Notes
Article history
The research reported in this issue of the journal was funded by PGfAR as project number RP-PG-0606-1151. The contractual start date was in August 2007. The final report began editorial review in May 2012 and was accepted for publication in May 2013. As the funder, the PGfAR programme agreed the research questions and study designs in advance with the investigators. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PGfAR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2013. This work was produced by Singh et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
It occurred to me that there was no difference between men, in intelligence or race, so profound as the difference between the sick and the well.
F Scott Fitzgerald, The Great Gatsby (p. 98)1
Chapter 1 Introduction and background
Compared with the white population, black and minority ethnic (BME) groups in the UK, especially young African Caribbean men, have higher rates of psychosis, experience more adverse pathways into care, are at greater risk of detention under the Mental Health Act (MHA)2 and are more likely to disengage with services over time, be less satisfied with their care and have poorer outcomes, with greater social exclusion. The conventional explanation for this is based on the notion of institutional racism within psychiatry. 3 However, this view has been challenged as providing simplistic explanations for complex underlying processes. 4
Ethnic differences in rates of psychosis and pathways to care are evident even in BME patients presenting with a first episode of psychosis (FEP);5,6 therefore, contributory factors must be operating before presentation to psychiatric services. These therefore need to be understood in a wider societal context. We have argued that ‘any potential solutions (to reduce such differences) must go beyond the health sector and involve statutory as well as voluntary and community agencies. The problem does not reside exclusively in psychiatry and hence the solutions cannot emerge from psychiatric services alone’ (p. 650, italics in original). 7
Early intervention services focus specifically on reducing the duration of untreated psychosis (DUP), enhancing therapeutic engagement and reducing social exclusion by providing care in community-based, low-stigma settings. 8 The UK has been at the forefront of developing early intervention services. There is also good evidence that specialist early intervention services demonstrate both clinical effectiveness and cost-effectiveness in improving the short- to medium-term outcomes of FEP. It is reasonable to assume that the assertive, community-based, non-coercive early intervention approach may specifically benefit BME patients. The Lambeth Early Onset trial9 found that BME patients were more likely to stay engaged with early intervention services than with generic community mental health teams (CMHTs). However, it is unclear whether generic early intervention services, as currently organised, meet the specific demands and challenges of providing care for BME patients.
The need for the ENRICH programme grew out of three strands of clinical need, policy imperatives and research evidence:
-
Adverse pathways to care in BME groups during FEP. Pathways to care are adverse in BME groups even in first presentation of a psychotic illness. 5,10 The three-centre Aetiology and Ethnicity in Schizophrenia and Other Psychoses study of FEP found that black patients were less likely to come to services through their general practitioner (GP) and more likely to come through criminal justice agencies and compulsory detention. In addition, family members were more likely to seek police help than medical help. 10,11 Hence, the determinants of these pathways need to be explored within the familial and wider societal context of BME patients. 12,13
-
Ethnic differences in compulsory detention rates. Detention rates for BME patients are high even for the FEP and they increase in later episodes. 6 This deteriorating relationship trajectory between BME patients and mental health services, with decreasing engagement and increasing detention rates over time, has been consistently demonstrated. 6,13–16 It is not clear, however, whether service-level intervention can reduce this detention rate and improve the engagement of BME patients.
-
Ethnic differences in outcomes and service satisfaction. BME patients, especially young black men, report less satisfaction with mental health services, with an increased number of previous admissions predicting greater dissatisfaction. 14 In the UK, the unemployment rate for patients suffering from psychosis has risen over the last 50 years and was 70–80% during the 1990s. 17 Service users and carer advocacy groups consider a return to work and occupation as one of the highest priorities for patients suffering from psychosis, which enhances their functional status and improves their quality of life. 18,19 BME patients may be doubly disadvantaged because of the combined effect of racism in the labour market and the stigma of mental illness.
The ENRICH programme aimed to develop the knowledge base essential for reducing, and if possible eliminating, ethnic differences in pathways to care in FEP. We proposed three studies conducted over 42 months of all service users referred to early intervention services in Birmingham. We wished to explore the cultural and family-related factors that facilitated or impeded access to health care. We planned to evaluate all MHA assessments to determine whether some BME patients had fewer community alternatives for care than other ethnic groups, thus leading to greater risk of detention. We wanted to seek the opinions of service users, carers, clinicians and other stakeholders on how early intervention services could become more appropriate for, and acceptable to, BME communities.
Chapter 2 Objectives and ethical considerations
The specific objectives of the programme, conducted as three distinct studies, were as follows:
-
Study 1: to understand ethnic differences in pathways to care in FEP by exploring cultural determinants of illness recognition, attribution and help-seeking among different ethnic groups.
-
Study 2: to evaluate the process of detention under the MHA and assess ethnic differences in the availability of alternative provision that could reduce the need for detention.
-
Study 3: to determine the appropriateness, accessibility and acceptability of generic early intervention services for different ethnic groups and establish the care needs and preferences of service users and other stakeholders.
In the original proposal we had also sought funding for two further studies:
-
Study 4: to understand pathways and predictors of social exclusion, especially vocational outcomes in FEP, and evaluate the effectiveness of early intervention services in enhancing social inclusion.
-
Study 5: to evaluate the longitudinal impact of early intervention services on engagement, satisfaction and coercion in FEP patients.
Funding for these studies was not approved.
Ethical considerations
Ethics approval
The Warwickshire Research Ethics Committee (WREC) gave ethical approval on 10 December 2008 subject to minor amendments. Amended documents were submitted and finally approved in February 2009. The study was approved by the Birmingham and Solihull Mental Health NHS Foundation Trust’s (BSMHFT) Research and Development Department on the 11 March 2009.
Birmingham City Council ethics
Originally we had planned to recruit patients into study 2 using data from social services, supplemented by data from home treatment teams. Although we had received ethical approval for this method from the WREC we were asked to seek separate ethical approval from an ethics committee run by Birmingham City Council (BCC). This committee did not accept WREC approval and did not agree to let us access their data set. After prolonged negotiations we received BCC approval on the 6 April 2009. We were given access to anonymised data; however, we had to pay a BCC staff member from our research funds to anonymise the data set for us. In addition, we had to seek separate BCC approval for the study 2 qualitative study; this was received on the 22 June 2010. Preparing the relevant documents and waiting for BCC approval led to a 9-month delay in data collection.
Chapter 3 Literature review
Social anthropological perspectives of health and illness suggest that a decision to seek care is, in part, mediated by beliefs about illness causality as well as the wider social and cultural networks. 16,20,21 There is evidence that some BME communities, especially those from African Caribbean and Asian backgrounds, attach greater stigma to mental illness, may attribute unusual behaviour to the individual rather than to an illness and seek police rather than medical help when dealing with an ill relative. 10 It is as yet unclear how such factors influence the observed ethnic differences in care pathways during FEP.
We reviewed the literature on ethnic and cultural determinants of help-seeking in serious mental disorders including the role of competing and contrasting explanatory models of mental illness held by BME service users and the role of stigma and shame in hindering access to care. We wished to determine whether mental health services consider the cultural, religious or spiritual needs of service users and their carers. We also conducted a systematic review and meta-analysis to explore correlates and predictors of ethnic differences in pathways to care in FEP.
Ethnic and cultural determinants of help-seeking
Culture and beliefs
Culture provides a framework for making sense of experience. 22 In the health-care context this is important because the ‘cultural interpretations of mental illness held by members of a society or social group (including mental health professionals) strongly influence their response to persons who are ill and both directly and indirectly influence the course of the illness’ (p. 233). 23 Explanatory models represent the concepts and frameworks utilised by people to describe the causes and course of their mental illness. 24 Littlewood25 makes a distinction between ‘etic’ models of medical perspectives, which are clinical/scientific explanations, and ‘emic’ models, which focus on patients’ perspectives based on the cultural understanding of subjective experience. Such explanatory models influence the perceived causation, recognition and treatment preferences that determine help-seeking attitudes and behaviours for mental illness20,21 and could therefore be implicated in delays in help-seeking.
Since 1994, the UK Department of Health has conducted national surveys that show fluctuations in the general population’s attitude to mental health. The most recent survey26 suggests a slight increase in positive attitudes towards those with mental illness compared with 2008,27 but current attitudes are not as positive as those in 2009. 28 It is difficult to pinpoint the cause in these fluctuations. Even though ethnicity status was collected, the reports do not highlight any differences in attitudes within ethnic groups. Hence, the survey does not explore the consequences of negative attitudes, such as the shame and stigma that exist within communities, or how religious beliefs may play a role in the attitudes and behaviour of a community. 29
Multiple explanatory models or multiple exploratory maps
Williams and Healy’s30 study of first-time presenters to mental health services showed that individuals move between varied and complex sets of beliefs and a variety of explanations are either held simultaneously or taken up and dismissed rapidly. Some people can move from one strongly held view to another relatively quickly and unproblematically, forming an exploratory map rather than an explanatory model. The authors state that ‘such beliefs should not be regarded as taking the form of a coherent explanatory model but rather as a map of possibilities, which provides a framework for the ongoing process of making sense and seeking meaning’ (p. 473). 30 Clearly, people’s cultural perspectives and interpretations of situations change too. Hence, explanatory models remain in use as long as they fit shared experiences,31 and experiences in turn shape cultural models over time.
Explanatory models in different ethnocultural groups
In studies examining the appropriateness of mental health services for Asian populations in the UK, the most frequently mentioned causes of mental health illness were social stress, family problems and the ‘will of God’. 32 Other attributions include ‘bad thoughts’, ‘lack of will power’ and ‘weakness in personality’. 33,34
McCabe and Priebe’s35 study exploring explanatory models in schizophrenia in the UK found that white patients cited biological causes of illness more often than African Caribbean, West African and Bangladeshi patients, and both Bangladeshi and West-African patients cited supernatural causes more frequently than white patients. Small qualitative studies have suggested that such supernatural explanatory models lead to help-seeking from traditional healers rather than mental health services. 36–38 However, there are few studies in the literature that have systematically explored cultural attribution in emerging psychosis and its relationship to help-seeking.
Lack of education and information are considered to be important factors related to supernatural explanations for mental illness, both amongst BME groups in the UK39 and in the developing world. Srinivasan and Thara40 found that, in urban India, families living with someone suffering from chronic schizophrenia subscribed to a supernatural causation of the illness, which the authors suggest occurs because of lack of information. However, other research shows that supernatural causes of schizophrenia are strongly held despite a medical knowledge of mental illness. 37,41 For instance, Das et al. 41 attempted to explore the effects of a structured educational programme on explanatory models of illness among relatives of people with schizophrenia in India. They found that many of the indigenous explanatory models persisted, especially those related to treatment (i.e. visiting traditional healers), despite the educational intervention. Dein and Sembhi39 found that age (as opposed to education) of subjects was the key variable, with younger patients more likely to consult traditional healers.
Spiritual and religious beliefs
Spirituality and religion are elusive concepts that are hard to define. 42 The Royal College of Psychiatrists43 defines spirituality as:
A distinctive, potentially creative and universal dimension of human experience arising both within the inner subjective awareness of individuals and within communities, social groups and traditions. It may be experienced as relationship with that which is intimately ‘inner’, immanent and personal, within the self and others, and/or as a relationship with that which is wholly ‘other’, transcendent and beyond the self. It is experienced as being of fundamental or ultimate importance and is thus concerned with matters of meaning and purpose in life, truth and values.
p. 24
Religion is an organised and communal activity, which encompasses most if not all aspects in definitions of spirituality, particularly in the context of belief in some sort of supernatural power, or God(s). Spirituality is more personal and individual in nature. 44,45 However, it is generally accepted that they overlap46 and that spirituality concerns anything that inspires a person, whether or not this is a formal religion.
In the UK’s changing and diverse society, people move across cultural boundaries and between faiths, or from belief to unbelief and then back to belief when a crisis occurs. 47 Research demonstrates that members of BME communities explicitly express their religious needs more than members of white communities. 48 Illness attributions, however, may not be bound to one particular religion. For instance, belief in demon possession as an explanation for mental illness has been noted in many Christian, Muslim and other communities in the UK. 49
In the study by Leavey et al. 50 on clergy contact with people with mental illness, both imams and Pentecostal pastors stated that they were often contacted by individuals or families who feared that ill health or misfortune had been provoked by a curse or witchcraft, or was the result of spirit possession. In such cases, prayer and religious rituals such as deliverance (exorcism) were considered to be the appropriate response. 50 Rabiee and Smith4 also highlighted similar findings amongst Somalian carers and users of mental health services in Birmingham.
In the UK, > 50% of service users say that spirituality helps them to cope with ill health and should be nurtured. 51 In light of the focus on spirituality in mental health care, the Royal College of Psychiatrists has set up a Special Interest Group in Spirituality (www.rcpsych.ac.uk/college/specialinterestgroups/spirituality.aspx; accessed July 2013). This group produces guidance on the relationship between spirituality and psychiatry, and the practicalities of addressing spirituality in psychiatric care. The Department of Health also produced a report highlighting the value of religion and belief in health, and the duty of professionals to respect and value belief systems in care planning and delivery. 52
Stigma and shame
‘Stigma’ is a mark or discredit that sets a person aside from others. 53 Human beings have a basic need to obtain or maintain a positive self-concept (ego-defence). 54 Research has demonstrated that stigmatising attitudes towards mental illness are particularly pervasive and harmful to those experiencing mental health problems, devaluing and discrediting self-identity. 55 Stigma and shame have been heavily implicated in poor help-seeking behaviour. 56 The fear of being labelled ‘mad’ or being perceived as mentally ill can lead to sufferers distancing themselves from others in their social roles and interactions. 56 Social distance is a measurement of an individual’s readiness to inter-relate with a target person in a variety of relationships. 57 Studies have shown that those with previous extensive communications with individuals experiencing mental health problems feel the need for less social distance than those with limited or no experience of such difficulties. 57
Evidence also suggests that urbanicity and cultural beliefs have an effect on levels of social distance. High levels of urbanicity and cultural beliefs in supernatural reasons for mental illness have been related to increased levels of social distance. 58 The fear of mental illness and people with mental health problems acts as a barrier in engaging with services, which can bring about stigmatised attitudes towards mental health and cause delays in help-seeking. 59 As the clergy in the Leavey et al. 50 study acknowledge, profoundly stigmatising community attitudes towards mental illness can result in religious rather than psychiatric help-seeking for such cases.
Systematic review of ethnic differences in pathways to care in first-episode psychosis
The primary aim of this systematic review was to explore ethnic differences in pathways to care exclusively during FEP and to explore factors that influence these differences. This review is split into two parts: the first will descriptively review the literature, exploring ethnic variation in pathways to care and associated factors; the second will report the meta-analysis, exploring ethnic variation in compulsory hospitalisation and criminal justice agency and GP involvement.
Search strategy and methodological appraisal
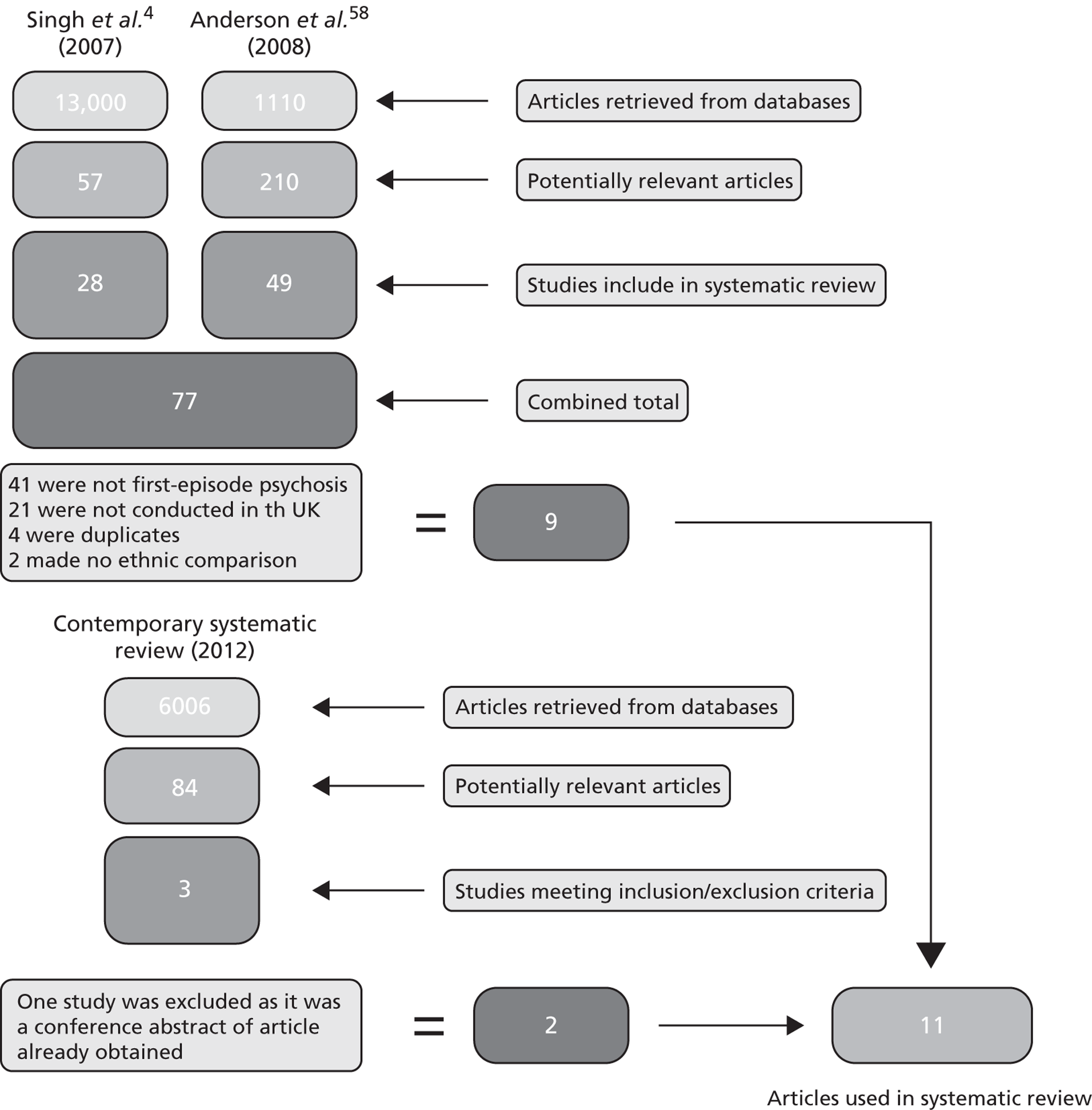
A comprehensive search strategy was developed to identify all studies in the UK that had explored ethnic variation in pathways to care during FEP (see Appendix 2). Singh et al. 6 had previously conducted a systematic review exploring ethnic differences under the MHA 1983, and Anderson et al. 60 conducted a systematic review exploring pathways to care during FEP. As these overlapped for the purpose of this review, relevant articles from these two reviews were carried forward (Figure 1). An additional literature review was conducted, extending the time period of these previous reviews. Bibliographic databases [MEDLINE, Web of Science, PsycINFO, Google Scholar, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Electronic Theses Online Service (EThOS) – British Library and The Cochrane Library] were searched from May 2005 to December 2011.
FIGURE 1.
Flow chart of the amalgamation of the current search with the previous systematic reviews exploring ethnic variation in pathways to care during FEP.
Inclusion criteria included:
-
studies including FEP-only cohorts
-
studies conducted in England and Wales
-
studies conducting an ethnic comparison between two or more groups
-
studies conducting a comparison of at least one pathway to care outcome (e.g. compulsory hospital admission, GP involvement, criminal justice agency involvement).
Exclusion criteria included:
-
data used in previous articles
-
data from first-contact studies, with no specification of episode
-
qualitative papers
-
studies not in English.
Of the roughly 6000 journal articles retrieved, three61–63 met the overall inclusion criteria of our review. These were added to the 9 articles10,11,15,64–70 identified through the two previous reviews, giving a total of 12 studies. However, further examination revealed that one of these61 was a conference abstract of a paper that had already been retrieved and it was therefore excluded. Our review therefore consisted of 11 studies10,11,15,62–70 that had explored ethnic variation in pathways to care in FEP patients. These studies are listed in Table 1.
| Study | Sample size for each ethnic group (n) | Total sample size (n) | City | Adjustment for confounders | Recording of ethnicity | Quality score (max. 11) |
|---|---|---|---|---|---|---|
| Harrison et al. 198964 | African Caribbean 42; non-African Caribbean 89 | 131 | Nottingham | Diagnosis, gender, age | Third-party reports | 5 |
| Chen et al. 199165 | African Caribbean 40; non-African Caribbean 40 | 80 | Nottingham | Diagnosis | Medical records, source not specified | 4 |
| Birchwood et al. 199266 | White British 74; Asian British 30; African Caribbean British 50 | 154 | Birmingham | Diagnosis | Census rated | 6 |
| King et al. 199467 | White 39; Asian 11; black 38; ‘other’ 5 | 93 | London | Diagnosis | Self-reported/census categorisation | 4 |
| Cole et al. 199568 | White 39; black 38; ‘other’ 16 | 93 | London | Diagnosis, absence of a help-seeker, lack of GP involvement | Census rated | 8 |
| Burnett et al. 199970 | White 38; African Caribbean 38; Asian 24 | 100 | London | Diagnosis | Self-reported/census categorisation | 7 |
| Goater et al. 199915 | White 39; black 38; ‘other’ 16 | 93 | London | Age, gender, unemployment, risk to others, diagnosis, criminal justice referrals, self-initiated help-seeking | Self-reported/census categorisation | 6 |
| Harrison et al. 199969 | African Caribbean 33; ‘other’ 133 | 166 | Nottingham | Diagnosis | Third-party reports | 2 |
| Brunet 200362 | White 16; black 37; Asian 30; ‘other’ 8 | 91 | Birmingham | Diagnosis | Not reported | 5 |
| Morgan et al. 200510,11 | White British 237; African Caribbean 128; black African 64; white ‘other’ 33 | 462 | London and Nottingham | Age, gender, unemployment, risk to others, criminal justice referrals, self-initiated help-seeking, diagnosis | Self-reported/census categorisation | 10 |
| Chaudhry et al. 200863 | White British 24; South Asian 24 | 48 | Lancashire | Diagnosis | Not reported | 4 |
Quality rating
The 11 studies were evaluated for methodological quality using a review tool described by Bhui et al. 13 Essentially, the tool is a scoring system, appraising each study on four domains: sample size, adjustment for confounders, measurement of ethnicity and choice in ethnic comparison (see Appendix 3). Studies are scored on each domain, with the individual scores summed (maximum 11). Higher scores reflect better methodological quality.
From each study, two types of information were extracted: (1) ethnic variation in pathways to care (ethnic differences in compulsory hospital admission, criminal justice agency involvement and GP involvement) and (2) empirically supported explanations offered for these differences.
Ethnic differences in pathways to care during first-episode psychosis
Several studies included in the review confirmed that BME patients had higher rates of MHA detention, more contact with criminal justice agencies and less involvement of GPs in the care pathway. We also identified other ethnicity-related differences that have received less attention in research. Burnett et al. 70 reported that Asian patients had a higher level of domiciliary visits than white and African Caribbean patients. Morgan et al. 10 reported significantly higher levels of domiciliary visits for African Caribbean patients than for white patients. In 35% of these visits the police were involved, suggesting that these were usually crisis referrals. In Manchester, Chaudhry et al. 63 reported that South Asian patients were more likely to have community mental health services as their first contact to seek help whereas white patients had more inpatient admissions as entry into care. Cole et al. 68 reported that white patients were more likely than black and Asian patients to make first contact with a duty psychiatrist.
Four areas that may influence ethnic variation in pathways to care were also identified in the literature. These are differences in clinical presentation, delays in help-seeking, the role of social networks and cultural attribution of emerging illness:
-
Clinical factors. Harrison et al. 64 reported ethnic differences in both clinical presentation and manifest behaviour during FEP. Informants (family, friends and clinicians) reported that African Caribbean patients were more likely to show neglect in social functioning, personal appearance and hygiene, suggesting greater impairment. African Caribbean patients were also more likely to be perceived as being a danger to themselves and more likely to commit violent attacks than patients from other groups. Chen et al. 65 reported that African Caribbean patients presented more frequently to services with behavioural disturbances and agitation (collectively defined as violence, extreme bizarre behaviour, threatening behaviour and absconding) than non-African Caribbean patients. There was also a trend towards more affective psychosis and fewer substance-related psychoses amongst the African Caribbean sample than amongst the white patients. Morgan et al. 11 reported that African Caribbean patients were significantly more likely than patients from other ethnic groups to be involved in a violent incident and/or to be perceived as threatening by others leading to inpatient admission. There were no differences in DUP between African Caribbean and other ethnic groups.
-
Delays in help-seeking. Harrison et al. 64 reported that 40% of African Caribbean patients made contact with services < 1 week before psychiatric contact, compared with 1% of the non-African Caribbean sample (p < 0.001). There was no difference in symptom duration between the two groups but, once African Caribbean patients had made contact with services, psychiatric intervention occurred much sooner than amongst the non-African Caribbean sample, suggestive of crisis referral.
-
Social networks. Surprisingly little attention has been paid to the role of social and family networks in influencing pathways to care. Harrison et al. 64 reported lower levels of past relative contact amongst African Caribbean patients than amongst those from non-African Caribbean groups [χ2 = 5.22, degrees of freedom (df) = 1, p < 0.05].
-
Illness recognition and cultural attribution. This important variable has also received minimal attention in studies of pathways into care for FEP. Harrison et al. 64 asked informants (carers) to explain the cause of their patient’s current problems. Carers of African Caribbean patients were significantly more likely to attribute cause to ‘faulty biology’ or ‘substance misuse’ than carers of non-African Caribbean patients (χ2 = 4.7, df = 1, p < 0.03). About one-third (35%) of the African Caribbean carers viewed the illness as the result of personal character/lifestyle choices, compared with 50% of non-African Caribbean carers. However, this difference was not statistically significant. Only one African Caribbean carer mentioned a supernatural cause, compared with three non-African Caribbean patients. When carers were asked what they thought the nature of the problem was, both groups frequently cited mental illness.
Meta-analyses
Compulsory hospital admission
Each of the 12 studies made ethnic comparisons of the rates of compulsory hospital admission during FEP. Two studies10,11 used the same data set in this comparison and so only one of these studies was included. Meta-analyses were conducted by pooling the odds ratios (ORs) across seven studies. 10,62,64–66,68,70 The remaining studies were excluded as they either descriptively reported ethnic differences or did not include raw data. Given the variation in how BME groups were categorised in individual studies, we decided to conduct multiple comparisons to ensure meaningful ethnic comparisons. Four separate meta-analyses were conducted: (1) black Caribbean compared with white British patients, (2) black Caribbean compared with non-black Caribbean patients, (3) black (i.e. black African, black Caribbean, black ‘other’) compared with non-black patients and (4) Asian compared with non-Asian patients. Studies were included more than once in each analysis when multiple ethnic comparisons were made.
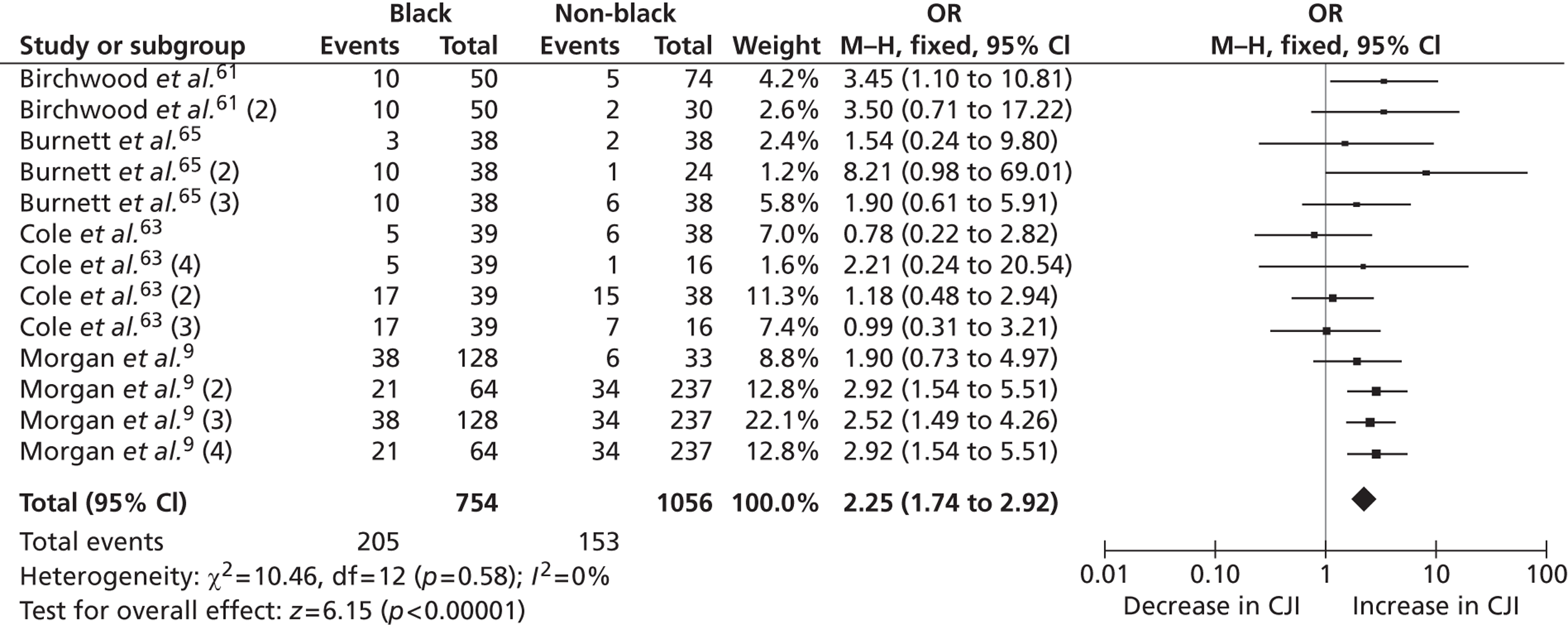
Criminal justice agency involvement
The review also investigated ethnic differences in criminal justice agency involvement. We defined this as any contact with either judicial agencies or law enforcement agencies. Of the 12 studies, five11,64,66,68,70 had explored ethnic differences in relation to criminal justice agency involvement. Of these, four64,66,68,70 were of ‘moderate’ methodological quality and one was rated ‘high’. 11 Two separate sources of data were extracted from the articles by Cole et al. 68 and Burnett et al. 70 as they used two independent measures of criminal justice agency involvement. In total, two separate meta-analyses were conducted to explore ethnic variations in criminal justice agency involvement: (1) black Caribbean compared with non-black Caribbean patients and (2) black (i.e. black African, black Caribbean, black ‘other’) compared with non-black patients. All articles except that by Harrison et al. 64 were included multiple times as the authors made comparisons between multiple ethnic groups.
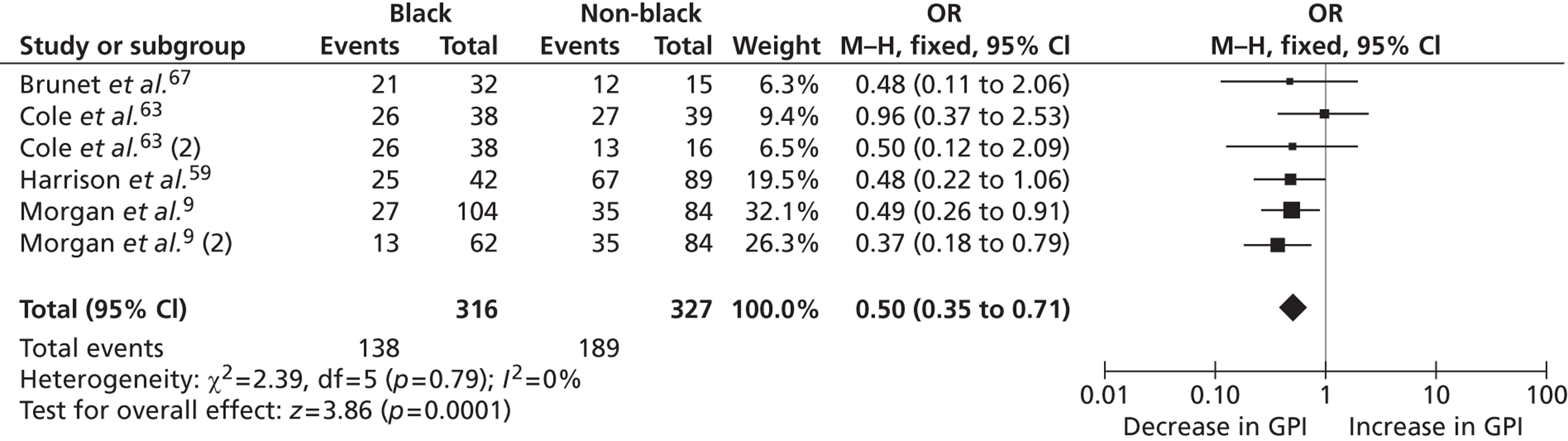
General practitioner involvement
Four studies11,64,68,70 explored ethnic differences in use of GP referral in pathways to care. Of these, one11 was rated high on methodological quality and the others were rated moderate. The study by Burnett et al. 70 used two measurements of GP referral, one by family members and the other by the patients themselves. Because of the lack of clarity surrounding how GP referral was determined in this study, we excluded it from the analyses.
Results of the systematic review
Compulsory hospital admission
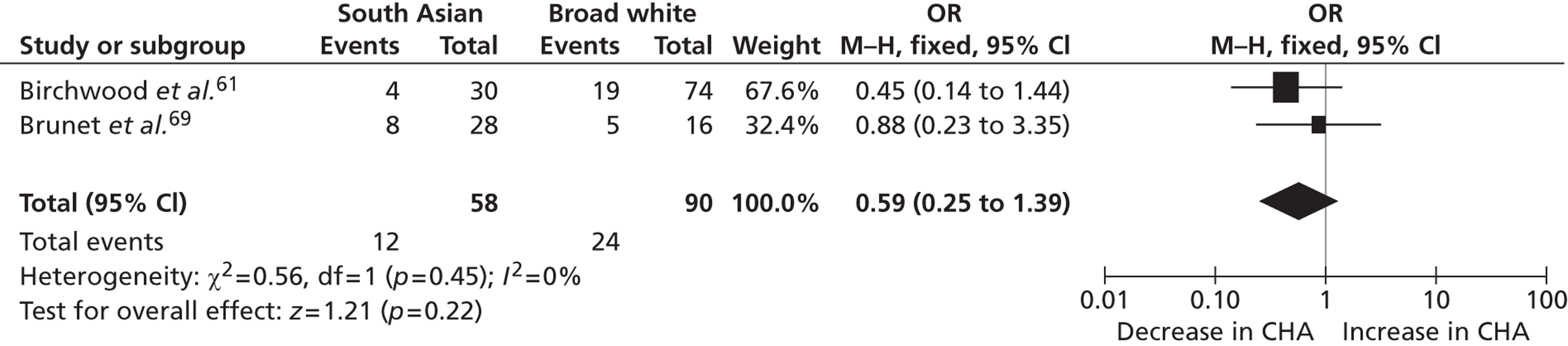
The results of the meta-analysis showed that black Caribbean patients were significantly more likely to be compulsorily detained during FEP. Specifically, black Caribbean patients were 2.39 times more likely to be detained than white British patients [95% confidence interval (CI) 1.62 to 3.52, p = 0.0001, Figure 2] and 2.13 times more likely to be detained than non-black Caribbean patients (95% CI 1.64 to 2.76, p = 0.00001, Figure 3). This finding was also true for broadly defined black patients (black Caribbean, black African and black ‘other’ patients) compared with non-black patients (2.33, 95% CI 1.85 to 2.93, p = 0.00001, Figure 4) but not for Asian patients compared with white patients (0.59, 95% CI 0.25 to 1.39, p = 0.22, Figure 5).
FIGURE 2.
Forest plot for studies included in the comparison of black Caribbean patients and white British patients for compulsory hospital admission.
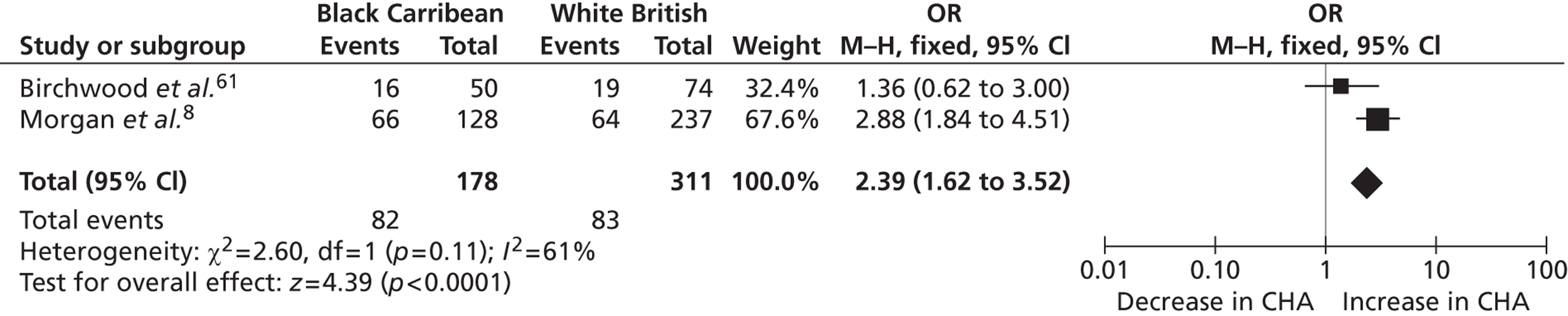
FIGURE 3.
Forest plot for studies included in the comparison of black Caribbean patients and non-black Caribbean patients for compulsory hospital admission.
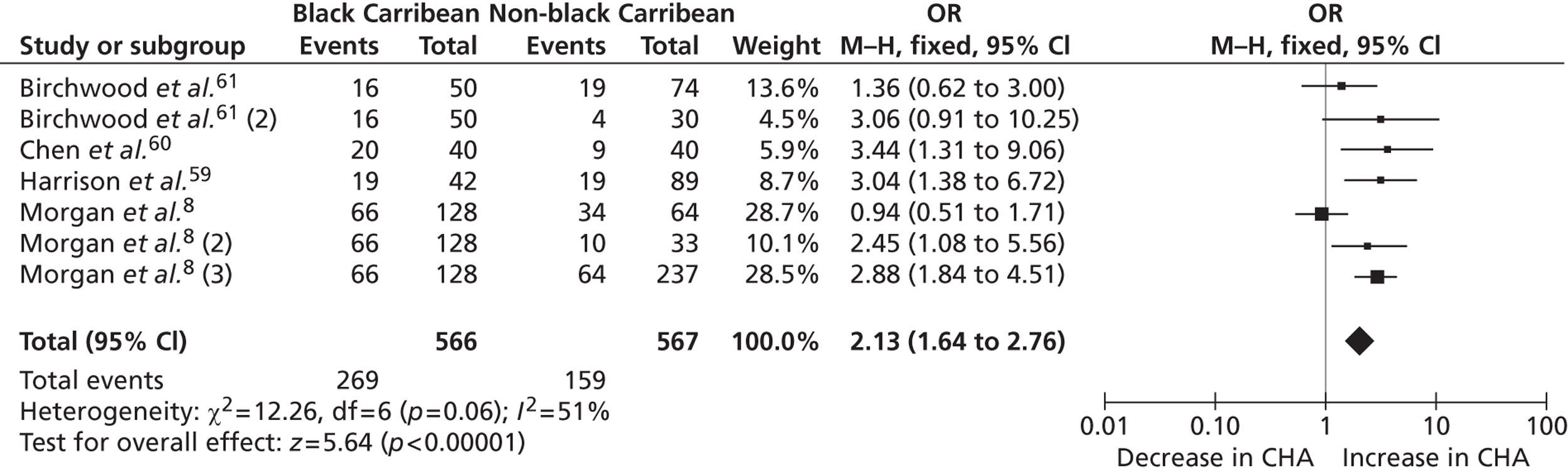
FIGURE 4.
Forest plot for studies included in the comparison of broadly defined black patients and non-broadly defined black patients for compulsory hospital admission.
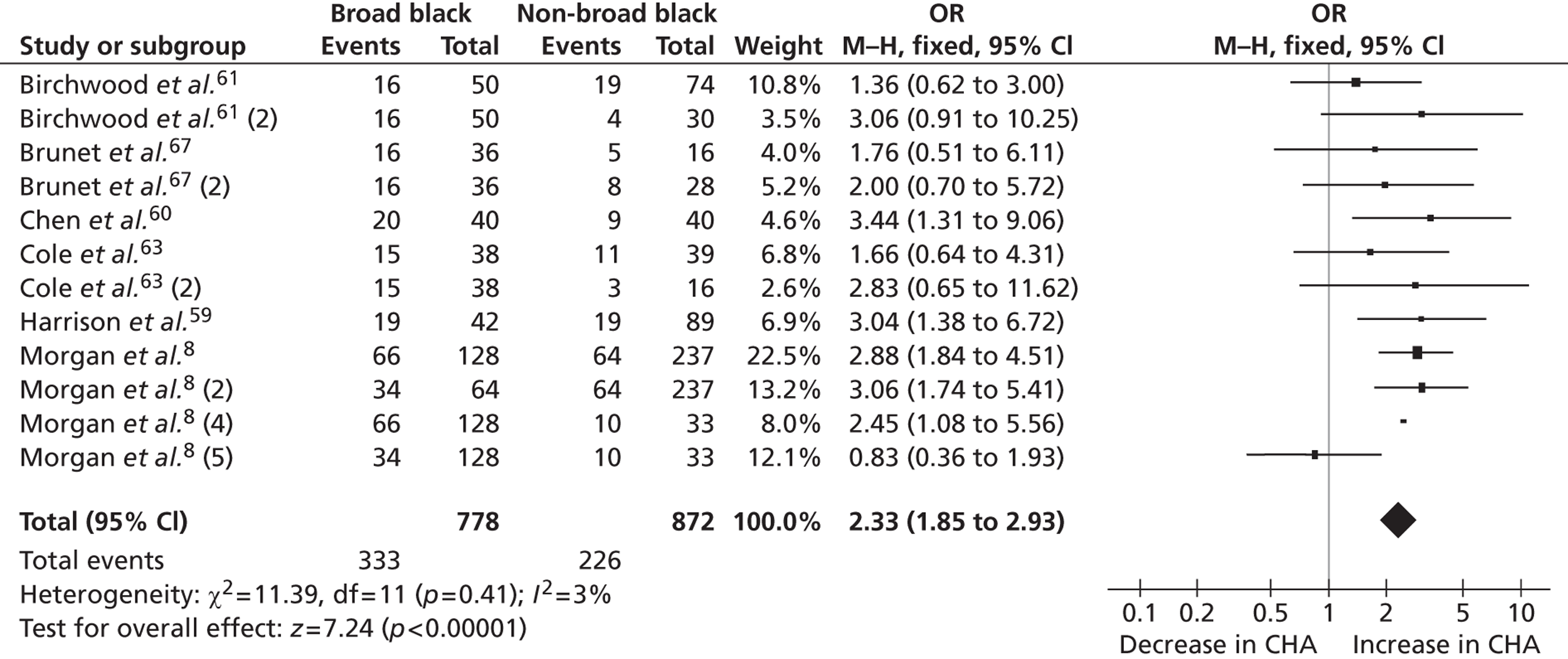
FIGURE 5.
Forest plot for studies included in the comparison of Asian patients and white patients for compulsory hospital admission.
The following explanations were offered for ethnic variation in compulsory hospital admission.
Harrison et al. 64 found that compulsory hospital admission was significantly higher amongst black Caribbean women than amongst other British women. However, no differences were found for men across different ethnic groups. In addition, when ethnic comparisons were made for those aged < 30 years only, the increased rate of admission amongst black Caribbean patients was reduced. The authors suggested that gender and age may account for the increased detention levels amongst some BME groups.
The findings of the study by Morgan et al. 10 were in direct contrast to those of the study by Harrison et al. 64 In this study, African Caribbean men were 4.75 times more likely to experience compulsory hospital admission then white British patients (95% CI 2.41 to 9.38, p < 0.0001). Such a difference was not found for either African Caribbean women or the entire black African group. In relation to age, the authors found a higher level of compulsory hospital admissions amongst younger African Caribbean patients.
Morgan et al. 10 attempted to control for confounders using two logistic regression models. In addition to ethnicity, the first model included employment status, criminal justice agency referral, perceived risk to others, self-initiated help-seeking and diagnosis with detention as the outcome variable. In the second model, an additional interaction effect term ‘African Caribbean ethnicity against gender’ was included. The results of the first analysis demonstrated that, in addition to African Caribbean and black African ethnicity, unemployment, manic psychosis, perceived risk to others, criminal justice agency referral and self-initiated help-seeking all predicted compulsory hospital admission. In the second analysis, with the interaction effect term included, African Caribbean men were 3.52 times more likely to be detained, a rate that was higher than the unadjusted rate. Being unemployed, perceived as being a risk to others, affective psychosis and self-initiated help-seeking also remained significant in the model. It seems, therefore, that, amongst men, being African Caribbean significantly increases the risk of being detained.
Criminal justice agency involvement
The results of the meta-analyses showed that black Caribbean patients were roughly twice as likely as non-African Caribbean patients to experience criminal justice agency involvement in their pathways to care during FEP [odds ratio (OR) 2.05, 95% CI 1.51 to 2.80, p < 0.00001, Figure 6]; similarly, black patients (broadly defined) were roughly twice as likely as non-black patients to experience criminal justice agency involvement in their pathways to care during FEP (OR 2.25, 95% CI 1.74 to 2.92, p < 0.00001, Figure 7).
FIGURE 6.
Forest plot for studies included in the African Caribbean vs. non-African Caribbean comparison of criminal justice agency involvement.
