him to the service. It took him a day to go through all the educational stuff – what he needed to learn before taking the test. Then the following week he came to the service again and did the test. He passed. He’s now got his qualification and he was offered the job.
He’s actually amazed about that, he’s very proud. He’s really looking forward to starting his new job, and it’s going to help him out money-wise too. He now tells me when he’s had a drink and we just chat about this, I just keep saying to him ‘don’t let it escalate, do you know what I mean, because you’ve got everything going for you there’.
We have a really good relationship. He’s said how much I’ve been there for him, that I’d never turn my back on him, that I have always carried on supporting him, so I’ve had some really nice texts off him. Like this one:
Thanks for all your help today and every other day, you’ve made times for me, wouldn’t be here without your help, much appreciated, William.
And then I put, ‘cheers mate but remember we have done this as a team, good to see you’.
And then last week he texted me:
this is the first time I’ve celebrated with fish and chips and not drugs or alcohol, thank you.
And I put ‘bet it was more rewarding mate, proud of you, have a good weekend.’.
And then he texted to say he had gotten drunk and said he had let everyone down. I put:
that all depends on if you keep repeating the mistake or deal with it and remember you never let me down, will call later. I am at the gym, off work today.
And I’ve just put this morning:
leave message when you get this and I will call you, don’t worry about things it’s happened, what have I always said? Your next move is the most important and anything you want to talk about, I am here.
I think he was worried that when he left the service that he wouldn’t get the support and that I wouldn’t be there to support him, but we have still been meeting every couple of weeks. William often says nice little things like ‘thanks for your help today and every day’ and about not giving up on him.
Christie
I met Christie in one of the services that I work in. I had seen her around and I’d had brief chats with her. Her previous Support Worker in that service had left and it wasn’t clear who would replace them. I also learnt that she was in between CPNs and in between psychiatrists. I got a sense from her that she felt like she used to have quite a lot of support in place – then she got a tenancy and she was floating about and not feeling supported anywhere. She now felt a bit sidelined, but she was still struggling a lot with drug issues and had an ongoing volatile situation with her ex-partner.
She was the first person I started working with. I offered to do some work with her and see how we got on; she was open and welcoming to that. I’ve done a lot of one-to-ones with her – giving her the space to talk with someone who will listen. Initially, I spent a lot of time helping with practical stuff, including ironing out some benefits issues and supporting her and reassuring her that it was going to be all right.
I encouraged her to attend groups, which she did on and off. It sometimes felt like she would pull away or do reasonably well for a short period of time and then an ex-partner or some specific mates would come to stay or drop in, and she’d relapse and she’d be using again sporadically. So I did quite a lot of very informal relapse prevention work and a bit of anger management support as well.
I have found connecting with Christie relatively easy. She is very open and forthcoming. Our contact fluctuated a lot in the beginning and still can, although, it seems to have settled into its own pattern, so it doesn’t worry me. She is also much more settled now.
I have found working with Christie and witnessing her progress a privilege. It’s been nice to build that relationship. She will share some stuff that I get the sense she doesn’t share with most people. She listens to my opinion on things and doesn’t get defensive if I challenge some of her attitudes. She is open to it and we can both just be quite upfront.
A good proportion of the progress she’s made I don’t feel that I’ve had that much to do with, although I may have done in a roundabout way. For example, I encouraged her to go to a different service and meet some different people. I think this has had a big impact and opened her world up a bit. It’s shown her that there is other support out there and you have to put your best foot forward and go out and get it – you have to get a bit uncomfortable to go and investigate it because it’s not all going to come to you.
Christie’s made significant progress with her using. She is now having longer and more frequent contact with her child. She is more stable on her prescription after going up the dosage slightly – she was reluctant to do this at first because she was worried that they would put her back on testing with a daily pick-up, but this didn’t happen. I attended a few GP appointments with her, telling her about my experience of working with doctors and my perception of the doctor’s attitude, which was really positive and supportive – this helped her to make the decision to increase her dose.
