Notes
Article history
The research reported in this issue of the journal was funded by PGfAR as project number RP-PG-0707-10123. The contractual start date was in April 2009. The final report began editorial review in July 2014 and was accepted for publication in July 2015. As the funder, the PGfAR programme agreed the research questions and study designs in advance with the investigators. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PGfAR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Membership of the following committees was declared: Professor M Morgan: National Black, Asian and Minority Ethnic Transplant Alliance; Professor B Farsides: UK Donation Ethics Committee; Professor Gurch Randhawa: UK Donation Ethics Committee; Human Tissue Authority; National Institute for Health and Care Excellence Evidence Update Group (Organ Donation Guidelines); National Black, Asian and Minority Ethnic Transplant Alliance; Transplant 2020 Stakeholder Group (chairperson).
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by Morgan et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction and background
Developments in transplantation
Solid organ transplantation is described as one of the most remarkable therapeutic advances in medicine during the past 60 years, with significant benefits for patient survival and quality of life. 1 In 1954, the first successful kidney transplantation was undertaken between identical twins, and between 1962 and 1967 the first successful transplants of the kidney, heart, lung, pancreas and liver from the organs of deceased donors were performed. However, the discovery of ciclosporine (Neoral®, Novartis) (the first targeted immunosuppressive drug), and its commercial availability from 1982, is regarded as marking the beginning of the modern era of transplantation with its substantial benefits for graft survival. 2 Currently, over 93% of kidneys from deceased donors and 83% of heart transplants are functioning well after 1 year and many continue to function for at least 10 years. 3
The population’s need for transplantation has steadily increased, with an estimated increase of 8% per year in the numbers of people requiring a transplant in the UK. 4 This increasing need reflects both the ageing population and the increasing scope and success of transplant surgery, which itself increases clinical need. Thus, although 4212 solid organ transplants were performed in the UK in 2012/13, as of 31 March 2013 there were 7332 patients on the active transplantation list. 3 In addition, a total of 466 patients died during 2012/13 while on an active waiting list and a further 766 were removed from the list as a result of deteriorating health and ineligibility for transplant. 3 Altogether, 82% of patients were waiting for a kidney transplant, with 62% of kidney transplants currently involving a kidney from a deceased donor.
Long waiting times for transplantation are associated with reduced quality of life and increased mortality risks. Moreover, transplantation not only has substantial benefits for patients and families but also is generally cost-effective for the NHS, particularly for the large numbers of people with end-stage renal failure (ESRF). On 1 April 2009, there were 6920 patients with ESRF waiting for a transplant, with the majority on dialysis, at an estimated total cost of around £193M per year. If all of these patients received a transplant, the approximate cost is estimated at £41M per year, representing a saving to the NHS of £152M per year. 5
Donation and transplantation among minority ethnic groups
The problem of long waiting times is of particular significance for the Asian population (mainly people of Indian, Pakistani and Bangladeshi heritage) and the black population (mainly people of Caribbean and African origin). These ethnic groups make up around 10.6% of the UK population but accounted for 27% of patients waiting for a kidney transplant and had a median waiting time for a kidney-only transplant in 2013 of over 1400 days, representing nearly 1 year longer than for the general adult population. 3
One major factor explaining the over-representation of ethnic minorities on kidney transplant waiting lists is their relatively high level of need, reflecting a high incidence of chronic kidney disease and ESRF, with risk of ESRF for the black and South Asian populations three to four times that of the general population. 6 The other main determinant of the waiting list and long waiting times for transplantation relates to the supply side in terms of the availability of organs for transplantation. Although the rate of living donation among minority ethnic groups is comparable to that of the general population, the rate of deceased donation is much lower, with just 4% of all deceased donors being of black or South Asian ethnicity. 3
This low rate of deceased donation is of particular significance for minority ethnic groups given requirements for matching human leucocyte antigen (HLA) tissue type and blood group. Matching these aims to reduce risks of graft rejection and the amount of immunosuppressive drugs required with their associated risks of severe side effects. However, for members of ethnic minorities with a HLA tissue type and blood group that is less common in the general population, the effect is to restrict the potential donor pool and thus increase waiting times for transplantation. This situation identifies the importance of increasing organ donation among minority ethnic groups. It has also led to questioning of the merits of further relaxing the criteria for matching employed by the NHS given the advances in immunosuppression, although recognising that immunosuppressive drugs carry risks of cancers, cardiovascular disease and other severe side effects. 7,8
Reducing the gap between need and supply
One approach to bringing demand for transplantation and availability into equilibrium among minority ethnic groups is through more effective detection and management of diabetes, hypertension and renal disease, thus preventing the onset of chronic kidney disease, which is associated with high rates of type 2 diabetes, obesity and hypertension. 9,10 There is also some evidence of a lower quality of diabetes and renal care, and of patient compliance, among South Asian and African/Caribbean populations, thus increasing risks of renal failure. Reducing demand for transplantation through improving both primary and secondary prevention is therefore an important strategy in improving individuals’ quality of life and reducing risks of ESRF and the need for kidney transplantation. Clinical guidelines and incentive-based care schemes in the UK therefore now focus on tackling cardiovascular risk and renal disease progression in all patients with chronic kidney disease. 11–13
The other main approach to bringing demand and availability into equilibrium is to increase supply through increasing both rates of registration on the Organ Donor Register (ODR) and family consent to donation. It is estimated that 3.5% of the black, Asian and minority ethnic (BAME) population are on the ODR, compared with one-third of the white population. 3 The main source of registration is through checking the appropriate box on applications for a driving licence (58% registrations by March 2013), followed by applications to register with a general practice (21% registrations), with other sources including online registration or applying for a passport or a Boots Advantage Card. 14 However, ethnicity is recorded for only 18% of registrations, mainly because of some sources for sign-up not recording ethnicity, with estimates of the ethnic composition of the ODR therefore derived from limited data. 14
For people who die in an intensive care unit (ICU) or emergency department and are identified as potential donors, family consent is required for donation to proceed. In the UK, in 2012/13, only 33% of bereaved ethnic minority families consented to donation (56 donors), compared with 61% of eligible white donor families (1155 donors). 15 Family consent rates are significantly higher when their deceased relative is on the ODR (or if their deceased relative’s wishes are otherwise known), although currently 10% of families override the wishes of a relative who has joined the ODR. 15
The low rate of deceased organ donation among minority ethnic groups in the UK has parallels with the situation in other countries, including the USA and Canada (see Chapters 2 and 3). There are also similarities with the less studied topic of blood donation, with 5% of the eligible UK population donating blood, of whom just 3% are from the Asian, African and Caribbean communities. 16 This again raises issues of matching, as blood group B is more prevalent among Asian and black communities, whereas blood group U negative is almost entirely found among African and Caribbean populations.
In summary, BAME groups in the UK have a relatively high need for transplantation mainly because of a high rate of ESRF. These groups also experience long waiting times for kidney transplantation associated with a low donation rate and thus a shortage of well-matched organs with implications for quality of life and survival. One approach to address this and thus reduce inequalities in transplantation is through the improvement of primary and secondary prevention to reduce rates of ESRF. The other approach is to increase donation rates among minority ethnic communities.
Donation policies
The situation of high levels of unmet need and long waiting times for transplantation among minority ethnic groups occurs within a system in which the need for transplantation continues to increase and far outstrips availability. For example, in 2006 the UK ranked 14th out of 18 countries with a donation rate per million population (pmp) of 12.9, compared with 35.5 pmp in Spain. 4 Since 2006, the position in the UK has improved, with a donation rate of 19.1 pmp by 2013, although this is still lower than in many other European countries. 15 This national situation thus forms the broader context within which the particular needs of minority ethnic groups require to be addressed.
The Organ Donation Taskforce (ODT) was set up in 2006 to provide advice on how best to address the relatively low transplantation and donation rate in the UK. The taskforce initially considered the requirements and likely impact of redesigning services while retaining the current model of informed consent (opt-in system). The opt-in system enshrines individual autonomy and choice, with individuals able to indicate their willingness to donate their organs should the situation arise by joining the ODR. For those who are identified as a potential donor, their relatives are asked for their consent to donation.
The ODT report Organs for Transplant4 was published in January 2008 and set out 14 recommendations for redesigning the organ donation services while retaining an opt-in system. In addition, the ODT set up an independent Working Group to examine the likely impact of moving to a system of presumed consent (opt out) that involves an assumption of donation unless individuals opt out. The range of evidence assembled by the Working Group to consider the merits of a change to a presumed consent system identified a complex situation, particularly with ‘hard’ and ‘soft’ versions of both informed and presumed consent that vary in their provision for relatives to influence the donation decision (Box 1). 17
‘Soft’ version: it is normal practice to let relatives know if a person has registered on the ODR and doctors can decide not to proceed if there is opposition from relatives (e.g. current UK).
‘Hard’ version: individuals can decide if they wish to opt in and relatives are not able to oppose a deceased person’s wishes.
Presumed consent model‘Hard’ version: doctors can remove organs from every adult who dies unless a person has registered to opt out (e.g. Austria) OR the person belongs to a group that is defined by law as being against an opt-out system (e.g. Singapore, where Muslims chose to opt out as a group).
‘Soft’ version: in some countries relatives are allowed to tell doctors not to take organs, but it is up to the relatives to tell doctors because the doctors may not ask them (e.g. Belgium). In other countries it is good practice for doctors to ask relatives for their agreement at the time of death (e.g. Spain).
Evidence that is often cited to support a shift to presumed consent is the increased rates of deceased donation following implementation of a presumed consent model. However, Rithalia et al. 18 concluded, based on a detailed review of the evidence, that changes in the system of donation have often been accompanied by educational campaigns and improvements in infrastructure and that these changes may have formed the major catalyst leading to increased donation rates. 18 This view is supported by Dr Rafael Matesanz, President of the Spanish National Transplant Organisation,19 who cast doubt on the impact of presumed consent in achieving the high donation rates in Spain, noting that whereas informed consent was introduced in 1979 in Spain, donation rates only significantly increased from 1989 following the major redesign of donation services.
Further difficulties in the interpretation of between-country variations area arise from the wide range of other factors that influence rates of donation, including the level of mortality rates from road traffic accidents, overall health expenditure, religion, education and transplant infrastructure. Important exceptions to the generally positive association between presumed consent and donation rates have also been noted, including the situation in Sweden where presumed consent was introduced in 1996 but the country continued to have one of the lowest donation rates in Europe.
The Working Group reported in September 200817 and concluded that evidence for a change to presumed consent was not sufficiently robust to support this shift, although acknowledging, ‘The question of whether or not changing to an opt-out system for organ donation is right for the UK is a finely balanced one . . .’17 (p. 4). The potential downsides of such a move were identified as including the potential negative impacts on the relationship of trust between clinicians and their patients and families, the importance for both recipient and donor families that organs are freely given as a ‘gift’ and the possibility that some groups may opt out (or may need provision not to be included), together with practical, cost and security issues of setting up and running a system of presumed consent. 17 Thus, on balance, it was concluded that, ‘moving to an opt-out system at this time may deliver real benefits but carries a significant risk of making the current situation worse’ (p. 5).
The UK has, therefore, retained a system of informed consent and during 2008–13 implemented the ODT’s 14 recommendations. 4 These recommendations were influenced by both the successful ‘Spanish model’19 and service redesign in the USA. 20 They aimed to increase donation and hence transplantation rates through both public campaigns and the redesign of hospital donation services. The latter aimed to achieve better identification of potential donors, increased family consent rates, more effective organ retrieval, and more efficient allocation and use of donated organs.
These wider national issues provide a context for a focus on the particular issues for minority ethnic groups who received specific consideration in relation to increasing organ donation and transplantation rates with the ODT’s recommendation 13 stating:
There is an urgent requirement to identify and implement the most effective methods through which organ donation and the ‘gift of life’ can be promoted to the general public and to the BME [black and minority ethnic] population
Paragraph 1.474
This sentiment was subsequently echoed by the Nuffield Bioethics Council report ‘Human bodies: donation for medicine and research’,21 which acknowledged that ‘BME [black and minority ethnic] populations are significantly less likely to become donors (across a range of different forms of bodily material)’ and argued that ‘a stewardship state has a direct responsibility to explore the reasons why some populations are hesitant to donate, and if appropriate to take action to promote donation’ (p. 16). 21 A co-ordinating voice is now also provided by the recently formed National Black, Asian and Ethnic Minority Transplant Alliance (www.nbta-uk.org.uk/) that brings together the NHS Blood and Transplant (NHSBT) and a number of charities, with the aim of increasing donor numbers and attitudes to donation and transplantation within the BAME population.
Whereas the policy in England, Northern Ireland and Scotland continues to be one of increasing donation on a voluntary basis, Wales is introducing a system of presumed consent in 2015, albeit a ‘soft’ version. 22 Wales will, therefore, provide a pilot test case of this model, including issues of the responses of ethnic and faith groups.
Another approach to increasing donation rates is the Israeli system of giving priority for transplantation surgery to those previously registered as a donor for 3 years. 23 It is argued that this could serve as an impetus for ethnic minorities who would have an even longer wait under a prioritisation system if they do not commit. 24 However, such a prioritisation system raises ethical issues of coercion, constraints or strategic behaviour. 25,26 It also requires ample public awareness of embedding incentives in a new allocation system plus assuring that registration details are up to date. Translating such a policy into practice in the UK is, therefore, acknowledged to raise both ethical and administrative difficulties.
England, Northern Ireland and Scotland have continued to support an opt-in system of donation and aim to achieve increased donation rates within this voluntary system. The present programme aimed to contribute to this objective by providing guidance to increase the acceptability and effectiveness of both national campaigns to increase registration and family consent with particular reference to minority ethnic groups.
Chapter 2 Overview of the research
The research programme referred to as Donation, Transplantation and Ethnicity (DonaTE) took up the challenge relating to ethnic minorities identified by recommendation 13 of the ODT report. 4 The main objectives of the programme were therefore to:
-
identify barriers to registration as an organ donor and family consent to deceased donation among minority ethnic groups of African/Caribbean and Asian descent
-
develop and pilot a hospital-based intervention to enhance quality of care and consent rates.
Our research examined issues of both registration and family consent to donation. Family consent is the key determinant of deceased donation in an opt-in system but whether or not the patient has expressed their wishes and is registered on the ODR has an important influence on family decision-making. For example, in the UK in 2012/13, 90% of all families whose relative was registered on the ODR consented to donation, but 60% of families where the deceased was not on the ODR. 15 This has led to a move towards reducing the rights of families to reject donation where their relative has expressed their wishes by joining the ODR, thus increasing the importance of registration. 15
Components of the research programme
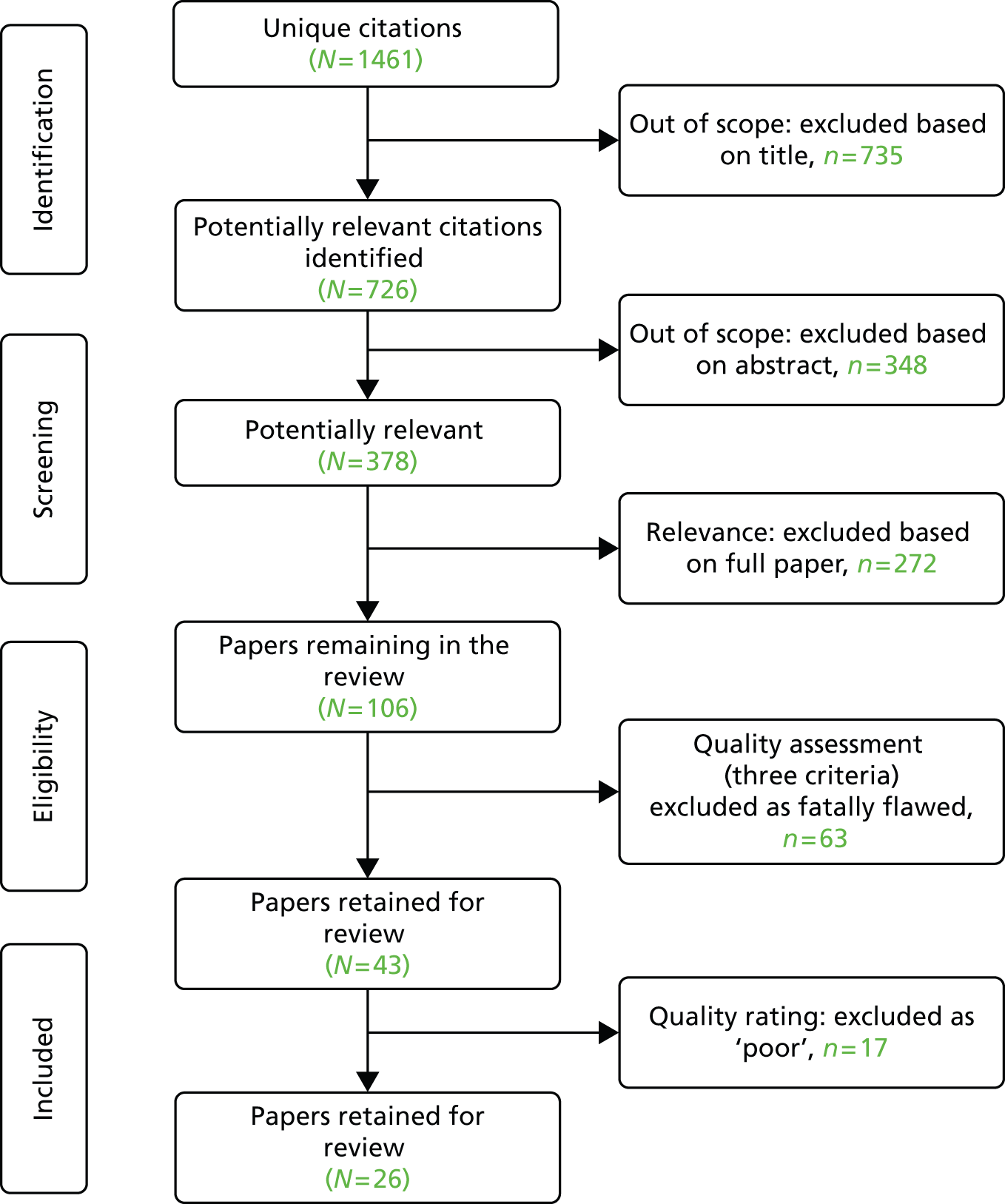
The research involved three phases comprising seven linked studies as indicated in Figure 1.
FIGURE 1.
Overview of the DonaTE programme of research.
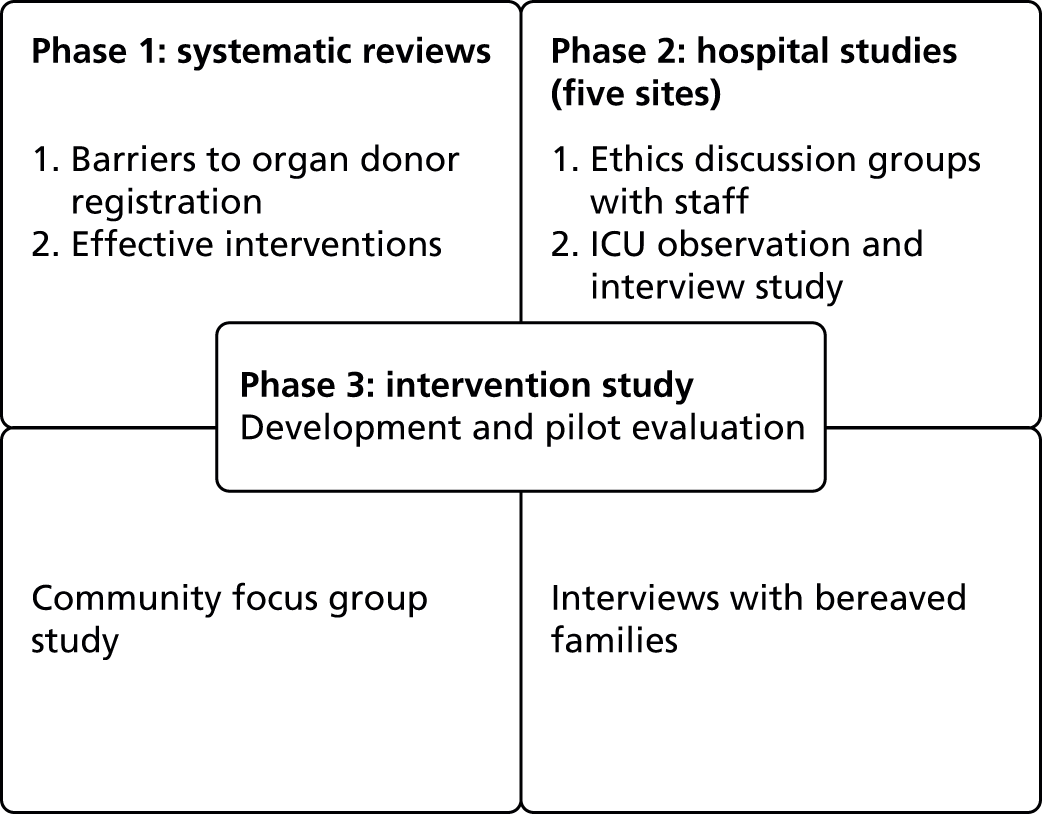
The first community-level phase involved a systematic review to examine the current knowledge regarding attitudes and practices to ODR among minority ethnic groups based on studies undertaken in both the UK and North America. This was followed by a study based on 22 focus groups, which aimed to respond to gaps in knowledge identified by the systematic review. The final phase of the community-based research comprised a second systematic review to identify the characteristics of those interventions demonstrated to be effective in achieving increased knowledge and/or registration as an organ donor among minority ethnic groups.
The second hospital-level phase examined issues of consent to donation by families from minority ethnic groups. This focused on the structures and practices that may influence family decision-making and examined the perspectives and practices of different groups of professionals involved in caring for families, namely clinicians, specialist nurses for organ donation (SNODs), bedside nurses and hospital chaplains, and also elicited the experiences of bereaved families themselves. This phase involved several forms of data collection: interviews with ICU staff; observation of the work of SNODS, ethics discussion groups (EDGs) with a range of staff, and interviews with bereaved families at least 3 months post bereavement.
The third phase of developing and piloting a professional development package drew on data collected in earlier phases of the research, particularly the hospital-based studies, to develop a professional development package. This package is designed to influence the attitudes, motivation and skills in cross-cultural communication of junior ICU staff, so as to enhance staff confidence and the quality of support provided to minority ethnic families.
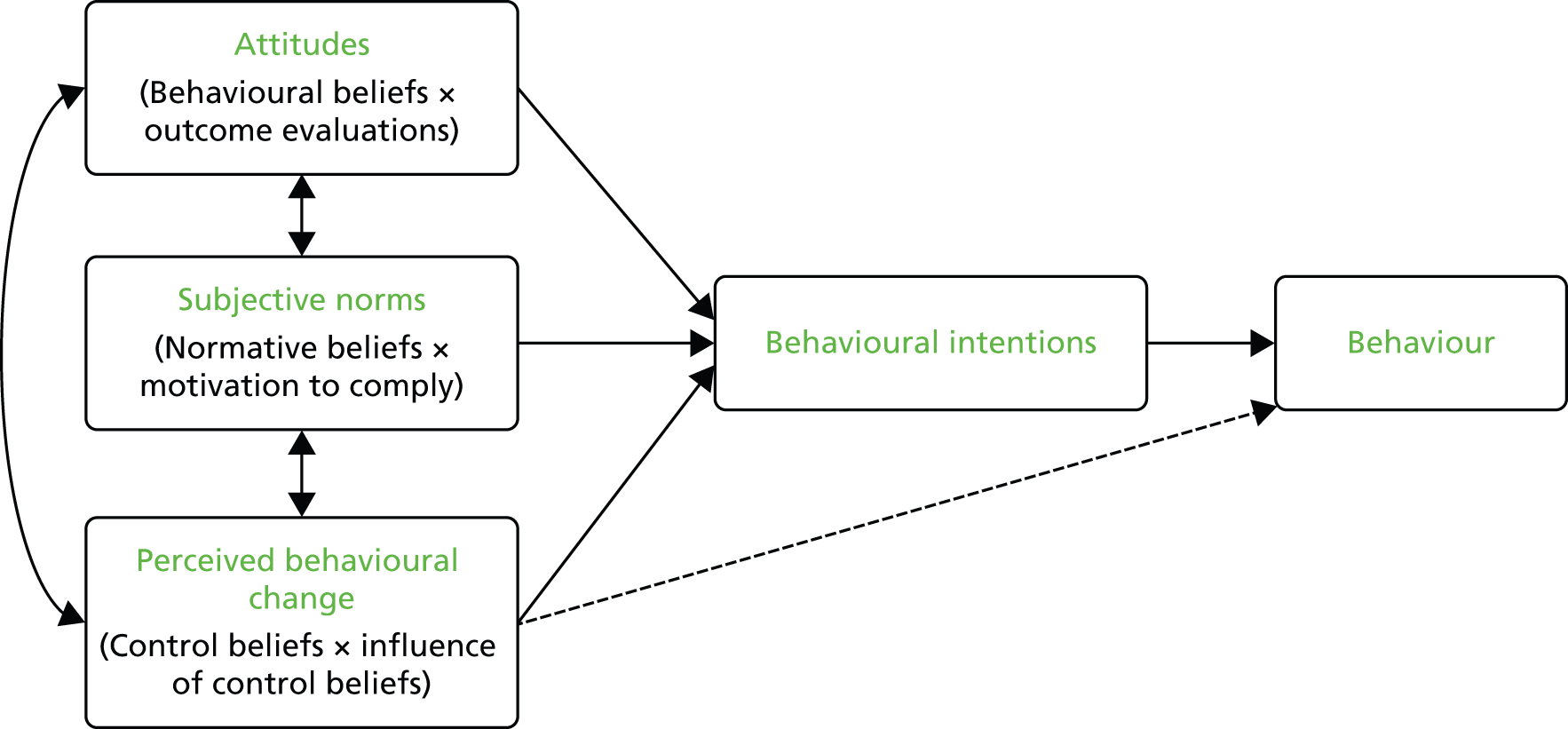
The package comprises a main video, short family drama and a workbook based on principles of behavioural change integral to Ajzen’s theory of planned behaviour (TPB). 27 Evaluation involved piloting the package with groups of ICU staff with before-and-after studies to examine outcomes in terms of rates of family consent and changes in staff attitudes factors and skills.
Data analysis
Both the focus groups and hospital studies involved qualitative methods. The discussions and interviews were audio-recorded and fully transcribed. Formal analysis involved, first, entering data into NVivo9 (QSR International, Warrington, UK) and reading and re-reading transcripts to identify major issues for analysis. Data relating to these key issues were initially coded line by line followed by grouping into categories. For the hospital interview and observational study, this coding and analysis was undertaken separately in relation to three areas of enquiry that were managed and written up as separate themes. These were hospital staff’s beliefs and practices in relation to supporting patients from minority ethnic groups, factors limiting the SNODs’ participation in collaborative donation discussions with families and hospital chaplains’ perception of their role in end-of-life care.
Analysis involved comparisons both between and within ethnic groups in the focus groups, and between study sites and staff groups for the hospital data, with the aim of identifying similarities and explain differences in practices at both community and hospital levels. Emerging explanations and interpretations were checked with subsequent data and, when necessary, by re-reading the original transcripts. Interpretations were also checked through informal discussions with ICU staff and the lay advisory group.
Evaluation of the intervention involved quantitative data analysis. Details of the before-and-after design and analysis of the TPB questionnaire and family consent rates are given in Chapter 5.
Approach to ‘ethnicity’
This research responds to a policy aim of increasing rates of deceased donation among minority ethnic groups, which, in turn, has benefits of reducing waiting times for transplantation for minority ethnic groups and thus improving quality of life and survival. However, this approach with its emphasis on changing the practices of ethnic minorities as fundamental to achieving a positive gain runs the risk of problematising ethnic groups and what Ahmed and Bradby28 refer to ‘cultural racism’. In contrast, we sought to achieve a more contextualised approach based on the following aims and assumptions:
-
We attempted to reflect the range of influences that potentially shape ethnic patterning by studying not only an individual’s knowledge and beliefs but also encompassing wider conditions and practices that may facilitate or form barriers to deceased donation. Thus, whereas the initial community-based research mainly focused on an individual’s awareness and beliefs regarding organ donation (informed by the synthesis of existing studies), we also examined issues relating to effective interventions and the provision of services. In particular, the hospital-based research shifts the focus from the beliefs and practices of minority ethnic groups to the perceptions and practices of different groups of staff that may impact on the quality and acceptability of end-of-life care and thus have implications for families’ consent to donation.
-
We also aimed to move beyond the notion of static and homogeneous ethnic groups associated with broad census classifications and instead sought to take account of the contingent and changing nature of ethnicity, acknowledging how this varies in relation to particular sets of social circumstances and responses of the wider society that often leads, over time, to changes in both individual and collective ethnic identities. For example, the focus group study aimed to examine beliefs and practices associated with country of origin, faith, length of residence in the UK, age and gender, etc. This study also allowed for linguistic diversity with discussions with older South Asian groups being conducted by bilingual researchers familiar with the community languages and cultural practices.
The wider UK policy context
The DonaTE research was undertaken over the period September 2009–January 2014 (initial 48-month period extended by 4 months because one researcher was on maternity leave for 1 year). The research, therefore, took place in an evolving policy context that involved gradual implementation across the country of the Taskforce’s 14 recommendations4 under the direction of a Taskforce Implementation group and in conjunction with NHSBT as the new national organ donation organisation. The research therefore aimed to provide information to inform strategies to address the needs of minority ethnic groups. This included identifying barriers to full implementation of the SNODs’ role in engaging in early contact with families and their participation in the donation discussion and exploring issues with doctors, nurses, hospital chaplains and the hospital Organ Donation Committee (ODC).
The various changes introduced over the period 2008–2013 were successful in achieving the government’s target of increasing donation by 50%. However, this target was largely reached through a greater number of approaches made to potential donors after circulatory (or cardiac) death (DCD), with the UK now having one of the highest rates of DCDs, accounting for 42% of all donation, with donation after brain stem death (DBD) accounting for 57% of donations. In contrast, there was little change in consent rates, with the overall family consent rate remaining fairly stable at 57%. 15 Increasing the family consent rate, including among minority ethnic groups, therefore, remains a key policy objective. This is reflected in NHSBT’s new policy document, Taking Organ Transplantation to 2020, which identifies increasing family consent as the ‘single most important strategy’ (p. 15). 15
The DonaTE programme, therefore, links with the continuing policy priority in England, Northern Ireland and Scotland of increasing donation rates within an informed consent model through further community campaigns and changes in donation services. The current goals, as set out in Taking Organ Donation to 2020, are to increase the authorisation/consent rate to > 80% by 2020 and achieve a deceased donor transplant rate of 74 pmp (increasing from 49 pmp). 15
Structure of the report
The research studies are presented in the next three chapters. Chapter 3 describes three community-based studies that focus on registration as an organ donor and Chapter 4 describes three studies examining issues relating to family consent to donation. Chapter 5 then describes the development of the professional development package that draws on these earlier studies and outlines its piloting and evaluation with groups of ICU staff.
Chapter 6 brings together the different elements to provide an overview of the programme and considers the implications of the findings for practice and for further research. It also includes a discussion and assessment of some of the particular challenges of undertaking research in this area to assist future studies.
Each phase of the research benefited from input by DonaTE’s lay advisory group, whose recruitment and activities are described in Chapter 6, Public engagement and dissemination. Academic dissemination to date through publications and conference presentations is also listed in Chapter 6.
Ethics approval
The National Ethics Service Hampstead granted approval for the programme of research (REC 09/H0720/134). Following initial approval amendments were submitted as the research progressed. Research and development (R&D) approval was granted by all NHS trusts involved in the research. The hospital-based fieldwork initially involved five trusts (increased from four trusts in original application) with a sixth added to complete the EDGs. The bereaved family study then expanded beyond the six study sites, given difficulties of recruiting ethnic minorities who had been approached about donation to include 40 trusts identified by NHSBT as having one or more families from mixed or minority ethnic groups consenting to donation in 2011/12.
Chapter 3 Community studies: registration as an organ donor
Introduction
This chapter describes three community-based studies that examined issues relating to the particularly low rates of registration as a donor among minority ethnic groups. These were:
-
a systematic review to identify current knowledge and gaps in knowledge of the barriers to organ donor registration among minority ethnic groups
-
a focus group study to examine the knowledge and attitudes of members of five ethnic minorities, namely people of Indian, Pakistani, Bangladeshi, Nigerian and Caribbean descent, and identify variations within these groups by age, generation and gender
-
a systematic review to identify the characteristics of effective community-based interventions to increase registration as a donor among minority ethnic groups based on UK and North American literature.
Study 1: systematic review of barriers to organ donor registration among minority ethnic groups
Abstract
This systematic review aimed to identify current research knowledge relating to community attitudes and barriers to organ donor registration among minority ethnic groups in the UK and North America. A systematic search of databases, websites and hand searching was conducted, followed by assessment of relevance and quality. Altogether, 26 papers29–53 (14 quantitative, 12 qualitative) were retained. Note that one of the retained papers is unpublished (Poonia J. South Asian and Black Organ Donation Research Project: Key Findings. Prepared for Central Office of Information on behalf of UK Transplant London NHSBT; 2006).
The synthesis followed the methods of narrative synthesis and it initially involved separate syntheses of the quantitative and qualitative studies, followed by their integration. This focused on five key barriers to registering as a donor: (1) knowledge of organ donation and registration; (2) talking with family about donation; (3) faith and cultural beliefs; (4) bodily concerns; and (5) issues of trust.
Lack of knowledge about the need for deceased donation and transplantation among ethnic minority groups, and how to register as a donor was identified as a key barrier that continues to be highly prevalent. Faith barriers mainly related to uncertainty about their faith’s position and the need for guidance rather than the belief that donation was prohibited. Religious uncertainty was particularly common among people of Islamic faith, whereas issues of trust in allocation procedures and in doctors were most common among the black populations. Specific gaps identified included a lack of explanation of the continuing low knowledge despite campaigns focusing on ethnic minorities; the very limited investigation of how beliefs and practices may vary with age; place of birth or socioeconomic status; and lack of attention to possible structural barriers, including perceptions of the accessibility of registration and needs for discussion regarding registration as an organ donor to supplement media campaigns.
Rationale and review question
Community-based studies in the UK and North America examining barriers to registering as an organ donor among ethnic minorities have been published in a range of clinical, health service and social science journals, with little attempt to integrate this literature. A key initial objective was, therefore, to undertake a systematic review of community-based research to identify current knowledge and existing gaps.
The specific review question was, ‘What are the barriers to organ donor registration and willingness to become a donor among minority ethnic groups?’
In this context, the term ‘barrier’ refers to a range of individual- and service-level factors that inhibit registration and willingness to become an organ donor. Individual-level barriers potentially include religious beliefs, cultural expectations and sociodemographic characteristics (e.g. age, gender or social position). Service-level barriers relate to aspects of the infrastructure and pertain to awareness, acceptability and accessibility of the processes of registration. The participants were regarded as belonging to visible minority ethnic groups in the countries where the studies were undertaken.
Review methods
Design of review: a systematic search was undertaken, followed by the procedures of narrative synthesis described by Popay et al. 54 This adopts an interpretive approach to synthesis while retaining the rigour of traditional systematic reviews and provides a range of tools through which quantitative and qualitative studies can be descriptively explored and synthesised.
Narrative synthesis involves four broad phases:
-
Phase 1: systematic search and quality appraisal.
-
Phase 2: preliminary synthesis – initial description of the results of the included studies and identification of factors that have influenced the results reported.
-
Phase 3: exploring relationships and main synthesis – this goes beyond simple description and focuses on exploring relationships in greater detail. Methods depend on the nature of the data and questions to be addressed.
-
Phase 4: assessing the robustness of the synthesis – this relates to assessment of both methodological and theoretical quality.
Phase 1: systematic search and quality appraisal
Specific inclusion criteria for the review are shown in Box 2.
Country: UK and North America – a systematic review of modifiable risk factors for organ donation identified most current research on the topic as conducted in these countries. 23
Type of donation: deceased organ donation.
Ethnicity: focus on a visible (non-white) ethnic minority or analysis of one or more minority ethnic groups.
Date: studies published between January 1980 and 2010. A preliminary Google Scholar (https://scholar.google.co.uk) of relevant research indicated that most studies were undertaken from the 1990s, given the increased development of transplantation services over the past 20 years. An ethnic question was also first asked in the 1991 UK census. 55
Language: relevant papers in all languages were to be included. However, the systematic review of modifiable risk factors by Simpkin et al. 56 indicated that nearly all papers would be in the English language.
Research design: both quantitative and qualitative studies were included to encompass the cross-disciplinary and methodologically pluralistic nature of research on the topic.
Age: ≥ 18 years. The focus is exclusively on adults given that people aged < 18 years require parental agreement for donation.
Setting: non-hospital.
Barriers: include attitudes, knowledge, beliefs, faith, trust, motivation, access, worry, understanding and fear.
Source: reproduced with permission from Morgan M, Kenten C, Deedat S. Attitudes to deceased organ donation and registration as a donor among minority ethnic groups in North America and the U.K.: a synthesis of quantitative and qualitative research. Ethn Health 2013;18:367–90. 57
Systematic search: databases were searched during November and December 2010 (Box 3, name of host databases in bold). Relevant websites were also searched [i.e. Google (Google Inc., Mountain View, CA, USA), Department of Health website] and key journals searched by hand. Experts in the field were contacted regarding recently published or ongoing projects and grey literature.
Ovid: MEDLINE, EMBASE, PsycINFO, Health Management Information Consortium (HMIC), Transplant Library Database, Social Policy & Practice.
Web of Science: Science Citation Index Expanded (SCI-EXPANDED), Social Sciences Citation Index (SSCI), Arts & Humanities Citation Index (A&HCI), Conference Proceedings Citation Index-Science (CPCI-S), Conference Proceedings Citation Index-Social Science & Humanities (CPCI-SSH).
Cambridge Scientific Abstracts (CSA) Illumina: Applied Social Sciences Index and Abstracts (ASSIA), Sociological Abstracts, Education Resources Information Center (ERIC).
EBSCOhost: International Bibliography of the Social Sciences (IBSS), Cumulative Index to Nursing and Allied Health Literature (CINAHL).
Scopus.
WebsitesGoogle, Department of Health website.
Other searchesKey journals, grey literature, contact made with experts in the field.
Source: reproduced with permission from Morgan M, Kenten C, Deedat S. Attitudes to deceased organ donation and registration as a donor among ethnic groups in North America and the U.K.: a synthesis of quantitative and qualitative research. Ethn Health 2013;18:367–90. 57
It was not possible to obtain all relevant grey literature commissioned by NHSBT and undertaken by a range of private research companies. Although we attempted to get access to full reports of these reviews via senior staff at NHSBT, via the market research companies commissioned by NHSBT to conduct research and from the Central Office of Information, none of these organisations was prepared to share this information.
The search strategy was written in conjunction with an information specialist. Terms employed reflected previous and current phrasing associated with deceased donation (e.g. cadaveric and deceased donation included), and included a range of terms to identify the correct populations across the UK, USA and Canada. Specific ethnic categories were those attributed in the papers reviewed. Following the initial MEDLINE search, this was slightly modified to be applicable to other databases (see the medical subject heading search terms in Appendix 1).
The initial database and grey literature searches yielded a total of 2185 returns, reducing to 1461 following deduplication. These papers were initially screened for relevance based on the title and abstract, and those failing to meet the inclusion criteria were excluded. When it was not possible to determine relevance from the title or abstract, the full-text papers were retrieved and assessed. The main reasons for exclusion were that studies related only to children (students were included), were conducted in a country other than the UK, USA or Canada, focused on living donation/donors or on transplantation or treatment/follow-up rather than donor issues. Following relevance assessment 106 papers were retained (Figure 2).
Quality assessment
This was undertaken by two authors, with any differences discussed and a consensus reached. Papers were initially assessed using three of five criteria proposed to identify ‘fatally flawed papers’ that are applicable to both qualitative and quantitative research. 58 These were (1) are the aims and objectives of the research clearly stated?; (2) is the research design clearly specified and appropriate for the aims and objectives of the research?; and (3) is there a clear account of the process by which their findings were produced?
Following this initial assessment, 43 papers (17 qualitative and 26 quantitative) were retained. The 17 qualitative papers were further were assessed using two criteria that focus on the quality of analysis and interpretation identified by Dixon-Woods et al. 58 These criteria were (1) are enough data displayed to support the interpretations and conclusions? and (2) is the method of analysis appropriate and adequately explicated? This assessment resulted in three qualitative papers rated as ‘sound’ (sufficient in-depth data and interpretation), eight papers as ‘adequate’ and six papers rated as ‘poor’ on at least one criterion.
The 26 quantitative papers retained were reviewed at this stage using questions specifically designed to assess survey research:59 (1) Is the response rate adequate to ensure response bias is not a problem? (2) Are sample size or power calculations reported? (3) Is the survey method likely to introduce significant bias? (4) Are reporting of the results of analyses adequate? and (5) Is the statistical analysis appropriate?59 Altogether, 11 quantitative papers were rated as ‘adequate’, three papers were rated as ‘sound’ and 12 papers were rated as ‘poor’ on two or more criteria.
The 12 quantitative and six qualitative papers rated as ‘poor’ were further assessed as ‘thick’ or ‘thin’, based on their descriptive and interpretive content. 60 This resulted in the retention of one qualitative paper otherwise rated as ‘poor’ because limited methodological detail was available. A total of 14 quantitative and 12 qualitative papers were therefore retained for the synthesis (see Figure 2 and Appendix 2). 29–53 See also summary of included studies in Appendix 2, Table 16.
Approach to synthesis
The preliminary synthesis initially involved making descriptive summaries of the characteristics and methods of each paper. Grouping and clustering was then undertaken to describe the set of retained papers.
Parallel syntheses of the 14 quantitative and 12 qualitative papers were undertaken and the two syntheses were then juxtaposed to develop an integrated synthesis. The key barriers identified from the quantitative data provided the initial framework for this synthesis, with the findings then elaborated with the qualitative data and explanations developed.
Results
A detailed synthesis is published in Morgan et al. 57 The characteristics of included studies are shown in Appendix 2 and the main findings are briefly summarised below.
Phase 2: preliminary synthesis (grouping and clustering of studies)
Only five retained studies were published prior to 2000,33,34,38,41,53 reflecting the fairly recent growth in transplantation and deceased organ donation. Altogether, 15 studies were conducted in the USA,29–34,37,39,41,47–50,52,53 and these were primarily quantitative surveys to identify self-reported donation attitudes and behaviour among African Americans. The three Canadian studies were all qualitative and examined barriers relating to native, Chinese and Indo Canadians. 42–44 Seven of the eight UK studies were also qualitative (focus groups or semistructured interviews)35,36,38,40,46,51 and studied black African, black Caribbean and South Asian (Indian, Pakistani, Bangladeshi) ethnic groups, with just one quantitative survey in south London. 45
The papers focused on knowledge and attitudes, with a lack of attention to the effects of access to information or sources of registration, although such barriers have been identified as common in disadvantaged communities in the USA. 61
Phase 3: main synthesis and relationships
Knowledge
The most commonly studied barrier in quantitative studies was respondents’ knowledge about the need for organ donation or the process of registration. Knowledge was generally identified as lower among ethnic minorities than in the white population. Some studies showed that this held after adjusting for age and education,45 although adjustment for education or other socioeconomic variables was rare. However, two US studies37,41 that employed composite knowledge scores reported no significant difference in scores between black, white or Asian medical students,37 or between African American and Hispanic participants. 41 These differing findings may reflect the nature of study samples, with ethnicity often interacting with social disadvantage to contribute to relatively low knowledge.
Talking with family
Families’ awareness of the deceased’s wishes regarding donation is of considerable importance in an opt-in system, in which donation requires the consent of next of kin. However, two quantitative37,47 studies in the USA identified ethnic minorities as significantly less willing than the general population to talk with their family about organ donation. In the UK, similar differences in willingness to talk with family were reported, with black African, African Caribbean and South Asian minority groups being significantly less likely than the general white population to have discussed the topic of organ donation with friends or family, following adjustment for age, gender and number of years in education. 45
Qualitative studies identified several reasons for a lack of willingness to talk with family about organ donation, including superstitions around talking about death, parents not wanting to think about their children dying and concerns about offending elders. 40 The older generation were also less likely to support organ donation as it was generally not part of their traditions and their views could have a dominant influence. For example, black Africans in the UK described a fear of family rejection if they went against their views on this issue,36 and a study of Indian Sikhs indicated that the younger generation felt a duty to respect the wishes of their elders, particularly during bereavements. 38
Faith and cultural beliefs
Two quantitative studies41,47 identified African Americans and Hispanics as significantly more likely than white Americans to regard organ donation as contrary to their religious beliefs, as did a study comparing UK minority groups (black Caribbean, black African and South Asian) with the white population. 45 In contrast, a study of medical students did not identify the statement ‘donation is against religious viewpoints’ as a significant predictor of willingness to donate among African American and Asian American medical students compared with white medical students. 37 Similarly, religious objections were not identified as a significant predictor of willingness to donate among black and white Seventh-day Adventist students in the USA after adjusting for race, gender, age and a range of attitudinal barriers to donation. 32 Evidence of the influence of religion on willingness to donate was therefore mixed, possibly reflecting both differences between faith groups and the varying significance of faith for different age and socioeconomic groups.
Although people of Islamic faith are generally regarded as less likely to view deceased donation as acceptable, one study (Poonia et al. , unpublished) identified differences in knowledge and views between Muslims in the south and those in the north of England. Those in the north were less likely to consider organ donation and were described as a group for whom ‘religion defines who they are, colours all aspects of their daily life’, and were thus characterised by a strong ethnic/faith identity. 40 However, another key characteristic of respondents’ accounts was their uncertainty as to whether or not their faith permitted organ donation or has a single standpoint on the issue. 38,40
Bodily concerns
Concerns about the body took various forms that, in part, linked with faith and cultural beliefs, particularly a belief in the need for an intact body for the afterlife but also reflected general fears and feelings of disgust and concerns about bodily disfigurement that were particularly prevalent among ethnic minorities. 29,32,37,41,45
Uncertainty about their faith’s stance to the body remaining intact following death formed a particular concern for those of Islamic faith40 (Poonia et al. , unpublished), but was also raised by other ethnic and faith groups. 39,43,44,53 Other concerns related to donation interfering with traditional death rituals and practices involving appropriate care of the body after death42 or delaying burial and the body being ‘put to rest’. 39 In addition, a qualitative study in the UK identified respondents of second and third generation Caribbean origin as having an idealised desire that their body should return intact to their ‘home’ country for burial, which reflected the importance for them of reconciling a divided identity at death by returning home with their body intact. 46
Issues of trust
Trust involved various aspects. One key concern was trust in the fairness of the organ allocation system, with African Americans being less likely than white respondents to regard organs as allocated fairly and more likely to be allocated to the ‘rich and famous’. 37,47,50
Studies in the USA37,50 and a survey in the UK45 also indicated that black Caribbean and black African respondents in the UK and African Americans were significantly less likely than white correspondents to ‘feel confident that medical teams would try as hard to save the life of a person who had agreed to donate their organs’ (adjusting for age, gender and education), and were significantly more likely to worry that donated organs may be used ‘without consent for other purposes like medical research’. 45
Qualitative studies also provided further evidence of fairly widespread concerns among all ethnic groups that less would be done to save their life if they were known to be an organ donor. 35,38,46,53
Phase 4: robustness of the synthesis
This synthesis is one of a small number of reviews that have integrated quantitative and qualitative research and thus bring together studies that differ in their design, measures and study populations. These differences limited precise comparisons, although the inclusion of both types of data enabled a more detailed understanding of beliefs and practices.
Retained studies were, however, mainly ‘thin’ in interpretive content, thus restricting the possibility of more complete explanatory models. This may partly reflect the particular challenges of research in this area, including the cultural taboos and fears surrounding death and notions of organ donation, as well as people not having previously engaged in discussion of this topic.
Despite acknowledged limitations of the research, there was evidence of commonalities in attitudes and beliefs across race/ethnic groups, particularly the similarities between African Americans beliefs and those of the black population in the UK, as well as evidence of some variations between ethnic groups.
Conclusions
The review identified a number of consistent themes regarding barriers to donation.
-
Knowledge of deceased donation: this was fairly limited among all sections of the population, although minority ethnic groups in both the UK and North America demonstrated relatively low awareness and knowledge about needs for donation and how to register. Low knowledge was associated with less willingness both to register as a donor and to talk with their family about donation.
