Notes
Article history
The research reported in this issue of the journal was funded by PGfAR as project number RP-PG-0407-10029. The contractual start date was in July 2008. The final report began editorial review in December 2013 and was accepted for publication in March 2015. As the funder, the PGfAR programme agreed the research questions and study designs in advance with the investigators. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PGfAR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Neil Marlow reports personal fees from Novartis (Basel, Switzerland), Shire plc (Dublin, Ireland) and GlaxoSmithKline plc (Middlesex, UK), outside the submitted work.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by Field et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
Choice of topic
At the time that this programme grant was conceived, in 2007, the intention was to improve understanding of some of the key contributors to the high rates of early childhood morbidity and mortality in the UK. This broad aim remains relevant as, although progress has been made in the intervening years, these same themes appeared in the 2012 Chief Medical Officer’s (CMO’s) report published in October 2013. 1
When planning the research it was clear that it would not be possible to target all of the factors that contribute to early childhood mortality and morbidity, but our intention, and the linking theme of the work, was to focus on important areas of practice and/or policy in which knowledge and understanding were lacking. Therefore, the original application was focused on three topic areas.
Perinatal and early childhood mortality rates
Although UK stillbirth, neonatal and infant mortality rates had generally reduced over previous decades, it was clear that there were wide health inequalities in these rates across the country2 and overall stillbirth rates had demonstrated much more limited change. 3 Furthermore, it was recognised that UK rates for each of these measures were high compared with those in similar developed countries. 4
Premature birth was known to be the major component of both neonatal and infant mortality, accounting for approximately 50% of neonatal deaths,2 with very preterm birth (< 33 completed weeks’ gestation) account for most of the deaths. Previous data from our group demonstrated that rates of delivery of < 33 weeks were particularly high in the UK, and we also found that rates of very premature birth doubled when the least deprived areas of the country were compared with the most deprived. 5 However, at the start of this programme there was little information about the extent to which variation around the country was explained by differences in other causes of early death such as congenital anomaly or, indeed, other aspects of how and where premature infants were managed.
Late and moderately preterm birth
Late and moderately preterm (LMPT) birth is defined as birth between 32 and 36 completed weeks’ gestation. At the time of our application this area was largely unstudied in the UK and yet, numerically, LMPT babies remain the largest group of preterm babies. 6,7 In particular, we did not know whether or not deprivation had the same influence on these babies or if most of them were born because it was considered safer to end a pregnancy in which some complication had arisen. Perhaps more importantly, we knew little about the degree to which these babies contributed to early childhood mortality and morbidity. Better understanding of the risks attached to delivery at this gestation was seen as important in helping families and clinicians in the management of high-risk pregnancies in which delivery between 32 and 36 weeks’ gestation was seen as an option.
Our third stream of work was intended to explore the use of biochemical markers to identify women early in pregnancy who were at high risk of preterm delivery. This stream was considered unlikely to deliver benefit to the NHS within 3–5 years [a prerequisite for National Institute for Health Research (NIHR) programme grants] and hence this stream was not funded.
Therefore, the report of the programme that follows describes the outputs from two streams of work.
Stream 1
This stream was designed to focus on an analysis of stillbirth and early childhood mortality rates, with the aim of improving understanding of the different influences on these rates in the UK. The work relied heavily on both routine data and more specialist data collected for other purposes.
Stream 2
This stream focused on the contribution of the group of babies born at 32–36 weeks’ gestation to both early mortality and morbidity. This work was based on a cohort of babies born LMPT and a random set of term-born control infants.
Developments during the course of the programme grant
In terms of the work focused on early childhood mortality, developments/new information during the course of the programme reinforced the need for more detailed studies to take place. In particular, in the years leading up to 2010 the NHS had a key target of reducing the health inequalities in infant mortality by 10%. 8 Despite this, health inequalities were widening at the time this programme commenced. A lack of understanding of the major influences on both neonatal and infant mortality was identified at a Department of Health workshop as one of the major difficulties in achieving the target. Therefore, even if one sets aside the huge importance to individuals and communities in reducing neonatal and infant mortality, there remains a need to understand the public health and societal influences that lead to both the UK’s relatively high rates of death in early life and the associated health inequalities. In particular:
-
the scale of the impact of deprivation on the published rates
-
the effect of cultural and religious differences between communities which, for example, could influence the management of antenatally identified severe congenital anomalies
-
the extent to which public health interventions could influence particular causes of death (such as sudden infant death syndrome).
Without such an understanding it was simply not possible to develop a rational approach to reducing perinatal and early childhood mortality rates.
During the period of the programme grant, a range of studies focusing on LMPT babies were published from around the world, but particularly in the USA, where such babies were growing in number. However, most of these studies were small and retrospective and without the opportunity to combine data about antenatal events, neonatal course and subsequent development. Certainly no such studies have emerged from the UK.
New questions did arise, in particular regarding the extent to which LMPT births contribute to the overall burden of morbidity resulting from prematurity. Routine data from Scotland9 demonstrated a link to an increased incidence of special educational need in babies born LMPT, but it remained unclear whether this was a generic risk attached to all babies born at these gestations or whether the affected babies represented a specific subset that could be identified (and potentially targeted for intervention) in the antenatal or neonatal period.
Therefore, the aims and objectives of the programme, which are set out at the start of the report from each stream, remained both topical and relevant.
Chapter 2 Understanding inequalities in cause-specific infant mortality (stream 1)
Aim
The aim of stream 1 was to understand the recent widening inequalities in infant mortality rates (death in the first year of life) by exploring cause-specific mortality, gestation and deprivation.
Objectives
Original objectives
-
To investigate if excess infant deaths related to prematurity have increased in more deprived areas.
-
To investigate how inequalities in cause-specific infant, neonatal and perinatal mortality have changed over time.
-
To explore health inequalities in neonatal and perinatal mortality among very preterm infants and to identify whether or not service use varies with deprivation.
-
To explore risk factors for mortality in the neonatal and perinatal period.
-
To develop newly defined cause-specific mortality targets for primary care trusts (PCTs) accounting for variations in case mix.
Deviations from the original planned research
The original research plan focused on one of the key determinants of inequality in neonatal mortality: deaths related to immaturity, including detailed analyses of these deaths to improve understanding of the reason(s) for these inequalities using detailed regional data. Results from early analyses indicated that another key element of the socioeconomic inequalities associated with infant mortality is congenital anomalies. Deaths as a result of a congenital anomaly accounted for the largest proportion of the deprivation gap in neonatal mortality attributable to a single cause, and also represented a significant proportion of the deprivation gap in stillbirths. It seemed clear that understanding how these inequalities related to congenital anomalies arose was key to implementing effective public health interventions to reduce socioeconomic inequalities in infant and neonatal mortality. The objectives of the study were, therefore, modified in order to allow a detailed exploration of the underlying reasons behind these issues, looking particularly at the impact of variations in patterns of termination of pregnancy for congenital anomaly on rates of stillbirth, live birth and neonatal mortality. It was felt that this should take higher priority, as little research has been undertaken in this area. The presence of the East Midlands and South Yorkshire Congenital Anomalies Register (EMSYCAR) within the same research team facilitated this analysis.
As a priority, our research planned to look at adjusting infant mortality rates at a local level for differences in case mix, particularly socioeconomic deprivation. This was intended to aid policy-makers and commissioners working in PCTs to reliably assess how they compared with other regions with broadly similar population case mix and hence assess whether or not appropriate packages of care could be implemented in their region to improve outcomes. However, it was apparent on close inspection of the data when embarking on this work that there were major differences in the reporting of live births of infants aged 22 and 23 weeks’ gestation. Based on international research, variations in birth registration practices have been shown to have a major influence on infant mortality rankings and there was clearly a need to assess the scale of this issue in the UK in order that ‘real’ variations in performance could be separated from those arising as a result of artefactual/administrative differences. Therefore, it seemed essential to explore the available data for the UK on the variation in the registration of births of infants at 22 and 23 weeks of gestation and the impact of this variation on infant mortality.
Amended objectives
-
To investigate socioeconomic inequalities in cause-specific neonatal mortality rates in England (study 1).
-
To investigate socioeconomic inequalities in cause-specific stillbirth rates in England (study 2).
-
To explore the reasons underlying cause-specific inequalities in mortality (study 3).
-
To improve comparisons of mortality between health regions accounting for variations in case mix (study 4).
Study 1: investigating socioeconomic inequalities in cause-specific neonatal mortality in England
Background
Despite overall improvements in mortality and neonatal care, in the UK 17 babies die just before, during or just after birth every day, with around 6500 deaths per year. 10 Wide socioeconomic inequalities exist in stillbirth and neonatal mortality, with significantly higher rates in the most deprived areas of England. 11 The UK government made major attempts to tackle socioeconomic inequalities in infant mortality by setting a public service agreement target in 2003 to reduce the relative deprivation gap in England and Wales by 10% by 2010. 8 However, the deprivation gap in all-cause mortality, rather than narrowing, showed evidence of widening. 12 The limitations of all-cause mortality analyses meant that it was not clear how this widening gap was influenced by changes in the underlying trends in specific causes of death.
Preterm birth is the main cause of neonatal and infant mortality, accounting for two-thirds of neonatal deaths in England. 2 Rates of very preterm birth have increased over time in the UK and internationally5,13 and, as these rates are generally higher in more deprived areas of the UK,5 it is likely that this is associated with an increase in the absolute numbers of excess deaths relating to deprivation. Such an effect clearly has the potential to result in a widening of the health inequalities in infant mortality. Therefore, this research was designed to unpick the socioeconomic inequalities in all-cause mortality, by exploring cause-specific trends over time, and identify major potentially modifiable risk factors for mortality.
This study provided a detailed exploration of socioeconomic inequalities in infant and neonatal mortality in England using routinely available data sets.
Objective
To investigate socioeconomic inequalities in cause-specific neonatal and infant mortality in England.
Methods
Description of data sets utilised
In order to achieve this objective, analyses utilised data at a national level to explore health inequalities in cause-specific infant, neonatal and perinatal mortality. As this study was based on routinely collected data that were anonymised, there was no requirement for ethics approval. The study focused on the 12-year period of 1 January 1997 to 31 December 2008 and utilised several national data sets.
National (England) data: mortality
Individual-level data on all neonatal deaths (death before 28 days of life) of singleton infants born to mothers resident in England between 1 January 1997 and 31 December 2008 came from the Centre for Maternal Child Enquiries (CMACE; www.cmace.org.uk), which until 2011 collected neonatal mortality data as part of its national perinatal mortality surveillance work, funded by the National Patient Safety Agency. Originally, CMACE and its predecessor organisation collected data for all stillbirths and infant deaths; however, from 1 January 2004, CMACE data collection was limited to stillbirths and neonatal mortality, although data for late fetal losses at 22 and 23 weeks’ gestation were collected until 3 December 2006. The cessation of collection of postneonatal mortality data prevented analyses of infant mortality for the whole 12-year period. However, sensitivity analyses were undertaken using information on infant mortality in 1997–2003 to assess the differences in patterns between neonatal and infant mortality. Data included cause of death, type of death (i.e. stillbirth, late fetal loss, neonatal death or postneonatal death), gestation, date of birth, mother’s age, sex of the infant, birthweight, ethnic group, multiplicity and the mother’s lower super output area (LSOA) of residence an area used in the 2001 and 2011 UK censuses,14 covering around 1500 households. Only neonatal and postneonatal deaths with a valid LSOA were included; otherwise, no deprivation score could be assigned, but this excluded only 1% of deaths.
Classification of causes of deaths
For the national data on mortality, a local CMACE co-ordinator initially classified deaths using the extended Wigglesworth hierarchical classification system. 15 A CMACE regional manager then checked them with reference to post-mortem and coroner’s reports, when available. Finally, CMACE carried out central cross-validation checks to ensure consistency.
In this report, for neonatal deaths (i.e. live births ending in a death before 28 days of life) and postneonatal deaths (deaths up until 1 year of life) the Wigglesworth classification has been used but has been expanded for deaths caused by immaturity, on the basis of gestational age at birth (< 24 weeks, 24–27 weeks and 28–36 weeks). Accidental deaths were grouped with ‘other specific conditions.’ Unfortunately, because of the changes in the classification systems used by CMACE over the time period, 1997–2008, neonatal death data classified by Wigglesworth cause of death (Box 1) were available only from 1997 to 2007, as in 2008 CMACE implemented a new cause of death classification that was not comparable with previous years of data. Therefore, for analyses involving cause of death, 11 years of data were available (1997–2007) but, for analyses of overall mortality, 12 years of data were available.
Congenital anomaly.
Intrapartum event.
Immaturity (< 24 weeks).
Immaturity (24–27 weeks).
Immaturity (28–36 weeks).
Infection.
Accidents and other specific causes.
Sudden infant death.
Denominator data: live births
Ideally, individual-level birth denominator data were required from the NHS Numbers For Babies (NN4B) project. This data set was established in 2005 and part of the financial rationale for its implementation was to provide denominator live-birth data, including gestational age (not previously available in England) for easy access by researchers. However, this aim had not been achieved and the data set was not routinely available in a timely manner. Additionally, because of confidentiality issues, data for analysis were not available at the individual level and linkage and so, unfortunately, were not usable for these analyses. After a lengthy period of unproductive negotiation, a decision was made to resort to using Office for National Statistics (ONS) birth registrations for calculating mortality rates. As no gestational age information is included in these data, this limited the detailed analyses of issues relating to prematurity. Furthermore, as a result of regulatory stipulations associated with access to ONS data, it was not possible to obtain individual-level data on live births. Birth data were, therefore, obtained in two separate ways in order to facilitate the different analyses to be undertaken. First, the number of live births by year of birth and LSOA of residence were obtained to enable the calculation of mortality rates by LSOA. These data allowed exploration of trends over time. A second data set, used primarily for study 3, was obtained from the ONS on live births with additional information on birthweight, mother’s age, sex and multiplicity of birth. These data were available only in an aggregated form providing data for deprivation deciles of LSOAs across England.
Measurement of socioeconomic deprivation
Previous government targets in England and Wales measured the relative deprivation gap by using a classification of socioeconomic group based on the father’s occupation. 12 This excluded both infants whose parents had never worked and those who were solely registered by the mother. This led to the exclusion of a significantly at-risk group. Consequently, this method of measurement of socioeconomic group is inadequate. Ideally, individual measures of socioeconomic deprivation would have been used. However, as the overall aim of this programme was to utilise routine data to assess and monitor socioeconomic inequalities, an area-level measure of deprivation was chosen to fulfil this role. Therefore, socioeconomic inequalities were measured by using the Index of Multiple Deprivation (IMD) for 200416 at the LSOA level.
This measure of multiple deprivation is made up of seven domain indices at the LSOA level, which relate to (1) income deprivation; (2) employment deprivation; (3) health deprivation and disability; (4) education; (5) skills and training deprivation; (6) barriers to housing and services; and (7) living environment deprivation and crime. LSOAs are the smallest areas for which these deprivation data are available; although some degree of heterogeneity exists within them, the small size of the areas (only 1500 residents) limits this.
All LSOAs in England were ranked by deprivation score. They were then weighted by its population of births (using the live-birth denominator data) and divided into 10 groups with approximately equal populations of births in each from 1 (least deprived) to 10 (most deprived). Thus, when calculating mortality rates, if stillbirth or neonatal mortality was the same for all deprivation groups, a similar number of neonatal deaths would be expected in each of the 10 groups. This approach offered the potential not only to monitor mortality but also to allow targeted interventions at an area level in the future.
Data linkage
The national infant mortality and stillbirth data were provided with LSOA codes. The IMD 200416 was then linked to the mortality data matching on LSOA code, facilitating the linkage to the LSOA-level ONS birth denominator data set by LSOA-level code. The second, more detailed ONS births data set was linked using deprivation decile, multiplicity of birth, mother’s age, sex of the baby and the PCT of residence at birth.
Statistical analyses
The aim of these analyses was to explore the deprivation gap in neonatal and infant mortality over time, first at an all-cause level and then by specific cause to unpick the key causes of death that related to socioeconomic inequalities in mortality. In order to explore trends by socioeconomic deprivation neonatal mortality rates for each cause of death by deprivation decile and time period were calculated. Analyses were undertaken solely for singleton births in this study because, in relation to multiple births, a variety of factors (such as differential access to fertility treatment) affects the rate at which multiple births occur and, in addition, multiple births are associated with both a higher mortality rate and additional specific causes of death.
Exploring the deprivation gap
Poisson regression models17 were used to assess trends in mortality by deprivation decile over time, fitting separate models for all-cause mortality and each specific cause of neonatal mortality. Previous UK targets for reducing socioeconomic inequalities in infant mortality8 have been based on the relative deprivation gap identified in 2003. In the work carried out within this programme, in order to co-ordinate with the national targets, the relative deprivation gap was measured by fitting a linear trend between deprivation decile and mortality, and calculating the mortality rate ratio between the most deprived and least deprived deciles which is similar in approach to the relative index of inequality. 18 Significant change in the relative deprivation gap over time was assessed by fitting a separate deprivation effect for each time period. Reductions in neonatal mortality over time were explored by relative change (percentage reduction in mortality rate by deprivation decile).
Investigating both the relative and absolute deprivation gap can provide a better understanding of time trends in socioeconomic inequalities. For example, if a condition is relatively common, a small relative gap may be associated with a large absolute difference in rates. Adjusting for the underlying prevalence can ignore important changes in the absolute deprivation gap. Therefore, absolute changes in stillbirth and neonatal mortality over time by deprivation decile (difference in neonatal mortality per 10,000 births by deprivation decile) were calculated to assess improvements in mortality. The delta method was used to calculate confidence limits. 19 Excess mortality associated with deprivation was estimated as a percentage by separately applying the stillbirth rate and neonatal mortality rate in the least deprived decile to the total population divided by the total number of deaths observed. The proportion of the deprivation gap for both all-cause stillbirth and all-cause neonatal mortality explained by each cause for each time period was calculated. For each specific cause, the neonatal mortality rates in the least deprived decile and the most deprived decile for each time period were calculated using the Poisson regression models. The absolute difference between these two rates was calculated and expressed as a proportion of the absolute difference in rates for all causes combined.
Results
Deprivation gap in all-cause neonatal mortality over time
Between 1997 and 2007, a total of 18,524 neonatal deaths of singleton infants were notified to CMACE All-cause neonatal mortality decreased over time from 31.4 per 10,000 live births (1997–9) to 25.1 per 10,000 live births (2006–7), but this differed by deprivation group. In absolute terms, rates were significantly higher in the most deprived areas (Table 1). Between 1997–9 and 2006–7 rates decreased more in the least deprived decile than in the most deprived decile (most deprived decile, 7.4 fewer deaths per 100,00 births; least deprived decile, 5.6 fewer deaths per 10,000 births). However, the relative reduction in mortality over time was smaller in the most deprived decile (17%) than in the least deprived decile (26%), leading to a widening of the deprivation gap. Table 2 details the regression equation for all-cause mortality. In 1997–9 infants risk of neonatal death in the most deprived decile was twice that in the least deprived [mortality rate ratio 2.08, 95% confidence interval (CI) 1.92 to 2.27], and this gap widened significantly over time, reaching a peak of 2.68 in 2003–5 before slightly narrowing to 2.35 in 2006–7. Consequently, the percentage of excess deaths associated with deprivation increased over the time period from 32.3% (1997–9) to 51.0% (2003–5) and then decreased to 37.5% (2006–7). Consequently, there was no evidence of an overall reduction over the time period to achieve the relevant NHS targets.
| Cause of death | Deprivation decile | Mortality per 10,000 live births | Reduction in mortality from 1997–9 to 2006–7 | ||||
|---|---|---|---|---|---|---|---|
| 1997–9 | 2000–2 | 2003–5 | 2006–7 | Relative change, % (95% CI) | Absolute change per 10,000 births (95% CI) | ||
| All causes | Least deprived | 20.8 | 18.3 | 16.9 | 14.9 | 26.1 (18.9 to 32.7) | 5.55 (3.89 to 7.21) |
| Most deprived | 46.4 | 46.6 | 43.5 | 35.9 | 16.7 (10.4 to 22.6) | 7.41 (4.49 to 10.32) | |
| Cause-specific deaths | |||||||
| Congenital anomaly | Least deprived | 5.7 | 3.9 | 4.0 | 4.1 | 31.3 (16.9 to 43.3) | 1.60 (0.81 to 2.39) |
| Most deprived | 12.4 | 12.4 | 10.5 | 10.5 | 9.5 (–4.6 to 21.7) | 1.05 (–0.45 to 2.56) | |
| Intrapartum events | Least deprived | 2.4 | 2.7 | 3.1 | 2.2 | 15.6 (–9.4 to 34.9) | 0.45 (–0.23 to 1.13) |
| Most deprived | 3.6 | 2.5 | 3.2 | 2.6 | 29.4 (9.9 to 44.6) | 1.17 (0.37 to 1.96) | |
| Immaturity < 24 weeks’ gestation | Least deprived | 2.6 | 3.5 | 2.9 | 2.7 | 1.9 (–22.4 to 21.4) | 0.06 (–0.58 to 0.69) |
| Most deprived | 8.6 | 10.7 | 11.2 | 9.3 | –4.0 (–22.0 to 11.3) | –0.35 (–1.76 to 1.07) | |
| Immaturity 24–27 weeks’ gestation | Least deprived | 4.9 | 3.4 | 3.1 | 2.7 | 44.7 (31.4 to 55.4) | 2.19 (1.44 to 2.94) |
| Most deprived | 9.9 | 8.0 | 7.4 | 6.1 | 35.1 (22.9 to 45.4) | 3.24 (2.00 to 4.48) | |
| Immaturity 28–36 weeks’ gestation | Least deprived | 1.0 | 1.1 | 0.8 | 0.5 | 56.8 (32.3 to 72.4) | 0.81 (0.42 to 1.21) |
| Most deprived | 3.0 | 1.8 | 2.4 | 0.9 | 60.4 (42.3 to 72.8) | 1.63 (1.03 to 2.23) | |
| Infection | Least deprived | 1.8 | 1.4 | 1.3 | 1.2 | 24.6 (–1.9 to 44.3) | 0.49 (–0.02 to 0.99) |
| Most deprived | 3.7 | 4.2 | 3.7 | 3.1 | –5.2 (–33.0 to 16.8) | –0.20 (–1.11 to 0.72) | |
| Accidents and other specific causes | Least deprived | 1.8 | 0.9 | 1.0 | 0.8 | 10.7 (–24.5 to 35.9) | 0.17 (–0.32 to 0.66) |
| Most deprived | 2.8 | 3.2 | 2.6 | 2.4 | 7.2 (–23.0 to 29.9) | 0.19 (–0.53 to 0.91) | |
| Sudden infant death | Least deprived | 0.3 | 0.9 | 0.3 | 0.4 | 6.8 (–69.0 to 48.6) | 0.03 (–0.21 to 0.27) |
| Most deprived | 1.4 | 1.3 | 1.1 | 0.5 | 40.3 (6.9 to 61.7) | 0.62 (0.11 to 1.14) | |
| Variable | Coefficient | SE | 95% CI |
|---|---|---|---|
| Constant | 0.002 | < 0.001 | |
| Year (2000–2) | 0.85 | 0.035 | 0.78 to 0.92 |
| Year (2003–5) | 0.77 | 0.032 | 0.71 to 0.84 |
| Year (2006–7) | 0.74 | 0.035 | 0.67 to 0.84 |
| Deprivation decile | 2.08 | 0.089 | 1.92 to 2.27 |
| Deprivation decile year (2000–2) | 1.22 | 0.076 | 1.08 to 1.37 |
| Deprivation decile year (2003–5) | 1.29 | 0.081 | 1.14 to 1.46 |
| Deprivation decile year (2006–7) | 1.13 | 0.081 | 0.98 to 1.30 |
Deprivation gap in specific-cause neonatal mortality over time
The next step was to explore these deaths in more detail by investigating the cause-specific mortality. Immaturity was the most common cause (45.4%), followed by congenital anomalies (24.5%), intrapartum events (10.8%), infection (9.8%), accidents and other specific causes (7.1%), and sudden infant deaths (3.0%). The number of deaths increased with increasing deprivation for each cause, although the magnitude of this increase varied by cause. With the exception of deaths due to immaturity of < 24 weeks’ gestation, neonatal mortality fell over time for all causes, with the greatest falls seen for immaturity of 24–27 and 28–36 weeks’ gestation.
For five of the eight causes of death [congenital anomalies, immaturity (< 24 weeks and 24–27 weeks), infection and accidents and other specific causes], there was a larger relative fall in mortality over time in the least deprived decile than in the most deprived decile, although this was only statistically significant for congenital anomalies (Table 3). For these causes and immaturity (28–36 weeks) the trend in the deprivation gap over time was similar to all-cause neonatal mortality, with an initial two- to threefold ratio deprivation gap in 1997–9 (neonatal mortality rate ratio range 1.70–2.98) which increased up to 2003–5 (range 2.17–4.14) followed by a slight narrowing in 2006–7 (range 1.72–3.16) (see Table 3). The widest deprivation gap was seen for death due immaturity of < 24 weeks’ gestation, with the risk of death in the most deprived decile in 1997–9 being threefold that in the least deprived decile; the increased risk of death rose to over fourfold in 2003–5 and fell again slightly to threefold in 2006–7. As the absolute mortality did not fall over this time period, this widening of the deprivation gap led to the deaths due to immaturity of < 24 weeks’ gestation representing a larger proportion of all deaths in 2006–7 (21.7%) than in 1997–9 (16.9%).
| Cause of death | 1997–9, mortality rate ratio (95% CI) | 2000–2, mortality rate ratio (95% CI) | 2003–5, mortality rate ratio (95% CI) | 2006–7, mortality rate ratio (95% CI) | Test for interaction between deprivation and year |
|---|---|---|---|---|---|
| All causes | 2.08 (1.92 to 2.27) | 2.53 (2.32 to 2.77) | 2.68 (2.45 to 2.93) | 2.35 (2.10 to 2.63) | p = 0.0004 |
| Cause-specific deaths | |||||
| Congenital anomaly | 2.16 (1.82 to 2.56) | 2.92 (2.43 to 3.51) | 3.06 (2.54 to 3.70) | 2.85 (2.27 to 3.58) | p = 0.0264 |
| Intrapartum events | 1.37 (1.07 to 1.76) | 1.15 (0.87 to 1.53) | 1.21 (0.94 to 1.56) | 1.15 (0.82 to 1.61) | p = 0.7817 |
| Immaturity < 24 weeks’ gestation | 2.98 (2.42 to 3.67) | 3.28 (2.66 to 4.05) | 4.14 (3.40 to 5.06) | 3.16 (2.47 to 4.04) | p = 0.1217 |
| Immaturity 24–27 weeks’ gestation | 1.88 (1.57 to 2.25) | 2.49 (2.03 to 3.06) | 2.38 (1.94 to 2.92) | 2.21 (1.68 to 2.91) | p = 0.1779 |
| Immaturity 28–36 weeks’ gestation | 1.88 (1.35 to 2.62) | 1.74 (1.16 to 2.59) | 3.22 (2.10 to 4.95) | 1.72 (0.93 to 3.18) | p = 0.1393 |
| Infection | 1.92 (1.45 to 2.54) | 2.66 (2.00 to 3.53) | 2.17 (1.57 to 3.00) | 2.68 (1.88 to 3.83) | p = 0.3333 |
| Accidents and other specific causes | 1.70 (1.23 to 2.35) | 2.29 (1.65 to 3.18) | 2.71 (1.92 to 3.83) | 1.77 (1.18 to 2.65) | p = 0.1987 |
| Sudden infant death | 3.62 (2.15 to 6.07) | 2.47 (1.49 to 4.07) | 2.08 (1.26 to 3.43) | 2.32 (1.14 to 4.73) | p = 0.4806 |
Rates of intrapartum death and sudden infant death showed fell more among the most deprived decile than in the least deprived, leading to a non-significant narrowing of the deprivation gap in mortality of these causes. However, these deaths constituted only 13.5% of deaths, and their impact on all-cause mortality was small. Deaths due to intrapartum events showed the narrowest deprivation gap (ranging from 1.15 to 1.37 across the time period). Consequently, the reduction in deaths if the rates seen in the least deprived decile were applied across all deciles was small, ranging from 6.8% to 14.8%. In contrast, the deprivation gap for sudden infant deaths was the widest seen for any specific cause in 1997–9 (mortality rate ratio 3.62). This showed a non-significant decrease over time to 2.32 in 2006–7. Sudden infant deaths would have been reduced by over half in 1997–9 if mortality rates for the least deprived decile were applied to the whole population, compared with a reduction of just over one-third in 2006–7.
Graphical approach to understanding the deprivation gap
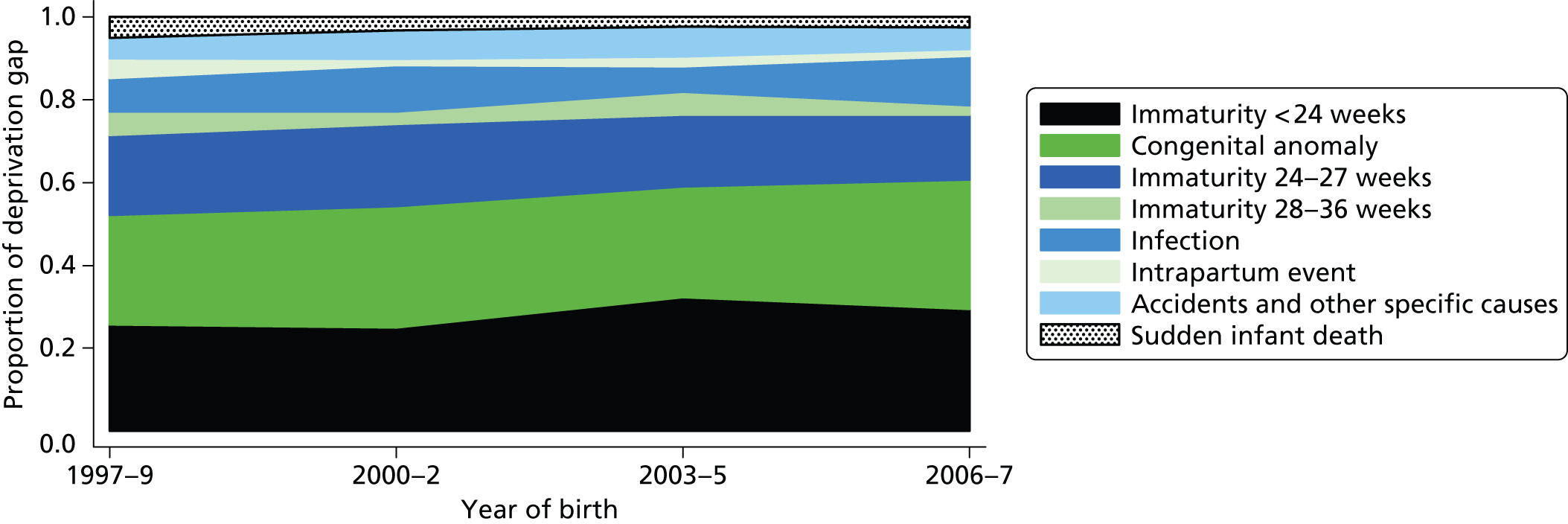
In order to best convey the cause-specific socioeconomic inequalities in mortality, a graphical approach was chosen. Figure 1 demonstrates the percentage of the deprivation gap in all-cause neonatal mortality explained by each specific cause. The width of the bands is directly related to the proportion of the deprivation gap in neonatal mortality that each cause accounts for. This graph clearly demonstrates that deaths due to immaturity (babies of < 24, 24–27 and 28–36 weeks’ gestation) and congenital anomalies explain the majority of the deprivation gap in all-cause mortality. Thus, all deaths due to immaturity and congenital anomalies combined accounted for 77% of the deprivation gap in 1997–9, rising to a peak of 81.9% in 2003–5 and then declining again to 79% in 2006–7. This increase in the proportion of the deprivation gap explained by prematurity and congenital anomalies was due to a combination of a widening deprivation gap in mortality for these causes, the high proportion of deaths due to these causes and a lack of decline in mortality due to immaturity at < 24 weeks. The remaining causes (sudden infant death, intrapartum events, infection, accidents and other causes) account for only 20% of the deprivation gap. Their reduced impact is partially related to their relatively smaller contribution to overall mortality, but also the narrow deprivation gap in mortality for intrapartum deaths. The percentage of the gap explained by sudden infant deaths fell over time from 5% (1997–9) to 2.5% (2006–7).
FIGURE 1.
Proportion of the deprivation gap in all-cause neonatal mortality rates explained by each cause of death over time. Reproduced from Smith et al.,20 © 2010, British Medical Journal Publishing Group, under the terms of the Creative Commons Attribution Non-Commercial Licence (CC BY-NC 2.0), which permits use, distribution and reproduction in any medium, provided the original work is properly cited, the use is non-commercial and is otherwise in compliance with the licence.
Sensitivity analyses
Sensitivity analyses of infant mortality rates (1997–2003) showed extremely similar trends in the deprivation gap over time for all-cause mortality and death from each specific cause, but deprivation gaps for individual causes of death tended to be higher than for neonatal mortality overall. In 1997–9, sudden infant deaths explained 20% of the deprivation gap in all-cause infant mortality, but this declined to 8% by 2003. In contrast, immaturity and congenital anomalies accounted for 53% of the deprivation gap in 1997–9, increasing to 73% in 2003, similar to the percentage seen in neonatal mortality. Hence, although the percentage of infant deaths due to each cause differed from neonatal deaths in 1997–9, over time the patterns became increasingly similar as immaturity and congenital anomalies played a greater role.
Conclusions
Key findings
-
As there was a decrease in neonatal mortality over the period 1997–2007, the relative deprivation gap (the ratio of mortality in the most deprived decile to that in the least deprived decile) increased, particularly for deaths related to congenital anomalies and immaturity.
-
Almost 80% of the relative deprivation gap in all-cause mortality was explained by premature birth and congenital anomalies.
Limitations and strengths
Availability of death data
This work focused on neonatal mortality, as data on gestation-specific postneonatal deaths after 2003 were not available. However, patterns in infant mortality in 1997–2003 were extremely similar to those seen for neonatal mortality, with a slightly wider deprivation gap.
Individual-level socioeconomic data
No routine data on individual risk behaviour, lifestyle, health and ethnicity were available for the mothers included in this work. Inevitably this has limited the extent of the conclusions that can be drawn and has the potential to have introduced a degree of confounding. For example, epidemiological work using individual-level data has shown wide differences in stillbirth rates associated with maternal smoking during pregnancy, hypertension and maternal obesity. Neonatal deaths are also known to be more common in sole registrations. The lack of individual-level data also meant that it was not possible to identify women who had had more than one neonatal death over the time period. However, while women who had had a neonatal death were more likely to have a recurrence, the proportion of neonatal deaths that were likely to have shown this pattern was low and, therefore, negligible in terms of our findings.
Despite these caveats, provided the results are treated with caution and trends are not extrapolated beyond the time period under study, our methods are relatively straightforward and provide a way for health service planners to monitor the latest trends in mortality.
Implications for policy and practice
Although targets were set to reduce inequalities in infant mortality by 2010 in the UK,8 the deprivation gap did not narrow. Cause-specific analyses provide more detailed information, highlighting the contribution of each causal group and the impact of interventions or changes in society over time.
In the absence of cause-specific analyses various identifiable actions were recommended in England and Wales to reduce the deprivation gap in infant mortality by the target 10% (Dr Marilena Korkodilos, Specialist Public Health Services at Public Health England, 2010, personal communication). These are, in order of magnitude of anticipated reduction:
-
increasing breastfeeding rates and reducing obesity in the routine and manual group
-
reducing rates of smoking during pregnancy
-
alleviating overcrowded housing
-
reducing teenage conceptions.
However, while these were all laudable aims, it seems clear from the work presented here that, unless interventions target specifically the risk of very premature birth and potentially lethal congenital abnormalities, the impact on the deprivation gap is likely to be minor. For example, even accounting for the higher rates of infant mortality due to sudden infant death compared with neonatal mortality, based on our findings the contribution to the total mortality gap is simply too small to have a significant impact. The situation is somewhat different for smoking, as there is evidence to suggest that smoking is an important factor in the aetiology of preterm birth and, as a consequence, infant mortality. 21 The potential impact of reducing obesity and teenage pregnancy is less clear, in terms of existing evidence. However, smoking, obesity and teenage pregnancy have all been the subject of longstanding public health campaigns of limited success and the UK suggested goals required major behavioural changes. Our lack of understanding about the everyday environmental influences on the risk of preterm birth and major congenital abnormalities appears to be a significant impediment to the development of a rational strategy for diminishing the influence of deprivation on measures of early childhood mortality. Research has previously demonstrated the importance of immaturity in the UK compared with other European countries22 and the March of Dimes has highlighted the problem in global terms. 13 Tackling the wide deprivation gap among those less born at than 24 weeks’ gestation is likely to be achievable not through further progress in neonatal care but only through prevention. The need for a greater understanding of the mechanistic link between deprivation and prematurity is a major research priority, which would then allow a focus on primary preventative strategies to reduce the rate of prematurity itself. Our lack of understanding about the influence of health inequality in relation to major congenital anomalies deserves no less attention.
These findings point to ways in which our understanding of the social influences on early childhood mortality rates in particular localities might be improved, for example:
-
The annual cause-specific mortality should be measured and overall neonatal and infant mortality rates should be reviewed. Cause-specific analyses provide much greater insight into socioeconomic inequalities in neonatal mortality on a global level, thus facilitating each country’s/area’s understanding of its early childhood mortality rates and identifying appropriate interventions for prioritisation.
-
The use of the father’s occupational class to assess socioeconomic group should be avoided, as this excludes single mothers from analyses, a significant at-risk group. Area-level deprivation measures offer an inexpensive and quick way to continue monitoring inequalities. However, the collection of, and timely access to, comprehensive individual-level information for neonatal deaths and denominator data would be a further improvement.
-
Improved data linkage between large routine data sets such as NN4B would facilitate considerable improvement in the research related to socioeconomic inequalities in infant mortality.
-
Greater focus should be placed on the influence of preterm birth and congenital anomalies in neonatal mortality.
-
Strategies for reducing socioeconomic inequalities should focus on the prevention of preterm birth rather than improvements in neonatal care, particularly for babies born before 24 weeks’ gestation.
Recommendations for future research
-
There is a great need for a greater understanding of the mechanistic link between deprivation and prematurity. In order to reduce socioeconomic inequalities in neonatal mortality rates, there needs to be a shift in focus from targeting risk factors that have a minimal effect on prematurity rates to major primary prevention strategies for preterm birth.
-
The methods proposed here for monitoring inequalities in neonatal mortality provide a quick and straightforward way of monitoring socioeconomic inequalities in the future. However, the collection of, and timely access to, comprehensive individual-level information for neonatal deaths is required to confirm the findings at an individual level.
Study 2: investigating socioeconomic inequalities in cause-specific stillbirth in England
Background
Although there have been considerable improvements in health care in developed countries, stillbirth remains a common adverse pregnancy outcome,23 and in the UK rates have been particularly high. 24 This issue appears to be intractable and, in contrast to the improvements seen in neonatal mortality, there has been little or no reduction in rates of stillbirth over time. 3 This has led to an increase in the contribution of stillbirths to perinatal mortality. Consequently, stillbirth is a major public health burden that is frequently overlooked, since stillbirths are often excluded from international comparisons of maternal and infant health. 25,23
This burden has not affected all groups alike. Socioeconomic inequalities in stillbirth rates have been found in the UK and internationally,24,26,27 with women in deprived areas at higher risk of stillbirth. These deprivation differences persist even after adjusting for factors such as attendance at antenatal appointments or previous reproductive history. 28 Inequalities in stillbirth in England and Wales have existed for many years and research based on data from 1981–92 showed no signs of them diminishing. 29
Little is known about the differences in the deprivation gap by specific causes of stillbirth in the UK. Stillbirths are an extremely diverse group, with a variety of possible causes potentially resulting in a stillbirth. Consequently, identifying specific causes of stillbirth is extremely difficult. However, stillbirth is known to be linked to factors such as placental abruption, congenital anomalies and intrapartum events. It has been noted that the deprivation gap is different for different causes of neonatal mortality20 and it is likely that this is also true for stillbirths. Neasham et al. 30 investigated the extended perinatal mortality rate and noted that increased deprivation was associated with increased mortality as a result of non-chromosomal anomalies. Guildea et al. 27 noted a deprivation gap in unexplained antepartum stillbirths. However, these and other studies have been based on relatively small populations and addressed a limited number of causes.
In the UK, the Stillbirth and Neonatal Death Society (SANDS) has campaigned for further research into stillbirth, and in particular the extent to which deprivation is a risk factor for stillbirth. 31 As discussed above, successive UK governments have made major attempts to tackle socioeconomic inequalities in infant mortality culminating with the setting of a public service agreement target in 2003 to reduce the relative deprivation gap in England and Wales by 10% by 2010. 8 However, these targets neglected the issue of socioeconomic inequalities in stillbirth. Furthermore, the boundaries between early neonatal deaths and stillbirth are in many cases extremely blurred. There has been no recent evidence relating to the effect of deprivation on the overall stillbirth rate or indeed whether or not the deprivation gap has changed over time. An analysis of socioeconomic inequalities in stillbirth in England using routinely available data sets in conjunction with the analyses of neonatal deaths allowed a more detailed picture of socioeconomic inequalities in relation to early-life mortality.
Objective
The aim was to investigate socioeconomic inequalities in cause-specific stillbirth rates in England.
Methods
Description of data sets utilised
In order to achieve these objectives, analyses utilised national-level data to explore health inequalities in cause-specific stillbirths. As this study was based on routinely collected data that were anonymised, there was no requirement for ethics approval. The study focused on the 12-year period between 1 January 1997 and 31 December 2008, and utilised several national data sets.
Individual-level data on all singleton stillbirths (infants born at ≥ 24 weeks’ gestation and showing no signs of life at birth) born to mothers resident in England between 1 January 1997 and 31 December 2008 were obtained from the CMACE, which had collected neonatal mortality and stillbirth data as part of its national perinatal mortality surveillance work funded by the National Patient Safety Agency until 2012. Data included cause of death, gestation, date of birth, mother’s age, sex of the infant, birthweight, ethnic group, multiplicity and mother’s place of residence (LSOA). Only stillbirths with a valid LSOA were included as, otherwise, no deprivation score could be assigned, but this excluded only 1% of deaths.
Classification of causes of deaths
For the national data on stillbirth, a local CMACE co-ordinator initially classified deaths using the obstetric (Aberdeen) classification system32 for stillbirths (Table 4). A CMACE regional manager then checked them with reference to post-mortem and coroner’s reports when available. Finally, CMACE carried out central cross-validation checks to ensure consistency.
| Category | Comprised deaths due to |
|---|---|
| Congenital anomalies | Neural tube defects |
| Other anomalies | |
| Pre-eclampsia | Pre-eclampsia without antepartum haemorrhage |
| Pre-eclampsia complicated by antepartum haemorrhage | |
| Antepartum haemorrhage | Antepartum haemorrhage with placenta praevia |
| Antepartum haemorrhage with placental abruption | |
| Antepartum haemorrhage of uncertain origin | |
| Mechanical | Cord prolapsed or compression with vertex or face presentation |
| Other vertex or face presentation | |
| Breech presentation | |
| Oblique or compound presentation, uterine rupture, etc. | |
| Maternal disorder | Maternal hypertensive disease |
| Other maternal disease | |
| Maternal infection | |
| Miscellaneous | Isoimmunisation because of rhesus or other antigens |
| Neonatal infection | |
| Other neonatal infection | |
| Specific fetal condition | |
| Unexplained antepartum (SGA) | Unexplained antepartum (birthweight ≤ 10th percentile) |
| Unexplained antepartum (not SGA) | Unexplained antepartum (birthweight > 10th percentile) |
| Unclassifiable | Unclassified |
| Missing |
Several of the rarer classification groups of the obstetric (Aberdeen) classification system were combined. As so many deaths were in the unexplained antepartum deaths category, these were then divided on the basis of birthweight (≤ 10th percentile or > 10th percentile), resulting in nine categories (see Table 4). Similar to the situation for neonatal deaths, data on stillbirths, with information on cause of death according to the Aberdeen classification, were available for only 8 years (i.e. from 1 January 2000 to 31 December 2007).
Denominator data: live births
The ONS birth registrations were combined with CMACE data on stillbirths to obtain a denominator of all births, used for calculating stillbirth rates. As there is no gestational age information in these data, this limited the detailed analyses of prematurity. As discussed in the analyses of neonatal deaths, birth data were obtained on the number of live births by year of birth and LSOA of residence in order to calculate mortality rates by LSOA. This allowed exploration of trends over time.
Measurement of socioeconomic deprivation
The same methodology was used for measuring socioeconomic deprivation as in the analyses of neonatal deaths, utilising routine data to assess and monitor socioeconomic inequalities. The IMD for 200416 at the LSOA level enabled allocation of a deprivation score to all infants with a valid postcode. These data were obtained from the ONS.
As for the analyses of neonatal deaths, all LSOAs in England were ranked by deprivation score. The LSOAs were then weighted by their population of births (using all births as a denominator) and divided into 10 groups with approximately equal populations of births in each from 1 (least deprived) to 10 (most deprived). Thus, when calculating mortality rates, if stillbirth rates were the same for all deprivation groups, a similar number of stillbirths would be expected in each decile.
Data linkage
National stillbirth data were provided with LSOA codes. The IMD 200416 was then linked to the mortality data matching on LSOA code. These data were then linked to the LSOA-level ONS birth denominator data set by LSOA-level code.
Statistical analyses
First, analyses were undertaken at an all-cause level and then by specific cause to identify the key causes of death that related to socioeconomic inequalities in stillbirth. In order to explore trends by socioeconomic deprivation, stillbirth rates were calculated for each cause of death by deprivation decile and time period. Analyses were undertaken for singleton births only, as, in relation to multiple births, a variety of factors (such as differential access to fertility treatment) affect the rate at which multiple births occur and, in addition, it is known that multiple births are associated with both a higher mortality rate and additional specific causes of death.
Exploring the deprivation gap
As for the analyses of neonatal mortality, Poisson regression models were used to assess trends in mortality by deprivation decile over time,17 fitting separate models for all-cause mortality and each specific cause of death for stillbirths. As discussed, UK targets for reducing socioeconomic inequalities in infant mortality8 were based on the relative deprivation gap, to avoid the influence of the underlying prevalence. The relative deprivation gap was assessed by fitting a linear trend between deprivation decile and mortality and calculating the mortality rate ratio between the most deprived and least deprived deciles, which is similar in approach to the relative index of inequality. 18 Significant change in the relative deprivation gap over time was assessed by fitting a separate deprivation effect for each time period. Reductions in stillbirth over time were assessed by calculating the relative change (percentage reduction in stillbirth rate by deprivation decile).
Once again the absolute change in the outcome (in this case stillbirth) was calculated over time by deprivation decile to assess improvements in mortality. The delta method was used to calculate confidence limits. 19 Excess mortality associated with deprivation as a percentage was estimated by separately applying the stillbirth rate in the least deprived decile to the total population and dividing that by the total number of stillbirths observed. The proportion of the deprivation gap in all-cause stillbirth rates explained by each cause was calculated for each time period. Then for each specific cause, the stillbirth rate was estimated in the least deprived decile and the most deprived decile for each time period by using the regression models. The absolute difference in these two rates was then calculated and expressed as a proportion of the absolute difference in rates for all causes combined.
Results
Deprivation gap in all-cause stillbirth rates over time
From 2000 to 2007, 21,472 singleton stillbirths were reported to CMACE; of these, LSOA was missing in 120 (0.6%) and cause of death was missing or unclassifiable in 919 (4.3%), leaving 20,433 for analyses. First, the overall rate of stillbirth over time and by deprivation was assessed (Table 5). The overall stillbirth rate was 4.4 per 1000 births and there was no evidence of a change in stillbirth rate over time (2000–3 rate, 4.4 per 1000; 2004–7, 4.4 per 1000; p = 0.80). The total number of stillbirths in each deprivation decile increased as deprivation increased, with the number in the most deprived decile approximately double that in the least deprived. Women from the most deprived decile were twice as likely to experience a stillbirth of any cause than those from the least deprived (rate ratio 2.1, 95% CI 2.0 to 2.2; p < 0.0001). There was no evidence that this changed over time.
| Variable | Coefficient | SE | 95% CI |
|---|---|---|---|
| Constant | 0.0004 | < 0.001 | |
| Year (2004–7) | 0.991 | 0.029 | 0.94 to 1.05 |
| Deprivation decile | 2.117 | 0.068 | 1.99 to 2.25 |
| Deprivation decile year (2004–7) | 0.999 | 0.045 | 0.91 to 1.09 |
Deprivation gap in cause-specific stillbirth rates
Looking at stillbirths by cause of death (Table 6) revealed that antepartum deaths of unknown cause accounted for the highest percentage of stillbirths [59.2%: 21.3% small for gestational age (SGA); 37.9% not SGA] followed by antepartum haemorrhage (13.0%); maternal disorders (9.1%); congenital anomalies (7.8%); pre-eclampsia (4.2%) and mechanical issues during labour (2.4%). The remaining 4.3% were due to miscellaneous or unclassified reasons and were excluded from the Poisson regression analyses.
| Cause of death | Deprivation decile (1 = least deprived, 10 = most deprived) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | Total | |
| Live births | 463,148 | 464,092 | 464,487 | 465,295 | 465,814 | 466,377 | 467,227 | 467,767 | 468,144 | 469,044 | 4,661,395 |
| Stillbirths | |||||||||||
| All cause | 1489 | 1526 | 1642 | 1783 | 1991 | 2099 | 2372 | 2647 | 2760 | 3043 | 21,352 |
| Cause-specific stillbirths | |||||||||||
| Congenital anomalies | 106 | 111 | 116 | 114 | 159 | 132 | 184 | 229 | 258 | 258 | 1667 (7.8) |
| Pre-eclampsia | 60 | 66 | 70 | 71 | 80 | 96 | 121 | 112 | 111 | 107 | 894 (4.2) |
| Antepartum haemorrhage | 141 | 152 | 185 | 229 | 261 | 287 | 302 | 366 | 372 | 478 | 2773 (13.0) |
| Mechanical | 52 | 40 | 46 | 46 | 51 | 67 | 52 | 55 | 47 | 56 | 512 (2.4) |
| Maternal disorder | 130 | 126 | 157 | 156 | 190 | 181 | 222 | 258 | 275 | 251 | 1946 (9.1) |
| Miscellaneous (including isoimmunisation) | 26 | 32 | 37 | 31 | 25 | 32 | 38 | 47 | 42 | 47 | 357 (1.7) |
| Unknown antepartum (SGA) | 293 | 290 | 351 | 385 | 374 | 438 | 527 | 574 | 613 | 709 | 4554 (21.3) |
| Unknown antepartum (not SGA) | 650 | 682 | 635 | 701 | 790 | 802 | 874 | 942 | 960 | 1051 | 8087 (37.9) |
| Unclassifiable | 31 | 27 | 45 | 50 | 61 | 64 | 52 | 64 | 82 | 86 | 562 (2.6) |
There was no evidence of trends of increasing or decreasing rates of stillbirth over time for any specific cause (Table 7); however, the deprivation gap varied by cause. Mechanical issues during labour was the only specific cause for which there was no evidence of a deprivation gap [relative risk (RR) 1.2, 95% CI 0.9 to 1.5]. All other causes of stillbirth showed a significant deprivation gap, varying from a 1.7- to a 3.1-fold difference. The widest deprivation gap was seen for deaths due to antepartum haemorrhage; women from the most deprived decile were 3.1 (95% CI 2.8 to 3.5) times more likely to experience stillbirth of this cause than those from the least deprived decile. Wide deprivation gaps were also seen for deaths due to congenital anomalies (rate ratio 2.8, 95% CI 2.4 to 3.3) and maternal disorders such as hypertension (RR 2.2, 95% CI 1.9 to 2.5). The deprivation gap was wider for stillbirths of infants who were SGA (RR 2.5, 95% CI 2.3 to 2.7) than for those who were not SGA (RR 1.7, 95% CI 1.5 to 1.8; p = 0.26) (see Table 4). The percentage excess deaths of all causes related to deprivation was 33%, suggesting in total one-third more stillbirths were observed than would have been expected if the stillbirth rate for all deprivation groups were the same as that for the least deprived decile.
| Cause of death | Deprived decile | Rates of stillbirth per 10,000 births (95% CI) | Change in mortality from 2000–3 to 2004–7 (95% CI) | ||
|---|---|---|---|---|---|
| 2000–3 | 2004–7 | Absolute change per 10,000 births | Relative change (%) | ||
| All stillbirths (N = 20,433) | Least deprived | 29.3 (28.1 to 30.5) | 29.3 (26.0 to 32.9) | –0.3 (–2.0 to 1.4) | 1.0 (0.9 to 1.0) |
| Most deprived | 61.9 (59.9 to 64.0) | 61.2 (59.3 to 63.2) | –0.7 (–3.5 to 2.2) | 1.0 (0.9 to 1.0) | |
| Cause-specific stillbirths | |||||
| Congenital anomalies (n = 1667; 8.1%) | Least deprived | 2.0 (1.8 to 2.4) | 1.7 (1.1 to 2.6) | –0.1 (–0.5 to 0.4) | 1.0 (0.8 to 1.2) |
| Most deprived | 6.3 (5.6 to 7.0) | 5.2 (4.6 to 5.8) | –1.1 (–2.0 to -0.2) | 0.8 (0.7 to 1.0) | |
| Pre-eclampsia (n = 894; 4.4%) | Least deprived | 1.4 (1.2 to 1.7) | 1.4 (0.8 to 2.5) | –0.2 (–0.6 to 0.2) | 0.9 (0.7 to 1.1) |
| Most deprived | 2.8 (2.4 to 3.3) | 2.4 (2.1 to 2.9) | –0.4 (–1.0 to 0.2) | 0.9 (0.7 to 1.1) | |
| Antepartum haemorrhage (n = 2773; 13.6%) | Least deprived | 3.3 (2.9 to 3.7) | 3.1 (2.2 to 4.3) | –0.2 (–0.7 to 0.3) | 0.9 (0.8 to 1.1) |
| Most deprived | 10.5 (9.7 to 11.4) | 9.2 (8.5 to 10.1) | –1.2 (–2.4 to –0.1) | 0.9 (0.8 to 1.0) | |
| Mechanical (n = 512; 2.5%) | Least deprived | 0.9 (0.7 to 1.2) | 0.7 (0.3 to 1.4) | 0.2 (–0.2 to 0.5) | 1.2 (0.8 to 1.6) |
| Most deprived | 1.3 (1.0 to 1.6) | 1.1 (0.9 to 1.4) | –0.2 (–0.5 to 0.2) | 0.9 (0.6 to 1.2) | |
| Maternal disorder (n = 1946; 9.5%) | Least deprived | 2.5 (2.2 to 2.8) | 2.2 (1.5 to 3.2) | 0.5 (–0.03 to 1.0) | 1.2 (1.0 to 1.4) |
| Most deprived | 5.9 (5.3 to 6.6) | 6.1 (5.5 to 6.7) | 0.2 (–0.7 to 1.1) | 1.0 (0.9 to 1.2) | |
| Unknown antepartum (SGA) (n = 4554; 22.3%) | Least deprived | 6.0 (5.5 to 6.6) | 6.1 (4.7 to 7.8) | –0.2 (–0.9 to 0.6) | 1.0 (0.9 to 1.1) |
| Most deprived | 14.9 (13.9 to 16.0) | 14.7 (13.7 to 15.7) | –0.2 (–1.6 to 1.2) | 1.0 (0.9 to 1.1) | |
| Unknown antepartum (not SGA) (n = 8087; 39.6%) | Least deprived | 13.5 (12.6 to 14.3) | 15.2 (12.7 to 18.3) | –0.3 (–1.5 to 0.8) | 1.0 (0.9 to 1.1) |
| Most deprived | 20.9 (19.7 to 22.1) | 23 (21.9 to 24.2) | 2.1 (0.5 to 3.8) | 1.1(1.0 to 1.2) | |
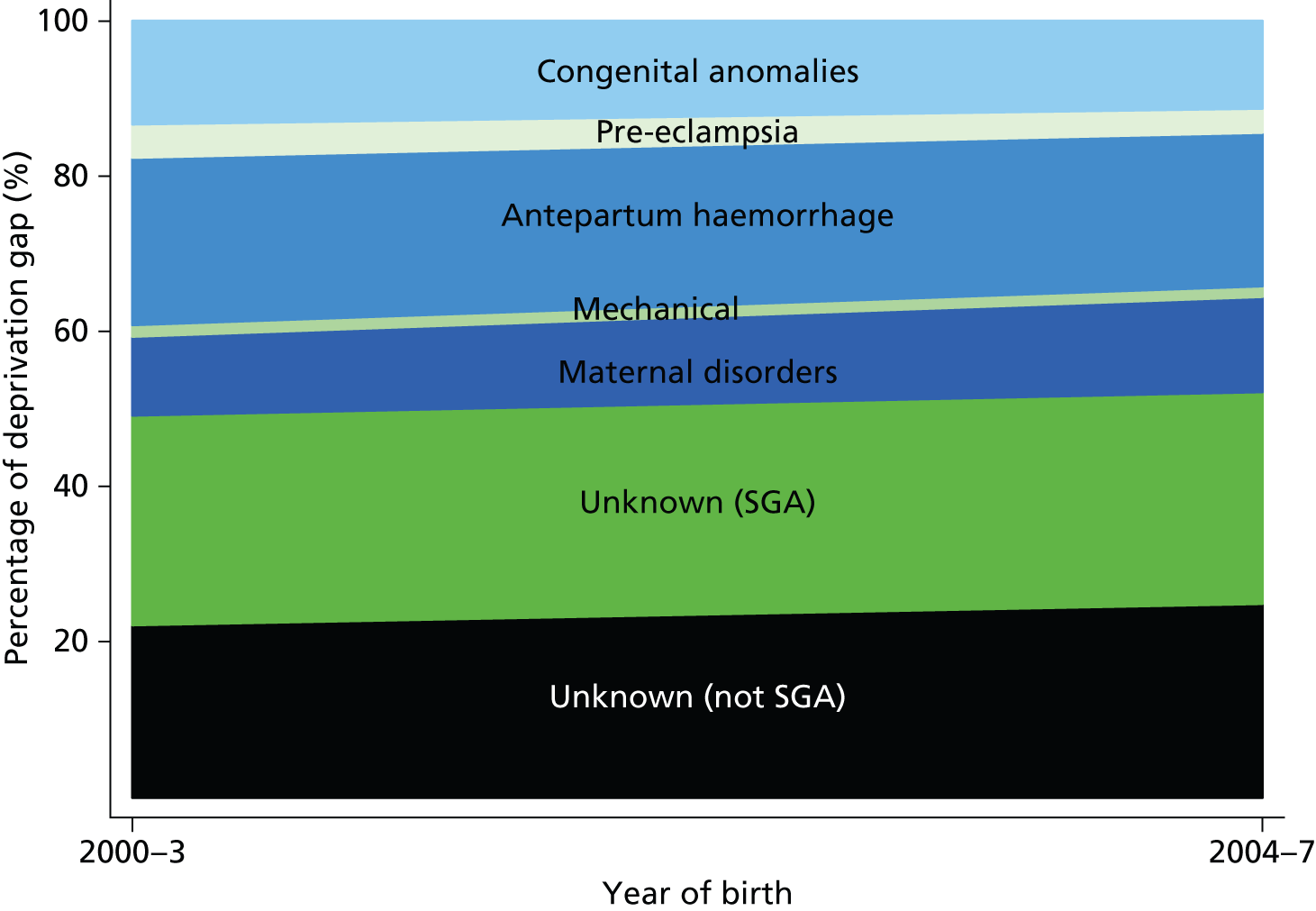
Graphical approach to understanding the deprivation gap
Again, in order to best illustrate the cause-specific socioeconomic inequalities in stillbirth, a graphical approach was chosen. Figure 2 demonstrates the percentage of the deprivation gap in all-cause stillbirth mortality explained by each specific cause estimated from the Poisson regression models. This figure highlights that those deaths due to unexplained antepartum events account for 50% of the deprivation gap. Although, overall, among unexplained antepartum deaths, the proportion of infants who were SGA were smaller than the proportion who were not (22.3% SGA and 39.6% not SGA), the SGA group explains more of the deprivation gap. This is because the deprivation gap was wider for stillbirth infants who were SGA (RR 2.5, 95% CI 2.3 to 2.7) than for those who were not SGA (RR 1.7, 95% CI 1.5 to 1.8). There was no evidence of a change in the proportion of the deprivation gap explained by any of the different causes over time, which can be seen by the lack of change in the gradient of the lines representing each specific cause. Mechanical causes are seen to constitute a very small, insignificant proportion of the deprivation gap.
FIGURE 2.
Proportion of the deprivation gap in all-cause stillbirth rates explained by each cause of death over time. Reproduced from Seaton et al. 33 © 2012, British Medical Journal Publishing Group, under the terms of the Creative Commons Attribution Non-Commercial Licence (CC BY-NC 2.0), which permits use, distribution and reproduction in any medium, provided the original work is properly cited, the use is non-commercial and is otherwise in compliance with the licence.
Conclusions
Key findings
-
Rates of stillbirth were twice as high in the most deprived decile as in the least deprived.
-
This wide gap remained constant over time and was not diminishing.
-
There was a significant deprivation gap for most specific causes of stillbirth.
-
Unexplained antepartum stillbirths accounted for 50% of the deprivation gap.
Limitations and strengths
Classification of deaths
A limitation of much stillbirth research, including this work, is that many stillbirth classifications, such as the obstetric (Aberdeen) classification,32 classify the majority of stillbirths as occurring for unknown reasons and hence further analysis to improve understanding is restricted. Alternative classifications of these deaths were not available for this work as for the time period under study national routinely collected data in England used only the Aberdeen classification for stillbirth. There are currently 35 published classification systems for stillbirth,25 many relying on advanced diagnostics that are not globally available. These systems are not comparable and there has been a strong case made to have one universal system for all countries. 34 Consequently, there has been a call for a consensus on definitions and classifications in order to better understand the causes of stillbirth. 24 Alternative systems, such as the classification of stillbirth by relevant condition at death (ReCoDe)35 or the Cause of Death and Associated Conditions (CODAC)36 classification, provide a possible cause of death for approximately 85% of stillborn infants, providing greater insight to guide those developing interventions to reduce future mortality.
Individual-level socioeconomic data
As discussed in the analyses of neonatal deaths, data on individual risk behaviour, lifestyle, health and ethnicity were not available for the mothers included in this work as it has been in other research. Inevitably, this has limited the extent of our conclusions and has the potential to have produced a degree of confounding. For example, epidemiological research using individual-level data has shown wide differences in stillbirth rates associated with maternal smoking during pregnancy24 and maternal obesity. 37 Stillbirths are also known to be more common in sole registrations. 38 In women from deprived areas of Scotland, maternal smoking status accounted for 38% of the inequalities seen in stillbirths. 21 The lack of individual-level data also meant that it was not possible to identify women who had more than one stillbirth over the time period. However, as women who have had a stillbirth are more likely to have a recurrence, the proportion of stillbirths that are likely to show this pattern is low and, therefore, negligible in terms of our findings.
Despite this, provided the results are treated cautiously and trends are not extrapolated beyond the time period under study, our methods are relatively straightforward and provide a way for health service planners to monitor up-to-date trends in stillbirth.
Implications for policy and practice
Cause-specific analyses provide more detailed information, highlighting the contribution of each causal group to deprivation differentials and the impact of interventions or changes in society over time.
Recent reductions in the stillbirth rate in other high-income countries24 suggest that there exist modifiable risk factors and that by the introduction of targeted interventions, an improvement in stillbirth rates could be seen, in particular the early identification of close monitoring of fetal movements. 39 Maternal smoking may be targeted successfully to impact on the rate of stillbirths, but effective tools to reduce maternal obesity and rates of teenage pregnancy are currently lacking. 40 Smoking, obesity and teenage pregnancy have all been the subject of longstanding public health campaigns of limited success and the UK suggested goals require major behavioural changes.
Some practical measures could help in improving our understanding of the role of deprivation in relation to stillbirth:
-
Cause-specific socioeconomic inequalities in stillbirth should be monitored annually.
-
Avoid the use of the father’s occupational class to assess socioeconomic group, as this excludes single mothers from analyses, a significant at-risk group. Area-level deprivation measures offer an inexpensive quick way to continue monitoring inequalities.
-
Improved data linkage between large routine data sets such as NN4B would facilitate considerable improvement in the research related to socioeconomic inequalities in infant mortality.
-
The implementation of an improved, internationally adopted, classification system would enhance the ability to identify other modifiable risk factors. In addition, such a system would facilitate the implementation of appropriate targets and interventions and reduce the proportion of stillbirths assigned to unknown causes.
Recommendations for future research
-
The lack of change in stillbirth rates in the UK and the persistent wide socioeconomic inequalities highlights the need for further research to understand this intractable problem.
-
Assessment of the impact of recent professional recommendations on the classification of births after 24 weeks’ gestation known to have died earlier as ‘late fetal losses’.
Study 3: exploring the reasons underlying cause-specific inequalities in mortality – congenital anomalies
Background
Socioeconomic inequalities in deaths associated with congenital anomaly
Following the national work on understanding socioeconomic inequalities in neonatal mortality and stillbirth, it became apparent that a key area of concern was the widening gap in socioeconomic inequalities in neonatal mortality relating to congenital anomalies. Deaths as a result of a congenital anomaly accounted for the largest proportion of the deprivation gap in neonatal mortality due to a single cause, and also represented a significant proportion of the deprivation gap in stillbirths. Understanding how these inequalities relating to congenital anomalies arose seemed key to implementing effective public health interventions to reduce socioeconomic inequalities in infant and neonatal mortality.
