Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 11/148/01. The contractual start date was in March 2014. The draft report began editorial review in July 2016 and was accepted for publication in January 2017. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Mark Gabbay reports grants from the National Institute for Health Research (NIHR) during the conduct of the study and membership of the Health Technology Assessment (HTA) Devices Topic Identification Development and Evaluation board. Rod Taylor reports membership of HTA Themed Call and HTA Efficient Study Designs Boards.
Disclaimer
This report contains transcripts of interviews conducted in the course of the research and contains language that may offend some readers.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2017. This work was produced by Gabbay et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
In 2012, the National Institute for Health Research (NIHR) Health Technology Assessment (HTA) programme invited research teams to submit proposals to evaluate the clinical effectiveness and cost-effectiveness of an intervention to integrate debt counselling and advice within a primary care setting (HTA commission call number 11/148). The research question set out in the commissioning brief was ‘Does the provision of debt counselling and advice in primary care improve the health and well-being of people with depression and related debt problems compared with usual GP care?’. 1
In response to this call, we designed an adaptive, parallel, two-group, multicentre randomised controlled trial [Debt Counselling for Depression in Primary Care: an adaptive randomised controlled pilot trial (DeCoDer)] with a nested mixed-methods process and economic evaluation.
The purpose of our trial was to deliver an intervention for patients with depression and worries about debt within a primary care setting. The intervention was debt advice from a Citizens Advice Bureau (CAB) advisor that incorporated a shared biopsychosocial assessment by a general practitioner (GP) and debt advisor. We planned to evaluate this intervention in terms of its clinical effectiveness and cost-effectiveness, collecting data at baseline and at 4 and 12 months, to compare mental health, well-being and cost-effectiveness outcomes. We also planned to assess the acceptability and accessibility of the intervention, and facilitators of and barriers to recovery through both quantitative and qualitative data collection. We conducted an internal pilot trial to test the procedures, recruitment processes and operational strategies planned for use in the main trial, so that we could identify and resolve any problems and thereby assess the feasibility of continuing with the main trial. As a result of issues related to practice recruitment, trial set-up and participant recruitment, the target sample size for the pilot trial was not achieved according to the pre-defined stopping rules. After consultation with the NIHR HTA, the trial was stopped and data collection was completed at 4 months for those already recruited at that stage.
Given that the study failed to reach its recruitment target and was terminated early during the internal pilot phase, and therefore did not progress to main trial, we report here the findings of the pilot trial including descriptive statistics [mean and standard deviation (SD)] for the primary, secondary and economic outcomes by group, at baseline, and at 4- and 12-month follow-up (when available). We also present the findings of our qualitative analyses concerning participants’ experiences of debt and depression, the intervention and their involvement in the trial. Using the normalisation process theory (NPT) approach,2 we report some of the potential barriers to and facilitators of implementing the intervention in practice.
We also report in detail the recruitment process and outcomes, our comparison of cluster versus individual randomisation and the various challenges we faced in trial set-up and in recruiting general practices and participants to the study. Our account provides key learning points that will be particularly beneficial to future researchers planning randomised controlled trials with hard-to-reach and vulnerable groups in primary care. This group of patients is typically those who are suffering the greatest health inequalities and it is, therefore, important for the future of research design to understand how we can access such patients and maximise data collection in these populations.
We note at this point that by the time the current study had been approved for funding and was ready to commence recruitment, an advice service provided by CAB had already been commissioned by the Clinical Commissioning Group in one of the three study sites. In April 2012, the Clinical Commissioning Group in this site agreed to pilot as part of their primary mental health care strategy, a CAB service called the ‘Advice on Prescription Programme’. The proposed model, new for primary mental health care, included a ‘practical offer’ of advice based in primary care aimed at the most vulnerable patients. This service offered quality-assured advice on benefits, debt, housing and employment support. The service was originally piloted in nine GP surgeries from April 2012 to March 2013 and then rolled out across all practices from April 2013, following independent evaluation. 3
The service continued throughout the current pilot trial period and was aimed at people who were at risk of developing mental health problems as a result of their circumstances. Although this service differed from that proposed in the pilot trial, it is evidently possible that the availability of this service within general practices might have contributed to the difficulties we encountered recruiting general practices to the study in this particular research site.
Scientific background
History of the problem
Depression is estimated to affect 5–19% of adults at any one time. 4,5 Depression is a common presentation in primary care. 6 However, research suggests that only around 2.5% of patients are formally recorded by GPs as having active depression or depressive symptoms. 7,8 Alongside anxiety and stress, depression is considered the most common cause of prolonged work absenteeism,9 as well as presenteeism (working below normal capacity when unwell). Recent work on the cause of sickness absence indicates that the proportion of absence due to mild to moderate mental health problems is increasing. 10 Mental ill health is estimated to cost the UK economy £40B per year overall. 11,12
Around 16% of the UK population is estimated to be struggling with personal debt,13 and there is increasing evidence of a link between debt and poor mental health. 14,15 In a recent study on the association between suicide and the 2008–10 economic recession in England, Barr et al. 16 identified a link between rising episodes of suicide and rising debts.
The changing composition of debt and the rise of debt problems
Indebtedness and poverty are endemic in Great Britain,17 particularly in areas of deprivation and high unemployment, and the economic downturn has only further exacerbated these problems. A report by Lucchino and Morelli18 found that the difference in consumption growth and income growth was largest among those on the lowest incomes. The authors concluded that people in the lowest income decile appeared to be reliant on credit to maintain consumption. Similarly, a UK study that analysed data from clients seen by the then Consumer Credit Counselling Service (now called StepChange) found high debt-to-income ratios in households with incomes of up to £13,500. These households held unsecured debts worth 20% more than their annual net income. 19
In a recent study examining the relationship between the increasing number of food banks across the UK and current austerity, it was found that food banks were more likely to open up in areas of higher unemployment and those most affected by welfare cuts and benefits sanctions. 20
Summary of management of depression in primary care
Most episodes of depression are managed in primary care, following the National Institute for Health and Care Excellence-recommended four-step approach. 7 This involves a range of low-intensity interventions including social prescribing to support lifestyle changes (e.g. for exercise), short-term talking therapies and antidepressants for more persistent symptoms. However, a recent HTA trial21 found a marginal benefit of selective serotonin reuptake inhibitors (antidepressants) for new cases of mild to moderate depression managed in primary care over treatment as usual (TAU). Consequently, many questions remain about the most cost-effective ways to manage depression. 7
Current debt advice services: issues and gaps
In 2013, the Money Advice Service reported that nearly one in five adults in the UK was affected by problem debt. 22 There has been a sharp rise in demand for debt advice. A recent survey found a 56% increase in demand for debt advice in the 3 years since 2012. 23 The last few years have seen an increase in the number of ‘priority’ debts, including housing, utilities and government debts (issues about benefits and tax credit overpayments, social fund debts, child support arrears and magistrate court fines), and a decrease in non-priority debts. 24 Between 2005–6 and 2014–15, the number of priority debts that CAB provided advice for more than doubled, whereas personal loan and credit card debt (non-priority debts) over the same period more than halved since their peak in 2008. 24
Recognising the increasing burden of indebtedness and the link between debt and mental ill health outlined in the Foresight Report,25 the UK government now provides web-based advice and guides on debt management, highlighting a range of providers. 26 Debt advice services are, therefore, now freely available from commercial, public and third-sector providers. Topping this list is CAB, a charity-based service that is widely available across the UK in > 3500 locations and provides support to > 2.5 million people per year. 27 Its principal online recommended site is provided by the government, funded by a statutory levy from the financial services industry and backed by a national advertising campaign (the Money Advice Service; www.moneyadviceservice.org.uk/). However, currently there is no robust evidence regarding the impact of these services on mental health outcomes or their cost-effectiveness. Furthermore, those with depression, especially those from socioeconomically deprived groups, may be particularly likely to find such online services insufficient or inaccessible (because of travel cost, low mood, poor information technology skills and no/low access to information technology and telephone); therefore, a locally accessible, nationally provided advice service was thought, at the time of our application submission, to be a potentially important way to provide easier access to those with the greatest need. Debt is more common among poorer populations, and is a problem in around one in four of those experiencing mental health problems. This group with mental health problems make up 50% of those with debt overall. 28,29 The strategic economic case for providing debt advice for people experiencing mental health problems has been made in recent influential reports, and the intervention we proposed in the current study fell within the suggested service provision costs and model. 30,31
Relationship between debt and depression
A clinical knowledge summary on assessing people with depression advises recording psychosocial factors ‘contributing to the development of depression’;32 at the top of the list are employment and financial worries. In discussing the relationship between debt and depression, it is important to stress that the debt relates to financial liability that is large in relation to income and is difficult or impossible to repay. 33
Social surveys have consistently found a negative correlation between unsecured personal debt and subjective measures of happiness and life satisfaction. 34,35 One debt charity found that debt affected people’s sleep and concentration at work, and put a strain on family relationships. 23 Another debt charity, Citizens Advice, released data suggesting that 60% of its clients had received a mental health diagnosis within the previous 6 months and that in 56% of cases its debt advisors felt that their clients’ mental state had a negative impact on their ability to make ‘reasonable decisions’ about credit. 36
A survey by Mind37 identified an increase in rates of debt among people with mental health problems. This report suggests that a two-way relationship can exist between debt and mental health. Of those people surveyed, nearly three-quarters thought that their mental health problems had made their debt worse. This rose to more than four-fifths among those in problem debt, which was defined as occurring ‘where an individual is two or more consecutive payments behind with a bill or repayment’ (p. 1). 37 In addition, almost 9 out of 10 of those in problem debt said that they thought that their financial difficulties had made their mental health problem(s) worse.
A recent meta-analysis on the relationship between personal unsecured debt and health38 found a significant relationship between debt and depression. The authors identified psychological elements, such as worry and stress, hopelessness, and locus of control, as potentially playing a role in mediating the relationship.
In a large household survey, Bridges and Disney39 found a strong association between depression and self-reported indebtedness and financial stress. They also found a weaker link between the onset of depression and subsequent financial difficulties. Although they found no direct association between objective measures of depression and debt, the authors did find an indirect association via subjective indicators of financial well-being.
Fitch et al. 40 conducted a systematic narrative analysis of peer-reviewed literature on the relationship between personal debt and mental health. They found that indebtedness may contribute to the development of mental health difficulties and mediate accepted relationships between those difficulties and poverty and low income.
Drawing on data from a national household survey, Gathergood41 has explored some of the causal links between problem debt and depression and has introduced the idea of social norm effects. He concluded that exogenous factors, such as the level of social stigma in relation to debt, may have both positive and negative effects on the links between debt and depression.
In conclusion, the literature suggests that social and psychological factors may mediate the relationship between debt and depression, in either direction. Longitudinal research is needed to explore aspects of the relationship between debt and depression further, such as (the direction of) causality and the specific mechanisms and mediators that are involved. This may help in developing appropriate policies and practices to help (depressed) people avoid and manage problem debt, and to prevent and treat depression in those with debt. Research would also help identify which type of intervention works best for whom.
Aims and objectives of the main trial
As reported above, the early termination of this study in the pilot phase precluded statistical evaluation of the clinical effectiveness and cost-effectiveness of the intervention. However, we were able to address most of key objectives of the main trial in a modified form, as detailed below in italics.
The objectives of the main trial were:
-
to compare depression between intervention and control groups – we report descriptive statistics (mean and SD) at baseline and at 4 and 12 months, when available
-
to compare anxiety, mental well-being, debt/financial status, satisfaction, health-related quality of life and societal costs between intervention and control groups – we report descriptive statistics (mean and SD) at baseline and at 4 and 12 months, when available
-
to explore outcomes referred to in (1) and (2) in terms of the following potential predictors – substance misuse problems, self-esteem, life events and difficulties, hope, optimism, resilience and attribution style – we report descriptive statistics only
-
to determine core outcome domains and measures using the Core Outcome Measures in Effectiveness Trials initiative approach to define a standard outcome measure for mental health trials in deprived and hard-to-reach groups in primary care, adapted to this specific study – we make tentative recommendations only
-
to manualise debt assessment, joint comprehensive assessment (GP/patient/CAB) and counselling intervention for use within the intervention – we undertook limited testing
-
to recruit new and chronic/recurrent cases from a variety of practices and populations to enhance generalisability – we could not address
-
to undertake a mixed-methods process evaluation to assess fidelity of intervention (using NPT) and explore reasons for observed outcome differences and relationships between depression, anxiety, debt, stigma, shame and psychosocioeconomic factors; triangulating economic, psychological factors analysis and qualitative interview data – we have partially addressed
-
to undertake knowledge exchange events to inform adoption into care pathways (implementation) – we will undertake a reduced dissemination plan
-
to work closely with service users in research/patient and public involvement (PPI) groups across the study sites to inform trial methodology, intervention development, aspects of analysis and the implementation of preparatory work – we addressed in full
-
to recruit a virtual group of commissioners, providers and health and well-being board members to check willingness to commission the intervention and advise on domains and measures – we undertook a modified activity
-
to work with CAB leads, GPs and PPI advisors on developing the intervention and comprehensive assessment, qualitative topic guides and aspects of data analysis – we addressed in full.
Aims and objectives of the pilot trial
The aim of the pilot trial was to test the procedures, recruitment processes and operational strategies that were planned for use in the main trial and to identify and resolve any problems in continuing with the main trial. We addressed this aim and all of the following objectives of the pilot trial:
-
to confirm methods for recruitment of practices
-
to test the ability to recruit patients via the proposed approaches
-
to confirm the acceptability of the study interventions
-
to confirm acceptability of data collection (outcome measures)
-
to assess contamination and confirm the randomisation method for the main trial
-
to assess the level of participant attrition
-
to check the robustness of data collection systems
-
to identify and resolve potential difficulties in implementing the shared assessment
-
to assess intervention fidelity.
Intervention: theory and development
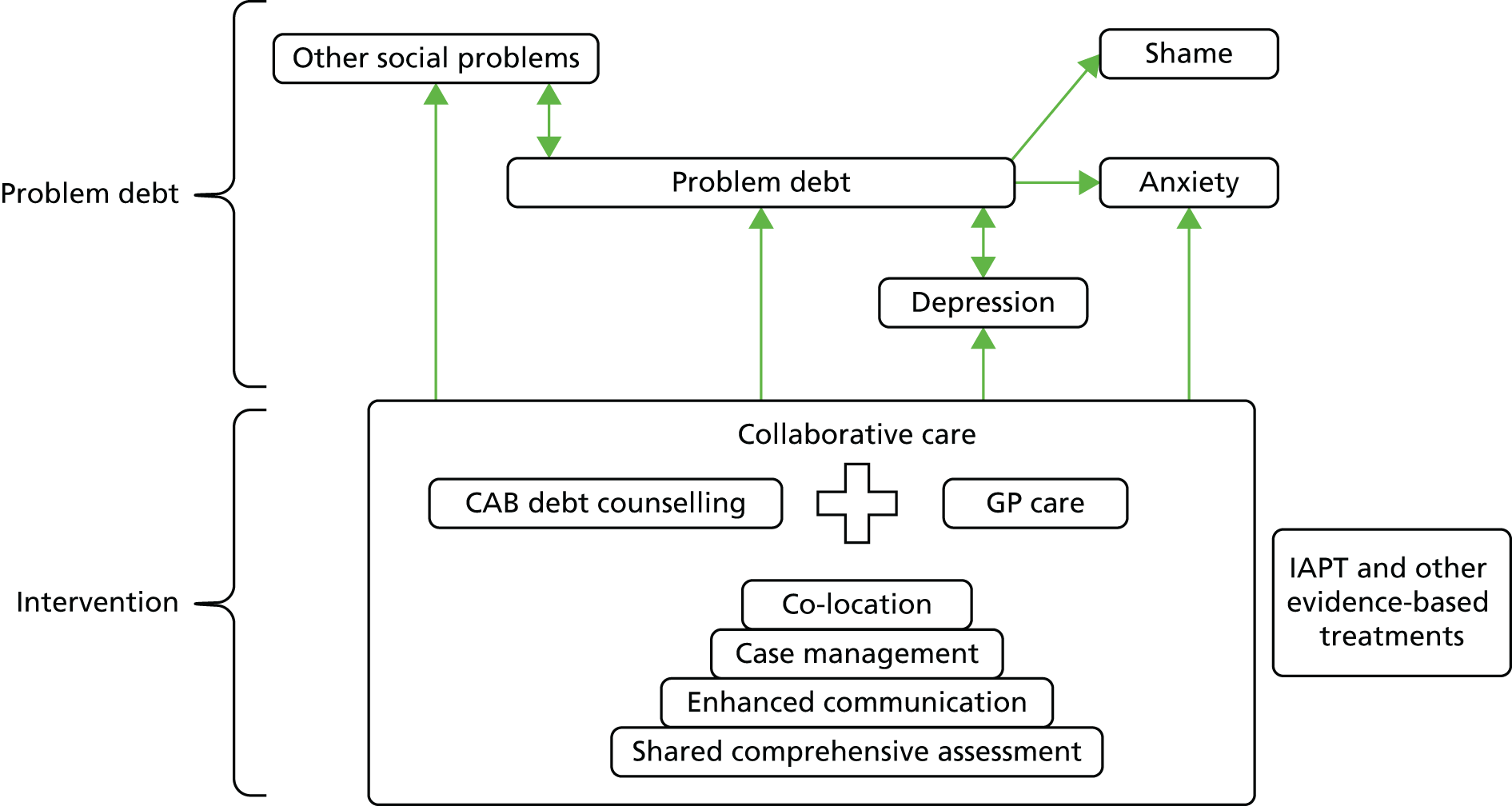
Our intervention was informed by the principles of collaborative care. 42,43 The principles of collaborative care include (1) adopting a multiprofessional approach (e.g. a GP plus at least one other professional), (2) a structured management plan, (3) scheduled patient follow-up and (4) enhanced interprofessional communication. A collaborative approach to patient care has been shown to improve quality of life, healthy behaviours, self-efficacy and other health outcomes. 44 In addition, our intervention aimed to redress inequalities and promote social inclusion of marginalised groups. 45 Our intervention was based on the assumption that social context plays an important role for mental illness onset and recovery, particularly in the case of debt and depression. 40
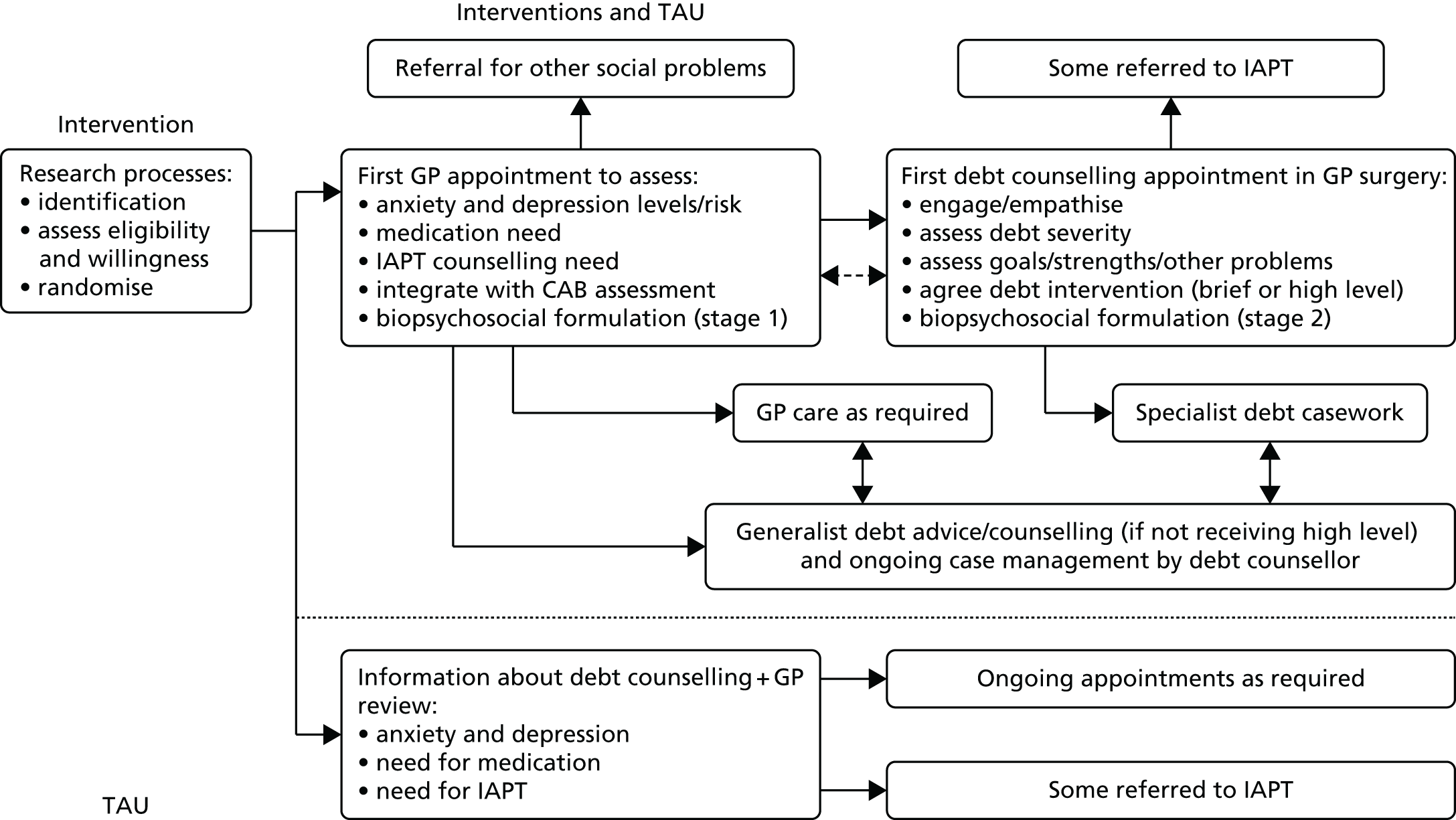
Our intervention brought together two existing services: (1) primary care mental health services provided by general practices, supplemented by Improving Access to Psychological Therapies (IAPT) services in England, and in Wales a variety of counselling and psychological therapies services; and (2) debt counselling provided by third-sector providers, such as CAB (see Figure 1).
Our model of debt advice – debt advice provided by CAB advisors – was distinct from many of the commercially available offers of debt consolidation as the focus of our intervention was on face-to-face debt advice, assessing the level and urgency of debts and arrears, and then triaging clients to specific detailed advice on debt or money management.
Liaison has been shown to be an important element of collaborative care and shared care more generally. 46 In developing the intervention we considered that communication would be enhanced through a comprehensive assessment that was cocreated by, and shared among, the patient, CAB advisor and GP. The purpose of the shared comprehensive assessment (SCA) was to combine social, psychological, environmental, economic and medical perspectives with personal goals, in the production of a biopsychosocial management plan. We developed a SCA form for sharing of information between GPs and CAB advisors with input from GPs, CAB advisors and managers and service users (see Appendix 1).
The active parts of our intervention as a whole were the combining of primary care treatment of depression with the addition of debt counselling and a comprehensive shared assessment, supported by the co-location of GP and debt advisor in primary care; the additional pathways of care; enhanced communication between the GP and debt advisor; and case management for participants (see Appendix 2). Figure 1 summarises all the aspects of the intervention and TAU options, whereas Table 1 summarises and compares the contributions of the GP and CAB advisor within the intervention. Figure 2 maps the key components of this approach: co-location, shared assessment and enhanced interdisciplinary communication.
FIGURE 1.
Intervention diagram.
| GP | CAB advisor |
|---|---|
| Undertake initial part of shared assessment and complete form (estimated to take up to 20 minutes – double appointment slot) | Undertake CAB section of shared assessment |
| Commitment to share care and decisions with the CAB advisor, with patient at the centre of care | Commitment to share care and decisions with the GP, with patient at the centre of care, sharing information with GP as part of structured agreed plan, plus informal case liaison as required |
| Share additional information with CAB advisor as appropriate (using shared comprehensive GP follow-up form) as part of structured management plan and enhanced communication between GP/CAB | Case manage patient and work with GP team to encourage engagement and retention within the planned intervention taking account of contexts of shame, stigma and chaotic life circumstances, the patient and their attendances during intervention |
| Work with patient and CAB advisor to encourage engagement and retention within plan in contexts of shame, stigma and chaotic life circumstances | Support patient to devise and deliver solutions to debt problems sensitive to mental health contexts |
FIGURE 2.
Conceptual map of the intervention and potential impact for individuals.
Process evaluation
We used semistructured interviews with participants, GPs and CAB staff to evaluate the process of integrating the intervention within primary care. We adopted a NPT approach2 to data analysis, which focuses on the various actors, objects and context of the intervention (see Chapter 2, Intervention process evaluation, Data analysis, for more detail of this approach).
Chapter 2 Methods
Pilot trial design
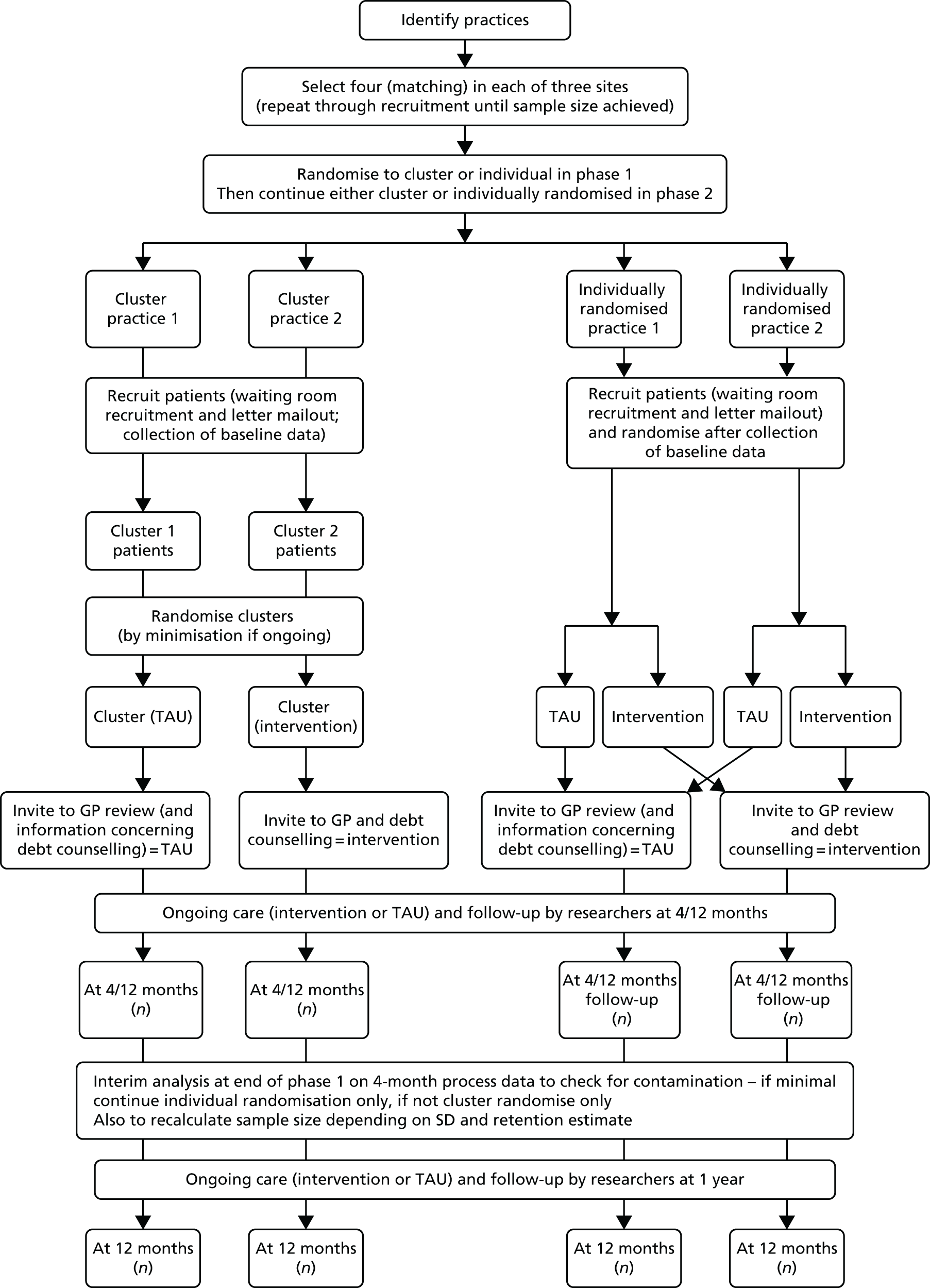
We designed an adaptive, parallel, two-group, pragmatic randomised controlled trial with 1 : 1 allocation to intervention or TAU control, with a planned mixed-methods process and economic evaluation. During the pilot trial we assessed intervention fidelity and any implementation problems, seeking to resolve any issues without change to the intervention so that data collected in the pilot trial could be used in the final analysis at the end of the full trial. We used both individual and cluster randomisation methods in the pilot trial to assign participants to the intervention or the control arm (see Table 1), with the aim of using individual-level randomisation in the main trial (should it have gone ahead) if the pilot trial showed no substantive evidence of contamination (crossover of the intervention between trial arms).
Changes to trial protocol and methods
We undertook several revisions of the protocol and study methods over the course of the pilot trial in response to the differing issues we encountered. This was within the parameters of the adaptive design within which we anticipated a degree of iterative protocol development in the internal pilot phase. The changes to the protocol and methods (listed in this section) were approved by the NIHR HTA programme, the University of Liverpool (research sponsor), Research Ethics Committee North West, in Preston, and the local research management and governance offices [Clinical Research Network (CRN), North West Coast (lead CRN), Royal Devon and Exeter NHS Foundation Trust and Abertawe Bro Morgannwg University Health Board].
Changes to exclusion criteria
Following confirmation from CAB that participants could be visited in their own home by CAB advisors, we removed ‘housebound’ from the exclusion criteria.
Following early contacts with interested patients, we made an addition to the study exclusion criteria to exclude patients (prior to consent) who did not wish to take up support for debt/money worries provided via the general practice. This was to ensure that potential participants were clear about what their participation might involve, and that we consented into the study only those who were interested in receiving support for their money worries through this route.
