Notes
Article history
The research reported in this issue of the journal was funded by PGfAR as project number RP-PG-1212-20019. The contractual start date was in March 2015. The final report began editorial review in May 2021 and was accepted for publication in September 2022. As the funder, the PGfAR programme agreed the research questions and study designs in advance with the investigators. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PGfAR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
Copyright © 2023 Gillard et al. This work was produced by Gillard et al. under the terms of a commissioning contract issued by the Secretary of State for Health and Social Care. This is an Open Access publication distributed under the terms of the Creative Commons Attribution CC BY 4.0 licence, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. See: https://creativecommons.org/licenses/by/4.0/. For attribution the title, original author(s), the publication source – NIHR Journals Library, and the DOI of the publication must be cited.
2023 Gillard et al.
Synopsis
Note: some text in the synopsis below has been reproduced from the published study protocol [Gillard S, Bremner S, Foster R, Gibson SL, Goldsmith L, Healey A, et al. Peer support for discharge from inpatient to community mental health services: study protocol clinical trial (SPIRIT Compliant). Medicine 2020;99(10):e19192]. This is an open access article distributed under the Creative Commons Attribution License 4.0 (CCBY), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited. See https://creativecommons.org/licenses/by/4.0/. The text below includes minor additions and formatting changes to the original text.
Background
Discharge from psychiatric inpatient care
People recently discharged from psychiatric hospital often fail to continue with treatment,1 relapse and are readmitted. 2 For example, in the UK it has been reported that 36% of inpatients with psychotic disorders are readmitted within 1 year of discharge,3 while in New Zealand the readmission rate of all psychiatric inpatients has been reported at 41%. 4 A high proportion of people are readmitted shortly after discharge, with an Australian study of over 35,000 people admitted to psychiatric hospital finding that nearly a fifth of all psychiatric inpatients (half of all people readmitted) were readmitted in the first month post discharge,5 and a UK study of nearly 8000 people observing 15% readmissions within 3 months of discharge. 6 People recently discharged are also at risk of suicide and self-harm with, globally, suicide rates in the first 3 months after psychiatric discharge 100 times the suicide rate in the general population, and suicidal thoughts and behaviours 200 times the level in the general population. 7 In the UK, post-discharge suicides are most frequent in the first week after discharge, with 15% of all suicides nationally among people within 3 months of a psychiatric discharge. 8 Evidence suggests that lack of follow-up care post discharge9 and lack of continuity of care from hospital to community are predictors of early readmissions,10 with, conversely, higher levels of follow-up from community mental health services post discharge predicting lower readmission rates. 11 Systematic review evidence suggests that interventions supporting transition from inpatient to community mental health care are feasible and likely to be cost-effective. 9 Two of the studies reviewed evaluated multidisciplinary transitional discharge interventions that included peer support components. 12,13
Peer support in mental health services
Origins of peer support in mental health services are twofold. First, there is a decades-old tradition of self-help in Europe and North America, underpinned by a ‘helper therapy principle’14 that is perhaps best exemplified by the 12-step programmes of Alcoholics Anonymous and related programmes, having more recently proliferated into mental health care with the emergence of organisations such as Depression Alliance and the Hearing Voices Network. Second, peer support work in mental health grew out of reactions to negative and coercive mental health treatment15 with, by the 1970s, people building programmes focused on self-advocacy and campaigning where people focused on helping each other, acknowledging that their experiences and life stories could be a source of important knowledge. Since then peer support has gradually moved into the mainstream of mental health service provision, with state-funded and approved mental health service providers increasingly employing and training peer support workers – people with their own experiences of mental distress and of using mental health services – to role-model living well with mental illness and embody hope in the future, and to improve the ‘recovery focus’ of mental health services. 16 Peer workers (PWs) have been employed in a variety of roles in the NHS in the UK, most typically as peer healthcare assistants in inpatient settings or as peer community support workers in Community Mental Health Teams (CMHTs), with a focus on telling their ‘recovery story’ alongside enacting a more conventional support worker role. 17
Peer support for discharge
An observational pilot of a transitional discharge intervention delivered wholly by PWs has shown promise,18 while comparison group studies of community-based peer support programmes have also reported reductions in readmissions19 and longer community tenure20 compared to traditional services alone. A pilot trial of a community-based peer mentoring intervention for people with a history of recurrent psychiatric hospitalisation reported fewer readmissions for people receiving peer mentoring over a 9-month period, compared to community treatment as usual. 20 In another trial, among participants who engaged with treatment, fewer people receiving assertive community treatment (ACT) from a consumer-staffed ACT team reported being hospitalised than those receiving care from a non-consumer ACT team, although length of follow-up varied between participants and was not reported. 21
The evidence base for peer support in mental health services
While this evidence suggests that interventions employing PWs might offer a strategy for improving the outcomes of discharge, meta-analyses of trials of a range of peer support interventions have indicated little difference in outcomes for people receiving peer support, either in comparison to treatment as usual or to similar support provided by other mental health workers, once data from across trials are pooled. 22,23 Those systematic reviews have also pointed to the heterogeneity of the peer support evaluated, issues with the quality of trials, an absence of formal studies of cost-effectiveness, and a lack of reporting of how peer support is designed to bring about change in comparison to other forms of mental health support. In particular, inadequate randomisation and sequence generation processes,22 lack of blinding of assessors, risk of bias resulting from missing data, and selective or incomplete reporting of outcomes measured were identified as trial quality issues that need to be addressed. 23
Processes and principles of peer support
A wider literature, including qualitative and observational research, has indicated that organisational factors supporting the implementation of peer support into practice in mental health services might impact on its effectiveness. Issues such as clarity of job description,24,25 access to appropriate training and support,26 shared expectations of the PW role25,27 and preparation and training for the team that will be working alongside PWs28 have all been identified as important facilitators of the introduction of the PW role. It has been noted how the distinctiveness of peer support, in comparison to other forms of mental health care, can be lost in a formal environment of statutory mental health services if those organisational conditions are not met. 27,29,30
The distinctiveness of peer support has been attributed to the particular qualities of peer-to-peer relationships in contrast to the conventional clinician-patient relationships: peer-to-peer relationships are underpinned by a sense of connection between peers based on a recognition of shared experiences;31 reciprocity in the relationship whereby both parties learn from each other;32 and the validation and exchange of experiential, rather than professionally-acquired, knowledge. 33 In previous research by the team we developed a general change model for peer support in mental health services31 that underpins, theoretically, the development and implementation of both our peer support for discharge intervention and our evaluation. Elsewhere, a more recent review of peer support in mental health services concluded that a lack of attention to fidelity to the core principles underpinning peer support limits the usefulness of current peer support research to policy makers and practitioners. 34
Impact of peer support on peer workers
A parallel body of research has identified potential benefits and challenges for people working in a PW capacity. It has been suggested that peer support might enhance personal recovery for PWs, but can also be a source of stress, with mental health professionals voicing concern that the PWs they work alongside might relapse and be hospitalised because of the stresses of the role. 16 A review of qualitative research about PWs’ experiences of peer support indicated improvements in confidence, self-esteem and social contacts for PWs. 35 However, more recently, a survey of 84 PWs working in a range of mental health services in one state in the United States (US) USA found that PWs experienced difficulties including poor financial compensation, limited employment opportunities, work stress, the emotional stress of helping others and in maintaining personal wellness, with 44% of the sample reporting having experienced a relapse in their mental health while working as a PW. 36 It is important to understand and evaluate the impact of working in a peer support capacity in order to ensure that implementation of peer support into mental health services is both safe and rewarding for PWs.
Rationale
Mental health policy and workforce initiatives in higher income countries are driving the introduction of PWs into statutory mental health services despite these uncertainties in the evidence base. 22,23 As such, there is a need for high-quality trials of peer support that specify, model and evaluate the distinctive processes whereby peer support brings about change in specific contexts and settings, as well as for good health economic evaluation. This study aims to address those limitations in the current evidence base while providing clear evidence of the effectiveness and cost-effectiveness of a PW intervention to enhance discharge from inpatient to community mental health care.
The research programme
Aims
The overarching aim of this programme of applied research was to enhance the experience of discharge from psychiatric inpatient care for mental health service users, preventing unnecessary readmission and reducing costs. The specific aim of the programme was to manualise, pilot and trial a peer support intervention to enhance discharge from inpatient to community mental health care, significantly reducing readmissions and the associated cost of care. The detailed research objectives of the programme were:
-
to refine an empirically and theoretically grounded model that explains how peer support interventions impact on outcomes for service users post-discharge
-
to develop and manualise a peer support intervention to enhance discharge
-
to develop an index to assess the fidelity of peer support interventions
-
to conduct a high-quality randomised controlled trial (RCT) of the intervention
-
to establish the effectiveness and cost-effectiveness of a peer support intervention to enhance discharge
-
to explore the impact on PWs of providing peer support for discharge.
This programme also aimed to deliver applied outputs that will enable mental health service providers in the NHS to effectively and cost-effectively integrate peer support into the mental health discharge pathway, including: the ENRICH training programme and intervention handbook, providing implementation guidance for managers and commissioners in the NHS, and our principles-based peer support fidelity index.
Work packages
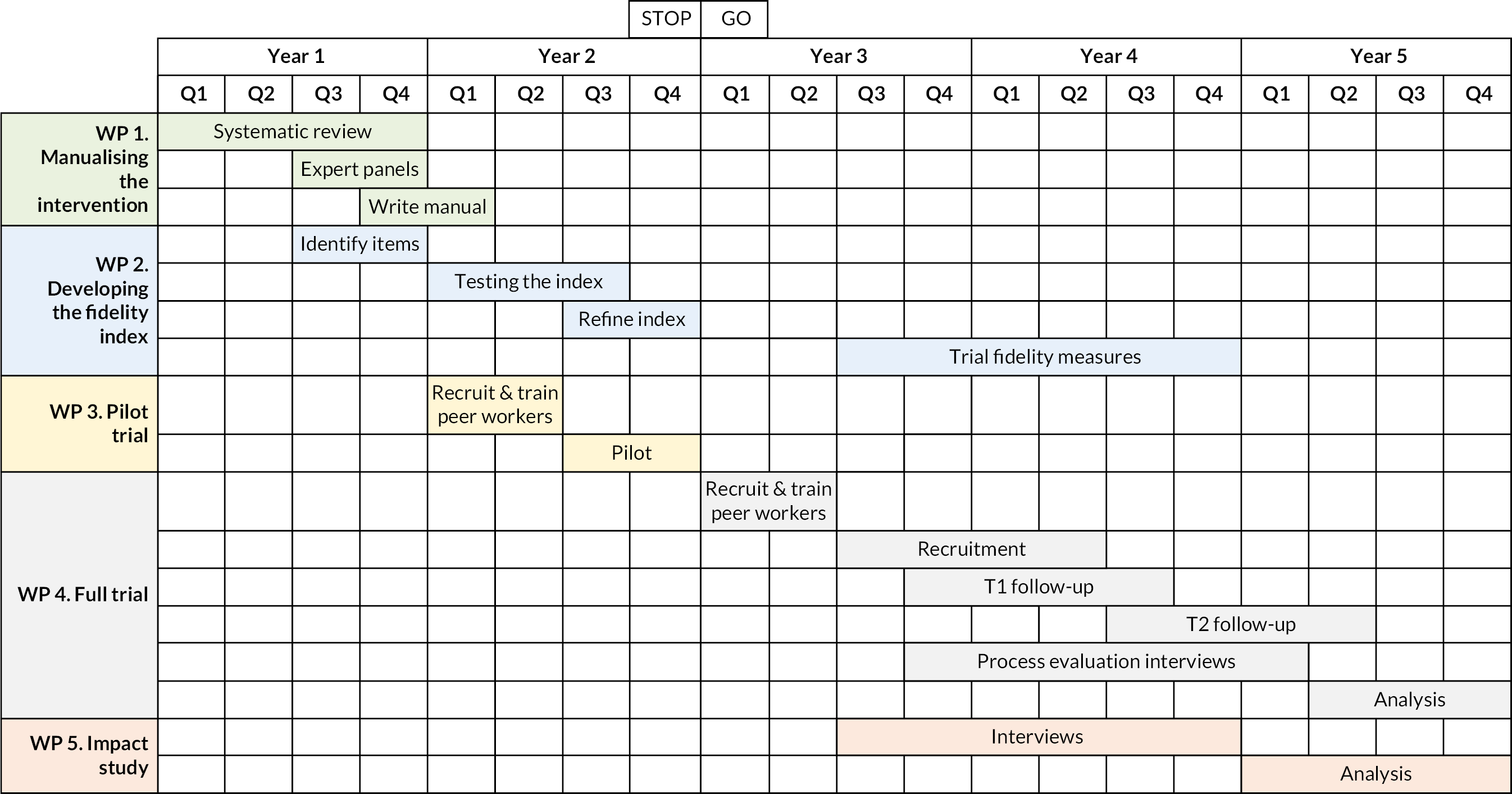
The ENRICH programme comprised five interlinked work packages (WP) that addressed the aims listed above (see Figures 1 and 2).
FIGURE 1.
Research pathway diagram.
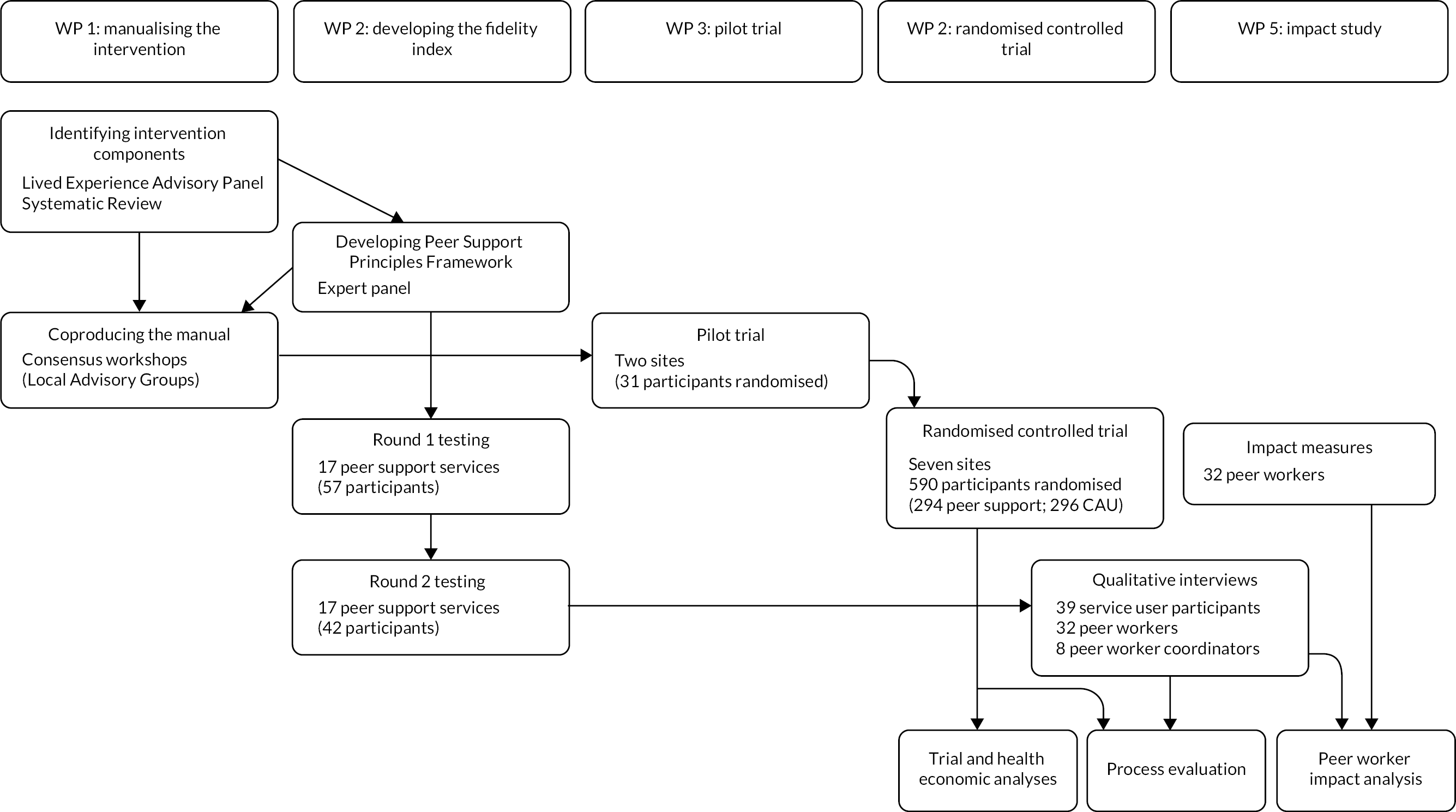
FIGURE 2.
Overview of the programme.
WP1. Manualising the ENRICH intervention
WP1 comprised two main pieces of work. First, a systematic review of the evidence for one-to-one peer support in mental health services was undertaken to refine the model underpinning the intervention, identify intervention components and establish the effectiveness of one-to-one peer support intervention. Second, we worked with expert panels, at study site and national levels, to identity and prioritise intervention components, and to develop and refine the ENRICH training programme and peer support handbook for the trial in WP4.
WP2. Developing the peer support fidelity index
A fidelity index was developed, and its psychometric properties and acceptability tested, and used in the WP4 trial to assess the extent to which the peer support intervention was implemented to principles underpinning peer support.
WP3. Pilot trial
An internal pilot trial of the intervention was conducted in two sites using the protocol for the full RCT to test procedures for recruitment, randomisation, allocation to and delivery of intervention, and collection of data. A clear set of stop-go rules was used to determine whether the programme proceeded to full trial, and if any procedures needed to be refined.
WP4. Randomised controlled trial
A fully powered superiority trial, comparing peer support for discharge plus care as usual (CAU), with CAU only at discharge from inpatient psychiatric care, was conducted to establish the effectiveness and cost-effectiveness of the ENRICH peer support intervention. This WP also comprised a substantial mixed methods process evaluation that used measures of process as well as in-depth qualitative interviews with trial participants, PWs and their supervisors [peer worker co-ordinators (PWCs)] to explore, quantitatively and qualitatively, the processes of peer support.
WP5. Impact study
A mixed method, longitudinal cohort study using standardised measures and in-depth interviews with PWs delivering the peer support intervention explored the impact of the role on well-being and employment outcomes for PWs.
Setting
The programme took place in adult acute psychiatric inpatient and community mental health service settings in mental health NHS trusts in England. Two trusts [South West London (SWL) & St George’s Mental Health NHS Trust and East London (ELN) NHS Foundation Trust] took part in the pilot study, with five additional trusts joining for the full trial and subsequent WPs (Central and North West London NHS Foundation Trust; Sussex Partnership NHS Foundation Trust; Surrey and Borders Partnership NHS Foundation Trust; Birmingham and Solihull Mental Health NHS Foundation Trust; Bradford District Care NHS Foundation Trust). Two other trusts – Dorset HealthCare University NHS Foundation Trust and South West Yorkshire Partnership NHS Foundation Trust – were involved in WP1 of the programme but were unable to remain involved for the full trial.
Population
The primary population of the research was adult inpatients of psychiatric hospital wards (acute admission wards and their equivalents) who had had at least one previous admission in the preceding 2 years. Secondary populations included the PWs employed to implement the intervention and their supervisors (PWC).
Ethical approval
A single application for NHS research ethics approval was made for all WPs. The programme was approved by the UK National Research Ethics Service, Research Ethics Committee London – London Bridge on 10 May 2016, reference number 16/LO/0470.
Governance
The Chief Investigator, Programme Manager and trial statistician reported regularly to an independent Programme Steering Committee (PSC) and an independent Data Management and Ethics Committee (DMEC). Oversight from a patient and public perspective was provided by a Lived Experience Advisory Panel (LEAP) as well as service user representation on the PSC and DMEC.
Changes to the funded programme
Changes to the funded programme were minimal. In WP1 we split the systematic review into two outputs. We initially prioritised data extraction of components of peer support to inform development of the intervention. We returned to the review and updated searches once the WP4 trial had completed recruitment (and more researcher resource was available). This was to our advantage as a sufficient number of new trials of peer support had been published in the interim to enable us to undertake a meta-analysis.
There were no major changes to the WP4 trial that required ethical approval. Minor changes to recruitment procedures were made following the pilot trial that did require amendment to ethical approval.
As noted in Process evaluation – predictors of engagement with peer support below, because we did not observe a positive effect on primary outcome, we were not able to undertake the structured equation modelling we had intended, to explore pre-specified change mechanisms. Given that our complier average causal effect (CACE) analysis had indicated a relationship between engagement with intervention and outcome, we instead undertook an analysis of pre- and post-randomisation predictors of engagement. Similarly, in Process evaluation – peer support and change in mental health services – the qualitative component of the process evaluation – instead of exploring our pre-specified mechanisms we used our qualitative dataset to refine the change model for peer support in mental health services that underpinned the intervention (thus remaining consistent with our original objectives).
Work package 1 Manualising the ENRICH peer support intervention
In this work package we aimed to address objectives 1 and 2 of the programme:
-
to refine an empirically and theoretically grounded change model that explains how peer support interventions impact on outcomes for service users post discharge
-
to develop and manualise a peer support intervention to enhance discharge.
We sought to build on what is already known about peer support interventions in order to refine our trial protocol and develop an intervention that would improve on the existing evidence base for peer support in mental health services. In previous research undertaken by the team we had developed a general change model for peer support in mental health services31 and had identified some of the key components that might comprise a PW intervention supporting discharge. 25,27 We undertook two main strands of work to fulfil these objectives:
-
a systematic review of research evaluating one-to-one peer support in mental health services
-
co-design and consensus work with advisory groups comprising people involved in delivering, developing, leading and working alongside peer support services in NHS mental health services.
Systematic review of one-to-one peer support in mental health services
Existing systematic reviews of peer support in mental health services were not indicative of clear effects on outcome based on the evidence available at the time reviews were conducted, pointing to a high degree of heterogeneity of peer support interventions (reviews included one-to-one and group peer support, and peer-led services that comprised multiple elements) and to the generally low quality of trials undertaken to date. 22,23 We undertook a systematic review focusing on one-to-one peer support in mental health services. The review asked the following questions:
-
What are the components of one-to-one peer support interventions?
-
What are the outcomes of one-to-one peer support interventions?
-
How are the processes of peer support associated with change?
The review protocol was registered with the International Prospective Register of Systematic Reviews, identifier: CRD42015025621. 37 We undertook searches and reported the review in two stages, the first stage of which is summarised in Co-design and consensus work to develop the peer support intervention below.
White et al.38
We produced a second review, addressing questions 2 and 3 above (outcomes and process of peer support). Work on this second review was delayed while we undertook the main trial, with searches subsequently undertaken up to 13 June 2019. The full method for the search is described in the paper. 38 The search identified 23 papers reporting 19 RCTs comparing a range of one-to-one peer support interventions with either CAU or an active control arm. Fourteen trials provided data for meta-analysis of nine different outcomes. We found that one-to-one peer support in mental health services has a small but statistically significant benefit for individual recovery [standardised mean difference (SMD) 0.22, 95% confidence interval (CI) 0.01 to 0.42; p = 0.042] and empowerment (SMD 0.23, 95% CI 0.04 to 0.42; p = 0.020). There was no effect on clinical outcomes such as symptoms or hospitalisation; the risk of being hospitalised was reduced by 14% for those receiving peer support but was non-significant [risk ratio (RR) 0.86, 95% CI 0.66 to 1.13].
In subgroup analyses we explored the extent to which processes of peer support impact change in outcome; we compared the effect on outcome of peer support provided in addition to CAU with peer support where PWs acted as ‘substitutes’ for other workers providing similar support, and compared the effect of peer support interventions where there were high levels of support for PWs with interventions where support for PWs was low. This indicated that peer support had a significantly greater effect on social network support (Qint = 4.27, p = 0.039) where peer support was delivered in addition to CAU (SMD = 0.23) compared to when it was provided as a substitute intervention (SMD = −0.30). We note in the review the continued heterogeneity in peer support interventions and in outcomes assessed in trials, and the importance of ensuring that the constructs that are assessed relate to the mechanisms and processes of the peer support that is being evaluated. 38
Co-design and consensus work to develop the peer support intervention
Marks et al.39
The intervention was developed in three sequential stages – (1) generating intervention components; (2) producing the intervention handbook; (3) piloting the intervention. Experiential knowledge was integrated through the development process, with several members of the research team identifying as service user or survivor researchers, or working as PWs. Our LEAP and a Local Advisory Group (LAG) at each study site also included people with experiences of using mental health services and peer support (see Table 3). Development closely followed the Medical Research Council complex interventions guidance. 40 The methods and results are summarised in Appendix 1, including the first stage of the systematic review identifying components of peer support interventions.
The ENRICH peer support for discharge intervention
The intervention development process resulted in the production of a detailed handbook and manualised training programme for peer support for discharge from inpatient mental health care, described in detail in our trial protocol paper. 41 People receiving the intervention are offered at least one face-to-face contact with a PW in hospital prior to discharge and, once discharged, a weekly meeting with the PW for 10 weeks, stepping down to three subsequent fortnightly meetings. Meetings are flexible in length, typically ranging from 60 to 90 minutes, supplemented by phone calls and text messages. Initial meetings focus on building a relationship, with subsequent meetings making flexible use of the skills and tools covered in the training (see below). There is emphasis on enabling the supported peer (SP) to access available social support, rather than the PW directly providing support. PWs could attend discharge and care planning meetings and appointments with care professionals at the SP’s request.
The handbook provides PW and PWC role descriptions, specifies the support and supervision PWs receive, and details preparation sessions for clinical teams where the peer support takes place. The training programme comprises 8 weekly 6-hour training sessions, plus employment support, hospital visits and structured feedback. Training covers guidance and practice for PWs in using their own experience-based knowledge, and use of a range of structured tools and exercises focused on building individual strengths and engaging with activities in the community (e.g. personal asset mapping, goal setting, and discharge, recovery and crisis planning).
Work package 2 Developing a peer worker fidelity index
Developing the index
To improve the utility of the evidence base, measurement of fidelity to peer support principles in trials of peer support has been called for. 34 This WP reports the development and testing of a fidelity index for one-to-one peer support in mental health services, designed to assess fidelity to principles that characterise the distinctiveness of peer support.
Gillard et al.42
An iterative process of developing and testing the fidelity index is described in detail in this report. A draft index was developed using expert panels including service user researchers and people doing peer support, with fidelity criteria generated for each of the peer support principles identified in WP1 and index items written as a means of testing criteria. Two rounds of testing took place in 24 mental health services providing peer support in a range of settings. Fidelity was assessed through interviews with PWs, their supervisors (PWCs) and people receiving peer support. Index items were rated by members of the research team, with responses tested for spread and internal consistency, and independently double rated for inter-rater reliability. Feedback from interviewees and service user researchers was used to refine both the content of the index and the rating procedure.
A fidelity index for one-to-one peer support in mental health services was produced with good psychometric properties. Fidelity is assessed in four principles-based domains – building trusting relationships based on shared lived experience; reciprocity and mutuality; leadership, choice and control; building strengths and making connections to community – and is separately assessed for the set-up and ongoing delivery of peer support, while an overall score can also be generated.
We conclude that the index offers the potential to improve the evidence base for peer support in mental health services, enabling future trials to assess fidelity of interventions to peer support principles, and giving service providers a means of ensuring that peer support retains its distinctive qualities as it is introduced into mental health services. We suggest that further testing of the internal structure of the index is necessary to fully establish the psychometric properties of the index, for example through a confirmatory factor analysis, and testing the construct validity for the index by exploring the relationship between fidelity scores and outcomes that might be expected to be associated with fidelity.
Fidelity in the ENRICH trial
We report, descriptively, fidelity at site level and over time in the WP4 ENRICH trial, and (graphically) association between measurement of fidelity and outcomes in the trial. As can be seen in Figure 3, fidelity was consistently reasonably good at set-up across sites, which might be expected as all sites were using the same handbook and training manual and had the support of the study team to do so. There were some inconsistencies in set-up scores in the SWL site, but it is noted that the PWC was absent at the site for much of the set-up period which may have been disruptive. Scores were lower in the Sussex (SSX) site where PWs were employed by a third-sector organisation that had a long tradition of peer support and so may have used a more idiosyncratic approach to supporting PWs.
FIGURE 3.
Fidelity set-up scores by site. BMS, Birmingham and Solihull; SAB, Surrey and Borders.
