Notes
Article history
The contractual start date for this research was in January 2022. This article began editorial review in April 2023 and was accepted for publication in November 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The Health Technology Assessment editors and publisher have tried to ensure the accuracy of the authors’ article and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
Permissions
Copyright statement
Copyright © 2024 Maddocks et al. This work was produced by Maddocks et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2024 Maddocks et al.
Background
Functional loss (also called activity limitation or disability) is defined as an inability to perform necessary or desired tasks. 1 This is typically operationalised as occurring in terms of the inability to perform activities of daily living: from more basic self-care tasks, such as bathing and dressing, to instrumental activities requiring more complex planning and thinking, such as safety awareness, taking medications, social participation and managing money and bills. 1–3 Life-limiting illness(es) and accompanying symptoms (e.g. pain, fatigue, breathlessness, anxiety, depression or cognitive dysfunction) commonly contribute to functional loss and a consequent need for help, support or supervision. 4–6 While functional loss often occurs late in the course of disease for people with cancer, those with non-cancer conditions (e.g. chronic respiratory diseases or heart failure) and multiple long-term conditions experience functional loss earlier in the disease trajectory,7,8 with periods of acute worsening that fluctuate over time. 9–11 Both sudden and progressive loss of ability can cause crises that precipitate hospital or care home admission12 and result in distress and suffering related to loss of usual roles and routines, independence, choice and sense of dignity. 13–15
Rehabilitation is a set of interventions designed to address functional loss, promote activity and preserve functional reserve and social participation. 16,17 It is characterised by cycles of nested treatment, which are reviewed and refined over time and typically delivered by a multidisciplinary team. 18 As people age and increasingly live with multiple long-term conditions, trajectories of functional loss become more variable and unpredictable giving rise to additional complexities for rehabilitation delivery. 19 Challenges in rehabilitation include weighing up potential treatment benefits and burden, aligning care to individuals’ priorities and being responsive to fluctuating needs across multiple domains of health. 20–22 Palliative rehabilitation focuses on relief and reduced impact from distressing/disruptive symptoms (e.g. breathlessness or fatigue)23 and managing or minimising the impact of geriatric syndromes (e.g. frailty or sarcopenia). 24
Within the fields of palliative medicine and geriatric medicine, a spectrum tends to exist where palliative medicine focuses on symptoms and geriatric medicine focuses on function. 25 Both share commitment to person-centeredness, communication, education and multiprofessional working. Rehabilitation is recognised as essential within both palliative and geriatric care: it can reverse and slow functional loss, which may not only improve quality of life but may also cut ongoing costs relating to care, admissions and complications. 26–28 Examples of specific interventions include techniques to manage persistent symptoms and adjustment work around loss (in palliative care),29–31 comprehensive assessment and management of geriatric syndromes (in geriatric care)32–34 and environmental adaption and assistive technologies. 35–37 Yet, access to these services is often inequitable, and individual teams’ capacity to deliver evidence-based rehabilitation interventions is highly variable. 27,38
Despite limited life expectancy, or uncertain ability to benefit from interventions, palliative rehabilitation services have often been not provided or dis-investment has occurred due to limited resources and competing priorities. 39–41 Such decisions are rarely supported by rigorous needs assessment or evaluation of effectiveness and cost effectiveness partly because these are methodologically difficult in this context. As a result, optimal ways to integrate the best of palliative and geriatric rehabilitation towards the end of life are currently unknown. Clinical trials and conventional health economic approaches may not be sufficient, at least on their own, and new methodologies have been suggested to answer these questions more meaningfully and in a way that supports service development and commissioning. To address these challenges, it is imperative that diverse expertise is brought together. 42 We therefore aimed to establish and grow a research partnership around the topic area of functional loss and rehabilitation in palliative and end-of-life care.
Objectives
-
Establish and develop a multidisciplinary, cross-peciality collaborative research partnership that includes geographic populations historically underserved by research activity.
-
Generate key research questions in relation to functional loss and rehabilitation in palliative care by collaborating with professional and public stakeholders.
-
Co-design and submit high-quality competitive research proposals to future National Institute for Health and Care Research (NIHR) calls on palliative and end-of-life care.
-
Share topic and methodological expertise to jointly address the complexities of rehabilitation interventions within palliative and end-of-life care, including their rigorous evaluation, and pathways to implementation.
-
Build capacity and capability to deliver nationally generalisable studies of rehabilitation interventions in palliative and end-of-life care, across health and social care, and voluntary and community organisations in partnership with patients and their families.
Objective 1 – Establishing the partnership
The Palliative Care Rehabilitation Partnership was established by professionals from across England and Scotland with a focus around the topic area of functional loss and rehabilitation in palliative and end-of-life care. The partnership contained multidisciplinary professionals with complementary areas of expertise and experience in complex palliative and geriatric research, physiotherapy, nursing, palliative medicine and psychology. The project adopted the term ‘partnership’ to describe the expectation of collaboration among researchers, clinical academics, clinicians, students and patient and public involvement (PPI) members. The partnership leads, who were the main representatives from the collaborator sites (Figure 1), steered activities such as workshops and training and were responsible for promoting the partnership to local people and infrastructure. Individuals who participated in any of the partnership activities were considered partners.
FIGURE 1.
Partnership leads, expertise and linked infrastructure.
