Notes
Article history
The research reported in this issue of the journal was funded by PGfAR as project number RP-PG-0606-1086. The contractual start date was in August 2007. The final report began editorial review in October 2013 and was accepted for publication in April 2015. As the funder, the PGfAR programme agreed the research questions and study designs in advance with the investigators. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PGfAR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by Morrison et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Background
Mental disorder and mental illness are two of the most significant burdens on society in terms of personal distress, disability and economic cost. There are currently more people on incapacity benefit than there are unemployed, with 40% having incapacity due to a primary mental health problem and a further 10% having a secondary mental health problem. 1 Our focus on mental health, and specifically psychosis, is clearly consistent with priorities and needs, as psychosis is associated with significant personal, social and economic costs, and psychosis accounts for a large proportion of the national health and social care budget. 2 Suicide risk and behaviour in patients with psychosis is a significant and serious clinical and social problem. Approximately 4–10% of patients suffering from schizophrenia will eventually kill themselves. 3 Suicide ideation and attempts are common, with over half of all patients having a history of attempted suicide or having significant suicidal ideation at any one time. 4,5 Suicidal ideation and planning are important steps that lead to an attempt of self-harm that may lead to death with previous unsuccessful suicide attempts increasing risk for later successful suicide. 3,6 Similarly, bipolar disorder (BD) affects over 1 million people in England alone and has a prevalence rate of around 2%. 7,8 In addition to repeated periods of mania and depression, most individuals with BD experience extended periods of distressing subsyndromal mood symptoms between episodes. 9–11 Consequently, BD has significant impact emotionally and functionally12 and is a substantial financial burden to society with a recent estimated cost to the English economy at £5.2B per annum. 8
Access to psychological treatments is a government priority; recently Lord Layard highlighted the challenge presented by mental health and recommended the provision of psychological treatments. 13 Although psychological intervention approaches for psychosis such as cognitive–behavioural therapy (CBT) have been demonstrated to be effective and recent National Institute for Health and Care Excellence (NICE) guidelines for schizophrenia and BD have recommended that people be offered CBT,14,15 there are a number of limitations to the delivery of CBT in routine services. 16 Such limitations are the widespread lack of trained therapists means that provision of this type of intervention is limited; the refusal rate for participating in trials of cognitive–behavioural therapy for psychosis (CBTP) is relatively high, suggesting that not all service users wish to engage in current modes of delivery of this therapy; there is some concern that the focus of CBT interventions for psychosis have been overly restrictive; and that such CBT does not necessarily target the priorities identified by service users.
Recovery-orientated services are recommended across treatment settings in adult mental health and specifically in the implementation guidance for specialist and community teams, but with little evidence base to support this. Recovery from psychosis is a relatively new concept given that psychotic disorders have historically been thought of as a severe and enduring mental illness. 17 However, research over the last two decades has begun to challenge these assumptions and it is becoming more accepted that people can, and do, recover from psychosis. 18 Clinical recovery relates to the absence of symptoms whereas the meaning of recovery to service users is much broader and recovery is seen as a process,19 having many aspects such as empowerment and quality of life. 20–22 It is also evident that there is not always a relationship between symptoms and recovery. 19 The dominant approach to identifying psychological mechanisms involved in recovery from psychosis has focused on cognitive deficits (deficiencies in intellectual functioning and basic information processes such as attention and memory). 23 Most investigations have considered attentional problems to be central to schizophrenia and BD but, despite consistent findings of poor performance in patients,24 the precise role of deficits in psychosis remains unclear. Deficits are apparent on all tasks24,25 and performance is similar in patients meeting criteria for BD and schizophrenia. 26,27 Furthermore, the severity of cognitive deficits does not predict positive symptoms,25 although they do predict social functioning. 28 Recent studies have shown that the relationship between gross cognitive functioning and social functioning is mediated by social–cognitive skills (the ability to understand social situations and respond appropriately),29 but the implications of this research for the process of recovery have hardly been studied.
Although there is an increasing recovery literature for individuals with experience of psychosis, there has been little or no research of this type specifically targeted at individuals with a diagnosis of BD. As with psychosis in general, most individuals with a bipolar diagnosis will continue to experience psychiatric symptoms despite psychiatric treatment. 11 However, as the recovery literature increasingly shows, individual definitions of recovery are diverse and rarely focus on eradication of symptoms.
Some authors have suggested that there is a lack of ‘empirical’ literature on recovery and that ‘no empirical conceptualisations of recovery have been published’. 30 Although recovery is being studied with increasing frequency, a recent literature search revealed that there are few instruments that measure recovery from the service users’ perspective in comparison to those that measure symptoms and measurement of symptoms has not benefited from user involvement. 31,32
With respect to psychological predictors of recovery, cognitive deficits might be expected to impact on the recovery domain of rebuilding life (involving re-establishing positive relationships and meaningful daily activities), whereas cognitive biases are more likely to be implicated in rebuilding the self and hope for the future. Consistent with this, research has found that service users who experience paranoia shift their beliefs about the extent to which they deserve persecution unpredictably over time and that these changes are associated with changes in self-esteem and attributional processes. 33 In the case of bipolar patients, research suggests that coping strategies, which seem to affect the stability of self-esteem, differ between different phases of the disorder. 34 Dynamical models have the potential to explain why systems of interacting cognitive processes sometimes settle in stable states that are resistant to perturbation (which might be taken as an indicator of recovery).
Recovery from psychosis clearly involves the planning for the future and ensuring future well-being. Feelings of loss and lowered expectations for future achievements can lead to depression and feelings of hopelessness. 35 Thus, part of the recovery process involves the challenges of remaining optimistic and fulfilling full potential and well-being. While there is clearly a strong evidence base for CBTP, including much of our own work,36–41 research indicates that CBTP does not significantly reduce suicide behaviour;42 thus, the development of CBT for suicide prevention is a priority. There are also other limitations with respect to the delivery of CBTP mentioned above, so alternative modes of delivery need to be explored. The most recent study of CBT for relapse prevention in BD found that there was a significant interaction between the number of episodes and the outcome, with only those with fewer episodes benefiting significantly. 43 To date, no CBT interventions have been specifically designed for delivery to individuals early in their illness course.
It is clear that mental health problems, including psychosis, suicide and BD, are a significant burden for society. National guidelines recommended a recovery-orientated approach with psychological interventions, such as CBT, be offered as part of routine practice. However, further research to investigate the psychological mechanisms of recovery in psychosis, suicide and BD would be beneficial to inform the development of evidence-based recovery-focused psychological interventions. Consideration of effective modes of delivery for psychological interventions as well as service user choice and preference are essential.
Aims
To complete a series of linked projects with the aim of understanding and promoting recovery from psychosis and BD, in a manner that is acceptable to and empowering of service users.
Objectives and research questions
Our research programme consisted of six linked project themes, each of which were designed to further our understanding of recovery. Objectives for each theme were:
-
to develop a valid and acceptable service user designed tool to assess the severity of multiple dimensions of experiences of psychosis
-
to determine levels of consensus around the service user-defined recovery concept
-
to confirm the psychological factors that are associated with recovery from psychosis and examine the longitudinal course of such factors
-
to develop and evaluate cognitive–behavioural approaches to guided self-help and group therapy for recovery, taking patient preferences into account
-
to develop and evaluate a cognitive–behavioural approach to understanding and preventing suicide in people with psychosis
-
to understand the process of recovery from BD and to develop and evaluate a cognitive–behavioural approach to recovery from a first episode of BD.
An additional aim of the programme as a whole was the development, within the lifetime of the programme, of key deliverables that will be important to the NHS, namely user-defined measures of recovery and symptoms, manuals for telephone-assisted CBT, recovery groups, CBT for suicide prevention, CBT for early BD and assessment of barriers to recovery. It can be noted that the original title of the research application was psychological approaches to understanding and promoting recovery from psychosis; the title of this report changed to incorporate the emphasis on BD as well as psychotic disorders as this is a more accurate reflection of the aims and programme content.
Service user involvement in research
Involving service users in research has been advocated for many years and has been implemented to some degree in many areas. Increasing such involvement and inclusion is important for a number of reasons.
First, professional researchers may not always effectively address the personal priorities or preferences of research participants and so collaborative consultation with service users can be helpful in focusing and shaping research to be more clinically meaningful and ethically sound. Second, service users often report that they would value the opportunity to meet and speak with others who have similar experiences and so including user researchers within research teams can help to increase such opportunities for research participants and may improve participants’ personal engagement. Third, recognising the inherent value of personal insight that service users can bring to research can help to improve service users’ own self-worth, individually and collectively. This may be an especially important aim as people who experience psychosis commonly report reduced self-esteem and disempowerment as a result of their experiences, or their treatment.
The Recovery Research Programme has fully integrated service user involvement from the outset by including two service users as grant holders, employing two part-time service user researchers throughout the programme, including 10 service users as consultants and setting up a bimonthly service user reference group [service user reference group (SURG)]. The service user researchers conducted all of the individual qualitative interviews and led the analyses of these data. They also delivered elements of peer support within the patient preference trial (PPT). The role of the service user consultants and service user reference group was to act in a consultative and advisory capacity, making recommendations on a variety of elements including the content and conduct of studies. The service user reference group was co-ordinated by a service user researcher with support from the research programme manager and administrator. Service users were paid for their time and travel expenses both for attending the meeting and preparation/reading time. The group met at a regular time and day on a bimonthly basis (every other month) throughout the programme. All SURG meetings were minuted and items for action or suggestions for amendments to studies were taken to individual project teams. Any amendments made were documented and fed back to the SURG. If suggestions made by SURG were not able to be accommodated, reasons for this decision were still fed back to the group and discussed.
The SURG agreed that they would be involved with:
-
reporting on progress of service user involvement in individual research projects (each person involved represents one project)
-
supporting and representing other service users involved in individual projects in any issues that arise from their involvement
-
responding to any requests for input from individual academics/recovery programme meetings
-
being consulted about any ‘add on’ projects to the recovery programme
-
being involved in the recruitment of staff.
Some key contributions of the SURG to individual studies included reviewing all of the topic guides for the qualitative interview studies, advocating strongly for a preference trial design in the PPT, providing input to the development of the self-help recovery guide in the PPT and developed the distress management protocol for the programme. A review of the service user involvement in the Recovery Research Programme was conducted by a service user researcher (and co-ordinator of SURG). The review highlighted that SURG has functioned well as a group and that their involvement had benefited the research and the individuals involved. It was felt that opinions of service users were taken seriously and had a wider impact including being nationally recognised as an example of good practice for service user involvement. It was noted that future service user involvement should continue to improve communications between all members of the research team (including service users) as well as involving service users from the outset in planning and standardising service user involvement for each study.
Conduct of the research programme
It was important that the research programme was conducted in a cohesive way that allowed consistency across the studies in terms of staff training and supervision, cross-programme meetings, standard operating procedures (SOPs), provision of trial management to the bipolar and suicide prevention trials and a cross-programme Data Monitoring Committee (DMC). This enabled the programme to be conducted in an efficient and effective way. The chief investigator (APM), programme co-ordinator (HL) and programme manager (MW) contributed to the provision of these cross-programme aspects. Individual project leads (GH, RPB, CB, NT and SHJ) were responsible for the conduct of the studies within their themes, as well as decisions regarding data analysis (in conjunction with the programme statisticians: GD and NS) and decisions regarding dissemination and publication of findings within their themes.
Enabling cross-learning: staff training, supervision and cross-programme meetings
To enable cross-learning and consistency across the research programme, staff were trained and supervised centrally. Weekly group supervision meetings were held with the researchers to monitor adherence to the study protocol and SOPs, as well as monthly meetings to ensure consistent scoring and inter-rater reliability for the assessment measures used across the programme. In addition, project leads met regularly to discuss progress on the individual studies in order for shared learning to take place across the studies.
Standard operating procedures
Standard operating procedures were created across the programme as a whole to facilitate consistency, quality and integrity of routine activities within the research studies. This included producing procedures for recruitment, randomisation, safe working, management of distress and risk, data quality and safety reporting. SOPs were generally prepared by the trial manager and approved by the project leads before being shared with programme staff via a secure web-based portal hosted by the National Institute for Health Research (NIHR). This ensured the SOPs were current, version controlled and accessible from any location. SOPs minimised variation across the studies and promoted quality through consistent implementation even if personnel changes occurred during the lifespan of the study. Compliance with SOPs was monitored directly by supervisors and line managers.
In addition to the SOPs for each study and across the programme as a whole, the service user reference group suggested the addition of a distress management protocol which included offering a follow-up telephone call to all participants to ensure that they had not experienced any distress following the research assessment. If any distress was reported the researcher would check immediate safety and well-being, followed by signposting to the appropriate clinical care team or seeking consent to share this with the participant’s clinical care team. Additionally, the distress protocol recommended that assessments were not conducted on a Friday afternoon owing to the possibility of the participant feeling distressed over the weekend and unable to easily contact their clinical care team.
Data Monitoring Committee
The DMC was set up to review the safety and efficacy of the research studies, with a particular focus on the clinical trials of therapeutic interventions. The DMC consisted of an independent clinician and statistician, and was attended by the programme co-ordinator/trial manager to provide updates and the programme statistician to consult on the statistical aspects of the studies. Meetings were held twice a year with additional ad-hoc meetings or teleconferences when necessary to review adverse events. It was agreed that the DMC would review recruitment and retention and monitor safety and adverse events.
Cross-programme recruitment
There was a procedure for the facilitation of cross-recruitment between several of the individual studies to ensure that participants who were keen to take part in more research were offered the opportunity to do so. While many participants took part in more than one study, their data from previous studies were not generally utilised (i.e. each study was independent and built on the findings of previous phases). When possible in the time frames required for valid assessments, data could be reutilised to minimise participant burden. However, in practice this was not possible for most participants owing to the short validity periods of standardised clinical assessments. The only exception to this was the study examining longitudinal predictors of recovery in psychosis, which utilised data from the clinical trials to examine change over time.
Cross-programme measures
There was an attempt to utilise similar measures across studies in order to allow comparisons to be made and to maximise the possibility of combining samples when appropriate (e.g. in the study examining longitudinal predictors of recovery in psychosis, which utilised data from the clinical trials to examine change over time). The Questionnaire about the Process of Recovery (QPR) was used throughout the programme, often as the primary outcome in a clinical trial, or as the dependent variable when examining predictors of recovery. Initial studies used the original 22-item version as this was what was available. It became apparent that the psychometric properties were not ideal for measuring recovery as a unitary and independent construct. In the first study for which this was required, which examined psychosocial and neuropsychiatric predictors of recovery, an individualised statistical analysis was conducted that resulted in a combined measure that utilised the visual analogue scale ratings in combination with five QPR items. Subsequent studies used a 15-item version of the QPR, which was one-dimensional and had improved psychometric properties [but this had not been available to the earlier studies (those before 2013)].
Structure of this report
Chapters 2–7 of this report presents findings from each of the six linked themes. Each chapter includes a brief background to the theme followed by subsections representing each phase of the project. Subsections for each phase consist of a brief overview of the objectives, methodology, results and discussion. The final chapter brings together all of the findings from the six themes, includes an overview of the development of key deliverables that will be important to the NHS and discusses implications for future research and clinical practice.
Changes to protocol or original proposal
The original plan of research was titled ‘Psychological approaches to understanding and promoting recovery from psychosis’. The original proposal outlined six key objectives and the methods used to achieve these objectives as follows:
-
Development of a valid and acceptable tool to assess the severity of multiple dimensions of psychotic experiences that can be reliably used by service users and further validation of a user-led measure of recovery. To achieve this objective the original proposal contained three phases to this research:
-
Qualitative interviews conducted by, and with, services users to generate items relating to the experience of psychotic symptoms.
-
Q-sort methodology to generate potential themes and items for the new measure.
-
Investigation of the psychometric properties of the new scale (including test–retest reliability and concurrent and predictive validity).
-
-
Confirmation of psychological factors that are associated with recovery from psychosis and examination of the longitudinal course of such factors.
-
A cross-sectional study exploring the relationship between cognitive functioning and social functioning, and assessment of the extent to which cognitive functioning and cognitive biases are associated with subjective domains of recovery of importance to patients.
-
A longitudinal assessment of cognitive processes in recovered and non-recovered schizophrenia spectrum patients including an experience sampling method (ESM) study of stability in these processes.
-
Examination of predictors of recovery. Based on the results from phases 1 and 2, production of a final battery of variables most closely linked to the process of recovery, and testing of their ability to predict specific domains in the patients participating in two of the trials. In each trial, the assessment battery was administered at inception and at 6-month follow-up. This is to enable the prospective assessment of predictors of recovery.
-
Production of a manual for the recovery prediction battery. Based on the results from phases 1–3, the optimum combination of measures were chosen to include in a brief, transdiagnostically valid battery designed to assess intrapsychic impediments to recovery. A manual describing the final battery and summarising our findings would be made available to clinicians and researchers elsewhere.
-
-
Development and evaluation of cognitive–behavioural approaches to guided self-help and group therapy for recovery, taking patient preferences into account.
-
Development of the self-help manual. The recovery manual was developed in a manual format by a multidisciplinary group of mental health professionals and users informed from both the recovery literature and cognitive–behaviourally oriented treatments for people with psychosis.
-
Piloting the manual, estimating effect size and study of patient preferences. Participants were randomly allocated to the manual plus telephone condition or treatment as usual (TAU). Baseline and post-treatment assessments were completed in the same manner as in the proposed PPT. Detailed feedback about the manual and telephone support was requested from participants.
-
An additional sample of service users meeting the inclusion criteria above were interviewed as to their hypothetical preferences in terms of treatment condition.
-
The PPT. The three conditions to be evaluated in the PPT were TAU, manual plus low support (telephone support), manual plus high support (telephone and group).
-
-
Development and evaluation of a cognitive–behavioural approach to understanding and preventing suicide in people with psychosis.
-
To investigate the psychological architecture that drives suicide behaviour, including information processing biases, suicide schema and appraisal systems using information processing tasks such as autobiographical memory tasks to investigate bias, standardised assessment to investigate appraisal and schema.
-
To derive a method of assessing this architecture through semistructured interviews that will have clinical utility.
-
To formulate and develop a manualised cognitive–behavioural treatment programme for suicide prevention in psychosis and to test the clinical acceptance and feasibility of this intervention. It was hypothesised that the treatment would be acceptable, feasible and reduce suicide behaviour.
-
At the end of the programme, to be in position to design a clinical trial to test the efficacy of the intervention.
-
-
Understanding the process of recovery from BD and the development and evaluation of a cognitive–behavioural approach to recovery from a first episode of BD.
-
A qualitative study to identify the key themes associated with recovery in individuals who have a diagnosis of BD.
-
On the basis of the information collected in phase 1, a questionnaire was constructed to conduct a quantitative study of recovery from BD. This study evaluated the reliability and validity of the measure.
-
To evaluate a CBT-based recovery intervention for individuals with a first diagnosis of BD.
-
-
The development, within the lifetime of the programme, of key deliverables which will be important to the NHS, namely user-defined measures of recovery and symptoms, manuals for telephone-assisted CBT, recovery groups, CBT for suicide prevention, CBT for first episode BD and assessment of barriers to recovery.
First, it can be noted that the original title of the research application was ‘Psychological approaches to understanding and promoting recovery from psychosis’; the title of this report changed to incorporate the emphasis on BD as well as psychotic disorders as this is a more accurate reflection of the aims and programme content.
An additional objective was added to this list during the course of the research programme (see Chapter 3) to examine consensus around conceptualisations of recovery. It was felt that this was a valuable addition to underpin the studies in this research programme and provide further clarity on the concept of recovery.
It should also be noted that the original plans for the Chapter 6 studies on recovery and suicide did not include the qualitative study (phase 1) to examine the subjective experience of participating in this type of research. However, based on service user feedback and suggestions from the SURG, the team decided to add this phase to explore service user perceptions and inform the conduct of the future studies.
Finally, the original proposal stated that the outcome of the Chapter 4 studies on understanding psychological and social predictors of recovery would be an assessment battery and manual for assessment and prediction of recovery. However, this aim proved to be unrealistic given the idiosyncratic nature of recovery, the differences between clinical populations and the diversity of approaches used to capture information about recovery. However, we have included a section at the end of the conclusion of Chapter 4 that addresses recommendations for the measurement of recovery.
Chapter 2 User-defined conceptualisation and measurement of recovery in psychosis
Background
Recovery has become an increasingly popular and important concept for mental health service providers and policy-makers following guidance in a number of government policies and the national service framework. 44 Despite this, a working definition of the concept of recovery has never been formalised.
Consequently, current approaches to defining and measuring recovery in mental health utilise a variety of approaches. For example, traditional models tend to focus on symptoms while other models are concerned with a sense of well-being regardless of symptoms. Davidson et al. 45 outlines this as two superseding models. Similarly, although measurement of recovery is sometimes concerned with only a single factor approach, such as assessment of symptoms, relapse rates or functioning,46,47 others consider recovery to be a multifactorial long-term process incorporating hope for the future rebuilding self and rebuilding life. 19 Alternative approaches have assessed recovery as a set of internal and external conditions. 48 Despite the diverse nature of understandings of the concept itself, the term recovery has become widely used and recognised by professionals and service users alike. This highlights the importance of aiming for a shared understanding of recovery to prevent misapplication and miscommunication.
Recovery from psychosis has traditional been viewed as achieving symptom alleviation. 49 The gold standard in research investigating therapies, treatments and medications would be large clinical studies such as randomised controlled trials (RCTs), which aim to reduce frequency of symptoms. The primary outcome measure in RCTs investigating CBT50–52 and medication53,54 has been symptom change scores using standardised psychiatric interviews. Similarly, mental health services often use the criteria of symptom alleviation as a benchmark for demonstrating effective practice, adopting the benchmark from RCTs.
As a result of this focus on symptom change, a number of measures of symptomatic recovery have been developed including the Positive and Negative Syndrome Scale (PANSS55) and the Brief Psychiatric Rating Scale. 56 Symptoms have been shown to cause reduction in social and daily functioning as well as leading to distress,47,57 demonstrating the need to consider symptoms of psychosis when examining recovery. Although these measures have been shown to be reliable and useful in assessments of outcome in psychosis, they may not be considered by service users to reflect the multifactorial nature of recovery from psychosis. Other unidimensional approaches to measuring recovery from psychosis have included relapse reduction,58 for which rehospitalisation, remission and reoccurrence of symptoms are taken into account. 59 Periods without hospitalisation and remission of symptoms are used as indicators of periods in recovery. 59
Alternatively, services have increasingly turned to assessment of quality of life as a measurement of recovery in psychosis. 60 This approach integrates more of the elements of service user-defined recovery such as a range of life domains and individual values. 61 Measures such as the Global Assessment of Functioning (GAF62) scale and the Quality of Life Scale63 are commonly used. Research studies often use these measures alongside the more traditional symptom and relapse measures. 64
Although there has been a wealth of research developing these measures and utilising them in RCTs and other studies, few have examined whether or not these outcomes are relevant and meaningful to service users and their definitions of recovery. A recent review of measures of recovery31 included examination of acceptability to service users and found that only one measure had been developed in collaboration with service users to specifically to measure recovery from psychosis: the QPR. 32 Further psychometric testing of the QPR was recommended. This measure was utilised throughout the Recovery Research Programme allowing future examination of psychometric properties and utility as well as further exploration of whether or not it covers key recovery themes as defined by service users.
Service user-defined recovery has been examined in a recent meta-analysis26 which identified five processes that are important to recovery: (1) personal and self-empowerment; (2) motivational processes including hope; (3) developing competencies such as seeking knowledge and making sense of distress; (4) social and community participation; and (5) utilising available resources, including services and voluntary support agencies. Development of a measure that takes into account these factors and other elements which service users highlight as essential to recovery, as well as their relationship to symptoms, would further our understanding of recovery and the ability of services to effectively measure recovery-focused outcomes.
In order to develop a measure of recovery that incorporates dimensions of symptoms, but which is meaningful and relevant to service users, resolution around the meaning of recovery must first be addressed. This would then progress to developing and validating a service user generated measure, which would encompass this definition. The psychometric properties of this measure would then be established. This chapter includes three distinct phases of a study to address this deficit. This study aims to alleviate uncertainty about the concept of recovery by adopting an inclusive approach, scrutinising factors that are important to a multidimensional approach to recovery before using this information to develop a service user generated, self-report scale to assess recovery in relation to symptoms in psychosis. The three phases to this study include (1) a qualitative approach to exploring service user experiences of recovery; (2) a Q-methodology approach to further refine what factors are important to service user definitions of recovery; and (3) utilisation of information from phases 1 and 2 to develop a service user designed measure of recovery in relation to symptoms of psychosis and establish its psychometric properties.
Phase 1: conceptualisation and perceptions of recovery from psychosis – a service users perspective
This research was previously published as Wood L, Price JF, Morrison AP, Haddock G. Conceptualisation of recovery from psychosis: a service-user perspective. Psychiatrist 2010;34:65–47065 and much of this text has been reproduced with permission from the Royal College of Psychiatrists.
Objectives
This study aimed to explore peoples’ subjective experiences of recovery using interpretative phenomenological analysis (IPA) to elicit data from participants.
Method
Participants
Participants were invited to take part in the study if they had experience of psychosis in the last year, were aged 16–65 years and were currently in contact with mental health services. Exclusion criteria included not being able to speak English, not able to give informed consent and having taken part in other research with the past 6 months. Participants were recruited from statutory care providers across the Greater Manchester West Mental Health NHS Foundation Trust. Recruitment was conducted until the research team felt that saturation of themes was achieved.
Design
The study utilised a semistructured interview approach, with an interview schedule developed by a clinical psychologist and service user researcher (GH and MK). A service user group facilitated generation of questions surrounding personal background, experience of symptoms, recovery and impacts of symptoms. These questions were piloted with three service users and amendments were made following their feedback. The final version included the following headings: information on initial contact with mental health services, background on personal experiences, current experiences, what they felt had changed over time/recovered, how they feel they have changed (over time/recovered, ways of coping, impacts and changes to their life).
Procedure
Recruitment for the study took place in early intervention services (EISs), assertive outreach (AO) teams and community mental health teams (CMHTs). Participants were given a minimum of 24 hours to read the information sheet before being asked to sign a consent form. A service user researcher conducted the majority of the interviews (75%). All interviews were audio-recorded and transcribed verbatim by the service user researcher and research assistant in order to help familiarise themselves with the data.
Analysis
Interpretative phenomenological analysis66 is an approach to qualitative research with a focus on how an individual makes sense of an event or phenomenon. IPA involves collecting information from participants, in this case using interviews, on a given experience and how the individual has interpreted and made sense of that experience. IPA was utilised to explore the data in this study, as it is well suited to the exploration of subjective experience. 66 A core concept of IPA is that the analyst should become immersed in the data66 to enable the researcher to gain an insider perspective. This was achieved by listening to the audio-recorded interviews and reading through the final transcripts a number of times. Two researchers analysed all the interviews independently and extracted pertinent themes. The third researcher acted as a mediator if there was any disagreement.
Results
Eight people were interviewed (six males and two females) with an age range of 24–35 years. All had experiences of delusions and/or hallucinations within the last 12 months and six were recruited from EISs and two were from CMHTs.
Initially, 132 themes were generated from the interviews, which were condensed into 50 clear themes that were representative of the expansive concourse. The process of condensing these themes involved identifying overlapping and repetitive items and reaching consensus about removal of these items. These were then fine-tuned to remove themes that were felt to reflect the same concepts as others. The final 50 themes broadly covered eight areas of recovery: symptoms, emotional aspects, the self, behaviour, services and support, coping mechanisms, social functioning and occupational aspects. From these eight broad themes, a logical grouping of four superordinate themes emerged.
The four superordinate themes were described as ‘impacts on mental health’, ‘self-change and adaptation’, ‘social redefinition’ and ‘individualised coping mechanisms’. These themes were underpinned by change, highlighting that recovery is a process, not an end point. These themes each had two further subthemes that consisted of smaller themes (Box 1).
-
Preoccupation with experiences.
-
The content of experiences.
-
The frequency of experiences.
-
The duration of experiences.
-
Amount of distress.
-
Conviction.
-
Overcoming depression and low mood.
-
Feeling of happiness and enjoyment.
-
Overcoming anxiety and stress.
-
Overcoming anger and frustration.
-
Changes in the amount of emotions experienced.
-
Stable living conditions.
-
Job seeking and maintaining employment.
-
Financial stability.
-
Being less withdrawn and isolated.
-
Finding the ability to trust others.
-
Taking part in meaningful activities and hobbies.
-
Developing and depending on relationships with friends and loved ones.
-
Increasing social activity.
-
Overcoming being judged and stigmatised.
-
Positive self-beliefs.
-
Redefining who you are.
-
Feeling less vulnerable.
-
Overcoming embarrassment.
-
Regaining personal freedoms and rights.
-
Having a positive outlook for the future.
-
Improvements in sleep.
-
Energy and lethargy.
-
Motivation for change.
-
Reduction in self-harm and suicidal ideation.
-
Regaining independence.
-
Changes in drug and alcohol use.
-
Benefits of medication.
-
Benefits of therapies.
-
Peer support.
-
Support from loved ones and/or friends.
-
Receiving help from mental health services.
-
Concerns over side effects of medication.
-
Importance of spirituality/religion.
-
Help seeking with experiences.
-
Recognising the early signs of becoming unwell.
-
Being able to cope with experiences.
-
Understanding your experiences and/or diagnosis.
-
Feeling empowered over your experiences.
-
Having control over experiences.
-
Thinking clearly about experiences.
-
Having control over own thoughts.
Theme 1: impacts on mental health
All people interviewed discussed alleviation of symptoms and/or negative emotions as key to their recovery. Participants discussed specific changes in symptom characteristics as well as changes in their emotional state.
Reduction in symptoms of psychosis
All participants considered a change in symptom characteristics as important to their recovery.
. . . they’re not as aggressive as they were when the were really bad . . . they were really, really nasty and they used to really upset me but they’re not as bad anymore . . .
(Reflecting the importance of the subordinate theme of ‘the content of experiences’.)
Emotional changes
Affective and emotional changes are often associated with experiences of psychosis:
. . . it was definitely the most difficult time I’ve ever experienced, and I’ve had depression since, on and off since I was 14 maybe. But it [the depression that coincided with the psychosis] was far worst than that.
(Showing the importance of the ‘overcoming depression and low mood’.)
Theme 2: self-change and adaptation
Experience of psychosis was shown to have great impact on one’s self. The themes illustrated the importance of overcoming psychosis and being able to regain self-identity.
Personal change and belief
Interviewees described negative self-belief and negative personal change since experiencing psychosis. Their previous self wanted to be redefined in spite of current experiences:
I feel better about myself now, the voices used to make me feel like a rubbish person, they made me feel like I wasn’t worth anything, now I can control this I feel better about myself.
(The theme ‘ positive self-beliefs’ was key to personal change and belief.)
Behavioural change
The research also identified a number of behavioural changes; participants expressed the importance of motivation, independence, and changing harmful behaviours:
‘I think I’m over most of it you know, but I think there’s still little things, like a routine of looking after myself which can sometimes suffer, . . . sometimes my appearance can get quite bad’
(Illustrating the self-care is key to subordinate theme ‘regaining independence’)
Theme 3: social redefinition
Mental health problems were shown to have a direct impact on an individuals’ social role. Redefining and reconciling their social circumstances was frequently spoken about in all interviews.
Occupational change
Changes in finance, work, and living arrangements are acknowledged to be great stressors to individuals with and without mental health problems. A return to these situations was identified as a struggle but something that people do want to tackle:
Not having much luck getting a job at the moment which is quite frustrating really.
I was in lots of debt and it was stressing me out.
(Illustrating subordinate themes ‘job seeking and maintaining employment’ and ‘financial stability’ are main occupational issues.)
Relationship/social behaviour
Social isolation, the breakdown of social networks, judgement and stigmatisation is often a common with mental health experiences. It was important to interviewees to rebuild these networks and relationships to assist in recovery:
One of the main things [that made me feel better] is the support that my family gave me really, although it was strained at times, after a while, not at first but after a while they would understand what I was going through.
(All interviewee’s supported the theme ‘developing and depending on relationships with loved ones.)
Theme 4: individualised coping mechanisms
Developing an individualised coping mechanism was considered important to all people interviewed. By accessing support and treatment, people were able to assist their recovery. Furthermore, gaining insight and understanding was also shown to be important.
Support and treatment
Interviewees had diverse views about what support and treatment they found beneficial illustrating the individuality in appropriate support and treatment:
And [care co-ordinator] has been a great help, you know working through everything . . . and the team [were helpful].
(Subordinate theme ‘receiving help from the mental health services’ was important to some interviewee’s recovery.)
Understanding and control
Understanding and coping with experiences was highlighted by all interviewees as important to their recovery. However, each individual had different approaches and found a range of things helpful:
I would have to think something rational and take control of my own beliefs and it was really empowering.
(This quote reflects the need for subordinate theme ‘having control over experiences’.)
Discussion
This study found four main themes that are important to consider when conceptualising recovery: impacts on mental health, self-change and adaptation, social redefinition and adapting an individual coping style. The study also supported previous research that found recovery is felt to be a process rather than an end point and that recovery in psychosis is multidimensional.
All participants felt the four themes were important to recovery, although there was varied emphasis placed on each theme by each individual. Consistent with previous research, this highlights the complexities of conceptualising recovery and indicates that recovery is not an outcome with clear-cut differences between recovered and not recovered.
Self-change and adaptation was often felt to be central to recovery. Changes to character, personality and identity were noted by all participants and reduced motivation, energy and confidence were often reported. Previous research19 has indicated that rebuilding the self understandably plays a key part in recovery and this study emphasises the importance of consideration of this factor in therapy and research.
Participants did report that symptom alleviation had a major impact of their recovery, highlighting the importance of symptoms as an indicator of outcome. However, participants found that symptoms are important in conjunction with a range of other factors. Indeed, for some service users there may be a continued presence of symptoms but without their negative impacts.
It may be of particular interest that the emotional impacts of having psychosis were also identified. The effects on depression, anxiety, anger and frustration illustrate that emotional change is also important to consider. This could have significant implications for measurement of outcomes that do not typically take factors such as anger and frustration into account.
The social impact of psychosis was also common throughout the themes and is often noted as a key area of recovery. Financial stability, living arrangements and employment status were affected by having experienced psychosis for the majority of participants. Participants discussed a decrease in social activity, feeling alone and isolated and the huge impacts that psychosis had on relationships with loved ones. Services that aim to be recovery orientated should consider the continued need for social relationships and impacts on social behaviour.
An important implication of the findings of this study is the need to understand recovery using a holistic approach, which incorporates personal factors as well as symptoms. Social and personal change and coping styles should be considered alongside symptom alleviation, with equal importance being given to each factor. Assessment tools that take into account the important element of symptom alleviation alongside these broader personal and social themes would be desirable with consideration of the impact that these experiences have on life.
The main strength of this research is that the majority of the interviews were carried out by a service user researcher. As the service user researcher had shared experience with the interviewee, it could be expected that richer and more detailed information may have been elicited. This has been illustrated in other service-user-led studies about recovery19 and impacts of diagnosis. 67
In contrast, one main limitation to the study was also the service user researcher conducting the majority of the interviews. The service user researcher felt that his personal experiences influenced the direction and data extracted by the interview process. The central role of the researcher in interpreting qualitative data is a core feature of IPA. The supervisory process and reflections of the service user researcher in discussion with both colleagues and members of the SURG provided a forum for the researcher to balance their own views with those of others, in relation to both the conduct of interviews and the analysis of the transcripts.
In conclusion, this study has demonstrated that recovery is a multifaceted process that incorporates symptoms, social factors, personal adaption and development of individualised coping mechanisms. Future research as well as development of services and therapy should consider these four factors with equal weighting of importance to create a more holistic approach to recovery.
Phase 2: exploring service users perceptions of recovery from psychosis – a Q-methodological approach
This research was previously published as, and much of this text has been reproduced with permission from, Wood L, Price JF, Morrison AP, Haddock G. Exploring service users perceptions of recovery from psychosis: a Q-methodological approach. Psychol Psychother 2013;86:245–61,68 John Wiley & Sons. © 2012 The British Psychological Society.
Objectives
This study aimed to explore, using Q-methodology, the factors important to service users in relation to recovery from psychosis.
Method
Development of the Q-sort
Q-methodology is undertaken in a number of steps. 69 First, a database of relevant codes (Q-concourse) is developed. This usually consists of a large database of diverse information from a variety of sources about the topic being examined. The Q-concourse was developed from two main sources: themes identified from the interviews conducted in phase 1 and also from existing literature. This Q-concourse codes are then grouped together to form a final set of descriptive themes. These are then translated into statements cards (this is called the Q-set). An initial set of 132 codes was condensed into 52 clear themes that were representative of the expansive concourse by a multidisciplinary team that included service users. These themes were then categorised by the research team and deemed to broadly cover eight areas of recovery: symptoms, emotional aspects, social functioning, the self, cognitions, services, coping mechanisms and occupational aspects. Participants (known as the P-set) are required to sort these statements in order of importance in relation to one another using a forced normal distribution table.
Participants
Forty participants were identified as being required to take part in the study, which was deemed to be a sufficient number for a study of this design based on previous research. 69,70 The inclusion criteria for the participants in the study were: aged between 18 and 65 years, experienced delusions and/or hallucinations for at least 1 year and in contact with a statutory mental health service in Greater Manchester in the North West of England.
Participants’ self-report demographics are outlined in Table 1. Participants’ diagnoses were self-report, with the majority (40%) reporting a diagnosis of schizophrenia, or experience of psychosis (20%).
| Total sample (N = 40) | Factor 1 (N = 8) | Factor 2 (N = 10) | Factor 3 (N = 9) | Factor 4 (N = 5) | |
|---|---|---|---|---|---|
| Age (years) (SD; range) | 36.97 (12.01; 20–65) | 38.63 (13.43; 27–65) | 35.60 (10.81; 25–59) | 32.22 (11.61; 20–58) | 34.25 (14.10; 20–53) |
| Delusions, n (%) | 32 (75) | 6 (75) | 7 (70) | 8 (88.9) | 5 (100) |
| Average duration of delusion (months) (range) | (3–360) | 160 (12–120) | (3–164) | (24–360) | (12–184) |
| Hallucinations, n (%) | 27 (67.5) | 6 (75) | 6 (60) | 4 (44.5) | 5 (100) |
| Average duration of hallucination (months) (range) | (3–360) | 152 (9–120) | (3–240) | (18–360) | (12– 84) |
| Gender, n (%) | |||||
| Male | 25 (62.5) | 1 (12.5) | 7 (70) | 8 (88.9) | 3 (60) |
| Female | 15 (37.5) | 7 (87.5) | 3 (30) | 1 (11.1) | 2 (40) |
| Nationality, n (%) | |||||
| White | 35 (87.5) | 8 (100) | 9 (90) | 9 (100) | 4 (80) |
| Black | 3 (7.5) | 0 (0) | 1 (10) | 0 (0) | 0 (0) |
| Asian | 1 (2.5) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Other | 1 (2.5) | 0 (0) | 0 (0) | 0 (0) | 1 (20) |
| Employment status, n (%) | |||||
| Unemployed | 35 (87.5) | 5 (62.5) | 9 (90) | 8 (88.9) | 5 (100) |
| Student | 2 (5) | 2 (25) | 1 (10) | 1 (11.1) | 0 (0) |
| Employed | 2 (5) | 1 (12.5) | 0 (0) | 0 (0) | 0 (0) |
| Other | 1 (2.5) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Education level, n (%) | |||||
| Primary/secondary | 18 (45) | 3 (37.5) | 4 (40) | 5 (55.6) | 1 (20) |
| Further/higher | 22 (55) | 5 (62.5) | 6 (60) | 4 (44.4) | 4 (80) |
| Marital status, n (%) | |||||
| Single | 25 (62.5) | 4 (50) | 6 (60) | 7 (77.8) | 3 (60) |
| In a relationship | 10 (2.5) | 1 (12.5) | 3 (30) | 2 (22.2) | 2 (40) |
| Separated/divorced | 3 (7.5) | 2 (25) | 0 (0) | 0 (0) | 0 (0) |
| Other | 2 (5) | 1 (12.5) | 1 (10) | 0 (0) | 0 (0) |
Procedure
Participants were shown the Q-sort matrix (Figure 1) and given 52 shuffled statement cards (the Q-set). They were asked to read through them thoroughly to ensure they understood them before sorting the cards into three piles, one that represented things that were important to their recovery, one for things that were not important and ones that they were not sure about. They were then asked to consider the ‘most important’ pile and pick the two most important statements and place them on the far right of the grid (column 12), they were then asked to pick the three next most important and place it onto column 11, and so forth until they placed all the most important cards onto the grid. The same procedure was repeated with the least important pile and the not sure pile until the table was full. Participants were given the opportunity to move the statements around until they were happy with their final sort and were asked follow-up questions about the reasoning behind the rating of the two highest and two lowest items, if they thought any recovery items were missing, and for any further comments.
FIGURE 1.
Q-sort response matrix.

Data analysis
A Q-method software package (PQ method version 2.11; Kent State University, Kent, OH; URL: http://schmolck.userweb.mwn.de/qmethod/pqmanual.htm) was used to analyse the data. Principal component analysis (PCA) with varimax rotation was implemented to sort factors and to explain the maximum amount of variance. Q-method analysis factors groups of people together as opposed to items in traditional factor analysis.
Results
Q-method analysis resulted in a four-factor solution that 32 out of the 40 participants loaded on. These other eight participants were excluded from the factor arrays and do not contribute to the interpretations detailed below. In the Q-sort people are factor analysed instead of items. Therefore, to explain the most variance we had to lose eight participants from the factor analysis to come up with a factor solution that explained the most variance in recovery views. With this type of analysis, a loss of participant data cannot be avoided. The factor solution explained 36% of the variance and had an Eigenvalue of 2.74. Eight participants loaded onto factor 1 (accounting for 10% of the variance), 10 participants loaded onto factor 2 (10%), nine participants loaded onto factor 3 (9%) and five people loaded onto factor 4 (7%). Factors identified will be referred to as ‘viewpoints’.
Most important viewpoints of recovery
All 52 items were endorsed (placed in columns 9–12) by at least two of all 40 participants (5%). The number of endorsements and percentage of endorsements are shown in Table 2.
| Statement | Numbers endorsing each statement (9, 10, 11, 12) | |
|---|---|---|
| n | % | |
| 35. How much support I get from loved ones in helping with my experiences | 26 | 65 |
| 45. How much I have changed as a person/personality since I have had these experiences | 21 | 52.5 |
| 33. How my experiences effect my relationships with friends and loved ones | 18 | 45 |
| 31. How my experiences effect how positive I am for the future | 17 | 42.5 |
| 1. How depressed my experiences make me feel | 16 | 40 |
| 26. How my experiences effect how happy I feel | 14 | 35 |
| 49. How concerned I am of the side effects of taking medication for my experiences | 13 | 32.5 |
| 42. How clearly I can think about my experiences | 13 | 32.5 |
| 40. How much I feel mental health services are helpful with my experiences | 13 | 32.5 |
| 34. How much I understand my experiences | 13 | 32.5 |
| 29. How trusting of others I am as a result of my experiences | 13 | 32.5 |
| 15. How helpful I feel my medication is with my experiences | 13 | 32.5 |
| 39. How bothered I am about the stigma/being judged about my experiences | 12 | 30 |
| 27. How anxious or stressed I am from my experiences | 12 | 30 |
| 25. How well I was able to recognise the early signs of becoming unwell | 12 | 30 |
| 22. How my experiences have effect my memory and concentration | 12 | 30 |
| 17. How convinced I am that my experiences are real | 12 | 30 |
| 41. How my experiences alter my ability to control my own thoughts | 11 | 27.5 |
| 30. How much I socialise as a result of my experiences | 11 | 27.5 |
| 3. How unpleasant my experiences/voices are | 11 | 27.5 |
| 28. How withdrawn I am as a result of my experiences | 11 | 27.5 |
| 2. How much I dwell on my experiences | 11 | 27.5 |
| 19. How my experiences effect the quality/and or amount of sleep I get | 11 | 27.5 |
| 47. My ability to find work as a result of my experiences | 10 | 25 |
| 11. How positive I view my experiences to be | 10 | 25 |
| 51. How motivated I feel about changing my experiences | 9 | 22.5 |
| 43. The amount to which I can cope with my experiences | 9 | 22.5 |
| 37. How ashamed and/or embarrassed I feel about my experiences | 9 | 22.5 |
| 23. How my experiences effect my ability to look after myself | 9 | 22.5 |
| 21. How my experiences effect the amount of anger and frustration I feel | 9 | 22.5 |
| 13. The amount I think about harming myself as a result of my experiences | 9 | 22.5 |
| 5. How much control I have over my experiences | 8 | 20 |
| 48. How financially stable I am as a result of my experiences | 8 | 20 |
| 18. The amount of support I get from other service users | 8 | 20 |
| 16. How helpful I feel psychological therapies are with my experiences | 8 | 20 |
| 46. My living arrangements as a result of my experiences | 7 | 17.5 |
| 20. How my experiences effect my personal freedoms and rights | 7 | 17.5 |
| 12. How much religion/spirituality was involved with my experiences | 7 | 17.5 |
| 9. How loud my voices are | 6 | 15 |
| 50. How vulnerable I feel as a result of my experiences | 6 | 15 |
| 44. In alcohol and drug use that worsens my experiences | 6 | 15 |
| 4. How pleasant my experiences/voices are | 6 | 15 |
| 10. My belief that my experiences come from my own mind | 6 | 15 |
| 7. How much time in my life they take up | 5 | 12.5 |
| 52. How concerned I am that my experiences will happen again | 5 | 12.5 |
| 38. How my experiences effect the amount of emotion I feel | 5 | 12.5 |
| 32. How enjoyable I find hobbies/activities as a result of my experiences | 5 | 12.5 |
| 8. Amount to which my voices are inside my head compared to outside my head | 4 | 10 |
| 6. How often my experiences happen | 4 | 10 |
| 14.How my experience effect how energetic I feel | 3 | 7.5 |
| 36. How empowered I feel over my experiences | 2 | 5 |
| 24. How active I was in seeking help with my experiences | 2 | 5 |
Interpretation of viewpoints
The Q-sort resulted in four viewpoints: collaborative support and understanding, emotional change though social and medical support, regaining functional and occupational goals, and self-focused recovery. The correlations between the factor scores indicated no overlap between factors.
Tables for each factor array, indicating where all statements were ranked for all four viewports are provided in Table 3.
| Viewpoint 1 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| –6 | –5 | –4 | –3 | –2 | –1 | 0 | 1 | 2 | 3 | 4 | 5 | 6 |
| 9. How loud my voices are | 8. Amount to which my voices are inside my head compared to outside | 3. How unpleasant my experiences/voices are | 4. How pleasant my experiences/voices are | 1. How depressed my experiences make me feel | 14. How my experiences effect how energetic I feel | 12. How much religion/spirituality there was involved with my experiences | 10. My belief that my experiences come from my own mind | 30. How much I socialise as a result of my experiences | 15. How helpful I feel my medication is with my experiences | 5. How much control I have over my experiences | 16. How helpful I feel psychological therapies are with my experiences | 31. How my experiences effect how positive I am for the future |
| 44. In alcohol and drug use that worsens my experiences | 13. The amount I think about harming myself as a result of my experiences | 7. How much time in my life they take up | 37. How ashamed or embarrassed I feel about my experiences | 2. How much I dwell on my experiences | 22. How my experiences effect my memory and concentration | 33. How my experiences effect my relationships with friends/loved ones | 24. How active I was seeking help with my experiences | 19. How my experiences effect the quality/and or amount of sleep | 17. How convinced I am that my experiences are real | 11. How positive I view my experiences | 34. How much I understand my experiences | 40. How much I feel mental health services are helpful with my experiences |
| 6. How often my experiences happen | 21. How my experiences effect the amount of anger/frustration I experience | 45. How much I have changed as a person/personality since I have had my experiences | 27. How anxious or stress I am from my experiences | 28. How withdrawn I am as a result of my experiences | 38. How my experiences effect the amount of emotion I feel | 29. How trusting of others I am as a result of my experiences | 20. How my experiences effect my personal freedoms and rights | 43. The amount to which I can cope with my experiences | 18. The amount of support I get from other service users | 35. How much support I get from loved ones in helping with my experiences | ||
| 46. My living arrangements as a result of my experiences | 47. My ability to find work as a result of my experiences | 42. How clearly I can think about my experiences | 50. How vulnerable I feel as a result of my experiences | 39. How bothered I am about the stigma/being judged about my experiences | 32. How enjoyable I find hobbies/activities as a result of my experiences | 23. How my experiences effect my ability to look after myself | 51. How motivated I feel about changing my experiences | 25. How well I was able to recognise the early signs of becoming unwell | ||||
| 49. How concerned I am of that side effects of taking medication | 52. How concerned I am that my experiences will happen again | 41. How my experiences alter my ability to control my own thoughts | 36. How empowered I feel over my experiences | 26. How my experiences effect how happy I feel | ||||||||
| 48. How financially stable I am as a result of my experiences | ||||||||||||
| Viewpoint 2 | ||||||||||||
| –6 | –5 | –4 | –3 | –2 | –1 | 0 | 1 | 2 | 3 | 4 | 5 | 6 |
| 12. How much religion/spirituality there was involved with my experiences | 16. How helpful I feel psychological therapies are with my experiences | 8. Amount to which my voices are inside my head compared to outside | 4. How pleasant my experiences/voices are | 18. The amount of support I get from other service users | 5. How much control I have over my experiences | 7. How much time in my life they take up | 13. The amount I think about harming myself as a result of my experiences | 2. How much I dwell on my experiences | 3. How unpleasant my experiences/voices are | 27. How anxious or stress I am from my experiences | 1. How depressed my experiences make me feel | 26. How my experiences effect how happy I feel |
| 44. In alcohol and drug use that worsens my experiences | 24. How active I was seeking help with my experiences | 9. How loud my voices are | 34. How much I understand my experiences | 30. How much I socialise as a result of my experiences | 14. How my experiences effect how energetic I feel | 23. How my experiences effect my ability to look after myself | 21. How my experiences effect the amount of anger/frustration I experience | 6. How often my experiences happen | 33. How my experiences effect my relationships with friends/loved ones | 29. How trusting of others I am as a result of my experiences | 15. How helpful I feel my medication is with my experiences | 35. How much support I get from loved ones in helping with my experiences |
| 46. My living arrangements as a result of my experiences | 10. My belief that my experiences come from my own mind | 47. My ability to find work as a result of my experiences | 32. How enjoyable I find hobbies/activities as a result of my experiences | 17. How convinced I am that my experiences are real | 25. How well I was able to recognise the early signs of becoming unwell | 38. How my experiences effect the amount of emotion I feel | 22. How my experiences effect my memory and concentration | 41. How my experiences alter my ability to control my own thoughts | 31. How my experiences effect how positive I am for the future | 45. How much I have changed as a person/personality since I have had my experiences | ||
| 11. How positive I view my experiences | 48. How financially stable I am as a result of my experiences | 36. How empowered I feel over my experiences | 19. How my experiences effect the quality/and or amount of sleep | 37. How ashamed or embarrassed I feel about my experiences | 43. The amount to which I can cope with my experiences | 28. How withdrawn I am as a result of my experiences | 50. How vulnerable I feel as a result of my experiences | 40. How much I feel mental health services are helpful with my experiences | ||||
| 42. How clearly I can think about my experiences | 20. How my experiences effect my personal freedoms and rights | 39. How bothered I am about the stigma/being judged about my experiences | 51. How motivated I feel about changing my experiences | 49. How concerned I am of that side effects of taking medication | ||||||||
| 52. How concerned I am that my experiences will happen again | ||||||||||||
| Viewpoint 3 | ||||||||||||
| –6 | –5 | –4 | –3 | –2 | –1 | 0 | 1 | 2 | 3 | 4 | 5 | 6 |
| 8. Amount to which my voices are inside my head compared to outside | 28. How withdrawn I am as a result of my experiences | 17. How convinced I am that my experiences are real | 11. How positive I view my experiences | 12. How much religion/spirituality there was involved with my experiences | 21. How my experiences effect the amount of anger/frustration I feel | 7. How much time in my life they take up | 13. The amount I think about harming myself as a result of my experiences | 22. How my experiences effect my memory and concentration | 29. How trusting of others I am as a result of my experiences | 15. How helpful I feel my medication is with my experiences | 35. How much support I get from loved ones in helping with my experiences | 19. How my experiences effect the quality/and or amount of sleep |
| 9. How loud my voices are | 3. How unpleasant my experiences/voices are | 4. How pleasant my experiences/voices are | 18. The amount of support I get from other service users | 16. How helpful I feel psychological therapies are with my experiences | 31. How my experiences effect how positive I am for the future | 9. How loud my voices are | 24. How active I was seeking help with my experiences | 27. How anxious or stress I am from my experiences | 44. In alcohol and drug use that worsens my experiences | 23. How my experiences effect my ability to look after myself | 33. How my experiences effect my relationships with friends/loved ones | 47. My ability to find work as a result of my experiences |
| 36. How empowered I feel over my experiences | 6. How often my experiences happen | 26. How my experiences effect how happy I feel | 20. How my experiences effect my personal freedoms and rights | 34. How much I understand my experiences | 14. How my experiences effect how energetic I feel | 1. How depressed my experiences make me feel | 2. How much I dwell on my experiences | 45. How much I have changed as a person/personality since I have had my experiences | 30. How much I socialise as a result of my experiences | 46. My living arrangements as a result of my experiences | ||
| 38. How my experiences effect the amount of emotion I feel | 41. How my experiences alter my ability to control my own thoughts | 25. How well I was able to recognise the early signs of becoming unwell | 42. How clearly I can think about my experiences | 32. How enjoyable I find hobbies/activities as a result of my experiences | 43. The amount to which I can cope with my experiences | 39. How bothered I am about the stigma/being judged about my experiences | 50. How vulnerable I feel as a result of my experiences | 37. How ashamed or embarrassed I feel about my experiences | ||||
| 5. How much control I have over my experiences | 52. How concerned I am that my experiences will happen again | 40. How much I feel mental health services are helpful with my experiences | 48. How financially stable I am as a result of my experiences | 49. How concerned I am of that side effects of taking medication | ||||||||
| 51. How motivated I feel about changing my experiences | ||||||||||||
| Viewpoint 4 | ||||||||||||
| –6 | –5 | –4 | –3 | –2 | –1 | 0 | 1 | 2 | 3 | 4 | 5 | 6 |
| 9. How loud my voices are | 3. How unpleasant my experiences/voices are | 6. How often my experiences happen | 50. How vulnerable I feel as a result of my experiences | 51. How motivated I feel about changing my experiences | 5. How much control I have over my experiences | 49. How concerned I am of that side effects of taking medication | 45. How much I have changed as a person/personality since I have had my experiences | 52. How concerned I am that my experiences will happen again | 7. How much time in my life they take up | 46. My living arrangements as a result of my experiences | 11. How positive I view my experiences | 20. How my experiences effect my personal freedoms and rights |
| 19. How my experiences effect the quality/and or amount of sleep | 13. The amount I think about harming myself as a result of my experiences | 27. How anxious or stress I am from my experiences | 47. My ability to find work as a result of my experiences | 24. How active I was seeking help with my experiences | 15. How helpful I feel my medication is with my experiences | 17. How convinced I am that my experiences are real | 4. How pleasant my experiences/voices are | 48. How financially stable I am as a result of my experiences | 14. How my experiences effect how energetic I feel | 2. How much I dwell on my experiences | 12. How much religion/spirituality there was involved with my experiences | 28. How withdrawn I am as a result of my experiences |
| 21. How my experiences effect the amount of anger/frustration I feel | 8. Amount to which my voices are inside my head compared to outside | 16. How helpful I feel psychological therapies are with my experiences | 33. How my experiences effect my relationships with friends/loved ones | 18. The amount of support I get from other service users | 23. How my experiences effect my ability to look after myself | 30. How much I socialise as a result of my experiences | 1. How depressed my experiences make me feel | 39. How bothered I am about the stigma/being judged about my experiences | 26. How my experiences effect how happy I feel | 22. How my experiences effect my memory and concentration | ||
| 10. My belief that my experiences come from my own mind | 35. How much support I get from loved ones in helping with my experiences | 40. How much I feel mental health services are helpful with my experiences | 32. How enjoyable I find hobbies/activities as a result of my experiences | 25. How well I was able to recognise the early signs of becoming unwell | 42. How clearly I can think about my experiences | 31. How my experiences effect how positive I am for the future | 38. How my experiences effect the amount of emotion I feel | 34. How much I understand my experiences | ||||
| 43. The amount to which I can cope with my experiences | 37. How ashamed or embarrassed I feel about my experiences | 29. How trusting of others I am as a result of my experiences | 44. In alcohol and drug use that worsens my experiences | 41. How my experiences alter my ability to control my own thoughts | ||||||||
| 36. How empowered I feel over my experiences | ||||||||||||
Viewpoint 1: collaborative support and understanding
This viewpoint (n = 8) consisted of people who felt that positive and collaborative engagement with others and services was key to their recovery. This group of people was positively motivated to overcome their experiences and willingly accepted help from others to achieve this. This group did not focus on the negative aspects of having a mental health problem. Aspects such as ‘the amount of alcohol and drug use that worsens my experiences’ (−6), ‘the amount I think about harming myself as a result of my experiences’ (−5) and similar aspects were not considered important.
Viewpoint 2: emotional change through social and medical support
This viewpoint (n = 10) consisted of people who considered emotional stability through support and treatment as a key factor to the recovery process. The affective impacts of having psychosis were prioritised whereas the symptoms of psychosis were not considered as important. This group do not find the psychiatric characteristics of symptoms or occupational aspects of any importance.
Viewpoint 3: regaining functional and occupational goals
This viewpoint (n = 9) consisted of people who considered functional and occupational goals as key to their recovery. It was important to this group of people to regain life functioning and aspects that hindered this process were considered important to change in their recovery. This group did not find the internal cognitive aspects important.
Viewpoint 4: self-focused recovery
This viewpoint (n = 5) consisted of people who were internally focused in recovery. Aspects found important to this group involved the self and feelings of isolation. It seemed this group felt persecuted and unsupported by services and felt that they could only be dependent on themselves for recovery. Aspects that were not important to this group appeared to relate to support from others and psychiatric aspects of symptoms.
Additional feedback
Five participants left additional feedback outlining how they found completing the questionnaire and how useful the Q-sort was in helping understand their experiences. All feedback was positive about the procedure.
Discussion
Results suggest that there are different aspects to recovery from psychosis that are not necessarily linked to alleviation or removal of symptoms. Furthermore, it highlights the importance of ensuring that treatment is idiosyncratic in facilitating people’s recovery.
The four-factor solution provides an interesting insight into recovery and the different types of recovery styles. Four Q-sorts were generated: collaborative support and understanding, emotional change through social and medical support, regaining functional and occupational goals, and self-focused recovery.
The qualitative feedback obtained from the questionnaire illustrated that a number of participants found that the Q-sort helped them further understand their recovery, indicating that the recovery Q-sort may be a therapeutic tool in its own right. The identification of four different recovery styles highlights the importance of tailoring care packages to individual needs. Arguably, people that loaded onto the first three viewpoints may benefit from therapies such as CBT, which are goal orientated, collaborative, person-centred and utilise guided discovery. Those who support ‘self-focused recovery’ may need a more self-directed recovery programme to assist empowerment and self-change.
Utilisation of Q-methodology allowed for the recovery themes to be examined by a wider group of service users. It would therefore be hoped that these four recovery viewpoints are representative of the service user population as a whole. It is interesting to note that two of the viewpoints appeared to be endorsed predominantly by one sex (females predominantly endorsed collaborative support and understanding, whereas males predominantly endorsed regaining functional and occupational goals); future research could examine whether or not this finding is replicable and valid, and may indicate the importance of examining sex differences in recovery styles. The main limitation of the study was that the factor solution only explained 36% of the variance, with eight people not loading onto any factors. Therefore, it is acknowledged that only tentative interpretations can be drawn from the results. However, this research lays a platform for further research into this area.
Phase 3: the Subjective Experiences of Psychosis Scale – psychometric evaluation of a scale to assess outcome in psychosis
This research was previously published as Haddock G, Wood L, Watts R, Dunn G, Morrison AP, Price J. The Subjective Experiences of Psychosis Scale (SEPS): psychometric evaluation of a scale to assess outcome in psychosis. Schizophr Res 2011;133:244–971 and much of this text has been reproduced with permission from Elsevier.
Objectives
This project aimed to develop a service-user-generated, valid, reliable, multidimensional tool to assess dimensions of symptoms of psychosis that can be used to assess and monitor experiences of psychosis.
Method
Development of the Subjective Experiences of Psychosis Scale
Potential items for the new scale [the Subjective Experiences of Psychosis Scale (SEPS)] came from three sources: (1) items identified from the existing literature on outcomes within mental health; (2) themes generated from phase 1; and (3) material generated from phase 2. A total of 146 items were identified from these methods which were reduced down to 52 items within three distinct categories: (1) impact of experiences of psychosis on mental health and well-being; (2) impact of support (such as treatment, support from friends and family, alcohol) on experiences of psychosis; and (3) severity of different dimensions of experiences of psychosis (e.g. frequency and pleasantness). Both positive and negative aspects of experiences of psychosis were identified in all three categories.
This initial draft scale was further scrutinised for content and face validity by a SURG resulting in the following changes: reducing the number of items to eliminate redundant or repeated items, introducing a scoring method that represented both the positive and negative aspects of psychosis for all items, including a scored example and rewording the instructions.
These modifications resulted in a 45-item self-report scale, consisting of three subscales assessing positive and negative aspects of experience of psychosis. Subscale 1 was ‘positive impacts of experiences’ and ‘negative impacts of experiences’, respectively, (31 items each), subscale 2 was ‘positive impact of support’ and ‘negative impact of support’ on experiences of psychosis (eight items each) and subscale 3 was ‘positive dimensions’ (two items) and ‘negative dimensions’ of experiences of psychosis (four items). Items were scored from 1 (not at all) to 5 (very much) with the addition of a ‘not applicable’ box for subscale 2.
Participants
Participants were required to meet the following inclusion criteria:
Materials
Measurement of symptoms of psychosis was assessed using the PANSS55 and PSYRATS. 72 Depression, hopelessness, anxiety and self-esteem were assessed using the Calgary Depression Scale,73 Beck Hopelessness Scale (BHS74), Beck Anxiety Inventory (BAI75) and the Self-Esteem Rating Scale (SERS76), respectively. Functioning was assessed using the GAF scale. 77 In addition, we explored how the SEPS related to self-reported progress in recovery from psychosis and using the QPR. 32 All measures have been shown to have good reliability and validity with psychosis samples.
Procedure
Participants were recruited from mental health teams in the north-west of England via mental health professionals. The study was carried out over three stages. Stage 1 required participants to fill out the SEPS and self-report measures and participate in PANSS and PSYRATS interviews. Data from stage 1 were used to carry out a PCA and investigation of internal consistency and concurrent validity of the SEPS. In stage 2, which was completed 1–2 weeks later, participants completed the SEPS again to investigate test–retest reliability.
In stage 3, which involved exploration of the SEPS in relation to the other measures over time, participants were required to repeat the assessments carried out in stage 1. Participants were given the option to take part in any, or all, of the stages.
Statistical analysis
An initial PCA was carried out on the SEPS and the internal consistency of identified subscales was computed using Cronbach’s alpha. Intraclass correlations (ICCs) and Spearman’s rank-order correlation analysis were used to examine test–retest reliability, concurrent validity and sensitivity to change between the SEPS and the other measures.
Results
One hundred participants took part in the study and participation in different aspects of the research are shown in Table 4 along with the demographic details of the sample.
| PCA and internal consistency (n = 100) | Test–retest (n = 35) | Concurrent validity (n = 75) | Sensitivity to change (n = 30) | |
|---|---|---|---|---|
| Sex | ||||
| Male | 75 | 27 | 59 | 22 |
| Female | 25 | 8 | 16 | 8 |
| Age (years) | ||||
| Mean (SD) | 38.14 (10.23) | 37.25 (10.23) | 37.79 (10.63) | 38.40 (10.42) |
| Range | 18–65 | 19–63 | 18–65 | 19–65 |
| Marital status | ||||
| Single | 72 | 27 | 53 | 22 |
| Married | 6 | 2 | 5 | 1 |
| Partner | 12 | 0 | 8 | |
| Cohabiting | 0 | 2 | 0 | 3 |
| Separated/divorced | 9 | 3 | 8 | 3 |
| Widowed | 1 | 1 | 1 | 1 |
| Employment status | ||||
| Unemployed | 77 | 25 | 58 | 22 |
| Voluntary work | 5 | 1 | 3 | 1 |
| Student | 8 | 4 | 7 | 3 |
| Full time | 5 | 3 | 4 | 2 |
| Part time | 1 | 0 | 0 | 0 |
| Retired | 3 | 2 | 2 | 2 |
| Home worker | 1 | 0 | 1 | 0 |
| Ethnicity | ||||
| White | 85 | 30 | 63 | 27 |
| Asian | 5 | 1 | 3 | 1 |
| Black | 5 | 1 | 4 | 1 |
| Other | 5 | 3 | 5 | 1 |
Initial data scrutiny
From the initial pool of items for the SEPS examined in stage 1, items with very low endorsements (< 20% of sample) and either high or low inter item correlations (< 0.200 or > 0.900) were removed. In addition, items with low test–retest scores and which contributed to a decrease in internal consistency were examined further. Together with these considerations and initial PCA feedback from participants and from the SURG, a number of items were removed resulting in a final number of 41 items on which all subsequent analyses were carried.
Principal component analysis: in the first instance, the data set was checked for suitability of PCA by examining the correlation matrix to ensure no multicollinearity or singularity. A PCA was then performed on each of the three SEPS subscales using varimax rotation. From examination of the scree plots and Eigenvalues, all three analyses resulted in two-factor solutions, with loadings > 0.4 taken as significant. The subscales and factors defined in this analysis were used in all further psychometric analyses. The three subscales had 29, 6 and 6 items, respectively. Each subscale consisted of two factors positive and negative items. Total variance explained by these subscales was relatively low.
Subscale 1: impact of experiences
Two factors contributed to 40.13% of explained variance, with factor 1 (‘positive impacts of experiences of psychosis’) contributing to 21.54% of the variance and factor 2 (‘negative impacts of experiences of psychosis) contributing to 18.59% of the variance.
Subscale 2: impact of support
Two factors contributed to 54.29% of the total variance explained, with factor 1 (‘positive impact of support on experiences of psychosis) contributing to 29.49% of the variance and factor 2 (‘negative impact of support on experiences of psychosis) contributing to 24.80% of the variance.
Subscale 3: dimensions of experiences of psychosis
The two identified factors explained 60.12% of cumulative variance; factor 1 (‘negative dimensions of experiences of psychosis) contributed to 33.47% of the variance, and factor 2 (‘positive dimensions of experiences of psychosis’) contributed to 26.65% of the variance.
Reliability
Cronbach’s alpha statistics were calculated for each subscale and these ranged from acceptable to good (Table 5). ICCs, using a two-way random model and absolute agreement were also computed to provide further evidence for the reliability of the SEPS. All subscales within the SEPS showed moderate to good ICCs (see Table 5). Furthermore, the positive and negative aspects of each subscale were not significantly correlated with each other, although there was a moderate correlation between the positive and negative support items (ρ = 0.364; p < 0.01).
| Subscale | Internal consistency (n = 100) | ICC (n = 35) | Confidence intervals (n = 35) | Baseline (n = 35) (SD) | Retest (1–2 weeks) (n = 35) (SD) | Spearman’s ρ (significance) (n = 35) |
|---|---|---|---|---|---|---|
| Subscale 1 | ||||||
| Positive impact | 0.95 | 0.461** | 0.151 to 0.687 | 57.80 (25.83) | 58.63 (28.28) | 0.558** |
| Negative impact | 0.93 | 0.829** | 0.689 to 0.909 | 71.46 (24.87) | 68.37 (25.46) | 0.827** |
| Subscale 2 | ||||||
| Positive support | 0.80 | 0.323 | –0.014 to 0.592 | 12.89 (6.63) | 12.94 (6.66) | 0.359* |
| Negative support | 0.79 | 0.657** | 0.417 to 0.812 | 7.83 (4.29) | 7.86 (5.12) | 0.575** |
| Subscale 3 | ||||||
| Positive dimensions | ρ = 0.535** | 0.736** | 0.536 to 0.858 | 4.40 (1.87) | 4.49 (2.06) | 0.723** |
| Negative dimensions | 0.66 | 0.640** | 0.391 to 0.801 | 13.40 (3.35) | 12.40 (3.47) | 0.606** |
Test–retest means, standard deviations (SDs) and correlation coefficients of the subscale scores of the SEPS are also shown in Table 5. The subscales had good retest reliability overall although the positive support subscale was only moderate. The majority of individual items in the subscales also indicated good retest reliability with only five items with correlations below 0.2.
Validity
Means and SDs for all measures are shown in Table 6. The relationship between the SEPS and measures of symptoms of psychosis, affect, esteem, function and recovery can also be found in Table 6.
| Measure | Mean (SD) (n = 75) | Range (n = 75) |
|---|---|---|
| SEPS | ||
| Subscale 1 | ||
| Positive impact | 56.80 (25.85) | 29–119 |
| Negative impact | 68.77 (24.72) | 29–127 |
| Subscale 2 | ||
| Positive support | 14.09 (6.54) | 1–30 |
| Negative support | 7.84 (4.87) | 1–22 |
| Subscale 3 | ||
| Positive dimensions | 4.60 (2.09) | 2–10 |
| Negative dimensions | 12.81 (3.90) | 4–20 |
| PANSS | ||
| Positive | 14.69 (4.33) | 9–26 |
| Negative | 13.52 (4.23) | 7–26 |
| General | 29.49 (6.58) | 17–47 |
| Total | 57.71 (11.92) | 33–88 |
| PSYRATS | ||
| Auditory hallucinations | 25.06 (7.42) | 11–37 |
| Delusions | 12.38 (5.41) | 3–22 |
| Calgary Depression Scale | 5.72 (4.39) | 0–17 |
| QPR | ||
| Intrapersonal subscale | 58.60 (11.18) | 29–84 |
| Interpersonal subscale | 18.40 (2.63) | 11–25 |
| Total | 77.00 (12.57) | 45–109 |
| BHS | 12.76 (5.58) | 1–20 |
| BAI | 17.43 (12.88) | 0–56 |
| SERS | ||
| Positive self-esteem | 41.45 (13.08) | 11–70 |
| Negative self-esteem | 32.91 (11.42) | 10–58 |
| GAF scale | ||
| Symptoms | 34.23 (8.13) | 21–57 |
| Functioning | 41.49 (9.83) | 25–70 |
| Total | 34.21 (8.13) | 21–60 |
Relationship between the Subjective Experiences of Psychosis Scale and psychosis symptom measures
The positive impacts of experiences and positive impact of support were not correlated with any of the symptom measures. However, there was a modest, negative correlation between the positive dimensions items of subscale 3 and the PSYRATS delusions subscale.
Negative impacts of experiences showed small to moderate correlations with all PANSS subscales apart from the PANSS negative subscale. There were moderate correlations with PSYRATS auditory hallucinations and delusions subscales. There were no significant correlations between negative support and any symptom measures. A similar picture to subscale 1 was observed for the negative dimensions of experiences, with moderate correlations with all PANSS and PSYRATS subscales but no correlation between the PANSS negative subscale.
Relationship between the Subjective Experiences of Psychosis Scale and measures of affect, esteem, functioning and recovery
The positive impacts of experiences and positive impact of support were not correlated with any measures. However, positive dimensions showed small, positive correlations with progress on recovery on the intrapersonal and interpersonal subscales of the QPR and showed a moderate positive correlation with self-esteem on the SERS positive subscale.
Negative impacts of experiences correlated moderately with depression, intrapersonal aspects of recovery, hopelessness, anxiety and self-esteem (both positive and negative subscales of the SERS). Negative impact of support was not correlated with any affect or functioning measures other than a small, positive correlation with anxiety. A similar picture to the impact of experiences subscale was observed for negative dimensions, with small to moderate correlations with depression, intrapersonal aspects of recovery, hopelessness, anxiety and negative self-esteem. In addition, there was also a moderate relationship between negative dimensions of symptoms and lower functioning on the GAF scale (Table 7).
| Measure | Positive impact | Negative impact | Positive support | Negative support | Positive dimensions | Negative dimensions |
|---|---|---|---|---|---|---|
| PSYRATS hallucinations | –0.050 | 0.593** | –0.080 | 0.136 | –0.060 | 0.551** |
| PSYRATS delusions | –0.106 | 0.374** | –0.135 | –0.003 | –0.280* | 0.473** |
| PANSS positive | 0.115 | 0.269* | –0.770 | 0.046 | –0.029 | 0.535** |
| PANSS negative | 0.083 | 0.149 | 0.023 | 0.104 | –0.077 | –0.097 |
| PANSS general | –0.023 | 0.435** | –0.062 | 0.081 | –0.036 | 0.373** |
| PANSS total | 0.035 | 0.356** | –0.100 | 0.084 | –0.050 | 0.339** |
| Calgary Depression Scale | –0.109 | 0.408** | –0.071 | 0.152 | 0.005 | 0.333** |
| QPRIntra | 0.150 | –0.493** | 0.214 | –0.122 | 0.291* | –0.330** |
| QPRInter | –0.104 | –0.146 | 0.120 | –0.022 | 0.278* | –0.058 |
| QPR total | 0.120 | –0.467** | 0.216 | –0.120 | 0.322** | –0.307** |
| BHS | –0.047 | 0.392** | –0.126 | 0.053 | –0.192 | 0.258* |
| BAI | –0.059 | 0.439** | 0.153 | 0.269* | 0.020 | 0.370** |
| SERS positive | –0.181 | –0.326** | 0.087 | –0.045 | 0.335** | –0.204 |
| SERS negative | –0.059 | 0.506** | –0.038 | 0.170 | –0.166 | 0.301** |
| GAF scale symptoms | –0.094 | –0.202 | –0.120 | –0.047 | –0.041 | –0.394** |
| GAF scale functioning | –0.064 | –0.145 | –0.041 | –0.092 | 0.094 | –0.209 |
| GAF scale total | –0.039 | –0.154 | –0.053 | –0.024 | 0.048 | –0.314** |
Sensitivity to change of the Subjective Experiences of Psychosis Scale
Sensitivity to change was derived by calculating the change in score (baseline score minus follow-up score) on each measure. The change scores for each section within the SEPS were then correlated with all measures, which can be found in Table 8.
| Positive impact | Negative impact | Positive support | Negative support | Positive dimensions | Negative dimensions | |
|---|---|---|---|---|---|---|
| PSYRATS hallucinations | 0.029 | 0.262 | –0.027 | 0.202 | 0.172 | 0.455 |
| PSYRATS delusions | 0.062 | 0.365 | –0.082 | 0.196 | 0.235 | 0.394* |
| PANSS positive | –0.246 | 0.123 | –0.153 | 0.040 | 0.147 | 0.125 |
| PANSS negative | 0.076 | 0.355 | 0.153 | 0.282 | 0.270 | 0.169 |
| PANSS general | –0.024 | 0.436* | –0.175 | 0.259 | –0.044 | 0.385* |
| PANSS total | –0.040 | 0.431* | –0.084 | 0.281 | 0.121 | 0.333 |
| Calgary Depression Scale | –0.204 | 0.304 | –0.327 | 0.002 | –0.058 | 0.243 |
| QPRIntra | –0.215 | –0.408* | –0.014 | –0.441* | –0.176 | –0.175 |
| QPRInter | –0.013 | –0.283 | 0.291 | –0.137 | 0.075 | –0.268 |
| QPR total | –0.201 | –0.463** | 0.103 | –0.407* | –0.135 | –0.210 |
| BHS | –0.046 | 0.158 | 0.225 | 0.167 | –0.194 | 0.200 |
| BAI | –0.125 | –0.077 | –0.283 | –0.317 | –0.085 | –0.019 |
| SERS positive | –0.010 | –0.635** | –0.145 | –0.309 | 0.216 | –0.527** |
| SERS negative | 0.008 | 0.113 | 0.357 | 0.200 | 0.085 | 0.086 |
| GAF scale symptoms | 0.066 | –0.054 | 0.064 | –0.191 | –0.128 | –0.188 |
| GAF scale functioning | 0.042 | –0.307 | 0.003 | –0.344 | 0.034 | –0.207 |
| GAF scale total | 0.052 | –0.089 | 0.016 | –0.141 | –0.047 | –0.165 |
Relationships between change on the Subjective Experiences of Psychosis Scale and psychosis symptom measures
Change in the positive subscales did not correlate with change in any symptom measures. Change in negative impacts of experiences showed moderate, positive correlations with the PANSS general subscale and total PANSS scores. Change in negative support did not correlate with change on any of the psychosis measures. Change in negative dimensions showed moderate correlations with delusion severity measured by the PSYRATS delusions scale and with the PANSS general subscale scores.
Relationship between change on the Subjective Experiences of Psychosis Scale and measures of affect, esteem, functioning and recovery
There was no relationship between change in the positive aspects of any subscale and any other measures. Negative aspects on the SEPS were related to esteem and progress in recovery and suggested that increases in negative impact, poor support and increase in self-reported symptoms was related to decreases in self-esteem and recovery.
Feedback and distress
Participants took between 5 and 30 minutes to complete the SEPS. Ninety-nine participants (99%) rated the degree of distress experienced from completing the SEPS. Seventy-five participants (75%) reported that they experienced no distress from completing the scale. Fourteen (14%) reported experiencing ‘a little’ distress, five (5%) reported ‘moderate’ distress and 5 (5%) rated ‘quite a lot’ of distress. When distress was disclosed, the researcher debriefed the participant, ensuring they had the opportunity to discuss any concerns and consent was sought to share this information with the participant’s clinical team if this was considered appropriate.
Discussion
The SEPS is a reliable and valid self-report measure of psychosis experiences. It has been developed with the direct input of service users, both in terms of project design and investigation and in the development of the content and format of the measure to ensure that the items and presentation reflect their experience of psychosis. The scale is easy to use, takes a relatively short time to complete and appears to be extremely meaningful for many service users. It has good retest reliability and the subscales have good internal consistency. Although the total variance explained by the two-component solution is relatively low, negative factors on the SEPS related well to widely used objective interview measures of psychosis such as the PANSS55 in relation to concurrent experiences and change over time. These are important aspects when evaluating outcome and they emphasise the validity of this method of self-report assessment of psychosis experiences.
The scale covers distinct areas that have been outlined in previous service user informed research. For example, social, relationship and support factors, which have been outlined as key areas for recovery from psychosis19 and which play an important role in service provision. 14 In addition, the scale also assesses specific characteristics of symptoms, some of which are included in other scales; however, the items in this scale are the dimensions that service users highlight as being most relevant. The diverse subscales of the SEPS cover a vast array of topics not yet scrutinised in a single measure, thus illustrating its comprehensiveness. These complex dimensions are essential when aiming to understand idiosyncratic experiences of psychosis and is in keeping with the idiosyncratic nature of the recovery process. 19
In addition, the development of the scale highlighted the importance of considering the positive impacts of psychosis experiences, an area not addressed in other outcome scales for psychosis. The psychometric investigation revealed that the positive aspects of psychosis are not solely the converse of the negative aspects but are independent and salient aspects that relate more to positive self-esteem and progress in relation to recovery than to psychosis symptomatology. This is consistent with other findings which have reported on positive functions of psychosis. For example, some people who hear voices report associated benefits such as companionship or comfort. 78,79
Further investigation of the role of positive aspects of psychosis is needed; however, the findings here suggest that assessing and monitoring positive as well as negative aspects of symptoms may be important to fully document an individual’s recovery profile. In addition, the exploratory analyses with measures of affect, esteem, recovery and functioning highlighted the close relationship between psychosis experiences and these phenomena, implying that these issues need to be considered in treatment delivery.
There are a number of limitations to this study. One of the main limitations was the moderate sample size used for psychometric testing. Test–retest reliability and sensitivity to change analysis used only 35 and 30 participants, respectively. Furthermore, PCA was carried out with 100 participants when it is often recommended that 10 times the number of items is required for an adequate sample size. 80 Additionally, alternative means of determining the component structure of the measure (such as parallel analysis) could have resulted in an alternative number of components to extract, therefore, future confirmatory studies could utilise this approach.
In addition, although the sample represented the users of mental health services within the geographical area where recruitment took place, this may not be representative of the population in general. The sample consisted of mainly white, British males. The low proportion of female participants and those from ethnic minorities suggest limitations in the generalisability of these findings.
Finally, the SEPS is a self-report tool for which participants are required to make a subjective judgement about their experience of psychosis. Although this is a strength of the tool in that it could be argued that self-reporting perceptual experiences is more likely to provide a true representation of the experience than one provided by an observer, it is also a potential weakness. Self-report methods are subject to a number of responder biases that may lead to data inaccurately reflecting the construct being measured and may result in overinflated relationships between variables. 81 The findings should be interpreted in the light of these limitations.
Despite these limitations, the SEPS appears to be a valid and reliable self-report measure of both positive and negative aspects of psychosis experiences including the impact of such experiences, support that improved or exacerbated such experiences and dimensions of such experiences. As this measure was developed in collaboration with service users at each stage of the research process, this ensures that it can be used to assess and monitor important aspects of psychosis experiences that are relevant to users own concerns, which may help mental health professionals to engage people in services and to develop and monitor meaningful outcomes.
Conclusions
The research studies within this chapter aimed to explore user-defined conceptualisation and measurement of recovery in psychosis. A key objective was to develop a measure of recovery in psychosis that was meaningful and relevant to service users, and incorporated dimensions of symptoms. To achieve this objective the research was split into three phases:
-
a qualitative approach to explore service user experiences of recovery
-
a Q-methodology approach to further refine what factors are important to service user definitions of recovery
-
utilisation of information from phases one and two to develop a service user designed measure of recovery in relation to symptoms of psychosis and establish its psychometric properties.
