Notes
Article history
The research reported in this issue of the journal was funded by PGfAR as project number RP-PG-0606-1335. The contractual start date was in August 2007. The final report began editorial review in April 2015 and was accepted for publication in December 2015. As the funder, the PGfAR programme agreed the research questions and study designs in advance with the investigators. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PGfAR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by Perez et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
SYNOPSIS
Setting the scene
Psychotic illnesses such as schizophrenia and related conditions are a major concern for individuals, for society and for the NHS; they cause enormous disability and are expensive to treat. Developments in interventions have been slow. We have a clearer picture of the role of psychological therapies but the relative benefits of newer, expensive antipsychotic drugs remain uncertain. 1 However, services to deliver these interventions have changed over the last decade. For example, seminal work from around the world has led to the widespread adoption in the UK of crisis resolution and home treatment services for people with enduring mental illness such as schizophrenia, as set out in the NHS Plan. 2 In addition, a simple but radical idea concerning early-intervention services (EISs) and the evolution of psychosis through at-risk mental states has shaped service developments. Work by our research team and others has shown early developmental antecedents to psychosis. 3 As the illness becomes manifest, non-specific signs such as anxiety and depression develop and short-lived individual psychotic features form a prodrome to the full psychotic syndrome that may endure for months or even years before people seek help or receive treatment. This duration of untreated psychosis (DUP) is inversely related to outcome. Treatment in the prodrome (shortening DUP) may prevent the development of severe illness, improve outcome and lead to recovery in many cases. 4
In addition to our disease focus on psychosis, this programme aimed to address a strategic issue for applied research and development (R&D) in the NHS. Although considerable amounts of clinical and social information data are processed daily within NHS and social care services, this information is disconnected from research so that it cannot be used to answer strategic questions. Many R&D developments are making important progress, but we wanted this programme to advance knowledge and understanding further by providing tools and a blueprint for connecting information, clinicians and patients in the search for the best services and interventions.
The problem we decided to tackle is cultural as well as structural.
Importance and relevance of the programme
Evidence for early intervention
At the time that our programme application was submitted the evidence base for EISs was emerging but was far from conclusive and, as ever, models successful in one area may not be suitable for another. Nevertheless, a clear blueprint was contained in the NHS Mental Health Policy Implementation Guide5 and recent years have seen the rapid development of EISs across England for young adults aged 14–35 years; hence, individual-level randomised controlled trials (RCTs) of the effectiveness of early intervention are unlikely to be possible in England.
Epidemiology of high risk for psychosis
However, it was still not clear how early we should intervene as the natural history or epidemiology of individuals at high risk (HR) for psychosis was unspecified. As we began to appreciate the huge variability in the incidence of psychotic illness across different areas and communities in the UK,6 it became clear that EIS planning was significantly hindered, with the likelihood of serious mistakes from over- and underprovision because the demand was not clear. EISs in some cities are overwhelmed whereas those in affluent suburban areas have capacity to spare.
The evidence–policy–practice gap
Identification of HR individuals was difficult and unfamiliar for staff in health and social care settings, let alone in education and other arenas where more applied research was required. We knew little about the causes of psychosis in individuals and could not fully explain the major variations in risk between regions. We aimed to close these gaps with this programme of applied epidemiological and observational research and a simple application of the cluster randomised controlled trial (cRCT) design (see Work package 3).
In addition to having been involved in independently funded trials of psychosocial interventions aimed at earlier intervention,7 we had shown in our service that many people at an early stage of their psychotic illness have major cognitive problems that may underpin disability and be a realistic target for new interventions. 3 They also contribute to problems in functional outcome that are regarded by service users as more important than the symptoms and phenomena that professionals focus on. This functional recovery is what is important to people with psychosis, and we aimed to develop simple, patient-focused measures that could be used in everyday practice.
Unmet needs
There were gaps between the policy blueprint for EISs and existing evidence bases in epidemiology and prognosis. Furthermore, we highlighted the overarching gap between clinical practice and routine applied research.
We intended to exploit both the natural variance in our trust catchment area (Cambridgeshire and Peterborough), which covers an enormous range of demographic, social and environmental characteristics, and the planned and unplanned variation in service developments over time. With the help of recently developed statistical models for observational data we planned to build causal inferences from our observations.
We have an EIS called CAMEO [see www.cameo.nhs.uk (accessed 18 January 2016)] that includes two sister teams serving Cambridge and South Cambridgeshire, the deprived rural Fenland areas, prosperous market towns and the deprived inner-city areas of Peterborough. Our social and service variations give us sufficient capacity traction to ask, and answer, relevant questions.
By developing work from previous epidemiological and health services research studies, current descriptive research and work in our flagship EIS, CAMEO, we aimed to develop a programme of rolling observational studies and comparisons that could indicate what works and what does not work, and where a more formal RCT is needed (see Work package 3 and Work package 5). We were fully aware of the strengths and weaknesses of observational designs and considered them as complementary methods to randomised designs to address relevant questions, funded through appropriate schemes. However, we included one cluster randomised element in this programme to tell us more about HR individuals and how to detect them (see Work package 4).
Innovation
One problem with HR mental states, despite their topicality, is that we knew little (nothing) about their epidemiology. Therefore, planning services was difficult. Population-based studies suggest that individual psychotic symptoms are common in young adults. 8 However, few people appear particularly disabled by a single symptom and, although they are linked with later development of psychotic illness, the vast majority of sufferers do not seek help; we do not know how these responses are related to illness. We needed to establish the epidemiology of early psychosis through case definitions such as, but not restricted to, HR, to foster appropriate help seeking and referrals.
Later in the illness it is clear that the incidence of diagnosable psychotic disorders varies hugely in terms of age, sex, ethnic mix and social geography of local communities. We had already shown marked heterogeneity in incidence according to age, sex, ethnicity and place in the three-centre Aetiology and Ethnicity in Schizophrenia and Other Psychoses (ÆSOP) study. 6 This has huge implications for EIS planners, for resource allocation decisions and for understanding where, when and why people become unwell. However, these findings are yet to be applied in a way that makes them immediately relevant to other places in the UK. Therefore, we investigated this in our diverse population and produced a service planning tool for the NHS to use nationwide (see Work package 3).
Original aims, objectives and outputs and eventual achievements
Our primary aim was to improve the identification, diagnosis and outcome of emerging and incident psychotic illness through a programme of research applied to service developments in our mental health trust. A secondary aim was to establish a system for applied R&D embedded in NHS services.
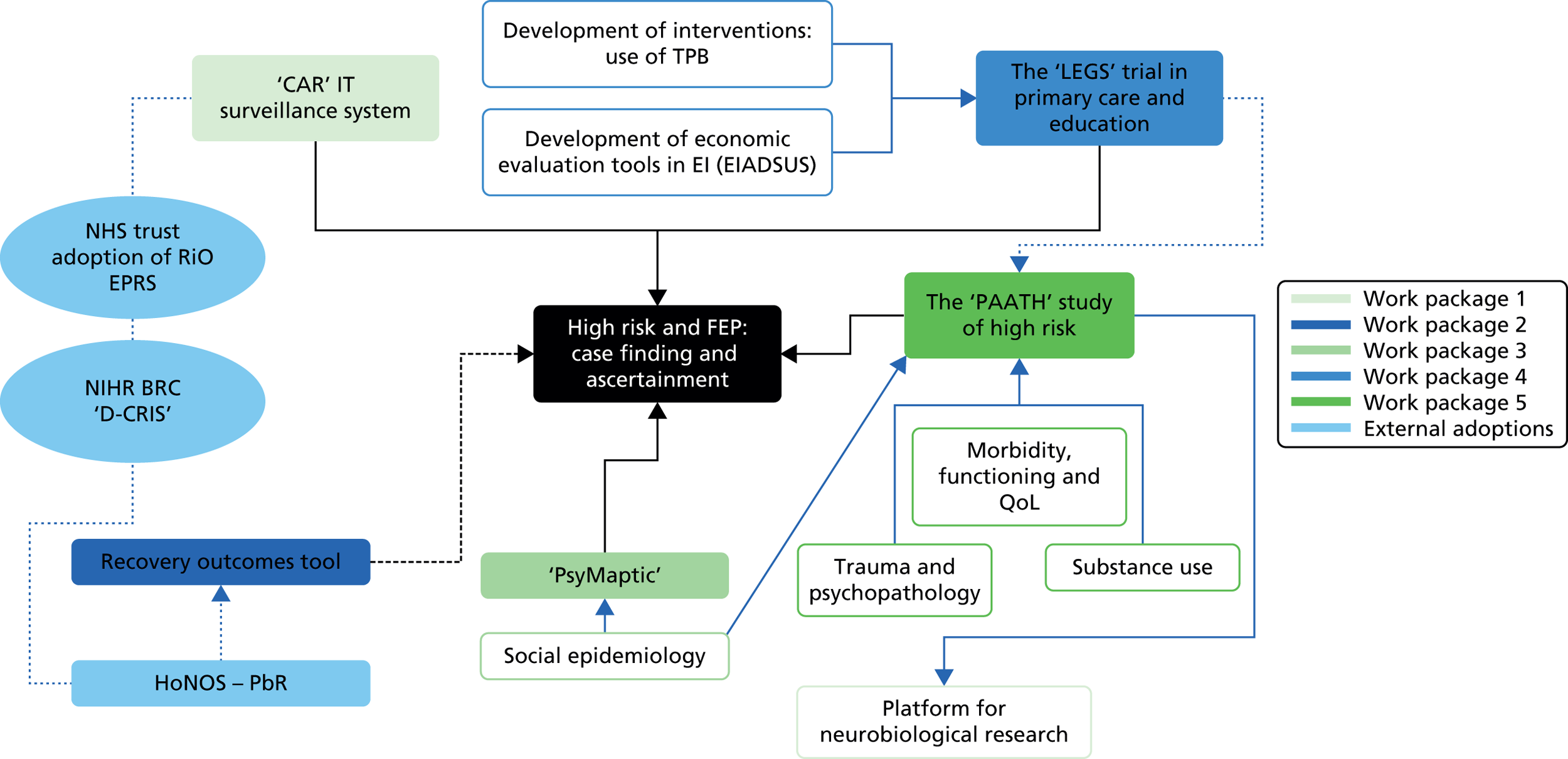
We consider that we achieved both of these aims in broad terms through a series of inter-related work packages (Figure 1), including the results of our cRCT on the identification and diagnosis of psychosis in primary care already informing NHS England commissioning guidance (see Work package 4); clinical studies on people with clinical HR mental states, function and quality of life (see Work package 5); a tool to predict the incidence of psychosis in geographical areas also informing front-line commissioning (see Work package 3); and evidence of successful embedding of researchers in clinical teams.
FIGURE 1.
Diagram depicting the whole programme and its inter-relationships. BRC, Biomedical Research Centre; CAR, Client Assessment Register; CRIS, Clinical Record Interactive Search; D-CRIS, Clinical Record Interactive Search (Collaboration Programme); EI, early intervention; EIADSUS, Early Intervention Adult Services Use Schedule; FEP, first-episode psychosis; HoNOS-PbR, Health of the Nation Outcome Scales – payment by results; IT, information technology; LEGS, Liaison with Education and General practiceS; NIHR, National Institute for Health Research; PAATH, Prospective Analysis of At-risk mental states and Transitions into psycHosis; QoL, quality of life; RiO EPRS, RiO electronic patient record system; TPB, theory of planned behaviour. The neurobiological research associated with this programme was funded by the Medical Research Council and the Wellcome Trust.
These successes are evidenced by our outputs for the objectives we set ourselves to achieve our aims. These are outlined below in advance of our fuller description of each work package, but here we also note where the objectives of our original programme were unsuccessful:
-
To define the incidence and social epidemiology of psychotic disorders and those at HR for psychosis in Cambridgeshire and Peterborough and establish cohorts for research that will allow us to understand causes and target services.
Overall, this objective was achieved successfully in work package 3 (see Work package 3), with impact beyond Cambridgeshire and Peterborough to the national level. Research into the social and macrolevel environmental risk factors for first-episode psychosis (FEP) (see Appendices 1 and 2) led to the development of the PsyMaptic prediction tool [see www.psymaptic.org/ (accessed 18 January 2016) and Appendix 3], already in use by commissioners and incorporated into the NHS England commissioning guidance for EISs published in 2015. 9 In terms of causes of psychosis at this level, the work has defined and used the differences in incidence of psychosis in different localities such as population density and proportion of people in a community from black and minority ethnic groups, as well as other factors. Thus, the programme has informed national efforts to target EISs at a local level. This spatial epidemiology was extended to HR for the first time (see Appendix 4).
The case ascertainment and assessment processes that we embedded within the NHS EIS, CAMEO, to underpin this epidemiological programme (see objective 2) also supported the Liaison with Education and General practiceS (LEGS) cRCT. The cohorts of patients with HR states have been used to support mechanistic and causal research projects funded through alternative sources, complementing our applied research; these are described in Work package 5.
-
To design reliable (efficient), brief and valid assessment procedures for case mix, service use and outcome for longitudinal studies of these clinical populations and to make these data available for prognostic research to study service variations.
This objective was underpinned by work packages 1 and 2 (see Work package 1 and Work package 2), in which there was mixed success. Some aspects did not go ahead whereas others developed in unforeseen but important ways.
We describe in work package 1 the development of the Client Assessment Register (CAR), a user-friendly, computerised system that was used by clinicians and researchers within the team using local information technology (IT) systems and support. Our original ambition was to move this to a trust-wide mental health information system, not funded through the programme, to support routine clinical measurement at baseline and outcome, supporting the kind of observational studies in routine care that we had outlined in the application. In common with virtually all mental health trusts and most NHS trusts of any type, the implementation of a new IT system capable of supporting clinical work, management and research was problematic and protracted; it became clear early on that our plan would not be possible as our host trust decided to invest in the RiO electronic patient record system (EPRS) to meet its clinical and business needs.
However, National Institute for Health Research (NIHR) funding in the mental health Biomedical Research Centre (BRC) at the South London and Maudsley (SLAM) NHS trust led to a prototypic system, the Clinical Record Interactive Search (CRIS) system, developed to provide researchers with regulated access to anonymised information extracted from electronic clinical records systems [see www.slam.nhs.uk/about/core-facilities/cris (accessed 19 January 2016)]. Originally designed for the SLAM electronic system, CRIS has now been extended as Clinical Record Interactive Search (Collaboration Programme) (D-CRIS) to five mental health trusts including the Cambridgeshire and Peterborough NHS Foundation Trust (CPFT), our host, and is running on our RiO electronic record system in shadow form. Thus, we were not able to implement this element of the programme, which itself was a major piece of IT development. However, this has been achieved at greater scale through larger investments in the SLAM NIHR BRC, and is being implemented in our trust at the time of writing.
As we describe in work package 2, our original intention was to use the information to develop an outcome assessment measure with considerable input from patients. Soon after we began the programme all NHS mental health trusts began to be encouraged to adopt the Health of the Nation Outcome Scales (HoNOS),10 later further developed for use as the ‘case mix’ adjustment for payment by results (PbR) funding of mental health services (HoNOS-PbR) (treating people with more severe disorders and greater needs attracting greater funding from commissioners and vice versa). Understandably, our host NHS trust was keen to move wholesale to this measure, something that we supported even though it made some of our programme redundant. Payment by results is not yet fully implemented as such.
-
To investigate the factors associated with transition from at-risk mental states to psychosis syndromes (true positives) and to characterise false-positive referrals.
-
To investigate the barriers to, and promoters of, functional recovery in at-risk mental states and early psychosis, in particular with relation to substance misuse.
Work packages 4 and 5 underpinned the achievement of these two objectives, with the LEGS cRCT generating referrals of FEP or HR participants (true positives) or those with a range of other disorders (false positives). Standardised assessments and instruments such as the Comprehensive Assessment of At-Risk Mental States (CAARMS)11 interview and the Mini-Neuropsychiatric Interview (MINI)12 were used to classify individuals’ mental health problems into psychiatric diagnoses.
The finding of the LEGS cRCT (see Work package 4) that a high-intensity liaison approach between primary and secondary care doubled, as we hypothesised, referrals of FEP and HR mental states combined, of FEP alone and of HR individuals alone (the last of these not reaching statistical significance) is important; moreover, it saved money. Our combination of clinical effectiveness and cost-effectiveness methodology used in the trial was praised in a commentary that accompanied the publication of the LEGS trial13 and the results were incorporated in the new NHS England commissioning guidance for early intervention in psychosis. 9
The cross-sectional follow-up of the cohort of people with HR mental states assembled through the true-positive referrals from the LEGS trial, collectively known as the Prospective Analysis of At-risk mental states and Transitions into psycHosis (PAATH) study (see Work package 5) was a success. The finding that people with mental states thought to put them at HR of psychosis almost invariably had one and often two non-psychotic diagnoses changes the way that we think about these presentations in that we should treat the disorders that they have (largely depression and anxiety), not the disorder that we think they may get (psychosis). Risk factors such as childhood maltreatment/trauma were investigated as was drug use.
-
To evaluate a range of effective interventions and service configurations that vary across our large mental health trust aimed at improving early identification outcome and promoting recovery.
This objective was achieved in a narrow sense through the LEGS cRCT (see Work package 4), which compared two specific approaches to liaison between primary and secondary care in the identification and referral of new-onset psychosis and HR states and set these in the context of practice as usual (PAU). Our broader aim to have routine measures of baseline state and outcomes embedded in practice throughout our trust and supported by an effective IT system was not achieved, largely for the reasons outlined in our comment on objective 2. No mental health trust has this yet in routine practice although it, and the aspiration for ongoing, real-time observational assessment of alternative interventions delivered through different service configurations, remains on the horizon in mental health, particularly through developments such as CRIS, as it does in other areas of health care. Randomised designs on such a platform, most likely with adaptive methods to maximise both short-term patient benefit and long-term improvements in care, remain over the horizon but are being discussed at a conceptual level. 14
The research elements that we employed to achieve our objectives are described in the work packages of this report. The publication outputs are mostly included as appendices (Table 1).
| Programme objectives | Synopsis: research development | Description of programme outputs |
|---|---|---|
| To define the incidence and social epidemiology of psychosis | Work package 3: incidence and social epidemiology of psychosis (see Work package 3) | Appendices 1 – 4 |
| To design reliable, brief and valid assessment procedures | Work package 1: IT systems (see Work package 1) | CAR IT surveillance system and CRIS (external adoption) |
| Work package 2: development of a tool to measure recovery (see Work package 2) | HoNOS-PbR (external adoption) | |
| To investigate the factors associated with transition from HR | Work package 5: follow-up of referrals of individuals identified as being at HR for psychosis (see Work package 5) | Appendices 9 – 12 |
| To investigate the barriers to, and promoters of, functional recovery in HR | Work package 5: follow-up of referrals of individuals identified as being at HR for psychosis (see Work package 5) | Appendices 9 – 12 |
| To evaluate a range of effective interventions and service configurations | Work package 4: detecting and refining referrals of individuals at HR for psychosis (see Work package 4) | Appendices 5 – 8 |
Patient and public involvement throughout the programme
As outlined in our programme grant application, we have a strong commitment to public involvement in research in the context of a mental health partnership trust and therefore patient and public involvement (PPI) has been paramount.
Involvement has been prominent in all phases. It forms a blueprint for our service development within CAMEO. We stress our commitment to research as a means of improving practice in the initial information materials that service users and their carers receive. All are invited to take part in research with the emphasis on this being entirely their own decision. We have a high (> 50%) prevalence of people becoming involved so we can tailor our research to answer questions that are relevant to them. We run dissemination ‘research groups’ for our service users and carers, keeping them informed and promoting discussion of new ideas, methods and projects. We always have a carer (family) and/or a user on interview panels for research staff when there is patient contact.
In the current programme a service user’s mother sparked the idea of working with general practitioners (GPs) and schools to try to improve detection and referral. PPI was vital for the development of the information sheets and assessment tools that we designed; if the tools were not useful to patients, they were not useful at all.
The pilot study that informed our LEGS trial (see Work package 4) interventions included 84 GPs and a similar number of teachers outside the trial area. Their contributions and comments were a significant asset in the development of interventions based on the theory of planned behaviour (TPB)15 and within the Medical Research Council framework for the development and evaluation of complex interventions. 16
As part of the high-intensity intervention for general practices and colleges, educational digital versatile discs (DVDs) were produced (see Work package 4). They required input and advice from service users and college students. Two GPs, two teachers, two service users, two college students and one professor of psychiatry participated in developing the content of the scripts and production. These DVDs have been highly regarded by GPs and teaching staff participating in the LEGS trial.
All primary care practitioners and teachers involved in the LEGS trial have had the opportunity to contribute with comments and impressions through a biannual newsletter. These comments were taken into account to facilitate the practical implementation of the trial, except when they could potentially affect aspects related to methodological aspects of the study protocol.
With regard to the follow-up of HR referrals (the PAATH study; see Work package 5), we developed a comprehensive database to collect relevant epidemiological, clinical, functional and quality of life information. One of the peer support workers working in the CAMEO clinical team, where this research is embedded, participated in the design of the database and has facilitated its use enormously. His clinical knowledge and experience as a service user contributed to making it meaningful and easy to analyse. He has closely worked with our IT project manager and psychometrician.
Our research team, particularly JP, has built up innovative partnerships with mental health charities such as Squeaky Gate, an extraordinary and creative charity that empowers people with mental health problems through music and the arts [see www.squeakygate.org.uk (accessed 19 January 2016)], especially during the so-called Squeaky Gate Galas featuring ‘Inside an Unquiet Mind’ that usually take place in Cambridge during the annual Science Festival. This has been an excellent collaboration to publicise research such as the LEGS cRCT (see Work package 4) and the PAATH study (see Work package 5). These performances are open to the general public. For example, last year more than 500 people watched these plays. They were very well received by the public and also had a significant repercussion in the scientific literature. Indeed, the EMBO Journal, from Nature publishing group, invited us to write an article on this new venture. 17
The significant evolution of PPI in research during the last few years has been challeging at times as we had to adjust our initial objectives and plans to new and more desirable requirements. However, we feel that this progression has eventually become seamless. Now, we would naturally have included a service user or carer with research experience as a co-applicant, but at the time that the application for this programme was submitted current guidance did not recommend this; things have moved on. However, we included GPs and sought teachers’ advice in our steering groups and, as set out above, have included PPI: a patient and carer have helped with the construction of this report, including having some detailed input to the Abstract, Plain English summary and Scientific Summary.
We are committed to disseminating our results using all possible channels to reach patients and the public. We have excellent links with charities (see above) and third-sector organisations such as Rethink [see www.rethink.org/ (accessed 20 January 2016)]. We also have excellent relationships with commissioners who will advise about the best way to communicate findings that emerged from this programme. We will also provide information about the results to participants with their approval and will organise meetings to feed back our findings. We have a programme arranged to execute our strategy to further disseminate results to the public.
