Notes
Article history
The contractual start date for this research was in October 2020. This article began editorial review in March 2023 and was accepted for publication in November 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The Health Technology Assessment editors and publisher have tried to ensure the accuracy of the authors’ article and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Webb et al. This work was produced by Webb et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Webb et al.
Background and introduction
Coronavirus disease 2019 (COVID-19) is a new disease caused by the SARS-CoV-2 virus, first discovered in Wuhan, China, in December 2019,1 which has caused global disease, suffering and disruption. Most people infected with the virus will have mild or moderate respiratory or viral symptoms; however, some become seriously ill and require hospital-based treatment. Individuals who develop severe illness due to COVID-19 tend to be older people with comorbidities such as cardiovascular disease, chronic respiratory disease, diabetes and cancer. 2
As well as studying COVID-19 symptoms, risk factors, management and mortality, it is important to know how COVID-19 affects quality of life (QOL). Knowing the impact on QOL gives a holistic picture of the burden of COVID-19 on the patient experience. It is also an important factor in knowing how to guide care to support patients’ needs. Furthermore, vast resources have been spent on combating COVID-19, with estimates of over US$7 billion in research and development funding being made available in the first 9 months of the pandemic. 3 QOL data underpin examinations of how cost-effective interventions that aim to tackle COVID-19 are, by reducing the risks of hospitalisation, intensive care unit (ICU) admission, ventilation, etc., and/or by aiding recovery.
There has been research focusing on the QOL of people with COVID-19 following discharge from hospital, with a systematic review including 21 studies. 4 There have also been studies on how Long COVID-19 affects QOL, with reviews summarising the findings. 5,6 However, we are not aware of any summaries of findings for QOL for patients hospitalised with COVID-19, and this study seeks to fill this gap by providing an overview of research in this area. QOL for hospitalised patients with COVID-19 is important to study alongside post-hospitalised/long COVID-19 patients, as they are the people most impacted during the acute phase of the disease. Thanks to the delivery of large, rapid randomised controlled trials,7,8 there is now much more knowledge about how best to prevent and treat COVID-19, including widespread vaccination,9,10 and the distribution of disease severity in hospitals has consequently changed over time. As novel diagnostics and therapeutics continue to emerge, it is important to understand the evolving burden of disease and impact on QOL for individuals hospitalised with COVID-19.
Quality of life is typically measured using questionnaires, ideally completed by the individual with the disease in question, typically including generic questions which capture the individual’s physical, psychological and social capabilities. Another reason it is important to examine the research on QOL for patients hospitalised with COVID-19 is that collecting data on patient-reported outcome measures (PROMs) in hospitals during the peak of the pandemic presented a logistical challenge, with the protection of patients and staff rightly taking priority.
Aims and objectives
The aim of this paper is to provide an overview of studies reporting QOL data for individuals who are hospitalised with COVID-19, and the methods they used. This will reveal the best currently available evidence on COVID-19 inpatients’ QOL. It will also give an overview of how QOL research progressed throughout the course of the pandemic, given the challenges involved. Finally, the review will highlight where knowledge gaps exist in relation to QOL for people hospitalised with COVID-19, as well as providing recommendations for research practice during future health crises.
Methods
Search terms were developed with reference to Arber et al. 11 by two authors, one a health economist (EW) and one an information specialist (NK). The search terms centred around the concepts of hospital patients, COVID-19 and health utility measures, including quality-adjusted life-years (QALYs), disability-adjusted life-years (DALYs) and survey measures such as EQ-5D, the Short Form (36) Health Survey (SF-36) and the Health Utilities Index (HUI). A full list of search strategies is included in the Appendix. The following databases were searched in May 2022, with searches re-run in December, from database inception to 7 December 2022: EMBASE (Classic and Ovid), Ovid MEDLINE®, Scopus and Web of Science (Core Collection, SCI-EXPANDED 1900+, SSCI 1900+, A&HCI 1975+, CPCI-S 1900+, CPCI-SSH 1900+, ESCI 2015). We did not apply limits for language or publication date to the search. The search was peer-reviewed by a second information specialist using the PRESS checklist. 12
Search results were stored and deduplicated in an EndNote library. Titles and abstracts were initially screened for inclusion in full-text review, after which the selected full texts were screened for inclusion in the data extraction process. Screening was done by one health economist author (EW).
The inclusion criteria were:
-
reporting on original research
-
English language full text available
-
includes quantitative data specifically for inpatients with COVID-19.
Pre-prints and conference abstracts were included, but editorials, letters and commentaries were not. Likewise, review papers, protocols, secondary analyses and animal and laboratory studies were excluded. Studies only reporting results for pooled samples of COVID-19 inpatients and non-COVID-19 inpatients were not included. Studies were included if they used published utility values for conditions other than COVID-19, provided these utilities were used to represent QOL for COVID-19 inpatients within the context of that study. So, for example, cost–utility analyses of interventions for COVID-19 inpatients were eligible for inclusion, even if the utility values were taken from patients with other conditions.
Three authors (EW, DH, BS) used a data extraction form to extract information on the studies’ methods and key results. The data extraction form is provided as Report Supplementary Material 1.
Extracted data were analysed using narrative synthesis.
Equality, diversity and inclusion
Inclusive language was used throughout the manuscript. Studies from many different countries, including low- or middle-income countries, met the inclusion criteria. Patient and public involvement co-researchers were involved throughout the project.
Results
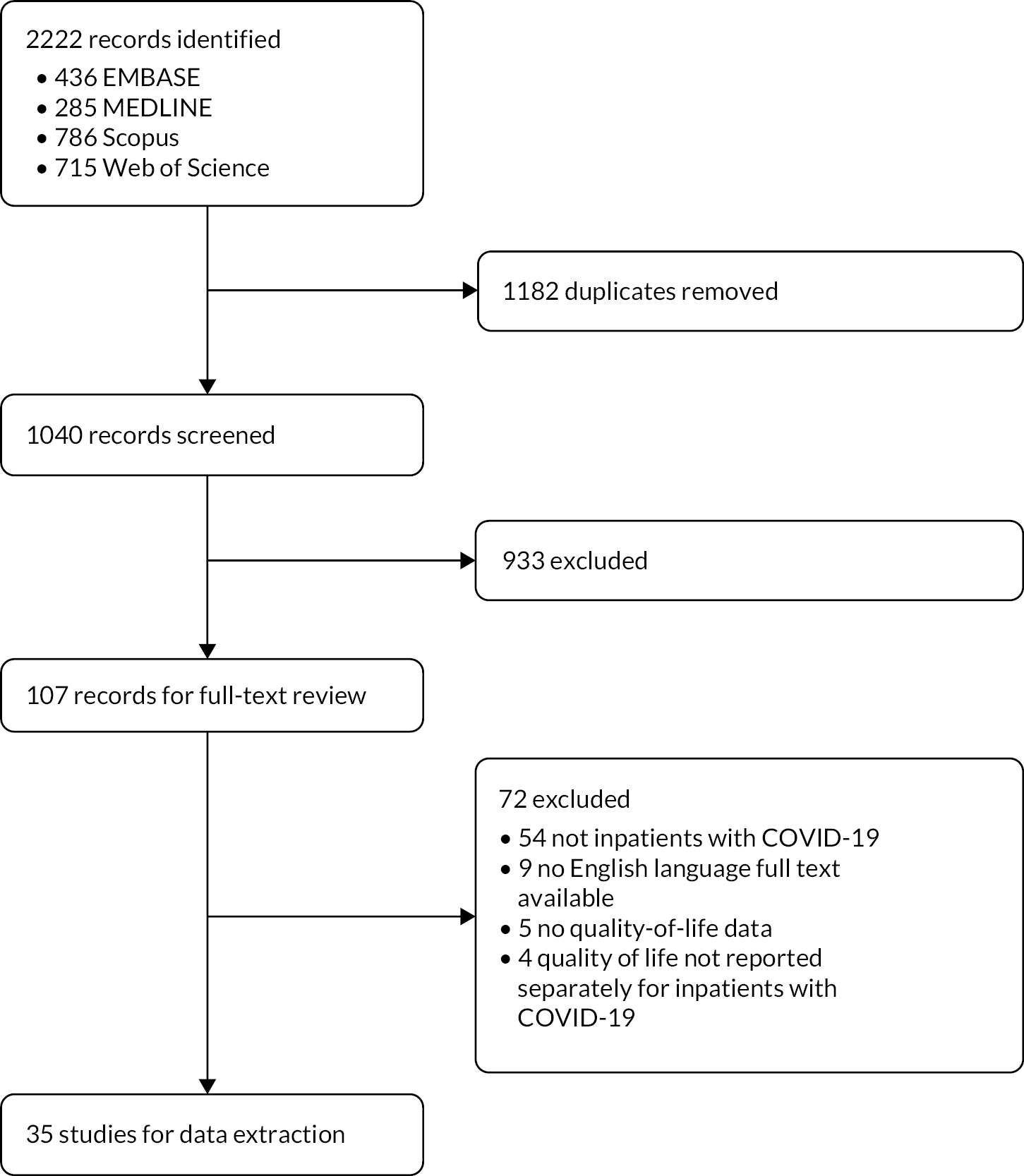
Figure 1 gives a PRISMA diagram of the search results and paper identification. The final search identified 2222 records with 1040 unique records after deduplication. There were 107 records selected for full-text review, out of which 35 studies were selected for data extraction. Table 1 summarises the individual studies, with all extracted data available as Report Supplementary Material 1.
FIGURE 1.
PRISMA diagram.