She is currently seeking some support for an eating disorder, which seems to have become more problematic as the substance use has declined. She has started volunteering at a local stables, which she is really enjoying. It has rekindled a childhood passion that she had. I think her life looks very different from what it did 6 or 7 months ago. There is still a lot of stuff that could do with looking at and being healed, some of which I am probably not the best placed to try and facilitate, but I can be a go-between, hopefully.
Christie wants to stay drug free, to continue volunteering and to stay involved with the stuff that she is doing. She lights up when she talks about it all, so I just think that’s a no-brainer – that’s something to keep pursuing. She wants to keep building on her family relationships, and engage with support for mental health and her eating disorder.
She often says to me ‘I know there is no point bullshitting you’. The relationship is strong enough to know that there is no judgement in any of it. But think the other part is just almost a realisation: ‘I can’t blag you, like, if I wanted to, or if I felt I needed to I probably couldn’t pull it off anyway. Because you can’t bullshit a bullshitter! You have been there so I can’t get around you; I might as well just tell you this is what I’ve been up to!’
After our most recent meet-up, Christie texted me and said ‘thanks for talking to me about my weight and eating. I feel no one else wants to listen, so I really appreciated you sitting with me when I phoned today [a service]’.
Sean
I was referred to Sean after he’d been discharged from hospital. I started to work with him through informal meet-ups and phone contact. He felt discriminated against in one of his appointments and he was having issues accessing the aftercare he needed. When I met him, he was homeless. He was using drugs sporadically and he was struggling with pain management.
When we started off, contact was a bit sporadic. It took time to build trust. I feel like he was a little bit sceptical to start with. I think there was a patch of time where what was going on and what was said was going on were two totally different things. And it almost just played itself out. Some stuff kind of came up and sparked Sean to re-engage and potentially put a bit more effort in himself and a bit more honesty.
In that time I didn’t want to challenge him too strongly. I wanted to allow him space to think and to keep the door and offer open. I knew that it would shift, but knew it wasn’t going to shift when I wanted it to – it was almost just playing the waiting game and allowing that, which did happen. There was a lot of learning in this for me as well – to just allow a process to run its course a bit really, I think, and not try and meddle in it too much.
Our relationship now is good and a lot more straightforward. We have regular meet-ups. We made a homeless application. I accompanied him to the doctors and helped him to get these appointments. We made a PIP [Personal Independence Payment] application and I supported him to the assessment, which was successful. He goes to groups at one of the services. I made a referral and supported him to a service to get him signed up for some training – we are in the middle of that process just now. We’ve sorted his bus pass out and I’m encouraging him to regularly bid for new tenancies.
Early on, he was a bit fragile and the focus was on meeting up and getting him a cuppa. But I think that was probably some of the most meaningful work, and that probably laid the groundwork for him wanting to re-engage after that little bit of patchy time.
Sean is much more settled now. He’s in a relationship. He’s looking a lot better. He’s put on quite a bit of weight. He’s drug free. He enjoys attending the group session and always has a really good input to it. I think his confidence has improved quite a lot. And I get a sense that he’s thinking more about the future and where he might go next, as opposed to where he’s been and feeling stuck. This is just lovely to see.
He’s working towards employment and training – looking at using his time meaningfully and finding stuff to get his teeth stuck into, really. I think when we first started working together he thought his life was a done deal. I think he thought his past was going to define his future and that he was going to be restrained by that and not ever break out of that. I think this will be a big part, hopefully, of him realising that this is not the case.
We have spoken about that kind of stuff he wants to do – to remain drug free, to possibly start a voluntary position in the near future if we can see something that he’d like to get involved in. His new relationship is really important to him too. I think he’s starting to find his voice and some aspirations for the future and realise that there is a big wide world out there and there is a right life and a calling and a passion with his name on it if he wants to come out and find it.
He’s sent me some nice texts to thank me for my support. One is:
I hope you feel good about this positive change in me you’ve played the most important part I am grateful to you.
And then another one is:
you’ve been a good rock to me I respect that. Too many gave up on me, you hadn’t, I enjoyed today, I knew when we first spoke that I respected you.