Changes to participant recruitment procedures
Our original intention was that CRN staff would support research assistants (RAs) in handing out flyers (advertising the study) and expression of interest (EOI) forms to patients in general practice waiting rooms. As a result of resource issues, CRNs were unable to support these activities, so we approached general practices to ask if their staff would be willing to hand out flyers/EOI forms; following necessary approvals, general practice staff (including reception staff) in some practices did this. The potential benefits of this change were twofold: first, if all patients were simply handed the flyer at reception, patients would not feel like they were being singled out in the waiting room; and, second, patients would still be able to receive information about the research when RAs were not in the practice, ensuring that as many patients as possible were given the opportunity to be made aware of the study and register their interest. We also made a change to the information pack sent out to patients by post, namely adding the advertisement flyer. This meant that patients could read the brief summary information in the flyer and decide whether or not they were interested in the study before they went on to read through the much more detailed participant information sheet.
Change to requirement for general practitioners to check identified patient lists
Towards the end of the pilot trial we changed the directive for GPs to check patient lists generated from practice database searches to a neutral suggestion that GPs may choose whether or not to check the patient list. The reasons for this change were twofold. First, although all GPs received similarly worded advice, our experience showed that individual GPs were checking patient lists in very different ways. Some were looking at records in great detail and excluding substantial numbers of potential participants, some of whom might have been eligible to participate and were potentially being denied the opportunity. Other GPs adopted much narrower exclusion criteria, simply confirming no errors in coding and that a patient’s participation was not impractical (e.g. because they were recently bereaved, terminally ill or sleeping rough). We considered the ethical issues regarding this change, and felt that, although the original protocol was based on the idea that GPs should exclude those patients whom they deemed unsuitable for us to approach, it was also equally valid that patients make this choice for themselves on reading the flyer and letter of invitation. Second, based on recruitment rates at that time, we needed to increase considerably the number of patients approached by letter, at least doubling the number of patients we had originally planned to approach in each practice. We were already aware that some GPs were struggling to find time to check the number of patients originally planned, resulting in delays to patient recruitment. This difficulty would have been further compounded by increasing numbers of patients for review. In the event, this change was introduced just before the trial was closed, so only one practice was recruited after the change came into effect, and it was not possible to judge the impact of this change on recruitment delays.
Change to mail-out procedure
Following a request from one practice, we introduced the option for practices to use the Docmail® v2.0 (CFH Docmail Ltd, Radstock, UK) service for sending out the information pack to patients, but this practice was the only one to adopt this method. It did not result in any important delays or additional complexities to recruitment.
Practice identification, recruitment and training
In the pilot trial, we planned to recruit 12 general practices across the three research centres (with an average of approximately 10,000 patients per practice). Two of these practices were to be those in which GP members of the research team were based. Using these two sites early in the pilot enabled the GP academics on the study team to closely monitor how the systems worked within their practices. This facilitated feedback from colleagues about problems, enablers and barriers to delivering the study, thus informing team discussions about adaptations during the pilot. The remaining practices were randomly selected (by the study statistician) from the full list of practices at each site. All practices were matched according to whether situated in high- or low-deprivation communities and practice size (large/medium/small).
Identified practices were initially approached by CRN staff (and in one centre by research staff) and sent an invitation letter with brief information about the study (see Appendix 3). We followed up this initial communication with a telephone call (from the CRN officer or a member of the research team, if appropriate) to ascertain if the practice was interested in the study. When a practice declined to participate, the study statistician identified further matched practices.
When a practice registered interest in participating in the study, we arranged a meeting between GPs/practice staff and members of the research team to discuss this. In some sites, CRN staff also attended practice meetings to discuss the support they could provide to practices.
No financial incentives were offered to practices for taking part in the study. Service support costs were reimbursed for meetings with the research team, for administrative activities carried out by practice staff (e.g. practice database searches) and for a GP’s time spent checking patient lists, and excess treatment costs were met for GPs delivering the shared assessment component of the intervention. Control GPs did not receive any payment for providing TAU and handing out the two debt advice leaflets to participants in the control arm of the trial.
Following paired practices’ agreement to take part, we informed practices of their allocation and asked them to select the GPs and staff members who would be involved in the study. Principal investigators and/or research managers arranged further meeting(s) with GPs and selected staff for the purposes of training, and CAB staff met with GPs and practice staff (when appropriate) to explain the debt advice process and what this would entail. We provided GPs with a study pack containing supporting documentation including a participant pathway flow diagram (see Appendix 4), a protocol guidance sheet (relevant to practice allocation) (see Appendices 5 and 6), a serious adverse events form (see Appendix 7), a copy of the study debt advice leaflet (see Appendix 8), a copy of the Royal College of Psychiatrists’ debt advice leaflet47 and the SCA form (see Appendix 1), when appropriate. For intervention practices we also discussed the shared biopsychosocial assessment and stressed that this was an important component of the intervention, intended to support case management by the CAB advisor and facilitate the sharing of relevant key elements of the history and progress. We sent GPs and relevant practice staff a link and login to the password-protected study website, and training was provided using test data. Research managers and/or RAs provided ongoing support for GPs and practice staff via telephone calls, e-mail communications and further visits to the practice.
Trial participants: selection and recruitment
Patients with a history of depression (with or without anxiety) within the last 12 months and who also had worries about personal debt were identified through participating general practices at the study centres.
Inclusion and exclusion criteria
Patients were eligible to take part if they:
-
were aged ≥ 18 years
-
scored ≥ 14 on the Beck Depression Inventory II (BDI-II)
-
had worries about personal debt.
Patients were excluded from taking part if they:
-
were actively suicidal or psychotic and/or severely depressed and unresponsive to treatment
-
were experiencing severe problems with addiction to alcohol or illicit drugs
-
were unable or unwilling to give written informed consent to participate in study
-
were currently participating in another research study including follow-up data collection phase
-
had received CAB debt advice in the past 12 months
-
did not want support about debt or money worries provided through the general practice.
Participant recruitment
We recruited patients to the study via two approaches.
-
GP database searches and letter mail-out: practice database searches were conducted by CRN officers or practice staff to identify adult patients potentially with current depression or who had depression-related treatment in the last 12 months. GPs subsequently screened generated patient lists to exclude any patients they deemed inappropriate for the study (with one exception after a protocol amendment, see Change to requirement for general practitioners to check identified patient lists). Practices sent a standard introductory pack (including covering letter, advertisement flyer, participant information sheet, EOI form and freepost envelope) (see Appendices 9–12) to potentially eligible patients.
-
Waiting room recruitment: publicity posters (see Appendix 13) were displayed in the waiting rooms of participating general practices and flyers with attached EOI forms (see Appendices 10–12) were placed around the practice waiting room. Flyers/EOI forms were also handed out by study RAs in practice waiting rooms, and in some practices by practice staff. Interested patients were able to either hand the completed EOI form back to the RA or return it at a later date in the freepost envelope provided.
Participant eligibility checking and consent
On receipt of a completed EOI form, local RAs contacted the respondent by telephone to discuss the study and assess initial eligibility (i.e. that the patient had worries about debt that they were personally responsible for, was not currently taking part in any other research, had not received debt advice from the CAB in the past 12 months and was interested in receiving support for money worries provided via their general practice). If, after this, the patient was still interested in taking part in the study (and eligible at this point), the RA arranged a date and time to meet with the patient to complete the formal consent to participate process, including obtaining formal written consent (see Appendix 14), a final-stage eligibility check (completing the BDI-ll) and the collection of baseline data (Table 2). Participants scoring < 14 on the BDI-ll were advised that they were not eligible to take part in the study, thanked for their time and willingness to participate, and given the same two debt advice leaflets as those given to study participants.
| Data/measure | Baseline | 4 months | 12 months |
|---|---|---|---|
| Demographic (age, sex, deprivation score, etc.) | ✓ | ||
| BDI-II | ✓ | ✓ | ✓ |
| Alcohol Use Disorders Identification Test (AUDIT) | ✓ | ✓ | ✓ |
| Drug Abuse Screening Test (DAST) | ✓ | ✓ | ✓ |
| Beck Anxiety Inventory (BAI) | ✓ | ✓ | ✓ |
| Short Warwick–Edinburgh Mental Wellbeing Scale (SWEMWBS) | ✓ | ✓ | ✓ |
| Client Service Receipt Inventory (CSRI) (adapted for trial) | ✓ | ✓ | ✓ |
| EuroQol-5 Dimensions-5 levels (EQ-5D-5L) | ✓ | ✓ | ✓ |
| Manchester Short Assessment of Quality of Life questionnaire (MANSA) | ✓ | ✓ | ✓ |
| Stanford Presenteeism Scale | ✓ | ✓ | ✓ |
| CAB/Control Debt Assessment and Outcomes questionnaire | ✓ | ✓ | ✓ |
| General Satisfaction Questionnaire (GSQ) | ✓ | ||
| Hope Trait Scale | ✓ | ✓ | |
| Life Events and Difficulties Schedule-short (LED-S) | ✓ | ✓ | |
| Other as Shamer scale (OAS) | ✓ | ✓ | |
| Response Style Questionnaire-24 (RSQ-24) | ✓ | ✓ | |
| Qualitative interviews | |||
| Participant purposive sample | ✓ | ✓ | |
| Professional (GP/CAB staff) purposive sample | Once all participant consultations complete | ||
Outcomes of pilot trial
Assessment of approach to practice recruitment
We assess our approach to practice recruitment by comparing figures for number of practices approached versus number recruited (see Table 4), and we record the reasons why practices declined to participate (see Table 5). We also evaluate our recruitment approach by recording the time (in days) from the initial contact with each practice to the practice’s recruitment (see Table 6). We also report findings from a focus group analysis on trial processes (barriers to and facilitators of recruitment of practices) and information recorded by CRN staff and study team members.
Assessment of ability to recruit patients via proposed recruitment approaches
We assess the two approaches to participant recruitment (database search and letter mail-out vs. waiting room recruitment) by comparing the number of participants recruited via each approach (see Table 9). We report the number of participants recruited during the pilot stage of the trial compared with target recruitment (see Table 12) and we report the conversion rate from participants returning an eligible EOI to being randomised into the study (see Table 10). We report reasons for dropout, ineligibility and loss to follow-up rates (Figure 3) and we compare the cost per returned EOI form between the two recruitment approaches (see Table 11).
FIGURE 3.
Trial flow diagram.
Assessment of contamination
We assessed contamination based on self-reported information about receipt of CAB advice provided by participants at the 4- and 12-month follow-up visits. We report the proportion of control participants within each site with an individual allocation receiving CAB advice versus those in cluster-allocated control sites receiving CAB advice.
Assessment of patient satisfaction with intervention
We assessed participants’ satisfaction with the intervention based on data from the self-report General Satisfaction Questionnaire (GSQ) collected at 4-month follow-up and from participants’ reported experiences of the intervention during the qualitative interview.
Assessment of acceptability of data collection (outcome measures)
We assessed acceptability of data collection (outcome) measures based on participants’ reported experiences (from qualitative data) of data collection measures and from RAs’ feedback about comments of participants at the time of the assessment.
Assessment of intervention fidelity
Intervention fidelity was assessed based on information from the clinician and CAB advisor qualitative interviews.
Assessment of data collection systems and data completeness
Data collection and entry systems
Data were collected using paper-based participant booklets and researcher-completed case report forms (CRFs). Paper documents were sent to Peninsula Clinical Trials Unit (PenCTU) so that the data could be entered into a password-protected database. Data were double entered (by two independent staff members) and then compared by standard scripts for any errors. All errors were checked back to the original forms or queried with sites and then corrected. Data were centrally tracked using a web-based trial management system. Microsoft SQL Server 2014 (Microsoft Corporation, Redmond, WA, USA) was used as the database software behind the websites.
Data completeness
Data that were ‘missed’ were chased when appropriate and, if still missing, were marked as such. Pre-defined rules (as recommended in the relevant literature and supporting documentation) were employed for dealing with missing data; for example, for the main outcome (BDI-II), if the missing count of items was ≥ 10 the total score was computed.
Data exports
Various reports for study management were created in Microsoft Access® v15.0 (Microsoft Corporation, Redmond, WA, USA) and Microsoft Excel® v15.0 (Microsoft Corporation, Redmond, WA, USA) using tables linked directly to the website data. These links were read only. Data were extracted from the website using Microsoft Access. The data were complemented by an export dictionary, which listed all the fields and their possible values and meanings.
Participant outcomes
Primary outcome and measurement
The primary outcome was severity of depression measured using the 21-item self-report BDI-II. 48 All measures of mood are essentially self-reported; although a person’s demeanour, dress and behaviour can tell us something about their internal emotional status, their mood cannot be directly observed. It can be argued, therefore, that instruments such as the Hamilton Rating Scale for Depression, which are applied by professionals, are no more valid than those that are completed directly by patients. Furthermore, it has been shown that a professional rating of a person’s emotional state adds nothing of value over and above a self-report. 49 Thus, the BDI-II is commonly used to assess depression in primary care mental health studies.
The BDI-II was completed by participants at baseline and at the 4- and 12-month (for participants completing their participation before the trial was closed down) follow-up assessments. Participants were classified according to the following categories: 14–19 points (mild depression), 20–28 points (moderate depression) and > 28 points (severe depression).
Secondary outcomes and measurement
The secondary outcomes included psychological well-being, health-related quality of life, cost-effectiveness, participant satisfaction and explanatory factors. For data collection time points for secondary outcome measures, see Table 2. We discussed the proposed data collection plan with a panel of NHS commissioners to ensure that the types of data we were planning to collect were considered relevant to influencing commissioning decisions, and to confirm that a positive trial result had the potential to positively influence service commissioning (as per the HTA brief).
Measures of psychological well-being
-
The Beck Anxiety Inventory (BAI),50 a 21-item self-report measure, was used to assess severity of anxiety. The BAI was chosen for consistency with the BDI-II.
-
The Short Warwick–Edinburgh Mental Wellbeing Scale (SWEMWBS)51 was used to measure aspects of positive psychological function, covering both hedonic (e.g. positive feelings and emotions) and eudaimonic (e.g. positive functioning) aspects. The SWEMWBS is a shortened version consisting of seven of the original 14 items. The SWEMWBS was chosen for inclusion in the North West Mental Wellbeing survey and identified as the psychological well-being indicator in the government’s Public Health Outcomes Framework. 52
Measures of health-related quality of life
-
The EuroQol-5 Dimensions-5 levels (EQ-5D-5L)53 is a well-known and commonly used generic measure of health status. It is used to measure outcomes in clinical effectiveness, cost-effectiveness and population health studies. 54 It is a patient-reported outcome measure in the Patient Reported Outcome Measures programme run by NHS England. 55 A key feature of the EQ-5D-5L is the ability to generate ‘utilities’ for health states (reflecting the preferences of the general public), which can be used to estimate quality-adjusted life-years (QALYs).
-
The Manchester Short Assessment of Quality of Life questionnaire (MANSA)56 was chosen because it is preferred by service users, is more specific for mental health studies and has good reliability and validity. 56
Measures of health and social care utilisation
-
A version of the Client Service Receipt Inventory,57 together with a comprehensive ‘guide’ describing all the resource use items, was adapted for this study population and used to measure NHS and social services resource use, and also contact with criminal justice services.
Employment factors
-
Work-related issues were measured by self-report (absence and partial work). We decided against a primary care records ‘Fitnote’ search, as the Medical Certificate of Fitness for Work (MED 3s) is a recommendation not a measure of actual absence, with modified or partial work subject to employer agreement.
-
Impact of health problems on work performance was measured using the Stanford Presenteeism Scale-6 items (SPS-6). 58
Record of personal debt issues
We recorded priority and non-priority debts in participants’ CRFs at all three assessment points (baseline, 4 months and 12 months). Priority debts are those that must be dealt with first because of the sanctions available to priority creditors in the event of non-payment; such debts include mortgage or rent arrears, secured loans, council tax, gas/electricity, child support, income tax, fines, value-added tax, hire purchase and telephone arrears. Non-priority debts are those debts for which the only course of recovery action is to sue the client in the county court. They do not involve the legal sanctions that are available in response to priority debts, such as eviction or service disconnection. Generally speaking, therefore, all other types of debt are non-priority and include, but are not limted to, credit cards, personal loans, charge cards, catalogues, personal debts to family and friends, doorstep-collected loans, credit sale agreements, trading cheques and vouchers.
We chose to record priority and non-priority debts as opposed to absolute amount of debt because comparing the absolute amount of debt at baseline and outcome is less important than comparing the extent of arrears and priority debts. The risks from debt may be reduced, alongside the associated worries, without the absolute amount necessarily also reducing; it is the potentially serious consequences that often provoke distress and the resolution of these that provides relief, even though the outstanding amounts may remain. Study RAs were provided with guidance from the CAB in recording priority and non-priority debts.
Service satisfaction
Service satisfaction was measured with the GSQ. 59 The GSQ was chosen because it is a brief measure with good psychometric properties and has been used before in studies of people with mental health problems.
Measures of substance misuse
-
Alcohol use was measured with the self-report version of the Alcohol Use Disorders Identification Test (AUDIT). 60 We chose to use the AUDIT because it is a well-recognised and widely adopted measure of alcohol consumption in primary care, and its reliability and validity have been established.
-
Illicit drug use was measured with an adapted version of the Drug Abuse Screening Test. 61 We chose this measure because it is simple and relevant, and widely used in the USA; there is no UK-specific equivalent.
Record of life events and difficulties
Life events and difficulties were assessed using the Life Events and Difficulties Schedule-short (LED-S). 62 The LED-S is a researcher-led semistructured interview schedule that has been widely used and acknowledges the difference between the respondent’s personal reported actual reaction to a stressor and the ‘contextual’ severity of that stressor, namely how severely most people in the respondent’s biographical circumstances (or ‘context’) would be expected to react to an event with those same ramifications. Raters have to undergo detailed training and lengthy manuals of examples of various types of events and ongoing difficulties to inform their ratings of the tape-recorded interviews. It pays special attention to dating of stressors in relation to symptoms, and can be used in both quantitative and qualitative research.
Life events and difficulties were assessed for the 12 months prior to baseline assessment and for the period between baseline and the 4-month follow-up assessment.
Research assistants received extensive training in LED-S from Tirril Harris, one of the authors of this monograph and co-applicant on the grant, who is an original author of the LED-S. All RAs attended an initial intensive training session with Tirril Harris and had the opportunity to undertake practise LED-S interviews with members of the public with a history of depression and debt. Tirril Harris also conducted consensus meetings with RAs throughout the data collection period to discuss and advise on coding of LED-S data. Further guidance and support was provided by Tirril Harris via telephone and e-mail to support RAs in coding of LED-S data.
Explanatory measures
Research on the relationship between debt and psychological distress consistently suggests that the relationship between distress and subjective measures of debt severity is stronger than that with objective measures. For example, Drentea and Reynolds63 analysed data from a large two-wave panel survey in the USA. Their analysis found that although debt (uniquely among the socioeconomic variables studied) was significantly related to a clinically valid measure of depression, the strength of the relationship did not vary as a function of individuals’ financial position; that is, being in debt was experienced as bad irrespective of its objective severity. In a British study, Bridges and Disney39 analysed the UK Families and Children Survey. They identified a strong positive association between subjective debt problems and self-reported mental health difficulties in the family, which persisted when objective financial circumstances were controlled for; hence, they concluded that ‘only a weak link exists between “objective” measures of the financial position of the household and psychological stress’. 39
Given these and other findings, it was felt important to include measures of psychological factors that might plausibly mediate the debt–distress relationship within the DeCoDer study, because this would offer the possibility of exploring within-group variability in outcomes. However, research evidence bearing directly on the question of which constructs might be most significant to perceptions of debt severity was limited. Hypotheses were therefore generated on the basis of psychological mechanisms known to be implicated in depression in other settings.
We had planned to assess three psychological constructs, each having been strongly associated with depression in previous work and that might reasonably be hypothesised to mediate the debt–depression relationship. As a result of the early closure of the trial and smaller than anticipated sample size, mediational analyses were not possible, but we report instead descriptive data for the following three constructs.
-
Hopelessness: the feeling of little or no hope for the future has long been associated with both depression and suicide. An analysis of the British National Survey of Psychiatric Morbidity in 2011 suggested that hope/hopelessness may be a strong mediating factor in the relationship between self-reported debt problems and suicidal ideation. 64 A positive association between suicidal ideation and self-reported indebtedness and a ‘strong indirect effect through hopelessness’ has been described previously. 64 There are two widely used psychometric instruments to measure hope: the Adult Hope Scale65 and the Beck Hopelessness Inventory. 66 These measures conceptualise hope in slightly different ways. The latter measures hopelessness in terms of just negative expectations about the future, whereas the former conceptualises hope in terms of a sense of agency (feeling that it is possible to effect change in one’s life) and a pathway (having the ability to find a solution to the problem). The Adult Hope Scale was, therefore, better suited to the current trial, as a central aspect of the intervention was helping people to see practical ways to better manage their finances.
-
Shame: depression has been associated with the experience of negative social comparison, such as comparing oneself unfavourably to someone else or imagining their judgement. 67 There is evidence that debt problems may cause people to judge themselves negatively compared with others. For example, Gathergood41 found that people in debt were more likely to experience mental health problems if they lived in areas where the wider prevalence of debt problems was low. We used the Other as Shamer scale (OAS)68 (a psychometric instrument developed in order to measure external shame) to assess a participant’s beliefs about how others evaluate the self. The OAS is conceptualised as a trait measure, reflecting an individual’s characteristic and global beliefs about how they are viewed. We decided to use this measure, instead of the originally proposed Attributional Style Questionnaire, because the OAS appeared to capture more accurately the experience of being judged negatively by other people – hypothesised as a mediating factor in the debt–depression relationship.
-
Rumination: rumination is defined as ‘repetitively focusing on one’s symptoms of distress and the circumstances surrounding these symptoms’. 69 Rumination is strongly associated with depression70 and impairs problem-solving ability. 71 Ruminating on debt is likely to increase negative affect and limit the extent to which individuals are able to conceive ways to improve their financial situation. We assessed rumination with the Response Style Questionnaire-24,72 the most commonly used measure of depressive rumination. 73
Sample size
For the full trial we estimated that we would require 135 patients per arm in order to have 90% power to detect a clinically meaningful difference in the primary outcome of 3.5 BDI-II units between groups at 5% two-sided alpha (based on a SD of 9). 74 To allow for a cluster (practice-level) allocation of patients, we inflated the sample size by a design effect of 1.45 (assuming an intracluster correlation coefficient of 0.05 and an average cluster size of 10). 75 Based on this proposed sample size for the full trial, we proposed a sample size of 120 patients for the pilot trial, randomised to intervention and control (TAU) arms, nested by individual or cluster randomisation. Given its early termination, the study did not progress to a full trial and achieved a recruited patient sample size of 61 patients (32 in the intervention group and 29 in the TAU group) in the pilot phase.
Trial interventions
Treatment as usual plus two debt advice leaflets
Following randomisation, participants assigned to TAU were contacted by their general practice to arrange an initial consultation with the GP participating in the study. We asked practices to arrange this initial GP assessment within 1 week of the participant being randomised, whenever possible. During this initial appointment, GPs managed participants in line with their trial arm allocation, conducting an initial assessment (or review for those already in treatment) of both anxiety and depression, discussing treatment options and/or progress (medication/psychological therapy) and negotiating an ongoing management plan. We advised GPs that TAU could include a referral to the local IAPT service and might normally include up to 12 further GP contacts; they were also free to refer participants to other treatment/services as they deemed appropriate (see Appendices 5 and 6). We also asked TAU GPs to hand out the study debt advice leaflet (see Appendix 8) and the Royal College of Psychiatrists’ debt advice leaflet. 47 GPs were asked to record all non-attendances in the password-protected study website and to make reasonable attempts to recontact patients to check if they wished to rebook their appointment with the GP.
Intervention: treatment as usual plus primary care-based Citizens Advice Bureau debt advice plus two debt advice leaflets
Following randomisation, participants assigned to the intervention arm of the trial were contacted by their general practice to arrange an initial consultation with the GP participating in the study. We asked practices to arrange this initial GP assessment within 1 week of the participant being randomised whenever possible. During this initial trial appointment, GPs conducted the same patient assessment and review as for TAU participants. In addition, intervention GPs were asked to confirm the participant’s willingness to continue in the trial and obtain their written consent for completion of the SCA form (see Appendix 1), sharing of information with CAB advisor and referral for an appointment with a CAB advisor. The signed SCA form was retained by the practice and participants were offered a printed copy. As in the TAU arm, we asked intervention GPs to hand out the two debt advice leaflets to participants during the consultation (see Appendices 5 and 6 for intervention GP protocol). We asked GPs to record all non-attendances on the password-protected study website and to make reasonable attempts to recontact participants to check if they wished to rebook the GP appointment.
When participants agreed to CAB referral, CAB advisors contacted participants to arrange an initial assessment appointment. We asked CAB advisors to arrange the initial appointment within 2 weeks of receipt of the referral whenever possible. The advisors were asked to case manage the participants and send them appointment reminders as required.
The aim of the initial CAB appointment was to assess the severity of debt and other social problems, and to draw up a management plan. At the end of the assessment there was an agreement regarding whether the participant required a higher-level debt counselling intervention or the basic debt counselling provision. The CAB intervention was implemented utilising protocols (see Appendix 15 for the CAB advisor protocol), manuals, training and organisational agreements. Appointments between the CAB advisor and participant usually took place at the participant’s own general practice (to facilitate liaison between GP and CAB services), although CAB advisors visited some participants at alternative venues at the request of the participant. More detailed information about the CAB advisor and GP roles is provided in section 4.1 of the protocol (see Appendix 2).
We followed up all participants who were still willing to participate in the study but did not wish to be contacted by a CAB advisor, as planned per protocol. We asked GPs (or agreed member of practice staff) and CAB advisors to access the password-protected study website following appointments with participants to record study-specific information (e.g. dates of scheduled appointments, and if and when participants attended).
Randomisation
Demographic information (size and deprivation index score) for all general practices in the three study localities was sent to the study statistician (RST). General practices in each locality were matched on their size (‘small’, < 3500 patients; ‘medium’, 3500–8000 patients; ‘large’, > 8000 patients) and deprivation index score76 (‘not deprived’ indices of multiple deprivation score of ≤ 21.7, ‘deprived’ score of > 21.7, where 21.7 is the UK 2010 average score) before being randomised to intervention or control arms either at the cluster (practice) or individual (patient) level (see Table 1).
The randomisation sequences and matching was computer generated and undertaken by the study statistician.
In practices allocated to individual patient allocation, a member of the research team (usually the RA) gained informed consent and then accessed the password-protected randomisation website developed by PenCTU and entered participant details. Once data entry was complete, participant allocation was automatically generated by the computer but did not appear on the screen, thereby maintaining RA blinding.
When a general practice dropped out post randomisation, we replaced it with a practice of similar size and deprivation index by matching it with practices on a waiting list. Practice staff in the cluster randomisation arms were not informed about their allocation before they agreed to participate in the trial.
Individual randomisation procedure
Following the obtaining of informed consent and the completion of the baseline assessment, RAs accessed the password-protected study website (designed by PenCTU) and entered the required participant details (including general practice and participating GP’s e-mail address) in order to generate the participant’s allocation and study number. The participant’s study number was visible to the RA on the database screen but the participant’s allocation was not, thereby maintaining blinding of the RA who was conducting the participant assessments. This randomisation procedure triggered an automatic e-mail to an identified member of the practice staff, informing them of the participant’s allocation. This e-mail identified the participant by their initials and unique trial number. Based on this information, the practice staff (and study GP) were able to identify the participant when they accessed the web-based password-protected study database.
We maintained separation between GPs seeing TAU and intervention participants within individual randomisation sites in an effort to reduce the risk of contamination. A member of the practice staff forwarded the automatic e-mail to the appropriate study GP (intervention or control GP), and the participant’s personal details were retrieved from the password-protected study website so that practice staff could call the patient to arrange an appointment with that GP at the practice.
Cluster randomisation procedure
Participants recruited from cluster-randomised practices were registered into the study as soon as possible after giving their written consent and completing the baseline assessment. The RA accessed the password-protected study website and entered the required participant details (including general practice and participating GP’s e-mail address) in order to register the participant on the trial. This process triggered an automatic e-mail to the relevant member of the practice staff, confirming the participant’s consent and registration. The same administrative process was undertaken as for individual randomised patients: a member of practice staff accessed the web-based password-protected study database to retrieve the participant’s personal details so that they could call the participant to arrange an appointment with a named GP at the practice.
Blinding
In the pilot trial both researchers and participants were kept blind to practice and participant allocation.
Researcher blinding
Researchers conducting assessment interviews were not informed of participant allocation. RAs entered the same information into the study website for all participants and were unaware which participants had been individually randomised and which participants were from cluster practices. At the start of each visit, RAs explained to participants that they did not know what type of debt advice the participant had received and requested that this not be discussed during the visit to avoid RA unblinding. Instead, participants self-completed a questionnaire about the debt advice they had received (see Appendix 16), which they then placed in a sealed envelope so that the RA did not see the questionnaire. The sealed envelope was sent to PenCTU along with the participant’s other data to be entered onto the study database by PenCTU staff. If the RA was inadvertently made aware of the participant’s trial arm during the assessment visit, ‘unblinding’ was recorded on the participant’s CRF at the time of the data collection visit. Practices were advised that researchers carrying out the assessment interviews were blind to participant/practice allocations and that they should refrain from referring to participants’ allocations in discussions with RAs. Local research managers liaised with the practice on matters related to practice and participant allocation (e.g. training about the referral process and use of the study database).
Participant blinding
Participants were also blind to their allocation. The reason for not telling participants whether they were in the intervention or TAU arm of the trial was the belief that there was genuine equipoise about the benefits of the intervention versus GPs providing TAU plus signposting with advice leaflets about managing debt.
To maintain participant blinding, the participant information sheet explained that the study was evaluating different ways of providing debt advice but did not refer to ‘intervention’ and ‘control’ groups. The information sheet explained that participants would be ‘randomly allocated’ to a particular way of providing debt advice. The information sheet made it clear that one type of debt advice was referral to a CAB advisor and that this type of advice would not be available to all, but this was not identified as an ‘intervention’. GPs told patients their trial allocation during their initial consultation, explaining that they had been allocated to receive debt advice from a CAB advisor or that they were to receive two debt advice leaflets. GPs were asked not to refer to ‘intervention’ or ‘control’ arms in discussions with participants.