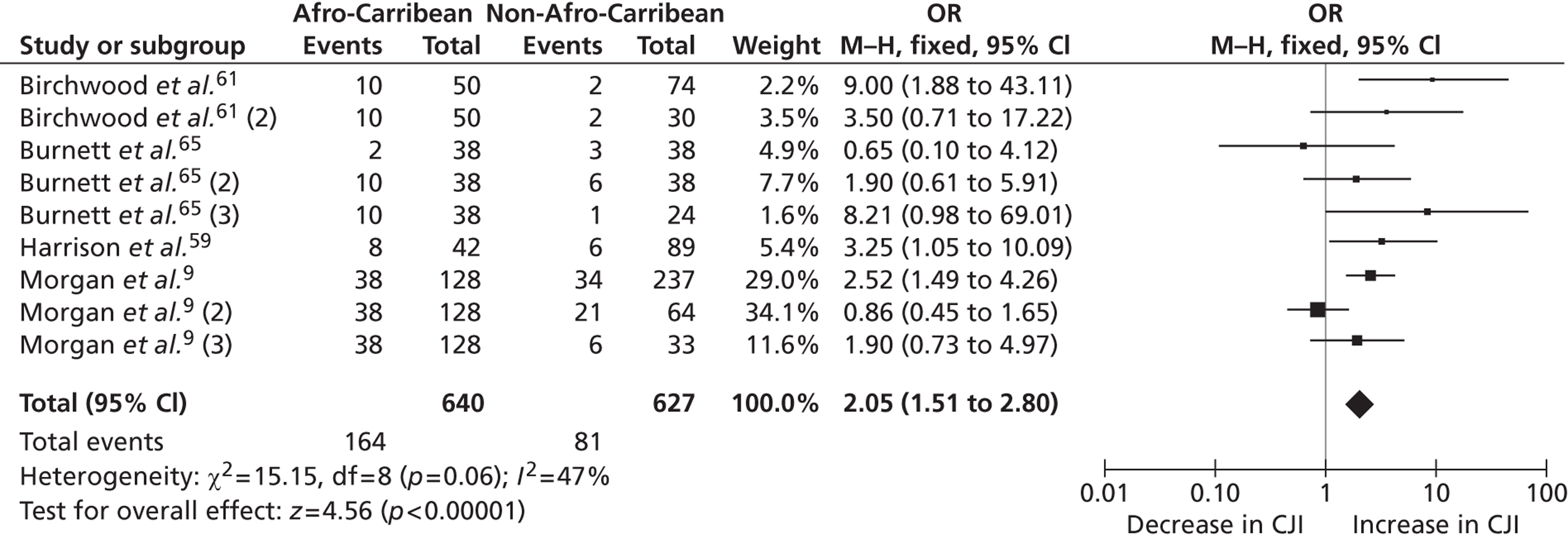
FIGURE 7.
Forest plot for studies included in the broad black vs. non-black comparison of criminal justice agency involvement.
Of the five studies, only Morgan et al. 11 explored the determinants of these differences. First, the authors calculated the unadjusted ORs for all variables that predicted criminal justice agency involvement in addition to ethnicity. The results showed that unemployment, living status, diagnosis and family involvement were all associated with criminal justice agency involvement. In a multiple regression model, black African ethnicity no longer remained significant, suggesting that these variables accounted for the increased criminal justice agency involvement amongst this group.
General practitioner referral
The results of the meta-analyses suggested that black patients were significantly less likely than non-black patients to have GP involvement in their pathway to care during FEP (OR 0.51, 95% CI 0.35 to 0.72, p = 0.0001, Figure 8).
FIGURE 8.
Forest plot for studies included in the comparison of broadly defined black patients and non-broadly defined black patients for GP involvement.
Morgan et al. 10 demonstrated that, when confounders such as living circumstances, gender, help-seeking patterns and family involvement were controlled for, the odds of excess detention in black patients were significantly reduced.
Findings from the systematic review
Overall, our review provides strong evidence for ethnic differences in pathways to care during FEP. In particular, black and African Caribbean patients are significantly more likely to experience adverse pathways to care during first presentation. There is no clear pattern in the predictors of such ethnic differences, although younger age, male gender, low level of social support and clinical differences in level of risk account for some of the observed ethnic differences in compulsory detention and criminal justice agency involvement.
There is some evidence, mainly from small qualitative studies, that mental health help-seeking amongst BME groups is strongly influenced by culturally mediated attributions of mental disorders, in particular religious and spiritual attributions, and by stigma and shame within BME communities.
To the best of our knowledge, no study has attempted to explore attributions and help-seeking behaviour in emerging psychosis to determine whether or not these might explain some of the ethnic differences in pathways to care. In particular, inter- and intra-ethnic differences have not been explored; instead, BME groups have been compared as homogeneous entities with a homogeneous and contrasting white population. These lacunae in our knowledge were the drivers for evidence gathering that is the ENRICH programme.
Chapter 4 Study 1: determinants of ethnic variation in pathways to care during first-episode psychosis
Abstract
Introduction: Black and minority ethnic patients in the UK are known to experience adverse pathways into care for FEP. Several explanations have been offered for these differences, ranging from institutional racism in psychiatry to differences in clinical presentation. However, the role of culturally mediated attributions of emerging symptoms in psychosis and how these influence help-seeking has not been explored in a systematic manner.
Methods: A prospective cohort of all consenting, newly accepted first-episode of psychosis patients was approached to take part in an in-depth semistructured interview using the Nottingham Onset Schedule (NOS), the Emerging Psychosis Attribution Schedule (EPAS) and the Amended Encounter Form. Qualitative analyses were conducted on a subsample of NOS interviews, stratified by ethnicity.
Results: A total of 132 patients were recruited (45 white, 35 black, 43 Asian and nine ‘other’ patients). There were no ethnic differences in duration of untreated psychosis and duration of untreated illness. Duration of untreated psychosis was not related to illness attribution; long duration of untreated psychosis was associated with patients being young (< 18 years) and living alone. During the prodromal phase of the illness, ‘social world’ attributions were most common and patients sought help from health agencies. With the emergence of psychotic symptoms, BME patients and carers, in particular British Asians, were significantly more likely to have ‘supernatural’ attributions and seek faith-based help.
Conclusions: Culturally mediated attributions of emerging symptoms of psychosis are an important and hitherto unexplored variable that may explain ethnic differences in pathways to care.
Aims and objectives
This mixed-methods study used both quantitative and qualitative approaches to assess ethnic variation in the process of help-seeking during FEP. The overall aim of the study was to understand ethnic variation in pathways to care in FEP by exploring sociocultural determinants of illness recognition, attribution and help-seeking among different ethnic groups. The specific research questions were as follows:
-
Are there ethnic differences in how patients and their carers recognise and understand early signs of psychosis?
-
Are such differences a function of cultural factors such as explanatory models of illness or are these related to socioeconomic status, deprivation and isolation?
-
Do biological as opposed to psychological or social explanatory models of illness predict early medical help-seeking and shorter DUP?
Quantitative study 1
Methodology
Patients were recruited from the early intervention services of the BSMHFT. The trust provides psychiatric care for the geographical area of Birmingham and the neighbouring borough of Solihull. All participants in this study were recruited from the early intervention service in Birmingham as the Solihull early intervention service was not yet established at the time of study commencement.
Birmingham city has a population of 1,073,045 (BCC, census and population data 2012) from diverse socioeconomic, ethnic and cultural backgrounds. The 2011 ethnic breakdown of the city population was estimated as 53.1% white, 4.4% Caribbean, 2.8% African and 22.5% South Asian; the remainder were from ‘other’ ethnic groups (see Appendix 4). 71 The Birmingham early intervention service provides comprehensive community-based care for all people aged between 16 and 35 years experiencing a FEP. Specialist Child and Adolescent Mental Health Services (CAMHS) nurses also work in this service in collaboration with local CAMHS services for patients aged < 16 years.
Sample
All patients attending the Birmingham early intervention service (within the BSMHFT) who were able to give informed consent were invited to participate in the study. Researchers regularly screened all new referral lists for potential participants. Each eligible participant’s community psychiatric nurse (CPN) was approached to determine whether the patient was well enough to take part in terms of symptoms, general well-being and recovery. If the CPN felt that the patient was suitable, the information sheet and consent form were given to the CPN to give to the patient. If the patient agreed to meet the research team, a researcher contacted the patient to explain the study and answer any questions. The initial contact with the research team took place at a venue suitable for the patient, including in the patient’s home if requested. During the consenting process, participants were also asked if the research team could invite a carer to participate in the study. The definition of a carer for the purpose of this study was someone who had played an important role in the major decisions related to the service user’s journey to care and was identified thus by the patient. Separate informed consents were obtained from patients and their carers.
Recruitment of cases
The early intervention service in Birmingham is a highly research-active service. During the 2-year period of data collection, various other research projects were being conducted, including studies carried out by medical, clinical psychology and PhD students. It is likely that this affected patient recruitment, as care co-ordinators often reported that their patients were unwilling to engage with further lengthy assessments, or were too busy with other commitments to engage with another study. Although we approached all consecutive cases over this time, we did not recruit all eligible cases as participation was voluntary. Patients who refused initially were approached once more for participation. After the second refusal they were not approached again. We made comprehensive notes detailing reasons for non-participation. For illustrative purposes, we describe here the reasons for non-participation from one early intervention services team: 34.4% were recruited, 19.4% declined as they were not interested in research, 17.9% were unsuitable to give informed consent, 7.5% were not recruited because they were not engaging clinically with services, 6% refused without specifying a reason and the remainder refused for other reasons.
Over the 2-year study period, 499 patients were accepted into early intervention services. Of these, 31.5% were white, 20.9% were black, 36.1% were Asian and 11.4% were from other ethnic groups. In total, 66.3% of the participants were male and the average age of the sample was 22.59 years.
To ensure that our sample was representative, comparisons were made between participants recruited into the ENRICH study and the 2-year total early intervention service (EIS) intake (Table 2).
| Ethnic group | Proportion of ethnic group in cohort (%) | Mean age of ethnic group (years) | Male (%) | |||
|---|---|---|---|---|---|---|
| 2-year EIS intake | ENRICH sample | 2-year EIS intake | ENRICH sample | 2-year EIS intake | ENRICH sample | |
| White | 31.5 | 34.1 | 21.97 | 23.13 | 64.30 | 80.00 |
| Black | 20.9 | 26.5 | 22.92 | 22.17 | 67.30 | 68.60 |
| Asian | 36.1 | 32.6 | 21.82 | 23.72 | 69.40 | 72.10 |
| Other | 11.4 | 6.5 | 24.91 | 21.00 | 59.60 | 66.70 |
Measures
Data were collected using the following measures.
Sociodemographics
Data were recorded on age, gender, ethnicity, religious affiliation, living and employment status, postcode and occupation. The service user general information sheet is provided in Appendix 5. Ethnicity was recorded in two ways. First, participants were asked to describe their ethnicity in their own words. This was recorded verbatim. Second, a list of census categories was presented to participants and they were asked to select the category that best represented their ethnic group. As there was consistency across the sample between these two methods, the standardised census categorisation method was used in the analysis. From this, the following four groups were created for analyses:
-
white (white British, white Irish, white ‘other’)
-
black (black/black British Caribbean, black/black British African)
-
Asian (Asian/Asian British Pakistani, Asian/Asian British Indian, Asian/Asian British Bangladeshi)
-
‘other’ (mixed white/black Caribbean, mixed ‘other’).
Nottingham Onset Schedule
The NOS72 is a short guided interview and rating schedule for establishing the chronology and components of symptom development in a FEP. The patient’s history is collected before the interview from medical notes and clinical correspondence to develop a preliminary timeline. This timeline is then used with the patient (and the carer if available) to guide the NOS interview. Once all available information is collected, a final timeline and the following four time points are derived (see Appendix 6):
-
Prodrome. The onset of prodrome is defined as the phase of illness from the emergence of prodromal symptoms to the development of psychotic disorder. Prodromal symptoms usually include non-specific disturbance of mood, thinking, behaviour, perception and functioning. For such symptoms to be considered as part of the psychotic illness there should be no return to premorbid functioning following onset of these symptoms.
-
First psychotic symptom. Unequivocal presence of one or more positive psychotic symptoms, rating 2 (minimal) or 3 (mild) on the Positive and Negative Syndrome Scale (PANSS), characterised by the definite presence of the symptom, which, though clearly evident, occurs only occasionally or intrudes on daily life mildly. In some cases this phase of illness may not be easily separated from the preceding phase.
-
Definite diagnosis. A rating of ≥ 4 on any one of the positive symptoms from the PANSS or a group of positive symptoms on the PANSS with a collective rating of ≥ 7, not including those scored as 1 (absent). Symptoms should have occurred for at least 1 week (transition into psychosis).
-
Date of start of antipsychotics at adequate dosage. Adequate dosage is defined as evidence that medication is being taken at ≥ 75% of the prescribed dosage and for ≥ 75% of the prescribed time. Compliance may be assumed when a patient is on home treatment or is hospitalised and there is no record of non-compliance. When a patient has initially been non-compliant, the start date of treatment recommencement and compliance is used.
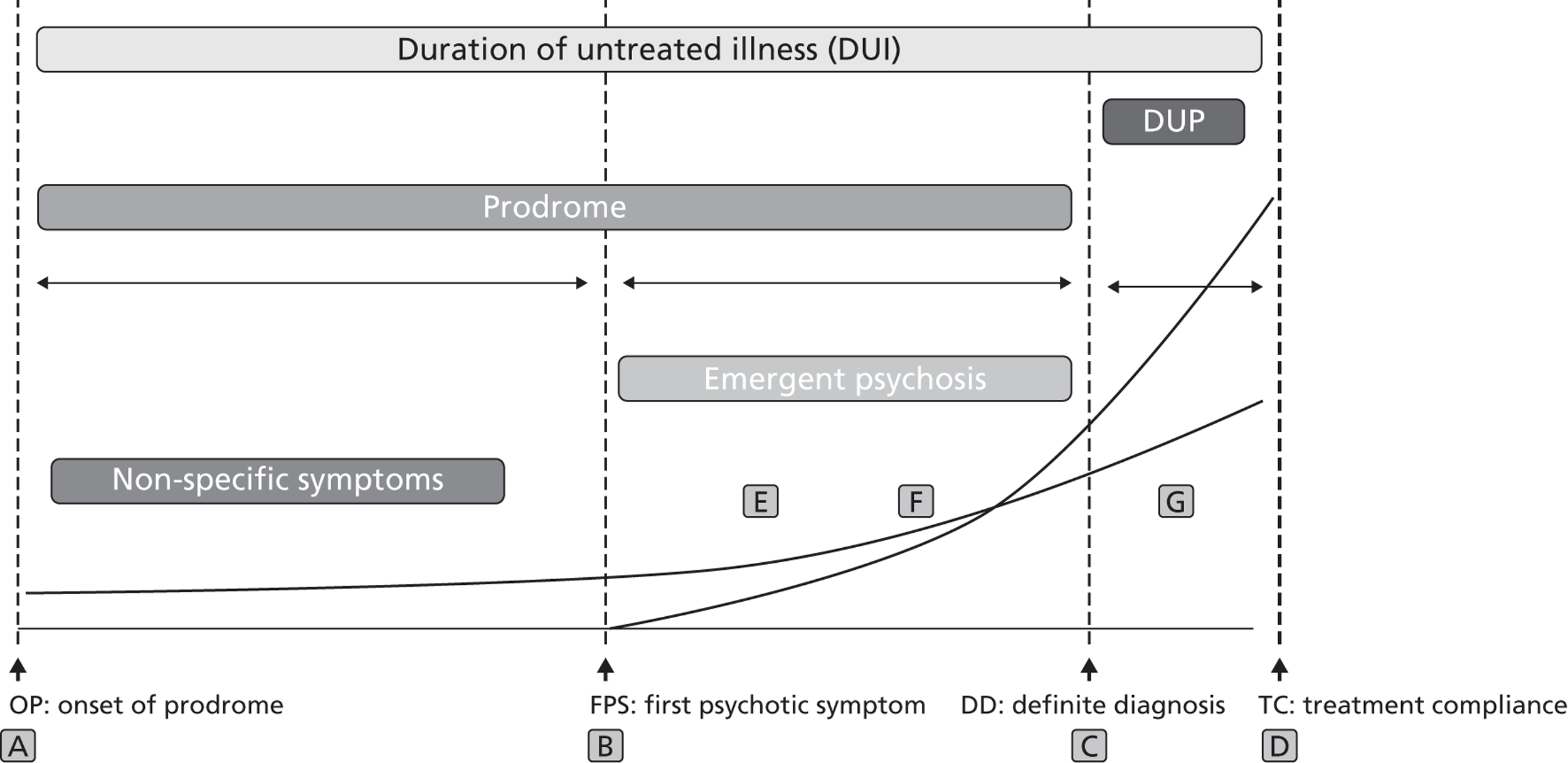
Once these time points had been established, three illness phases were created, as illustrated in Figure 9:
-
prodrome (early phase of illness between points A and C)
-
DUP (period of FEP, between points C and D)
-
duration of untreated illness (DUI) (between points A and D).
FIGURE 9.
Components in the development of FEP, as established by the NOS. Note: the thin black lines running horizontally represent the unfolding of symptoms through the various stages.
The NOS has high test–retest and inter-rater reliability72 and is a standard measure for DUP in several early intervention services. 73
Emerging Psychosis Attribution Schedule
In the original ENRICH programme proposal, we intended to use the Short Explanatory Model Interview (SEMI)74 to capture how participants attributed the causes of their symptoms. After further consideration we realised that the tool had two limitations. The first was that its terminology was overtly medical, which the research team felt might bias the responses of participants with non-medical explanations and attributions. Second, the SEMI is a cross-sectional method and does not distinguish symptom attribution during early and later stages of the disorder.
We decided to develop a specific schedule to complement the NOS interview, using a similar approach as SEMI but capturing symptom attribution over time and without a medical bias. The EPAS is a semistructured interview guide, implementation protocol and coding manual used to elicit attributional responses of symptoms identified during the NOS (see Appendix 7). Both patients and carer-informants are asked to recall how they attributed a symptom at the time the symptom first appeared, as recalled during the NOS interview. Individual responses are then categorised into one of six broad groups, loosely based on the anthropological work of Cecil Helman21 on cultural beliefs of illness:
-
Within the individual. Attributions that locate the origin of ill health within, or arising from within, the individual. Here, attributions are likely to refer to psychological and/or physiological causes, genetic or hereditary factors and factors relating to the sufferer’s personality or character.
-
The natural world. Relating the cause of the illness to natural occurrences, such as germs/infections or environmental agents/toxins. In addition, attributions described as reactions to accidents, injuries or medicinal/illicit drug use are included here.
-
The social world. Related to factors in the sufferer’s social world, such as other people or social experiences and adverse events.
-
The supernatural world. Emanating from non-natural domains, such as interactions with supernatural forces, superhuman influences, spiritual possession and supernatural punishment.
-
Unawareness of symptoms. This category was specifically developed to capture responses in which no attribution of causation was reported, despite the participant being aware of symptoms.
-
Cannot code. When no attributions were made or attributions did not fit with the categories above.
All responses were then grouped and assigned to either the prodromal or the psychotic phase of illness (see above for definition).
The inter-rater reliability of the EPAS was determined. A total of 15 randomly selected transcripts of symptom attribution interviews were coded by two researchers. In all, 64 separate attribution statements were elicited across the transcripts, which both researchers independently coded into one of the six codes. Before coding, both researchers were trained in attribution coding and were familiar with the EPAS coding manual. Inter-rater agreement was good between researchers, achieving a kappa coefficient of 0.763 across all elicited attributions.
Illness encounters and pathways to care
Although several pathways to care measures are available,5 we could not identify an illness encounter tool that specifically met the needs of this study. We therefore used an amended version of the encounter form from Gater et al. 75 in which an interview and coding protocol were created to ensure consistency between researchers (see Appendix 8). As with the NOS, all medical notes and correspondence are collated into a timeline detailing the patient’s journey to psychiatric care. This is presented to the patient and carer-informant and they are asked to confirm that it is correct as well as describe any other help-seeking avenues (illness encounters) that they may have used. Participants are specifically asked to recall help-seeking during the prodromal phase of the illness, as medical records rarely capture such information. Likewise, third-sector/voluntary and faith-based illness encounters are specifically asked for. From this, three main sets of data are established:
-
Encounter type – the types of contact that each participant made on his or her pathway to psychiatric services (e.g. faith organisation, mental health services, local GP, police).
-
Help-seeking initiation – the person(s) responsible for the initiation of the encounter contact (patient own choice, joint decision with family/friends or family choice alone).
-
Help-seeking support – people who attended each encounter (patient on his or her own, with family and friends, or family/friends on their own).
All researchers were trained on this measure before study commencement.
Data collection procedure
After a patient had consented to participate in the study, a date, time and location for the interview were agreed between the patient and the researcher. Before the assessment began, patients were asked whether the interview could be digitally audio recorded. If they declined, one of the two researchers present at the interview conducted the interview to complete the schedules and the other made comprehensive notes for later scrutiny.
Before appointments, researchers screened medical records to create NOS, EPAS and Encounter timelines. During the interviews, participants were reminded about the reasons for the assessments and any queries/concerns were addressed. Once the sociodemographic data had been collected, the NOS and EPAS were administered. In addition, researchers listened carefully for instances of participants giving spontaneous attributions during the NOS phase of the interview. Finally, help-seeking attempts and pathways to care were determined using the ENRICH encounter form. The same procedure was followed in interviews with carers/informants.
Data coding and storage
After the interviews, two researchers rated the schedules to agree the final timelines, attributions and pathways to care. Causal attribution data were coded into categorical variables and clustered into developmental phases identified by the NOS (i.e. prodrome and FEP). Carer-informant and patient data remained separate through this process. After coding, all information was electronically input onto a secure clinical database (openCDMS), designed and hosted especially for the study by the Heart of England Mental Health Research Network (MHRN). The database is a secure password-protected interface that allows multiple researchers to input data simultaneously onto one database. Data were then output into SPSS Statistics version 20.0 (IBM Corp., Armonk, NY, USA) data files for analysis.
Data analysis
The data were analysed in an agreed sequence. We first explored ethnic variation in sociodemographic variables, clinical variables such as DUP, help-seeking and encounter variables, and symptom attributions. Descriptive statistics were used to identify trends, which were then subjected to statistical testing. Second, we identified ethnic differences in relation to pathway to care encounters using the chi-squared test. Third, we attempted to understand the determinants of these differences. Unadjusted ORs were calculated for all variables against each pathway to care encounter that was shown to have some association with ethnicity in the previous phase. Factors shown to influence these outcomes were taken forward into a logistic regression model, in addition to ethnicity, in the final and fourth stage.
Attribution analyses
It was clear, even during data collection, that participants gave multiple, sometimes conflicting, symptom attributions during both the early and the later stages of illness. We therefore devised a system to give a proportional score for each attribution type. For each illness phase (prodrome and DUP), the number of attributions given for each attribution category was divided by the overall number of attributions in that phase and then multiplied by 100. A standardised score, interpreted simply as a percentage, was therefore calculated for each of the five attribution types for each participant. When an ethnic comparison was made, the mean scores for each group were used. An example of the attribution scoring method is shown in Box 1.
Participant ENR089 gave eight attributions in total during her interview, five for prodromal symptoms and three for psychotic ones. During the prodromal phase of the illness, one was ‘within the individual’, three were in the ‘social world’ and one was in the ‘natural world’. During the psychotic phase of the illness she gave one ‘social world’, one ‘natural world’ and one ‘unaware’ attribution.
Attribution scoring matrix| Attribution category | Prodrome score | Psychosis score |
|---|---|---|
| Within the individual | 1/5 × 100 = 20 | 0/3 × 100 = 0 |
| Social world | 3/5 × 100 = 60 | 1/3 × 100 = 33.3 |
| Natural world | 1/5 × 100 = 20 | 1/3 × 100 = 33.3 |
| Supernatural world | 0/5 × 100 = 0 | 0/3 × 100 = 0 |
| Unawareness of symptoms | 0/5 × 100 = 0 | 1/3 × 100 = 33.3 |
During the prodromal phase of the illness, participant ENR89 gave predominantly ‘social world’ attributions (60%) followed by ‘within the individual’ (20%) and ‘natural world’ (20%) attributions equally. During the psychotic phase of the illness she gave ‘social world’, ‘natural world’ and ‘unaware’ attributions equally (33.3%).
Encounter analyses
The same approach was used for comparisons between each of the encounter variables. For each, we divided the number of reported categories within that variable by the overall number of help-seeking attempts. A score was then derived, which was comparable between participants and across groups when group averages were taken (e.g. participant A made 10 help-seeking attempts during the psychotic phase of her illness; three of these were with her local GP and therefore her GP help-seeking score is 30%). Further details are provided in Box 2.
Participant ENR04 made a total of 10 encounter contacts in his pathways to care. In total, he made three visits to the GP, was referred to his local CMHT, sought help from a local pastor, went to the A&E department twice, was hospitalised, was placed on home treatment and finally came into the care of early intervention services. Once coded under the ENRICH encounter coding system, patient ENR04 made five GP/A&E encounters, one faith encounter, three mental health service encounters and one early intervention encounter.
Attribution scoring matrix| Attribution category | Encounter score |
|---|---|
| Mental health service encounters | 3/10 × 100 = 30 |
| Faith encounters | 1/10 × 100 = 10 |
| GP/A&E encounters | 5/10 × 100 = 50 |
| Early intervention encounters | 1/10 × 100 = 10 |
| Voluntary and third-sector organisation encounters | 0/10 × 100 = 0 |
In this case, this patient predominantly sought help within primary care and emergency services. It is also clear that he made no contact with third-sector and voluntary organisations.
Help-seeking analyses
Finally, we attempted to explore ethnic variation in help-seeking initiation and help-seeking support. In doing so, we calculated a proportional score for ‘within each participant’ and ‘within each group’. Higher scores reflect a higher rate of occurrence than lower scores. The following scores were calculated:
-
help-seeking initiation scores:
-
patient only: the proportion of help-seeking initiated solely by the patient
-
patient and family: the proportion of help-seeking initiated jointly by patients and carers
-
family and friends only: the proportion of help-seeking initiated by family and friends only
-
encounter contact approached client: the proportion of help-seeking initiated by services (police and compulsory admission).
-
-
help-seeking social support scores:
-
patient only: the proportion of encounters attended by the patient alone
-
patient and family: the proportion of encounters attended by both patient and family members
-
family only: the proportion of encounters attended by family members only.
-
It is important to note that these scores are not percentages because they do not add up to 100, as not every participant can be categorised.
Deprivation levels
Postcodes were collected from each participant during the interviews. In cases in which participants had recently moved, the postcode of their residency during their psychotic illness was requested. The English Indices of Deprivation (IMD) 201076 is a composite measure of deprivation in England scoring geographical location (postcode proxies) based on income level, employment, health and disability, education, skills and training, barriers to housing and services, crime, and living environment. Postcode deprivation scores were categorised into decile, with the bottom decile representing the highest levels of deprivation and the top the lowest. Each participant was then assigned to one IMD decile category, which was then used to explore ethnic differences.
Results
A total of 132 participants were recruited from early intervention services in Birmingham over a 2-year period (2008–10). Of these, 45 (34.1%) were categorised as white, 35 (26.5%) as black, 43 (32.6%) as Asian and nine (6.8%) as ‘other’. Table 3 shows the sociodemographic profile of the sample. Participants predominantly were male (73.5%), were young [20.73 years, standard deviation (SD) 5.53 years], had a psychotic disorder (schizophrenia 68.9%) and were born in the UK (81.8%).
| Characteristic | White (n = 45), n (%) | Black (n = 35), n (%) | Asian (n = 43), n (%) | Other (n = 9), n (%) | p-value |
|---|---|---|---|---|---|
| Gender: male | 36 (80.0) | 24 (68.6) | 31 (72.1) | 6 (66.7) | 0.643 |
| Age at assessment (mean years) | 23.13 | 22.71 | 23.72 | 21 | 0.320 |
| Educational achievement | |||||
| To school level | 22 (48.9) | 20 (57.1) | 22 (51.2) | 4 (44.4) | 0.960 |
| Beyond school level | 23 (51.1) | 15 (42.9) | 21 (48.8) | 5 (55.6) | |
| Religious affiliation | |||||
| Christianity | 15 (33.3) | 29 (82.9) | 0 (0.0) | 5 (55.6) | – |
| Other | 0 (0.0) | 1 (2.9) | 3 (7.0) | 0 (0.0) | |
| Islam | 1 (2.2) | 1 (2.9) | 36 (83.7) | 1 (11.1) | |
| None | 29 (64.4) | 4 (11.4) | 4 (9.3) | 3 (33.3) | |
| Not practising religion | 38 (84.4) | 16 (45.7) | 11 (25.6) | 6 (66.7) | – |
| Migrant generation | |||||
| First generation | 1 (2.2) | 13 (37.1) | 13 (30.2) | 1 (11.1) | – |
| Second generation | 0 (0.0) | 8 (22.9) | 24 (55.8) | 4 (44.4) | |
| Third generation | 1 (2.2) | 14 (40.0) | 6 (14.0) | 3 (33.3) | |
| Not applicable | 43 (95.6) | 0 (0.0) | 0 (0.0) | 1 (11.1) | |
| Country of birth | |||||
| Africa | 0 (0.0) | 4 (11.4) | 0 (0.0) | 0 (0.0) | 0.160 |
| Caribbean | 0 (0.0) | 8 (22.9) | 0 (0.0) | 0 (0.0) | |
| Other | 1 (2.2) | 0 (0.0) | 0 (0.0) | 1 (11.1) | |
| South Asia | 0 (0.0) | 0 (0.0) | 10 (23.3) | 0 (0.0) | |
| UK | 44 (97.8) | 23 (65.7) | 33 (76.7) | 8 (88.9) | |
| Marital status | |||||
| Married/cohabiting | 3 (6.7) | 1 (2.9) | 9 (20.9) | 0 (0.0) | 0.081 |
| Single | 42 (93.3) | 34 (97.1) | 34 (79.1) | 9 (100) | |
| Living status | |||||
| Alone | 8 (17.8) | 17 (48.6) | 4 (9.3) | 5 (55.6) | – |
| With family/friends/others | 37 (82.2) | 18 (51.4) | 39 (90.7) | 4 (44.4) | |
| Age at onset (years) | |||||
| < 18 | 15 (33.3) | 12 (34.3) | 16 (37.2) | 5 (55.6) | – |
| > 18 | 30 (66.7) | 23 (65.7) | 27 (62.8) | 4 (44.4) | |
| Not in work or education at time of onset | 18 (40.0) | 14 (40.0) | 16 (37.2) | 4 (44.4) | 0.978 |
| IMD | |||||
| Bottom 10% | 16 (35.6) | 16 (50.0) | 28 (68.3) | 6 (75.0) | – |
| 10–20% | 10 (22.2) | 7 (21.9) | 6 (14.6) | 2 (25.0) | |
| 20–30% | 5 (11.1) | 5 (15.6) | 2 (4.9) | 0 (0.0) | |
| 40%+ | 14 (31.1) | 4 (12.5) | 5 (12.2) | 0 (0.0) | |
There were very few demographic differences between the ethnic groups; however, there was some variation in religious affiliation and practice. In total, 83.7% of the Asian sample reported having a religious affiliation to Islam and 82.9% of the black sample reported a religious affiliation to Christianity; 64.4% of the white group declared no religious affiliation at all. In relation to religious practice, 74.4% of the Asian participants, 54.3% of the black participants and 15.6% of the white participants practiced a religion. On the whole, deprivation levels in the cohort were high, with the whole sample falling into the bottom 40% of national deprivation levels. About two-thirds (68.3%) of the Asian sample were in the bottom 10% in comparison to 50.0% of the black sample and 35.6% of the white sample (see Table 3).
In total, 71 carers were recruited of whom 28 (39.4%) were white, 16 (22.5%) were black, 23 were Asian (32.4%) and four (5.6) were in the ‘other’ group (Table 4). Like the patients, there were clear differences between religious affiliation and practice, with 20 carers (87%) from the Asian group having a religious affiliation to Islam and 15 carers (53.6%) from the white group and 14 (87.5%) carers from the black group having a religious affiliation to Christianity. The majority of the black and Asian carers but not the white carers reported that they did practice a religion (see Table 4).
| Characteristic | White (n = 28), n (%) | Black (n = 16), n (%) | Asian (n = 23), n (%) | Other (n = 4), n (%) | p-value |
|---|---|---|---|---|---|
| Gender: male | 4 (14.3) | 5 (31.3) | 7 (30.4) | 0 (0.0) | 0.287 |
| Age at assessment (mean years) | 43.89 | 43.19 | 43.95 | 46.67 | – |
| Educational achievement | |||||
| To school level | 13 (46.4) | 7 (43.8) | 12 (52.2) | 2 (50.0) | 0.958 |
| Beyond school level | 15 (53.6) | 9 (56.3) | 11 (47.8) | 2 (50.0) | |
| Religious affiliation | |||||
| Christianity | 15 (53.6) | 14 (87.5) | 0 (0.0) | 3 (75.0) | – |
| Other | 2 (7.1) | 1 (6.3) | 2 (8.7) | 1 (25.0) | |
| Islam | 0 (0.0) | 0 (0.0) | 20 (87.0) | 0 (0.0) | |
| None | 11 (39.3) | 1 (6.3) | 1 (4.3) | 0 (0.0) | |
| Not practising religion | 23 (82.1) | 4 (25.0) | 2 (8.7) | 2 (50.0) | – |
| Migrant generation | |||||
| First generation | 1 (3.6) | 6 (37.5) | 12 (52.2) | 1 (25.0) | – |
| Second generation | 0 (0.0) | 8 (50.0) | 10 (43.5) | 2 (50.0) | |
| Third generation | 0 (0.0) | 2 (12.5) | 1 (4.3) | 0 (0.0) | |
| Not applicable | 27 (96.4) | 0 (0.0) | 0 (0.0) | 1 (25.0) | |
| Country of birth | |||||
| Africa | 0 (0.0) | 2 (12.5) | 0 (0.0) | 0 (0.0) | – |
| Caribbean | 0 (0.0) | 6 (37.5) | 0 (0.0) | 0 (0.0) | |
| Other | 1 (3.6) | 0 (0.0) | 0 (0.0) | 1 (25.0) | |
| South Asia | 0 (0.0) | 0 (0.0) | 17 (73.9) | 0 (0.0) | |
| UK | 27 (96.4) | 8 (50.0) | 6 (26.1) | 3 (75.0) | |
| Marital status | |||||
| Married/cohabiting | 14 (50.0) | 10 (62.5) | 16 (69.6) | 0 (0.0) | – |
| Single | 14 (50.0) | 6 (37.5) | 7 (30.4) | 4 (100.0) | |
| Living status | |||||
| Alone | 2 (7.1) | 0 (0.0) | 0 (0.0) | 0 (0.0) | – |
| With family/friends/others | 26 (92.9) | 16 (100.0) | 23 (100.0) | 4 (100.0) | |
Ethnic comparison of clinical variables
The descriptive statistics of the clinical factors for each ethnic group are shown in Table 5.
| White (n = 45), n (%) | Black (n = 35), n (%) | Asian (n = 43), n (%) | Other (n = 9), n (%) | p-value | |
|---|---|---|---|---|---|
| DUP (median dichotomised) | |||||
| Short | 26 (57.8) | 18 (51.4) | 18 (41.9) | 4 (44.4) | 0.500 |
| Long | 19 (42.2) | 17 (48.6) | 25 (58.1) | 5 (55.6) | |
| DUP (6-month cut-off) | |||||
| Short | 19 (42.2) | 13 (37.1) | 16 (37.2) | 1 (11.1) | – |
| Long | 26 (57.8) | 22 (62.9) | 27 (62.8) | 8 (88.9) | |
| Prodrome length | |||||
| Short | 16 (35.6) | 20 (57.1) | 26 (60.5) | 5 (55.6) | 0.920 |
| Long | 29 (64.4) | 15 (42.9) | 17 (39.5) | 4 (44.4) | |
| DUI | |||||
| Short | 18 (40.0) | 19 (54.3) | 24 (55.8) | 5 (55.6) | 0.432 |
| Long | 27 (60.0) | 16 (45.7) | 19 (44.2) | 4 (44.4) | |
| Diagnosis | |||||
| Broad schizophrenia | 27 (60.0) | 27 (77.1) | 30 (69.8) | 7 (77.8) | – |
| Depressive psychosis | 14 (31.1) | 7 (20.0) | 9 (20.9) | 2 (22.2) | |
| Manic psychosis | 2 (4.4) | 0 (0.0) | 1 (2.3) | 0 (0.0) | |
| Missing | 2 (4.4) | 1 (2.9) | 3 (7.0) | 0 (0.0) | |
Duration of untreated illness
Overall, the median DUI in our sample was 1095 days (mean 1454.7 days, SD 1416 days, range 8–8093 days). We dichotomised DUI using the median into two categories: long DUI (> 1095 days) and short DUI (≤ 1095 days). In our sample, 60% of the white group had a long DUI whereas the other groups had a predominantly short DUI (see Table 5). However, across the four groups, there was no significant difference in DUI length (χ2 = 2.750, df = 3, p = 0.432).
Prodrome length
Overall, the median prodrome length was 365 days. As with the DUI data, we dichotomised prodrome length into two groups: long prodrome length (> 365 days) and short prodrome length (≤ 365 days). Two-thirds (64%) of the white sample had a long prodrome length whereas in the BME groups the prodrome length was predominantly short (see Table 5). However, again, no significant difference was observed across all ethnic groups (χ2 = 6.436, df = 3, p = 0.092). When individual BME groups were compared with the white group, a significantly shorter prodrome length was found for both the black group (B = 0.414, 95% CI 0.167 to 1.024, p = 0.05) and the Asian group (B = 0.361, 95% CI 0.152 to 0.856, p = 0.02).
Duration of untreated psychosis
Duration of untreated psychosis was analysed using two methods. The first method dichotomised DUP by the overall median. The median DUP for the overall sample was 357 days (11.9 months) and so the group was split into long DUP (> 357 days) and short DUP (≤ 357 days). Second, DUP was dichotomised using a 6-month cut-off (182.62 days). This is because of recent evidence that the critical DUP length that influences FEP outcome is 6 months; Drake et al. 77 have found poor recovery trajectories for those patients with a DUP > 6 months.
No significant ethnic differences in DUP length were observed based on median DUP dichotomy (χ2 = 2.368, df = 3, p = 0.500). Likewise, no significant differences were observed based on DUP dichotomised using a 6-month cut-off (χ2 = 3.110, df = 3, p = 0.375).
Encounter pathways
The descriptive statistics of the encounter pathways for each ethnic group are shown in Table 6. During the psychotic phase of illness there was a clear trend in the types of encounters that each group made during their pathways to care. In relation to faith encounters (spiritual and religious), 41.9% of Asian patients made contact with such services at least once, compared with 20.0% of the black group, 11.1% of the ‘other’ group and 0.0% of the white group. This difference was statistically significant (χ2 = 24.813, df = 3, p = 0.0001). Overall, black patients were 11 times more likely (B = 11.00, 95% CI 1.28 to 94.26, p = 0.029) and Asian patients were almost 32 times more likely (B = 31.680, 95% CI 3.99 to 251.72, p = 0.001) to experience faith encounters during their psychotic phase of illness than white patients.
| Encounter | White (n = 45), n (%) | Black (n = 35), n (%) | Asian (n = 43), n (%) | Other (n = 9), n (%) | p-value |
|---|---|---|---|---|---|
| At least one faith encounter | 0 (0.0) | 7 (20.0) | 18 (41.9) | 1 (11.1) | 0.0001 |
| At least one criminal Justice agency encounter | 11 (24.4) | 16 (45.7) | 14 (32.6) | 4 (44.4) | 0.217 |
| At least one third-sector, education or social welfare encounter | 7 (15.6) | 9 (25.7) | 5 (11.6) | 3 (33.3) | 0.243 |
| At least one incidence of general practice involvement | 30 (66.7) | 18 (51.4) | 30 (69.8) | 7 (77.8) | 0.271 |
| At least one A&E encounter | 17 (37.8) | 17 (48.6) | 8 (18.6) | 3 (33.3) | 0.043 |
| At least one compulsory detention | 10 (22.2) | 20 (57.1) | 13 (30.2) | 3 (33.3) | 0.011 |
| Median number of encounters in prodrome | 1 | 1 | 0 | 1 | – |
| Median number of encounters in FEP | 5 | 5 | 6 | 6 | – |
We also explored the interaction between ethnicity and criminal justice agency involvement and crisis (A&E) presentations. Almost half (45.7%) of the black group had at least one criminal justice agency encounter during the psychotic phase of illness compared with one-third (32.6%) of Asian patients and a quarter (24.4%) of white patients. The black group was roughly twice as likely to experience criminal justice agency involvement then the white group (B = 2.603, 95% CI 1.006 to 6.737, p = 0.049).
Black patients had the highest number of A&E encounters, with 48.6% making contact with services on one or more occasions during their psychotic episode; comparative figures for the Asian and white groups were 18.6% and 37.8% respectively (χ2 = 8.130, df = 3, p = 0.043). Asian patients were less likely to experience A&E encounters in their pathways to care (B = 0.376, 95% CI 0.142 to 0.999, p = 0.050) than white patients. No difference was found between the white and black groups (B = 1.556, 95% CI 0.635 to 3.810, p = 0.334). Black patients were less likely to make GP contact; however, no statistically significant differences were observed for GP contact between the three groups (χ2 = 3.912, df = 3, p = 0.271).
Finally, we explored ethnic variation in the use of compulsory hospital admission. Table 6 shows that 57.1% of black patients experienced compulsory hospital admission compared with 22.2% of white patients, 30.2% of Asian patients and 33.3% of ‘other’ patients. These differences were significant (χ2 = 11.235, df = 3, p = 0.011). Comparison with white patients, black patients were almost five times more likely to be compulsorily detained (B = 4.667, 95% CI 1.768 to 12.318, p = 0.002).
Rank order of help-seeking encounters
We further explored ethnic variation in the rank order of help-seeking encounters within each ethnic group. In doing so, we decided to use the encounter scoring system (see Box 2) to prevent ethnic variation in the total number of encounters score biasing our interpretation of the data. The results demonstrated that, during the prodrome phase of the illness, all three ethnic groups were most likely to seek help from NHS services (GPs and A&E departments). However, after NHS contact, black patients were more likely to seek help through community/voluntary organisations whereas white patients utilised specialised mental health services and Asian patients utilised faith organisations.
During the psychotic phase of illness there was similarity between the groups. All groups most often consulted mental health services. The second and third commonest help-seeking agencies were early intervention services and general health-care services (GPs and A&E). Criminal justice agency involvement ranked fourth for the black, white and ‘other’ ethnic groups whereas faith organisations ranked fourth for the Asian group.
Help-seeking behaviours: help-seeking initiation and help-seeking support
We also explored ethnic variation in help-seeking behaviours, exploring phase-wise differences in help-seeking initiation within the patients’ social networks. A summary of who suggested that help should be sought is provided in Table 7. It can be seen that, during the prodromal phase of illness, participants from the black group were more likely to initiate help-seeking on their own whereas, for white and Asian patients, family members were most likely to seek help on their behalf. However, during the psychotic phase of the illness, help-seeking was predominantly initiated by the encounter contact (previous referrals) in all three groups, followed by the family members/friends or the patient (in the case of the ‘other’ group). This suggests that the referral system in health care is the main driver of the pathways to care following the emergence of psychosis.
| Person(s) suggesting help-seeking | Prodromal phase (proportional score) | Psychotic phase (proportional score) | ||||||
|---|---|---|---|---|---|---|---|---|
| White | Black | Asian | Other | White | Black | Asian | Other | |
| Patient only | 13.70 | 19.52 | 7.36 | 33.33 | 11.17 | 11.87 | 10.05 | 20.92 |
| Patient and family member | 3.78 | 5.71 | 1.16 | 0.00 | 1.17 | 1.35 | 6.05 | 1.59 |
| Family member only | 19.67 | 14.29 | 12.98 | 22.22 | 15.71 | 18.47 | 18.81 | 18.22 |
| Initiation by encounter contact | 2.22 | 4.29 | 4.65 | 11.11 | 3.56 | 2.79 | 2.84 | 5.00 |
| Referred through previous encounter | 10.26 | 5.71 | 2.91 | 11.11 | 56.65 | 59.07 | 52.31 | 42.87 |
| Not known | 8.15 | 1.90 | 5.81 | 0.00 | 6.90 | 3.60 | 2.96 | 11.40 |
We also explored ethnic variation in the social support available to each group during the help-seeking process, exploring who attended each appointment during the pathway to care. For all groups, help was mainly sought solely by the patient during the prodromal phase. This was followed by attendance by carers and patients jointly. During the psychotic phase, however, help-seeking was mainly a joint process by patient and carers. There were no significant differences between the ethnic groups. A summary of these results is provided in Table 8.
| Person(s) attending encounter | Prodromal phase | Psychotic phase | ||||||
|---|---|---|---|---|---|---|---|---|
| White | Black | Asian | Other | White | Black | Asian | Other | |
| Patient only | 36.67 | 29.52 | 16.28 | 44.44 | 13.11 | 11.35 | 10.71 | 10.48 |
| Patient and family/friend | 18.37 | 15.71 | 12.60 | 33.33 | 79.03 | 83.13 | 79.72 | 89.52 |
| Family/friend only | 2.74 | 4.29 | 3.68 | 0.00 | 3.42 | 2.66 | 2.21 | 0.00 |
Symptom attributions
We explored ethnic variation in symptom attribution during each phase of the illness. We omitted the patients from the ‘other’ ethnic category as small numbers made it difficult to make meaningful comparisons.
Patients’ and carers’ attribution frequency
First, we compared ethnic variation in attribution frequency across the prodrome and psychotic phases of illness. In both the carer sample and the patient sample, it was evident that the majority of participants gave more than one attribution during both phases of the illness (Table 9). A Kruskal–Wallis test was used to see if there were any ethnic differences in attribution frequency. In the patient group, no significant differences were found between the groups for either the prodromal (H = 5.247, df = 2, p = 0.073) or the psychotic (H = 1.145, df = 2, p = 0.564) phases of illness. This was also true for carers for both the prodromal (H = 0.160, df = 2, p = 0.923) and the psychotic (H = 0.493, df = 2, p = 0.782) phases of illness.
| Group | Illness phase | Median | Mean | SD | Minimum | Maximum | 95% CI |
|---|---|---|---|---|---|---|---|
| Carers | Prodromal | 2.00 | 2.40 | 1.38 | 0 | 6 | 1.88 to 2.93 |
| Psychotic | 2.00 | 1.91 | 1.50 | 0 | 8 | 1.52 to 2.30 | |
| Patients | Prodromal | 2.00 | 1.84 | 2.00 | 0 | 6 | 1.60 to 2.07 |
| Psychotic | 2.00 | 1.67 | 1.08 | 0 | 5 | 1.47 to 1.85 |
Carers’ attribution of prodromal symptoms
There was similarity in how the carers in the three ethnic groups attributed symptoms during the prodromal phase of the illness (Figure 10). For all three groups, ‘social world’ attributions were most often cited followed by those ‘within the individual’. Both the black and white sample cited ‘natural’ causes third whereas Asian carers cited ‘supernatural’ reasons third. We further sought to explore any significant differences between the three ethnic groups across all five attribution types. A one-way analysis of variance (ANOVA) was used to compare differences in attribution scores; however, no significant differences were observed (Table 10).