The research within this chapter provided additional support for previous studies suggesting recovery is a multifaceted process that should be understood and supported using a holistic approach. For example, the first phase found four main themes that are important to consider when conceptualising recovery: impacts on mental health, self-change and adaptation, social redefinition and adapting an individual coping style. This highlights the need to consider coping styles and social and personal change alongside symptom alleviation, with equal importance being given to each factor. An important implication of this study was the need for assessment tools, which take into account the important element of symptom alleviation alongside the broader personal and social themes with consideration of the impact that these experiences have on the lives of service users.
The second phase suggested similar factors which are important in recovery: collaborative support and understanding, emotional change through social and medical support, regaining functional and occupational goals, and self-focused recovery. Interestingly, a number of participants found that the Q-sort technique helped them further understand their recovery, indicating that the recovery Q-sort could be utilised as a therapeutic tool in its own right. In support of phase 1 of this research, this study also highlighted the importance of tailoring care packages to individual needs.
Taking the findings from phases 1 and 2 into account, the final phase of this research was to develop and validate a measure of recovery in relation to symptoms of psychosis: the SEPS. The SEPS was shown to be a reliable and valid self-report measure of experiences of psychosis. It was developed with direct input from service users, both in terms of project design and investigation, and in the development of the content and format of the measure to ensure that the items and presentation reflect their experience of psychosis. The scale is easy to use, takes a relatively short time to complete and appears to be extremely meaningful for many service users. It has good retest reliability and the subscales have good internal consistency. Additionally, the scale highlights the importance of considering the positive impacts of psychosis experiences, an area not addressed in other outcome scales for psychosis. It appears that positive aspects of psychosis are not solely the converse of the negative aspects, but are independent and salient aspects that relate more to positive self-esteem and progress in relation to recovery than to psychosis symptomatology. Further investigation of the role of positive aspects of psychosis is needed; however, the findings here suggest that assessing and monitoring positive as well as negative aspects of symptoms may be important to fully document an individual’s recovery profile.
In conclusion, the research in this chapter has confirmed that recovery in psychosis is a multifaceted process and highlights the importance of the positive and negative aspects of experiences of psychosis. The research has led to the development of a user-defined measure that has been shown to be reliable and valid, as well as meaningful and relevant to service users. The use of the recovery Q-sort and the SEPS measure may help mental health professionals to engage people in services and to develop and monitor meaningful outcomes and user-defined recovery.
Chapter 3 What does recovery mean to service users with experience of psychosis? A Delphi study with experts by experience
This research has been published previously as Recovery in psychosis: a Delphi study with experts by experience [published online ahead of print April 12 2014]. Schizophr Bull 2014. 82 Reproduced under the guidance of Oxford University Press.
Background
Mental health services typically define recovery from psychosis in terms of absence of symptoms, decreases in duration of hospital admissions and reduced rate of rehospitalisation. 83 Clinical research trials often attempt to quantify recovery by demonstrating significant improvements in symptoms and other so-called ‘deficits’ to the degree that they could be considered within the ‘normal’ range. 84 In stark contrast, service users conceptualise recovery very differently to this,18 believing that recovery is a unique process rather than an end point with key recovery themes including hope, rebuilding self and rebuilding life. 19 Many qualitative studies and service user accounts demonstrate these similar themes of recovery and indicate that there is potential for all individuals to recover to some extent. 20
This new found optimism about the potential for recovery from psychosis has been adopted in various health policies,85–89 which have a focus on collaborative working between clinicians and service users, rebuilding lives with or without ongoing symptoms and recognising the importance of hope and empowerment. Despite this recognition of what may be required for recovery-oriented mental health services, it is not always clear how health professionals can provide effective recovery-oriented services that can be evaluated for their performance in supporting people to recover. 90
Various measures of service user-defined recovery have been developed over the last two decades, with items covering a variety of themes including hope, confidence and empowerment, awareness and understanding, help seeking, social support and goals or purpose. 31 Only two measures have been developed specifically to measure service user-defined recovery from psychosis: the Psychosis Recovery Inventory91 and the QPR. 92 None of the user-defined recovery measures has been adopted as a routine outcome measure in mental health services in the UK to date, although various services are piloting local measures. There is continued debate about whether or not recovery can be measured as an outcome when it is defined as a process, although it has been suggested that if measurement of recovery is a collaborative process involving service users and clinicians, it could be a feasible and valid method for evaluation of effective recovery-oriented services. 30
Although there has been a reasonable level of agreement that mental health services should aim to be recovery-oriented and that it is possible to measure the effectiveness of these services, the problem of reaching consensus about what we mean by recovery and producing a definition that is acceptable to service users, while being practical and achievable by clinicians and services, has yet to be resolved. There is a multitude of service user accounts of recovery93–96 and qualitative studies exploring recovery,19,97,98 which identify various common themes but most, if not all, conclude that recovery is a unique process that can be different for everyone. This makes it extremely difficult for clinicians and services to provide recovery-oriented services. The extent to which service users agree about what constitutes recovery and what helps their recovery has yet to be explored.
Various methods and techniques can be employed to help reach consensus about a given debated topic. 99 One such technique is the Delphi method, which is a systematic process of engaging a group of ‘experts’ in the chosen field in two or more rounds of questionnaires, with the aim of identifying items which the panel agree are important to the chosen topic. The Delphi method has been utilised previously to identify essential elements in schizophrenia care,100 indicators of relapse,101 essential elements of EISs,102 first aid guidelines for psychosis103 and components of CBTP. 104
Expert panels used in the Delphi method usually consist of expert clinicians and academics, although two studies to date have also utilised small groups of service users. 103,105 On the topic of recovery from psychosis, it could be argued that service users themselves are the experts. Indeed, many of the documents that endorse the recovery approach accept that it should be defined by service users. Many NHS initiatives aim to view the patient as the expert106 and mental health services are increasingly taking this approach of valuing service users as ‘experts on their own experience’. 107
This study utilises the Delphi methodology to consult a large group of service users about what recovery means to them. The aim of the study was determine the level of consensus regarding service user conceptualisations of recovery.
Method
Participants
Participants who took part in this Delphi exercise were services users who identified themselves as having experience of psychosis. Participants were included in the study if they have (or have had in the past) experience of psychosis, are over the age of 16 years and are able to understand English. Participants were recruited via convenience sampling through mental health services (including CMHTs and EISs), non-NHS groups/voluntary groups and networks, and advertising of the study by leaflets, posters, e-mail networks, websites, social media and local media (including press releases). This study was supported by the Mental Health Research Network who provided clinical studies officers to advertise and recruit participants using the methods described above. Recruitment took place across seven trusts in the North West of England: Cheshire and Wirral Partnership NHS Foundation Trust, Cumbria Partnership NHS Foundation Trust, Greater Manchester West Mental Health NHS Foundation Trust, Lancashire Care NHS Foundation Trust, Manchester Mental Health and Social Care Trust, Mersey Care NHS Trust and 5 Boroughs Partnership NHS Foundation Trust.
Procedure and analysis
This study was approved by the National Research Ethics Service Committee East Midlands. The Delphi process consisted of three stages based around those identified by Langlands et al. 103
Stage 1
Elements identified as pertinent to the definition or conceptualisations of recovery from psychosis were identified through a literature search of journals, policy documents, recovery measures and websites. This list was reviewed by the authors and collated into an initial list of statements (n = 141). Owing to the complexities of including a large panel of service users as the experts to be consulted, the authors decided to use a smaller panel of service users (a local service user reference group with 10 members, all of whom have personal experience of psychosis and using mental health services) during stage 1 to further refine this initial statement list. This resulted in the addition of a further three items, rewording of several items to increase acceptability to service users (e.g. including the word ‘experiences’ alongside ‘symptoms’ and removing the word ‘illness’ where possible) and deletion of seven items which were felt by the service users to be duplications.
Stage 2
In this stage the finalised list of 137 statements from stage 1 was collated and formatted into an online questionnaire and an alternative paper version. A demographics sheet was added to collect data on age, sex, mental health trust, diagnosis and length of diagnosis. Participants were given the option to state ‘prefer not to say’ for all demographic items. Participants were also asked if they would like to provide a postal or e-mail address so they could be invited to take part in the final stage of the study, although this was optional to allow complete anonymity if preferred.
Participants were then asked to rate the importance of each item on the statement list, in relation to defining recovery from psychosis, on a 5-point Likert scale (1 – essential, 2 – important, 3 – do not know/depends, 4 – unimportant and 5 – should not be included). A total of 426 participants completed the stage 2 questionnaire, although 45 were not included in the final sample (26 were deemed to be ineligible owing to reporting no experience of psychosis, 14 people did not complete the questionnaire, one person added a note to say they had already completed the study before and four people posted the questionnaire after the deadline). Results from the remaining 381 eligible participants were entered into an anonymised database and analysed by obtaining group percentages.
In accordance with the methods used by Langlands et al. 103 the following criteria were used to determine items for inclusion, exclusion and rerating.
-
Items rated by 80% or more participants as essential or very important to defining or conceptualising recovery are included as standard.
-
Items rated as essential or important to defining or conceptualising recovery by 70–79% of respondents in stage 2 were rerated in stage 3.
-
Any statements that did not meet the above two conditions were excluded.
This resulted in the inclusion of 71 items, the exclusion of 30 items and 36 items to be rerated in stage 3.
Stage 3
In stage 3, participants were asked to rerate only those items that 70–79% of respondents had rated as essential or important during stage 2 (n = 36 items). Two hundred and six participants provided contact details to be invited to take part in stage 3. The majority of participants opted to be sent a postal paper version rather than complete the questionnaire online. A total of 154 postal questionnaires were distributed in stage 3 and 52 participants were sent the online questionnaire link. One hundred participants completed the final stage resulting in a further 23 statements being included and 13 statements being excluded.
Results
Table 9 provides an overview of the demographic information collected during stages 2 and 3.
| Characteristics | Stage 2 (n = 381) | Stage 3 (n = 100) |
|---|---|---|
| Sex | ||
| Male | 223 (59.6%) | 43 (43%) |
| Female | 151 (39.6%) | 56 (56%) |
| Not stated | 7 (1.8%) | 1 (1%) |
| Age (years) | ||
| 17–20 | 7 (1.8%) | 1 (1%) |
| 21–29 | 53 (13.9%) | 9 (9%) |
| 30–39 | 94 (24.7%) | 16 (16%) |
| 40–49 | 108 (28.3%) | 29 (29%) |
| 50–59 | 72 (18.9%) | 27 (27%) |
| 60 or older | 40 (10.5%) | 17 (17%) |
| Not stated | 7 (1.8%) | 1 (1%) |
| Diagnosis | ||
| Schizophrenia | 152 (39.9%) | 32 (32%) |
| BD | 66 (17.3%) | 28 (28%) |
| Prefer not say | 62 (16.3%) | 11 (11%) |
| Other | 26 (6.8%) | 8 (8%) |
| Psychosis | 24 (6.3%) | 8 (8%) |
| Depression | 20 (5.2%) | 1 (1%) |
| Schizoaffective disorder | 16 (4.2%) | 5 (5%) |
| No diagnosis | 15 (3.9%) | 7 (7%) |
| Length of diagnosis | ||
| Within the last year | 36 (9.4%) | 5 (5%) |
| 1–4 years ago | 64 (16.8%) | 15 (15%) |
| 5–10 years ago | 78 (20.5%) | 25 (25%) |
| More than 10 years ago | 177 (46.5%) | 50 (50%) |
| Not stated/no diagnosis | 26 (6.8%) | 5 (5%) |
A total of 94 items were retained in the final statement list after being rated as important or essential by > 80% of participants. No items reached consensus for not being included (rated as should not be included by > 80% of participants). Figure 2 illustrates the number of items which were included, rerated and excluded at each round of the study.
FIGURE 2.
Summary of items included, rerated and excluded at each stage.
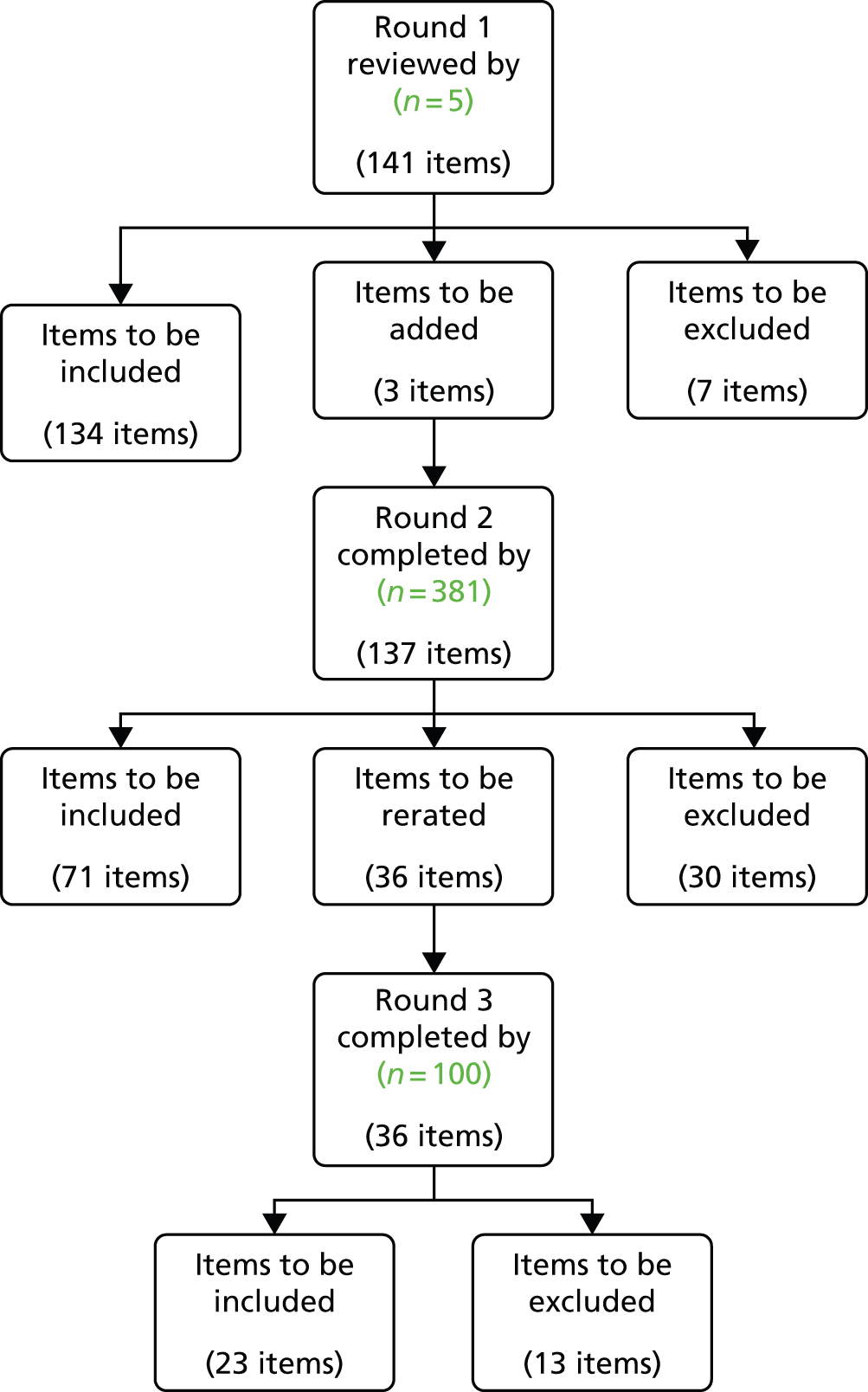
The final 94 items were divided into four categories: defining recovery (n = 19 items), factors that help recovery (n = 43 items), factors that hinder recovery (n = 11 items) and factors that show someone is recovering (n = 21 items).
Tables 10–13 show the final statements in their respective category, with percentage of participants who rated the item as essential or important. Items with extremely high consensus obtained in stage 2 (> 90%) are highlighted in green. The percentage in brackets represents the responses of participants who reported a diagnosis of schizophrenia, schizoaffective disorder or psychosis. Only one of the differences in percentage agreements between the sample as a whole and this subgroup was significant [item ‘Believing that something good will happen eventually’ χ2(2, N = 100) = 4.822 p = 0.028; indicating that this item was less important to those in this subgroup than the sample as whole]. Table 14 shows the items that were excluded in stages 2 and 3.
| Item | Stage included | Percentage agreement, n (%) |
|---|---|---|
| Recovery is the achievement of a personally acceptable quality of life | 2 | 91 (89) |
| Recovery is feeling better about yourself | 2 | 91 (90) |
| Recovery is a return to a state of wellness | 2 | 89 (87) |
| Recovery is the process of regaining active control over one's life | 2 | 88 (86) |
| Recovery is being happy with who you are as a person | 2 | 87 (86) |
| Recovery is a way of living a satisfying, hopeful and contributing life, even with the limitations caused by symptoms/experiences of psychosis | 2 | 87 (85) |
| Recovery is about building a meaningful and satisfying life, as defined by the person themselves, whether or not there are ongoing or recurring symptoms or problems | 2 | 86 (84) |
| Recovery is knowing that you can help yourself become better | 2 | 86 (82) |
| Recovery is the unique journey of an individual living with mental health problems to build a life for themselves beyond illness | 2 | 85 (82) |
| Recovery is learning how to live well in the context of continued mental health problems | 2 | 84 (82) |
| Recovery is understanding how to control the symptoms of psychosis | 2 | 83 (83) |
| Recovery is when there is meaning and purpose to life | 2 | 83 (82) |
| Recovery is a process of changing one's orientation and behaviour from a negative focus on a troubling event, condition or circumstance to the positive restoration, rebuilding, reclaiming or taking control of one's life | 2 | 83 (82) |
| Recovery is believing that you can meet your current personal goals | 2 | 82 (81) |
| Recovery involves the development of new meaning and purpose in one's life as one grows beyond the catastrophic effects of mental health problems | 3 | 89 (89) |
| Recovery is a process or period of recovering | 3 | 88 (89) |
| Recovery is a deeply personal, unique process of changing one's attitudes, values, feelings, goals, skills and roles | 3 | 88 (84) |
| Recovery is accepting that mental health problems/symptoms/experiences are a part of the whole person | 3 | 86 (84) |
| Recovery is regaining optimum quality of life and having satisfaction with life in disconnected circumstances | 3 | 81 (86) |
| Item | Stage included | Percentage agreement, n (%) |
|---|---|---|
| Having a good, safe place to live | 2 | 96 (95) |
| Having the support of others | 2 | 94 (93) |
| Having a good understanding of your mental health problems | 2 | 94 (89) |
| Living in the kind of place you like | 2 | 91 (92) |
| Knowing what helps you get better | 2 | 91(89) |
| Knowing how to take care of yourself | 2 | 91 (90) |
| Recognising the positive things you have done | 2 | 90 (87) |
| Knowing that there are mental health services that do help | 2 | 90 (89) |
| Working on things that are personally important | 2 | 89 (89) |
| Being strongly motivated to get better | 2 | 89 (88) |
| Being able to identify the early warning signs of becoming unwell | 2 | 89 (88) |
| Having a positive outlook on life | 2 | 88 (87) |
| Having a plan for how to stay or become well | 2 | 88 (87) |
| Having goals/purpose in life | 2 | 87 (86) |
| Accomplishing worthwhile and satisfying things in life | 2 | 87 (86) |
| Being able to develop positive relationships with other people | 2 | 87 (83) |
| Knowing that there are things that you can do that help you deal with unwanted symptoms/experiences | 2 | 86 (82) |
| Being able to handle stress | 2 | 85 (85) |
| Feeling part of society rather than isolated | 2 | 85 (83) |
| Being hopeful about the future | 2 | 85 (83) |
| Learning from mistakes | 2 | 85 (85) |
| Accepting that you may have set backs | 2 | 85 (82) |
| Being able to come to terms with things that have happened in the past and move on with life | 2 | 84 (83) |
| Receiving treatment for distressing/unusual thoughts and feelings | 2 | 84 (81) |
| Taking medication as prescribed | 2 | 84 (83) |
| Having healthy habits | 2 | 83 (84) |
| Having a desire to succeed | 2 | 82 (82) |
| Health professionals and service users working collaboratively as equals | 2 | 82 (84) |
| Knowing that even when you don’t care about yourself, other people do | 2 | 82 (81) |
| Spending time with people to feel connected and better about yourself | 2 | 82 (80) |
| Being able to fully understand mental health problems/experiences | 2 | 80 (79) |
| Having courage | 2 | 80 (80) |
| Allowing personalisation or choice within health services | 2 | 80 (77) |
| Knowing that even when you don’t believe in yourself, other people do | 2 | 80 (78) |
| Knowing that you can handle what happens next in your life | 3 | 90 (89) |
| Knowing that all people with experience of psychosis can strive for recovery | 3 | 88 (86) |
| Being able to make sense of distressing experiences | 3 | 85 (82) |
| Making a valuable contribution to life | 3 | 84 (86) |
| Knowing that recovery from mental health problems is possible no matter what you think may cause them | 3 | 83 (82) |
| When services understand/consider the culture and beliefs of the individual | 3 | 83 (82) |
| Continuing to have new interests | 3 | 81 (75) |
| Knowing that you are the person most responsible for your own improvement | 3 | 80 (84) |
| Being able to assert yourself | 3 | 80 (82) |
| Item | Stage included | Percentage agreement, n (%) |
|---|---|---|
| When health services do not provide help and support to recover | 2 | 84 (83) |
| When a person feels lost or hopeless for much of the time | 2 | 82 (79) |
| When a person feels isolated or alone even when with family of friends | 2 | 81 (77) |
| When a person feels discriminated against or excluded from the community because of mental health problems | 3 | 91 (93) |
| Health professionals who do not accept that their views are not the only way of looking at things | 3 | 89 (93) |
| The impact of a loved one’s mental health problems on their family | 3 | 88 (82) |
| When a person can’t find the kind of place you want to live in | 3 | 87 (84) |
| When a person deliberately stopping taking medication although the doctor recommends taking it regularly | 3 | 83 (80) |
| Medication that can affect concentration and memory | 3 | 83 (87) |
| When no one will employ the person owing to past mental health problems | 3 | 81 (84) |
| When other people are always making decisions about the person’s life | 3 | 80 (80) |
| Item | Stage included | Percentage agreement, n (%) |
|---|---|---|
| When the person is able to find time to do the things they enjoy | 2 | 93 (93) |
| When the person is able to ask for help when they need it | 2 | 92 (90) |
| When the person can trust themselves to make good decisions and positive changes in life | 2 | 92 (88) |
| When the person knows when to ask for help | 2 | 91 (89) |
| When the person is able to take control of aspects of their life | 2 | 90 (87) |
| When the person feels reasonably confident that they can manage their mental health problems | 2 | 90 (87) |
| When the person is able to actively engage with life | 2 | 90 (88) |
| When the person feels like they are coping well with mental or emotional problems on a day to day basis | 2 | 89 (88) |
| When symptoms/experiences of psychosis interfere less and less with daily life | 2 | 88 (87) |
| When the person is able to define and work towards achieving a personal goal | 2 | 88 (87) |
| When fear doesn’t stop the person from living the life they want to | 2 | 85 (80) |
| When the person knows a great deal about coping strategies | 2 | 85 (84) |
| When symptoms/experiences of psychosis don’t get in the way of doing things they want or need to do | 2 | 84 (83) |
| When the person finds places and situations where they can make friends | 2 | 83 (82) |
| When the person feels in touch with their own emotions again | 2 | 83 (79) |
| When the person knows a great deal about their own symptoms/experiences | 2 | 82 (80) |
| When the person knows a great deal about their treatment options | 2 | 82 (79) |
| When the person is able to access independent support | 2 | 81 (75) |
| When coping with mental health problems is no longer the main focus of a person’s life | 2 | 81 (76) |
| When the people who are important to someone are actively supporting their mental health treatment | 2 | 81 (83) |
| When symptoms/experiences of psychosis are a problem for shorter periods of time each time they occur | 3 | 85 (84) |
| Defining recovery | Stage excluded | Percentage agreement, n (%) |
|---|---|---|
| Recovery is the intended consequence of the skilful use of the full range of effective treatments | 2 | 65 (63) |
| Personal recovery can occur in the context of continuing symptoms/experiences | 2 | 64 (65) |
| Recovery is to fully return to how a person was before they were unwell | 2 | 57 (60) |
| Recovery is an act of obtaining usable resources from apparently unusable sources (e.g. in psychosis where the experience itself has personal value) | 2 | 46 (45) |
| Recovery is a spontaneous and natural event | 2 | 35 (37) |
| Recovery is having an idea of who you want to become | 3 | 67 (66) |
| Factors that help recovery | ||
| Knowing that although your symptoms may get worse, you can handle it | 2 | 69 (65) |
| Meeting people who have had similar experiences | 2 | 69 (67) |
| Feeling able to take chances in life | 2 | 69 (64) |
| When services allow the individual to decide if and when to begin the recovery process and direct it | 2 | 68 (67) |
| Having a variety of friends | 2 | 68 (70) |
| Having faith | 2 | 64 (67) |
| Knowing that things happen for a reason | 2 | 53 (51) |
| Being with people at a church, temple or prayer meeting who understand the journey to recovery | 2 | 37 (38) |
| Understanding that recovery does not mean going back to the way things used to be | 3 | 79 (73) |
| Believing that something good will eventually happen | 3 | 75 (64)a |
| Factors that hinder recovery | ||
| Recovering from the consequences of mental health problems is sometimes more difficult than recovering from the problem itself | 2 | 68 (65) |
| Lack of access to peer support (which means support from other people who have personal experience of mental health problems) | 2 | 67 (63) |
| Stigma associated with mental health problems | 2 | 66 (67) |
| When health services do not allow an individual to direct the recovery process | 2 | 64 (60) |
| When a person’s family try to control their treatment too much | 2 | 63 (60) |
| Lack of access to service user led education and training | 2 | 62 (57) |
| Mental health services which promote dependency on services (rather than independence from services) | 2 | 62 (59) |
| An ‘expert’ and ‘patient’ relationship between health professional and service user (rather than a partnership/collaboration) | 2 | 62 (61) |
| Taking medication itself is like having a handicap | 2 | 52 (53) |
| Medication that can slow people down physically and mentally | 3 | 79 (78) |
| Feeling like life has been ruined by mental health problems | 3 | 78 (78) |
| Feeling angry about what has happened in the past | 3 | 69 (60) |
| Factors that show recovery | ||
| When the person feels their experiences have made them more sensitive towards others | 2 | 69 (72) |
| When the person hasn’t been rehospitalised in the last 4 to 6 months | 2 | 69 (65) |
| When the person talks to someone outside of their family regularly | 2 | 69 (68) |
| When the person feels their recovery has helped challenge other peoples views about getting better | 2 | 68 (70) |
| When the person hasn’t had a relapse of symptoms in the last 4 to 6 months | 2 | 68 (66) |
| When the person actively seeks information on mental health problems/experiences from different sources (e.g. books, internet) | 2 | 63 (63) |
| When the person can control whether they relapse or not by will power | 2 | 55 (56) |
| When the person enjoys sex again | 2 | 51 (47) |
| When you regularly spend time doing an activity with or for another person (not including self care/personal home maintenance) | 3 | 79 (76) |
| When the person has thought about a relapse prevention plan | 3 | 79 (73) |
| When the person feels their experiences have changed them for the better | 3 | 78 (76) |
| When the person is taking their medication as prescribed most of the time | 3 | 78 (80) |
| When the person knows a great deal about the medication available to them | 3 | 74 (69) |
| When the person is actively participating in self-help or service user run activities | 3 | 69 (60) |
| When symptoms/experiences of psychosis don’t bother the person too much | 3 | 68 (69) |
Discussion and conclusions
This is the first study to attempt to reach a consensus about understanding recovery from psychosis. It is also one of a small number of studies that consult services users as experts on their own experiences. 103,105 A high level of consensus was reached for a range of items, which were deemed important in defining recovery, understanding what helps and hinders recovery and what would show that someone is recovering.
In line with other studies involving service user-defined recovery, this study also found that the concept of rebuilding life, self and hope is essential in defining recovery. 19 In contrast with previous studies exploring service user-defined recovery, the Delphi methodology allowed collation of views from a large sample of individuals with psychosis. Although it was agreed that recovery is a unique process that is different for each individual, the Delphi method allows us to identify areas of recovery which appear to be the same for the majority of people. In the subsection for defining recovery, the highest level of consensus was reached for ‘recovery is the achievement of a personally acceptable quality of life’ and ‘recovery is feeling better about yourself’. This indicates the importance of routine measures of quality of life and self-esteem when evaluating recovery-oriented services as well as a focus on working with service users to improve quality of life and esteem rather than a focus solely on symptoms and relapse prevention. Service users did not feel that items such as ‘recovery is to fully return to how a person was before they were unwell’ or ‘recovery is to have an idea of you want to become’ were important to defining recovery so these items were removed from the final list.
Service users endorsed a number of factors which may facilitate their recovery, with the highest levels of agreement reached for environmental factors (such as a safe place to live), social support and items focusing on personal understanding of mental health problems and recovery. The role of services was also deemed to be important, although it was knowledge that there are services which can help with mental health problems which was rated the highest, rather than the impact of the services or treatments on offer per se. Personal factors such as having goals and purpose, hope for the future and motivation/desire to succeed were also felt to be important, in agreement with previous research. 19,97,98 Factors such as ‘knowing that although your symptoms may get worse, you can handle it’ and ‘meeting people who have had similar experiences’ were not felt to be helpful to recovery for everyone so these items were removed.
There was less agreement about what factors may hinder recovery. Participants agreed that lack of services to provide help and support would hinder recovery as well as feeling lost hopeless or isolated. Participants also highlighted stigma as a potential barrier to recovery, including discrimination such as not being able to gain employment. Interestingly, although a high proportion of people felt that not taking medication as prescribed could hinder recovery, the same proportion of people also felt that side effects of medication, such as concentration problems and memory loss, could also hinder recovery. As highlighted in previous research addressing treatment choice,108 knowledge of treatment options is an important factor for services to consider as well as the need to address this conflict of believing that compliance with medication is essential to recovery, while also believing that the side effects may prevent recovery. Allowing treatment choice both in terms of alternative medications which may produce less side effects, but also non-pharmacological options such as CBT, may help to promote recovery.
The final section of the Delphi study addressed which items people felt would show someone was recovering. As discussed, several measures of recovery from psychosis have already been developed based on service user accounts91 and one measure was designed collaboratively with service users. 92 However, no previous studies have been able to ask a large sample of service users to rate the importance of items included in these measures and other similar measures of recovery. This study found a high level of consensus from service users about what would show that someone is recovering. Service users felt that engaging in and enjoying activities was essential, as well as feeling able to make ‘good’ decisions in life. Items around effective help-seeking behaviours (such as knowing when and how to ask for help) were also important to recovery. As well as being able to ask for help, having personal skills to manage or cope with day-to-day life were also rated highly. As could be expected, reduced impact of symptoms on daily life were seen as evidence of the recovery process although they were only ninth in the ranked list of factors that show someone is recovering. It may be important for services to rethink their approach to viewing reduction in symptoms as a key outcome for mental health. Participants did not feel that factors such as reduced hospitalisation or relapses were essential for demonstrating recovery.
There are several limitations to this study. First, recruitment only took place across the north-west of England, which may mean that results are not representative of other areas of the UK or in other countries. Service users in different areas may have access to different types of services and/or have varying levels of knowledge regarding recovery. Indeed, a number of postal questionnaires for this study were returned with notes about the individual’s service and how they had never heard about the potential for recovery. Future research could investigate these varying levels of awareness of recovery and how this impacts on what service users want for their own recovery.
Another limitation is the heterogeneity of diagnoses in the sample. The study was primarily aimed at individuals with experience of psychosis and as a result of initial feedback on the design of the study from a group of service users, a decision was made not to exclude participants based on diagnosis. It would have also been difficult in practical terms to exclude people based on the diagnosis they have been given owing to the anonymity in the study and the nature of the online study option. Instead of using diagnosis as an exclusion criteria, the study asked a screening question about whether or not the individual defined themselves as having experience of psychosis. As can be seen in the participant characteristics table, this resulted in individuals who had received a wide variety of diagnoses taking part in the study. Although each question reiterated that the study was asking about relevance to recovery from psychosis, it may be that participants prioritised their own experiences when thinking about the concept of recovery. Therefore, the results of this study may represent a more transdiagnostic approach to understanding recovery. However, percentage agreements for the sample as whole compared with the percentage agreement for participants reporting a diagnosis of schizophrenia, schizoaffective disorder or psychosis, were generally very similar and only one of the differences was significant. The significant difference was found for item ‘believing something good will eventually happen’, although both the schizophrenia subgroup and the sample as whole did not feel this item should be included overall. Future research could aim to explore this issue further by recruiting specifically through clinicians to identify only those groups with a particular diagnosis, although this would potentially exclude some service users. An alternative approach may be to ask people which difficulties they are currently prioritising. Although the variety of diagnoses in the study could be seen as a limitation, it was also interesting to note the number of people with a diagnosis of BD that chose to take part in the study, despite it being advertised as a study about recovery from psychosis. This may be a reflection of the high proportion of people with a diagnosis of BD who experience psychosis. 15 This interest in the concept of recovery and willingness to participate in the study may pave the way for a similar study in the future that explores recovery by diagnosis type.
It may also be interesting for future studies to explore differences in recovery conceptualisations and goals throughout the recovery process. The majority of participants in this study, particularly in the final stage, had established diagnoses (> 5 years) so further investigation of the impact of length of time since diagnosis or first experience of psychosis would not have been appropriate. However, it would be useful for this area to be examined further to understand recovery for those with recent onset of symptoms and experiences compared with those with more established diagnoses and experiences. This would ensure that services are effectively geared towards their client groups. For example, EISs may require a different approach to CMHTs.
Although research has indicated that it is essential for recovery to be defined by service users themselves, it is also important to consider the views of clinicians working in mental health services. Without some agreement between clinicians and services users, or at least some adoption by clinicians of what is important to service users when understanding recovery, mental health services will struggle to effectively meet the needs of its client group. It would be interesting to ask clinicians to rate similar statements about recovery and examine agreement between the two groups. Ultimately, it will be up to services and the clinicians within those services to understand what is important to their service users, and to take this on board when offering treatment and ongoing support.
There are many implications from the results of this study. First, service users agreed that awareness and understanding of recovery was essential. Collaborative approaches to this training by clinicians and service users would best promote the recovery approach. Similarly, the audience for this training may include clinicians, service users and carers who want to understand more about recovery from psychosis and other mental health problems. Continued evaluation and development of such a training programme would be important to assess their impact on learning outcomes. Any training package should be made easily accessible to the target audience, utilising a variety of formats such as web based training or workshops.
This study also acts a starting point for identifying service user priorities regarding recovery. It is apparent that less focus on reducing relapse and more promotion of quality of life and achievement of personal goals are required for truly recovery-oriented services. This work, alongside traditional approaches to symptom reduction and increased personal coping and life skills, may be effective. Similarly recovery oriented services should ensure that communities are aware of the services on offer and should actively promote recovery awareness.
Finally, further consideration of the measurement of recovery should be undertaken. This study is the first of its kind to approach a large group of individuals with personal experience of psychosis and ask them what they believe demonstrates that someone is recovering. This may be a useful technique to develop user informed tools for measuring the effectiveness of recovery-oriented services. Identification of treatment and support priorities for recovery followed by routine measurement and audit of these priorities may indicate the effectiveness of services. This may also enable a comparison of services across the UK to ensure that there is equality of access to high-quality effective services. There is potentially scope to utilise the items rated as essential or important to service users as an audit tool for benchmarking of services.
Similarly, the items rated as essential or important to ‘show that someone is recovering’ may provide a useful tool for measuring individual recovery. There are several measures already developed for this purpose; however, none has undergone a similar process of consulting service users about their applicability and importance. The items could be used as a stand-alone tool for an individualised assessment of the recovery process and goals. There may also be potential for the items to be developed and used as a patient-reported outcome measure (PROM) to assess service user’s own views on their mental health and recovery. Use of PROMs in the field of mental health have been shown to be particularly positive, suggesting further exploration of a recovery-related PROM would be beneficial.
Future research should consider exploring recovery across a range of diagnoses as well as consulting clinicians about their views on recovery. This study demonstrates it is feasible and helpful to consult service users on topics such as recovery. The fact that such a large number of individuals with a variety of mental health problems and experiences were willing and keen to take part in this study, opens up the possibility of encouraging service users to share their views to have a real impact on the services they receive. This would give them a stake in making services successful and promoting recovery awareness. Similar research in other areas of the UK and in other countries may also be beneficial to assess cross-cultural differences in approaches to, and definitions of, recovery.
Chapter 4 Understanding psychological and social predictors of recovery
Background
Despite recent interest in the concept of recovery from psychosis, there remains no clear and unambiguous definition among the users of mental health services, clinicians and academics. It has been argued that extrapolating definitions of recovery from the physical health arena to the domain of severe and enduring mental illness would mean that few people would ever experience full recovery,17 although this has been disputed. 109 Within a biomedical framework, recovery has been defined in terms of symptom remission, decreases in the duration of hospital admissions and reduced rate of rehospitalisation. 83 However, a purely symptom-focused definition of recovery has often been shown to be unrelated to social and occupational functioning. 109,110
Narrative accounts of recovery formulated by service users with experience of psychosis liken the concept to a personal journey93 or process of growth and change. 111 These accounts have been supplemented by qualitative studies utilising a more scientific approach to elicit general themes from semistructured interviews. 97,98 One recent study involving the users of mental health services revealed themes of rebuilding life, rebuilding self and having hope for a better future as being important in the definition of recovery, as well as highlighting the deeply personal nature of the process. 19 Such idiosyncrasy and nonlinearity have also been noted in subsequent studies. 112,113 A review of experiential accounts of recovery111 attempted to pull together the previous qualitative accounts revealing a model of recovery involving four measurable processes: hope, re-establishment of identity, finding meaning and taking of responsibility.
The difficulties in definition and measurement of recovery, created by both the distance from biomedical conceptualisations and the inherent variability in a subjective recovery journey, have been noted. 31,111 However, various measures have been developed and validated within clinical samples and there are two that measure recovery specifically in people with experience of psychosis: the Psychosis Recovery Inventory91 and the QPR. 32 This difference in consumer and clinical conceptualisations of recovery has been highlighted in a study that explored the correlation of outcome measures of recovery from the two perspectives. 114 The authors did not find much of a relationship between clinical and consumer-defined recovery, strongly suggesting that routinely used measures of outcome may not assess important aspects of recovery which are meaningful for the service user.
On the other hand, there is a significant body of research examining psychosocial and neuropsychiatric factors that are associated with recovery from psychosis. Quantitative assessment of personal recovery from psychosis based on such research has shown that measures of recovery and quality of life are often associated with measures of psychological functioning such as well-being, emotional disturbance and self-esteem. 32 A study of 161 patients with severe mental illness (schizophrenia, BD and depression) found a strong association between empowerment and recovery,115 and a longitudinal study of 128 patients with a diagnosis of schizophrenia found that internal locus of control was associated with long-term recovery. 116
Studies of predictors of recovery using more traditional psychiatric definitions focused on symptom remission or non-recurrence have found that neuropsychiatric factors are relevant. For example, a study on 436 patients with schizophrenia spectrum diagnoses117 found that better insight was associated with good outcomes (defined as a single episode with no persistent symptoms); however, other evidence suggests that increasing insight is often associated with poor outcomes such as greater suicidality in people with psychosis. 118 Neurocognitive deficits have also been examined in relation to dimensions of recovery and have been found to be associated with social behaviour deficits, but not with subjective quality of life. 23
Several studies have found both psychosocial and neuropsychiatric factors to be associated with recovery and related concepts such as quality of life. A study of 201 patients with a diagnosis of schizophrenia showed that psychological factors (optimism, personal agency and internal stigma), as well as symptoms, explained a large proportion of the variance in quality-of-life ratings. 119 Multiple factors including both psychiatric (symptoms and intellectual functioning) and psychosocial (self-esteem and optimism) were found to be related to recovery in 103 individuals meeting criteria for schizophrenia spectrum disorders. 120
The main limitation of this existing research is that it relies almost entirely on cross-sectional data. To overcome this, ESMs allow such psychological processes to be explored longitudinally both day to day and moment to moment. The ESM is a type of intensive diary technique, which requires participants to repeatedly record their experiences and the context in which they occur, typically many times a day over several days. Diary reports are typically cued electronic devices, such as pre-programmed digital watches, personal digital assistants or mobile phone apps. It has been used often to record psychotic symptoms such as hallucinations and delusions in everyday life121,122 and to explore the role in mental illness of such processes as negative affect and stress sensitivity (e.g. Myin-Germeys et al. 123 and Myin-Germeys and van Os124).
A recent study125 used ESM in 177 patients with schizophrenia spectrum diagnoses to demonstrate that negative affect played a significant role in both symptomatic remission status (a traditional approach to defining recovery) and real-life functioning in everyday life (a more user-orientated definition); this raises the possibility that emotion could be a mediating factor between psychosocial and neuropsychiatric variables and recovery.
The present exploratory study aims to address the gap in knowledge regarding judgements of recovery, associated factors and predictors. It will explore factors associated with subjective judgements of recovery in people with experience of psychosis before examining psychosocial and neuropsychiatric predictors of recovery judgements in both a cross-sectional and longitudinal sample. This information will be used to develop and carry out a study that will use the ESM to examine recovery judgements and associated factors on a momentary basis over the period of a week. This will allow examination of whether or not, and to what extent, patients’ recovery judgements are stable over time and whether or not the same kind of psychosocial factors that have been shown to be associated with recovery judgements in cross-sectional studies, for example self-esteem and hope for the future predict recovery judgements longitudinally.
Phase 1: subjective judgements of perceived recovery from psychosis
This research has been published previously as Subjective judgements of perceived recovery from psychosis by Beck R, et al. Journal of Mental Health Col.21:6 (2012) pp. 556–66. 126 This is an Accepted Manuscript of an article published by Informa Healthcare in Journal of Mental Health on 2012, available online: http://informahealthcare.com/doi/full/10.3109/09638237.2012.710765.
Objectives
This study aimed to elicit subjective judgements of recovery utilising different approaches to its measurement. This study also aimed to investigate the association between recovery judgements and psychological and social factors.
Method
Participants
Data for the present study are a secondary analysis of a large study of psychosocial and neuropsychiatric predictors of recovery from psychosis. 127 Participants were aged 16–65 years, with a schizophrenia spectrum diagnosis as well as sufficient level of English literacy to complete the measures and the capacity to provide informed consent. A total of 122 participants entered the study (88 male, 34 female), four of whom completed only half of the measures. The majority of participants were white British (84.4%). Diagnoses, confirmed using ICD-10 checklists were as follows: schizophrenia (n = 75), schizoaffective disorder (n = 10), substance-induced psychosis (n = 5), unspecified non-organic psychosis (n = 15), acute and transient psychotic disorder (n = 12), persistent delusional disorder (n = 4) and post-partum psychosis (n = 1).
Measures
The Process of Recovery from Psychosis Questionnaire32
The QPR is a 22-item questionnaire, which was collaboratively developed with service users. The questionnaire measures subjective recovery in two domains: intrapersonal functioning (17 items) and interpersonal functioning (five items). An example of an item on the intrapersonal scale is ‘I have been able to come to terms with things that have happened to me in the past and move on with my life’ and the interpersonal scale, ‘meeting people who have had similar experiences makes me feel better’. Participants rate their agreement with statements on a 5-point Likert scale rating from ‘strongly disagree’ to ‘strongly agree’. Respondents may score between 0 and 88. The subscales have good internal consistency and test–retest reliability over short periods. 32 Cronbach’s alpha coefficients for the intrapersonal and interpersonal scales for this sample were α = 0.94 and α = 0.66, respectively.
Dichotomous recovery question
Appended to the QPR, participants were asked: ‘Do you consider that you have recovered from your illness? (Yes/No)’.
Recovery Analogue Scale
Appended to the QPR: ‘Please place a cross on the line below to indicate the extent to which you think you have recovered from your illness’ (10-cm analogue scale with left anchor ‘completely recovered’ and right anchor ‘not recovered at all’) to gauge the extent to which participants believe they are recovered.
Beck Hopelessness Scale
The BHS74 is a 20-item self-report scale assessing negative expectations about the future. Participants respond ‘true’ or ‘false’ to the items and responses are summed to obtain a total hopelessness score (range = 0–20). Cronbach’s alpha value for this sample was α = 0.92.
The Brief Self-Esteem Rating Scale – Short Form
The SERS76 is a 20-item measure of explicit self-esteem, assessing both positive (10 items) and negative (10 items) beliefs about the self. Participants rate how often each of the statements reflect their feelings about the self, on a 7-point Likert scale of ‘never’ to ‘always’. Cronbach’s alpha values for the positive and negative scales for this sample were α = 0.92 and α = 0.91, respectively.
Hospital Anxiety and Depression Scale
The Hospital Anxiety and Depression Scale (HADS)128 is a 14-item self-report measure. Of these items, seven assess depression, while the remaining seven items assess anxiety, over a period of the preceding week. Cronbach’s alpha coefficients for the anxiety and depression scales for this sample were α = 0.86 and α = 0.83, respectively.
Procedure
Prior to commencement of the study, a dedicated service user panel was consulted on all aspects of design, including wording of information sheets, inclusion of questionnaires, length of assessments, semantic concerns and appropriate amount of payment. Participants were recruited from CMHTs, inpatient settings, early intervention (EI) teams and the voluntary sector to ensure heterogeneity in experience of psychosis and service provision in the Greater Manchester area. Individuals were approached via their care co-ordinator. Those who were interested in taking part were briefed about the study and provided with a participant information sheet. They were then given a minimum of 24 hours to decide whether or not to take part. On agreeing to take part, a research assistant met with the participant to take informed consent and administer questionnaires, over a single visit or two visits at the participant’s request. Participants were remunerated for their time.
Statistical analyses
Chi-squared tests were performed in order to examine the association between sociodemographic variables and self-selected group (‘recovered’ vs. ‘not recovered’). For these purposes, sociodemographic variables were transformed into dichotomous variables using the following criteria: not in education, employment or training (NEET) status: (1 = NEET; 2 = in education, employment or training); marital status (1 = married/cohabiting; 2 = not living with a partner); religiosity (1 = no religious beliefs, 2 = religious beliefs); level of education [1 = compulsory education (primary/secondary) only; 2 = further education post age 16 years]; mental health provider (1 = EISs, 2 = other community services). Data were analysed using Predictive Analytics SoftWare statistics 18 [Statistical Package for the Social Sciences (SPSS) Inc., Chicago, IL, USA]. All variables were scrutinised before inferential analysis and valid parametric analysis were conducted. Correlational analyses were performed to determine the association between recovery measures. Correlations were also calculated between each of the recovery measures and the psychological variables: positive and negative self-esteem, hopelessness, anxiety and depression. Regression analyses using forward entry were conducted with our recovery measures as dependent variables.
Results
Demographic characteristics for the sample are shown in Table 15. Table 16 provides an overview of means and SDs of scores on each recovery measure. On the dichotomous recovery measure, ‘do you feel you have recovered from your illness? Yes/No’, 41.8% (n = 57) of participants responded yes, placing themselves in the ‘recovered’ group, while 58.2% (n = 71) of participants responded no, placing themselves in the ‘not recovered’ group. In order to explore the consistency between the measures of recovery, the data were explored visually with histograms of scores on Recovery Analogue Scale (RecA) for each of the dichotomous recovery question groups (Figure 3). The ‘not recovered’ group displayed a wider range of responses on the analogue scale, while the responses of those in the ‘recovered’ group clustered around the top end of the analogue scale. Additionally, a scatterplot (Figure 4) demonstrates the association between recovery percentage scores and QPR total scores, split by ‘recovered’ and ‘not recovered’ self-selected grouping.
| Sample characteristic | % (n) |
|---|---|
| Age (years) | Mean 35.5 ± 11.5 |
| Sex | Male 72.1 (88) |
| Female 27.9 (34) | |
| Ethnicity | White 84.4 (103) |
| Asian 5.7 (7) | |
| Black 5.7 (7) | |
| Mixed 4.1 (5) | |
| Schooling | Primary 20.5 (25) |
| Secondary 32 (39) | |
| Further 31.1 (38) | |
| Higher 16.4 (20) | |
| Marital status | Single 82.8 (101) |
| Married/common law 9 (11) | |
| Separated/divorced 8.2 (10) | |
| Employment status | Employed 4 (5) |
| Unemployed 79.6 (97) | |
| Student 5.7 (7) | |
| Volunteer 8.2 (10) | |
| Retired 2.5 (3) | |
| Religious belief | None 50.1 (61) |
| Christian 37.7 (46) | |
| Muslim 4.9 (6) | |
| Other 7.3 (9) |
| Minimum | Maximum | Mean | SD | |
|---|---|---|---|---|
| Recovery percentage | 0.00 | 100.00 | 61.62 | 24.67 |
| QPRIntra | 8.00 | 68.00 | 44.67 | 12.68 |
| QPRInter | 5.00 | 20.00 | 13.92 | 3.07 |
| QPR total score | 21.00 | 88.00 | 58.59 | 14.67 |
FIGURE 3.
Histograms to show the distribution of scores on the analogue scale gauging recovery percentage, split by dichotomous ‘yes/no’ recovery measure.
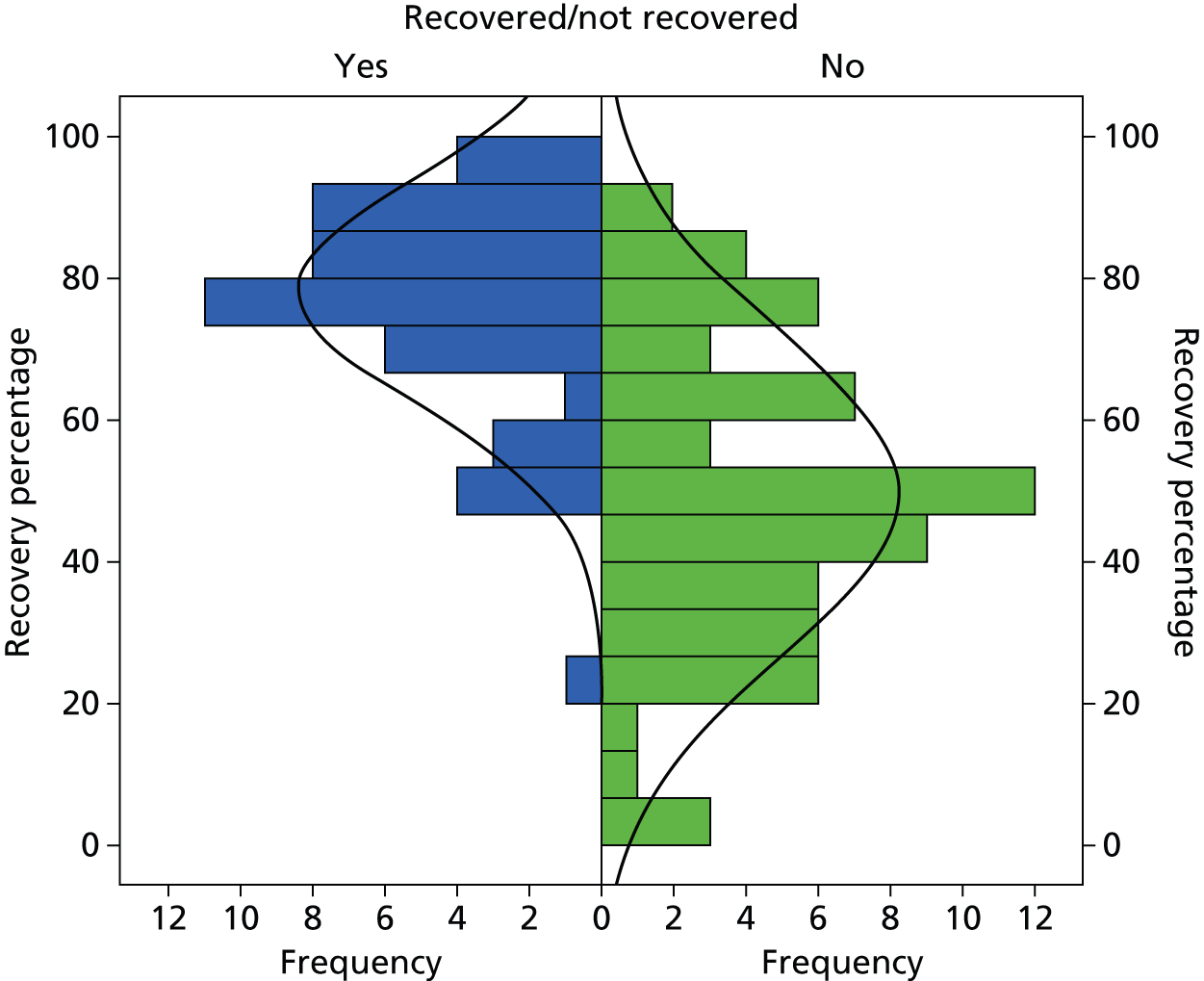
FIGURE 4.
Scatterplot to show the correlation between recovery percentage and QPR total scores, split by dichotomous ‘yes/no’ recovery measure.
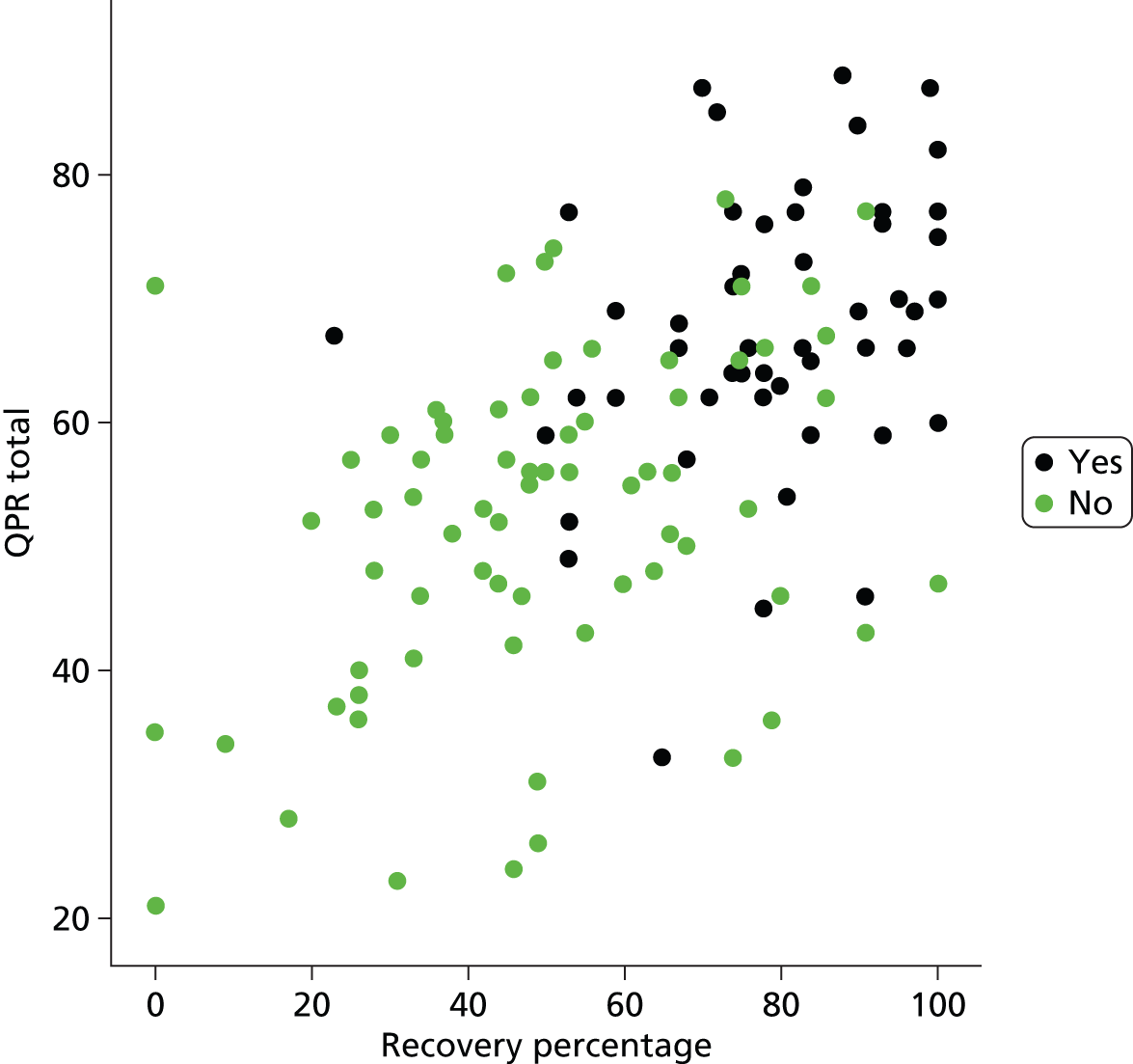
All measures of recovery were found to be significantly correlated with each other (Table 17).
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Recovered/not recovered | – | 0.581** | 0.542** | 0.240** | –0.534** | –0.420** | –0.486** | 0.419** | 0.393** |
| 2. Recovery Percentage | – | – | 0.582** | 0.187* | –0.551** | –0.572** | –0.524** | 0.444** | 0.350** |
| 3. QPR Intrapersonal | – | – | – | 0.580** | –0.630** | –0.705** | –0.792** | 0.629** | 0.677** |
| 4. QPR Interpersonal | – | – | – | – | –0.187* | –0.322** | –0.386** | 0.162 | 0.394** |
| 5. HADS Anxiety | – | – | – | – | – | 0.699** | 0.627** | –0.754** | –0.468** |
| 6. HADS Depression | – | – | – | – | – | – | 0.743** | –0.695** | –0.635** |
| 7. BHS Total | – | – | – | – | – | – | – | –0.661** | –0.638** |
| 8. SERS negative | – | – | – | – | – | – | – | – | 0.605** |
| 9. SERS positive | – | – | – | – | – | – | – | – | – |
Each recovery measure was significantly correlated with all of the psychological variables, with the exception of Questionnaire about the Process of Recovery interpersonal subscale (QPRInter) score and negative self-esteem (r = − 0.162, not significant). Chi-squared analyses were conducted to establish whether or not there were any significant relationships between the sociodemographic characteristics and responses of yes/no on the dichotomous recovery variable. No significant associations were found between the dichotomous recovery variable and each of the demographic variables: sex {χ2 [degrees of freedom (df) 1] = 0.54, not significant}, NEET status [χ2 (df 1) = 0.07, not significant], marital status [χ2 (df 1) = 0.37, not significant], religiosity [χ2 (df 1) = 0.50, not significant], level of education [χ2 (df 1) = 1.90, not significant], mental health provider [χ2 (df 1) = 2.80, not significant].
A Pearson correlation between age and self-selected grouping revealed a significant correlation, showing older age to be associated with the ‘not recovered’ group (r = − 0.25; p < 0.05). Age was also correlated with recovery percentage (r = − 0.28; p < 0.01) and Questionnaire about the Process of Recovery intrapersonal subscale (QPRIntra) scores (r = − 0.23; p < 0.05). In order to further investigate the contribution of psychological factors to subjective recovery judgements in people with experience of psychosis, three regression analyses were conducted. First, in order to investigate the contribution of self-esteem (positive and negative), mood (anxiety and depression) and optimism to self-rated recovery, a multiple regression analysis was performed using hierarchical direct entry with the RecA as the dependent variable. The multiple R was 0.63 and significant [F(5,112) = 13.99; p < 0.001]. The adjusted R2 was 0.37 indicating that a moderate amount of the variance was accounted for by these predictor variables. Summary statistics for the regression are shown in Table 18.
| Sample characteristic | β | t-test | p-value |
|---|---|---|---|
| SERS negative | −0.082 | −0.659 | 0.512 |
| SERS positive | −0.019 | −0.180 | 0.857 |
| BHS | −0.181 | −1.520 | 0.132 |
| HADS Anxiety | −0.279 | −2.261 | 0.026 |
| HADS Depression | −0.332 | −2.590 | 0.011 |
Second, a multiple regression analysis was performed using hierarchical direct entry with the same predictor variables and QPRIntra as the dependent variable. The multiple R was 0.86 and significant [F(5,113) = 59.21; p < 0.001]. The adjusted R2 was 0.72 indicating that a large amount of the variance was accounted for by these predictor variables. Summary statistics for the regression are shown in Table 19.
| Sample characteristic | β | t-test | p-value |
|---|---|---|---|
| SERS negative | −0.043 | −0.519 | 0.605 |
| SERS positive | 0.289 | 4.122 | 0.000 |
| BHS | −0.428 | −5.449 | 0.000 |
| HADS Anxiety | −0.247 | −3.033 | 0.003 |
| HADS Depression | −0.090 | −1.062 | 0.290 |
Finally, a logistic regression analysis was performed using direct entry with the dependent variable being the dichotomous recovery rating and the predictor variables as above. The final results of this analysis (Table 20) showed a significant model (χ2 = 50.6, df = 5; p < 0.001), with anxiety (odds ratio = 1.33; p < 0.001) and positive self-esteem (odds ratio = 0.94; p < 0.05) being the significant predictors.
| Sample characteristic | β | SE | Odds ratio | p-value |
|---|---|---|---|---|
| SERS negative | 0.015 | 0.031 | 10.015 | 0.627 |
| SERS positive | –0.060 | 0.030 | 0.942 | 0.044* |
| BHS | 0.147 | 0.075 | 10.159 | 0.051 |
| HADS Anxiety | 0.281 | 0.087 | 10.325 | 0.001* |
| HADS Depression | -0.092 | 0.097 | 0.912 | 0.344 |
Discussion
The correlations between the measures of recovery suggest that, in general terms, the measures are comparable and fulfil the intention of tapping into the construct of recovery. The significant correlations between the measures of recovery and the psychological factors suggest that higher levels of self-esteem and hope, along with lower levels of depression and anxiety, were associated with more positive judgements of recovery across the disparate measures. Chi-squared analyses did not reveal any significant associations of sociodemographic characteristics with the dichotomous recovery outcome variable, suggesting that these social factors were not implicated in the subjective recovery judgements of our sample. Visual inspection of the data regarding different methods of measuring recovery judgements also show general consistency in within-person ratings across all measures; however, the range of scores between individuals on the correspondent measures were widely dispersed.
The data, split by the self-selected ‘recovered’ or ‘not recovered’ groupings, showed a trend towards those scoring higher on the QPR rating themselves higher on the analogue scale. Those in the ‘not recovered’ group show a wider range of responses on the analogue scale, while the ratings of those in the ‘recovered’ group cluster around the top end of the analogue scale. The responses of both the ‘recovered’ and ‘non-recovered’ group on the analogue scale are shown to be normally distributed, with the ‘recovered’ group displaying a higher mean. Furthermore, there were several notable outliers endorsing a ‘yes’ judgement to recovery, yet rating themselves comparatively low on the analogue scale or vice versa. Such variations in within-person responding across measures of recovery are of interest; it appears that individuals tend to discriminate between dichotomous and continuous responses, for instance, endorsing the ‘not recovered’ status yet scoring high on an analogue scale. This is indicative of differing personal thresholds for the definition of ‘recovered’ and provides empirical evidence consistent with a perspective of recovery as a personal journey that does not necessarily have an end point. Thus, the conclusions from first-person reports and qualitative studies19,93 appear generalisable. People appear to hold an individual representation of what it means to be recovered.
These individual representations may explain the differences in within-person ratings on the dichotomous versus analogue measures and may be associated with stable dispositional characteristics. Given that self-esteem was a significant correlate, individual characteristics such as trait-like optimism or perfectionism and other attributes associated with self-esteem, may be important in making judgements of recovery. If judgements of recovery are likely to fluctuate, as noted by narrative accounts describing recovery as dynamic, it is likely that certain people may be mindful to their status as liable to change when making an overall judgement. Indeed, several participants commented on how some days they do feel recovered and other days do not, finding it difficult to make a cross-sectional judgement.
The idiosyncratic nature of recovery judgements reported here is consistent with the literature. It may also help to explain the differing emphases found in tools designed to measure recovery, as well as having implications for the use of these tools in clinical practice and the need for further research to examine whether or not the measures are sensitive to change over time. As noted earlier, personal narratives of recovery and many of the measures of recovery include hope as a central theme19,97,98 and this is reflected in our results of this study, which show a significant association between hope and subjective judgements of recovery. The association between recovery and emotion/self-esteem is consistent with research linking aspects of recovery from psychosis to levels of anxiety and depression. 32 The findings from the regression analyses are also consistent with the literature, again supporting the generalisability of the small qualitative studies and first-person accounts, and suggest significant overlap between self-ratings of recovery and self-esteem, mood and hope about the future. Given that this pattern of results was most comprehensive for the QPR scale, with all three components being associated with recovery, and with over 70% of the variance being explained, it may be that this approach to measuring recovery may be the most fruitful.
There are some methodological limitations that need to be considered. The study utilised self-report methodology, with participants being required to read and complete all the measures themselves (with help from a researcher if needed). The usual problems with regard to understanding the scale items and biases in responding thus apply. In particular, the anchoring of the analogue recovery scale could be considered counter intuitive and confusing, with ‘most recovered’ being the left anchor. The study employed a cross-sectional design, allowing associations to be made but no causation and temporal nature of effects can be determined. For analyses involving sociodemographic factors, these were transformed into dichotomous variables to undertake chi-squared analysis, which did not reveal any significant associations with subjective judgements of recovery. Measurement of social factors in a more precise, ordinal fashion would allow more powerful analysis, which may demonstrate the importance of such factors. Prospective longitudinal research methods could examine fluctuations in the recovery process over time and response to treatments, while innovative methodologies such as ESMs could examine the day-to-day variation in recovery judgements and how these are related to psychological and environmental factors. Judgements about recovery from psychosis, while showing a trend, are idiosyncratic. Thus, subjective recovery can be regarded as an internal concept, variable between individuals, and appearing to be personally defined. Within-person discrepancies in responding across disparate measures further show the importance of subjectivity in interpretation and definition. Here, the addition of a concurrent qualitative assessment would be desirable in supplementing the findings with richer, more detailed, data potentially indicating the most pertinent factors for consumer recovery.
There may not be a ‘one size fits all’ measure of recovery, which could go some way to explaining the lack of a ‘gold standard’ in measurement to date. The general agreement that the construct is open to personal interpretation having multiple facets that differ in amplitude between individuals should be embraced in clinical settings, which are increasingly taking a focus on the promotion of recovery. Such a working model for care also builds on embedded positive concepts in mental health practice, including building on personal strengths and promoting diversity. As an example, the collaborative recovery model129 represents such an approach, with an emphasis on nurturing constructs associated with recovery such as hope, autonomy and goal ownership. The regular assessment of recovery judgements would help to evaluate the extent to which services are recovery oriented and also help individuals to monitor their progress.
The strong association between recovery and psychological factors, such as self-esteem, optimism and emotional disturbances, also highlights the importance of assessment and monitoring of these factors. It also raises that possibility that psychological interventions specifically focused on factors such as self-esteem in people with psychosis130 may be ideally suited to the facilitation of recovery. Recognition of the association of such factors with levels of subjective recovery could help to foster collaborative identification of personal difficulties, agreement of shared goals and identification of targets for mental health service provision.
Phase 2: psychosocial and neuropsychiatric predictors of subjective recovery from psychosis
This research was previously published as, and much of this text has been reproduced from, Morrison AP, Shryane N, Beck R, Heffernan S, Law H, McCusker M, et al. Psychosocial and neuropsychiatric predictors of subjective recovery from psychosis. Psychiatry Res 2013;208:203–9,127 with permission from Elsevier.
Objectives
This study aimed to investigate factors associated with subjective judgements of recovery from psychosis, examining how both psychosocial and neuropsychiatric factors are related to subjective perceived recovery and how such predictors are mediated via the experience of negative emotions. Our primary hypothesis was that the relationship between perceived recovery and such predictors will be mediated via the experience of negative emotions.
Method
Participants
Participants were aged 16–65 years, with a schizophrenia spectrum diagnosis with a sufficient level of English literacy to complete the measures and capacity to provide informed consent. At study entry, there were 122 participants (88 male, 34 female), four of whom completed only some of the measures. The majority were white British (84.4%). Diagnoses, confirmed using ICD-10 checklists, were as follows: schizophrenia (n = 75), schizoaffective disorder (n = 10), substance-induced psychosis (n = 5), unspecified non-organic psychosis (n = 15), acute and transient psychotic disorder (n = 12), persistent delusional disorder (n = 4) and post-partum psychosis (n = 1). Participants were recruited from EISs (n = 40), other community-based mental health teams (n = 81) and an inpatient unit (n = 1).
Measures
Measures of recovery
The Process of Recovery from Psychosis Questionnaire32
The QPR is a 22-item questionnaire that was collaboratively developed with service users. The questionnaire measures subjective recovery in two domains: intrapersonal functioning and interpersonal functioning. Participants rate their agreement with statements on a 5-point Likert scale ranging from ‘strongly disagree’ to ‘strongly agree’. The subscales have good internal consistency and test–retest reliability with participants with experience of psychosis. 32 Cronbach’s alpha value for the intrapersonal and interpersonal scales for this sample are α = 0.94 and α = 0.66, respectively. It was chosen for this study because it assesses constructs such as hope, empowerment, self-understanding and integration with social networks, which have been shown to be central to user-defined recovery from psychosis.
Recovery Analogue Scale
Appended to the QPR was the following: ‘please place a cross on the line below to indicate the extent to which you think you have recovered from your illness’ (10-cm analogue scale with left anchor ‘Completely recovered’ and right anchor ‘Not recovered at all’). This was to provide a 0–100 visual analogue scale rating of the extent to which participants believed they were recovered (i.e. another dimension of self-defined recovery).
Psychosocial measures
The Self-Esteem Rating Scale – Short Form76
The Self-esteem Rating Scale (SERS)76 is a 20-item measure of explicit self-esteem, assessing both positive (10 items) and negative (10 items) beliefs about the self. Participants rate how often each of the statements reflects their feelings about the self, on a 7-point Likert scale of ‘Never’ to ‘Always’. Cronbach’s alpha values for the positive and negative scales for this sample are α = 0.92 and α = 0.91, respectively.
Hospital Anxiety and Depression Scale128
The HADS is a 14-item self-report measure. Of these items, seven assess depression, while the remaining seven items assess anxiety, over a period of the preceding week. Cronbach’s alpha values for anxiety and depression scales for this sample are α = 0.86 and α = 0.83, respectively.
Multidimensional Locus of Control Scale131
The Multidimensional Locus of Control Scale is a 24-item locus of control questionnaire with three subscales measuring internality (α in the present study = 0.57), belief in powerful others (α = 0.76) and belief in chance (α = 0.76). Responses to items on this questionnaire are obtained on 5-point scales (‘agree strongly‘, ’agree somewhat‘, ‘neither agree nor disagree‘, ‘disagree somewhat’ and ‘disagree strongly’).
Neuropsychiatric measures
Positive and Negative Syndromes Scale
The PANSS55 is a clinician-administered 30-item semistructured interview consisting of seven items assessing positive symptoms (e.g. hallucinations, delusions, conceptual disorganisation), seven items assessing negative symptoms (e.g. blunted affect, passive/apathetic social avoidance) and 16 items assessing global psychopathology (e.g. depression, anxiety, lack of insight, guilt). All items are scored between 1 (not present) and 7 (severe). A number of studies have demonstrated the reliability and validity of the PANSS. 55 PANSS raters (RB, SH) were trained using a standardised approach and had good reliability. Given the overlap between the global psychopathology subscale and our other measures [e.g. HADS, Insight Scale (IS)], we only utilised the positive and negative symptom subscales.
Birchwood Insight Scale
Insight was measured with the IS,132 which is an 8-item self-report scale designed to be sensitive to change and which captures three widely accepted dimensions of insight: perceived need for treatment, awareness of illness and relabelling of symptoms as pathological. Higher scores indicate greater levels of insight. In this study the scale had an alpha coefficient of 0.66.
Brief Assessment of Cognition in Schizophrenia
The Brief Assessment of Cognition in Schizophrenia (BACS)133 is a battery of neurocognitive tests that assesses the aspects of neurocognition found to be most impaired and most associated with outcome in patients with a diagnosis of schizophrenia (general cognitive performance, working memory and executive functioning). The BACS requires about 30 minutes to complete and has high reliability.
Procedure
Prior to commencement of the study, a dedicated service user panel was consulted on all aspects of design, including wording of information sheets, inclusion of questionnaires, length of assessments, semantic concerns and appropriate amount of payment. Participants were recruited from CMHTs, inpatient settings, EI teams and the voluntary sector to ensure heterogeneity in experience of psychosis and service provision in the Greater Manchester area. Individuals were approached via their care co-ordinator. Those who were interested in taking part were briefed about the study and provided with a participant information sheet. They were then given a minimum of 24 hours to decide whether or not to take part. When an individual agreed to take part, a research assistant met with the participant to take informed consent and administer questionnaires, over a single visit or two visits at the participant’s request. Participants were remunerated for their time.
Statistical analyses
We hypothesised that recovery judgements, as measured by RecA, QPRIntra and QPRInter would form a single, latent dimension of recovery beliefs. We also hypothesised that the variables measuring negative emotion and related processes, namely anxiety, depression and negative self-esteem, would form a single latent dimension of negative emotion. We posited these measurement hypotheses as straightforward, robust and plausible ways of operationalising our multifaceted key constructs. If these hypotheses are supported, then the specification of the mediation model to test the primary hypothesis can be done in a structural equation modelling (SEM) framework using latent variables. Using latent variables allows for the separation of ‘true’ from ‘error’ (more accurately, ‘specific’) construct variance, giving the model greater statistical power and validity than using observed variables alone. 134
A series of factor analyses [exploratory factor analysis (EFA) and confirmatory factor analysis (CFA)] and SEM were specified to test our measurement modelling and mediation hypotheses. Using a SEM approach to estimating mediation models has been shown to reduce bias in the parameter estimates for the mediation effects and to give adequate power to detect mediation effects with samples as small as 100. 134 All models were fitted using Mplus 6.1 (Muthén & Muthén, Los Angeles, CA, USA) and estimated by maximum likelihood. Because of the sensitivity of mediation models to parametric assumptions and the modest sample size available in this study, we computed parameter standard errors (SEs) using bias-corrected bootstrapping based on 1000 bootstrap replications. 135 Latent variables in all factor models were statistically identified by setting the factor loading of one of the factor indicators to one. Alpha for hypothesis testing was set at 0.05 and all hypothesis tests were two-tailed.
To have confidence in hypothesis tests of parameter estimates, it is reasonable (though not strictly necessary) to require that an over-identified statistical model as a whole should provide a reasonable fit to the data. Model fit was assessed following the recommendation that a combination of the standardised root mean-square residual (SRMR) < 0.08 and the Cumulative Fit Index (CFI) > 0.95 provides an optimal trade-off between type I and type II errors in models estimated by maximum likelihood in smaller samples. 136
Results
Data from 12 participants had to be dropped because of missing data, leaving a final sample size of 110. Participant characteristics for the sample are shown in Tables 21 and 22.
| Variable | %, n |
|---|---|
| Sex | |
| Male | 72.1 (88) |
| Female | 27.9 (34) |
| Ethnicity | |
| White | 84.4 (103) |
| Asian | 5.7 (7) |
| Black | 5.7 (7) |
| Mixed | 4.1 (5) |
| Schooling | |
| Primary | 20.5 (25) |
| Secondary | 32 (39) |
| Further | 31.1 (38) |
| Higher | 16.4 (20) |
| Marital status | |
| Single | 82.8 (101) |
| Married | (11) |
| Separated | 8.2 (10) |
| Employment status | |
| Employed | 4 (5) |
| Unemployed | 79.6 (97) |
| Student | 5.7 (7) |
| Volunteer | 8.2 (10) |
| Retired | 2.5 (3) |
| Religious belief | |
| None | 50.1 (61) |
| Christian | 37.7 (46) |
| Muslim | 4.9 (6) |
| Other | 7.3 (9) |
| Variable | Mean | SD |
|---|---|---|
| Age (years) | 35.5 | 11.5 |
| Months of untreated psychosisa | 37.7 | 74.6 |
| Months in most recent therapyb | 6.9 | 11.3 |
| RecA | 61.6 | 24.7 |
| QPRIntra recovery | 44.6 | 12.7 |
| QPRInter recovery | 13.9 | 3.1 |
| Dep | 6.2 | 4.3 |
| Anx | 9.0 | 5.0 |
| Negative self-esteem (SEn) | 32.6 | 12.6 |
| PANSS positive symptoms (Pos) | 15.5 | 5.6 |
| PANSS negative symptoms (Neg) | 14.6 | 4.8 |
| MLCSi | 28.5 | 4.0 |
| IS | 10.4 | 3.0 |
| BACS | 23.8 | 5.9 |
Measurement model of recovery
The unidimensional CFA model of QPRIntra, QPRInter and RecA proved to be a poor one. Although RecA and QPRIntra were well correlated (r = 0.58), RecA and QPRInter were not (r = 0.19). Although no formal measures of goodness of fit were available for this just identified unidimensional CFA model1, the estimated solution was improper, with negative residual variances for the interindicator and a non-positive-definite hessian matrix. The a priori measurement hypothesis for recovery was therefore rejected. We subsequently embarked on exploratory psychometric analysis of the QPR, to search for a coherent subset of the 22 QPR items that would reflect the desired notion of recovery beliefs. This use of exploratory, as opposed to a priori confirmatory, measurement modelling runs the risk of capitalising on chance and sampling variability. However, our goal here was only to find an internally reliable and interpretable set of recovery beliefs; the measurement model was not selected based on its providing a good fit with the other variables that would comprise the mediation model.
A two-factor EFA model of the 22-item QPR was estimated by maximum likelihood. Model fit statistics were somewhat mixed, the CFI indicating moderate but not close fit (CFI = 0.91), the SRMR indicating close fit (SRMR = 0.05), but the chi-squared test resoundingly significant [χ2 (df 188) = 308.46; p < 0.01]. Neither varimax, oblimin nor geomin rotation could recover an approximate simple structure for the two factors, with many items having significant loadings on both factors. Using the oblique geomin rotation (suitable when item complexity is high, i.e. items load on more than one factor), only two out of the five items considered a priori comprising the interpersonal subscale had strong loadings on only the second (i.e. ‘interpersonal’) factor.
The hypothesised two-factor solution did not appear well supported in these data. However, a subset of the QPR items had strong loadings (> 0.7) on just one of the factors, and we decided to use these items as a unidimensional scale of recovery beliefs. These items were: (1) ‘I feel better about myself’, (2) ‘I feel able to take chances in life’, (6) ‘I feel that my life has purpose’, (12) ‘I can take charge of my life’ and (19) ‘I can actively engage with life’. Alpha reliability for these items was 0.88.
A second unidimensional CFA model was fitted by maximum likelihood, using these five QPR items and RecA as indicators. Model fit statistics were excellent [χ2 (9) = 11.42, p = 0.25; CFI = 0.99; SRMR = 0.03]. All standardised factor loadings were highly significant and between 0.61 (RecA) and 0.79 (Questionnaire about the Process of Recovery item number 12). This factor was labelled Recov.
Measurement model of negative emotion
Anxiety, depression, and negative self-esteem were well correlated, between r = 0.66 and r = 0.72. A unidimensional CFA model of these three indicators was estimated. As stated above, overall goodness of fit statistics are not available for such a just identified model. However, with standardised factor loadings all highly significant (depression 0.78, negative self-esteem 0.83 and anxiety 0.86), the hypothesis of unidimensionality was clearly plausible. This factor was labelled Nemo.
Joint model of recovery and emotion
A joint CFA model of Recov and Nemo was fitted, to further test the measurement reliability of these constructs as operationalised above. Two correlated latent factors were specified, each factor indicated uniquely by the variables listed above, with no cross-loadings. Model fit statistics for this now over-identified model were good, indicating close fit between the model and the data [χ2 (26) = 53.70, p < 0.01; CFI = 0.96; SRMR = 0.05].
The correlation between the recovery and emotion factors was very high, r = –0.83 (SE = 0.05), casting some doubt on the discriminant validity of these two related constructs. We, therefore, fitted two further models in an ad hoc test of the dimensionality of the recovery and negative emotion constructs. The first model was a unidimensional CFA model, the single latent factor indicated by all nine of the Recov and Nemo variables. The second model had two latent factors. The first factor was again a general factor, indicated by all nine variables. The second factor was indicated by the Nemo variables only and would, therefore, represent any correlations among these variables not accounted for by the general factor. The two factors were specified as uncorrelated, the association between the latent factors being represented by the cross-loadings on the Nemo variables. These two models were nested, meaning that the parameters of the first (unidimensional) model were a subset of those in the second model. The improvement in fit of the second model over the first model could therefore be formally tested using a likelihood ratio chi-squared test.
The likelihood ratio chi-squared test was significant [χ2LR (3) = 41.90; p < 0.01], the second factor improving model fit significantly and supporting the hypothesis of separate recovery and negative emotion factors, despite their high correlation.
Latent mediation model of recovery on predictors, mediated by negative emotion
Finally, we specified a SEM mediation model to test our primary hypothesis. Recov was the dependent variable and Nemo the mediator. Both the dependent and mediator variables were regressed on the predictor variables Pos, Neg, Multidimensional Locus of Control Scale – internality subscale (MLCSi), BACS and IS. This was, therefore, a model of partial mediation, with direct effects of the predictors on the dependent variable as well as indirect effects via the mediator (Figure 5).