| Study | Design | N analysed | Quality-of-life measures | Quality-of-life values | Quality-of-life conclusions |
|---|---|---|---|---|---|
| Akinci and Basar13 | Cross-sectional | 189 | PSQI; HADS | 87 had PSQI < 5, 102 had PSQI>=5; 17% of good sleepers above HADS anxiety threshold vs. 9% for poor sleepers (p = 0.131); 29% of good sleepers above HADS depression threshold vs. 52% for poor sleepers (p = 0.010) | COVID-19 patients with poor sleep were more likely to be above the HADS depression scale |
| Bayrak and Çadirci14 | Prospective cohort study | 122 | World Health Organization Quality of Life-OLD (WHOQOL-OLD) | Overall WHOQOL-OLD total score = 41.5 (27.0–69.0). For those who survived (n = 111), total score = 42.0 (20.01–69.0). For non-survivals, total score = 21.0 (17.0–38.0) | QOL scores were significantly lower in the non-survivors on the first day of hospitalisation |
| Bounoua et al.15 | Cross-sectional | 85 | SF-36 | Not clear | COVID-19 negatively affected QOL, with lower SF36 scores with severe and critical COVID-19 compared to moderate; age, comorbidities and residual symptoms were associated with QOL |
| Carta and Conversano16 | Economic evaluation | 1000 (simulated) | Published values for influenza/pneumonia | Base utility 0.851; hospitalised with no supplemental oxygen 0.581; hospitalised with supplemental oxygen 0.5; hospitalised patients with non-invasive ventilation 0.23; hospitalised with invasive ventilation 0.05 | |
| Chakrabarti17 | Cross-sectional | 590 | PHQ-9; ISI | 40.1% had a PHQ-9 score over 24 indicating depression; depression was more likely among older people; females; unmarried/separated people; people with substance abuse issues and comorbidities; 28.8% of patients had ISI scores above 14 indicating insomnia; 5% indicated suicidal ideation | COVID-19 had a major psychological impact on patients |
| Cleary et al.18 | Economic evaluation | N/A | DALYs: YLL from actuarial study, disability weights from GBDS severe lower respiratory tract infection/pneumoconiosis | Severe patients: disability weight 0.13, illness duration 1.5 months; critical patients: disability weight 0.41, duration of illness 2 months | |
| Congly et al.19 | Economic evaluation | N/A | Published values for influenza/influenza (H1N1)2009 | Base utility 0.851; severe COVID-19 0.23; moderate COVID-19 0.5616 | |
| Covino et al.20 | Prospective cohort study | 368 | EQ-5D-5L | All cases (n = 368) = 8[5,10]. Survived (n = 236) = 9[7,13]. The group is also split by who had a stable QOL over time and those who QOL worsened to look for associations | Factors most influencing a decrease in QOL were found to be the female sex, frailty status before COVID-19, age group and overall pre-existing EQ-5D-5L value |
| Dijk et al.21 | Economic evaluation | N/A | Published HUI values for SARS; published EQ-5D-3L values for post-ICU/post-hospitalised patients | ICU 0.050; hospital ward 0.500; recovered from ICU 0.677; recovered from hospital ward 0.880 | |
| Gloeckl et al.22 | Prospective cohort | 50 | SF-66; PHQ-9; GAD-7 | For mild/moderate patients: SF-36 mental (31.8 vs. 31.7) and physical (48.6 vs. 54.2) components not significantly different pre/post intervention. For severe/critical patients: SF-36 physical component not significantly different pre/post intervention (30.2 vs. 34.7), mental component score significantly different (38.5 vs. 52.9, p < 0.001); PHQ-9 score significantly improved (4 vs. 7, p = 0.002); GAD-7 score significantly deteriorated (4 vs. 5, p = 0.021) | Pulmonary rehabilitation can improve QOL for patients with severe/critical COVID-19 |
| Gunes and Sensoy23 | Cross-sectional | 94 | PSQI; ESS; ISI | 55.1% of confirmed COVID-19 patients had bad sleep quality (PSQI > 5) compared to 33.1% of suspected COVID-19 patients (p = 0.02); no significant differences between groups were seen for ESS or ISI | ‘[T]he psychosomatic aspect of this epidemic should not be overlooked and patients must be evaluated in detail in respect of sleep’ |
| Hayden et al.24 | Prospective cohort | 105 | EQ-5D-5L | Median EQ-5D-5L level sum was 11.65 pre intervention and 9.23 post intervention (p < 0.001); EQ-VAS improved pre/post intervention (medians 50.01 vs. 68.05, p < 0.001); PHQ-9 improved pre/post intervention (medians 4.39 vs. 2.69, p < 0.001); GAD-7 improved pre/post intervention (medians 6.39 vs. 4.00, p < 0.001) | Pulmonary rehabilitation can improve quality of life for patients with COVID-19 |
| He et al.25 | Cross-sectional | 9 (expert panel); 2702 (patients) | DALYs: disability weights from expert panel. | Highest disability weight was 0.399 for severe expiratory dyspnoea; lowest disability weight was 0.004 for mild cough and sore throat; mean synthetic DALY was 2.29, mean daily DALY was 0.18 | COVID-19 disease burden was higher for women than men, and higher in the younger than the older population |
| Huang et al.26 | Prospective cohort | 74 | SSS-8; mMRC; PSQI | SSS-8, mMRC and PSQI scores declined over time | Symptomatic burden of COVID-19 and sleep quality improves over time up to 1 month post discharge |
| Jovanoski et al.27 | Economic evaluation | N/A | Published utility values for Clostridioides difficile | Base utility: 0.9442-0.0027*age; non-hospitalised COVID-19 disutility: 0.19; hospitalised COVID-19 disutility: 0.61 | |
| Kairu et al.28 | Economic evaluation | 20,836 | DALYs: disability weights from GBDS severe respiratory infection/ICU admission | Severe patients: disability weight 0.133; critical patients: disability weight 0.655 | |
| Karaogullarindan et al.29 | Case-control | 71 COVID, 71 non-COVID | PSQI; BDI; BAI | 53.5% of COVID patients had poor sleep quality compared to 43.0% of non-COVID patients (p = 0.011); 66.2% of COVID patients had positive anxiety symptoms compared to 59.2% of non-COVID patients (p = 0.088); 63.4% of COVID patients had positive depression symptoms compared to 57.0% of non-COVID patients (p = 0.127); disparities were worse for older patients | Poor sleep quality, anxiety and depression were observed for COVID-19 inpatients aged > 65 |
| Kelton et al.30 | Economic evaluation | N/A | Published values for C. difficile and other unspecified conditions | Base utilities ranged from 0.922 for 18- to 29-year-olds to 0.736 for aged 80+; COVID-19 symptom disutility –0.190; mechanical ventilation disutility –0.600; non-invasive ventilation disutility –0.500; supplemental oxygen disutility –0.400; medical care without oxygen disutility –0.300 | |
| Kokhan et al.31 | Prospective cohort study | 38 | EQ-5D-3L | On the 21st day of the rehabilitation programme, the quality of life of the project participants questionnaire improved by 15.7% (from 8.9 ± 0.6 to 7.5 ± 0.5 points) | QOL scores improved over time for those undertaking the walking therapy intervention |
| Kowal et al.32 | Economic evaluation | N/A | Published utility values | Unclear | N/A |
| J Li et al.33 | Non-randomised controlled trial | 75 | SIM-C; PSQI; HADS | Mindfulness intervention significantly improved SIM-C scores from 30.1 to 35.2 (p < 0.001), no significant difference for standard of care (29.4 vs. 31.2); Anxiety score: no significant differences in either group (14.1 vs. 12.9, p = 0.084 for intervention, 13.6 vs. 13.3, p = 0.629 for control); Depression score: significant improvement for intervention (14.1 vs. 12.5, p = 0.038) but not control (14.0 vs. 13.5, p = 0.568); PSQI: significant improvement for intervention (12.9 vs. 9.4, p < 0.001) but not control (13.4 vs. 11.9, p = 0.150) | Mindfulness meditation improved sleep quality and depression |
| X Li et al.34 | Cross-sectional | 66 | SDS; SAS; PSQI | 27.6% were above SDS depression threshold; 22.7% were above SAS anxiety threshold; 25.5% had poor sleep | COVID-19 inpatients had mental health and sleep quality problems |
| Moretti et al.35 | Cross-sectional study | 23 | mBDS | 8 patients (34.8%) had no dyspnoea, 3 (13.04%) had mild dyspnoea, 10 (43.5%) had severe dyspnoea, 1 (4.3%) had very severe dyspnoea and 1 (4.3%) had critical dyspnoea | mBDS scores were moderately correlated with reduced muscle power functions (ICF code: b730, p = 0.041) and walking (ICF code: d450, p = 0.011) |
| Moseholm et al.36 | Prospective cohort study | 95 | HADS; PSS-10; ISI; HTQ; SF-36 | Baseline mean HADS-D score was 6.54; HADS-D scores were lower at 3-month (3.71, p < 0.001) and 6-month (3.29, p < 0.001) follow-up; baseline mean HADS-A score was 5.87; HADS-A scores were lower at 3-month (3.90, p < 0.001) and 6-month (3.93, p < 0.001) follow-up; baseline mean PSS scores were 11.11, with no significant changes at 3-month (11.47, p = 0.67) or 6-month follow-up (10.93, p = 0.95); baseline mean ISI scores were 8.58, with no significant changes at 3-month (9.41, p = 0.67) or 6-month follow-up (7.33, p = 0.95); 81% had no PTSD symptoms at baseline, with 82% at 3-month and 84% at 6-month follow-up; baseline mean SF-12 mental component was 46.35; SF-12 mental component did not change significantly at 3-month follow-up (46.42, p = 0.40) but was significantly higher at 6-month follow-up (49.33, p = 0.03); baseline mean SF-12 physical component was 42.39; SF-12 physical component did not change significantly at 3-month follow-up (42.48, p = 0.42) but was significantly higher at 6-month follow-up (46.26, p < 0.01) | A high proportion of patients hospitalised with COVID-19 experienced psychological distress |
| Ohsfeldt et al.37 | Economic evaluation | N/A | Published values for influenza/C. difficile | Base utilities ranged from 0.922 for 18- to 29 year-olds to 0.736 for aged 80+; COVID-19 symptom disutility –0.190; mechanical ventilation disutility –0.600; non-invasive ventilation disutility –0.500; supplemental oxygen disutility –0.400; medical care without oxygen disutility –0.300 | |
| Oksuz et al.38 | Economic evaluation | 78 | Published values for unspecified conditions | Standard of care disutility: –0.515; remdesivir disutility: –0.341 | |
| Ouanes et al.39 | Case-control study | SF-36 | SF-36 physical component scores were 58.1 (inpatients), 58.2 (quarantined) and 57.2 (general population) with no significant differences; SF-36 mental component scores were 51.2 (inpatients), 49.5 (quarantined) and 47.9 (general population) with general population significantly lower than the other two groups | COVID-19 patients’ QOL was better than expected, possibly due to support, access to mental health care and enhanced resilience on recovering from COVID-19 | |
| Pass et al.40 | Retrospective cohort study | 123 COVID; 3610 non-COVID | EQ-5D-3L | EQ-5D-3L values were higher for non-COVID-positive patients than COVID-positive patients (0.701 vs. 0.291, p = 0.001) | A COVID-19 infection was associated with reduced QOL |
| Rafia et al.41 | Economic evaluation | N/A | Published values for influenza/C. difficile | Utility value for patients undergoing invasive ventilation assumed to be 0; hospitalised, not on oxygen disutility –0.36; hospitalised on oxygen disutility –0.58; increased comorbidities at entry disutility –0.116; 1-year post-discharge disutility –0.097 | |
| Samushiya et al.42 | Cross-sectional study | 119 | HADS; PSQI; MFI-20 | 11% of patients had HADS anxiety subscale scores above 8; 4% of patients had HADS depression subscale scores above 8; 73% of patients had MFI-12 scores above 20; 27% of patients had PSQI scores above threshold for sleep disorders | COVID-19 inpatients had poor mental health, fatigue and sleep quality; QOL = health-related quality of life |
| Sheinson et al.43 | Economic evaluation | N/A | Published values for survivors of acute respiratory distress syndrome/unspecified conditions | Base utilities ranged from 0.920 for 18- to 29-year-olds to 0.740 for aged 80+; COVID-19 symptom disutility –0.270; mechanical ventilation disutility –0.560; oxygen support without ventilation disutility –0.360; no oxygen support disutility –0.110 | |
| Tapan et al.44 | Cross-sectional study | 105 | PSQI; HADS | Patients with severe COVID-19 had worse sleep quality than those with non-severe COVID-19 (PSQI 12.64 vs. 8.43, p < 0.001), worse HADS anxiety subscale score (13.18 vs. 8.01, p < 0.001) and worse HADS depression subscale scores (11.76 vs. 9.00, p < 0.001) | Patients with COVID-19 had sleep quality and mental health problems, which were worse for patients with a more severe form of the disease |
| Taskesen et al.45 | Cross-sectional study | 100 inpatients, 100 outpatients | CPTS-RI; CDI; SCARED | CDI values were comparable for inpatients/outpatients (7.34 vs. 10.13; p = 0.13); inpatient CPTS-RI was significantly lower than outpatient (10.7 vs. 16.63, p = 0.01); SCREAM values were not significantly different for inpatients and outpatients (15.64 vs. 14.8, p = 0.57) | COVID-19 can have psychopathological effects on paediatric patients |
| Whittington et al.46 | Economic evaluation | N/A | Published values for influenza/C. difficile | COVID-19 symptom disutility –0.190; mechanical ventilation disutility –0.600; non-invasive ventilation disutility –0.500; supplemental oxygen disutility –0.400; medical care without oxygen disutility – 0.300 | |
| Wimmer et al.47 | Prospective cohort study | 61 | Fatigue Severity Scale-7 (FSS-7); HADS; EQ-5D-5L | No significant differences were seen between baseline and discharge for FSS-7 (2.8 vs. 2.9, p = 0.970) or HADS-A (5.0 vs. 4.0, p = 0.142); significant improvements were seen between baseline and discharge for HADS-D (4.0 vs. 3.0, p = 0.026), EQ-VAS (52.3 vs. 67.4, p < 0.001) and EQ-5D-5L index value (0.554 vs. 0.749, p < 0.001) | Neurorehabilitation improves QOL for patients with severe neurological symptoms following COVID-19 |
Figure 2 illustrates which geographical contexts the studies were set in. Four out of six inhabited continents were represented, with no studies coming from Oceania or South America. The most common country was the USA, with just over a quarter of all studies (N = 9).
FIGURE 2.
Which country studies took place in.