FIGURE 10.
Bar chart showing ethnic variation in carers’ attribution scores during the prodromal phase of illness.
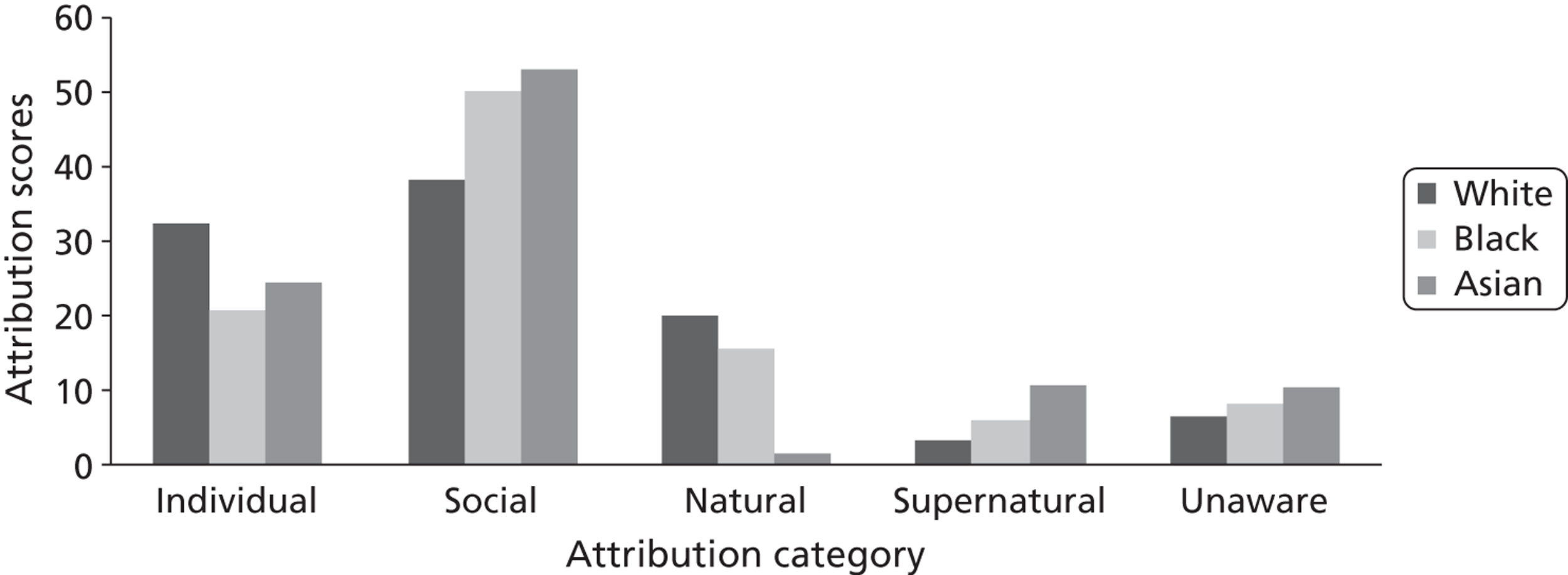
| Attribution type phase wise | Patient group (%) | Carer group (%) | ||||||
|---|---|---|---|---|---|---|---|---|
| White (n = 4) | Black (n = 35) | Asian (n = 43) | p-value | White (n = 25) | Black (n = 13) | Asian (n = 21) | p-value | |
| Prodromal phase | ||||||||
| Within the individual | 16.00 | 11.48 | 21.45 | 0.414 | 32.35 | 20.77 | 24.44 | 0.762 |
| The social world | 38.77 | 50.73 | 37.25 | 0.395 | 38.12 | 49.74 | 53.05 | 0.446 |
| The natural world | 10.98 | 6.30 | 6.25 | 0.816 | 20.00 | 15.40 | 1.67 | 0.114 |
| The supernatural world | 1.61 | 2.48 | 5.88 | 0.404 | 3.19 | 5.96 | 10.56 | 0.296 |
| Unaware | 32.64 | 29.01 | 29.17 | 0.845 | 6.34 | 8.15 | 10.28 | 0.762 |
| Other/none given | ||||||||
| Psychotic phase | ||||||||
| Within the individual | 16.24 | 11.72 | 16.20 | 0.770 | 61.81 | 37.08 | 27.65 | 0.017 |
| The social world | 7.48 | 6.51 | 2.78 | 0.502 | 22.22 | 29.73 | 18.72 | 0.699 |
| The natural world | 5.64 | 8.85 | 5.09 | 0.758 | 8.68 | 12.08 | 12.70 | 0.846 |
| The supernatural world | 8.08 | 13.02 | 40.74 | 0.000 | 0.00 | 0.00 | 33.09 | 0.000 |
| Unaware | 62.56 | 59.90 | 35.19 | 0.009 | 5.21 | 16.94 | 1.96 | 0.088 |
| Other/none given | 0.00 | 0.00 | 0.00 | 2.08 | 4.17 | 5.88 | 0.773 | |
Carers’ attribution of psychotic symptoms
In contrast to the prodromal phase of illness, there was divergence in attribution scores across ethnic groups during the psychotic phase (Figure 11). White carers’ most dominant attribution type was ‘within the individual’ whereas Asian carers’ most dominant attribution was the ‘supernatural world’. Similar to the white group, black carers attributed the cause of symptoms predominantly to factors ‘within the individual’; however, they scored much higher for factors within the social world then either of the other two groups (see Table 10 for more details).
FIGURE 11.
Bar chart showing ethnic variation in carers’ attribution scores during the psychotic phase of illness.
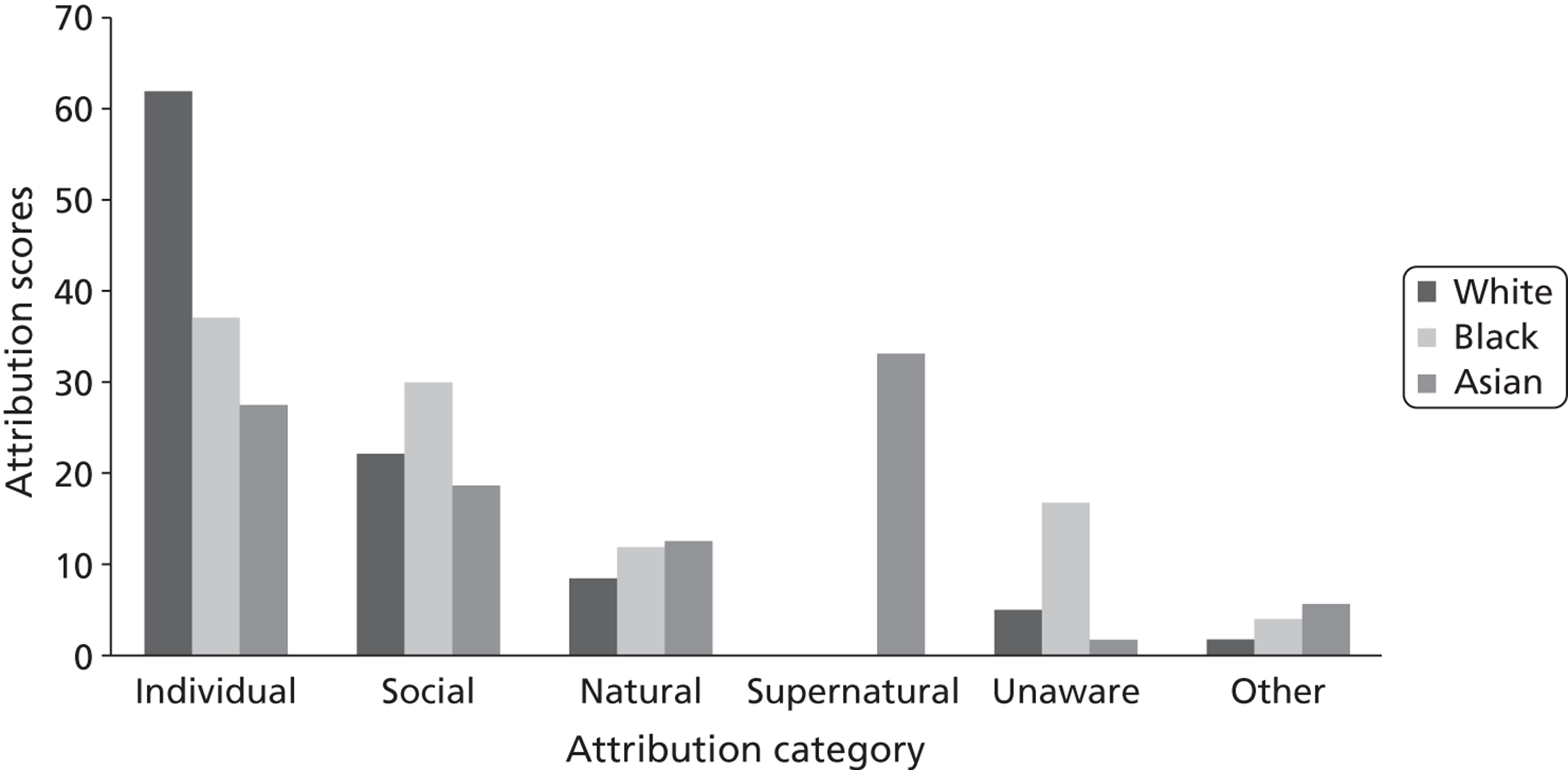
The results from the one-way ANOVA showed statistically significant differences between the three groups for ‘within the individual’ (F2,50 = 4.456, p = 0.017) and ‘supernatural world’ scores (F2,50 = 10.433, p < 0.001) during psychosis. White carers were statistically more likely then Asian carers to attribute the cause of psychosis ‘within the individual’ (p = 0.18). Likewise, Asian carers were statistically more likely than both black (p = 0.002) and white (p < 0.001) carers to attribute the cause of psychotic symptoms to factors within the ‘supernatural world’.
Patients’ attribution of prodromal symptoms
The attribution types were ranked equally by the three ethnic groups. As with the carer data, ‘social world’ attributions were most often cited during the pre-psychotic phase of illness followed by being ‘unaware’, ‘within the individual’, ‘natural world’ and finally ‘supernatural world’ attributions (Figure 12 and see Table 10). No significant differences were observed between the groups.
FIGURE 12.
Bar chart showing ethnic variations in patients’ attribution scores during the prodromal phase of illness.
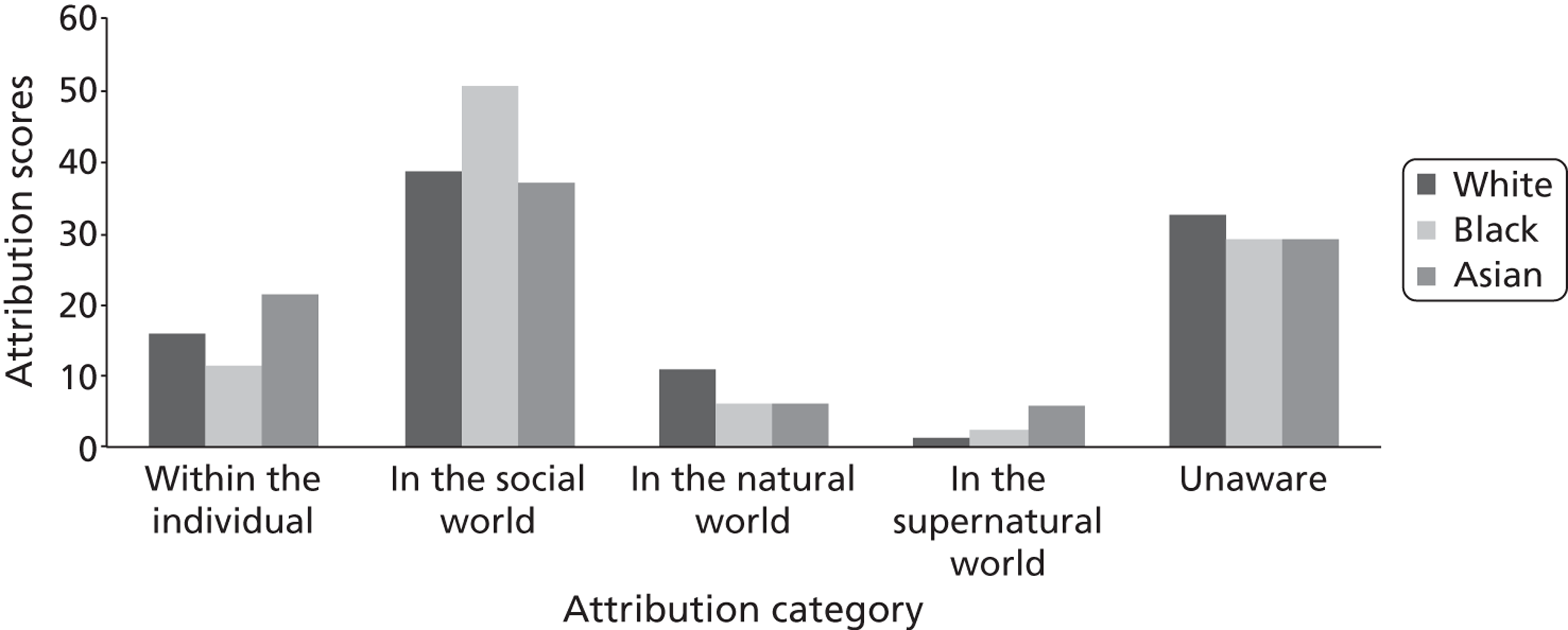
Patients’ attribution of psychotic symptoms
During the psychotic phase of illness, most of the patients reported being unaware of the cause of their symptoms (Figure 13). The highest attribution score for Asian patients was for the ‘supernatural world’ (40.74) compared with values for this attribution of 13.02 for black patients and 8.08 for white patients.
As shown in Table 10, the results of the ANOVA showed that there was a significant difference between the three groups in the scores for the ‘supernatural world’ (F2,104 =12.394, p = 0.000) and being ‘unaware’ [F2,104 = 4.893, p = 0.009]. Specifically, Asian patients were significantly less likely to be unaware of their symptoms than both black (p = 0.45) and white (p = 0.14) patients and significantly more likely to give ‘supernatural world’ attributions.
FIGURE 13.
Bar chart showing ethnic variations in patients’ attribution scores during the psychotic phase of illness.
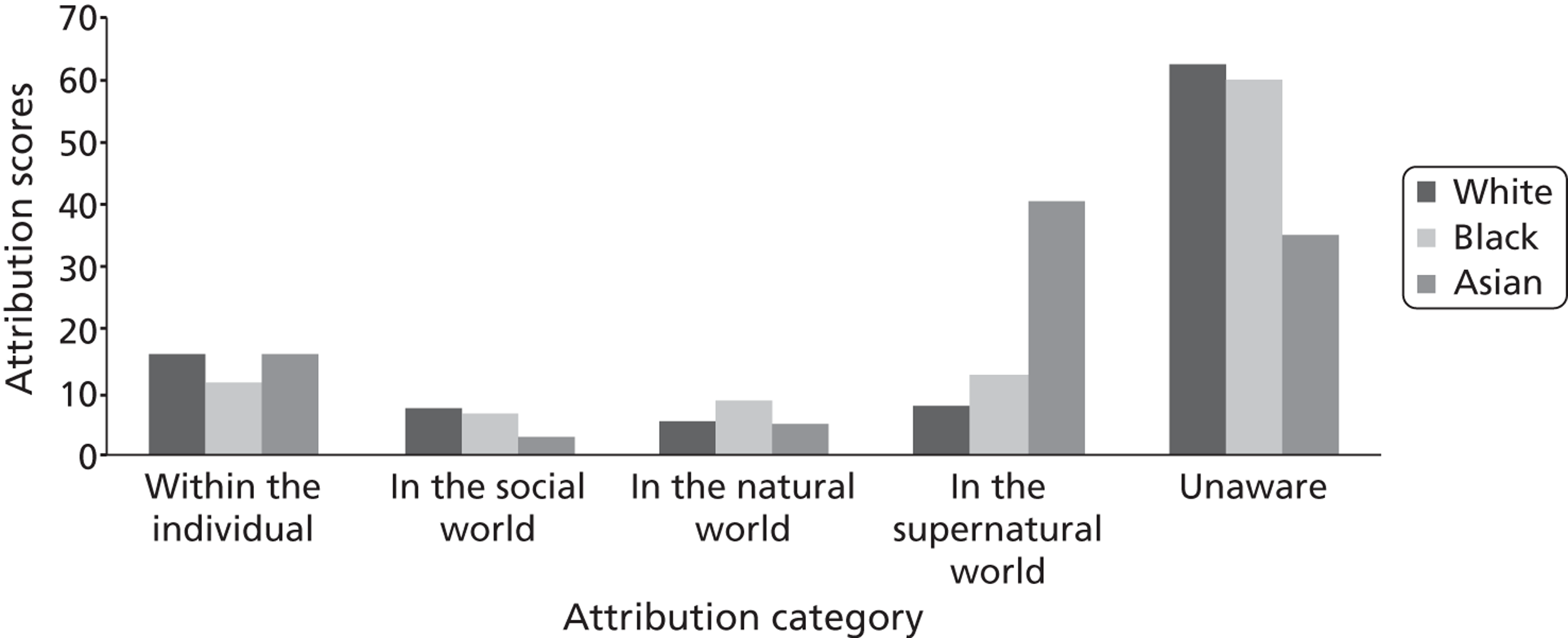
Change in patients’ attributions over time
Finally, we attempted to explore how patients’ attributions changed over time, using the Wilcoxon non-parametric test statistic (Table 11). For all three groups, during the prodromal phase, ‘social world’ attributions were most dominant. However, there was a change of scores during the psychotic phase of the illness, with a significant reduction in this attribution. Conversely, ‘supernatural’ scores increased over time between the prodromal and psychotic phases of illness for all three groups. However, this was most noticeable in the Asian and black groups. For all three groups, ‘within the individual’ was one of the most stable attribution types, seeing no change over time. These trends are illustrated in Figures 14–16.
| Attribution type | Prodromal phase (%) | Psychotic phase (%) | p-value | Test statistic | Standard error |
|---|---|---|---|---|---|
| Asian patients | |||||
| Unaware | 29.17 | 35.19 | 0.465 | 147.00 | 38.987 |
| Individual | 21.45 | 16.20 | 0.696 | 75.00 | 19.196 |
| Social | 37.25 | 2.78 | 0.000 | 151.00 | 20.724 |
| Natural | 6.25 | 5.09 | 0.680 | 9.00 | 3.640 |
| Supernatural | 5.88 | 40.74 | 0.000 | 185.00 | 24.523 |
| Black patients | |||||
| Unaware | 29.01 | 59.90 | 0.001 | 16.00 | 26.540 |
| Individual | 11.48 | 11.72 | 0.389 | 24.00 | 6.964 |
| Social | 50.74 | 6.51 | 0.001 | 173.00 | 24.418 |
| Natural | 6.30 | 8.85 | 0.273 | 2.00 | 2.739 |
| Supernatural | 2.47 | 13.02 | 0.028 | 1.00 | 5.906 |
| White patients | |||||
| Unaware | 32.28 | 62.56 | 0.002 | 70.00 | 43.656 |
| Individual | 16.00 | 16.24 | 0.958 | 67.00 | 19.203 |
| Social | 38.77 | 7.48 | 0.000 | 269.00 | 32.753 |
| Natural | 10.63 | 5.64 | 0.043 | 15.00 | 3.708 |
| Supernatural | 2.32 | 8.08 | 0.017 | 0.00 | 5.870 |
FIGURE 14.
Line graph showing attribution score change between phases for Asian patients.
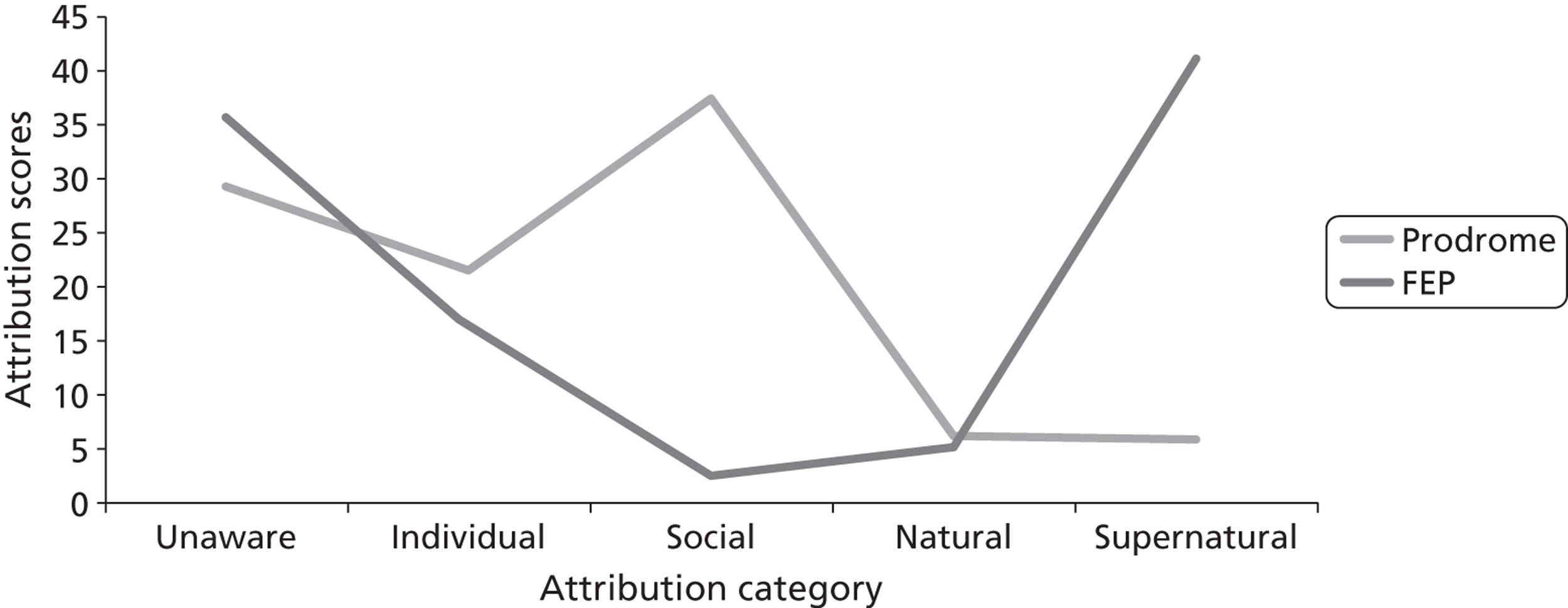
FIGURE 15.
Line graph showing attribution score change between phases for black patients.
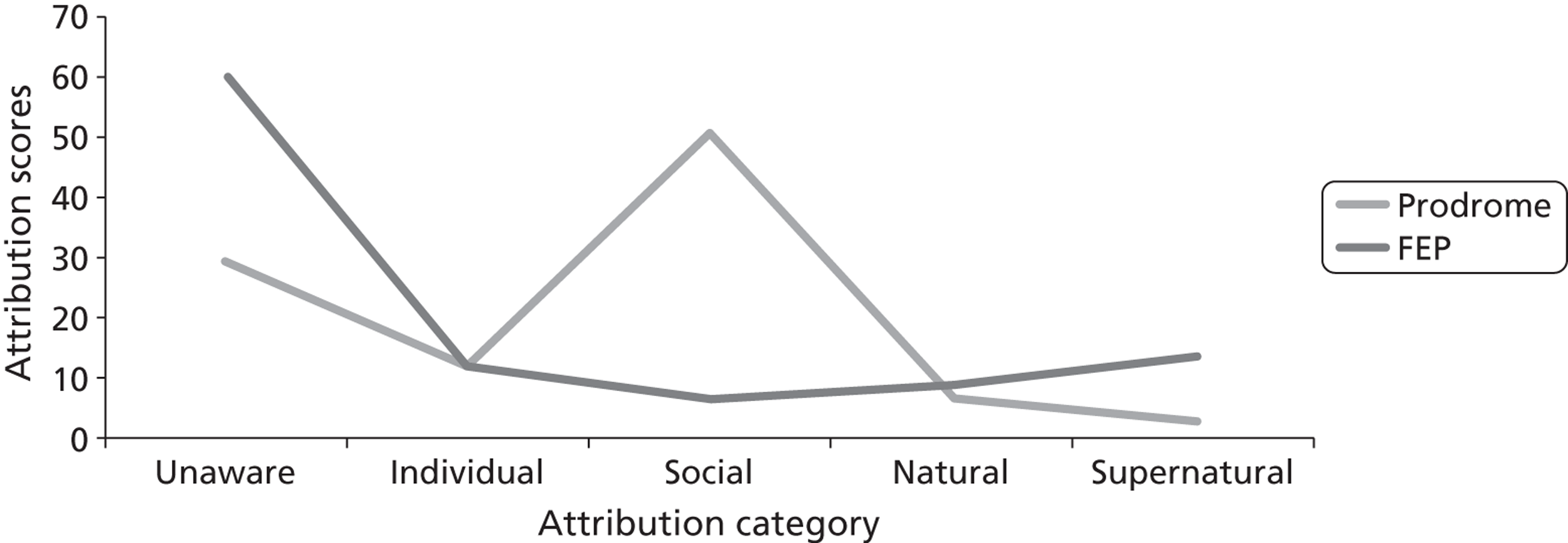
FIGURE 16.
Line graph showing attribution score change between phases for white patients.
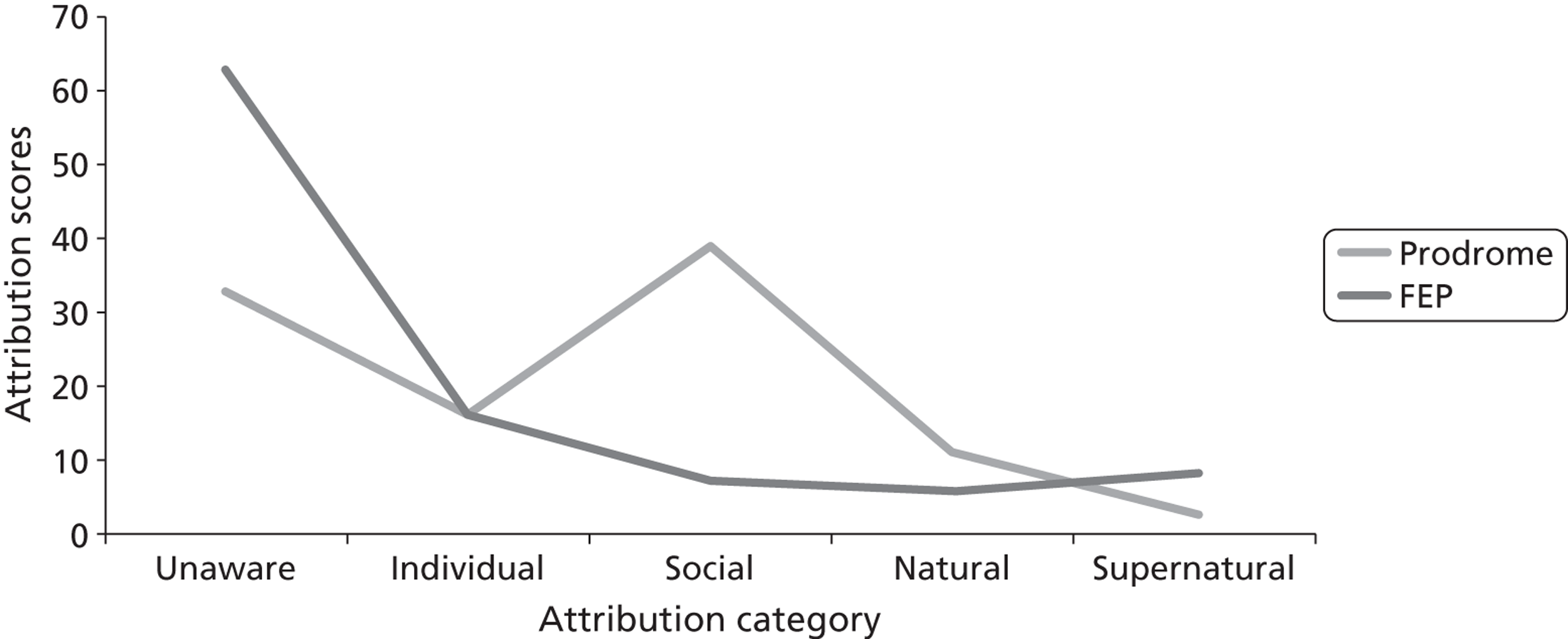
Duration of untreated psychosis and attributions
As we found no ethnic difference in DUP, we decided to identify which variables in our data predicted long DUP. We conducted a logistic regression using variables having some putative association with DUP, including biomedical attribution (‘within the individual’) (Table 12). Rather than using the continuous attribution scoring system, we created a new dichotomous variable for ‘within the individual’ attributions in both phases. Median scores were used as a cut-off point. Of the six variables included in the model, only age and living status remained significant. Being young at the time of psychosis onset (< 18 years) and living alone significantly predicted long DUP (> 6 months), independent of biomedical attribution score.
| Variable | OR | 95% CI for OR | p-value |
|---|---|---|---|
| Ethnicity | |||
| White | 1 | ||
| Black | 0.988 | 0.350 to 2.789 | 0.982 |
| Asian | 1.344 | 0.530 to 3.406 | 0.533 |
| Other | 2.970 | 0.304 to 28.987 | 0.349 |
| Gender | |||
| Female | 1 | – | |
| Male | 1.650 | 0.663 to 4.106 | 0.282 |
| Age | |||
| ≥ 18 years at onset | 1 | – | |
| < 18 years at onset | 6.293 | 2.438 to 16.242 | 0.000 |
| Living status | |||
| Not alone | 1 | – | |
| Alone | 2.763 | 1.009 to 7.565 | 0.048 |
| ‘Within the individual’ attribution during prodrome | |||
| Below median | 1 | ||
| Above median | 0.604 | 0.229 to 1.595 | 0.309 |
| ‘Within the individual’ attribution during FEP | |||
| Below median | 1 | ||
| Above median | 1.623 | 0.599 to 4.400 | 0.341 |
Summary findings from quantitative study 1
Overall, these findings can be summarised as follows:
-
We confirmed previous reports of the greater risk of MHA detention, more criminal justice involvement and more A&E presentations amongst black service users than amongst white and Asian groups.
-
There were no ethnic differences in DUP and DUI in FEP.
-
DUP was not related to illness attribution; long DUP was associated with patients being young and living alone. Therefore, length of treatment delay by itself does not account for adverse and coercive pathways reported for BME groups.
-
Patients from all ethnic groups hold multiple attribution types; simple notions that certain ethnic groups possess only one explanatory model should therefore be dismissed as in reality the process is much more complex.
-
During the prodromal phase, all three ethnic groups had similar attributions, considering the prodromal symptoms to be a reaction to social adversity. All three ethnic groups were likely to seek help from health organisations, including from GPs.
-
Black patients were most likely to seek help on their own during the prodromal phase whereas, in the case of white patients, their family members did the majority of the help-seeking.
-
With the emergence of psychotic symptoms, Asian carers and users were most likely to attribute symptoms to faith-based or supernatural explanations and seek help from faith-based organisations. Some black patients also changed to supernatural explanations, which influenced their care pathways, but this was only in a small proportion of cases.
-
Asian patients were significantly less likely to have A&E involvement and significantly more likely to have faith encounters in their pathways to care than white patients. Black patients were also more likely than white patients to have faith-based help-seeking encounters.
-
Help-seeking during the psychotic phase was primarily initiated by family members and carers.
Qualitative study 1
Aim and objectives
The aim of this study was to qualitatively explore how service users and their families make sense of the emerging symptoms of psychosis and initiate help-seeking. The objectives of the qualitative component of the research were twofold:
-
to understand the dynamic, social and cultural processes that determine help-seeking behaviour and encounters with statutory services
-
to explore ethnic differences in stigma, mistrust or suspicion of services.
Methodology
As NOS interviews are semistructured and allow qualitative exploration of narrative accounts, secondary analysis was conducted on NOS interview transcripts. Thematic analysis was conducted in which lower-order themes were collated in each of the transcripts. These themes were compared across the transcripts and further cross-cutting themes were developed.
Sample
Participants were a part of the larger quantitative cohort from study 1. These participants (users and carers) are described in the first part of this chapter and were recruited from early intervention services. During the quantitative phase of the study, patients and carers were given the choice whether or not to have their NOS interviews recorded. Of those who agreed, a subset of cases for which both the carer and the patients audio files were available was randomly selected for the qualitative phase of the study. In addition, one Asian participant who did not have a carer was included because he gave an extremely rich account of his pathways to care. Once this subset had been achieved, a research fellow purposefully identified a mixture of cases that were representative of the wider population. Special attention was given to ensure that key factors were a part of the interviews selected, including important variables such as long and short DUPs, a mixture of encounter types and involvement of both medical and non-medical help-seeking.
A total of 14 carer–patient interview dyads were selected from the full sample. The ethnic make-up of those interviewed was five black service users and five black carers; five Asian service users and four Asian carers; and four white service users and four white carers (Table 13). In total, 13 service user and 12 carer interviews were analysed.
| Case no. | ENR0 | Ethnicity | Carer–patient relationship | DUP (days) | GP involvement | Compulsory admission |
|---|---|---|---|---|---|---|
| 1 | ENR04 | White British | Mother–son | 4 | Yes | No |
| 2 | ENR033 | White British | Mother–son | 89 | Yes | Yes |
| 3 | ENR093 | White British | Mother–daughter | 28 | Yes | Yes |
| 4 | ENR056 | White British | Boyfriend–girlfriend | 1757 | Yes | No |
| 5 | ENR013 | Black Caribbean | Brothers | 5 | Yes | No |
| 6 | ENR014 | Black Caribbean | Mother–son | 1979 | Yes | Yes |
| 7 | ENR06 | Black Caribbean | Mother–daughter | 270 | Yes | No |
| 8 | ENR073 | Black Caribbean | Mother–daughter | 2620 | Yes | No |
| 9 | ENR09 | Black Caribbean | Sisters | 138 | Yes | Yes |
| 10 | ENR028 | Asian Pakistani | Mother–son | 164 | No | Yes |
| 11 | ENR026 | Asian Pakistani | Brothers | 920 | Yes | No |
| 12 | ENR021 | Asian Pakistani | NA | 2089 | Yes | No |
| 13 | ENR059 | Asian Pakistani | Mother–daughter | 7 | Yes | Yes |
| 14 | ENR050 | Asian Pakistani | Mother–daughter | 25 | Yes | No |
Data analysis
All semistructured interviews were recorded and transcribed with line numbers, resulting in typed transcripts of the narratives from each participant and their carer. Each interview was coded separately by two different researchers. The researchers:
-
Listened to transcripts via the audio files to familiarise themselves with the nature and context of the interviews.
-
Read and reread the transcripts to highlight statements relevant to the two main study objectives. Each highlighted item was then given a code name describing the theme or the process being described. Codes were transferred into a single Word document (Microsoft Corporation, Redmond, WA, USA) to produce a series of subcategories clustered by ethnic grouping.
-
Produced a written description for each of the subcategories compiled, with case and line numbers used to illustrate different points.
-
Derived higher-order themes with cross-cutting themes running through all of the transcripts. Finally, subthemes of the non-cross-cutting themes that were unique to different ethnic subgroups were saved separately to explore anything unique about the experiences of a particular ethnic subgroup.
-
To enhance rigour and methodological quality, the two researchers carried out this process by consensus coding to increase accuracy and reduce bias in any single researcher’s subjective interpretation of the data.
Results
Objective 1: to understand the dynamic, social and cultural processes that determine help-seeking behaviour and encounters with statutory services
Cross-cutting themes across the three ethnic groups
One of the most revealing findings of the qualitative data was the role that family members played in finding help, especially when service users reached crisis point. Within this there were ethnic differences with regard to which family member intervened and the types of familial networks they tapped into for finding help. Most white respondents sought help in consultation with members from the nuclear family, whereas in the black and Asian cohort help was sought in consultation with larger family networks (aunts, uncles, grandparents, cousins). For example, in the ENR09 case (a black British African Caribbean woman), the entire extended family (mother, father, brother, sister and an aunt) was involved in help-seeking:
Interviewer: So how did that go on then? What were the kinds of mechanisms that got her to the hospital? Did you call the GP?
Carer: It was my mum’s sister. My mum contacted my sister. Well, we were out and we were like visiting my sister and she was asking for any good doctors that she knows and she recommended her own GP and so mum referred [patient’s name] through my auntie’s GP.
Almost all British Pakistanis sought help through religious agencies and, in some cases, understood that the problem was medical only when somebody external to the larger kinship network intervened:
Interviewer: So 2006, 2007, it was around the end of college and beginning of summer time? So how often were these incidents happening when he was talking [to himself] in the bathroom?
Carer: On a daily basis. It was ridiculous. You know, we’d always catch him. Then my mother; she did try like . . . You know, obviously our religion. We do like . . . it’s not an exorcism or nothing. It’s just kind of like a blessing. We took him to all sorts of Maulvis [cleric] and stuff and paid a lot of money and stuff.
ENR026, Asian/Asian British Pakistani carer
The white sample on the other hand never sought help from religious or cultural sources. Two of the black Caribbean cases consulted the church about the distress that they and their family members were going through; however, this was not as common as in the Pakistani group.
The second cross-cutting theme that emerged was marked ethnic differences in the meaning of psychological distress. The majority of white parents recognised the early signs of psychological dysfunction as a ‘serious problem’ that required medical intervention. ENR033 was a white male whose symptoms had worsened gradually over time. His mother, despite believing that this was due to excessive cannabis use, was able to pick up on the changes and speak about the transition when ‘real’ help was required:
Interviewer: And until that point you thought it was linked to cannabis at the time?
Carer: I started to think that he was going to need some serious help. I did not know where to go and I didn’t know how to sort of suggest it to him because again he would go online and do all this self-diagnosis. He’s never told me actually what he read, but he was saying to ‘I know exactly what the problem is now’ and he was hyperactive and it was just opposite of what he had been. He was down here and up here and I know about bipolar and stuff and I thought this is just not good.
Ethnic minority carers on the other hand tended to ‘normalise’ symptoms, relating these to life events or giving them a supernatural/religious explanation. For example, one Pakistani mother thought that her son’s paranoid behaviour was due to the trouble that he had faced in the area they were living in. She believed that once his initial fear had subsided, his behaviour would settle and return to normal. Similarly, black carers, despite perceiving a change in a family member, did not attribute it to a mental illness. For example, ENR014, a black male, had been socially withdrawn for almost 3 years. His family members did not appreciate the change in his behaviour until he became aggressive:
Interviewer: So, did you notice the change two or three years ago?
Carer 1: Yes, he has been up and down and some days he would shout at us and some days his sister, he is frustrated and aggressive.
Interviewer to service user’s sister: And so, do you agree with your mum that it was around November 2007 that things changed, or was it before that?
Carer 2: Not really, no.
Carer 1: We hadn’t noticed if it did.
Pakistani service users often had multiple attributions; help was sought from the agency thought to be most appropriate for a particular attribution. For example, a young Pakistani man failed to seek medical help because he had a religious framework that both confirmed his symptom as spiritual in origin and legitimised the use of spiritual intervention:
Interviewer 1: So, you actually experienced these things? You did not think it was because of an illness? Or was it something spiritual?
Service user: That is what I am thinking it could be something spiritual, that is what I was thinking.
Interviewer 1: You think it was spiritual, elaborate on this for me?
Service user: Because I had one of these taweez [amulets] and that is for taking the spiritual thing away from you and protect you.
Interviewer 2: Why did you get the taweez and why did you get it in the first place?
Service user: In the first place the reason why I got it was because I thought there was an evil spirit around me, because every time I used to wake up in the night, I used to feel as if there was something pressing down on me and my chest.
ENR021
This young man saw a spiritual leader from the local mosque not only during the early stages of the illness but also when he was in hospital. His family brought the spiritual leader to the hospital and conducted rituals and also gave him a new taweez and held prayers. They also promised to conduct various sacrifices at religious shrines in their village in Pakistan if his health improved.
In some interviews with Black Caribbean participants, the role of multiple frameworks of attribution was also evident. The family of ENR09, a young British Caribbean woman, prayed for her both in Jamaica and in England as they struggled to deal with her distress. Although some family members felt that this would help, younger members of the family thought that this was not likely to be beneficial, suggesting important intergenerational differences in attributions.
There were also other instances in which service users and their families tapped into faith networks and used holy water and anointing oils to find relief. In some cases, when religion was the dominant attribution for understanding the changes in behaviour, even symptoms of psychosis were ‘normalised’ as just being life. For instance, in the ENR09 case, when the service user talked about speaking with God, family members understood it within a religious framework:
Okay, the way I looked at it was like music was speaking to her in the spiritual sense. That is how I saw it. From my eyes, she was like telling me to be quiet because she really needs to take everything in.
ENR09, black Caribbean carer
In sharp contrast, white service users and carers did not have spiritual attributions and did not seek any kind of spiritual intervention.
One of the themes that ran across the qualitative interviews was how stressful life events were used to interpret psychological distress. Often, stressful life events preceded or occurred alongside emerging symptoms, making it difficult for carers to differentiate illness from reaction. For example, the mother of ENR073, a black Caribbean woman, said:
She had given birth for the second time, did not have money, was in a relationship with a man who gave her drugs and was abusive, hence when she started isolating herself, I thought, she has had enough. I actually started looking after the children so that she can have some free time.
Similarly, a white carer said:
He had struggled with diabetes, was not doing well at school, his friends had left the neighbourhood, the band he used to play for no longer met. Our marriage had broken, I just thought he is a young lad and is not very happy. He also smoked cannabis and I knew all along that was doing him the utmost damage.
ENR033
With Asian service users and carers it was very similar, for example the case of ENR059, a young British Pakistani woman. Her sister was a doctor and played a key role in finding her help, but she had ignored her initial symptoms, thinking:
She was not happy with her university situation, had lost her job and was generally not getting on well at home as the family was not happy that she had dropped out of the university and was not able to get her fees back.
This contextualising of psychological distress as a reaction to stressful life events was therefore observed in most narratives across all ethnic groups.
The narratives also showed ethnic differences in coping during emerging psychosis. Black Caribbean patients attempted to deal with psychological and emotional dysfunction on their own. For example, ENR06, in talking about her initial period of distress, said: ‘The way I dealt with it at the time was a lot like, because I know I can put up on a hard front if I want to and I think, that is what I started to do’.
Similarly, ENR014, a black service user said: ‘I was coping as people expected you to get on. They did not know that I was raped and abused and was not feeling great about myself’. Isolating oneself also became a way of coping, ENR026, a British Pakistani man, said: ‘I started keeping to myself, as I did not want them to laugh at me’.
The white narratives revealed that, despite the struggle of coping with the illness, having a medical explanation helped service users find the resources within themselves and avoid becoming isolated or having to put up a front.
Across all ethnic groups, families made significant changes in helping the ill person cope with distress. These included moving out of the family home to live with the user to monitor his mental state and provide care (a white mother); ensuring that the user had personal space and asking family members to make accommodation for the changing behaviour (a Pakistani mother); and making job changes such as a black mother working night shifts to look after the service user’s children during the day.
Ethnic differences were observed in the ways in which crises unfolded and were dealt with, relating to illness attribution. ENR014, a young black Caribbean man, had been hearing voices. He followed his mother to his uncle’s house and was told by his mother to go back home. While on his way home he saw a police vehicle and asked the police to drop him home as he was hearing voices and was distressed. When they did not take him seriously he got angry and hit a policeman, ending up in services through the criminal justice system. In a different case, a young British Asian man (ENR026) came to services only after the postman reported to neighbours the chaotic state of his house, which he had witnessed while delivering a parcel. This prompted the neighbours to call the police for help. The police involvement then triggered medical consultation. In both of these cases, family members did not attribute the change in the service users to an illness that needed medical intervention.
Families with a biomedical attribution, mainly white, were able to find help through their GPs or through NHS Direct; however, even in some of these cases help was received only after a crisis occurred.
Even in cases in which the dominant model of understanding was essentially religious, there was a great deal of ambivalence in service users’ narratives as they constantly searched for explanations for their experiences. A young British Pakistani man (ENR026) told us: ‘My parents gave me a taweez [amulet], but I did not believe that it could take things away’. His parents brought his amulet back while he was in hospital while he was still hearing voices (after an episode at the police station in which he lost his amulet). He had initially attributed everything that happened at the police station and the subsequent hospitalisation to the loss of the amulet, but realised that things did not change dramatically after the amulet was brought back. Another young British Pakistani man (ENR021) who had a religious attribution became unsure of this over time:
And that could be the reason [referring to jinn] that day when they tried to cut my throat. It can be quite scary when I think about it so that’s why I try to keep it in the past you see. And there’s quite a lot of things I still don’t understand, I still would like to know more but it’s best to keep it where it is because the more you dig into it the worse it can get . . . I question it. I wonder whether sometimes it is Satan or is it me?
Objective 2: to explore ethnic differences in stigma, mistrust or suspicion of services
Carers from ethnic minority backgrounds were dissatisfied with services more often than white carers, even though white carers had similar difficulties as non-white carers in accessing care. With the Asian carers, the dissatisfaction was partly related to anxiety about not knowing what was causing the illness and also to worries about not getting the right care. For example, the mother of ENR050 kept taking her daughter to the GP and struggled to understand why the GP took so long to come up with a diagnosis and provide her daughter with the right help:
Researcher: So, they referred you to CAMHS?