The relatively low knowledge among minority ethnic groups has persisted despite campaigns in the UK since 1999 that have specifically focused on increasing knowledge and encouraging registration as an organ donor among minority ethnic groups (see Table 2). This raises questions of the reasons for lack of awareness and how campaigns could be more effective.
-
Attitudinal and cultural barriers: a common barrier for many African Americans and for the black UK populations was a pervasive lack of trust in the health-care system, which was reflected in concerns regarding inappropriate withdrawal of treatment and perceived inequities in the allocation of organs. This perception may be shaped by their shared histories and feelings of marginalisation, together with the significant inequalities in access to health-care resources in the USA.
For many people of Pakistani and Bangladeshi ethnicity, their faith beliefs formed the most significant barrier. However, rather than regarding Islam as prohibiting organ donation, respondents often felt uncertain and expressed the need for guidance from faith leaders. This situation exists despite jurisdiction rulings stating that Islam permits organ donation. 62 Lack of awareness of such formal authority has also been shown to extend to individual faith leaders, who differ in their interpretations and views on this topic. 63
The review also identified important gaps in knowledge. First, ethnic groups were mainly treated as discrete and largely homogeneous groups whose attitudes and beliefs are at variance with a socially desired practice, with little attention given to either variations within ethnic groups by age/generation or education/socioeconomic status, or to the ways in which age and social disadvantage may interact with ethnicity to influence knowledge and beliefs about organ donation. Second, there was little attempt to explain the lack of knowledge about organ donation among ethnic minorities or to consider possible structural barriers to practices, including access to information and sources of registration, although these have been identified as contributing to spatial variations in overall donation rates in the USA. 61
Study 2: focus group study – beliefs and attitudes to registration
Abstract
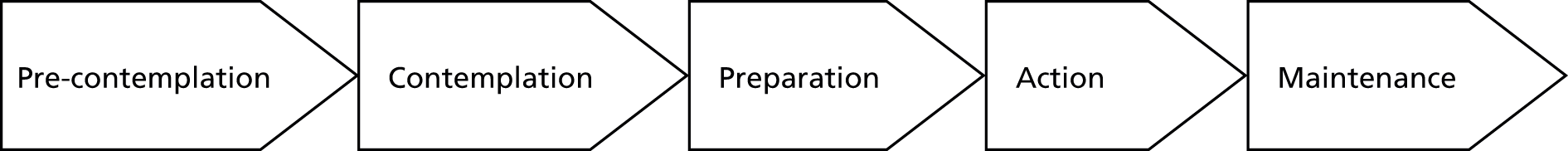
This study had two main aims: (1) to explain the continuing low knowledge regarding organ donation and registration as a donor among minority ethnic groups and (2) to identify similarities and variations in beliefs and practices between and within ethnic groups. Data collection involved a brief questionnaire and 22 focus groups comprising six ethnic/faith groups (who identified as Nigerian Christian, Caribbean Christian, Indian Sikh, Indian Hindu, Pakistani Islamic and Bangladeshi Islamic). Separate groups were held for older and younger members of each ethnic group, and for men and women among older South Asian groups. Discussion was facilitated by the use of vignettes. Sessions were recorded and transcript data analysed qualitatively. The discussions indicated that participants varied in their position on the ‘pathway’ towards registration as a donor; however, the majority were at a ‘pre-contemplation’ stage, despite ongoing campaigns to promote organ donor registration. We explain this by drawing on Schutz’s theory of relevance. 64 This describes a filtering process in which information that lacks perceived relevance to participants’ lives and which does not relate to their ‘stock of knowledge’ often ‘passes by unnoticed’. Second, we examined perceived barriers to deceased donation and the ways in which these were influenced by ethnic background, age, length of time in the UK and other life circumstances, thus leading to considerable heterogeneity within ethnic groups. The implications of these findings are considered for approaches to increasing knowledge and changing attitudes to deceased donation.
Background
A series of national campaigns have focused specifically on raising awareness of the need for organ donors among minority ethnic groups. These began in 1999 with a campaign focusing on the South Asian community, followed by three further national campaigns (Table 1). The campaigns differed in their specific theme/strapline, but all aimed to increase knowledge and change attitudes, and thus influence practices among minority ethnic groups. The campaigns generally involved national adverts, local radio shows and leaflets distributed to health centres, community centres, social centres, places of worship, etc. In 2010, they also included street plays in areas with relatively high BAME populations.
| Years | Organisation | Title | Target |
|---|---|---|---|
| 1999–2001 | Department of Health | South Asian community organ donation campaign | South Asians |
| 2002–5 | UK Transplant | Be part of the solution | Black population |
| 2006–7 | NHSBT | Can we count on you? | Black and South Asian |
| 2009–10 | NHSBT (Prove It campaign) | If you believe in organ donation, prove it | General population (2009), BAME groups (2010) |
| 2011–12 | NHSBT | Real people, real lives, real action | General population and BAME groups |
National campaigns have been supported by considerable local activity that is often targeted on specific ethnic and faith groups. The extent of this activity has not been documented, but it appears to have increased significantly since 2009, particularly through the activities of ODCs associated with NHS trusts.
Aims
This study aimed to address two key issues raised by the prior systematic review of the literature:
-
Why is there a continuing low level of knowledge about deceased donation and registration as a donor despite public campaigns focusing on minority ethnic groups?
-
How do beliefs and attitudes to organ donation and registration vary between and within different ethnic groups with a particular focus on African (Nigerian), Caribbean and South Asian (Indian, Pakistani and Bangladeshi) populations, particularly in terms of the influence of cultural and religious barriers?
We also initially aimed to elicit views regarding the possible introduction of a system of presumed consent in the UK; however, neither the participants’ level of knowledge nor the time available for focus groups enabled us to do this.
Design and method
Focus groups were selected as the method of data collection, as they have the advantage of encouraging debate about a topic that is not normally discussed and for which people may have limited knowledge. Addressing this topic as a group may also be more comfortable compared with the one-to-one situation of a personal interview.
Participant recruitment
Our research protocol identified the need to employ a recruitment company with experience of engaging people from minority ethnic groups in academic research, given the demands of recruitment and a limited timescale. We identified a company that had a network of local fieldworkers and was willing to undertake only the recruitment stage, with our team then conducting the groups and undertaking the analysis.
The recruitment strategy (Table 2) aimed to allow beliefs and attitudes to be examined both between and within ethnic groups. Separate focus groups were, therefore, conducted with people of Indian, Pakistani, Bangladeshi, Caribbean and Nigerian ethnic origin (the Nigerian and Nigerian British population was selected representing the largest proportion of the black African population in the UK). 65 These ethnic groups were also divided into younger (18–40 years) and older age groups (≥ 41 years). For the South Asian groups, separate groups were held for men and women to reflect cultural traditions and promote discussion among participants.
| Age | 18–40 years and ≥ 41 years |
| Gender | Male and female |
| Ethnicity | Indian, Pakistani, Bangladeshi, Afro-Caribbean and West African |
| Religion | Islam, Hindu, Christianity and Sikh |
| South Asian recruitment boroughs | Brent, Tower Hamlets, Harrow, Newham |
| Caribbean and Nigerian recruitment boroughs | Croydon, Southwark, Lambeth, Lewisham |
The recruitment company was tasked with recruiting participants in line with our stratified sampling and to organise suitable locations for holding the discussions. Initially we hoped to recruit some groups outside the London area; however, the logistics of recruitment resulted in our recruiting groups from the eight London boroughs with the greatest ethnic minority populations. With the exception of the African and Caribbean groups, recruitment of a particular minority group took place in single boroughs, where a significant proportion of the population was made up of the ethnic minority groups under study as identified by Ethnic Group Projections for 2010. 65 Table 2 shows which boroughs each ethnic group were recruited from.
Agency fieldworkers were of the same ethnicity, faith and gender as the population to be recruited, and often resided within in the recruitment borough, thus benefiting from local knowledge, recruited the participants. Recruitment occurred on a door-to-door basis, in the street, at places of worship and community organisation, and through snowballing.
The recruitment company was supplied with a brief information sheet for potential respondents, which outlined the purpose of the research, what to expect if participating, assurances of confidentiality and the promise of expenses (£25). Potential participants were invited to contact the researcher if they wished to discuss any aspect of the research before making up their mind to join the study.
The aim was to recruit 10 participants for each focus group to ensure that approximately eight participants attended. Altogether, just over two-thirds of those recruited attended the focus groups, with attrition between recruitment and attending the event being greater among Caribbean and Nigerian populations (Table 3).
| Ethnicity | Recruited | Attended | |
|---|---|---|---|
| Number | Number | Percentage of recruited | |
| Bengali | 49 | 45 | 92 |
| Caribbean | 41 | 19 | 46 |
| Indian Gujarati | 44 | 37 | 84 |
| Indian Punjabi | 45 | 40 | 89 |
| Nigerian | 70 | 31 | 44 |
| Pakistani | 62 | 36 | 58 |
| Total | 311 | 208a | 67 |
Throughout the recruitment process the research team was in close contact with the company to provide feedback and to ensure that the high level of attendance was achieved, with participants drawn from our designated minority ethnic groups and age groups. The split between employing a specialist company for recruitment and facilitating the focus groups ourselves seemed to work well.
Non-English-language groups
Recognising that English was likely to be a second or third language for some members of the older generation, we employed bilingual fieldworkers with experience of conducting qualitative research to facilitate the discussion with older Pakistani groups in Urdu, older Bangladeshi groups in Sylheti, older Indian Hindu groups in Gujarati and Indian Sikh groups in Punjabi.
A training session was held to brief the fieldworkers and familiarise them with the topic guide. The DonaTE team also developed an annotated version of the focus group topic guide that explained the rationale for the questions being asked in each section and gave an indicative list of potential topics to probe further (see Appendix 4). The day also included training on the conduct and facilitation of focus groups. These sessions provided ‘top tips’ for effective facilitation and covered issues such as how to break the ice, managing dominant participants and dealing with the ‘group expert’. This phase of training also involved discussion of what areas to prompt and probe and how to do this effectively. The training day also allowed an opportunity to consider issues in translating the topic across languages when direct translations of words associated with organ donation are not available or the concepts around donation are unfamiliar. As the final stage of training, the fieldworkers were observed in facilitating practice focus groups involving other members of the group.
Topic guide and vignettes
The topic guide covered individual knowledge and attitude towards organ donation, wider social benefits, and religious and moral issues regarding donation (see Appendix 4).
Piloting the topic guide confirmed that participants knew little about deceased donation and had little direct experience of the situations in which organs are requested to be donated or required for transplantation. When initially asked about organ donation, they therefore mainly talked positively about the benefits of transplantation and any conversation about donation was mainly situated within narratives of doing a good deed and saving the life of another, reflecting prevailing narratives of organ donation/transplantation in the media.
In an attempt to prompt more detailed discussion, we revised the topic guide and included factual information about donation to introduce each section, including information on the disparities in donation and consent between the general population and minority groups (see Appendix 4). We also developed vignettes that required participants to consider how they might behave in a particular donation situation and how they would advise a friend faced with a similar situation (Figure 3).
FIGURE 3.
Vignette scenarios relating to registering as a donor. Reproduced with permission from Morgan M, Deedat S, Kenten C. ‘Nudging’ registration as an organ donor: Implications of changes in choice contexts for socio-cultural groups. Curr Sociol 2015:63:714–28. 66
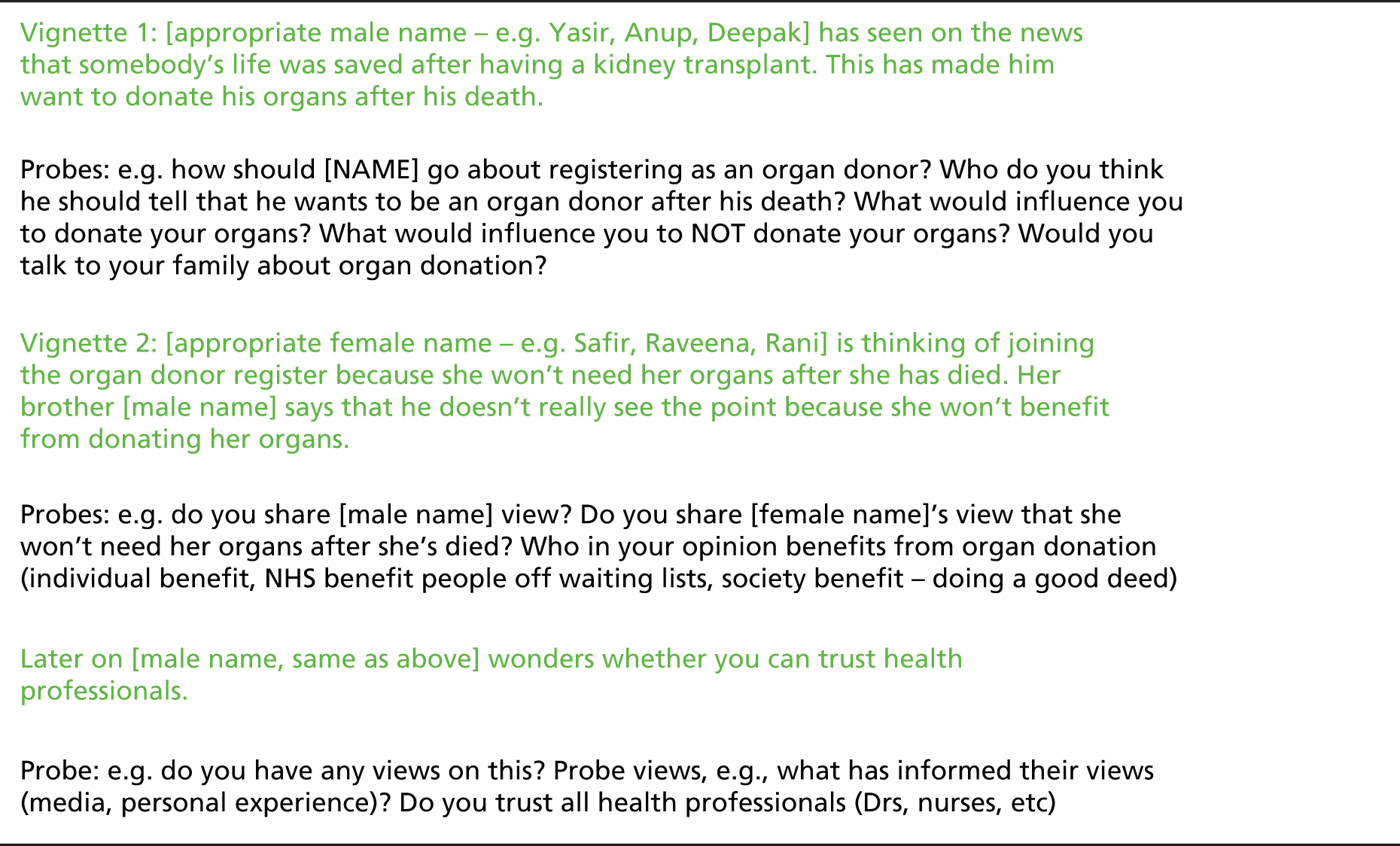
The vignettes were informed by the literature and campaigns to promote organ donation. We also sought feedback from our lay advisory group to ensure that the situations depicted seemed plausible and comprehensible. Those attending the meeting felt that the topic guide and vignettes were appropriate and a few minor comments were incorporated. The decision to stratify by gender for the younger Indian, Bangladeshi and Pakistani groups was not regarded as necessary but at that stage it was too late to alter the recruitment strategy to reflect this sentiment.
Two vignettes are considered in this chapter and relate directly to registering as an organ donor. A third vignette focused on issues of family consent to donation. This was less successful in promoting discussion as participants were becoming tired and lacked understanding of the donation process within ICUs that required a new set of information. Moreover, their over-riding concern and almost sole focus of discussion was about whether or not you know if someone is really dead or may come back to life.
Conducting the focus groups
A total of 22 focus groups were held over 3 months (March–May 2010). Two researchers (CK and SD) facilitated 14 groups. The other eight community language groups were facilitated by bilingual fieldworkers, with a researcher also present to ensure that the groups ran smoothly and clarify any questions that the group might have about organ donation.
The focus groups were conducted in community spaces that were local to and often known by the participants and were also close to public transport. The groups were mainly held in the late afternoon/evenings or weekends, as this was the most convenient times for the participants. Each lasted 60–90 minutes. Participants received £25 in cash to cover expenses that they incurred attending the group. It was clear that, for some, this payment was an incentive to participation.
At the start of the group, the researcher provided an overview of the study and explained how the focus group would proceed. Written consent was obtained and a short questionnaire completed to provide summary sociodemographic information (see Appendix 5).
Data analysis
The bilingual fieldworkers interpreted and transcribed their focus group discussions into English. Other audio-recordings were transcribed verbatim by a professional transcriber and checked for precision by CK and SD. Listening to the transcripts and reading them for accuracy of transcription aided the identification of potentially relevant analytical concepts and patterns of response across groups.
To assist the analytical process, each transcript was imported into the qualitative software package NVivo (version 9). Analysis and interpretation occurred concurrently with data collection. Initial line by line coding was undertaken, with the responses grouped into categories that related to the five themes identified in the systematic review of barriers to donation. However, the analysis was not intended to be limited to these themes, with emphasis also given to the variations within and between groups, as well as to emerging thematic categories and interpretations.
Findings
Characteristics of participants
Table 4 summarises the characteristics of participants (see Appendix 6). Of the participants, students, retirees and those caring for family accounted for 29%. In general, the sample was biased towards the lower occupational and socioeconomic groups, with those employed (44%) mainly being in low-skilled or semi-skilled occupations, such as taxi drivers, security guards, and teaching and kitchen assistants. An exception was the group of younger Indian Hindu women, several of whom were in professional occupations, including an engineer and a general practitioner (GP).
| Focus group numbers | Ethnic group and age (years) | Number of participants | Place of birth | Work | Know person waiting for or had transplant |
|---|---|---|---|---|---|
| 11 | Caribbean (Christian), 18–40 | 8 | UK, n = 7 Jamaica, n = 1 |
Employed, n = 5 Care for family, n = 1 Student, n = 2 |
2/8 |
| 2 and 20 | Caribbean (Christian), > 40 | 19 | UK, n = 3 Jamaica, n = 6 Barbados, n = 2 St Kitts, n = 1 Guyana, n = 1 Sierra Leone, n = 1 Not stated, n = 5 |
Employed, n = 6 Care for family, n = 3 Unemployed, n = 6 Retired, n = 4 |
6/19 |
| 13 and 22 | African (Nigerian Christian), 18–40 | 21 | UK, n = 5 Nigeria, n = 16 |
Employed, n = 13 Care for family, n = 1 Student, n = 7 |
2/21 |
| 21 | African (Nigerian Christian), > 40 | 11 | UK, n = 1 Nigeria, n = 8 Not stated, n = 2 |
Employed, n = 6 Unemployed, n = 4 Not stated, n = 1 |
1/11 |
| 7 and 8 | Pakistani, 18–40 | 27 | UK, n = 6 Pakistan, n = 16 India, n = 1 Bangladesh, n = 1 Kenya, n = 2 Russia, n = 1 |
Employed, n = 9 Care for family, n = 8 Student, n = 5 Unemployed, n = 5 |
4/27 |
| 15 and 16 | Pakistani, > 40 | 16 | UK, n = 1 Pakistan, n = 11 Not stated, n = 4 |
Employed, n = 2 Care for family, n = 6 Unemployed, n = 1 Retired, n = 2 Not stated, n = 5 |
0/16 |
| 3 and 4 | Bangladeshi, 18–40 | 26 | UK, n = 7 Bangladesh, n = 15 Not stated, n = 4 |
Employed, n = 9 Student, n = 8 Unemployed, n = 9 |
2/26 |
| 17 and 18 | Bangladeshi, > 40 | 21 | Bangladesh, n = 15 Not stated, n = 6 |
Employed, n = 8 Care for family, n = 3 Unemployed, n = 5 Retired, n = 5 |
1/21 |
| 5 and 6 | Indian Hindu, 18–40 | 20 | UK, n = 1 India, n = 18 Zambia, n = 1 |
Employed, n = 13 Care for family, n = 1 Student, n = 6 |
5/20 |
| 12 and 14 | Indian Hindu, > 40 | 19 | India, n = 14 Yemen, n = 3 Kenya, n = 1 Not stated, n = 1 |
Employed, n = 3 Care for family, n = 3 Student, n = 1 Unemployed, n = 9 Retired, n = 2 Not stated, n = 1 |
0/19 |
| 9 and 10 | Indian Sikh, 18–40 | 22 | UK, n = 11 India, n = 8 Tanzania, n = 1 Not stated, n = 2 |
Employed, n = 18 Care for family, n = 1 Student, n = 2 Unemployed, n = 1 |
4/22 |
| 19 and 23 | Indian Sikh, > 40 | 18 | India, n = 16 Not stated, n = 2 |
Employed, n = 8 Care for family, n = 7 Unemployed, n = 2 Retired, n = 1 |
1/18 |
The participants included a high proportion of recent migrants; of the 202 who stated their place of birth, 79% were born outside the UK. These characteristics of relatively low socioeconomic status and a high proportion of overseas born people are fairly typical of areas with a high multiethnic population.
Knowledge about organ donation
A small number of people attending each focus group knew someone who was waiting for a transplant or who had received a transplant; however, few people were sure they had definitely joined the ODR. An exception was four highly educated Hindu women who had signed up to the ODR following participation in a cord blood donation project at a London hospital that led to their knowledge and interest in donation. Another rather larger group were unsure if they had checked the relevant box agreeing to be registered as an organ donor when renewing their passport, applying for a driving licence or applying for a Boots Advantage Card.
With few exceptions, individuals tended to reflect positively and with some enthusiasm about the abstract notions of donation and transplantation, with responses frequently situated within narratives of doing a good deed and saving the life of another. However, when asked to discuss the first vignette and to share their opinions or what they knew about organ donation, their responses were limited:
I don’t have knowledge on it to be honest. I’ve never looked it up to be honest, nothing really – I don’t know anything about it, all I know is that they take things out of your body.
Bengali Muslim woman, 18–40 years
When asked about how they would go about registering on the ODR, most participants’ responses drew on what Schutz64 terms ‘cook book knowledge’. This refers to ‘recipes’ for dealing with routine matters encountered in daily life that can be drawn on by individuals when faced with new or unfamiliar situations. For example, given their lack of awareness and knowledge of how and where to register as a potential organ donor, participants suggested logical places where it would be assumed individuals should or could possibly register. These tended to be local hospitals or GP surgeries. As registration was perceived to be a medical matter and an important decision, registering in a ‘health space’ was regarded as appropriate and to have the advantage of the opportunity to ask questions about an unfamiliar topic:
And I think, you know, with the GP you’ve been, hopefully, with that GP for a long time, they know all your history . . . trust is built over time, you know, it’s, you go with all your personal issues, and so yes the trust is definitely there.’
Indian Sikh woman, 18–40 years
Awareness of the shortage of organs was also limited. Across the groups, a number of participants (both older and younger) were of the opinion that the NHS holds a store of organs within hospitals that would be available for transplant when required. Within this context there was little imperative to register as an organ donor as they perceived there to be abundant stores of organs available.
Oh, sorry, I don’t know much about it, but do they freeze these until someone needs them?
Nigerian Christian woman, 18–40 years
. . . my organs may be removed after my death and put in a freezer box for a while. Doctors may use these organs from the freezer box later . . .
Bengali Muslim man, ≥ 41 years
If they don’t find a person [suitable recipient], they will put it [donated organ], keep it in a freezer for a long time.
Bengali Muslim man, 18–40 years
Explaining low knowledge
The national ‘Prove it’ campaign focused on minority ethnic groups in 2010 and coincided with the focus group study (see Table 1). However, few respondents were aware of this or of any other campaign. We believe this lack of awareness is because organ donation has limited ‘topical relevance’ for the majority of participants. Schutz64 described the notion of ‘topical relevance’ as something that is imbued with meaning for an individual because it stands out for them (p. 125). Schutz described individuals as structuring their knowledge into zones of relevance, which decrease in degrees of clarity and precision as they move outwards from areas of personal concern. Within this context, the potential exists for information that is not perceived by an individual as ‘topically relevant’, in terms of being of close personal concern and relating to their existing ‘stock of knowledge’, to ‘pass by unnoticed’ rather than being actively rejected. This lack of personal relevance was often reflected in participants’ accounts:
. . . you see leaflets and cards in everywhere like surgeries, and you don’t really give it that much importance . . .
Bengali Muslim woman, 18–40 years
Yes exactly the thought [of registering as a donor] has been there when you’ve read a poster or something but as soon as you walk away from that poster . . . as soon it comes in it goes out . . .
Indian Sikh man, 18–40 years
Analysis of participants’ accounts identified several reasons why organ donation campaigns lacked topical relevance for them.
Lack of direct personal experiences
Participants often cited an absence of any direct personal experiences of donation or transplantation, with the topic seeming remote for them:
I’ve seen lots of adverts, seen loads of donor cards and even been given them but not done anything . . . well . . . I think if it was somebody close who I loved or really felt for that would influence me a lot more than maybe the advertising.
Pakistani Muslim man, ≥ 41 years
Although across the focus groups, 14% of participants indicated that they knew of someone who had received a transplant or was waiting for one, but this direct personal experience did not necessarily guarantee their joining the ODR, or produce a lasting sense of motivational relevance.
. . . I never thought about it [organ donation] until then [when best friend had a transplant], and I haven’t really thought about it since . . .
Caribbean Christian woman, 18–40 years
Thus, it appeared that knowing of somebody who had received or was waiting for a transplant was not enough to increase topical relevance and motivation. In particular, several participants referred to what they regarded as the lack of visibility of donation within the wider community and thus the absence of a prompt that could direct and focus for their attention. As one Pakistani male participant commented,
We don’t have a much experience in our community doing anything like that [organ donation]. I never heard anything.
Pakistani Muslim man, ≥ 41 years
This lack of experience and familiarity with organ donation was particularly marked among the older participants, who observed that it was not part of their childhood or culture, which affected both their own engagement with the topic and their transmission of information to the next generation:
. . . from the time I was a little lad growing up in Barbados it [organ donation] was nothing that was ever discussed. So, and then again, raising my own children, it is nothing that I more or less spoke to them about. So it’s not part of my culture, the circumstances in which I was brought up, that more or less would have prevent me from even giving it a thought.
Caribbean Christian man, ≥ 41 years
Some of the younger participants, particularly from the black community, also suggested that their limited awareness of organ donation reflected their feeling of being outsiders and not yet full members of the society:
. . . people in the UK, like Africans in the UK, Caribbeans in the UK, Asians in the UK, fine, they’ve been in the UK, they’ve heard about it, they’ve seen what is from across the road. They’re not on the same side as like the whites in the UK that kind of grew up in the whole thing. So they are still watching over it from the other side of the fence. Yes they are seeing it but it’s something that has not really, is not really part of them, their lives or completely accepted. They see it happening, fine, but it’s still is a strange process.
Nigerian Christian man, 18–40 years
Perceived lack of relevance for own community
Caribbean and African groups regarded organ donation as having greater relevance for ‘white people’ than for ethnic minorities. One explanation for this was in terms of a perceived visual absence of black people and ethnic minorities more generally in narratives of transplantation conveyed through the media. This is illustrated by an exchange between three Caribbean women:
Woman 1: . . . if they promote it more [organ donation and greater need for kidneys among BAME], we would sit back and think, we would be more aware of it, ‘Oh, our race needs a transplant,’ but as you said, you look on the TV [television], the majority of the people on TV who need transplants, is white people.
Woman 2: You know, they don’t show an Asian, they don’t show a Chinese.
Woman 3: Yes, I think, why should I give them my kidney, what for?
Caribbean Christian women, 18–40 years
Nigerian male participants also very much perceived organ donation as a ‘white issue’ and explained that this was because white people are not as strong and so have a greater need for transplantation, whereas black people’s organs were stronger:
So naturally the thing is, black people, we don’t believe in it [deceased donation], because we believe we are strong.
Nigerian Christian man, 18–40 years
I won’t need an organ donor, I’m black, and all my organs are strong. It’s only the white people’s organs that are not strong.
Nigerian Christian man, 18–40 years
It was notable that when the Nigerian groups were shown a picture used by a national campaign of a black man in a blue hospital gown looking very ill with a cannula in his neck, they did not identify with this man at all, as they did not expect an African man to be weak and sick.
Competing priorities and relevance
For some people, particularly among the Asian focus groups, there was a sense that the day-to-day rhythm of their working lives did not afford opportunities or provide any prompts to think about organ donation.
. . . if you work 9 to 5, you’re not going to have this discussion [about registering as a donor].
Indian Sikh man, 18–40 years
Our lifestyle is such that you put it aside and think you will do it one day but you don’t actually get round to do it.
Indian Hindu woman, ≥ 41 years
Never discuss it. You know we talk about politics other stuff, cricket . . . you know. They seem to be more important in our lives with all the 20/20 cricket we talk about but we don’t talk about . . . the discussion never happens, never seem to think about it [organ donation].
Indian Hindu man, 18–40 years
As several participants noted, having immediate access to registration would increase their likelihood of doing it. For example, a young Hindu man observed:
I think if someone said to me, ‘Right here’s the form’ I would do it. But I think, again, is just time, just going out and there are far more important things to do.
Indian Hindu man, 18–40 years
Coming to a decision about organ donation was also described as a gradual process of change, often ignited by a personal experience. However, unresolved questions could inhibit actually joining the ODR as this Caribbean participant explained:
black people have just recently started to come to terms with cremation, it’s a process that probably with more education, more knowledge, it will start. [It’s] a generation thing because I think my children would probably be more willing to go along that road. I am starting to turn the corner, because I have seen so many friends and family, on dialysis and needing organs. But it does raise a kind of question mark in your mind, as to how it is [organs] allocated.
Caribbean Christian woman, ≥ 41 years
Stages on the donation pathway
The majority of focus group participants were at the early ‘pre-contemplation’ stage of Prochaska and Velicer’s67 transtheoretical model of behaviour change (TTM), with little knowledge of donation or its relationship with transplantation (Figure 4). In contrast, the small group of Indian Hindu women had achieved an ‘action’ stage and joined the ODR, having being prompted by cord blood donation and had discussed this with their spouse, thus providing further maintenance of their wishes. Another group appeared to be at a contemplation stage, but either had some unresolved worries or, as in the case of many younger Indian Hindu and Sikh participants, regarded other things in their lives as having greater priority. However, it appeared that this group would be likely to take action in response to a ‘prompt’, such as the availability of easy and immediate access to registration. In addition, some older members of the Asian community felt that trying to register online could be too difficult given a lack of familiarity with this and their limited English.
Stages of change adapted for organ donation
Pre-contemplation: have not considered registering as a donor.
Contemplation: considered organ donation but not taken steps towards registration or addressing unresolved issues.
Preparation: able to recognise the benefits of registration and have taken action to find out more.
Action: expressed their wishes about donation by joining the ODR or discussed wishes with immediate family/kin.
Maintenance: occasionally reinforce statement of wishes to family members/kin.
Explaining negative attitudes
The second vignette was designed to elicit views and attitudes towards organ donation by presenting a scenario that prompted discussion regarding the pros and cons of registering as an organ donor (see Figure 3). For those with little knowledge who were thus at a pre-contemplation stage, these were not attitudes that currently influenced their behaviour but had the potential to do so in the future.
It was notable that participants were generally positive about the benefits that organ donation has to deliver to others. However, there was a distinct variation across the groups in salient uncertainties viewed as barriers to joining the ODR. Thematic coding of the data revealed that the most pertinent uncertainties revolved around issues pertaining to religious permissibility (most commonly among Muslim participants) and issues of trust among Caribbean participants.
Religion and belief in the permissibility of organ donation
All faiths in the UK formally support deceased organ donation with permission, care and respect, based on interpretations of scriptures that emphasise ‘selfless giving’. 68 Research commissioned by the ODT’s Independent Working Group to examine the potential impact of an opt-out system on different cultural groups included interviews with 26 representatives of the main faith groups. This indicated that the majority opinion in their faith or belief group was to permit organ donation, with some actively supporting it, although interviewees were keen to stress that there is a broad spectrum of opinion on organ donation within each faith and belief group, and that consequently it is difficult to speak on behalf of an entire group. 63 Similarly, the focus groups indicated that there was considerable uncertainty among the lay population concerning the permissibility of organ donation with differences occurring both between and within ethnic/faith groups.
Many of these participants were not aware of the religious permissibility of donation but nevertheless tended to regard deceased donation positively. As this older Pakistani man explained:
I’ve never discussed it. I’ve never read anything about it in the Quran. I’ve never heard anything . . . I mean I’m not deeply religious I have to say. I don’t know what the situation is [in terms of permissibility of organ donation]. In my own essence, I think it is a very noble pious thing. Your death gives life to somebody else. I don’t know what the Islamic religious viewpoint, what Islam says about it.
Pakistani Muslim man, ≥ 41 years
The few who had taken steps to look into the Islamic view on organ donation had done so following the situation where a close family member required a kidney transplant. However, they did not appear to have found a clear answer. As this Bengali woman explained:
Initially I was keen, but then I found out in terms of, like I said about religion and everything, you may not be allowed – and that’s the reason I’ve been doing a lot of research on whether I’m allowed or not, because I want to be able to donate if I am, because I don’t want that to go to waste, but if I’m not, then I don’t want to go against everything that I believe in, in terms of my religion.
Bengali Muslim woman, 18–40 years
Individuals in both the Bengali and Pakistani groups were happy to discuss organ donation within the focus groups and to consider whether or not organ donation could be seen as a permissible act. Several participants were also able to draw on a particular line from the Quran, which states that ‘if anyone saves a life, it shall be as though they had saved the lives of all mankind’ (surah 5, verse 32). Those aware of this verse were more confident in believing that organ donation could be an acceptable act within Islam:
[T]here’s actually a verse in the Quran, which is in the fifth chapter, 32nd verse, I think, if I remember. It says, if you save one life, and this is anybody, Muslim or non-Muslim, save one person, it’s equivalent to saving the whole of humankind, and, you know, that’s a big thing. So definitely, to save another person is a great thing . . . although in Islam it teaches that you shouldn’t harm yourself, harm your body, and obviously to give you an operation would do that, but if it means saving someone else’s life, that’s a bigger thing. So you can, you can take that smaller evil to make up for something which is a lot better. And definitely, if it’s a small operation to save someone’s life, yes definitely.
Pakistani Muslim man, 18–40 years
More generally, the view that saving a life is the most important consideration was common, with the older generation often referring to the scriptures to justify this:
A lot of scholars are saying it is permissible in Islam to donate your organs after your death. If you can help someone to live after your death, that is allowed. It is a great reward.
Pakistani Muslim woman, ≥ 41 years
In contrast, younger people generally talked about the value of saving a life without linking this specifically to the scriptures:
I don’t know much about it . . . but I think it’s a good idea if it means that, you know, obviously you’re dead, so you’re dead, but if your organs can go to something useful and save someone’s life, I think that is a good thing.
Pakistani Muslim man, 18–40 years
I think if it can help someone, that’s great isn’t it? I mean it’s saving a life.
Bangladeshi Muslim man, 18–40 years
However, there was also evidence of a range of views, with some people, particularly among the older groups, believing that ‘Islam does not give permission, so we need to follow that command’ and sometimes referring to organ donation as representing desecration of the body, which is expressly forbidden in Islam.
We’re not allowed to and I mean after we die, we are told that our soul becomes to – I mean, belongs to God. And we‘re not allowed to hurt our body because obviously if you’re going to donate, they cut you up and take, you know. So we’re just not supposed to hurt ourselves because our body is not ours any more. And I think that is the number one thing.
Bengali Muslim, female 18–40 years
However, whereas small numbers held such definite views of a lack of permissibility, many others discussed the fact that views about organ donation are based on an interpretation of the scriptures and noted that there is no single view among the faith leaders. As this Bengali woman explained:
I wouldn’t say it’s easy . . . people have different opinions and people say different things. So you’d have to be careful who you would go to and – ‘cos there will be some scholars that would probably say, ‘No,’ and he won’t even explain himself, ‘No.’ So you’d have to look it up through books as well as, you know, maybe [go to] someone you trust.
Bengali Muslim, woman 18–40 years
Several of the younger Muslim participants also suggested that members of their community, including Imams, confuse aspects of culture with religion and as a consequence cultural practice influences religious edicts:
But scholars don’t go on culture, I hope not though anyway, but they go with what is taught to them and what they learn from what they read. They don’t, they’re not supposed to go by culture. I mean we live with our cultures and mix it in with our religion. That’s where we go wrong, but where the scholars are concerned, they’re not allowed to put in their culture – maybe it happens, because they are human too. But that’s not religion. So they might misinform somebody else as well, but that’s, you know, a mistake from maybe God as well.
Pakistani Muslim woman, 18–40 years
The thing is if you go to every mosque, every mullah will say ‘no’. But they are not the people, they are not the scholars. I mean it says in the Quran to help people and save people, so I don’t understand why the Mullah say ‘no’.
Bangladeshi Muslim man, 18–40 years
Participants of Islamic faith therefore held differing views of the significance of Islam for donation, ranging from belief in the value of saving a life as the most important consideration to views that deceased donation was not permissible. However, there was also evidence of a questioning of traditional faith views particularly by younger Muslim participants, who often emphasised the general value of saving a life, with some also commenting that a shift towards westernised views was taking place.
Issues of religious writings and permissibility did not appear to be of significance for views of deceased donation among these participants. Instead there was a common belief that they were expected by their religion to do good for others and for the society, with organ donation following death regarded as an important aspect of this. Typical statements were:
The faith I believe in . . . there’s nothing that I’ve heard that we’re not allowed.
Indian Hindu man, 18–40 years
Our beliefs teaches us that however you can help somebody you should, if it improves someone’s situation then it’s very good.
Indian Hindu woman, ≥ 41 years
The religion itself promotes do unto others as you would have done to us. If you can help in doing good you should, whether you do it in life or death.
Indian Sikh man, 18–40 years
Positive influences on attitudes to donation included a familiarity with cremation (in contrast to traditional burial among Muslims), and a clear distinction made between the body and the soul. As these two younger Sikh men explained:
The body is just a vessel carrying the soul and that’s it.
Yes, exactly, so essentially, as much as I want to cremate it whole and keep it whole, there’s nothing left, so if that nothing can be put to good use, then why not.
Both Indian Sikh and Hindu participants regarded donation as having benefits both for those who donate and for the recipient. In personal terms:
It’s very important, comforting even to know your body can help someone, for example that my eyes will be helping someone to see after I’m gone.
Indian Sikh woman, ≥ 41 years
. . . you have those scales where you do good things and bad things, and when you go to heaven God assesses your good things and your bad things. So that [donation] could be one of the good things you do.
Indian Sikh woman, 18–40 years
In the case of Sikh and Hindu participants, their religion thus appeared to exert a positive influence on attitudes to donation. However, as they noted, the topic was rarely discussed or considered right to talk about, particularly with older family members. There were also differing views of personal autonomy; some younger people regarded donation as a personal decision, although one that the family should know about, whereas others felt that they would need to make sure that their family was comfortable with their decision and that they would not go ahead and register as a donor if their family was not comfortable with this.
Both older and younger participants from these ethnic/faith backgrounds regarded organ donation as a personal choice rather than governed by religious scriptures.
All Christians agree that you don’t need organs when dead – the spirit lives on and if you can prolong life that is a good thing . . . it’s a personal choice rather than religious decision.
Nigerian Christian man, 18–40 years
I have no problem, no religious problem with that. You are not killing someone, just being to prolong somebody’s life, innit?
Caribbean Christian man, ≥ 41 years
Most of these participants were in favour of donation, emphasising that you are going to die anyway and that donation is a way of helping others rather than just having your body decompose. However, a small number of older members expressed concerns about the afterlife and described growing up with the belief that you are required to return to God with everything you came with:
I think if something was missing from you when you die when you come back you will get sick and die.
Caribbean Christian woman, ≥ 41 years
However, most people of black Christian origin did not raise any religious barriers to deceased donation, and for many their religious teachings had a positive effect on their views of donation. The exception was a small number of older members who were concerned that their body should remain whole. Similarly, some of the younger participants thought their families would not approve of donation, reflecting traditional views of burying the body whole.
Trust and mistrust
Of particular salience among Afro-Caribbean participants were issues relating to trust. This partly related to the fair allocation of organs, with a common perception that white people would be privileged in terms of allocation:
I think the reason why the Afro-Caribbean not giving, because they don’t think that – it is fear because they think that even if we all come together and say we’re willing to give, we’re going to be the last one to get, right . . . Suppose 50 people have something wrong with their inside and they are 50 white, OK are they going to choose half of this and half of that? I think that they are going to go with the white one first and then whatever left, then the black one get it, then the Afro-Caribbean get it. That is what I think anyway, that’s the reason why they don’t go for it.
Caribbean Christian woman, ≥ 41 years
. . . I mean I am starting to turn the corner, because I have seen so many friends and family, you know, on dialysis and needing organs. But I mean, as Maureen just said, it does raise a kind of question mark in your mind, as to how it is allocated.
Caribbean Christian woman, ≥ 41 years
Additionally, Afro-Caribbean participants commonly vocalised a concern that donated organs may be used ‘without consent for other purposes like medical research’. In addition, they questioned whether doctors ‘will do all they can to save you’ or ‘just cut my body and take stuff’ (Caribbean Christian man, ≥ 41 years).
South Asian and Nigerian participants, in contrast, described generally trusting the UK medical system and having few worries about misuse of organs or unethical allocation practices in the NHS compared with systems back home.
. . . here [in the UK] I’d be a donor because the system is protected to a reasonable level. But If I go to Africa I will never be a donor, no way, because I don’t trust the system . . . In the UK I think I have the confidence in how it’s [organ retrieval, treatment of the body] being done especially in the NHS, I’m not saying its 100% but at least to a reasonable level, at least I’ll give them 85–90% if not more than that.
Nigerian Christian man, 18–40 years
Other beliefs and concerns
Participants identified a number of other beliefs and concerns that could enter into decisions regarding donation. For Muslims, a key issue was the need to be buried within 24 hours, which is recognised to present problems for donation and coroners’ inquests. General worries also included a dislike of the body being cut, as well as the notion that the dead body can feel pain and that this can even be more intensely felt by a dead person. A few people also voiced concerns about disfigurement and not looking normal if the body is displayed in an open casket, although most realised that donors would be presented so that they did not look different. Other worries related to general notions of tempting fate by joining the ODR.
There were, therefore, often a variety of influences that shaped views of donation and willingness to register as a donor, although for the small number of Muslims who believed donation was not permissible, this formed the single key concern.
Conclusions
-
This study offers a conceptually and empirically grounded explanation of why poor knowledge about organ donation and the ODR persists among many ethnic minorities despite a number of targeted health promotion campaigns over the last decade. We drew on Schutz’s64 theory of relevance to argue that information in the public domain about organ donation often passes people by unnoticed because their messages do not resonate with participants’ public or private life worlds. Organ donation, therefore, represents an issue of minimal topical relevance for many people who thus remain at a pre-contemplation stage, whereas for others the main issues were the presence of particular worries or concerns about donation or a lack of priority given to registration in their busy lives.
-
A key requirement is therefore to gain a better understanding of where groups are situated along the donation ‘pathway’ and to undertake a targeted approach. This requires responding to the particular constraints of different groups to directly address their beliefs and concerns.
-
Analysis of differences between ethnic/faith groups and between age groups indicated that although faith and cultural beliefs are often identified as a primary cause of non-registration and low donation rates, there is evidence of varying views and impacts of faith. For some, particularly those of Sikh and Hindu faith, their faith often formed a positive force shaping attitudes to donation. For others, their faith was perceived as having little impact on donation decisions. For example, for participants of Caribbean and Nigerian origin, their Christian faith was generally not identified as having a direct influence on donation decisions, which was regarded as a personal decision shaped by precepts for life that include the need to be altruistic and do good for others. Similarly, many Pakistani Muslims had few faith-related concerns, whereas a small number of people of Islamic faith, particularly of Bengali origin, regarded Islam as prohibiting donation, although a more common view among Bengali Muslim participants was that of uncertainty regarding the permissibility of donation and a need for guidance.
-
There was some evidence of generational changes, with younger people among all ethnic groups being less likely to regard donation as a faith-related issue compared with their parents. However, younger participants of Indian and Hindu origin felt a need to follow their parents’ wishes, whereas younger people of Caribbean and Nigerian origin were more likely to regard organ donor registration as a personal decision.
-
Issues of trust in doctors and the health system were of particular importance for the Caribbean respondents, who often raised concerns about the allocation procedure. This rarely featured in the accounts articulated by South Asian ethnic groups or Nigerian respondents, with both these groups emphasising their trust in the NHS, including in relation to organ donation and contrasting this favourably with the situation in their home country.
-
A strongly held view, particularly among the Caribbean participants, was that they would like the opportunity to have a personal discussion with a doctor or practice nurse regarding donation. When asked about registration they speculated that primary care would be where they would need to go.
-
Ease of access to registration was identified as of particular importance for those people who were willing to register, particularly younger people of Sikh and Hindu faith for whom other activities of life often took priority.
-
Some older participants with a low educational level regarded the notion of registration as complex and were uncertain about doing this online and whether their English would be sufficient or not.
-
Very few people were sure that they had registered as a donor but some people were uncertain if they had registered when obtaining a driving licence, passport or joining a general practice or applying for a Boots Advantage Card and would have liked to have had a registration card.
Study 3: systematic review – effective interventions to increase organ donor registration
Abstract
This systematic review aimed to identify the particular characteristics of effective interventions in terms of increased knowledge of organ donation and rates of registration. The review initially involved a systematic search followed by assessment of relevance and quality. This resulted in 18 papers29,69–85 retained for synthesis (17 papers from the USA29,69–84 and one from the UK85). These were a mix of cluster randomised trials and before-and-after evaluations. An interpretive synthesis was undertaken to examine the effectiveness of interventions and to identify the characteristics associated with implementing a particular intervention to maximum effect. This indicated that media interventions alone were not effective in achieving change in willingness or intention to register as an organ donor. Educational interventions were more effective in achieving change, with characteristics associated with successful change among minority ethnic groups, including a strong interpersonal element, a focus on the populations’ specific concerns, messages that are delivered by a trained member of the local community in familiar environments and immediate access to registration.
Rationale and review question
The focus group study indicated that despite campaigns to promote knowledge about organ donation and registration as a donor among minority ethnic groups, the level of knowledge remains poor. This raises questions of the characteristics of effective interventions.
We conducted the first systematic review of evaluated community-based interventions that aimed to increase organ donor knowledge and registration among minority ethnic groups. The specific question addressed was, ‘What are the characteristics of interventions that have been successful in increasing a range of outcomes relating to deceased organ donation among minority ethnic groups?’
Methods
A systematic search was undertaken with databases initially searched in December 2009 and refreshed in November 2012 (Table 5). Hand checking of relevant publications and direct contacts with experts were also undertaken.
| Databases | |
|---|---|
| Ovid | MEDLINE, EMBASE, PsycINFO |
| EBSCOhost | CINAHL, Cochrane Central PubMed |
| Trials data bases | UKCRN, ClinicalTrials.gov, WHO International Clinical Trials Registry Platform, Health Services Research Projects in Progress |
| Websites | NHSBT (www.nhsbt.nhs.uk); Kidney Research (UK) www.kidneyresearchuk.org; US Department of Transplant (funded studies) www.organdonor.gov/dtcp/behaviour.html |
The search strategy was written in conjunction with an information specialist (see the medical subject heading terms, Appendix 7). Following the initial MEDLINE search this was slightly modified to be applicable to other databases. The inclusion criteria are shown in Table 6.
| Country | UK, North America |
| Date of publication | 1980–2012 |
| Ethnicity | Visible (non-white) ethnic minority |
| Design | Intervention, evaluation study |
| Outcomes | Verified registration, changes in knowledge about donation (knowledge of the relevance to ethnic minority populations and knowledge of the process of registration) and changes in willingness to donate and to discuss organ donation with family |
| Participants | Adults (≥ 18 years) |
| Setting | Community |
Relevance and quality assessment
Following initial deduplication, 557 articles remained. This was followed by a review of relevance that was conducted by two researchers based on title and abstract, and, if necessary, review of the full article. This process led to the retention of 18 papers for synthesis (Figure 5). 29,69–85 These papers were reviewed for quality as a measure of robustness rather than for purposes of exclusion. Quality assessment was based on the Effective Public Health Practice Project tool that is applicable to randomised controlled trials, quasi-experimental studies and uncontrolled studies, and has established content and construct validity. 87,88
FIGURE 5.
