Notes
Article history
The research reported in this issue of the journal was funded by PGfAR as project number RP-PG-0407-10044. The contractual start date was in July 2008. The final report began editorial review in June 2015 and was accepted for publication in November 2015. As the funder, the PGfAR programme agreed the research questions and study designs in advance with the investigators. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The PGfAR editors and production house have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the final report document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Pinki Sahota reports a Learning Curve Grant 2011 from Danone Baby Nutrition for infant dietary analysis. Helen Ball reports consultancy work to develop and test a safe infant sleep tool for NHS Lancashire and Blackpool, consultancy work to advise on bedside sleeping promotional materials for Kindred Agency (for NCT Bednest) and a grant from the Economic and Social Research Council (ESRC) for the Infant Sleep Information Source website.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by Wright et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Description of ethnic classification
Born in Bradford is a multiethnic cohort consisting of families from around the world. However, the main ethnic groups are of South Asian origin (Pakistani, Bangladeshi and Indian) and white British origin. The large majority of the South Asian-origin families are of Pakistani origin. Much research into South Asian health and well-being combines what are often very heterogeneous ethnic groups. A strength of Born in Bradford is the homogeneity of the largest ethnic group of Pakistani origin. Methodologically and statistically, the focus of much of the work in the programme has been on Pakistani and white British comparisons. For completeness some of the analyses include a third category of ‘other’ ethnicities, which includes non-Pakistani and non-white British children. When we refer to the terms ‘South Asian’ and ‘Pakistani’ we are referring to families of South Asian or Pakistani origin who have been born either in the UK or in South Asia or Pakistan.
SYNOPSIS
Childhood obesity is a major global public health threat. 1,2 Although overweight and obesity prevalence in some groups of children may be flattening or decreasing,3–5 overall prevalence remains high, particularly in children from minority ethnic groups. 6,7 Evidence from the UK and the USA shows that the prevalence of overweight and obesity in preschool children is > 33%. 8–10 Obesity acquired in childhood has been shown to persist into adulthood with over half of obese children growing up to be obese adults. 11 It is estimated that the direct cost of obesity to the NHS will be £2B by 2030 if the current trends continue. 12 The 2007 Foresight report13 estimated that the direct and indirect costs of child and adult obesity would rise to £27B by 2015.
Childhood obesity has a major impact on health and well-being in childhood and through to adult life. 14–17 Obese children experience poor health-related quality of life and low self-esteem18 and, although the contribution of obesity towards the risk of negative health outcomes such as cardiovascular disease (CVD) and diabetes is complex, evidence suggests a consistent positive association. 19,20
Children of South Asian origin are at particular risk of overweight and obesity, demonstrating greater central adiposity and insulin resistance than their European-origin counterparts for a given body mass index (BMI). 21–24 Evidence suggests that this fat–thin insulin-resistant phenotype is present at birth and that pregnancy is an important window of opportunity for obesity prevention. 25,26 The adoption of Western urban lifestyles that result from migration to the UK has the potential to increase the risk of rapid postnatal growth and obesity contributing to the higher risks of diabetes and CVD.
There is emerging evidence that early life environments are important in the aetiology of obesity. 27 Maternal gestational weight gain and gestational glucose metabolism, together with greater birthweight and rapid postnatal growth, are all associated with later obesity, although it is unclear if this is driven by causal mechanisms. 28–32 Infant weight gain is consistently associated with subsequent risk of childhood and adult obesity and this risk is particularly high for infants with very rapid weight gain [> 1.33 standard deviation score (SDS) or two centile band crossings]. 33 However, it is the social, behavioural and environmental influences on childhood obesity that offer most potential for modification of factors influencing obesity. 34–38 A recent review of systematic reviews of early determinants of obesity identified the following factors associated with an increased risk of childhood obesity: maternal smoking, short sleep duration, < 30 minutes of daily physical activity, consumption of sugar-sweetened drinks, screen viewing and parental feeding practices. 39 Importantly, however, the evidence of causality is not clear. 40 Thus, although reinforcement of positive health interventions such as breastfeeding should be encouraged, there is still much to learn regarding the impact it has on childhood obesity.