The substantive conclusions regarding our mediation hypotheses would be assessed using significance tests of the indirect effects (i.e. the product of the coefficients for the mediator regressed on the predictors and the outcome variable regressed on the mediator). Because indirect effects are based on products of parameters, confidence limits based on asymptotic (i.e. normal) theory are expected to be biased; we therefore used significance tests based on SEs computed using bias-corrected bootstrapping (1000 replications), as recommended. 135
Tables 23a–c show the results of the mediation model. The mediator, Nemo, had a very strong, negative and significant relationship with Recov, accounting for an R2 of 68%. Of the predictor variables, only MLCSi had a significant direct effect on Recov, with a positive relationship. MLCSi also had a significant, positive, indirect effect on Rec, which was composed of a negative relationship between MLCSi and Nemo and a negative relationship between Nemo and Rec. The only other significant indirect effect was for Pos, a negative relationship. Pos was positively associated with Nemo, which was negatively related to Recov. The standardised effect sizes of these significant mediation effects were –0.311 for Pos and 0.211 for MLCSi, corresponding, by Cohen’s rule of thumb, to ‘medium’ sized effects. 137 The R2 for Recov in the full model was very large, 72%. The majority of this was due to the R2 of 50% uniquely associated with the total indirect effects. 138
| Variable | Unstandardised direct effect | Bootstrap SE | p-value | Standardised direct effect |
|---|---|---|---|---|
| Nemo | –0.227 | 0.079 | 0.004 | –0.610 |
| Pos | –0.021 | 0.038 | 0.581 | –0.076 |
| Neg | –0.029 | 0.030 | 0.330 | –0.090 |
| MLCSi | 0.098 | 0.035 | 0.005 | 0.253 |
| BACS | 0.042 | 0.025 | 0.097 | 0.161 |
| IS | 0.005 | 0.035 | 0.883 | 0.010 |
| Variable | Unstandardised indirect effect | Bootstrap SE | p-value | Standardised indirect effect |
|---|---|---|---|---|
| Pos | –0.086 | 0.037 | 0.020 | –0.311 |
| Neg | –0.003 | 0.022 | 0.903 | –0.008 |
| MLCSi | 0.082 | 0.037 | 0.026 | 0.211 |
| BACS | –0.008 | 0.017 | 0.615 | –0.032 |
| IS | –0.055 | 0.034 | 0.103 | –0.107 |
| Variable | Unstandardised effect | Bootstrap SE | p-value | Standardised effect |
|---|---|---|---|---|
| Pos | 0.380 | 0.074 | 0.000 | 0.510 |
| Neg | 0.012 | 0.088 | 0.894 | 0.013 |
| MLCSi | –0.359 | 0.093 | 0.000 | –0.346 |
| BACS | 0.037 | 0.065 | 0.572 | 0.052 |
| IS | 0.243 | 0.127 | 0.055 | 0.175 |
A final model was fitted to check the robustness of these results to the possibly confounding effects of Sex (binary), Age (years), relationship status (single vs. not single) and employment status (NEET vs. not NEET). Both Recov and Nemo were regressed on these four extra predictors and the mediation model was rerun. Comparing the difference in model chi-squares between this and the original model using a likelihood ratio test found no significant improvement by including the four extra predictors [χ2LR (28) = 32.995; p = 0.236], and so presented no evidence of confounding by these variables. Zero-order correlations for the variables are provided in Table 24.
| Variable | RecA | QPRIntra | QPRInter | Dep | Anx | SEp | SEn | Pos | Neg | MLCSi | IS | BACS |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RecA | 1 | |||||||||||
| QPRIntra | 0.552 | 1 | ||||||||||
| QPRInter | 0.176 | 0.619 | 1 | |||||||||
| Dep | –0.547 | –0.698 | –0.348 | 1 | ||||||||
| Anx | –0.530 | –0.619 | –0.195 | 0.651 | 1 | |||||||
| SEp | 0.347 | 0.682 | 0.418 | –0.620 | –0.377 | 1 | ||||||
| SEn | –0.439 | –0.619 | –0.191 | 0.650 | 0.727 | –0.555 | 1 | |||||
| Pos | –0.440 | –0.533 | –0.217 | 0.458 | 0.556 | –0.315 | 0.449 | 1 | ||||
| Neg | –0.421 | –0.252 | –0.099 | 0.277 | 0.176 | –0.189 | 0.046 | 0.405 | 1 | |||
| MLCSi | 0.289 | 0.548 | 0.323 | –0.453 | –0.327 | 0.535 | –0.413 | –0.191 | 0.005 | 1 | ||
| IS | –0.221 | –0.170 | 0.006 | 0.163 | 0.280 | –0.075 | 0.256 | 0.125 | 0.011 | –0.144 | 1 | |
| BACS | 0.298 | 0.144 | 0.065 | –0.080 | –0.028 | –0.013 | 0.053 | –0.222 | –0.532 | –0.131 | 0.099 | 1 |
Discussion
We found that subjective recovery judgements were directly associated with negative emotion (anxiety, depression and negative self-esteem) and internal locus of control, lower levels of negative emotion and higher levels of internal locus of control were associated with higher judgements of recovery. We also found that positive symptoms and internal locus of control were indirectly associated with recovery judgements via their relationship with negative emotion. There was a trend towards such an indirect effect of insight on recovery judgements (higher insight associated with higher negative emotion). There did not appear to be any effect of negative symptoms or neurocognitive functioning on self-rated recovery or negative emotion.
These findings are broadly consistent with the findings of other studies of the relationship between psychosocial factors and broad definitions of recovery. Our demonstration that internal locus of control and negative emotion were directly related to recovery judgements is consistent with previous findings regarding the importance of locus of control, empowerment, optimism, self-esteem and personal agency. 115,116,119,120 However, our study, which is relatively unique in comprehensively assessing both psychosocial factors and neuropsychiatric factors, found no evidence for a relationship between negative symptoms or neurocognitive functioning and subjective recovery, which is compatible with the equivocal findings to date. We found that insight and positive symptoms were related to recovery judgements via their influence on negative emotion; thus, higher insight and psychosis symptoms may increase distress that has a negative influence on subjective recovery. It is possible that this relationship, in turn, may be mediated by the appraisal of symptoms and an individual’s explanatory framework or conceptualisation of illness. The finding regarding locus of control and insight are also compatible with research demonstrating that biological explanations of mental health problems tend to be associated with greater stigma and pessimism in comparison with psychosocial explanations in studies of both the general public139–141 and in relation to internalised stigma in people with psychosis. 142
Overall, our findings are consistent with recent models of recovery that encompassed processes such as hope, re-establishment of identity, finding meaning in life and taking responsibility. 111,143 Thus, it would appear that self-rated perceptions of recovery are related to increased control and reduced distress, rather than the severity of neurocognitive deficits or psychiatric symptoms. The relationship between severity of psychosis symptoms and increased insight and self-rated recovery judgements was mediated by the effect that they had on negative emotion (i.e. increasing distress). The lack of a relationship between recovery and both negative symptoms and neurocognitive deficits may be understandable given recent evidence suggesting that the impact of these processes on functioning may be mediated by defeatist beliefs about performance144 (which are likely to be associated with self-esteem, locus of control and negative emotions).
There are a number of methodological limitations to consider regarding this study. First, we had a relatively modest sample size. However, using a SEM approach to estimating the mediation effects and using bias-corrected bootstrapped SEs to evaluate the significance of these effects has been shown to give unbiased estimates and adequate statistical power for moderate effect sizes in samples as small as 100. 134,135 The size of the indirect, mediation effects in this study were large, suggesting that sample size and statistical power was not a critical issue. Second, our sample was also diagnostically heterogeneous, which may be problematic, for example if different groups conceptualise recovery very differently; however, we used multiple indicators of recovery and a latent variable measurement model to address measurement error, and the diverse sample should provide greater generalisability to clinical services and settings, which also have considerable diagnostic heterogeneity. The predominance of male participants may, however, adversely affect generalisability. Third, there are a number of assumptions that must be made if the significant associations found in the mediation model are to be interpreted as causal effects, including the absence of unmeasured confounding between the mediator and outcome variables. 145 Although our measurement model showed discriminant validity between the negative emotion mediator and recovery outcome, the fact that our research design was cross-sectional and that no instrumental variable for the mediator (i.e. one predicting emotion but not recovery) was available, does not give us a basis to make the assumption of lack of confounding. However, our results are consistent with a causal account and we are currently conducting a prospective study of recovery from psychosis to test this. In addition, recent attempts to develop broader criteria for defining recovery have included domains of functioning such as involvement in work or study, independent living and social networks,146–148 which were not utilised in our analysis. However, zero-order correlations revealed that such factors were not related to perceived recovery in our sample, so they were excluded from the model to avoid over-parameterisation. Finally, our choice of measures is subject to criticism; for example, some may argue we should have employed the five-factor solution of the PANSS, and many of our measures were self-report. Incorporation of other potentially relevant variables such as social cognition would be desirable in future research.
There are several clinical implications of this research. It suggests that we can measure recovery and negative emotion and that these are distinguishable, but related, concepts. The finding that internal locus of control is directly associated with recovery suggests that services should promote internality by involving service users as active agents in their own care, providing responsibility for decision-making and recognition of strategies within their control that contribute to positive outcomes. Recent web-based interventions to promote such empowerment have shown promise. 149 Characteristics of service models such as collaborative care, shared decision-making and promotion of self-management strategies should facilitate service user-defined recovery, although there are also some potential problems of promoting empowerment and involvement in decision-making in unresponsive settings. For example, a recent study showed decision-making training for people with psychosis resulted in their psychiatrists viewing them as more disruptive;150 therefore, such interventions should be applied within the context of concurrent systemic change.
Strategies targeted at reducing negative emotion and counteracting the negative effects of positive symptoms and increased insight, such as the provision of normalising explanations,151 reduction of internalised stigma152 and improvement of self-esteem130 should also promote recovery. Conversely, a reduction of the emphasis that services place on psychosis symptoms and traditional psychiatric insight, which can convey pessimistic messages of hopelessness and lack of personal agency, should be beneficial in promoting recovery.
Phase 3: longitudinal predictors of subjective recovery from psychosis
This research was previously published as, and reproduced from, Law H, Shryane N, Bentall RP, Morrison AP. Longitudinal predictors of subjective recovery in psychosis [published online ahead of print November 2015]. Br J Psychiatry 2015. http://bjp.rcpsych.org/content/early/2015/11/05/bjp.bp.114.158428)153
Objectives
This study aimed to explore longitudinal predictors of recovery with a particular focus on the role of negative emotion. We hypothesised that recovery at time 2 would be predicted by recovery at time 1 and negative emotion at time 1.
Method
Participants
Data for this study were collected throughout the recovery programme from all appropriate studies to create a comprehensive data set. Participants were recruited from EI teams, CMHTs, inpatient settings and voluntary services across the north-west of England. Participants were included in the data set if they were aged 16–65 years, had a diagnosis of schizophrenia spectrum disorder, sufficient understanding of the English language to allow them to complete the measures and the capacity to provide informed consent. A total of 110 participants were assessed at baseline and 6 months.
Measures
The Process of Recovery Questionnaire
The original version of the QPR92 is a 22-item self-report measure with two subscales which was developed collaboratively by a team of service user researchers and clinicians. Items are rated on a 5-point Likert scale ranging from ‘strongly disagree’ to ‘strongly agree’ and measure key service user-defined elements of recovery including hope, self-esteem, social integration and empowerment. Higher scores on the measure are indicative of recovery. A factor analysis of the psychometric properties of the QPR suggested an amended 15-item one-dimensional version of the measure provided the most interpretable and reliable solution. The 15-item total is used in this study; Cronbach’s alpha for the 15-item version in the sample used in this study is 0.947.
The Positive and Negative Syndrome Scale
The PANSS55 is a 30-item semistructured clinical interview including seven items to assess positive symptoms (such as hallucinations and delusions), seven items to assess negative symptoms (such as blunted affect and emotional withdrawal) and 16 items to assess global psychopathology (such as anxiety, guilt and depression). All items are rated from 1 (not present) to 7 (severe). The PANSS has been used in a variety of studies and has been shown to have good reliability and validity. 154
The Personal and Social Performance scale
The Personal and Social Performance (PSP) scale155 is a measure of functioning rated by an observer across four domains: socially useful activities, personal and social relationships, self-care and aggression. The scale has been shown to have adequate internal consistency (α = 0.76). 156 Total scores range from 1 to 100, with 100 indicating no functional difficulties. The majority of participants were rated for functioning using PSP. For a small number of participants (n = 27) the functioning subscale of the GAF scale77 was used instead. The GAF scale is also a measure of functioning which is used by an observer to rate symptoms, social, psychological and occupational functioning.
The Calgary Depression Scale for Schizophrenia
The Calgary Depression Scale for Schizophrenia73 is a nine-item scale with items rated on a 3-point Likert scale. Global scores range from 0 to 27. The scale measures items on depression, hopelessness, self-depreciation, guilty ideas of reference, pathological guilt, morning depression, early wakening, suicide and observed depression.
The Beck Hopelessness Scale
The BHS74 is a 20-item self-report measure designed by clinicians to measure thee dimensions of hopelessness: feelings of the future, loss of motivation and expectations. Statements are rated by participants as true or false for their attitudes over the last week. The psychometric properties of the BHS have been examined in various studies and the measure has been shown good reliability and validity. 157–159
The Self-Esteem Rating Scale – Short Form
The SERS76 is a 20-item self-report measure assessing both positive and negative beliefs about the self. Items are rated on a 7-point Likert scale ranging from ‘never’ to ‘always’. The scale demonstrated good internal consistency and reliability and adequate convergent validity. 76
Procedure
Recruitment took place across EI teams, CMHTs, inpatient settings and voluntary services across the Greater Manchester area to ensure heterogeneity of service provision and experience of psychosis. Potential participants were approached by the care team and offered information about the study. Interested participants were given a minimum of 24 hours to read the participant information sheet and decide whether or not to take part. Those who agreed to take part met with a researcher to complete a consent form and the baseline study measures. The researcher then attempted to contact all participants again 6 months later to repeat the set of measures in a follow-up assessment. Participants were recompensed for their time.
Statistical analysis
All models were fitted in Mplus version 7 (Muthén & Muthén, Los Angeles, CA, USA) and estimated by maximum likelihood. SEs were estimated using the Huber–White Sandwich estimator, robust to non-normality and heteroscedasticity in the outcome variables. Model log-likelihoods and the likelihood ratio tests were computed using Satorra–Bentler adjustments for non-normality. Nested models were compared using Satorra–Bentler-corrected likelihood ratio chi-squared tests.
Results
Sample characteristics
Demographic characteristics of the sample are shown in Table 25. The average age of participants was 37.3 (SD 11.62) years. Diagnoses at referral were schizophrenia (n = 50), schizoaffective disorder (n = 13), persistent delusional disorder (n = 7), unspecified non-organic psychosis (n = 4), and acute and transient psychotic disorder (n = 2). The remaining 30 participants had not been given a diagnosis but were experiencing psychosis. Participants were recruited from EISs (n = 27), other community-based mental health teams (n = 45) and an inpatient service (n = 1). Data on service type at referral were missing for 37 participants.
| Variable | % | n |
|---|---|---|
| Sex | ||
| Male | 69.1 | 76 |
| Female | 30.9 | 34 |
| Ethnicity | ||
| White | 83.6 | 92 |
| Asian | 8.2 | 9 |
| Black | 4.5 | 5 |
| Mixed | 3.6 | 4 |
| Marital status | ||
| Single | 78.2 | 86 |
| Married | 11 | 12 |
| Separated | 10.9 | 12 |
| Employment status | ||
| Employed | 7.3 | 8 |
| Unemployed | 76.4 | 84 |
| Student | 2.7 | 3 |
| Volunteer | 11 | 10 |
| Retired | 3.6 | 4 |
| Religious belief | ||
| None | 35.5 | 39 |
| Christian | 31.8 | 35 |
| Muslim | 10.9 | 12 |
| Other | 21.8 | 24 |
Model variables
Variables are sufficed 1 to indicate time 1 (baseline) assessments and 2 to indicate time 2 (6-month follow-up) assessments.
Core variables
-
Recovery 1 (Rec1) and recovery 2 (Rec2). This variable consisted of the 15-item total QPR score at time 1 or time 2, respectively.
-
Negative emotion (Nemo1 and Nemo2). A composite variable for negative emotion was constructed by taking the mean of scores from the Calgary Depression Scale and the SERS-N. The SERS-N is scored from 10 to 70 whereas the Calgary Depression Scale is scored from 0 to 27. To avoid the composite measure being dominated by the higher scores of the SERS-N, the raw SERS-N scores were divided by seven before taking the composite mean, which gave both contributing scales similar means and SDs.
Test variables
-
Symptoms (PANSS1 and PANSS2). A composite variable representing the overall mean of the seven positive, seven negative and 16 general PANSS scale items was created.
-
Hopelessness (Hopeless1 and Hopeless2). Total score from BHS was utilised.
-
Positive self-esteem (SERS-P1 and SERS-P2). Total score from the positive subscale of the SERS.
-
Functioning (Func1 and Func2). Functioning score utilised the PSP scale if available and the functioning subscale of the GAF scale if not.
Exogenous covariates
All of these variables were measured at time 1:
-
Age.
-
Education or employment. A binary variable indicating whether or not the participant was engaged in paid employment (full or part time), study or voluntary work (coded as 1) versus being unemployed, retired or in receipt of disability living allowance (coded as 0).
-
Marital status. A binary variable indicating whether or not the participant was married or living with a common-law spouse (coded as 1) versus being single, divorced or widowed.
-
Religious beliefs. A binary variable indicating whether or not the participant was a theist, that is believed in the existence of a deity (coded as 1).
-
Early intervention. A binary variable indicating whether or not the participant was recruited from an EIS.
Model of recovery and negative emotion
Both Rec and Nemo were highly correlated within time point (r = –0.66 in both time points). This correlation was reduced to r = –0.45 at time point 2, after controlling for the previous time point.
Table 26 shows that both recovery and negative emotion were significant predictors of recovery at time 2, but that only negative emotion was a significant predictor of negative emotion at time 2.
| Predictor of Rec2 | Ba | SE | p-value | βb |
|---|---|---|---|---|
| Rec1 | 0.26 | 0.08 | 0.001 | 0.35 |
| Nemo1 | –0.85 | 0.31 | 0.006 | –0.27 |
| Predictor of Nemo2 | Ba | SE | p-value | βb |
| Rec1 | –0.02 | 0.02 | 0.213 | –0.09 |
| Nemo1 | 0.64 | 0.07 | < 0.001 | 0.70 |
The R2 for recovery at time 2 was 31.8% and for negative emotion 58.3%. The large R2 for negative emotion at time 2 was mainly accounted for by its relationship with negative emotion in the previous time point.
Further development and testing of the model
The core model of recovery and negative emotion (as illustrated in Figure 6) was compared with test Models 2.1–2.4 using Satorra–Bentler corrected likelihood ratio chi-squared tests for nested models.
FIGURE 6.
Core model (Model 1): recovery and negative emotion at time 2 predicted by recovery and negative emotions at time 1.
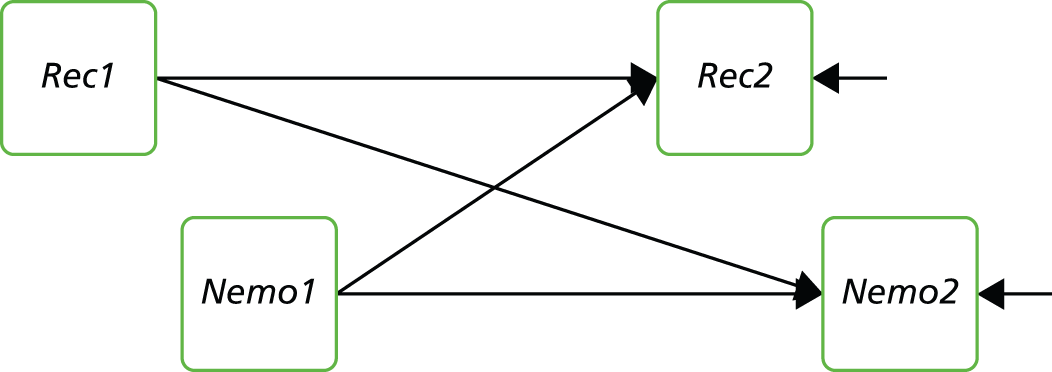
In each test model, the core model was added to by including extra predictors of the outcome variables (recovery and negative emotion at time 2). In Model 2.1, the extra predictors were the overall PANSS symptom scores at times 1 and 2. In Model 2.2 the extra predictors were hopelessness time 1 and hopelessness time 2 scores. Positive self-esteem was the extra predictor in Model 2.3 and functioning was included in Model 2.4.
Table 27 shows the results of the likelihood ratio tests comparing each of Models 2.1–2.4 with the core model.
| Parameters | Model log-likelihood | Likelihood ratio chi-squared vs. core model (Model 1) | p-value for likelihood ratio chi-squared | R2 improvement | |
|---|---|---|---|---|---|
| Model 1 | 9 | –592.30 | – | – | |
| Compared with | |||||
| Model 2.1: symptoms | 13 | –579.76 | 24.21 | < 0.001 | Rec2 7.1% Nemo2 5.8% |
| Model 2.2: hopelessness | 13 | –576.61 | 32.93 | < 0.001 | Rec2 14.3% Nemo2 4.7% |
| Model 2.3: positive SE | 13 | –578.56 | 22.75 | < 0.001 | Rec2 14.1% Nemo2 3.7% |
| Model 2.4: functioning | 13 | –584.71 | 16.08 | 0.003 | Rec2 7.6% Nemo2 2.6% |
All models improved on the fit of the core model, with the largest improvements seen in the prediction of recovery scores at time 2 owing to hopelessness and positive self-esteem.
A further model was then fitted, which combined the predictors that were tested separately in Models 2.1–2.4 into a single Model 2.5.
The parameter estimates for Model 2.5 are shown in Table 28.
| Predictor of Rec2 | Ba | SE | p-value | βb |
|---|---|---|---|---|
| Rec1 | 0.01 | 0.08 | 0.94 | 0.01 |
| Nemo1 | –0.09 | 0.38 | 0.81 | –0.03 |
| PANSS1 | –3.49 | 1.56 | 0.03 | –0.17 |
| Hopeless1 | –0.18 | 0.13 | 0.17 | –0.11 |
| SERS-P1 | 0.00 | 0.07 | 0.98 | 0.00 |
| Func1 | –0.09 | 0.06 | 0.12 | –0.15 |
| PANSS2 | –0.32 | 2.38 | 0.89 | –0.01 |
| Hopeless2 | –0.50 | 0.14 | 0.00 | –0.26 |
| SERS-P2 | 0.24 | 0.06 | 0.00 | 0.33 |
| Func2 | 0.14 | 0.07 | 0.05 | 0.23 |
| Predictor of Nemo2 | Ba | SE | p-value | βb |
| Rec1 | 0.00 | 0.02 | 0.93 | –0.01 |
| Nemo1 | 0.57 | 0.07 | 0.00 | 0.63 |
| PANSS1 | –0.57 | 0.47 | 0.22 | –0.09 |
| Hopeless1 | –0.03 | 0.04 | 0.40 | –0.07 |
| SERS-P1 | 0.02 | 0.02 | 0.26 | 0.09 |
| Func1 | –0.01 | 0.01 | 0.68 | –0.03 |
| PANSS2 | 1.46 | 0.62 | 0.02 | 0.21 |
| Hopeless2 | 0.11 | 0.04 | 0.01 | 0.20 |
| SERS-P2 | –0.04 | 0.02 | 0.02 | –0.19 |
| Func2 | 0.00 | 0.02 | 0.99 | 0.00 |
Recovery at time 2 was predicted significantly by symptoms at time 1 and hopelessness and positive self-esteem at time 2. After accounting for these influences, recovery at time 1 was no longer a significant predictor of recovery at time 2.
Negative emotion at time 1 was a significant predictor of negative emotion at time 2, along with symptoms, hopelessness and positive self-esteem at time 2.
Checking for endogeneity
There was a possibility that regressing closely related constructs on one another within each data collection time point would be stretching assumptions of exogeneity with regard to these constructs. To test for this we ran a model, Model 2.6, which regressed recovery and negative emotion at time 2 on the other test variables from time 1 only, not including the other time 2 variables as predictors.
From Table 29, we see that symptoms and positive self-esteem at time 1 are significant predictors of recovery beliefs at time 2, each with broadly equal magnitude. These predictors accounted for 44% of the variance in recovery at time 2.
| Predictor of Rec2 | Ba | SE | p | βb |
|---|---|---|---|---|
| Rec1 | 0.07 | 0.08 | 0.35 | 0.10 |
| Nemo1 | 0.08 | 0.41 | 0.86 | 0.02 |
| PANSS1 | –6.65 | 1.67 | 0.00 | –0.32 |
| Hopeless1 | –0.28 | 0.17 | 0.10 | –0.17 |
| SERS-P1 | 0.18 | 0.08 | 0.03 | 0.25 |
| Func1 | 0.03 | 0.04 | 0.43 | 0.06 |
| Predictor of Nemo2 | Ba | SE | p | βb |
| Rec1 | 0.00 | 0.02 | 0.92 | –0.01 |
| Nemo1 | 0.58 | 0.09 | 0.00 | 0.65 |
| PANSS1 | 0.61 | 0.44 | 0.17 | 0.10 |
| Hopeless1 | –0.02 | 0.04 | 0.59 | –0.05 |
| SERS-P1 | –0.02 | 0.02 | 0.21 | –0.09 |
| Func1 | –0.02 | 0.01 | 0.11 | –0.10 |
By far the strongest predictor of negative emotion at time 2 is the time 1 score on this variable. No other time 1 variables were significant predictors of negative emotion at time 2. The R2 for this model was 61%.
The fact that recovery and negative emotion have different sets of predictors is evidence in support of the fact that these are distinct constructs.
Checking for confounding
In the previous analyses, no attempt was made to control for the effects of potential demographic and other confounding factors. Such variables available in this study were age, sex, marital status, employment status, religious beliefs and whether or not the participant was drawn from an EI or other service.
Fitting the same series of models above, but this time conditioning the outcome variables (i.e. Rec2 and Nemo2) on these covariates, the pattern of model improvement was identical to that seen in Table 29(Table 30). In these models, the only variable that had any significant effects was sex.
| Parameters | Model log-likelihood | Likelihood ratio chi-squared test vs. Model 1 | p-value for likelihood ratio chi-squared test | |
|---|---|---|---|---|
| Model 1 | 21 | –581.01 | – | – |
| Compared with | ||||
| Model 2.1: symptoms | 25 | –568.52 | 27.07 | < 0.001 |
| Model 2.2: hopelessness | 25 | –565.50 | 32.76 | < 0.001 |
| Model 2.3: positive SE | 25 | –565.97 | 26.36 | < 0.001 |
| Model 2.4: functioning | 25 | –571.55 | 19.68 | 0.001 |
We decided to fit an additional model with sex as a predictor, but this time exploiting the fact that we could plausibly assume that sex was a truly exogenous variable and so include it as a predictor of both the time 1 and time 2 outcomes.
The results for this model, Model 3, are shown in Table 31.
| Predictor of Rec2 | Ba | SE | p-value | βb |
|---|---|---|---|---|
| Rec1 | 0.07 | 0.07 | 0.36 | 0.11 |
| Nemo1 | –0.19 | 0.39 | 0.63 | –0.07 |
| PANSS1 | –5.73 | 1.66 | 0.00 | –0.32 |
| Hopeless1 | –0.23 | 0.16 | 0.15 | –0.17 |
| SERS-P1 | 0.20 | 0.08 | 0.01 | 0.33 |
| Func1 | –0.01 | 0.04 | 0.91 | –0.01 |
| Male | –4.33 | 1.37 | 0.00 | –0.24 |
| Predictor of Nemo2 | Ba | SE | p-value | βb |
| Rec1 | 0.00 | 0.02 | 0.89 | –0.01 |
| Nemo1 | 0.55 | 0.09 | 0.00 | 0.67 |
| PANSS1 | 0.74 | 0.43 | 0.09 | 0.13 |
| Hopeless1 | –0.02 | 0.04 | 0.69 | –0.04 |
| SERS-P1 | –0.02 | 0.02 | 0.31 | –0.08 |
| Func1 | –0.02 | 0.01 | 0.06 | –0.15 |
| Male | –0.58 | 0.43 | 0.17 | –0.11 |
| Outcome variables, predicted by male | Ba | SE | p-value | βb |
| Rec1 | 0.74 | 2.66 | 0.78 | 0.03 |
| Nemo1 | –1.03 | 0.67 | 0.12 | –0.15 |
| PANSS1 | 0.14 | 0.09 | 0.14 | 0.14 |
| Hopeless1 | –0.69 | 1.31 | 0.60 | –0.05 |
| SERS-P1 | 4.08 | 2.80 | 0.15 | 0.14 |
| Func1 | –7.27 | 3.34 | 0.03 | –0.22 |
The pattern of significant results in Model 3 is identical to that in Model 2.6 with the notable exception that although sex is not a significant predictor of recovery beliefs at time 1, it is a significant and substantial predictor of recovery beliefs at time 2, with men having an average recovery score 4 points less than women. This is despite the fact that sex was not a significant predictor of negative emotion at either time point.
Discussion
This exploratory study found that subjective recovery scores at time 2 were predicted by negative emotion, positive self-esteem and hopelessness and, to a lesser extent, by symptoms and functioning at time 1. Additionally, current recovery score was predicted by current hopelessness and positive self-esteem. Current recovery score was not predicted by past recovery scores after accounting for past symptoms and current hopelessness and positive self-esteem.
The strongest predictor of negative emotion was past negative emotion. Other predictors of negative emotion included current scores for symptoms, hopelessness and positive self-esteem. The analysis supports the notion that recovery and negative emotion are distinct but related constructs, each with a distinct set of predictors.
The findings are consistent with the literature on defining recovery, which suggest that rebuilding the self and hope are key components of recovery. 19 The results also support previous research on recovery and related concepts such as quality of life. For example, in one study psychological factors such as hope and internalised stigma accounted for variance in ratings of quality of life,119 while a similar study found that psychosocial factors including self-esteem and optimism were related to recovery.
This present study also found that sex was a significant predictor of recovery, with men having lower recovery scores than women. The finding that men have generally lower recovery scores is consistent with previous research investigating the role of sex in outcomes for people with a diagnosis of schizophrenia. 160 However, the present finding is intriguing because sex was not a predictor of recovery beliefs at baseline, only at the 6-month point, suggesting possibly different processes at work for recovery beliefs of men and women. Sex was not a predictor of negative emotion at either time point, suggesting that the relationship between recovery and sex was not mediated by negative emotion. We could speculate on other processes, for example sample selection may have played a part if males and females find their ways into services at different rates at different stages of illness and recovery. In addition, this research only explored demographic categories of male and female. Further research using a more sociocultural approach to examine the sex roles and identity (see Nasser et al. 161 for review) may improve our understanding of the role of sex in both negative emotion and recovery.
There are a number of methodological limitations to the study. First, the study used a relatively modest sample size and all analyses are exploratory. Further research could examine a larger group that would allow for more extensive testing with a larger number of potential predictors and parameters. Second, the sample was mostly male and diagnostically heterogeneous, which may mean that conceptualisations of recovery were very different within the sample. However, the sample was recruited across a variety of services and settings to ensure it was representative of the target clinical population. Finally, although this study was fairly unique in assessing both neuropsychiatric and psychosocial factors that may predict recovery over time, the follow-up period was relatively short (6 months). Further research could aim to examine the course of recovery and associated predictors over a longer time frame.
Future research could also aim to examine the impact of insight on recovery judgements and explore the impact of insight on negative emotion. Previous research has suggested mixed results with regards to insight and recovery. For example, in one study improved insight was associated with improved outcomes,117 while other studies have suggested that increased insight can be associated with increased negative outcomes including greater suicidality. 118 Developing an understanding of the role of insight in relation to recovery and negative emotion would be beneficial.
There are several potential implications from this research. Interventions that aim to reduce negative emotion while promoting self-esteem and hope may be beneficial to promoting recovery. Strategies such as improvement of self-esteem130 and reduction of internalised stigma,152 for example, may lead to improved recovery outcomes. Emphasis in services should move away from traditional symptom and functioning approaches and towards a more psychosocial approach, which takes into account this key role of negative emotion on personal recovery outcomes.
Phase 4: how do I know if I am better? Judgements of recovery from psychosis in everyday life
Objectives
In this study, we used ESM to address two important questions about recovery judgements:
-
To explore whether or not, and to what extent, patients’ recovery judgements are stable over time. This question is important as instabilities in recovery judgements might compromise the assessment of patients’ subjective well-being, and might potentially have prognostic and treatment implications.
-
To test whether or not the same kind of psychosocial factors that have been shown to be associated with recovery judgements in cross-sectional studies, for example self-esteem and hope for the future, predict recovery judgements longitudinally over moment-to-moment situations in real life.
Method
Participants
This study was reviewed and approved by the NHS North West 10 Research Ethics Committee Greater Manchester North (REC reference 10/H1011/36) and was sponsored by the University of Bangor.
Sixty-eight service users meeting criteria for a diagnosis on the schizophrenia spectrum disorders (ICD-10 schizophrenia, delusional disorder, schizoaffective disorder and psychotic disorder not otherwise specified) were recruited into the present study. Service users were recruited from CMHTs, hospital inpatient wards and day hospitals across several trusts in the North West, including Greater Manchester West Mental Health NHS Foundation Trust, Cheshire and Wirral NHS, Pennine Care, 5 Boroughs Partnership, and Manchester Mental Health and Social Care Trust. Inclusion criteria were: aged between 16 (required for informed consent) and 65 years; being in current contact with mental health services; ability to provide informed consent; and sufficient competency in English to complete the assessments.
Procedure
Participants completed baseline clinical and questionnaire assessments and were then instructed to complete the ESM diaries. Some service user participants were later followed up at 3 and 6 months to assess changes in and stability of recovery; these data are not reported here.
Baseline measures
Positive and Negative Syndromes Scale162
The PANSS is a clinician-administered 30-item semistructured interview consisting of seven items assessing positive symptoms, seven items assessing negative symptoms and 16 items assessing global psychopathology (e.g. depression, anxiety, lack of insight, guilt). All items are scored between 1 (not present) and 7 (severe). A number of studies have demonstrated the reliability and validity of the PANSS. 163 PANSS raters (JD, PT, SA, SM) were trained using a standardised approach and had good reliability. Given the overlap between the global psychopathology subscale and our other measures (e.g. HADS, IS), we only utilised the positive and negative symptom subscales.
The Process of Recovery from Psychosis Questionnaire92
The QPR is a 22-item questionnaire that was collaboratively developed with service users. The questionnaire measures subjective recovery in two domains: intrapersonal functioning and interpersonal functioning. Participants rate their agreement with statements on a 5-point Likert scale rating from ‘strongly disagree’ to ‘strongly agree’. The subscales have good internal consistency and test–retest reliability over short periods. 92 However, the Cronbach’s alpha value for the intrapersonal and interpersonal scales in our sample were α = 0.936 and α = 0.656, respectively, the latter being relatively poor. Therefore, we utilised a 15-item total score that has been derived from factor analyses and shown to be superior to the two subscales; in our sample, the Cronbach’s alpha value for the 15-item total score was α = 0.930.
Participants were also asked to make a simple binary judgement, yes or no, about whether or not they considered themselves to be recovered.
The Brief Self-Esteem Rating Scale – Short Form76
The SERS is a 20-item measure of explicit self-esteem validated for use with patients with psychosis, assessing both positive (10 items) and negative (10 items) beliefs about the self. Participants rate how often each of the statements reflect their feelings about the self on a 7-point Likert scale of ‘never’ to ‘always’. Cronbach’s alpha values for the positive and negative scales for this sample are α = 0.919 and α = 0.908, respectively.
Hospital Anxiety and Depression Scale128
The HADS is a 14-item self-report measure. Of these items, seven assess depression, while the remaining seven items assess anxiety over a period of the preceding week. Cronbach’s alpha values for anxiety and depression scales for this sample are α = 0.859 and α = 0.834, respectively.
Experience sampling methodology
The ESM is a pseudorandom time sampling assessment that has previously demonstrated feasibility, validity and reliability in people diagnosed with psychosis. 121,123,164 All service user participants received an electronic digital watch to wear, which was programmed to bleep 10 times a day on a pseudorandom schedule between 07.30 and 22.00 over the course of 6 days. Participants were asked to complete a short diary around their recovery on hearing a bleep.
The items included in the ESM diary measured psychological experiences on a 7-point Likert scale. The items were adapted from our previous studies121,122,165 and integrated recovery-related variables including positive and negative affect, self-esteem, activity-related stress, self-efficacy, rumination, recovery status and savouring ability.
Measures of self-esteem (four items) and single-item measures of visual hallucinations, auditory hallucinations and current paranoia were taken from previous ESM studies. 121,122,165 From these studies we also took single-item measures of appraisals of symptoms: whether or not visual hallucinations were present, whether or not auditory hallucinations were pleasant and whether or not persecution was believed to be deserved. Two additional measures were piloted by a team of service user researchers before inclusion in the study.
Momentary recovery was generated as the mean of the three ESM recovery items: (1) ‘I felt limited by psychological problems’; (2) ‘I have worries about psychiatric problems’; and (3) ‘I have felt mentally well’. Items (1) and (2) were first reverse coded so the overall recovery score would be on a positive scale, that is higher values indicate better recovery. Momentary recovery was negatively skewed but residuals of the models seemed Normally distributed enough for the assumption to hold.
Three items derived from the BHS166 were included to measure hopelessness: ‘my future seems darks to me’, ‘I feel optimistic about the future’ and ‘the future seems vague and uncertain to me’.
Analysis
All analyses were performed in Stata version 11.0 (StataCorp LP, College Station, TX, USA) using the xtmixed command, and Mplus version 7.1 (Muthén & Muthén, Los Angeles, CA, USA). To test the factor structure of the predictor scales, we used a two-level CFA with participant and beep as the levels, postulating a one-factor solution for each scale to test that the items did load onto a single factor.
Fluctuations in scores were calculated as the absolute difference between ESM measures at two consecutive time points.
As the ESM measures have a three-level hierarchical structure (beeps nested within days nested within participant), we use multilevel modelling to account for the clustering in outcomes within participants. We fitted three-level random intercept models containing in the error structure: a random intercept for each participant, a random intercept for each day within a participant and a beep-specific error term.
In order to test the hypothesis that the ‘Right Now’ variables are correlated with recovery at time 1 we considered predictors and outcomes at concurrent entry points; the results will demonstrate if there is an association between the predictors and outcomes which, if significant, might suggest that they occur simultaneously. To test the hypothesis that the Right Now variables at time 0 predict recovery at time 1 lagged values of the predictors were used in the multilevel models instead of concurrent predictor values.
Results
Participant characteristics
A total of 80 service users took part in the study (Table 32 shows summary table of participant characteristics). Demographic information was missing for 10 participants. The majority of participants were referred based on having experience of psychosis but no diagnosis specified (n = 35, 58%), while 36.7% (n = 22) had a diagnosis of schizophrenia and 3 participants (5%) had a diagnosis of schizoaffective disorder.
| Characteristics | Service users (N = 68a), n (%) |
|---|---|
| Age (years), mean (SD) | 38.6 (10.6) |
| Sex (Male) | 36 (60.0) |
| Current living arrangements | |
| Spouse/partner | 7 (11.7) |
| Spouse/partner and children | 5 (8.3) |
| Alone | 22 (36.7) |
| Children | 4 (6.7) |
| Parents only | 7 (11.7) |
| Supported accommodation | 4 (6.7) |
| Other | 11 (18.4) |
| Marital status | |
| Single | 42 (70.0) |
| Married | 6 (10.0) |
| Separated | 2 (3.3) |
| Divorced | 8 (13.3) |
| Common law | 2 (3.3) |
| Religious beliefs | |
| Christianity | 28 (46.7) |
| Islam | 4 (6.7) |
| Judaism | 1 (1.7) |
| Buddhism | 0 |
| Theism | 5 (8.3) |
| Paganism | 1(1.7) |
| Atheism | 2 (3.3) |
| Other | 19 (31.7) |
| Ethnicity | |
| White | 48 (80.0) |
| Black | 5 (8.3) |
| Asian | 4 (6.7) |
| Other | 3 (5.6) |
| Schooling level | |
| Primary | 1 (1.7) |
| Secondary | 21 (35.0) |
| Further | 25 (41.7) |
| Higher | 13 (21.7) |
| Employment | |
| Full time | 3 (5.0) |
| Part time | 5 (8.3) |
| Unemployed | 13 (21.7) |
| Disabled | 29 (48.3) |
| Voluntary | 8 (13.3) |
| Retired | 1 (1.7) |
| Students | 1 (1.7) |
Summary data for completed measures can be seen in Table 33.
| Variable | Subscale | Mean (SD) | n |
|---|---|---|---|
| QPR total | 52.5 (9.04) | 68 | |
| PANSS | Positive | 12.6 (4.0) | 60 |
| Negative | 11.6 (3.5) | 60 | |
| General | 24.8 (5.9) | 60 | |
| SERS | Positive | 43.9 (11.8) | 60 |
| Negative | 33.7 (14.0) | 60 | |
| BHS total | 7.4 (5.4) | 60 | |
| PSP total | 73.2 (13.4) | 60 | |
Is there a relationship between baseline recovery and fluctuations in recovery?
We compared fluctuations in momentary recovery between groups defined according to whether their baseline ratings were ‘yes’ (recovered) or ‘no’ (Table 34). Baseline recovery was entered into the model as a fixed effect and allowing different residual variance of the two baseline recovery groups. The ‘recovered’ group at baseline have significantly higher mean recovery scores recorded in everyday life than the ‘not recovered’ group, but there was more variation in recovery in the ‘not recovered’ baseline group.
| Variable | Fixed effects | Random effects | ||||
|---|---|---|---|---|---|---|
| Coefficient | SE | p-value | Level | Variance | SE | |
| Baseline recovery (yes/no) | 0.77 | 0.38 | 0.043 | Person | 1.26 | 0.13 |
| Day | 0.51 | 0.03 | ||||
| Beep: not recovered | 0.71 | 0.01 | ||||
| Recovered | 0.50 | 0.02 | ||||
For the baseline QPR recovery (Table 35), the total baseline score (of the 15 items) was entered as a fixed effect. This score was then split into tertiles and entered into the random part of the model to allow the residual variance to be different for each group, as with the binary baseline recovery. Group 1 included total baseline scores of 30–49, group 2 scores of 50–56 and group 3 scores of 57–73. The results imply that for a unit increase in baseline QPR score, mean momentary recovery scores increase by 0.09. However, showing a similar pattern to the binary baseline recovery variable, there is more variation in momentary recovery judgements for those with lower baseline QPR scores than for those with higher baseline QPR scores.
| Variable | Fixed effects | Random effects | ||||
|---|---|---|---|---|---|---|
| Coefficient | SE | p-value | Level | Variance | SE | |
| Baseline QPR | 0.09 | 0.02 | 0.000 | Person | 1.04 | 0.12 |
| Day | 0.22 | 0.03 | ||||
| Group 1: low recovery | 0.57 | 0.03 | ||||
| Group 2: medium recovery | 0.49 | 0.03 | ||||
| Group 3: high recovery | 0.37 | 0.02 | ||||
Which experience sampling methodology variables correlate with current momentary recovery judgements?
Table 36 shows the relationship between momentary recovery judgements and individual ESM measures taken at the same time point. There are significant correlations between the concurrent variables and momentary recovery judgements. As expected, positive measures (self-esteem) are positively correlated with recovery, whereas the symptom measures are negatively correlated with recovery. For example, for a unit increase in self-esteem, momentary recovery increases by 0.38, whereas for a unit increase in hopelessness momentary recovery decreases by 0.35.
| Variable | Fixed effects | Random effects | ||||
|---|---|---|---|---|---|---|
| Coefficient | SE | p-value | Level | Variance | SE | |
| Self-esteem | 0.38 | 0.02 | 0.000 | Person | 1.06 | 0.20 |
| Day | 0.18 | 0.02 | ||||
| Beep | 0.46 | 0.01 | ||||
| Hopelessness | –0.35 | 0.02 | 0.000 | Person | 1.03 | 0.19 |
| Day | 0.17 | 0.02 | ||||
| Beep | 0.45 | 0.01 | ||||
| Visual hallucinations (I see phenomena) | –0.14 | 0.02 | 0.000 | Person | 1.53 | 0.28 |
| Day | 0.18 | 0.02 | ||||
| Beep | 0.49 | 0.02 | ||||
| Visual hallucinations (these are pleasant) | 0.17 | 0.03 | 0.000 | Person | 1.52 | 0.47 |
| Day | 0.07 | 0.03 | ||||
| Beep | 0.33 | 0.03 | ||||
| Auditory hallucinations (I hear voices) | –0.13 | 0.02 | 0.000 | Person | 1.51 | 0.28 |
| Day | 0.19 | 0.02 | ||||
| Beep | 0.48 | 0.02 | ||||
| Auditory hallucinations (these are pleasant) | 0.13 | 0.03 | 0.000 | Person | 1.42 | 0.38 |
| Day | 0.20 | 0.04 | ||||
| Beep | 0.43 | 0.03 | ||||
| Paranoia | –0.42 | 0.02 | 0.000 | Person | 0.75 | 0.14 |
| Day | 0.15 | 0.02 | ||||
| Beep | 0.45 | 0.01 | ||||
| Deservedness | –0.22 | 0.03 | 0.000 | Person | 1.30 | 0.24 |
| Day | 0.25 | 0.03 | ||||
| Beep | 0.48 | 0.01 | ||||
All of the current variables were entered into one model (Table 37), excluding the pleasantness of hallucinations and deservedness ratings for which there were not sufficient data (including these variables would cause the model to use only 145 observations whereas, excluding them the model uses 2273 observations). In this model, self-esteem, hallucinations (visual and auditory), and paranoid are all significantly associated with recovery judgements.
| Variable | Fixed effects | Random effects | ||||
|---|---|---|---|---|---|---|
| Coefficient | SE | p-value | Level | Variance | SE | |
| Self-esteem | 0.23 | 0.02 | 0.000 | |||
| Hopelessness | –0.18 | 0.02 | 0.000 | |||
| Visual hallucination | –0.07 | 0.02 | 0.003 | |||
| Auditory hallucinations | –0.06 | 0.02 | 0.002 | |||
| Paranoia | –0.26 | 0.02 | 0.000 | |||
| Person | 0.56 | 0.11 | ||||
| Day | 0.11 | 0.02 | ||||
| Beep | 0.40 | 0.01 | ||||
Do variables at the previous time point predict momentary recovery judgements?
Lagged variables for predictor ESM variables were generated, restricting lag to be within day. Each line in Table 38 corresponds to a separate model with the lagged variables as the predictors, controlling for baseline recovery group (yes/no binary judgement) as this was found to be a significant predictor of recovery scores in a previous analysis. It can be seen that self-esteem, hopelessness and the symptom measures (but not participants’ appraisals of their symptoms, as indicated by the pleasantness of their hallucinations or their beliefs about whether or not they deserved to be persecuted) predicted the extent to which they believed they were recovered.
| Variable | Fixed effects | Random effects | ||||
|---|---|---|---|---|---|---|
| Coefficient | SE | p-value | Level | Variance | SE | |
| Self-esteem | 0.15 | 0.03 | 0.000 | Person | 1.17 | 0.23 |
| Day | 0.18 | 0.02 | ||||
| Beep | 0.43 | 0.02 | ||||
| Hopelessness | –0.13 | 0.02 | 0.000 | Person | 1.19 | 0.23 |
| Day | 0.18 | 0.02 | ||||
| Beep | 0.43 | 0.02 | ||||
| Halluc1 (I see phenomena) | –0.06 | 0.03 | 0.045 | Person | 1.30 | 0.25 |
| Day | 0.16 | 0.02 | ||||
| Beep | 0.43 | 0.02 | ||||
| Halluc2 (these are pleasant) | –0.03 | 0.04 | 0.408 | Person | 1.02 | 0.34 |
| Day | 0.13 | 0.05 | ||||
| Beep | 0.29 | 0.03 | ||||
| Halluc3 (I hear voices) | –0.09 | 0.02 | 0.000 | Person | 1.21 | 0.24 |
| Day | 0.16 | 0.02 | ||||
| Beep | 0.43 | 0.02 | ||||
| Halluc4 (these are pleasant) | 0.02 | 0.03 | 0.486 | Person | 1.45 | 0.41 |
| Day | 0.19 | 0.04 | ||||
| Beep | 0.42 | 0.03 | ||||
| Paranoia | –0.19 | 0.03 | 0.000 | Person | 0.97 | 0.19 |
| Day | 0.17 | 0.02 | ||||
| Beep | 0.43 | 0.02 | ||||
| Deservedness | 0.02 | 0.03 | 0.499 | Person | 1.49 | 0.29 |
| Day | 0.20 | 0.03 | ||||
| Beep | 0.43 | 0.02 | ||||
Table 39 shows the results when all variables were entered into a single model, controlling for baseline recovery group. Again, because of the small number of observations for the symptom appraisal variables, these were excluded, enabling an analysis with 169 observations instead of 172. As can be seen, in this analysis all of the variables with the exception of visual hallucinations are significant predictors. Substantially similar results were obtained by using baseline QPR scores instead of the binary recovery classification.
| Variable | Fixed effects | Random effects | ||||
|---|---|---|---|---|---|---|
| Coefficient | SE | p-value | Level | Variance | SE | |
| Self-esteem | 0.12 | 0.03 | 0.000 | |||
| Hopelessness | –0.06 | 0.03 | 0.030 | |||
| Visual hallucinations | –0.02 | 0.03 | 0.624 | |||
| Auditory hallucinations | –0.07 | 0.02 | 0.002 | |||
| Paranoia | –0.11 | 0.03 | 0.000 | |||
| Baseline recovery | 1.04 | 0.26 | 0.000 | |||
| Person | 0.74 | 0.16 | ||||
| Day | 0.12 | 0.02 | ||||
| Beep | 0.43 | 0.02 | ||||
Sensitivity analysis
The results above include data from all participants regardless of the total number of observations completed per person. In line with common practice of only including data from participants who have completed at least one-third of the potential observation, a sensitivity analysis was conducted to identify any changes to the results. Analysis 3 (in which lagged variables were used to predict recovery judgements) was repeated including only participants who had completed at least 20 observations overall: 54 out of the 68 service users. Results were very similar to the full sample, with only a slight decrease in magnitude of the effect for each of the predictor variables. The only variable to significantly change was visual hallucinations, which now had an effect size of –0.05 (SE 0.03; p-value 0.056).
Discussion
To our knowledge, this is the first study to use experience-sampling methodology to explore the concept of recovery from psychosis in everyday life. We found that recovery judgements are variable in some patients but more stable in others, which is in keeping with the conceptualisation of recovery as an idiosyncratic process. 19,143 We also found that, generally, those who reported themselves as being recovered using the questionnaire measure at baseline reported higher levels of recovery when required to make those ratings in everyday life, which demonstrates a certain consistency in recovery judgements regardless of the methodology used; this is consistent with findings regarding use of different self-report approaches to defining recovery. 126 Those with lower baseline questionnaire recovery scores showed greater fluctuations in recovery judgements in everyday life. Hence, low baseline recovery is associated with instability of recovery judgements, which is an interesting finding, since stability would be expected to form part of any criteria by which people judge themselves or others to be recovered. Both concurrently and prospectively, self-esteem and hopelessness but also, less expectedly, symptoms (hallucinations and paranoia), predicted whether or not patients felt themselves to be recovered. In general, the effect sizes for self-esteem, hopelessness and paranoia were large compared with those for hallucinations. Thus, it would appear that self-esteem and hope are important factors in the recovery process, which confirms previous findings from both qualitative19,143 and quantitative127 studies. Previous research has indicated that the role of symptoms in recovery judgements appears to be indirect, mediated via the role of negative emotions such as anxiety and depression; it is possible that the strength of findings for paranoia may be due to the overlap with anxiety, as both are concerned with threat appraisals, but it may be that the interpersonal nature of paranoia as a symptom makes it more important to perceived recovery than hallucinatory experiences. It may also be that hallucinatory experiences as symptoms are less relevant to perceived recovery because they are, at times, pleasant, whereas it is unlikely that people would experience paranoid ideation as pleasant. The role of symptoms in subjectively perceived recovery is clearly relevant, but we require further research to clarify this.
A number of limitations of this study require acknowledgement. Despite methodological advantages of ESM over classical self-report measures,167 some researchers have voiced concerns regarding participants’ compliance with, and hence the reliability of, pencil and paper methods of experience sampling, recommending the use of electronic diaries. 168 Although this could be a serious limitation in studies employing predetermined entries, previous studies have demonstrated comparable compliance in electronic and paper diary studies, when using a random-entry design, which we employed in our study. There was a predominance of male participants in this study, which may affect generalisability. The average age of participants was 38.6 years which may indicate that further work to explore recovery from psychosis in EI populations would be beneficial because this age group may conceptualise and judge recovery differently to those with more established diagnoses. For a significant proportion of the sample, diagnosis was unconfirmed. Although experiences of psychosis were verified using the PANSS structured interviews, this is likely to have led to diagnostic heterogeneity that may be considered as a limitation of the study. However, this diagnostic heterogeneity is likely to be representative of the clinical populations accessing services.
There are a number of implications arising from this research. Future longitudinal research should further investigate the role of symptoms and psychological factors (such as negative affect, self-esteem and hope) in relation to perceived recovery over a longer time frame, in order to examine the casual and temporal relationships between such factors. Clinical implications include the desirability of using recent technology for monitoring of subjective recovery and related factors in everyday life (e.g. via mobile phone applications that could provide feedback to service users and care teams). The promotion of recovery in clinical services could be facilitated by regular assessment and monitoring of perceived recovery, as well as the incorporation of targets such as self-esteem, hope and positive affect into goals within care plans and service specifications or operational policies. The promotion of recovery within individuals could utilise psychosocial approaches to increase hope, self-esteem and mood; these could include individual or group therapies that are specifically focused on these issues, life skills courses (including education about definitions of recovery, recovery rates and recovery-related skills) or peer-delivered support.
Conclusions
The research studies in this chapter aimed to address the gap in knowledge regarding judgements of recovery, associated factors and predictors. The research was split into four phases:
-
an exploration of subjective judgements of recovery in people with experience of psychosis
-
a cross-sectional investigation of psychosocial and neuropsychiatric predictors of subjective recovery from psychosis
-
an examination of longitudinal predictors of subjective recovery
-
an ESM study to examine recovery judgements and associated factors.
The research in this chapter found further support for the idea that recovery is multifaceted and idiosyncratic, as well as having significant relationships with psychological factors such as self-esteem, hope and emotion. This research was the first to examine measurement and prediction of subjective recovery using a variety of approaches (including cross-sectional, longitudinal and moment-to-moment techniques).
The first phase found significant correlations between measures of recovery and psychological factors; higher levels of self-esteem and hope, along with lower levels of depression and anxiety, were associated with more positive judgements of recovery. The different methods of measuring recovery judgements (yes/no response, percentage agreement and QPR scores) highlighted a general consistency in within-person ratings across all measures; however, the ranges of scores between individuals were widely dispersed.
The second phase of this research found that subjective recovery judgements were directly associated with negative emotion (anxiety, depression and negative self-esteem) and internal locus of control; lower levels of negative emotion and higher levels of internal locus of control were associated with higher judgements of recovery. Positive symptoms and internal locus of control were indirectly associated with recovery judgements via their relationship with negative emotion. There did not appear to be any effect of negative symptoms or neurocognitive functioning on self-rated recovery or negative emotion. This research provided support for the measurement of recovery and negative emotion, and suggests that these are distinguishable, but related, concepts.
The third phase of the research found that subjective recovery scores at time 2 (6-month follow-up) were predicted by negative emotion, positive self-esteem, hopelessness and to a lesser extent by symptoms and functioning at time 1 (baseline assessment). Additionally, in support of the earlier phases of this research, current recovery score was predicted by current hopelessness and positive self-esteem. The strongest predictor of current negative emotion was past negative emotion. Other predictors of negative emotion included current scores for symptoms, hopelessness and positive self-esteem. The analysis provides further support for the notion that recovery and negative emotion are distinct but related constructs, each with a distinct set of predictors. It was also found that sex was a significant predictor of recovery, with men having lower recovery scores than women. The present finding is intriguing because sex was not a predictor of recovery beliefs at baseline, only at the 6-month point, suggesting that there may be different processes at work over time for recovery beliefs of men and women. Sex was not a predictor of negative emotion at either time point, suggesting that the relationship between recovery and sex was not mediated by negative emotion.
The final phase of this research was the first study to use ESM to explore the concept of recovery from psychosis in everyday life. Recovery judgements were found to be variable in some patients but more stable in others, which is in keeping with the conceptualisation of recovery as an idiosyncratic process. 19,143 Those with lower baseline questionnaire recovery scores showed greater fluctuations in recovery judgements in everyday life. Hence, low baseline recovery is associated with instability of recovery judgements, which is an interesting finding, as stability would be expected to form part of any criteria by which people judge themselves or others to be recovered. Both concurrently and prospectively, self-esteem and hopelessness but also, less expectedly, symptoms (hallucinations and paranoia), predicted whether or not patients felt themselves to be recovered. In general, the effect sizes for self-esteem, hopelessness and paranoia were large compared with those for hallucinations. Thus, it would appear that self-esteem and hope are important factors in the recovery process, which confirms previous findings from the earlier phases of this research and the current literature. 19,32,97,98,119,120
This research in this chapter is indicative of differing personal thresholds for the definition of ‘recovered’ and provides empirical evidence consistent with the idea that recovery is a personal journey that does not necessarily have an end point. It suggests that there may not be a ‘one size fits all’ measure of recovery and the idea of a personalised recovery approach should be embraced in clinical settings. Regular assessment of recovery judgements, as well as psychological factors such as self-esteem, optimism and emotional disturbance, would help to evaluate the extent to which services are recovery oriented and also help individuals to monitor their progress. The possibility of using recent technology for monitoring of subjective recovery and related factors in everyday life (e.g. via mobile phone applications that could provide feedback to service users and care teams) should also be considered.
The finding that internal locus of control is directly associated with recovery suggests that services should promote internality by involving service users as active agents in their own care, providing responsibility for decision-making and recognition of strategies within their control that contribute to positive outcomes. Strategies targeted at reducing negative emotion and counteracting the negative effects of positive symptoms and increased insight, such as the provision of normalising explanations,151 reduction of internalised stigma152 and improvement of self-esteem130 should also promote recovery. Conversely, a reduction of the emphasis that services place on psychosis symptoms and traditional psychiatric insight, which can convey pessimistic messages of hopelessness and lack of personal agency, should be beneficial in promoting recovery.
Overall, this work, in combination with the findings from Chapters 2, 3 and 6, suggest that measurement of recovery should be individually tailored to the preferences and needs of the service user and the service. The identification of such choices for the assessment of monitoring of subjective recovery should include consideration of the frequency of monitoring, the purpose of such assessment (e.g. to identify goals or to monitor change) and the specific aspects of recovery that are prioritised by the service user. For example, beginning with a generic self-report assessment of recovery [such as is provided by the QPR for people with psychosis or the Bipolar Recovery Questionnaire (BRQ) for those with BD] could be supplemented by a more detailed discussion of recovery targets and preferences (such as is provided by the Q-sort exercise in Chapter 2 or the Delphi-rating exercise in Chapter 3). Once these methods have elicited a more idiosyncratic operationalisation of recovery for that person, a more comprehensive assessment battery incorporating measures of self-esteem, hope and optimism, social functioning, locus of control, positive and negative emotion and the subjective impact of symptoms could be designed for that individual.
Chapter 5 Development and evaluation of cognitive–behavioural approaches to guided self-help and group therapy for recovery, taking preferences into account
Background
Treatment guidelines in the UK currently recommend psychological treatments for psychosis, such as CBT. 14 RCTs have consistently demonstrated the efficacy of such treatments. 71 Despite the high internal validity of these trials, external validity can be compromised by confounding variables such as effects of preference. 169 Service users typically have little choice about the mode and content of therapy and may be less likely to benefit from treatments they do not choose to receive. 170,171 Service user involvement in mental health and research trials is advocated,83,172,173 and allowing service user choice is increasingly highlighted as important. 18,19
The partially randomised preference trial design (PRPT174) has been used to enable treatment choice and overcome preference effects in evaluations of various treatments, including psychological therapy. 175 In PRPTs, participants are allocated to their preferred treatment if they have a strong preference and randomised if they do not express a strong preference and consent to randomisation. In comparison with a RCT, the PRPT design does have significant methodological limitations, which suggest that PRPT designs are often viewed as unsuitable, but if they are utilised attempts can be made to overcome some limitations by statistically adjusting for potential unmeasured biases, although this does not overcome their limitations fully. 176 PRPTs can also encounter difficulties when certain treatment options are favoured less than others,177 in particular TAU. 178 It is therefore useful to establish likely preferences prior to such a trial. 169
Trial participation decisions are complex and involve consideration of benefits to self and others. 179 Barriers to participation include inconvenience, treatment preferences, aversion to randomisation, uncertainties regarding treatments, concerns regarding information and consent, and clinicians acting as a barrier. 180 The likelihood of participation in schizophrenia treatment trials is influenced by perceptions of risk, personal benefits and altruistic reasons,181,182 although this has been little researched to date. Hypothetical willingness to participate in clinical trials ranges from 70% to 96%. 183 The majority of studies regarding specific psychological treatments for psychosis have focused on treatment outcomes and processes rather than content. 108 In a general review of preference trials,175 the proportion of participants willing to accept random allocation varied considerably (from 26% to 88%). Further exploration of treatment preferences and feasibility of the PRPT design for research investigating CBT would be beneficial.
Despite recommendations that CBT should be given to all individuals who experience psychosis,83 the implementation of CBP within NHS services is poor16 owing to a number of factors. First, the widespread lack of trained therapists means that provision of this type of intervention is limited. Second, the refusal rate for participating in trials of CBP is relatively high, suggesting that not all service users wish to engage in current modes of delivery of this therapy. There is also some concern that the focus of CBT interventions for psychosis have been overly restrictive and that CBT does not necessarily target the priorities identified by service users. Although there have been several developments of novel therapeutic approaches within primary care (such as stepped care and the use of computerised and telephone treatments),184,185 there has been little exploration of novel approaches within services for serious mental illness. However, these adapted CBT approaches may lend themselves well to this client group, who may have difficulty in accessing traditional face-to-face talking treatments and are more likely to have difficulty in attending and travelling to appointments. As a result, further exploration of the best way to deliver psychological support to those who experience psychosis is needed.
This study will address these concerns around service user treatment preferences and modes of delivery for psychological support. The first phase will begin by investigating hypothetical preferences for psychological treatment in a sample of individuals experiencing psychosis. This will provide information about the decision-making process as well as preferred modes of delivery for psychological therapy. The second phase will consist of a pilot study to explore implementation of the preferred modes of therapy including development of a recovery-focused self-help package. The information obtained in the first and second phase will be used to facilitate the final phase of this study: a PPT to evaluate the recovery-focused self-help package of treatment for people who experience psychosis.
Phase 1: preferences for psychological therapy in psychosis – trial participation, mode of treatment and willingness to be randomised
This research has been accepted for publication and reproduced with permission from Sumner K, Haddock G, Hartley S, Kilbride M, McCusker M, Pitt L, et al. Preferences for psychological therapy in psychosis: trial participation, mode of treatment, and willingness to be randomised. J Ment Health 2014;23:67–71. 186
This is an Accepted Manuscript of an article published by Informa Healthcare in Journal of Mental Health in 2014, available online: http://informahealthcare.com/doi/full/10.3109/09638237.2013.841865.
Objectives
This study aimed to examine preferences for hypothetical psychological treatment in a sample of people with experience of psychosis.
The objectives of the study were to examine:
-
participants’ decisions regarding trial participation and reasons
-
preferences for psychological therapy and reasons
-
associations between demographic/symptom characteristics and preferences.
Method
Participants
Participants were included in the study if they were aged 18–65 years, had sufficient English language skills, were in contact with mental health services, met ICD-10 criteria187 for non-affective psychosis and had been considered by their clinical team to be symptomatically stable for at least 1 month.
Recruitment
Participants were recruited from community secondary mental health services in three NHS trusts in the north-west of England. Of 119 service users identified by mental health professionals, 90 gave informed consent to take part. Participants were interviewed in their home or a clinical service base, receiving £10 as a token of appreciation.
Measures
Assessments included a sociodemographic questionnaire, the PANSS55 and the GAF77 scale. Inter-rater reliability was high for the PANSS [ICC coefficient 0.96, 95% confidence interval (CI) 0.93 to 0.98] and GAF scale (ICC coefficient 0.95, 95% CI 0.85 to 0.99).
Participants were provided with an information sheet (with counterbalanced presentation) describing hypothetical treatment options: (1) TAU, (2) self-help manual with telephone CBT and peer support (weekly 30-minute sessions for up to 6 months) in addition to TAU [self-help and telephone support (SHT)] or (3) as SHT plus a fortnightly 2-hour group support session for up to 6 months [self-help and group support (SHG)] facilitated by a psychological therapist and a peer supporter. TAU in secondary care mental health services typically consists of the provision of support by a care co-ordinator and monitoring of psychiatric medication. Telephone CBT has been shown to be equivalent to face-to-face CBT in other populations185 and provides increased flexibility about therapy contact which may be particularly helpful with this client group; it was offered as an option here as a way of maximising the flexibility for delivery of CBT. Participants were asked about their hypothetical preferences for participation in a future study, preferred treatment, willingness to be randomised and reasons for their choices. A qualitative interview method was chosen to ensure participants’ understanding and allow open-ended responses and clarification of reasons for preferences.
Data analysis
The data were analysed using SPSS version 17. Missing items were substituted with the mean when < 10% of the scale items were missing. Comparisons between the groups opting for each of the treatment options (TAU, SHT or SHG) were performed using chi-squared tests for categorical data, t-tests/analysis of variance (ANOVA) tests for parametric continuous data, and Mann–Whitney U-tests for non-parametric continuous data. Owing to the use of multiple comparisons, a stringent significance level of p < 0.01 was used.
Content analysis was used to explore reasons reported by participants for their choices, which involved categorising participants’ reasons into mutually exclusive themes188 following discussion with a researcher with lived experience of mental health challenges. The agreement between two raters (KS and SW) for each of the categories was as follows: willingness to participate, 84.4%; unwillingness to participate, 69.2%; preference for TAU, 70.6%; preference for SHT, 91.2%; preference for SHG, 73.8%; willingness to be randomised, 76.7%; and unwillingness to be randomised, 84.4%; ranging from acceptable to good. 189
Results
Sample
Ninety participants were included. The majority of participants were white (n = 77), male (n = 68), unemployed (n = 63) and met criteria for a diagnosis of schizophrenia (n = 59). The remainder met criteria for other ICD-10 defined non-affective disorders, for example schizoaffective disorder or delusional disorder. The mean age of participants was 37.22 years (SD 11.34 years; range 19–63 years). Means for the clinical measures were 28.6 (SD 7.32) for the PANSS general scale, 14.19 (SD 5.57) for the positive scale and 12.05 (SD 3.58) for the negative scale, and 47.98 (SD 12.90) for the GAF scale. The median number of years since first experience of psychosis was 8 years (range 1–34 years) and the median number of hospital admissions of participants was two (range 0 to ≥ 11 admissions).
Key findings
Participants’ willingness to participate in the proposed PRPT was high and SHT was the most popular option. Most participants reported that they would prefer not to agree to randomisation. The results are reported in further detail below, along with the results of the content analysis of participants’ reasons for their preferences.
Willingness to participate in the proposed PRPT
The majority of participants (90%, n = 81) stated that they would be willing to consider participating in a PRPT evaluating psychological therapy for psychosis. Results of the content analysis are reported in Table 40, which illustrates the diversity of participants’ views about participating in a psychological treatment trial.
| Major themes (frequency) | Examples | |
|---|---|---|
| Willingness to participate | ||
| 1. | Benefits to self (n = 46) | ‘Anything I can do that might help myself and prevent future relapses’ |
| 2. | Benefits to others (n = 42) | ‘It gives people a broader view of what’s happening with mental health problems’ |
| 3. | To gain information/knowledge/understanding (n = 17) | ‘It’s good to have more information from people who have had the experiences so I know what to do in the future’ |
| 4. | For an experience/activity/out of interest (n = 15) | ‘It’s something to do, I’m unemployed’ |
| 5. | Desire for social/normalising aspect/sharing experience (n = 15) | ‘I want to socialise with people’ |
| 6. | Positive view of therapy, manual or group support (n = 10) | ‘The telephone therapy sounds good’ |
| 7. | Dissatisfaction with current services (n = 2) | ‘Psychiatrists forget about you’ |
| Unwillingness to participate | ||
| 1. | Dislike of/lack of desire for aspect of treatment/therapy in general (n = 9) | ‘When I meet with authority figures I feel like more of a patient than a human being’ |
| 2. | Potential for distress (n = 2) | ‘Discussing my symptoms confuses and depresses me’ |
| 3. | Satisfaction with current treatment (n = 2) | ‘I’m happy with the level of support I receive at the moment and get quite a lot of support’ |
Preferences for treatment
Most of the participants who were willing to participate in the PRPT had a preference for therapy as opposed to TAU only (Table 41). The telephone support option (SHT) was favoured more than the telephone plus group support option (SHG). Results of the content analysis highlighting the reasons for this are displayed in Table 42.
| Preferred treatment (N = 81) | n | % |
|---|---|---|
| TAU | 18 | 22 |
| SHT | 35 | 43 |
| SHG | 27 | 33 |
| No preference | 1 | 1 |
| Major themes (frequency) | Examples | |
|---|---|---|
| TAU | ||
| 1. | Dislike of/lack of desire for aspect of therapy/therapy in general (n = 9) | ‘I like to be the one in control, I’m not a sociable person unless I’ve known someone for a while’ |
| 2. | Therapy viewed as unnecessary at present (n = 7) | ‘I don’t think CBT would do much to help my situation now, I’m beyond the stage where it would be needed’ |
| 3. | Satisfaction with current support (n = 5) | ‘Because it [usual treatment] works with me’ |
| 4. | Preference for manual alone (n = 5) | ‘I don’t need any telephone support, but having a guide on its own would be useful’ |
| 5 | Assist the research (n = 2) | ‘I want to help the study’ |
| Self-help with telephone support or SHT | ||
| 1. | Dislike of/lack of desire for group support (n = 31) | ‘I don’t like talking about problems in a group’ |
| 2. | Desire to receive therapy/therapy viewed as helpful (n = 16) | ‘It would be a standard telephone call each week, when I’m ill I do not seek help so this would be useful’ |
| 3. | Desire to receive self-help manual (n = 9) | ‘The self-help manual seems interesting’ |
| 4. | Group support unnecessary (n = 8) | ‘I don’t feel I need a group at this moment’ |
| Self-help with telephone and group support or SHG | ||
| 1. | Social aspect/normalising/sharing experiences (n = 19) | ‘I’m not over the moon about cognitive therapy but I like the idea of meeting people with the same experiences’ |
| 2. | Benefits to self/highest level of support is most beneficial (n = 17) | ‘I’d try anything that might help’ |
| 3. | To gain knowledge/information/understanding (n = 5) | ‘I need to know where I’m going and need to know more about things’ |
| 4. | For an experience/activity/out of interest (n = 3) | ‘Somewhere to go, something to do’ |
| 5. | Desire for group support (n = 5) | ‘The group will be useful and interesting’ |
Willingness to be randomised
Of the 81 participants who reported that they would consider taking part in the PRPT, the majority (57%, n = 46) said they would be unwilling to be randomised to treatment group. Results of the content analysis highlighting the reasons for this are shown in Table 43.
| Major themes (frequency) | Examples | |
|---|---|---|
| Willingness to be randomised | ||
| 1. | To assist the research/make a contribution (n = 14) | ‘To have the opportunity to take part means a lot, to make a contribution’ |
| 2. | No strong preference/no urgent need for additional support (n = 12) | ‘I don’t mind, it’s not a problem being chosen or not chosen’ |
| 3. | Positive view of randomness/chance/lack of decision-making (n = 10) | ‘I feel safer being randomly chosen’ |
| 4. | Belief in fairness/all deserve a chance (n = 5) | ‘Not everyone can get what they want when they want it’ |
| Unwillingness to be randomised | ||
| 1. | Lack of desire for/dislike of aspect of therapy/therapy in general (n = 27) | ‘I can’t see the point of the other preferences, they wouldn’t work for me, wouldn’t be productive’ |
| 2. | Desire to receive preferred option/to have a choice (n = 21) | ‘I might get high support and not want to take that and then I’d lose the option of low support’ |
| 3. | Allocation should be based on need/assessment (n = 4) | ‘An assessment should be made of a person to see what they actually need’ |
Characteristics associated with preferences
None of the assessed sociodemographic and clinical variables was found to be significantly associated with preferences for therapy or willingness to be randomised. Comparisons of those who were willing and unwilling to participate could not be performed owing to the low number who were unwilling (n = 9).
Discussion
Key findings
Hypothetical preferences indicated that willingness to participate in a PRPT of a cognitive–behavioural psychological treatment for psychosis was high in comparison with other psychiatric research studies. 183 Both personal and altruistic benefits were evident, as has been found in other research. 181 Reasons for potential participation included a desire to gain information or understanding, to have a new experience or activity, or to share experiences with others, suggesting that there may be gaps in service provision in these areas. Reasons for non-participation in the future trial largely reflected a negative view of the treatment offered, or satisfaction with current treatment, consistent with a cost–benefit analysis.
The majority of the sample had a preference for therapy in addition to TAU, consistent with previous research regarding psychological therapy for other mental health problems. 190 The telephone support condition (SHT) was more popular than the telephone plus group support option (SHG), although considerable numbers of participants opted for each. A substantial number of participants opted for TAU alone, in contrast with previous findings. 178 Many of those who opted for TAU in the current study reported perceived lack of need or desire for the additional therapy. Reasons for preferring SHT indicated a desire to receive therapy or gain information and the lack of desire for group support, often due to a specific dislike of group situations. In contrast, reasons for preferring SHG often reflected a positive view of the social or group support, or the higher level of support available. Notably, participants’ reasons for their treatment preferences showed wide individual variation.
Most participants reported unwillingness to be randomised, (in line with King et al. ’s175 review) and cited a desire to receive the preferred treatment or for allocation to be based on necessity, or therapy being viewed as unhelpful. Reasons for willingness to be randomly allocated included altruistic reasons, a personal positive belief in chance and the absence of a strong preference. Participants seemed able to understand randomisation despite previous research191 indicating that this may not be the case. None of the sociodemographic and clinical variables measured was significantly associated with preferences, supporting the need for an individualised approach.
Limitations
The sample may be biased owing to recruitment via mental health services, although it is likely that findings are generalisable to future similar trials. Further, the reported high rate of willingness to participate in the proposed PRPT may reflect participants’ general acceptance of research. Bespoke, non-validated measures were used to determine preferences, which is not ideal. In addition, hypothetical rather than actual preferences were assessed, although the two have been found to be relatively consistent. 192 It is possible that cognitive functioning (which was not assessed) and/or the presence of symptoms may have impacted on participants’ ability to make decisions. 193 However, participants were able to give coherent reasons for their preferences, and clinical severity was not related to preferences.
Implications for research and clinical practice
The findings indicate that many service users with experience of psychosis welcome choice about psychological treatment and highlight the importance of individual differences. Future research may involve the more detailed investigation of the PRPT design (including feasibility and statistical considerations and differences in outcomes compared with RCTs), in-depth qualitative research, development of standardised measures of preferences and interventions to improve the understanding of research. Finally, it would be of interest to determine whether or not the participants’ stated hypothetical preferences and reasons are reflected in real decisions.
This research adds to the growing literature regarding psychological treatment for individuals with experience of psychosis, for which the ethics of treatment choice may be particularly pertinent owing to the experience of marginalisation. The results indicate that preference trials are feasible in terms of overall popularity and proposed treatment options, including TAU. Randomisation was often viewed negatively; therefore, preference designs may enhance recruitment and prevent ‘resentful demoralisation’. 170 Preferences were not associated with any of the variables measured, suggesting that it is difficult to predict preferences on the basis of individual characteristics and that all service users should be supported to state their choices.
Phase 2: a proof of concept study of a recovery-focused self-help package for people with psychosis
Objectives
This study aimed to obtain information to facilitate the implementation of a PPT to evaluate a recovery-focused self-help package of treatment for people who experience psychosis.
The main objectives of the proof of concept study were as follows:
-
To determine the appropriateness and perceived usefulness of the manual and telephone help by monitoring the number of people who refuse participation, the number of sessions when clients are available, any problems arising concerning telephone access and from gaining feedback from clients participating in the study.
-
To determine in what ways the manual and delivery modes might be modified to increase the perceived appropriateness and usefulness of the manual and telephone help.
Method
Pilot study context and design
This self-help therapy and recovery proof of concept study constituted phase 2 of project 4 in the recovery programme of research. This followed from phase 1 work developing the self-help recovery guide for psychosis and exploring people’s hypothetical preferences for different levels of therapeutic support. The proof of concept study used a randomised design whereby participants were allocated to either receive TAU or extra therapeutic support in the form of the recovery guide plus telephone CBT provided in 30-minute sessions over 6 months, in addition to monthly peer support sessions. Participants met with a researcher at the start of the project and at 6 months and 12 months to assess their experiences, emotions, functioning and recovery using a range of measures.
Recruitment
The proof of concept study aimed to recruit 30 participants from three NHS trusts: Pennine Care, Greater Manchester West and Manchester Mental Health and Social Care Trust. Participants met the following inclusion criteria:
-
aged 18–65 years
-
in contact with mental health services
-
met ICD-10 criteria for non-affective psychosis (schizophrenia, schizophreniform disorder, schizoaffective disorder, delusional disorder)
-
at least 1 month of stabilisation if the person had experienced a symptom exacerbation in the last 6 months
-
able to provide written informed consent
-
able to read the self-help manual/assessments
-
able to use the telephone.
Results
In total, 29 participants were recruited over a 6-month period. Figure 7 details the recruitment progress of those initially identified as potentially eligible.
FIGURE 7.
Recruitment rates and refusals.
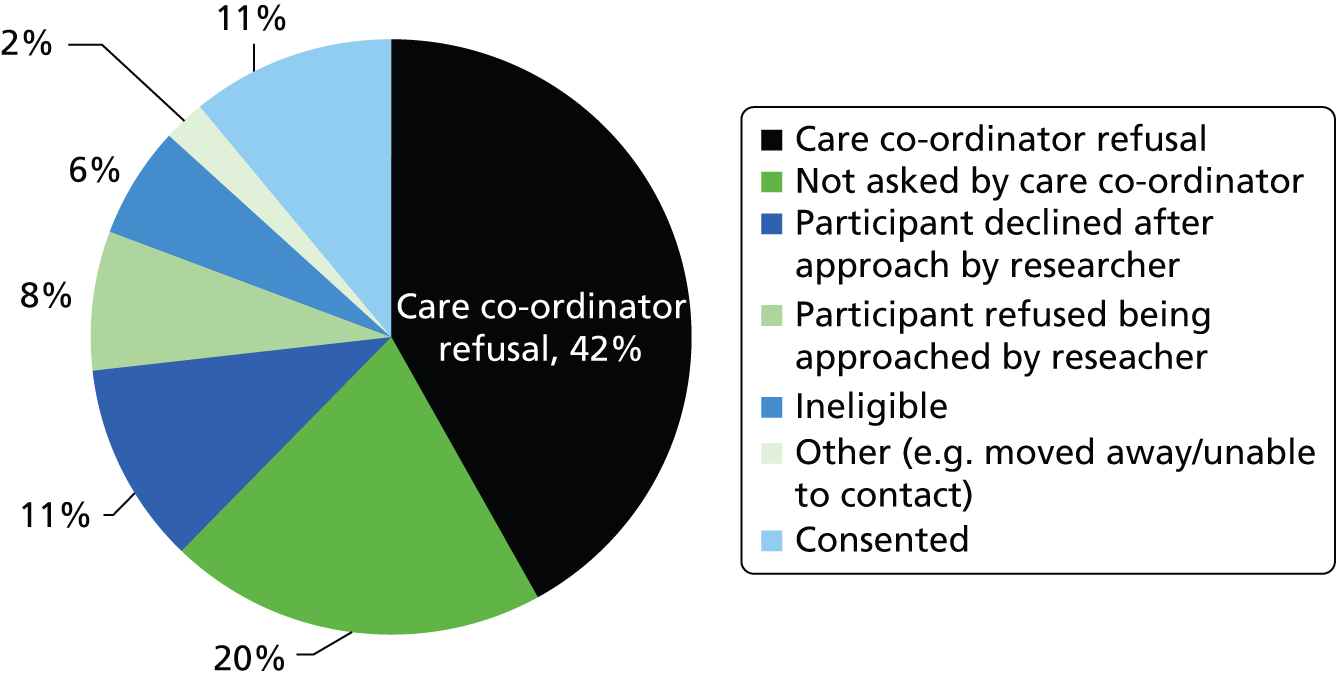
Retention and therapy uptake
Of the 29 people in the study at the start, 27 were followed up at 6 months and the full 29 were followed up at 12 months, demonstrating an excellent retention rate for the project as a whole.
As a result of the random allocation, 15 people continued with their TAU with no extra support provided by the project and 14 people were offered therapy and peer support sessions and the recovery guide.
Therapy session uptake
Of the whole therapy sample:
-
mean number of therapy sessions conducted: 14
-
mean number of therapy sessions offered: 17
-
mean per cent of therapy sessions conducted, of those offered: 79%
-
number of withdrawals from therapy: 5 (out of 14).
Among those who did not withdraw:
-
mean number of therapy sessions conducted: 17
-
mean per cent of therapy sessions offered: 20
-
mean per cent of therapy sessions conducted, of those offered: 87%.
Sections of the guide used
The session notes of those participants in therapy were reviewed in order to discern which guide sections were utilised. A summary of this information is provided in Figure 8, showing that most participants were able to utilise chapters 1 and 2 of the self-help guide, and a good proportion also used additional chapter 3 sections (chapter 1, What is Recovery from Psychosis, chapter 2, Making Sense of Yourself and chapter 3, Your Current Situation).