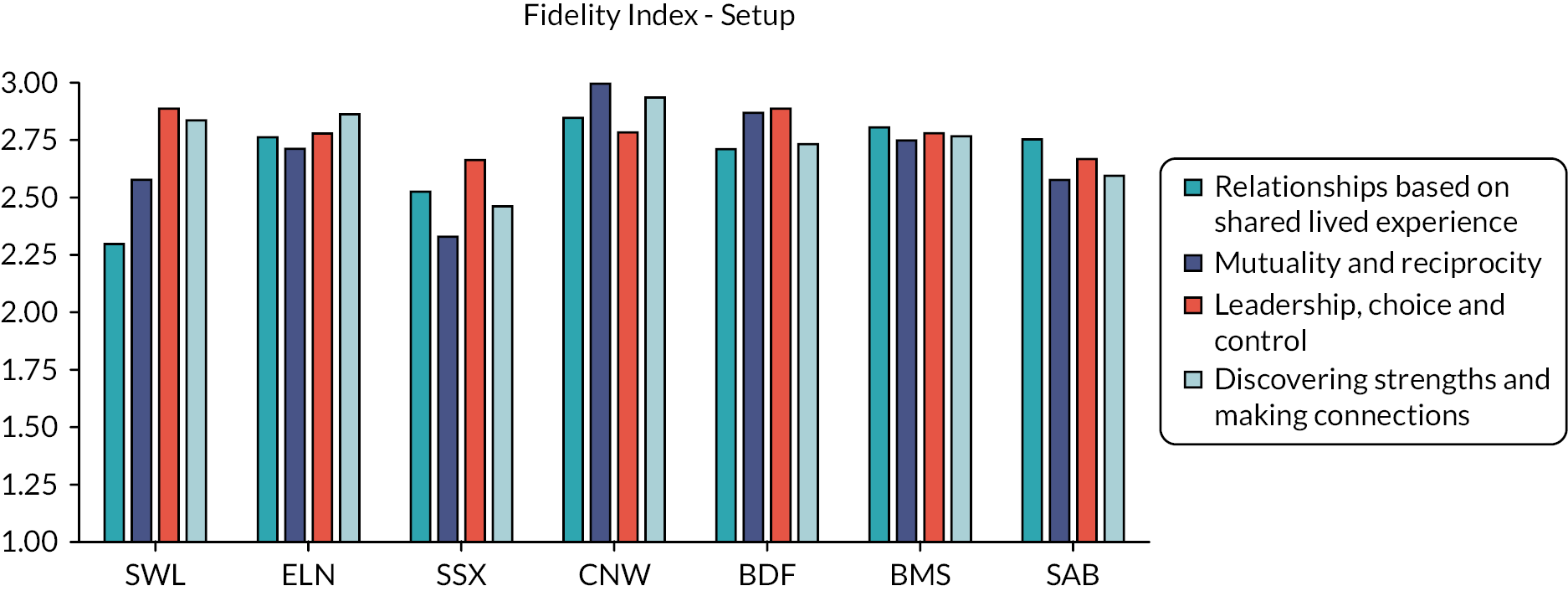
There was more variability in delivery scores, both between sites and over time (see Figures 4–7), with the exception of scores in domain 1 – relationships based on shared lived experience (see Figure 4) – which were generally high. The Central and North West London (CNW) site had consistently good scores in all delivery domains, with other sites showing more variability over time and lower scores in some domains.
FIGURE 4.
Fidelity delivery scores – relationship domain by site. BMS, Birmingham and Solihull; SAB, Surrey and Borders; T, timepoint.
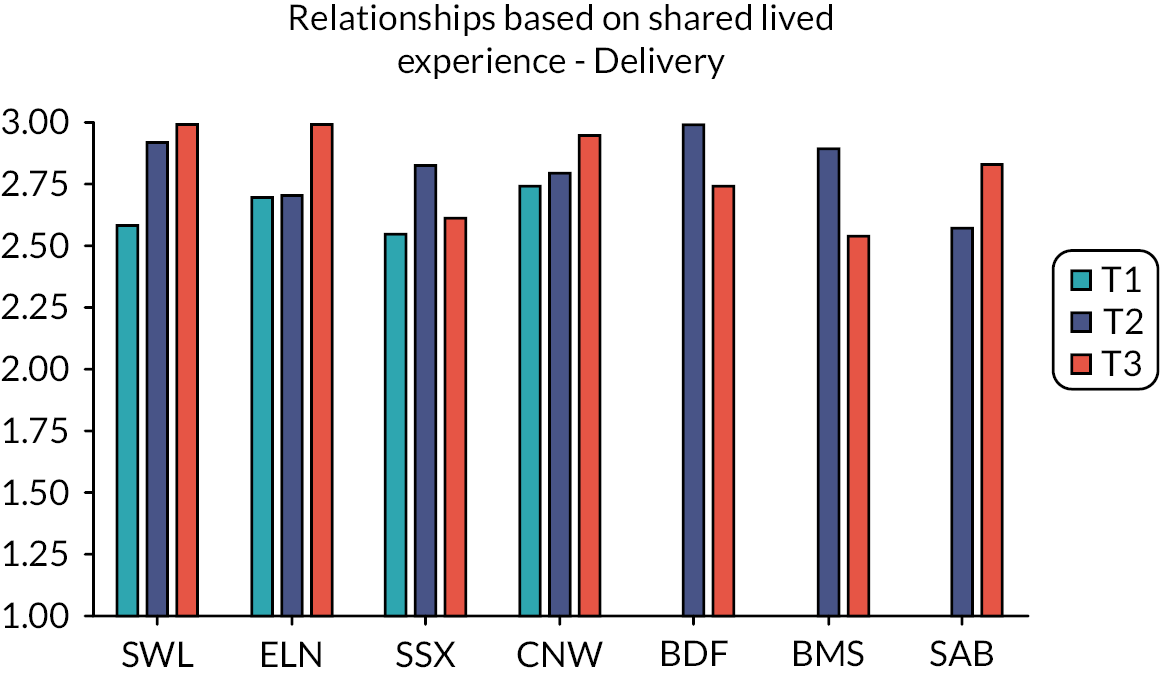
FIGURE 5.
Fidelity delivery scores – mutuality and reciprocity domain by site. BMS, Birmingham and Solihull; SAB, Surrey and Borders; T, timepoint.
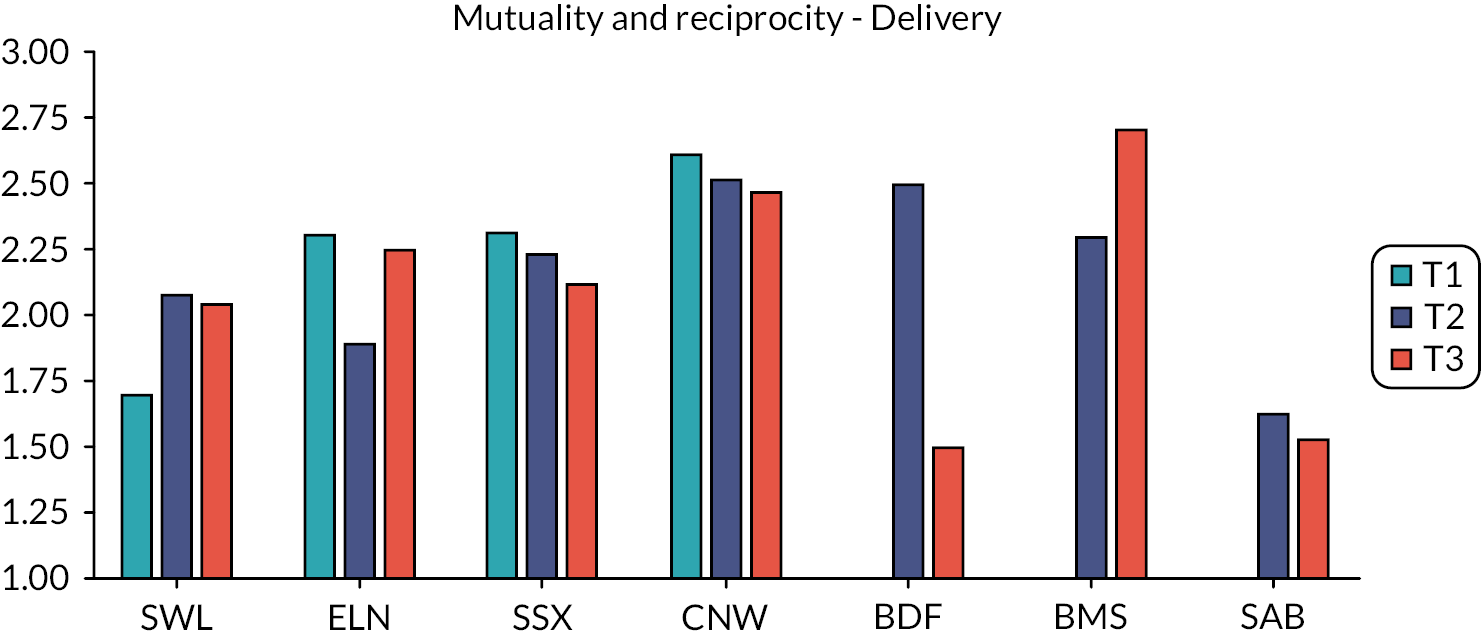
FIGURE 6.
Fidelity delivery scores – leadership, choice and control domain by site. BMS, Birmingham and Solihull; SAB, Surrey and Borders; T, timepoint.
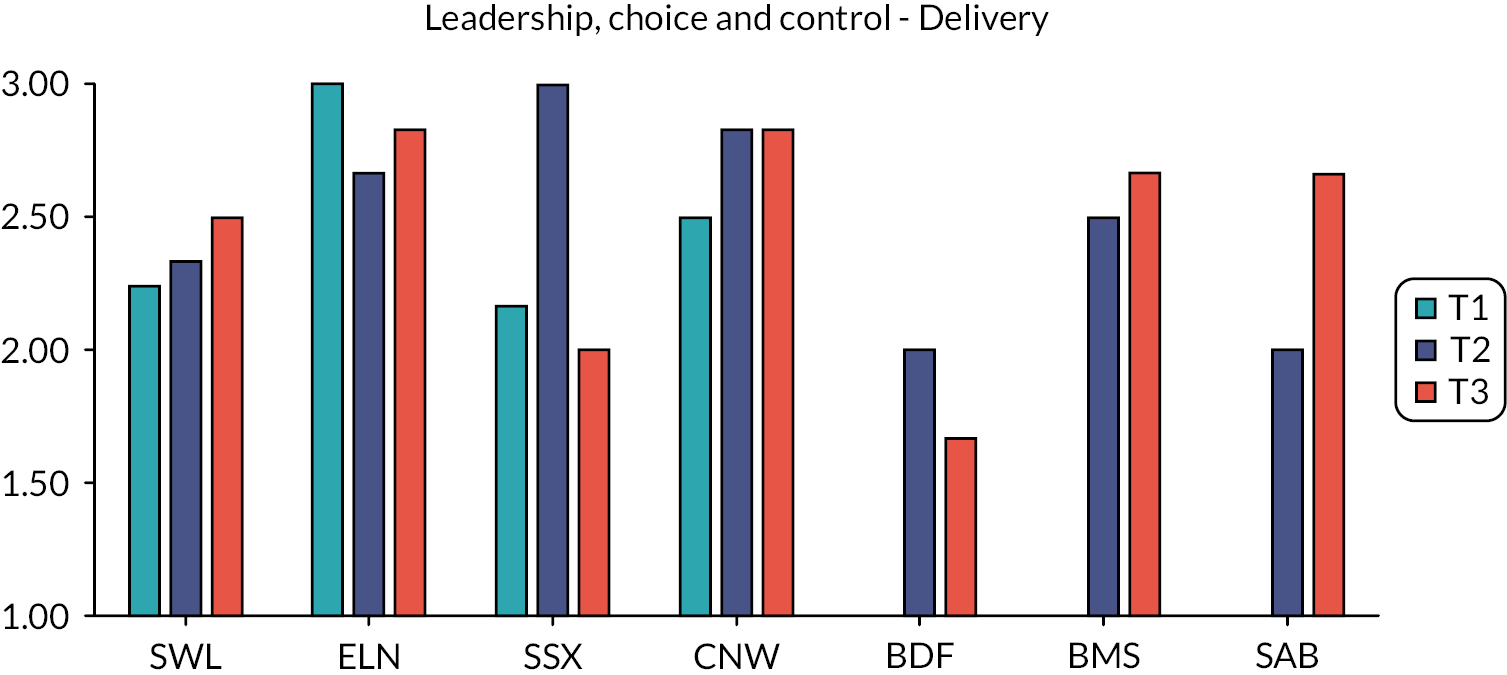
FIGURE 7.
Fidelity delivery scores – strengths and connections domain by site. BMS, Birmingham and Solihull; SAB, Surrey and Borders; T, timepoint.

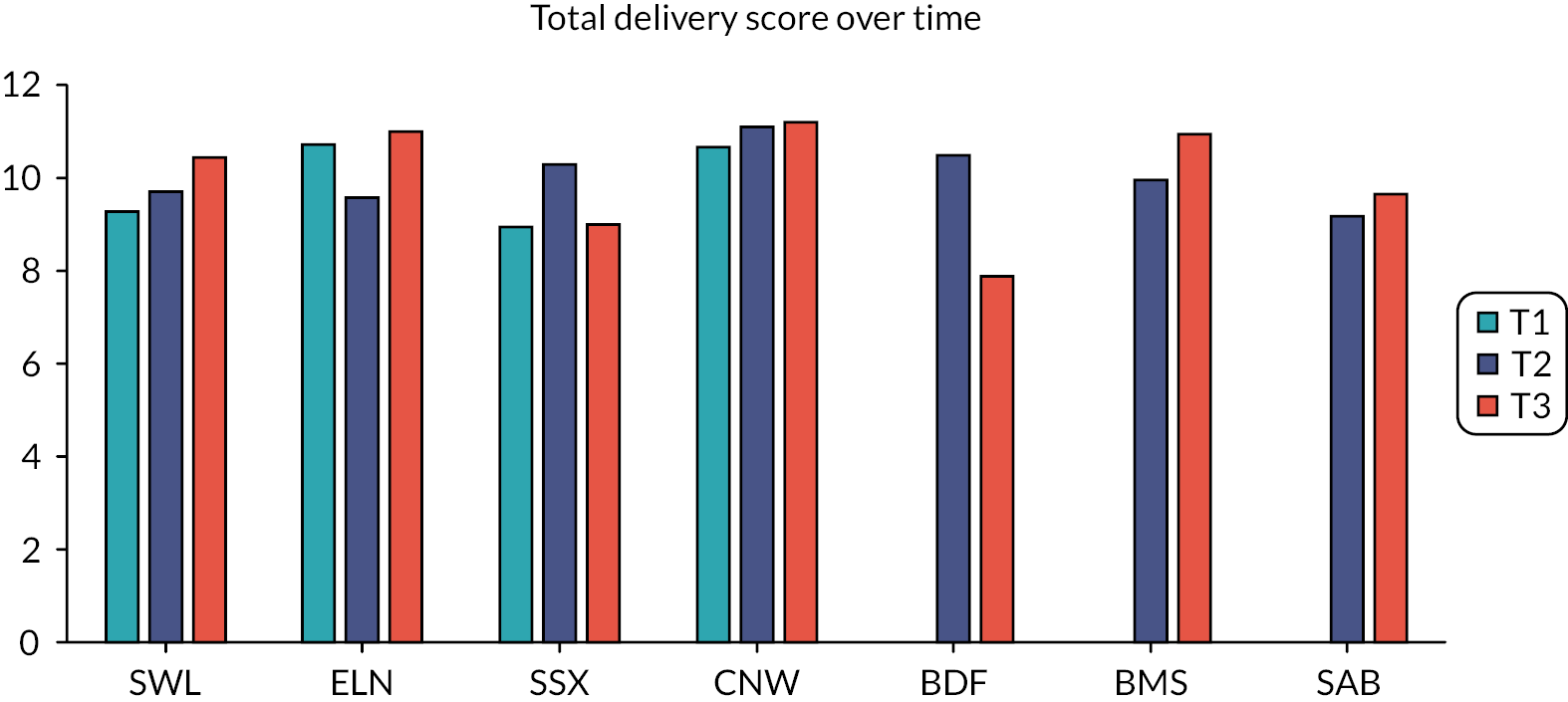
Total delivery score improved slightly at most sites over time (see Figure 8) with the exception of the SSX and Bradford (BDF) sites where total delivery score dropped from T2 to T3. SSX and BDF were the two sites where PWs were employed by a third-sector partner where, as noted above, a more independent way of working might have been in place.
FIGURE 8.
Change in total delivery score by site. BMS, Birmingham and Solihull; SAB, Surrey and Borders; T, timepoint.
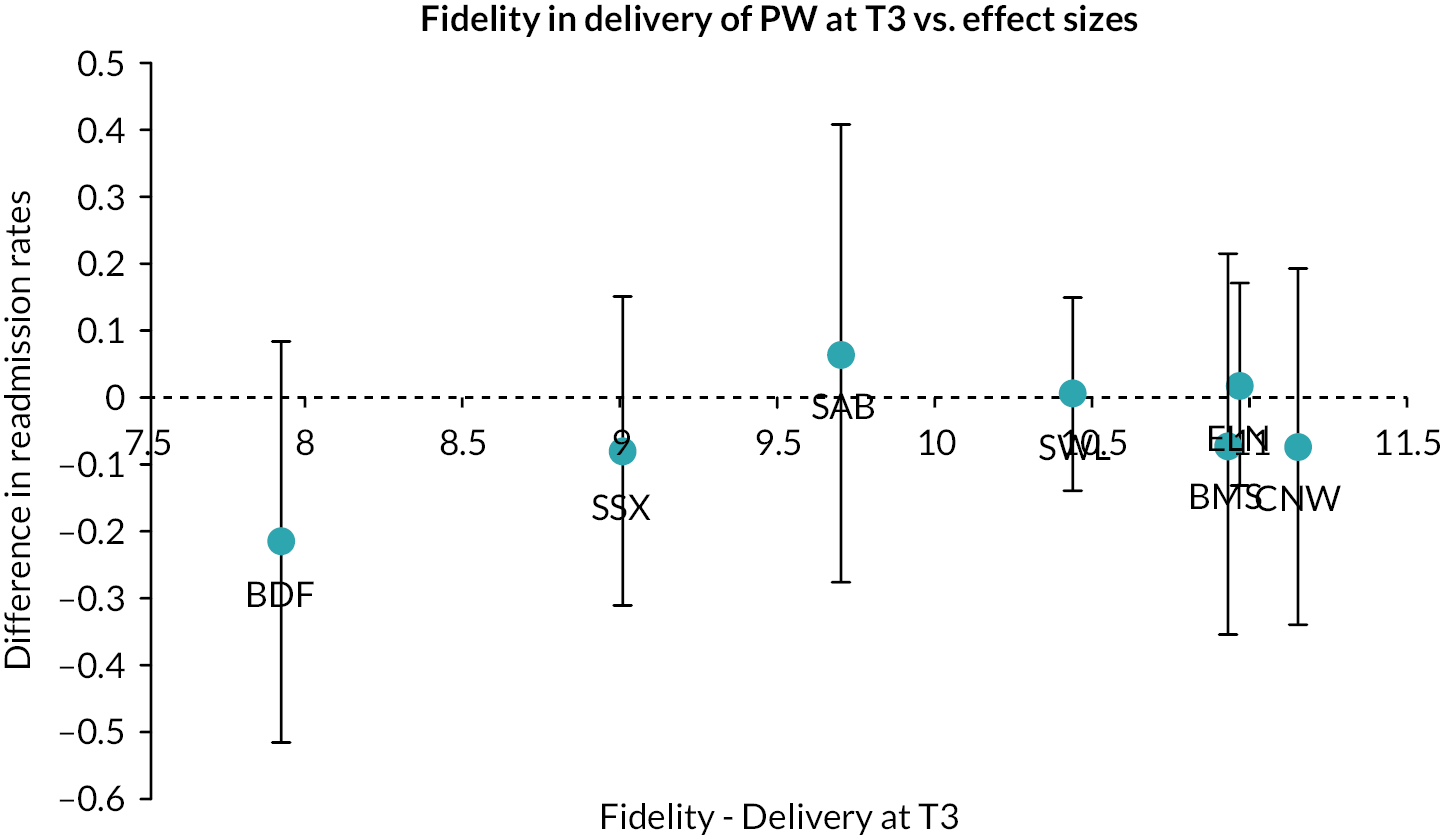
Figures 9 and 10 show no clear relationship, at site level, between effect and fidelity at set-up or T3. However, relationship between effect and total fidelity score – the most reliable score42 – is interesting. The two sites with lowest total fidelity – SSX and BDF, the two sites with third-sector providers – reported a difference in readmission rate favouring peer support. However, we note that these sites had low numbers of participants and therefore wide error bars. We observe, graphically, a trend in the relationship between fidelity and outcome (favouring peer support in sites where fidelity is higher) in the five sites where PWs were employed in the NHS. However, we note that error bars for all sites encompass no difference in outcome between peer support and control (and that the study was not powered to detect a difference at site level, our main trial reporting no site subgroup effect). While we cannot, as a result, be confident in these observations, it would be interesting to pool data from further peer support studies that made use of the fidelity index in order to further explore the relationship between fidelity and effect on outcome.
FIGURE 9.
Relationship between fidelity set-up score and primary outcome by site. BMS, Birmingham and Solihull; SAB, Surrey and Borders; T, timepoint.
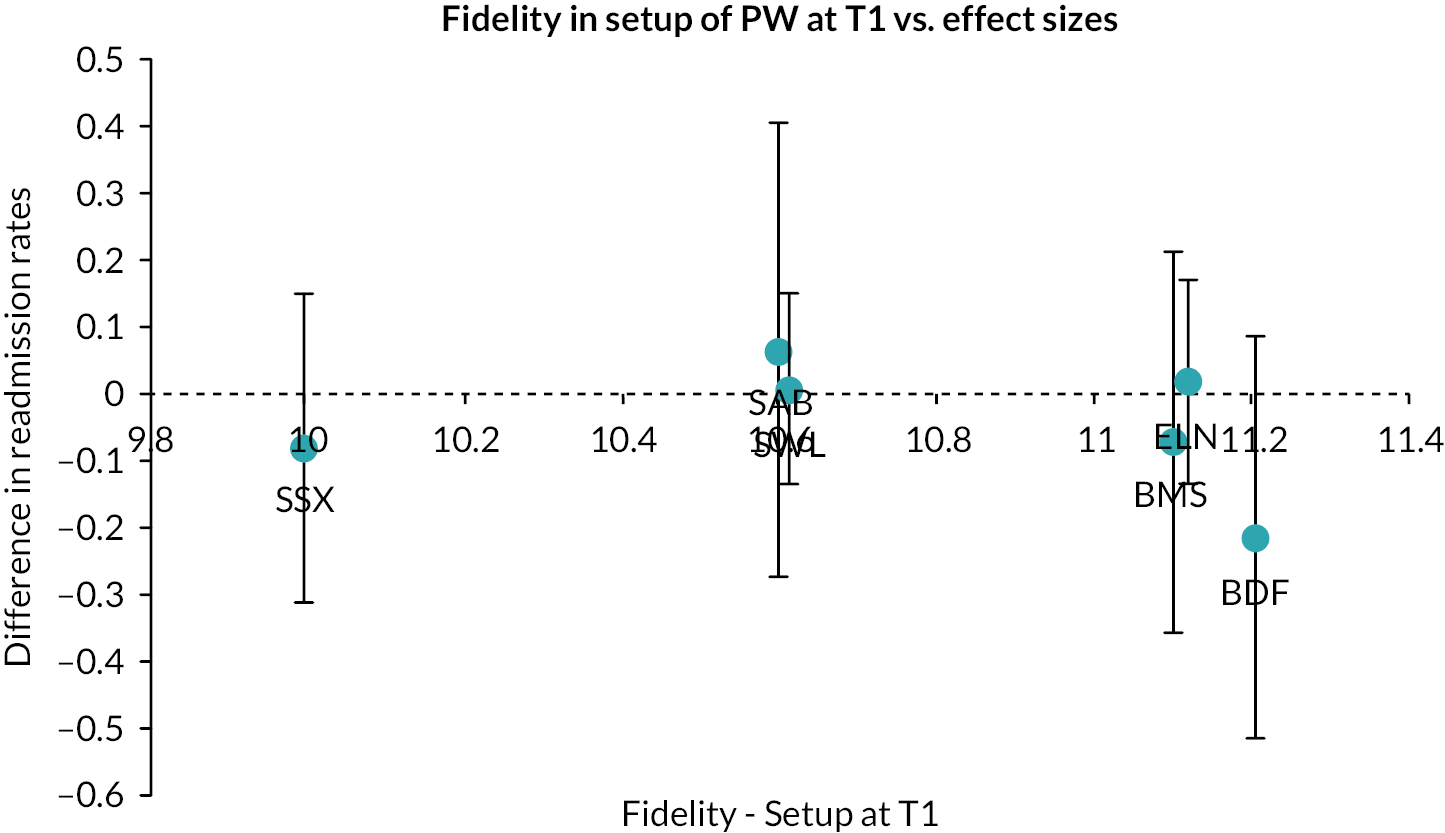
FIGURE 10.
Relationship between fidelity delivery score and primary outcome by site. BMS, Birmingham and Solihull; SAB, Surrey and Borders; T, timepoint.
Work package 3 Piloting the ENRICH peer support intervention
An internal pilot trial was conducted in two sites, SWL and ELN, following the same protocol as the full trial,41 commencing on 1 December 2016. The stop-go rules for the pilot trial were agreed by the PSC as follows:
-
to recruit a total of at least 32 participants to the pilot trial by end of February 2017 with a recruitment rate of 8 participants a month achieved in both sites for at least 2 months
-
to demonstrate 90% completeness of electronic patient record (EPR) data (including primary outcome) of all participants enrolled at end of pilot
-
to recruit, train and sustain a team of 2.0 full-time equivalent (FTE) PWs to deliver the intervention at each site.
Assessment of progression to full trial
Recruitment to the pilot trial at the two sites in the period leading up to the end of February 2017 was as follows (see Table 1):
| SWL | EL | Total for both sites | ||||
|---|---|---|---|---|---|---|
| Randomised | Randomised | Randomised | ||||
| Date | Number | Total | Number | Total | Number | Total |
| 1 December 2016 to 31 December 2016 | 3 | 3 | - | - | 3 | 3 |
| 1 January 2017 to 31 January 2017 | 9 | 12 | 7 | 7 | 16 | 19 |
| 1 February 2017 to 28 February 2017 | 8 | 20 | 4 | 11 | 12 | 31 |
Completeness of outcomes data, as collected using EPRs (patient notes) at both sites, of all participants enrolled to the study as of 8 February 2017, was as follows (see Table 2):
| Missing | Non-missinga | Total | |||
|---|---|---|---|---|---|
| n | (%) | n | (%) | n | |
| EPR data | 0 | (0) | 20 | (100) | 20 |
While the data collected here were baseline data, this was the same dataset that would be collected at 12 months follow-up (for the 12 months post discharge from index admission), including the primary outcome (psychiatric admission).
Both sites successfully recruited and trained a team of four PWs working to a total of 2.0 FTE per site. The ELN team comprised two PWs at 0.4 FTE each and two at 0.6 FTE each. The SWL team comprised three PWs at 0.4 FTE each and one at 0.8 FTE. The ELN team had one additional trained PW who could act as a reserve; the SWL team had two reserve PWs.
Actions to support progression
Rules two and three were met, and while rule one was met in the SWL site it was not met in the ELN site (and therefore narrowly missed overall). The PSC asked the study team to produce an analysis of barriers to recruitment and propose measures to improve recruitment. The flow of potential participants in the pilot trial at both sites is given in Figure 11 and Appendix 1, Figure 12 indicating reasons for potential participants not progressing. We spoke in depth to researchers [Research Assistants (RAs)], Clinical Studies Officers (CSOs) and clinical staff at each site to enable us to better understand these data. We proposed the following actions to improve recruitment going forward:
-
The proportion of patients eligible for the study was lower than we had anticipated. We would open the study on an additional ward at each site and take a flexible approach to the number of wards we would open at additional sites in the main trial.
-
We identified misunderstanding of eligibility criteria around potential risk to PW and likelihood of discharge in the next month. Members of the study team would make visits to participating wards as necessary to ensure that clinical staff were fully aware of eligibility criteria and recruitment processes.
-
Potential participants were lost between initial screening and confirmation of eligibility by the clinical team, or between confirmation of eligibility and first contact with a CSO, because patients could be discharged between weekly visits to the ward by CSOs. We increased the flexibility of the recruitment process so that RAs could liaise directly with the clinical team when the CSO was not present on the ward.
-
Some potential participants were declining to meet a RA after they had been first approached about involvement in the study. Members of the study team and/or PWs would attend weekly community meetings on wards to provide general information about the study.
The PSC received and reviewed our report and proposed actions, and recommended to the funder that the study progress to the main trial. We obtained NHS ethical approval for amendments to the study protocol and procedures as necessary.
Work package 4 Trialling the ENRICH peer support intervention
Randomised controlled trial
This WP aimed to establish the effectiveness of a PW intervention to reduce psychiatric readmission following discharge, as developed in WP1 above. We hypothesised that participants receiving peer support for discharge, in addition to CAU, would be significantly less likely to be readmitted in the year following discharge than participants receiving CAU only.
Gillard et al.41
The study was a parallel, two-group, individually randomised controlled superiority trial, with trial personnel (outcome assessors, data analysts) masked to allocation of participants. The study took place in the inpatient and community mental health services of seven NHS mental health trusts in England (sites). In five sites where participants were recruited from two inpatient facilities, and one site where recruitment was from three facilities, these were treated as single sites for stratification. A detailed trial protocol has been published;41 trial procedures are summarised only here.
The trial is registered with the ISRCTN clinical trial register, number ISRCTN 10043328,43 and was overseen by an independent steering committee and a data monitoring committee.