Flow diagram showing exclusions for interventions review. Reproduced from Deedat S, Kenten C, Morgan M. What are effective approaches to increasing rates of organ donor registration among ethnic minority populations: a systematic review. BMJ Open 2013;3:e003453 under the Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0). 86
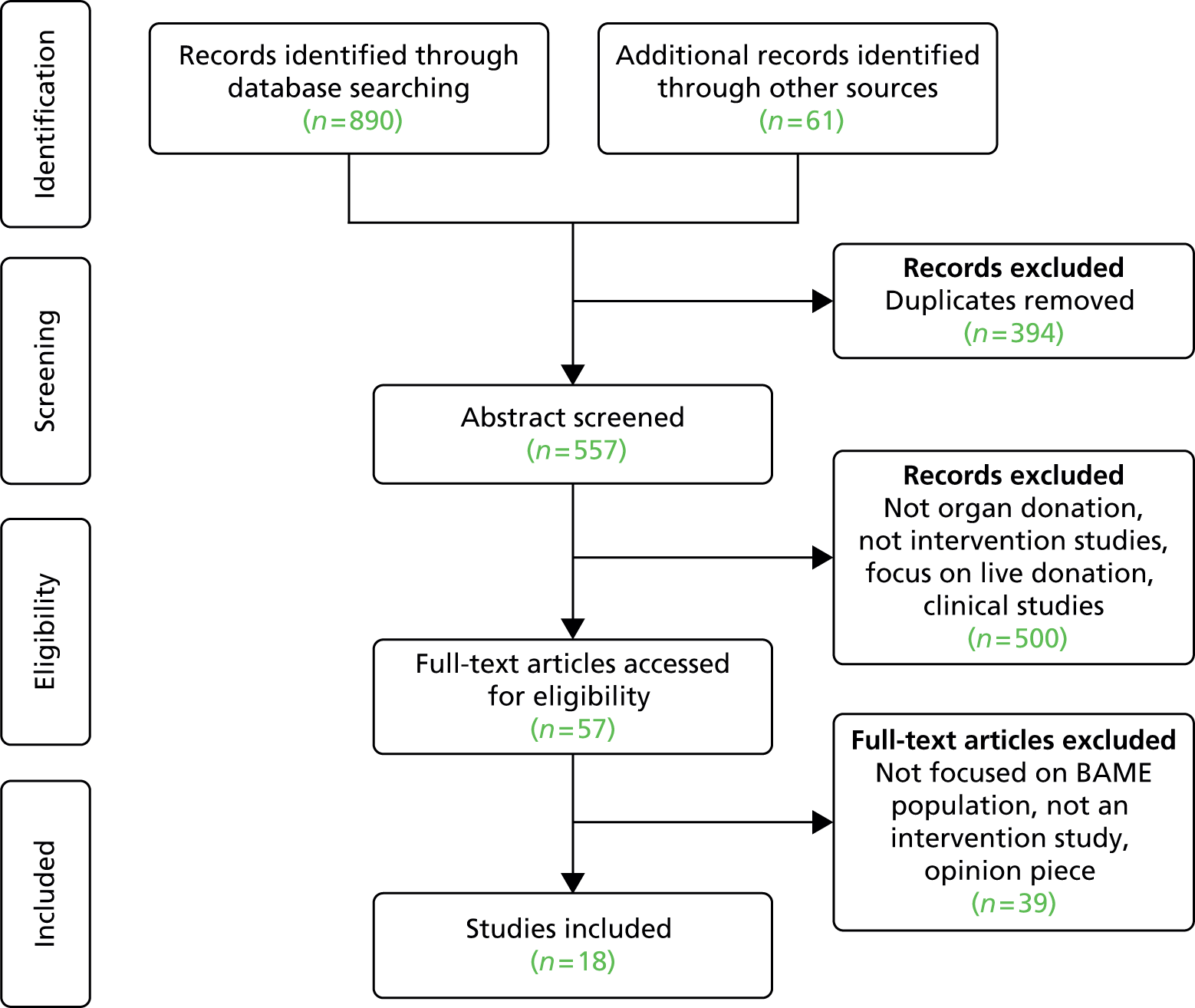
Results
Study characteristics
The 18 included studies29,69–85 are listed in Appendix 8 with their main characteristics summarised in Appendix 8, Table 17. These studies were all conducted between 1993 and 2012 and evaluated the effects of either an ethnically targeted mass media campaign or community-based education. All but one study85 was undertaken with ethnic minority populations in the USA, mainly African Americans or Hispanics. Most interventions published before 2009 adopted a pre- and post-evaluation design, whereas studies published since 2009 mainly employed a cluster randomised design. Outcomes assessed were verified registration, self-reported registration status or knowledge about organ donation (see Appendix 8, Table 17).
A detailed account of the findings is available86 and is briefly summarised here.
Educational interventions
A total of 11 papers reported educational interventions. 29,69,70,72–76,81,82,85 These interventions differed in their design and whether or not the outcome was verified enrolment on the ODR, changing knowledge or a shift towards greater readiness. However, shared characteristics of effective interventions were having a strong interpersonal element; being delivered by a range of individuals including recipient families, other trained lay individuals, or organ transplant and procurement staff; and being delivered in familiar settings, such as in a local church or a hairdresser salon, at community events or on a student campus.
The three main types of outcome evaluated in education interventions are considered below.
Enrolment on an Organ Donor Register
Verified enrolment was reported by three cluster randomised trials. 70,78,80 For all three interventions, the exposed group was significantly more likely to register than the controls.
Three further community educational studies with a follow-up or cross-sectional design reported strategies to increase organ donor registration. 71,76,85 These community educational studies identified important influences on registration such as the individual’s prior readiness and access to registration.
Changing knowledge
Three educational interventions focused on changing knowledge. 73,74,82 This was assessed by asking participants to indicate whether a range of statements regarding organ donation were ‘true’ or ‘false’. These included general knowledge statements about donation, knowledge of the relevance of donation to ethnic minority population, knowledge about the procurement and allocation of organs, religious and cultural knowledge about organ donation, and knowledge about the financial costs of organ donation. Ethnic minority transplant surgeons and donor/recipient families delivered presentations to participants.
Measured shift towards greater readiness
Two educational interventions were informed by the TTM67 and measured change in individual’s ‘readiness to become an organ donor’. 29,75 Both studies aimed to measure change across the five TTM stages from pre-contemplation to maintenance (see Figure 4). In Fahrenwald et al. ’s study,75 56.9% of participants progressed to a more advanced stage at post test and none regressed, whereas Arriola et al. 29 reported that intervention participants were 1.53 times more likely to be in a later stage of readiness than control participants.
Collaboration with members of the targeted ethnic population was undertaken to ensure the relevance and acceptability of the intervention. 29,75 For Arriola et al. 29 this involved a specific focus on religious objections to organ donation, involvement of the church pastors and the use of a well-known gospel choir to present the intervention video, whereas Fahrenwald et al. 75 included respected members of Native American tribes and their storytelling traditions to convey donation messages.
These studies provide evidence of positive movement towards readiness to become an organ donor, sign a donor card or talk to family members about their preferences, although whether those at a later stage of readiness actually signed a donor card or not is less clear. This issue is reflected in the UK community study where only a small proportion of participants who stated an intention to register in the future had done so at follow-up. 85
Mass media interventions
The seven media interventions attempted to detect changes in willingness or intention to join a donor register or sign a donor card. 71,77–80,82,83
Interventions that solely utilised mass media reported no significant change in intention or willingness to register an organ donor, despite focusing on a single ethnic group and undertaking formative research in the target population.
In contrast, a high level of success was achieved by one study78 that innovatively combined mass media techniques with interpersonal communication. This was conducted at vehicle licensing office in the USA, a setting in which individuals are able to join a state donor registry. To determine the effect of each component of the intervention on registrations, the campaign occurred in three stages, each lasting 3 months. The interpersonal component of the intervention was identified as accounting for the greatest increase in registrants, increasing from 444 in the year prior to 5588 in the post-campaign year. Overall, the combined effect of the intervention components increased donation by 700%.
Conclusions
-
This is the first systematic review of evaluated interventions to increase organ donor registration and knowledge of organ donation among minority ethnic groups, and identified 18 evaluated intervention studies29,69–85 focusing on ethnic minorities that were educational in nature, delivered in community settings or disseminated through mass media. All but one study were conducted in the USA. 85 This draws attention to the neglect of formal evaluation of interventions in this area in the UK despite the considerable local engagement.
-
Limitations of the review include the heterogeneity of study populations, measures and outcome variables employed, and the frequent use of non-validated measures of knowledge. It is also notable that few studies explicitly mentioned an attempt to connect with the target population during the developmental phase to assess acceptability. The reporting of important contextual information relating to the interventions was also sparse.
-
Despite limitations of evaluative research in this area, detailed analysis of both process and outcomes identified guidance for increasing the acceptability and effectiveness of interventions.
-
There was some evidence that media interventions successfully addressed knowledge gaps and misconceptions about organ donation. However, community-based educational interventions exhibited a higher level of success in terms of verified registration than those solely reliant on the mass media.
-
Characteristics of community educational interventions that were successful in increasing registration were identified as having a strong interpersonal element that focused on the particular concerns of the target population; being delivered by appropriately trained lay individuals from their own community; and undertaken in familiar environments. These characteristics are likely to be of particular significance for people at a contemplation or pre-contemplation stage. For people at later stages of the donation pathway, the availability of immediate access to registration is likely to be of particular importance in increasing motivation to register.
-
Implications of the three community-based studies
This section considers the implications of the two systematic reviews and focus group study for policy and practice, and for further research.
Implications for policy and practice
-
Differences in knowledge and faith cultural beliefs among ethnic/faith and age groups present a complex pattern and requires that messages are tailored to particular groups and their stage on the donation pathway. Success for those at a pre-contemplation stage may initially involve just a shift along the registration pathway, with actual registration for these groups often requiring multiple interventions that reinforce and build on each other over a period of time. In contrast, people who are far along the pathway may require only a small ‘nudge’ or ‘prompt’ to register as an organ donor through interventions involving behavioural prompts, cues to action and, when possible, an immediate opportunity to register.
-
Educational interventions are generally more effective than mass media campaigns to address attitudes and develop and allow messages to be tailored to the populations’ specific concerns. Characteristics of effective interventions include personalised case studies and delivery by trained lay individuals or community representatives in familiar settings to ensure their acceptability and resonance with the beliefs and identities of community members.
-
Many focus group participants, particularly of Caribbean origin, wished to discuss organ donation and joining the ODR with a practice nurse or GP, whom they regarded as accessible, trusted and well-qualified sources of advice, and thought registration should also be available at general practices but there are no data on the feasibility and cost-effectiveness of such a primary care-based approach could be assessed.
-
Many people were uncertain whether or not they had ticked the relevant donation box on their driving licence, Boots Advantage Card or passport application and preferred having the traditional donor card as confirmation of having joined the ODR.
-
Targeting campaigns could be assisted by more complete recording of ethnicity in relation to registration as a donor, as only 18% of registrations now have ethnicity recorded.
Implications for research
-
To date there has been little emphasis in the UK on the evaluation of community campaigns to build up knowledge of the format and delivery of effective strategies.
-
The effective targeting of campaigns requires knowledge of the stage on the ‘donation pathway’ of different ethnic groups, and variations by age and ethnicity/culture. This could be facilitated through a large survey or by adding questions to existing national surveys.
-
A better understanding of the interaction of age, ethnicity and socioeconomic status on organ donor registration could be achieved through electronic surveys conducted among employees of all grades in large organisations such as the Civil Service or large companies.
Chapter 4 Hospital studies and consent to donation
Overview of studies
This phase moves the focus from registration as a donor to examining issues of family consent to donation among minority ethnic groups.
The research comprised two studies to examine the perceptions and practices of groups of staff who form major stakeholders in the organ donation process (SNODs, clinicians and bedside nurses) while a third study focused on the perceptions and experiences of bereaved families. The three studies are detailed below.
Study 1: interview and observational study
This ethnographic-style study involved observation, informal discussion and interviews with a range of staff at the five study sites (NHS trusts). We report here on three key themes:
-
theme 1: attitudes and practices of ICU staff in providing end-of-life care to minority ethnic groups
-
theme 2: SNODs’ role and participation in consent discussions
-
theme 3: hospital chaplains and end-of-life care.
Study 2: ethics discussion groups
These groups aimed to engage in-group discussion of donation-related issues with mixed groups of staff in NHS trusts to identify their shared practices and institutional philosophy, as well as points of conflict and collaboration.
Study 3: interviews with bereaved families
This study aimed to elicit perceptions of end-of-life care and the organ donation process among bereaved families from mixed and minority ethnic groups, and was conducted at home at least 3 months post bereavement.
The hospital-based research (studies 1 and 2) was undertaken in two regions with the greatest density of ethnic minorities in the UK, namely the London and the Midlands regions.
In the original application we stated that we would base the hospital fieldwork on four NHS hospital trusts, with these sites being selected to include larger ICUs, in which organ donation was expected to be a more frequent occurrence, and included a mix of different types of ICUs, to ensure that we would include both donation after DBD and DCD. However, during the initial fieldwork we became aware that, despite focusing our research on areas with large ethnic minority populations, there were only small numbers of patients from minority ethnic groups who were admitted to ICUs, possibly partly reflecting their younger age structure. We, therefore, added a fifth site located in an area with a large and mixed multiethnic population with appropriate ethics and R&D permissions. The five study sites each included general ICUs that cover a range of diagnoses, cardiothoracic ICUs at three sites and two sites had neurological ICUs specialising in conditions such as stroke and brain haemorrhage.
We initially visited each site to outline the DonaTE programme with senior staff [particularly clinical leads for organ donation (CLODs), SNODs and matrons] and discuss the data collection. Assistance was also requested in contacting ICU staff and members of the trust’s ODC on our behalf. Up to 2 weeks prior to data collection we contacted consultants and nursing staff with links with the organ donation process, together with all members of the Chaplaincy and ODC, to inform them about the research and invite their participation.
The second study, EDGs, required the inclusion of an additional site (sixth site) to complete the required 10 discussion groups.
The third study, interviews with bereaved families, also involved substantially expanded recruitment to a total of 40 trusts. This was necessary given that there were only 56 donors from black and minority ethnic families in 2012/13. 3
The next sections present the detailed methods and findings for individual studies.
Study 1: interview and observational study
Overall aims and methods
This study focused on how the needs of ethnic minority families are met and the particular issues that arise for bedside nurses, SNODs and hospital chaplains in providing end-of-life care for minority ethnic groups.
Data were collected across five study sites (ICUs at NHS hospital trusts), with two researchers (CK and SD) spending 3 weeks at each site between July and December 2010. Data collection involved semistructured interviews, observation of the work of SNODs and informal discussions.
Study sites
The study was based in the London region and the Midlands, with these regions selected because they have the greatest density of ethnic minorities in the UK. The study sites selected within these regions were ones with the larger ICU, where organ donation was expected to be a more frequent occurrence.
All study hospitals were teaching hospitals with on average 42 designated ICU beds (range 36–56). All the sites had general ICUs that cover a range of diagnoses (e.g. stroke, heart attack, head injuries, accidents) as well as a range of specialist ICUs; four sites had specialist cardiothoracic units and two had specialist neurological units for conditions such as stroke and brain haemorrhage, with other sites catering for neurological patients on general ICUs.
Data collection
This involved a mix of non-participant observation, semistructured interviews and informal discussions at five study sites.
The researchers observed the activities of the units in short time slots (approximately 30 minutes) by ‘hanging around’ nurses stations, which were usually positioned with a view to covering most of the unit, or watching from a short distance the work of one or two of the unit staff at the bedside. This assisted the researchers in becoming familiar with key issues and activities of the ICU.
The researchers also ‘shadowed’ SNODs over several hours when a potential donor was identified on the unit, and observed four requests for family consent to organ donation with the family’s permission. These family approaches were observed at three of the study sites. In just one instance, the approach for consent to donation was observed for a family from an ethnic minority group. This reflected the relatively small number of families approached for consent over a 3-week fieldwork period and particularly the small number of patients from minority ethnic groups on the ICUs. This is not surprising, given that only 237 eligible ethnic minority donors were approached about donation in the UK 2012/13. 3
Field notes were taken during observations or shortly after and contributed to the overall data set.
A series of topic guides were developed and covered five core areas for each group of staff, with additional questions applicable to a particular staff group. The core areas covered were:
-
broad overview of work and responsibilities
-
involvement in the organ donation process
-
communication with relatives regarding futility/withdrawal of treatment, end-of-life care and approach to organ donation
-
involvement with families of minority ethnic groups
-
views of the roles/practices of the SNOD/CLOD.
All participants were provided with an information sheet and gave written consent prior to interview. Interviews ranged from about 10 minutes to 2 hours and were tape recorded with permission. Interviews were conducted on ICUs, in offices or a side room, or occasionally in the hospital cafe.
We originally envisaged undertaking 40 semistructured interviews with hospital staff. In practice, we conducted 107 interviews, although interviews with bedside nurses were mainly quite short. This increased number of interviews partly arose from the addition of an extra study site; however, it also reflected a shift in the balance of data collection, with a smaller emphasis given to the observational element, as the number of potential donors was quite small during the 3 weeks spent at each study site. We also increased the number of chaplains interviewed, as they appeared to be an under-researched group with potential for an increased contribution in this area (see Study 1: theme 3 – hospital chaplains and end-of-life care) (Table 7).
| Hospital staff | Number interviewed |
|---|---|
| Consultants | 21 |
| CLODs | 7 |
| Nurses | 28 |
| SNODs | 7 |
| Chaplains | 19 |
| ODC members | 25 |
| Total respondents | 107 |
Analysis
Audio-recorded interviews were transcribed in full and transcript data were managed using NVivo version 9 software. Full transcripts were read and coded for themes and subthemes. These related to identifying potential donors, providing support to families and managing visitors with particular reference to minority ethnic groups, treatment withdrawal and the donation discussion, and the roles and relationships of different groups of staff in relation to the organ donation process.
Many issues identified by staff, such as difficulties that sometimes occur for families in understanding that their relative is dead and agreeing to withdrawal of treatment, occurred among all ethnic groups. However, the next sections focus on three themes that emerged as being of particular potential significance for family consent to donation among minority ethnic groups:
-
theme 1: attitudes and practices of ICU staff in providing end-of-life care to minority ethnic groups
-
theme 2: SNODs’ role and participation in consent discussions
-
theme 3: hospital chaplains and end-of-life care.
Study 1: theme 1 – attitudes and practices of intensive care unit staff in end-of-life care
Abstract
This theme focuses on the attitudes and practices of individual ICU staff (bedside nurses, SNODs and clinicians) in providing end-of-life care for minority ethnic groups. It focuses particularly on issues identified by staff as problematic, particularly cross-cultural communication, managing large families and visitors, responding to faith/cultural requests, the use of chaplaincy services and overcoming language difficulties. Some variations in the way practices addressed these issues were identified between sites, reflecting differences in facilities, priorities and individual preferences of the clinicians. It was also noted that some members of all staff groups acknowledged uncertainties about approaching families from different cultural groups, with junior nurses at each of the study sites most often describing feelings of hesitancy in approaching a different cultural group. They were also particularly positive about training to enhance their confidence and skills in this area.
Aims
This theme describes the practices employed in ICUs to meet faith or cultural needs and to manage large families and numbers of visitors in terms of both access to the bed space and involvement in discussions of treatment withdrawal. It also pays particular attention to bedside nurses’ perceptions of their own confidence and skills in communicating with different cultural groups.
Background
The successful redesign of donation services in most countries, including Spain and the USA, has involved the appointment of staff with specific responsibilities for organ donation, including discussing donation choices with families. In the UK, a workforce of SNODs were appointed following recommendation 9 made by the ODT:4
The current network of Donation and Transplant Co-ordinators (DTC’s) should be expanded and strengthened through central employment by a UK-wide Organ Donation Organisation. Additional co-ordinators, embedded within critical care areas, should be employed to ensure a comprehensive, highly skilled, specialised and robust service.
At the time of fieldwork, 250 SNODs were employed by NHSBT (the national organisation with responsibility for blood and organ donation). SNODs are mainly drawn from senior intensive care nurses and are embedded within hospital trusts, and are on-call for other ICUs in the same region. SNODs are regarded as providing ‘a comprehensive, highly skilled, specialist and robust service’, and have responsibilities that extend beyond those of the previous donor transplant co-ordinators. Their role involves overseeing the donation process, from identification of a potential donor to organising and managing donation, including offering organs to transplant centres and co-ordinating the retrieval process. They also provide early and continuing contact with families, collaborate in donation discussions and conduct the Potential Donor Audit (PDA) that records the number of patients who could be solid organ donors and identifies reasons for non-referral and non-consent.
The role of the SNOD in the UK is supported by CLODs, who are clinicians (generally intensivists) with a part-time responsibility as ‘champion’ for organ donation within a hospital trust. This involves an educational and facilitative role to achieve the goal of normalising organ donation so that it becomes usual practice within the trust.
Although SNODs and CLODs have special responsibility for organ donation, it is recognised that the collective and co-ordinated behaviour of the wider multidisciplinary team involved in caring for patients and families on ICUs, particularly the bedside nurses, is also of importance in promoting a culture of organ donation and ensuring appropriate communication and responses to the needs of different patient and family groups.
Methods
The analysis of practices undertaken in ICUs and responses to minority ethnic groups is based on interview and observational data as previously described (see Study 1: interview and observational study, Overall aims and methods).
Findings
This section discusses professional practices in supporting families of different ethnic, cultural and faith backgrounds and focuses on the themes of accommodating faith-based needs and requests, overcoming communication barriers and managing families at the bedside. These findings often provided examples of how staff met the needs of diverse patients and families despite having little formalised cultural competency training.
Accommodating faith-based needs and requests
Consultants, nurses and SNODs all mentioned the role of faith and religious beliefs in terms of end-of-life care, and offering faith or religious support appeared to be a well-established practice among all the hospital study sites. Consultants and SNODs would often broach the subject to families directly as part of standard practice at either admission or end of life, or both. In some ICUs there was also an end-of-life care form that asked whether spiritual needs had been addressed or not, or if the family had been offered chaplaincy support.
Staff at two study sites mentioned how even people who describe themselves as not being religious would take up hospital chaplaincy, especially during withdrawal of treatment:
Variably, I would say probably about 60 or 70% of people take it up. I mean even if the patient isn’t religious, if there’s any question, they go for it. Sometimes they’ll say, ‘Oh no, he didn’t believe in all that, so no thank you.’ But I would say about 50, 60% of people do take it up actually yes.
Consultant, site 2
Staff described families for whom faith was significant for himself or herself or the patient as often wanting the support of a faith leader to be reassured that their decision regarding withdrawal of treatment was compatible with their own religious belief system. In addition, such contact often took away feelings of guilt when they supported the clinician’s view regarding withdrawal of treatment.
In addition to families being offered the services of the hospital chaplaincy, it was observed that they often sought the support of their local faith leaders, with this being most common among families of Islamic faith and African Christians.
And most of the local Muslims, they will want their imam from their own mosque to come in, or they won’t want a stranger. And I think most, most mosques, they’re not like, it’s not like Church of England where, you know, they are sort of fairly similar – I think there’s a lot of differences, and it’s more about the local society . . .
Consultant, site 5
Many of the Nigerian African families bring their own pastors. And they wouldn’t want to see a hospital chaplaincy, because they would believe in different things, operate in a somewhat different angle.
Consultant, site 2
Faith and religious support was also seen as a resource for staff, as faith representatives could help the families understand the futility of further treatment and accept the withdrawal of treatment or clarify their faith’s position on organ donation. These representatives were viewed as figures of authority through their spiritual knowledge and were also described by SNODs as having the authority to say things to families that SNODs sometimes felt unable to.
Generally, staff only spoke of the chaplains’ support in terms of assisting in treatment withdrawal and end-of-life care, given that the hospital chaplaincy helped only to facilitate the organ donation request at one study hospital. At this site, the chaplains addressed the families’ religious concerns and assured them that helping other people in this way was not against their religion.
Aside from calling on chaplaincy support or their own faith representatives, staff recounted how some families would observe a range of faith practices at the bedside, including prayers and chanting. Where feasible, a side room was arranged to accommodate this. Other requirements, especially for Muslim and Jewish families, related to wanting a quick burial for faith or cultural reasons with this otherwise forming a barrier to organ donation. However, interviewees from different study sites observed that fulfilling this request was not always possible if they were going for donation, or if it is a coroners’ case or death occurs at the weekend. However, when possible, they fulfilled particular requests and regarded this as an important aspect of providing individualised and family-centred care.
Overcoming communication barriers
Practices varied across the study sites in the provision of interpreters when this was required. Interpreters mentioned ranged from professional interpreters supplied by the hospital (in person or over the telephone), to other members of hospital staff, family members and occasionally a faith leader.
Staff tended to first mention using professional interpreters because they were seen as reliable in delivering the correct information to families. However, the availability of interpreters depended on the timing and demands on the service.
In cases for which professional interpreters could not be present, LanguageLine (www.languageline.com) could be used; however, most felt that this option was not ideal for dealing with sensitive situations like end-of-life care. They, therefore, often preferred to use other staff as interpreters, especially as the study hospitals employed a diverse workforce that could be called on to interpret if necessary:
Yes. We have great access to many doctors and nurses in this trust who are from millions of different countries. So we can access people at short notice if we need to, if there’s a problem with an interpreter service. There’s a list actually, I don’t know about each hospital, but our hospital here has a list of languages spoken and where you can find those people and if they happen to be on duty at the time, they are always helpful to come and speak.
SNOD, site 1
One hospital site was more likely to use staff as interpreters before professional services. This was both because hospital staff were more readily available than professional services and to also overcome the cost issue:
You try and find someone within the service who will translate for you, before you start looking to translation services because there’s a cost implication there, which is not your primary concern, but it has to be – we all need to think about these things. If a service needs to be provided, if that’s the way to do it, then that’s the way to do it. But you look at other options first.
Nurse, site 4
At all the study sites, family members would be used if there were no other options available. However, at one site (site 3) family members were mentioned as being involved before other staff members, whereas at other sites staff described family members as being unreliable interpreters, with the general practice in their units being that they should be avoided if possible. A particular concern was that family members would often filter things and withhold information to ‘protect’ the patient or other family members. Family members were, therefore, described as:
often interpreting what they think that the family wants to hear as opposed to what you’re saying, so wherever possible I use interpreters, staff as a second line but only when there’s absolutely nobody then a family member but then try to use a family member who’s much more remote from the immediate family members, so (a) because I think it’s unfair on the family members and (b) as I say because we can never guarantee what we tell them is what they tell their family.
Consultant, site 5
Similarly, a preference for using non-family members was echoed on another site:
Yes, I like to use non-family members if I can, so if there’s somebody on shift that may be can liaise a little bit, then I will try and get them involved. I’m not saying that I don’t trust family members, but I have, I have experienced before family members keeping information from the husband or the wife of the person that’s died. I have experienced them actually keeping information from them. Trying to protect them, but yes they don’t always keep them fully informed.
Nurse, site 4
There were only two examples of a faith leader acting as interpreter and in both instances was an imam.
Managing large families and numbers of visitors
There was a general perception that minority ethnic patients would be likely to have large numbers of visitors. This was regarded as particularly true of patients and families from the Asian subcontinent, with a cultural expectation that members of the community would come to the ICU to pay their respects. Several staff referred to 40 or 50 people and even over 100 people sometimes waiting to visit the patient. However, it was unclear how often such large numbers of people were actually present and how far this differed from other families in close-knit communities.
Different ways of managing large family numbers were described so to minimise disruption to the ward. This usually involved allowing only two people at the bed space, with staff frequently working with families to identify who were their close family members. In some cases a password system was then used to restrict access:
But basically we just keep to the two people at the bed space, we set up passwords so that only certain members of the family can come through, because otherwise their cousins, uncles, brothers, wife, daughter comes. And that’s the, that’s how we can say, ‘Well actually you can’t come in, because you don’t know the password, so you’re not immediate family.’ And we often have to get security to clear the ramp and around here, because they say that the higher up in the community they are, means the more people who will come.
Nurse, site 5
A further key issue related to who should be involved in decision-making, which, in many cases, was viewed as not simply a matter for the next of kin. As a SNOD explained:
. . . what I will do is I will identify who the key players are, and the key players might not be, you know, for example, with an Asian family or a Sri Lankan family, it won’t necessarily be the wife, but it will be male members of the family. You know, with the female members, particularly with some of the ethnic minority backgrounds, is very, very much kind of more emotionally related, you know, and ensuring that they’re prepared for the conversation. You know, ‘Is this a conversation you want to hear? It’s going to be distressing, please be prepared.’ You know, and for some of them, and it’s almost kind of guiding them not to be there. You know, ‘There will be decisions that need to be made, are you the person that’s going to make that decision?’ ‘No I’m not.’ ‘OK, well can you tell me who is?’
SNOD, site 5
However, ICU staff differed in their views of the numbers of people who should be involved in communication about futility and withdrawal of treatment or organ donation. Some staff felt that the more people involved in decision-making, the more room there was for disagreement, especially on the topic of organ donation, and so favoured smaller numbers of people being involved. As a SNOD explained:
The less people that you approach about organ donation, the better, because the less people are going to stick their oar in and have their, you know.
SNOD, site 1
Staff also wanted to keep family numbers smaller owing to space restrictions of waiting rooms:
And we do, we are very good here that we will limit it, and I mean you’ve seen the size of that room, it’s tiny. So we will only realistically have a maximum of six people. So we can minimise it through physical space. And we’ll do it that way. But yes we do try, but we do it . . .
SNOD, site 5
Another reason to limit the number of people was given because of different, and often more vocal, forms of emotional expression.
The problems in my experience, tend to come when you get a large group of people and then that’s when the sort of more extreme reactions can come out of that sort of – but generally trying to keep that group fairly small, to try and stop that – so you haven’t got someone wailing in each of the four corners of the room, then you can’t talk properly, you can’t get them to concentrate on what you’re trying to tell them . . . On one occasion I think there was certainly some extreme reactions from mostly the – like the female members of the extended family.
Nurse, site 3
Similarly, a CLOD observed:
Well, you know, one of my reasons for limiting the number of people in the room when I break bad news, is the deafening wailing that – you know, as long as you’re expecting it, that’s fine. I must admit I’ve learnt the hard way to make sure everyone is sitting down, because I have had a few people throw themselves on the floor . . . I think in some ways I think it’s far more healthy having a good loud release of emotions, than the Caucasian upper lip, you know, ‘Oh I’m sorry, I shed a tear doctor, how uncouth of me’! But, you know, ‘for God’s sake, it’s your husband that’s died, you’re allowed to wail a bit if you want.’ But no, I mean the only startling thing is, is that the amount of noise that sometimes is generated – I was going to disparagingly say, histrionics, but that’s not quite right, but the, you know the fainting and throwing to the ground that goes along with it sometimes. But again if you’re expecting that, it doesn’t take you by surprise, but I think, you know, I remember as a registrar, the first time I heard that, I was horrified and I was shouting for help.
CLOD, site 3
Whereas most staff sought to limit the number of family involved in discussion, a few favoured getting all close family members together for discussions about end of life. This was because they felt that restricting numbers may cause more problems later on when information was relayed to other members of the family.
I would say to the family that they need to bring in all the family members that they feel need to be present for a very important discussion about their relative . . . You have to allow the family that chance, that would be my view. Because you’re only storing up problems for yourself, because you – if you make the family prioritise family members for that conversation, you’re automatically making the family argue amongst themselves, but usually you can tell who the spokespeople are, very quickly.
Consultant, site 5
A consultant at another site explained:
Usually we try to get all of the close family together and just have a conversation once, because sometimes the families can be large and there will be people who take slightly different views or maybe have different questions and different issues they want to raise.
Consultant, site 2
However, problems of the limited space and facilities to accommodate large numbers of people were noted, especially in older hospitals where side rooms and family rooms are generally quite small.
Nurses’ perception of cross-cultural communication
Only one of 28 bedside nurses interviewed mentioned having received training relating to cross-cultural communication. Not surprisingly, given the lack of formal training and often limited experience of patients from minority ethnic groups, the nurses often felt it was difficult to approach families from a different ethnic group unless they had developed on-the-job experience of this. As one nurse explained:
I’m worked in London for, what, 6 years now. I’m not that familiar with different races, I come from the middle of the country where there’s farmer Giles and all the blooming same, you know. And to me it’s a fascinating world and I just, I just love being involved with the families. You just learn so much from it. To me it’s a whole life experience, not just a nursing experience. But equally, if I don’t understand that family very well I’d find it very difficult to, to go in and approach them.
Nurse site 2
The lack of formal training and experience meant that ICU staff often drew on social constructions of people from minority ethnic and faith groups different from their own. For some, a lack of contact and experience in supporting patients and families from minority ethnic groups meant that they were constructed as ‘other’. For example, following an informal discussion with a bedside nurse, the following field note was recorded:
In relation to what the participant (bedside nurse) terms ‘ethnics’ the family members of sick and dying patients on the unit were seen to be a serious problem, causing disruption to the unit and overcrowding the waiting room. She described these people as tending to have more than two kids and so it can mean too many family members would want to see the patient, causing disruption to the unit and overcrowding the waiting room.
Site 4, field note
There was also a view that people of Asian origin and the African Caribbean population may often not be approached for donation as they were seen as less likely to donate: ‘I think, because there’s a lot of experience of donation not being quite so favoured with the two ethnic groups (Asian and African–Caribbean). And it is probably a massive stereotype, because there are some from both groups that do.’ She went on to note that ‘there were also quite often quite a lot of real language barriers sometimes with some of the Muslim families that make it even more difficult’ (nurse 19, site 3).
However, experience of working with different families meant staff understandings often shifted from a more general view of ethnic groups to recognising the heterogeneity and individual variations within groups, as this nurse explained:
And I think that often the cultural things, it involves a little bit of working with the families as well and realising the families themselves have their own culture within them, and they may not go down the textbook route that this is what a Muslim family does and this is what a Christian family does and this is what a Buddhist family does. And trying to have the ability to be mature enough and confident enough that we can let that family take it the way they want it to go, as long as it meets within the law. I think that’s the bit that takes a bit more experience perhaps.
Nurse, site 2
Of those specifically asked about cultural competency training, most felt that it would be welcomed and that it would benefit the ICUs by preventing (unintentional) situations of insensitive care before they could occur. An example was described by a SNOD:
Well you see here on this unit, we don’t receive or not we don’t, the nurses don’t receive ethnicity and diversity training. We have a Muslim lady who had come back from theatre, and they won’t cover their head. And, you know, because they’ve had a brain operation, now OK fair enough that you have to take the head covering off, but, you know, it is reasonable that at some point, when they’re back, that actually you can make some attempt to cover up the person’s head. Now when that person starts to wake up and have their tubes out, they’ll be absolutely mortified to think that how long have they been like that. And nobody’s, and they’ll – and I’ve seen them grab, you know, like take pillowcases off the bed and try to cover themselves up. And the nurses are just oblivious to what’s going on and you think, ‘Bloody hell,’ you know. Just – and I don’t know, I mean I think that, that’s probably, you know, from a hospital perspective, something that we need to, you know, we need to look at. You know, how do our nurses deal with these patients?
SNOD, site 1
Conclusions
-
There is a lack of formal training in what is termed ‘cultural competency’, with individuals mainly relying on their ‘on-the-job’ experience to respond to people’s faith and culture in the provision of end-of-life care. However, junior nurses often had less experience, sometimes leading to what has been described as a ‘disabling hesitancy’ and inertia in their practice, particularly in situations where families are experiencing considerable emotional distress. 89 They thus welcomed training to increase their confidence in supporting families from minority ethnic groups and reduce stereotypical views.
-
Key aspects of care that were often regarded as problematic, and particularly in relation to minority ethnic groups, were managing large families and visitors in terms both of patient access and communication by clinicians, responding to language barriers and accommodating faith-based practices.
-
Variations in practices in terms of responding to the needs of ethnic/faith groups were often influenced by the hospital facilities and capacity as well as by established organisational practice and cost constraints. For example, the use of interpreters varied, with some hospitals more likely to use professional services, whereas some rely on staff first because of availability or cost, and others may use families because there is established precedent to do so. Similarly, being able to accommodate large family groups is influenced by the availability of side rooms off the main ICU ward and the size of family rooms. There were also differences between clinicians in their preferred practices, including their ways of managing large families, with some preferring to include a large family group so that all received information directly while others preferred a small group of close relatives.
-
It was common to offer chaplaincy services for withdrawal of treatment and formed an important example of how hospital staff aimed to meet the needs of people from different faith backgrounds. However, when feasible, staff also aimed to respond to particular requests that might be made by any families, reflecting the importance of achieving individualised care. Examples included families wishing to pray around the bed and requests for pieces of jewellery or other mementoes to be placed alongside the dying patient.
Study 1: theme 2 – specialist nurses for organ donation’s role in relation to families and the consent discussion
Abstract
The establishment of SNODs was a key aspect of service redesign that was introduced following the ODT report. Although SNODs receive specialist training in communication skills and aim to provide long contact with families, there is evidence that a significant number of donation requests continue to be undertaken by the clinician alone. This theme, therefore, examined the reasons for the lack of full implementation of the SNODs’ role and focused on both clinicians’ views and responses to the introduction of SNODs whose remit partially overlaps with the medical jurisdiction and the strategies employed by SNODs to embed their role within ICUs. This identified considerable variation in the degree of acceptance of SNODs and examines the varying personal, clinical and organisational factors that have led to the slow adoption of early referral to SNODs of potential donors and their participation in collaborative consent discussions.
Aims
To examine the SNODs’ role in relation to families including the constraints on early referral of a potential donor to SNODs and their opportunity to collaborate in donation discussions with families.
Background
Consultants were traditionally responsible for assessing patients’ suitability for donation and undertaking the donation discussion with families. However, it is now expected that the SNOD will participate in these activities. This involves being informed when brain stem testing for neurological death of a patient is planned or the futility of further treatment has been discussed with a patient’s next of kin. 4 The SNOD then checks the patients’ clinical suitability for donation and whether or not a patient is registered as a donor by consulting the ODR to which only the SNOD has access. Second, discussion of the possibility of organ donation with bereaved families was recommended by the ODT as ideally involving ‘collaboration’ between the consultant and SNOD, with this subsequently endorsed by the National Institute for Health and Care Excellence (NICE) guidelines, with the expectation that both the SNOD and the consultant would contribute and be present throughout the donation discussion. 89 Collaborative requesting has also been affirmed in local donation policies at trust level.
The routinely collected data support the positive effects of the involvement of SNODs, indicating that the consent rate is higher when a SNOD has been involved in a collaborative donation discussion with families than when this discussion is undertaken by the consultant alone. For example, in 2012/13, the consent rate was 65.8% when a SNOD was involved, compared with 36.7% when there was no SNOD involvement. 3 The difference was greatest for DCD donation. For example, in 2012/13, SNODs were involved in 71.3% of approaches, with this made up of 78.9% of DBD discussions and 66.7% of DCD consent discussions, reflecting a slight increase in involvement from earlier years. 3 However, as these figures indicate, a significant proportion of donation discussions continue to be undertaken by the clinician alone, although involvement of SNODs increased from 59.6% in 2010/11 to 71.3% in 2012/13.
The role of the SNOD impinges on the traditional medical jurisdiction, at least at its boundaries, and requires clinicians’ acceptance of the shift in responsibilities. However, consultants’ responses to this have not previously been explored.
Methods
This theme draws on the interview and observational data described in Study 1: theme 3 – hospital chaplains and end-of-life care.
Findings
The interviews indicated that all consultants welcomed the SNODs’ involvement in the administrative and nursing aspects of organ donation, including their role in organising the retrieval and offering process. However, they varied in their acceptance of those aspects of the SNODs’ role at the boundaries of their traditional medical jurisdiction. Views on this varied both within and between ICUs. This was reflected in differences in clinicians’ willingness to notify the SNOD of potential donors and to allow SNODs to participate in a collaborative donation discussion.
We distinguished three groups of consultants in terms of their response to SNODs and willingness to refer potential donors to the SNOD and engage in a collaborative consent discussion.
Acceptors
This refers to the group of ICU consultants who described how they worked with SNODs collaboratively, with this collaboration occurring whether the SNOD was embedded (i.e. based in the particular ICU) or attending the ICU on an on-call basis. They were happy for the SNODs to be around the unit and for nurses to refer potential donors to the SNOD, and described talking informally with the SNODs about patients who might undergo brain stem death tests. This group also recognised and valued the SNODs’ particular skills in supporting families and discussing choices regarding organ donation. This view is illustrated by a consultant who commented:
Yes I think it’s [SNOD] an essential role. I don’t see how the process could work without them. And they’ve got specialist knowledge that we don’t have, and they can stand independently away from the caring team, and only come on line, you know, in collaboration with us. And their role is clearly prescribed, yes, an essential role, essential role.
Consultant, site 4
These consultants thus appeared to have reached a point where they had come to trust the SNODs’ expertise:
And it’s interesting looking at 2 years of data that there’s some consultants of 2 years ago who were not doing collaborative [approaches], but now they’re doing all their approaches as collaborative. So it is a step-wise progression. I think it is just gaining that trust and knowing that, you know, the person you’re taking into the room for this difficult discussion, is going to be on the same page really.
CLOD, site 3
How a ‘collaborative’ approach actually worked in practice, however, varied between consultants, reflecting a situation in which although collaborative requesting is identified as an ideal model its precise form is not fully specified and is, therefore, open to local interpretation and negotiation. Collaborative requesting sometimes took the form of a ‘decoupled’ approach, whereby the consultant broke the bad news to kin, and explained the medical situation and futility, and the SNOD then approached the family to discuss consent for organ donation. Another model was for consultants and SNODs to work together in what might be viewed as a ‘fully collaborative’ approach, with consultants often describing how they drew on the SNODs’ experience to decide when to raise the topic of organ donation or decided between them how they would approach a particular family.
Resistors
This describes a diametrically opposed group and consisted of those consultants who rejected and vigorously resisted the central role of the new professional group of SNODs. When a request for donation was made to the next of kin these consultants were unlikely to allow the SNOD to be in the room at the time. Others sanctioned the SNODs’ presence, although the SNOD was not permitted to make any contribution to the discussion. The SNODs’ involvement in this situation was, therefore, mainly limited to checking to see if the patient was registered as a donor, and if consent was obtained they took formal written consent from the next of kin and organised the retrieval process.
The consultants we categorised as ‘resistors’ generally acknowledged the need for improvements in the system but regarded this as best achieved through the intensivists rather than SNODs:
So you need to give the responsibility for that to the people who have the power to deliver it. And that’s the intensivist.
Consultant, site 3
These consultants also viewed themselves as personally responsible for deciding whether or not, in their professional opinion, it was appropriate to ask the next of kin about organ donation, rather than accepting the current requirement and referring all potentially suitable patients. In particular, they emphasised that they sometimes regarded referral as inappropriate if they thought families had ‘been through enough already’ or were not likely to consent. They were also strongly resistant to the need to refer patients who they regarded as clearly clinically unsuitable for donation, despite the possibility that such patients might have at least one organ suitable for transplantation.
Other reasons given by consultants for resisting SNODs’ involvement was that they regarded themselves as best placed to discuss organ donation choices with kin. They explained that as they had already developed a rapport with the next of kin this made it more appropriate to undertake the consent discussion themselves and regarded this as preferable to introducing a stranger (the SNOD) at a time of acute grief. This view was often linked with feelings of their own personal responsibility to the patient and its extension to their next of kin:
I may be a bit old fashioned, but I still think that my duty is to the patient, and the relatives must see me as acting on behalf of the patient, not on behalf of getting organs for someone else, even though we all believe in that . . . I don’t like the idea of a transplant co-ordinator coming in and sort of hovering around the place, as we’ve occasionally had, when the patient isn’t yet formally dead.
Consultant, site 2
Although ‘resistors’ occurred across all types of ICU, there were particular issues for consultants who worked in general and cardiothoracic ICUs and thus cared for patients who could be potential donors after circulatory death. For these patients, judgements of suitability were more uncertain given the patients’ greater age and often multiple morbidities, and consultants often described how they were keen to do everything possible for the patient both for the benefit of the next of kin and to avoid litigation, even if this meant continuing drug treatments that would ultimately make the patient unsuitable for donation. Clinicians’ concerns regarding the patients’ suitability for donation and issues of the timing of withdrawal, therefore, related particularly to DCDs, and especially controlled DCDs. This involves organ retrieval following the planned limitation or withdrawal of cardiorespiratory treatments at the end of a critical illness from which a person will not recover and thus differs from the less problematic situation of uncontrolled DCD, which occurs when patients are not successfully resuscitated from cardiac arrest. The early involvement of the SNOD was, therefore, regarded as unhelpful in this situation and led to resistance to the SNODs’ completion of the PDA, which records reasons why a potential donation did not occur.
Controlled DCD has recently been subject to a number of guidance documents,90,91 including the recent policy document, Taking Organ Transplantation Towards 2020. 15 The UK Donation Ethics Committee (UKDEC)92 has also considered ethical questions that relate to how death is diagnosed, how decisions are made about end-of-life care and organ donation, and conflicts of interest between the donor and potential recipient. Recommendations have been put forward for nationally agreed protocols, including guidance for the withdrawal of life-sustaining treatment together with a scoring system to help predict the likelihood of death within a given time period so as to identify patients who would not be suitable for DCD. Such guidance may increase clarity and reduce the tensions and resistance that can occur in managing these patients and assessing suitability for donation.
Intermediate responses
This group of consultants was probably often in a transitional situation. They still retained authority over the whole donation process but were prepared to release a limited amount of ‘turf’ to the SNODs as their suspicions and uncertainties in the SNODs began to wane:
But I guess there was a little bit of resistance, because we felt to a degree that we were being spied upon or somebody was there to audit what we were doing and they’re just sat in that office next door. Now it certainly hasn’t turned out like that and I don’t feel that we’re being sort of observed. And I think that’s a good positive reflection on the transplant coordinators and the personalities, the personnel and personalities involved.
Consultant, site 4
These consultants recognised a partial contribution that SNODs can make to the process and thus permitted limited involvement. For example, when they identified a patient as a potential donor requiring brain stem testing, they often asked the SNOD to begin to check the patient’s suitability and whether or not they were on the ODR. However, whether or not this led to the SNODs having contact with the next of kin or being part of a collaborative approach to discussing organ donation was less certain and often depended on the consultants’ professional trust in the individual SNOD. Nevertheless, these consultants acknowledged some aspects of the SNODs’ role and the value that they may have in providing support for the next of kin:
[the SNOD] has made the whole process easier and they do offer some family counselling and support which is also very useful.
Consultant, site 3
At times this ‘intermediate’ group of consultants acknowledged that there were aspects of breaking bad news to the next of kin and proceeding to ask about organ donation that they found uncomfortable and suggested that this could be addressed by leaving the consultant to break the bad news and then handing over to the SNOD to raise the issue of organ donation, thus essentially considering a decoupled approach. As one consultant (site 5) noted, ‘I do quite like the idea of separating the two things. You know, a different person asking.’ However, the same consultant was hesitant about letting ‘any SNOD’ take on this role because of what they perceived as inconsistencies between individual SNODs’ interactions with the next of kin.
These consultants were, therefore, generally willing to ‘trial’ a SNOD, or more specifically an aspect of their skills set, and when they had previously worked with a SNOD and valued an aspect of their contribution were willing to build on this experience and allow the SNOD further involvement. The consultants’ trust was thus initially in the individual rather than the profession. However, it took time for these working relationships to develop in view of the mix of staff, shift patterns and organ donations being relatively unusual events. It was, therefore, often quite a time before the same consultant and SNOD worked together again, which may have contributed to the slow pace of change. Moreover, when this was not a successful experience for the consultant they would often then limit the role of the specific or any SNOD in future potential donations.
Explaining variations in clinicians’ responses
Each of the three types of responses occurred at each site and were also observed to occur within each ICU. More generally our analysis suggests that variations in consultants’ views and practices were influenced by a mix of personal, clinical and contextual factors, with these factors often interacting to produce a slow pace of change in what was a relatively infrequent event for individual consultants.
Personal characteristics of clinicians
Across the sites it was acknowledged that it was often, but not always, the very senior (older) and influential consultants who were the most resistant to changing their practices relating to organ donation and were sceptical about the significance of the role that the SNOD could play in the process. Many of these consultants also felt less comfortable personally with organ donation and in their communication on this topic, and for these reasons were often less willing to involve a SNOD.
Willingness to refer and engage in a collaborative discussion was also influenced by whether or not consultants knew the SNOD and their perceptions of the personality and experience of the SNOD. Many of the initial group of SNODs had previously worked as a fairly senior intensive care nurse on the ICU, although this situation has changed as new SNODs have been appointed.
Culture of intensive care units
Differences in the culture of donation between units often appeared to be influenced by the leadership provided by the CLOD. Some CLODs were very committed and active in their role of educating and normalising donation and formed true ‘champions’, whereas others had not necessarily sought the position of CLOD and were less enthusiastic, committed and active in this role.