It took some time for honesty to improve. I believe a constant offer of unconditional support made the difference between engaging with me properly and not.
Simon
I met Simon in passing at a service. He really stood out; he was quiet and he just seemed quite clean cut. He was quite sceptical of me and that was sort of exemplified when he overheard me talking to another member of staff. I was very new in the role and I said that I was struggling to get people to engage with me, or at least I was finding that difficult. He overheard and said something like ‘are the lab rats not playing ball?’ I approached him and said sorry if it had come across like that and I introduced myself.
At the time he was also using another service that I have connections with. But then he ended up in hospital and I got a referral. I met him in hospital and we had some quite good conversations there.
He’d jumped right out of his B&B window, in some sort of psychosis, likely from his attempted home detox. He was in a bad way – he had a broken back, pelvis, fractures everywhere. I met him a few times in the hospital, gave him some books and we spoke about spiritual stuff. He shared some of the stuff with me that had happened to him and what he’d been through. I just said that I would be willing to help him even if he didn’t sign up to the study, and I meant it.
Initially, I was trying to chase up stuff about what was going to happen after he got out of hospital, about what benefits he was on, social work and so on. He was homeless. At that time he was obviously in a physically bad way, but also psychologically, and feeling completely hopeless. I learned that he’d been on heroin for a number of years and had experienced lots of trauma and tragedies.
He was very grateful for the support that I was able to offer initially while he was in hospital. He seemed to light up a bit when I was there. We’d have a laugh about how terrible the situation was for him – that kind of black humour. I’d share a bit of my experience about the hopelessness and then getting into recovery and we’d discuss spiritual stuff. I’d try and use motivational interviewing a bit, which I think he tolerated! He’s quite a charming guy. He can be quite funny, so spending time with him was good. He’s an intelligent guy as well.
When he was discharged, he was given a hotel in a different part of the city. He had no bus pass, no money, no way to get any food, or to travel. He had a wheelchair with him, but he couldn’t wheel it very easily, given his injuries.
I picked him up to take him to get his scripts and I sorted and collected food parcels for him. I took him to a service to get his benefits sorted out and helped him to apply for alternative accommodation. I also took him to some recovery meetings. We got him a clothing grant too.
His physical recovery has been amazing, though I think he’s going to be left with a bit of damage. His benefits have been increased. He is being well supported by staff in his new accommodation. He is still using, but he’s on a prescription now. He has ups and downs with his using – when I see him he says he wants to quit for good, but then something gets in the way. I just need to continue to offer my hand of support, which I do. I call him a couple of times a week, probably, and that’s all he’s really wanting to do at the moment. He’s talking about moving away to another country and I’ve spoken to him about that – about fixing problems inside as well as outside.
He was emphatically grateful for the support I gave him at the beginning. He said ‘no one else would have helped, that I’ve just been left here and if it wasn’t for you I would, I would be worried that I would still be here’. I’ve heard him pulling up others if they’ve been critical of groups that I run. He’s always been aware that a lot of the times I’ve been going above and beyond, and he definitely appreciates that.
Ally
I met Ally very early on in one of the services I worked in. I introduced myself, and played with his dog.
He was immediately very open about his past trauma and the way that he’d been let down by people, particularly men. That sort of gave me a bit of licence to share a bit of my experience around personal trauma.
He had been using heroin for a long time. He was homeless – he had left his tenancy and was sleeping rough. He was very traumatised and his behaviour could be a bit unpredictable at times. He was very wary of other people and, if he felt threatened, he could be quite growly with people. He was physically unwell, with abscesses on his legs. He’d spent a lot of time in institutions and had experienced a lot of trauma.
I started to work with him immediately. He needed support to get on a script, which I gave him – it took a bit of time because he was so chaotic and because he wasn’t registered with a GP practice.
After my efforts to get him onto a script, he warmed to me a little more. We discussed the trauma he’d experienced, and he told me that he was very wary of male workers (he exclusively works with women). I am his only male worker and he says that is because I have no power over him – I treat him as an equal.