All new admissions to participating adult acute inpatient wards were screened for eligibility. Inpatients were eligible if they had at least one psychiatric admission in the preceding 2 years, were aged 18 years or older, were assessed by the ward clinical team as likely to be discharged within the next month and had capacity to give written informed consent to participate in the research. Patients were excluded if they had a diagnosis of any organic mental disorder, had a primary diagnosis of eating disorders, learning disability or drug or alcohol dependency (as recorded in clinical notes), or were assessed by the clinical team on the ward as presenting a current, substantial risk to a PW. Following completion of baseline assessments, consenting patients were randomised to treatment groups in a 1 : 1 ratio, stratified by site and diagnostic group (psychotic disorders, personality disorders, other eligible non-psychotic disorders). Measures to ensure protection of masking of assessors are detailed in the study protocol. 41
Participants in the intervention group received the peer support intervention, delivered one-to-one by a designated PW, a Discharge Information Pack and CAU at discharge. Participants were assigned a PW after allocation and prior to discharge by the site PWC who also provided support and supervision to the PW team. The peer support intervention, including the PW training programme, is specified in a handbook and described in detail in the trial protocol41 and summarised in Co-design and consensus work to develop the peer support intervention above. The Discharge Information Pack provided information about potentially useful statutory and voluntary sector services. CAU post-discharge from inpatient psychiatric care is mandated nationally in England as follow-up by community mental health services or primary care mental health team within 7 days of discharge. Within a week of discharge, a discharge summary should be sent by the inpatient team to the patient’s GP and others involved in developing their care plan, including information about why the patient was admitted and how their condition has changed during the hospital stay. A member of the CMHT or primary care mental health team to which the patient has been discharged will typically telephone or visit the patient within 1 week of discharge to make arrangements for their ongoing care. Participants in the control group received CAU and a copy of the Discharge Information Pack to control for any effect of access to information alone on outcome. We conducted the trial in sites where there was no offer of one-to-one peer support in either inpatient or community settings. In some sites group peer support was on offer, typically as peer-facilitated support groups in inpatient settings that people could ‘drop in’ to on an ad hoc basis. It is possible that participants in either peer support or control groups accessed group peer support. Stratification of randomisation by site was used in part to address this.
Data were collected at baseline (T0), and at 4 months (T1) and 12 months (T2) post-discharge from the index admission. Mental health service use data were extracted from the site EPR at baseline and 12 months. The primary outcome for the trial was psychiatric inpatient readmission in the 12 months post-discharge, including both formal and informal admissions. Secondary outcomes were number of voluntary admissions, involuntary admissions and total number of admissions, total number of days in hospital, time to first readmission, use of accident and emergency (A&E) services for a psychiatric emergency (measured as number of episodes of liaison psychiatry contact), and number of contacts with crisis resolution and home treatment teams in the year post discharge, plus standardised measures of psychiatric symptom levels, subjective quality of life, social inclusion, hope for the future and strength of social network, measured at end of intervention (4 months post discharge). Adherence to the intervention was assessed using a structured online survey completed by PWs following each contact. Serious adverse events (SAEs), as defined in the trial protocol,41 were recorded and followed up until the end of the 12-month follow-up.
We required a sample of 530 participants, allocated on a 1 : 1 ratio, to detect a reduction of 12% in readmission (from 34% to 22%) in the intervention group compared to the CAU group, with 80% power at the 5% significance level. This calculation allowed for clustering by PW in the intervention group only,44 assuming an intracluster correlation of 0.05 with an average cluster size of 10 participants. We inflated the sample size by 10% to allow for missing primary outcome data at follow-up,45 resulting in a final sample size of 590. All analyses were conducted according to the intention-to-treat (ITT) principle, meaning that all randomised participants with a recorded outcome were included in the analysis and analysed according to the group to which they were randomised. We also estimated the CACE for the intervention on the primary outcome46 (where compliers were participants who had at least two PW meetings, at least one of which was in the community following discharge). The CACE was estimated with a two-stage estimation procedure. In the first stage, a logistic regression of treatment receipt regressed on randomisation was conducted. In the second stage, a Poisson regression of the outcome on treatment receipt was conducted. The analysis was adjusted for the same covariates as the ITT analysis. A bootstrap (1000 samples) was used to obtain bias corrected and accelerated CIs. Subgroup analyses for the primary outcome were pre-specified: ethnicity (any black ethnicity, all other ethnicities); primary diagnosis at index admission (psychotic disorders, personality disorders, other eligible disorders); first language (English, other). Full details of the analyses undertaken are given in the trial protocol. 41
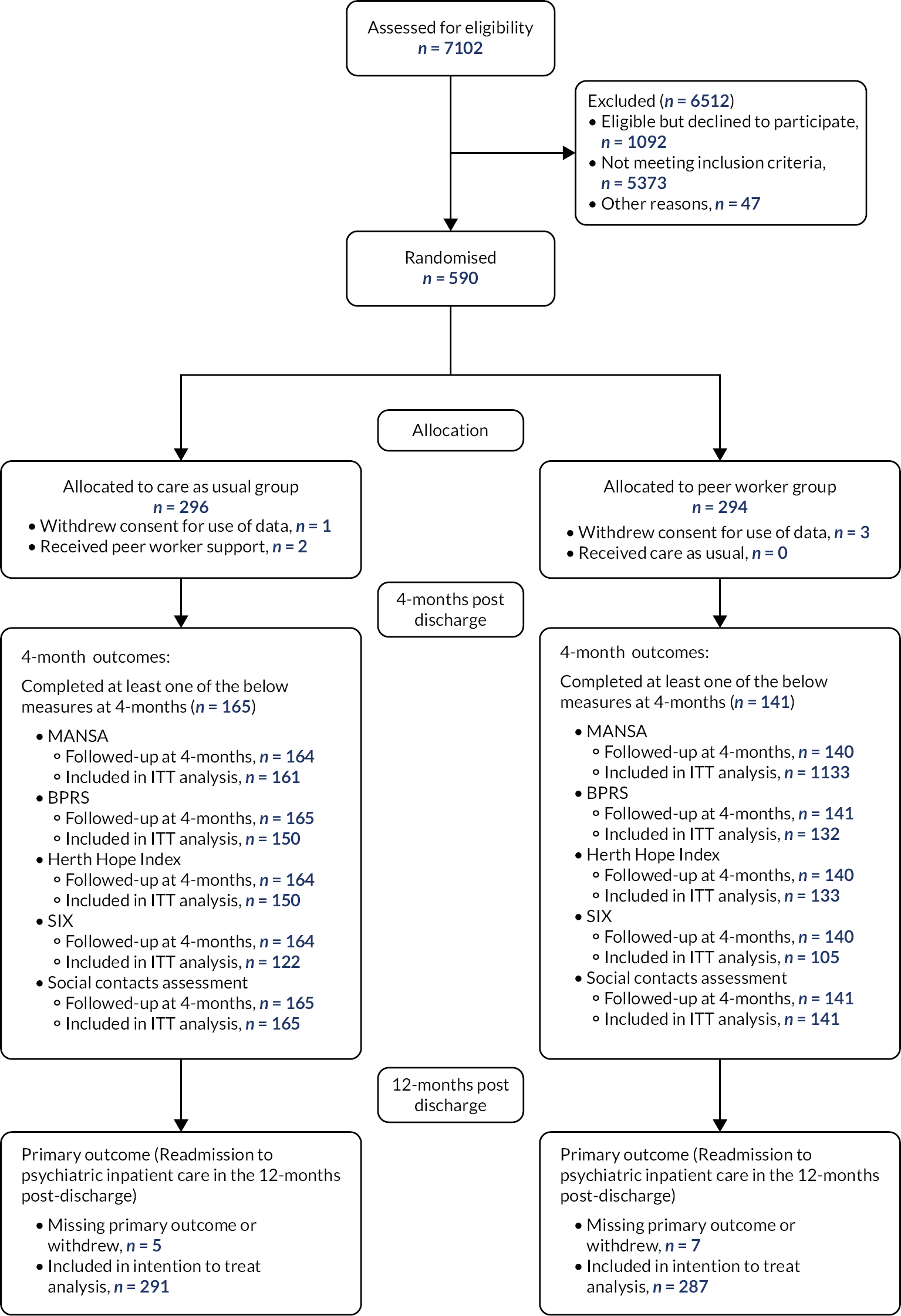
Gillard et al.47
Results for the trial are given here pending peer review and publication of the main trial paper. 47 We note that recruitment into the full trial at additional sites was delayed while we waited for approval for the checkpoint report at end of the pilot trial, and then as some sites secured approvals to employ PWs locally. A seventh site (in addition to the original six) was opened to support recruitment, with recruitment taking 6 months longer than originally planned. The target of 590 participants was successfully recruited, with flow of participants into the study given in Figure 11. Participant characteristics were well-balanced between groups (see Tables 3 and 4).
FIGURE 11.
Flow of participants in the ENRICH trial.
| Baseline characteristics | Number of patients with available data – n (%) | Summary measure | ||
|---|---|---|---|---|
| CAUa (n = 296) | PWb (n = 294) | CAU | PW | |
| Gender – n (%) | 292 (98.6) | 286 (97.3) | ||
| Female | 159 (54.5) | 147 (51.4) | ||
| Male | 130 (44.5) | 137 (47.9) | ||
| Transgender | 2 (< 1) | 1 (< 1) | ||
| Prefer not to say | 1 (< 1) | 1 (< 1) | ||
| Age (years) | 291 (98.3) | 280 (95.2) | ||
| Mean (SD) | 40.0 (13.1) | 39.4 (14.2) | ||
| Median (IQR) | 38 (31–50) | 38 (27–51) | ||
| Sexual orientation – n (%) | 290 (98.0) | 286 (97.3) | ||
| Bisexual | 26 (9.0) | 20 (7.0) | ||
| Gay | 6 (2.1) | 10 (3.5) | ||
| Heterosexual | 232 (80.0) | 239 (83.6) | ||
| Lesbian | 5 (1.7) | 5 (1.7) | ||
| Not completed/declined to answer | 21 (7.2) | 12 (4.2) | ||
| Diagnostic group – n (%) | 295 (99.7) | 291 (99.0) | ||
| F20–29 (schizophrenia, schizotypal and delusional disorders) | 134 (45.4) | 129 (44.3) | ||
| F60 (specific personality disorders) | 61 (20.7) | 58 (19.9) | ||
| Other eligible non-psychotic disorders | 100 (33.9) | 104 (35.7) | ||
| First language – n (%) | 288 (97.3) | 280 (95.2) | ||
| English | 243 (84.4) | 226 (80.7) | ||
| Other | 45 (15.6) | 54 (19.3) | ||
| Ethnicity – n (%) | 293 (99.0) | 283 (96.3) | ||
| Asian/Asian British | 32 (10.9) | 36 (12.7) | ||
| Black/African/Caribbean/Black British | 48 (16.4) | 46 (16.3) | ||
| Mixed/multiple ethnic groups | 18 (6.1) | 30 (10.6) | ||
| Other ethnic group | 5 (1.7) | 8 (2.8) | ||
| White | 190 (64.8) | 163 (57.6) | ||
| MANSAc | 292 (98.6) | 283 (96.3) | ||
| Mean (SD) | 3.9 (1.1) | 4.2 (1.1) | ||
| Median (IQR) | 4.0 (3.2–4.7) | 4.2 (3.4–4.8) | ||
| Objective social outcomes index (SIX)d | 251 (84.8) | 244 (83.0) | ||
| Mean (SD) | 3.2 (1.3) | 3.2 (1.3) | ||
| Median (IQR) | 3 (2–4) | 3 (2–4) | ||
| Herth Hope Index (HHI)e | 280 (94.6) | 275 (93.5) | ||
| Mean (SD) | 33.1 (7.9) | 33.1 (8.1) | ||
| Median (IQR) | 34 (28–39) | 34 (28–39) | ||
| Brief Psychiatric Rating Scale (BPRS)f | 268 (90.5) | 272 (92.5) | ||
| Mean (SD) | 36.6 (10.2) | 34.5 (9.9) | ||
| Median (IQR) | 36 (29–43) | 33 (27–41) | ||
| Pre-index admission characteristics (12 months prior to index admission) | Number of patients with available data – n (%) | Summary measure | ||
|---|---|---|---|---|
| CAU (n = 296) | PW (n = 294) | CAU | PW | |
| Number of admissions to psychiatric inpatient care – n (%) | 293 (99.0) | 291 (99.0) | ||
| 0 | 84 (28.7) | 101 (34.7) | ||
| 1 | 144 (49.1) | 130 (44.7) | ||
| 2 | 39 (13.3) | 35 (12.0) | ||
| 3 or more | 26 (8.9) | 25 (8.6) | ||
| Number of voluntary admissions – n (%) | 255 (86.1) | 258 (87.8) | ||
| 0 | 158 (62.0) | 166 (64.3) | ||
| 1 | 69 (27.1) | 56 (21.7) | ||
| 2 or more | 28 (11.0) | 36 (14.0) | ||
| Number of involuntary admissions – n (%) | 255 (86.1) | 258 (87.8) | ||
| 0 | 154 (60.4) | 161 (62.4) | ||
| 1 | 81 (31.8) | 79 (30.6) | ||
| 2 or more | 20 (7.8) | 18 (7.0) | ||
| Total length of stay over all admissions (calendar days) | 293 (99.0) | 291 (99.0) | ||
| Mean (SD) | 32.7 (48.0) | 28.9 (41.3) | ||
| Median (IQR) | 16 (0–42) | 14 (0–39) | ||
| Number of A&E attendances – n (%) | 293 (99.0) | 291 (99.0) | ||
| 0 | 123 (42.0) | 113 (38.8) | ||
| 1 | 64 (21.8) | 75 (25.8) | ||
| 2 | 37 (12.6) | 43 (14.8) | ||
| 3 or more | 69 (23.5) | 60 (20.6) | ||
| Number of crisis resolution or home treatment team contacts – n (%) | 293 (99.0) | 291 (99.0) | ||
| 0 | 72 (24.6) | 86 (29.6) | ||
| 1 | 45 (15.4) | 30 (10.3) | ||
| 2 | 15 (5.1) | 14 (4.8) | ||
| 3 or more | 161 (54.9) | 161 (55.3) | ||
In the PW group, 136 (47.4%) participants were readmitted to psychiatric inpatient care within 12 months post-index admission, and 146 (50.2%) in the CAU group (see Table 5). The unadjusted risk difference was −3% (95% CI −0.11 to 0.05; p = 0.5070) in favour of the peer support group. The adjusted relative risk of readmission in the ITT analysis was 0.97 (95% CI 0.82 to 1.14; p = 0.6777), and the adjusted odds ratio (OR) was 0.93 (95% CI 0.66 to 1.30). In the CACE analysis, the relative risk of readmission according to the natural indirect effect (RR 0.88, 95% CI 0.76 to 0.99) was lower than from the ITT analysis and was significant. In subgroup analyses, for participants of any black ethnicity the adjusted OR of readmission was 0.40 (95% CI 0.17 to 0.94), while for any other ethnicity the OR was 1.12 (95% CI 0.77 to 1.63; interaction p = 0.0305). No other subgroup effects were found (see Table 6).
| Primary outcome | Number of patients with available data and included in analysis – n (%) | Summary measure | Treatment effect (95% CI) | p-value | ||
|---|---|---|---|---|---|---|
| CAU (n = 296) | PW (n = 294) | CAU | PW | |||
| Readmission to psychiatric inpatient care in the 12 months post dischargea | 291 (98.3) | 287 (97.6) | 146 (50.2) | 136 (47.4) | 0.93 (0.66 to 1.30)b | 0.6777 |
| 0.97 (0.82 to 1.14)c | ||||||
| −0.03 (−0.11 to 0.05)d | 0.5070 | |||||
| Subgroup variable | Number of participants with available data and included in analysis – n (%) | Readmission to psychiatric inpatient care in the 12 months post discharge – n (%) | Adjusted OR (95% CI) | p-value for interaction | ||
|---|---|---|---|---|---|---|
| CAUa (n = 295/296) | PWb (n = 291/294) | CAU | PW | |||
| Ethnicityc,d | ||||||
| Black/African/Caribbean/Black British | 48/48 (100.0) | 46/46 (100.0) | 28/48 (58.3) | 17/46 (37.0) | 0.40 (0.17 to 0.94) | 0.0305 |
| Any other ethnicity | 241/245 (98.4) | 233/237 (98.3) | 117/241 (48.5) | 117/233 (50.2) | 1.12 (0.77 to 1.63) | |
| Diagnostic groupd | ||||||
| F20–29 (schizophrenia, schizotypal and delusional disorders) | 132/134 (98.5) | 128/129 (99.2) | 65/132 (49.2) | 54/128 (42.2) | 0.79 (0.48 to 1.31) | 0.6704 |
| F60 (specific personality disorders) | 59/61 (96.7) | 56/58 (96.6) | 35/59 (59.3) | 32/56 (57.1) | 0.98 (0.45 to 2.11) | |
| Other eligible non-psychotic disorders | 100/100 (100.0) | 103/104 (99.0) | 46/100 (46.0) | 50/103 (48.5) | 1.11 (0.63 to 1.95) | |
| First languaged,e | ||||||
| English | 240/243 (98.8) | 222/226 (98.2) | 124/240 (51.7) | 105/222 (47.3) | 0.88 (0.60 to 1.28) | 0.3055 |
| Other | 44/45 (97.8) | 54/54 (100.0) | 19/44 (43.2) | 28/54 (51.9) | 1.42 (0.62 to 3.23) | |
Observed differences in the secondary outcomes collected at 4 months were small and none were statistically significant (see Table 7). There were no statistically significant differences between the groups in any of the secondary outcomes assessed at 12 months (see Table 8). Adherence to the intervention was assessable in 268 (91.2%) participants with a mean of 1.8 [standard deviation (SD) = 2.9) face-to-face contacts with a PW in hospital, 4.4 (SD = 4.6) post discharge. Assessors were unmasked by 52/306 (17.0%) patients revealing their allocation during collection of secondary outcome data at 4 months (38 in the peer support group, 14 in the CAU group).
| Outcomes | Number of patients with available data and included in analysis – n (%) | Summary measure | Treatment effect (95% CI) | p-value | ||
|---|---|---|---|---|---|---|
| CAU (n = 296) | PW (n = 294) | CAU | PW | |||
| MANSA | 161 (54.4) | 133 (45.2) | 4.1 (1.0)a | 4.4 (0.9)a | 0.17 (−0.01 to 0.36)b | 0.0713 |
| BPRS | 150 (50.7) | 132 (44.9) | 31.7 (10.7)a | 29.5 (9.6)a | −0.59 (−2.70 to 1.52)b | 0.5832 |
| HHI | 150 (50.7) | 133 (45.2) | 32.3 (7.2)a | 33.8 (7.0)a | 0.50 (−0.80 to 1.79)b | 0.4529 |
| SIX | 122 (41.2) | 105 (35.7) | 3.2 (1.0)a | 3.2 (1.0)a | 0.10 (−0.13 to 0.34)b | 0.3778 |
| Social contacts assessment | 165 (55.7) | 141 (48.0) | 3 (1–4)c | 2 (1–5)c | 1.07 (0.85 to 1.34)d | 0.5607 |
| Outcomes | Number of participants with available data and included in analysis – n (%) | Summary measure | Treatment effect (95% CI) | p-value | ||
|---|---|---|---|---|---|---|
| CAU (n = 296) | PW (n = 294) | CAU | PW | |||
| Number of readmissions to psychiatric inpatient care in the 12 months post discharge | 291 (98.3) | 287 (97.6) | 1 (1–2)a | 1 (1–2)a | 0.95 (0.75 to 1.19)b | 0.6413 |
| Number of voluntary admissions to psychiatric inpatient care in the 12 months post dischargec | 253 (85.5) | 257 (87.4) | 1 (0–1)a | 1 (0–2)a | 1.07 (0.77 to 1.48)b | 0.7079 |
| Number of compulsory admissions to psychiatric inpatient care in the 12 months post dischargec | 253 (85.5) | 257 (87.4) | 1 (0–1)a | 1 (0–1)a | 0.88 (0.64 to 1.22)b | 0.4443 |
| Total length of stay over all readmissions (calendar days)c | 291 (98.3) | 287 (97.6) | 57 (27–128)a | 61 (26–99)a | 0.81 (0.51 to 1.29)b | 0.3783 |
| Number of separate episodes of liaison psychiatry contact in hospital A&Ec | 291 (98.3) | 287 (97.6) | 0 (0–1)d | 0 (0–1)d | 1.18 (0.84 to 1.66)b | 0.3351 |
| Number of crisis resolution and home treatment team contactsc | 291 (98.3) | 287 (97.6) | 3 (0–13)d | 2 (0–16)d | 0.90 (0.66 to 1.23)b | 0.5267 |
| Time to first readmission to psychiatric inpatient care (calendar days)c | 291 (98.3) | 287 (97.6) | 107 (46–180)a | 104 (36–201)a | 0.95 (0.75 to 1.20)e | 0.6563 |
There was a total of 67 SAEs reported in the trial (34 in the peer support group, 33 in the CAU group) from 51 participants (26 in the peer support group, 25 in the CAU group). One SAE in the peer support group, an incident of self-harm, was reported as related to the intervention. Number and type of SAEs included 12 deaths, none of which were reported as related to the study.
The trial indicated that one-to-one peer support for discharge from psychiatric inpatient care, offered in addition to CAU, did not have a significant effect on readmission when compared to CAU only. There were neither significant effects on any secondary service use outcomes in the year following discharge nor any reduction in symptom severity or benefit to psychosocial outcomes after 4 months. The CACE analysis indicated that a smaller proportion of participants in the peer support group who received a pre-defined minimal amount of the intervention were readmitted than participants in the control group who – according to the analysis – would also have received the minimal amount of peer support if such support had been offered to them. Additionally, compared to CAU, participants of any black ethnicity in the peer support group were significantly less likely to be readmitted than participants of any other ethnicity (see Table 6).
The study reflects findings from our systematic review of one-to-one peer support in a range of mental health service settings which suggests that, on the basis of pooled data from trials to date, peer support is unlikely to have an effect on psychiatric hospital admission, length of stay in hospital or clinical severity. 38 Engagement in the peer support intervention was low. However, the findings of the CACE analysis, suggesting that participants who engaged better may have benefited from the intervention, raised the question as to why engagement with the intervention was not more complete. We were encouraged that black participants were significantly less likely to be readmitted in the year post-discharge compared to control than those of any other ethnicity (see Table 6). While we need to better understand how and why peer support seemed to work better for this group of participants, this finding offers hope that peer support might help address persistent inequalities. 48,49
Predictors of readmission
A secondary aim of WP4 was to explore predictors of readmission across our sample. Of the 590 participants recruited to the study, EPR data, which provided all service use data, was available for 578 (98%). Of these 578 participants, 282 (49%) were readmitted within 1 year post discharge. Fifty-nine (10%) were readmitted in 30 days or less, 123 (21%) in 90 days or less.
The following variables were tested as predictors of readmission (binary outcome) and time to readmission (time to event outcome): age, gender, ethnicity, diagnosis, SIX, BPRS, Manchester Short Assessment of Quality of Life (MANSA), number of admissions in the previous year, number of compulsory admissions in the previous year, number of A&E attendances in the previous year, compulsory or voluntary index admission, length of index admission. Univariate analysis was carried out using logistic regression to estimate the relationship between each potential predictor and the readmission outcome. Those predictors found to be statistically significant (significance level = 5%) univariately were entered into a multiple logistic regression model. This strategy was followed for the time to readmission outcome using Cox regression.
Diagnosis, BPRS, MANSA, number of admissions in the previous year and number of A&E attendances in the previous year were found to be univariately associated with both outcomes. Number of compulsory admissions in the previous year and type of index admission (compulsory or voluntary) were also significantly associated with time to readmission. However, both variables had more than 10% missing data and so were not entered into the final regression models. All univariate analyses are reported in Report Supplementary Material 2.
In the multiple logistic regression model (n = 529) readmission was associated with higher BPRS (OR 1.03, 95% CI 1.01 to 1.05; p = 0.009) and number of admissions in the previous year (OR 1.32, 95% CI 1.10 to 1.57; p = 0.002). In the multiple Cox regression model (n = 529) shorter time to readmission was associated with higher BPRS [hazard ratio (HR) = 1.01, 95% CI 1.00 to 1.03; p = 0.031] and number of admissions in the previous year (HR=1.24, 95% CI 1.14 to 1.38; p < 0.001). These findings are in line with previous similar analyses (see Table 9). 50,51
| Readmission | Time to readmission | ||||||
|---|---|---|---|---|---|---|---|
| n | OR (95% CI) | p | HR (95% CI) | p | |||
| Socio-demographic and psychosocial variables | |||||||
| Age (years) | 563 | 1.0 (0.98 to 1.01) | 0.429 | 1.0 (0.99 to 1.01) | 0.383 | ||
| Gender | Female | 301 | 1 | 1 | |||
| Male | 264 | 0.9 (0.63 to 1.21) | 0.409 | 0.9 (0.69 to 1.10) | 0.259 | ||
| Ethnicity | Asian | 68 | 1 | 1 | |||
| Black | 94 | 1.0 (0.55 to 1.92) | 0.918 | 1.0 (0.65 to 1.60) | 0.939 | ||
| Mixed | 48 | 1.0 (0.45 to 2.00) | 0.896 | 1.0 (0.55 to 1.64) | 0.863 | ||
| Other | 12 | 2.3 (0.62 to 8.18) | 0.218 | 1.6 (0.74 to 3.50) | 0.228 | ||
| White | 346 | 1.1 (0.68 to 1.87) | 0.689 | 1.1 (0.75 to 1.60) | 0.624 | ||
| Social inclusion (SIX T0) | 488 | 1.1 (0.96 to 1.26) | 0.178 | 1.1 (0.96 to 1.16) | 0.255 | ||
| Quality of life (MANSA) | 568 | 0.9 (0.73 to 0.99) | 0.037 | 0.9 (0.79 to 0.98) | 0.017 | ||
| Clinical and service use variables | |||||||
| Diagnosis | F20–F29 | 260 | 1 | 1 | |||
| F60 (Specific personality disorder) | 115 | 1.7 (1.06 to 2.58) | 0.026 | 1.5 (1.13 to 2.05) | 0.006 | ||
| Other eligible non-psychotic disorders | 203 | 1.1 (0.74 to 1.54) | 0.745 | 1.1 (0.84 to 1.43) | 0.508 | ||
| Severity of symptoms (BPRS T0) | 533 | 1.03 (1.01 to 1.05) | 0.001 | 1.02 (1.01 to 1.03) | 0.001 | ||
| Index admission | Voluntary | 246 | 1 | 1 | |||
| Compulsory | 261 | 0.8 (0.54 to 1.08) | 0.126 | 0.8 (0.59 to 0.98) | 0.033 | ||
| Length of index admission (days) | 578 | 1.0 (1.00 to 1.00) | 0.113 | 1.0 (1.00 to 1.00) | 0.263 | ||
| Number of admissions in the year prior | 578 | 1.4 (1.20 to 1.65) | < 0.001 | 1.3 (1.21 to 1.41) | < 0.001 | ||
| Number of compulsory admissions in the year prior | 510 | 1.3 (0.99 to 1.61) | 0.058 | 1.2 (1.05 to 1.46) | 0.011 | ||
| Number of A&E attendances in the previous year | 578 | 1.1 (1.06 to 1.23) | 0.001 | 1.1 (1.04 to 1.10) | < 0.001 | ||
Health economic evaluation
Our primary economic analysis aimed to evaluate the impact of patient access to peer support for psychiatric discharge on the total cost of NHS mental health service utilisation over a 12-month period following hospital discharge, allowing for the cost of peer support itself.
Secondary economic analyses aimed:
-
to evaluate the cost-effectiveness of peer support based on cost and quality-adjusted life-year (QALY) outcomes observed for trial participants at 4 months post hospital discharge
-
to examine the association between exposure to peer support and wider service utilisation and costs over 4 months post discharge beyond costs attributable to contact with NHS mental health services.
Methods and results for this WP are summarised in Appendix 2. The primary analysis of total costs over 12 months and the secondary cost-effectiveness analysis at 4 months were carried out from an NHS mental health service perspective, though a wider ‘societal’ perspective was taken when analysing non-NHS mental healthcare costs over 4 months. Mental health service contacts for all trial participants were collected from EPRs for 12 months post discharge from the index hospital admission and over 12 months prior to the index admission. Non-NHS mental healthcare costs were collected by self-report at 4 months post discharge, as was health-related quality of life, measured using the EuroQol-5 Dimensions, five-level version instrument. 52 Number, type and length of contacts with PWs were collected using the online contact log completed by PWs after each contact. Total costs per trial participant were calculated using appropriate unit costs (see Appendix 2). All analyses were conducted on an ITT basis using a generalised linear modelling (GLM) with a logarithmic link function. 53 A ‘net benefit’ framework was used54 to evaluate whether the peer support intervention offered a cost-effective alternative to usual care after 4 months post-discharge from the index hospital admission using an appropriate cost-effectiveness threshold. As with the main clinical analysis, missing data from EPRs on service contacts and other patient covariates was not a serious problem; we assumed that it was ignorable and likely to be missing at random. Missing data on self-reported service contacts and quality of life at 4 months were more problematic – as self-report data are likely to be not missing at random, we did not seek to impute values where data were missing.
A cost analysis of mental health service contacts over a 12-month period following discharge from acute inpatient care showed that, on average and accounting for sampling error in the trial data, the addition of peer support to a patient’s care bundle prior to leaving hospital could reduce the average cost of mental health service contacts by more than £2500 per patient. This allows for the additional cost of peer support itself – a mean cost of around £540 per participant. Most of the cost advantage over follow-up was due to reductions in the cost of bed day utilisation. There was a moderate (18%) risk that usual care would be more favourable in cost terms. Over months, and considering patient quality of life outcomes as well as cost, peer support was also found to be cost-effective from an NHS mental health service perspective. This finding is driven in large part by lower total cost of mental health service contacts for trial participants over the first 4 months after leaving hospital. The expected QALY gains associated with peer support were marginal: a 0.002 QALY improvement per participant, equivalent to less than a single day in full health. Compared to the cost of NHS mental health care contacts, there was a relatively weak association between exposure to peer support and the cost of wider community-based and police-related service contacts over 4 months after leaving hospital, with much less pronounced differences in costs between intervention and control participants.
We conclude that peer support delivered to the type of population recruited to this study could lower costs of mental health care use principally arising from bed day utilisation, though there is a moderate degree of uncertainty associated with this conclusion. Based on quality-of-life data and QALY outcomes estimated at 4 months, there is also tentative evidence that this could be achieved without necessarily being harmful to patient outcomes.