Socioeconomic inequalities in congenital anomalies have been demonstrated in the rates of stillbirth and perinatal, neonatal and infant mortality. 20,30,41,42 Research had shown an increasing risk of non-chromosomal anomalies with increasing deprivation, in contrast to a decreasing risk of chromosomal anomalies. 43 This last finding was predominantly a result of the increased risk of chromosomal anomalies with increasing maternal age. However, the influence of socioeconomic deprivation along the pathway from antenatal detection to delivery and possible neonatal mortality was not fully understood because of the lack of clearly defined standardised data in the antenatal period. Countries that have introduced the use of prenatal diagnostic techniques and access to termination of pregnancy because of congenital anomaly have reported large reductions in neonatal mortality rates, in contrast to those countries with more restrictive policies on pregnancy termination. 44–47 Nevertheless, the impact of these secondary preventative measures might vary with socioeconomic deprivation in terms of access to, and timing of, antenatal detection services through to the provision of information, the interpretation of risk, and the consequent decision-making regarding continuation or termination of a pregnancy.
Evidence in this area is sparse. A systematic review of UK studies showed no evidence of social inequalities in the uptake of prenatal screening,48 whereas research in Northern Ireland,49 where there is no provision of termination services, showed inequalities in both the offer and the uptake of screening. Further research suggested that socioeconomic differentials in decision-making following antenatal detection are a result of maternal age differences. 50 The term ‘congenital anomaly’ covers a very wide spectrum from the relatively minor to those with an exceptionally poor prognostic outcome and it is secondary preventative measures targeted at the latter that have the potential to improve infant mortality rates.
A detailed analysis of regional data was undertaken to identify the underlying reasons behind the inequalities seen in the analyses of neonatal mortality and stillbirth. Data were used from a large population-based congenital anomaly register in England (EMSYCAR) covering about 10% of the births in England and Wales, for 1998–2007, to investigate socioeconomic inequalities in the risk of congenital anomalies with a poor prognosis from antenatal diagnosis to end of pregnancy. The impact of variations in rates of termination of pregnancy for congenital anomaly on rates of stillbirth, live birth and neonatal mortality associated with congenital anomaly were explored to aid understanding of the reasons for the widening socioeconomic inequalities in neonatal and infant mortality in England.
Objective
The objective was to explore the reasons underlying cause-specific inequalities in mortality.
Methods
Description of data sets
Regional data: congenital anomalies incidence and mortality
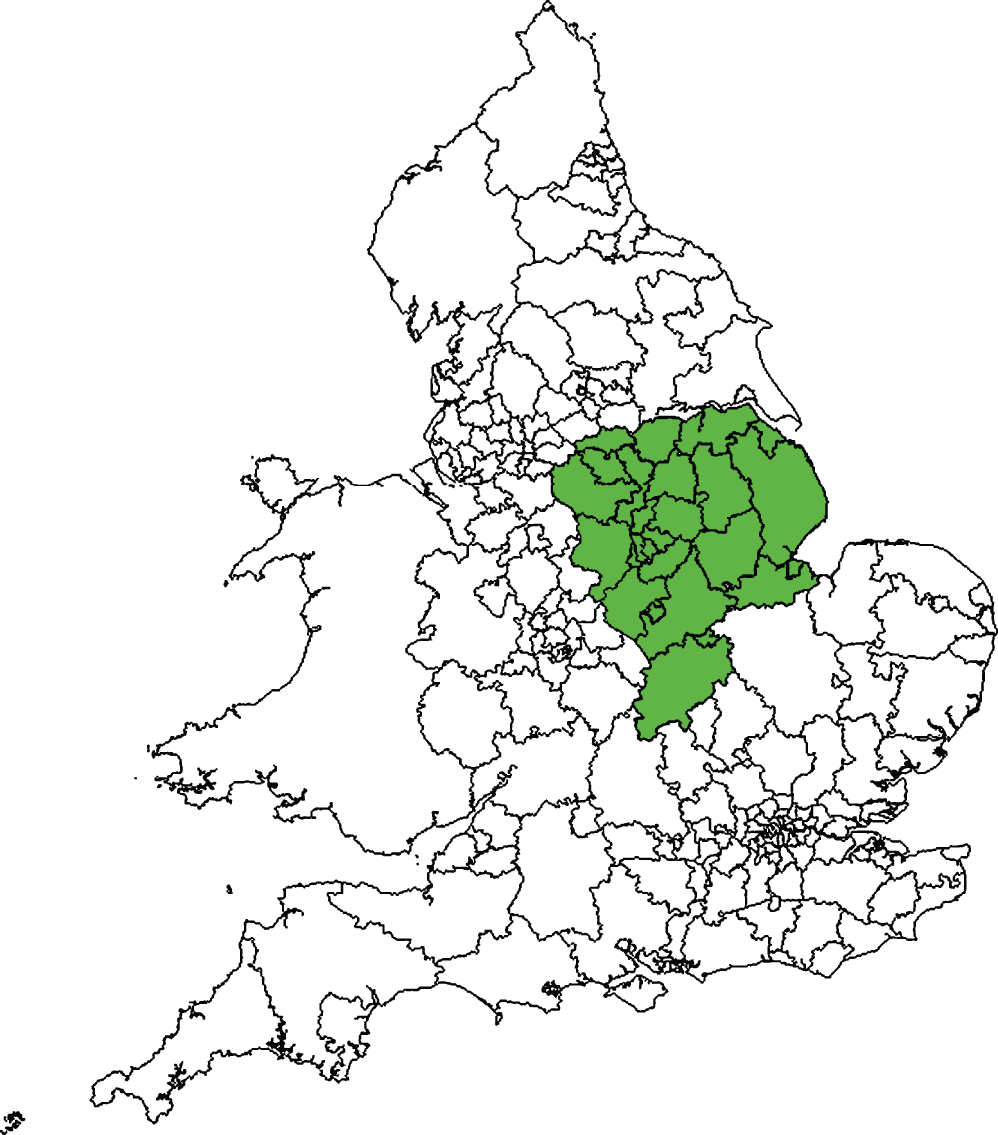
The EMSYCAR currently covers about 74,000 births annually (about one-tenth of all births in England and Wales), with around 2200 reported cases per year. The region covered by the register can be seen in Figure 3. Data for Northamptonshire, which joined the register only in 2003, were excluded, leaving a geographical area with about 60,000 births annually.
FIGURE 3.
English counties covered by the EMSYCAR.
This register is population based and includes all structural and chromosomal congenital anomalies in fetuses and infants of mothers living within the region at the time of delivery. It includes live births, stillbirths (from 24 weeks’ gestation), spontaneous fetal loss (before 24 weeks’ gestation) and termination of pregnancy for fetal anomaly at any gestational age. The register uses multiple sources of case ascertainment from within the care pathway, including antenatal ultrasonography, antenatal screening, delivery reports, birth notifications, pathology, cytogenetics, clinical genetics and paediatric surgery. All reported anomalies are coded in accordance with the International Classification Of Diseases, Tenth Edition (ICD-10). Information on maternal age and ethnicity, mother’s postcode of residence at delivery, end date of pregnancy and gestation at delivery were available from data collected by the register. The study included fetuses with an anomaly with an end of pregnancy date between 1 January 1998 and 31 December 2007. These data were linked to the ONS birth registrations and the Confidential Enquiry into Maternal and Child Health (CEMACH) data by LSOA to look at morbidity and mortality. Ideally, analyses would be based on the mother’s postcode at conception, but this was not available from the register. Analyses were therefore based on the mother’s postcode at delivery. To assess the potential impact of changes in the mother’s residence through the pregnancy on the observed socioeconomic inequalities, deprivation at antenatal detection and delivery was assessed separately for those fetuses for which this information was available (i.e. fetuses detected in the antenatal period when the mother opted to continue with the pregnancy).
Classification of congenital anomalies
The focus of the study was to investigate how socioeconomic inequalities arise along the care pathway from antenatal detection to delivery. Serious congenital anomalies were defined as those incompatible with life or associated with severe morbidity and for which screening systems are in place, leading to a precise antenatal diagnosis that allows parents to make an informed decision about continuation of the pregnancy. As a starting point, therefore, the 11 anomalies identified by the Fetal Anomaly Screening Programme (FASP)51 in the UK were used (Table 8). Two anomalies were excluded – cleft lip and gastroschisis – as they were much less likely to have a poor prognostic outcome. Only those anomalies associated with a unique ICD-10 code and for which there is a high level of certainty about an adverse prognosis were included. Nine anomalies met these criteria: two chromosomal anomalies (trisomy 13 and trisomy 18) and seven non-chromosomal anomalies (anencephaly, spina bifida, hypoplastic left heart, bilateral renal agenesis, lethal skeletal dysplasia, diaphragmatic hernia and exomphalos). For the majority of these, the FASP definition of the anomaly was directly related to an ICD-10 code. However, for cardiac anomalies this was much more difficult, as one ICD-10 code could relate to a less certain prognosis. Hypoplastic left heart was chosen as it is the main cardiac anomaly diagnosed antenatally for which prognosis is clear and recognised to be poor. In the case of fetuses registered with a chromosomal diagnosis, any coexisting congenital anomalies were considered as secondary to the underlying chromosomal problem, rather than separate non-chromosomal anomalies, as such associations are well established. Additional information on antenatal detection was obtained from the register on these selected anomalies, including the method and timing of diagnosis. An anomaly was deemed to be ‘antenatally detected’ if the date of detection of the exact, or a closely related, anomaly predated delivery or the date of detection of an antenatal soft marker related to the anomaly present at delivery predated the date of delivery. Ethnicity [classified into four groups: white British, Asian or Asian British (Indian), Asian or Asian British (Pakistani) and other or missing] was included in the regression models to assess whether or not the inclusion of ethnic group attenuated any observed socioeconomic inequalities in the rate of antenatal detection and termination of pregnancy.
| Anomaly | ICD-10 code | Total cases (N) | Antenatal detection, % (n) | Termination in cases detected antenatally, % (n) | Outcome of pregnancy for all cases | |||
|---|---|---|---|---|---|---|---|---|
| Termination, % (n) | Fetal loss and stillbirth, % (n) | Live birth (surviving > 28 days), % (n) | Neonatal death, % (n) | |||||
| Selected anomalies | ||||||||
| Anencephaly | Q000 | 257 | 97 (249) | 88 (218) | 85 (218) | 8 (20) | 0 (1) | 7 (18) |
| Spina bifida | Q050–9 | 339 | 90 (303) | 78 (235) | 70 (235) | 6 (20) | 22 (75) | 2 (8) |
| Hypoplastic left heart | Q234 | 171 | 85 (146) | 56 (82) | 48 (82) | 8 (14) | 25 (42) | 19 (33) |
| Bilateral renal agenesis | Q601/606 | 59 | 81 (48) | 85 (41) | 69 (41) | 15 (9) | 0 (0) | 15 (9) |
| Lethal skeletal dysplasia | Q771–3 | 45 | 82 (37) | 57 (21) | 47 (21) | 7 (3) | 33 (15) | 13 (6) |
| Diaphragmatic hernia | Q790 | 183 | 77 (140) | 29 (40) | 22 (40) | 8 (14) | 47 (86) | 23 (43) |
| Exomphalos | Q792 | 230 | 85 (195) | 56 (109) | 47 (109) | 15 (34) | 34 (77) | 4 (10) |
| Trisomy 18 | Q910–13 | 285 | 85 (242) | 81 (196) | 69 (196) | 13 (38) | 6 (18) | 12 (33) |
| Trisomy 13 | Q914–7 | 127 | 84 (107) | 83 (89) | 70 (89) | 16 (20) | 5 (6) | 9 (12) |
| Other anomalies audited by FASP | ||||||||
| Cleft lip | Q360–79 | 540 | – | – | 6 (33) | 3 (17) | 90 (484) | 1 (6) |
| Gastroschisis | Q793 | 278 | – | – | 6 (17) | 6 (16) | 87 (242) | 1 (3) |
| All selected anomalies | – | 1579 | 86 (1357) | 70 (944) | 60 (944) | 10 (158) | 20 (317) | 10 (160) |
| Other registered | – | 12,001 | – | – | 13 (1514) | 5 (550) | 80 (9579) | 3 (358) |
| Total registered | – | 13,580 | – | – | 18 (2458) | 5 (708) | 73 (9896) | 4 (518) |
Sensitivity analyses were undertaken to look at outcomes of pregnancy for anomalies not in the selected severe group to assess whether or not any major severe anomalies with poor outcome were being omitted from the analyses. These additional cases of congenital anomaly demonstrated exceptionally low rates of termination of pregnancy and neonatal mortality (see Table 8). Although 60% of pregnancies affected by the nine severe anomalies selected ended in a termination of pregnancy, only 13% of all pregnancies with other registered anomalies ended in termination. Furthermore, although 80% of pregnancies affected by the selected anomalies ended in a neonatal death, this was true for only 20% of pregnancies affected by all other registered anomalies. Evidently, these 20% of neonatal deaths are attributable to severe anomalies, such as cardiac anomalies, that are less well specified, but for the purpose of this analysis the nine anomalies specified here were deemed to be the most cohesive group.
Denominator data: live births
The birth denominator data, as used in the exploration of national trends in infant mortality, of ONS birth registrations by year of birth and LSOA of residence, were used in order to calculate mortality rates by LSOA. This allowed us to explore trends over time for the geographical region covered by the EMSYCAR data defined by PCT boundaries. Live births with additional information on birthweight, mother’s age, sex and multiplicity of birth were obtained from the ONS. These had to be obtained in an aggregated form and so deprivation deciles of LSOAs across England were specified and data were obtained on the number of live births by decile of deprivation, year of birth and PCT.
Data linkage
The regional data included postcode of the mother’s residence at registration of the congenital anomaly. These were linked to LSOA codes which enabled linkage with both the IMD 200416 and the ONS birth denominator data set.
Statistical analyses
A range of rates along the pathway from diagnosis of an anomaly in the antenatal period to birth and survival/death were calculated (selected anomalies refers to the nine selected FASP anomalies as defined in Table 8):
-
rate of selected anomalies in utero (all cases of selected anomalies whether identified in the antenatal period or at birth) (denominator: total live births, stillbirths and known late fetal losses and terminations of pregnancy, i.e. those registered with a fetal anomaly)
-
rate of antenatal detection (denominator: all cases of selected anomalies)
-
rate of termination of pregnancy because of fetal anomaly (denominator: antenatally detected cases)
-
rate of fetal loss or stillbirth with an anomaly (denominator: total live births, stillbirths, and known late fetal losses, i.e. those registered with a fetal anomaly)
-
rate of live births with an anomaly (denominator: total live births)
-
rate of neonatal mortality of infants with an anomaly (denominator: total live births).
Analyses were undertaken at the individual case (fetus or baby) level. Poisson regression models17 were used to assess trends in the six outcome measures described above by deprivation decile over time. The time period was divided into two sections: 1998–2002 and 2003–7. Data on terminated pregnancies and fetal losses before 24 weeks’ gestation were available only when they were associated with a congenital anomaly. Only these terminations and late fetal losses were included in the denominators for calculation of rates of anomalies in utero. Models were fitted for all anomalies combined and then separately for chromosomal and non-chromosomal anomalies. Interactions were explored to assess the change in the effect of deprivation over time. Maternal age (< 20 years, 20–24 years, 25–29 years, 30–34 years and > 35 years) was then included in the models to assess its influence on any observed socioeconomic inequality. Confidence limits were obtained using the delta method. 19
The effect of gestational age at detection of anomaly on termination of pregnancy was also assessed. Gestational age group was classified based on the standard timings of antenatal testing into four bands: ≤ 17 weeks’, 18–21 weeks’, 22–23 weeks’ and ≥ 24 weeks’ gestation.
In order to assess whether or not patterns in outcome of pregnancy by deprivation for the nine selected anomalies were similar to those for all registered anomalies, sensitivity analyses were undertaken using data on all registered congenital anomalies.
Results
There were 1712 separate registrations of the nine anomalies between 1998 and 2007, of which 1695 had full postcode and maternal age information (99%). These 1695 registrations represented 1472 fetuses with one of the nine selected anomalies and a further 107 fetuses with two or more of the nine anomalies, making 1579 fetuses in total (see Table 8).
Antenatal detection rates varied according to the type of congenital anomaly, ranging from 97% for anencephaly to 77% for diaphragmatic hernia. Of those antenatally detected, over 80% of pregnancies with a diagnosis of anencephaly, bilateral renal agenesis, trisomy 13 or trisomy 18 ended in termination and less than 6% of fetuses with these anomalies were live born and survived the neonatal period. Pregnancies in which the fetus was diagnosed with diaphragmatic hernia were least likely to be terminated (24%), but such fetuses accounted for one-quarter of the observed neonatal deaths relating to the nine anomalies. Just one in five fetuses with one of the nine selected anomalies were live born and survived the neonatal period, compared with four out of five for all other registered anomalies. Exploring the number of cases by ethnicity showed that, of fetuses with an anomaly, 84% (1159) were classified as ‘white,’ with the second largest ethnic groups being Pakistani (Asian or Asian British) (4%, 53 fetuses), and Indian (Asian or Asian British) (3%, 47 fetuses). Unfortunately, birth data were not available by ethnic group, but, according to census data for the register area, 2% of those aged 0–15 years were classified as Pakistani and 3% as Indian.
Socioeconomic inequalities following diagnosis of a congenital anomaly
Table 9 demonstrates that there was no evidence of a difference in the overall rate of registrations of the nine anomalies by deprivation (rate ratio comparing the most deprived decile with the least deprived decile 1.05, 95% CI 0.89 to 1.23). In 86% of cases, the anomaly was detected during the antenatal period and, similarly, there was no evidence that this varied with deprivation (rate ratio 0.99, 95% CI 0.84 to 1.17) or ethnicity (p = 0.913). However, termination of pregnancy when an anomaly was detected antenatally was substantially less common in the most deprived decile (63%) than in the least deprived decile (79%; rate ratio 0.80, 95% CI 0.65 to 0.97), and this finding was similar after adjusting for maternal age differences (rate ratio 0.79, 95% CI 0.65 to 0.97) but slightly attenuated after adjusting for differences in termination rates by ethnicity (rate ratio 0.86, 95% CI 0.70 to 1.05). This was because, although rates of termination were similar for mothers classified as white British (71%) and Indian (Asian or Asian British) (71%), they were considerably lower for Pakistani (Asian or Asian British) mothers (42%).
| Outcome measure | All selected anomalies (n = 1579) | |
|---|---|---|
| Unadjusted RRa (95% CI) | Adjusted RRa (95% CI) | |
| Registered cases per 10,000 births | 1.05 (0.90 to 1.23) | 1.22 (1.04 to 1.44) |
| % of all cases detected antenatally | 0.99 (0.84 to 1.17) | 0.99 (0.84 to 1.18) |
| % terminations in cases detected antenatally | 0.80 (0.65 to 0.98) | 0.79 (0.64 to 0.98) |
| Stillbirth or fetal loss per 10,000 births | 1.20 (0.74 to 1.97) | 1.57 (0.93 to 2.63) |
| Live birth per 10,000 live births | 1.61 (1.21 to 2.15) | 1.85 (1.36 to 2.50) |
| Neonatal deaths per 10,000 live births | 1.98 (1.20 to 3.27) | 2.23 (1.31 to 3.78) |
These socioeconomic variations in termination of pregnancy for congenital anomaly impacted greatly on socioeconomic inequalities in the rate of fetal loss, stillbirth and live birth associated with an anomaly and also subsequent neonatal death. Considering all of the selected anomalies combined, rate of stillbirth or fetal loss was 20% higher in the most deprived decile than in the least deprived decile while the rate of live birth was 61% higher and the rate of neonatal mortality was 98% higher. After adjusting for maternal age differences, socioeconomic inequality widened, with women of a similar age from the most deprived decile being 57% more likely to experience fetal loss or stillbirth, 85% more likely to give birth to a live infant and 123% more likely to have a baby who subsequently died in the neonatal period.
Exploring inequalities by type of anomaly
When looking at chromosomal and non-chromosomal anomalies separately (Table 10), the effect of deprivation differed, with women from the most deprived decile at increased risk of having a fetus with a non-chromosomal anomaly (rate ratio 1.41, 95% CI 1.17 to 1.70), but at reduced risk of a fetus with a chromosomal anomaly (rate ratio 0.52, 95% CI 0.39 to 0.69), compared with women from the least deprived decile. The greater risk of chromosomal anomalies was the result of differences in maternal age distribution between pregnant women from the most deprived and least deprived areas (women in the most deprived decile accounted for 25% of pregnant women > 35 years of age, whereas women in the least deprived decile accounted for 64% of this age group). As expected, the risk of chromosomal anomalies increased with increasing maternal age [women aged > 35 years were nearly five times more likely to carry a fetus with a chromosomal anomaly than younger mothers (rate ratio 4.96, 95% CI 4.12 to 5.98)]. In contrast, there was no evidence of a difference in the rates of non-chromosomal anomalies with maternal age (rate ratio 1.01, 95% CI 0.86 to 1.20). The age-adjusted RR for chromosomal anomalies showed no evidence of a difference in rate depending on deprivation level (rate ratio 0.85, 95% CI 0.63 to 1.15).
| Outcome measure | Non-chromosomal anomalies (n = 1118) | Chromosomal anomalies (n = 461) | ||
|---|---|---|---|---|
| Unadjusted RRa (95% CI) | Adjusted RRa (95% CI) | Unadjusted RRa (95% CI) | Adjusted RRa (95% CI) | |
| Registered cases per 10,000 births | 1.41 (1.17 to 1.70) | 1.43 (1.17 to 1.74) | 0.52 (0.39 to 0.69) | 0.85 (0.63 to 1.15) |
| % of all cases detected antenatally | 1.00 (0.82 to 1.23) | 1.01 (0.82 to 1.24) | 0.96 (0.70 to 1.31) | 0.97 (0.70 to 1.35) |
| % terminations in cases detected antenatally | 0.84 (0.66 to 1.08) | 0.82 (0.64 to 1.06) | 0.82 (0.57 to 1.17) | 0.82 (0.56 to 1.19) |
| Stillbirth or fetal loss per 10,000 births | 2.47 (1.26 to 4.86) | 2.57 (1.26 to 5.24) | 0.47 (0.22 to 1.00) | 0.85 (0.38 to 1.86) |
| Live births per 10,000 live births | 1.64 (1.20 to 2.24) | 1.78 (1.28 to 2.48) | 1.50 (0.74 to 3.04) | 2.21 (1.05 to 4.64) |
| Neonatal deaths per 10,000 live births | 2.30 (1.25 to 4.23) | 2.32 (1.22 to 4.42) | 1.44 (0.60 to 3.47) | 2.04 (0.81 to 5.14) |
Despite these differences in registrations of chromosomal and non-chromosomal anomalies, the socioeconomic differences in antenatal detection rates and terminations of pregnancy were similar for both chromosomal and non-chromosomal anomalies. There was no evidence of a difference in antenatal detection rates with deprivation for either chromosomal (rate ratio 0.96, 95% CI 0.70 to 1.31) or non-chromosomal anomalies (RR 1.00, 95% CI 0.82 to 1.23). The socioeconomic differences in rates of termination of pregnancy seen for chromosomal and non-chromosomal anomalies when considered separately were similar to those seen for all anomalies combined.
In contrast, the rate of live birth associated with a non-chromosomal anomaly was 64% higher in the most deprived decile than in the least deprived decile and neonatal mortality was 130% higher. Socioeconomic inequalities for chromosomal anomalies appeared slightly narrower and were not statistically significant. The rate of live birth with a chromosomal anomaly was 50% higher in most deprived decile than in the least deprived decile (compared with 64% in the case of non-chromosomal anomalies) and neonatal mortality were 44% higher (compared with 130% in the case of non-chromosomal anomalies). However, adjusting for the wide maternal age differences increased the socioeconomic inequality for chromosomal anomalies to 121% increased risk for a live birth with an anomaly and to 104% for a neonatal mortality associated with an anomaly.
Sensitivity analyses
Sensitivity analyses were also undertaken to compare the pattern of deprivation with outcome of pregnancy for all 13,580 registered cases of anomaly. This analysis showed a similar pattern to that for the nine selected anomalies with a poor prognosis. There was an increase in the risk of an anomaly among women from the most deprived areas (rate ratio 1.25, 95% CI 1.19 to 1.32) and a substantially lower rate of terminations (rate ratio 0.55, 95% CI 0.48 to 0.62), resulting in an increased rate of live birth (rate ratio 1.48, 95% CI 1.39 to 1.58) and neonatal death (rate ratio 1.98, 95% CI 1.49 to 2.63) associated with an anomaly.
Conclusions
Key findings
-
Rates of severe anomalies and method of detection were similar for all deprivation groups.
-
Rates of termination after antenatal diagnosis of a congenital anomaly were lower in the most deprived areas than in the least deprived.
-
This resulted in wide socioeconomic inequalities in live-born infants with a congenital anomaly and subsequent neonatal mortality.
Strengths and limitations
Classification of congenital anomalies
Alternative definitions of anomalies with a poor prognostic outcome could affect the results seen here. However, our sensitivity analyses of all registered cases of congenital anomaly showed similar findings to analyses of the nine selected anomalies. The work focused on those anomalies with a high detection rate through the fetal anomaly screening programme. The socioeconomic differences in the risk of live-born infants with an anomaly and neonatal deaths might be less marked for anomalies that are not routinely detected before birth as the differential rates of termination will not play a part. Other anomalies, such as Down syndrome, rely on accessing additional blood tests and amniocentesis for detection and have much lower rates of associated mortality. Such conditions might show greater socioeconomic inequalities in live births associated with an anomaly as there is greater potential for variation in access to screening and differences in interpretation of risk and, consequently, an increased likelihood of socioeconomic differences in decisions to terminate a pregnancy. Data from antenatal detection through to outcome of pregnancy are not available nationally in the UK or many other countries. Here, the work utilised the largest of the regional congenital anomaly registers in England, a large population-based register that covers 10% of England and Wales. As 10 years of data were explored, this covered around 600,000 births and provides detailed information from antenatal detection through to information on terminations, birth outcomes and neonatal mortality unavailable elsewhere. Although coverage of the UK population is incomplete, the data held by the nine regional registers that do exist are of the highest quality, and, since the demise of the National Congenital Anomaly System, are now the only source of information available for monitoring the incidence of congenital anomalies across the UK.
Although we have shown here that women of Pakistani (Asian or Asian British) ethnicity have much lower rates of termination than white British or Indian (Asian or Asian British) women, we were unable to investigate the important issues of religious beliefs and the acceptability of termination of pregnancy. Nevertheless, the ethnic differences seen here could partially reflect different attitudes to termination with religion. There is also discord in opinion within groups, and it is important that neither ethnicity nor religion is taken as a proxy for attitudes towards termination of pregnancy. Differences could be as a result of variations in the communication of risk and timing of detection as well as cultural or religious differences between ethnic groups.
Implications for policy and practice
Although this work concentrated on a specific region of the UK, it is likely that these results are generalisable to the whole of the UK. The FASP aims to ensure consistent provision across the UK, although there may be some variation between centres in the antenatal detection rates of the selected anomalies and differences in uptake of screening programmes. This is unlikely to impact substantially on socioeconomic differences in behaviour following detection of a suspected anomaly. In England, Scotland and Wales secondary prevention of anomalies through access to termination of pregnancy is available to all. Internationally, this is not universally the case, as access to termination of pregnancy varies, but these findings may be mirrored in countries with a similar policy to that of England on the termination of pregnancy.
The use of prenatal diagnostic techniques and access to termination of pregnancy for fetal anomaly has reduced neonatal mortality internationally, but this research has demonstrated that these secondary prevention measures have had a knock-on effect of an increase in the socioeconomic inequality in mortality.
Going forward, comparisons of infant mortality rates between regions would be improved by taking into account of the variation in rates of termination of pregnancy for severe congenital anomaly since this will impact greatly on observed crude mortality rates. National monitoring of socioeconomic variations in congenital anomalies would facilitate evaluation of services and this may be possible following the introduction (in England) of the planned national congenital anomaly register.
Recommendations for future research
-
It is vital that variations in congenital anomalies arising through the secondary prevention programmes based on screening and the uptake of termination of pregnancy do not detract from the importance of reducing inequalities in anomalies through primary prevention prior to conception as highlighted by Dolk. 53 Further research into the links between non-chromosomal anomalies and deprivation needs to be undertaken in order to identify primary prevention interventions.
-
A decision to continue a pregnancy associated with a serious congenital anomaly should not be thought of as a flawed choice and may relate to societal and cultural norms. However, it is important that the reported socioeconomic variations in rates of termination do not arise from systematic differences in the delivery of services such as access to timely detection services, communication of mortality and morbidity risk by health professionals and access to a termination of pregnancy. Future research into the reasons underlying the socioeconomic variations in continuation of pregnancies associated with serious congenital anomalies is needed.
Study 4: improving comparisons of mortality between health regions
Background
The aim of this work was to explore how targets could be developed for PCTs to account for the variation in population case mix. In the UK, the role of improving infant mortality has fallen to local commissioners (currently Clinical Commissioning Groups, but at the time of this work PCTs had this responsibility), who are responsible for health-care provision at a population level. PCT-level infant mortality rates have been compared with peer PCTs to adjust for variation attributable to risk factors such as socioeconomic deprivation, ethnicity and maternal age. Attention has then focused on whether or not the substantial residual variation results from the effectiveness of local antenatal or neonatal services, with calls for public health interventions to lower rates among PCTs perceived to be performing poorly. The intention of this work was to use information on socioeconomic deprivation, age profile, ethnicity and other factors54 to adjust crude infant mortality rates so that PCTs could be compared in a more appropriate manner and targets for reducing inequalities could be better assessed. One initial plan to look at these data was by gestational age, and it was immediately apparent that the numbers of deaths at < 24 weeks’ gestation varied greatly between PCTs, despite extremely similar case-mix profiles.
At an international level, variations in birth registration practices have been shown to have a major influence on infant mortality rankings55,56 and there is a need to distinguish between ‘real’ variations and those arising from artefactual differences. Registration disparities mainly relate to births of uncertain viability when definitions of late fetal death and live birth are particularly complicated. Changes in views on the limit of viability have led to increases in registered live births of < 24 weeks’ gestation. However, survival of these infants remains poor57–60 and they impact greatly on mortality rates, accounting for 20% of neonatal deaths in England. Situations in which significant differences exist in the interpretation of what constitutes a live birth between countries comparisons may be of limited value as standard published infant mortality rates include only live births and, in England, in particular, there is no legal requirement to register fetal deaths before 24 weeks’ gestation.
As became apparent from the PCT-level data, variation was evident between regions and the implications of this were unknown but likely to be similar to the impact seen at an international level, rendering comparisons between PCTs of infant mortality rates of limited value. Therefore, before such between-region comparisons were made, any differences resulting from variation in registration practices needed to be taken into consideration,61 and this research aimed to assess the best methods for achieving this.
Objective
The aim was to improve comparisons of mortality between health regions accounting for variations in case mix.
Methods
Description of data sets
Birth denominator data
As discussed in the analysis of neonatal deaths, access to the NN4B data set was extremely difficult, but for this work, data finally became available from the NN4B birth notifications data set, which includes all live birth and stillbirth registrations by gestation at birth. These detailed birth notification data commenced in 2005 and were available only for 2005–8 for this study. Owing to confidentiality issues, only aggregated data are made available several years after the time period of coverage. PCT-level data on all registered births and linked infant deaths (death before 1 year of life) in England by gestational age bands (< 24, 24–27, 28–32, 33–36 and ≥ 37 weeks) were obtained.
Four of the 151 PCTs were excluded because of high levels of missing gestational age data in the NN4B data set (13–82% missing, n = 14,917; 0.3% overall).
Infant deaths and late fetal loss data
The NN4B data were linked to ONS data on infant deaths for the period 2005–6. Additional CMACE data used in the national study of mortality on all neonatal deaths were also used here, including information on late fetal losses – babies born with no signs of life at 22+0–23+6 weeks’ gestation. From 24+0 weeks’ gestation these births would be certified and legally registered as a stillbirth; however, babies born with no signs of life at earlier gestations are not certified and, consequently, there is no legal registration process and so they are not included in the ONS births or deaths data. CMACE also collected national data on deaths at 22 and 23 weeks’ gestation until 31 December 2006, when data collection ceased. As information on late fetal losses was not available for the whole 4-year period covered by the NN4B data, an estimate was made based on doubling the numbers seen in 2005–6, but sensitivity analyses based on 2003–6 were also undertaken, and these suggested that there had been little change in the number of late fetal losses over time by PCT.
Data linkage
The ONS and NN4B data were linked by ONS to form a complete births and deaths data set. The late fetal loss data were then linked by PCT to provide PCT-level data on all registered births and linked infant deaths (death before 1 year of life) in England by gestational age (< 24, 24–27, 28–32, 33–36 and ≥ 37 weeks) for the period 1 January 2005 to 31 December 2008.
Statistical analyses
Very preterm birth rates
The aim of the work was to assess whether or not the proportion of live births by gestational age was similar across different PCTs. Registration of births in the UK is based on gestational age and not birthweight, so gestational age cut-off points for viability were used. Variation in delivery outcome and rate of very preterm birth (≤ 32 weeks’ gestation) were explored between PCTs using:
-
the gestation-specific birth rate for live-born infants (denominator: all live births)
-
the gestation-specific birth rate for all infants (denominator: all live and stillbirths and late fetal deaths)
-
the gestation-specific percentage of infants registered as live (denominator: gestation-specific live births and stillbirths/late fetal deaths).
For each measure, the median, interquartile range (IQR) and 90% percentile range were calculated by gestational age and PCT. Binomial regression models were fitted with PCT included as a random effect to compare the variation in gestation-specific rates between PCTs. These models enable the exploration of between-PCT variation in excess of that expected by chance, accounting for differences in sample size. The standard deviation (SD) of the random effect for PCTs was compared across different gestational ages, with a lower SD suggesting greater homogeneity between PCTs. Models were then adjusted for maternal age and ethnicity based on census data and socioeconomic deprivation, measured using the area-level IMD 2007 (population-weighted average of LSOAs in each PCT).
Infant mortality
The next step was to assess the impact of the variation in registration of births at > 24 weeks’ gestation on infant mortality rates. The median, IQR and 90% percentile range for the proportion of infant deaths at < 24 weeks’ gestation were calculated by PCTs to assess variation in the contribution of these deaths to overall infant mortality. For each PCT, standard infant death rates were calculated (denominator: all live births) and then recalculated excluding births for which clinical decision-making was most prone to variation (births < 24 weeks’ gestation). Sensitivity analyses excluding births < 28 weeks’ gestation were also undertaken. For each PCT, the absolute change in infant mortality and the change in rank before and after excluding preterm births < 24 weeks’ gestation were calculated. Changes in infant mortality were compared between PCTs with a high (≥ 50%) or low (< 50%) percentage of preterm births < 24 weeks’ gestation registered as live born.
Results
Variation in preterm birth rates
There were 2,535,855 live births, 13,112 stillbirths and 2382 estimated late fetal deaths across the 147 PCTs. First, the live-birth rate was assessed by gestational age to assess how the rate of preterm live birth varied between PCTs. Rates of extremely preterm births (< 24 weeks’ gestation) varied widely between PCTs (Figure 4). Binomial regression models confirmed this pattern of variation between PCTs (SD between PCT variation < 24 weeks, 0.29; 24–27 weeks, 0.17; 28–32 weeks, 0.11) (see Figure 4), with the rate of extremely preterm birth being six times higher in the top 5% of PCTs than in the lowest 5% (90th percentile range 0.31 to 1.91 per 1000 births). In the older gestational age groups, this variation decreased, with a twofold and 1.5-fold difference at 24–27 and 28–32 weeks’ gestation, respectively (90th percentile range: 24–27 weeks, 2.48 to 5.26; 28–32 weeks, 10.24 to 15.75). This pattern was confirmed by binomial regression models with decreases in the between-PCT SD with increasing gestation (SD between PCT variation < 24 weeks, 0.38; 24–27 weeks, 0.18; 28–32 weeks, 0.11). After adjusting for socioeconomic deprivation, ethnicity and the age distribution of women in the PCT, the between-PCT variation was reduced for the more mature births but remained high in the extremely preterm group.
FIGURE 4.
Median, IQR and 90th percentile range of rate of preterm birth (live births and all births) by gestational age for PCTs (log-scale). Reproduced from Smith et al. 62 © 2013, BMJ Publishing Group Ltd and the Royal College of Paediatrics and Child Health, under the terms of the Creative Commons Attribution Non-Commercial Licence (CC BY-NC 3.0), which permits use, distribution and reproduction in any medium, provided the original work is properly cited, the use is non-commercial and is otherwise in compliance with the licence.
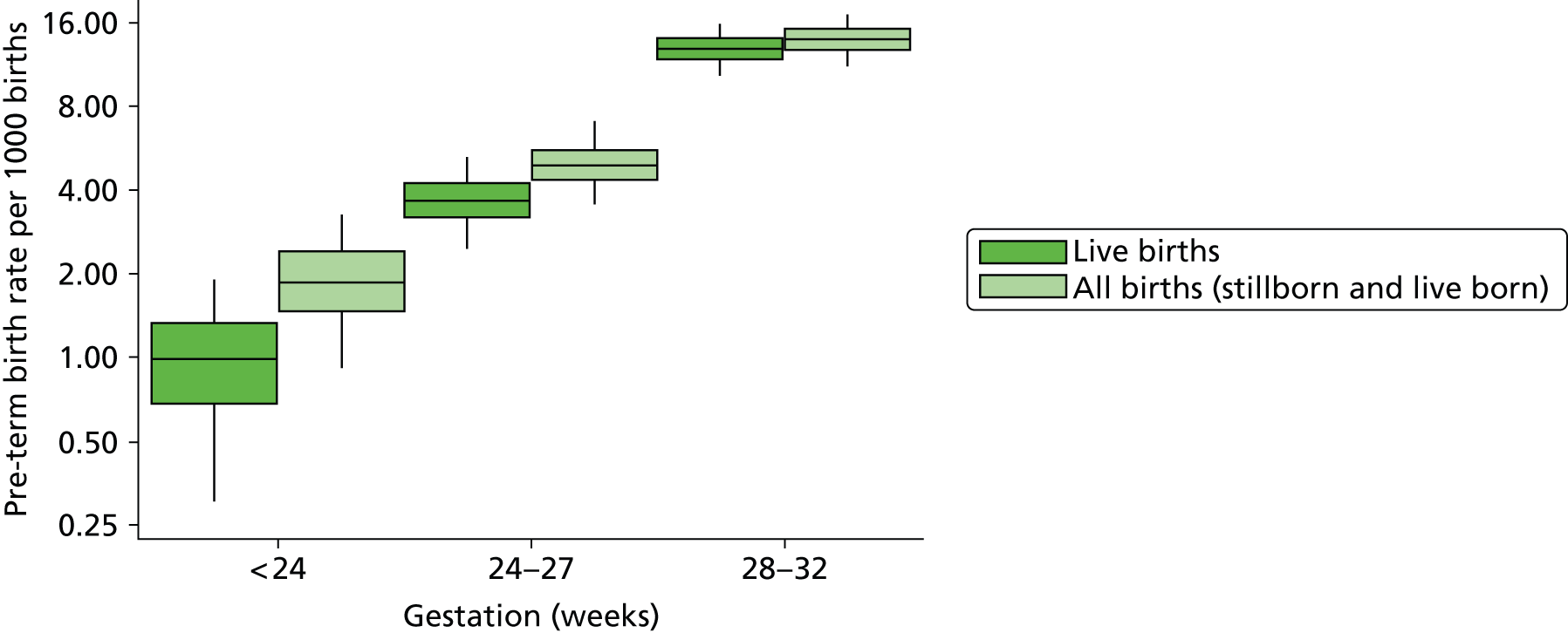
The next stage was to assess how the inclusion of fetal deaths and stillbirths affected the variation in the live-birth rate by gestational age. Including fetal deaths in the overall rate of very preterm birth (total births including fetal deaths) produced a reduction in the between-PCT variation in preterm births < 24 weeks’ gestation but little change at later gestations (see Figure 4). Binomial regression models confirmed this pattern of variation between PCTs (< 24 weeks, 0.29; 24–27 weeks, 0.17; 28–32 weeks, 0.11).
The proportion of births recorded as live showed an increase with increasing gestational age from 52.6% at < 24 weeks’ gestation to 73.9% at 24–27 weeks’ gestation and 91.9% at 28–32 weeks’ gestation, as would be expected as survival improves with increasing gestation (Figure 5). However, the variation at < 24 weeks’ gestation was wide with a 90% percentile range of 26.3% to 79.5%; that is, in the lower 5% of PCTs, around one-quarter of births were registered as live-born compared with over three-quarters in the upper 5% of PCTs. This variation reduced considerably with increasing gestation as seen in Figure 5 (90% percentile of range 24–27 weeks, 64.4% to 82.9%; 28–32 weeks, 88.5% to 95.4%). Binomial regression models again confirmed this pattern of decreasing between-PCT variation in the percentage of births registered as live-born with increasing gestation. Adjusting for PCT population characteristics resulted in little change in the between-PCT variation for all gestational age groups.
FIGURE 5.
Median, IQR and 90% percentile range for the percentage of preterm births registered as live-born by gestational age for PCTs (log-scale). Reproduced from Smith et al. 62 © 2013, BMJ Publishing Group Ltd and the Royal College of Paediatrics and Child Health, under the terms of the Creative Commons Attribution Non-Commercial Licence (CC BY-NC 3.0), which permits use, distribution and reproduction in any medium, provided the original work is properly cited, the use is non-commercial and is otherwise in compliance with the licence.
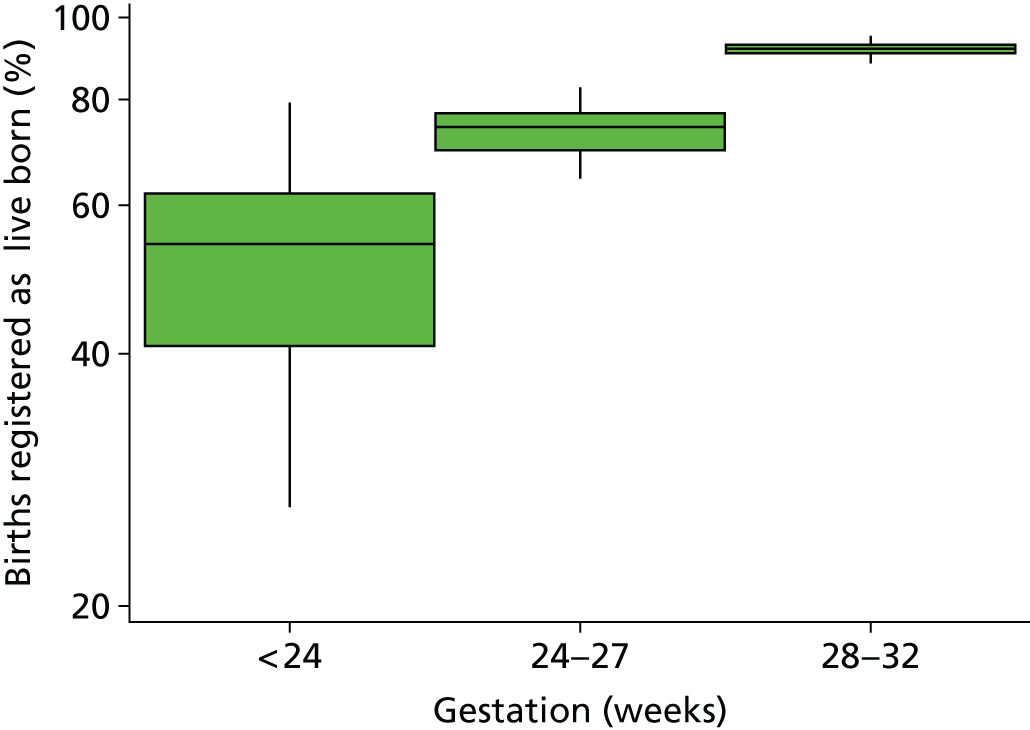
Impact of extremely preterm births on infant mortality rates
The overall infant mortality rate was 4.78 per 1000 live births (n = 12,083). This varied widely between PCTs from 2.34 to 8.93 per 1000 births. Despite making up only 1% of births, 19.5% of infant deaths arose from births < 24 weeks’ gestation. Between PCTs this varied considerably (90% percentile range 6.7% to 31.9%).
First, the impact of preterm births < 24 weeks on the actual rate of infant mortality was assessed. Comparing the overall infant mortality rate with the infant mortality rate excluding preterm births < 24 weeks’ gestation (Figure 6) showed a decrease in infant mortality of more than 1 death per 1000 births after exclusion of preterm births < 24 weeks’ gestation in 60 out of the 147 PCTs. Of these, 83% registered more than half of preterm births < 24 weeks’ gestation as live-born. Conversely, of those 87 PCTs which had a smaller decrease in infant mortality (≤ 1 death per 1000 births), only 43% had registered over half of preterm births < 24 weeks’ gestation as live-born.
FIGURE 6.
Overall infant mortality rate vs. infant mortality rate excluding infants of < 24 weeks’ gestation for PCT by percentage of births of < 24 weeks’ gestation registered as live-born. Lines indicate an absolute difference of one death and two deaths per 1000 live births. Reproduced from Smith et al. 62 © 2013, BMJ Publishing Group Ltd and the Royal College of Paediatrics and Child Health, under the terms of the Creative Commons Attribution Non-Commercial Licence (CC BY-NC 3.0), which permits use, distribution and reproduction in any medium, provided the original work is properly cited, the use is non-commercial and is otherwise in compliance with the licence.
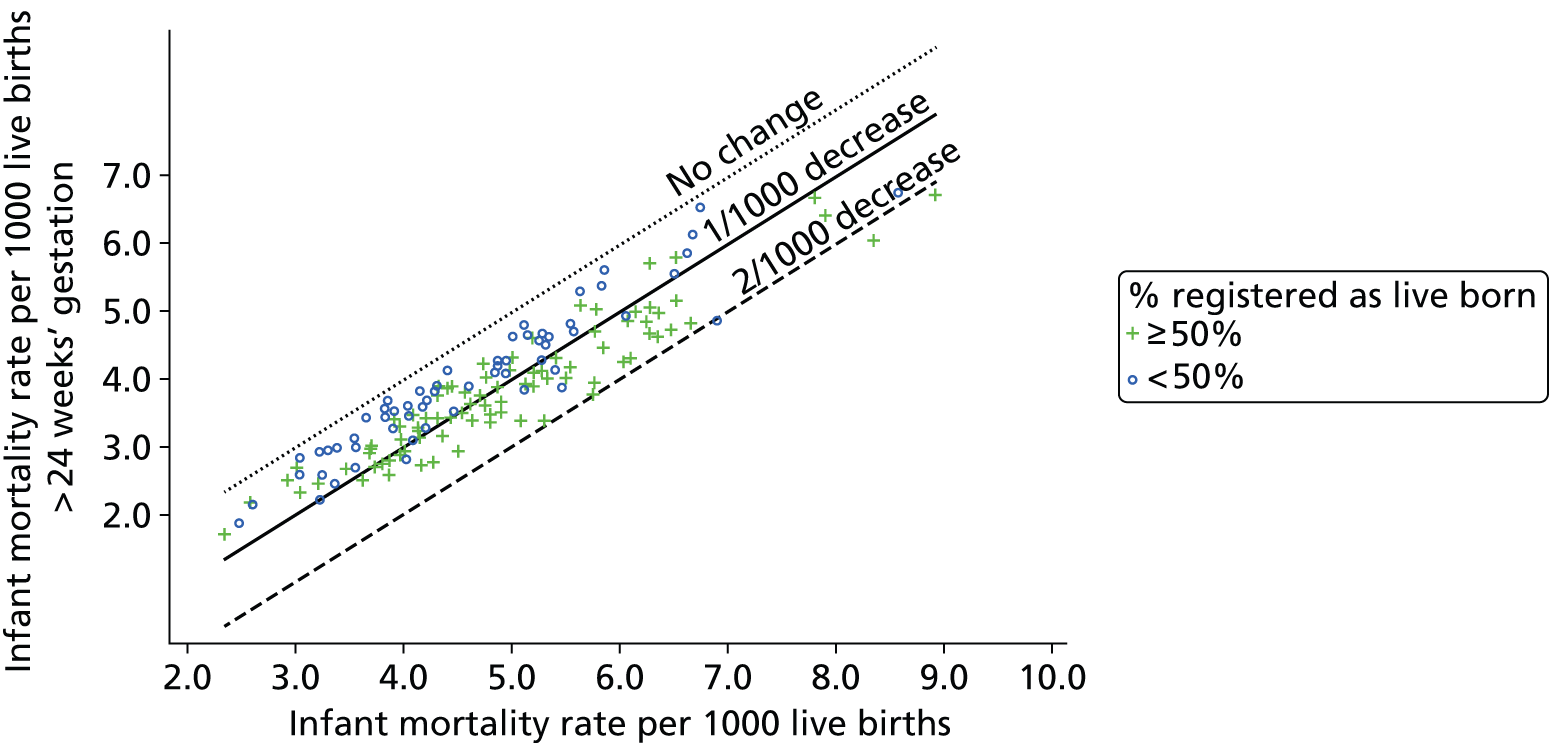
Second, as infant mortality rates are often used to rank PCTs’ performance, the impact of births at < 24 weeks’ gestation on rankings of infant mortality rates was assessed. After excluding preterm births at < 24 weeks’ gestation (Figure 7), PCTs that registered fewer than half of preterm births of < 24 weeks’ gestation as live-born fell a median of 12 places whereas those that registered at least half of births as live-born improved by a median of 4 places.
FIGURE 7.
Rank of overall infant mortality rate vs. rank of infant mortality excluding infants born at < 24 weeks’ gestation for PCTs by percentage of births at < 24 weeks’ gestation registered as live-born. Lines refer to an absolute increase and decrease of 20 places in rankings, 1 = lowest mortality rate, 147 = highest mortality rate. Reproduced from Smith et al. 62 © 2013, BMJ Publishing Group Ltd and the Royal College of Paediatrics and Child Health, under the terms of the Creative Commons Attribution Non-Commercial Licence (CC BY-NC 3.0), which permits use, distribution and reproduction in any medium, provided the original work is properly cited, the use is non-commercial and is otherwise in compliance with the licence.

Sensitivity analyses
Sensitivity analyses excluding infants < 28 weeks’ gestation showed similar findings. Further analyses using estimates of late fetal deaths, based on 1997–2006 data, showed a stronger relationship between the percentage of births registered as live-born < 24 weeks’ gestation and changes in both infant mortality rates and ranks when excluding births < 24 weeks’ gestation. Although missing gestational age data may be more common in earlier gestations, analyses assuming that the rate of missing data was 100 times higher in the earliest gestational age group (< 24 weeks) had little effect on the results.
Conclusions
Key findings
-
Wide between-PCT variation existed in extremely preterm birth (< 24 weeks’ gestation) rates.
-
Consequently, the percentage of infant deaths arising from these births varied.
-
Exclusion of births < 24 weeks’ gestation led to significant changes in infant mortality rankings of PCTs.
-
Infant death rates in PCTs in England are influenced by variation in the registration of births for which viability is uncertain.
Limitations and strengths
The variation in the rate of live births at < 24 weeks’ gestation and the proportion of births registered as live-born may reflect true underlying differences in the extremely preterm birth rate and fetal death rate between PCTs. However, after adjusting for underlying aetiological differences such as socioeconomic deprivation, ethnicity and maternal age, wide variation between PCTs persisted in this early gestational age group. Furthermore, it was not possible to attribute such between-PCT variation to any reported approach to care or improved overall outcomes in particular hospitals around England. These are the first analyses exploring variation in the registration of < 24-week gestation births and deaths and their impact on infant mortality in the UK. By utilising national data collected in a validated, systematic way, it provides a large reliable data set to assess variation between regions across England.
Implications for policy and practice
This work demonstrates that registration differences impact on within-country comparisons, as well as those between countries. In order to make direct comparisons in mortality, be it at international, regional or unit level, detailed validation and standardisation is essential to ensure that ‘like-with-like’ comparisons are being made, distinguishing ‘real’ variation from ‘artefacts’ that arise from reporting and registration differences. A standardised approach to the collection, calculation and presentation of mortality rates would reduce artefactual differences.
Despite improvements in care, variations in outcomes persist. Differences in management strategies and decisions regarding viability by a range of health-care professionals present at delivery are likely to be responsible for the wide variations in delivery outcome of extremely preterm infants. Such variation in management is likely to reflect not policy at the commissioner level but rather the approach of individual hospitals and their clinical teams. In the UK, the World Health Organization (WHO) definition of a live birth based on signs of life irrespective of gestational age is generally accepted for registration purposes. However, there are practical difficulties in interpreting true signs of life as well as subjective differences in judgements about the best outcome for parents. In the USA, where the WHO definition is accepted, research shows that nearly one-third of physicians include gestational age in their personal criteria for defining a live birth with definitions ‘open to subjective interpretation’.
Decisions over registration greatly affect parents in the UK, as late fetal deaths (< 24 weeks of gestation) are not officially registered. Following the death of a live-born baby of any gestation or stillbirth after 24 weeks’ gestation, all parents are entitled to a birth and death certificate, to maternity/paternity leave and pay, to child benefit for 8 weeks and to means-tested assistance with funeral expenses, and mothers receive free prescriptions and dental care for 1 year; in addition, the case will be referred to a coroner for investigation. In comparison, following a late fetal loss, parents will be eligible for none of these benefits. This is likely to have financial impacts since extremely preterm birth is considerably higher in socioeconomically deprived areas. There may also be emotional impacts related to these babies not being formally registered as births and deaths. This issue was highlighted by a House of Commons debate exploring the introduction of birth certificates for stillbirths (from 24 weeks’ gestation), lobbied for by parents. 63
It would seem sensible that, when comparing localities, infant and neonatal mortality rates are calculated excluding births less than 24 weeks’ gestation to ensure that ‘like-with-like’ comparisons are being made. However, this would mean the exclusion of up to one-third of infant deaths in some areas and ultimately it would seem wise to work towards reducing the variation in the registration of extremely preterm infants in England.
Since 2013, the national perinatal mortality surveillance system in the UK has aimed to collect data on all deaths (including babies born dead) at 22 and 23 weeks’ gestation. This step should not only improve our ability to investigate within-country differences in early-life mortality rates but also allow for direct international comparisons, particularly across Europe, where the vast majority of countries use the WHO definition of birth and register all pregnancy outcomes from 22 weeks’ gestational age. Such an approach would seem sensible for all developed countries.
Recommendations for future research
-
Research into understanding how this variation arises and standardising the implementation of guidelines regarding viability of infants of < 24 weeks’ gestational age is needed in order to tackle this variation and reduce its impact on both mortality rate comparisons and inequalities in parents’ access to benefits.
-
Detailed understanding is needed of the potential emotional impact on parents of certifying babies at 22 and 23 weeks’ gestation as neonatal deaths or fetal losses so that guidelines can be introduced to ensure that all parents are treated in the most appropriate way at this difficult time.
Chapter 3 The Late And Moderately preterm Birth Study
Background and rationale to the application
Introduction
The risks of very preterm birth (before 32 weeks’ gestation) have been extensively reported. It is well recognised that delivery at this very early stage of pregnancy is associated with substantial neonatal morbidity and mortality and with adverse long-term outcomes for the child. 64–67 Very preterm birth has, therefore, been the main focus of perinatal research for many years. In contrast, babies born between 32 and 36 weeks’ gestation have been understudied and, indeed, almost overlooked by researchers until recent years. As such, there is a relative paucity of data about the outcomes of these larger and more mature preterm infants. LMPT infants (32–36 weeks’ gestation) constitute a much larger group than very preterm infants, representing 6–7% of all births and around 75% of preterm births. In England and Wales, this represents around 40,000 babies each year. 68 Births in this group have increased disproportionately in recent years. In the USA, the years between 1990 and 2006 saw preterm births rise by more than 20%, from 7.3% to 9.1%, with the greatest rise being seen in births between 34 and 36 weeks’ gestation. Numbers of births at gestations below 34 weeks had increased by only 10%. 69
Increasing rates of LMPT births are likely to be influenced by a number of factors. These were not well understood, but it seemed reasonable to suppose that both increasing numbers of spontaneous deliveries and increasing obstetric intervention for maternal and fetal complications at this gestation might have contributed. The assumption, although untested, that late preterm infants were at much lower risk of significant morbidity than were babies born at < 32 weeks’ gestation may have led to a trend towards earlier intervention in pregnancies complicated by maternal pregnancy-related illness. In addition, improved obstetric care at earlier gestations allowed prolongation of some pregnancies in which early delivery was threatened to a stage when the risk of neonatal morbidity was perceived to be smaller (i.e. > 32 weeks). It seemed plausible, therefore, that the number of infants falling within this gestational age group might increase even further with obstetric intervention focused on minimising the risk of stillbirth close to term and reducing neonatal morbidity.
In the UK, at the time when this study was planned, there was no routine collection of perinatal or neonatal data for babies born at ≥ 32 weeks’ gestation and these infants were not routinely followed up after discharge from neonatal hospital care. There was a widely held belief that the outcomes for preterm infants born closer to term did not differ substantially from those of term-born infants. However, evidence was emerging to suggest that this might not be true. It became clear that prospective, comprehensive data collection for infants born LMPT was needed to clarify factors that contribute to preterm birth at these gestations and to provide contemporaneous information about outcomes of LMPT infants to inform parents and clinical management.
Terminology
Until 5–10 years ago, little attention was paid to standardising terminology relating to birth at 32–36 weeks’ gestation. Historically, such infants were often referred to as ‘near-term’, but other expressions, such as ‘moderate’, ‘mild’ and ‘marginally’ preterm, were also commonly used. In response to rapidly rising preterm birth rates and in order to better acknowledge the needs of this group, a workshop, sponsored by the National Institutes for Health (NIH) USA, was held (Optimizing Care and Outcome of the Near-term Pregnancy and Near-term Newborn Infants: a summary of the workshop sponsored by the National Institute of Child Health and Human Development). 70 This suggested that the use of ‘near-term’ should be abandoned, as this description did not adequately reflect the immaturity of these preterm infants and implied a greater degree of development than was appropriate. It was recommended that ‘late preterm’ should be used to denote birth between 34+0 and 36+6 weeks’ gestation. Some discrepancies in terminology remain, but there is now a greater consistency within the published literature. Late preterm birth has been accepted as birth between 34+0 and 36+6 weeks’ gestation. Although there has been no such consensus for a classification of birth between 32+0 and 33+6 weeks, ‘moderately preterm’ is now commonly used. We chose to adhere to these definitions, which are used throughout this report. When we describe issues relevant to the whole group we use the abbreviation LMPT.
Aetiology of late and moderately preterm birth
No single cause has been identified to explain why preterm birth occurs. Risk factors for delivery at very preterm gestations have been more extensively studied than those at more mature preterm gestations. A number of associations have been found that are thought to predispose women to deliver prematurely. 71–73 With respect to late and moderate prematurity, it was not known whether risk factors would be similar to those associated with very preterm birth or whether different influences may be important.
Maternal infection
Maternal systemic, genital and urinary tract infection and inflammation have been causally linked to preterm birth. 74,75 The risk of infective complications increases with pre-labour premature rupture of the membranes. Maternal chorioamnionitis has been implicated as a factor contributing to the poor neurodevelopmental76 and neurological77 outcomes in affected neonates. However, the proportion of pregnancies complicated by infection at later preterm gestations is unknown.
Socioeconomic deprivation
Material or social deprivation refers to a variety of conditions experienced by people who lack certain resources in relation to others in the community. 18 Material, social and financial deprivation, educational disadvantage and poor access to health-care services are often closely linked. Areas of interest with respect to preterm birth have been the impact of living conditions and working conditions, including physical aspects of work. 78 These and other experiences that result in stress are thought to contribute to preterm delivery in the extremely preterm group, with rates of preterm birth in the most deprived women rising to almost twice those of the least deprived. 5 Poor dental health is a common problem in socioeconomically deprived populations. 79 Maternal oral health has been shown to be important for overall health and periodontal disease during pregnancy has been associated with adverse pregnancy outcomes. 80,81 Much of the research linking socioeconomic status with preterm birth has been carried out with respect to extreme prematurity. 5,82 The influence of socioeconomic deprivation in women delivering at later preterm gestations remains unexplored.
Lifestyle
Many aspects of lifestyle are closely linked to levels of material and financial deprivation. Lack of access to financial resources can limit the choice of lifestyle and ability to access education and health care, making it extremely difficult to separate material and behavioural issues. A number of elements of maternal lifestyle during pregnancy may have either positive or adverse effects on the fetal growth or development in utero and may influence rates of congenital anomaly. Although results of studies are conflicting, stress during pregnancy and, in particular, during the early stages of pregnancy is also thought to be an important risk factor for adverse pregnancy outcomes. 83 Such stress may be related either to pregnancy-specific anxieties84 or to life events. Stress responses are frequently linked to financial poverty as people living in poverty have fewer resources, both financial and psychological, with which to respond to major life events.
Other key issues potentially associated with preterm birth and adverse fetal development reflect lifestyle choices such as risk-taking behaviours including smoking,85 excessive alcohol intake,86,87 recreational drug use88 and dietary intake. Women are encouraged to eat a ‘healthy’ diet during pregnancy. There is evidence from research to suggest that a cholesterol-lowering, or Mediterranean-style, diet reduces the risk of preterm delivery. 89–92 Women at lower risk were those who ate fish at least twice a week, used olive or rapeseed oil, ate five or more portions of fruit and vegetables a day, ate meat at most twice a week and drank no more than two cups of coffee a day. 90 However, others have shown no such association. Maternal caffeine intake during pregnancy has, in itself, been associated with an increased risk of spontaneous abortion. 93,94 The UK Foods Standards Agency recently reassessed its recommendations, and suggested that caffeine intake should be no more than 200 mg per day (approximately two cups of coffee or tea) because of an increased risk of fetal growth restriction (FGR). 95 The impact of these factors of maternal lifestyle has not been assessed with respect to LMPT birth.
Obstetric intervention
Expectant management of complications allows prolongation of pregnancy to a gestation at which morbidity due to major problems of prematurity lessens on the basis that, at some point, the balance of risk shifts in favour of delivery. As survival of infants born at > 34 weeks’ gestation is similar to that of those born at term, 34 weeks appears to have been adopted as the point at which the threshold for delivery changed for many obstetricians. There is, however, only limited objective evidence to support clinical practice for many aspects of obstetric management in threatened labour and delivery at later gestations.
Antenatal corticosteroids
Research on the use of antenatal corticosteroids (ANSs) to prevent lung disease of prematurity has focused on very preterm deliveries and these drugs are recommended for use only up to 34 weeks’ gestation. Despite some evidence to suggest neonatal benefit even in term deliveries,96 and guidance suggesting that they may be considered in threatened preterm labour beyond 34 weeks, the use of ANSs in late preterm deliveries is rare.
Tocolytic agents
The use of tocolytic agents is closely linked to attempts to prolong pregnancy in order to allow administration of steroids at earlier gestations. The use of these medications beyond 34 weeks’ gestation is not recommended. 97
Pre-labour premature rupture of membranes
The Royal College of Obstetricians and Gynaecologists’ recommendations state that delivery should be considered when rupture of the membranes occurs at 34 weeks’ gestation or later. 98 This recommendation was based on the increased risk of development of chorioamnionitis with expectant management. Only a limited number of studies have addressed this question, and more research is required to determine the optimal time of delivery.
Maternal complications
Pregnancy-induced hypertension and pre-eclampsia are the most common complications of pregnancy. Delivery at 34 weeks’ gestation or later has been recommended in severe cases,99 but data suggest that women with mild disease are also more likely to be delivered in the late preterm period. 100
Previous delivery by caesarean section
Rates of caesarean section (CS) have been increasing in both the UK and the USA. Vaginal delivery after previous CS carries additional risks for both mother and baby101,102 and concerns about safety have led to a decline in both the number of obstetricians offering a trial of labour and the number of mothers taking up this option. Most obstetricians delivered such women at 36–37 weeks’ gestation, but no clear guidelines existed indicating the optimal time for delivery.
Maternal medical conditions
There are a number of maternal chronic conditions (e.g. essential hypertension, diabetes, renal disease or connective tissue disorders) that may adversely affect either mother or fetus as pregnancy progresses. The contribution of such conditions to the proportion of late preterm births had not been fully elucidated, but it seems likely that the combination of late preterm birth with maternal morbidity will substantially increase the risk for newborn morbidity compared with term-born infants. 103
Intrauterine growth restriction
An estimated fetal weight below the 10th percentile for gestational age is associated with some chronic maternal medical conditions, placental disorders and fetal conditions such as chromosomal abnormalities and viral infections. Timing of delivery depends on both maternal and fetal condition; expectant management with close fetal monitoring is indicated and pregnancy is usually prolonged until at least 34 weeks unless monitoring indicates significant fetal compromise. However, the optimal timing for delivery for those who find continuous fetal monitoring reassuring has not been determined.
Oligohydramnios
Lower than expected volumes of amniotic fluid can occur because of a number of different pathologies, placing the fetus at increased risk. Close monitoring of the pregnancy is indicated, but the optimal management in the late preterm period has not been defined.
Multiple gestations
The incidence of twin and higher-order multiple pregnancies has increased, partly because of the increasing use of treatments for infertility. Multiple births are more likely to occur in the late preterm period because of higher rates of spontaneous preterm labour and complications of pregnancy. 104 According to data from the USA, the average gestational age at delivery of twins is 35.3 weeks and of triplets is 32.2 weeks. 105 There is evidence of increased risk of fetal death with increasing gestation in both monochorionic and dichorionic pregnancies. 106–108 At the time that this work was planned, the role of elective delivery in the LMPT period in multiple pregnancies was yet to be clarified.