The following statement is not strictly related to PPI but is a fair reflection of what the research team, along with PPI, accomplished in making materials successful and worthwhile in the LEGS cRCT. This feedback was sent to us by a nurse working in a large college of further education:
Cambridge Regional College (CRC) has a population of approximately 5000 full-time students. About 1/10 students are referred to/seek help at Student Services for emotional and mental health issues. The majority of our students are aged 16-25, and a large quantity come from challenging backgrounds (e.g. abuse, domestic violence, homelessness, and substance abuse etc). Consequently, there are high risks for students developing poor emotional health and (sometimes chronic) mental health issues. Early identification and referral is critical to the students’ well-being and ability to achieve their college goals. Participating in the LEGS trial has provided staff at CRC an opportunity to increase their knowledge and understanding of psychosis (clarification of the condition, and how and when it can present). Staff were extremely positive about the CAMEO training on September 8th 2011 (to which about 50 people attended); staff stated that it increased their confidence in detecting early symptoms (indicative of psychosis), and making referrals to appropriate professionals. The laminated posters/flyers (which were displayed in staff rooms and offices), are reported to be useful resources in reminding staff what to look out for. Prior to the LEGS trial, many tutors, teachers and staff found the term ‘psychosis’ intimidating, and were not confident in dealing with the issue. Since the LEGS trial this year, many staff have stated their overall response to psychosis has improved. As the mental health practitioner at the college, I have noticed an increase in the number of students being referred to Student Services with symptoms possibly pertaining to psychosis (e.g. delusions and hallucinations) this academic year. Staff have also been quicker to identify students with unusual presentation (e.g. uncharacteristic affect/behaviour, lack of concentration/attendance) and refer them to review and identify any core underlying issues. Over the last year, there has been a significant shift and improvement in attitudes and approaches to mental health at CRC, and the LEGS trial has played a part in this. As a result of this shift, more students have been able to have their needs assessed and (if necessary) receive the appropriate support and treatment. With the right interventions, more students have been able to complete their academic courses/qualifications this year. As a professional, it is my priority to support the early identification of mental health issues, so students have the best possible treatment and prognosis. I have made several referrals to CAMEO this year, and have been extremely pleased with the quick response and quality of CAMEO’s assessment and advice. The feedback from students referred to CAMEO has generally been very positive too. Students have expressed they feel ‘comfortable’ talking to the CAMEO team, and have appreciated having their issues ‘taken seriously’ and advised accordingly. For many students being referred to a specialist mental health agency is a scary experience (for many reasons e.g. ‘I must be crazy now’, and ‘doctors and diagnoses’ are often involved). However, CAMEO’s approach has reassured students, and many have been onto the CAMEO website for further information. Overall, Cambridge Regional College has benefited from participating in the LEGS trial, and looks forward to further information and involvement with CAMEO.
Work package 1: information technology systems
Development and implementation of the Client Assessment Register
In support of various data collection requirements for service outcomes, evaluation and research trials, we have developed and implemented a clinical surveillance system to identify and electronically record all cases of clinically relevant psychotic states. This information has been gathered through predetermined sets of assessment batteries that can be modified according to clinical or research requirements. The system integrates with the central care records system of the trust to avoid data redundancy. This process synchronises with the centralised system’s basic sociodemographic data on a daily basis. The data are only editable in the central system and several data validity checks are built into the system to ensure improved data quality.
The CAR system consists of a front-end application interface designed according to industry-acceptable development standards. The front end was developed in a Visual Basic Integrated Development Environment and works on a client–server topology (Figure 2). The database side of the system was developed in Microsoft Transact Structured Query Language (Transact-SQL) database format (Microsoft Corporation, Redmond, WA, USA) and uses an Open Database Connectivity (ODBC) client to connect and transmit data.
FIGURE 2.
Screenshot of the CAR constructed for the programme and available from the authors.

As a reporting function the CAR system also allows for data to be exported from the database into external data sources such as Microsoft Excel, for analysis and manipulation for statistical analysis.
To ensure that the system stays in line with future technological development we also created a mobile module for remote capturing and reporting of the CAR data. The enhancement allows service users and staff to remotely capture a specific battery of assessments on an iPad or any tablet device that can connect to the internet and have browsing capabilities. This is achieved through a web-based application that is enhanced using the Visual Basic.NET framework. The system also allows service users to enter data. Through the scoring system, staff can immediately access the outcome of particular self-assessments, which may have clinical implications. They can then act accordingly by putting the necessary procedures in place.
During the LEGS cRCT the system was supported and maintained by an appointed IT development and project manager. This staff member was also responsible for training members of staff and service users to ensure the best quality of data capture.
The team also had access to a trust-wide data library that stores the clinical documents of trust service users. The Clinical Documents Library is a bespoke web-based solution that provides a user-friendly, secure single point of access for all authorised users throughout the trust. The library stores clinical letters, reports and assessments against service user records.
An initial requirements report recognised that existing ways of sharing clinical documents at various locations presented inefficiencies and the recommended approach is consistent with the trust’s strategic vision and principles within the Way Ahead Programme [see www.wayaheadcare.co.uk/quality-assurance.php (accessed 20 January 2016)]. The following details some of the features of the new system:
-
enables service user records to be held at a central location
-
enables a single standardised way of storing and sharing clinical documents
-
provides a secure library of clinical documentation
-
is available to all authorised clinicians throughout the trust
-
reduces time spent by staff looking for documents
-
reduces data redundancy
-
provide electronic versions of clinical information.
As stated earlier, our final goal was to implement our CAR information system at a trust-wide level, not funded through the programme, to support routine clinical measurement at baseline and outcome. In common with virtually all mental health trusts and most NHS trusts of any type, the implementation of a new IT system capable of supporting clinical work, management and research was problematic and protracted; it became clear early on that our plan would not be possible as our host trust decided to invest in the RiO EPRS to meet its clinical and business needs.
However, the NIHR BRC for mental health at the SLAM NHS Foundation Trust developed a prototypic system, the CRIS system, to provide regulated access to anonymised data from electronic patient records systems (see www.slam.nhs.uk/about/core-facilities/cris). Although the CRIS system was initially designed for SLAM NHS Foundation Trust systems, it has now been implemented as D-CRIS in several mental health trusts, including CPFT, our host, where it is running on and shadowing the RiO EPRS. Thus, we were not able to extrapolate this element of our programme, which itself was a significant IT development that was already completed and significantly contributed to the success of this programme, especially the LEGS cRCT and the PAATH study. Nevertheless, this ambitious objective has been achieved through larger investments in CRIS/D-CRIS by the NIHR BRC for mental health.
Work package 2: development of a tool to measure recovery
With regard to work package 2, we proposed to develop psychometrically and practically acceptable instruments and test them in practice to understand predictors of and barriers to recovery. Through measurement innovation we intended to create tools and the culture that could sustain (indeed welcome) constant evaluation of service structure and interventions. We considered this fundamental to guide service planning. However, this was partly resolved with the gradual adoption during the programme of the HoNOS10 by our NHS trust. As stated in our application, this simple tool was already employed in Scandinavia and Australia, but not in the UK. Its eventual adoption by the NHS significantly reduced the importance and viability of this element in our research plan. Furthermore, HoNOS seem to possess satisfactory sensitivity and validity to be used in routine assessment within early-intervention programmes. 10 The HoNOS have become the basis of PbR for mental health (as HoNOS-PBR) nationally, and our trust was in line with others by adopting them. We were disappointed not to be able to produce a psychometrically sophisticated tool for use in clincal practice but delighted that the services are using a recognised tool.
Work package 3: incidence and social epidemiology of psychosis
In this work package we describe the administrative incidence (these are data not primarily collected for research purposes) and social epidemiology of psychotic disorders and HR for psychosis in Cambridgeshire and Peterborough. This was mainly intended to help understand the complex person–place interactions in the genesis of schizophrenia and other psychoses as a useful, less immediately applied but ultimately essential goal in terms of the future prevention of disability from such disorders.
To continue with our endeavour of understanding who we treat, where they come from, what is wrong, what we do for them and what happens to them, we built on our clinical and research experience in the local Cambridge EIS (CAMEO) as it expanded in stages to cover all of Cambridgeshire and Peterborough, a socially and ethnically diverse area of 800,000 people. By our alignment with other regional research projects, such as the Social Epidemiology of Psychosis in East Anglia study [SEPEA; see www.sepea.org (accessed 19 January 2016)], we also evaluated comparative epidemiological data for the whole of East Anglia.
These findings were compared with wider data that we have collected with other academic partners, such as the ÆSOP6 and East London First-Episode Psychosis (ELFEP)18 studies, to devise realistically complex statistical models of psychosis incidence.
As a result of this, we developed a web-deployed clinical epidemiology tool that will predict the numbers of people who will develop new psychotic illnesses by social geography, demographics and area, to facilitate future NHS planning. Any health economy will be able accurately to predict morbidity in its area, taking into account detailed characteristics of its population (available from census data). This will promote the right services in the right places.
In this context we also developed and implemented clinical surveillance and IT systems to identify and electronically record all cases of clinically relevant psychotic syndromes in Cambridgeshire and Peterborough, linking with routine data capture for the Mental Health Minimum Data Set (MHMDS) requirements. 19 This represented a culture change within a predominantly clinical service that we implemented successfully.
Incidence of psychosis in socially and ethnically diverse settings
See Appendix 1 for the published report of this work. 20
Research aims
The aim of this study was to compare the observed with the expected incidence of psychosis and delineate the clinical epidemiology of FEP using epidemiologically complete data from the CAMEO EIS over a 6-year period in Cambridgeshire for a mixed rural urban population.
Methods for data collection
Data came from a population-based study of FEP [International Classification of Diseases, 10th revision (ICD-10), F10–3921] in people aged 17–35 years referred between 2002 and 2007; the denominator was estimated from mid-year census statistics. Sociodemographic variation was explored by Poisson regression. Crude and directly standardised rates (for age, sex and ethnicity) were compared with pre-EIS rates from two major epidemiological FEP studies conducted in urban English settings. 6,18
Analysis
Incidence per 100,000 person-years was calculated with 95% confidence intervals (CIs). Incidence rate ratios (IRRs) were calculated (with 95% CIs) using Poisson regression to control for possible confounding. We conducted a sensitivity analysis on subjects with missing ethnicity data by repeating the Poisson regression four times, assuming that all such subjects belonged to the white British, non-British white, black and other ethnic groups in turn. The likelihood ratio test was applied to assess statistical interactions and model fit.
Key findings
There were 285 cases over 569,921 person-years (aged 16–35 years), yielding a crude incidence of 50.0 per 100,000 person-years (95% CI 44.5 to 56.2 per 100,000 person-years), higher than anticipated and comparable with estimates from more urban UK settings. These comparisons were with rates on which EISs were predicated and also with incidence rates from the two recent observational studies of FEP covering four urban catchment areas of the UK: east London and south-east London, Nottingham and Bristol. 6,18 These comparisons are shown in Figure 3.
FIGURE 3.
Comparison of crude and directly standardised incidence rates in Cambridgeshire and the four catchment areas of the ÆSOP6 and ELFEP18 studies. Directly standardised to the population of England aged 18–34 years estimated in the 2001 census. a, Data made available from the authors;18 b, data made available from the authors. 6
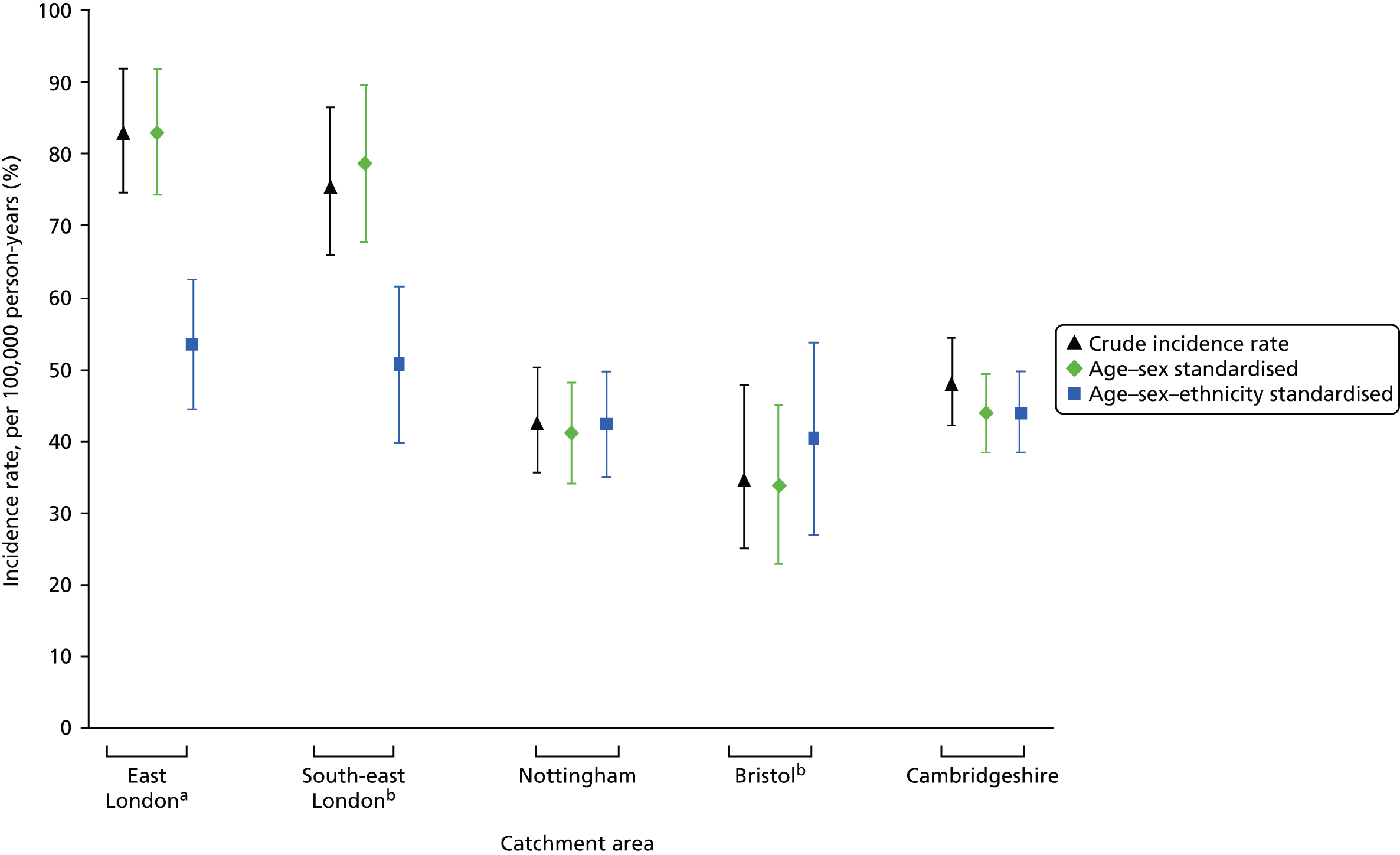
Rates in men were double those in women and declined with age for both sexes. After adjustment for age and sex, rates were elevated for people from black ethnic groups (IRR 2.1, 95% CI 1.1 to 3.8). The increased risk of psychosis among people of black ethnicities demonstrated in this study was smaller than that seen in other studies.
The administrative incidence of psychosis calculated from within an EIS in a mixed urban–rural setting was similar to estimates from city-based studies and higher than originally predicted when EISs were designed in the UK. The sociodemographic characteristics of incidence rates were also similar to those of more urban studies, including higher rates in black and ethnic minority groups, indicating that psychosocial and other phenomena contributing to this variation are not confined to urban populations. Adjustment of city rates for ethnic structure of the population reduced high city rates markedly, indicating the importance of this factor to the high burden of FEP in cities. This has implications not only for our understanding of the determinants of psychosis but also for service planning.
The crude incidence rates presented from the CAMEO EIS were more than three times higher than anticipated by the original service planning estimates from the Department of Health in 2001. Possible explanations for this are:
-
There has been little evidence on incidence in rural settings compared with urban areas, such that the assumptions about overall rates in the general population have simply been wrong.
-
EISs are particularly effective in eliciting referrals of true positives and engaging them long enough for assessments to be made. That said, the fact that we did not have a formal leakage study, as was undertaken in our comparison samples, suggests to us that those studies and general mental health services did not massively underestimate morbidity.
-
More rural areas may look like cities because of the uniformly high prevalence of cannabis use by young people in the UK.
-
The most obvious reason for the discrepancy between our data and the figure for EIS planning used in England (around 15 per 100,000 person-years) is that the latter is predicated largely on the incidence of schizophrenia whereas we know that only around one-third of FEP is classified as such at first presentation.
-
The incidence of psychosis is higher in young adults aged 14–35 years than in the population as a whole, and EISs are targeted at the former group.
Limitations
Because of the lack of routine incidence data at the time of the study, we were unable to compare incidence rates presented here with those in our study population prior to the start of the CAMEO service. This is necessary to determine precisely whether or not EISs do identify excess morbidity.
Incidence of psychosis across Eastern England
See Appendix 2 for the published report of this work. 22
Research aims
The aim of this research was to present the initial 18-month findings from the SEPEA study, a large, 3-year population-based FEP study of incepted incidence observed through five EISs.
Methods for data collection
We established a surveillance system to record sociodemographic and clinical data on all people aged 16–35 years resident within East Anglia who were referred to and accepted by our EIS with FEP over the 3 years from 1 August 2009. ICD-1021 clinical and research (OPCRIT23) diagnoses for psychotic disorder (F10–39) are established at 6 months and 3 years after referral.
Analysis
Poisson regression explored covariate effects. The full method is given in the online supplement [see http://bjp.rcpsych.org/content/suppl/2011/12/19/bjp.bp.111.094896.DC1.html (accessed 21 September 2014)].
Key findings
We identified 357 eligible subjects (incidence 45.1 per 100,000 person-years, 95% CI 40.8 to 49.9 per 100,000 person-years). Rates varied across the EISs but were two to three times higher than those on which services were commissioned.
Risk decreased with age, was nearly doubled among men and differed by ethnic group: it was doubled in people of mixed ethnicity but was lower for those of Asian origin than for the white British population (Table 2).
| Variable | Participants, n (%) | Denominator, n (%)a | Adjustedb relative risk (95% CI) |
|---|---|---|---|
| Total | 357 (100) | 838,574 (100) | – |
| EIS (n = 357) | |||
| Cambridgeshire, Peterborough and Royston | 122 (34.2) | 306,283 (36.5) | – |
| West Norfolk | 17 (4.8) | 41,765 (5.0) | – |
| Central Norfolk | 91 (25.5) | 219,860 (26.2) | – |
| Great Yarmouth and Waveney | 38 (10.6) | 69,218 (8.3) | – |
| Suffolk | 89 (24.9) | 201,448 (24.0) | – |
| Sex (n = 330) | |||
| Women | 115 (34.8) | 405,221 (48.3) | 1 |
| Men | 215 (65.2) | 433,353 (51.7) | 1.7 (1.4 to 2.2) |
| Age group (years) (n = 330) | |||
| 16–17 | 52 (15.8) | 71,929 (8.6) | 1 |
| 18–19 | 53 (16.1) | 88,976 (10.6) | 0.8 (0.6 to 1.2) |
| 20–24 | 118 (35.8) | 219,157 (26.1) | 0.7 (0.5 to 1.0) |
| 25–29 | 73 (22.1) | 213,385 (25.4) | 0.5 (0.3 to 0.7) |
| 30–35 | 34 (10.3) | 245,127 (29.2) | 0.2 (0.1 to 0.3) |
| Ethnicity (n = 330) | |||
| White British | 261 (79.1) | 671,588 (80.1) | 1 |
| White non-British | 21 (6.4) | 50,882 (6.1) | 1.2 (0.8 to 1.9) |
| Mixed ethnicity | 15 (4.5) | 17,364 (2.1) | 2.1 (1.3 to 3.6) |
| Black | 12 (3.6) | 18,471 (2.2) | 1.8 (1.0 to 3.3) |
| Asian | 12 (3.6) | 69,014 (8.2) | 0.5 (0.3 to 0.9) |
| Other ethnicities | 9 (2.7) | 11,255 (1.3) | 2.3 (1.2 to 4.5) |
Psychosis risk among ethnic minorities was lower than reported in urban settings, which has potential implications for aetiology if whatever factors increase risk in people from black and minority ethnic groups in cities are less potent, rare or absent in rural areas. Overall, our data suggest considerable psychosis morbidity in diverse, rural communities.
Development of a population-level prediction tool for the incidence of first-episode psychosis (PsyMaptic)
See Appendix 3 for the published report of this work. 24
Research aims
Although the true incidence of FEP varies enormously according to sociodemographic factors, a single estimate of population need was used universally for developing EISs in the UK. Therefore, we sought to develop a realistically complex, population-based prediction tool for FEP, based on precise estimates of epidemiological risk.
Methods for data collection
Data from 1037 participants in two cross-sectional population-based FEP studies6,18 were fitted to several negative binomial regression models to estimate risk coefficients across combinations of different sociodemographic and socioenvironmental factors. We applied these coefficients to the population at risk of a third, socioeconomically different region to predict the expected caseload over 2.5 years, where the observed rates of ICD-10 F10–39 FEP had been concurrently ascertained through EISs.
Analysis
The main outcome measure was observed counts compared with predicted counts [with 95% prediction intervals (PIs)] at EIS and local authority district (LAD) levels in East Anglia to establish the predictive validity of each model. For the full analysis see Appendix 3.
Key findings
The use of modelling with epidemiological data from two large studies of FEP in England6,18 produced accurate FEP forecasts.
Negative binomial regression models with age, sex, ethnicity and population density performed most strongly, predicting 508 FEP participants in EISs in East Anglia (95% PI 459 to 559 FEP participants) compared with 522 observed participants. This model predicted correctly in five out of six EISs and 19 out of 21 LADs.
Our data suggested that the original figure used to commission EISs probably overestimated the true incidence of FEP in rural areas and underestimated rates in urban settings.
The initial assessment of some people who do not require subsequent EIS care means that additional service resources will be required.
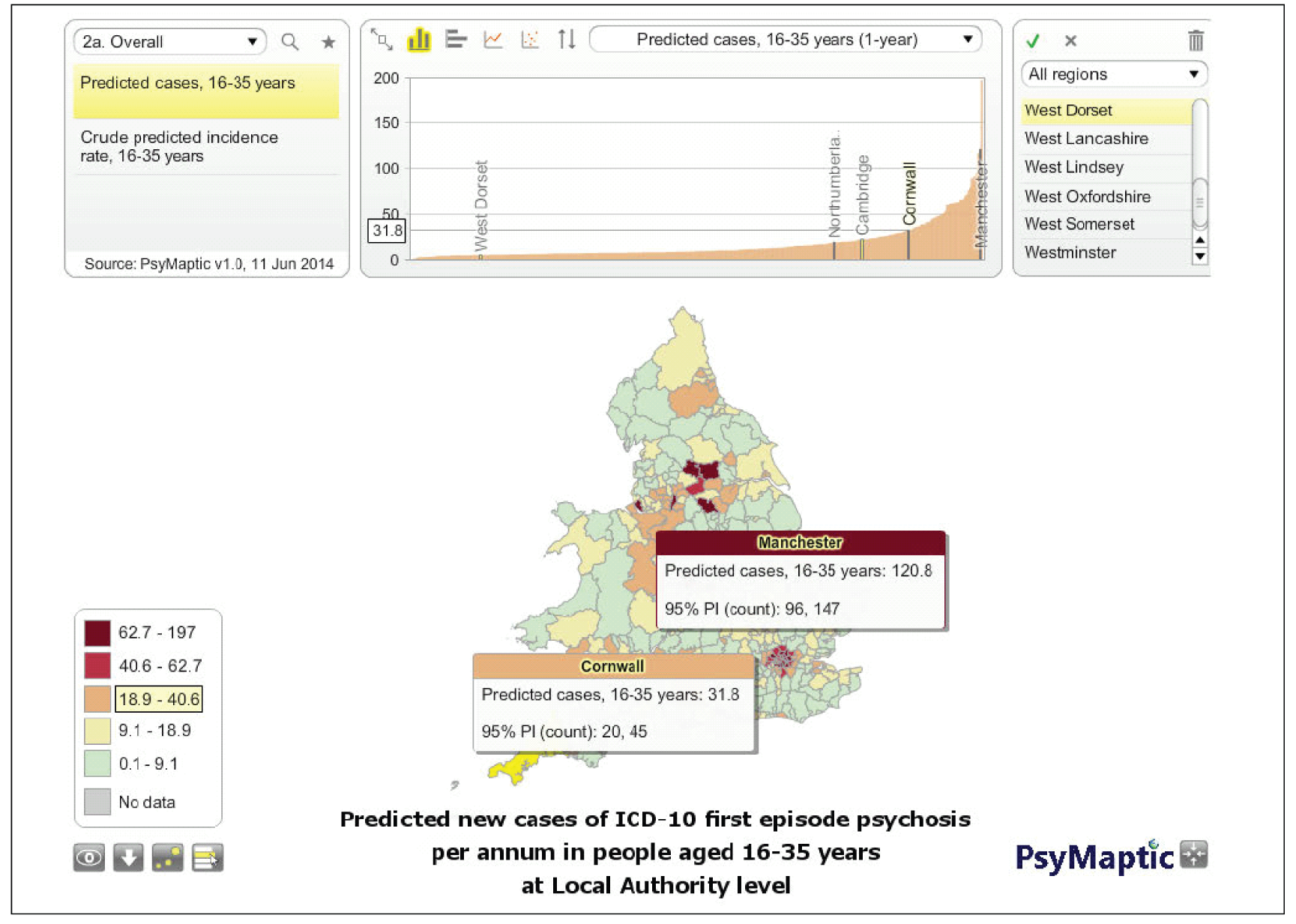
Successes
All models performed better than the current gold standard for EIS commissioning in England (716 cases, 95% PI 664 to 769 cases). We have developed a prediction tool for the incidence of psychotic disorders in England and Wales, made freely available online (see www.psymaptic.org/), to provide health-care commissioners with accurate forecasts of FEP based on robust epidemiology and anticipated local population need (Figure 4). This has already been used for service planning in London and, at the time of writing, is being used by NHS England to support the national early intervention waiting time standard and target. The work also appeared in the Annual Report of the Chief Medical Officer 2013 [see www.gov.uk/government/uploads/system/uploads/attachment_data/file/413196/CMO_web_doc.pdf (accessed 19 January 2016)].