Process evaluation – predictors of engagement with peer support
We originally proposed a process evaluation to explore three distinct mechanisms of peer support in our intervention, derived from a change model developed in earlier research:31
-
Peer workers role-model recovery, increasing levels of hope and enabling participants to function well in the community and so avoid hospital admission.
-
Peer workers build strong therapeutic relationships with participants and reduce their experiences of stigma within services, improving engagement with services, increasing planned service use and decreasing emergency service use and compulsory admission.
-
Positive experiences of relationship building with PWs decreases anticipation of stigma, enabling participants to strengthen social networks, and decrease emergency service use and compulsory admission.
The quantitative process evaluation reported here differs from what was planned in the programme protocol given the non-significant findings of the primary analysis. However, as noted in Randomised controlled trial, a CACE analysis indicated that participants who met the criteria for having received a minimal amount of the peer support intervention were significantly less likely to be readmitted in the year post-discharge than a counter-factual group of similar participants who were not offered peer support. With only 62% of participants engaging with the intervention, an understanding of engagement in peer support should be considered as part of a change model for peer support in mental health services. We therefore sought to identify pre-randomisation and pre-discharge predictors of engagement with peer support in the trial.
Methods and results for this WP are summarised in Appendix 3. We included all trial participants randomised to peer support in this analysis. Pre-randomisation and pre-discharge variables were obtained from baseline interviews, EPRs and PW contact logs. Logistic regression was used to model the relationship between the two groups of predictor variables and ‘engaged with peer support’, defined as having had at least two face-to-face contacts with the PW, at least one of which was in the community post discharge.
The change model informing the trial31 indicated that ‘building a trusting relationship based on shared lived experience’ was fundamental to the process of peer support. Our analysis supports that, suggesting that the length of first contact is positively associated with engaging with peer support, and participants who went on to engage with peer support experienced more relationship-building activity in that first contact. We had hypothesised that a longer period of time between joining the study and discharge, and more contacts with the PW during that period, would also support the relationship-building process and therefore engagement. However, not only were more pre-discharge contacts with the PW not associated with engagement, but the longer period pre discharge was associated with non-engagement. It might be that extended uncertainty about discharge arrangements was disruptive of the peer support relationship although we lack data to explain this finding. However, our findings do suggest that both length and quality of the first contact with the PW are key to engagement. (We note that the amount of relationship-building activity in the first contact was significantly associated with engagement when analysed separately – those who engaged with peer support had on average one more relationship-building activity than those who did not engage with peer support; OR 1.48, 95% CI 1.24 to 1.76 – but was no longer significant when included in the regression model, suggesting that length of first session and amount of relationship-building activity might be correlated).
We found that participants who identified as gay, lesbian or bisexual were significantly more likely to engage with peer support than heterosexual participants. This is an important finding given that people who are gay, lesbian or bisexual are more likely to experience mental health problems than the general population. 55 However, we had relatively few participants in this group and did not collect the data needed to explore this finding further. Future research should focus on the experiences of peer support for this group of people.
Process evaluation – peer support and change in mental health services
Given the lack of an effect on our primary outcome we did not explore hypothesised mechanisms explicitly in the qualitative component of the process evaluation. One of the programme objectives was ‘to refine an empirically and theoretically grounded model that explains how peer support interventions impact on outcomes for service users post-discharge’. To do this we explored, in depth, the peer support change model informing the trial31 from the perspective of trial participants and PWs.
We conducted a qualitative interview study using a ‘co-production’ approach designed to integrate the full range of perspectives on the research team – clinical, academic and experiential – into the interpretive process (see below). 56 We held a workshop with our LEAP to refine our original change model31 (see Appendix 1, Figure 14).
Service user participants were a subsample of trial participants allocated to peer support, interviewed at end of intervention. We aimed to recruit five trial participants at each of the seven sites and used a sampling framework to guide selection (see Appendix 2, Table 14), developed with the service user researcher team. PW participants were PWs delivering peer support as part of the trial, interviewed shortly after finishing training, and at 4 and 12 months after they had been in post. Interview schedules were informed by the literature on peer support cited above, including our earlier research on the processes31 and principles of peer support,57 the output of the LEAP workshop described above (see Appendix 1, Figure 14) and the experiential knowledge of members of the service user researcher team. All interviews were conducted by service user researchers, and they were audio recorded and transcribed verbatim.
Analysis took a hybrid inductive/deductive approach58 in two main stages. In the first stage we took a co-produced approach as a multidisciplinary team to developing, inductively, a semantic-level59 or descriptive thematic framework. Following processes that we had developed previously,56 members of the team, including service user researchers, clinical academics and social scientists, individually undertook preliminary analyses of a selection of interview transcripts. We then presented our emerging ideas to each other, with illustrative examples of data (verbatim quotes), while, through discussion, we combined and collapsed thematic ideas into coherent categories to produce a provisional coding framework that captured the diversity as well as shared aspects of our interpretation. We repeated this process a second time working with a further set of transcripts, refining the framework. The service user researcher team then used the framework to code the full set of interview transcripts, further refining the framework where transcripts contained data that did not fit existing codes. In the second, more deductive stage of the analysis process, we took a critical interpretive approach,60 seeking to use data from our interviews to critique and refine the change model that informed the research. A service user researcher (RF), working with the lead author (SG), identified codes in the final coding framework that related to each of the components in the revised change model (see Appendix 1, Figure 15), before re-coding those data to themes that reflected, or challenged and refined the components of the original change model. We retained inductive space in this process to identify new themes, enabling us to produce a final change model for peer support for discharge from inpatient psychiatric care.
A total of 39 trial participants were interviewed, with characteristics of the sample indicated in Report Supplementary Material 3, Appendix 2, Table 14. A total of 32 PW participants were interviewed across the seven sites after training, 20 of whom were interviewed again at 4 months and 21 at 12 months (see Appendix 4, Table 25). The coding framework developed following the first, inductive stage of the analysis process is given in Report Supplementary Material 3, Appendix 2, Table 16. The final, adapted change model for peer support for psychiatric discharge is shown in Report Supplementary Material 3, Appendix 1, Figure 16. Report Supplementary Material 3 reports data that illustrate each of the themes in the final change model, summarised in brief below.
-
Building trusting therapeutic relationships
As described in our original model, building a trusting, therapeutic relationship was the essential first step for successful peer support to take place.
-
Unique role – Participants described the PW role as being more informal and relaxed in comparison to other professional roles. PWs were seen as more authentic, less judgmental and willing to explore topics that others seemed uncomfortable with (e.g. experiences of psychosis or relationship problems). Authenticity and trust were conveyed through sharing lived experience (of mental illness and personal life); support peers (SPs – the trial participants) commented that PWs persevered and never gave up on them.
-
Unique relationship – Participants described the relationship they shared as unique, equal and non-directive. Communication was open, honest and non-judgmental so that SPs felt that they could truly be themselves and were able to say whatever they needed as power in the relationship felt balanced. The relationship had boundaries that provided a safer, more neutral space than with friends or family.
-
Whole-person approach – PWs took a whole-person approach towards each SP and the activities they did together. This included getting to know the individual without a focus on mental health, and the opportunity for mutual enjoyment and to explore interests together. PWs supported people with a variety of difficulties, including relationship problems, financial concerns and healthy routines.
-
Connecting socially
Once a therapeutic relationship had been established, participants described how PWs supported them towards living and functioning well in the community.
-
Embodying recovery and hope – SPs often described PWs as embodying successful recovery and hope, by coping well with symptoms or showing resilience through leading a successful life in spite of mental health. Sometimes PWs literally embodied connecting by going with the SP the first time they tried out a new activity.
-
Connecting to people – Participants described feeling more comfortable around other people since taking part in the peer support, which motivated them to socialise more and make new friends. PWs encouraged SPs to make healthy connections, either by motivating people to make new friends, or by supporting them to identify and avoid negative relationships.
-
Adapting back to society – Peer support subtly supported the process of adapting back to everyday life, whether this meant relearning appropriate cultural/societal norms or learning helpful daily living skills. These processes occurred through a combination of active guidance, renegotiating boundaries in the relationship or breaking complex social processes down into achievable steps.
-
Changing attitudes to community resources – Participants described increased confidence and motivation to try new activities, a desire to have more structure in daily living, confidence to go out and cope independently and to explore hobbies and interests.
-
Tailored recommendations – SPs valued and trusted the personalised recommendations that their PWs made and were more likely to try suggestions from PWs even if other people had previously made the same suggestions.
-
Interacting with services
Participants described the different ways that they felt towards, and used, statutory services since taking part in peer support, including increased willingness to use statutory services.
-
Role modelling interactions with statutory staff – PWs seemed to play an important role by role modelling communication with staff. SPs described feeling more able to talk to ward and community staff since the peer support.
-
‘Bridging the gap’ – Peer support increased communication and helped to build trust between SPs and their teams. PWs were often trusted to liaise with staff from statutory services on behalf of their SPs, thereby bridging the gap in communication.
-
Intrapersonal changes to ‘navigate the system’ – Participants described feeling more knowledgeable and confident about who to contact and where to go for support since spending time with their PW, whether that was statutory or voluntary services.
-
Social functioning
-
Intrapersonal changes towards others – SPs felt trust and motivation to make and maintain new relationships; they described wanting to go out more to be around people, joining groups and enjoying shared time with people.
-
Increased use of community resources – SPs were often more likely to explore community resources available to them; joining clubs, taking up hobbies and enrolling at colleges.
-
Intrapersonal changes towards self and future – Many participants described positive changes in their feelings of confidence, experienced more hope about the future, felt recovery was possible, described happiness and having more trust in others (including professionals).
-
Service use
-
Feelings towards services – SPs described having a better understanding of services, including how to navigate them if needed, as well as feeling they could trust and talk to staff members from services more easily since the peer support.
-
Service use – Participants often described having more knowledge and ability to use services since the peer support sessions. Some described using additional community services that they had learned about through peer support, such as voluntary sector support groups.
-
Barriers
-
Temporality – Many participants felt that the peer support did not last long enough. There were many examples of SPs saying that they had gone back to their ‘old ways’ since the peer support had finished. Many PWs agreed that further work could be achieved with more time.
-
Environmental and practical barriers – A variety of barriers were described, from ward environments to delayed discharge and illness severity. Some barriers were specific to statutory service culture, such as role confusion and integration into existing multidisciplinary team cultures, acting as a barrier to PWs’ ability to act as a link between SPs and statutory services.
-
Choice and control
Where the therapeutic relationship was strong, and the processes above were in place, then SPs’ overall sense of choice and control seemed to be increased, positively mediating processes of peer support.
-
Choice and control – Many SPs appreciated having choice and control during the peer support sessions, including feeling less pressure to talk if they felt uncomfortable.
-
Lack of choice and control – A lack of choice and control was experienced when the peer support relationship came to an end, despite endings happening gradually and with notice. Some SPs described feeling sad when the sessions ended, others a dependence on their PW.
-
Distinctiveness of peer support
Participants often made sense of peer support by comparing it to statutory care they had received.
-
Interpersonal interactions – Participants experienced a different approach to communication, empathy and relationship boundaries with their PWs compared to interactions with other staff.
-
Practical – Peer support compared favourably with other care that SPs had received, including: appointment length, waiting time, location, modality (text/call if wanted), contacts in between appointments and a lack of fixed agenda or measurement tools.
-
Confidentiality understood differently – Many SPs indicated that they trusted their PW to maintain confidentiality more than other professionals. The fact that PWs were not integrated into multidisciplinary teams was valued by some SPs as ensuring that confidentiality was maintained.
We note that interviews report largely positive experiences of peer support, attribute change to engaging in peer support and report a number of positive outcomes, personally, socially and in relation to mental health services. There was little indication that peer support was not well implemented, as we had planned it, although there could be practical barriers to providing and receiving peer support. The degree of choice and control people were able to exercise in the way that made use of peer support seemed to mediate the benefits of peer support for some people. We conclude that the detailed change model we develop here – see Report Supplementary Material 3 – improves on our original model31 and is potentially useful in informing the development of future peer support interventions and mental health services, and in the design of evaluations of peer support.
Work package 5 Studying the impact of peer support on peer workers
The objective of WP5 was to explore the impact of working as a PW on PW’s well-being and employment outcomes. We asked the following questions:
-
What is the impact of working as a PW on well-being and employment outcomes for PWs?
-
How do PWs and PWCs understand the impact of peer working on PW’s well-being and their ability to fulfil the role?
This was a mixed method, longitudinal study using standardised measures of outcome, structured questionnaires and semi-structured qualitative interviews with all 32 PWs who provided peer support in the trial. The methods and results for WP5 are summarised in Appendix 4. Measures of well-being and employment-related outcomes were collected after PWs had completed their training, and after they had been working in the PW role for 4 and 12 months. In-depth qualitative interviews about PWs’ experiences of the role were also conducted at each timepoint. Descriptive statistics for each outcome were compared by inspection with appropriate population norms. Paired t-tests were used to examine change in outcomes over time. Qualitative data were first analysed thematically as described in Process evaluation – peer support and change in mental health services above, contributing to the development of the codebook shown in Appendix 2, Table 16. Data were synthesised by exploring convergence and divergence between datasets,61 using qualitative interview data to illuminate quantitative findings or to elucidate tensions between analyses.
Peer workers in our study had well-being and employment-related outcomes that were similar to, if not slightly higher than, norms for other healthcare workers (and in particular, they were less burnt out) – reflecting findings among PWs in the USA62 and Australia63 – over the course of a year. PWs felt empowered by the role and that it had brought a new meaning and purpose to their lives, reflecting important aspects of wellness associated with peer support work in other research. High levels of satisfaction with the job were associated with pay and working conditions as well as a personal sense of satisfaction in and enjoyment of the work. For PWs in our study, at a rough estimate, sickness absence was around 4%, comparable with the 6% for all mental health staff in the NHS in the UK and certainly less than the 22% reported for all PWs in the NHS. 64
There were significant, small-to-medium reductions in some outcomes after PWs had been in post for around 4 months (well-being, personal satisfaction, satisfaction with workload and satisfaction with prospects) and a similar increase in burn out, although these changes were not maintained at 1 year. A US longitudinal study with PWs in veterans’ mental health services similarly observed an initial increase in burn out (at 6 months) that was not maintained at 1 year. 62 Qualitative data in our study suggest that initial positive scores, perhaps buoyed by the optimism associated with taking on a new role, might be tempered somewhat when the realities of the job sink in, but that as PWs become further accustomed to the role there is no continued decline. The implication of these findings for practice is that organisations employing PWs need to ensure that support and supervision, both practical and emotional, is in place to enable PWs to successfully adjust to the demands of the role. At 1 year, PWs remained worried about their career prospects, with many fixed-term contracts about to come to an end, while satisfaction with training was also lower, suggesting that ongoing support and career development for PWs was under-developed.
Peer workers in our study felt well-supported in the role, with supervision from PWCs and a sense of peer support from fellow PWs highly valued. In our trial, PWs were managed within their own peer support team, working across inpatient and community mental health services as necessary, rather than being embedded as part of the complement of the ward or community clinical team. This potentially circumvented many of the challenges associated with integrating into the clinical team that have been identified elsewhere. 65,66 However, the drawback of this arrangement was that PWs could feel that communication was poor with clinicians also working with the people they were supporting, leading to misunderstandings about what their role was25 and hampering their ability to provide the best possible support.
Patient and public involvement in the research
Patient and public involvement is described throughout this report. A number of co-investigators brought a service user researcher or PW perspective to the study team, and service user researchers were employed to contribute to the ongoing development of the study and to collect and analyse data, reflecting the research team’s track record in co-producing research from a range of clinical, academic and experiential perspectives. 56 Our approach to co-producing analysis of qualitative data is reported in Process evaluation – peer support and change in mental health services, while service user researchers also played a key role in the development of the fidelity measure reported in WP2. Service user researchers reflected that the approach they took to trial recruitment, disclosing their lived experience, enabled potential trial participants to feel comfortable and better able to make an informed decision about participation in the research, enhancing recruitment to the trial and enabling us to successfully recruit to target. We put comprehensive measures in place to support service user researchers, including group and individual reflective spaces provided by co-investigators who brought a wealth of expertise as highly experienced service user researchers, and a clinically-led supportive group space that was available during the WP4 trial. A LEAP met regularly to ensure that an experiential perspective informed the programme throughout, especially in developing the intervention (WP1) and the qualitative component of the process evaluation (Process evaluation – peer support and change in mental health services). LAGs, incorporating service user and PW perspectives, played a key role in developing the intervention (WP1). See Table 10 in Appendix 1 for details.
Goldsmith et al.67
We undertook novel work in incorporating experiential knowledge into the design and conduct of a RCT. In this paper we explore how service user researchers on the team and our LEAP, alongside clinicians and academics, contributed to key decisions in the design of the trial including: (1) identification of the trial population; (2) choice of psychometric measures and outcomes; (3) development of the trial statistical analysis plan (the LEAP worked with the trial statisticians and other members of the research team in defining minimum level of engagement in the intervention for the CACE analysis and in prioritising subgroups). The paper explores tensions between perspectives, and how these were resolved and informed decision-making, using reflective accounts from a range of team members.
Foster et al. (in development)
A second paper, currently in development, explores in-depth the experiences of service user researchers working on a RCT and in particular the tensions between the standardised demands of the methodology and the experiential knowledge that service user researchers brought to recruitment and data collection processes. A reflective log kept by service user researchers is systematically analysed, as is an additional set of interviews with trial participants about their experiences of recruitment, consent and data collection as part of enrolment to the trial. Experiences of support provided to service user researchers is also considered.
We reflect critically on patient and public involvement (PPI) in the programme. The abstract to this report summarises PPI in the programme alongside a summary of study aims, methods, results and conclusion. Clear indication is given of the theoretical underpinning to PPI in the programme, based on concepts of co-production in research56 and constructs of experiential knowledge. 33 In each work package the level and type of PPI involved, and who is involved, is specified. Capturing or measuring of PPI in the programme was limited. We refer above to one paper where we use a critical reflective approach to explore the impact of PPI on decision-making in the trial,67 and another paper still in development analysing a reflective log kept by service user researchers on their role in the trial and additional questions asked of trial participants about their experiences of recruitment to the trial. We did not undertake an economic assessment of PPI in the programme. We briefly consider how the methodological constraints of a clinical trial limit the space for meaningful PPI once the trial is underway, while noting the impact of PPI on development of the trial intervention. Our reflection on the impact of PPI on shaping key trial parameters offers potential contribution to theory. Our key learning from the programme is around ensuring that there is meaningful PPI at the earliest stage in trial protocol development.
Discussion
Our trial offers aclear and consistent indication that one-to-one peer support in addition to CAU did not have a significant effect on readmission as the primary outcome, or on any secondary outcome, including number of admissions, days in hospital, time to (first) readmission or emergency or crisis service use in the year following discharge. There was also no reduction in severity of psychiatric symptoms or benefit to psychosocial outcomes after 4 months. While the health economic analysis indicated some cost savings for peer support compared to control (and marginal gain in QALYs), these are modest.
However, the CACE analysis indicated that participants in the peer support group who had at least two peer support contacts, at least one of which was in the community post-discharge, were less likely to be readmitted than participants in the control group who might also have received this level of peer support if it had been offered to them. In addition, participants of any black ethnicity in the peer support group were significantly less likely to be readmitted than patients of any other ethnicity compared to control (see Table 6). Our trial addresses some of the methodological weaknesses of trials of peer support to date, as noted in the background section to this report,22,23 including robust procedures for concealment of allocation from assessors, complete reporting of outcomes and low levels of attrition at the primary endpoint, resulting in a robust primary analysis.
These findings reflect meta-analyses in our systematic review which suggest that peer support is unlikely to have an effect on psychiatric hospital admission, length of stay in hospital or clinical severity. 37 The review did indicate a modest positive effect on self-reported recovery and empowerment, however at the time we designed our trial, literature was indicative of potential impact on admission. Review findings therefore indicate the potential impact of peer support for discharge on psychosocial outcomes that were not assessed in our trial.
Level of engagement with peer support in the trial was arguably low, with 62% of participants in the peer support group having at least two contacts, at least one of which was in the community, and an overall mean of 6.2 face-to-face contacts per participant compared to a planned total of 14 contacts. However, our qualitative process evaluation indicated a high level of positive feedback on the peer support and no indication that the intervention had been implemented poorly. Fidelity scores suggested that peer support was well implemented at all sites and, while there was some inconsistency in delivery scores, there were no sites where fidelity of delivery was lower throughout the trial. We also bear in mind that choice and control over engaging with peer support was identified as a key principle underlying peer support,57 with peer support an offer rather than a prescription. A clinical trial, by definition, estimates the effect of an offer of an intervention and as such we consider this an important finding, rather than a limitation of the study.
There may be multiple reasons why over a third of participants chose not to take up the offer. First, participants might not have had an opportunity to establish a good relationship with their PW prior to discharge. Second, we recruited participants who were at high risk of readmission (i.e. people with a recent history of admissions,6 with over half of our sample having been admitted involuntarily prior to recruitment; Appendix 1, Table 10), who might have found it particularly hard to engage with peer support at the point of discharge. Our intervention allowed a high degree of flexibility in the activities that took place, and a more structured, manualised approach might have better met the needs of this group of people.
Nonetheless, as noted above, findings of the CACE analysis suggested that participants who did engage with more peer support may have benefited. Our quantitative process evaluation indicated that length of first session of peer support (and amount of relationship-building activity that took place in that first contact) was predictive of higher levels of engagement. Interestingly, matching of PW and the person they supported by gender, ethnicity or diagnostic group was not predictive of higher engagement. Our qualitative process evaluation refined our formative model of the mechanisms of peer support,31 with interview data from PWs and the people they supported offering good evidence to inform guidance and training to improve engagement with peer support.
We also note that participants of any black ethnicity were more likely to benefit from peer support compared to people not offered peer support than those of any other ethnicity. This is important because being of black ethnicity is a predictor of psychiatric readmission,49 and black people are over-represented in acute mental health care compared to the general population. 48 The sample size for the subgroup analysis was small so this finding should be treated with caution, but it offers a strong rationale for further research in this area.
Finally, we found in our PW impact study that well-being and employment outcomes were largely consistently good for PWs in the study, with levels of sick leave lower than indicative norms for PWs in the NHS in England generally. 64 PWs felt safe and well-supported in the role, benefitting from supervisors who were experienced PWs themselves, and from being part of stand-alone PW teams based alongside, rather than within, clinical teams. These findings offer valuable insight in optimal implementation of peer support as it is rolled out in the UK and beyond.
Reflections on the success of the programme
The main achievement of this programme is the successful, full recruitment to what is, to date, the largest trial of one-to-one peer support in mental health services internationally. Having completed a high-quality trial, we have made a major contribution to the evidence base for peer support in mental health services. Reflecting our systematic review and meta-analysis, the trial suggests more generally that peer support in mental health services should not be commissioned with the intention of impacting clinical outcomes such as hospitalisation and psychiatric symptoms. Nonetheless we successfully developed a comprehensive, theoretically and empirically grounded handbook and training programme for peer support in mental health services. Our CACE analysis, predictors of engagement study and ethnicity analysis all suggest the potential for the intervention to be effective for high-need groups. We also reflect that this is the first formal cost-effectiveness study of peer support in mental health services and so begins to fill that important gap in the evidence base.
Other elements of the programme make important contributions to the international literature on the implementation of peer support into mental health services. Our qualitative process evaluation provides detailed insight informing the refinement and further development of mental health peer support interventions, adding substantially to the still limited literature on the mechanisms and processes of peer support. This is complemented by our impact study which makes a novel contribution to an emerging literature by observing longitudinally, both quantitatively and qualitatively, the occupational impacts of working in a peer support capacity. Our fidelity study also offers a first in developing a reliable measure of fidelity to peer support principles in peer support interventions.
A further major success of the programme has been the comprehensive integration of experiential knowledge, from service user researchers and people involved in peer support, into the ongoing development and conduct of the programme, as reflected on above, ensuring that our findings respond to and offer insight into the priorities of people who receive care from mental health NHS trusts.
Limitations of the research
Our trial demonstrated strengths that had been noted as lacking in the existing evidence base. 22,23 These include robust procedures for randomisation and concealment of allocation from assessors, complete reporting of outcomes and low levels of attrition at the primary end-point. Completeness of primary and secondary outcomes data on the use of healthcare services was 99% – we had anticipated 90% – adding power to analyses. Conversely, our sample size calculation had assumed a readmission rate in the population of 34%, the observed readmission rate of nearly 50% overall therefore resulting in some reduction in statistical power. However, we note that our results are consistently negative with the sample size target having been met, resulting in a robust primary analysis. While the data obtained from clinical records were complete for almost all patients, we failed to interview around 48% of patients face to face at 4-month follow-up. Sensitivity analyses suggested that these data were unlikely to be missing at random, impacting the confidence we might have in our analysis of secondary, psychosocial outcomes.
We note that the economic analysis at 12-month follow-up was not designed to consider participant outcomes needed to facilitate a broader assessment of cost-effectiveness. As such, uncertainty as to whether the reduction in total costs associated with peer support over 12 months was achieved without any detriment to participant outcomes and quality of life over that period remains uncertain. Reduction in the cost of mental health service contacts were also found to be concentrated in the right tail of the cost distribution. While baseline adjustments to comparison were made, including allowance for the total cost of mental health care received over 12 months prior to index admission, it is possible that adjusted comparisons and randomisation did not adequately balance out differences between the trial arms in terms of factors driving lengthier and more costly admissions to hospital. About half of self-reported, non-mental health service contacts and quality of life data at 4 months were missing due to patients not being interviewed at follow-up. As self-report data are likely to be not missing at random, these analyses may have been subject to bias.
Finally, our impact study, with its relatively small sample, was weakened somewhat by data that were often incomplete at our two follow-up timepoints, limiting the power of our analyses and our ability to explore possible associations between outcomes, necessitating further confirmatory research.
Conclusions from the programme
In conclusion, this programme demonstrated that one-to-one peer support for patients at risk of readmission, offered prior to discharge from inpatient psychiatric care in addition to CAU, was not superior to CAU alone. The trial added our support to systematic review of peer support in a range of mental health service settings, indicating that peer support is not likely to impact significantly on psychiatric admission, days in hospital or severity of symptoms.
Experience of the intervention was largely very positive – there were few suggestions that peer support was not implemented as planned – and fidelity to principles underpinning peer support was generally high. Nonetheless, a large minority of people offered peer support chose not to engage with their PW. We conclude on the balance of evidence from across our programme that peer support should be carefully tailored to specific groups of people, including people from different black and minority ethnic communities, in order that the benefits of peer support, including to psychosocial aspects of care, are optimised.
Recommendations for future research
Our trial indicated that peer support for discharge, as we had designed it, was not superior to CAU. However, our CACE analysis indicated that the intervention was likely to have had an effect for participants who engaged in a minimum amount of peer support, and our study identifying predictors of engagement began to elucidate that. We may also have targeted a group of patients who found it particularly hard to engage with peer support at a difficult point in the care pathway and/or whom PWs found challenging to support. Taken together, these findings suggest that further research is needed to optimise implementation of peer support for discharge for this group of people.
Lesbian, gay and bisexual participants were more likely to engage in peer support, warranting further study to identify how peer support might address a need for these groups. Subgroup analysis also indicated that black participants were significantly more likely to benefit from the intervention than participants of any other ethnicity compared to control, although findings suggested that matching PWs and trial participants by ethnicity was not predictive of greater engagement in peer support; it was peer support provided ‘across difference’ that was successful in having this positive effect. Further research is needed to understand how and why this group benefited, especially given inequalities in mental health care experienced by black people. 48,49 In addition, while subgroup analyses did not indicate differences in outcome in relation to diagnostic group, our qualitative process evaluation did suggest that some participants felt that the benefits of peer support might have been enhanced by sharing of experiences and insight around specific experiences of mental health or of using specialist mental health services, indicating potential value in considering adaptation of the intervention to particular clinical settings. Our predictors of readmission analysis reflected research from elsewhere indicating that people with a diagnosis of personality disorder were more likely to be readmitted compared to people with other diagnoses,6 so it might be important to consider the potential role of peer support for this group of people.
Our systematic review and meta-analysis were indicative of modest but significant improvements in individual recovery and empowerment for peer support, compared to CAU – outcomes that we did not measure in our trial. In the trial we observed a small positive effect of peer support on subjective quality of life, but low rates of follow-up impacted statistical power. As such, the possibility remains that peer support in mental health services might offer benefits to psychosocial outcomes. We also established in our review that it was viable to analyse associations between the way in which peer support is implemented (including organisational support provided for peer support) and outcome, with our impact study indicating the importance of ongoing training and support to PWs. Further research, building on our process evaluation and impact studies, might usefully explore and establish how both psychosocial outcomes and implementation variables in the delivery of peer support are assessed in future evaluations of peer support in mental health services.
We note that further testing of our fidelity index, for example through a confirmatory factor analysis, might provide additional evidence of the validity of the index. This might be undertaken were the index to be applied to a larger sample in future studies. While consideration of fidelity in our trial hinted at possible association between fidelity score and outcome in some sites, to establish properly construct validity for the index it would be necessary to explore, robustly, the relationship between fidelity scores and outcomes that might be expected to be associated with fidelity. Again, this might be undertaken as part of further research to fully establish the psychometric properties of the index, perhaps pooling data from a number of studies with similar populations.
As has been noted, confirmation of findings of our impact study in relation to well-being and occupational outcomes for PWs might usefully be explored in a larger population. There is an opportunity to build on the qualitative component of the impact study to identify ongoing training and career development needs for PWs once they are in post, and to establish an organisational model that optimises the potential for peer support delivered either alongside or integrated into the multidisciplinary clinical team.
Finally, we would recommend that researchers working from an experiential perspective play a leading role in peer support research going forward, ensuring that future research is informed by the experiences, insights and priorities of people engaged in peer support.