Neonatal morbidity
Although they generally experience less severe and shorter-lived acute morbidities in the neonatal period than their more preterm counterparts, evidence is mounting to suggest that LMPT infants are at increased risk of a number of important neonatal conditions compared with term-born infants. These include respiratory distress,109 temperature instability,110 hypoglycaemia,111 jaundice112 and feeding difficulties. 113 These morbidities are likely to lead to longer initial hospital stays, and researchers in both the USA114 and the UK115 have also demonstrated that hospital readmission is more likely in this group of babies than in term-born infants.
Respiratory disease
As infants born at < 32 weeks’ gestation are at the highest risk of respiratory disease associated with prematurity, data reporting on rates and types of respiratory complications in more mature preterm infants were relatively sparse and there were no UK studies addressing this. Rubaltelli et al. 109 reported that the rate of any respiratory distress among infants born at 33–34 weeks’ gestation in Italian neonatal units (NNUs) was 20.6% and among those born at 35–36 weeks was 7.3%, compared with 0.6% in babies born at > 37 weeks. Wang et al. 110 compared outcomes of infants born at 35–36 weeks’ gestation between 1997 and 2000. In this study, 28.9% of late preterm infants experienced respiratory distress, compared with 5.3% of term-born infants. Similar results were reported by Escobar et al. 116 in 2006, with rates of 22.1%, 8.3% and 2.9% at 34, 35 and 36 weeks’ gestational age, respectively, in a retrospective review of the Kaiser Permanente cohort of babies in the USA. In this study, infants born at 35 weeks’ gestation were nine times more likely to be ventilated than those born at 38–40 weeks; infants born at 36 weeks were five times more likely to require ventilation. A retrospective single-centre study reported ventilation rates of 30%, 33% and 23%, at 34, 35 and 36 weeks’ gestational age, respectively. 117
Hypothermia
Temperature control and prevention of hypothermia form a part of routine newborn management. Wang et al. 110 found that 10% of late preterm infants required active management for hypothermia compared with term-born infants. Laptook and Jackson111 demonstrated increased susceptibility to cold stress in infants born at 34–37 weeks’ gestation. Temperature instability may be the presenting feature of other illness such as sepsis, but the frequency of, and factors associated with, hypothermia in LMPT infants in the UK has not been determined.
Hypoglycaemia
Hypoglycaemia is commonly encountered in neonatal care. The level of blood glucose that constitutes significant hypoglycaemia likely to impact on outcome is controversial for both term-born and preterm infants. 118,119 However, prevention of hypoglycaemia and its potential adverse neurodevelopmental effects is recognised as an important part of neonatal management. 120 Studies addressing hypoglycaemia in moderately and late preterm infants were few, but, in a retrospective review of records of more than 7000 infants, Wang et al. 110 observed hypoglycaemia three times as often in infants born at 35–36 weeks’ gestation as in term-born infants.
Feeding difficulties
Feeding represents one of the most basic skills that an infant must acquire in the neonatal period before discharge from hospital. Difficulties with feeding may influence length of hospital stay, early weight gain, glycaemic control and risk of infection. Sleepiness, difficulty with latching onto the breast and poor co-ordination of sucking and swallowing are all common causes of delay in establishing normal oral feeding in LMPT infants. 113 Wang et al. 110 found that 27% of late preterm infants, compared with 5% of term-born infants, required intravenous (i.v.) fluid administration. A substantial number, particularly those unable to feed enterally because of other conditions, may require a period of parenteral nutrition (PN). Although this may be necessary to meet nutritional requirements, it carries associated risks related to the PN itself and increased incidence of catheter-related infection with central venous line placement. As a result of the challenges of establishing breastfeeding in preterm infants, it is possible that mothers of such infants may be more likely to abandon breastfeeding than those delivering at term, although it is known that breast milk is the most appropriate nutrition for a newborn baby. Methods of feeding in LMPT babies at discharge from hospital and post discharge have not specifically been studied.
Jaundice
Prematurity places infants at an increased risk of hyperbilirubinaemia and the associated bilirubin encephalopathy (kernicterus) that can result from extremely high levels of serum bilirubin (SBR). It had been suggested that a trend towards earlier postnatal discharge of healthy newborn babies has led to an increased risk of severe jaundice secondary to postdischarge feeding difficulties and reduced monitoring in the first few days of life. In a study of hospital readmissions in the neonatal period,121 jaundice was one of the most common reasons for readmission; late preterm infants required readmission more frequently than did term-born infants. Bhutani et al. 112 studied cases reported to the Pilot Kernicterus Registry in the USA and found that late preterm babies were overrepresented in this registry, with breastfeeding being a significant risk factor.
Mortality
Worryingly, the observed risk of increased morbidity, as discussed above, seemed also to be associated with higher mortality rates in this group of infants than in those born at term. In 2000, Kramer122 assessed the contribution of ‘mild and moderate preterm birth’ to infant mortality and concluded that these infants had a high RR of death during infancy. Published infant mortality data for 2002 in the USA105 show that the mortality rate among babies born mild or moderately preterm is three times that of term-born infants. This was confirmed by Tomashek et al.,123 who found that early and late neonatal mortality were, respectively, six and three times higher, and infant mortality three times higher, among preterm infants than that of term-born infants. A substantial number of early deaths in both groups were related to congenital anomalies, but differences persisted even after exclusion of infants with anomalies.
Neurodevelopmental outcomes
A small number of published studies suggest that surviving LMPT infants may be at risk of significant later neurodevelopmental impairment. Results of a prospective follow-up study of 24 infants in 1987 indicated that preterm infants born between 34 and 36 weeks’ gestation had increased psychomotor developmental problems and, in particular, language difficulties when compared with term-born control children at 4 years of age. 124 In the UK, Huddy et al. 125 sought to quantify poor outcomes at school age among 176 infants born between 32 and 35 weeks’ gestation. Their results, based on parent and teacher reports, suggested that up to one-third of these infants had educational problems and required additional help at school. Hyperactivity was noted by both parents and teachers in 8% of the group and was associated with poor school performance. Using routinely collected maternal and infant data, the authors identified an association between early respiratory illness and poor school outcome. However, loss to follow-up in this study was substantial (34%), suggesting that the results might not represent the most reliable estimate of the true incidence of difficulties.
Other researchers studied outcomes of preterm infants deemed to be at low risk of neurodevelopmental impairment. Pasman et al. 126 studied 44 low-risk infants born at 25–34 weeks’ gestation and found that the subgroup of infants born between 31 and 34 weeks performed less well on neuropsychological testing than their term-born counterparts. Pietz et al. 127 assessed neurodevelopmental outcomes at 7 years of age in low-risk infants with birthweights of > 1000 g who were apparently normal during infancy. Although rates of severely subnormal test results were low in this group, there was an increased frequency of moderately subnormal performance. Caravale et al. 128 published results of 3- to 4-year follow-up of 30 neurologically normal children born between 30 and 34 weeks’ gestation. Compared with term-born controls matched for age, sex and parental educational and occupational status, these infants achieved significantly lower scores for tests of intellectual development, perceptual and motor abilities, language abilities, memory and attention.
Growth in infancy and childhood in infants born late or moderately preterm
Poor postnatal growth is well recognised in extremely preterm infants129 and is often characterised in terms of failure to achieve growth rates that would be expected for intrauterine development. 130
Little is known about nutrition and growth in relation to later development of LMPT babies. A study of postnatal growth in infants born at 30–34 weeks’ gestation suggested that intrauterine growth rates are rarely achieved in this group. 131 Pietz et al. 127 examined growth parameters in low-risk preterm infants at 20 months and 7 years of age. They found that more children in the preterm group than in the control group had weight, height and head circumference below the ninth percentile at 7 years. The proportion of children with weight below the third percentile increased significantly between the ages of 20 months and 7 years. Dodrill et al. 132 examined the long-term oral sensitivity and feeding skills in 20 low-risk infants born between 32 and 37 weeks’ gestation compared with matched full-term control infants. They found statistically significant differences between the groups at 11–17 months corrected age, with preterm infants showing delay in development. This delay was greater in infants who had received longer periods of nasogastric feeding.
The economic costs of late and moderately preterm birth
It is well recognised that preterm birth places a significant financial burden on parents, families and the health and educational services. Given the increased neonatal morbidity that is apparently experienced by LMPT infants, it seems likely that the cost of initial birth hospitalisation will be significantly higher for LMPT infants than for term-born infants. 133 The public health and economic impact of much larger numbers of survivors with less obvious physical, neuropsychological, educational and behavioural difficulties than those seen in extremely preterm infants should not be underestimated. Compared with infants born at term, it had been suggested that LMPT infants will have additional health-care needs and have more hospital admissions during childhood. 134 Among 263,000 infants born in California between 1992 and 2000, 15% of preterm infants required readmission to hospital in the first year of life, with infants born at 35 weeks’ gestation accounting for 25% of the total cost. Increased postdischarge health-care service utilisation had been seen in studies of very preterm infants in the UK. 134,135 As health-care costs are often ongoing in infants of any gestation with long-term problems, it seems likely that the need for special educational support in the LMPT gestational age group might be substantial and may not previously have been fully recognised.
The need for further research
As outcomes of LMPT babies are thought to be similar to those of term-born babies, clinical management of these infants is similar to that of infants born at ≥ 37 weeks’ gestation. Following publication in 2000, by Kramer et al. ,122 of the first findings of increased mortality in LMPT infants, there was a substantial upsurge in research interest between 2004 and 2006 in babies born at LMPT gestations. The results all pointed to an association between LMPT birth and outcomes that were worse than those of term-born infants. However, these studies were, for the most part, small and of a retrospective design and there was little consistency between them with respect to the gestational ages of the children studied. In addition, published studies were carried out in North America, with few European data and no UK data available. Researchers were beginning to question the accepted clinical approach to the care of such infants and calling for enhanced neonatal care, surveillance and follow-up in this group, similar to that which is routine in infants born extremely preterm. Given the much larger numbers of LMPT babies, this would present a considerable additional burden on health-care resources. There was, therefore, a clear and pressing need for large, contemporary studies to clarify outcomes for LMPT infants and to determine if and how these differ from those of term-born babies. As available data were then limited principally to retrospective reviews of large data sets, prospective work with the potential to identify antenatal and perinatal risk factors for LMPT birth was needed. In addition, further research was required to determine whether or not certain groups of babies might be at particularly high risk and if these groups might be amenable to targeted intervention to improve their outcomes. Although costs associated with preterm birth in general have been studied, there is little information available that specifically highlights the financial burden for parents and society that is attributable to early and ongoing support of infants born LMPT.
Aims and objectives of the Late And Moderately preterm Birth Study
Overall aim
The study aimed to clarify factors contributing to preterm delivery at 32+0–36+6 weeks’ gestation and to provide current information about outcomes of infants born at this gestation.
Specific objectives
Specific objectives were as follows:
-
to clarify the relative contributions of infection, deprivation, maternal lifestyle and obstetric intervention to LMPT birth
-
to inform the development of guidelines for the management of complicated pregnancies at 32–36 weeks’ gestation
-
to quantify early mortality and morbidity associated with late and moderate prematurity compared with that of control infants born at ≥ 37 weeks’ gestation
-
to identify perinatal or neonatal interventions with the potential to improve neonatal outcomes at hospital discharge and reduce infant mortality in infants born at 32–36 weeks’ gestation
-
to evaluate health-care needs and use of health-care resources in infants born at 32–36 weeks’ gestation
-
to estimate the economic costs of moderate and late prematurity, in order to inform and guide planning and configuration of children’s services.
Key questions and focused objectives
In order to meet the above objectives, we developed a number of more focused areas for study and key questions. These questions led to a series of focused objectives that are described in the relevant sections of this report. Some of these questions were relevant for more than one of the specific objectives.
-
To clarify the relative contributions of infection, deprivation, maternal lifestyle and obstetric intervention to LMPT birth:
-
What are the pre-pregnancy characteristics of mothers who delivered their babies at LMPT gestations?
-
What are the differences in characteristics between mothers delivering at LMPT gestations and those who deliver at ≥ 37 weeks’ gestation?
-
Which factors are likely to place women at higher risk of delivering LMPT?
-
What is the contribution of socioeconomic deprivation in LMPT birth, and are area-level deprivation effects explained by individual socioeconomic factors?
-
What are the differences between the outcomes of LMPT infants born to mothers who had non-spontaneous onset of labour with those whose mothers had spontaneous onset of labour?
-
-
To inform the development of guidelines for the management of complicated pregnancies at 32–36 weeks’ gestation:
-
What are the frequency and type of pregnancy-related complications affecting women who go on to deliver at LMPT gestations?
-
What are the differences in pregnancy-related complications between women delivering at LMPT gestations and those delivering at term?
-
What are the frequencies of assisted reproductive techniques, obstetric investigations and interventions in women delivering at LMPT gestations and how do these compare with those in women delivering at term?
-
What is the number of women having medical intervention for delivery prior to the onset of labour at LMPT gestations, compared with those at term?
-
-
To quantify early mortality and morbidity associated with late and moderate prematurity compared with that of control infants born at ≥ 37 weeks’ gestation:
-
What are the characteristics at birth of singletons and multiples born at LMPT gestations?
-
How do characteristics of LMPT babies at birth differ from those of babies born at ≥ 37 weeks’ gestation?
-
What is the incidence of congenital anomalies among LMPT babies compared with those born at term and what type of anomalies occur in this population?
-
How does mortality and morbidity associated with late and moderate prematurity compare with that of control infants born at ≥ 37 weeks’ gestation?
-
-
To identify perinatal or neonatal interventions with the potential to improve neonatal outcomes at hospital discharge and reduce infant mortality in infants born at 32–36 weeks’ gestation:
-
Which factors are likely to place women at higher risk of delivering LMPT?
-
What are the differences between the outcomes of LMPT infants born to mothers who had non-spontaneous onset of labour with those whose mothers had spontaneous onset of labour?
-
-
To evaluate health-care needs and use of health-care resources in infants born at 32–36 weeks’ gestation:
-
What are the health and respiratory outcomes of children born LMPT at 2 years of age?
-
What is the prevalence of cognitive and neurodevelopmental disability among children born LMPT?
-
What are the neonatal risk factors for neurodevelopmental disability at 2 years of age among children born LMPT?
-
What is the impact of LMPT birth on behavioural outcomes at 2 years of age?
-
-
To estimate the additional economic costs of moderate and late prematurity, in order to inform and guide planning and configuration of children’s services:
-
What are the economic costs between birth and initial hospital discharge associated with moderate and late prematurity?
-
What are the economic costs between birth and 2 years associated with moderate and late prematurity?
-
How are the economic costs associated with moderate and late prematurity distributed across sectors?
-
What other factors, clinical and sociodemographic, constellate with moderate and late prematurity in estimations of economic costs?
-
Study methods
Study participants
Eligibility
Our original plan was for recruitment to take place over a 1-year period between September 2009 and August 2010. All mothers who were resident in a geographically defined area of Leicestershire and Nottinghamshire and delivered babies at 32+0–36+6 weeks’ gestation were eligible to participate in the study with their babies. There were no exclusion criteria. We also identified a group of babies born at term (≥ 37 weeks’ gestation) during the same time period and geographical region that would be recruited as a control group.
However, towards the end of the proposed 12-month recruitment period it became apparent that the target sample size of 800 singleton births in each group was unlikely to be met. An extension of the recruitment period was agreed with the ethics committee and recruitment continued until 31 December 2010.
Participating centres
We used a population-based design for the study to allow evaluation of the risks and outcomes within a regional population. The geographical area covered by the study comprised rural and urban populations, as well as a diverse range of ethnicities and a wide socioeconomic spectrum. This avoided the bias introduced in hospital-based studies, which often leads to recruitment of a study population with artificially elevated risk compared with the population as a whole. Within the chosen geographical area around Leicester and Nottingham, there were four hospitals and one community birth centre that provided maternity services to the population. Two hospitals in Nottingham provided all levels of neonatal care, from intensive care to low-dependency or ‘special’ care, with a total of approximately 10,000 deliveries annually. In Leicester, where there are also approximately 10,000 deliveries in total each year, one hospital provided both neonatal intensive and low-dependency care while the other provided low-dependency care only. In each of the two cities a single team of consultant neonatologists working across the two hospital sites provided medical management of neonatal care. Therefore, although infants were cared for in four separate geographical locations, for the purposes of delivery of neonatal care, these could be regarded as two neonatal centres. Both centres were regional referral units for women with complicated pregnancies and/or neonates with postnatal problems requiring higher-level care. The community birth centre within the region catered for around 250 deliveries per year. The deliveries here that were included were to low-risk women in whom there had been no complications of pregnancy. In addition, a proportion of the lowest-risk pregnancies were represented by deliveries at home.
Definition of geographical boundaries for recruitment
For the purposes of this study a geographical area covered by these hospitals was defined that maximised the number of participants in the study but minimised the number of residents who would deliver in other units not participating in the study (Figure 8). The region covered by the study was well known to the researchers and has previously been the setting for a number of successful population-based research studies.
FIGURE 8.
Map of area of residence for eligibility for recruitment into the Late And Moderately preterm Birth Study.
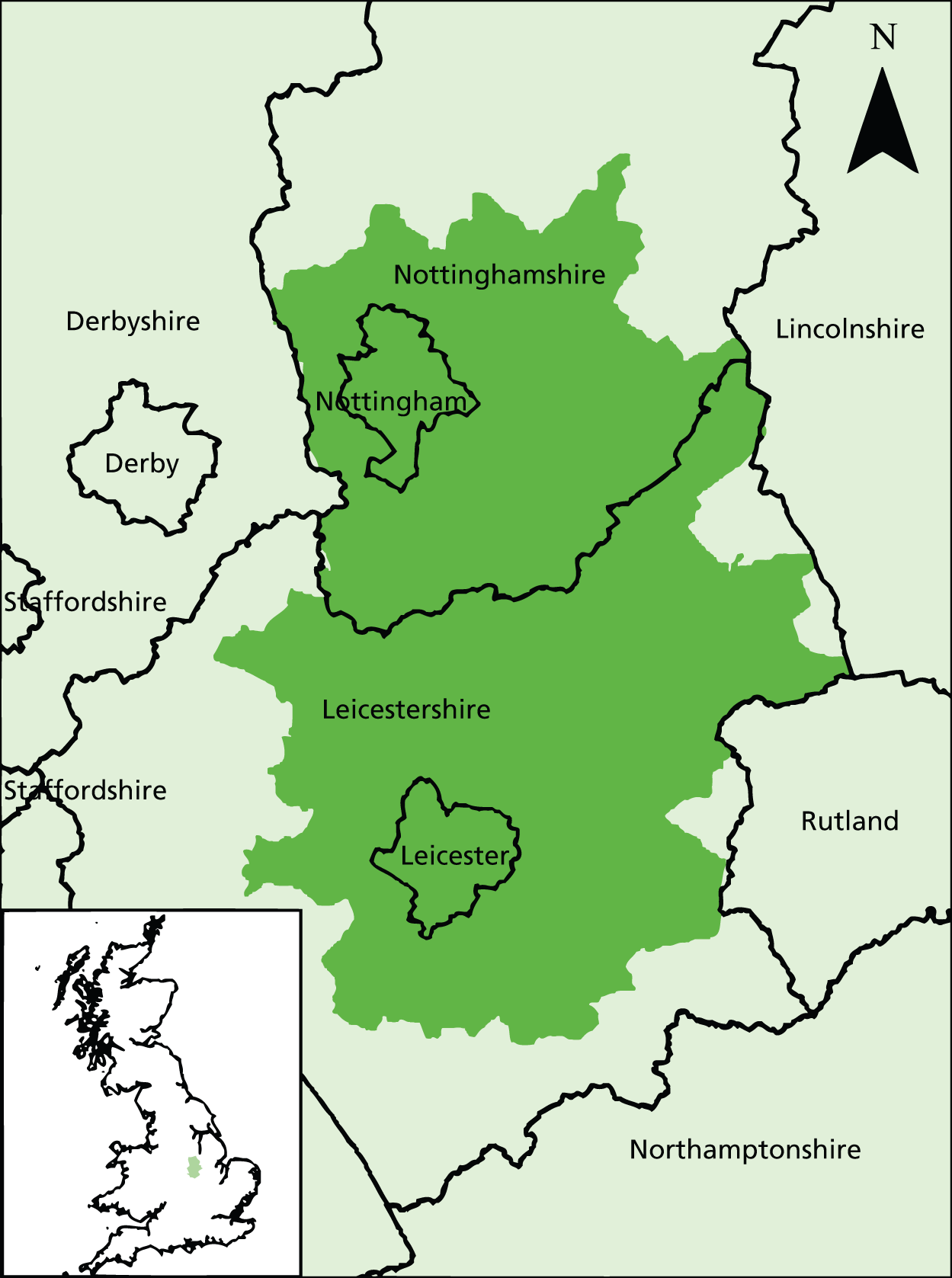
Data were obtained from the ONS for the hospital of birth for babies born in 2007 to mothers living in the postcode areas NG (Nottingham) and LE (Leicester). Based on these data, for each postcode sector (e.g. LE1 6) the percentage of births delivering at the five maternity units participating in the study was calculated. A cut-off point was then determined for the minimum percentage of births to occur in the five participating maternity units that would give at least 85% of all births in the total included area occurring in these units, that is to say that a cut-off point of 85% would mean that at least 85% of all births in each included postcode sector would deliver at one of the five participating delivery sites. The percentage of all births in the included area delivering to those five sites was actually much higher than this cut-off point as nearly all women living in close proximity to a participating hospital deliver there.
Based on these estimates, and the aim of including around 2000 singleton infants in the study, a cut-off point of 85% was decided on. This equated to 96.8% of births for the included postcode sectors actually occurring in the five participating hospitals, increasing to 99.2% when home births were included: that is, only 0.8% of births occurred in maternity units other than the five participating in the study.
Sample size
The sample size was based on detecting differences in rates of cognitive impairment and early rehospitalisation between the study and control groups of infants from singleton pregnancies. School-age follow-up of children in the EPICure study used a group of classroom controls,136 among whom the rate of cognitive impairment was 2%. There are no data for rates of cognitive impairment in moderately preterm infants in the UK. It was estimated that a rate of 5% cognitive impairment in our study group would be clinically relevant and justify targeted intervention in children’s health and education services. Oddie et al. 115 found that the rate of rehospitalisation in the first month of life in babies born at 35–37 weeks’ gestation was 6%, compared with 3% among term-born infants. A sample size estimation based on these figures predicted that recruitment of 800 singleton infants per group would allow detection of this difference in cognitive function with 90% power and in rehospitalisation with 80% power at the 5% significance level. To allow for potential non-consent and loss to follow-up, we decided to try to recruit 1000 singleton LMPT infants and 1000 singleton term-born infants.
In 2007, there were approximately 17,000 singleton births in the selected study area in Leicestershire and Nottinghamshire. Assuming that the proportion of births at 32+0–36+6 weeks’ gestation is 6–7%, it was anticipated there would be around 1000–1200 LMPT singleton births in 1 year. A minimum recruitment rate of 80% would give the required sample size.
Multiple births
To ensure inclusion into the study of sufficient term-born infants from multiple pregnancies it was decided to include all births at 32+0 weeks’ gestation or greater resulting from multiple pregnancies.
Selection of singleton control infants
Potential term-born control babies were identified using a pseudo-random sample of births obtained from ONS births data for 2007. For a random sample of 1000 births for the study area, ONS supplied information on the day of the week of birth, month of birth and place of delivery. A date and time of birth were then assigned to each of the births in this sample using known dates and time for births in Leicestershire obtained from the Child Health Registers for Leicester and Leicestershire and Rutland PCTs. These data were adjusted for day of the week to ensure an appropriate sampling of babies born at the weekend, as non-urgent induction of labour and CSs are more likely to be undertaken on a weekday.
This method overcomes the bias that may occur if more naive sampling methods are used, for example selecting the next term birth to occur at the maternity unit after a LMPT birth. 137,138 Such sampling methods would be likely to result in oversampling of high-risk term-born infants as these tend to be delivered in the sample places and at the same times as LMPT births; for example, no births would have been sampled from the midwifery-led unit.
Twelve births in the sample were excluded as they occurred at centres other than the five maternity units included in the Late And Moderately preterm Birth Study (LAMBS) or at home. Therefore, the 988 controls were used plus an additional 12 sampled from the 988 to make a pseudo-sample of 1000 controls. The list of potential control singleton births was then passed to the study midwives.
The birth to be included in the study was the first birth recorded at or after the time stated on the sample list. If there was uncertainty over which birth should be included because more than one birth occurred at the same time, then the NHS numbers of the mothers were examined and the infant included was the one born to the mother with the lowest final digit of NHS number. For example, if there were two eligible births to mothers with NHS numbers 2365892145 and 6523674352, then the mother with the latter number would be included. If the last digits were identical, then the next digit to the left would be used until there was a difference.
Recruitment to Late And Moderately Preterm Birth Study
Timing of recruitment
We aimed to recruit both study and control infants during their initial hospital stay following delivery. The length of this stay varied considerably depending on the gestational age and clinical condition of the baby at birth and the condition of the mother. In all centres, it was common for term-born infants to be discharged home at 6–12 hours following delivery if there was no medical indication for either mother or baby to remain in hospital. Infants at the lower end of the gestational range required admission to a NNU and longer hospital stays.
At the time of recruitment, the mothers were either on the delivery suite or on a postnatal ward depending on the anticipated length of hospital stay. If any mother was too sick to give consent in the period following delivery, this process was delayed until the obstetrician caring for her was happy that she was in a fit condition to be approached for consent.
Identification of eligible mothers and infants
Clinical staff on the delivery suite of each participating hospital identified infants born at 32–36 weeks’ gestation and informed a member of the research team. The research midwives referred each day to the list of dates and times on which to base recruitment of the control infants in order to identify the next infant born at ≥ 37 weeks’ gestation eligible to be recruited to the control group.
Consent
The Derbyshire NHS Research Ethics Committee (REC) approved the study design and methods. A team of six midwives who worked collaboratively across the centres carried out recruitment to the study. A research midwife attempted to approach all eligible mothers within the first 24 hours after the birth to provide them with an information sheet and obtain written informed consent for their participation. Mothers who were discharged before this initial contact could be made to present the study were contacted by a member of the clinical staff and, when possible, a home visit by a research midwife was arranged. The midwife obtained informed consent at this visit.
Written consent was obtained from parents of study and control infants for the following:
-
interview with a research midwife and completion of a maternal lifestyle questionnaire
-
collection, retention and analysis of pregnancy, perinatal and neonatal data
-
permission to send follow-up questionnaires at 6, 12, 18 and 24 months following the child’s birth.
Development of the Late And Moderately preterm Birth Study documentation
Parent information leaflets were designed to be given to parents by the research midwives following a verbal explanation of the study aims and methods. As relevant information for parents differed between the LMPT and term groups, two different leaflets were developed. In addition, our intention to recruit all eligible births, including stillbirths, necessitated the development of separate leaflets for bereaved parents. There were, therefore, four separate parent information leaflets. Those for bereaved parents were printed in a different colour from those for parents of live-born infants, to minimise the likelihood of error in distribution of the information. Similarly, separate consent forms for participation were developed for live births and stillbirths.
Data at recruitment and at all follow-up stages of the study were collected via a series of paper data collection forms. These comprised:
-
maternal interview questionnaire
-
maternal data collection form
-
neonatal data collection form
-
6-month follow-up parent questionnaire
-
12-month follow-up parent questionnaire
-
2-year follow-up parent questionnaire.
When possible, data were collected using items or scales that had been previously validated in other settings (e.g. national census, prior research studies). When this was not possible, specific questions were developed for the study following review of the relevant published literature. At the 2-year follow-up, all measures included were validated assessment tools; as such, these are not included in an appendix given copyright restrictions.
As the East Midlands is home to an ethnically diverse population, information sheets were also translated to into the most commonly encountered languages: Hindi, Urdu, Punjabi, Gujarati, Polish, French and Arabic. These versions were stored electronically to be accessible whenever they were needed for a potential participant.
Staff appointment and training
Midwives working on the LAMBS were interviewed, appointed and began their employment 4 months prior to the planned commencement of the study. This lead-in period was designed to allow ample time for new members of staff to obtain required permissions, complete induction and undergo appropriate study-specific training. Training was provided by the study principal investigator and project manager and included the following: good clinical practice training, familiarisation with study sites and clinical documentation, introduction to research methods, background information about neonatal research, prematurity and published data specifically addressing LMPT birth; and familiarisation with LAMBS documentation, safety issues and procedures related to research in the community and interview techniques. A period of observed data collection and practice interviews was included prior to the start of the study.
Accompanying manuals for each of the data collection forms were developed that were intended as guidance for those collecting data. These were provided to the research midwives in order to (1) standardise methods of data collection by ensuring that all those collecting data interpreted the questions in the same way and (2) to provide clear guidance in areas where uncertainty in interpretation was most likely to occur.
Data collection for the Late And Moderately preterm Birth Study
Perinatal data collection
Baseline data about all live births, stillbirths and neonatal deaths on delivery suite occurring at 32–36 weeks’ gestation were obtained from records of admissions and deliveries in each participating centre. Individual participant study data were extracted from medical notes by the research midwives and recorded using neonatal and maternal data collection forms (see Appendices 1 and 2).
Data relating to mothers’ general medical history, past obstetric history, antenatal care, labour and delivery were extracted from the mothers’ maternity records. Data relating to the neonatal stay for well term-born and late preterm infants who required no neonatal medical input were also obtained from the mothers’ maternity records. For infants who received medical care, either on the NNU or on the postnatal ward, neonatal medical and nursing records were consulted to extract data about the infant’s clinical course until hospital discharge.
In addition to obtaining data from medical records, research midwives interviewed each consenting mother using a semistructured questionnaire (see Appendix 1) to obtain sociodemographic details and information about her lifestyle, living and working conditions and antenatal health.
Follow-up data collection
After discharge from neonatal care, follow-up data were collected using a series of postal questionnaires. These were sent for parents to complete and return when the children reached 6 and 12 months of chronological age and 2 years corrected age (2Y-CA). Prior to sending all postal correspondence, infants were traced via the NHS Patient Demographic Service to ensure that they were alive and to obtain current contact details. Freepost envelopes were provided for parents to return questionnaires. A second copy of the questionnaire was mailed 2–3 weeks later if the study centre had not received a completed questionnaire.
Six months
The questionnaire at 6 months comprised items to assess their child’s use of health-care services, child-care costs and mothers’ general health (see Appendix 2). Questionnaires were posted to parents within 1 week of the date on which their child attained 6 months of age.
Twelve months
At 12 months of age, the same questionnaire was sent to obtain further longitudinal data relating to the use of health-care and social care services, with additional questions to determine whether or not the child had achieved key developmental milestones (see Appendix 3). Similar to the 6-month follow-up, questionnaires were mailed to parents within 1 week of the date on which their child reached 12 months of age and a second copy of the questionnaire was mailed 2–3 weeks later if a completed questionnaire had not been returned. However, at this follow-up, data were collected using a hierarchical mixed-mode approach. Parents who had not responded to two postal questionnaires were contacted by telephone, e-mail or text message to confirm that they had received the questionnaire and to offer the option to complete it as a telephone interview. Non-responders to postal questionnaires were therefore routinely offered the option of a telephone interview when contact could be made. At this time, parents were also given the opportunity to complete the 6-month questionnaire during the same telephone interview if this had not previously been returned. Up to three attempts were made to contact each family by telephone, e-mail or text message.
Two years
At 2 years, the child’s age at follow-up was corrected for prematurity. Data relating to health and neurodevelopmental outcomes were again collected using a hierarchical mixed-mode approach. Parents were mailed a questionnaire to complete 7–10 days prior to the day on which their child reached 2 years of age, corrected for prematurity. If the questionnaire was not received 10 days post 2Y-CA, parents were contacted by telephone, e-mail or text message to remind them to complete the questionnaire and to offer the option to complete it over the telephone at a time convenient to them. In addition, at this follow-up stage, a system for online completion of questionnaires was established to improve response rates. An identical format of the questionnaire was programmed online using SurveyMonkey® (SurveyMonkey, Palo Alto, CA, USA) and, if this option was selected, parents were e-mailed a web link to the questionnaire to be completed at their convenience. If parents could not be contacted by telephone, text or e-mail and the questionnaire had not been received 2 weeks post 2Y-CA, a second postal questionnaire was sent. A final attempt was made 1–2 weeks later to contact parents by telephone, text or e-mail to offer a telephone interview or online completion. A maximum of three attempts were made to contact each family by telephone, e-mail or text message.
Minimising loss to follow-up
To maintain parents’ interest in the study and minimise participant attrition, parents were sent a study newsletter when children were 6, 12 and 18 months of age and children were sent a first and second birthday card. Children were also sent a sticker activity sheet to play with while their parent completed the questionnaire. Partway through the study, a Facebook group (Facebook, Inc., Menlo Park, CA, USA) was also established in order to retain contact with the cohort. In order to protect the privacy of participants in the study, a closed group was established whereby parents could only join after confirming personal details held on study records. Parents were sent information about how to join the Facebook group with routine study communications. Questionnaire data were not collected via Facebook, but the private message system was used to maintain contact with families and send reminders to complete questionnaires. Regular updates and news about the study were also posted to members of the LAMBS Facebook group to maintain interest in the study. The Facebook link was included in all communication with parents of children in the study to remind them of the group’s existence. All communications via Facebook received an individual response from a member of the LAMBS research team. It was suggested that parents could post photographs or updates to the Facebook page to encourage participation and dialogue with the study team and other study families.
Data management and analyses
Data entry and management
A custom-made database was developed for initial study recruitment. This database was employed by study administrative staff throughout the study period to ensure that participant records were up to date at all stages of the study. Records of recruitment were cross-checked with birth registers in each maternity unit. This database was also used to monitor and record method of completion and receipt of follow-up questionnaires.
Further databases were developed for entry of data relating to each of the study data collection forms and parent questionnaires. All data were independently double entered into a computer database and any ambiguous data items were clarified by further review of the medical records. Implausible values were highlighted during data cleaning and checked.
Statistical analyses
All statistical analyses were undertaken using Stata 13 (StataCorp LP, College Station, TX, USA). Statistical significance was set at the 5% level for all analyses and no adjustment was made for multiple testing. 139
In all tables categorical variables are presented as n (%) and continuous variables are presented as either means (SD) or medians (range).
The potential predictive effects of mothers’ and babies’ characteristics on the probability of being born LMPT were quantified using estimated odds ratios (ORs), with 95% CIs and p-values.
Summary statistics of clinical outcomes are presented by study group, multiplicity and whether or not labour was spontaneous. Relative risks were estimated for each outcome by Poisson regression, with 95% CIs calculated using robust standard errors (SEs). 140,141
Odds ratios were used to estimate the association between the potential predictors and the probability of being born LMPT as this part of the study had a case–control design and, therefore, the direct estimation of RRs was not possible. 142 The investigation of clinical and neurodevelopmental outcomes, however, had a cohort study design, which allowed the estimation of RRs.
Non-response at the 2-year follow-up was investigated separately for term-born and LMPT children. The risk of non-response was calculated using Poisson regression with robust SEs for a variety of maternal and infant characteristics. For the categorical health, developmental and behavioural outcomes, the risk of the poor outcome occurring was investigated. RRs with 95% CIs were presented for the risk of the poor outcome in the LMPT compared with the term-born group. When not accounted for in the developmental score, adjustments were also made for sex of child, corrected age and socioeconomic status. When adjustment resulted in separation, this has been noted and estimates are not provided.
For continuous outcomes [measured using the Parent Report of Children’s Abilities – Revised (PARCA-R) and Brief Infant and Toddler Social–Emotional Assessment (BITSEA) scores], the mean difference with 95% CI between the term-born and LMPT children is presented using a linear model. Adjustments have been made for corrected age, socioeconomic status and sex of child.
Univariable associations with neurodevelopmental disability for LMPT children were calculated. The multivariable model was constructed by selecting the variables with a p-value of < 0.2 in the univariable analysis, excluding the IMD quartile because of its correlation with the socioeconomic score, into a model selection procedure using backwards stepwise selection. The final model chosen was that in which all included variables had a p-value of < 0.05.
Socioeconomic risk index
To facilitate exploration of the independent effect of preterm birth on developmental outcomes it was decided to devise a composite socioeconomic risk index (SES Index) based on the definition of socioeconomic risk outlined here and the socioeconomic risk factors identified. This was to enable adjustment for important social and economic factors that are known to influence cognitive and behavioural development. Similar indices have been used to adjust for social and economic factors in other studies exploring neurodevelopmental outcomes following preterm birth. Table 11 highlights the contribution of each risk factor to the composite score. Mother’s education was predominantly measured using the highest qualification from degree level to no qualifications, but was combined with information on age at leaving full-time education when this information was missing. Risk was scored as low risk (score = 0, degree or higher), mild risk [score = 1, advanced levels (A levels)], moderate risk [score = 2, General Certificate of Secondary Education (GCSE) grades A–C] and high risk (score = 4, GCSE grades D–G or none of the above). Occupation was also scored on this four-level scale, based on the National Statistics Socio-economic Classification (NS-SEC) gradings (see Table 11).
| Socioeconomic risk aspect | Indicator | Risk level | |||
|---|---|---|---|---|---|
| Low (score = 0) | Mild (score = 1) | Moderate (score = 2) | High (score = 3) | ||
| Education | Mother’s highest educational qualification If missing or unknown substitute with age at end of continuous education |
Degree or equivalent (≥ 19 years) | A Level or equivalent (18–21 years) | GCSE grades A–C or equivalent (16–17 years) | GCSE grade D or below or equivalent (< 16 years) |
| Occupation | Mother’s occupational status (NS-SEC analytic class) If ‘looking after family’ coded based on benefit claims |
Managerial, professional or administrative occupations | Intermediate, supervisory or small-employer occupations Looking after family (not claiming benefits) |
Routine or semiroutine occupations | Unemployed or never worked Looking after family (claiming income support/Jobseeker’s Allowance) |
| Social support | Cohabiting status | Living with a partner | – | Not living with a partner | – |
| Income | Car ownership | Access to at least one car in the household | – | No household access to car | – |
| Wealth | Home ownership | Owns home or has mortgage | – | Rents/part rents/rent free | – |
In addition, receipt of benefits was used as a proxy measure for assigning risk status for mothers who were unemployed and self-rated as looking after family, as such a large proportion of the population were looking after the family and did not state a previous occupation. Cohabiting status, car ownership and home ownership were scored at two levels: low risk (score = 0) and moderate (score = 2). A total score across the five variables was computed ranging from 0 to 12, which was then used to classify level or risk.
Maternal age was not included in the SES Index score as this is intrinsically linked with highest educational qualification and occupational status, thus placing young mothers at particularly high risk and older mothers at low risk.
Tertiles of risk were then calculated:
-
low risk = SES Index score of 0–2
-
moderate risk = SES Index score of 3–5
-
high risk = SES Index score of ≥ 6.
Exploratory analyses showed that, using these classifications, approximately one-third of mothers fell into each risk category. Overall, for 12 mothers data were missing for one of the variables, so for these the missing item was imputed with the mean of the remaining four variables for that child. For only one mother was more than one item missing, and thus this mother was excluded from analyses using the SES Index.
Study population
All births
Recruitment until the end of the original planned recruitment period comprised 685 LMPT singleton births and 730 singleton term-born births. Figure 9 shows final recruitment to the study and survival to discharge of recruited infants. During the 15-month extended period of recruitment, there were 20,321 births at or beyond 37 weeks’ gestation within the relevant geographical area and 1376 births between 32 and 36 weeks’ gestation. LMPT births accounted for 6.3% of all births during the study period.
FIGURE 9.
The Late And Moderately preterm Birth Study recruitment.
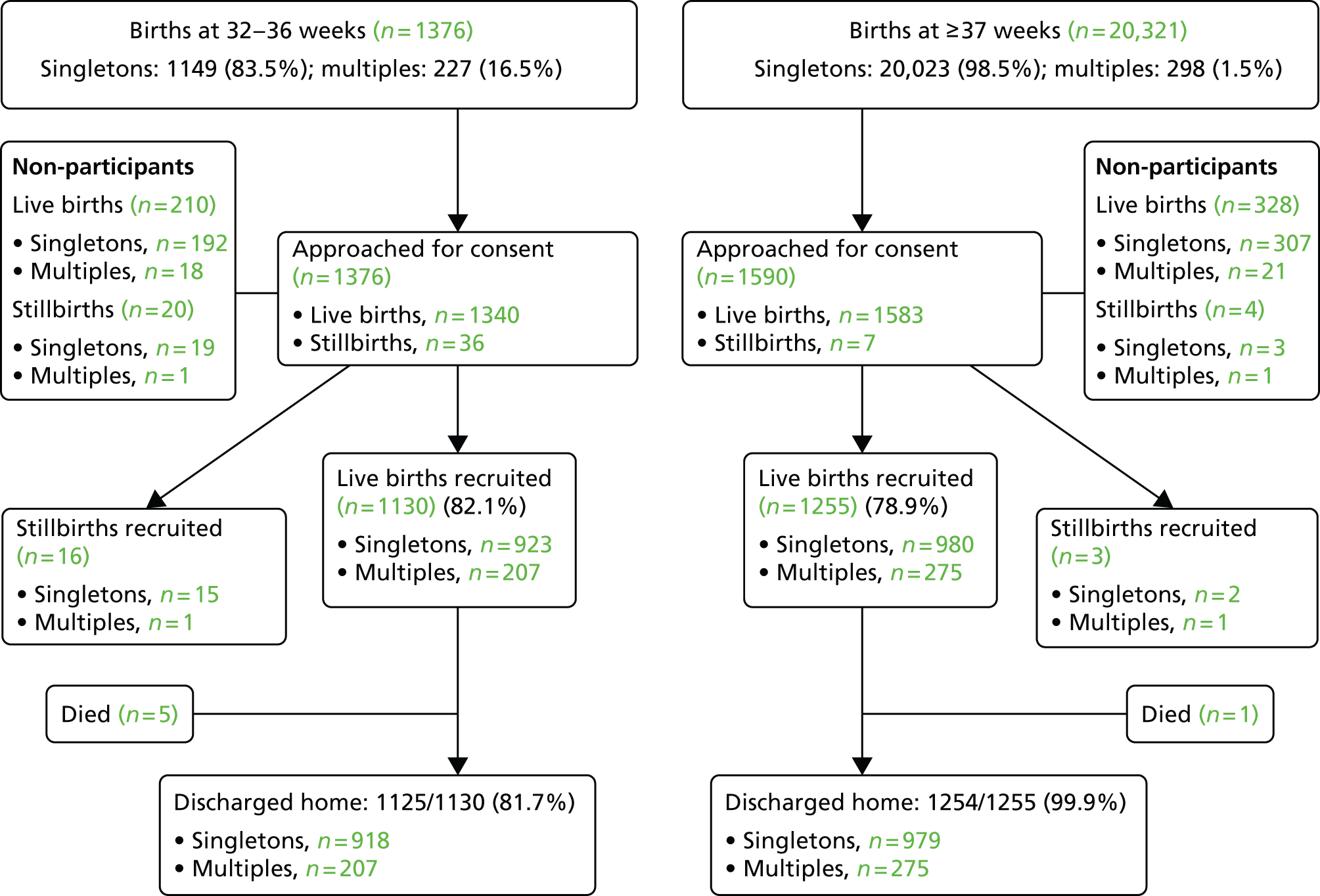
All 1376 births at LMPT gestations were eligible to participate and the control selection process identified 1590 term births within the study period that were eligible. Attempts were made to approach mothers of all these eligible infants, both live born and stillborn, to invite them to participate in the study. A total of 1146 out of 1376 (83%) LMPT and 1258 out of 1590 (79%) term births were included.
Singleton births
Singleton births accounted for 83.5% of all LMPT births during the study period and for 98.5% of births at ≥ 37 weeks’ gestation. Mothers of 1149 LMPT infants and 1192 term-born singleton infants were eligible for recruitment to the study and, of these, 938 (81.6%) and 982 (82.5%), respectively, agreed to participate.
Multiple births
Babies from multiple gestations accounted for 16.5% of LMPT births and for 1.5% of all births at ≥ 37 weeks’ gestation. In contrast to the recruitment of singletons, when eligible term births were sampled from the complete population of term singleton births, in the case of multiples, all those born at term were eligible as previously stated. Mothers of 226 LMPT and 298 term-born multiples were eligible to participate and, of these, 208 (92%) LMPT and 276 (92.6%) term-born babies were recruited.
Stillbirths
There were 36 stillbirths at LMPT gestation and seven stillbirths in the randomly selected group of deliveries at term. Of these, 16 were recruited to the LMPT group and three to the term-born group.
Non-participation
A record was maintained of numbers of women who declined to participate in the study. This record comprised only those data that were required to identify potential recruits (gestation, postcode and whether or not the pregnancy resulted in a live birth or stillbirth). When the reason for non-participation was articulated, the research midwife documented this.
Live births
Of all mothers of live-born infants, 210 (15.6%) in the LMPT group and 328 (20.7%) in the term group either declined participation or were unable to be contacted by the clinical staff following discharge from hospital. A reason for non-participation was given by 118 (56%) of the LMPT group and by 191 (58%) of the term group. The most common reason in both groups was a lack of interest in the research, which was the reason given by 45% of LMPT mothers and 36% of mothers delivering at term.
Stillbirths
As might be expected, mothers of stillborn infants were less likely to agree to participate in the study: 55% of mothers of preterm stillborn infants declined to participate, as did 57% of mothers of stillborn infants born at term. Many of these mothers did not wish to hear about or engage in research after this distressing experience, although most indicated that they were willing to be contacted at a later date. Therefore, in most cases, a period of time was allowed to elapse before the research midwives attempted to approach these women. For those who wished to speak to a research midwife shortly after their delivery, every effort was made to offer support and, when necessary, practical advice at this time. Mothers who had given permission to contact them after discharge were telephoned at least 2 weeks after the delivery and were not approached again if they declined at this time.
Deaths
There were six deaths in the postnatal period prior to discharge home. Of these, five were in LMPT group and one was in the term-born group. There were two further deaths following discharge from hospital: one term-born infant died before the 6-month follow-up and a further preterm infant died between 6 months and 1 year.
Characteristics of mothers delivering at late and moderately preterm gestations
Objectives
For singleton and multiple gestation pregnancies:
-
to describe pre-pregnancy characteristics of mothers who delivered their babies at LMPT gestations
-
to compare characteristics of mothers delivering at LMPT gestations with those who delivered at ≥ 37 weeks’ gestation
-
to describe characteristics of babies born at LMPT gestations
-
to compare characteristics of LMPT babies at birth with those of babies born at ≥ 37 weeks’ gestation
-
to determine the incidence and type of congenital anomalies among LMPT babies compared with those born at term.
Methods
Data obtained from mothers’ obstetric and delivery records were used, together with information gathered from mothers at the time of interview post delivery.
Measures
Obstetric data
Data collection focused on exploration of the impact of key sociodemographic factors on the incidence of LMPT birth and on outcomes of newborn infants. We studied the distribution of pre-pregnancy health factors, including body mass index (BMI) at the time of booking for antenatal care, pre-existing chronic health problems, diabetes mellitus and hypertension. We also looked at previous obstetric history, including whether or not this was the first pregnancy and if the mother had experienced a previous preterm birth.
Maternal interview data
The maternal interview (see Appendix 1) involved collection of sociodemographic data from all mothers. This included information on mothers’ age, ethnicity, civil status, occupation during pregnancy, working patterns and conditions, education, socioeconomic status and lifestyle.
The highest maternal educational qualification was classified into four categories: (1) degree or higher; (2) A levels; (3) GCSE grades A–C; and (4) GCSE grades D–G or none of the above. Occupations were classified into eight analytic classes which were collapsed into managerial or professional (classes I and II); intermediate occupations (classes III–V); routine and semiroutine occupations (classes VI and VII); and unemployed, retired and students (class VIII).
Mothers’ occupational status was classified using the NS-SEC (ONS143), with mothers who reported that they looked after their family full time classified separately. Other economic information obtained comprised receipt of means-tested benefits, access to a car, home ownership, self-reported financial status and information about day-to-day financial hardship. These were combined into the composite working condition risk score described above.
Data collected relating to mothers’ health comprised self-reported chronic health conditions. Socioeconomic factors included maternal lifestyle and risk-taking behaviour including the use of tobacco, alcohol or recreational drugs.
Delivery and neonatal data
Data collection included mode of delivery, gestation, birthweight, gender, FGR and the occurrence of major chromosomal or structural congenital anomalies. Mode of delivery included spontaneous vaginal delivery; assisted vaginal delivery, which included all instrumental deliveries with either cephalic or breech presentation; and CSs and whether or not this was preceded by labour. Deliveries in which vaginal instrumental delivery was attempted, but the baby was ultimately delivered by a CS were classified as CS. FGR was defined using a customised weight percentile of calculator [Gestation Related Optimal Weight (GROW) Customised Centile Calculators, v5.16; Gestation Network LTD, Birmingham, UK].
There is no universally accepted definition of a major congenital anomaly. For the purposes of this study, major structural and chromosomal anomalies were classified by clinical consensus and with reference to the classifications used by the EMSYCAR.
Results
There were 923 mothers who gave birth at LMPT gestation and 980 who gave birth at term to singleton infants recruited to the study. In terms of multiple births, 103 mothers whose pregnancy ended in delivery at LMPT gestation and 138 that delivered their babies at ≥ 37 weeks’ gestation joined the study.
The characteristics of mothers of all LMPT and term-born singleton infants participating in the LAMBS are shown in Table 12 for singleton births and in Table 13 for multiple births. These tables include those whose babies were born with major structural and/or chromosomal congenital anomalies. Maternal characteristics were compared between the LMPT and term groups.
| Characteristic | Term | LMPT | OR (95% CI) for LMPT | p-value |
|---|---|---|---|---|
| n (%) | 980 (51.5) | 923 (48.5) | – | – |
| Age at time of baby’s birth (years), n (%) | ||||
| < 20 | 55 (5.6) | 51 (5.5) | 0.94 (0.62 to 1.42) | 0.76 |
| 20–24 | 187 (19.1) | 186 (20.2) | 1.01 (0.77 to 1.31) | 0.97 |
| 25–29 | 266 (27.1) | 263 (28.5) | Baseline | – |
| 30–34 | 278 (28.4) | 266 (28.8) | 0.97 (0.76 to 1.23) | 0.79 |
| ≥ 35 | 194 (19.8) | 156 (16.9) | 0.81 (0.62 to 1.07) | 0.14 |
| Unknown | 0 (0.0) | 1 (0.1) | – | – |
| Ethnicity, n (%) | ||||
| White | 759 (77.5) | 661 (71.6) | Baseline | – |
| Mixed | 19 (1.9) | 30 (3.3) | 1.81 (1.01 to 3.26) | 0.046 |
| Asian or Asian British | 142 (14.5) | 171 (18.5) | 1.38 (1.08 to 1.77) | 0.01 |
| Black or black British | 48 (4.9) | 49 (5.3) | 1.17 (0.77 to 1.77) | 0.50 |
| Chinese or other ethnic group | 11 (1.1) | 12 (1.3) | 1.25 (0.54 to 2.86) | 0.59 |
| Missing | 1 (0.1) | 0 (0.0) | – | – |
| Cohabitation, n (%) | ||||
| Living as part of a couple | 849 (86.6) | 755 (81.8) | 0.69 (0.54 to 0.88) | < 0.003 |
| Single | 130 (13.3) | 168 (18.2) | Baseline | – |
| Unknown | 1 (0.1) | 0 (0.0) | – | – |
| Consanguineous relationship, n (%) | ||||
| Yes | 26 (2.7) | 23 (2.5) | 0.94 (0.53 to 1.66) | 0.83 |
| No | 951 (97.0) | 896 (97.1) | Baseline | – |
| Missing | 3 (0.3) | 4 (0.4) | – | – |
| Highest educational qualification, n (%) | ||||
| Degree or equivalent – codes 4 and 5 | 333 (34.0) | 245 (26.5) | Baseline | – |
| A level or equivalent – code 3 | 227 (23.2) | 224 (24.3) | 1.34 (1.05 to 1.72) | 0.02 |
| GCSE grades A–C or equivalent – code 2 | 252 (25.7) | 262 (28.4) | 1.41 (1.11 to 1.80) | 0.005 |
| GCSE grade D or below or equivalent – codes 1 and 0 | 164 (16.7) | 190 (20.6) | 1.57 (1.20 to 2.06) | 0.001 |
| Unknown | 4 (0.4) | 2 (0.2) | – | – |
| Occupational status during pregnancy, n (%) | ||||
| Managerial and professional – codes 1 and 2 | 285 (29.1) | 220 (23.8) | Baseline | |
| Intermediate – codes 3, 4 and 5 | 201 (20.5) | 180 (19.5) | 1.16 (0.89 to 1.52) | 0.28 |
| Routine and manual – codes 6 and 7 | 150 (15.3) | 132 (14.3) | 1.14 (0.85 to 1.53) | 0.38 |
| Never worked or unemployed – code 8 | 117 (11.9) | 150 (16.3) | 1.66 (1.23 to 2.24) | 0.001 |
| Looking after family – code 9 | 219 (22.4) | 236 (25.6) | 1.40 (1.08 to 1.80) | 0.01 |
| Missing | 8 (0.8) | 5 (0.5) | – | – |
| BMI at booking, n (%) | ||||
| Normal | 478 (48.8) | 479 (51.9) | Baseline | – |
| Underweight | 37 (3.8) | 49 (5.3) | 1.32 (0.84 to 2.07) | 0.22 |
| Overweight | 240 (24.5) | 225 (24.4) | 0.94 (0.75 to 1.17) | 0.56 |
| Obese | 184 (18.8) | 126 (13.7) | 0.68 (0.52 to 0.89) | 0.004 |
| Not known | 41 (4.2) | 44 (4.8) | – | – |
| Previous preterm delivery, n (%) | ||||
| Yes | 51 (5.2) | 175 (19.0) | 4.26 (3.07 to 5.91) | < 0.001 |
| No | 929 (94.8) | 748 (81.0) | Baseline | – |
| Unknown | 0 (0.0) | 0 (0.0) | – | – |
| Primigravida, n (%) | ||||
| Yes | 371 (37.9) | 361 (39.1) | 1.06 (0.87 to 1.28) | 0.56 |
| No | 609 (62.1) | 561 (60.8) | Baseline | – |
| Unknown | 0 (0.0) | 1 (0.1) | – | – |
| Any chronic health problem, n (%) | ||||
| Yes | 306 (31.2) | 360 (39.0) | 1.41 (1.16 to 1.71) | < 0.001 |
| No | 674 (68.8) | 563 (61.0) | Baseline | – |
| Unknown | 0 (0.0) | 0 () | – | – |
| Smoking during pregnancy, n (%) | ||||
| Yes | 204 (20.8) | 252 (27.3) | 1.44 (1.16 to 1.78) | 0.001 |
| No | 776 (79.2) | 666 (72.2) | Baseline | – |
| Unknown | 0 (0.0) | 5 (0.5) | – | – |
| Recreational drug use during pregnancy, n (%) | ||||
| Yes | 12 (1.2) | 19 (2.1) | 1.69 (0.82 to 3.51) | 0.16 |
| No | 967 (98.7) | 904 (97.9) | Baseline | – |
| Unknown | 1 (0.1) | 0 (0.0) | – | – |
| SES Index, n (%) | ||||
| Low risk | 365 (37.2) | 283 (30.7) | Baseline | – |
| Medium risk | 292 (29.8) | 270 (29.3) | 1.19 (0.95 to 1.50) | 0.13 |
| High risk | 323 (33.0) | 370 (40.0) | 1.48 (1.19 to 1.84) | < 0.001 |
| Missing | 0 (0.0) | 0 (0.0) | – | – |
| Alcohol in pregnancy, n (%) | ||||
| Yes | 416 (42.5) | 367 (39.8) | 0.89 (0.74 to 1.08) | 0.23 |
| No | 563 (57.5) | 555 (60.1) | Baseline | |
| Unknown | 1 (0.1) | 1 (0.1) | – | |
| Pre-pregnancy diabetes, n (%) | ||||
| Yes | 8 (0.8) | 32 (3.5) | 4.36 (2.00 to 9.52) | < 0.001 |
| No | 972 (99.2) | 891 (96.5) | Baseline | – |
| Unknown | 0 (0.0) | 0 (0.0) | – | – |
| Pre-pregnancy hypertension, n (%) | ||||
| Yes | 11 (1.1) | 26 (2.8) | 2.55 (1.25 to 5.20) | 0.01 |
| No | 969 (98.9) | 897 (97.2) | Baseline | – |
| Unknown | 0 (0.0) | 0 (0.0) | – | – |
| Characteristic | Term | LMPT | OR (95% CI) for LMPT | p-value |
|---|---|---|---|---|
| n (%) | 138 | 103 | – | – |
| Age at time of baby’s birth (years), n (%) | ||||
| < 20 | 1 (0.7) | 10 (9.7) | 14.00 (1.68 to 116.49) | 0.015 |
| 20–24 | 16 (11.6) | 9 (8.7) | 0.79 (1.68 to 2.07) | 0.63 |
| 25–29 | 35 (25.4) | 25 (24.3) | Baseline | – |
| 30–34 | 41 (29.7) | 37 (35.9) | 1.26 (0.64 to 2.49) | 0.50 |
| ≥ 35 | 45 (32.6) | 22 (21.4) | 0.68 (0.33 to 1.41) | 0.30 |
| Unknown | 0 (0.0) | 0 (0.0) | – | – |
| Ethnicity, n (%) | ||||
| White | 105 (76.1) | 84 (81.6) | Baseline | – |
| Mixed | 4 (2.9) | 3 (2.9) | 1.25 () | 0.93 |
| Asian or Asian British | 17 (12.3) | 9 (8.7) | 0.66 () | 0.35 |
| Black or black British | 12 (8.7) | 5 (4.9) | 0.52 () | 0.24 |
| Chinese or other ethnic group | 0 (0.0) | 1 (1.0) | a | a |
| Unknown | 0 (0.0) | 1 (1.0) | a | a |
| Cohabitation, n (%) | ||||
| Living as part of a couple | 126 (91.3) | 89 (86.4) | 0.50 (0.21 to 1.19) | 0.12 |
| Single | 10 (7.3) | 14 (13.6) | Baseline | – |
| Unknown | 2 (1.6) | 0 (0.0) | – | – |
| Consanguineous relationship, n (%) | ||||
| Yes | 5 (3.6) | 0 (0.0) | a | a |
| No | 133 (96.4) | 103 (100.0) | a | a |
| Highest educational qualification, n (%) | ||||
| Degree or equivalent – codes 4 and 5 | 67 (48.6) | 38 (36.9) | Baseline | – |
| A level or equivalent – code 3 | 31 (22.5) | 21 (20.4) | 1.19 (0.60 to 2.36) | 0.61 |
| GCSE grades A–C or equivalent – code 2 | 25 (18.1) | 23 (22.3) | 1.62 (0.81 to 3.24) | 0.17 |
| GCSE grade D or below or equivalent – codes 1 and 0 | 14 (10.1) | 21 (20.4) | 2.64 (1.21 to 5.80) | 0.015 |
| Unknown | 1 (0.7) | 0 (0.0) | – | – |
| Occupational status during pregnancy, n (%) | ||||
| Managerial and professional – codes 1 and 2 | 55 (39.9) | 40 (38.8) | Baseline | – |
| Intermediate – codes 3, 4 and 5 | 20 (14.5) | 12 (11.7) | 0.83 (0.36 to 1.88) | 0.65 |
| Routine and manual – codes 6 and 7 | 23 (16.7) | 16 (15.5) | 0.96 (0.45 to 2.04) | 0.91 |
| Never worked or unemployed – code 8 | 7 (5.1) | 15 (14.6) | 2.94 (1.10 to 7.89) | 0.032 |
| Looking after family – code 9 | 33 (23.9) | 20 (19.4) | 0.83 (0.42 to 1.66) | 0.60 |
| Unknown | 0 (0.0) | 0 (0.0) | – | – |
| BMI at booking, n (%) | ||||
| Normal | 68 (49.3) | 56 (54.4) | Baseline | – |
| Underweight | 4 (2.9) | 5 (4.9) | 1.52 (0.39 to 5.92) | 0.55 |
| Overweight | 38 (27.5) | 21 (20.4) | 0.67 (0.35 to 1.27) | 0.22 |
| Obese | 24 (17.4) | 12 (11.7) | 0.61 (0.28 to 1.32) | 0.21 |
| Not known | 4 (2.9) | 9 (8.7) | – | – |
| Previous preterm delivery, n (%) | ||||
| Yes | 3 (2.2) | 8 (7.8) | 3.79 (0.98 to 14.66) | 0.054 |
| No | 135 (97.8) | 95 (92.2) | Baseline | – |
| Unknown | 0 (0.0) | 0 (0.0) | – | – |
| Primigravida, n (%) | ||||
| Yes | 51 (37.0) | 39 (37.9) | 1.04 (0.61 to 1.76) | 0.89 |
| No | 87 (63.0) | 64 (62.1) | Baseline | – |
| Unknown | 0 (0.0) | 0 (0.0) | – | – |
| Any chronic health problem, n (%) | ||||
| Yes | 45 (32.6) | 34 (33.0) | 1.02 (0.59 to 1.75) | 0.95 |
| No | 93 (67.4) | 69 (67.0) | Baseline | – |
| Unknown | 0 (0.0) | 0 (0.0) | – | – |
| Smoking during pregnancy, n (%) | ||||
| Yes | 23 (16.7) | 26 (25.2) | 1.69 (0.90 to 3.18) | 0.10 |
| No | 115 (83.3) | 77 (74.8) | Baseline | – |
| Unknown | 0 (0.0) | 0 (0.0) | – | – |
| Recreational drug use during pregnancy | ||||
| Yes | 0 (0) | 4 (3.9) | a | a |
| No | 137 (99.3) | 99 (96.1) | a | a |
| Unknown | 1 (0.7) | 0 (0.0) | – | – |
| SES Index, n (%) | ||||
| Low risk | 71 (51.5) | 44 (42.7) | Baseline | – |
| Medium risk | 37 (26.8) | 24 (23.3) | 1.05 (0.55 to 1.98) | 0.89 |
| High risk | 30 (21.7) | 35 (34.0) | 1.88 (1.02 to 3.48) | 0.044 |
| Missing | 0 (0.0) | 0 (0.0) | – | – |
| Alcohol in pregnancy, n (%) | ||||
| Yes | 80 (58.0) | 67 (65.1) | 0.73 (0.43 to 1.25) | 0.25 |
| No | 57 (41.3) | 35 (34.0) | Baseline | – |
| Unknown | 1 (0.7) | 1 (1.0) | – | – |
| Pre-pregnancy diabetes, n (%) | ||||
| Yes | 2 (1.5) | 0 (0.0) | a | a |
| No | 136 (98.6) | 103 (100.0) | a | a |
| Unknown | 0 (0.0) | 0 (0.0) | – | – |
| Pre-pregnancy hypertension, n (%) | ||||
| Yes | 1 (0.7) | 1 (1.0) | 1.34 | 0.84 |
| No | 137 (99.3) | 102 (99.0) | Baseline | – |
| Unknown | 0 (0.0) | 0 (0.0) | – | – |
Maternal age and ethnicity
The distribution of ages of mothers at the time of delivery was similar between groups, with the majority (57.3%) of mothers of singleton infants being between 25 and 35 years of age. Compared with the reference group (aged 25–29 years), much smaller proportions of teenage mothers and older mothers (> 35 years) delivered at LMPT gestations, but these differences did not reach statistical significance. No particular age band was associated with increased odds of delivering a singleton baby at LMPT gestation.
The odds of LMPT delivery were significantly increased in mothers of multiple births delivering at < 20 years of age, but the numbers of these women were extremely small, with only one in the term group.
The majority of the mothers of infants in both LMPT (71.6%) and term (77.5%) groups were of white British origin. Women of Asian and Asian British origin formed the next largest group, comprising 18.5% of mothers delivering LMPT and 14.5% of those delivering at ≥ 37 weeks’ gestation. The odds of these women delivering LMPT babies were significantly increased (OR 1.38, 95% CI 1.08 to 1.77; p = 0.01) compared with those of white origin. Odds of LMPT delivery were also increased in women of mixed racial origin, although the number of these women in the cohort were small (1.9% and 3.3% for LMPT and term births, respectively).
Maternal socioeconomic characteristics
Living as part of a couple was associated with significantly lower odds of delivering a singleton LMPT infant than was being a single parent (OR 0.69, 95% CI 0.54 to 0.88; p < 0.01). The number of mothers whose relationships were consanguineous was small, but similar in both groups of singleton births. Similar analysis was not possible for multiple pregnancies as there were only five mothers who were in consanguineous relationships.
With respect to maternal education, comparisons between levels of education were against the reference group comprising those women who had attained the highest level of educational qualification (degree or equivalent). When compared with this group, all those with lower levels of education had significantly increased odds of delivering at LMPT gestation. There was an inverse relationship between mothers’ highest education level and odds of LMPT birth, with the lowest educational group being at highest risk. A similar pattern was seen for mothers having multiple births, with those in the lowest educational group having significantly increased odds of delivering LMPT (OR 2.64, 95% CI 1.21 to 5.80; p = 0.015).
For occupational status during pregnancy, comparisons were made against the reference group of managerial and professional occupations. Compared with this group, all other groups had increased odds of delivering LMPT infants, and these differences were statistically significant in the case of those who had never worked or were unemployed (OR 1.66, 95% CI 1.23 to 2.24; p = 0.001), and in women who reported that they were looking after their family on a full-time basis (OR 1.40, 95% CI 1.08 to 1.81; p = 0.01). Within the group of multiple births, those who had never worked or were unemployed had increased odds of LMPT delivery (OR 2.94, 95% CI 1.10 to 7.89; p = 0.032)
Using the derived SES Index, as described previously, the odds of delivering LMPT were increased within the high-risk socioeconomic group compared with the low-risk group (OR 1.48, 95% CI 1.19 to 1.84; p < 0.001). Although the pattern was similar for multiple births, the difference between the high- and low-risk groups was of more marginal statistical significance (p = 0.044).