Interventions to prevent obesity
Despite the public health threat of obesity there is a notable gap in the research evidence on effective interventions to prevent and treat obesity, particularly in early childhood and in South Asian populations. 41
Systematic review evidence42–49 has found that efforts to prevent obesity have shown disappointing results, which may be for the following reasons:
-
intervention schemes not guided by a robust evidence-based development process and not rooted in behaviour change theory
-
intervention strategies not tailored to the most important and modifiable behaviours
-
inadequate strategies to change family, environmental and extrinsic factors in combination with health education strategies aimed at personal behaviours
-
lack of careful pre-testing and formative evaluation procedures before larger-scale implementation
-
lack of involvement of stakeholders in intervention development, resulting in reduced engagement.
One explanation for the disappointing results of randomised controlled trials (RCTs) in terms of reducing obesity in schoolchildren is that they begin too late. Body composition and feeding patterns may become established in infancy, providing a potentially critical period for intervention. 50 Systematic reviews of obesity prevention in early childhood provide support for targeting interventions in early childhood but highlight the limited quantity and quality of the mostly US research. 45,46 Specific gaps in the evidence include the lack of family studies and studies that attempt to improve professional–family interaction, the dearth of evidence on the effectiveness of interventions in ethnic groups and the absence of economic evaluations.
There is a good theoretical51 and empirical33,36,52–56 basis for developing obesity prevention interventions in early childhood as unfavourable health behaviours are established in early childhood and are good predictors of subsequent behaviours. It is likely, therefore, that early childhood provides a unique and circumscribed opportunity to promote health and prevent obesity. However, there is a paucity of evidence about safe and effective interventions in preschool children. 57 A systematic review of studies to prevent obesity in children aged 0–5 years found that interventions varied widely although most were multifaceted in their approach. 58 These interventions have been found to be feasible and acceptable and there was evidence to suggest that behaviours that contribute to obesity can be positively impacted in this age group, particularly with the involvement of parents and the targeting of skills and competencies rather than just knowledge. A systematic review of qualitative studies on behaviours related to childhood obesity found that many parents felt that strategies to promote healthy weight should start in early life and also identified the importance of targeting the wider family rather than the parents alone. 59 Studies have also suggested that an intervention delivered within a parenting programme that focuses on parenting skills and style will have an enduring impact on the development of children’s healthy eating and activity patterns. 60,61
Born in Bradford
This programme harnessed the research potential of the new Born in Bradford (BiB) study, a longitudinal multiethnic birth cohort study aiming to examine the impact of environmental, psychological and genetic factors on maternal and child health and well-being. 62 Bradford is a city in the north of England with high levels of socioeconomic deprivation and ethnic diversity. Approximately half of the births in the city are to mothers of South Asian origin. Women were recruited to the BiB study while waiting for their glucose tolerance test, a routine procedure offered to all pregnant women registered at the Bradford Royal Infirmary at 26–28 weeks’ gestation. For those consenting, a baseline questionnaire was completed during an interview with a study administrator.
The baseline questionnaire for the mothers was transliterated into Urdu and Mirpuri using a standardised process so that words and phrases corresponded to the original English version. As Mirpuri does not have a written form, trained bilingual interviewers administered the transliterated questionnaires to Mirpuri speakers.
The full BiB study recruited 12,453 women during 13,776 pregnancies between 2007 and 2010 and the cohort is broadly characteristic of the city’s maternal population. Ethical approval for the BiB1000 data collection was granted by the Bradford Research Ethics Committee (reference number 07/H1302/112).