Limitations
Although our models provide estimates of the expected clinical burden of FEP in the community, services may see a broader range of psychopathology, consuming resources, or incepted rates may be influenced by supply-side organisational factors.
It was not possible to validate our prediction tool in settings outside of England and Wales or for specific psychotic disorders. As data become available we will assess the use of our prediction tool in other settings and for disorders.
Social and spatial heterogeneity in psychosis proneness
See Appendix 4 for the published report of this work. 25
Research aims
To test whether spatial and social neighbourhood patterning of people at HR of psychosis differs from that of FEP participants or control subjects (healthy volunteers; HVs) and to determine whether or not exposure to different social environments is evident before disorder onset.
Methods for data collection
First-episode psychosis participants were identified through the SEPEA study. HR participants were identified as part of the PAATH study, which ran in parallel to the SEPEA study in CAMEO. Control participants were identified from an embedded project within the SEPEA study, the European Union Gene–Environment Interaction (EU-GEI) study [see www.eu-gei.eu/ (accessed 19 January 2016)], an international, multicentre case–sibling–control study of gene–environment interactions in schizophrenia and other psychoses in people aged 18–64 years. Using a NIHR Primary Care Research Network (PCRN) initiative designed to assist with recruitment of participants from primary care for research, HVs who met the inclusion criteria (aged 18–64 years; no previous history of psychosis) were randomly selected from 10 GP practice patient lists within the Cambridgeshire and Peterborough catchment area.
Analysis
We tested differences in the spatial distributions of representative samples of individuals with FEP, HR participants and HVs and fitted two-level multinomial logistic regression models, adjusted for individual-level covariates, to examine group differences in neighbourhood-level characteristics. For full techniques see Appendix 4.
Key findings
The spatial distribution of HVs (n = 41) differed from that of HR participants (n = 48; p = 0.04) and FEP participants (n = 159; p = 0.01), whose distribution was similar (p = 0.17). Risk in FEP and HR groups was associated with the same neighbourhood-level exposures: proportion of single-parent households [FEP adjusted odds ratio (aOR) 1.56, 95% CI 1.00 to 2.45; HR aOR 1.59, 95% CI 0.99 to 2.57), ethnic diversity (FEP aOR 1.27, 95% CI 1.02 to 1.58; HR aOR 1.28, 95% CI 1.00 to 1.63) and multiple deprivation (FEP aOR 0.88, 95% CI 0.78 to 1.00; HR aOR 0.86, 95% CI 0.76 to 0.99).
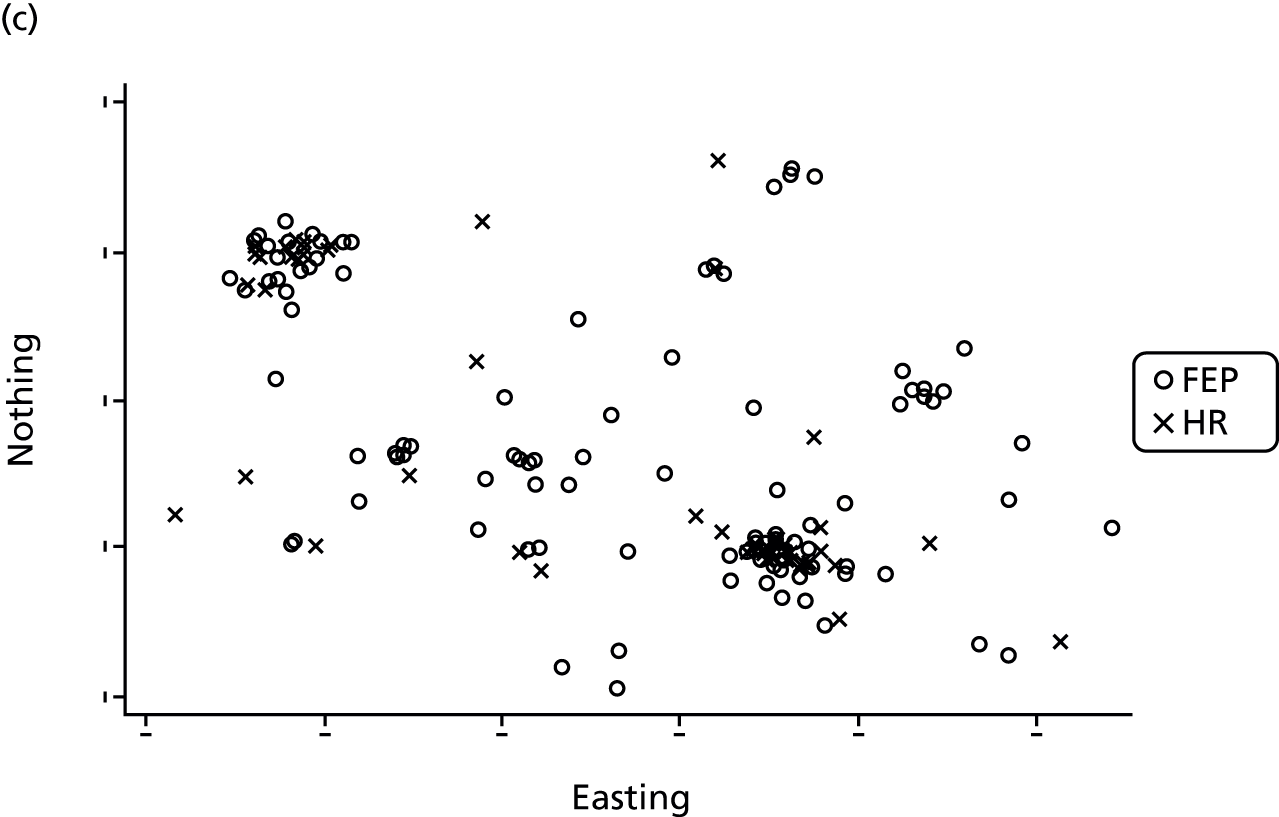
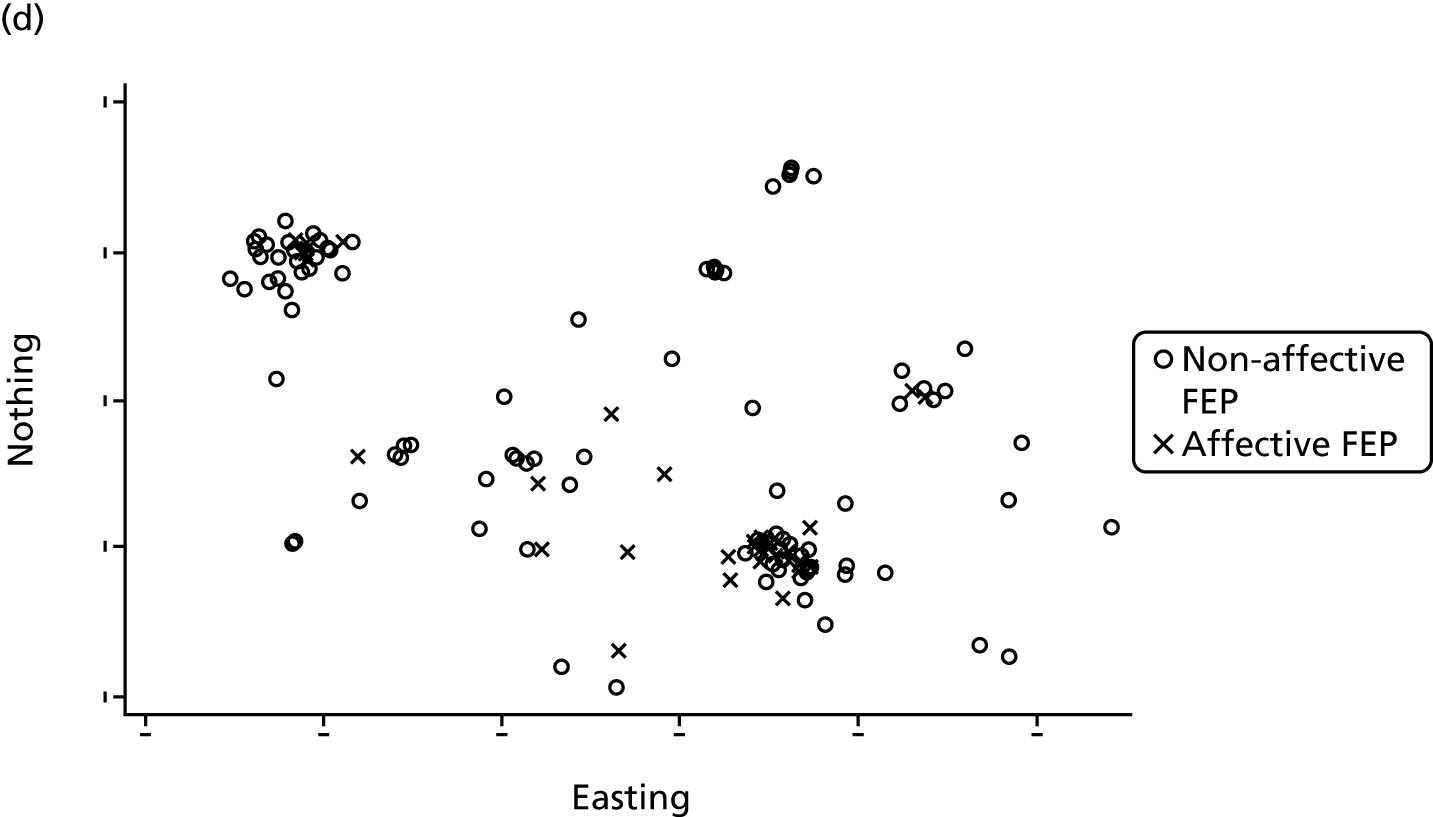
The pattern of elevated risk at the neighbourhood level was similar for both HR and FEP participants relative to HVs (Figure 5).
FIGURE 5.
Spatial locations of participants by status. The spatial distribution of control subjects (HVs) was significantly different from that of both (a) people with FEP (p = 0.01) and (b) the HR group (p = 0.04) under a two-dimensional M-test. There was no statistically significant difference in the spatial distribution of (c) FEP and HR participants (p = 0.17). The spatial distribution of (d) people with non-affective FEP and people with affective FEP was also significantly different from each other (p = 0.01). Locations are based on postcode centroid at first contact. Axis scales are plotted according to British National Grid co-ordinates of residential postcode at first contact, but the co-ordinates and scale have been removed to preserve sample anonymity.

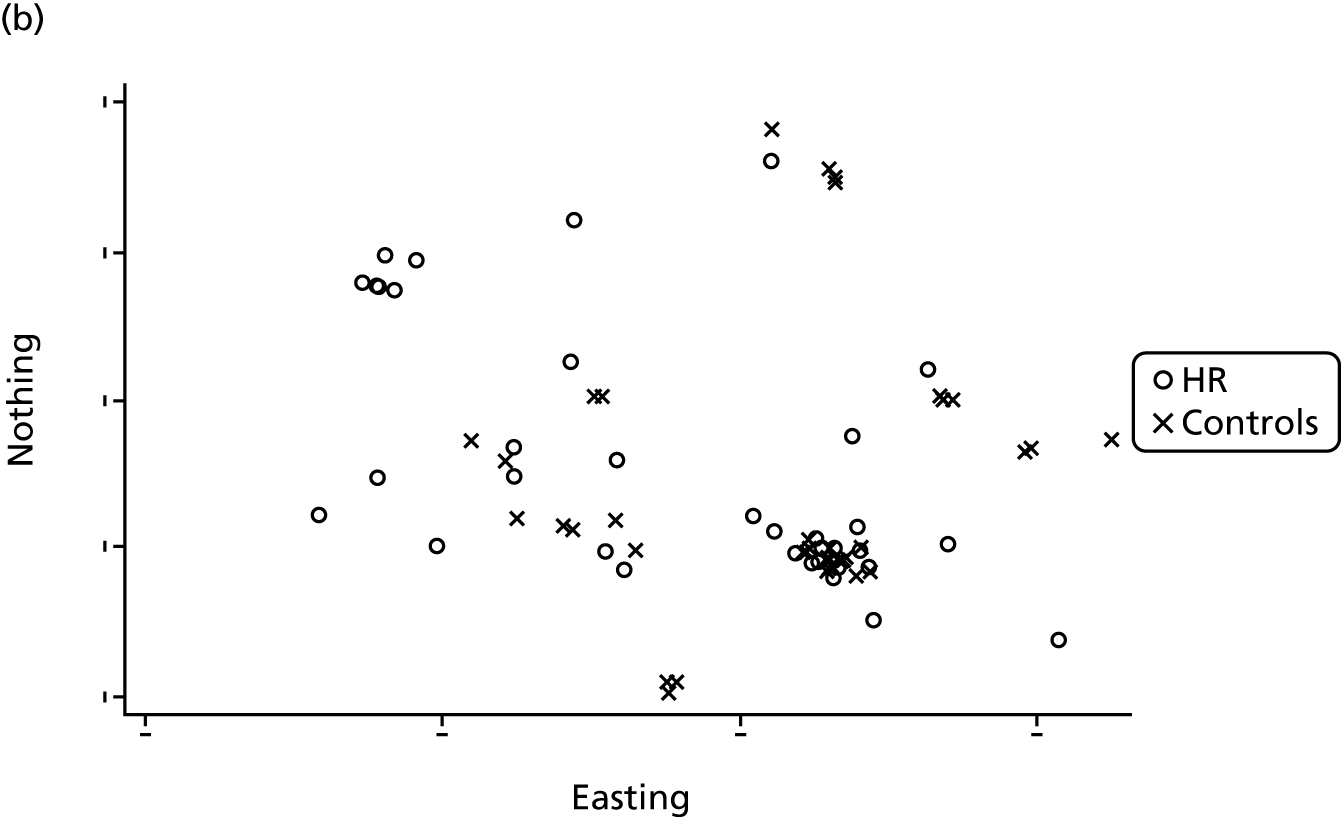
Social drift may begin earlier in the prodromal phase or expose people to greater socioenvironmental adversities, which increase psychosis proneness.
Limitations
This multilevel study used cross-sectional data to compare social and spatial differences in the three groups in a defined catchment area; we did not have longitudinal data on transition to psychosis in HR participants.
The odds ratios were conservative because, although the control subjects and the population at risk were similar in sociodemographic terms, they came from more densely populated neighbourhoods. The sample of HVs and HR participants was relatively small in this study.
Work package 4: detecting and refining referrals of individuals at high risk for psychosis
Liaison with Education and General practiceS to detect and refine referrals of people with at-risk mental states for psychosis
International efforts to decrease the stigma of psychosis and solicit self- and other referrals have exploited print and television media for public information campaigns, as well as educating members of relevant occupational groups. In this context we compared techniques to identify this important population, ensuring a representative sample of HR individuals for our research and finding a cost-effective way to ascertain this group for EISs to work with subsequently.
We called this initiative LEGS. We employed a cluster randomised approach to finding out which, if any, of two methods of finding HR individuals works best. We targeted those aged 16–35 years registered in and attending primary care (although the intervention will affect a broader age range) and those aged 16+ years in further education in our county. The units randomised (primary care practices and age 16+ educational institutions) in Cambridgeshire and Peterborough were balanced for social deprivation before randomisation using Index of Deprivation scores. 26 We tested whether or not a simple ‘postal’ campaign, co-ordinated from an office, was more clinically effective and cost-effective than a more elaborate and expensive system of personal liaison by health professionals with the primary care practices and the 16+ educational institutions.
The aim of both interventions was to sensitise staff working in primary care practices and 16+ educational institutions to the nature and likely manifestation(s) of common psychotic symptoms or mental states that put individuals at risk, as defined by existing definitions and established general population screening tools applied in current government epidemiological surveys. Those identified can be referred to their local EIS.
Clinical effectiveness and cost-effectiveness of tailored intensive liaison between primary and secondary care to identify individuals at risk of a first psychotic illness: a cluster randomised controlled trial
The complex educational intervention used in this trial required a number of developmental stages before implementation and evaluation. Here we outline key findings, successes, challenges, limitations and recommendations for future research for each of the stages.
Development of the educational intervention to improve detection of high-risk mental states and first-episode psychosis
A detailed description of this developmental stage has been published (see Appendix 5). 27
First, we investigated what education was required and on what to base our low-intensity intervention (a leaflet sent by post) and the high-intensity, fact-to-face and video package supported by a member of staff. The TPB15 was selected to guide the design of the educational intervention. Use of the TPB requires the development of a questionnaire to identify and measure specific beliefs associated with each of the theory’s constructs: intention, attitude, subjective norm and perceived behavioural control (PBC). The beliefs are then targeted with strategies designed to influence behaviour. Strengthening GPs’ intentions to identify individuals at HR was predicted to increase the likelihood that they would identify and refer those at risk.
Research aims
The aim of this stage was to describe the development and psychometric evaluation of a questionnaire designed to identify and measure factors that influence the identification of individuals at HR for psychosis in primary care. This informed the design of the LEGS educational intervention to help GPs and primary care physicians detect these individuals.
Methods for data collection
Following standard TPB guidelines28 a 106-item preliminary questionnaire was constructed using a semistructured discussion group with eight GPs to elicit commonly held beliefs about identifying HR individuals. The questionnaire was distributed to 400 GPs in 38 practices across 12 counties in England, not including Cambridgeshire and Peterborough where we intended to run the trial.
Analysis
A polytomous graded response model29 was used to identify redundant items and assess the validity of the questionnaire. Factor analysis was used to assess the structural conformity of the final questionnaire with the TPB. Cronbach’s alphas were calculated to determine the reliability of the final questionnaire. Path analysis was conducted to assess the ability of the TPB’s constructs to predict intention and reveal the percentage of variance explained by intention.
Key findings
Indirect measures were well constructed and adequately covered the breadth of the measured construct. Items within all direct measures measured the corresponding construct satisfactorily. The alpha values confirmed improvement for each of the constructs in the reduced version of the questionnaire with the exception of intention, which remained the same. The final instrument consisted of 73 items and showed acceptable reliability (α = 0.77–0.87) for all direct measures. All of the direct measures of the TPB significantly predicted intention, accounting for 35% of the variance. Subjective norm (perceived professional influences) was the strongest predictor of intention. GPs had positive intentions and attitudes towards identifying individuals at HR for psychosis. The foremost motivational factors for GPs were their perceptions of whether or not other GPs identify HR individuals and whether significant others (e.g. patients, colleagues, health-care system) approved or disapproved of identification.
Successes
Theory underpinned the design of all components of the educational intervention: the understanding of the GPs’ behaviour, the development of the measures and the attempt to change behaviour. We confirmed the feasibility, reliability and acceptability of a TPB-based questionnaire to identify GPs’ beliefs and intentions concerning the identification of individuals at HR for psychosis.
Theory-based interventions provide an understanding of what works and thus are a basis for developing better theory across different contexts, populations and behaviours. They could, and should, be used more in the NHS where innovation often requires education and behaviour change by staff.
Challenges
The average time taken to complete the questionnaire was 16 minutes. Most of the declining GPs and some of the participating GPs mentioned that the length of the questionnaire was off-putting.
Limitations
The response to the pilot was very low: only 82 (20.5%) GPs returned questionnaires. The cost and time investments were high for such a low return.
Recommendations for future research
The recommendation that an original TPB questionnaire is developed every time a new behaviour is studied,28 or the same behaviour is studied in a new population, suggests that similar methodology can be used to help GPs in the identification of other pathologies and in a variety of mental health settings. Further application of the TPB in the NHS has already been mentioned.
Design of the educational intervention
Methods for data collection
The information collated from the pilot questionnaire identified specific barriers that we targeted with strategies designed to change clinical practice with respect to identifying HR individuals in primary care.
Key findings
This theory-based information could be important for improving the efficiency of referral pathways and contributing to a reduction in the DUP. We had a clear structure on which to base our low-intensity leaflet intervention and our high-intensity face-to-face and video approaches.
Successes
Mapping theoretical constructs to behaviour change techniques provided a clear framework for process analysis and increased the ability of the intervention to accomplish the desired outcome of motivating GPs to identify individuals at HR.
It was invaluable to have a guide to the different behaviour change techniques, with definitions that addressed different behavioural determinants linked to theoretical constructs. This allowed us to select the most appropriate intervention strategies for GPs.
Challenges
The mapping of theoretical constructs to behaviour change techniques was complex and time-consuming. However, this systematic approach ensured that the behaviour change techniques and delivery methods targeted the theoretical determinants of GPs’ behaviour directly.
We learnt from the pilot that individual clinicians have very different levels of knowledge about psychosis and mental health in general. Therefore, it was important to ‘pitch’ the presentation at the right level so as not to be condescending but at the same time ensure a basic level of understanding. Achieving this balance proved extremely difficult, especially given the time restraints of the 60-minute sessions. Trying to explain the complexities of the at-risk concept in a concise way but also making it educationally appropriate for both GPs and practice nurses took many drafts. Again, it was helpful to have comments from GP colleagues regarding the presentation to guide us before we approved the final version.
Limitations
Ensuring that the leaflet was specific enough to capture all possible at-risk symptoms [attenuated symptoms, family vulnerability and BLIPS (Brief Limited Intermittent Psychotic Symptoms)] without being too sensitive and producing numerous ‘false-positive’ referrals was a dilemma. Despite utilising many sources of information, including GPs practising outside the trial area, the resulting leaflet proved a little too sensitive.
Recommendations for future research
Few studies have used the TPB to predict intention to take part in an intervention. Such an application could provide valuable information about how best to recruit GPs into future studies.
Implementation of the high-intensity intervention
Successes
The PCRN was useful in terms of accessing surgeries for participation history and informing them about the study. It provided us with the Research Information Sheet for Practices (RISP). The focus of this was provision of information about the practical implications of the research for the participating GPs (What, Where, How often, etc.). This proved more useful than the trial information sheet, which, although detailed and well structured, did not cover enough of the practical details that were required to help practices reach a decision about whether or not to participate.
Having an out-of-area GP review and critique the educational materials proved invaluable for establishing the appropriate pitch and tone and reviewing the content of the intervention.
Three dedicated research and liaison practitioners (RLPs) were specifically recruited for the trial [one man, two women; mean age 45.5 years, standard deviation (SD) 4.7 years]. All were experienced mental health professionals (one psychologist, one nurse, one social worker). They acted as facilitators between secondary and primary mental health services as it is proposed that this is a fundamental role in helping individuals and teams to understand what they need to change and how they need to change it, to translate evidence into practice. Each RLP was responsible for delivering the high-intensity intervention to the surgeries within one of the three geographical areas in Cambridgeshire covered by the trial. The RLPs found that showing empathy (understanding the nature of school/practice life) was central in building a relationship with the teachers/GPs. Face-to-face meetings at the point of consent facilitated this.
A beneficial approach was conveying the research as an important medium through which problems that were relevant for a GP’s daily practice could be understood and solutions to the problems could be generated. Flexibility when arranging presentations (i.e. offering more than one session to accommodate all staff) was important for optimising participation.