Type of donation
Other differences occurred between the neurological ICUs, in which brain stem testing provides a clear time of death for the patient, and a general or cardiothoracic ICU in which decisions regarding the timing of withdrawal of treatment and the interventions facilitating DCDs are often more difficult. Many concerns regarding DCDs raised by consultants in our study are currently being addressed with the aim of achieving a professional consensus on the ethical and legal issues relating to DCDs and developing agreed standards of practice together with protocols for local implementation. These developments may, therefore, have a key influence in facilitating change.
Responses by specialist nurses for organ donation
The SNODs were aware that consultants had the power to limit their claims to practice and of the varying responses of individual consultants. They also recognised that given the considerable autonomy of consultants in the NHS there was often little opportunity to achieve full engagement in their role through formal channels. SNODs, therefore, often relied on informal strategies to shift boundaries in their favour and as a way of ‘getting things accomplished’.
The informal strategies employed by SNODs included a range of non-verbal and positioning approaches to make their presence visible to ICU staff; this involved walking through the unit and talking to the bedside nurses and the clinical staff to make their presence felt and increase their opportunities for inclusion. They also valued having desk space on or close to the ICU to increase their visibility and accessibility, and sometimes used visibility strategically in situations when there was a potential donor on the ICU but they knew that the particular consultant might not automatically include a SNOD. In this situation:
we’ll be more visible. And we will have more discussions with them, just to make them aware that we actually here.
SNOD, site 5
The SNODs also often attended handovers as a way of enhancing their visibility and knowing if any patients were likely to be brain stem tested and whether or not organ donation would be considered.
The SNODs’ visibility and accessibility and their contact with other ICU staff sometimes led to ‘strategic alliances’, which were particularly valuable when ICU consultants were reluctant to refer a patient or to consider organ donation. In these circumstances a member of ICU staff, such as a bedside nurse or the nurse in charge, might informally inform the SNOD about a particular patient and the SNOD could then investigate further and talk to the consultant about the patient.
Negotiated approaches by SNODs sometimes benefited from support of the CLOD, who could use their peer-to-peer negotiations with their clinical colleagues to endorse the value of the SNOD and provide them with an entry point. For example, a CLOD described the value of ‘opportunistic chats’ with his consultant colleagues and explained that it was then up to the SNOD to take this forward and make further progress.
Conclusions
-
Implementation of the SNODs’ full role in relation to families is only gradually being achieved. This reflects a situation in which acceptance of the SNODs’ activity in areas that were traditionally within the medical jurisdiction varies between individual consultants with the lack of a fully ‘collective acceptance’ that is ICU or trust wide. There are also marked regional variations. Figures for 2012/13 indicated that collaborative involvement of SNODs in donation discussions varied from a high of 80.4% in South Central (London area) to a low of 40.5% in the South West. 3
-
None of the trust sites reflected a linear development of the SNODs’ involvement for the ICU as a whole. Instead clinicians categorised as ‘acceptors’, ’intermediate’ and ‘resistors’ appeared to occur concurrently on an ICU. This reflects a more general finding of the varying speed of uptake of innovations, which is influenced by the interests of consultants and other health professionals interacting with the organisational and cultural context. 93
-
Factors identified as contributing to lack of acceptance of the SNODs’ full involvement with families and their collaboration in consent discussions included the beliefs of clinicians in their personal competence in communicating with families; their experience of working with individual SNODs; perceptions of their own responsibilities to families; and the clinical and ethical issues surrounding controlled DCDs. There were also often perceptions of a conflict between the SNODs’ interests and role in conducting the PDA and what clinicians viewed as best practices for patients undergoing planned limitation or withdrawal of cardiorespiratory treatments.
-
Evidence that consent rates are higher when the donation discussion is collaborative indicates that increasing the proportion of family discussions conducted collaboratively would have a major impact on family consent rates.
Study 1: theme 3 – hospital chaplains and end-of-life care
Abstract
Hospital chaplains from different faith groups were interviewed as forming part of the multidisciplinary ICU team. Given the limited knowledge regarding the role of the hospital chaplains, we examined how they viewed their role in supporting patients and families from different faith groups. This identified the importance of generic chaplaincy work, offering spiritual support to patients and families in terms that are not informed by religion. All saw themselves as making a contribution to end-of-life care and most were supportive of deceased donation but had limited knowledge of its processes and practices. Scope was identified for greater involvement of hospital chaplains both within the hospital setting and in the community, with appropriate training and contractual requirements.
Aims
To explore the perceptions and practices of a diverse sample of hospital chaplains regarding end-of-life care and organ donation.
Background
NHS chaplaincy is emerging as an allied health profession that covers a range of religions and spiritual orientations. Hospital chaplains aspire to be relevant to the whole population of health-care users and have a potentially important contribution in supporting patients and families at the end of life as part of the multidisciplinary team. 94,95
Hospital chaplaincy teams in major British cities involve chaplains from different religious backgrounds and spiritual practices to reflect the local population, working in part-time and full-time capacities, both as volunteers and on a salaried basis. As with other allied health professions, NHS chaplains’ work is described and managed in secular rationalist and humane terms, without reference to religious doctrine.
In principle, a chaplain from any faith background can become the lead chaplain with responsibility for managing the chaplaincy team. In practice, it is likely that lead chaplains will continue to be from Christian traditions for the immediate future since salaried chaplains from minority faiths are recent and currently often part-time appointments.
Research from the USA suggests that the chaplains’ role in supporting patients’ decision-making around end-of-life care makes a measurable difference to outcomes. 96 It may also be expected that the chaplains’ role may, for some, influence donation decisions.
At a national level, all religious groups in the UK provide support for organ donation. 4 In contrast, a study of religious leaders identified some variations in individual’s views of the acceptability of deceased donation. 97 However, little is known about the views and practices of hospital chaplains from different faith groups.
Our research included chaplains as part of the broader category of ICU staff involved in the process of deceased organ donation. The key role that chaplains can play was emergent during our research and they were therefore analysed as a separate group. We were some way from reaching data saturation with these interviews, which limited the comparisons possible between faith leaders. Nevertheless, the data contributes to the very small literature in this area (for published paper from these data see Bradby et al. 98) and identifies hospital chaplains as a potentially important resource whose role could be expanded.
Methods
Semistructured interviews were held with 19 chaplains across five hospital trusts as part of the larger study of the study hospitals.
Recruitment
Interviews were sought via the lead chaplain at each of the five hospital trusts. The lead chaplains then contacted other chaplains in person or via e-mail to extend the invitation to be interviewed. Of those who were not interviewed and when reasons were given, these were a lack of time particularly for those in part-time employment; a lack of interest in or knowledge of organ donation; and a perception that the topic was not relevant to their role.
Interviews
Every participant received a study information sheet and signed a consent form. The interviews were semistructured and covered the following topics: the role of the hospital chaplain, involvement in ICU; expected death/funeral practices of the faith; the faith’s views towards deceased organ donation; their involvement in the organ donation process and experience of supporting the next of kin at this time; whether or not they felt equipped to support the next of kin in these circumstances; if they had any links with SNODs or the CLOD; their view of the priority given to organ donation within the trust; any further involvement they would like; and their personal views towards organ donation.
Most of the interviews were conducted in the relevant hospital’s chaplaincy offices and were audio-recorded with permission. One interview was conducted in an intensive care ward room. One chaplain declined to be recorded and written notes were made, and one chaplain was interviewed on the telephone. The interviews ranged in length from 20 minutes to nearly 2 hours.
Findings
Characteristics of the sample
The 19 chaplains interviewed were drawn from a range of faiths, and comprised both men and women and those employed both part and full time, with length of service ranging from 2 months to over 20 years (Table 8). Of the eight Christian chaplains, three were lead or senior chaplain.
| Faith | Number interviewed | Number declined |
|---|---|---|
| Anglican | 2 | 4 |
| Methodist | – | 1 |
| Roman Catholic | 4 | 1 |
| Free Church | 2 | 1 |
| Jewish | 2 | – |
| Buddhist | 2 | – |
| Islamic | 6 | 1 |
| Hindu | 1 | 1 |
| Sikh | – | 1 |
| All faiths | 19 | 10 |
Chaplaincy work
The idea of generic chaplaincy work in terms of offering spiritual support to patients and their families in terms that are not informed by religion was a feature of Hindu, Muslim and Anglican chaplains’ work. This reflected a situation in which patients often did not want to talk about religion at all but needed support and a ‘general chat’ and to have their ‘spirits lifted’. As a Muslim chaplain (respondent 4) explained:
We’re not actually there to quote Islam on to them. 50% of the patients I see, they don’t talk about religion . . . We’re more there for comforting. We’re not there for bringing any religion for them.
Chaplains from minority faiths frequently reflected on how their own work did not necessarily follow the patterns established by Christian chaplains. For example, whereas Anglican, Catholic and Jewish chaplains may be attached to a particular church or synagogue, imams do not belong to a specific mosque although they may attend prayers at a particular mosque. However, it is the teacher they follow which is of more significance in defining their religious practice. An imam also does not have a specific pastoral responsibility to visit Muslims who pray at the same mosque and Muslim patients, therefore, rarely asked for a local imam to attend a patient’s bedside, nor did they necessarily request a chaplain.
As the idea of chaplaincy as a source of spiritual support in hospital is novel for Muslims, Hindus and Buddhists, chaplains from these faiths explained that ideas are still developing as to how chaplains can best serve patients from their own religious background.
Chaplains and end-of-life care
Chaplains from all religious groups represented in this study saw themselves as making contributions to end-of-life care. This partly consisted of providing support for the family and kin by being able ‘to have a different kind of conversation’ around death, to listen and to comfort. They also acted as the intermediary between the family and hospital staff in terms of resolving clashes between patients and medical staff, accompanying patients to difficult meetings with clinicians, and enabling patients to have difficult conversations by offering explanations in lay terms and/or in an appropriate minority language. This was described as providing ‘a moral voice’ to pose questions in the patient’s interests. As a Roman Catholic chaplain (respondent 15) explained:
I sometimes raise questions that families have raised to me. So in that circumstance, I’m almost a little bit of a voice, like for the families, for the parents. You know, sometimes also, you know a bit of a moral voice, you know to raise a question mark when I think it needs to be raised.
Chaplains reported that clinical staff were sometimes grateful for their presence when discussing the withdrawal of treatment with a family and noted instances of supportive co-operation with clinical colleagues at such times. As an Anglican lead chaplain (respondent 17) explained:
We’re here obviously with a religious hat on. We’re also working within the NHS, working within the institution. So we’re working in a multidisciplinary context. We have to support our colleagues.
Although communication during end-of-life care was important across the different religions represented by chaplains, the specifics of patients’ expectations around the time of death brought out key differences. For three Catholic chaplains and one Pentecostalist chaplain, a key part of their role was to offer the sacrament and anoint a patient with oil prior to an operation. This could be done only by an ordained priest and was described as taking significant time. Prayers said for the dying and the dead in Islamic, Jewish, Sikh and Hindu traditions can be recited by any believer, with no particular call for a learned or scholarly person. Thus, although Muslim and Jewish chaplains would not be called to a dying patient with the urgency that applies for Pentecostalist and Catholic patients, they nonetheless saw discussions with patients and their families about end-of-life care as part of their remit.
Organ donation: perceptions and practices
Chaplains, with a couple of exceptions were, in principle, supportive of efforts to increase awareness of the issues around deceased organ donation within their own hospital. Support for this was typically couched in terms of donation being ethically sound and death not being hastened by the process. However, only three chaplains interviewed knew the SNOD in their hospital, and these three were all members of the ODC, all were Christian, all ordained and all senior (senior Catholic chaplain, lead Anglican chaplain, a Canon). In contrast, the other chaplains were not aware that a SNOD’s role existed in their hospital and had very limited knowledge regarding the process and practices of organ donation. This limited knowledge is doubtless explained in some measure by the very limited active engagement that CLODs and SNODs had with minority chaplains because of their clinical focus.
In contrast to a general acceptance of the principle of organ donation, a chaplain who was also a Catholic priest (respondent 19) reported that he would advise patients against deceased organ donation. He reasoned that one could never be sure that the act of removing an organ had not hastened the donor’s death. He felt that a Catholic could ‘legitimately accept an organ because, at the time when it’s being given to them, it’s already there’, although there was no religious duty to accept a donated organ.
A Muslim chaplain (respondent 4) said that he felt deceased donation was unacceptable both in religious terms and to him personally. This chaplain had not been involved in discussions about organ donation with patients and, like other chaplains, he emphasised that if asked to advise he would describe what he saw as the relevant religious rulings and leave the decision-making to the family. The other Muslim chaplains all expressed doubts about deceased organ donation in more equivocal terms, weighing up the pros and cons and unable to adopt a definitive position for or against.
In considering whether or not organ donation could ever be acceptable, Catholic and Muslim chaplains discussed whether or not the religious exhortation against the mutilation of bodies could be outweighed by the greater purpose of saving a person’s life. While a Catholic chaplain said that seeing people dying while waiting for organs to become available had persuaded him to support organ donation, like other pro-donation chaplains, he was very specific about the conditions that made donation acceptable. For Muslim chaplains, the Islamic principle of respecting and preserving human life, while important, could not tip their views towards outright and unqualified support for deceased organ transplantation because of the principles of modesty and respect for the dying body.
Development of hospital chaplains’ role relating to organ donation
Clinical staff sometimes called on chaplains to speak with a family about allowing the withdrawal of treatment; this led to some concern about being too closely associated with clinicians in the context of deceased organ donation as chaplains did not wish to be seen as overtly promoting organ donation. An Anglican chaplain, who was himself registered as an organ donor, said he did not want to be seen as yet another team member who was setting out to persuade families in favour of donation and cited a family, in shock about their daughter’s imminent death, who had felt that the donation team were ‘preying’ on a dying patient, impatient to harvest her organs.
By contrast, an Anglican (respondent 17) and a Muslim chaplain (respondent 13) voiced the suspicion that Muslim families were not approached regarding organ donation as their refusal was presumed. A Jewish chaplain reported that two Jewish parents, who he thought probably would have agreed to donate their son’s organs, had not been approached; hence, a possible donation was missed. This suggests that misplaced cultural sensitivity or fear of refusal is excluding Jewish and Muslim families from discussions about organ donation at the end of life.
While two pro-donation lead chaplains saw their profession as well placed to initiate discussions about organ donation (respondents 1 and 17), a Muslim part-time chaplain (respondent 4) pointed out that he had limited time and resources for his existing workload, without taking on the complexities of a conversation about organ donation.
Despite misgivings about being too closely associated with organ donation, chaplains broadly supported the removal of organisational or prejudicial barriers to deceased organ donation. The necessity of good information was emphasised by a Muslim chaplain who was herself equivocating over whether or not donation was acceptable under Islam. She pointed out that a single case or even the rumour of a case of organs being removed marginally before death had actually occurred, whether in the UK or abroad, could undermine people’s faith in the practice (respondent 13).
A lack of positive stories about organ donation among Muslims was attributed to the presumed reluctance of Muslims to speak out about receiving cadaver-donated organs, as people with successful transplant did not speak out for fear of being judged Haram (unacceptable). Persuading imams of the Halal (acceptable) nature of organ transplantation was therefore felt to be the most important task in making deceased organ donation more widely acceptable among Muslims. One chaplain (respondent 5) suggested a seminar for British-based imams in which organ donation is discussed in terms of being the ‘last great deed before they meet their Lord’. If the argument could be framed in terms of the virtue of saving a life, ‘save one life and you save all humanity’, then organ donation could be Halal and even be seen as an obligation and not just a virtuous act.
An authoritative ruling on the acceptable nature of deceased donation was, however, not expected, given that there is no single authoritative body representing all British Muslims. As most imams currently working in Britain were brought up overseas, and also studied overseas, they tend to follow the traditions of their place of origin. Muslim chaplains contrasted Saudi Arabia, where scholars have declared some deceased organ donation to be Halal, with South Asian and African traditions, where organ donation is deemed Haram. As ‘home-grown’ British scholars of Islam become more influential the debate might become what one Muslim chaplain termed ‘more open-minded’.
Muslim chaplains made various other suggestions to promote an open conversation about deceased organ donation. These included introducing donor and recipient families to those imams who are currently against deceased organ donation, and offering posthumous anaesthesia during organ retrieval to allay fears of the soul’s prolonged suffering.
Conclusions
-
Minority faith hospital chaplains, like the patients and families that they look after, demonstrated limited knowledge regarding the process of deceased donation and donor registration and the procedures in their own hospital. Few minority faith chaplains had been involved with patients’ deceased organ donation, an experience that was most common among the Anglican chaplains interviewed. In addition, only senior and ordained Christian chaplains who sat on a hospital ODC knew of the SNODs, suggesting that minority faith chaplains are not being included in organ donation discussions in their own place of work. Chaplains’ attitudes to organ donation were also by no means homogeneous by religion. Even in this small-scale study, the views of the six Muslim and the four Roman Catholic chaplains interviewed varied within and between religious affiliations.
-
Chaplains described a majority of their conversations with patients as not focused on religion, with chaplains therefore seen as people who are well qualified to be able to reflect on the various interests at stake in discussing end-of-life care.
-
There is scope for greater involvement of hospital chaplains in relation to end-of-life care and organ donation. This is supported by the NICE guidelines on organ donation, which recommend that the multidisciplinary team should include ‘. . . local faith representative(s) where relevant when approaching families for consent’. 99 This requires being inclusive of different faith groups, although the often part-time nature of the hospital appointment of many chaplains from minority religions often limits the scope for engaging in this role.
-
The position in the community of most ethnic minority chaplains together with their interest in the topic of deceased organ donation suggests there may be capacity to develop conversations about organ donation in community settings where the implications of religious affiliation, cultural practice and identity are lived out. This community-based role has been recognised by the Faith Engagement and Organ Donation Action Plan undertaken in collaboration with NHSBT. 100
Study 2: ethics discussion groups
Abstract
Ten EDGs were held (five with doctors and nurses, and five with members of the local ODC) to examine views and practices regarding their responsibility to BAME families and wider engagement in the community. This involved a total of 58 participants. Discussion raised issues of equity, solidarity and reciprocity in the giving and receipt of organs by minority ethnic groups. This included considering the implications of different policies and practices, and ways of influencing attitudes at a hospital level among ethnic minorities and so as to achieve NHSBT’s goal of making donation a key priority within trusts and as being ‘usual as opposed to unusual’.
Aims
To engage in group discussion of donation-related issues with mixed groups of staff to identify their underlying beliefs and attitudes, their shared practices and institutional philosophy, as well as points of conflict and collaboration and differences between local cultures and practices at study sites.
Background
Recommendation 13 of the ODT report4 states that ‘There is an urgent requirement to identify and implement the most effective methods through which organ donation and the “gift of life” can be promoted to the general public, and specifically to the BAME population’. The tenor of this recommendation may be taken to suggest that the work needs to be done at an academic and/or societal level rather than within the hospital. However, it is important to acknowledge two points in relation to this recommendation.
First, recommendation 13 needs to be considered alongside recommendation 4 of the report, which states that ‘All parts of the NHS must embrace organ donation as a usual, not an unusual event. Local policies, constructed around national guidelines, should be put in place. Discussions about donation should be part of all end-of-life care when appropriate. Each Trust should have an identified clinical donation champion and a Trust donation committee to help achieve this’. To exclude BAME patients from this agenda could be seen as discriminatory, particularly given the widespread claim that being able to donate is a valuable opportunity. Furthermore, when a trust serves a sizeable BAME community, making donation ‘usual as opposed to unusual’ and ‘part of core NHS business’ will necessarily entail engaging the BAME community and then ensuring that particular families are given the opportunity to discuss donation as part of their loved one’s end-of-life care. Second, in the period covered by this research NHSBT and UKDEC were working to ensure that information was being produced in conjunction with members of BAME groups. A National BAME Transplant Alliance was launched in 2012 to provide an umbrella for groups committed to encouraging donation. It was, therefore, important to capture the views of experienced practitioners on the conceptual frameworks informing this work. It was also important to establish whether or not they saw the task of promoting donation within BAME groups as work that should continue at the bedside.
Even if the efforts to promote donation had translated into more BAME members signing on to the ODR, they would still fall in to the category of ‘pioneers’ and their families might not have moved as far along the road to accepting donation. This means that even if a member of the BAME community was identified as a potential willing donor, there would be crucially important work to be done in the hospital setting to ensure that this wish was not overridden by a family objection.
Given these two considerations it becomes crucially important to understand how individual trusts characterise their experience of working with BAME donor families and how they view their responsibilities to BAME families when seeking to promote and support donation more widely within their areas. It is also important to understand the barriers they envisage in fulfilling this task, especially given that ODT recommendations have clearly identified ways in which different types of barrier might be removed. So, for example, any lingering ethical concerns could be taken to the UKDEC, and importantly, resource or organisational issues could and should be reported to the trusts via their ODC or to NHSBT via the embedded SNODs and CLODs.
For these reasons, it is important to understand how practitioners and those involved in the governance of donation at a hospital level understand and approach donation within BAME communities.
Methods
Recruitment
We initially contacted the CLOD and the SNOD to request for their assistance in contacting ICU staff and members of the trusts ODCs to participate in the EDGs. The CLOD usually circulated an e-mail on our behalf and when e-mail addresses were provided to the research team the general invitation was followed up with direct emails to consultants and other appropriate staff.
Discussion groups
A total of 10 groups were held, five with nurses and clinicians (or in one case nurses alone). Each group included people in junior and senior grades. The other five groups consisted of members of the ODC. Given the difficulties in arranging the EDGs and because we were only able to hold a doctors and nurses group at one of our original five sites and only an ODC members group at another site, we decided to include a sixth site where we held EDGs for both groups.
The numbers of people attending the groups were not known in advance as availability depended on the demands of the unit. EDGs were held in a meeting room close to the ICU. Groups with ODC staff were mainly held following an ODC meeting to facilitate attendance.
Conducting ethics discussion groups
The attendees were provided at the outset with a participant information sheet, a brief verbal introduction to the research programme and aims of the EDG. They were also asked to sign a consent form and to keep the proceedings confidential.
It is important to note that the EDGs were not focus groups as traditionally understood. Discussions were conducted in an open manner with the facilitator following and exploring themes that emerged, based on the approach of a philosophy seminar in which participants are asked to consider issues such as the value they attach to different concepts and choices. The EDGs also differed from interviews in that the facilitator (BF, a philosopher in our study team with long experience of facilitating similar groups addressing ethical issues in health-care settings) followed up contributions with probes informed by her philosophical orientation. Unusually, participants were asked to be prepared to explain and defend their positions and when appropriate to challenge those of the institution or other professionals in the group. Moreover, BF’s approach and focus was guided by reading transcripts of interviews already undertaken with staff at the study site.
It is a feature of this methodological approach that made the discussion schedule unique to each EDG. The topics for discussion were chosen by reading the interview transcripts of staff at the study site and identifying themes and issues for further exploration. In practice a number of themes were identified as common to all groups but there was also the opportunity to discuss issues of particular local interest and or novel points raised by individual interviewees. In the latter case care was taken not to reveal the source of the issue.
In the EDGs the discussion began with introductions and ground rules and then explored issues that the interview data suggested that participants would feel comfortable to be challenged on. As the discussion progressed more contentious issues were introduced and as more groups were interviewed there was also the possibility of using references to earlier discussions to take groups into new areas. By the end of the process all groups had covered a broadly similar range of issues but the emphasis, time spent and resulting discussion differed dependent on the interests of the group starting out, their prioritisation of issues, their willingness and ability to defend their views and challenge one another, and finally whether or not they felt a need or desire to reach agreement and/or consensus.
Nine groups were facilitated by a health-care ethicist (BF), one by a social scientist (CK) and eight were attended by the programme lead (MM). All discussions were recorded with participants’ permission. Groups lasted for about 90 minutes, with some people coming to join the group or leaving to fit with demands of their job.
Analysis
Both the interview and EDG recordings were fully transcribed and entered into NVivo version 9. For our analysis of the individual interview and EDG transcripts, we used thematic analysis following close readings of the transcripts. The themes reported here emerged from this analysis as the study proceeded and were discussed in our team meetings. All quotes are referred to using an EDG number or interview number.
Findings
The findings draw on material from the 10 EDGs that each comprised between 3 and 15 participants with a total of 59 participants (Table 9) that were carried out between October 2011 and September 2012. Data from the EDGs are supplemented in this section by material from individual interviews conducted between July and December 2010 as described in Chapter 3.
| Site | Doctors and nurses EDGs | Members of ODC EDGs |
|---|---|---|
| Site 1 | N = 7 Specialist registrar (n = 2), senior house officer (n = 1), senior sister palliative care (n = 1), staff nurse ITU (n = 2), medical student (n = 1) |
N = 6 SNOD (n = 2), CLOD (n = 1), ICU consultant (n = 1), neurological ICU nurse (n = 1), sister general ICU (n = 1) |
| Site 2 | N = 3 CLOD (n = 1), SNOD (n = 1), nurse (n = 1) |
– |
| Site 3 | N = 4 CLOD (n = 1), SNOD (n = 2), staff nurse (n = 1) |
N = 4 Sister (n = 1), SNOD (2), consultant (n = 1) |
| Site 4 | – | N = 6 Matron (n = 2), chairperson ODC (n = 1), CLOD (n = 1), neurological ICU nurse (n = 1), sister general ICU (n = 1) |
| Site 5 | N = 5 Nurse (n = 4), SNOD (n = 1) |
N = 5 Consultant (n = 1), nurse (n = 2), SNOD (n = 1), chaplain (n = 1) |
| Site 6 | N = 15 Junior/senior doctor (n = 5), consultant (n = 1), CLOD (n = 1), nurse (n = 4) |
N = 4 SNOD (n = 3), consultant (n = 1) |
Shortage and scarcity of organs
Underpinning these discussions was the construction of a ‘shortage’ of organs for transplant because more people will need to be recipients than the number willing (and able) to donate organs. Given the statistics available through NHSBT most staff took this claim to be relatively uncontroversial in pure numerical terms and most were comfortable to quote commonly available statistics without comment or criticism, including a specific and even more serious scarcity of organs available for members of BAME groups. There was a further tendency within the groups to move quickly on from the fact of shortage to discuss the barriers to donation from suitable donors within the same BAME groups.
The biggest group that we face difficulty with in terms of acceptance . . . was obviously amongst Middle Eastern and Asian minorities, but also amongst very strict Jewish faith. And pretty much the, the ‘no’ rate was 100%.
EDG site 1, doctors and nurses
I don’t know of any single Muslim family during the 6 months I was there, so maybe 10 to 15 times, the success rate was zero.
EDG site 1, doctors and nurses
The significance of the lack of BAME donors was connected to the need to find the best HLA tissue match for optimal transplant outcomes:
It’s like bone marrow, like all other things, how many of the people who are actually donating, agreeing to donation and how many of them are the recipients? So you would find that the South East Asian, you know, the tissue typing and stuff is quite specific. There’s better acceptance rates or recipients would have better acceptance rates if you get it from the same Asian matched or whatever group that you are in.
EDG site 3, ODC
However, there was a slight difference of opinion on the extent to which HLA tissue matching is essential to good transplant outcomes. For example, one group discussed how because of improvements to anti-rejection drugs the need to match donors and recipients ‘is probably not medically as true now as it was probably 15 years ago’ (EDG site 5, ODC).
This has been recognised to some extent in recent practice guidance,101 for example, in changes in HLA matching criteria and in acknowledging the impact of more effective immunosuppressant drugs, although these drugs are associated with high risks, including risks of cancer. 102
It is interesting to note that participants did not choose to interpret the scarcity of ‘suitable’ organs in anything other than a clinical/scientific sense. A suitable organ was seen as one with a chance of being a good match that is one which would work well when transplanted irrelevant of origin or destination. Donating to ‘one’s own group’ was seen as necessary or preferable only because of the clinically relevant issues raised by matching donors from different ethnic groups. There was no suggestion that prospective recipients were concerned about receiving organs from within their own group and there was no sense in which people were thought to be waiting for an ‘ethnically suitable match’. Unlike the discourse in fields such as sperm and embryo donation or xenotransplantation, there was no discussion of the potential unsuitability of donation across ethnic groups owing to concern for group identity or controversial issues such as ‘contamination’. An exception to this was a case reported in one of the EDGs:
I was speaking to one of my colleagues who is a very devout Muslim and he’s of the opinion that . . . a Muslim can only accept an organ from another Muslim. Whereas he can donate to anyone, but recipient wise, it must be from the right donor.
EDG site 5, ODC
By restricting the concept of ‘suitability’ to the very narrow clinical interpretation of the term, clinicians were at the same time able to acknowledge scarcity and the reasons for it without having to take on the full ethical implications raised by the possibility of there being a perceived ‘free rider problem’.
For as long as low rates of donation within a particular group disadvantage that group alone, there is the potential for the problem to be minimised or hidden, particularly if the groups’ interests are generally harder to highlight and defend. However, if it comes to be the case that the scarcity could be addressed by utilising the good offices of people outside the group, the nature of the issue changes. You could now have a group that does not do what it takes to help themselves, but rather relies on others to do it for them. There then emerges a negative rhetoric familiar within liberal politics (‘scroungers’ vs. ‘taxpayers’), which demands a response.
The assumption of scarcity was, therefore, an important element of the ethical context within which people saw themselves operating. However, the clinical limitations within which they were currently operating provided them with a way of avoiding some of the really difficult issues. The ‘groups’ in question could be understood in terms of differing clinical need (tissue type) as opposed to differing donation practices. Race, ethnicity and other forms of shared identity could be put to one side, as there was little or no evidence of people wanting to receive from only ‘their own’ and only a few notorious cases of people wishing to direct their donations on what could be seen as discriminatory grounds.
The shortage of suitable organs was seen as in large part attributed to a failure of sufficient members of BAME communities to donate compounded by a higher possibility of family veto within BAME communities. It was interesting to note that within the EDGs there was little willingness to ‘own’ the issue of scarcity or be the focus of a solution, with responsibility being given to others ‘outside the hospital’ to raise awareness, build community engagement and encourage donation. SNODs cited lack of time and resource, and, in some cases, expressed regret at what could be done if they only had time to ‘get out of the hospital’. Having said this, there was a clear acknowledgement of the need to approach BAME families and to do so in an appropriate manner to create the best possible chance of donation once the situation arose.
The clinical/scientific interpretation of scarcity is comfortable because it insulates the clinician from confronting the full extent of justice-related issues raised by the free rider problem. By stating that the problem of scarcity arises because people from within certain groups need to receive an organ of a particular tissue type and these organs are in short supply because of low rates of donation within that group, the problem is contained within the group, the solutions in terms of meeting the needs of individual patients reside with the group. If you accept that a possible response to this is to remove the clinical/scientific barrier to transplant by minimising the need for in-group donation, you allow for the possibility of members of the community benefiting from donations outside the community, when their own community has failed to respond.
Approaching black and minority ethnic families
There was a prevalent view that approaching BAME families might be seen as more challenging. Reference was made to the size of some family groups, the problem with identifying a key informant/decision-maker, language barriers and different patterns of bereavement, etc. Having acknowledged the problem of an initial approach, staff went on to consider the terms within which an approach might be framed. For some staff, there was ambivalence about whether families should be approached in ways that are informed by knowledge of different cultural beliefs and practices, or whether they should be approached in the same way as the families of all other patients:
I think you need to be able to know people’s cultures and the different cultures there are around, so then you know how you can approach the organ donation. You know – well actually we were saying that you approach everybody the same, but it would be good to know more about people’s cultures.
EDG site 5, nurses
Several participants echoed this feeling of not having correct or sufficient cultural and/or religious knowledge, as well as a fear of offending families:
The barrier is definitely not knowing their culture . . . Not knowing if you can approach that, if it’s appropriate or not . . . like do I discuss organ donation with these families, do they agree with it, do they believe in it, would it offend their religion or, you know . . .
EDG site 5, nurses
I’ve seen reluctance from senior consultants or even staff that they won’t even broach the subject because they don’t want to offend or . . . they don’t know if people are aware of the importance of it if they’ve come from a different culture, if they’re new to the country and things . . . they won’t necessarily know about it.
EDG site 5, nurses
A similar obstacle was the fear of being perceived as being discriminatory in their treatment of BAME families.
I think there are times when, especially with BAME communities, there’s a fear of how to engage, a fear of getting it wrong, and then, you know, the fear of being branded racist if something went wrong.
EDG site 5, ODC
On the whole, members of staff who participated in our programme of research were careful not to use stereotypes about particular groups or religions, and pointed out the importance of recognising diversity within such categories. To some staff, the extent of diversity even within particular ethnic or religious groups could work against the idea that culturally specific approaches could be formulated, since they could not be sure of being sufficiently appropriate for all families within a particular category. Some participants talked about all people being individuals and commented that it was not helpful to think in terms of ethnic groups having either different or shared group beliefs.
They also recognised that views often differed between generations, with examples mainly given of Asian families:
I do a lot of, we do a lot of open days and we have an awful lot of young Bengali, I would say sort of teenagers, early sort of – between sort of 13 to 17/18. And they’re all interested in organ donation, and some of them have come up to me and said, ‘Yes I’m very keen, but my family . . .’ – that’s the thing, you see, you’ve got a generational thing going on. So the young ones are getting it, they are getting it.
EDG site 5, nurses
Discussions around the approach to families raised a number of ethical issues, some of which staff clearly found difficult to discuss openly. As in previous studies that have adopted the EDG approach, there was a shared sense among many of the health-care professionals that religious- or faith-based objections hold a special force in a health-care setting. This, in turn, meant that the default response might be to accept an individual or family’s view without question or challenge if it is presented in terms of a faith-based objection or demand. This may be even more prevalent when the health-care professional is unfamiliar with the tenets of the belief and/or when the group in question is perceived as particularly vulnerable to misunderstanding and/or prejudicial views.
The wish to neither stereotype nor make assumptions based on ethnicity or group membership was clearly stated, yet it is possible to move beyond a crude and reductionist form of profiling to acknowledging that cultural and religious factors will combine with age, class, education, etc., to provide some clues to a family’s preferred way of doing things. Although no two families of any type are the same, and all should be treated appropriately, it was clear that a wish not to discriminate could potentially translate into a tendency not to pay due regard to morally relevant differences across and within groups. Another interesting finding from the groups was the fact that health-care professionals from BAME groups were not necessarily feeling any better equipped to approach the families in question.
Reciprocity
As previously mentioned, when there appears to be inequity in the provision and consumption of social goods there is the potential for injustice specifically through the notion of free riders (people who benefit without contributing even though they could). At the time of the groups, there was a growing interest in the concept of reciprocity as a potential response to this issue both within the professional literature and in the media as a result of policy decisions in Israel.
Some staff were aware of the use of officially produced materials relying on reciprocity-based scenarios.
I worked at [x hospital] recently and . . . I noticed there was a lot of posters up with different ethnic minorities with a, you know, ‘I’m on the transplant list, if something happened to me I would want, I’m waiting for kidneys, if I were well I would donate mine,’ or something, you know, something. And it was quite clearly, they had three posters, one each from different ethnic group . . . some of them were those posters where you had the person well and then you had the person who is ill . . . it felt very targeted actually, the ethnic minority and the ‘here I am well,’ and the reciprocal, you know, ‘if I’m on the register, I expect that I would give anything I could’.
EDG site 1, doctors and nurses
However, there was a caution expressed in relation to the use of publicity material with several members of staff reporting that they had observed the removal of advertisements targeting BAME patients and families in waiting rooms. This was linked to anecdotal claims that this approach could be counterproductive:
So there’s some evidence to show that currently in these, in the communities, the advertising potentially is counterproductive because people, you know, have an instinctive reaction to it and then reinforce their prejudices.
EDG site 6, ODC
A member of an ODC put the problem in economic terms:
There is a business case for it . . . one of the things I want to do, you know, my involvement with this committee, is to take this message out to communities and just say, ‘Look it’s in your interests that you are involved in this.’ And there was one meeting I went to last year and I actually said to a lot of BAME communities there that, ‘Look if you don’t wise up, people in your community are just going to die, it’s as simple as that’.
EDG site 4, ODC
Some of those in favour of making special efforts to encourage organ donation amongst BAME families commented that families might be more willing to consider donation if they believed someone they knew or at least someone from their own ethnic group could benefit. So, for example, one strategy could be:
educating people to say that if your relative does donate organs, it’s not just going to an English person, it may go to another person who you know or somebody else who has renal failure.
EDG site 5, nurses
People will respond to that, it’s our people who want organs. It’s kind of something about your being mine, you being us, and therefore it will help you and therefore it will help one of our own.
EDG site 5, ODC
These comments suggest that an appeal to solidarity with people from the same ethnic background, or people with the same disease, could be the basis on which to make an approach to BAME families for donations. However, participants acknowledged that it might not always be possible to trump fundamental resistance. One consultant recounted how he had tried this approach with the family of a patient in ‘resus’ (resuscitation) with no success:
I specifically used the, the little hook that, you know, ‘her kidneys will usually match with people who are similar to you.’. . . But obviously that was a refusal as well . . . that was a Muslim family . . . that was the first I’d tried the little, you know, ‘It’s like her, because of her genetics, her organs would go to help someone who’s likely to be of a similar race to you’. . . but it didn’t really – so I don’t know the ideal way to approach really. I suppose, watch this space.
Site 3, consultant interview
Within the EDGs it was seen that the notion of reciprocity allowed for an acknowledgement of the scarcity problem while still containing it in the manner achieved by the clinical criteria-based discussion above. Thus, an appeal can be made to community solidarity that can be respectably and legitimately defended, because the clinical facts mean that your donation is likely to go to someone within your community. This moral convenience is unlikely to persist, however, as it is also in the interests of the community to conduct research and introduce new practices to minimise the impact of tissue types on the success rates of transplanted organs. The question then arises whether or not it is morally defensible to seek to raise organ donation within BAME groups by appealing to solidarity and the wish to benefit one’s own if that would only be possible through the introduction of some form of directed donation. There was no support for this step within the EDGs, but there was some sympathy for the wider case for societal rather than group reciprocity, such that if you do not give you should not receive, with the acknowledgement that this could further disadvantage BAME groups in the absence of an increase in donation rates.
Unwillingness to donate
The EDGs were keen to speculate on why for members of some groups there was a reluctance to give organs despite there being a willingness to receive them. A suggestion was that an asymmetry in giving and receiving organs could be explained in relation to Muslim patients by the belief among this group that the body should not be ‘cut up’, which overrides the consideration of benefiting other people; and on the other hand the belief that transplants are made possible without the need for personal agency because:
Allah has given them an organ to save their lives.
EDG site 5, nurses
One of the consultants, talking about a Muslim family who had declined donation, commented on how far the concept of belonging to a wider society might apply for such families:
I think that there’s not the same sense of community. In the same way as I’ve described a fiduciary relationship, which begins with the patient, moves to the family and goes out into the wider society, I don’t think they have that same sense of wider society. I think their view of society is the family, and I think that’s where the walls stop.’
Site 3, consultant interview
This view chimes with the reported experience of some members of staff who had been involved in the field of live organ donation; anecdotally they reported that while some African-Caribbean families will participate in live organ donation within the family it was rare, if not unknown, for members of this community to come forward to donate beyond the family.
Although these are clearly not robust data on which to build conclusions, it is important to understand the shared understandings and ‘stories’ that circulate within medical teams. An assumption that people from certain communities ‘don’t donate unless to their own’ in the narrowest of senses might well have an impact on the willingness of staff to approach such families. This might also have an impact at a policy level with the problem being seen as structural and insurmountable, as well as culturally and religiously sensitive. Similarly, another consultant thought that in some very:
. . . isolated cultural communities, they would either want organ donation, only to have them if it’s one of their own, or they can’t see the benefit because they’re very locked in communities, they don’t perceive the rest of communities outside their own, to be given a gift. And they very much feel that, you know, they’re the ones who need everything. And they’ve not prepared to move beyond that.
Site 5, consultant interview
Staff felt that a further reason for questioning targeted approaches was that this strategy could be perceived as being associated with directed donation (i.e. donation solely for the benefit of specific groups or identified individuals), which is prohibited by UK regulations. These regulations are specifically designed to ensure fairness in the allocation of organs and to ensure that morally irrelevant factors such as race or even the football team one supports do not become factors in limiting the scope of a person’s donation.
Some staff warned against ‘tiptoeing in the direction of selected donation’ and commented that it was important not to move away from the idea of pooled donation. In this view, donations should be seen in terms of contributing to the greater society, not just for the benefit of a particular group. In turn, there was a feeling among some practitioners that even the suggestion of direction to a community member by dint of tissue matching should be avoided.
Taking but not giving organs
Staff did not avoid the conclusion that the lack of available organs was due, in significant part, to low donation rates within BAME groups and they were also prepared to invite members of the communities, including those on waiting lists for transplant, to reflect on this fact. Having rejected any notion of explicit directed donation within communities and in the absence of a united call for the introduction of a reciprocity model, such as that introduced in Israel,23 there were several calls for better community-based education specifically highlighting the unmet need and utilising the possibility for community-based altruism.
As one consultant described the situation:
I believe a large population of those waiting for a right match are from the ethnic minority. And they are waiting the longest, and that’s because a right match is not found, and that’s because the donation pool is not as big. I think the community should know those figures rather than just saying, ‘We are doing good for mankind . . . And then we could then give the community a real perspective of what the actual scale of the problem is . . . But I feel that that message is not conveyed yet . . . If we came out with a figure to say, ‘Look guys, organ donation is difficult in this community because it has to be appropriately matched and your, your sort of ethnic minority are the longest waiting, and there is X many thousands of patients waiting.’ I think that is when it hits home.
Site 3, consultant interview
Similarly, other participants thought that BAME families should be informed of the situation and invited to think about reciprocal benefits when the possibility of donation arises, for example by saying:
‘If it is one of your relatives on the waiting list, they will wait longer because your community are less likely to donate.’ That sounds like putting the guilt factor in, but it’s the truth.
EDG site 6, ODC
However, two consultants, while generally supportive of increasing understanding at a community level, were not happy with using this approach in the ICU:
It’s not the time when you’re discussing the issue about organ donation with the relatives. You can’t say, ‘Oh did you know so many people are waiting?’ because it’s completely not the right time to do it. But yes, it could be done in outpatients . . . So that those who are on dialysis or in end-stage renal failure, their relatives can learn to say, ‘Actually yes,’ you know, yes I think there is a role for hospitals to play as part in community education.
Site 3, consultant interview
Participants varied in terms of their propensity to judge those who would receive but not donate an organ. In an interview with a consultant the term ‘double standards’ was used to describe a potential recipient being willing to be saved by transplanted organs, but not being willing to agree to donation:
I think that people born and bred in this country probably have thought at some stage, ‘Well, you know, if I needed a heart, I’d have one, if I needed a kidney, I’d have one, I wouldn’t refuse to be a recipient, just on the basis that I’m so and so religion.’ And, you know, if they’ve been through that thought process, then when it comes to saying, ‘Well I’m happy to be an organ donor,’ they would be I aware, I think, of the double standards involved in that.
Site 4, consultant interview
Some staff commented on why reciprocity perspectives might not sit well with BAME families. For example, there was some anecdotal evidence that some people from BAME families have a belief that one day they will be returning ‘home’, so they do not want to donate in the UK. One member of staff commented that this was a view he could relate to:
I think the majority of them don’t want to know, don’t want to get involved because I sense that these people are here temporarily. I think, you know, minority ethnic minorities are here . . . some of them are in transition. So they come here to work for how many years and they have in mind that they will retire and go home. So it’s nothing that they would like to get involved, like ‘Why would I want to register as a donor here, I’m going home.’. . . I see from my own perspective, I would donate anywhere obviously, but in my head one day I’ll move and I won’t be here. So if I just had that in mind I’d go, ‘No’, if I had to tick a box because I’m going home.
EDG site 5, nurses
This could be read as an expression of alienation or a sense of not ‘belonging’, and, therefore, not feeling that there is a commitment from the wider society to people from BAME groups as citizens that they would wish to reciprocate. A consultant made a similar comment:
They need to build from the ground up, the idea that transplantation is a benefit to everyone, because maybe . . . if you’re in any minority group and you can see the establishment as being not there for you really, even if you’re using it, it can be still a cultural perception that it’s more for other people than it is for you.
Site 2, consultant interview
So although many of the staff considered issues that could be conceptualised in terms of solidarity and reciprocity in relation to the value of donating and receiving organs, there was acknowledgement from their experiences and knowledge of their patients and their families that these were not necessarily priority values in the minds and belief systems of those families. They were also prepared to situate a consideration of societal reciprocity (as the ethically defensible model) alongside issues of community identity and membership, bodily integrity, and historical and future affiliations, which came together to provide a complex picture of the ethically appropriate context for donation.
Conclusions
-
Health-care providers and policy-makers have a strong concern not to appear discriminatory in either attitudes or actions, which is at root a commitment to a fundamental equality. However, the notion of equality is sometimes crudely drawn such that health-care professionals are fearful of being seen to ‘treat people differently’ when that is precisely what the principle of equality sometimes requires. The important issue is that people are treated differently for morally relevant reasons and in the interests of securing a just and equal outcome.
-
Gift giving and exchange, or reciprocity, have long been regarded as key aspects of the concept of solidarity and are often cited in discussions of blood and organ donation. 103 An appeal to the idea of solidarity with the needs of members of one’s own ethnic group may seem straightforward but can easily be problematised. 104 For example, it is crucial to recognise the heterogeneity of social groups, the interplay between individual values and collective values held by particular groups, and differences in attitudes according to types of tissue being considered for donation. 105 It is particularly important to engage both health-care professionals and community members with these issues, which will become all the more stark as medical expertise develops and renders cross-community donation unproblematic.
-
Some believed that an appeal to the specific ‘shortage’ of donated organs from BAME groups might prompt more willingness to express a wish to donate by registering on the ODR. Others felt that an understanding of scarcity would encourage families of patients in end-of-life care to consider donation and at least be open to an approach. Both groups advocated a robust ‘educative’ approach, but there was a clear resistance to bringing such discussions to the bedside and a sense of powerlessness in terms of their own capacity to contribute to efforts outside the hospital.
-
Questions were raised about the best way of putting the scarcity message across, as professionals did not want to be perceived as discriminating among or between patients on the basis of ethnicity. It is, therefore, important to remain committed to community-based and community-informed initiatives, which build on shared values, and acknowledge and respond to the shared concerns of particular groups while also acknowledging that this is part of and not apart from the overriding aim of addressing scarcity UK-wide. As such, it is also integral to the goal of making discussion and consideration of organ donation a component of excellent end-of-life care across the NHS.
-
Clinicians were clear that the task of moving families towards acceptance of donation in the absence of a clear expression of wishes was significant, and more often than not was unachievable. Yet, ethically, this must been seen to apply to all patients irrespective of race, ethnicity or religion with the ‘likely possibility’ (sic) of donation referring to only the manner of death and other clinical factors. To accept upfront the unlikelihood of donation on grounds of ethnicity or religion would be to accept the status quo in relation to hard-to-reach groups and would perpetuate the scarcity of organs within those groups.
-
Feedback from participants underlined the value placed on being given the opportunity to discuss sensitive issues in a safe and constructive setting, with the general view that staff working in ethically challenging areas should be given a regular opportunity to discuss and reflect on practice in a confidential and non-judgemental setting.
Relationship with overall programme
The reporting of findings from the EDGs may not immediately reflect the distinctiveness of the approach with some of the findings looking similar to those achievable through a less searching process. However, the important difference with the EDGs is that they reveal and then explore important commonalities and differences in the way staff perceive and respond to an issue. As a result people can leave the group feeling a number of different ways. They may be more confident in their positions because they have defended them successfully. They will thereby know that their ideas, beliefs and or actions have stood up to scrutiny, and they may even have persuaded some colleagues to think differently. In other cases people will know that they have been effectively challenged, that their views do not sit happily with the prevailing culture and/or their practices may be out of step with what others think is required to deal with a problem. On some occasions a whole group might be challenged to rethink what has become familiar and comfortable to them.
In terms of approaching BAME families, participants were very honest and open about the barriers and their reluctance and/or inability to address them, with the EDGs complementing the individual interviews by drawing out the ethical and moral dimensions surrounding their relationships with BAME patients and families.
Consideration of the welfare of BAME members on the transplant list made it clear that such families needed to be approached, although it was felt that families from minority ethnic groups would be particularly unprepared for the issue of donation arising and that staff might be particularly ill-equipped to make the first approach to raise the possibility. The specific features of the case determined by the ethnicity of the family and potential donor were those of unpreparedness, lacked of shared cultural knowledge and understanding, and a consequent fear of being perceived insensitive and/or discriminatory.