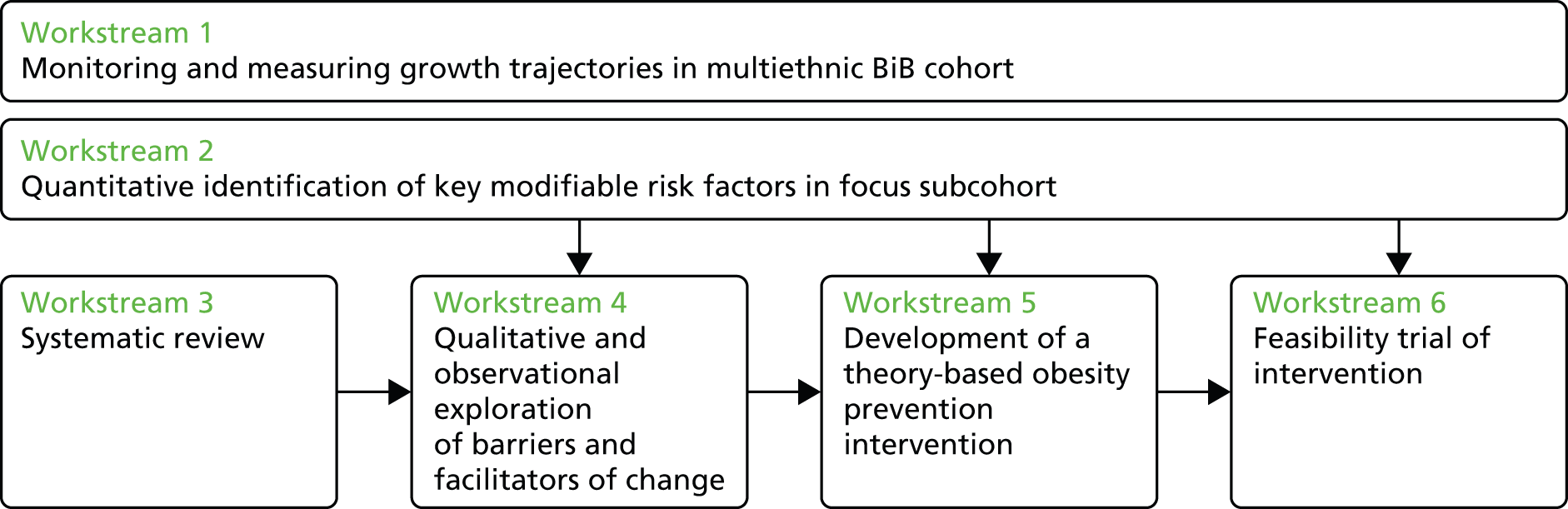
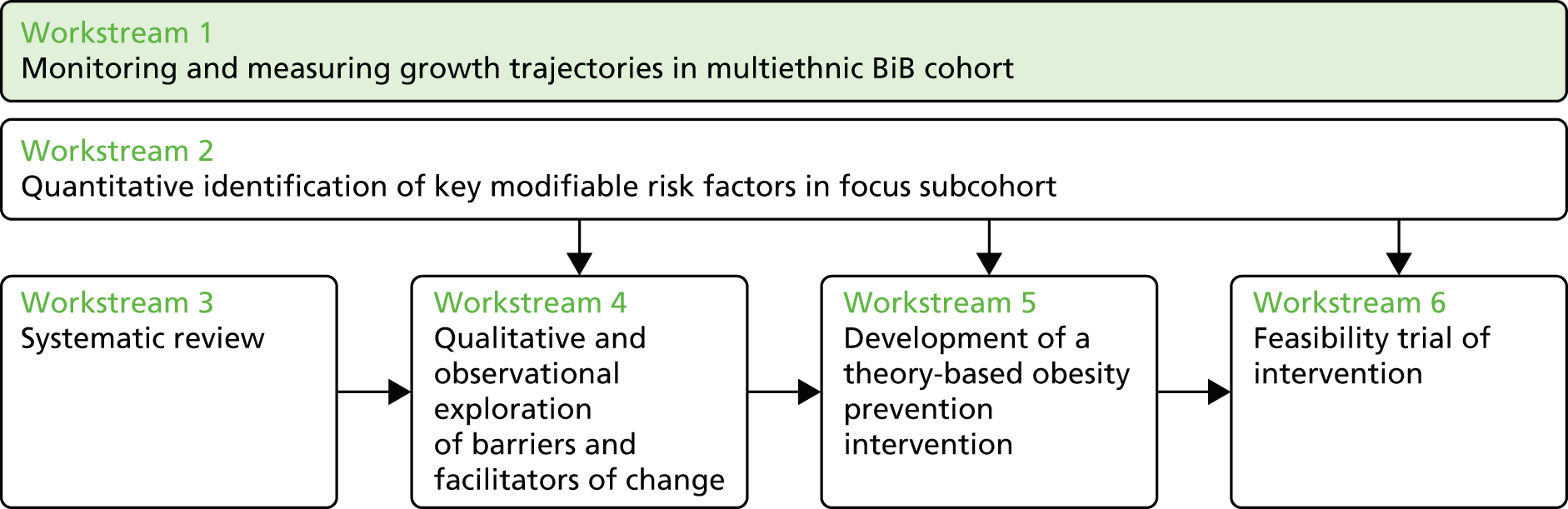
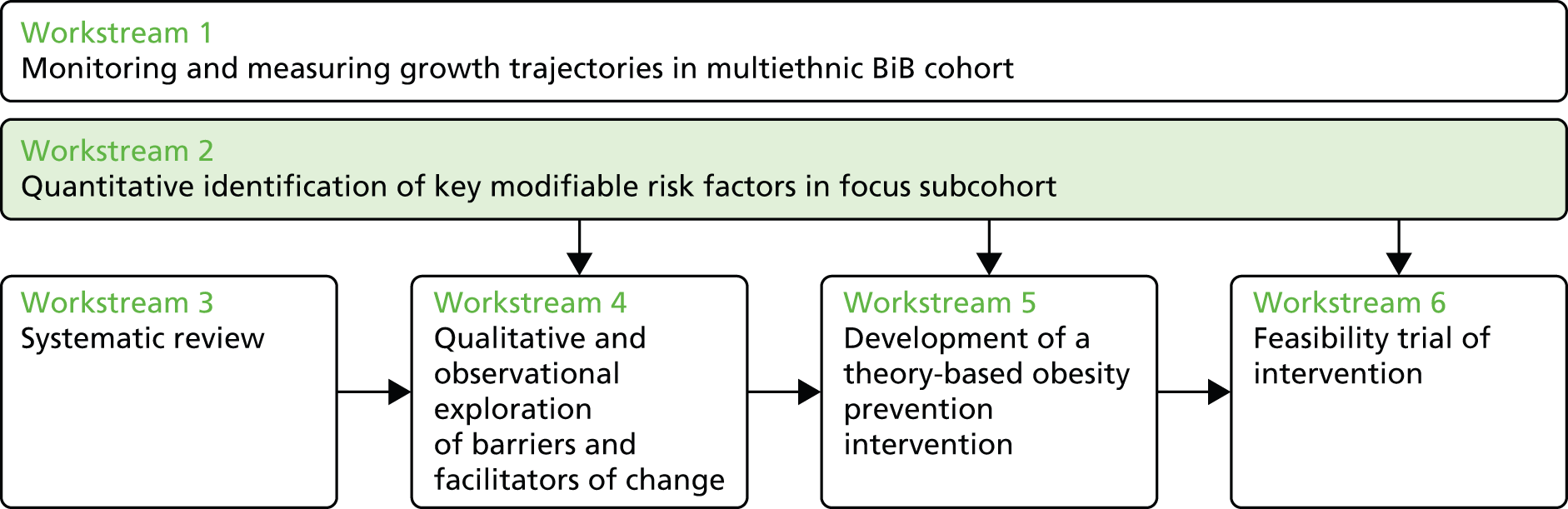
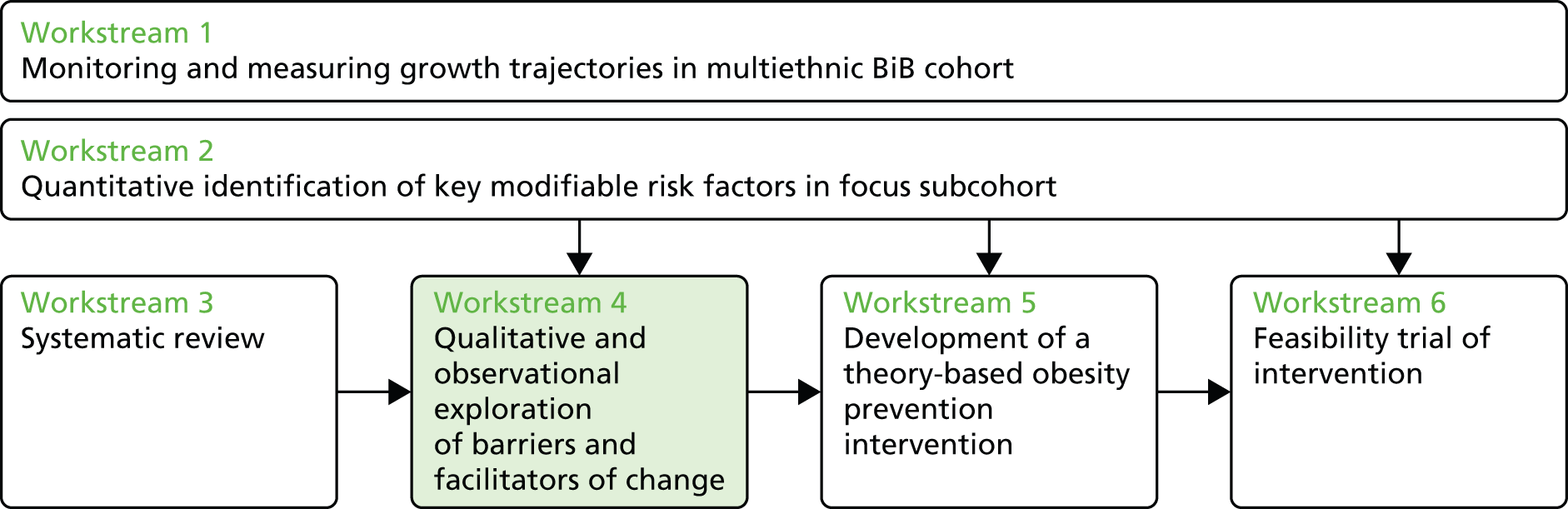
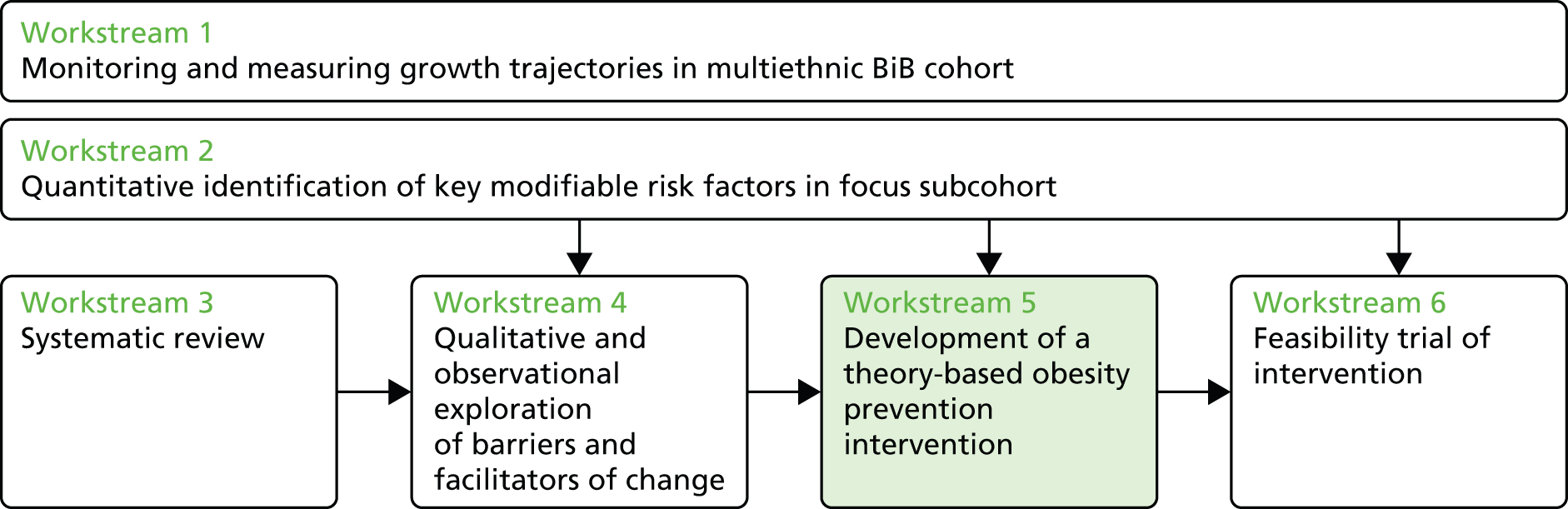
An applied research programme on childhood obesity
The aim of this National Institute for Health Research (NIHR) programme was to study the patterns and aetiology of childhood obesity in a multiethnic population and use this evidence to develop a tailored obesity prevention intervention.
The design and development of effective interventions requires a robust empirical evidence base to identify the right targets (modifiable behaviours) for preventing obesity and the right timing (in growth trajectory) for implementing the intervention. We set out to measure and analyse data on growth trajectories in a multiethnic population alongside assessment of hypothesised modifiable environmental and behavioural risk factors for obesity. Our intention was to determine whether or not the relative impact of any modifiable risk factor differs between South Asian and European-origin populations and to assess whether or not mechanisms for change differ between communities.