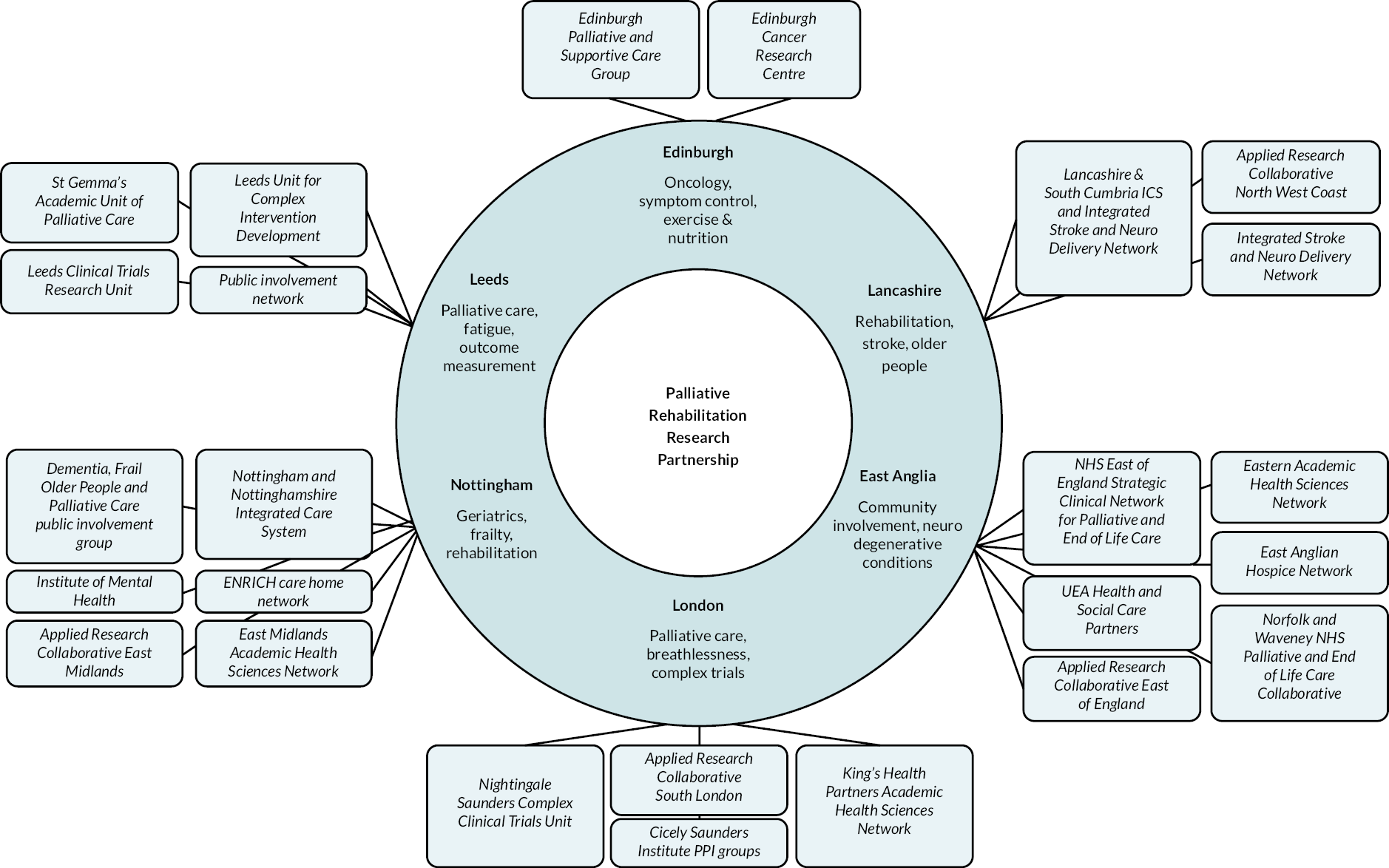
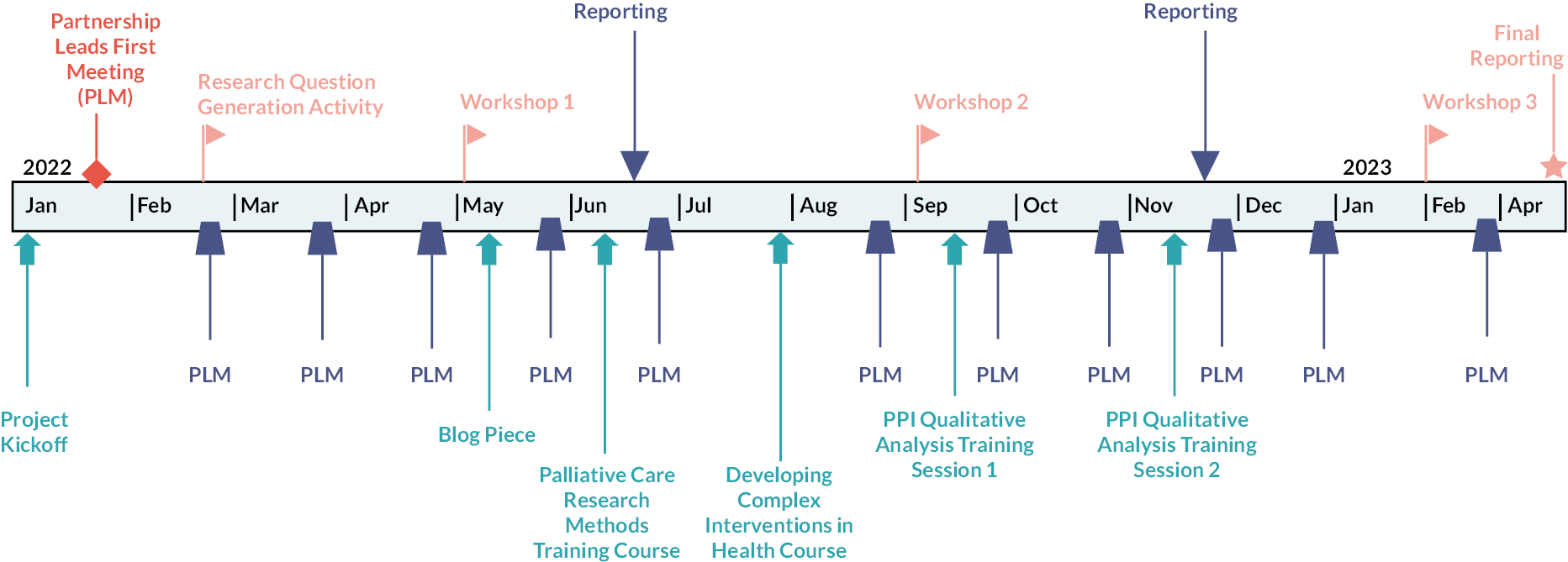
The partnership was successfully established through an initial launch meeting, development of an online presence and creating platforms for joint working. We recruited a diverse group of multidisciplinary, cross-speciality professionals spanning England and Scotland, with insight into the local geographical populations and areas under-represented in research. The partnership was promoted via the Applied Research Collaboration (ARC) National Leads for Palliative and End of Life Care, local ARCs and the Council for Allied Health Professions Research to encourage clinicians, students and PPI members to engage. The partnership created a shared online workspace via Microsoft SharePoint, which provided the partnership leads with the means to collectively work on projects and share information. Additionally, the partnership leads collectively met monthly via Microsoft Teams to discuss partnership activities and to share updates on key deliverables. Partnership activities were shared with and open to any professional or public member with an interest in research and care relating to functional loss in palliative care and towards the end of life. An overview of the partnership’s key activities is summarised in Figure 2.
FIGURE 2.
Summary of partnership activities.
Objective 2: Research question generation
The partnership commenced its activities by conducting a research question generation activity, utilising a modified version of the Child Health and Nutrition Initiative methodology43 to gather and score questions related to functional loss and rehabilitation towards the end of life. This was completed as a stakeholder activity (rather than a research study), and therefore research ethics approval was not required.
A management group, comprising all the partnership leads, and a stakeholder’s group consisting of researchers, clinical academics, clinicians, experts by experience, patients and family members were created. The stakeholder’s group were recruited through the partnership leads’ affiliations and networks, established public involvement groups and key research publications as well as snowballing through additional recommendations from those invited to participate.
The research question generation and prioritisation process comprised five key stages: defining, sourcing, synthesising, scoring and analysis/dissemination. The management group specified the scope and prioritisation criteria for the research question generation exercise. The questions were devised by using the following scope aligned with the topic and NIHR principles:
-
Adults with advanced disease experiencing, or at risk of, functional loss.
-