Carer: So, CAMHS came later. Every time I took her to the GP (every 2–3 weeks) they told me nothing was wrong but I told her I can see changes in her; she is losing weight, she looks weak, she does not eat. They then did a blood test. I was really upset and began to cry, telling them that I knew her and would not bring her out for no reason. I was really upset and began to cry.
In certain cases, carers, both black and Asian, did not appreciate or understand the need for police involvement:
I don’t understand why he should be taken to the police station and kept overnight. He had done nothing. He needed the doctor not the police. They kept him there all night and he showed us bruises on his back from the police manhandling . . . . They told us there was no bed available. How can they tell us that there is no bed available in any hospital in Birmingham? There are so many hospitals in Birmingham, why are there no seats? After three days we got a phone call from London that he was in hospital there. The atmosphere in the hospital made his condition worse as he had never witnessed anything of that sort before. We don’t really know if he needed hospitalisation. Nobody ever told us anything. He had marks on him. He told me that the police had hit him. They should not treat him like that [mother starts crying].
ENR026, carer
The family had a religious/cultural explanation of their son’s illness and found it difficult to understand why their son was taken to the police station. When the researchers met them they wanted to forget the episode as a ‘blip’ and to ‘move on’ as their son had recovered. They were also worried about his marriage prospects and did not want this incident to get in the way of future alliances from respectable families.
The lack of availability of beds, an unfamiliar hospital environment and being taken to the police station before getting care were recurrent themes in ethnic minority interviews. African Caribbean service users who had come into care through the criminal justice system felt that they were never taken seriously:
I stopped a police car and I told them that I don’t feel well and I need some help, so could they drop me home as I am hearing all of these voices. They never took me seriously and I must have went in like a tangent and they started putting handcuffs on my wrists and that lot and I was flipping out, like kicking them in their faces and then they took me to the police station. From the police station, I had to go to the court and that is where I was slashing my wrists. I was clearly unwell. If they had taken me home maybe I would not have to go to the prison and then to the hospital.
ENR014, service user
The white British narratives also reported similar difficulties and delays in finding the right help at the right time; however unlike BME users and carers, white users and carers did not mistrust services.
Summary findings from qualitative study 1
This qualitative study confirmed and reinforced several findings from the quantitative study. These include:
-
The key drivers for help-seeking in FEP were family members and carers.
-
There were ethnic differences in which family member intervened and the types of familial networks tapped into for finding help. Most white respondents sought help in consultation with members from the nuclear family, whereas black British and British Asian respondents sought help in consultation with larger family networks (aunts, uncles, grandparents, cousins) and through community organisations.
-
Users and carers held multiple and sometimes competing attributions for the emerging symptoms and altered behaviour of FEP.
-
Many service users access or receive help only when a crisis point is reached. Even when carers have a predominantly biomedical attribution for psychotic symptoms, medical help is not sought until a crisis point is reached.
-
Many Asian and some black carers strongly believe in supernatural and faith-based explanations for the symptoms of FEP. There were important intergenerational differences, with second-generation Asians less likely to consider supernatural causes as adequately explaining the altered behaviour in the service users.
-
Attributing the symptoms of emerging psychosis to life events and social adversity can hinder medical help-seeking by providing a ‘normalising’ explanation.
-
All three ethnic groups experienced difficulties in accessing medical help; however, BME service users and carers mistrusted the services whereas white service users and carers did not.
Findings from study 1 are discussed in detail in Chapter 7 in the context of the overall ENRICH programme findings and their interoperation.
Chapter 5 Study 2: ethnicity and detention under the Mental Health Act
Abstract
Background: Black and minority ethnic patients have frequently been reported to be disproportionately detained under the MHA. Most studies have been conducted in a detained population. A more appropriate denominator for determining disproportionality is the population assessed under the MHA, only some of whom get detained.
Method: A prospective study of all MHA assessments (April 2009–March 2010) was conducted. Information was gathered on sociodemographic and clinical details, availability of community alternatives and outcome of assessment. In a randomly selected cohort (five per ethnic group), qualitative exploration was conducted of carer preceptions of the MHA assessment process.
Results: The sample consisted of 1115 assessments made on 863 individuals (some assessed more than once) with a mean age of 40.12 (SD 14.75) years, 60.3% of whom were men. These assessments led to 709 detentions (63.6%). Compared with the BSMHFT service user population and population estimates for Birmingham, BME individuals were significantly more likely to be assessed and detained. However, in a logistic regression model, detention was related to a diagnosis of mental illness, presence of risk and level of social support, but not ethnicity. Carers found the MHA process stressful, even when they understood the need for the process and agreed with its outcome. Police presence during MHA assessments was particularly stressful, and black carers perceived a racial bias in police involvement.
Conclusion: We found no evidence that ethnicity was a predictor of detention in those assessed under the MHA.
Introduction
Black and minority ethnic groups are disproportionately detained under the MHA in the UK. A recent systematic review6 concluded that BME patients experience higher rates of detention under the MHA than white patients. Meta-analysis of pooled data found that black patients were 3.35 times more likely, and Asian patients were 2.06 times more likely, to be detained than white patients. The review also noted that higher-quality studies are less likely than low- or medium-quality studies to report an excess of black detentions. However, meta-analysis showed that, even for high-quality studies, detention rates for BME patients remain about 2.5 times those for white patients.
Five main categories of explanations emerged from the 49 studies included in the review:
-
explanations related to patient characteristics, such as a higher rate of psychosis and greater risk of harm to self or others in BME patients
-
explanations related to clinical differences, such as more challenging behaviour and less compliance with medication in BME patients
-
service-related explanations, for example misdiagnosis, under-recognition of illness, lower referral rates, racial discrimination and stereotyping
-
explanations related to cultural characteristics, such as cultural differences in explanatory models of illness and greater stigma in BME groups
-
explanations related to the patient–service interface, for example BME alienation and mistrust of services and poorer engagement.
Overall, racial stereotyping and discrimination against BME patients was the most often cited explanation (15 papers, 31%), followed by alienation, dissatisfaction, negative perceptions and mistrust of psychiatric services (in 28% of studies), perception of BME patients as being more violent (24%), higher rates of psychosis (22%), delay in help-seeking and poor social support (18%) and misdiagnosis, under-recognition of illness and lower referral rates to services (16%). If the perception of BME patients as being more violent or at greater risk is considered as part of the racial stereotyping/racism category, then this ‘race-based’ explanation was offered in 53% of the studies. There was no primary evidence provided by any study to confirm any of these explanations, and some papers presented data that suggested that the ethnicity excess did not appear significant once confounders such as age, gender, diagnosis and risk were accounted for.
The appropriate denominator population for determining predictors of detention is the population who is assessed under the MHA not the subgroup who are detained, as studying the latter does not allow exploration of differences in the two groups (detained vs. not detained). The two groups may differ in, for instance, the availability of community alternatives to avoid detention. However, there are no studies in the psychiatric literature of patients assessed under the MHA 2007 in the UK. Factors related to higher rates of detention of BME patients under the MHA could be explored by evaluating the outcomes of MHA assessments. 6
The aims of the present study were to answer two questions:
-
Are there ethnic differences in the proportions of patients undergoing MHA assessments in a given year?
-
What are the clinical, sociodemographic, ethnic and risk-related predictors of detention as an outcome of MHA assessments?
Quantitative study 2
Methodology
Data were collected on all MHA assessments conducted between April 2009 and March 2010. A MHA assessment was defined as a clinical encounter in which an approved social worker (ASW, as defined in the MHA 198378) or an approved mental health professional (AMHP, as defined in the MHA 20072) has been involved or invited, or in which at least one medical recommendation has been completed, regardless of the outcome of the assessment (detention, voluntary admission or no admission).
Ethnicity
Self-assigned ethnicity is recorded on both MHA monitoring forms and in medical records. Four broad ethnic groups were created for the purpose of the analysis: white (including Irish and other Europeans), black Caribbean and black African, Asian (including Indian, Pakistani, Bangladeshi and Sri Lankan) and ‘other’ (including Chinese and Vietnamese). Mixed-race individuals were included in the ‘other’ category if they were not assigned to the black, white or Asian categories on the MHA monitoring form or in medical records.
Risk
Data on risk were obtained from MHA monitoring forms using the following categories: self-harm, self-neglect, deterioration in mental state, harm to other people, harm to property and harm to vulnerable others.
Data sources
Details of the MHA assessment are recorded by the AMHP using two forms, SS101 and CR6B (see Appendix 9). The SS101 records basic demographic information about the service user assessed, as well as basic information about location of assessment, current legal status under the MHA and outcome of assessment.
The CR6B form provides:
-
details of the last/previous admission
-
the circumstances leading to assessment/reassessment
-
a record of interviews and discussions (a) with the service user, (b) with regard to the assessment of risk to the service user and others, (c) with nearest relatives and others and (d) with doctors and other professional staff
-
the service user’s social situation, including (a) accomodation, (b) employment situation and (c) family and social relationships
-
the reason for the decision, including consideration of alternatives, advance decision and appropriate medical treatment.
Data were collected under the following headings:
-
setting of the assessment – where the assessment was conducted (venue, day, time), the individuals (including discipline and role) involved in the assessment and whether a carer/family member was present
-
patient characteristics – sociodemographic variables such as age, gender, self-ascribed ethnicity, residential status, level of community and social support; and clinical variables including diagnosis, type and magnitude of risk and the compatibility of clinical presentation with legal criteria for detention
-
service characteristics – local bed availability, availability of alternatives to detention and provision of specialist outreach services
-
factors determining outcome – including diagnosis, risk, alternative community treatment being available, the home treatment team able to manage the service user in the community, and voluntary admission from the service user.
Data collection
Before starting data collection, researchers arranged a meeting with the ASWs/AMHPs in the BSMHFT to describe the study, answer any queries and request that ASWs/AMHPs ensure that the SS101 and CR6B forms were completed in as much detail as possible. After some initial ambivalence related to whether the study was a way of scrutinising clinical practice, ASWs/AMHPs became willing and enthusiastic supporters of the project. Data were collected through the CR6B forms from AMHPs/ASWs and cross-checked against electronic patient notes. This information was collated and encoded at each site using PASW Statistics (version 18.0, SPSS Inc., Chicago, IL, USA). A copy of the coding manual can be found in Appendix 10.
The research team made weekly contact with the clinical teams, including on-call clinicians and crisis resolution/home treatment teams at each site, to identify all MHA assessments conducted in the previous week. Details of the MHA assessments are recorded by the AMHPs using the CR6B form. The format of the form and the level of detail varied depending on the site of collection and the AMHP recording the information. To ensure consistent and reliable data collection, a consistent coding regime was used (see Appendix 10) and all assessments were cross-checked with the data set of MHA assessments held by social services. For each site, patient electronic databases were utilised to ensure that as much information as possible was supplied to the research team by the AMHPs. Information from the assessment documentation was coded and input using SPSS statistical analysis software (SPSS Inc, Chicago, IL, USA).
Results
Sample
In the year April 2009–March 2010, 1115 MHA 20072 assessments were conducted in the BSMHFT. These 1115 assessments were made on 863 individuals (some of whom were assessed more than once during the study period) having a mean age of 40.12 (SD 14.75) years and of whom 60.3% were men. Of the 1115 assessments, 709 led to detentions (63.6%). The ethnic profile of those assessed was 51% white British, 14.8% Asian/Asian British Pakistani, 13.9% black/black British Caribbean, 7% black/black British African, 5.6% Asian/Asian British Indian, 1.6% Asian/Asian British Bangladeshi, 2.5% mixed ethnicity, 3.1% ‘other’ and 0.5% refused to say. Of the individuals assessed, 443 (51.3%) had had a previous hospital admission. Substance misuse was reported in 295 (34.2%) individual cases. The diagnostic composition of the cohort was 48.1% schizophrenia, schizotypal and delusional disorders [International Classification of Diseases, Tenth Edition (ICD-10)79 diagnostic codes F20–29], 25.3% mood (affective) disorders (F30–F39) and 4.8% disorders of adult personality and behaviour (F60–F69).
Ethnicity and frequency of assessments
Table 14 provides the numbers of individuals assessed (total n = 863) within the different ethnic groups compared with the total number of service users accessing BSMHFT services in 2009–10 (total n = 52,063) and the ethnic population estimates for Birmingham in 2009 (www.birmingham.gov.uk) for each group. The results reveal that a significantly greater proportion of patients accessing the BSMHFT from a BME background than those from a white British background were assessed under the MHA (χ2 = 415.0842, df = 5, p < 0.001). There were significant differences between the ethnic groups in the proportion of MHA assessments compared with the ethnic population estimates for Birmingham in 2009 (χ2 = 335.8437, df = 5, p < 0.001).
| Ethnic group | Population | n | Assessed as % of population |
|---|---|---|---|
| White British | Assessed under the MHA 2007 | 439 | – |
| Service users accessing the BSMHFT 2009–10 | 35,403 | 1.24 | |
| Birmingham population estimate for 2009 (×1000) | 699.7 | 0.06 | |
| Asian/Asian British Pakistani | Assessed under the MHA 2007 | 128 | – |
| Service users accessing the BSMHFT 2009–10 | 3761 | 3.40 | |
| Birmingham population estimate for 2009 (×1000) | 99.8 | 0.13 | |
| Asian/Asian British Indian | Assessed under the MHA 2007 | 48 | – |
| Service users accessing the BSMHFT 2009–10 | 1791 | 2.68 | |
| Birmingham population estimate for 2009 (×1000) | 59.4 | 0.08 | |
| Asian/Asian British Bangladeshi | Assessed under the MHA 2007 | 14 | – |
| Service users accessing the BSMHFT 2009–10 | 562 | 4.62 | |
| Birmingham population estimate for 2009 (×1000) | 25.5 | 0.29 | |
| Black/black British Caribbean | Assessed under the MHA 2007 | 120 | – |
| Service users accessing the BSMHFT 2009–10 | 2598 | 4.62 | |
| Birmingham population estimate for 2009 (×1000) | 41 | 0.29 | |
| Black/black British African/African ‘other’ | Assessed under the MHA 2007 | 60 | – |
| Service users accessing the BSMHFT 2009–10 | 724 | 8.29 | |
| Birmingham population estimate for 2009 (×1000) | 26.6 | 0.23 |
Ethnicity and detention
Of the 863 individuals assessed, 561 were detained at least once. Table 15 provides the number of detentions for each ethnic group as well as the proportion (%) of detentions within each ethnic group compared with the total number of service users (n = 52,063) accessing the BSMHFT in 2009–2010 and the ethnic population estimates for Birmingham in 2009.
| Ethnic group | Population | n | Detained as % of population |
|---|---|---|---|
| White British | Detained under the MHA 2007 | 307 | – |
| Service users accessing the BSMHFT 2009–10 | 35,403 | 0.87 | |
| Birmingham population estimate for 2009 (×1000) | 699.7 | 0.04 | |
| Asian/Asian British Pakistani | Detained under the MHA 2007 | 88 | – |
| Service users accessing the BSMHFT 2009–10 | 3761 | 2.30 | |
| Birmingham population estimate for 2009 (×1000) | 99.8 | 0.09 | |
| Asian/Asian British Indian | Detained under the MHA 2007 | 30 | – |
| Service users accessing the BSMHFT 2009–10 | 1791 | 1.68 | |
| Birmingham population estimate for 2009 (×1000) | 59.4 | 0.05 | |
| Asian/Asian British Bangladeshi | Detained under the MHA 2007 | 13 | – |
| Service users accessing the BSMHFT 2009–10 | 562 | 2.31 | |
| Birmingham population estimate for 2009 (×1000) | 25.5 | 0.05 | |
| Black/black British Caribbean | Detained under the MHA 2007 | 87 | – |
| Service users accessing the BSMHFT 2009–10 | 2598 | 3.35 | |
| Birmingham population estimate for 2009 (×1000) | 41 | 0.21 | |
| Black/black British African/African ‘other’ | Detained under the MHA 2007 | 36 | – |
| Service users accessing the BSMHFT 2009–10 | 724 | 4.97 | |
| Birmingham population estimate for 2009 (×1000) | 26.6 | 0.14 |
Chi-square analysis revealed significant differences in detention rates under the MHA between the different ethnic groups when compared with the total number of patients accessing the BSMHFT (χ2 = 259.7323, df = 5, p < 0.001) and the ethnic population estimates for Birmingham in 2009 (χ2 = 232.3088, df = 5, p < 0.001).
Post hoc analysis
Post hoc analysis was conducted to investigate the differences between all of the ethnic groups in rates of assessment and detention within the two denominator populations of BSMHFT service users (Table 16) and the ethnic population estimates for Birmingham in 2009 (Table 17). Compared with patients accessing the BSMHFT, a significantly larger proportion of patients from a BME background were assessed and detained than white British/white ‘other’ patients. Within the BME groups, patients of black/black British African/African ‘other’ ethnicity were significantly more likely to be assessed and detained than those from any other ethnic group (see Table 16).
| Ethnic group | Proportion assessed (95% CI) (%) | Proportion detained (95% CI) (%) |
|---|---|---|
| White British/white ‘other’ | 1.2 (1.1 to 1.4) | 1.2 (1.1 to 1.4) |
| Asian Pakistani | 3.4a (2.9 to 4.0) | 3.4a (2.9 to 4.0) |
| Asian Indian | 2.7a (2.0 to 3.6) | 2.7a (2.0 to 3.6) |
| Asian Bangladeshi | 2.5 (1.4 to 4.2) | 2.5a (1.4 to 4.2) |
| Black Caribbean | 4.6a (3.9 to 5.5) | 4.6a (3.9 to 5.5) |
| Black African/‘other’ | 8.3a (6.4 to 10.6) | 8.3a (6.4 to 10.6) |
| Ethnic group | Proportion assessed (95% CI) (%) | Proportion detained (95% CI) (%) |
|---|---|---|
| White British/white ‘other’ | 0.06 (0.057 to 0.069) | 0.04 (0.039 to 0.049) |
| Asian Pakistani | 0.13a (0.107 to 0.153) | 0.09a (0.071 to 0.109) |
| Asian Indian | 0.08 (0.060 to 0.108) | 0.05 (0.035 to 0.073) |
| Asian Bangladeshi | 0.05 (0.031 to 0.095) | 0.05 (0.028 to 0.090) |
| Black Caribbean | 0.29a (0.244 to 0.351) | 0.21a (0.171 to 0.263) |
| Black African/‘other’ | 0.23a (0.174 to 0.292) | 0.14a (0.096 to 0.189) |
Compared with the ethnic population estimates for Birmingham in 2009, a significantly larger proportion of individuals of Asian/Asian British Pakistani, Black/black British Caribbean and Black/black British African/African ‘other’ ethnicity were assessed and detained than individuals of white British/white ‘other’ ethnicity (see Table 17). Within the BME groups, individuals of black/black British African/African ‘other’ and black/black British Caribbean ethnicity were significantly more likely to be assessed and detained than those of Asian/Asian British Pakistani/Indian and Bangladeshi ethnicity. In addition, individuals of Asian/Asian British Pakistani ethnicity were significantly more likely to be assessed than those of Asian/Asian British Bangladeshi ethnicity.
Ethnicity, multiple assessments and multiple detentions
Table 18 shows the mean (range) number of times assessed and detained for each ethnic group. Because of the non-normal distribution of data for multiple assessments and multiple detentions, Kruskal–Wallis one-way ANOVA was used to test for overall differences. There were no ethnic differences between multiple assessments (χ2 = 3.815, df = 5, p = 0.576) and multiple detentions (χ2 = 5.248, df = 5, p = 0.386).
| Ethnic group | Mean (range) times assessed | Mean (range) times detained |
|---|---|---|
| White British | 1.28 (1–6) | 0.83 (0–4) |
| Asian/Asian British Pakistani | 1.35 (1–4) | 0.88 (0–3) |
| Asian/Asian British Indian | 1.35 (1–4) | 0.77 (0–3) |
| Asian/Asian British Bangladeshi | 1.36 (1–3) | 1.00 (0–2) |
| Black/black British Caribbean | 1.32 (1–4) | 0.88 (0–3) |
| Black/black British African/African ‘other’ | 1.25 (1–3) | 0.72 (0–2) |
Predictors of assessment and detention
Univariate analyses were conducted to identify sociodemographic and clinical variables that statistically differed between ethnic groups (Table 19). Because of the small numbers in some BME groups, we pooled the ethnicity data into broad black, white and Asian groups. Six variables were checked for co-linearity with each of the five other factors using Pearson’s correlation and then used to model detention. A logistic regression model was constructed to predict the outcome of a patient’s mental health assessment (either ‘resulted in detention’ or ‘no detention’) using SPSS statistical analysis software. Variables were entered into the model and identified as categorical when appropriate. The ENTER method was used to force inclusion of all factors into the final model in which model coefficients could be easily compared. Variables with more than two categories were tested for significance both as combined factors and as individual categories, which allows the overall effect of the variable to be captured alongside the effects of each category. ORs and 95% CIs were computed for each individual category.
| Variable | OR | 95% CI for OR | p-value |
|---|---|---|---|
| At least one risk | |||
| No | 1 | ||
| Yes | 2.553 | 1.923 to 3.390 | 0.000a |
| Ethnic group | |||
| White | 1 | ||
| Black | 0.945 | 0.688 to 1.297 | 0.727 |
| Asian | 0.972 | 0.714 to 1.324 | 0.859 |
| Other | 0.676 | 0.388 to 1.178 | 0.167 |
| Diagnosis | |||
| Psychopathic disorder | 1 | ||
| Mental impairment | 0.796 | 0.238 to 2.662 | 0.711 |
| Mental illness | 1.650 | 1.059 to 2.570 | 0.027b |
| Comorbidity | 0.846 | 0.379 to 1.886 | 0.682 |
| None | 0.237 | 0.107 to 0.523 | 0.000a |
| Age (years) | |||
| < 35 | 1 | ||
| ≥ 35 | 1.540 | 1.203 to 1.971 | 0.001a |
| Living status | |||
| With family/friends | 1 | ||
| Living alone | 1.147 | 0.863 to 1.524 | 0.345 |
| Supported living | 0.571 | 0.334 to 0.978 | 0.041b |
| No fixed abode | 1.190 | 0.581 to 2.439 | 0.634 |
| Gender | |||
| Male | 1 | ||
| Female | 1.277 | 0.992 to 1.643 | 0.057 |
In the total assessed population, detention was predicted by having a mental illness, the presence of risk, age > 35 years and living in supported accommodation. Ethnicity was not a predictor of detention under the MHA (Table 20). We repeated the analysis restricting the ethnicity breakdown to the three largest groups, which also had the most disproportionate rates of assessment and detention under the MHA. These were the Pakistani, black Caribbean and black African groups. Compared with the white group, ethnicity was still not an independent predictor of detention.
| Variable | OR | 95% CI for OR | p-value |
|---|---|---|---|
| Presence of risk | |||
| Yes | 7.658 | 3.008 to 19.495 | 0.000a |
| Ethnic group | |||
| White | 1 | 0.395 | |
| Black | 0.922 | 0.629 to 1.352 | 0.678 |
| Asian | 0.941 | 0.635 to 1.395 | 0.764 |
| Other | 0.560 | 0.290 to 1.083 | 0.085 |
| Diagnosis | |||
| Psychopathic disorder | 1 | 0.000a | |
| Mental impairment | 3.518 | 1.439 to 8.598 | 0.006 |
| Mental illness | 7.039 | 1.523 to 32.524 | 0.012 |
| Comorbidity | 6.835 | 3.136 to 14.898 | 0.000 |
| None | 4.867 | 1.655 to 14.319 | 0.004 |
| Age (years) | |||
| < 35 | 1 | ||
| ≥ 35 | 0.660 | 0.487 to 0.896 | 0.008a |
| Living status | |||
| With family/friends | 1 | 0.018b | |
| Living alone | 1.142 | 0.821 to 1.588 | 0.431 |
| Supported living | 0.456 | 0.254 to 0.820 | 0.009 |
| No fixed abode | 1.242 | 0.556 to 2.777 | 0.597 |
| Gender | |||
| Male | 1 | ||
| Female | 1.210 | 0.896 to 1.633 | 0.214 |
Summary findings from quantitative study 2
-
Greater proportions of the BME groups, particularly the black Caribbean and black African groups, are assessed and detained under the MHA than of the white group. This is true both when the denominator is the general population and when the denominator is the population currently receiving care from secondary mental health services.
-
When age, diagnosis, risk and level of social support are accounted for, ethnicity is not an independent predictor of MHA detention.
-
The ‘disproportionate’ excess of BME service users in the detained population is likely to be the result of underlying differences in rates of illness, presence of risk and level of social support.
Qualitative study 2
While collecting the quantitative data for this study we observed major inter- and intra-ethnic differences between the five broad groups (Pakistani, Indian, Caribbean, white British and African). For example, Caribbean and Pakistani service users had a higher number of Section 3 detentions. The data also showed that Indian service users were more likely to accept informal community treatment. To explore the underlying reasons for such cultural and ethnic differences in the outcomes of assessment, a triangulation approach was used and qualitative data were collected from carers, AMHPs and Section 12 doctors.
Methodology
Pilot and development of topic guides
Separate topic guides were devised for each of the groups to be interviewed (carers, AMHPs and Section 12 doctors). To devise the topic guides for the professionals, informal interviews were conducted with the operational leads (service managers) of four areas within the BSMHFT. The analysis of these interviews shaped the development of the topic guides. The questions for the qualitative interviews with carers were devised on the basis of our quantitative findings and the aims of the qualitative component of the research. Each of these topic guides was approved by the ethical lead of social services for Birmingham and Solihull.
Sample
The study team stratified the quantitative data set by ethnicity and then randomly selected five cases from each of the ethnic groups. Contact was made with care co-ordinators to obtain permission to contact service users. Contact was then made with service users and verbal consent received (the date of the verbal consent was recorded) to contact their carers and respective professionals involved in the assessment process. If the service user declined participation, further potential participants were randomly selected from the cohort of users of the same ethnicity. Once verbal consent was received, contact was made with carers by telephone and also a letter was sent explaining the study. Once carer interviews were conducted, contact was made with the professionals and interviews were conducted across the trust at their venue of choice.
Interviews were conducted by two researchers with both researchers making detailed ethnographic notes about the major themes emerging in the interview. These notes provided the context and background to the larger thematic analysis to follow. All interviews except one were audio recorded (one Caribbean carer did not give us permission to record the interview). Extensive notes were taken by the second interviewer while the lead interviewer asked questions. The interviewers typed up these notes together to maintain accuracy in representation. The same procedure was followed in the professional interviews. The professionals were given notice and details about the episodes that the researchers were going to speak to them about. Some of them used medical notes to remind themselves about the details around the outcomes of the assessments. In some cases, researchers provided professionals with the CR6B form for the assessment to assist them with remembering the details of the case.
Results
Recruitment
A total of 46 service users were contacted from the five different ethnic groups. The black African group and the British Indian group were the hardest to engage, with most refusals coming from the British Indian group. The study failed to recruit from the black African sample as some of them were clinically unwell or had moved away.
A total of 11 service users consented for us to contact their carers – five British Pakistani, two British Caribbean, one British Indian, one white British and two mixed parentage (one white–Asian, one black Caribbean–white) service users (Table 21). Although mixed parentage was not part of our inclusion criteria, these service users were included in the final analysis because EPEX (electronic medical records database) identified these cases as white and black and once we met the respective carers we realised that they were of mixed lineage.
| Carer | Outcome | Ethnicity of carer |
|---|---|---|
| C1 | Section 3 | Mixed (white and Asian) |
| C2 | Section 3 | British Pakistani |
| C3 | Section 3 | British Pakistani |
| C4 | Section 3 | British Pakistani |
| C5 | Section 2 | White British |
| C6 | Section 2 | British Pakistani |
| C7 | Intensive community treatment | British Pakistani |
| C8 | Section 3 | British Caribbean |
| C9 | Section 2 | British Indian |
| C10 | Section 3 | British Caribbean |
| C11 | Section 3 | Mixed (black and white) |
In seven out of the 11 cases, the outcome was detention under Section 3 and in three cases the outcome was detention under Section 2; in the other case the outcome was intensive community treatment. Eight of the 11 carers were women (mothers and partners) and three were men (one brother and two fathers).
Once the carer interviews had been conducted, the Section 12 doctors and AMHPs present at the MHA assessments were tracked to complete the case study. Tracking professionals was a major challenge as some had moved jobs or felt too busy to participate. A total of six AMHP interviews and four Section 12 doctor interviews were conducted (Tables 22 and 23 show the ethnic breakdown of the AMHPs and Section 12 doctors respectively), making a total of 21 interviews for the qualitative component of study 2. There were three cases in the entire data set for which all three interviews were conducted (carer, AMHP and Section 12 Doctor). These interviews were analysed separately and treated as complete cases.
| AMHP | Ethnicity |
|---|---|
| AMHP1 | African Caribbean |
| AMHP2 | African Caribbean |
| AMHP4 | British Pakistani |
| AMHP8 | British Pakistani |
| AMHP9 | British Indian |
| AMHP10 | British Pakistani |
| Section 12 doctor | Ethnicity |
|---|---|
| SD2 | White British |
| SD4 | White ‘other’ |
| SD7 | White British |
| SD9 | Middle Eastern |
Data analysis
All interviews were recorded and transcribed with line numbers, resulting in typed transcripts of the narratives produced by the carers, AMHPs and Section 12 doctors.
Each interview was coded separately by two different researchers. Thematic analysis was conducted across the interview sets collected.
The researchers:
-
Listened to the transcripts via audio file to familiarise themselves with the nature and context of the interviews.
-
Read and reread the transcripts to highlight statements relevant to the two main study objectives. Each highlighted item was then given a code name describing the theme or the process being described.
-
Transferred the codes into a single Word document to produce a series of subcategories clustered by ethnic grouping.
-
Produced a written description for each of the subcategories compiled, with case and line number used to illustrate different points.
-
Finally, higher-order themes were derived, which included cross-cutting themes running through all transcripts.
Subthemes of the non-cross-cutting themes that were unique to different ethnicity subgroups were also saved separately to deduce whether there was anything unique about the experiences of a particular ethnicity, carer or service provider that needed to be reported to understand the uniqueness of the process.
A senior member of the study team with expertise in qualitative data analysis went over the preliminary coding, which allowed us to collapse categories and also question some of the generalisations that the researchers had made in relation to the themes.
The data were manually coded and each theme was colour coded across transcripts. To enhance rigour and methodological quality, the two researchers carried out this process by consensus coding to increase accuracy and reduce bias in any single researcher’s subjective interpretation of the data.
To protect anonymity each participant was given a letter(s) code and assigned a number as follows:
-
carers: C1–11
-
section 12 doctors: SD2, 4, 7 and 9
-
AMHPs: AMHP1, 2, 4, 8, 9 and 10
-
the numbering of the AMHPs and Section 12 Doctors mirrors the cases that they were attached to, that is, AMHP2 and SD2 correspond to the case involving carer 2.
Two approaches to data analysis were used. In the first, the material collected from each of the groups was analysed separately and grouped under broad headings; in the second, the cases for which all three groups were interviewed were treated as a separate group and any discrepancies in accounts were examined.
Results
The following three broad themes emerged from the analysis of data in relation to carers’ experiences of undergoing MHA assessments: (1) experience with services, (2) shame, stigma and discrimination and (3) culture, religion and coping.
Carers’ experiences of services
Help-seeking and difficulties in accessing care through primary care
Six of the 11 carers interviewed spoke about the GP being the first port of call, and that they found that GPs did not have a very good understanding of mental illness. C9 (British Indian) repeatedly visited the GP describing his son’s symptoms. The GP kept asking him to bring his son to the surgery and did not accept that the son’s mental health problems stopped him from leaving the house. Similarly, a Caribbean carer (C8) said: ‘No, I contacted the GP, GP did not take it seriously and within a few days, he was arrested and sent to Winson Green prison’.
Only two cases found it relatively easy to find help and had no problems accessing help from mental health services. These service users were already within and known to mental health services.
Help was often obtained only after the service user reached a ‘crisis point’, as this white mother described:
I took him to the GP, he sent him straight away to Centre X, we went in there, I said, ‘I want you to keep him’, and they said, ‘No, we’ll just give him tablets’, and everything, but I really wanted them to keep him.
C1
The next day she tried reaching out to different agencies for help: ‘For whatever reason he just would not leave me alone. So I took him to my mum’s Sunday morning and I phoned up different agencies who couldn’t help me, in the end they told me to phone . . .’.
Two carers told us how they contacted the mental health teams, described the symptoms and people came around, for example: ‘It was easy, I noticed the signs and called her care coordinator and the home treatment team came along’ (C2). But the same carer had to go through distress and manage her husband at home as there was no bed available:
Researcher: How long did it take to find him a bed?
Carer: Almost two weeks.
Researcher: Were they monitoring him at home? Were they coming to see him?
Carer: Yes, to give him his medication to make sure. But with my husband it would be a hit and miss, sometimes he’d be there all the time for them to assess him. And they know that this was a regular pattern. He’ll never be at home, and then I was worrying that it’s not just his mental health. He is also a diabetic, he could be anywhere. He could be on the streets; he could have gotten himself into trouble. Because he causes a lot of fights and also borrows money and gambles. I was walking in egg shells.
During this period she went and saw her GP as she physically could not cope and she was given sleeping medication to help her sleep. Her children were sent to her extended family as she did not want them to be a part of the stress that they were going through.
Hence, help-seeking was not a straightforward process and was mediated by the service user’s history of mental illness. GP contact delayed help-seeking for first-time help-seekers.
Experience of the Mental Health Act
Family members across the sample found the MHA process very stressful, but felt that it was the right outcome as they could not manage their family member at home. The majority of them found the police presence very distressing. Although the police were involved in the majority of the assessments within the sample, it was the Caribbean carers who felt that there was a racial bias to police involvement: ‘Yes, the police were involved, he was reluctant to go inside the ambulance. There was a lot of hoo haa, to get him in. I sort of expected it for black lads and all that you know’ (C8 African Caribbean mother). This mother believed the harsh process was due to her son being black: ‘is how it goes, doesn’t it?’.
Another Asian carer spoke about it being a ‘long drawn out process’, which turns into a public spectacle every time it happens:
So many people came, social workers, doctors, two police vans, so many people just outside. The people in the surrounding see it and are looking at what is going on. He also feels that he is surrounded by it. He was questioning them, why are you coming to my property.
C4
Another Caribbean carer felt strongly about how the police treat black men with certain postcodes. She did not understand why her son needed to go to the police station if he was unwell and needed to be hospitalised. She was worried that he might be killed in custody:
I know, he did not trust me and did not want me involved in the assessment process. But, I was worried as I had heard what happens to men who are taken into mental health services. I also knew that it was unsafe to keep him at home as I felt threatened and I just had to let them take him. I did not feel that I was a part of the sectioning process. Even when he was in hospital, I felt that things were not communicated to me. I made a formal complaint about it and did not receive a very good response from a manager from my own community.
C10
However, a Pakistani carer did not feel that there was a racial element in the process:
Yes because the doctor said the way she was acting, and it’s dangerous for her, that she’s cutting herself and all the arguing, not staying in, she’s just, sometimes she just, you know that day she was just, open the door and run and go there, in front of the car or, using bad language to other people.
C6
In this case, although the carer was not happy with the lack of explanation, he thought that police involvement was warranted as his daughter posed a threat to herself and the family could not manage her at home.
Intraservice experience
Whereas GPs’ misrecognition of symptoms was a dominant theme in delays in help-seeking, once within mental health services users did not have problems in finding help. The only theme that stood out in the data was the lack of continuity of care once within services:
It would help if they did not discharge him and his relapses were monitored closely. The way the system works is that once you see the signs, you start all over again. We know he is sick and needs to be looked after.
C2
In two cases in which users were on supervised community treatment orders (CTOs), these were perceived to be less disruptive and ensured continuity of care from the same set of professionals: ‘I think it [CTO] works for him. He is out, we are less worried about him, but he also gets looked after’ (C4, mother).
Carer burden
Carer burden and deterioration in carer mental health were dominant themes. Although most of the carers were asked by services if they needed support to cope, few admitted getting help as finding help for the ill member of the family was their main priority: ‘Whatever I got would not have worked because, it was something that happened to me that I had to deal with and get through, and I was offered support but I haven’t, I never took it ’ (C1, white mother).
Carers also reported a deterioration in their own health as the service user got better:
I just had to be. I was probably stronger when it happened, than afterwards. I think, as he got better I got worse, cause I could let myself.
C1, white mother
But, when so many people come and take him away, I find that hard. It pains me and causes me a lot of distress. But, they also come in and say sorry to me for causing distress . . . It has made me ill. I am also taking medication for depression. I had a lot of trouble and then I went to the doctor and she is lovely. She told me, that I had depression and so I should be taking medication at night.
C4, British Pakistani mother
It was a rollercoaster for myself. Because I don’t know what to do, I don’t know how it’s going to pan out. What’s going to happen, and then you’ve got a grown man. Crying so much in front of you, ranting and raving, you just don’t know what to do. Then he becomes quiet, he has no interest in life. Then you wonder how is it going to turn out . . . I didn’t get no support, no I was just forgotten. But then I’m that kind of person that says as long as they are concentrating on him, I am happy.
C2
Dissatisfaction with services
Our sample showed ethnic differences in the level of satisfaction with services. Whereas one white British carer felt totally supported by services, the two Caribbean carers were not happy with services. C8 (Caribbean carer) thought that services did not take culture and cultural needs into consideration and that the quality of care would be different if the psychiatrist was from a similar background:
I don’t really think she got us. She did not get him. He would be better off with a black psychiatrist. His care co-ordinator is of the same ethnicity, but that is no use to us as he has no power. She [psychiatrist] makes all the decisions.
Across all ethnic groups family members wanted more than just medical intervention for their family members:
They discharged him, did not give me much information on how to deal with him and I felt lost. When he first came out, the mental health services were doing various things with him, there just wasn’t enough of it. He needed more stimulation.
C1, white mother
They medicate her, she is like a zombie. Sometimes you just need talking and that can cure. To take out of her mind that she is mentally ill and to empower her so that she can look after herself. Not just sitting here all day or laying about, and just giving her medicine, medicine, medicine. Medicine is not everything. You need advice as well.
C7, Pakistani father
Actually work groups, apprenticeships instead of just giving him medication and then leaving him, Because I can’t do it, I have a full-time job, there needs to be someone who is more hands on with him.
C8, African Caribbean carer
Shame, stigma and discrimination
There was a clear ethnic difference in the way that stigma and shame were perceived by Asian and Caribbean carers. Most Asian carers did not think that shame and stigma were a problem within the community. On the contrary, they felt supported by the community and their families:
No. It is an illness. I have diabetes too, why should I be ashamed of it?
C4, Pakistani carer
My family is so big that I don’t really need the community. But, it does not really matter. They have been supportive and have been feeling bad for us.
C6, Indian father
Another Pakistani carer described how the neighbours and extended family came around for support and read prayers and conducted other rituals with the aim of finding relief.
Although family members did not feel ashamed about their relative having a diagnosis of mental illness, some of them felt ashamed to acknowledge the presence of the mentally ill person in their household in front of others:
It is hard because she is a girl. I don’t want the marriage prospects of my other children to be ruined because she is like this and hence she stays with my parents, so it is not embarrassing for us when she runs out of the street.
C7, Pakistani father
One daughter, the one after him, is a social worker and she understands it and is sympathetic. But, the other daughter, she is eighteen and she is not very happy to have him around when her friends come over.
C8, black Caribbean mother
In the Caribbean group, one carer was selective in telling her family and friends about her son’s illness as she perceived stigma from the community: ‘My family members, only those who understand and have some knowledge know about it. Even with friends, I have had to be a bit selective’ (C8, black Caribbean mother). Also:
The Christian Black church environment is less helpful. People kind of give sympathy, but no practical help. They wanted to know not because they wanted to help me but because they were curious. I asked them not to call me during the day as my husband was suffering from panic attacks and they were not understanding of this. I had to walk away.
C10, Caribbean carer
Overall, it seemed that stigma was higher within the Caribbean community than within the Asian community.
Culture, religion, illness explanation and coping
None of the carers we interviewed attributed signs of distress to solely religious or cultural reasons. There were instances in which service users, when unwell, thought that they were possessed by jinn or cases in which people in the extended family thought that the illness could be attributed to religious or cultural reasons. Although most carers recognised symptoms from previous family history or linked the illness to taking drugs, called it ‘thinking oddly’ or recognised it as a clearly medical problem, help-seeking was not delayed by a different explanatory model of illness. One carer thought that it could be attributed to religious reasons but over time realised that it was linked to cannabis intake and had no religious connotations. Some of the service users, on the contrary, while unwell, believed that they could be possessed by spirits and others accused their family members of casting spells and carrying out black magic. It is interesting to note that, despite the fact that carers did not have strong religious explanations for distress, a lot of them sought refuge in religion in the hope of finding peace. A Pakistani carer told us:
I believed it, but my husband did not. I have a cousin in Saudia and she is from Karachi, she knows someone there. She told me that he is being followed by these bad things. She asked me to read the last two suras [verses] of the Quran. She asked me to read them forty-one times for forty-one days and I did that and I did not see any change in him [laughs aloud]. Then my husband said, that it is an illness. But, then I told him that the Quran has answers to this as well and I keep reading the Quran. But, it is not necessary that it is just that thing. It is good to pray.
C4
Another Pakistani carer felt hugely supported by her faith: ‘When I do my prayers, I find the inner strength to deal with his illness. When I am not praying, my family know that I am not coping’ (C2).
A Caribbean carer told us: ‘I shut myself to the people from the church as I found their interference difficult but continued praying as that was the only way I could cope. My faith became stronger and helped me cope’ (C10).
Professionals’ views and experiences
Aims
Professional interviews aimed to understand:
-
the determinants of, or the reasons for, the outcome of the assessment
-
the mechanics of decision-making
-
their perceptions of ethnic inequalities and the role of ethnicity and culture in mediating the illness experience.
Note on analysis/limitations of the study
Professional interviews were harder to conduct because of time pressures and hence not all of the professionals interviewed could be asked the same set of questions. Instead of organising the material under each of the broader aims, researchers took a decision to summarise the cross-cutting themes that emerged from interviews with AMHPs and Section 12 doctors seperately.
Outcome of the assessment
The dominant form of language that influenced decision-making was ‘clinical’ and about ‘risk’. Even in cases in which social workers were critical of professional practice, ‘risk’ was the dominant area around which the discussion of decision-making and outcomes was constructed:
Yes I think, I think we were all agreed that we were concerned about the level of risk to wife and potential risk to public. So we were definitely concerned about the risk of aggression. I think, again and just from what I recall, I think there was some discussion about the whole fact that he was hearing voices and whether this was, psychosis or religion and yes, I think it was Dr [name] that was one of the Section 12 doctors.
AMHP10
They [A&E staff] were worried about his own safety and also the safety of the people in the A&E department.
AMHP4
He wasn’t aggressive at all but he expressed ideas that his grandmother might be sexually interfering with a niece and he also expressed that he had thoughts of children, sexual ideas towards children, but it was limited what he said but he was very, very distressed by those kinds of thoughts. It was apparent that there were levels of risk regarding his risk to others because of the aggression that he displayed at his grandmother’s house. There seemed that there may be a risk to himself because he kind of had a self-loathing about having these thoughts about children, which he couldn’t actually control.
AMHP1
Because the parents were leaving [to go to India for a while]. So we decided that we needed to do something with this guy, you know, we can’t leave him in his bedroom, you know, the risks. We weighed up the risks and did we feel that he was gonna be safe, while other people were looking after him and doing his food and stuff like that, so we decided to do a Mental Health Act assessment.
AMHP8
Despite the fact that ‘risk’ was the dominant area around which the discussion of the outcome was constructed, and how it was constructed varied from case to case, decision-making did take alternatives to detention into account as well as deploying the ‘least restrictive options’.
One social worker, talking about the decision-making process around a service user who was new to the services, said:
We did balance up whether or not we could manage him on home treatment and the thought was that given the risk and given the unknown risk, because the idea about children, we weren’t sure whether he would act on them or he had acted on them. We didn’t feel that the risk could be managed at home with his family, so we thought the best thing to do was to bring him into a safe environment.
AMHP1
This discussion about options was something that occurred in each of the cases discussed.
Understanding the outcome process: role of religion and culture
Culture and religious backgrounds were flagged up as important components mediating the illness experience. Clinicians’ understanding came from their own ethnic experience, but also from working in the city where they learned from the practice of engagement with diverse communities. While emphasising the importance of distinguishing between culture and ethnicity, the emphasis was on understanding culture as upbringing, which is contextually constructed.
A black Caribbean social worker told us:
I think you have to look at ethnicity, but also at culture as well, because when people talk about ethnicity, an example I’ll give you is that we have African colleagues on my team. Their understanding of what Caribbean culture is, is not the same, whereas people think other people will think both of you are non-white, so you may understand what I’m saying, but their cultural ideas are not the same as Caribbean.
AMHP1
The importance of making distinctions between psychotic symptoms and normal religious beliefs was also emphasised. For a lot of the people who practise religion, it was normal to talk in terms of God talking to them or God revealing things to them as this was considered to be a part of their religious beliefs. AMHP1 cites the example of a man who was a strong practising Christian and whose wife was cheating on him who said that God had revealed it to him, which could be interpreted as delusional from the perspective of Western biomedicine.
In a similar vein, a British Indian social worker told us that generational differences in language and vocabulary around distress within the South Asian community need to be taken into consideration. She emphasised tapping into cultural nuances, getting as much information as possible and working with the families to achieve the best outcome for the ill person and the family:
I’ve worked in a multiculture society for many years so I feel I’ve got an understanding of when, when that’s out of the ordinary. I think the key messages remain the same whatever culture you work in, that you get corroborative information from people who, you know, we’re just, we just have some information on something, we need to always involve other people who have other pieces of the jigsaw.
AMHP9
Ethnic matching
Although all social workers had interesting takes on culture, religion, language and ethnicity, they were of the opinion that ethnic matching was not always a solution. AMHP1, talking about her experiences of working with people from her community, was of the opinion that sometimes it can get in the way of professional practice. She told us:
That is a tricky one. While I want to say, it works, there is always an assumption that since you are from the same background the outcome will be desirable to family members and the ill person. That can make your place uncomfortable as a professional trying to do their job. Also, sometimes you have to deal with lack of trust of professionals when you are working in the same settings. That is really tricky.