Maternal lifestyle
The majority of women in both study groups had a BMI within the normal range. Compared with those with booking weight within the normal range, however, those women whose weight fell within the obese range were less likely to deliver a LMPT baby (OR 0.68, 95% CI 0.52 to 0.89; p = 0.004). This was not the case for multiple births.
Smoking during pregnancy was associated with increased odds of delivery at LMPT gestation (OR 1.44, 95% CI 1.16 to 1.78; p = 0.001) in singleton but not in multiple pregnancies. The number of women who reported the use of recreational drugs was very small, but in this study this did not carry any increased risk of LMPT delivery. Alcohol use in pregnancy was also not associated with increased odds of LMPT delivery in either singleton or multiple pregnancies.
Previous preterm birth and pre-pregnancy health
Nineteen per cent of mothers of LMPT singleton infants had experienced a previous preterm delivery, compared with 5.2% of mothers delivering at term (OR 4.26, 95% CI 3.07 to 5.91). In the small number of multiple pregnancies in which the mother had previously had a preterm birth, there was a trend towards increased odds, but this did not reach statistical significance, and CIs were wide (OR 3.79, 95% CI 0.98 to 14.66). Women for whom this was the first pregnancy, regardless of whether this was a singleton or a multiple birth, were not at increased risk of delivering at LMPT gestations.
A large number of women delivering singletons reported having had chronic health problems during pregnancy (39.0% of LMPT singleton births and 31.2% of term births). Those reporting chronic health problems had increased odds of LMPT birth (OR 1.41, 95% CI 1.17 to 1.70; p < 0.001) compared with those who did not. Among mothers having multiple births, the proportion was similar for LMPT (33.0%) and term (32.6%) groups.
Specifically, pre-pregnancy diabetes and pre-pregnancy hypertension were associated with LMPT delivery in singleton pregnancies [OR 4.36, 95% CI 2.00 to 9.52 (p < 0.01), and OR 2.56, 95% CI 1.25 to 5.20, respectively]. The numbers of women having multiple pregnancies who had suffered from either of these conditions prior to becoming pregnant were too small to be suitable for analysis.
The characteristics of live-born singleton babies, including those with congenital anomalies, are shown in Table 14. The birth characteristics of 923 LMPT and 980 term-born singleton babies are compared. There were no statistically significant differences in the number of male babies or in the proportion of first-born infants. There were twice as many congenital anomalies in the LMPT group, but this difference did not reach statistical significance. LMPT babies were significantly more likely to have been affected by intrauterine growth restriction (OR 1.95, 95% CI 1.51 to 2.51; p = 0.001). Compared with spontaneous vaginal deliveries, LMPT babies were more likely to be born following pre-labour CSs (OR 2.17, 95% CI 1.67 to 2.81; p < 0.001) and significantly less likely to have an assisted vaginal delivery (OR 0.71, 95% CI 0.54 to 0.93; p = 0.014).
| Characteristic | Term | LMPT | OR (95% CI) for LMPT | p-value |
|---|---|---|---|---|
| N (%) | 980 (51.5) | 923 (48.5) | – | – |
| Birthweight (g), median (range) | 3420 (1980 to 5160) | 2480 (1120 to 4960) | – | – |
| Male sex, n (%) | 503 (51.3) | 512 (55.5) | 1.18 (0.99 to 1.41) | 0.07 |
| Major congenital anomalies, n (%) | 8 (0.8) | 16 (1.7) | 2.14 (0.91 to 5.03) | 0.08 |
| Birthweight below the 10th fetal percentile, n (%) | 113 (11.5) | 187 (20.3) | 1.95 (1.51 to 2.51) | 0.001 |
| First born, n (%) | ||||
| Yes | 437 (44.6) | 434 (47.0) | 1.12 (0.93 to 1.34) | 0.24 |
| No | 537 (54.8) | 478 (51.8) | Baseline | – |
| Unknown | 6 (0.6) | 11 (1.2) | – | – |
| Mode of delivery, n (%) | ||||
| Spontaneous vaginal | 616 (62.9) | 524 (56.8) | Baseline | – |
| Assisted vaginal | 167 (17.0) | 101 (10.9) | 0.71 (0.54 to 0.93) | 0.014 |
| CS, during labour | 89 (9.1) | 99 (10.7) | 1.31 (0.96 to 1.78) | 0.089 |
| CS, not in labour | 108 (11.0) | 199 (21.6) | 2.17 (1.67 to 2.81) | < 0.001 |
There were 207 LMPT and 275 live term-born infants from multiple pregnancies and their birth characteristics are shown in Table 15. As for singletons, there were no statistically significant differences in gender or in the proportion of first-born infants. Although a significant difference is seen for congenital anomalies, with LMPT having increased odds of being affected (OR 9.59, 95% CI 1.17 to 78.56; p = 0.035), this must be interpreted with caution because of the small numbers and very wide CIs. In contrast to singleton births, multiples were more likely to be delivered by CS after the onset of labour but, similar to singletons, the odds of assisted vaginal delivery in the LMPT group were reduced compared with spontaneous vaginal delivery (OR 0.40, 95% CI 0.21 to 0.75; p = 0.004).
| Characteristic | Term | LMPT | OR (95% CI) for LMPT | p-value |
|---|---|---|---|---|
| N (%) | 275 (57.1) | 207 (42.9) | – | – |
| Birthweight (g), median (range) | 2720 (1250 to 4120) | 2200 (1098 to 3390) | – | – |
| Male sex, n (%) | 148 (53.8) | 97 (46.9) | 0.76 (0.53 to 1.09) | 0.13 |
| Major congenital anomalies, n (%) | 1 (0.4) | 7 (3.4) | 9.59 (1.17 to 78.56) | 0.035 |
| Birthweight below the 10th fetal percentile, n (%) | 117 (42.6) | 73 (35.3) | 0.74 (0.51 to 1.07) | 0.11 |
| First born, n (%) | ||||
| Yes | 126 (45.8) | 106 (51.2) | 1.24 (0.86 to 1.78) | 0.24 |
| No | 149 (54.2) | 101 (48.8) | Baseline | – |
| Unknown | 0 (0.0) | 0 (0.0) | – | – |
| Mode of delivery, n (%) | ||||
| Spontaneous vaginal | 65 (23.6) | 50 (24.2) | Baseline | – |
| Assisted vaginal | 65 (23.6) | 20 (9.7) | 0.40 (0.21 to 0.75) | 0.004 |
| CS, during labour | 39 (14.2) | 57 (27.5) | 1.90 (1.10 to 3.29) | 0.022 |
| CS, not in labour | 106 (38.5) | 80 (38.7) | 0.98 (0.61 to 1.57) | 0.94 |
Stillbirths
There were 16 recruited stillbirths in the LMPT group and three in the term group. The very small numbers of stillbirths occurring within the study period, and even smaller number of recruits in this group, means that meaningful analysis of the data collected for these mothers and their babies was not possible. However, the characteristics of the participating mothers and their stillborn infants are detailed in Table 16.
| Characteristics | Term | LMPT |
|---|---|---|
| Maternal characteristics | ||
| N (%) | 3 (15.6) | 16 (84.2) |
| Age at time of baby’s birth (years), n (%) | ||
| < 20 | 0 (0.0) | 2 (12.5) |
| 20–24 | 0 (0.0) | 5 (31.3) |
| 25–29 | 1 (33.3) | 4 (25.0) |
| 30–34 | 2 (66.7) | 3 (18.8) |
| ≥ 35 | 0 (0.0) | 2 (12.5) |
| Unknown | 0 (0.0) | 0 (0.0) |
| Ethnicity, n (%) | ||
| White | 3 (100.0) | 10 (62.5) |
| Mixed | 0 (0.0) | 0 (0.0) |
| Asian or Asian British | 0 (0.0) | 5 (31.3) |
| Black or black British | 0 (0.0) | 0 (0.0) |
| Chinese or other ethnic group | 0 (0.0) | 0 (0.0) |
| Unknown | 0 (0.0) | 1 (6.3) |
| Cohabitation, n (%) | ||
| Living as part of a couple | 2 (66.7) | 13 (81.3) |
| Single | 1 (33.3) | 2 (12.5) |
| Unknown | 0 (0.0) | 1 (6.3) |
| Consanguineous relationship, n (%) | ||
| Yes | 0 (0.0) | 0 (0.0) |
| No | 3 (100.0) | 15 (93.7) |
| Unknown | 0 (0.0) | 1 (6.3) |
| Highest educational qualification, n (%) | ||
| Degree or equivalent – codes 4 and 5 | 2 (66.7) | 4 (25.0) |
| A level or equivalent – code 3 | 0 (0.0) | 2 (12.5) |
| GCSE grades A–C or equivalent – code 2 | 1 (33.3) | 6 (37.5) |
| GCSE grade D or below or equivalent – codes 1 and 0 | 0 (0.0) | 3 (18.8) |
| Unknown | 0 (0.0) | 1 (6.3) |
| Occupational status during pregnancy, n (%) | ||
| Managerial and professional – codes 1 and 2 | 1 (33.3) | 3 (18.8) |
| Intermediate – codes 3, 4 and 5 | 1 (33.3) | 3 (18.8) |
| Routine and manual (%) – codes 6 and 7 | 1 (33.3) | 2 (12.5) |
| Never worked or unemployed – code 8 | 0 (0.0) | 0 (0.0) |
| Looking after family – code 9 | 0 (0.0) | 7 (43.8) |
| Unknown | 0 (0.0) | 1 (6.3) |
| BMI at booking, n (%) | ||
| Normal | 1 (33.3) | 6 (37.5) |
| Underweight | 0 | 1 (6.3) |
| Overweight | 2 (66.7) | 5 (31.3) |
| Obese | 0 | 3 (18.8) |
| Not known | 0 | 1 (6.3) |
| Previous preterm delivery, n (%) | ||
| Yes | 0 (0.0) | 3 (18.8) |
| No | 3 (100.0) | 13 (81.2) |
| Unknown | 0 (0.0) | 0 (0.0) |
| Primigravida, n (%) | ||
| Yes | 0 (0.0) | 2 (12.5) |
| No | 3 (100.0) | 13 (81.3) |
| Unknown | 0 (0.0) | 1 (6.3) |
| Any chronic health problem, n (%) | ||
| Yes | 1 (33.3) | 6 (37.5) |
| No | 2 (66.7) | 10 (62.5) |
| Unknown | 0 (0.0) | 0 (0.0) |
| Smoking during pregnancy, n (%) | ||
| Yes | 1 (66.7) | 5 (31.3) |
| No | 2 (33.3) | 10 (62.5) |
| Unknown | 0 (0.0) | 1 (6.3) |
| Recreational drug use during pregnancy, n (%) | ||
| Yes | 0 (0.0) | 0 (0.0) |
| No | 3 (100.0) | 15 (93.8) |
| Unknown | 0 (0.0) | 1 (6.3) |
| First born, n (%) | ||
| Yes | 1 (33.3) | 4 (25.0) |
| No | 2 (66.7) | 12 (75.0) |
| Unknown | 0 (0.0) | 0 (0.0) |
| Mode of delivery, n (%) | ||
| Spontaneous vaginal | 1 (33.3) | 11 (68.8) |
| Assisted vaginal | 1 (33.3) | 2 (12.5) |
| CS, during labour | 1 (33.3) | 2 (12.5) |
| CS, not in labour | 0 | 0 (0.0) |
| Unknown | 0 | 1 (6.3) |
| Infant characteristics | ||
| n (%) | 3 (15.8) | 16 (84.2) |
| Male sex, n (%) | 0 (0.0) | 12 (75.0) |
| Major congenital anomalies, n (%) | 0 (0.0) | 0 (0.0) |
| Birthweight below tenth fetal percentile, n (%) | 1 (33.3) | 6 (37.5) |
There were 15 singleton stillbirths in the LMPT group and two in the term group. There was one stillborn infant in each group that was from a twin pregnancy. There were no stillbirths in higher-order multiple births and in no case were both twins stillborn.
One mother consented to participate in the study following the birth of her baby that was known to have died in utero, but, when contacted at a later date to arrange an interview, she was too distressed to participate. Therefore, data for this case were available only from the mother’s maternity records and some data items were missing.
One stillbirth was the result of elective feticide in a twin pregnancy at 33 weeks’ gestation. This baby was included in the study, as the birth fulfilled the eligibility criteria. Documentation at the time of the feticide suggested that the decision for this course of action was taken because of antenatal detection of multiple fetal anomalies, but no further details were available about the nature of these anomalies.
Discussion
In singleton pregnancies, previous preterm birth and pre-pregnancy health were factors that were associated with the highest odds of delivering at LMPT gestation. Khatibi et al. 144 found that increased maternal pre-pregnancy BMI increased the risk of both early and late preterm delivery. In contrast, this current study found decreased odds of LMPT delivery in obese mothers.
Women with diabetes or hypertension that originated prior to pregnancy were at particular risk. Carter et al. 145 also found an increase in late preterm birth among women with pre-gestational diabetes mellitus. Catalano and Sacks146 suggest that the risk of intrauterine death at term, even in women with well-controlled diabetes, is significant, but whether the risk is different in those with chronic rather than pregnancy-related disease is not clear. Kase et al. 147 reported that one-third of women with chronic hypertensive disease delivered before 37 weeks’ gestation, with more than half of these being in the late preterm period. There is only limited evidence regarding management of women with chronic diseases in pregnancy and the relative benefits and risks associated with early delivery. Among the other reported illnesses, a very large range of problems was cited, including conditions with a very wide spectrum of severity such as ‘depression’, ‘back problems’ and ‘asthma’. No relationship between chronic disease and multiple LMPT birth were demonstrated, but the number of multiple pregnancies was relatively small.
In this study we saw a larger proportion of congenital anomalies in both singletons and multiples in the LMPT group than in the term-born group. Although this was not a statistically significant finding, it is possible that the differences would reach significance if examined in a larger cohort. Intrauterine growth restriction was more common in the LMPT infants and it is likely that, for many of these babies, their poor growth would have been the indication for early delivery.
Conclusions
Key findings
-
There was an inverse relationship between mothers’ highest education level and odds of LMPT birth in both singleton and multiple pregnancies, with the lowest educational group being at highest risk.
-
Mothers of Asian origin had increased odds of LMPT delivery than in those women whose ethnicity was white.
-
Living as part of a couple during pregnancy was associated with lower odds of LMPT delivery than being single.
-
Previous preterm delivery was associated with a fourfold increase in the odds of LMPT delivery compared with delivery at term.
-
Maternal hypertension and diabetes originating prior to pregnancy were associated with two and four times increased odds of delivering at LMPT gestations, respectively, compared with term births.
-
LMPT babies are more likely to be affected by intrauterine growth restriction than those born at term.
Strengths and limitations
The population-based nature of the study and inclusion of 80% of eligible mothers allowed recruitment from a socially and culturally diverse population. In addition, our study was able to recruit a large proportion of all births of twins and higher multiples. However, although study information was available in multiple languages for women from ethnic minorities, for the most part those with a limited understanding of English chose not to participate and this may have influenced our results with respect to analyses based on ethnicity.
We have identified an association between LMPT singleton delivery and previous preterm delivery, although from our data we are unable to determine whether this increased risk is related to previous LMPT birth or previous delivery at lower gestations.
In our study, information about specific pre-pregnancy diseases and any other chronic illnesses was ascertained by self-report at interview. It is well recognised that self-report may lead to either under- or over-reporting of conditions, although this effect is likely to occur in both study groups. No attempt has been made to determine the severity of these problems, but further subclassification of the conditions with respect to the likelihood of impact on pregnancy outcomes may be helpful.
Implications for practice
Although there is currently limited evidence for interventions to prevent preterm birth, our findings suggest that targeted counselling and/or care for a number of groups at risk of delivering at LMPT gestations may be appropriate. These include women who are likely to have difficulties accessing medical care, such as those with lower levels of education and those from ethnic minority communities. Women with longstanding chronic diseases may also benefit from enhanced medical surveillance or input to minimise the impact of their disease during pregnancy and optimise outcomes. However, the efficacy of targeted counselling and/or surveillance has not yet been tested and would require evaluation.
A number of sociodemographic factors were found to be associated with LMPT birth in both singletons and multiples. The impact and implications for these in singleton births are discussed in detail in a following section.
Future research
Further investigation of common and important pre-pregnancy medical conditions is warranted to clarify factors that place women at increased risk of LMPT delivery and determine whether targeted or general counselling, interventions and education can improve pregnancy outcomes for specific groups. Currently, information is limited about factors influencing spontaneous onset of labour at LMPT gestations and the role that maternal medical conditions play in this. There also remains a paucity of data about pregnancies in which pre-existing disease exerts an influence on the progress of pregnancy or well-being of the baby either directly, or by precipitating or exacerbating pregnancy-related complications. Exploration of this is necessary to guide obstetric decision-making in situations in which either expectant management or early delivery is an option, but the optimal course of action is uncertain.
Complications of pregnancy and obstetric intervention
Objectives
-
To describe the frequency and type of pregnancy-related complications affecting women who go on to deliver at LMPT gestations.
-
To compare pregnancy-related complications in women delivering at LMPT gestations with those delivering at term.
-
To describe the frequency of assisted reproductive techniques (ARTs), obstetric investigations and interventions in women delivering at LMPT gestations and compare these with women delivering at term.
Methods
Detailed data about each mother’s pregnancy, obstetric interventions during pregnancy, administration of antenatal steroids and induction of labour were extracted from her maternity records. Information about ARTs for this pregnancy was obtained from the interview with the mother.
Details of the statistical methods are given in Data management and analyses.
Measures
Pregnancy-related data collection was focused upon exploration of the impact of several key factors on the incidence of LMPT birth. Clinical factors affecting the mother and/or the fetus during pregnancy or labour were explored.
Maternal complications included pre-eclampsia, infection, gestational diabetes and prolonged rupture of membranes (PROM). Pre-eclampsia was defined as proteinuric hypertension with or without other symptoms. Prolonged rupture of the membranes was considered to be significant if the time between membrane rupture and delivery was > 24 hours. Maternal systemic infection during pregnancy was defined as illness when positive cultures were obtained from the mother’s blood. During labour, raised maternal C-reactive protein (CRP) levels of > 5 mg/l or pyrexia of > 37.5 °C were regarded as clinical evidence of maternal systemic infection and/or chorioamnionitis.
Complications affecting the fetus included intrauterine FGR, abnormalities of umbilical Doppler studies, meconium staining of the liquor, abnormalities on cardiotocography (CTG) and umbilical cord prolapse. Fetal growth restriction was defined using the GROW software. As umbilical vessel Doppler studies are performed only in pregnancies in which there are concerns about placental insufficiency and effects on fetal growth or fetal well-being, this investigation would have been indicated in only a limited proportion of women. Abnormal umbilical Doppler studies were defined as those in which the end-diastolic flow in the umbilical arteries was determined to be absent or reversed. We did not collect data regarding the length of time these findings were present or whether the findings were constant or intermittent in nature.
Many different abnormalities can affect the results of CTG during labour. We collected data for all possible abnormalities including fetal tachycardia, early, late or variable decelerations of the fetal heart rate, sustained fetal bradycardia and other abnormalities not specified. However, CTG is not performed in all women during labour. When it was clear that no cardiotocographic trace could be obtained, either because CTG was not performed or for other reasons, this was documented.
Data collected about ARTs included information about a range of techniques: ovulation induction using clomifene, follicle-stimulating hormone or other means, intrauterine insemination, donor insemination, in vitro fertilisation, intracytoplasmic sperm injection and reversal of sterilisation. However, because of the number of women having ARTs was small, the different methods were not separated for analysis.
Details about amniocentesis, if performed, were recorded, together with the reason for performing the investigation (maternal age, suspected chromosomal or other anomaly) and whether the results were normal or abnormal. In the case of chorionic villous sampling (CVS), we recorded whether the result was normal or abnormal.
A complete course of antenatal steroids was defined as either two doses of betamethasone, 12 hours apart, or two doses of dexamethasone, 24 hours apart. An incomplete course was defined as one dose of either drug. The date and time of the last dose prior to delivery were recorded and whether or not multiple courses had been administered.
Results
Maternal and fetal complications occurring during pregnancy or labour are shown in Table 17 for 938 LMPT deliveries and 982 term deliveries. Stillbirths and pregnancies in which fetal anomalies were diagnosed, either antenatally or in the neonatal period, are included.
| Complication | Term | LMPT | OR (95% CI) for LMPT | p-value |
|---|---|---|---|---|
| Maternal complications during pregnancy | ||||
| N (%) | 982 (51.2) | 938 (48.9) | – | – |
| Systemic infection, n (%) | ||||
| Yes | 3 (0.3) | 5 (0.5) | 1.77 (0.42 to 7.41) | 0.44 |
| No | 972 (99.0) | 917 (97.8) | Baseline | – |
| Unknown | 7 (0.7) | 16 (1.7) | – | – |
| Pre-eclampsia, n (%) | ||||
| Yes | 36 (3.7) | 128 (13.7) | 4.16 (2.84 to 6.10) | < 0.001 |
| No | 940 (95.7) | 803 (85.6) | Baseline | – |
| Unknown | 6 (0.6) | 7 (0.87) | – | – |
| Gestational diabetes, n (%) | ||||
| Yes | 31 (3.2) | 41 (4.4) | 1.41 (0.87 to 2.26) | 0.16 |
| No | 949 (96.6) | 893 (95.2) | Baseline | – |
| Unknown | 2 (0.2) | 4 (0.4) | – | – |
| Prolonged rupture of membranes > 24 hours, n (%) | ||||
| Yes | 70 (7.1) | 217 (23.1) | 3.91 (2.94 to 5.21) | < 0.001 |
| No | 900 (91.7) | 713 (76.0) | Baseline | – |
| Unknown | 12 (1.2) | 8 (0.9) | – | – |
| Maternal complications during labour | ||||
| Raised CRP level of > 5 mg/l, n (%) | ||||
| Yes | 3 (0.3) | 33 (3.5) | 11.85 (3.62 to 38.79) | < 0.001 |
| No | 943 (96.0) | 875 (93.3) | Baseline | – |
| Unknown | 36 (3.7) | 30 (3.2) | – | – |
| Raised temperature > 37.5 °C, n (%) | ||||
| Yes | 45 (4.6) | 55 (5.9) | 1.30 (0.87 to 1.95) | 0.20 |
| No | 931 (94.8) | 875 (93.3) | Baseline | – |
| Unknown | 6 (0.6) | 8 (0.9) | – | – |
| Fetal complications | ||||
| Fetal growth restriction < 10th percentile,b n (%) | ||||
| Yes | 113 (11.5) | 193 (20.6) | 1.99 (1.55 to 2.56) | < 0.001 |
| No | 869 (88.5) | 745 (79.4) | Baseline | – |
| Unknown | 0 (0.0) | 0 (0.0) | – | – |
| Abnormal umbilical Doppler studies, n (%) | ||||
| Yes | 2 (0.2) | 25 (2.7) | 13.4 (3.17 to 56.80) | < 0.001 |
| No | 980 (99.8) | 913 (97.3) | Baseline | – |
| Unknown | 0 (0.0) | 0 (0.0) | – | – |
| Meconium-stained liquor, n (%) | ||||
| Yes | 129 (13.1) | 43 (4.6) | 0.32 (0.22 to 0.45) | < 0.001 |
| No | 844 (86.0) | 886 (94.5) | Baseline | – |
| Unknown | 9 (0.9) | 9 (1.0) | – | – |
| CTG abnormality, n (%) | ||||
| Yes | 427 (43.5) | 466 (49.7) | 1.28 (1.07 to 1.54) | 0.007 |
| No | 555 (56.5) | 472 (50.3) | Baseline | – |
| Unknown | 0 (0.0) | 0 (0.0) | – | – |
| Umbilical cord prolapse, n (%) | ||||
| Yes | 0 (0.0) | 4 (0.4) | a | a |
| No | 978 (99.6) | 931 (99.3) | a | a |
| Unknown | 4 (0.4) | 3 (0.3) | – | – |
Maternal complications
Women with systemic infection during pregnancy were no more likely to deliver at LMPT gestations than at term. However, when a raised CRP level was documented during labour, this was associated with odds of LMPT delivery that were 11 times greater than the odds of delivering at term (OR 11.85, 95% CI 3.62 to 38.79; p < 0.001). In contrast, women with a documented temperature of > 37.5 °C during labour were no more likely to deliver early. These results must be interpreted with caution. CRP level is generally regarded as a reasonably sensitive biochemical marker of the presence of infection, but is not measured in all women, so this finding is likely to reflect a group of women in whom infection was suspected. We do not have data for women in whom a CRP was measured, but was not found to be elevated, or for those in whom it was never measured. Modest fever of > 37.5 °C is less sensitive than a raised CRP level and can be caused by other, non-pathological, factors such as the ambient environmental temperature or the use of epidural anaesthesia in labour. Had data collection been limited to a more extreme value for mothers’ temperature, this may have produced different results.
Pre-eclampsia was also associated with increased odds of LMPT delivery, with affected women being four times more likely to delivery LMPT than at term (OR 4.16, 95% CI 2.84 to 6.10; p < 0.001). In addition, women who delivered LMPT infants were more likely than those delivering at term to have experienced rupture of the amniotic membranes > 24 hours prior to delivery. Gestational diabetes affected < 5% of women in each group and was not associated with increased odds of LMPT delivery compared with delivery at term.
Fetal complications
Fetal growth restriction and abnormal antenatal umbilical Doppler studies are closely related and are both likely to lead to decisions to deliver an affected infant prematurely. It is, therefore, not a surprising finding that, in this study, using univariable analysis, both were associated with increased odds of LMPT delivery [FGR: OR 1.99, 95% CI 1.55 to 2.56 (p < 0.001); abnormal Doppler: OR 13.4, 95% CI 3.17 to 56.80 (p < 0.001)]. Fetal growth restriction is likely to be the more reliable measure of the two, as it is impossible to know, with any degree of certainty, how many mothers in either group would have had abnormal studies if these had been performed. The uncertainty and the effect of small numbers are reflected in wide CIs for this measure.
Cardiotocographic abnormalities of any kind were common in both LMPT and term deliveries, with > 40% of all women in each group having some documented CTG abnormality during labour. However, abnormalities were more commonly documented in LMPT deliveries and this was associated with increased odds of LMPT delivery (OR 1.28, 95% CI 1.07 to 1.54; p < 0.007) compared with deliveries at term.
Meconium staining of the liquor was significantly less common in LMPT deliveries (OR 0.32, 95% CI 0.22 to 0.45; p < 0.001), which is an expected finding, as fetal distress associated with the passage of meconium in utero is principally a concern for women during labour at term, and in particular for post-term births (> 41 weeks’ gestation).
Umbilical cord prolapse was seen in only four (0.4%) LMPT deliveries and in no term deliveries, and so further analysis was not possible for this variable.
Assisted reproductive techniques and obstetric intervention
Table 18 shows the numbers of pregnancies that were the result of ARTs, and the number that required obstetric investigation or intervention in terms of amniocentesis, CVS or administration of ANSs for threatened preterm delivery and induction of labour. All mothers, including those delivering multiples, stillbirths and infants with congenital anomalies, are included. This comprised 1041 mothers delivering LMPT and 1120 delivering at term.
| Investigation/intervention | Term | LMPT | OR (95% CI) for LMPT | p-value |
|---|---|---|---|---|
| Number of mothers, N (%) | 1120 (51.8) | 1041 (48.2) | – | – |
| Assisted reproductive techniques, n (%) | ||||
| Yes | 67 (6.0) | 47 (4.5) | 0.74 (0.51 to 1.10) | 0.13 |
| No | 1053 (94.0) | 994 (95.5) | Baseline | – |
| Amniocentesis, n (%) | ||||
| Yes | 14 (1.3) | 17 (1.6) | 1.32 (0.65 to 2.59) | 0.45 |
| No | 1103 (98.5) | 1017 (97.7) | Baseline | – |
| Unknown | 3 (0.3) | 7 (0.7) | – | – |
| CVS, n (%) | ||||
| Yes | 1 (0.01) | 5 (0.5) | 5.39 (0.63 to 46.24) | 0.12 |
| No | 1110 (99.1) | 1029 (98.9) | Baseline | – |
| Unknown | 9 (0.79) | 7 (0.7) | – | – |
| Administration of ANSs, n (%) | ||||
| Yes | 16 (1.4) | 273 (26.2) | 24.63 (14.75 to 41.12) | < 0.001 |
| No | 1100 (98.2) | 762 (73.2) | Baseline | – |
| Unknown | 4 (0.4) | 6 (0.6) | – | – |
| Induction of labour, n (%) | ||||
| Yes | 304 (27.1) | 232 (22.3) | 0.77 (0.63 to 0.94) | 0.009 |
| No | 812 (72.5) | 806 (77.4) | Baseline | – |
| Unknown | 4 (0.4) | 3 (0.3) | – | – |
There were 47 (4.5%) births following ARTs in the LMPT group and 67 (6%) in the term group. This difference was not statistically significant. There were also no differences between the groups in the number of women undergoing amniocentesis or CVS during their pregnancy. Both investigations were carried out in only very small numbers of women; this was particularly true for CVS, and CIs were wide.
As expected, the number of women receiving ANSs was significantly higher in the LMPT group (26.2%), although a small proportion (1.4%) of mothers who went on to deliver at ≥ 37 weeks’ gestation had been given corticosteroids for anticipated preterm delivery at some stage in their pregnancy (OR 24.63, 95% CI 14.75 to 41.12; p > 0.001). Induction of labour was less common in mothers who delivered their babies at LMPT gestations.
Discussion
We saw higher rates of LMPT delivery in women with prolonged rupture of the amniotic membranes. Other researchers have also identified PROM as being more common in LMPT deliveries. 148,149 Labour has often been induced between 34 and 37 weeks’ gestation in women in the hope of avoiding problems in the neonate. However, the results of the recently published PPROMEXIL (Preterm Prelabour Rupture Of Membranes Expectant Management versus Induction of Labour) trial150 suggest that induction of labour carries no benefit over expectant management. Pre-eclampsia is another common reason for medically indicated delivery, when the well-being of the fetus is in jeopardy because of maternal illness. Although delivery may be indicated at any time during pregnancy for very severe disease, the report of the HYpertension and Pre-eclampsia Intervention Trial At Term (HYPITAT) trial151 recommends induction of labour at 37 weeks’ gestation in women with mild pre-eclampsia. There is little evidence to suggest that earlier delivery for pre-eclampsia improves outcomes for either the mother or the baby. 152 An increase in LMPT birth in mothers with pre-eclampsia has been reported, but in our study we sought only to determine the presence, not the severity, of pre-eclampsia. In contrast to others,145 we found no increased risk of LMPT birth in women with gestational diabetes.
Cardiotocographic abnormalities were detected in large numbers of women in both groups. It is possible that this finding was affected by a degree of bias, as women in whom preterm delivery is anticipated are more likely to be hospitalised prior to delivery and, therefore, are more likely to undergo CTG at this time. In addition, although efforts were made to distinguish those women in whom CTG had been performed and was normal from those in whom CTG was not carried out, this proved difficult. It is possible that CTG was not carried out in a substantial proportion of the large number of women in whom no abnormality was reported, and it cannot be presumed that CTG would be normal in these women. Further analysis of the more severe abnormalities that might be expected to adversely affect the fetus may be more discriminating.
Fetal growth restriction was commoner in LMPT deliveries and, in a large proportion of these, is likely to have been the main indication for early delivery. As expected, this is reflected in a larger proportion of women in this group having abnormal antenatal umbilical Doppler studies. The documented rates are likely to be an underestimate of the occurrence of abnormal Doppler studies, as it is likely that FGR was not identified antenatally in some women,153 who, therefore, may not have undergone Doppler ultrasonography.
Conclusions
Key findings
-
Pregnancies ending in LMPT delivery are more likely to have been affected by PROM, pre-eclampsia and FGR than are pregnancies that continue to term.
Implications for practice
The results of this study highlight for obstetric clinicians the increased likelihood of LMPT delivery in pregnancies complicated by pre-eclampsia, FGR and infection. Both expectant management and early delivery carry competing risks, with the risk of stillbirth at one end of the spectrum and the risk of neonatal morbidity at the other. As the optimal time for delivery has not yet been determined, options for management of these women at this stage of pregnancy should be approached with careful consideration of all factors.
Strengths and limitations
We have collected a wide range of obstetric information about mothers delivering at LMPT gestations and the in utero well-being of babies in order to determine factors that are associated with LMPT birth. We have shown that LMPT delivery is more common in pregnancies affected by complications. It was, however, beyond the scope of this study to explore the decision-making processes of obstetric teams that led to LMPT delivery in those in whom delivery was elective or semielective, and this is likely to play a crucial part in rates of LMPT birth and variation in these.
Future research
There is a need for further research into the management of complicated pregnancies at LMPT gestations and, in particular, to define optimum management of women who develop pre-eclampsia. The role of infection and inflammation in LMPT delivery and the value of clinical markers in guiding decisions to deliver require clarification.
There have been few studies of the outcomes of pregnancies affected by common complications with the aim of identifying the point at which the risk of in utero demise exceeds the risk of neonatal morbidity and thus justifies LMPT delivery. Exploration is needed to allow more detailed understanding of the obstetric decisions that lead to LMPT delivery.
Socioeconomic risk factors for late and moderately preterm birth
Background
The main objective of this study was to better understand the impact of socioeconomic risk factors on LMPT birth at both an area and individual level. Stream 1 highlighted that almost 80% of the relative deprivation gap in all-cause neonatal mortality is a result of premature birth and congenital anomalies. Understanding the link between deprivation and preterm birth is vital in order to identify interventions to reduce preterm birth in the future. One key way of doing this is to unpick socioeconomic inequalities in health seen at an area level by exploring individual socioeconomic risk factors.
Both area-level factors of socioeconomic risk and single individual measures of income and education have been shown to be associated with very preterm delivery in the UK5 and other developed countries. 13 However, there has been less exploration of its effect specifically at later gestations.
When socioeconomic factors are explored in most analyses, there is a focus on attributing socioeconomic differences to variations in lifestyle and health-related behaviours. These single measures of education or income do not allow exploration of the multidimensional nature of socioeconomic risk. Individuals with equivalent education or income may have considerably different available resources (house ownership, car ownership, access to benefits). In this analysis the focus was on understanding the impact of socioeconomic risk factors on LMPT birth from a multidimensional standpoint, exploring a range of socioeconomic indicators. A major challenge in exploring the influence of socioeconomic deprivation on health outcomes is how best to define the concept of ‘socioeconomic deprivation’ and identify measurable indicators. These issues are discussed here, but with a focus on the impact of socioeconomic factors to assess the impact of deprivation on preterm birth in the UK, rather than the impact of lifestyle and health behaviours.
Objective
-
To clarify the contribution of socioeconomic deprivation in LMPT birth, and assess whether or not area-level deprivation effects are explained by individual socioeconomic factors.
Methods
Area-level socioeconomic risk
As in stream 1, area-level socioeconomic risk was calculated using the IMD 2010. 154 This measure of multiple deprivation is made up of seven domain indices at the LSOA level, which relate to income deprivation, employment deprivation, health deprivation and disability, education, skills and training deprivation, barriers to housing and services, and living environment deprivation and crime. LSOAs are the smallest areas for which these deprivation data are available; although some degree of heterogeneity will exist within them, the small size of the areas (only 1500 residents) limits this. IMD 2010 was linked to the LAMBS data constructed on LSOA of residence based on the mother’s postcode at the time of birth.
These data were obtained from the ONS and linked to the maternal data by LSOA. All LSOAs in England were ranked by deprivation score. They were then weighted by their population of births (using the live-birth denominator data) and divided into five groups, with approximately equal populations of births in each, from 1 (least deprived) to 5 (most deprived).
Individual-level socioeconomic risk
In order to operationalise the concept of socioeconomic risk, a multidimensional approach was taken, aiming to encapsulate five key areas of importance: (1) education; (2) occupation; (3) income; (4) wealth; and (5) social support. Indicators were then incorporated into the maternal interview to reflect these five aspects of socioeconomic risk.
Education was measured by collecting information on mother’s highest qualification and also age at leaving continuous education. Occupation was measured by both detailed questions on mother’s occupation during pregnancy and receipt of Jobseeker’s Allowance. Mother’s socio-occupational status was then classified using the NS-SEC (ONS143) based on the information collected in the maternal interview. Occupations were classified into eight analytic classes, which were collapsed into managerial or professional (classes I and II), intermediate occupations (classes III–V), routine and semiroutine occupations (classes VI and VII), and unemployed, retired and students (class VIII). Mothers who reported that they looked after their family full time were classified separately. Income was measured by the collection of occupation data but also was based on household access to a car, which is thought to reflect current income. It was decided not to ask for detailed information on personal income, as this was thought to reduce response rates. Wealth and long-term income was measured based on whether or not the mother was a home owner. Finally, social support was measured based on whether or not the mother was living with someone as a couple during the majority of the pregnancy.
Sociodemographic data
Demographic data were also collected in the maternal interview including mother’s age and ethnic group. Mother’s age was categorised into four groups: (1) < 20 years; (2) 20–29 years; (3) 30–39 years; and (4) ≥ 40 years. Ethnic group was based on groups used in the census: white; mixed; Asian or Asian British; black or black British; and Chinese or other ethnic group.
Statistical analyses
The aim of this work was to explore whether or not area-level socioeconomic deprivation was related to LMPT birth and then to try to unpick any inequalities by identifying whether or not individual socioeconomic-level factors explained observed variations.
First, univariable analyses were undertaken to explore the relationship with area-level deprivation and the five aspects of socioeconomic risk and rate of LMPT birth. Analyses were restricted to singleton births because differential access to fertility treatment may lead to a higher incidence of multiple births in less deprived areas. Following univariable analysis, multivariable unconditional logistic regression was used to examine the independent relationship between area- and individual-level socioeconomic risk factors and LMPT and to generate adjusted ORs with their 95% CIs. Variables likely to confound the relationship between socioeconomic position and LMPT were identified a priori based on evidence from the published literature and the results of univariable analysis (i.e. ethnicity and maternal age).
Model building using unconditional logistic regression was then undertaken based on LMPT as the outcome and including all five measures of individual socioeconomic risk, and area-level socioeconomic risk. Ethnicity and maternal age were also included, as there was a priori evidence that these factors were related to LMPT birth. Adjusted ORs were obtained for each risk factor and compared with the unadjusted ORs to assess the relative importance of the effect to LMPT birth. The individual effect of each variable on the fit of the data was assessed using the likelihood ratio test.
Finally, models were fitted to compare the effect of including the SES Index of combined socioeconomic risk with a model of the significant individual indicators to assess whether or not this combined score accounted for a greater amount of variation in LMPT births than the individual risk factors, as it reflected a multiplicative effect of the individual factors. These models were both adjusted for ethnicity and maternal age.
Results
Data were available on 938 singleton LMPT births and 982 singleton term-born controls. Univariable analyses showed area-level deprivation to be significantly associated with LMPT birth (Table 19). A total of 33.1% of LMPT infants were born to mothers living in the most deprived quintile, compared with 27.7% of term-born infants. This equated to an increased odds of 49% of delivering LMPT for those mothers from the most deprived quintile. All of the five individual socioeconomic risk factors were seen to be significantly associated with gestation at birth.
| Indicator | Term-born controls, n (%) | LMPT births, n (%) | Chi-squared test p-value |
|---|---|---|---|
| Area-level deprivation quintile | |||
| 1 (least deprived) | 177 (18.1) | 135 (14.5) | 0.003 |
| 2 | 172 (17.6) | 122 (13.1) | Missing = 10 |
| 3 | 135 (13.8) | 146 (15.7) | – |
| 4 | 222 (22.7) | 221 (23.7) | – |
| 5 (most deprived) | 271 (27.7) | 309 (33.1) | – |
| Highest educational qualification | |||
| Degree or equivalent | 335 (34.1) | 249 (26.6) | 0.002 |
| A level or equivalent | 227 (23.1) | 226 (24.1) | Missing = 7 |
| GCSE grades A–C or equivalent | 252 (25.7) | 267 (28.5) | – |
| GCSE grade D or below or equivalent | 164 (16.7) | 193 (20.6) | – |
| NS-SEC occupational status | |||
| Managerial or professional | 286 (29.1) | 222 (23.7) | 0.003 |
| Intermediate | 202 (20.6) | 183 (19.5) | Missing = 11 |
| Routine and manual | 150 (15.3) | 134 (14.3) | – |
| Unemployed | 192 (19.6) | 247 (26.3) | – |
| Looking after the home | 145 (14.8) | 148 (15.8) | – |
| Cohabiting status | |||
| Living with partner | 850 (86.6) | 767 (81.8) | 0.004 |
| Not living with partner | 131 (13.3) | 170 (18.1) | Missing = 2 |
| Access to a car | |||
| Yes | 775 (78.9) | 668 (71.2) | < 0.001 |
| No | 204 (20.8) | 270 (28.8) | Missing = 3 |
| Home ownership | |||
| Owns with/without mortgage | 479 (48.8) | 238 (43.6) | 0.027 |
| Rents/lives rent free | 503 (51.2) | 526 (56.1) | Missing = 3 |
Table 19 shows that, compared with those mothers delivering at term, mothers who delivered LMPT were more likely to have a very low educational level (GCSE grade D or below: LMPT, 20.7%; term, 16.7%); to be unemployed (LMPT, 26.3%; term, 19.6%); to not be living with a partner (LMPT, 18.1%; term, 13.3%); to not own a car (LMPT, 28.8%; term, 20.4%); and to not own their own home (LMPT, 56.1%; term, 51.2%).
These socioeconomic factors were then explored in a multivariable model (excluding 25 cases with missing information: 969 term-born controls and 926 LMPT) (Table 20). Demographic factors were included in the model, including maternal age and ethnicity, but only ethnicity was seen to be significantly related to LMPT birth (p = 0.0153). Adjusting for socioeconomic factors showed a considerable reduction in the odds of being born LMPT for those mothers from the most deprived areas, from an OR of 1.49 before adjustment to an OR of 1.13 after adjustment, and this effect was no longer significant. After adjustment for demographic factors, the only individual factor to show a significant association with LMPT birth was car ownership (p = 0.0227). Mothers without a car were at 37% increased odds of delivering LMPT than those with access to a car (OR 1.37, 95% CI 1.04 to 1.79). There was no evidence of a relationship for education (p = 0.2010), occupation (p = 0.7108), home ownership (p = 0.5914) or cohabitation (p = 0.2734) in the multivariable model. In order to overcome the issue of correlation between the five individual factors, a model with the combined SES Index was then compared with a model adjusting only for car ownership (both models adjusted for maternal age and ethnicity). This showed that women from the most deprived tertile, who were more likely to be unemployed, single parents, poorly educated and not own a car or a house, were at 50% increased odds of delivering LMPT (OR 1.50, 95% CI 1.21 to 1.87). However, the change in deviance for this model was smaller (χ2 = 13.31 on 2 degrees of freedom) than the change seen when adjusting for car ownership (χ2 = 15.61 on 1 degree of freedom) and was not therefore seen to explain any additional variation compared with the single indicator of car ownership.
| Indicator | Unadjusted OR | p-value | Adjusted OR | p-value | ||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |||
| Area-level deprivation quintile | ||||||
| 1 (least deprived) | 1 | – | 0.003 | 1 | – | 0.20 |
| 2 | 0.93 | 0.67 to 1.28 | – | 0.91 | 0.65 to 1.26 | – |
| 3 | 1.42 | 1.03 to 1.96 | – | 1.35 | 0.97 to 1.89 | – |
| 4 | 1.31 | 0.98 to 1.75 | – | 1.06 | 0.77 to 1.46 | – |
| 5 (most deprived) | 1.49 | 1.13 to 1.97 | – | 1.13 | 0.82 to 1.56 | – |
| Highest educational qualification | ||||||
| Degree or equivalent | 1 | – | 0.002 | 1 | – | – |
| A Level or equivalent | 1.34 | 1.05 to 1.71 | – | 1.30 | 0.99 to 1.70 | 0.20 |
| GCSE grades A–C or equivalent | 1.43 | 1.12 to 1.81 | – | 1.29 | 0.97 to 1.71 | – |
| GCSE grade D or below or equivalent | 1.58 | 1.21 to 2.06 | – | 1.34 | 0.96 to 1.86 | – |
| NS-SEC occupational status | ||||||
| Managerial or professional | 1 | – | 0.002 | 1 | – | 0.71 |
| Intermediate | 1.17 | 0.90 to 1.53 | – | 1.03 | 0.77 to 1.37 | – |
| Routine and manual | 1.16 | 0.87 to 1.55 | – | 0.95 | 0.68 to 1.32 | – |
| Unemployed | 1.67 | 1.29 to 2.15 | – | 1.19 | 0.83 to 1.70 | – |
| Looking after the home | 1.32 | 0.99 to 1.76 | – | 0.98 | 0.70 to 1.38 | – |
| Cohabiting status | ||||||
| Living with partner | 1 | 0.004 | 1 | 0.27 | ||
| Not living with partner | 1.44 | 1.12 to 1.84 | 1.18 | 0.88 to 1.58 | ||
| Access to a car | ||||||
| Yes | 1 | – | 0.0001 | 1 | – | 0.02 |
| No | 1.54 | 1.04 to 1.90 | – | 1.37 | 1.04 to 1.79 | – |
| Home ownership | ||||||
| Owns with/without mortgage | 1 | – | 0.027 | 1 | – | 0.59 |
| Rents/lives rent free | 1.22 | 1.02 to 1.47 | – | 0.91 | 0.72 to 1.16 | – |
| Mother’s age (years) | ||||||
| < 20 | 1 | – | 0.706 | 1 | – | 0.47 |
| 20–29 | 1.05 | 0.71 to 1.56 | – | 1.37 | 0.89 to 2.10 | – |
| 30–39 | 0.94 | 0.63 to 1.41 | – | 1.44 | 0.91 to 2.26 | – |
| ≥ 40 | 0.89 | 0.49 to 1.64 | – | 1.31 | 0.68 to 2.52 | – |
| Ethnicity | ||||||
| White | 1 | – | 0.028 | 1 | – | 0.025 |
| Mixed | 1.79 | 1.00 to 3.22 | – | 1.75 | 0.94 to 3.27 | – |
| Asian or Asian British | 1.41 | 1.10 to 1.80 | – | 1.47 | 1.12 to 1.92 | – |
| Black or black British | 1.16 | 0.77 to 1.75 | – | 0.99 | 0.63 to 1.53 | – |
| Chinese or other ethnic group | 1.24 | 0.54 to 2.83 | – | 1.51 | 0.64 to 3.58 | – |
Discussion
Key findings
-
Women from the most deprived areas had a 49% higher risk of delivering LMPT than of delivering at term.
-
After adjusting for individual-level socioeconomic factors, there was no significant association with area deprivation and LMPT birth.
-
Not having access to a car had the strongest association with LMPT, with mothers at 37% increased odds of LMPT.
-
Area- and individual-level socioeconomic factors did not explain the increased odds of Asian or British Asian women delivering an LMPT infant. Some of the apparent socioeconomic inequalities at the univariate level may be because of this higher rate of LMPT birth among Asian or Asian British women, who are more likely to be more deprived.
Strengths and limitations
Many research studies exploring socioeconomic inequalities in preterm birth are limited to area-level measures of deprivation. Here it has been possible to explore both area- and individual-level socioeconomic risk factors and assess the impact on LMPT birth with a rich source of data on these risk factors. Almost all respondents answered the socioeconomic questions in the maternal data set and so missing data were not a significant problem. Lack of access to a car showed the strongest relationship with LMPT birth, but there was strong correlation between all of the five individual socioeconomic risk factors. However, the SES Index, combining all five indicators of socioeconomic risk, did not account for any more of the variation in LMPT risk.
Data are available only for responders to the study. Study response has been shown to be related to socioeconomic status in a variety of studies, including the national census, and so the responders in this study are likely to be less deprived than all eligible study participants. Therefore, the socioeconomic effects seen here may be underestimated.
Implications
Socioeconomic inequalities exist in LMPT birth at both area and individual level. The effect of socioeconomic deprivation on very preterm birth rates appears to continue into LMPT gestations. This suggests that the burden of LMPT is greater in more deprived areas and is likely to lead to a greater burden of mortality, morbidity and adverse long-term outcomes in these areas owing to differential rates of LMPT birth.
In studies of socioeconomic deprivation, area measures are generally used as a proxy for individual risk. Consequently, as in this work and a recently published Italian study,155 there appears to be no residual influence of area-level deprivation after adjusting for individual measures, as there is often misclassification of deprivation at the area level. However, in studies from the USA and Canada, a consistent area-level deprivation effect has been shown even after accounting for individual-level behavioural and medical risk factors,156,157 which suggests that there may be geographical differences in access to good health care.
Interestingly, although all of the individual socioeconomic risk factors explored showed a relationship with LMPT birth at the univariable level, only lack of access to a car was significant after adjusting for other variables. This socioeconomic risk factor showed a stronger association than education, occupation, house ownership or cohabiting status. Lack of access to a car may reflect access to short-term income, but may also reflect ability to physically access services.
These data suggest that reducing the burden of disease as a result of LMPT birth will have to involve targeted, disease-specific preventative interventions in high-risk pregnancies. However, for low-risk groups, population-level public health action is needed to address risk factors for preterm birth associated with social deprivation.
Future research
The LAMBS collected rich and diverse data on socioeconomic risk, but also on lifestyle and health behaviours, stress and work conditions. The next stage of this research will be to understand how these factors are related to the observed socioeconomic inequalities seen here, exploring modifiable risk factors that may reduce the incidence of LMPT birth in the future. It is likely that the relationship between low socioeconomic group and LMPT may be explained by the clustering of lifestyle factors and health-related behaviours among socioeconomically deprived women. Both Danish and Swedish population-based studies have shown a reduction in the educational/socioeconomic status gradient in risk of preterm birth after adjustment for lifestyle factors including smoking. 158,159 Using data from the LAMBS we can extend these analyses to assess the impact of these risk factors on LMPT birth and assess whether or not the effects are similar to those seen at earlier gestations.
Neonatal outcomes in infants born late and moderately preterm
Background
Although outcomes of very preterm (< 32 weeks’ gestation) infants have been extensively studied, there have been few prospective studies exploring the outcomes of infants born at more mature preterm gestations. In particular, the number of infants in the LMPT population in the UK who require neonatal specialist care has not been clarified and there is a paucity of research into the influence of plurality on neonatal outcomes in the preterm population in general. In the LMPT group this is potentially even more important, as multiple births are over-represented in this population. Management of LMPT babies has, until recently, been similar to that of term-born babies, but there has been little guidance for clinicians with respect to the understanding of differences in the incidence of morbidity between these two groups. We chose to study a range of important morbidities that are known to present commonly in infants born close to term and at term, and investigations that are also commonly performed in these infants.
Objectives
-
To describe and quantify early mortality and morbidity associated with late and moderate prematurity compared with that of infants born at ≥ 37 weeks’ gestation.
-
To compare outcomes of singleton infants with those of twins and higher-order multiples born at LMPT gestations.
Methods
Outcome data for LMPT and term-born infants were obtained from hospital records. For infants in either group who did not require admission to a NNU, specific neonatal medical records may not have been generated. In these cases, data were obtained from the mothers’ maternity records. For infants receiving care in a NNU, data were extracted from the neonatal medical and nursing records and observation charts.
Clinical outcomes of live-born infants are presented for those without congenital anomalies, because of the likelihood of anomalies having a major effect on many common outcomes, both during the neonatal stay and at discharge. As it is known that neonatal outcomes differ between infants from singleton or multiple pregnancies, multiple births were analysed separately from singleton births.
Measures
Neonatal data collection focused on determining the range of important short-term outcomes during the neonatal hospital stay and at hospital discharge in LMPT compared with term-born infants. Deaths during the neonatal period were recorded. When available, the cause of death and findings at post-mortem were obtained. For surviving infants, the total length of hospital neonatal stay was calculated from the day of birth to the day of discharge. For those admitted for specialist neonatal care, the number of days spent in a NNU was recorded. For infants discharged home on the day of birth, or infants born at home, this was recorded as 0 days. Data were obtained for congenital anomalies and for important conditions highlighted in the literature and observed in clinical practice as those most commonly affecting this population. These included resuscitation at delivery, respiratory outcomes and the need for respiratory support, surgical intervention, feeding outcomes including rates of breastfeeding and nutritional support, hypoglycaemia, jaundice, hypothermia and systemic infection.
Information collected about resuscitation included the administration of facial oxygen, intermittent positive-pressure ventilation (IPPV) via a facemask and endotracheal intubation. IPPV via a facemask or endotracheal tube and the use of drugs at resuscitation were classed as active resuscitation. The presence of respiratory distress, hypoglycaemia, hypothermia, jaundice and suspected infection were documented in babies for which this required either review by a member of the medical team or admission to a NNU. For babies affected by these conditions, the lowest recorded blood sugar level, highest SBR level and whether the baby required phototherapy or exchange transfusion, and the lowest temperature below 36.5 °C were recorded. Hypoglycaemia was defined as a blood sugar level of < 2.5 mmol/l and significant hypoglycaemia as < 2.0 mmol/l. Hypothermia was defined as a temperature of < 36.5 °C and severe hypothermia as a temperature of < 36.0 °C. Active management of hypothermia was defined as intervention using a heated mattress, incubator or overhead heater. Suspected infection was recorded for any infant who received investigation for infection with blood cultures, urine cultures or lumbar puncture to obtain cerebrospinal fluid for microbiological investigation. Proven infection was recorded for infants for whom a positive culture was obtained from one of these normally sterile body fluids.
Common investigations performed in babies during the neonatal hospital stay were recorded. These included radiological investigations [chest radiography, cranial ultrasound scan and magnetic resonance imaging (MRI)], screening for infection, electroencephalography (EEG), chromosomal studies and any other significant investigation.
The summary outcomes at the time of discharge from neonatal hospital care were recorded according to the number of days or part days for which a particular type of care or intervention was required. Respiratory outcomes included the number of days of respiratory support including mechanical ventilation via an endotracheal tube and non-invasive ventilation (nasal continuous positive airways pressure and methods of biphasic non-invasive ventilation], and the number of days of oxygen therapy via incubator, nasal cannulae or headbox. For each day, the highest level of support was recorded as follows: mechanical ventilation > non-invasive ventilation > oxygen therapy. Nutritional outcome data collected were for the number of days of PN administration, number of days of clear i.v. fluid administration and the day of attaining full oral feeds (not feeding via a nasogastric tube (NGT)]. When no nutritional support was required and the baby fed fully by bottle or breast from birth, the day of attaining full feeds was recorded as day 0. The type of milk feed and method of feeding at hospital discharge was also recorded. For infants receiving any maternal breast milk during their hospital stay, the last date on which breast milk was given was recorded, together with whether or not there was exclusive breastfeeding or mixed feeding at discharge.
Mortality and morbidity
Mortality
Deaths were uncommon in the study group, but six babies died before discharge from hospital. Of these, five had been born at LMPT gestations and one at term, but the difference in the number of deaths between the two groups was not statistically significant. Four deaths occurred within the first week of life, one of which was of a term-born baby, and there were two deaths at more than 28 days of life. Table 21 shows the gestational ages of these infants at birth, the postnatal day of death and the cause of death.
| Gestation at birth | Postnatal day of death | Cause of death |
|---|---|---|
| LMPT | ||
| 36 weeks | 1 day | Hydrops fetalis |
| 34 weeks | 1 day | Pulmonary hypoplasia |
| 32 weeks | 7 days | Pulmonary haemorrhage |
| 34 weeks | 32 days | Hypoplastic left heart syndrome |
| 32 weeks | 78 days | Acute renal failure |
| Necrotising enterocolitis | ||
| Bowel obstruction | ||
| Septo-optic dysplasia | ||
| Term | ||
| 40 weeks | 4 days | Hyperammonaemia |
Congenital anomalies
There were 23 babies in the LMPT group and nine babies in the term-born group with major congenital anomalies or chromosomal disorders. Table 22 shows the range of congenital anomalies seen and numbers of affected babies in both groups.
| Anomaly | Numbers of babies | |
|---|---|---|
| Term | LMPT | |
| Oesophageal atresia and tracheo-oesophageal fistula | 0 | 5 |
| Gastroschisis | 0 | 4 |
| Hirschsprung’s disease | 1 | 0 |
| Cleft lip ± cleft palate | 2 | 2 |
| Skeletal dysplasia | 1 | 1 |
| Congenital heart disease | 0 | 4 |
| Chromosomal anomaly | 3 | 2 |
| Congenital infection | 1 | 1 |
| Neural tube defect | 0 | 1 |
| Pulmonary hypoplasia | 0 | 1 |
| Other unspecified major structural abnormality or syndrome | 1 | 2 |
| Total | 9 | 23 |
Clinical outcomes for singletons
Table 23 shows outcomes during the neonatal hospital stay for live-born, normally formed singleton infants. Outcomes are compared between LMPT (n = 907) and term-born infants (n = 972).
| Outcome | Term | LMPT | RR (95% CI) for outcome | p-valuea |
|---|---|---|---|---|
| Number of babies, n (%) | 972 (51.7) | 907 (48.3) | – | – |
| Deaths before discharge, n (%) | 1 (0.1) | 3 (0.3) | – | – |
| Any active resuscitation at birth, n (%) | 72 (7.4) | 159 (17.5) | 2.37 (1.82 to 3.08) | < 0.001 |
| Endotracheal intubation at birth, n (%) | 8 (0.8) | 30 (3.3) | 4.02 (1.85 to 8.72) | < 0.001 |
| Length of hospital stay (days), median (range) | 2 (0–25) | 5 (1–78) | ||
| All newborn care given on postnatal ward, n (%) | 910 (93.6) | 505 (55.7) | 0.58 (0.55 to 0.62) | < 0.001 |
| Any care in a NNU, n (%) | 43 (4.4) | 402 (44.3) | 9.82 (7.27 to 13.27) | < 0.001 |
| Maximum level of respiratory support | ||||
| Mechanical ventilation, n (%) | 8 (0.8) | 75 (8.3) | – | – |
| Non-invasive respiratory support, n (%) | 1 (0.1) | 36 (4.0) | – | – |
| Oxygen therapy, n (%) | 7 (0.7) | 32 (3.5) | – | – |
| No respiratory support, n (%) | 956 (98.4) | 764 (84.2) | – | – |
| Ventilation and/or non-invasive respiratory support, n (%) | 9 (0.9) | 107 (11.8) | 12.74 (6.49 to 25.01) | < 0.001 |
| Days of ventilation and/or non-invasive respiratory support, median (range) | 3 (1–4) | 2 (1–26) | – | – |
| Fluids and nutrition | ||||
| i.v. fluids, n (%) | 20 (2.1) | 243 (26.8) | 13.02 (8.33 to 20.36) | < 0.001 |
| Days of i.v. fluids, median (range) | 2.5 (1 to 10) | 2 (1 to 14) | – | – |
| PN, n (%) | 3 (0.3) | 32 (3.5) | 11.43 (3.51 to 37.21) | < 0.001 |
| Days of PN, median (range) | 3 (3 to 3) | 5.5 (1 to 60) | – | – |
| Days to full oral suck feeds, median (range) | 0 (0–19) | 0 (0–95) | – | – |
| Nasogastric feeding at discharge, n (%) | 0 (0.0) | 3 (0.3) | a | a |
| Breastfeeding | ||||
| Any breast milk given, n (%) | 717 (73.8) | 582 (64.2) | 0.87 (0.82 to 0.92) | < 0.001 |
| Receiving breast milk at discharge, n (%) | 701 (72.2) | 524 (58.0) | 0.80 (0.75 to 0.86) | < 0.001 |
| Exclusively breastfed at discharge, n (%) | 632 (65.1) | 355 (39.3) | 0.60 (0.55 to 0.66) | < 0.001 |
| Investigations | ||||
| Cranial ultrasound scan, n (%) | 13 (1.3) | 63 (7.0) | 5.19 (2.88 to 9.37) | < 0.001 |
| MRI scan, n (%) | 5 (0.5) | 8 (0.9) | 1.71 (0.56 to 5.22) | 0.34 |
| Chest radiography, n (%) | 22 (2.3) | 175 (19.3) | 8.52 (5.52 to 13.16) | < 0.001 |
| Screening for infection, n (%) | 48 (4.9) | 322 (35.5) | 7.19 (5.38 to 9.60) | < 0.001 |
| Morbidities | ||||
| Culture-positive infection, n (%) | 0 (0.0) | 17 (1.9) | – | – |
| Jaundice requiring phototherapy, n (%) | 6 (0.6) | 199 (21.9) | 35.54 (15.85 to 79.68) | < 0.001 |
| Hypothermia (temperature of < 36.0 °C), n (%) | 11 (1.1) | 83 (9.2) | 8.09 (4.34 to 15.07) | < 0.001 |
| Hypoglycaemia (blood sugar level of < 2.0 mmol/l), n (%) | 8 (0.8) | 61 (6.7) | 8.17 (3.93 to 16.98) | < 0.001 |
| Neonatal encephalopathy grade II/III, n (%) | 4 (0.4) | 4 (0.4) | 1.07 (0.27 to 4.27) | 0.92 |
Resuscitation at birth
Compared with term-born babies, those born at LMPT gestations were more than twice as likely to require active resuscitation at birth (RR 2.37, 95% CI 1.82 to 3.08; p < 0.001), and were four times more likely to require endotracheal intubation (RR 4.02, 95% CI 1.85 to 8.72; p < 0.001).
Respiratory outcomes
The majority of babies in both the LMPT (84.2%) and term (98.4%) groups did not require any form of respiratory support. However, the risk of needing mechanical ventilation and/or non-invasive respiratory support in the LMPT group was more than twice that of infants born at term (RR 12.74, 95% CI 6.49 to 25.01; p < 0.001). Ventilatory support was required by 8.3% of LMPT infants, compared with < 1% of term-born infants. Non-invasive support was the maximum level of respiratory support given in 4% of LMPT infants and 0.1% of term-born infants. Oxygen therapy was required in 3.5% of LMPT infants, compared with only 0.7% of those born at term.
Nutritional outcomes
The proportion of babies requiring i.v. fluids was higher in the LMPT group than in the term-born group (RR 13.02, 95% CI 8.33 to 20.36; p < 0.01). The use of PN was also more common in LMPT infants (RR 11.43, 95% CI 3.51 to 37.21; p < 0.001) and the duration of i.v. fluids and nutrition use was also greater in the LMPT group. LMPT babies took longer than their term-born counterparts to attain full oral feeding by breast or bottle. Three infants in the LMPT group were fed via a NGT when they were discharged from hospital, compared with no infants in the term group.
With respect to breastfeeding, LMPT infants were less likely to receive any breast milk during their neonatal stay than infants born at term (64.2% vs. 73.8%; RR 0.87, 95% CI 0.82 to 0.92; p < 0.001). This proportion decreased during the neonatal stay in both groups, but fell more in the LMPT babies than in the term babies. The proportion of babies receiving any breast milk at the time of hospital discharge was 72.2% in the term group, compared with only 58% in the LMPT group. Exclusive breast milk feeding at discharge was seen in 65.1% of the term-born babies, but in fewer than half of the LMPT babies (65.1% vs. 39.3%; RR 0.60, 95% CI 0.55 to 0.66; p < 0.001).
Admission to neonatal unit and neonatal morbidity
Late and moderately preterm infants were almost 10 times more likely to be admitted to a NNU than babies in the term-born group (RR 9.82, 95% CI 7.27 to 13.27; p < 0.001). They were also at significantly higher risk of a number of common neonatal morbidities including hyperbilirubinaemia [that was of a level requiring management with phototherapy (RR 35.54, 95% CI 15.85 to 79.68; p < 0.001)], severe hypothermia (RR 8.09, 95% CI 4.34 to 15.07; p < 0.01) and severe hypoglycaemia (RR 8.17, 95% CI 3.93 to 16.98; p < 0.001). The incidence of neonatal encephalopathy of moderate or severe severity (grades II and III) was similar in the two groups.
Clinical investigations performed during the neonatal stay
In general, LMPT infants were more likely to undergo investigation than term-born babies. With respect to radiological examinations, LMPT babies were eight times more likely to have chest radiography performed (RR 8.52, 95% CI 5.52 to 13.16; p < 0.001) than term-born babies, and were also more likely to have had a cranial ultrasound scan performed (RR 5.19, 95% CI 2.88 to 9.37; p < 0.001). However, the number of MRI scans did not differ between the groups.
Screening for suspected infection was carried out in more than one-third of LMPT infants, compared with < 5% of those born at term (RR 7.19, 95% CI 5.38 to 9.60; p < 0.001). This yielded a positive culture in only 17 LMPT infants (5% of those tested). None of the infants born at ≥ 37 weeks’ gestation had a culture-positive infection.
Length of hospital stay
Three LMPT babies and one term-born baby died before discharge. For those infants surviving to discharge, the total length of hospital stay was greater in the infants born LMPT.