Implications for policy and practice
The main implication of the programme, taken as a whole, for policy and practice is that peer support for discharge should not be commissioned with the expectation that it will significantly reduce readmission for patients at risk of readmission (i.e. those with previous admissions), although a modest reduction in days spent in hospital in the year post-discharge for those offered peer support (compared to control) does indicate a cost-saving for service providers of about £2500 per person.
The results of our systematic review indicate that one-to-one peer support in mental health services should not be commissioned with the expectation that it will significantly reduce hospitalisation (admissions or days in hospital) or improve clinical outcomes (symptoms). However, when considering the implications of all the evidence considered in our review, we suggest that decisions about implementing peer support in specific clinical contexts should be driven by subsequent systematic reviews that are focused on particular clinical populations. Results of our review do indicate that one-to-one peer support might be commissioned with the expectation that it improves individual recovery and empowerment (and potentially also strength of social network where peer support is provided in addition to CAU). The same caveat applies – that subsequent systematic reviews focused on particular populations are necessary to confirm these findings in specific clinical contexts.
Our programme is indicative of the potential of peer support as a strategy for reducing health inequalities. We found that peer support was significantly more likely to be of benefit to black service users at discharge compared to service users of other ethnicities, and that lesbian, gay and bisexual service users were most likely to engage in peer support once it was offered. These findings imply that mental health service providers might, subject to the best available evidence around targeting and tailoring peer support, consider implementing peer support as an approach to improving access, experience and outcomes of mental health care for specific disadvantaged populations.
Finally, our review, impact, fidelity and process evaluations all lend support to suggestions made elsewhere in the literature that the effectiveness of peer support is associated with how well PWs are supported at an organisational level. The implication for practice is that mental health service providers make use of the best available evidence on additional training for PWs once they are in post, career development pathways for PWs, and should consider how best peer support might work alongside or within clinical teams. We note the central role that experiential knowledge played in the development of our peer support intervention, implying that people directly involved in providing and making use of peer support might play a leading role in optimising the development and delivery of peer support going forward.
Acknowledgements
This report is dedicated to the late Ruth Chandler. Ruth was one of the originators of this programme and brought a tireless energy and commitment to the research. She was also one of the UK’s leading advocates of service user involvement in research and is sorely missed by our research team and many other people besides.
We would like to thank our participants for their time and for allowing us to intrude on their lives, and to acknowledge the spirit and enthusiasm of our PWs, and the expertise and dedication of our PWCs.
We would also like to acknowledge the principal investigators, clinical studies staff and clinical teams, as well as the LAGs who supported the programme at each site.
We would especially like to thank our Programme Steering Committee, chaired by Professor Helen Killaspy, our Data Management & Ethics Committee, chaired by Professor Martin Webber, and the members of our LEAP for their collective wisdom and support.
Contributions of authors
Steve Gillard (https://orcid.org/0000-0002-9686-2232) led this programme of research, conceived the programme, was part of the programme management team, undertook systematic reviews, led intervention development and undertook qualitative analyses.
Rhiannon Foster (https://orcid.org/0000-0003-3490-0624) undertook systematic reviews, led intervention development, led participant recruitment and data collection and undertook qualitative analyses.
Sarah White (https://orcid.org/0000-0003-2468-6193) conceived the programme, undertook systematic reviews and statistical analyses for the fidelity study, process evaluation and impact study.
Andrew Healey (https://orcid.org/0000-0003-2013-3161) conceived the programme, was part of the programme management team and undertook health economic analyses.
Stephen Bremner (https://orcid.org/0000-0003-0790-7070) conceived the programme, was part of the programme management team and undertook trial analyses.
Sarah Gibson (https://orcid.org/0000-0002-7595-0874) conceived the programme, was part of the programme management team, led on patient and public involvement in the programme, co-ordinated the LEAP and provided support to intervention development.
Lucy Goldsmith (https://orcid.org/0000-0002-6934-1925) led participant recruitment and data collection and undertook the CACE analysis.
Mike Lucock (https://orcid.org/0000-0003-0968-5475) conceived the programme.
Jacqueline Marks (https://orcid.org/0000-0002-1235-8945) managed the programme, including the trial, was part of the programme management team, undertook systematic reviews, led intervention development, provided additional support to implementation of the intervention, led participant recruitment and data collection and undertook qualitative analyses.
Rosaleen Morshead (https://orcid.org/0000-0003-0741-0750) undertook systematic reviews, led participant recruitment and data collection and undertook qualitative analyses.
Akshaykumar Patel (https://orcid.org/0000-0002-0640-9937) undertook trial analyses.
Shalini Patel conceived the programme and provided support to intervention development.
Julie Repper (https://orcid.org/0000-0001-6748-6402) conceived the programme and provided support to intervention development.
Miles Rinaldi (https://orcid.org/0000-0003-3822-1434) conceived the programme and provided support to intervention development.
Alan Simpson (https://orcid.org/0000-0003-3286-9846) conceived the programme and provided support to intervention development.
Michael Ussher (https://orcid.org/0000-0002-0995-7955) conceived the programme and provided support to intervention development.
Jessica Worner conceived the programme, provided support to intervention development and additional support to implementation of the intervention.
Stefan Priebe (https://orcid.org/0000-0001-9864-3394) provided mentorship, conceived the programme and was part of the programme management team.
Ruth Chandler conceived the program, led on patient and public involvement in the programme, co-ordinated the LEAP and provided support to intervention development.
All authors contributed to, read and approved the final version of this report.
Publications
Gillard S, Banach N, Barlow E, Byrne J, Foster R, Goldsmith L, et al. Developing and testing a principle-based fidelity index for peer support in mental health services. Soc Psychiatry Psychiatr Epidemiol 2021;19:1–9. URL: https://link.springer.com/article/10.1007/s00127-021-02038-4
Gillard S, Bremner S, Foster R, Gibson SL, Goldsmith L, Healey A, et al. Peer support for discharge from inpatient to community mental health services: Study protocol clinical trial (SPIRIT Compliant). Medicine 2020;99(10):e19192. URL: https://journals.lww.com/md-journal/Fulltext/2020/03060/Peer_support_for_discharge_from_inpatient_to.13.aspx
Gillard S, Bremner S, Patel A, Goldsmith L, Marks J, Foster R, et al. Peer support for discharge from inpatient mental health care versus care as usual in England (ENRICH): a parallel, two-group, individually randomised controlled trial. The Lancet Psychiatry 2022;9(2):125–36. URL: www.sciencedirect.com/science/article/pii/S2215036621003989
Gillard S, Foster R, Gibson S, Goldsmith L, Marks J, White S. Describing a principles-based approach to developing and evaluating peer worker roles as peer support moves into mainstream mental health services. Ment Health Soc Incl 2017;21(3):133–43. URL: www.emerald.com/insight/content/doi/10.1108/MHSI-03-2017-0016/full/html
Gillard S, White S, Marks J, Foster R. A systematic narrative synthesis of the evidence for one-to-one peer support interventions in mental health. PROSPERO 2015:CRD42015025621. URL: www.crd.york.ac.uk/prospero/display_record.php?RecordID=25621 (accessed 6 January 2022).
Goldsmith LP, Morshead R, McWilliam C, Forbes G, Ussher M, Simpson A, et al. Co-producing randomized controlled trials: How do we work together? Front Sociol 2019;4:21. URL: www.frontiersin.org/articles/10.3389/fsoc.2019.00021/full?fbclid=IwAR0He8NQGYB4M6KaPc6i8TJ3CX6zyhmwBsNfpWmWJXQnyE_kowXQ1lGnwA0
Marks J, Foster R, Gibson S, Simpson A, Rinaldi M, Repper J, et al. Development of a peer support intervention to improve the experience and outcomes of discharge from inpatient to community mental health care: the role of experiential knowledge in a coproduced approach. BMC Res Notes 2021;14:320. URL: https://bmcresnotes.biomedcentral.com/articles/10.1186/s13104-021-05735-0
Gillard S, Marks J. Peer support for discharge from inpatient to community mental health services. URL: www.isrctn.com/ISRCTN10043328 (accessed 6 January 2022).
White S, Foster R, Marks J, Morshead R, Goldsmith L, Barlow S, et al. The effectiveness of one-to-one peer support in mental health services: a systematic review and meta-analysis. BMC Psychiatry. 2020;20(1):1–20. URL: https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-020-02923-3
Ethics statement
This programme was approved by the UK National Research Ethics Service, Research Ethics Committee London – London Bridge on 10/05/2016, reference number 16/LO/0470.
Data-sharing statement
All data from this programme are available on reasonable request to the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health and Care Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, CCF, PGfAR or the Department of Health and Social Care. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the PGfAR programme or the Department of Health and Social Care.
References
- Qurashi I, Kapur N, Appleby L. A prospective study of noncompliance with medication, suicidal ideation, and suicidal behavior in recently discharged psychiatric inpatients. Arch Suicide Res 2006;10:61-7. https://doi.org./10.1080/13811110500318455.
- Craig TJ, Fennig S, Tanenberg-Karant M, Bromet EJ. Rapid versus delayed readmission in first-admission psychosis: quality indicators for managed care?. Ann Clin Psychiatry 2000;12:23-38. https://doi.org./10.3109/10401230009147117.
- Burns T, Rugkåsa J, Molodynski A, Dawson J, Yeeles K, Vazquez-Montes M, et al. Community treatment orders for patients with psychosis (OCTET): a randomised controlled trial. The Lancet 2013;381:1627-33. https://doi.org/10.1016/S0140-6736(13)60107-5.
- Wheeler A, Moyle S, Jansen C, Robinson E, Vanderpyl J. Five-year follow-up of an acute psychiatric admission cohort in Auckland, New Zealand. N Z Med J 2011;124:30-8.
- Li X, Srasuebkul P, Reppermund S, Trollor J. Emergency department presentation and readmission after index psychiatric admission: a data linkage study. BMJ Open 2018;8.
- Tulloch AD, David AS, Thornicroft G. Exploring the predictors of early readmission to psychiatric hospital. Epidemiol Psychiatr Sci 2016;25:181-93.
- Chung DT, Ryan CJ, Hadzi-Pavlovic D, Singh SP, Stanton C, Large MM. Suicide rates after discharge from psychiatric facilities: a systematic review and meta-analysis. JAMA Psychiatry 2017;74:694-702.
- NCISH . The National Confidential Inquiry into Suicide and Homicide by People with Mental Illness. Annual Report July 2013 2013. http://documents.manchester.ac.uk/display.aspx?DocID=37595 (accessed 6 January 2022).
- Vigod SN, Kurdyak PA, Dennis CL, Leszcz T, Taylor VH, Blumberger DM, et al. Transitional interventions to reduce early psychiatric readmissions in adults: systematic review. Br J Psychiatry 2013;202:187-94. https://doi.org/10.1192/bjp.bp.112.115030.
- Durbin J, Lin E, Layne C, Teed M. Is readmission a valid indicator of the quality of inpatient psychiatric care?. J Behav Health Serv Res 2007;34:137-50.
- Mark T, Tomic KS, Kowlessar N, Chu BC, Vandivort-Warren R, Smith S. Hospital readmission among medicaid patients with an index hospitalization for mental and/or substance use disorder. J Behav Health Serv Res 2013;40:207-21.
- Reynolds W, Lauder W, Sharkey S, Maciver S, Veitch T, Cameron D. The effects of a transitional discharge model for psychiatric patients. J Psychiatr Ment Health Nurs 2004;11:82-8. https://doi.org/10.1111/j.1365-2850.2004.00692.x.
- Forchuk C, Reynolds W, Sharkey S, Martin ML, Jensen E. The transitional discharge model: comparing implementation in Canada and Scotland. J Psychosoc Nurs Ment Health Serv 2007;45:31-8.
- Reissman F. The ‘helper’ therapy principle. Soc Work 1965;10:27-32.
- Mead S, MacNeil C. Peer Support: A Systemic Approach 2005. www.intentionalpeersupport.org/wp-content/uploads/2014/02/Peer-Support_A-Systemic-Approach.pdf (accessed 6 January 2022).
- Repper J, Carter T. A review of the literature on peer support in mental health services. J Ment Health 2011;20:392-411.
- Repper J. Peer Support Workers: Theory and Practice. London, UK: Centre for Mental Health, NHS Confederation; 2013.
- Lawn S, Smith A, Hunter K. Mental health peer support for hospital avoidance and early discharge: An Australian example of consumer driven and operated service. J Ment Health 2008;17:498-50.
- Davidson L, Chinman M, Sells D, Rowe M. Peer support among adults with serious mental illness: a report from the field. Schizophr Bull 2006;32:443-50. https://doi.org/10.1093/schbul/sbj043.
- Min SY, Whitecraft J, Rothbard AB, Salzer MS. Peer support for persons with co-occurring disorders and community tenure: a survival analysis. Psychiatr Rehabil J 2007;30:207-13.
- Sledge EH, Lawless M, Sells D, Wieland M, O’Connell MJ, Davidson L. Effectiveness of peer support in reducing readmissions of persons with multiple psychiatric hospitalizations. Psychiatr Serv 2011;62:541-4.
- Pitt V, Lowe D, Hill S, Prictor M, Hetrick SE, Ryan R, et al. Consumer-providers of care for adult clients of statutory mental health services. Cochrane Database Syst Rev 2013.
- Lloyd-Evans B, Mayo-Wilson E, Harrison B, Istead H, Brown E, Pilling S, et al. A systematic review and meta-analysis of randomised controlled trials of peer support for people with severe mental illness. BMC Psychiatry 2014;14.
- Kemp V, Henderson AR. Challenges faced by mental health peer support workers: Peer support from the peer supporter’s point of view. Psychiatr Rehabil J 2012;35:337-40.
- Gillard SG, Edwards C, Gibson SL, Owen K, Wright C. Introducing peer worker roles into UK mental health service teams: a qualitative analysis of the organisational benefits and challenges. BMC Health Serv Res 2013;13.
- Tse S, Tsoi EW, Wong S, Kan A, Kwok CF-Y. Training of mental health peer support workers in a non-western high-income city: preliminary evaluation and experience. Int J Soc Psychiatry 2014;60:211-8.
- Gillard S, Holley J, Gibson S, Larsen J, Lucock M, Oborn E, et al. Introducing new peer worker roles into mental health services in England: comparative case study research across a range of organisational contexts. Adm Policy Ment Health and Ment Health Serv Res 2015;42:682-94.
- Schmidt LT, Gill KJ, Pratt CW, Solomon P. Comparison of service outcomes of case management teams with and without a consumer provider. Am J Psychiatr Rehabil 2008;11:310-29.
- Stewart S, Watson S, Montague R, Stevenson C. Set up to fail? Consumer participation in the mental health service system. Australas Psychiatry 2008;16:348-53.
- Faulkner A, Kalathil J. The Freedom to be, the Chance to Dream: Preserving User-led Peer Support in Mental Health. London: Together for Mental Wellbeing; 2012.
- Gillard S, Gibson SL, Holley J, Lucock M. Developing a change model for peer worker interventions in mental health services: a qualitative research study. Epidemiol Psychiatr Sci 2015;24:435-45.
- Mead S, Filson B. Mutuality and shared power as an alternative to coercion and force. Ment Health Soc Incl 2017;21:144-52.
- Oborn E, Barrett M, Gibson S, Gillard S. Knowledge and expertise in care practices: the role of the peer worker in mental health teams. Sociol Health Illn 2019;41:1305-22.
- King A, Simmons M. A systematic review of the attributes and outcomes of peer work and guidelines for reporting studies of peer interventions. Psychiatr Serv 2018;69:961-77.
- Walker G, Bryant W. Peer support in adult mental health services: a meta-synthesis of qualitative findings. Psychiatr Rehabil J 2013;36:28-34.
- Ahmed A, Hunter K, Mabe A, Tucker SJ, Buckley PF. The professional experiences of peer specialists in the Georgia Mental Health Consumer Network. Community Ment Health J 2015;51:424-36.
- Gillard S, White S, Marks J, Foster R. n.d. www.crd.york.ac.uk/prospero/display_record.php?RecordID=25621 (accessed 6 January 2022).
- White S, Foster R, Marks J, Morshead R, Goldsmith L, Barlow S, et al. The effectiveness of one-to-one peer support in mental health services: a systematic review and meta-analysis. BMC Psychiatry 2020;20:1-20.
- Marks J, Foster R, Gibson S, Simpson A, Rinaldi M, Repper J, et al. Development of a peer support intervention to improve the experience and outcomes of discharge from inpatient to community mental health care: the role of experiential knowledge in a coproduced approach. BMC Res Notes 2021;14.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Medical Research Council Guidance . Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337.
- Gillard S, Bremner S, Foster R, Gibson SL, Goldsmith L, Healey A, et al. Peer support for discharge from inpatient to community mental health services: Study protocol clinical trial (SPIRIT Compliant). Medicine (Baltimore) 2020;99.
- Gillard S, Banach N, Barlow E, Byrne J, Foster R, Goldsmith L, et al. Developing and testing a principle-based fidelity index for peer support in mental health services. Soc Psychiatry Psychiatr Epidemiol 2021;19:1-9.
- ISRCTNregistry . Peer Support for Discharge from Inpatient to Community Mental Health Services n.d. www.isrctn.com/ISRCTN10043328 (accessed 6 January 2022).
- Roberts C, Batistatou E, Roberts SA. Design and analysis of trials with a partially nested design and a binary outcome measure. Stat Med 2016;35:1616-36.
- Priebe S, Yeeles K, Bremner S, Lauber C, Eldridge S, Ashby D, et al. Effectiveness of financial incentives to improve adherence to maintenance treatment with antipsychotics: cluster randomised controlled trial. BMJ 2013;347.
- Dunn G, Emsley R, Liu H, Landau S, Green J, White I, et al. Evaluation and validation of social and psychological markers in randomised trials of complex interventions in mental health: a methodological research programme. Health Technol Assess 2015;19:1-115.
- Gillard S, Bremner S, Patel A, Goldsmith L, Marks J, Foster R, et al. ENRICH trial study group . Peer support for discharge from inpatient mental health care versus care as usual in England (ENRICH): a parallel, two-group, individually randomised controlled trial. Lancet Psychiatry 2022;9:125-36.
- Bhui K, Halvorsrud K, Nazroo J. Making a difference: ethnic inequality and severe mental illness. Br J Psychiatry 2018;213:574-8.
- Halvorsrud K, Nazroo J, Otis M, Brown Hajdukova E, Bhui K. Ethnic inequalities and pathways to care in psychosis in England: a systematic review and meta-analysis. BMC Med 2018;16.
- Hariman K, Lam J, Leung SK, Lui SS. Clinical risk model to predict 28-day unplanned readmission via the accident and emergency department after discharge from acute psychiatric units for patients with psychotic spectrum disorders. BJPsych Open 2020;6.
- Tan JHP, Conlon C, Tsamparli A, O’Neill D, Adamis D. The association between family dysfunction and admission to an acute mental health inpatient unit: a prospective study. Ir J Psychol Med 2019;12:1-11.
- Herdman M, Gudex C, Lloyd A, Janssen MF, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727-36.
- McCullagh P, Nelder J. Generalised Linear Models. London: Chapman and Hall/CRC; 1989.
- Stinnett AA, Mullahy J. Net health benefits: a new framework for the analysis of uncertainty in cost-effectiveness analysis. Med Decis Making 1998;18:S68-80.
- Plöderl M, Tremblay P. Mental health of sexual minorities. A systematic review. Int Rev Psychiatry 2015;27:367-85.
- Gillard S, Simons L, Turner K, Lucock M, Edwards C. Patient and public involvement in the coproduction of knowledge: reflection on the analysis of qualitative data in a mental health study. Qual Health Res 2012;22:1126-37.
- Gillard S, Foster R, Gibson S, Goldsmith L, Marks J, White S. Describing a principles-based approach to developing and evaluating peer worker roles as peer support moves into mainstream mental health services. Ment Health Soc Incl 2017;21:133-43.
- Fereday J, Muir-Cochrane E. Demonstrating rigor using thematic analysis: A hybrid approach of inductive and deductive coding and theme development. Int J Qual Methods 2006;5:80-92.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101.
- Mason J. Qualitative Researching. Thousand Oaks, CA: SAGE Publications Ltd; 2017.
- Creswell JW, Klassen AC, Plano Clark VL, Smith KC. Best practices for mixed methods research in the health sciences. Bethesda, Maryland: National Institutes of Health; 2011.
- Park SG, Chang BH, Mueller L, Resnick SG, Eisen SV. Predictors of employment burnout among VHA peer support specialists. Psychiatr Serv 2016;67:1109-15.
- Scanlan JN, Still M, Radican J, Henkel D, Heffernan T, Farrugia P, et al. Workplace experiences of mental health consumer peer workers in New South Wales, Australia: a survey study exploring job satisfaction, burnout and turnover intention. BMC Psychiatry 2020;20.
- National Workforce Stocktake of Mental Health Peer Support Workers in NHS Trusts. Health Educ 2020. www.hee.nhs.uk/sites/default/files/documents/NHS%20Peer%20Support%20Worker%20Benchmarking%20report.pdf (accessed 22 September 2023).
- Otte I, Werning A, Nossek A, Vollmann J, Juckel G, Gather J. Challenges faced by peer support workers during the integration into hospital-based mental health-care teams: Results from a qualitative interview study. Int J Soc Psychiatry 2020;66:263-9.
- Voronka J. The mental health peer worker as informant: performing authenticity and the paradoxes of passing. Disabil Soc 2019;34:564-82.
- Goldsmith LP, Morshead R, McWilliam C, Forbes G, Ussher M, Simpson A, et al. Co-producing randomized controlled trials: How do we work together?. Front Sociol 2019;4.
- Bartholomew LK, Parcel GS, Kok G, Gottlieb NH, Schaalma HC, Markham CC, et al. Planning Health Promotion Programs: An Intervention Mapping Approach. San Francisco, CA: Jossey-Bass; 2011.
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013;46:81-95.
- Wood JR, Wood LE. Card sorting: current practices and beyond. J Usability Stud 2008;4:1-6.
- Ericsson KA, Simon HA. How to study thinking in everyday life: contrasting think-aloud protocols with descriptions and explanations of thinking. Mind, Culture, and Activity 1998;5:178-86.
- Trevillion K, Domoney J, Pickles A, Bick D, Byford S, Heslin M, et al. Depression: an exploratory parallel-group randomised controlled trial of Antenatal guided self-help for WomeN (DAWN): study protocol for a randomised controlled trial. Trials 2016;17.
- PSSRU . Unit Costs of Health and Social Care 2019 n.d. www.pssru.ac.uk/project-pages/unit-costs/unit-costs-2019/ (accessed 6 January 2022).
- NHS England . National Cost Collection for the NHS n.d. www.england.nhs.uk/national-cost-collection/ (accessed 6 January 2022).
- Heslin M, Callaghan L, Barrett B, Lea S, Eick S, Morgan J, et al. Costs of the police service and mental healthcare pathways experienced by individuals with enduring mental health needs. Br J Psychiatry 2017;210:157-64.
- NICE . Position Statement on Use of the EQ-5D-5L Value Set for England (Updated October 2019) n.d. www.nice.org.uk/about/what-we-do/our-programmes/nice-guidance/technology-appraisal-guidance/eq-5d-5l (accessed 6 January 2022).
- Dolan P. Modeling valuations for EuroQol health states. Med Care 1997;35:1095-108.
- Van Hout B, Janssen MF, Feng Y-S, Kohlmann T, Busschbach J, Golicki D, et al. Interim scoring of the EQ5D-5L: mapping the EQ5D-5L to EQ5D-3L value sets. Value in Health 2012;15:708-15.
- Beecham J, Knapp M. Measuring Mental Health Needs. London: Gaskell; 1992.
- Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, et al. The Warwick-Edinburgh mental well-being scale (WEMWBS): development and UK validation. Health Qual Life Out 2007;5:1-3.
- Traynor M, Wade B. The development of a measure of job satisfaction for use in monitoring the morale of community nurses in four trusts. J Adv Nurs 1993;18:127-36.
- Temkin-Greener H, Gross D, Kunitz SJ, Mukamel D. Measuring interdisciplinary team performance in a long-term care setting. Med Care 2004;42:472-81.
- Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory. Palo Alto, CA: Consulting Psychologists Press; 1981.
- Taggart F. WEMWBS Population Norms in Health Survey for England Data 2011 n.d. www.corc.uk.net/media/1243/wemwbs_populationnorms2011.pdf (accessed 6 January 2022).
- Schaufeli WB, Bakker AB, Hoogduin K, Schaap C, Kladler A. On the clinical validity of the Maslach Burnout Inventory and the Burnout Measure. Psychol Health 2001;16:565-82.
- Wade BE. The job satisfaction of health visitors, district nurses and practice nurses working in areas served by four trusts: year 1. J Adv Nurs 1993;18:992-1004.
Appendix 1 Developing the ENRICH peer support for discharge intervention
| Research team | Lived experience advisory panel | Local advisory groups | |
|---|---|---|---|
| Number of people involved | 14 | 13 | 48 (6 groups: average of 8 members per group) |
| Stage of process | 1, 2, 3 | 1, 2 | 2 |
| Types of expertise (number of team members) |
|
|
|
Methods
Stage 1: Generating intervention components
The systematic review and expert workshops were used to identify potential components, following an intervention mapping approach. 68 Components were given a short label and a descriptor, and mapped on to five domains: (1) Recruitment and Role Description; (2) Training; (3) Delivery; (4) Supervision and Support; (5) Organisation and Team.
Systematic review. Procedures for the review are as described in Systematic review of one-to-one peer support in mental health services above. 38 For the purposes of intervention development, papers reporting studies of any design were included, from database inception until end of April 2015, where they reported description of intervention components. In addition, grey literature – unpublished evaluations and experiential testimonies – were identified using a snowball approach through emails to contacts known to be working in peer support. A member of the LEAP screened each article with decisions checked by the first author. Data detailing peer support components were extracted from included studies and coded to the five intervention domains.
Expert workshops. Workshops were held with the LEAP and the research team to suggest potential components for the intervention. A third workshop was held with five members of the research team to consider how a taxonomy of behaviour change techniques (BCT)69 might be relevant to peer support in mental health services. Again, components were mapped on to the five domains, and where similar components were identified from different sources these were coded together.
Stage 2: Producing the intervention handbook
Prioritising components. LAGs were convened in each of six study sites (mental health trusts). LAGs prioritised components using a card sort exercise structured into the five domains. 70 A large visual grid was produced with five columns labelled with the five domains and cards were printed for each component comprising a name and brief definition. Components identified by three or more sources in stage 1 (e.g. LEAP, team and review) were considered core to the intervention and those cards were placed within relevant domains on the grid. LAGs were given the remaining set of cards and invited to discuss the relevance and importance of each in the context of peer support and mental health service delivery locally. LAGs were asked to prioritise and identify up to five more components to add to each domain of the grid. Notes were made of LAG discussions, including the rationale for prioritising components. The research team produced a single grid based on the output from all LAGs. Components were discounted from further discussion (not included on the grid) if not prioritised by any LAGs, added as core components (added to the grid) if prioritised by a majority of LAGs, or otherwise retained for further discussion.
Producing and refining the intervention ‘blueprint’. Using output from the LAGs we produced a blueprint of the intervention in the form of a flow diagram, specifying the processes of recruiting PWs, training, delivering the intervention, and support received by PWs. The blueprint included all components retained for discussion, as well as the full set of core components, so that local implementation issues could be considered. In a second round of meetings, LAGs were presented with the flow diagram and invited to discuss the blueprint using well-established talk-aloud approaches. 71 Discussion began at the top left of the flow diagram (recruiting PWs) and proceeded sequentially, including consideration of alternative pathways as appropriate, with LAGs to consider the appropriateness of each component, reflecting on practicalities of implementing and supporting the intervention locally. Again, notes were made of all discussions.
Drafting the intervention handbook. The output of LAG meetings was used to draft the ENRICH intervention handbook and PW training programme. Development of the intervention was also informed by our ‘peer support principles’ (see below). Further workshops with the LEAP and research team were held to inform writing the handbook and training content.
Stage 3: Piloting the intervention
A pilot randomised controlled trial of the intervention was conducted in two study sites to test feasibility of delivering trial procedures and implementation of the intervention (see WP3 below). Following the pilot, feedback workshops were held with the PWCs who trained and supervised PW teams at both sites, and the PWs who had delivered the peer support at one site, exploring their experiences and views on what worked well and what might be improved about the training and other aspects of the peer support. Workshops were semi-structured discussions rather than formal focus groups, inviting participants to feedback on any issues arising in their experiences of delivering the peer support. Changes were made to the handbook and training programme, based on the feedback, following a further research team workshop.
Gillard et al.57
Work with our LEAP and the service user researchers on the team indicated the importance of not just identifying components of peer support, but also ensuring that values underpinning peer support, that make it distinct from other forms of mental health support,31 should inform the development of the intervention. In our literature search,39 we also extracted data from studies reporting the values underlying peer support which we analysed thematically. We held a workshop with a National Expert Panel (NEP) comprising 10 people with personal experience of peer support, of developing peer-led services or of doing research about peer support from an experiential perspective which generated a further set of themes. We did this in three stages, first inviting NEP members to, independently, identify five items each which they felt, in their experience, were important values that define the distinctiveness of peer support. We then asked NEP members to share their items and, through discussion, to group those items into themes where items were meaningfully similar. Finally, we asked the NEP to produce a title and a brief definition for each value.
Through an iterative process of discussion and writing between the research team and the panel, we mapped those two sets of themes on to each other in order to produce a set of principles (including extended definitions) which supported the implementation of those values into practice in a peer support intervention (see Appendix 1, Figure 12).
FIGURE 12.
Principles of peer support.