Another social worker said that one had to go beyond ethnicity and engage with cultural upbringing as matching colour did not mean anything: ‘Being black does not mean we are similar. It’s about our culture, our upbringing’ (AMHP2).
Another social worker with a British Indian background demonstrated how understanding the cultural context worked in a particular case:
There was a greater issue between the father and the daughter-in-law, you know his [son’s] wife, and he just couldn’t stand the fact that they were together again, and I had to ask him to back off, you know, that he’s a grown man, ‘Your son is a grown man, he can make his own decisions’. ‘But he’s always making the wrong decisions’. ‘It doesn’t matter if he’s making the wrong decisions, if he wants to, [Name].’ You know, I had to plain talk with him in my language that it’s none of his business, if the husband and wife want to get together, yeah, and it was very difficult for the father to take that on board.
AMHP9
She felt that she had used her knowledge of culture and language but also her rapport with the family to assert herself in a helpful and constructive way.
On the whole, the opinion around ethnic matching was mixed, with the black social workers being ambivalent and the South Asian social worker demonstrating that it could be helpful.
Medical perspective compared with social work perspective
Social workers commented on a generational difference in the attitudes of Section 12 doctors, with the older generation not wanting to be questioned and expecting social workers to be ‘rubber stampers’:
Sometimes it is that they’ve already done the medical recommendation or they haven’t involved you, but then obviously in terms of looking for your second doctor, you don’t go for the ones who are rubber stampers. There is this attitude of we know what is best, you just sign the dotted line. I have walked into assessments and questioned the outcome many times. It does not always happen, but there are some oldies, who are set in their ways.
AMHP1
Culture/ethnicity and its impact on the outcome of assessment
Most medics emphasised that assessment was a ‘culturally neutral’ process:
If I feel that the patient is necessary for him to be detained for the best interest, best, and health and to protect others, I don’t look into the shade and type of the person, straight away I will section them, if it is necessary and if the other measures all fail look at the patient, as a person. To me what matters is that whether, and I just the same to the families, I just listen to the views of the other team members, but to me, whatever ethnic group, if I feel there’s a mental illness and that person need to be in hospital, I will do it whatever the pressure on me will be.
SD9
Another Section 12 doctor felt that certain communities had unrealistic expectations of services and sought help elsewhere when these expectations were not met:
I think expectations are part of the problem, I’m not saying it’s the entire problem, but you haven’t cured him. You are the doctor. You haven’t cured him and sometimes you have to say, oh well, I’m not God here. There are limitations to what I can do. Whether or not we haven’t been able to explain those limitations, or we are unable to get to them in a realistic way, it’s a possibility, I’m not saying, some of them they have their own perceptions. I’ve got a Somali patient which I will be very surprised if the mother doesn’t take him to one of the healers tomorrow because she doesn’t believe her son have any psychiatric problem, it’s all about magic, black magic.
SD4
Views on black and minority ethnic over-representation in mental health services
Over-representation was not considered to be a problem, given the demographic profile of Birmingham, and was even thought to be improving:
I think that the general trend is that actually over-representation is coming down and down because I remember there was a couple of studies in 1980s with Professor [name] of [name of city] that they actually saw, 1980s the Black Afro-Caribbean 13 times more at risk of actually just being detained and 10 years later it actually came down to eight times more than a white Caucasia.
SD7
Summary findings from qualitative study 2
-
There are clear differences in MHA experiences between carers whose family members are known to services and those who present for the first time. The former receive unproblematic access to care; the latter feel that the system does not respond to their concerns in a timely and appropriate manner.
-
Help arrives only following a crisis and early warning signs are usually ignored by services, particularly GPs.
-
Carers find the MHA process very stressful, even when they understand the need for the process and agree with its outcomes.
-
Carers feel that their own mental health has suffered because of the burden of care.
-
Police presence during MHA assessments is particularly stressful, and black carers perceive a racial bias in police involvement.
-
Stigma and shame appear to be greater in the black community than in the Asian community. Asian carers find shared spiritual explanations within the community a source of comfort and support.
-
Cultural attributions change over time; in established illness medical explanations become more dominant but supernatural explanations continue to provide culturally appropriate meaning.
-
Amongst clinicians, risk assessment and management are the paramount drivers of MHA assessment and outcomes.
-
Although all clinicians agree on the importance of cultural and ethnic factors in assessments, social workers place a greater emphasis on these in practice whereas medics see themselves as ‘culturally neutral’.
-
There is no consensus on the need for ethnicity matching in the MHA assessment process.
Chapter 6 Study 3: appropriateness, accessibility and acceptability of generic early intervention services for different ethnic groups
Abstract
Aim: Study 3 aimed to determine the appropriateness, accessibility and acceptability of generic early intervention services for different ethnic groups and establish the care needs and preferences of service users and other stakeholders.
Method: Focus groups (n = 13) were conducted with early intervention service users (n = 22), carers (n = 11), community and voluntary sector organisation representatives (n = 6), commissioners (n = 10), early intervention professionals (n = 9) and spiritual care representatives (n = 8).
Results: Service users and carers had multiple explanatory models of illness, which are often competing and contrasting. For many BME groups, help-seeking involved support from faith/spiritual healers, before seeking medical intervention. This continued even during engagement with early intervention services. Early intervention services were considered accessible and appropriate and were largely perceived as being positive and caring and as taking into account the cultural and ethnic background of users and carers. No specific changes were needed or demanded from the current model of early intervention services to make it more culturally appropriate. BME service users did not seek BME-specific measures or interventions; they wanted to be able to share their spiritual/religious and cultural beliefs with mental health service professionals in an open manner without being judged. There was no demand for ethnic or gender matching between users and clinicians. Instead, users and carers wanted competent and caring clinicians, regardless of gender or ethnicity. Lack of appropriate interpretation services is a key barrier for some BME carers and users.
Conclusion: Newer ways of collaboration between the NHS and non-medical, particularly faith, organisations is needed to improve pathways to care for BME service users and carers.
Aim
The aim of study 3 was to determine the appropriateness, accessibility and acceptability of generic early intervention services for different ethnic groups and establish the care needs and preferences of service users and other stakeholders.
Method
This study’s methodology takes a constructionist approach in contrast to the objectivist and data-driven approaches of the studies 1 and 2. Here, knowledge about subjective social reality is derived from describing and interpreting people’s definitions of it, by using ethnographic methods,80 for example interviewing, focus group discussions or observation, to understand how people make sense of their world.
Focus groups
Focus groups are a form of group interview in which participants are selected because they are a purposive, although not necessarily representative, sample of a specific population, with the group being ‘focused’ on a given topic. Focus groups are increasingly popular in health research for ‘exploring what individuals believe or feel as well as why they behave in the way they do’ (p. 655). 81
Focus groups were coducted with service users, carers, health professionals, key stakeholders from voluntary sector and community groups, commissioners and representatives of spiritual care. All focus groups used a topic guide developed around the key questions: ‘How appropriate and accessible are generic early intervention services for the specific ethnic and cultural needs of BME communities in Birmingham? How can these be improved?’ The topic guide was developed after discussion with the project steering group. Cultural appropriateness, accessibility and acceptability of early intervention services was explored within several domains, including:
-
user choice
-
importance of, assessment of and perceived respect for cultural needs
-
availability of interpreters and information leaflets in different languages
-
ethnic mix of the treating teams and services
-
local provision of culturally appropriate ‘talking therapies’.
Users and carers were specifically asked about their perceptions of the relevance and importance of cultural and ethnic factors in the care received from the early intervention service within Birmingham. Each focus group was faciliated by the same senior researcher to ensure consistency of aproach. She was accompanied by a note-taker who observed and recorded the non-verbal interactions and documented the general content of the discussion to aid later analysis of the data. Debriefing meetings were held immediately after each focus group between the senior researcher and the note-taker at which throughts and perceptions about the content of discussions were recorded. Before conducting focus group interviews, a pilot focus group with service users and one with carers were conducted to test the topic guide and assess the feasibility of the focus group and the time required for carrying out the main interview.
Sociodemographic information sheet
Service users and carers were asked to complete a basic sociodemographic information sheet recording age, date of birth, gender, ethnicity, religious affiliation, living and employment status, postcode and other demographics (see Appendices 2 and 8).
Ethnicity was recorded in two ways. First, participants were asked to describe their ethnicity in their own words. This was then recorded on the demographics information sheet verbatim. Second, a list of census categories was presented to participants and they were asked to check the box that they felt best represented their ethnic group.
Procedure for all focus groups
Before each focus group the facilitator described the study and asked participants again if they were happy to participate. Participants were asked to sign a consent form. All participants were asked if the focus group could be audio recorded and whether they were happy for anonymised quotes to be used in the report and any future publications.
Sample
An initial mapping excerise was conducted from November 2009 to April 2010 to identify voluntary and community organisations that served BME mental health service users and their carers across Birmingham. Advice on the sources to access such information was initially sought through discussion with steering group members.
Between February 2010 and April 2010, the research team presented the study aims and objectives across all four teams at early intervention multidisciplinary team meetings and asked members to identify suitable BME users and carers. Presentations were also made to service user and carer groups, such as a football group and dance group for early intervention services users, Birmingham carer and user groups across Birmingham (e.g. Ashram Support 4 U, a monthly carer support group), a Women of Culture event (led locally by women in the community but a regionally driven organisation) and the refugee mental health conference (organised by PrideStart). Researchers also attended a number of regional and national events and sought advice from the Programme Manager of Wellbeing, Heart of Birmingham, Teaching Primary Care Trust (Public Health Directorate). As an outcome of this, a newsletter about ENRICH 3 was circulated through Lunchbox (internal e-newsletter for Heart of Birmingham staff) and CASCADE (internal e-newsletter for Birmingham East and North staff) in October 2010. Potential service users and carers were also identified from study 1 and contacted as above (see Procedure for all focus groups).
Mapping
A total of 138 organisations were identified as having a BME focus out of a possible 487. Table 24 highlights the numbers of organisations that were identified.
| Source | No. of organisations identified | No. of organisations with a BME focus |
|---|---|---|
| The BSMHFT intranet (accessed November 2009) (www.bsmhft.nhs.uk/service-user-and-carer/group/) | 48 | 3 |
| Lists provided by senior community development workers | 306 | 98a |
| MIND resource directory | Out of date, produced in 2007 | |
| Report: Irish mental health in Birmingham: what is appropriate and culturally competent primary care?82 | Out of date, produced in 2007 | |
| Report: Being understood, being respected: an evaluation of the statutory and voluntary mental health service provision in Birmingham for members of the Black African and Black African-Caribbean communities4 | Out of date, produced in 2006 | |
| BarberShop Magazine, Issue 3, Spring 2010 | 104 | 8 |
| Digbeth Trust (a source of development funding and support for grass roots voluntary and community organisations in Birmingham and the West Midlands seeking to develop community facilities and services) | 29 | 29 |
| Meeting between carers and mental health joint commissioners, April 2010 | Did not attend but study leaflets distributed | No response |
The BSMHFT intranet ‘Find a Local Group’ page was accessed in November 2009. There were 48 local user and carer organisations listed at that time; out of these, only three organisations had a BME focus. Unfortunately, two of these were no longer functioning. Details of all of the relevant voluntary and community organisations are listed in Appendix 10.
Recruitment of the sample
When convening focus groups, we aimed to represent the ethnic mix within each locality in the city. A maximum number of 10 participants were recruited for each focus group. Before commencement of the focus group, service users and carers were also asked to complete the sociodemographic information sheet. Focus groups lasted up to 90 mintues and all those participating were provided with refreshments. In addition, participating service users and carers were given £10 as a token of appreciation for their time.
In total, 13 focus groups were convened. Six service user groups were conducted, including service users from the four early intervention service teams across Birmingham East and North, East and West (Heart of Birmingham) and South. These included people from a variety of ethnic backgrounds. Three carer focus groups were conducted with current carers of BME service users who accessed the early intervention service in Birmingham. Four separate focus groups were also conducted with service providers across Birmingham. These included:
-
professionals working within the early intervention service in Birmingham
-
West Midlands commissioners
-
voluntary and commnity group representatives across Birmingham
-
spiritual care representatives within the trust.
Preliminary data analysis highlighted the importance of understanding how issues of religion and spirituality were addressed in early intervention services. Hence, it was decided that a separate focus group be conducted with representatives of the spiritual care team within the trust.
All participants agreed for focus group discussions to be recorded. However, one service user, one carer and two professionals declined to have any direct quotes used in the report or any arising publications.
Recruitment
Service user focus groups
Following the presentations, each team appointed a member of staff (usually an assistant psychologist) to act as a main point of contact for each team. This team member would liaise with care co-ordinators to confirm whether any suitable service users could be identified and then inform the research team. These individuals were called/e-mailed on a fortnightly basis over a period of approximately 12 weeks. Only one individual was identified through this process.
Because of the lack of response from professionals at the early intervention service it was decided that a researcher would visit the early intervention service base once a week (generally after multidisciplinary team meetings) and speak to service managers and clinicians directly. This proved to be the most successful method of gaining information about potential participants. Initially, care co-ordinators asked any potential participants if they were happy to take part in study 3. If a potential participant agreed to be contacted by the researchers, one of the research team telephoned him or her to briefly inform him or her of the study and explain that a letter of invitation along with more detailed information would be sent in the post. This was followed by a telephone call from the research team to confirm whether he or she was willing to participate in the study. Figure 17 shows the recruitment process for service users.
FIGURE 17.
Attrition chart: recruitment route for service users.
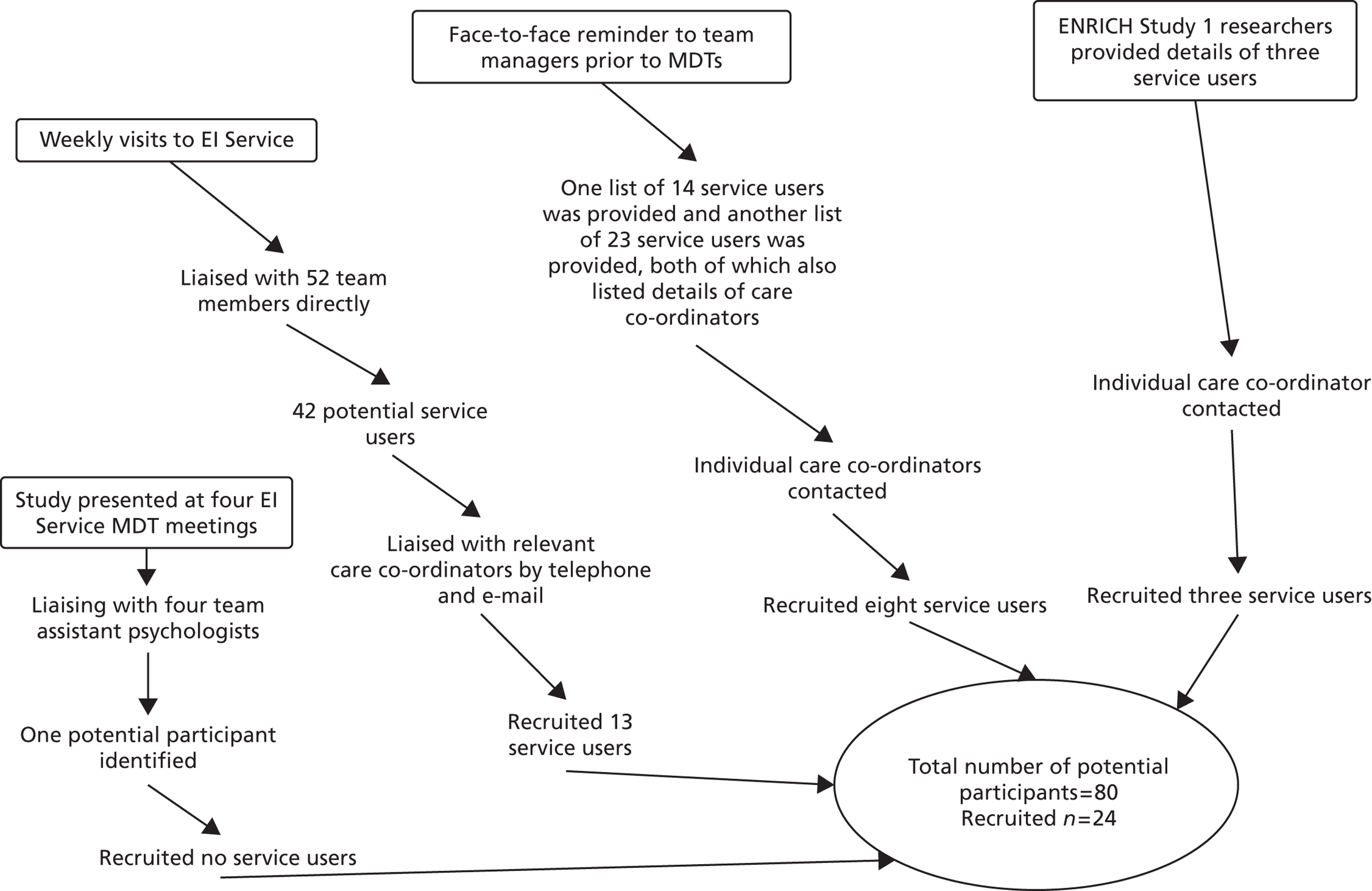
In total, 80 potential participants were identified of whom 24 (including the pilot) were recruited to the study. The main reasons for non-participation were service users declining participation and not meeting the inclusion criteria because they were not from a BME group.
Carer focus groups
Potential carer participants were idenitifed from a range of sources including two voluntary/community organisations, the ENRICH programme study 1 team, service users (who had participated in the service user focus groups), a PhD student and one care co-ordinator from the early intervention service. Intitally, the agreement of service users was sought before carers were approached. Once service users agreed to participate, the same procedure used for recruiting service users was used to recruit carers.
In total, 14 carers were recruited of whom three did not meet the inclusion criteria for particpation in the study and therefore formed the pilot carer focus group. These three carers were idenitifed by a voluntary/community organisation as being suitable for the study. Details of the numbers of carers contacted and the 11 recruited for the three focus groups are shown in Figure 18.
FIGURE 18.
Attrition chart: recruitment route for carers.
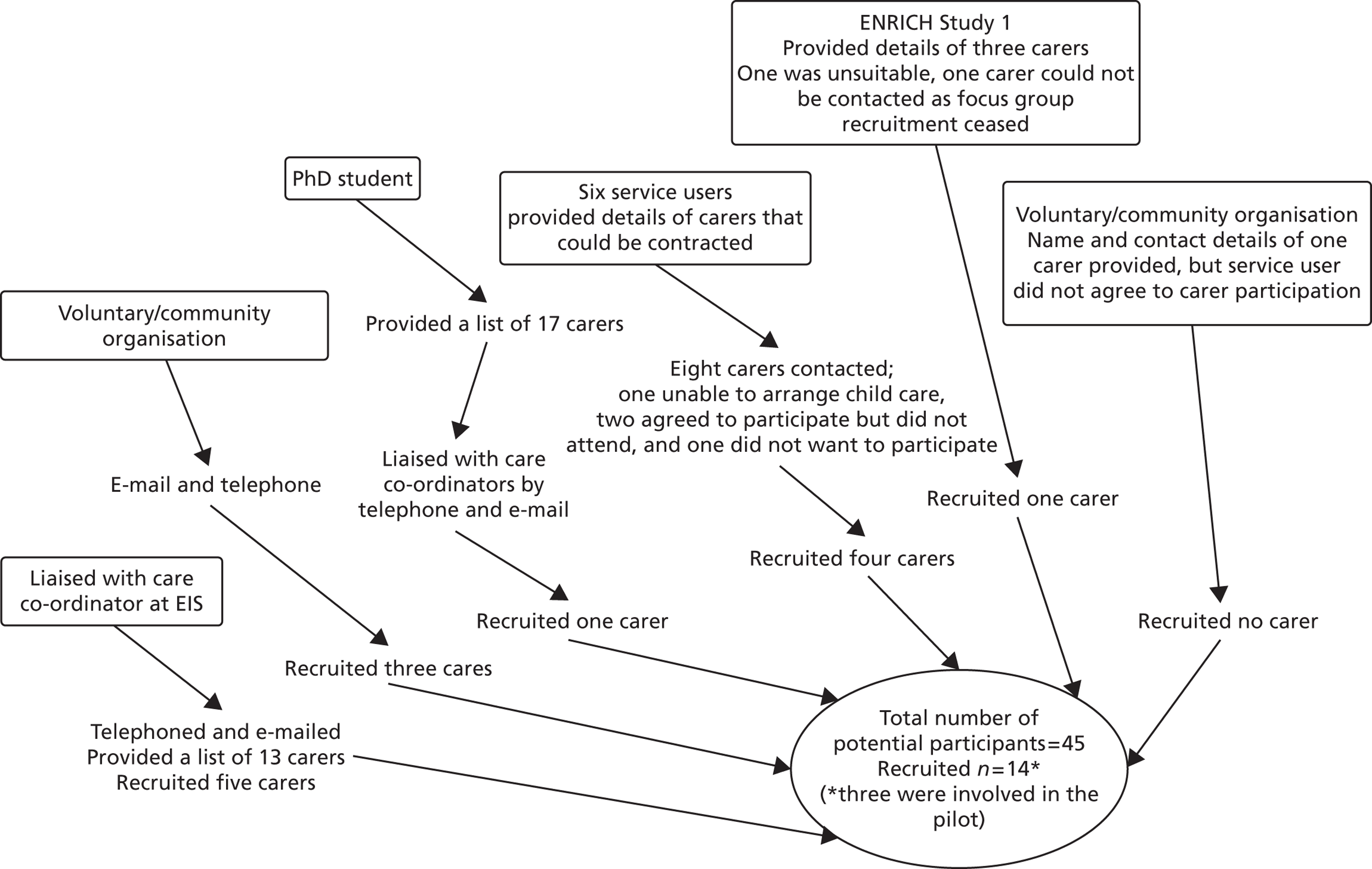
Focus group with voluntary and community organisation representatives
All 40 voluntary organisations identifed (see Appendix 12) as serving BME mental health service users and carers (see Mapping) were contacted by one of the research team. Initially, organisations were telephoned and then the study information sheet and leaflet were e-mailed or posted to the relevant individual at each organisation. This was followed up by a telephone call inviting members to attend a focus group and asking for verbal consent along with an e-mail confirming the focus group details, asking the recipient for a confirmation e-mail of attendance or non-attendance. When the researchers did not receive a response an additional telephone call was made to confirm attendance.
Out of the 40 organisations contacted, representatives from six agreed to participate. Of the six, only two had an understanding of the early intervention service. Most organisations were unaware of the early intervention service and its remit.
Focus group with commissioners
To ensure that commissoners took part in a focus group, the principal investigator liaised with the lead for the West Midlands comissioners group. It was decided that the focus group be held at the end of the commisionners’ regular monthly meeting. Before this, the senior researcher sent study 3 information sheets and leaflets to the lead comissioner for distribution. All 10 commissioners who were present at the meeting agreed to participate.
Focus group with professionals
An e-mail was circulated to all early intervention service staff members (n = 90) and the senior researcher visited each individual team base to discuss the study. Nine interested clinicians were finally recruited.
Focus group with spiritual care representatives
In liaison with the head of spiritual care in the BSMHFT, a total of 11 spiritual care representatives were contacted. Eight representatives were finally recruited.
Characteristics of the sample
Table 25 shows the numbers of participants in the 13 focus groups (this excludes the pilot).
| Focus group | No. of participants | No. of focus groups | Gender | Ethnicity | Religious affiliation |
|---|---|---|---|---|---|
| Service usersa | 22 | 6 | 12 M, 10 F | 9 Asian/Asian British – Pakistani, 5 black/black British – Caribbean, 3 mixed white and black Caribbean, 3 black/black British – African, 1 ‘other’, 1 Asian/Asian British – Bangladeshi | 11 Muslim, 6 Christian, 2 no faith, 3 ‘other’ (includes one service user who described himself as having ‘belief in one God’) |
| Carers | 11 | 3 | 3 M, 8 F | 3 Asian/Asian British – Pakistani, 5 black/black British – Caribbean, 1 black/black British – African, 1 mixed white and black African, 1 white British | 7 Christian (of whom 2 stated that they were Catholics), 3 Muslim, 1 did not respond |
| Voluntary sector | 6 | 1 | NR | NR | NR |
| Commissioners | 10 | 1 | NR | NR | NR |
| Early intervention service professionals | 9 | 1 | NR | NR | NR |
| Spiritual care | 8 | 1 | NR | NR | NR |
| Total | 66 | 13 | 33 | 33 | 33 |
Analysis
Each interview was transcribed verbatim and audio taped. Analysis was conducted using a thematic approach83 to systematically code, classify and organise the focus group content into key themes and subthemes. This is based on a thematic approach and also drawing on Krueger and Casey framework analysis. 84 Intially, each line of the transcript was numbered and then printed and read by two members of the research team to identify recurring concepts and categories. These transcripts were then reread to identify how these concepts and categories formed the basis of a conceptual thematic framework. This framework was used to code and classify data, and was then modified and refined throughout the analysis to reflect the content and issues expressed by respondents across all focus groups. These coded categories were then sorted into broader core themes based on similarlity and content. Illustrative quotes are provided to aid transparency of categorisation and theme representation.
To protect anonymity, every participant in each focus group was given a letter code (as below) and assigned a number:
-
service users: SU
-
carers: C
-
professionals: P
-
voluntary and community organisations: V
-
commissioners: COM
-
spiritual care representatives: SC.
The results are presented and discussed using the following thematic framework, generated from the data and by revisiting the original proposal:
-
help-seeking
-
culture and beliefs
-
social stigma and shame
-
experience of using the early intervention service
-
recreation of self
-
how to improve accessibility, acceptability and appropriateness.
When applicable, the results are presented under the thematic headings for each of the six stakeholder groups.
Results
Help-seeking
All service users and carers were asked how they, or the person they cared for, came to be using early intervention services. The other stakeholder groups were asked about their opinions of the factors that may delay or facilitate BME service users and their carers accessing early intervention services.
Crisis
The majority of service users reached mental health services through a ‘crisis’. Even in cases in which carers recognised the need for medical help, help was not sought until service users reached a ‘crisis’ point. For most, help was not sought until the patient was perceived as dangerous either to themselves or to others:
Three times I called 999 to come and help me, they said he’s not a small boy, this boy I said I was fearing will die, so it went all like that on Saturday and I was thinking, he ran in the cold, he opened all the windows, it was very cold. He told me he had clothes on, so later I had to call the police then they came, no I called the ambulance and I told them that he was going to died, I have made a note of all the calls I have made.
C3, black British female
Carers experienced frustration, anger and emotional turmoil as a result of not being able to access appropriate mental health services sooner: ‘It’s so upsetting though isn’t it like because when you talk about it, it still hits you that you’ve had to struggle to get that help’ (C13, mixed white and black African female).
Accessing services through crisis meant that quite often patients were detained under the MHA in community settings, leading to additional distress because of shame and social stigma (see Social stigma and shame). Police presence was generally viewed as negative. The general consensus held by spiritual care representatives was that every effort needs to be made to make legal detention ‘a private event’:
No, it’s better to go, not with the ambulance but maybe a private car, not drive up with an ambulance and you know this, they don’t like that. That will make them more aggressive, okay, but with a private car, they go with a chaplin or a priest and, get the person somewhere private, and then section the person. But they shouldn’t do it in the community, that’s one, especially in the BME community. Once they see an ambulance pull up at the gate, you know, people will start to look out through their windows, people will start to come across, they don’t like that.
SC5
Invisible carers
The majority of carers raised concerns about the failure of GPs to listen to and address their concerns: ‘Why is it such a battle to get them to recognise what the parent is saying you know I was so angry, that’s my child, I know my child’ (C12, black British Caribbean female).
In some cases, GPs were not happy for carers to speak on behalf of service users and preferred to speak to service users directly. However, carers were frustrated with this and believed that they had to speak on behalf of service users as quite often service users were ‘in denial’ and had little insight:
They should do right, so there’s no point them sitting back telling us as a parent we’re not the ones to speak the volume. Yes we are the ones to speak the volumes because the child or the person that’s sick cannot identify, ‘I’m sick’, they are in denial. They know that these people are in denial because they don’t know that is an illness.
C12, black British Caribbean female
In some cases, carers obtained appropriate medical support by exaggerating service users’ symptoms: ‘I got the police involved, we called the police, something’s wrong, I had to tell lies . . . he’s going to do something because he’s talking about the Taliban’ (C12, black British Caribbean female).
Help was also sought through alternative avenues such as through the local radio station (C12, black British Caribbean female), by writing to a local MP (C13, mixed white and black African female) and, in one case, by contacting a tenant support officer who contacted the early intervention service (C14, black British Caribbean female).
Carers and voluntary and community organisation representatives believed that GPs needed further training in detecting the symptoms of mental illness and in understanding that carers were best placed to detect any changes in behaviour (symptoms) of the service user. The consensus was that GPs lacked knowledge of appropriate mental health services (including voluntary and community organisations) and failed to signpost service users or provide appropriate treatment or ensure adequate follow-up:
I think when we go to see the doctor, the doctor needs to know what we tell them, what our problem is and to understand and you know, know the diagnosis straight away almost, or something along that line.
C13, mixed white and black African female
I mean for me, I work with carers so we have to look after the carers, you know, and this is what they say time and time again, you know, and they know, the person, more than the doctors, more than, anybody else, so surely they should be listened to.
V20
That is a big worry, because sometimes you have to look into professional and the providers, because provider is directly working with the service users, so I mean, commissioning side as well, they don’t have much knowledge about mental health, I’m not quite happy with the GP services, or the GP is not qualified on mental health, without listening they’re prescribing the medication, plus they’re not explaining them, what will be the side effects of this medication.
V16
The majority of voluntary and community organisation representatives also stated that carers needed support. Some carers had their own mental health problems and financial worries but were unaware that as ‘carers’ they were entitled to certain benefits and support:
The main problem that service users, carers have, is the mental health, secondly it’s financial, thirdly it’s housing and, so these are regular issues that will crop up with everybody you see, it, if, mentally they’re fine, they’ve got problems with their finances, their benefits, you know, at the moment, in the next years, everybody’s gonna be affected, so they’re worried, they’re worried now, what’s gonna happen in 2 years. Also with the housing, a lot of issues are neighbours, you know, that have anti-social behaviour . . . and it adds to their mental health and their worries.
V20
The avenues available to deal with carer issues were generally deemed to be insufficient because of recent government cutbacks.
Service users who were unable to obtain appropriate support were often left reliant on family and friends. This was not necessarily deemed beneficial when those called on for support lacked knowledge and understanding of mental illness and the appropriate services available for treatment:
If your family and friends around you don’t know what to do and you’re relying on them, to try and support you, it’s really difficult, because, I mean they didn’t know what to do . . . if they . . . haven’t got any professional help for it, you’re stuck.
V15
Mistrust of services
Some commissioners, early intervention professionals and voluntary and community organistion representatives felt that BME communities mistrusted services and that this contributed to a delay in help-seeking:
Asian community or African Caribbean community think, well, we’re gonna lose all control over this, because they’ll take us on a path where we may not want, we may not want medication, we may not want this, we may not want that, but then they lose control don’t they? And then you get child protection issues coming in . . . And I think there is an element of losing control . . . And you hide them in the community as well, until it’s really too late, you know, and then it comes to crisis point.
COM6
I think they . . . some of the African Caribbean community . . . [take] a very rational view that mental health services are punitive, they’re sectioning a lot of them . . . isn’t that the cycle where therefore people don’t come forward until they’re at their most critical and key stages. Therefore when they do come forward it’s likely to be the police bringing them in, which is, is it half of the admissions for African Caribbean male is, is by the police, which, which goes to prove that, you get that cycle, it just goes to prove that’s what mental health systems do for you. And if you’re an African Caribbean man you don’t go anywhere near them, so you, so it kind of, so it’s breaking that.
COM4
They suggested that trust could be established by promoting services within local communities: ‘I feel that when they’ve got trust in an organisation, it’s brilliant, they’ll always land on your doorstep, and especially if there are local communities promoting it and saying, “I’ve accessed it and its brilliant”’ (V15).
Voluntary and community organisations also regarded themselves as having a key role in empowering services users, by educating them about treatment and support options as well as self-management techniques, which ultimately gave them a sense of independence:
They [service users] have to look into the self-management and self-care. You have to be independent, you should not be dependent on people, because they don’t get any support from family members . . . we are building and we are empowering the women to build the confidence.
V16
Culture and beliefs
All service users and their carers held multiple explanatory models and ‘exploratory maps’ of illness, which were often competing and contrasting as well as interchangeable. Some carers cited religious and cultural beliefs as explanations for intial symptoms of mental illness, such as supernatural forces or black magic. For others, fear of being unwell had an important role in consolidating beliefs in religious and cultural explanations of illness. Religion gave them a sense of structure and purpose, and a framework within which to understand emerging symptoms:
Right and this went on for a period of time where it was getting worse for him, myself I started to think as a black person there was something wrong, I thought there’s a ghost in the place.
C12, black British Caribbean female
If I did I didn’t go through what I did, I wouldn’t be as humble or as worshipping of God as I am or as grateful as I am now to God. So I’m kind of, I’m actually a grateful person and a very lucky person because to go through what I went through it goes to show that I’m in God’s memory, God hasn’t forgotten me you know.
SU20, Asian British Pakistani male
Voluntary and community representatives felt strongly that religious and cultural explanations of symptoms were a key factor in delaying help-seeking amongst BME groups:
When there’s an issue about, you know, like, ‘Oh she’s, this person’s possessed, or that, or there’s something wrong’, ‘Oh, go to the Imam’, or, you know, like I know a lot of women say to me, ‘Oh I phoned up the helpline on one of the TV’s, Islamic TV’s’, ‘I’ve spoken to the Imam over the phone’.
V15
There’s a lot of, this thing about black magic and . . . possessions and things . . . you know, ‘We feel somebody’s done something to us, who do we go to?’ . . . so at that point . . . do I say to them, ‘Okay, maybe you need to go to mental health service’, . . . people are just quite. . . quick to judge, you know, a slight calamity in the family or a slight thing happens, you know, they’re quite quick to say, ‘Okay it must have been the neighbours who’ve done something to me’, you know, or, ‘Somebody’s come and possessed him’.
V20
Other explanations for the delay in help-seeking included perceived gender roles: ‘with them [Irish men] it’s mainly the issue of, because they’re men, they’re less likely to ask for the help, so, that’s, in their culture, I think it’s the sort of macho type, figure that they’re trying to portray’ (V17).
The role of faith
For some carers, their spiritual and religious beliefs and support system were paramount for their own psychosocial well-being and that of the service users:
I have had support from the Church, my friends, I have people who organise prayer for me, pray for him you know. All these things you know when I don’t have the strength on my own, you know at times you can be so down that you cannot open your mouth to pray, at that time, you need people to pray for you.
C3, black British African female
For the majority of service users and carers such as family members as well as community members and friends, faith played an important role in help-seeking. Help-seeking included visiting multiple faith and spiritual healers:
Something’s breathing on him, how can it be possible that he’s feeling something directly blowing into his face and got my son to start thinking something. So of course I did the right thing . . . we got a vicar, I took him up to the flat, he blessed the place and as a black person that’s what’s we’d done.
C12, black British Caribbean female
I thought I would take any help I could get . . . I know you’re supposed to believe in God but I did actually believe that he’s a person of God and he’s got some spiritual thing with him to help me.
SU7, Asian British Pakistani female
In their quest for faith/spiritual healing some carers were willing to travel to other cities and countries to seek the support of more ‘powerful’ faith/spiritual healers:
I believed to be honest that the vicar just wasn’t strong enough, powerful enough to me . . . I actually went to another Church which was a Catholic Church because we believe in the Catholic people, if you’re blessed by a Catholic Priest or what so ever, they are much stronger and powerful.
C12, black British Caribbean female
My mom, cos she was from . . . well is from Pakistan, their like I’ll take you to Pakistan and you’ll get better, I’ll take you to the ‘Delbar’ like spiritual [healer].
SU13, Asian British Pakistani female
For the majority of service users who sought the support of faith/spiritual healers, this practice proved to be beneficial: ‘I went to see him again just to get like duaa and stuff with special power and stuff as well . . . I found that useful, it kind of like calmed me down and helped me’ (SU7, Asian British Pakistani female).
Some service users also continued to visit faith healers after coming to early intervention services: ‘like I always go to his [faith healer] talks now once a week, and he talks to you’ (SU20, Asian British Pakistani male).
However, a few service users also talked about the negative aspects of visiting faith/spiritual healers. These individuals discussed their experiences of being the victims of ‘charlatans’:
He asked me for £500 . . . I actually went to the cash point withdrew £500, . . . he gave me that egg anyway and he goes when you gonna go somewhere far, throw it over you shoulder and pray for what you want and don’t look back and walk away and don’t go back there again.
SU13, Asian British Pakistani female
The issue of service users being on the receiving end of such ‘fake experts’ was also raised by spiritual care representatives.
A minority of commissioners stated that it was not just BME service users who favoured seeking support from faith leaders. One gave examples of similar faith-based help-seeking from the indigenous white population:
I think in Staffordshire we have a very low BME population . . . And I think it’s just the point of, the first point of contact, for a lot of our communities [white British], isn’t the GP or isn’t anything like that, it is very much, you know, churches and, and . . ., you know, some of our local churches, actually, support people with what, you know, what we would regard as quite sort of severe mental health issues, and they never actually come into, services, because, actually, the, the community worker, the volunteer goes out at two o’clock in the morning and goes there at, you know, six in the morning, to make sure people are having their breakfast and all sorts of things like that, and they, they sort of support people, in that way really.
COM9
A few commissioners also went on to suggest that the mental well-being of BME service users was much higher than that of the indigenous white population as a result of having ‘stronger social networks’ and avenues for alternative help-seeking and support:
The mental well-being of the BME population is much higher than the white population and, the significant . . . reasons for that being, that the social networks are, much stronger and where they go for support and other things like that and there are actually quite some differences, and, particularly between Polish and the South Asian as well.
COM9
In contrast to this, a minority of professionals stressed that those who were in receipt of family support had a longer DUP as carers ‘absorbed stresses’. Equally, those deemed as not having any support had a far shorter DUP and came in to services far sooner:
The longest kind of DUPs if you like the ones where you’ve got the family support and they absorb a lot of the stresses going on. The ones that are found very quickly usually are the ones without a family . . . and these guys are found running out into the street being very positive with their thing, because they’ve got nobody there supporting them and helping them through that thing.
P5
This view was also reiterated by a few voluntary and community representatives. They stated that it was lack of knowledge and understanding held by family members that resulted in BME service users having a longer DUP:
It was a case that you were stuck in a cycle, so if your family and friends around you don’t know what to do and you’re relying on them, to try and support you, it’s really difficult, because, I mean they didn’t know what to do.’
V15
Some carers did not discuss the issue of mental illness with their faith community because of fear of facing negative reactions as a result of lack of knowledge and understanding:
No I didn’t tell the church, I kept it secret from the church members, I didn’t tell them. I don’t think they would have understood.
C14, black British Caribbean female
I didn’t tell the church, I go to church as well, I don’t think they could help you know, they wouldn’t understand.
C1, black British Caribbean male
Ambiguity and uncertainty/interchangeable belief systems
There was also evidence of ambiguity and uncertainty in relation to both explanations of symptoms and cultural understandings of mental illness, especially amongst second-generation service users who felt that their parents and community members believed in black magic whereas they were unsure:
Yeah and people say I was [victim of] black magic and I don’t know.
SU21, Asian British Pakisitani male
I still don’t quite understand why I got ill . . . they say my sister-in-law . . . is evil . . . They say that but how can she be like that?
SU22, Asian British Pakistani male
Some service users thought that they were being punished for bad deeds and that they were in fact victims of ‘karma’:
I don’t know if someone could explain to me what’s happened, what is it, maybe I’ve done something wrong because I felt all this happened because I’ve done wrong in my life.
SU22, Asian British Pakistani male
It’s karma yeah, it is karma where in the sense if you do bad, you’ve just got to be always good and have a positive outlook and then worship God and remember God as you can because I did go a bit arrogant I was doing kick boxing and I was winning and I was suffering and stuff but it didn’t bother me, my ego was higher than anything I thought I was indestructible and to the point where I didn’t believe in God.
SU20, Asian British Pakistani male
Cultural beliefs often competed and contrasted with medical or genetic explanations:
My mother believes that cure will come from God, that God will come through and I believe that as well, obviously medicine is here for a reason as well so . . .
SU15, Asian British Pakistani female
Because they [parents] were confused . . . they’d go in a spiritually way and say okay we’ll call a pir [holy man] or . . . we’ll deal with it that way or we’ll call the doctor and they decided to call the doctor.
SU22, Asian British Pakistani male
Even when service users and carers recognised that substance and alcohol abuse were potential causes of developing psychosis these beliefs were interchangeable with cultural/religious belief systems:
I totally agree with what she’s saying it’s true I do hear voices cos I smoked cannabis . . . I’ve cut down but I used to smoke heavy didn’t I but I’ve cut back now . . ., I do hear voices strongly when I smoked.
SU12, mixed white and black Caribbean male
As soon as we smoke weed or we have alcohol we’re not pure, our bodies are not pure so we are prone to attack from evil forces.
SU20, Asian British Pakistani male
Knowledge and understanding
Lack of knowledge and understanding was highlighted as a key barrier to delaying appropriate help-seeking by commissioners and voluntary and community organisation representatives: ‘it’s not that they don’t, don’t want to access the service, it’s just they don’t even know about the services. They’re not aware of it for one’ (V18). However, commissioners believed that this issue was partly being addressed by community development workers through their role as ‘peer educators’ (COM4):
But our Mental Health Trust has community development workers, so I’d like to think that part of their role is, they should know about the EIS [early intervention service], we work for that organisation, and their job is to go out and raise awareness of mental health. So I’m not saying that’s a whole answer but, you know, I do think it’s part of their role to, you know, because they do know that EI [early intervention] exists whereas the vast majority of professionals, GPs are like, wouldn’t know what an EIS was.
COM7
Social stigma and shame
The fear of social stigma and shame emerged as a key factor in delayed help-seeking in all focus groups, particularly in the Asian communities:
In certain minority cultures, mental health needs are stigmatised a lot more than they are, even in Western, in Western cultures. So there may be either reluctance or unwillingness to recognise, the early stages of psychosis and what they are.
COM3
I want to start using the word ‘shame’ because, that’s how the patients feel, but because of the culture around them, they, they feel, a failure, they feel, labelled, they feel they’re doing the wrong thing . . . and because of the, attitude of the local community, they, they then feel very fearful of, of coming out or meeting anybody. And the whole thing goes round in a circle and gets bigger and bigger, see what I mean?
SC7
It’s not just the BME community, it’s the wider community, but obviously the BME community . . . it affects them even more, cause, you know, your honour, your status, your privilege, you know, it all depends on your state of mind and what you provide to society, you know, unfortunately they tend to be less tolerant if you do have a mental illness, no matter what you do, people will look your illness first and then look at your job title, so they can even dismiss a Prime Minister if he has got a mental health problem, so that’s the level, you know, the stigma, so, you know, so people quite rightly hide it or deny it, for that reason.
V20
Voluntary and community organistation representatives and spiritual care representatives emphasised that the label of mental illness held repercussions for carers and family members, affecting marriage prospects and positions within communities: ‘Sometimes people think mental health is kind of a disease that will catch people’ (V16). A few spiritual care representatives reiterated this point by giving examples of how they faced social stigma by working with mental health service users:
Unfortunately, stigma is not only with them with us as well, one of my friends, . . . he said, ‘If you work in a mental hospital, you must have been affected by it, and I don’t like to be affected by you’.
SC6
Equally, a voluntary and community representative stated that the stigma held around the label of mental illness was a factor in why BME communities failed to attend local mental health awareness-related events:
Because I find that there’s a really big issue with engaging with, in workshops, cause that’s what we’re there for, to do the workshops, but they won’t come, like you’ll find, there’s an issue, cause as soon as you advertise a workshop, and say, you know, you have to almost hide the fact you’re not gonna be talking about mental health.
V15
As a result of this, it was feared that people who needed the support of services were failing to reach services until they reached a crisis point:
From what I’ve learnt there’s a huge amount of mental illness out there in the community which is not being picked up, and I hadn’t picked it up before, it’s only now that I work in this area that I’ve realised how much there is.
V20
The negative community attitudes towards mental illness were believed to be influenced by a lack of understanding of the impact of mental illness on an individual’s life/self-identity or the symptomology/prognosis for those with a mental illness. As one service user stated: ‘[They don’t understand] the actual problems that people get and how horrible it can be . . . They don’t know how to identify it as well (SU7, Asian British Pakistani female).
Experience of early intervention services
Accessibility
On the whole, service users and carers were positive about the early intervention service. Although the majority of service users accessed mental health care after a crisis, once they were in receipt of the service it was generally viewed as appropriate, accessible and accomodating in terms of service users’ needs:
No flaw, no disappointment, even in the night when we call, they were always there.
C1, Asian British Pakistani female
He said don’t worry we’ll look after your daughter, don’t worry and he explained everything, he said don’t worry about the lift or anything we’ll provide the transport and come to see her in the house. If you’ve got no transport someone will come here to pick her up and take her to our office and we think this is the best thing.
C2, Asian British Pakistani male
Early intervention professionals were considered to be understanding, respectful and accomodating: ‘They are very friendly, as soon as they walk in the house it’s like they adapt to the environment in the sense that this is an Asian/Muslim family so we have got to be open to suggestions’ (SU22, Asian British Pakistani male).
None of the focus group participants felt that early intervention services had to change to meet BME needs; instead, the issues raised were seen as generic to mental health care.
User choice
The majority of service users were not given a choice in terms of the gender or ethnic background of the professionals who they came in to regular contact with (e.g care co-ordinators). However, for most service users this was not a problem provided that professionals were competent in their job and treated them with respect. All service users were unanimous that early intervention services should consider language needs and provide interpreters when needed.
Continuity/discontinuity of care
One of the key negative aspects of the early intervention service was the high levels of staff turnover. Service users and carers formed strong relationships with early intervention service staff (particularly care co-ordinators) and became anxious when there were staff changes: ‘my son is already worrying. It’s worrying because he’s saying when [care co-ordinator] gone because to him [care co-ordinator] everything right now’ (C12, black British Caribbean female).