Convincing the practice leads that participation in the trial would benefit individual GPs, the practice as a whole and most importantly the patients was a key factor in gaining consent to participate in the research. Another successful strategy included emphasising that, by taking part in the trial, GPs could potentially be saving themselves and the practice time because the intervention would allow them to quickly and accurately judge whether or not a young person required a specialist assessment of symptoms. The GPs could see how this would benefit everyone involved.
The GPs were also concerned about what would happen to the individuals who they referred to CAMEO. Assurance that all those identified as being at risk would be invited into the PAATH study for 2 years of mental state monitoring and easy access to a CAMEO psychiatrist if there was any concern about symptoms deteriorating also helped them see the benefits of participating in the trial. We were also able to emphasise that patients without a diagnosis of HR would have a thorough mental health assessment and would then receive appropriate referral on to other services.
Challenges
The trial did not directly involve patients; therefore, it was assumed that only the agreement of practices in the high-intensity arm would be needed for the distribution of leaflets and for their participation in the educational sessions. However, despite discussions with previous members of the Cambridgeshire 1 Research Ethics Committee (REC) about this matter, the committee stipulated that formal consent was required from all invited surgeries, regardless of which arm of the trial they were assigned to. This led to an unexpected long delay in the roll-out of the trial, with contacts, sometimes visits, needing to be arranged with > 100 practices, ultimately resulting in our being granted an 18-month no-cost extension to our programme by the NIHR. The upside was more time to develop the theory-based interventions prior to the trial beginning.
This is a relevant point to place a general comment about our programme. We had to manage challenging situations, a protracted ethical review and subsequent adjustments to our protocol. All of these were ultimately beneficial (see in particular the PAATH study in Work package 5), other than the requirement to gain consent from practices to take part in the cRCT. That reduced our sample size but allowed a PAU comparator in those practices that did not consent, and we retained sufficient power to reject our null hypothesis and confirm the hypothesis of doubling referrals with uncanny accuracy. In retrospect, we would have benefited from a Programme Steering Group as is now required by the NIHR, but we drew on valuable advice from the Central Commissioning Facility and from the late Professor Helen Lester, who inspired some of our programme and was generous with her advice.
The recruitment process was lengthy and at times extremely frustrating. Busy GPs were difficult to contact directly but practice managers were good liaison intermediaries. However, many of the practice managers were very protective of the GPs’ time and were occasionally more negative about the likelihood of the practice participating than were the GPs when we eventually spoke to them. It took many attempts to persuade some practice managers to facilitate discussion of the research trial at team meetings, despite the fact that information had already been sent to the lead GPs within the practices.
The time commitment required to participate in the trial was a key issue for GPs. Reassurance that participation involved essentially just the 2 hours of educational sessions over the whole 2 years of the trial, for which the practice would receive income, was helpful in motivating them to participate.
Recommendations for future research
As has become evident in much health research, the process of ethical review can be protracted and frustrating for researchers. GPs’ negative attitudes, concerns and ambivalent feelings should be elicited and addressed with recruitment strategies.
We relied on the assumption that lead GPs would read the trial information sheet, discuss it with their colleagues and decide whether or not they wanted to participate. It became apparent during the trial that this was not always the case, as many GPs with other demands on their time did not know about our trial. A more advantageous approach could be to advertise the trial with individual GPs prior to gaining consent.
Implementation of the Liaison with Education and General practiceS cluster randomised controlled trial with general practices
The full protocol for this trial has been published. 30
Research aims
Our main aim was to test the null hypothesis that, in terms of the effectiveness and cost-effectiveness of detecting individuals at HR aged 16–35 years, a theory-based educational intervention for primary care was not different from a postal information campaign co-ordinated from an office in a secondary care-based EIS (CAMEO). The journal, Trials, where we published the protocol, insisted on this null construction, which is not easy to follow.
Formulated in a positive manner, this cRCT compared two different approaches to liaising with primary care to increase detection and early referral of people at HR to a specialist early-intervention team for young people with psychosis. We predicated the sample size and power on a doubling of HR and FEP referrals by the high-intensity intervention.
Methods for data collection
General practices were randomly allocated into two groups to establish which is the most effective and cost-effective way to identify people at HR for psychosis. One group received postal information about the local EIS, including how to identify young people who may be in the early stages of a psychotic illness. The second group received the same information plus an additional ongoing theory-based educational intervention with dedicated liaison practitioners to train clinical staff at each site.
The primary outcome was count data per practice site on the number of HR referrals to a county-wide specialist EIS (CAMEO). This was conducted over a 2-year period. All referrals during the duration of the trial were assessed clinically by the study team and stratified into those who met criteria for HR or FEP according to the CAARMS11 (true positives) and those who did not fulfil such criteria (false positives).
Analysis of the effectiveness of the intervention
Given that the main outcome (referrals per practice) was count data, the yield, our primary statistical approach was Poisson regression. Results were adjusted for surgery size and the number of GPs working in each site was considered as a covariate in the model. We also employed Pearson’s chi-squared test and Fisher’s exact test to compare demographic characteristics of the general practices. All of the analyses were performed using the statistical package R (version 3.0.0; the R Foundation for Statistical Computing, Vienna, Austria).
Analysis of the cost-effectiveness of the intervention
Decision-analytic modelling was used to investigate the cost-effectiveness of the high- and low-intensity interventions compared with PAU. A decision tree was constructed in Microsoft Excel 2013 to model the care pathways of the young people in the trial and assess the costs and effects over 2 years associated with the two active interventions and PAU. The costs of (a) the high- and low-intensity interventions, (b) diagnosing referrals who did not meet criteria for HR or FEP (false positives), (c) diagnosing and treating identified HR and FEP cases (true positives) and (d) the subsequent treatment of HR and FEP cases who were not identified (false negatives) were included.
Results of the Liaison with Education and General practiceS cluster randomised controlled trial
The results from this trial have been published online (see Appendix 7). 31
Key findings on the effectiveness of the intervention
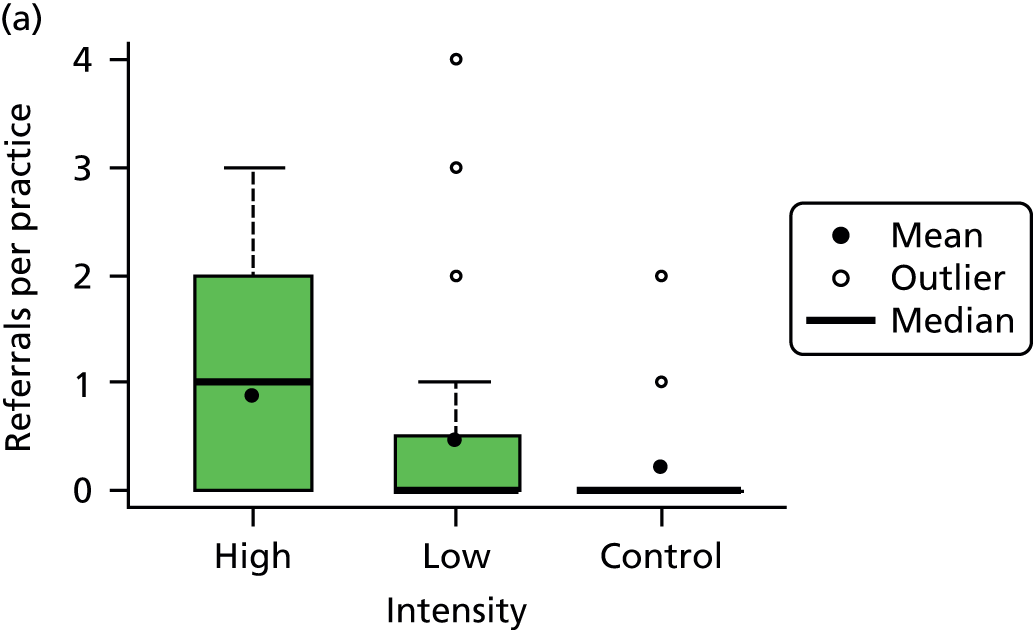
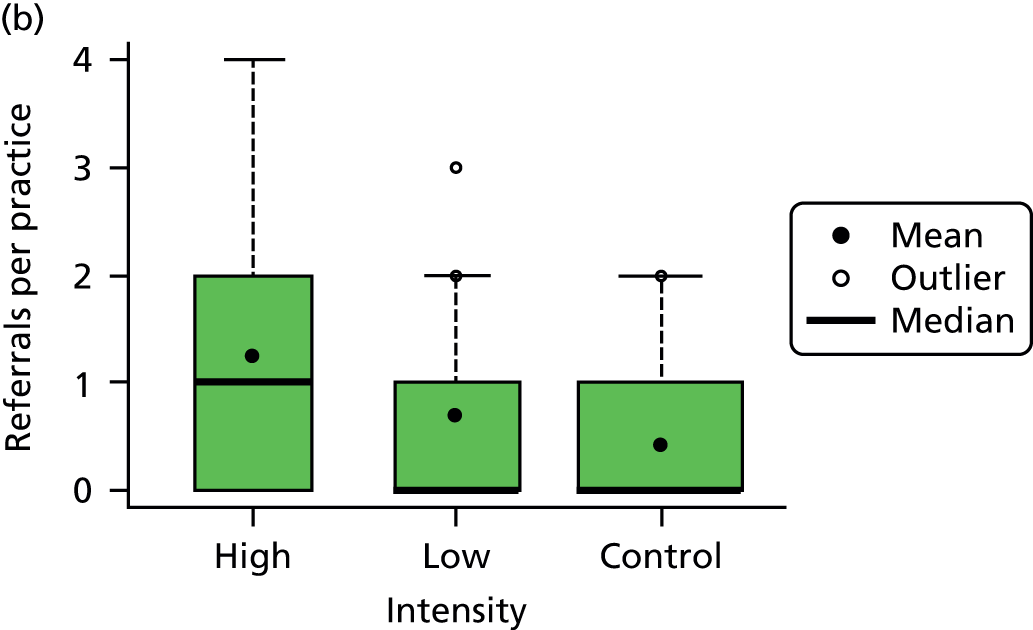
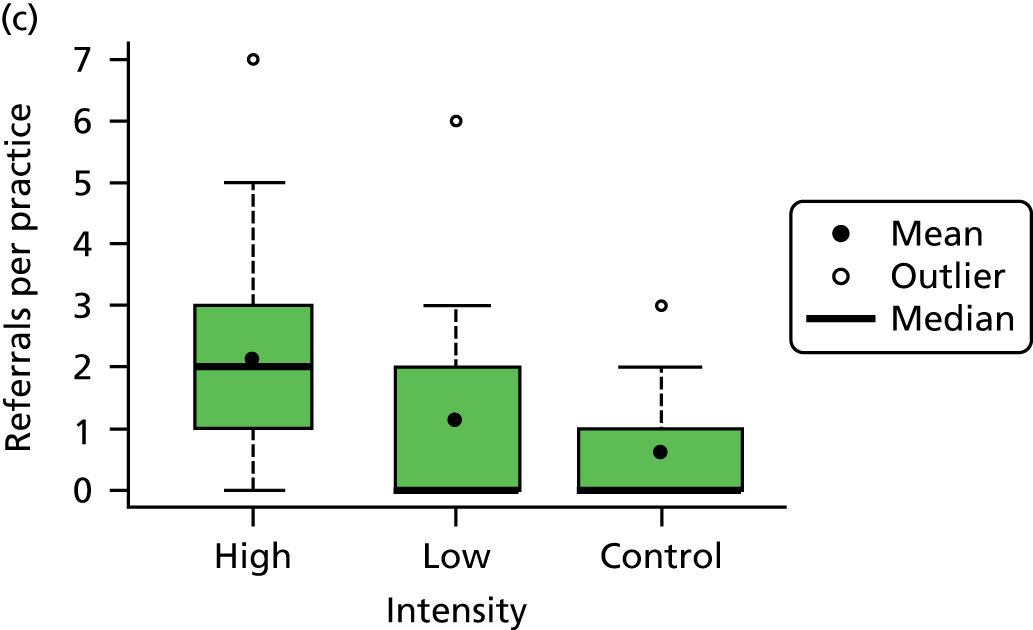
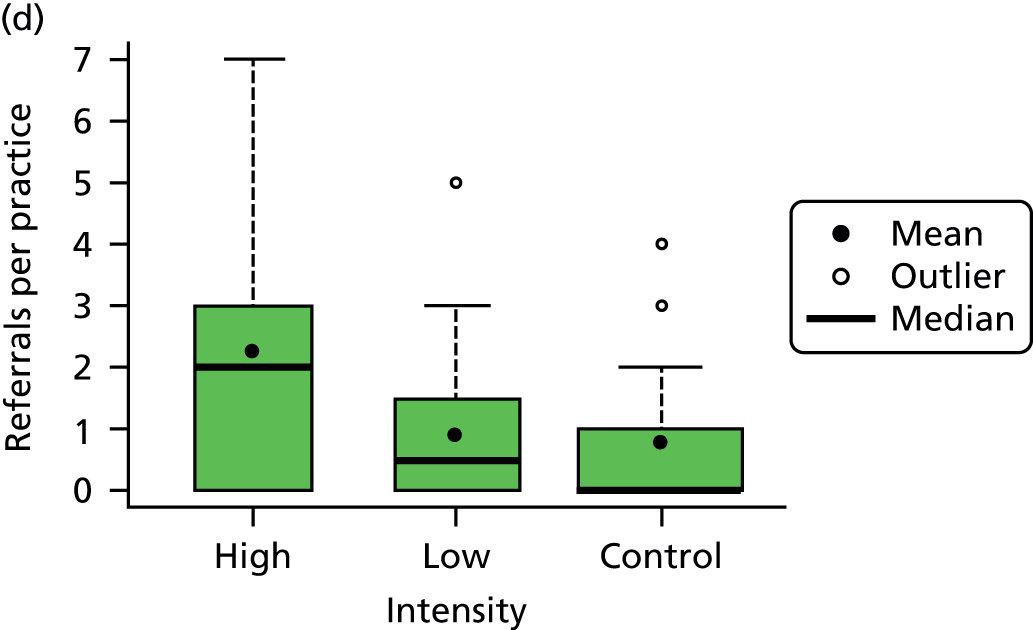
The intervention succeeded in raising awareness of potential psychotic symptoms. Between 22 December 2009 and 7 September 2010, 54 of 104 eligible practices provided consent and between 16 February 2010 and 11 February 2011 these practices were randomly allocated to the interventions (28 to the low-intensity intervention and 26 to the high-intensity intervention); the remaining 50 practices constituted the PAU group. Two high-intensity practices were excluded from the analysis. In the 2-year intervention period, high-intensity practices referred more FEP cases than low-intensity practices [mean (SD) 1.25 (1.2) for high intensity vs. 0.7 (0.9]) for low intensity; IRR 1.9, 95% CI 1.05 to 3.4; p = 0.04], although the difference was not statistically significant for individuals at HR of psychosis [mean (SD) 0.9 (1.0) for high intensity vs. 0.5 (1.0) for low intensity; IRR 2.2, 95% CI 0.9 to 5.1; p = 0.08]. For HR and FEP cases combined, high-intensity practices referred both more true-positive [mean (SD) 2.2 (1.7) for high intensity vs. 1.1 (1.7) for low intensity; IRR 2.0, 95% CI 1.1 to 3.6; p = 0.02] and more false-positive [mean (SD) 2.3 (2.4) for high intensity vs. 0.9 (1.2) for low intensity; IRR 2.6, 95% CI 1.3 to 5.0; p = 0.005] cases. Most of these (68%) were referred on to appropriate services. Referral patterns did not differ between low-intensity and PAU practices (Figure 6).
FIGURE 6.
Comparison of the distribution of referrals by intervention group. (a) HR; (b) FEP; (c) true positives; and (d) false positives. Lower hinge = 25th centile; upper hinge = 75th centile; line = median; filled dots = means; open dots = outliers.
Key findings on the cost-effectiveness of the intervention
Details of the quantitative economic results and how this part of the trial was conducted can be found at www.thelancet.com/cms/attachment/2035390784/2050868157/mmc1.pdf (accessed 19 January 2016).
Total cost per true-positive referral in the 2-year follow-up was £26,785 in high-intensity practices, £27,840 in low-intensity practices and £30,007 in PAU practices. The lower cost was attributable to fewer false negatives (HR and FEP cases that are not identified), which are assumed to be associated with treatment costs at a later point. The high-intensity intervention was the most cost-effective strategy.
Interpretation
This intensive intervention to improve liaison between primary and secondary care for people with early signs of psychosis was clinically effective and cost-effective. Increasing the resources aimed at managing the primary–secondary care interface provides clinical and economic value in this setting.
Successes
In the south of the county, mental health services were cohesive and the early-intervention team was well established. Generally speaking, the GPs in the south of the county were much better informed about the CAMEO team and what it could offer patients. As a result, they were more open to participating in research connected to psychosis.
The GPs were willing to discuss their patients in detail with each other at the two educational sessions. As a general rule, the GPs responded well to the facts and figures used to illustrate the main points within both the presentations and the DVD. Comments were made about how useful the DVD would be for training GPs and disseminating the information to colleagues who were unable to attend the presentations. As a ‘continuing professional development’ session, many of the GPs and practice nurses were positive about the educational intervention that they attended.
Notably, as with PsyMaptic (see Work package 3), NHS England is currently using these results in its strategy to implement waiting time standards and targets for EISs nationally.
Challenges
General practitioners’ perceptions of the poor relationships between primary care and secondary mental health services was a barrier to participation and the building of relationships with the RLPs. In the north of the county, EISs were relatively new and historically there had been difficult relationships between primary care and local mental health services. Attitudes in the north of the county towards the liaison aspect of the trial and the potential outcome of referrals to CAMEO were rather negative in comparison with attitudes in the south. During some of the educational interventions, several GPs were quite adversarial and extremely critical of mental health services in general. However, the process of the study appeared to help this and the GPs had, after all, agreed to take part.
It took GPs between 15 and 30 minutes to complete the TPB questionnaire. Many of them found it arduous and complained that it was too lengthy. The RLPs had to work hard to justify the displeasure that some of the GPs felt at having to complete such a long questionnaire. Much effort was made to explain why such a questionnaire was being used and how much of an essential part of the research it was. However, this remained the most consistent criticism of the interventions delivered.
During the 60-minute sessions it was a challenge to deliver the presentation, complete questionnaires and leave some time for questions at the end. Some GPs were very keen to discuss particular patients, whether or not they had HR symptoms. The numbers of clinicians who did attend the sessions was always fewer than the numbers practising at the individual surgeries.
During the first educational intervention, some GPs commented that they had not seen any patients with suspected HR symptoms since receiving the leaflet and were rather dismissive of how relevant this all was to their everyday experiences of young people and their problems. To address this, the importance of identifying the early signs of psychosis was emphasised in the DVD by the chief investigator of the trial, Professor P Jones, Head of Psychiatry at Cambridge University. He used the example of ‘crushing chest pain’ as an analogy for the importance and urgency of identifying and treating psychotic symptoms because of the devastating, long-term effects of untreated psychosis on the individual. This aspect of the DVD did generate discussion with some groups of GPs and provided an opportunity to emphasise again how the long-term effects of a psychotic illness should be avoided at all costs.
To facilitate further reinforcement of the symptoms that GPs should be looking for in young people, practices in the high-intensity group were given specific details about the symptoms of the HR patients who they referred. These were provided in the initial assessment feedback document and in the updates for each of the follow-up assessments. GPs rarely commented on this more detailed feedback during the second educational intervention.
There were mixed responses to the DVD. Some GPs found it very helpful; however, some found it to be repetitive because of similar material in the ‘revision’ presentation.
Limitations
A variety of reasons were given for non-attendance at the sessions. These ranged from being on duty to sickness or being on annual leave. Our strategy to address this was to offer practices multiple visits. This facilitated the maximum number of clinicians attending each session. At some surgeries GPs could not stay for the whole session because of clinical commitments; therefore, it is possible that some GPs missed vital information. Another consequence was that not all of the surgeries had a comparable educational experience and this could have had some effect on the results of the trial. We used an intention-to-treat approach for the analysis.
General practitioners rarely telephoned RLPs to discuss particular patients or symptoms, despite being encouraged to do so at every opportunity during the course of the trial. We suspect that their decisions to refer did not depend on the minutiae and finer points of psychopathology that interest secondary mental health care. If the number of RLPs was scaled down or RLPs were removed from the high-intensity intervention it could have been more cost-effective; however, this is conjecture.
Sufficient copies of the laminated version of the leaflet were sent to each practice that each GP could receive his or her own copy before the date of the intervention. When we asked the GPs about their experiences of using the leaflet it was rather disappointing to discover that many of them had not used it and in some practices had not seen it at all. In some cases this seemed to be an administrative error; the leaflets may have arrived at the practice but had not been distributed to the individual GPs. Some of the lead GPs took responsibility for this; in other practices it was the responsibility of the practice manager. Clearly, in some cases our leaflets remained in the postal noise, not being recognised as signal.
Recommendations for future research
Many of the GPs were doubtful about being able to refer accurately. They considered that many of the signs and symptoms that could indicate risk are also present in other mental health illnesses such as anxiety, depression or obsessive–compulsive disorder. This issue was revealed in the pilot study; therefore, we had focused on encouraging the GPs to keep their ‘HR radar’ on when interviewing a young person. We specified that they should use the leaflet to help them ask the relevant ‘probing’ questions, which would guide their referral practice. Their lack of confidence, despite these strategies, is an issue that needs to be addressed in future research.
During the course of the trial many GPs expressed that (1) they would rather have had an electronic version of the leaflet or (2) specific at-risk symptoms should have been included in their nationwide, web-based illness identification tool, which is available to all GPs. This would have been a good idea.
The trial did not measure how long the intervention effect endures or calculate the optimal number of sessions required. This information is important to enable a balance between intervention effectiveness and cost-effectiveness while maintaining identification of HR and FEP individuals.
The Liaison with Education and General practiceS cluster randomised controlled trial: liaison with 16+ educational institutions to detect and refine referrals of people with at-risk mental-states for psychosis
The aims, methods for data collection and analyses for the cRCT with 16+ educational institutions replicated the work with primary care practices but in a different setting. Briefly, we used the TPB to assess teachers’ baseline knowledge and motivation to change behaviour regarding pupils with HR mental states. We developed a low-intensity intervention and a high-intensity ‘teach the teachers’ intervention that we compared in a cRCT.
In our programme we made the primary care trial the priority and, because of disappointing initial results in the educational setting, have completed this educational work later. The follow-up period for counting referrals has now come to an end and we are analysing the data. Here, we outline key findings, successes, challenges, limitations and recommendations for future research for each of the completed stages.
A detailed description of this developmental stage has been published (see Appendix 8). 32
Development of the educational intervention
Methods for data collection
An elicitation phase revealed beliefs underlying teachers’ motivations to detect HR students and informed the construction of a preliminary 114-item questionnaire incorporating all constructs outlined in the TPB. To define the determinants of teachers’ intention to identify HR students, 75 teachers from secondary and further education institutions in 12 counties surrounding Cambridgeshire completed the questionnaire. A psychometric model of item response theory was used to identify redundant items and produce a reduced questionnaire of 44 items that would be acceptable to teachers.
Analysis
A psychometric evaluation of the questionnaire was conducted. The polytomous graded response model was used to examine the validity items within direct and indirect measures and to inform decisions regarding the removal of items. Cronbach’s alpha coefficient was used to assess the internal consistency of the direct measures of attitude, subjective norm and PBC. The relationship between intention and the indirect and direct measures was investigated using path analysis.
Key findings
The average time taken to complete the TPB questionnaire was 20 minutes. The majority of the teachers (63%) reported never having attended any kind of mental health training during their careers.
Indirect measures were well constructed and adequately covered the breadth of the measured construct with the exception of PBC. Items within all direct measures measured the corresponding construct satisfactorily. Only one item within direct subjective norms, direct PBC, showed a factor validity of < 0.5. Cronbach’s alphas for the reduced questionnaire showed acceptable internal consistency.