FIGURE 8.
Sections of the guide used.
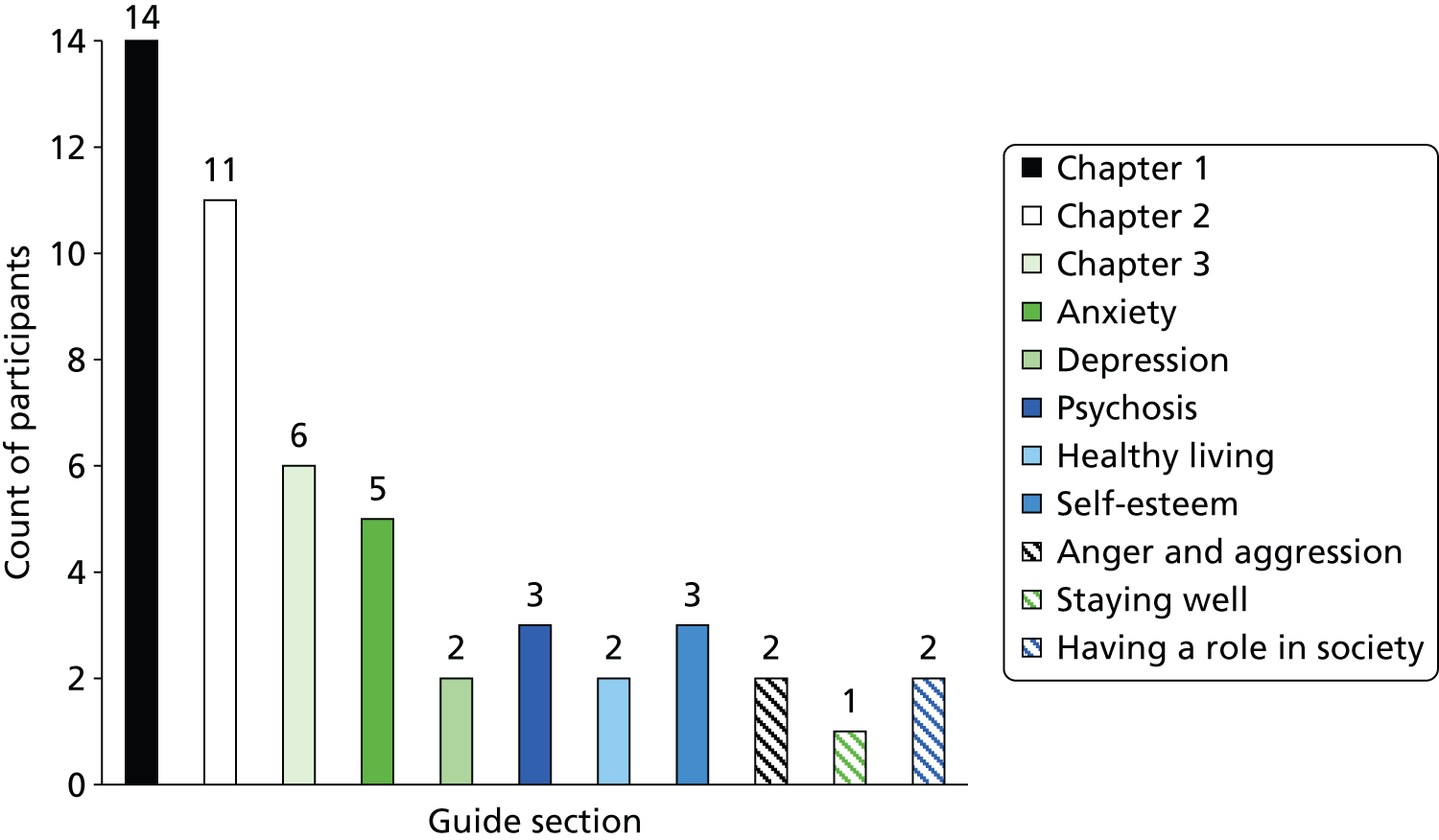
Quantitative analyses
An additional aim of the pilot study was to assess the potential impact of the guide and therapy on people’s functioning, recovery and experiences of psychosis.
The primary outcome was a measure of recovery; the QPR. 32 Analysis of the data showed that there were no significant differences between the therapy and TAU groups on the QPR measure at baseline, 6 months or 12 months. Other measures showed variations in their initial starting scores and change scores. Allocation group (i.e. TAU vs. therapy) significantly predicted 12-month follow-up scores while controlling for baseline scores on measures of negative self-esteem, depression, negative symptoms of psychosis and general symptoms of psychosis. Those in the therapy condition had higher mean scores on these measures at 12 months, which suggested the possibility that the additional therapy (consisting of a combination of the recovery guide, telephone-delivered CBT and peer support) actually hindered recovery. When we only included those people in the therapy group that had more than five therapy sessions in total, only the effects for negative self-esteem and general symptoms of psychosis remained significant.
The possibility that this intervention was delaying recovery was considered by the study team and the independent DMC. However, it was decided that the small sample size of the study made it difficult to make any firm conclusions on the basis of these analyses. Given that the preference design of the next phase meant that people were able to choose which arm of the trial they were allocated to and the qualitative feedback (see Qualitative feedback) was largely positive, it was decided that the next phase was merited.
Qualitative feedback
Feedback interviews were conducted by a service user researcher with four participants receiving telephone therapy. The interviews explored participants’ views on the guide (Table 44), telephone therapy (Table 45), reasons for taking part, peer support (Table 46), CBT model and suggestions for changes. A selection of comments on therapy, the guide and peer support is provided below (roughly proportionate to the total amount of comments in each category). Many suggestions were incorporated in revisions for the current trial, including reducing the amount of text, reducing the number of rating scales to complete, adding more blank copies of formulation diagrams and tables, offering longer and more telephone sessions and offering group sessions.
| Positives | Negatives |
|---|---|
| Good to see other people I could identify withWritten in clear and easy to understand languageBeing able to work at your own pace was goodProvided different techniques for getting betterGot a sense of pride, sense of achievement, another string to your bowIt has been a great help. I do feel it has aided me in my first steps to recovery. If I hadn’t got the guide and help – I don’t know where I would be now – I think things would probably have got a lot worse | A lot of reading in the first few sections which I wasn’t keen onI didn’t like the scales, I could be a 5 on one day and the next day I could be a 2. I left a lot of them blank. I am not keen on them personallyA bit more demanding than I thought – filling in the different sections and thinking about my mental health |
| Positives | Negatives |
|---|---|
| Easier in some ways than face to face – can put phone down and stop talking, have a cigarette and coffee if nervousMeeting person (therapist and peer supporter) helps you touch base and get an image of the personBuilt a positive relationship with therapist despite being wary to start with about telephone therapyFelt it helped – could get my point across, therapist made some good suggestions and helped with the guide | Hard getting used to talking to someone on phone but got used to itWould prefer face to face therapy – you don’t get face to face contact – can’t read body language |
| Positives | Negatives |
|---|---|
| Nice to have someone prepared to listenGives you a different angle from the therapy angle to talk more generally and not as structured a conversationGood that is unstructured because I can say what I want but bad if you don’t know what you are going to talk aboutGave me a sense of camaraderie | Found it quite stressful at time but not right not to have itFrequencies of contact not as great so could be stressful |
Conclusions
Attrition from the study was low and uptake of sessions offered was high, providing support for the appropriateness of the materials and mode of delivery. Moreover, qualitative feedback indicated a high degree of satisfaction from service users who participated in the therapy and provided useful information on how the materials and therapy delivery might be changed in order to better meet service user needs. The small sample size of the study makes it difficult to make any conclusions about the efficacy of the therapy in terms of service user outcomes.
Phase 3: a preference trial of recovery-focused cognitive–behavioural therapy for psychosis delivered over the telephone with support from a self-help guide and group sessions (Self-help Therapy and Recovery Trial)
Objectives
This study aimed to evaluate a self-help recovery intervention that was jointly developed and delivered by service users and CBT therapists, in the context of a PPT.
The Self-help Therapy and Recovery Trial (STAR-T) aimed to bring together factors of recovery, CBT, service user involvement and patient preference to evaluate a self-help recovery intervention that was jointly developed and delivered by service users and CBT therapists, in the context of a PPT for individuals who experience psychosis.
Method
Participants
Recruitment was undertaken in three North West England NHS Trusts: Greater Manchester West Mental Health NHS Foundation Trust, Manchester Mental Health and Social Care Trust and Five Boroughs Partnership NHS Foundation Trust.
Participants met the following inclusion criteria:
-
ICD-10 diagnosis of a schizophrenia spectrum disorder
-
aged 18–65 years
-
in contact with mental health services
-
able to use the telephone
-
able to read English
-
able to provide written informed consent
-
at least 1 month of stabilisation if the person has experienced a symptom exacerbation in the last 6 months.
Design
The STAR-T trial had three arms: TAU, low-support treatment (self-help recovery guide plus weekly CBT sessions delivered over the phone) and high-support treatment (the same as the low-support treatment, plus group therapy sessions). Participants were able to either choose their preferred treatment arm or they could choose to be randomised to treatment.
Procedure
Informed, written consent was obtained from all participants prior to the initiation of any assessment. All participants were given a payment of £10 for each assessment set as a token of appreciation.
Assessments were carried out at three time points: baseline, 9 months after baseline (post therapy) and a final follow-up at 15 months after baseline. Following the completion of the assessment procedures, participants were contacted by the trial manager, who conducted a semistructured interview to ascertain participants’ preferences for allocation. Participants were provided with an information sheet listing the four options (TAU, low-support treatment, high-support treatment or randomisation) and a short description of each. Based on the information gathered during this interview, participants were either allocated to their preferred therapy option or randomised to receive one of the therapy options. Randomisation was conducted remotely by an independent clinical trials unit and was performed using random permuted blocks.
Measures
Trial feasibility outcome: we will consider whether or not the trial design permitted the planned comparisons between randomised and non-randomised participants.
Primary outcome measure: QPR. 92
Secondary outcome measure: SEPS. 71
Other measures: included those of general symptom severity, delusion and hallucination severity, depression and anxiety. General symptom severity was assessed using the PANSS55,154,194 and delusion and hallucination severity was assessed using the PSYRATS,72 with PANSS scores. 195
Sociodemographic information was gathered relating to ethnicity, living arrangements, employment or education, marital status and religious beliefs.
Intervention
There were three intervention arms in the current study: TAU, low support and high support. TAU consisted of participants receiving their usual care only, alongside assessment visits at baseline, 9 months and 15 months. The low-support and high-support interventions were both provided in addition to usual care and assessments over 9 months. Low support consisted of the provision of the recovery guide, alongside weekly recovery-focused cognitive–behavioural therapy (RfCBT) sessions, which lasted approximately 45 minutes and were delivered over the telephone.
The recovery guide is a supported self-help resource that includes two core chapters (relating to the meaning of recovery, goals, resources and understanding the development of problems) and two chapters with numerous optional sections to facilitate work on overcoming obstacles (such as anxiety, paranoia, low self-esteem) or reaching wider recovery goals (such as finding employment, enjoying oneself and relaxing, developing social networks). The recovery guide was developed over approximately 1 year. It was produced in collaboration with both service users and staff from community-based mental health teams including EISs and CMHTs. Focus groups were held with both sets of participants in order to elicit what relevant questions such a guide should address and what kind of information would be useful in addressing these topics. In addition, several service users read drafts of the individual sections of the guide and provided extensive feedback in both written form and via additional focus groups. Participants were given the opportunity to work on the guide independently and also within telephone therapy sessions. Participants in phase 1 of the trial also received up to five sessions of peer support, provided by a researcher with lived experience of mental health challenges and delivered over the telephone.
The high-support arm consisted of all of the same elements of the low-support arm, with the addition of group sessions. Group sessions were delivered over 6 months of the 9-month therapy window and were offered roughly every 2 weeks, lasting 2 hours. Participants in the high-support arm attended a local group alongside two facilitators: a therapist and a researcher with lived experience of mental health challenges. The sessions followed the ethos of the recovery guide, exploring issues relating to recovery, cognitive–behavioural principles, normalising experiences and also provided a venue for participants to share ideas and experiences.
Therapy manuals for the purpose of replication and the fidelity scale used to assess therapist adherence to the intervention are available from the first author.
Analysis
The aim of the analysis was to evaluate the effects of the interventions and to assess whether or not they were unaffected by the mechanism of treatment selection (that is, by patient preference or random allocation). In the absence of significant numbers of participants accepting randomisation (see Preferences) this aspect of the analysis plan had to be abandoned. The outcome data were analysed using appropriate regression (analysis of covariance) models in order to assess the effects of treatment receipt, regardless of the mechanism of treatment selection, using several baseline covariates to allow for any possible confounding of the effect of treatment receipt on outcome. All analyses were carried out using Stata.
Results
The primary outcome analysis is provided in Table 47, as well as the demographic and therapy allocation data.
| Variable | n | % |
|---|---|---|
| Age (years) | ||
| Mean 36, SD 10.9 | ||
| Sex | ||
| Male | 60 | 63 |
| Female | 35 | 37 |
| Ethnicity | ||
| White | 76 | 80 |
| Black/minority ethnic group | 13 | 14 |
| Mixed race | 4 | 4 |
| Not reported | 2 | 2 |
| Occupation | ||
| Employed/studying | 24 | 73 |
| Not working/studying | 69 | 25 |
| Not reported | 2 | 2 |
| Education | ||
| Education post 16 years | 51 | 44 |
| No education post 16 years | 42 | 54 |
| Not reported | 2 | 2 |
| Living arrangements | ||
| Alone | 60 | 63 |
| With family members/partner | 31 | 33 |
| Supported accommodation | 2 | 2 |
| Not reported | 2 | 2 |
| Martial status | ||
| Married/civil partnership/cohabiting | 10 | 11 |
| Single | 83 | 87 |
| Not reported | 2 | 2 |
| Diagnosis | ||
| Schizophrenia | 39 | 41 |
| Schizoaffective disorder | 12 | 13 |
| Psychosis NOS | 35 | 36 |
| Delusional disorder | 3 | 3 |
| Paranoid schizophrenia | 6 | 6 |
| BD | 1 | 1 |
| Clinical team | ||
| CMHT | 59 | 62 |
| EIS | 36 | 38 |
Preferences
Figure 9 shows the distribution of chosen treatment choices within the trial. Three participants were randomised to treatment arm while the rest were allocated to their therapy of preference.
FIGURE 9.
Treatment allocation on the basis of stated preferences.

A total of 89 subjects chose (n = 86) or were randomised (n = 3) to treatment. Of those who were randomised, one participant was allocated to each group. One subject who chose TAU but changed to low support was assigned to their original choice (i.e. TAU) for the provision of summary statistics and all the analyses.
In order to evaluate the predictors of patient treatment choice, a multinomial regression model was fitted with a trinary outcome (TAU, low support or high support) for the 86 subjects who chose their therapy. The model included the following treated as quantitative variables: age, education, baseline scores for PANSS positive and PSP, and sex as a categorical variable. The relative risk ratio was significant for PANSS positive at baseline for the high support vs. TAU outcomes (p = 0.046) and sex was marginally significant for this comparison (p = 0.063).
Primary outcomes analyses
In all outcome analyses the baseline score was entered as a covariate along with baseline PANSS positive and PSP totals. Consistent with the choice model above, age, education and sex were also included in each linear regression model.
Table 48 shows the estimated treatment effects from fitting models to the three primary outcomes at 9 and 15 months as choice or randomisation to therapy.
| Month 9 | Treatment comparison | Treatment difference (score difference) | SE | p-value | 95% CI lower | 95% CI upper |
|---|---|---|---|---|---|---|
| QPR | Overall | 0.577 | ||||
| LS–TAU | –2.42 | 2.90 | 0.406 | –8.22 | 3.38 | |
| HS–TAU | –3.28 | 3.61 | 0.367 | –10.50 | 3.94 | |
| HS–LS | –0.86 | 3.68 | 0.817 | –8.23 | 6.51 | |
| HS and LS–TAU | –2.70 | 2.61 | 0.304 | –7.93 | 2.52 | |
| QPRIntra | Overall | 0.576 | ||||
| LS–TAU | –1.76 | 2.40 | 0.466 | –6.56 | 3.04 | |
| HS–TAU | –2.89 | 2.95 | 0.332 | –8.80 | 3.02 | |
| HS–LS | –1.13 | 3.03 | 0.71 | –7.19 | 4.93 | |
| HS and LS–TAU | –2.14 | 2.15 | 0.324 | –6.45 | 2.16 | |
| QPRInter | Overall | 0.501 | ||||
| LS–TAU | –0.84 | 0.71 | 0.242 | –2.26 | 0.58 | |
| HS–TAU | –0.45 | 0.88 | 0.616 | –2.21 | 1.32 | |
| HS–LS | 0.39 | 0.88 | 0.659 | –1.38 | 2.16 | |
| HS and LS–TAU | –0.71 | 0.64 | 0.274 | –2.00 | 0.58 | |
| Month 15 | Treatment comparison | Treatment difference | SE | p-value | 95% CI lower | 95% CI upper |
| QPR | Overall | 0.821 | ||||
| LS–TAU | 1.83 | 3.02 | 0.548 | –4.25 | 7.91 | |
| HS–TAU | 1.54 | 3.96 | 0.699 | –6.42 | 9.50 | |
| HS–LS | –0.29 | 3.95 | 0.942 | –8.23 | 7.65 | |
| HS and LS–TAU | 1.75 | 2.77 | 0.531 | –3.82 | 7.31 | |
| QPRIntra | Overall | 0.753 | ||||
| LS–TAU | 1.99 | 2.64 | 0.453 | –3.31 | 7.30 | |
| HS–TAU | 0.94 | 3.62 | 0.796 | –6.34 | 8.22 | |
| HS–LS | –1.05 | 3.65 | 0.775 | –8.39 | 6.29 | |
| HS and LS–TAU | 1.71 | 2.42 | 0.483 | –3.16 | 6.58 | |
| QPRInter | Overall | 0.361 | ||||
| LS–TAU | –0.09 | 0.71 | 0.903 | –1.51 | 1.34 | |
| HS–TAU | 1.15 | 0.90 | 0.208 | –0.66 | 2.97 | |
| HS–LS | 1.24 | 0.91 | 0.18 | –0.58 | 3.06 | |
| HS and LS–TAU | 0.30 | 0.66 | 0.653 | –1.02 | 1.62 |
Considering all three treatment groups at 9 months, there was no evidence of an overall treatment effect for the QPR total primary outcome (p = 0.58). For QPR total, the adjusted mean difference comparing high support to low support was –0.86 units meaning that on average the high-support group were less recovered on QPR but this was not significant (p = 0.82). Comparing high support and low support with TAU, the adjusted mean difference was –2.70 units, that is, on average the ‘extra’ support group were less recovered on QPR, but this was not significant (p = 0.30).
At 15 months there was no overall treatment effect for QPR total (p = 0.82). The adjusted mean difference comparing high support with low support was –0.29 units meaning that on average the high-support group were less recovered than low support but this was not significant (p = 0.94). The estimated mean difference between ‘extra’ support and TAU was 1.75, but non-significant (p = 0.53).
Missing primary outcome data and sensitivity analyses
The extent of missing follow-up QPR total data is shown in Table 49. For each treatment allocation, a separate logistic regression model was fitted using the same covariates as in the choice and standard outcomes model to predict who provided QPR total outcome data 9 months after baseline completion. Each model was used to generate an expected probability of providing outcome data and the reciprocal of this estimated probability was used as an inverse probability weight for use in sensitivity analyses of the 9-month primary QPR outcome. The same procedure was undertaken for the intrapersonal and interpersonal QPR subscales. These steps were repeated for the coprimary data at 15 months.
| Month | TAU, n (%) | LS, n (%) | HS, n (%) |
|---|---|---|---|
| 9 | 6 (18.2) | 7 (21.2) | 10 (43.5) |
| 15 | 10 (30.3) | 10 (30.3) | 12 (52.2) |
This method assumes that for subjects with a particular combination of baseline covariates the value of the outcome is independent of whether observed or not (‘missing at random’ assumption). The results of fitting the regression models with inverse probability weights showed no evidence of significant difference between these results and the basic approach.
Secondary outcomes analyses
The same basic analyses were performed on a pre-specified selection of secondary outcomes: four out of the six SEPS subscales and PANSS positive and negative subscales; the results are shown in Table 50. Inverse probability weight sensitivity analyses were not performed. The only significant result was for the SEPS negative experience outcome at 15 months for which there was an estimated difference in adjusted means comparing high support with TAU of 16.85 units (95% CI 1.36 to 32.35; p = 0.03) (Table 51).
| Variable | Treatment comparison | Treatment differencea | SE | p-value | 95% CI lower | 95% CI upper |
|---|---|---|---|---|---|---|
| SEPS | Overall | 0.792 | ||||
| Positive impacts of experiences | LS–TAU | 2.97 | 7.41 | 0.691 | –11.91 | 17.84 |
| HS–TAU | 6.58 | 9.84 | 0.507 | –13.17 | 26.32 | |
| HS–LS | 3.61 | 9.73 | 0.712 | –15.92 | 23.14 | |
| HS and LS–TAU | 3.97 | 6.84 | 0.564 | –9.75 | 17.69 | |
| SEPS | Overall | 0.905 | ||||
| Negative impacts of experiences | LS–TAU | –1.31 | 4.17 | 0.754 | –9.69 | 7.06 |
| HS–TAU | 0.93 | 5.13 | 0.856 | –9.36 | 11.23 | |
| HS–LS | 2.25 | 5.32 | 0.674 | –8.43 | 12.92 | |
| HS and LS–TAU | –0.54 | 3.72 | 0.884 | –8.01 | 6.93 | |
| SEPS | Overall | 0.593 | ||||
| Positive dimensions of psychosis | LS–TAU | –0.18 | 0.66 | 0.788 | –1.49 | 1.14 |
| HS–TAU | 0.68 | 0.84 | 0.422 | –1.01 | 2.37 | |
| HS–LS | 0.86 | 0.84 | 0.313 | –0.83 | 2.55 | |
| HS and LS–TAU | 0.08 | 0.60 | 0.892 | –1.13 | 1.29 | |
| SEPS | Overall | 0.294 | ||||
| Negative dimensions of psychosis | LS–TAU | 1.56 | 1.04 | 0.140 | –0.53 | 3.64 |
| HS–TAU | 1.42 | 1.32 | 0.285 | –1.22 | 4.07 | |
| HS–LS | –0.13 | 1.30 | 0.919 | –2.75 | 2.48 | |
| HS and LS–TAU | 1.52 | 0.95 | 0.116 | –0.39 | 3.42 | |
| PANSS | Overall | 0.553 | ||||
| Positive | LS–TAU | 0.02 | 0.80 | 0.981 | –1.59 | 1.63 |
| HS–TAU | 1.05 | 1.03 | 0.311 | –1.01 | 3.10 | |
| HS–LS | 1.03 | 1.04 | 0.325 | –1.05 | 3.11 | |
| HS and LS–TAU | 0.34 | 0.74 | 0.647 | –1.13 | 1.81 | |
| PANSS | Overall | 0.385 | ||||
| Negative | LS–TAU | –0.89 | 0.92 | 0.339 | –2.74 | 0.96 |
| HS–TAU | 0.70 | 1.25 | 0.580 | –1.81 | 3.20 | |
| HS–LS | 1.59 | 1.24 | 0.204 | –0.89 | 4.06 | |
| HS and LS–TAU | –0.47 | 0.87 | 0.593 | –2.20 | 1.27 |
| Outcome | Treatment comparison | Treatment differencea | SE | p-value | 95% CI lower | 95% CI upper |
|---|---|---|---|---|---|---|
| SEPS | Overall | 0.389 | ||||
| Positive impacts of experiences | LS–TAU | –2.40 | 7.72 | 0.758 | –17.94 | 13.15 |
| HS–TAU | 12.09 | 10.54 | 0.257 | –9.13 | 33.31 | |
| HS–LS | 14.49 | 10.55 | 0.176 | –6.74 | 35.72 | |
| HS and LS–TAU | 1.49 | 7.25 | 0.838 | –13.09 | 16.08 | |
| SEPS | Overall | 0.094 | ||||
| Negative impacts of experiences | LS–TAU | 6.46 | 6.04 | 0.290 | –5.69 | 18.61 |
| HS–TAU | 16.85 | 7.70 | 0.034 | 1.36 | 32.35 | |
| HS–LS | 10.39 | 8.27 | 0.215 | –6.26 | 27.05 | |
| HS and LS–TAU | 9.92 | 5.40 | 0.073 | –0.95 | 20.79 | |
| SEPS | Overall | 0.881 | ||||
| Positive dimensions of psychosis | LS–TAU | –0.19 | 0.64 | 0.772 | –1.47 | 1.10 |
| HS–TAU | 0.22 | 0.81 | 0.792 | –1.42 | 1.85 | |
| HS–LS | 0.40 | 0.81 | 0.624 | –1.23 | 2.04 | |
| HS and LS–TAU | –0.06 | 0.58 | 0.915 | –1.23 | 1.11 | |
| SEPS | Overall | 0.153 | ||||
| Negative dimensions of psychosis | LS–TAU | 1.00 | 1.05 | 0.349 | –1.12 | 3.11 |
| HS–TAU | 2.66 | 1.37 | 0.058 | –0.09 | 5.41 | |
| HS–LS | 1.66 | 1.43 | 0.251 | –1.22 | 4.54 | |
| HS and LS–TAU | 1.52 | 0.95 | 0.118 | –0.40 | 3.44 | |
| PANSS | Overall | 0.451 | ||||
| Positive | LS–TAU | 1.03 | 1.11 | 0.361 | –1.21 | 3.26 |
| HS–TAU | 1.70 | 1.45 | 0.245 | –1.21 | 4.61 | |
| HS–LS | 0.68 | 1.42 | 0.636 | –2.18 | 3.54 | |
| HS and LS–TAU | 1.22 | 1.03 | 0.240 | –0.84 | 3.28 | |
| PANSS | Overall | 0.971 | ||||
| Negative | LS–TAU | –0.20 | 0.93 | 0.831 | –2.07 | 1.67 |
| HS–TAU | 0.03 | 1.31 | 0.982 | –2.60 | 2.66 | |
| HS–LS | 0.23 | 1.28 | 0.860 | –2.35 | 2.81 | |
| HS and LS–TAU | –0.14 | 0.87 | 0.869 | –1.89 | 1.60 |
Discussion
Unfortunately, as the trial was unable to compare treatment effects, both with and without randomisation to treatment, the data analysis had to be based on what, in effect, was an underpowered observational study, subject to all of the threats to its validity that such a study entails. It appears that, although patients had a strong preference for particular treatments, there is little evidence that it had any effect on their outcomes. The interventions appeared to be ineffective despite the likely selection effects (confounding) induced by letting the participants have their preferred treatment. The failure to randomise also has important implications for future evaluations of these interventions and there is little to suggest that an appropriately designed randomised trial would be feasible.
The STAR-T trial is the first PPT to be conducted with people who experience psychosis and, therefore, service user preferences, in terms of therapy allocation, are of particular interest. Only 3 out of the 89 participants chose to be randomised, showing that participants had strong preferences about their treatment. This finding suggests that services may need to assess treatment preferences and offer increased flexibility in what they offer, to provide service users with informed choice and involve individuals in collaborative health-care decisions, as recommended by national guidelines for the treatment of psychosis. 14 However, it is also worth noting that, although the participants were able to choose their form of treatment, our trial showed little evidence that such choices effected outcomes or engagement.
Historically, people who experience psychosis may not have been involved in many treatment decisions, despite the majority of patients being able to make safe and appropriate choices about their treatment. 196 However, informed and shared decision-making can increase feeling of empowerment and positive self-esteem197 to key aspects of user-defined recovery from psychosis. 19 It seems likely that if individuals are receiving a treatment they have chosen, uptake rates will be higher and may also aid the process of recovery, as well as improving therapeutic relationships with clinical staff; however, we did not observe this in our trial.
Treatment preferences within the trial were surprisingly balanced, with a third of participants choosing their TAU, suggesting that many participants were happy with the treatment they were receiving and did not want any additional psychological support. These were found to be the main reasons for participants not choosing therapy in a qualitative study of theoretical patient preferences completed by Sumner et al. 186 in preparation for the STAR-T trial. This has additional clinical implications and reflects the fact that not everyone feels they would benefit from psychological therapy.
Within this trial, there were no significant differences in outcome between groups. However, at the 15-month follow-up, the majority of participants remained stable regardless of treatment group. Given that this is a group with typically high rates of relapse,198 it is possible that by choosing their own treatment, people received the level of support they needed and this was sufficient to keep them stable over a significant period of time; however, it is also likely that people remained stable owing to the benefits associated with participation in a clinical trial. 199
Attendance rates in the high-support group were particularly poor and this may be owing to a number of issues. The concept of low-support therapy (self-help manual and telephone support) was originally appealing to many services users as it meant therapy could be received at home and at a time that was convenient for them. Therefore, it may be the case that although participants liked the idea of receiving additional support through the high-support group therapy sessions, practical access and organisational issues may have affected attendance. In addition, those who chose high-support therapy were more likely to have increased positive symptoms (compare with those who chose TAU). This may have been why these individuals felt the need for additional support but may have also added to access difficulties.
In addition, while many individuals may have liked the idea of receiving additional support, the social aspects of the group therapy may have been difficult for some individuals. Future work should consider ways in which participants could receive extra help, without the potential pressure of a group situation, perhaps through additional one-on-one sessions with a service user researcher (with lived experience of psychosis) or through additional telephone sessions.
High-support therapy was chosen by the fewest number of participants and also had the highest rates of attrition. This, combined with the lack of significant treatment effects, may reflect that although having treatment choice was acceptable to service users, the therapy itself may need additional refinements. However, the findings from this trial show that people who experience psychosis have strong preferences about treatment and services should consider additional flexibility in treatment options, as well as shared decision-making, to accommodate this. The concept of service user-defined recovery remains somewhat subjective and it may be the case that the outcome measures were not sufficiently sensitive to individual changes during the trial. It is also possible that the power was underpowered to detect such changes; however, our results suggest that the interventions, as currently developed, did not effect recovery outcomes. Therefore, further work is needed to develop and refine recovery-focused treatment strategies, in order to ensure we have evidence-based psychological interventions, which are focused on the preferences and needs of service users.
Conclusions
This chapter contained studies that aimed to explore service user treatment preferences and modes of delivery of psychological support. The research was conducted in three phases:
-
an investigation of hypothetical preferences for psychological treatment in a sample of individuals experiencing psychosis
-
a pilot study to explore implementation of the preferred modes of therapy including development of a recovery-focused self-help package
-
a PPT to evaluate the recovery-focused self-help package of treatment for people who experience psychosis.
The research studies within this chapter are the first to explore treatment preferences in relation to recovery. The studies also contributed to the development of a collaboratively designed supported self-help resource known as the recovery guide. The recovery guide is a supported self-help resource that includes two core chapters (relating to the meaning of recovery, goals, resources and understanding the development of problems) and two chapters with numerous optional sections to facilitate work on overcoming obstacles (such as anxiety, paranoia, low self-esteem) or reaching wider recovery goals (such as finding employment, enjoying oneself and relaxing, developing social networks).
The first phase of this research found that, hypothetically, participants were willing to participate in a partially randomised preference trial of a cognitive–behavioural psychological treatment for psychosis, with reasons for potential participation including a desire to gain information or understanding, to have a new experience or activity, or to share experiences with others. Reasons for non-participation in the future trial largely reflected a negative view of the treatment offered or satisfaction with current treatment, consistent with a cost–benefit analysis.
The majority of the sample had a preference for therapy in addition to TAU and the telephone support condition (SHT) was more popular than the telephone plus group support option (SHG), although considerable numbers of participants opted for each. A substantial number of participants opted for TAU alone and reported a perceived lack of need or desire for the additional therapy. Participants’ reasons for their treatment preferences showed wide individual variation. Most participants reported unwillingness to be randomised (in line with the review by King et al. 175) and cited a desire to receive the preferred treatment or for allocation to be based on necessity, or therapy being viewed as unhelpful. None of the sociodemographic and clinical variables measured was significantly associated with preferences, supporting the need for an individualised approach.
The second phase of this research was a pilot study to evaluate the feasibility of the therapy package and modes of delivery. Attrition from the study was low and uptake of sessions offered was high, providing support for the appropriateness of the materials and mode of delivery. Moreover, qualitative feedback indicated a high degree of satisfaction from service users who participated in the therapy and provided useful information on how the materials and therapy delivery might be changed in order to better meet service user needs. The small sample size of the study makes it difficult to make any conclusions about the efficacy of the therapy in terms of service user outcomes.
The final phase of this research utilised the information on patient preferences and modes of delivery of therapy from the first two phases, to conduct a partially randomised preference trial. Only 3 out of the 89 participants in the study chose to be randomised, showing that participants had strong preferences about their treatment. Unfortunately, as the trial was unable to compare treatment effects, both with and without randomisation to treatment, the data analysis had to be based on what, in effect, was an underpowered observational study, subject to all of the threats to its validity that such a study entails. It appears that, although patients had a strong preference for particular treatments, there is little evidence that it had any effect on their outcomes. The interventions appeared to be ineffective despite the likely selection effects (confounding) induced by letting the participants have their preferred treatment. The failure to randomise also has important implications for future evaluations of these interventions and there is little to suggest that an appropriately designed randomised trial would be feasible.
The research in this chapter indicates that many service users with experience of psychosis welcome choice about psychological treatment, suggesting that services may need to assess treatment preferences and offer increased flexibility in what they offer, to provide service users with informed choice and involve individuals in collaborative health-care decisions, as recommended by national guidelines for the treatment of psychosis. 14 However, it is also worth noting that, although the participants were able to choose their form of treatment, our trial showed little evidence that such choices effected outcomes or engagement. The research also highlights the importance of individual differences and adds to the growing literature regarding psychological treatment for individuals with experience of psychosis, for which the ethics of treatment choice may be particularly pertinent owing to the experience of marginalisation. Feedback from participants suggests that the recovery guide may be a useful resource for provision of supported self-help in clinical services.
Chapter 6 Development and evaluation of a cognitive–behavioural approach to understanding and preventing suicide in people with psychosis
Background
Suicide and suicide behaviour are of substantial public and social concern. It is well established that risk of suicide is considerably elevated in those suffering from schizophrenia and psychosis. 6,200,201 Suicide ideation and suicide attempts are common, with up to 50% of patients experiencing suicidal ideation at any point in time or having a history of previous attempts. 3,6 The psychological processes underlying suicidal ideation, as well as resilience to suicide, are key areas for research in order to advance our understanding of suicide behaviour.
It is assumed that there is a progressive continuum from ideation, intent, action and completion. 200 Thus, suicidal ideation is a risk factor for self-harm and completed suicide and a legitimate clinical target in its own right. A meta-analysis of cognitive–behavioural interventions to reduce suicide behaviour202 demonstrated that individual, but not group, CBT was effective in significantly reducing suicide behaviour in adults, but not adolescents, in the short and medium term. This result held despite considerable variability both in the target populations and in the CBT interventions. However, there is a paucity of studies that have attempted to diminish suicide behaviour in psychosis, despite the well established high risk in this group. CBTP reduces positive and negative symptoms of psychosis, depression and anxiety but has less effect on hopelessness203 and suicidality. 42 Psychological interventions are most likely to be successful when they are clearly derived from a theoretical understanding of underlying mechanisms. 200,204 Advances in understanding the cognitive architecture underpinning suicidality have resulted in the development of empirically validated theoretical models, such as the Schematic Appraisal Model of Suicide (SAMS),204,205 which was modified from the Cry of Pain model. 206 The SAMS has three core psychological components, namely the presence of negative information processing biases, extensive ‘suicide schema’ and a negative and suicide-focused appraisals system. 204 To date, empirical evidence supports a multitiered appraisals system together with the operation of suicide schema in people experiencing suicidality, psychosis and post-traumatic stress disorder. 207–210 The Cognitive–Behavioural Suicide Prevention in Psychosis (CBSPp)211 was founded on the SAMS. Thus, the specific cognitions targeted by CBSPp are information processing biases and appraisals of defeat, entrapment, emotional dysregulation, social isolation and poor interpersonal problem-solving. 211 Although CBSPp arose from work with psychosis and post-traumatic stress disorder, it has the potential to be applied transdiagnostically. 211
Further research to investigate the efficacy of CBSPp is warranted. However, there are reservations about research among individuals diagnosed with schizophrenia,212 which have been endorsed by both psychiatrists and service users alike. 213 These participants may be at further risk from experiencing distress when the research concerns sensitive subjects such as trauma or suicide. 214 Further investigation of the experience of participants diagnosed with schizophrenia spectrum disorders, particularly when taking part in research on the topic of suicide is therefore warranted.
This chapter describes the three study phases used to develop and investigate the efficacy of CBSPp. First, a qualitative, open-ended methodology was employed to explore the nature and variety of the negative and positive experiences reported by participants taking part in a clinical study researching psychosis and suicide. This study was conducted based on recommendations from the SURG on the importance of investigating the feasibility and acceptability of asking people with experience of psychosis and suicidality to take part in research trials. The study was designed to assess potential feasibility for the main trial and to inform the nature and conduct of the subsequent phases of this project. In the second phase, psychological processes underlying suicide behaviour and resilience factors in a sample of participants with schizophrenia spectrum disorders were investigated. Phase 1 was used to inform the methodology and feasibility of the CBSPp RCT and phase 2 was used to inform the development of the CBSPp intervention. Finally, the third phase utilised a RCT to evaluate the CBSPp.
Phase 1: the subjective experience of participation in schizophrenia research
This research was previously published as, and much of this text is reproduced with permission from, Taylor PJ, Awenat Y, Gooding P, Johnson J, Pratt D, Wood A, et al. The subjective experience of participation in schizophrenia research: a practical and ethical issue. J Nerv Ment Dis 2010;198:343–8. 215
Objectives
This study aimed to investigate the subjective experiences of research participation in individuals with a diagnosis of a psychotic disorder. The focus was on the experiences of participants taking part in a clinical study researching psychosis and suicide.
Method
Participants
The sample consisted of 79 outpatients from the Greater Manchester area who consented to take part in a larger study investigating psychological factors predicting vulnerability to suicide (mean age = 42.3 years, SD = 11.7 years; 23 women). All participants met the following inclusion criteria: (1) a chart diagnosis (ICD-10) of a schizophrenia spectrum disorder; (2) being over the age of 18 years; (3) psychosis not caused primarily by drug misuse or organic disorder; (4) currently not at very high risk of suicide as judged by their keyworker or other appropriate health-care professional; and (5) capable of providing informed consent as judged by their keyworker or other appropriate health-care professional. The majority of participants had a diagnosis of schizophrenia (n = 72, 91.1%). The remainder had received diagnoses of other schizophrenia spectrum disorders (e.g. schizoaffective disorder, atypical psychosis, and psychosis not otherwise specified). The majority of participants were white British (n = 63, 79.7%), with the remainder being either mixed British (n = 6, 7.6%), Asian (n = 3, 3.8%), Afro-Caribbean (n = 1, 1.3%), or other (n = 4, 5.1%). Ethnicity data were missing for two participants.
Measures
A feedback form was provided to allow written feedback about the experience of taking part in the study. This form included three open questions, beneath which there was space for participants to respond: Question 1, How did you find it talking about the issues raised in the study? Question 2, What was your general experience like, taking part in this study? Question 3, How do you feel about research in this area? Questions 1 and 2 both assessed participant’s personal experiences of the research. The focus of the first question was on participant’s reactions to the content of the research, whereas the second question looked at the overall experience of the research process. The third question assessed general views and attitudes towards clinical psychological research. There was also room for participants to provide any additional comments. The question number is displayed in parenthesis next to all quotes cited in this article. The form was completed by the participant with a researcher present to provide support and answer questions.
Procedure
The larger study was the first in a planned series looking at factors conferring vulnerability to suicidality in schizophrenia. This research was reviewed and approved by an NHS research ethics committee. Informed consent was obtained from all participants before taking part in the study. Participants were informed that their responses would be kept confidential except in circumstances where they suggested they were going to harm themselves or somebody else, in which case a relevant member of their care team would be informed. The study lasted between an hour and an hour and a half with a researcher present throughout. The study involved completing a range of self-report measures, tasks and a clinical interview assessing negative cognitions, attitudes and psychopathology, including depression and suicidality. At the end of the study, each participant was asked to provide feedback about their experience during the study on the form provided, in particular noting down anything they liked, disliked or found distressing about the study.
Qualitative thematic analysis
The use of qualitative thematic analysis has been advocated within psychology as an analytic tool because of its inherent methodological and theoretical flexibility216,217 allowing the identification and interpretation of central themes emerging from the data. The main aim of this analysis was to uncover key themes reflecting participants’ opinions, motivations, and experiences of taking part in the research. In this instance an inductive, exploratory approach was employed. A realist stance underlined this analysis, whereby participants’ responses were assumed to reflect genuine aspects of their experience, motivations, and views. The qualitative analysis was initially conducted by two members of the research team: a service user with personal experience of having a severe and enduring mental health condition, currently working as an Honorary Research Fellow within the Division of Clinical Psychology (University of Manchester) and a Doctoral student in clinical psychology. Responses to each question on the feedback form were studied separately in turn, with responses reread multiple times to identify key features. Data were then hand sorted and responses with similar content were gathered together into categories, which were then divided into emerging themes. Questions raised in Polit and Hungler’s218 qualitative content analysis framework (e.g. ‘What is going on here?’, ‘What is this?’, ‘What does this mean?’) were applied to each item of data to aid the process of coding and analysis. Themes were then studied and interpretations applied. Themes were based on the prevalence of particular patterns within the data, but also in terms of relevance and importance of these patterns to the research aims. 217 Further examination, checking and group discussion were carried out by the remaining members of the research team. A single item of data contributed to < 1 theme in some cases. The results were also discussed with the SURG at the University of Manchester. SURG is a body of service users who aid in the development and conduct of mental health research both through providing consultation and feedback and actively conducting research themselves. Consultation of this group provided a form of member checking of the interpretations made by the research team, as advocated by Glaser and Strauss,219 to assure qualitative validity and rigor.
Results
Descriptive statistics
Six (7.6%) participants failed to provide any feedback. Reasons for this were not formally recorded, but anecdotally the most common reason cited was that participants had nothing they wanted to say. A further three participants completed the feedback form for questions 1 and 2, but left the third question blank and a single participant did not respond to question 1 alone. Responses to each question were rated for the presence of negative and positively valenced content. Table 52 reports the frequency of positive and negative content in responses to each question. It should be noted that some responses included both positive and negative content [e.g., ‘I found it interesting although difficult at times (Q1)’, ‘Quite depressing, overall positive (Q1)’] and were subsequently rated separately for both positive and negative content. This was only apparent in three cases for the first question and one for the second question. If a conservative approach is taken, whereby these mixed responses are classified just as negative, then for the first question, 33 (41.8%) responses were positive and 12 (15.2%) responses negative, whereas for the second question, 36 (45.6%) responses were positive and 7 (8.9%) responses negative. These results are very similar to those obtained when positive and negative elements were considered separately (see Table 52). A second independent judge rated a subset of the responses (n = 47, 59.5%). Inter-rater agreement between judges was good, with kappa scores averaging at κ = 0.92. These are reported by question and valence in Table 52. The remainder of responses were neutral in content [e.g., ‘Okay (Q1)’, ‘All right (Q1)’, ‘I didn’t mind, it was fine (Q1)’].
| Question | Positive, n (%) | Inter-rater agreement (k) | Negative, n (%) | Inter-rater agreement (k) |
|---|---|---|---|---|
| How did you find it talking about the issues raised in the study? | 36 (45.6) | 0.90 | 12 (15.2) | 0.88 |
| What was your general experience like taking part in this study? | 38 (48.1) | 0.90 | 7 (8.9) | 1.00 |
| How do you feel about research in this area? | 48 (60.8) | 0.85 | 2 (2.5) | 1.00 |
Thematic analysis
Five key themes were identified through the qualitative analysis of the feedback data. These themes were reviewed and validated by members of a SURG. A summary of these themes and associated responses is displayed in Table 53.
| Themes | Responses |
|---|---|
| Altruism | Overall positive, enjoyed helping. It was okay, glad that they did it (Q2) |
| If it helps people with illness I am all for research (Q3) | |
| Good, how else will the helpers help people without understanding (Q3) | |
| Very interesting and helpful for other sufferers (Q3) | |
| Little bit more help for people like me (Q3) | |
| If it helps other people in the long run then it’s worth it (Q3) | |
| Happy to help others (additional comments) | |
| I hope it(s) benefitiol (beneficial) to mental health | |
| Good idea to maybe think 1 d you could stop these problems for people (Q3) | |
| Good because people need help (Q3) | |
| I feel like it is helping other’s if it stop’s somebody from comiting (committing) suicide. It’s a good thing (Q3) | |
| I was glad to help (Q3) | |
| Helpful on both sides (Q3) | |
| The value of research | Necessary and needed (Q3) |
| Very important (Q3 × 3) | |
| Worthwhile (Q3) | |
| Think it’s a good thing (Q3) | |
| Think it’s great (Q3) | |
| Good thing (Q3) | |
| It’s something that needs to be done. Psychology is in it’s infancy (Q3) | |
| Very good idea (Q3) | |
| Very useful (Q3) | |
| Should be more research (Q3) | |
| Could be quite useful (Q3) | |
| About time (additional comments) | |
| More researches should be done (additional comments) | |
| Positive and promising (Q3) | |
| Important (Q3) | |
| The research is necessary and ongoing (Q3) | |
| It’s one way of finding out about things (Q3) | |
| Not enough of it (Q3) | |
| Worthwhile (Q3) | |
| I agree (Q3) | |
| Therapeutic | It helps me with my problems when discussing issues with my health (Q1) |
| Comfortable, makes me aware of myself (Q1) | |
| Helpful (Q1) | |
| Released (Q1) | |
| The interview reminded me of some of my problems in the past, but I found it helpful to talk about them (Q1) | |
| Didn’t bother me, glad to get it out of my system (Q1) | |
| Very good, it helps me gain clarity (Q2) | |
| Made me think (Q2) | |
| I felt released and calm (Q2) | |
| Helpt (helped) me (Q2) | |
| Very helpful (Q2) | |
| I really enjoyed it, remembered a lot of things in my life (Q2) | |
| Said things I’ve not said to my psychiatrist, because it’s confidential it was a bit of a release (Q2) | |
| I felt quite comfortable talking about my issues. The suicide attempt was a few months ago, but being asked these question(s) makes me realise I’m not alone and my thought and emotion are quite common (Q1) | |
| Great. The talking did me good (Q2) | |
| Great, I feel much better now I can open up about things that have happened in my life. Before, I couldn’t let it out and that made me depressed (Q1) | |
| Very easy. Especially feeling you can confide. To tell the truth (Q1) | |
| Brilliant. Good therapy (Q1) | |
| I found it quite therapeutic (Q1) | |
| Therapeutic (Q2) | |
| Relaxing (Q2) | |
| Enjoyable experience | Alright, enjoyed doing it (Q2) |
| Fun (Q2) | |
| I enjoyed it (Q2) | |
| I am enjoying myself thoroughly all question and find that good think with one and another (Q3) | |
| I enjoyed the session with Judith and Peter (additional comments) | |
| Enjoyed the experience (Q1) | |
| I enjoyed the first part of the course (Q1) | |
| I found it quite enjoyable (Q3) | |
| Enjoyed it (Q1) | |
| Negative experiences | Alright. Asking questions about the devil were distressing (Q1) |
| Quite depressing (Q1) | |
| Distressing to some degree (Q1) | |
| I found it interesting although difficult at times (Q1) | |
| Always difficult to talk about, overall okay (Q1) | |
| I was scared at first, but alright during the study (Q2) | |
| Not good to some degree (Q2) | |
| Anxious, didn’t like cards or words (Q2) | |
| Felt a bit nervous (Q1) | |
| It was a bit difficult for me to talk about my issues but I had no problems with it (Q1) | |
| I was a bit nervous but the researcher was friendly and explained the research process to me (Q2) | |
| Fine, a little difficult when asked to talk about my ‘breakdown’ (Q1) | |
| I got very tired (Q2) | |
| Difficult (Q1, Q3) | |
| A little bit difficult, but on the whole OK (Q1) | |
| Uneasy (Q1) | |
| Hard, OK (Q1) | |
| On the whole alright, but I had some difficulty thinking of the memories (Q2) | |
| Find it hard to bother with (Q3) |
Altruism
This theme included comments that revealed a desire to participate in the research not particularly for personal gain, but rather for ‘the greater good’ of others in the future: ‘Happy to help others (additional comment)’, ‘If it helps other people in the long run then it’s worth it (Q3)’, and ‘I was glad to help (Q3)’. Sometimes this included a particular desire to help those with similar experiences and mental health problems to the participants themselves: ‘Very interesting and helpful for other sufferers (Q3)’, ‘If this helps people with illness I am all for research (Q3)’, ‘A little bit more help for people like me (Q3)’, and ‘Good, how else will the helpers help people without understanding (Q3)’.
Value of being involved in research
This theme captured positive comments related to the value and benefits of research in general. This theme is distinct from the previous one in that responses were not linked to a specific motive for participating in research. Responses reflected the belief that clinical research was a worthwhile and valuable pursuit: ‘Worthwhile (Q3)’, ‘Very important (Q3)’, was necessary ‘Necessary and needed (Q3)’, ‘It’s something that needs to be done, psychology is in its infancy (Q3)’, ‘The research is necessary and ongoing (Q3)’, and of which more is required ‘More research should be done (additional comment)’, ‘Should be more research (Q3)’, ‘Not enough of it (Q3)’.
Therapeutic effect
Many service users described a personal therapeutic effect that they associated with taking part in the research: ‘It helps me with my problems when discussing issues with my health (Q1)’, ‘I felt quite comfortable talking about my issues. The suicide attempt was a few months ago, but being asked these question(s) makes me realise I’m not alone and my thoughts and emotions are quite common (Q1)’, ‘Brilliant. Good therapy (Q1)’, and ‘Therapeutic (Q2)’. In particular, a subset of participants suggested the interview had cathartic properties, expressing a feeling of relief and release related to talking to the researcher about their mental health problems and experiences: ‘Didn’t bother me, glad to get it out of my system (Q1)’, ‘I felt released and calm (Q2)’, and ‘Very easy. Especially feeling you can confide. To tell the truth (Q1)’. In one instance, awareness of the confidentiality of the research was highlighted as an important factor in allowing the participant to talk openly and experience catharsis: ‘I said things that I have not said to my psychiatrist, because it’s confidential it was a bit of a release (Q2)’. Therapeutic gains were linked to other psychological domains, including enhanced awareness of past problems ‘The interview reminded me of some of my problems in the past, but I found it helpful to talk about them (Q1)’ and increased self-awareness ‘Makes me aware of myself (Q1)’, and ‘Very good, it helps me gain clarity (Q2)’.
Enjoyable experience
A number of participants simply reported that they enjoyed taking part in the study ’Alright, enjoyed doing it (Q2)’, ‘Fun (Q2)’, ‘I enjoyed the session with Judith & Peter (the researchers) (additional comment)’, and ‘I found it quite enjoyable (Q3)’.
Negative experiences
Seventeen participants raised points that reflected negatively on their experience of being involved in the study: ‘Quite depressing (Q1)’, ‘Distressing to some degree (Q1)’, and ‘I got very tired (Q2)’. Participant’s negative experiences included difficulty and distress associated with disclosure and discussion of their mental health difficulties: ‘It was a bit difficult for me to talk about my issues, but I had no problems with it (Q1)’, ‘Fine, a little difficult when asked to talk about my ‘breakdown’ (Q1)’, and ‘Always difficult to talk about, overall okay (Q1)’. It should be noted in the above responses that despite the instances of distress, participants asserted that they found this questioning and the research generally acceptable. In one instance, this distress was linked in particular to a discussion about the participant’s auditory hallucinations in which they would hear the devil, suggesting a particular sensitivity to this topic: ‘Asking questions about the devil were distressing (Q1)’. Negative experiences also included anxiety and nervousness ‘Felt a bit nervous (Q1)’, ‘Anxious, didn’t like cards or words (Q2)’, although two participants also suggested these feelings could be successfully allayed: ‘I was a bit nervous but the researcher was friendly and explained the research process to me (Q2)’, and ‘I was scared at first, but alright during the study (Q2)’. Three responses suggested a sixth theme, which was the need to be heard, whereby participants indicated that their involvement in the research process gave them ‘a voice’ or an opportunity to talk openly about their experiences: ‘It gave me a chance to tell my story (Q2)’, ‘It’s about time we were asked (Q3)’, and ‘It enabled me to talk about something I know a little about (Q1)’. This theme was underrepresented in the data, but was considered interesting and could be an area of focus for future research.
Discussion
The current study aimed to investigate the subjective experiences of taking part in research for participants with a diagnosis of a psychotic disorder. The findings of this study are largely positive. Negative content was apparent in only a minority of responses, with prevalence ranging between 2.5% and 15.2% across questions. In contrast, positive content was more frequent, with prevalence ranging between 45.6% and 60.8% across questions. These findings are in line with a recent review suggesting a similar prevalence of negative and positive reactions to research in patient samples. 214 The qualitative analysis of feedback responses allowed an investigation into the nature and range of individuals’ experiences during the study. This analysis supports previous qualitative findings that research can have a number of benefits for those who participate. These include a sense of catharsis and therapeutic gain and a perception of helping others. 220,221 It should be clarified that the therapeutic effect reported by participants reflects their subjective experiences. Whether or not this therapeutic effect endures after the study and translates into a genuine improvement in well-being requires further investigation. The theme of therapeutic effect may stem in part from the unique interpersonal context of the research. The research environment may provide a context in which issues pertaining to mental health and suicide can be discussed in a confidential, open and non-judgemental way. Fear of treatment and involuntary hospitalisation may prevent some service users from discussing aspects of their mental health with health-care professionals,222,223 whereas for others certain issues may not be raised in routine assessments. 224 The research environment may differ in that the focus is not primarily on treatment, and confidentiality is emphasised along with the boundaries of this confidentiality. Consequently, some participants may see research as an additional forum to voice their problems, which lies outside of the usual context of care and treatment. Of course, research cannot be seen to provide any form of alternative to participants’ standard care. The current study also supports past findings that patients with diagnoses of schizophrenia predominantly express positive views about mental health research, viewing it as an important and valuable endeavour,213 and rating the possible benefit to others as an important reason for participating. 213,225 This motivation for participation in mental health research has also been endorsed by other populations, such as bereaved parents. 220 Anxiety and nervousness surrounding participation was also reported; however, it seems that for a few participants at least, these feelings were only present at the beginning of the study and were successfully reduced once the study began. It seems likely that the researcher may play an important role in quelling such anxieties, through careful explanation of the study procedure and identification of any particular concerns. Other negative experiences included distress and difficulty linked with the disclosure and discussion of personal mental health problems. The specific features of the study content that lead to distress may be idiosyncratic, reflecting personal sensitivities to certain topics. 221 Consequently, it may not always be possible to ascertain who will or will not be distressed by a particular feature of the study and, therefore, raises the importance of having adequate procedures in place for dealing with instances of participant distress. Such procedures need to be flexible enough to deal with the potential variation in the nature and degree of distress experienced. In the study from which the current feedback was taken, these procedures involved concluding the study with a detailed and interactive debriefing. This included a brief task designed to restore positive mood through encouraging a focus on the participant’s favoured activities and positive characteristics. This study also made use of multiple follow-up calls to assess individuals’ well-being after the study. In two instances, these calls led to concerns about a participant’s well-being. In these cases, these concerns were passed on to the participant’s keyworker or other relevant health-care professional with the participant’s consent. Maintaining strong links with a participant’s care team was therefore another important factor in managing participant distress. Interestingly, negative responses were more frequent for the first two questions, which assessed personal experiences of the research, than the third, which assessed more general views towards clinical psychological research. This suggests participants may experience distress related to particular aspects of the study, but still maintain the overall value of such research. This possibility is supported by the observation that a number of participants reporting distress also stated in the same response that they found the study acceptable.
It is therefore relevant for future research of this nature to recognise that participants may hold mixed and dissonant views of this nature. These results may have implications for how informed consent is obtained. It is important for a potential participant to be fully aware of the nature and content of the study, particularly when the focus is on personal mental health issues, as this is an area some may find distressing. An awareness of this content will allow individuals to predict the degree of distress that the study may cause them and subsequently whether or not to participate. In the current study, participants were provided with information sheets at least 24 hours before consent was sought. These outlined the study procedure and content, and provided examples of the questions participants would be asked. Unfortunately, it was beyond the scope of the current study to assess participant’s satisfaction with the informed consent process, although this is an important issue that has received attention elsewhere (e.g. Anderson and Mukherjee226).
Adequate debriefing procedures are important after research, including encouragement of participant feedback, so that negative experiences can be identified and discussed with the researcher. Such debriefings may also have an educational or informative value to participants. 227 Considering the finding that many participants may engage in research with altruistic motives, a reiteration of the research’s purpose and aims may also be beneficial, allowing participants to determine whether or not their involvement has been worthwhile. As a final point, researchers should show caution in describing the possible benefits of research participation. Although positive experiences are frequent, they cannot be guaranteed and research should not be viewed in any way as a substitute for clinical therapeutic interventions. Several limitations of this study need to be recognised. First, it is possible that some participants may have been uncomfortable or in other ways unwilling to report on the negative aspects of their experience. This may partly account for the low rates of such experiences apparent in the feedback responses. In such cases participants may have provided neutral responses, rather than describe their true negative experiences. Similarly, negative responses that were intermixed with neutral content [e.g., ‘Always difficult to talk about, overall okay (Q1)’] may simply reflect participants trying to ameliorate the impact of their negative comments (or soften the blow). Still, such acquiescent or deferential responding seems less likely to account for the substantial numbers of positive responses identified in the study. Second, the written feedback format resulted in often quite terse responses from participants. It is likely a semistructured interview methodology would have provided a deeper and more detailed exploration of participant’s experiences. However, participants had already endured 1–1.5 hours of questions and an additional detailed interview may have overburdened some individuals. Future research investigating participant distress could employ semistructured interviews conducted a few days following the study, so as to assess the ongoing impact of participation on the individual. The questions used in this study could inform future studies exploring the issues and experiences involved when participating in research studies.
Phase 2: investigating the psychological mechanisms underlying suicide behaviours – the role of defeat, entrapment and resilience
This research was previously published as Taylor PJ, Gooding PA, Wood AM, Johnson J, Pratt D, Tarrier N. Defeat and entrapment in schizophrenia: The relationship with suicidal ideation and positive psychotic symptoms. Psychiatr Res 2010;178:244–8;209 and Johnson J, Gooding PA, Wood AM, Tarrier N. Resilience as positive coping appraisals: Testing the schematic appraisals model of suicide (SAMS). Behav Res Ther 2010;48:179–86,205 and much of this text is reproduced with permission from Elsevier.
Objectives
First, this study aimed to test whether or not perceptions of defeat and entrapment mediate the relationship between positive symptoms of psychosis and suicidal ideations. The second aim of the study was to explore resilience to suicide, in particular whether or not positive self-appraisals buffer the impact of hopelessness.
Method
Participants and procedure
A total of 90 participants were recruited from CMHTs, AO teams, EISs and voluntary organisations across the North West. Participants were included in the study if they met the following criteria: (1) a clinical diagnosis based on ICD-10 criteria for schizophrenia spectrum disorder; (2) aged ≥ 18 years or over; (3) English speaking; (4) currently not considered to be an acute and serious suicide risk by their key worker or appropriate health-care professional; and (5) able to provide informed consent as judged by their keyworker or appropriate health-care professional. Participants were excluded from the study if drug use or organic disorder was judged to be the major cause of the psychosis. Participants were referred by their key worker or other health-care professional and completed the study measures in one or two sessions. This study was approved by a national research ethics committee prior to commencing.
Measures
Entrapment
The entrapment scale228 comprises 16 items assessing feelings of being trapped by internal and external events (e.g. ‘I feel trapped inside myself’). Items are rated on a 5-point scale ranging from ‘Not at all like me’ to ‘Extremely like me’. No previous reports of internal consistency for this measure in a psychosis group could be found. The alpha coefficient for the current study was 0.95.
Defeat
The defeat scale228 comprises 16 items assessing perceptions of defeat including those of failed struggle and low social rank (e.g. ‘I feel that I am one of life’s losers’). Items are rated for their prevalence in the past week, on a 5-point scale ranging from ‘Never’ to ‘Always/all the time’. No previous reports of internal consistency for this measure in a psychosis group could be found. The alpha coefficient for the current study was 0.86.
Resilience
The Resilience Appraisals Scale (RAS205) is a 12-item scale consisting of three four-item subscales assessing positive self-appraisals. These subscales focus on appraisals of perceived ability to cope with emotions, perceived ability to cope with difficult situations and perceived ability to gain social support. Items for the emotion coping scale include ‘I can handle my emotions’ and ‘In difficult situations, I can manage my emotions’. Items for the situation coping subscale include ‘I can usually find a way of overcoming problems’ and ‘If faced with a set-back, I could probably find a way round the problem’, and items for the social support subscale include ‘My family or friends are very supportive of me’ and ‘If I were to have problems, I have people I could turn to’. Responses are scored on a 5-point scale ranging from ‘Strongly disagree’ to ‘Strongly agree’. Johnson et al. 205 have found the scale to have a robust three factor structure and report evidence of convergence with other measures of appraisals. Findings also suggest scores are distinct from measures of current life stress. 205 Alpha reliabilities were 0.88 for the total scale, 0.92 for the emotion coping subscale, 0.92 for the situation coping subscale and 0.93 for the social support subscale. 205
Hopelessness
The BHS74 comprises 20 true or false items assessing the prevalence of hopelessness in the past week (e.g. ‘My future seems dark to me’). This measure has a reported alpha coefficient of 0.93 and a test–retest reliability of r = 0.85 over 3 weeks. 229 This measure has been used extensively in individuals diagnosed with schizophrenia (e.g. Tarrier et al. 230 and White et al. 231).
Suicidal ideation
The Beck Suicidal Ideation Scale (BSS232) is a 21-item scale assessing the prevalence of suicidal ideation, planning and intent in the past week and previous attempt history. For each item, participants choose between three responses of increasing suicidal ideation (e.g. ‘I have no desire to kill myself’; ‘I have a moderate to strong desire to kill myself’). In previous research in a sample with psychosis the BSS has demonstrated an alpha coefficient of 0.96 and test–retest reliability over 1 week of r = 0.88. 233
Symptoms of psychosis
The Brief Psychiatric Rating Scale Expanded version (BPRS-E234,235) is a 24-item interviewer-rated assessment of psychopathological symptoms. Each item refers to a particular symptom and is rated for frequency and severity on a 7-point scale ranging from 1 (‘not present’) to 7 (‘extremely severe’). For the purposes of the current study, separate positive and depressive symptom total scores were calculated by summing scores on the relevant item (i.e. positive symptoms = unusual thought content, suspiciousness, bizarre behaviour, grandiosity, hallucinations, hostility; depression = depression; anxiety, guilt, self-neglect, somatic concern), based on empirically identified components. 63 The suicide subscale was excluded from the depressive symptoms total score to avoid confounding depression with suicidal ideation. The positive and depressive symptom components were found to have alpha coefficients of 0.74 and 0.75, respectively. Ratings were made by one of two doctoral-level students or a trainee clinical psychologist. ICC coefficients between the three raters for a subset of interviews (n = 19) ranged between 0.87 and 0.92, suggesting good inter-rater reliability.
Analysis
Defeat and entrapment as mediators of the relationship between positive symptoms and suicide behaviours
The hypothesised mediational model was tested via SEM. Covariances were analysed via SPSS Amos version 7.0 (IBM, Chicago, IL, USA) using maximum-likelihood estimation. 236 In this model defeat and entrapment were represented as a single latent variable (referred to as defeat/entrapment hereafter). The chi-squared goodness-of-fit statistic was scaled to compensate for the small sample using a formula by Bartlett. 237 Monte Carlo simulations have found this scaled chi-square to function acceptably in models with sample sizes to parameter ratios of 5 : 1. 238 A significant value (p < 0.05) of this statistic suggests poor fit.
Model fit was also assessed via combinational rules found to minimise type I and type II errors suggesting cut-off scores of < 0.09 for the SRMR and > 0.95 for the CFI as indicants of good fit. 136
Mediation was formally tested via bootstrapping with 1000 random samples. This method involves generating CIs through a process of random resampling. Bootstrapping provides an alternative test of mediation to the commonly used Sobel test that is suitable for smaller samples. 239
Positive self-appraisals as moderators of the relationship between hopelessness and suicidal ideation
Initially, correlation analyses were carried out to explore associations between key variables. A hierarchical regression analysis was then conducted to examine whether or not positive self-appraisals measured by the RAS moderated the association between hopelessness and suicidal ideation. In the first step of this analysis, hopelessness scores were entered into the regression model. In the second step, RAS scores were entered. In the third step, the interaction term between hopelessness and the RAS was entered. At each step, standardised variables were used to avoid multicollinearity. 240 If the addition of the interaction term in the third step added significant predictive variance to the regression model, it indicated a moderating effect of positive self-appraisals as measured by the RAS on the association between hopelessness and suicidal ideation. 241 This analysis was then repeated for each of the subscales of the RAS to investigate whether or not positive self-appraisals of emotion coping, situation coping and social support would have a moderating impact when examined in isolation.
Results
Participant characteristics
A sample of 90 participants was initially recruited for the study. Of these, six failed to meet diagnostic criteria and six had substantial missing data and were therefore excluded. This resulted in a final sample of 78 participants (23 female; mean age = 42.5 years, SD = 11.8 years) with diagnoses of schizophrenia (n = 71, 91.0%), schizoaffective disorder (n = 4, 5.1%), psychosis not otherwise specified (n = 2, 2.6%), and atypical psychosis (n = 1, 1.3%) in accordance with ICD-10 criteria. The majority of participants were white (n = 63, 80.8%), mixed British (n = 6, 7.7%), Asian (n = 3, 3.8%), Afro-Caribbean (n = 1, 1.3%) and other (n = 4, 5.1%). Ethnicity data were missing for one participant. Participants had an average duration of illness of 17.5 years (SD = 11.0 years). Age, sex and duration of illness were not significantly associated with suicidal ideation (p > 0.05). Only 22 participants (28.2%) reported no history of suicide attempts, with 17 (21.8%) reporting a single attempt and 39 (50.0%) reporting multiple past attempts, ranging in number from 2 to 11. No record was taken of the nature or severity of these attempts. Descriptive statistics and correlations for the measures used are reported in Table 54. Multicollinearity was not a problem in the data (tolerance > 0.2242), although defeat and entrapment were highly correlated (r = 0.85), supporting the decision to analyse these as a single latent variable. One further participant was later excluded from the analysis on positive self-appraisals owing to missing data for the resilience measure.
| Model variable | Untransformed | Transformeda | Defeat | Entrapment | Positive Symptoms | Hopelessness | Depression | ||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||||||
| 1. Suicidal ideation | 5.64 | 6.67 | 1.91 | 1.43 | 0.52 | 0.56 | 0.29 | 0.53 | 0.51 |
| 2. Defeat | 28.56 | 16.02 | 0.85 | 0.35 | 0.71 | 0.61 | |||
| 3. Entrapment | 24.67 | 18.55 | 0.49 | 0.70 | 0.64 | ||||
| 4. Positive symptoms | 13.10 | 5.95 | 3.53 | 0.79 | 0.32 | 0.46 | |||
| 5. Hopelessness | 7.41 | 5.51 | 2.45 | 1.20 | 0.64 | ||||
| 6. Depression | 12.18 | 4.91 | 2.41 | 0.43 | |||||
Defeat and entrapment as mediators of the relationship between positive symptoms and suicide behaviours
The hypothesised mediation model with associated fit indices, standardised regression weights and multiple squared correlations is displayed in Figure 10. This model fit the data well and all direct paths were significant (p < 0.05). The results of the bootstrap analysis suggested that the indirect effect of positive symptoms on suicidal ideation was also significant; p = 0.002 (95% CI 0.14 to 0.39). The above model assumed full mediation, for which no direct effect of positive symptoms on suicidal ideation remained after accounting for perceptions of defeat/entrapment. In order to test this assumption, a second partial mediation model was calculated and compared with the full mediation model. The models were compared in terms of improvement in the scaled chi-squared statistic and Akaike information criterion (AIC). It has been suggested that differences of ≤ 2 on the AIC provide substantial support for the more parsimonious model. 243 The partial mediation model failed to demonstrate a significant improvement in fit, χ2−K (1) = 0.02, not significant, AIC = 1.98, providing support for the more parsimonious full mediation model.
FIGURE 10.
Model depicting full mediation of positive symptoms on suicidal ideation via defeat/entrapment. Rectangles represent observed variables in the model. Defeat and entrapment have been used as indicators of a single latent variable, represented by an oval.

In order to test the robustness of the mediation model, the analysis was repeated controlling for the effect of hopelessness (BHS) and depressive symptoms (BPRS-E). The model continued to demonstrate good fit, χ2−K (4, n = 78) = 5.54; p = 0.24, SRMR = 0.02, CFI = 0.99. All direct and indirect paths remained significant and standardised coefficients differed by β ≤ 0.30.
Secondary analysis
A secondary exploratory analysis was undertaken to examine the individual positive symptoms that contributed most to suicidal ideation. Correlations between individual positive symptoms and suicidal ideation are reported in Table 55.
| Symptoms | Correlation (rs) |
|---|---|
| Hostility | 0.15 |
| Grandiosity | −0.14 |
| Suspiciousness | 0.42* |
| Hallucinations | 0.23* |
| Delusions | 0.15 |
| Bizarre behaviour | 0.11 |
Only suspiciousness and hallucinations were significantly associated with suicidal ideation. In order to investigate whether or not the link between these individual symptoms and suicidal ideation was mediated by perceptions of defeat and entrapment, a SEM was calculated with suspiciousness and hallucinations as predictors, defeat/entrapment as a mediator and suicidal ideation as an outcome variable. Suspiciousness and hallucinations had means of 2.72 (SD = 1.76) and 3.00 (SD = 2.14), respectively. Prior to the analysis, the variable suspiciousness was square root transformed to correct for mild positive skew, resulting in a mean of 1.56 (SD = 0.53). This model with associated fit indices, standardised regression weights and multiple squared correlations is displayed in Figure 11. The model fit the data well and all direct paths were significant, with the exception of the direct effect of hallucinations on defeat/entrapment. The indirect effect of suspiciousness on suicidal ideation was also significant (95% CI 0.18 to 0.46; p = 0.002), but not the indirect effect of hallucinations on suicidal ideation (95% CI −0.05 to 0.20; p = 0.28).
FIGURE 11.
Model depicting full mediation of suspiciousness and hallucinations on suicidal ideation via defeat/entrapment.

Positive self-appraisals as moderators of the relationship between hopelessness and suicidal ideation
Descriptive statistics and zero-order correlations
Zero-order correlations, means and SDs for the variables are displayed in Table 56. Results suggested that hopelessness scores were moderately correlated with suicidal ideation. Similarly, positive self-appraisals according to the RAS were found to be moderately inversely correlated with suicidal ideation, as were the two RAS subscales of emotion coping and situation coping. There was no correlation between the social support subscale of the RAS and suicidal ideation. Inverse correlations between hopelessness, total RAS scores and each of the RAS subscales were also found.
| Variable name | Untransformed mean (SD)a | Transformed mean (SD)a | Hopelessness (BMS) | Positive self-appraisals (RAS) | Emotion Coping Appraisals subscale (RAS Emo) | Situation Coping Appraisals subscale (RAS Situ) | Social Support Appraisals subscale (RAS Social) |
|---|---|---|---|---|---|---|---|
| 1. Suicidality (BSS)b | 5.60 (6.73) | 1.88 (1.45) | 0.54** | –0.47** | –0.53** | –0.42** | –0.11 |
| 2. Hopelessness (BHS)b | 7.21 (5.47) | 2.41 (1.19) | –0.56** | –0.50** | –0.49** | –0.32** | |
| 3. Positive self-appraisals (RAS) | 42.75 (9.80) | 0.89** | 0.83** | 0.60** | |||
| 4. Emotion Coping Appraisals subscale (RAS Emo) | 13.14 (4.67) | 0.71** | 0.30** | ||||
| 5. Situation Coping Appraisals subscale (RAS Situ) | 13.31 (4.17) | 0.19 | |||||
| 6. Social Support Appraisals subscale (RAS Social)b | 16.30 (3.80) | 3.00 (0.85) |
Regression analyses
As can be seen in Table 57, positive self-appraisals measured according to the RAS were found to moderate the association between hopelessness and suicidal ideation. Once hopelessness scores had been entered, positive self-appraisals predicted suicidal ideation both in addition to hopelessness, β = –0.252, and when interacting with hopelessness, β = –0.218, supporting a moderating impact of self-appraisals on hopelessness.
| Moderator variable | Step | Variable entered | β | SE β | Total R2 ΔR2 | |
|---|---|---|---|---|---|---|
| Positive Self–Appraisals (RAS) | 1 | BHS | 0.536*** | 0.097 | 0.287 | |
| 2 | BHS | 0.395** | 0.115 | 0.331 | 0.044* | |
| 3 | RAS | –0.252* | 0.115 | 0.367 | 0.036* | |
| BHS | 00.396** | 0.112 | ||||
| RAS BHS–RAS interaction | –0.269* | 0.1130.107 | ||||
| –0.218* | ||||||
| Emotion Coping Appraisals (RAS Emo) | 1 | BHS | 0.536*** | 0.097 | 0.287 | |
| 2 | BHS | 0.360** | 0.106 | 0.380 | 0.092** | |
| RAS Emo | –0.351** | 0.106 | ||||
| 3 | BHS | 0.389*** | 0.104 | 0.419 | 0.039* | |
| RAS Emo | –0.311** | 0.105 | ||||
| BHS – RAS | –0.228* | 0.103 | ||||
| Emo | ||||||
| interaction | ||||||
| Situation Coping Appraisals (RAS Situ) | 1 | BHS | 0.536*** | 0.097 | 0.287 | |
| 2 | BHS | 0.437*** | 0.110 | 0.318 | 0.031 | |
| RAS Situ | –0.203 | 0.110 | ||||
| 3 | BHS | 0.442*** | 0.109 | 0.342 | 0.024 | |
| RAS Situ | –0.194 | 0.109 | ||||
| BHS – RAS | –0.174 | 0.107 | ||||
| Situ | ||||||
| interaction | ||||||
| Social Support Appraisals (RAS Social) | 1 | BHS | 0.536*** | 0.097 | 0.287 | |
| 2 | BHS | 0.558*** | 0.103 | 0.292 | 0.005 | |
| RAS Social | 0.071 | 0.103 | ||||
| 3 | BHS | 0.553*** | 0.104 | 0.295 | 0.003 | |
| RAS Social | 0.067 | 0.104 | ||||
| BHS – RAS | 0.065 | 0.109 | ||||
| Social | ||||||
| interaction | ||||||
From Figure 12 it can be seen that for those with high levels of positive self-appraisals, increased hopelessness corresponded with only minimal increases in suicidal ideation.
FIGURE 12.
Resilience Appraisals Scale moderate hopelessness (BHS) to predict suicidality (BSS).
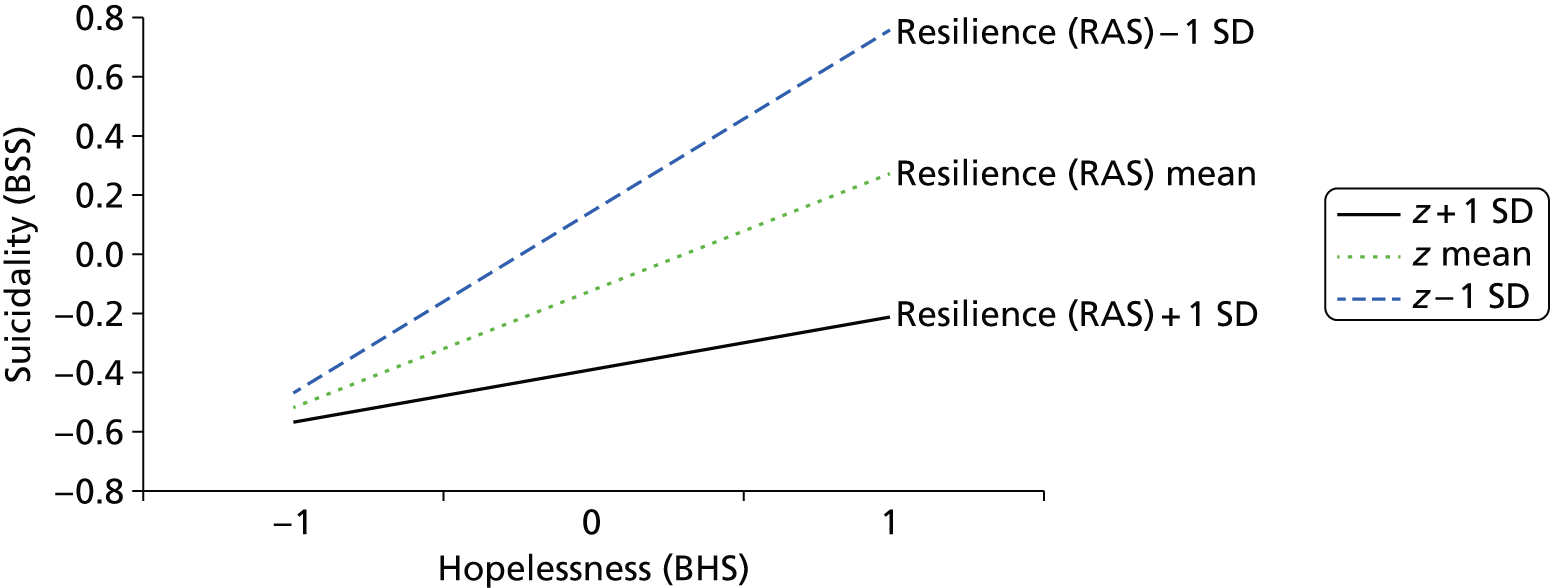
Subscales of the Resilience Appraisals Scale
Next, each of the RAS subscales was examined as a moderator of hopelessness. A significant moderating impact was found for the subscale of emotion coping, which predicted suicidal ideation both in addition to hopelessness scores, β = –0.351, and also interactively with hopelessness β = –0.228. As shown in Figure 13, this pattern was similar to that found for the overall scale and suggests that for those who are high on emotion coping appraisals, there is minimal increase in suicidal ideation at higher levels of hopelessness. By contrast, neither the situation coping subscale nor the social support subscale was found to predict suicidal ideation either in addition to hopelessness, or in interaction with hopelessness.
FIGURE 13.
Appraisals of emotion coping ability (RAS Emotion Coping subscale) moderate hopelessness (BHS) to predict suicidality (BSS).
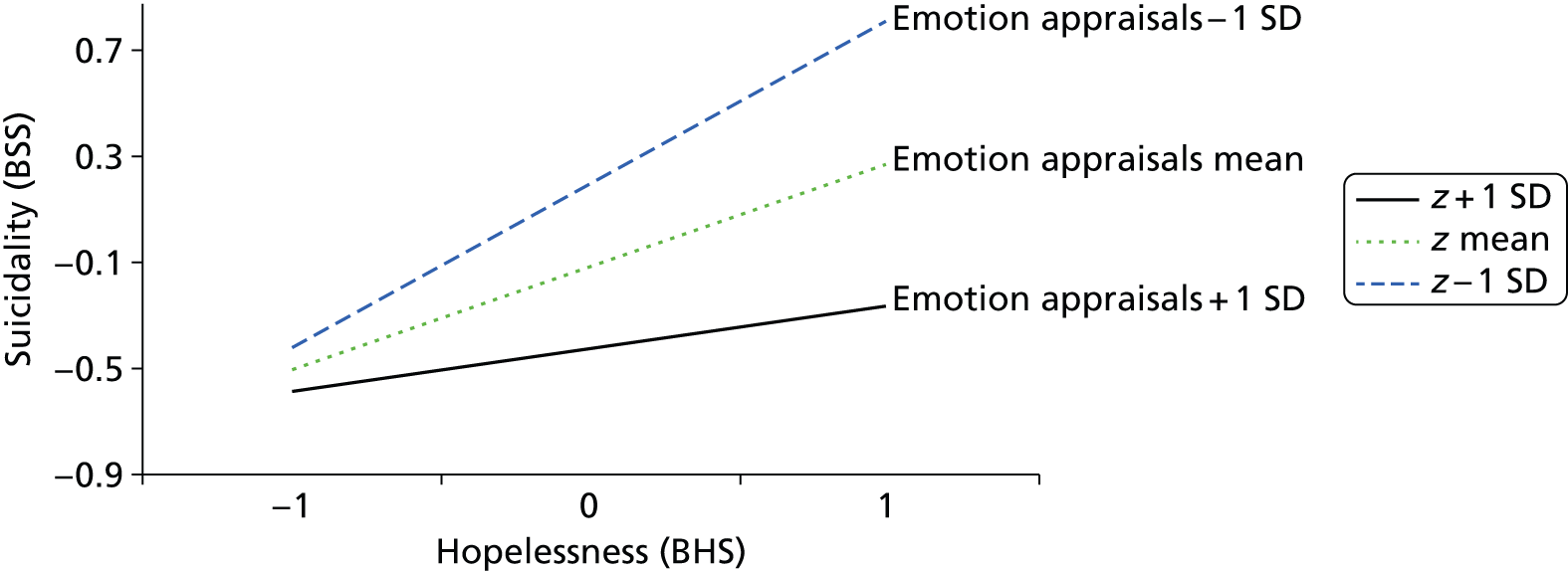
Discussion
Defeat and entrapment as mediators of the relationship between positive symptoms and suicide behaviours
It was found that perceptions of defeat and entrapment, conceptualised as a single variable, accounted for a large proportion (31%) of the variance in suicidal ideation. As hypothesised, defeat and entrapment fully mediated the association between positive symptom severity and suicidal ideation. This result held while controlling for levels of hopelessness and depression suggesting it was robust and not simply an artefact of the conceptual overlap between variables. An additional exploratory analysis revealed that suspiciousness in particular was related to suicidal ideation and that this effect was also fully mediated by defeat and entrapment.