Study 3: interviews with bereaved families
Abstract
This is the first UK study to examine the experiences of bereaved families from minority ethnic groups in relation to deceased donation. However, as a result of restrictions on identifying families who did not consent to organ donation, the study was limited to 13 families who did consent to organ donation. These families regarded communication with ICU staff to have been of a high standard and appreciated the clear, honest and accurate information with frequent updates and the opportunity to ask questions. They also appreciated the lack of pressure to make a donation decision but would have liked further follow-up information regarding the progress of the recipient.
Aims
To elicit bereaved families’ experience of communication and support in ICUs, including their perceptions of the discussion regarding organ donation and the influences on their decision-making.
Background
A fundamental requirement in achieving higher levels of organ donation is to ensure that families feel well supported and satisfied that everything possible was done for their relative and that they felt that the timing and process of the consent discussion were appropriate. Considerable research has been undertaken in the USA to examine the characteristics of donor and non-donor families and reasons for non-donation based on a structured telephone interview106 and chart reviews,107,108 with these studies including both consenting and declining families. Important influences on consent to donation were identified as including prior knowledge of the patients’ views, having more contact with requesting staff, viewing the requestor as sensitive to their needs and experiencing an optimal request pattern, which corresponds with the findings of qualitative interview studies with families in the UK. 109–111
Black families in the USA, as in the UK, are less likely to consent to donation. A study by Siminoff et al. ,112 based on a chart review at nine trauma hospitals in the USA, indicated that non-consent was partly linked with families’ experiences of care, with black families less likely to have spoken with an organ procurement representative, being given fewer opportunities to consider the decision with a health-care provider, and having less knowledge of their family members wishes, while they also expressed less favourable attitudes to donation and the health-care system. These findings regarding knowledge and attitudes correspond with our prior review of influences on registration as a donor among minority ethnic groups. 27 However, to date there has been no direct information on the experiences of bereaved families from minority ethnic groups in the UK in terms of interactions with ICU staff, or of reasons for their non-consent.
Methods
Study sites
The initial application implied that only bereaved families at five NHS trusts in the London region who met the inclusion criteria would be invited to take part in the study. However, in 2012, only 56 of the 1212 donors in the UK came from black, Asian or other minority ethnic groups and thus constituted a very small group. Owing to a small sample and an expected low participation rate, recruitment was subsequently extended to include the top 20 English hospital trusts in terms of numbers of approaches to BAME families for organ donation and we also approached the five remaining London trusts (of which all but two were able to participate). This involved 23 additional sites, giving 28 sites in total. This required that each of these trusts became a patient identification centre (PIC), which permits clinicians or clinical units to identify and refer potential participants to external research teams without requiring a full governance review.
Subsequently, it was clear that 28 sites were unlikely to provide sufficient participants and NHSBT provided data that identified a further 18 trusts as having one or more consenting kin from an ethnic minority group; of these, 12 trusts participated and PIC applications were completed. A total of 40 trusts were therefore involved.
Identifying potential participants
The most comprehensive way to identify and contact potential participants was via NHSBT, which retains records of all organ donors and next of kin contact details, unless no further communication was requested.
The intention was to initially employ a retrospective approach and invite the next of kin or family member who had or had not consented to organ donation to take part in an interview, if they fulfilled the following inclusion criteria:
-
adult donor (aged ≥ 18 years)
-
died on ICU [or accident and emergency (A&E)]
-
recorded as being from a minority ethnic group or mixed background or family
-
next of kin did or did not consent to deceased organ donation.
The expected number of participants at the time of submitting the grant was 20–24, ideally split between consenting and non-consenting families.
It was proposed that both consenting and non-consenting families would be retrospectively recruited via NHSBT. However, NHSBT’s governance requirements mean that it does not centrally retain the details of families who were approached but declined organ donation and asking hospitals to search their records was not regarded as feasible owing to the length of time this would take and the finite length of the programme. Considerable contact and negotiation occurred with NHSBT to try to overcome this problem; however, this did not prove feasible. Instead, an alternative recruitment strategy was suggested that involved the prospective recruitment of non-consenting families. The two recruitment strategies are described below.
Families who have consented to organ donation (retrospective)
The leader of the London SNODs centrally identified families at the selected hospitals who had consented to organ donation within the last calendar year and who were not less than 3 months post bereavement. SNODs then sent families fulfilling the study inclusion criteria a study recruitment pack provided by the DonaTE team. This included a cover letter from the SNOD, a letter from the study team and a patient information sheet that outlined the study. No less than 5 days after the recruitment packs were sent out, the SNOD telephoned potential participants to ask if they had any queries about the research and whether or not they would be willing to take part in an interview and for their contact details to be passed on to the DonaTE team, who would then contact them to arrange an interview at a mutually convenient time.
Families who did not consent to organ donation (prospective)
Families who were approached to give consent to donation (prospective) were also informed by the SNOD about the bereaved family study and asked whether or not they would be prepared to receive an information pack in 6 weeks’ time. The SNOD also emphasised that receiving a pack did not oblige them to take part in the study. When this was agreed a pack was posted out 6 weeks post bereavement. One week later the SNOD telephoned the next of kin to ask if they would be willing to take part in the study and agree to the SNOD passing their contact details to the DonaTE programme researchers.
The retrospective and prospective recruitment began in September 2011 and concluded in September 2012. Overall, 74 next of kin were invited to take part, of whom 23 (14 consenting and nine non-consenting) agreed to receive the information pack. Altogether 13 agreed (17.5%) to be interviewed, and these were all from consenting families.
Recruitment delays
Recruitment for this study was very time-consuming with considerable researcher time involved. This partly reflected the substantially expanded number of study sites (see Methods, Study sites), together with the need to include a prospective component, which required a substantial amendment to be submitted to the Research Ethics Committee. Recruitment began in September 2011, with the final recruitment packs sent out in September 2012.
Interviews
Additional training was undertaken by the researchers to prepare them to interview the bereaved, a group with whom neither had previously conducted research. They attended a training course, ‘It’s hard to talk about it: taking the risk of opening a can of worms’, at Sobell House, Oxford. This focused on difficult conversations about the end of life and death, primarily aimed to prepare those who work in hospices.
All participants preferred to be interviewed at home. The topic guide was structured chronologically to guide the participants through their experience (see Appendix 8). It covered:
-
background information about the donor and events surrounding their hospital admission
-
impressions of the hospital, diagnosis and communication
-
potential treatment withdrawal/breaking bad news
-
approach for consent for organ donation including how this was explained, discussions with family and decision-making
-
DBD- and DCD-specific questions
-
end-of-life practices
-
consent paperwork
-
reflections on the donation decision and taking part in the research.
All participants received a participant information sheet and signed a consent form before the start of the interview. The interviews were all conducted at home as preferred by participants. They were audio-recorded (with permission) and designed to last 60–90 minutes.
It was made clear to the participants that they could have a break during the interview or could stop the interview at any time if they found this too distressing. The researchers took information from local bereavement counselling services and ensured that the participant was all right before they left.
After each interview the participant was sent a thank you letter together with a brief post-interview feedback questionnaire that was returned to the chief investigator. These feedback responses were extremely positive, with the participants regarding the researcher as most understanding and feeling very comfortable talking with them. They also reported that they were able to cope with the length of the interview and, although recounting a particularly distressing time, they generally found it helpful to have talked about their experiences.
Findings
Characteristics of participants
There were a total of 17 participants, with three interviews involving more than one person. Altogether four participants were a spouse of the deceased, seven a parent (mainly mother), three a sibling and three a child of the deceased. Participants were predominantly of Indian origin and mainly Hindu and Christian faith (Table 10).
| Reference | Gender | Ethnicity of participant | Faith of participant | Relationship to donor | Ethnicity of donor |
|---|---|---|---|---|---|
| 1 | M | Indian | Hindu | Brother | Indian |
| 2 | F | Indian | Jain | Wife | Indian |
| 3 | F | White British | Catholic | Mother | White British/Asian |
| 4 | F | Caribbean | Christian | Mother | Caribbean |
| 5 | M | White British | Christian | Husband | Malaysian |
| 6 | F | Filipino | Catholic | Mother | Jamaican/Malaysian |
| 7 | F | Indian | Hindu | Mother | Indian |
| 8 | F, F | Caribbean | Christian | Mother, sister | Caribbean |
| 9 | M | Indian | Christian | Son | Indian |
| 10 | M, F, F | Indian | Hindu | Father, mother, sister | Indian |
| 11 | F, F | Indian | Hindu | Wife, daughter | Indian |
| 12 | M | Sri Lankan | Hindu | Son | Sri Lankan |
| 13 | M | White British | Christian | Husband | Jamaican |
Initial communication
The events leading to their relative’s hospital admission were unexpected and the result of, for example, heart attacks, aneurysms or accidents. The initial contact and communication from the staff varied. Those whose relatives were admitted to A&E and remained there reported waiting a considerable time before being informed about their relative’s condition and were not happy with this situation:
The doctor who was in charge, you know . . . I kept asking because I wasn’t sure what was happening. And didn’t say anything until about 3 hours, that that’s what’s happened. But they had told me that he’s not well.
Respondent 2: wife, Indian, Jain
Participants were aware that an admission to intensive care implied that the prognosis was unlikely to be good, but their initial contact with and impressions of the hospital were generally positive and often supported by existing knowledge of the hospital’s reputation:
I knew that for head injuries, he was in very good hands at [name of hospital]. So from the medical point of view, I was, there wasn’t a better [place] that he could be. So we knew that he was at the right hospital with the right teams presumably looking after him on that evening.
Respondent 1: brother, Indian, Hindu
Relatively soon after admission to an ICU the participants reported meeting with an ICU consultant who updated them on their relative’s condition and they appreciated the honest communication that they received:
I don’t know, he was a surgeon, he was still in his scrubs, he was quite matter of fact. Honest, I mean that’s what you want, I mean you don’t want to be given false hope, do you really, you know.
Respondent 10: sister, Indian, Hindu
Subsequent communication from the ICU staff appeared to demonstrate good practice that was characterised by talking to the family in a private space (away from the communal waiting room), explaining the patient’s condition clearly, assuring them they were doing all they could and ensuring the relatives were comfortable to ask any questions they may have:
At the [hospital] they was so, it just seems that no stone was left unturned. Everything was done to clearly let us know and to assure us there was nothing.
Respondent 3: mother, white British, Catholic
Being near to the patient and being able to spend time at their bedside was important for all of the participants and other family members and was usually facilitated by the ICU staff. However, when the family was updated about the patient’s condition this often took place in a small family room that often could not accommodate everyone the family wished to be present, although the efforts of staff to identify and allocate another larger room were appreciated.
Breaking bad news
During the patient’s time on ICU the participants reported conversations with the consultant to receive updates about their relative’s condition and prognosis. The participants appreciated receiving accurate and honest information but reported disbelief about the seriousness of the patient’s condition particularly if their physical appearance looked ‘normal’.
The communication of the ICU staff communication with the families was reported to be clear and usually delivered in a way that the family understood, with a space provided for the family to ask additional questions that the staff were happy to answer. Respondents also commented favourably on the efforts to facilitate end-of-life care in a way that was sympathetic and empathetic to the family and their situation:
So it’s like everybody done everything from their heart. So there is no complaints about it. There’s no mistakes or something. So whatever they’re doing is very good.
Respondent 12: son, Sri Lankan, Hindu
Diagnosis of death
While participants’ specific recollection of what they were told about brain stem tests varied, most reported understanding the concept of brain stem death and knowing that a ventilator was ‘breathing’ for the patient. The same level of explanation may not have been circulated to wider family and friends, who perceived the patient was alive:
Well some of our family relations didn’t believe she’s dead because they said, ‘There’s breath,’ so I said, ‘Yes it is artificial breath because they don’t want to upset you straightaway, that’s why they kept her breathing.’ But some of the people say, ‘No she’s not dead, there is still breath.’ I said, ‘Yes I know there’s a breath . . . because it’s artificial breath.’
Respondent 12: husband, Sri Lankan, Hindu
One inconsistency is whether or not families are invited to observe the brain stem test, which was often a way of assuring themselves that their relative was dead.
From the sample, three patients were DCD donors and all ‘died in time’ for donation to proceed. The participants reported receiving a clear explanation about how death would occur including the body’s physical reactions and the need to move swiftly to theatre after the patient had been declared dead for organ retrieval to proceed.
Approach for consent
After families had accepted the death of their relative, at an appropriate juncture, organ donation was raised, usually with the next of kin. The approach was often led by the SNOD, although for at least two families in this sample, they were initially asked about organ donation by a consultant. Regardless of who made the approach the families felt this was done sensitively. Differences occurred in how organ donation was seen to be presented to the families who reported, for example, organ donation presented as a way for their relative to live on or to save or improve the lives of others. Three families distinctly remembered being told that if they donated their relative’s organs these were likely to go to someone of the same ethnic background. This was not reported as influencing their donation decisions. However, one family felt they might have been slightly misled when they learnt that the recipient of a donated organ had gone to someone from a different ethnicity.
One family reported feeling under pressure by the ICU staff to consent to donation but other families described and appreciated being given time to think about organ donation and discuss this with their family, particularly when their initial reaction was one of uncertainty. Although a few families initial reaction to organ donation was ‘no’, after being given time to think about organ donation and usually having discussed this with other family members, they decided to consent. The families welcomed the lack of pressure to make a decision, so that they could make a decision that was right for them and their relative.
No there was no pressure. We could step back at any stage. However, she explained that, ‘Once we go into the theatre, that’s it, it’s their right after that stage, but up until that door opens and we wheel her inside there, you can step down at any stage.’ And that’s what I liked about the whole process with them, you know, just the respect, the way they spoke about her, the way things were done.
Respondent 8: mother, black Caribbean, Christian
Making the donation decision
Two patients were on the ODR, with their wishes therefore known and respected. However, other patients had not discussed organ donation or their wishes with their families, with the decision, therefore, left with the next of kin. In this situation there was little discord reported between family members when organ donation was suggested and if initially discord occurred, donation was eventually supported with the final decision usually taken by just one person, often the (legal) next of kin. However, this person sought the views of other family and friends who were broadly in favour and made it clear that they would support the final choice the next of kin made.
In considering organ donation and coming to a decision, the participants thought about what the patient would have done and often involved reference to what the donor was like as a person:
And then what I had to do was put myself in my daughter’s position, think of my child. And I based it upon what would [daughter’s name] have done? And knowing [daughter’s name] she would give away everything, [daughter’s name] would give away everything. And that’s what I based it on.
Respondent 8: mother, black Caribbean, Christian
Perhaps unexpectedly, several families raised organ donation themselves with the ICU staff. This arose as either they knew of someone needing or having received a transplant or they had a wider awareness of the need for transplants via the media. For example, one family described seeing an organ donation leaflet in the family waiting room. Underlying their support for organ donation was a desire to help others live and a belief that it is what their relative would have wanted or supported, even if they did not know their wishes:
I think it’s just when you hear a lot of people needs kidney and everything, you know, you hear so many things on the telly. I usually watch the programmes all the time, the hospital programmes and things like that, and I see how many people, you know, the people who need all these organs, and how difficult it is in here. So I would have thought that that would have been something that I’ve done for other people’s life.
Respondent 2: wife, Indian, Hindu
After consenting to organ donation, family and friends usually spent time with the patient at the bedside to say their goodbyes. This was often facilitated by the SNOD in negotiation with the ICU and supported by the bedside nurse. In addition, some families reported wanting to carry out particular faith or cultural practices, for example, praying at the bedside, which was relatively easy to facilitate for other families, compromises were found so they could fulfil practices without compromising the unit or the care of other patients. For example, for a Malaysian Buddhist family the burning of a talisman had to take place in a designated area of the hospitals’ car park rather than at the bedside. If a compromise was required, the participants were happy to go along with this.
As well as meeting practical, emotional, faith and cultural needs, the families were offered a memento of their relative. These ‘mementos’ vary by hospital and are arranged by the SNOD. The most common mementos are handprints or a lock of hair; with less common items including photographs of tattoos, footprints and for a paediatric donor casts of their feet.
Post donation
It is usual for the SNOD to telephone the next of kin or a nominated contact to tell them that the organ retrieval is complete and later to send a letter outlining which organs were suitable for transplants with a brief descriptor about the recipient. The families were pleased to learn that their relatives’ organs had saved or improved the lives of others, albeit strangers who they would never meet.
On the first anniversary of the patient’s donation, the SNOD usually sends an anniversary card to the next of kin, again thanking them and updating them on the progress of recipient(s). However, in practice, not all the participants had received further contact from the SNOD, and would have generally have appreciated an update just to know that the recipients of their donated organs were healthy and getting on with their lives.
Conclusions
Strengths and limitations
This is the first UK study to ascertain the experiences of minority ethnic groups in relation to deceased donation. With just 13 participants who consented to donation it is not possible to argue that saturation was reached in the analysis of this group, although there are consistencies across the data reflecting good communication practices and experiences despite the tragic circumstances. The most significant limitation was being unable to retrospectively contact non-consenting next of kin. This group forms the majority of the minority ethnic groups who have been approached for consent for organ donation, and without access to this group we were unable to identify the reasons for not consenting to organ donation. It is not known if commonly cited reasons for not consenting such as faith or cultural practices hold true or if other reasons influence this decision. Without this knowledge barriers cannot be addressed and these may continue to prohibit organ donation.
Families’ positive views of experiences
Among the group of consenting families the quality of the communication between the ICU staff and the families was reported to be of a high standard. Families appreciated clear, honest and accurate information about their relative’s condition after admission and subsequent updates, often in a private space. They felt comfortable, were able to ask questions at any point and recognised the time consultants and nursing staff spent with them. Consultants broke bad news and explained how the patient would die or be declared dead with sensitivity and clarity often after earlier conversations about a poor prognosis, which had prepared the family for bad news.
Families’ perceptions of gaps in services
Families would have liked the offer of observing brain stem death tests when these were carried out, but this did not always occur. There was room for improving communication with families who came via or remained in A&E when it appeared to take some time before the family were spoken to by clinicians. This is likely to be a significant future issue with A&E departments, regarded as a further source of potential organ donors. Families often heard nothing about the organ recipients without asking and would like to be automatically updated on how they were doing unless they had opted out of further contact.
Implications of the hospital studies
Implications for policy and practice
-
Bedside nurses were positive about the provision of training in cross-cultural communication.
-
Clinicians’ often limited SNODs’ involvement and participation in ‘collaborative’ requesting, with this partly arising from uncertainties surrounding withdrawal of treatment in controlled circulatory death as well as perceptions of their own role and responsibilities.
-
Many hospital chaplains expressed interest in receiving training to support families in organ donation decisions. They potentially form an important resource, although this role would be limited by other demands on their time.
-
The positive influence of interpersonal support on families’ donation decisions is in line with NHSBT’s recommendation to pilot a peer support scheme in ICUs with a large ethnic minority population. 15
Implications for research
-
Further research is required to achieve a better understanding of the reasons for non-consent to donation among ethnic minority families. This might be initially based on secondary analysis of detailed information on reasons for refusal now recorded by SNODs. More in-depth primary research could also be undertaken with permission given by NHSBT to approach bereaved families on a retrospective basis.
-
It is important that research-based evaluation examining both process and outcomes forms part of the piloting of new schemes, such as proposals for peer support, so as to expand the limited UK evidence base and guide future implementation.
Chapter 5 Development and pilot evaluation of a professional development package
Abstract
This chapter describes the development and evaluation of a professional development package to increase the confidence and competence of ICU staff, particularly bedside nurses, in supporting families from different cultural backgrounds. The storyboard for the digital versatile disk (DVD) drew on the interviews with ICU staff and the community focus group study. It examines the varying beliefs and responses of ethnic minorities and best practices in relation to five key dimensions: emotional expression; faith and culture; the family; language and communication; and anxieties about donation. Presentation of material relating to each of these dimensions was framed by Ajzen’s TPB,27 which that identifies attitudes towards the behaviour, subjective norms and perceived behavioural change as influencing intentions and behavioural practices. The research team worked with a production company to develop the storyboard into a package comprising a main video and short family drama plus accompanying workbook to encourage reflection and personal plans. This has been presented to groups of nurses, clinicians and SNODs, with assessment comprising feedback forms completed at the end of the session, a before-and-after evaluation with TPB questionnaires (baseline and 3 months) and assessment of the impact on family consent rates. The results were encouraging, although further evaluation is required with larger numbers of participants.
Aims
To develop and undertake a pilot evaluation of the training package designed to increase the confidence and skills of ICU staff in communicating with patients and families from different cultural groups.
Background
There is evidence from previous studies that the perceived quality of communication and support during end-of-life care is an important factor influencing family consent as well as satisfaction with the donation discussion itself,109,111 thus identifying the way in which the multidisciplinary team contributes to increasing donation rates. However, there is currently no provision for formal ‘cultural competency’ training in the NHS. This was noted by NICE which commented in relation to cancer services that professionals may be poorly skilled in communicating effectively in ethnically diverse settings. 99 This contrasts with the situation in the USA, where considerable emphasis is given to training in cultural competence and often forms a mandatory aspect of medical and nursing training. This requirement was introduced as part of a wider strategy to reduce ethnic disparities in health and is based on the view that health-care services that are respectful of and responsive to the health beliefs, practices, and cultural and linguistic needs of diverse patients can help bring about positive health outcomes. 113
Not surprisingly, given the lack of training in cross-cultural communication in the NHS, the DonaTE ICU studies identified junior nurses as often experiencing some hesitancy in fully engaging with families from minority ethnic groups at a time of considerable emotional distress. Moreover, at times, some ICU staff drew on social constructions of people from minority ethnic and faith groups different from their own that portrayed them as ‘other’ and often as significantly different from the majority (white) population (see Chapter 3). Our training package (‘Life after death: supporting organ donation choices for ethnic minority families’) therefore aimed to challenge the sometimes fixed notions of faith, culture or ethnicity that were discussed during the interviews.
Running through the package is a portrayal of ethnic groups as heterogeneous and to be understood by the audience as fluid rather than static. We aimed to achieve this through providing culturally relevant background information, with an emphasis on differences both within and between minority ethnic groups, as well as generic skills in providing patient- and family-centred care. This corresponds with a broad approach to what is often referred to as ‘cultural competence’ which emphasises the importance of individual’s confidence, motivation and skills in achieving what Cooper and Roter114 describe as ‘the ability of individuals to establish effective interpersonal & working relationships that supersede cultural difference’. This is therefore closely aligned with notions of patient-centred care that involves acquiring some background knowledge of a specific cultural group, together with attitudes and skills that are universally relevant. 115 This contrasts with the more traditional concept of the provision of ‘culturally fitting care’ that involves matching a person’s needs based on an understanding of the clients’ culture in terms of caring actions, health-care information and knowledge particular to each culture. 116 Such a ‘fact file’ approach to assumed cultural characteristics of ethnic groups fails to capture the diverse and fluid nature of culture and ethnicity and may lead to reifying existing racial categories rather than achieving the intention of deconstructing barriers to health care. 117,118
Structure of training package
We structured the training package around five ‘dimensions’ identified in the hospital study as key aspects of the interaction with families that presented particular challenges to staff in providing end-of-life care. These can be viewed as generic issues that apply across ICUs and are therefore likely to have generalisability and longevity. The five ‘DonaTE dimensions’ were:
-
emotional expression, in terms of specific expressions of emotion when told their relative would not live and how to respond to this
-
faith, religion and cultural beliefs, in terms of uncertainty about any specific end-of-life requirements or practices in relation to the body that might be required, and how to ask families about these and faith-based needs and concerns regarding organ of donation
-
extended family and visitors, in terms of considering issues that may arise regarding large numbers of visitors and the need to establish the core family group which may differ from the traditional formal hierarchy of biological relationships
-
language and communication, in terms of ensuring a clear understanding on both sides, and when English was not a first language, and how interpretation could be organised if required
-
knowledge and anxieties about organ donation, in terms of awareness of common myths and misconceptions with advice on how to address these and who to ask or discuss with.
Application of Ajzen’s theory of planned behaviour
Our approach to behavioural change was informed by Ajzen’s TPB. 27 This is a social cognition model that has been widely employed to predict health behaviours and is regarded as a powerful and predictive model. 119
The TPB views practices as influenced by intentions that, in turn, are a product of three sets of factors:
-
whether or not the person is in favour of doing it (‘attitude’)
-
how much the person feels social pressure to do it (‘subjective norm’)
-
whether or not the person feels in control of the action in question (‘perceived behavioural change’).
By changing these three ‘predictors’, it is possible to increase the chance that the person will intend to do a desired action and thus increase the chance of the person actually doing it (Figure 6).
The TPB constructs form a set of cross-cutting themes that framed the content of each of the five DonaTE dimensions and targeted attitudes, beliefs about social norms and self-efficacy in managing the manifestations of each dimension.
For example, in terms of ‘emotional expression’ the DVD sought to:
-
change the participants’ attitude to different forms of emotional expression, by explaining the varied and unpredictable range of emotional responses to being informed about withdrawal of treatment or brain stem death and encourage acceptance of the full range of emotional response as normal within cultural and ethnic groups (attitudes)
-
emphasise the importance of a team approach and identify the role of nurses in supporting families in these situations (subjective norms)
-
provide advice to encourage within participants the belief that they possessed the skills and knowledge to manage the full range of emotional expression they may experience in responding to patients from minority ethnic communities.
There were many strong examples for all dimensions that could not be included owing to time constraints. However, the final content was viewed as conveying the practicalities, and, importantly, the care with which the consultants and nurses support families at times of acute bereavement, and also recognised that choices about organ donation are rarely a simple or easy decision for families to make.
Storyboard to screen
Having developed our approach to the training intervention we produced a detailed storyboard that aimed to have clear messages. Following interviews we selected a production company with previous experience of working with academics to produce DVDs for dissemination, training and teaching.
The company and the research team worked together on further development of the storyboard, with a key challenge being to simplify messages while retaining intended meanings. The research team also had at least one member present during recordings which enabled us to observe the potential content, and if necessary adjust questions asked of talking heads. The DonaTE team then reviewed the interview material and first edited line by line and made suggestions for material to be included, as well as discussing the content and key messages with the director to ensure that the edited content reflected our intended messages. We also invited several health-care professionals and members of the public with experience of transplantation or end-of-life care to view an early edit of the DVD and provide any comments, with these contributing to the final version.
Each of the five dimensions used a ‘talking heads’ approach, in which a person talks to the camera with their head and upper body visible on screen and giving the impression that the person is directly talking to the audience. Rather than relying on actors we mainly drew on health professionals as ‘talking heads’ (two consultants, two ICU nurses, one SNOD, four hospital chaplains of different faiths and three lay people with experience of transplantation or organ donation) as they were able to recount their own personal experiences and reflections and provide authentic voices. All talking heads came over as warm, caring and approachable. They also expressed the value of providing appropriate support to families and for the ICU staff to work as a team to ensure that a family’s needs are identified and that as far as possible these are met. In addition, they also emphasised that staff need to take a non-judgemental approach and stressed the importance of looking beyond a specific identity (e.g. faith or ethnic group) and being aware of the similarities and differences within and between groups.
Components of the professional development package
The package has three components:
-
A core factual programme (30-minute DVD): this addresses issues of ethnicity and needs for transplantation, followed by discussion relating to each of our five DonaTE dimensions. The latter emphasises the three influences on behavioural intentions of attitude towards the behaviour, subjective norm and perceived behavioural change (see Figure 6). This includes contributions by consultants, nurses, specialist nurses, hospital chaplains, transplant patients and families that are structured by a medical presenter who guides the audience and recaps on the key messages. These messages are summarised for each dimension in Box 4.
This addresses the five DonaTE dimensions.
1. Emotional expression – people respond in different ways to acute grief; some individuals and families rarely show their grief outwardly, whereas others may engage in loud crying or wailing and sometimes show physical anguish through for example banging their head.
What you can do – supporting individuals and families requires being prepared for a range of reactions and allowing individual expression while ensuring safety and a lack of harm.
2. Faith, religious and cultural beliefs – no faith prohibits organ donation but there are many different views and beliefs at a community level, and many myths and misconceptions exist. Some people believe that donation is not permitted by their faith or are uncertain about the requirements of their faith, with such views forming a significant factor in organ donation decisions. For some families (or family members) it is also important to fulfil specific faith or cultural practices at or around the time of death.
What you can do – avoid making assumptions regarding individuals’ faith and cultural beliefs, as people of the same faith may differ in their understandings and the significance of faith and culture for them. There is therefore a need to identify their beliefs and provide information required to make informed choices. This may involve asking families if they would like a chaplain to visit them or their relative and also when possible facilitating particular faith-based requirements.
3. Extended family and visitors – both the immediate family and often other visitors wish to visit the patient in the ICU. If this involves a large number of people at any one time this may need to be managed both to retain access for key family members and to limit disruption to staff, other patients and their visitors.
What you can do – work with the family to ensure appropriate access to the patient for family members and other visitors. Practical arrangements may involve a rota for visitors, or using a password to access the patient. It is important to identify (rather than assume) who are the key decision-makers in relation to consent to donation and to ensure their close involvement.
4. Language and communication – staff and family communication needs to be clear and technical terms avoided or explained clearly to avoid misunderstandings and particularly when English may not be a first language. Good communication also requires establishing a rapport and building trust.
What you can do – check that key family members or decision-makers understand the information they have been given. One technique is to ask then to explain to you what they understand about the patient’s condition and prognosis. The development of a rapport and trust is also influenced by frequent updates, the consistency of communication (and communicator) and exploring and responding to fears and concerns.
5. Anxieties about organ donation – organ donation generally raises many questions and anxieties for the family. The unfamiliar environment of ICU and often the unanticipated situation often exacerbates these. Key issues for relatives often relate to whether or not donation will delay the funeral and if donation is compatible with treating the deceased with dignity and respect.
What you can do – answer the families’ questions, or find another person who can, such as the SNOD who has detailed knowledge regarding organ donation.
-
Three-part structured drama (10-minute DVD): this aims to reinforce the five dimensions and provides a more detailed understanding of families’ experiences by dipping in and out of a longer-term narrative. Each of the dimensions discussed in the main programme were therefore subtly included in key conversations. The family drama portrays the consultant, SNOD and ICU nurse preparing to talk to the family, followed by the breaking of bad news and the family talking about organ donation. This short drama provides the audience with an opportunity to think about the perspective of the family as whole and in relation to individual family members. We were aware of a perception that people from Islamic backgrounds are least likely to consent to organ donation for a range of personal, faith and cultural reasons and therefore chose to depict a Pakistani Muslim family. The family was played by six actors who portrayed a young woman whose husband was shown in an ICU bed being cared for by a nurse, his brother, her parents and a person referred to as ‘uncle’.
-
Workbook for self-learning: this contains background information about organ donation that depicts the potential outcome as worthwhile in terms of increased organs for transplant, thus justifying a positive attitude (see Appendix 11). The worksheets also asked participants to reflect on the content of the DVD and their own experience, with the aim of assisting ICU staff in recognising and developing their own skills and competence to achieve high-quality individualised end-of-life care across cultural groups on their own units. The final worksheet then asked the participants to devise short-, medium- and longer-term aims to help put these aims into practice, thus targeting perceived behavioural change. An example might be to find out more about the faith and cultural backgrounds of the patients from the majority and minority ethnic, faith or cultural groups they most often see in ICUs, with this varying across the UK.
Pilot evaluation
Sessions to trial the DVD were held with small groups of mainly four to eight ICU staff (range 2–12) from December 2012 to June 2013. Participants were initially given an information sheet and completed a consent form and a baseline TPB questionnaire (see Appendix 12). It was not possible for staff to view and undertake the full package owing to time constraints. Only 1-hour time slots were available, and about 20 minutes of this time was taken up with completing consent forms and the baseline TPB questionnaire. Therefore, following a brief introduction by the facilitator (MM or researcher) the participants viewed the main DVD programme. This was followed by a short discussion of the material run by the facilitator and completion of a feedback form. Three months later the participants received the follow-up TPB questionnaire electronically.
In practice, it was very difficult to recruit participants, particularly as educational sessions had been cut back and duty nursing staff are often engaged in one-to-one care and then go directly home at the end of their shift. The unpredictable demands of ICUs also presented difficulties, and on several occasions we had arranged a session and turned up at the ICU only to find all the staff were occupied by an emergency. Staff were also sometimes bleeped and had to leave midway through the session. However, for the future, the aim is for the package to form part of ICU training when it will be feasible to show and discuss both the main video and family drama, and undertake exercises in the workbook.
In total, the training intervention was provided to 99 participants across 15 sessions and included nurses, SNODs, consultants and other doctors (see Table 12).
Outcomes
Feedback questionnaires
Methods
The one-page feedback questionnaire comprised six structured questions with 7-point Likert scales and two open answer questions, plus questions on the respondents’ experience of organ donation and job category (see Appendix 12). Responses on the Likert rating scales were categorised as positive (rating 5, 6 or 7), intermediate (rating 4) and negative (rating 1, 2 or 3) (the scale was flipped around for questions 3, 4 or 5 to take account of the difference in wording).
A total of 66 participants completed feedback forms at the end of the session. Respondents comprised a mix of bedside nurses of various grades (bands 3–7), student nurses, SNODs and doctors (a mix of consultants, specialist registrars and training grades). Apart from the SNODs and consultants, few had any experience of organ donation.
Findings
Altogether, 83% of responses to the structured questions were positive, 11% intermediate and 6% negative. The only question with < 82% positive responses related to the length of the session, with only 65% regarding this as ‘about right’ and 31% as too long (Table 11).
| Questions and grouped responses | All (n = 66) | Nurse (n = 28) | Student nurse (n = 10) | SNOD (n = 13) | Doctor (n = 15) |
|---|---|---|---|---|---|
| 1. How much of the session was relevant to your work on ICU?a | |||||
| Positive | 60 (92%) | 27 (96%) | 10 (100%) | 11 (92%) | 12 (80%) |
| Intermediate | 3 (5%) | 0 | 0 | 1 (8%) | 2 (13%) |
| Negative | 2 (3%) | 1 (4%) | 0 | 0 | 1 (7%) |
| 2. Will the training session be useful in your work on ICU?a | |||||
| Positive | 53 (82%) | 24 (86%) | 10 (100%) | 10 (83%) | 9 (60%) |
| Intermediate | 3 (5%) | 1 (4%) | 0 | 0 | 2 (13%) |
| Negative | 9 (14%) | 3 (11%) | 0 | 2 (17%) | 4 (27%) |
| 3. Was the session presented clearly by the facilitator?a | |||||
| Positive | 55 (85%) | 23 (82%) | 10 (100%) | 11 (92%) | 11 (73%) |
| Intermediate | 8 (12%) | 3 (11%) | 0 | 1 (8%) | 4 (27%) |
| Negative | 2 (3%) | 2 (7%) | 0 | 0 | 0 |
| 4. Was the film content clear and easy to understand? | |||||
| Positive | 59 (89%) | 26 (93%) | 10 (100%) | 12 (92%) | 11 (73%) |
| Intermediate | 4 (6%) | 2 (7%) | 0 | 0 | 2 (13%) |
| Negative | 3 (5%) | 0 | 0 | 1 (8%) | 2 (13%) |
| 5. Was the length of the session | |||||
| Too long (negative) | 20 (31%) | 3 (11%) | 2 (20%) | 4 (31%) | 11 (73%) |
| Just right (positive) | 42 (65%) | 23 (85%) | 7 (70%) | 8 (62%) | 4 (27%) |
| Too short (negative) | 3 (5%) | 1 (4%) | 1 (10%) | 1 (8%) | 0 |
| 6. Has the session made you think about supporting next of kin?a | |||||
| Positive | 53 (82%) | 26 (93%) | 10 (100%) | 8 (67%) | 9 (60%) |
| Intermediate | 6 (9%) | 1 (4%) | 0 | 2 (17%) | 3 (20%) |
| Negative | 6 (9%) | 1 (4%) | 0 | 2 (17%) | 3 (20%) |
Examples of free answer comments given by nurses to the question of ‘What aspects of the training were well done?’ were:
the video was very interesting, especially the look at different faiths.
Nurse
Religious faiths – made me think about utilising faith leaders for advice.
Nurse
Covered several actual problems I have encountered re [regarding] next of kin and end of life/communication
Student nurse
As a student nurse we come across a lot about end of life care and been left to deal with patients’ relatives fears on our own sometimes don’t know what to do just observing.
Student nurse
I would love to be added to a mailing list for future training/or conferences regarding organ donation. I have enjoyed today’s session – thank you.
Student nurse
Specialist nurses for organ donation comments mainly related to the value for training purposes:
Clear and concise. Perfect for those new to ICU.
Very clear with good parts.
Clear, useful, inoffensive film.
Doctors also noted that the video provided a good introduction and covered important aspects simply and clearly. Particularly positive aspects identified were the ‘broad range of opinions/professional participants’, ‘dealing with sensitivity of handling the family’, ‘the belief of different faith groups’, and ‘the video of donor recipients’.
Negative comments mainly related to the length of time required to complete the baseline TPB questionnaire and what was seen by some as the confusing mix of positive and negative statements in this questionnaire. However, some nurses indicated that they would have liked a longer training session, which is envisaged when the full package is employed.
A further indicator of the quality of the presentation was the nomination of the DVD for a national Learning on Screen award, 2014, in which it was highly commended.
In summary, feedback ratings were high for relevance, usefulness and clear presentation by all professional groups. Nurses also commented that it filled an important gap for them, and both SNODs and doctors commented on its value for training.
Before-and-after evaluation of changes in theory of planned behaviour constructs
Methods
Development of the TPB questionnaire for the evaluation followed the manual for TPB questionnaire construction. 120 This requires that the four constructs of attitudes, subjective norms, perceived behavioural change and behavioural intentions are populated with questions of relevance for the study, with each question using a 7-item Likert scale (Appendix 12).
Analysis for the TPB questionnaire comprised five stages: (1) description of the characteristics of participants; (2) exploration of the psychometric properties of the scale; (3) descriptive analysis of TPB variables; (4) exploration of change in TPB variables; and (5) exploration of relationships between TPB variables.
Findings
Pre-intervention sample
The intervention sample comprised 58 bedside nurses, 22 doctors, of whom half were consultants, and 19 SNODs (Table 12). On average the SNODs had spent the greatest time working on an ICU and bedside nurses the least. Altogether 57 were of all forms of Christian faith, with small numbers of other faiths, 14 were agnostic/atheist or Pagan and 20 did not identify a religion or faith. There was also a mix of ethnicities and people born in UK or abroad, particularly among bedside nurses (see Table 12).
| Characteristics | SNODs (n = 19) | Nurses (n = 58) | Doctors (n = 22) |
|---|---|---|---|
| Length of time working on this ICU (months) | |||
| Mean (SD) | 4.3 (3.6) | 3.0 (8.6) | 3.8 (6.2) |
| Range | 0–12 | 0–20 | 0–26 |
| Length of time working on any ICU (months) | |||
| Mean (SD) | 10.8 (8.1) | 3.0 (6.1) | 7.2 (7.1) |
| Range | 2–35 | 0–27 | 0–27 |
| Religion or faith | |||
| Agnostic/atheist/Pagan | 4 | 7 | 3 |
| Christian (all forms) | 10 | 33 | 12 |
| Buddhist | 0 | 0 | 1 |
| Hindu | 0 | 1 | 2 |
| Islam | 0 | 2 | 0 |
| Judaism | 1 | 1 | 0 |
| Sikh | 1 | 1 | 0 |
| None stated | 3 | 13 | 4 |
| Country of birth | |||
| UK | 13 | 47 | 20 |
| Other | 6 | 11 | 2 |
| In the last 3 months I have . . . | |||
| Supported the next of kin during end-of-life care | 18 | 27 | 20 |
| Been involved in the care of an organ donor | 19 | 10 | 14 |
Exploration of psychometric properties of the theory of planned behaviour scale
The TPB questionnaire was designed to encompass six subscales reflecting the constructs in the TPB as follows:
-
attitudes towards organ donation
-
subjective norms – normative beliefs about subjective norms
-
subjective norms – motivation to comply with subjective norms
-
perceived behavioural change – control beliefs
-
perceived behavioural change – influence of control beliefs
-
behavioural intentions.
An item analysis of each subscale was conducted for the data from the pre-intervention completion of the scale (n = 99) according to the procedure suggested by Anastasi. 121 Specifically, for each subscale, items that were, at the design phase, identified as reverse scored were scored in that way. Corrected item-total correlations were then calculated for items within the scale in order to identify items that appeared to be inconsistent with the scale (defined as a corrected item-total correlation < 0.3). Cronbach’s alpha for the scale including the remaining items was calculated to determine the internal consistency of the scales. Scale scores were calculated by summing the items that made up each scale and dividing by the number of items in the scale.
All subscales achieved a satisfactory level of internal consistency (see Appendix 13). However, lower levels of internal consistency were found for the subscale assessing perceived beliefs about subjective norms and beliefs about the individual’s ability to control the behaviour of talking about organ donation. Overall, the subscales were found to have satisfactory levels of internal consistency and were used as the basis for analysis of the impact of the intervention.
Pre-intervention subscale scores of participants by professional group
The pre-intervention scores for participants in three occupational groups were compared (see Appendix 14). Significant differences between the groups emerged for four subscales:
-
SNODs had the most positive attitudes towards organ donation among individuals from minority ethnic communities, whereas the other nurses were the least positive.
-
All three groups had similar levels of belief about the subjective norms in regard to seeking organ donation from minority ethnic communities. However, both SNODs and nurses expressed high levels of willingness to comply with such norms, with doctors being less willing overall.
-
All three groups expressed high levels of understanding of their role in seeking consent for donation but the SNODs felt more positive that those beliefs would influence their behaviour, probably reflecting their specialist role in family discussions.
-
Intentions to seek consent for organ donation from individuals from minority ethnic communities were highest among the SNODs and nurses and significantly lower among doctors.
Pre- and post-intervention responses to the theory of planned behaviour questionnaire
The follow-up questionnaires were distributed electronically [via SurveyMonkey® (www.surveymonkey.com)] 3 months following the initial session and sent out in March–September 2013.
The 3-month follow-up responses were received from only 21 of the 99 intervention participants (21%). They comprised 12 nurses of the 77 SNODs (21%) and 9 doctors of the 22 (41%). No SNODs completed the follow-up questionnaire. Scores for initial and follow-up questionnaires for TPB sets of factors are shown for the nurses (see Appendix 15) and doctors (see Appendix 16).
For both bedside nurses and doctors, the only significant change following training was in attitudes towards seeking organ donation from individuals from minority ethnic communities, with both professional groups being more positive in their attitudes following training.
There are several possible reasons for why only attitudes changed following the intervention:
-
The intervention was designed as a three-part package with the DVD designed to address attitudes and knowledge, whereas the interactive elements and planning components were designed to change perceptions of behavioural control and subjective norms. Unfortunately, given the time pressure on staff and the length of the DVD, it often proved impossible to include the more interactive elements and planning components in the time allocated for the training.
-
It is highly likely that the participants had no opportunities to change the way that they thought about and practised seeking organ donation over the 3 months, as seeking organ donation is a rare event and even rarer where consent is sought from an individual from a minority ethnic community.
-
The lack of impact may also partly reflect awareness on the part of participants of the structural barriers to practising what they learned from the intervention.
Correlation of theory of planned behaviour constructs with behavioural intention
To explore the relationship between the components of the TPB and behavioural intentions, Spearman’s correlations were calculated across the participants at the pre-intervention stage (Table 13).
| TPB constructs | Correlation with behavioural intention |
|---|---|
| Attitudes towards organ donation | 0.27 (p = 0.007) |
| Subjective norms – normative beliefs about subjective norms | 0.36 (p < 0.001) |
| Subjective norms – motivation to comply with subjective norms | 0.30 (p = 0.002) |
| Perceived behavioural change – control beliefs | 0.03 (p = 0.765) |
| Perceived behavioural change – influence of beliefs | 0.18 (p = 0.081) |
Attitudes towards organ donation and the subjective norm components were predictive of intention to seek consent for organ donation, which further suggests that the impact on practices may increase over time.
Outcomes for consent rates
The PDA, which is completed by the SNODs at each hospital to record the numbers and outcomes for eligible donors, was used to examine the impact of the intervention on family consent rates.
Methods
Routine data
Potential Donor Audit data were provided by NHSBT for two time periods, pre intervention (December 2011–November 2012) and post intervention (June 2013–May 2016), for six study sites (four London study sites, one West Midlands and one East Midlands) together with aggregated data for all other hospitals in London, West Midlands and East Midlands strategic health authorities. These data identified numbers of eligible donors, numbers of eligible donors whose families were approached and numbers of eligible donors whose families gave consent for three ethnic categories: white, BAME (black and Asian) and not known.
Analysis
These data were first aggregated for the four individual intervention hospitals in the London region to give three regions. The proportions of donor families who (1) were approached as a percentage of those eligible and (2) gave consent as a percentage of those approached were calculated. Summary data were then calculated by ethnicity and time period. Individuals whose ethnicity was recorded as ‘not known’ were not included in any analysis owing to the small numbers (3% for the proportion approached and 1.5% for the proportion who gave consent).
Simple differences in proportions were calculated to summarise the changes in rates pre and post intervention in the different regions and ethnic groups. A mixed-effects model was employed to estimate the effect of the intervention while allowing for regression to the mean (intervention vs. control regions) and ethnicity. For this analysis we fitted normal errors two-level regression models to the proportion approached and the proportion that gave consent. The distribution of the residuals was confirmed to be normal. Region fitted as a random effect and time period (pre/post intervention), ethnicity (white/BAME) and intervention/control were modelled as fixed effects. An interaction test was used to determine whether or not there was a difference in the time period effect by ethnic group. Results are presented as difference in proportions (as percentages) with 95% confidence intervals (CIs).
Results
The numbers of eligible donors and families approached decreased slightly between the pre- and the post- intervention periods for both the white and BAME populations, whereas the consent rate among those approached increased, with the increase being particularly large for the BAME population [(11 percentage points increase in consent compared with nearly 7 percentage points among the white population (Table 14)].
| Ethnicity | Time period | Eligible number | Approached | Family consented | ||
|---|---|---|---|---|---|---|
| Number | % eligible | Number | % approached | |||
| White | Pre | 891 | 625 | 70.1 | 363 | 58.0 |
| Post | 1185 | 762 | 64.3 | 494 | 64.8 | |
| BAME | Pre | 229 | 162 | 70.7 | 48 | 29.6 |
| Post | 289 | 197 | 68.1 | 80 | 40.6 | |
| Not known | Pre | 91 | 36 | 39.5 | 11 | 2.7 |
| Post | 99 | 18 | 68.1 | 4 | 22.2 | |
| Total | Pre | 1211 | 823 | 67.9 | 422 | 51.2 |
| Post | 1573 | 977 | 62.1 | 578 | 59.1 | |
For white families approached, there was an improvement in consent rates from pre to post intervention in both the intervention (three percentage points increase) and the control hospitals (8 percentage points increase). The increase in rates was more marked in the BAME families, with an increase of 12 percentage points (intervention) and 10 percentage points (control). Neither the increase in the intervention nor the increase in the control hospitals was statistically significant (p = 0.15 and 0.11, respectively) (see Appendix 17).
We believe the observed similarity of consent rates in the intervention and control groups among the BAME might have been partly explained by contamination of the control sites, given the considerable movement of SNODs between study sites and our presenting the DonaTE project at regional meetings of SNODs. In addition, a number of local initiatives focusing on increasing donation rates among the BAME community were taking place at hospitals across the study regions.
A post-hoc analysis was therefore conducted to pool the intervention and control hospitals. This showed that the pooled change from pre to post intervention was statistically significant (pooled difference 11%, 95% CI 1.2% to 21%; p = 0.03). However, this must be interpreted cautiously as this is a subgroup analysis and does not allow for either the variations between regions or, importantly, regression to the mean (i.e. the possibility that rates would have increased with or without the intervention because of some other factor).
When the approach rate was modelled, this showed no firm evidence for a difference between the intervention and the control areas (difference in percentages 4.5%, 95% CI –5% to 14%) after adjusting for the time period and ethnicity (Table 15). Overall, the approach rates were lower after the intervention when other factors were allowed for and this was borderline significant (difference –8.4%, 95% CI –17% to 0.2%). The analysis confirmed the difference in approach rates between the white and the BAME donors (difference –8.4%, 95% CI –17% to 0.2%).
| Predictor variable (fixed effects) | Adjusted difference in percentages | 95% CI | p-value |
|---|---|---|---|
| Approach rate | |||
| Intervention – control hospital | 4.5% | –5.0% to 14.0% | 0.35 |
| Post intervention – pre intervention | –8.4% | –17.0% to 0.2% | 0.055 |
| BAME – white ethnicity | –8.4% | –17.0% to 0.2% | 0.055 |
| Consent rate | |||
| Intervention – control hospital | –6.3% | –18.6% to 6.0% | 0.31 |
| Post intervention – pre intervention | 7.2% | –4.0% to 18.5% | 0.21 |
| BAME – white ethnicity | –26.1% | –37.3% to –14.8% | < 0.001 |
In the model for the consent rate, the period effect was quite large, 7.2 percentage points (95% CI –4.0% to 18.5%), but this was not statistically significant after allowing for the variations in regions, the difference between the intervention and the control hospitals, and ethnicity. The interaction effect for the period effect by ethnicity was tested but was not significant (p = 0.54). There was, therefore, no statistical evidence that the period effect varied by ethnic group and so further subgroup analysis is not permitted. The analysis again showed the large effect of ethnicity with –21 percentage points difference in mean rates (95% CI –4.0% to 18.5%; p < 0.001). The multivariable analysis, therefore, while not conclusive, is suggestive of an intervention effect of approximately 7 percentage points with an upper confidence limit of 19%.