Perceived behavioural control was the strongest predictor of intention, followed by attitude. Subjective norm did not predict intention. Collectively, the direct measures explained 37% of the variance of intention to identify HR for psychosis. Mean scores for direct measures were just above the mid-scale score for intention and attitude and just below the mid-scale score for subjective norm and PBC.
Teachers considered identifying students at HR for psychosis a worthwhile behaviour and would attempt identification during the school day and believed that their peers or superiors might not approve of them identifying at-risk students. The greatest source of social pressure came from the senior management team within 16+ educational institutions. Teachers’ confidence and control over identification were low.
Increasing awareness and understanding of mental health issues emerged as the most important source of personal positive beliefs. The lack of access to information, knowlege and resources could hinder teachers‘ identification behaviour. Teachers’ perceptions of how confident they are that they are capable of identification and how much control they have over identification were prominent motivational factors.
Our questionnaire proved to be reliable, with the analysis supporting the predictive power of intention within the TPB model.
Successes
We have confirmed the feasibility, reliability and acceptability of a TPB-based questionnaire to identify teachers’ beliefs and intentions concerning the identification of individuals at HR of psychosis.
Limitations
Despite strenuous efforts, the response rate to our questionnaire was very low: only 75 teachers (9.5%) returned the questionnaire of the 793 invited. External validity could have been undermined if respondents differed systematically from non-respondents, which they probably did. The potential limitations of using self-report measures must be considered when interpreting the results as acquiescence and social desirability may have been influencing factors.
Recommendations for future research
Objective measures of behaviour should be incorporated in future research to avoid reliance on self-report.
The questionnaire length would be a limiting factor for TPB studies with teachers; therefore, options for reducing the number of items should be explored in future research.
Design of the educational intervention
Successes
Work with ‘consultant’ teachers from outside the trial area was very important so that the language used about symptoms could be assessed and deemed to be at an appropriate level for non-medical staff.
Challenges
Teaching teachers was quite a daunting prospect for the RLPs. Achieving the balance between an appropriately academic language for a group of professional teachers and recognising that many teachers would have very little or no knowledge at all about psychosis required many revisions of the presentation material. Describing psychosis and HR symptoms had to be approached differently for the teaching staff as they had no clinical knowledge. Success in presenting this kind of intervention required the open acknowledgement of differing levels of knowledge and understanding about mental health problems. As both nurses and teaching staff would be present at the educational sessions, the needs of these two different professional roles needed to be addressed within the presentations.
It was important not to present the material as all encompassing but rather as an introduction to the subject, covering all of the essential information. Therefore, further information was made available through a recommended reading list, references and a paper copy of the presentation. This material was included in packs that were distributed at the end of the presentations.
Teachers were not able to refer directly to a secondary mental health team but had to refer through school and college nursing staff. It was necessary to contact the nurses’ local area team prior to the roll-out of the intervention to ensure that the referral procedure was in accordance with existing referral practices. This also prepared the nursing staff for the possible increase in number of referrals. Each individual institution’s referral procedures were respected, rather than dictating a county-wide protocol for the study.
It was also necessary to stress the importance of discussing any referral with the student, to establish that consent had been given for information sharing.
Implementation of the high-intensity intervention
Successes
The consent visit to 16+ educational institutions to discuss the trial seemed to considerably improve awareness of the EIS and the importance of not missing what could be the signs and symptoms of a developing mental illness in students who were not performing to expected levels. At the initial contact with 16+ educational institutions the response from most of the head teachers was extremely positive. The majority could see the importance of identifying students early to prevent serious illness from developing.
Many of the teachers were interested in the content of the presentations, asking pertinent questions. Positive recurring themes were:
-
the opportunity to discuss students who they recognised could be HR cases
-
a genuine enlightenment by the discussion of symptoms
-
awareness, for the first time, that there is a service that specialises in the assessment and treatment of young people with psychosis.
The nurses and pastoral support staff felt more confident when talking to students because of the leaflet and what they had learnt from the presentations.
Challenges
As stated in the previous section, many of the teachers were interested in the content of the presentations, asking pertinent questions. Negative recurring themes, that are themselves findings, included:
-
the teachers held strong views that identifying HR symptoms in students was not part of a teacher’s role
-
a reluctance to take on this extra ‘pastoral’ responsibility
-
a feeling that the content of the presentations was too medical and health related
-
a level of genuine anxiety about whether or not they should even attempt to identify HR symptoms.
Attempting to speak to the head teachers of some 16+ educational institutions proved difficult, with one school telling us that ‘we don’t have that kind of problem in this school!’ Conversely, other head teachers expressed an eagerness to be in the high-intensity group so that their staff could receive the high-intensity intervention. Many of the head teachers had not heard of the CAMEO service although others had through previous experience of having one or two students with psychotic disorders in their college.
Head teachers expressed a desire to have a ‘youth-focused’ service to which to refer students when necessary. Therefore, it was necessary to stress that referrals would be appropriate only for those who may be at risk of developing psychosis, not for those with any mental health problems generally. Having said that, our primary care trial suggests that this course of action may have benefits.
It became apparent that there were going to be few opportunities within the timetables of 16+ educational institutions to allow staff to be present all together for the presentations. The RLPs were able to reassure the head teachers that they could be as flexible as required to deliver the intervention. Solutions included delivering the intervention out of teaching hours or during lunch breaks or having the option of multiple sessions (one of the interventions was delivered at 0830 in the morning to accommodate as many teachers as possible).
Distributing and collecting the questionnaires at the educational sessions was challenging as the groups consisted of up to 50 teachers. At some of the larger groups extra research staff helped to facilitate this aspect of the presentations.
These larger numbers also meant that waiting for all of the teachers to complete the questionnaire became a problem, with small groups of teachers chatting among themselves before the rest had finished. This became quite disruptive and it took some time to retrieve the attention of those attending in order to continue with the second part of the presentation. Completing the questionnaire elicited some protesting, but it was stressed that this was very much a part of the research and essential to measuring the change in referral behaviour before and after the interventions.
Many teachers raised the subject of substance misuse-related psychosis. They were interested to know whether or not the use of substances would increase the likelihood of psychotic symptoms and whether or not this would be an exclusion criterion for referral to CAMEO. We reassured them that students who may have symptoms following alcohol or substance use should not be excluded from referral for assessment by CAMEO.
Limitations
There were several hundred teachers at some of the colleges and this made it almost impossible to know whether or not the leaflets had been distributed effectively to all staff. It is possible that a proportion of the teaching staff did not see, or have regular access to, the leaflet.
Recommendations for future research
Leaflet distribution should be monitored and verified in future interventions with 16+ educational institutions. Identifying and fitting in research with the rhythm of teachers’ professional development (e.g. ‘Baker days’) would be useful. That said, as with the GPs, teachers’ time is increasingly pressured and so finding innovative ways to generate research-based knowledge is a challenge.
We have completed the collection of data from the teachers involved in the LEGS trial. We plan to analyse these data over the next 6 months.
Supplement to the original research proposal: the Prospective Analysis of At-risk mental states and Transitions into psycHosis study
Rationale
The original design of the LEGS trial was to assess all referrals generated by the surgeries and schools in all three arms. These young people have often remained under GPs caseloads or unidentified in schools, with likely deterioration of functioning and academic tasks because of non-specific symptoms of psychosis. The individuals who were identified as HR would be offered 3-monthly follow-ups to assess their progress and monitor any transitions to FEP. Depending on the level of severity and particular needs, true HR cases would also be offered ‘signposting’ to appropriate teams. Non-true HR cases would also be discussed and referred to more appropriate mental health teams according to symptoms and needs. However, the Cambridgeshire 1 REC granted approval on the basis that the liaison with primary care and educational institutions and follow-up of ensuing referrals was divided into separate studies. This resulted in the design of the PAATH study. This was used to enhance the programme. This new work package, created as a result of a decision by an ethics committee, was added to the programme and represented a remarkable enhancement of the original grant application through an efficient use of available resources. We present it as work package 5.
Work package 5: follow-up of referrals of individuals identified as being at high risk for psychosis
The Prospective Analysis of At-risk mental states and Transitions into psycHosis
Research aims
The first aim of this study was to establish the prevalence of transition from HR mental states into FEP. We then aimed to describe and compare the characteristics of people with HR mental states who transitioned into FEP and the characteristics of those who did not. This would facilitate effective responses with better assessments and more focused interventions. Secondary objectives included various epidemiological and clinical analyses that would (1) contribute to an enhanced delineation of people at HR who are more likely to develop a full psychotic illness and (2) allow comparisons between people at HR and HVs, especially with regard to possible causal factors tied to sociodemographic and comorbid clinical characteristics, substance use and trauma history. Finally, we aimed to describe the morbidity and the effect on social functioning and quality of life of HR states, which are sometimes seen by services as merely predictors of FEP rather than as highly troublesome mental health conditions themselves.
Methods for data collection
All individuals at HR for psychosis living and detected in Cambridgeshire and Peterborough, including those identified by GPs or 16+ educational institutions in the LEGS cRCT, were offered a systematic follow-up in the context of this prospective, naturalistic study. Participants between the ages of 16 and 35 years were referred to our offices through a number of different routes (GPs, schools, relatives, friends). Candidates were initially assessed by both a psychiatrist and an experienced non-medical clinician trained in the CAARMS questionnaire,11 which is used to detect individuals at HR for psychosis. This was already routine practice in the CAMEO EIS. Individuals who met criteria for HR were invited to take part in the study and written consent was obtained.
A total of 60 help-seeking HR participants were followed up for 2 years from the initial referral date. Interestingly, all help-seeking HR individuals referred to us were willing to be followed up in the context of this study. However, as stated below, we encountered difficulties in retaining some of them for the whole follow-up period. During this period they were asked to attend nine interviews (at baseline and then every 3 months until the end of the study) at which they completed structured interviews and questionnaires under the direction of a clinical researcher. These questionnaires targeted different domains such as sociodemographic characteristics, diagnosis, psychiatric morbidity, trauma history, substance use and functioning, among others. The interviews took place in our CAMEO offices in Cambridge and Peterborough, at GP practices or in participants’ homes.
A random sample of 60 HVs matched for age (16–35 years), sex and geographical location was recruited by using the Postcode Address File® (PAF) provided by the Royal Mail. Addresses within the same three-digit postcodes as those of cases were picked at random and sent a letter inviting residents aged 16–35 years to participate. This methodology for finding comparison subjects had been successfully used in the ÆSOP study. 6
Healthy volunteers underwent the same battery of questionnaires at baseline, 1 year and the end of the follow-up period unless they were, themselves, diagnosed as HR. In this case they would be offered the same number of interviews, questionnaires and possible clinical interventions as the HR individuals. HVs were offered £50 as a reward for taking part in the study and an incentive of £50 if they completed the interviews. Table 3 provides a sociodemographic comparison between HR and HV participants in the PAATH study.
| Sociodemographic characteristics | HR participants (n = 60) | HVs (n = 60) | p-value |
|---|---|---|---|
| Age at study entry (years), median (min., max., SD) | 19.89 (16.41, 30.21, 2.38) | 22.60 (16.18, 35.57, 5.68) | < 0.001a |
| Sex, n (%) | |||
| Male | 31 (51.7) | 26 (43.3) | 0.465b |
| Female | 29 (48.3) | 34 (56.7) | 0.465b |
| Ethnicity, n (%)c | |||
| White | 56 (93.3) | 55 (91.7) | 1.000b |
| Mixed | 2 (3.3) | 2 (3.3) | 1.000b |
| Asian | 1 (1.7) | 2 (3.3) | 1.000b |
| Black | 1 (1.7) | 1 (1.7) | 1.000b |
| Occupational status, n (%)d (n = 7 with missing data) | |||
| Unemployed | 20 (33.3) | 8 (13.3) | 0.004b |
| Employed | 8 (13.3) | 27 (45.0) | 0.001b |
| Students | 25 (41.7) | 25 (41.7) | 0.575b |
Challenges of the Prospective Analysis of At-risk mental states and Transitions into psycHosis study
The process of identifying participants
Young people referred to and assessed by CAMEO but who were not experiencing a FEP were offered a follow-up interview including an assessment using the CAARMS to confirm or refute whether or not they met the criteria for HR for psychosis. Those who met the criteria were invited to another interview at which the outcome of their assessment was explained and they were provided with information about participation in the PAATH study. The study was explained in detail, drawing attention to the fact that there would be no treatment or intervention. It was also explained that participants would be seen over a period of 24 months, once every 3 months, undergoing mental state monitoring in the form of a selection of psychometric tools. It was difficult to describe the required involvement without sounding as though the participants were being asked to give up their time for no obvious advantage or direct therapeutic benefit. No payment was offered to participants but it was explained that by participating in the research they would have their symptoms monitored very carefully. Should the symptoms worsen they could be seen promptly by the psychiatrist leading the research. This provided some incentive because they would be seen much sooner without having to go through the usual route of referral by their GP back into secondary services.
Participant attrition
We implemented a variety of strategies to retain participant involvement in the PAATH study. Despite achieving a good rapport with many of the participants, keeping in touch with them after the baseline session and encouraging them to continue the 3-monthly assessment sessions was a real challenge. This was probably in part because they were generally a mobile, transient young population.
Lack of clinical follow-up by mental health services
Although a high proportion of those meeting the criteria for HR were signposted on to other services for support [e.g. Improving Access to Psychological Therapies (IAPT) service or locality mental health teams], some participants did not engage with the other service at the outset or soon dropped out. Therefore, members of the research team may have been the only mental health professionals seeing the young person. We implemented protocols to take clinical risk issues into account. Clear guidelines were followed, should any clinical crisis occur. However, because the CAMEO team is not funded to work with HR individuals it did create confusion with regard to clinical responsibility. Other mental health teams could mistakenly believe the participant to be under the care of the CAMEO team rather than participating solely in a research study, despite our best efforts to make it very clear in our clinical documentation that this was not the case. Some PAATH participants would inform other mental health professionals that they were ‘under CAMEO’, erroneously giving the impression that they were being treated, without understanding the confusion that this created. To try and solve this potential confusion, we sent a clear explanation of the situation of the participants with regard to clinical responsibility to any mental health professionals involved and to the participants’ GPs. Standard letters were sent out to the referrers or to our clinical colleagues in other secondary care teams as appropriate.
Respondent fatigue
At baseline and thereafter at 6-monthly intervals a batch of 10 assessment tools was administered to each participant. This process took approximately 2 hours for each participant. It was difficult at times to keep the participants engaged with such a lengthy session. Several of the assessment tools contained similar questions despite assessing different aspects of the participants’ mental health and this caused frustration for the participants. Moreover, several of the tools themselves were lengthy, especially some of the self-completing assessments. At times, much encouragement and support was required to ensure that participants completed all of the assessments. We always tried to complete the whole batch in one session to prevent the possibility that participants would drop out, resulting in missing data.
The potential therapeutic effect of monitoring
It was inevitable that working relationships would be formed between the participants and the research clinicians during the months of assessment. Seeing someone every 3 months for 2 years resulted in significant monitoring of their mental health. This resulted in a certain amount of understanding of their current situation and any issues or difficulties that they were having in their lives. Although no overt or deliberate therapeutic intervention was provided, the continuity of contact and necessary interest in the participants’ well-being resulted in a relationship that it could be argued was therapeutic in itself and this may have influenced the course of the participants’ illness to some degree.
For the researchers it became increasingly frustrating that we were seeing many young people for whom there was no appropriate service available. Services are still divided between child and adolescent and adult mental health teams. Therefore, young people have no access to a service that provides specialist, non-stigmatising and youth-friendly approaches to working with mental health problems in young adults.
Referrals to Improving Access to Psychological Therapies in primary care
The majority of young HR individuals that we evaluated and followed up over the course of our programme indicated a strong preference to be treated in primary care rather than in a specialist mental health service. Interestingly, during our programme the NHS implemented in primary care one of the most important innovations in mental health services in recent decades: the IAPT programme [see www.iapt.nhs.uk (accessed 19 January 2016)]. This programme massively increased access to psychological treatments for anxiety and depression in primary care across England, promoting the use of talking therapies based on cognitive–behavioural therapy (CBT) approved by the National Institute for Health and Care Excellence (NICE).
Given the high prevalence of depression and anxiety in the HR individuals assessed in our services, we made a number of referrals (n = 66) to IAPT services. Many of them (n = 22; 33%) were not accepted because IAPT therapists were not appropriately trained to provide psychological therapies to people experiencing psychotic-like experiences, even if these were in the context of depression and anxiety. Of those who were accepted (n = 44; 67%) for treatment by IAPT services, a significant proportion (n = 25; 57%) disengaged after one or two therapy sessions. This uncovered the need to tailor IAPT CBT to engage and treat individuals with these clinical presentations, enhancing engagement, assessment of complex problems and management of psychotic-like experiences by de-catastrophising and normalising, as also recommended in NICE guidelines for schizophrenia. 33
Prevalence of transition from high risk to first-episode psychosis over 2 years
Key findings
Only three out of 60 (5%) of our HR sample made a full transition to a psychotic disorder based on structured clinical diagnosis (10% when CAARMS11 criteria were employed) over the 2-year follow-up period. This was an unexpectedly low figure given our prior beliefs at the beginning of the programme in 2008, but is in line with the results of other studies published over recent years, including the Early Detection and Intervention Evaluation for people at risk of psychosis (EDIE-Two) study,7 a RCT of CBT for young people with HR mental states in which we were a study site. Overall, the transition in the intervention and control groups was < 10%. This is a really important finding for young people with HR mental states – they are not at very HR of transition to a FEP over 2 years and the term ‘high risk’ is almost a misnomer. Rather, services can focus on the mental health problems that they have in addition to their psychotic experiences, largely depression and anxiety (see Psychiatric morbidity in the high-risk sample).
Thus, it is important not only to pay attention to the evolution of HR individuals but also to thoroughly understand the type and severity of the psychopathology and the psychological and demographic characteristics of these presentations as an independent morbid population cluster. The development of specific care pathways or beneficial interventions for this population is urgently required.
Strengths
The epidemiologically principled design, the standardised assessment with the CAARMS11 and the 2-year follow-up are particular strengths of this study.
Limitations
The study is relatively small with low precision in the prevalence of transitions to FEP. Recruiting a sample large enough to lead to a step change in power and precision (e.g. 10 times as many) would be a huge challenge requiring multicentre working. Participation in the PAATH study could indirectly involve the provision of non-specific clinical care. One-to-one sessions with a supportive research clinician every 3 months could reduce stress and subsequently the likelihood of conversion into frank psychotic disorders. This may have reduced the number of transitions.
Recommendations for future research
The inclusion of a follow-up component in future research in this area with a more sophisticated approach to outcome than merely HR, FEP or normal is recommended. These states all have a wide range of expression, with a kaleidoscopic variability over the medium term in some people. Studies equipped to capture this would allow the relationships between psychotic experiences and other psychopathology to be more clearly understood and more effective management to be devised.
Psychiatric morbidity in the high-risk sample
See Appendix 9 for the published report of this work. 34
Research aims
To ensure that appropriate care pathways and interventions are put in place that benefit people at HR for psychosis, the type and severity of psychopathology in this group must be understood. The aims of this study were to describe the clinical and functional characteristics of young people at HR for psychosis. We compared their level of global functioning, occupational status and quality of life with those of a sample of HVs recruited from the same geographical area.
Methods for data collection
We collected sociodemographic information, clinical morbidity measures including the Positive and Negative Syndrome Scale (PANSS),35 the Beck Depression Inventory version II (BDI-II),36 the Beck Anxiety Inventory (BAI),37 the Young Mania Rating Scale (YMRS)38 and the Yale–Brown Obsessive Compulsive Scale (YBOCS),39 functioning measures including the Global Assessment of Functioning (GAF)40 and occupational status, as well as subjective quality of life measured by the Manchester Short Assessment of Quality of Life (MANSA)41 for 60 HR individuals and 45 HVs. Although the final sample total for the HV group in the PAATH study was 60, this paper was published before recruitment was complete; therefore, the HV sample includes only 45 participants.
Analysis
All comparisons were made using the chi-squared test or Fisher’s exact test for categorical variables and the t-test or Mann–Whitney U-test for continuous variables.
Key findings
Individuals at HR are a heterogeneous group with members commonly having more than one psychiatric disorder, mainly depression and/or anxiety or anxiety-related states such as obsessive–compulsive disorder. In contrast with previous cohorts, individuals at clinical HR in our sample were affected by mild psychotic symptoms. In addition to psychotic symptoms, a wide range of serious psychiatric disorders, suicidal ideation/intention, depressive and anxiety symptoms, low levels of quality of life and employment status impede the global functioning of those at HR.
High-risk individuals had poorer functioning with significantly lower GAF scores for symptoms and disability than HVs (both p < 0.001). There was a statistically significant higher prevalence of moderate/severe depression (p < 0.001 and p = 0.025, respectively), anxiety (p < 0.001), obsessive–compulsive behaviours (p < 0.001) and suicidality (p < 0.001) in HR individuals than in HVs. Therefore, a HR mental state may be associated not only with an increased risk for psychosis but also other psychiatric disorders (Table 4). Indeed, linked psychometric analyses by the authors (JS, JP, TJC and PBJ) in other population samples indicated that psychotic experiences measure the severe end of a common mental distress factor, which is consistent with these results. 42
| Clinical characteristicsa | HR participants (n = 60) | HVs (n = 45) | p-value |
|---|---|---|---|
| PANSS, mean (SD) (n = 6) | |||
| Positive | 13.1 (3.2) | 7.1 (0.5) | < 0.001b |
| Negative | 12.4 (5.0) | 7.8 (0.9) | < 0.001b |
| General psychopathology | 32.7 (7.0) | 16.3 (1.3) | < 0.001b |
| Sum of all items | 58.2 (12.1) | 31.3 (1.9) | < 0.001b |
| BDI-II (n = 11) | |||
| Sum of all items, mean (SD) | 29.9 (12.8) | 5.6 (5.5) | < 0.001b |
| Suicidality (score 1–3), n (%) | 36 (72.0) | 4 (9.1) | < 0.001c |
| Depression subgroup, n (%) | < 0.001c | ||
| Minimal (score 0–13) | 5 (10.0) | 39 (88.6) | < 0.001c |
| Mild (score 14–19) | 8 (16.0) | 3 (6.8) | 0.167c |
| Moderate (score 20–28) | 10 (20.0) | 2 (4.5) | 0.025c |
| Severe (score 29–63) | 27 (54.0) | 0 (0) | < 0.001c |
| BAI (n = 15) | |||
| Sum of all items, mean (SD) | 28.2 (11.9) | 6.7 (5.6) | < 0.001b |
| Anxiety subgroup, n (%) | < 0.001c | ||
| Minimal (score 0–7) | 2 (4.2) | 29 (67.4) | < 0.001c |
| Mild (score 8–15) | 5 (10.4) | 9 (20.9) | 0.165c |
| Moderate (score 16–25) | 12 (25.0) | 5 (11.6) | 0.102c |
| Severe (score 26–63) | 29 (60.4) | 0 (0) | < 0.001c |
| YMRS (n = 7) | |||
| Sum of all items, mean (SD) | 3.9 (4.1) | 0.5 (1.2) | 0.001b |
| YBOCS (n = 13) | |||
| Having obsession, n (%) | 37 (77.1) | 2 (4.5) | < 0.001c |
| Having compulsion, n (%) | 34 (70.8) | 1 (2.3) | < 0.001c |
| Sum of all items, mean (SD) | 20.1 (5.8) | 5.3 (1.5) | < 0.001b |
| Severity subgroups, n (%) | < 0.001c | ||
| Subclinical (score 0–7) | 2 (5.4) | 3 (100) | 0.001d |
| Mild (score 8–15) | 5 (13.5) | 0 (0) | 0.001d |
| Moderate (score 16–23) | 20 (54.1) | 0 (0) | 0.231d |
| Severe (score 24–31) | 9 (24.3) | 0 (0) | 1.000d |
| Extreme (score 32–40) | 1 (2.7) | 0 (0) | 1.000d |
This prominently poor global functioning and quality of life (Table 5) combined with a significant risk of suicidality justifies special attention from mental health services to develop appropriate care pathways.
| Functioning and quality of life measuresa | HR participants (n = 60) | HVs (n = 45) | p-value |
|---|---|---|---|
| GAF, mean (SD) (n = 3) | |||
| Symptoms | 45.4 (8.9) | 86.6 (3.8) | < 0.001b |
| Disability | 48.6 (9.4) | 86.7 (3.6) | < 0.001b |
| Occupational status, n (%) (n = 7)c | 0.061d | ||
| Unemployed | 20 (37.7) | 8 (17.8) | 0.029d |
| Employed | 16 (30.2) | 22 (48.9) | 0.058d |
| Student | 17 (32.1) | 15 (33.3) | 0.895d |
| MANSA, mean (SD) (n = 11) – satisfied with: | 3.8 (1.0) | 5.6 (0.6) | < 0.001e |
| Life as a whole today | 3.4 (1.5) | 5.6 (1.0) | 0.001e |
| Health | 3.5 (1.4) | 5.4 (1.1) | < 0.00e |
| Present mental health | 3.0 (1.4) | 6.2 (0.8) | < 0.00e |
| Job (if working) | 4.1 (1.8) | 5.4 (1.4) | 0.011e |
| Not working (if not working) | 3.7 (1.7) | 4.0 (1.9) | 0.532e |
| Financial situation | 3.5 (1.5) | 4.6 (1.5) | 0.001e |
| Leisure activities | 3.9 (1.9) | 5.6 (1.3) | < 0.00e |
| Number of friends | 4.2 (1.8) | 5.8 (1.0) | < 0.001e |
| Relationships with friends | 4.5 (1.7) | 5.7 (0.9) | < 0.001e |
| Personal safety | 4.0 (1.6) | 5.8 (0.9) | < 0.001e |
| Accommodation | 4.6 (1.7) | 6.0 (1.2) | < 0.001e |
| People one lives with (if living with other) | 4.7 (1.4) | 6.1 (0.9) | < 0.001e |
| Living alone (if living alone) | 4.0 (–) | – | – |
| Relationship with family | 4.0 (1.4) | 5.6 (1.0) | < 0.001e |
| Life overall | 3.0 (1.4) | 5.8 (0.9) | < 0.001e |
Limitations
A chronicity criterion should have been used to determine any differences in psychopathological profiles between individuals with longer and shorter durations of HR symptoms.