Research ideas should be relevant to a UK context.
-
Research projects should deliver findings that could be implemented into practice within 3–5 years.
Once the scope had been established, the stakeholder’s group were e-mailed to inform about the objectives and context of the research question generation exercise and were invited to participate. Members who expressed an interest in participating were subsequently invited to generate and submit research questions via e-mail or an online form. PPI members were offered support in sharing their research ideas and developing those into a research question format if they preferred.
The proposed research questions were collated by the management group and were made available to the stakeholder’s group for 4 weeks, who were invited to score the proposed research questions in relation to the prioritisation criteria via a digital or paper form. The stakeholder’s group were asked to score research questions against five criteria:
-
Answerability – Is the proposed research question answerable?
-
Effectiveness – Will the research question lead to intervention that effectively addresses functional loss in advanced disease?
-
Feasibility – Is the research question feasible based on current knowledge, capacity and resources?
-
Burden reduction – Will the proposed research lead to a significant burden reduction for patients, carers and families?
-
Equity – Will the research bring about changes that favour patients equitably?
Research question scoring
The stakeholders scored each domain of the research question by using the following scoring system: 0 (unlikely to meet criterion), 0.5 (not sure if it can meet the criterion) and 1 (likely to meet the criterion). PPI members were offered additional support to complete the scoring and were offered the option of alternative completion formats (larger print paper copies) and a simplified scoring system, if they preferred, using just one of the five criteria (burden reduction). Participants were asked to leave a blank score if they were unable to judge the criterion due to a lack of knowledge on the subject. Additionally, members were provided with the opportunity to input free text comments via the online form to relay any constructive feedback and to express their interest in a proposed question. This information was consequently shared with the individual(s) who proposed the question, with the aim of introducing members with a shared interest in a given topic area. For each research question submitted, mean scores from individual responses across the five prioritisation criteria were calculated, giving an overall ‘Research Priority Score’. The scores were gathered using Microsoft Excel and transformed into a percentage to make them more interpretable.