Conclusions
Piloting of the intervention was limited to the main DVD together with a brief introduction by the facilitator to the training package at the beginning and a short discussion at the end. This limited version was used, as it was necessary to complete consent forms and baseline questionnaires plus the training and feedback within the 1-hour slots available.
Our interim findings based on this limited version indicate that the training package is acceptable and useful to ICU staff and that when fully implemented is likely to impact on staff practices and to be associated with significantly increased donation rates among the BAME families. However, our experience emphasises the difficulties of evaluation that often occur in a real-world situation, reflecting the combination of time constraints, staff changes and low returns of follow-up questionnaires, contamination between intervention and control groups, and the effects of external influences such as other BAME activities. For the future, further evaluation should be undertaken with the full package.
Although the training package was designed for bedside nurses there has been considerable interest in its use by hospital chaplains as part of the development in their professional training. Several community organisations have also asked to include the main DVD in their discussions of organ donation to inform their audience about donation and transplantation, and emphasised the value for recipients, particularly in addressing community issues of trust in health professionals and the health system. We expect use by different audiences will increase following its availability on the National Institute for Health Research (NIHR) YouTube (YouTube, LLC, San Bruno, CA, USA) website at (www.youtube.com/watch?v=ueaR6XYkeVM&feature=youtu.be).
Chapter 6 Discussion of all elements
We have successfully completed a programme of research that responds to the challenge set out by the ODT on the need to understand and promote organ donation among the general public and specifically the BAME population. 4 Our work has examined issues relating to both the ODR and family consent among minority ethnic groups, with findings presented to formal bodies including an All-Party Parliamentary Committee and public engagement events as well as disseminated through academic publications and conferences (see Dissemination). The research programme has also produced the first training package in cultural competence in the NHS with this forming a key outcome.
There were many challenges in conducting this programme of research, particularly as it involves multiethnic- and ICU-based research. We resolved most of the challenges with time and innovative approaches but also recognised that there were limitations to what was practically feasible. We have therefore drawn on our experience of the realities of conducting the research with the aim of offering some guidance for future research in this or related areas in which similar issues may arise. We then provide an overview of the findings across the various community- and hospital-based studies and provide recommendations for future research.
Reflections on methods
The research involved substantial qualitative research to examine both public and professional perspectives, including 22 focus groups with different ethnic and age groups to examine attitudes and beliefs regarding organ donation, and ICU-based research involving observation and interviews with range of professional groups across five trusts, together with systematic reviews. The findings of the various studies were then drawn on to develop and undertake a preliminary evaluation of a DVD-based professional development package.
This section briefly considers four main challenges presented by the research and how these were addressed.
Recruiting minority ethnic groups
This was a particular challenge for the focus group study, with each focus group session requiring the participation of about eight people from a particular ethnic and age group, with separate groups for older (≥ 40 years) and younger (18–40 years) age groups. We achieved recruitment in our specified categories through recruiting in areas with a high multiethnic population and employing a specialist company who had local fieldworkers in different areas of London. We also ensured that the focus groups were held in easily accessible locations, with access to bus routes, and expenses of £25 were offered to participants. This seemed an appropriate level of reward to attract interest but not to unduly influence recruitment, with many attending because of their interest in finding out more about the topic.
However, recruitment in multiethnic areas influenced the characteristics of the sample, which was characterised by a preponderance of first-generation migrants and manual socioeconomic groups. Analysis of the significance of socioeconomic position was thus limited by the participation of a relatively small number of people in managerial and professional occupations, while multiethnic communities in London may also not necessarily be representative of other communities in different parts of the country.
Conducting 22 focus groups across five ethnic groups and engaging participants in a discussion of knowledge and attitudes to deceased donation was in itself a considerable achievement. However, for future research a greater geographic and socioeconomic spread is important and could be achieved through recruiting employees of large organisations, including NHS trusts and large companies rather than taking a community-based approach.
Discussing an unfamiliar topic
It was difficult to discuss registration as an organ donor, as this is rarely a topic for either public or private discussion and is one about which participants had little knowledge. We therefore revised the topic guide and provided some basic information to ensure that everyone had a certain necessary level of knowledge about each topic. We also developed vignettes to focus and guide the discussion.
Vignettes involving short scenarios have mainly been employed in quantitative research to explore respondents’ preferences and choices. There was, therefore, little guidance available on practical aspects of developing and using vignettes in qualitative research when they have mainly been employed as an ‘icebreaker’ rather than as a tool to facilitate discussion of the unfamiliar. The approach we adopted involved fairly simple vignettes in which two participants (who were given names to reflect the ethnicity of the particular focus group participants) were depicted as holding differing views. Two vignettes relating to registration as a donor were very successful in stimulating a focused discussion. However, vignette fatigue then seemed to occur, which may have been influenced by the fact that the third vignette involved a rather different situation of family consent at a hospital level and, therefore, required new information. The participants also found difficulty in thinking past their worry of whether the patient would be really dead or might recover. The use of an alternative form of stimulus material would therefore probably have been better in this context, although moving from the community level to the hospital situation was probably too big a shift in the circumstances.
It is possible that a group approach resulted in some bowing to social pressure among participants to unite opinion. However, clear differences between group members were also evident and the vignettes often promoted quite animated discussions. Overall we felt that the group approach was preferable in researching this unfamiliar and rarely discussed topic, with members gaining support from each other and debating topics, whereas one-to-one interviews in this situation might have led to embarrassing and non-productive situations.
Conducting research within intensive care units
Gaining the participation of ICU staff in the research required considerable time in liaising with both medical and nursing ‘gatekeepers’, including CLODs, team and regional leads for SNODs, and matrons. Initially we probably did not allow sufficient time for these conversations or for follow-up contact prior to data collection.
Not surprisingly there were differences in the level of co-operation and support for the research between sites. At some sites we experienced a very high level of support for interviews, and clinical and nursing staff also generously participated in the video as ‘talking heads’. At other sites participation in the research was much more difficult to organise as reflected in our decision to add a new site (sixth site) to complete the EDGs and evaluate the intervention.
The main phase of the research involved two researchers spending 3 weeks at each site (NHS trust). This provided flexibility in conducting interviews and the opportunity to gain familiarity with the culture and practice of ICUs. However, some senior staff found it difficult to make time for the interviews alongside their other duties and others were not sufficiently interested in organ donation to take part. Conducting interviews with ICU nurses was also particularly difficult owing to their job demands. Those in bedside nurse roles often provide care on a one-to-one basis within ICU units and go home directly following a shift. Interviews with nurses were therefore often conducted while patients were undergoing diagnostic tests off the unit, or between discharge and admission of patients. On several occasions when the researchers had arranged to interview nurses this was not possible because of pressures on the unit. However, despite these various difficulties, we conducted 108 interviews across the five study sites.
The EDGs required attendance at fixed sessions and therefore proved more difficult to organise. This reflected the realities of ICUs in terms of the unpredictable nature of the work and one-to-one nursing. Some planned sessions for EDGs, therefore, had to be cancelled at the last minute because of emergency admissions, which significant increased the fieldwork time. Professor Farsides noted that setting up EDGs with ICU staff (particularly doctors and nurses) proved far more difficult than in any other health service situation in which she has previously undertaken this method.
Cutbacks in protected educational sessions for nursing staff occurred during the project and presented particular difficulties for evaluation of the training package. The research requirement to complete baseline questionnaires that operationalised the TPB took at least 15 minutes, with the time left in a 1-hour session therefore being sufficient only to introduce the main programme, show the programme and have a brief discussion. This reality of limited time was not fully expected. Further difficulties occurred in relation to the follow-up TPB questionnaire, with nurses leaving for new posts and lack of e-mail access at work contributing to the low response rate to the follow-up questionnaire, together with the general problems associated with a relatively long questionnaire required by the TPB.
Our experience to some extent reflects more general differences between research in community and research in organisational settings. However, the nature of ICU work also means that staff have very particular job demands.
Recruiting for the bereaved family study
A very small number of ethnic minority families are approached for donation, with only 96 black and minority ethnic families approached for consent to organ donation in the UK in 2009/10. It was therefore necessary to go beyond the London hospitals to obtain a sample, and we approached a total of 40 sites (hospital trusts). R&D approvals were undertaken for these additional sites through the PIC system that had been set up to simplify the R&D process. However, trusts often lacked knowledge of how the PIC system worked, which created substantial delays. There was also a lack of consistency by trusts in the information requested from SNODs, such as obtaining their curriculum vitae or obtaining signatures from senior staff. A large number of regional groups also required the researchers to attend a meeting to describe the study and requirements for recruitment.
On average we needed to call each trust three times for them to be aware of the study or answer queries and to follow-up on progress. Many trusts also did not know they had to upload the final approval letter required for full approval and to begin data collection. The time for PICs to be approved by individual trusts was between 2 weeks and several months (see Chapter 4).
A further unexpected difficulty arose in recruiting non-consenting families. Whereas prior UK research had involved both consenting and non-consenting families (Sque M, Walker W, Long-Sutehill T, Morgan M, Randhawa G, Warrens A. Bereaved Families’ Experiences of Organ and Tissue Donation, and Perceived Influences on their Decision Making. University of Wolverhampton; 2013, unpublished),109,122 NHSBT’s governance procedures and protocols do not allow retention of the details of non-consenting families. These families could not, therefore, be identified retrospectively and approached for the study. After much discussion with NHSBT, we followed a recommended prospective study procedure. This was time-consuming to set up as it involved an ethics amendment and attending regional team meetings to request the participation of embedded SNODs working in participating NHS trusts and to brief them on the process and disseminate recruitment packs.
The prospective approach was time-consuming and not surprisingly the SNODs often felt uncomfortable about asking families who had declined to consent if they would be willing to receive information about the research. In total, 74 recruitment packs were sent out, including nine to non-consenting families, but this did not result in the participation of any non-consenting families. Our experience is similar to that of a recent bereaved family study with the white population, which also undertook the recommended prospective approach without success (Sque M, Walker W, Long-Sutehill T, Morgan M, Randhawa G, Warrens A. Bereaved Families’ Experiences of Organ and Tissue Donation, and Perceived Influences on their Decision Making. University of Wolverhampton; 2013, unpublished).
Overview of studies
The next sections describe the three groups of studies, the community studies, the hospital-related studies and the intervention for ICU staff, and consider the links and integration between studies.
Community studies
This phase involved three linked studies: a systematic review of barriers to registration as a donor, a focus group study and a further systematic review of effective interventions to increase donation rates.
The first systematic review highlighted issues that were examined in more detail in the focus groups, including the reasons for the consistent finding of low knowledge, and the variations in bodily concerns and faith beliefs regarding donation among different ethnic/faith and age groups. The focus group findings regarding the large group of people at a pre-contemplation stage and the small numbers of other people who were further along the donation pathway also raised issues for effective interventions in relation to different locations along the donation pathway that were considered in the second systematic review.
Knowledge
Both the systematic review of barriers to organ donor registration among minority ethnic groups in the UK and USA and the focus group study identified low knowledge about organ donation and registering as a donor as a key barrier. This occurred despite recent campaigns in the UK that aimed specifically to promote organ donor registration among minority ethnic groups. People often remained at an initial ‘pre-contemplation stage’, with organ donation not being something they had thought about. However, our research went beyond merely reporting on this situation, with the focus group study leading to a conceptually and empirically grounded explanation of why poor knowledge about organ donation and organ donor registration persists despite a number of targeted campaigns.
Drawing on Schutz’s64 theory of relevance we argued that the existence of large numbers of people at a pre-contemplation stage reflected a situation in which national campaigns to increase knowledge and promote registration as a donor among minority ethnic groups were not perceived as ‘relevant’ as they did not link with individuals’ stock of knowledge or priorities. The messages therefore often ‘passed them by’ as part the general filtering information that we all engage in, rather than being actively rejected. Reasons for a lack of perceived relevance were identified as including a lack of familiarity with organ donation in their home country, a belief particularly among black African men that their organs were ‘strong’ and that organ donation and transplantation were therefore not of relevance to their group, and a general view that transplantation and the need for organs was depicted in the media as largely a problem for white people.
Faith and attitudinal barriers
The focus groups confirmed and extended our understanding of attitudinal barriers to registering as a donor by identifying the significance of particular barriers for different ethnic/faith and age groups. For example, people of Islamic faith were most likely to identify uncertainties, or occasionally prohibitions, arising from their faith. However, there was also some evidence among the younger generations of their awareness of different schools of thought and the confusion that exists between religion and culture, thus identifying the heterogeneity and fluidity of ethnic groups.
Whereas ‘faith’ is often regarded as a general barrier to donation, few focus group participants from Christian, Sikh or Punjabi groups regarded their faith beliefs as a barrier. Indeed their faith often appeared to form a positive force encouraging an altruistic approach that extended to deceased donation, particularly among Sikh and Hindu participants.
Personal autonomy
A theme running through accounts by the younger generation was the increasing emphasis on individual autonomy and choice that was not constrained by religion or by the views of their elders, although this was also often accompanied by a concern to avoid family conflict and upset. These beliefs correspond with the current policy emphasis, which suggests that the family should not be able to overrule donation if the patient is registered on the ODR and has thus made their own wishes known. 15 It also identifies the fluidity and changing beliefs among ethnic groups with attitudes and beliefs of younger people associated with fewer faith/cultural barriers to deceased donation.
Effective interventions
The focus groups identified the importance of identifying the target groups’ stage of change (stage on the donation pathway) and designing appropriate interventions in relation to their circumstances.
For those at an early pre-contemplation stage on the donation pathway, the synthesis identified educational interventions (or combined educational and mass media approaches) as most effective in increasing knowledge and achieving a shift along the donation pathway, with important characteristics being a strong interpersonal element, delivered by trained members of the lay community, and including personal case studies of both donors and recipients from their own communities which address key concerns.
Other groups comprised those who were aware of the message regarding the importance of organ donation and of joining the ODR but had not acted, either because of worries and concerns or because their level of motivation was not sufficiently high to make this a priority. For example, younger men of Indian descent often explained that they had not joined the ODR because they were occupied with work and other interests and that these took priority in their lives. For this group, a small ‘nudge’, including immediate access to registration, may prompt action.
Hospital-related studies
This part of the research programme examined professional and organisational practices within ICUs that have implications for family consent to donation. This was based on detailed observational- and interview-based research undertaken on ICUs at five NHS trusts. The initial interviews with ICU staff were important in identifying issues to be examined in more detail through additional interviews (e.g. with hospital chaplains) and issues to be probed (e.g. the reasons for clinicians’ reluctance to involve SNODs), as well directing observation of SNODs’ activities.
Organisational practices
Intensive care units generally described similar challenges in relation to different ethnic/faith groups, including managing large numbers of family members and visitors, responding to language difficulties and to varying forms of emotional expression and meeting faith-based needs. Local resources, including the opportunity for engaging interpreters, the availability of facilities to cater for the wider family and visitors and the availability of hospital chaplains from different faiths, led to variations between sites in how particular needs were met.
Junior nurses
A widely held view was of a lack of training and preparation to enable them to meet the needs of families from different cultural groups. This was acknowledged to sometimes lead to hesitancy in communicating with families from different cultural groups, especially at a time of considerable emotional distress. Junior nurses also had little familiarity with the organ donation process, as this is not a common occurrence, and they welcomed more knowledge and training in these areas.
Specialist nurses for organ donation
This professional group was established following recommendations of the ODT4 and is experienced in responding to the needs of families from different cultural backgrounds reflecting its specialised role. However, its training does not specifically cover issues of cross-cultural communication or of ethnicity and donation rates/needs for transplantation and there is therefore scope to include training in these aspects.
Specialist nurses for organ donation differed in the opportunities that they had to fulfil their full role. This arose from differences in whether or not an early referral of potential donors was made to SNODs, thus allowing them to begin to establish contact with families and undertake preliminary work relating to the donation process. Such referrals often depended on consultants’ views of the appropriate role and responsibilities of SNODs and, thus, their willingness to involve them at an early stage.
There are known to be differences in whether or not consultants involve SNODs in consent discussions with families; the present study examined the reasons for this in detail. The responses and practices of some consultants indicated that they were very positive about the SNODs and collaborated at all stages (‘acceptors’). In contrast some consultants (‘resistors’) were reluctant to accept the SNODs’ involvement outside traditional nursing and administrative tasks. A third group of consultants (‘intermediate’) were identified as probably in a transitional situation, as they often accepted the involvement of a particular SNOD but not the enhanced role of SNODs in general.
The reluctance of some consultants to involve SNODs partly reflected their own personal characteristics, which included a general resistance to change, particularly among the older consultants, together with a lack of knowledge and appreciation of the training and expertise of SNODs. Other influences related to aspects of the local environment, including the leadership provided by CLODs and the general culture of the ICU. There were also differences associated with the type of donation, with consultants generally being much more receptive to SNODs’ involvement in relation to DBDs following conclusive brain stem tests. In contrast, there was more tension with the role of the SNOD with uncontrolled DCD, when the decision to withdraw cardiorespiratory treatments and the timing of death are less certain and may involve a balance between the needs of patients and families, and those of a potential recipient. In this situation, clinicians often preferred not to involve a SNOD and emphasised their priorities and responsibilities in acting in the interests of the patient and family.
Hospital chaplains
This refers to chaplains of all faith groups with a full- or part-time hospital appointment. Chaplains provide support to patients and families and were often valued by ICU staff in communicating with families but had little knowledge specifically about organ donation.
Hospital chaplains comprise a group in the process of developing as a professional specialty, with discussions taking place regarding specialised training in hospital work. They have potential for an expanded role, particularly in relation to families from minority ethnic groups, with this involving both supporting families during end-of-life care and also promoting awareness of organ donation and addressing perceived barriers within faith groups at a community level.
Bereaved families
The small group of bereaved consenting families from minority ethnic groups who were interviewed were very positive regarding the kindness and consideration shown by ICU staff and the quality of care their relative experienced. Such positive views and experiences are likely to have impacted favourably on their consent to donation. The only critical comments related to the initial time spent by some in A&E departments and limited communication that occurred when this was the entry point. Families also described varying practices regarding brain stem testing, with some families wanting the opportunity to attend but this was not offered. Some families would also have valued follow-up information about how the recipient was getting on being provided automatically for the first few years.
Professional development package
There is a recognised need for training to increase the cultural confidence and competence of junior ICU staff. The DonaTE professional development package forms a key outcome of the research and is the first NHS training package that is designed to increase cultural competence. The three-part package aims to enhance motivation, skills and confidence in supporting families from minority ethnic groups and provides guidance on best practices. The training comprises a DVD with a main programme, plus a separate family drama that reinforces the key messages, together with a workbook that encourages reflection and personal plans.
The variations identified by the focus groups among different ethnic/faith and age groups informed a central theme of the DVD that emphasised the heterogeneity of ethnic groups and the importance of avoiding stereotypical assumptions. The hospital studies both supported the need for training and informed the content of the training package in terms of the focus on five key areas that were perceived to be particular challenges for staff (DonaTE dimensions), namely the varying forms of emotional expression; faith and cultural beliefs and practices; managing large families; language and communication; and anxieties about donation. These therefore formed central elements of the training package.
The training package is primarily aimed to address the training needs of bedside nurses, although we are aware that other groups of ICU staff have some similar concerns regarding communicating with minority ethnic groups about organ donation. However, focusing on a particular staff group allowed the training package to be designed to closely match the needs of this group. There has, however, been interest in the main DVD programme from hospital chaplains who view this as a informative for chaplains working in ICUs and supporting patients and families from different cultural backgrounds. Community groups have also found the programme helpful in promoting trust in the health professionals regarding donation among minority ethnic groups.
Further evaluation is, however, required to assess the impacts of the full DonaTE professional development package on attitudes, skills and behavioural intentions, together with participants’ feedback so as to guide and fine tune its implementation, including the facilitators approach to delivery.
Summary of main findings
Community studies and registration as an organ donor
-
Ethnic minorities are at different stages on the ‘pathway’ to registration, with large numbers remaining at an initial ‘pre-contemplation’ stage despite national media campaigns focusing specifically on minority ethnic groups.
-
Campaign images and messages were often not perceived by ethnic minorities to apply to their lives and experiences, with this mainly reflecting the lack of a relevant prior stock of knowledge to draw on, perceptions of transplantation as a ‘white’ issue and a cultural belief in the bodily strength of their own ethnic group. The importance of specific factors in limiting perceived ‘relevance’, however, varied in relation to ethnic background, age, gender and length time in UK.
-
Four main attitudinal barriers were identified as reducing motivation to register as a donor: faith and cultural beliefs, bodily concerns, willingness to talk with family, and trust in health professionals and the health system. However, there was a considerable variation in the content and importance of these concerns for different ethnic/faith and age groups, particularly in relation to the influence of faith and cultural beliefs.
-
The synthesis of interventions provides guidance for the design of more effective campaigns. Community-based education campaigns were identified as more effective in increasing organ donor registration than media campaigns alone, particularly for people at pre-contemplation or early contemplation phases. Characteristics of effective educational interventions included delivery in familiar community settings, involving a strong interpersonal element, presented by trained lay individuals, and the availability of immediate access to registration.
Hospital studies and family consent to donation
-
Intensive care unit staff often lacked confidence in communicating with ethnic minority families particularly at times of emotional distress. This was most commonly reported by junior bedside nurses who also specifically identified a need for training.
-
The continuing significant proportion of consent discussions undertaken by the clinician alone rather than a collaborative discussion with SNODs was explained by clinicians’ beliefs in their own expertise and responsibility, a lack of trust in SNODs, the culture of the ICU and lack of any formal requirement to engage in recommended collaborative discussions. The particular uncertainties and requirements of donations after cardiac death also led to clinicians not wishing to involve a SNOD.
-
Hospital chaplains’ perception of their role and involvement in end-of-life care identified the potential for some members of this group to be a resource in supporting families during end-of-life care with appropriate training, although for others this would be limited by their part-time hospital appointments.
-
Health-care providers and policy-makers had a strong concern not to appear discriminatory in either attitudes or actions, which is at root a commitment to a fundamental equality. However, the notion of equality is sometimes crudely drawn such that health-care professionals are fearful of being seen to ‘treat people differently’ when that is precisely what the principle of equality sometimes requires. The important issue is that people are treated differently for morally relevant reasons and in the interests of securing a just and equal outcome.
Professional development intervention
-
The DVD was nominated for the national Learning on Screen Awards, 2014 and feedback from ICU staff was also very positive.
-
The before-and-after evaluation identified a significant positive effect on attitudes but no effect on subjective norms and perceived behavioural change.
-
The comparison of intervention and non-intervention sites did not identify a significant intervention effect, although the short time period and possible crossover effects limited this comparison.
Implications for policy and practice
Community level
-
Community interventions are most effective when informed by the population’s ‘stage of change’, with initial ‘success’ for those at a pre-contemplation stage often involving a shift along the registration pathway, whereas actual registration often requires multiple interventions that reinforce each other over a period of time. However, people further along the pathway who have reached an action stage may require only a limited ‘nudge’ or ‘prompt’ to register as an organ donor and, when possible, an immediate opportunity to register.
-
Interventions focusing on a ‘pre-contemplation’ stage or those with negative attitudes benefit from greater use of personalised case studies and messages being delivered by trained lay individuals or community representatives in familiar settings.
-
Many focus group participants, particularly of Caribbean origin, wished to discuss organ donation and joining the ODR with a practice nurse or GP, whom they regarded as accessible, trusted and well-qualified sources of advice, and to have access to registration at general practices. However, the feasibility and cost-effectiveness of this primary care-based approach has not been assessed.
-
The views of Islamic faith leaders regarding permissibility have an important influence on the views practices of the older generation, and it is important to achieve a consensus regarding key statements (fatwa).
-
Many people were uncertain whether or not they had ticked the relevant donation box on their driving licence, Boots Advantage Card or passport application and preferred a donor card as confirmation of being on the ODR.
-
Increasing the ease and accessibility of organ donor registration, such as through completing postcards at shopping centres, could increase accessibility for busy people and reduce complexity for older groups, those less familiar with the internet or those with more limited English.
-
The spatial targeting of campaigns would be assisted by more complete recording of ethnicity in relation to registration as a donor (only 18% of registrations now have ethnicity recorded).
Hospital level
-
The DonaTE training package was designed to be used as part of ICU induction or ongoing education delivered by SNODs or by critical care networks to increase the cultural confidence and competence of junior ICU staff. However, it has also been of interest to community organisations to increase knowledge and trust in donation and is available on NIHR’s YouTube website: (www.youtube.com/watch?v=ueaR6XYkeVM&feature youtu.be). An accompanying workbook for ICU nurses is available from Professor Morgan (myfanwy.morgan@kcl.ac.uk).
-
Addressing clinicians’ views and concerns regarding ‘collaborative requesting’ may reduce barriers to SNODs’ involvement, with significant benefits for consent rates.
-
Hospital chaplains form a resource to address families’ concerns about organ donation at both a hospital and community level with appropriate training.
-
Participants in the EDGs valued the opportunity to discuss sensitive issues in a safe and constructive setting, including different approaches to increasing donor numbers, particularly of BAME groups. The general view was that staff working in ethically challenging areas would benefit from a regular opportunity to discuss and reflect on practice in a confidential and non-judgemental setting. An example of this is the successful introduction of Schwartz Centre Rounds® that enable NHS staff to get together once a month to reflect on the stresses and dilemmas that they have faced while caring for patients. 123
Implications for further research
Promoting organ donor registration
-
Despite the considerable and growing community-based activity to increase organ donation in the UK these initiatives are rarely evaluated. A greater emphasis on evaluation is required to increase knowledge of successful community campaigns and requires to be given greater priority.
-
Identifying the stage on the ‘donation pathway’ and barriers of different ethnic/faith groups and variations by age is important for effective targeting and requires either a large purpose-designed survey or adding questions to existing national surveys.
-
A better understanding of the interaction of ethnicity and socioeconomic status on organ donor registration could be achieved through wider data collection, such as through electronic surveys conducted among employees at different levels of large organisations, such as the Civil Service and the NHS.
-
The impacts of access to GPs and primary care nurses to discuss organ donation and registration could be piloted in multiethnic areas, and its acceptability, training requirements and impacts addressed through a mixed-methods study to include qualitative interviews with the different stakeholders (GPs, nurses and patients) and cost-effectiveness analyses.
-
There is a need to ensure that ethnicity is recorded on all sources of registration (currently recorded for only 18% of registrations), while spatial analysis of these data would assist in targeting local campaigns.
-
It is important to examine the introduction of presumed consent in Wales in terms of community knowledge and acceptability, responses by ethnic/faith groups and cost-effectiveness.
Family consent to donation
-
Information is required regarding the reasons for non-consent to donation among ethnic minority families. This might be achieved through secondary analysis of data recorded by SNODs of reasons for refusal and through research with permission to approach bereaved families on a retrospective basis.
-
The importance of interpersonal support for a family’s donation decision links with the recommendation by NHSBT of the value of the piloting of a peer support scheme in ICUs with a large ethnic minority population, with this requiring a process/outcomes evaluation and guidance for future implementation. 17
-
Hospital chaplains have received limited attention but form an important potential resource in supporting families. A questionnaire survey would be valuable to establish views of all UK hospitals chaplains regarding their role in end-of life care, their views of organ donation, their desire for training and specific aspects of interest, and the balance between their hospital- and community-based work.
Wider implications
Many of our findings, although focusing on ethnic minorities, are applicable more broadly. For example, there is considerable scope to increase donation rates among the general population, with many members of the general UK population knowing little about organ donation; however, this group accounts for a rather smaller percentage of the general population than minority ethnic groups. 45 Similarly, many members of white ethnic groups experience worries and anxieties about donation and may have concerns about trusting health professionals, although the prevalence of these issues are again lower than among minority ethnic groups. 45
At a hospital level, issues relating to the full embedding of SNODs’ role and their collaboration in donation discussions as well as the quality support provided during end-of-life care are similarly of general significance.
These commonalities mean that many of the recommendations for further research and policy are applicable more generally, including the importance of targeting those at different stages on the donation pathway, the characteristics of effective community interventions and the importance of support at a hospital level. The NHSBT policy is, therefore, to seek to increase the number of people, from all sections of the UK’s multiethnic and multifaith population, who consent to and authorise organ donation in their life. 15 The main differences arise from specific faith beliefs and practices that are regarded as presenting particular constraints on organ donation and are most common among older people particularly of Islamic faith. The current policy is therefore to work in partnership with faith leaders and communities as part of a broader educational and promotional strategy that encompasses all sections of society. 100
Public engagement and dissemination
Public engagement
Our primary engagement activity focused on involving patients and the public as a lay advisory group in each of the main phases of our research, with meetings held to review materials and receive comments. In addition, a member of Donor Family Network was a co-investigator and fully involved as a member of the project group, contributing particularly to the bereaved family interviews and training film. However, we went beyond these forms of consultation and collaboration, with the lay advisory group providing the impetus for two public engagement events.
This section describes the setting up and activities of the lay advisory group and the two public engagement events that were held.
Lay advisory group
The initial inclusion criteria for becoming a member of the lay advisory group were people who belonged to BAME group and had either been involved in a discussion to donate the organs of a relative, received a transplant or had an interest in the topics of organ donation and transplantation. Recruitment proved difficult, as organ donation and transplantation are not common experiences, especially for minority ethnic groups. There was also the added barrier of death and organ donation being taboo subjects and not usually discussed.
In April 2010, we were able to recruit four people to the lay advisory group. To bolster membership we undertook a second round of recruitment in July 2012, and expanded the inclusion criteria to include those who had experienced the death of a family member in an ICU. In addition, we advertised for recruitment more broadly. This led to the involvement of 11 people, of whom eight remained as active group members until the end of the programme in 2013.
We employed various materials and methods to try to reach target audiences. We designed an A4 flyer for print and distributed this through our networks, such as key contacts at Guy’s and St Thomas’ NHS Foundation Trust, University of Wolverhampton and the programme’s co-investigators. We worked with the Biomedical Research Centre to ensure that our promotional materials would be clear and appropriate; members of the public made revisions of materials during a ‘Getting involved in research’ training day at the Biomedical Research Centre. We also sent this flyer in a recruitment pack (with a more detailed information sheet and accompanying covering letter) to six local community organisations of which we had no previous contact. We created an advertisement for the group on INVOLVE’s People in Research website, uploading our recruitment material text on to their website submission template.
Publicising the group through online networks specialising in ethnicity and health was found to be the most successful method of recruitment. We first posted a call for interest via the ethnicity and health Jisc mailing list, which at the time had a membership of 566 professionals working in academic, NHS and local government sectors who ‘continually strive to improve the health of minority ethnic groups’. The e-mail was then reposted on two other mailing lists – the Child and Adolescent Mental Health Services list (108 members) and Higher Education Admin Equal Opportunities List (446 members) – and the Race Equality Foundation’s website. We received 15 responses to the advert through the mailing lists, although four people did not fulfil the inclusion criteria.
The 11 group members comprised women (n = 8) and men (n = 3) from black Caribbean, black African and South Asian backgrounds, identified as Christian, Hindu, Muslim and as having no religion. Most of the members came from the Greater London area, with two from outside London (Bradford and Wolverhampton). Three members had family members who were waiting for a transplant or are a transplant recipient, one person had received a transplant, three people had family members die in an ICU, one person was involved in a discussion to donate the organs of a relative, and three people were interested in the topic and improving health outcomes for people of minority ethnic backgrounds. This group was small but manageable in terms of co-ordinating schedules for meetings and ensuring that all members had an opportunity to contribute to the discussions.
The primary involvement activities for the lay advisory group have been reviewing programme materials and providing feedback and suggestions at four meetings held at different stages of the programme.
At the first meeting in April 2010, we discussed the proposed topic guide and vignettes for the focus groups. Two members were able to attend the meeting in person. The materials were sent to three other members who could not attend the meeting and were telephoned to discuss their comments. Overall, we received positive comments, particularly about the vignettes as a way for people to think and engage with a topic about which they may have little knowledge.
In February 2011, we invited the members to comment on the topic guide for interviews to be conducted with bereaved family members. Owing to various commitments of the members, it was not possible to meet in person, and information was therefore sent via e-mail with discussion and comments received via e-mail/telephone. The response was positive, with participants commenting favourably on the idea of discussing directly with bereaved family members and regarded the 3-month post bereavement time for contacting families as appropriate. They were also reassured about the participants receiving a follow-up phone call the next day to see they were all right.
In September 2012, we had meeting with the newly recruited and larger advisory group. The meeting was arranged to be in the afternoon at Guy’s Hospital, as this time was best for all the participants, and the venue was accessible for members with restricted mobility and provided public prayer facilities. Members had their travel to the meeting reimbursed and we provided refreshments and cakes.
At the meeting they were put into small groups based on their relationship to the inclusion criteria and were asked to review the storyboard for our training intervention in the meeting based on their personal experiences. We incorporated their main points into our training intervention, for example suggestions for how the family waiting areas should look on the video, the amount of information health professionals should give families and possible sensitivities arising from the portrayal of particular minority groups.
In November 2012, we had a follow-up meeting at Guy’s Hospital and showed the completed DVD programme to the advisory group. The content was well received, with members agreeing the content was educative and culturally aware, although members felt that the health-care professionals who contributed did not sufficiently reflect the ethnic diversity within the NHS in terms of visible minorities. The final meeting ended with suggestions for the next steps. These included the advisory group producing materials on involving the public from minority ethnic groups in research and possible educational events to target the public and community groups to raise awareness about joining the ODR. This latter suggestion led to applying for small amounts of additional funding from special engagement funds provided by King’s College London (KCL) and University College London (UCL) to hold public events.
In addition to seeking advice from our lay advisory group we obtained advice from health professionals. This included meeting with a group of former ICU nurses at Wolverhampton University to review and comment on the storyboard and the drama scenario, based on their experiences of working with families from minority ethnic backgrounds. They suggested additions to the intervention that were incorporated into the script, such as examples of how staff can support each other during the organ donation consent process (‘huddle scene’). We also consulted with a member of the Donor Family Network for their views on how best to incorporate the donor family perspective, which was subsequently included within the DVD.
The main challenge was to recruit people from minority ethnic groups who also had links with transplantation and/or organ donation. This involved considerable time given to the public and patient involvement aspects and significantly benefited from a dedicated part-time (80% full-time equivalent) member of staff who not only undertook administrative activities but also specifically had responsibility for the patient and public involvement activities. This meant that relationships could be established with the lay advisory group and that ongoing pastoral support could be provided to develop the group and activities further.
We found there was little guidance available regarding effective methods for recruiting minority ethnic groups. However, we found that the most successful method of recruitment was through websites, particularly the ethnicity and health Jisc mailing list, which at the time had a membership of 566 professionals working in a variety of settings. We also kept in touch with the lay advisory group and collaborators between meetings and updated them on our progress and other news and events through sending out four DonaTE newsletters.
Overall the public and patient involvement component of the programme both fulfilled and successfully extended its original remit, developing from reviewing research materials and activities to include two collaborative and user-led public events. These engaged larger public audiences in issues of organ donation and transplantation and the importance of people from minority ethnic groups joining the ODR.
Public engagement events
We held two public engagement events that stemmed from the interests of members of our lay advisory group.
King’s College London event: Who Would You Give Your Heart To?
We applied for a small funding grant from KCL’s public engagement department to hold an event targeted at the public. The event aimed to raise the topic of organ donation and engage with people from BAME communities in developing interventions based on their knowledge and experiences.
Funding for public engagement events was introduced as a new scheme in the university and so our event was among the very first to be organised. As a result, there were no strict criteria for proposed events other than it was to engage the public in KCL research, cost less than £1000 and be written up in a short report, with photographs, for use on the university website and promotional materials. We planned a half-day workshop to cost a maximum of £500, which would include presentations, an activity for the participants, publications and refreshments (see Appendix 6).
We advertised the event with a flyer and distributed to number of networks, including Guy’s and St Thomas’ NHS Foundation Trust; King’s College Hospital; KCL; Kidney Patient Association; NHSBT; National Black, Asian and Minority Ethnic Transplant Alliance; the ethnicity and health Jisc mailing list; and 10 third-sector organisations: Community Action Southwark, Southwark Healthwatch, Chinese Healthy Living Centre, Midaye, Al Hasaniya Women’s Group, Migrant and Refugee Forum, Maslaha, Race Equality Foundation, Runnymede Trust and the Arbour.
We found that networks related to organ donation and transplantation were the most successful channels for getting interest in the event. The National Black, Asian and Minority Ethnic Transplant Alliance’s contact mailing list produced the most registrations for attendance, followed by direct invitations from the co-ordinator (JS), referrals from friends and family, people’s employers (Guy’s and St Thomas’ Hospital Trust and King’s College Hospital) and through the NHSBT Facebook (Facebook, Inc., Menlo Park, CA, USA) page.
As with other activities on the programme, we had difficulty reaching our target attendance of 40 people. However, this worked out for the best as our first choice venue closed for refurbishment in the beginning of June and our second choice venue could not fit more than 25 people comfortably.
Our 17 attendees came from eight ethnic and five faith backgrounds (Christian, Hindu, Islamic, Jain and no religion) and ranged from 18 to 68 years old. Of the attendees, 11 were already signed up to the ODR and no one was opposed to donating their organs.
The workshop was split into two parts, presentations to provide the attendees with some relevant background information and then application of the points of the presentations in an activity.
First, Professor Myfanwy Morgan gave a 15-minute presentation on the DonaTE programmes studies on minority ethnic organ donation with specific reference to the literature review on barriers to joining the ODR, the community study based on 22 focus groups with people from different ethnic and faith backgrounds and the hospital data collected via interviews with doctors and nurses working in ICUs.
This was followed by a 10-minute presentation by Dr Sarah Deedat on a systematic review of literature on evaluated organ donation registration health interventions. This presentation focused on what has shown to work primarily in the USA to encourage people to think about organ donation and to join an ODR.
The goal of the workshop was to engage the public in creating interventions that would motivate people from minority ethnic groups to sign up to the ODR in the UK, based on the criteria of success identified in the narrative synthesis. For this, participants worked in groups with an advisory group member, with each table having 60 minutes to work together to design an intervention. Each group was given instructions and a pack of materials to work with to create two posters – one summary and one visual – to represent their intervention. The pack contained markers, coloured paper, glue, scissors, newspapers, magazines and relevant photo clippings. After the task, the tables presented their work to the whole group. The interventions presented included:
-
collaborative working between local faith groups and medical professionals to create donor champions to educate congregants about organ donation and to improve consent rates in hospitals
-
educational sessions at schools delivered by donor families, recipients and medical professionals to increase knowledge and get discussions going between pupils and their parents
-
informational stand on health issues related to transplantation/organ donation at events (e.g. Notting Hill Carnival family day) delivered by recipient families, celebrities, medical professionals
-
session at a local music festival to target young people.
Feedback forms were included with participants’ materials and completed at the end of the session. They indicated that people came to the event to learn more, because they had a personal experience with the issues or had an interest in BAME communities and communication strategies. The following quotations are some reflections on the event that show the variation of people’s motivation to attend:
I think it was engaging interesting and definitely is food for thought!! I have learned a few more things.
Meeting interesting people, hearing different views, increase knowledge.
A way to develop community champions who are passionate about the subject.
All participants ticked ‘yes’ to a question of whether or not they felt able to contribute and several commented on the pleasant relaxed atmosphere, describing the event as very ‘open’ with people able to ask questions easily. The participants’ only criticism was that they would have liked to explore what brought other participants to the event. We had not expected that people would want time during the session to share their personal and professional experiences on the issue as this event was promoted for general members of the public and no background knowledge was necessary to participate. However, as only a minority of people are on the ODR or affected by donation or transplantation and the topic is often considered taboo, it is perhaps not surprising that they would have been interested in hearing more of other participants’ experiences.
Our recommendation for planning future sessions would be allow for time slippage as the workshop overran by 30 minutes owing to waiting for attendees to arrive and because when they engaged with the activity they requested extra time to finish their poster. This meant that there was no time at the end for scheduled networking and reflecting on professional and personal experiences. It was also notable that people had heard about the event in different ways and it is therefore important to use a variety of sources to disseminate information about such events.
University College London Grand Challenges
A second opportunity for holding public engagement events came as a user-led initiative of the DonaTE lay advisory group member Cecil Thompson, who works as a research associate at UCL and is chairperson of the UCL Race Equality Group. DonaTE became a co-applicant for UCL’s Grand Challenge Awards for public engagement in research with UCL’s Race Equality Group, Department of Surgery and Department of Medical Education, and Royal Free Hospital’s Renal Transplant Unit. The award (£5000) was to hold a 1-day conference on minority ethnic organ donation, two informational assemblies in primary schools, two events targeted to community organisations and to train medical students as donor champions.
Involvement of DonaTE with the Grand Challenge programme of work was mainly directed at organising the day conference, ‘Organ Donation Amongst Ethnic Minorities: A Grand Challenge’ at the Royal Free Hospital on 7 July 2013. This included consulting on dissemination materials, creating an UCL/Royal Free staff survey on organ donation, developing the conference programme and potential speakers, and giving presentations on the day.
The conference was held on a Saturday in July. There were approximately 70 people at the start of the conference, with numbers dropping to 30 after lunch for the workshops. The participants included nurses, SNODs, UCL medical students, academics, people working in minority ethnic community groups and patients (both organ donors and recipients).
The conference featured presentations on different aspects of organ donation, including talks by Sally Johnson (Director of Organ Donation and Transplantation at NHSBT) on the progress so far, Gurch Randhawa (from the University Bedfordshire and co-investigator on DonaTE), on recent engagement activities undertaken in local communities, Sarah Deedat (DonaTE researcher) on successful campaigns and interventions (Study 1b), Neerja Jain introduced Kidney Research UK’s peer educator programme and Amanda Gibbon (Lay Chairperson, Local ODC at University College Hospital) on ethical perspectives of international organ donor registration models.
After lunch, conference attendees choose from four workshops: setting up a peer educator project, creating a successful intervention (Jessica Sims – DonaTE co-ordinator), learning the clinical aspects of donation and transplantation or learning about public engagement projects in schools by the Royal Free Hospital.
Conclusions
The lay advisory group and lay member of the programme team made valuable contributions to the research programme and also helped to facilitate wider dissemination of the topic through public events. However, there was little available practical information to guide us, particularly in terms of recruitment. Messages that arise from our experience are:
-
recruiting groups with relatively low numbers in the population requires using multiple sources with a particular emphasis on relevant websites
-
a dedicated part-time co-ordinator is valuable in developing public and patient engagement activities, maintaining links with participants and providing support
-
it is important to allow adequate time for group work and contacts among the participants, with potential slippage if possible being allowed for.
Dissemination
A range of dissemination activities occurred throughout the programme to facilitate the progress of the programme. These included 32 presentations to regional and local groups of SNODs and clinicians. The main public/policy and academic dissemination activities are described below.
Public/policy dissemination
NHS Blood and Transplant
We have had regular contact with NHSBT head office and discussed our findings regarding barriers to joining the ODR and effective approaches to increase organ donor registration. We also had a teleconference with a market research group appointed to develop NHSBT’s forthcoming national campaign.
Presentations to facilitate ongoing work included informal meetings with key ‘gatekeepers’ to initially set up the hospital-based studies and 17 presentations to groups of SNODs in different parts of the country to gain acceptance of a prospective approach to bereaved ethnic minority families. We also presented on several occasions at regional team meetings in London, Leeds and Birmingham to inform them about the ongoing research and discuss the findings.
We continue to be involved in meetings with SNODs to disseminate the professional development package (providing DVDs, workbooks for participants and guides for facilitators), with the aim of actively encouraging and facilitating use of the package as part of ICU training for junior staff and thus reducing the implementation gap.
House of Commons
We presented written and oral evidence to an All-Party Parliamentary Committee for Sickle Cell and Thalassaemia for a meeting on Blood and Organ Donations on April 2013 chaired by Diane Abbott MP.
The presentation provided research evidence to support three ‘Asks’:
-
The need to create a bank of personal case studies of families of organ donors and recipients from a range of relevant communities to promote the perceived relevance and acceptability of deceased donation among minority ethnic groups and thus increase the effectiveness of campaigns. This could be undertaken and collated in association with NHSBT.
-
The need identified to be able to access personal responses to common questions about organ donation in primary care settings and opportunities to register in health-related spaces (GP surgeries, hospitals and pharmacies). This requires additional training for primary care staff through professional bodies and piloting of cost-effectiveness.
-
The need to provide training for new ICU staff to enable them to better support families from minority ethnic groups and reduce avoidable barriers to consent. A training package to fulfil this has been developed by the DonaTE programme and is available for rollout.
It was agreed that targeting BAME populations for organ donation was about utilising different areas of communication in cost-effective and innovative ways, and targeting the importance of the messenger as well as the message. The All-Party Parliamentary Group secretariat planned to circulate the ‘DonaTE’ summary sheet.
Professor Morgan gave a talk on ’Barriers to decreased organ donation among black and South Asian minority ethnic groups’ at the All-Party Parliamentary Group meeting on 9 March 2016, Delivering the UK Stem Cell Strategy Improving Equity of Access for Black, Asian and Minority Ethnic Patients, chaired by David Burrows MP and Mark Tami MP.
Media
We received a request from ITV, which wanted to gain an insight into officially conducted BAME research that gives a sociological view on why the percentage of black and Asian donors is so low, so that its presenter could have a full picture of the issue. We provided information derived from the focus groups to address two issues: first, why people often do not join the ODR, and register their willingness to be a donor if they die and fulfil the criteria to be considered as a potential donor; and second, why families often decline when approached for consent to donating their deceased relatives’ organs.
Information was presented on both issues with illustrative quotations from the DonaTE research.
Academic dissemination
Publications
Morgan M, Deedat S, Kenten C. ‘Nudging’ registration as an organ donor: implications of socio-cultural variations in knowledge and attitudes. Curr Sociol 2015;63:714–28.
Morgan M, Kenten C, Sims J, Newton T. Improving Communication and Consent for Organ Donation Among Minority Ethnic Groups: Development and Evaluation of a Hospital Based Intervention. In Weimar W, Boss MA, Busschbach JJV, editors. Organ Transplantation: Ethical, Legal and Psychosocial Aspects – Expanding the European Platform. Lengerich, Germany: PABST Science Publishers; 2014.
Deedat S, Kenten C, Morgan M. What are effective approaches to increasing rates of organ donor registration among minority ethnic populations: a systematic review. BMJ Open 2013;3:e003453.
Bradby H, Kenten C, Deedat S, Morgan M. ‘Having a different conversation around death.’ Diverse hospital chaplains’ views on end of life care. Ethn Health 2013;18:367–90.
Morgan M, Kenten C, Deedat S. Attitudes to deceased organ donation and registration as a donor among minority ethnic groups in North America and the UK: a synthesis of quantitative and qualitative research. Ethn Health 2013:18;367–90.
Sims JM, Kenten C, Deedat S, Randhawa G, Morgan M. Overcoming Barriers to Registering as an Organ Donor among Minority Ethnic Groups. London: Race Equality Foundation; 2012.
Morgan M, Deedat S, Kenten C. Explaining Low Rates of Organ Donation Among Minority Ethnic Groups. In Weimar W, Boss MA, Busschbach JJV, editors. Organ transplantation: Ethical, Legal and Psychosocial Aspects – Expanding the European Platform. Lengerich, Germany: PABST Science Publishers; 2011. pp. 99–106.
Main conference presentations
International
Morgan M. Explaining low rates of organ donation among ethnic minorities: a holistic approach. Ethical, Legal and Psychosocial Aspects of Organ Transplantation, Second Ethical, Legal and Psychosocial Aspects of Transplantation (ELPAT) Congress, Rotterdam, April 2010.
Morgan M, Deedat, S, Kenten C. The framing of ethnicity in public campaigns to promote organ donation in the UK. Fourth Invitational Ethical, Legal and Psychosocial Aspects of Transplantation (ELPAT) Working Group Meeting, Berlin, November 2011.