The study was cross-sectional and therefore it was not possible to identify causal relationships between the HR state, psychiatric morbidity and impaired functioning.
Recommendations for future research
Rather than exclusively focusing on the treatment and/or prevention of psychosis, clinical interventions with individuals at HR identified in EISs should aim at targeting a broader range of psychopathology, especially mood and anxiety symptoms.
Substance use
See Appendix 10 for the published report of this work. 43
Research aims
The role of substance use in the development of HR for psychosis or its impact on the transition to full psychotic presentations is overlooked in the literature. The aim of this study was to describe in detail past and current substance use in HR individuals and compare this profile with that of a random sample of HVs recruited from the same geographical area.
Methods for data collection
We recorded information on alcohol and substance use profiles for both groups, including identification of abuse/dependence and influence on psychotic-like experiences. Additionally, differences between HR individuals and HVs were assessed for sex, ethnicity, occupational status, age of lifetime first substance use and prevalence and frequency of substance use.
Analysis
To compare the two groups a two-sample t-test was used for age and Fisher’s exact test was used for sex, ethnicity and occupational status. Fisher’s exact test was also used for assessing the differences between substance use distributions and patterns. The Wilcoxon signed-rank test was employed for non-normally distributed continuous variables (age of lifetime first substance use, frequency of substance use). Box plots were used for graphical representation of the differences in frequency of substance use.
Key findings
High-risk individuals were significantly younger than HVs when they started using alcohol and drugs (p = 0.014). This may be important as harmful effects of drugs may differ according to brain development, with younger brains and minds being more vulnerable to deleterious effects. The prevalence of HR substance use was generally similar to that of HV substance use except for past polydrug use, which was higher for HR individuals. HR polydrug users experimented with a wider range of substances than HV polydrug users. Choice of substance was similar when comparing HR individuals’ and HVs’ current and past use. Alcohol was the most frequently reported substance used in both groups. This was different from previous findings in which cannabis was the most commonly used substance. 44 Cannabis was the most widely used drug in both groups, the use of other illicit substances being considerably lower; the least used substances for both groups were sedatives and opiates.
None of the HR individuals or HVs met the criteria for a Diagnostic and Statistical Manual of Mental Disorders, 4th edition, text revision (DSM-IV TR)45 substance use disorder or dependence. Thus, the HR substance use profile in our sample was significantly different from that of FEP patients in our region at the time of their referral to CAMEO. The pattern of comparatively low use in people with HR mental states could have some influence on psychotic-like experiences but not on transition to a frank psychotic disorder.
The main difference between HR individuals and HVs was the frequency of substance use. Current frequency of use was significantly higher in HR individuals than in HVs for alcohol (p = 0.001) and cannabinoids (p = 0.03) (Figure 7). None of our HR group used cannabis daily. This was contrary to many reports in the literature regarding HR individuals, in which around 60% of participants used these substances. 44 Frequency of substance use for HR individuals was similar for current and past use whereas HVs were more likely to have had a period in the past when they used these substances more frequently (see Figure 7). This sustained substance use over a protracted period could be more deleterious than a shorter period of increased use. The higher frequency of substance use in HR individuals combined with a significantly younger age of first use could contribute to the development of psychotic-like experiences.
FIGURE 7.
Frequency of substance use in HR individuals and HVs in the PAATH study. (a) Current frequency of substance use; and (b) past frequency of substance use.
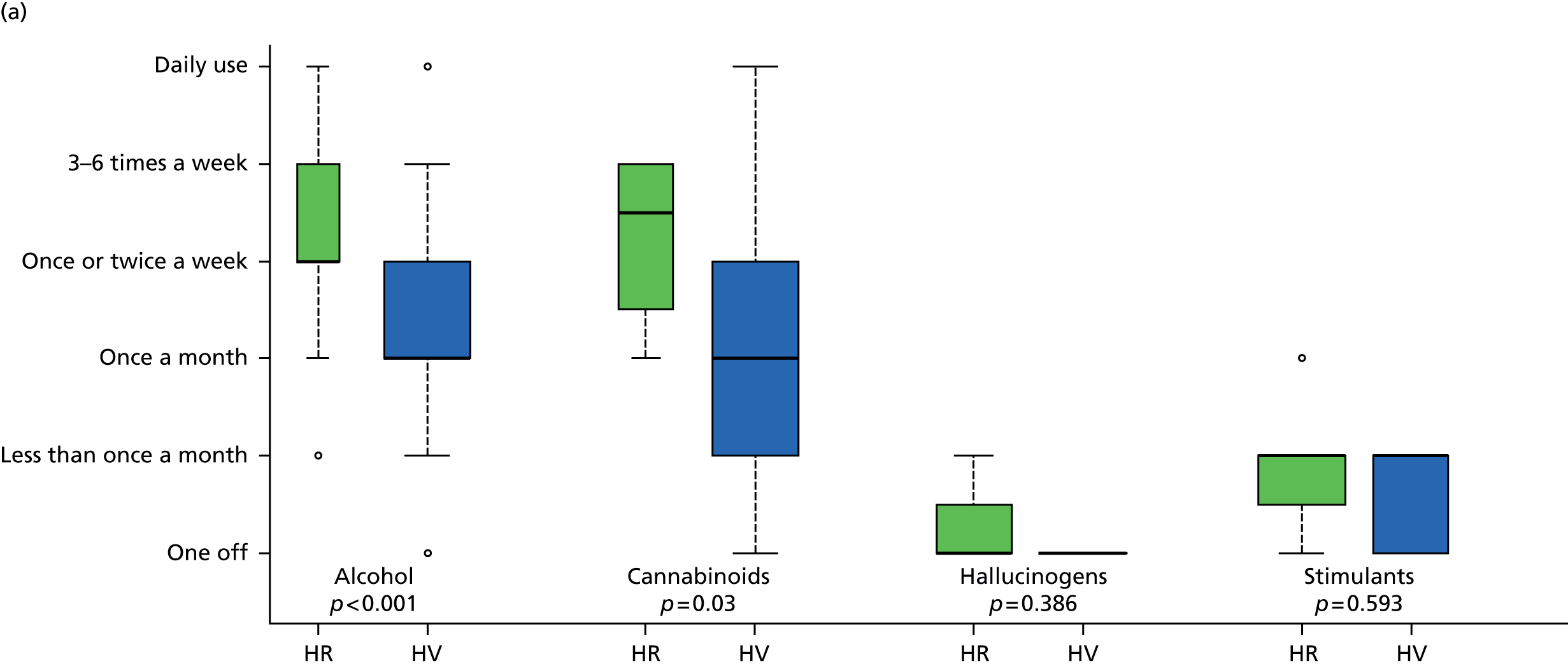

Limitations
The short follow-up period in this study could explain the low transition rate. In addition, the 3 monthly follow-ups may have been therapeutic and consequently reduced the likelihood of transition. The sociodemographic differences between our groups could also have influenced the findings. HVs were significantly older than HR individuals. In addition, as male sex is associated with substance use in patients and psychotic disorders in the general population, the slightly higher proportion of males in the HR group may have influenced the substance use profiles.
Recommendations for future research
The pattern of substance use by each individual following their referral to CAMEO was not closely monitored. Future research should include a prospective follow-up to show any changes in patterns of substance use and identify any associations with incidence of psychotic experiences over time.
Substance use in HR individuals requires a greater emphasis and a more detailed consideration in future studies. All of our studies are from secondary analyses in a relatively small sample; the younger age of onset of use in the HR group may be important and, chiming with findings from other studies44 including birth cohorts, merits further enquiry at clinical and biological levels.
History of psychological, physical and sexual trauma
See Appendix 11 for the published report of this work. 46
Research aims
Differences in the experience of trauma such as severity, frequency and age at trauma exposure could result in different responses among individuals and explain the likelihood of developing particular psychiatric symptoms. The aim of this study was to compare the characteristics of the trauma history between young people at HR for psychosis and a sample of HVs recruited from the same geographical area to determine which are more likely to be associated with HR mental states.
Methods for data collection
The Trauma History Screen (THS)47 was used to enable an assessment of the number and perceived intensity of adverse life events and age at trauma exposure. The BDI-II36 and BAI37 were also used to assess the relationship between these factors and depression and anxiety.
Analysis
Fisher’s exact test was used to compare demographic information and negative binomial regression was used for the comparison of the total number of traumas and the age at which trauma occurred.
Poisson regression and the t-test were used to compare individual traumas and the intensity of trauma respectively. Relationships between age at which trauma occurred, number and intensity of traumas, BDI-II score and BAI score were explored with Pearson correlations. Logistic regression was used to assess the influence of age at trauma exposure and the intensity and number of traumas with regard to the presence of HR mental states. We also presented graphical comparisons of both groups using box plots.
Key findings
High-risk participants had a higher incidence of trauma and reported repeated exposure to trauma compared with HVs. Traumatic events involving physical abuse with intention to harm accounted for the largest proportion of reported trauma for both groups and showed the largest difference between HVs and HR participants. Traumatic events involving sexual abuse were uncommon in both groups.
High-risk participants experienced significantly more traumatic events than HVs (p ≤ 0.001) but equivalent distress in relation to these events. Although up to 70% of individuals endorsed experiencing distress, in both groups 30–40% of traumatic experiences were not considered to be emotionally distressing. There was only a single case of post-traumatic stress disorder in the whole sample. The perceived intensity of trauma could be a future predictor of psychopathology other than psychosis.
First incidents of trauma and the total number of traumas (p < 0.001) occurred at an earlier age for HR participants, who also experienced significantly more traumas during the developmental period between the ages of 0 and 8 years (p ≤ 0.001) (Figure 8). HVs experienced more traumas between the ages of 25 and 35 years and higher instances of trauma occurred between the ages of 9 and 24 years than between the ages of 0 and 8 years. Both incidences of trauma and age at which trauma occurred were the most likely predictors of becoming HR, not the degree of distress reported as a result of the trauma. Higher age for trauma exposure and lack of sexual abuse could be ameliorating factors for the HR individuals in this study.
FIGURE 8.
Box plots showing (a) the distribution of traumatic events; (b) the intensity of trauma; and (c) the age at trauma exposure for HR and HV participants in the PAATH study.

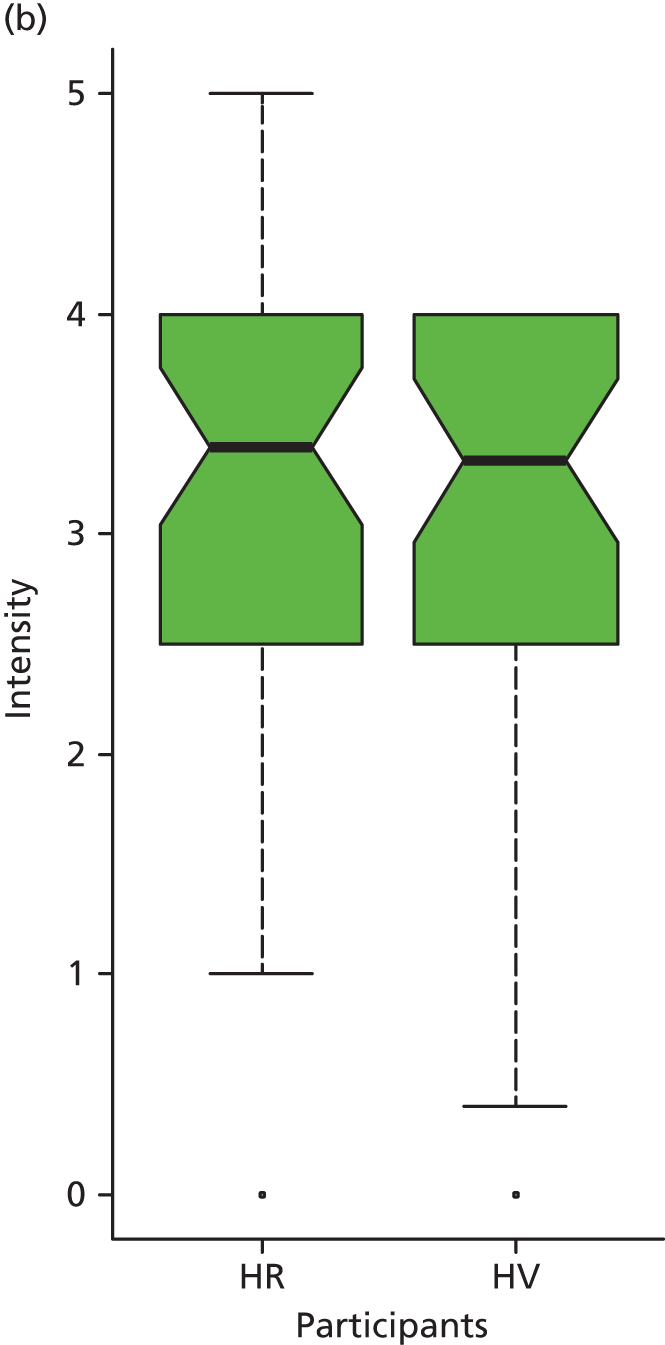
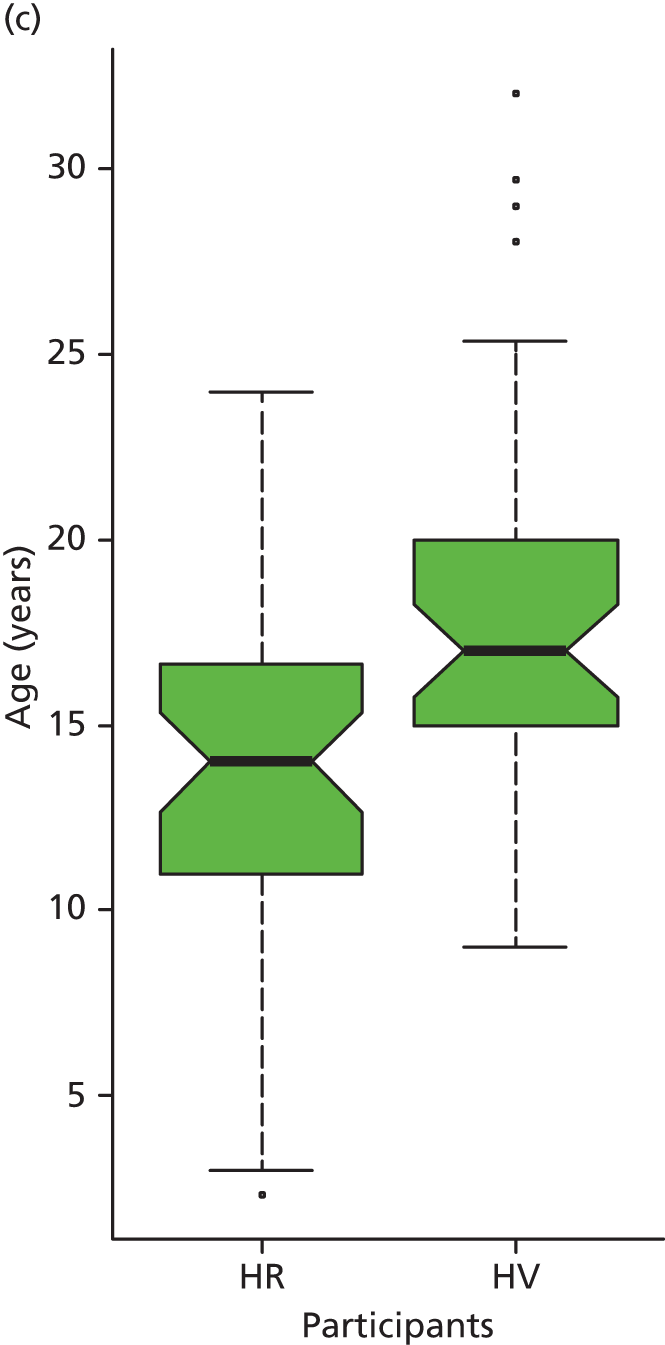
Higher levels of anxiety (p ≤ 0.001) and depression (p ≤ 0.001) were found in our HR group. Combined with the very low transition rates to date, this could be interpreted as a lack of diagnostic specificity and predictive value in the HR model. A HR mental state is not necessarily a specific marker for psychosis. The prevalent co-presence of anxiety and depression in this group indicates that trauma may play a role in this manifestation of symptoms.
Limitations
Trauma was measured only using the respondents’ subjective information and not corroborated by independent information. Using a combination of methods would yield the most accurate record of trauma. A valid measure of distress should have been used to elucidate any relationships between distress, trauma, anxiety and psychotic experiences/symptoms.
Although the THS47 does examine trauma involving physical abuse as a child and events that induce feelings of fear, helplessness and horror, there is no specific question concerning bullying. It is possible that a large proportion of traumatic experiences were missed because of this omission.
Recommendations for future research
We need to understand the emotional impact of trauma on the subjective perceptions of the individual. This can extend our understanding of why particular events cause traumatic stress in particular individuals.
To enable differentiation between psychotic-like experiences that may reflect dissociative responses to trauma and genuine prodromal psychotic presentations, trauma characteristics in individuals at clinical HR should be thoroughly assessed routinely.
First-rank symptoms
See Appendix 12 for the published report of this work. 48
Research aims
Kurt Schneider49 considered certain types of psychotic experience of first-rank importance in deciding whether or not a psychotic syndrome was schizophrenia. These ‘first-rank symptoms’ (FRSs) remain influential in operational diagnostic criteria today, but there is little work evaluating their significance in HR mental states or even whether or not they occur there at all. Would they predict transition from HR to FEP?
The aims of this study were to describe (1) the prevalence of FRSs among individuals at HR; (2) the association between FRSs and transition to full-blown psychosis; and (3) the level of adjustment of individuals at HR and with FRSs during their childhood (aged 6–11 years) in terms of social and academic functioning. Comparisons were made between a sample of individuals at HR who were referred to an EIS and HVs recruited from the same geographical area.
Methods for data collection
All subjects were assessed by senior research clinicians using the MINI12 and the PANSS. 35 FRSs were defined according to Kurt Schneider’s49 original classification and information was collected from the PANSS,35 CAARMS11 and clinical reports. Early premorbid functioning was measured using the Premorbid Adjustment Scale (PAS). 50 We grouped individuals by number and type of FRSs and analysed transitions to full-blown psychosis over a 2-year follow-up period. We also correlated the general social and functional adjustment of these individuals during their childhood (aged 6–11 years) with the future development of HR mental states and FRSs.
Analysis
Fisher’s exact test was used for comparing the categorical sociodemographic variables; for age the t-test was used. The Wilcoxon signed-rank test was used to compare PAS domains between HR individuals and HVs. Fisher’s exact test was also used to investigate associations between the FRSs in HR individuals and transitions to psychosis.
Key findings
At least one FRS was present in 43.3% of HR individuals and 21.6% of HR individuals had more than one FRS. Auditory hallucinations and passivity experiences were the most commonly reported (Figure 9).
FIGURE 9.
Distribution and frequency of FRSs in HR individuals in the PAATH study.
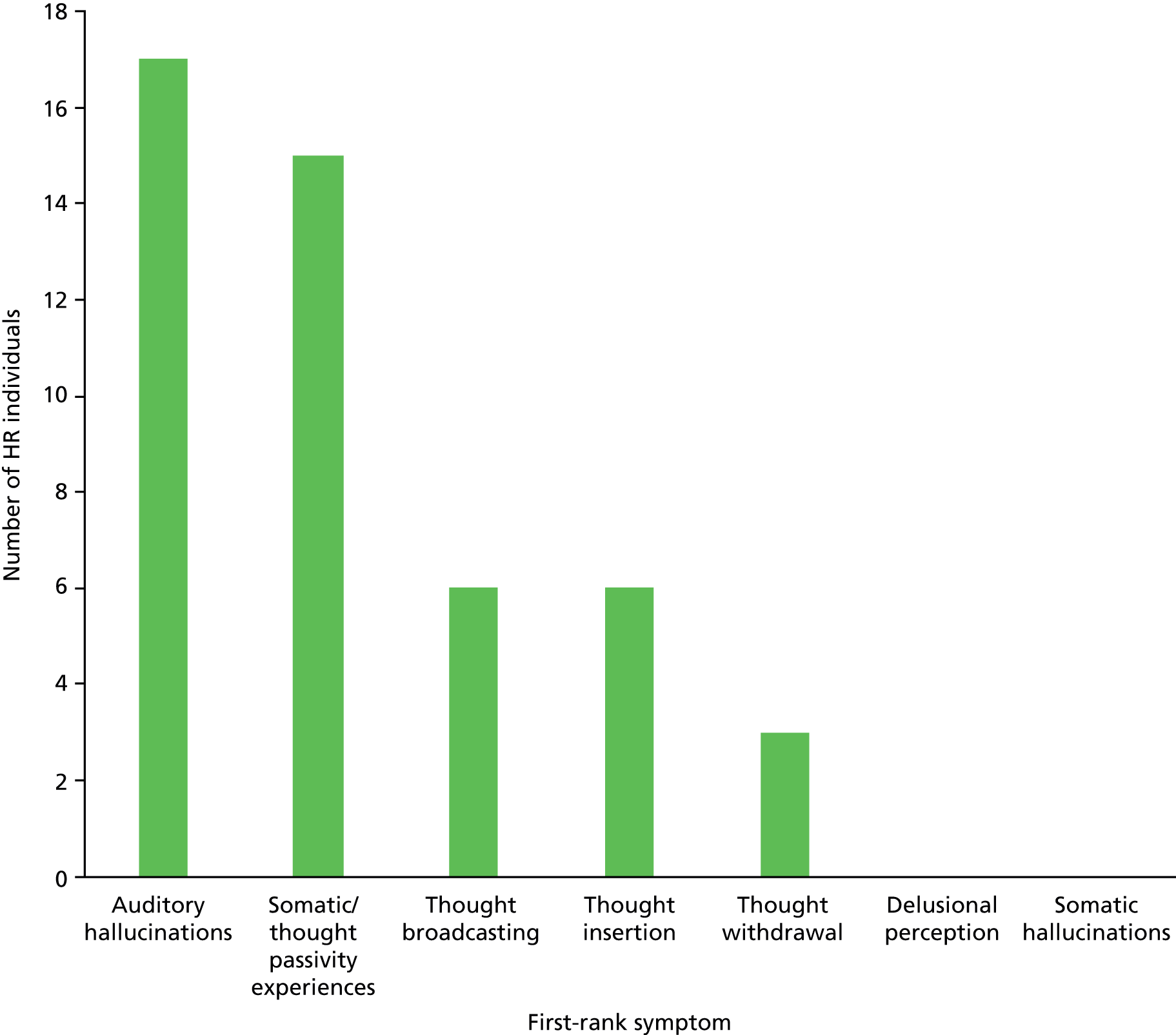
Except for passivity experiences, the presence of one or more FRS was not significantly associated with transition to FEP. Compared with HVs, HR individuals, especially those with FRSs, had poorer premorbid functioning and adjustment as children across educational, social and peer relationship domains; however, this was not associated with FEP 2 years later (Figure 10).