Continuity of care was important; in particular; having the same care co-ordinator was vital, as long as the service user had a good relationship with him or her.
High turnover of staff meant that service users had to repeat details of events. Repeating details of the negative events that had occurred leading up to developing mental illness to different professionals was often described as ‘traumatic’ and was considered to have a detrimental effect on the well-being of the service user: ‘For me it was a negative thing because I wasn’t confident enough to disclose to someone who is new so I had to withdraw a bit’ (SU5, black British African female).
Early intervention service staff roles and responsibilities
Service users and carers talked about their relationships with early intervention service staff, particularly their care co-ordinators. For some, there appeared to be confusion over the role of care co-ordinators. A few service users described care co-ordiantors as ‘friends’ – ‘We get on like friends. I’d see her as a friend really’ (SU7, Asian British Pakistani female) – whereas others were suspicious of care co-ordinators’ motives and suggested that this was all part of a method employed by professionals to create a rapport and obtain information – ‘To get you to trust them basically so they try and become your friend . . . I don’t see them as that no. Not really, their working people that are doing their job’ (SU10, black British Caribbean female).
Most service users discussed their care plans with care co-ordinators and the services that would be provided to them and considered early intervention staff to be accessible and accommodating:
They called at my house . . . they called me before coming, the booked appointment to ask if I would be available at home or college so then.
SU3, Asian British Pakistani female
Yeah I was given [option], they would ask me how often do you want us to visit you or if you don’t want us to come to your house, how often do you want to come to early intervention.
SU5, black British African female
However, there were a few cases in which service users believed that this was not the case: ‘Excuse me, they never gave me a plan like which dates they want to come’ (SU6, black British African male).
A minority of carers were also frustrated with the care co-ordinators. One carer believed that he had no support from the early intervention service. He did not find the carer support group useful as no action was taken about concerns he raised with regards to his son’s welfare and ‘life circumstances’:
Sometimes I phone up and I leave messages and they don’t get back to me . . . Once I have phoned him and he turned the phone off so I told [service user] to tell him that he should speak to me and I want to see him, he don’t come.
C4, black British Caribbean male
A positive aspect of early intervention was that the service was accommodating and considerate of the service users’ individual and cultural needs. For instance, the doctor could visit service users at home or they could go to an alternative clinic in a different area and early intervention would provide them with transport to get there. This was also reiterated by voluntary and community organisation representatives:
In the community where, the stigma, basically, attached to the mental health issues and it, you know, they provide a service where they pick up people from home and drop them off at home. But a lot of their clients won’t like to be dropped off or picked up from home, you have to drop them off round the corner or something.
V20
However, professionals also recognised that, although attempts were being made to work more holistically, case load, time and financial constraints meant that it was diffciult to provide a bespoke person-centred approach that considered all cultural needs.
Withholding information
In general, when service users were continuing to seek support from traditional healers (i.e. faith/spiritual) they did not disclose this to early intervention professionals. They believed that professionals (i.e. care co-ordinators and doctors) would not understand their views/perceptions of health and well-being, or the use of traditional remedies for the treatment of distress or illness, including psychological and emotional difficulties, within a spiritual framework:
Just that . . . we can’t blame them because they’re upbringing is like Westernised, they can’t understand if we talk about jinn’s.
SU20, Asian British Pakistani male
Something that me and my family talk about.
SU7, Asian British Pakistani female
Similarly, spiritual care representatives stated that they received only ‘occasional referrals’ from early intervention services and that service users were reluctant to disclose their faith and the associated religious practices and beliefs because of a fear that this would be misconstrued by professionals as being part of their mental illness. The general consensus was that service users’ spiritual/religious and cultural beliefs needed to be considered when building a care plan and providing person-centred care:
When you hear somebody saying, ‘that they want to be washed in the blood of Jesus’. That’s enough to make a lot of psychiatrists really quite nervous. But, from a particular faith, and, particularly a cultural expression of faith, that would be something that you would hear week in, week out, in a perfectly ordinary service of worship. There’s nothing unusual about that phrase. And it certainly falls well within the norm, of what might be practised by those, who are not mentally unwell.
SC8
Cultural appropriateness
The majority of professionals recognised that great variation exists between and within cultures held by service users in terms of explanations of mental illness and preferred treatment options. It was acknowldeged that these needed to be considered in the care plan approach taken. Professionals appeared respectful and considerate of what might be deemed culturally appropriate behaviour, including perceived traditional gender roles amongst certain BME groups. One professional discussed the complexities of working with diverse ethnic groups and conflicting and changing gender roles and life paths, which meant that she had to develop treatment plans that remained respectful of families’/carers’ wishes and benefited the service users:
I think sometimes, a big focus on thinking that everyone’s got to be in jobs or in training, that can be equally inappropriate for some of the girls [from Asian backgrounds] or lead to conflict where you could be getting in a real battle where we might have some of our girls who actually want to live a more Westernized life, and there’s already that conflict in the family and I think you’ve got to be careful not to sort of, side too much so you’re actually causing a lot of tension within the family, because that has happened where, for instance we wanted to take somebody out to build up their confidence, and then the family members have been a bit worried about where are you going to take this person, is it going to be mixed day centre for instance or going to somewhere like a respite unit, that needs careful handling as well.
P6
A major concern expressed by professionals and voluntary and community organisation representatives was the availability of appropriate interpreters. Professionals stressed that the quality, reliability and competence of interpreters were questionable:
I’m not sure what level or degree of training these people have in mental health . . . the service user was very angry and conveyed that he really wanted to belt this guy because he was so objectionable, to what the client was expressing, which really undoes a lot of the work that we do with engagement.
P2
Other professionals talked about their experiences of interpreters overstepping professional boundaries and behaving inappropriatley:
I’ve been out with an interpreter once, and one of the things that we were trying, we were trying to basically persuade this young person to take medication, and he said, ‘Well let me persuade it’ and then the whole boundaries of that interpreting role, which was competently inappropriate, and it was just quite, well really unprofessional.
P6
There were concerns that interpreters might breach confidentiality if they were from the same close-knit BME community, you don’t always take it on board that people know of people, who know people.
P3
In relation to the point raised by professionals around social stigma (see Social stigma and shame), professionals recognised that, although some information around individuals’ beliefs and values was collated through the health and social care assessment, ‘this was underutiliesed’ (P5, P6), the main reason being workload and time constraints.
Treatment, support and recovery
All carers were positive about the treatment provided by early intervention services, particularly in terms of the positive affect of medication:
[Name] has got a lot better in himself in that way I think the injection and the support he has been getting.
C5, white British female
I find it helpful like they give you medication to calm him down and counselling.
C11, black British Caribbean male
However, the majority of service users were unhappy with their medication: ‘I’ve told them that I want to come off this [medication] . . . I don’t think it’s really helping me anymore’ (SU4, black British Caribbean male).
The main frustration for service users was that medication/treatment did not provide a cure, hence the service was only seen as partially effective: ‘the medication is good and everything but it’s not taking away the illness . . . I want the cure you know, we want the cure you know’ (SU6, black British African male). As a result, some service users sought advice about alternative treatments from other service users: ‘I’m just waiting until I come off those and then I will ask them about the next medication . . . I . . . was told . . . by someone else they just said it might help me . . . one of the other service users’ (SU4, black British Caribbean male).
Professionals acknowledged that the internet had made information accessible and service users were knowledgable about treatment options as well as about the ingredients in certain medications. This meant that service users whose religious practice and beliefs forbade the consumption of pork or pork products refused to take medication that contained such ingredients: ‘some of the medication they do have pork fat for example in them and they [service users] are very cautious about taking this sort of medication’ (P6). Professionals acknowledged this but also stated that they were unaware of the alternative treatments/medication available.
The majority of service users did not see the potential benefits of talking therapies (i.e. counselling, psychotherapy); again, this was because they could not see the immediate benefits. Some voluntary and community representatives urged the need for efforts to educate service users about the benefits of such therapies and the need to make these culturally appropriate: ‘whenever I refer so many clients to the, for the counselling services, they said, ‘I didn’t find it quite useful’, and we are encouraging them to understand, what is counselling about’ (V16).
Examples of what were deemed to be appropriate talking therapies were given, for instance, one voluntary and community representative mentioned the Lateef Project, a Muslim telephone counselling service. However, the majority of voluntary and community organisation representatives stressed that services geared towards BME service users needed to consider the individual needs of the service user not just his or her assumed preferences based on his or her religious identity:
But I have a client who go into anxiety, right, she even, though she don’t pick the phone at home, once the phone rings, she get panic, she don’t want to, right, and she always have that kind of fear, ‘somebody’s listening my conversation’.
V16
In terms of culturally appropriate treatment or the care plan approach taken with BME service users the majority of professionals stated that they learned through experience as opposed to any official training:
I’ve never had a day of dedicated cultural awareness [training, other than the 1-day trust cultural and diversity training] . . . so I’ve learned through blunders I’ve made. Through asking families, from colleagues. I suppose the first thing I would do like for instance the first time I work with a family, from a Pakistani Muslim family, was talk to a colleague from that culture and say, come on, give us a clue, or what shouldn’t I say for a start.
P6
Professionals highlighted that, although the service had made attempts to set up carer support groups and these were open to all carers, only black female carers (namely mums) were accessing them. The process of encouraging Asian carers to access such groups was viewed as ‘difficult’ and ‘culturally insensitive’ because of the social stigma of having the label of mental illness:
We try to get something in our team going for some of the mums and this was with a lot of the Pakistani and Bengali community but the point is, in a culture where mental illness is so taboo, the idea of getting people to talk about it, in itself isn’t really culturally sensitive. Because there are some groups aren’t there for that client group, I know one of the CMHTs runs a group for carers but they call it a sewing group, and it’s not a sewing group it’s a support group, but that’s what they do, to enable people to get that support without the stigma.
P6
Some service users and carers also stressed that the early intervention service played a pivotal role in providing a support system for service users post recovery, that is, support in terms of developing life skills and reintegration into the community. For these individuals, the early intervention service was considered to be key in providing the support needed for service users to maintain esstential life skills such as independence and vocational attainment: ‘He is doing voluntary work now; he’s living in his own flat now’ (C14, black British Caribbean female).
Creating a new self
Coming to terms with mental illness was a difficult process for all service users. It challenged the way that they felt about themselves and how they related to others. This was reiterated by spiritual care representatives who suggest that:
They [service users] internalise that shame, yeah, so they actually, they can’t, I mean, they can’t accept being given a diagnosis because that seems to be the worse thing possible, that, you know, the most awful thing that could possibly happen to them is that they could be told they’re mentally ill.
SC7
In an attempt to maintain a positive sense of self, in most cases there was a period of conscious and/or unconscious denial of reality and resistance to accepting illness. As one spiritual care representative stated: ‘But this [is] denial . . . I, witness it every day . . . people say, “Oh I’m not sick, these tablet make me sick”‘ (SC6).
Some service users did not accept that they were unwell and began normalising symptoms and developing coping strategies/explanations to maintain a sense of normality: ‘Yeah I just thought you know what I am who I am and I think I control my own destiny and then God probably gave me this’ (SU20, Asian British Pakistani male). This was often followed by anger and grief: ‘But I don’t want them [voices] to be there because I was never like this. I can’t live hearing some people talking’ (SU5, black British African female).
Returning to a state of psychosocial well-being was a difficult process. Becoming well often resulted in the ‘rejection of the old self’ and ‘acceptance of the new self’ in terms of exercising personal agency by abstaining from behaviours and practices such as drinking, smoking cannabis and spending time with friends who were involved in such activities. Early intervention service staff were considered to play a useful role in aiding the creation of new social networks, through activities and events arranged for service users.
How to improve accessibility, acceptability and appropriateness
In all stakeholder focus groups, discussion was held around how the accessibility, acceptability and appropriateness of early intervention services could be improved for BME communities.
Educate and raise awareness
The majority of service users and carers stressed the need for early intervention services to educate carers and raise awareness about mental Illness in terms of causes, symptoms and affects. Service users belived that more work needed to be undertaken to educate BME communities across generations:
Maybe educating Asian people again about mental health problems because a lot of them don’t understand it, even like the young generation people. I’ve got some Asian friends and they don’t really understand it so I never bothered telling them.
SU7, Asian British Pakistani female
There was a consensus amongst voluntary and community representatives that BME service users were more likely to seek spiritual/religious and/or cultural explanations of symptoms as opposed to medical explantaions because of a lack of knowledge and understanding. As a result, the majoirty of voluntary and community represntatives and a minority of spiritual care representatives suggested that faith healers such as imams also needed to develop knowledge about the symptoms of mental illness and the services available so that they could recognise and signpost individuals appropriately:
Well, I think this is where it’s important that the health-care professionals and the psychiatrists or consultants and the nurses, work with the Imams and try and understand Islamic perspective on mental health. Or if the Imam does not have enough knowledge, that they train the Imam . . . these are the things that one needs to look at, right, which would differentiate from, someone, suddenly going into this transit of speaking in tongues [or becoming mentally unwell].
SC1
The information currently available regarding early intervention services and mental health services in general was not accessible for all. Carers suggested that any information should be printed in an accessible lay format ensuring that language barriers and individuals’ levels of understanding are considered: ‘You know, for the Jamaican community and the Asian people, I don’t think there is enough information, but it’s not just information it’s the understanding of English’ (C5, white British female).
Collaborative working with voluntary and community organisations
Commissioners stated that voluntary and community organisations were ‘key partners’ in terms of engaging with communities. Community development workers were also highlighted as playing a key role in bridging the gap between the local BME communities and services by raising awareness of the mental health services that are available.
However, professionals were not liaising with community development workers and had little knowledge of the voluntary or community sector organisations available in the local areas (see Treatment, support and recovery). They also lacked the capacity and time to explore such options; instead, they stated that an up-to-date directory with details of such services needed to be made available:
Yes, everything is a secret in Birmingham . . . you’ve got to learn, you’ve got to find this person, then word of mouth and then you meet people they’re really knowledgeable and helpful and you cling onto them, don’t you? Because you know they’re going to help you with lots of stuff. But there’s no obvious way of finding stuff.
P6
Time constraints and large caseloads meant that there was little opportunity for professionals to network with voluntary and community organisation representatives.
Lack of funding and resources
Although the importance of voluntary and community organisations was acknowledged, commissioners felt that the funding for such services was limited:
We fund to do a bit of counselling to BME communities and then there’s others that might be funded say through the NHS or the City Council to provide broader services, to do with well-being. And then there’s others that we wouldn’t fund, but nevertheless are key for us, because as you said, people who are working directly with the local communities.
COM8
The majority of voluntary and community representatives were frustrated and anxious about changes in the health service. A key point of frustration was the lack of local culturally appropriate respite provision:
The Commissioner was giving the funding, they were, they purchased the service and we were the provider, but still I’ve noticed that they never, ever come and visit the service, and my concern was, how they were monitoring the service? . . . without seeing the Project, they just cross out.
V16
The majority of voluntary and community organisation representatives also stated that their role in service provision, health promotion and dissemination of information needed to be recognised and valued by statutory services. Suggestions were made about how to reduce barriers to and delays in help-seeking, such as provision of services within GP practices, and early intervention services commissioning voluntary and community services:
It will be a really good idea for GP to purchase those services and those voluntary organisations work alongside with the GP, so it will be less work for the GP . . . if, early intervention can purchase the service, direct from us we can provide the service.
V16
The consensus was that more funding needed to be made available from the Department of Health to sustain voluntary and community organisations.
Summary findings from study 3
-
As in study 1, the findings from study 3 confirm that BME populations have multiple explanatory models of illness, which are often influenced by family and friends, but that these are also competing and contrasting, both in relation to explanations of symptoms and in relation to cultural understandings of mental illness.
-
These explanatory models influence initial help-seeking (i.e. seeking the support of faith leaders as opposed to mental health professionals).
-
Voluntary sector and community organisations believe that BME communities have a poorer understanding of mental illness, appropriate pathways into care and the role of interventions such as psychotherapy and counselling.
-
GP failure to address carer concerns delays access to appropriate services.
-
In the absence of appropriate help through medical pathways, some BME groups, particularly the African Caribbean carers, resort to exaggerating risk or seeking help from the police, leading to criminal justice involvement in pathways to care.
-
Crisis points are often the drivers of help-seeking, regardless of biomedical attributions or understanding of the illness.
-
BME groups are more likely to have a supernatural or faith-based attribution for mental illness.
-
Faith-based help-seeking can provide comfort to carers and users but can also lead to delays in accessing medical help and sometimes financial exploitation of the family.
-
Stigma and shame of mental illness are prominent reasons for delay in accessing care. Such stigma can also occur within faith groups leading to marginalisation of users/carers.
-
There are prominent intergenerational differences in spiritual attributions with the second- and third-generation BME population less likely to have such attributions.
-
Early intervention services are considered accessible and appropriate, and are perceived to be largely positive and caring and to take into account the cultural and ethnic background of users and carers.
-
No specific changes need to be made to the current model of early intervention services to make it more culturally appropriate for BME groups.
-
BME service users are not asking for BME-specific measures; they (like all service users) want to be able to share their spiritual/religious and cultural beliefs with mental health service professionals in a open manner without being judged.
-
There is no demand for ethnic or gender matching between users and clinicians; instead, users and carers want competent and caring clinicians, regardless of gender or ethnicity.
-
Lack of appropriate interpretation services is a key barrier for some BME carers and users.
-
Improving services for BME groups requires (1) an improved understanding of mental illness and routes into mental health care for BME communities, (2) raising awareness of the different treatment modalities available and (3) achieving (1) and (2) through statutory organisations working more closely with voluntary and community organisations.
Chapter 7 Discussion
It is a guiding principle of mental health policy that service users should exercise choice and control over their treatment and be subjected to the least restrictive form of care. 85 This principle stands in stark contrast to the rising use of compulsory treatment under the MHA in England and Wales, which rose by 15% from 1993 to 2003. 86,87 There is particular concern that BME populations experience more adverse pathways into mental health care5,6,13 and have higher rates of coercion and poorer engagement with services. 6 This group is also more likely to suffer from serious mental disorders such as psychosis. 88 The Delivering Race Equality programme89 specifically recommended a coherent programme of work for achieving equality of access, experience and outcomes for BME service users. However, such improvements cannot be achieved without first understanding the real reasons behind ethnic differences in pathways to care.
The conventional explanation for ethnic differences is based on the notion of institutional racism within psychiatry. 3,90–92 However, this view has been challenged as providing simplistic explanations for complex processes. 7 Ethnic differences are evident even at first presentation of psychosis; therefore, contributory factors must operate before presentation to psychiatric services and these need to be understood in a wider social context.
In their systematic review of ethnicity and detention, Singh et al. 6 suggested that many potential explanations for ethnic differences in pathways to care had not been fully explored. The more appropriate denominator population for determining predictors of detention (including BME status) is the population who is assessed under the MHA, not the subgroup who is detained. Yet there are no studies in the psychiatric literature on patients assessed under the MHA. There is therefore a clear need for an in-depth evaluation of the process of detention using a denominator population of all those assessed rather than all those detained, as studying the latter does not allow exploration of ethnic differences in the availability of alternatives to detention, which can be studied only at the point of assessment. There is very little research on cultural determinants of illness recognition and attribution, users’ and carers’ care service preferences and the role of alternative community-based strategies in improving satisfaction, promoting adherence, reducing detention rates and enhancing outcomes.
Psychiatric research has studied pathways to care using two contrasting approaches: a medicoepidemiological approach, which explores the empirical relationship between service utilisation and factors affecting such utilisation; and a socioanthropological approach, which studies the dynamic social and interpersonal processes that affect help-seeking. However, no studies have attempted to integrate these two types of approaches. No interventions have so far been identified that clearly reduce coercive mental health treatment for BME service users. The paucity of such evidence has hindered the development of service-level interventions with the potential to improve mental health care for BME service users. It is also unclear whether generic early intervention services meet the specific demands and challenges of providing care for BME patients.
The ENRICH programme was designed to produce the evidence base necessary to understand and reduce, or hopefully eliminate, ethnic differences in pathways to care in FEP. In a series of three linked multimethod studies, we examined pathways to care and MHA assessment for patients in the BSMHFT. Study 1 determined the ethnic and cultural determinants of help-seeking in FEP by conducting quantitative assessments and in-depth qualitative interviews with services users and carers on how emerging psychosis is recognised, symptoms attributed and help sought. Study 2 explored ethnic differences in the process and outcome of MHA application, focusing on assessments rather than detentions, and determining predictors of detention as an outcome of assessment. In study 3, focus groups of services users, carers, clinicians and other key stakeholders discussed the appropriateness, accessibility and acceptability of generic early intervebtion services in meeting the specific needs of BME patients.
We will first summarise the findings from the three ENRICH programme studies and then present the findings as answers to specific research queries. Finally, we discuss the implications of our findings.
Study 1 on attributions and help-seeking in a prospective cohort of all FEP cases in Birmingham had the following findings:
-
It confirmed previous reports of the greater risk of MHA detention, more criminal justice involvement and more A&E presentations amongst black service users than among white and Asian service users.
-
It found no ethnic differences in DUP and DUI in FEP. DUP was not related to illness attribution; long DUP was associated with patients being young (< 18 years) at the time of psychosis onset and living alone. Therefore, length of treatment delay by itself does not account for adverse and coercive pathways reported for BME groups.
-
Patients from all ethnic groups hold multiple attributions for the emerging symptoms of psychosis – the idea that certain ethnic groups possess only one explanatory model can be dismissed. In reality, the attribution process is complex, context dependent, fluid and dynamic and changes over time, especially following contact with services. There were also intergenerational differences in attributions, particularly in the British Asian group.
-
During the prodromal phase, all three ethnic groups had similar attributions, considering prodromal symptoms to be a reaction to social adversity. All three ethnic groups sought help from health services, mainly GPs. Black patients were most likely to seek help on their own whereas, in the case of white patients, their family did the majority of the help-seeking.
-
With the emergence of psychotic symptoms, Asian carers and users were most likely to attribute symptoms to faith-based or supernatural explanations and seek help from faith organisations. Some black patients also changed to supernatural explanations, which influenced their care pathway, but this was in a smaller proportion of cases.
-
Asian patients were significantly less likely to have A&E involvement and significantly more likely to have faith encounters in their pathways to care than white patients. Black patients were also more likely to have faith-based help-seeking encounters than white patients.
-
Although the key drivers for help-seeking in FEP were family members and carers, there were ethnic differences with regard to which family member intervened and the types of familial networks that were tapped into for finding help. Most white respondents sought help in consultation with members from the nuclear family whereas, in the black British and British Asian cohort, help was sought in consultation with the larger family networks (aunts, uncles, grandparents, cousins) and through community organisations.
-
Many service users accessed or received help only when a crisis point was reached. Even when carers had a predominantly biomedical attribution for psychotic symptoms, medical help was not sought until a crisis point was reached.
-
Attributing the symptoms of emerging psychosis to life events and social adversity can hinder medical help-seeking by providing a ‘normalising’ explanation.
-
All three ethnic groups experienced difficulties in accessing medical help. However, only BME service users and carers and not white service users and carers mistrusted services, even though both groups reported similar difficulties and delays in finding the right help at the right time.
Study 2 on the outcome of MHA assessments in a prospective cohort in the BSMHFT over 1 year found that:
-
A greater proportion of BME groups, particularly the black Caribbean and black African groups, than of the white group were assessed and detained under the MHA. This was true when the denominator was both the general population and the population currently receiving care from secondary mental health services.
-
When age, diagnosis, risk and level of social support were accounted for, ethnicity was not an independent predictor of MHA detention. The ‘disproportionate’ excess of BME groups in the detained population is likely to be the result of underlying differences in rates of illness, presence of risk and level of social support.
-
There were clear differences between the MHA experiences of carers whose ill family members were known to services and the MHA experiences of carers of those who presented for the first time. The former received relatively unproblematic access to care; the latter felt that the system did not respond to their concerns in a timely and appropriate manner. Help arrived only following a crisis and early warning signs were usually ignored by services, particularly by GPs.
-
Carers found the MHA process very stressful, even when they understood the need for the process and agreed with its outcome. Police presence during MHA assessments was particularly stressful and black carers perceived a racial bias in police involvement. Carers felt that their own mental health had suffered because of the burden of care.
-
Stigma and shame appeared to be higher in the black community than in the Asian community. Asian carers found shared spiritual explanations within the community to be a source of comfort and support.
-
Cultural attributions changed over time; in established illness, medical explanations became more dominant but supernatural explanations continued to provide culturally appropriate meaning.
-
Amongst clinicians, risk assessment and management were the paramount drivers of MHA assessment and outcome. Although all clinicians agreed on the importance of cultural and ethnic factors in assessments, social workers placed a greater emphasis on these in practice whereas medics perceived themselves as ‘culturally neutral’.
-
There was no consensus on the need for ethnicity matching in the MHA assessment process.
Study 3 on the cultural appropriateness, accessibility and acceptability of generic early intervention services for specific BME needs found that:
-
BME populations had multiple explanatory models of illness, which were often influenced by family and friends, but these models were also competing and contrasting. These explanatory models influenced initial help-seeking (e.g. seeking the support of faith healers as opposed to mental health professionals). Crisis points were often the drivers of help-seeking, regardless of biomedical attributions or understanding of the illness.
-
In the absence of appropriate help through medical pathways some BME groups, particularly the African Caribbean carers, resorted to exaggerating risk or seeking help from the police, leading to criminal justice involvement in pathways to care.
-
GP failure to address carer concerns delayed access to appropriate services.
-
Faith-based help-seeking can provide comfort to carers and service users but can also lead to delays in accessing medical help and sometimes financial exploitation of the family. There were prominent intergenerational differences in spiritual attributions, with the second- and third-generation BME populations less likely to have such attributions.
-
The stigma and shame of mental illness were important reasons for the delay in accessing care for some in the BME groups. Such stigma could also occur within faith groups leading to marginalisation of users/carers.
-
Early intervention services were considered accessible and were perceived to be positive and caring and to take into account the cultural and ethnic background of users and carers. No specific changes were demanded or felt to be needed in the current model of early intervention services to make it more culturally appropriate for BME groups. BME service users were not asking for BME-specific measures; they wanted to be able to share their spiritual/religious and cultural beliefs with mental health service professionals in an open manner without being judged.
-
There was no demand for ethnic or gender matching between users and clinicians; instead, users and carers wanted competent and caring clinicians, regardless of gender or ethnicity.
-
A lack of appropriate interpretation services was considered a key barrier for some BME carers and users.
-
Improving services for BME groups required (1) an improved understanding of mental illness and routes into mental health care for BME communities, (2) raising awareness of the different treatment modalities available and (3) achieving points (1) and (2) through statutory organisations working more closely with voluntary and community organisations.
Strengths and limitations
Before we present our findings as answers to specific research questions, it is important to consider the limitations of our study methods and some relative strengths. Although we collected a prospective cohort of all FEP cases for study 1, we managed to recruit only around 50% of all referrals to early intervention services during the study period. The main reason for failure to recruit was service users not being well enough to give informed consent. There is a possibility that our sample in study 1 is not truly representative of the total early intervention service population. However, the profile of our included cohort is very similar to the profile of the overall early intervention service population in the BSMHFT. Therefore, it is unlikely that we systematically missed patients from any particular ethnic group. Although we collected data for study 2 using multiple sources of information, we may have missed some cases. However, there is no reason to believe that we would have missed data on specific BME groups leading to a systematic bias in our findings. Finally, for study 3, although we endeavoured to achieve wide participation from several key stakeholders, the cohort who participated may not represent all of the BME groups of interest. In particular, disenfranchised or marginalised groups, who are most likely to have received poorer care, may have selectively chosen not to participate in our study.
A final limitation of this study is one that is common to most ethnicity studies: the ‘homogenising’ of ethnic groups, which conceals important intra-ethnic differences. We have used very broad categories of white, black and Asian in this study and, as study 2 shows, there are important differences between British citizens of Indian, Pakistani and Bangladeshi origins. In study 1, the majority of the ‘Asian’ sample was from a relatively homogeneous Kashmiri/Pakistani origin. In study 3, we attempted to invite participants from diverse ethnic groups. We also did not distinguish between ethnicity and culture, for example an attribution such as belief in jinn is a cultural and religious phenomenon rather than an ethnic one. Hence, our findings must be interpreted with caution when applied to ethnic groups not included in our study.
To the best of our knowledge this is the first study that has quantified cultural attributions in a prospective cohort of patients with FEP (study 1). Study 2 is the first ever study of MHA assessments (not only detentions) in the UK. We therefore have unique data sets to explore new hypotheses and answer as yet unanswered questions. Between them the data collection team spoke English, Urdu, Punjabi, Hindi, Konkani, Gujurati, Bengali and Pothwari. Hence, we were able to collect qualitative data from users and carers in their mother tongues with all but one participant (who spoke Arabic and needed an interpreter). We believe that this allowed us to build a rapport and win trust with study participants and to faithfully capture their views.
Do the ENRICH findings explain ethnic differences in pathways to care?
Several hypotheses have been proposed for the excess detention rate and more adverse pathways to care for BME patients. These can broadly be divided into those that are rooted in the service response, such as racial stereotyping, labelling and discrimination and institutional racism, and misdiagnosis, poorer recognition and lower referral to mental health care; and those that lie within BME groups such as higher rates of psychosis, greater propensity to risk, greater stigma of mental illness and mistrust of services leading to delayed help-seeking. The ENRICH programme was able to test some of these hypotheses and also some previously unexplored domains of BME pathways to care. The specific questions we were able to answer are as follows.
Is there a delay in help-seeking amongst black and minority ethnic groups?
We found no ethnic differences in any aspect of treatment delay as measured by the NOS. Ethnic groups in Birmingham did not differ in length of prodrome, DUI or DUP. The key predictors of long DUP were young age and living alone. These two are correlates of early- and insidious-onset psychotic disorders, which are known to be associated with longer DUP and poorer outcome. 93,94 Our findings also confirm the results of other recent studies that have found no ethnic differences in DUP. 10 There may be subgroups of BME patients who have a longer DUP related to attributions and non-medical help-seeking, as discussed below. Measurement of DUP and DUI may not help understand important ethnic differences in pathways to care or help-seeking or differential rates of coercive service contacts.
Are there cultural and ethnic differences in attributions of emerging psychosis?
We found that users and carers had multiple, sometimes competing and contrasting, attributions of mental illness. 30,39 There was no simple dichotomy within or between different ethnic groups between biomedical and supernatural attributions. Attributions were fluid and changed over time, as in study 2, in which carers of patients with long-established illness changed their attributions increasingly to a biomedical explanation. However, when we focused on the dominant attributions, there were clear ethnic differences in how emerging illness, particularly psychotic symptoms, is understood within a cultural framework. Service users with an Asian background were significantly more likely to attribute symptoms to supernatural and faith-based explanations. 36,37,41 This was also true for some black African and Caribbean users and carers. By contrast, white users and carers had predominantly biomedical attributions for emerging symptoms, supporting previous similar findings on schizophrenia. 35
Do culturally mediated attributions of illness influence help-seeking? If so, do these explain ethnic differences in pathways to care?
We confirmed the results of previous qualitative studies showing that culturally mediated attributions do influence help-seeking. 36–39 During the prodromal phase, all ethnic groups attribute their symptoms to stressful life events or factors within themselves. As psychotic symptoms emerge and Asian carers change their attributions to a supernatural cause, they seek help from faith organisations for their ill relatives. There are intergenerational differences, with the younger generation less likely to attribute symptoms to supernatural causes. However, as the key initiators for help-asking during the psychotic phase are family and carers, Asian patients are much more likely to have faith-based encounters. This can sometimes lead to delays in receiving medical care and even financial exploitation of families already struggling with the burden of care of the mentally ill.
Supernatural attributions can also provide a sense of meaning and faith-based help-seeking can be a source of comfort for carers and service users. 50 Many continue to have faith-based encounters even after coming into contact with mental health services. However, they sometimes do not feel able to share this important part of their lives with their clinicians for risk of being negatively judged.
In the psychiatric literature, there is considerable disagreement and debate about whether clinical care should take religion and spirituality into account when management plans or interventions are being devised. 49 Although some argue for proactively including service users’ religious and spiritual perspectives and experiences in the initial assessment and therapy,95 other caution against it. Crossley and Salter’s96 study of clinical psychologists’ experience of addressing spiritual beliefs in therapy found that, although some practitioners reported a proactive approach, others waited for users to raise spiritual issues on the assumption that if these were significant users would mention them without prompting. Mayers et al. 97 found that users were unwilling to disclose such information during assessment because of the fear that it might be evaluated negatively.
Our findings suggest that users and carers will seek faith-based help and, rather than judge it as at best a distraction and at worst a hindrance, mental health services need to work with faith-based organisations more closely so that the supportive aspects of faith-based encounters can be sustained but the potential for delays be reduced or avoided (see Chapter 8). An assessment of a user’s religious or spiritual beliefs and experiences may need to unfold progressively within the context of a secure therapeutic relationship. 98
Are biomedical as opposed to spiritual/faith-based attributions associated with quicker and more appropriate access to care?
We found no evidence that biomedical attributions were associated with quicker or easier access to care. White carers predominantly had biomedical attributions for both the prodromal and the psychotic phases of illness. They were also most likely to seek help from health-care agencies including GPs. However, psychiatric help was usually sought or obtained only at a crisis point. Some of this was due to GP delay in recognition of emerging symptoms of psychosis and some was because of patient reluctance to seek help despite family concerns. General practice is the ‘front door’ of health services, including mental health care. A large majority of GPs have no postgraduate mental health training and they often have negative opinions about providing care for people with schizophrenia. 99 GPs believe that they contribute little to the care of people with serious mental illness in general and that the incidence of FEP is too low to warrant more active involvement. 100 Lester et al. 101 recruited 110 practices to assess the effect of an educational intervention for GPs on referral rates to early intervention services and on DUP for young people with FEP. Interestingly, they found that training GPs about FEP was insufficient to alter referral rates to early intervention services or to reduce the DUP.
There are two important caveats to the finding of no relationship between attribution type and DUP. First, our study is of a relatively small sample and may not have had the power to detect such a relationship. Second, our findings suggest that the mechanism of treatment delay in psychosis is complex and multifaceted and may not be related primarily to BME differences in delay in help-seeking. Emerging evidence points to delays within the secondary care system, with patients with FEP who are referred to CMHTs having particularly long delays in reaching early intervention services. 102 We have not explored the important dimension of delays within the secondary care system in this report; however, we will do so in further analyses of the data.
Are black and minority ethnic patients disproportionately detained?
The over-representation of BME groups amongst people detained under the MHA has been an integral part of a wider charge that UK psychiatry is ‘institutionally racist’. 3,91 Senior figures such as the previous mental health ‘tsar’103 and successive presidents of the Royal College of Psychiatrists104,105 have accepted institutional racism as the cause of ethnic differences in the UK. One report (p. 6)106 has emphasised that:
Black people mistrust and often fear services, and staff are often wary of the Black community, fearing criticism and not knowing how to respond, and fearful of young Black men. The cycle is fuelled by prejudice, misunderstanding, misconceptions and sometimes racism.
A Department of Health89 report stated that ‘mental health services in the UK do not take account of BME values, and that mental health professionals needed training to deliver care in a culturally competent way’ (p. 13).
Studies have indeed found a higher number of detained BME patients than white patients in inpatient services. 6,13,16 A systematic review and meta-analysis6 found that, compared with white patients, Asian patients are twice as likely and black patients are nearly four times as likely to be detained. The most commonly cited explanations for these differences are ‘race related’, with the excess attributed to discrimination, labelling and stereotypes of BME patients among psychiatrists. These explanations are not backed by robust evidence. The politically contentious and charged nature of the racism accusation has led to considerable effort and resources being invested to ensure that mental health services deliver racial equality of outcomes. A major policy initiative, Delivering Race Equality,89 was launched in 2005, which explicitly aimed to reduce ‘the disproportionate rates of compulsory detention of BME service users in inpatient units’ (p. 4). In the run-up to the MHA 2007 amendments, similar concerns were expressed that the changes in the law would have a disproportionately negative impact on BME patients. 107
We found that a greater proportion of BME patients was assessed and detained under the MHA than could be accounted for from their population numbers, both in the general population and within the subgroup receiving care under secondary mental health services. These differences were most prominent for the black Caribbean, black African and British Pakistani groups. However, when confounders such as age, diagnosis, risk and level of social support were taken into account, ethnicity was not an independent predictor of MHA detention. The two key predictors of detention in those assessed under the MHA, a diagnosis of mental illness and the presence of risk, are also two of the three prerequisites for detaining an individual under the MHA, the third one being no alternative to hospital admission.
It could be argued that BME patients are more likely to be considered risky, that is, clinician assessment of risk is biased by stereotypical or racist attitudes towards minority patients. This is difficult to test in MHA assessments, which are often conducted in difficult circumstances with clinicians having to balance clinical needs, manage risk and comply with the law. A 1990 case vignette study of psychiatrists in the UK108 found that black men were perceived to be more at risk of violence, although psychiatrists were less likely to diagnose schizophrenia in black cases.
A decade later, a much larger study found that psychiatrists did not rate black patients as more violent than white patients. 109 Whether the second study represents a genuine change in perceptions, a greater sensitivity to race-based questions or a better ability to hide racial prejudice remains unanswered. The possibility of racial stereotyping in clinical assessments therefore cannot be decidedly refuted. However, there is no evidence to confirm it either. Racial stereotyping and discrimination within services continue to be the dominant explanations for perceived ethnic inequalities, and have become ‘true’ simply by the act of repetition. 7,110
Studies from Canada, the USA and Belgium have shown that legislation that was introduced to decrease the use of psychiatric detention resulted in a paradoxical increase in involuntary hospitalisation. 111 Despite the efforts of several European countries to reform their mental health laws to better protect patients, rates of detention are generally increasing. 112 Even when clinicians’ judgements are consistent with the law, unexplained variations in decision-making exist, influenced by factors such as clinician characteristics, local service provision, community support for patients, patient ethnicity, age and education and attitudes to mental health. 111,113–115
Although the exact reasons for increasing detention rates have not been delineated, our findings suggest one possibility: the increasing risk aversion in clinical practice. Clinicians in our study highlighted how risk assessment and management is increasingly the focus of their concern in MHA assessments. In addition, bed availability was also a crucial issue for some Birmingham service users, who sometimes had to wait for a bed to be allocated even after a MHA recommendation for detention had been made.
The rate of MHA detentions has increased synchronously with the rate of reduction in the number of psychiatric beds within the NHS. 116,117 Many previous studies of the excess detention of BME patients have been from London, which may not be representative of other areas of the UK. A large study of 22 psychiatric hospitals in England found no association between ethnicity and patient perceptions of coercion at admission or during the first 4 weeks of inpatient stay. However, the treating mental health trust was strongly associated with patient experience of coercion. 118 BME patients, particularly black patients, were more likely to be in hospitals that were perceived to be more coercive, with both black and white patients within these hospitals feeling coerced. This is an effect of service culture and resources rather than patient ethnicity.
Our findings suggest that the MHA does what it should: ensures that people with serious mental disorders who are at risk are provided with the care that they need within the law. However, it is also true, as found in our qualitative study, that users and carers find MHA detention to be a very stressful process, even when they agree that admission under the MHA is the correct outcome. The involvement of the police in particular was very distressing for carers and users. It is imperative that services attempt to make mental health-care provision as non-coercive as possible (see Chapter 8).
Are generic early intervention services accessible, acceptable and culturally appropriate to meet the specific needs of black and minority ethnic groups?
In-depth interviews and focus groups with service users, their carers, service providers and commissioners all confirmed that BME users and carers have positive view of early intervention services. Early intervention services were perceived to be accessible, supportive, acceptable and culturally appropriate. When users or carers had concerns about the cultural appropriateness of services, these were related to mental health services in general rather than to early intervention services in particular. Service users and carers were clear that no specific changes needed to be made to early intervention services to meet BME needs.
A few service users did express dissatisfaction with the high level of staff turnover in early intervention services. It was also clear that, although BME service users were not asking for BME-specific measures, BME service users (like all service users) wanted to be able to share their spiritual/religious and cultural beliefs with mental health service professionals in an open manner without being judged. However, the fear of negative reactions and/or a lack of understanding prevented service users who were seeking support from faith or spiritual healers whilst attending early intervention services from disclosing this to early intervention service professionals. This fear is not unfounded because, as our evidence suggests, early intervention service professionals receive limited spiritual/religious and cultural awareness training.
An important issue emerged with regard to BME needs in mental health care: the availability and quality of interpreters. The UK has never had a coherent policy on standards of interpreting in health care or in any other part of the public sector. 119 The training and practice standards for professional interpreters are not statutory. As Cambridge et al. 119 highlight, ‘Interpreting, translation and language support (ITALS) must be delivered to a highly trained professional standard, and yet ITALS remains a neglected area of provision in British healthcare’ (p. 121). Clearly, training needs to be put in place for any interpreters employed by the trust. This should give them the knowledge to translate medical jargon appropriately, but it should be explicit that the role of interpreters is translation only and confidentiality of all should also be respected.
Do black and minority ethnic groups mistrust mental health services?
We found some evidence from our qualitative interviews and focus groups that some service users and carers, particularly those from black Caribbean backgrounds, perceived a racial bias in the service response or when police were involved in a mental health assessment. Strikingly, white patients and carers had similar negative experiences of mental health care but did not attribute this to race or racism. This leads to an interesting query: is racism within services simply a matter of perception, or is there a systematic bias and difference in how services deal with BME patients? The argument about racial bias in services is based on reported higher rates of psychosis in BME groups, higher rates of detention, greater use of medication and electroconvulsive therapy and lower use of psychological therapies, and greater restraint and seclusion, leading to lower levels of satisfaction with services.
The evidence backing these assertions is flimsy at best. Rates of psychosis are indeed higher for BME groups with no evidence of misdiagnosis88,120 and this seems to be a migration effect rather than a racial one, with societal deprivation and adversity experienced by migrant groups leading to higher rates of psychosis. 121,122 Ethnicity is not a predictor of seclusion, restraint or emergency medication. 123 There are no differences in prescribing between black and white patients in the UK,124,125 and white patients are about twice as likely as black patients in the UK to receive electroconvulsive therapy. 126 Even the reported dissatisfaction with services amongst BME groups is unconfirmed. In a large national survey of 26,555 respondents, black patients were more likely than white patients to have had better access to a community psychiatric nurse and care plan than white patients, who had better access than Asian patients. 127 Black and Asian patients had poorer access to talking therapies; however, it was unclear whether this was because these groups were offered talking therapies less often or because they accepted them less often. We have previously argued that repeated charges of institutional racism in psychiatry act as a self-fulfilling prophecy whereby BME patients expect services to be discriminatory and hence avoid seeking help. 7 The ENRICH programme findings lend some support to this: for similar poor experience of mental health care, BME users and carers attribute it to race-based discrimination unlike white patients. BME patients often live in deprived areas with poor mental health care; but this care is poor for everyone in that area. Services need to improve for all patients; a BME focus simply distorts the debate in a ‘racial’ manner without doing anything to improve care for the mentally ill. 128,129
Is there a need or demand for black and minority ethnic-specific services or ethnicity matching between patients and clinicians?
Such has been the concern about ethnic differences in mental health care that some have even argued for ethnic-specific services for BME patients. 130 Although seemingly helpful, this suggestion is based on several untested assumptions, for example ethnic differences in pathways are entirely the result of the service response and can improve only when services are BME led; all members of an ethnic group (howsoever defined) need one particular kind of service; ethnicity and culture are such impermeable barriers between people that only ethnically matched clinicians and patients can work together; and BME service users are dealt with differently by mental health services and this is perceived as racism by BME service users and hence they demand BME-specific services.
Our findings argue against BME-specific services. BME users and carers repeatedly asked for competent and compassionate care and to be treated as individuals rather than group members, regardless of the gender or ethnicity of the clinician or the service provider. Other studies that have specifically explored the role of institutional racism in mental health care have also found that BME users and carers predominantly want good care from competent clinicians. 131
Chapter 8 Conclusions
We are restricting our conclusions to the implications of the study findings for health care and are making no recommendations about policy and clinical care, as required by National Institute for Health Research guidelines for authors. We have previously argued that:
Any potential solutions to reduce ethnic differences must go beyond the health sector and involve statutory as well as voluntary and community agencies. The problem of ethnic differences in mental health does not reside exclusively in psychiatry and hence the solutions cannot emerge from psychiatric services alone.
p. 6507
The ENRICH programme findings confirm this assertion.
The most important implication of the ENRICH studies is that statutory health-care organisations need to work closely with community groups to improve pathways to care for BME service users. Voluntary and community organisations are key partners for engaging BME communities. The main purposes of such collaborations should be to raise community awareness with regard to the recognition and treatment of mental disorders, available services and interventions, and pathways to mental health care; and most importantly to reduce mistrust between services and communities. Statutory and voluntary/community organisations need to jointly develop community engagement projects within local communities and faith-based organisations, as well as schools, colleges, youth or community clubs and universities. These could include ‘well-being events’, such as stalls manned by mental health and public health promotion professionals as well as local BME voluntary and community organisations. Any information regarding available services needs to be ‘culturally sensitive’, that is, produced in formats that take into account the diversity of BME languages and the multitude of explanatory models held within BME groups. Other avenues for raising mental health awareness could include ‘human libraries’ in which BME service users and/or carers could share their narratives with local communities. Alternatively, statutory and voluntary and community organisations could work with service users and carers to produce DVDs about their experiences of mental illness. Extracts of these narratives could be exhibited within local BME community avenues as well as local museums and libraries, and DVDs could be made freely available on request. Internet-based discussion forums and websites are another potential tool for engagement with BME groups, particularly the youth.
The most important research recommendation from the ENRICH studies is the need to develop and evaluate models for community awareness programmes that are effective in improving access to care. Evidence for the effectiveness of such programmes in reducing DUP is patchy. 132 However, the ENRICH studies found that measurement of DUP alone does not capture the complexity of help-seeking in psychotic disorders and does not help elucidate critical BME differences in pathways to care. Rather than universal public education campaigns, researchers and practitioners need to develop public awareness programmes that are specifically focused on BME groups and test whether help-seeking pathways such as faith encounters can be targeted for reducing treatment delays and preventing adverse pathways. Such campaigns also need BME-specific strategies to raise knowledge and understanding of mental disorders and treatment while combating social stigma and shame. If such interventions are shown to be effective in reducing stigma, increasing mental health awareness, promoting trust between BME communities and mental health services and reducing coercive experiences of care right at the start of the illness, we could make long-term changes to outcomes by ensuring sustained engagement and treatment for those amongst our BME communities who need ongoing care but who are often reluctant to seek it.