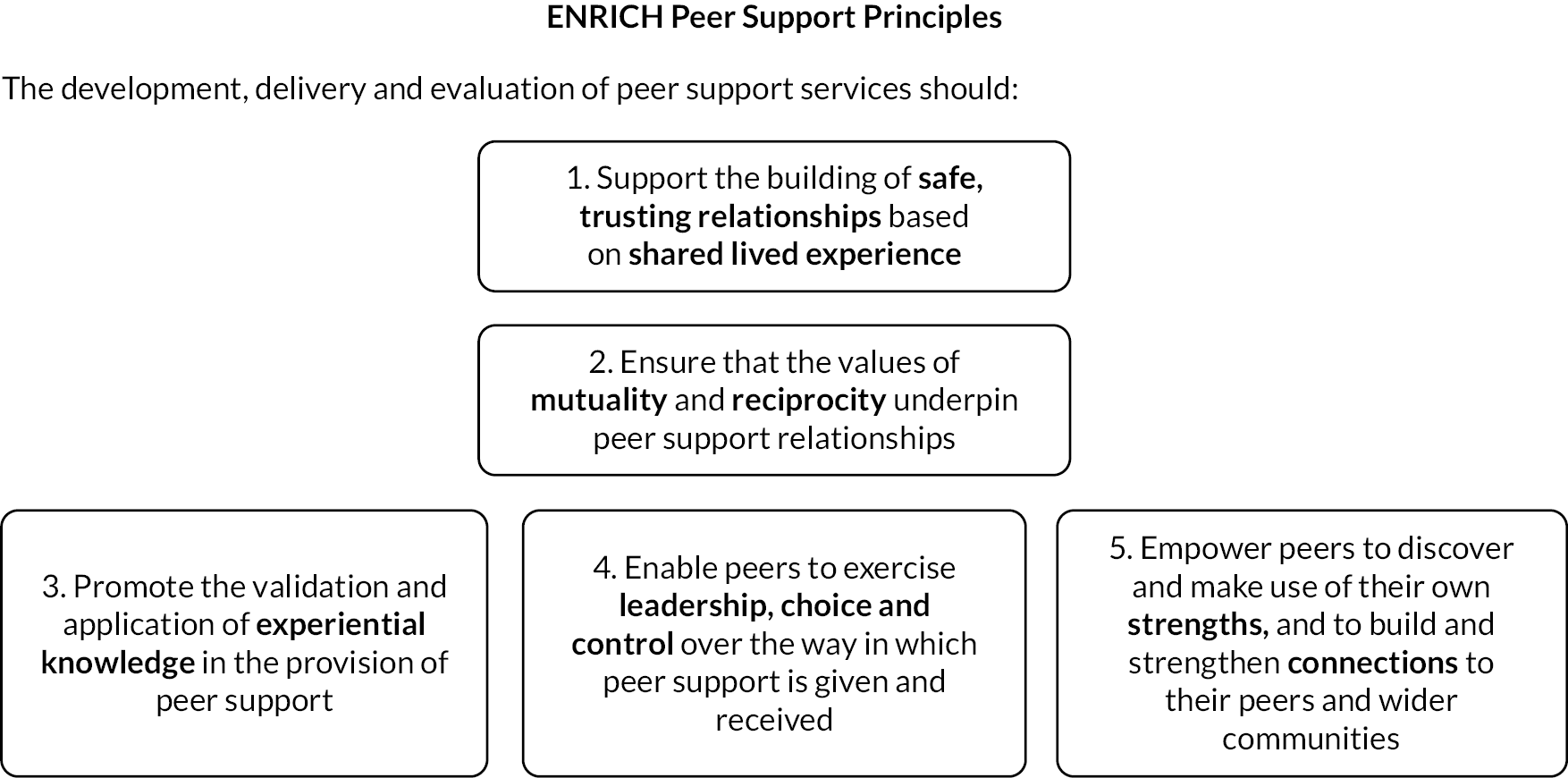
Results
Stage 1: Generating intervention components
A total of 3800 studies were identified in the literature search, of which 97 were included in the review, 85 peer-reviewed and 12 from grey literature (see Appendix 1, Figure 13). Components generated by the literature review and expert workshops were mapped on to the five intervention domains (see Appendix 1, Table 11). Forty-four components were identified in the review (including 6 from grey literature), 29 by the LEAP, 37 by the research team and 6 from the BCT workshop; a total of 66 distinct components, once similar components were combined. Twelve core components, identified by three or more sources, are identified with an asterisk in Appendix 1, Table 11.
FIGURE 13.
Flow diagram of studies in the WP1 literature review.
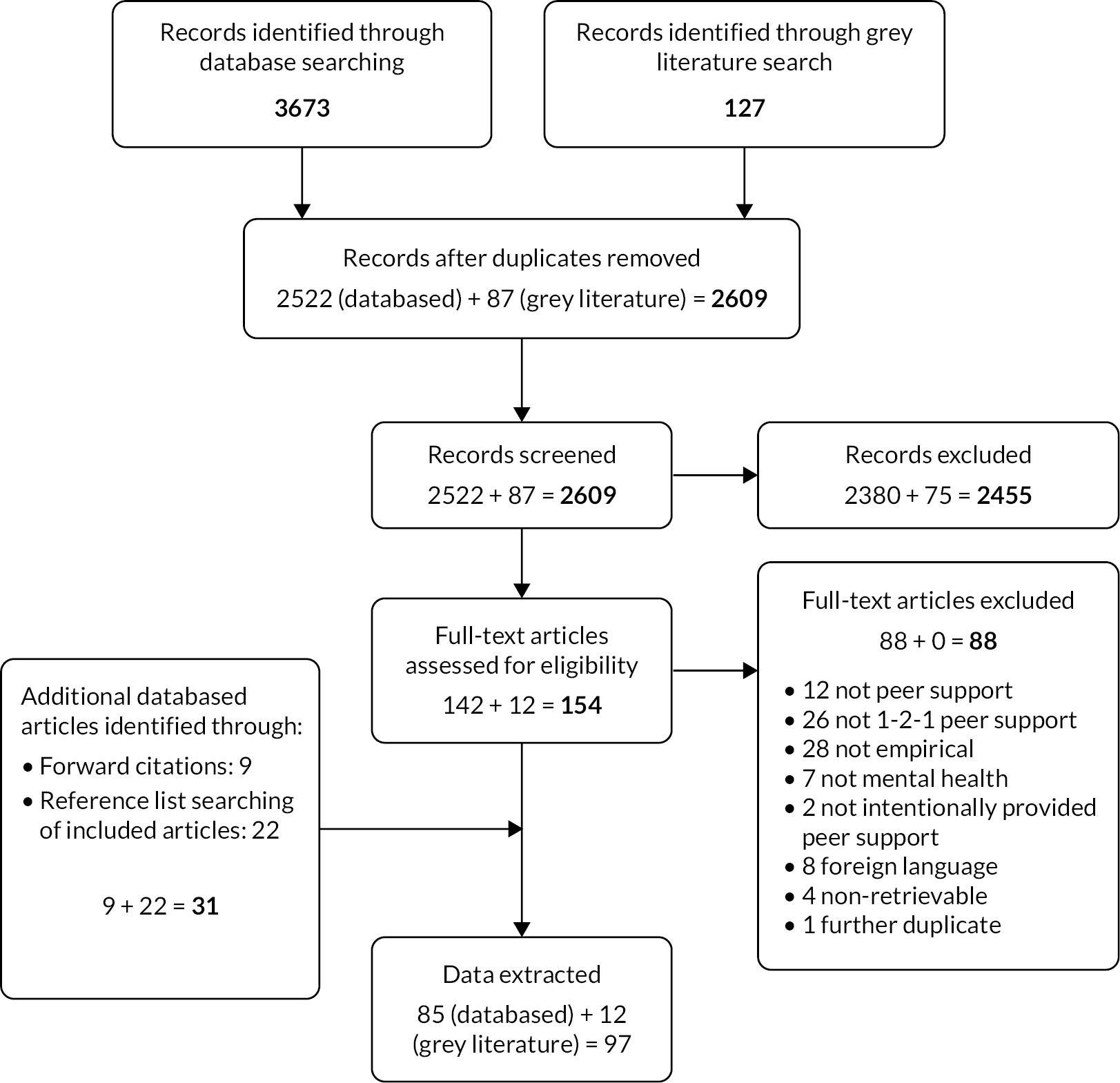
| Domain | Label | Descriptor | Source |
|---|---|---|---|
| Domain 1: Recruitment and role description | Person specification to include definition of lived experience | LEAP | |
| Person specification to include having been an inpatient | Desirable rather than essential criteria | LEAP | |
| Person specification to include the ability to reflect on personal experiences | Personal experiences of mental distress, recovery, and giving and receiving support | LEAP, Review | |
| Peer leadership in recruitment and interview process essential | Ideally should be the PWC | LEAP, Review | |
| Person specification to include ability to record and report | LEAP, Review | ||
| Interview to ask how working as a PW fits with future career aspirations | LEAP | ||
| Person specification to include knowledge of living and using services locally | LEAP | ||
| Recruitment process to take the form of a whole day event or open day | Potential PWs to engage in observed, scenario-based group and pairs work etc. during the day, not just a one-to-one interview | Team, Review | |
| Recruitment is to training (not to job) | Sufficient people recruited to training to allow for drop-out/people not moving into a job, plus a reserve (approx. double the number required for posts) | Team, Review | |
| Person specification to include having completed recovery training/have a recovery plan | Not essential, but to be a requirement of training if not already in place | Team | |
| aRole description clearly describes peer’s approach around discovering and enabling service user’s strengths, empowering the individual to build their own support network post discharge | Note the peer should not become a substitute for that network for a limited period (linked to competencies in training) | LEAP, BCTs, Review | |
| aRole description to focus on identifying, signposting and, where requested by service user, accompanying to activities/support/opportunities using locally developed resource pack | Resource pack linked to local resource mapping session in training; to include (a) things the individual did before admission, (b) new things; peer to have sufficient flexibility in the role to attend activities as appropriate | LEAP, Team, Review | |
| Role description to clearly indicate expectations of the role, with service user to be provided with information sheet clearly indicating expectation of the peer support role | Noting that role is not about the peer being an advocate or a generic support worker | LEAP | |
| Person specification to include strong interpersonal skills, interest in helping others etc., to be tested at interview | Review | ||
| Recruitment by advertisements in services/organisations that might employ peers | Review | ||
| Letters of reference required at recruitment | Can be character references in the absence of work references | Review | |
| Homework and/or tests (quizzes) as part of the assessment process | Review (grey lit.) | ||
| Pre-screening telephone interview prior to invitation to recruitment day | Assessing how comfortable people are talking about their mental health, scenarios around providing support etc. | Review | |
| Domain 2: Training | Training to include work-based placements | Including working alongside existing peers | Team, Review |
| Training to include standard Trust induction | Note: this might include Trust’s standard breakaway training etc. although peers would not be required to use this as part of their role | Team | |
| Training to include locally led ‘community asset mapping’ session | Team, LEAP | ||
| Training to incorporate locally developed/delivered sessions where these cover required skills/competencies | LEAP, Review | ||
| Training to have at least some minimal level of accreditation | LEAP | ||
| aTraining (and supervision) to include a focus on boundaries and managing relationships | For example, on blurred friendship line, especially where there is a pre-existing friendship or there is an attraction between peer and service user | LEAP, Team, Review | |
| Training to include session on preparing for the workplace | For example, working on the ward, plus basics around use of phones, office etc. | Team, Review | |
| Training (and supervision) to include a focus on keeping yourself well and safe at work | Including the well-being and mental health of the peer | Team, Review | |
| aTraining (and supervision) to include appropriate sharing of lived experience to role model post-discharge experience | Linked to competencies in training | Team, BCTs, Review, LEAP | |
| aTraining to be co-delivered by experienced PWs | In similar roles (if not the same) | LEAP, Team, Review | |
| Training to include cultural competence, gender issues etc. | Review | ||
| Training to include competence around addressing stigma | Review | ||
| Training (and supervision) for peer in discussing difficult issues | For example, suicidality, self-harm, drug taking, sexual abuse etc. | Team | |
| aTraining to cover key communication and supporting self-management skills | Peer has a range of core skills, – for example reflective listening, summarising, goal-planning etc. – to use in addition to sharing of lived experience | LEAP, BCTs, Review, Team | |
| aTraining structured around core set of values-based competencies | Exercises and assessments to cover each competency (for example mutuality, reciprocity, non-directive working, validating etc.) | Team, BCTs, Review | |
| Assessments during and at end of training around each key competency | Including role play type assessments plus readiness to work interview; used to decide who moves from training to full or reserve role | Team, Review | |
| aTraining (and supervision) to include comprehensive coverage of working with risk and safety | Including decision-making about what and when to handover to clinical team; if PWC does not have clinical experience, appropriate clinical link person should be identified in the Trust | LEAP, Team, Review | |
| Domain 3: Delivery of peer support | Peers to accompany people on home visits/leave while still in hospital, and meet people in their homes while living in the community | Where possible, to support reconnecting with people and places; only where a preference for that is expressed by the service user; must conform to employer’s lone working policy | Team, LEAP |
| aPeers to be part of formal discharge meeting/care planning meetings where invited by the service user | To accompany, support and enable (not to advocate) | LEAP, Team, Review | |
| Initial contact on the ward to focus on listening to the service user and relationship building | Focus on building trust, building a rapport, not on the peer telling their story (appropriate sharing of lived experience to make a connection) | LEAP, Team | |
| aPeer to support/enable optional use of service user-owned discharge plan, crisis plan and personal recovery plan | Discharge tool to focus on what service user wants/does not want post-discharge, rather than prescriptive planning of activities; all tools, can use locally available or any suitable strengths-based tools | LEAP, Team, BCTs, Review | |
| First meeting with peer post-discharge should be in addition to follow-up by community team | Not instead of or part of that statutory meeting | LEAP | |
| Clear guidance for peers on telephone, text, email and social media contact | Team | ||
| Matching of peers to service user by key demographics, experience of services and/or hobbies & interests | As far as possible given size of PW team | Review | |
| Peers direct service users to appropriate online resources | Including information sites, mental health discussion forums, online self-management/psychosocial education etc. | Review | |
| Peer encourages involvement of ‘significant others’ in any personal/recovery/crisis planning | Review | ||
| Peers will only write in (Trust) clinical notes what is agreed with service user | Team, Review | ||
| Health lifestyle and health promotion included in training/delivery | Review (grey lit.) | ||
| Medication and symptom management included in training/delivery | Review (grey lit.) | ||
| Messages linked to recovery planning/goal setting sent by PW using text or email | Review (grey lit.) | ||
| PW to help service user to complete self-assessment and monitoring tools | Review (grey lit.) | ||
| aPreparation for ending the support to be on the agenda from the outset | Contact reducing from weekly to fortnightly towards the end of peer support, training and supervision to include working with attachment, therapeutic relationship, endings etc. (including ending of individual sessions as well as support relationship) | LEAP, BCTs, Team, Review | |
| The PW fulfils a ‘navigator’ role, helping service user assess health and social care needs, identify providers, make appointments and accompany as necessary | Review (grey lit.) | ||
| Domain 4: Support and supervision (Note: a number of components included in training domain also apply to supervision) | Regular peer-to-peer support meeting | Sharing of experiences, strategies etc. by peers, plus opportunity to recognise successes in the workplace etc. | LEAP, Team |
| Group supervision for peers from PWC | With option of one-to-one supervision always available | Team | |
| Appropriate support always accessible when supervision (PWC) is not available | By phone or face to face, including when PWC is unavailable, so peer is never left isolated holding a difficult issue | LEAP, Review | |
| Supervision from someone with lived experience essential | Included in the person specification for the PWC (note: if a suitable individual is not available locally for the role, external supervision from a peer should be resourced, in addition to line management from within the Trust) | LEAP, Team | |
| PWCS to undertake their own recovery planning | Team | ||
| PWCs should have access to learning sets with people in the same/equivalent roles | Either locally or more widely if necessary | Team | |
| Development programme in place for people moving into reserve roles | To include, at a minimum, a monthly development meeting plus opportunities for placements in, for example, local recovery college and help in applying for other (voluntary or paid) peer roles | Team | |
| Domain 5: Team and organisational support | PWs require a ‘team base’ | Including access to office space; somewhere they feel safe and can take time out, meet and build supportive relationships with colleagues (flexibility locally re most appropriate location) | Team, Review |
| Links to good employment support services | Can be in the Trust or local voluntary sector provider | Team, LEAP | |
| aWard and community teams – including managers – should receive a team preparation session co-delivered by peers working locally | Focus on role of peer support alongside current service delivery | Team, LEAP, Review | |
| PWC, and where possible peers, should visit wards/teams as part of set-up | To establish communication, explain processes, address expectations etc. | Team, Review | |
| Peer support for discharge should be embedded in Trust’s recovery strategy, strategic development, planning documents etc. | Team, Review | ||
| Clinical team preparation sessions should involve team members identifying the assets that PWs will bring | Not a teaching session; use of appropriate tools | Team | |
| Employment of peers on the workforce should be integrated into HR policies | Review, Team |
Stage 2: Producing the intervention handbook
Prioritising components. Following the first round of LAGs, 6 components were discounted, 19 added as core components (see Appendix 1, Table 12), and 29 retained for further discussion.
| 1: Recruitment and role description | 2: Training | 3: Delivery of peer support | 4: Supervision and support | 5: Organisational and team support |
|---|---|---|---|---|
| aRole description clearly describes peer’s approach around discovering and enabling service user’s strengths, empowering the individual to build their own support network post discharge | aTraining (and supervision) to include a focus on boundaries and managing relationships | aPeers to be part of formal discharge meeting/care planning meetings where invited by the service user | Regular group supervision for PW team from PWC | aWard and community teams – including managers – should receive a team preparation session co-delivered by peers working locally |
| aRole description to focus on identifying, signposting and, where requested by service user, accompanying to activities/support/opportunities using locally developed resource pack | aTraining (and supervision) to include appropriate sharing of lived experience to role model post-discharge experience | aPeer to support/enable optional use of service user-owned discharge plan, crisis plan and personal recovery plan | Appropriate support always accessible when supervision (PWC) is unavailable | PWs require a ‘team base’ |
| Person specification to include the ability to reflect on personal experiences | aTraining to be co-delivered by experienced PWs | aPreparation for ending the support to be on the agenda from the outset | PWC, and where possible PWs, should visit wards/teams at part of set-up | |
| Peer leadership in recruitment and interview process essential | aTraining to cover key communication and supporting self-management skills | Initial contact on the ward to focus on listening to the service user and relationship building | Peer support for discharge should be embedded in the Trust’s strategies | |
| Role description to clearly indicate expectations of the role, with service user to be provided with information sheet clearly indicating expectation of the peer support role | aTraining structured around core set of values-based competencies | First meeting between PW and service user post-discharge should be in addition to follow-up by community team | Clinical team preparation sessions should involve team members identifying the assets that PWs will bring | |
| aTraining (and supervision) to include comprehensive coverage of working with risk and safety | Employment of PWs on the workforce should be integrated into HR policies | |||
| Training to include standard Trust induction | ||||
| Training to include locally led ‘community asset mapping’ session | ||||
| Existing locally developed training sessions included in PW training where these cover required skills/competencies | ||||
| Training (and supervision) to include a focus on keeping yourself well and safe at work | ||||
| Training to include specific focus on experience of the discharge ‘transition’ | ||||
| Training to include cultural competence, gender, religious, cultural issues etc. | ||||
| Training (and supervision) for PW in discussing difficult issues |
Producing and refining the intervention blueprint. The flow diagram used in the walkthrough exercises in the second round of LAGs is shown in Appendix 1, Figure 14.
FIGURE 14.
Flow diagram depicting intervention blueprint.
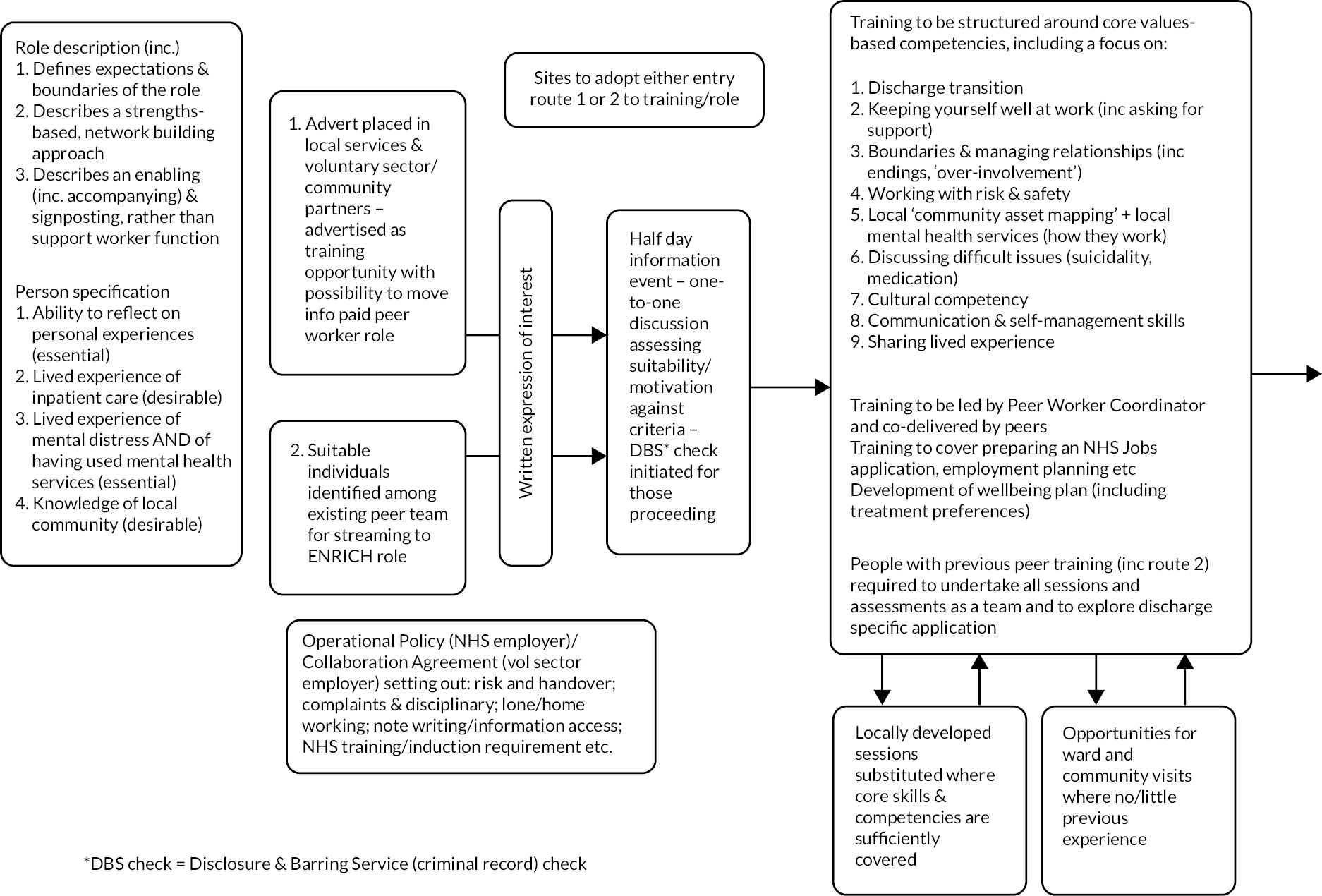
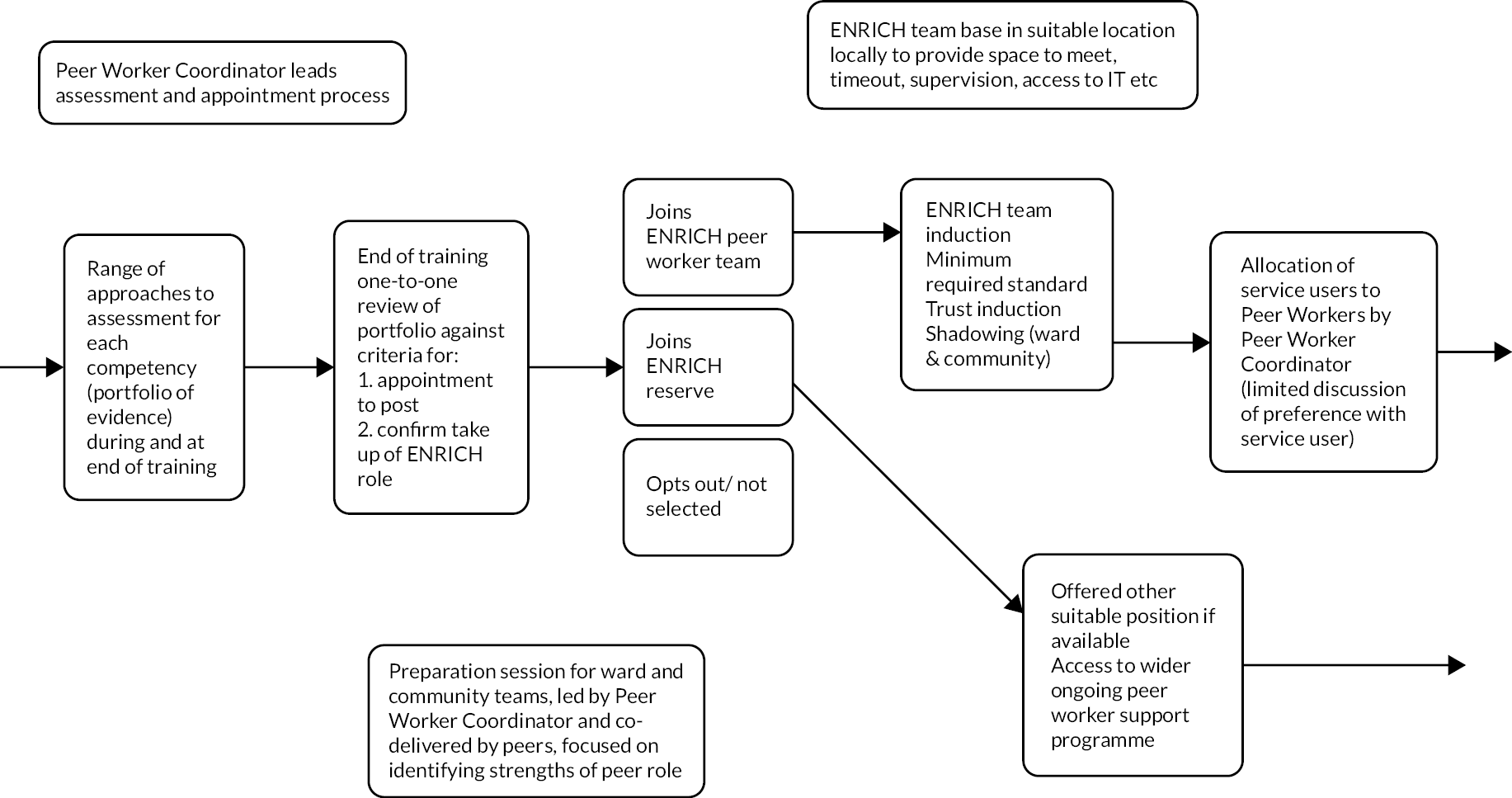
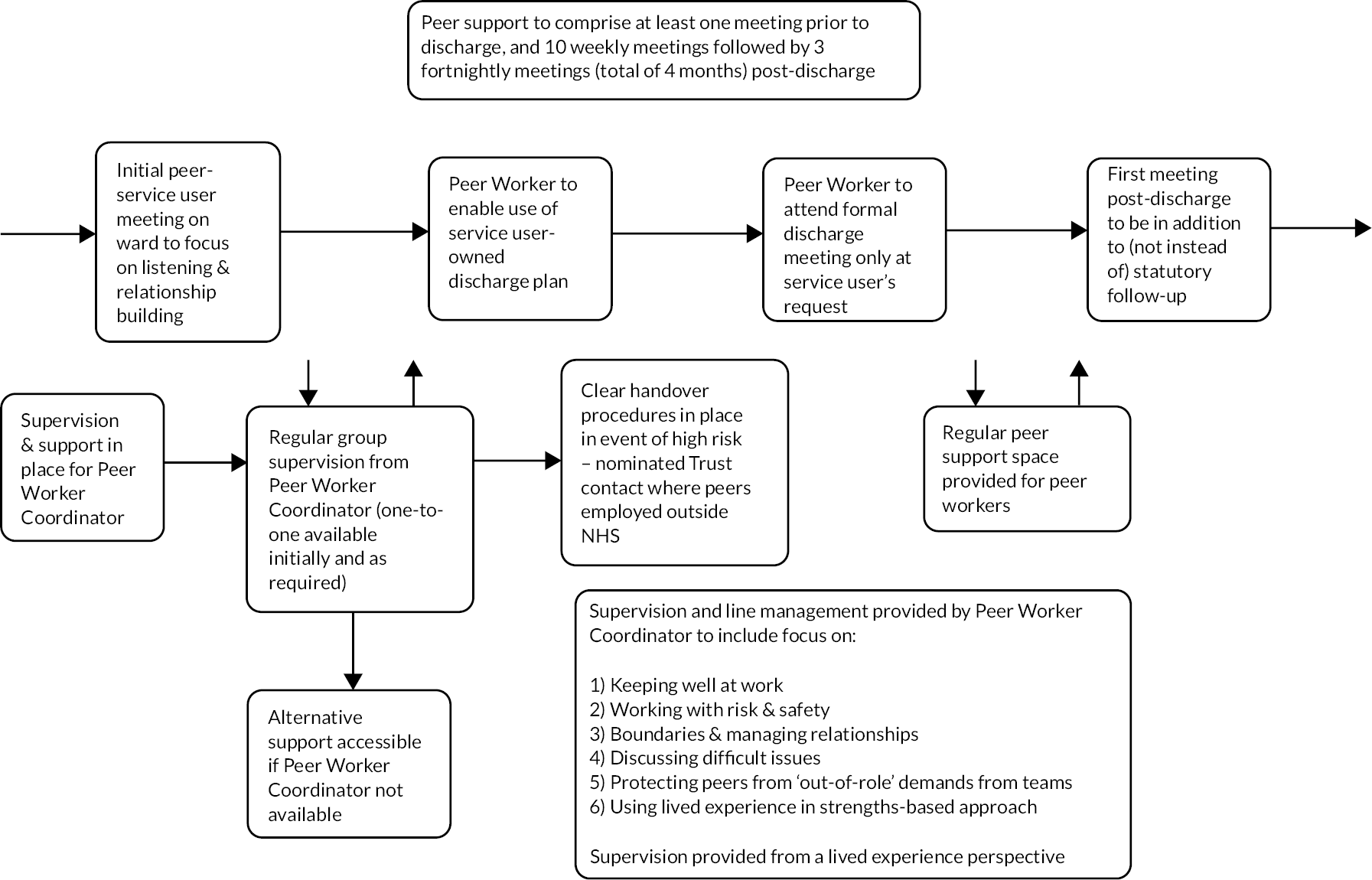

Drafting the intervention handbook. A detailed handbook was produced specifying a full set of procedures defining PW and the PWC roles, recruitment process, training, support and supervision for PWs, and how the peer support is delivered in hospital and in the community (see Appendix 1, Table 13).