FIGURE 10.
Comparison of PAS domains (aged 6–11 years) between HR individuals, HVs and a subgroup of HR individuals with FRSs in the PAATH study. Q1: sociability and withdrawal; Q2: peer relationships; Q3: scholastic performance; Q4: adaptation to school.
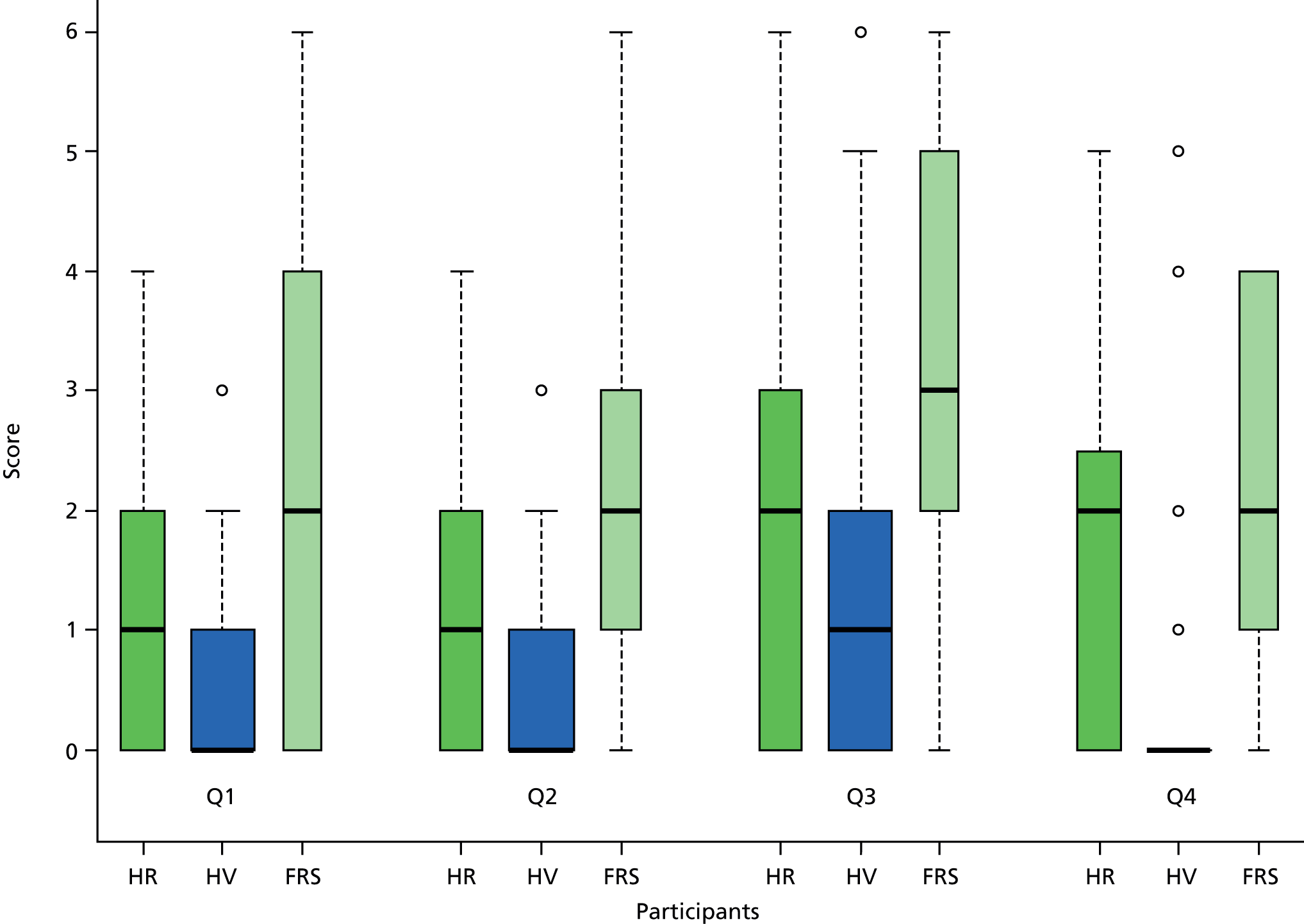
Strengths
The study was controlled, including both HVs and help-seeking HR individuals. The longitudinal design and high retention rates over 2 years made it possible to address the limitations associated with cross-sectional studies.
Limitations
The sample size did not allow further adjustment for comorbid mental disorders, which may have shed light on specific associations between level of impairment and increased risk for non-psychotic mental disorders.
It was possible that early premorbid adjustment was subject to recall bias because of the retrospective measure employed. In addition, conversion rates to psychosis could have been higher if follow-up had been longer than 2 years.
Studies with larger samples will be required to replicate findings regarding associations between specific FRSs and future conversions to psychosis, especially the relevance of those FRSs that were absent in our sample (somatic hallucinations and delusional perceptions).
Insights from the clinical team
In Appendix 13 we include a subjective view from the researchers and clinicians who were on the ground delivering the programme and collecting the data. We share this perspective, which could be acquired only through the process of operationalising this programme, reflecting on the merit, worth and significance of our work and providing insights that we hope will guide future research.
Inter-relation between aspects of the programme
It is noteworthy that the elements of our research plan mostly run in parallel, reinforcing each other to successfully achieve most of our aims by the time that this programme ended.
We also significantly enhanced some aspects of the programme through an efficient use of available resources. For example, we systematically followed all individuals at HR for psychosis in the context of a separate, naturalistic, observational design, which is described in Work package 5. Furthermore, this study was linked with several epidemiological and neurobiological research projects, representing an example of efficiencies in science.
The Prospective Analysis of At-risk mental states and Transitions into psycHosis study as an example of efficiency in health research
As previously mentioned, the PAATH study enhanced the original grant application through an efficient use of available resources. This study was not only aligned with other epidemiological projects (see Work package 3) but also nurtured neurobiological projects, creating a remarkably efficient research network around it that included backwards translation to investigate biological mechanisms underlying the HR state. HR individuals have not often been studied and so this group of 60 research volunteers represented a remarkable resource for other studies. This development was particularly important as the programme grant application did not consider cognitive or neurobiological examinations in the HR sample, which would add valuable information and provide a more comprehensive evaluation of this population cluster. Thus, the NIHR funding had an impact beyond our programme.
Some of these more biological projects that rely on our programme are briefly described in the following sections, including the title, chief investigator and aims. All of these projects were adopted onto the NIHR portfolio.
Neurobiological factors underlying the onset of psychosis
Chief investigators
Professor Philip McGuire and Dr Paul Allen, Institute of Psychiatry, London, UK.
Funder
Wellcome Trust, UK.
Aims
The key objective of this study is to examine the relationship between the medial temporal lobe and glutamatergic, gamma-aminobutyric acid (GABA)ergic and dopaminergic dysfunction in people at HR of psychosis. A further aim is to determine whether or not neuroimaging measures of these factors can be used in a clinical setting to predict the risk of later transition to psychosis in individuals at HR for psychosis.
The influence of cortisol levels on cognitive function and psychotic symptoms in patients with at-risk mental states for psychosis
Chief investigators
Professors Paul Fletcher and Ian Goodyer with Dr Veronika Dobler, University of Cambridge, Cambridge, UK.
Funder
Wellcome Trust, UK.
Aims
The proposed research focuses on particular aspects of the stress–diathesis model by further defining cognitive deficits and exploring the differential impact of variation in circulating cortisol levels (as a biological marker of stress) on current cognitive function in HR. This will be examined in three inter-related studies:
-
study 1 – the influence of physiologically induced stress on cognitive function in patients with at-risk mental states for psychosis and age- and sex-matched controls
-
study 2 – cognitive and perceptual processing deficits in HR
-
study 3 – functional magnetic resonance imaging (fMRI) analysis of brain responses during reward learning processes before and after the induction of stress in HR individuals and age- and sex-matched control subjects.
The learning study
Chief investigator
Dr Graham Murray, University of Cambridge, Cambridge, UK.
Funder
Medical Research Council, UK.
Aims
This study aims to identify brain regions involved in simple learning tasks in patients and HVs using fMRI. Any group differences may inform on both the neurophysiological and the neuropsychological features of mild psychosis. Better insights into these features will be of benefit to patients and their families in making sense of otherwise strange and potentially frightening symptoms and will lead to more informed and appropriate use of currently available treatments and may ultimately lead to novel pharmacological and/or psychological treatments for psychosis.
Summary
This applied health research programme focused on case finding and case ascertainment for psychosis. It was embedded in clinical services with the aim of improving the planning and delivery of those services. Most of our research programme was carried out in our EIS, CAMEO, in the CPFT, in general practices and in sixth-form educational colleges across the county of Cambridgeshire and the city of Peterborough, UK. We also extended some elements of our research to the whole of the East of England. Our overall conclusions from the research are expressed below as implications for practice, set out for each work package, but we begin with some overall comments and reflections on the programme.
To support and facilitate data collection, outcome evaluations and randomised trials in the programme, we successfully developed an IT clinical surveillance system (CAR; see Work package 1). We recorded in CAR all HR and FEP cases identified over the course of our programme. This provided a useful blueprint to connect information from patients, services, clinicians and researchers. In fact, our programme consisted of five inter-related work packages that helped us understand the socioepidemiology of psychosis and HR mental states, as well as better identify these clinical presentations in primary care and educational institutions.
The main component of our programme was the LEGS cRCT (see Work package 4), in which we educated GPs about HR and FEP and encouraged them to identify and refer young people with these mental states to CAMEO so that they could receive specialist attention or be signposted to other services, if required. Our new theory-based intervention demonstrated that additional expenditure, through the use of tailored intensive liaison between primary and secondary care to identify and help with the referral of individuals with early signs of psychosis, adds clinical and economic value. Such research linking GPs, colleges and mental health services, with input from a NHS trust and university, was challenging but very rewarding. It helped different organisations in the public sector understand each other and, in so doing, helped young people with emerging mental disorders. We are still analysing the results from the educational colleges.
The LEGS cRCT was successfully implemented but we had to manage challenging situations along the way, several of which provide useful lessons. Ethical approval for a cluster trial is a good example. Based on discussions with former REC members, we assumed that only the agreement of practices in the intervention arm would be needed to undertake certain elements of the trial, such as educational sessions. In normal practice it would be up to one organisation to agree with another how they interacted; we had hoped simply to randomise this process. However, in the research context the ethics committee stipulated that formal consent was required from all invited general practices, regardless of which arm of the trial they were assigned to. With > 100 practices to work with and, in many cases, visit, this resulted in a delay in implementing the trial, which required an 18-month no-cost extension that was finally granted by the NIHR. In the future, early liaison with the REC would be recommended at the design phase of the programme.
In addition, the REC considered that the follow-up of young people at HR referred from the LEGS trial, another objective of our programme, had to be carried out as a separate study that required a different REC application and, in consequence, another NHS governance process. Again, careful liaison with the REC at the design stage, before the application was submitted to the NIHR, would have negated this problem.
Nevertheless, clearing what seemed like hurdles at the time ultimately enhanced the programme. For example, the delay in the implementation of the LEGS trial allowed extra time to develop the theory-based educational intervention. A number of practices refused to take part in the research, which reduced our sample size but allowed those general practices that did not consent to make up a PAU comparator, so we retained sufficient statistical power. In addition, by separating the follow-up of individuals at HR from the LEGS trial, we developed a new, naturalistic, observational study, which was not included in our initial application, involving a thorough, systematic follow-up of these young people: the PAATH study (see Work package 5).
In the PAATH study we followed those identified as being at HR to determine how many would develop a full psychotic illness over 2 years. Interestingly, only 5% of the HR participants made a transition to psychosis, which made it difficult to define or elicit factors associated with conversions (because of very low statistical power). The study was able to contribute to a new understanding of the mental health problems, mainly depression and anxiety, suffered by people at HR, beyond the simple fact that they were experiencing psychotic phenomena. Furthermore, we showed that they had a significant history of psychological trauma during their childhood and adolescence. Indeed, we consider that the PAATH study contributed to the growing evidence suggesting relationships between depression, anxiety and psychotic experiences in young people without psychotic disorders. The HR mental state is not necessarily simply a harbinger of psychotic illness but a marker of previous psychological trauma, depression and anxiety in people with marked functional impairment.
When we studied the geographical distribution of HR individuals in comparison with that of HVs and those with FEP across Eastern England, the pattern of elevated risk at the neighbourhood level was similar for both HR and FEP participants relative to HVs, suggesting either that social drift, when it happened, began in the prodromal phase or that the exposure of young people to higher socioeconomic deprivation increased the risk of psychosis. This finding formed part of a wider work package (see Work package 3) in which we looked into the incidence of psychosis across Eastern England and social and epidemiological factors associated with variations in incidence rates. A series of epidemiological studies, including the SEPEA study in the Eastern region, helped us develop a prediction tool for the incidence of psychotic disorders in England and Wales, made freely available online (see www.PsyMaptic.org) to provide health-care commissioners with accurate forecasts of FEP incidence based on robust epidemiology and anticipated local population need.
We successfully completed most components of our programme but we did not develop a tool to understand predictors of and barriers to recovery in FEP as we had initially planned. This aspect of the programme was deemed to be redundant because of the adoption of the HoNOS by our host NHS trust and throughout the NHS, particularly the version amended to support funding of services according to their activity and outcomes (PbR). At the time this appeared to undermine the importance and viability of this element of our programme but, as we have noted elsewhere, PbR for mental health services is not yet implemented at the time of writing this report and the research may indeed have been useful.
Recommendations for future research
We have set out a series of specific recommendations for future research in each of our work packages. Our general recommendation refers to the particular challenges and unsuccessful elements of the programme, intimately linked with the complex and evolving nature of the NHS. In retrospect, we would have benefited from a Programme Steering Group as is now required by the NIHR. Better intelligence regarding the agenda for changes in the NHS would have helped to mitigate if not avoid some of the challenges that we encountered. In our opinion, the Programme Steering Group membership should include not only academic advisors but also trust board-level executive members, ensuring direct dialogue so that the research programme is fully embedded in the NHS host’s business agenda.
Implications for practice
The outputs produced by this programme are already having a significant impact on clinical practice and commissioning in the NHS.
PsyMaptic, our prediction tool for the incidence of psychotic disorders in England and Wales, appeared in the Annual Report of the Chief Medical Officer 2013 and is already being used for service planning in the UK. Also, the findings from the LEGS cRCT, whose methodology and economic modelling were praised by the author of a commentary on our work in The Lancet,13 have recently been included in the commissioning guidelines9 for early intervention in psychosis in the UK. Both PsyMaptic and the LEGS cRCT are in line with the 2014 announcement from the UK government of patient waiting time targets being extended to mental health in general and HR and FEP patients in particular. 51 Furthermore, we significantly added evidence to a new understanding of the HR mental state in young people. Only one in 20 participants in the PAATH study moved into a psychotic illness. This is far fewer than initially anticipated but is in line with, and forms part of, a recently accumulating body of evidence. Furthermore, the majority of the entire HR group suffered from depression and anxiety meriting clinical attention and impinging on their daily function. Many of this group had experienced significant psychological or physical abuse, which requires careful exploration and resolution given that these traumatic events may play a central role in the causation of the mental distress. Thus, such people with psychotic experiences but without a psychotic illness should receive timely, appropriate and effective help for their current mental health problems, ideally in a non-stigmatising clinical setting such as primary care, rather than just monitoring to see whether or not they develop a full psychotic illness. This view inspired a new application to the NIHR for a successor programme.
Acknowledgements
The authors thank staff, users and families within CPFT’s CAMEO services for their help and support in the prosecution of this research programme as well as those who contributed to the production of this report.
Contributions of authors
Jesus Perez was the principal investigator, Michelle Painter was the project manager and Peter B Jones was the chief investigator for this programme. Tim Croudace and Peter B Jones designed the programme. James B Kirkbride led the analysis, data extrapolation and interpretation of the epidemiological studies. He also led the development of the PsyMaptic tool. Debra A Russo elaborated the theoretical basis of the LEGS intervention and collected the data for the pilots in educational institutions and primary care. All authors contributed to the development of educational materials within the LEGS trial. Jan Stochl and Tim J Croudace conducted the sample size calculations, statistical analysis and random assignment of participants. Gillian F Shelley and Carolyn M Crane implemented the LEGS interventions and conducted the PAATH assessments. Gillian F Shelley and Carolyn M Crane also contributed insights from the clinical team. Jesus Perez, Debra A Russo and Peter B Jones drafted the report. All authors provided a critical review and final approval of the report.
Data sharing statement
All available data can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, CCF, NETSCC, PGfAR or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PGfAR programme or the Department of Health.
References
- Jones PB, Barnes TR, Davies L, Dunn G, Lloyd H, Hayhurst KP, et al. Randomized controlled trial of the effect on quality of life of second- vs. first-generation antipsychotic drugs in schizophrenia: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study (CUtLASS 1). Arch Gen Psychiatry 2006;63:1079-87. http://dx.doi.org/10.1001/archpsyc.63.10.1079.
- The NHS Plan: A Plan for Investment, a Plan for Reform. London: Department of Health; 2000.
- Barnett JH, McDougall F, Xu MK, Croudace TJ, Richards M, Jones PB. Childhood cognitive function and adult psychopathology: associations with psychotic and non-psychotic symptoms in the general population. Br J Psychiatry 2012;201:124-30. http://dx.doi.org/10.1192/bjp.bp.111.102053.
- Marshall M, Lewis S, Lockwood A, Drake R, Jones P, Croudace T. Association between duration of untreated psychosis and outcome in cohorts of first-episode patients: a systematic review. Arch Gen Psychiatry 2005;62:975-83. http://dx.doi.org/10.1001/archpsyc.62.9.975.
- The Mental Health Policy Implementation Guideline. London: Department of Health; 2001.
- Kirkbride JB, Fearon P, Morgan C, Dazzan P, Morgan K, Tarrant J, et al. Heterogeneity in incidence rates of schizophrenia and other psychotic syndromes: findings from the 3-center ÆSOP study. Arch Gen Psychiatry 2006;63:250-8. http://dx.doi.org/10.1001/archpsyc.63.3.250.
- Morrison AP, French P, Stewart SL, Fowler D, Gumley AI, Birchwood M, et al. Early detection and intervention evaluation for people at risk of psychosis: multisite randomised controlled trial. BMJ 2012;344. http://dx.doi.org/10.1136/bmj.e2233.
- Kelleher I, Keeley H, Corcoran P, Wigman JT, Devlin N, Ramsay H, et al. Clinico-pathological significance of psychotic experiences in non-psychotic young people: evidence from four population-based studies. Br J Psychiatry 2012;201:26-32. http://dx.doi.org/10.1192/bjp.bp.111.101543.
- NHS England . Guidance on New Mental Health Standards Published 2015. www.england.nhs.uk/2015/02/mh-standards/ (accessed 22 January 2016).
- Preti A, Pisano A, Cascio MT, Galvan F, Monzani E, Meneghelli A, et al. Validation of the Health of the Nation Outcome Scales as a routine measure of outcome in early intervention programmes. Early Interv Psychiatry 2012;6:423-31. http://dx.doi.org/10.1111/j.1751-7893.2011.00329.x.
- Yung AR, Yuen HP, McGorry PD, Phillips LJ, Kelly D, Dell’Olio M, et al. Mapping the onset of psychosis: the Comprehensive Assessment of At-Risk Mental States. Aust N Z J Psychiatry 2005;39:964-71. http://dx.doi.org/10.1080/j.1440-1614.2005.01714.x.
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998;59:22-33.
- Kearns B. Improved Identification of People at Risk of Psychosis: Is It Value for Money? 2015. www.thelancet.com/pdfs/journals/lanpsy/PIIS2215-0366(15)00175-3.pdf (accessed 22 January 2016).
- Angus D. Fusing randomized trials with big data: the key to self-learning health care systems?. JAMA 2015;314:767-8. http://dx.doi.org/10.1001/jama.2015.7762.
- Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process 1991;50:179-211. http://dx.doi.org/10.1016/0749-5978(91)90020-T.
- Medical Research Council . Developing and Evaluating Complex Interventions: New Guidance 2008. www.mrc.ac.uk/documents/pdf/complex-interventions-guidance/ (accessed 23 January 2016).
- Critchlow HM, Herrington P, Gunton S. Inside an unquiet mind. Music and science join forces to explore mental ill health. EMBO Rep 2012;13:95-9. http://dx.doi.org/10.1038/embor.2011.255.
- Coid JW, Kirkbride JB, Barker D, Cowden F, Stamps R, Yang M, et al. Raised incidence rates of all psychoses among migrant groups: findings from the East London first episode psychosis study. Arch Gen Psychiatry 2008;65:1250-8. http://dx.doi.org/10.1001/archpsyc.65.11.1250.
- Health and Social Care Information Centre . Mental Health and Learning Disabilities Data Set 2013. www.hscic.gov.uk/mhldds (accessed 19 January 2016).
- Cheng F, Kirkbride JB, Lennox BR, Perez J, Masson K, Lawrence K, et al. Administrative incidence of psychosis assessed in an early intervention service in England: first epidemiological evidence from a diverse, rural and urban setting. Psychol Med 2011;41:949-58. http://dx.doi.org/10.1017/S0033291710002461.
- The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization; 1992.
- Kirkbride JB, Stubbins C, Jones PB. Psychosis incidence through the prism of early intervention services. Br J Psychiatry 2012;200:156-7. http://dx.doi.org/10.1192/bjp.bp.111.094896.
- Rucker J, Newman S, Gray J, Gunasinghe C, Broadbent M, Brittain P, et al. OPCRIT+: an electronic system for psychiatric diagnosis and data collection in clinical and research settings. Br J Psychiatry 2011;199:151-5. http://dx.doi.org/10.1192/bjp.bp.110.082925.
- Kirkbride JB, Jackson D, Perez J, Fowler D, Winton F, Coid JW, et al. A population-level prediction tool for the incidence of first-episode psychosis: translational epidemiology based on cross-sectional data. BMJ Open 2013;3. http://dx.doi.org/10.1136/bmjopen-2012-001998.
- Kirkbride JB, Stochl J, Zimbrón J, Crane CM, Metastasio A, Aguilar E, et al. Social and spatial heterogeneity in psychosis proneness in a multilevel case–prodrome–control study. Acta Psychiatr Scand 2014;132:283-92. http://dx.doi.org/10.1111/acps.12384.
- Department for Communities and Local Government . English Indices of Deprivation 2010 2010. http://data.gov.uk/dataset/index-of-multiple-deprivation/ (accessed 22 January 2016).
- Russo DA, Stochl J, Croudace TJ, Graffy JP, Youens J, Jones PB, et al. Use of the theory of planned behaviour to assess factors influencing the identification of individuals at ultra-high risk for psychosis in primary care. Early Interv Psychiatry 2012;6:265-75. http://dx.doi.org/10.1111/j.1751-7893.2011.00296.x.
- Francis JJ, Eccles MP, Johnston M, Whitty P, Kaner E, Smith L, et al. Constructing Questionnaires Based on the Theory of Planned Behaviour. A Manual for Health Services Researchers. Newcastle upon Tyne: Centre for Health Services Research, Newcastle University; 2004.