This monograph describes the results of our findings linked to the original programme objectives (a full list of publications arising from our programme of work can be found in Acknowledgements, Publications).
Recruitment of the BiB1000 cohort to investigate childhood obesity
-
Objective 1a: a 10% subsample of the BiB cohort was recruited for intensive follow-up to collect data on modifiable risk factors and growth. Data were collected from the 10% subsample through home visits by bilingual researchers, who administered survey instruments for behavioural measures and undertook anthropometry assessments.
Modelling growth trajectories and obesity risk
-
Objective 1b: the programme established research-calibre routine data collection on growth monitoring in a deprived, biethnic population through strengthening routine surveillance and monitoring growth trajectories.
Ethnic differences in obesity risk factors
-
Objective 2a: the focus for this objective was to describe ethnic differences in obesity risk factors to inform a culturally sensitive intervention.
Early risk factors for childhood obesity
-
Objective 2b: the focus for this objective was to identify modifiable behaviours and environmental risk factors that could be targeted in future interventions.
Systematic review of diet and physical activity interventions to prevent or treat obesity in South Asian children and adults
-
Objective 3: the focus for this objective was to conduct a systematic review of diet and physical activity interventions to prevent or treat obesity in South Asian children and adults.
Investigation of social and environmental determinants of childhood obesity
-
Objective 4: the focus for this objective was to determine appropriate intervention targets. Qualitative interviews, observational methods, geospatial mapping and nutritional audits were undertaken to explore determinants of feeding practices; cultural and social differences in feeding practices; the influence of key stakeholders; beliefs, attitudes and practices in relation to obesity, diet and exercise; perceptions in the South Asian community about childhood obesity; access to fast-food retailing; and eating patterns.
Development of an obesity prevention intervention
-
Objective 5: evidence from current and previous interventions was supplemented by a survey of nationally relevant work. Intervention mapping was used to select an appropriate theoretical foundation, identify change objectives and design the intervention and implementation. Field testing of candidate components for an intervention strategy was undertaken to test their feasibility and acceptability.
Exploratory trial of the obesity prevention intervention
-
Objective 6: the ultimate aim of the programme was to design an innovative community/family-based intervention to improve modifiable behaviours in both parent and child. The aim of the exploratory trial was to inform a definitive (Phase III) randomised trial that could be implemented within the NHS. The exploratory trial assessed the feasibility and acceptability of the intervention; eligibility, consent and recruitment rates; the acceptability of the randomisation process; and follow up rates. Outcomes were collected to inform the components and delivery of the intervention, estimate the effect size and test and validate outcome measures.
Programme management
A quarterly steering group of all 12 co-applicants and additional expert advisors was established to oversee the implementation of the research programme. An independent trials management group consisting of Julie Walker (clinical manager), Kim Cocks (statistician and triallist) and Tracy Wood (local authority parenting expert) was established in 2012 to provide monitoring and scrutiny of the feasibility trial.
Helen Ball and her team from Durham University joined the programme to support the study of sleep in early life. Aziz Sheikh and his team at Edinburgh University joined the programme to support the development of a culturally adapted intervention. Kate Tilling and Laura Howe from Bristol University joined the programme to provide expertise in the use of multilevel linear spline and latent class modelling of early life trajectories. Darren Greenwood from Leeds University joined the team to provide support for the dietary analysis. Kath Kiernan from York University provided expert support for the exploration of the association of parenting practices with obesity. Sally Barber from the Bradford Institute for Health Research joined the team to provide expertise on physical activity.
Clinical engagement
The programme was set up to promote strong clinical engagement in the research. Such engagement was fundamental to the success of the programme. Support from health visitors from Bradford District Care Trust was required to ensure high-quality additional routine postnatal measurements. Support from the midwives at Bradford Teaching Hospitals NHS Foundation Trust was required for the successful recruitment of pregnant women to the pilot trial. Close involvement of local dieticians and public health consultants was required for the development of the intervention. Finally, close partnership with Barnado’s and Family Links was essential for the delivery of the intervention.