Clinical outcomes for infants from multiple births
Table 24 shows the outcomes during the neonatal hospital stay for live-born infants without congenital anomalies who were from multiple pregnancies. There were 200 LMPT infants and 274 infants born at ≥ 37 weeks’ gestation.
| Outcome | Term | LMPT | RR (95% CI) for outcome | p-valuea |
|---|---|---|---|---|
| Number of babies, n (%) | 274 (57.8) | 200 (42.2) | – | – |
| Deaths before discharge, n (%) | 0 (0.0) | 0 (0.0) | – | – |
| Any active resuscitation at birth, n (%) | 31 (11.3) | 41 (20.5) | 1.81 (1.18 to 2.79) | 0.007 |
| Endotracheal intubation at birth, n (%) | 2 (0.7) | 3 (1.5) | 2.06 (0.35 to 12.21) | 0.43 |
| Length of hospital stay (days), median (range) | 4 (1–26) | 6.5 (2–35) | – | – |
| All newborn care given on postnatal ward, n (%) | 251 (91.6) | 114 (57.0) | 0.62 (0.55 to 0.71) | < 0.001 |
| Any care in a NNU, n (%) | 23 (8.4) | 86 (43.0) | 5.12 (3.36 to 7.81) | < 0.001 |
| Maximum level of respiratory support | ||||
| Mechanical ventilation, n (%) | 1 (0.4) | 17 (8.5) | – | – |
| Non-invasive respiratory support, n (%) | 1 (0.4) | 11 (5.5) | – | – |
| Oxygen therapy, n (%) | 1 (0.4) | 4 (2.0) | – | – |
| No respiratory support, n (%) | 271 (98.9) | 168 (84.0) | – | – |
| Ventilation and/or non-invasive respiratory support, n (%) | 2 (0.7) | 28 (14.0) | 19.18 (4.62 to 79.70) | < 0.001 |
| Total days of ventilation and/or non-invasive respiratory support, median (range) | 1 (1–1) | 2 (1–5) | – | – |
| Fluids and nutrition | ||||
| i.v. fluids, n (%) | 10 (3.7) | 54 (27.0) | 7.40 (3.86 to 14.18) | < 0.001 |
| Days of i.v. fluids, median (range) | 1.5 (1–3) | 2 (1–9) | – | – |
| PN, n (%) | 0 (0.0) | 7 (3.5) | a | a |
| Days of PN, median (range) | 0 (0–0) | 4 (1–9) | – | – |
| Days to full oral suck feeds, median (range) | 0 (0–31) | 0 (0–106) | – | – |
| Nasogastric feeding at discharge, n (%) | 0 (0.0) | 1 (0.5) | a | a |
| Breastfeeding | ||||
| Any breast milk given, n (%) | 196 (71.5) | 126 (63.0) | 0.88 (0.77 to 1.00) | 0.058 |
| Receiving breast milk at discharge, n (%) | 177 (64.6) | 107 (53.5) | 0.83 (0.71 to 0.97) | 0.018 |
| Exclusively breastfed at discharge, n (%) | 111 (40.5) | 49 (24.5) | 0.60 (0.46 to 0.80) | < 0.001 |
| Investigations | ||||
| Cranial ultrasound scan, n (%) | 3 (1.1) | 13 (6.5) | 5.94 (1.71 to 20.58) | 0.005 |
| MRI scan, n (%) | 2 (0.7) | 2 (1.0) | 1.37 (0.19 to 9.66) | 0.75 |
| Chest radiography, n (%) | 10 (3.7) | 42 (21.0) | 5.75 (2.96 to 11.20) | < 0.001 |
| Screening for infection, n (%) | 16 (5.8) | 70 (35.0) | 5.99 (3.59 to 10.00) | < 0.001 |
| Morbidities | ||||
| Culture-positive infection, n (%) | 1 (0.36) | 2 (1.00) | 2.74 (0.45 to 30.08) | 0.41 |
| Jaundice requiring phototherapy, n (%) | 4 (1.5) | 31 (15.5) | 10.62 (3.80 to 29.63) | < 0.001 |
| Hypothermia (temperature of < 36.0 °C), n (%) | 7 (2.6) | 13 (6.5) | 2.54 (1.03 to 6.27) | 0.042 |
| Hypoglycaemia (blood sugar level of < 2.0 mmol/l), n (%) | 3 (1.1) | 6 (3.0) | 2.28 (0.55 to 9.46) | 0.15 |
| Neonatal encephalopathy grade II/III, n (%) | 0 (0.0) | 0 (0.0) | – | – |
Resuscitation at birth
Compared with term-born multiples, LMPT multiples were more likely to require active resuscitation at birth (RR 1.81 95% CI 1.18 to 2.79; p = 0.007), but were no more likely to need endotracheal intubation.
Respiratory outcomes
As was the case with singleton births, high percentages of multiples in both groups did not receive any respiratory support (LMPT 84% and term 98.9%). Mechanical ventilation, non-invasive respiratory support and oxygen therapy were each required by only one baby in the term-born multiples group. However, 17 babies (8.5%) of LMPT multiples were ventilated and 11 (5.5%) and 4 (2%), respectively, needed non-invasive support and oxygen therapy. Among the multiple births, the risk of LMPT infants needing mechanical ventilation and/or non-invasive respiratory support was significantly higher than that of infants born at term (RR 19.18, 95% CI 4.62 to 79.70; p < 0.001). It should be noted that the small numbers for this analysis result in wide CIs.
Nutritional outcomes
Among infants from multiple births, the number of babies requiring any kind of nutritional support was small in both groups. No term-born infant required either PN or feeding by NGT, and only seven (3.5%) LMPT infants required PN and only one (0.5%) required feeding by NGT. More than one-quarter of LMPT infants required i.v. fluids, which was a significantly higher proportion than in the term-born group (RR 7.40, 95% CI 3.86 to 14.18; p < 0.001).
There were lower rates of breastfeeding among the LMPT multiple births than in the term-born group. A smaller percentage of LMPT than of term-born babies received any breast milk, but this difference did not reach statistical significance. However, a similar pattern of decline as seen in the singletons led to a significantly smaller proportion of LMPT multiples receiving breast milk at discharge (RR 0.83, 95% CI 0.71 to 0.97). Less than one-quarter of LMPT multiples were fed exclusively on the mother’s breast milk at discharge and, compared with term-born multiples, this was a highly significant difference (RR 0.60, 95% CI 0.46 to 0.80; p < 0.001).
Admission to neonatal unit and neonatal morbidity
Late and moderately preterm infants from multiple births were five times more likely to be admitted to a NNU than babies in the term-born group (RR 5.12, 95% CI 3.36 to 7.81; p < 0.001). Their risk of jaundice requiring phototherapy was also 10 times higher than that of term-born multiples (RR 10.62, 95% CI 3.80 to 29.63; p < 0.001), and they were twice as likely to have severe hypothermia (RR 2.54, 95% CI 1.03 to 6.27; p = 0.042). There was no increased risk for hypoglycaemia among LMPT multiples and neonatal encephalopathy was not seen in any baby from a multiple birth.
Clinical investigations performed during the neonatal stay
Late and moderately preterm infants from multiple births were more likely to under chest radiography (RR 5.75 95% CI 2.96 to 11.20; p < 0.001) and a cranial ultrasound (RR 5.94, 95% CI 1.71 to 20.58; p < 0.001) than term-born babies. The number of MRI scans performed was the same in both groups.
Screening for suspected infection was carried out in 35% of LMPT multiples, compared with only 5.8% of those born at term (RR 5.99, 95% 3.59 to 10.00; p < 0.001), but only two (1%) LMPT babies and one (36%) term-born baby were subsequently found to have positive cultures.
Length of hospital stay
All live-born infants from multiple births survived until discharge from hospital, but among these infants the average neonatal hospital stay was longer in the LMPT group than in the term-born group.
Comparison between the outcomes of late and moderately preterm singletons and multiples
Differences between LMPT singleton infants and those from multiples are shown in Table 25. For the majority of outcomes, there were no differences observed between singletons and multiples in this study. Neither group was more likely than the other to require resuscitation at birth, respiratory support or admission to a NNU. There was less jaundice (RR 0.71, 95% CI 0.50 to 1.00; p = 0.049) and a non-significant trend towards less hypoglycaemia (RR 0.45, 95% CI 0.20 to 1.02; p = 0.055) in the multiples than in the singletons.
| Outcome | Singletons | Multiples | RR for outcome (95% CI) | p-valuea |
|---|---|---|---|---|
| Number of babies, n (%) | 907 (81.9) | 200 (18.1) | – | – |
| Deaths before discharge, n (%) | 3 (0.3) | 0 (0.0) | a | a |
| Any active resuscitation at birth, n (%) | 159 (17.5) | 41 (20.5) | 1.17 (0.86 to 1.59) | 0.32 |
| Length of hospital stay, days, median (range) | 5 (1 to 78) | 6.5 (2 to 35) | – | – |
| Any care in a NNU, n (%) | 402 (44.3) | 86 (43.0) | 0.97 (0.81 to 1.16) | 0.74 |
| Ventilation and/or non-invasive respiratory support, n (%) | 107 (11.8) | 28 (14.0) | 1.19 (0.81 to 1.75) | 0.39 |
| Total days of ventilation and/or non-invasive respiratory support, median (range) | 2 (1–26) | 2 (1–5) | – | – |
| Fluids and nutrition, median (range) | ||||
| Days of i.v. fluids | 2 (1–14) | 2 (1–9) | – | – |
| Days of PN | 5.5 (1–60) | 4 (1–9) | – | – |
| Days to full oral suck feeds | 0 (0–95) | 0 (0–106) | – | – |
| Breastfeeding, n (%) | ||||
| Any breast milk given | 582 (64.2) | 126 (63.0) | 0.98 (0.87 to 1.10) | 0.76 |
| Receiving breast milk at discharge | 524 (58.0) | 107 (53.5) | 0.92 (0.80 to 1.06) | 0.26 |
| Exclusively breastfed at discharge | 355 (39.3) | 49 (24.5) | 0.62 (0.48 to 0.81) | < 0.001 |
| Morbidities, n (%) | ||||
| Culture-positive infection | 16 (1.8) | 2 (1.0) | 0.57 (0.31 to 2.45) | 0.45 |
| Jaundice requiring phototherapy | 199 (21.9) | 31 (15.5) | 0.71 (0.50 to 1.00) | 0.049 |
| Hypothermia (temperature of < 36.0 °C) | 84 (9.3) | 13 (6.5) | 0.70 (0.40 to 1.23) | 0.22 |
| Hypoglycaemia (blood sugar level of < 2.0 mmol/l) | 61 (6.7) | 6 (3.0) | 0.45 (0.20 to 1.02) | 0.055 |
| Neonatal encephalopathy grade II/III | 4 (0.4) | 0 (0.0) | – | – |
Although equal numbers of babies in each group received some breast milk during their hospital stay and at the time of discharge, multiples were significantly less likely to be exclusively breastfed at discharge than were singletons. However, it is likely that, rather than a difference between characteristics of the babies, this is more reflective of a difference in the ability of mothers of multiples to produce sufficient milk for all their babies compared with mothers of singletons.
Obstetric intervention and neonatal outcomes of late and moderately preterm singleton infants
Background
This and other studies have shown that infants born at LMPT gestations are at increased risk of adverse outcomes in the neonatal period compared with infants born at term. These adverse outcomes span a number of different areas. However, current understanding of these differences is limited and it is not known to what degree poorer outcomes are related to prematurity per se or how much may be related to problems that occur during pregnancy and subsequently lead to medically indicated preterm delivery. We sought to compare the outcomes of infants born LMPT following spontaneous onset of labour with the outcomes of infants delivered prior to the onset of labour as a result of intervention by obstetricians, that is induction of labour or CS. In order to gain some information about the relative effects of obstetric intervention and prematurity, we have also compared outcomes in these subgroups within the term-born group of infants.
Objectives
-
To determine the numbers of women in whom delivery prior to the onset of labour, at LMPT gestations or at term, was the result of medical intervention.
-
To compare the outcomes of LMPT infants born to mothers who had non-spontaneous onset of labour with those whose mothers had spontaneous onset of labour.
Methods
Data regarding the onset of labour were obtained from the mothers’ maternity records. Data for the outcomes of LMPT and term-born infants were obtained from hospital records as previously described. Clinical outcomes of live-born infants without congenital anomalies are presented because of the likelihood of antenatal diagnosis of a major congenital anomaly contributing to the decision-making with respect to induction of labour or delivery by CS. In view of the different mechanisms leading to delivery in singleton and multiple births, singletons only are included in these analyses. Home births are included.
Measures
Spontaneous onset of labour was recorded when the onset of uterine contractions was spontaneous and when this led to delivery by any mode. When the onset of labour contractions was medically induced or where delivery by CS was carried out without prior contractions, the onset of labour was classed as non-spontaneous.
Results
Clinical outcomes of live-born LMPT and term-born babies without anomalies are shown in Tables 26 and 27, respectively, according to whether onset of labour in the mothers was spontaneous or non-spontaneous.
| Outcome | Spontaneous | Non-spontaneous | RR (95% CI) | p-valuea |
|---|---|---|---|---|
| Number of babies, n (%) | 525 (57.9) | 382 (42.1) | – | – |
| Deaths before discharge, n (%) | 1 (0.2) | 2 (0.5) | – | – |
| Birthweight (g), median (range) | 2520 (1240–3950) | 2380 (1120–4960) | – | – |
| Gestation (weeks), median (range) | 35+6 (32+0–36+5) | 35+6 (32+0–36+5) | – | – |
| Any active resuscitation at birth, n (%) | 76 (14.5) | 83 (21.7) | 1.50 (1.13 to 1.99) | 0.005 |
| Length of hospital stay (days), median (range) | 4 (1–74) | 6 (1–78) | – | – |
| Any care in a NNU, n (%) | 201 (38.3) | 200 (52.4) | 1.37 (1.18 to 1.58) | < 0.001 |
| Ventilation and/or non-invasive respiratory support, n (%) | 45 (8.6) | 62 (16.2) | 1.89 (1.32 to 2.72) | 0.001 |
| Total days of ventilation and/or non-invasive respiratory support, median (range) | 2 (1–7) | 2 (1–26) | – | – |
| Mode of delivery | ||||
| Spontaneous vaginal, n (%) | 386 (73.5) | 129 (33.7) | – | – |
| Assisted vaginal, n (%) | 75 (14.3) | 26 (6.8) | – | – |
| CS, during labour, n (%) | 64 (12.2) | 34 (8.9) | – | – |
| CS, not in labour, n (%) | – | 193 (50.5) | – | – |
| Unknown, n (%) | – | – | – | – |
| Fluids and nutrition | ||||
| i.v. fluids, n (%) | 113 (21.5) | 130 (34.0) | 1.58 (1.28 to 1.96) | 0.005 |
| Days of i.v. fluids, median (range) | 2 (1–14) | 2 (1–12) | – | – |
| PN, n (%) | 9 (1.7) | 23 (6.0) | 1.36 (1.64 to 7.51) | 0.001 |
| Days of PN, median (range) | 3 (1–6) | 7 (1–60) | – | – |
| Days to full oral suck feeds, median (range) | 0 (0–93) | 0 (0–95) | – | – |
| Morbidities | ||||
| Culture-positive infection, n (%) | 10 (1.9) | 6 (1.6) | 0.82 (0.30 to 2.25) | 0.71 |
| Jaundice requiring phototherapy, n (%) | 118 (22.5) | 81(21.2) | 0.94 (0.73 to 1.21) | 0.65 |
| Hypothermia (temperature of < 36.0 °C), n (%) | 39 (7.4) | 45 (11.8) | 1.59 (1.05 to 2.39) | 0.027 |
| Hypoglycaemia (blood sugar level of < 2.0 mmol/l), n (%) | 31 (5.9) | 30 (7.9) | 1.33 (0.82 to 2.16) | 0.25 |
| Neonatal encephalopathy grade II/III, n (%) | 2 (0.4) | 2 (0.5) | 1.37 (0.19 to 9.72) | 0.75 |
| Outcome | Spontaneous | Non-spontaneous | RR for outcome (95% CI) | p-valuea |
|---|---|---|---|---|
| Number of babies, n | 640 (65.8) | 332 (34.2) | – | – |
| Deaths before discharge, n (%) | 1 | – | – | |
| Birthweight (g), median (range) | 3420 (2150–4850) | 3431 (1980–5160) | – | – |
| Gestation (weeks), median (range) | 40+1 (37+0–43+4) | 39+5 (37+0–42+6) | – | – |
| Any active resuscitation at birth, n (%) | 44 (6.9) | 28 (8.4) | 1.23 (0.78 to 1.93) | 0.38 |
| Length of hospital stay (days),b median (range) | 2 (0–14) | 3 (1–25) | – | – |
| Any care in a NNU, n (%) | 22 (3.4) | 21 (6.3) | 1.84 (1.03 to 3.30) | 0.04 |
| Ventilation and/or non-invasive respiratory support, n (%) | 5 (0.8) | 4 (1.2) | 1.54 (0.42 to 5.71) | 0.65 |
| Total days of ventilation and/or non-invasive respiratory support,c median (range) | 3 (1–4) | 3 (2–4) | – | – |
| Mode of delivery | ||||
| Spontaneous vaginal, n (%) | 484 (75.6) | 127 (38.3) | – | – |
| Assisted vaginal, n (%) | 106 (16.6) | 60 (18.1) | – | – |
| CS, during labour, n (%) | 50 (7.8) | 39 (11.8) | – | – |
| CS, not in labour, n (%) | – | 106 (31.9) | – | – |
| Unknown, n (%) | – | – | – | – |
| Fluids and nutrition | ||||
| i.v. fluids, n (%) | 10 (1.6) | 10 (3.0) | 1.93 (0.81 to 4.59) | 0.14 |
| Days of i.v. fluids, median (range) | 2 (1–6) | 3 (1–10) | – | – |
| PN, n (%) | 2 (0.3) | 1 (0.3) | 0.96 (0.09 to 10.6) | 0.98 |
| Days of PN, median (range) | 3 (3,3) | 3 (3,3) | – | – |
| Days to full oral suck feeds, median (range) | 0 (0–9) | 0 (0–19) | – | – |
| Morbidities | ||||
| Culture-positive infection, n (%) | 0 (0.0) | 0 (0.0) | a | a |
| Jaundice requiring phototherapy, n (%) | 3 (0.5) | 3 (0.9) | 1.93 (0.39 to 9.51) | 0.42 |
| Hypothermia (temperature of < 36.0 °C), n (%) | 5 (0.8) | 7 (2.1) | 2.70 (0.86 to 8.44) | 0.088 |
| Hypoglycaemia (blood sugar level of < 2.0 mmol/l), n (%) | 2 (0.3) | 7 (2.1) | 6.75 (1.41 to 32.32) | 0.017 |
| Neonatal encephalopathy grade II/III, n (%) | 3 (0.5) | 1 (0.3) | 0.64 (0.07 to 6.16) | 0.70 |
Non-spontaneous onset of labour occurred in 42.1% of LMPT and 34.2% of term births. Of these, 50.5% of LMPT infants and 31.9% of term-born infants were delivered by CS not preceded by labour. Birth gestations for infants following spontaneous and non-spontaneous labours were similar within both groups. LMPT infants whose mothers had not spontaneously laboured were more likely to receive resuscitation (RR 1.50, 95% CI 1.13 to 1.99; p = 0.005), to be admitted to a NNU (RR 1.37, 95% CI 1.18 to 1.58; p < 0.001) and to require respiratory intervention with either mechanical ventilation or non-invasive respiratory support (RR 1.89, 95% CI 1.32 to 2.72; p = 0.001) than those whose mothers had laboured spontaneously. For those admitted, duration of NNU stay was longer (median 4 days, range 1–77 days vs. median 6 days, range 1–78 days; p < 0.001). In term-born infants there were no differences in these outcomes between medically indicated and spontaneous preterm deliveries.
With respect to common morbidities, hypothermia was seen more commonly in LMPT babies following non-spontaneous onset of labour and hypoglycaemia was also more common in the non-spontaneous group. There were no other significant differences in the morbidities explored.
Discussion
Our results show that infants born at LMPT gestations are at significantly increased risk of most adverse neonatal outcomes compared with their term-born counterparts. This includes the need for intervention at delivery, admission to NNUs and common morbidities. We were unable to demonstrate a statistically significant increase in mortality in this group, although there were more deaths in the LMPT babies. Our findings are in line with other published findings, both those from studies conducted before the LAMBS began recruitment6,109,110,113,116,160 and those from studies have reported results during the course of this study. 161–170 Breastfeeding rates of both singletons and multiples were poor in the LMPT group and worsened during the course of the neonatal stay .
Delivery following obstetric intervention is more likely to occur at LMPT gestations than at term. Non-spontaneous onset of labour at LMPT gestations is associated with more neonatal morbidity than delivery following spontaneous labour, but these associations are not present when comparisons are made between groups of term-born infants according to the type of onset of labour. Indications for delivery have not yet been analysed. However, in the LMPT group it is likely that a greater proportion of obstetrically induced deliveries occur as a result of illness in either the mother or fetus. In contrast, a proportion of deliveries beyond 37 weeks’ gestation will occur because the pregnancy has reached post-term gestation. As there are differences between the two LMPT groups that are not present in the term-born groups, our findings suggest that adverse outcomes in LMPT infants are related not only to the effects of prematurity itself, but also to the indications for delivery. Further exploration of indications for delivery may reveal groups at particularly high risk for adverse neonatal and long-term outcomes.
Conclusions
Key findings
-
Infants born at LMPT gestations are at a significantly greater risk of neonatal morbidity than infants born at term.
-
For most adverse outcomes, there is no difference in the effect between singletons and multiples born at LMPT gestations.
-
Late and moderately preterm babies are less likely to receive maternal breast milk than those born at term.
-
Non-spontaneous onset of labour at LMPT gestations is associated with more neonatal morbidity than delivery following spontaneous onset of labour.
-
The effects of prematurity at LMPT gestations are compounded by effects relating to complications leading to medically indicated delivery.
Strengths and limitations
We have recruited a large population of LMPT infants and have collected detailed data for a wide range of outcomes. Data were collected either during the infants’ neonatal hospital stay or as soon as possible after discharge, minimising error and missing data. However, we were unable to recruit 100% of infants and it is possible that selection bias may have occurred if mothers of specific groups of infants declined to participate, for example if the baby was extremely sick or so well that very early discharge from hospital was possible. This may have led to both over- and under-estimation of effects.
Implications for practice
There is a need to examine current practice with regard to neonatal care for LMPT babies, as these babies have historically been cared for in a similar way to those born at term. Our findings and those of other researchers, in identifying increased risks of multiple common and important neonatal morbidities, should prompt consideration of whether or not current models of care are the most appropriate for this group. It may be that a greater level of surveillance following delivery or earlier intervention in some cases may lead to improved outcomes and shorter hospital stays, and this should be explored. Changes in clinical practice, if required in this large group of babies, are likely to be costly in terms of both resources and personnel, and careful planning would be needed to ensure that the highest risk groups are identified and targeted when possible.
Observation of poorer breastfeeding rates in LMPT babies is worrying, particularly as the longer duration of hospital stay in this group might be expected to allow greater support for mothers wishing to breastfeed their babies. As these babies appear to constitute a group at high risk of breastfeeding failure, targeted support in establishing and maintaining breastfeeding may lead to improvement in rates of breastfeeding at discharge.
High rates of obstetric intervention for delivery in LMPT babies and our finding of worse outcomes in this group suggested that greater caution may need to be exercised in determining the optimum timing for delivery in complicated pregnancies.
Future research
Having identified a higher risk of adverse neonatal outcomes in LMPT babies, future research is required to determine how much of this observed risk relates to immaturity and how much to the reasons for the early delivery. In this way, it may be possible to highlight certain groups for whom there may be scope to intervene and improve early outcomes. The identification of poorer breastfeeding rates in LMPT babies warrants urgent work to explore the factors influencing the initiation and maintenance of breastfeeding in this group and whether or not this can be improved with a different model of care. Ongoing work in this group is needed to determine whether problems in the neonatal period affect very large numbers of LMPT infants or whether they are confined to smaller, high-risk groups. Our findings of higher rates of morbidity in infants following medically indicated delivery rather than spontaneous onset of labour suggest that the latter explanation may be likely, with these infants forming one higher-risk group. Follow-up of the cohort will be crucial to indicate whether or not adverse neonatal outcomes translate into adverse outcomes in childhood and beyond.
Health and developmental outcomes at 2 years of age following late and moderately preterm birth
Background
Follow-up of the LAMBS cohort at 2Y-CA was conducted to determine health and developmental outcomes of infants born at LMPT gestations to guide screening, follow-up and intervention efforts and to identify potential intervention strategies. There is a well-documented risk for adverse health, neurodevelopmental and behavioural sequelae171–173 among children born very preterm (i.e. < 32 weeks’ gestation). Recent studies have suggested that the constellation of health and developmental problems associated with very preterm birth extends across birth at LMPT gestations, exerting a significant but smaller impact on long-term outcomes. 174–177 However, results are inconsistent; some have reported no difference from term-born controls178 and there appears to be a significant moderating effect of socioeconomic risk among this group of children. 175 To further existing knowledge and guide the provision of evidence-based long-term care for children in the UK, we sought to identify the range and prevalence of adverse outcomes following LMPT birth. In particular, we sought to determine whether or not LMPT birth confers additional risk over socioeconomic factors alone and to identify risk factors for adverse neurodevelopmental outcomes at 2 years of age.
Objectives
-
Explore the health and respiratory outcomes of children born LMPT at 2 years of age.
-
Identify the prevalence of cognitive impairment and neurodevelopmental disability among children born LMPT.
-
Identify neonatal risk factors for neurodevelopmental disability at 2 years of age among children born LMPT.
-
Evaluate the impact of LMPT birth on behavioural outcomes at 2 years of age.
Methods
Measures
Data relating to health, respiratory, neurodevelopmental, cognitive and behavioural outcomes were collected via parental reporting. A study questionnaire combining standard parent report measures and additional items to address health issues associated with preterm birth was developed. To assess general health, parents were asked to rate their children’s health in comparison with other children of the same age using a 4-point scale (excellent, good, fair or poor). Respiratory outcomes were assessed using forced-choice questions relating to the frequency of wheezing (never, occasionally, frequently or every day), type (preventer or reliever) and frequency of inhaler use (never, occasionally, frequently or every day), and prescription of steroids for wheezing (yes or no). Neurological outcomes were assessed using forced-choice questions relating to whether or not the child had experienced seizures over the last year (none, febrile only or neurological seizures) and prescription for anticonvulsant medication (yes or no).
To assess neurodevelopmental outcomes, parents were asked whether or not the child had been given a diagnosis of cerebral palsy (CP) and three forced-choice items were used to assess the child’s vision, hearing and neuromotor function. Responses were used to identify the severity of functional impairment (none, mild, moderate, severe) within each domain. Children were classified as having neurosensory impairment (NSI) if they had a moderate or severe impairment in any one of these three domains (irrespective of the diagnosis of CP). These questionnaire items were designed to map onto standard criteria for classifying neurodevelopmental outcomes at 2 years of age. 179
Cognitive development was assessed using the PARCA-R, a parent questionnaire of cognitive and language development. 180,181 Raw scores were summed to provide a subscale score for non-verbal cognition (NVC; range 0–34) and language development (range 0–124). These were then summed to provide a total parent report composite (PRC) score (range 0–158). The PARCA-R has excellent concurrent validity with gold standard developmental tests and PRC scores of < 49 have good diagnostic utility, with ≥ 80% sensitivity and specificity, for identifying very preterm children with developmental delay at 2 years of age. 180,181 Therefore, PRC scores of < 49 were used to identify children with suspected developmental delay in the present study. If fewer than four items were missing on the NVC scale, these items were replaced by the average NVC item score at the individual level. If more than five items were missing from the PARCA-R NVC scale, these children were excluded (n = 6). For 21 children whose first language was not English and whose parent was unable to complete the language section of the questionnaire, summary scores were not computed but cognitive impairment was classified using the NVC subscale alone, from which scores of < 22 were used to identify developmental delay corresponding with NVC scores of < 2.5th percentile of the term-born group. Classifications of cognitive impairment were combined with the NSI classification to determine the proportion of children with composite neurodevelopmental disability (defined as a moderate/severe impairment in vision, hearing, motor or cognitive function). 179
Behavioural outcomes were measured using the BITSEA,182 a norm-referenced parent report screener for social–emotional development and behavioural problems in children aged 1–3 years. The problem subscale comprises 31 items to assess problems such as aggression, defiance, hyperactivity, negative emotionality, anxiety and withdrawal, from which a summed total problem score is computed, with higher scores indicating greater problems. The competence subscale comprises 11 items to assess social–emotional abilities such as empathy, prosocial behaviours and compliance, from which a total competence score is computed, with lower scores indicating lesser competence. Behaviour problems (problem scores ≥ 75th percentile) and delayed social–emotional competence (competence scores ≤ 15th percentile) were identified using published age- and gender-specific norm-referenced cut-off points. 182 The questionnaire also comprises two questions to elicit level of parental concern about their child’s socioemotional and language development. The BITSEA has good test–retest reliability, inter-rater reliability and internal consistency, and positive screens have been shown to predict behaviour problems and psychiatric disorders at school age in both term-born and very preterm children. 182,183
Statistical analyses
Non-response at 2 years was investigated separately for LMPT and term-born children. The risk of non-response was calculated using Poisson regression with robust SEs for maternal and infant characteristics listed in Table 28. To assess the effect of LMPT birth on long-term outcomes, RRs with 95% CIs are presented for the risk of adverse outcomes in the LMPT group compared with the term-born controls. RRs adjusted for sex, corrected age at assessment and socioeconomic status are also presented. When adjustment resulted in separation this has been noted and estimates are not provided. For the BITSEA scores, the mean difference with 95% CIs between term-born and LMPT children is presented using a linear model both crude and after adjustment for corrected age, socioeconomic status and sex. To identify predictors of adverse outcomes in LMPT children, univariable associations with neurodevelopmental disability were calculated. To identify independent risk factors, a multivariable model was then constructed selecting variables with a p-value of < 0.2 in the univariable analysis, (excluding IMD quartile because of its correlation with the SES Index score) into a model selection procedure using backwards stepwise selection. The final model chosen was that in which all included variables had a p-value of < 0.05.
| Characteristic | Term-born controls | LMPT infants | ||||||
|---|---|---|---|---|---|---|---|---|
| Responders | Non-responders | RR (95% CI) | p-value | Responders | Non-responders | RR (95% CI) | p-value | |
| Mothers | (n = 696) | (n = 420) | – | – | (n = 596) | (n = 424) | – | – |
| Age at baby’s birth (years), n (%) | ||||||||
| ≤ 20 | 17 (2.4) | 39 (9.3) | 1.78 (1.42 to 2.23) | < 0.001 | 19 (3.2) | 42 (9.9) | 1.84 (1.47 to 2.31) | < 0.001 |
| 20–24 | 96 (13.8) | 106 (25.2) | 1.34 (1.11 to 1.63) | 0.003 | 89 (14.9) | 105 (24.8) | 1.45 (1.19 to 1.77) | < 0.001 |
| 25–29 | 182 (26.2) | 117 (27.9) | Baseline | – | 178 (29.9) | 106 (25.0) | Baseline | – |
| 30–34 | 212 (30.5) | 107 (25.5) | 0.86 (0.70 to 1.06) | 0.14 | 194 (32.6) | 108 (25.5) | 0.96 (0.77 to 1.19) | 0.70 |
| ≥ 35 | 189 (27.2) | 50 (11.9) | 0.53 (0.40 to 0.71) | < 0.001 | 115 (19.3) | 63 (14.9) | 0.95 (0.74 to 1.22) | 0.68 |
| Unknown | – | 1 (0.2) | – | – | 1 (0.2) | – | – | – |
| Ethnic group, n (%) | ||||||||
| White | 574 (82.5) | 288 (68.7) | Baseline | – | 467 (78.4) | 276 (65.1) | Baseline | – |
| Mixed | 8 (1.1) | 15 (3.6) | 1.95 (1.43 to 2.67) | < 0.001 | 12 (2.0) | 21 (5.0) | 1.71 (1.30 to 2.25) | < 0.001 |
| Asian or Asian British | 77 (11.1) | 82 (19.6) | 1.54 (1.29 to 1.84) | < 0.001 | 88 (14.8) | 89 (21.0) | 1.35 (1.14 to 1.61) | 0.001 |
| Black or black British | 30 (4.3) | 30 (7.1) | 1.50 (1.14 to 1.96) | 0.003 | 22 (3.7) | 31 (7.3) | 1.57 (1.23 to 2.01) | < 0.001 |
| Chinese or other ethnic group | 7 (1.0) | 4 (1.0) | 1.09 (0.50 to 2.39) | 0.83 | 6 (1.0) | 7 (1.7) | 1.45 (0.67 to 2.42) | 0.16 |
| Missing | – | 1 (0.2) | – | – | 1 (0.2) | – | – | – |
| SES Index, n (%) | ||||||||
| Low risk | 342 (49.1) | 94 (22.4) | Baseline | – | 259 (43.5) | 65 (15.3) | Baseline | |
| Medium risk | 211 (30.3) | 118 (28.1) | 1.66 (1.32 to 2.09) | < 0.001 | 186 (31.2) | 106 (25.0) | 1.81 (1.39 to 2.36) | < 0.001 |
| High risk | 143 (20.6) | 208 (49.5) | 2.75 (2.25 to 3.35) | < 0.001 | 151 (25.3) | 253 (59.7) | 3.12 (2.84 to 3.93) | < 0.001 |
| English not first language, n (%) | 86 (12.5) | 81 (19.9) | 1.38 (1.15 to 1.65) | < 0.001 | 86 (14.6) | 80 (19.2) | 1.20 (1.00 to 1.44) | 0.01 |
| Poor mental health,a n (%) | 71 (10.2) | 49 (11.7) | 1.10 (0.87 to 1.38) | 0.44 | 70 (11.8) | 70 (16.5) | 1.24 (1.03 to 1.49) | 0.023 |
| Poor general health,b n (%) | 35 (5.0) | 31 (7.4) | 1.27 (0.97 to 1.66) | 0.08 | 48 (8.1) | 56 (13.2) | 1.34 (1.10 to 1.63) | 0.003 |
| Infants | (n = 771) | (n = 482) | (n = 651) | (n = 472) | ||||
| Gestational age (weeks), mean (SD) | 39.3 (1.4) | 39.0 (1.4) | 0.91 (0.87 to 0.96) | < 0.001 | 34.9 (1.2) | 35.0 (1.2) | 1.05 (0.99 to 1.1) | 0.13 |
| Birthweight (kg), mean (SD) | 3.3 (0.5) | 3.2 (0.6) | 0.80 (0.71 to 0.91) | 0.001 | 2.4 (0.5) | 2.4 (0.5) | 0.98 (0.85 to 1.12) | 0.74 |
| Major congenital anomalies, n (%) | 5 (0.7) | 4 (0.8) | 1.16 (0.56 to 2.41) | 0.70 | 11 (1.7) | 9 (1.9) | 1.07 (0.66 to 1.75) | 0.78 |
| Fetal growth restriction (< third percentile),c n (%) | 51 (6.6) | 44 (9.1) | 1.22 (0.97 to 1.54) | 0.08 | 70 (10.8) | 66 (14.0) | 1.18 (0.98 to 1.42) | 0.09 |
| Multiple births, n (%) | 151 (19.6) | 124 (25.7) | 1.23 (1.06 to 1.44) | 0.01 | 111 (17.1) | 95 (20.1) | 1.12 (0.95 to 1.33) | 0.18 |
| Any respiratory support,d n (%) | 8 (1.0) | 3 (0.6) | 0.71 (0.27 to 1.86) | 0.48 | 92 (14.1) | 54 (11.4) | 0.86 (0.69 to 1.08) | 0.20 |
| Intracranial abnormality,e n (%) | 5 (0.7) | 4 (0.8) | 1.16 (0.56 to 2.41) | 0.70 | 7 (1.1) | 3 (0.6) | 0.71 (0.28 to 1.84) | 0.48 |
| Any breast milk at discharge,f n (%) | 594 (77.3) | 292 (60.7) | 0.63 (0.55 to 0.73) | < 0.001 | 410 (63.1) | 228 (48.4) | 0.71 (0.61 to 0.82) | < 0.001 |
Results
Two-year follow-up rates
At 2Y-CA, seven (0.6%) LMPT children had died, the parents of eight (0.7%) had withdrawn them from the study and two (0.2%) children had moved into closed foster care precluding ongoing follow-up. Of the remaining 1113 LMPT children eligible for follow-up at 2 years, the parents of two (0.2%) refused to complete a study questionnaire, and we did not receive follow-up data from the parents of 460 (41.3%) children, despite numerous attempts to contact them. Thus, follow-up data were ultimately received for 651 (58.5%) infants born LMPT (Figure 10); excluding deaths, this equates to a follow-up rate of 58.0% of the total LMPT cohort.
FIGURE 10.
Follow-up rates and retention of the LAMBS cohort to 2Y-CA.
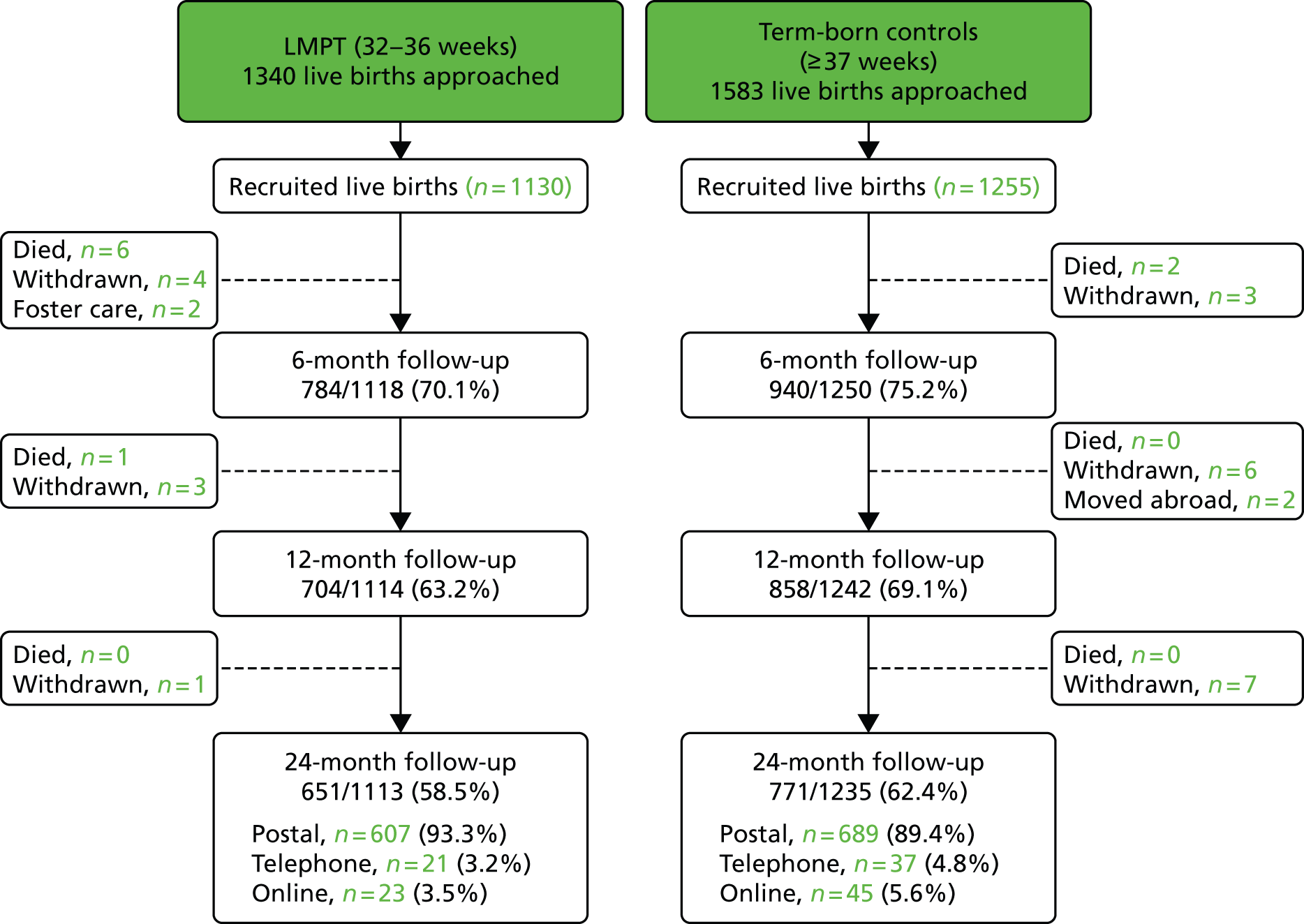
Of term-born infants, two (0.2%) had died, the parents of 16 (1.3%) children had withdrawn them from the study, and the parents of two (0.2%) had moved abroad, leaving 1235 children eligible for follow-up at 2Y-CA. Of these term-born infants, the parents of three (0.2%) infants refused to complete a study questionnaire, and we did not receive follow-up data from the parents of 461 (37.3%) children. The parents of 771 returned questionnaires, equating to a follow-up rate of 62.4% (see Figure 10) of eligible term-born children and, excluding deaths, 61.5% of the term-born cohort recruited. For all subsequent analyses, infants with major congenital anomalies were excluded; this equated to 638 responders in the LMPT group and 765 among the term-born controls.
Analysis of non-responders
Previous research has shown that non-responders to follow-up in preterm cohorts typically have higher medical and socioeconomic risk than those who respond to study questionnaires or formal evaluations. 185,186 To examine the effect of loss to follow-up on outcomes at 2 years, maternal and infant characteristics of non-responders were analysed for both LMPT and term-born children (see Table 28). Among infants born LMPT, all the maternal characteristics examined were significantly associated with non-response to follow-up at 2 years. Specifically, mothers who did not respond to follow-up were more likely to be younger (i.e. aged < 25 years), to have higher socioeconomic risk and poorer mental and general health, to be of non-white ethnic origin and not to speak English. The greatest risk was associated with socioeconomic deprivation, with those with medium- and high-risk SES Index scores being, respectively, 1.8 (95% CI 1.4 to 2.4) and 3.1 (95% CI 2.8 to 3.9) times more likely than those with low risk to be non-responders (see Table 28). Of all the infant characteristics examined, not receiving any breast milk at discharge was the only significant factor associated with non-response; this is likely to be a marker of higher social risk among those mothers not completing study questionnaires.
Analysis of factors associated with non-response in term-born controls produced similar results in terms of maternal characteristics, with non-responders more likely to be younger (aged < 25 years) or older mothers (aged ≥ 35 years), to have higher socioeconomic risk and to be of non-white ethic origin and not to speak English. However, there was no association with response to follow-up in terms of mothers’ self-reported general and mental health. Again, the greatest risk was associated with socioeconomic deprivation, with those with medium- and high-risk SES Index scores being, respectively, 1.7 (95% CI 1.3 to 2.1) and 2.8 (95% CI 2.3 to 3.4) times more likely than those with low risk to be non-responders. As in the LMPT group, not receiving any breast milk at discharge was significantly associated with non-response. In addition, mothers who gave birth to more than one baby and mothers of babies born at lower gestational age or of low birthweight were more likely to be non-responders (see Table 28).
Discussion
The factors associated with non-response were similar between the groups and indicate that non-responders to follow-up at 2 years were more likely to be from families with higher demographic risk and socioeconomic deprivation. As these factors are associated with poor neurodevelopmental outcomes, the results presented hereafter may underestimate the true prevalence of adverse outcomes in the LMPT and term-born populations; however, the effect of this is likely to be similar between groups. Our later discussion and conclusions have thus been tempered accordingly.
Health, respiratory and neurological outcomes
Among those without congenital anomalies, health and respiratory outcomes for LMPT infants and term-born controls are shown in Table 29. RRs for adverse outcomes among LMPT infants are reported both unadjusted and adjusted for sex and SES Index (low, middle and high risk).
| Outcome | Term (n = 765) | LMPT (n = 638) | Unadjusted | Adjusteda | ||
|---|---|---|---|---|---|---|
| RR (95% CI) | p-value | RR (95% CI) | p-value | |||
| General health | ||||||
| Poor health,b n (%) | 2.35 (1.44 to 3.84) | 0.001 | 2.26 (1.38 to 3.70) | 0.001 | ||
| Excellent | 468 (61.2) | 358 (56.1) | – | – | – | – |
| Good | 274 (35.8) | 234 (36.7) | – | – | – | – |
| Fair | 22 (2.9) | 44 (6.9) | – | – | – | – |
| Poor | 1 (0.1) | 1 (0.2) | – | – | – | – |
| Missing | – | 1 (0.2) | – | – | – | – |
| Respiratory outcomes | ||||||
| Frequent wheeze,c n (%) | 0.89 (0.45 to 1.75) | 0.729 | 0.85 (0.43 to 1.68) | 0.64 | ||
| Never | 594 (77.7) | 439 (68.8) | – | – | – | – |
| Occasionally | 152 (19.9) | 183 (28.7) | – | – | – | – |
| Frequently | 16 (2.1) | 11 (1.7) | – | – | – | – |
| Every day | 3 (0.4) | 3 (0.5) | – | – | – | – |
| Missing | – | 2 (0.3) | – | – | – | – |
| Uses an inhaler, n (%) | 1.38 (1.10 to 1.73) | 0.005 | 1.36 (1.09 to 1.70) | 0.007 | ||
| Uses a preventer | 8 (1.1) | 4 (0.6) | – | – | – | – |
| Uses a reliever | 90 (11.8) | 108 (16.9) | – | – | – | – |
| Uses both | 19 (2.5) | 23 (3.6) | – | – | – | – |
| Missing | 1 (0.1) | – | – | – | – | – |
| Frequent inhaler use,d n (%) | 0.77 (0.39 to 1.55) | 0.47 | 0.73 (0.37 to 1.46) | 0.38 | ||
| Never | 653 (85.4) | 515 (80.7) | – | – | – | – |
| Occasionally | 84 (11.0) | 107 (16.8) | – | – | – | – |
| Frequently | 7 (0.9) | 5 (0.8) | – | – | – | – |
| Every day | 13 (1.7) | 8 (1.3) | – | – | – | – |
| Missing | 8 (1.1) | 3 (0.5) | – | – | – | – |
| Steroids used, n (%) | 47 (6.2) | 49 (7.7) | 1.25 (0.85 to 1.84) | 0.26 | 1.21 (0.82 to 1.80) | 0.33 |
| Neurological outcomes | ||||||
| Seizures in past year,e n (%) | 1 (0.1) | 2 (0.3) | 2.41 (0.22 to 26.49) | 0.473 | 2.31 (0.22 to 24.22) | 0.49 |
| Prescribed anticonvulsant, n (%) | 2 (0.3) | 1 (0.2) | 0.60 (0.05 to 6.60) | 0.676 | 0.52 (0.05 to 4.97) | 0.57 |
Overall, LMPT infants were at 2.4 times (95% CI 1.4 to 3.8 times) increased risk of poorer parent-reported general health than infants born at term. Notably, this increase was not evidenced in terms of ‘poor’ health, but instead there was an excess of LMPT infants reported as having ‘fair’ health. A similar pattern of results was evidenced for respiratory outcomes. Although LMPT infants did not have frequent wheeze more often than infants born at term (RR 0.89, 95% CI 0.45 to 1.75; p = 0.72), there was an excess of LMPT infants with occasional wheeze (29% vs. 20%) and a reduction in the proportion who were reported as never wheezing compared with infants born at term (69% vs. 78%). Similarly, although more LMPT infants had been prescribed an inhaler by 2 years of age (RR 1.38, 95% CI 1.10 to 1.73; p = 0.005), they did not have a higher rate of frequent inhaler use than term-born infants (RR 0.77 95% CI 0.39 to 1.55; p = 0.47); there was an increase only in occasional inhaler use, and LMPT infants had not been prescribed more corticosteroids than term-born controls, indicating no excess of severe respiratory problems. Similarly, there was no excess of neurological sequelae in LMPT infants: they were no more likely than term-born infants to have had seizures in the past year or to have been prescribed anticonvulsant medication (see Table 29). Adjustment for potential confounders of the association between outcomes and LMPT birth did not alter the statistical significance of results for any health, respiratory or neurological outcome (see Table 29).
Discussion
Taken together these results indicate that there is an excess of mild health problems among infants born LMPT and that severe adverse health outcomes are as rare among this group as they are in the general population. These findings are commensurate with other recent population-based studies of long-term outcomes in children born LMPT in which an increase in mild health and respiratory problems has been observed. 167,174,187 This contrasts with the well-documented outcomes of very preterm infants in which there is a significantly increased risk for severe respiratory and neurological problems. 171,188 Increases in even mild health problems should not be underestimated, as these can have a significant impact at the population level given the large numbers of babies born LMPT. 7,174,189 Whether the observed increase in inhaler use reflects a true increase in respiratory symptoms or a potential prescription bias among preterm children requires elucidation with detailed clinical studies to confirm the validity of these parent reports. However, others have demonstrated impaired lung function at school age in children born LMPT,174,187 suggesting that these children may be at risk of respiratory problems. Further detailed studies of long-term respiratory function are needed to better define outcomes in this area. Later follow-up of this cohort will also enable an investigation of the long-term functional significance of these findings.
Neurodevelopmental outcomes
Neurodevelopmental outcomes for LMPT and term-born children are shown in Table 30. RRs were adjusted for potential confounders (sex, corrected age and SES Index) when possible.
| Neurodevelopmental outcome | Term (n = 765) | LMPT (n = 638) | Unadjusted | Adjusteda | ||
|---|---|---|---|---|---|---|
| RR (95% CI) | p-value | RR (95% CI) | p-value | |||
| Composite outcomes | ||||||
| NSI,b n (%) | 2 (0.3) | 10 (1.6) | 6.00 (1.32 to 27.28) | 0.021 | – | – |
| Neurodevelopmental disability,c n (%) | 77 (10.1) | 101 (15.9) | 1.57 (1.19 to 2.07) | 0.001 | 1.42 (1.08 to 1.86) | 0.011 |
| Domains of impairment | ||||||
| Hearing impairment, n (%) | 9 (0.0) | 3 (0.5) | – | – | – | – |
| Vision impairment, n (%) | 9 (0.0) | 2 (0.3) | – | – | – | – |
| Motor impairment, n (%) | 2 (0.3) | 5 (0.8) | 3.00 (0.58 to 15.41) | 0.19 | – | – |
| CP, n (%) | 4 (0.5) | 0 (0.0) | – | – | – | – |
| Cognitive impairment,d n (%) | 76 (10.0) | 99 (15.6) | 1.56 (1.18 to 2.06) | 0.002 | 1.41 (1.07 to 1.85) | 0.013 |
As in the term-born population, the prevalence of moderate/severe NSI was very low, with < 1% of LMPT children having functional hearing, visual or neuromotor impairment. When RRs could be computed, these showed no significant difference from term-born controls. When these were combined as a composite measure, overall there was a significantly increased risk for NSI among LMPT children compared with controls (1.6% vs. 0.3%; RR 6.00; 95% CI 1.32 to 27.28). Among the LMPT group, no parents reported that their child had received a diagnosis of CP compared with 0.5% of the term-born population (see Table 30).
Cognitive problems were more frequent, in general, and there was a significantly increased risk of cognitive impairment, which was present in 16% of LMPT children compared with 10% of term-born children (RR 1.56, 95% CI 1.18 to 2.06). There was also a significant difference in mean PARCA-R scores between LMPT children and controls (term: mean 94.5, SD 33.3; LMPT: mean 88.9, SD 36.0; unadjusted mean difference –5.61, 95% CI –9.28 to -1.95, p = 0.003; adjusted mean difference –4.16, 95% CI –7.70 to -0.63, p = 0.021). The distribution of PRC scores was similar in both the LMPT and term-born children, but there appeared to be a general shift to the left, resulting in an excess of LMPT children with scores below the cut-off point for cognitive impairment (Figure 11).
FIGURE 11.
Frequency distribution of PARCA-R PRC scores in LMPT and term-born children. Higher scores indicate better cognitive development. The vertical line indicates the cut-off point for identifying cognitive impairment.
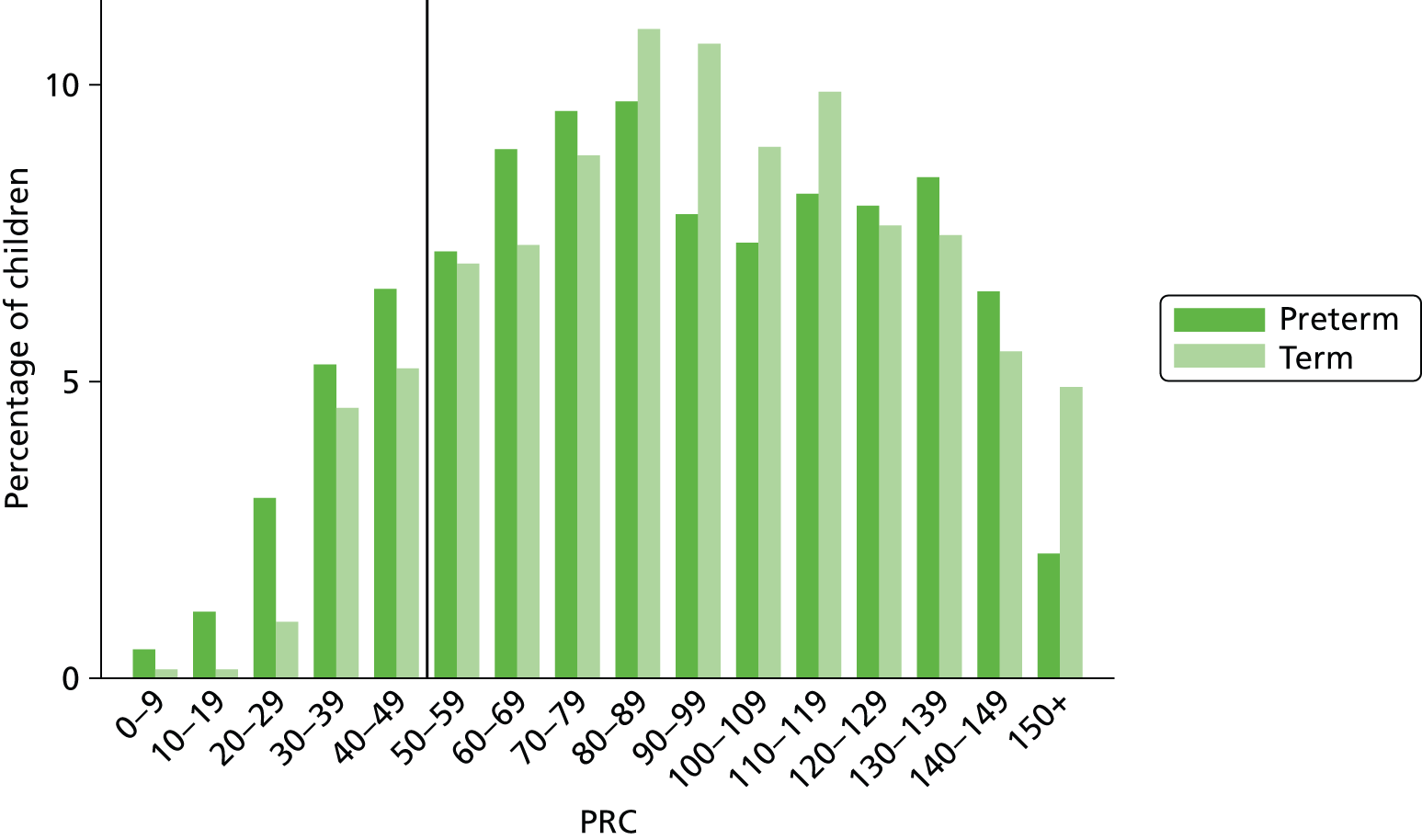
When cognitive impairment was combined with NSI, LMPT children were at significantly increased risk of moderate/severe neurodevelopmental disability compared with term-born controls (RR 1.57, 95% CI 1.19 to 2.07). This was almost exclusively the result of cognitive impairment, with only two additional LMPT children and one additional control having neurodevelopmental disability over cognitive impairment alone (see Table 30). The adjusted RR for neurodevelopmental disability was 1.42 (95% CI 1.08 to 1.86).
Discussion
Although these results indicate that there is a significantly increased risk of functional NSIs in LMPT children compared with those born at term, these were rare and affected only 1.6% of LMPT children. This represents a marked reduction in adverse neurosensory outcomes compared with children born very preterm and extremely preterm. 171,188 The rate of CP was also higher among term-born controls than those born LMPT (0.5% vs. 0%, respectively). However, the statistical significance of this could not be assessed given the low prevalence. Moreover, diagnoses were reported by parents and not confirmed in this sample. Given that CP diagnoses often become clinically apparent only at this age, additional cases of mild CP may become evident at later stages of follow-up.
In contrast, 16% of LMPT children had moderately to severely delayed cognitive development, compared with 10% of term-born controls. Thus, although the RR (1.6) was lower than for NSI (6.00), the absolute impact of cognitive difficulties is likely to be greater at a population level given the higher prevalence of these outcomes. Early cognitive difficulties are an important indicator of an individual’s childhood achievement and future life chances. 190 Moreover, cognitive problems in very preterm children have been shown to persist throughout childhood and adolescence and to have a profound impact on academic attainment and the need for special educational intervention. 191,192 Thus, it might be predicted that LMPT children will have higher rates of special educational needs and poor school performance as shown in recent studies. 9,175
Historically, cognitive problems in very preterm children have proven difficult to ameliorate and numerous neonatal and early developmental interventions have met with limited success; even when these show early benefits, these are rarely sustained beyond the period of intervention delivery. 193 However, a number of studies, including the large-scale US Infant Health and Development Program (IHDP), have reported beneficial effects of intervention for relatively larger babies with birthweight of 2001–2500 g, which may suggest that LMPT infants could benefit from early intervention. 194–197 Olds et al. 198 have identified particular benefit from interventions in families of low socioeconomic status. It is not clear to what extent cognitive problems identified at 2 years represent impaired function or developmental delays and whether or not there is the potential for catch-up over the preschool years. Longer-term follow-up of this cohort is needed to determine how these cognitive problems evolve over time and the long-term significance of these early outcomes for later educational attainment. The efficacy of early intervention programmes requires investigation in this population. Given the size of the LMPT population, intervention and follow-up for all may be prohibitive in terms of the cost and resources required. Thus, it is important to identify an at-risk subgroup in order to target resources to those in greatest need. As such, we also investigated risk factors for adverse neurodevelopmental outcomes among LMPT children.
Risk factors for neurodevelopmental disability in children born late and moderately preterm
In order to identify children at greatest risk of adverse outcomes, we explored the association of obstetric and neonatal factors with the presence of neurodevelopmental disability at 2Y-CA. As shown in Table 31, children whose mothers were of non-white ethnic origin, non-English speaking or of higher socioeconomic risk, or who smoked or took recreational drugs during pregnancy, or who had pre-pregnancy hypertension or pre-eclampsia were significantly more likely to have neurodevelopmental disability. Raised CRP levels during pregnancy were also marginally associated with disability (p < 0.1). LMPT children who were conceived via infertility treatment were less likely to have neurodevelopmental disability at 2 years. Of the neonatal factors analysed, being male, being resuscitated at birth and not having any breast milk at discharge were significantly associated with the risk of neurodevelopmental disability. These variables predominantly appear to be markers of high sociodemographic risk or hypertensive disease, either before or during pregnancy. The greatest impact was found for recreational drug use during pregnancy, pre-pregnancy hypertension and higher SES Index, each of which as associated with a three- to fourfold increased risk of disability.
| Variable | n (%) with neurodevelopmental disability | RR (95% CI) | p-value | |
|---|---|---|---|---|
| Risk factor present | Risk factor absent | |||
| Obstetric factors | ||||
| Mother’s age (years) | ||||
| < 20 | 4 (20.0) | 97 (16.0) | 1.39 (0.54 to 3.59) | 0.49 |
| 20–24 | 19 (21.6) | 82 (15.5) | 1.50 (0.88 to 2.56) | 0.14 |
| 25–29 | 26 (14.4) | 75 (16.8) | Baseline | – |
| 30–34 | 26 (12.1) | 75 (18.2) | 0.84 (0.51 to 1.40) | 0.51 |
| ≥ 35 | 26 (21.1) | 75 (14.9) | 1.47 (0.90 to 2.41) | 0.13 |
| Non-white ethnic group | 29 (23.2) | 72 (14.4) | 1.61 (1.10 to 2.37) | 0.015 |
| Non-English-speaking at home | 22 (27.5) | 79 (14.6) | 1.88 (1.24 to 2.84) | 0.003 |
| SES Index | ||||
| Low risk | 20 (7.1) | 81 (23.5) | Baseline | – |
| Medium risk | 37 (19.2) | 64 (14.7) | 2.71 (1.62 to 4.53) | < 0.001 |
| High risk | 44 (29.0) | 57 (12.0) | 4.10 (2.51 to 6.69) | < 0.001 |
| Conceived via infertility treatment | 1 (1.85) | 100 (17.4) | 0.11 (0.02 to 0.75) | 0.024 |
| Pre-pregnancy diagnosed diabetes | 4 (19.1) | 97 (16.0) | 1.19 (0.48 to 2.93) | 0.70 |
| Pre-pregnancy diagnosed hypertension | 7 (46.7) | 94 (15.3) | 3.04 (1.72 to 5.39) | < 0.001 |
| Smoked during pregnancy | 32 (25.2) | 69 (13.8) | 1.85 (1.27 to 2.68) | 0.001 |
| Alcohol drank during pregnancy | 40 (14.1) | 61 (17.7) | 0.79 (0.55 to 1.15) | 0.22 |
| Recreational drugs used during pregnancy | 6 (50.0) | 95 (15.4) | 3.24 (1.79 to 5.88) | < 0.001 |
| Pre-eclampsia | 25 (26.9) | 76 (14.2) | 1.89 (1.27 to 2.81) | 0.002 |
| Infection (positive culture) during pregnancy | 11 (24.4) | 86 (15.2) | 1.61 (0.93 to 2.80) | 0.089 |
| Gestational diabetes | 5 (21.7) | 96 (15.8) | 1.38 (0.62 to 3.06) | 0.43 |
| Pre-labour rupture of membranes > 24 hours prior to delivery | 21 (17.2) | 80 (15.8) | 1.09 (0.70 to 1.69) | 0.70 |
| Antinatal corticosteroids given | 24 (13.9) | 77 (16.9) | 0.82 (0.54 to 1.26) | 0.37 |
| Labour induced | 27 (20.3) | 74 (14.9) | 1.37 (0.92 to 2.04) | 0.12 |
| Raised CRP level during labour | 7 (29.2) | 94 (15.6) | 1.84 (0.96 to 3.53) | 0.067 |
| Normal vaginal delivery | 48 (15.2) | 53 (17.0) | 0.89 (0.63 to 1.28) | 0.54 |
| Cord pH of ≤ 7.1 | 5 (25.0) | 96 (15.8) | 1.55 (0.70 to 3.46) | 0.28 |
| Absent or reversed end diastolic flow | 5 (19.2) | 96 (16.0) | 1.21 (0.54 to 2.71) | 0.65 |
| Neonatal factors | ||||
| Male | 79 (23.4) | 22 (7.6) | 3.10 (1.98 to 4.84) | < 0.001 |
| Gestational age (weeks) | ||||
| 36 | 52 (19.2) | 49 (13.7) | Baseline | – |
| 35 | 19 (11.5) | 82 (17.7) | 0.60 (0.37 to 0.98) | 0.041 |
| 34 | 16 (14.8) | 85 (16.7) | 0.77 (0.46 to 1.29) | 0.32 |
| 33 | 9 (19.2) | 92 (15.8) | 1.00 (0.53 to 1.89) | 0.99 |
| 32 | 5 (13.5) | 96 (16.2) | 0.70 (0.30 to 1.65) | 0.42 |
| Multiple birth | 11 (10.3) | 90 (17.3) | 0.60 (0.33 to 1.07) | 0.085 |
| Birthweight | ||||
| > 10th percentile for gestation and sex | 87 (15.7) | 14 (19.4) | Baseline | – |
| > third and ≤ 10th percentile for gestation and sex | 8 (20.0) | 93 (15.8) | 1.28 (0.67 to 2.45) | 0.46 |
| ≤ third percentile for gestation and sex | 6 (18.8) | 95 (15.9) | 1.20 (0.57 to 2.53) | 0.64 |
| Fetal growth restrictiona | 25 (17.2) | 76 (15.7) | 1.10 (0.73 to 1.65) | 0.66 |
| APGAR score of < 5 at 5 minutes | 0 (0) | 101 (16.2) | – | – |
| Resuscitated at birth | 28 (24.8) | 73 (14.2) | 1.75 (1.19 to 2.57) | 0.005 |
| Any respiratory support receivedb | 18 (21.4) | 83 (15.3) | 1.40 (0.89 to 2.21) | 0.14 |
| Neonatal seizures | 0 (0) | 101 (16.1) | – | – |
| Intracranial abnormalityc | 1 (20.0) | 100 (16.1) | 1.25 (0.21 to 7.27) | 0.81 |
| Jaundice requiring phototherapy | 4 (8.3) | 97 (16.7) | 0.48 (0.19 to 1.26) | 0.14 |
| Antibiotics given | 39 (18.8) | 92 (15.9) | 1.18 (0.63 to 2.20) | 0.60 |
| Any breast milk at discharged | 48 (12.2) | 53 (22.9) | 0.53 (0.37 to 0.76) | 0.001 |
Given the correlation between these factors, multivariable analyses were conducted to identify independent predictors of neurodevelopmental disability in LMPT children. As shown in Table 32, eight factors emerged as risk factors. Being male, being resuscitated at birth, having a mother who had pre-pregnancy hypertension or pre-eclampsia or who used recreational drugs during pregnancy was associated with a 1.5- to 2.5-fold increased risk of disability. Socioeconomic deprivation was also independently associated with disability, with risk of disability increasing with increasing deprivation. In addition, having a mother who did not speak English and not having had breast milk at discharge were also associated with disability.
| Variable | RR (95% CI) | p-value |
|---|---|---|
| Male infant | 2.60 (1.66 to 4.06) | < 0.001 |
| Pre-pregnancy diagnosed hypertension | 2.42 (1.44 to 4.04) | 0.001 |
| SES Index | ||
| Medium risk | 2.25 (1.31 to 3.85) | 0.003 |
| High risk | 3.33 (2.00 to 5.57) | < 0.001 |
| Non-English-speaking | 1.87 (1.20 to 2.93) | 0.006 |
| Any breast milk at discharge | 0.63 (0.43 to 0.92) | 0.016 |
| Any respiratory support | 1.59 (1.03 to 2.46) | 0.035 |
| Pre-eclampsia | 2.16 (1.45 to 3.22) | < 0.001 |
| Recreational drugs used during pregnancy | 2.39 (1.48 to 3.84) | < 0.001 |
Discussion
These findings will aid in the identification of a subgroup of infants at high risk for disability following LMPT birth. It should be noted that these results are likely to reflect the association with cognitive outcomes, as 98% of LMPT children with disability were classified as such on the basis of a cognitive impairment. The association of these factors with neurodevelopmental disability is not unexpected given their well-documented association with both neonatal and long-term neurodevelopmental outcomes in both term-born and preterm children. These associations are also borne out in other studies in which resuscitation at birth, sociodemographic factors and pre-eclampsia, in particular, have been independently associated with long-term outcomes in this population. 175,199,200 Not receiving any breast milk at discharge, either expressed or by breastfeeding, was associated with disability at 2 years. The impact of breastfeeding on infant development has been widely reported, although the mechanisms for this association remain unclear in both term-born and preterm infants. 201,202
Promisingly, a number of these factors may be amenable to intervention. For example, improving access to community health-care services, supporting breastfeeding and providing developmental support for infants born into high socioeconomic risk may serve to improve cognitive and thus neurodevelopmental outcomes; this has been suggested by results for infants in the US IHDP, in which heavier babies, rather than those with very low birthweight, appeared to benefit most from intervention. 194,196,197 Education and intervention strategies to minimise recreational drug use during pregnancy or provide enhanced antenatal surveillance for these mothers may also be beneficial. The timing of delivery for mothers with pre-eclampsia may also impact on outcomes, and efforts to target optimal timing of delivery for these babies may help to reduce the prevalence of poor long-term outcomes. Future analyses are needed to explore the interaction of socioeconomic factors with outcome, in more detail, to attempt to identify those children at greatest risk. In particular, an exploration of potential interactions between the neonatal and obstetric variables examined may aid in identifying a high-risk subgroup of children born LMPT.