The activity generated a variety of research ideas, with some ideas being more refined and developed than others. A total of 82 research ideas were submitted by 35 people; out of which, 37 research ideas considered a variety of interventions for people with a specific life-limiting condition, with the top 5 being cancer, dementia, stroke, motor neurone disease and frailty. The remaining 45 research ideas considered the impact of interventions in patients with any advanced disease. Among the proposed research questions, 23 questions suggested possible interventions and outcomes to be measured. These included assessing the efficacy of modalities such as exercise, nutrition, electrotherapy, psychosocial strategies and the use of robotics in reducing functional decline, minimising the impact of fatigue and improving quality of life for patients and their families. Figure 3 captures key themes from the research questions submitted to depict the suggested populations, interventions, comparisons and outcomes.
FIGURE 3.
Word cloud depicting the population, intervention, comparison and outcomes from the submitted research questions.

On average each question was scored by 15 people (Table 1) and received 5 free-text responses. A mean of 4 people expressed an interest for each question submitted, with one question generating an interest from 13 individuals. Notably, research questions scored highest on the ‘answerability’ domain while most concerns were raised around ‘effectiveness’ and ‘equity’. Research questions and scores were shared with all participants and disseminated in a report via e-mail. The generated scores and free text comments allowed members to strengthen their research proposals by identifying areas requiring development prior to attending the partnership’s first workshop.
| Question | Mean | Median | Interquartile range (IQR) |
|---|---|---|---|
| Answerability | 0.68 | 0.74 | 0.26 (0.57–0.83) |
| Effectiveness | 0.60 | 0.63 | 0.27 (0.47–0.73) |
| Feasibility | 0.64 | 0.67 | 0.18 (0.58–0.76) |
| Burden reduction | 0.65 | 0.68 | 0.21 (0.54–0.75) |
| Equity | 0.60 | 0.62 | 0.21 (0.50–0.71) |
| Across all five domains | 0.63 | 0.65 | 0.20 (0.56–0.76) |
Objectives 3 and 4: Research proposal development
Through a series of three workshops, the partnership supported the transformation of research ideas, generated through the research question activity, towards full proposals. Workshops were conducted via Zoom with academic, clinical and PPI representation at each. We welcomed presentations from anyone who had submitted a research question. Additionally, the workshops welcomed participants who were actively working on research proposals related to the partnership’s objectives. This approach aimed to encourage broader engagement and collaboration within the community interested in functional loss and rehabilitation in palliative care.
Workshop 1: shaping the proposal
Workshop 1 provided presenters with the opportunity to share their initial research ideas with the group. Each presenter was allocated 20 minutes and asked to prepare for the session by considering the aims and objectives of their research idea and by building upon the feedback that had been given from the research question generation exercise. Presenters were requested to refrain from using jargon during their presentations so that all members in the workshop would be able to actively participate and contribute. The workshop comprised facilitated discussions, where attendees considered the potential issues around delivery of the project, identified expertise needed to answer the proposed research question and identified key stakeholders that would need to be consulted. Each presenter received verbal and written feedback, which was offered to further develop research ideas.
The partnership’s first workshop was held virtually on 24 May 2022 and was attended by 30 people: 11 researchers, 4 clinical academics, 9 clinicians and 6 PPI members. A total of six research ideas were presented. Research topics included rehabilitation decisions in the frail older population, management of fatigue, sharing prognostic information with patients and families, supporting mobility in patients at end of life, palliative care for patients with cerebral palsy and engaging informal carers in a patient’s rehabilitation. The workshop generated varied discussion between attendees, with a wide range of suggestions put forward to presenters to consider while further developing their proposals. Feedback from attendees was collated and sent to each presenter, with several recurring themes. Attendee feedback emphasised the significance of considering the perspectives and expectations of both the patient and their family during palliative rehabilitation. It also stressed the need to ensure that research questions were pertinent to the current issues facing patients and that research projects were supported by multidisciplinary, multiprofessional and PPI representation.
The first workshop received positive feedback from attendees, with feedback highlighting the importance of collaborative partnerships and the benefit of meaningful engagement with relevant stakeholders, such as PPI members. Attendees suggested that subsequent workshops could be improved by ensuring that any materials used during the session be made available beforehand to allow for sufficient time to consider questions and feedback.
Workshop 2: strengthening the study methodology
With support from methodologists, the second workshop aimed to develop the early research ideas that had been presented during the first workshop by considering the following components of proposals: study design, methodologies to be employed, outcomes to be measured, intervention theory and analysis plans. Each presenter was allocated 30 minutes to discuss their proposal designs. Through facilitated discussions, attendees were asked to comment on the feasibility of the study, recruitment, ethical and other practical considerations of the methodology to be employed. Presenters were provided with verbal and written feedback from the group, received individual support from methodologists and were encouraged to continue developing their research proposals.
The partnership’s second online workshop was held on 13 September 2022 and was attended by 24 people: 13 researchers, 4 clinical academics, 2 clinicians and 5 PPI members. Three presenters shared the progress and development of their respective research idea since the first workshop. Topics that were revisited were rehabilitation decisions in the frail older population, supporting mobility in patients at end of life and palliative care for patients with cerebral palsy. The workshop provided a forum for sharing of ideas and identified methodological considerations that needed to be addressed by presenters. Examples of feedback given to presenters included the need to carefully consider the inclusion and exclusion criteria of research ideas, to consider the individual components of any complex intervention, to identify the primary outcome tool to be used to measure change and to understand the rationale for palliative care services in the defined population.