Data collection
Participant assessment visits were undertaken at baseline and at 4 and 12 months (for some participants who had reached this stage when the study was closed) (see Table 2). Data were collected through a combination of participant self-report and researcher-led questioning. Booklets containing self-complete measures were handed to participants at the start of each assessment visit. Researcher-administered measures were entered into study-specific CRFs by the RAs. The order of completion of the measures was predetermined, giving consideration to the sensitive nature of some questionnaires (see Appendix 17). The original CRF pages and self-complete booklets were sent to PenCTU for double-data entry onto a password-protected database. Double-entered data were compared for discrepancies using a stored procedure, and discrepant data were checked and verified with RAs who retained a photocopied version of the CRF. Participants were able to complete data measures (see Table 2) over more than one visit if they preferred to do so. However, subsequent visits were required to be completed within 1 week of the first assessment visit. Participants received a £10 voucher at the end of each assessment (baseline and 4 and 12 months) as a form of recognition of their participation in the study.
Baseline data collection
All participants (with consent) had the LED-S component of the baseline assessment visit audio-recorded. The participant’s unique trial number was included on all parts of all participant data collection booklets and CRFs.
Follow-up data collection
Further data collection visits (before the closure of data collection) were completed at 4 and 12 months after the baseline assessment visit (see Table 2). Follow-up data collection visits were completed as close as possible to the follow-up due date (generated by a computer). If participants did not want or were unable to complete follow-up visits, we asked them if they would be willing to complete the primary outcome measure (BDI-II) by telephone.
Quantitative data analysis
Statistical analysis
Given that the study did not progress to a full trial and achieved a reduced sample size in the pilot trial phase, we were not powered to undertake an inferential statistical comparison of outcomes between intervention and control groups. Instead, outcomes findings are reported descriptively (means and SDs, or numbers and percentages) for primary and secondary outcomes for the two groups at baseline and at 4 and 12 months post randomisation. Using the Consolidated Standards of Reporting Trials (CONSORT) framework, we provided a detailed summary of the flow of participants through the study from approach to participation to 4- and 12-month follow-up for those completed before close-down.
Health economics analysis
The ‘true’ cost of the intervention has been estimated using CAB standard rates for the NHS. The CAB also provided their records to confirm the time taken to complete the intervention. Given the reduced sample size in the pilot trial, the focus of the health economics analysis is descriptive: we present a summary of mean QALYs, health-care utilisation and costs by group. No incremental cost per QALY analysis was undertaken; instead, we have undertaken a disaggregated analysis of costs and consequences.
Participant qualitative data collection and analysis
Data collection
We originally planned to conduct two qualitative interviews (one at baseline and one 4 months later) with 30–45 participants (10–15 from each of the three research sites). As a result of early closure of the trial and the smaller than anticipated sample size in the pilot trial, only 23 participants had been recruited for a qualitative interview at the point of trial closure (see Table 39).
We selected participants for qualitative interview by first identifying participants who had registered their interest in taking part in qualitative interviews on the main study consent form. As participant recruitment was gradual and baseline qualitative interviews had a timeline for completion within 2–4 weeks of baseline assessment visits, it was agreed with the qualitative research team that the first six participants registering their interest in a qualitative interview would all be contacted for interview. Subsequently, participants were purposively sampled based on their age, sex, BDI-II score and allocation. We also sought to ensure that there was representation in the qualitative sample from each of the three study sites and, whenever possible, at least one participant from each general practice. One of the three research sites started participant recruitment much later than the other two sites; consequently, only five participants were recruited from this site before the trial was closed down. All five participants registered their interest in a qualitative interview and so all were approached by a study RA for interview.
Research assistants contacted participants by telephone, e-mail or letter to check if they were still interested in taking part in a qualitative interview and, if they were, to arrange a date and time for the interview. Not all participants who were contacted to participate in qualitative interviews actually completed an interview (see Chapter 6, Participants). We asked participants taking part in qualitative interviews to complete a further consent form specific to the qualitative interview that included providing consent for the use of anonymised quotations (see Appendix 18). The qualitative interviews were conducted by different study RAs from those conducting the assessment interviews to avoid unblinding. Interviews took place face to face and in a setting convenient for the participant. Interviews were audio-recorded with the participant’s consent and were anonymised during transcription. Transcripts were identified by the participant’s unique trial number and each participant was assigned a pseudonym.
Baseline qualitative interview
We conducted the baseline qualitative interview with the aid of a topic guide (see Appendix 19). This topic guide was developed by the qualitative team, including the service user lead, and refined iteratively. The baseline interview adopted a semistructured approach, commencing with a broad opening question inviting participants to tell their story about their experience of money worries. This was followed up with additional prompts (as appropriate) to explore participants’ biographies of depression, anxiety and debt, and the impact of these on their lives. The interview also explored participants’ experiences relating to the practical aspects of debt (e.g. contact with creditors).
Four-month follow-up qualitative interview
We conducted a further topic-guided (see Appendix 19) interview with participants 4 months later. The 4-month topic guide was developed using the same approach used to develop the baseline topic guide. The follow-up interview was semistructured in form and enquired about developments since the participant’s baseline interview, including any changes in debt and depression, and any possible influences on changes in mental distress. We also asked participants about their experiences of the intervention (as appropriate) and involvement in the trial. We explored in particular each participant’s acceptability of the intervention, assessment visits with the researcher and outcome measures, and views about costs in terms of time and convenience with respect to study participation.
Data transcription and management
Digital audio-recordings were transcribed by an independent professional transcriber. The recordings were transcribed verbatim, although it was agreed that brief pauses and verbal idiosyncrasies (e.g. ‘er’) would not be transcribed. The reason for any significant pause in the interview (e.g. where participant left the room for any reason or the audio-recording was paused) was recorded in brackets on the transcript. In addition to participant identification number, participants’ age, sex and a pseudonym were added during transcription. When participants referred to another individual by name, the other individual’s relationship to the participant was inserted instead for purposes of anonymity. When direct reference was made to the name of a service or place, this was replaced with a generic term such as ‘hospital’ or ‘GP’. Qualitative RAs subsequently checked the transcripts against the audio-recording for accuracy and the recordings were then deleted. For ease of management and coding, transcript data were imported into NVivo version 10 (QSR International, Warrington, UK).
Data analysis
The first five transcripts were read and underwent open coding77 by members of the qualitative team, and emerging concepts were discussed. We transformed the data through an iterative process of reading and rereading transcripts, working actively with the data to develop a framework that enabled conceptual development of the data. The framework included both in vivo concepts (concepts using the participants’ own words)77 and researcher-generated concepts. Through a further process of axial coding, a sense of the relationships between concepts was developed. 77
One member of the qualitative team conducted a subsample analysis focusing specifically on the phenomenological experience of debt and the psychological mechanisms linking these to the experience of distress. 78
Intervention process evaluation
Data collection
In each of the three research centres we interviewed a number of GPs and CAB advisors about their experiences of participating in the trial. GPs and CAB advisors were provided with an information sheet (see Appendix 20) prior to the interview and completed a consent form (see Appendix 21) before the start of the interview.
The interviews with GPs and CAB advisors were topic guided (see Appendix 19) and semistructured in form. The topic guide was developed with the professional members of the team (CAB and GPs plus the qualitative team and PPI lead) and followed the NPT framework approach. We explored clinicians’ and CAB advisors’ experiences of implementing the intervention, their views about the processes involved and their thoughts about the feasibility of integrating the intervention into everyday practice, including any potential barriers to or facilitators of this.
Data analysis
The components of the intervention were analysed following the rationale of NPT. 2 NPT underpinned the exploration of the behavioural mechanisms that inhibit the routine incorporation of interventions in everyday practice. It provides a rigorous conceptual framework to identify, describe and understand interactions between participants’ contribution (i.e. the things that they do) and the capabilities offered by the intervention. Most specifically, NPT pays attention to the intervention’s workability and integration within the workflow and context in which the intervention is undertaken. The analysis of the interviews encompasses an interpretation based on the understanding of the wider research project.
Patient and public involvement
Service user involvement has been integral to the DeCoDer trial. In this section we detail the different ways in which service users have contributed to the development and progression of the trial throughout its course.
Pre-funding preparation
The research team co-applicant leading on public involvement has been involved with the trial from the outline bid stage. Early engagement and involvement of service users was facilitated through the NIHR Research Design Service North West PPI fund. This fund supported our initial meetings with Liverpool Mental Health Consortium and the chief investigator presented the proposed study to the former NIHR North West Mental Health Research Network Service User Research Panel to discuss the trial and obtain feedback on the potential value of such a service, and possible concerns individuals who had personal experience of such difficulties might hold. Through the PPI lead co-applicant, contact was also made with PPI groups in the other two research centres before funding. Feedback from these service users influenced our intervention design, data collection protocol and recruitment strategy. Service users commented on the proposed intervention, informed by their personal experiences of debt and mental health problems. They reviewed the various proposed data collection instruments and options being considered, and recommended alternatives based on their views on both the acceptability and relevance of various options being suggested, and the overall burden of data completion.
Post-funding preparatory work
Our PPI lead co-applicant was involved in frequent communications (e-mail, teleconference and face-to-face meetings) to develop study protocols (including the safety protocol) and participant documentation. Participant information sheets and consent forms were based on templates provided by our PPI lead. Service user representatives reviewed participant-related documentation (including, but not limited to, the advertisement poster, flyer, debt advice leaflets, participant information sheet and assessment questionnaires). We amended documentation in light of their comments, including making changes to the advertisement poster. The service user group advised that, although they were happy with the assessment questionnaires for the pilot trial, any opportunity to reduce the number of questionnaires for the full trial would be welcomed.
Service user representatives from the former Mental Health Research Network Service User Research Panel were involved in training study RAs, namely by taking part in practice assessment interviews and meeting with RAs to discuss the sensitivities involved in conducting interviews about depression and debt.
Our PPI lead co-applicant attended the research ethics committee review meeting along with the chief investigator and the trial manager.
Throughout progression of the pilot trial
Throughout the course of the pilot trial changes to the study protocol and documentation were discussed with the PPI lead co-applicant. Discussions included those concerning our close-down plan and our proposal to complete 12-month follow-up assessment visits with all participants recruited to the pilot trial, although the funder did not endorse this. Our PPI lead co-applicant has also contributed to the analysis of participant qualitative data.
Report writing, academic paper preparation and dissemination
The PPI co-applicant on the team has been involved in the production of the final report to HTA, including preparation of the Plain English summary and preparation of the end-of-study information sheet for pilot trial participants (see Appendix 22). He will continue to be involved in dissemination activities and preparation of academic papers.
Ethics approval and research management and governance approval
The study was reviewed and approved by NHS Research Ethics Committee North West – Preston (reference 14/NW/0230). Site-specific assessments were completed by NIHR CRN – North West Coast, Royal Devon and Exeter Foundation Trust, and Abertawe Bro Morgannwg University Health Board, and all of the necessary approvals were granted. All substantial amendments were reviewed and approved by the above bodies, and letters of assurance were provided.
Sponsorship
The study sponsor is the University of Liverpool.
Chapter 3 Implementation of the pilot trial
Introduction
In this chapter we detail the challenges we faced in setting up the internal pilot trial, including the recruitment and set-up of general practices and the recruitment of participants. We sought to recruit general practices to the pilot trial during a time of considerable change and flux both at the practice level, as it was a period of upheaval within general practice,79 and in terms of NIHR infrastructure support systems, following the transition from primary care research networks to local CRNs, with considerable staffing turnover and resource strain. The practices themselves were under particular stress as they were largely situated in deprived areas and reflected the known imbalance between primary care demand and resources. 80,81 Our target population – people with depression who had worries about debt – is known to be a vulnerable group in society who are often hard to reach and engage. We sought to recruit representatives from this hard-to-reach group from deprived areas at a time when they were under considerable personal stress (in debt and depressed/anxious).
Focus group analysis
Two focus groups were undertaken by a researcher in February 2015 as part of an independent investigation of factors that had either hindered or enhanced the progress of the DeCoDer trial. The focus groups were conducted with a sample of study team members from each of the three trial sites. Semistructured qualitative interviews, informed by a topic guide, focused on key stages of study design: recruitment of patients and general practices; progression from baseline visit/randomisation to intervention/control; progression from baseline to 4- and 12-month follow-up; communication, within and across research teams, and local CRN support; and causes of delays/barriers to trial progression and recruitment. The overall aim of the focus groups was to access narrative voices of those involved in the design and delivery of the trial, including the different roles played by each team member. Each focus group lasted approximately 3 hours. Digitally recorded discussions were transcribed and coded to identify dominant themes and areas of divergence. Group discussions were lively and informative. The data were analysed in terms of discursive strands, but issues were intricately interwoven, capturing the multiple realities of undertaking large-scale, collaborative projects.
Communication was identified as potentially problematic in the engagement, recruitment and retention aspects of the trial. However, when effectively managed, and there was clear evidence of this, interpersonal relations played a key role in progress. Mental health distress and financial stresses constructed the sample group as a ‘hard-to-reach’ population: chaotic lives mediated by crisis and comorbidity. Health inequalities impacted in poorer neighbourhoods where general practices, confronted by statutory requirements of regulatory monitoring and target-driven services, were less likely to prioritise research. Time was lost in the ‘setting-up’ and ‘signing-up’ phases of general practice recruitment owing to contractual and higher-level administrative issues, which for one site generated frustration and substantial delays. Staff acting as a ‘gatekeeper’ to individual GPs proved a significant impediment, as did staffing issues/workload and variable levels of support from CRNs. In this context, ‘doctor-to-doctor talk’ proved helpful, and there was a feeling that any disinclination of GPs to participate signalled powerlessness rather than lack of interest.
The recruitment of patients was compromised by a number of factors, such as the vulnerability of the client group, the physical space of waiting rooms and the complexity of primary care services in which privatisation, private finance initiatives and moves towards multiprovider facilities presented challenges. The period between ‘expression of interest’ and ‘conversion’ was described as a process rather than procedure, requiring sensitive management and flexibility. Similarly, baseline screening and home visit interviews had to account for the often difficult circumstances of the individual. Overall, it was acknowledged that trial complexities were underestimated in the proposal but, despite slower than expected progress, commitment and enthusiasm of participants was without question.
Pilot trial challenges and issues
We encountered a range of issues in setting up and delivering the pilot trial as we had originally envisaged. These issues could be broadly categorised as (1) organisational- and governance-level issues, (2) study design issues, (3) capacity issues and (4) participant engagement issues.
Organisational- and governance-level issues
Contractual processes
Delays in contracting for the study had a major impact on project start-up, particularly in one of the three study sites. From the contract start date (1 March 2014) it took 33 days for the collaborative agreement to be signed off by the funder and a further 134 days for the collaborative agreement to be signed off between the host organisation and collaborating institutions. This had serious implications for one of the three research sites in particular, as it was not permitted by its institution to proceed with research staff recruitment without the finalised, fully executed collaborative agreement. Although locally based co-investigators were able to make progress with site recruitment, further administrative delays at this site after collaborative agreement sign-off, specifically local post-award administration processing and recruitment permissions, resulted in essential research staff (local trial manager and RA) finally coming into post a full 12 months after the official start date for the study. This left little time for recruitment of practices and participants at this site before the trial was officially closed to recruitment, with the first trial participant being recruited at this site almost 6 months after the original timetabled end date for pilot trial recruitment.
Approval timelines for substantial amendments
Our study was funded as an ‘adaptive’ trial design, and we undertook a number of protocol and documentary amendments (five in all) throughout the course of the pilot trial as we worked through the various issues as they arose. These amendments required funder, sponsor, research ethics and research governance approval. Although review processes are often described as running in ‘parallel’, in reality approvals are sequential: the research sponsor requiring funder approval before proceeding, research ethics committee requiring sponsor approval before proceeding and research governance offices requiring research ethics committee approval before providing final approval. In our experience, research ethics approval and lead CRN approval was expedited fairly swiftly; however, the timeline from initial approach to the funder for review of the amendment to final local governance approval was variable. In one instance, the timeline from submitting a substantial amendment to the funder, to the final local Research and Development office approval was 49 days (Table 3). Consequently, implementing necessary changes in the tight time frame of a pilot trial was not facilitated by the approval processes at the time. It is also of note that the shorter timelines reported were only possible through constant monitoring and engagement with the different review organisations, and a willingness on their part to expedite reviews in fewer than the 35 days that they are legitimately afforded for local site reviews.
Study design issues
Recruiting general practices to the pilot trial proved to be much more difficult than we had originally envisaged. One of the factors that contributed to this difficulty and the extended time taken to recruit (and then train) practices was the requirement to recruit pairs of matched practices. This requirement is recommended to add robustness to intervention trial designs; in particular, it can help reduce baseline difference between participants in cluster trials in which practices rather than participants are randomised. Nevertheless, it led to substantial delays in undertaking necessary training and preparatory work in practices before participant recruitment could begin. In one research site there was a 6-month delay between a practice agreeing to take part and the arrangement of necessary (before participant recruitment) practice-based activities, while we recruited a suitable matched practice (see Table 6). In fact, recruitment to the trial was closed before this practice was actually able to get started. At a time when practices face staff shortages, Care Quality Commission inspections and changing expectations as new innovations in care and targets are being introduced, delays in progressing practice set-up would have probably resulted in some practices becoming disengaged with the study had we progressed to full trial. This design issue would have needed to be resolved to avoid practices withdrawing from the study before they had even started recruitment.
A further issue concerned the size of the available practice pool in one research site, which was relatively small and so quickly exhausted, requiring a substantial amendment to approach practices in neighbouring areas. Given the aforementioned review timelines, this requirement was less than ideal.
Capacity issues
Further issues that hampered both practice recruitment and set-up concerned capacity within practices and the CRN teams. Both practice staff and GPs had competing clinical and administrative workloads that severely constrained their availability to complete required practice-based activities before participant recruitment. This was further compounded by the limited resources (in terms of time and expertise) in some local CRNs. These issues had serious implications for both recruitment and retention of practices, and completion of practice-based activities (practice meetings, practice training, practice database searches, GP list checks, mail merging/envelope stuffing) that were required to progress participant recruitment.
It is of note that practice capacity/staffing issues were also the reason most often cited by practices for declining to participate in the trial (see Table 5). Current practice workload coupled with limited capacity was also offered as an explanation for early withdrawal from the pilot trial by two participating practices, both of which withdrew before reaching their target participant number. The timing of general practice recruitment was identified as an important factor in terms of likely sign-up, recruitment of practices before Christmas being less successful than after Easter owing to a combination of fluctuating workload and the aforementioned constraints. Before the pilot trial was closed, we were planning to widen the recruitment areas and start to sign up practices in advance of the full trial as an adaptation to the design. This was to ensure that we would have sufficient practices signed up before opening up to the full-trial recruitment phase.
It was also evident that activities that were required to be undertaken by participating practices as part of the letter mail-out approach to participant recruitment took much longer than anticipated because of either research capacity issues or competing priorities within practices. For example, practice database searches (required to identify potential participants for study pack mail-out) had to be completed by practice or CRN staff. This was because research staff were not permitted to access patient records before participant consent was obtained. Completing this activity was particularly problematic in one research site where neither the practice staff nor the CRN had the capacity to conduct the database search, leading to substantial delays in participant recruitment via the letter mail-out approach.
Once patient lists had been generated through practice database searches, GPs were (prior to a substantial amendment) required to check patient lists to exclude patients whom they deemed it would be inappropriate to approach. The limited availability of GPs to check patient lists because of their clinical workload meant that this activity took far longer than had been anticipated. Some GPs had to complete the list check over a number of sessions because of the time taken in checking lists, with some GPs undertaking extremely thorough reviews. The maximum number of days from an initial database search to the completion of GP list check was 87, although the quickest GP managed this in 4 days (see Table 6).
Finally, letter mail-outs were also delayed in some practices as a result of limited availability of practice administrative staff to undertake mail-merge and envelope stuffing, with the number of days from GP list check to mail-out completion ranging from 5 in one practice to 56 in another. Overall time from initial contact to first randomisation ranged from 89 to 320 days, with three of the practice sites never getting to consent a participant before the trial closed (see Table 6).
Although local CRNs were supportive of the study and were involved in many initial approaches to general practices and attending practice meetings in some centres, growing pressures on local CRN officers meant that their availability to support the trial became increasingly limited. In particular, local CRNs were unable to support recruitment of participants via the waiting room approach. This meant that recruitment from practice waiting rooms was limited by the availability of local RAs, recruitment via the waiting room being possible only when RAs were not busy contacting interested participants or undertaking assessment interviews. In addition, in one site the CRN was unable to support practice or participant recruitment until the first general practice had been recruited. This ‘rule’ delayed CRN support for the study in this site.
Participant engagement issues
We sought to offer flexibility in terms of the methods by which we contacted participants following their initial register of interest from the letter mail-out or waiting room approach. The EOI form returned by participants included a number of options for future contact (telephone/text/letter/e-mail) and patients were also able to indicate a preferred time to be contacted (see Appendix 12). Nevertheless, researchers experienced considerable difficulty in contacting some patients following an initial EOI, with 29 (13.4%) of 216 patients who returned eligible EOI forms being subsequently non-contactable (see Figure 4). There were also some issues in completing assessment visits that had been arranged, with a number of patients cancelling (some rebooking) or failing to be in/show up for the baseline assessment. These patients are likely to be among the most vulnerable patients on a practice list and also, because of their debt, more likely to avoid answering calls. Although these issues were not wholly surprising given the very difficult circumstances that many people were probably experiencing, they did have an impact on participant recruitment and lead to delays in entering patients into the study.
Remedial actions: did they have an impact?
In light of the challenges we faced in recruiting general practices and participants to the pilot trial, we undertook a number of amendments to the protocol and methods for the study, as detailed previously in Chapter 1. It is of note that not all of the changes that we proposed were implemented as anticipated and, therefore, it is possible that not all were as successful as might have been expected. For example, we had hoped that practice staff (in particular reception staff) would hand out study flyers to consecutive adult patients at reception and that this would bolster the distribution of the flyers during periods when the study RAs were not available to carry out waiting room recruitment. However, although this amendment to recruitment processes had been approved, some practices were reluctant to engage in this activity because of either competing task and time pressures or concerns regarding the sensitive nature of the research and potential patient responses. Practices that did agree to distribute the flyers did not consistently hand them out to all adult patients who approached the reception desk. Once these inconsistencies had been identified, through conversations with staff or observation while recruiting on site, this activity was withdrawn from practices in which it was an issue to avoid reception staff ‘cherry picking’ ‘suitable’ patients to receive flyers.
The removal of the requirement for GPs to check patient lists before mail-out was approved only shortly before recruitment closed; it was not possible, therefore, to assess the impact of this change on participant recruitment timelines.
Summary and recommendations for future research
We faced a number of challenges during the internal pilot trial that could be largely categorised into one of four key areas: (1) organisational and governance-level issues, (2) study design issues, (3) capacity issues and (4) participant engagement issues. Although some of these issues spanned all three research sites, other issues were more site specific. We sought to address these issues through a number of protocol and method amendments that were in and of themselves time-consuming in the tight time constraints of a pilot trial. Our experiences of both practice and patient recruitment highlight the considerable challenges of recruiting in a primary care setting within the current health-care and research funding climate.
In one site, CRNs provided training to administrative staff about the importance of taking part in research. This was part of the CRN remit as they were seeking to offer training to support GPs in becoming more research active. In light of the issues we experienced in some practices, we would fully endorse CRNs providing such training to practices, in particular those practices that are new to research. It is likely that where practices are new to research, so too will be their patients; thus, having practice staff (including administrative staff) who are confident about responding to patient queries about research would be likely to benefit patient recruitment to research.
The population of patients we sought to recruit face many and complex difficulties, indicated by our quantitative and qualitative data (see Chapters 4 and 6, respectively). Consequently, these participants required considerable flexibility in order to facilitate their participation in research. This flexibility, and the extended timelines required to facilitate it, were not conducive with the constraints of a short pilot trial time frame.
As we seek to build robust evidence on the impact of interventions among vulnerable populations who may be harder to reach, consideration needs to be given to the complexity and additional time needed in trial designs, and the associated cost implications. The risk is that underserved populations will continue to be underserved by research as well, unless additional resources are granted to meet their additional needs and complexities.
Chapter 4 Pilot trial results: statistical analysis
Introduction
We report here our findings with regard to the pilot trial objectives.
Given that the study did not progress to a full trial and achieved a reduced sample size in the pilot trial phase, outcomes findings are reported descriptively (means and SDs, or numbers and percentages) for primary and secondary outcomes for the two groups at baseline and at 4 and 12 months post randomisation.
Practice recruitment
Recruitment process
Of 67 practices approached, 14 failed to respond to our invitation, 40 declined participation, one was excluded and 12 were recruited to the trial (Table 4). The main reason given by practices for declining to participate was current staffing/resource issues, with a number reporting staff absence due to sickness, key staff leaving the practice or new staff having just joined (Table 5).
| Site | Number of practices (%) | ||||
|---|---|---|---|---|---|
| Approached | That did not respond | Declined | Excluded | Recruited | |
| North-west England | 16 | 7 (43.7) | 5 (31.3) | 0 (0.0) | 4 (25.0) |
| South-west England | 9 | 2 (22.2) | 2 (22.2) | 1 (11.1) | 4 (44.4) |
| South Wales | 42 | 5 (11.9) | 33 (78.6) | 0 (0.0) | 4 (9.5) |
| Total | 67 | 14 (20.9) | 40 (59.7) | 1 (1.5) | 12 (17.9) |
| Reason for decline | Site, n (%) | Total, n (%) | ||
|---|---|---|---|---|
| North-west England | South-west England | South Wales | ||
| Staffing/resource issues | 4 (80.0) | 1 (50.0) | 14 (42.4) | 19 (47.5) |
| Too busy currently | 1 (20.0) | 0 (0.0) | 4 (12.1) | 5 (12.5) |
| Practice in a period of change | 0 (0.0) | 0 (0.0) | 4 (12.1) | 4 (10.0) |
| Not interested in the study | 0 (0.0) | 0 (0.0) | 4 (12.1) | 4 (10.0) |
| No reason given | 0 (0.0) | 1 (50.0) | 7 (21.2) | 8 (20.0) |
| Total | 5 | 2 | 33 | 40 |
Arranging an initial meeting with practices to discuss the study was a protracted process, with the period from initial letter/e-mail contact to practice meeting ranging from 22 to 135 days (Table 6).
| Site/practice | Initial contact to practice meeting (days) | Practice meeting to training (days) | Practice meeting to first database search (days) | First database search to first list check (days) | First list check to first mail-out (days) | Mail-out to first randomisation (minimum) (days) | Mail-out to first randomisation (maximum) (days) | Initial contact to first randomisation (days) |
|---|---|---|---|---|---|---|---|---|
| 101 | 28 | 65 | 57 | 4 | 10 | 14 | 20 | 113 |
| 102 | 53 | 62 | 55 | 0 | 24 | 14 | 14 | 146 |
| 107 | 85 | 30 | 30 | –a | –a | 20 | 34 | 213 |
| 108 | 70 | 29 | 20 | 8 | 30 | 13 | 20 | 141 |
| 203 | 64 | 189 | 108 | 87 | 56 | 13 | 13 | 315 |
| 204 | 64 | 189 | 108 | –b | –c | –c | –c | –c |
| 205 | 29 | 90 | 56 | 26 | 8 | 35 | 35 | 264 |
| 206 | 135 | 137 | 75 | 86 | 3 | 15 | 21 | 320 |
| 209 | 64 | 395d | 343 | –e | –e | –f | –f | –f |
| 310 | 27 | 28 | 50 | 0 | 5 | 14 | 14 | 96 |
| 311 | 22 | 35 | 35 | 1 | 11 | 20 | 20 | 89 |
| 3g | 44 | NC | 42 | 0 | –f | –f | –f | –f |
| 3g | 38 | NC | 159h | –f | –f | –f | –f | –f |
As noted previously, arranging necessary practice activities in advance of participant recruitment was not without its difficulties. In the case of recruitment by letter mail-out, in addition to arranging an initial meeting with the practices to discuss the study and completing practice training, there were challenges in completing the database search to identify patients, the GP list check to exclude patients and the administrative mail-out activities. These resulted in longer than anticipated timelines to participant recruitment, with the number of days from practice meeting to the randomisation of the first patient by letter mail-out ranging from 67 to 251 days across practices (see Table 6).
Practice and general practitioner demographics
Ten practices participated in the study. Of these, seven identified themselves as a city practice, two identified as suburban and one identified as rural. Practice list size ranged from 2800 to 28,500, with a mean of 9306.7 and a SD of 7194.5. All practices reported that they were training practices and seven were registered as research ready or linked to a primary care network.