These results support the SAMS model which argues that negative appraisals result in perceptions of defeat and entrapment in psychosis. These in turn lead to suicidal ideation. 204 Defeat and entrapment, defined as perceptions of loss or rejection without escape or likelihood of improvement,228 may represent one particularly maladaptive psychological response to the difficulties posed by living with psychosis, which may provoke suicidal ideation and behaviour as a means of escape or protest. 206
The current study supports the link between the severity of positive symptoms of psychosis, in particular experiences of suspiciousness or paranoia, and suicidal ideation. 244–246 Moreover, it was found that this relationship was explained by perceptions of defeat and entrapment, which were amplified as symptoms became increasingly distressing and enduring. Suspiciousness may be particularly entrapping and defeating as such experiences can carry a sense of ongoing personal threat and negative implications concerning social rank. 247 It is possible that paranoia represents a psychosis-specific risk factor for suicide that functions along side other transdiagnostic factors, such as depression. 200 This possibility requires further investigation.
It could be that the current results concerning defeat and entrapment are simply an artefact of the demoralisation syndrome identified in some individuals diagnosed with schizophrenia. This syndrome, which follows an individual’s negative awareness of the impact of the illness on their goals and future aspirations, has also been associated with suicide248,249 and shares some conceptual similarities with defeat and entrapment. However, this explanation is unlikely, as hopelessness and depression are proposed as key symptomatic features of the demoralisation syndrome in schizophrenia248,249 and both of these variables were controlled for in the current analyses.
The results of this study raise the possibility that perceptions of defeat and entrapment could be used alongside better established indicators of suicide such as depression and hopelessness200,230,250–253 to identify patients diagnosed with schizophrenia who are at heightened risk of suicide. Further investigation of the utility of defeat and entrapment in predicting suicidal behaviour is therefore warranted. The results also suggest that psychological therapies aimed at reducing suicidal ideation in individuals diagnosed with schizophrenia could focus specifically on reducing perceptions of defeat and entrapment, alongside interventions aimed more directly at alleviating clients’ symptoms. Psychosocial interventions, including psychotherapy, have been suggested as one important approach in the prevention of suicide in individuals diagnosed with schizophrenia. 253 A recent meta-analysis has also supported the overall efficacy of CBT in suicide prevention. 202 CBT may therefore provide one useful framework within which perceptions of defeat and entrapment could be targeted. 254 A more detailed discussion of therapeutic approaches to dealing with defeat and entrapment in psychosis is described elsewhere. 204
Positive self-appraisals as moderators of the relationship between hopelessness and suicidal ideation
Positive self-appraisals moderated the impact of hopelessness, such that individuals with high levels of positive self-appraisals were significantly less likely to experience suicidal ideation even at the highest levels of hopelessness. When specific types of self-appraisals were examined in isolation, appraisals of emotion coping ability appeared to moderate the impact of hopelessness, but appraisals of situation coping and social support did not show this moderating impact.
These results support previous research that suggests that positive self-appraisals may confer resilience against risk, reducing the likelihood that risk will lead to suicidal thoughts. 255 Interest into concepts of suicide resilience has grown in recent years, but generally this research has explored potential resilience factors by examining their direct linear association with suicidal thoughts,256,257 which does not demonstrate a buffering or resilience role for the variable. Instead, resilience needs to be understood as a separate dimension to risk, which can exist alongside it, acting to attenuate the likelihood that risk will lead to suicidality. By finding an interaction between positive self-appraisals and hopelessness in a sample of individuals with schizophrenia-spectrum diagnoses, the current results both support these previous findings and expand on them in four main ways.
First, the current results indicate that positive self-appraisals may also be a resilience factor for clinical populations, specifically for individuals with schizophrenia-spectrum disorders, who are at particularly high risk of suicidality. 258,259 Risk factors for suicidality have been studied extensively for this group and a range of factors have been found to increase the likelihood of suicide. 6,253 One of the strongest psychological factors is hopelessness. 260,261 Although an understanding of risk factors can increase the prediction of suicide risk and inform clinical interventions, it is limited. The current results suggest that some factors can act as buffers and that when they are studied in interaction with risk, they can increase predictive validity. This may improve identification of individuals who are at risk from suicide and reduce the number of false positives.
Second, the present study investigated an interaction between positive self-appraisals and hopelessness. Previously, positive self-appraisals were studied in relation to life events in a student sample,255 but as life events may not be an accurate predictor of suicide amongst individuals with psychosis200 the current study focused on a clinical risk factor, namely, hopelessness. The finding that positive self-appraisals can also buffer against hopelessness demonstrates that their buffering impact is not limited to life events and suggests that positive self-appraisals may be an important resilience factor for a range of risk factors. Although this will need to be explored by further research, the current findings suggest that positive self-appraisals could be an important resilience factor.
Third, the present study used a concept of suicide resilience based on the Schematic Appraisals Model of Suicide (SAMS204). This model suggests that cognitive biases and a suicide schema interact with appraisals of the self and the situation to lead to suicidal thoughts and behaviours. In particular, the self-appraisals construct is thought to have a central role, impacting on all other relevant processes. This suggests that positive self-appraisals could be especially beneficial, potentially buffering against maladaptive processes taking place elsewhere in the model. Johnson et al. 255 found support for this proposed central role of positive self-appraisals among a student sample and the current study extends this by finding further evidence for the importance of the self-appraisal construct among individuals with psychosis-spectrum disorders. This suggests that the processes described by the SAMS may be relevant among both clinical and non-clinical samples and supports other findings which identify the SAMS as a useful framework for understanding suicidality among individuals with psychosis spectrum disorders. 209
Fourth, by exploring each of the subscales of the positive appraisals measure (RAS255) the current findings indicate which types of positive self-appraisals may be relevant for individuals with non-affective psychosis. The measure comprises three subscales designed to capture an individual’s appraisal of their ability to cope with their emotions, their ability to cope with difficult situations and their ability to gain social support. When each of these subscales was studied, the only one found to moderate the impact of hopelessness was ability to cope with emotions. This subscale is designed to reflect an individual’s confidence in their ability to manage their emotions and contains items such as ‘I can handle my emotions’ and ‘In difficult situations, I can manage my emotions’. The present results suggest that although the overall construct of the self-appraisal may be relevant, emotion coping appraisals could be a key aspect of resilience.
Interestingly, the present study found that although scores on the appraisals of social support and appraisals of situation coping subscales were moderately correlated with suicidal ideation, when entered into a regression analysis they did not predict suicidality either in addition to, or when interacting with, hopelessness. This may appear counterintuitive, as research from previous studies has suggested that social support and aspects related to situation coping, such as problem-solving can reduce the likelihood of suicidality (e.g. Hawton et al. 6 and Chang262). One possible explanation for this finding is that although emotion coping appraisals can moderate hopelessness when considered in isolation, social support and problem-solving confidence could have a compensatory impact on each other. This would imply that high levels of one could compensate for low levels of the other and this possibility is supported by the finding that although neither subscale was a buffer when considered in isolation, the overall appraisals scale was significant. It should be noted that this suggestion is tentative and further research is necessary before any conclusions can be drawn.
Limitations and future research
There were four main limitations to the study. First, it was cross-sectional, which limits the extent to which findings can be interpreted for causality; longitudinal research in the future would allow exploration of causality. Second, the study was examining psychological processes and resilience on suicidal thoughts and not completed suicide. Some research has suggested that these are distinct phenomena that may need to be studied separately;263 however, other research has found that suicidal thoughts and behaviours exist on a continuum with completed suicide, which suggests they may share underlying mechanisms and be a relevant criterion through which to investigate suicidality and suicide prevention strategies. 264–266 Third, owing to ethical guidelines, the study did not include participants who were judged to be an acute and serious suicide risk and so results may not generalise to this subpopulation. Despite this, participants who were actively suicidal were included and the results can be expected to generalise to the large majority of individuals with psychosis. The final caveat of this study is the relatively small sample size; however, the models depicted met recommendations of over five participants per parameter being estimated. 267,268 Replication of the present results in a larger sample would still be beneficial for strengthening the generalisability of these results.
Future research would also benefit from the further refinement and exploration of the defeat and entrapment construct in relation to psychosis. This should involve additional investigation of the phenomenology of this construct and its operationalisation within the context of psychosis. The use of a case–control methodology to further investigate defeat and entrapment in relation to suicide would also be of interest. Such research would be beneficial in confirming the present findings and determining whether or not they extend to completed suicide.
Implications for clinical practice
When assessing individuals for suicide risk, it may be important to account for the presence of resilience factors in addition to risk factors and to be mindful that some factors, such as the self-appraisal, may alter the impact of risk. The self-appraisals investigated by the study concerned the individual’s view of their ability to cope and can be understood as reflecting a form of self-efficacy. 269 In particular, appraisals of ability to cope with emotions appeared to have a buffering impact and could be a key aspect to focus on. For individuals who have a low level of positive self-appraisals, risk factors such as hopelessness may be particularly deleterious and such individuals may be regarded as especially high risk. By contrast, for individuals who are high on positive self-appraisals, hopelessness may cease to be considered a risk factor for suicidal ideation. This is not to suggest that it should not be monitored as it could still have relevance to psychological well-being and clinical symptomatology, but it should not be considered to be a relevant predictor for suicidal thoughts and behaviours in this group.
In addition, as positive self-appraisals can alter the impact of clinical risk factors, these may be an important aspect to incorporate into clinical interventions. Reducing an individual’s level of risk is an important part of any suicide treatment programme, and practical interventions, such as the removal of firearms, potentially lethal substances and other means of suicide, can have a strong impact on likelihood of suicide. 270 However, the present results suggest that developing positive self-appraisals may indirectly reduce the likelihood of suicide risk by attenuating the impact of risk. Thus, they may represent a particularly beneficial area to target when conducting treatment interventions. Tarrier and Gooding271 suggest that the use of techniques such as positive data logging, in which clients record specific examples of times they have demonstrated positive qualities, may be useful in developing a more positive self-concept.
Phase 3: a randomised controlled trial of Cognitive–Behavioural Prevention of Suicide in psychosis
This research was previously published as Tarrier N, Kelly J, Maqsood S, Snelson N, Maxwell J, Law H, Dunn G, Gooding P. 2014. The cognitive behavioural prevention of suicide in psychosis: A clinical trial. Schizophr Res 2014;156:204–10272 and much of this text is reproduced with permission from Elsevier.
Objectives
This study aimed to evaluate the Cognitive–Behavioural Prevention of Suicide in psychosis protocol (CBPSp).
Specifically, it was hypothesised that CBSPp in addition to TAU would have significant advantages over TAU alone in reducing (1) measures reflecting suicidal behaviour including hopelessness and (2) measures associated with other symptom clusters of psychosis including depression, thought disorder and low self-esteem.
Method
This was a single-blind RCT that aimed to test the feasibility and potential efficacy of a novel intervention (CBSPp) designed to reduce suicidal behaviours in those suffering from schizophrenia spectrum disorders. Participants assigned to the treatment condition in addition to TAU were compared with those allocated to a TAU condition alone. Ethical approval was obtained from Stockport Research Ethics Committee (08/H1012/97).
Participants
Between April 2009 and October 2010, CMHTs, EI teams and AO teams across four National Mental Health Service trusts, including Greater Manchester West, Manchester Mental Health and Social Care, Pennine Care and Five Boroughs in the north-west of England, were approached to facilitate recruitment. Participants were recruited into the study if they were (1) aged between 18 and 65 years; (2) had a Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition (DSM-IV) diagnosis of schizophrenia, schizophreniform disorder, schizoaffective disorder, delusional disorder or psychotic disorder not otherwise specified; (3) identified as having previous suicide attempts or experiencing current suicidal ideation; (4) under the care of an appropriate clinical team and currently in contact with mental health services; (5) receiving appropriate antipsychotic medication; and (5) not currently receiving CBT or other empirically validated psychological treatments. Participants were excluded if they (1) currently suffered serious suicidal intent and were currently considered a danger to themselves by their clinical team; (2) had a primary diagnosis of bipolar depression or substance induced psychosis; and (3) suffered from an organic brain disease.
Procedure
Mental health staff identified potential participants on their caseload who met the recruitment criteria. Once diagnosis was confirmed and written consent was obtained, the baseline assessments were administered by research assistants, independent of therapy. Following the baseline assessment, participants were randomised using a clinical data management system and allocated to either the experimental treatment group in which participants were to receive CBSPp in addition to TAU or the control in which participants were to receive only TAU. Randomisation was controlled by staff not directly linked to the trial to ensure independence and blindness to the trial allocation arms. Participants were informed of the randomisation outcome via a letter, which also contained a note reminding them not to disclose any information about their care or treatment during assessments, which would break the blind requirement. In cases for which the research assistants were unblinded, protocols were followed whereby blinds were documented and the assessment packs were to be scored by another research assistant. Masking was further maintained by ensuring that therapists and research assistants were located in different offices so that therapy files and assessment data were stored separately. In addition, clinical staff were repeatedly instructed not to disclose any knowledge of therapy or group allocation to assessors. Participants who were allocated to the treatment arm were then contacted by one of the trial therapists to arrange their first session. Therapists were given a copy of the completed baseline assessments prior to starting their therapy sessions to aid their clinical formulations and prevent unnecessary repetition of questioning of participants. Participants were assessed at baseline and then at 4- and 6-month follow-up time points. Prior to each assessment point, care co-ordinators were approached by a member of the research team to obtain a comprehensive risk assessment.
A routine telephone follow-up call was made the day after each assessment and 7 days later to ensure that the assessments had not caused any distressing after-effects for the participant. Therapists and assessors received regular (every 2 months) clinical supervision.
Measures and assessments
Standardised measures consisting of a short semistructured clinical interview and self-report questionnaires were used.
Primary outcome measures
These were measures of suicidal thoughts, behaviours and hopelessness, specifically:
The Adult Suicidal Ideation Questionnaire273
The Adult Suicidal Ideation Questionnaire (ASIQ) is a 25-item self-report questionnaire that assesses suicidal intent in adults. Respondents report the frequency of thoughts about death in the last month using a 7-point Likert scale (almost every day; couple of times a week; about once a week; couple of times a month; about once a month; I had this thought before, but not in the past month; I never had this thought).
The Suicide Probability Scale274
The Suicide Probability Scale (SPS) consists of 36 statements with four subscales [hopelessness (12 items), suicidal ideation (eight items), negative self-evaluation (nine items) and hostility (seven items)]. Responses are measured on a 4-point Likert scale (none or a little of the time, some of the time, good part of the time, most or all of the time).
Beck Scale for Suicide Ideation275
The BSS is a 21-item self-report questionnaire, which explores the presence and severity of suicidal intent. Higher scores indicate greater suicidal ideation. The measure has a reliability of 0.90 with inpatient samples and 0.87 with outpatient samples and test–retest reliability of 0.54.
Secondary outcome measures
These were included to reflect mood, symptoms of psychosis and associated outcomes:
Training and monitoring/supervising trial therapists
Trial therapists were two clinical psychologists (JK and JM) who had extensive experience in delivering CBTP. Prior to the commencement of the trial, the therapists received extensive training to familiarise them with the therapy manual. During the trial, group supervision with the treatment developer (NT) was provided on a fortnightly basis and peer supervision occurred on a weekly basis.
Intervention
Cognitive–Behavioural Suicide Prevention in Psychosis was based on a treatment manual202,211 and was derived from an explanatory model of suicide behaviour: the SAMS. 204 The intervention consisted of three phases to address and change the three components of the SAMS. Modification of:
-
information processing biases
-
appraisals, with a focus on defeat, entrapment, social isolation, emotional dysregulation and interpersonal problem-solving
-
suicide schema.
In addition, the sessions focused on the processes thought to underlie resilience to suicide. The psychological therapy consisted of up to 24 individual therapy sessions delivered twice a week across 12 weeks at a convenient location for the participant (usually their home). Telephone contact or SMS messaging was utilised when, and if, appropriate to support the therapy sessions.
Statistical analysis
All analyses were carried out using Stata. Random effects (i.e. random intercepts) models for repeated measures data were fitted to both 4- and 6-month outcome variables with the baseline value of the outcome variable being used as a covariate (allowing for a follow-up time by covariate interaction in all models). Stata’s xtreg command was used. After preliminary examination of the data, treatment effects were assumed to be the same for both follow-up times, the estimate of the effect of treatment arising from fitting the random effect model being that which is common to both follow-up times. Because most, if not all, of the outcomes were positively skewed, CIs for the treatment effects were routinely estimated through the use of the bootstrap,276 using the percentiles based on the results of 1000 replications (using the trial participant as the sampling unit).
Results
Of the 131 potentially eligible participants, 49 were randomised, 25 to CBSPp plus TAU and 24 to TAU alone (Figure 14). Of the CBSPp group, 16 participants were reassessed at 4 months and 17 were reassessed at 6 months. In the TAU alone group, 19 were reassessed at 4 months and 18 were reassessed at 6 months (see Figure 14).
FIGURE 14.
Flow diagram of recruitment and treatment allocation.
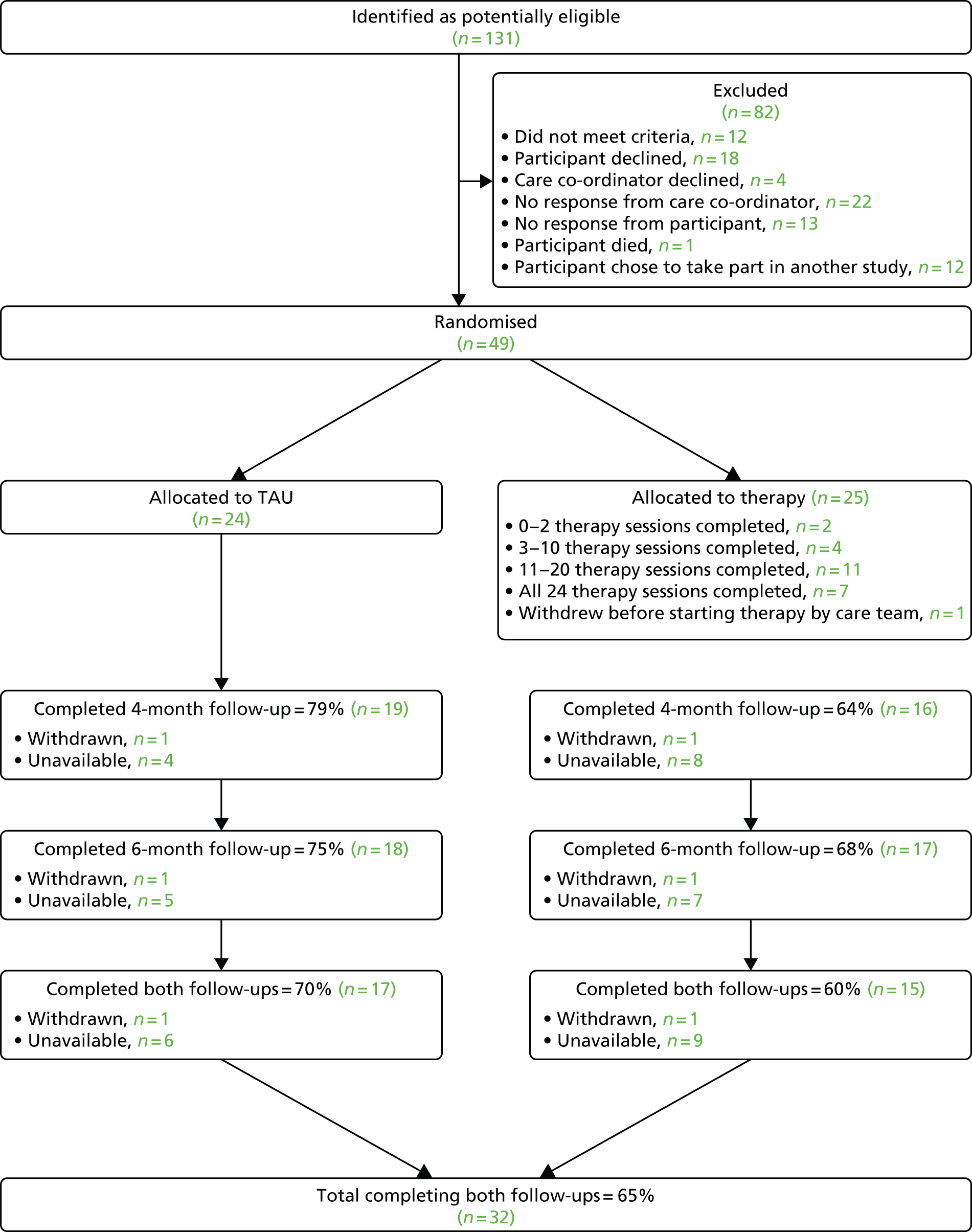
The mean age of the sample overall was 34.9 years (SD = 13.1 years) and 31 out of the 49 participants were male. The mean age of the participants in the CBSPp and TAU alone conditions were 32.6 years (SD = 11.7 years) and 37.3 years (SD = 14.2 years), respectively, a difference which was not significant. Forty-two participants were white (UK), one was white (non-UK), one was black (UK African), one was black (UK/Caribbean African), two were Chinese, and two were of mixed ethnic background. Thirty-six participants were single, two were married, four were divorced and seven were in common law marriages. A total of 2, 30, 15 and 2 participants had completed UK primary, secondary, further and higher education levels, respectively, as their highest level of educational qualification. The majority of the sample (n = 35) were unemployed. Twenty-nine participants were atheist, 14 were Christians, one was a Hindu, four did not specify a religion and there were missing data for one individual. Fifteen participants had attempted suicide once, 27 had attempted suicide twice or more and seven had not previously attempted suicide. Twenty-two participants were recruited from EI services, 26 were recruited from CMHTs and one was recruited from AO teams. Schizophrenia (n = 18), schizoaffective disorder (n = 8), persistent delusional disorder (n = 3), other (psychosis not otherwise specified) (n = 10) and unable to capture data/missing data (n = 10) were the primary diagnoses. The vast majority of primary and secondary outcome measures were significantly intercorrelated (Table 58).
| Outcome variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Suicidal ideation | 0.76** | 0.59** | 0.83** | 0.46** | 0.52** | 0.69** | 0.44** | –0.55** | 0.58** | 0.60** | 0.47** | 0.30* | –0.53** | –0.50** | –0.38** | |
| 2. Suicide probability (SPS) | 0.87** | 0.86** | 0.78* | 0.80* | 0.75** | 0.71** | –0.75** | 0.56** | 0.60** | 0.41** | 0.34* | –0.59** | –0.56** | –0.48** | ||
| 3. Hopelessness (SPS) | 0.61** | 0.63** | 0.65** | 0.63** | 0.65** | –0.74** | 0.43** | 0.55** | 0.28 | 0.27 | 0.47** | 0.46** | 0.41** | |||
| 4. Ideation (SPS) | 0.57** | 0.55** | 0.74** | 0.62** | –0.61** | 0.57** | 0.59** | 0.40** | 0.38** | –0.62** | –0.59** | –0.41** | ||||
| 5. Negative self evaluation (SPS) | 0.57** | 0.67** | 0.64** | –0.72** | 0.44** | 0.44** | 0.32* | 0.29* | –0.40** | –0.38** | –0.48** | |||||
| 6. Hostility (SPS) | 0.47** | 0.49** | –0.50** | 0.38** | 0.37** | 0.33* | 0.14 | –0.42** | –0.39** | –0.34* | ||||||
| 7. Calgary Depression Scale | 0.64** | –0.72** | 0.62** | 0.69** | 0.47** | 0.40** | –0.57** | –0.54** | –0.60** | |||||||
| 8. Hopelessness (BHS) | –0.70** | 0.51** | 0.59** | 0.36** | 0.34* | –0.59** | –0.58** | –0.41** | ||||||||
| 9. Self-esteem | –0.57** | –0.62** | –0.34* | –0.43** | 0.47** | 0.44* | 0.58** | |||||||||
| 10. PANSS | 0.90** | 0.87** | 0.73** | –0.82** | –0.80** | –0.45** | ||||||||||
| 11. PANSS general | 0.70** | 0.55** | –0.78** | –0.76** | –0.51** | |||||||||||
| 12. PANSS positive | 0.49** | –0.77** | –0.75** | –0.31* | ||||||||||||
| 13. PANSS negative | –0.46** | –0.37** | 0.36* | |||||||||||||
| 14. GAF scale total | 0.99** | 0.41** | ||||||||||||||
| 15. GAF scale symptoms | 0.36* | |||||||||||||||
| 16. GAF scale disability |
As can be seen from Table 59, the repeated measures regression model indicated that there were significant improvements in the primary outcome measures of suicidal ideation (ASIQ, treatment effect = –12.30, SE 6.30, 95% CI –24.30 to –0.14), suicidal probability (SPS, treatment effect = –7.00, SE = 3.90, 95% CI –15.50 to 0.00) and hopelessness (subscale of the SPS, treatment effect = –3.80, SE = 1.70, 95% CI –7.30 to –0.50) at the follow-up periods. Suicidal ideation, the probability of suicide and feelings of hopelessness significantly decreased in the Treatment group compared with the TAU group.
| Variable | Baseline | 4 months | 6 months | |||
|---|---|---|---|---|---|---|
| Primary outcomes | Treatment (n = 25) | TAU (n = 24) | Treatment (n = 16) | TAU (n = 19) | Treatment (n = 17) | TAU (n = 18) |
| Suicidal ideation (ASIQ)a | 54.1 (38.8) | 57.4 (38.1) | 37.1 (33.6) | 40.9 (40.5) | 29.6 (31.3) | 41.5 (34.9) |
| Suicide probability (SPS)a | 84.8 (23.1) | 83.2 (24.6) | 67.3 (23.3) | 73.2 (21.8) | 67.5 (19.6) | 70.3 (20.4) |
| SPS suicidal ideation | 23.0 (7.8) | 20.8 (10.0) | 15.6 (7.7) | 16.7 (8.3) | 16.7 (8.6) | 15.9 (8.0) |
| SPS hopelessnessa | 27.5 (8.7) | 26.4 (9.4) | 19.9 (8.3) | 22.8 (8.0) | 20.0 (7.1) | 22.9 (7.8) |
| SPS negative self-evaluation | 18.5 (3.6) | 19.9 (3.8) | 16.8 (3.5) | 17.9 (4.2) | 16.0 (3.1) | 18.2 (4.7) |
| SPS hostility | 15.8 (7.3) | 16.1 (5.8) | 15.0 (6.8) | 15.8 (6.8) | 14.8 (5.2) | 13.3 (5.5) |
| Secondary outcomes | ||||||
| Depression (Calgary Depression Scale)a | 8.6 (4.9) | 9.4 (4.9) | 4.2 (4.1) | 8.5 (6.5) | 4.0 (3.8) | 7.2 (5.2) |
| Self-esteema | 68.0 (24.6) | 67.6 (25.3) | 88.0 (27.0) | 77.3 (24.7) | 90.3 (21.9) | 73.4 (25.3) |
| PANSS totala | 58.7 (10.4) | 61.6 (16.4) | 49.8 (12.3) | 58.1 (17.1) | 47.9 (11.9) | 53.9 (12.8) |
| PANSS generala | 31.3 (5.2) | 31.5 (7.8) | 24.3 (5.6) | 29.0 (9.0) | 24.4 (6.6) | 27.1 (7.8) |
| PANSS positivea | 14.8 (4.8) | 16.1 (5.2) | 14.0 (5.9) | 15.2 (5.5) | 12.4 (4.9) | 14.9 (4.0) |
| PANSS negative | 12.6 (2.6) | 14.0 (5.5) | 11.6 (2.9) | 14.0 (5.6) | 11.1 (2.3) | 11.9 (3.1) |
| GAF total | 28.7 (7.5) | 30.4 (9.1) | 34.0 (8.5) | 36.6 (15.6) | 39.2 (19) | 35.7 (12.0) |
| GAF symptoms | 31.2 (13.0) | 33.9 (17.0) | 42.8 (22.2) | 43.2 (24.8) | 47.5 (26.3) | 37.5 (15.5) |
| GAF disability | 43.2 (11.1) | 42.8 (9.3) | 44.1 (5.4) | 47.2 (12.3) | 46.9 (15.5) | 44.9 (8.4) |
Analysis of the secondary outcome measures indicated significant improvements in depression (treatment effect = –3.3, SE = 1.0, 95% CI –5.3 to –1.4), self-esteem (treatment effect = 14.5, SE = 4.9, 95% CI 5.0 to 24.3), positive and negative symptom total scores (PANSS, treatment effect = –7.1, SE = 2.1, 95% CI –11.3 to –2.0), PANSS general symptoms scores (treatment effect = –4.5, SE = 1.2, 95% CI –6.8 to –2.1), PANSS positive symptoms scores (treatment effect = –1.6, SE = 0.8, 95% CI –3.0 to –0.1), and GAF scale symptom scores (treatment effect = 8.3, SE = 4.0, 95% CI 0.6 to 15.8). It should be noted that scores did not improve for the treatment relative to the TAU alone group for PANSS negative symptom scores nor for the GAF scale total or disability scores, BHS hopelessness score or BSS score.
Discussion
In general, there were improvements on all measures over the trial. CBSPp in addition to TAU successfully, and significantly, reduced the primary and secondary outcome measures compared with TAU alone. That is, subjective measures of suicidal ideation, estimated probability of suicide and hopelessness (as measured by the SPS) were improved as were the associated outcomes of depression, self-esteem, symptoms of psychosis overall, positive and general symptoms of psychosis, and the GAF scale symptoms score. There were no significant group differences in negative symptoms or measures of overall functioning and disability using the GAF scale. Thus, it is important to note that the intervention not only improved suicidal thoughts and behaviours but also improved some of the known risk factors for suicide, such as depression and symptoms of psychosis. Previous reports on the reduction of suicide behaviours have tended to be secondary reports of larger studies, which have had more global clinical aims. For example, one study277 conducted an evaluation of an integrated community treatment including assertive community treatment, antipsychotic medication, psychoeducational family treatment and social skills training with people experiencing first episodes of psychosis. Similarly, the Study of Cognitive Reality Alignment Therapy in Early Schizophrenia (SoCRATES) trial42 was an evaluation of CBT with recent onset schizophrenia aimed to speed recovery in those suffering an acute episode of psychosis. Thus, both of these studies included retrospective evaluations of suicide behaviour in trials that did not have a sole and dedicated aim to reduce such behaviour. Therefore, the current study differed markedly from previous published studies in that the intervention was derived directly from a theoretical understanding and an empirically validated model of the psychological mechanisms underlying suicide behaviour. The core mechanisms that have been identified involve negatively biased attentional processes, negative appraisals of defeat, entrapment, social support, emotional regulation and problem-solving, and the presence of an extensive suicide schema. 207–211 The trial was carried out explicitly to target these underlying psychological mechanisms and thus reduce suicide behaviour. 211 Evidence from other work has shown in those experiencing psychosis that CBT without this targeted development was disappointing in ameliorating suicidality;42 however, this issue should be investigated with a full-scale RCT. There are a number of major difficulties in evaluating suicidal prevention interventions. First, morbidity as a result of self-harm, although all too frequent, is an impractical and ethically problematic outcome measure for a small clinical trial. Therefore, it was necessary to investigate suicide behaviour by examining suicidal thoughts as a more frequently occurring proxy outcome measure. Moreover, suicidal ideation is subjectively distressing and, thus, can be considered a legitimate target in its own right. Second, the ethical requirements of administering a clinical study, especially one involving an untried therapeutic intervention, preclude the participation of those who are considered to be at current high probability of self-harm or acutely suicidal. Understandable as this is, it means that the study focused on risk factors such as history of past attempts or current ideation. A third, and related, issue is whether or not participation in suicide research is distressing or endangering to those with ongoing suicidal thoughts. This is not supported by a study in which we elicited feedback from 79 service users who had participated in suicide related research. The results indicated that overall feedback was positive, and negative feedback was rare. 215 This study has a number of weaknesses. The trial was small and not all participants were available at follow-up assessments. We used a simple design in which we compared CBSPp plus TAU with TAU alone. Future work would benefit from systematically comparing different forms of interventions, such as supportive counselling, to both a CBSPp condition and a waiting list control. The follow-up periods were relatively short at 4 and 6 months. On the positive side, this was an adequately powered trial of a manualised novel treatment to address an important clinical life-threatening problem, with independent and masked random allocation, and independent and masked assessments, using standardised measures with an at risk population recruited from a geographical cohort using public health services. The trial hypotheses were supported and there were no evident adverse effects. The trial was the first of its kind and, thus, was an indication of feasibility as well as estimating the efficacy of the novel treatment.
Conclusions
The research in this chapter aimed to develop and evaluate a cognitive–behavioural approach to understanding and preventing suicide in people with psychosis. The research was broken down into three phases:
-
a qualitative exploration of the subjective experience of participation in schizophrenia research
-
an investigation of the psychological mechanisms underlying suicide behaviours: the role of defeat, entrapment and resilience
-
a RCT of CBSPp.
This chapter described a series of studies to investigate suicidality in people with experience of psychosis, leading to an understanding of the mechanisms that underlie suicide behaviours and the development of a cognitive–behavioural intervention for this population.
The first phase of this research indicated that participants are willing to take part in research and discuss potentially sensitive topics such as psychosis and suicide. Additionally, feedback suggested a number of benefits for those who participate, including a sense of catharsis and therapeutic gain and a perception of helping others. It appears that the research environment may provide a context in which issues pertaining to mental health and suicide can be discussed in a confidential, open and non-judgemental way. This phase of the research provided a sound basis for further exploration of the topic of suicide in people who experience psychosis.
The second phase of the research investigated mechanisms underlying suicide behaviours to inform the development of the CBSPp. This study suggested that defeat and entrapment fully mediated the association between positive symptom severity and suicidal ideation. Defeat and entrapment, defined as perceptions of loss or rejection without escape or likelihood of improvement,228 may represent one particularly maladaptive psychological response to the difficulties posed by living with psychosis, which may provoke suicidal ideation and behaviour as a means of escape or protest. 206 This suggests that psychological therapies aimed at reducing suicidal ideation in individuals diagnosed with schizophrenia could focus specifically on reducing perceptions of defeat and entrapment, alongside interventions aimed more directly at alleviating clients’ symptoms.
Additionally, this phase of the research found that positive self-appraisals moderated the impact of hopelessness such that individuals with high levels of positive self-appraisals were significantly less likely to experience suicidal ideation even at the highest levels of hopelessness. When specific types of self-appraisals were examined in isolation, appraisals of emotion coping ability appeared to moderate the impact of hopelessness, but appraisals of situation coping and social support did not show this moderating impact. This suggests that positive self-appraisals may be an important aspect to incorporate into clinical interventions, particularly the possibility of developing positive self-appraisals to indirectly reduce the likelihood of suicide risk by attenuating the impact of risk.
The final phase of the research used the information gathered in phases 1 and 2 to inform the development of the CBSPp and evaluate this intervention in a RCT. This trial is the first study to date that utilised an intervention that has been derived directly from a theoretical understanding and an empirically validated model of the psychological mechanisms underlying suicide behaviour. The core mechanisms that have been identified involve negatively biased attentional processes, negative appraisals of defeat, entrapment, social support, emotional regulation and problem-solving and the presence of an extensive suicide schema. 207–211 The trial was carried out explicitly to target these underlying psychological mechanisms and so, reduce suicide behaviour.
The trial results showed that CBSPp, in addition to TAU, successfully and significantly reduced the primary and secondary outcome measures compared with TAU alone. That is, subjective measures of suicidal ideation, estimated probability of suicide and hopelessness (as measured by the SPS) were improved as were the associated outcomes of depression, self-esteem, symptoms of psychosis overall, positive and general symptoms of psychosis and the GAF scale symptoms score. There were no significant group differences in negative symptoms or measures of overall functioning and disability using the GAF scale. Thus, it is important to note that the intervention not only improved suicidal thoughts and behaviours but also improved some of the known risk factors for suicide, such as depression and symptoms of psychosis.
Chapter 7 Development and evaluation of recovery-focused cognitive–behavioural therapy for individuals with early bipolar disorder
Background
Bipolar disorder affects over one million people in England alone and has a prevalence rate of around 2%. 7 In addition to repeated periods of mania and depression, most individuals with BD experience extended periods of distressing subsyndromal mood symptoms between episodes. 9–11 Consequently, BD has a significant impact emotionally and functionally12 and constitutes a substantial financial burden to society with a recent estimated cost to the English economy at £5.2B per annum. 8 NICE has recommended the provision of structured psychological therapy for individuals with BD. 15 To date, controlled trials of structured psychological therapy have focused on individuals with a chronic BD. 278,279
Although it might seem logical to focus interventions on individuals with established illness course, recent psychological models of BD suggest otherwise. It has been argued that associative mechanisms build up over repeated mood episodes in BD such that later episodes are both more readily triggered by psychosocial circumstances previously linked to mood changes and are also less likely to be mediated by cognitive processes. 280–282 This suggests that cognitive–behavioural interventions may be more powerful when applied earlier in the illness course before strong associative links to bipolar emotional states are established. Consistent with this research a recent study of CBT for relapse prevention in BD found a significant benefit only for those with fewer episodes in a post hoc analysis. 43 Additionally, there is evidence that individuals with earlier onset of BD tend to have worse clinical outcomes, leading to calls for more timely detection and intervention. 283,284 Despite the arguments in favour of earlier treatment, there have been no RCT evaluations to date of CBT for BD specifically targeted at individuals early in their illness course.
Research into the longer-term outcomes of pharmacological and psychological interventions for BD has concentrated on symptom reduction and relapse prevention;278,285,286 thus, there is increasing interest in experience of recovery,287 which is now reflected in government mental health policy in England (Department of Health New Horizons,87 Department of Health Journey to Recovery288). Research in psychosis indicates that reduction in symptoms of psychosis is not a necessary requirement for the experience of recovery. 19,22,111 It has also been argued by consumers that recovery in BD is not always associated with symptomatic change. 95 To date there have been very few studies that have explored this issue systematically. Studies that have explored how individuals with BD stay well have focused primarily on methods by which relapse is avoided and have defined recovery in terms of symptom reduction, rather than focusing on the subjective process of recovery. 289,290 Additionally, studies have focused mainly on individuals with long-term diagnosis of BD neglecting exploration of how these processes develop earlier on in the course of the disorder. No study has explored experiences of recovery from the perspective of the participants early in the course of their BD.
Similarly, individuals with personal experience of severe mental illness, including BD, express dissatisfaction with the notion that symptom and relapse reduction are the primary targets of clinical practice. Instead, service users argue for the importance of personal recovery outcomes. 19,95,291 Although clinical recovery contributes to this process, the emphasis for many people is on social and functional recovery outcomes. Understanding and endorsement of this recovery perspective by clinical professionals can lead to significant benefits in terms of greater service user empowerment, enhanced use of collaborative care models (including advanced directives) and tailoring of clinical interventions which together enhance social and functional outcomes. 292–296 However, there have been very few studies that have explored recovery experiences systematically in BD. Some qualitative studies have explored how individuals with BD stay well, focusing primarily on methods by which relapse is avoided, rather than on the subjective process of recovery, highlighting the importance of both medication and psychosocial support in the context of active condition management by the individual. 289,290 Although clinically helpful, such reports define recovery in terms of symptom reduction and avoidance of relapse thus missing the more idiosyncratic personal recovery experiences that are often most important to service users. They also do not incorporate research which indicates that trajectories of symptomatic and functional improvement are often different297,298 and that some individuals with significant residual symptoms can achieve high levels of functioning. 299 Furthermore, such approaches do not offer researchers or clinicians a time-efficient tool to assess recovery in relation to new treatments or routine clinical practice. The QPR has recently been developed, which explores intrapersonal and interpersonal aspects of recovery from psychosis as a process32 and has already been adopted as the primary outcome measure for a cluster RCT of a recovery-focused approach to CMHT care. 300 However, despite the promise of this measure, it was not developed to capture the unique experiences of individuals with BD, including its varied and fluctuating nature and the need to balance experience across phases of mania, depression and euthymia. For example, in people with BD, there is a risk that high levels of optimism, involvement in meaningful activities and social interactions and self-confidence may actually be indicative of mental health problems in a way that is unlikely for people with psychosis.
In light of this, the current study begins by exploring the subjective experience of recovery in the early stages of BD. This information will then be used to develop and evaluate a service-user informed measure of recovery in BD (the BRQ). The final phase of this study will use an adapted CBT intervention for individuals within the first 5 years since onset of BD. An earlier version of this intervention has already proved to be acceptable and feasible in a single case series of seven bipolar participants. 301 The present trial builds on this pilot work in a RCT feasibility study, but also extends the intervention to incorporate a clear focus on recovery outcomes (RfCBT) as measured by the BRQ. The intervention used in this study was developed using evidence-based principles for effective psychological interventions for BD279 previous pilot case series work301 and through qualitative interviews, focus group work and consultation with individuals with experience of BD.
Phase 1: recovery in the early stages of bipolar disorder
Objectives
This study aimed to identify the range and nature of subjective recovery experiences in a group of individuals with recent onset BD.
Method
Participants
Over a period of 4 months, nine individuals with a diagnosis of BD were recruited from mental health services and service user groups in the north-west of England. Participants were asked to complete a demographic sheet, two self-report measures of mood [Beck Depression Inventory302 (BDI) and the Internal States Scale (ISS);303,304 Table 60]. Diagnosis was confirmed with the Structured Clinical Interview for DSM-IV Disorders (SCID). 305
| Participant | Age (years) | Sex | Ethnicity | Diagnosis | Number of years since diagnosis | BDI score | ISS-W | ISS-A | ISS-PC | ISS-D |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 35 | Male | White British | Bipolar 1 disorder | 2 | 12 | 181 | 180 | 161 | 30 |
| 2 | 39 | Male | White British | Bipolar 2 disorder | 4 | 8 | 219 | 60 | 34 | 0 |
| 3 | 43 | Female | White British | Bipolar 1 disorder | 0 | 3 | 235 | 323 | 35 | 10 |
| 4 | 24 | Male | White British | Bipolar 1 disorder | 3 | 15 | 147 | 40 | 59 | 12 |
| 5 | 61 | Female | White British | Bipolar 1 disorder | 0 | 0 | 204 | 81 | 77 | 28 |
| 6 | 43 | Female | White British | Bipolar 1 disorder | 2 | 9 | 153 | 121 | 92 | 17 |
| 7 | 24 | Female | White British | Bipolar 1 disorder | 5 | 0 | 200 | 171 | 63 | 0 |
| 8 | 56 | Female | White British | Bipolar 1 disorder | 0 | 3 | 235 | 385 | 35 | 0 |
| 9 | 37 | Female | White British | Bipolar 1 disorder | 3 | 11 | 212 | 64 | 37 | 11 |
Inclusion criteria
Participants were included in the study if they had received a diagnosis of BD I or II (according to SCID criteria) in the previous 5 years and felt that they could reflect on their experiences of recovery in BD. Participants were aged between 18 and 65 years at the time of interview.
Exclusion criteria
Individuals were excluded if they were currently experiencing acute major depression or mania or had experienced an acute mood episode of either type in the 2 months prior to interview. The presence of subsyndromal mood symptoms did not preclude recruitment.
Interview procedure
A topic guide was used for each interview to provide a provisional structure (including possible open-ended questions) but was intended to be flexible and did not dictate the direction of the interview or resultant themes. The topic guide was developed by the authors in consultation with a reference group of past and present service users with personal experience of BD. Service user feedback concerned the relevance and appropriateness of the questions to the consideration of recovery and related issues. Issues covered in the interview included past experiences of BD, strategies or ways of coping with BD, participant definitions of recovery in BD, experiences of recovery and factors that were helpful or unhelpful in recovery. All interviews were conducted in person and, depending on the participant’s preference, took place either at the participants’ homes or at their local mental health services. Interviews lasted 1 hour on average and were audio-recorded for later analysis.
Analysis
Interview recordings were transcribed verbatim and analysed using the qualitative method of IPA. 66,306 IPA aims to describe, explore and understand the individual experiences of participants and attempts to capture the meanings that particular phenomena hold for them. The central interpretative role of the researchers in analysing and making sense of these experiences is recognised as part of IPA. Therefore, this method is consistent with the primary aim of the present study to explore the subjective experience of recovery and the idiographic nature of recovery definitions, over and above externally imposed assumptions of what recovery is and how it occurs.
Data were analysed by three authors: a clinical academic with a psychological perspective, an academic researcher and a non-clinical academic with expertise in qualitative methodology. Consistent with the procedures described by Smith et al. ,66 each of the first three transcripts were analysed in detail by each researcher independently. This preliminary information on key themes was then reviewed in detail by the researchers as a group to construct key themes for each participant. These agreed theme sets were then evaluated and integrated by the group of researchers to provide indicative themes that informed (but did not restrict) the subsequent analysis of the remaining transcripts. To ensure the reliability and validity of the analysis, authors met regularly to compare their independent analyses of transcripts. As a further step, the reference group of service users were consulted on both the validity of the interpretation of participant quotes and on the developing themes that emerged. Superordinate themes were identified from clustering of connected themes that most strongly reflected participants’ perspectives on recovery related issues.
Results
The five key themes that emerged from participant accounts are described below.
Mood experiences as understandable and manageable
Participants described a process of coming to see their mood experiences as developing from a combination of early experiences, developing personality and ongoing life events. Many participants described having reached an understanding of how these elements interact and how their patterns of interaction with the world and others might have an impact on their vulnerability to develop mood symptoms in the future. This includes appreciating how early experiences had shaped the way they perceived the world in some cases:
I think some of the work I did with the psychologists when I got under the EI team allowed me to make a bit of sense of perhaps from some of the things that had happened early on in my life. There were some quite traumatic events early on in my life . . . I guess maybe some of the things that had happened to me previously in life had given me a lot of beliefs that perhaps were brought to the fore when I was, when my mood was kind of all over the place.
Participant 1
For others, examples of enduring traits were identified including setting high standards for one’s self, taking on too much or being a perfectionist which they related to potential for the development of mood symptoms:
I think one of the problems I have is erm I set my standards really high and when I fail it’s an excuse to beat myself up, it’s an excuse, well which leads to depression or it’s an excuse to work even harder which is going to push me the other way into hypomanic or mixed episode.
Participant 9
A lot of people I know with bipolar are included in this, are very much perfectionists and blame themselves when things aren’t going right and I’ve sort of, I’ve tried to stop [laughs] worrying about every little detail of things.
Participant 2
This process of making mood experiences understandable enabled participants to develop a stronger sense that such experiences could also be managed rather than having a ‘life of their own’:
I always felt that, certainly with, particularly with depression, that it controlled me, rather than me having any control over it at all, so it happened to me and it was done to me, but I think now I don’t have that belief I believe I have the control over it from having the diagnosis and doing the work subsequently.
Participant 1
Developing resources to self-manage health
The development over time of strategies that enabled participants to take more effective control of their own mood typically had a profound impact on their beliefs in their own self-efficacy. Changes in self-efficacy beliefs were often illustrated by contrasting current coping behaviour with previous, less effective, ways of managing mood in which they would ‘charge on’ with it, or ‘go straight steaming a head through it’ (which are active strategies that may exacerbate mania) (participant 4), or would ‘sit it out’ and wait for it to disappear (passive strategies that may exacerbate low mood). There was general acknowledgement of a central role of the individual in managing care from diverse sources (including medication, therapy, family, support groups, psychoeducation, etc.) to enhance mood stability and mental health:
I’ve got management tools of how to deal with the old me and that’s what I didn’t have before cause I’ve got much more insight and I can now learn how to deal with those things and how to control it rather than being that all over the place whirl wind, cause I wasn’t just a whirlwind, I was, it was a very broad whirlwind [laughs].
Participant 3
Change in balance of care from perceived dependence on others to increased autonomy and independence was regarded as an important facet of recovery
You know as everyone’s erm been around monitoring me, and I’ve been monitoring myself, you know, its about finding your triggers, what makes these things erm just what makes them happen really and once you identify them then you can go around them and you know you just don’t go straight steaming a head through it.
Participant 4
Being able to look after yourself, being able to look after the house, [. . .] err being healthy, not having to rely on professionals or medication.
Participant 8
Recovery involved more than solely gaining mood stabilisation. Mood stability was conceptualised as aiding progress towards a more complete recovery but not as indicating recovery in and of itself:
I don’t think any clinical measure [of mood stability] really means much. I mean it may be a means to an end but it’s certainly not at the end.
Participant 2
Access to personally meaningful activity
Access to personally meaningful activities was highly valued by participants in relation to their recovery. For some participants this involved becoming involved in activities that they have previously engaged in before the onset of their BD. For some participants this included becoming involved in activities that they engaged in before the onset of their BD, such as going back to a valued job or undertaking previously enjoyed hobbies:
I just feel like I’m getting back to how I used to be before the whole section thing and the huge mania . . . just more happy, happier you know erm, more productive, I’ve been writing songs again which I haven’t done for, you know, since the whole 60 songs in 2 days thing.
Participant 4
It reminded me that I can do all that stuff, I was beginning to wonder at what point if my brain was completely fried and all the things I was able to do ten years ago, if I could still do that at all in terms of being professional about things, and understanding finances and erm company structures and all that sort.
Participant 2
For other participants, recovery involved taking on of new roles, for example in the context of work or volunteering:
I started to feel better about myself, I started to engage in more of the stuff that the early intervention team offered. Like the STR’s there ran a football group, so I started to go and play football again and there was opportunities to go and volunteer . . . I felt that I made quite quick steps recovery wise because of that, and I really hold that as a strong belief now, that just those meaningful activities that put your self-respect back, have got a massive effect on your recovery.
Participant 1
It was engagement in these activities that had a profound impact on how participants saw themselves, helping them ‘feel productive’, regain confidence and realise their own self-worth. Lessons learned from these activities in turn aided the (re)building of the self:
I think two trips combined have really taught me to sort out you know, what matters and what doesn’t matter and not to get stressed out about things that you can’t do anything about, don’t get yourself stressed out because it is just going to lead to, if I let it build up it’ll just lead to another episode so I think I have changed and I think my travelling has got a lot to do with that.
Participant 9
Recovery as a life long process
Recovery was typically conceptualised as an ongoing process without a definite end point. In parallel with recovery was an awareness of continuing vulnerability to mood fluctuations and a continuing need to monitor mood to remain in recovery:
I feel like I’m well on the road to recovery, but I also don’t want to be naïve in thinking this is me bomb proof like, for the rest of my life. [. . .] I still feel vulnerable to mental health problems and I think I probably always need to keep a check on mood.
Participant 1
I mean from what I’ve read there’s always going to be ups and downs eventually, so I guess it’s just remaining mindful that, yeah I have been ill and I’m probably more, more than the average person, more susceptible to becoming ill again so I’ve got to watch out for it and just yeah take it easy and look after myself.
Participant 4
An additional element to this theme was awareness that hypomanic states continued to be both appealing and seductive:
How important it is to not chase your highs, just to sort of sit on them rather than let them lead you know erm, whereas before I just used to push it as far as I could go, and then that’s when I’d get into trouble or when things would start to fall apart, whereas now I realised that, it’s really hard though cause they’re so seductive and you just want to go along with them.
Participant 7
When it’s mixed or manic or hypomanic, it’s very very difficult because as soon as you get an upsurge in energy with those sorts of episodes it’s like ‘yeah great I can do this, I can do that, oh I’m going to do this, I’m going to do that blah blah blah blah’ you know ‘I’m going to climb mountains and I’m going to swim oceans’ [laughs] you know what I mean, it’s, and it’s easy to turn a blind eye to the warning signs of those types of episodes.
Participant 9
Discussion
Although there have been studies that have explored the ways in which individuals achieve mood stabilisation, this is the first study of the understanding of recovery and recovery-related experiences from the perspectives of individuals with recent onset BD.
It is clear that participants engaged in active processes linking their understanding of themselves with their symptom experiences. This development of enhanced understanding over time was regarded as important in providing participants with the tools to manage their mood symptoms. In addition to active mood management strategies, people typically associated increased self-efficacy more widely with recovery. This was often marked by a transition from relying on a wide range of formal and informal sources of support early in recovery to more strategic and lower use of these resources as recovery progressed. It also seemed that recovery was facilitated when people moved from unhelpful active or passive coping behaviours to more functional, balanced coping methods consistent with cognitive–behavioural understandings of BD. 278 A wider aspect of recovery was highlighted in the role of engaging in activities that were personally meaningful. People either found these activities important in defining themselves as distinctly different from their pre-bipolar self or found value in activities that were consistent with returning to their original view of themselves. There was also evidence that recovery was perceived to be a dynamic process rather than movement towards a fixed end point. As such most participants reported progressing through recovery while at the same time holding a sense of vulnerability to future episodes, which could be moderated by awareness of this risk.
Previous research
Consistent with previous research, the present study indicates varied impacts of BD. Michalak and Murray307 identified both positive and negative effects of BD on quality of life. Studies of ‘staying well’ in BD have indicated roles for life style management, warning sign detection/mania avoidance medication and use of support services. 289,290 These reports defined wellness in terms of absence of relapse and recruited their sample on the basis of being out of episode for ≥ 2 years. The current study finds the processes involved in recovery may be different. First, experience of recovery was not limited to individuals with extensive symptom-free periods. Second, the role of medication did not emerge as a theme in relation to recovery. Third, the specific importance of meaningful activity is highlighted in recovery in contrast with previous wellness research. In a mixed psychiatric group, a staged model of recovery was reported from acknowledgement/acceptance of illness initially through learning about the illness to later stages of building independence and quality of life. 308 In contrast, here a staged process of this type would not describe the varied recovery paths reported. The similarities between the findings of our study and those of recovery from psychosis are notable,19,22,111 with recovery identified as a process or journey that involves increased self-efficacy and understanding of self as well as reintegration with life, social inclusion and active participation in meaningful roles.
Strengths and limitations
Consistent with guidelines for IPA research, the sample for this study is not large but was selected to be homogeneous with respect to diagnosis and relatively recent onset. Although drawn from a range of NHS and service user settings across the north-west, this sample is not intended to be formally representative of all early onset bipolar service users. Therefore, it is important to be cautious about generalising these findings too widely. However, the sample provided a series of rich and diverse themes illustrative of the complex recovery paths that people with BD negotiate. Care was taken to engage service users in the planning and process of the study and comparison of independent analyses of interviews was used to ensure reliability and validity of analyses.
Implications
Services should note that even relatively early in the course of BD, people report a wide range of recovery experiences. Recovery in this group is an ongoing process that is facilitated by flexible provision of formal and informal care. A crucial aspect of this process is access to activity that is personally meaningful to the individual, whether that be paid employment, voluntary work or hobbies. The diversity of routes through the recovery process and the partial independence of recovery from symptom reduction presents clinical challenges. Services need to support individualised assessment of recovery process in the patients under their care. Services could promote recovery in a number of ways: provision of optimistic, normalising information could facilitate people viewing mood swings and BD as both understandable and manageable; increasing adaptive coping would also promote recovery (this could include use of medication, use of cognitive–behavioural methods such as evaluation of problematic appraisals and behavioural experiments, and use of lifestyle interventions such as sleep hygiene, exercise and minimising substance use); provision of meaningful activities and promotion of ordinary lives by services should also assist recovery, as could structured assessments, goal-setting and social and vocational interventions designed to facilitate re-engagement with employment, education and training.
Future research should explore the relationships between the patterns observed in the current study and those present in individuals with a more established history of BD. Assessment of recovery processes within services would be facilitated by the development of a quantitative self-report measure informed by research of this type, in a similar way to the user-informed recovery measure that has been developed for use with people with psychosis. 32
Phase 2: the Bipolar Recovery Questionnaire – psychometric properties of a quantitative measure of recovery experiences in bipolar disorder
This research was previously published as Jones S, Mulligan LD, Higginson S, Dunn G, Morrison AP. The bipolar recovery questionnaire: psychometric properties of a quantitative measure of recovery experiences in bipolar disorder. J Affect Disord 2013;147:34–43309 and much of this text is reproduced with permission from Elsevier.
Objectives
This study reports on the development of a new measure: the BRQ.
The study aimed to determine whether or not the BRQ is (1) internally consistent and reliable; (2) logically associated with measures of mental health symptoms (negative associations with depressive and manic mood symptoms, positive association with well-being); and (3) logically associated with measures of functioning and growth (positive associations with improved functioning and growth).
Method
Item generation methods
Potential items for the new scale (the BRQ) were generated based on both a review of recovery literature in severe mental illness and specifically in BD and from the phase 1 qualitative study of individuals with BD using an interpretative framework approach to explore personal definitions, experiences and accounts of recovery. Based on these sources, 45 items were drafted by the authors intending to capture personal understanding of self and symptoms, the role of the individual and sense of personal agency in the process of recovery, developing meaning through active engagement in the social/occupational world and finally to identify recovery as a dynamic process rather than a static goal.
Item reduction methods
After initial generation, all candidate items were first reviewed by a service user reference group and item wordings amended when required on the basis of this review. No items were removed at this stage. Items were then further reviewed and scrutinised for content and face validity by clinicians, academics and service user consultants involved in this project. Of the 18 experts contacted, 13 responded, rating each item on Likert scales ranging from 1 (not at all) to 5 (a great deal), for relevance to recovery (how relevant is the item to recovery in BD?) and comprehensibility (how comprehensible is the item? Is it easy to understand?). Any candidate items with an average rating of < 4 for relevance to recovery were eliminated from the item pool (n = 11). Items with an average rating of < 4 for comprehensibility were considered for rewriting (n = 2). After rewording, these items were rerated by one of the experts who offered original feedback. Both were rated as suitably comprehensible and relevant to recovery (i.e. > 4) and so were included in the final item pool. The final item pool was then reviewed and approved by the service user reference group for this project. The final BRQ scale for psychometric investigation consisted of 36 items (see Appendix 12). Each item is scored on a 100-mm visual analogue scale from 0 to 100 anchored by ‘strongly disagree’ (0)’, disagree’ (25), ‘agree’ (75) and ‘strongly agree’ (100). Total BRQ score is calculated by summing individual scores across all items of which 12 are reverse scored (i.e. strongly disagree would indicate a score of 100, and strongly agree would indicate a score of zero). Higher BRQ total scores indicate a higher degree of self-rated recovery. The scale consists of a mixture of positively and negatively keyed items to guard against acquiescence responding biases in which the participant may tend towards repeatedly giving high or low ratings on items independent of item content. 310
Participants
Participants were included in the study if they met criteria for a diagnosis of BD I or II, confirmed using the SCID. 305 Participants had to be aged 18–65 years old and sufficiently fluent in English to be able to complete the BRQ and other study measures.
Individuals were excluded if they were currently experiencing an acute episode of major depression or mania, or had experienced either in the month prior to assessment. This led to the exclusion of one potential participant.
Procedure
Participants were recruited via mental health services and service user groups across the north-west of England. Ethical approval for the study was granted by a local NHS research ethics committee, which operated in accordance with the Declaration of Helsinki. 311 Depending on individual participant preference, assessments were either completed at the participants’ homes or at local mental health services. Following a SCID interview to confirm diagnostic status and to confirm absence of a current acute mood episode, participants then completed the following measures together with the BRQ.
Symptom measures
Observer rated
Bech–Refaelsen Mania Scale (MAS):312 the MAS is an observer-rated measure of mania severity, scored over 11 items. The MAS is a widely validated scale and evidence exists for its internal consistency (α = 0.80–0.90). 313
Hamilton Rating Scale for Depression (HDRS):314 the HDRS is an observer-rated measure of depression severity, scored over 17 items. The HDRS has been shown to have a high degree of scale reliability and evidence exists for its concurrent and discriminant validity. 315,316
Self-report
Beck Depression Inventory – Second Edition (BDI-II):302 the BDI-II is a self-report inventory of depression severity, scored over 21 items. The scale has good psychometric properties, including test–retest reliability of 0.65–0.85 in depressed adults over periods of 1–3 weeks. 302
Internal States Scale:303 the ISS is a well-established self-report measure of bipolar symptomatology, scored across four subscales assessing Internal States Scale activation (ISS-A), Internal States Scale perceived conflict (ISS-PC), Internal States Scale well-being (ISS-W) and Internal States Scale depression (ISS-D). The ISS has been shown to have excellent psychometric properties across two studies. 303,304
Functioning and growth measures
Observer rated
Personal and Social Performance scale:155 the PSP is an observer-rated measure of functioning, scored across four domains assessing socially useful activities, personal and social relationships, self-care and aggression. The internal consistency of the overall scale has been shown to be adequate (α = 0.76). 156
Self-report
Medical Outcomes Study Short Form Health Survey:317 the Medical Outcomes Study Short Form Health Survey is a self-report measure of mental and physical health functions cored over 12 items. The mental health and physical health summary components of the Medical Outcomes Study Short form Health Survey demonstrate good psychometric properties (α = 0.88 and 0.86, respectively). 318
Post-traumatic growth inventory (PTGI):319 the PTGI is a 21-item self-report measure of positive outcomes following traumatic experiences. The psychometric properties of the PTGI total score are good (α = 0.90). 319,320
Psychometric analysis
Internal consistency of the BRQ was computed using Cronbach’s alpha (α). External validity was assessed by analysing cross-sectional relationships between BRQ scores and the self-reported and observer-rated measures described above (see Symptom measures, Observer rated and Self-report). Power calculations revealed that 60 participants were sufficient to detect correlational relationships of ≥ 0.4 between BRQ and measures of interest with alpha set at 0.01 and beta at 0.8. This threshold was deemed sufficient to ensure that items of potential significance associated with BRQ were not missed. To more rigorously assess the unique associations between measures of symptoms and function and BRQ scores, those measures that were significantly associated with BRQ were entered together into a series of regression analyses to explore the variance accounted for by each, one exploring the variance explained by symptom measures and a second, exploring the variance explained by measures of growth and functioning. Significant predictors from these initial analyses were then entered into a final regression analysis to explore the specific measures that uniquely predicted recovery. Kolmogorov–Smirnov (KS) tests were used to assess the distributions of data for questionnaire totals and subscales. None of the scales deviated significantly from normality.
Results
Participants
Sixty participants were recruited, comprising 26 males (43%) and 34 females (57%) aged between 19 and 63 years (mean age 42.37 years, SD 11.42 years). Fifty-two participants (87%) had a diagnosis of BD I and the remainder had a diagnosis of BD II (13%). Twenty-eight participants completed the BRQ for a second time 4 weeks later for reliability testing. The majority of participants were not in employment despite half the sample having completed tertiary education. Over half of the participants had experienced seven or more episodes of depression and/or mania. A full description of participant demographics is reported in Table 61.
| Variable | Total sample (n = 60) |
|---|---|
| Age (years) | |
| Mean (SD) | 42.34 (11.42) |
| Range | 19–63 |
| Sex | |
| Male | 26 |
| Female | 34 |
| Ethnicity | |
| White | 57 |
| Asian | 1 |
| Black | 1 |
| Other | 1 |
| Marital status | |
| Single | 22 |
| Married | 18 |
| Cohabiting | 5 |
| Divorced/separated | 14 |
| Widowed | 1 |
| Education attainment | |
| Secondary education | 26 |
| Further education | 12 |
| Higher education | 22 |
| Employment status | |
| Full time, part time or voluntary | 27 |
| Disabled/Disability Living Allowance | 26 |
| Student | 5 |
| Retired | 1 |
| Unemployed | 1 |
| Diagnosis | |
| BD I disorder | 52 |
| BD II disorder | 8 |
| Number of previous episodes of mania or hypomania | |
| 0–6 | 27 |
| 7–11 | 10 |
| 12–29 | 10 |
| > 30 | 11 |
| Unknown | 2 |
| Number of previous episodes of depression | |
| 0–6 | 20 |
| 7–11 | 13 |
| 12–29 | 13 |
| > 30 | 11 |
| Unknown | 3 |
Reliability
Internal consistency
Cronbach’s alpha was calculated for the 36-item scale. Internal reliability analyses showed that the BRQ had a good to excellent consistency (α = 0.875),321 and in no case did deleting an item lead to a significant improvement in the internal reliability of the scale (change α > 0.02). Across all the items, endorsement in the low range (0–10) ranged from 0% to 16.7%. In the moderate range (11–50) endorsements ranged from 3.3% to 51.7% and from 38.3% to 96.7% in the higher range (51–100). For total BRQ scores, skewness and kurtosis were acceptable, with values not substantially greater than zero, and within the limits of skewness < 2 and kurtosis < 7. 322,323
Test–retest reliability
Test–retest reliability was computed by comparing initial BRQ scores (time 1) with those completed 4 weeks later (time 2) in 28 participants of the total sample (47%). The results yielded strong relationships between time 1 and time 2 BRQ scores, indicating excellent test–retest reliability (r = 0.866; p < 0.001).
Validity
Relationship between Bipolar Recovery Questionnaire recovery score and symptom measures
The BRQ and symptom scores are presented in Table 62. Relationships between total BRQ score and symptom measures are illustrated in Table 63. Bivariate correlations indicated that BRQ total score correlated negatively with HDRS, BDI and ISS depression scores as well as ISS activation and perceived conflict. A significant positive association was identified between BRQ and ISS well-being. The bivariate association between BRQ and MAS was not significant (p < 0.05). Associations were also explored between BRQ total score and specific depression (HDRS-D) and elevated mood items [Bech–Refaelsen Mania Scale – mood items (MAS-M)]. The BRQ score was significantly negatively associated with both mood items.
| Variable | n | Mean | SD |
|---|---|---|---|
| BRQ | 60 | 2357.7 | 414.0 |
| HDRS | 59 | 6.5 | 6.1 |
| MAS | 59 | 1.9 | 2.6 |
| BDI | 59 | 14.5 | 11.8 |
| ISS-PC | 59 | 81.7 | 71.0 |
| ISS-W | 59 | 131.1 | 69.4 |
| ISS-A | 59 | 97.9 | 82.0 |
| ISS-D | 59 | 45.9 | 42.0 |
| IDQ-D | 59 | 20.1 | 8.2 |
| IDQ-N | 59 | 27.2 | 6.8 |
| IDQ-E | 59 | 6.5 | 3.2 |
| HIQ-H | 59 | 24.5 | 8.2 |
| HIQ-N | 59 | 23.2 | 6.1 |
| HIQ-E | 59 | 4.7 | 4.1 |
| SF12-P | 59 | 45.3 | 11.0 |
| SF12-M | 59 | 39.9 | 11.7 |
| PSP | 59 | 67.6 | 11.5 |
| Variable | BRQ | HDRS | HDRS-D | MAS | MAS-M | BDI | ISS-PC | ISS-W | ISS-A | ISS-D |
|---|---|---|---|---|---|---|---|---|---|---|
| BRQ | ||||||||||
| HDRS | –0.495** | |||||||||
| HDRS-D | –0.456** | |||||||||
| MAS | –0.144 | 0.434** | ||||||||
| MAS-M | –0.304* | –0.118 | –0.236 | 0.519** | ||||||
| BDI | –0.665** | 0.752** | 0.685** | 0.373** | –0.172 | |||||
| ISS-PC | –0.448** | 0.375** | 0.301* | 0.358** | –0.155 | 0.563** | ||||
| ISS-W | 0.525** | –0.391** | –0.415** | 0.013 | 0.350** | –0.398** | –0.261* | |||
| ISS-A | –0.289* | 0.254 | 0.171 | 0.514** | 0.135 | 0.390** | 0.548** | 0.160 | ||
| ISS-D | –0.459** | 0.577** | 0.522** | 0.347** | –0.074 | 0.550** | 0.470** | –0.620** | 0.171 | |
| PTGI | 0.591** | –0.104 | –0.179 | 0.144 | 0.364** | –0.298* | –0.126 | 0.368** | 0.022 | –0.275* |
Relationship between Bipolar Recovery Questionnaire recovery score and measures of appraisals, growth and functioning
Appraisal, growth and functioning scale scores are presented in Table 62. Relationships between total BRQ score and functioning and growth measures are presented in Table 64.
| Variable | BRQ | PTGI | SF12-P | SF12-M | SF12-WB |
|---|---|---|---|---|---|
| BRQ | |||||
| PTGI | 0.591** | ||||
| SF12-P | 0.058 | –0.238 | |||
| SF12-M | 0.561** | 0.290* | –0.102 | ||
| SF 12-WB | 0.549** | 0.323* | 0.125 | 0.728** | |
| PSP | 0.489** | 0.239 | 0.344** | 0.548** | 0.481** |
Bivariate correlations indicated that BRQ total score was significantly positively associated with PSP score, Medical Outcomes Study Short Form – mental health and PTGI. BRQ total score was also specifically associated with an index of positive well-being composed of two Short Form questionnaire-12 items (SF-12) items: (1) calm and peaceful and (2) energy. Bivariate correlations were also conducted to assess the relationships between total BRQ score and individual items of PTGI to explore which elements of post-trauma growth were most related to recovery (Table 65). There were significant associations with 15 out of the 21 PTGI items with the highest associations (> 5) with items 10 (I know better that I can handle difficulties), 12 (I am better able to accept the way things work out), 19 (I have discovered that I’m stronger than I thought I was), 2 (I have a greater appreciation of the value of my own life), 3 (I developed new interests) and 4 (I have a greater feeling of self-reliance).
| PTGI item | BRQ |
|---|---|
| PTGI1: ‘I changed my priorities about what is important in life’ | 0.061 |
| PTGI2: ‘I have a greater appreciation of the value of my own life’ | 0.514** |
| PTGI3: ‘I developed new interests’ | 0.457** |
| PTGI4: ‘I have a greater feeling of self-reliance’ | 0.464** |
| PTGI5: ‘I have a better understanding of spiritual matters’ | 0.355** |
| PTGI6: ‘I more clearly see that I can count on people in times of trouble’ | 0.185 |
| PTGI7: ‘I established a new path for my life’ | 0.401** |
| PTGI8: ‘I have a greater sense of closeness with others’ | 0.369** |
| PTGI9: ‘I am more willing to express my emotions’ | 0.083 |
| PTGI10: ‘I know better that I can handle difficulties’ | 0.627** |
| PTGI11: ‘I am able to do better things with my life’ | 0.532** |
| PTGI12: ‘I am better able to accept the way things work out’ | 0.573** |
| PTGI13: ‘I can better appreciate each day’ | 0.454** |
| PTGI14: ‘New opportunities are available which would not have been otherwise’ | 0.365** |
| PTGI15: ‘I have more compassion for others’ | 0.288* |
| PTGI16: ‘I put more effort into my relationships’ | 0.231 |
| PTG17: ‘I am more likely to try to change things which need changing’ | 0.381** |
| PTGI18: ‘I have a stronger religious faith’ | 0.307* |
| PTGI19: ‘I have discovered that I’m stronger that I thought I was’ | 0.524** |
| PTGI20: ‘I learned a great deal about how wonderful people are’ | 0.096 |
| PTGI21: ‘I better accept needing others’ | 0.101 |
Predictors of total Bipolar Recovery Questionnaire recovery score
To explore more specifically which measures were uniquely associated with BRQ recovery score multiple regressions with blockwise entry were conducted. Based on the variance inflation factor and tolerance statistics, there were no concerns about multicollinearity. Plots did not indicate any concerns about homoscedasticity, and standardised residuals were normal. First, each clinical symptom measure with a significant bivariate correlation with total BRQ score was entered into the first equation. The overall regression equation was significant [F(6,52) = 10.613; p < 0.0001]. The regression equation indicated that BDI total score (standardised β = 0.503, t = 3.096; p < 0.01) and ISS-W score (standardised β = 0.423, t = 3.234; p < 0.01) contributed significantly to the variance in BRQ score. Both BDI and ISS-W score each contributed to BRQ variance. In combination the two variables explained another 5% of variance in BRQ score, explaining 21% in total. Second, each growth and functioning measure with a significant bivariate correlation with total BRQ score was entered into another regression equation. The overall regression equation was significant [F(3,55) = 22.261; p < 0.0001]. The equation indicated that PTGI total score (standardised β = 0.448, t = 4.708; p < 0.001), PSP score (standardised β = 0.221, t = 2.028; p < 0.047) and mental health score of the Medical Outcomes Study Short Form health Survey (standardised β = 0.310, t = 2.805; p < 0.005) contributed significantly to the variance in total BRQ score. PTGI score contributed 17% to BRQ variance, PSP 3% and Medical Outcomes Study Short Form health Survey contributed 7%. In combination the three variables explained another 27% of variance in BRQ score, explaining 54% in total. Third, using the significant predictors of BRQ total score from both clinical symptom measures (regression 1) and appraisals, growth and functioning measures (regression 2), a further regression equation with blockwise entry was conducted. The overall regression equation was significant [F(5,53) = 20.457; p < 0.0001]. The regression equation indicated that PTGI total (standardised β = 0.363, t = 4.114; p < 0.001), ISS-W (standardised β = 0.199, t = 2.173; p < 0.05) and BDI total (standardised β = 0.401, t = 3.097; p < 0.001) contributed significantly to the variance in total BRQ score. PTGI contributed 11% to BRQ variance; ISS-W contributed 3% and BDI score contributed 6%. In combination the three variables explained another 9% of variance in BRQ score, explaining 29% in total. A final regression was conducted to explore which of the PTGI items was uniquely associated with BRQ total score. All six PTGI items with a bivariate correlation of 0.5 or higher were entered into the regression. The overall regression equation was significant [F(6,52) = 9.536; p < 0.0001]. One item contributed significantly to variance in BRQ score; 10 (I know better that I can handle difficulties) (standardised β = 0.384, t = 2.63; p < 0.01) and a second showed a non-significant trend; 12 (I am better able to accept the way things work out) (standardised β = 0.212, t = 1.84; p < 0.1). Item 10 alone explained 6% of variance in BRQ score; item 12 explained a further 3%. Total variance in BRQ score explained by all six items individually and in combination was 52%.
Discussion
Although the importance of personal recovery in mental health is increasingly widely recognised there has been little research into this area in relation to BD. BRQ is the first self-report tool specifically designed to capture the subjective experience of recovery in individuals with BD. In line with Anthony’s287 proposal that recovery experiences are highly personal and multifaceted, the BRQ items were informed by prior qualitative research on the nature and experience of recovery in BD. 291 Item relevance and comprehensibility was also reviewed by clinical, research and consumer experts to refine the final version of BRQ. Current findings indicate that the questionnaire is internally consistent and reliable over time. Significant associations were observed with mood symptoms and, as expected, recovery was associated with lower levels of manic and depressive symptoms and higher levels of well-being. The one mood measure that was not significantly associated with BRQ was the MAS, which may be owing to very low mania scores in the current sample. Additionally, when associations were explored between BRQ and MAS elevated mood item and HRDS depressed mood item, both correlations were significant, consistent with the pattern of increased recovery being linked to lower mania and improved depression. Additionally BRQ was also associated with improvements in overall functioning, improved mental health, improved positive well-being, experience of personal growth and improved overall functioning recovery was associated with the majority of the items from the PTGI, with particularly strong associations with items concerned with a stronger sense of being able to cope with challenges and greater acceptance of how life can work out. Regression analysis indicated among the measures of mood that self-rated depression and well-being were unique associates of recovery. Conversely, among measures of functioning and growth, both personal growth, improved overall functioning and positive mental health were unique associates of recovery. When these variables were combined a final regression indicated that personal growth, well-being and self-reported depression contributed uniquely to explained variance in BRQ score. The results indicate the BRQ is not solely a measure of either functioning or mood symptoms but appears to capture a combination of these elements consistent with both personal reports of individuals with BD and with Anthony’s wider definition of recovery. Neil et al. 32 also found significant associations between their QPR and measures of health and quality of life in their sample of participants with psychosis. However their study did not look specifically at the relative contributions of symptoms and functioning to recovery experiences. A further regression analysis of the relationships between specific PTGI items and BRQ indicated that only one item (I know better that I can handle my difficulties) was a unique associate suggesting the potential importance of confidence in one’s own resources in recovery in this group.
The current findings suggest that BRQ has potential as a method for economically evaluating recovery outcomes in research studies and clinical practice for people with BD. Employing both types of measure in such studies offers important opportunities to understand more about which treatments are beneficial for clinical and personal recovery, respectively, with a view to developing treatment programmes that offer an optimal balance between these elements.
There are limitations to the current study. First, the size of the sample meant that PCA was not appropriate. For future research, it would be appropriate to explore the factor structure of the BRQ in a larger samples to understand more about whether it contains subscales with particular relationships to symptoms or functioning. Second, although the BRQ was reliable over a period of 1 month in the current sample, it would be helpful to again replicate this finding in a larger sample than that available in the current study. Third, although the sample was drawn from across the north-west of England and from a range of different services it is not yet established how generaliseable the current findings are to the wider UK or international groups of people with BD.
It is also recognised that BRQ is a self-report tool and, therefore, captures the subjective experiences of individuals. This is strength in terms of definitions of recovery which highlight its individualised, personal and subjective nature. Although more objective observer rated tools are available for the assessment of clinical recovery, it is unclear whether or not this is possible for personal recovery. The current findings indicate that personal recovery and clinical recovery are linked but not synonymous for individuals with BD.
In conclusion, BRQ was developed with extensive input from individuals with personal experience of BD in recognition of the importance of identifying personally defined recovery experience. The resulting questionnaire appears to be a reliable and valid measure of recovery in BD. Although further research is indicated to finalise BRQ’s factor structure, it has promise as a tool for research and clinical practice and is currently being evaluated as an outcome measure in a RCT of new psychological intervention for BD.
Phase 3: a randomised controlled trial of recovery-focused cognitive–behavioural therapy for individuals with early bipolar disorder
The design of this research has previously been published as Jones S, Mulligan LD, Law H, Dunn G, Welford M, Smith G, et al. A randomised controlled trial of recovery focused CBT for individuals with early bipolar disorder. BMC Psychiatry 2012;12:204. 324 Much of this text is reproduced from Jones et al. © 2012 Jones et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This research was previously published as Jones S, Smith,G, Mulligan LD, Lobban F, Law H, Dunn G, et al. Recovery-focused cognitive–behavioural therapy for recent-onset bipolar disorder: randomised controlled pilot trial. Br J Psychiatry 2015;206:58–66 and much of this text has been reproduced with permission from the Royal College of Psychiatrists. 325
Objectives
The primary objective of this trial was to establish the acceptability and feasibility of a new CBT-based intervention (RfCBT), designed in collaboration with individuals with early BD to improve clinical and personal recovery outcomes.
Main research questions:
-
to demonstrate feasibility of recruitment and consenting procedures, adherence to protocol and retention to both arms of the trial across assessment, intervention and follow-up periods
-
to provide parameter estimates of clinical outcomes with respect to, recovery, bipolar relapse, mood, cognitive style, quality of life, functioning, hope, stigma and self-esteem, post-traumatic growth and medication adherence.
Method
This study was a rater-blind RCT that compared up to 18 hours of RfCBT plus TAU for BD with TAU.
Participants
Recruitment took place across 11 NHS trusts in the north-west of the UK. CMHTs, out-patient clinics, GP surgeries, primary care mental health teams and voluntary services were approached to identify potential participants. Participants were recruited into the study if they met the inclusion criteria of DSM-IV diagnosis of primary BD with onset in last 5 years;305 sufficient understanding of written and spoken English in order to provide consent, engage with interviews and use the intervention; and aged between 18 and 65 years. Participants were not included if they were assessed to be manic, hypomanic, depressed or mixed episode currently or in the last 4 weeks. As the primary purpose of the study was to evaluate the feasibility and acceptability of delivering the proposed intervention a formal power calculation is not appropriate. It has been estimated that 30 participants per group will be sufficient to be able to reliably determine primary feasibility outcomes. The recruitment target was set at 72 participants in total to allow for expected attrition rates.
Procedure
Care co-ordinators, research nurses and research development officers were approached in order to contact potential participants in the first instance. Potential participants were offered a participant information sheet by their care co-ordinators or the research team, outlining the study and their role should they wish to take part. Care co-ordinators and other relevant health professionals were informed of a participant’s involvement in the study subject to participant consent. If a participant did not wish for their GP or care co-ordinator to be informed about their involvement in the study, this did not prevent their participation and contact details of all health professionals involved in their care were still taken in case of any clinical adverse events during the study.
After the initial baseline assessment, eligible participants were randomised to via the independent Clinical Trials Unit at The Christie NHS Foundation Trust, Manchester, with minimisation on number of bipolar episodes and level of current mood symptoms (including depression and mania). These minimisation variables were selected as there is preliminary evidence that clinical outcomes are better in BD for individuals with fewer episodes43 and with less severe mood problems at inception (although this research is clearest with respect to symptoms of depression, the high rates of manic symptoms found in individuals in depressed states indicates the importance of allowing for both affective poles326,327). Participants were randomised to receive RfCBT plus TAU or TAU alone. After randomisation, participants were followed up for a period of up to 15 months. In addition to regular (3-monthly) assessments to evaluate bipolar relapse, recovery and observer-rated mood, additional clinical outcome and process measures were completed at baseline and then at 6-monthly intervals.