Workshop 3: refining the proposals
The final workshop intended for members of the partnership to present their draft research proposals and receive final verbal and written feedback from the group prior to NIHR submission. However, in response to feedback from interested attendees, the format was kept flexible to incorporate people at different stages of proposal development. Presenters were allocated 30 minutes to present their proposal, followed by an open question and answer session. Facilitated discussions helped attendees evaluate various aspects of the proposal, which was built upon discussions and themes from the second workshop.
The partnership’s final workshop was held online on 9 February 2023 and was attended by 14 people: 6 researchers, 3 clinical academics and 5 PPI members. Two members presented their research proposals. One project aimed to evaluate the impact of exercise and nutrition in people with cancer, while the other wished to explore palliative rehabilitation in the context of older adults with frailty. Both projects generated interest from attending PPI members in participating in the research. Feedback on the proposals included recommendations for recruiting participants while ensuring diversity in the study populations and addressing implementation failures of research in clinical practice and provided suggestions to reduce such failures.
Objective 5: Building capacity and capability
Service mapping
Health and social care services for functional loss vary widely across locations in both goals and delivery (restorative, adaptive or prosthetic) and organisational structures. This is the case across community health care, intermediate care, acute and mental health hospitals as well as hospices and care home settings. Numerous specialties are involved, including primary care, rehabilitation and therapies, and also different medical disciplines, including geriatric medicine and palliative care.
The partnership aimed to map services catering to functional loss for individuals approaching end of life, including evaluating their capability and capacity as well as identifying barriers and facilitators to accessing these services. The partnership sought to investigate the extent to which these services were aware of rehabilitation requirements towards end-of-life care as well as their management of access, prognostication, prioritisation, effectiveness, adverse effects, treatment burden, communication, shared decision-making and advance care planning. However, during the partnership’s activities, several challenges arose in current service mapping due to a lack of shared understanding of ‘palliative rehabilitation’. In response to this, the partnership took a more conceptual approach to this exercise.
To contribute towards a better shared conceptualisation of palliative rehabilitation, the team channelled their insights from discussions throughout the partnership into an academic commentary piece. The commentary summarises the particular challenges in how rehabilitation is perceived in the context of palliative and end-of-life care, including the need to challenge assumptions focused on restoration and recovery of abilities and ideas around ‘no rehabilitation potential’. It calls for approaches that include adaptation and assistance in the context of functional decline as well as flexibility to take individualised, goal-based approaches that focus on what is important to the person and their family.
Training opportunities
The partnership lends itself to the ‘virtual community of practice’ model,44 as it was established by a range of individuals with complementary skills and expertise that aimed to advance knowledge around functional loss and rehabilitation in palliative care. This approach shares similarities with other approaches such as the ‘virtual learning community’ model,44 but has more of an emphasis on sharing knowledge between participants with a shared research area.
The partnership aimed to understand and strengthen capacity and capability by providing structured training, opportunities for knowledge exchange via workshops and ensuring clinicians partaking within the partnership were provided with protected time and mentorship. The partnership offered funded structured training and development opportunities for members, with focused learning that builds on NIHR open online courses on ‘improving health care through clinical research’ and ‘what is health research?’. The partnership extended the invitation to attend training to students, clinicians and PPI members. In summary:
-
Two PhD students were supported to attend the Palliative Care Research Methods course jointly delivered by the Association of Palliative Medicine and Palliative Care Research Society. The course ran over 3 weeks and supported them in developing skills in palliative research.
-
Four clinicians were supported to attend ‘Developing Complex Interventions to Improve Health’, a 1-day course run by the University of Sheffield. The course explored the different approaches that can be used to answer complex questions within health care and provided examples of how clinicians may apply these methods to a clinical context. One clinician stated that ‘the course covered important ground and detailed the latest developments. I enjoyed the interactive components, and the pre-reading helped set the scene.’
-
Six PPI members partook in a two-part online qualitative analysis training session, delivered over the course of two 3-hour sessions by one of the partnership leads. The course covered the theory behind qualitative methods, considered the strengths and limitations of qualitative research and provided an overview of thematic analysis. The PPI training was well received with one participant stating that ‘although I had little knowledge of qualitative analysis, I found the training informative and useful.’
Clinical academic mentorship
The partnership offered mentorship to two clinical academics and provided them with protected time to develop research projects and proposals. The partnership recognised the importance of protected time for front-line clinical academics, as studies indicate that these individuals often lack the necessary time to apply their clinical and academic expertise to promote clinically driven research. 45–47 One clinical academic commented that:
The partnership provided me with access to and support from world leading academics in the field of palliative care. They helped me understand different methodologies, gave me the time and space to reflect on methodological and theoretical challenges in developing robust programmes of research. As an early career researcher this has been immensely valuable.
Patient and public involvement
Alongside the outlined activities, the partnership also took up several other capacity building exercises. The involvement of PPI members was embedded within all partnership activities, including the research generation activity and proposal development. Two PPI members and an academic from the partnership collaboratively wrote a blog piece for the NIHR, which reflected on their experiences from partaking within the first partnership workshop. 48 Outside of these activities, PPI members were encouraged to join the various existing networks and ongoing activities, such as the National ARC Palliative and End of Life Care PPI workshops. Partnership leads also shared their expertise and good practice in involvement with other members of the partnership and helped link up partners with additional PPI expertise where helpful.