Behavioural outcomes
Behavioural outcomes were assessed using the BITSEA parent report questionnaire from which both continuous and categorical outcomes were derived for the presence of behaviour problems and delays in socioemotional competence. Analyses are presented unadjusted and after adjustment for age, sex and socioeconomic status (Table 33).
| Behavioural outcome | Term (n = 765) | LMPT (n = 638) | Unadjusted | Adjusteda | ||
|---|---|---|---|---|---|---|
| Scale scores | Mean (SD) | Mean (SD) | Mean difference (95% CI) | p-value | Mean difference (95% CI) | p-value |
| Problem score | 9.22 (6.52) | 9.81 (6.58) | 0.59 (–0.10 to 1.29) | 0.094 | 0.28 (–0.38 to 0.95) | 0.41 |
| Competence score | 17.20 (2.96) | 16.62 (3.40) | –0.58 (–0.91 to –0.25) | 0.001 | –0.44 (–0.77 to -0.12) | 0.008 |
| Problems or delays | n (%) | n (%) | RR (95% CI) | p-value | RR (95% CI) | p-value |
| Behaviour problems | 139 (18.3) | 132 (21.0) | 1.15 (0.93 to 1.42) | 0.20 | 1.07 (0.87 to 1.32) | 0.52 |
| Delayed competence | 142 (18.6) | 167 (26.5) | 1.42 (1.17 to 1.73) | < 0.001 | 1.36 (1.12 to 1.65) | 0.002 |
| Problems or delay | 231 (30.3) | 236 (37.2) | 1.23 (1.06 to 1.42) | 0.006 | 1.17 (1.01 to 1.35) | 0.032 |
| Parental concerns | n (%) | n (%) | RR (95% CI) | p-value | RR (95% CI) | p-value |
| Concerned about behaviour | 10 (1.3) | 9 (1.4) | 1.08 (0.44 to 2.64) | 0.868 | 0.92 (0.38 to 2.27) | 0.86 |
| Concerned about language | 18 (2.4) | 25 (3.9) | 1.66 (0.92 to 3.02) | 0.094 | 1.53 (0.85 to 2.76) | 0.158 |
Although there was a trend towards higher problem scores in LMPT children (p < 0.1), there was no statistically significant difference in the mean BITSEA problem scores. In contrast, LMPT children had significantly lower competence scores than term-born controls both before and after adjustment for confounders (adjusted mean difference –0.44, 95% CI –0.77 to –0.12; p = 0.008). When the BITSEA scores were compared with age- and sex-standardised norms, overall, LMPT children were significantly more likely to have a behaviour problem or delay, present in 37% of LMPT children, compared with 30% of controls (adjusted RR 1.17, 95% CI 1.01 to 1.35). However, although significantly more LMPT children had delays or deficits in socioemotional competence (adjusted RR 1.36, 1.12 to 1.65; p = 0.002), there was no excess of behavioural problems in this group. Despite the delays in socioemotional development observed among LMPT children, parents did not report more frequent concerns about their child’s behaviour or language development (see Table 33).
Discussion
The BITSEA problem scale assesses internalising difficulties, externalising problems, dysregulation, atypical behaviours and maladaptive behaviours. The results of this study indicate that children born LMPT were not at increased risk of these problems at 2 years of age. This was a somewhat unexpected finding. Very preterm birth (< 32 weeks) is associated with an increased risk of attention deficit/hyperactivity disorders, emotional disorders and autism spectrum disorders,173 the cluster of which has been termed the ‘preterm behavioural phenotype’. 203 These disorders are present in around 25% of very preterm children at school age and are considered to have a neurodevelopmental origin in this population. 203 Moreover, these problems are already evident on parent-reported behavioural screening questionnaires in the pre-school years. 204–208 If the constellation of behavioural outcomes associated with very preterm birth extends across birth at LMPT gestations, we would expect to find increased parent-reported behaviour problems at 2 years, albeit with less severity and lower prevalence. This finding may thus be indicative of a different behavioural profile among LMPT children from that among those born very preterm.
We did, however, find that LMPT children had delayed socioemotional development compared with term-born peers and that this was not accounted for by the higher socioeconomic risk status of families with LMPT children. The BITSEA competence scale assesses aspects of social relatedness that develop early in childhood, including compliance with adult expectations and requests, attention skills, mastery motivation, imitation and play and pro-social interactions. Delays in early socioemotional competence have been associated with later social, emotional and behaviour problems and disorders in both preterm and term-born children. 183,207,209 Thus, although it is reassuring that early behaviour problems were not evident at 2 years of age, the increase in poor socioemotional competence raises concerns about the risk for longer-term problems in this population. In particular, follow-up of this cohort is needed to determine whether these early findings are indicative of deficits in social and emotional competence and associated risk for long-term difficulties, or whether these represent early delays from which there may be developmental catch-up. In addition, it is well documented that parental mental health is associated with behavioural outcomes in their offspring and with family socioeconomic status and adversity. 210 The impact of parental mental health and other maternal obstetric and neonatal factors on LMPT children’s behavioural outcomes requires further investigation to determine whether or not services can be targeted to subgroups of children at greatest risk. If behavioural outcomes are socially mediated to a greater extent in LMPT children than those born very preterm, there may be potential for parenting interventions to improve outcomes in this population.
Conclusions
Key findings
-
Parents report that children born LMPT have poorer health than children born at term and are more likely to be prescribed inhalers. These findings are indicative of an increase in minor health conditions and respiratory symptoms rather than severe health, respiratory or neurological outcomes.
-
Children born LMPT have a six times higher risk of NSIs than children born at term. However, the absolute impact of these impairments is minimal compared with the increased risk of cognitive difficulties, which are present in 16% of children born LMPT.
-
Late and moderately preterm children are more likely to have delayed socioemotional development at 2 years of age. Although parents do not report concern about these early delays/deficits, these may be indicative of longer-term peer relationship difficulties and mental health problems.
-
The excess of socioemotional delays in the absence of behaviour problems may be indicative of a different behavioural profile following LMPT birth compared with children born very preterm.
-
The significant increase observed in adverse health, cognitive and socioemotional outcomes is not accounted for by the association of LMPT birth with higher socioeconomic risk.
-
Risk factors for poor neurodevelopmental disability in LMPT children include high socioeconomic risk, male sex, maternal hypertensive disease before or during pregnancy, antenatal recreational drug use and not feeding breast milk at discharge from hospital. These factors may be amenable to intervention for improving long-term outcomes in this population.
Strengths and limitations
Despite intensive efforts and resources directed at improving response rates to follow-up at 6, 12 and 24 months, this still remained at approximately 60%. Analysis showed that non-responders had higher socioeconomic and demographic risk than responders, and thus we may have underestimated the true prevalence of developmental problems in this study. Although the effect of selective dropout was similar in both groups, we intend to carry out multiple imputations to assess the impact of non-response bias on the prevalence of key adverse outcomes at 2Y-CA.
Given the size of the cohort, individual assessments were not possible at 2Y-CA and thus we opted to conduct follow-up using validated parent report measures. The utility of these for identifying children with poor longer-term outcomes requires investigation to determine the predictive validity of infant assessments in this population. The prospective nature of this study enabled us to collect important demographic, obstetric and neonatal information and thus we were able to adjust for the effects of socioeconomic deprivation on developmental outcomes at 2 years. Although multivariable analyses showed that NSI, cognitive impairment and delayed socioemotional competence were significantly increased after adjustment for our composite SES Index, there may be a significant interaction between preterm birth and socioeconomic factors. In particular, greater affluence and lower social risk may have a greater impact on outcomes in the LMPT population, potentially ‘protecting’ infants from the risks conferred by LMPT birth. As a priority, we intend to carry out further analyses to explore factors that mediate the relationship between LMPT birth and adverse developmental outcomes and the interaction of socioeconomic factors with the predictors of disability examined above. In addition, we intend to carry out further analyses to determine whether or not we can identify a subgroup of LMPT children at greatest risk of adverse outcomes in order to aid in decision-making around the time of birth and to help target follow-up and early intervention efforts.
Implications for practice
The results of the 2-year follow-up study may be used by obstetric practitioners in decision-making when considering the likely long-term outcomes of delivery of pregnancies at LMPT gestations. Information about developmental difficulties may also be used to counsel parents about the potential long-term outcomes for their child. This may aid in shared decision-making around delivery and also in raising awareness of the potential for long-term developmental problems, particularly in terms of cognitive and socioemotional development. Our patient and public involvement (PPI) work has identified that parents feel that community health-care workers lack specialist knowledge about the developmental and caregiving needs of babies born at LMPT gestations. Thus, the results of this study may be important in informing community paediatricians and health-care practitioners about outcomes for children born LMPT and for the need to carry out surveillance for developmental problems among these children.
The increased prevalence of cognitive and socioemotional difficulties at 2 years may warrant follow-up over the early years. Given the low prevalence of neurodevelopmental disorders and the size of the LMPT population, this may be best delivered by community health-care services rather than by neonatal services, as is currently the model of provision for children born very preterm. Low-cost alternatives to developmental assessments may be appropriate for this population, for which parent questionnaires may prove valuable. Enhanced antenatal surveillance for pregnant women at highest risk of pre-eclampsia and socioeconomic deprivation and ongoing developmental and educational support for mothers post discharge may also be beneficial for their infants who are born at LMPT gestations.
Future research
There is a need to assess the validity of the PARCA-R for predicting longer-term outcomes to determine its use as a clinical screening measure in children born LMPT. Longer-term follow-up of this cohort will be imperative to determine how early cognitive problems evolve over time and whether or not there is developmental plasticity in LMPT children. This will also enable an assessment of whether or not delays in early socioemotional development manifest as behavioural problems or peer relationship difficulties later in childhood.
Work to evaluate the efficacy of early parenting interventions for improving cognitive and socioemotional development in this population is needed. Given that we have identified an increase in problems in this group at 2 years, there is a need to develop, implement and evaluate potential follow-up schemes for families and children born LMPT that are feasible in such a large group of children. Detailed clinical studies are warranted to further explore and validate our findings relating to an observed excess of mild respiratory symptoms in this group of children. The impact of maternal mental health on behavioural outcomes in this population also requires exploration.
Costs of late and moderately preterm birth
Objectives
-
To determine the economic costs between birth and initial hospital discharge associated with LMPT birth.
-
To determine the economic costs between birth and 2 years associated with LMPT birth.
-
To determine how the economic costs associated with LMPT birth are distributed across sectors.
-
To identify how other factors, clinical and sociodemographic, constellate with LMPT birth in estimations of economic costs.
Methods
Measurement of resource use and costs
Relevant resource items were integrated into the perinatal and follow-up data collection instruments described previously. The neonatal and maternal data collection forms captured a comprehensive profile of resource use by each infant, encompassing length of stay by intensity of care, surgeries, investigations, procedures, drugs, consumables, transfers and post-mortem examinations until final hospital discharge or death (whichever was earliest). Resource inputs were valued using a combination of primary research, based on established accounting methods, and data collated from secondary national tariff sets. 211,212 All costs were expressed in pounds sterling and reflected values for the financial year 2010–11.
The total length of stay (total inpatient hospital days) was computed as the total number of hospital days until first discharge to home or death. This total incorporated any hospital stays following interhospital transfers that may have occurred. Postnatal costs for the mothers were based on the method of delivery and costs assigned using data from the NHS Reference Costs 2010–11. 212 Detailed information was available on the interventions and feeding received by infants in the NNU including number of days on oxygen, number of days on a ventilator, number of days of non-invasive respiratory support, number of days of PN and number of days of i.v. fluids. A clinician involved with the study (EMB) used this daily information on interventions and feeding to map the time spent in the NNU into days by level of neonatal care (special, high dependency or intensive). The cost of neonatal care was calculated for each infant by multiplying the length of stay in special care, high-dependency care or intensive care by the per diem cost of the corresponding level of care using data from the NHS Reference Costs 2010–11. 212 Non-routine investigations excluded from these per diem costs were identified by study clinicians and these were valued using a combination of primary and secondary costs. For situations in which these costs were not available from national tariffs, clinicians were asked to identify the staff and material inputs required for these investigations. Staff time was valued using the Unit Costs of Health and Social Care 2012. 211 The costs of surgeries were calculated by assignment of surgical procedures to relevant Healthcare Resource Group (HRG) codes and application of unit costs from national tariffs. 212 Transfers were recorded whenever an infant was transported from a general hospital to a specialist hospital for neonatal critical care, from a specialist centre to a general hospital, or from a specialist centre to a higher-level centre, and were valued using costs from the NHS Reference Costs 2010–11. 212 Post-mortem costs were based on data from secondary sources. 213 Table 34 contains for a list of resource values and their sources for the period from birth to initial hospital discharge.
| Resource use measures | Unit cost (£) | Source |
|---|---|---|
| Mode of delivery | ||
| Spontaneous vaginal | 1206 | NHS Reference Costs 2010–11 212 |
| Spontaneous vaginal and induction | 1594 | NHS Reference Costs 2010–11 212 |
| Forceps | 1624 | NHS Reference Costs 2010–11 212 |
| Forceps and induction | 2116 | NHS Reference Costs 2010–11 212 |
| Ventouse | 1624 | NHS Reference Costs 2010–11 212 |
| Ventouse and induction | 2116 | NHS Reference Costs 2010–11 212 |
| Ventouse and forceps | 1624 | NHS Reference Costs 2010–11 212 |
| Ventouse and forceps and induction | 2116 | NHS Reference Costs 2010–11 212 |
| Assisted breech | 2178 | NHS Reference Costs 2010–11 212 |
| Assisted breech and induction | 2783 | NHS Reference Costs 2010–11 212 |
| CS, during labour | 3236 | NHS Reference Costs 2010–11 212 |
| CS, not in labour | 2622 | NHS Reference Costs 2010–11 212 |
| Ventouse and forceps and CS | 3236 | NHS Reference Costs 2010–11 212 |
| Forceps and CS | 3236 | NHS Reference Costs 2010–11 212 |
| CS with eclampsia, pre-eclampsia or placenta praevia | 5253 | NHS Reference Costs 2010–11 212 |
| Home birth | 1067 | Birthplace in England Collaborative Group214 |
| Investigations | ||
| Cranial ultrasound scan | 53 | NHS Reference Costs 2010–11 212 |
| Electroencephalography | 93 | NHS Reference Costs 2010–11 212 |
| MRI | 98 | NHS Reference Costs 2010–11 212 |
| Chromosomal studies | 589 | NHS Reference Costs 2010–11 212 |
| Other investigations | Various | NHS Reference Costs 2010–11 212 |
| Surgery/operations, n (%) | Various procedures | NHS Reference Costs 2010–11 212 |
| Hospital transfer | ||
| To lower intensity | 255 | NHS Reference Costs 2010–11 212 |
| To higher intensity | 1028 | NHS Reference Costs 2010–11 212 |
| Post-mortem | 620 | Birthplace in England Collaborative Group214 |
| Neonatal care | ||
| Transitional care | 402 | NHS Reference Costs 2010–11 212 |
| Special care | 489 | NHS Reference Costs 2010–11 212 |
| High-dependency care | 823 | NHS Reference Costs 2010–11 212 |
| Intensive care | 1186 | NHS Reference Costs 2010–11 212 |
As part of the battery of research instruments completed at the follow-up points (6 months, 1 year and 2 years), the main parent was asked to complete detailed postal questionnaires about their child’s resource utilisation over the previous period. The 6-month questionnaire covered the child’s resource utilisation between initial hospital discharge and 6 months; the 1-year questionnaire covered the child’s resource utilisation between 6 and 12 months; and the 2-year questionnaire covered the child’s resource utilisation between their first and second birthdays. The questionnaires were piloted to ascertain their acceptability, ease of comprehension and reliability and reminder letters were sent to parents to increase the response and completion rates. The data collected from the main parent included their child’s use of hospital inpatient, day care and outpatient services, community health and social care services, and medicines and drugs, and also recorded adaptations to the home, provision of special equipment and parental lost productivity attributable to the child’s health status, over the relevant time horizons. Resource inputs were valued using a combination of primary research, based on established accounting methods, and data collated from secondary national tariff sets211,212 (GBP, 2011 prices).
The use of hospital-based services over the period between initial hospital discharge and 2 years included inpatient admissions, use of hospital day-care services, paediatric outpatient department appointments, other outpatient department appointments and visits to accident and emergency units. Inpatient admissions over this time horizon were delineated by type and duration of neonatal or paediatric care and valued using per diem costs extracted from the NHS Reference Costs 2010–11. 212 Use of other hospital-based care was valued by applying unit costs extracted from national tariffs. 211 The use of community-based care included routine appointments (immunisations, weight checks and developmental checks), general practitioner (GP) or practice nurse appointments, physiotherapy contacts, walk-in health-care centre visits and telephone calls to NHS Direct. Costs for these community-based services were calculated by applying unit costs from national tariffs211 to resource volumes. A list of all medications prescribed was extracted from the resource use questionnaires and items were identified for inclusion in the economic analysis. This list included musculoskeletal, central nervous system, gastrointestinal, infections, skin, eye, cardiovascular, respiratory, ear, nose, oropharynx and endocrine system drugs, as well as nutrition and blood vitamins, food additives and borderline substances. NHS net prices per milligram for these medications were obtained from the British National Formulary for Children (BNFC). 215 Costs for individual infants were estimated based on their reported doses and frequencies if these were available, or otherwise on an assumed daily dose based on BNFC215 recommendations. Drugs cost were delineated in terms of different child age groups when the recommended daily dosage obtained from the BNFC215 varied by age (i.e. < 6 months, 6–12 months, 12–24 months). In estimating these costs, we assumed an average weight of 4.3 kg for children at 1 month, 7.7 kg for children at 6 months and 11.8 kg for children at 24 months. 216 Other costs captured in the study included adaptations to the home, provision of special equipment and parental lost productivity. Adaptations to the child’s home as a result of the child’s health status encompassed changing plugs, redecoration, heating alterations, sanitation, change of flooring, house extensions and purchase of humidifiers and equipment to ensure child safety. Cost estimates for these adaptations were informed by information obtained from the international electronic commerce company Amazon (Amazon.com Inc., Seattle, WA, USA; UK version). Adaptations such as house extensions and redecorations were guided by estimated prices provided by private building companies. Special equipment and aids required by the LAMBS infants over the course of follow-up fell into the following broad categories: breathing support equipment, feeding/breastfeeding equipment, chairs/mattresses and room ventilation equipment. Unit costs for these items were informed by information obtained from the international electronic commerce company Amazon (UK version). The costs to parents of taking time off work to care for the infant(s) were estimated by applying gender-specific median earnings data217 to occupational classifications derived from the self-reported employment information. A list of resource values and their sources for the period between initial hospital discharge and 24 months is provided in Table 35. All costs occurring beyond the first year after birth were discounted using the UK recommended discount rate of 3.5%. 220
| Resource use measure | Unit cost (£) | Source |
|---|---|---|
| Hospital care | ||
| Inpatient admissions | Based on HRG code | NHS Reference Costs 2010–11 212 |
| Admission to day care | 133 | NHS Reference Costs 2010–11 212 |
| A&E visits | 117 | Unit Costs of Health and Social Care 2012 211 |
| Paediatric outpatient department visits | 131 | Unit Costs of Health and Social Care 2012 211 |
| Other outpatient department visits | 163 | Unit Costs of Health and Social Care 2012 211 |
| Community care | ||
| Routine 6-week check | 43 | NHS Reference Costs 2010–11 212 |
| Immunisations | 27 | NHS Reference Costs 2010–11 212 |
| Weight checks | 43 | NHS Reference Costs 2010–11 212 |
| Health visitor visits | 43 | NHS Reference Costs 2010–11 212 |
| Hearing/developmental checks | 43 | NHS Reference Costs 2010–11 212 |
| GP visits | 36 | Unit Costs of Health and Social Care 2012 211 |
| Practice nurse visits | 12 | Unit Costs of Health and Social Care 2012 211 |
| Community paediatrician visits | 131 | Unit Costs of Health and Social Care 2012 211 |
| Physiotherapy visits | 35 | Unit Costs of Health and Social Care 2012 211 |
| Community nurse visits | 50 | Unit Costs of Health and Social Care 2012 211 |
| Speech and language therapist visits | 34.5 | Unit Costs of Health and Social Care 2012 211 |
| Occupational therapist visits | 34.5 | Unit Costs of Health and Social Care 2012 211 |
| Walk-in centre contacts | 38 | NHS Reference Costs 2010–11 212 |
| Telephone calls to NHS Direct | 28 | NHS Direct: Operating Costs 218 |
| Any prescribed medications | Various | BNF for Children 2013–14;215 Prescription Cost Analysis – England, 2011219 |
| Other | ||
| Time off work | Based on derived occupational code | ONS 2011217 |
| Provided with special equipment | Various | Self-report, commercial prices |
| Adaptations to home | Various | Self-report, commercial prices |
Analysis of resource use and cost data
Maternal and neonatal characteristics and resource use items were summarised by gestational age at birth meta-group (moderate or late preterm vs. term). Differences between groups were analysed using t-tests for continuous variables and chi-squared test for categorical variables. Mean (SE) costs by cost category and mean (SE) total costs were estimated by gestational age at birth status for each meta-group. Total costs were estimated both from a NHS and Personal Social Services (PSS) perspective and from a broader societal perspective. Cost comparisons for moderate or late preterm versus term infants were carried out using Student’s t-tests. Differences in mean costs and their corresponding CIs were estimated for moderate or late preterm versus term infants. Non-parametric bootstrap220 estimates based on 1000 replications were also calculated for these differences in mean costs and their CIs.
Regression modelling was used to estimate the relationship between gestational age at birth and total costs. The models were estimated using both ordinary least squares (OLSs) and generalised linear models (GLMs). 221 For the GLMs, a gamma distribution and log-link function for costs was selected on the basis of its Akaike information criterion (AIC)222 statistic compared with alternative distributional forms (e.g. Gaussian, inverse Gaussian and Poisson distributional families) and link functions (e.g. identity link function). The modified Parks test223 was also used in an iterative manner to identify the preferred distributional family, and the last estimable model in the processes adopted was the GLM with gamma distribution and log-link. The first set of regression models were estimated with total NHS and PSS costs, from birth to initial hospital discharge (or death), representing the dependent variable in all analyses. Covariates considered in these regression analyses (referents in brackets) included gestational age birth status [(term), moderate or late preterm]; place of delivery [(centre A, centre B), other], mode of delivery [(spontaneous vaginal), assisted/instrumental, CS while in labour, CS not in labour]; baby status [(alive), stillbirth, early neonatal death, late neonatal death, infant death]; multiplicity [(singleton), multiple]; gender [(male) female]; SGA [> first decile, (≤ first decile of customised fetal weight224)]; congenital anomaly [yes, (no)]; first born [yes, (no)]; maternal age (continuous); maternal BMI [(normal), underweight, overweight, obese]; maternal ethnicity [(white), mixed, Asian or Asian British, black or black British, Chinese or other]; mother’s highest educational qualification [(higher degree), degree, A levels vocational level 3 and equivalent, GCSE grades A*–C vocational level 2 and equivalent, GCSE grades D–G vocational level 1 and below, qualification level unknown, no qualifications]; marital civil status [(living as part of a couple), not living as part of a couple]; social class based on the mother’s occupational status [(managerial and professional), intermediate, routine and manual, never worked and long-term unemployed, looking after family]; home ownership [(owner-occupied), renting, living rent free]; pre-pregnancy maternal European Quality of Life-5 Dimensions (EQ-5D)184 utility score; maternal chronic health problems [(no), yes]; socioeconomic deprivation [a composite indicator of socioeconomic deprivation for each postcode sector was derived using the 2010 IMD, which uses census-derived indicators of income, education, employment, environment, health and housing at small-area level]225 [(first quintile), second quintile, third quintile, fourth quintile, fifth quintile]; maternal recreational drug use during pregnancy [(no), yes]; maternal smoking during pregnancy [(no), yes]; previous premature birth [(no), yes]; and maternal drinking during pregnancy [(no), yes]. Table 36 contains a list of independent variables used in the regression models.
| Variable | Categories for categorical variables, referent in brackets |
|---|---|
| Gestational age status | (Term), late and moderately preterm |
| Place of delivery | Neonatal service A, neonatal service B, other |
| Mode of delivery | (Spontaneous vaginal), assisted/instrumental, CS during labour, CS not in labour |
| Baby status | (Alive), stillbirth, early neonatal death, late neonatal death, infant death |
| Multiplicity | (Singleton), multiple |
| Gender | (Male), female |
| SGA | (No), yes |
| Congenital anomaly | (No), yes |
| First born | (No), yes |
| Maternal age | |
| Maternal BMI | (Normal), underweight, overweight, obese |
| Maternal ethnicity | (White), mixed, Asian or Asian British, black or black British, Chinese or other, not known |
| Highest qualification | (Higher degree), degree, A Levels, vocational level 3 and equivalent, GCSE grades A*–C, vocational level 2 and equivalent, GCSE grades D–G, vocational level 1 and below, qualification level unknown, no qualifications, not known |
| Marital civil status | (Living as part of a couple), not living as part of a couple |
| Socioeconomic classification | (Managerial and professional occupations), intermediate occupations, routine and manual occupations, never worked and long-term unemployed, looking after family, not known |
| Home ownership | (Own), rent, lives rent free |
| EQ-5D utility score | |
| Chronic health problems | (No), yes |
| Deprivation score | (First quintile), second quintile, third quintile, fourth quintile, fifth quintile |
| Recreational drugs during pregnancy | (No), yes |
| Smoke during pregnancy | (No), yes |
| Previous premature baby | (No), yes |
| Drink during pregnancy | (No), yes |
The first model (model 1) explored the impact of infant and birth characteristics on economic costs; the second model (model 2) included additional maternal sociodemographic and maternal lifestyle characteristics; and the third model (model 3) built on model 2 and included two additional variables (previous premature birth and maternal drinking during pregnancy) for which there was a high proportion (60.1%) of missing data.
A second set of regression models was also estimated with total societal costs, from birth to 24 months (or death), representing the dependent variable in the analyses. The first of these models (model 4) contained all of the covariates included in model 1 except for the baby status variable and the second model (model 5) included all of the covariates included in model 2 except for baby status and maternal BMI. These covariates were excluded from the analyses as they precluded estimation of GLMs and we wanted to present results for comparable models using alternative estimators. As per the birth to initial hospital discharge analyses, the models were estimated using both OLSs and GLMs. 221 Two sets of analyses were conducted: the first used cases in which there were cost data available at all time points (complete cases), and the second used the inverse probability weighting method226,227 (using the same set of covariates in model 5) to adjust for the presence of censored data.
All estimates were additionally recalculated following weighting of the random sample of term births to adjust for the oversampling of term multiple births. All analyses were estimated using Stata version 11.
Results
Descriptive statistics
The maternal and infant characteristics of the study population are presented in Table 37. Of 1376 eligible infants born at 32–36 weeks’ gestation in the East Midlands region over the study time frame, 1146 (83%) were recruited; 1258 infants born at ≥ 37 weeks’ gestation (79% of all eligible) acted as controls. The corresponding number of mothers who gave birth to these infants was 1041 for the LMPT group and 1120 for the term group.
| Variable | Late and moderate preterm, 32–36 weeks | Term, ≥ 37 weeks | Term, ≥ 37 weeks reweighteda | p-valueb |
|---|---|---|---|---|
| Number of mothers | 1041 | 1120 | 1120 | – |
| Maternal age (years), mean (SD) | 29.33 (5.85) | 29.79 (5.96) | 29.53 (5.87) | 0.031 |
| BMI, n (%) | ||||
| Normal | 546 (52.45) | 534 (47.68%) | (49.82%) | 0.014 |
| Underweight | 49 (4.71) | 40 (3.57) | (3.81) | |
| Overweight | 262 (25.17) | 290 (25.89) | (26.45) | |
| Obese | 143 (13.74) | 212 (18.93) | (19.92) | |
| Not known | 41 (3.94) | 44 (3.93) | (3.93) | |
| Ethnicity, n (%) | ||||
| White | 752 (72.24) | 863 (77.05) | (77.17) | 0.013 |
| Mixed | 33 (3.17) | 25 (2.23) | (2.24) | |
| Asian or Asian British | 186 (17.87) | 159 (14.20) | (14.45) | |
| Black or black British | 54 (5.19) | 60 (5.36) | (4.93) | |
| Chinese or other ethnic group | 11 (1.06) | 9 (0.80) | (0.82) | |
| Not known | 5 (0.48) | 4 (0.36) | (0.41) | |
| Marital/civil status, n (%) | ||||
| Living as part of a couple | 856 (82.23) | 976 (87.14) | (86.60) | 0.12 |
| Single | 184 (17.68) | 141 (12.59) | (13.28) | |
| Not known | 1 (0.10) | 3 (0.27) | (0.12) | |
| Age (years) completed education, mean (SD) | 18.43 (2.97) | 18.74 (3.08) | 18.65 (3.00) | 0.003 |
| Not known, n (%) | 6 (0.58) | 7 (0.63) | – | – |
| Highest educational qualification, n (%) | ||||
| Higher degree | 95 (9.13) | 134 (11.96) | (10.88) | 0.001 |
| Degree | 173 (16.62) | 245 (21.88) | (21.24) | |
| A level | 209 (20.08) | 212 (18.93) | (19.04) | |
| GCSE grades A*–C | 252 (24.21) | 253 (22.59) | (23.37) | |
| GCSE grades D–G | 111 (10.66) | 88 (7.86) | (8.42) | |
| Qualification level unknown | 82 (7.88) | 88 (7.86) | (7.93) | |
| No qualifications | 94 (9.03) | 75 (6.70) | (6.72) | |
| Not known | 25 (2.40) | 25 (2.23) | (2.43) | |
| Occupational status during pregnancy, n (%) | ||||
| Employed | 609 (58.50) | 738 (65.89) | (65.23) | < 0.001 |
| Unemployed | 123 (11.82) | 84 (7.50) | (8.10) | |
| Caring for family | 263 (25.26) | 252 (22.50) | (22.32) | |
| Full-time student | 31 (2.98) | 33 (2.95) | (3.04) | |
| Long-term sick or disabled | 11 (1.06) | 7 (0.63) | (0.71) | |
| Not known | 4 (0.38) | 6 (0.54) | (0.60) | |
| IMD deprivation score, n (%) | ||||
| First quintile | 179 (17.20) | 255 (22.77) | (22.25) | < 0.001 |
| Second quintile | 196 (18.83) | 237 (21.16) | (21.09) | |
| Third quintile | 219 (21.04) | 211 (18.84) | (18.37) | |
| Fourth quintile | 232 (22.29) | 205 (18.30) | (18.98) | |
| Fifth quintile | 215 (20.65) | 212 (18.93) | (19.32) | |
| NS-SEC, n (%) | ||||
| Managerial and professional occupations | 262 (25.17) | 341 (30.45) | (29.23) | 0.001 |
| Intermediate occupations | 177 (17.00) | 202 (18.04) | (18.68) | |
| Routine and manual occupations | 168 (16.14) | 193 (17.23) | (17.11) | |
| Never worked and long-term unemployed | 165 (15.85) | 124 (11.07) | (11.85) | |
| Looking after family | 263 (25.26) | 252 (22.50) | (22.32) | |
| Not known | 6 (0.58) | 8 (0.71) | (0.80) | |
| Home ownership, n (%) | ||||
| Own | 464 (44.57) | 561 (50.09) | (48.87) | 0.001 |
| Rent | 514 (49.38) | 493 (44.02) | (44.94) | |
| Lives rent free | 60 (5.76) | 66 (5.89) | (6.19) | |
| Not known | 3 (0.29) | 0 (0) | 0 (0) | |
| EQ-5D-3L utility score, mean (SD) | 0.94 (0.14) | 0.96 (0.13) | 0.96 (0.13) | 0.001 |
| Chronic health problems, n (%) | ||||
| No | 783 (75.22) | 900 (80.36) | (80.63) | < 0.001 |
| Yes | 255 (24.50) | 219 (19.55) | (19.26) | |
| Not known | 3 (0.29) | 1 (0.09) | (0.11) | |
| Previous preterm baby, n (%) | ||||
| No | 433 (41.59) | 632 (56.43) | (56.04) | < 0.001 |
| Yes | 192 (18.44) | 59 (5.27) | (5.58) | |
| Not known | 416 (39.96) | 429 (38.30) | (38.39) | |
| Recreational drugs during pregnancy, n (%) | ||||
| No | 1017 (97.69) | 1106 (98.75) | (98.67) | 0.002 |
| Yes | 23 (2.21) | 12 (1.07) | (1.21) | |
| Not known | 1 (0.10) | 2 (0.18) | (0.11) | |
| Smoking during pregnancy, n (%) | ||||
| No | 753 (72.33) | 893 (79.73) | (79.26) | 0.14 |
| Yes | 282 (27.09) | 227 (20.27) | (20.74) | |
| Not known | 6 (0.58) | |||
| Drinks alcohol during pregnancy, n (%) | ||||
| Drinks more than 5 units per day | 408 (39.19) | 475 (42.41) | (42.61) | 0.062 |
| Never | 363 (34.87) | 431 (38.48) | (38.54) | |
| Less than once per month | 26 (2.50) | 24 (2.14) | (2.33) | |
| 1–2 days per month | 10 (0.96) | 5 (0.45) | (0.51) | |
| 1–2 days per week | 4 (0.38) | 6 (0.54) | (0.51) | |
| 3–4 days per week | – | 1 (0.09) | (0.01) (0.20) | |
| 5 or more days per week | 1 (0.10) | 2 (0.18) | (0.51) | |
| Not known | 4 (0.38) | 6 (0.54) | – | |
| Number of infants | 1146 | 1258 | – | – |
| Gestational age in completed weeks, median (range) | 35 (32–36) | 39 (37–43) | – | – |
| Mean (SD) | 34.93 (1.22) | 39.18 (1.40) | 39.59 (1.24) | – |
| Birthweight (g), median (range) | 2420 (820–4960) | 3280 (520–5160) | – | – |
| Mean (SD) | 2415.99 (506.24) | 3275.02 (557.18) | 3418.01 (502.47) | < 0.001 |
| Missing, n (%) | 1 (0.1) | – | – | – |
| Below 10th birth weight percentile at birth, n (%) | 144 (12.6) | 115 (9.1) | (6.9) | 0.003 |
| Below 10th fetal weight percentile at birth, n (%) | 305 (26.6) | 281 (22.3) | (15.8) | 0.006 |
| Male sex, n (%) | 621 (54.2) | 651 (51.8) | (51.3) | 0.002 |
| Baby status, n (%) | ||||
| Alive | 1123 (98.0) | 1253 (99.6) | (99.6) | 0.002 |
| Stillbirth | 16 (1.4) | 3 (0.2) | (0.2) | |
| Early neonatal deaths (within first 7 days) | 3 (0.3) | 1 (0.1) | (0.1) | |
| Late neonatal death (8–28 days of life) | 1 (0.1) | – | – | |
| Infant death (≥ 29 days of life) | 3 (0.3) | 1 (0.1) | (0.1) | |
| Multiplicity, n (%) | ||||
| Singleton | 938 (81.9) | 982 (78.1) | (98.2) | 0.027 |
| Twins | 196 (17.1) | 276 (21.9) | (1.8) | |
| Triplets | 12 (1.1) | – | – | |
| Congenital anomaly, n (%) | 22 (1.9) | 9 (0.7) | (0.7) | 0.002 |
| First born, n (%) | 544 (47.5) | 564 (44.8) | (44.6) | 0.002 |
Comparisons of demographic characteristics of the mothers by birth status (LMPT vs. term) revealed that there were significant differences in all characteristics with the exception of maternal age, ethnicity, maternal recreational drug use during pregnancy and maternal drinking during pregnancy. The characteristics of the infants are presented by gestational age status (moderately or late preterm vs. term). The mean gestational age at birth for the combined LMPT group and for the term group was 34.9 (SD 1.2) weeks and 39.59 (SD 1.2) weeks, respectively. The proportion of singletons was 82 for the combined LMPT group and 98 for the term group. Two per cent of the LMPT infants had a congenital anomaly compared with one for the term group. There were significant differences in the characteristics of the infants by gestational age at birth status (LMPT or term) across all variables with the exception of gender and whether or not the infant was first born.
Resource use
Resource use measures and their values between birth and initial hospital discharge are summarised in Table 38 for the comparator groups. The mean duration of the initial hospitalisation was 2.64 (SD 2.40) days for term-born infants, whereas the LMPT infants had a substantially longer mean stay of 9.15 (SD 17.8) days (p < 0.001). LMPT infants also spent longer in the NNU on average, with a mean length of stay of 4.45 (SD 8.79) days, compared with 0.24 (SD 1.68) days for the term-born infants (p < 0.001). The LMPT infants also had higher rates of resource use across all other resource categories compared with term-born infants (see Table 35).
| Variable | Late and moderate preterm, 32–36 weeks | Term, ≥ 37 weeks | Term, ≥ 37 weeks reweighteda | p-valueb |
|---|---|---|---|---|
| Number of infants | 1146 | 1258 | ||
| Mode of delivery, n (%) | ||||
| Spontaneous vaginal | 607 (53.0) | 702 (55.8) | (62.5) | 0.006 |
| Assisted/instrumental | 101 (8.8) | 213 (16.9) | (16.8) | |
| CS labour | 158 (13.8) | 129 (10.3) | (9.2) | |
| CS not in labour | 279 (24.4) | 214 (17.0) | (11.5) | |
| Not known | 1 (0.1) | |||
| Place of delivery, n (%) | < 0.001 | |||
| Centre A | 674 (58.8) | 661 (52.5) | (52.4) | |
| Centre B | 459 (40.1) | 570 (45.3) | (45.0) | |
| Other | 13 (1.1) | 27 (2.2) | (2.5) | |
| Any active resuscitation at birth, n (%) | 211 (18.4) | 104 (8.3) | (7.5) | < 0.001 |
| NNU admission, n (%) | 494 (43.1) | 67 (5.3) | (4.5) | < 0.001 |
| Length of neonatal stay (days), median (range) | 0 (0–101) | 0 (0–26) | – | – |
| Length of neonatal stay (days), mean (SD) | 4.45 (8.79) | 0.27 (1.84) | 0.24 (1.68) | < 0.001 |
| Maximum respiratory support required, n (%) | ||||
| Mechanical ventilation | 120 (10.5) | 13 (1.0) | (1.1) | < 0.001 |
| Non-invasive respiratory support | 100 (8.7) | 6 (0.5) | (0.4) | < 0.001 |
| Nasal cannula oxygen | 101 (8.8) | 16 (1.3) | (1.4) | < 0.001 |
| No respiratory support | 942 (82.2) | 1234 (98.1) | (98.0) | < 0.001 |
| PN, n (%) | 64 (5.6) | 7 (0.6) | (0.6) | < 0.001 |
| i.v. fluids, n (%) | 332 (29.0) | 36 (2.9) | (2.6) | < 0.001 |
| Length of hospital stay (days), median (range) | 5 (0–369) | 2 (1 –33) | – | – |
| Mean (SD) | 9.15 (17.80) | 2.97 (2.48) | 2.64 (2.40) | < 0.001 |
| Surgery/operations, n (%) | 18 (1.6) | 1 (0.1) | (0.1) | < 0.001 |
| Hospital transfer, n (%) | ||||
| None | 1099 (95.9) | 1257 (99.9) | (99.9) | 0.13 |
| To lower intensity | 34 (3.0) | 1 (0.1) | (0.0) | |
| To higher intensity | 13 (1.1) | – | – | |
| Post-mortem, n (%) | 10 (0.9) | 3 (0.2) | (0.3) | < 0.001 |
| Other investigations, n (%) | 139 (12.1) | 45 (3.6) | (2.8) | < 0.001 |
| Number of investigations, n (%) | ||||
| One | 93 (8.1) | 29 (2.3) | (2.3) | < 0.001 |
| Two | 25 (2.2) | 6 (0.5) | (0.3) | |
| Three or more | 21 (1.8) | 10 (0.8) | (0.9) | |
| Transitional care received, n (%) | 270 (23.6) | 16 (1.3) | (0.3) | 0.003 |
| Length of transitional care stay (days), median (range) | 0 (0 to 21) | 0 (0 to 10) | – | < 0.001 |
| Length of transitional care stay (days), mean (SD) | 1.44 (3.05) | 0.06 (0.58) | 0.02 (0.32) | |
| Special care received, n (%) | 679 (59.3) | 80 (6.4) | (4.6) | < 0.001 |
| Length of special care stay (days), median (range) | 0 (0 to 45) | 0 (0 to 26) | – | < 0.001 |
| Length of special care stay (days), mean (SD) | 3.91 (6.82) | 0.24 (1.69) | 0.20 (1.45) | |
| High-dependency care received, n (%) | 117 (10.2) | 5 (0.4) | (0.4) | < 0.001 |
| Length of high-dependency care stay (days), median (range) | 0 (0 to 307) | 0 (0 to 7) | – | < 0.001 |
| Length of high-dependency care stay (days), mean (SD) | 0.68 (9.40) | 0.01 (0.25) | 0.02 (0.28) | |
| Intensive care received, n (%) | 108 (9.4) | 11 (0.9) | (1.0) | < 0.001 |
| Length of intensive care stay (days), median (range) | 0 (0 to 32) | 0 (0 to 4) | – | < 0.001 |
| Length of intensive care stay (days), mean (SD) | 0.34 (1.92) | 0.02 (0.23) | 0.02 (0.26) | |
Resource use measures and their values between initial hospital discharge and 24 months are presented in Table 39 for the comparator groups. For the period between initial hospital discharge and 6 months, the proportion of infants using hospital-based services was significantly higher for LMPT infants than for term-born infants for all categories of hospital services (p < 0.05). The proportion of infants accessing community-based care services was significantly higher for LMPT infants for all categories of community services except GP visits. The proportion of parents taking time off work to care for their child and the proportion of infants provided with special equipment was significantly higher in the LMPT group.
| Variable | Late and moderate preterm, 32–36 weeks | Term, ≥ 37 weeks | Term, ≥ 37 weeks reweighteda | p-valueb |
|---|---|---|---|---|
| Post discharge to 6 months | ||||
| Number of infants | 781 | 939 | ||
| Hospital care | ||||
| Inpatient admissions, n (%) | 230 (29.45) | 162 (17.25) | (16.46) | < 0.001 |
| Number of admissions, mean (SE) | 0.27 (0.02) | 0.16 (0.01) | 0.15 (0.01) | < 0.001 |
| Cumulative inpatient length of stay, mean (SE) | 0.74 (0.10) | 0.35 (0.10) | 0.34 (0.11) | < 0.001 |
| Cumulative inpatient length of stay, median (IQR) | 0.00 (0.00) | 0.00 (0.00) | – | – |
| Admission to day care, n (%) | 186 (23.88) | 121 (13.00) | (12.08) | < 0.001 |
| Number of admissions, mean (SE) | 0.25 (0.02) | 0.13 (0.01) | 0.12 (0.01) | < 0.001 |
| A&E visits, n (%) | 199 (25.61) | 176 (18.90) | (18.01) | < 0.001 |
| Mean visits (SE) | 0.26 (0.02) | 0.18 (0.01) | 0.17 (0.01) | < 0.001 |
| Other outpatient department visits, n (%) | 251 (32.35) | 189 (20.28) | (19.74) | < 0.001 |
| Mean visits (SE) | 0.52 (0.04) | 0.27 (0.02) | 0.27 (0.02) | < 0.001 |
| Community care | ||||
| Routine 6-week check, n (%) | 754 (96.92) | 914 (97.86) | (98.32) | 0.004 |
| Immunisations, n (%) | 767 (98.46) | 925 (99.04) | (99.05) | < 0.001 |
| Immunisations, n, mean (SE) | 2.21 (0.03) | 2.35 (0.03) | 2.33 (0.03) | 0.001 |
| Weight checks, n (%) | 736 (94.60) | 880 (94.12) | (94.35) | 0.017 |
| Weight checks, n, mean (SE) | 5.55 (0.15) | 4.91 (0.12) | 4.83 (0.11) | < 0.001 |
| Health visitor visits, n (%) | 733 (94.22) | 854 (91.43) | (91.10) | < 0.001 |
| Health visitor, mean visits (SE) | 3.75 (0.12) | 3.10 (0.08) | 3.02 (0.08) | < 0.001 |
| GP visits, n (%) | 549 (70.38) | 651(69.70) | (71.00) | 0.089 |
| GP, mean visits (SE) | 1.47 (0.07) | 1.35 (0.05) | 1.32 (0.05) | 0.001 |
| Community paediatrician visits, n (%) | 44 (5.67) | 29 (3.12) | (3.05) | < 0.001 |
| Community paediatrician, mean visits (SE) | 0.08 (0.01) | 0.04 (0.01) | 0.05 (0.01) | < 0.001 |
| Physiotherapy visits, n (%) | 22 (2.83) | 16 (1.72) | (1.29) | 0.004 |
| Physiotherapy, mean visits (SE) | 0.04 (0.01) | 0.03 (0.01) | 0.02 (0.01) | 0.001 |
| Community nurse visits, n (%) | 34 (4.38) | 31 (3.33) | (3.06) | 0.001 |
| Community nurse, mean visits (SE) | 0.12 (0.03) | 0.05 (0.01) | 0.05 (0.01) | < 0.001 |
| Walk-in centre contacts, n (%) | 119 (15.32) | 135 (14.50) | (15.00) | 0.049 |
| Walk-in centre, mean contacts (SE) | 0.19 (0.02) | 0.14 (0.01) | 0.15 (0.01) | 0.001 |
| Telephone calls to NHS Direct, n (%) | 207 (26.68) | 217 (23.31) | (23.43) | < 0.001 |
| Telephone calls to NHS Direct, mean (SE) | 0.31 (0.02) | 0.25 (0.02) | 0.26 (0.02) | < 0.001 |
| Any prescribed medications, n (%) | 411 (52.69) | 467 (49.73) | (50.86) | 0.012 |
| Time off work, n (%) | 98 (12.55) | 55 (5.86) | (5.13) | < 0.001 |
| Days off work, mean (SE) | 1.99 (1.02) | 0.19 (0.04) | 0.19 (0.04) | < 0.001 |
| Days off work, median (IQR) | 0.00 (0.00) | 0.00 (0.00) | – | – |
| Provided with special equipment, n (%) | 45 (5.76) | 19 (2.02) | (2.29) | < 0.001 |
| Adaptations to home, n (%) | 6 (0.77) | 9 (0.96) | (0.95) | < 0.001 |
| 6–12 months | ||||
| Number of infants | 703 | 856 | ||
| Hospital care | ||||
| Inpatient admissions, n (%) | 92 (13.09) | 89 (10.43) | (11.35) | 0.38 |
| Inpatient admissions, number of admissions, mean (SE) | 0.11 (0.01) | 0.08 (0.01) | 0.09 (0.01) | 0.005 |
| Cumulative inpatient length of stay, mean (SE) | 0.38 (0.20) | 0.11 (0.02) | 0.13 (0.03) | < 0.001 |
| Cumulative inpatient length of stay, median (IQR) | 0.00 (0.00) | 0.00 (0.00) | – | – |
| Admission to day care, n (%) | 74 (10.53) | 61 (7.13) | (7.53) | 0.002 |
| Admission to day care, number of admissions, mean (SE) | 0.24 (0.03) | 0.18 (0.02) | 0.20 (0.02) | 0.004 |
| A&E visits, n (%) | 152 (21.62) | 155 (18.11) | (20.28) | 0.056 |
| A&E, mean visits (SE) | 0.49 (0.04) | 0.42 (0.03) | 0.47 (0.03) | 0.18 |
| Other outpatient department visits, n (%) | 160 (22.76) | 139 (16.24) | (15.88) | < 0.001 |
| Other outpatient department, mean visits (SE) | 0.55 (0.04) | 0.43 (0.04) | 0.44 (0.04) | < 0.001 |
| Community care | ||||
| Immunisations, n (%) | 622 (88.48) | 710 (82.94) | (85.00) | 0.006 |
| Immunisations, mean (SE) | 2.05 (0.05) | 2.06 (0.04) | 2.12 (0.04) | 0.019 |
| Weight checks, n (%) | 599 (85.21) | 722 (84.35) | (84.43) | < 0.001 |
| Weight checks, mean (SE) | 2.64 (0.09) | 2.80 (0.08) | 2.84 (0.09) | 0.001 |
| Health visitor visits, n (%) | 512 (72.83) | 603 (70.44) | (70.38) | < 0.001 |
| Health visitor, mean visits (SE) | 1.97 (0.07) | 1.93 (0.06) | 1.96 (0.06) | 0.51 |
| Hearing/developmental checks, n (%) | 405 (57.61) | 475 (55.49) | (55.83) | < 0.001 |
| Hearing/developmental checks, mean (SE) | 1.31 (0.05) | 1.35 (0.05) | 1.37 (0.05) | < 0.001 |
| GP visits, n (%) | 523 (74.40) | 612 (71.50) | (71.97) | < 0.001 |
| GP visits, mean visits (SE) | 2.04 (0.07) | 1.98 (0.06) | 2.00 (0.06) | 0.008 |
| Community paediatrician visits, n (%) | 51 (7.25) | 32 (3.74) | (4.26) | 0.001 |
| Community paediatrician, mean visits (SE) | 0.17 (0.03) | 0.11 (0.02) | 0.12 (0.02) | 0.002 |
| Physiotherapy visits, n (%) | 19 (2.70) | 10 (1.17) | (1.05) | < 0.001 |
| Physiotherapy, mean visits (SE) | 0.09 (0.03) | 0.04 (0.02) | 0.04 (0.02) | < 0.001 |
| Community nurse visits, n (%) | 27 (3.84) | 22 (2.57) | (2.25) | 0.002 |
| Community nurse, mean visits (SE) | 0.10 (0.02) | 0.07 (0.02) | 0.06 (0.02) | 0.001 |
| Walk-in centre contacts, n (%) | 124 (17.64) | 147 (17.17) | (17.87) | 0.15 |
| Walk-in centre, mean contacts (SE) | 0.42 (0.04) | 0.40 (0.03) | 0.43 (0.03) | 0.08 |
| Telephone calls to NHS Direct, n (%) | 195 (27.74) | 233 (27.22) | (28.07) | 0.11 |
| Telephone calls to NHS Direct, mean (SE) | 0.65 (0.04) | 0.64 (0.04) | 0.67 (0.04) | 0.036 |
| Any prescribed medications, n (%) | 330 (46.94) | 405 (47.31) | (47.95) | 0.009 |
| Time off work, n (%) | 163 (23.19) | 179 (20.91) | (20.75) | < 0.001 |
| Days off work, mean (SE) | 1.15 (0.27) | 0.89 (0.14) | 0.91 (0.15) | < 0.001 |
| Days off work, median (IQR) | 0.00 (0.00) | 0.00 (0.00) | – | – |
| Provided with special equipment, n (%) | 26 (3.70) | 14 (1.64) | (1.77) | < 0.001 |
| Adaptations to home, n (%) | 3 (0.43) | 9 (1.05) | (1.03) | < 0.001 |
| 12–24 months | ||||
| Number of infants | 651 | 771 | ||
| Hospital care | ||||
| Inpatient admissions, n (%) | 88 (13.52) | 66 (8.56) | (8.39) | |
| Number of admissions, mean (SE) | 0.16 (0.02) | 0.10 (0.01) | 0.10 (0.01) | < 0.001 |
| Cumulative inpatient length of stay, mean (SE) | 0.89 (0.56) | 0.25 (0.07) | 0.28 (0.08) | < 0.001 |
| Cumulative inpatient length of stay, median (IQR) | 0.00 (0.00) | 0.00 (0.00) | – | < 0.001 |
| Paediatric outpatient department visits, n (%) | 123 (18.89) | 102 (13.23) | (14.38) | – |
| Paediatric outpatient department, mean visits (SE) | 0.20 (0.02) | 0.14 (0.01) | 0.15 (0.01) | < 0.001 |
| A&E visits, n (%) | 184 (28.26) | 169 (21.92) | (22.38) | 0.001 |
| A&E, mean visits (SE) | 0.29 (0.02) | 0.22 (0.02) | 0.23 (0.02) | < 0.001 |
| Other outpatient department visits, n (%) | 124 (19.05) | 90 (11.67) | (12.36) | < 0.001 |
| Other outpatient department, mean visits (SE) | 0.20 (0.02) | 0.12 (0.01) | 0.13 (0.01) | < 0.001 |
| Community care | ||||
| GP visits, n (%) | 524 (80.49) | 582 (75.49) | (75.76) | < 0.001 |
| GP, mean visits (SE) | 0.95 (0.03) | 0.87 (0.02) | 0.86 (0.02) | < 0.001 |
| Practice nurse visits, n (%) | 128 (19.66) | 161 (20.88) | (20.51) | 0.004 |
| Practice nurse, mean visits (SE) | 0.20 (0.02) | 0.21 (0.02) | 0.21 (0.02) | 0.001 |
| Community paediatrician visits, n (%) | 23 (3.53) | 19 (2.46) | (2.28) | < 0.001 |
| Community paediatrician, mean visits (SE) | 0.04 (0.01) | 0.03 (0.01) | 0.03 (0.01) | < 0.001 |
| Physiotherapy visits, n (%) | 23 (3.53) | 13 (1.69) | (1.76) | < 0.001 |
| Physiotherapy, mean visits (SE) | 0.06 (0.02) | 0.03 (0.01) | 0.03 (0.01) | < 0.001 |
| Speech and language therapist visits, n (%) | 41 (6.30) | 13 (1.69) | (1.46) | < 0.001 |
| Speech and language therapist, mean visits (SE) | 0.09 (0.02) | 0.02 (0.00) | 0.02 (0.00) | < 0.001 |
| Occupational therapist visits, n (%) | 8.00 (1.23) | 4.00 (0.52) | (0.63) | 0.002 |
| Occupational therapist, mean visits (SE) | 0.03 (0.01) | 0.01 (0.01) | 0.01 (0.01) | 0.001 |
| Community nurse visits, n (%) | 14.00 (2.15) | 22.00 (2.85) | (2.91) | < 0.001 |
| Community nurse, mean visits (SE) | 0.03 (0.01) | 0.03 (0.01) | 0.03 (0.01) | 0.010 |
| Walk-in centre contacts, n (%) | 170 (26.11) | 179 (23.22) | (24.27) | 0.007 |
| Walk-in centre, mean contacts (SE) | 0.27 (0.02) | 0.23 (0.02) | 0.24 (0.02) | 0.005 |
| Telephone calls to NHS Direct, n (%) | 204 (31.34) | 190 (24.64) | (24.82) | < 0.001 |
| Telephone calls to NHS Direct, mean (SE) | 0.32 (0.02) | 0.25 (0.02) | 0.26 (0.02) | < 0.001 |
| Other services, n (%) | 44 (6.76) | 25 (3.24) | (3.37) | < 0.001 |
| Other services, mean (SE) | 0.08 (0.01) | 0.06 (0.02) | 0.06 (0.02) | 0.001 |
| Any prescribed medications, n (%) | 359 (55.15) | 436 (56.55) | (56.91) | < 0.001 |
| Time off work, n (%) | 183 (28.11) | 200 (25.94) | (23.88) | 0.006 |
| Days off work, mean (SE) | 2.02 (0.33) | 1.19 (0.12) | 1.16 (0.11) | < 0.001 |
| Days off work, median (IQR) | 0.00 (2.00) | 0.00 (0.50) | – | – |
| Provided with special equipment, n (%) | 17 (2.61) | 14 (1.82) | (1.93) | < 0.001 |
| Adaptations to home, n (%) | 5 (0.77) | 3 (0.39) | (0.31) | 0.004 |
The proportion of infants attending hospital day care and outpatient hospital departments between 6 and 12 months was significantly higher in the LMPT group than in the term group. The mean number of contacts with hospital outpatient departments was significantly higher for LMPT infants than for term-born infants. The proportion of infants using community-based immunisation services, paediatrician services, and physiotherapy services was also significantly higher for LMPT infants over this period, as was the proportion of infants provided with special equipment.
The proportion of infants admitted to hospital, attending a paediatric outpatient department or attending other outpatient hospital departments between 12 and 24 months was significantly higher in the LMPT group than in the term group. The mean number of contacts with hospital-based accident and emergency services and other outpatient hospital departments over this period was also significantly higher in the LMPT group, as was the mean number of contacts with GP services, community-based physiotherapy and speech and language therapy services, and NHS Direct services.