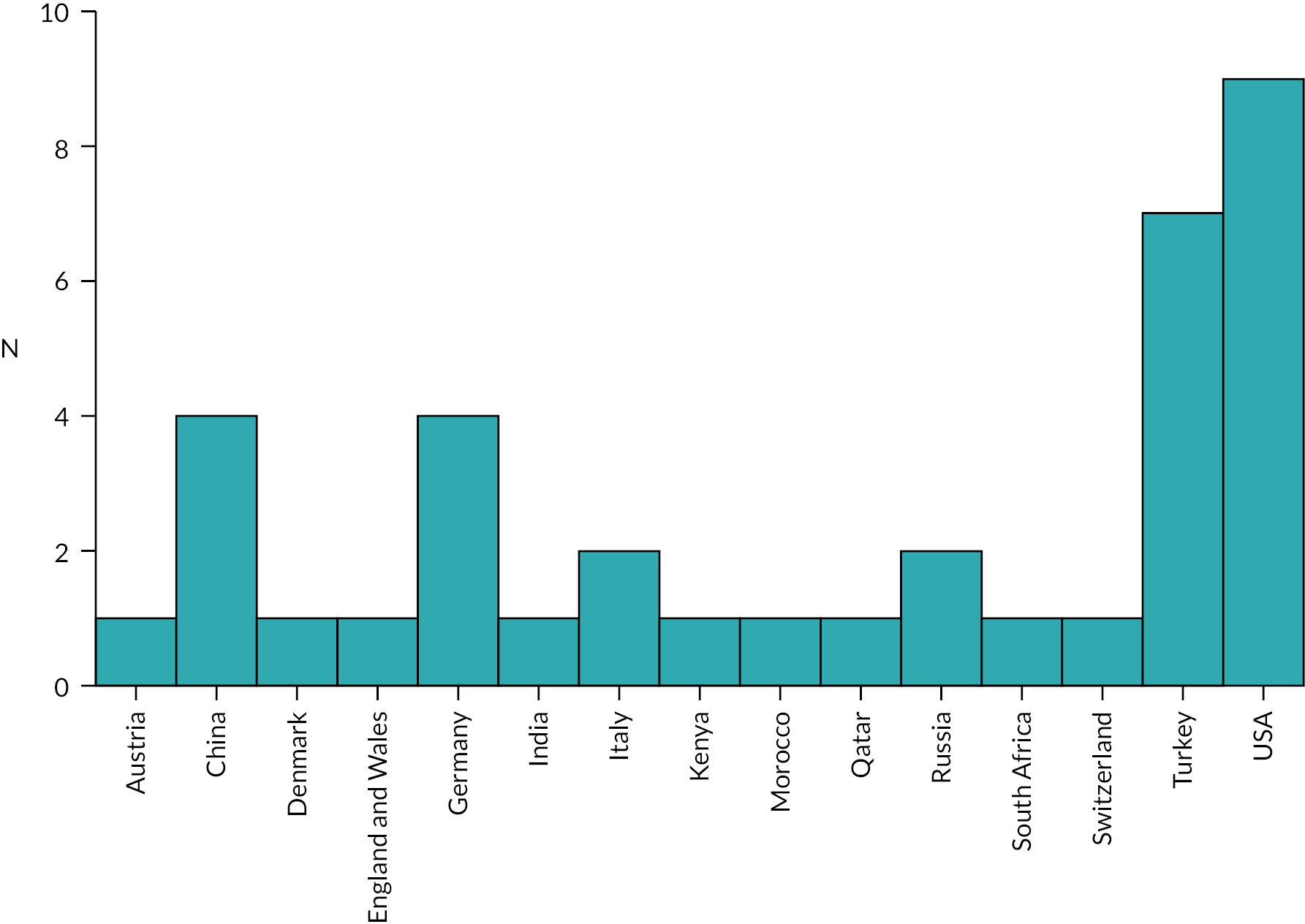
Figure 3 shows which study designs were chosen. The most common design was economic evaluation (N = 13) followed by cross-sectional (N = 10). Figure 3 also illustrates what approaches were taken for economic evaluation. Most (N = 8) used a decision tree, with almost half (N = 6) using a Markov model. 48 These modelling approaches were often combined, with a decision tree representing the hospitalisation phase, followed by a Markov process representing the rest of a patient’s life post discharge, with transitions between ill health, recovery and death. In two studies21,46 a value of information analysis was performed.
FIGURE 3.
(a) Frequency of using study design; (b) frequency that economic evaluation studies used different modelling approaches.
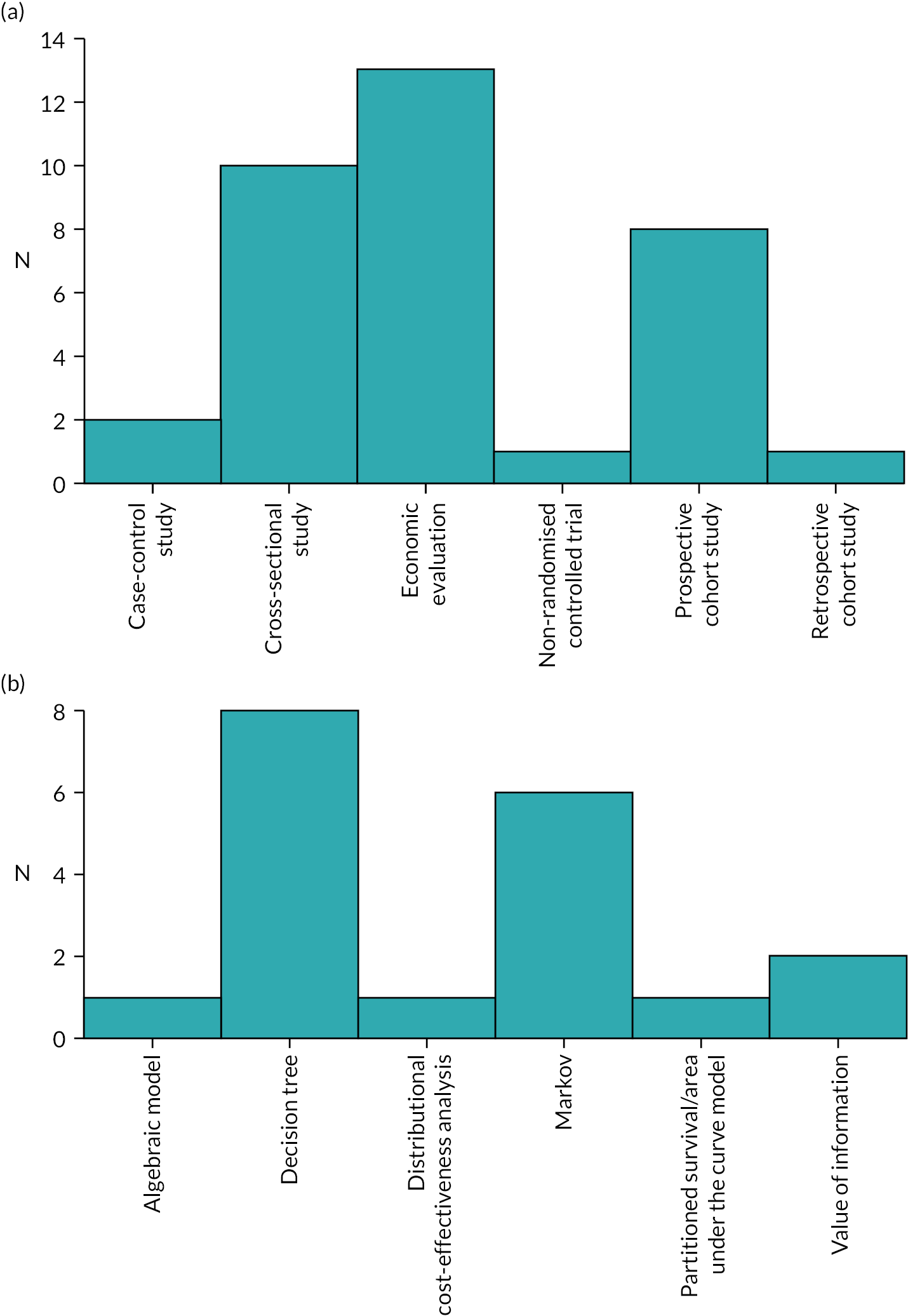
Table 2 gives details about the various QOL measures employed by studies and Figure 4 illustrates how frequently they were used. Most (N = 13) used published utility values, all of which were economic evaluations. Four studies27,37,41,46 used values for influenza to represent mild/moderate COVID-19 and values for patients with Clostridioides difficile infection to represent more severe illness. Two other studies used values for influenza to represent less severe COVID-19 cases and values for either influenza H1N1 (swine flu)19 or pneumonia16 to represent more severe cases. Kelton et al. 30 used values for patients with C. difficile infection and Sheinson et al. 43 used utility values from people with severe acute respiratory syndrome (SARS). Dijk et al. 21 used published HUI values for SARS for patients hospitalised with COVID-19, and published EQ-5D-3L values to represent QOL in post-ICU and post-hospitalisation patients. Two studies reported DALYs for patients using published disability weights from the Global Burden of Disease (GBD) study. 49 One used weights for severe lower respiratory tract infection to represent severe COVID-19 inpatients, and pneumonia to represent critical inpatients;18 the other used severe respiratory tract infection for severe patients, but weights for ICU admission for critical patients. 28 In four studies, it was unclear what conditions some or all published utility values came from. 30,32,38,43 A single study25 used a nine-member expert panel to estimate COVID-19 disability weights for calculating DALYs.
| Survey | Abbreviation | Description | Reference |
|---|---|---|---|
| Beck Anxiety Inventory | BAI | 21-item measure of anxiety severity | 50 |
| Beck Depression Inventory | BDI | 21-item measure of depression severity | 51 |
| Child Depression Inventory | CDI | 10-item measure of child psychological health | 52 |
| Child Post-Traumatic Stress Disorder Reaction Index | CPTS-RI | 48-item structured interview assessing child’s trauma history | 53 |
| Epworth Sleepiness Scale | ESS | 8-item measure of sleepiness | 54 |
| EQ-5D | EQ-5D | Generic health-related quality of life measure with three-level (EQ-5D-3L) and five-level (EQ-5D-5L) versions | 55 |
| Generalised Anxiety Disorder-7 | GAD-7 | Condition-specific measure assessing generalised anxiety disorder | 56 |
| Harvard Trauma Questionnaire | HTQ | Checklist measuring exposure to traumatic events | 57 |
| Hospital Anxiety and Depression Scale | HADS | 14-item scale measuring anxiety and depression separately | 58 |
| Insomnia Severity Index | ISI | 7-item scale measuring sleep quality | 59 |
| Modified Borg Dyspnea Scale | mBDS | 10-point scale measuring breathing difficulties | 60 |
| Modified Medical Research Council Dyspnea Scale | mMRC | 5-item scale measuring severity of dyspnoea symptoms | 61 |
| Multidimensional Fatigue Inventory | MFI-20 | 20-item measure of fatigue | 62 |
| Patient Health Questionnaire-9 | PHQ-9 | 9-item scale used to diagnose mental health disorders | 63 |
| Perceived Stress Scale | PSS-10 | 10-item measure of stress | 64 |
| Pittsburgh Sleep Quality Index | PSQI | 19-item measure of sleep quality and disturbances | 65 |
| Screen for Child Anxiety Related Disorders | SCARED | 41-item measure of anxiety in children | 66 |
| Self-rating Anxiety Scale | SAS | 20-item measure of anxiety disorder symptoms | 67 |
| Self-rating Depression Scale | SDS | 20-item measure of depression disorder symptoms | 68 |
| Short Form (36) Health Survey | SF-36 | Generic health-related quality-of-life measure | 69 |
| Short Inventory of Mindfulness Capability | SIM-C | 12-item measure of the describing, act-aware and non-judging factors of mindfulness | 70 |
| 8-item Somatic Symptom Scale | SSS-8 | 8-item measure of somatic symptom burden, short version of the Patient Health Questionnaire-15 | 71 |
| World Health Organization Quality of Life – Older Adults Module | WHOQOL-OLD | 24-item measure of quality of life in older people | 72 |
FIGURE 4.
Frequency of using different quality-of-life measures. BAI, Beck Anxiety Inventory; BDI, Beck Depression Inventory; CDI, Child Depression Inventory; CPTS-RI, Child Post-Traumatic Stress Reaction Index; DALY, disability-adjusted life-year; ESS, Epworth Sleepiness Scale; GAD-7, Generalised Anxiety Disorder-7; HADS, Hospital Anxiety and Depression Scale; HTQ, Harvard Trauma Questionnaire; ISI, Insomnia Severity Index; mBDS, modified Borg Dyspnea Scale; MFI-20, Multidimensional Fatigue Inventory; mMRC, modified Medical Research Council Dyspnea Scale; PHQ-9, Patient Health Questionnaire-9; PSQI, Pittsburgh Sleep Quality Index; PSS-10, Perceived Stress Scale; SAS, Self-rating Anxiety Scale; SCARED, Screen for Child Anxiety Related Disorders; SDS, Self-rating Depression Scale; SF-36, Short Form-36; SIM-C, Short Inventory of Mindfulness Capability; SSS-8, 8-item Somatic Symptom Scale; WHOQOL-OLD, World Health Organization Quality of Life Instrument – Older Adults Module.