Measures and assessments
A summary of measures and their respective time points can be found in Table 66.
| Assessment | 0 weeks (baseline) | 3 months (telephone assessment) | 6 months | 9 months (telephone assessment) | 12 months | 15 months (telephone assessment) |
|---|---|---|---|---|---|---|
| BRQ | ✓ | ✗ | ✓ | ✗ | ✓ | ✗ |
| Time to bipolar relapse: weekly LIFE scores (SCID LIFE) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| HDRS | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Bech–Refaelsen Mania Scale (MAS) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| BDI | ✓ | ✗ | ✓ | ✗ | ✓ | ✗ |
| ISS | ✓ | ✗ | ✓ | ✗ | ✓ | ✗ |
| Brief Quality of Life in Bipolar Disorder Questionnaire | ✓ | ✗ | ✓ | ✗ | ✓ | ✗ |
| PSP | ✓ | ✗ | ✓ | ✗ | ✓ | ✗ |
| Stephenson Medication Adherence Interview | ✓ | ✗ | ✓ | ✗ | ✓ | ✗ |
Primary clinical outcomes
Hypotheses for the primary clinical outcomes were that RfCBT would (1) increase self-reported recovery as measured by the BRQ;309 (2) increase time to bipolar relapse measured by the SCID, research version (SCID DSM-IV: SCID Life);328 and (3) reduce mood symptoms as measured by HDRS314 and Bech-Rafaelsen Mania Scale. 312
Secondary outcomes
Hypotheses for secondary outcomes were that RfCBT would improve (1) self-reported mood symptoms as measured by the BDI-II302 and ISS;303 (2) quality of life and social functioning as measured by Personal and Social Functioning Scale155 and the Brief Quality of Life in Bipolar Disorder Questionnaire;307 and (3) medication adherence measured by the Stephenson Medical Adherence Questionnaire. 329
Measures to assess therapeutic alliance and adherence
Engagement in therapy was assessed by means of the Working Alliance Inventory (WAI) (Short Form, therapist and client versions). 330 Treatment fidelity was assessed by both the Cognitive Therapy Scale Revised Version331 and the RfCBT fidelity scale specifically designed for the current study.
Individual recovery-focused cognitive–behavioural therapy intervention
The RfCBT intervention was informed by current evidence for components of effective CBT interventions279 as well as findings from a completed case series of CBT for first diagnosis bipolar clients301 supporting importance of flexible engagement, allowing time for full consideration of meaning of diagnosis to the client, engaging in coping skills reviews around subsyndromal exacerbations as well as prior episodes and considering the role of appraisals of fluctuations in affect. Therapy manual development was also informed by qualitative interviews with individuals about their experiences of recovery in BD and focus groups with individuals with BD to consult on the draft content, format and supporting materials for the RfCBT intervention. The intervention was delivered by mental health professionals trained to British Association for Behavioural and Cognitive Psychotherapies (BABCP) accreditation level in CBT or equivalent. Duration of therapy was up to 18 hours delivered over a period of approximately 6 months at client’s homes or mental health facilities according to client preference. Initial sessions were weekly, with later sessions fortnightly and typically lasted 45–60 minutes.
The following elements are contained within the RfCBT manual and reflect elements typically addressed in the course of therapy, although the relative emphasis on each element is informed by the client’s formulation:
-
introducing the recovery approach to clients
-
collection of information about current and historical mood and functioning
-
meaning and relevance of diagnosis
-
identification of recovery informed therapy goals
-
initial formulation of relationships between mood experiences and progress towards recovery goals
-
identification and application of CBT techniques to address and facilitate positive coping
-
consideration of wider functioning issues in relation to recovery
-
development and completion of recovery plan
-
sharing lessons from therapy with key stakeholders.
The therapy approach differs from standard CBT for BD in the following ways:
-
explicit focus on eliciting client-focused goals rather than presuming a target of relapse prevention
-
formulation driven idiosyncratic approach rather than applying a very similar model of bipolar experience across clients
-
freedom to work within whatever model the client brings
-
openness to address functioning and comorbidity issues as well as mood problems.
Treatment as usual in both groups was typically characterised by routine medication (mood stabilisers, antipsychotics and antidepressants). Participants received their medical care either through primary or secondary services. In the latter case, most participants received maintenance appointments for their responsible clinician and support from a care co-ordinator via a CMHT.
Statistical analysis
Feasibility
As the primary purpose of the study was to evaluate the feasibility and acceptability of delivering the proposed intervention, a formal power calculation comparing treatment groups was not essential. With 72 subjects in total, the study was able to estimate a follow-up rate of 75% with precision ± 10%.
Clinical outcomes
All analyses were carried out using Stata. All therapy effects were estimated using a random effects (random intercepts) model, assuming that the effects were the same for each follow-up times (having first checked that there was no significant therapy by follow-up time interaction). The baseline value of the relevant outcome measure was used as a covariate. The intention-to-treat principle was followed throughout. If there had been a significant number of participants not attending their allocated sessions, this would have been supplemented by estimation of the therapy effects in those participants who actually receive the intervention via estimation of the Complier-Average Causal Effect;332,333 however, this proved to be unnecessary. Time to relapse was assessed by survival analysis (differences between groups being evaluated using the log-rank test and hazard ratios were estimated using a Cox proportional hazards model). Missing data were assumed to be missing at random (ignorable) and automatically allowed for in fitting the random effects or analysis of covariance models. 334
Results
Feasibility outcomes
Key feasibility outcomes for this study were recruitment, retention and participation in the intervention for those in the treatment arm. Participant flow is indicated in Figure 15. Of 128 screened for eligibility, 67 individuals were randomised to RfCBT or TAU. Of those who were not randomised, the majority declined the opportunity to participate (n = 35), the remainder did not meet study criteria owing to duration of illness > 5 years (n = 14), currently in an episode (n = 6), > 65 years (n = 2) and already participating in another intervention study (n = 1).
FIGURE 15.
Follow-up rates including partial data.
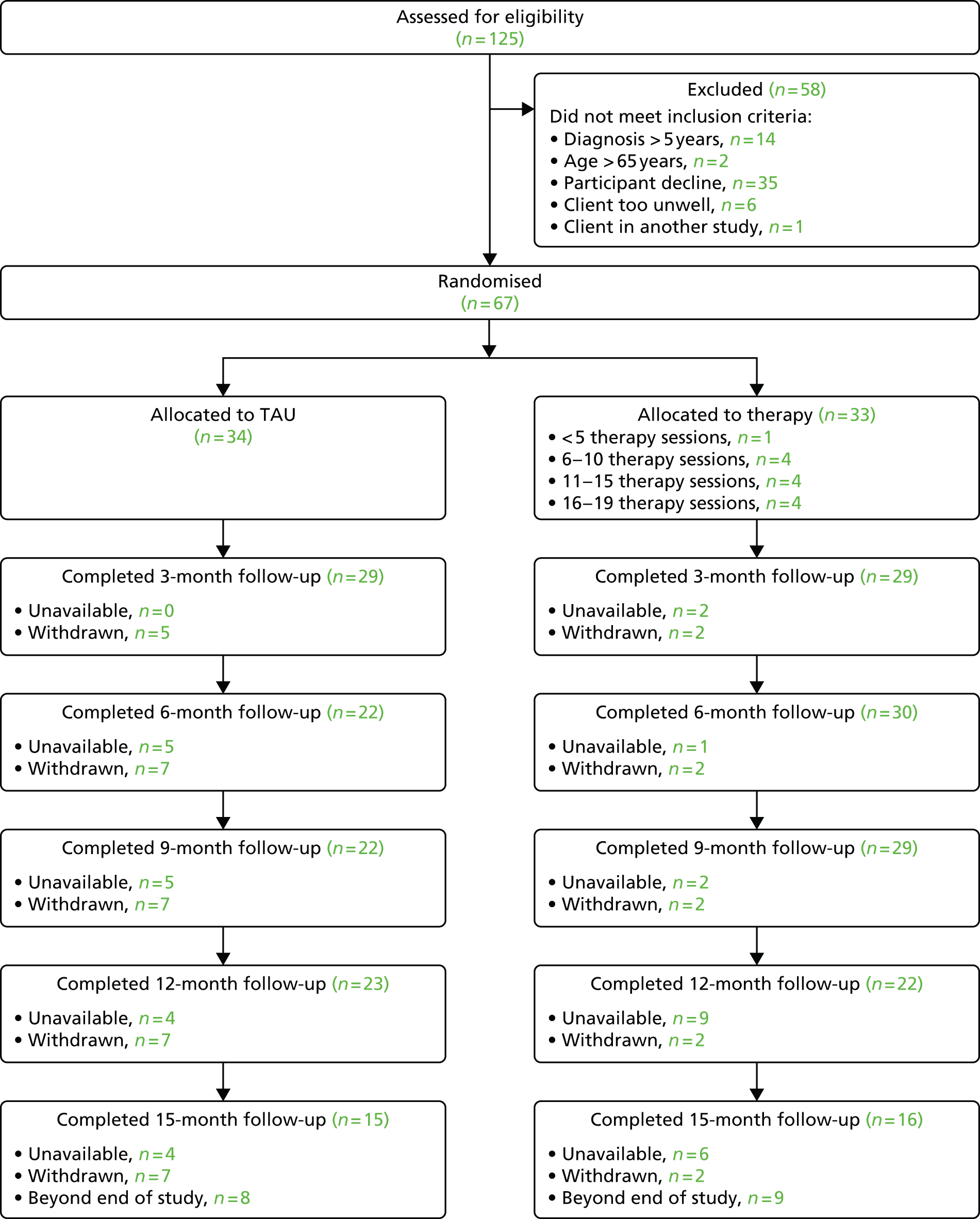
Of the 67 participants randomised, 77% were retained to end-of-therapy follow-up at 6 months, 76% to 9 months’ follow-up and 67% at 12 months’ follow-up. The 15-month follow-up period was tapered as the funding for the study terminated before this assessment became due for 17 of the participants. Of those eligible, 61% completed the 15-month follow-up.
Of the 33 participants allocated to RfCBT, 32 attended at least six sessions with a mean of 14.15 (SD 4.21) sessions overall. Working alliance as rated by therapists was 56.55 (SD 4.94) at session 4; 58.84 (SD 4.76) at session 8 and 61.76 (SD 4.84) at session 17. At each stage of therapy clients ratings were higher than those of therapists: session 4, 64.72 (SD 7.01); session 8, 66.35 (SD 7.66) and 71 (SD 5.51). Both sets of alliance ratings are comparable with those observed for psychological therapy in mild and complex patient groups. 335,336 Therapist protocol adherence was independently assessed for 33 randomly selected session tapes. Adherence to the therapy protocol was 91% (recovery fidelity scale) while mean score for Cognitive Therapy Scale – Revised was 35.4 (SD 7.9) which is above established threshold criteria for competence. 337 Recovery fidelity and Cognitive Therapy Scale – Revised scores were moderately but significantly correlated (r = 0.467; p < 0.006).
Participants were, on average, under 40 years of age, predominantly female on both arms and had received their formal clinical diagnosis of BD within the last 2–3 years. The majority of participants had a diagnosis of bipolar 1 disorder with the remainder BD II (Table 67). Participants in both groups were receiving a mixture of antidepressants, mood stabilisers and antipsychotics. Care team arrangements were similar with both the majority of both groups receiving care from a CMHT or primarily from a psychiatrist. A minority of participants in both groups were under the care of their GP. There were no significant differences between arms on any of these variables.
| Characteristics | TAU (n = 34) | Therapy (n = 33) |
|---|---|---|
| Age (years), mean (SD) | 39.9 (10.4) | 38.3 (12.8)a |
| Sex (female), n (%) | 22 (64.7) | 25 (75.8)b |
| Age of bipolar diagnosis (years), mean (SD) | 37.4 (10.2) | 35.9 (12.7)c |
| Diagnosis | ||
| Bipolar 1 disorder, n (%) | 29 (85.3) | 24 (72.7)d |
| Bipolar 2 disorder, n (%) | 5 (14.7) | 9 (27.3) |
| Medication at baseline | ||
| Antidepressant, n (%) | 17 (50) | 14 (42)e |
| Mood stabiliser, n (%) | 22 (65) | 14 (42)f |
| Antipsychotic, n (%) | 21 (62) | 20 (61)g |
| Care team | ||
| CMHT, n (%) | 24 (70) | 19 (58) |
| Psychiatrist, n (%) | 3 (9) | 4 (12) |
| GP, n (%) | 7 (21) | 10 (30) |
Table 68 provides supplementary demographic information concerning marital status, ethnicity, schooling, employment, previous episodes and hospitalisations. The two arms of the trial did not differ on any of these variables.
| Variable | TAU group, n (%) | Therapy group, n (%) |
|---|---|---|
| Marital status | ||
| Single | 13 (38.2) | 6 (18.2)a |
| Married | 6 (17.6) | 15 (45.5) |
| Separated | 3 (8.8) | 1 (3.0) |
| Divorced | 7 (20.6) | 4 (12.1) |
| Cohabiting | 5 (14.7) | 7 (21.2) |
| Ethnicity | ||
| White | 32 (94) | 32 (97)b |
| Black | 1 (2.9) | 1 (3.0) |
| Asian | 1 (2.9) | 0 |
| Age on leaving education (years), mean (SD) | 17.9 (2.6) | 17.6 (2.5)c |
| Schooling level | ||
| Primary | 3 (8.8) | 3 (9.1)d |
| Secondary | 9 (26.5) | 13 (39.4) |
| Further | 11 (32.4) | 8 (24.2) |
| Higher | 11 (32.4) | 9 (27.3) |
| Employment | ||
| Full time | 12 (35.3) | 11 (33.3)e |
| Part time | 1 (2.9) | 5 (15.2) |
| Unemployed | 18 (52.9) | 16 (48.5) |
| Voluntary | 1 (2.9) | 1 (3.0) |
| Retired | 2 (5.9) | 0 |
| Number of previous major depressive episodes, n (%) | ||
| None | 0 | 1 (3.0) |
| 1–6 | 19 (59.4) | 16 (48.5) |
| > 6 | 13 (40.6) | 16 (48.5) |
| Number of previous manic episodes, n (%) | ||
| 1–6 | 26 (81.3) | 21 (63.6)f |
| > 6 | 6 (18.8) | 12 (36.4) |
| Number of hospital admissions, n (%) | ||
| None | 10 (30.3) | 10 (30.3)g |
| 1–6 | 23 (69.7) | 22 (66.7) |
| > 6 | 0 | 1 (3.0) |
Baseline measure scores
Both groups had low levels of depression and mania at baseline consistent with entry criterion of being out of a current mood episode. Recovery scores on the BRQ and self-reported quality of life were lower in both groups were lower in both groups than has been reported in previous samples. 307,309
Primary clinical outcomes
Random effects models were used to estimate the effect of treatment compared with TAU on BRQ from baseline to follow-up. There was a greater recovery score in RfCBT at follow-up than TAU [310.87 (SE 120.34); 95% CI 75.00 to 546.74; p = 0.010]. There was no interaction between this effect and follow-up point (6 or 12 months). As Table 69 indicates, not all participants completed self-report questionnaires at assessment points despite providing relapse data in each case (BRQ data: 98% of potential sample at baseline, 90% at 6 months, 82% at 12 months).
Follow-up data on relapse were available for 58 participants (29 from each of the two treatment arms). Participants were followed up for a period of up to 15 months, during which time 32 were known to have experienced a relapse of either depression or mania (20 TAU vs. 12 RfCBT). Kaplan–Meier estimates of time to first recurrence are presented in Figure 16. Median survival times for TAU and RfCBT were 18 weeks (95% CI 8 to 40 weeks) and 56 weeks (95% CI 28 to ∞ weeks), respectively. Estimated mean survival times were 37 weeks for TAU and 86 weeks for RfCBT. The difference in time to recurrence was statistically significant (χ2 = 7.64; p < 0.006); estimated hazard ratio 0.38 (95% CI 0.18 to 0.78).
FIGURE 16.
Kaplan–Meier estimates of time to first depressive or manic recurrence over up to 60 weeks follow-up.
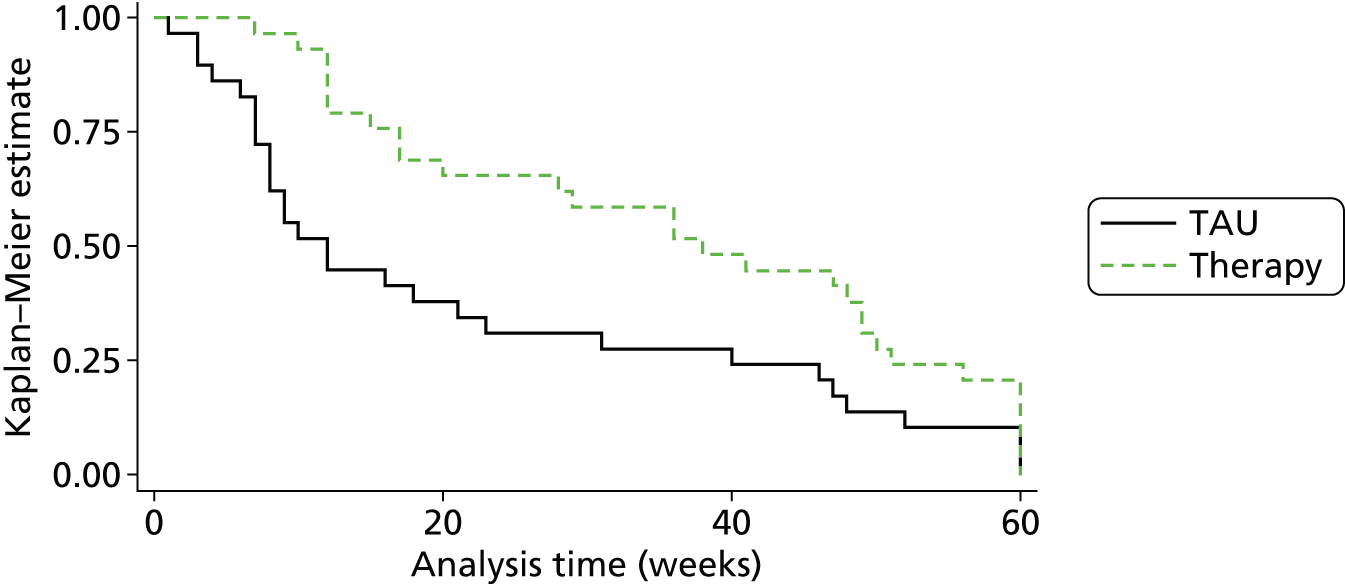
During the follow-up period, 30 patients experienced a depressive relapse (19 TAU vs. 11 RfCBT). Kaplan–Meier estimates of time to first depressive recurrence are presented in Table 3. Median survival times for TAU and RfCBT were 18 weeks (95% CI 8 to 47 weeks) and 60 weeks (95% CI 29 to ∞ weeks), respectively. Estimated mean survival times were 37 weeks for TAU and 78 weeks for RfCBT. The difference in time to recurrence rates was statistically significant (χ2 = 7.63; p < 0.006); estimated hazard ratio 0.37 (95% CI 0.18 to 0.77).
Manic relapses were less common, occurring in 13 of the participants (10 TAU vs. 3 RfCBT). Kaplan–Meier estimates of time to first manic recurrence are presented in Figure 17. Median survival times for TAU and RfCBT were 33 weeks (95% CI 23 to 58 weeks) and 60 weeks (95% CI 53 to ∞ weeks), respectively. Estimated mean survival times were 42 weeks for TAU and 76 weeks for RfCBT. This difference in time to recurrence was statistically significant (χ2 = 6.77; p < 0.009); estimated hazard ratio 0.38 (95% CI 0.19 to 0.79).
FIGURE 17.
Kaplan–Meier estimates for time to first manic recurrence over up to 60 weeks follow-up.
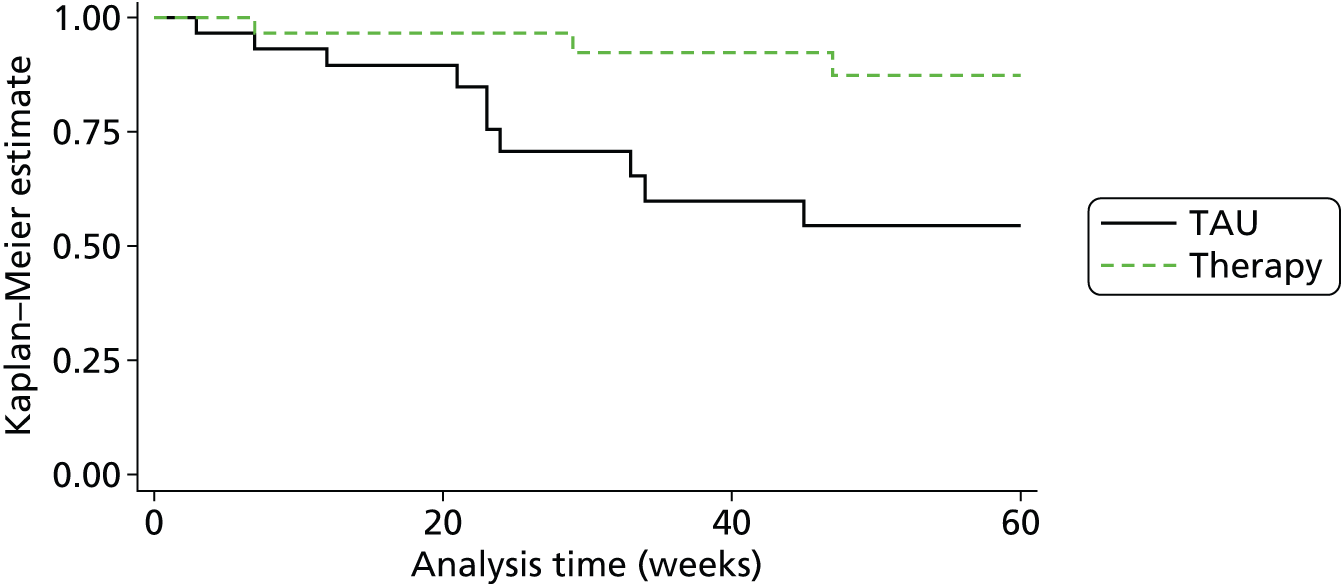
Comparisons were also made for average mood symptoms (Hamilton Depression Rating Scale and Bech-Rafaelsen Mania Scale) across the follow-up period (Figure 18). There was no significant impact of RfCBT compared with TAU on depressive [–0.98 (SE 1.37), 95% CI –3.66 to 1.71] or manic symptoms [–0.66 (SE 0.53), 95% CI –1.69 to 0.37] across the follow-up period, although the direction of effect favoured RfCBT in both cases. There is an elevation in mean HRSD score at 15-month follow-up but the actual score remains below clinical threshold and width of error bars indicates that this is unlikely to be a precise point estimate.
FIGURE 18.
Observer-rated depression and mania rating scores.
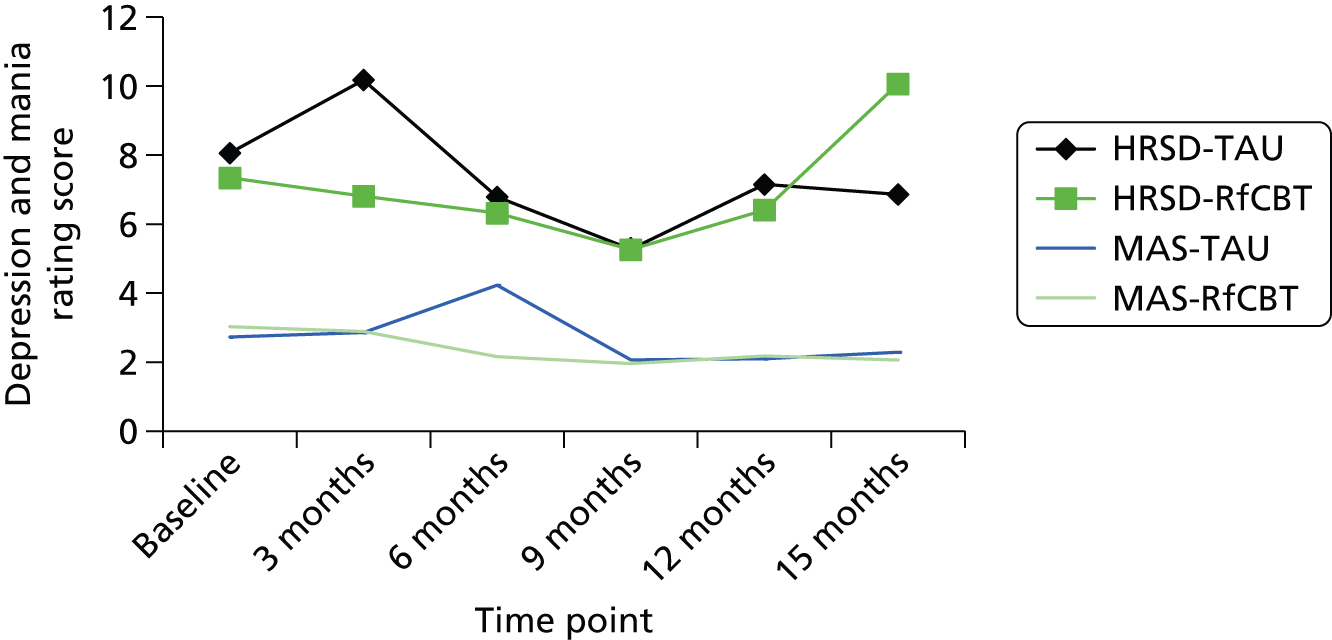
Secondary clinical outcomes
Random-effects models were used to estimate the effect of treatment compared with TAU on quality of life (Brief Quality of Life in Bipolar Disorder Questionnaire), social functioning (PSP), self-reported mood symptoms (BDI and ISS), and medication adherence between baseline and follow-up. Table 69 provides summary data for each measure across assessment points.
| Variable | TAU | RfCBT | ||||
|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | |
| BRQ T1 | 33 | 1934.57 | 543.85 | 33 | 1797.39 | 454.80 |
| BRQ T2 | 21 | 2082.57 | 518.58 | 26 | 2378.92 | 578.26 |
| BRQ T3 | 15 | 2193.40 | 357.74 | 22 | 2351.41 | 462.02 |
| QoL BD T1 | 33 | 36.73 | 11.59 | 33 | 35.91 | 8.76 |
| QoL BD T2 | 21 | 38.14 | 14.27 | 26 | 42.30 | 9.03 |
| QoL BD T3 | 15 | 39.67 | 7.60 | 22 | 42.27 | 7.34 |
| PSP T1 | 32 | 71.59 | 16.31 | 32 | 69.16 | 16.98 |
| PSP T2 | 19 | 64.89 | 24.0 | 22 | 75.73 | 19.52 |
| PSP T3 | 16 | 77.13 | 15.78 | 18 | 78.49 | 18.10 |
| ISS-A-T1 | 32 | 118.22 | 96.70 | 33 | 115.91 | 90.98 |
| ISS-A-T2 | 19 | 100.32 | 98.37 | 24 | 81.96 | 77.89 |
| ISS-A-T3 | 15 | 93.26 | 76.87 | 22 | 93.86 | 101.93 |
| ISS-W-T1 | 32 | 128.59 | 85.82 | 33 | 132.09 | 73.47 |
| ISS-W-T2 | 19 | 157.00 | 62.63 | 24 | 165.88 | 69.25 |
| ISS-W-T3 | 15 | 153.60 | 78.90 | 22 | 162.14 | 78.00 |
| BDI T1 | 33 | 19.00 | 14.85 | 33 | 19.39 | 13.23 |
| BDI T2 | 20 | 13.60 | 13.00 | 26 | 13.58 | 14.91 |
| BDI T3 | 15 | 14.87 | 14.20 | 22 | 14.41 | 21.98 |
For Quality of Life in Bipolar Disorder Questionnaire and PSP there were trends towards greater quality of life and improved social functioning in RfCBT at follow-up compared with TAU Quality of Life in Bipolar Disorder Questionnaire (QoL BD): estimated treatment effect 4.83 (SE 2.50), 95% CI –0.07 to 9.74; p = 0.054; PSP: estimated treatment effect 11.24 (SE 6.79), 95% CI –2.09 to 24.56; p = 0.099]. There was no interaction between either effect and follow-up points (6 or 12 months) for either measure.
There was no evidence for a significant differential treatment effect between RfCBT and TAU on self-reported mood symptoms although, in all cases, the direction of effect favoured RfCBT [ISS-A: estimated treatment effect –2.79 (SE 17.98), 95% CI –37.86 to 32.27; p = 0.88; ISS-W: estimated treatment effect 8.09 (SE 17.04), 95% CI –25.32 to 41.51; p = 0.635; BDI: estimated treatment effect –0.88 (SE 3.43), 95% CI –7.59 to 5.84; p = 0.798].
Discussion
This is the first study to evaluate the impact of RfCBT for early BD. RfCBT was developed in partnership with individuals with lived experience of bipolar consistent with Mental Health Research Network good practice guidelines,338 including service user involvement in qualitative work on recovery experiences, development of a recovery outcome measure and structure and format of the RfCBT intervention itself. This level of engagement of individuals with personal experience of BD is consistent with the model of recovery approaches as being empowering, individualised and grounded in the individual’s own priorities and needs. RfCBT differs from standard CBT in that there is an explicit focus on eliciting client goals, which may not include relapse prevention as a primary goal, whereas in CBT this target is assumed for all clients. There is also a strong emphasis on formulation rather than applying a very similar model of bipolar experience across clients, so the client route through therapy is different depending on their needs, giving the therapist freedom to work with whatever model the client brings but in the context of offering evidence-based approaches. Therapists are also explicitly permitted to focus on issues around functioning and comorbidity as well as mood problems.
Findings provide preliminary evidence in support of both feasibility and effectiveness in this client group. With respect to feasibility outcomes, it proved possible to recruit participants for this study and we reached 94% of the target figure of 72. The primary reason for the 6% shortfall was participants becoming unwell between initial screening and baseline. Retention to follow-up assessments was balanced across both arms of the study and within 10% of the 75% target to the 12-month follow-up.
Participants in the therapy arm engaged with RfCBT attending an average of 14 therapy sessions with 32 out of 33 clients attending at least six sessions. Both client and therapist ratings of working alliance were consistent with clients experiencing the therapy as worthwhile. Therapy adherence ratings indicated that the therapy delivered was consistent with CBT good practice principles and also with the more flexible recovery focus of RfCBT.
In terms of primary clinical outcomes, RfCBT significantly improved personal ratings of recovery at both 6- and 12-month follow-up assessments compared with TAU. RfCBT also significantly increased time to any relapse and time to both depressive and manic relapses (if relapses occurred). Time to any relapse was increased by 38 weeks, time to depressive relapse by 42 weeks and time to manic relapse by 27 weeks compared with TAU. In contrast, RfCBT had no significant impact on observer ratings of residual symptoms of depression or mania. Both HRSD and MAS scores were low throughout the study. For HRSD, scores ranged from mild depression to no depression across follow-ups, whereas on average for MAS, mania scores indicated absence of mania throughout.
Secondary clinical impact of RfCBT appeared to be stronger on functional than symptomatic outcomes. Thus, quality of life and social functioning were numerically improved in RfCBT compared with TAU, the differences approached (but did not meet) statistical significance at the 5% level. There were no group differences on self-reported mood. Both groups scored in the no mania range on ISS-A throughout the study, whereas for ISS-W both groups scored as mildly depressed at baseline, but outside the clinical range at both follow-up points. Scores on the BDI indicated mild-minimal depression throughout the study period.
Comparison to other studies
Previous studies of CBT have varied in their impact on time to relapse. Lam et al. 278 reported a significant effect over 12 months, while Ball et al. 339 reported a trend (for depressive relapse), both favouring CBT in increasing survival time. In contrast, neither the Scott et al. 43 nor Meyer et al. 340,341 studies identified any benefit of CBT in relation to survival times to relapse. A post hoc finding from the Scott et al. 43 study was that that higher number of previous episodes was associated with worse outcomes leading to a suggestion that earlier intervention might be more appropriate. Consistent with this our trial of RfCBT with individuals within 5 years of diagnosis found strong effects on relapse. A recent study of enhanced relapse prevention delivered by non-specialist CMHT staff indicated improvements in relapse outcomes compared with TAU, but these did not reach statistical significance. 328 It is of interest that the current study did not primarily focus on relapse prevention but yet obtained strong impact on relapse compared with previous research. No other studies have specifically explored recovery outcomes in BD so it is not possible to make direction comparisons for this variable.
Strengths of the study include targeting a clearly defined sample who are currently poorly served by available interventions, namely individuals with recent onset BD. It is also the first therapy for BD that explicitly aims to enhance recovery outcomes which are valued by service users. Additionally, we have not assumed expert clinician knowledge of the nature of recovery in BD, but rather grounded the intervention in the experience and knowledge that service users have offered us with respect to recovery. The study also recruited from across NHS primary and secondary care settings and through self-referral so that findings should are more representative than those that solely focus on specialist mental health settings, as only a subset of individuals with BD are in such settings long term. 342
Limitations
There are weaknesses to the study that would need to be addressed in a definitive trial. First, there is no active treatment control group so that any indications of effectiveness need to be interpreted with caution as we will not know whether possible benefits are a function of this specific treatment or structured treatment in general. Second, it was only possible to follow up a proportion of the sample for 15 months. Longer follow-ups would be helpful to indicate more definitively whether or not this intervention impacts on relapse as well as recovery.
Clinical implications
Despite these challenges, if the current study indicates that RfCBT is feasible and has potential clinical benefits, it will be an important step towards developing evidence-based recovery interventions for people with BD that have been lacking until now.
Conclusions
This chapter explored the experience and process of recovery in individuals with BD. The research was conducted in three phases:
-
an exploration of the subjective experience of recovery in the early stages of BD
-
development, coproduction and evaluation of a service user informed measure of recovery in BD (the BRQ)
-
a RCT of RfCBT for individuals with early BD.
The research described within this chapter is the first series of studies to explore recovery and recovery-related experiences from the perspectives of individuals with recent onset BD. Consistent with findings throughout this research programme in relation to recovery in psychosis, these studies also highlighted that recovery in BD is an ongoing process that is facilitated by personally meaningful activity and appears to be only partially related to symptom reduction.
The first phase of this research elicited four key themes regarding subjective recovery experiences in individuals with experience of recent onset BD: mood experiences as understandable and manageable; developing resources to self-manage health; access to personally meaningful activity; and recovery as a lifelong process. This highlighted the importance of addressing these areas to promote recovery within services, as well as the need to develop a quantitative self-report measure informed by research of this type, in a similar way to the user-informed recovery measure that has been developed for use with people with psychosis. 32
As a result of the findings from phase 1, the second phase of this research went on to develop the first self-report tool specifically designed to capture the subjective experience of recovery in individuals with BD. Items on the BRQ were directly informed by the prior qualitative research in phase 1 on the nature and experience of recovery in BD and were further refined through consultation with SURG and a survey of users, clinical and academic experts. The BRQ was evaluated and the results indicated that the questionnaire is internally consistent and reliable over time. Significant associations were observed with mood symptoms and, as expected, recovery was associated with lower levels of manic and depressive symptoms and higher levels of well-being. Personal growth, well-being and self-reported depression contributed uniquely to explained variance in BRQ scores. These findings suggest that the BRQ is not solely a measure of either functioning or mood symptoms, but appears to capture a combination of these elements consistent with both personal reports of individuals with BD and with Anthony’s wider definition of recovery. 287 The findings from phase 2 suggest that the BRQ has potential as a method for economically evaluating recovery outcomes in research studies and clinical practice for people with BD.
The themes identified in phase 1 of this research were then used to inform the development of a recovery-focused cognitive–behavioural intervention for early BD. This RfCBT was evaluated in a RCT conducted as phase 3 of this research. The BRQ measure that was developed in phase 2 was used as a main outcome measure for evaluating the intervention. RfCBT differs from standard CBT in that there is an explicit focus on eliciting client goals, which may not include relapse prevention as a primary goal, whereas in CBT this target is assumed for all clients. There is also a strong emphasis on formulation rather than applying a very similar model of bipolar experience across clients, so the client route through therapy is different depending on their needs, giving the therapist freedom to work with whatever model the client brings but in the context of offering evidence-based approaches.
Findings from the RCT in phase 3 provide preliminary evidence in support of both feasibility and effectiveness of RfCBT in this client group. RfCBT significantly improved personal ratings of recovery at both 6- and 12-month follow-up assessments compared with TAU. RfCBT also significantly increased time to any relapse and time to both depressive and manic relapses (if relapses occurred). This suggests that RfCBT is feasible and has potential clinical benefits, which may be an important step towards developing evidence-based recovery interventions for people with BD that have been lacking until now.
Chapter 8 Discussion
Summary of results
This programme of research has provided significant advances in our understanding and facilitation of recovery from psychosis and BD. A summary of key findings can be seen in Table 70. In terms of conceptualisation and measurement of user-defined recovery, we have demonstrated the reliability and validity of the BRQ (see Chapter 7) and the SEPS (see Chapter 2), which can be used to evaluate perceived recovery in BD and the impact (both positive and negative) of dimensions of symptoms on recovery in psychosis. These scales can be used to evaluate outcome from treatment and reflect the multidimensional experience of psychosis (including both positive and negative aspects) and BD. Qualitative research found that recovery is felt to be a process rather than an end point and that recovery in psychosis is multidimensional and identified four main themes that are important to consider when conceptualising recovery in psychosis: impacts on mental health, self-change and adaptation, social redefinition, and adapting an individual coping style (see Chapter 2). Our research also suggests that there are different aspects to recovery from psychosis that are not necessarily linked to alleviation or removal of symptoms. Furthermore, it highlights the importance of ensuring that treatment is idiosyncratic in facilitating people’s recovery. The four viewpoints identified by the Q-sort provide an interesting insight into recovery and the different types of recovery styles: collaborative support and understanding, emotional change through social and medical support, regaining functional and occupational goals, and self-focused recovery (see Chapter 2).
| Chapter | Study | Phase | Key findings |
|---|---|---|---|
| 2 | User-defined conceptualisation and measurement of recovery in psychosis | 1. Conceptualisation and perceptions of recovery from psychosis: a service users perspective65 |
|
| 2. Exploring service users perceptions of recovery from psychosis: a Q-methodological approach68 |
|
||
| 3. The SEPS: psychometric evaluation of a scale to assess outcome in psychosis71 |
|
||
| 3 | What does recovery mean to service users with experience of psychosis? A Delphi study with experts by experience82 | N/A |
|
| 4 | Understanding psychological and social predictors of recovery | 1. Subjective judgements of perceived recovery from psychosis126 |
|
| 2. Psychosocial and neuropsychiatric predictors of subjective recovery from psychosis127 |
|
||
| 3. Longitudinal predictors of subjective recovery from psychosis153 |
|
||
| 4. How do I know if I’m better? Judgements of recovery from psychosis in everyday lifea |
|
||
| 5 | Development and evaluation of cognitive–behavioural approaches to guided self-help and group therapy for recovery, taking preferences into account | 1. Preferences for psychological therapy in psychosis: trial participation, mode of treatment, and willingness to be randomised186 |
|
| 2. A pilot study of a recovery-focused self-help package for people with psychosisb |
|
||
| 3. A preference trial of recovery-focused CBPT delivered over the telephone with support from a self-help guide and group sessions (STAR-T)c |
|
||
| 6 | Development and evaluation of a cognitive–behavioural approach to understanding and preventing suicide in people with psychosis | 1. The Subjective Experience of Participation in Schizophrenia Research215 |
|
| 2. Investigating the psychological mechanisms underlying suicide behaviours: the role of defeat, entrapment and resilience205,209 |
|
||
| 3. A RCT of CBSPp272 |
|
||
| 7 | Development and evaluation of RfCBT for individuals with early BD | 1. Recovery in the early stages of BDd |
|
| 2. The BRQ: psychometric properties of a quantitative measure of recovery experiences in BD309 |
|
||
| 3. A RCT of RfCBT for individuals with early BD324 |
|
In Chapter 3 our consensus study examining service user-defined recovery found a surprisingly high level of agreement (given the idiosyncratic nature of individual recovery journeys) about factors that define recovery, factors which help recovery, factors that hinder recovery and factors that demonstrate that someone is recovering. The themes from this consultation highlighted key areas that are important to service users: knowledge including an understanding of mental health problems as well as coping and help seeking skills such as ‘knowing what helps you get better’; social support and relationships, as well as support from mental health services; choice and control, including having control of life and symptoms, as well as control and choice surrounding treatment options; having goals, meaning, and purpose in life; quality of life, even in the context of continued symptoms and mental health problems; having hope for the future and feeling positive about yourself and your future, as well as self-esteem; and having a good, safe place to live.
In Chapter 4, we have found consistent psychological factors that are associated with recovery from psychosis, including negative emotions, hope and self-esteem. Concurrently, moment to moment in everyday life and prospectively over 6 months, these factors predict subjective recovery judgements. Symptoms also seem to be related to perceived recovery, although this appears to occur over time rather than cross-sectionally.
In Chapter 5, our work on cognitive–behavioural approaches to guided self-help and group therapy for recovery, has demonstrated that service users had strong preferences for treatment. The Patient Preference Design was shown to be unfeasible in a study of this size and nature. It also appears that, although patients had a strong preference for particular treatments, there is little evidence that they had any effect on their outcomes. The interventions appeared to be ineffective despite the likely selection effects (confounding) induced by letting the participants have their preferred treatment, suggesting the interventions require significant additional improvements. The failure to randomise also has important implications for future evaluations of these interventions and there is little to suggest that an appropriately designed randomised trial would be feasible.
Our work on a cognitive–behavioural approach to understanding and preventing suicide in people with psychosis (see Chapter 6) has shown that the relationship between positive symptoms of psychosis and suicidal ideation is mediated by perceptions of defeat and entrapment while positive self-appraisals were found to buffer the impact of hopelessness. Our RCT showed that CBSPp was superior to TAU on the primary outcomes of suicidal ideation and hopelessness and on secondary outcomes of depression, symptoms of psychosis and self-esteem.
In Chapter 7, our work on recovery from BD found some striking similarities from a service user perspective to the conceptualisation of recovery from psychosis; however, there was a greater emphasis on the role of medication and symptoms in perceived recovery. We developed the BRQ with extensive input from individuals with personal experience of BD and the resulting questionnaire appears to be a reliable and valid measure of recovery in BD. Our RCT of a cognitive–behavioural approach to recovery from a first episode of BD has shown that RfCBT is feasible and has potential clinical benefits for people with BD, demonstrating improvements in personal ratings of recovery and time to relapse for both depressive and manic relapses.
Deliverables for the NHS
This programme of research has resulted in a number of deliverables for the NHS that will improve services and patient experience. The Q-sort developed in our work on understanding recovery (see Appendix 7) can be utilised for the idiosyncratic assessment and generation of recovery goals. This can be used to facilitate a conversation that focuses on collaborative support and understanding, emotional change though social and medical support, regaining functional and occupational goals, and self-focused recovery; these goals can be prioritised in relation to their importance to the service user.
Similarly, the SEPS (see Appendix 8) can be used for the assessment and monitoring of positive and negative aspects of symptoms that are relevant to user-defined recovery; this represents a significant advance on traditional psychiatric interviews that focus solely on presence or absence of symptoms and their severity. A revised version of the QPR (incorporating 15 items in a single recovery factor along with a visual analogue scale and a dichotomous recovery question: see Appendix 13) will also be valuable to mental health services and service users in assessing and monitoring progress throughout individual recovery journeys. The BRQ (see Appendix 12) can be utilised for similar purposes for people with BD, rather than psychosis, and also represents a significant advance for this population.
The factors that help and hinder recovery identified from our consensus study can be utilised in a checklist that could be used by services to evaluate how recovery-focused they are and to use for benchmarking of services. These checklists (see Appendix 9) could also be rated by service users on a regular basis to ensure meaningful feedback on services and to monitor the effects of service development and redesign, which is highly relevant in the current NHS context. The experience sampling diaries (see Appendix 10) could be used to monitor recovery in everyday life and it is likely that these could be utilised to develop technological applications using smart phones or tablets that could be helpful in providing clinical services with data for assessment and outcome purposes.
We have produced three treatment manuals that will be of benefit to NHS staff and which will contribute to the dissemination of recovery-focused approaches. The manual for the cognitive–behavioural approach to suicide prevention has been published211 and is, therefore, widely available. The recovery guide that we produced for the preference trial will provide a valuable resource for clinical staff and service users and carers. The recovery guide (see Appendix 11) is a supported self-help resource that includes two core chapters (relating to the meaning of recovery, goals, resources and understanding the development of problems) and two chapters with numerous optional sections to facilitate work on overcoming obstacles (such as anxiety, paranoia, low self-esteem) or reaching wider recovery goals (such as finding employment, enjoying oneself and relaxing, developing social networks). Although the specific methods of support (telephone-delivered and group therapy) did not appear to represent significant benefits over TAU, participant and staff feedback about the content of the manual has been very positive. The RfCBT manual for BD will also provide a valuable resource for psychological therapists working with this population.
Finally, given that mood, self-esteem, locus of control and hope were all related to recovery, we would recommend that the measures we employed within this research programme (HADS for anxiety and depression, SERS-Short Form for self-esteem, BHS for hope and Multidimensional Locus of Control Scale for locus of control) be added to the SEPS and QPR or BRQ to represent a comprehensive assessment of recovery-related factors.
Overall limitations
The methodologies employed throughout this programme of research have a number of advantages and disadvantages that need to be considered before making any firm conclusions or generalisations from the findings. Although these are discussed in detail in each of the respective chapters of this report, it is acknowledged that there are additional general limitations that apply to the research as a whole.
First, it is important to consider the participant samples within the studies and the methods used to recruit them. The research in this report mostly consisted of individuals referred by their care teams. This may have led to biases in the recruitment process, with care teams selecting individuals who they believed were suitable or appropriate for the research studies, which would limit the generalisability of results. Similarly, this report includes three clinical trials that offered some form of therapy. This could be seen as biasing the sample to individuals who are actively help-seeking, able and willing to commit to a trial for a considerable number of months and are deemed suitable for a research trial by their care team. This could lead to a sample of participants with particular unique characteristics (such as motivated or high-functioning individuals) and consequently reduce the generalisability of results. In addition, the small numbers of service users that are not particularly diverse who were used to generate themes or items for general measures of recovery is potentially problematic. An alternative approach would have been to deliberately select a maximum variance sample.
Similarly, it is acknowledged that the majority of participants in these studies were white British, which may have limited the relevance of findings to individuals from other backgrounds. The lack of ethnic diversity in our samples would suggest that caution is applied in generalising to other cultures and ethnic backgrounds. Future cross-cultural research could investigate whether or not the concept of recovery, as operationalised in our research measures, is valid in other settings.
It also possible that some of the variability in experiences and responses to interventions could be accounted for by comorbid symptoms or diagnoses. Future research could aim to explore the impact of comorbidity on recovery experiences and the effectiveness of interventions.
In addition, it is acknowledged that missing data may have limited statistical power, increased the possibility of type II error and resulted in a biased sample. Missing data were not imputed for any of the studies within this report; rather, cases were deleted when data were missing for ≥ 20% of items on particular scale. In cases for which < 20% of items on a scale were missing, responses were prorated. Although acknowledging that this is a limitation of the studies, it is also important to note that priorities must be with reducing participant burden and ensuring that all participation and responses to each question are voluntary. Longitudinal studies and research trials can be particularly high burden for participants and this is a key ethical consideration for any such research. More specifically, it is important to recognise that despite the work on reaching a consensus on conceptualisations of recovery, understanding of recovery is vastly variable and can even vary within an individual and from moment to moment. Similarly, experiences of psychosis and episodes of BD can vary significantly and, therefore, recovery may be different following each episode. Future research should aim to explore these differences within individuals.
As discussed earlier in the introduction to this report (see Chapter 1, Cross-programme measures), the QPR was used throughout the research programme, often as the primary outcome in a clinical trial or as the dependent variable when examining predictors of recovery. During the course of the research programme, it became apparent that the psychometric properties were not ideal for measuring recovery as a unitary and independent construct. Individualised statistical analysis was conducted that resulted in a combined measure that utilised the visual analogue scale ratings in combination with five QPR items in Chapter 4 and subsequent studies used a 15-item version of the QPR, which was one-dimensional and had improved psychometric properties (but this had not been available to the earlier studies).
Similarly, several studies explored the relationships between negative emotion and recovery. Within different studies, self-esteem and hopelessness are utilised as components of the negative emotion construct or independently of negative emotion depending on the specific research questions and the statistical properties of the associations between these constructs. For example, if the primary research question was to address the relationship between symptoms, recovery and negative emotion, then such constructs would be used to produce the best latent measure of negative emotion; however, if the primary research question was to determine the relationship between moment-to-moment changes in self-esteem, optimism, negative emotion and recovery, then these variables would be treated separately as long as it was statistically valid to do so.
Finally, the theme of research on BD in Chapter 7 highlighted the importance of post-traumatic growth and its relationship to recovery. Further consideration of post-traumatic growth for people with experience of psychosis would have been useful and may have contributed to our understanding of recovery and our evaluations of the recovery-focused interventions.
Future research
There are a variety of implications for future research that have arisen from this programme and these will be described, but the order does not imply prioritisation of these implications. A summary of these future research suggestions is provided in Table 71. Given the clear feasibility of the cognitive–behavioural approaches to recovery from BD and the prevention of suicide in psychosis, definitive trials should be conducted. These trials should compare the clinical effectiveness and cost-effectiveness of the psychological intervention alone with TAU using an adequately powered study with a randomised controlled design. Key outcomes should include recovery, symptoms, relapse rates, quality of life, treatment acceptability, social functioning and the cost-effectiveness of the interventions.
| Chapter | Study | Phase | Future research |
|---|---|---|---|
| 2 | User-defined conceptualisation and measurement of recovery in psychosis |
|
|
| 3 | What does recovery mean to service users with experience of psychosis? A Delphi study with experts by experience | N/A |
|
| 4 | Understanding psychological and social predictors of recovery |
|
|
| 5 | Development and evaluation of cognitive–behavioural approaches to guided self-help and group therapy for recovery, taking preferences into account |
|
|
| 6 | Development and evaluation of a cognitive–behavioural approach to understanding and preventing suicide in people with psychosis |
|
|
| 7 | Development and evaluation of RfCBT for individuals with early BD |
|
|
| 8 | Overall programme discussion |
|
The further refinement of the delivery of the recovery guide would also be beneficial. This could include the possibility of traditional individual therapy to support service users in navigating and implementing the guide, or the use of peer support could be explored. The development of interventions that specifically aim to increase the positive aspects of psychotic symptoms would also be expected to increase perceived recovery. In addition, it would be important to evaluate the use of the Q-sort set as a recovery-focused goal-setting intervention. The development and evaluation of these interventions should begin with pilot or feasibility studies, before progressing to definitive multisite RCTs if warranted. Care should be taken to ensure appropriate comparison groups and outcome measures are selected.
The factors that help and hinder recovery, which were identified by our consensus study, should be evaluated at both individual and service level with large-scale quantitative research. The evaluation of training packages on the topic of understanding and promoting recovery that incorporate the results from this programme and are jointly delivered by service users and clinicians would be beneficial. These studies could utilise qualitative evaluations in addition to quantitative methods, including RCTs. Further work on the understanding of the development of patient preferences would be helpful for service planning and the design and conduct of future clinical trials. Additional research that seeks to understand the role of preferences and other factors (e.g. causal explanations and health beliefs) in the uptake of, and response to, treatment would also be important. Similarly, the development and evaluation of methods to help service users to make informed choices and express treatment preferences would be valuable in facilitating recovery and promoting autonomy and empowerment.
Clinical implications
There are a variety of clinical implications that have emerged from this research programme and these will be described, but the order does not imply prioritisation of these implications. Clearly, it will be important for services to regularly assess and monitor recovery in a multimodal way at both the individual and service level. The facilitation of collaborative conversations about recovery, focusing on factors that help and hinder recovery for that person (possibly using the checklist as a prompt), as well as identification of idiosyncratic recovery goals (possibly using the Q-sort card set), is also likely to help make services more acceptable and effective in achieving outcomes that are prioritised by service users and carers. Similarly, at a service level, attempts could be made to decrease factors that hinder recovery and to increase factors that promote recovery. It is also important to note that psychotic experiences are not always associated with distress and may be identified as a positive experience by service users (e.g. the companionship that is at times provided by auditory hallucination in those who hear voices).
Services may also endeavour to deliver specific interventions which target factors that have consistently been shown to affect recovery. These could include interventions aimed at improving mood and reducing negative affect (such as evidence-based psychological therapies, activity scheduling and physical exercise); promoting self-esteem (such as compassion-focused therapy and CBT); development of an internal locus of control and optimism about the future (such as provision of optimistic, recovery-focused psychosocial explanations of mental health problems and the use of cognitive–behavioural strategies); reduction of defeat and entrapment appraisals (such as CBT); and optimal management of symptoms (such as evidence-based pharmacological and psychological treatments, including an evaluation of the advantages and disadvantages of such symptoms).
The trials of cognitive–behavioural approaches to suicide prevention in psychosis and recovery from the early phases of BD are encouraging and suggest that these options could be considered for people presenting with such problems. However, before such treatments can be routinely recommended in treatment guidelines, we would need definitive trials with adequate statistical power.
The introduction of informed choices in a standard way, providing service users and carers with sufficient information to be able to do so, and in the context of mental health services that welcome and facilitate such choices would represent a major step forward in the treatment of psychosis and BD. It is clear that many people hospitalised with psychosis retain treatment decision-making capacity343 and a recent review regarding choice and decision-making in people using mental health services concluded that service users clearly want to be offered choices about their treatment rather than just offered medication. 344 This has led to recent calls for choice between treatments and less reliance on the exclusive use of medication for people with psychosis, as well as the suggestion that some decisions to refuse or discontinue antipsychotic medication may represent a rational informed choice rather than an irrational decision owing to lack of insight or symptoms such as suspiciousness. 345 Such choices have been recommended within recent NICE guidelines. 346
The similarities in the themes highlighted between psychosis and BD would suggest that many of the implications could be generic for people with serious mental health problems. However, the themes for people with psychosis seemed to have less emphasis on the biogenetic model, medication and symptoms, which suggests that different explanatory frameworks may be required to best engage service users and ensure that services can act effectively as a platform on which to deliver acceptable and evidence-based interventions. Perhaps choice of causal models could also be embraced within services.
Acknowledgements
Acknowledgement to the Service User Consultants and individual members of the Service User Reference Group, Yvonne Awenat, Rory Byrne, Ellen Hodson, Sam Omar, Liz Pitt, Jason Price, Tim Rawcliffe and Yvonne Thomas, for their work on this research programme.
The research team recognise that the terms and language used in this report are not universally endorsed. When differences of opinion arose in this report preparation the team decided to use the term that was endorsed by the majority while also respecting the views of others.
On behalf of the recovery programme team
Sehar Ahmed, Yvonne Awenat, Christine Barrowclough, Rosie Beck, Richard Bentall, Katherine Berry, Rory Byrne, Lelsey-Ann Carter, Gabriel Davies, Kim Drummond, James Dudley, Graham Dunn, Richard Emsley, Paul French, Patricia Gooding, Gillian Haddock, Samantha Hartley, Suzanne Heffernan, Sally Higginson, Ellen Hodson, Fiona Holland, Judith Johnson, Steven Jones, James Kelly, Martina Kilbride, Heather Law, Janet Maxwell, Monica McCusker, Anthony Morrison, John Mulligan, Lee Mulligan, Craig Murray; Sandra Neil, Sam Omar, Elizabeth Pitt, Daniel Pratt, Jason Price, Tim Rawcliffe, Zoe Rivers, Nick Shyrane, Gina Smith, Natasha Snelson, Katherine Sumner, Nicholas Tarrier, Pamela Taylor, Peter Taylor, Christopher Taylor, Yvonne Thomas, Filippo Varese, Rachel Watts, Mary Welford, Alex Wood, Lisa Wood, and Sarah Woodward.
Contributions of authors
Anthony P Morrison was the chief investigator for the programme grant and contributed methodological and/or practical advice to all components of the research programme as well as having overall responsibility for the conduct of the research programme. He contributed to the design, conduct, data analysis and interpretation of many of the studies and took joint lead on writing this report.
Heather Law was research co-ordinator for the programme with responsibility for management of studies and research assistants. She was responsible for trial management for the suicide prevention and recovery from BD studies and contributed to co-ordination and practical advice for the programme as a whole and publications arising from the research. She contributed to the design, conduct, data analysis and interpretation of many of the studies and took joint lead on writing this report. She also led the consensus study theme and the longitudinal study in the psychosocial predictors of recovery theme. She supervised and co-ordinated recruitment, contributed to training of research staff and was responsible for staff management and overall co-ordination of the studies.
Christine Barrowclough was the principal investigator for the first two phases of the PPT project. She contributed to the design, conduct, data analysis and interpretation of many of the studies within the preference trial theme and contributed to drafts of the papers for publication emerging from that theme as well as to this report. She participated in preparation of the treatment protocol and the training and supervision of the therapists and research assistants for this theme.
Richard P Bentall was the principal investigator for the psychosocial predictors of recovery projects. He contributed to the design, conduct, data analysis and interpretation of many of the studies within this theme and contributed to drafts of the papers for publication emerging from that theme as well as to this report.
Gillian Haddock was the principal investigator for the understanding and measuring recovery theme and for the final phase of the PPT project. She contributed to the design, conduct, data analysis and interpretation of all of the studies within these themes and contributed to drafts of the papers for publication emerging from these themes as well as to this report. She participated in preparation of the treatment protocol and the training and supervision of the therapists and research assistants for these themes.
Steven H Jones was the principal investigator for the understanding and promoting recovery from BD theme. He contributed to the design, conduct, data analysis and interpretation of all of the studies within this theme and contributed to drafts of the papers for publication emerging from this theme as well as to this report. He participated in preparation of the treatment protocol and the training and supervision of the therapists and research assistants for this theme.
Martina Kilbride was a service user researcher who was an applicant on the original application and, therefore, the design of the studies and themes. She contributed to the design, conduct, data analysis and interpretation of many of the studies within the preference trial theme. Unfortunately Martina died during the programme so was unable to contribute to drafts of this report; however, given her contribution all authors wished to include her.
Elizabeth Pitt is a service user researcher who was an applicant on the original application and, therefore, the design of the studies and themes. She contributed to the design, conduct, data analysis and interpretation of many of the studies within the preference trial theme and contributed to drafts of the papers for publication emerging from this theme as well as to this report.
Nicholas Shryane was the statistician for many of the empirical studies in the programme. He advised on statistical aspects of these projects, developed the analysis plans and performed the statistical analyses.
Nicholas Tarrier was the principal investigator for the suicide prevention theme. He contributed to the design, conduct, data analysis and interpretation of all of the studies within this theme and contributed to drafts of the papers for publication emerging from this theme as well as to this report. He participated in preparation of the treatment protocol and the training and supervision of the therapists and research assistants for this theme.
Mary Welford was the programme manager for the research programme. She contributed to the design, conduct, data analysis and interpretation of many of the studies within the programme and contributed to drafts of many papers for publication emerging from this programme as well as to this report. She participated in preparation of the treatment protocols for the clinical trials and the training and supervision of the therapists within all of the trials in the programme. She was responsible for clinical staff management and overall co-ordination of the therapist resource across the programme.
Graham Dunn was the trial statistician for all clinical trials in the programme. He advised on randomisation and all statistical aspects of the clinical trials, developed the analysis plans and performed the statistical analyses.
Publications
Wood L, Price JF, Morrison AP, Haddock G. Conceptualisation of recovery from psychosis: a service-user perspective. Psychiatrist 2010;34:65–470
Wood L, Price JF, Morrison AP, Haddock G. Exploring service users perceptions of recovery from psychosis: a Q-methodological approach. Psychol Psychother 2013;86:245–61.
Haddock G, Wood L, Watts R, Dunn G, Morrison AP, Price J. The Subjective Experiences of Psychosis Scale (SEPS): psychometric evaluation of a scale to assess outcome in psychosis. Schizophr Res 2011;133:244–9.
Law H, Morrison AP. Recovery in Psychosis: A Delphi Study With Experts by Experience. Schizophrenia Bulletin. 2014;40(6):1347-55.
Beck R, Heffernan S, Law H, McCusker M, Bentall RP, Morrison AP. Subjective judgements of perceived recovery from psychosis. J Mental Health 2012;21:556–66.
Morrison AP, Shryane N, Beck R, Heffernan S, Law H, McCusker M, et al. Psychosocial and neuropsychiatric predictors of subjective recovery from psychosis. Psychiatry Res 2013;208:203–9.
Law H, Shryane N, Bentall RP, Morrison AP. Longitudinal predictors of subjective recovery in psychosis [published online ahead of print November 2015]. Br J Psychiatry 2015.
Sumner K, Haddock G, Hartley S, Kilbride M, McCusker M, Pitt L, et al. Preferences for psychological therapy in psychosis: trial participation, mode of treatment, and willingness to be randomised. J Ment Health 2014;23:67–71.
Taylor PJ, Awenat Y, Gooding P, Johnson J, Pratt D, Wood A, et al. The subjective experience of participation in schizophrenia research: a practical and ethical issue. J Nerv Ment Dis 2010;198:343–8.
Taylor PJ, Gooding PA, Wood AM, Johnson J, Pratt D, Tarrier N. Defeat and entrapment in schizophrenia: The relationship with suicidal ideation and positive psychotic symptoms. Psychiatr Res 2010;178:244–8.
Johnson J, Gooding PA, Wood AM, Tarrier N. Resilience as positive coping appraisals: Testing the schematic appraisals model of suicide (SAMS). Behav Res Ther 2010;48:179–86.
Tarrier N, Kelly J, Maqsood S, Snelson N, Maxwell J, Law H, et al. 2014. The cognitive behavioural prevention of suicide in psychosis: A clinical trial. Schizophr Res 2014;156:204–10.
Jones S, Mulligan LD, Higginson S, Dunn G, Morrison AP. The bipolar recovery questionnaire: psychometric properties of a quantitative measure of recovery experiences in bipolar disorder. J Affect Disord 2013;147:34–43.
Jones S, Mulligan LD, Law H, Dunn G, Welford M, Smith G, et al. A randomised controlled trial of recovery focused CBT for individuals with early bipolar disorder. BMC Psychiatry 2012;12:204.
Jones S, Smith,G, Mulligan LD, Lobban F, Law H, Dunn G, et al. Recovery-focused cognitive–behavioural therapy for recent-onset bipolar disorder: randomised controlled pilot trial. Br J Psychiatry 2015;206:58–66.
Data sharing statement
Owing to ethical constraints at the time of the research and the complexity of the databases used, the data access is currently limited. For further information on how the data may be accessed, please contact Anthony P Morrison.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, CCF, NETSCC, PGfAR or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PGfAR programme or the Department of Health.
References
- State of the Nation Report: Poverty, Worklessness and Welfare Dependency in the UK. London: Cabinet Office; 2010.
- The Economic and Social Costs of Mental Health Problems in 2009/10. London: Centre for Mental Health; 2010.
- Palmer BA, Pankratz VS, Bostwick JM. The lifetime risk of suicide in schizophrenia: a reexamination. Arch Gen Psychiatry 2005;62:247-53. http://dx.doi.org/10.1001/archpsyc.62.3.247.
- Breier A, Schrieber JL, Dyer J, Pickar D. National institute of mental health longitudinal study of chronic schizophrenia: prognosis and predictors of outcome. Arch Gen Psychiatry 1991;48:239-46. http://dx.doi.org/10.1001/archpsyc.1991.01810270051007.
- Harkavy-Friedman JM, Restifo K, Malaspina D, Kaufmann CA, Amador XF, Yale SA, et al. Suicidal behaviour in schizophrenia: characteristics of individuals who had and had not attempted suicide. Am J Psychol 1999;156:1276-8.
- Hawton K, Sutton L, Haw C, Sinclair J, Deeks JJ. Schizophrenia and suicide: systematic review of risk factors. Br J Psychiatry 2005;187:9-20. http://dx.doi.org/10.1192/bjp.187.1.9.
- Merikangas KR, Akiskal HS, Angst J, Greenberg PE, Hirschfeld RMA, Petukhova M, et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the national comorbidity survey replication. Arch Gen Psychiatry 2007;64:543-52. http://dx.doi.org/10.1001/archpsyc.64.5.543.
- McCrone S, Cotton S, Jones L, Hawkins TA, Costante J, Nuss M. Depression in a rural, free clinic providing primary care: prevalence and predictive factors. Arch Psychiatr Nurs 2007;21:291-3. http://dx.doi.org/10.1016/j.apnu.2007.06.009.
- Solomon DA, Leon AC, Coryell WH, Endicott J, Li C, Fiedorowicz JG, et al. Longitudinal course of bipolar I disorder duration of mood episodes. Arch Gen Psychiatry 2010;67:339-47. http://dx.doi.org/10.1001/archgenpsychiatry.2010.15.
- Judd LL, Akiskal HS, Schettler PJ, Endicott J, Maser J, Solomon DA, et al. The long-term natural history of the weekly symptomatic status of bipolar I disorder. Arch Gen Psychiatry 2002;59:530-7. http://dx.doi.org/10.1001/archpsyc.59.6.530.
- Judd LL, Akiskal HS, Schettler PJ, Coryell W, Endicott J, Maser JD, et al. A prospective investigation of the natural history of the long-term weekly symptomatic status of bipolar II disorder. Arch Gen Psychiatry 2003;60:261-9. http://dx.doi.org/10.1001/archpsyc.60.3.261.
- Judd LL, Schettler PJ, Solomon DA, Maser JD, Coryell W, Endicott J, et al. Psychosocial disability and work role function compared across the long-term course of bipolar I, bipolar II and unipolar major depressive disorders. J Affect Disord 2008;108:49-58. http://dx.doi.org/10.1016/j.jad.2007.06.014.
- Layard R. Mental Health: Britain’s Biggest Social Problem? n.d.
- Core Interventions in the Treatment and Management of Schizophrenia in Primary and Secondary Care (Update). London: NICE; 2009.
- Bipolar Disorder: The Management of Bipolar Disorder in Adults, Children and Adolescents, In Primary and Secondary Care. London: NICE; 2006.
- Prytys M, Garety PA, Jolley S, Onwumere J, Craig T. Implementing the NICE guideline for schizophrenia recommendations for psychological therapies. A qualitative analysis of the attitudes of CMHT staff. Clinical Psychol Psychot 2011;18:48-59. http://dx.doi.org/10.1002/cpp.691.
- Whitwell D. Recovery Beyond Psychiatry. London: Free Association; 2005.
- Bellack AS. Scientific and consumer models of recovery in schizophrenia: concordance, contrasts, and implications. Schizophr Bull 2006;32:432-42. http://dx.doi.org/10.1093/schbul/sbj044.
- Pitt L, Kilbride M, Nothard S, Welford M, Morrison AP. Researching recovery from psychosis: a user-led project. Psychiatr Bull 2007;31:55-60. http://dx.doi.org/10.1192/pb.bp.105.008532.
- Davidson L. Living Outside Mental Illness: Qualitative Studies of Recovery in Schizophrenia. New York, NY: New York University Press; 2003.
- Jerrell JM, Cousins VC, Roberts KM. Psychometrics of the recovery process inventory. J Behav Health Ser R 2006;33:464-73. http://dx.doi.org/10.1007/s11414-006-9031-5.
- Resnick SJ, Rosenheck RA, Lehman AF. An exploratory analysis of correlates of recovery. Psychiatr Serv 2004;55:540-7. http://dx.doi.org/10.1176/appi.ps.55.5.540.
- Smith TE, Hull JW, Goodman M, Hedayat-Harris A, Willson DF, Israel LM, et al. The relative influences of symptoms, insight, and neurocognition on social adjustment in schizophrenia and schizoaffective disorder. J Nerv Ment Dis 1999;187:102-8. http://dx.doi.org/10.1097/00005053-199902000-00006.
- Heinrichs R, Zakzanis KK. Neurocognitive deficit in schizophrenia: a quantitative review of the evidence. Neuropsychology 1998;12:426-45. http://dx.doi.org/10.1037/0894-4105.12.3.426.
- Keefe R, Poe, M, Walker, TM, Harvey PD. The relationship of the Brief Assessment of Cognition in Schizophrenia (BACS) to functional capacity and real-world functional outcome. J Clin Exp Neuropsychol 2006;28:260-9. http://dx.doi.org/10.1080/13803390500360539.
- Fleming K, Green MF. Backward masking performance during and after manic episodes. J Abnorm Psychol 1995;104:63-8. http://dx.doi.org/10.1037/0021-843X.104.1.63.
- Nuechterlein K, Dawson M, Ventura J, Miklowitz D, Konishi G. Information processing abnormalities in the early course of schizophrenia and bipolar disorder. Schizophr Res 1991;5:195-6. http://dx.doi.org/10.1016/0920-9964(91)90069-4.
- Green MF. Schizophrenia from a Neurocognitive Perspective: Probing the Impenetrable Darkness. Boston, MA: Allyn and Bacon; 1998.
- Addington JSH, Addington D. Facial affect recognition: a mediator between cognitive and social functioning in psychosis. Schizophr Res 2006;85:142-50. http://dx.doi.org/10.1016/j.schres.2006.03.028.
- Resnick SJ, Fontana A, Lehman A, Rosenheck RA. An empirical conceptualisation of the recovery orientation. Schizophr Res 2005;75:119-28. http://dx.doi.org/10.1016/j.schres.2004.05.009.
- Law H, Morrison AP, Byrne R, Hodson E. Recovery from psychosis: a user informed review of self-report instruments for measuring recovery. J Mental Health 2012;21:192-207. http://dx.doi.org/10.3109/09638237.2012.670885.
- Neil ST, Kilbride M, Pittb L, Nothard S, Welford M, Sellwood W, et al. The questionnaire about the process of recovery (QPR): a measurement tool developed in collaboration with service users. Psychosis 2009;2:88-91. http://dx.doi.org/10.1080/17522430902913450.
- Melo SS, Taylor J, Bentall RP. Poor me versus bad me paranoia and the instability of persecutory ideation. Psychol Psychother 2006;79:271-87. http://dx.doi.org/10.1348/147608305X52856.
- Bentall RP, Myin-Germeys I, Smith A, Knowles R, Jones SH, Smith T, et al. Hypomanic personality, stability of self-esteem and response styles to negative mood. Clin Psychol Psychother 2011;18:397-410. http://dx.doi.org/10.1002/cpp.780.
- Birchwood M, Mason R, MacMillan F, Healy J. Depression, demoralization and control over psychotic illness: A comparison of depressed and non-depressed patients with a chronic psychosis. Psychol Med 1993;23:387-95. http://dx.doi.org/10.1017/S0033291700028488.
- Tarrier N, Lewis S, Haddock G, Bentall R, Drake R, Kinderman P, et al. Cognitive-behavioural therapy in first-episode and early schizophrenia. 18-month follow-up of a randomised controlled trial. Br J Psychiatry 2004;184:231-9. http://dx.doi.org/10.1192/bjp.184.3.231.
- Tarrier N, Yusupoff L, Kinney C, McCarthy E, Gledhill A, Haddock G, et al. Randomised controlled trial of intensive cognitive behaviour therapy for patients with chronic schizophrenia. BMJ 1998;317:303-7. http://dx.doi.org/10.1136/bmj.317.7154.303.
- Barrowclough C, Haddock G, Lobban F, Jones S, Siddle R, Roberts C, et al. Group cognitive behaviour therapy for schizophrenia: randomised controlled trial. Br J Psychiatry 2006;189:1-7. http://dx.doi.org/10.1192/bjp.bp.106.021386.
- Barrowclough C, Haddock G, Tarrier N, Lewis SW, Moring J, O’Brien R, et al. Randomized controlled trial of motivational interviewing, cognitive behavior therapy, and family intervention for patients with comorbid schizophrenia and substance use disorders. Am J Psychiatry 2001;158:1706-13. http://dx.doi.org/10.1176/appi.ajp.158.10.1706.
- Haddock G, Barrowclough C, Tarrier N, Moring J, O’Brien R, Schofield N, et al. Cognitive-behavioural therapy and motivational intervention for schizophrenia and substance misuse. 18-month outcomes of a randomised controlled trial. Br J Psychiatry 2003;183:418-26. http://dx.doi.org/10.1192/bjp.183.5.418.
- Morrison AP, French P, Walford L, Lewis SW, Kilcommons A, Green J, et al. Cognitive therapy for the prevention of psychosis in people at ultra-high risk: randomised controlled trial. Br J Psychiatry 2004;185:291-7. http://dx.doi.org/10.1192/bjp.185.4.291.
- Tarrier N, Haddock G, Lewis S, Drake R, Gregg L, So CTG. Suicide behaviour over 18 months in recent onset schizophrenic patients: the effects of CBT. Schizophr Res 2006;83:15-27. http://dx.doi.org/10.1016/j.schres.2005.12.846.
- Scott J, Paykel E, Morriss R, Bentall R, Kinderman P, Johnson T, et al. Cognitive-behavioural therapy for severe and recurrent bipolar disorders: randomised controlled trial. Br J Psychiatry 2006;188:313-20. http://dx.doi.org/10.1192/bjp.188.4.313.
- National Service Framework for Mental Health. London: Department of Health; 1999.
- Davidson L, O’Connel M, Tondora J, Styron T, Kangas K. The top ten concerns about recovery encountered in mental health system transformation. Psychiatr Serv 2006;57:640-5. http://dx.doi.org/10.1176/ps.2006.57.5.640.
- Pilling S, Bebbington P, Kuipers E, Garety P, Geddes J, Martindale B, et al. Psychological treatments in schizophrenia: II. Meta-analyses of randomized controlled trials of social skills training and cognitive remediation. Psychol Med 2002;32:783-91. http://dx.doi.org/10.1017/S0033291702005640.
- Addington J, Penn D, Woods SW, Addington D, Perkins DO. Social functioning in individuals at clinical high risk for psychosis. Schizophr Res 2008;99:119-24. http://dx.doi.org/10.1016/j.schres.2007.10.001.
- Jacobson N, Greenley D. What is recovery? A conceptual model and explication. Psychiatr Serv 2001;52:482-5. http://dx.doi.org/10.1176/appi.ps.52.4.482.
- Silverstein SM, Bellack AS. A scientific agenda for the concept of recovery as it applies to schizophrenia. Clin Psychol Rev 2008;28:1108-24. http://dx.doi.org/10.1016/j.cpr.2008.03.004.
- Kuipers E, Fowler D, Garety P, Chisholm D, Freeman D, Dunn G, et al. London-East Anglia randomised controlled trial of cognitive-behavioural therapy for psychosis. III: follow-up and economic evaluation at 18 months. Br J Psychiatry 1998;173:61-8. http://dx.doi.org/10.1192/bjp.173.1.61.
- Sensky T, Turkington D, Kingdon D, Scott JL, Scott J, Siddle R, et al. A randomized controlled trial of cognitive-behavioral therapy for persistent symptoms in schizophrenia resistant to medication. Arch Gen Psychiatry 2000;57:65-72. http://dx.doi.org/10.1001/archpsyc.57.2.165.
- Jackson C, Trower P, Reid I, Smith J, Hall M, Townend M, et al. Improving psychological adjustment following a first episode of psychosis: a randomised controlled trial of cognitive therapy to reduce post psychotic trauma symptoms. Behav Res Ther 2009;47:454-62. http://dx.doi.org/10.1016/j.brat.2009.02.009.
- Gitlin M, Nuechterlein K, Subotnik KL, Ventura J, Mintz J, Fogelson DL, et al. Clinical outcome following neuroleptic discontinuation in patients with remitted recent-onset schizophrenia. Am J Psychiatry 2001;158:1835-42. http://dx.doi.org/10.1176/appi.ajp.158.11.1835.
- McGlashan TH, Zipursky RB, Perkins D, Addington J, Miller T, Woods SW, et al. Randomized, double-blind trial of olanzapine versus placebo in patients prodromally symptomatic for psychosis. Am J Psychiatry 2006;163:790-9. http://dx.doi.org/10.1176/ajp.2006.163.5.790.
- Kay SR, Fiszbein LA, Opler LA. The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophr Bull 1987;13:261-76. http://dx.doi.org/10.1093/schbul/13.2.261.
- Overall J, Gorham DR. The brief psychiatric rating scale. Psychol Rep 1962;10:799-812. http://dx.doi.org/10.2466/pr0.1962.10.3.799.
- Peters E, Myin-Germeys I, Williams S, Greenwood K, Kuipers E, Scott J, et al. Appraisals, psychotic symptoms and affect in daily life. Schizophr Res 2008;98:180-1. http://dx.doi.org/10.1016/j.schres.2007.12.424.
- Garety PA, Fowler DG, Freeman D, Bebbington P, Dunn G, Kuipers E. Cognitive-behavioural therapy and family intervention for relapse prevention and symptom reduction in psychosis: randomised controlled trial. Br J Psychiatry 2008;192:412-23. http://dx.doi.org/10.1192/bjp.bp.107.043570.
- Harrow M, Grossman LS, Jobe TH, Herbener ES. Do patients with schizophrenia ever show periods of recovery? A 15-year multi-follow-up study. Schizophr Bull 2005;31:723-34. http://dx.doi.org/10.1093/schbul/sbi026.
- Malla AK NR, McLean TS, McIntosh E. impact of phase specific treatment of first episode psychosis on Wisconsin quality of life index. Acta Psychiatr Scand 2001;103:355-61. http://dx.doi.org/10.1034/j.1600-0447.2001.00200.x.
- Felce D, Perry J. Quality of life: its definition and measurement. Res Dev Disabil 1995;16:51-74. http://dx.doi.org/10.1016/0891-4222(94)00028-8.
- Drake RE, McHugo GJ, Xie H, Fox M, Packard J, Helmstetter B. Ten-year recovery outcomes for clients with co-occurring schizophrenia and substance use disorders. Schizophr Bull 2006;32:464-73. http://dx.doi.org/10.1093/schbul/sbj064.
- Heinrich DW HT, Carpenter WT. Quality of life scale: an instrument for rating the schizophrenic deficit scale. Schizophr Bull 1984;10:388-98. http://dx.doi.org/10.1093/schbul/10.3.388.
- Lewis S, Tarrier N, Haddock G, Bentall R, Kinderman P, Kingdon D, et al. Randomised control trial of cognitive behaviour therapy in early schizophrenia: acute-phase outcomes. Br J Psychiatry 2002;181:91-7. http://dx.doi.org/10.1192/bjp.181.43.s91.
- Wood L, Price JF, Morrison AP, Haddock G. Conceptualisation of recovery from psychosis: a service-user perspective. Psychiatrist 2010;34:65-470. http://dx.doi.org/10.1192/pb.bp.109.027409.
- Smith JA, Flowers P, Larkin M. Interpretative Phenomenological Analysis: Theory Method and Research. London: Sage; 2009.
- Pitt L, Kilbride M, Welford M, Nothard S, Morrison AP. Impact of a diagnosis of psychosis: user-led qualitative study. Psychiatr Bull 2009;33:419-23. http://dx.doi.org/10.1192/pb.bp.108.022863.
- Wood L, Price JF, Morrison AP, Haddock G. Exploring service users perceptions of recovery from psychosis: a Q-methodological approach. Psychol Psychother 2013;86:245-61. http://dx.doi.org/10.1111/j.2044-8341.2011.02059.x.
- Brown S. Political Subjectivity: Applications of Q Methodology in Political Science. New Haven, CT: Yale University Press; 1980.
- Stainton Rogers R, Smith JA, Harre R, Langenhove LV. Rethinking Methods in Psychology. Thousand Oaks, CA: Sage; 1995.
- Haddock G, Wood L, Watts R, Dunn G, Morrison AP, Price J. The Subjective Experiences of Psychosis Scale (SEPS): psychometric evaluation of a scale to assess outcome in psychosis. Schizophr Res 2011;133:244-9. http://dx.doi.org/10.1016/j.schres.2011.09.023.
- Haddock G, McCarron J, Tarrier N, Faragher EB. Scales to measure dimensions of hallucinations and delusions: the Psychotic Symptom Rating Scales (PSYRATS). Psychol Med 1999;29:879-89. http://dx.doi.org/10.1017/S0033291799008661.
- Addington D, Addington J, Schissel B. A depression rating scale for schizophrenics. Schizophr Res 1990;3:247-51. http://dx.doi.org/10.1016/0920-9964(90)90005-R.
- Beck AT, Weissman A, Lester D, Trexler L. The measurement of pessimism: the Hopelessness Scale. J Consult Clin Psychol 1974;42:861-5. http://dx.doi.org/10.1037/h0037562.
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol 1988;56:893-7. http://dx.doi.org/10.1037/0022-006X.56.6.893.
- Lecomte T, Corbiere M, Laisne F. Investigating self-esteem in individuals with schizophrenia: relevance of the Self-Esteem Rating Scale-Short Form. Psychiatry Res 2006;143:99-108. http://dx.doi.org/10.1016/j.psychres.2005.08.019.
- Hall RCW. Global assessment of functioning: a modified scale. Psychosomatics 1995;36:267-75. http://dx.doi.org/10.1016/S0033-3182(95)71666-8.
- Romme M, Escher A. Hearing voices. Schizophr Bull 1989;15:209-16. http://dx.doi.org/10.1093/schbul/15.2.209.
- Miller LJ, O’Connor E, DiPasquale T. Patients’ attitudes toward hallucinations. Am J Psychiatry 1993;150:584-8. http://dx.doi.org/10.1176/ajp.150.4.584.
- Field A. Discovering Statistics Using SPSS. London: Sage Publications; 2005.
- Razavi T. Self-Report Measures: An Overview of Concerns and Limitations of Questionnaire Use in Occupational Stress Research (Discussion Papers in Accounting and Management Science). Southampton: University of Southampton School of Management; 2001.
- Law H, Morrison AP. Recovery in psychosis: a Delphi study with experts by experience. Schizophrenia Bulletin 2014;40:1347-55. http://dx.doi.org/10.1093/schbul/sbu047.
- Schizophrenia: Core Interventions in the Treatment and Management of Schizophrenia in Adults in Primary and Secondary Care (Updated Edition). London: NICE; 2010.
- Schrank B, Slade M. Recovery in psychiatry. Psychiatr Bull 2007;31:321-5. http://dx.doi.org/10.1192/pb.bp.106.013425.
- Guiding Statement on Recovery. Leeds: National Institute for Mental Health in England; 2005.
- Position Statement on the Use of the Concept of Recovery. Washington, DC: American Psychiatric Association; 2005.
- New Horizons: A Shared Vision for Mental Health. London: Department of Health; 2009.