General practitioner characteristics
We asked the sites to identify a trial lead GP for cluster sites and a pair for individual randomisation sites (one for intervention appointments, the other for TAU participants). Fourteen GPs had seen at least one participant. This sample of GPs was generally older and there was a predominance of male GPs. The majority of GPs were in full-time posts, were a principal/partner in the practice and had a Membership of the Royal College of General Practitioners or a Fellowship of the Royal College of General Practitioners qualification. Just over half had worked in a psychiatric post (Table 7).
| Characteristics | GP sample (N = 14), n (%) |
|---|---|
| Age band (years) | |
| 20–30 | 1 (7.1) |
| 31–40 | 2 (14.3) |
| 41–50 | 5 (35.7) |
| 51–60 | 6 (42.9) |
| Sex | |
| Male | 9 (64.3) |
| Female | 5 (35.7) |
| Professional status | |
| Full-time post | 10 (71.4) |
| A principal/partner in the practice | 11 (78.6) |
| Have MRCGP/FRCGP | 12 (85.7) |
| Have worked in a psychiatric post | 8 (57.1) |
Availability of services for treatment of depression
Practices were asked to record the availability of a number of services for depression for their practice population. Interestingly, IAPT services were not considered to be readily available by any practice and four practices failed to enter a response for that service (Table 8).
| Services for treatment of depression | Availability, n (%) | ||||
|---|---|---|---|---|---|
| Readily available | Available with some difficulty | Available with great difficulty | Not available | Not completed, n (%) | |
| Psychiatrist | 0 (0) | 6 (60) | 2 (20) | 1 (10) | 1 (10) |
| Community psychiatric nurse | 0 (0) | 3 (30) | 4 (40) | 1 (10) | 2 (10) |
| Psychologists | 0 (0) | 3 (30) | 4 (40) | 0 (0) | 3 (30) |
| Psychiatric social worker | 0 (0) | 1 (10) | 3 (30) | 3 (30) | 3 (30) |
| Counsellor | 1 (10) | 6 (60) | 2 (20) | 0 (0) | 1 (10) |
| IAPT | 0 (0) | 3 (30) | 1 (10) | 2 (20) | 4 (40) |
Participant recruitment
Assessment of ability to recruit participants by recruitment approaches
We assessed the two recruitment approaches (letter mail-out vs. waiting room recruitment) by comparing numbers of participants recruited to the study with costs of recruitment. Across the three research sites, 4121 letters were mailed out to potential participants, 127 eligible EOI forms were returned and 43 participants were randomised (Table 9). In comparison, across the three research sites 3367 flyers (with attached EOI forms) were distributed in general practice waiting rooms, 89 eligible EOI forms were returned and 18 participants were randomised (see Table 9). Conversion rate from eligible EOI to randomised participants was greater from mail invitations than from waiting room recruitment, with 34% of eligible EOIs from letter mail-out being converted to randomised participants versus 20% from waiting room recruitment approaches (Table 10). Although letter mail-out yielded more randomised participants, this approach was more expensive than waiting room recruitment in terms of cost per returned EOI (Table 11). However, when comparing cost per randomised patient (rather than returned EOI), letter mail-out was marginally cheaper than waiting room recruitment (see Table 11). It is also important to note that 33 EOIs from mail-out approaches, compared with just three EOIs from waiting room recruitment, could not be progressed owing to the early closure of the trial. These 36 EOIs had the potential to become randomised patients and this ratio difference is likely to have further widened the difference in cost between the two recruitment approaches.
| Site/practice | Recruitment method | |||||||
|---|---|---|---|---|---|---|---|---|
| Letter mail-out | Waiting room | |||||||
| Letters mailed out (n) | EOI forms returned, n (%)a | Eligible EOI forms, n (%)a | Patients randomised, n (%)a | Flyers distributed (n) | EOI forms returned, n (%)a | Eligible EOI forms, n (%)a | Patients randomised, n (%)a | |
| 101 | 640 | 32 (5) | 30 (4.7) | 11 (1.7) | 181 | 14 (7.7) | 13 (7.2) | 3 (1.7) |
| 102 | 300 | 12 (4) | 12 (4) | 7 (2.3) | 173 | 8 (4.6) | 8 (4.6) | 1 (0.6) |
| 107 | 537 | 11 (2) | 11 (2) | 4 (0.75) | 557 | 15 (2.7) | 12 (2.1) | 6 (1.08) |
| 108 | 239 | 4 (1.7) | 4 (1.7) | 3 (1.3) | 514 | 9 (1.7) | 9 (1.7) | 1 (0.2) |
| 203 | 192 | 10 (5.2) | 8 (4.2) | 2 (1.04) | 130 | 7 (5.4) | 7 (5.4) | 1 (0.77) |
| 204b | 0 | –c | –c | –c | 332 | 25 (7.5) | 21 (6.3) | 4 (1.2) |
| 205 | 583 | 12 (2.1) | 12 (2.1) | 4 (0.7) | 355 | 13 (3.7) | 11 (3.09) | 1 (0.3) |
| 206 | 189 | 11 (5.8) | 11 (5.8) | 8 (4.2) | 88 | 8 (9.09) | 7 (7.9) | 0 |
| 209b | 632 | 18 (2.8) | 16 (2.5) | –d | –d | –d | –d | –d |
| 310 | 578 | 22 (3.8) | 18 (3.1) | 1 (0.2) | 275 | 1 (0.36) | 1 (0.36) | 1 (0.36) |
| 311 | 231 | 6 (2.6) | 5 (2.2) | 3 (1.3) | 762 | 0 | 0 | 0 |
| Total | 4121 | 138 (3.3) | 127 (3.08) | 43 (1.04) | 3367 | 100 (3) | 89 (2.6) | 18 (0.53) |
| Site/practice | Recruitment method | |||
|---|---|---|---|---|
| Letter mail-out | Waiting room | |||
| Eligible EOI returned, (n) | Patients randomised, n (%) | Eligible EOI returned (n) | Patients randomised, n (%) | |
| 101 | 30 | 11 (36.7) | 13 | 3 (23.1) |
| 102 | 12 | 7 (53.3) | 8 | 1 (12.5) |
| 107 | 11 | 4 (36.4) | 12 | 6 (50.0) |
| 108 | 4 | 3 (75.0) | 9 | 1 (11.1) |
| 203 | 8 | 2 (25.0) | 7 | 1 (14.3) |
| 204 | –a | –a | 21 | 4 (19.1) |
| 205 | 12 | 4 (33.3) | 11 | 1 (9.1) |
| 206 | 11 | 8 (72.7) | 7 | 0 |
| 209 | 16 | –b | –b | –b |
| 310 | 18 | 1 (5.5) | 1 | 1 (100) |
| 311 | 5 | 3 (60.0) | 0 | 0 |
| Total | 127 | 43 (33.9) | 89 | 18 (20.2) |
| Recruitment method | |||||
|---|---|---|---|---|---|
| Letter mail-out | Waiting room | ||||
| Item | n | Cost (£) | Item | n | Cost (£) |
| Packs | 3882 | 5127.04 | Flyers | 3367 | 208.75 |
| Pre-paid envelopes | 4121 | 235.76 | EOIs | 3367 | 208.75 |
| Administrator time (hours) | 38.82 | 446.43 | Receptionist time (sessions) | 3 | 195.00 |
| Searches | 11 | 385.98 | Pre-paid envelopes | 100 | 5.72 |
| Patient list check | 9 | 1040.00 | Researcher time (hours) | 170 | 2949.50 |
| Mail merge | 10 | 943.92 | Returned envelopes | 10 | 29.50 |
| Docmail® | 1 | 103.56 | PIS | 100 | 24.80 |
| Returned envelopes | 138 | 40.71 | |||
| Total cost | 8323.40 | Total cost | 3622.02 | ||
| Number of EOIs | 138 | Number of EOIs | 100 | ||
| Cost per EOI | 60.31 | Cost per EOI | 36.22 | ||
| Patients randomised | 43 | Patients randomised | 18 | ||
| Cost per randomised patient | 193.57 | Cost per randomised patient | 201.22 | ||
We compared actual recruitment against target recruitment. Our planned target was to recruit 120 participants over a period of 6 months from July to December 2014. At the end of this 6-month recruitment period we had randomised 19 patients, 15.8% of the target randomisation (Table 12). We continued to recruit to the study through January to June 2015, when stopping rules were invoked following a meeting with NIHR HTA. In discussion, it was agreed that patients who already had a baseline assessment visit booked would be permitted to complete their assessment and recruited to the study. We recruited our final participant in August 2015, giving a final sample size of 61 participants, 50.8% of our original target randomisation figure for the internal pilot trial (see Table 12).
| Month | Month number | Target randomisation (n) | Actual randomisation (n) | Target cumulative randomisation (n) | Actual cumulative randomisation, n (%) |
|---|---|---|---|---|---|
| June 2014 | 1 | 0 | 0 | 0 | 0 (0.0) |
| July 2014 | 2 | 6 | 0 | 6 | 0 (0.0) |
| August 2014 | 3 | 6 | 0 | 12 | 0 (0.0) |
| September 2014 | 4 | 18 | 2 | 30 | 2 (6.7) |
| October 2014 | 5 | 30 | 2 | 60 | 4 (6.7) |
| November 2014 | 6 | 30 | 7 | 90 | 11 (12.2) |
| December 2014 | 7 | 30 | 8 | 120 | 19 (15.8) |
| January 2015 | 8 | – | 5 | 120 | 24 (20.0) |
| February 2015 | 9 | – | 4 | 120 | 28 (23.3) |
| March 2015 | 10 | – | 7 | 120 | 35 (29.2) |
| April 2015 | 11 | – | 3 | 120 | 38 (31.7) |
| May 2015 | 12 | – | 9 | 120 | 47 (39.2) |
| June 2015 | 13 | – | 9 | 120 | 56 (46.7) |
| July 2015 | 14 | – | 4 | 120 | 60 (50.0) |
| August 2015 | 15 | – | 1 | 120 | 61 (50.8) |
Participant flow
Figure 4 is the CONSORT diagram showing participant flow through the trial. The CONSORT diagram provides summary figures for numbers of patients assessed for eligibility, declines, exclusions, allocation and completion of 4-month follow-up data collection. Tables 13–15 provide a breakdown of reasons for decline, reasons why patients did not meet inclusion criteria and reasons why patients did not participate in the pilot trial, respectively.
FIGURE 4.
The CONSORT diagram showing participant flow from initial eligibility assessment through to 4-month follow-up.
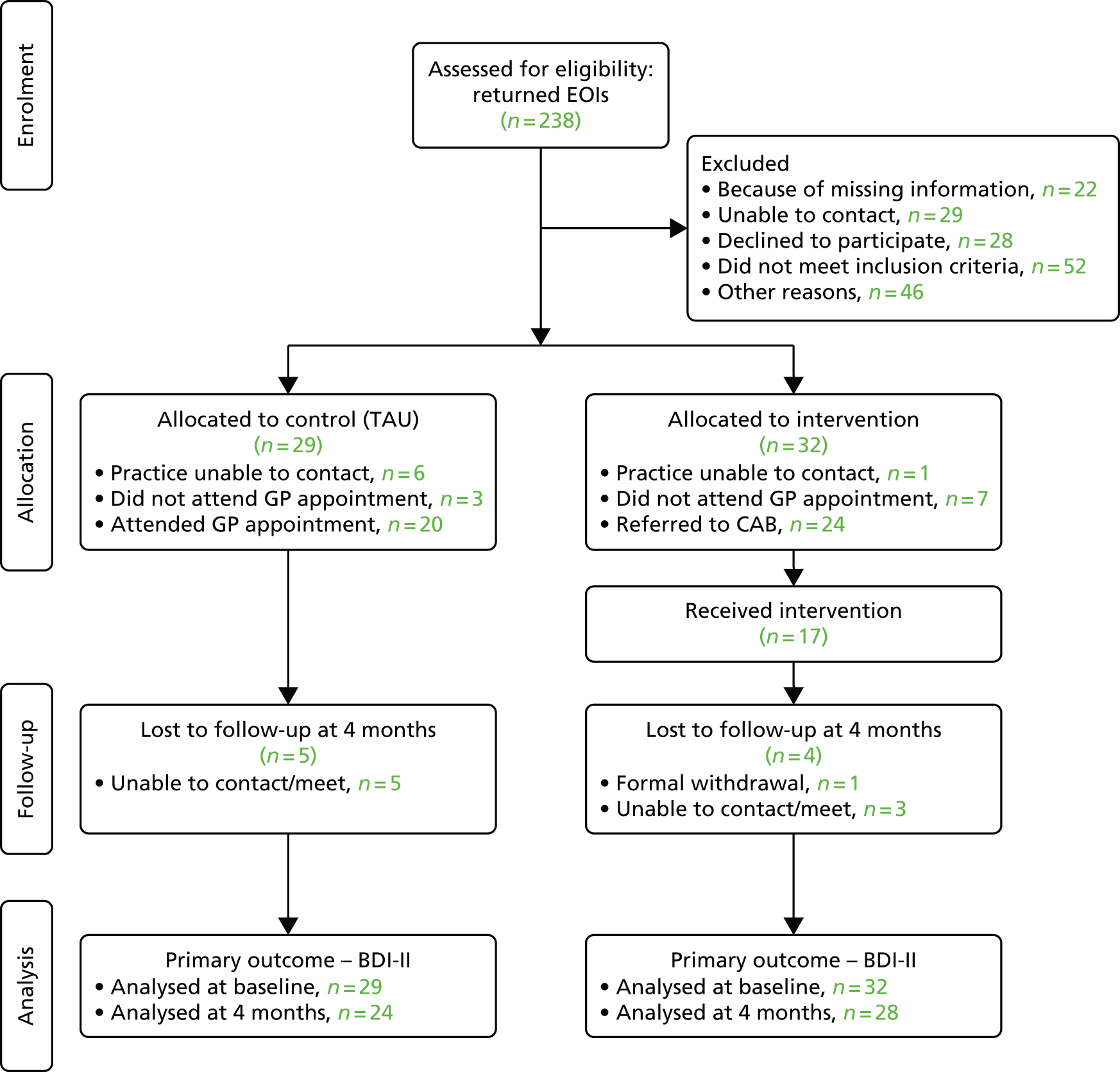
| Reasons | n |
|---|---|
| Does not want to take part in research | 2 |
| Unable to take part because of time commitment | 5 |
| Baseline cancelled/no show at baseline unable to recontact or decided no | 13 |
| Decided no longer interested | 8 |
| Total | 28 |
| Reasons | n |
|---|---|
| Currently taking part in another research study | 2 |
| Debt advice form CAB in last 12 months | 10 |
| Does not have low mood/depression | 9 |
| Does not want debt advice via general practice | 3 |
| Not worried about debt or no debt | 25 |
| BDI-II score of < 14 at baseline assessment | 3 |
| Total | 52 |
| Reasons | n |
|---|---|
| Baseline risk assessed then unable to recontact/did not wish to continue | 3 |
| Baseline split over more than one visit: unable to recontact to complete | 1 |
| Withdrawn by GP | 1 |
| General practice no longer able to take participants into the study | 3 |
| Change of location/general practice pre baseline | 2 |
| HTA decision to close trial: unable to progress to baseline | 36 |
| Total | 46 |
Participant characteristics
Of 61 participants randomised into the study, 26 (42.6%) were male and 35 (57.4%) were female. The mean age of the participants was 46 years (SD 12.8 years; range 21–79 years). Fifty-nine (96.8%) participants reported their ethnicity as white and two (3.2%) reported it as ‘other’. Fourteen (23%) participants were married, four (6%) were cohabiting, six (10%) were in a relationship, 31 (51%) were single and six (10%) reported their marital status as ‘other’. Nine (14.8%) participants were in paid work, two (3.3%) were in training/education, 29 (47.5%) were not working because of long-term illness or disability, three (4.9%) were looking after the home, eight (13.1%) were unemployed and actively seeking employment, four (6.6%) were retired and six (9.8%) recorded their employment status as ‘other’.
Severity of depression
Mean BDI-II score across participants at baseline was 35.2 (SD 8.1; range 14–53). The great majority of participants recorded BDI-II scores in the severe range (Figure 5), with a score of 14–19 indicating mild depression (two participants, 3%), a score of 20–28 indicating moderate depression (six participants, 10%) and a score of > 28 indicating severe depression (53 participants, 87%).
FIGURE 5.
Severity of depression across the whole sample.
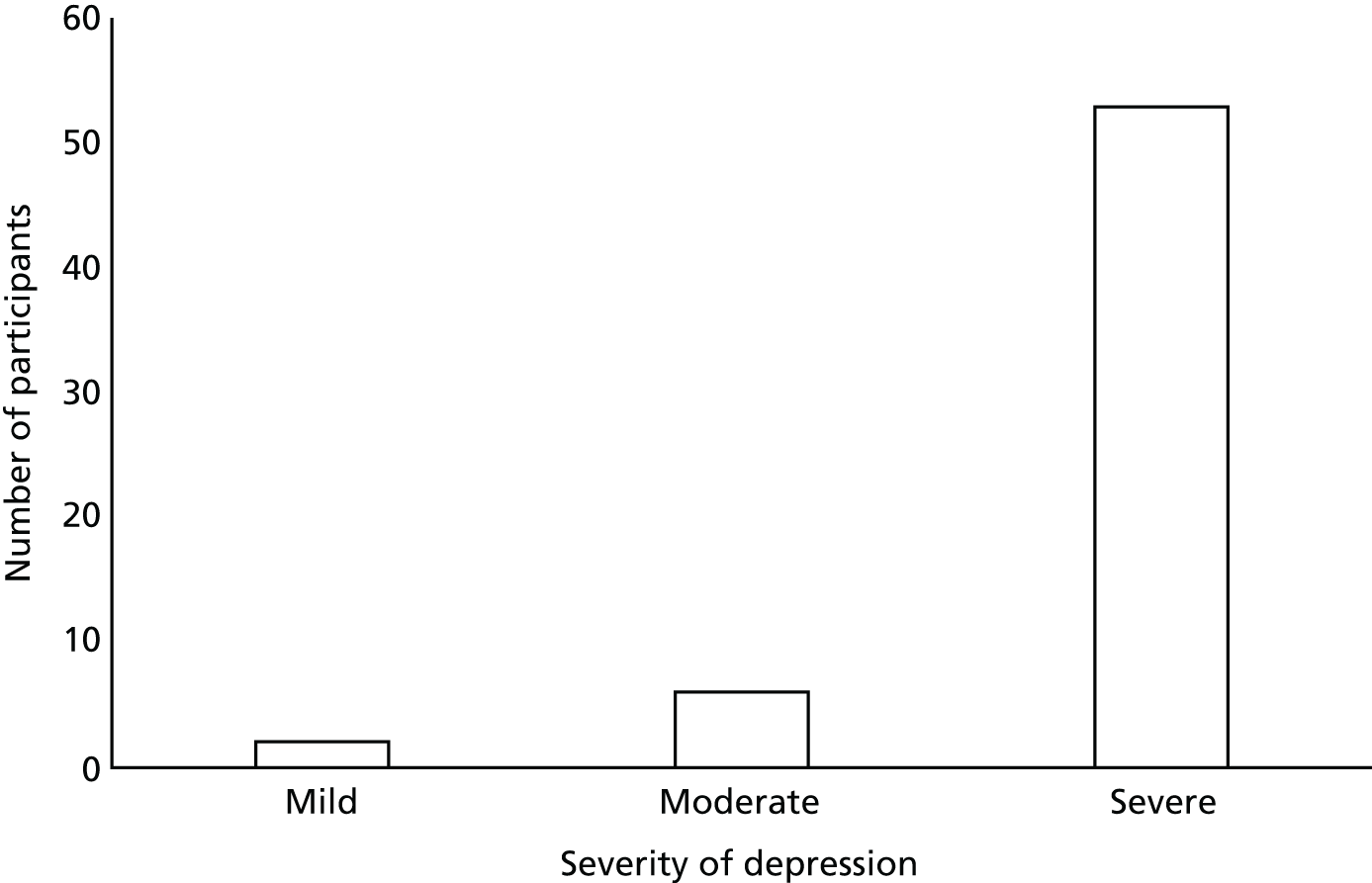
Comparison of participant characteristics by recruitment approach: letter mail-out versus waiting room recruitment
Table 16 provides a summary comparison of participant characteristics by the two recruitment methods. Although equal numbers of male and female participants were recruited by the waiting room method, 61% of those recruited by letter mail-out were female. More single participants than cohabitees (72% vs. 67%) were recruited by letter mail-out, as were more participants who were not employed (84% vs. 78%). However, in light of the relatively small numbers, there is no evidence of significant sample skewing between the two methods of recruitment.
| Baseline characteristic | Recruitment method | |
|---|---|---|
| Letter mail-out | Waiting room | |
| Sex, n (%) | ||
| Male (N = 26) | 17 (39.5) | 9 (50.0) |
| Female (N = 35) | 26 (60.5) | 9 (50.0) |
| Age (years), mean (SD) | 46.3 (13.2) | 44.4 (11.9) |
| Ethnicity, n (%) | ||
| White (N = 59) | 43 (100.0) | 16 (88.9) |
| Other (N = 2) | 0 (0.0) | 2 (11.1) |
| Cohabiting status, n (%) | ||
| Cohabiting (N = 18) | 12 (27.9) | 6 (33.3) |
| Not cohabiting (N = 43) | 31 (72.1) | 12 (66.7) |
| Employment, n (%) | ||
| Employed (N = 11) | 7 (16.3) | 4 (22.2) |
| Not employed (N = 50) | 36 (83.7) | 14 (77.8) |
| Mean depression score (SD) | 35.8 (8.3) | 33.8 (8.1) |
| Severity of depression, n (%) | ||
| Mild (N = 2) | 2 (4.7) | 0 (0.0) |
| Moderate (N = 6) | 2 (4.7) | 4 (22.2) |
| Severe (N = 53) | 39 (90.6) | 14 (77.8) |
Comparison of participant characteristics by allocation
Table 17 summarises participant characteristic by allocation. There was a greater proportion of female participants in the control arm than in the intervention arm (69% vs. 47%). The mean ages of the groups were similar [mean age in control arm, 45.5 (SD 15.0) years; mean age in intervention arm, 46.4 (SD 10.6) years]. Of those participants who were employed, almost two-thirds were in the intervention arm of the study, although these constituted only 18% of the whole sample. Although the majority of the sample recorded their ethnicity as white, both of the participants who did not were in the intervention arm of the trial. The vast majority of the sample recorded BDI-II scores at baseline that fell within the severe range; however, both participants with scores that fell within the mild range were in the intervention arm of the trial (see Table 17).
| Baseline characteristic | Trial arm | |
|---|---|---|
| Control (TAU) | Intervention | |
| Age (years), n [mean] (SD) | 29 [45.5] (15.0) | 32 [46.4] (10.6) |
| Sex, n (%) | ||
| Male (N = 26) | 9 (31.0) | 17 (53.1) |
| Female (N = 35) | 20 (69.0) | 15 (46.9) |
| Ethnicity, n (%) | ||
| White (N = 59) | 29 (100.0) | 30 (93.7) |
| Other (N = 2) | 0 (0.0) | 2 (6.3) |
| Cohabiting status, n (%) | ||
| Cohabiting (N = 18) | 9 (31.0) | 9 (28.1) |
| Not cohabiting (N = 43) | 20 (69.0) | 23 (71.9) |
| Employment, n (%) | ||
| Employed (N = 11) | 4 (13.8) | 7 (21.9) |
| Not employed (N = 50) | 25 (86.2) | 25 (78.1) |
| Severity of depression, n (%) | ||
| Mild (N = 2) | 0 (0.0) | 2 (6.3) |
| Moderate (N = 6) | 3 (10.3) | 3 (9.4) |
| Severe (N = 53) | 26 (89.7) | 27 (84.3) |
Assessment of contamination
We assessed contamination based on self-report information about receipt of debt advice provided by participants at the 4- and 12-month assessment visits. The original criterion for determining evidence of contamination was ‘10 or more of the individually randomised TAU participants from among the 30 individually randomised control participants seeking debt advice, providing this is at least twice as common among individually versus cluster randomised controls’. At the time recruitment to the trial closed, only 29 participants had been allocated to the control arm of the trial, with 18 participants from cluster control practices and 11 participants individually randomised. Of the 18 cluster controls, 13 completed the debt advice question at 4-month follow-up, with one participant reporting having received debt advice. Of the 11 individually randomised controls, 10 completed the debt advice question at 4-month follow-up, with one participant reporting having received debt advice. Only four control participants completed a 12-month follow up, all were individually randomised controls. None reported receiving debt advice in the preceding 8 months. Although the figures are small, based on the definition above, there was no evidence of serious contamination within the participants individually randomised to the control arm of the trial. We would therefore have employed individual randomisation for the full trial.
Assessment of unblinding
Unblinding of RAs (when it occurred) was recorded on the participant CRF. There were four definite cases (one control participant and three intervention participants) in which RAs were unblinded to participant allocation at 4-month follow-up. There were also a further four cases (all intervention participants) in which RAs were unsure whether or not they had been unblinded – either because there had been some reference to practice allocation or because participants had referred to CAB – but it was unclear whether this was for the study or if the participant was seeing CAB independently. No additional unblinding occurred at the 12-month follow-up point.
Assessment of data collection systems and data completeness
We checked through the clinical trials unit for missing data in all files from baseline, 4- and 12-month follow-up. In each case, although there were some missing answers in a few questionnaires, most were fully completed where relevant (e.g. high ‘missing rate’ in Stanford presenteeism scale owing to low levels of employment among participants).
Primary and secondary outcome analysis: descriptive statistics
Although we include available data for all three data collection points (baseline and 4- and 12-month follow-up), we will not comment on the 12-month data because of the small imbalanced numbers of participants at 12 months.
Primary outcome
Table 18 shows mean BDI-II scores in the control and intervention groups at both baseline and 4-month follow-up. The mean scores in all groups at all time points continue to fall within the moderate (20–28) or severe (> 28) depression range.
| Trial arm | Time point, n [mean] (SD) | ||
|---|---|---|---|
| Baseline | 4 months | 12 months | |
| Control | 29 [36.6] (7.9) | 24 [29.0] (11.3) | 4 [31.8] (20.3) |
| Intervention | 32 [33.9] (8.4) | 28 [25.7] (9.9) | 18 [25.4] (8.8) |
Secondary outcomes
Psychological well-being
Anxiety and well-being were assessed using the BAI and the SWEMWBS, respectively. Table 19 shows the mean anxiety scores for control and intervention groups at baseline and follow-up, and Table 20 shows the mean SWEMWBS scores for control and intervention groups at baseline and follow-up.
| Trial arm | Time point, n [mean] (SD) | ||
|---|---|---|---|
| Baseline | 4 months | 12 months | |
| Control | 27 [28.2] (13.0) | 23 [22.4] (11.8) | 4 [32.0] (19.9) |
| Intervention | 31 [25.4] (13.3) | 26 [24.9] (14.0) | 18 [22.0] (14.1) |
| Trial arm | Time point, n [mean] (SD) | ||
|---|---|---|---|
| Baseline | 4 months | 12 months | |
| Control | 17 [16.3] (4.9) | 22 [17.9] (4.3) | 4 [14.5] (6.0) |
| Intervention | 28 [17.6] (4.7) | 25 [18.6] (4.3) | 17 [20.1] (4.8) |
Employment factors
Employment factors were assessed with participants’ self-reported absence from work due to sickness and with the SPS-6 questionnaire assessing the impact of health problems on work. Table 21 shows the percentage of participants in the control and intervention groups reporting a sickness absence at baseline and follow-up. At both baseline and follow-up a greater percentage of the intervention group reported sickness absence. Table 22 shows mean scores on the SPS-6 for control and intervention groups. The possible presenteeism score ranges from 6 to 30, with lower scores indicating less presenteeism. Both groups, thus, have moderate presenteeism average scores with little change at follow-up.
| Trial arm | Time point, n [mean] (SD) | ||
|---|---|---|---|
| Baseline | 4 months | 12 months | |
| Control | 5/10 (50.0) | 4/11 (36.4) | No data |
| Intervention | 8/10 (80.0) | 5/9 (55.6) | 1/2 (50) |
| Trial arm | Time point, n [mean] (SD) | ||
|---|---|---|---|
| Baseline | 4 months | 12 months | |
| Control | 10 [18.2] (4.9) | 11 [16.1] (5.5) | No data |
| Intervention | 17 [17.9] (5.0) | 14 [17.0] (5.4) | 6 [19.0] (4.5) |
Service satisfaction
Participant service satisfaction was assessed with the GSQ, with higher scores indicating greater satisfaction. Table 23 shows mean scores between groups on the GSQ at 4-month follow-up, with little difference in mean scores for control and intervention groups, suggesting no evidence of relatively lower satisfaction with either approach.
| Trial arm | Time point, n [mean] (SD) |
|---|---|
| 4 months | |
| Control | 22 [47.4] (9.2) |
| Intervention | 25 [46.0] (10.6) |
Substance misuse
Alcohol and illicit drug use was assessed with the AUDIT questionnaire and Drug Use Questionnaire, respectively. Table 24 presents mean scores for alcohol consumption. Clinically, those scoring 8–15 would be offered advice on reducing hazardous drinking, those scoring 16–19 would be offered a more structured brief intervention and those scoring ≥ 20 would be considered potentially dependent drinkers. At all data collection points, the mean score in the intervention group is higher than in the control group; indeed, the mean score of persistently > 20 in the intervention group who completed the full AUDIT score suggests that many of these were dependent drinkers. The proportions of hazardous (or more) drinkers were comparable between the control and intervention samples at baseline, dropping after 4 months among controls (from 38% to 29%) but rising among the intervention group (from 34% to 50%).
| AUDIT score | Time point, n [mean] (SD) | ||
|---|---|---|---|
| Baseline | 4 months | 12 months | |
| Control | |||
| Qu 1–3 | 18 [1.4] (1.6) | 17 [1.4] (1.7) | 2 [2.0] (2.8) |
| Qu 1–10 | 11 [13.6] (9.6) | 7 [15.4] (9.8) | 2 [11.5] (6.4) |
| All | 29 [6.0] (8.4) | 24 [5.5] (8.3) | 4 [6.8] (6.8) |
| Intervention | |||
| Qu 1–3 | 21 [2.0] (1.7) | 13 [1.9] (1.8) | 9 [2.0] (1.7) |
| Qu 1–10 | 11 [21.7] (12.7) | 13 [23.9] (10.1) | 9 [21.3] (12.0) |
| All | 32 [8.8] (12.0) | 26 [12.9] (13.3) | 18 [11.7] (13.0) |
Table 25 shows mean scores between groups for illicit drug use. The mean score for illicit drug use is higher in the intervention group at all data collection points. Table 26 shows the comparison between the control and intervention groups for illicit drug use by severity category. No participant in the control arm scored within the severe range for illicit drug use, compared with two participants scoring within the severe range at some point across the data collection points.
| Treatment arm | Time point, n [mean] (SD) | ||
|---|---|---|---|
| Baseline | 4 months | 12 months | |
| Control | 6 [1.3] (0.5) | 6 [1.8] (1.2) | 2 [1.5] (0.7) |
| Intervention | 8 [3.0] (3.0) | 12 [3.6] (3.0) | 5 [4.8] (3.9) |
| Severity category | Time point, n/N (%) | ||
|---|---|---|---|
| Baseline | 4 months | 12 months | |
| Control | |||
| Low | 6/6 (100.0) | 5/6 (83.3) | 2/2 (100.0) |
| Moderate | 0/6 (0.0) | 1/6 (16.7) | 0/2 (0.0) |
| Substantial | 0/6 (0.0) | 0/6 (0.0) | 0/2 (0.0) |
| Severe | 0/6 (0.0) | 0/6 (0.0) | 0/2 (0.0) |
| Intervention | |||
| Low | 5/8 (62.5) | 6/12 (50.0) | 2/5 (40.0) |
| Moderate | 1/8 (12.5) | 4/12 (33.3) | 1/5 (20.0) |
| Substantial | 1/8 (12.5) | 0/12 (0.0) | 1/5 (20.0) |
| Severe | 1/8 (12.5) | 2/12 (16.7) | 1/5 (20.0) |
Quality of life
Quality of life was assessed with MANSA, with higher scores indicating better quality of life. Table 27 shows that at both time points there was some difference in mean quality-of-life scores between groups, with the mean score at baseline being lower among the controls, but rising by 8.8 versus 3.3 in the intervention group to give a higher mean score at 4 months.