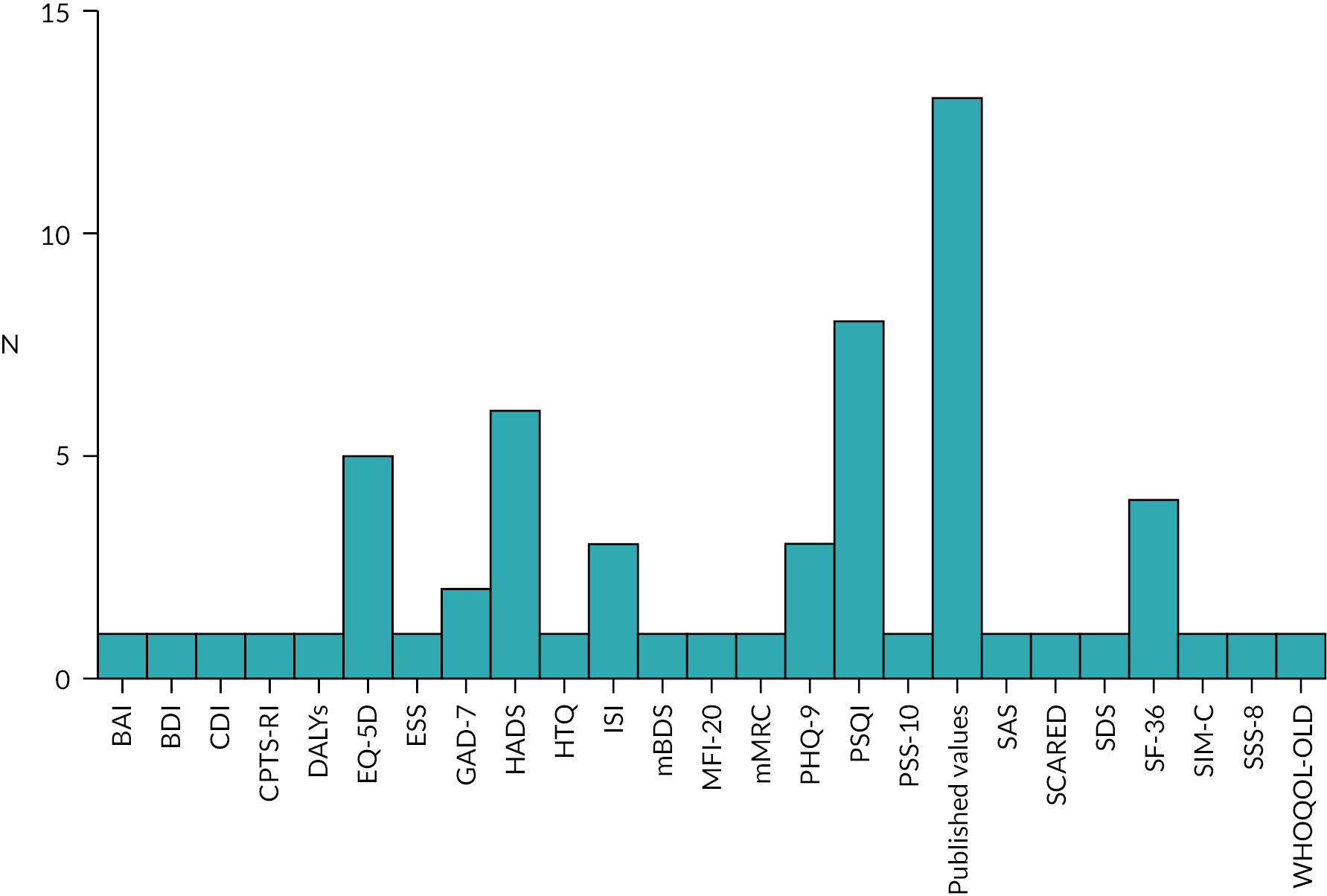
Twelve studies17,22,24,26,29,33,34,36,42,44,45,47 used 12 different mental health-related measures: the Patient Health Questionnaire-9 (PHQ-9; N = 3), the Hospital and Anxiety Depression Scale (HADS; N = 2), Generalised Anxiety Disorder-7 (GAD-7; N = 2), the Beck Anxiety Inventory (BAI; N = 1), the Beck Depression Inventory (BDI; N = 1), the Child Depression Inventory (CDI, N = 1), the Child Post-Traumatic Stress Reaction Index (CPTS-RI; N = 1), the Harvard Trauma Questionnaire (HTQ; N = 1), the Perceived Stress Scale (PSS-10; N = 1), the Screen for Child Anxiety Related Disorders (SCARED; N = 1), the Self-Rating Anxiety Scale (SAS; N = 1) and the Self-Rating Depression Scale (SDS; N = 1). Twelve studies used one or more sleep-related QOL measures,13,17,23,26,29,33-36,42,44,47 with the most popular being the Pittsburgh Sleep Quality Index (PSQI; N = 8).
Considering generic health measures, four studies>15,22,36,39 used the Short Form (36) Health Survey (SF-36) and five studies20,24,31,40,47 used EQ-5D, of which two used EQ-5D-3L and three used EQ-5D-5L. Two studies using EQ-5D assessed inpatient rehabilitation programmes24,31 and one looked at patients seen 7 days after undergoing surgery for a proximal femur fracture. 40 Thus, although they qualify for inclusion in this review due to reporting QOL data for inpatients with COVID-19, they did not collect data from patients in the acute phase of the disease. The remaining study20 collected only data from those aged over 80.
Figure 5 shows how many COVID-19 inpatients were analysed by each study. The median number of participants was 97.5 and the mean was 1096.25. The mean was far higher due to two outliers, He et al. 25 and Kairu et al.,28 who included 2702 and 20,836 patients, respectively. These numbers were achieved by reporting DALYs calculated using years of life lost from routine data and disability weights from either published values or a nine-member expert panel.
FIGURE 5.
Analysis sample sizes of COVID-19 inpatients.
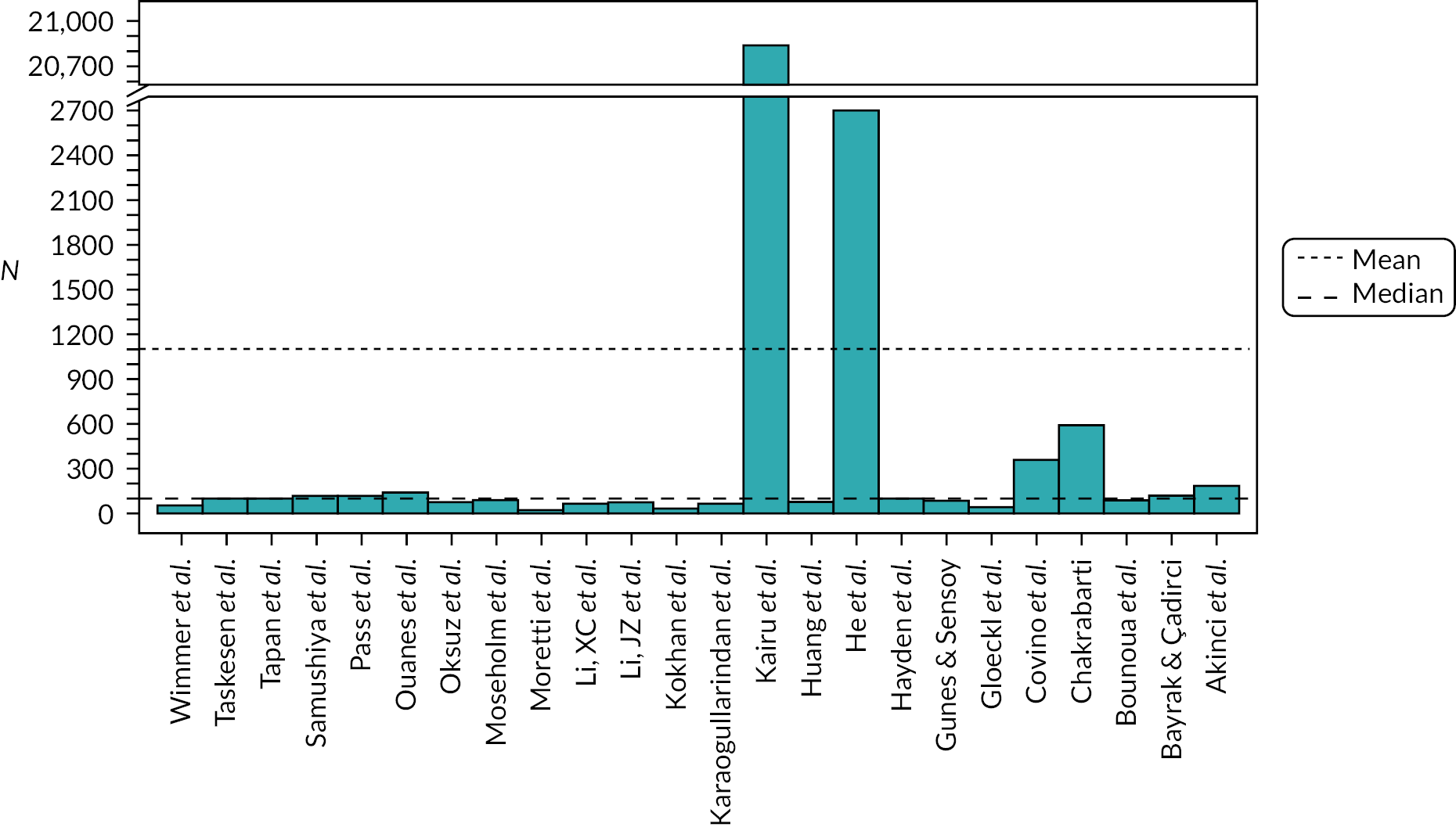
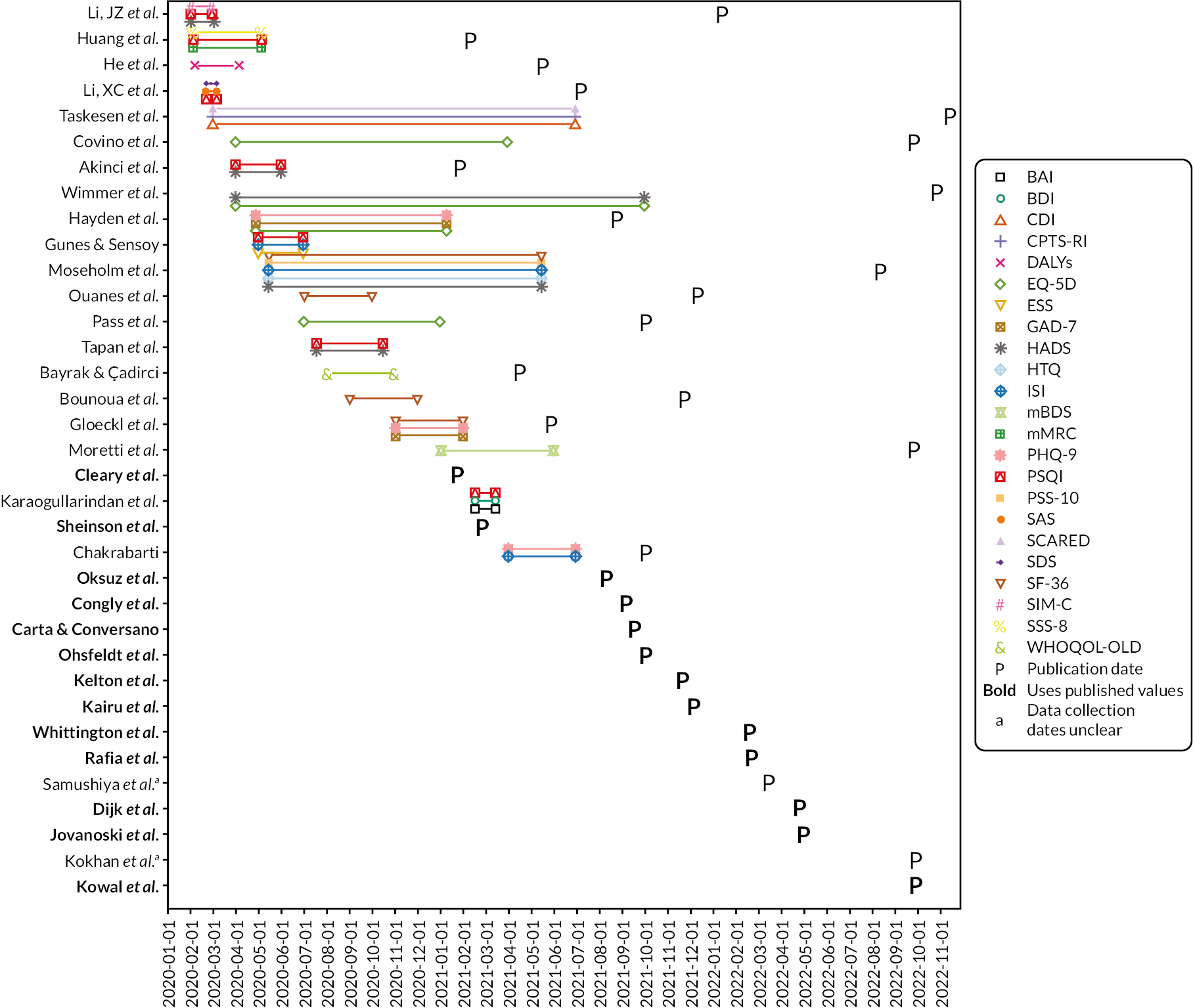
Figure 6 shows a timeline of when studies collected data and publication dates (where only the month of data collection start/stop is given, we assumed collection started on the first and/or ended on the last day of the relevant month). The earliest data collection started in February 202033 and seven other studies also began collection in the first half of 2020,13,23–26,29,34 with the majority using sleep and/or mental health-related measures. The first study to be published was Cleary et al.,18 who used published utility values. The first study to be published which reported data collected from COVID-19 inpatients was Akinci et al.,13 who used PSQI and HADS.
FIGURE 6.
Timeline of data collection and study publication dates.