Acknowledgements
The ENRICH study was funded by the National Institute for Health Research Programme Grants for Applied Research programme.
We are very grateful to all of our service users, carers and members of stakeholder organisations who generously gave us their time for this study.
The ENRICH team would like to thank Jeremy Patton, Michael Kay, Paul Dolan, Paul McDonald, Audrey Smith, Laura Daly, Sarah Thorpe and the MHRN Heart of England Hub. We would also like to thank all of the honorary researchers who supported the study team: Saimah Yasmin, Gagandeep Chohan, Marta Wanat and Mehmoona Ashiq.
ENRICH study team
Professor Swaran Singh, Dr Zoebia Islam, Mr Luke Brown, Dr Rubina Jasani, Dr Ruchika Gajwani, Ms Shabana Akhtar, Ms Charlene Jones, Ms Madeline Parkes, Mr Nathan Worthington-Williams, Dr Helen Parsons, Professor Fatemeh Rabiee, Professor Max Birchwood, Professor Helen Lester and Dr Hannah Bradby.
Steering group
Professor Tom Burns and Professor Paula McGee (Joint Chairs), Professor Swaran Singh, Dr Zoebia Islam, Mr Luke Brown, Dr Rubina Jasani, Dr Ruchika Gajwani, Professor Fatemeh Rabiee-Khan, Professor Max Birchwood, Professor Helen Lester, Dr Hannah Bradby, Ms Shabana Akhtar, Ms Charlene Jones, Ms Madeline Parkes, Bishop Joe Aldred, Dr Jo Barber, Dr Neil Deuchar, Mr Derek Smith, Ms Shahana Ramsden, Dr Peter Lewis, Ms Tara Moran, Ms Ranjeet Sangheera, Professor Nigel Stallard, Mr Raja Khan, Mr Roger Telfia and Mr Nathan Worthington-Williams.
Contributions of authors
Professor Swaran Singh is the Principal Investigator and the guarantor of this report. He is the Head of the Division of Mental Health and Wellbeing, Warwick Medical School and Honorary Consultant Psychiatrist at the BSMHFT. Professor Singh was involved in all stages of the study, from inception to final submission.
Dr Zoebia Islam is a Senior Research Fellow and the ENRICH Programme Co-ordinator. She contributed to the literature review, collected data and conducted analysis for study 3, contributed to the interpretation of the results and assisted in the overall writing of the report.
Mr Luke Brown is a Research Fellow and PhD student on the ENRICH study based at the Research and Innovation Department, BSMHFT. He contributed to the literature review, the methods and assessment tools for study 1, data collection (both quantitative and qualitative), the quantitative analysis for study 1, the interpretation of the results for study 1 and the writing up of the final report.
Dr Ruchika Gajwani is a Clinical Psychology Trainee in Birmingham. She was a Research Fellow on the study and contributed to the methods and design for studies 1 and 2, data collection and analysis for study 2 (quantitative) and the writing up of the final report.
Dr Rubina Jasani is a Lecturer at Manchester University. She was a Senior Research Fellow on the study and contributed to the conception and design of, and data collection and analysis for, qualitative studies 1 and 2.
Professor Fatemeh Rabiee is Professor of Public Health Promotion at Birmingham City University. She contributed to the design and analysis of all of the qualitative studies, the interpretation of their results and the writing up of the final report.
Dr Helen Parsons is a Research Fellow and Statistician at Warwick University. She contributed to the quantitative analysis for studies 1 and 2, the interpretation of the results and the writing up of the final report.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, CCF, NETSCC, PGfAR or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PGfAR programme or the Department of Health.
References
- Fitzgerald FS. The Great Gatsby. New York, NY: Infobase Publishing; 2010.
- London: The Stationary Office; 2007.
- Sashidharan SP. Institutional racism in British psychiatry. Psychiatr Bull 2001;25:244-7. http://dx.doi.org/10.1192/pb.25.7.244.
- Rabiee F, Smith P. Being understood, being respected; an evaluation of the statutory and voluntary mental health service provision in Birmingham for members of the black African and black African-Caribbean communities. Birmingham: Faculty of Health and AFCAR, University of Central England; 2007.
- Singh SP, Grange T. Measuring pathways to care in first-episode psychosis: a systematic review. Schizophr Res 2006;81:75-82. http://dx.doi.org/10.1016/j.schres.2005.09.018.
- Singh SP, Greenwood N, White S, Churchill R. Ethnicity and the Mental Health Act 1983 – systematic review. Br J Psychiatry 2007;191:99-105.
- Singh P, Burns T. Race and mental health: there is more to race than racism. BMJ 2006;333:648-51. http://dx.doi.org/10.1136/bmj.38930.501516.BE.
- Tait L, Birchwood M, Trower P. Predicting engagement with services for psychosis: insight, symptoms and recovery style. Br J Psychiatry 2003;182:123-8. http://dx.doi.org/10.1192/bjp.182.2.123.
- Craig TK, Garety P, Power P, Rahaman N, Colbert S, Fornells-Ambrojo M, et al. The Lambeth Early Onset (LEO) team: randomised controlled trial of the effectiveness of specialised care for early psychosis. BMJ 2004;329:1067-70. http://dx.doi.org/10.1136/bmj.38246.594873.7C.
- Morgan C, Mallett R, Hutchinson G, Bagalkote H, Morgan K, Fearon P, et al. Pathways to care and ethnicity. I: sample characteristics and compulsory admission – report from the AESOP study. Br J Psychiatry 2005;186:281-9.
- Morgan C, Mallett R, Hutchinson G, Bagalkote H, Morgan K, Fearon P, et al. Pathways to care and ethnicity. 2: source of referral and help-seeking – report from the AESOP study. Br J Psychiatry 2005;186:290-6.
- Bhui K, Bhugra D, Goldberg D. Causal explanations of distress and general practitioners’ assessments of common mental disorder among Punjabi and English attendees. Soc Psychiatry Psychiatr Epidemiol 2002;37:38-45. http://dx.doi.org/10.1007/s127-002-8212-9.
- Bhui K, Stansfeld S, Hull S, Priebe S, Mole F, Feder G. Ethnic variations in pathways to and use of specialist mental health services in the UK – systematic review. Br J Psychiatry 2003;182:105-16. http://dx.doi.org/10.1192/bjp.182.2.105.
- Parkman S, Davies S, Leese M, Phelan M, Thornicroft G. Ethnic differences in satisfaction with mental health services among representative people with psychosis in south London: PRiSM study 4. Br J Psychiatry 1997;171:260-4. http://dx.doi.org/10.1192/bjp.171.3.260.
- Goater N, King M, Cole E, Leavey G, Johnson-Sabine E, Blizard R, et al. Ethnicity and outcome of psychosis. Br J Psychiatry 1999;175:34-42. http://dx.doi.org/10.1192/bjp.175.1.34.
- Morgan C, Mallett R, Hutchinson G, Leff J. Negative pathways to psychiatric care and ethnicity: the bridge between social science and psychiatry. Soc Sci Med 2004;58:739-52. http://dx.doi.org/10.1016/S0277-9536(03)00233-8.
- Marwaha S, Johnson S, Bebbington P, Stafford M, Angermeyer MC, Brugha T, et al. Rates and correlates of employment in people with schizophrenia in the UK, France and Germany. Br J Psychiatry 2007;191:30-7. http://dx.doi.org/10.1192/bjp.bp.105.020982.
- Drake RE, Becker DR. The individual placement and support model of supported employment. Psychiatr Serv 1996;47:473-5.
- Cook JA, Razzano L. Vocational rehabilitation for persons with schizophrenia: recent research and implications for practice. Schizophr Bull 2000;26:87-103. http://dx.doi.org/10.1093/oxfordjournals.schbul.a033448.
- Kleinman A. Concepts and a model for the comparison of medical systems as cultural systems. Soc Sci Med Part B Med Anthropol 1978;12:85-93. http://dx.doi.org/10.1016/0160-7987(78)90014-5.
- Helman C. Culture, health and illness. London: Hodder Arnold; 2007.
- Much N, Smith JA, Harré R, Van Langenhove L. Rethinking psychology. London: Thousand Oaks, CA: Sage Publications; 1995.
- Good BJ. Studying mental illness in context: local, global, or universal?. Ethos 1997;25:230-48. http://dx.doi.org/10.1525/eth.1997.25.2.230.
- Sewell H. Spirituality and mental health. Brighton: Pavilion Publishing; 2011.
- Littlewood R. From categories to contexts: a decade of the ‘new cross-cultural psychiatry’. Br J Psychiatry 1990;156:308-27. http://dx.doi.org/10.1192/bjp.156.3.308.
- Attitudes to mental illness 2010 report. London: Department of Health; 2010.
- Attitudes to mental illness 2008 research report. London: Department of Health; 2008.
- Attitudes to mental illness 2009 research report. London: Department of Health; 2009.
- Our voice: the Pakistani community’s view of mental health and mental health services in Birmingham. Kingston upon Thames: Rethink; 2007.
- Williams B, Healy D. Perceptions of illness causation among new referrals to a community mental health team: ‘explanatory model’ or ‘exploratory map’?. Soc Sci Med 2001;53:465-76. http://dx.doi.org/10.1016/S0277-9536(00)00349-X.
- Strauss C, Quinn N. A cognitive theory of cultural meaning. Cambridge: Cambridge University Press; 1997.
- Hatfield B, Mohamad H, Rahim Z, Tanweer H. Mental health and the Asian communities: a local survey. Br J Soc Work 1996;26:315-36. http://dx.doi.org/10.1093/oxfordjournals.bjsw.a011098.
- Narikiyo TA, Kameoka VA. Attributions of mental-illness and judgements about help seeking among Japanese-American and white American students. J Counseling Psych 1992;39:363-9. http://dx.doi.org/10.1037//0022-0167.39.3.363.
- Suan LV, Tyler JD. Mental-health values and preference for mental-health resources of Japanese-American and Caucasian-American students. Prof Psychol Res Pract 1990;21:291-6. http://dx.doi.org/10.1037//0735-7028.21.4.291.
- McCabe R, Priebe S. Explanatory models of illness in schizophrenia: comparison of four ethnic groups. Br J Psychiatry 2004;185:25-30. http://dx.doi.org/10.1192/bjp.185.1.25.
- Zafar S, Syed R, Tehseen S, Gowani S, Waqar S, Zubair A, et al. Perceptions about the cause of schizophrenia and the subsequent help seeking behavior in a Pakistani population – results of a cross-sectional survey. BMC Psychiatry 2008;8. http://dx.doi.org/10.1186/1471-244X-8-56.
- Banerjee G, Roy S. Determinants of help-seeking behaviour of families of schizophrenic patients attending a teaching hospital in India: an indigenous explanatory model. Int J Soc Psychiatry 1998;44:199-214. http://dx.doi.org/10.1177/002076409804400306.
- Razali SM, Khan UA, Hasanah CI. Belief in supernatural causes of mental illness among Malay patients: impact on treatment. Acta Psychiatr Scand 1996;94:229-33. http://dx.doi.org/10.1111/j.1600-0447.1996.tb09854.x.
- Dein S, Sembhi S. The use of traditional healing in South Asian psychiatric patients in the UK: interactions between professional and folk psychiatries. Transcult Psychiatry 2001;38:243-57.
- Srinivasan TN, Thara R. Beliefs about causation of schizophrenia: do Indian families believe in supernatural causes?. Soc Psychiatry Psychiatr Epidemiol 2001;36:134-40. http://dx.doi.org/10.1007/s001270050302.
- Das S, Saravanan B, Karunakaran K, Manoranjitham S, Ezhilarasu P, Jacob K. Effect of a structured educational intervention on explanatory models of relatives of patients with schizophrenia: randomised controlled trial. Br J Psychiatry 2006;188:286-7. http://dx.doi.org/10.1192/bjp.bp.104.007245.
- Cook CCH. Addiction and spirituality. Addiction 2004;99:539-51. http://dx.doi.org/10.1111/j.1360-0443.2004.00715.x.
- Cook CC, Powell A, Sims ACP. Spirituality and psychiatry. London: RCPsych Publications; 2009.
- Hall DE, Meador KG, Koenig HG. Measuring religiousness in health research: review and critique. J Relig Health 2008;47:134-63. http://dx.doi.org/10.1007/s10943-008-9165-2.
- Frey BB, Daaleman TP, Peyton V. Measuring a dimension of spirituality for health research. Res Aging 2005;27:556-77. http://dx.doi.org/10.1177/0164027505277847.
- Mytko JJ, Knight SJ. Body, mind and spirit: towards the integration of religiosity and spirituality in cancer quality of life research. Psychooncology 1999;8:439-50. http://dx.doi.org/10.1002/(SICI)1099-1611(199909/10)8:5<439::AID-PON421>3.3.CO;2-C.
- Parkes M. Report on the place of spirituality in mental health. National Spirituality and Mental Health Forum, 14 February 2011 n.d. www.nmhdu.org.uk/. /-report-on-the-place-of-spirituality-in-mental-health (accessed 10 May 2012).
- Sproston K, Nazroo J. Ethnic minority psychiatric illness rates in the community (EMPIRIC). London: The Stationary Office; 2002.
- Poole R, Cook CCH. Praying with a patient constitutes a breach of professional boundaries in psychiatric practice. Br J Psychiatry 2011;199:94-8. http://dx.doi.org/10.1192/bjp.bp.111.096529.
- Leavey G, Loewenthal K, King M. Challenges to sanctuary: the clergy as a resource for mental health care in the community. Soc Sci Med 2007;65:548-59. http://dx.doi.org/10.1016/j.socscimed.2007.03.050.
- Fallot RD. Spirituality and religion in psychiatric rehabilitation and recovery from mental illness. Int Rev Psychiatry 2001;13:110-16. http://dx.doi.org/10.1080/09540260120037344.
- Delivering race equality in mental health: a review. London: Department of Health; 2009.
- Byrne P. Psychiatric stigma. Br J Psychiatry 2001;178:281-4. http://dx.doi.org/10.1192/bjp.178.3.281.
- Deal M. Disabled people’s attitudes toward other impairment groups: a hierarchy of impairments. Disabil Soc 2003;18:897-910. http://dx.doi.org/10.1080/0968759032000127317.
- Goffman E. Stigma; notes on the management of spoiled identity. Englewood Cliffs, NJ: Prentice-Hall; 1963.
- Corrigan PW, Green A, Lundin R, Kubiak MA, Penn DL. Familiarity with and social distance from people who have serious mental illness. Psychiatr Serv 2001;52:953-8. http://dx.doi.org/10.1176/appi.ps.52.7.953.
- Link BG, Yang LH, Phelan JC, Collins PY. Measuring mental illness stigma. Schizophr Bull 2004;30:511-41. http://dx.doi.org/10.1093/oxfordjournals.schbul.a007098.
- Adewuya A, Makanjuola R. Lay beliefs regarding causes of mental illness in Nigeria: pattern and correlates. Soc Psychiatry Psychiatr Epidemiol 2008;43:336-41. http://dx.doi.org/10.1007/s00127-007-0305-x.
- Breaking the cycles of fear: a review of the relationship between mental health services and African and Caribbean communities. London: Sainsbury Centre for Mental Health; 2002.
- Anderson KK, Fuhrer R, Malla A. The pathways to mental health care of first-episode psychosis patients: a systematic review. Psychol Med 2010;40:1585-97. http://dx.doi.org/10.1017/S0033291710000371.
- Williams P, Tarrant CJ, Window S, Boot D, Bagalkote H, Jones PB. Are there ethnic group differences in pathways to care for psychosis?. Schizophr Res 2000;41. http://dx.doi.org/10.1016/S0920-9964(00)90715-1.
- Brunet K. Treatment delay in first episode-psychosis: service configuration, pathways to care and the psychology of help seeking. Birmingham: Univeristy of Birmingham; 2003.
- Chaudhry IB, Htay T, Qureshi M, Koch S, Bork N, Chaudhry N, et al. Does ethnicity influence use of psychiatric services in early psychosis?. Early Interv Psychiatry 2008;2.
- Harrison G, Holton A, Neilson D, Owens D, Boot D, Cooper J. Severe mental disorder in Afro-Caribbean patients: some social, demographic and service factors. Psychol Med 1989;19:683-96. http://dx.doi.org/10.1017/S0033291700024284.
- Chen E, Harrison G, Standen P. Management of first episode psychotic illness in Afro-Caribbean patients. Br J Psychiatry 1991;158:517-22. http://dx.doi.org/10.1192/bjp.158.4.517.
- Birchwood M, Cochrane R, Macmillan F, Copestake S, Kucharska J, Carriss M. The influence of ethnicity and family structure on relapse in first-episode schizophrenia. A comparison of Asian, Afro-Caribbean, and white patients. Br J Psychiatry 1992;161:783-90. http://dx.doi.org/10.1192/bjp.161.6.783.
- King M, Coker E, Leavey G, Hoare A, Johnson-Sabine E. Incidence of psychotic illness in London: comparison of ethnic groups. BMJ 1994;309:1115-19. http://dx.doi.org/10.1136/bmj.309.6962.1115.
- Cole E, Leavey G, King M, Johnson-Sabine E, Hoar A. Pathways to care for patients with a first episode of psychosis. A comparison of ethnic groups. Br J Psychiatry 1995;167:770-6. http://dx.doi.org/10.1192/bjp.167.6.770.
- Harrison G, Amin S, Singh S, Croudace T, Jones P. Outcome of psychosis in people of African-Caribbean family origin. Population-based first-episode study. Br J Psychiatry 1999;175:43-9. http://dx.doi.org/10.1192/bjp.175.1.43.
- Burnett R, Mallett R, Bhugra D, Hutchinson G, Der G, Leff J. The first contact of patients with schizophrenia with psychiatric services: social factors and pathways to care in a multi-ethnic population. Psychol Med 1999;29:475-83. http://dx.doi.org/10.1017/S0033291798008125.
- Birmingham City Council . 2011 Population Census n.d. www.birmingham.gov.uk/cs/Satellite?blobcol=urldata&blobheader=application%2Fpdf&blobheadername1=Content-Disposition&blobkey=id&blobtable=MungoBlobs&blobwhere=1223530606141&ssbinary=true&blobheadervalue1=attachment%3B+filename%3D649122web_2011_Key_Statistics_for_Birmingham_%28profile%29_v4.pdf (accessed 16 June 2013).
- Singh SP, Cooper JE, Fisher HL, Tarrant CJ, Lloyd T, Banjo J, et al. Determining the chronology and components of psychosis onset: the Nottingham Onset Schedule (NOS). Schizophr Res 2005;80:117-30. http://dx.doi.org/10.1016/j.schres.2005.04.018.
- Fisher H, Theodore K, Power P, Chisholm B, Fuller J, Marlowe K, et al. Routine evaluation in first episode psychosis services: feasibility and results from the MiData project. Soc Psychiatry Psychiatr Epidemiol 2008;43:960-7. http://dx.doi.org/10.1007/s00127-008-0386-1.
- Lloyd KR, Jacob KS, Patel V, St Louis L, Bhugra D, Mann AH. The development of the Short Explanatory Model Interview (SEMI) and its use among primary-care attenders with common mental disorders. Psychol Med 1998;28:1231-7. http://dx.doi.org/10.1017/S0033291798007065.
- Gater R, Almeida E, Sousa DB, Barrientos G, Caraveo J, Chandrashekar CR, et al. The pathways to psychiatric care: a cross-cultural study. Psychol Med 1991;21:761-74. http://dx.doi.org/10.1017/S003329170002239X.
- Department for Communities and Local Government . English Indices of Deprivation 2010 2011. www.gov.uk/government/publications/english-indices-of-deprivation-2010 (accessed July 2013).
- Drake R, Haley C, Akhtar S, Lewis SW. Causes and consequences of duration of untreated psychosis in schizophrenia. Br J Psychiatry 2000;177:511-15. http://dx.doi.org/10.1192/bjp.177.6.511.
- London: The Stationary Office; 1983.
- The ICD-10 classification of mental and behavioural disorders: clinical classification of mental and behavioural disorders: descriptions and diagnostic guidelines. Geneva: WHO; 1992.
- Morgan G, Smircich L. The case for qualitative research. Acad Manag Rev 1980;5:491-500. http://dx.doi.org/10.2307/257453.
- Rabiee F. Focus-group interview and data analysis. Proc Nutr Soc 2004;63:655-60. http://dx.doi.org/10.1079/PNS2004399.
- McGee P. Irish mental health in Birmingham: what is appropriate and culturally competent primary care. Birmingham: Birmingham City University; 2008.
- Ritchie R, Spencer L, Bryman A, Burgees R. Analysing qualitative data. London: Routledge; 1994.
- Krueger R, Casey MA. Focus groups: a practical guide. London: Sage; 2009.
- Department of Health . Equity and Excellence: Liberating the NHS 2010. www.official-documents.gov.uk/document/cm78/7881/7881.pdf (accessed 22 July 2013).
- Dressing H, Salize HJ. Compulsory admission of mentally ill patients in European Union Member States. Soc Psychiatry Psychiatr Epidemiol 2004;39:797-803.
- Salize HJ, Dressing H. Epidemiology of involuntary placement of mentally ill people across the European Union. Br J Psychiatry 2004;184:163-8. http://dx.doi.org/10.1192/bjp.184.2.163.
- Morgan C, Dazzan P, Morgan K, Jones P, Harrison G, Leff J, et al. First episode psychosis and ethnicity: initial findings from the AESOP study. World Psychiatry 2006;5:40-6.
- Department of Health . Delivering Race Equality in Mental Health Care: An Action Plan for Reform Inside and Outside Services and the government’s Response to the Independent Inquiry into the Death of David Bennett 2005. http://webarchive.nationalarchives.gov.uk/20130107105354/http:/www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4100773 (accessed July 2013).
- Sashidharan SP, Francis E. Racism in psychiatry necessitates reappraisal of general procedures and Eurocentric theories. BMJ 1999;319. http://dx.doi.org/10.1136/bmj.319.7204.254.
- McKenzie K, Bhui K. Institutional racism in mental health care. BMJ 2007;334:649-50. http://dx.doi.org/10.1136/bmj.39163.395972.80.
- McKenzie K, Chakraborty A. Racial discrimination and mental illness. Br J Psychiatry 2003;182:77-82. http://dx.doi.org/10.1016/S0924-9338(02)80385-6.
- Marshall M, Lewis S, Lockwood A, Drake R, Jones P, Croudace T. Association between duration of untreated psychosis and outcome in cohorts of first-episode patients: a systematic review. Arch Gen Psychiatry 2005;62:975-83. http://dx.doi.org/10.1001/archpsyc.62.9.975.
- Perkins D, Gu H, Boteva K, Lieberman J. Relationship between duration of untreated psychosis and outcome in first-episode schizophrenia: a critical review and meta-analysis. Am J Psychiatry 2005;162:1785-804. http://dx.doi.org/10.1176/appi.ajp.162.10.1785.
- Pargament KI. Spiritually integrated psychotherapy: understanding and addressing the sacred. New York: Guilford Press; 2007.
- Crossley JP, Salter DP. A question of finding harmony: a grounded theory study of clinical psychologists’ experience of addressing spiritual beliefs in therapy. Psychol Psychother Theory Res Pract 2005;78:295-313. http://dx.doi.org/10.1348/147608305X26783.
- Mayers C, Leavey G, Vallianatou C, Barker C. How clients with religious or spiritual beliefs experience psychological help-seeking and therapy: a qualitative study. Clin Psychol Psychother 2007;14:317-27. http://dx.doi.org/10.1002/cpp.542.
- Coyle A, Lochner J. Religion, spirituality and therapeautic practice. Psychologist 2011.
- Lawrie SM, Martin K, McNeill G, Drife J, Chrystie P, Reid A, et al. General practitioners’ attitudes to psychiatric and medical illness. Psychol 1998;28:1463-7. http://dx.doi.org/10.1017/S0033291798007004.
- Bindman J, Johnson S, Wright S, Szmukler G, Bebbington P, Kuipers E, et al. Integration between primary and secondary services in the care of the severely mentally ill: patients’ and general practitioners’ views. Br J Psychiatry 1997;171:169-74. http://dx.doi.org/10.1192/bjp.171.2.169.
- Lester H, Birchwood M, Freemantle N, Michail M, Tait L. REDIRECT: cluster randomised controlled trial of GP training in first-episode psychosis. Br J Gen Pract 2009;59:e183-90. http://dx.doi.org/10.3399/bjgp09X420851.
- Birchwood M, Connor C, Lester H, Patterson P, Freemantle N, Marshall M, et al. Reducing duration of untreated psychosis: care pathways to early intervention in psychosis services. Br J Psychiatry 2013;203:58-64.
- Leason K. Mental health ‘tsar’ admits services suffer from institutional racism. Community Care 2003;1481:18-9.
- Cox JL. Commentary: institutional racism in British psychiatry. Psychiatr Bull 2001;25:248-9. http://dx.doi.org/10.1192/pb.25.7.248.
- Hollins S, Moodley P. Racism in Mental Health n.d. www.bmj.com/cgi/eletters/333/7569/648. (accessed 2006).
- Keating F, Robertson D, McCulloch A, Francis E. Breaking the circles of fear: a review of the relationship between mental health services and African and Caribbean communities. London: Sainsbury Centre for Mental Health; 2002.
- Patel K, Heginbotham C. Race equality, human rights and mental health legislation: recent developments in England and Wales. S Afr J Psychiatr 2007;13:76-8.
- Lewis G, Croft-Jeffreys C, David A. Are British psychiatrists racist?. Br J Psychiatry 1990;157:410-15. http://dx.doi.org/10.1192/bjp.157.3.410.
- Minnis H, McMillan A, Gillies M, Smith S. Racial stereotyping: survey of psychiatrists in the United Kingdom. BMJ 2001;323:905-6. http://dx.doi.org/10.1136/bmj.323.7318.905.
- Singh SP. Shooting the messenger: the science and politics of ethnicity research. Br J Psychiatry 2009;195:1-2. http://dx.doi.org/10.1192/bjp.bp.108.058685.
- Bagby RM, Thompson JS, Dickens SE, Nohara M. Decision making in psychiatric civil commitment: an experimental analysis. Am J Psychiatry 1991;148:28-33.
- Zinkler M, Priebe S. Detention of the mentally ill in Europe – a review. Acta Psychiatr Scand 2002;106:3-8. http://dx.doi.org/10.1034/j.1600-0447.2002.02268.x.
- Hotopf M, Wall S, Buchanan A, Wessely S, Churchill R. Changing patterns in the use of the Mental Health Act 1983 in England, 1984–1996. Br J Psychiatry 2000;176:479-98. http://dx.doi.org/10.1192/bjp.176.5.479.
- Lorant V, Depuydt C, Gillain B, Guillet A, Dubois V. Involuntary commitment in psychiatric care: what drives the decision?. Soc Psychiatry Psychiatr Epidemiol 2007;42:360-5. http://dx.doi.org/10.1007/s00127-007-0175-2.
- Wall S, Hotopf M, Wessely S, Churchill R. Trends in the use of the Mental Health Act: England, 1984–96. BMJ 1999;318:1520-1. http://dx.doi.org/10.1136/bmj.318.7197.1520.
- Keown P, Holloway F, Kuipers E. The impact of severe mental illness, co-morbid personality disorders and demographic factors on psychiatric bed use. Soc Psychiatry Psychiatr Epidemiol 2005;40:42-9. http://dx.doi.org/10.1007/s00127-005-0842-0.
- Keown P, Weich S, Bhui KS, Scott J. Association between provision of mental illness beds and rate of involuntary admissions in the NHS in England 1988–2008: ecological study. BMJ 2011;343. http://dx.doi.org/10.1136/bmj.d3736.
- Bennewith O, Amos T, Lewis G, Katsakou C, Wykes T, Morriss R, et al. Ethnicity and coercion among involuntarily detained psychiatric in-patients. Br J Psychiatry 2010;196:75-6. http://dx.doi.org/10.1192/bjp.bp.109.068890.
- Cambridge J, Singh SP, Johnson M. The need for measurable standards in mental health interpreting: a neglected area. Psychiatrist 2012;36:121-4. http://dx.doi.org/10.1192/pb.bp.110.031211.
- Fearon P, Kirkbride JB, Morgan C, Dazzan P, Morgan K, Lloyd T, et al. Incidence of schizophrenia and other psychoses in ethnic minority groups: results from the MRC AESOP study. Psychol Med 2006;36:1541-50. http://dx.doi.org/10.1017/S0033291706008774.
- Cantor-Graae E, Pedersen CB, McNeil TF, Mortensen PB. Migration as a risk factor for schizophrenia: a Danish population-based cohort study. Br J Psychiatry 2003;182:117-22.
- Selten JP, Bhugra D, Leff J, Fernando S, Eagles JM, Barlett A, et al. Psychotic illness in ethnic groups. BMJ 2004;310:331-3. http://dx.doi.org/10.1136/bmj.310.6975.331b.
- Gudjonsson GH, Rabe-Hesketh S, Szmuckler G. Management of psychiatric in-patient violence: patient ethnicity and use of medication, restraint and seclusion. Br J Psychiatry 2004;184:258-62. http://dx.doi.org/10.1192/bjp.184.3.258.
- Connolly A, Rogers P, Taylor D. Antipsychotic prescribing quality and ethnicity: a study of hospitalized patients in south east London. J Psychopharmacol 2007;21:191-7. http://dx.doi.org/10.1177/0269881107065899.
- Connolly A, Taylor D. Ethnicity and quality of antipsychotic prescribing among in-patients in south London. Br J Psychiatry 2008;193:161-2. http://dx.doi.org/10.1192/bjp.bp.108.050427.
- Department of Health . Engaging and Changing. Developing Effective Policy for the Care and Treatment of Black and Minority Ethnic Detained Patients 2003. www.doh.gov.uk/changeagentteam (accessed 10 September 2013).
- Raleigh VS, Irons R, Hawe E, Scobie S, Cook A, Reeves R, et al. Ethnic variations in the experiences of mental health service users in England: results of a national patient survey programme. Br J Psychiatry 2007;191:304-12. http://dx.doi.org/10.1192/bjp.bp.106.032417.
- Singh SP. Institutional racism in psychiatry: lessons from inquiries. Psychiatr Bull 2007;31:363-5. http://dx.doi.org/10.1192/pb.bp.106.013953.
- Murray R, Fearon P. Searching for racists under the psychiatric bed: commentary on … institutional racism in psychiatry. Psychiatr Bull 2007;31:365-6. http://dx.doi.org/10.1192/pb.bp.107.016303.
- Cannon M, McKenzie K, Sims ACP, Bhui K, Sashidharan SP. Should there be separate psychiatric services for ethnic minority groups?. Br J Psychiatry 2003;182:10-2.
- Weich S, Griffith L, Commander M, Bradby H, Sashidharan SP, Pemberton S, et al. Experiences of acute mental health care in an ethnically diverse inner city: qualitative interview study. Soc Psychiatry Psychiatr Epidemiol 2012;47:119-28. http://dx.doi.org/10.1007/s00127-010-0314-z.
- Lloyd-Evans B, Crosby M, Stockton S, Pilling S, Hobbs L, Hinton M, et al. Initiatives to shorten duration of untreated psychosis: systematic review. Br J Psychiatry 2011;198:256-63. http://dx.doi.org/10.1192/bjp.bp.109.075622.
Appendix 1 Protocol
Ethnicity, Detention and Early Intervention: Reducing Inequalities and Improving outcomes for Black and Ethnic Minority (BME) Patients: The ENRICH Programme
Funded by NIHR £920,000; duration 42 months
PI Professor Swaran Singh, University of Warwick
Summary
Black and Minority Ethnic (BME) patients in the UK, especially young Afro-Caribbean men, suffer from disproportionately high rates of psychosis and coercive care, with poorer access, experience and outcomes than White patients. Institutional racism in psychiatry is often cited as a cause, but since such differences are present even when BME individuals first present to mental health care, some of the reasons must lie in the wider social context. Early Intervention in Psychosis (EI) services are designed to improve access and provide effective and evidence-based care in low-stigma, community settings. We wish to evaluate the effectiveness of such services in specifically improving the experience of care and outcomes of BME patients.
We propose a series of three, high quality projects within Birmingham, which is renowned for its EI service for young people with psychosis. The service is being extended to the entire city and has developed strategic partnerships with NGOs and BME community groups. Over 42 months, we will evaluate the care and outcomes of all service users referred to EI services in Birmingham. We will explore what culture and family related factors facilitate or impede access to health care. We will evaluate all Mental Health Act assessments to determine whether some BME patients have fewer community alternatives of care than other ethnic groups, thus leading to greater chance of detention. We will seek the opinions of service users, carers, clinicians and other stakeholders on how EI services can become more appropriate and acceptable to BME communities. We will evaluate the outcomes of all early psychosis on experience outcomes of care, especially vocational outcomes, to demonstrate that over time, BME patients have similar levels of engagement, non-coercive care, satisfaction with services and quality of recovery as any other patient group. We will demonstrate that innovative models of collaboratove working between mental health services, voluntary sector and community groups can transform the experience of care and outcomes in BME groups, thus reducing detention rates and promoting social inclusion. During its lifetime itself, the programme will help services deliver better care and ensure that BME service users do not have different or worse outcomes.
Background
BME patients in the UK, especially young Afro-Caribbean men, have high rates of psychosis [1], experience adverse pathways into care [2], are at greater risk of detention under the Mental Health Act (MHA) [3], are more likely to disengage over time [4], be less satisfied with their care [5] and thereby have poorer outcomes, with greater social exclusion. The conventional explanation for these inequalities is based on the notion of institutional racism within psychiatry [8, 9]. However this view has recently been challenged as providing simplistic explanations for complex processes [10]. Ethnic inequalities are evident even at first presentation of psychosis; therefore contributory factors must operate prior to presentation to psychiatric services and need to be understood in a wider context. We have further argued that ‘any potential solutions must go beyond the health sector and involve statutory as well as voluntary and community agencies. The problem does not reside exclusively in psychiatry and hence the solutions cannot emerge from psychiatric services alone’ [10].
Early Intervention (EI) services are expected to impact favourably upon ethnic inequalities by focussing specifically on therapeutic engagement [11], reducing social exclusion by targeting vocational disabilities, and providing care in community-based, low stigma settings. The development of such services in the UK has been patchy and uneven, despite recommendation from DH that there should be 50 such services in the country by 2004 [7]. Even where services are available, it is unclear whether generic EI services meet the specific demands and challenges of providing care for BME patients.
This programme of work aims to develop the knowledge base essential to reverse ethnic inequalities in care and outcome of psychotic disorders. We aim to evaluate the effectiveness of innovative models of care in transforming the experience of mental health care for BME patients. We wish to demonstrate that strategic partnerships between health services, social care and voluntary sectors can reduce ethnic inequalities and ensure that over time, outcomes of BME patients converge rather than diverge from other ethnic groups.
This programme is timely and relevant to several pressing concerns and priorities within the NHS. These include
-
Delivering Race Equality: The document Delivering Race Equality [6] recommends a coherent programme of work for achieving equality of access, experience and outcomes for BME service users. Most research and clinical effort for improving BME patient care has focussed on generic services dealing with chronic, enduring mental disorders. Disabilities set in early in psychosis and the first three years are the ‘critical period’ when interventions are most effective and often not available [12]. To achieve equality of access and outcomes for BME patients, attention needs to shift to providing effective care in early psychosis.
-
Developing Early Intervention in Psychosis Services: EI services are of demonstrable value in maintaining engagement and improving outcomes in FEP [13, 14]. However to ensure that generic EI services meet the specific needs of BME communities, and are equally appropriate, accessible and acceptable, we need to establish care needs and preferences of service users and carers from different ethnic groups.
-
Reducing Social Exclusion: The Social Exclusion Unit Report [15] highlights the importance of EI services in reducing barriers to employment. Social exclusion is the explanatory framework within which service users and BME communities most often describe their interaction with health services, perceiving fewer employment opportunities perceived as a major contributor to exclusion [16]. EI services can, and prioritise social recovery, particularly reintegration into mainstream education or employment.
-
Developing NHS–NGO partnerships: The NHS confederation call for collaborations between NHS and NGOs [17] can be best tested in EI services with existing partnerships. Birmingham has strategic partnerships already in place with NGOs which specialise in working with BME groups providing respite homes, support staff and vocational input into Birmingham EI services.
Our programme of work is relevant to all these priorities. By understanding the mechanisms behind adverse pathways to care and evaluating the effectiveness of collaborations between healthcare and other agencies in improving user experience and outcome, we aim to demonstrate that the DRE ambitions can be achieved.
Since ethnic inequalities in care and outcome of psychosis are evident even in the first episode [18, 19] and trusts are expected to develop EI services for FEP, this is an opportune moment for research focus and clinical effort to shift to BME patients with early psychosis.
-
Detention and FEP: Our recent systematic review [3] emphasised the need for evaluating of the process of detention, using a denominator population of all those assessed, rather than all those detained since studying the latter does not allow exploration of ethnic differences in the availability of alternatives to detention which could avoid the need for detention.
-
Pathways to care in FEP: Our other recent review of pathways in FEP [2] highlighted the limitations of the two diverse ways that pathways have so far been studied: a medico-epidemiological approach, and a socio-anthropological approach. In the absence of integration between these two approaches, no interventions have been identified which alter adverse pathways for BME users. In particular the role of service-level interventions in improving access and reducing detention rates has not been evaluated.
-
Social inclusion and vocation recovery: Vocational recovery is a necessary precondition for social inclusion. However, there is little available information on the pathways to vocational loss and recovery in early psychosis and no evidence to support any particular vocational strategy in FEP. Even less is known about strategies that facilitate return to education. A Cochrane review has confirmed that placing patients in competitive employment immediately whilst providing on-the-job support (Individual Support and Placement, IPS) is more effective than pre-vocational training in helping service users obtain competitive employment [20].
Our programme is ideally placed to explore all these areas. An inception cohort of FEP in a multi-ethnic area, managed by an established EI service with NGO collaboration, will be longitudinally assessed to establish the determinants of ethnic inequalities and evaluate the effectiveness of EI services. We will demonstrate that divergent trajectory of BME groups can be made convergent with other ethnic groups, thereby reducing inequalities of access, satisfaction and outcomes.
-
Adverse pathways to care in BME groups: Pathways to care are adverse in BME groups even in first presentation of a psychotic illness [2, 18, 19]. The three-centre AESOP study of FEP found Black patients with FEP were less likely to be engaged with their GP and their family members were more likely to seek police rather than medical help [18, 19]. Hence the determinants of these pathways must be explored within familial and wider societal context of BME patients [21, 22].
-
Ethnic differences in detention rates: Detention rates for BME patients are high even in the first psychotic episode and increase in latter episodes [3]. This trajectory of deteriorating relationship between BME patients and mental health services, with decreasing engagement and increasing detention rates over time, has now been well replicated in research [3–5, 22, 23]. It is not clear however whether some service level intervention can reduce this detention rate and improve engagement of BME patients.
-
Ethnic inequalities in health outcomes and service satisfaction: BME patients, especially young Black men, report lesser satisfaction with mental health services, with the number of previous admissions predicting greater dissatisfaction [5]. In the UK unemployment rates for patients suffering from psychosis have risen over the last 50 years and were 70–80% during 1990s [24]. Service users and carer advocacy groups consider return to work and occupation as one of their highest priorities; one that enhances their functional status and improves their quality of life [25, 26] BME patients are doubly disadvantaged due to the combined effect of racism in the labour market and the stigma of mental illness.
Our programme will establish the determinants of ethnic inequalities in pathways to care and detention rates. We will examine change in healthcare of BME patients with FEP over three years in Birmingham EI services. We will demonstrate that novel ways of joint working between health, social and voluntary sectors can reduce detention rates, improve engagement, enhance recovery, increase user satisfaction and reduce social exclusion of BME patients. The programme will have a direct impact on both improved health care and on better health care delivery.
The R&D department at BSMHFT departments has worked closely with the universities of Warwick, Birmingham and Central England. We have support from key members of all organisations involved in the programme (see applicant list and research team). We have conducted a series of outcome studies in FEP and piloted pathways projects in FEP and EI services in Birmingham and London [2, 27–29]. We were commissioned by DH Policy Research Programme (2005–9) to undertake national study (National EDEN programme) which is evaluating the implementation of early intervention on key outcomes in differently configured EI services across sites in England. Findings from National EDEN project (to be completed 2008) will inform the development of this programme. Our programme is significantly different from the EDEN evaluation. We are specifically focussing on BME service users and their needs and outcomes by following up the cohort for the entire three-years in a multi-ethnic area, rather than the limited one-year follow-up in EDEN. We have already carried out high quality qualitative work in the area of access, widening participation, evaluation in the area of health care, ethnicity and early psychosis. [30–33]
Pilot work: We have conducted pilot audits to determine referral rates to EI services across Birmingham (expected annual rate 300 new cases/per year). We have piloted and implemented the use of structured assessments as part of routine clincal care. We are currently undertaking a qualitative study in BSMHFT funded by CSIP to explore ethnic differences in pathways into and out of crisis. This project involves users, carers and staff in the three Crisis Resolution Home Treatment teams in the Heart of Birmingham PCT. We are also mapping service provision in both the statutory and voluntary sectors and undertaking in-depth interviews with a wide range of service providers. Preliminary data from research by one of the applicants (FR) has helped us develop strong links with local voluntary and community organisations, who strongly support efforts to bridge the gap and creating trust between users, carers and statutory service providers. Before starting the main studies, we will conduct pilot projects on recruitment and assessment of disengaged/dissatisfied users and carers to ensure adequate data collection from a group that is traditionally lost to follow-up.
Aims & Objectives
We propose three, linked, high-quality projects which will identify the determinants of ethnic inequalities in first-episode psychosis (FEP) and evaluate service-level interventions that ensure that BME users do not have divergent trajectories of outcome as compared to other groups.
The specific objectives of the programme are:
-
To understand ethnic differences in pathways to care in FEP by exploring cultural determinants of illness recognition, attribution and help-seeking among different ethnic groups.
-
To evaluate the process of detention under the Mental Health Act (MHA) and assess ethnic differences in the availability of alternative provision which could reduce the need for detention.
-
To determine the appropriateness, accessibility and acceptability of generic early intervention (EI) services for different ethnic groups and establish care needs and preferences of service users and other stakeholders.
Research Plan
We propose a series of three, linked projects over over 42 months in Birmingham and Solihull Mental Health Foundation Trust (BSMHFT). Before starting the specific projects, we will map existing BME service provision, identify and contact key stakeholders, and create a data base for both routine data collection and future sample ascertainment. Some aspects of the projects will be conducted in parallel while others will be informed by results as these emerge. These results will be integrated into ongoing service delivery, creating a feedback loop that ensures service improvement during the lifetime of the programme. Our overall aim is to transform the care received by BME patients with early psychosis and eliminate, or at least significantly diminish, ethnic inequalities in early psychosis.
Programme Plan
Mapping of service provision, identification of key stakeholders and creation of database: The DRE Focussed Implementation Site (FIS) Evaluation Project (SW is PI) is mapping all statutory and non-statutory organisations working with BME service users across 8 sites in the UK. BSMHFT is one such site and we will access data on BSMHFT organisations to map local services and key stakeholders.
We will create a minimum data set for routine data collection on all patients with FEP referred to EI services in Birmingham. Data will be collected on socio-demographic indices including measures of deprivation; clinical measures of onset (Nottingham Onset Schedule NOS [28]) clinical presentation: Positive and Negative Symptom scale PANSS [34]), insight ITAQ [35], resource utilisation including number of admissions, inpatient days and use of the Mental Health Act, engagement with services (SOLES [36]). We have piloted and implemented the use of these structured assessments. These are now used with all EI service users by clinicians during regular patient reviews. Ethnicity will be measured along several dimensions including self-assigned ethnicity, place of birth, country of parent’s birth, religion, language, cultural affiliation and shared sense of belonging to an ethnic group [37].
The service map and data set will be used for sample ascertainment and recruitment for individual projects. We will conduct pilot projects for recruitment into qualitative interviews which will inform and improve our sample ascertainment methods.
At the end of the programme we will have serial quantitative and qualitative data collected over three years on all patients referred to EI services in BSMHFT. This data set will be explored to compare trajectories of outcomes between different ethnic groups. Our results will be compared with results from other outcome data sets such as MiDATA covering all London EI Services [38] and historical outcome data from literature on other FEP cohorts [13, 14, 29, 39]. Although ethnicity is the focus of this research project, this data set will also serve as an important resource for future research on other aspects of FEP.
The specific projects will include:
Study 1. Ethnic and cultural determinants of help-seeking in first-episode psychosis
Background and Aims:
While it is well established that BME users have adverse pathways to care; it is less clear what socio-cultural and ethnic influences determine these pathways. Institutional racism, often cited as a cause, does not explain why pathways are adverse even in FEP, since these users have no prior experience of mental health care. Explanations are likely to lie in wider social and family influences which impact upon help-seeking, illness recognition and symptom attribution. There is evidence that some BME communities, especially those from Afro-Caribbean background, stigmatise mental illness more heavily, attribute unusual behaviour to the individual rather than to an illness [40, 41] and seek police rather than medical help when dealing with an ill relative [19].
This mixed methods study will use both quantitative and qualitative approaches to assess ethnic variations in help-seeking in FEP. The specific research questions will be:
-
Are there ethnic differences in the recognition of early signs of psychosis and help-seeking behaviours?
-
Are such differences a function of cultural factors such as explanatory models of illness or are these more closely related to socio-economic status, deprivation and isolation?
-
Do biological as opposed to psychological or social explanatory models of illness predict early medical help-seeking and shorter duration of untreated psychosis (DUP)?
Methodology:
Study design: A cohort of FEP patients and their families (one key carer per patient) presenting to EI services will be interviewed individually to determine how the early changes of psychosis are understood and attributed by the patient and the family, what help-seeking processes are initiated, by whom, and with what outcomes. We will specifically explore the issues of stigma, mistrust or suspicion of services and treatment and perceptions of discrimination and prejudice from services.