At one point, it was so cold outside that we were both worried for his safety and so we tried to find dog-friendly accommodation. This wasn’t possible, so I spent a day trying to get his dog separately looked after to get Ally off the streets.
He spent quite a bit of time with me. He came to group sessions and we’d get coffees and we sorted out his housing situation. I got his dog a vet appointment, despite him having no ID [identification] for her, and I’m looking into the possibility of getting her trained as a therapet with him.
He ended up in prison for a few months. While he was in prison, I visited him and wrote him letters. I handed him in some cash to keep him going with essentials. He actually gave me a hug when we said goodbye at the visit and that sort of sat with me for a couple of days, as it was quite something.
During his sentence, he had a hearing in court. I waited outside for 3 hours because I wanted him to see that I was there, but then I was told that the policy has changed, and when someone gets released from court, they go back to the prison, and no one told me. It was annoying but I just wanted him to see me waiting outside, there for him.
We sorted out his housing situation again when he got out. I think he struggles with continually feeling let down, and his agitation can become more visible in our interactions – but that’s fine – I just see a hurt person, and sometimes we do have a laugh as well. I can see the graft he is willing to put in to improve his situation. Like, even walking down the street just a couple of days ago from his accommodation to come and see me, when he is struggling so much physically and mentally.
We’ve got his PIP reinstated and him signed up for Universal Credit. He’s got a safe place to stay and I’m helping him with his script again.
He wants to do some volunteering. He wants to not use drugs or to only smoke weed. He said that, on his second day out of prison, he cooked up a hit after his first night out, but then he started trembling, so much so that he was just terrified. So he just squirted it out, and then he smoked it that night. He just wants to be able to just smoke weed and get to that point.
He appreciates the extra stuff that I’ve done to try and make sure that he’s OK, to try to help, and he thanks me for all that. I get a lot from this and from working with him.
Glossary
- Disclosure and Barring Service
- Often in the context of ‘Disclosure and Barring Service check’ for working with vulnerable individuals/groups.
- Lifehouse
- Salvation Army-managed residential setting/hostel.
- Protecting Vulnerable Groups
- Often in the context of ‘Protecting Vulnerable Groups check’ for working with vulnerable individuals/groups.
List of abbreviations
- A&E
- accident and emergency
- B&B
- bed and breakfast
- CARE
- Consultation and Relational Empathy
- CHI
- Community Health Index
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- CPN
- community psychiatric nurse
- EbyE
- Experts by Experience
- EQ-5D
- EuroQol-5 Dimensions
- ETHOS
- European Typology of Homelessness and Housing Exclusion
- GAD-7
- Generalised Anxiety Disorder-7
- GDPR
- General Data Protection Regulation
- GP
- general practitioner
- LGBTQ+
- lesbian, gay, bisexual, transgender, queer, + includes any individual who feels that they do not fit into these categories, including intersex and asexual individuals
- MAP
- Maudsley Addiction Profile
- NICR
- NHS, Invasive or Clinical Research
- NIHR
- National Institute for Health Research
- NPS
- novel psychoactive substance
- NPT
- normalisation process theory
- OST
- opioid substitution therapy
- PHQ-9
- Patient Health Questionnaire-9 items
- PHQ-ADS
- Patient Health Questionnaire Anxiety and Depression Scale
- PIE
- psychologically informed environment
- PIP
- Personal Independence Payment
- PN
- Peer Navigator
- PPI
- patient and public involvement
- PVG
- Protecting Vulnerable Groups
- RAND SF-36
- RAND Corporation Short Form survey-36 items
- RCT
- randomised controlled trial
- SACASR
- Salvation Army Centre for Addiction Services and Research
- SD
- standard deviation
- SDF
- Scottish Drugs Forum
- SHARPS
- Supporting Harm Reduction through Peer Support
- SSG
- Study Steering Group
- SURE
- Substance Use Recovery Evaluator
- TSA
- The Salvation Army