Deedat, S, Kenten C, Morgan M. ‘I’ve never had to think or even talk about it’: exploring the unfamiliar using vignettes with focus groups. European Sociological Association, Annual Conference, Geneva, September 2011.
Kenten C, Deedat S, Randhawa G, Morgan M. Dying to donate? Family, generation and organ donation in the UK. European Sociological Association, Annual Conference, Geneva, September 2011.
Morgan M, Kenten C, Deedat S. Shaping individual choice for public benefit: promoting deceased organ donation in a system of informed consent. International Sociological Association Forum, Buenos Aires, August 2012.
Morgan M, Bradby H. Religion, organ donation and disparities in transplantation among minority ethnic groups in the UK. International Sociological Association, XVII World Congress of Sociology, Yokohama, Japan, July 2014.
Morgan M, Kenten C, Sims J. Life after death: supporting organ donation choices among minority ethnic families (An ICU training video). Fifth Invitational Ethical, Legal and Psychosocial Aspects of Transplantation (ELPAT) Working Group Meeting, Sicily, 2–4 November, 2012.
National
Morgan M, Jones R. Organ donation and ethnic minorities: community attitudes and challenges for health care. European Society for Medical Sociology, Annual Conference, Lisbon, August 2009.
Kenten C, Deedat S, Morgan M. Scaling the barriers to organ donor registration and organ donation. Royal Geographical Society, Annual Conference, London, September 2010.
Kenten C, Deedat S, Morgan M. If you don’t laugh you cry: organ donation and ICUs. Royal Geographical Society, Annual Conference, London, September 2011.
Kenten C, Sque M, Morgan M. Varying meanings of the ‘family’ in the context of death and organ donation on intensive care units. British Sociological Association’s Death, Dying and Bereavement Study Group’s symposium, Death and the Family, 19 November 2012, London.
Kenten C, Deedat S, Morgan M. Failed nurses or an essential resource? The embedding of specialist nurses for organ donation within intensive care units. British Sociological Association, Annual Conference, Leeds, April 2012.
Morgan M. Normalising organ donation registration and consent: insights from the DonaTE programme. University of Wolverhampton and Wolverhampton NHS Trust, June 2013.
Morgan M, Kenten C, Deedat S, Sims J. DonaTE: Overview and key messages. Meeting of National Black, Asian and Minority Ethnic (BAME) Transplant Alliance (NBTA), June 2013.
Acknowledgements
The DonaTE team are most grateful to Jane Griffiths, Regional Manager for SNODs (London and Northern Ireland Region), for her generous support and facilitation of the project over several years and to Dr Paula Aubrey, who subsequently took on this role for the final stages of the research. We also thank Jeanette Foley for her valuable assistance with co-ordinating the bereaved family study in London, Dr Hannah Bradby for analysis of the chaplains#x02019; interviews and preparing a paper, Dr Kathryn Ehrich for her contribution to the analysis of the transcripts for the EDGs and Rebecca Moss for her analysis of organisational aspects.
We thank the NHS clinical and nursing staff, hospital chaplains, SNODs and members of the ODC at our six study sites together with patients and families for their most generous participation in the research.
Contributions of authors
Professor Myfanwy Morgan was the chief investigator and is guarantor of the report. She is Professor of Medical Sociology, Department of Primary Care and Public Health Sciences at KCL. Professor Morgan was involved in all stages of the research from inception to final submission and was mainly responsible for drafting the report.
Dr Charlotte Kenten was a research fellow on the DonaTE study. She jointly undertook data collection for the community and hospital studies, and contributed to data analysis and drafts. Dr Kenten had particular responsibility for the bereaved family study, liaison with regional teams, and development and production of the professional training package.
Dr Sarah Deedat was a research associate on the DonaTE study. She jointly undertook data collection phase for the community and hospital studies, and contributed to data analysis and drafts. Dr Deedat had particular responsibility for conducting the systematic review of effective interventions.
Professor Bobbie Farsides is Professor of Clinical and Medical Ethics, Brighton and Sussex Medical School. She facilitated the EDGs and was co-author of this chapter.
Professor Tim Newton is Professor of Health Psychology at the Dental Institute, KCL. He contributed to development of the professional training package and led on the construction, analysis and write up of the TPB-based questionnaire assessment.
Professor Gurch Randhawa is Professor of Diversity at the University of Bedfordshire. He contributed particularly to development of the focus group study and recruiting bilingual fieldworkers.
Ms Jessica Sims was a co-ordinator/researcher on the DonaTE study from 2011. She had particular responsibility for recruitment and activities of the lay advisory group and dissemination of the study to local agencies. She also contributed to the design and production phase of the professional training package and co-authored the public engagement section.
Professor Magi Sque is Professor of Clinical Practice and Innovation, University of Wolverhampton and Wolverhampton NHS Trust. She contributed particularly to the bereaved family study.
Other members of the programme team
Dr Debasish Bannerjee is a consultant at St George’s NHS Trust specialising in renal medicine and transplantation. He facilitated both project development and fieldwork.
Professor Roger Jones is a Emeritus Professor at KCL and Editor of the British Journal of General Practice. He undertook a key role while at KCL in the early development of the research and programme application.
Professor Janet Peacock is a Professor of Medical Statistics, Department of Primary Care and Public Health Sciences, KCL. She joined the study in 2010 and analysed and wrote up the statistical outcomes data.
Dr John Scoble is the Clinical Director of Renal and Urological Services, Guy’s and St Thomas’ NHS Trust and provided a clinical and policy perspective throughout the research.
Pauline Weaver represented the Family Donor Network and provided valuable lay input to the research.
Data sharing statement
All data can be obtained from the corresponding author (Professor M Morgan).
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, CCF, NETSCC, PGfAR or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PGfAR programme or the Department of Health.
References
- Linden PK. History of solid organ transplantation and organ donation. Crit Care Clin 2009;25:165-84. http://dx.doi.org/10.1016/j.ccc.2008.12.001.
- Sims TW, Good EW. The next generation of medications for kidney transplant patients. Crit Care Nurs Clin North Am 2002;14:99-109. http://dx.doi.org/10.1016/S0899-5885(03)00041-8.
- NHS Blood and Transplant . Organ Donation and Transplantation – Activity Figures 2013 n.d. www.organdonation.nhs.uk/statistics/downloads/annual_stats.pdf (accessed 10 September 2014).
- Organs for Transplants: A Report from the Organ Donation Taskforce. London: Department of Health; 2008.
- NHS Blood and Transplant . Cost-Effectiveness of Transplantation 2009 n.d. www.organdonation.nhs.uk/newsroom/fact_sheets/cost_effectiveness_of_transplantation.asp (accessed 2 September 2014).
- Roderick PJ, Raleigh VS, Hallam L, Mallick NP. The need and demand for renal replacement therapy in ethnic minorities in England. J Epidemiol Comm Health 1996;50:334-9. http://dx.doi.org/10.1136/jech.50.3.334.
- Cecka MJ. Significance of histocompatibility in organ transplantation. Curr Opin Organ Transplant 2007;12:402-8. http://dx.doi.org/10.1097/MOT.0b013e3281c55d8c.
- Johnson RJ, Fuggle SV, Mumford L, Bradley JA, Forsythe JL, Rudge CJ, et al. A new UK 2006 national kidney allocation scheme for deceased heart beating donor kidneys. Transplantation 2010;89:387-94. http://dx.doi.org/10.1097/TP.0b013e3181c9029d.
- Forouhi NG, Merrick D, Goyder E, Ferguson BA, Abbas J, Lachowycz K, et al. Diabetes prevalence in England, 2001 – estimates from an epidemiological model. Diabetic Med 2006;23:189-97. http://dx.doi.org/10.1111/j.1464-5491.2005.01787.x.
- Gholap N, Davies M, Patel K, Sattar N, Khunti K. Type 2 diabetes and cardiovascular disease in South Asians. Prim Care Diabet 2011;5:45-56. http://dx.doi.org/10.1016/j.pcd.2010.08.002.
- Randhawa G. Achieving Equality in Organ Donation and Transplantation in the UK – Challenges and Solutions. London: Race Equality Foundation and Department for Communities and Local Government; 2011.
- Wilkinson E, Randhawa G, Roderick P, Rehman T, Abubacker T. The impact of quality improvement initiatives on diabetes care among south Asian people. Diabetes Prim Care 2011;12:90-8. http://dx.doi.org/10.5301/jn.5000037.
- Marks A, MacLeod C, McAteer A, Murchie P, Fluck N, Cairns W, et al. Chronic kidney disease, a useful trigger for proactive primary care? Mortality results from a large UK cohort. Fam Pract 2012;30:282-9. http://dx.doi.org/10.1093/fampra/cms079.
- National Black, Asian and Minority Ethnic Transplant Alliance . Report on Black, Asian and Minority Ethnic Organ Donation and Transplantation Data 2012. www.kidney.org.uk/documentlibrary/NBTA-BAME_donation-transplant_data-oct12.pdf (accessed April 2015).
- Department of Health . Taking Organ Transplantation to 2020: A Detailed Strategy 2013. www.nhsbt.nhs.uk/to2020/get-the-strategy/ (accessed 2 September 2014).
- British Broadcasting Corporation . Ethnic Groups Urged to Give Blood 2013. news.bbc.co.uk/1/hi/health/4160110.stm (accessed 22 April 2014).
- The Potential Impact of an Opt Out System for Organ Donation in the UK. London: Department of Health; 2008.
- Rithalia A, McDavid C, Suekaman S, Myers L, Sowden A. Impact of presumed consent for organ donation rates: a systematic review. BMJ 2009;338. http://dx.doi.org/10.1136/bmj.a3162.
- Matesanz R, Dominguez-Gil B, Coll E, de la Rosa G, Marazuela R. Spanish experience as a leading country: what kind of measures were taken?. Transpl Int 2011;24:333-43. http://dx.doi.org/10.1111/j.1432-2277.2010.01204.x.
- Shafer TJ, Wagner D, Chessare J, Schall MW, McBride V, Zampiello FA, et al. US organ donation breakthrough collaborative increases organ donation. Crit Care Nurs Q 2008;31:190-21. http://dx.doi.org/10.1097/01.CNQ.0000325044.78904.9b.
- Nuffield Council on Bioethics . Human Bodies: Donation for Medicine and Research 2011. http://nuffieldbioethics.org/wp-content/uploads/2014/07/Donation_full_report.pdf (accessed 2 August 2013).
- British Broadcasting Corporation . Welsh Government’s ‘Opt Out’ Organ Donor Consultation 2011. www.bbc.co.uk/news/uk-wales-politics-15625285 (accessed 20 March 2014).
- Lavee J, Ashkenazi T, Gurman G, Steinberg D. A new law for allocation of donor organs in Israel. Lancet 2010;375:1131-3. http://dx.doi.org/10.1016/S0140-6736(09)61795-5.
- Sharif A. Prioritising existing donors to receive organs would boost donation from ethnic minorities. BMJ 2013;347. http://dx.doi.org/10.1136/bmj.f5036.
- Cronin AJ, Douglas JF. Directed and conditional organ donation: laws and misconceptions. Med Law Rev 2010;18:275-301. http://dx.doi.org/10.1093/medlaw/fwq019.
- Siegal G. Making the case for directed organ donation to registered donors in Israel. Israel J Health Policy Res 2014;3. http://dx.doi.org/10.1186/2045-4015-3-1.
- Ajzen I. The theory of planned behavior. Organ Behav Hum Dec 1991;50:179-211. http://dx.doi.org/10.1016/0749-5978(91)90020-T.
- Ahmed W, Bradby H. Ethnicity and health: key themes in a developing field. Curr Sociol 2008;56:47-56. http://dx.doi.org/10.1177/0011392107084378.
- Arriola K, Robinson DH, Thompson NJ, Perryman JP. Project ACTS: an intervention to increase organ and tissue donation intentions among African Americans. Health Educ Behav 2009;37:264-74. http://dx.doi.org/10.1177/1090198109341725.
- Atkins L, Davis K, Holtzman SM, Durand R, Decker PJ. Family discussion about organ donation among African Americans. Prog Transplant 2003;13:28-32. http://dx.doi.org/10.7182/prtr.13.1.fkn1288817056711.
- Boulware LE, Ratner LE, Cooper LA, Sosa JA, LaVeist TA, Powe NR. Understanding disparities in donor behaviour: race and gender differences in willingness to donate blood and cadaveric organs. Med Care 2002;40:85-9. http://dx.doi.org/10.1097/00005650-200202000-00003.
- Cort M, Cort D. Willingness to participate in organ donation among black Seventh–day Adventist college students. J Am Coll Health 2008;56:691-7. http://dx.doi.org/10.3200/JACH.56.6.691-697.
- Creecy RF, Wright R. Correlates of willingness to consider organ donation among blacks. Soc Sci Med 1990;31:1229-32. http://dx.doi.org/10.1016/0277-9536(90)90128-F.
- Creecy RF, Wright R, Berg WE. Discriminators of willingness to consider cadaveric kidney donation among black Americans. Soc Work Health Care 1992;18:93-105. http://dx.doi.org/10.1300/J010v18n01_06.
- Davis C, Randhawa G. ‘Don’t know enough about it!’: awareness and attitudes towards organ donation and transplantation among the black Caribbean and black African population in Lambeth, Southwark and Lewisham, United Kingdom. Transplantation 2004;78:420-5. http://dx.doi.org/10.1097/01.TP.0000128341.81362.0F.
- Davis C, Randhawa G. The influence of religion on organ donation and transplantation among the black Caribbean and black African population – a pilot study in the United Kingdom. Ethn Dis 2006;16:281-5.
- Edwards TM, Essman C, Thornton JD. Assessing racial and ethnic differences in medical student knowledge, attitudes and behaviours regarding organ donation. J Natl Med Assoc 2007;99:131-7.
- Exley C, Sim J, Reid N, Jackson S, West N. Attitudes and beliefs within the Sikh community regarding organ donation in a pilot study. Soc Sci Med 1996;43:23-8. http://dx.doi.org/10.1016/0277-9536(95)00320-7.
- Fahrenwald NL, Stabnow W. Sociocultural perspective on organ and tissue donation among reservation-dwelling American Indian adults. Ethn Health 2005;10:341-54. http://dx.doi.org/10.1080/13557850500168826.
- Hayward C, Madill A. The meanings of organ donation: Muslims of Pakistani origin and white English nationals living in North England. Soc Sci Med 2003;57:389-401. http://dx.doi.org/10.1016/S0277-9536(02)00364-7.
- McNamara P, Guadagnoli E, Evanisko MJ, Beasley C, Santiago-Delpin EA, Callender CO, et al. Correlates of support for organ donation among three ethnic groups. Clin Transplant 1999;13:45-50. http://dx.doi.org/10.1034/j.1399-0012.1999.t01-2-130107.x.
- Molzahn AE, Starzomski R, McDonald M, O’Loughlin C. Aboriginal beliefs about organ donation: some Coast Salish viewpoints. Can J Nurs Res 2004;36:100-28.
- Molzahn AE, Starzomski R, McDonald M, O’Loughlin C. Chinese Canadian beliefs toward organ donation. Qual Health Res 2005;15:82-98. http://dx.doi.org/10.1177/1049732304270653.
- Molzahn AE, Starzomski R, McDonald M, O’Loughlin C. Indo-Canadian beliefs regarding organ donation. Prog Transplant 2005;15:233-9. http://dx.doi.org/10.7182/prtr.15.3.j57370x38l782124.
- Morgan M, Hooper R, Mayblin M, Jones R. Attitudes to kidney donation and registering as a donor among ethnic groups in the UK. J Public Health (Oxf) 2006;28:226-34. http://dx.doi.org/10.1093/pubmed/fdl045.
- Morgan M, Mayblin M, Jones R. Ethnicity and registration as a kidney donor: the significance of identity and belonging. Soc Sci Med 2008;66:147-58. http://dx.doi.org/10.1016/j.socscimed.2007.
- Morgan SE, Miller JK, Arasaratnam LA. Similarities and differences between African Americans’ and European Americans’ attitudes, knowledge, and willingness to communicate about organ donation. J Appl Soc Psychol 2003;33:693-715. http://dx.doi.org/10.1111/j.1559-1816.2003.tb01920.x.
- Morgan SE. Many facets of reluctance: African Americans and the decision (not) to donate organs. J Natl Med Assoc 2006;98:695-703.
- Sherman NC, Sherman MF, Smith RJ, Rickert-Wilbur P. Disgust sensitivity and attitudes towards organ donation among African-American college students. Psychol Rep 2001;89:11-23. http://dx.doi.org/10.2466/pr0.2001.89.1.11.
- Siminoff LA, Burant CJ, Ibrahim SA. Racial disparities in preferences and perceptions regarding organ donation. J Gen Intern Med 2006;21:995-1000. http://dx.doi.org/10.1007/BF02743151.
- Smith G, Saxena S, Car J, Jain N, Reece P, Dulku H, et al. Appendix E, Becoming an Organ Donor: Oral Histories of People from Three Ethnic Backgrounds. London: Department of Health; 2008.
- Terrell F, Moseley KL, Terrell AS, Nickerson KJ. The relationship between motivation to volunteer, gender, cultural mistrust, and willingness to donate organs among Blacks. J Natl Med Assoc 2004;96:53-60.
- Wheeler MS, O’Friel M, Cheung AHS. Cultural beliefs of Asian-Americans as barriers to organ donation. J Transplant Coord 1994;4:146-50.
- Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews: A Product from the ESRC Methods Programme. Version 1. Swindon: ESRC Methods Programme; 2006.
- Office for National Statistics . United Kingdom Census 1991 n.d. www.ons.gov.uk/ons/guide-method/census/1991-and-earlier-censuses/1991-census-data/index.html (accessed 1 December 2014).
- Simpkin AL, Robertson LC, Barber VS, Young JD. Modifiable factors influencing relatives’ decision to offer organ donation: systematic review. BMJ 2009;338. http://dx.doi.org/10.1136/bmj.b991.
- Morgan M, Kenten C, Deedat S. Attitudes to deceased organ donation and registration as a donor among minority ethnic groups in North America and the U.K.: a synthesis of quantitative and qualitative research. Ethn Health 2013;18:367-90. http://dx.doi.org/10.1080/13557858.2012.752073.
- Dixon-Woods M, Cavers D, Agarwal S, Annandale E, Arthur A, Harvey J, et al. Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Med Res Methodol 2006;6. http://dx.doi.org/10.1186/1471-2288-6-35.
- Crombie I. The Pocket Guide to Critical Appraisal. London: BMJ Publishing Group; 1996.
- Arai L. Preventing Accidents in Children: How Can we Improve our Understanding of What Really Works? Exploring Methodological and Practical Issues in the Systematic Review of Factors Affecting the Implementation of Child Injury Prevention Initiatives. London: Health Development Agency; 2003.
- Healy K. Last Best Gifts: Altruism and the Market for Human Blood and Organs. Chicago, IL: University of Chicago Press; 2006.
- Islam Question and Answer . Ruling on Organ Donation 2014. http://islamqa.info/en/107690 (accessed 10 June 2013).
- Randhawa G, Brocklehurst A, Pateman R, Kinsella S, Parry V. Religion and organ donation: the views of UK faith leaders. J Relig Health 2012;51:743-51. http://dx.doi.org/10.1007/s10943-010-9374-3.
- Schutz A. Reflections on the Problem of Relevance. New Haven, CT: Yale University Press; 1970.
- Office of National Statistics . Census Gives Insight into Characteristics of London’s Population; 2012 n.d. www.ons.gov.uk/ons/dcp29904_291554.pdf (accessed 16 April 2012).
- Morgan M, Deedat S, Kenten C. ‘Nudging’ registration as an organ donor: Implications of changes in choice contexts for socio-cultural groups. Curr Sociol n.d.;63:714-28. http://dx.doi.org/10.1177/0011392115590086.
- Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot 1997;12:38-4. http://dx.doi.org/10.4278/0890-1171-12.1.38.
- NHS Blood and Transplant . Religious Perspectives on Organ Donation n.d. www.organdonation.nhs.uk/how_to_become_a_donor/religious_perspectives/index.asp (accessed 10 June 2013).
- Allen MD, Stillwater B, Siegel JT, Alvaro EM. Understanding Organ Donation: Applied Behavioral Science Perspectives. Chichester: Wiley-Blackwell; 2010.
- Alvaro EM, Jones SP, Robles AS, Siegel J. Hispanic organ donation: impact of a Spanish-language organ donation campaign. J Natl Med Assoc 2006;98:28-35.
- Alvaro EM, Siegel JT, Jones SP. Increasing organ donor registration rates by providing an immediate and complete registration opportunity: an experimental assessment of the IIFF model. Psychol Health Med 2011;16:686-94. http://dx.doi.org/10.1080/13548506.2011.564353.
- Andrews AM, Zhang N, Magee JC, Chapman R, Langford AT, Resnicow K. Increasing donor designation through black churches: results of a randomized trial. Prog Transplant 2012;22:161-7. http://dx.doi.org/10.7182/pit2012281.
- Callender CO, Hall MB, Branch D. An assessment of the effectiveness of the Mottep model for increasing donation rates and preventing the need for transplantation – adult findings: program years 1998 and 1999. Semin Nephrol 2001;21:419-28. http://dx.doi.org/10.1053/snep.2001.23778.
- Cárdenas V, Thornton JD, Wong KA, Spigner C, Allen MD. Effects of classroom education on knowledge and attitudes regarding organ donation in ethnically diverse urban high schools. Clin Transplant 2010;24:784-93. http://dx.doi.org/10.1111/j.1399-0012.2009.01200.x.
- Fahrenwald NL, Belitz C, Keckler A. ‘Tribes sharing life’: an organ donation educational intervention for American Indian tribal college and university students. West J Nurs Res 2011;33:901-15. http://dx.doi.org/10.1177/0193945911401431.
- Feeley TH, Anker AE, Watkins B, Rivera J, Tag N, Volpe L. A peer-to-peer campaign to promote organ donation among racially diverse college students in New York City. J Natl Med Assoc 2009;101:1154-62. http://dx.doi.org/10.1016/S0027-9684(15)31112-3.
- Frates J, Bohrer CG, Thomas D. Promoting organ donation to Hispanics: the role of the media and medicine. J Health Community 2006;11:683-98. http://dx.doi.org/10.1080/10810730600934542.
- Harrison TR, Morgan SE, King AJ, Williams EA. Saving lives branch by branch: the effectiveness of driver licensing bureau campaigns to promote organ donor registry sign-ups to African Americans in Michigan. J Health Community 2011;16:805-19. http://dx.doi.org/10.1080/10810730.2011.552001.
- Hebert PL, Rivera J, Eng K, Lee R, Seto-Yee RN. Understanding Organ Donation: Applied Behavioral Science Perspectives. Chichester: Wiley-Blackwell; 2010.
- Radosevich DM, Larson SM, Scott T, Jones C, Tenle W, Gunderson S, et al. Understanding Organ donation: Applied Behavioral Science Perspectives. Wiley-Blackwell; 2010.
- Resnicow K, Andrews AM, Beach DK, Kuhn L, Krein SL, Chapman R, et al. Randomized trial using hair stylists as lay health advisors to increase donations in African Americans. Ethn Dis 2010;20:276-81.
- Salim A, Berry C, Ley EJ, Schulman D, Navarro S, Zheng L, et al. A focused educational program after religious services to improve organ donation in Hispanic Americans. Clin Transplant 2012;26:e634-40. http://dx.doi.org/10.1111/ctr.12036.
- Salim A, Berry C, Ley EJ, Schulman D, Navarro S, Chan LS. Utilizing the media to help increase organ donation in the Hispanic American population. Clin Transplant 2011;25:E622-8. http://dx.doi.org/10.1111/j.1399-0012.2011.01505.x.
- Thornton JD, Alejandro-Rodriguez M, León JB, Albert JM, Baldeon EL, De Jesus LM, et al. Effect of an iPod video intervention on consent to donate organs: a randomized trial. Ann Intern Med 2012;156:483-90. http://dx.doi.org/10.7326/0003-4819-156-7-201204030-00004.
- Buffin J, Little R, Jain N, Warrens AN. A peer outreach initiative to increase the registration of minorities as organ donors. Clin Kidney J 2015;8:623-8. http://dx.doi.org/10.1093/ckj/sfv066.
- Deedat S, Kenten C, Morgan M. What are effective approaches to increasing rates of organ donor registration among ethnic minority populations: a systematic review. BMJ Open 2013;3. http://dx.doi.org/10.1136/bmjopen-2013-003453.
- Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.0. The Cochrane Collaboration; 2008.
- Jackson N, Waters E. Guidelines for Systematic Reviews in Health Promotion and Public Health Taskforce . Criteria for the systematic review of health promotion and public health interventions. Health Promot Int 2005;20:367-74. http://dx.doi.org/10.1093/heapro/dai022.
- Organ Donation for Transplantation: Improving Donor Identification and Consent Rates for Deceased Organ Donation. London: NICE; 2011.
- Manara AR, Murphy PG, O’Callaghan G. Donation after circulatory death. Br J Anaesth 2012;108:i108-i21. http://dx.doi.org/10.1093/bja/aer357.
- British Transplant Society and Intensive Care Society . United Kingdom Guidelines: Transplantation from Donors After Deceased Circulatory Death; 2013. www.bts.org.uk/Documents/Guidelines/Active/DCD%20for%20BTS%20and%20ICS%20FINAL.pdf (accessed September 2014).
- An Ethical Framework for Controlled Donation after Circulatory Death. London: Academy of Medical Royal Colleges; 2011.
- Ashford J, Eccles M, Bond S, Hall J, Bond J. Improving health care through professional behaviour change. Clin Gov 1999;1:14-23. http://dx.doi.org/10.1108/14664109910297146.
- James J, Cottle E, Hodge RD. Registered nurse and health care chaplains experiences of providing the family support person role during family witnessed resuscitation. Intens Crit Care Nurs 2011;27:19-26. http://dx.doi.org/10.1016/j.iccn.2010.09.001.
- Kernohan WG, Waldron M, McAfee C, Cochrane B, Hasson F. An evidence base for a palliative care chaplaincy service in Northern Ireland. Palliat Med 2007;21:519-25. http://dx.doi.org/10.1177/0269216307081500.
- Flannelly K, Emanuel L, Handzo G, Galek K, Silton N, Carlson M. A national study of chaplaincy services and end-of-life outcomes. BMC Palliat Care 2012;11. http://dx.doi.org/10.1186/1472-684X-11-10.
- Randhawa G, Brocklehurst A, Pateman R, Kinsella S, Parry V. ‘Opting-in or opting-out?’--the views of the UK’s faith leaders in relation to organ donation. Health Policy 2010;96:36-44. http://dx.doi.org/10.1016/j.healthpol.2009.12.012.
- Bradby H, Kenten C, Deedat S, Morgan M. ‘Having a different conversation around death’: diverse hospital chaplains’ views on end-of-life care. Ethn Health 2013;18:530-43. http://dx.doi.org/10.1080/13557858.2013.828832.
- Cancer Service Guidance: Improving Supportive and Palliative Care for Adults with Cancer. London: NICE; 2004.
- Randhawa G. NHSBT . Faith Engagement and Organ Donation Action Plan 2014. www.organdonation.nhs.uk/pdfs/faith_action_plan.pdf (accessed 11 December 2015).
- Martins L, Fonseca I, Sousa S, Matos C, Santos J, Dias L, et al. The influence of HLA mismatches and immunosuppression on kidney graft survival: an analysis of more than 1300 patients. Transplant Proc 2007;39:2489-93. http://dx.doi.org/10.1016/j.transproceed.2007.07.033.
- Campistol JM. Minimizing the risk of post transplant malignancy. Transplant Proc 2009;87:19-22. http://dx.doi.org/10.1097/TP.0b013e3181a07a57.
- Titmuss R. The Gift Relationship from Human Blood to Social Policy. London: Allen & Unwin; 1970.
- Prainsack B, Buyx A. Solidarity: Reflections on an Emerging Concept in Bioethics. London: Nuffield Council on Bioethics; 2011.
- Hoeyer K. Donors perceptions of consent to and feedback from biobank research: time to acknowledge diversity?. Pub Health Genomics 2010;13:345-52. http://dx.doi.org/10.1159/000262329.
- Rodrigue JR, Cornell DL, Howard RJ. Organ donation decision: comparison of donor and nondonor families. Am J Transplant 2006;6:190-8. http://dx.doi.org/10.1111/j.1600-6143.2005.01130.x.
- Siminoff LA, Arnold RM, Hewlett J. The process of organ donation and its effect on consent. Clin Transplant 2001;15:39-47. http://dx.doi.org/10.1034/j.1399-0012.2001.150107.x.
- Siminoff LA, Gordon N, Hewlett J, Arnold RM. Factors influencing families’ consent for donation of solid organs for transplantation. JAMA 2001;286:71-7. http://dx.doi.org/10.1001/jama.286.1.71.
- Sque M, Long T, Payne S. Organ donation: key factors influencing families’ decision-making. Transplant Proc 2005;37:543-6. http://dx.doi.org/10.1016/j.transproceed.2004.11.038.
- Ormrod JA, Ryder T, Chadwick RJ, Bonner SM. Experiences of families when a relative is diagnosed brain stem dead: understanding of death, observation of brain stem death testing and attitudes to organ donation. Anaesthesia 2005;60:1002-8. http://dx.doi.org/10.1111/j.1365-2044.2005.04297.x.
- Haddow G. Donor and nondonor families’ accounts of communication and relations with healthcare professionals. Prog Transplant 2004;14:41-8. http://dx.doi.org/10.7182/prtr.14.1.r3510160u371qj20.
- Siminoff LA, Lawrence RH, Arnold RM. Comparison of black and white families’ experiences and perceptions regarding organ donation requests. Crit Care Med 2003;31:146-51. http://dx.doi.org/10.1097/00003246-200301000-00023.
- Diette GB, Rand C. The contributing role of health-care communication to health disparities for minority patients with asthma. Chest 2007;132:802S-9S. http://dx.doi.org/10.1378/chest.07-1909.
- Cooper LA, Roter DL, Smedley BD, Stith AY, Nelson AR. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2002.
- Saha S, Beach MC, Cooper LA. Patient centeredness, cultural competence and healthcare quality. J Nat Med Assoc 2008;100:1275-85. http://dx.doi.org/10.1016/S0027-9684(15)31505-4.
- Beach MC, Price EG, Gary TL, Robinson KA, Gozu A, Palacio A, et al. Cultural competence: a systematic review of health care provider educational interventions. Med Care 2005;43:356-73. http://dx.doi.org/10.1097/01.mlr.0000156861.58905.96.
- Carpenter-Song EA, Nordquest Schwallie M, Longhofer J. Cultural competence reexamined: critique and directions for the future. Psychiatr Serv 2007;58:1362-5. http://dx.doi.org/10.1176/ps.2007.58.10.1362.
- Culley L. Transcending transculturalism? Race, ethnicity and health-care. Nurs Inq 2006;13:144-53. http://dx.doi.org/10.1111/j.1440-1800.2006.00311.x.
- Armitage C, Conner M. Efficacy of the theory of planned behaviour: a meta-analytic review. Br J Soc Psychol 2001;40:471-99. http://dx.doi.org/10.1348/014466601164939.
- Francis J, Eccles M, Johnston M, Walker A, Grimshaw J, Foy R, et al. Constructing Questionnaires Based on the Theory of Planned Behaviour: A Manual for Health Service Researchers. Newcastle: Centre for Health Services Research; 2004.
- Anastasi A. Psychological Testing. New York, NY: Macmillan; 1976.
- Sque M, Long T, Payne S, Allardyce D. Why relatives do not donate organs for transplants: ‘sacrifice’ or ‘gift of life’?. J Adv Nurs 2008;61:134-44. http://dx.doi.org/10.1111/j.1365-2648.2007.04491.x.
- Expansion of Groundbreaking Scheme to Support NHS Staff. London: Department of Health; 2013.
Appendix 1 Medical subject heading terms (MEDLINE) for systematic review of barriers to organ donor registration
This text has been reproduced with permission from Morgan M, Kenten C, Deedat S. Attitudes to deceased organ donation and registration as a donor among minority ethnic groups in North America and the U.K.: a synthesis of quantitative and qualitative research. Ethn Health 2013;18:367–90.
Date range searched: January 1980 to January 2010.
Date of search: April 2010.
-
exp “Tissue and Organ Procurement”/
-
exp “Tissue and Organ Harvesting”/
-
((cadaver or deceased) adj2 donor*).ti,ab.
-
((postmortem or post mortem) adj2 donor*).ti,ab.
-
((deceased or dead) adj2 donor*).ti,ab.
-
((organ or organs) adj3 donor*).ti,ab.
-
((transplant or transplantation) adj donor*).ti,ab.
-
((cadaver or deceased) adj2 (donat* or harvest*)).ti,ab.
-
((postmortem or post mortem) adj2 (donat* or harvest*)).ti,ab.
-
((deceased or dead) adj2 (donat* or harvest*)).ti,ab.
-
((organ or organs) adj3 (donat* or procure* or harvest*)).ti,ab.
-
or/1-11
-
Living Donors/
-
(“non cadaveric” or “living don*”).ti,ab.
-
(“blood donor” or “blood donation” or “blood donors”).ti,ab.
-
(tissue adj3 donor*).ti,ab.
-
(tissue adj3 (donat* or procure* or harvest*)).ti,ab.
-
12 not (13 or 14 or 15 or 16 or 17)
-
African Continental Ancestry Group/ or Ethnic Groups/
-
Indians, North American/
-
African Americans/ or Asian Americans/
-
“native american*”.tw.
-
(race or racial or ethnic* or native american* or native canadian* or native alaskan* or american indian* or canadian indian* or amerind* or negro* or afro* or african* or black or blacks or arab* or asian* or chinese or japanese or oriental* or thai* or philipino* or filipino* or taiwanese* or indian* or bengali* or kashmiri* or gujarati* or tamil* or bangladeshi* or pakistani* or sri lankan* or hispanic* or latino* or nonwhite* or non-white* or multiracial or multi-racial).tw.
-
Hispanic Americans/
-
Mexican Americans/
-
ethnic groups/
-
or/19-26
-
(culture or cultural or faith* or relig* or sikh* or hindu* or muslim* or islam* or christian* or catholic* or judaism or jew* or buddhis* or jehovah* or evangelical or evangelist* or adventist* or pentacostal).tw.
-
(barrier* or prohibit* or custom or customs or factor* or interest* or disinterest* or objection* or opposition or decision* or decide or deciding or allow* or agree* or disagree* or willing* or unwilling or moral* or ethics or ethical or attitude* or behaviour* or behavior* or knowledge or education* or opinion* or belief* or emotion* or motivat* or demotivat* or choice* or acceptab* or accessib* or inaccessib* or regist* or provision or availab* or aware* or perception or perceive* or view* or perspective* or inhibit* or influenc* or fear* or misunderstanding or misunderstood or consent or reluctant or reluctance or disparity or disparities or family or families or relative*).tw.
-
Great Britain/
-
(“united kingdom” or UK or england or scotland or wales or ireland).mp. [mp=title, original title, abstract, name of substance word, subject heading word, unique identifier]
-
“new south wales”.mp.
-
31 not 32
-
30 or 33
-
united states.mp.
-
(“united kingdom” or UK or england or scotland or wales or ireland).in.
-
new south wales.in.
-
36 not 37
-
(usa or “united states of america” or “north america”).in.
-
“north America”.mp.
-
(“central america” or “south america”).mp.
-
(“central america” or “south america”).in.
-
34 or 35 or 38 or 39 or 40
-
43 not (41 or 42)
-
28 or 29
-
exp Health Education/ or exp Health Knowledge, Attitudes, Practice/ or Health Behavior/ or exp Attitude to Health/ or Attitudes to Death/ or Prejudice/ or Healthcare Disparities/
-
Physician-Patient Relations/
-
45 or 46 or 47
-
18 and 27 and 44 and 48
-
limit 49 to yr=“1980 -Current”
-
“black market”.tw.
-
50 not 51
Appendix 2 Studies included in review of barriers to organ donor registration
| Author, date | Country | Sample size (response rate, %) | Participants | Aims | Sampling/recruitment | Data collection |
|---|---|---|---|---|---|---|
| Arriola et al. 200929 | USA | 425 (n/r) | Churches in a metropolitan area. 425 black adults, aged ≥ 18 years | To explore the association between different types of knowledge related to donation and transplantation, and donation intentions via ones driver’s license, a donor card or sharing ones wishes with family | Recruited from churches in a large metropolitan area | Questionnaire |
| Atkins et al. 200330 | USA | 375 (n/r) | Random-digit dialling (African Americans only) | To explore the inclination of African Americans to engage in family discussion about organ donation | African American adults sampled at random by telephone | Questionnaire |
| Boulware et al. 200231 | USA | 485 (84%) | 114 black females, 46 black males, 110 white females and 69 white males. Participants were aged 18–75 years | To assess race and gender differences in willingness to donate | Study population defined as all residents living in 14 ZIP codes in the Baltimore metropolitan area. Households sampled using random-digit selection | Telephone questionnaire |
| Cort and Cort 200832 | USA | 334 (n/r) | Two colleges. Seventh-day Adventist students. African American students (n = 182) and white (n = 152). Male = 41% | To compare the power of religious socialisation with racial socialisation with regard to willingness to consider organ donation | Questionnaires completed in classroom | Questionnaire |
| Creecy and Wright 199033 | USA | 217 (82%) | High school in the south-eastern United States. All participants classified as African American. Females = 57% of the sample | To identify correlates of willingness to consider cadaveric kidney donation among black Americans | Participants selected through systematic random sampling of black high school and university students | Questionnaire |
| Creecy et al. 199234 | USA | 217 (82%) | High school in the south-eastern United States. All participants classified as African American. Females = 57% of the sample, males = 43% of the sample | To identify discriminators of willingness to consider cadaveric kidney donation among black Americans | Participants selected through systematic random sampling of black high school and university students | Questionnaire |
| Davis and Randhawa 200435 | UK | 120 (n/a) | 120 black African and black Afro-Caribbean participants, aged 18–60+ years | To assess the current awareness of organ donation and transplantation among black African and African Caribbean populations | Advertised by posters in the community and personal invitations to residents. Letters sent to > 200 community groups and churches | Focus groups |
| Davis and Randhawa 200636 | UK | 120 (n/a) | 120 black African and black Afro-Caribbean participants. Men and women aged 18–60+ years | To examine the influence of religion on the extent and direction of public attitudes towards organ donation in black African and black Caribbean population | Advertised using posters in the community and personal invitations to residents. Letters were sent to > 200 community groups and churches | Focus groups |
| Edwards et al., 200737 | USA | 500 (93%) | First and second year medical students attending one of three Ohio medical schools, January–April 2005. White 77%, Asian 13%, black 8%, Latino 3% | Assessment of medical students’ knowledge and attitudes to determine their preparedness to encourage organ donation | Questionnaire distributed to medical students | Questionnaire |
| Exley et al. 199638 | UK | 22 (n/a) | 22 Sikh participants (male, n = 9; female, n = 13) | To examine the reluctance of one South Asian community in Coventry to organ donation | Local community and primary care settings | In-depth interviews |
| Fahrenwald and Stabnow, 200539 | USA | 217 (n/a) | 21 American Indians (female, n = 15; male, n = 6), aged 21–82 years | To understand the sociocultural patterns that influence decisions about organ and tissue donation among American Indian adults | Snowballing within the community | Interviews |
| Hayward and Madill, 200340 | UK | 27 (n/a) | Muslim women (n = 5), white English women (n = 9), Muslim men (n = 5), white men (n = 8).7 out of 10 Muslim participants were first generation. English participants were matched on occupational class with Muslim participants | To understand the meanings of organ donation with particular emphasis on donating eyes and hearts. Comparing people across gender and two ethnic groups | Women recruited through community centres. Men recruited face to face and through word of mouth | Focus groups |
| McNamara et al. 199941 | USA | 6080 (45%) | 4880 white respondents, 634 African American respondents and 566 Hispanic respondents. White: 48% male, average age 43 years | To assess the influence of several independent (knowledge, trust, bodily disfigurement) variables on willingness to donate | Stratified list-assisted random digit design to select households. Adults randomly selected using the most recent birthday technique. Booster sample of Hispanic and African American households | Telephone interview conducted by Gallup |
| Molzahn et al. 200442 | Canada | 39 (n/a) | 39 Chinese Canadian men and women. 15 participated in an interview (10 women and five men). This group were mixed in terms of generation. 24 individuals participated in a focus group | To explore the values and beliefs regarding organ donation of Chinese Canadians | Purposive and snowballing sampling | Interviews and focus groups |
| Molzahn et al. 200543 | Canada | 14 (n/s) | 13 Aboriginal Canadians (Coast Salish), (women n = 8, men n = 6). Age: 25–63 years | To explore the values and beliefs regarding organ donation of Coast Salish people living in British Columbia, Canada | Snowball sampling of English speaking adults | Interviews |
| Molzahn et al. 200544 | Canada | 40 (n/a) | 40 Indo-Canadians. 15 participants in the interviews (seven women and eight men). All first generation immigrants. 25 individual (19 women and six men) participated in the focus groups. The majority were first generation Canadians | To explore the values and beliefs regarding organ donation among Indo-Canadian people living in British Columbia | Purposive and snowballing sampling | Interviews and focus groups |
| Morgan et al. 200645 | UK | 1903 (84%) | Attendees at for general practices in London. White, n = 808 (52.6%), black Caribbean, n = 338 (22.0%), black African, n = 192 (12.5%), South Asian (Indian, Bangladeshi, Pakistani and other Asian), n = 33 (2.1%), other ethnic minorities/mixed races, n = 165 (10.7%) | To examine attitudes to kidney donation and registering as a donor among ethnic groups in the UK | Patients attending four general practices in South London were recruited into the study by a fieldworker | Questionnaire |
| Morgan et al. 200846 | UK | 12 (n/a) | 14 participants (nine women and five men), South East London (second or third generation Caribbean immigrants). Aged 21–48 years. Participants mainly from skilled and semi-skilled occupations | To understand the ways in which the self-identity and experiences of the Caribbean community shaped perceptions and attitudes to kidney donor registration | Purposive and snowballing sampling | In-depth interviews |
| Morgan et al. 200347 | USA | 798 (50%) | 710 (89%) white, 8% African American, 1% Hispanic, 1% Asian, 1% other | To examine similarities and differences between African Americans’ and European Americans’ attitudes, knowledge, and willingness to communicate about organ donation | Employees of a large national corporation | Questionnaire |
| Morgan 200648 | USA | 311 (n/r) | n = 310 African American. Female respondents = 59.4% of sample | To understand reluctance among African Americans and influence on donation decisions | Questionnaires distributed through regional community organisation and outreach managers at the regional organ procurement organisation | Questionnaire |
| Poonia J et al. 2006 (unpublished) | UK | 12 mini discussion groups and two friendship pairs (n/a) | First, second and third generation men and women of Bangladeshi, Pakistani, Indian and black Caribbean origin. Numbers in groups not given | To inform health promotion campaigns by examining attitudes to organ donation among different ethnic groups and generations | Not reported | Interviews and focus groups |
| Sherman et al. 200149 | USA | 241 (n/r) | African American: men (n = 94), women (n = 147). Mean age: 20.3 years | To examine the influence of disgust on attitudes to organ donation among African American students | Students completed survey during psychology classes. Participation was voluntary | Questionnaire |
| Siminoff et al. 200650 | USA | 1283 (60%) | Households in Ohio: African American, n = 312; white, n = 971 | To identify reasons for lower organ donation rates by African Americans by examining death, donation and transplantation | Residential random-digit dial sample frames. Adults in the household were randomly selected by selecting the adult with the most recent birthday | Telephone questionnaire |
| Smith et al. 200851 | UK | 50 (n/a) | 50 participants: 15 South Asian (9 females and 6 males); 19 white British/Irish (12 females, 7 males), 16 African Caribbean (10 females, 6 males) | To explore how people from three ethnic backgrounds who held a positive attitude towards organ donation had integrated the concept into their ethnic identity | Various sources of community recruitment | Oral history style interviews |
| Terrell et al. 200452 | USA | 120 (89%) | Black psychology students at a predominantly white university. Black male students n = 35, black female students, n = 75 | To examine the relative potential contribution of cultural mistrust to respondents’ willingness to participate in the organ donation system | Participants recruited from a large University in Dallas Fort Worth | Questionnaire |
| Wheeler et al. 199453 | USA | 29 (n/a) | 29 participants: 11 Japanese, 10 Chinese and 8 Filipino. 12 men and 17 women. Age range 18–50 years | To describe the attitudes and beliefs of Asian–Americans living in Hawaii concerning organ donation | Telephone recruitment | Focus groups |
List of papers included in review of barriers to organ donor registration
Arriola K, Robinson DH, Thompson NJ, Perryman JP. Project ACTS: an intervention to increase organ and tissue donation intentions among African Americans. Health Educ Behav 2009;37:264–74. 29
Atkins L, Davis K, Holtzman SM, Durand R, Decker PJ. Family discussion about organ donation among African Americans. Prog Transplant 2003;13:28–32. 30
Boulware LE, Ratner LE, Cooper LA, Sosa JA, LaVeist TA, Powe NR. Understanding disparities in donor behaviour: race and gender differences in willingness to donate blood and cadaveric organs. Med Care 2002;40:85–95. 31
Cort M, Cort D. Willingness to participate in organ donation among black Seventh–day Adventist college students. J Am Coll Health 2008;56:691–7. 32
Creecy RF, Wright R. Correlates of willingness to consider organ donation among blacks. Soc Sci Med 1990;31:1229–32. 33
Creecy RF, Wright R, Berg WE. Discriminators of willingness to consider cadaveric kidney donation among black Americans. Soc Work Health Care 1992;18:93–105. 34
Davis C, Randhawa G. ‘Don’t know enough about it!’: awareness and attitudes towards organ donation and transplantation among the black Caribbean and black African population in Lambeth, Southwark and Lewisham, United Kingdom. Transplantation 2004;78:420–5. 35
Davis C, Randhawa G. The influence of religion on organ donation and transplantation among the black Caribbean and black African population – a pilot study in the United Kingdom. Ethn Dis 2006;16:281–5. 36
Edwards TM, Essman C, Thornton JD. Assessing racial and ethnic differences in medical student knowledge, attitudes and behaviours regarding organ donation. J Natl Med Assoc 2007;99:131–7. 37
Exley C, Sim J, Reid N, Jackson S, West N. Attitudes and beliefs within the Sikh community regarding organ donation in a pilot study. Soc Sci Med 1996;43:23–8. 38
Fahrenwald NL, Stabnow W. Sociocultural perspective on organ and tissue donation among reservation-dwelling American Indian adults. Ethn Health 2005;10:341–54. 39
Hayward C, Madill A. The meanings of organ donation: Muslims of Pakistani origin and white English nationals living in North England. Soc Sci Med 2003;57:389–401. 40
McNamara P, Guadagnoli E, Evanisko MJ, Beasley C, Santiago-Delpin EA, Callender CO, et al. Correlates of support for organ donation among three ethnic groups. Clin Transplant 1999;13:45–50. 41
Molzahn AE, Starzomski R, McDonald M, O’Loughlin C. Aboriginal beliefs about organ donation: some Coast Salish viewpoints. Can J Nurs Res 2004;36:100–28. 42
Molzahn AE, Starzomski R, McDonald M, O’Loughlin C. Chinese Canadian beliefs toward organ donation. Qual Health Res 2005;15:82–98. 43
Molzahn AE, Starzomski R, McDonald M, O’Loughlin C. Indo-Canadian beliefs regarding organ donation. Prog Transplant 2005;15:233–9. 44
Morgan M, Hooper R, Mayblin M, Jones R. Attitudes to kidney donation and registering as a donor among ethnic groups in the UK. J Public Health (Oxf) 2006;28:226–34. 45
Morgan M, Mayblin M, Jones R. Ethnicity and registration as a kidney donor: the significance of identity and belonging. Soc Sci Med 2008;66:147–58. 46
Morgan SE, Miller JK, Arasaratnam LA. Similarities and differences between African Americans’ and European Americans’ attitudes, knowledge, and willingness to communicate about organ donation. J Appl Soc Psychol 2003;33:693–715. 47
Morgan SE. Many facets of reluctance: African Americans and the decision (not) to donate organs. J Natl Med Assoc 2006;98:695–703. 48
Poonia J. South Asian and Black Organ Donation Research Project: key findings. Prepared for Central Office of Information on behalf of UK Transplant. London: NHSBT. Unpublished; 2006.