| Trial arm | Time point, n [mean] (SD) | ||
|---|---|---|---|
| Baseline | 4 months | 12 months | |
| Control | 29 [41.8] (13.1) | 24 [50.6] (10.5) | 4 [43.2] (11.6) |
| Intervention | 32 [44.1] (11.6) | 27 [47.4] (12.9) | 18 [52.4] (11.6) |
Life events and difficulties
The presence of life events and difficulties known to be associated with depression, and positive events and reduction in difficulties associated with improvement in psychological well-being, were assessed with the LED-S. At baseline, there appeared to be some difference between groups in the reporting of life events and difficulties, with a greater percentage of the intervention group reporting a severe event or severe financial event in the 12 months prior to baseline. However, a greater percentage of the intervention group also reported a fresh start event in the 12 months prior to baseline. A greater percentage of the control group reported a financial fresh start event, a difficulty reduction, a financial difficulty reduction, a positive experience and a positive financial experience in the 12 months prior to baseline (Table 28). At the 4-month follow-up a greater percentage of the control group reported having experienced a severe event, a fresh start event and a positive experience between baseline and 4-month follow-up, suggesting that the intervention had no effect on experiences relieving stress. There was little difference between the groups on any other indices at 4-month follow-up (see Table 28). Comparing the mean number of events and difficulties between groups, Table 29 shows little difference between the control and intervention groups in the mean number of events and difficulties occurring in the 12 months prior to baseline and between baseline and 4-month follow-up.
| Events and difficulties | Severe event or difficulty occuring, n/N (%) | |
|---|---|---|
| In the 12 months prior to baseline | Between baseline and 4 months | |
| Participants reporting a severe event | ||
| Control | 16/29 (55.2) | 12/24 (50.0) |
| Intervention | 21/32 (65.6) | 10/27 (37.0) |
| Participants reporting a severe financial event | ||
| Control | 5/29 (17.2) | 2/24 (8.3) |
| Intervention | 8/32 (25.0) | 2/27 (7.4) |
| Participants reporting a fresh start event | ||
| Control | 9/29 (31.0) | 9/24 (37.5) |
| Intervention | 12/32 (37.5) | 7/27 (25.9) |
| Participants reporting a financial fresh start | ||
| Control | 2/29 (6.9) | 0/24 (0.0) |
| Intervention | 1/32 (3.1) | 0/27 (0.0) |
| Participants reporting any difficulty reduction | ||
| Control | 13/29 (44.8) | 1/24 (4.1) |
| Intervention | 8/32 (25.0) | 1/27 (3.7) |
| Participants reporting any financial difficulty reduction | ||
| Control | 13/29 (44.8) | 1/24 (4.1) |
| Intervention | 8/32 (25.0) | 1/27 (3.7) |
| Participants reporting any positive experience | ||
| Control | 18/29 (62.1) | 9/24 (37.5) |
| Intervention | 17/32 (53.1) | 7/27 (25.9) |
| Participants reporting any positive financial experience | ||
| Control | 3/29 (10.3) | 2/24 (8.3) |
| Intervention | 1/32 (3.1) | 1/27 (3.7) |
| Events and difficulties | Event or difficulties occuring, n [mean] (SD) | |
|---|---|---|
| In the 12 months prior to baseline | Between baseline and 4 months | |
| Mean number of severe events | ||
| Control | 29 [1.7] (2.7) | 24 [1.1] (1.6) |
| Intervention | 32 [1.6] (1.7) | 27 [0.8] (1.7) |
| Mean number of severe financial events | ||
| Control | 29 [0.3] (0.8) | 24 [0.2] (0.7) |
| Intervention | 32 [0.3] (0.5) | 27 [0.1] (0.5) |
| Mean number of provoked difficulties | ||
| Control | 29 [2.9] (1.3) | 24 [2.4] (1.1) |
| Intervention | 32 [2.7] (1.2) | 27 [2.2] (1.2) |
| Mean number of financial provoked difficulties | ||
| Control | 29 [0.7] (0.4) | 24 [0.7] (0.5) |
| Intervention | 32 [0.8] (0.4) | 27 [0.8] (0.5) |
| Mean number of severe provoking events | ||
| Control | 29 [4.6] (3.4) | 24 [3.5] (2.6) |
| Intervention | 32 [4.3] (2.4) | 27 [3.0] (2.2) |
| Mean number of severe financial provoking events | ||
| Control | 29 [1.0] (1.0) | 24 [0.9] (0.9) |
| Intervention | 32 [1.1] (0.6) | 27 [0.9] (0.7) |
| Mean number of fresh starts | ||
| Control | 29 [0.5] (0.8) | 24 [0.5] (0.8) |
| Intervention | 32 [0.5] (0.8) | 27 [0.3] (0.6) |
| Mean number of financial fresh starts | ||
| Control | 29 [0.4] (0.2) | 24 [0.1] (0.3) |
| Intervention | 32 [0.0] (0.0) | 27 [0.04] (0.2) |
The proportions of participants with severe financial events and difficulties in the past 12 months are higher than in most studies, but this is unsurprising given that such an experience was a sample selection criterion. Proportions with other types of severe events and difficulties are similar to those in other studies with inner-city working-class participant samples.
Explanatory measures
Hopelessness
Table 30 shows some differences between the two groups in mean score, and agency and pathway subscale, with controls recording lower mean scores (i.e. lower propensity to believe themselves able to effect change in their lives and believe themselves able to find solutions to problems) at both time points than the intervention group.
| Trial arm and variables | Time point, n [mean] (SD) | |
|---|---|---|
| Baseline | 4 months | |
| Control | ||
| Agency | 27 [14.2] (5.3) | 24 [17.4] (6.8) |
| Pathway | 27 [16.1] (5.6) | 24 [19.4] (5.9) |
| Total | 27 [55.3] (11.7) | 24 [61.9] (13.0) |
| Intervention | ||
| Agency | 32 [16.0] (6.5) | 25 [16.1] (7.6) |
| Pathway | 32 [18.5] (7.0) | 26 [18.7] (7.1) |
| Total | 32 [58.9] (12.3) | 25 [58.5] (13.9) |
Shame
Table 31 shows some difference between the two groups in mean score on the OAS scale, with controls recording higher mean scores (i.e. greater propensity to experience feelings of shame arising from the perceived negative judgement of others) at both time points than those in the intervention group.
| Trial arm | Time point, n [mean] (SD) | |
|---|---|---|
| Baseline | 4 months | |
| Control | 29 [37.5] (12.2) | 24 [36.4] (14.6) |
| Intervention | 31 [33.7] (15.5) | 26 [31.3] (15.8) |
Rumination
Table 32 shows little difference between the two groups in mean Response Style Questionnaire-24 scores for rumination at both baseline and 4-month follow-up.
| Trial arm | Time point, n [mean] (SD) | |
|---|---|---|
| Baseline | 4 months | |
| Control | 29 [29.0] (7.9) | 23 [27.5] (8.1) |
| Intervention | 32 [27.8] (8.0) | 26 [27.9] (8.0) |
Comparing perceptions between groups of debt contribution to low mood and low mood contribution to debt
Participants completed a question asking whether or not they thought that their money difficulties contributed to their experience of low mood/depression/anxiety and, conversely, whether or not they thought that low mood/depression/anxiety had a negative impact on their money difficulties. If participants answered affirmatively to the first question, they then rated, on a scale of 1–10 (where 1 was ‘hardly at all’ and 10 was ‘completely’), the contribution of money difficulties to low mood/depression/anxiety and, conversely, the contribution of low mood/depression/anxiety to money difficulties. Table 33 shows the mean contribution scores by group. The means in all instances suggest that the majority of the sample felt that debt contributed substantially to their low mood/anxiety and conversely that low mood/depression contributed substantially to their money difficulties, with little difference between groups. This bidirectional interaction reflects previous research (see Chapter 1, Relationship between debt and depression) and our qualitative findings (see Chapter 6).
| Trial arm | Time point, n/N [mean] (SD) | ||
|---|---|---|---|
| Baseline | 4 months | 12 months | |
| Debt contributes to low mood | |||
| Control | 26/28 [7.6] (2.1) | 21/24 [7.6] (1.8) | 4/4 [6.5] (3.1) |
| Intervention | 21/21 [7.6] (1.7) | 24/27 [7.6] (1.5) | 14/18 [7.3] (2.4) |
| Low mood contributes to debt | |||
| Control | 25/28 [7.7] (2.3) | 21/24 [7.1] (2.4) | 3/4 [8.0] (1.0) |
| Intervention | 19/21 [7.6] (1.9) | 21/27 [8.0] (1.4) | 13/18 [8.2] (1.8) |
Chapter 5 Pilot trial results: health economics analysis
Descriptive analysis: health and social care utilisation and personal debt
Given the small sample size and unbalanced 12-month follow-up samples, we comment mainly on the data collected at baseline and 4-month follow-up.
Inpatient data
No participant listed any use of long-stay or rehabilitation inpatient hospital services over the 3 months prior to study entry, or at either of the two follow-up time points. Overall, the number of participants with use of inpatient hospital services was low; moreover, the number of inpatient contacts in the 3-month period directly preceding baseline and each of the two follow-up data collection points was low within both the control and intervention groups. Inpatient service use was reported mostly as acute and as occurring prior to the baseline visit for all participants, with 10% of participants in the control group reporting acute medical visits, compared with 6% of the intervention group. Acute surgical inpatient contacts were reported by 7% of the control group, compared with 3% of the intervention group. Only one person (3%) from the intervention group reported acute inpatient service use for mental health services; this admission took place in the 3 months preceding baseline, with a reported number of 41 inpatient days. A minority of the acute admissions were via the accident and emergency (A&E) department, with 14% of admissions taking place via this route for the control group, compared with 11% of acute admissions for the intervention group. Only one participant from each group reported inpatient service use in the 3 preceding months at 4-month follow-up; both were for acute service use of medical or surgical nature, rather than for mental health services.
Outpatient (ambulatory) hospital services
As can be seen in Table 34, there is little difference in the percentage of participants attending for physical health care from either the control or the intervention group. The number of participants reporting physical health-care appointments was in both groups higher in the 3 months preceding the 12-month follow-up assessment than at the 4-month follow-up, but the differences between baseline and 4-month follow-up are small. At baseline, a greater percentage of participants from the intervention group (21%) than from the control group (10%) report outpatient care for mental health. However, during the 3 months preceding the 4-month follow-up, both groups’ use of outpatient care falls, the intervention group falls to 7% from 22%, compared with 8% from 10% among the control. Similarly, the percentage of participants reporting A&E appointments changes between the groups at baseline and 4 months, with both groups reporting a small rise, but the overall numbers are small (range 7–13%).
| Type of appointment | Data collection point | |||||
|---|---|---|---|---|---|---|
| Baseline (N = 61) | 4 months (N = 51) | 12 months (N = 22) | ||||
| Control (n = 29) | Intervention (n = 32) | Control (n = 24) | Intervention (n = 27) | Control (n = 4) | Intervention (n = 18) | |
| Physical | ||||||
| Participants with appointments, n (%) | 15 (51.7) | 17 (53.1) | 12 (50.0) | 14 (51.9) | 3 (75.0) | 12 (66.7) |
| Number of appointments across participants, mean (SD) | 2.6 (2.5) | 3.4 (5.1) | 2.9 (2.8) | 1.9 (1.7) | 4.0 (1.7) | 2.4 (1.9) |
| Mental health | ||||||
| Participants with appointments, n (%) | 3 (10.3) | 7 (21.9) | 2 (8.3) | 2 (7.4) | 1 (25.0) | 1 (5.6) |
| Number of appointments across participants, mean (SD) | 3.0 (3.5) | 4.0 (4.4) | 2.0 (0.0) | 1.0 (0.0) | 1.0 (–) | 2.0 (–) |
| A&E | ||||||
| Participants with appointments, n (%) | 2 (6.9) | 3 (9.4) | 3 (12.5) | 3 (11.1) | 1 (25.0) | 3 (16.7) |
| Number of appointments across participants, mean (SD) | 4.0 (2.8) | 1.3 (0.58) | 1.0 (0.0) | 1.7 (1.2) | 1.0 (–) | 1.0 (0.0) |
Community-based day services
Table 35 shows that at baseline and at 4-month follow-up a greater percentage of intervention group participants than control group participants reported attending community-based services for mental health care. A greater percentage of intervention group participants than control group participants consistently reported attending community-based alcohol/substance misuse services at each data collection point, but this falls substantially among the intervention participants at 4 months compared with baseline or the 12-month follow-up (7% vs. 18% and 28%, respectively).
| Type of appointment | Data collection point | |||||
|---|---|---|---|---|---|---|
| Baseline (N = 61) | 4 months (N = 51) | 12 months (N = 22) | ||||
| Control (n = 29) | Intervention (n = 32) | Control (n = 24) | Intervention (n = 27) | Control (n = 4) | Intervention (n = 18) | |
| Mental healtha | ||||||
| Participants with appointments, n (%) | 3 (10.3) | 6 (18.8) | 3 (12.5) | 7 (25.9) | 2 (50.0) | 3 (16.7) |
| Number of appointments across participants, mean (SD) | 1.0 (0.0) | 6.5 (3.6) | 6.0 (4.0) | 3.6 (4.2) | 2.5 (2.1) | 9.3 (14.4) |
| Alcohol/substance misuseb | ||||||
| Participants with appointments, n (%) | 1 (3.5) | 6 (18.8) | 0 (0.0) | 2 (7.4) | 0 (0.0) | 5 (27.8) |
| Number of appointments across participants, mean (SD) | 2.0 (–) | 21.2 (38.0) | – | 56 (62.2) | – | 20.2 (23.7) |
Primary care contacts
The percentage of participants reporting a primary care contact is similar between the control and intervention groups at baseline and 4-month follow-up (Table 36), with nearly all participants reporting at least one GP contact, as one might expect in view of the study design and population.
| Type of contact | Data collection point | |||||
|---|---|---|---|---|---|---|
| Baseline (N = 61) | 4 months (N = 51) | 12 months (N = 22) | ||||
| Control (n = 29) | Intervention (n = 32) | Control (n = 24) | Intervention (n = 27) | Control (n = 4) | Intervention (n = 18) | |
| All primary care contacts | ||||||
| Participants with contact, na (%) | 27 (93.1) | 31 (96.9) | 23 (95.8) | 24 (88.9) | 4 (100.0) | 15 (83.3) |
| Contacts, meanb,c (SD) | 5.8 (4.5) | 3.8 (2.3) | 4.1 (3.1) | 3.4 (2.7) | 3.5 (1.3) | 4.6 (3.6) |
| Time spent with clinician across participants (minutes), meanb,c (SD) | 88.3 (81.7) | 55.4 (43.2) | 53.9 (42.2) | 58.8 (58.4) | 33.8 (14.9) | 86.0 (89.1) |
| GP contacts | ||||||
| Participants with contact, na (%) | 27 (93.1) | 31 (96.9) | 23 (95.8) | 24 (88.9) | 4 (100.0) | 15 (83.3) |
| Contacts, meanb,c (SD) | 5.4 (4.4) | 3.4 (2.0) | 3.8 (2.8) | 3.4 (2.7) | 2.8 (1.3) | 4.5 (3.5) |
| Time spent with GP across participants (minutes), meanb,c (SD) | 79.6 (77.9) | 48.0 (37.0) | 50.3 (41.6) | 58.8 (58.4) | 26.3 (14.9) | 79.3 (78.2) |
Priority and non-priority debts
Table 37 shows the number of participants with priority and non-priority debts by allocation. Although there is some variation between groups in the percentage of participants reporting priority debts at baseline and 4-month follow-up, the average number of priority debts per participant is similar between groups at each time point. At baseline and 4-month follow-up a greater percentage of participants in the control group report having non-priority debts than in the intervention group. The proportion of participants reporting a priority debt at 4 months falls more among control participants (from 72% to 50%) than among intervention participants (from 81% to 74%), although there is a greater reduction in the mean number of priority debts (mean reduction at 4 months, intervention 0.8 vs. control 0.4).
| Type of debt | Data collection point | |||||
|---|---|---|---|---|---|---|
| Baseline (N = 61) | 4 months (N = 51) | 12 months (N = 22) | ||||
| Control (n = 29) | Intervention (n = 32) | Control (n = 24) | Intervention (n = 27) | Control (n = 4) | Intervention (n = 18) | |
| Priority | ||||||
| Participants with priority debts, n (%) | 21 (72.4) | 26 (81.3) | 12 (50.0) | 20 (74.1) | 4 (100.0) | 14 (77.8) |
| Number of priority debts across participants, mean (SD) | 3.5 (2.2) | 3.2 (2.4) | 3.9 (1.8) | 3.1 (1.6) | 3.3 (1.5) | 2.6 (1.6) |
| Non-priority | ||||||
| Participants with non-priority debts, n (%) | 27 (93.1) | 25 (78.1) | 20 (83.3) | 19 (70.4) | 2 (50.0) | 15 (83.3) |
| Number of non-priority debts across participants, mean (SD) | 3.6 (3.4) | 2.7 (1.4) | 2.3 (1.6) | 2.5 (1.0) | 1.0 (0.0) | 2.6 (1.4) |
Criminal justice system
Table 38 shows the number of participants who reported, via the Client Service Receipt Inventory, criminal justice system contacts in the 3 months preceding each of the baseline, 4-month follow-up and 12-month follow-up assessments. Only a small percentage of participants from both groups reported police contacts at baseline and at 4-month follow-up. One participant from each group reported ‘spending the night in a prison cell’ in the 3 months preceding baseline, but no further reports of such incidents were presented at 4-month follow-up in either group. A small percentage of participants in each group reported having civil court appearances at baseline and at 4-month follow-up. No participant reported having any criminal court appearances. Only one participant from the intervention group reported receiving a psychiatric assessment ‘in custody’; this took place in the 3 months preceding baseline and we have not included these data in Table 38.
| Type of contacta | Data collection point | |||||
|---|---|---|---|---|---|---|
| Baseline (N = 61) | 4 months (N = 51) | 12 months (N = 22) | ||||
| Control (n = 29) | Intervention (n = 32) | Control (n = 24) | Intervention (n = 27) | Control (n = 4) | Intervention (n = 18) | |
| Police | ||||||
| Participants with contacts, n (%) | 1 (3.4) | 2 (6.2) | 1 (4.2) | 3 (11.1) | 1 (25.0) | 3 (16.7) |
| Number of contacts across participants, mean (SD) | 1.0 (–) | 2.0 (1.4) | 2 (–) | 3.7 (1.5) | 1 (–) | 2.3 (2.3) |
| Night in prison cell | ||||||
| Participants with contacts, n (%) | 1 (3.4) | 1 (3.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Number of contacts across participants, mean (SD) | 1 (–) | 1 (–) | – (–) | – (–) | – (–) | – (–) |
| Civil court appearance | ||||||
| Participants with contacts, n (%) | 2 (6.9) | 2 (6.3) | 0 (0.0) | 1 (3.7) | 1 (25.0) | 2 (11.1) |
| Number of contacts across participants, mean (SD) | 1.5 (0.7) | 1 (0.0) | – (–) | 1 (–) | 1 (–) | 1 (0.0) |
Citizens Advice Bureau contacts
A total of 32 participants were allocated to the intervention arm to receive CAB debt advice. Of these, 19 had some form of communication with the CAB, two participants chose not to take up the service and 17 went on to receive CAB debt advice. Of the 17 participants receiving CAB advice, 10 (59%) had a single CAB appointment, five (30%) had two appointments and a small number had three or four appointments (12% and 6%, respectively). Across the 17 participants, a total of 28 appointments took place. Most appointments were completed face to face at the participant’s own general practice (71%), with four appointments (14%) taking place at CAB premises. Appointments lasted an average of 57 minutes (range 10–90 minutes).
Health-related quality of life
The data produced three samples of participants: those with baseline data (n = 61: control, n = 29; intervention, n = 32), those who also had data from 4-month follow-up (n = 50: control, n = 24; intervention, n = 26) and those who had complete-case data at 12 months (n = 22: control, n = 4; intervention, n = 18). The data described later (see Figures 6 and 7) consider each sample (in isolation) at the three data collection points. Results from all participants, as represented by group allocation of control and intervention, are presented.
One data point was imputed for one participant to facilitate retention within the 12-month follow-up sample; the data point was rescored using data from a participant with a similar pattern of response across the EQ-5D-5L dimensions. Data at 4 months were spoiled for one participant and so only baseline data were included.
The EQ-5D-5L Crosswalk Index Value Calculator (version 2) was used to calculate the EQ-5D-5L index values and the following formula was used to calculate QALYs from the EQ-5D-5L administered at baseline and at 4-month follow-up:
The formula was extended to calculate QALYs from the EQ-5D-5L administered at baseline and the two follow-up time points (4 and 12 months):
EurolQol-5 Dimensions UK population norms
In this study the EQ-5D-5L version was used; currently, there are no data for the UK population norms from the five-level version, and the comparison made here is in reference to the EuroQol-5 Dimensions-3 levels (EQ-5D-3L). For the purposes of the comparisons shown here, the potential differences in values from the three- and five-level versions are unlikely to lead the reader to draw erroneous conclusions about the study population and UK norms. The norms were originally calculated by Kind et al. 82 from a sample of 3395 participants within the UK and recently reproduced in a study by Janssen and Szende. 83 As the number of people reporting severe problems is usually a small proportion of the general population, it is common to sum the reported levels of problems. 83 In the case of the EQ-5D-3L, this means that levels 2 and 3 are summed to create two categories of ‘no problems’ and ‘problems’ for each of the five dimensions. As the opportunity to observe changes in the reported level of problems is more refined for the EQ-5D-5L, no such categorising of ‘no problems’ relative to ‘problems’ has been conducted for the DeCoDer sample in an effort to demonstrate the nuances of change that transpired across the three data collection periods. For both the index values (total and by domain) and visual analogue scale (VAS) scores, the study population can be seen to score substantially below UK norms.
EurolQol-5 Dimensions health states by group allocation
As can be seen from Figure 6, across the two groups most participants at baseline reported some problems (levels 2–5/’slight’ to ‘extreme’) in all five EurolQol-5 Dimensions (EQ-5D) dimensions of mobility (54.4%), self-care (39.6%), usual activity (82.0%), pain/discomfort (73.8%) and anxiety/depression (98.4%). Anxiety/depression was consistently reported at a higher level (‘moderate to extreme’) across groups (78.7%), along with usual activity (55.8%) and pain/discomfort (49.2%). Self-care (60.7%) and mobility (45.5%) were the dimensions in which most participants reported ‘no problems’. Similar patterns of reporting were seen within both the control (n = 29) and intervention (n = 32) groups, although the proportion of participants reporting higher levels (levels 4–5) of mobility problems was higher in the control group (62.1%) than in the intervention group (43.7%), and similarly for usual activity (89.7% and 75.0%, respectively). Some variation in reported levels of problems can be seen across and within groups, as well as between data collection points.
FIGURE 6.
Percentage of participants in the control and intervention groups reporting level of problems at each data collection point, from level 1, ‘no problems’, to level 5, ‘extreme problems’, by dimension alongside UK population norms. A greater percentage indicates more participants reporting at this level. (a) Mobility; (b) self-care; (c) usual activities; (d) pain/discomfort; and (e) anxiety/depression.