- Samejima F. Estimation of latent ability using a response pattern of graded scores. Psychometrika Monogr Suppl 1969;34:100-14.
- Perez J, Russo DA, Stochl J, Byford S, Zimbron J, Graffy JP, et al. Comparison of high and low intensity contact between secondary and primary care to detect people at ultra-high risk for psychosis: study protocol for a theory-based, cluster randomized controlled trial. Trials 2013;14. http://dx.doi.org/10.1186/1745-6215-14-222.
- Perez J, Jin H, Russo DA, Stochl J, Painter M, Shelley G, et al. Clinical effectiveness and cost-effectiveness of tailored, intensive liaison between primary and secondary care to detect individuals at risk of a first psychotic illness (the LEGS study): a cluster-randomised controlled trial. Lancet Psychiatry 2015;2:984-93. http://dx.doi.org/10.1016/S2215-0366(15)00157-1.
- Russo DA, Stochl J, Painter, M, Shelley GF, Jones PB, Perez J, et al. Use of the theory of planned behaviour to assess factors influencing the identification of students at clinical high-risk for psychosis in 16+ education. BMC Health Serv Res 2015;15. http://dx.doi.org/10.1186/s12913-015-1074-y.
- Psychosis and Schizophrenia in Adults: Prevention and Management. London: NICE; 2014.
- Hui C, Morcillo C, Russo DA, Stochl J, Shelley GF, Painter M, et al. Psychiatric morbidity, functioning and quality of life in young people at clinical high risk for psychosis. Schizophr Res 2013;148:175-80. http://dx.doi.org/10.1016/j.schres.2013.05.026.
- Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 1986;13:261-76. http://dx.doi.org/10.1093/schbul/13.2.261.
- Beck AT, Steer RA, Ball R, Ranieri W. Comparison of Beck Depression Inventories-IA and -II in psychiatric outpatients. J Pers Assess 1996;67:588-97. http://dx.doi.org/10.1207/s15327752jpa6703_13.
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol 1998;56:893-7. http://dx.doi.org/10.1037/0022-006X.56.6.893.
- Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: reliability, validity and sensibility. Br J Psychiatry 1978;133:429-35. http://dx.doi.org/10.1192/bjp.133.5.429.
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, et al. The Yale–Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch Gen Psychiatry 1989;46:1006-11. http://dx.doi.org/10.1001/archpsyc.1989.01810110048007.
- Endicott J, Spitzer RL, Fleiss JL, Cohen J. The global assessment scale. A procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry 1976;33:766-71. http://dx.doi.org/10.1001/archpsyc.1976.01770060086012.
- Priebe S, Huxley P, Knight S, Evans S. Application and results of the Manchester Short Assessment of Quality of Life (MANSA). J Soc Psychiatry 1999;45:7-12. http://dx.doi.org/10.1177/002076409904500102.
- Stochl J, Khandaker GM, Lewis G, Perez J, Goodyer IM, Zammit S, et al. Mood, anxiety and psychotic phenomena measure a common psychopathological factor. Psychol Med 2015;45:1483-93. http://dx.doi.org/10.1017/S003329171400261X.
- Russo DA, Stochl J, Painter M, Jones PB, Perez J. Substance use in people at clinical high-risk for psychosis. BMC Psychiatry 2014;14. http://dx.doi.org/10.1186/s12888-014-0361-1.
- Addington J, Case N, Saleem MM, Auther AM, Cornblatt BA, Cadenhead KS. Substance use in clinical high risk for psychosis: a review of the literature. Early Interv Psychiatry 2014;8:104-12. http://dx.doi.org/10.1111/eip.12100.
- Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychiatric Association; 2000.
- Russo DA, Stochl J, Painter M, Dobler V, Jackson E, Jones PB, et al. Trauma history characteristics associated with mental states at clinical high risk for psychosis. Psychiatry Res 2014;220:237-44. http://dx.doi.org/10.1016/j.psychres.2014.08.028.
- Carlson EB, Smith SR, Palmieri PA, Dalenberg C, Ruzek JI, Kimerling R, et al. Development and validation of a brief self-report measure of trauma exposure: the Trauma History Screen. Psychol Assess 2011;23:463-77. http://dx.doi.org/10.1037/a0022294.
- Morcillo C, Stochl J, Russo DA, Zambrana A, Ratnayake N, Jones PB, et al. First-rank symptoms and premorbid adjustment in young individuals at increased risk of developing psychosis. Psychopathology 2015;48:120-6. http://dx.doi.org/10.1159/000369859.
- Schneider K. Clinical Psychopathology. New York, NY: Grune & Stratton; 1959.
- Larsen TK, Friis S, Haahr U, Johannessen JO, Johannessen JO, Melle I, et al. Premorbid adjustment in first-episode non-affective psychosis: distinct patterns of pre-onset course. Br J Psychiatry 2004;185:108-15. http://dx.doi.org/10.1192/bjp.185.2.108.
- Mental Health Services: Achieving Better Access by 2020. London: Department of Health; 2014.
Appendix 1 Administrative incidence of psychosis assessed in an early intervention service in England: first epidemiological evidence from a diverse, rural and urban setting
© Cambridge University Press 2010. The online version of this article is published within an Open Access environment subject to the conditions of the Creative Commons Attribution-NonCommercial-ShareAlike licence <http://creativecommons.org/licenses/by-nc-sa/2.5/>. The written permission of Cambridge University Press must be obtained for commercial re-use.
Appendix 2 Psychosis incidence through the prism of early intervention services
© Royal College of Psychiatrists. This paper accords with the Wellcome Trust Open Access policy and is governed by the licence available at http://www.rcpsych.ac.uk/pdf/Wellcome%20Trust%20licence.pdf.
Appendix 3 A population-level prediction tool for the incidence of first-episode psychosis: translational epidemiology based on cross-sectional data
© 2016 Copyright Clearance Center, Inc. All Rights Reserved. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-commercial License, which permits use, distribution, and reproduction in any medium, provided the original work is properly cited, the use is non commercial and is otherwise in compliance with the license. See: http://creativecommons.org/licenses/by-nc/2.0/ and http://creativecommons.org/licenses/by-nc/2.0/legalcode.
Appendix 4 Social and spatial heterogeneity in psychosis proneness in a multilevel case–prodrome–control study
© 2014 The Authors. Acta Psychiatrica Scandinavica Published by John Wiley & Sons Ltd.
Appendix 5 Use of the theory of planned behaviour to assess factors influencing the identification of individuals at ultra-high risk for psychosis in primary care
© 2011 Blackwell Publishing Asia Pty Ltd.
Appendix 6 Comparison of high and low intensity contact between secondary and primary care to detect people at ultra-high risk for psychosis: study protocol for a theory-based, cluster randomized controlled trial
© 2013 Perez et al.; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Appendix 7 Clinical effectiveness and cost-effectiveness of tailored intensive liaison between primary and secondary care to identify individuals at risk of a first psychotic illness (the LEGS study): a cluster-randomised controlled trial
© Perez et al. Open Access article distributed under the terms of CC BY.
Appendix 8 Use of the theory of planned behaviour to assess factors influencing the identification of students at clinical high-risk for psychosis in 16+ education
© 2015 Russo et al. Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Appendix 9 Psychiatric morbidity, functioning and quality of life in young people at clinical high risk for psychosis
© 2013 The Authors. Published by Elsevier B.V. All rights reserved
Appendix 10 Substance use in people at clinical high-risk for psychosis
© 2014 Russo et al.; licensee BioMed Central. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly credited. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Appendix 11 Trauma history characteristics associated with mental states at clinical high risk for psychosis
© 2014 The Authors. Published by Elsevier Ireland Ltd.This is an open access article under the CCBY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/3.0/).
Appendix 12 First-rank symptoms and premorbid adjustment in young individuals at increased risk of developing psychosis
© 2015 S. Karger AG, Basel. This is an Open Access article licensed under the terms of the Creative Commons Attribution-NonCommercial 3.0 Unported license (CC BY-NC) (www.karger.com/OA-license), applicable to the online version of the article only. Distribution permitted for non-commercial purposes only.
Appendix 13 Insights from the clinical team
Observations concerning our high-risk cohort
To ensure the reliability of the CAARMS scores, each assessment was discussed at length by the research team in an inter-rater reliability meeting, scored individually and recorded before a consensus was reached. The identity of each case was anonymised to eliminate bias.
The identification of HR for the purposes of the LEGS trial and the PAATH study was decided at the inter-rater reliability meeting. This process of assessment provided consistent symptom ratings and therefore reliable decisions over the period of the study. As knowledge, experience and understanding grew, this also greatly contributed to both the clinical team’s and the research team’s understanding of the complexity of psychotic symptoms.
Clinical and consensus decisions were discussed with the research consultant psychiatrist and trial co-ordinator (consultant psychologist) at a pre-(CAMEO) clinical meeting. There were many instances when a score was ‘over threshold’, that is, psychotic according to the CAARMS algorithm, but the general presentation did not necessarily fit with the CAMEO clinical team’s criteria for inclusion on its caseload and continued care. However, the CAARMS scores, detailed feedback and clinical discussions all contributed positively to enhancing the decision-making within the CAMEO clinical team meetings. The extended assessments improved both the research team’s and the clinical team’s knowledge and understanding of the relationship between psychotic symptoms and disorders and the accurate identification of a first episode of psychosis. The CAMEO team have continued to use the CAARMS as part of the assessment process as it has proved to be a useful tool in understanding the intensity, frequency and level of distress of symptoms.
The young people seen during the research presented to their GP or another professional with symptoms that indicated the early stages of a psychotic illness. It became apparent that this is a complex group. The psychotic symptoms were often comorbid with depression, anxiety, obsessive–compulsive disorder or traits of a variety of personality disorders.
These patients tended to be very impaired by their symptoms as identified (as determined in Appendix 7). It was common to find that they were not achieving their potential generally and that they struggled in their relationships with others. Many of the young people who we assessed continue to suffer negative symptoms. They continue to have extremely poor social networks and may become (or remain) dependent, both financially and emotionally, on their parents or partners. They may be underachieving academically or in their careers because of the mental health difficulties that they experience. It was also evident that they had a higher than average risk of suicide or self-harming behaviours.
One of the most worrying aspects of this troubled group of patients is that very often they do not engage well with offers of support from adult mental health services.
Participants presented with a degree of subthreshold psychotic symptoms, which complicated their general mental health presentation. This caused complications for them at the beginning of their pathway into care because their presenting symptoms did not easily fit into the available adolescent or adult mental health services.
Participants described a variety of symptoms and were not a homogeneous group. It was rarely clear, from one interview, what the diagnosis was. Although they did not meet criteria for a psychotic illness, many young people had subthreshold symptoms for psychosis that could range from infrequent but frightening auditory and visual hallucinations to paralysing social anxiety or moderate levels of paranoia. Common problems included loss of concentration, sleep difficulties and increasing social isolation. Notably, all of these symptoms are present in other mental health disorders or are characteristics of young people at a difficult stage of their lives.
The assessments were potentially therapeutic in themselves. The more detailed second assessment session allowed for more trust to be built up and often resulted in further disclosure of symptoms; it certainly led to a better understanding of symptoms. This may have been because the CAARMS assessments were usually conducted on a one-to-one basis and in most cases with a familiar clinician. This allowed for an improved ‘alliance’ between the young person and the interviewer during the CAARMS assessment. This second detailed interview reassured participants that they were being taken seriously and that their experience was being validated by a professional.
More often than not, those assessed as having subthreshold symptoms of psychosis required some psychological therapy. Referring a young person with psychotic symptoms on to psychological services was sometimes problematic. The majority of services located within primary care were not resourced to deal with young people who have psychotic symptoms as part of their presenting problems. The secondary mental health services that do work with people experiencing hallucinations or delusions were completely overwhelmed and were unable to spend the time on engagement that this group of patients requires. This resulted in patients not being seen or followed up by the secondary services. It was challenging to address the issue of where to treat this group of patients while considering putting their best interests first.
For the first part of the trial, the CAMEO team agreed that those who crossed the threshold on CAARMS should have an extended assessment period to consider their differential diagnosis and clinical needs. More often than not these patients were discharged to their GP after a period of 3–6 months having benefited from the enhanced treatment within an EIS. Subsequently, as changes within the mental health trust necessitated stricter criteria, people with psychotic symptoms over the threshold for psychosis on the CAARMS but not a suspected psychotic disorder were referred to another secondary or primary care team for treatment of another primary disorder. Therefore, they did not receive this specialist care.
As a group of professionals who have monitored young people with HR symptoms for at least 5 years, we would contend that this patient group represents an unmet need within mental health services. We could be preventing some young people from ever crossing that threshold into full-blown psychosis, enabling them to escape the hugely debilitating, costly and distressing experience of having a psychotic illness. Furthermore, we could be intervening, giving age-appropriate psychoeducation, treatment and support to all those who may never cross that threshold and who just simply carry on experiencing a subthreshold level of psychotic symptoms. This HR group of patients, mostly aged between 16 and 25 years, were at a crucial time in their lives. We have observed that they need as much help and support as those who are more unwell and who fit more neatly into the traditional psychiatric diagnoses.
Critique of the Comprehensive Assessment of At-Risk Mental States
Conviction about beliefs
Assessing the level of conviction about a belief is central to establishing where on the spectrum of psychosis the symptoms lie. Rating the percentage of conviction, both at the time of experiencing the thought and afterwards, would help to clarify this.
If someone is suffering from social anxiety, they may have total conviction that people are talking about them. In this case it is the oddness or unusualness of the belief in context that is important to understand, although this is complex when many delusional ideas have some basis in reality anyway.
Insight
It is always important to assess level of insight into the unusual thought or belief. Insight can range from someone knowing that they are thinking erroneously but not being able to stop to not being able to even consider any alternative explanation. This seems to significantly vary naturally in people, depending on resourcefulness and intelligence. Conversely, concrete thinking can lead to rather fixed beliefs.
Unusual thought content
There was a strong tendency for individuals to answer the question at the beginning of the CAARMS, ‘Have you felt that something odd is going on that you can’t explain?’, with a description of all of the symptoms that distress them most. This can distract from the process and almost never elicited delusional mood.
The manner in which the questions are worded allows misinterpretation of the answers about delusional mood. Many people answer this by describing symptoms of derealisation, for example that they feel separate from the world, as if they are in a bubble. Some people experience significant derealisation or dissociation as a result of anxiety or trauma that arguably should score higher on the CAARMS (as a perceptual abnormality) than a ‘3’, that is, low-level symptoms and the severity properly assessed. A better example could also be associated with these phenomena.
Others express that they feel that the world is going to end or that something bad is going to happen and have felt that for years. Delusional mood, however, apart from being rare, is a time-limited precursor to a delusion. It is a self-referential alienation from the environment, for example that everything is ‘set up for you like you’re in a theatre’, as opposed to the detachment of the emotional component from the perception or ‘as if it’s a stage set’.
Non-bizarre ideas
Paranoia is difficult to assess as it is possible to have extreme fixed beliefs around others wishing you harm without having any delusional explanation of the scenario.
The CAARMS does not fully explore the person’s belief system around the paranoid thinking. Identifying (1) whether or not there is a wider delusional system into which the paranoid thought fits and (2) whether the person believes that he or she is the sole target or if everyone around him or her is also suffering the same problems helps rate more accurately the extent of the delusional belief.
It is necessary to establish the context of the belief to determine whether or not it is triggered by a real situation. If someone thinks that there are people out to get him or her, he or she may be part of a violent or criminal social network in reality.
It is quite common to find people who have a single unusual belief about themselves that may relate to another mental health diagnosis, such as body dysmorphic disorder. The question of whether or not dysmorphia is delusional is contentious.
Obsessional thinking and beliefs can seem very much like delusions and are not clearly differentiated on the CAARMS. People with these beliefs can normally retain some understanding that their thoughts are odd. Enquiring about other obsessional aspects of the person’s presentation will aid understanding of this.
Perceptual abnormalities
The most frequent reason why participants crossed the threshold on the CAARMS was that perceptual abnormalities reached the threshold for psychosis for more than a week. If this was the only symptom, often the clinical team did not regard these participants as having a first episode of psychosis. This created an important dilemma as they were also over the threshold for not ‘HR’ according to the CAARMS and therefore did not meet the PAATH study criteria.
Hallucinations can also be related to a disturbance of mood or trauma, an indicator of a schizotypal presentation or emotional instability. The presence of hallucinations with no other psychotic symptoms may be an indicator that the person is not primarily suffering a psychotic illness. For these reasons it is useful to assess the possible comorbidity of other disorders that can include the experience of psychotic or psychotic-like symptoms such as trauma, post-traumatic stress disorder, social anxiety, depression, obsessive–compulsive disease or various personality traits.
Understanding the origin of the voice experienced is important:
-
Does it sound like the person’s own thoughts?
-
Might it be their own thoughts?
-
Are they attributed to someone else?
-
Do they know who the voice belongs to?
-
Is the voice heard internally or in external space?
Assessing the level of distress that perceptual abnormalities elicit is crucial. Some people are not distressed by hearing voices and it can be a positive protective experience.
The perceptual abnormalities scale does not adequately describe the difference between subthreshold and threshold for psychosis. For example, where on the scale can you rate a shouting voice that cannot be understood but which is distressing? Or a vague outline of a male figure jumping towards the person with claw hands? Another point on the scale below threshold would resolve this dilemma.
Disorganised speech
We assessed only a very few people with recognisable disorganised speech. It was characterised generally by ‘flight of ideas’, ‘pressure of speech’, tangentiality and only very rarely by poverty of speech, all of which could be possible indicators of thought disorder.
We believe that disorganised speech symptoms are not adequately covered in the CAARMS, especially as the severity of the CAARMS disorganised speech component is the strongest predictor of transition to frank psychosis. Of those we assessed with these observable symptoms, the majority went on to be diagnosed with psychosis.
Much time can be spent discussing someone’s slight subjective communication difficulties and there is a case for scoring only what can be seen objectively: mild disconnected speech.
Risk
Because the rating of suicidality and self-harm is combined, it makes a true assessment of the level of risk to self very difficult to determine. The two behaviours should be rated separately to provide any meaningful indication of risk.
Duration of symptoms
There is a group of people, mostly with a range of personality traits including schizotypy, who have suffered from symptoms since childhood or early adolescence, especially hallucinations but also persistent overvalued ideas. In our experience these people are not at risk of becoming delusional or of having a psychotic disorder as their beliefs and experiences have been stable for a long period.
Applying the parameters that (1) the symptoms under assessment should have been present for < 5 years or (2) there is evidence of the symptoms worsening would help avoid labelling someone as psychotic when he or she has another primary problem.
Other psychotic-like symptoms
Dissociation as a result of anxiety or trauma can cause significant distress; arguably it could score on the CAARMS.
The criteria for BLIPS are problematic. Florid psychotic symptoms, especially if the picture is not complicated by drug use or an organic presentation that resolves within a week, were rare.
Cultural context
Asking questions to find out whether a patient’s relatives or friends might feel the same can eliminate the misidentification of paranoid or delusional thinking. We experienced the following scenarios:
-
Families having cultural beliefs around seeing ghosts or spirits that can influence a person’s explanation of his or her experiences.
-
Individuals were part of a social group in which violence and harassment were common.
-
Religious beliefs caused difficulties when assessing whether or not someone had a delusional belief, in particular cross-cultural misinterpretations of someone’s belief system.
The CAARMS does refer to these issues in the ‘Guidelines for rating’ but there should be a prompt within the individual sections for this.
Level of symptoms
There is no evidence, from our experience or from the literature, to support the possibility that mild symptoms, however often they are experienced, are associated with a risk of psychosis. Therefore, we suggest excluding on all of the scales the lowest level of possible ‘at-risk’ symptoms (i.e. level 3).
Global Assessment of Functioning
The GAF is included in the CAARMS to establish the level of functioning in relation to the ‘trait plus state’ criteria. It would be helpful to include prompting questions to elicit this information, especially with respect to mood, anxiety and work.
Conclusion
As the brief version of the CAARMS focuses on particular symptoms, it does not cover the wider clinical picture and this is an issue that needs to be considered when deciding whether someone has a psychotic illness or attenuated psychotic symptoms.
If the use of the CAARMS is preceded by a good knowledge of symptomatology and there is an assumption of clinical skills being used in the assessment process, there is less need for detail and explanation. However, its use by research assistants in RCTs will inevitably lead to inaccuracies.
The CAARMS provides a useful backbone for assessing psychotic symptoms. Its limitations as a tool are mostly concerned with the complexity of the symptoms to be assessed and the current lack of understanding of who is at risk of developing psychosis.
To understand this group of patients, assessing who makes a ‘transition’ to psychosis may be the wrong question. Is it not better to ask what these people suffer from and what happens to them over time? Do they primarily have a depressive or anxiety-related illness?
In our experience, using the CAARMS to assess attenuated symptoms has not led to a greater understanding of who is prodromal for psychosis.
It would be beneficial to use a wider system for training and concordance to ensure accurate use. We had to develop our own guidelines for consistent use internally.
For future research we consider that two baseline CAARMS, a month apart and before consent, would go some way to eliminating ‘false’ transitions, for example if someone disclosed a symptom the second time that CAARMS questions were asked which was not newly experienced. Establishing a rapport may take more than one session. On many occasions, at the second meeting, people disclosed further symptoms, having established trust and having the knowledge that they were being taken seriously.
It is important not to lose track of the point – that ideally we would predict who is prodromal rather than who has psychotic-like symptoms.
List of abbreviations
- ÆSOP
- Aetiology and Ethnicity in Schizophrenia and Other Psychoses
- aOR
- adjusted odds ratio
- BAI
- Beck Anxiety Inventory
- BDI-II
- Beck Depression Inventory version II
- BLIPS
- Brief Limited Intermittent Psychotic Symptoms
- BRC
- Biomedical Research Centre
- CAARMS
- Comprehensive Assessment of At-Risk Mental States
- CAR
- Client Assessment Register
- CBT
- cognitive–behavioural therapy
- CI
- confidence interval
- CPFT
- Cambridgeshire and Peterborough NHS Foundation Trust
- cRCT
- cluster randomised controlled trial
- CRIS
- Clinical Record Interactive Search
- D-CRIS
- Clinical Record Interactive Search (Collaboration Programme)
- DUP
- duration of untreated psychosis
- DVD
- digital versatile disc
- EIS
- early-intervention service
- ELFEP
- East London First-Episode Psychosis
- EPRS
- electronic patient record system
- FEP
- first-episode psychosis
- fMRI
- functional magnetic resonance imaging
- FRS
- first-rank symptom
- GAF
- Global Assessment of Functioning
- GP
- general practitioner
- HoNOS
- Health of the Nation Outcome Scales
- HoNOS-PbR
- Health of the Nation Outcome Scales – payment by results
- HR
- high risk
- HV
- healthy volunteer
- IAPT
- Improving Access to Psychological Therapies
- ICD-10
- International Classification of Diseases, 10th revision
- IRR
- incidence rate ratio
- IT
- information technology
- LAD
- local authority district
- LEGS
- Liaison with Education and General practiceS
- MANSA
- Manchester Short Assessment of Quality of Life
- MINI
- Mini-Neuropsychiatric Interview
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- PAATH
- Prospective Analysis of At-risk mental states and Transitions into psycHosis
- PANSS
- Positive and Negative Syndrome Scale
- PAS
- Premorbid Adjustment Scale
- PAU
- practice as usual
- PBC
- perceived behavioural control
- PbR
- payment by results
- PCRN
- Primary Care Research Network
- PI
- prediction interval
- PPI
- patient and public involvement
- R&D
- research and development
- RCT
- randomised controlled trial
- REC
- Research Ethics Committee
- RLP
- research and liaison practitioner
- SD
- standard deviation
- SEPEA
- Social Epidemiology of Psychoses in East Anglia
- SLAM
- South London and Maudsley
- THS
- Trauma History Screen
- TPB
- theory of planned behaviour
- YBOCS
- Yale–Brown Obsessive Compulsive Scale
- YMRS
- Young Mania Rating Scale