Sample: A cohort of up to 120 (estimated) FEP patients and their families (one key carer per patient [Total n = 120 estimated]) presenting to EI services will be interviewed individually. In these interviews, along with routine structured assessments described above, data will also be collected on five additional measures (listed below) in order to fufill the study objectives.
A purposive sample of FEP patients (n = 30) and their families (one key carer per patient) will also be drawn from this cohort of patients (and their carers) to participate in in-depth individual interviews. We will ensure that participants include a range of socio-demographic backgrounds including age, gender, ethnicity and economic indices.
Data collection: Interviews will be held at the interviewees’ home or a neutral setting if this is preferred. It is anticipated that the interviews will take approximately 60–120 minutes each with patients and carers. Carers will be interviewed separately unless requested otherwise.
Along with routine structured assessments described above, data will also be collected on:
-
Nottingham Onset Schedule [28]: This semi-structured interview identifies the emerging signs and symptoms of early psychosis and acts as a template upon which help-seeking endeavours of the patient and carers are mapped in a reliable manner. A Psychosis Causal Beliefs Coding System (PCBCS) (developed from the SEMI [37] and Helman 1994 [42]) will be included as part of NOS in order to develop an understanding of patients and carers attributions to symptoms and help-seeking.
-
Inventory of Attitudes towards Seeking Mental Health Services (IASMHS) [43]: This is a self-report questionnaire that aims to develop an understanding of patients’ attitudes towards help-seeking from Mental Health Services.
-
Beliefs About Causes of Mental Illness (BACMI) [44]: This is a cross-cultural questionnaire devised to understand beliefs about mental illness within the Chinese and the British context. This questionnaire has been amended (with due permission) to fit the context in Birmingham.
-
Beliefs About Treatment of Mental Illness (BATMI) [44]: This cross-cultural questionnaire elicits patients and their carers beliefs about the treatment of mental illness.
-
The Stigma Scale [45]: This is a standardised measure devised on the basis of service users experiences and views of stigma to mental illness.
-
ITAQ (The insight scale) [35]: This scale assesses insight into dimensions of recognition of need for recognition and treatment of illness.
Analysis:
With permission from the participants, each interview will be transcribed verbatim and analysed using Krueger’s framework and Rabiee’s guidelines [30]. Quantitative data from NOS will be explored to determine the relationship between socio-demographic and clinical variables and service utilisation. Attributions collected as part of the NOS will coded using Leeds Attribution Coding Schedule (LACS) [46]. The beliefs and attitudes questionnaires are standardised measures which allow us to quantify attitudes and beliefs towards mental health services. The Research Team has been provided adequate training to carry out the same. A triangulation of data generated from different methods mentioned above will allow an in-depth understanding of the dynamic social, cultural and interpersonal processes that affect help-seeking and the interplay between these processes and local healthcare system. We shall specifically explore whether a bio-medical attribution of causation for early signs of psychosis predicts help-seeking through medical agencies, shorter DUP and less adverse pathways to care as opposed to a social explanatory model.
Outcomes:
The study outcome will include an understanding of the socio-cultural determinants of recognition of illness and help-seeking behaviour in FEP, including intra-ethnic differences. We will identify ‘malleable’ variables in care pathways that lend themselves to service-level interventions and ensure improved access to care. We will also develop family and community psycho-education strategies and intervention to reduce the stigma of mental illness, improve community understanding of the identification, causes and treatment of psychosis, and minimise barriers to help-seeking in early psychosis.
Study 2. Determinants of ethnic differences in the process and outcome of Mental Health Act (MHA) assessments
Background and Aims:
The true denominator population for determining predictors of detention (including BME status) is the population which is assessed under the MHA, not the subgroup which is detained, since studying the latter does not allow exploration of differences in the availability of community alternatives to avoid detention [3]. Yet there is no study in psychiatric literature on patients assessed under the MHA. This study will prospectively evaluate the outcomes of all MHA assessments over one year. A sub-sample of assessments will undergo in-depth evaluation by researchers who will interview users, carers and clinicians to identify the determinants of the detention, including ethnic differences in the availability of community alternatives to inpatient admission.
The specific research questions will be:
-
Are there ethnic differences in the proportions of patients undergoing MHA assessments in a given year?
-
What are the clinical, sociodemographic, ethnic and risk-related predictors of detention as an outcome of MHA assessments?
-
Do ethnic groups differ in the availability of community alternatives (statutory and voluntary) which could reduce need for in-patient detention?
Methodology:
Study design: A prospective study of all MHA assessments conducted in one year using social services and MHA office records. In-depth evaluation of a subsample of MHA assessments to determine clinical, sociodemographic and ethnic predictors of detention as an outcome of assessment.
Study sample: About 150 patients are detained under the MHA each year in BSMHFT. The rate of assessment is likely to be 1.5 to 2 times the detained population. About 250–300 MHA assessments will therefore form the study sample. We will purposely select a subsample of these assessments for in-depth qualitative assessments of the process of detention and the determinants of the final decision, including both detained patients and those in whom detention was not the final outcome.
Study method: All psychiatric and social work services in the study area will be contacted with a letter explaining the purpose of the study and asking them to record data on all MHA assessments they conduct, regardless of whether the assessment resulted in detention or not. A data collection tool will be developed specifically for the study to include data on diagnosis, ethnicity, objective and subjective measures of risk, level of social support, outcome of assessment and the availability and use of community alternatives to detention. A researcher will ring all clinical teams once a week and ask the team manager about any MHA assessments conducted in the previous week. For all assessments thus identified, the MHA tool will be sent to the psychiatrist and social worker involved, and responses sought with periodic reminders.
A subsample of MHA assessments, ensuring wide socioeconomic, geographic and ethnic representation, and including both detained and not-detained patients, will be evaluated in depth by researchers who will interview the psychiatrist (n = 20) and social worker (n = 20) involved in the assessment and a carer (n = 20) of the service user. We will therefore have 20 case studies with a total of 60 interviews. Carers interviews will explore themes of stigma, shame, mistrust and fear of services and treatment modalities, perceptions of discrimination, and the availability and acceptability of alternatives to traditional in-patient care which could have avoided detention. Interviews with psychiatrists and social workers will explore the clinical determinants of their reason to detain the patient, including perceived level of risk, local provision of alternatives to in-patient care and risk-aversion due to concerns about adverse events were the patient not to be detained.
Data Analysis:
For all MHA assessments, ethnic differences in assessment and detention rates will be explored and correlated with sociodemographic and clinical characteristics of the sample. These will be proportions and percentages for categorical data; means and standard deviations for continuous data when parametric assumptions are met; and medians and interquartile ranges for other continuous data and for ordinal variables. Logistic regression will be conducted to determine predictors of detention with age, gender, diagnosis, risk, social support and ethnicity as independent variables to establish the independent effect of ethnicity on detention when other risk factors are taken into account.
Qualitative data: All interviews will be audio taped with permission and fully transcribed. Field notes will be made immediately after each interview to complement data collection. We expect that data saturation will be reached in these 60 interviews. Two experienced researchers will each read the transcripts and field notes and construct a preliminary thematic coding framework. Disagreements during this process will be discussed until a consensus is achieved. Deviant cases will be actively sought throughout the analysis and emerging ideas and themes modified in response. Nvivo (QRS release 2.0) will be used to manage data more effectively and transparently with data organised into initial and then higher codes that provide insight into identified themes.
Outcomes:
The primary study outcome will be the socio-cultural and ethnic determinants of MHA assessment outcomes, especially ethnic differences in the availability and acceptability of alternatives to inpatient admission. Secondary outcomes will include ethnic variations in rates of MHA assessments and clinical risk factors that influence coercion. Qualitative analysis will yield information on how encounters between healthcare providers and service users and carers, who often hold conflicting explanatory systems about health and illness, can be negotiated to avoid coercion. We will develop conceptual models and good practice guidelines that bring together very different views of reality: a biomedical versus a biographical approach to the events that lead to the MHA detentions.
Study 3. Determining the appropriateness and acceptability of EI services for different ethnic groups
Background and Aims:
The NHS Policy Implementation Guide [7] recommended the development of 50 Early Intervention in Psychosis (EI) services in the UK by April 2004, each catering for about 1 million populations each. A detailed plan outlines the structure, function and focus of these services. However, such ‘one size fits all’ model may not take into account differences in local population needs and preferences [47]. In particular it is not clear whether such generic services meet the specific demands and challenges of providing care for BME patients.
This study will explore the appropriateness, accessibility and acceptability of generic EI services for different ethnic groups within Birmingham to better understand care needs and preferences of service users and clinicians. We will also develop ethnically-appropriate outcome measures that can be used both in EI services and more broadly within mental health services.
Methodology:
Study design: Focus groups of service users, carers, health professionals and key stakeholders from voluntary sector and community groups will be conducted at several sites ensuring wide ethnic representation and moderated by members of the research team. Focus group topic guides will be developed from in-depth interviews with service users, carers, professionals, community organisations and a literature review. We will address themes of trust, alliance, ethnic sensitivity, cultural barriers to help-seeking, perception of unmet need and alternative provisions to improve BME users engagement and experience of services.
Sample: Participants will be drawn from the database of service users and the preliminary mapping exercise. User and carer groups will be homogenous in that professionals will be excluded, to allow users to express themselves freely in the absence of service providers. Special consideration will be given in the composition of the groups to issues of language and stigma, whereby users/carers may not wish to be with others from their own community. Since our priority is to promote creativity and the emergence of innovative ideas in service development, all other groups will be of mixed composition. A maximum number of 10 participants will be recruited for each focus group to allow generating a variety of perspectives. The focus groups will be convened as follows:
-
Six service user groups, two to be held at each geographical location in BSMHFT (HOB, South and North-East EI services). These will include people from a variety of ethnic backgrounds and perspectives on explanatory models, treatment and service provision in early psychosis.
-
Three carer groups, one from each site (as above). Purposive selection will be used to ensure a variety of sociodemographic and ethnic characteristics and experiences.
-
Three service provider groups, consisting of primary and secondary care providers and commissioners, mental health clinicians and members of NGO/voluntary sector.
The topic for each of these focus groups will be ‘How appropriate and accessible are generic EIS services for the specific ethnic and cultural needs of BME communities in Birmingham? How can these be improved?’ Cultural appropriateness and accessibility of services will be explored within several domains including user choice; importance, assessment and perceived respect for cultural needs; availability of interpreters and information leaflets in different languages; ethnic mix of the treating teams and services; and local provision of culturally appropriate ‘talking therapies’. Users and carers will be specifically asked about their perception of the relevance and importance of cultural and ethnic factors in the care received from EI services. For service improvement, preliminary findings from study 1 and 2 on pathways into care and coercive treatment will be briefly presented as a basis for a discussion. The discussion will focus on ethnic differences and determinants of pathways into care, predictors of detention, and ideas for innovative community alternatives to traditional in-patient care. The focus groups will be of approximately one and a half hours’ duration.
Analysis and outcomes:
Each interview will be transcribed verbatim and if, permitted by participants, audio-taped. Data will be analysed using Krueger’s framework and Rabiee’s guidelines [30] to identify themes that will inform about appropriateness and acceptability of EI services for different ethnic groups. We will develop ethnically appropriate and culturally-sensitive outcome measures for performance managing mental health services and ensuring that DRE expectations are met. We will produce guidelines on why and how EI services should be modified for the needs of the BME communities.
Research Team:
The research team consists of internationally recognised leaders in the field of ethnicity research, early intervention, epidemiology, health services evaluation, qualitative research, statistics, and senior managers from the trust, NGOs and BME community groups. Professor Singh has conducted research in early psychosis and ethnicity and developed EI services recognised for their vocational outcomes [15]. Professor Birchwood has led EI research and service development nationally and internationally, and was recently awarded the Richard Wyatt Award by the International Early Psychosis Association. Professor Weich co-directs the National Centre for Research in Ethnicity and Mental Health at Warwick Medical School and is the PI on the evaluation of Focussed Implementation Site Programme. Professor Lester is a GP, Professor of Primary Care Mental Health, the primary care lead of MHRN and mental health co-lead within the National School of Primary Care Research. Dr Bradby is a sociologist with expertise in mental health issues of BME communities. Professor Rabiee is a Professor of Public Health Promotion with interests in health and social policy, health inequalities and health promotion. Her current DH funded project is evaluating mental health services for Black African and Black-Caribbean communities in Birmingham. Professor Stallard is Professor of Medical Statistics at Warwick Medical School with expertise in statistical aspects of the design and analysis of clinical trials. Dr Deuchar is the Medical Director of BSMHFT. Roger Telfia is the Chief Executive of Future Health and Social Care, a partner NGO in the project. Ms Doherty leads the mental health section of Focus Futures, our other NGO partner. Ms Sanghera is regional NIMHE Race Equality Lead for the West Midlands. Mr Khan is an ex-service user who now works for Future Health and Social Care.
The research will be executed by a team of researchers, who have prior experience in conducting mental health research and are equipped with both qualitative and quantitative research skills. Dr. Zoebia Islam (Study Co-ordinator) has conducted research in the areas of disability, race, childhood and black and minority health and mental health issues. Dr. Rubina Jasani (Research Fellow), has conducted prior ethnographic with ethnic minorities both in India and the UK (within mental health settings). Dr. Ruchika Gajwani (Research Fellow) has undertaken a PhD in Psychology on pathways to emotional dysfunction in young people at Ultra-High-Risk for developing psychosis. Mr. Luke Brown (Research Associate) has masters of research degree in Clinical Psychology and has conducted research on suicide in psychosis and perceptions and prevalence of violence against psychiatric staff, from ‘mentally’ ill patients. Mr. Brown is also undertaking a PhD in Psychiatry.
Anticipated Outcomes:
The major outcome of this programme will be a demonstration that ethnic inequalities in access, experience and outcomes of mental health care for BME patients can be abolished or significantly reduced by services working innovatively and in collaboration with the voluntary and community sectors. We will develop an understanding of ethnic and cultural factors that influence help-seeking and factors that influence detention. We will develop conceptual models and good practice guidelines on how encounters between healthcare providers and service users and carers, who often hold conflicting explanatory systems about health and illness, can be negotiated to avoid coercion. We will establish the appropriateness, accessibility and acceptability of generic EI services for different ethnic groups and understand care needs and preferences of service users and clinicians. We will develop ethnically-appropriate outcome measures that can be used both in EI services and more broadly within mental health services. We will develop a clearer understanding of what contributes to social exclusion of BME service users with FEP and what promotes inclusion. The findings from the programme will inform community education programmes, family intervention strategies and interventions to improve patient engagement with services.
The outputs of this programme will include a series of high quality academic papers which will be submitted to high impact peer-reviewed journals and at high profile national and international conferences. We will also seek to disseminate our findings in a variety of other media that are more accessible to the wider NHS community and general public. This includes writing articles for journals that target specific NHS Management audiences including the Health Service Journal and publications from the voluntary sector. We will ensure that our findings are disseminated to mental health service user and carer communities and will use our strong connections with the MHRN regionally and nationally e.g. work with the Service User Research Group in England (SURGE) and with Rethink to ensure that this happens. The findings will also be disseminated through electronic media using university, mental health trust and service user websites.
The heath impact of the programme will be to help reduce the multiple health inequalities experienced by BME patients. Within its lifetime, the programme should be able to show that divergent trajectory of BME groups can be made convergent with other ethnic groups, thereby reducing inequalities of access, satisfaction and outcomes, particularly in terms of pathways to care, use of the MHA, clinical, social and vocational outcomes and social exclusion. It should lead to improvement in the quality of life for patients and their families. It may also lead to improvements at a health economy level, given the exceptionally high cost of untreated or inadequately treated psychosis.
Ethical Implications:
Patients with FEP are a potentially vulnerable group. We have a strong track record of working with young people with FEP in both clinical and research settings. In particular, we are mindful of key ethical issues of patient choice and the need to be entirely non-coercive in recruiting patients into research. There are particular ethical concerns about recruiting detained patients and their families, many of whom may be traumatised by the detention process. We will take special consideration of this while approaching patients for participation, ensuring that patients are only approached when clinically well, able and willing to give informed consent. We will also be mindful of any patients’ reluctance to talk about racism and discrimination, and also of the concerns about stigma of mental illness within BME communities when recruiting for focus group participants. For any patient or carer who wishes to be interviewed or exclude any staff from a particular ethnic background, we will provide alternatives as far as possible and feasible. Also, if any service user/carer decides to withdraw from the study, their information will be withdrawn and destroyed from the study with immediate effect.
The Trust’s research governance strategy and practice was recently audited and endorsed by the Strategic Health Authority. We will seek full ethical approval before initiating any data collection. Only trained or supervised researchers holding a Trust/NHS contract (honorary or full) will be allowed to contact potential participants. Recruitment of participants for interviews will be facilitated by their care co-ordinators. If potential participants agree to take part, written consent will be obtained and the original consent form will be kept on file. All researchers will be trained in sensitive and empathic interviewing style and closely supervised. Patient data will be anonymised and held on encrypted systems so as not to compromise the Data Protections Act (1998). Professor Singh will act as custodian for the data and will also supervise destroying the data five years after the completion of the study. Systems will be set up for reporting and managing any adverse events or misconduct during the studies.
References
- Fearon P., . Incidence of schizophrenia and other psychoses in ethnic minority groups: results from the MRC AESOP Study. Psychol Med 2006:1-10.
- Singh S.P., Grange T. Measuring pathways to care in first-episode psychosis: a systematic review. Schizophr Res 2006;81:75-82.
- Greenwood N., Singh S.P., Churchill R. Ethnicity and Mental Health Act 1983: A systematic review. London: DOH; 2006.
- Goater N., . Ethnicity and outcome of psychosis. British Journal of Psychiatry 1999;175:34-42.
- Parkman S., . Ethnic differences in satisfaction with mental health services among representative people with psychosis in south London: PRiSM study 4. British Journal of Psychiatry 1997;171:260-4.
- Sashidharan S. Institutional racism in British psychiatry. Psychaitric Bulletin 2001;25:244-7.
- Fernando S. Mental health, race and culture. Basingstoke: Palgrave Macmillan; 2001.
- Singh S.P., Burns T. Race and Mental Illness: There is More to race than Racism. BMJ 2006;333:648-51.
- Tait L., Birchwood M., Trower P. Adapting to the challenge of psychosis: personal resilience and the use of sealing-over (avoidant) coping strategies. Br J Psychiatry 2004;185:410-5.
- DOH . The Mental Health Policy Implementation Guide 2001. URL: www.dh.gov.uk,.
- DOH (2005) . Delivering Race Equality in Mental Health Care: An Action Plan for Reform Inside and Outside Services and the Government’s Response to the Independent Inquiry into the Death of David Bennett n.d. URL: http://www.dh.gov.uk/PublicationsAndStatistics/Publications/PublicationsPolicyAndGuidance/PublicationsPolicyAndGuidance.
- Birchwood M., Todd P., Jackson C. Early intervention in psychosis. The critical period hypothesis. Br J Psychiatry Suppl 1998;172:53-9.
- Craig T.K., . The Lambeth Early Onset (LEO) Team: randomised controlled trial of the effectiveness of specialised care for early psychosis. BMJ 2004;329.
- Petersen L., . A randomised multicentre trial of integrated versus standard treatment for patients with a first episode of psychotic illness. BMJ 2005;331.
- Mental Health and Social Exclusion 2004. London: Social Exclusion Unit, The Deputy Prime Ministers Office; n.d.
- McLean C., Campbell C., Cornish F. African-Caribbean interactions with mental health services in the UK: experiences and expectations of exclusion as (re)productive of health inequalities. Soc Sci Med 2003;56:657-69.
- NHS Confederation 2006. URL: http://www.nhsconfed.org/influencing/public_health_and_partnership.asp.
- Morgan C., . Pathways to care and ethnicity. 1: Sample characteristics and compulsory admission. British Journal of Psychiatry 2005;186:281-9.
- Morgan C., . Pathways to care and ethnicity. 2: Source of referral and help-seeking. British Journal of Psychiatry 2005;186:290-6.
- Crowther R., . Vocational rehabilitation for people with severe mental illness. Cochrane Database Syst Rev 2001.
- Bhui K., Bhugra D. Explanatory models for mental distress: implications for clinical practice and research. British Journal of Psychiatry 2002;181:6-7.
- Bhui K., . Ethnic variations in pathways to and use of specialist mental health services in the UK. Systematic review. British Journal of Psychiatry 2003;182:105-16.
- Morgan C., . Negative pathways to psychiatric care and ethnicity: the bridge between social science and psychiatry. Social Science and Medicine 2004;58:739-52.
- Marwaha S., Johnson S. Schizophrenia and employment – a review. Soc Psychiatry Psychiatr Epidemiol 2004;39:337-49.
- Becker D.R., . Job preferences of clients with severe psychiatric disorders participating in supported employment programs. Psychiatr Serv 1996;47:1223-6.
- Cook J.A., Razzano L. Vocational rehabilitation for persons with schizophrenia: recent research and implications for practice. Schizophr Bull 2000;26:87-103.
- Skeate A., . Duration of untreated psychosis and pathways to care in first-episode psychosis. Investigation of help-seeking behaviour in primary care. Br J Psychiatry Suppl 2002;43:s73-7.
- Singh S.P., . Determining the chronology and components of psychosis onset: The Nottingham Onset Schedule (NOS). Schizophr Res 2005;80:117-30.
- Singh S.P., . Three-year outcome of first-episode psychoses in an established community psychiatric service. British Journal of Psychiatry 2000;176:210-6.
- Rabiee F. Focus-group interview and data analysis. Proceedings of the Nutrition Society 2004;63:655-60.
- Lester H., Tritter J.Q., Sorohan H. Patients’ and health professionals’ views on primary care for people with serious mental illness: focus group study. BMJ 2005;330.
- Rabiee F, T. D. Widening Participation-Increasing Access to Higher Education for Muslim Women. Birmingham: University of Central England and Birmingham University; 2000.
- Richardson C., Rabiee F. ‘A Question of Access’ – an exploration of the factors influencing the health of young males aged 15–19 living in Corby and their use of health care services. Health Education Journal 2001;60:3-6.
- Singh S.P. Ethnicity in psychiatric epidemiology: need for precision. British Journal of Psychiatry 1997;171:305-8.
- Fisher H., . MIDATA: A clinician-based assessment package for evaluating early intervention services. Schizophrenia Research 2006;86.
- Singh S.P., O’Brien. The development and validation of the SOLES, a new scale measuring engagement with . . Journal of Mental Health 2009.
- Lloyd K.R., . The development of the Short Explanatory Model Interview (SEMI) and its use among primary-care attenders with common mental disorders. Psychol Med 1998;28:1231-7.
- Singh S.P., . Developing early intervention services in the NHS: a survey to guide workforce and training needs. Psychiatr Bull 2003;27:254-8.
- Kay S.R., Fiszbein A., Opler L.A. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 1987;13:261-76.
- O’Brien A. Engagement in Psychosis (unpublished MD thesis), in Mental Health 2006.
- Ruggeri M., . Development, internal consistency and reliability of the Verona Service Satisfaction Scale–European Version. EPSILON Study 7. European Psychiatric Services: Inputs Linked to Outcome Domains and Needs. Br J Psychiatry Suppl 2000:s41-8.
- Helman C.G. Culture, Health and Illness. Oxford: Butterworth-Heinemann; 1994.
- Mckenzie C., Knox V.J., Gelkoski W.L., Macaulay H.L. An Adaptation and Extension of the Attitudes Toward Seeking Professional Psychological Help Scale. Journal of Applied Social Psychology 2004;34:2410-35.
- Furnham A., Wong L. A cross-cultural comparison of British and Chinese beliefs about the causes, behaviour, manifestations and treatment of schizophrenia. Psychiatry Research 2007;151:123-38.
- King M, Dinos S., Shaw J., Watson R, Stevens S, Passetti F., et al. The Stigma Scale: development of a standardised measure of the stigma of mental illness. British Journal of Psychiatry 2007;190:8-254.
- Stratton P., Munton T., Hanks H., Heard D, Davidson C. Leeds Attributional Coding System Manual. Leeds: Leeds Family Therapy and Research Centre, Department of Psychology; 1988.
- Glasby J, Lester HE, B. J. Cases for change in adult mental health services. London: Department of Health; 2003.
Appendix 2 Sources used in the contemporary systematic review (2012)
A bibliographic database search was conducted to identify studies that explored ethnic differences in the use of the MHA in the UK. As the literature surrounding this was extensive, a search strategy was employed to identify existing systematic reviews from the following bibliographic databases: MEDLINE, Web of Science, PsycINFO, Google Scholar, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Electronic Theses Online Service (EThOS) – The British Library and The Cochrane Library. In addition, the search terms used were split into the following categories:
-
Mental Health Act terms [MHA, Detention, Hospital$]
-
mental illness/psychiatric conditions terms [exp. Schizophrenia and Disorders with Psychotic Features/ OR exp. Affective Disorders, Psychotic/ OR?psychosis.mp OR?psychotic disorder$.mp OR severe mental illness$.mp] AND [exp. Health Services Accessibility/ OR pathways to care.mp OR?pathways to mental health care.mp OR pathways to health care.mp OR pathways to psychiatric care.mp OR pathways to services.mp OR pathways to mental health services.mp OR pathways to health services.mp OR pathways to psychiatric services.mp] [First-Episode Psychosis]
-
compulsory detention terms
-
ethnicity terms [Ethnic$, Ethnic Minorit$, Black, Afro-Caribbean, Black-Caribbean, Asian, White-British]
-
pathway to care-related terms [Pathway to care, Pathways to care, service usage, service utilization].
Appendix 3 Scoring system for methodological quality of papers included in the meta-analysis
| Sample source and size | Score | Adjustment for confounding variables | Score | Ethnicity categorisation | |||
|---|---|---|---|---|---|---|---|
| Quality | Score | Use in the analysis | Score | ||||
| Routine data (e.g. health authority, GP list data) | 0 | None | 0 | Third-party reports (e.g. ward staff categorisation, name-based methods, skin colour methods) | 0 | Inappropriate ethnic groups combined for major study outcomes (black vs. all others) or poor method of collecting ethnicity data | 0 |
| Project-specific data: < 30 cases in ethnic groups for major outcomes | 1 | Age and/or gender | 1 | Self-reported ethnicity or use of census categories | 1 | Lumping of groups: reasonable combinations of groups collected by census/self-report method | 1 |
| Project-specific data: > 30 cases in ethnic groups for major outcomes | 2 | Diagnosis or disease severity (give 1 point if this sample is selected by diagnosis) | 1 | All analysis done on ethnic groups without amalgamation, and self-report/census categories for categorisation | 2 | ||
| Project-specific data: > 500 | 3 | Comorbidity and risk factors for outcome of interesta | 1–3 | ||||
| Maximum possibleb | 3 | 5 | 1 | 2 | |||
Appendix 4 Population census data 2011
Appendix 5 Service user general information sheet
Appendix 6 The Nottingham Onset Schedule
Appendix 7 The Emerging Psychosis Attribution Schedule
| Within the individual | In the social world |
|---|---|
| 1. Brain malfunctioning 2. Problems of mind 3. Personality/a part of who they are 4. Physiological or biological malfunction 5. Genetic/hereditary 6. Other within the individual causal beliefs |
10. Negative sexual experiences during childhood 11. Negative physical experiences during childhood 12. Negative psychological experiences during childhood 13. Negative sexual experiences during adulthood 14. Negative physical experiences during adulthood 15. Negative psychological experiences during adulthood 16. Lack of social support networks 17. Conflict with culturally defined norms 18. Economic and financial issues 19. Family disturbances 20. Death of loved one 21. Other social causal beliefs |
| In the natural world | In the supernatural world |
| 7. Medicine and narcotic use/abuse 8. As the result of accident or injury 9. Invasion of germs/infections |
22. Punishment for sins/wrongdoings by a supernatural force 23. Possession by jinn/bhoot/demons/sprits within 24. Supernatural human influence 27. Science-based occurrences outside the natural realms 26. Conspiracy against the individual 25. Interaction with a supernatural force 28. Other supernatural, cultural, spiritual attributions |
| 66. I thought it was normal: the participant thought that symptoms and symptom-related behaviour was not abnormal 77. Was not aware of it at the time: participant states that they were not aware of symptoms at the time that they were experiencing them 88. Can’t code 99. No causal belief given: participants were unable to give a causal belief 100. Other |
|
Appendix 8 Amended encounter form
Appendix 9 The SS101 and CR6B forms
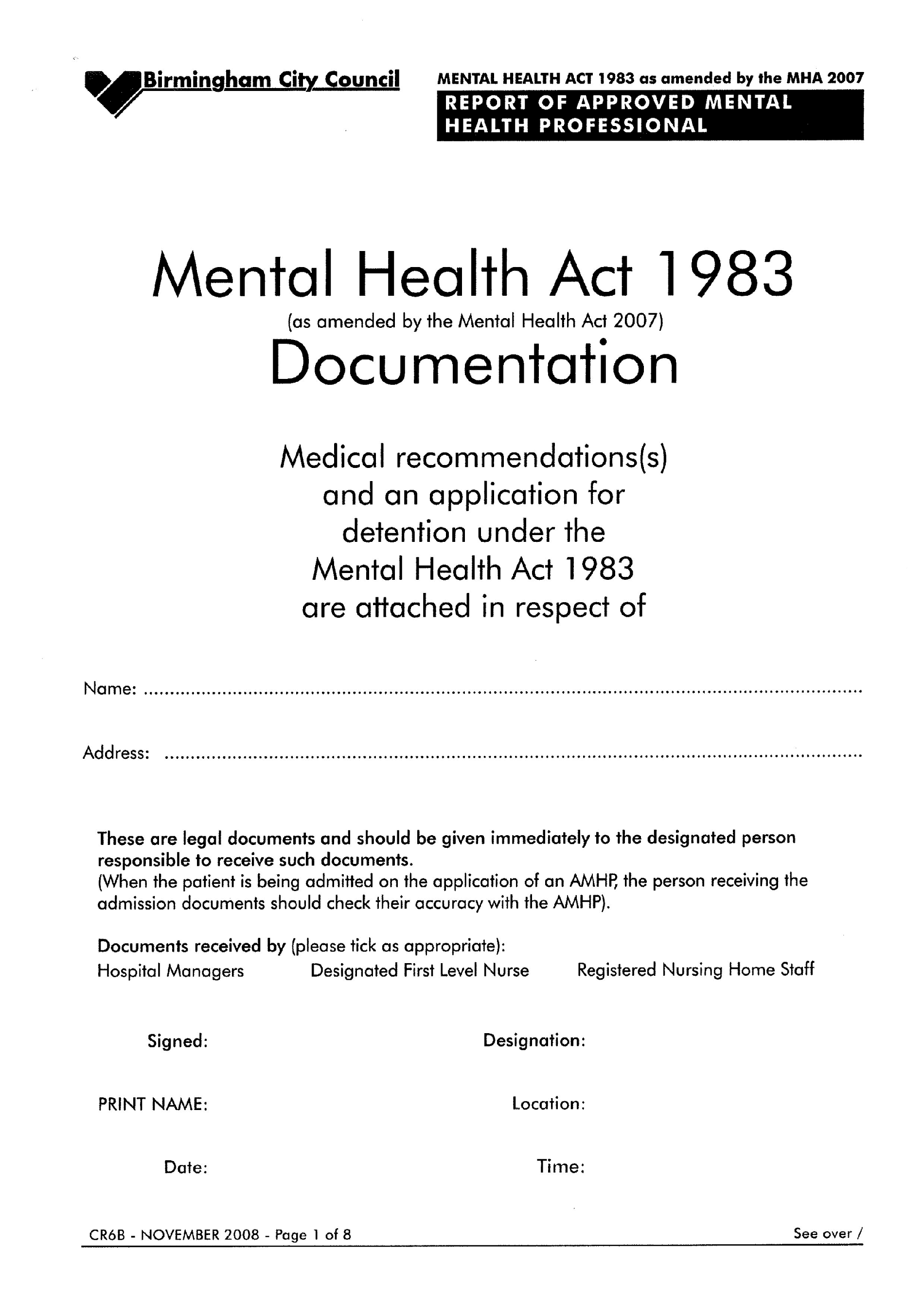
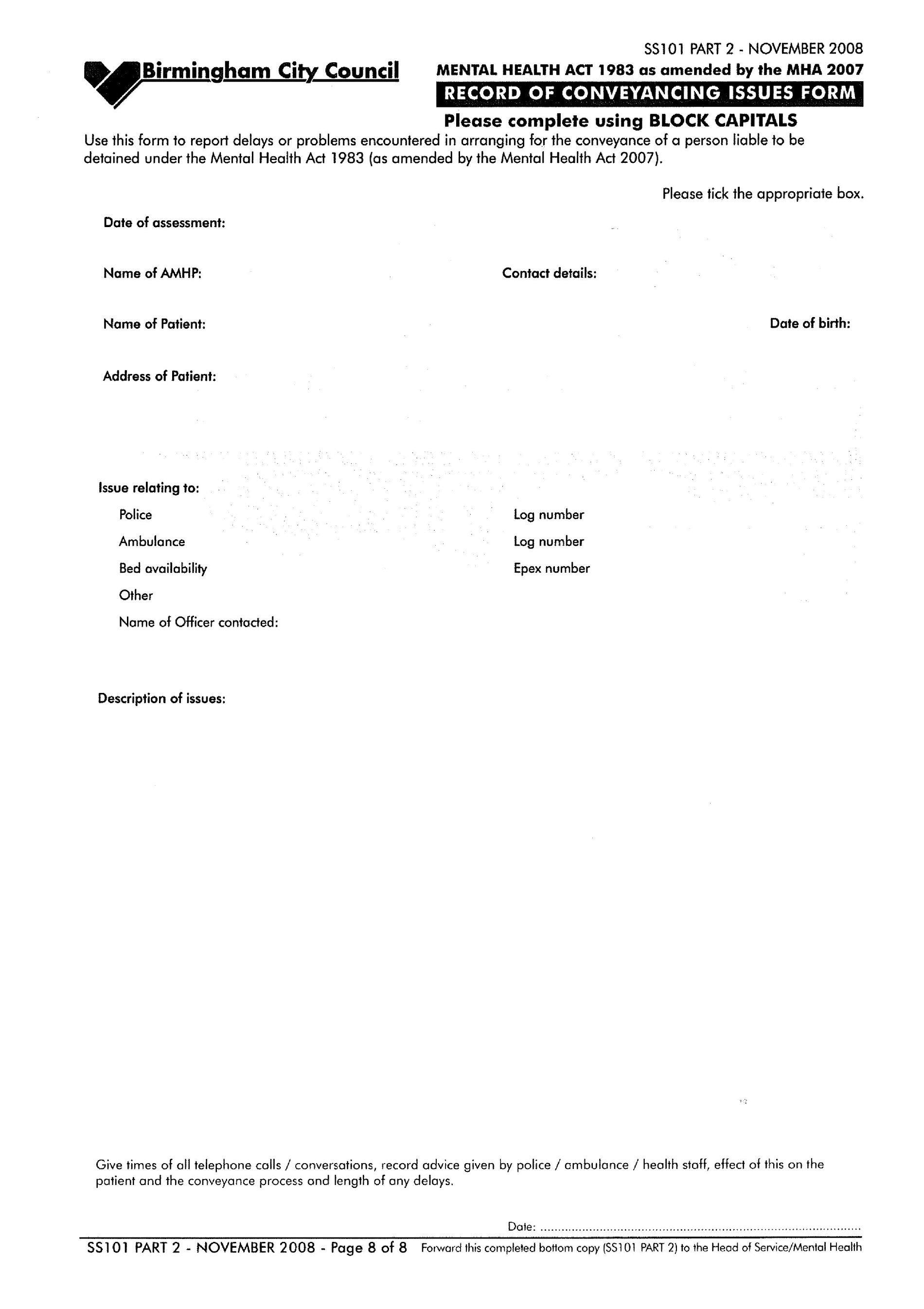
Appendix 10 Coding manual for ENRICH study 2
Assessment and service user details
Social circumstances
Mental health history
Risk
Risk as recorded explicitly by the AMHP on the CR6B form. The AMHP may have made the judgement of risk through conversation with attending doctors or other professionals or through conversation with family members/carers/friends and/or appropriate members of the public.
Persons present at the time of assessment
The following persons were recorded as being present at the time of assessment if they were detailed as being present by the AMHP on the CR6B form:
-
service user’s responsible clinician
-
assessing Section 12 doctor 1
-
assessing Section 12 doctor 2
-
community psychiatric nurse
-
force medical examiner or forensic medical examiner
-
service-user’s GP
-
ASW/AMHP (always present)
-
carer – family member
-
carer – friend
-
police officer
-
other (specified).
Nearest relative – notification of the assessment and subsequent action to the nearest relative recorded. Reasons for not notifying the nearest relative were also recorded.
Outcome of the assessment
The outcome of the assessment was recorded from the information on the CR6B form. Options included:
-
no psychiatric intervention
-
informal community treatment
-
informal admission
-
Section 2
-
Section 3
-
Section 4
-
not admitted – guardianship
-
admitted – guardianship
-
renewal of guardianship
-
regrading not implemented
-
inappropriate referral
-
other (specify)
-
no bed available*
-
not admitted to hospital (specify)
-
CTO
-
CTO revoked
-
assessment not completed
-
Section 2 recommendation but no bed available*
-
Section 3 recommendation but no bed available*
-
informal admission but no bed available*
-
discharged.
* Details of the bed availability were recorded, along with the section or informal admission recommended. If a bed was unavailable and the person was subsequently managed in the community, the outcome was recorded as not detained. However, if a bed was unavailable at the time of assessment but one became available later the same day or at a later date, the outcome would be recorded as the one recommended in the notes (section or informal admission).
Specify outcome
A ‘specify outcome’ variable followed the ‘outcome’ variable in which details of the outcome were recorded from the CR6B form or EPEX as applicable.
Reasons for outcome: not detained
Data were collected from the CR6B form on the alternatives to detention that were put in place at the time of the assessment. Multiple reasons could be listed as alternatives.
Alternatives to detention included the following factors:
Reasons for outcome: detained
Data were collected from the CR6B on the reasons for detention that were recorded at the time of the assessment. Multiple reasons could be listed.
Reasons for detention included the following factors:
Diagnosis
Four further variables were added to the end of the database including:
Notes
Any additional notes found on the CR6B form, EPEX, RiO or Jade that would illuminate or justify the nature of the recordings for all variables on the database were recorded by the research team.
Appendix 11 Carer general information sheet
Appendix 12 Voluntary and community organisations
| Voluntary/community organisation | Address/contact details |
|---|---|
| Afghan Youth & Family Association | 14 Halescroft Square, Northfield, Birmingham, B31 1HF Tel: 0121 243 4007 E-mail: Reza11afg@yahoo.com |
| Amina Women’s Group | Farhana Tel: 07966 142844 |
| Ashiana Community Project | 21–25 Grantham Road, Sparkbrook, Birmingham, B11 1LU Stefan Jones Tel: 0121 687 6767 |
| Ashram Housing Association | Fairgate House, 205 Kings Road, Tyseley, Birmingham, B11 2AA Tel: 0300 111 7000 E-mail: gurjitk@ashramha.org.uk |
| Asian Resource Centre | 110 Hamstead Road, Handsworth, Birmingham, B20 2QS E-mail: barc@asianresource.org.uk Web: www.asianresource.org.uk |
| Aston Parish Church | Witton Lane, Birmingham, B6 6QA Tel: 0121 327 3880 |
| The A-Team, Birmingham’s Primary Care Alcohol & Healthy Living Service | 113 Griffins Brook Lane, Bournville, Birmingham, B30 1QN Tel: 0121 475 8885 E-mail: Rene.cross@nacro.org, Sue.vincent@rapt.org.uk Web: www.alcoholservices-ateam.org.uk |
| AXIS BME Carer Groups | 198–200 Albert Road, Handsworth, Birmingham, B21 9JT Philomena Mcauley Tel: 0121 773 2922, 07818 510709 E-mail: philomena.mcauley@birmingham.gov.uk |
| Azaadi Community Drug Team | 296 Washwood Heath Road, Birmingham, B8 2UL |
| Birmingham Central Synagogue | 133 Pershore Road, Birmingham, B5 7PA Tel: 0121 440 4044 E-mail: sgrey@bhamjcc.co.uk |
| Birmingham Chinese Society | Tel: 0121 685 8510 E-mail: amycui@ccc-b.org.uk, MANDY.TSANG@REACHTHECHARITY.ORG.UK |
| Birmingham Irish Mental Health Forum | Ted Ryan E-mail: Mr.organisation@yahoo.co.uk |
| Birmingham LINk Make it Happen! | Gateway Family Services CIC, Radclyffe House, 66–68 Hagley Road, Birmingham, B16 8PF Tel: 0121 456 7820 E-mail: Andrew.john@gatewayfs.org |
| Birmingham Somali Welfare | Tel: 0121 440 8616, 07918 4019129 |
| BME Mental Health Community Development Worker Team | 4th Floor, Waterlinks House, Richard Street, Aston, Birmingham, B7 4AA New address: Suit 202, 2nd floor, CIBA Building, 146 Hagley Rd, Birmingham, B16 9NX Samina Arshad (mental health model of care improvement and development project manager) Tel: 0121 465 5178 E-mail: Samina.arshad@benpct.nhs.uk |
| Connexions Direct | Sara Brasington |
| Coping Opportunities Partnership Equality (COPE), Black Mental Health Foundation | 408 Aston Lane, Aston, Birmingham, B6 6QL Tel: 0121 551 7984 E-mail: admin@contactfamilycentre.org.uk |
| Council of Black Led Churches | St Georges Community Hub, Great Hampton Row, Birmingham, B19 3JG |
| Fairbridge West Midlands | 79 Warick St, Digbeth, Birmingham, B12 0NH Tel: 0121 773 1538 E-mail: Philip.rattigan@fairbridge.org.uk |
| Golden Hillock Community Day Centre | 107–111 Golden Hillock Road, Small Heath, Birmingham, B10 0DP Tel: 0121 753 2838 |
| Golden Hillock Mosque | 150 Golden Hillock Road, Small Heath, Birmingham, B10 0DX Zahida Evans, Amjad Rusool Tel: 0121 773 7277 E-mail: Imran.talib@ghamkolsharif.org |
| Green Lane Masjid | 20 Green Lane, Small Heath, Birmingham, B9 5DB Qari Zakaulllah E-mail: info@greenlanemasjid.org Monday and Wednesday mornings between 0930 and 1200 |
| Guru Nanak Nishkam Sevak Jatha | 18–20 Soho Road, Handsworth, Birmingham, B21 9BH Tel: 0121 515 4299 E-mail: info@mca.org |
| KIK IT (culturally sensitive multilingual drug support services) | 153 Stratford Road, Sparkbrook, Birmingham, B11 1AH Diana Laurence Tel: 0121 771 1119 E-mail: kikit@ashianacp.org.uk |
| Mashriq Challenge | Mashriq Challenge Resource Centre, Mashriq MCRC Ltd, 131 Soho Hill, Hockley, Birmingham, B19 1AT Salma Lokath Tel: 0121 551 5478 |
| Midlands Vietnamese Community Association | Handsworth, Birmingham, B19 1DA Tel: 0121 554 9685 E-mail: Mvrca1982@yahoo.com |
| MIND | Julie Wilson Tel: 0121 608 8001 E-mail: juliewilson@birminghammind.org |
| MYTIME | Tel: 0121 766 6699 |
| Northside Welcome Centre | 176 Streetly Road, Erdington, Birmingham, B23 7AL Saptal Singh Tel: 0121 377 6136 Open between 1000 and 1400 |
| Piece of Mind | Tel: 0121 243 1270 |
| Rehab UK | Suzanne Ashby Tel: 0121 616 3900 E-mail: suzanneashby@rehabuk.org |
| Rethink | 9 St Michaels Court, Victoria Street, West Bromwich, B70 8ET Idrees Kiyani (mental health recovery worker) Tel: 07918 192853 E-mail: Idrees.kayani@rethink.org |
| RSVP: Rape and Sexual Violence Project | Lisa Thompson Tel: 0121 200 1695 E-mail: rsvp@fsmail.net |
| Saathi House | 49 Bevington Road, Birmingham, B6 6HR Peyara Begum Tel: 0121 328 0013 Fax: 0121 328 0081 |
| Shakeelas, Saltley Fellowship User Day Centre | Elaine Lucas Tel: 0121 327 3223 |
| SIFA Fireside | Ground Floor, 18–28 Lower Essex Street, Birmingham, B5 6SN 122 Pershore Street, Birmingham, B5 6PA Beth Wood, mental health project worker Tel: 0121 666 7023 Fax: 0121 622 7250 Email: office@sifafireside.co.uk, bethwood@sifafireside.co.uk |
| Sikh Youth Service | Khalsa House, 4 Holyhead Road, Handsworth, Birmingham, B21 OLT Charan Singh Tel: 0121 554 8034 |
| Start Again Project | Jonathan Reece Tel: 07565 244317 E-mail: Johnathan.reece@start-again.co.uk |
| Unity FM | Stratford Road, Sparkhill, B11 1AR Hussein E-mail: studio@unityfm.net, Nassar25@hotmail.co.uk |
| Women Acting in Today’s Society | Marion Clarke (counsellor) Chris Tee (Chinese women support and development worker) Tel: 0121 713 1676 Web: www.waitsaction.org |
List of abbreviations
- AMHP
- approved mental health professional
- ANOVA
- analysis of variance
- ASW
- approved social worker
- BCC
- Birmingham City Council
- BME
- black and minority ethnic
- BSMHFT
- Birmingham and Solihull Mental Health NHS Foundation Trust
- CAMHS
- Child and Adolescent Mental Health Services
- CI
- confidence interval
- CMHT
- community mental health team
- CPN
- community psychiatric nurse
- CTO
- community treatment order
- df
- degrees of freedom
- DUI
- duration of untreated illness
- DUP
- duration of untreated psychosis
- EPAS
- Emerging Psychosis Attribution Schedule
- FEP
- first-episode psychosis
- GP
- general practitioner
- IMD
- English Indices of Deprivation
- MHA
- Mental Health Act
- MHRN
- Mental Health Research Network
- NOS
- Nottingham Onset Schedule
- OR
- odds ratio
- PANSS
- Positive and Negative Syndrome Scale
- SD
- standard deviation
- SEMI
- Short Explanatory Model Interview
- WREC
- Warwickshire Research Ethics Committee