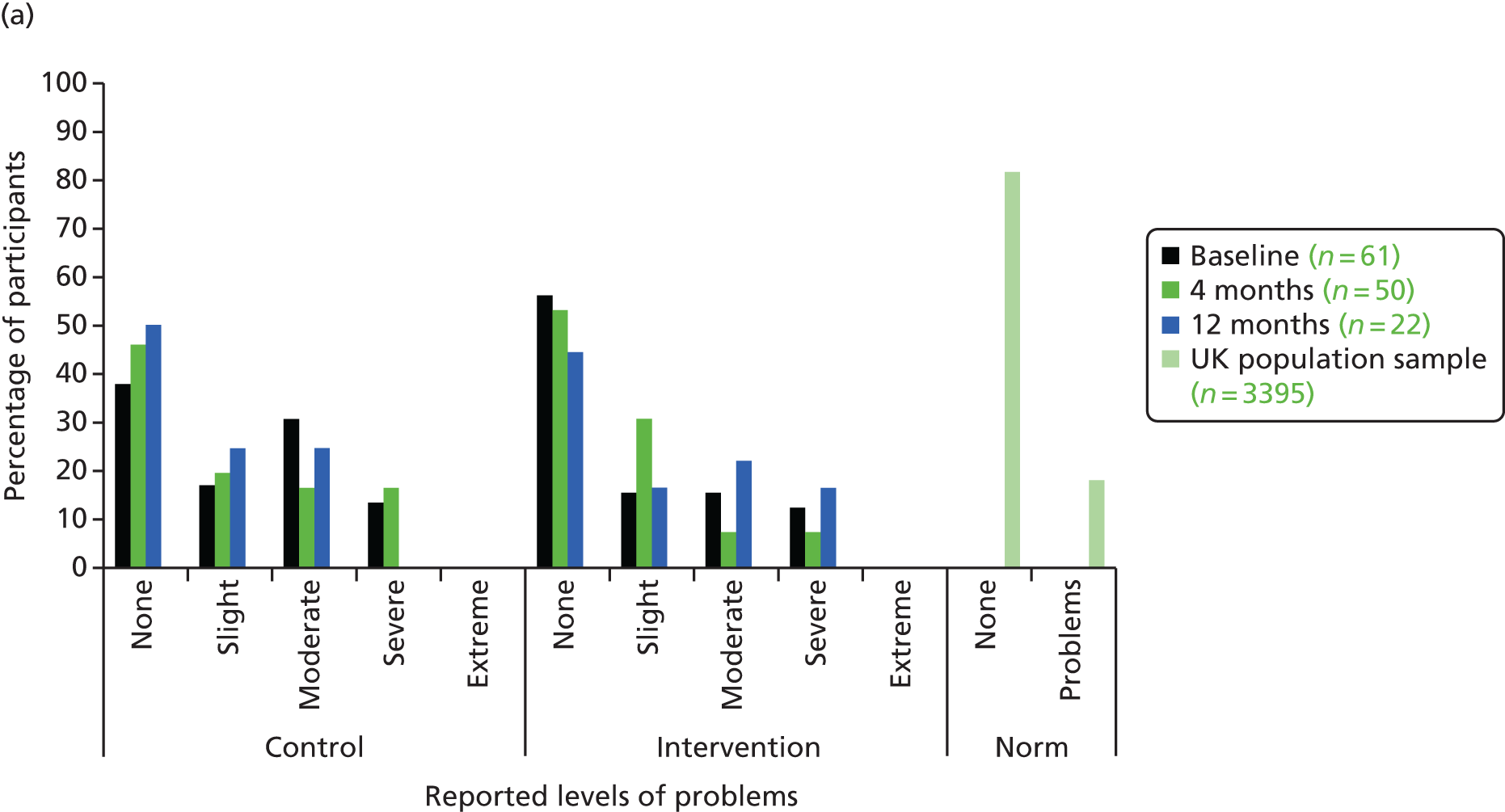
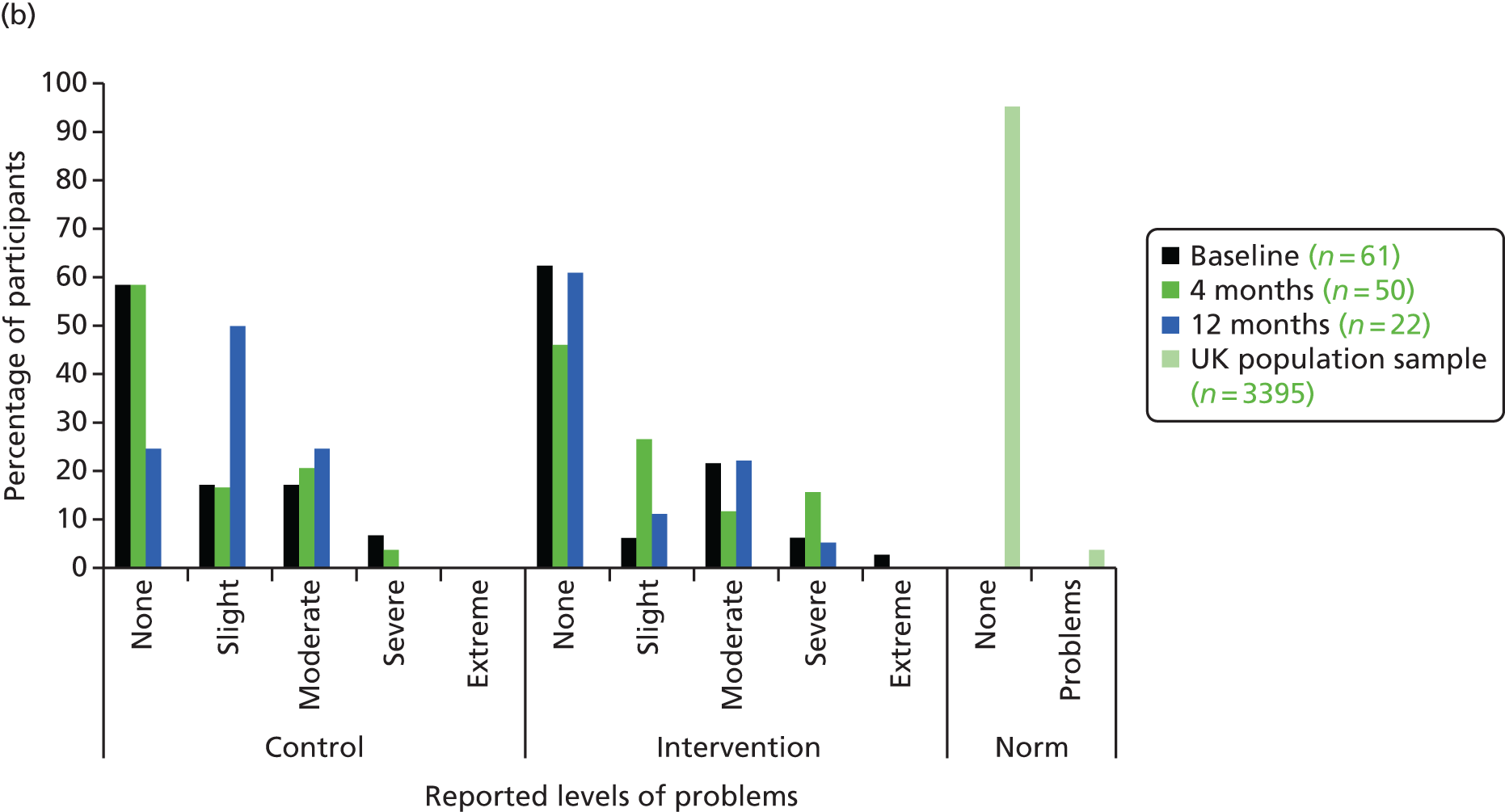
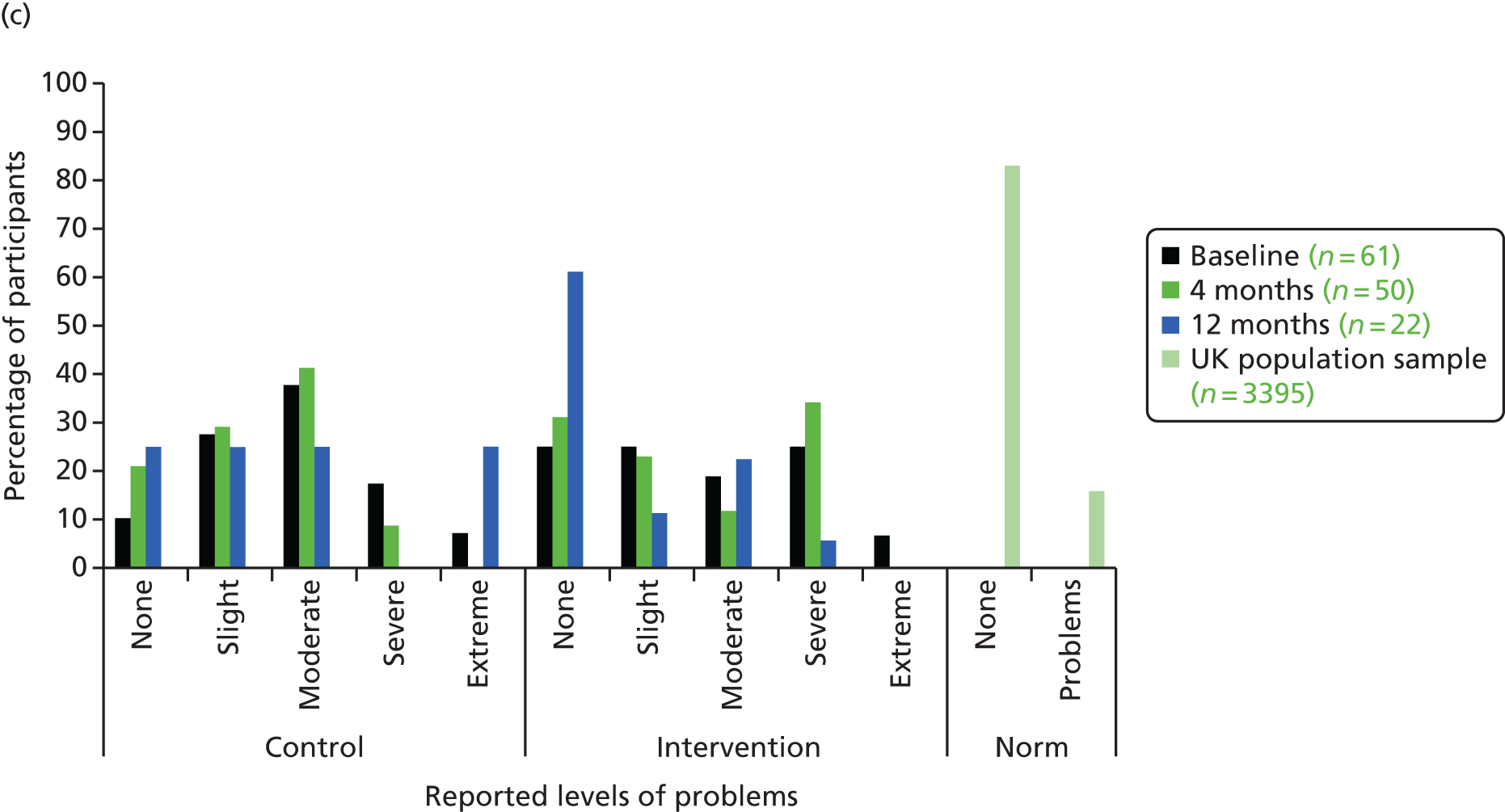
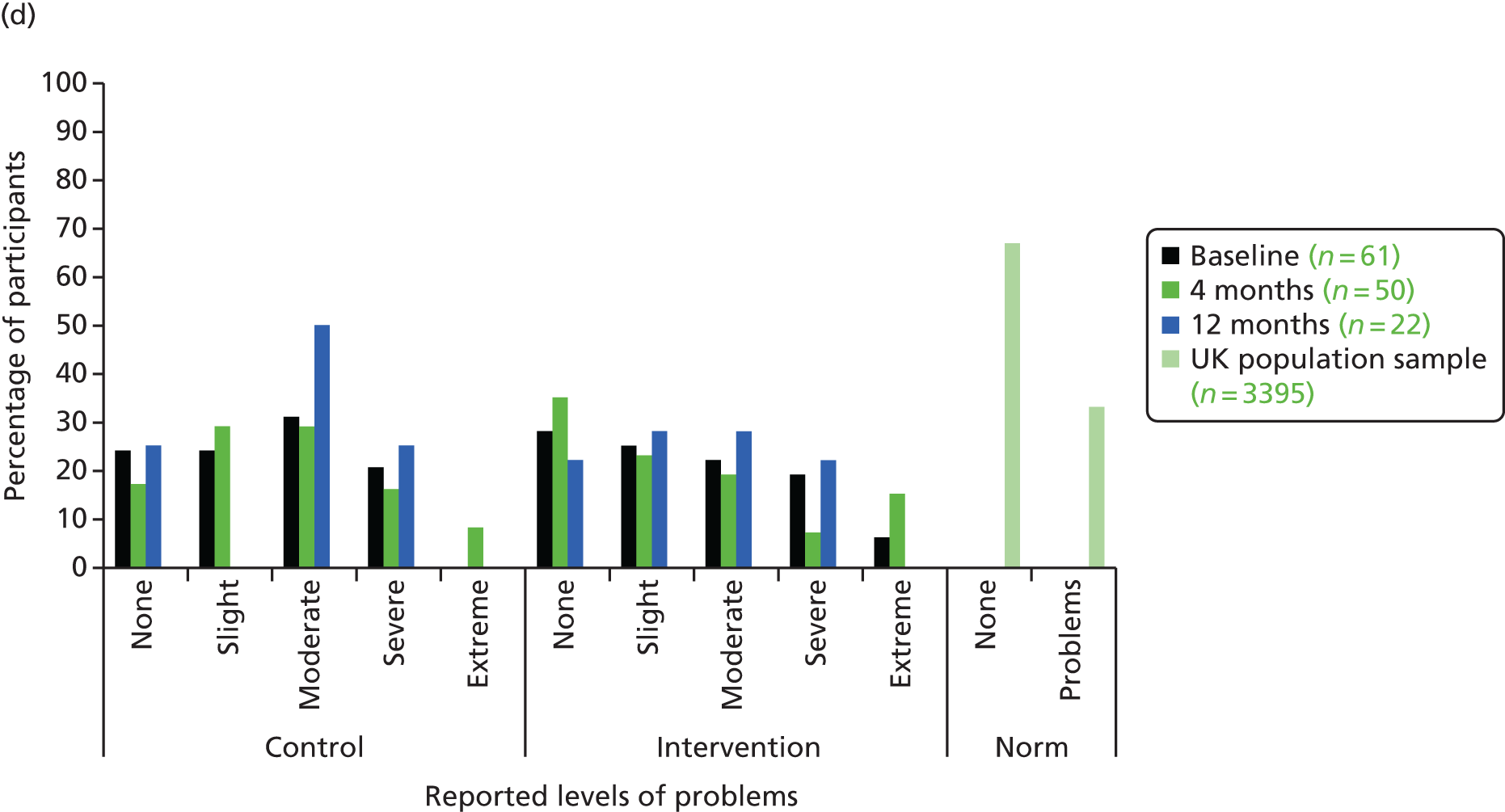
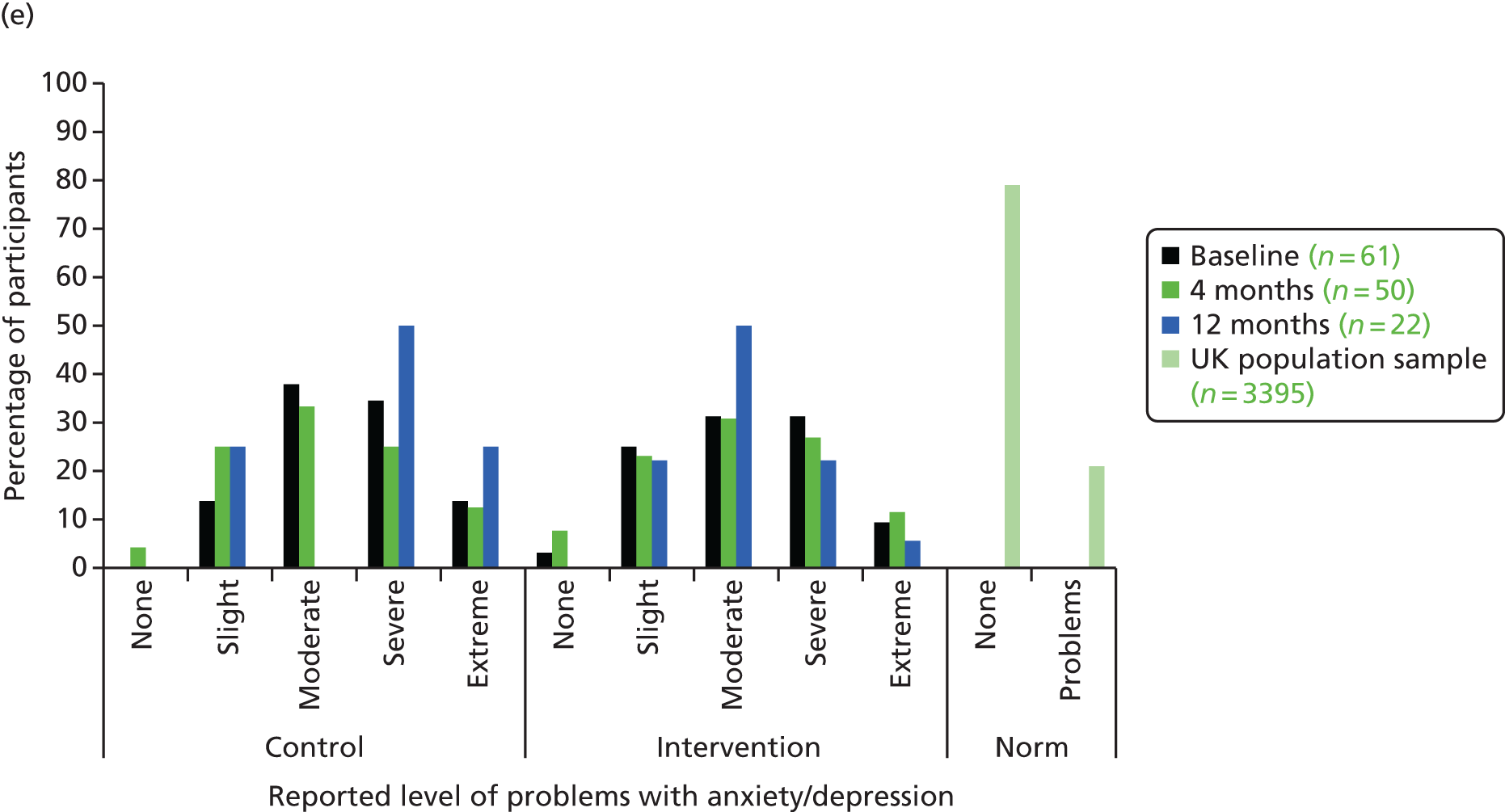
EurolQol-5 Dimensions visual analogue scale and index value by group allocation
The EQ-5D VAS scores (range 0–100) were rescaled for comparability with index values (range 0–1) by dividing scores by 100 (e.g. a VAS score of 45 = 45/100 = 0.450).
As can be seen in Figure 7, at baseline the control group report marginally higher EQ-5D index values than the intervention group (0.497 and 0.468, respectively), whereas the control group’s VAS scores are marginally lower than those of the intervention group (0.450 and 0.522, respectively). Across both groups the index value score and the VAS reports appear to be consistent in representing similar health-state valuations.
FIGURE 7.
Mean EQ-5D index and VAS scores (rescaled) for participants in the control and intervention groups at each time point alongside UK population norms. Higher scores indicate a better quality of life.

Summary: health economics
The results are purely descriptive and, with such a small sample size, we are cautious about drawing conclusions. However, it seems clear that at baseline the study population are ‘users’ of health services and there is an imbalance at baseline. In a full randomised controlled trial, adjustment for baseline use and other factors may be required. There were some participants who had contact with criminal justice services, so in order for a full picture of impact on services to be captured, those conducting future studies should be mindful of collecting these data as well as the health and social care contacts.
The EQ-5D data reflect the impact on health-related quality of life that the study participants experienced as a consequence of debt and depression; we see that, on the mental health domain, around 80% of the study sample report ‘moderate’, ‘severe’ or ‘extreme’ problems with anxiety and depression. This is relative to a UK norm of around 20% reporting some problems with anxiety and depression. We noted that 7% of our participants reported that they had no problems with depression or anxiety at baseline, even though all reached the BDI-II threshold for depression.
Chapter 6 Qualitative findings
Introduction
Chapter 6 is divided into two main components. First, we provide summary information about the patient participant sample and present findings from the analysis of patient participant interviews. Second, in Intervention process evaluation we present the findings from the analysis of clinician and CAB advisor participant interviews with regard to the intervention process evaluation component of the study.
Participants
Of the 61 participants recruited to the study, 57 (93.4%) registered their interest in taking part in the qualitative component of the study. Of these 57 participants, 34 (59.6%) were selected for interview at the time recruitment to the study was closed. Of the 34 participants selected, 23 (67.6%) actually went on to complete a qualitative interview.
Of the 23 participants interviewed, just over half had been allocated to the intervention arm of the study, and 65% were female. As with the overall sample, the majority of participants taking part in an interview were categorised as having severe depression. The ages of participants ranged from 23 to 71 years, with a mean age of 47 years. All participants taking part in a qualitative interview were given a pseudonym (Table 39).
| Baseline depression severitya | Age groupb | Pseudonym |
|---|---|---|
| Intervention | ||
| Female | ||
| Severe | Older | Angela |
| Severe | Older | Natalie |
| Severe | Older | Anne |
| Severe | Older | Paula |
| Severe | Older | Laura |
| Severe | Younger | Karen |
| Severe | Younger | Lucy |
| Mild | Older | Jane |
| Male | ||
| Severe | Older | Mike |
| Severe | Older | Mark |
| Severe | Older | John |
| Severe | Older | James |
| Control | ||
| Female | ||
| Severe | Older | Emma |
| Severe | Older | Sophie |
| Severe | Younger | Amy |
| Severe | Younger | Emily |
| Moderate | Older | Alice |
| Moderate | Older | Jill |
| Moderate | Younger | Susan |
| Male | ||
| Severe | Older | Pete |
| Severe | Older | David |
| Severe | Older | Christopher |
| Severe | Younger | Steve |
Of the 23 participants that took part in a baseline qualitative interview, 19 (82.6%) also completed a 4-month follow-up interview.
Introduction to findings
The purpose of undertaking participant interviews was threefold. First, we wanted to gain a better understanding of participants’ lived experience of debt and depression, and the relationship between these experiences. Second, we wanted to explore participants’ experience of the intervention. Third, we wanted to explore participants’ experience of involvement in the trial, including the acceptability of trial processes and outcome measures. We take each of these purposes in turn in presenting the findings of the qualitative analysis.
The lived experience of debt and depression: a story of complexity
Participants’ biographies of debt and depression reflected the highly individualised and complex social, psychological and contextual arena in which debt and depression was experienced.
Although each participant described a unique constellation of experience, important concepts and patterns could be identified that spanned individualised experience.
Trajectories into unmanageable debt
Most participants were able to identify key trigger points/events that shifted them from a position of financial security or manageable debt into a position of unmanageable debt: debts that participants considered there to be little hope of them being able to address within the context of their circumstances at that time. Trigger events often heralded a loss or reduction in household income, as described by Anne and Natalie:
Then he [partner] started with depression then he couldn’t work, so then I was paying everything and then I started getting into debt again.
Anne
Before I was divorced when I was married to him, he would buy the kids things you know, and help them along and what have you, well after I was divorced I still tried to do that, and using the credit card and that you know and buying stuff for the kids . . . that is how it started.
Natalie
Psychological impact of unmanageable debt
The psychologically damaging effects of unmanageable debt were clearly articulated by participants; these included, but were not limited to, pervasive worry, threat and fear, a sense of entrapment, demotivation and low mood/depression. It was apparent that these negative psychological experiences were intimately entwined and compounded by other social and contextual influences. Pervasive worry, for example, was linked by participants to their expressed feelings of low mood/depression:
It [debt] it worries you to the point where you know you are sitting here every day thinking am I going to be here next week you know what I mean . . . debt was a killer it really was, I would sit here and I would be in buckets all day all night.
Pete
Your central heating because you are worrying in case you put that on, you are worrying in case your electricity, worrying in case and that is where the depression comes in on the financial side.
David
Many a day many a time I sat here . . . what are you going to do for food, what are you going to eat today. And there will be no leccy [electricity] then what’s the point going out for work, or what is the point [name] it is going to be the same, the same, the motivation, the self-esteem, it is just rock bottom and then the depression sets in.
Mark
Contextual influences
The context of unmanageable debt contributed substantially to participants’ experience of unmanageable debt and depression. In particular, participants’ social and life roles (and activities) featured heavily in their descriptions of debt impact. Such activities appeared to be integral to participants’ psychological well-being and the loss or severe limitation of these (due to lack of finances) was identified as a barrier to life enjoyment and a key contributor to feelings of low mood and depression:
[Mates] are enjoying themselves . . . going to festivals whatever, enjoying themselves with their mates . . . I can’t afford even just to even think about . . . that kind of stuff . . . debt is the wall and I can’t climb over it and enjoy myself.
Steve
The financial depression or whatever you want to call it, money worries or that does revolve around that. Where you pick your grandkids up, and or you don’t pick them up because you say to your lad or your daughter or whatever, listen you make an excuse because you haven’t got the money you know.
David
But it feels like so often I am having to sacrifice not even, not even big luxuries just kind of like little bits of money just to you know for, to get by really so that is, that is depressing . . . waiting for your life to actually begin in a way . . . I can’t afford to have fun.
Lucy
Responses of others
How other individuals, in particular family members, responded to participants’ money difficulties also influenced how participants felt about their current situation (and themselves), with negative responses from others further compounding participants’ psychological distress:
. . . and this is why now I won’t tell my family because they can’t just go oh, right come here then let’s, let’s help let’s have a look it is, well why didn’t you just ring them up, why didn’t you just fill it in, why didn’t you just . . . and this is the bit that makes you feel even more inadequate, makes the depression worse, and makes you put things off more.
Anne
Iatrogenic systems and processes
A subtheme that linked to ‘responses of others’ was the approaches taken by some creditors, debt collection agencies and benefits agencies. Participants described the negative effects of being hounded by debt collection agencies and experiencing what they perceived to be an uncaring approach of some agencies. These negative experiences further compounded participants’ psychological distress in the context of unmanageable debt:
I had horrible letters saying about coming here and they [debt collectors] did come here too which was very disturbing.
Emma
It was a like a big black cloud that was over me . . . it was a nightmare you know what I mean that was another one where I didn’t want to wake up of a morning . . . I was just getting hounded and I kept thinking I am going to walk out the door here now and have these bailiffs on me.
Mike
It took 7 weeks before they could actually start processing the claim, and I thought, 7 weeks with not a **** penny no gas, no electric . . . It was just a **** nightmare with all of them . . . and I was stuck in the middle, suffering.
Pete
It feels like they [local authorities] don’t care . . . I was in hospital on my own, I don’t have a partner to go for me, and when I came out of hospital I wasn’t well enough to go . . . how can I get the bus to the one-stop shop . . . I am going to appeal it but then I think, when that [claim] gets rejected that is going to knock me down again.
Amy
Multiple stigma
Also closely linked to others’ responses were participants’ perceptions of how others viewed them in relation to the problems that they were experiencing. Having depression, being unemployed, being on benefits and being in debt were all identified as stigmatising experiences by some participants:
I haven’t got a job and I am getting money from taxpayers so then again I am getting I feel like I am scum almost because we’re stigmatised the unemployed aren’t we at the moment, so it is that doesn’t make you feel good either.
Steve
A small number of participants were concerned about how they would be viewed in their parenting role because of the stigma they believed to be associated with mental health, and this had implications for accessing help:
You get the mental health awareness days and stuff I am jumping on that a bit more now whereas I used to ignore it because I didn’t want to class myself in that category because of the stigma . . . I was always scared . . . I think that is why I haven’t even gone and told anyone the issues because I thought the kids would get taken off me.
Jane
They put me for a referral for a mental health screening I didn’t go back . . . I don’t know it worries me. Because I have got my daughter and I am on my own, I am worried they are going to label me as incapable of parenting.
Emily
Concomitant difficulties
Other concurrent difficulties, for example physical health difficulties, relationship difficulties and addictions, also contributed to participants’ distress, acting both independently of and in combination with money difficulties to further compound feelings of worry and low mood:
My next big step is the finances the gambling that is hard, very, very hard . . . but other problems you have like in not being able to put your heating on in the winter, not being able to go out because of my ailments of my medical grounds . . . just an ongoing thing . . . it is depressing. Very depressing.
David
What am I going to do when the winter comes because it is cold then isn’t it. And I have got diabetes, I am cold at the best of times. You know but, it is only the worrying, not having money to pay my bills.
Angela
And then my depression following the breakup was about the breakup it wasn’t, well it didn’t help with the fact I didn’t have any money.
Amy
Trapped and demotivated
Participants described how their experiences left them feeling trapped and demotivated. They further described how demotivation, coupled with an expressed desire to escape (if only momentarily) from the misery of debt, could, in turn, affect their engagement with debt issues:
It is like a vicious circle because I just can’t win and if I think I have found a solution, then it comes down to the money and I don’t have the money and then to get money it means getting a loan and no one is going to give me a loan because of my credit because I have never paid nothing back. So there isn’t, I feel like . . . there is no answer, I can’t be bothered let’s just not bother.
Emily
And then you get more and more into the depression you just don’t think about money and then you think about it, you get more upset and you just block it out it is like a, just it doesn’t matter, it is not important, we will just pretend it doesn’t matter.
Amy
Linked to a sense of entrapment was a sense of dependency, which was closely aligned by a number of participants to other negative experiences including feelings of embarrassment, guilt and shame:
Once the disability was lost I just, it was just I couldn’t really I had to borrow money and I was embarrassed about it . . . Because I never asked money in my life.
John
But food bank no it is not a good, I mean it is a good idea, for people who need the food you know what I mean but, it made me feel worse knowing I had to go.
Pete
If I don’t get back to work I have no . . . I will have absolutely no option but to throw myself upon somebody’s mercy and that feels horrible to me I don’t like it, it is not very good for my self-esteem either.
Laura
Complexity and a vicious cycle of debt and depression
The overarching theme that encapsulated the myriad of experiences, influences and interactions reflected in participants’ stories of debt and depression was that of complexity; complexity in terms of the multiplicity of difficulties described by participants and the complexity of the interaction between these difficulties and debt and psychological distress. For those participants experiencing the greatest complexity in their lives, their experience was one that was characterised by a deeply entrenched vicious cycle of debt and depression:
It [debt] has made me ill, it [debt] is like a disease like I have caught something and I can’t get shut of it. You know what I mean it is going to be with me until the day that I die, it is not a debt I can see me ever getting out of . . . the [tablets] are supposed to help with the stem of the thoughts, and they are not working again at the minute but this is because the debt now is mounting . . . to deal with debt you need to be healthy . . . my mind is not healthy, my body is not healthy.
Paula
Depression and loneliness, and the isolation thinking back to what I had and what I am doing now I drink because of my past . . . there was times I would pack up the drinking and then but sitting in the misery of basically getting by every fortnight . . . I am hoping that I can get back around the [work] but at the moment I am just, continuing drinking as you can see . . . and then that is where my depression comes in.
Mark
Priorities for change
For many participants, not having to worry about money was a key hope for the future and commonly employment was seen as the favoured route out of money difficulties. However, participants also identified a number of important barriers to achieving this, including (1) the current employment climate, (2) the wage trap and (3) physical and mental health difficulties:
Yes and earning enough money that I don’t have to worry do you know what I mean, I am sick of it . . . I would want a job that you think right [name] you know you are going to be working 10 hours a day, 6 days a week 60 hours a week . . . don’t give me a job that is 20 hours a week, minimum wage because I know I am going to be struggling.
Mark
I am trying for work you know, but you don’t know how hard it is . . . how many knockbacks I have had now and it just disheartens you really bad.
Mike
So this is the longest I have ever been unemployed and I think because of the length of time now it is making me a bit frightened about going back to work.
Anne
Although many participants identified having more money (and linked to that employment) as a key route out of debt and psychological distress, it was clearly apparent from the issues participants raised that considerable support would be required in achieving this goal. It was also apparent that for those participants experiencing a multitude of interconnected difficulties, a detailed and highly co-ordinated package of support would be required if the vicious and debilitating cycle of debt and depression was to be broken.
A number of participants pointed to the importance of an understanding and supportive approach to addressing money difficulties in the context of mental health difficulties:
I went for my medical and they put me on the ESA [Employment and Support Allowance] so I am still like kind of employment seeking but not as stressful as the job seekers yes. Just a bit more understanding . . . they are dead helpful.
Jane
They [creditors] do burn your head up but it would be nice if they sat down with you, and spoke about it like we are speaking about it now and come to some plan and then I wouldn’t be like that.
Mike
But the doctor can just sort of like send a letter to whoever, who it is because I don’t think they do that, and just say to them you know this person is suffering at the moment, and what is happening has made it worse. They accept that it is their fault, but could you just sort of ease up a little bit, maybe give a bit of breathing space . . . I mean that would be a nice solution.
Christopher
Participant experience of the intervention
Although participants did not go into great detail about their experiences of the intervention, a number provided examples of the ways in which they believed CAB advice had started to help them to address the difficulties that they were experiencing with debt.
Engagement and information sharing
Two key concepts in this respect were engagement and being informed. Several participants described how CAB advisors had engaged with creditors on their behalf and, as such, had started an important dialogue so that participants could progress their engagement with debt issues:
Well I wouldn’t have got this point unless I had all the advice and doing the, and phone calls and all ringing them up and things, I wouldn’t have got anywhere otherwise.
Emma
I think actually when I go to see [CAB advisor] next week, I think I am going to ask her to between us draft a letter, maybe because this is where if I am left to do it myself I will keep putting it off and putting it off.
Anne
The second way in which participants had found CAB advice beneficial was helping participants to identify and access financial support or discretionary payments:
Yes a big help [CAB advice]. I wouldn’t have known anything about you know. Because they don’t tell you what you’re entitled to in benefits or anything like that, if you’ve got depression.
Natalie
For increasing my money . . . the information they [CAB advisor] gave me was really useful like I said and they started the ball rolling with the [organisation].
James
[CAB advisor] filled in a [form] for me which is a discretionary housing benefit that you are, well some people are entitled to and some aren’t basically and [CAB advisor] filled it in, explaining my mental health issues and the trouble that I was facing financially and I got my [payment] through.
Paula
Psychological benefit of intervention
A small number of participants indicated some psychological benefit from their meeting(s) with CAB advisors:
I don’t need, feel I need to yet [take advice] but I felt very reassured and hopeful. It lifted me up a bit that there was, I wasn’t on my own and I didn’t have to struggle with it on my own. There was help.
Laura
See I haven’t paid it for years. So I am going to end up to here and she [CAB advisor] said no, she said there is only so many years they can go back, so all this information was like, it took a weight off my shoulders.
Jane
In a similar vein, participants who spoke about their consultation with GPs indicated that what was most important about the consultation was that the GP was showing interest in, understanding of and concern for their difficulties:
I think before if you owed money like I didn’t feel the GP would be interested in that particular reason . . . feel that that has changed yes because [GP] did ask me . . . I felt better that he’d asked rather than me just come and pour out all the information.
James
I think that was quite helpful. I think the fact that they [GP] were perhaps more receptive to debt and depression going hand in hand and one feeding into the other.
Lucy
But she [GP] was nice and like she understood.
Jill
I could tell him [GP] anything, and I know it wouldn’t go any further. Which is sometimes a big help . . . Makes me feel better. Because I always say well at least someone’s concerned at what is going on in my life even though no one else is bothered.
Angela
However, one participant described how the consultation with the GP had provided an opportunity to discuss a change in her antidepressant treatment, and another explained how it had led to progress in investigating other concurrent health concerns:
I was a bit unsure about getting referred to my doctor but ended up what happened is I saw a different doctor, who I originally registered with and the good thing that came out of that, is I am changing my antidepressants.
Anne
They are keeping an eye on me anyway as well the general practitioner . . . well yes (what GP is doing helpful), they arranged the X-ray . . . I have got to have a scan done because that was normal . . . he [GP] said it is inside, in your bones probably arthritis like I had in my knee 12 months ago . . . so I want to get that sorted.