For studies where it was clear what mode was used for data collection, two used paper surveys,25,44 six collected responses online,17,26,34,39,42,45 three collected responses via phone36,39,42 and one used in-person interviews. 23,36
In general, studies found that being an inpatient with COVID-19 negatively affected QOL and, in particular, many studies found a negative impact on mental health13,17,29,34,42,44 and/or sleep quality. 13,17,23,26,29,33,34,42,44 However, many studies did not formally include a comparator group of those without COVID-19, making it difficult to isolate the causal effect of the disease. This is particularly problematic with sleep quality and anxiety where hospitalisation for any condition may be expected to have an impact. A differential impact on some groups was found by several studies, in particular older inpatients,15,20,29 women20,25 and those with comorbidities. 20 The four studies examining inpatient rehabilitation programmes22,24,31,47 all showed a significant post-intervention improvement in QOL compared to baseline.
Discussion
The results show that collecting data on COVID-19 inpatients’ QOL was feasible, even in the early stages of the pandemic. Given the disruption that the pandemic caused to healthcare systems, as well as wider society, this is an encouraging finding for QOL research.
It is positive that many studies were from low- or middle-income countries. However, sample sizes, especially for studies collecting data directly from patients, were often relatively low, with a median of under 100. In addition, many studies were cross-sectional. While this design provides much useful information, it is difficult to get a picture of how QOL has varied over the course of the COVID-19 pandemic.
A large fraction of the included studies used sleep and/or mental health-related survey instruments. However, there was a lack of consensus on what survey measures to use, with a large number employed. Some variation was clearly necessary, for example using child-specific instruments for studies in children, but the wide variety of surveys used hinders comparison of results across different studies.
While sleep and mental health are undoubtedly important topics, there is a lack of data on the overall QOL impact of being hospitalised with COVID-19. For example, only five studies used the EQ-5D measure commonly used in other areas of health research. Only one study targeted the general population of people hospitalised with COVID-19, with the others targeting specific sub-populations (older people,20 those undergoing surgery40 or people in rehabilitation programmes24,31).
The paucity of general QOL data for people hospitalised in the acute phase of the disease meant that economic evaluations used published utility values of disability weights for people with other conditions. This represents a serious knowledge gap, especially given the demonstrated feasibility of collecting such data. Research to fill this gap would be useful, not just for economic evaluation, but also to see what the impact of being hospitalised with COVID-19 is on people’s QOL, and what aspects of health are most affected.
The latest date on which any included study was open for data collection was September 2021, although results from some studies which collected data at later time points may not yet be available. COVID-19 has evolved during the course of the pandemic and widespread vaccination has also reduced the probability of serious illness for those infected. 73–75 Several studies have looked at how QOL evolved for the general population76,77 or for specific groups such as carers. 78–80 However, the large number of survey measures used and the fact that generic measures were in a minority makes it difficult to track how the pandemic’s evolution has impacted QOL for COVID-19 inpatients.
Several studies examined a group of COVID-19 inpatients, but without also measuring QOL for a comparison group of individuals without the condition. This made it difficult to quantify the impact of being hospitalised with COVID-19, since there was no counterfactual to measure a decrement against. Several other studies had a cross-sectional design, which is a common approach and can give valuable insight. However, a longitudinal design can give additional information, albeit usually with greater resource costs.
A strength of our paper is that we jointly developed a search strategy involving those with health economic experience, but also information specialist expertise. We also searched a wide range of databases. This approach maximised our chances of finding all relevant studies.
While our systematic searches were an advantage, it is a weakness of this study that it is not a systematic review, and no protocol was registered in advance. This may potentially have introduced some bias into our findings. There were limitations to the conclusions that could be drawn from the external data. For example, it was not possible to synthesise data from the included studies to find values representing QOL for COVID-19 inpatients on a full health = 1, dead = 0 scale. Many included studies used published values for people with other conditions. Those that did survey patients used a wide range of measures that were difficult or impossible to directly compare, and often comparison groups were not included. There was also a wide range of settings studied, from ICU to inpatient rehabilitation. A final limitation to the extracted data is that it was often difficult to distinguish between people hospitalised due to COVID-19 and those hospitalised for another reason who had also acquired a COVID-19 infection (although given the time frame of most studies, patients were likely to mostly consist of the former group). Yet it is also a strength of our study that examining the above limitations has allowed us to make recommendations both for future COVID-19 and QOL research and for methodological approaches to measuring the QOL impact of future health crises.
Conclusion
We conclude by summarising some recommendations for COVID-19-related research, as well as for research during future health crises. On the former topic, we recommend that such data be collected longitudinally, so that the QOL impact for patients hospitalised with COVID-19 can be assessed as the disease progresses throughout its acute phase. Several economic evaluations of COVID-19 treatments exist which use utility values from patients with other conditions. The cost-effectiveness of such treatments should be reassessed using data collected from COVID-19 patients.
In future health crises, researchers should be aware of early opportunities to collect QOL data from hospitalised patients, given the feasibility demonstrated during COVID-19. There should also be an effort on behalf of the research community to co-ordinate as much as possible, to enhance comparability of results between studies and to ensure that important knowledge gaps do not arise.
Additional information
CRediT contribution statement
Edward Webb: Conceptualisation (equal), Data curation (lead), Investigation (equal), Methodology (joint lead), Software (lead), Visualisation (lead), Writing – original draft (lead), Writing – editing and reviewing (lead). Natalie King: Investigation (equal), Methodology (joint lead), Writing – editing and reviewing (supporting). Daniel Howdon: Data curation (supporting), Investigation (supporting), Writing – editing and reviewing (supporting). Enitan D Carrol: Conceptualisation (supporting), Funding acquisition (joint lead), Writing – editing and reviewing (supporting). Joanne Euden: Funding acquisition (equal), Project administration (lead), Writing – editing and reviewing (supporting). Philip Howard: Funding acquisition (equal), Writing – editing and reviewing (supporting). Philip Pallmann: Funding acquisition (equal), Writing – editing and reviewing (supporting). Martin J Llewelyn: Funding acquisition (equal), Writing – editing and reviewing (supporting). Emma Thomas-Jones: Funding acquisition (equal), Writing – editing and reviewing (supporting). Bethany Shinkins: Conceptualisation (equal), Data curation (supporting), Funding acquisition (equal), Investigation (supporting), Supervision (lead), Writing – original draft (supporting), Writing – editing and reviewing (supporting). Jonathan Sandoe: Conceptualisation (supporting), Funding acquisition (joint lead), Writing – editing and reviewing (supporting). Robert West: Funding acquisition (equal). Lucy Brookes-Howell: Funding acquisition (equal). Paul Dark: Funding acquisition (equal). Neil Powell: Funding acquisition (equal). Tamas Szakmany: Funding acquisition (equal). Mahableshwar Albur: Funding acquisition (equal). David Partridge: Funding acquisition (equal). Thomas Hellyer: Funding acquisition (equal). Helena Parsons: Funding acquisition (equal). Susan Hopkins: Funding acquisition (equal). Margaret Ogden: Funding acquisition (equal). Dominic Shaw: Funding acquisition (equal). Stacy Todd: Funding acquisition (equal). Stuart Bond: Funding acquisition (equal).
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/ATPR4281.
Primary conflicts of interest: None declared.
Data-sharing statement
Full extracted data are provided as Report Supplementary Material 1. All requests for data should be directed to the corresponding author.
Ethics statement
Research approval for the PEACH study was provided by the Health Research Authority (HRA) and Health and Care Research Wales (HCRW). Ethics approval was provided by West Midlands – Solihull Research Ethics Committee (REC Reference 21/WM/0052).
Information governance statement
The University of Leeds is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under the Data Protection legislation, The University of Leeds is the Data Controller, and you can find out more about how we handle personal data, including how to exercise your individual rights, and the contact details for our Data Protection Officer are here: https://dataprotection.leeds.ac.uk/.
Study registration details
This study is registered as ISRCTN66682918.
Department of Health and Social Care disclaimer
This publication presents independent research commissioned by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, MRC, NIHR Coordinating Centre, the HTA programme or the Department of Health and Social Care.
Funding
This article presents independent research funded by the National Institute for Health and Care Research (NIHR) Health Technology Assessment (HTA) programme as award number NIHR132254. The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the HTA programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HTA programme or the Department of Health and Social Care.
This article reports on one component of the research award Evidence of quality of life for hospitalised patients with COVID-19: a scoping review. For more information about this research please view the award page [https://www.fundingawards.nihr.ac.uk/award/NIHR132254].
About this article
The contractual start date for this research was in October 2020. This article began editorial review in March 2023 and was accepted for publication in November 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The Health Technology Assessment editors and publisher have tried to ensure the accuracy of the authors’ article and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
This article was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Copyright
Copyright © 2024 Webb et al. This work was produced by Webb et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
List of abbreviations
- BAI
- Beck Anxiety Inventory
- BDI
- Beck Depression Inventory
- CDI
- Child Depression Inventory
- COVID-19
- coronavirus disease 2019
- CPTS-RI
- Child Post-Traumatic Stress Reaction Index
- DALY
- disability-adjusted life-year
- EQ-5D
- EuroQol-5 Dimensions
- EQ-5D-3L
- EuroQol-5 Dimensions, three-level version
- GAD
- generalised anxiety disorder
- GBD
- Global Burden of Disease
- HADS
- Hospital and Anxiety Depression Scale
- HTQ
- Harvard Trauma Questionnaire
- HUI
- Health Utilities Index
- ICU
- intensive care unit
- PHQ-9
- Patient Health Questionnaire-9
- PROM
- patient-reported outcome measure
- PSQI
- Pittsburgh Sleep Quality Index
- PSS
- Perceived Stress Scale
- QALY
- quality-adjusted life-year
- QOL
- quality of life
- SAS
- Self-rating Anxiety Scale
- SCARED
- Screen for Child Anxiety Related Disorders
- SDS
- Self-rating Depression Scale
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/ATPR4281).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
References
- Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497-506.
- World Health Organization . COVID-19: Vulnerable and High Risk Groups 2023. www.who.int/westernpacific/emergencies/covid-19/information/high-risk-groups (accessed 3 August 2023).
- Organisation for Economic Co-operation and Development . OECD Science, Technology and Innovation Outlook 2021 2021.
- Nandasena H, Pathirathna M, Atapattu A, Prasanga P. Quality of life of COVID 19 patients after discharge: systematic review. PLOS ONE 2022;17.
- Malik P, Patel K, Pinto C, Jaiswal R, Tirupathi R, Pillai S, et al. Post‐acute COVID‐19 syndrome (PCS) and health‐related quality of life (HRQoL): a systematic review and meta‐analysis. J Med Virol 2022;94:253-62.
- Michelen M, Manoharan L, Elkheir N, Cheng V, Dagens A, Hastie C, et al. Characterising long COVID: a living systematic review. BMJ Glob Health 2021;6.
- Horby P, Landray M, Haynes R, Juszczak E, Baillie K, Jaki T. Randomised Evaluation of COVID-19 Therapy (RECOVERY): Study Protocol. Oxford: University of Oxford; 2020.
- Butler CC, Hobbs FR, Gbinigie OA, Rahman NM, Hayward G, Richards DB, et al. Molnupiravir plus usual care versus usual care alone as early treatment for adults with COVID-19 at increased risk of adverse outcomes (PANORAMIC): an open-label, platform-adaptive randomised controlled trial. Lancet 2022;401:281-93.
- Watson OJ, Barnsley G, Toor J, Hogan AB, Winskill P, Ghani AC. Global impact of the first year of COVID-19 vaccination: a mathematical modelling study. Lancet Infect Dis 2022;22:1293-302.
- World Health Organization . Global COVID-19 Vaccination Strategy in a Changing World, July 2022 Update 2022.
- Arber M, Garcia S, Veale T, Edwards M, Shaw A, Glanville JM. Performance of Ovid MEDLINE search filters to identify health state utility studies. Int J Technol Assess Health Care 2017;33:472-80.
- McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol 2016;75:40-6.
- Akinci T, Melek Basar H. Relationship between sleep quality and the psychological status of patients hospitalised with COVID-19. Sleep Med 2021;80:167-70. https://doi.org/10.1016/j.sleep.2021.01.034.
- Bayrak M, Cadirci K. The associations of life quality, depression, and cognitive impairment with mortality in older adults with COVID-19: a prospective, observational study. Acta Clin Belg 2022;77:588-95. https://doi.org/10.1080/17843286.2021.1916687.
- Bounoua F, Khannous A, Moubachir H, Serhane H. Evaluation of the quality of life in patients treated for COVID-19 at the Hassan II hospital in Agadir using the MOS SF-36 questionnaire. Eur Respir J 2021;58. https://doi.org/10.1183/13993003.congress-2021.PA299.
- Carta A, Conversano C. Cost utility analysis of Remdesivir and Dexamethasone treatment for hospitalised COVID-19 patients: a hypothetical study. BMC Health Serv Res 2021;21. https://doi.org/10.1186/s12913-021-06998-w.