Sherman NC, Sherman MF, Smith RJ, Rickert-Wilbur P. Disgust sensitivity and attitudes towards organ donation among African-American college students. Psychol Rep 2001;89:11–23. 49
Siminoff LA, Burant CJ, Ibrahim SA. Racial disparities in preferences and perceptions regarding organ donation. J Gen Intern Med 2006;21:995–1000. 50
Smith G, Saxena S, Car J, Jain N, Reece P, Dulku H, et al. The Potential Impact of an Opt-out System for Organ Donation in the UK – A Report from the Organ Donation Taskforce. Annex M (Cultural Working group). Appendix E, Becoming an Organ Donor: Oral Histories of People from Three Ethnic Backgrounds. London: Department of Health; 2008. 51
Terrell F, Moseley KL, Terrell AS, Nickerson KJ. The relationship between motivation to volunteer, gender, cultural mistrust, and willingness to donate organs among Blacks. J Natl Med Assoc 2004;96:53–60. 52
Wheeler MS, O’Friel M, Cheung AHS. Cultural beliefs of Asian-Americans as barriers to organ donation. J Transplant Coord 1994;4:146–50. 53
Appendix 3 Preferred Reporting Items for Systematic Reviews and Meta-Analyses checklist: systematic review of barriers to organ donor registration
| Section/topic | Number | Checklist item | Reported on page number |
|---|---|---|---|
| Title | |||
| Title | 1 | Identify the report as a systematic review, meta-analysis, or both | 11 |
| Abstract | |||
| Structured summary | 2 | Provide a structured summary including, as applicable: background; objectives; data sources; study eligibility criteria, participants, and interventions; study appraisal and synthesis methods; results; limitations; conclusions and implications of key findings; systematic review registration number | 11 |
| Introduction | |||
| Rationale | 3 | Describe the rationale for the review in the context of what is already known | 12 |
| Objectives | 4 | Provide an explicit statement of questions being addressed with reference to participants, interventions, comparisons, outcomes, and study design (PICOS) | 12 |
| Methods | |||
| Protocol and registration | 5 | Indicate if a review protocol exists, if and where it can be accessed (e.g. web address), and, if available, provide registration information including registration number | No |
| Eligibility criteria | 6 | Specify study characteristics (e.g. PICOS, length of follow-up) and report characteristics (e.g. years considered, language, publication status) used as criteria for eligibility, giving rationale | 13 |
| Information sources | 7 | Describe all information sources (e.g. databases with dates of coverage, contact with study authors to identify additional studies) in the search and date last searched | 14 |
| Search | 8 | Present full electronic search strategy for at least one database, including any limits used, such that it could be repeated | See Appendix 1 |
| Study selection | 9 | State the process for selecting studies (i.e. screening, eligibility, included in systematic review, and, if applicable, included in the meta-analysis) | 14–15 |
| Data collection process | 10 | Describe method of data extraction from reports (e.g. piloted forms, independently, in duplicate) and any processes for obtaining and confirming data from investigators | n/a |
| Data items | 11 | List and define all variables for which data were sought (e.g. PICOS, funding sources) and any assumptions and simplifications made | Available in Morgan et al.57 |
| Risk of bias in individual studies | 12 | Describe methods used for assessing risk of bias of individual studies (including specification of whether this was done at the study or outcome level), and how this information is to be used in any data synthesis | 15 |
| Summary measures | 13 | State the principal summary measures (e.g. risk ratio, difference in means) | n/a |
| Synthesis of results | 14 | Describe the methods of handling data and combining results of studies, if done, including measures of consistency (e.g. I2) for each meta-analysis | n/a |
| Risk of bias across studies | 15 | Specify any assessment of risk of bias that may affect the cumulative evidence (e.g. publication bias, selective reporting within studies) | 15 |
| Additional analyses | 16 | Describe methods of additional analyses (e.g. sensitivity or subgroup analyses, meta-regression), if done, indicating which were pre-specified | n/a |
| Results | |||
| Study selection | 17 | Give numbers of studies screened, assessed for eligibility, and included in the review, with reasons for exclusions at each stage, ideally with a flow diagram | 15 |
| Study characteristics | 18 | For each study, present characteristics for which data were extracted (e.g. study size, PICOS, follow-up period) and provide the citations | See Appendix 2 |
| Risk of bias within studies | 19 | Present data on risk of bias of each study and, if available, any outcome level assessment (see Item 12) | n/a |
| Results of individual studies | 20 | For all outcomes considered (benefits or harms), present, for each study: (a) simple summary data for each intervention group (b) effect estimates and confidence intervals, ideally with a forest plot | n/a |
| Synthesis of results | 21 | Present results of each meta-analysis done, including confidence intervals and measures of consistency | n/a |
| Risk of bias across studies | 22 | Present results of any assessment of risk of bias across studies (see Item 15) | 18 |
| Additional analysis | 23 | Give results of additional analyses, if done (e.g. sensitivity or subgroup analyses, meta-regression [see Item 16]) | n/a |
| Discussion | |||
| Summary of evidence | 24 | Summarise the main findings including the strength of evidence for each main outcome; consider their relevance to key groups (e.g. health-care providers, users, and policy-makers) | 16–17 |
| Limitations | 25 | Discuss limitations at study and outcome level (e.g. risk of bias), and at review-level (e.g. incomplete retrieval of identified research, reporting bias) | 18 |
| Conclusions | 26 | Provide a general interpretation of the results in the context of other evidence, and implications for future research | 18 |
| Funding | |||
| Funding | 27 | Describe sources of funding for the systematic review and other support (e.g. supply of data); role of funders for the systematic review | Part of overall NIHR programme |
Appendix 4 Focus group topic guide (annotated with instructions for facilitators)
Appendix 5 Focus group questionnaire
Appendix 6 Characteristics of focus group participants
| Focus group number | Ethnicity, age (years), gender, language | Number of participants | Average age (years) (range) | Place of birth | Work | Know someone waiting for or received a transplant |
|---|---|---|---|---|---|---|
| 11 | Caribbean, 18–40, mixed, English | 8 | 31 (21–41) | UK, n = 7 Jamaica, n = 1 |
Employed, n = 5 Student, n = 2 Care for family, n = 1 |
2/8 |
| 2 | Caribbean, ≥ 40, mixed, English | 7 | 54 (28–71) | Jamaica, n = 5 Barbados, n = 1 Not stated, n = 1 |
Unemployed, n = 3 Care for family, n = 1 Retired, n = 3 |
2/7 |
| 20 | Caribbean, ≥ 40, mixed, English | 12 | 52 (44–76) | UK, n = 3 Barbados, n = 1 St Kitts, n = 1 Guyana, n = 1 Jamaica, n = 1 Sierra Leone, n = 1 Not stated, n = 4 |
Employed, n = 6 Unemployed, n = 3 Care for family, n = 2 Retired, n = 1 |
4/12 |
| 13 | African, 18–40 mixed, English | 9 | 31 (20–40) | Nigeria, n = 9 | Employed, n = 6 Student, n = 3 |
2/9 |
| 22 | African 18–40, mixed, English | 12 | 22 (19–49) | UK, n = 5 Nigeria, n = 7 |
Employed, n = 7 Student, n = 4 Care for family, n = 1 |
0/12 |
| 21 | African, ≥ 40, mixed, English | 11 | 48 (38–58) | UK, n = 1 Nigeria, n = 8 Not stated, n = 2 |
Employed, n = 6 Unemployed, n = 4 Not stated, n = 1 |
1/11 |
| 8 | Pakistani, 18–40, male, English | 9 | 30 (22–43) | UK, n = 3 Pakistan, n = 4 India, n = 1 Kenya, n = 1 |
Employed, n = 6 Unemployed, n = 1 Student, n = 2 |
0/9 |
| 16 | Pakistani, ≥ 40, male, Urdu | 6 | 56 (50–69) | UK, n = 1 Pakistan, n = 4 Not stated, n = 1 |
Employed, n = 2 Unemployed, n = 1 Retired, n = 2 Not stated, n = 1 |
0/9 |
| 7 | Pakistani, 18–40, female, English | 18 | 32 (19–58) | UK, n = 3 Pakistan, n = 12 Kenya, n = 1 Russia, n = 1 Bangladesh, n = 1 |
Employed, n = 3 Unemployed, n = 4 Student, n = 3 Care for family, n = 7 |
4/18 |
| 15 | Pakistani, ≥ 40, female, Urdu | 10 | 48 (44–60) | Pakistan, n = 7 Not stated, n = 3 |
Unemployed, n = 4 Care for family, n = 6 |
0/10 |
| 4 | Bangladeshi, 18–40, male, English | 15 | 29 (19–40) | Bangladesh, n = 11 Not stated, n = 4 |
Employed, n = 4 Unemployed, n = 4 Student, n = 7 |
1/15 |
| 18 | Bangladeshi, ≥ 40, male, Sylheti | 10 | 47 (36–58) | Bangladesh, n = 8 Not stated, n = 2 |
Employed, n = 6 Unemployed, n = 2 Not stated, n = 2 |
0/10 |
| 3 | Bangladeshi, 18–40, female, English | 11 | 29 (21–41) | Bangladesh, n = 3 UK, n = 7 Not stated, n = 1 |
Employed, n = 5 Unemployed, n = 5 Student, n = 1 |
2/11 |
| 17 | Bangladeshi, ≥ 40, female, Sylheti | 11 | 46 (33–58) | Bangladesh, n = 7 Not stated, n = 4 |
Employed, n = 4 Unemployed, n = 3 Care for family, n = 3 Retired, n = 1 |
1/11 |
| 6 | Indian, Hindu, 18–40, male, English | 10 | 28 (18–45) | UK, n = 1 India, n = 8 Zambia, n = 1 |
Employed, n = 5 Student, n = 5 |
2/10 |
| 14 | Indian, Hindu ≥ 40, male, Guajarati | 10 | 50 (50–61) | Yemen, n = 3 India, n = 7 |
Employed, n = 2 Unemployed, n = 5 Student, n = 1 Care for family, n = 1 Retired, n = 1 |
2/10 |
| 5 | Indian, Hindu women, 18–40, English | 10 | 31 (26–40) | India, n = 10 | Employed, n = 8 Student, n = 1 Care for family, n = 1 |
3/10 |
| 12 | Indian, Hindu women, ≥ 40, Guajarati | 9 | 52 (45–63) | India, n = 7 Kenya, n = 1 Not stated, n = 1 |
Employed, n = 1 Unemployed, n = 4 Care for family, n = 2 Retired, n = 1 Not stated, n = 1 |
2/9 |
| 10 | Indian Sikh, 18–40, male, English | 10 | 34 (18–40) | UK, n = 7 Tanzania, n = 1 Not stated, n = 1 |
Employed, n = 9 Student, n = 1 |
2/10 |
| 19 | Indian Sikh, ≥ 40, male, Punjabi | 9 | 54 (44–62) | India, n = 7 Not stated, n = 2 |
Employed, n = 7 Unemployed, n = 2 |
1/9 |
| 9 | Indian Sikh, 18–40, female, English | 12 | 33 (26–50) | India, n = 7 UK, n = 3 Norway, n = 1 Not stated, n = 1 |
Employed, n = 8 Unemployed, n = 1 Student, n = 1 Care for family, n = 1 |
2/12 |
| 23 | Indian Sikh, ≥ 40, female, Punjabi | 9 | 55 (44–68) | India, n = 9 | Employed, n = 1 Care for family, n = 7 Retired, n = 1 |
0/9 |
Appendix 7 Medical subject heading terms (MEDLINE) for systematic review of effective interventions
This text is reproduced from Deedat S, Kenten C, Morgan M. What are effective approaches to increasing rates of organ donor registration among ethnic minority populations: a systematic review. BMJ Open 2013;3:e003453 under the Creative Commons Attribution-NonCommercial 4.0 International (CC BY-NC 4.0). 86
Date range searched: January 1980 to January 2012.
Date of search: March 2012.
-
randomized controlled trial/ or clinical trial/ or controlled clinical trial/ or multicenter study/ or single blind method/ or double blind method/ or random allocation/ or chi square distribution/ or control groups/ or Cross-Sectional Studies/ or Cohort Studies/
-
(randomized controlled trial or controlled clinical trial or multicenter study).pt.
-
(random adj2 allocat*).tw.
-
(control* adj2 (clinical or group* or trial* or study or studies or design* or methods or random*)).ti,ab.
-
((multicent* or multi-cent* or multisite? or multi-site?) adj (study or studies or trial*)).ti,ab.
-
(random* or quasi* or “before and after”).ti,ab.
-
randomized controlled trials as topic/ or clinical trials as topic/
-
((single or double or treble or triple) adj (blind* or mask*)).tw.
-
chi-square?.ti,ab.
-
Chi-Square Distribution/
-
Research Design/
-
Matched-Pair Analysis/
-
matched pair*.ti,ab.
-
Meta-Analysis/
-
meta analy*.ti,ab.
-
“Outcome Assessment (Health Care)”/
-
(outcome* stud* or intervention* stud*).ti,ab.
-
Intervention Studies/
-
follow up studies/ or pilot projects/ or prospective studies/
-
Evaluation Studies as Topic/
-
Evaluation Studies/
-
(effective adj3 intervention*).ti,ab.
-
(evaluat* adj3 intervention*).ti,ab.
-
(outcome* adj3 measure*).ti,ab.
-
primary outcome*.ti,ab.
-
secondary outcome*.ti,ab.
-
Comparative Study/
-
evaluat*.tw.
-
or/1-28
-
exp “Tissue and Organ Procurement”/
-
((cadaver or deceased or dead) adj2 (donor* or donat*)).ti,ab.
-
((organ or organs) adj3 (donor* or donat*)).ti,ab.
-
((cadaver or deceased) adj2 (donat* or donor*)).ti,ab.
-
((postmortem or post mortem) adj2 (donat* or donor*)).ti,ab.
-
(“organ donor” or “organ donors” or “organ donation”).ti,ab.
-
or/30-35
-
Indians, North American/
-
African Americans/ or Asian Americans/
-
“native american*”.tw.
-
(race or racial or ethnic* or native american* or native canadian* or native alaskan* or american indian* or canadian indian* or amerind* or negro* or afro* or african* or black or blacks or arab* or asian* or chinese or japanese or oriental* or thai* or philipino* or filipino* or taiwanese* or indian* or bengali* or kashmiri* or gujarati* or tamil* or bangladeshi* or pakistani* or sri lankan* or hispanic* or latino* or nonwhite* or non-white* or multiracial or multi-racial).tw.
-
Hispanic Americans/
-
Mexican Americans/
-
ethnic groups/
-
(culture or cultural or faith* or relig* or sikh* or hindu* or muslim* or islam* or christian* or catholic* or judaism or jew* or buddhis* or jehovah* or evangelical or evangelist* or adventist* or pentacostal).tw.
-
Minority Groups/
-
Continental Population Groups/
-
Asian Continental Ancestry Group/
-
Asian Continental Ancestry Group/ or African Continental Ancestry Group/ or Ethnic Groups/
-
british asian*.tw.
-
british african*.tw.
-
or/37-50
-
29 and 36 and 51
-
(consent* adj3 (increas* or accept* or participat* or encourag* or facilitat* or influenc* or promot* or chang* or focus* or motivat*)).tw.
-
informed consent/
-
cultural competency/
-
decision making/
-
Communication/ or Communication Barriers/
-
Communications Media/
-
(media or message* or communicat* or television or radio or broadcast* or internet or campaign* or program* or leaflet* or questionnaire* or literature or pamphlet* or resource*).tw.
-
((register* or registration) adj3 (increas* or accept* or encourag* or facilitat* or influenc* or promot* or chang* or focus* or motivat*)).tw.
-
((register* or registration or registry or registries) adj3 (increas* or accept* or encourag* or facilitat* or influenc* or promot* or chang* or focus* or motivat*)).tw.
-
(intervention* or multiintervention* or multi-intervention* or postintervention* or post-intervention* or preintervention* or pre-intervention*).tw.
-
Patient Education Handout/ or Health Education/ or Education/ or Patient Education as Topic/
-
Patient Participation/ or intention/
-
Attitude to Health/
-
Health Knowledge, Attitudes, Practice/
-
“Attitude of Health Personnel”/
-
Health Personnel/ed [Education]
-
Health Policy/ or “Delivery of Health Care”/
-
(policy or policies or practice or practices).tw.
-
or/53-70
-
29 and 36 and 51 and 71
-
(“tissue donor” or “tissue donors” or “tissue donation”).tw.
-
72 not 73
-
*living donors/
-
74 not 75
Added line 77 as a double safety check to see if the live donor papers included any live and dead donors – 2 selected.
-
74 not 76
-
from 77 keep 16,30
Appendix 8 Summary of studies included in review of effective interventions
| Author and country | Demographic sample size | Study design | Mode of delivery | Results | Outcomes | Theoretical framework | Database |
|---|---|---|---|---|---|---|---|
| Allen and Stillwater 2010,69 USA | Alaskan native, health staff (n = 54) and students (n ≤ 200) | Before-and-after study (education) | PowerPoint® presentation and video focused on issues about organ donation and Alaskan natives | Improved knowledge and positive attitude towards donation and intention to register post test | Knowledge and intention to register as a donor | Not mentioned | Hand search of book |
| Alvaro et al. 2006,70 USA (pertains to study II reported in paper) | Hispanic | Before-and-after study (education) | On alternate weeks, employees of the local organ procurement organisation offered the attendees at a flea market an immediate opportunity to register or information about organ donation | Participants offered an immediate opportunity to register rather than just information about organ donation were significantly more likely to register (86% vs. 54%) | Verified registration | The IIFF model (Immediate opportunity, information, focused engagement and favourable activation) | MEDLINE |
| Alvaro et al. 2011,71 USA | Hispanic, n = 2401 | Before-and-after study (media campaign) | Television and radio adverts highlighted positive impact of transplantation on Hispanic individuals and substantial efforts by doctors to save the life of a potential donor | Greater reporting of pro-donation beliefs and family discussion post intervention | Self-reported registration status. No validated measures of attitude and willingness to organ donations | Not mentioned | EMBASE and MEDLINE |
| Andrews et al. 2012,72 USA | African American intervention n = 622; control n = 632 | Cluster randomised (education) | Members of the congregation undertook discussions with lay health advisors about organ donation. A DVD was designed to address organ donation barriers for African Americans | Increase in verified enrolment on donor registry in intervention group. No increase in knowledge observed | Verified enrolment on donor registry | Not mentioned | PubMed |
| Arriola et al. 2009,29 USA | African American intervention n = 175; control n = 162 | Cluster randomised(education) | Video and written materials mailed to participants | Greater readiness to sign a donor card, register through a driver’s licence or talk to family about wishes in the intervention group | Readiness to express donation intent through a driver’s licence, donor card and discussion with family | TTM | EMBASE, PubMed and MEDLINE |
| Buffin et al. 2015,85 UK | Multiethnic, n = 806 | Cross-sectional evaluation (education) | Peer educators trained to deliver health promotion about organ donation | Increase in the percentage of people signed up to the ODR | Registration | Not mentioned | Author contact |
| Callender et al. 2001,73 USA | Multiethnic n = 914 | Before-and-after study (education) | Presentation about organ donation delivered by transplant recipients, donors, individuals on transplant lists health-care professionals who are ethnically similar to the target population | Improvements in knowledge and attitudes towards organ donation, high reporting of willingness to discuss organ donation with family | Willingness to donate organs for oneself and loved ones after death. No valid measures to assess attitudes to organ donation | Not mentioned | EMBASE |
| Cárdenas et al. 201074 USA | Multiethnic intervention n = 96; control n = 91 | Cluster randomised (education) | Transplant surgeons and young recipients gave a presentation followed by a Q&A session and video | Knowledge increase post intervention was the strongest predictor of positive change in opinion about organ donation | Knowledge, attitudes and awareness of organ donation | None mentioned | MEDLINE |
| Fahrenwald et al. 2011,75 USA | American Indians n = 1580 | Before-and-after study (education) | Outreach co-ordinators facilitate delivery to small groups who were required to read and discuss a one-page brochure. This was followed by a 13-minute video and a group discussion facilitated by the co-ordinator | Significant change in stage of motivational readiness to become an organ donation post intervention | Stage of motivational readiness to serve as an organ donor | TTM | PubMed |
| Feeley et al. 2009,76 USA | Multiethnic | Before-and-after study (education) | Peer educators delivered a range of campus-based activities | Increased donor registration | Self-reported registration | Not mentioned | MEDLINE |
| Frates et al. 2006,77 USA | Hispanic, n = 4500 | Before-and-after study (media campaign) | Prime-time television and radio slots | Year-on-year increase in Hispanic organ donation consent rates | Consent rates from organ procurement organisation. No valid measures to assess attitudes to organ donation | TTM | EMBASE, MEDLINE and PsycINFO |
| Harrison et al. 2011,78 USA | African American, n = 626,771 | Before-and-after study (media campaign) | Billboards in the vicinity of vehicle licensing offices and radio adverts. Trained volunteers with links to donation at vehicle licensing offices to engage in conversation | Overall 700% increase above baseline in sign up to the donor register. The magnitude of the increase was greatest when one-to-one promotion was combined with other medium | Verified registration | Communication design | PubMed |
| Hebert et al. 2010,79 USA | Chinese American, n = 1134 | Before-and-after study (media campaign) | Media campaign. Grass roots community outreach | Significant increase in stated intention to donate in the intervention area vs. the control area | Joining a donor registry; express a desire to become an organ donor; communicating wishes to family | Not mentioned | Hand search of book |
| Radosevich et al.,80 USA | African American, n = 465 | Before-and-after study (media campaign) | Media campaign conveyed through television, radio, targeted print media. Donor families and health-care professionals were interviewed on television and radio | Significant increase in knowledge and attitude about organ donation post campaign | No significant change in intention and willingness to become a donor | Theory of reasoned action | Hand search of Book |
| Resnicow et al. 2010,81 USA | African American, intervention n = 1370; control n = 1419 | Cluster randomised (education) | Hairstylists trained as lay health advisors used motivational interviewing to discuss organ donations with customers | Participants receiving the intervention were four times more likely to join the register than the controls | Self-reported donation status. Verified enrolment on state registry | Not mentioned | PubMed and EMBASE |
| Salim et al. 2012,82 USA | Hispanic, n = 341 | Before-and-after study (education) | Presentation about the need for transplant and information about donation led by a local organ procurement organisation | Increase in knowledge, perceptions and beliefs. No difference willingness to discuss donation with family or intent to donate | Change in knowledge and attitude. Donation intent | Not mentioned | PubMed |
| Salim et al. 2011,83 USA | Hispanic, n = 1052 | Before-and-after study (media campaign) | Prime-time television and radio slots | Improved knowledge post campaign when compared with baseline | Awareness, perception and belief about organ donation | Not mentioned | EMBASE and MEDLINE |
| Thornton et al., 2012,84 USA | Multiethnic intervention, n = 443; control n = 509 | Cluster randomised (media campaign) | 5-minute video about organ donation prior to collecting driver’s licence. Controls obtained licence in the usual manner | Cases more likely to register as donors compared with controls (76% vs. 54%) | Verified enrolment on donor registry | Not mentioned | EMBASE |
List of studies included in review of effective interventions
Allen MD, Stillwater B. Organ donation and transplantation: a new tradition of sharing for Alaska natives. In Siegel JT, Alvaro EM, editors. Understanding Organ Donation: Applied Behavioral Science Perspectives. Chichester: Wiley-Blackwell; 2010. pp. 83–97. 69
Alvaro EM, Jones SP, Robles AS, Siegel J. Hispanic organ donation: impact of a Spanish-language organ donation campaign. J Natl Med Assoc 2006;98:28–35. 70
Alvaro EM, Siegel JT, Jones SP. Increasing organ donor registration rates by providing an immediate and complete registration opportunity: an experimental assessment of the IIFF model. Psychol Health Med 2011;16:686–94. 71
Andrews AM, Zhang N, Magee JC, Chapman R, Langford AT, Resnicow K. Increasing donor designation through black churches: results of a randomized trial. Prog Transplant 2012;22:161–7. 72
Arriola K, Robinson DH, Thompson NJ, Perryman JP. Project ACTS: an intervention to increase organ and tissue donation intentions among African Americans. Health Educ Behav 2009;37:264–74. 29
Callender CO, Hall MB, Branch D. An assessment of the effectiveness of the Mottep model for increasing donation rates and preventing the need for transplantation – adult findings: program years 1998 and 1999. Semin Nephrol 2001;21:419–28. 73
Cárdenas V, Thornton JD, Wong KA, Spigner C, Allen MD. Effects of classroom education on knowledge and attitudes regarding organ donation in ethnically diverse urban high schools. Clin Transplant 2010;24:784–93. 74
Fahrenwald NL, Belitz C, Keckler A. ‘Tribes sharing life’: an organ donation educational intervention for American Indian tribal college and university students. West J Nurs Res 2011;33:901–15. 75
Feeley TH, Anker AE, Watkins B, Rivera J, Tag N, Volpe L. A peer-to-peer campaign to promote organ donation among racially diverse college students in New York city. J Natl Med Assoc 2009;101:1154–62. 76
Frates J, Bohrer CG, Thomas D. Promoting organ donation to Hispanics: the role of the media and medicine. J Health Community 2006;11:683–98. 77
Harrison TR, Morgan SE, King AJ, Williams EA. Saving lives branch by branch: the effectiveness of driver licensing bureau campaigns to promote organ donor registry sign-ups to African Americans in Michigan. J Health Community 2011;16:805–19. 78
Hebert PL, Rivera J, Eng K, Lee R, Seto-Yee RN. Improving Organ Donations in Chinese Communities in New York. In Understanding Organ Donation: Applied Behavioral Science Perspectives. Chichester: Wiley-Blackwell; 2010. pp. 199–131. 79
Radosevich DM, Larson SM, Scott T, Jones C, Tenle W, Gunderson S, et al. The effectiveness of the donate life – African American campaign in Minneapolis-St Paul. In Siegel JT, Alvaro EM, editors. Understanding Organ donation: Applied Behavioral Science Perspectives. Wiley-Blackwell; 2010. pp. 64–82. 80
Resnicow K, Andrews AM, Beach DK, Kuhn L, Krein SL, Chapman R, et al. Randomized trial using hair stylists as lay health advisors to increase donations in African Americans. Ethn Dis 2010;20:276–81. 81
Salim A, Berry C, Ley EJ, Schulman D, Navarro S, Zheng L, et al. A focused educational program after religious services to improve organ donation in Hispanic Americans. Clin Transplant 2012;26:e634–40. 82
Salim A, Berry C, Ley EJ, Schulman D, Navarro S, Chan LS. Utilizing the media to help increase organ donation in the Hispanic American population. Clin Transplant 2011;25:E622–8. 83
Thornton JD, Alejandro-Rodriguez M, León JB, Albert JM, Baldeon EL, De Jesus LM, et al. Effect of an iPod video intervention on consent to donate organs: a randomized trial. Ann Intern Med 2012;156:483–90. 84
Buffin J, Little R, Jain N, Warrens AN. A peer outreach initiative to increase the registration of minorities as organ donors. Clin Kidney J 2015;8:623–8. 85
Appendix 9 Preferred Reporting Items for Systematic Reviews and Meta-Analyses checklist: systematic review of effective interventions
| Section/topic | Number | Checklist item | Reported on page number |
|---|---|---|---|
| Title | |||
| Title | 1 | Identify the report as a systematic review, meta-analysis, or both | 36 |
| Abstract | |||
| Structured summary | 2 | Provide a structured summary including, as applicable: background; objectives; data sources; study eligibility criteria, participants, and interventions; study appraisal and synthesis methods; results; limitations; conclusions and implications of key findings; systematic review registration number | 36 |
| Introduction | |||
| Rationale | 3 | Describe the rationale for the review in the context of what is already known | 36 |
| Objectives | 4 | Provide an explicit statement of questions being addressed with reference to participants, interventions, comparisons, outcomes, and study design (PICOS) | n/a |
| Methods | |||
| Protocol and registration | 5 | Indicate if a review protocol exists, if and where it can be accessed (e.g. web address), and, if available, provide registration information including registration number | No |
| Eligibility criteria | 6 | Specify study characteristics (e.g. PICOS, length of follow-up) and report characteristics (e.g. years considered, language, publication status) used as criteria for eligibility, giving rationale | 37 |
| Information sources | 7 | Describe all information sources (e.g. databases with dates of coverage, contact with study authors to identify additional studies) in the search and date last searched | 36 |
| Search | 8 | Present full electronic search strategy for at least one database, including any limits used, such that it could be repeated | See Appendix 7 |
| Study selection | 9 | State the process for selecting studies (i.e. screening, eligibility, included in systematic review, and, if applicable, included in the meta-analysis) | 37 |
| Data collection process | 10 | Describe method of data extraction from reports (e.g. piloted forms, independently, in duplicate) and any processes for obtaining and confirming data from investigators | n/a |
| Data items | 11 | List and define all variables for which data were sought (e.g. PICOS, funding sources) and any assumptions and simplifications made | n/a |
| Risk of bias in individual studies | 12 | Describe methods used for assessing risk of bias of individual studies (including specification of whether this was done at the study or outcome level), and how this information is to be used in any data synthesis | 37 |
| Summary measures | 13 | State the principal summary measures (e.g. risk ratio, difference in means) | n/a |
| Synthesis of results | 14 | Describe the methods of handling data and combining results of studies, if done, including measures of consistency (e.g. I2) for each meta-analysis | n/a |
| Risk of bias across studies | 15 | Specify any assessment of risk of bias that may affect the cumulative evidence (e.g. publication bias, selective reporting within studies) | n/a |
| Additional analyses | 16 | Describe methods of additional analyses (e.g. sensitivity or subgroup analyses, meta-regression), if done, indicating which were pre-specified | n/a |
| Results | |||
| Study selection | 17 | Give numbers of studies screened, assessed for eligibility, and included in the review, with reasons for exclusions at each stage, ideally with a flow diagram | 37 |
| Study characteristics | 18 | For each study, present characteristics for which data were extracted (e.g. study size, PICOS, follow-up period) and provide the citations | See Appendix 8 |
| Risk of bias within studies | 19 | Present data on risk of bias of each study and, if available, any outcome level assessment (see Item 12) | n/a |
| Results of individual studies | 20 | For all outcomes considered (benefits or harms), present, for each study: (a) simple summary data for each intervention group (b) effect estimates and confidence intervals, ideally with a forest plot | n/a |
| Synthesis of results | 21 | Present results of each meta-analysis done, including confidence intervals and measures of consistency | n/a |
| Risk of bias across studies | 22 | Present results of any assessment of risk of bias across studies (see Item 15) | n/a |
| Additional analysis | 23 | Give results of additional analyses, if done [e.g. sensitivity or subgroup analyses, meta-regression (see Item 16)] | n/a |
| Discussion | |||
| Summary of evidence | 24 | Summarise the main findings including the strength of evidence for each main outcome; consider their relevance to key groups (e.g. health-care providers, users, and policy-makers) | 38–9 |
| Limitations | 25 | Discuss limitations at study and outcome level (e.g. risk of bias), and at review level (e.g. incomplete retrieval of identified research, reporting bias) | 39 |
| Conclusions | 26 | Provide a general interpretation of the results in the context of other evidence, and implications for future research | 39 |
| Funding | |||
| Funding | 27 | Describe sources of funding for the systematic review and other support (e.g. supply of data); role of funders for the systematic review | Part of overall NIHR programme |
Appendix 10 Topic guide for bereaved family interviews
-
Prior to recording: re-cap of the research and the information the participant has received.
-
Ensure participant aware CK/SD are researchers not counsellors.
-
Take written consent.
-
Ensure the participant has a person to support them after the researcher leaves.
-
Ensure participant is happy to begin.
Background
Could you tell me a little about [name]?
What were they like as a person?
What role did they play in the family?
When did you become aware that something had happened to [name]?
Hospital
Which hospital was [name] admitted to?
Did [name] move hospitals during the course of [their] treatment?
Can you tell me what happened when you first arrived at intensive care? (or A&E)
-
First impressions of the unit?
-
Who was with you?
-
Which of the medical staff spoke with you?
-
Where did they speak to you (bedside, ward, relatives room, office)?
-
What did they discuss with you?
-
How did you feel about this discussion (e.g. any information given, the manner in which the discussion was carried out, chance to ask questions and have them answered, etc.)?
-
Who else came to the hospital (immediate family, extended family, friends)?
At what point after [name] was admitted were you aware that their outlook/prognosis was poor? (Hours, days, weeks?)
Potential of treatment withdrawal
When were you told that [name] would not recover?
Can you tell me what you remember about this conversation?
-
Who talked to you about the fact that [name] would not recover?
-
How did they explain [name] situation?
-
Who was with you at this time (family)?
-
Was anyone else present, e.g. other medical staff and did they say or do anything?
-
Where did the conversation take place?
How long did it take you/other family members to recognise that further treatment would not save [name]’s life?
Thinking back to this conversation, how well do you think this information was explained to you?
-
Was everything explained clearly to you?
-
Were you given time to ask questions?
-
Did you or any of your family have any questions? What were these?
-
Probe on trust – did you question whether this information was correct?
-
How do you feel you and your family were treated by the staff (sensitive, caring, rushed)?
Were you offered any spiritual or religious support or similar from outside the hospital?
-
If yes, what was the type and form of that support (talk, practical, faith based e.g. prayer)?
Donation after brain stem death only
How was the fact that [name] was ‘brain stem dead’ explained to you?
Did you have any questions about this?
How were the brain stem death tests explained to you?
Were you offered the opportunity to observe the Doctor carrying out these tests?
Approaching organ donation
Can you tell me when organ donation was first mentioned?
-
How was this explained and by whom?
-
What was your reaction?
Had you ever discussed organ donation with [name]?
Did [name] have any views towards organ donation?
Which family members did you discuss donating [name] organs with?
-
What were the views within the family?
-
Any areas of agreement/disagreement? Was a consensus reached?
-
What were the views of older and younger members of your family?
-
Did you have any questions about organ donation (did you ask these, were they answered)?
-
Did you have any concerns about organ donation?
-
Where were you when you were discussing whether or not to agree to donation (waiting room, bedside, not at hospital)?
-
Were any of the doctors or nurses present when you were discussing this?
-
How long did it take you to decide what you wanted to do?
Did you ever feel any pressure to make a decision one way or the other?
What did you decide re: organ donation?
How did you come to this decision?
Were there any particular influences in this decision?
-
Family (who, what was their view, who had the final say)?
-
Cultural?
-
Faith?
-
Time pressure (family e.g. funeral considerations or clinical)?
-
How did this influence your decision (explore)?
What happened next?
Were you and other members of the family able to spend time with [name]?
Was there anything you or a family member wanted done for [name] at this point or closer to their death or just after?
-
Family, e.g. jewellery?
-
Cultural, e.g. wearing something/washing the body?
-
Faith, e.g. prayers?
Why was it important that these things were done? (This is normal practice, generation specific, gender specific.)
Were these requests carried out?
Where was this and did you feel this space was appropriate?
Death and circulatory (or cardiac) death only
How did the medical staff explain how they would withdraw treatment and how they would diagnose death?
Was any time frame given re: when [name] would die?
Can you tell me about when [name] died?
-
Was this what you expected?
Where did [name] die?
Death by brain stem death only
How did the medical staff explain how they would proceed and how they would diagnose death?
How did you feel about [name] body functions being maintained by the ventilator when they had been certified dead by brain stem testing?
Ask to all
Can I ask more broadly, for a relative who hasn’t died in intensive care or in hospital, what would be the normal things that you would like for that person?
-
Practices normal to the family?
-
Anything gender specific?
-
Cultural practices?
-
Faith practices?
Decided to donate
Can you tell me about the paperwork that needed to be completed for donation?
-
What did you agree to being donated?
-
What did you not want to be donated? Why
How well do you feel you were supported in your decision-making?
What time-scale were you given for [name] to be taken to the operating theatre?
Were you able to spend time with [name]?
Were you offered any mementos, e.g. hand prints, etc.?
-
Where was this and did you feel this space was appropriate (private, quiet)?
What did you do when [name] went to theatre?
After [name] had donated their organs, have you had any contact with staff from intensive care (meet in person, phone call, letter)?
Do you know what happened to [name] organs?
Was any follow-up discussed with you by the specialist nurse for organ donation/transplant co-ordinator?
Reflections
How did you feel about the care and treatment that [name] and the family received while in hospital (General reflection of overall care at the hospital)?
What was the best thing about the way you were approached to consider organ donation?
What do you wish they had done differently (and how)?
How do you now feel about your donation decision?
Taking part in research
Just to finish with, we’re interested in why people agree to take part in a research interview.
How did you feel about receiving a letter inviting you to participate in this study?
Did you discuss your participation in this interview with anyone else/other family members?
Why were you willing to take part in this interview?
Exit
Is there anything else you would like to tell me about your experience?
Offer any bereavement information, referral, etc.?
Will give follow-up telephone call within 24–48 hours (arrange a convenient time)
Expect a letter of thanks and a short questionnaire evaluation of the interview
If you would like a summary of research (will remind in letter).
Thank you for your time.
Appendix 11 Workbook for training intervention
Appendix 12 Evaluation questionnaires for DonaTE training intervention
Appendix 13 Internal consistency of subscales of the theory of planned behaviour questionnaire
| Subscale | Number of items | Cronbach’s alpha for scale |
|---|---|---|
| Attitudes towards organ donation | 30 | 0.938 |
| Subjective norms – normative beliefs about subjective norms | 5 | 0.610 |
| Subjective norms – motivation to comply with subjective norms | 4 | 0.839 |
| Perceived behavioural change – control beliefs | 4 | 0.626 |
| Perceived behavioural change – influence of control beliefs | 8 | 0.851 |
| Behavioural intentions | 10 | 0.886 |
Appendix 14 Subscale cores for the participants who completed the pre-intervention questionnaire by professional group (scores range from –3 to +3)
| TPB constructs | SNODs (n = 19) | Nurses (n = 58) | Doctors (n = 22) | Significance |
|---|---|---|---|---|
| Attitudes towards organ donation | ||||
| Mean (SD) | 2.0 (0.93) | (0.82) | 1.5 (0.8) | < 0.001 |
| Median | 2.3 | 1.1 | 1.5 | |
| Range | –1.2 to 2.8 | –1.8 to 2.5 | –0.4 to 2.8 | |
| Subjective norms – normative beliefs about subjective norms | ||||
| Mean (SD) | 1.6 (0.69) | 1.4 (0.72) | 0.7 (0.93) | 0.16 |
| Median | 1.8 | 1.2 | 0.8 | |
| Range | 0.6 to 2.8 | 0.2 to 3.0 | –1.6 to 2.2 | |
| Subjective norms – motivation to comply with subjective norms | ||||
| Mean (SD) | 2.1 (1.11) | 2.2 (0.81) | 1.8 (0.90) | 0.002 |
| Median | 2.5 | 2.5 | 2.0 | |
| Range | –0.8 to 3.0 | –0.5 to 3.0 | –1.0 to 3.0 | |
| Perceived behavioural change – control beliefs | ||||
| Mean (SD) | 0.6 (0.93) | 0.7 (1.00) | 0.8 (1.0) | 0.85 |
| Median | 0.5 | 0.8 | 0.4 | |
| Range | –0.5 to 2.5 | –1.8 to 3.0 | –0.8 to 2.8 | |
| Perceived behavioural change – influence of beliefs | ||||
| Mean (SD) | 1.7 (0.60) | 0.6 (0.91) | 0.9 (0.77) | < 0.001 |
| Median | 1.8 | 0.6 | 1.0 | |
| Range | 0.3 to 2.8 | –1.4 to 2.6 | –0.9 to 2.1 | |
| Behavioural intentions | ||||
| Mean (SD) | 2.1 (0.74) | 2.0 (0.79) | 1.4 (1.0) | 0.019 |
| Median | 2.1 | 2.2 | 1.3 | |
| Range | 0.6 to 3.0 | –0.1 to 3.0 | –1.1 to 3.0 | |
Appendix 15 Pre- and post-intervention scores for the theory of planned behaviour constructs by professional group (nurses only) (scores range from –3 to +3)
| Nurses (n = 12) | Pre intervention (n = 12) | Post intervention (n = 12) | Wilcoxon signed-rank test |
|---|---|---|---|
| Attitudes towards organ donation | |||
| Mean (SD) | 0.99 (0.56) | 1.46 (0.54) | 0.04 |
| Median | 0.80 | 1.55 | |
| Subjective norms – normative beliefs about subjective norms | |||
| Mean (SD) | 1.42 (0.90) | 1.41 (1.12) | 0.72 |
| Median | 1.20 | 1.40 | |
| Subjective norms – motivation to comply with subjective norms | |||
| Mean (SD) | 2.17 (1.12) | 2.09 (1.24) | 0.95 |
| Median | 2.62 | 2.75 | |
| Perceived behavioural change – control beliefs | |||
| Mean (SD) | 1.06 (0.79) | 0.85 (0.78) | 0.33 |
| Median | 1.00 | 1.00 | |
| Perceived behavioural change – influence of beliefs | |||
| Mean (SD) | 0.26 (0.91) | 0.76 (0.62) | 0.11 |
| Median | 0.13 | 0.84 | |
| Behavioural intentions | |||
| Mean (SD) | 1.79 (0.86) | 1.62 (0.70) | 0.45 |
| Median | 1.95 | 1.69 | |
Appendix 16 Pre- and post-intervention scores on the theory of planned behaviour constructs by professional group (doctors only)
| Doctors (n = 9) | Pre intervention (n = 7) | Post intervention (n = 7) | Wilcoxon signed-rank test |
|---|---|---|---|
| Attitudes towards organ donation | |||
| Mean (SD) | 0.98 (0.76) | 1.46 (0.85) | 0.04 |
| Median | 1.10 | 1.70 | |
| Subjective norms – normative beliefs about subjective norms | |||
| Mean (SD) | 1.43 (1.20) | 1.46 (1.52) | 0.91 |
| Median | 2.0 | 2.00 | |
| Subjective norms – motivation to comply with subjective norms | |||
| Mean (SD) | 0.77 (0.45) | 1.11 (0.41) | 0.20 |
| Median | 0.80 | 1.20 | |
| Perceived behavioural change – control beliefs | |||
| Mean (SD) | 0.75 (1.32) | 0.36 (0.71) | 0.50 |
| Median | 0.25 | 0.25 | |
| Perceived behavioural change – influence of beliefs | |||
| Mean (SD) | 0.69 (0.66) | 0.52 (0.92) | 0.60 |
| Median | 0.75 | 0.63 | |
| Behavioural intentions | |||
| Mean (SD) | 0.86 (1.07) | 0.90 (1.14) | 0.87 |
| Median | 1.00 | 0.80 | |
Appendix 17 Eligible donor families who were approached and gave consent by intervention/control, region, ethnicity and time period
| Area | Hospital sites | Pre- and post-intervention proportions by ethnicity | |||||
|---|---|---|---|---|---|---|---|
| White ethnicity: pre intervention | White ethnicity: post intervention | White ethnicity: post intervention – pre intervention | BAME ethnicity: pre intervention | BAME ethnicity: post intervention | BAME ethnicity: post intervention – pre intervention | ||
| Approach rate | |||||||
| London | Intervention | 88% (135/153) | 78% (154/197) | –10% | 85% (61/72) | 74% (54/73) | –11% |
| Control | 69% (169/246) | 64% (214/333) | –4% | 69% (71/103) | 69% (96/140) | 0% | |
| Birmingham | Intervention | 77% (41/53) | 83% (35/42) | 6% | 56% (9/16) | 52% (11/21) | –4% |
| Control | 68% (175/259) | 55% (194/355) | –13% | 54% (13/24) | 67% (24/36) | 13% | |
| Leicester | Intervention | 80% (20/25) | 56% (22/39) | –24% | 50% (2/4) | 25% (1/4) | –25% |
| Control | 55% (85/155) | 65% (143/219) | 10% | 60% (6/10) | 73% (11/15) | 13% | |
| All | Intervention | 85% (196/231) | 76% (211/278) | –9% | 78% (72/92) | 67% (66/98) | –11% |
| Control | 65% (429/660) | 61% (551/907) | –4% | 66% (90/137) | 69% (131/191) | 3% | |
| Consent rate | |||||||
| London | Intervention | 60% (81/135) | 68% (105/154) | 8% | 31% (19/61) | 43% (23/54) | 12% |
| Control | 59% (100/169) | 66% (142/214) | 7% | 30% (21/71) | 39% (37/96) | 9% | |
| Birmingham | Intervention | 68% (28/41) | 66% (23/35) | –3% | 22% (2/9) | 36% (4/11) | 14% |
| Control | 59% (103/175) | 63% (122/194) | 4% | 23% (3/13) | 33% (8/24) | 10% | |
| Leicester | Intervention | 50% (10/20) | 27% (6/22) | –23% | 0% (0/2) | 0% (0/1) | 0% |
| Control | 48% (41/85) | 67% (96/143) | 19% | 50% (3/6) | 73% (8/11) | 23% | |
| All | Intervention | 61% (119/196) | 64% (134/211) | 3% | 29% (21/72) | 41% (27/66) | 12% |
| Control | 57% (244/429) | 65% (360/551) | 8% | 30% (27/90) | 40% (53/131) | 10% | |
Glossary
- Approach rate
- The percentage of potential donor families approached for consent or to authorise donation.
- Black, Asian and minority ethnic group
- A term often used in the UK to describe people of non-white descent.
- Black population
- UK census category that comprises people of Caribbean and African descent.
- Clinical lead for organ donation
- The clinician at each trust who has responsibility for providing clinical leadership on organ donation within the hospital and championing improvements as a part-time role.
- Consent rate
- The consent/authorisation rate is based on eligible donors whose family were formally approached for consent/authorisation for donation. The consent/authorisation rate is the proportion of these families who consented to/authorised solid organ donation.
- Donors after brain death
- Patients in whom death was confirmed following neurological tests and in whom there were no absolute or relative medical complications to solid organ donation.
- Donors after brain stem death
- Donation following certification of death following neurological criteria.
- Donors after circulatory death
- Patients in whom imminent death was anticipated and treatment was withdrawn, and in whom there were no absolute or relative medical contraindications to solid organ donation.
- Intensive care unit
- Specialist hospital wards that provide treatment and monitoring for people in a critically ill or unstable condition. Intensive care units are also sometimes known as critical care units or intensive therapy departments.
- NHS Blood and Transplant
- Established as a Special Health Authority in England and Wales in October 2005, with responsibilities across the UK in relation to organ transplantation. Its remit is to provide a reliable and efficient supply of blood, organs and associated services to the NHS.
- Organ Donation Committee
- The national Organ Donation Committee provides guidance to NHS Blood and Transplant on the implementation of policies relating to organ donation. Local networks of Organ Donation Committees at hospital trust level aim to ensure that robust policies are in place to maintain best practice alongside national guidance in all aspects of end-of-life care and donation practices, and to promote knowledge and awareness of donation and its benefits throughout the trust and wider community. Local Organ Donation Committees comprise clinical staff from across the hospital as well as non-clinical staff and generally include donor family representatives.
- Potential Donor Audit
- The national Potential Donor Audit is an audit completed by specialist nurses for organ donation and aims to determine the potential number of solid organ donors in the UK and to collect data on why particular patients did not become solid organ donors.
- South Asian
- UK census classification of people of Indian, Pakistani and Bangladeshi heritage. From 2011, this census category also includes people self-identified as Chinese.
- Specialist nurse for organ donation
- Specialist nurses who are employed by NHS Blood and Transplant and are trained to provide the donor service to over 300 hospitals across the UK. They have responsibilities in four main areas: approaching families about donation; managing and co-ordinating the donation and offering process; supporting the clinical lead and donation committee; and carrying out the Potential Donor Audit.
- UK Research Ethics Committee
- An organisation that considers both general and specific ethical issues relating to the field of organ donation and transplantation, and provides independent advice to clinicians, policy leads and others as appropriate including relevant issues referred by local Organ Donation Committees.
List of abbreviations
- A&E
- accident and emergency
- BAME
- black, Asian and minority ethnic
- CI
- confidence interval
- CLOD
- clinical lead for organ donation
- DBD
- donation after brain stem death
- DCD
- donation after circulatory (or cardiac) death
- DonaTE
- Donation, Transplantation and Ethnicity
- DVD
- digital versatile disk
- EDG
- ethics discussion group
- ESRF
- end-stage renal failure
- GP
- general practitioner
- HLA
- human leucocyte antigen
- ICU
- intensive care unit
- KCL
- King’s College London
- NHSBT
- NHS Blood and Transplant
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- ODC
- Organ Donation Committee
- ODR
- Organ Donor Register
- ODT
- Organ Donation Taskforce
- PDA
- Potential Donor Audit
- PIC
- patient identification centre
- pmp
- per million population
- R&D
- research and development
- SNOD
- specialist nurse for organ donation
- TPB
- theory of planned behaviour
- TTM
- transtheoretical model of behavioural change
- UCL
- University College London
- UKDEC
- UK Donation Ethics Committee