Emma
Participant experience of involvement in the trial
Opportunity to talk
A key theme in participants’ descriptions of their experience of involvement in the trial, and, in particular, with regard to researcher interviews, was ‘unloading’. A number of participants described how talking to the researcher had provided them with an opportunity to talk about the difficulties that they were experiencing that they would be unlikely to feel able to discuss with known others:
But sometimes for me to try and unload some pressure from myself a lot of my gambling I tend to bottle up because I find it is embarrassing. So being able to talk, about certain things and to maybe relate openly to somebody like yourself and the other lady.
David
Just to get it off my, you know the guilt, because I feel guilty for owing this money to the banks . . . it was total like this, relaxation you know, it was a bit of therapy for me to tell you the truth.
Mike
Engagement and reflection
For a number of participants, interviews with researchers also provided a space within which they themselves could engage with and reflect on the difficulties that they were experiencing:
It has helped me work through things because you have to think about what impact has that had on everything and it does, it has had a knock-on effect on, on everything.
Amy
It has helped, and it will help yes definitely because it helped, well one you know when I am talking things through with you or just explaining, I am quite good at reflecting, and as I am talking it is like therapy a bit.
Laura
Issues with involvement
Although the opportunity to engage with and reflect on difficulties was identified as beneficial by a number of participants, for Paula there was a downside to the completion of some questionnaires, as she describes in the following quotation:
That [questionnaires] irritates me . . . because it is a constant question of what I am like, what are my thoughts, what is my emotions, how would you describe and that irritates me. Because then I have got to think and then it is not a nice, that is not the nice part of the process to be honest with you because that delves too deep, far too deep than sometimes I am prepared to go.
Paula
Forced choices
Both Anne and Paula reflected on the forced choice response of many questionnaires. Both considered this to be problematic because it meant that their responses did not accurately reflect how they were feeling at that time:
Not so much the questions that they are asking it is how you can answer them. There is never on quite a few occasions there was never a tick box that I could have safely said well actually yes that is how I am feeling.
Anne
I just think on some of them [questionnaires] there is not the right answer there to answer it by you can’t put it down in sometimes always never . . . it doesn’t tell you exactly, you can’t express exactly how you are feeling on them.
Paula
Question relevance
Christopher questioned the relevance of some of the questions included in the context of a study about debt and depression:
I think last time there was a sexual question, to do with partners or whether you have random partners or something I can’t remember what the question was, it is irrelevant . . . I answered it but then I thought, you know is that really necessary to do with debt.
Christopher
Language complexity
Several participants noted the complexity of the language used in some of the questionnaires, which was a contributory factor to some overly long interviews:
For me it wasn’t [a struggle], but I did think there was, if you were . . . if reading wasn’t a real strong point you would find it difficult. That is what I thought, some people might find it difficult because and some of the questions were quite complex in some ways.
Laura
I didn’t understand a lot of the questions so she [researcher] was having to interpret them . . . and that probably it probably went longer than what it should have done.
David
Interviews too long
As noted in the previous section, some interviews took longer than anticipated. Although many participants did not consider time commitment an issue, several commented on interview length:
Yes they all right, they are fine. When they’re 3 hours it’s a bit . . .
Natalie
I just turned round to [researcher 1] and said is it OK that I am going this slow and she went yes but I didn’t finish it. She had to come back the next day to finish it off.
Mike
Proposed changes
When invited to comment about possible changes for future research, participants suggested little change. However, and not surprisingly, two participants advocated reducing the length of the data collection visit and one indicated that the significant commitment required on the part of participants warranted greater financial remuneration. Certainly participants appreciated the recognition of their involvement with the receipt of a shopping voucher:
The shorter interviews are better . . . yes, perhaps shorter interviews but that’s all.
Natalie
I want to help, and everything else, but my advice, or my opinion is it is far better to have 2 or 3 × 2 hours.
David
If I am being honest . . . if you want to go into somebody’s life so personally and in depth, in depth I just think that you know maybe . . . probably more of a monetary encouragement if I am being honest.
Christopher
I have enjoyed participating. Particularly like the £10 voucher . . . I saved the last ones, because I want to buy myself something for my birthday.
Anne
I quite like the £10 voucher, only because I feel like I don’t get anything . . . Although it wouldn’t be necessary for me I would have done it anyway. But it is nice.
Laura
Intervention process evaluation
The intervention process evaluation focused on the qualitative analysis of semistructured interviews with a sample of seven GPs and four CAB advisors who participated in the trial. The purpose of the interviews was to check fidelity to the model and the impact of participation on clinician and CAB advisor attitudes and practices, using the framework of NPT. 2
Analysis
The analysis focused on three specific components of the intervention as originally conceived (see Figure 7): (1) co-location of CAB advisors in general practices, (2) GPs’ assessment of debt and depression, and (3) enhanced communication between GPs and CAB advisors.
Co-location of Citizens Advice Bureau advisors in general practices
General practitioners and CAB advisors unanimously agreed that patients would benefit from having a debt advisor based within general practices:
But there is no doubt that every general practice should have a debt advice service, you know, that is an obvious place for them to be.
Interview 9, GP
Yes because you know the GP can pick up, you know, identify that the client has got debt, and we are going to the surgery to see and we get all that side of it has worked well with the referrals coming in, we contact the client, go to the surgery to see that has been quite seamless I think so I don’t see why it couldn’t expand, we couldn’t see more clients in that way.
Interview 4, CAB advisor 1
This finding shows that the co-location of the CAB advisor in primary care is an intervention that is normalised and, therefore, it could be integrated in the daily routine of general practices.
General practitioner’s biopsychosocial assessment of debt and depression
General practitioners conducted the assessment for debt and depression in the fashion of an ordinary consultation for depression:
I asked to come in to talk about debt or something or, so, so from my point of view probably they weren’t any different than what I normally do as a first depression kind of consultation. So it is quite a long consultation, there is like you know 20 minutes probably maybe a bit longer, I put them at the end of my list, so I could run over a bit more if I needed to rather than just have 10 minutes.
Interview 1, GP
It was apparent, therefore, that although incorporating discussion of debt into the consultation was feasible, addressing debt was time-consuming and not something that fitted easily within the constraints of a single GP appointment slot. The issue of time was also raised by GPs when they provided feedback on the SCA form, whose length and complexity was not considered helpful in keeping the consultation concise:
OK so, yes it was too long. And things like you know what are your three most important individualised goals? That is hard for anyone to say, and then you know, in what, in what aspect of my life and obviously you are talking about debt so actually, well get rid of the debt is going to be it isn’t it but, but you know goals for everything in the future that just becomes a sort of like a, a game they have to play so I didn’t find that helpful.
Interview 3, GP
The only barriers again you see there is a difference between running a study and running it in real life, so the only big barrier for me would be (a) the form that I had to fill in that was too long, so that needed to be refined to a one-sheet job.
Interview 9, GP
Although the inclusion of the SCA form raises the issue of time management, it was apparent that the consultation per se followed the routine of a clinical assessment for depression, demonstrating that the intervention was normalised within the GP’s usual practice:
[. . .] It is almost like a first depression consultation then isn’t it? The first time when you see them. So it is more like a kind of, finding out how they are and going back to the beginning a bit of why they were depressed and that could then lead on to talking about counselling if they had not thought about it, and discussions about things like that rather than, just being on medication.
Interview 1, GP
No [the consultation was not different] but it was really nice for me to know that I had something that I could offer you know because previously I just wasn’t aware of, or so much aware of, I would not, it wasn’t on my radar so much to specifically ask about debt.
Interview 5, GP
Enhanced communication between general practitioners and Citizens Advice Bureau advisors
A SCA form was developed in the start-up phase of the trial to facilitate sharing of information between GPs and CAB advisors, with participant consent. Providing feedback on the form, GPs and CAB advisors show a sense of uncertainty about what information should be shared and whether or not that information was helpful:
Does it help them to know what this person’s medical problems are, it might do. That would be interesting to know whether it helped them or made it harder sometimes you know. Because even if you put the diagnosis down, does that help the CAB advisor deal with them in a better way I don’t know. It might do.
Interview 3, GP
Encouraged the, you know the doctor to maybe write more and it might have encouraged us to write a bit more on there as well. I think that might have been something that could have been useful to have a look at in a little bit more depth.
Interview 4, CAB advisor
It was, therefore, apparent that both GPs and CAB advisors were somewhat tentative about their input into the shared assessment form and whether or not it facilitated collaborative care. One GP provided a possible solution to this issue:
I guess there is probably training issues for the people that are doctors that are involved, the clinicians that are involved as to what information is key on the forms and I guess the conversation with CAB about like I said before, how useful, what bits are key that they really want and you know how much is too much, how much is not enough a bit more of a conversation.
Interview 2, GP
The above statement indicated that some training and an ongoing dialogue between professionals (i.e. GPs and CAB advisors) could facilitate collaborative care. However, it was apparent that CAB advisors felt that there were no opportunities to engage in such a dialogue with GPs currently when attending general practices:
So I know that they already have CAB advisors in some doctor’s surgeries, and I don’t think they have any, any avenue of speaking to the doctors so there should be something in place.
Interview 10, CAB advisor
Following CAB advisors’ point of view, the issue of communication between GPs and CAB advisors was informed by their individual experience in one site, of GP’s reservations about engaging in conversations about depression:
I did feel like, the big, big stumbling block was I don’t necessarily feel like all the GPs were on board. And I don’t necessarily feel like it was necessarily, I get they are busy and I get that, but obviously we are busy as well, but I don’t think it was necessarily promoted in a way that was . . . when we go to meetings and stuff there was a bit of hesitation I think in people saying I don’t necessarily want to ask my client, my patient if they have anxiety or depression.
Interview 7, respondent 1, CAB advisor
As one CAB advisor suggested, the issue of communication between CAB advisors and GPs may have arisen because the component of co-location was not embedded within the practice:
But I suppose if I was seeing three or four clients throughout the day I would spend the day in the surgery and you would be in the kitchen making a, I am thinking of one surgery in particular where, I have seen people milling about in and out of the kitchen you would be part of that I suppose you could be part of that wouldn’t you and speak to people and get to know people. But because it has only been in and out for one person, I haven’t actually met any GPs just reception staff really.
Interview 4, CAB advisor
Despite this barrier in communication, there was willingness among CAB advisors to move forward and progress communication with GPs:
Let’s face it, we understand our topic a lot better than they do but then, they understand their topic a lot better than we do [laughs] so you know and that, so I think there was a difficulty there really and maybe having a bit more awareness of each other.
Interview 7, respondent 1, CAB advisor
It is almost like we are two pieces of a jigsaw and actually unless you are put together you can’t see the whole picture.
Interview 7, respondent 2, CAB advisor
Although CAB advisors addressed their concern about communication directly, this point appeared somewhat overlooked by GPs. One GP did refer to collaborative care, suggesting that adopting a form of communication familiar to GPs to raise awareness around mental health and as a reminder of services would be beneficial:
I think for health professionals to be more aware from my bitter experience if you don’t keep reminding them, and I put myself in this group, you forget, you forget that the service is there. So at least bi-annually, at least every other year or yearly it would not harm for a short, sharp blast across GP education systems, there is one once a month in this area . . . a short presentation, these are the patients we saw last year, this number committed suicide, this number had depression but weren’t seen for over 12 months . . . so really hard-hitting facts . . . there is nothing quite like a bit of peer review, peer pressure, say oh flipping heck if that practice can do it [laughs] why aren’t we you know.
Interview 9, GP
Although CAB advisors are appreciative of liaising with GPs and co-location should facilitate planned (i.e. telephone conversations, meetings, etc.) and written conversations (i.e. assessment form), communication between these two professional groups is partial. This shows that the component of enhanced communication was not normalised. The above statement highlights the importance of utilising existing approaches to communication that are familiar to GPs, such as peer review communication that is grounded in evidence, to remind GPs about available services and embed them within the everyday general practice.
In summary, the analysis of GP and CAB advisor interviews showed that although co-location of CAB advisors in general practices and GPs’ assessment for debt and depression were normalised, enhanced verbal communication between GPs and CAB advisors was not. This is because communication between these professionals is limited by a lack of co-location, small numbers of shared patients and a relative unfamiliarity with each other and the ways of working.
Chapter 7 Discussion and conclusions
The study failed to reach its recruitment target and was terminated early during the internal pilot phase, and, therefore, it did not progress to main trial. This report describes the study rationale, methods and findings of the pilot phase of this study, and implications for future research in this area.
The following discussion focuses largely on a discussion of the challenges we faced in seeking to implement the trial as originally envisaged and provides learning points for future researchers. We will, in addition, discuss our qualitative data findings. These provide a valuable insight and points of learning both for future research and for those seeking to support people living with debt and depression. Finally, we briefly discuss the descriptive and health economics data.
Feasibility
Premature closure of trial at pilot stage
Ultimately, this trial ended prematurely because of the failure to recruit both practices and participants to time and target. The view of NIHR was that the trial would ultimately fail to recruit sufficient participants with the resources and time available. Although the requirement to recruit 50% of the target population was ultimately achieved, the stopping rule for target recruitment was invoked because achieving this target took twice as long as the intended time frame (12 months rather than 6 months). Below we discuss the various challenges we faced that meant that the time frame for participant recruitment turned out, ultimately, not to be realistic given the current funding and primary care climate, and that we sought to recruit participants from a vulnerable and hard-to-reach group.
Research environment
In a multicentre trial, the lead organisation sets up the original agreements with the funder, and then subcontractual arrangements are agreed with the other centres. We found that this protracted process added many months to the time taken to finalise legal and financial agreements across all centres. Finalising ethics and other governance arrangements, which could not be completed in individual sites until the teams were set up (even if, theoretically, all centres can open once host sponsorship and permissions are granted), further delayed participant recruitment. Research teams in each centre need to build working relationships within their sites to run a trial effectively, liaising with the local research support and governance teams covering their sites. All of these processes eat into the tight time frame of a pilot trial.
Unless organisations are prepared to employ staff in advance of finalisation of all contractual and financial resources, significant delays in getting staff and other resources in place to set up and run a study can occur. This was a particular issue in one of our three research centres, which was able to employ its full complement of staff only once all financial systems were fully in place. This resulted in a 12-month delay in that centre, such that it just started recruiting participants only as the pilot trial came to a close. We had planned for 40 participants to be recruited from each of the three centres; in the end they achieved 36, 20 and 5. Near the closure, however, recruitment was accelerating. A further 36 EOI forms that were submitted towards the end of the pilot phase could not be converted to randomised participants because of the closure of participant recruitment. Almost half of these interested patients were from the delayed set-up centre.
A further problem was the reorganisation of NIHR research networks between developing and delivering the trial. This reorganisation meant that some of the anticipated practical network support that we had envisaged was not available, which increased the hands-on recruitment expectations for the core team and practice staff and, in particular, had implications for completing practice database searches and waiting room recruitment activities.
The challenge of recruiting general practitioner practices and completing research-related tasks
With hindsight, this was not a good time to be conducting a trial among a hard-to-reach vulnerable group through primary care, with general practice under pressure from external inspections being introduced (Care Quality Commission), problems with staff recruitment and increasing expectations of target-driven expanding service delivery, such as extended opening hours, intermediate care expansion and a new contract. Fewer practices than anticipated offered to support the trial. Many practices required frequent calls and reminders, and some failed to return calls or e-mails. In one, although the local staff were interested, the parent company refused permission for the practice to become a site. Because of the approach to practice recruitment (selected using random sampling by the study statistician in matched pairs) new practices could be approached only once practices had refused, with some taking weeks to provide a simple ‘no’, which delayed approach to further practices. We would have dropped the pairing of practices in the main trial as any theoretical benefits were outweighed by fewer practices being available to participate and additional delays. In many participating practices, the pressure of core NHS work and the number and pace of practice changes, and the resulting pressure on meeting agendas, meant that organising initial practice meetings to discuss the study, the necessary training and other research-related activities (once practices had agreed to participate) took months rather than weeks. Once practices signed up, the mode of participation varied significantly: some were highly co-operative, others failed to check lists for months and one checked lists so assiduously (in order to organise care better for depression) that delays were significant and many patients were excluded. The average time from initial practice contact to first randomisation ranged from 8 to 46 weeks (mean 27 weeks), with three practices failing to recruit any participants (one despite a large mail-out). One of the practices met with the study team only 7 weeks before study closure.
It was important to keep in regular e-mail or telephone contact with practice research leads once they expressed an interest, and weekly once we had held our initiating meeting to check for progress and to troubleshoot any emerging problems and delays with them. GPs were not keen on receiving newsletters or other formal updates as they felt that these would remain unread.
Adapting to change
An advantage of an adaptive design is that it enables adjustments to be made once a pilot has started, linked to a priori agreed rules for changing the trial design as it proceeds. In DeCoDer this included changes to trial information sheets, mechanisms for publicising the trial to patients and GP list searches, determining the need for cluster or individual randomisation in a full trial. However, what works well in some sites is less straightforward in others, and indeed within sites. This is particularly likely with large practice teams who work differently and have varying individual beliefs and expectations, which have a greater relative impact in non-routine work such as research recruitment and study support. There was a wide variation in the interpretation of list checking by GPs, with some just excluding a tiny fraction and others excluding far more, which introduces sample bias. For most practices, GPs struggled to find the 2–3 hours they needed to check the patient search lists before mail-outs, which took from 0 to 87 days, the average delay being > 3 weeks, nearly one-third of the total time we had anticipated to spend recruiting in each practice. On balance, we decided to allowed GPs to choose whether or not they needed to check lists before mail-outs. One practice did receive a complaint from a patient who did not consider themselves to be suffering from depression as described in the letter, so we made the wording in the invitation letter more neutral to reduce the risk of causing inadvertent offence. However, every change in trial design, even if small, needs to be approved, in sequence, by the funder, the sponsor, ethics and governance, all of which require full paperwork including a revised protocol with marked changes. Even with the most efficient systems, this takes at least 4–6 weeks from seeking permission to instigating change across all sites.
Participant recruitment
The baseline data suggest that although we were able to recruit the target hard-to-reach vulnerable patients with depression and debt, this took longer than anticipated. Most participants had severe depression as assessed by the BDI-II. It is not surprising that patients with debt and depression were difficult to recruit, as they are less likely to respond to contacts – as highlighted during qualitative interviews. We tested two main methods of recruitment, mail-outs signed by GPs from practice list searches and waiting room recruitment. The return rates in terms of participants randomised were low for both methods at 1% recruited per letter posted and 0.5% per leaflet distributed, respectively. Although the EOI return was comparable at 3% for both methods, the conversion to consent rate was double within the letter method compared with the waiting room method. This was not surprising as we anticipated a proportion of those agreeing face to face in the waiting room, perhaps in an effort to please, would change their mind after reflection. In terms of cost, this was around £200 per consented participant in both methods.
We anticipated a 20% dropout rate at 4 months; in the event this was 17% among controls but only 12.5% among intervention patients. However, the research team had to work hard to achieve this, with many participants requiring frequent contacts and sometimes repeat visits to complete data collection. People in debt tend to avoid communication by letter or telephone in case these are associated with their debts, and this is exacerbated by the low motivation that occurs in depression. Although the 12-month follow-up was incomplete due to early study closure, the indications were that dropout at 12 months would be below 20% as well. We believe this was because of the relationship formed between participants and researchers through the baseline assessment. Our belief in this respect was grounded in data from qualitative interviews, with many participants expressing how they valued the contact and interest in them and their lived experiences.
It is of note that after randomisation only 69% in TAU and 75% in the intervention group attended a GP appointment for allocation. Of the latter, 71% actually received the intervention after allocation, representing 53% of those allocated to see a CAB advisor. More than this proportion, however, continued within the trial (83% in TAU and 88% in CAB intervention). This failure to make and attend appointments reflects the difficulties faced by such patients during episodes of crisis and distress. Certainly our qualitative findings demonstrate the sheer complexity of difficulties experienced by some participants. We did try to mitigate this by adopting a case management approach for CAB advisors to support the participants referred to them but, as described in Chapter 1, Intervention: theory and development, and Chapter 2, Practice identification, recruitment and training, such patients are often shy of unknown contacts, fearing that they relate to debts. It was not uncommon in qualitative interviews for participants to mention that they avoid telephone calls and leave letters unopened. Some participants referred to pawning items in times of particular hardship and this included, for one participant, their mobile phone. Other difficulties and commitments also impacted some participants’ engagement with the research at one time or another.
The overall feasibility of a randomised controlled trial approach
Funding and time constraints
On reflection, the recruitment target for the pilot was overoptimistic in that, unless all our assumptions about setting up times and site recruitment were realised, recruitment was always likely to fall below target, despite the best efforts of the research team. This is probably true if it is expected that conducting a complex intervention trial among vulnerable, hard-to-reach populations in primary care can be undertaken without enhanced investment over other primary care trials. A higher rate of investment is needed to widen the pool of sites to recruit from, and to account for, more intensive participant support to engage with the study and maintain contact through to trial completion.
Constraints of trial design
In terms of trial design, the expectation of robust methods to achieve grant funding and ethical approval (e.g. balanced matching, testing cluster vs. individual randomisation, list checking, complexity of approvals for even minor protocol changes within an adaptive design) further add to delays in achieving recruitment. Our experience was that many practices struggled to support the steps required for recruitment, not least due to the rising workload for the NHS and problems recruiting clinical staff, particularly for practices in inner-city areas, where more vulnerable and hard-to-reach patients are likely to be registered. Our current ethos demands that changes in service design and investment in new treatments will only take place if robust research is available to support them. This means that if randomised controlled trials are not undertaken in hard-to-reach populations, we risk further increasing the health inequalities gap, as trials will focus on easier populations and problems.
Cluster versus individual randomisation
We did not find any evidence of contamination of the intervention between control and intervention participants in practices where individuals were randomised, with only one participant in each control group seeing a CAB advisor (which was one of the options outlined in the leaflets) during the study for debt advice. There was no evidence of GPs recommending CAB to those in control groups. Thus, we would not have recommended a cluster design for the full trial. Perhaps the additional costs associated with this approach are better diverted to increasing the number of sites to improve the chances of achieving recruitment to time and target. This pilot examination of cluster versus individual randomisation was one of the successes of this trial. Cluster randomised trials are potentially weaker designs than those in which participants are individually randomised, mainly because of the need to inflate the sample size and the potential for imbalance in participants’ characteristics at baseline. Despite our slow recruitment, we showed that an innovative examination of each method is possible at the outset of a trial and could save funds in cases when a more expensive cluster randomised method can be avoided.
Summary qualitative findings
The debt–depression relationship
Participants’ stories of debt and depression highlighted the complexity of influences (psychological, social and contextual) that contributed to both the impact of debt and the relationship between debt and psychological distress. These influences compounded participants’ feelings of depression, contributed to participants’ disengagement with debt issues and, ultimately, contributed to an ongoing cycle of debt and depression. Participants’ stories of debt and depression indicated a bidirectional relationship, with unmanageable debt contributing to negative feelings (including anxiety and depression) and psychological distress impacting participants’ engagement with debt issues through psychological and behavioural avoidance. Participants’ quantitative ratings of the contribution of debt to psychological distress and psychological distress to money difficulties gave us more evidence on this relationship, with the majority of participants indicating that debt contributed to anxiety and depression, and anxiety and depression contributed to their debt problems.
It is of note that many of the psychological impacts reported by participants are also features of depression. It was impossible to delineate psychological distress as a consequence of unmanageable debt from the experience of depression per se, such was the complexity of participants’ lived experience of debt and depression.
Evaluation of the intervention
Participants allocated to the intervention arm of the trial were largely positive about their experience. Two aspects of CAB involvement were identified as particularly helpful. First, the CAB advisor role acting as a conduit between the participants and other agencies, to facilitate communication and negotiation about debt issues. Second, identifying possible sources of additional financial support and discretionary payments. A small number of participants viewed their appointment with the GP as psychologically supportive, providing validation for their concerns and evidence of GPs’ interest in their current difficulties.
General practitioner and CAB advisor experience and views about the intervention provided positive feedback, but also a number of caveats concerning the feasibility of implementing the intervention, as originally conceived, into day-to-day practice. Although co-location of services was welcomed on both sides, the anticipated benefit in terms of a collaborative approach to care through informal liaison between GPs and CAB advisors was not realised. It was suggested that the sporadic nature of CAB advisor attendance at GP surgeries (as a result of the small sample size and intermittent nature of participant recruitment), coupled with current working practices in general practice, meant that the CAB service was unable to become embedded within the fabric of the practice. Although the psychosocial assessment conducted by all GPs was normalised within the consultation, it was noted that this extended appointment duration, particularly in the intervention arm in which GPs were required to complete detailed information for sharing with CAB advisors. Consequently, this particular aspect of the intervention was not considered to be workable within the confines of a single GP appointment.
Participants’ experience of involvement in the trial
Participants were largely positive about their involvement in the trial. A particular benefit of involvement was identified as the opportunity to talk to researchers about the difficulties that they were experiencing (a possible confounder had the full trial gone ahead).
With regard to feasibility and acceptability of the outcome measures, it was apparent that the number of outcome measures (and their form and content) was problematic for some participants – adding considerably to the time taken for completion of interviews. Furthermore, several participants questioned the forced choice responses of questionnaires, which did not capture the reality of their experience. Both of these issues raise questions about the use of validated questionnaires that are often viewed as gold standard approaches to the assessment of effectiveness in randomised controlled trials. Thus, there are competing expectations of comprehensive data collection to maximise the opportunities to understand not only if an intervention works (primary outcomes), but also why, and for whom, it does or does not (secondary measures), versus caring for participants and reducing dropout by not overburdening them.
Outcomes
Summary of descriptive statistics
We have presented only descriptive analyses as a result of the small sample size. It is important to note that, although a number of participants commented on the burden of data collection in our qualitative interviews, the data collection was sufficiently comprehensive to be able to provide data for nearly all participants for each of the measures at all time points, although we did have to impute some missing values. However, we would have been likely to reduce the burden for the main trial, as data collection usually took nearly 3 hours rather than the 2 hours we had anticipated. For example, although theoretically we would have wanted to know about absenteeism and presenteeism, because this important outcome is often ignored in randomised controlled trials, the low employment rates among the sample suggest this was often irrelevant and confusing for participants who were in receipt of welfare (Job Seeker’s Allowance or Employment and Support Allowance). We would probably have also undertaken only the explanatory measures among a subsample (Hope Trait, Other as Shamer and Response Style Questionnaire).
Snyder et al. 65 reported data from samples of US college students, outpatients receiving psychological treatment and psychiatric inpatients of a state hospital. Mean agency, pathway and total scores for the student group were A12.61, P12.61 and T25.24, respectively; for the outpatient sample these were A11.27, P11.33 and T22.60, respectively; and for the inpatient sample were A11.25, P11.25 and T23.11, respectively. However, these data are not directly comparable to scores in the present study because they are based on the four-point response scale originally used in the Adult Hope Scale. This was later revised to the eight-point format utilised in DeCoDer; however, no comparable studies of depressed populations were found that also used this format.
Gilbert84 reported data on the OAS from a UK sample of students (screened as below the clinical threshold for depression on the Centre for Epidemiological Studies Depression Scale) and patients who had been hospitalised as a result of severe depression (mean BDI-II scores of 29). The mean OAS score for the student group was 22.5 and for the depressed group was 45.2. The group means in the present study fall somewhere between these two, which would be consistent with participants in the DeCoDer trial experiencing mild to moderate levels of depression. However, the mean BDI-II score at baseline and 4 months’ follow-up is higher than that for students with severe depression in the Gilbert study. 84 Thus, there is little evidence that debt is perceived as a particularly shameful state of affairs, as measured with the OAS, as the mean scores are broadly similar to those seen in people who are experiencing similar levels of depression. Nevertheless, shame remains a key cognitive concomitant of a depressed mood.
The group means for rumination are again broadly consistent with, or slightly lower than, comparable scores in people experiencing a depressed mood. 70 As with shame, there is little specific evidence of rumination as a problematic element in the presentation of people in debt, over and above the levels of rumination normally observed in depressed people. Nevertheless, rumination, like shame, remains a key cognitive concomitant of a depressed mood. That is, both rumination and shame are commonly present in depressed individuals, and are seen here. There is little evidence, however, that indebted depressed people have higher levels of either shame or rumination than people who are depressed but are not in debt.
Our results do indicate that we were successful in recruiting the target group in terms of mental health problems and life events being at the most severe end of a primary care population.
Summary of health economics data
The small sample limits the level of interpretation and analysis of the data collected to description only. However, our findings did suggest that some adjustment would be required in a full trial to account for resource use in the period prior to baseline, as these were imbalanced between the TAU and intervention groups. We also suggest that any future study should account for criminal justice contacts as part of a representative economic factor data collection within this type of population. Our EQ-5D data also support the finding that we were recruiting our target vulnerable population with health-related quality-of-life scores that matched against peer norms.
Lessons learned for future trials
-
Take into account the barriers to and facilitators of trials for individuals with common mental health problems and social disadvantage.
-
Consider carefully the number of outcome measures beyond the primary outcome, balancing learning against burden.
-
Consider which outcome measures to use – not necessarily the ones that everyone else uses.
-
Consider adding criminal justice contacts as an economic factor in such populations.
-
Where it is unclear whether or not there is likely to be crossover of the intervention between experimental and control participants (contamination), consider a pilot phase of cluster versus individual randomisation in which this can be assessed.
-
Ensure that trial centres are willing to recruit staff early, even if that is in advance of final subcontract agreements being in place, to minimise delays in starting the trial.
Lessons learned for developing the intervention
-
Needs to be clear expectations of each party/service in the collaboration – in this case what information is considered helpful/required.
-
Time commitment: the referral processes/information required needs to fit within the constraints of a normal GP appointment.
-
Raise awareness through usual channels of GP communication, embedding in general practice consciousness.
-
Alternative approaches to interventions for individuals with common mental health problems and social disadvantage need to be considered.
Implications
This pilot trial indicates that it is possible to recruit and retain vulnerable and stigmatised hard-to-reach patients to a primary care trial. However, we suggest that the recruitment site base needs to be wider than anticipated for other trials, and the population and inner-city practices they are registered with requires more intense support and investment of time to achieve recruitment to time and target than is usually required for complex intervention trials in primary care. The complexity of their problems suggests that a more comprehensive intervention than debt advice alone is required to support the recovery of patients with debt and depression.