- Supporting Recovery in Mental Health. London: NHS Confederation; 2012.
- Opportunities for a New Mental Health Strategy. London: Future Vision Coalition; 2010.
- Essock S, Sederer L. Understanding and measuring recovery. Schizophr Bull 2009;35:279-81. http://dx.doi.org/10.1093/schbul/sbn185.
- Chen EY, Tam DK, Wong JW, Law CW, Chiu CP. Self-administered instrument to measure the patient’s experience of recovery after first-episode psychosis: development and validation of the Psychosis Recovery Inventory. Aust N Z J Psychiatry 2005;39:493-9. http://dx.doi.org/10.1080/j.1440-1614.2005.01609.x.
- Neil ST, Kilbride M, Pitt L, Nothard S, Welford M, Sellwood W, et al. The questionnaire about the process of recovery (QPR): a measurement tool developed in collaboration with service users. Psychosis 2009;1:145-55. http://dx.doi.org/10.1080/17522430902913450.
- Deegan PE. Recovery: the lived experience of rehabilitation. Psychosoc Rehabil J 1988;11:11-9. http://dx.doi.org/10.1037/h0099565.
- Leete E. How I perceive and manage my illness. Schizophr Bull 1989;15:197-200. http://dx.doi.org/10.1093/schbul/15.2.197.
- Mead S, Copeland ME. What recovery means to us: consumers’ perspective. Community Ment Health J 2000;36:315-28. http://dx.doi.org/10.1023/A:1001917516869.
- Ridgeway P. Restoring psychiatric disability: learning from first person recovery narratives. Psychiatr Rehabil J 2001;24:335-43. http://dx.doi.org/10.1037/h0095071.
- Smith MK. Recovery from a severe psychiatric disability: findings of a qualitative study. Psychiatr Rehabil J 2000;24:149-58. http://dx.doi.org/10.1037/h0095105.
- Spaniol L, Wewiorski NJ, Gagne C, Anthony WA. The process of recovery from schizophrenia. Int Rev Psychiatry 2002;14:327-36. http://dx.doi.org/10.1080/0954026021000016978.
- Jones J, Hunter D. Qualitative research: consensus methods for medical and health services research. BMJ 1995;311:376-80. http://dx.doi.org/10.1136/bmj.311.7001.376.
- Fiander M, Burns T. Essential components of schizophrenia care: a Delphi approach. Acta Psychiatr Scand 1998;98:400-5. http://dx.doi.org/10.1111/j.1600-0447.1998.tb10105.x.
- Burns T, Fiander M, Audini B. A Delphi approach to characterising ‘relapse’ as used in UK clinical practice. Int J Soc Psychiatry 2000;46:220-30. http://dx.doi.org/10.1177/002076400004600308.
- Marshall M, Lockwood A, Lewis S, Fiander M. Essential elements of an early intervention service for psychosis: the opinions of expert clinicians. BMC Psychiatry 2004;4. http://dx.doi.org/10.1186/1471-244X-4-17.
- Langlands RL, Jorm AF, Kelly CM, Kitchener BA. First aid recommendations for psychosis: using the Delphi method to gain consensus between mental health consumers, carers, and clinicians. Schizophr Bull 2008;34:435-43. http://dx.doi.org/10.1093/schbul/sbm099.
- Morrison A, Barratt A. What are the components of CBT for psychosis? A Delphi study. Schizophr Bull 2010;36:136-42. http://dx.doi.org/10.1093/schbul/sbp118.
- Byrne R, Morrison A. Service users’ priorities and preferences for treatment of psychosis: a user-led Delphi study. Psychiatr Serv 2014;65:1167-9. http://dx.doi.org/10.1176/appi.ps.201300289.
- The Expert Patient: A New Approach to Chronic Disease Management for the 21st Century. London: Department of Health; 2001.
- Recent Advances in Understanding Mental Illness and Psychotic Experiences. Leicester: British Psychological Society; 2000.
- Byrne R, Davies L, Morrison AP. Priorities and preferences for the outcomes of treatment of psychosis: a service user perspective. Psychosis 2010;2:210-17. http://dx.doi.org/10.1080/17522430903456913.
- Harding CM, Brooks GW, Ashikaga T, Strauss JS, Breier A. The Vermont longitudinal study of persons with severe mental illness, II: long-term outcome of subjects who retrospectively met DSM-III criteria for schizophrenia. Am J Psychiatry 1987;144:727-35. http://dx.doi.org/10.1176/ajp.144.6.727.
- Strauss JS, Carpenter WT. Prediction of outcome in schizophrenia. III. Five-year outcome and its predictors. Arch Gen Psychiatry 1977;34:159-63. http://dx.doi.org/10.1001/archpsyc.1977.01770140049005.
- Andresen R, Oades L, Caputi P. The experience of recovery from schizophrenia: towards an empirically validated stage model. Aust N Z J Psychiatry 2003;37:586-94. http://dx.doi.org/10.1046/j.1440-1614.2003.01234.x.
- Ng RM, Pearson V, Chen EE, Law CW. What does recovery from schizophrenia mean? Perceptions of medical students and trainee psychiatrists. Int J Soc Psychiatry 2011;57:248-62. http://dx.doi.org/10.1177/0020764009354833.
- Noiseux S, Ricard N. Recovery as perceived by people with schizophrenia, family members and health professionals: a grounded theory. Int J Nurs Stud 2008;45:1148-62. http://dx.doi.org/10.1016/j.ijnurstu.2007.07.008.
- Andresen R, Caputi P, Oades LG. Do clinical outcome measures assess consumer-defined recovery?. Psychiatry Res 2010;177:309-17. http://dx.doi.org/10.1016/j.psychres.2010.02.013.
- Lloyd C, King R, Moore L. Subjective and objective indicators of recovery in severe mental illness: a cross-sectional study. Int J Soc Psychiatry 2010;56:220-9. http://dx.doi.org/10.1177/0020764009105703.
- Harrow M, Hansford BG, Astrachan-Fletcher EB. Locus of control: relation to schizophrenia, to recovery, and to depression and psychosis – a 15-year longitudinal study. Psychiatry Res 2009;168:186-92. http://dx.doi.org/10.1016/j.psychres.2008.06.002.
- Rosen K, Garety P. Predicting recovery from schizophrenia: a retrospective comparison of characteristics at onset of people with single and multiple episodes. Schizophr Bull 2005;31:735-50. http://dx.doi.org/10.1093/schbul/sbi017.
- Kim CH, Jayathilake K, Meltzer HY. Hopelessness, neurocognitive function, and insight in schizophrenia: relationship to suicidal behavior. Schizophr Res 2003;60:71-80. http://dx.doi.org/10.1016/S0920-9964(02)00310-9.
- Ho WWN, Chiu MYL, Lo WTL, Yiu MGC. Recovery components as determinants of the health-related quality of life among patients with schizophrenia: structural equation modelling analysis. Aust N Z J Psychiatry 2010;44:71-84. http://dx.doi.org/10.3109/00048670903393654.
- Lysaker PH, Ringer J, Maxwell C, McGuire A, Lecomte T. Personal narratives and recovery from schizophrenia. Schizophr Res 2010;121:271-6. http://dx.doi.org/10.1016/j.schres.2010.03.003.
- Thewissen V, Bentall RP, Lecomte T, van Os J, Myin-Germeys I. Fluctuations in self-esteem and paranoia in the context of everyday life. J Abnorm Psychol 2008;117:143-53. http://dx.doi.org/10.1037/0021-843X.117.1.143.
- Oorschot M, Lataster T, Thewissen V, Bentall RP, Delespaul P, Myin-Germeys I. Temporal dynamics of visual and auditory hallucinations. Schizophr Res 2012;140:77-82. http://dx.doi.org/10.1016/j.schres.2012.06.010.
- Myin-Germeys I, van Os J, Schwartz JE, Stone AA, Delespaul PAEG. Emotional reactivity to daily stress in psychosis. Arch Gen Psychiatry 2001;58:1137-44. http://dx.doi.org/10.1001/archpsyc.58.12.1137.
- Myin-Germeys I, van Os J. Stress-reactivity in psychosis: evidence for an affective pathway to psychosis. Clin Psychol Rev 2007;27:409-24. http://dx.doi.org/10.1016/j.cpr.2006.09.005.
- Oorschot M, Lataster T, Thewissen V, Lardinois M, Van Os J, Delespaul P, et al. Symptomatic remission in psychosis and real-life functioning. Schizophr Bull 2013;39. http://dx.doi.org/10.1192/bjp.bp.111.104414.
- Beck R, Heffernan S, Law H, McCusker M, Bentall RP, Morrison AP. Subjective judgements of perceived recovery from psychosis. J Mental Health 2012;21:556-66. http://dx.doi.org/10.3109/09638237.2012.710765.
- Morrison AP, Shryane N, Beck R, Heffernan S, Law H, McCusker M, et al. Psychosocial and neuropsychiatric predictors of subjective recovery from psychosis. Psychiatry Res 2013;208:203-9. http://dx.doi.org/10.1016/j.psychres.2013.05.008.
- Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 1983;67:361-70. http://dx.doi.org/10.1111/j.1600-0447.1983.tb09716.x.
- Oades L, Deane F, Crowe T, Lambert WG, Kavanagh D, Lloyd C. Collaborative recovery: an integrative model for working with individuals who experience chronic and recurring mental illness. Aust Psychiatry 2005;13:279-84. http://dx.doi.org/10.1111/j.1440-1665.2005.02202.x.
- Hall PL, Tarrier N. The cognitive-behavioural treatment of low self-esteem in psychotic patients: a pilot study. Behav Res Ther 2003;41:317-32. http://dx.doi.org/10.1016/S0005-7967(02)00013-X.
- Levenson H. Activism and powerful others: distinctions within the concept of internal-external control. J Pers Assess 1974;38:377-83. http://dx.doi.org/10.1080/00223891.1974.10119988.
- Birchwood M, Smith J, Drury V, Healy J, Macmillan F, Slade M. A self-report insight scale for psychosis: reliability, validity and sensitivity to change. Acta Psychiatr Scand 1994;89:62-7. http://dx.doi.org/10.1111/j.1600-0447.1994.tb01487.x.
- Keefe RSE, Goldberg TE, Harvey PD, Gold JM, Poe MP, Coughenour L. The brief assessment of cognition in schizophrenia: reliability, sensitivity, and comparison with a standard neurocognitive battery. Schizophr Res 2004;68:283-97. http://dx.doi.org/10.1016/j.schres.2003.09.011.
- Cheung GW, Lau RS. Testing mediation and suppression effects of latent variables: bootstrapping with structural equation models. Organ Res Method 2007;11:296-325. http://dx.doi.org/10.1177/1094428107300343.
- MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: distribution of the product and resampling methods. Multivar Behav Res 2004;39:99-128. http://dx.doi.org/10.1207/s15327906mbr3901_4.
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling 1999;6:1-55. http://dx.doi.org/10.1080/10705519909540118.
- Cohen J. Statistical Power Analysis for the Behavioural Sciences. London: Lawrence Erlbaum Associates; 1988.
- Fairchild AJ, MacKinnon DP, Taborga MP, Taylor AB. R2 effect-size measures for mediation analysis. Behav Res Methods 2009;41:486-98. http://dx.doi.org/10.3758/BRM.41.2.486.
- Read J, Harre N. The role of biological and genetic causal beliefs in the stigmatisation of ‘mental patients’. J Mental Health 2001;10:223-35. http://dx.doi.org/10.1080/09638230123129.
- Read J, Haslam N, Sayce L, Davies E. Prejudice and schizophrenia: a review of the ‘mental illness is an illness like any other’ approach. Acta Psychiatr Scand 2006;114:303-18. http://dx.doi.org/10.1111/j.1600-0447.2006.00824.x.
- Lincoln TM, Arens E, Berger C, Rief W. Can antistigma campaigns be improved? A test of the impact of biogenetic vs psychosocial causal explanations on implicit and explicit attitudes to schizophrenia. Schizophr Bull 2008;34:984-94. http://dx.doi.org/10.1093/schbul/sbm131.
- Pyle M, Stewart SLK, French P, Byrne R, Patterson P, Gumley A, et al. Internalized stigma, emotional dysfunction and unusual experiences in young people at risk of psychosis. Early Intervention in Psychiatry 2015;9:133-40. http://dx.doi.org/10.1111/eip.12098.
- Leamy M, Bird V, Le Boutillier C, Williams J, Slade M. Conceptual framework for personal recovery in mental health: systematic review and narrative synthesis. Br J Psychiatry 2011;199:445-52. http://dx.doi.org/10.1192/bjp.bp.110.083733.
- Grant PM, Beck AT. Defeatist beliefs as a mediator of cognitive impairment and negative symptoms in schizophrenia. Schizophr Bull 2009;35:798-806. http://dx.doi.org/10.1093/schbul/sbn008.
- Sobel ME. Identification of causal parameters in randomized studies with mediating variables. J Educ Behav Stat 2008;33:230-51. http://dx.doi.org/10.3102/1076998607307239.
- Torgalsboen AK. Full recovery from schizophrenia: the prognostic role of premorbid adjustment, symptoms at first admission, precipitating events and gender. Psychiatry Res 1999;88:143-52. http://dx.doi.org/10.1016/S0165-1781(99)00077-3.
- Albert N, Bertelsen M, Thorup A, Petersen L, Jeppesen P, Le Quack P, et al. Predictors of recovery from psychosis: Analyses of clinical and social factors associated with recovery among patients with first-episode psychosis after 5 years. Schizophr Res 2011;125:257-65. http://dx.doi.org/10.1016/j.schres.2010.10.013.
- Harvey PD, Bellack A. Toward a terminology for functional recovery in schizophrenia: is functional remission a viable concept?. Schizophr Bull 2009;35:300-6. http://dx.doi.org/10.1093/schbul/sbn171.
- Alvarez-Jimenez M, Bendall S, Lederman R, Wadley G, Chinnery G, Vargas S, et al. On the HORYZON: moderated online social therapy for long-term recovery in first episode psychosis. Schizophr Res 2013;143:143-9. http://dx.doi.org/10.1016/j.schres.2012.10.009.
- Hamann J, Mendel R, Meier A, Asani F, Pausch E, Leucht S, et al. ‘How to speak to your psychiatrist’: shared decision-making training for inpatients with schizophrenia. Psychiatr Serv 2011;62:1218-21. http://dx.doi.org/10.1176/ps.62.10.pss6210_1218.
- Kingdon DG, Turkington D. Preliminary report: the use of cognitive behaviour therapy and a normalizing rationale in schizophrenia. J Nerv Ment Dis 1991;179:207-11. http://dx.doi.org/10.1097/00005053-199104000-00005.
- Lucksted A, Drapalski A, Calmes C, Forbes C, DeForge B, Boyd J. Ending self-stigma: pilot evaluation of a new intervention to reduce internalized stigma among people with mental illnesses. Psychiatr Rehabil J 2011;35:51-4. http://dx.doi.org/10.2975/35.1.2011.51.54.
- Law H, Shryane N, Bentall RP, Morrison AP. Longitudinal predictors of subjective recovery in psychosis. Br J Psychiatry 2015. http://dx.doi.org/10.1192/bjp.bp.114.158428.
- Kay SR, Opler LA, Lindenmayer J-P. Reliability and validity of the Positive and Negative Syndrome Scale for schizophrenia. Psychiatry Res 1988;23:99-110. http://dx.doi.org/10.1016/0165-1781(88)90038-8.
- Morosini PL, Magliano L, Brambilla L, Ugolini S, Pioli R. Development, reliability and acceptability of a new version of the DSM-IV Social Occupational Functioning Assessment Scale (SOFAS) to assess routine social functioning. Acta Psychiatr Scand 2000;101:323-9.
- Kawata AK, Revicki DA. Psychometric properties of the Personal and Social Performance scale (PSP) among individuals with schizophrenia living in the community. Qual Life Res 2008;17:1247-56. http://dx.doi.org/10.1007/s11136-008-9400-z.
- Nunn KP, Lewin TJ, Walton JM, Carr VJ. The construction and characteristics of an instrument to measure personal hopefulness. Psychol Med 1996;26:531-45. http://dx.doi.org/10.1017/S0033291700035613.
- Dyce JA. Factor structure of the Beck Hopelessness Scale. J Clin Psychol 1996;52:555-8. http://dx.doi.org/10.1002/(SICI)1097-4679(199609)52:5<555::AID-JCLP10>3.0.CO;2-D.
- Young MA, Halper IS, Clark DC, Scheftner W, Fawcett J. An item-response theory evaluation of the Beck Hopelessness Scale. Cognitive Ther Res 1992;16:579-87. http://dx.doi.org/10.1007/BF01175143.
- Goldstein JM, Tsuang MT, Faraone SV. Gender and schizophrenia: implications for understanding the heterogeneity of the illness. Psychiatry Res 1989;28:243-53. http://dx.doi.org/10.1016/0165-1781(89)90205-9.
- Nassar EH, Walders N, Jankins JH. The Experience of Schizophrenia: what’s gender got to do with it? A critical review of the current status of research on schizophrenia. Schizophr Bull 2002;28:351-62. http://dx.doi.org/10.1093/oxfordjournals.schbul.a006944.
- Kay SR, Opler LA. The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophr Bull 1987;13:507-18. http://dx.doi.org/10.1093/schbul/13.2.261.
- Kay SR, Opler LA, Fiszbein A. Reliability and validity of the Positive and Negative Syndrome Scale for schizophrenics. Psychiatry Res 1988;23:276-86. http://dx.doi.org/10.1016/0165-1781(88)90038-8.
- Myin Germeys I, Krabbendam L, Jolles J, Delespaul PA, van Os J. Are cognitive impairments associated with sensitivity to stress in schizophrenia? An experience sampling study. Am J Psychiatry 2002;159:443-9. http://dx.doi.org/10.1176/appi.ajp.159.3.443.
- Udachina A, Varese F, Oorschot M, Myin-Germeys I, Bentall RP. Dynamics of self-esteem in ‘poor-me’ and ‘bad-me’ paranoia. J Nerv Ment Dis 2012;200:777-83. http://dx.doi.org/10.1097/NMD.0b013e318266ba57.
- Beck A, Weissman A, Lester D, Trexler L. The measurement of pessimism: the Hopelessness Scale. J Consult Clin Psychol 1974;42:861-5. http://dx.doi.org/10.1037/h0037562.
- Delespaul P. Assessing Schizophrenia in Daily Life: The Experience Sampling Method. Maastricht: Universitaire Pers Maastricht; 1995.
- Kimhy D, Myin-Germeys I, Palmier-Claus J, Swendsen J. Mobile assessment guide for research in schizophrenia and severe mental disorders. Schizophr Bull 2012;38:386-95. http://dx.doi.org/10.1093/schbul/sbr186.
- Howard L, Thornicroft G. Patient preference randomised controlled trials in mental health research. Br J Psychiatry 2006;188:303-4. http://dx.doi.org/10.1192/bjp.188.4.303.
- Bradley C. Patients’ preferences and randomised trials. Lancet 1996;347:1118-19. http://dx.doi.org/10.1016/S0140-6736(96)90317-7.
- Janevic MR, Janz NK, Dodge JA, Lin X, Pan W, Sinco BR, et al. The role of choice in health education intervention trials: a review and case study. Soc Sci Med 2003;56:1581-94. http://dx.doi.org/10.1016/S0277-9536(02)00158-2.
- Involvement Works. The Second Report of the Standing Group on Consumers in NHS Research. London: Department of Health; 1999.
- Treatment Choice in Psychological Therapies and Counselling. London: Her Majesty’s Stationery Office; 2001.
- Brewin CR, Bradley C. Patient preferences and randomised clinical trials. BMJ 1989;299:313-15. http://dx.doi.org/10.1136/bmj.299.6694.313.
- King M, Nazareth I, Lampe F, Bower P, Chandler M, Morou M, et al. Impact of participant and physician intervention preferences on randomized trials: a systematic review. J Am Med Assoc 2005;293:1089-99. http://dx.doi.org/10.1001/jama.293.9.1089.
- Gemmell ID G. The statistical pitfalls of the partially randomized preference design in non-blinded trials of psychological interventions. Int J Methods Psychiatr Res 2011;20:1-9. http://dx.doi.org/10.1002/mpr.326.
- Brocklehurst P. Partially randomised patient preference trials. BJOG 1997;104:1332-5. http://dx.doi.org/10.1111/j.1471-0528.1997.tb10999.x.
- Ward E, King M, Lloyd M, Bower P, Sibbald B, Farrelly S, et al. Randomised controlled trial of non-directive counselling, cognitive-behaviour therapy, and usual general practitioner care for patients with depression. I: clinical effectiveness. BMJ 2000;321:1383-8. http://dx.doi.org/10.1136/bmj.321.7273.1383.
- Locock L, Smith L. Personal benefit, or benefiting others? Deciding whether to take part in clinical trials. Clin Trials 2011;8:85-93. http://dx.doi.org/10.1177/1740774510392257.
- Ross S, Grant A, Counsell C, Gillespie W, Russell I, Prescott R. Barriers to participation in randomised controlled trials: a systematic review. J Clin Epidemiol 1999;52:1143-56. http://dx.doi.org/10.1016/S0895-4356(99)00141-9.
- Roberts LW, Warner TD, Brody JL, Roberts B, Lauriello J, Lyketsos C. Patient and psychiatrist ratings of hypothetical schizophrenia research protocols: assessment of harm potential and factors influencing participation decisions. Am J Psychiatry 2002;159:573-84. http://dx.doi.org/10.1176/appi.ajp.159.4.573.
- Roberts LW, Warner TD, Hammond KG, Hoop JG. Views of people with schizophrenia regarding aspects of research: study size and funding sources. Schizophr Bull 2006;32:107-15. http://dx.doi.org/10.1093/schbul/sbj022.
- Zullino D, Conus P, Borgeat F, Bonsack C. Readiness to participate in psychiatric research. Can J Psychiatry 2003;48:480-4.
- Marks IM, Mataix-Cols D, Kenwright M, Cameron R, Hirsch S, Gega L. Pragmatic evaluation of computer-aided self-help for anxiety and depression. Br J Psychiatry 2003;183:57-65. http://dx.doi.org/10.1192/bjp.183.1.57.
- Lovell K, Cox D, Haddock G, Jones C, Raines D, Garvey R, et al. Telephone-administered cognitive behaviour therapy for the treatment of obsessive compulsive disorder: randomised controlled noninferiortiy trial. BMJ 2006;333. http://dx.doi.org/10.1136/bmj.38940.355602.80.
- Sumner K, Haddock G, Hartley S, Kilbride M, McCusker M, Pitt L, et al. Preferences for psychological therapy in psychosis: trial participation, mode of treatment, and willingness to be randomised. J Ment Health 2014;23:67-71. http://dx.doi.org/10.3109/09638237.2013.841865.
- The ICD-10 Classification of Mental and Behavioural Disorders. Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization; 1992.
- Bernard HR, Ryan GW. Analyzing Qualitative Data: Systematic Approaches. Thousand Oaks, CA: Sage Publications; 2010.
- Krippendorff K. Content analysis: an introduction to its methodology. JASA 1984;79. http://dx.doi.org/10.2307/2288384.
- Bedi N, Chilvers C, Churchill R, Dewey M, Duggan C, Fielding K, et al. Assessing effectiveness of treatment of depression in primary care. Br J Psychiatry 2000;177:312-18. http://dx.doi.org/10.1192/bjp.177.4.312.
- Featherstone K, Donovan JL. Random allocation or allocation at random? Patients’ perspectives of participation in a randomised controlled trial. BMJ 1998;317:1177-80. http://dx.doi.org/10.1136/bmj.317.7167.1177.
- Halpern SD, Metzger DS, Berlin JA, Ubel PA. Who will enrol? Predicting participation in a phase II AIDS vaccine trial. J Acquir Immune Defic Syndr 2001;27:281-8. http://dx.doi.org/10.1097/00126334-200107010-00011.
- Kovnick JA, Appelbaum PS, Hoge SK, Leadbetter RA. Competence to consent to research among long-stay inpatients with chronic schizophrenia. Psychiatr Serv 2003;54:1247-52. http://dx.doi.org/10.1176/appi.ps.54.9.1247.
- Kay SR, Opler LA, Fiszbein A. The Positive and Negative Syndrome Scale (PANSS) rating manual. Social and Behavioural Sciences Documents 1986;17:28-9.
- Drake R, Haddock G, Tarrier N, Bentall R, Lewis S. The Psychotic Symptom Rating Scales (PSYRATS): Their usefulness and properties in first episode psychosis. Schizophr Res 2007;89:119-22. http://dx.doi.org/10.1016/j.schres.2006.04.024.
- Torrey WC, Drake RE. Practicing shared decision making in the outpatient psychiatric care of adults with severe mental illnesses: redesigning care for the future. Community Ment Health J 2010;46:433-40. http://dx.doi.org/10.1007/s10597-009-9265-9.
- McCabe R, Saidi M, Priebe S. Patient-reported outcomes in schizophrenia. Br J Psychiatry 2007;191:S21-8. http://dx.doi.org/10.1192/bjp.191.50.s21.
- Eisner E, Drake R, Barrowclough C. Assessing early signs of relapse in psychosis: review and future directions. Clin Psychol Rev 2013;33:637-53. http://dx.doi.org/10.1016/j.cpr.2013.04.001.
- Braunholtz D, Edwards SJ, Lilford RJ. Are randomized clinical trials good for us (in the short term)? Evidence for a ‘trial effect’. J Clin Epidemiol 2001;54:217-24. http://dx.doi.org/10.1016/S0895-4356(00)00305-X.
- Bolton C, Gooding P, Kapur N, Barrowclough C, Tarrier N. Developing psychological perspectives of suicidal behaviour and risk in people with a diagnosis of schizophrenia: we know they kill themselves but do we understand why?. Clin Psychol Rev 2007;27:511-36. http://dx.doi.org/10.1016/j.cpr.2006.12.001.
- Caldwell CB, Gottesman II. Schizophrenics kill themselves too: a review of risk factors for suicide. Schizophr Bull 1990;16:571-90. http://dx.doi.org/10.1093/schbul/16.4.571.
- Tarrier N, Taylor K, Gooding P. Cognitive-behavioural interventions to reduce suicidal behaviour: a systematic review and meta-analysis. Behav Modif 2008;32:77-108. http://dx.doi.org/10.1177/0145445507304728.
- Wykes T, Steel C, Everitt B, Tarrier N. Cognitive behavior therapy for schizophrenia: effect sizes, clinical models, and methodological rigor. Schizophr Bull 2008;34:523-37. http://dx.doi.org/10.1093/schbul/sbm114.
- Johnson J, Gooding P, Tarrier N. Suicide risk in schizophrenia: explanatory models and clinical implications, the Schematic Appraisal Model of Suicide (SAMS). Psychol Psychother 2008;81:55-77. http://dx.doi.org/10.1348/147608307X244996.
- Johnson J, Gooding PA, Wood AM, Tarrier N. Resilience as positive coping appraisals: testing the schematic appraisals model of suicide (SAMS). Behav Res Ther 2010;48:179-86. http://dx.doi.org/10.1016/j.brat.2009.10.007.
- Williams JMG. Cry of Pain. London: Penguin; 1997.
- Panagioti M, Gooding PA, Tarrier N. Hopelessness, defeat, and entrapment in posttraumatic stress disorder: their association with suicidal behavior and severity of depression. J Nerv Ment Dis 2012;200:676-83. http://dx.doi.org/10.1097/NMD.0b013e3182613f91.
- Pratt D, Gooding P, Johnson J, Taylor P, Tarrier N. Suicide schemas in non-affective psychosis: an empirical investigation. Behav Res Ther 2010;48:1211-20. http://dx.doi.org/10.1016/j.brat.2010.08.005.
- Taylor PJ, Gooding PA, Wood AM, Johnson J, Pratt D, Tarrier N. Defeat and entrapment in schizophrenia: the relationship with suicidal ideation and positive psychotic symptoms. Psychiatry Res 2010;178:244-8. http://dx.doi.org/10.1016/j.psychres.2009.10.015.
- Taylor PJ, Wood AM, Gooding P, Tarrier N. Appraisals and suicidality: the mediating role of defeat and entrapment. Arch Suicide Res 2010;14:236-47. http://dx.doi.org/10.1080/13811118.2010.494138.
- Tarrier N, Gooding P, Pratt D, Kelly J, Awenat Y, Maxwell J. Cognitive Behavioural Prevention of Suicide in Psychosis: A Treatment Manual. London: Routledge; 2013.
- Wilson ST, Stanley B. Ethical concerns in schizophrenia research: looking back and moving forward. Schizophr Bull 2006;32:30-6. http://dx.doi.org/10.1093/schbul/sbj023.
- Roberts LW, Warner TD, Brody JL. Perspectives of patients with schizophrenia and psychiatrists regarding ethically important aspects of research participation. Am J Psychiatry 2000;157:67-74. http://dx.doi.org/10.1176/ajp.157.1.67.
- Jorm AF, Kelly CM, Morgan AJ. Participant distress in psychiatric research: a systematic review. Psychol Med 2007;37:917-26. http://dx.doi.org/10.1017/S0033291706009779.
- Taylor PJ, Awenat Y, Gooding P, Johnson J, Pratt D, Wood A, et al. The subjective experience of participation in schizophrenia research: a practical and ethical issue. J Nerv Ment Dis 2010;198:343-8. http://dx.doi.org/10.1097/NMD.0b013e3181da8545.
- Bowling A. Research Methods in Health. Buckingham: Open University Press; 2000.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. http://dx.doi.org/10.1191/1478088706qp063oa.
- Polit D, Hungler BP. Essentials of Nursing Research. Philadelphia, PA: Lippincott-Raven; 1997.
- Glaser B, Strauss A. The Discovery of Grounded Theory: Strategies for Qualitative Research. Chicago, IL: Aldine; 1967.
- Dyregrov K. Bereaved parents’ experience of research participation. Soc Sci Med 2004;58:391-400. http://dx.doi.org/10.1016/S0277-9536(03)00205-3.
- Hutchinson SA, Wilson ME, Wilson HS. Benefits of participating in research interviews. J Nurs Scholarsh 1994;26:161-4. http://dx.doi.org/10.1111/j.1547-5069.1994.tb00937.x.
- Hahm H, Segal S. Failure to seek healthcare among the mentally ill. Am J Orthopsychiatry 2005;75:54-62. http://dx.doi.org/10.1037/0002-9432.75.1.54.
- Sussman LK, Robins LN, Earls F. Treatment-seeking for depression by black and white Americans. Soc Sci Med 1987;24:187-96. http://dx.doi.org/10.1016/0277-9536(87)90046-3.
- Jobes DA, Nelson KN, Peterson EM, Pentiuc D, Downing V, Francini K, et al. Describing suicidality: An investigation of qualitative SSF responses. Suicide Life-Threat Behav 2004;34:99-112. http://dx.doi.org/10.1521/suli.34.2.99.32788.
- Roberts LW, Warner TD, Anderson CT, Smithpeter MV, Rogers MK. Schizophrenia research participants’ responses to protocol safeguards: recruitment, consent, and debriefing. Schizophr Res 2004;67:283-91. http://dx.doi.org/10.1016/S0920-9964(03)00101-4.
- Anderson KK, Mukherjee SD. The need for additional safeguards in the informed consent process in schizophrenia research. J Med Ethics 2007;33:647-50. http://dx.doi.org/10.1136/jme.2006.017376.
- Brody JL, Gluck JP, Aragon AS. Participants’ understanding of the process of psychological research: debriefing. Ethics Behav 2000;10:13-25. http://dx.doi.org/10.1207/S15327019EB1001_2.
- Gilbert P, Allan S. The role of defeat and entrapment (arrested flight) in depression: an exploration of an evolutionary view. Psychol Med 1998;28:585-98. http://dx.doi.org/10.1017/S0033291798006710.
- Holden RR, Fekken GC. Test-retest reliability of the Hopelessness Scale and its items in a university population. J Clin Psychol 1988;44:40-3. http://dx.doi.org/10.1002/1097-4679(198801)44:1<40::AID-JCLP2270440108>3.0.CO;2-P.
- Tarrier N, Barrowclough C, Andrews B, Gregg L. Risk of non-fatal suicide ideation and behaviour in recent onset schizophrenia. The influence of clinical, social, self-esteem and demographic factors. Soc Psychiatry Psychiatr Epidemiol 2004;39:927-37. http://dx.doi.org/10.1007/s00127-004-0828-3.
- White RG, McCleery M, Gumley AI, Mulholland C. Hopelessness in schizophrenia: the impact of symptoms and beliefs about illness. J Nerv Ment Dis 2007;195:968-75. http://dx.doi.org/10.1097/NMD.0b013e31815c1a1d.
- Beck AT, Steer RA. Manual for Beck Scale for Suicidal Ideation. New York, NY: Psychological Corporation; 1991.
- Pinninti N, Steer RA, Rissmiller DJ, Nelson S, Beck AT. Use of the Beck Scale for Suicide Ideation with psychiatric inpatients diagnosed with schizophrenia, schizoaffective, or bipolar disorders. Behav Res Ther 2002;40:1071-9. http://dx.doi.org/10.1016/S0005-7967(02)00002-5.
- Ventura J, Green MF, Shaner A, Liberman RP. Training and quality assurance with the Brief Psychiatric Rating Scale: ‘The drift busters.’. Int J Methods Psychiatr Res 1993;3:221-44.
- Dingemans PMAJ, Linszen DH, Lenior ME, Smeets RMW. Component structure of the expanded Brief Psychiatric Rating Scale (BPRS-E). Psychopharmacology 1995;122:263-7. http://dx.doi.org/10.1007/BF02246547.
- Arbuckle J. Amos 7.0 User’s Guide. Spring House, PA: AmosDevelopment Corporation; 2006.
- Bartlett M. Tests of significance in factor analysis. Br J Psychol 1950;3:77-85. http://dx.doi.org/10.1111/j.2044-8317.1950.tb00285.x.
- Nevitt J, Hancock GR. Evaluating small sample approaches for model test statistics in structural equation modeling. Multivar Behav Res 2004;39:439-78. http://dx.doi.org/10.1207/S15327906MBR3903_3.
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Metodsh Instr 2004;36:717-31. http://dx.doi.org/10.3758/BF03206553.
- Frazier PA, Tix AP, Barron KE. Testing moderator and mediator effects in counseling psychology research. J Couns Psychol 2004;51:115-34. http://dx.doi.org/10.1037/0022-0167.51.2.157.
- Cohen J, Cohen P. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences. Hillsdale, NJ: Erlbaum; 1983.
- Menard S. Applied Logistic Regression Analysis. Sage University Paper Series on Quantitative Applications in the Social Sciences. Thousand Oaks, CA: Sage; 1995.
- Burnham KP, Anderson DR. Multimodel inference: understanding AIC and BIC in model selection. Sociological Method Res 2004;33:261-304. http://dx.doi.org/10.1177/0049124104268644.
- Fenton WS, McGlashan TH, Victor BJ, Blyler CR. Symptoms, subtype, and suicidality in patients with schizophrenia spectrum disorders. Am J Psychiatry 1997;154:199-204. http://dx.doi.org/10.1176/ajp.154.2.199.
- Heila H, Isometsa ET, Henriksson MM, Heikkinen ME, Marttunen MJ, Lonnqvist JK. Suicide victims with schizophrenia in different treatment phases and adequacy of antipsychotic medication. J Clin Psychiatry 1999;60:200-8. http://dx.doi.org/10.4088/JCP.v60n0311.
- Saarinen PI, Lehtonen J, Lonnqvist J. Suicide risk in schizophrenia: An analysis of 17 consecutive suicides. Schizophr Bull 1999;25:533-42. http://dx.doi.org/10.1093/oxfordjournals.schbul.a033399.
- Freeman D, Garety PA, Bebbington PE, Smith B, Rollinson R, Fowler D, et al. Psychological investigation of the structure of paranoia in a non-clinical population. Br J Psychiatry 2005;186:427-35. http://dx.doi.org/10.1192/bjp.186.5.427.
- Drake RE, Cotton PG. Depression, hopelessness and suicide in chronic schizophrenia. Br J Psychiatry 1986;148:554-9. http://dx.doi.org/10.1192/bjp.148.5.554.
- Restifo K, Harkavy-Friedman JM, Shrout PE. Suicidal behavior in schizophrenia: a test of the demoralization hypothesis. J Nerv Ment Dis 2009;197:147-53. http://dx.doi.org/10.1097/NMD.0b013e318199f452.
- Siris SG. Suicide and schizophrenia. J Psychopharmacol 2001;15:127-35. http://dx.doi.org/10.1177/026988110101500209.
- Montross LP, Zisook S, Kasckow J. Suicide among patients with schizophrenia: a consideration of risk and protective factors. Ann Clin Psychiatry 2005;17:173-82. http://dx.doi.org/10.1080/10401230591002156.
- Schwartz-Stav O, Apter A, Zalsman G. Depression, suicidal behavior and insight in adolescents with schizophrenia. Eur Child Adolesc Psychiatry 2006;15:352-9. http://dx.doi.org/10.1007/s00787-006-0541-8.
- Pompili M, Lester D, Grispini A, Innamorati M, Calandro F, Iliceto P, et al. Completed suicide in schizophrenia: evidence from a case-control study. Psychiatry Res 2009;167:251-7. http://dx.doi.org/10.1016/j.psychres.2008.03.018.
- Swallow SR, Sloman L, Gilbert P. Subordination and Defeat: An Evolutionary Approach to Mood-disorders and Their Therapy. Mahwah, NJ: Lawrence Erlbaum Associates; 2000.
- Johnson J, Gooding PA, Wood AM, Taylor PJ, Pratt D, Tarrier N. Resilience to suicidal ideation in psychosis: Positive self-appraisals buffer the impact of hopelessness. Behav Res Ther 2010;48:883-9. http://dx.doi.org/10.1016/j.brat.2010.05.013.
- Osman A, Gutierrez PM, Muehlenkamp JJ, Dix-Richardson F, Barrios FX, Kopper BA. Suicide resilience inventory-25: development and preliminary psychometric properties. Psychol Rep 2004;94:1349-60. http://dx.doi.org/10.2466/pr0.94.3.1349-1360.
- Rutter PA, Freedenthal S, Osman A. Assessing protection from suicidal risk: psychometric properties of the suicide resilience inventory. Death Stud 2008;32:142-53. http://dx.doi.org/10.1080/07481180701801295.
- Cavanagh JTO, Carson AJ, Sharpe M, Lawrie SM. Psychological autopsy studies of suicide: a systematic review. Psychol Med 2003;33:395-40. http://dx.doi.org/10.1017/S0033291702006943.
- Conwell Y, Duberstein PR, Cox C, Herrmann JH, Forbes NT, Caine ED. Relationships of age and axis I diagnoses in victims of completed suicide: a psychological autopsy study. Am J Psychiatry 1996;153:1001-8. http://dx.doi.org/10.1176/ajp.153.8.1001.
- Ahrens B, Linden M. Is there a suicidality syndrome independent of specific major psychiatric disorder? Results of a split half multiple regression analysis. Acta Psychiatr Scand 1996;94:79-86. http://dx.doi.org/10.1111/j.1600-0447.1996.tb09829.x.
- Ran MS, Xiang MZ, Mao WJ, Hou ZJ, Tang MN, Chen EYH, et al. Characteristics of suicide attempters and nonattempters with schizophrenia in a rural community. Suicide Life-Threat Behav 2005;35:694-701. http://dx.doi.org/10.1521/suli.2005.35.6.694.
- Chang EC. Examining the link between perfectionism and psychological maladjustment: social problem solving as a buffer. Cognitive Ther Res 2002;26:581-95. http://dx.doi.org/10.1023/A:1020329625158.
- Kessler RC, Berglund P, Borges G, Nock M, Wang PS. Trends in suicide ideation, plans, gestures, and attempts in the United States, 1990–1992 to 2001–2003. J Am Med Assoc 2005;293:2487-95. http://dx.doi.org/10.1001/jama.293.20.2487.
- Funahashi T, Ibuki Y, Domon Y, Nishimura T, Akehashi D, Sugiura H. A clinical study on suicide among schizophrenics. Psychiatry Clin Neurosci 2000;54:173-9. http://dx.doi.org/10.1046/j.1440-1819.2000.00655.x.
- Hawton K, Arensman E, Wasserman D, Hulten A, Bille-Brahe U, Bjerke T, et al. Relation between attempted suicide and suicide rates among young people in Europe. J Epidemiol Community Health 1998;52:191-4. http://dx.doi.org/10.1136/jech.52.3.191.
- Mann JJ, Waternaux C, Haas GL, Malone KM. Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry 1999;156:181-9.
- Bentler PM, Chou C-P. Practical issues in structural modelling. Sociological Method Res 1987;16:78-117. http://dx.doi.org/10.1177/0049124187016001004.
- Kline RB. Principles and Practice of Structural Equation Modelling. New York, NY: The Guilford Press; 1998.
- Bandura A. Social Learning Theory. Oxford: Prentice-Hall; 1977.
- Lewis G, Hawton K, Jones P. Strategies for preventing suicide. Br J Psychiatry 1997;171:351-4. http://dx.doi.org/10.1192/bjp.171.4.351.
- Tarrier N, Gooding P, Pratt D, Kelly J, Awenat Y, Maxwell J. Cognitive Behavioural Prevention of Suicide in Psychosis: A Treatment Manual. Hove: Routledge; 2013.
- Tarrier N, Kelly J, Maqsood S, Snelson N, Maxwell J, Law H, et al. The cognitive behavioural prevention of suicide in psychosis: a clinical trial. Schizophr Res 2014;156:204-10. http://dx.doi.org/10.1016/j.schres.2014.04.029.
- Reynolds WM. Adult Suicidal Ideation Questionnaire: Professional Manual. Odessa, FL: Psychological Assessment Resources; 1991.
- Cull JG, Gill WS. Suicide Probability Scale. Los Angeles, CA: Western Psychological Services; 1982.
- Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: the scale for suicide ideation. J Consult Clin Psychol 1979;47:343-52. http://dx.doi.org/10.1037/0022-006X.47.2.343.
- Efron B, Tibshirani RJ. Introduction to the Bootstrap. London: Chapman & Hall; 1993.
- Nordentoft M, Jeppesen P, Abel M, Kassow P, Petersen L, Thorup A, et al. Opus study: Suicidal behaviour, suicidal ideation and hopelessness among patients with first-episode psychosis. One-year follow-up of a randomised controlled trial. Br J Psychiatry 2002;181:S98-106. http://dx.doi.org/10.1192/bjp.181.43.s98.
- Lam DH, Watkins ER, Hayward P, Bright J, Wright K, Kerr N, et al. A randomized controlled study of cognitive therapy for relapse prevention for bipolar affective disorder: outcome of the first year. Arch Gen Psychiatry 2003;60:145-52. http://dx.doi.org/10.1001/archpsyc.60.2.145.
- Miklowitz D, Goodwin G, Bauer M, Geddes J. Common and specific elements of psychosocial treatments for bipolar disorder: a survey of clinicians participating in randomized trials. J Psychiatr Pract 2008;14:77-85. http://dx.doi.org/10.1097/01.pra.0000314314.94791.c9.
- Barnard PJ. Bridging between basic theory and clinical practice. Behav Res Ther 2004;42:977-1000. http://dx.doi.org/10.1016/j.brat.2004.04.002.
- Jones SH. Circadian rhythms, multilevel models of emotion and bipolar disorder – an initial step towards integration?. Clin Psychol Rev 2001;21:1193-209. http://dx.doi.org/10.1016/S0272-7358(01)00111-8.
- Jones S, Mansell W, Waller L. Appraisal of hypomania-relevant experiences: development of a questionnaire to assess positive self-dispositional appraisals in bipolar and behavioural high risk samples. J Affect Disord 2006;93:19-28. http://dx.doi.org/10.1016/j.jad.2006.01.017.
- Lish JDD-MS, Whybrow PC, Price RA, Hirschfeld RM. The National Depressive and Manic-depressive Association (DMDA) survey of bipolar members. J Affect Disord 1994;31:281-94. http://dx.doi.org/10.1016/0165-0327(94)90104-X.
- Baldessarini RJ, Tondo L, Vazquez GH, Undurraga J, Bolzani L, Yildiz A, et al. Age at onset versus family history and clinical outcomes in 1,665 international bipolar-I disorder patients. World Psychiatry 2012;11:40-6. http://dx.doi.org/10.1016/j.wpsyc.2012.01.006.
- Geddes JR, Burgess S, Hawton K, Jamison K, Goodwin GM. Long-term lithium therapy for bipolar disorder: systematic review and meta-analysis of randomized controlled trials. Am J Psychiatry 2004;161:217-22. http://dx.doi.org/10.1176/appi.ajp.161.2.217.
- Colom F, Vieta E, Sanchez-Moreno J, Palomino-Otiniano R, Reinares M, Goikolea JM, et al. Group psychoeducation for stabilised bipolar disorders: 5-year outcome of a randomised clinical trial. Br J Psychiatry 2009;194:260-5. http://dx.doi.org/10.1192/bjp.bp.107.040485.
- Anthony WA. Recovery from mental illness: the guiding vision of the mental health service system in the 1990s. Psychosoc Rehabil J 1993;16:11-23. http://dx.doi.org/10.1037/h0095655.
- The Journey to Recovery – The Government’s Vision for Mental Health Care. London: Department of Health; 2001.
- Russell SJ, Browne JL. Staying well with bipolar disorder. Aust N Z J Psychiatry 2005;39:187-93. http://dx.doi.org/10.1080/j.1440-1614.2005.01542.x.
- Mansell W, Powell S, Pedley R, Thomas N, Jones SA. The process of recovery from bipolar I disorder: a qualitative analysis of personal accounts in relation to an integrative cognitive model. Br J Clin Psychol 2010;49:193-215. http://dx.doi.org/10.1348/014466509X451447.
- Jones S, Higginson S, Murray C, Morrison AP. Recovery Experiences in Bipolar Disorder. Manchester: Proceedings of The British Association for Behavioural and Cognitive Psychotherapy Annual Conference; 2010.
- Berk M, Berk L, Castle D. A collaborative approach to the treatment alliance in bipolar disorder. Bipolar Disord 2004;6:504-18. http://dx.doi.org/10.1111/j.1399-5618.2004.00154.x.
- Flood C, Byford S, Henderson C, Leese M, Thornicroft G, Sutherby K, et al. Joint crisis plans for people with psychosis: economic evaluation of a randomised controlled trial. BMJ 2006;333:729-32. http://dx.doi.org/10.1136/bmj.38929.653704.55.
- Henderson C, Flood C, Leese M, Thornicroft G, Sutherby K, Szmukler G. Effect of joint crisis plans on use of compulsory treatment in psychiatry: single blind randomised controlled trial. BMJ 2004;329:136-8. http://dx.doi.org/10.1136/bmj.38155.585046.63.
- Simon D, Willis CE, Harter M, Edwards A, Elwyn G. Shared Decision-Making in Healthcare: Achieving Evidence Based Patient Choice. New York, NY: Oxford University Press; 2009.
- Recovery is for All: Hope, Agency and Opportunity in Psychiatry. A Position Statement by Consultant Psychiatrists. London: SLAM/SWLSTG; 2010.
- Chengappa KNR, Hennen J, Baldessarini RJ, Kupfer DJ, Yatham LN, Gershon S, et al. Recovery and functional outcomes following olanzapine treatment for bipolar I mania. Bipolar Disord 2005;7:68-76. http://dx.doi.org/10.1111/j.1399-5618.2004.00171.x.
- Martinez-Aran A, Vieta E, Torrent C, Sanchez-Moreno J, Goikolea JM, Salamero M, et al. Functional outcome in bipolar disorder: The role of clinical and cognitive factors. Bipolar Disord 2007;9:103-13. http://dx.doi.org/10.1111/j.1399-5618.2007.00327.x.
- Murray G, Michalak EE. Quality of life in patients with bipolar disorder: defining and measuring goals. Psychiatr Times 2007;24:24-6.
- Slade M, Bird V, Le Boutillier C, Williams J, McCrone P, Leamy M. REFOCUS Trial: protocol for a cluster randomised controlled trial of a pro-recovery intervention within community based mental health teams. BMC Psychiatry 2011;11. http://dx.doi.org/10.1186/1471-244X-11-185.
- Jones SH, Burrell-Hodgson G. Cognitive-behavioural treatment of first diagnosis bipolar disorder. Clin Psychol Psychother 2008;15:367-77. http://dx.doi.org/10.1002/cpp.584.
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clin Psychol Rev 1988;8:77-100. http://dx.doi.org/10.1016/0272-7358(88)90050-5.
- Bauer MS, Crits-Christoph P, Ball WA, Dewees E, McAllister T, Alahi P, et al. Independent assessment of manic and depressive symptoms by self-rating: scale characteristics and implications for the study of mania. Arch Gen Psychiatry 1991;48:807-12. http://dx.doi.org/10.1001/archpsyc.1991.01810330031005.
- Bauer MS, Vojta C, Kinosian B, Altshuler L, Glick H. The Internal State Scale: replication of its discriminating abilities in a multisite, public sector sample. Bipolar Disord 2000;2:340-6. http://dx.doi.org/10.1034/j.1399-5618.2000.020409.x.
- First MB, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS. Structured Clinical Interview for DSM-IV Axis I Disorders, Research Version, Patient Edition. Washington DC: American Psychiatric Press, Inc.; 1997.
- Smith JA, Osborn M, Smith JA. Qualitative Psychology: A Practical Guide to Research Methods 51–80. Thousand Oaks, CA: Sage Publishing; 2003.
- Michalak EE, Murray G. Development of the QoL.BD: a disorder-specific scale to assess quality of life in bipolar disorder. Bipolar Disord 2010;12:727-40. http://dx.doi.org/10.1111/j.1399-5618.2010.00865.x.
- Young S, Ensing D. Exploring recovery from the perspective of people with psychiatric disabilities. Psychiatr Rehabil J 1999;99:219-32. http://dx.doi.org/10.1037/h0095240.
- Jones S, Mulligan LD, Higginson S, Dunn G, Morrison AP. The bipolar recovery questionnaire: psychometric properties of a quantitative measure of recovery experiences in bipolar disorder. J Affect Disord 2013;147:34-43. http://dx.doi.org/10.1016/j.jad.2012.10.003.
- Jackson DN, Berg IA. Response Set in Personality Assessment. Chicago, IL: Aldine; 1967.
- Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. Tokyo, Japan: 29th World Medical Association General Assembly; 1975.
- Bech P, Rafaelsen OJ, Kramp P, Bolwig TG. The mania rating scale: scale construction and inter-observer agreement. Neuropharmacology 1978;17:430-1. http://dx.doi.org/10.1016/0028-3908(78)90022-9.
- Bech P, Baastrup PC, De Bleeker E, Ropert R. Dimensionality, responsiveness and standardization of the Bech-Rafaelsen mania scale in the ultra-short therapy with antipsychotics in patients with severe manic episodes. Acta Psychiatr Scand 2001;104:25-30. http://dx.doi.org/10.1034/j.1600-0447.2001.00244.x.
- Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry 1960;23:59-62. http://dx.doi.org/10.1136/jnnp.23.1.56.
- Carroll BJ, Fielding JM, Blashki TG. Depression rating scales – critical review. Arch Gen Psychiatry 1973;28:361-6. http://dx.doi.org/10.1001/archpsyc.1973.01750330049009.
- Knesevich JW, Biggs JT, Clayton PJ, Ziegler VE. Validity of Hamilton Rating-Scale for Depression. Br J Psychiatry 1977;131:49-52. http://dx.doi.org/10.1192/bjp.131.1.49.
- Ware JE, Kosinski M, Keller SD. A12-item short-form health survey-construction of scales and preliminary tests of reliability and validity. Med Care 1996;34:220-33. http://dx.doi.org/10.1097/00005650-199603000-00003.
- Stewart AL, Hays RD, Ware JE. The MOS short-form general health survey-reliability and validity in a patient population. Med Care 1988;26:724-32. http://dx.doi.org/10.1097/00005650-198807000-00007.
- Tedeschi RG, Calhoun LG. The posttraumatic growth inventory: measuring the positive legacy of trauma. J Trauma Stress 1996;9:455-72. http://dx.doi.org/10.1002/jts.2490090305.
- Jaarsma TA, Pool G, Sanderman R, Ranchor AV. Psychometric properties of the Dutch version of the post traumatic growth inventory among cancer patients. Psycho Oncol 2006;15:911-20. http://dx.doi.org/10.1002/pon.1026.
- George EL, Miklowitz DJ, Richards JA, Simoneau TL, Taylor DO. The comorbidity of bipolar disorder and axis II personality disorders: prevalence and clinical correlates. Bipolar Disord 2003;5:115-22. http://dx.doi.org/10.1034/j.1399-5618.2003.00028.x.
- Curran PJ, West SG, Finch JF. The robustness of test statistics to nonnormality and specification error in confirmatory factor analysis. Psychol Methods 1996;1:16-29. http://dx.doi.org/10.1037/1082-989X.1.1.16.
- Tabachnick BG, Fidell LS. Using Multivariate Statistics. Boston, MA: Allyn and Bacon; 2001.
- Jones S, Mulligan LD, Law H, Dunn G, Welford M, Smith G, et al. A randomised controlled trial of recovery focused CBT for individuals with early bipolar disorder. BMC Psychiatry 2012;12. http://dx.doi.org/10.1186/1471-244X-12-204.
- Jones S, Smith G, Mulligan LD, Lobban F, Law H, Dunn G. Recovery-focused cognitive–behavioural therapy for recent-onset bipolar disorder: randomised controlled pilot trial. Br J Psychiatry 2015;206:58-66. http://dx.doi.org/10.1192/bjp.bp.113.141259.
- Goldberg JF, Perlis RH, Bowden CL, Thase ME, Miklowitz DJ, Marangell LB, et al. Manic symptoms during depressive episodes in 1,380 patients with bipolar disorder: findings from the STEP-BD. Am J Psychiatry 2009;166:173-81. http://dx.doi.org/10.1176/appi.ajp.2008.08050746.
- Perlis RH, Ostacher MJ, Patel JK, Marangell LB, Zhang H, Wisniewski SR, et al. Predictors of recurrence in bipolar disorder: primary outcomes from the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). Am J Psychiatry 2006;163:217-24. http://dx.doi.org/10.1176/appi.ajp.163.2.217.
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, et al. The longitudinal interval follow-up evaluation. A comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry 1987;44:540-8. http://dx.doi.org/10.1001/archpsyc.1987.01800180050009.
- Stephenson B, Rowe BH, Haynes RB, Macharia WM, Leon G. The rational clinical examination. Is this patient taking the treatment as prescribed?. J Am Med Assoc 1993;269:2779-81. http://dx.doi.org/10.1001/jama.1993.03500210079036.
- Tracey TJ, Kokotovic AM. Factor structure of the Working Alliance Inventory. Psychol Assess 1989;1:207-10. http://dx.doi.org/10.1037/1040-3590.1.3.207.
- Blackburn I-M, James IA, Milne DL, Baker C, Standart S, Garland A, et al. The revised cognitive therapy scale (CTS-R): psychometric properties. Behav Cogn Psychother 2001;29:431-46. http://dx.doi.org/10.1017/S1352465801004040.
- Dunn G, Maracy M, Dowrick C, Ayuso-Mateos JL, Dalgard OS, Page H, et al. Estimating psychological treatment effects from a randomised controlled trial with both non-compliance and loss to follow-up. Br J Psychiatry 2003;183:323-31. http://dx.doi.org/10.1192/bjp.183.4.323.
- Loeys T, Goetghebeur E. A causal proportional hazards estimator for the effect of treatment actually received in a randomized trial with all-or-nothing compliance. Biometrics 2003;59:100-5. http://dx.doi.org/10.1111/1541-0420.00012.
- Frangakis C, Rubin DB. Addressing complications of intention-to-treat analysis in the combined presence of all-or-none treatmentnon compliance and subsequent missing outcomes. Biometrika 1999;86:365-79. http://dx.doi.org/10.1093/biomet/86.2.365.
- Busseri MA, Tyler JD. Interchangeability of the working alliance inventory and working alliance inventory, short form. Psychol Assess 2003;15:193-7. http://dx.doi.org/10.1037/1040-3590.15.2.193.
- Davidson K, Norrie J, Tyrer P, Gumley A, Tata P, Murray H, et al. The effectiveness of cognitive behavior therapy for borderline personality disorder: results from the Borderline Personality Disorder Study of Cognitive Therapy (BOSCOT) trial. J Personal Disord 2006;20:450-65. http://dx.doi.org/10.1521/pedi.2006.20.5.450.
- Keen AJ, Freeston MH. Assessing competence in cognitive-behavioural therapy. Br J Psychiatry 2008;193:60-4. http://dx.doi.org/10.1192/bjp.bp.107.038588.
- Service User Involvement in the UK Mental Health Research Network. London: Mental Health Research Network; 2005.
- Ball J, Mitchell PB, Corry JC, Skillecorn A, Smith M, Malhi GS. A randomized controlled trial of cognitive therapy for bipolar disorder: focus on long-term change. J Clin Psychiatry 2006;67:277-86. http://dx.doi.org/10.4088/JCP.v67n0215.
- Meyer T, Hautzinger M. Cognitive behaviour therapy and supportive therapy for bipolar disorders: relapse rates for treatment period and 2-year follow-up. Psychol Med 2012;42:1429-39. http://dx.doi.org/10.1017/S0033291711002522.
- Lobban F, Taylor L, Chandler C, Tyler E, Kinderman P, Kolamunnage-Dona R, et al. Enhanced relapse prevention for bipolar disorder by community mental health teams: cluster feasibility randomised trial. Br J Psychiatry 2010;196:59-63. http://dx.doi.org/10.1192/bjp.bp.109.065524.
- Merikangas KR, Jin R, He JP, Kessler RC, Lee S, Sampson NA, et al. Prevalence and correlates of bipolar spectrum disorder in the World Mental Health Survey Initiative. Arch Gen Psychiatry 2011;68:241-51. http://dx.doi.org/10.1001/archgenpsychiatry.2011.12.
- Owens GS, Richardson G, David AS, Szmukler G, Hayward P, Hotopf M. Mental capacity to make decisions on treatment in people admitted to psychiatric hospitals: cross sectional study. BMJ 2008;337. http://dx.doi.org/10.1136/bmj.39580.546597.BE.
- Warner L, Mariathasan J, Lawton-Smith S, Samele C. A Review of the Literature and Consultation on Choice and Decision-making for Users and Carers of Mental Health and Social Care Services. London: The King’s Fund/Sainsbury Centre for Mental Health; 2006.
- Morrison AP, Hutton P, Shiers D, Turkington D. Antipsychotics: is it time to introduce patient choice?. Br J Psychiatry 2012;201:83-4. http://dx.doi.org/10.1192/bjp.bp.112.112110.
- Psychosis and Schizophrenia in Children and Young People: Recognition and Management. London: NICE; 2013.
- Harding CM, Zahniser JH. Empirical correction of seven myths about schizophrenia with implications for treatment. Acta Psychiatr Scand 1994;90:140-6. http://dx.doi.org/10.1111/j.1600-0447.1994.tb05903.x.
- Green MF, Nuechterlein KH. Should schizophrenia be treated as a neurocognitive disorder?. Schizophr Bull 1999;25:309-19. http://dx.doi.org/10.1093/oxfordjournals.schbul.a033380.
- Medalia A, Thysen J. Insight into neurocognitive dysfunction in schizophrenia. Schizophr Bull 2008;34:1221-30. http://dx.doi.org/10.1093/schbul/sbm144.
- Myin-Germeys I, Delespaul PAEG, de Vries MW. Schizophrenia patients are more emotionally active than is assumed based on their behaviour. Schizophr Bull 2000;26:847-53. http://dx.doi.org/10.1093/oxfordjournals.schbul.a033499.
- Myin-Germeys I, Krabbendam L, Jolles J, Delespaul PAEG, van Os J. Are cognitive impairments associated with sensitivity to stress in schizophrenia? An experience sampling study. Am J Psychiatry 2002;159:443-9. http://dx.doi.org/10.1176/appi.ajp.159.3.443.
- Thewissen V, Myin-Germeys I, Bentall RP, de Graaf R, Vollenberg W, van Os J. Instability in self-esteem and paranoia in a general population sample. Soc Psychiatry Psychiatr Epidemiol 2007;42:1-5. http://dx.doi.org/10.1007/s00127-006-0136-1.
- Glen T, Whybrow PC, Rasgon N, Grof P, Alda M, Baethge C, et al. Approximate entropy of self-reported mood prior to episodes in bipolar disorder. Bipolar Disord 2006;8:424-9. http://dx.doi.org/10.1111/j.1399-5618.2006.00373.x.
- Melo S, Corcoran R, Shryane N, Bentall RP. The persecution and deservedness scale. Psychol Psychother 2009;82:247-60. http://dx.doi.org/10.1348/147608308X398337.
- Chadwick P, Lees S, Birchwood M. The revised Beliefs About Voices Questionnaire (BAVQ-r). Br J Psychiatry 2000;177:229-32. http://dx.doi.org/10.1192/bjp.177.3.229.
- Stip E, Caron J, Renaud S, Pampoulova T, Lecomte Y. Exploring cognitive complaints in schizophrenia: the subjective scale to investigate cognition in schizophrenia. Compr Psychiatry 2003;44:331-40. http://dx.doi.org/10.1016/S0010-440X(03)00086-5.
- Beck AT, Brown G, Berchick RJ, Stewart BL, Steer RA. Relationship between hopelessness and ultimate suicide: a replication with psychiatric outpatients. Am J Psychiatry 1990;147:190-5. http://dx.doi.org/10.1176/ajp.147.2.190.
- Kaney S, Bentall RP. Persecutory delusions and attributional style. Br J Med Psychol 1989;62:191-8. http://dx.doi.org/10.1111/j.2044-8341.1989.tb02826.x.
- Bentall RP, Kinderman P, Howard R, Blackwood N, Cummins S, Rowse G, et al. Paranoid delusions in schizophrenia and depression: the transdiagnostic role of expectations of negative events and negative self-esteem. J Nerv Ment Dis 2008;196:375-83. http://dx.doi.org/10.1097/NMD.0b013e31817108db.
- Bartholomew K, Horowitz LM. Attachment styles among young adults: a test of a four-category model. J Pers Soc Psychol 1991;61:226-44. http://dx.doi.org/10.1037/0022-3514.61.2.226.
- Treynor W, Gonzalez R, Nolen-Hoeksema S. Rumination reconsidered: a psychometric analysis. Cognitive Ther Res 2003;27:247-59. http://dx.doi.org/10.1023/A:1023910315561.
- Goldberg D, Huxley P. Common Mental Disorders: A Bio-Social Model. London: Routledge; 1992.
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol 1986;51:1173-82. http://dx.doi.org/10.1037/0022-3514.51.6.1173.
- Dickerson SS, Kemeny ME. Acute stressors and cortisol responses: a theoretical integration and synthesis of laboratory research. Psychol Bull 2004;130:355-91. http://dx.doi.org/10.1037/0033-2909.130.3.355.
- Norman RMG, Malla AK. Dysphoric mood and symptomatology in schizophrenia. Psychol Med 1991;21:897-903. http://dx.doi.org/10.1017/S0033291700029883.
- Kernis M. Toward a conceptualization of optimal self-esteem. Psychol Inq 2003;14:1-26. http://dx.doi.org/10.1207/S15327965PLI1401_01.
- Tschacher W, Scheier C, Hashimoto Y. Dynamical analysis of schizophrenia courses. Biol Psychiatry 1997;41:428-37. http://dx.doi.org/10.1016/S0006-3223(96)00039-X.
- Bech P, Bowlig TG, Kramp P, Rafaelsen OJ. The Bech-Rafaelsen Mania Scale and the Hamilton Depression Scale. Acta Psychiatr Scand 1979;59:420-30. http://dx.doi.org/10.1111/j.1600-0447.1979.tb04484.x.
- Cassidy F, Forest K, Murry M, Carroll BJ. A factor analysis of the signs and symptoms of mania. Arch Gen Psychiatry 1998;55:27-32. http://dx.doi.org/10.1001/archpsyc.55.1.27.
- Tamminga CA, Davis JM. The neuropharmacology of psychosis. Schizophr Bull 2007;33:937-46. http://dx.doi.org/10.1093/schbul/sbm063.
- Craddock N, Owen MJ. The beginning of the end of the Kraepelinian dichotomy. Br J Psychiatry 2005;186:364-6. http://dx.doi.org/10.1192/bjp.186.5.364.
- van der Gucht E, Morriss R, Lancaster G, Kinderman P, Bentall RP. Psychological processes in bipolar affective disorder: Negative cognitive style and reward processing. Br J Psychiatry 2009;194:146-51. http://dx.doi.org/10.1192/bjp.bp.107.047894.
- Carver CS, White TL. Behavioral inhibition, behavioral activation, and affective responses to impending reward or punishment: the BIS/BAS Scales. J Pers Soc Psychol 1994;67:319-33. http://dx.doi.org/10.1037/0022-3514.67.2.319.
- Greenwald AG, McGhee DE, Schwartz JLK. Measuring individual differences in implicit cognition: the implicit association test. J Pers Soc Psychol 1998;74:1464-80. http://dx.doi.org/10.1037/0022-3514.74.6.1464.
- McKay R, Langdon R, Coltheart M. The defensive function of persecutory delusions: an investigation using the implicit association test. Cognit Neuropsychiatry 2007;12:1-24. http://dx.doi.org/10.1080/13546800500363996.
- Moritz S, Werner R, von Collani G. The inferiority complex in paranoia readdressed: a study with the Implicit Association Test. Cognit Neuropsychiatry 2006;11:402-15. http://dx.doi.org/10.1080/13546800444000263.
- Tarrier N, Lewis S, Haddock G, Bentall RP, Drake R, Dunn G, et al. 18-month follow-up of a randomized controlled trial of cognitive-behaviour therapy in first episode and early schizophrenia. Br J Psychiatry 2004;184:231-9. http://dx.doi.org/10.1192/bjp.184.3.231.
- Applegate E, El-Deredy W, Bentall RP. Reward responsiveness in psychosis-prone groups: hypomania and negative schizotypy. Pers Individ Diff 2009;47:452-6. http://dx.doi.org/10.1016/j.paid.2009.04.017.
- Clinical Guidelines for Bipolar Disorder. London: NICE; 2006.
- Mead S, Copeland ME. What Recovery Means to Us. New York, NY: Pelnum Publishing; 2000.
- Jones S. Psychotherapy of bipolar disorder: a review. J Affect Disord 2004;80:101-14. http://dx.doi.org/10.1016/S0165-0327(03)00111-3.
- Beck AT, Steer RA. Beck Depression Inventory. San Antonio, TX: The Psychological Corporation; 1987.
- Neff K. Self-compassion: an alternative conceptualization of a healthy attitude toward oneself. Self Identity 2003;2:85-101. http://dx.doi.org/10.1080/15298860309032.
- Scott J, Gutierrez MJ. The current status of psychological treatments in bipolar disorders: a systematic review of relapse prevention. Bipolar Disord 2004;6:498-503. http://dx.doi.org/10.1111/j.1399-5618.2004.00153.x.
Appendix 1 Protocol for Chapter 2 studies
Appendix 2 Protocol for Chapter 3 study
A DELPHI STUDY WITH SERVICE USERS – WHAT DOES RECOVERY MEAN TO SERVICE USERS WITH EXPERIENCE OF PSYCHOSIS?
Aim
The overall aim of this study is to determine the extent of the consensus among service users on the meaning of recovery from psychosis.
Objectives
-
To produce a list of statements related to the definition and conceptualisation of recovery from psychosis as identified through a search of the literature.
-
To circulate this list of statements to a service user focus group for consultation.
-
To format the list of statements into an online survey to be circulated more widely among people with experience of psychosis for extensive consultation.
-
Based on the above consultation process, to identify areas of consensus relating to the conceptualisation of recovery and extrapolate other key themes emerging from the survey.
Background
The word psychosis describes a common set of experiences including hearing voices, seeing things, unusual thoughts and unusual beliefs. Many people will have these experiences to some degree, but for some people experience of psychosis may interrupt or disturb daily activities or cause distress. Medically, psychosis is usually understood as a symptom of a psychiatric disorder such as schizophrenia, and from the traditional medical paradigm, people who experience psychosis are not expected to get better or recover.
Recovery in the field of mental health is a relatively new concept and encompasses ‘recovering’ in the traditional sense of ‘feeling well again’ but also acknowledging that recovery is a personal process involving rebuilding life, rebuilding self and hope for a better future (Pitt et al. , 2007), rather than purely focusing on symptom reduction. 19 Within the academic literature, service users themselves have led the ‘recovery movement’ by publishing personalised accounts of their recovery. This has brought a new sense of optimism for health professionals and service users alike. Health services and policy makers have taken on board this positive approach to mental health by advocating services which are recovery orientated.
Despite this interest in adopting a ‘recovery approach’, there is still no universally accepted and unambiguous definition of recovery. The word has a completely different meaning to service users compared with clinicians and academics. Generally the term recovery implies a cure or healing after illness or injury and a return to the normal condition. However, based on this connotation, few people with severe mental illness would ever be fully recovered. 17
The service user movement in conceptualising recovery has moved away from professional classifications towards self-definition. Service users view recovery as something very different to clinicians18 and are not limited to purely considering recovery as the absence of symptoms, disability or reduction in the use of mental health services. 76 There is a strong belief that recovery is different for everyone and that it is a complex process rather than an outcome or end point. 19
As part of a larger project titled ‘Understanding recovery in psychosis’, this study will aim to address the gap in the literature by exploring what recovery from psychosis means to service users. Service users should be recognised as ‘experts on their own experiences’ (British Psychological Society, 2000) and as such this study will consult a large number of service users about what recovery means to them.
This study will use a method known as the Delphi process which aims to elicit the opinions of a group of experts and reach a consensus on a given topic. In this case, the topic is defining and conceptualising recovery from psychosis and the group of experts will be service users with experience of psychosis.
Method
Participants
Participants will be recruited via convenience sampling through mental health services (including Community Mental Health Teams and Early Intervention Services), non-NHS groups/voluntary groups and networks (such as MIND, RETHINK and the Hearing Voices Network), and advertising of the study by leaflets, posters, e-mail networks and voluntary organisations websites, social media and local media (including press releases). This is to ensure the study is advertised as widely as possible allowing as many people as possible to submit their views.
It is also hoped that recruitment can also make use of a new pilot system being implemented at Greater Manchester West Mental Health NHS Foundation Trust. This system (called FAIR-Free Access to Involvement in Research) allows all service users to opt in to hearing about possible research studies. The R&D department send letters to service users who have asked to hear about research. The letters do not give details of the research study itself but allow people to contact the research team directly for more information.
Participants will be included in the study if they have (or have had in the past) experience of psychosis, are over the age of 16 and are able to understand English.
Demographic details including age, gender, location and mental health diagnosis or description will be collected.
Participants who express an interest in the study will have the option of having the study information and link e-mailed directly to them to facilitate easy access to the study website. Participants who do not have access to the computer will be offered a paper copy of the survey to allow them to take part.
Participants who request a paper copy of the survey will also be given a paper version of the consent form. Participants completing the survey online will complete an online declaration which reminds them that once they submit their responses they are agreeing to take part in the research.
Procedure
The Delphi process will consist of three stages:
Stage 1
Elements identified as pertinent to the definition or conceptualisation of recovery from psychosis will be identified through a literature search and collated into a list of statements. This list will then be sent via e-mail and post to a panel of service users (experts by their experiences) to take part in this initial consultation phase. Those who agree to take part will be asked to rate, add to and amend the list of statements. Any amendments and new items (except duplications) will be added to the list to form the questionnaire for the next stage.
Stage 2
The finalised statement list from the first stage will be collated and formatted into an online questionnaire (with a paper alternative made available). Participants will be asked to rate the importance of each item, in relation to defining recovery, on a five point Likert scale (1-essential, 2-important, 3-do not know/depends, 4-unimportant and 5-should not be included). Responses to this stage of the consultation are analysed to inform the final round of questionnaires. At this stage, participants are asked if they would like to provide a contact e-mail or postal address so that they are able to take part in the final stage of the consultation.
Stage 3
In stage 3, participants will be asked to re-rate only those items that 70–79% of respondents had rated as essential or important during stage 2. The questionnaire will take exactly the same format as above, but will only include items which were rated as essential or important by 70–79% of the stage 2 respondents.
Materials
Materials will include advertising posters and leaflets, information sheets, consent, consent forms and the statement list in questionnaire format. These will be made available in an online and paper version where possible.
Analysis
Survey responses were recorded in a secure anonymised database and analysed by obtaining group percentages. The following cut-off points were used in relation to inclusion, re-rating and exclusion criteria for the items:
-
Items rated by 80% or more participants as essential or very important to defining or conceptualising recovery are included as standard.
-
Items rated as essential or important to defining or conceptualising recovery by 70–79% of respondents in stage 2 will be re-rated in stage 3.
-
Any statements that did not meet the above 2 conditions were excluded.
Potential risks/ethical issues
It is not envisaged that there will be any risks or ethical issues from taking part in this research.
Confidentiality
Participation in this study is completely anonymous. Responses are submitted online without entering any personal identifiable information or on an anonymised paper version. All responses are anonymous.
Right to withdraw
Participants are free to withdraw at any time without detriment to their care and this will be made clear on the information sheets and consent forms.
Data storage
Data will be held (in accordance with University of Manchester policy) for 5 years after the last publication of the study or for 10 years, whichever is the greater. Consent forms will be retained as essential documents, but personal contact details will be deleted following stage 3 of the study.
Appendix 3 Protocol for Chapter 4 studies
PSYCHOLOGICAL FUNCTIONING AND SUBJECTIVE RECOVERY VERSION 5/23RD SEPTEMBER 2009
Background
Most research on the long-term course of severe mental illness (including randomized controlled trials) has defined outcome in terms of symptoms or symptomatic relapse. However, this narrow focus is problematic for two main reasons. First, symptomatic outcomes (e.g. as measured using interview schedules such as the Positive and Negative Syndromes Scale; PANSS) correlate very poorly with other types of outcome, such as social, occupational110 or cognitive functioning. 28 Hence, it is possible for a person with psychosis to experience a complete remission of symptoms while continuing to experience enduring social disability, or to function well socially and occupationally despite persisting symptoms. Second, it has become increasingly recognised that patients’ conceptions of recovery often differ from those of professionals. For example, in a recent qualitative study it was found that service users tended to define recovery in terms of rebuilding life, rebuilding self and hope for a better future,19 Hence it has been argued that recovery should be seen as:
A deeply personal, unique process of changing one’s attitudes, values, feelings, goals, skills, and/or roles. It is a way of living a satisfying, hopeful, and contributing life, even with limitations caused by the illness. Recovery involves the development of new meaning and purpose in one’s life287
and that, when considered in this way, recovery is much more common than has previously been thought. 347
This realisation has resulted in services in Britain and North America moving towards a ‘recovery model’ of service provision. Although it is not always clear what this means, services of this kind tend to promote an optimistic view of mental health outcomes encourage patients to develop their own understanding of what recovery means, and help patients to find the best way of achieving their personally defined goals. However, this development has been impeded by a lack of understanding of subjectively defined recovery or how it relates to important dimensions of psychological functioning. 18 Given this reconceptualization, work is required in order to determine what factors determine recovery judgements. Why do some patients regard themselves as recovered whereas others do not? So far very little research has addressed this issue and our hypotheses are therefore necessarily speculative.
For example, although many investigators have been at pains to define recovery in ways that do not include symptoms, it remains possible that patients’ appraisals about their symptoms (e.g. the extent to which the symptoms are seen as intrusive and uncontrollable) affect whether or not they see themselves as well (H1). Given that research shows that many psychotic patients suffer from mild cognitive impairment and that this influences social functioning,348 it is also possible that recovery judgements are related to either current cognitive ability (H2) or appraisals of cognitive ability (H3) (which may be uncorrelated). 349 In frequently used tests of cognitive ability it has been shown that patients are able to improve on their score, becoming comparable to controls through repetition of the task (Bellack et al. , 1990) or by the inclusion of a monetary incentive (Green et al. , 1992). As it is possible that incentivised performance is a better indicator of cognitive ability than unincentivised performance, we will also investigate whether the inclusion of a monetary reward improves the ability of cognitive tests to predict subjective recovery (H4). It has also been shown that emotion-related processes play an important role in psychosis, with acutely ill patients showing extreme stress-sensitivity. 350,351 As stress sensitivity is likely to affect coping, it would not be surprising if this kind of emotional instability affected recovery judgements (H5). Finally, recent research has shown that instability in psychological processes may be more important than overall level of psychological functioning in people with severe mental illness; for example self-esteem is highly unstable (as indicated by moment-to-moment fluctuations) in patients in with paranoid delusions121 and individuals who later develop paranoid beliefs. 352,353 have shown that, in bipolar patients, approximate entropy (a statistical measure of chaotic fluctuations in affect) indicates an imminent relapse and, if this is the case in schizophrenia spectrum patients, it might be expected that instability of emotional and social functioning will be associated with negative judgements about recovery (H6).
To test H1-H4, we will conduct a cross-sectional study in which patients with schizophrenia spectrum disorders will be asked to complete four different measures of subjective recovery, together with objective measures of clinical functioning, measures of emotional functioning and subjective measures of clinical functioning. We will investigate associations between the four measures of recovery and use regression analysis to examine whether symptoms, cognitive and emotional functioning predict recovery status. In a second study with a subsample (subject to a separate ethics application), we will use the Experience Sampling Method (ESM) to test H5 and H6 by examining the stability of affect and social cognition in relation to recovery status.
Study design
Participants
A minimum of 120 patients meeting criteria for a lifetime diagnosis of DSM-IV schizophrenia spectrum disorders (schizophrenia, delusional disorder, schizoaffective disorder, psychotic disorder NOS) will be recruited to the study. We will be seeking to recruit a sample that is heterogeneous with respect to severity of symptoms, social functioning, duration of illness, and subjective appraisal of recovery status. Hence, we will use a broad recruitment strategy, approaching patients in hospital wards, day hospitals and CMHTs.
We will also recruit a convenience sample of 40 healthy control participants from NHS and university academic staff, informal contacts and from local fire services, approximately matched with the patient participants for age, sex and educational attainment (fire personnel tend to be good matches with patients of key demographic variables). (These participants will complete only some of the assessments – see below.)
Recovery appraisal measures
We will measure recovery appraisals using three measures, which will be administered only to the patient participants:
The Process of Recovery from Psychosis Questionnaire (QPR) is a 22-item questionnaire measuring subjective recovery in two domains: intrapersonal functioning and interpersonal functioning. The subscales have good internal consistency and test–retest reliability over short periods. 32
Additional recovery questions
Two additional questions will be appended to the QPR; participants will be asked: ‘Do you consider that you have recovered from your illness?’ (YES/NO); and ‘Please place a cross on the line below to indicate the extent to which you think you have recovered from your illness’ (10 cm analogue scale with left anchor ‘Completely recovered’ and right anchor ‘Not recovered at all’).
Objective clinical measures (to be administered to all participants)
The Positive and Negative Syndrome Schedule162 will be used to assess current symptoms. This is a structured clinical interview yielding ratings of the severity of thirty symptoms over the previous week and is used to calculate three composite scores: positive symptoms, negative symptoms, and general psychopathology. Researchers will receive training in the administration of the schedule and will be required to achieve the recommended lever of reliability (no scores deviating greater than 1 point from the scores of expert raters). Additional questions will be included from the Psychotic Symptoms Rating Scale (Psyrats; Haddock et al. , 1999). An observable measure of functioning, the Personal and Social Performance Scale (Nasrallah et al. , 2008, will also be included). Administration takes approximately 50 minutes.
Antipsychotic mediation dose will be recorded and converted to chlorpromazine equivalents, using standard tables. (These values will be zero for the healthy controls).
Brief Assessment of Cognition in Schizophrenia (Keefe et al. , 2004) is a 30-minute battery designed to be administrable by researchers without formal training in neuropsychology, which includes measures of verbal memory, attention, working memory, motor speed, verbal fluency and executive function. The BACS has been shown to have good test–retest reliability, to correlate with more extensive batteries, and to predict daily living skills in patients diagnosed as suffering from schizophrenia. One of the BACS subscales, the Tower of London (a measure of executive functioning) will be administered twice, once without and once with monetary reinforcements (20p per correct response).
Subjective appraisals of clinical functioning
The Persecution and Deservedness Scale354 (all participants) is a 20-item questionnaire measuring severity of persecutory ideation and the extent to which persecution is believed to be deserved.
The Interpretations of Voices Inventory355 (all participants) is a 35-item scale with three subscales measuring beliefs about voice-hearing.
The Subjective Experiences of Psychotic Symptoms Scale (SEPPS; Haddock et al. in prep) (patient participants only) is a recently developed 47-item scale designed to measure how much patients’ lives are affected by their symptoms.
The Subjective Scale to Investigate Cognition in Schizophrenia (SSICS)356 (all participants) is a 21-item scale measuring subjective cognitive deficits.
The Insight Scale132 (patient participants only) is a 10-item scale measuring perceived need for treatment.
Emotional Functioning (all participants).
Beck Hopeless Scale357 is a 20-item scale measuring negative thoughts about the future.
The Brief Self-esteem Rating Scale76 is a 20-item scale with good reliability which has been shown to be a valid measure of positive and negative self-esteem in psychotic patients.
The Acceptance and Avoidance Questionnaire-II (AAQ-II) is a 10-item scale with good reliability that measures intolerance of unpleasant thoughts and emotions. We have found that it is a strong predictor of paranoid beliefs in non-clinical samples (Udachina, et al. in submission).
Multidimensional locus of control scale131 is a reliable 24-item scale measuring dimensions of internality, belief in powerful others and belief in chance. In previous studies358 it has been found that paranoid patients scored abnormally highly on the ‘powerful others’ subscale.
Anticipation of future threats359 is a simple questionnaire in which individuals are asked, first, to state how often 7 common positive (e.g. a friend helps you), 7 neutral (e.g. you receive a letter) and 7 common negative events (e.g. a friend ignores you) have occurred over the last month. Participants are then asked to rate the future probability of these events for themselves and ‘other people’ using seven point analogue scales.