- Chakrabarti S. Mental health in hospitalised COVID 19 patients in quarantine during second wave in a south Indian private teaching hospital. J Multidiscip Healthc 2021;14:2777-89. https://doi.org/10.2147/JMDH.S330812.
- Cleary SM, Wilkinson T, Tamandjou Tchuem CR, Docrat S, Solanki GC. Cost-effectiveness of intensive care for hospitalized COVID-19 patients: experience from South Africa. BMC Health Serv Res 2021;21. https://doi.org/10.1186/s12913-021-06081-4.
- Congly SE, Varughese RA, Brown CE, Clement FM, Saxinger L. Treatment of moderate to severe respiratory COVID-19: a cost-utility analysis. Sci Rep 2021;11. https://doi.org/10.1038/s41598-021-97259-7.
- Covino M, Russo A, Salini S, De Matteis G, Simeoni B, Pirone F, et al. Long-term effects of hospitalization for COVID-19 on frailty and quality of life in older adults >=80 years. J. Clin. Med. 2022;11. https://doi.org/10.3390/jcm11195787.
- Dijk SW, Krijkamp EM, Kunst N, Gross CP, Wong JB, Hunink MGM. Emerging therapies for COVID-19: the value of information from more clinical trials. Value Health 2022;27. https://doi.org/10.1016/j.jval.2022.03.016.
- Gloeckl R, Leitl D, Jarosch I, Schneeberger T, Nell C, Stenzel N, et al. Benefits of pulmonary rehabilitation in COVID-19: a prospective observational cohort study. ERJ Open Res 2021;7. https://doi.org/10.1183/23120541.00108-2021.
- Gunes A, Sensoy B. Sleepiness, insomnia, and sleep quality of hospitalized patients with coronavirus disease-2019: sleep scale evaluation. J Turk Sleep Med 2022;9:11-5. https://doi.org/10.4274/jtsm.galenos.2021.39974.
- Hayden MC, Limbach M, Schuler M, Merkl S, Schwarzl G, Jakab K, et al. Effectiveness of a three-week inpatient pulmonary rehabilitation program for patients after COVID-19: a prospective observational study. Int J Environ Res Public Health 2021;18. https://doi.org/10.3390/ijerph18179001.
- He M, Li X, Tan Q, Chen Y, Kong Y, You J, et al. Disease burden from COVID-19 symptoms among inpatients at the temporary military hospitals in Wuhan: a retrospective multicentre cross-sectional study. BMJ Open 2021;11. https://doi.org/10.1136/bmjopen-2021-048822.
- Huang S, Zhuang W, Wang D, Zha L, Xu X, Li X, et al. Persistent somatic symptom burden and sleep disturbance in patients with COVID-19 during hospitalization and after discharge: a prospective cohort study. Med Sci Monit 2021;27. https://doi.org/10.12659/MSM.930447.
- Jovanoski N, Kuznik A, Becker U, Hussein M, Briggs A. Cost-effectiveness of casirivimab/imdevimab in patients with COVID-19 in the ambulatory setting. J Manag Care Spec Pharm 2022;28:555-65. https://doi.org/10.18553/jmcp.2022.21469.
- Kairu A, Were V, Isaaka L, Agweyu A, Aketch S, Barasa E. Modelling the cost-effectiveness of essential and advanced critical care for COVID-19 patients in Kenya. BMJ Glob 2021;6. https://doi.org/10.1136/bmjgh-2021-007168.
- Karaogullarindan A, Erkan SO, Tuhanioglu B, Kuran G, Gorgulu O. Sleep quality in patients over 65 years of age in the Covid-19 pandemic. Turk Geriatri Dergisi 2021;24:381-90. https://doi.org/10.31086/tjgeri.2021.235.
- Kelton K, Klein T, Murphy D, Belger M, Hille E, McCollam PL, et al. Cost-effectiveness of combination of Baricitinib and Remdesivir in hospitalized patients with COVID-19 in the United States: a modelling study. Adv Ther 2022;39:562-82. https://doi.org/10.1007/s12325-021-01982-6.
- Kokhan S, Kolokoltsev M, Vorozheikin A, Gryaznykh А, Romanova E, Guryanov M, et al. Physical rehabilitation of patients with post-COVID syndrome. J Phys Educ Sport 2022;22:2005-11. https://doi.org/10.7752/jpes.2022.09255.
- Kowal S, Ng CD, Schuldt R, Sheinson D, Cookson R. The impact of funding inpatient treatments for COVID-19 on health equity in the United States: a distributional cost-effectiveness analysis. Value Health 2022;26:216-25. https://doi.org/10.1016/j.jval.2022.08.010.
- Li J, Zhang YY, Cong XY, Ren SR, XM T. Wu JF 5-min mindfulness audio induction alleviates psychological distress and sleep disorders in patients with COVID-19. World J Clin Cases 2022;10:576-84. https://doi.org/10.12998/wjcc.v10.i2.576.
- Li X, Cai Q, Jia Z, Liu L, Zhou Y, Zhang B, et al. The correlation between mental health status, sleep quality, and inflammatory markers, virus negative conversion time among patients confirmed with 2019-nCoV during the COVID-19 outbreak in China: an observational study. Medicine 2021;100. https://doi.org/10.1097/MD.0000000000026520.
- Moretti A, Belfiore A, Bianco M, Liguori S, Paoletta M, Toro G, et al. Functioning issues in inpatients affected by COVID-19-related moderate pulmonary impairment: a real-practice observational study. J Int Med Res 2022;50. https://doi.org/10.1177/03000605221126657.
- Moseholm E, Midtgaard J, Bollerup S, Apol AD, Olesen OB, Jespersen S, et al. Psychological distress among hospitalized COVID-19 patients in Denmark during the first 12 months of the pandemic. Int J Environ Res Public Health 2022;19. https://doi.org/10.3390/ijerph191610097.
- Ohsfeldt R, Kelton K, Klein T, Belger M, Mc Collam PL, Spiro T, et al. Cost-effectiveness of Baricitinib compared with standard of care: a modeling study in hospitalized patients with COVID-19 in the United States. Clin Ther 2021;43:1877-93.e4. https://doi.org/10.1016/j.clinthera.2021.09.016.
- Oksuz E, Malhan S, Gonen MS, Kutlubay Z, Keskindemirci Y, Jarrett J, et al. Cost-effectiveness analysis of Remdesivir treatment in COVID-19 patients requiring low-flow oxygen therapy: payer perspective in Turkey. Adv Ther 2021;38:4935-48. https://doi.org/10.1007/s12325-021-01874-9.
- Ouanes S, Al-Amin H, Hussein NB, Khan F, Al Shahrani A, David P, et al. Physical and psychosocial well-being of hospitalized and non-hospitalized patients with COVID-19 compared to the general population in Qatar. Front Psychiat 2021;12. https://doi.org/10.3389/fpsyt.2021.792058.
- Pass B, Vajna E, Knauf T, Rascher K, Aigner R, Eschbach D, et al. Registry for Geriatric Trauma (ATR-DGU) . COVID-19 and proximal femur fracture in older adults: a lethal combination? An analysis of the Registry for Geriatric Trauma (ATR-DGU). J Am Med Dir Assoc 2022;23:576-80. https://doi.org/10.1016/j.jamda.2021.09.027.
- Rafia R, Martyn-St James M, Harnan S, Metry A, Hamilton J, Wailoo A. A cost-effectiveness analysis of Remdesivir for the treatment of hospitalized patients with COVID-19 in England and Wales. Value Health 2022;25:761-9. https://doi.org/10.1016/j.jval.2021.12.015.
- Samushiya MA, Kryzhanovsky SM, Ragimova AA, Berishvili TZ, Chorbinskaya SA, Ivannikova EI. Psychoemotional disorders and sleep impairments in patients with COVID-19. Neurosci Behav Physiol 2022;52:231-5. https://doi.org/10.1007/s11055-022-01229-z.
- Sheinson D, Dang J, Shah A, Meng Y, Elsea D, Kowal S. A cost-effectiveness framework for COVID-19 treatments for hospitalized patients in the United States. Adv Ther 2021;38:1811-31. https://doi.org/10.1007/s12325-021-01654-5.
- Tapan OO, Tapan U, Alasan F, Akgul AF, Genc S. Factors that affect sleep quality in hospitalized patients with COVID-19 pneumonia. J Turk Sleep Med 2022;9:51-6. https://doi.org/10.4274/jtsm.galenos.2021.86648.
- Taskesen B, Kardas O, Yilmaz K. Evaluation of depression, anxiety and posttraumatic stress response levels of children and adolescents treated with COVID-19. Eur J Pediatr 2022;182:567-74. https://doi.org/10.1007/s00431-022-04713-3.
- Whittington MD, Pearson SD, Rind DM, Campbell JD. The cost-effectiveness of Remdesivir for hospitalized patients with COVID-19. Value Health 2022;25:744-50. https://doi.org/10.1016/j.jval.2021.11.1378.
- Wimmer C, Egger M, Bergmann J, Huge V, Muller F, Jahn K. Critical COVID-19 disease: clinical course and rehabilitation of neurological deficits. Front Neurol 2022;13. https://doi.org/10.3389/fneur.2022.1012685.
- Briggs A, Sculpher M. An introduction to Markov modelling for economic evaluation. PharmacoEcon 1998;13:397-409.
- Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020;396:1204-22.
- Beck AT, Epstein N, Brown G, Steer R. Beck Anxiety Inventory. J Consult Clin Psychol 1993;56:893-7.
- Beck AT, Steer RA, Brown GK. Beck Depression Inventory. New York: Harcourt Brace Jovanovich; 1987.
- Kovacs M. Child Depression Inventory. Person Individ Diff 1992. https://doi.org/10.1037/t19482-000.
- Steinberg AM, Brymer MJ, Decker KB, Pynoos RS. The University of California at Los Angeles Post-Traumatic Stress Disorder Reaction Index. Curr Psychiatry Rep 2004;6:96-100.
- Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 1991;14:540-5.
- Group TE. EuroQol: a new facility for the measurement of health-related quality of life. Health Pol 1990;16:199-208.
- Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006;166:1092-7.
- Mollica RF, Caspi-Yavin Y, Bollini P, Truong T, Tor S, Lavelle J. The Harvard Trauma Questionnaire: validating a cross-cultural instrument for measuring torture, trauma, and posttraumatic stress disorder in Indochinese refugees. J Nerv Ment Dis 1992;180:111-6.
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361-70.
- Morin CM. Insomnia: Psychological Assessment and Management. New York: Guilford Press; 1993.
- Muza SR, Silverman MT, Gilmore GC, Hellerstein HK, Kelsen SG. Comparison of scales used to quantitate the sense of effort to breathe in patients with chronic obstructive pulmonary disease. Am Rev Respir Dis 1990;141:909-13.
- Fletcher CM, Elmes PC, Fairbairn AS, Wood CH. Significance of respiratory symptoms and the diagnosis of chronic bronchitis in a working population. Br Med J 1959;2:257-66.
- Smets E, Garssen B, Bonke B, De Haes J. The Multidimensional Fatigue Inventory (MFI) psychometric qualities of an instrument to assess fatigue. J Psychosom Res 1995;39:315-25.
- Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr Ann 2002:509-15. https://doi.org/10.3928/0048-5713-20020901-06.
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav 1994;10:385-96. https://doi.org/10.2307/2136404.
- Buysse DJ, Reynolds CF III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 1989;28:193-21.
- Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, et al. The Screen for Child Anxiety Related Emotional Disorders (SCARED): scale construction and psychometric characteristics. J Am Acad Child Adolesc Psychiat 1997;36:545-53.
- Zung WW. A rating instrument for anxiety disorders. Psychosomatics 1971;12:371-9. https://doi.org/10.1016/S0033-3182(71)71479-0.
- Zung WW. A self-rating depression scale. Arch Gen Psychiatry 1965;12:63-70.
- Hays RD, Sherbourne CD, Mazel RM. The rand 36‐item health survey 10. Health Econ 1993;2:217-27.
- Duan W, Li J. Short Inventory of Mindfulness Capability. Front Psychol 2016. https://psycnet.apa.org/doi/10.1037/t58213-000.
- Gierk B, Kohlmann S, Kroenke K, Spangenberg L, Zenger M, Brähler E, et al. The Somatic Symptom Scale–8 (SSS–8): a brief measure of somatic symptom burden. JAMA Intern Med 2014;174:399-407.
- Power M, Quinn K, Schmidt S. WHOQOL-OLD Group . Development of the WHOQOL-old module. Qual Life Res: Int J Qual Life Asp Treat Care Rehabil 2005;14:2197-214.
- Knoll MD, Wonodi C. Oxford–AstraZeneca COVID-19 vaccine efficacy. Lancet 2021;397:72-4.
- Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med 2020;383:2603-15.
- Heath PT, Galiza EP, Baxter DN, Boffito M, Browne D, Burns F, et al. 2019nCoV-302 Study Group . Safety and efficacy of NVX-CoV2373 Covid-19 vaccine. N Engl J Med 2021;385:1172-83.