| Chapter | Content |
|---|---|
| 1.0 What is ENRICH? | 1.1 Why peer support for discharge? 1.2 What is the ENRICH project and why do we need it? 1.3 The ENRICH research team |
| 2.0 Peer support for discharge – a principles-based approach | 2.1 Developing the principles framework 2.2 Applying the framework in ENRICH peer support for discharge |
| 3.0 Developing the ENRICH peer support handbook | 3.1 Generating ideas 3.2 Arriving at a consensus 3.3 Piloting the handbook |
| 4.0 The ENRICH PW role | 4.1 Role description 4.2 Person specification 4.3 Working pattern and flexibility 4.4 Remuneration |
| 5.0 The PWC role | 5.1 Role description and person specification 5.2 Duties and responsibilities 5.3 Remuneration 5.4 Support and supervision for the PWC 5.5 Cover in the absence of the PWC |
| 6.0 Peer worker recruitment process | 6.1Pathway 1 – advertising and recruiting new PWs 6.2Pathway 2 – assigning PWs from existing peer workforce 6.3Advertising the role 6.4Information event and pre-training meeting 6.5Role of training assessment in recruitment process 6.6Job application and interview 6.7Employment and welfare support 6.8Appointment to role/appointment to reserve 6.9Disclosure and Barring Service (DBS) checks and Occupational Health 6.10Recruitment numbers |
| 7.0 The ENRICH training programme | 7.1 Structure of training programme (a principles-based approach) 7.2 Delivery of training (role of the PWC) 7.3 Content of training sessions 7.4 Use of local training modules 7.5 Feedback and reflection 7.6 Assessment methods 7.7 Site visits |
| 8.0 Accessing patient notes | 8.1 Peer workers with access to electronic patient notes 8.2 Peer workers without access to electronic patient notes |
| 9.0 Induction | 9.1 Peer worker team induction 9.2 NHS induction 9.3 Ward visits and shadowing |
| 10.0 Preparing NHS teams | 10.1 Ward and community team preparation workshops |
| 11.0 Supervision and support for PWs | 11.1 Group supervision 11.2 Individual supervision 11.3 Absence of PWC 11.4 Risk, safety and handover 11.5 Access to peer support for peers 11.6 Peer worker well-being plan 11.7 Team base |
| 12.0 Pairing of PWs and service users | 12.1 The research process (allocation to peer support) 12.2 PWC preference meeting with service user |
| 13.0 Delivery on the ward | 13.1 First meeting 13.2 Frequency, location and duration of meetings 13.3 Use of service user-owned discharge plan 13.4 Peer worker involvement in formal discharge planning 13.5 Peer worker relationship to ward team 13.6 Risk, safety and handover |
| 14.0 Delivery in the community | 14.1 First meeting post-discharge 14.2 Frequency, location and duration of meetings 14.3 Lone/home working 14.4 Telephone and social media contact 14.5 Use of service user-owned plans and tools 14.6 Accompanying 14.7 Peer worker relationship to CMHTss 14.8 Ten-week step down 14.9 Endings 14.10 ENRICH PW Code of Ethics 14.11 Readmission to hospital during community-based peer support |
| 15.0 Peer worker absence | 15.1 Short-term cover (within team) 15.2 Long-term cover (reserve PWs) 15.3 Support and induction for reserve PWs |
An 8-day, manualised training programme was developed, underpinned by 10 knowledge and skill sets derived from components prioritised to the training domain in stage 2, and the peer support principles. 57 The resulting training matrix (see Appendix 1, Figure 15) guided writing and development of training materials. Each training day comprised session plans, slides, handouts, exercises and other materials.
FIGURE 15.
ENRICH training matrix.
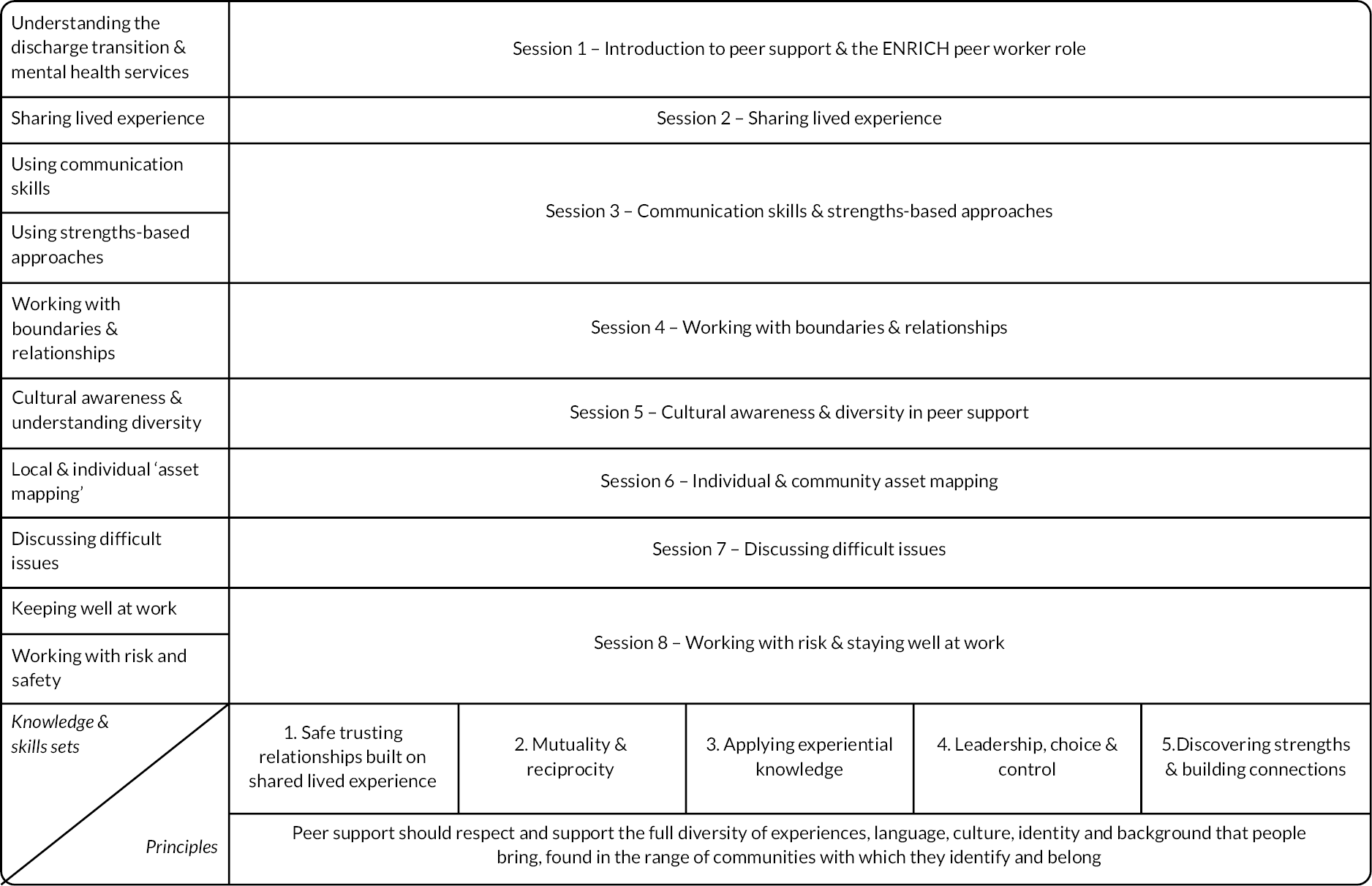
Stage 3: Piloting the intervention
Five PWCs involved in delivering training at both pilot sites attended a feedback workshop, with one PWC providing individual feedback. Four of five PWs at one site attended a workshop. Feedback was used to make amendments to the training and aspects of the handbook on recruitment of PWs and post-training support (see Appendix 1, Figure 16).
FIGURE 16.
Feedback from the pilot trial.
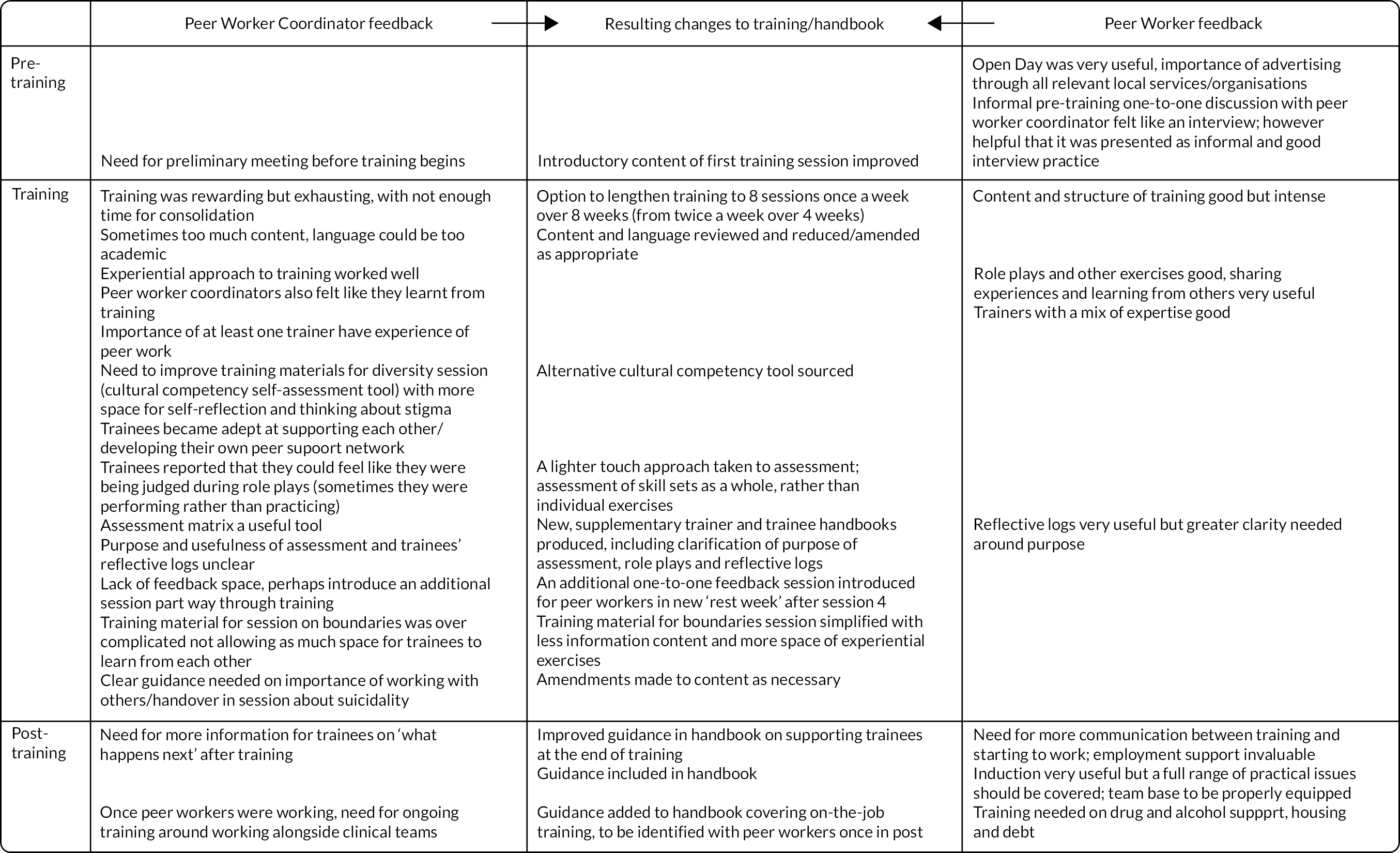
Appendix 2 Health economic evaluation
Data
Service contacts
The primary health economic analysis and secondary cost-effectiveness analysis at 4 months were carried out using EPRs data supplied by participating mental health trusts. This included all recorded NHS hospital- and community-based mental health service contacts and psychiatric bed days utilised by trial participants up to 12 months post discharge from the index hospital admission and over the 12 months prior to the index admission. The PW contact log was used to record face-to-face contacts between PWs and trial participants.
For the secondary analysis of costs relating to wider service use, a version of the Adult Service Use Schedule (AD-SUS)72 was administered to collate trial participant self-reported contacts with services not delivered by NHS mental health providers, including: primary care, hospital for non-psychiatric reasons, social worker, voluntary sector services, private therapists and contacts with the police for any reason, including number of times placed in custody. The AD-SUS was administered at baseline with reference to the 3-month period prior to index admission; and at 4 months post discharge reference for that period.
Unit costs
Unit costs required for costing service contacts were obtained from the Unit Costs of Health and Social Care published annually by the Personal Social Services Research Unit73 and NHS Reference costs. 74 The unit cost of police contacts and police custody were based on costs reported by Heslin and colleagues. 75
An estimate of the cost per minute of face-to-face contact between peer support workers and trial participants was developed specifically for this study. Activity logs relating to a sample period of 10 working days were completed by PWs and the PWCs. These were used to identify the ratio between face-to-face and non-face-to-face time allocated to a specific patient, including time spent by PWCs training PWs, and subsequently to estimate a cost per hour of face-to-face contact inclusive of costs of training and non-face-to-face contact time. PW and PWC time was costed using the appropriate corresponding NHS salary grading (reported with relevant salary ‘on-costs’ in the Unit Costs of Health and Social Care). 73 Additional overhead costs and capital costs related to employment were applied proportionately in accordance with unit costs reported for similar professionals in the Unit Costs of Health and Social Care. 74
Cost and outcome measurement
The total cost per trial participant was calculated as the sum of costs attributed to all community- and hospital-based contacts made over 12 months from the date of discharge from the index admission (for the primary cost analysis) or over 4 months post discharge date (for the secondary cost-effectiveness analysis). Costs were also split into those relating to: CMHT contacts; psychiatric bed days; crisis team and A&E contacts (summed together); and all other service contacts.
For the secondary analysis of wider service costs over 4 months post hospital discharge, the number of self-reported contacts for each trial participant was multiplied by the relevant unit cost. For this analysis, costs were divided into total community-based service contacts and the total cost of contacts made with the police, including the cost of police custody. Costs of peer support were excluded from the secondary analysis of wider service costs. Health-related quality of life outcomes converted to a 4 month ‘QALY’ equivalent were measured using the EuroQol-5 Dimensions, five-level version (EQ-5D-5L) instrument. 52 Following recent guidance issued by National Institute of Health and Care Excellence (NICE),76 health states reported by trial participants were mapped back on to the health state valuation system applicable to the 3-level version of the EQ-5D. 77 The cross-mapping utilised the algorithm reported by Van Hout and colleagues. 78
Analysis
All analyses were conducted on a complete case basis and restricted to randomised participants included in the analysis samples at 4 months and 12 months used for the clinical evaluation (see Appendix 2, Table 17). Missing data from EPRs on service contacts and other patient covariates was not a serious problem and, in line with the main clinical analysis, we assumed that it was ignorable and likely to be missing at random. Missing data on self-reported service contacts and quality of life at 4 months were more problematic due to patients not being interviewed at follow-up – as self-report data is likely to be not missing at random, we did not seek to impute values where data were missing. For the primary analysis (12-month cost of mental health service contacts) complete cost data were available for n = 537 participants (91% of those randomised); complete health state utility data required for a complete case cost-effectiveness analysis were available for n = 289 participants (49% of those randomised); and for secondary analysis of the cost of wider service contacts, complete data on the cost of community service contacts at 4 months were available for n = 291 participants (49% of those randomised) and n = 293 (50% randomised participants) for cost of police contacts.
Multivariate modelling: costs and health state utilities
The estimation of differences in the mean total cost of mental health service use over 12 months (for the primary analysis) and over 4 months post discharge (for the secondary cost-effectiveness analysis) for intervention and control participants was undertaken using GLM with a logarithmic link function. 53 Total cost for each period was regressed on a dummy variable identifying treatment allocation (1 = Peer support; base category = usual care) and additional ‘baseline’ covariates: ethnicity; trial site; diagnostic group; total cost of mental health service contacts over 12 months prior to the index admission. The sub-categories of cost defined above were also modelled (over 12 months only) using the same approach. Wider service costs over 4 months were modelled similarly with total community-based costs and total costs of police contacts modelled separately. Utility scores applicable to EuroQol-5 Dimensions, three-level version (EQ-5D-3L) health states were also analysed using GLM framework using a log-link. Covariates included ethnicity, diagnostic group, number of previous psychiatric admissions, trial site and baseline utility scores.
Cost-effectiveness analysis at 4 months: combining costs and QALY outcomes
A ‘net benefit’ framework was used54 to evaluate whether the peer support intervention offered a cost-effective alternative to usual care after 4 months post discharge from the index hospital admission. For the ‘base case’ analysis, we adopted a cost-effectiveness threshold of £20,000 per QALY gained. This is the lower end of the range currently used by NICE (£20,000 to £30,000) when assessing health programme cost-effectiveness.
Uncertainty in cost-effectiveness analysis
For the primary analysis of costs over the 12 month follow-up, non-parametric bootstrap sampling was performed to facilitate an evaluation of uncertainty in relation to the estimated incremental effect of the PW intervention on total costs over 12 months arising from trial sampling error. The probability of drawing an incorrect conclusion about cost impact of peer support based on this expected value was determined with reference to the proportion of the bootstrap incremental values that are either negative or positive. We also present 95% confidence limits using values at the 97.5th and 2.5th percentiles of the distribution.
Results
Primary analysis
Appendix 2, Table 14 presents descriptive statistics for the cost of mental health service contacts measured over 12 months post discharge from hospital separately for intervention and control participants, including the cost of participant contacts with peer support workers. A positive mean cost of PW support is shown for the control arm of the trial on account of two trial participants receiving the intervention in error.
| PW intervention | CAU | |||||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Min-max value | N | Mean | SD | Min-max value | N | |
| PW intervention | £536 | £528 | £0 to £2574 | 251 | £5 | £84 | £0 to £1434 | 296 |
| Service contacts | ||||||||
| CMHTs | £1523 | £1273 | £0 to £8083 | 287 | £1749 | £1768 | 0 to £19,883 | 291 |
| Crisis teams | £571 | £1060 | £0 to £8050 | 287 | £554 | £949 | £0 to £6600 | 291 |
| A&E (psychiatric-related contacts) | £273 | £709 | £0 to £5278 | 287 | £225 | £569 | £0 to £4669 | 291 |
| Psychiatric bed days | £15,937 | £28,520 | £0 to £211,560 | 287 | £21,366 | £40,027 | £0 to £242,529 | 291 |
| Day services | £107 | £758 | £0 to £11,470 | 287 | £324 | £2724 | 0 to £44,020 | 291 |
| Liaison psychiatry | £126 | £408 | £0 to £3660 | 287 | £95 | £367 | £0 to £3294 | 291 |
| Psychological treatment | £401 | £2156 | £0 to £21,279 | 287 | £453 | £2511 | £0 to £36,849 | 291 |
| Psychotherapy | £47 | £472 | £0 to £5925 | 287 | £17 | £278 | £0 to £4740 | 291 |
| Psychiatric assessment | £22 | £129 | £0 to £1212 | 287 | £22 | £229 | £0 to £3636 | 291 |
| Street triage | £3 | £19 | £0 to £180 | 287 | £2 | £13 | £0 to £120 | 291 |
| Criminal justice liaison | £7 | £120 | £0 to £2040 | 287 | £0 | £0 | - | 291 |
| Place of safety (Section 136) | £233 | £913 | £0 to £9560 | 287 | £181 | £1293 | £0 to £20,313 | 291 |
| Forensic psychiatry | £31 | £396 | £0 to £2040 | 287 | £13 | £104 | £0 to £1435 | 291 |
| Community drug and alcohol team | £0 | £0 | - | 287 | £22 | £259 | £0 to £3857 | 291 |
| Occupational therapy service | £101 | £553 | £0 to £7802 | 287 | £161 | £684 | £0 to £6889 | 291 |
| Perinatal mental health | £13 | £173 | £0 to £2784 | 287 | £13 | £172 | £0 to £2784 | 291 |
| All other services | £315 | £1324 | £0 to £13,640 | 287 | £318 | £4182 | £0 to £71,192 | 291 |
| Total cost over follow-up (including intervention cost) | £19,807 | £29,133 | £5 to £215,698 | 246 | £25,519 | £41,449 | £0 to £247,372 | 291 |
Appendix 2, Table 15 contains the main results from the primary analysis carried out on total costs of mental health service contacts over 12 months, inclusive of the costs of contacts with peer support workers in the intervention group. Adjusting for baseline covariates, exposure to peer support was associated with a reduction in mean total costs of £2631 (95% CI −£21,546 to £3845) – this amounted to a 10% reduction in mean total costs over 12 months post hospital discharge compared to usual care (95% CI −31% to 15%). Given sampling uncertainty there was an estimated 82% probability that peer support was associated with lower total costs over 12 months (or an 18% chance that usual care was the lower cost alternative).
| Total cost (including cost of intervention)a | N | |
|---|---|---|
| % effect (95% CI) | −10% (−31% to 15%) | 527 |
| Mean cost difference (95% CI) | −£2631 (−£21,546 to £3845) | |
| Probability total cost PW < CAU | 82% | |
| Service contact sub-categories b | ||
| CMHT contacts | N | |
| % effect of PW intervention (95% CI) | −8% (−21% to 7%) | 527 |
| Mean cost difference (95% CI) | −£132 (−£380 to £137) | |
| Psychiatric bed days | N | |
| % effect of PW intervention (95% CI) | −17% (−39% to 12%) | 527 |
| Mean cost difference (95% CI) | −£3765 (−£9696 to −£2167) | |
| Crisis team and A&E contacts combined | N | |
| % effect of PW intervention (95% CI) | 2% (−22% to 34%) | 527 |
| Mean cost difference (95% CI) | £17 (−£209 to £243) | |
| All other service contacts | N | |
| % effect of PW intervention (95% CI) | −4% (−38% to 46%) | 527 |
| Mean cost difference (95% CI) | −£65 (−£690 to £560) | |
Multivariate analysis undertaken on sub-categories of cost suggests that most of the cost reduction associated with peer support arose from reduced cost of bed day utilisation (estimated reduction in bed day costs of −£3765, 95% CI −£9696 to −£2167), although peer support was also associated with an 8% reduction in the costs of CMHT contacts (95% CI −21% to 7%).
Sensitivity analysis
Estimated treatment effects using multi-level (GLM) random intercepts model resulted in only marginal differences in the standard errors estimated around treatment effects and the predicted difference in mean total costs between intervention and control participants.
Two additional post hoc sensitivity analyses were also conducted on the primary analysis of 12-month total costs. First, we evaluated whether the exclusion of the estimated reduction in costs of community mental team contacts associated with peer support made any difference to the estimated differences in total cost. While there was a small reduction in effect of peer support on total cost over 12 months when CMHT costs were excluded, much of the intervention effect on mean total costs over 12 months was retained, again suggesting that most of the overall effect on total costs can explained by a reduction in bed day utilisation.
Second, we tested the sensitivity of the estimated reduction in total costs over 12 months to the exclusion of bed day costs above the 95th percentile of the cost distribution. As total costs have a distribution with a long right tail (a comparatively small percentage of participants generating a disproportionate volume of cost over follow-up), it is plausible that the observed effect of peer support at the sample mean will be driven by prevention of lengthier and more costly psychiatric admissions. We found that exclusion of the participants in the top 5% of bed day costs substantially diminished estimated reduction in mean total costs associated with peer support to £549 (compared to the ‘full’ effect of −£2631).
Secondary analysis
Appendix 2, Table 16 presents the baseline covariate adjusted EQ-5D-3L health state utility values for intervention and control participants at 4 months post hospital discharge. These differences amount to a gain of just 0.002 QALYs over 4 months for the intervention over the control group (95% CI −0.01 to 0.01) – an improvement equivalent to less than one extra day spent in full health. As at 12 months, exposure to peer support was associated with lower total costs of mental health service contacts over 4 months (again inclusive of the incremental costs associated with peer support) – a reduction in mean costs of −£2066 (95% CI −£24,158 to £1155).
| Mean | 95% CI | N | |
|---|---|---|---|
| PW intervention | 0.65 | (0.55 to 0.76) | 130 |
| CAU | 0.63 | (0.54 to 0.73) | 159 |
Appendix 2, Table 17 presents the combined analysis of QALY and cost outcomes over 4 months at a cost-effectiveness threshold of £20,000. The expected incremental net benefit (INB) of peer support (expressed in QALY units) is positive (0.11 QALYs, 95% CI −0.08 QALYs to 1.29 QALYs). Given sampling error, there is a 75% chance that this conclusion is correct (or conversely a 25% probability that usual care was the more cost-effective alternative).
| Mean (% effect) | 95% CI | ||
|---|---|---|---|
| Incremental total cost | −£2066 (−17%) | −£24,158 to £1155 | |
| Incremental QALYs | 0.003 (2%) | (−0.032 to 0.032) | |
| Cost-effectiveness | CET = £20,000 (base case) | CET = £30,000 | CET = £13,000 |
| Incremental net benefit per patient exposed to PW | 0.11 QALYs | 0.07 QALYs | 0.15 QALYs |
| 95% CI | −0.08 QALYs to 1.29 QALYs | −0.06 QALYs to 0.86 QALYs | −0.09 QALYs to 2.04 QALYs |
| Probability that PW is a cost-effective alternative to CAU at 4 months | 75% | 75% | 76% |
The expected incremental net benefit of peer support remains positive over all values of the cost-effectiveness threshold (see Appendix 2, Table 17) with little variability in estimated uncertainty.
Appendix 2, Table 18 contains descriptive statistics for the costs of wider service contacts. Appendix 2, Table 19 presents estimated differences in the costs of wider service contacts between intervention and controls, adjusting for baseline covariates. The mean cost of self-reported community-based service and police-related contacts was estimated to be £51 (95% CI −£164 to £265) and £53 (−£43 to £149) higher for intervention participants respectively.
| PW intervention | CAU | |||||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Min-max value | N | Mean | SD | Min-max value | N | |
| Community-based service contacts | £631 | £1035 | £0 to £6228 | 138 | £617 | £883 | £0 to £5950 | 160 |
| Contact with police (including custody) | £127 | £311 | £0 to £1170 | 136 | £113 | £295 | £0 to £1296 | 163 |
| Mean difference | 95% CI | N | |
|---|---|---|---|
| Community-based service contacts | £51 | −£164 to £265 | 291 |
| Contact with police (including police custody) | £53 | −£43 to £149 | 293 |
Appendix 3 Predictors of engagement with peer support
Methods
Participants
All trial participants who had been randomised to the PW group and who had a known allocated PW were included in this analysis.
Data
The dependent variable, ‘engaged with PW’, was defined in the CACE analysis as participants who had at least two PW meetings, at least one of which was in the community post-discharge.
Pre-randomisation and pre-discharge predictor variables were obtained from a number of sources: baseline research interview which was conducted prior to randomisation, EPR extracted by site information management personnel for the period 12 months pre-index admission and a PW contact log completed using an online survey after each attempted contact.
Pre-randomisation predictor variables were: index admission type (compulsory/voluntary), sexual orientation (heterosexual/not heterosexual), gender, diagnosis (using stratification variable), ethnicity (black/other), age, social inclusion (SIX), severity of symptoms (BPRS), hope, number of admissions in year prior to index admissions, treatment stigma barriers to accessing care evaluation, severity of anticipated stigma and count of life areas of stigma questionnaire on anticipated discrimination (QUAD).
Pre-discharge predictor variables were: matching characteristics between participant and PW, relationship-building in first contact, length of first contact with PW (minutes), days between recruitment and discharge and whether the participant had two or more PW contacts pre discharge.
To calculate the ‘matching characteristics’, variable intermediate variables were calculated to indicate whether allocated PWs matched participants on age (matching within age bands: 18–35, 36+), gender, ethnicity (matched within ethnicity groups; Asian, black, mixed, other and white) and diagnosis (matched with diagnosis categories: psychotic disorder, personality disorder, other diagnosis). The variable ‘matching characteristics’ was calculated as the sum of the four characteristics PWs and participants may have matched on, giving a possible range of 0–4.
For each contact PWs indicated which of the following activities were covered in the contact: using your own lived experience, learning from the lived experience of the person you are supporting, negotiating (or renegotiating) the boundaries in your relationship, accompanying or ‘being alongside’ the person you are supporting, using active listening skills. Using these data, ‘relationship-building’ was calculated as the count of these activities covered in the first contact between PW and participant and had a possible range of 0–5.