Acknowledgements
Contributions of authors
All co-applicants (Mark B Gabbay, Richard Byng, Rod S Taylor, Caryn Matthews, Tirril Harris, Paula Byrne, Suzanne Edwards, Richard Emsley, Lucy Frith, Peter Huxley, Peter Kinderman, Michael King, Carl May, Ceri Phillips, Tim Rawcliffe and Sam Thompson) were involved in the conceptualisation and design of the study. All authors have contributed to the development of this report and commented on the final drafts. In addition, specific contributions are as detailed below.
Mark B Gabbay (Professor, General Practice) had overall responsibility for delivery of the trial and has been responsible for the drafting, collating and editing of all sections of the report, including writing the initial drafts of Chapters 2–4, 6 and 7.
Adele Ring (Post-doctoral Researcher/Trial Manager, Health Services Research) had responsibility for the day-to-day management of the trial and local site management at the north-west England site, contributed to the developed of the SCA intervention and GP guidance documents, collaborated with colleagues at PenCTU on the development of the study website, carried out the qualitative field work in the north-west England site, conducted qualitative data coding and analysis of participant transcripts, and has been responsible for the drafting, collating and editing of all sections of the report, including writing initial drafts of all chapters except for Chapter 5.
Richard Byng (Professor, Primary Care Research) had responsibility for leading the study at that the south-west England site, developed the SCA intervention and GP guidance documents, and contributed to the analysis of clinician and CAB advisor interviews and write-up of process evaluation section of Chapter 6.
Pippa Anderson (Acting Head and Director Swansea Centre for Health Economics, Health Economics) developed the combined statistical and health economics analysis plan, had responsibility for leading the study at the site in South Wales, conducted the health economic analysis and led on the drafting of Chapter 5, and contributed to the writing of Chapters 3 and 4.
Rod S Taylor (Professor, Health Services Research) was responsible for randomisation of practices, developed the combined statistical and health economics analysis plan, conducted the statistical analysis and produced data tables, and contributed to the drafting of Chapters 4 and 5.
Caryn Matthews (Chief Executive Officer, South Liverpool CAB) provided managerial oversight for the CAB service – liaising across sites with local CAB managers and advisors, was involved in general practice engagement in relation to CAB referral process and procedures at the north-west England site, contributed to the development of study documentation regarding the intervention and contributed to the writing of Chapter 1.
Tirril Harris (Honorary Research Fellow, Psychology and Social Science) trained RAs in the LED-S, provided ongoing expert advice and support to RAs in relation to LED-S identification and coding and LED-S analysis, and contributed to drafting Chapters 2 and 4.
Vashti Berry (Senior Research Fellow, Trial Manager, south-west England site) was responsible for day-to-day management of the trial at the south-west England site, and contributed to the development of the SCA intervention and GP guidance documents.
Paula Byrne (Lecturer, Health Services Research) developed the qualitative component of the study and contributed to qualitative data analysis of participant transcripts and drafting of Chapter 6.
Elliot Carter (Data Programmer, PenCTU) was responsible for data programming, including development of the study database and website.
Pam Clarke (RA, Health Services Research) recruited participants and conducted assessment interviews and LED-S coding in the north-west England site, contributed to the literature review (including management of references) for the report, drafted the end of study information sheet for participants, prepared report appendices and contributed to the preparation of Chapters 1, 3 and 4.
Laura Cocking (Senior Data Manager, PenCTU) was responsible for data management, including the development of all participant data collection forms and the development of the study database and website in collaboration with PenCTU colleagues.
Suzanne Edwards (Senior Lecturer, Medical Education) provided day-to-day support in the management of the trial at the site in South Wales, contributed to the development of the SCA intervention and GP guidance documents, developed the qualitative component of the study, contributed to the qualitative analysis of participant transcripts and contributed to the drafting of Chapter 6.
Richard Emsley (Senior Lecturer, Biostatistics) led the development of causal analysis for the original application.
Mauro Fornasiero (RA, Primary Care Research) carried out the qualitative analysis of clinician/CAB advisor interviews and wrote the draft process evaluation section of Chapter 6.
Lucy Frith (Reader, Social Science and Bioethics) developed the qualitative component of the study and contributed to the qualitative data analysis of participant transcripts and drafting of Chapter 6.
Shaun Harris (RA, Health Economics) conducted the health economic analysis, supporting Pippa Anderson and contributed to the drafting of Chapter 5.
Peter Huxley (Professor, Mental Health Research) contributed to the secondary outcomes design and analyses.
Siw Jones (Chief Executive Officer, North Liverpool CAB) supported Caryn Matthews in her CAB management role and contributed to the development of study documentation regarding the intervention.
Peter Kinderman (Professor, Clinical Psychology) led the psychological modelling component of the original application and contributed to the drafting of Chapter 2.
Michael King (Professor, Mental Health Sciences) advised on the overall design of the study and has worked with Rod Taylor on the statistical analysis.
Liv Kosnes (Research Officer, Trial Manager, south Wales) was responsible for the day-to-day management of the trial in the site in South Wales, carried out the qualitative fieldwork at the site in South Wales, and contributed to the health economic analysis and the drafting of Chapters 3 and 5.
Daniel Marshall (RA) contributed to the development of the SCA intervention and GP guidance documents, and undertook data collection in the south-west England site.
Dave Mercer (Lecturer, Mental Health) conducted the focus group interviews, undertook the independent analysis of focus group interviews and produced a written report for NIHR HTA programme as part of the regular progress report process.
Carl May (Professor, Healthcare Innovation) developed the process evaluation component of the trial and contributed to the NPT analysis.
Debbie Nolan (CAB Manager) supported Caryn Matthews in her CAB management role and contributed to the development of study documentation regarding the intervention.
Ceri Phillips (Professor, Health Economics) developed the original health economics and cost-effectiveness analysis plan for the application.
Tim Rawcliffe (Patient Public Involvement Co-applicant) led service user involvement in the study and has been involved in all stages of the study. He commented on all substantial amendments and liaised with patient and public representatives in the development and review of all participant-related documentation. He drafted the lay summary, contributed to the qualitative data analysis and the drafting of Chapter 6, and to the finalisation of the end of study participant information sheet.
Alexandra V Sardani (RA) recruited participants and conducted participant assessment data collection and LED-S coding in the site in South Wales.
Elizabeth Shaw (Research Associate, Clinical Psychologist) recruited participants and conducted participant assessment data collection and LED-S coding in the south-west England site.
Sam Thompson (Doctor, Psychology) carried out some of the qualitative field work in the north-west England site and contributed to qualitative data analysis, literature summaries and the drafting of Chapters 2 and 7.
Jane Vickery (Senior Trial Manager, PenCTU) provided mentorship for Adele Ring and contributed to document development in the set-up phase of the trial.
Brian Wainman (Data Manager, PenCTU) was responsible for data cleaning, scoring, preparation of data for the CONSORT diagram and contributed to Chapter 2.
Mark Warner (Assistant Data Manager, PenCTU) was responsible for data monitoring, checking and query resolution.
Additional acknowledgements
We would like to thank participants and practices for agreeing to participate in the trial.
We also wish to thank a number of individuals at the study sites who undertook specific activities to support completion of the pilot trial. Nicole Williams, Liz Brignal and Margaret Hart provided administrative support. Chris Shiels undertook data scoring of several measures. Ken Linkman provided support with the bibliography. Isabelle la Hausse de Lalouviere assisted with the updating of the literature review. Stacy Harrison instigated practice recruitment at the South Wales site and Sam Groves undertook several data collections at that site. We also wish to thank researchers undertaking qualitative interviews at the south-west England site, CRNs for supporting the trial, CAB and the Trial Steering Committee.
Data sharing statement
Electronic records will be stored in a Structured Query Language (SQL) Server database, stored on a restricted access, secure server maintained by Plymouth University. The website will be encrypted using Secure Sockets Layer. Direct access to the trial data will be restricted to members of the research team and the CTU, with access granted to others on request. Access to the database will be overseen by the CTU data manager and trial manager. Those interested in accessing the data should contact the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- NIHR HTA Programme . Provision of Debt Counselling in Primary Care for People With Depression and Related Debt Problems 2002. www.journalslibrary.nihr.ac.uk/programmes/hta/1114801/#/documentation (accessed 30 May 2017).
- May C, Finch T. Implementing, embedding, and integrating practices: an outline of normalization process theory. Sociology 2009;43:535-54. https://doi.org/10.1177/0038038509103208.
- CAB Advice in Health Centres Pilot Evaluation Report. Liverpool: Praxis Evaluation and Research; 2013.
- Beaumont J, Thomas J. Measuring National Well-being, Health, 2012. London: ONS; 2012.
- King M, Nazareth I, Levy G, Walker C, Morris R, Weich S, et al. Prevalence of common mental disorders in general practice attendees across Europe. Br J Psychiatry 2008;192:362-7. http://dx.doi.org/10.1192/bjp.bp.107.039966.
- Goldberg DP, Huxley P. Common Mental Disorders: A Bio-social Model. London: Tavistock/Routledge; 1992.
- Depression in Adults: The Treatment and Management of Depression in Adults. London: NICE; 2009.
- Rait G, Walters K, Griffin M, Buszewicz M, Petersen I, Nazareth I. Recent trends in the incidence of recorded depression in primary care. Br J Psychiatry 2009;195:520-4. http://dx.doi.org/10.1192/bjp.bp.108.058636.
- Shiels C, Gabbay MB. Patient, clinician, and general practice factors in long-term certified sickness. Scand J Public Health 2007;35:250-6. https://doi.org/10.1080/14034940601072364.
- Gabbay M, Shiels C, Hillage J. Factors associated with the length of fit note-certified sickness episodes in the UK. Occup Environ Med 2015;72:467-75. http://dx.doi.org/10.1136/oemed-2014-102307.
- Sainsbury Centre for Mental Health Policy . Mental Health at Work: Developing the Business Case 2007. www.impact.ie/wp-content/uploads/2015/07/Mental-Health-at-Work.pdf (accessed 30 June 2016).
- Lelliott P, Tulloch S, Boardman J, Harvey S, Henderson M, Knapp K. Mental Health and Work DWP Report 2008. www.dwp.gov.uk/docs/hwwb-mental-health-and-work.pdf (accessed 30 June 2016).
- Morawiec J, Little S, Kinloch C. A Picture of Over-indebtedness. London: Money Advice Service; 2016.
- Ford E, Clark C, McManus S, Harris J, Jenkins R, Bebbington P, et al. Common mental disorders, unemployment and welfare benefits in England. Public Health 2010;124:675-81. http://dx.doi.org/10.1016/j.puhe.2010.08.019.
- Riumallo-Herl C, Basu S, Stuckler D, Courtin E, Avendano M. Job loss, wealth and depression during the Great Recession in the USA and Europe. Int J Epidemiol 2014;43:1508-17. http://dx.doi.org/10.1093/ije/dyu048.
- Barr B, Taylor-Robinson D, Scott-Samuel A, McKee M, Stuckler D. Suicides associated with the 2008-10 economic recession in England: time trend analysis. BMJ 2012;345. http://dx.doi.org/10.1136/bmj.e5142.
- Chamberlain E. Household Debt Inequalities. London: Office for National Statistics; 2016.
- Lucchino P, Morelli S. Inequality, Debt and Growth. London: Resolution Foundation; 2012.
- The Financial Inclusion Centre . Report 1: Debt and Household Incomes 2011. http://inclusioncentre.co.uk/wordpress29/wp-content/uploads/2011/08/Report_Debt_and_household_incomes.pdf (accessed 30 June 2016).
- Loopstra R, Reeves A, Taylor-Robinson D, Barr B, McKee M, Stuckler D. Austerity, sanctions, and the rise of food banks in the UK. BMJ 2015;350. http://dx.doi.org/10.1136/bmj.h1775.
- Kendrick T, Chatwin J, Peveler R, Moore M, Mander H, Dowrick C, et al. Randomised controlled trial to determine the clinical effectiveness and cost-effectiveness of selective serotonin reuptake inhibitors plus supportive care, versus supportive care alone, for mild to moderate depression with somatic symptoms in primary care: the THREAD (THREshold for AntiDepressant response) study. Health Technol Assess 2009;13. https://doi.org/10.3310/hta13220.
- Indebted Lives, the Complexities of Life in Debt. London: Money Advice Service; 2013.
- StepChange . Over 7 Million Brits Kept Awake by Money Worries 2016. www.stepchange.org/Infographics/NeedtoSleep.aspx (accessed 1 February 2017).
- The State of Debt Collection: The Case for Fairness in Government Debt Collection Practice. London: Citizens Advice; 2016.
- The Government Office for Science . Foresight Mental Capital and Wellbeing Project (2008): Final Project Report 2008. www.gov.uk/government/uploads/system/uploads/attachment_data/file/292450/mental-capital-wellbeing-report.pdf (accessed 30 June 2016).
- Gov.uk . Options for Paying Off Your Debts 2016. www.gov.uk/options-for-paying-off-your-debts/overview (accessed 12 January 2017).
- Citizens Advice . Our Annual Report and Accounts 201415 2015. www.citizensadvice.org.uk/Global/Public/About%20us/Annual%20report/Citizens-Advice-annual-report-2014-15.pdf (accessed 30 June 2016).
- Jenkins R, Bebbington P, Brugha T, Bhugra D, Farrell M, Coid J, et al. Mental disorder in people with debt in the general population. Public Health Medicine 2009;6:88-92.
- Fitch C, Simpson A, Collard S, Teasdale M. Mental health and debt: challenges for knowledge, practice and identity. J Psychiatr Ment Health Nurs 2007;14:128-33. https://doi.org/10.1111/j.1365-2850.2007.01053.x.
- Kuyken W, Byford S, Taylor RS, Watkins E, Holden E, White K, et al. Mindfulness-based cognitive therapy to prevent relapse in recurrent depression. J Consult Clin Psychol 2008;76:966-78. http://dx.doi.org/10.1037/a0013786.
- Knapp M, McDaid D, Evans-Lacko S, Fitch C, King D, Knapp M, et al. Mental Health Promotion and Mental Illness Prevention: The Economic Case. London: Department of Health; 2011.
- Clinical Knowledge Summary: Depression. London: NICE; 2015.
- Wagmiller RL. Debt and Assets Among Low-income Families. Columbia, OH: National Center for Children in Poverty; 2003.
- Brown S, Taylor K, Price SW. Debt and distress: evaluating the psychological cost of credit. J Econ Psychol 2005;26:642-63. https://doi.org/10.1016/j.joep.2005.01.002.
- Cummins RA, Eckersley R, Lo SK, Okerstrom E, Davern M, Woerner J. Australian Unity Wellbeing Index Survey 11: Report 11.0: The Wellbeing of Australians-personal Financial Debt. Part A: The Report, Part B: Appended Tables. Melbourne, VIC: Australian Unity Limited; 2012.
- Six in Ten People in Debt Affected by Mental Health Problems. London: Citizens Advice; 2014.
- Mind . Still in the Red: Update on Debt and Mental Health 2011. www.mind.org.uk/media/273468/still-in-the-red.pdf (accessed 30 June 2016).
- Richardson T, Elliott P, Roberts R. The relationship between personal unsecured debt and mental and physical health: a systematic review and meta-analysis. Clin Psychol Rev 2013;33:1148-62. http://dx.doi.org/10.1016/j.cpr.2013.08.009.
- Bridges S, Disney R. Debt and depression. J Health Econ 2010;29:388-403. http://dx.doi.org/10.1016/j.jhealeco.2010.02.003.
- Fitch C, Hamilton S, Bassett P, Davey R. The relationship between personal debt and mental health: a systematic review. Ment Health Rev J 2011;16:153-66. https://doi.org/10.1108/13619321111202313.
- Gathergood J. Debt and depression: causal links and social norm effects. Econ J 2012;122:1094-114. https://doi.org/10.1111/j.1468-0297.2012.02519.x.
- Gunn J, Diggens J, Hegarty K, Blashki G. A systematic review of complex system interventions designed to increase recovery from depression in primary care. BMC Health Serv Res 2006;6. https://doi.org/10.1186/1472-6963-6-88.
- Von Korff M, Gruman J, Schaefer J, Curry SJ, Wagner EH. Collaborative management of chronic illness. Ann Intern Med 1997;127:1097-102. https://doi.org/10.7326/0003-4819-127-12-199712150-00008.
- Franek J. Self-management support interventions for persons with chronic disease: an evidence-based analysis. Ont Health Technol Assess Ser 2013;13:1-60.
- Marmot M. Fair Society, Healthy Lives. London: Institute of Health Equity, University College London; 2010.
- Lester H. Shared care for people with mental illness: a GP’s perspective. Adv Psychiatr Treat 2005;11:133-9. https://doi.org/10.1192/apt.11.2.133.
- Dean S. Debt and Mental Health. London: Royal College of Psychiatrists; 2012.
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996.
- Lewis G, Pelosi AJ, Glover E, Wilkinson G, Stansfeld SA, Williams P, et al. The development of a computerized assessment for minor psychiatric disorder. Psychol Med 1988;18:737-45. https://doi.org/10.1017/S0033291700008448.
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol 1988;56:893-7. https://doi.org/10.1037/0022-006X.56.6.893.
- Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, et al. The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation. Health Qual Life Outcomes 2007;5. https://doi.org/10.1186/1477-7525-5-63.
- Public Health England . Public Health Outcomes Framework n.d. www.phoutcomes.info (accessed 1 February 2017).
- Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727-36. http://dx.doi.org/10.1007/s11136-011-9903-x.
- Devlin NJ, Krabbe PF. The development of new research methods for the valuation of EQ-5D-5L. Eur J Health Econ 2013;14:1-3. http://dx.doi.org/10.1007/s10198-013-0502-3.
- Health and Social Care Information Centre . Patient Reported Outcome Measures (PROMs) in England – 2011–2012, Special Topic, EQ-5D Index Analysis 2014. www.hscic.gov.uk/catalogue/PUB14079 (accessed 30 June 2016).
- Priebe S, Huxley P, Knight S, Evans S. Application and results of the Manchester Short Assessment of Quality of Life (MANSA). Int J Soc Psychiatry 1999;45:7-12. https://doi.org/10.1177/002076409904500102.
- Beecham J, Knapp M, Thorncroft D. Measuring Mental Health Needs. London: Gaskell; 2001.
- Koopman C, Pelletier KR, Murray JF, Sharda CE, Berger ML, Turpin RS, et al. Stanford presenteeism scale: health status and employee productivity. J Occup Environ Med 2002;44:14-20. https://doi.org/10.1097/00043764-200201000-00004.
- Huxley PJ, Mohamad H. The development of a General Satisfaction Questionnaire for use in programme evaluation. Social Work Soc Sci Rev 1991;3:63-74.
- Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The Alcohol Use Disorders Identification Test – Guidelines for Use in Primary Care. Geneva: World Health Organization, Department of Mental Health and Substance Dependence; 2001.
- Gavin DR, Ross HE, Skinner HA. Diagnostic validity of the drug abuse screening test in the assessment of DSM-III drug disorders. Br J Addict 1989;84:301-7. https://doi.org/10.1111/j.1360-0443.1989.tb03463.x.
- Brown GW, Bifulco A, Harris TO. Life events, vulnerability and onset of depression: some refinements. Br J Psychiatry 1987;150:30-42. https://doi.org/10.1192/bjp.150.1.30.
- Drentea P, Reynolds JR. Neither a borrower nor a lender be: the relative importance of debt and SES for mental health among older adults. J Aging Health 2012;24:673-95. http://dx.doi.org/10.1177/0898264311431304.
- Meltzer H, Bebbington P, Brugha T, Jenkins R, McManus S, Dennis MS. Personal debt and suicidal ideation. Psychol Med 2011;41:771-8. http://dx.doi.org/10.1017/S0033291710001261.
- Snyder CR, Harris C, Anderson JR, Holleran SA, Irving LM, Sigmon ST, et al. The will and the ways: development and validation of an individual-differences measure of hope. J Pers Soc Psychol 1991;60:570-85. https://doi.org/10.1037/0022-3514.60.4.570.
- Beck AT, Steer RA, Beck JS, Newman CF. Hopelessness, depression, suicidal ideation, and clinical diagnosis of depression. Suicide Life Threat Behav 1993;23:139-45.
- Gilbert P, Allan S, Trent DR. Involuntary subordination or dependency as key dimensions of depressive vulnerability?. J Clin Psychol 1995;51:740-52.
- Goss K, Gilbert P, Allan S. An exploration of shame measures – I: the Other as Shamer scale. Pers Individ Diff 1994;17:713-17. https://doi.org/10.1016/0191-8869(94)90149-X.
- Nolen-Hoeksema S, McBride A, Larson J. Rumination and psychological distress among bereaved partners. J Pers Soc Psychol 1997;72:855-62. https://doi.org/10.1037/0022-3514.72.4.855.
- Nolen-Hoeksema S. The role of rumination in depressive disorders and mixed anxiety/depressive symptoms. J Abnorm Psychol 2000;109:504-11. https://doi.org/10.1037/0021-843X.109.3.504.
- Lyubomirsky S, Kasri F, Zehm K. Dysphoric rumination impairs concentration on academic tasks. Cogn Ther Res 2003;27:309-30. https://doi.org/10.1023/A:1023918517378.
- Nolen-Hoeksema S, Morrow J. A prospective study of depression and posttraumatic stress symptoms after a natural disaster: the 1989 Loma Prieta Earthquake. J Pers Soc Psychol 1991;61:115-21. https://doi.org/10.1037/0022-3514.61.1.115.
- Watkins ER. Constructive and unconstructive repetitive thought. Psychol Bull 2008;134:163-206. http://dx.doi.org/10.1037/0033-2909.134.2.163.
- Ward E, King M, Lloyd M, Bower P, Sibbald B, Farrelly S, et al. Randomised controlled trial of non-directive counselling, cognitive-behaviour therapy, and usual general practitioner care for patients with depression. I: clinical effectiveness. BMJ 2000;321:1383-8. https://doi.org/10.1136/bmj.321.7273.1383.
- Adams G, Gulliford MC, Ukoumunne OC, Eldridge S, Chinn S, Campbell MJ. Patterns of intra-cluster correlation from primary care research to inform study design and analysis. J Clin Epidemiol 2004;57:785-94. https://doi.org/10.1016/j.jclinepi.2003.12.013.
- Department for Communities and Local Government . English Indices of Deprivation 2015 2015.
- Corbin J, Strauss A. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. London: Sage; 2008.
- Thompson S. Understanding the Relationship Between Debt Problems and Psychological Distress 2015.
- Calnan M, Wainwright D, Forsythe M, Wall B, Almond S. Mental health and stress in the workplace: the case of general practice in the UK. Soc Sci Med 2001;52:499-507. https://doi.org/10.1016/S0277-9536(00)00155-6.
- Mackay D, Sutton M, Watt G. Deprivation and volunteering by general practices: cross sectional analysis of a national primary care system. BMJ 2005;331:1449-51. https://doi.org/10.1136/bmj.331.7530.1449.
- Watt G. Deep End Steering Group . GPs at the deep end. Br J Gen Pract 2011;61:66-7. http://dx.doi.org/10.3399/bjgp11X549090.
- Kind P, Hardman G, Macran S. UK Population Norms for EQ-5D. York: Centre for Health Economics, University of York; 1999.
- Janssen B, Szende A, Szende A, Janssen B, Labases J. Self-Reported Population Health: An International Perspective Based on EQ-5D. Netherlands: Springer; 2014.
- Gilbert P. The relationship of shame, social anxiety and depression: the role of the evaluation of social rank. Clin Psychol Psychother 2000;7:174-89. https://doi.org/10.1002/1099-0879(200007)7:3<174::AID-CPP236>3.0.CO;2-U.
Appendix 1 Shared comprehensive assessment forms
Appendix 2 Intervention protocol
Appendix 3 Invitation letter to general practitioners
Appendix 4 Participant pathway
FIGURE 8.
Pathway of participants through pilot trial.
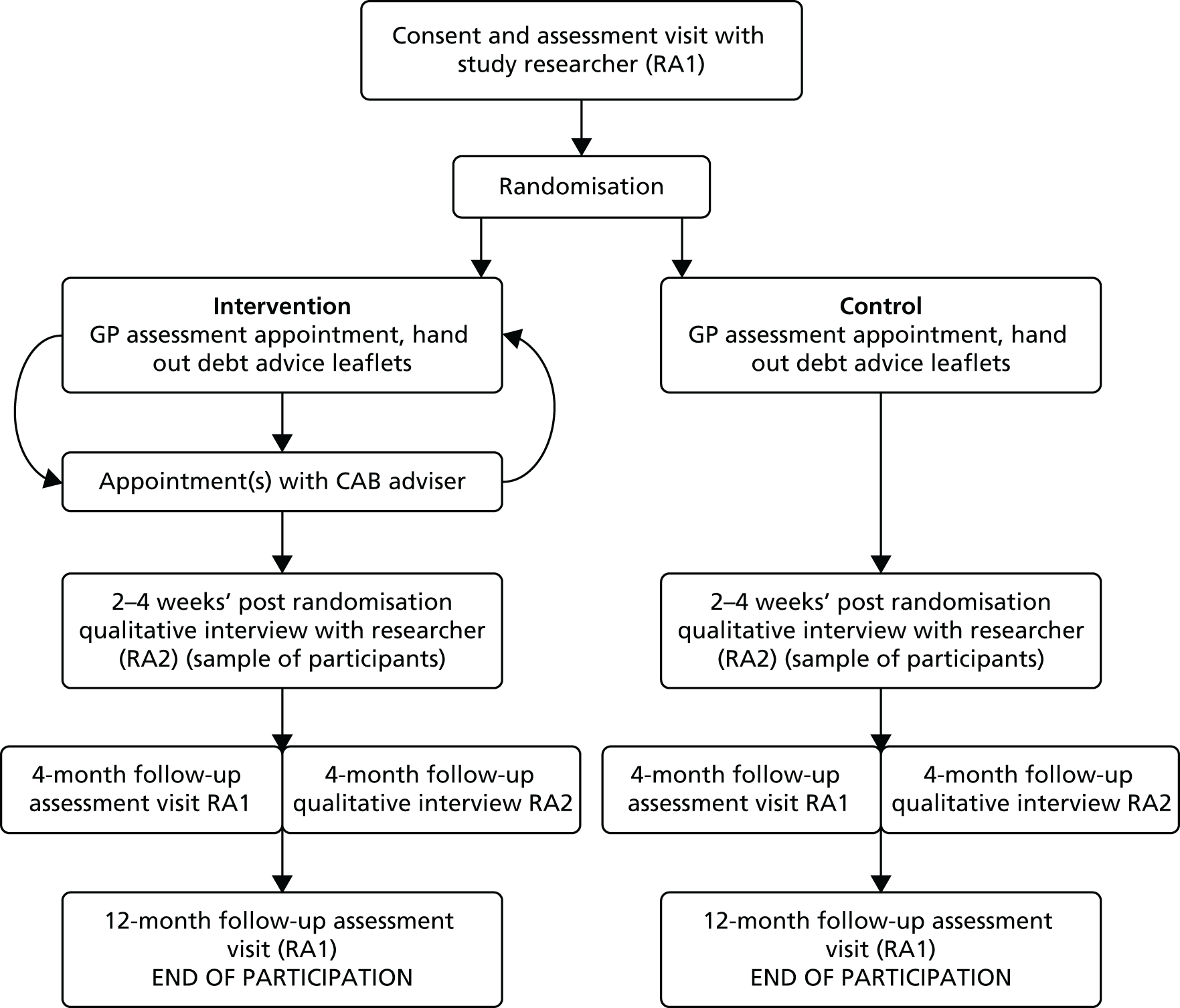
Appendix 5 Research protocols for general practitioners in the control arm
Appendix 6 Research protocol for general practitioners in the intervention arm
Appendix 7 Serious adverse events form
Appendix 8 Debt advice leaflet
Appendix 9 Patient letter
Appendix 10 General practitioner practice flyer
Appendix 11 Participant information sheet
Appendix 12 Expression of interest form
Appendix 13 Publicity poster
Appendix 14 Participant consent form
Appendix 15 Citizens Advice Bureau advisor protocol
Appendix 16 Debt advice questions
Appendix 17 Baseline visit overview (from case report form)
Appendix 18 Participant qualitative interview consent form
Appendix 19 Qualitative interview topic guides
Participant topic guide (baseline) version 1.3
Participant topic guide (4-month follow-up) version 1.1
Topic guide for professionals (control arm)
Topic guide for professionals (intervention arm) version 1.3
Appendix 20 Information sheet for professionals
Appendix 21 Interview consent form (professionals)
Appendix 22 End of study participant information sheet
List of abbreviations
- A&E
- accident and emergency
- AUDIT
- Alcohol Use Disorders Identification Test
- BAI
- Beck Anxiety Inventory
- BDI-II
- Beck Depression Inventory II
- CAB
- Citizens Advice Bureau
- CONSORT
- Consolidated Standards of Reporting Trials
- CRF
- case report form
- CRN
- Clinical Research Network
- DeCoDer
- Debt Counselling for Depression in Primary Care: an adaptive randomised controlled pilot trial
- EOI
- expression of interest
- EQ-5D
- EuroQol-5 Dimensions
- EQ-5D-3L
- EuroQol-5 Dimensions-3 levels
- EQ-5D-5L
- EuroQol-5 Dimensions-5 levels
- GP
- general practitioner
- GSQ
- General Satisfaction Questionnaire
- HTA
- Health Technology Assessment
- IAPT
- Improving Access to Psychological Therapies
- LED-S
- Life Events and Difficulties Schedule-short
- MANSA
- Manchester Short Assessment of Quality of Life questionnaire
- NIHR
- National Institute for Health Research
- NPT
- normalisation process theory
- OAS
- Other as Shamer scale
- PenCTU
- Peninsula Clinical Trials Unit
- PPI
- patient and public involvement
- QALY
- quality-adjusted life-year
- RA
- research assistant
- SCA
- shared comprehensive assessment
- SD
- standard deviation
- SPS-6
- Stanford Presenteeism Scale-6 items
- SWEMWBS
- Short Warwick–Edinburgh Mental Wellbeing Scale
- TAU
- treatment as usual
- VAS
- visual analogue scale