- Herrera MS, Elgueta R, Fernández MB, Giacoman C, Leal D, Marshall P, et al. A longitudinal study monitoring the quality of life in a national cohort of older adults in Chile before and during the COVID-19 outbreak. BMC Geriatr 2021;21:1-12.
- Ishikawa H, Kato M, Kiuchi T. Declines in health literacy and health-related quality of life during the COVID-19 pandemic: a longitudinal study of the Japanese general population. BMC Publ Health 2021;21:1-9.
- Willner P, Rose J, Stenfert Kroese B, Murphy GH, Langdon PE, Clifford C, et al. Effect of the COVID‐19 pandemic on the mental health of carers of people with intellectual disabilities. J Appl Res Intel Disab 2020;33:1523-33.
- Mak HW, Bu F, Fancourt D. Mental health and wellbeing amongst people with informal caring responsibilities across different time points during the COVID-19 pandemic: a population-based propensity score matching analysis. Perspectives in Public Health 2023;143:275-84. https://doi.org/10.1177/175791392211049.
- Whitley E, Reeve K, Benzeval M. Tracking the mental health of home-carers during the first COVID-19 national lockdown: evidence from a nationally representative UK survey. Psychol Med 2021;53:1096-105.
- AUHE Information Specialists . Checking for Duplicates Guidance 2016.
Appendix
We searched the following academic databases for quantitative measures of quality of life in patients hospitalised with COVID-19 on 6 May 2022, with searches re-run on 7 December 2022:
-
EMBASE Classic + EMBASE (Ovid) 1947 to 6 December 2022
-
Ovid MEDLINE® ALL 1946 to 6 December 2022
-
Scopus
-
Web of Science Core Collection; SCI-EXPANDED 1900+, SSCI 1900+, A&HCI 1975+, CPCI-S 1900+, CPCI-SSH 1900+, and ESCI 2015 + searched simultaneously.
Searches were developed for the concepts: COVID-19, health utility measures and hospital patients. Subject headings and free text words were identified for use in the search concepts by the information specialist and project team members. Further terms were identified and tested from known relevant papers.
For the QOL measures concept, we based our search on the MEDLINE precision maximising health utilities filter (FSF3) designed by Arber et al. 11 with the addition of extra QOL measurement tools. The search was then translated into the other databases. We did not apply limits for language or publication date to the search. The search was peer-reviewed by a second information specialist using the PRESS checklist. 12 Duplicates were removed automatically and manually using Academic Unit of Health Economics, University of Leeds guidance. 81
Search strategies
EMBASE Classic + EMBASE <1947 to 6 December 2022>
Search date: 7 December 2022
-
quality-adjusted life year/ 32,963
-
(quality-adjusted or adjusted life year$).ti,ab,kf. 31,924
-
(qaly$ or qald$ or qale$ or qtime$).ti,ab,kf. 25,432
-
(illness state$1 or health state$1).ti,ab,kf. 13,894
-
(hui or hui1 or hui2 or hui3).ti,ab,kf. 2939
-
(multiattribute$ or multi attribute$).ti,ab,kf. 1462
-
(utility adj3 (score$1 or valu$ or health$ or cost$ or measur$ or disease$ or mean or gain or gains or index$)).ti,ab,kf. 30,140
-
utilities.ti,ab,kf. 14,439
-
exp ‘quality of life assessment’/ 98,410
-
(eq-5d or eq5d or eq-5 or eq5 or euro qual or euroqual or euro qual5d or euroqual5d or euro qol or euroqol or euro qol5d or euroqol5d or euro quol or euroquol or euro quol5d or euroquol5d or eur qol or eurqol or eur qol5d or eur qol5d or eur?qul or eur?qul5d or euro$ quality of life or european qol).ti,ab,kf. 28,819
-
(euro$ adj3 (5 d or 5d or 5 dimension$ or 5dimension$ or 5 domain$ or 5domain$)).ti,ab,kf. 8407
-
(sf36$ or sf 36$ or sf thirtysix or sf thirty six).ti,ab,kf. 44,163
-
(time trade-off$1 or time tradeoff$1 or tto or timetradeoff$1).ti,ab,kf. 3381
-
standard gamble/ or time trade-off method/ 451
-
or/1-14 [Health utilities based on Arber et al. Health State Utilities FSF3 Precision maximising] 206,779
-
disability-adjusted life year/ 3742
-
(DALY? or disability-adjusted life year$).ti,ab,kf. 7098
-
(HALY? or health-adjusted life year$).ti,ab,kf. 654
-
(sf20$ or sf 20$ or sf twenty).ti,ab,kf. 585
-
(sf12$ or sf 12$ or sf twelve).ti,ab,kf. 11,252
-
(sf8$ or sf 8$ or sf eight).ti,ab,kf. 1321
-
‘health-related quality of life’.ti,ab,kf. 81,885
-
(HRqol or HR-QOL or HRQL or HR QL).ti,ab,kf. 42,963
-
or/16-23 [additional QOL terms] 103,844
-
15 or 24 [expanded Utility and QALY terms] 265,737
-
exp *coronavirus disease 2019/ 229,750
-
(coronavirus-19 or covid19 or covid-19 or covid 2019).ti,ab,kf. 304,433
-
exp *Severe acute respiratory syndrome coronavirus 2/ 35,387
-
(sars-cov2 or sars-cov-2 or sarscov2 or sarscov-2 or Sars-coronavirus2 or Sars-coronavirus-2 or SARS-like coronavirus*).ti,ab,kw. 117,021
-
or/26-29 [Covid 19 simplified] 340,238
-
25 and 30 3312
-
exp hospital patient/ 230,238
-
((hospital* or in-hospital) adj2 patient*).ti,ab,kf. 226,115
-
(inpatient* or in-patient*).ti,ab,kf. 3,392,878
-
or/32-34 [inpatients] 3,560,099
-
31 and 35 703
-
exp juvenile/ not exp adult/ 2,824,192
-
36 not 37 688
-
limit 38 to conference abstract 252
-
38 not 39 [Covid inpatient QALYs] 436
Ovid MEDLINE(R) ALL <1946 to 6 December 2022>
Search date: 7 December 2022
-
Quality-Adjusted Life Years/ 15,263
-
(quality-adjusted or adjusted life year$).ti,ab,kf. 22,040
-
(qaly$ or qald$ or qale$ or qtime$).ti,ab,kf. 13,846
-
(illness state$1 or health state$1).ti,ab,kf. 7970
-
(hui or hui1 or hui2 or hui3).ti,ab,kf. 1882
-
(multiattribute$ or multi attribute$).ti,ab,kf. 1232
-
(utility adj3 (score$1 or valu$ or health$ or cost$ or measur$ or disease$ or mean or gain or gains or index$)).ti,ab,kf. 19,091
-
utilities.ti,ab,kf. 8946
-
(eq-5d or eq5d or eq-5 or eq5 or euro qual or euroqual or euro qual5d or euroqual5d or euro qol or euroqol or euro qol5d or euroqol5d or euro quol or euroquol or euro quol5d or euroquol5d or eur qol or eurqol or eur qol5d or eur qol5d or eur?qul or eur?qul5d or euro$ quality of life or european qol).ti,ab,kf. 16,100
-
(euro$ adj3 (5 d or 5d or 5 dimension$ or 5dimension$ or 5 domain$ or 5domain$)).ti,ab,kf. 5598
-
(sf36$ or sf 36$ or sf thirtysix or sf thirty six).ti,ab,kf. 25,754
-
(time trade-off$1 or time tradeoff$1 or tto or timetradeoff$1).ti,ab,kf. 2276
-
or/1-12 [Arber et al. Health State Utilities FSF3 Precision maximising] 89,086
-
Disability-Adjusted Life Years/ 153
-
(DALY? or disability-adjusted life year$).ti,ab,kf. 5576
-
Healthy Life Expectancy/ 42
-
(HALY? or health-adjusted life year$).ti,ab,kf. 681
-
(sf20$ or sf 20$ or sf twenty).ti,ab,kf. 429
-
(sf12$ or sf 12$ or sf twelve).ti,ab,kf. 6600
-
(sf8$ or sf 8$ or sf eight).ti,ab,kf. 738
-
‘health-related quality of life’.ti,ab,kf. 56,432
-
(HRqol or HR-QOL or HRQL or HR QL).ti,ab,kf. 26,447
-
or/14-22 [additional QALY terms] 69,438
-
13 or 23 [expanded Utility and QALY terms] 137,390
-
COVID-19/ 202,332
-
(coronavirus-19 or covid19 or covid-19 or covid 2019).ti,ab,kf. 279,370
-
SARS-CoV-2/ 143,349
-
(sars-cov2 or sars-cov-2 or sarscov2 or sarscov-2 or Sars-coronavirus2 or Sars-coronavirus-2 or SARS-like coronavirus*).ti,ab,kf. 106,989
-
or/25-28 [covid 19 simplified] 313,388
-
24 and 29 1615
-
Inpatients/ 28,233
-
((hospital* or in-hospital) adj2 patient*).ti,ab,kf. 123,506
-
(inpatient* or in-patient*).ti,ab,kf. 2,129,575
-
or/31-33 [inpatients] 2,214,076
-
30 and 34 [in patients - all] 285
Scopus
Search date: 7 December 2022
-
((TITLE-ABS-KEY ((hospital* OR in-hospital) PRE/2 patient*)) OR (TITLE-ABS-KEY (inpatient* OR ‘in-patient*’))) AND ((TITLE-ABS-KEY (‘sars-cov2’ OR ‘sars-cov-2’ OR sarscov2 OR ‘sarscov-2’ OR ‘sars-coronavirus2’ OR ‘sars-coronavirus-2’ OR ‘sars-like coronavirus*’)) OR (TITLE-ABS-KEY (‘coronavirus-19’ OR covid19 OR ‘covid 19’ OR ‘covid 2019’))) AND (((TITLE-ABS-KEY (daly* OR ‘disability-adjusted life year*’)) OR (TITLE-ABS-KEY (‘healthy life expectancy’)) OR (TITLE-ABS-KEY (haly* OR ‘health-adjusted life year*’)) OR (TITLE-ABS-KEY (sf20* OR ‘sf 20*’ OR ‘sf twenty’)) OR (TITLE-ABS-KEY (sf12* OR ‘sf 12*’ OR ‘sf twelve’)) OR (TITLE-ABS-KEY (sf8* OR ‘sf 8*’ OR ‘sf eight’)) OR (TITLE-ABS-KEY (‘health-related quality of life’)) OR (TITLE-ABS-KEY (hrqol OR hr-qol OR hrql OR ‘hr ql’))) OR ((TITLE-ABS-KEY (hui OR hui1 OR hui2 OR hui3)) OR (TITLE-ABS-KEY (‘time trade-off*’ OR ‘time tradeoff*’ OR tto OR timetradeoff*)) OR (TITLE-ABS-KEY (sf36* OR ‘sf 36*’ OR ‘sf thirtysix’ OR ‘sf thirty six’)) OR (TITLE-ABS-KEY (euro* PRE/3 (‘5 d’ OR 5d OR ‘5 dimension*’ OR 5dimension* OR ‘5 domain*’ OR 5domain*))) OR (TITLE-ABS-KEY (eq-5d OR eq5d OR eq-5 OR eq5 OR ‘euro qual’ OR euroqual OR ‘euro qual5d’ OR euroqual5d OR ‘euro qol’ OR euroqol OR ‘euro qol5d’ OR euroqol5d OR ‘euro quol’ OR euroquol OR ‘euro quol5d’ OR euroquol5d OR ‘eur qol’ OR eurqol OR ‘eur qol5d’ OR ‘eur qol5d’ OR eur?qul OR eur?qul5d OR ‘euro* quality of life’ OR ‘european qol’)) OR (TITLE-ABS-KEY (utilities)) OR (TITLE-ABS-KEY (utility PRE/3 (score* OR valu* OR health* OR cost* OR measur* OR disease* OR mean OR gain OR gains OR index*))) OR (TITLE-ABS-KEY (multiattribute* OR ‘multi attribute*’)) OR (TITLE-ABS-KEY (‘illness state*’ OR ‘health state’)) OR (TITLE-ABS-KEY (qaly* OR qald* OR qale* OR qtime*)) OR (TITLE-ABS-KEY (‘quality-adjusted’ OR ‘adjusted life year*’)))) 786 results [#22 AND #25 AND #28]