Equality, diversity and inclusion
The partnership was committed to equality, diversity and inclusion during all activities. To achieve this, the partnership actively sought participation from a diverse range of stakeholders, including clinicians, researchers and PPI members, ensuring that voices from different backgrounds and experiences were heard and valued. Additionally, the partnership’s training opportunities and mentorship programmes were designed to be inclusive and accessible to individuals from various backgrounds and levels of expertise.
Reflections on partnership working
The partnership leads collectively met to discuss the key learning points after establishing the partnership. There was a mutual consensus that the partnership provided opportunities to gain new perspectives by bringing together individuals from across the country, each with their own unique skills, expertise and experiences. It provided junior researchers with the opportunity to be part of the iterative process of proposal development as well as provided opportunities to network with a more diverse group of experts. The workshops in particular were considered to be successful and of benefit, and would be recommended for future partnerships. The workshops provided the opportunity for presenters to be supported with their proposal development, brought together various professionals from a range of disciplines and specialisations and allowed PPI members to share their personal experiences and insights. The partnership leaders identified some administrative challenges during the set-up phase of the partnership, including those related to contracting with use of generic research governance templates by partners and sites. These difficulties were likely due to the novel nature of the partnership and being among the first to receive this NIHR funding. Moreover, the clinical academics without backfilled time found it challenging to create and develop proposals alongside their usual responsibilities. Future initiatives looking to encourage new collaborations with clinical academics may need to prioritise additional resources to support the time required. Through the workshops, the partnership has supported the development of at least three research proposals in preparation for submission to NIHR and other public funding calls. These include streams taking part in the NIHR themed call for Palliative and End of Life Care and fellowships.
Conclusion
During a 15-month period, the Palliative Care Rehabilitation Partnership was established and facilitated a series of workshops to aid members developing, refining and transforming their research ideas into research proposals for submission to NIHR funding calls. Furthermore, the partnership engaged in a range of activities such as conceptually mapping palliative rehabilitation services, promoting training opportunities for students, clinicians and PPI members as well as granting clinical academics protected time to undertake research activities. As a result of the opportunities made possible by the partnership, a network has been formed that will continue to collaborate on, and support research related to, functional loss and rehabilitation in palliative and end-of-life care.
Additional information
CRediT contribution statement
Matthew Maddocks (https://orcid.org/0000-0002-0189-0952): Conceptualisation (equal), Funding acquisition (lead), Methodology (lead), Supervision (lead), Visualisation (supporting), Writing – original draft (supporting), Writing – editing and reviewing (supporting). Lisa Jane Brighton (https://orcid.org/0000-0003-0516-0102): Conceptualisation (equal), Data curation (lead), Funding acquisition (supporting), Methodology (supporting), Project administration (lead), Visualisation (supporting), Writing – original draft (supporting), Writing – editing and reviewing (supporting). Louise Connell (https://orcid.org/0000-0002-0629-2919): Conceptualisation (equal), Funding acquisition (supporting), Methodology (supporting), Writing – editing and reviewing (supporting). Alison Cowley (https://orcid.org/0000-0001-6858-475X): Conceptualisation (equal), Funding acquisition (supporting), Methodology (supporting), Writing – editing and reviewing (supporting). Barry Laird (https://orcid.org/0000-0002-2807-6192): Conceptualisation (equal), Funding acquisition (supporting), Methodology (supporting), Writing – editing and reviewing (supporting). Guy Peryer (https://orcid.org/0000-0003-0425-6911): Conceptualisation (equal), Funding acquisition (supporting), Methodology (supporting), Writing – editing and reviewing (supporting). Carmine Petrasso (https://orcid.org/0009-0002-1462-5960): Conceptualisation (equal), Data curation (supporting), Project administration (supporting), Visualisation (lead), Writing – original draft (lead), Writing – editing and reviewing (supporting). Lucy Ziegler (https://orcid.org/0000-0001-9563-5014): Conceptualisation (equal), Funding acquisition (supporting), Methodology (supporting), Writing – editing and reviewing (supporting). Rowan Harwood (https://orcid.org/0000-0002-4920-6718): Conceptualisation (equal), Funding acquisition (lead), Methodology (supporting), Supervision (supporting), Writing – editing and reviewing (supporting).
Disclosure of interests
Full disclosure of interests: Completed ICMJE forms for all authors, including all related interests, are available in the toolkit on the NIHR Journals Library report publication page at https://doi.org/10.3310/PTHC7598.
Primary conflicts of interest: Matthew Maddocks is supported by a NIHR Career Development Fellowship (CDF-2017-10-009). Matthew Maddocks and Lisa Jane Brighton are supported by the National Institute for Health and Care Research (NIHR) Applied Research Collaboration South London (NIHR ARC South London) at King’s College Hospital NHS Foundation Trust. Rowan Harwood is the chief editor for Age and Ageing journal and has been previously supported by the following NIHR grants: NIHR134221, RP-DG-0611-10013, RP-PG-0614-20007, 13/114/93, PB-PG-0110-21229, 97/17/16, NIHR135262, 13/75/01, 08/1809/227, PB-PG-0613-31012, RP-PG-0407-10147, NIHR202338 and 15/11/16.
Data-sharing statement
For inquiries or requests related to data sharing, please contact the corresponding author.
Ethics statement
None of the activities were classified as research therefore no ethical approval was required.
Information governance statement
King’s College London is committed to handling all personal information in line with the UK Data Protection Act (2018) and the General Data Protection Regulation (EU GDPR) 2016/679. Under the Data Protection legislation, King’s College London is the Data Controller, and you can find out more about how we handle personal data, including how to exercise your individual rights and the contact details for our Data Protection Officer here (https://www.kcl.ac.uk/professional-services/business-assurance/data-protection-introduction-data-losses-and-reporting).