Relationships Questionnaire360 is a two-minute questionnaire measuring security of current attachment relations. Participants read four brief vignettes describing different styles of relating to others. They are asked to chose the description which best describes them, and then to rate how similar they are to each description using 7 point analogue scales.
Brooding subscale of the Ruminative Responses Scale361 is a 5-item questionnaire measure of rumination, which has been shown to predict persistence of negative affect.
Hospital Anxiety and Depression Scale128 is a 14-item questionnaire with subscales for anxiety and depression.
The measures will be administered over two sessions separated by a few days, with the PANSS, QPR, SEPSS, BHS, LeComte, and PSYRATS administered on the first session and all remaining measures administered on the subsequent session.
Analysis
Patterns of association and concordance between the four measures of recovery will be examined through the use of the kappa statistic.
We will divide patients in to ‘recovered’ and non-recovered’ groups by means of a median split of QPR. We will then conduct two-way sex x group (recovered, non-recovered, healthy controls) ANOVAs on key psychological variables. We will normalise any data as required using the appropriate transformation and, in the event of group differences in age and educational attainment, include these as covariates.
We will use a multiple regression approach to analysing predictors of recovery, first centering and normalising scores for predictor and outcome variables. Prior to analysis, we will seek to reduce the number of predictor variables using appropriate techniques (e.g. PCA). For example, given that depression and anxiety measures typically correlate by about 0.6 in both clinical and non-clinical samples362 we will almost certainly collapse the two HADS scales into a single measure of dysphoria. A final analysis incorporating all three measures of recovery will involve the use of a structural equation model to evaluate whether the predictors are common to the four or whether there are specific influences.
We will use the method of363 to study potential mediational affects between objective measures (e.g. positive symptoms on the PANSS; cognitive functioning on the BACS) and perceived recovery, using the relevant subjective appraisal measures (e.g. subjective impact of symptoms measured by the SEPPS; subjective cognitive functioning measured by the SSICS) as mediators.
However, one of the frequently unrecognised difficulties for the interpretation of these analyses is the possibility of confounding between putative mediator and final outcome (i.e. variables that have an influence on both). We will therefore attempt to identify and condition on potential confounders, and also investigate the possibility of the use of instrumental variable methods to allow for the effects of unmeasured confounders (see Dunn and Bentall, 2007).
UNDERSTANDING RECOVERY IN EVERYDAY LIFE: AN EXPERIENCE SAMPLING STUDY VERSION 8: 20TH DECEMBER 2011
Most research on the long-term course of severe mental illness (including randomized controlled trials) has defined outcome in terms of symptoms or symptomatic relapse. However, this narrow focus is problematic for two main reasons. First, symptomatic outcomes (e.g. as measured using interview schedules such as the Positive and Negative Syndromes Scale; PANSS) correlate very poorly with other types of outcome, such as social, occupational110 or cognitive functioning. 28 Hence, it is possible for a person with psychosis to experience a complete remission of symptoms while continuing to experience enduring social disability, or to function well socially and occupationally despite persisting symptoms. Second, it has become increasingly recognised that patients’ conceptions of recovery often differ from those of professionals. For example, in a recent qualitative study it was found that service users tended to define recovery in terms of rebuilding life, rebuilding self and hope for a better future. 19 Hence it has been argued that recovery should be seen as:
A deeply personal, unique process of changing one’s attitudes, values, feelings, goals, skills, and/or roles. It is a way of living a satisfying, hopeful, and contributing life, even with limitations caused by the illness. Recovery involves the development of new meaning and purpose in one’s life287
and that, when considered in this way, recovery is much more common than has previously been thought. 347
This realisation has resulted in services in Britain and North America moving towards a ‘recovery model’ of service provision. Although it is not always clear what this means, services of this kind tend to promote an optimistic view of mental health outcomes, encourage patients to develop their own understanding of what recovery means, and help patients to find the best way of achieving their personally defined goals. Unfortunately, this development has been impeded by a lack of understanding of subjectively defined recovery or how it relates to important dimensions of psychological functioning. 18 Given this reconceptualization, work is required to determine what factors determine recovery judgements. Are recovery judgements stable over time, or do patients fluctuate in their judgements about mental wellness? Why do some patients regard themselves as recovered whereas others do not? So far very little research has addressed this issue. Our study is therefore designed to address a series of hypotheses that are necessarily speculative.
Mood and self-esteem
In healthy individuals, challenges to self-esteem are the most potent elicitors of secretion of the stress hormone cortisol. 364 Research using various diary methods has shown that exacerbations of positive symptoms are preceded by increases in negative mood and decreases in self-esteem. 121,365 Service users report that a positive sense of self is an important component of being recovered. 19 Together, these findings suggest a close association between self-esteem and mental well-being. A complication is that self-esteem is a complex process, and it is therefore important to distinguish between explicit self-esteem, conscious judgements about how we feel about ourselves at a particular moment, and implicit self-esteem, that is more enduring beliefs about our self-worth that we may not be aware of for much of the time. 366 It seems likely that explicit self-esteem will be associated with immediate judgements of wellness, whereas implicit self-esteem will be a better predictor of long-term mental health (H1). To test this hypothesis we will administer appropriate measures of explicit and implicit self-esteem, and also assess self-esteem in daily life using the experience sampling method (ESM), a sophisticated diary methodology.
Childhood trauma, dissociation and hallucinations
It is commonly believed that most auditory hallucinations are to be considered a psychotic symptom, whereas some are dissociative experiences (Moskowitz and Cortens, 2008).However, recent findings suggest that not only do auditory hallucinations (AH) not have to occur as a symptom of a psychotic disorder, but that AH and dissociation are aetiologically associated (Moskowitz and Cortens, 2008). Studies investigating both non-clinical (Glickson and Barret, 2003; Morrison and Peterson, 2003) and clinical populations (Perona-Garcelán et al. , 2008) have found strong associations between hallucination-proneness and dissociative experiences. Furthermore, research has repeatedly noted a relationship between experience of childhood trauma and dissociation (Glaser, van Os, Portegijs, and Myin-Germeys et al. , 2003; Myin-Germeys, et al. , 2003) and AH (Read and Argyle, 1999; Ross, Anderson, and Clark, 1994). Due to the associations observed between childhood trauma and AH and dissociation, it would be beneficial to investigate whether a mediating relationship between these factors exists – they may be important in conceptualising recovery, or be potential mediators in recovery trajectories (traumatic life experiences, ability to self-soothe an appraisal of symptoms). It is expected that dissociation will mediate the relationship between childhood trauma scores and hallucination-proneness. To test this hypothesis we will administer measures of child abuse and trauma, hallucination-proneness and dissociative experiences.
Interpretation of hallucinations
Research suggests that the emotional and behavioural consequences of hallucinatory experiences may not be caused by the content, but by the beliefs about the experience (Chadwick and Birchwood, 1994). Wells and Butler (1997) proposed that positive beliefs about hallucinations are associated with efforts to engage with the experience, whereas negative beliefs about hallucinations are thought to be associated with unhelpful coping strategies. Furthermore, studies have shown that hallucinatory experiences are not reserved to those diagnosed with psychotic disorders, but occur in the non-clinical population also (Verdoux and van Os, 2002). These findings indicate that hallucinations are not necessarily pathological, and in some cases can be a positive experience, depending on the individuals own interpretation; therefore a further understanding could be beneficial to improved support in recovery. Based on the aforementioned research, it is expected that the individuals’ interpretation of their voices will be related to the positivity of the experience. To test this hypothesis, a scale measuring the individuals’ interpretation of their hallucinations as well as measures of self-esteem, mood, depression and assessment of everyday self-esteem and mood using experience sampling methodology will be used.
Self-compassion
Self-compassion is a strong predictor of well-being (Neff 2003). Compassion Focused Therapy (CFT) aims to increase self-compassion and was recently shown to result in recovery-focused outcomes with a group of 4 people experiencing negative and malevolent voices. Interestingly, CFT resulted in much less threat associated with voice hearing experiences, and an increase in desire to engage in social relationships (Mayhew and Gilbert, 2008). Self-Compassion is thought to reflect a well developed affiliative soothing system – a form of positive emotion with a specialised neural pathway (Depue and Morrone Stupinsky, 2005). This forms the basis of a sense of connection to others; thus reducing the malevolence in all social relationships, both with voices and with other people. We therefore predict self-compassion will be associated with lower distress in relation to voices (H1) and a lower levels of paranoia about other people (H2).
Dynamic aspects of recovery
Recent research has also emphasized the dynamic and changing nature of psychosis, and that the process of symptomatic recovery is often unpredictable and formally (in the mathematical sense) chaotic. 367 In a study by353 it was shown that, in bipolar patients, approximate entropy (a statistical measure of chaotic fluctuations in affect) indicates an imminent relapse, and it seems likely that the same will be true of patients with diagnoses in the schizophrenia spectrum. Hence, instability in psychological processes may be more important than overall level of psychological functioning in people with severe mental illness. Consistent with this idea, we have shown that mood and self-esteem are highly unstable (as indicated by moment-to-moment fluctuations) in patients in with paranoid delusions121 and in individuals who later develop paranoid beliefs. 352 No study to date has investigated the stability of feelings of subjective wellness (momentary feelings of well-being) or how these relate to changes in mood or reward processing. We expect that patients who believe themselves to be recovered will show more stable judgements of subjective wellness than those who do not believe themselves to be recovered (H3), and that experiences of subjective wellness will be influenced by mood and savouring in everyday life (H4). We also predict that those who show highest entropy in their self-esteem and mood scores will feel themselves to be less recovered, and will make more use of services, on long-term (6 month) follow-up. The use of ESM will allow us to test these hypotheses.
Our overall approach will be to conduct a study in which patients with schizophrenia spectrum disorders will be asked to complete four different measures of subjective recovery, together with measures of clinical functioning, sensitivity to reward stimuli, self-esteem, and level of occupational and social functioning. Some of these measures will be interview based, some questionnaires, and some by ESM. ESM is a means of collecting information pertaining to the context and content of the daily life experiences of individuals, which we have previously used successfully with patients suffering from psychosis. 121 Participants are issued with a signalling device, for instance a sports watch or hand held electronic device similar to a personal digital assistant. The device provides alerts at pseudo random intervals as programmed by the researcher. On the signal the participant is required to complete a diary entry. The strength of the method thus is its ecological validity; information is sampled at the moment an experience occurs and in the environments participants typically inhabit. This avoids potential distortions associated with questionnaires that rely on retrospective judgments. It also allows many samples to be made in one day so intra-individual variation in data can be investigated.
In the cross-sectional phase of the study, we will compare the patients with healthy controls on all of our measures. Within the patient groups, we will examine the stability of recovery judgements over time and the stability of affect and social cognition in relation to recovery status.
At monthly intervals and at 6 months we will reassess, with patients only, recovery judgements, symptoms and social functioning, as well as use of services over the follow-up period. This will allow us to test whether entropy in affect and self-esteem in phase 1 predicts these outcomes.
Study design
Participants
80 people meeting criteria for a diagnosis of ICD-10 schizophrenia spectrum disorders (schizophrenia, delusional disorder, schizoaffective disorder, psychotic disorder) will be recruited to the study. We will be seeking to recruit a sample that is heterogeneous with respect to severity of symptoms, social functioning, duration of illness, and subjective appraisal of recovery status. Hence, we will use a broad recruitment strategy, approaching patients in hospital wards, day hospitals and CMHTs. Participants will complete a baseline recovery measure allowing us to separate them into two groups: (1) 40 who consistently describe themselves as recovered on three measures (a yes/no judgment, analogue scale and QPR); (2) 40 who consistently describe themselves a not recovered on the same three measures.
A healthy control group of 40 will also be recruited opportunistically from NHS statutory staff, non-academic university staff and through participant panels at the School of Psychological Sciences at the University of Manchester and the School of Psychology at the University of Bangor. This group will be screened using the Positive and Negative Symptoms of Schizophrenia scale (PANSS) to ensure that they are not experiencing any psychotic symptoms. They will also be asked whether they have at any time in the past been treated for psychiatric disorder; and an affirmative answer will result in exclusion from the study.
In phase 1, participants will complete a series of questionnaires followed by a 6-day diary of individual experiences at ten pseudo-random time points throughout the day separated by at least fifteen minutes. By means of this methodology, we will measure environmental context, and psychological experiences in everyday life.
Phase 1 baseline questionnaires
Recovery appraisal measures
We will measure recovery appraisals using three measures:
The Process of Recovery from Psychosis Questionnaire (QPR) is a 22-item questionnaire measuring subjective recovery in two domains: intrapersonal functioning and interpersonal functioning. The subscales have good internal consistency and test–retest reliability over short periods. 32
Additional recovery questions. Two additional questions will be appended to the QPR; participants will be asked: ‘Do you consider that you have recovered from your illness?’ (YES/NO); and ‘Please place a cross on the line below to indicate the extent to which you think you have recovered from your illness’ (10 cm analogue scale with left anchor ‘Completely recovered’ and right anchor ‘Not recovered at all’).
Objective clinical measures
The Positive and Negative Syndrome Schedule162 will be used to assess current symptoms. This is a structured clinical interview yielding ratings of the severity of thirty symptoms over the previous week and is used to calculate three composite scores: positive symptoms, negative symptoms, and general psychopathology. Researchers will receive training in the administration of the schedule and will be required to achieve the recommended lever of reliability (no scores deviating greater than 1 point from the scores of expert raters). Additional questions will be included from the Psychotic Symptoms Rating Scale (Psyrats; Haddock et al. , 1999). An observable measure of functioning, the Personal and Social Performance Scale (Nasrallah et al. , 2008) will also be included. Administration takes approximately 50 minutes. Furthermore, additional questions about age of onset, state of remission and description of symptoms regarding hallucinations and paranoia will be included.
Antipsychotic mediation dose will be recorded and converted to chlorpromazine equivalents, using standard tables.
Hamilton Rating Scale for Depression (HRSD)314 is a 21-item questionnaire used to rate the severity of symptoms of depression such as low mood, insomnia, agitation, anxiety and weight loss. Researchers choose the possible responses to each question by interviewing the patient and by observing the patient's symptoms.
Bech-Rafaelsen Mania Scale368 is a short interview measure of manic symptoms that is designed to be administered with the HRSD. We are including this measure because there is consistent evidence of overlap between manic symptoms and psychosis at the phenomenological (e.g. 369) neuropharmacological370 and genetic371 level. Furthermore, we have found that mania and hypomania are related to excessive reward responsivity. 372 Hence, any attempt to investigate the role of reward processes in psychosis must consider comorbid hypomanic/manic symptoms.
Self-report scales
The Persecution and Deservedness Scale (PaDS354) a 10-item measure of paranoid thinking, which we are including because the PANSS does not record some aspects of paranoia (e.g. whether the participant feels that persecution is deserved) adequately for our purposes.
Behavioural Activation System Scale (BAS373) is a 24-item yes/no measure of subjective reward sensitivity. We have reduced this to a 14-item BAS only scale in the interest of reducing unnecessary questions; the study is not concerned with findings from the BIS scale.
Self-Esteem Rating Scale–Short Form (SERS; Lecomte et al. 2006) is a measure of explicit self-esteem comprising 20 Likert-based items: 10 positive statements about the self that provide a measure of positive self-esteem; and 10 negative statements about the self that provide a measure of negative self-esteem. The SERS has demonstrated good validity, internal consistency, and test–retest reliability in the general population and in those with schizophrenia. 76
Implicit Associations Test (IAT374) is a computerised test that is the most widely used assessment of implicit self-esteem. A large body of literature supports its validity and it has recently been successfully used in studies investigating implicit self-esteem in individuals psychosis. 375,376 Stimulus words, which are positive and negative personality traits, are presented in the middle of the computer screen and respondents are required to sort them into categories at the two different sides of the screen by pressing buttons on the corresponding sides of the keyboard. If a participant makes an error, a red cross appears on the screen and participants are asked to respond by correcting the error.
The version we will use will comprise eight blocks of trials. The first two blocks are practice blocks in which participants are required to practice sorting words into ‘me’ and ‘other’ categories. The categories swap sides between blocks one and two, in order to allow practice sorting ‘me’ and ‘other’ words to both sides. The third and fourth blocks are practice blocks in which participants are required to practice sorting words into ‘bad’ and ‘good’ categories. Again, the categories are swapped between sides between blocks.
The last four blocks participants are required to sort the two sets of stimuli at once. Therefore in these blocks, a ‘me’ or ‘other’ word or a ‘bad’ or ‘good’ word might appear in the centre of the screen. In two of the blocks, individuals are asked to sort ‘me’ and ‘good’ words to the same side and ‘other’ and ‘bad’ words to the same side (congruent conditions). In the other two blocks, they are asked to sort ‘me’ and ‘bad’ words to the same side and ‘other’ and ‘good’ words to the same side (incongruent conditions). The categories swap sides between the two congruent blocks and between the two incongruent blocks to control for any differences in sorting to either side. Implicit self-esteem is calculated by subtracting response times for the congruent conditions from the response times for the congruent conditions.
The Acceptance and Avoidance Questionnaire-II (AAQ-II) is a 10-item scale with good reliability that measures intolerance of unpleasant thoughts and emotions. We have found that it is a strong predictor of paranoid beliefs in nonclinical samples (Udachina, et al. in submission).
Beck Hopeless Scale357 is a 20-item scale measuring negative thoughts about the future.
The Stigma Scale (King et al. , 2007) is a 28-item scale measuring perceived discrimination, disclosure and positive aspects about mental health problems.
The Child Abuse and Trauma Scale (Sanders and Becker-Launsen, 1995) is a 38-item multidimensional measure of the perceived degree of stress and trauma experienced at childhood. Additional questions will be added following the CATS to ask whether the participant has been asked questions about traumatic experiences in early life, how they feel about being asked, and whether they have been offered help. A supporting leaflet will also be provided to those who have experienced sexual or physical abuse containing contacts and information on where to get additional support.
The revised Dissociative Experiences Scale (Carlson and Putnam, 1993) is a 28-item self-report measure designed to assess dissociative experiences in both clinical and non-clinical populations.
The revised Launay-Slade Hallucination Scale (Bentall and Slade, 1985) is a 12-item self-reported scale of hallucinatory proneness.
The Interpretations of Voices Inventory (Morrison et al. , 2002) is a 26-item self-report measure designed to assess positive and negative interpretations of auditory hallucinations.
The Self-Compassion Scale (SCS; Neff, 2003 a,b). is a 26-item scale designed to accurately measure self-compassion as conceptualised in Buddhist teachings. The scale includes subscales for the following: self-kindness (5 items), self-judgment (5 items), Common Humanity (4 items), Isolation (4 items), Mindfulness (4 items); and an Over-Identification subscale (4 items). Responses are given on a 5-point Likert scale, ranging from 1 = Almost never, to 5 = Almost always. All 6 subscales have been shown to be highly inter-correlated and confirmatory factor analysis determined that a single higher order factor of self-compassion explained these inter-correlations (Neff, 2003). The SCS has been demonstrated to have good internal consistency reliability (.92) as well as good test–retest reliability (r=.93) (Neff, 2003).
Experience sampling method
ESM, which we have successfully used with patients with severe mental illness,121 is a method of measuring cognitive and emotional functioning in everyday life. Participants wear electronic wrist-watches or use a palm computer programmed to bleep 10 times a day on a pseudorandom schedule between 7.30 am and 10 pm. Participants are asked to complete a short diary (taking approximately 2 minutes) on hearing a bleep. Participants are asked to wear the watches or use the palm computers for 6 days.
The procedure can cope with a high level of missing data; we will include data from any participant with > 19 diary entries. Multilevel modelling, with repeated measures regression analysis will be used to analyse reported activities and subjective responses, variations in these variables, and causal relationships between them.
Items measuring psychological experiences in the diary are typically on a 7-point Likert scale. As in our previous studies, we will include questions measuring affect (positive and negative) self-esteem, activity-related stress and self-efficacy. We have adapted our existing diaries to include questions on the following recovery-related variables: rumination, recovery status and savouring ability. Each diary entry typically takes about 2 minutes to complete.
Phase 2 follow-up assessments
At 6 months, clinical participants will be interviewed with the PANSS, and also asked to complete the QPR with additional recovery questions. They will also be asked to complete a simple service receipt schedule (based on our previous work with the SoCRATES trial377) which will record the following information: (a) total number of appointments with CPNs, psychiatrists and other mental health workers over the 6 month period; (b) total number of primary care appointments over the 6 month period; and (c) total number of days spent in day hospital, inpatient facilities, or under section.
At the 3-month follow-up point prior to the 6-month follow-up, a briefer interview focusing on subjective well-being will be conducted over the telephone. This will consist of the mood, self-esteem questions from the ESM, together with the QPR questions reworded so that they cover the past month. We will also ask a short schedule of qualitative questions regarding subjective well-being.
Safe working
Please refer to ‘Recovery Programme Safe Working Practices – Project 2 Version (latest version 01.03.2011)’.
Distress procedure
In the event of a participant experiencing distress during the study, please follow procedures outlined on page 17 of ‘Recovery Programme Safe Working Practices – Project 2 Version (latest version 01.03.2011)’.
Analysis
Patient participants will be divided into two groups, subjectively recovered vs. non-recovered, on the basis of a median split of QPR scores. We will compare these groups on the baseline questionnaire measures and IAT using analysis of variance. We have conducted power calculations for these analyses using our own data from studies either published or in submission.
Based on data collected by378 expected scores for the three groups on the BAS total scores are shown in Table 72 below (all figures rounded to nearest integer), based on extrapolation from extreme scores in a large (N > 300) healthy sample. Estimated scores for the SERS are based on actual patient vs. healthy control comparisons in a pilot study (N = 24 patients and 12 healthy controls) conducted recently in Bangor.
| Non-recovered | Recovered | Controls | ||||
|---|---|---|---|---|---|---|
| Measure | Mean | SD | Mean | SD | Mean | SD |
| BAS total | 14 | 2 | 16 | 2 | 18 | 2 |
| SERS negative | 43 | 17 | 37 | 9 | 26 | 9 |
Sample sizes were estimated using G*power software. Assuming a power of 0.8 and an alpha of 0.01, we will require only 8 participants to detect differences in BAS total (ES = 0.82). For SERS (ES = 0.54) 18 are required in each group.
Participants will only be retained for the analyses of the ESM data if they have > 19 completed data points (in practice, we have found that we loose about 5% of patients because of the failure to meet this minimum requirement). Summary scores, e.g. mean scores for self-esteem, positive affect, negative affect, and also fluctuations in mood and affect using momentary (change from last recording), daily (maximum and minimum scores within the day) and weekly (within-participant SD in scores) can be compared between groups using a standard analysis of variance approach. This can also be done with values for approximate entropy (ApEn), which we will calculate separately for positive affect, negative affect and self-esteem using standard methods. 353
A multilevel modelling approach is required to investigate the relationship between subjective recovery and psychological processes by modelling stability of processes using momentary (change from last recording), daily (maximum and minimum scores within the day) and weekly (within-participant SD in scores). Data will be analysed using maximum likelihood random coefficient models to minimise loss to attrition by ensuring that we make full use of participants who provide incomplete data (under an assumption of MAR missing data mechanism). It is difficult to calculate power estimates for this approach, but we note that previous studies, e.g. 123 and 121 have reported group differences in stability of self-esteem and stress sensitivity with total samples of 42–60 patients. Hence, including 40 in each group is a conservative approach.
We will use regression with selected baseline measures (e.g. SERS scores, ApEn for self-esteem, BAS) to predict outcomes defined in terms of positive symptoms at 6 months, total service utilisation over the follow-up period, and average QPR scores over the follow-up period. A widely accepted convention is that 10 participants are required for each predictor variable, allowing us to chose up to 8 predictors;137 Norman, 1994). With this number of predictors, we will be able to detect effect sizes of 0.29 or more with an alpha of 0.01 and a power of 0.80.
Appendix 4 Protocol for Chapter 5 studies
PROTOCOL VERSION 3 22/12/10 EVALUATION OF DIFFERENT LEVELS OF SUPPORT IN USING A RECOVERY GUIDE FOR PEOPLE WITH PSYCHOSIS AND THE IMPACT OF CHOICE ON OUTCOMES
Introduction
Although recent government guidelines (National Institute for Clinical Effectiveness, 2004) have recommended that people with persistent psychosis be supported using psychological intervention approaches such as cognitive–behaviour therapy, the widespread current lack of trained therapists to deliver this type of intervention means that provision of this type of intervention is likely to be limited. As a result, exploration of how this support can be provided to the greatest numbers of people is urgently needed. One way that is currently being explored within other domains is the stepped care approach first described in the United States in relation to the delivering of health care within primary care. Stepped care assumes that the least restrictive treatment or the minimum of therapist time is delivered that still brings about a significant improvement to the individual receiving it (Bower and Gilbody, 2005).
The stepped care approach has been examined in the UK in relation to the development of services for people with non-psychotic disorders. Much of this has been related to cognitive–behavioural interventions that appear to lend themselves well to a stepped care approach. For example, using CBT oriented bibliography (Cuijpers, 1997), computerised treatment (Marks et al. , 2003), telephone treatment (Lovell et al. , 2006) as well as face to face contact and ’full-blown’ CBT. Despite these developments within the primary care domain, little has been little explored within services for people with severe mental illness. However, these CBT approaches may well lend themselves extremely well to this client group whose ability to access ‘traditional talking treatments’ may be limited by lack of availability and by their difficulty in attending and travelling to travel to clinics.
One recent study, carried out by our group, has evaluated the applicability of one such approach with service users with psychosis. This study used a CBT oriented Recovery Guide with support from a CBT therapist delivered over the phone (over 6 months) and evaluated its impact using qualitative and quantitative methods. A comparison no intervention group was included although this was a small pilot trial, not a randomised controlled trial. Findings revealed that the approach was acceptable to the majority of participants (n = 15) and there were few drop-outs. Qualitative feedback from therapists and participants indicated that the content of the guide was relevant and that the support provided by telephone was useful and appropriate for providing support for the guide (Pitt et al. , 2009). However, findings revealed that some participants would prefer different levels of support in the use of the guide, for example, some would have preferred face to face therapy support rather than delivered over the telephone.
This qualitative finding was also confirmed by other methods. A study investigating the factors contributing to service user’s preferences for levels of psychological treatment was also carried out (n = 90 Gerrard et al. , 2009). Service users were presented with detailed information about the Recovery Guide and about different levels of therapy support for using the guide (low support = telephone support; high support = telephone therapy plus group support). Service users were asked to say whether they would be willing to take part in a trial involving these types of interventions, to say whether they would be willing to be randomised and to indicate whether they had a preference for treatment and is so, what treatment they would prefer (none, low support or high support) if they were to take part. Findings revealed that 90% would be willing to take part in a trial of psychological treatments although 57% of the participants said they were unwilling to be randomised. In addition, 22% said that if they were to take part they would prefer not to receive the psychological treatment. Of those who preferred treatment, 43% said they would prefer low support and 33% said they would prefer high support. These findings suggest that service users have strong preferences about the type of psychological treatments they would prefer.
These preferences have not been taken into account in previous psychological treatment trials although such preferences can make the interpretation of outcomes and their implementation in services problematic as variables related to preference may also be related to outcome (e.g. Janevic et al. , 2003). First, service users may either refuse to enter trials in case they do not receive their preferred treatment, or they may drop out of trials early because they are unhappy with the condition they have been allocated. Second, people may have feel resentful and demoralised (Bradley, 1993) if they do not get their preferred treatment choice, whereas those randomised to choice may have a morale boost. Such effects make the efficacy of the actual treatments difficult to evaluate. In order to take account of patient preferences, partially randomised PPTs where patients with treatment preferences are allowed their treatment without randomisation and those who do not have preference are randomised in the usual way have been suggested (Brewin and Bradley, 1989).
Clearly there are methodological problems with PPTs, the chief being that any comparison that uses non randomised groups is potentially unreliable because of unknown confounds (e.g. differences at baseline such as previous treatment history that might influence perceptions of effectiveness of treatments offered). However, ways of reducing the impact of such problems include: performing at least one comparison of the ‘true’ randomised arms alone; collecting information on potential confounds including ascertaining reasons for choice, then adjusting for these where the analysis includes non randomised people; using randomisation status (random/non-random) as a covariate in analyses. Because of the information required about patient preferences, it is therefore important to conduct adequate assessments about patient choice prior to conducting the preference trial.
In the case of the proposed trial we would argue that the potential benefits of a PPT outweigh the methodological problems, particularly as the preparatory work on patient choice has been conducted and the adjustments suggested above are included in the design and analysis. Such benefits include the likelihood that we will be able to recruit people who would otherwise refuse to take part in a traditional RCT and thus the sample will be more representative of all service users. A PPT will also improve the external validity of the trial and will likely be more commensurate with the nature of service users seen in routine practice. Moreover, the information about patient preferences and outcomes will inform services not only about the efficacy of treatments but also about patient preferences and likely take up of alternative methods of treatment delivery.
Aims
As this is a trial which allows the participant choice about the treatment they receive, it is expected that similar impacts will be seen across all three groups in the trial regardless of whether they receive therapy or not. With this in mind, specific aims are:
-
To evaluate the feasibility and acceptability of the Recovery Guide (Barrowclough et al. , 2009) when provided with either low or high support for people with psychosis.
-
To assess the relative impact of the guide in relation to low and high support and no- treatment1 on psychotic symptoms, affect, well-being and functioning.
-
To investigate the role of emotion and beliefs in relation to recovery.
As a result it is hypothesised that:
-
The Self-Help Recovery Guide will be acceptable and feasible to use by service users with psychosis as judged by retention in the treatment (assuming retention of 70%) and from qualitative interviews and this will not differ between those receiving high and low support.
-
There will be significant improvements in the disruption and distress caused by psychosis, affect, functioning and well-being and effect sizes will be comparable across groups (both no treatment and high and low support).
Exploratory aims also include:
-
To evaluate the impact of the two different modes of treatment on the working alliance between client and therapist.
-
To explore the relationship between change in symptoms, compassion, affect and cognitive processes associated with emotion in relation to recovery.
-
To explore the relationship between core schema and the experience of psychosis.
*As this is a pilot study and not a definite trial, estimates of the impact of treatment will be explored so that effect sizes can guide subject numbers required to carry out a subsequent study of effectiveness.
Method
Participants
Participants will meet the following inclusion criteria:
-
ICD-10 diagnosis of schizophrenia, schizophreniform disorder, schizoaffective disorder, delusional disorder or psychotic disorder (not otherwise specified).
-
Receiving mental health services in North West NHS trust of (insert 5 names).
-
Able to give informed consent.
Potential participants will be excluded if they have a primary organic disorder.
Participants who do not speak/read English will be excluded as the assessment measures, interview schedules and Recovery Guide are in English and we do not have the means to translate these.
Participants experiencing an acute exacerbation of symptoms requiring inpatient or other changes to treatment are unable to take part in the study.
Recruitment
Recruitment will take place in 4 mental health trusts and through voluntary groups within the North West of England. Within the mental health trusts, care coordinators, responsible medical officers, etc. will be provided with information about the study by the research team and will be asked to share this with potential participants. In addition, information providing sessions will be provided by the research teams to recruitment sites. If participants wish to be approached to receive more information about the research, a risk assessment will be carried out with the Care Coordinator. This assessment will then inform the best way to approach participants. They will then be approached and provided with information about the study. They will be given 24 hours to consider the information and, if they wish to proceed will be asked to sign a consent form. Once the participant has given consent, the Research Assistants will carry out an initial screen to ensure that the participant meets inclusion criteria. Participants meeting criteria will then be assessed using the battery of measures listed below. Participants will be recruited from voluntary groups using a similar procedure. Voluntary group organisations will be approached to publicise the research to their members and the project team will conduct information providing sessions. Interested members will be asked whether they would be willing to allow the research team to liaise with their Mental Health Care Coordinator (or clinical team). If yes, the Care coordinator will be approached to ensure that there is continuity between the Research Team and Clinical Services and to allow the appropriate risk assessment to be carried out. These participants will then be approached in the manner described above.
Measures
Primary outcome
Recovery: The Questionnaire Promoting Recovery from Psychosis (QPR; Neill et al. , 2009) and Service User Experience of Psychosis Scale (SEPS; Haddock et al. , 2009). Two self-report measures assessing different aspects of the impact of psychosis.
Secondary outcomes
-
Symptoms of psychosis
-
Positive and Negative Syndrome Schedule (positive and negative scales only; PANSS; Kay et al. , 1989),
-
Psychotic Symptom Rating Scales (PSYRATS; Haddock et al. , 1999) and recordings of symptom content. These are semistructured interviews aimed at eliciting and describing participants’ experience of psychosis
-
Calgary Depression Scale (Addington and Addington, 2001). This is a semistructured interview aimed at eliciting and describing participants’ experience of depression
-
-
The substance use section of The Opiate Treatment Index (OTI) (Darke et al. , 1992). This is a measure of substance use severity and is in the form of a structured interview that lasts approximately 5–10 minutes.
-
Questions relating to contact with services:
-
When was your first contact with mental health services?
-
When was your first contact with mental health services for reasons to do with psychosis?
-
-
Emotion and emotional processes (all self-report questionnaires)
-
Beck Anxiety Inventory (BAI; Beck et al. , 1988)
-
Positive Facets Scale (WHO-QOL; WHOQOL Group, 1998)
-
Metacognition in emotion scales (comprising scales of rumination worry, etc.)
-
-
Self-beliefs: Brief Core Schema Scales (ref) and the LeCompte Self-Esteem Scale (LeCompte et al. , 2006). These are self-report questionnaires.
-
Compassion scale (Neff, 2003b)
-
Personal and Social performance Scale (PSP; Morosini et al. , 2000)
-
Demographic questionnaire
-
Types of positive affect scale (Gilbert 2008).
It is anticipated that the interview based assessments will take approximately 40–45 minutes, and the questionnaires will take approximately 30 minutes to complete. All measures (1 to 6) will be administered at baseline, 9 and 15 months by an RA blind to treatment condition. In order to ensure that participants are comfortable in completing the interviews and assessments, they will be given the option of completing them over more than one session. In addition, the general scale of the PANSS will not be administered reducing the interview time for completing the symptom assessments to approximately 40 minutes rather than 1.5 hours.
Other measures
In addition, in order to assess therapeutic alliance, preference for psychological treatment and gain feedback on the experience of taking part, participants will also be asked to complete:
-
Interview about preference for psychological treatment (PPT). These interviews will be used to explain the options for psychological treatment and to facilitate the service user making an informed choice about what treatment they would prefer.
-
Working Alliance Inventory a self-report questionnaire of the therapeutic alliance completed by service users and their therapists.
-
Qualitative assessments of the experience of using the Self-Help Recovery Guide with Service Users and Care Coordinators.
The WAI and PPT scales will be administered by a therapist or Service User Researcher, trial manager or another worker allied to the trial who is not blind to treatment group, at a separate time to the other assessments. The PPT will be administered at baseline only and the WAI will be administered at session 3 and session 12 (where appropriate). Qualitative interviews will be carried out following the end of therapy by Service User Researchers. This aspect of the project will be guided by topic guides developed and used in piloting of the guide and by thematic analysis approaches (e.g. Braun and Clarke, 2006).
Procedure
Following recruitment, all participants will complete the above assessments (apart from the PPT and WAI scales) with an independent Research Assistant who will remain blind to treatment received. Participants will then complete the PPT scales with a therapist, service user researcher or trial manager. These scales will determine the preference they have for the type of psychological therapy they wish to receive. Once completed, if participants wish to participate in therapy they will be allocated a CBT therapist who will make initial contact to commence therapy (either low or high support; see below for details). Therapy will take place over 9 months and will consist of up to 30 sessions approximately once per week. Participants will then be followed up at 9 and 15 months by the RA blind to treatment condition and assessed using the measures described above (apart from PPT and WAI scales). Qualitative interviews will take place (n = 6–10 participants per treatment arm and 8–10 Care Coordinators) after therapy is completed. In addition, interviews with up to 8 participants form the different treatment arms and geographical locations will be conducted prior to therapy period commencement. Data will be stored on NHS or university premises in locked cabinets. All participants will be allocated a code number and records will be anonymised.
Therapy
Clients who choose to receive therapy will have the opportunity to choose whether they receive high or low support therapy.
-
Low support: this therapy will be delivered over 9 months and will consist of the following
-
Receive a copy of the Self-Help Recovery Guide (Barrowclough et al. , 2009). This guide is a comprehensive self-help guide to recovery designed and written with clinicians and service users. It has been piloted in earlier work and has been shown to be acceptable and feasible for service users to use with some support.
-
Support for the guide will be delivered in up to 30 weekly sessions provided by a cognitive–behaviour therapist who will facilitate the participant to use the guide during telephone sessions. The CBT therapist will telephone the participant on a number of their choice and will provide help and guidance in sessions lasting approximately 45 minutes.
-
-
High support: this therapy will also be delivered over 9 months. It will consist of all the components of low support i.e. participants will receive:
-
A copy of the Self-Help Recovery Guide
-
Up to 30 telephone sessions with a CBT therapist.
-
However, in addition, participants will also receive additional support in the form of group sessions. These will be co-facilitated by CBT therapists and Service user researchers and will run approximately fortnightly over the 9 month period (approximately 15 sessions). The groups will provide additional guidance and support in the use of the Recovery Guide and will allow participants to meet other Service Users who are using the guide. The group sessions will consist of a mixture of information provision, discussion of topics in the guide and peer support.
Data and statistical analysis
All analyses will be carried out under the direction of Professor Graham Dunn from the Biomedical and Statistics Unit of the University of Manchester. Participants will be randomised to psychological treatment using remote randomisation by telephone administered by the Christie Hospitals Trials Unit using a randomised permuted blocks procedure. In relation to sample size, a trial of size 120 (80 in the intervention group and 40 controls) will have a power of about 85% to detect a true standardised effect size of 0.60, using an independent groups t-test with two-sided significance level of 0.05. Feasibility, acceptability and retention will be estimated by proportions of total sample with 95% confidence intervals. Impact of the interventions will be assessed using an analysis of co-variance allowing for co-variates that would have a potential confounding effect on treatment outcome when people choose their treatment of choice.
Appendix 5 Protocol for Chapter 6 studies
COGNITIVE–BEHAVIOURAL SUICIDE PREVENTION FOR PSYCHOSIS (CBSPP), 24/04/2015, VERSION 3 PROTOCOL
Background
Psychotic disorders often cause extreme distress to patients and carers, are often associated with life long disability and a high risk of suicide, and are associated with substantial costs to individuals, health and social care services and the nation. The heightened risk for completed suicide in people with a diagnosis of schizophrenia has been well documented (e.g. Caldwell and Gottesman, 1990; 1992; Harris and Barraclough, 1997; Heila, Isometsa, Henriksson et al. , 1997). Estimates indicate that between nearly 5 and 10 patients in every 100 will kill themselves (Caldwell and Gottesman, 1990; Palmer, Pankratz, and Bostwick 2005). These estimates vary depending on the methodology, either proportional mortality (the percentage of the dead who died by suicide: approximately 10%) or case fatality (the percentage of the original sample who died by suicide: approximately 4%), used for the estimation of life time risk (Palmer et al. , 2005). Suicidal ideation and suicide attempts are common with as many as half of all patients with schizophrenia experiencing suicidal ideation at any point in time or having a history of attempts (Fenton, 2000; Fenton McGlashan, Victor and Blyler 1997; Harkavy-Friedman et al. , 2003; Kontaxakis et al. , 2004; Nieto, Vieta, Gasto, Vallejo and Cirera, 1992; Tarrier, Barrowclough, Andrews and Gregg, 2004; Tarrier, Khan, Carter and Picken, 2007a). It has been argued that suicidal ideation and planning are important steps that lead to an attempt of self-harm that may lead to death (Kontaxakis et al. , 2004) with previous unsuccessful suicide attempts increasing the risk for later successful suicide (Hawton, Sutton, Haw, Sinclair, and Deeks, 2005).
A body of literature has identified a number of socio-demographic and clinical factors which are predictive of increased suicide risk in the general population and which also apply to schizophrenia. These include being male, of younger age, being socially isolated, misusing substances, being depressed and/or hopeless, having previously attempted suicide, and having a family history of suicide (Caldwell and Gottesman, 1990; De Hert and Peuskens, 2000; Hawton, et al. , 2005; Joiner and Rudd, 2000; Pinikahana, 2003; Sher, 2006; Sinclair, Mullee, King, and Baldwin, 2004; Tandon and Jibson, 2003; Tremeau, 2005; Verdoux, et al. , 1999; Tarrier et al. , 2006). Being within 5-10 years of diagnosis and with an illness course characterised by multiple relapses, deterioration or repeated brief hospitalisations, low adherence to treatment and less than an optimal duration of hospitalisation also contribute to suicide risk (Hawton et al. , 2005; Herings and Erkins, 2003; Kuo, Tsai, Lo, Wang, and Chen, 2005; Potkin et al. , 2003; Qin and Nordentoft, 2005). Although descriptively useful, focusing on these types of clinical and demographic risk profiles is problematic for two reasons. First, from a clinical perspective, it offers limited assistance during assessment because the risk factors are common and identify a relatively large group of people (e.g. Drake and Cotton, 1986; Westermayer, Harrow and Marengo, 1991; Young, Neuchterlein, Mintz et al. , 1998). Second, the approach is atheoretical (Bolton, Gooding, Kapur, Barrowclough and Tarrier, 2007). Even though researchers have identified psychologically relevant variables, and have offered post-hoc interpretations invoking psychological factors (e.g. Hawton et al. , 2005; Joiner, Brown and Wingate, 2005), there have been few well-articulated and empirically tested models or approaches to explaining suicidal behaviour in schizophrenia. Similar criticisms have also been levelled at suicide research in general (see O'Connor and Sheehy, 2001).
Numerous studies have shown that psychotic symptoms are influenced by understandable psychological processes that can sometimes be changed by psychological treatments such as cognitive–behaviour therapy (CBT) (Tarrier and Wykes, 2004; Wykes et al. , 2008). Studies of patients’ own experiences show that recovery must be conceived of in much broader terms than symptom remission; recovery is an ongoing process, in which building a positive sense of self, learning how to pursue a meaningful life and maintaining hopefulness may be the most important components. There is evidence that the absence of hope is a major factor determining patients’ decisions to commit suicide. The aim of this project is to evaluate a suicide prevention intervention (Cognitive–Behavioural Suicide Prevention for Psychosis; CBSPp) developed from our on-going research to understand the cognitive architecture of suicide behaviour in patients suffering a psychosis.
This research is part of an NHS (NIHR) funded programme grant (RECOVERY) the aim of which is to conduct a series of linked investigations, including small-scale randomized trials, to: (a) develop a meaningful and patient-centred measure of recovery; (b) study psychological processes that impeded or assist the process of recovery in different domains; (c) investigate the causes of patient suicide and identify methods of preventing suicide; (d) evaluate individual, group and self-help psychological interventions to maximise recovery in patients with schizophrenia; and (e) assess the extent to which our research and treatment findings from schizophrenia patients can be applied to patients with bipolar disorder, who have been less often studied. The research programme will culminate in recommendations for more effective and patient-centred assessment and treatment strategies. We have an excellent track record in conducting research which has been directly translated into improvements in NHS service provision, and this programme will lead to the dissemination of clinical strategies that more effectively promote psychological well-being, bringing substantial benefits to patients, the public and the NHS.
There is very consistent evident from RCTs and systematic reviews that cognitive–behavioural therapy for psychosis (CBTp) results in significant clinical benefits of reduced psychotic symptoms, reduced depression and anxiety and improved functioning (Wykes et al. , 2008). Meta-analysis indicates that generic CBTp does not improve hopelessness (Wykes et al. , 2008) and although a large multicentred trial of CBTp with acutely ill patients indicated a reduction of suicide behaviour in the long term this result was not significant. We propose, that notwithstanding the clinical benefits of CBTp, it is necessary to modify and refine a CBT intervention to reduce and prevent suicide behaviour, and that this intervention should be based upon a theoretical understanding of the psychological mechanisms underlying suicide behaviour. Suicide is not a random event it happens for a reason and we have moved some way in understanding the reasons underlying suicide behaviour in psychotic patients.
Williams has produced a theoretical model of suicide, the Cry of Pain model, which describes the psychological conditions under which suicide is likely to occur and possible intervention strategies. Tarrier and colleagues have applied this model to psychotic patients) and elaborated upon the psychological architecture specific to psychosis including the appraisal of situation (including psychotic experiences and symptoms), self and future (Bolton et al. , 2007; Johnson, Gooding and Tarrier et al. , 2008). We suggested a modification to the Cry of Pain which replaces concepts of defeat, entrapment and lack of rescue with a four stage appraisal process in conjunction with information processing biases and suicidal schema. Thus there are three important elements within the explanation of suicide behaviour in our model, The Schematic Appraisal Model of Suicide (SAMS): 1) biases in information processing; 2) appraisal; and 3) suicide schema. Our experimental research so far (Ethics applications; 08/H1012/21, 08/H1012/39, and 08/H1012/22) has supported the SAMS model (Tarrier et al. , 2007 a; b; Johnson, Tarrier and Gooding, 2008). Thus, significant advances have been made in this theoretical understanding so that a series of confirmatory studies are required to formalise the targeting of a specific psychological architecture that increases risk of suicide.
Our preventative intervention is based on our theoretical model and on the favourable results of our systematic review and meta-analysis of CBT approaches to suicide prevention across all disorders and patient groups (Tarrier, Taylor and Gooding, 2008).
Our programme of intervention evaluation follows MRC guidelines on the evaluation of complex interventions: The phases distinguished were; 1) pre-clinical or theoretical, 2) phase 1 or modelling, 3) phase 2 or exploratory trial, 4) phase 3 or main or definitive RCT, 5) phase 4 or long term implementation (MRC, 2000). We have progressed through phases 1 and 2 and now intend to carry out a phase 2 or exploratory trial.
Based upon our explanatory model of suicide behaviour in psychotic patients the CBSPp intervention will consist of three phases to each address and change the three aspects of the model. These are: 1) methods to change information processing biases; 2) methods to change appraisals; and, 3) methods to change suicide schema. These methods are an amalgam of clinical techniques already used in clinical practice. Treatment will take place over 12 weeks. Patients will be seen twice weekly. In addition to this trial, participants will also be recruited to test one particular aspect of the intervention in a brief, additional and optional session. This session will test the Broadminded Affective Coping (BMAC) procedure, which involves the recall of a positive memory. This is usually incorporated into therapy, but this session will aim to examine the effectiveness of the procedure when it is in isolation. Participants who have had previous suicide attempts, will also be invited to take part in a qualitative interview exploring the key themes associated with peoples personal accounts of their experience of suicidal behaviour. The aim of the qualitative interview is to explore whether individuals’ own descriptions of their experiences are in line with the suggested cognitive architecture of suicide behaviour in psychosis, and also to investigate whether any additional themes emerge.
A treatment manual has been produced with feedback from the service user consultant involved in the RECOVERY project (Tarrier and Gooding, 2008). Initial application with service users indicates that the treatment is feasible and both acceptable to, and welcomed by, service users.
Participants
50 participants will need to be recruited into the trial to allow for 25 to be allocated to each treatment group, allowing for drop outs we intend to recruit 60 patients. 60 participants will also be recruited into the session which tests the BMAC procedure. Taking part in this session is not mandatory or exemptive for being part of the trial. 8-10 participants who have had previous suicide attempts will also be recruited into the qualitative interview. Taking part in this interview is not mandatory or exemptive for being part of the trial. Participants will be identified through their care co-ordinators. They will be included if they have: 1) a DSM IV diagnosis of schizophrenia, schizophreniform disorder, schizoaffective disorder, delusional disorder or psychotic disorder not otherwise specified (NOS); 2) have had previous suicide attempts or current suicidal ideation; 3) are not currently acutely suicidal or considered a danger to themselves or others; 4) are receiving appropriate anti-psychotic medication; 5) are under the care of an appropriate clinical team and have contact with mental health service.
Methodology
The 12-week trial
Design
The 12 week trial will be an exploratory randomised controlled trial to test the feasibility and assess the potential efficacy of a suicide prevention programme(CBSPp) with patients suffering from schizophrenia and schizophrenia-spectrum disorders. The comparison will be between patients receiving CBSPp in addition to treatment as usual (TAU) and TAU alone.
The primary outcome measures will be an assessment of suicide behaviour (Beck Scale for Suicidal Ideation (BSS) and The Suicide Probability Scale (SPS) and hopelessness (Beck Hopelessness Scale, BHS) at the end of the intervention and at follow-up. Secondary outcomes will be of psychotic symptoms, social adjustment, self-esteem and recovery measures.
Measures
Core recovery measures of the RECOVERY Programme
-
Questionnaire about the process of Recovery (QPR) (Neil, S.T; 2007 Unpublished Doctoral Thesis Submitted to The University of Liverpool. Publication in process)
-
Self-Esteem rating Scale (SERS) (LeCompte et al. , 2006)
-
Beck Hopelessness Scale (BHS) (Beck, 1987)
-
Calgary Depression Scale for Schizophrenia; Addington et al. , 1990)
-
The Subjective Experiences of Psychotic Symptoms Scale (SEPSS).
Core symptom measures
-
Positive and Negative Symptom Scale (PANSS; Kay et al. , 1989) to assess severity of symptoms
-
PSYRATS (Haddock et al. , 1999) to assess control over symptoms
-
Global assessment of functioning (DSM IV, 1994) to assess overall functioning
-
Beck Anxiety Inventory (BAI; Beck et al. , 1988).
Suicide Behaviour
-
Beck Scale for Suicidal Ideation (BSS; Beck, Kovacs and Weissman, 1979)
-
Suicide Probability Scale (SPS; Cull and Gill, 1988)
-
Adult Suicidal Ideation Questionnaire (ASIQ; Reynolds, 1991b).
Patient notes will be examined at recruitment, 3 and 6 months to assess for suicide attempts, serious incidents and clinical deterioration.
Patients who are receiving the intervention will also be interviewed using a cognitive–behavioural formulation (standard clinical practice) regarding the determinants of suicide behaviour. In addition those patients who have received the intervention will be asked to give feedback on their experience of the intervention and comment on its helpfulness, benefit or otherwise.
Procedure
Patients will be identified through their care co-ordinator and approached by a research assistant to explain the study and obtain informed consent. Once consented patients will be assessed with the measures described above and then they will be randomised to one of two groups, the experimental; treatment or control group by an independent trials unit. Those allocated to the experimental treatment will receive CBSPp as described in the manual in addition to treatment as usual (TAU). The control group will receive TAU alone. All patients will be re-assessed at 3 months and at 6 months. All patients will be included in the analyses as randomised.
BMAC session
Design
Participants will be randomly allocated to taking part in either the BMAC or a control task. The primary outcome measure will be positive and negative effect experienced following the task, 2 hours later, and 2 days later.
Measures of mood
-
Positive and Negative Affect Scales (PANAS; Watson, Clark and Tellegen, 1988)
-
Visual Analogue Scales of six mood states (happiness; sadness; defeat; frustration; energy; calmness).
Tasks
-
BMAC: This procedure involves the assisted recall and re-experiencing of a past positive memory. That is, participants are asked to remember a positive past experience, then are guided through the recall of images, sensations and emotions associated with the memory. The procedure begins with some relaxation exercises and ends with a debriefing session, and altogether should take around 20-30 minutes. More detailed instructions can be found in a forthcoming paper by Tarrier (in submission).
-
Control task: This will require participants to recall a positive memory and write about this.
Procedure
Participants will be recruited in the same manner as for the controlled trial, and can take part in this session in addition to the trial if they choose.
At the beginning of the session participants will be asked to read a separate participant information sheet and to complete a separate consent form (attached). At the beginning of the session, participants will first be asked to complete measures of mood. Following this they will either take part in the BMAC procedure, or a control task. The control task requests participants to recall a past positive memory and write it down. All participants will then complete the same measures of mood again. 2 hours later, participants will be re-contacted by phone and asked to complete the measures of mood a third time. Finally, two days later, participants will be re-contacted by phone and asked to complete measures of mood a fourth time.
Qualitative interview
Procedure
Participants will be recruited in the same manner as for the controlled trial, and those participants who have had a previous suicide attempt can take part in this interview in addition to the trial if they choose.
The recommended approach for IPA is to employ a semistructured interview, which in this case will focus on individual’s experience of suicidal behaviour. The project service user reference group will be consulted to ensure the relevance and appropriateness of target questions in the semistructured interview. All interviews will be tape recorded and transcribed verbatim. Each transcript will be read and subjected to content analysis to identify themes. Emerging themes from each report will be discussed with the research team to ensure agreement.
Potential risks
There is concern that for those suffering a mental disorder and especially psychosis that taking part in research is a burden and may have aversive consequences detrimental to their health. Jorm, Kelly and Morgan (2007) carried out a systematic review of 46 studies which examined distress following participation in research. They examined studies of both non-patient and patient populations that involved the assessment of psychiatric state or associated risk factors. They found that a minority of participants became distressed immediately after participation, with distress more likely in studies of traumatic experiences. There was little indication of adverse long-term impact. Positive reactions to participation were more common than negative reactions, and participants who reported distress may also have a positive evaluation of the research. There was little evidence of a causal role of participation leading to persistent distress, including research on suicidality. In a study of adult participants suffering severe mental illness (Boothroyd, 2000), almost all (96%) reported positive experience. Negative experiences were also reported in the form of anxiety (9%), fear of disclosure (17%) and regarding questions as invasive (17%). From the available evidence it is possible to conclude that the vast majority of participants rate the experience as positive although some experience emotional distress and have some concerns regarding the process, this is largely mild and short lived.
Maintenance of confidentiality and data storage
The responses given in the experiment will be coded by participant number and not by any form of personal identity. Only age and gender will be collected. Participant responses are therefore entirely confidential as they will not be associated with personal identity information.
Appendix 6 Protocol for Chapter 7 studies
AN EXPLORATORY RANDOMISED CONTROLLED TRIAL OF A COGNITIVE–BEHAVIOURAL THERAPY-BASED RECOVERY INTERVENTION FOR EARLY BIPOLAR DISORDER. VERSION 6, 23/10/2012
A trial of a recovery intervention for early Bipolar Disorder – Lead Steven Jones Protocol
Background
Recently the National Institute for Clinical Excellence Bipolar Guideline recommended that individual structured psychological treatment is offered to individuals with a diagnosis of bipolar disorder. 379 Their review of the evidence concluded that psychological interventions (primarily cognitive–behavioural therapy (CBT)) which included psychoeducation, stabilisation of social rhythms, detecting and coping with early signs of an affective episode, and enhancement of general coping skills are associated with reductions in relapse risk in individuals with a diagnosis of bipolar disorder. To date all published studies of structured psychological therapy have focused on individuals with a chronic bipolar disorder. For example, participants in the Lam, Watkins, Hayward, et al. (2003) study had experienced a mean of 5.8 depressive and 5.5 manic episodes. Indeed, it might appear logical that an intervention requiring significant therapist time is best reserved for individuals with an established illness course. However the most recent study of CBT for relapse prevention in bipolar disorder found that there was a significant interaction between number of episodes and outcome, with only those with fewer episodes benefiting significantly. 43 This finding would also be consistent with recent psychological models of bipolar disorder which have proposed that associative mechanisms build up over repeated mood episodes such that later episodes are both readily triggered by psychosocial circumstances previously linked to mood changes and are also less likely to be mediated by cognitive processes (Barnard, 2004; Jones, 2001, Jones, Mansell and Waller, 2005). This suggests that cognitive–behavioural interventions may be more powerful when applied earlier in the illness course before strong associative links to bipolar emotional states are established. Nevertheless, to date no cognitive–behaviour therapy interventions have been specifically designed for delivery to individuals early in their illness course. Our group has therefore devised an adapted CBT intervention for individuals after first diagnosis of bipolar disorder. This has proved to be acceptable and feasible in a single case series of 7 bipolar participants (Jones and Burrell-Hodgson, 2008). Substantial reductions in subsyndromal symptoms were observed during intervention and six month follow-up along with changes in appraisal styles and stability of sleep/wake cycles. This suggests that psychological intervention for individuals early in their course of bipolar disorder is both effective and acceptable to service users. A key feature of this project will therefore be to further develop this cognitive–behavioural approach for individuals early in their course of bipolar disorder.
The recovery literature in mental health research increasingly shows that individual definitions of recovery are diverse and rarely focus solely on the eradication of symptoms. Two mental health professionals with personal experience of bipolar disorder380 proposed the following as key facets of a recovery scenario for bipolar disorder: hope for the future, taking personal responsibility for health, education and learning, self-advocacy for personally relevant support and mutual social and peer support. A qualitative analysis of the experience of recovery in the early stages of bipolar disorder carried out by our group during phase 1 of the study (REC reference number: 08/H1013/77) found similar themes which included; making sense of self and symptoms, the centrality of the self in recovery: changing self-efficacy, and consolidating the self in recovery through personally meaningful activity. Therefore, a second feature of the project will be to incorporate into the intervention, the key recovery principles found in our group’s qualitative analysis of recovery.
It is also important that we have appropriate tools for the assessment of recovery relevant outcomes in individuals with bipolar disorder so that new interventions and routine service outcomes can be assessed with respect to factors which are valued by individual service users. The recovery themes found in phase 1 of the study have been used to inform the development of an assessment tool to measure recovery, the Bipolar Recovery Questionnaire (BRQ), which aims to assess aspects of recovery that are important and meaningful to service users. The BRQ has been found to be an acceptable tool for service users, and has been shown to be a reliable and valid measure. Therefore, in order to ensure that outcomes in the trial are assessed with respect to aspects of recovery that are valued by service users, the BRQ will constitute one of the primary outcome measures of the trial.
Participants
Participants will be identified from care co-ordinators and psychiatrists in mental health services, from GP’s in primary care sites, and also from voluntary sectors.
Participants will have either; received a clinical diagnosis of bipolar disorder within the last 5 years or meet DSM criteria for first episode mania within the last 5 years, or hypomania (with a previous episode of major depression) within the last 5 years (confirmed by SCID interview. 305 Individuals who are current inpatients will not be recruited into the trial until they are discharged to the community. All participants will enter the trial when neither acutely depressed nor manic. However, on the basis of previous longitudinal research it is expected that significant levels of subsyndromal symptoms will be present.
Trial design and outcomes
A rater blind randomised controlled trial is proposed. As this is an exploratory trial we wish to determine effect sizes for the primary and secondary outcome measures to inform the development of a definitive study. Primary outcomes are time to bipolar relapse and self-reported recovery score. Secondary outcomes are levels of affective and psychotic symptoms, level of functioning, levels depressive and hypomanic appraisal style, levels of hope, stigma and self-esteem, changes in medication adherence, and levels of self-compassion and positive affect.
Individual recovery-focused CBT intervention
The intervention has been developed through collaboration between a multidisciplinary group of mental health professionals and service users with experience of bipolar disorder. Focus groups have taken place with individuals who took part in the first phase of the project (the qualitative analysis of recovery themes) to ensure that the intervention is appropriate and acceptable to individuals early in the course of bipolar disorder. Furthermore, a service user consultation group have also been consulted on the development of the intervention (as well as the design of the study as a whole).
The elements of the intervention have been informed by 3 sources:
-
Current evidence for components of effective CBT interventions which include mood monitoring and awareness, regularisation of routines, enhancing prodromal coping and problem-solving training. 381
-
Our case series study of first diagnosis bipolar clients, which indicates the importance of maintaining a very flexible engagement approach, allowing time for full consideration of meaning of diagnosis to the client, engaging in coping skills reviews around subsyndromal exacerbations as well as prior episodes and considering the role of appraisals of fluctuations in affect.
-
The recovery relevant elements found in phase 1 and agreed by the multidisciplinary group which include making sense of self and symptoms, changing self-efficacy, and consolidating the self in recovery through personally meaningful activity.
The intervention will be delivered by mental health professionals trained to BABCP accreditation level in CBT. Therapy will consist of up to 18 sessions delivered over a period of approximately six months and delivered either at client’s homes or mental health facilities according to client preference. Initial session will be weekly, with later sessions fortnightly. Sessions will be typically 45–60 minutes long. The competency of the therapist will be assessed using two therapist fidelity measures.
Therapist fidelity measures
-
The Cognitive Therapy Scale – Revised (CTS-R; Blackburn, James, Milne, Baker, Standart, Garland and Reichelt, 2001) is a measure of therapist adherence to cognitive therapy. It covers many areas of therapist competence, including agenda setting and adherence, feedback, collaboration, pacing and efficient use of time, interpersonal effectiveness, eliciting of appropriate emotional expression, eliciting key cognitions, eliciting and planning behaviours, guided discovery, conceptual integration, application of change methods and homework setting. Each of these performance areas are rated on a 7 point Likert scale ranging from 0–6, 0 indicating minimal adherence, and 7 indicating maximum adherence and skill. Therapy sessions will be audio-taped and reviewed by the principal investigator or a suitably qualified member of the research team. The CTS-R has received good psychometric support (Blackburn et al. , 2001).
-
The Working Alliance Inventory – Short Form (WAI-S) (Tracey and Kokotovic, 1989) is a 12 item questionnaire that measures the strength of the therapeutic alliance between both therapist and client, on a 7 point Likert scale ranging from 1 (never) to 7 (always). The WAI-S measures 3 dimensions of alliance, namely, bond, goals, and tasks. Two versions of the WAI-S will be used; one specific for the client, and one for the therapist, both of which will be administered twice across the 18 therapy sessions. All clients will be given the choice of whether to complete the questionnaire immediately or outside the therapy session. They will similarly be provided with an addressed and sealed envelope (to ensure confidentiality) and have the choice of whether to return this to the therapist, or send this by post to the principal investigator. The WAI-S has received psychometric support, has good overall internal consistency (α=.94), and good internal consistency for each dimension of alliance, including bond (α=.84), goals (α=.88) and tasks (α=.90) (Tracey and Kokotovic, 1989).
Schedule of assessments
Follow-up will period will be 15 months from initial randomisation for the majority of participants (a small minority will only receive a 12 month follow up period due to restrictions in project timescales). In addition to regular (3 monthly) assessments to evaluate bipolar relapse, assessment of recovery, bipolar symptoms and functioning will also be conducted at inception, end of treatment and follow-up (6 and 12 months).
Measurement of primary outcomes
-
Time to bipolar relapse: measured using analysis of DSM-IV episodes (mania, hypomania, mixed affective episode or major depression) defined according to DSM criteria using SCID-LIFE assessed every 3 months from baseline,328 an approach which our group have already successfully employed to evaluate primary outcome in the recent MRC trial of CBT for chronic and severe bipolar disorder. 43
-
Self-reported recovery score will be assessed using the Bipolar Recovery Questionnaire developed in phase 2 of the same project (REC ref: 08/H1013/77), administered at inception and then every six months until the end of the study period.
Measurement of secondary outcomes
Self-report and observer rated assessments of bipolar symptomatology, functioning and of cognitions associated with bipolar disorder, applied at inception and then six monthly to the end of follow-up, namely:
-
Beck Depression Inventory (Second Edition), (BDI-II) – The BDI-II382 (is a 21 item self-report inventory that assesses for symptoms of depression. Total score cut offs are: 0–9 (normal/minimal depression), 10–18 (mild depression), 19–26 (moderate depression), and > 26 (severe depression).
-
Internal States Scale (ISS) – This is a 15 item self-report questionnaire that assesses for symptoms of mania and depression. It comprises four subscales, these being activation (ISS-ACT), perceived conflict (ISS-PC), well-being (ISS-WB) and depression (ISS-DEP). Each statement is rated based on how the individual has felt in the past 24 hours. A cut off score of 200 on activation scale has been validated as indicative of the presence of (hypo)mania. 303
-
Hamilton depression rating scale(HRDS) – The HDRS314 is another observer rated measure based on clinical observation that assesses for seventeen symptoms of depression. Total HDRS score is categorised as follows: < 10 (no depression), 10–13 (mild depression), 14–17 (mild to moderate depression) and > 17 (moderate to severe depression).
-
MAS – The MAS312 is an observer rated measure that assesses for eleven symptoms of mania or hypomania based on observations during clinical interview. The total MAS score is categorised as follows: 0–5 (no mania), 6–9 (hypomania), 10–14 (probable mania) and > 15 (definite mania).
-
Personal and Social Performance Scale (PSP). The PSP is an observer-rated measure of severity of personal and social dysfunction which assesses functioning in four main areas: 1) socially useful activities; 2) personal and social relationships; 3) self-care; and 4) disturbing and aggressive behaviours. Operational criteria to rate the levels of disabilities are defined for. Good inter-rater reliability has been reported (Morosini et al. , 2000).
-
Hypomanic Interpretations Questionnaire (HIQ). The HIQ (Jones, Mansell and Waller, 2006) is a 10 item self-report questionnaire which evaluates appraisals for 10 common hypomania-relevant experiences each followed by two explanations; (1) positive self-dispositional appraisals (HIQ-H) and (2) normalising appraisal (HIQ-NE). Participants also indicated using a yes/no scale whether they had experienced each situation in the preceding three months. The HIQ has been found to have good internal reliability; HIQ-H α=0.87 and HIQ-NE α=0.76 (Jones, Mansell and Waller, 2006).
-
Interpretation of Depression Questionnaire (IDQ). The IDQ (Jones and Day, 2008) is a 10 item self-report questionnaire analogous in structure to the HIQ, which evaluates appraisals of depression-relevant situations each followed by two explanation; (1) negative self-dispositional (IDQ-D); and (2) normalising appraisals (IDQ-N). Participants complete a yes/no scale indicating whether they had experienced each situation in the preceding three months.
-
The Brief Quality of Life in Bipolar Disorder (QoL.BD; Michalak and Murray, in press) is a 12 item disorder-specific quality of life measure in Bipolar Disorder. Each item is rated on a 5 point Likert scale (1= strongly disagree, 5= strongly agree). Initial field testing of the Quality of Life in Bipolar Disorder supports use of the instrument as a feasible, reliable and valid disorder-specific QoL measure for BD (Michalak and Murray, in press).
-
Post Traumatic Growth Inventory (PTGI). The PTGS (Tedeschi and Calhoun, 1996) is a 21-item self-report measure of positive outcomes following traumatic experiences. Each item is rated on a 6-point Likert format scale (0 = “I did not experience this change as a result of my crisis” 5 = “I experienced this change to a very great degree as a result of my crisis”). The total score can range from 0–105, with higher scores indicating greater growth. Five subscales can also be scored: (a) Relating to Others, (b) New Possibilities, (c) Personal Strength, (d) Spiritual Change, and (e) Appreciation of Life. The psychometric properties of the PTGI have been found to be adequate; Relating to Others α= .89, New Possibilities α= ,89, Personal Strength α= .84, Spiritual Change α= .65, Appreciation of Life α= .89. (Jaarsma, Pool, Sanderman and Ranchor, 2006).
-
Self-Esteem Rating Scale- Short Form (SERS; Lecomte et al 2006) is a measure of explicit self-esteem comprising 20 Likert-based items: 10 positive statements about the self that provide a measure of positive self-esteem; and 10 negative statements about the self that provide a measure of negative self-esteem. The SERS has demonstrated good validity, internal consistency, and test–retest reliability in the general population and in those with schizophrenia (Lecomte, Corbiere, and Laisne, 2006).
-
Herth Hope Index (HHI; Herth, 1992) is a 12 item questionnaire that measures feelings of hope on a 4 point Likert scale, ranging from 1 (strongly disagree) to 4 (strongly agree). Participants are instructed to rate each statements in terms of how they are feeling at the present time, resulting in a total hope score ranging from 12-48. Higher scores indicate a greater degree of hope. The HHI has been shown to have good internal consistency (α=.97), validity and good test re-test reliability (r=.91) (Herth, 1992).
-
Self-Esteem and Stigma Questionnaire (SESQ; Hayward, Wong, Bright and Lam, 2002) is a 14-item questionnaire measuring two important constructs in Bipolar disorder; self-esteem (6 items) and stigma (8 items). All items are scored on a 6-point Likert scale ranging from 1 (strongly agree) to 6 (strongly disagree), with lower scores in the self-esteem scale indicating higher confidence and self-esteem, and higher scores in the stigma scale indicating higher feelings of stigmatisation. The psychometric properties for the SESQ have been found to be adequate; for both self-esteem (α=.71) and stigma scales (α=.79) (Hayward et al. , 2002).
-
Stephenson Medication Adherence Interview (SMAI; Stephenson, Rowe, Haynes, Macharia, and Leon, 1993) is a short structured interview that assesses change in medication adherence over the last week, and previous month. The SMAI contains 7 questions overall, assessing current medication, missed medications and medication overuse, and the possible reasons behind such activity. The SMAI has been used in numerous RCTs and is considered a reliable and insightful measure of medication adherence (Scott and Pope, 2002).
-
Self-Compassion Scale (SCS)383 is a validated 26 item measure that assesses how individuals typically act towards themselves in times of difficulty. The SCS is composed of 6 subscales, including self-kindness (5 items), self-judgment (5 items), common humanity (4 items), isolation (4 items), mindfulness (4 items) and over-identification (4 items).Each item is rated on a 5 point Likert scale ranging from 1 (almost never) to 5 (almost always). The SCS has been shown to have good test–retest reliability (r = .90), and discriminant validity with other self-esteem measures (Neff, 2003).
-
The types of Positive Affect Scale (TPAS; Gilbert et al. , 2008) is a validated 18 item measure that assesses the frequency to which people experience positive feelings. The TPAS consists of 3 subscales, including active positive affect (8 items), relaxed positive affect (6), and safe/warmth positive affect (4 items). Respondents are asked to rate 18 positive ‘feeling’ words on a 5 point Likert scale to indicate how characteristic it is of them, ranging from 0 (not characteristic of me) to 4 (very characteristic of me). The scale has proven to have good psychometric properties for all subscales, with Cronbach’s alpha scores ranging from .73-.83 (Gilbert et al. , 2008).
Power
The proposed sample size will permit us to make reasonable estimates of feasibility of patient recruitment and consent to participate, adherence to protocol, retention within both arms across assessment, intervention and follow-up periods and outcome parameter estimates. In addition, we will be able to determine if the intervention is acceptable to service users. Therefore, our outcomes will include information regarding acceptability and feasibility, retention rates in the two arms of the study, and effect size estimates for proposed primary and secondary outcome measures. Professor Dunn, our trialist and statistician, has confirmed that the proposed sample size is suitable for these purposes. The research team will be able to then use this important information to mount a subsequent definitive pragmatic trial soon after programme completion, should the pilot study justify such an application. It would not provide value for money for DH/NHS to conduct a large scale RCT at this stage, since the feasibility data has yet to be collected, and cognitive–behavioural interventions with a first episode bipolar population have not been attempted under research conditions. As this form of intervention is new it is not possible to provide power calculations based on directly relevant previous trials. An indication of possible power for the proposed trial was obtained through calculations informed by the results of the recent studies of CBT for chronic bipolar disorder43,278 and a recent meta-analysis. 384 With 60 patients a two-tailed chi-squared test will have 64% power to detect an absolute difference in twelve-month (post-treatment) relapse rates of 25% (from 40% for TAU to 15% for CBT). We intend to enter 72 into the trial to allow for 20% drop outs.
Analysis plan
All treatment effects will first be estimated using the intention-to-treat principle, supplemented by estimation of the treatment effects in those participants who actually receive the intervention via estimation of the Complier-Average Causal effect. 332,333 Time to relapse will be assessed by survival analysis (using either proportional hazard or accelerated life-time models). Each of the secondary outcome measures will be analysed with analysis of covariance through the use of generalised linear models (the data distribution and link function being dependent upon the outcome under consideration). Adjustments for missing data will be made assuming that the missing data mechanism is either ignorable or latently ignorable. 334
Appendix 7 Q-sort package (see Chapter 2)
Q-sort items

1. How depressed my experiences make me feel.
2. How much I dwell on my experiences.
3. How unpleasant my experiences/voices are.
4. How pleasant my experiences/voices are.
5. How much control I have over my experiences.
6. How often my experiences happen.
7. How much time in my life they take up.
8. Amount to which my voices are inside my head compared to outside my head.
9. How loud my voices are.
10. My belief that my experiences come from my own mind.
11. How positive I view my experiences to be.
12. How much religion/spirituality was involved with my experiences.
13. The amount I think about harming myself as a result of my experiences.
14. How my experience effect how energetic I feel.
15. How helpful I feel my medication is with my experiences.
16. How helpful I feel psychological therapies are with my experiences.
17. How convinced I am that my experiences are real.
18. The amount of support I get from other service users.
19. How my experiences effect the quality/and or amount of sleep I get.
20. How my experiences effect my personal freedoms and rights.
21. How my experiences effect the amount of anger and frustration I feel.
22. How my experiences have effect my memory and concentration.
23. How my experiences effect my ability to look after myself.
24. How active I was in seeking help with my experiences.
25. How well I was able to recognise the early signs of becoming unwell.
26. How my experiences effect how happy I feel.
27. How anxious or stressed I am from my experiences.
28. How withdrawn I am as a result of my experiences.
29. How trusting of others I am as a result of my experiences.
30. How much I socialise as a result of my experiences.
31. How my experiences effect how positive I am for the future.
32. How enjoyable I find hobbies/activities as a result of my experiences.
33. How my experiences effect my relationships with friends and loved ones.
34. How much I understand my experiences.
35. How much support I get from loved ones in helping with my experiences.
36. How empowered I feel over my experiences.
37. How ashamed and/or embarrassed I feel about my experiences.
38. How my experiences effect the amount of emotion I feel.
39. How bothered I am about the stigma/being judged about my experiences.
40. How much I feel mental health services are helpful with my experiences.
41. How my experiences alter my ability to control my own thoughts.
42. How clearly I can think about my experiences.
43. The amount to which I can cope with my experiences.
44. In alcohol and drug use that worsens my experiences.
45. How much I have changed as a person/personality since I have had these experiences.
46. My living arrangements as a result of my experiences.
47. My ability to find work as a result of my experiences.
48. How financially stable I am as a result of my experiences.
49. How concerned I am of the side effects of taking medication for my experiences.
50. How vulnerable I feel as a result of my experiences.
51. How motivated I feel about changing my experiences.
52. How concerned I am that my experiences will happen again.
Appendix 8 The subjective experience of psychosis scale (see Chapter 2)
Appendix 9 Delphi study checklists (see Chapter 3)
Checklist: what helps recovery?
Having a good, safe place to live.
Having the support of others.
Having a good understanding of your mental health problems.
Living in the kind of place you like.
Knowing what helps you get better.
Knowing how to take care of yourself.
Recognising the positive things you have done.
Knowing that there are mental health services that do help.
Working on things that are personally important.
Being strongly motivated to get better.
Being able to identify the early warning signs of becoming unwell.
Having a positive outlook on life.
Having a plan for how to stay or become well.
Having goals/purpose in life.
Accomplishing worthwhile and satisfying things in life.
Being able to develop positive relationships with other people.
Knowing that there are things that you can do that help you deal with unwanted symptoms/experiences.
Being able to handle stress.
Feeling part of society rather than isolated.
Being hopeful about the future.
Learning from mistakes.
Accepting that you may have set backs.
Being able to come to terms with things that have happened in the past and move on with life.
Receiving treatment for distressing/unusual thoughts and feelings.
Taking medication as prescribed.
Having healthy habits.
Having a desire to succeed.
Health professionals and service users working collaboratively as equals.
Knowing that even when you don’t care about yourself, other people do.
Spending time with people to feel connected and better about yourself.
Being able to fully understand mental health problems/experiences.
Having courage.
Allowing personalisation or choice within health services.
Knowing that even when you don’t believe in yourself, other people do.
Knowing that you can handle what happens next in your life.
Knowing that all people with experience of psychosis can strive for recovery.
Being able to make sense of distressing experiences.
Making a valuable contribution to life.
Knowing that recovery from mental health problems is possible no matter what you think may cause them.
When services understand/consider the culture and beliefs of the individual.
Continuing to have new interests.
Knowing that you are the person most responsible for your own improvement.
Being able to assert yourself.
Checklist: what hinders recovery?
When health services do not provide help and support to recover.
When a person feels lost or hopeless for much of the time.
When a person feels isolated or alone even when with family of friends.
When a person feels discriminated against or excluded from the community because of mental health problems.
Health professionals who do not accept that their views are not the only way of looking at things.
The impact of a loved one’s mental health problems on their family.
When a person cannot find the kind of place you want to live in.
When a person deliberately stopping taking medication although the doctor recommends taking it regularly.
Medication that can affect concentration and memory.
When no one will employ the person owing to past mental health problems.
When other people are always making decisions about the person’s life.
Checklist: what shows that someone is recovering?
When the person is able to find time to do the things they enjoy.
When the person is able to ask for help when they need it.
When the person can trust themselves to make good decisions and positive changes in life.
When the person knows when to ask for help.
When the person is able to take control of aspects of their life.
When the person feels reasonably confident that they can manage their mental health problems.
When the person is able to actively engage with life.
When the person feels like they are coping well with mental or emotional problems on a day to day basis.
When symptoms/experiences of psychosis interfere less and less with daily life.
When the person is able to define and work towards achieving a personal goal.
When fear doesn’t stop the person from living the life they want to.
When the person knows a great deal about coping strategies.
When symptoms/experiences of psychosis don’t get in the way of doing things they want or need to do.
When the person finds places and situations in which they can make friends.
When the person feels in touch with their own emotions again.
When the person knows a great deal about their own symptoms/experiences.
When the person knows a great deal about their treatment options.
When the person is able to access independent support.
When coping with mental health problems is no longer the main focus of a person’s life.
When the people who are important to someone are actively supporting their mental health treatment.
When symptoms/experiences of psychosis are a problem for shorter periods of time each time they occur.
Appendix 10 Example page from Experience Sampling Methodology diary (see Chapter 4)
Appendix 11 Sample pages from the self-help recovery guide 9 (see Chapter 5)
Appendix 12 The Bipolar Recovery Questionnaire (see Chapter 7)
Appendix 13 The Questionnaire about the Process of Recovery (used throughout the research programme)
List of abbreviations
- AIC
- Akaike information criterion
- ANOVA
- analysis of variance
- AO
- assertive outreach
- ASIQ
- Adult Suicidal Ideation Questionnaire
- BABCP
- British Association for Behavioural and Cognitive Psychotherapies
- BACS
- Brief Assessment of Cognition in Schizophrenia
- BAI
- Beck Anxiety Inventory
- BD
- bipolar disorder
- BDI
- Beck Depression Inventory
- BDI-II
- Beck Depression Inventory – Second Edition
- BHS
- Beck Hopelessness Scale
- BPRS-E
- Brief Psychiatric Rating Scale Expanded version
- BRQ
- Bipolar Recovery Questionnaire
- BSS
- Beck Suicidal Ideation Scale
- CBSPp
- Cognitive–Behavioural Suicide Prevention in Psychosis
- CBT
- cognitive–behavioural therapy
- CBTP
- cognitive–behavioural therapy for psychosis
- CFA
- confirmatory factor analysis
- CFI
- Cumulative Fit Index
- CI
- confidence interval
- CMHT
- community mental health team
- df
- degrees of freedom
- DMC
- Data Monitoring Committee
- DSM-IV
- Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition
- EFA
- exploratory factor analysis
- EI
- early intervention
- EIS
- early intervention service
- ESM
- experience sampling methodology
- GAF
- Global Assessment of Functioning
- HADS
- Hospital Anxiety and Depression Scale
- HDRS
- Hamilton Rating Scale for Depression
- HIQ
- Hypomanic Interpretations Questionnaire
- ICC
- intraclass correlation
- ICD-10
- International Classification of Diseases, Tenth Edition
- IDQ
- Interpretations of Depression Questionnaire
- IPA
- interpretative phenomenological analysis
- IS
- Insight Scale
- ISS
- Internal States Scale
- ISS-A
- Internal States Scale activation
- ISS-D
- Internal States Scale depression
- ISS-PC
- Internal States Scale perceived conflict
- ISS-W
- Internal States Scale well-being
- MAS
- Bech–Refaelsen Mania Scale
- MAS-M
- Bech–Refaelsen Mania Scale – mood items
- MLCSi
- Multidimensional Locus of Control Scale – internality subscale
- NEET
- not in education, employment or training
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- PANSS
- Positive and Negative Syndrome Scale
- PCA
- principal component analysis
- PPT
- patient preference trial
- PROM
- patient-reported outcome measure
- PRPT
- partially randomised preference trial design
- PSP
- Personal and Social Performance Scale
- PSYRATS
- Psychotic Symptoms Rating Scale
- PTGI
- post-traumatic growth inventory
- QPR
- Questionnaire about the Process of Recovery
- QPRInter
- Questionnaire about the Process of Recovery interpersonal subscale
- QPRIntra
- Questionnaire about the Process of Recovery intrapersonal subscale
- RAS
- Resilience Appraisals Scale
- RCT
- randomised controlled trial
- RecA
- Recovery Analogue Scale
- RfCBT
- recovery-focused cognitive–behavioural therapy
- SAMS
- Schematic Appraisal Model of Suicide
- SCID
- Structured Clinical Interview for DSM-IV Disorders
- SD
- standard deviation
- SE
- standard error
- SEM
- structural equation modelling
- SEPS
- Subjective Experiences of Psychosis Scale
- SERS
- Self-Esteem Rating Scale
- SERS-N
- Self-Esteem Rating Scale, Negative subscale
- SHG
- self-help and group support
- SHT
- self-help and telephone support
- SoCRATES
- Study of Cognitive Reality Alignment Therapy in Early Schizophrenia
- SOP
- standard operating procedure
- SPS
- Suicide Probability Scale
- SPSS
- Statistical Package for the Social Sciences
- SRMR
- standardised root mean-square residual
- STAR-T
- Self-help Therapy and Recovery Trial
- SURG
- service user reference group
- TAU
- treatment as usual
- WAI
- Working Alliance Inventory
- WAI-S
- Working Alliance Inventory – Short Form