-
(TITLE-ABS-KEY ((hospital* OR in-hospital) PRE/2 patient*)) OR (TITLE-ABS-KEY (inpatient* OR ‘in-patient*’)) 2,538,425 results [#26 OR #27 Inpatients]
-
TITLE-ABS-KEY ((hospital* OR in-hospital) PRE/2 patient*) 233,554 results
-
TITLE-ABS-KEY (inpatient* OR ‘in-patient*’) 2,415,526 results
-
(TITLE-ABS-KEY (‘sars-cov2’ OR ‘sars-cov-2’ OR sarscov2 OR ‘sarscov-2’ OR ‘sars-coronavirus2’ OR ‘sars-coronavirus-2’ OR ‘sars-like coronavirus*’)) OR (TITLE-ABS-KEY (‘coronavirus-19’ OR covid19 OR ‘covid 19’ OR ‘covid 2019’)) 415,224 results [23 OR #24 COVID –simple]
-
TITLE-ABS-KEY (‘sars-cov2’ OR ‘sars-cov-2’ OR sarscov2 OR ‘sarscov-2’ OR ‘sars-coronavirus2’ OR ‘sars-coronavirus-2’ OR ‘sars-like coronavirus*’) 173,817 results
-
TITLE-ABS-KEY (‘coronavirus-19’ OR covid19 OR ‘covid 19’ OR ‘covid 2019’) 402,727 results
-
((TITLE-ABS-KEY (daly* OR ‘disability-adjusted life year*’)) OR (TITLE-ABS-KEY (‘healthy life expectancy’)) OR (TITLE-ABS-KEY (haly* OR ‘health-adjusted life year*’)) OR (TITLE-ABS-KEY (sf20* OR ‘sf 20*’ OR ‘sf twenty’)) OR (TITLE-ABS-KEY (sf12* OR ‘sf 12*’ OR ‘sf twelve’)) OR (TITLE-ABS-KEY (sf8* OR ‘sf 8*’ OR ‘sf eight’)) OR (TITLE-ABS-KEY (‘health-related quality of life’)) OR (TITLE-ABS-KEY (hrqol OR hr-qol OR hrql OR ‘hr ql’))) OR ((TITLE-ABS-KEY (hui OR hui1 OR hui2 OR hui3)) OR (TITLE-ABS-KEY (‘time trade-off*’ OR ‘time tradeoff*’ OR tto OR timetradeoff*)) OR (TITLE-ABS-KEY (sf36* OR ‘sf 36*’ OR ‘sf thirtysix’ OR ‘sf thirty six’)) OR (TITLE-ABS-KEY (euro* PRE/3 (‘5 d’ OR 5d OR ‘5 dimension*’ OR 5dimension* OR ‘5 domain*’ OR 5domain*))) OR (TITLE-ABS-KEY (eq-5d OR eq5d OR eq-5 OR eq5 OR ‘euro qual’ OR euroqual OR ‘euro qual5d’ OR euroqual5d OR ‘euro qol’ OR euroqol OR ‘euro qol5d’ OR euroqol5d OR ‘euro quol’ OR euroquol OR ‘euro quol5d’ OR euroquol5d OR ‘eur qol’ OR eurqol OR ‘eur qol5d’ OR ‘eur qol5d’ OR eur?qul OR eur?qul5d OR ‘euro* quality of life’ OR ‘european qol’)) OR (TITLE-ABS-KEY (utilities)) OR (TITLE-ABS-KEY (utility PRE/3 (score* OR valu* OR health* OR cost* OR measur* OR disease* OR mean OR gain OR gains OR index*))) OR (TITLE-ABS-KEY (multiattribute* OR ‘multi attribute*’)) OR (TITLE-ABS-KEY (‘illness state*’ OR ‘health state’)) OR (TITLE-ABS-KEY (qaly* OR qald* OR qale* OR qtime*)) OR (TITLE-ABS-KEY (‘quality-adjusted’ OR ‘adjusted life year*’))) Show less 794,919 results [#21 OR #12 All QOL measures]
-
(TITLE-ABS-KEY (daly* OR ‘disability-adjusted life year*’)) OR (TITLE-ABS-KEY (‘healthy life expectancy’)) OR (TITLE-ABS-KEY (haly* OR ‘health-adjusted life year*’)) OR (TITLE-ABS-KEY (sf20* OR ‘sf 20*’ OR ‘sf twenty’)) OR (TITLE-ABS-KEY (sf12* OR ‘sf 12*’ OR ‘sf twelve’)) OR (TITLE-ABS-KEY (sf8* OR ‘sf 8*’ OR ‘sf eight’)) OR (TITLE-ABS-KEY (‘health-related quality of life’)) OR (TITLE-ABS-KEY (hrqol OR hr-qol OR hrql OR ‘hr ql’)) 81,375 results [or/13-20 additional QOL]
-
TITLE-ABS-KEY (hrqol OR hr-qol OR hrql OR ‘hr ql’) 28,146 results
-
TITLE-ABS-KEY (‘health-related quality of life’) 61,618 results
-
TITLE-ABS-KEY (sf8* OR ‘sf 8*’ OR ‘sf eight’) 1003 results
-
TITLE-ABS-KEY (sf12* OR ‘sf 12*’ OR ‘sf twelve’) 7128 results
-
TITLE-ABS-KEY (sf20* OR ‘sf 20*’ OR ‘sf twenty’) 652 results
-
TITLE-ABS-KEY (haly* OR ‘health-adjusted life year*’) 1976 results
-
TITLE-ABS-KEY (‘healthy life expectancy’) 853 results
-
TITLE-ABS-KEY (daly* OR ‘disability-adjusted life year*’) 9278 results
-
(TITLE-ABS-KEY (hui OR hui1 OR hui2 OR hui3)) OR (TITLE-ABS-KEY (‘time trade-off*’ OR ‘time tradeoff*’ OR tto OR timetradeoff*)) OR (TITLE-ABS-KEY (sf36* OR ‘sf 36*’ OR ‘sf thirtysix’ OR ‘sf thirty six’)) OR (TITLE-ABS-KEY (euro* PRE/3 (‘5 d’ OR 5d OR ‘5 dimension*’ OR 5dimension* OR ‘5 domain*’ OR 5domain*))) OR (TITLE-ABS-KEY (eq-5d OR eq5d OR eq-5 OR eq5 OR ‘euro qual’ OR euroqual OR ‘euro qual5d’ OR euroqual5d OR ‘euro qol’ OR euroqol OR ‘euro qol5d’ OR euroqol5d OR ‘euro quol’ OR euroquol OR ‘euro quol5d’ OR euroquol5d OR ‘eur qol’ OR eurqol OR ‘eur qol5d’ OR ‘eur qol5d’ OR eur?qul OR eur?qul5d OR ‘euro* quality of life’ OR ‘european qol’)) OR (TITLE-ABS-KEY (utilities)) OR (TITLE-ABS-KEY (utility PRE/3 (score* OR valu* OR health* OR cost* OR measur* OR disease* OR mean OR gain OR gains OR index*))) OR (TITLE-ABS-KEY (multiattribute* OR ‘multi attribute*’)) OR (TITLE-ABS-KEY (‘illness state*’ OR ‘health state’)) OR (TITLE-ABS-KEY (qaly* OR qald* OR qale* OR qtime*)) OR (TITLE-ABS-KEY (‘quality-adjusted’ OR ‘adjusted life year*’)) 738,857 results [or/1-11 Arber et al. Health State Utilities FSF3 Precision maximising]
-
TITLE-ABS-KEY (‘time trade-off*’ OR ‘time tradeoff*’ OR tto OR timetradeoff*) 4189 results
-
TITLE-ABS-KEY (sf36* OR ‘sf 36*’ OR ‘sf thirtysix’ OR ‘sf thirty six’) 29,327 results
-
TITLE-ABS-KEY (euro* PRE/3 (‘5 d’ OR 5d OR ‘5 dimension*’ OR 5dimension* OR ‘5 domain*’ OR 5domain*)) 11,323 results
-
TITLE-ABS-KEY (eq-5d OR eq5d OR eq-5 OR eq5 OR ‘euro qual’ OR euroqual OR ‘euro qual5d’ OR euroqual5d OR ‘euro qol’ OR euroqol OR ‘euro qol5d’ OR euroqol5d OR ‘euro quol’ OR euroquol OR ‘euro quol5d’ OR euroquol5d OR ‘eur qol’ OR eurqol OR ‘eur qol5d’ OR ‘eur qol5d’ OR eur?qul OR eur?qul5d OR ‘euro* quality of life’ OR ‘european qol’) Show less 19,652 results
-
TITLE-ABS-KEY (utilities) 643,014 results
-
TITLE-ABS-KEY (utility PRE/3 (score* OR valu* OR health* OR cost* OR measur* OR disease* OR mean OR gain OR gains OR index*)) 29,903 results
-
TITLE-ABS-KEY (multiattribute* OR ‘multi attribute*’) 15,559 results
-
TITLE-ABS-KEY (hui OR hui1 OR hui2 OR hui3) 5075 results
-
TITLE-ABS-KEY (‘illness state*’ OR ‘health state’) 12,568 results
-
TITLE-ABS-KEY (qaly* OR qald* OR qale* OR qtime*) 14,986 results
-
TITLE-ABS-KEY (‘quality-adjusted’ OR ‘adjusted life year*’) 35,680 results
Web of Science Core Collection
Search date: 7 December 2022
Performed a simultaneous search of the following databases:
-
Science Citation Index Expanded (SCI-EXPANDED)–1900–present
-
Social Sciences Citation Index (SSCI)–1900–present
-
Arts & Humanities Citation Index (AHCI)–1975–present
-
Conference Proceedings Citation Index – Science (CPCI-S)–1990–present
-
Conference Proceedings Citation Index – Social Science & Humanities (CPCI-SSH)–1990–present
-
Emerging Sources Citation Index (ESCI)–2015–present.
Data updated 5 December 2022
-
‘quality-adjusted’ OR ‘adjusted life year*’ (Topic) Results: 21,592
-
qaly* OR qald* OR qale* OR qtime* (Topic) Results: 13,741
-
‘illness state*’ OR ‘health state’ (Topic) Results: 7234
-
hui OR hui1 OR hui2 OR hui3 (Topic) Results: 3535
-
multiattribute* OR ‘multi attribute*’ (Topic) Results: 11,488
-
utility NEAR/3 (score* OR valu* OR health* OR cost* OR measur* OR disease* OR mean OR gain OR gains OR index*) (Topic) Results: 41,056
-
utilities (Topic) Results: 476,812
-
eq-5d OR eq5d OR eq-5 OR eq5 OR ‘euro qual’ OR euroqual OR ‘euro qual5d’ OR euroqual5d OR ‘euro qol’ OR euroqol OR ‘euro qol5d’ OR euroqol5d OR ‘euro quol’ OR euroquol OR ‘euro quol5d’ OR euroquol5d OR ‘eur qol’ OR eurqol OR ‘eur qol5d’ OR ‘eur qol5d’ OR eur?qul OR eur?qul5d OR ‘euro* quality of life’ OR ‘european qol’ (Topic) Results: 17,634
-
euro* NEAR/3 (‘5 d’ OR 5d OR ‘5 dimension*’ OR 5dimension* OR ‘5 domain*’ OR 5domain*) (Topic) Results: 6128
-
sf36* OR ‘sf 36*’ OR ‘sf thirtysix’ OR ‘sf thirty six’ (Topic) Results: 30,354
-
‘time trade-off*’ OR ‘time tradeoff*’ OR tto OR timetradeoff* (Topic) Results: 3609
-
#11 OR #10 OR #9 OR #8 OR #7 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1 Results: 55,1076 [based on arber HSU precision maximising]
-
daly* OR ‘disability-adjusted life year*’ (Topic) Results: 7348
-
‘healthy life expectancy’ (Topic) Results: 592
-
haly* OR ‘health-adjusted life year*’ (Topic) Results: 1857
-
sf20* OR ‘sf 20*’ OR ‘sf twenty’ (Topic) Results: 347
-
sf12* OR ‘sf 12*’ OR ‘sf twelve’ (Topic) Results: 6651
-
sf8* OR ‘sf 8*’ OR ‘sf eight’ (Topic) Results: 810
-
‘health-related quality of life’ (Topic) Results: 63,430
-
hrqol OR hr-qol OR hrql OR ‘hr ql’ (Topic) Results: 27,090
-
#20 OR #19 OR #18 OR #17 OR #16 OR #15 OR #14 OR #13 Results: 80,329 [additional QALY terms]
-
#21 OR #12 Results: 608,391 [All QALY]
-
‘coronavirus-19’ OR covid19 OR ‘covid 19’ OR ‘covid 2019’ (Topic) Results: 348,006
-
‘sars-cov2’ OR ‘sars-cov-2’ OR sarscov2 OR ‘sarscov-2’ OR ‘sars-coronavirus2’ OR ‘sars-coronavirus-2’ OR ‘sars-like coronavirus*’ (Topic) Results: 105,265
-
#24 OR #23 Results: 370,141 [COVID]
-
inpatient* OR ‘in-patient*’ (Topic) Results: 2,184,563
-
(hospital* OR in-hospital) NEAR/2 patient* (Topic) Results: 177,489
-
#26 OR #27 Results: 2,297,088 [inpatients]
-
#22 AND #25 AND #28 Results: 715 [QALY in covid hospital patients]