Funding
This article presents independent research funded by the National Institute for Health and Care Research (NIHR) Health Technology Assessment programme as award number NIHR135171. The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the Health Technology Assessment programme or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the HTA programme or the Department of Health and Social Care.
This article reports on one component of the research award Establishing a research partnership to investigate functional loss and rehabilitation towards the end of life. For more information about this research please view the award page (https://www.fundingawards.nihr.ac.uk/award/NIHR135171)
About this article
The contractual start date for this research was in January 2022. This article began editorial review in April 2023 and was accepted for publication in November 2023. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The Health Technology Assessment editors and publisher have tried to ensure the accuracy of the authors’ article and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this article.
This article was published based on current knowledge at the time and date of publication. NIHR is committed to being inclusive and will continually monitor best practice and guidance in relation to terminology and language to ensure that we remain relevant to our stakeholders.
Copyright
Copyright © 2024 Maddocks et al. This work was produced by Maddocks et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaption in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
List of abbreviations
- ARC
- Applied Research Collaboration
- NIHR
- National Institute for Health and Care Research
- PPI
- patient and public involvement
References
- Lunney JR, Lynn J. Trajectories of disability in the last year of life. N Engl J Med 2010;363.
- Lunney JR, Lynn J, Foley DJ, Lipson S, Guralnik JM. Patterns of functional decline at the end of life. JAMA 2003;289:2387-92.
- Neo J, Fettes L, Gao W, Higginson IJ, Maddocks M. Disability in activities of daily living among adults with cancer: a systematic review and meta-analysis. Cancer Treat Rev 2017;61:94-106.
- Fettes L, Bone AE, Etkind SN, Ashford S, Higginson IJ, Maddocks M. Disability in basic activities of daily living is associated with symptom burden in older people with advanced cancer or chronic obstructive pulmonary disease: a secondary data analysis. J Pain Symptom Manage 2021;61:1205-14.
- Fettes L, Neo J, Ashford S, Higginson IJ, Maddocks M. Trajectories of disability in activities of daily living in advanced cancer or respiratory disease: a systematic review. Disabil Rehabil 2020;44:1790-801.
- Gill TM, Han L, Leo-Summers L, Gahbauer EA, Allore HG. Distressing symptoms, disability, and hospice services at the end of life: prospective cohort study. J Am Geriatr Soc 2018;66:41-7.
- Gill TM, Gahbauer EA, Leo-Summers L, Murphy TE. Recovery from severe disability that develops progressively versus catastrophically: incidence, risk factors, and intervening events. J Am Geriatr Soc 2020;68:2067-73.
- Lunney JR, Albert SM, Boudreau R, Ives D, Newman AB, Harris T. Fluctuating physical function and health: their role at the end of life. J Palliat Med 2019;22:424-6.
- Gill TM, Gahbauer EA, Han L, Allore HG. Trajectories of disability in the last year of life. N Engl J Med 2010;362:1173-80.
- Stolz E, Gill TM, Mayerl H, Rásky E, Freidl W. Trajectories of late-life disability vary by the condition leading to death. J Gerontol A Biol Sci Med Sci 2021;76:1260-4.
- Stolz E, Gill TM, Mayerl H, Freidl W. Short-term disability fluctuations in late life. J Gerontol B Psychol Sci Soc Sci 2019;74:e135-40.
- Gettel CJ, Venkatesh AK, Leo-Summers LS, Murphy TE, Gahbauer EA, Hwang U, et al. A longitudinal analysis of functional disability, recovery, and nursing home utilization after hospitalization for ambulatory care sensitive conditions among community-living older persons. J Hosp Med 2021;16:469-75.
- Chochinov HM, Hassard T, McClement S, Hack T, Kristjanson LJ, Harlos M, et al. The landscape of distress in the terminally ill. J Pain Symptom Manage 2009;38:641-9.
- Singer PA, Martin DK, Kelner M. Quality end-of-life care: patients’ perspectives. JAMA 1999;281:163-8.
- Steinhauser KE, Christakis NA, Clipp EC, McNeilly M, McIntyre L, Tulsky JA. Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA 2000;284:2476-82.
- Grund S, Gordon AL, van Balen R, Bachmann S, Cherubini A, Landi F, et al. European consensus on core principles and future priorities for geriatric rehabilitation: consensus statement. Eur Geriatr Med 2020;11:233-8.
- Wade DT. What is rehabilitation? An empirical investigation leading to an evidence-based description. Clin Rehabil 2020;34:571-83.
- Cheville AL, Morrow M, Smith SR, Basford JR. Integrating function-directed treatments into palliative care. PM R 2017;9:S335-46.
- Morgan DD, Tieman JJ, Allingham SF, Ekström MP, Connolly A, Currow DC. The trajectory of functional decline over the last 4 months of life in a palliative care population: a prospective, consecutive cohort study. Palliat Med 2019;33:693-70.
- Khizar B, Harwood RH. Making difficult decisions with older patients on medical wards. Clin Med (Lond) 2017;17:353-6.
- Javier NS, Montagnini ML. Rehabilitation of the hospice and palliative care patient. J Palliat Med 2011;14:638-48.