Statistical analysis
Logistic regression was used to model the relationship between the two groups of predictor variables and ‘engaged with peer support’ dependent variable. Results are reported with ORs and 95% CIs.
Results
Two hundred and ninety-four participants were allocated to the peer support group. Three of these participants withdrew their data. Of these, 265 (90%) had a known allocated PW.
Descriptive data
The sample had a mean age of 39.7 years (SD = 14.0) with a range from 18 to 74 years. There were similar numbers of male (48.3%) and female (51.4%) participants with one identifying as transgender. Just over half of the sample was white, 144/257 (56%) and 43/257 (16.7%) were black. Two hundred and seventeen participants were heterosexual. The largest diagnostic group in this sample was the psychotic disorders group (44.5%). Approximately half of participants (50.8%) had been admitted under a compulsory admission. In the year prior to the index admission, participants had a median of 1 psychiatric admission.
Engagement with peer support
Sixty-two per cent (163/265) of participants received peer support as defined as having had at least two PW meetings, at least one of which was in the community following discharge. For the 163 who engaged with peer support their mean number of face-to-face contacts was 9.1 (median = 9; SD = 4.7) ranging from 2 to 22. Post discharge they had a mean number of face-to-face contacts equal to 7.1 (median = 7; SD = 4.0) ranging from 1 to 15.
Pre-randomisation predictors of engagement
Descriptive statistics of the pre-randomisation variables being tested as predictors are reported in Appendix 3, Table 20, split by engaged with PW group. These are accompanied by the parameter estimates of the logistic regression model. It can be seen that the only demographic characteristic predictive of engaging with peer working is sexual orientation, heterosexual participants being 70% less likely to engage with PW than non-heterosexual participants, OR 0.3 (95% CI 0.08 to 0.87; p = 0.029).
| n | Engaged (%) | Not engaged (%) | OR (95% CI) n = 180 | p-value | ||
|---|---|---|---|---|---|---|
| Index admission | Voluntary | 122 | 80 (52) | 42 (45) | 1 | 0.248 |
| Compulsory | 126 | 75 (48) | 51 (55) | 0.7 (0.32 to 1.34) | ||
| Sexual orientation | Not heterosexual | 43 | 34 (21) | 9 (9) | 1 | 0.029 |
| Heterosexual | 217 | 126 (78) | 91 (91) | 0.3 (0.08 to 0.87) | ||
| Gender | Female | 133 | 84 (53) | 49 (50) | 1 | 0.684 |
| Male | 125 | 75 (47) | 50 (50) | 0.9 (0.44 to 1.72) | ||
| Diagnosis | F20–F29 | 118 | 70 (43) | 48 (47) | 1 | 0.451 |
| F60 (Specific personality disorder) | 51 | 29 (18) | 22 (22) | 0.6 (0.21 to 1.73) | ||
| Other eligible non-psychotic disorders | 96 | 64 (39) | 32 (31) | 0.6 (0.31 to 1.36) | ||
| Ethnicity | Other | 214 | 139 (87) | 75 (77) | 1 | 0.222 |
| Black | 43 | 21 (13) | 22 (23) | 0.6 (0.26 to 1.34) | ||
| n | Mean (SD) | Mean (SD) | ||||
| Age (years) | 255 | 40.2 (14.5) | 38.8 (13.2) | 1.0 (0.99 to 1.03) | 0.417 | |
| Social inclusion (SIX T0) | 220 | 3.2 (1.3) | 2.9 (1.4) | 1.2 (0.89 to 1.50) | 0.273 | |
| Severity of symptoms (BPRS T0) | 248 | 33.0 (9.2) | 35.1 (9.7) | 1.0 (0.94 to 1.02) | 0.404 | |
| Hope (HHI T0) | 249 | 33.1 (8.1) | 33.4 (8.3) | 1.0 (0.97 to 1.07) | 0.530 | |
| Admissions in year prior to index admission | 265 | 1.0 (1.3) 1.0 | 1.1 (1.2) 1.0 | 1.0 (0.75 to 1.27) | 0.860 | |
| Treatment stigma (BACE T0) | 254 | 1.3 (0.85) | 1.4 (0.84) | 1.2 (0.78 to 1.95) | 0.366 | |
| Severity of anticipated stigma (QUAD T0) | 258 | 1.4 (0.6) | 1.4 (0.5) | 1.0 (0.43 to 2.35) | 0.984 | |
| Count of life areas of stigma (QUAD T0) | 258 | 10.8 (3.9) | 10.9 (3.6) | 1.0 (0.88 to 1.12) | 0.946 | |
This model was repeated twice, (1) removing SIX and (2) removing count of life areas of stigma (QUAD). SIX was removed as this variable had the most missing data, its removal increasing n to 210. The QUAD variable was removed as the two versions of the scale, mean and count of life areas, were highly correlated, r = 0.73. These two models produced results consistent with the reported model in Appendix 3, Table 20. Little’s test was non-significant, indicating there was no evidence that data were not missing completely at random indicating that a complete case analysis is appropriate.
Pre-discharge predictors of engagement
Looking at the individual characteristics that may match or not between the participant and their PW it can be seen in Appendix 2, Table 19 that there is no evidence that matching on age, gender, ethnicity or diagnosis impacts on whether the participant engages with the PW. These are incidental matches – no attempt was made to match on characteristics apart from gender if a participant expressed a preference or if this was indicated as necessary by a member of the participant’s clinical team. The individual matching variables were not analysed further.
| n | Engaged (%) | Not engaged (%) | p-value | |
|---|---|---|---|---|
| Matched on age group | 231 | 70 (50) | 49 (54) | 0.477 |
| Matched ethnicity | 254 | 78 (49) | 49 (52) | 0.697 |
| Matched gender | 251 | 87 (56) | 51 (53) | 0.642 |
| Matched diagnosis | 265 | 53 (33) | 31 (30) | 0.718 |
Appendix 3, Table 22 reports the results of the logistic regression model exploring the association between predictors relevant to the instigation of the peer support relationship. It can be seen that a shorter time between recruitment and discharge and a longer duration of first contact with PW is associated with being more likely to ‘engage with peer support’. Relationship-building is nearly significant at the 5% level with those who engaged with peer support having on average 1 more relationship-building activity than those who did not engage with peer support.
| n | Engaged | Not engaged | OR (95% CI) n = 247 | p-value | |
|---|---|---|---|---|---|
| 2 or more contacts on ward pre-discharge | 265 | 66 (40.5%) | 35 (34.3%) | 1.5 (0.76 to 2.96) | 0.242 |
| Mean (SD) | Mean (SD) | ||||
| Degree of matching 0–4 | 265 | 1.8 (1.0) | 1.8 (1.0) | 1.0 (0.76 to 1.38) | 0.867 |
| Relationship-building – first contact | 248 | 3.2 (1.4) | 2.2 (1.8) | 1.2 (0.99 to 1.58) | 0.065 |
| Length of first contact (minutes) | 247 | 49.0 (30.4) | 29.0 (24.0) | 1.02 (1.00 to 1.04) | 0.010 |
| Time between enrolment and discharge (days) | 265 | 27.1 (37.4) | 66.6 (134.7) | 0.99 (0.98 to 1.00) | 0.002 |
Appendix 4 Peer worker impact study
Data collection
Interviews took place after training and induction into the role (T1) and after 4 months (T2) and 12 months in post (T3). At T1 only the interview included structured questions collecting socio-demographic data. At T1 and T3 questions were asked about mental health and physical health service use for the preceding 3 months using a modified version of the Client Services Receipt Inventory (CSRI). 79 At all three time points participants were asked to complete the Warwick-Edinburgh Mental Wellbeing Scale,80 Job Satisfaction Measure,81 Interdisciplinary Team Process and Performance in Long-Term Care82 and Maslach Burnout Inventory. 83 Data on days absent from work and length of employment for each PW was collected from the PWC at each site. Number of contacts with each person supported by each PW was collected from an online contact log completed by PWs after each contact.
Peer workers completed a qualitative interview, lasting about an hour, with a service user researcher at each timepoint. Interviews at T1 explored PWs’ experiences of recruitment to the role and training received and initial experiences of being part of a PW team. Interviews at T2 and T3 explored PWs experiences of providing peer support, reflection on how training helped them prepare for the role, challenges and rewards of the role, experiences of the PW team and working alongside clinical teams, experiences of support and supervision, and reflections on staying well at work. The interview at T3 also considered future work aspirations and opportunities.
Data analysis
Normative data were chosen for the general population (well-being) or a large sample (> 500) of healthcare professionals from the UK (job satisfaction and burn out) or USA (interdisciplinary team working). Comparison of the outcomes for PWs to normative samples was by inspection rather than statistical test. To examine change in outcomes over a year, paired t-test analyses were conducted comparing T1 to T3 data and T1 to T2 data.
Qualitative data were first analysed as described in Process evaluation – peer support and change in mental health services above, with data from impact study interviews with PWs contributing to the development of the analytical codebook (see Report Supplementary Material 3). Our approach to data synthesis sought to merge analyses by exploring convergence and divergence between datasets. 61 Where quantitative analysis was of interest, we revisited qualitative data either to illuminate quantitative findings or, where there were tensions between datasets, to understand how PWs might articulate their experiences differently.
Results
Participant characteristics are reported in Appendix 4, Table 23. The 32 PWs were in post for 17.7 months on average ranging from 6.1 to 31.6 months. The mean number of hours worked per week was 17.8 hours, ranging from 10 to 30 hours per week. PWs reported a mean of 6.8 days sick leave, ranging from 0 to 65 days with 12 PWs reporting no sick leave. PWs supported a mean of 9.7 people each, ranging from 1 to 39 people. Number of completed face-to-face contacts ranged from 2 to 273, with a mean of 56.1 contacts per PW and a total of 1682 contacts over the course of the study. Health service use for the 3 months prior to T1 are given in Appendix 4, Table 24.
| n | n (%) | ||
|---|---|---|---|
| Site | South West London | 32 | 5 (15.6) |
| East London | 7 (21.9) | ||
| Sussex | 6 (18.8) | ||
| Central & North West London | 5 (15.6) | ||
| Bradford | 3 (9.4) | ||
| Birmingham | 3 (9.4) | ||
| Surrey & Borders | 3 (9.4) | ||
| Gender | Male | 32 | 10 (31.3) |
| Female | 21 (65.6) | ||
| Prefer not to say | 1 (3.1) | ||
| Sexual orientation | Bisexual | 31 | 3 (9.7) |
| Lesbian/Gay | 2 (6.5) | ||
| Heterosexual | 22 (71.0) | ||
| Prefer not to say | 4 (12.9) | ||
| Ethnicity | White British | 30 | 20 (66.7) |
| White Irish | 3 (9.0) | ||
| White other | 2 (6.7) | ||
| Arab | 1 (3.1) | ||
| Black/Black British African | 1 (3.1) | ||
| Asian/Asian British Pakistani | 1 (3.1) | ||
| Mixed white & Asian | 1 (3.1) | ||
| Mixed other mixed background | 1 (3.1) | ||
| Highest education level | Secondary school | 25 | 7 (28.0) |
| More than secondary school | 10 (40.0) | ||
| University graduate | 4 (16.0) | ||
| Postgraduate | 4 (16.0) | ||
| Marital status | Married | 25 | 3 (12.0) |
| Single | 16 (64.0) | ||
| Divorced | 2 (8.0) | ||
| In a relationship | 4 (16.0) | ||
| Religion | No religion | 28 | 14 (50.0) |
| Christian | 8 (28.6) | ||
| Muslim | 3 (10.7) | ||
| Religion not stated | 3 (10.7) | ||
| English is first language | 25 | 24 (96.0) | |
| Has child under 18 years living in household | 23 | 1 (4.3) | |
| Mean (SD) Min-Max | |||
| Age | 27 | 42.9 (9.0) 26.0–59.0 | |
| Length of time in post, months | 32 | 17.7 (8.2) 6.1–31.6 | |
| Number of contracted hours per week | 30 | 17.8 (5.6) 10.0–30.0 | |
| Number of days sick leave | 30 | 7.7 (13.8) 0.0–55.0 | |
| Number of peers | 30 | 9.7 (8.0) 1.0–40.0 | |
| Number of completed FTF contacts | 30 | 56.1 (54.0) 2.0–273.0 | |
| T1 (n = 32) | T3 (n = 21) | |
|---|---|---|
| Inpatient stay (physical health) | 1 | 0 |
| A&E visit (physical health) | 4 | 2 |
| Outpatient visit (mental health) | 5 | 2 |
| Psychiatrist | 7 | 3 |
| CMHT | 13 | 6 |
| Crisis & home treatment team | 0 | 0 |
| Counselling/psychotherapy | 4 | 7 |
| GP | 13 | 10 |
| Primary care nurse | 8 | 6 |
| Recovery college | 9 | 6 |
| Other community-based well-being groups/services | 0 | 6 |
Measures of well-being, job satisfaction, multidisciplinary team working and burn out
Data were available for 20 PWs at T2 and 21 at T3. Descriptive statistics are reported in Appendix 4, Table 25. The well-being of the PWs remained fairly constant over the year, marginally lower than the general population norm. The job satisfaction subscales and overall score mean values were higher than norm values apart from satisfaction with pay and prospects subscales. Interdisciplinary Team Scale subscales were higher than norm values across the three timepoints apart from team effectiveness and workplace resources. Mean scores of Maslach Burnout Inventory subscales indicate lower levels of burn out and depersonalisation, and slightly higher levels of personal effectiveness than norms.
| T1 | T2 | T3 | ||||||
|---|---|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | Norm | ||
| WEMWBS – well-being a | 32 | 49.8 (9.07) 28.0–70.0 | 20 | 47.7 (9017) 32.0–69.0 | 21 | 48.7 (11.73) 25.0–68.0 | 51.6 (8.71) | |
| Measure of job satisfaction | Personal satisfaction | 29 | 4.3 (0.72) 1.5–5.0 | 17 | 4.2 (0.51) 3.3–5.0 | 19 | 4.2 (0.64) 3.2–5.0 | 3.7 (0.65) |
| Satisfaction with workload | 30 | 3.9 (0.76) 1.8–5.0 | 17 | 3.8 (0.62) 2.5–4.9 | 19 | 3.8 (0.78) 2.6–5.0 | 3.1 (0.77) | |
| Satisfaction with professional support | 31 | 4.5 (0.53) 3.0–5.0 | 17 | 4.5 (0.58) 3.4–5.0 | 19 | 4.4 (0.82) 1.8–5.0 | 3.6 (0.69) | |
| Satisfaction with training | 29 | 3.9 (0.74) 1.6–5.0 | 17 | 3.8 (0.92) 2.4–5.0 | 19 | 3.6 (0.86) 2.2 −5.0 | 3.2 (0.92) | |
| Satisfaction with pay | 30 | 3.5 (1.14) 1.0–5.0 | 17 | 3.4 (1.23) 1.0–5.0 | 20 | 3.5 (1.10) 1.0–5.0 | 3.4 (0.66) | |
| Satisfaction with prospects | 30 | 3.5 (0.92) 1.2–5.0 | 17 | 3.5 (1.00) 1.7–5.0 | 19 | 3.1 (1.10) 1.0–4.8 | 3.4 (0.66) | |
| Satisfaction with standards of care b | 29 | 4.0 (0.62) 2.8–5.0 | 17 | 4.0 (0.65) 2.3–5.0 | 19 | 3.9 (0.89) 2.2–5.0 | ||
| Overall satisfaction | 30 | 3.9 (0.66) 1.9–5.0 | 17 | 3.9 (0.60) 3.0–4.7 | 20 | 3.7 (0.74) 2.6–5.0 | 3.44 (0.53) | |
| Multidisciplinary team survey c | Leadership | 31 | 4.2 (0.66) 2.2–5.0 | 20 | 4.4 (0.47) 3.3–4.9 | 21 | 4.1 (0.62) 2.7–5.0 | 3.8 (0.77) |
| Team cohesion | 32 | 4.3 (0.84) 1.6–5.0 | 20 | 4.3 (0.47) 3.3–5.0 | 21 | 4.2 (0.93) 1.7–5.0 | 4.0 (0.73) | |
| Communication | 31 | 4.1 (0.57) 2.5–5.0 | 20 | 4.0 (0.60) 2.8–5.0 | 21 | 3.8 (0.93) 1.5–5.0 | 3.6 (0.69) | |
| Co-ordination | 31 | 4.2 (0.66) 1.8–5.0 | 20 | 4.2 (0.61) 2.8–5.0 | 21 | 4.1 (0.86) 1.7–5.0 | 3.9 (0.75) | |
| Conflict management | 27 | 3.8 (0.49) 2.8–4.7 | 20 | 3.8 (0.35) 3.2–4.4 | 20 | 3.7 (0.45) 2.7–4.3 | 3.6 (0.66) | |
| Team effectiveness | 26 | 4.0 (0.36) 3.0–4.4 | 20 | 3.9 (0.40) 3.0–4.4 | 19 | 3.7 (0.59) 2.3–4.4 | 4.2 (0.69) | |
| Workplace conditions | 31 | 3.7 (0.83) 1.4–5.0 | 19 | 3.9 (0.73) 2.2–5.0 | 20 | 3.8 (0.80) 2.4–5.0 | 3.2 (0.91) | |
| Workplace resources | 27 | 3.6 (1.01) 1.6–5.0 | 18 | 3.6 (0.89) 1.6–5.0 | 18 | 3.5 (0.74) 2.2–5.0 | 3.8 (0.86) | |
| Maslach burnout inventory d | Burn out | 32 | 8.6(9.27) 0.0–39.0 | 20 | 9.8 (7.84) 0.0–28.0 | 21 | 11.8 (9.72) 1.0–32.0 | 19.7 (9.6) |
| Depersonalisation | 32 | 3.0 (3.61) 0.0–14.0 | 20 | 4.4 (3.90) 0.0–16.0 | 21 | 4.7 (4.07) 0.0–14.0 | 8.9 (7.4) | |
| Personal achievement | 23 | 39.3 (7.34) 18.0–48.0 | 19 | 38.7 (6.90) 24.0–48.0 | 19 | 37.5 (11.2) 17.0–56.0 | 35.8 (7.6) | |
Change in service use
Appendix 4, Table 24 indicates very little change in use of services for both mental and physical health from T1 to T3, with the exception of an increase in use of counselling and psychotherapy, and new use of a range of community-based well-being services, including attending community and faith-based groups.
Change in outcomes
Change in outcomes from T1 to T2, and T1 to T3 is reported in Appendix 4, Table 26. Between baseline and 4 months follow-up there was a statistically significant decrease of nearly 4 points in well-being, a medium effect size, 0.56. However, over the course of the year there was no significant change in well-being. There was a statistically significant decrease in some job satisfaction subscales at the 4-month follow-up; personal satisfaction (medium effect size, 0.50), satisfaction with workload (small effect size, 0.31) and satisfaction with prospects (small effect size, 0.33). This decrease in satisfaction with prospects continued over the year with T1 to T3 scores reducing by 0.45 points, a statistically significant change (small – medium effect size, 0.43). Over the course of the year there was also a statistically significant decrease in satisfaction with training (small – medium effect size, 0.46). There was no statistically significant change in any of the Multidisciplinary Team subscales at T2 or T3. Of note however is the relatively large effect size for a decrease in the Communication subscale of 0.86 to T3. Examining the Maslach Burnout Inventory, there was a significant increase in depersonalisation at both T2 and T3, the increase occurring in the first 4 months and seemingly maintained to T3 (small-medium effect size to T2, −0.48).
| T1–T2 | T1–T3 | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| n | Change (95% CI) | p-value | ES | n | Change (95% CI) | p-value | ES | ||
| WEMWBS – well-being | 20 | 3.9 (0.67 to 7.13) | 0.020 | 0.56 | 21 | 1.00 (−3.46 to 5.46) | 0.645 | 0.09 | |
| Measure of job satisfaction | Personal satisfaction | 16 | 0.2 (0.00 to 0.44) | 0.044 | 0.50 | 19 | 0.09 (−0.28 to 0.46) | 0.625 | 0.11 |
| Satisfaction with workload | 16 | 0.2 (0.06 to 0.39) | 0.012 | 0.31 | 19 | 0.14 (−0.12 to 0.40) | 0.283 | 0.17 | |
| Satisfaction with professional support | 17 | 0.1 (−0.03 to 0.32) | 0.099 | 0.24 | 20 | 0.19 (−0.15 to 0.53) | 0.254 | 0.33 | |
| Satisfaction with training | 17 | 0.2 (−0.11 to 0.58) | 0.168 | 0.32 | 20 | 0.39 (0.03 to 0.76) | 0.036 | 0.46 | |
| Satisfaction with pay | 16 | 0.0 (−0.28 to 0.33) | 0.859 | 0.00 | 19 | 0.04 (−0.32 to 0.40) | 0.820 | 0.04 | |
| Satisfaction with prospects | 16 | 0.3 (0.09 to 0.42) | 0.004 | 0.33 | 19 | 0.45 (0.01 to 0.89) | 0.047 | 0.43 | |
| Satisfaction with standards of Care | 16 | 0.0 (−0.30 to 0.28) | 0.940 | 0.00 | 19 | 0.13 (−0.21 to 0.48) | 0.434 | 0.22 | |
| Overall satisfaction | 17 | 0.1 (−0.01 to 0.29) | 0.069 | 0.19 | 20 | 0.23 (−0.04 to 0.50) | 0.096 | 0.31 | |
| Multidisciplinary team survey | Leadership | 20 | 0.0 (−0.30 to 0.25) | 0.857 | 0.00 | 21 | 0.07 (−0.26 to 0.40) | 0.677 | 0.12 |
| Team cohesion | 20 | 0.1 (−0.35 to 0.47) | 0.757 | 0.14 | 21 | 0.04 (−0.51 to 0.60) | 0.880 | 0.05 | |
| Communication | 20 | 0.2 (−0.05 to 1.60) | 0.131 | 0.38 | 21 | 0.37 (−0.03 to 0.76) | 0.069 | 0.86 | |
| Co-ordination | 20 | 0.1 (−0.18 to 0.41) | 0.417 | 0.18 | 21 | 0.20 (−0.25 to 0.66) | 0.363 | 0.36 | |
| Conflict management | 20 | 0.1 (−0.17 to 0.28) | 0.616 | 0.17 | 21 | 0.13 (−0.09 to 0.36) | 0.235 | 0.22 | |
| Team effectiveness | 19 | 0.1 (−0.04 to 0.34) | 0.122 | 0.32 | 20 | 0.20 (−0.11 to 0.50) | 0.191 | 0.48 | |
| Workplace conditions | 18 | 0.0 (−0.40 to 0.38) | 0.952 | 0.00 | 20 | −0.01 (−0.49 to 0.47) | 0.965 | −0.01 | |
| Workplace resources | 18 | 0.1 (−0.57 to 0.69) | 0.840 | 0.11 | 20 | 0.00 (−0.38 to 0.38) | 0.982 | 0.00 | |
| Maslach burnout inventory | Burn out | 20 | −2.0 (−4.00 to 0.02) | 0.052 | −0.27 | 21 | −2.71 (−5.89 to 0.46) | 0.090 | −0.26 |
| Depersonalisation | 20 | −1.5 (−2.60 to −0.42) | 0.009 | −0.48 | 21 | −1.29 (−2.51 to −0.06) | 0.040 | −0.32 | |
| Personal achievement | 14 | 1.7 (−1.00 to 4.41) | 0.192 | 0.27 | 13 | 3.23 (−0.94 to 7.40) | 0.117 | 0.48 | |
Qualitative results
Overall levels of well-being and employment outcomes
Participants articulated a positive sense of well-being, attributing both feeling and functioning well aspects of well-being to the PW role:
For me it was about having the opportunity to be able to help others and to be able to realise that I was a human being who was valued, and it was an empowering experience to be able to now be in a position to contribute and have a meaningful fulfilling role in life again by supporting others.
(BMS-PW01-T1)
In general, satisfaction with the PW role was reported as high, participants were pleased that the role was, in most cases, properly salaried and they were, at least initially, optimistic about future job prospects:
This has been my first paid job in probably eight years I think … It’s been the most fantastic experience, I’ve absolutely loved it.
(SWL-PW05-T3)
… maybe gain some more experience, maybe go on to a more senior role or managerial role. I’d like to do some training development for my own personal growth. And maybe go on to peer training.
(CNW-PW04-T1)
A strong and supportive sense of team within the peer support team was evident in a number of interviews:
Supervision has been a really nice way to end the week because we all come together and we discuss ideas and issues and explore ways to make things better to improve our practice. I do enjoy working with my other peer workers as well, they’re really nice. We get on really well and I think having the people that you surround yourself with at work and a good work environment is really essential to your mental health.
(CNW-PW02-T2)
However, a sense of disconnect with the work of clinical teams might have contributed to the slightly lower team effectiveness and resources scores:
… it’s been a bit blurred about what our role is as peer support workers [when] there hasn’t been a care co-ordinator or other support workers involved with a particular peer that you are working with. I think sometimes you are a little bit forced into helping with things like accommodation … and that’s not your role.
(CNW-PW01-T2)
PWs, by and large, did not report feeling burnt out in their work, and also experienced a high degree of personal effectiveness in the role:
… so previously when I was at [name of service] they were very long days and it’s a crisis service so it’s extremely busy and you just don’t stop all day so I was tired. But this role, because it’s completely different, it’s good for me, it’s pushing me and I think it’s having a better impact on my well-being.
(BDF-PW03-T1)
Low levels of de-personalisation were indicated by enthusiasm about interpersonal relations and working alongside others, especially where the work was emotionally demanding:
… as soon as I walked on the ward … I was like, ‘I want to be back here on the ward with all these people’ … every time I come into work, the more I’m around people … it’s just like I’m on a complete high … It’s just so positive.
(ELN-PW01-T1)
Change in outcomes
Well-being
Qualitative data from T2 indicate that, perhaps once the excitement following training had gone and the realities of the work confronted PWs, well-being could be challenged:
Well the level of responsibility and the level of freedom has surprised me. In a good way predominantly but it does have its moments. I think remote working is quite difficult or can be … you can feel left with quite a lot of difficult feelings.
(CNW-PW02-T2)
Job satisfaction
PWs did voice concerns about managing workload as the project progressed:
… trying to work my hours and not try and work too much beyond them. That is quite a struggle I have to say and I do find because I work part-time and it’s quite difficult to fit everything into the designated days and the timetabling when particular peers say ‘oh well, we need you to send a text’ or ‘call me’ the day before we are meeting … it’s quite easy for the peer role to bleed into other days.
(CNW-PW02-T2)
Some PWs found it difficult when the people they were supporting did not engage with the peer support, leaving them underemployed at times:
How to deal with non-engaging clients and you just, it is frustrating because you want to help them. You think the person would benefit … you are prevented a little bit from taking on too many new clients because they might suddenly decide to re-engage so that’s a tricky one.
(BDF-PW02-T2)
PWs remained hopeful that they would find future employment but did voice concern as fixed term contracts were coming to an end:
I’m hoping that once our contracts are up or not furthered or whatever more opportunities will come.
(SSX-PW05-T2)
Team working
Peer workers continued to value good communication within the PW team, but also felt that improved communication with clinical teams involved in the care of the people they were supporting would be beneficial:
… part of that is also communicating to a supervisor or colleague what is going on is helpful because then you can get that support or support someone else.
(CNW-PW01-T2)
… what you find is sometimes having that engagement, that rapport with them [clinical teams] is actually very supportive of one another … it’s about working together and it’s not about stepping on anyone’s shoes … we’re all supposed to be reading off the same page.
(CNW-PW04-T2)
Burn out
One PW described measures put in place with their manager to address the demands of the role:
I like connecting with people in life. So that’s why when I was feeling this intensity I said there was a burn out … and my manager said ‘what would help you’? and I said ‘I still need to continue to connect with people, I don’t want time off, but I just don’t want to connect as intensely as I was doing.’ So they needed someone to promote the project so me going out now and doing presentations was a win-win situation …
(ELN-PW04-T2)
List of abbreviations
- A&E
- accident and emergency
- ACT
- assertive community treatment
- AD-SUS
- Adult Service Use Schedule
- BCT
- behaviour change technique
- BDF
- Bradford
- BPRS
- Brief Psychiatric Rating Scale
- CACE
- complier average causal effect
- CAU
- care as usual
- CI
- confidence interval
- CMHT
- Community Mental Health Team
- CNW
- Central and North West London
- CSO
- Clinical Studies Officer
- DMEC
- Data Management and Ethics Committee
- ELN
- East London
- EPR
- electronic patient record
- FTE
- full-time equivalent
- GLM
- generalised linear modelling
- HHI
- Herth Hope Index
- HR
- hazard ratio
- IQR
- interquartile range
- ITT
- intention to treat
- LAG
- Local Advisory Group
- LEAP
- Lived Experience Advisory Panel
- MANSA
- Manchester Short Assessment of Quality of Life
- NICE
- National Institute of Health and Care Excellence
- OR
- odds ratio
- PSC
- Programme Steering Committee
- PW
- peer worker
- PWC
- peer worker co-ordinator
- QALY
- quality-adjusted life-year
- QUAD
- questionnaire on anticipated discrimination
- RA
- Research Assistant
- RCT
- randomised controlled trial
- RR
- risk ratio
- SAE
- serious adverse event
- SD
- standard deviation
- SIX
- objective social outcomes index
- SMD
- standardised mean difference
- SP
- supported peer
- SSX
- Sussex
- SWL
- South West London
Notes
Supplementary material can be found on the NIHR Journals Library report page (https://doi.org/10.3310/LQKP9822).
Supplementary material has been provided by the authors to support the report and any files provided at submission will have been seen by peer reviewers, but not extensively reviewed. Any supplementary material provided at a later stage in the process may not have been peer reviewed.