Economic costs
Economic costs to initial hospital discharge or death (whichever was earliest) are summarised in Table 40 for LMPT infants and for term-born infants. Mean costs were significantly higher for LMPT infants than for term-born infants across all cost categories. Mean total costs were estimated at £5533 (SE £310) for the combined LMPT group compared with £1864 (SE £36) for infants born at term. The mean cost difference (LMPT vs. term) was £3668 (bootstrap 95% CI £3129 to £4361; p < 0.0001).
| Variable | LMPT, 32–36 weeks | Term, ≥ 37 weeks reweighteda | Mean differenceb (95% CI) | Bootstrapped difference (95% CI) | p-valuec |
|---|---|---|---|---|---|
| Number of infants | 1146 | 1258 | |||
| Postnatal cost (£), mean (SE) | 1985.26 (25.54) | 1708.54 (19.25) | 276.72 (211.76 to 341.68) | 277.15 (213.68 to 342.13) | < 0.001 |
| Neonatal cost (£), mean (SE) | 3449.17 (298.51) | 146.45 (27.54) | 3302.71 (2714.38 to 3891.05) | 3293.67 (2825.30 to 3934.87) | < 0.001 |
| Other costs (£), mean (SE) | |||||
| Transfer | 19.23 (3.44) | 0.02 (0.05) | 19.21 (12.47 to 25.96) | 18.99 (12.25 to 26.62) | < 0.001 |
| Post-mortem | 5.41 (1.70) | 1.86 (0.97) | 3.55 (–0.40 to 7.50) | 3.56 (–0.40 to 7.50) | 0.078 |
| Surgery | 46.86 (15.58) | 0.81 (0.73) | 46.05 (15.45 to 76.65) 19.14 | 46.23 (17.17 to 79.77) | 0.003 |
| Investigations | 25.91 (3.48) | 6.76 (1.69) | 19.15 (11.40 to 26.88) | 18.96 (11.55 to 26.88) | < 0.001 |
| Total (other costs) | 97.41 (17.53) | 9.45 (2.49) | 87.96 (53.15 to 122.76) | 87.43 (56.70 to 125.35) | < 0.001 |
| Total birth to discharge hospital costs (£), mean (SE) | 5532.62 (309.73) | 1864.38.03 (36.49) | 3668.24 (3055.84 to 4280.64) | 3663.68 (3129.48 to 4361.64) | < 0.001 |
Economic costs between initial hospital discharge and 24 months or death (whichever was earliest) are presented in Table 41 for LMPT infants and for term-born infants by cost category and follow-up period. For the period between initial hospital discharge and 6 months, all hospital care category costs were significantly higher for LMPT infants. Over this period NHS and PSS costs (LMPT: £1107 vs. term: £773; p < 0.001) and societal costs (LMPT: £1165 vs. term: £810; p < 0.001) were significantly higher for LMPT infants than for term-born infants. For the period between 6 and 12 months, all categories of hospital care costs were significantly higher for LMPT infants, with the exception of accident and emergency costs. All categories of community care costs were significantly higher for LMPT infants with the exception of health visitor and walk-in centre costs. Total NHS and PSS costs (LMPT: £798 vs. term: £682; p = 0.001) and total societal costs (LMPT: £822 vs. term: £790; p = 0.028) remained significantly higher among LMPT infants over this period. For the period between 12 and 24 months, total NHS and PSS (LMPT: £820 vs. term: £289; p < 0.001) and total societal costs (LMPT: £1029 vs. term: £393; p < 0.001) remained significantly higher among LMPT infants.
| Variable | LMPT, 32–36 weeks | Term, ≥ 37 weeks | Term, ≥ 37 weeks reweighteda | p-valueb |
|---|---|---|---|---|
| Post discharge to 6 months | ||||
| Number of infants | 781 | 939 | ||
| Hospital care costs (£), mean (SE) | ||||
| Inpatient care | 379.18 (44.36) | 192.59 (36.51) | 185.38 (39.68) | < 0.001 |
| Other outpatient department | 84.04 (6.22) | 44.71 (3.82) | 43.93 (3.92) | < 0.001 |
| A&E | 30.69 (2.45) | 21.55 (1.74) | 20.23 (1.70) | < 0.001 |
| Day care | 32.70 (2.54) | 16.75 (1.60) | 15.55 (1.54) | < 0.001 |
| Community care costs (£), mean (SE) | ||||
| Routine checks | 31.57 (0.43) | 33.79 (0.37) | 33.83 (0.37) | < 0.001 |
| Immunisations | 59.79 (0.89) | 63.40 (0.73) | 62.87 (0.74) | 0.001 |
| Weight checks | 238.50 (6.37) | 210.97 (4.99) | 207.84 (4.88) | < 0.001 |
| Health visitor | 161.11 (5.11) | 133.49 (3.59) | 129.92 (3.65) | < 0.001 |
| Other GP | 52.78 (2.51) | 48.74 (1.96) | 47.60 (1.71) | 0.001 |
| Community paediatrician | 10.30 (1.82) | 6.19 (1.47) | 6.43 (1.58) | < 0.001 |
| Physiotherapy | 1.46 (0.38) | 0.99 (0.32) | 0.86 (0.33) | 0.001 |
| Community nurse | 6.06 (1.55) | 2.70 (0.55) | 2.29 (0.50) | < 0.001 |
| Walk-in centre | 7.27 (0.81) | 5.34 (0.52) | 5.65 (0.56) | 0.001 |
| Calls to NHS Direct | 8.51 (0.65) | 7.02 (0.48) | 7.07 (0.49) | < 0.001 |
| Medication costs (£), mean (SE) | 3.99 (0.52) | 3.82 (0.90) | 3.88 (1.01) | 0.007 |
| Lost earnings (£), mean (SE) | 50.74 (18.43) | 5.99 (1.57) | 6.23 (1.66) | < 0.001 |
| Special equipment costs (£), mean (SE) | 4.86 (1.95) | 2.17 (1.64) | 0.80 (0.51) | 0.003 |
| Adaptation costs (£), mean (SE) | 1.26 (0.73) | 23.78 (12.85) | 29.85 (14.54) | 0.001 |
| NHS and PSS costs (£), mean (SE) | 1107.95 (52.07) | 792.05 (39.82) | 773.32 (42.51) | < 0.001 |
| Societal costs (£), mean (SE) | 1164.81 (57.18) | 824.00 (42.22) | 810.20 (45.22) | < 0.001 |
| 6–12 months | ||||
| Number of infants | 703 | 856 | 856 | |
| Hospital care costs (£), mean (SE) | ||||
| Inpatient care | 167.66 (65.34) | 67.79 (10.44) | 76.97 (11.44) | < 0.001 |
| Other outpatient department | 89.88 (6.82) | 70.52 (6.55) | 71.67 (6.91) | < 0.001 |
| A&E | 57.14 (4.55) | 49.16 (3.71) | 55.33 (3.91) | 0.18 |
| Day care | 31.84 (3.75) | 23.34 (3.00) | 25.95 (3.20) | 0.004 |
| Community care costs (£), mean (SE) | ||||
| Immunisations | 55.38 (1.24) | 55.51 (1.17) | 57.25 (1.20) | 0.019 |
| Weight checks | 113.32 (3.82) | 120.44 (3.62) | 122.31 (3.70) | 0.001 |
| Health visitor | 84.61 (3.04) | 83.06 (2.64) | 84.45 (2.79) | 0.51 |
| Hearing/developmental checks | 56.20 (2.12) | 58.25 (1.97) | 58.80 (2.00) | 0.001 |
| Other GP | 73.52 (2.59) | 71.20 (2.17) | 72.08 (2.17) | 0.008 |
| Community paediatrician | 22.64 (3.36) | 14.07 (2.84) | 16.10 (3.09) | 0.002 |
| Physiotherapy | 3.17 (0.94) | 1.47 (0.64) | 1.48 (0.70) | < 0.001 |
| Community nurse | 5.09 (1.10) | 3.62 (0.80) | 3.25 (0.79) | 0.001 |
| Walk-in centre | 15.84 (1.47) | 15.36 (1.19) | 16.29 (1.24) | 0.083 |
| Calls to NHS Direct | 17.96 (1.23) | 17.79 (1.03) | 18.50 (1.05) | 0.036 |
| Medication costs (£), mean (SE) | 3.46 (0.90) | 1.54 (0.21) | 1.69 (0.22) | < 0.001 |
| Lost earnings (£), mean (SE) | 22.56 (3.83) | 76.35 (40.94)) | 91.20 (45.93) | 0.001 |
| Special equipment costs (£), mean (SE) | 1.78 (0.75) | 0.87 (0.39) | 1.00 (0.43) | 0.001 |
| Adaptation costs (£), mean (SE) | 0.10 (0.07) | 24.30 (14.88) | 16.44 (14.02) | 0.005 |
| NHS and PSS costs (£), mean (SE) | 797.72 (72.11) | 653.13 (22.26) | 682.10 (23.91) | 0.001 |
| Societal costs (£), mean (SE) | 822.17 (72.99) | 754.65 (57.20) | 790.73 (62.89) | 0.028 |
| 12–24 months | ||||
| Number of infants | 651 | 771 | 771 | |
| Hospital care costs (£), mean (SE) | ||||
| Inpatient care | 651.44 (494.01) | 152.46 (47.99) | 162.68 (51.14) | < 0.001 |
| Paediatric outpatient department | 25.50 (2.19) | 18.73 (1.84) | 19.13 (1.83) | 0.001 |
| Other outpatient department | 31.24 (2.60) | 20.13 (2.11) | 20.74 (2.13) | < 0.001 |
| A&E | 33.04 (2.12) | 25.83 (1.76) | 25.50 (1.72) | < 0.001 |
| Community care costs (£), mean (SE) | ||||
| Other GP | 33.16 (0.91) | 31.29 (0.82) | 29.78 (0.78) | < 0.001 |
| Practice nurse | 2.28 (0.18) | 2.57 (0.18) | 2.45 (0.18) | 0.001 |
| Community paediatrician | 5.48 (1.28) | 3.81 (1.00) | 3.53 (0.99) | < 0.001 |
| Physiotherapy | 2.17 (0.53) | 0.88 (0.28) | 0.91 (0.28) | < 0.0001 |
| Speech and language therapist | 3.06 (0.54) | 0.60 (0.17) | 0.51 (0.15) | < 0.001 |
| Occupational therapist | 0.92 (0.37) | 0.37 (0.21) | 0.43 (0.22) | 0.001 |
| Community nurse | 1.60 (0.51) | 1.61 (0.35) | 1.46 (0.31) | 0.010 |
| Walk-in centre | 9.76 (0.65) | 8.88 (0.58) | 8.97 (0.57) | 0.005 |
| Calls to NHS Direct | 8.63 (0.52) | 22.18 (1.47) | 6.85 (0.44) | < 0.001 |
| Other services | 9.62 (1.54) | 4.30 (1.04) | 3.91 (0.86) | < 0.001 |
| Medication costs (£), mean (SE) | 1.96 (0.53) | 2.29 (0.51) | 2.23 (0.50) | < 0.001 |
| Lost earnings (£), mean (SE) | 186.97 (40.07) | 102.84 (10.92) | 101.62 (11.07) | < 0.001 |
| Special equipment costs (£), mean (SE) | 1.10 (0.40) | 1.34 (0.53) | 1.50 (0.56) | 0.006 |
| Adaptation costs (£), mean (SE) | 20.68 (11.39) | 0.70 (0.65) | 0.83 (0.70) | < 0.001 |
| NHS and PSS costs (£), mean (SE) | 819.87 (495.59) | 280.74 (50.28) | 289.08 (53.48) | < 0.001 |
| Societal costs (£), mean (SE) | 1028.62 (497.57) | 385.61 (55.88) | 393.02 (59.27) | < 0.001 |
Economic costs from birth to 24 months or death (whichever was earliest) are presented by cost category in Table 42 for LMPT infants and for term-born infants. The costs are presented for complete cases: that is, for those infants in whom cost data available were available at all follow-up periods. Mean total neonatal care costs, total hospital care costs, total NHS and PSS costs, and total societal costs were significantly higher for LMPT infants than for term-born infants. There were no significant differences in mean total community care costs, medication costs, lost earnings, special equipment costs, and adaption costs between the two groups. Mean (SE) total societal costs were estimated at £8123 (£586) for the combined LMPT group, compared with £3784 (£138) for children born at term. The mean cost difference (LMPT vs. term) was £4340 (bootstrap 95 CI £3142 to £5568; p < .0001).
| Variable | LMPT, 32–36 weeks | Term, ≥ 37 weeks reweighteda | Mean differenceb (95% CI) | Bootstrapped difference (95% CI) | p-valuec |
|---|---|---|---|---|---|
| Number of infants | 594 | 716 | |||
| Neonatal care costs, mean (SE) | 3765.83 (531.84) | 172.66 (39.32) | 3593.17 (2546.47 to 4639.86) | 3602.08 (2736.07 to 4828.16) | < 0.001 |
| Hospital care costs, mean (SE) | 3025.75 (150.76) | 2402.00 (89.16) | 623.75 (271.02 to 976.48) | 623.75 (312.76 to 1015.15) | 0.001 |
| Community care costs, mean (SE) | 1039.47 (22.34) | 1005.24 (16.72) | 34.23 (–22.35 to 90.80) | 33.18 (–22.35 to 89.13) | 0.23 |
| Medication costs, mean (SE) | 7.92 (0.98) | 7.99 (1.42) | 0.26 (–3.69 to 3.53) | 0.04 (–3.36 to 3.36) | 0.96 |
| Lost earnings, mean (SE) | 255.51 (49.08) | 155.86 (21.74) | 99.65 (–7.47 to 206.77) | 98.73 (7.12 to 210.45) | 0.06 |
| Special equipment costs, mean (SE) | 5.11 (1.15) | 3.32 (1.06) | 1.79 (–1.17 to 4.75) | 1.79 (–1.25 to 4.89) | 0.23 |
| Adaptation costs, mean (SE) | 23.72 (12.49) | 36.70 (32.26) | –12.98 (–86.90 to 60.94) | –11.96 (–97.38 to 43.78) | 0.73 |
| Total NHS and PSS costs, mean (SE) | 7838.96 (594.14) | 3587.89 (124.52) | 4251.07 (3085.50 to 5416.65) | 4240.47 (3071.09 to 5439.71) | < 0.001 |
| Total societal costs, mean (SE) | 8123.29 (586.42) | 3783.76 (137.97) | 4339.53 (3157.78 to 5521.28) | 4328.64 (3142.18 to 5568.14) | < 0.001 |
Regression models for economic costs
Birth to initial hospital discharge
Table 43 shows the results of three generalised linear regression models on total NHS and PSS costs to initial hospital discharge or death (whichever was earliest). The first model explores the impact of infant and birth characteristics on cost, while the second and third models also include maternal sociodemographic and lifestyle characteristics to explore if they additionally influence initial hospitalisation costs. Gestational age at birth status acted as the main exposure in these models. When compared with term-born infants, model 1 shows that the mean (SE) cost ratio for LMPT infants was 2.39 (0.08). Infants born in service B hospitals generated higher initial hospitalisation costs than those born in the service A hospitals, with a mean (SE) cost ratio of 1.20 (0.04). As expected, the method of delivery had a significant bearing on costs; infants born by assisted/instrumental delivery, CS during labour and CS not in labour had mean cost ratios of 1.31, 2.10, and 2.16, respectively, compared with the reference group of infants born by spontaneous vaginal delivery. Infants who were SGA had a mean cost ratio of 1.22 compared with the reference group of infants who were not SGA. Infants born with a congenital anomaly had a mean cost ratio of 5.33 compared with the reference group of infants born without congenital anomalies. Gender (male), whether or not the baby was first born, survival status and multiplicity did not have significant effects on total birth to initial hospital discharge costs. The addition of maternal sociodemographic and maternal lifestyle variables in models 2 and 3 had no significant impact on these findings.
| Variable | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| Relative cost (SE) | p > |t| | Relative cost (SE) | p > |t| | Relative cost (SE) | p > |t| | |
| Gestational age status (reference: term) | ||||||
| Late and moderate preterm | 2.39 (0.08) | < 0.001 | 2.30 (0.07) | < 0.001 | 2.15 (0.12) | < 0.001 |
| Place of delivery (reference: centre A) | ||||||
| Centre B | 1.20 (0.04) | < 0.001 | 1.17 (0.04) | < 0.001 | 1.09 (0.05) | 0.079 |
| Other | 1.19 (0.12) | 0.101 | 0.97 (0.08) | 0.759 | 0.95 (0.10) | 0.65 |
| Mode of delivery (reference: spontaneous vaginal) | ||||||
| Assisted/instrumental | 1.31 (0.06) | < 0.001 | 1.31 (0.05) | < 0.001 | 1.39 (0.11) | < 0.001 |
| CS, during labour | 2.10 (0.09) | < 0.001 | 2.24 (0.09) | < 0.001 | 2.06 (0.14) | < 0.001 |
| CS, not in labour | 2.16 (0.10) | < 0.001 | 2.26 (0.10) | < 0.001 | 2.09 (0.12) | < 0.001 |
| Baby status (reference: alive) | ||||||
| Stillbirth | 0.73 (0.11) | 0.039 | 0.78 (0.12) | 0.116 | 0.82 (0.14) | 0.25 |
| Early neonatal death | 1.42 (0.61) | 0.418 | 1.39 (0.59) | 0.443 | 2.47 (0.43) | < 0.001 |
| Late neonatal death | 0.84 (0.04) | < 0.001 | 0.87 (0.07) | 0.102 | 0.00 (–) | |
| Infant death | 2.79 (1.68) | 0.087 | 2.90 (1.81) | 0.088 | 0.72 (0.14) | 0.097 |
| Multiplicity (reference: singleton) | ||||||
| Multiple | 0.90 (0.05) | 0.079 | 0.83 (0.04) | 0.001 | 0.81 (0.07) | 0.012 |
| Gender (reference: male) | 0.98 (0.03) | 0.503 | 0.99 (0.03) | 0.797 | 0.97 (0.04) | 0.47 |
| Small for gestational agea (reference: no) | 1.22 (0.07) | < 0.001 | 1.22 (0.06) | < 0.001 | 1.29 (0.11) | 0.004 |
| Congenital anomaly (reference: no) | 5.33 (1.53) | < 0.001 | 5.47 (1.40) | < 0.001 | 5.52 (1.43) | < 0.001 |
| First born (reference: no) | 1.06 (0.04) | 0.096 | 1.04 (0.04) | 0.242 | 1.04 (0.07) | 0.56 |
| Maternal age | 1.00 (0.00) | 0.920 | 1.00 (0.01) | 0.81 | ||
| Maternal BMI (reference: normal) | ||||||
| Underweight | 0.96 (0.07) | 0.567 | 0.87 (0.08) | 0.14 | ||
| Overweight | 0.99 (0.04) | 0.876 | 1.05 (0.07) | 0.42 | ||
| Obese | 0.96 (0.04) | 0.231 | 0.99 (0.05) | 0.92 | ||
| Maternal ethnicity (reference: white) | ||||||
| Mixed | 1.02 (0.15) | 0.892 | 1.04 (0.24) | 0.88 | ||
| Asian or Asian British | 0.94 (0.04) | 0.214 | 0.92 (0.10) | 0.42 | ||
| Black or black British | 0.94 (0.06) | 0.392 | 1.02 (0.13) | 0.90 | ||
| Chinese or other | 0.93 (0.10) | 0.500 | 1.20 (0.20) | 0.27 | ||
| Not known | 1.02 (0.13) | 0.870 | 0.95 (0.11) | 0.66 | ||
| Highest qualification (reference: higher degree) | ||||||
| Degree | 0.93 (0.05) | 0.139 | 0.95 (0.07) | 0.46 | ||
| A levels, vocational level 3 and equivalent | 0.99 (0.05) | 0.809 | 0.97 (0.08) | 0.72 | ||
| GCSE grades A*–C, vocational level 2 and equivalent | 1.05 (0.07) | 0.451 | 1.11 (0.11) | 0.30 | ||
| GCSE grades D–G, vocational level 1 and below | 1.04 (0.08) | 0.653 | 1.00 (0.12) | 0.99 | ||
| Qualification level unknown | 0.96 (0.06) | 0.528 | 1.10 (0.12) | 0.35 | ||
| No qualifications | 1.03 (0.08) | 0.736 | 1.03 (0.13) | 0.82 | ||
| Not known | 1.22 (0.16) | 0.145 | 0.87 (0.14) | 0.40 | ||
| Marital civil status (referent: living as part of a couple) | 1.02 (0.07) | 0.773 | 1.07 (0.10) | 0.46 | ||
| NS-SEC (reference: managerial and professional occupations) | ||||||
| Intermediate occupations | 0.98 (0.05) | 0.642 | 1.03 (0.07) | 0.62 | ||
| Routine and manual occupations | 0.97 (0.05) | 0.601 | 1.04 (0.08) | 0.55 | ||
| Never worked and long-term unemployed | 0.99 (0.06) | 0.841 | 1.05 (0.10) | 0.58 | ||
| Looking after family | 0.96 (0.05) | 0.468 | 1.04 (0.07) | 0.59 | ||
| Not known | 0.81 (0.08) | 0.039 | 1.02 (0.11) | 0.82 | ||
| Home ownership (reference: own) | ||||||
| Rent | 1.07 (0.04) | 0.055 | 1.03 (0.06) | 0.52 | ||
| Lives rent free | 1.01 (0.07) | 0.919 | 0.83 (0.12) | 0.17 | ||
| EQ-5D utility score | 0.99 (0.12) | 0.923 | 1.08 (0.18) | 0.63 | ||
| Chronic health problems (reference: no) | 0.95 (0.03) | 0.133 | 0.95 (0.05) | 0.33 | ||
| Deprivation score (reference: first quintile) | ||||||
| Second quintile | 1.04 (0.04) | 0.331 | 0.97 (0.05) | 0.63 | ||
| Third quintile | 1.11 (0.05) | 0.026 | 1.08 (0.08) | 0.25 | ||
| Fourth quintile | 1.07 (0.06) | 0.217 | 1.13 (0.10) | 0.17 | ||
| Fifth quintile | 1.05 (0.05) | 0.309 | 1.02 (0.09) | 0.82 | ||
| Recreational drugs during pregnancy (reference: no) | 1.12 (0.15) | 0.416 | 0.98 (0.16) | 0.91 | ||
| Smoke during pregnancy (reference: no) | 0.91 (0.04) | 0.056 | 0.92 (0.07) | 0.26 | ||
| Previous premature baby (reference: no) | 1.17 (0.08) | 0.03 | ||||
| Drink during pregnancy (reference: no) | 1.00 (0.05) | 0.99 | ||||
| Constant | 7.12 (0.03) | < 0.001 | 7.11 (0.17) | < 0.001 | 7.07 (0.26) | < 0.001 |
| n | 2403 | 2281 | 958 | |||
| Adjusted R2 | 42,224.36 | 40,131.38 | 16,599.23 | |||
Table 44 contains the corresponding results for the OLS regressions. Model 1 shows that, even after controlling for infant and birth characteristics, LMPT birth increased costs by an average of £3006 (SE £234; p < 0.0001), in comparison with birth at full term. The same patterns of statistical significance present in the corresponding GLM are found in this OLS model. Similarly, the addition of maternal sociodemographic and maternal lifestyle variables in models 2 and 3 had no significant impact on these findings.
| Variable | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| Coefficient (SE) | p > |t| | Coefficient (SE) | p > |t| | Coefficient (SE) | p > |t| | |
| Gestational age status (reference: term) | ||||||
| Late and moderate preterm | 3006.44 (236.73) | < 0.001 | 2813.45 (195.33) | < 0.001 | 2396.23 (331.87) | < 0.001 |
| Place of delivery (reference: centre A) | ||||||
| Centre B | 647.61 (254.68) | 0.011 | 670.24 (239.42) | 0.005 | 437.83 (289.57) | 0.13 |
| Other | 1251.14 (356.31) | < 0.001 | 576.12 (365.21) | 0.115 | 204.86 (486.45) | 0.67 |
| Mode of delivery (reference: spontaneous vaginal) | ||||||
| Assisted/instrumental | 476.88 (213.26) | 0.025 | 453.09 (219.18) | 0.039 | 797.6 (333.63) | 0.017 |
| CS, during labour | 2335.05 (235.06) | < 0.001 | 2698.3 (291.28) | < 0.001 | 2288.85 (377.14) | < 0.001 |
| CS not in labour | 3554.03 (639.83) | < 0.001 | 3736.14 (703.97) | < 0.001 | 2407.36 (372.74) | < 0.001 |
| Baby status (reference: alive) | ||||||
| Stillbirth | –1538.09 (402.27) | < 0.001 | –1036.85 (547.27) | 0.058 | –1174.17 (685.38) | 0.087 |
| Early neonatal death | –5069.66 (6019.95) | 0.400 | –5482.15 (5791.83) | 0.344 | 2327.38 (886.67) | 0.009 |
| Late neonatal death | –435.57 (292.01) | 0.136 | –69.5 (685.3) | 0.919 | 0.00(-) | |
| Infant death | 17,327.97 (13056.93) | 0.185 | 16,560.15 (13477.4) | 0.219 | –1723.72 (1305.56) | 0.18 |
| Multiplicity (reference: singleton) | ||||||
| Multiple | –964.42 (526) | 0.067 | –1169.74 (470.98) | 0.013 | –806.43 (483.75) | 0.096 |
| Gender (reference: male) | 159.89 (306.52) | 0.602 | 165.35 (302.06) | 0.584 | –344.12 (280.05) | 0.21 |
| Small for gestational age (reference: no)a | 750.75 (439.71) | 0.088 | 760.29 (448.64) | 0.090 | 1074.5 (627.41) | 0.087 |
| Congenital anomaly (reference: no) | 20,847.47 (9240.88) | 0.024 | 22,025.33 (9765.91) | 0.024 | 17,999.29 (5310.01) | 0.001 |
| First born (reference: no) | 485.23 (267.82) | 0.070 | 342.54 (204.04) | 0.093 | 60.92 (397.78) | 0.87 |
| Maternal age | –4.96 (26.69) | 0.853 | –1.41 (43.31) | 0.97 | ||
| Maternal BMI (reference: normal) | ||||||
| Underweight | –586.96 (522.23) | 0.261 | –674.68 (549.06) | 0.21 | ||
| Overweight | –347.94 (303.08) | 0.251 | 130.91 (355.27) | 0.71 | ||
| Obese | –704.39 (360.31) | 0.051 | –235.85 (302.98) | 0.43 | ||
| Maternal ethnicity (reference: white) | ||||||
| Mixed | –1314.74 (1355.45) | 0.332 | –641.3 (1585.53) | 0.68 | ||
| Asian or Asian British | –14.86 (289.82) | 0.959 | –216.89 (457.6) | 0.63 | ||
| Black or black British | 41 (698.33) | 0.953 | 1574.4 (1772.62) | 0.37 | ||
| Chinese or other | –234.88 (480.43) | 0.625 | 784.1 (662.85) | 0.23 | ||
| Not known | 654.12 (775.22) | 0.399 | –185.67 (615.76) | 0.76 | ||
| Highest qualification (reference: higher degree) | ||||||
| Degree | –242.44 (293.33) | 0.238 | –5.18 (314.24) | 0.98 | ||
| A levels, vocational level 3 and equivalent | 238.34 (367.6) | 0.517 | 11.24 (314.92) | 0.97 | ||
| GCSE grades A*–C, vocational level 2 and equivalent | 271.13 (356.88) | 0.447 | 532.61 (412.15) | 0.19 | ||
| GCSE grades D–G, vocational level 1 and below | 1149.1 (1060.21) | 0.279 | 508.18 (879.86) | 0.56 | ||
| Qualification level unknown | –295.54 (427.07) | 0.489 | 466.53 (401.05) | 0.24 | ||
| No qualifications | 185.86 (443.23) | 0.675 | 233.9 (626.01) | 0.70 | ||
| Not known | 857.85 (610.14) | 0.160 | –248.76 (1000.89) | 0.80 | ||
| Marital civil status (reference: living as part of a couple) | 606.99 (870.1) | 0.485 | 698.69 (667.36) | 0.29 | ||
| NS-SEC (reference: managerial and professional occupations) | ||||||
| Intermediate occupations | –85.97 (279.29) | 0.758 | 142.59 (302.4) | 0.63 | ||
| Routine and manual occupations | 21.03 (292.56) | 0.943 | 576.22 (475.32) | 0.22 | ||
| Never worked and long-term unemployed | 674.69 (780.38) | 0.387 | 474.83 (501.23) | 0.34 | ||
| Looking after family | –47.92 (315.91) | 0.879 | 457.52 (398.87) | 0.25 | ||
| Not known | –294.44 (676.08) | 0.663 | 539.09 (614.68) | 0.38 | ||
| Home ownership (reference: own) | ||||||
| Rent | 388.66 (231.18) | 0.093 | –85.67 (252.83) | 0.73 | ||
| Lives rent free | –448.39 (726.37) | 0.537 | –726.56 (609.72) | 0.23 | ||
| EQ-5D utility score | –442.12 (974.97) | 0.650 | 1005.81 (1568.31) | 0.52 | ||
| Chronic health problems (reference: no) | 203 (420.2) | 0.629 | 249.31 (308.3) | 0.41 | ||
| Deprivation score (reference: first quintile) | ||||||
| Second quintile | 349.86 (275.16) | 0.204 | 20.76 (276.58) | 0.94 | ||
| Third quintile | 951.9 (577.34) | 0.099 | 375.34 (391.62) | 0.33 | ||
| Fourth quintile | 194.56 (260.96) | 0.456 | 380.15 (377.65) | 0.31 | ||
| Fifth quintile | –72.67 (310.32) | 0.815 | –56.38 (431.34) | 0.89 | ||
| Recreational drugs during pregnancy (reference: no) | 134.92 (614.57) | 0.826 | –174.4 (806.73) | 0.82 | ||
| Smoked during pregnancy (reference: no) | –887.12 (658.49) | 0.178 | –635.99 (560.96) | 0.25 | ||
| Previous premature baby (reference: no) | 1062.72 (490.45) | 0.03 | ||||
| Drink during pregnancy (reference: no) | 180.35 (262.81) | 0.49 | ||||
| Constant | 285.73 (262.61) | 0.277 | 574.88 (1303.54) | 0.659 | –724.58 (2479.41) | 0.77 |
| n | 2403 | 2281 | 958 | |||
| Adjusted R2 | 0.2162 | 0.2296 | 0.3448 | |||
Birth to 24 months
Table 45 shows the results of two generalised linear regression models on total cost from birth to 24 months or death (whichever was earliest). The results are presented for complete cases, i.e. for those infants for whom cost data were available at all follow-up periods. The first model (model 4) explores the impact of infant and birth characteristics on total societal costs, while the second model (model 5) also includes maternal sociodemographic and lifestyle characteristics to explore whether or not they additionally influence societal costs. Gestational age at birth status acted as the main exposure in these models. Model 4 shows that, compared with term-born infants, the mean (SE) cost ratio for LMPT birth was 1.70 (0.08). Infants born in service B hospitals generated higher initial hospitalisation costs than those born in the service A hospitals, with a mean (SE) cost ratio of 1.12 (0.05). Infants born by assisted/instrumental delivery, CS during labour and CS not in labour had mean cost ratios of 1.15, 1.51, and 1.74, respectively, compared with the reference group of infants born by spontaneous vaginal delivery. Infants born with a congenital anomaly had a mean cost ratio of 4.56 compared with the reference group of infants born without congenital anomalies. Infants who were first born had a mean cost ratio of 1.1 compared with the reference group of infants who were not first born. Gender (male), whether or not the baby was SGA and multiplicity did not have significant effects on total birth to 24 months costs. The addition of maternal sociodemographic and maternal lifestyle variables in model 5 had no significant impact on these findings.
| Variable | Model 4 | Model 5 | ||
|---|---|---|---|---|
| Cost ratio (SE) | p > |t| | Cost ratio (SE) | p > |t| | |
| Gestational age status (reference: term) | ||||
| Late and moderate preterm | 1.70 (0.08) | < 0.001 | 1.72 (0.07) | < 0.001 |
| Place of delivery (reference: centre A) | ||||
| Centre B | 1.12 (0.05) | 0.005 | 1.1 (0.05) | 0.026 |
| Other | 0.95 (0.1) | 0.627 | 1.03 (0.13) | 0.83 |
| Mode of delivery (reference: spontaneous vaginal) | ||||
| Assisted/instrumental | 1.15 (0.06) | 0.009 | 1.17 (0.06) | 0.002 |
| CS, during labour | 1.51 (0.08) | < 0.001 | 1.49 (0.08) | < 0.001 |
| CS, not in labour | 1.74 (0.1) | < 0.001 | 1.72 (0.09) | < 0.001 |
| Multiplicity (reference: singleton) | ||||
| Multiple | 1.03 (0.07) | 0.627 | 1.03 (0.07) | 0.63 |
| Gender (reference: male) | 0.96 (0.04) | 0.270 | 0.96 (0.04) | 0.25 |
| Small for gestational age (reference: no)a | 1.08 (0.07) | 0.213 | 1.08 (0.06) | 0.16 |
| Congenital anomaly (reference: no) | 4.56 (1.48) | < 0.001 | 4.42 (1.18) | < 0.001 |
| First born (reference: no) | 1.1 (0.04) | 0.020 | 1.1 (0.05) | 0.028 |
| Maternal age | 1.01 (0.00) | 0.072 | ||
| Maternal ethnicity (reference: white) | ||||
| Mixed | 1.04 (0.16) | 0.80 | ||
| Asian or Asian British | 0.93 (0.07) | 0.30 | ||
| Black or black British | 1.04 (0.13) | 0.72 | ||
| Chinese or other | 1.32 (0.18) | 0.03 | ||
| Not known | 0.69 (0.12) | 0.028 | ||
| Highest qualification (reference: higher degree) | ||||
| Degree | 0.99 (0.06) | 0.92 | ||
| A levels, vocational level 3 and equivalent | 1.06 (0.07) | 0.41 | ||
| GCSE grades A*–C, vocational level 2 and equivalent | 1.06 (0.09) | 0.49 | ||
| GCSE grades D–G, vocational level 1 and below | 0.95 (0.09) | 0.60 | ||
| Qualification level unknown | 1.08 (0.1) | 0.40 | ||
| No qualifications | 1.01 (0.11) | 0.94 | ||
| Not known | 1 (0.22) | 0.99 | ||
| Marital civil status (reference: living as part of a couple) | 0.87 (0.06) | 0.038 | ||
| NS-SEC (reference: managerial and professional occupations) | ||||
| Intermediate occupations | 0.97 (0.06) | 0.55 | ||
| Routine and manual occupations | 1.07 (0.08) | 0.36 | ||
| Never worked and long-term unemployed | 0.94 (0.07) | 0.39 | ||
| Looking after family | 0.88 (0.07) | 0.09 | ||
| Not known | 0.75 (0.17) | 0.20 | ||
| Home ownership (reference: own) | ||||
| Rent | 1.07 (0.06) | 0.23 | ||
| Lives rent free | 1.09 (0.1) | 0.35 | ||
| EQ-5D utility score | 0.78 (0.12) | 0.10 | ||
| Chronic health problems (reference: no) | 0.94 (0.04) | 0.15 | ||
| Deprivation score (reference: first quintile) | ||||
| Second quintile | 1.08 (0.06) | 0.17 | ||
| Third quintile | 1.06 (0.07) | 0.37 | ||
| Fourth quintile | 1.02 (0.07) | 0.81 | ||
| Fifth quintile | 1.09 (0.08) | 0.25 | ||
| Recreational drugs during pregnancy (reference: no) | 0.98 (0.14) | 0.86 | ||
| Smoked during pregnancy (reference: no) | 1.11 (0.08) | 0.159 | ||
| Constant | 7.96 (0.05) | < 0.001 | 7.91 (0.24) | < 0.001 |
| n | 1310 | 1310 | ||
| AIC | 24,854.06 | 24,893.99 | ||
Table 46 contains the corresponding results for the OLS regressions.
| Variable | Model 4 | Model 5 | ||
|---|---|---|---|---|
| Coefficient (SE) | p > |t| | Coefficient (SE) | p > |t| | |
| Gestational age status (reference: term) | ||||
| LMPT | 2849.72 (330.08) | < 0.001 | 2923.23 (340.99) | < 0.001 |
| Place of delivery (reference: centre A) | ||||
| Centre B | 663.18 (290.98) | 0.023 | 569.49 (297.32) | 0.05 |
| Other | 162.96 (516.51) | 0.752 | 223.4 (659.21) | 0.73 |
| Mode of delivery (reference: spontaneous vaginal) | ||||
| Assisted/instrumental | 605.84 (295.97) | 0.041 | 703.43 (294.25) | 0.01 |
| CS, during labour | 2152.88 (385.27) | < 0.001 | 1952.1 (424.43) | < 0.001 |
| CS, not in labour | 3143.88 (575.15) | < 0.001 | 2905.82 (703.63) | < 0.001 |
| Multiplicity (reference: singleton) | ||||
| Multiple | 571.21 (594.65) | 0.337 | 523.82 (592.83) | 0.37 |
| Gender (reference: male) | –238.42 (284.75) | 0.403 | –265.84 (331.38) | 0.42 |
| Small for gestational agea (reference: no) | 569.58 (463.99) | 0.220 | 672.68 (457.53) | 0.14 |
| Congenital anomaly (reference: no) | 19,210.29 (7614.32) | 0.012 | 19,197.8 (7291.8) | 0.009 |
| First born (reference: no) | 368.74 (328.21) | 0.261 | 494.44 (328.1) | 0.13 |
| Maternal age | 93.2 (49.61) | 0.06 | ||
| Maternal ethnicity (reference: white) | ||||
| Mixed | 59.75 (2289.7) | 0.97 | ||
| Asian or Asian British | –382.05 (438.67) | 0.38 | ||
| Black or black British | 2286.8 (2868.13) | 0.42 | ||
| Chinese or other | 1223.63 (646.08) | 0.05 | ||
| Not known | –1286.54 (737.4) | 0.08 | ||
| Highest qualification (reference: higher degree) | ||||
| Degree | 453.73 (365.68) | 0.21 | ||
| A levels, vocational level 3 and equivalent | 783.94 (452.23) | 0.08 | ||
| GCSE grades A*–C, vocational level 2 and equivalent | 564.54 (475.57) | 0.23 | ||
| GCSE grades D–G, vocational level 1 and below | 1402.66 (1551.93) | 0.36 | ||
| Qualification level unknown | 250.72 (638.87) | 0.69 | ||
| No qualifications | 762 (733.08) | 0.29 | ||
| Not known | 84.75 (1132.25) | 0.94 | ||
| Marital civil status (reference: living as part of a couple) | –957.4 (646.8) | 0.13 | ||
| NS-SEC (reference: managerial and professional occupations) | ||||
| Intermediate occupations | –264.08 (371.96) | 0.47 | ||
| Routine and manual occupations | 451.3 (583.1) | 0.43 | ||
| Never worked and long-term unemployed | –715.64 (575.48) | 0.21 | ||
| Looking after family | –932.63 (614.4) | 0.12 | ||
| Not known | –1472.1 (997.3) | 0.14 | ||
| Home ownership (reference: own) | ||||
| Rent | 647.71 (431.4) | 0.13 | ||
| Lives rent free | 654.94 (632.71) | 0.30 | ||
| EQ-5D utility score | –1777.27 (1672.07) | 0.28 | ||
| Chronic health problems (reference: no) | –251.48 (498.62) | 0.61 | ||
| Deprivation score (reference: first quintile) | ||||
| Second quintile | 482.39 (380.1) | 0.20 | ||
| Third quintile | 456.52 (557.57) | 0.41 | ||
| Fourth quintile | 8.61 (407.49) | 0.98 | ||
| Fifth quintile | 199.87 (540.81) | 0.71 | ||
| Recreational drugs during pregnancy (reference: no) | 127.57 (949.43) | 0.89 | ||
| Smoked during pregnancy (reference: no) | 459.54 (483.82) | 0.34 | ||
| Constant | 2475.13 (386.56) | < 0.001 | 535.75 (2488.64) | 0.83 |
| n | 1310 | 1310 | ||
| Adjusted R2 | 0.2778 | 0.2998 | ||
Table 47 shows the results of two generalised linear regression models on total cost from birth to 24 months or death (whichever was earliest) using the inverse probability weighting method226,227 to account for the presence of censored data. The same two models were estimated as for the complete case analyses (see Table 46). The same patterns of statistical significance present in model 4 for the complete case analysis are found in model 4 for the weighted data. The addition of maternal sociodemographic and maternal lifestyle variables in model 5 resulted in some significant effects. For example, an unknown maternal ethnicity status resulted in a mean cost ratio of 0.69 compared with the white reference group. Maternal occupational status reported as looking after the family was associated with reduced societal costs to 24 months. Table 48 contains the corresponding results for the OLS regressions.
| Variable (unit) | Model 4 | Model 5 | ||
|---|---|---|---|---|
| Cost ratio (SE) | p > |t| | Cost ratio (SE) | p > |t| | |
| Gestational age status (reference: term) | ||||
| Late and moderate preterm | 1.65 (0.08) | < 0.001 | 1.67 (0.08) | < 0.001 |
| Place of delivery (reference: centre A) | ||||
| Centre B | 1.11 (0.05) | 0.016 | 1.08 (0.05) | 0.09 |
| Other | 1.00 (0.11) | 0.971 | 1.1 (0.15) | 0.51 |
| Mode of delivery (reference: spontaneous vaginal) | ||||
| Assisted/instrumental | 1.16 (0.08) | 0.024 | 1.16 (0.07) | 0.01 |
| CS, during labour | 1.52 (0.09) | < 0.001 | 1.49 (0.09) | < 0.001 |
| CS, not in labour | 1.73 (0.1) | < 0.001 | 1.71 (0.09) | < 0.001 |
| Multiplicity (reference: singleton) | ||||
| Multiple | 1.13 (0.09) | 0.140 | 1.11 (0.08) | 0.17 |
| Gender (reference: male) | 0.96 (0.04) | 0.329 | 0.96 (0.04) | 0.35 |
| Small for gestational agea (reference: no) | 1.05 (0.06) | 0.413 | 1.07 (0.06) | 0.26 |
| Congenital anomaly (reference: no) | 4.47 (1.46) | < 0.001 | 4.50 (1.31) | < 0.001 |
| First born (reference: no) | 1.12 (0.05) | 0.014 | 1.11 (0.06) | 0.03 |
| Maternal age | 1.01 (0.00) | 0.09 | ||
| Maternal ethnicity (reference: white) | ||||
| Mixed | 0.88 (0.15) | 0.43 | ||
| Asian or Asian British | 0.94 (0.06) | 0.34 | ||
| Black or black British | 1 (0.11) | 0.97 | ||
| Chinese or other | 1.25 (0.16) | 0.09 | ||
| Not known | 0.69 (0.1) | 0.01 | ||
| Highest qualification (reference: higher degree) | ||||
| Degree | 0.99 (0.06) | 0.89 | ||
| A levels, vocational level 3 and equivalent | 1.07 (0.08) | 0.37 | ||
| GCSE grades A*–C, vocational level 2 and equivalent | 1.08 (0.1) | 0.39 | ||
| GCSE grades D–G, vocational level 1 and below | 0.9 (0.09) | 0.29 | ||
| Qualification level unknown | 1.09 (0.1) | 0.35 | ||
| No qualifications | 0.98 (0.11) | 0.88 | ||
| Not known | 1.14 (0.33) | 0.64 | ||
| Marital civil status (reference: living as part of a couple) | 0.93 (0.07) | 0.33 | ||
| NS-SEC (reference: managerial and professional occupations) | ||||
| Intermediate occupations | 0.97 (0.06) | 0.67 | ||
| Routine and manual occupations | 1.04 (0.08) | 0.64 | ||
| Never worked and long-term unemployed | 0.95 (0.08) | 0.55 | ||
| Looking after family | 0.85 (0.07) | 0.04 | ||
| Not known | 0.8 (0.16) | 0.25 | ||
| Home ownership (reference: own) | ||||
| Rent | 1.09 (0.06) | 0.12 | ||
| Lives rent free | 1.08 (0.1) | 0.41 | ||
| EQ-5D utility score | 0.8 (0.11) | 0.11 | ||
| Chronic health problems (reference: no) | 0.94 (0.04) | 0.20 | ||
| Deprivation score (reference: first quintile) | ||||
| Second quintile | 1.08 (0.07) | 0.23 | ||
| Third quintile | 1.06 (0.07) | 0.39 | ||
| Fourth quintile | 1.02 (0.08) | 0.82 | ||
| Fifth quintile | 1.08 (0.08) | 0.31 | ||
| Recreational drugs during pregnancy (reference: no) | 1.18 (0.2) | 0.32 | ||
| Smoke during pregnancy (reference: no) | 1.02 (0.07) | 0.78 | ||
| Constant | 7.96 (0.05) | < 0.001 | 7.89 (0.24) | < 0.001 |
| n | 1310 | 1310 | ||
| AIC | 45,007.86 | 45,026.75 | ||
| Variable | Model 4 | Model 5 | ||
|---|---|---|---|---|
| Coefficient (SE) | p > |t| | Coefficient (SE) | p > |t| | |
| Gestational age status (reference: term) | ||||
| Late and moderate preterm | 2590.13 (298.65) | < 0.001 | 2687.85 (308) | < 0.001 |
| Place of delivery (reference: centre A) | ||||
| Centre B | 603.13 (283.01) | 0.033 | 459.85 (284.09) | 0.10 |
| Other | 228.01 (637.28) | 0.721 | 271.02 (775.9) | 0.72 |
| Mode of delivery (reference: spontaneous vaginal) | ||||
| Assisted/instrumental | 594.69 (353.2) | 0.092 | 677.75 (331.85) | 0.04 |
| CS, during labour | 2145.89 (417.96) | < 0.001 | 1964.81 (440.47) | < 0.001 |
| CS, not in labour | 3129.18 (510.89) | < 0.001 | 2904.41 (641.87) | < 0.001 |
| Multiplicity (reference: singleton) | ||||
| Multiple | 334.77 (412.93) | 0.418 | 1025.23 (608.72) | 0.09 |
| Gender (reference: male) | 1158.28 (648.8) | 0.074 | –290.74 (335.99) | 0.38 |
| Small for gestational agea (reference: no) | –205.6 (267.77) | 0.443 | 468.38 (434.28) | 0.28 |
| Congenital anomaly (reference: no) | 18,945.89 (7182.38) | 0.008 | 19,105.01 (7076.49) | 0.007 |
| First born (reference: no) | 446.71 (312.44) | 0.153 | 512.91 (324.59) | 0.11 |
| Maternal age | 75.15 (42.62) | 0.07 | ||
| Maternal ethnicity (reference: white) | ||||
| Mixed | –1069.04 (1603.89) | 0.50 | ||
| Asian or Asian British | –340.33 (411.43) | 0.40 | ||
| Black or black British | 1410.5 (1688) | 0.40 | ||
| Chinese or other | 871.35 (643.08) | 0.17 | ||
| Not known | –1596.68 (734.38) | 0.03 | ||
| Highest qualification (reference: higher degree) | ||||
| Degree | 447.5 (373.72) | 0.23 | ||
| A levels, vocational level 3 and equivalent | 807.38 (431.17) | 0.06 | ||
| GCSE grades A*–C, vocational level 2 and equivalent | 753.11 (487.08) | 0.12 | ||
| GCSE grades D–G, vocational level 1 and below | 939.04 (1217.42) | 0.44 | ||
| Qualification level unknown | 363.03 (626.09) | 0.56 | ||
| No qualifications | 618.47 (720.22) | 0.39 | ||
| Not known | 702.8 (1501.19) | 0.64 | ||
| Marital civil status (reference: living as part of a couple) | –474.06 (506.58) | 0.35 | ||
| NS-SEC (reference: managerial and professional occupations) | ||||
| Intermediate occupations | –271.81 (391.55) | 0.48 | ||
| Routine and manual occupations | 56.96 (551.7) | 0.91 | ||
| Never worked and long-term unemployed | –683.91 (533.95) | 0.20 | ||
| Looking after family | –993.27 (578.7) | 0.08 | ||
| Not known | –1198.81 (885.51) | 0.17 | ||
| Home ownership (reference: own) | ||||
| Rent | 770.74 (387.29) | 0.04 | ||
| Lives rent free | 635.45 (568.31) | 0.26 | ||
| EQ-5D utility score | –1213.95 (1140.8) | 0.28 | ||
| Chronic health problems (reference: no) | –256.26 (411.92) | 0.53 | ||
| Deprivation score (reference: first quintile) | ||||
| Second quintile | 465.48 (411.43) | 0.25 | ||
| Third quintile | 494.82 (543.18) | 0.36 | ||
| Fourth quintile | 81.36 (413.29) | 0.84 | ||
| Fifth quintile | 234.19 (483.66) | 0.62 | ||
| Recreational drugs during pregnancy (reference: no) | 1661.19 (1189.57) | 0.16 | ||
| Smoked during pregnancy (reference: no) | –70.56 (415.8) | 0.86 | ||
| Constant | 2470.45 (323.2) | < 0.001 | 705.93 (1996.84) | 0.72 |
| n | 1310 | 1310 | ||
| Adjusted R2 | 0.2748 | 0.2953 | ||
Discussion
A recent study that reviewed the published evidence on the economic consequences of LMPT birth found sparse evidence on this topic. 228 No previous published studies have, to our knowledge, estimated the costs associated with LMPT birth in a UK setting. This study set out to estimate the economic costs associated with LMPT birth on the basis of a prospective population-based study in a geographically defined area of central England.
Conclusions
Key findings
-
During the initial hospitalisation, LMPT infants have higher rates of resource use than term-born infants across all hospital service resource categories.
-
Mean costs are significantly higher for LMPT infants than for term-born infants across all categories of hospital services.
-
The mean cost difference between our main comparator groups (LMPT vs. term) for the period until initial hospital discharge was £3668 (bootstrap 95% CI £3129 to £4362; p < .0001). This cost difference was accentuated when the time horizon for the economic analysis was extended to 2 years (cost differences for NHS £4083, PSS £34, other costs £101 and societal costs £4340).
Strengths and limitations
The main strengths of this study lie in the fact that it was based on a large geographically determined prospective population cohort, included a term comparison group and captured a comprehensive profile of resource use, encompassing use of hospital inpatient, day care and outpatient services, community health and social care services, medicines and drugs, adaptations to the home, provision of special equipment and parental lost productivity between birth and 2 years. Furthermore, the rigorous costing methodology applied followed national guidance for health economic evaluation purposes. 220,229
A number of caveats need to be borne in mind by readers. First, because the study was based in the geographical area of the East Midlands, it may not be representative of the UK population as a whole. Nevertheless, as we were able to collect information about the numbers of infants that were not recruited, together with baseline denominators in terms of ‘all births’, it has still been possible to create reasonable estimates for the population, which should be suitable for generalisation. Second, our study considered only hospitalisation costs during the period between birth and initial hospital discharge, whereas a broader societal perspective for economic costs over this initial time horizon might also appropriately consider costs borne by parents and informal carers. A recent structured review of the economic costs associated with preterm birth highlighted the importance of non-health-care costs associated with the initial period of hospitalisation, such as parental travel costs and those associated with lost parental productivity, and it is likely that these categories of costs are relevant to some families and carers of children born either moderately or late preterm. 230 Third, the study covered a time horizon of birth to 2 years, whereas a longer time horizon could have captured the economic consequences of potential longer-term sequelae, such as physical, neuropsychological and behavioural difficulties. The economic consequences of LMPT birth are likely to be ongoing in infants with long-term adverse sequelae and it is possible that the need for special educational support in this group is substantial but not yet fully recognised.
Implications for practice
Compared with birth at full term, LMPT birth is associated with significant additional costs during the period of the initial hospitalisation and over the first 2 years of life. Clinical decision-makers and budgetary and service planners should recognise the overall economic impact of LMPT birth in their service planning, as well as the potential contribution of clinical and sociodemographic factors to future public sector and broader societal costs. The results of our study should be considered for use within economic evaluations of preventative or treatment interventions for LMPT birth, or as inputs to studies attempting to model the economic costs of preterm birth throughout childhood.
The two neonatal services involved in this study generated significantly different costs associated with the care of LMPT babies. This is mirrored in clinical differences reported in previous sections. Rationalising the approach to care could result in very significant saving given that there are around 40,000 births each year in the UK at LMPT gestations.
Challenges and lessons learned from conducting the Late And Moderately preterm Birth Study
Improving response rates
Obtaining responses to postal questionnaires from parents of participating children was challenging and time-consuming. At recruitment, we asked parents for details of an additional contact to improve opportunities for follow-up, since we believed that this would be a very mobile population. Although this is a tried and tested approach to maximising follow-up, we had only limited success with this strategy from the outset, as large numbers of mothers did not feel comfortable in providing additional contact details of friends or relatives. This appeared to be related to the perceived nuisance caused to people by unwanted or irrelevant calls and may reflect disquiet with the ease with which multiple agencies are now able to contact individuals, with or without explicit consent. However, this reluctance on the part of participants reduced our ability to follow up a number of children beyond the neonatal period.
Families with young children are busy and have limited time to complete postal questionnaires, particularly when their children reach 1 or 2 years of age and both parents may again be working. In order to maximise our chances of contacting families who had failed to return postal questionnaires, we used telephone, text messaging and e-mail. We found a preference among some families for completing the questionnaire on the telephone, and these interviews also provided the opportunity to check contact details regularly.
The use of these additional methods of follow-up necessitated a review of administrative staffing, because of the time-consuming nature of this personal and individualised contact. Additional members of staff were employed at various points during the course of the study. This was necessary both to maximise opportunities for contacting parents and to allow a high degree of flexibility in the timing of calls to families, of which many expressed a wish to be telephoned to complete questionnaires at particular times of the day or evening.
We also faced a challenge related to new technology in that parents were often reluctant to respond to calls to their mobile phones or landlines that were displayed on their handset as ‘blocked call’ or ‘withheld number’. Mobile telephones were therefore purchased for use by study team members solely for the purpose of contacting families for which this appeared to be a difficulty. Text messaging was also possible and proved highly successful in avoiding this problem.
During the follow-up phase of the LAMBS, we received a number of requests from parents who wished to complete follow-up questionnaires in an online format. We therefore introduced this option at the 2-year follow-up, providing a web link via e-mail for individuals who expressed the desire to use this. A number of parents took advantage of this opportunity and these, together with telephone interviews, increased our response rate by five individuals at 2 years.
At the 6-month follow-up, parents had to contact the research team to complete their questionnaire by telephone interview. However, by the time of the 12-month follow-up questionnaire, with the additional staff, we were able to routinely contact them to ‘chase’ missing questionnaires and offer telephone interview or online completion. Therefore, from that point onwards, we were operating a true mixed mode approach in response to these identified needs. The introduction of additional methods in response to parents’ wishes appears to have had a positive effect, as our greatest loss to follow-up was in the first 6 months and contact has been more consistently maintained since that stage (see Figure 10). For each change or addition to methods of contacting parents, approval was sought from the REC and the participating NHS trusts.
Recruitment and follow-up for ethnic groups
Barriers caused by lack of availability of interpreters for mothers who had limited knowledge of English were a significant issue. Although information sheets were translated into all the common local languages, these were rarely used and parents instead chose either to rely on family members who spoke English or, more often, to decline participation. This is a substantial challenge in areas in which there is a high ethnic minority population. When face-to-face communication was possible, with or without the support of family members, this proved sufficient to allow understanding of the study at the recruitment stage. However, obtaining responses from these families to written questionnaires was often difficult. Telephone conversations were extremely challenging and often had to be abandoned when adequate understanding could not be assured. However, response rates among ethnic minority families were generally improved by offering telephone interviews.
Maintaining the cohort
In order to maintain interest in the study among participating families, we felt that it was necessary to have some means of communicating on a more informal basis. However, funding limitations precluded more regular postal correspondence.
The advent of social media has provided both opportunities and challenges for longitudinal research in young families. Facebook is a popular avenue of communication among young parents, and we sought to capitalise on this by creating a LAMBS Facebook group. However, in order to be of use to the research team, this required, and continues to require, a high level of input to maintain an active, informative site that maintains the interest of participants without compromising their privacy.
In order to thank mothers for their involvement in the study at the recruitment stage, following the interview, each mother was given a cotton bag displaying the LAMBS logo. This was designed to maintain awareness of the study and encourage parents to remember that they were participating. Birthday cards were sent to children at 1, 2 and 3 years. A colourful picture sheet with stickers was included with the questionnaire at 2 years and a suggestion made that this was used to occupy the child while parents completed the questionnaire. This proved extremely popular with parents and the study Facebook page was used by a number of mothers to respond with thank-you messages to the study team for this and for their child’s birthday cards.
Patient and public involvement
Engaging young parents and families with small children proved extremely challenging. It had been our intention to develop a ‘panel’ of parent advisors from those participating in the study. We envisaged that this group would attend regular but infrequent meetings and would use e-mail to comment on study documentation, provide feedback on the conduct of the study and guide the research team on areas for future research. However, although a considerable number of parents expressed interest in acting in this role during telephone conversations with members of the study team, we were unable to identify any parents who said that they would be willing to attend meetings, despite the fact that travel and child care expenses were offered. All parents who were approached indicated that they would not have sufficient time to devote to this. All indicated that they would be willing to engage in e-mail correspondence to help with this. However, when e-mails were distributed, responses were not received.
We then chose, instead, to use our Facebook page as a means of engaging parents. We initially invited them to attend a ‘coffee morning’ to give feedback on the study and provided a play specialist to entertain the children if they wished to bring them. Although approximately 10 parents indicated that they would attend, only two mothers came. Nevertheless, they provided very helpful comment and feedback. Parents who were unable to attend suggested that we posted questions on the Facebook page. This was much more successful and, in response to specific questions posted on the page, a number of responses were received and some discussion between parents was also generated. Although these efforts came too late to have an effect on the LAMBS conduct, input from these parents has been extremely helpful in providing guidance in prioritising areas for future work according to parents’ needs.
Summary
Over recent years there has been increasing concern about the short- and long-term outcomes of babies born LMPT. Historically, these babies have constituted a relatively understudied group, with the largest proportion of studies originating in North America since 2006. Subsequently, in the UK there have been a number of retrospective studies exploring outcomes in this group using data from large regional and national cohort studies. However, the LAMBS is the first UK population-based study of its kind, from a birth cohort designed with the specific aim of exploring issues associated with birth at these gestations.
We recruited a high proportion of all LMPT births, together with a control group of a similar number of babies born at ≥ 37 weeks’ gestation, and examined a wide range of risk factors and outcomes; these included maternal health, socioeconomic status and lifestyle factors, neonatal and early childhood outcomes and associated health-care costs. In doing so, we have identified a number of factors that confer an increased risk of delivery at LMPT gestations. These relate mainly to low levels of maternal education, socioeconomic deprivation and maternal health before and during pregnancy. For infants born LMPT, compared with their term-born counterparts, we have shown significantly increased risk for a range of adverse neonatal outcomes. These include the requirement for specialist neonatal care and prolonged neonatal hospital stay associated with increased neonatal morbidity. Furthermore, we have shown that an increased risk of problems persists into infancy and early childhood, with a greater proportion of children born LMPT experiencing health, cognitive and socioemotional difficulties.
Our findings support the findings of retrospective studies both in the USA and in the UK that these infants represent a group that is at higher risk than previously appreciated. Although LMPT babies experience less severe illness than infants born before 32 weeks’ gestation, they constitute a much larger group and represent around 75 of all preterm births. The effects of even modestly increased morbidity in such a large proportion of infants should not be underestimated in terms of the health and social care services required to support them as they grow older. As might be expected, given the increased incidence of problems in this group, we have also been able to demonstrate significantly increased costs associated with their care in the first 2 years of life.
A large proportion of LMPT birth occurs as a result of a decision on the part of obstetric clinicians. Decision-making in complicated pregnancies has been, to a great extent, based on the premise that outcomes for LMPT babies did not differ substantially from those of term-born infants. The findings of previous studies, and those from the LAMBS, suggest that this perception has been erroneous, and this necessitates further exploration of the factors that influence such decisions. The view that LMPT birth was relatively ‘benign’ has meant that few researchers have pursued exploration of the optimal time of delivery at LMPT gestations in which pregnancy is complicated by problems such as hypertensive disease of pregnancy and pre-eclampsia. However, our results suggest that delivery associated with these conditions may have effects for babies that extend beyond the neonatal period. We have begun to explore whether these adverse effects are related to immaturity owing to early delivery or the effects of maternal illness, but this requires further requires investigation and clarification.
The detailed information that we have collected relating to the antenatal, perinatal, neonatal and childhood periods places us in a position to explore the relationship between early factors and later outcomes in greater depth, and this will be a priority. Such exploration is required to identify modifiable risk factors and to inform guidance about the management of women and their babies affected by either spontaneous or medically indicated delivery.
Our cohort will provide an ideal opportunity for long-term follow-up in this group of children to determine whether or not they remain at increased risk at school age and whether this risk remains static or changes with time. As the risks of LMPT birth constitute a newly recognised entity, few studies have the capacity to monitor the outcomes for these individuals into later childhood and adolescence, and to relate these outcomes to influences during the antenatal and perinatal periods and the early years. As children grow and develop within different family and educational settings, these two environments will exert an influence on the long-term outcomes and it will be important to identify further factors that set those with adverse outcomes apart. Our ongoing aim is to capture the progress of these children in order to identify potential mechanisms that may be amenable to modification to optimise management at every point and maximise the potential of young people following LMPT birth.
Chapter 4 Discussion
This programme of work was originally conceived in recognition of the huge impact of prematurity on individuals, the NHS and society in general. The focus of research, at the time of the application, had been very much one of optimising the management of mothers presenting in preterm labour and dealing with the consequences of very preterm birth. This situation continues.
Preterm birth is a major problem, with implications across many aspects of health and social care, and hence it seemed important to try to focus on key aspects of the topic as a whole trying to:
-
understand how the impact of prematurity differed across the UK as it was clear that routine statistics were compromised by a number of aspects regarding how they were collected and presented
-
understand better the drivers and impact of LMPT births – who are the major contributors to the socioeconomic burden
-
explore avenues that might provide a means of preventing preterm birth – despite its economic importance there is still no credible primary prevention strategy.
We were funded to carry out the first two strands of work and these have been successfully completed.
Many of the findings of the stream focused on better understanding childhood mortality are already being implemented. The work of the LAMBS, as well as the detailed findings, offers routes to improved care of these babies at lower costs for the NHS as well the opportunity to prevent some of the long-term consequences of prematurity. However, both streams of work repeatedly flag the association between premature birth and deprivation both in relation to the occurrence of premature babies and their on-going problems. There are also clear indications that, despite our tendency to categorise preterm birth into different groups (extreme, very, LMPT), there is almost certainly a continuum of risk with many shared aetiological influences. Therefore, although continuing to deal with preterm babies in the most appropriate fashion remains a priority, the lack of a primary prevention strategy should command no less attention.
Impact
Our work on understanding socioeconomic inequalities in infant mortality has provided important information regarding ways to tackle these inequalities and to improve the future monitoring of socioeconomic inequalities in the UK, both at a national and at a regional level. This work has been disseminated through publications,20,33,52,62,231,232 workshops with directors of public health and presentations at relevant national and international conferences.
The work targeting LMPT births was completed just 3 months before the end of the grant and just 9 months before submission of this report. As a result, the work on LMPT birth will continue to be refined in terms of publications and influence on policy from this point on (the end of 2013). Nonetheless, there have already been a number of important publications189,233–236 and to date there have already been approximately 40 ‘engagement activities’ at which lessons from the work have been shared with both parents and relevant health professionals. Presentations have been given to national and international conferences to academics, midwives, obstetricians, neonatologists, health-care commissioners and policy-makers involved in provision of care for babies in the UK and internationally. At a local level we have fed back the findings of our work on mortality rates directly to Midlands-based directors of public health.
Synergies
Our work focused on important topics around the common theme of preventing mortality and morbidity in early life. Subsequently, this was supported by the CMO’s report for 2012 (published October 2013), which makes a very similar case for a change in policy towards prevention in order to deal with a range of challenges in childhood. 237
Additional synergy between the research streams was seen, as socioeconomic influences emerged strongly in both streams as perhaps offering the most obvious way in which to impact early childhood mortality and morbidity. The most obvious biological link to socioeconomic status, seen in both streams of work, related to the risk of preterm birth, which in the CMO’s 2012 report was estimated to cost the country £2.48B per year. However, we have identified the impact of socioeconomic factors to be far wider, including in relation to the risk of certain major congenital anomalies occurring, the nature of the population most likely to generate LMPT babies and its influence on the long-term development of children born LMPT.
The impact of ethnicity and cultural beliefs was also seen across both streams of work. Increased rates of stillbirth, LMPT birth and, through congenital anomalies, infant deaths have been demonstrated. Within the LAMBS cohort, recruitment showed differential participation according to ethnic group. These findings are probably mediated in a number of ways, including through decreased access to health-care resources, language difficulties and the effects of consanguinity. We were, however, unable to explore the effects of cultural and religious beliefs in these populations.
Key findings
Key issues that have emerged include:
-
There are widening socioeconomic inequalities in infant mortality. Approximately 70% of all infant deaths are the result of either preterm birth or a major congenital abnormality. These causes explain the majority of the deprivation gap.
-
Among women from the most deprived areas, the risk of preterm birth is double that of the least deprived groups in society.
-
Although responsible for < 1% of all births, babies born before 24 weeks’ gestation account for 20% of infant mortality.
-
The recording of babies born before 24 weeks’ gestation as live births shows very marked differences around the country, as if such babies subsequently die their deaths are registered. In contrast, babies born dead at this gestation are not included at all in routine statistics.
-
Although rates of severe congenital anomalies in utero were similar across all deprivation groups, women from the most deprived areas are significantly less likely to opt for termination than the least deprived, resulting in a significantly greater number of babies born alive with a serious congenital anomaly in the most deprived groups in society. The reason(s) for the differential rate of termination is not clear.
-
Risk of LMPT birth is greatest in the most deprived groups within society.
-
Compared with children born at term, babies born LMPT are at increased risk of poorer health and developmental outcomes, particularly delayed cognitive and socioemotional development.
-
The risk of adverse outcomes of children born LMPT is amplified by socioeconomic factors, with the greatest risk being for those born to the most deprived families.
-
Developmental surveillance and early intervention may be beneficial for LMPT infants at greatest risk, including those born to mothers with high antenatal and social risk.
-
During the first 24 months of life, each child born LMPT generates approximately £3500 of additional health and societal costs and around 40,000 such babies are born each year in the UK.
-
We identified significant differences in the average in-hospital costs generated by the two neonatal services involved in this study while caring for LMPT babies.
Patient and public involvement
Throughout the time that the programme of work was under way the team developed a range of alliances in relation to PPI, and this enthusiastic involvement of patients and the public benefited our research strongly. These were primarily:
-
A close working relationship with the national charities Bliss (‘for babies born too small, too soon, too sick’) and SANDS.
-
A whole range of interactions with families from the large cohorts involved in the LAMBS. These included face-to-face meetings in small groups, e-mail forums and a Facebook group.
In relation to this programme of work, the parents have been particularly helpful in planning interactions to maximise follow-up. However, as results started to emerge they were also very helpful in planning and supporting applications for further research, including the Research for Patient Benefit (RfPB)-funded LAMBS-II.
Our experiences of trying to engage with parents directly (as opposed to the charities, which could be approached on a more structured basis) taught us that it was necessary to tailor our approach to meet their needs. We thought we had done just that in our early attempts to meet small groups of parents. However, it was only later, when meetings were arranged in soft-play centres that catered fully for the needs of young children and their parents in a familiar, safe and relaxed setting, that we achieved the higher numbers we were hoping for. It is our intention to continue to use this approach/setting in future PPI engagement events and we have developed good links with these venues to support our future events. We have experimented with the use of social media in an attempt to seek wider engagement but the group attracted to this type of approach tended to be the better educated middle-class families rather than those from the otherwise hard-to-reach groups we intended to target.
The work was disseminated to a lay audience through the incorporation of the findings of socioeconomic inequalities in infant mortality into a series of Health Infancy Roadshows for parents held at children’s centres aiming to convey the main risk factors for infant mortality to pregnant women and teenage mothers living in deprived areas with high rates of infant mortality. Findings have also been disseminated to a lay audience including interviews for television (‘Central News’ on BBC1), radio (including ‘The Today Programme’ on BBC Radio 4; BBC Radio Leicester) and national newspapers (the Guardian, The Times and the Mirror).
Limitations
We have highlighted methodological issues relating to the research in the relevant earlier sections. However, the following points merit particular emphasis:
-
The results from the LAMBS cohort represent the earliest analysis from this aspect of the programme. More detailed analysis has since been carried out. 238
-
Maintaining high rates of follow-up in neonatal studies has been an increasing problem in the UK for the last 10 years. Although the rates achieved here were acceptable, they were less than we would have liked to have achieved and occurred despite the use of multiple methods of ascertainment. We will subsequently publish a more detailed analysis of the potential impact on the findings of those ‘lost to follow-up’. It seems clear that parents are more likely to accept face-to-face ‘assessment’ with feedback than questionnaire-based follow-up.
-
Despite the recurring theme of socioeconomic status in relation to both streams, it was only in relation to the LAMBS cohort that individual-level data were available. The lack of individual data in the routine data sources is likely to have reduced the size of the associations that were detected.
-
Given the large contribution of ethnic minorities to the population within the area in which the LAMBS was conducted, our results may not be fully generalisable to all parts of the UK.
The findings of one stream of work centred on improving understanding of routine statistics relating to early childhood mortality rates and these results have already influenced some aspects of policy.
The various outcomes indicated that unadjusted figures, even for geographically defined populations, needed guarded interpretation unless they were adjusted for key confounders. Some of the necessary adjustments could be made relatively easily, for example by applying government area-level indices of deprivation to adjust for ‘social mix’. However, variation in the practice of deciding whether the most immature babies are born alive or dead is much more complex to deal with. These complexities are far more testing when the population being considered is that from an individual trust, as opposed to a geographically defined population, as the trust population will have been subject to a whole range of biases related to not only geography but also the nature of its services. This makes ‘fair comparison’ to other apparently similar trusts very complex.
In 2012, a number of the original programme grant applicants successfully bid, as part of a co-operative, to take on the work of the Healthcare Quality Improvement Partnership’s maternal, neonatal and infant (mortality and morbidity) clinical outcome review programme (MNI-CORP). The relevant individuals lead on the perinatal aspects of the work and have already modified the data set to facilitate adjustment for the confounding influences identified by the work of the programme grant. It is intended in addition that future reports of the MNI-CORP will focus on commissioning group populations rather than trusts, although we acknowledge that initially both types of output will be required in order to provide some continuity with previous work.
In relation to the LAMBS cohort, the early results have highlighted a number of important findings that will almost certainly impact policy and practice in the next 3–5 years. In relation to decisions to deliver ‘at-risk pregnancies’ at these gestations, early indications are that the outlook for most babies is good, but that for some groups (we are currently focusing on those in which maternal hypertensive disease was the reason for early delivery being considered) the chances of ‘developmental delay’ being present as the child grows are increased. Hence the findings will be important to obstetricians managing women in which early delivery is seen as a reasonable treatment option.
In the neonatal period the size of the LMPT population means that LMPT infants consume significant resources either within the NNU or on the postnatal ward. It emerged from this study, which involved primarily two large neonatal services, that there were very diverse approaches to management that led to quite different patterns of resource use (the difference was significant). There are clearly important savings that could be made from rationalising the care of these babies that will be informed by the results of our studies.
It is in relation to the later development of these babies that probably the most important findings are emerging. It appears that babies born to the most affluent families have a reduced risk of significant developmental problems at 2 years of age compared with those babies born to mothers from more deprived backgrounds. One approach to dealing with this finding would be to try to manage delivery based on the mother’s socioeconomic status; however, this seems totally impractical. A more realistic option would be to view such developmental delay as ‘preventable’ and to screen and instigate early intervention in children at greatest risk for adverse outcomes. Although such an approach has largely failed in very preterm children, we have identified that the pattern of behavioural difficulties in LMPT children appears to be different. The findings from some intervention studies in more mature babies would suggest that such an approach could alter the developmental trajectory of these children.
Implications for practice
-
Continued exploration of socioeconomic inequalities in neonatal mortality and stillbirth would facilitate greater understanding of associated socioeconomic inequalities in health, both nationally and at a local level.
-
Commissioners and others responsible for clinical governance should be cautious when reviewing unadjusted early-life mortality rates, particularly when these relate to individual trusts.
-
Monitoring of inequalities in infant mortality by specific cause in the future would be facilitated by high-quality data collection at a national level.
-
When more sophisticated analysis is not possible, the exclusion of babies of < 24 weeks’ gestation from routine analyses would be a sensible compromise.
-
Neonatal services should consider the care they offer to babies born LMPT to ensure that it is appropriate to their needs and the risks that they face.
-
For women considering delivery of their baby at a LMPT gestation, evidence indicates that:
-
There is an increased risk of developmental problems, but that increased risk is very small.
-
The risk of developmental problems appears to differ depending on the reason for LMPT delivery. The nature of the developmental problems affecting these babies appears to be primarily cognitive, social and emotional.
-
The nature of the developmental problems seen in children born at LMPT gestations is different from that seen in babies born very preterm and hence approaches to follow-up, assessment and support need to reflect these differences.