- Morgan DD, Currow DC, Denehy L, Aranda SA. Living actively in the face of impending death: constantly adjusting to bodily decline at the end-of-life. BMJ Support Palliat Care 2017;7:179-88.
- Cheraghlou S, Gahbauer EA, Leo-Summers L, Stabenau HF, Chaudhry SI, Gill TM. Restricting symptoms before and after admission to hospice. Am J Med 2016;129:754.e7-15.
- Morgan DD, Cerdor PA, Brown A, Currow DC. Falls in palliative care. J Palliat Med 2015;18:827-8.
- Evans CJ, Ison L, Ellis-Smith C, Nicholson C, Costa A, Oluyase AO, et al. Service delivery models to maximize quality of life for older people at the end of life: a rapid review. Milbank Q 2019;97:113-75.
- Beard JR, Officer A, de Carvalho IA, Sadana R, Pot AM, Michel JP, et al. The World report on ageing and health: a policy framework for healthy ageing. Lancet 2016;387:2145-54.
- Gimigliano F, Negrini S. The World Health Organization ‘Rehabilitation 2030: a call for action’. Eur J Phys Rehabil Med 2017;53:155-68.
- Wade DT. The future of rehabilitation in the United Kingdom National Health Service: Using the COVID-19 crisis to promote change, increasing efficiency and effectiveness. Clin Rehabil 2021;35:471-80.
- Henson LA, Maddocks M, Evans C, Davidson M, Hicks S, Higginson IJ. Palliative care and the management of common distressing symptoms in advanced cancer: pain, breathlessness, nausea and vomiting, and fatigue. J Clin Oncol 2020;38:905-14.
- Maddocks M, Brighton LJ, Farquhar M, Booth S, Miller S, Klass L, et al. Holistic services for people with advanced disease and chronic or refractory breathlessness: a mixed-methods evidence synthesis. Health Serv Delivery Res 2019;7:1-104.
- Percival C, Hussain A, Zadora-Chrzastowska S, White G, Maddocks M, Wilcock A. Providing nutritional support to patients with thoracic cancer: findings of a dedicated rehabilitation service. Respir Med 2013;107:753-61.
- Gordon AL, Witham MD, Henderson EJ, Harwood RH, Masud T. Research into ageing and frailty. Future Healthc J 2021;8:e237-42.
- Harwood RH, Enguell H. End-of-life care for frail older people. BMJ Support Palliat Care 2019;12:e293-8.
- Janssen DJ, McCormick JR. Palliative care and pulmonary rehabilitation. Clin Chest Med 2014;35:411-21.
- Funch A, Kruse NB, la Cour K, Peoples H, Waehrens EE, Brandt A. The association between having assistive devices and activities of daily living ability and health-related quality of life: an exploratory cross-sectional study among people with advanced cancer. Eur J Cancer Care (Engl) 2019;28.
- Gill TM, Baker DI, Gottschalk M, Peduzzi PN, Allore H, Byers A. A program to prevent functional decline in physically frail, elderly persons who live at home. N Engl J Med 2002;347:1068-74.
- Nottelmann L, Jensen LH, Vejlgaard TB, Groenvold M. A new model of early, integrated palliative care: palliative rehabilitation for newly diagnosed patients with non-resectable cancer. Support Care Cancer 2019;27:3291-300.
- Cieza A, Causey K, Kamenov K, Hanson SW, Chatterji S, Vos T. Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2021;396:2006-17.
- Eva G, Morgan D. Mapping the scope of occupational therapy practice in palliative care: a European Association for Palliative Care cross-sectional survey. Palliat Med 2018;32:960-8.
- Runacres F, Gregory H, Ugalde A. ‘The horse has bolted I suspect’: a qualitative study of clinicians’ attitudes and perceptions regarding palliative rehabilitation. Palliat Med 2017;31:642-50.
- Wosahlo P, Maddocks M. Benchmarking the provision of palliative rehabilitation within the hospice setting. Palliat Med 2015;29:477-8.
- Enguell H, Harwood RH. What palliative care can learn from geriatric medicine. Br J Hosp Med (Lond) 2019;80:86-90.
- Rudan I, Gibson J, Kapiriri L, Lansang MA, Hyder AA, Lawn J, et al. Child Health and Nutrition Research Initiative (CHNRI) . Setting priorities in global child health research investments: assessment of principles and practice. Croat Med J 2007;48:595-604.
- Bos N, Zimmerman A, Olson J, Yew J, Yerkie J, Dahl E, et al. From shared databases to communities of practice: a taxonomy of collaboratories. J Comput-Mediat Commun 2007;12:652-72.
- Trusson D, Rowley E, Bramley L. A mixed-methods study of challenges and benefits of clinical academic careers for nurses, midwives and allied health professionals. BMJ Open 2019;9.
- Newington L, Wells M, Adonis A, Bolton L, Bolton Saghdaoui L, Coffey M, et al. A qualitative systematic review and thematic synthesis exploring the impacts of clinical academic activity by healthcare professionals outside medicine. BMC Health Serv Res 2021;21.
- Jones D, Keenan AM. The rise and rise of NMAHPs in UK clinical research. Future Healthc J 2021;8:e195-7.
- Bayly J, Ogeden M, Kumar R. Collaboration and Knowledge-Sharing to Address Functional Loss Towards the End of Life 2022. https://arc-sl.nihr.ac.uk/news-insights/blog-and-commentary/collaboration-and-knowledge-sharing-address-functional-loss (accessed 15 January 2024).