-
Future research
As a result of this programme of work a range of new research questions emerged and funding to pursue some of these has already been sought or is in place:
-
Understanding the socioeconomic variation in termination rates following detection of a severe congenital anomaly during pregnancy (University of Leicester PhD studentship). This will allow full investigation of the variation identified here with the aim of making recommendations for appropriate improvements in care.
-
Understanding decision-making regarding the interpretation of signs of life at the limit of viability to identify how to reduce variation in practice across the UK and inequalities in access to financial benefits for parents (a funded NIHR Career Development fellowship).
-
Longer-term follow-up of the LMPT cohort to determine how early cognitive and socioemotional problems evolve over time and whether or not there is developmental plasticity in LMPT children. This will also enable an assessment of whether delays in early socioemotional development manifest as behaviour problems or peer relationship difficulties later in childhood.
-
Evaluate the efficacy of early parenting interventions for improving cognitive and socioemotional development in the LMPT population.
-
Evaluating the efficacy and acceptability of developmental screening and follow-up in children born LMPT (NIHR RfPB-funded study).
-
Develop, implement and evaluate potential follow-up schemes for families and children born LMPT.
-
Investigation of ways in which rates of premature birth can be prevented.
-
Understanding obstetric decision-making regarding delivery at LMPT gestations.
-
Investigation of the most appropriate approach to the neonatal care of babies born LMPT.
-
Investigation of strategies to alter the developmental trajectory of at-risk LMPT children.
-
Development of strategies to support breastfeeding in babies born LMPT.
Acknowledgements
We are indebted to the families who took part in the LAMBS and wish to thank them for their contribution and support for the study. We also thank the members of the LAMBS team for their contribution to the successful running of this study: Laura Berry, Wanda Cunningham, Julie Faulkes, Ian Gallimore, Janet Hood, Samantha Hunt, Juliet Jones, Helen Jukes, Dianne Meecham, Frances Mielewczyk, Peter Perry and Nisha Sikotra (administrators); Martin Perkins (information technology officer); Janice Findlay, Kay Khan, Carol Liptrot, Carol McCormick, Emma Savage and Yvonne Toomassi (midwives); Samarita Blaggan and Alexa Guy (research associates, psychology); Kamran Khan (research fellow, health economics); Jon Dorling (consultant neonatologist, Nottingham University Hospital NHS Trust); Penny MacParland (consultant obstetrician, University Hospitals of Leicester NHS Trust); Kathryn Fairbrother (Leicestershire, Northamptonshire and Rutland Comprehensive Local Research Network); and Catherine Ashman-Lee (research governance, University Hospitals of Leicester NHS Trust).
Contributions of authors
David Field (Professor of Neonatal Medicine) led the overall programme, contributing to all work packages, and led the work leading to production of the final report.
Elaine Boyle (Senior Lecturer in Neonatal Medicine) led the LMPT birth work and coauthored the sections of the report focused on this stream.
Elizabeth Draper (Professor of Paediatric and Perinatal Epidemiology) provided epidemiological input to the whole programme and provided editorial input to the final report.
Alun Evans (Research Associate, Medical Statistics) carried out components of analysis for the LMPT birth sections of the final report.
Samantha Johnson (Senior Research Fellow, Developmental Psychology) led the neurodevelopmental assessment work of the LMPT birth stream and coauthored the sections of the report focused on this stream.
Kamran Khan (Research Fellow, Health Economics) carried out significant aspects of the health economic assessment and coauthored the health economic sections of the report.
Bradley Manktelow (Senior Research Fellow, Medical Statistics) provided leadership of the analysis of the LMPT birth work and contributed in addition to the analysis included in the early childhood mortality stream.
Neil Marlow (Professor of Neonatal Medicine) provided specialist neurodevelopmental advice to the LMPT birth work and provided input to sections of the report focused on this stream.
Stavros Petrou (Professor of Health Economics) led the health economic work and coauthored the health economic sections of the report.
Catherine Pritchard (Consultant, Public Health) provided managerial/public health input to the programme and contributed to production of the final report.
Sarah Seaton (Research Associate, Medical Statistics) carried out components of analysis for the LMPT birth sections of the final report.
Lucy Smith (research fellow, medical statistics) led the early childhood mortality stream work and coauthored the sections of the report focused on this stream and the socioeconomic aspects of LMPT birth.
Data sharing statement
Data from this study are available on completion of the appropriate data sharing request form available from timms@leicester.ac.uk.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, CCF, NETSCC, PGfAR or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PGfAR programme or the Department of Health.
References
- Department of Health . Annual Report of the Chief Medical Officer 2012. Our Children Deserve Better: Prevention Pays n.d. www.gov.uk/government/uploads/system/uploads/attachment_data/file/255237/2901304_CMO_complete_low_res_accessible.pdf (accessed 8 October 2015).
- Moser K. Gestation-specific infant mortality by social and biological factors among babies born in England and Wales in 2006. Health Stat Q 2009;42:78-87. http://dx.doi.org/10.1057/hsq.2009.18.
- Perinatal Mortality 2009. London: CMACE; 2010.
- Judge K. Inequalities in infant mortality: Patterns, trends, policy responses and emerging issues in Canada, Chile, Sweden and the United Kingdom. Health Sociol Rev 2009;18:12-24. http://dx.doi.org/10.5172/hesr.18.1.12.
- Smith LK, Draper ES, Manktelow BN, Dorling JS, Field DJ. Socioeconomic inequalities in very preterm birth rates. Arch Dis Child Fetal Neonatal Ed 2007;92:F11-14. http://dx.doi.org/10.1136/adc.2005.090308.
- Raju TN. Late-preterm births: challenges and opportunities. Pediatrics 2008;121:402-3. http://dx.doi.org/10.1542/peds.2007-2357.
- Raju TN. The problem of late-preterm (near-term) births: a workshop summary. Pediatr Res 2006;60:775-6. http://dx.doi.org/10.1203/01.pdr.0000246074.73342.1e.
- Tackling Health Inequalities: A Programme for Action. London: The Stationery Office; 2003.
- MacKay DF, Smith GC, Dobbie R, Pell JP. Gestational age at delivery and special educational need: retrospective cohort study of 407,503 schoolchildren. PLOS Med 2010;7. http://dx.doi.org/10.1371/journal.pmed.1000289.
- SANDS (Stillbirth and Neonatal Death Society) . Why 17? n.d. www.uk-sands.org/campaigns/our-campaigns/why-17 (accessed 8 October 2015).
- Marmot M. Fair Society, Healthy Lives: The Marmot Review: Strategic Review of Health Inequalities in England Post-2010. London: UCL Institute of Health Equity; 2010.
- Review of the Health Inequalities Infant Mortality PSA Target. London: DH; 2007.
- White Paper on Preterm Birth: The Global and Regional Toll. New York, NY: March of Dimes Foundation; 2009.
- Office for National Statistics . Super Output Area (SOA) n.d. www.ons.gov.uk/ons/guide-method/geography/beginner-s-guide/census/super-output-areas--soas-/index.html (accessed 8 October 2015).
- Keeling JW, MacGillivray I, Golding J, Wigglesworth J, Berry J, Dunn PM. Classification of perinatal death. Arch Dis Child 1989;64:1345-51. http://dx.doi.org/10.1136/adc.64.10_Spec_No.1345.
- Noble M, Wright G, Dibben C, Smith G, McLennan D, Anttila C, et al. Indices of Deprivation 2004: Report to the Office of the Deputy Prime Minister. London: Neighbourhood Renewal Unit; 2004.
- Lumley T, Kronmal R, Ma S. Relative Risk Regression in Medical Research: Models, Contrasts, Estimators, and Algorithms 2006. http://biostats.bepress.com/uwbiostat/paper293 (accessed 1 December 2013).
- Shaw M, Galbardes B, Lawlor D, Lynch J, Wheeler B, Davey Smith G. The Handbook of Inequality and Socioeconomic Position. Bristol: Policy Press; 2007.
- Oehlert GW. A note on the delta method. Am Stat 1992;46:27-9.
- Smith LK, Manktelow BN, Draper ES, Springett A, Field DJ. An investigation of the nature of socioeconomic inequalities in neonatal mortality: a population based study. BMJ 2010;341. http://dx.doi.org/10.1136/bmj.c6654.
- Gray R, Bonellie SR, Chalmers J, Greer I, Jarvis S, Kurinczuk JJ, et al. Contribution of smoking during pregnancy to inequalities in stillbirth and infant death in Scotland 1994–2003: retrospective population based study using hospital maternity records. BMJ 2009;339. http://dx.doi.org/10.1136/bmj.b3754.
- Field D, Draper ES, Fenton A, Papiernik E, Zeitlin J, Blondel B, et al. Rates of very preterm birth in Europe and neonatal mortality rates. Arch Dis Child Fetal Neonatal Ed 2009;94:F253-6. http://dx.doi.org/10.1136/adc.2008.150433.
- Goldenberg R, McClure E, Bhutta ZA, Belizan J, Reddy U, Rubens C. Stillbirths: the vision for 2020. Lancet 2011;377:1798-805. http://dx.doi.org/10.1016/S0140-6736(10)62235-0.
- Flenady V, Middleton P, Smith GC, Duke W, Erwich JJ, Khong TY, et al. Stillbirths: the way forward in high-income countries. Lancet 2011;377:1703-17. http://dx.doi.org/10.1016/S0140-6736(11)60064-0.
- Lawn JE, Blencowe H, Pattinson R, Cousens S, Kumar R, Ibiebele I, et al. Stillbirths: Where? When? Why? How to make the data count?. Lancet 2011;377:1448-63. http://dx.doi.org/10.1016/S0140-6736(10)62187-3.
- Dummer TJ, Parker L. Changing socioeconomic inequality in infant mortality in Cumbria. Arch Dis Child 2005;90:157-62. http://dx.doi.org/10.1136/adc.2003.036111.
- Guildea ZE, Fone DL, Dunstan FD, Sibert JR, Cartlidge PH. Social deprivation and the causes of stillbirth and infant mortality. Arch Dis Child 2001;84:307-10. http://dx.doi.org/10.1136/adc.84.4.307.
- Stephansson O, Dickman P, Johansson A, Cnattingius S. The influence of socioeconomic status on stillbirth risk in Sweden. Int J Epidemiol 2001;30:1296-301. http://dx.doi.org/10.1093/ije/30.6.1296.
- Dummer T, Dickinson H, Pearce M, Charlton M, Parker L. Stillbirth risk with social class and deprivation: no evidence for increasing inequality. J Clin Epidemiol 2000;53:147-55. http://dx.doi.org/10.1016/S0895-4356(99)00169-9.
- Neasham D, Dolk H, Vrijheid M, Jensen T, Best N. Stillbirth and neonatal mortality due to congenital anomalies: temporal trends and variation by small area deprivation scores in England and Wales, 1986–96. Paediatr Perinat Epidemiol 2001;15:364-73. http://dx.doi.org/10.1046/j.1365-3016.2001.0379a.x.
- Saving Babies’ Lives. London: SANDS; 2009.
- Baird D, Walker J, Thomson AM. The causes and prevention of stillbirths and first week deaths. III. A classification of deaths by clinical cause; the effect of age, parity and length of gestation on death rates by cause. J Obstet Gynaecol Br Emp 1954;61:433-48. http://dx.doi.org/10.1111/j.1471-0528.1954.tb07507.x.
- Seaton SE, Field DJ, Draper ES, Manktelow BN, Smith GC, Springett A, et al. Socioeconomic inequalities in the rate of stillbirths by cause: a population-based study. BMJ Open 2012;2. http://dx.doi.org/10.1136/bmjopen-2012-001100.
- Mullan Z, Horton R. Bringing stillbirths out of the shadows. Lancet 2011;377:1291-2. http://dx.doi.org/10.1016/S0140-6736(11)60098-6.
- Gardosi J, Kady SM, McGeown P, Francis A, Tonks A. Classification of stillbirth by relevant condition at death (ReCoDe): population based cohort study. BMJ 2005;331:1113-17. http://dx.doi.org/10.1136/bmj.38629.587639.7C.
- Froen JF, Pinar H, Flenady V, Bahrin S, Charles A, Chauke L, et al. Causes of death and associated conditions (CODAC): a utilitarian approach to the classification of perinatal deaths. BMC Pregnancy Childbirth 2009;9. http://dx.doi.org/10.1186/1471-2393-9-22.
- Kristensen J, Vestergaard M, Wisborg K, Kesmodel U, Secher NJ. Pre-pregnancy weight and the risk of stillbirth and neonatal death. BJOG 2005;112:403-8. http://dx.doi.org/10.1111/j.1471-0528.2005.00437.x.
- Messer J. An analysis of the socio-demographic characteristics of sole registered births and infant deaths. Health Stat Q 2011;50:79-107. http://dx.doi.org/10.1057/hsq.2011.9.
- The Lancet . Preterm birth: crisis and opportunity. Lancet 2006;368. http://dx.doi.org/10.1016/S0140-6736(06)69080-6.
- Cnattingius S, Stephansson O. The challenges of reducing risk factors for stillbirths. Lancet 2011;377:1294-5. http://dx.doi.org/10.1016/S0140-6736(11)60027-5.
- Oakley L, Maconochie N, Doyle P, Dattani N, Moser K. Multivariate analysis of infant death in England and Wales in 2005–06, with focus on socio-economic status and deprivation. Health Stat Q 2009;42:22-39. http://dx.doi.org/10.1057/hsq.2009.15.
- Olesen C, Thrane N, Ronholt AM, Olsen J, Henriksen TB. Association between social position and congenital anomalies: a population-based study among 19,874 Danish women. Scand J Public Health 2009;37:246-51. http://dx.doi.org/10.1177/1403494808100938.
- Vrijheid M, Dolk H, Stone D, Abramsky L, Alberman E, Scott JE. Socioeconomic inequalities in risk of congenital anomaly. Arch Dis Child 2000;82:349-52. http://dx.doi.org/10.1136/adc.82.5.349.
- Liu S, Joseph KS, Kramer MS, Allen AC, Sauve R, Rusen ID, et al. Relationship of prenatal diagnosis and pregnancy termination to overall infant mortality in Canada. J Am Med Assoc 2002;287:1561-7. http://dx.doi.org/10.1001/jama.287.12.1561.
- Garne E, Loane M, Dolk H, De Vigan C, Scarano G, Tucker D, et al. Prenatal diagnosis of severe structural congenital malformations in Europe. Ultrasound Obstet Gynecol 2005;25:6-11. http://dx.doi.org/10.1002/uog.1784.
- Davidson N, Halliday J, Riley M, King J. Influence of prenatal diagnosis and pregnancy termination of fetuses with birth defects on the perinatal mortality rate in Victoria, Australia. Paediatr Perinat Epidemiol 2005;19:50-5. http://dx.doi.org/10.1111/j.1365-3016.2004.00620.x.
- van der Pal-de Bruin KM, Graafmans W, Biermans MC, Richardus JH, Zijlstra AG, Reefhuis J, et al. The influence of prenatal screening and termination of pregnancy on perinatal mortality rates. Prenat Diagn 2002;22:966-72. http://dx.doi.org/10.1002/pd.442.
- Rowe RE, Garcia J, Davidson LL. Social and ethnic inequalities in the offer and uptake of prenatal screening and diagnosis in the UK: a systematic review. Public Health 2004;118:177-89. http://dx.doi.org/10.1016/j.puhe.2003.08.004.
- Alderdice F, McNeill J, Rowe R, Martin D, Dornan J. Inequalities in the reported offer and uptake of antenatal screening. Public Health 2008;122:42-5. http://dx.doi.org/10.1016/j.puhe.2007.05.004.
- Schechtman KB, Gray DL, Baty JD, Rothman SM. Decision-making for termination of pregnancies with fetal anomalies: analysis of 53,000 pregnancies. Obstet Gynaecol 2002;99:216-22. http://dx.doi.org/10.1016/S0029-7844(01)01673-8.
- Kirwan D. NHS Fetal Anomaly Screening Programme: 18+0 to 20+6 Weeks Fetal Anomaly Scan National Standards and Guidance for England. Exeter: NHS Fetal Anomaly Screening Programme; 2010.
- Smith LK, Budd JLS, Field DJ, Draper ES. Socioeconomic inequalities in outcome of pregnancy and neonatal mortality associated with congenital anomalies: a population based study. BMJ 2011;343. http://dx.doi.org/10.1136/bmj.d4306.
- Dolk H. What is the ‘primary’ prevention of congenital anomalies?. Lancet 2009;374. http://dx.doi.org/10.1016/S0140-6736(09)61411-2.
- Freemantle N, Wood J, Griffin C, Gill P, Calvert MJ, Shankar A, et al. What factors predict differences in infant and perinatal mortality in primary care trusts in England? A prognostic model. BMJ 2009;339. http://dx.doi.org/10.1136/bmj.b2892.
- Draper ES. Evaluating and comparing neonatal outcomes. Arch Dis Child Fetal Neonatal Ed 2010;95:F158-9. http://dx.doi.org/10.1136/adc.2008.148213.
- Kramer MS, Platt RW, Yang H, Haglund B, Cnattingius S, Bergsjo P. Registration artifacts in international comparisons of infant mortality. Paediatr Perinat Epidemiol 2002;16:16-22. http://dx.doi.org/10.1046/j.1365-3016.2002.00390.x.
- Field DJ, Dorling JS, Manktelow BN, Draper ES. Survival of extremely premature babies in a geographically defined population: prospective cohort study of 1994–9 compared with 2000–5. BMJ 2008;336:1221-3. http://dx.doi.org/10.1136/bmj.39555.670718.BE.
- Tommiska V, Heinonen K, Lehtonen L, Renlund M, Saarela T, Tammela O, et al. No improvement in outcome of nationwide extremely low birth weight infant populations between 1996–1997 and 1999–2000. Pediatrics 2007;119:29-36. http://dx.doi.org/10.1542/peds.2006-1472.
- Vanhaesebrouck P, Allegaert K, Bottu J, Debauche C, Devlieger H, Docx M, et al. The EPIBEL study: outcomes to discharge from hospital for extremely preterm infants in Belgium. Pediatrics 2004;114:663-75. http://dx.doi.org/10.1542/peds.2003-0903-L.
- Kamoji VM, Dorling JS, Manktelow BN, Draper ES, Field DJ. Extremely growth-retarded infants: is there a viability centile?. Pediatrics 2006;118:758-63. http://dx.doi.org/10.1542/peds.2005-2399.
- Richardus JH, Graafmans WC, Verloove-Vanhorick SP, Mackenbach JP. The perinatal mortality rate as an indicator of quality of care in international comparisons. Med Care 1998;36:54-66. http://dx.doi.org/10.1097/00005650-199801000-00007.
- Smith L, Draper ES, Manktelow BN, Pritchard C, Field DJ. Comparing regional infant death rates: the influence of preterm births < 24 weeks of gestation. Arch Dis Child Fetal Neonatal Ed 2013;8:F103-7. http://dx.doi.org/10.1136/fetalneonatal-2011-301359.
- House of Commons Daily Hansard . Amendment of the Law Relating to Abortion n.d. www.publications.parliament.uk/pa/cm200708/cmhansrd/cm080520/debtext/80520-0015.htm (accessed 27 October 2015).
- Costeloe KL, Hennessy EM, Haider S, Stacey F, Marlow N, Draper ES. Short term outcomes after extreme preterm birth in England: comparison of two birth cohorts in 1995 and 2006 (the EPICure studies). BMJ 2012;345. http://dx.doi.org/10.1136/bmj.e7976.
- Wood NS, Costeloe K, Gibson AT, Hennessy EM, Marlow N, Wilkinson AR. The EPICure study: growth and associated problems in children born at 25 weeks of gestational age or less. Arch Dis Child Fetal Neonatal Ed 2003;88:F492-500. http://dx.doi.org/10.1136/fn.88.6.F492.
- Wood NS, Marlow N, Costeloe K, Gibson AT, Wilkinson AR. Neurologic and developmental disability after extremely preterm birth. EPICure Study Group. N Engl J Med 2000;343:378-84. http://dx.doi.org/10.1056/NEJM200008103430601.
- Vohr BR, Wright LL, Dusick AM, Mele L, Verter J, Steichen JJ, et al. Neurodevelopmental and functional outcomes of extremely low birth weight infants in the National Institute of Child Health and Human Development Neonatal Research Network, 1993–1994. Pediatrics 2000;105:1216-26. http://dx.doi.org/10.1542/peds.105.6.1216.
- Moser K, Macfarlane A, Chow YH, Hilder L, Dattani N. Introducing new data on gestation-specific infant mortality among babies born in 2005 in England and Wales. Health Stat Q 2007;34:13-27.
- Martin JA, Kung HC, Mathews TJ, Hoyert DL, Strobino DM, Guyer B, et al. Annual summary of vital statistics: 2006. Pediatrics 2008;121:788-801. http://dx.doi.org/10.1542/peds.2007-3753.
- Raju TN, Higgins RD, Stark AR, Leveno KJ. Optimizing care and outcome for late-preterm (near-term) infants: a summary of the workshop sponsored by the National Institute of Child Health and Human Development. Pediatrics 2006;118:1207-14. http://dx.doi.org/10.1542/peds.2006-0018.
- Ananth CV, Vintzileos AM. Epidemiology of preterm birth and its clinical subtypes. J Matern Fetal Neonatal Med 2006;19:773-82. http://dx.doi.org/10.1080/14767050600965882.
- Ananth CV, Vintzileos AM. Maternal–fetal conditions necessitating a medical intervention resulting in preterm birth. Am J Obstet Gynecol 2006;195:1557-63. http://dx.doi.org/10.1016/j.ajog.2006.05.021.
- Leitich H, Bodner-Adler B, Brunbauer M, Kaider A, Egarter C, Husslein P. Bacterial vaginosis as a risk factor for preterm delivery: a meta-analysis. Am J Obstet Gynecol 2003;189:139-47. http://dx.doi.org/10.1067/mob.2003.339.
- Christiaens I, Zaragoza DB, Guilbert L, Robertson SA, Mitchell BF, Olson DM. Inflammatory processes in preterm and term parturition. J Reprod Immunol 2008;79:50-7. http://dx.doi.org/10.1016/j.jri.2008.04.002.
- Romero R, Gomez R, Chaiworapongsa T, Conoscenti G, Kim JC, Kim YM. The role of infection in preterm labour and delivery. Paediatr Perinat Epidemiol 2001;15:S41-56. http://dx.doi.org/10.1046/j.1365-3016.2001.00007.x.
- Costantine MM, How HY, Coppage K, Maxwell RA, Sibai BM. Does peripartum infection increase the incidence of cerebral palsy in extremely low birthweight infants?. Am J Obstet Gynaecol 2007;196:e6-8. http://dx.doi.org/10.1016/j.ajog.2007.01.009.
- Sun Y, Vestergaard M, Christensen J, Nahmias AJ, Olsen J. Prenatal exposure to maternal infections and epilepsy in childhood: a population-based cohort study. Pediatrics 2008;121. http://dx.doi.org/10.1542/peds.2007-2316.
- Bonzini M, Coggon D, Palmer KT. Risk of prematurity, low birthweight and pre-eclampsia in relation to working hours and physical activities: a systematic review. Occup Eviron Med 2007;64:228-43. http://dx.doi.org/10.1136/oem.2006.026872.
- Jamieson LM, Thomson WM. Adult oral health inequalities described using area-based and household-based socioeconomic status measures. J Public Health Dent 2006;66:104-9. http://dx.doi.org/10.1111/j.1752-7325.2006.tb02564.x.
- Boggess KA. Society for Maternal-Fetal Medicine Publications Committee . Maternal oral health in pregnancy. Obstet Gynaecol 2008;111:976-86. http://dx.doi.org/10.1097/AOG.0b013e31816a49d3.
- Khader Y, Al-shishani L, Obeidat B, Khassawneh M, Burgan S, Amarin ZO, et al. Maternal periodontal status and preterm low birth weight delivery: a case–control study. Arch Gynecol Obstet 2009;279:165-9. http://dx.doi.org/10.1007/s00404-008-0696-2.
- Smith LK, Draper ES, Manktelow BN, Field DJ. Deprivation and infection among spontaneous very preterm births. Obstet Gynaecol 2007;110:325-9. http://dx.doi.org/10.1097/01.AOG.0000270158.57566.2f.
- Hobel CJ, Goldstein A, Barrett ES. Psychosocial stress and pregnancy outcome. Clin Obstet Gynaecol 2008;51:333-48. http://dx.doi.org/10.1097/GRF.0b013e31816f2709.
- Lobel M, Cannella DL, Graham JE, DeVincent C, Schneider J, Meyer BA. Pregnancy-specific stress, prenatal health behaviors, and birth outcomes. Health Psychol 2008;27:604-15. http://dx.doi.org/10.1037/a0013242.
- Jaddoe VW, Troe EJ, Hofman A, Mackenbach JP, Moll HA, Steegers EA, et al. Active and passive maternal smoking during pregnancy and the risks of low birthweight and preterm birth: the Generation R Study. Paediatr Perinat Epidemiol 2008;22:162-71. http://dx.doi.org/10.1111/j.1365-3016.2007.00916.x.
- Ernhart CB, Wolf AW, Linn PL, Sokol RJ, Kennard MJ, Filipovich HF. Alcohol-related birth defects: syndromal anomalies, intrauterine growth retardation, and neonatal behavioral assessment. Alcohol Clin Exp Res 1985;9:447-53. http://dx.doi.org/10.1111/j.1530-0277.1985.tb05581.x.
- Sokol RJ, Janisse JJ, Louis JM, Bailey BN, Ager J, Jacobson SW, et al. Extreme prematurity: an alcohol-related birth effect. Alcohol Clin Exp Res 2007;31:1031-7. http://dx.doi.org/10.1111/j.1530-0277.2007.00384.x.
- Phupong V, Darojn D. Amphetamine abuse in pregnancy: the impact on obstetric outcome. Arch Gynecol Obstet 2007;276:167-70. http://dx.doi.org/10.1007/s00404-007-0320-x.
- Mikkelsen TB, Osterdal ML, Knudsen VK, Haugen M, Meltzer HM, Bakketeig L, et al. Association between a Mediterranean-type diet and risk of preterm birth among Danish women: a prospective cohort study. Acta Obstet Gynecol Scand 2008;87:325-30. http://dx.doi.org/10.1080/00016340801899347.
- Haugen M, Meltzer HM, Brantsaeter AL, Mikkelsen T, Osterdal ML, Alexander J, et al. Mediterranean-type diet and risk of preterm birth among women in the Norwegian Mother and Child Cohort Study (MoBa): a prospective cohort study. Acta Obstet Gynecol Scand 2008;87:319-24. http://dx.doi.org/10.1080/00016340801899123.
- Khoury J, Haugen G, Tonstad S, Froslie KF, Henriksen T. Effect of a cholesterol-lowering diet during pregnancy on maternal and fetal Doppler velocimetry: the CARRDIP study. Am J Obstet Gynecol 2007;196.
- Khoury J, Henriksen T, Christophersen B, Tonstad S. Effect of a cholesterol-lowering diet on maternal, cord, and neonatal lipids, and pregnancy outcome: a randomized clinical trial. Am J Obstet Gynecol 2005;193:1292-301. http://dx.doi.org/10.1016/j.ajog.2005.05.016.
- Rasch V. Cigarette, alcohol, and caffeine consumption: risk factors for spontaneous abortion. Acta Obstet Gynecol Scand 2003;82:182-8. http://dx.doi.org/10.1034/j.1600-0412.2003.00078.x.
- Weng X, Odouli R, Li DK. Maternal caffeine consumption during pregnancy and the risk of miscarriage: a prospective cohort study. Am J Obstet Gynecol 2008;198. http://dx.doi.org/10.1016/j.ajog.2007.10.803.
- Pregnant Women Advised to Limit Caffeine Consumption. London: Foods Standards Agency; 2008.
- Stutchfield P, Whitaker R, Russell I. Antenatal Steroids for Term Elective Caesarean Section Research Team . Antenatal betamethasone and incidence of neonatal respiratory distress after elective caesarean section: pragmatic randomised trial. BMJ 2005;331. http://dx.doi.org/10.1136/bmj.38547.416493.06.
- Clinical Guideline No 1(B)Tocolytic Drugs for Women in Preterm Labour. London: RCOG; 2002.
- Clinical Guideline No. 44: Preterm Prelabour Rupture of Membranes. London: RCOG; 2006.
- Clinical Guideline No.10(A): The Management of Severe Pre-eclampsia/Eclampsia. London: RCOG; 2006.
- Sibai BM. Preeclampsia as a cause of preterm and late preterm (near-term) births. Semin Perinatol 2006;30:16-9. http://dx.doi.org/10.1053/j.semperi.2006.01.008.
- Landon MB, Hauth JC, Leveno KJ, Spong CY, Leindecker S, Varner MW, et al. Maternal and perinatal outcomes associated with a trial of labor after prior cesarean delivery. N Engl J Med 2004;351:2581-9. http://dx.doi.org/10.1056/NEJMoa040405.
- Smith GC, Pell JP, Cameron AD, Dobbie R. Risk of perinatal death associated with labor after previous cesarean delivery in uncomplicated term pregnancies. J Am Med Assoc 2002;287:2684-90. http://dx.doi.org/10.1001/jama.287.20.2684.
- Shapiro-Mendoza CK, Tomashek KM, Kotelchuck M, Barfield W, Nannini A, Weiss J, et al. Effect of late-preterm birth and maternal medical conditions on newborn morbidity risk. Pediatrics 2008;121:e223-32. http://dx.doi.org/10.1542/peds.2006-3629.
- Lee YM, Cleary-Goldman J, D’Alton ME. The impact of multiple gestations on late preterm (near-term) births. Clin Perinatol 2006;33:777-92. http://dx.doi.org/10.1016/j.clp.2006.09.008.
- Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Menacker F, Munson ML. Births: final data for 2002. Natl Vital Stat Rep 2003;52:1-113.
- Barigye O, Pasquini L, Galea P, Chambers H, Chappell L, Fisk NM. High risk of unexpected late fetal death in monochorionic twins despite intensive ultrasound surveillance: a cohort study. PLOS Med 2005;2. http://dx.doi.org/10.1371/journal.pmed.0020172.
- Kahn B, Lumey LH, Zybert PA, Lorenz JM, Cleary-Goldman J, D’Alton ME, et al. Prospective risk of fetal death in singleton, twin, and triplet gestations: implications for practice. Obstet Gynaecol 2003;102:685-92. http://dx.doi.org/10.1016/S0029-7844(03)00616-1.
- Sairam S, Costeloe K, Thilaganathan B. Prospective risk of stillbirth in multiple-gestation pregnancies: a population-based analysis. Obstet Gynaecol 2002;100:638-41. http://dx.doi.org/10.1016/S0029-7844(02)02174-9.
- Rubaltelli FF, Dani C, Reali MF, Bertini G, Wiechmann L, Tangucci M, et al. Acute neonatal respiratory distress in Italy: a 1-year prospective study. Italian Group of Neonatal Pneumology. Acta Paediatr 1998;87:1261-8. http://dx.doi.org/10.1111/j.1651-2227.1998.tb00949.x.
- Wang ML, Dorer DJ, Fleming MP, Catlin EA. Clinical outcomes of near-term infants. Pediatrics 2004;114:372-6. http://dx.doi.org/10.1542/peds.114.2.372.
- Laptook A, Jackson GL. Cold stress and hypoglycemia in the late preterm (‘near-term’) infant: impact on nursery of admission. Semin Perinatol 2006;30:24-7. http://dx.doi.org/10.1053/j.semperi.2006.01.014.
- Bhutani VK, Johnson L. Kernicterus in late preterm infants cared for as term healthy infants. Semin Perinatol 2006;30:89-97. http://dx.doi.org/10.1053/j.semperi.2006.04.001.
- Adamkin DH. Feeding problems in the late preterm infant. Clin Perinatol 2006;33:831-7. http://dx.doi.org/10.1016/j.clp.2006.09.003.
- Escobar GJ, Greene JD, Hulac P, Kincannon E, Bischoff K, Gardner MN, et al. Rehospitalisation after birth hospitalisation: patterns among infants of all gestations. Arch Dis Child 2005;90:125-31. http://dx.doi.org/10.1136/adc.2003.039974.
- Oddie SJ, Hammal D, Richmond S, Parker L. Early discharge and readmission to hospital in the first month of life in the Northern Region of the UK during 1998: a case cohort study. Arch Dis Child 2005;90:119-24. http://dx.doi.org/10.1136/adc.2003.040766.
- Escobar GJ, Clark RH, Greene JD. Short-term outcomes of infants born at 35 and 36 weeks’ gestation: we need to ask more questions. Semin Perinatol 2006;30:28-33. http://dx.doi.org/10.1053/j.semperi.2006.01.005.
- Vachharajani AJ, Dawson JG. Short-term outcomes of late preterms: an institutional experience. Clin Pediatr 2009;48:383-8. http://dx.doi.org/10.1177/0009922808324951.
- Boluyt N, van Kempen A, Offringa M. Neurodevelopment after neonatal hypoglycemia: a systematic review and design of an optimal future study. Pediatrics 2006;117:2231-43. http://dx.doi.org/10.1542/peds.2005-1919.
- Rozance PJ, Hay WW. Hypoglycemia in newborn infants: features associated with adverse outcomes. Biol Neonate 2006;90:74-86. http://dx.doi.org/10.1159/000091948.
- Garg M, Devaskar SU. Glucose metabolism in the late preterm infant. Clin Perinatol 2006;33:853-70. http://dx.doi.org/10.1016/j.clp.2006.10.001.
- Tomashek KM, Shapiro-Mendoza CK, Weiss J, Kotelchuck M, Barfield W, Evans S, et al. Early discharge among late preterm and term newborns and risk of neonatal morbidity. Semin Perinatol 2006;30:61-8. http://dx.doi.org/10.1053/j.semperi.2006.02.003.
- Kramer MS, Demissie K, Yang H, Platt RW, Sauve R, Liston R. The contribution of mild and moderate preterm birth to infant mortality. Fetal and Infant Health Study Group of the Canadian Perinatal Surveillance System. J Am Med Assoc 2000;284:843-9. http://dx.doi.org/10.1001/jama.284.7.843.
- Tomashek KM, Shapiro-Mendoza CK, Davidoff MJ, Petrini JR. Differences in mortality between late-preterm and term singleton infants in the United States, 1995–2002. J Pediatr 2007;151:450-6.
- Holmqvist P, Regefalk C, Svenningsen NW. Low risk vaginally born preterm infants: a 4 year psychological and neurodevelopmental follow-up study. J Perinat Med 1987;15:61-72. http://dx.doi.org/10.1515/jpme.1987.15.1.61.
- Huddy CL, Johnson A, Hope PL. Educational and behavioural problems in babies of 32–35 weeks’ gestation. Arch Dis Child Fetal Neonatal Ed 2001;85:F23-8. http://dx.doi.org/10.1136/fn.85.1.F23.
- Pasman JW, Rotteveel JJ, Maassen B. Neurodevelopmental profile in low-risk preterm infants at 5 years of age. Eur J Paediatr Neurol 1998;2:7-17. http://dx.doi.org/10.1016/1090-3798(98)01000-7.
- Pietz J, Peter J, Graf R, Rauterberg-Ruland I, Rupp A, Sontheimer D, et al. Physical growth and neurodevelopmental outcome of nonhandicapped low-risk children born preterm. Early Hum Dev 2004;79:131-43. http://dx.doi.org/10.1016/j.earlhumdev.2004.05.001.
- Caravale B, Tozzi C, Albino G, Vicari S. Cognitive development in low risk preterm infants at 3–4 years of life. Arch Dis Child Fetal Neonatal Ed 2005;90:F474-9. http://dx.doi.org/10.1136/adc.2004.070284.
- Cooke RJ, Ainsworth SB, Fenton AC. Postnatal growth retardation: a universal problem in preterm infants. Arch Dis Child Fetal Neonatal Ed 2004;89:F428-30. http://dx.doi.org/10.1136/adc.2001.004044.
- Clark RH, Thomas P, Peabody J. Extrauterine growth restriction remains a serious problem in prematurely born neonates. Pediatrics 2003;111:986-90. http://dx.doi.org/10.1542/peds.111.5.986.
- Blackwell MT, Eichenwald EC, McAlmon K, Petit K, Linton PT, McCormick MC, et al. Interneonatal intensive care unit variation in growth rates and feeding practices in healthy moderately premature infants. J Perinatol 2005;25:478-85. http://dx.doi.org/10.1038/sj.jp.7211302.
- Dodrill P, McMahon S, Ward E, Weir K, Donovan T, Riddle B. Long-term oral sensitivity and feeding skills of low-risk preterm infants. Early Hum Dev 2004;76:23-37. http://dx.doi.org/10.1016/j.earlhumdev.2003.10.001.
- Kirkby S, Greenspan JS, Kornhauser M, Schneiderman R. Clinical outcomes and cost of the moderately preterm infant. Adv Neonatal Care 2007;7:80-7. http://dx.doi.org/10.1097/01.ANC.0000267913.58726.f3.
- Petrou S. The economic consequences of preterm birth during the first 10 years of life. BJOG 2005;112:S10-15. http://dx.doi.org/10.1111/j.1471-0528.2005.00577.x.
- Petrou S, Mehta Z, Hockley C, Cook-Mozaffari P, Henderson J, Goldacre M. The impact of preterm birth on hospital inpatient admissions and costs during the first 5 years of life. Pediatrics 2003;112:1290-7. http://dx.doi.org/10.1542/peds.112.6.1290.
- Marlow N, Wolke D, Bracewell MA, Samara M, Group EPS. Neurologic and developmental disability at 6 years of age after extremely preterm birth. N Engl J Med 2005;352:9-19. http://dx.doi.org/10.1056/NEJMoa041367.
- Clarke M, Clayton D. The design and interpretation of case-control studies of perinatal mortality. Am J Epidemiol 1981;113:636-45.
- Draper ES, Kurinczuk JJ, Abrams KR, Clarke M. Assessment of separate contributions to perinatal mortality of infertility history and treatment: a case-control analysis. Lancet 1999;353:1746-9. http://dx.doi.org/10.1016/S0140-6736(98)08500-6.
- Rothman KJ. No adjustments are needed for multiple comparisons. Epidemiology 1990;1:43-6. http://dx.doi.org/10.1097/00001648-199001000-00010.
- McNutt LA, Wu C, Xue X, Hafner JP. Estimating the relative risk in cohort studies and clinical trials of common outcomes. Am J Epidemiol 2003;157:940-3. http://dx.doi.org/10.1093/aje/kwg074.
- Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol 2004;159:702-6. http://dx.doi.org/10.1093/aje/kwh090.
- Deeks J. When can odds ratios mislead? Odds ratios should be used only in case-control studies and logistic regression analyses. BMJ 1998;317:1155-6. http://dx.doi.org/10.1136/bmj.317.7166.1155a.
- Standard Occupational Classification 2010: Volume 3 The National Statistics Socio-economic Classification User Manual. London: Palgrave Macmillan; 2010.
- Khatibi A, Brantsaeter AL, Sengpiel V, Kacerovsky M, Magnus P, Morken NH, et al. Prepregnancy maternal body mass index and preterm delivery. Am J Obstet Gynecol 2012;207. http://dx.doi.org/10.1016/j.ajog.2012.06.002.
- Carter MF, Fowler S, Holden A, Xenakis E, Dudley D. The late preterm birth rate and its association with comorbidities in a population-based study. Am J Perinatol 2011;28:703-7. http://dx.doi.org/10.1055/s-0031-1280592.
- Catalano PM, Sacks DA. Timing of indicated late preterm and early-term birth in chronic medical complications: diabetes. Semin Perinatol 2011;35:297-301. http://dx.doi.org/10.1053/j.semperi.2011.05.003.
- Kase BA, Carreno CA, Blackwell SC, Sibai BM. The impact of medically indicated and spontaneous preterm birth among hypertensive women. Am J Perinatol 2013;30:843-8. http://dx.doi.org/10.1055/s-0033-1333676.
- Lim JJ, Allen VM, Scott HM, Allen AC. Late preterm delivery in women with preterm prelabour rupture of membranes. J Obstet Gynaecol Can 2010;32:555-60.
- Laughon SK, Reddy UM, Sun L, Zhang J. Precursors for late preterm birth in singleton gestations. Obstet Gynaecol 2010;116:1047-55. http://dx.doi.org/10.1097/AOG.0b013e3181f73f97.
- van der Ham DP, van der Heyden JL, Opmeer BC, Mulder AL, Moonen RM, van Beek JH, et al. Management of late-preterm premature rupture of membranes: the PPROMEXIL-2 trial. Am J Obstet Gynecol 2012;207. http://dx.doi.org/10.1016/j.ajog.2012.07.024.
- Koopmans CM, Bijlenga D, Groen H, Vijgen SM, Aarnoudse JG, Bekedam DJ, et al. Induction of labour versus expectant monitoring for gestational hypertension or mild pre-eclampsia after 36 weeks’ gestation (HYPITAT): a multicentre, open-label randomised controlled trial. Lancet 2009;374:979-88. http://dx.doi.org/10.1016/S0140-6736(09)60736-4.
- Barton JR, Barton LA, Istwan NB, Desch CN, Rhea DJ, Stanziano GJ, et al. Elective delivery at 34(0/7) to 36(6/7) weeks’ gestation and its impact on neonatal outcomes in women with stable mild gestational hypertension. Am J Obstet Gynecol 2011;204.
- Kunzel W, Misselwitz B. Unexpected fetal death during pregnancy--a problem of unrecognized fetal disorders during antenatal care?. Eur J Obstet Gynecol Reprod Biol 2003;110:S86-92. http://dx.doi.org/10.1016/S0301-2115(03)00177-5.
- McLennan D, Barnes H, Noble M, Davies J, Garratt E, Dibben C. The English Indices of Deprivation 2010. London: Department for Communities and Local Government; 2011.
- Chiavarini M, Bartolucci F, Gili A, Pieroni L, Minelli L. Effects of individual and social factors on preterm birth and low birth weight: empirical evidence from regional data in Italy. Int J Public Health 2012;57:261-8. http://dx.doi.org/10.1007/s00038-011-0311-3.
- DeFranco EA, Lian M, Muglia LA, Schootman M. Area-level poverty and preterm birth risk: a population-based multilevel analysis. BMC Public Health 2008;8. http://dx.doi.org/10.1186/1471-2458-8-316.
- Auger N, Roncarolo F, Harper S. Increasing educational inequality in preterm birth in Québec, Canada, 1981–2006. J Epidemiol Community Health 2011;65:1091-6. http://dx.doi.org/10.1136/jech.2009.102350.
- Morgen CS, Bjork C, Andersen PK, Mortensen LH, Nybo Andersen AM. Socioeconomic position and the risk of preterm birth – a study within the Danish National Birth Cohort. Int J Epidemiol 2008;37:1109-20. http://dx.doi.org/10.1093/ije/dyn112.
- Raisanen S, Gissler M, Saari J, Kramer M, Heinonen S. Contribution of risk factors to extremely, very and moderately preterm births – register-based analysis of 1,390,742 singleton births. PLOS ONE 2013;8. http://dx.doi.org/10.1371/journal.pone.0060660.
- McIntire DD, Leveno KJ. Neonatal mortality and morbidity rates in late preterm births compared with births at term. Obstet Gynaecol 2008;111:35-41. http://dx.doi.org/10.1097/01.AOG.0000297311.33046.73.
- Cheng YW, Kaimal AJ, Bruckner TA, Halloran DR, Caughey AB. Perinatal morbidity associated with late preterm deliveries compared with deliveries between 37 and 40 weeks of gestation. BJOG 2011;118:1446-54. http://dx.doi.org/10.1111/j.1471-0528.2011.03045.x.
- Hibbard JU, Wilkins I, Sun L, Gregory K, Haberman S, . Consortium on Safe Labor . Respiratory morbidity in late preterm births. J Am Med Assoc 2010;304:419-25. http://dx.doi.org/10.1001/jama.2010.1015.
- Picone S, Paolillo P. Neonatal outcomes in a population of late-preterm infants. J Matern Fetal Neonatal Med 2010;23:S116-20. http://dx.doi.org/10.3109/14767058.2010.509921.
- Weng YH, Chiu YW, Cheng SW, Hsieh MY. Risk assessment for adverse outcome in term and late preterm neonates with bilirubin values of 20 mg/dL or more. Am J Perinatol 2011;28:405-12. http://dx.doi.org/10.1055/s-0031-1274506.
- Bastek JA, Sammel MD, Rebele EC, Srinivas SK, Elovitz MA. The effects of a preterm labor episode prior to 34 weeks are evident in late preterm outcomes, despite the administration of betamethasone. Am J Obstet Gynecol 2010;203. http://dx.doi.org/10.1016/j.ajog.2010.02.065.
- Cohen-Wolkowiez M, Moran C, Benjamin DK, Cotten CM, Clark RH, Benjamin DK, et al. Early and late onset sepsis in late preterm infants. Pediatr Infect Dis J 2009;28:1052-6. http://dx.doi.org/10.1097/INF.0b013e3181acf6bd.
- Colin AA, McEvoy C, Castile RG. Respiratory morbidity and lung function in preterm infants of 32 to 36 weeks’ gestational age. Pediatrics 2010;126:115-28. http://dx.doi.org/10.1542/peds.2009-1381.
- Kerstjens JM, Bocca-Tjeertes IF, de Winter AF, Reijneveld SA, Bos AF. Neonatal morbidities and developmental delay in moderately preterm-born children. Pediatrics 2012;130:e265-72. http://dx.doi.org/10.1542/peds.2012-0079.
- Khashu M, Narayanan M, Bhargava S, Osiovich H. Perinatal outcomes associated with preterm birth at 33 to 36 weeks’ gestation: a population-based cohort study. Pediatrics 2009;123:109-13. http://dx.doi.org/10.1542/peds.2007-3743.
- Kitsommart R, Janes M, Mahajan V, Rahman A, Seidlitz W, Wilson J, et al. Outcomes of late-preterm infants: a retrospective, single-center, Canadian study. Clin Pediatr 2009;48:844-50. http://dx.doi.org/10.1177/0009922809340432.
- Saigal S, Doyle LW. An overview of mortality and sequelae of preterm birth from infancy to adulthood. Lancet 2008;371:261-9. http://dx.doi.org/10.1016/S0140-6736(08)60136-1.
- Johnson S. Cognitive and behavioural outcomes following very preterm birth. Semin Fetal Neonatal Med 2007;12:363-73. http://dx.doi.org/10.1016/j.siny.2007.05.004.
- Johnson S, Wolke D. Behavioural outcomes and psychopathology during adolescence. Early Hum Dev 2013;89:199-207. http://dx.doi.org/10.1016/j.earlhumdev.2013.01.014.
- Boyle EM, Poulsen G, Field DJ, Kurinczuk JJ, Wolke D, Alfirevic Z, et al. Effects of gestational age at birth on health outcomes at 3 and 5 years: population based cohort study. BMJ 2012;344. http://dx.doi.org/10.1136/bmj.e896.
- Quigley MA, Poulsen G, Boyle E, Wolke D, Field D, Alfrievic Z, et al. Early term and late preterm birth are associated with poorer school performance at age 5 years: a cohort study. Arch Dis Child Fetal Neonatal Ed 2012;97:F167-73. http://dx.doi.org/10.1136/archdischild-2011-300888.
- de Jong M, Verhoeven M, van Baar AL. School outcome, cognitive functioning, and behaviour problems in moderate and late preterm children and adults: a review. Semin Fetal Neonatal Med 2012;17:163-9. http://dx.doi.org/10.1016/j.siny.2012.02.003.
- Loe IM, Lee ES, Luna B, Feldman HM. Behavior problems of 9–16 year old preterm children: biological, sociodemographic, and intellectual contributions. Early Hum Dev 2011;87:247-52. http://dx.doi.org/10.1016/j.earlhumdev.2011.01.023.
- Gurka MJ, LoCasale-Crouch J, Blackman JA. Long-term cognition, achievement, socioemotional, and behavioral development of healthy late-preterm infants. Arch Pediatr Adolesc Med 2010;164:525-32. http://dx.doi.org/10.1001/archpediatrics.2010.83.
- Report of a BAPM/RCPCH Working Group: Classification of Health Status at 2 Years as a Perinatal Outcome. London: BAPM; 2008.
- Johnson S, Marlow N, Wolke D, Davidson L, Marston L, O’Hare A, et al. Validation of a parent report measure of cognitive development in very preterm infants. Dev Med Child Neurol 2004;46:389-97. http://dx.doi.org/10.1017/S0012162204000635.
- Johnson S, Wolke D, Marlow N. Developmental assessment of preterm infants at 2 years: validity of parent reports. Dev Med Child Neurol 2008;50:58-62. http://dx.doi.org/10.1111/j.1469-8749.2007.02010.x.
- Briggs-Gowan MJ, Carter AS. Brief Infant-Toddler Social and Emotional Assessment. San Antonio, TX: Harcourt Assessment Inc.; 2006.
- Briggs-Gowan MJ, Carter AS. Social-emotional screening status in early childhood predicts elementary school outcomes. Pediatrics 2008;121:957-62. http://dx.doi.org/10.1542/peds.2007-1948.
- EuroQol Group . EuroQol – a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199-208. http://dx.doi.org/10.1016/0168-8510(90)90421-9.
- Johnson S, Fawke J, Hennessy E, Rowell V, Thomas S, Wolke D, et al. Neurodevelopmental disability through 11 years of age in children born before 26 weeks of gestation. Pediatrics 2009;124:e249-57. http://dx.doi.org/10.1542/peds.2008-3743.
- Tin W, Fritz S, Wariyar U, Hey E. Outcome of very preterm birth: children reviewed with ease at 2 years differ from those followed up with difficulty. Arch Dis Child Fetal Neonatal Ed 1998;79:F83-7. http://dx.doi.org/10.1136/fn.79.2.F83.
- Kotecha SJ, Watkins WJ, Paranjothy S, Dunstan FD, Henderson AJ, Kotecha S. Effect of late preterm birth on longitudinal lung spirometry in school age children and adolescents. Thorax 2012;67:54-61. http://dx.doi.org/10.1136/thoraxjnl-2011-200329.
- Moore T, Hennessy EM, Myles J, Johnson SJ, Draper ES, Costeloe KL, et al. Neurological and developmental outcome in extremely preterm children born in England in 1995 and 2006: the EPICure studies. BMJ 2012;345. http://dx.doi.org/10.1136/bmj.e7961.
- Boyle JD, Boyle EM. Born just a few weeks early: does it matter?. Arch Dis Child Fetal Neonatal Ed 2013;98:F85-8. http://dx.doi.org/10.1136/archdischild-2011-300535.
- Feinstein L, Duckworth K. Development in the Early Years: Its Importance for School Performance and Adult Outcomes. London: Centre for Research on the Wider Benefits of Learning, Institute of Education, University of London; 2006.
- Johnson S, Hennessy E, Smith R, Trikic R, Wolke D, Marlow N. Academic attainment and special educational needs in extremely preterm children at 11 years of age: the EPICure study. Arch Dis Child Fetal Neonatal Ed 2009;94:F283-9. http://dx.doi.org/10.1136/adc.2008.152793.
- Mathiasen R, Hansen BM, Andersen AM, Forman JL, Greisen G. Gestational age and basic school achievements: a national follow-up study in Denmark. Pediatrics 2010;126:e1553-61. http://dx.doi.org/10.1542/peds.2009-0829.
- Spittle AJ, Orton J, Doyle LW, Boyd R. Cochrane review: early developmental intervention programs post hospital discharge to prevent motor and cognitive impairments in preterm infants. Evid Based Child Health 2008;3:145-206. http://dx.doi.org/10.1002/ebch.209.
- McCarton CM, Brooks-Gunn J, Wallace IF, Bauer CR, Bennett FC, Bernbaum JC, et al. Results at age 8 years of early intervention for low-birthweight premature infants. The Infant Health and Development Program. J Am Med Assoc 1997;277:126-32. http://dx.doi.org/10.1001/jama.1997.03540260040033.
- McCormick MC, Brooks-Gunn J, Buka SL, Goldman J, Yu J, Salganik M, et al. Early intervention in low birth weight premature infants: results at 18 years of age for the Infant Health and Development Program. Pediatrics 2006;117:771-80. http://dx.doi.org/10.1542/peds.2005-1316.
- McCormick MC, McCarton C, Brooks-Gunn J, Belt P, Gross RT. The Infant Health and Development Program: interim summary. J Dev Behav Pediatr 1998;19:359-70. http://dx.doi.org/10.1097/00004703-199810000-00009.
- Brooks-Gunn J, Liaw FR, Klebanov PK. Effects of early intervention on cognitive function of low birth weight preterm infants. J Pediatr 1992;120:350-9. http://dx.doi.org/10.1016/S0022-3476(05)80896-0.
- Olds DL, Holmberg JR, Donelan-McCall N, Luckey DW, Knudtson MD, Robinson J. Effects of home visits by paraprofessionals and by nurses on children: follow-up of a randomized trial at ages 6 and 9 years. JAMA Pediatr 2013;168:114-21. http://dx.doi.org/10.1001/jamapediatrics.2013.3817.
- Odd DE, Emond A, Whitelaw A. Long-term cognitive outcomes of infants born moderately and late preterm. Dev Med Child Neurol 2012;54:704-9. http://dx.doi.org/10.1111/j.1469-8749.2012.04315.x.
- Talge NM, Holzman C, Wang J, Lucia V, Gardiner J, Breslau N. Late-preterm birth and its association with cognitive and socioemotional outcomes at 6 years of age. Pediatrics 2010;126:1124-31. http://dx.doi.org/10.1542/peds.2010-1536.
- Anderson JW, Johnstone BM, Remley DT. Breast-feeding and cognitive development: a meta-analysis. Am J Clin Nutr 1999;70:525-35.
- Heikkila K, Sacker A, Kelly Y, Renfrew MJ, Quigley MA. Breast feeding and child behaviour in the Millennium Cohort Study. Arch Dis Child 2011;96:635-42. http://dx.doi.org/10.1136/adc.2010.201970.
- Johnson S, Marlow N. Preterm birth and childhood psychiatric disorders. Pediatr Res 2011;69:11R-8R. http://dx.doi.org/10.1203/PDR.0b013e318212faa0.
- Clark CA, Woodward LJ, Horwood LJ, Moor S. Development of emotional and behavioral regulation in children born extremely preterm and very preterm: biological and social influences. Child Dev 2008;79:1444-62. http://dx.doi.org/10.1111/j.1467-8624.2008.01198.x.
- Elgen SK, Leversen KT, Grundt JH, Hurum J, Sundby AB, Elgen IB, et al. Mental health at 5 years among children born extremely preterm: a national population-based study. Eur Child Adolesc Psychiatry 2012;21:583-9. http://dx.doi.org/10.1007/s00787-012-0298-1.
- Scott MN, Taylor HG, Fristad MA, Klein N, Espy KA, Minich N, et al. Behavior disorders in extremely preterm/extremely low birth weight children in kindergarten. J Dev Behav Pediatr 2012;33:202-13. http://dx.doi.org/10.1097/DBP.0b013e3182475287.
- Treyvaud K, Doyle LW, Lee KJ, Roberts G, Lim J, Inder TE, et al. Social-emotional difficulties in very preterm and term 2 year olds predict specific social-emotional problems at the age of 5 years. J Pediatr Psychol 2012;37:779-85. http://dx.doi.org/10.1093/jpepsy/jss042.
- Woodward LJ, Moor S, Hood KM, Champion PR, Foster-Cohen S, Inder TE, et al. Very preterm children show impairments across multiple neurodevelopmental domains by age 4 years. Arch Dis Child Fetal Neonatal Ed 2009;94:F339-44. http://dx.doi.org/10.1136/adc.2008.146282.
- Treyvaud K, Ure A, Doyle LW, Lee KJ, Rogers CE, Kidokoro H, et al. Psychiatric outcomes at age seven for very preterm children: rates and predictors. J Child Psychol Psychiatry 2013;54:772-9. http://dx.doi.org/10.1111/jcpp.12040.
- Laucht M, Esser G, Baving L, Gerhold M, Hoesch I, Ihle W, et al. Behavioral sequelae of perinatal insults and early family adversity at 8 years of age. J Am Acad Child Adolesc Psychiatry 2000;39:1229-37. http://dx.doi.org/10.1097/00004583-200010000-00009.
- Curtis L. Unit Costs of Health and Social Care 2012. Canterbury: PSSRU, University of Kent; 2012.
- NHS Reference Costs 2010–2011. Appendix 1 NHS Trusts Reference Costs. London: DH; 2011.
- Schroeder E, Petrou S, Patel N, Hollowell J, Puddicombe D, Redshaw M, et al. Cost effectiveness of alternative planned places of birth in woman at low risk of complications: evidence from the Birthplace in England national prospective cohort study. BMJ 2012;344. http://dx.doi.org/10.1136/bmj.e2292.
- Birthplace in England Collaborative Group . Perinatal and maternal outcomes by planned place of birth for healthy women with low risk pregnancies: the Birthplace in England national prospective cohort. BMJ 2011;343. http://dx.doi.org/10.1136/bmj.d7400.
- BNF for Children 2013–2014. London: BMJ Group, Pharmaceutical Press, and RCPCH Publications; 2013.
- The WHO Growth Standards. Geneva: WHO; 2009.
- Annual Survey of Hours and Earnings. ONS; 2012.
- House of Commons Daily Hansard . NHS Direct: Operating Costs n.d. www.publications.parliament.uk/pa/cm200708/cmhansrd/cm081021/text/81021w0033.htm#08102160000093 (accessed 1 December 2013).
- Health and Social Care Information Centre . Prescription Cost Analysis – England, 2011 n.d. www.hscic.gov.uk/pubs/prescostanalysis2011 (accessed 1 December 2013).
- Guide to the Methods of Technology Appraisal. London: NICE; 2008.
- McCullagh P, Nelder JA. Generalized Linear Models. London: Chapman & Hall; 1989.
- Akaike H, Petrov BN, Caski F. Proceedings of the Second International Symposium on Information Theory. Budapest: Akadémiai Kiadó; 1973.
- Manning WG, Mullahy J. Estimating log models: to transform or not to transform?. J Health Econ 2001;20:461-94. http://dx.doi.org/10.1016/S0167-6296(01)00086-8.
- Gardosi J. Customised assessment of fetal growth potential: implications for perinatal care. Arch Dis Child Fetal Neonatal Ed 2012;97:F314-7. http://dx.doi.org/10.1136/fetalneonatal-2012-301708.
- Noble M, McLennan D, Wilkinson K, Whitworth A, Barnes H, Dibben C. The English Indices of Deprivation 2007. London: Communities and Local Government; 2008.
- Baser O, Gardiner JC, Bradley CJ, Yuce H, Given C. Longitudinal analysis of censored medical cost data. Health Econ 2006;15:513-25. http://dx.doi.org/10.1002/hec.1087.
- Baser OGJ, Bradley CJ, Given CW. Estimation from censored medical cost data. Biom J 2004;46:351-63. http://dx.doi.org/10.1002/bimj.200210036.
- Petrou S, Khan K. Economic costs associated with moderate and late preterm birth: primary and secondary evidence. Semin Fetal Neonatal Med 2012;17:170-8. http://dx.doi.org/10.1016/j.siny.2012.02.001.
- Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. BMJ 2013;346. http://dx.doi.org/10.1136/bmj.f1049.
- Petrou S, Eddama O, Mangham L. A structured review of the recent literature on the economic consequences of preterm birth. Arch Dis Child Fetal Neonatal Ed 2011;96:F225-32. http://dx.doi.org/10.1136/adc.2009.161117.
- Smith LK, Draper ES, Field D. Long-term outcome for the tiniest or most immature babies: survival rates. Semin Fetal Neonatal Med 2013;19:72-7. http://dx.doi.org/10.1016/j.siny.2013.11.002.
- Rattihalli R, Smith L, Field D. Prevention of preterm births: are we looking in the wrong place? The case for primary prevention. Arch Dis Child Fetal Neonatal Ed 2012;97:F160-1. http://dx.doi.org/10.1136/archdischild-2011-301096.
- Boyle E, Johnson S, Draper ES, Manktelow B, Seaton S, Smith LK, et al. Population-Based Prospective Study of Babies Born at 32–36 Weeks of Gestation: Neonatal Outcomes of Singleton Births From the Late And Moderate Preterm Birth Study (LAMBS) n.d.
- Boyle E, Johnson S, Draper ES, Manktelow B, Seaton S, Smith LK, et al. Neonatal Outcomes of Singletons and Twins Born at 32–36 Weeks of Gestation: Results from the Late And Moderate Preterm Birth Study (LAMBS) n.d.
- Boyle EM, Johnson S, Draper ES, Manktelow B, Seaton S, Dorling J, et al. A prospective population-based study of birth at 32–36 weeks’ gestation: neonatal outcomes from the Late and Moderate Preterm Birth Study (LAMBS). Pediatr Res 2011;70. http://dx.doi.org/10.1038/pr.2011.529.
- Boyle EM, Johnson S, Draper ES, Manktelow B, Seaton S, Smith LK, et al. Neonatal Outcomes Following Birth at 32–36 Weeks’ Gestation: The Late And Moderate Preterm Birth Study (LAMBS) n.d.
- Strelitz J. The Economic Case for a Shift to Prevention n.d. https://gov.uk/government/uploads/system/uploads/attachment_data/file/252653/33571_2901304_CMO_Chapter_3.pdf (accessed 27 October 2015).
- Khan KA, Petrou S, Dritsaki M, Johnson SJ, Manktelow B, Draper ES, et al. Economic costs associated with moderate and late preterm birth: a prospective population-based study. BJOG 2015;122:1495-505.
Appendix 1 The Late And Moderately preterm Birth Study maternal interview
Appendix 2 The Late And Moderately preterm Birth Study 6-month questionnaire
Appendix 3 The Late And Moderately preterm Birth Study 12-month questionnaire
Appendix 4 The Late And Moderately preterm Birth Study obstetric data collection form
Appendix 5 The Late And Moderately preterm Birth Study neonatal data collection form
Glossary
- Antenatal detection
- Identification of a congenital anomaly prior to birth.
- Antenatal soft marker
- Ultrasound findings that are indicative of an increased risk of an underlying fetal anomaly.
- Early neonatal death
- The death of a live-born infant before 7 completed days of life.
- Fetal loss
- Death before 24 weeks’ gestation (late fetal loss refers to births at 22 and 23 weeks’ gestation).
- Infant death
- Death of a live-born infant before 1 year of life.
- Late and moderately preterm
- Birth between 32 and 36 weeks’ gestation.
- Late neonatal death
- Death of a live-born infant between 7 and 28 days of life.
- Lower super output area
- A census-based geographical area relating to approximately 1500 residents.
- Neonatal death
- Death of a live-born infant before 28 completed days of life.
- Neurodevelopment disability
- A moderate to severe impairment of communication, visual, hearing, neuromotor or cognitive function.
- Neurosensory impairment
- A moderate to severe impairment of communication, visual, hearing or neuromotor function.
- Perinatal death
- A stillbirth or early neonatal death.
- Postneonatal death
- Death of a live-born infant after 28 days and before 1 year of life.
- Stillbirth
- Death after 24 weeks’ gestation.
List of abbreviations
- 2Y-CA
- 2 years corrected age
- AIC
- Akaike information criterion
- A level
- advanced level
- ANS
- antenatal corticosteroid
- ART
- assisted reproductive technique
- BITSEA
- Brief Infant and Toddler Social–Emotional Assessment
- BMI
- body mass index
- BNFC
- British National Formulary for Children
- CI
- confidence interval
- CMACE
- Centre for Maternal and Child Enquiries
- CMO
- Chief Medical Officer
- CP
- cerebral palsy
- CRP
- C-reactive protein
- CS
- caesarean section
- CTG
- cardiotocography
- CVS
- chorionic villous sampling
- EEG
- electroencephalography
- EMSYCAR
- East Midlands and South Yorkshire Congenital Anomaly Register
- EQ-5D
- European Quality of Life-5 Dimensions
- FASP
- Fetal Anomaly Screening Programme
- FGR
- fetal growth restriction
- GCSE
- General Certificate of Secondary Education
- GLM
- generalised linear model
- GP
- general practitioner
- GROW
- Gestation Related Optimal Weight software
- HRG
- Healthcare Resource Group
- ICD-10
- International Classification of Diseases, Tenth Edition
- IHDP
- Infant Health and Development Program
- IMD
- Index of Multiple Deprivation
- IPPV
- intermittent positive-pressure ventilation
- IQR
- interquartile range
- i.v.
- intravenous
- IVH
- intraventricular haemorrhage
- LAMBS
- Late And Moderately preterm Birth Study
- LMPT
- late and moderately preterm
- LSOA
- lower super output area
- MNI-CORP
- maternal, neonatal and infant (mortality and morbidity) clinical outcome review programme
- MRI
- magnetic resonance imaging
- NGT
- nasogastric tube
- NIHR
- National Institute for Health Research
- NN4B
- NHS Numbers for Babies project
- NNU
- neonatal unit
- NSI
- neurosensory impairment
- NS-SEC
- National Statistics Socio-economic Classification
- NVC
- non-verbal cognition
- OLS
- ordinary least squares
- ONS
- Office for National Statistics
- OR
- odds ratio
- PARCA-R
- Parent Report of Children’s Abilities – Revised
- PCT
- primary care trust
- PN
- parenteral nutrition
- PPI
- patient and public involvement
- PRC
- parent report composite score
- PROM
- prolonged rupture of membranes
- PSS
- Personal Social Services
- REC
- Research Ethics Committee
- RfPB
- Research for Patient Benefit
- RR
- relative risk
- SANDS
- Stillbirth and Neonatal Death Society
- SBR
- serum bilirubin
- SD
- standard deviation
- SE
- standard error
- SES Index
- Socioeconomic Risk Index
- SGA
- small for gestational age
- WHO
- World Health Organization