Patient and public involvement
The BiB1000 study has benefited from extensive experience of patient and public involvement within the Bradford Institute for Health Research. This has included the use of a panel of 10 people representing the local patient community who meet regularly (3-monthly) to participate in all stages of the research process, including identifying priorities, helping to write lay summaries, reviewing methodology and supporting translational work. Panel members work in pairs to provide peer support but also meet collectively to discuss general and specific issues. The BiB study has a strong focus on wider community engagement, with regular newsletters, birthday cards, picnics and art exhibitions. One of the great strengths of the study is the close involvement of the photographer Ian Beesley and the poet Ian McMillan, whose work is featured here and in the appendices of this report.
@BiBresearch (Twitter, Inc., San Francisco, CA, USA)

Born in Bradford (Facebook, Inc., Menlo Park, CA, USA) (www.facebook.com/BornInBradford/)



Recruitment and data collection for the BiB1000 cohort to investigate childhood obesity
The BiB1000 study was established to help enable a deep and extensive understanding of the predictors of and influences on health-related behaviours and to develop a culturally specific obesity prevention intervention. Here we describe the methodology and characteristics of the study participants; this work has been published as a separate paper. 63
All mothers recruited to the full BiB study between August 2008 and March 2009 who had completed the baseline questionnaire were approached to take part in the BiB1000 study during their routine 26- to 28-week glucose tolerance test. Those not attending this appointment were approached elsewhere during routine hospital attendances. A sample size of 1080 was calculated based on the ability to detect a clinically significant difference in infant growth of 0.67 SDS (one centile band) in weight at age > 1 year. Based on data from the Cole UK charts,64 we needed a minimum sample of 36 participants in any analysis group for length and a minimum of 67 participants for weight (β = 0.80; α = 0.05). Stratification by gender and ethnicity meant that we required a minimal sample of 280 at the completion of the preschool study. Allowing for a 5% annual attrition rate, we therefore required a total sample of 1080 births. However, to account for the higher anticipated attrition rate in a deprived multiethnic population, the plan was to oversample the population by up to 60%. Ethical approval was obtained from the Bradford Research Ethics Committee (reference number 07/H1302/112) and all participants provided written informed consent prior to inclusion in the research.
Bilingual study administrators who were trained in anthropometry collected baseline information from mothers using a structured questionnaire in the home, at hospital-based clinics and at local children’s centres. Participants were followed up at 6, 12, 18, 24 and 36 months.
The questionnaire measures included were selected based on hypothesised correlations with exposures and childhood obesity. As this was an exploratory study in a largely untested population, many of these hypotheses were driven by a combination of evidence from ‘similar’ populations in the literature and agreement by the scientific and clinical teams. Baseline data collection for the BiB study was pilot tested with a group of expectant mothers in the Bradford Royal Infirmary Maternity Unit for clarity, duration and acceptability. Except for assessment of dietary intake in infants, additional follow-up measures were not piloted in advance of data collection. However, their acceptability was determined within the BiB1000 cohort and amended as appropriate. The intended food frequency questionnaire for infants was pilot tested in children’s centres and this led to slight modifications to the clarification of items to ensure that foods were culturally representative (e.g. chapattis included within bread products).
Infant weight was measured at birth by midwives and infant head circumference, mid-upper arm circumference, abdominal circumference, subscapular skin fold and triceps skin fold were measured within the first 24 hours following delivery by paediatricians and midwives who were trained in measurement techniques according to written guidelines.
Postnatal measures of infant weight, length, head circumference and abdominal circumference were collected as part of routine practice by health visiting teams. Additional measures of weight, length, head circumference, abdominal circumference and skinfolds were taken by specially trained BiB1000 study health workers at follow-up visits.
Maternal weight was measured at all assessments, maternal height was measured at baseline and BMI was derived from the antenatal booking weight (at ≈12 weeks of pregnancy) and baseline height.
The majority of the demographic data were obtained using structured questionnaires. Items were generated and modified from the Millennium cohort study,65 Growing up in Australia,66 the 2001 census67 and the European Prospective Investigation into Cancer and Nutrition (EPIC)68 questionnaires.
Behavioural measures were collected as part of the structured administered follow-up questionnaires, including feeding style and practices, parental and infant diet, mental health, parental and infant activity, sleep patterns, home food availability, parenting practices and other health behaviours (e.g. smoking, alcohol consumption). Validated questionnaires were used when available, although appropriate ethnic modifications were made and tested using expertise within Bradford (e.g. diet questionnaires were modified based on 24-hour recall data collected from parents in Bradford alongside input from Bradford dieticians).
A full set of questionnaires used for all follow-up assessments can be found on our website [see www.borninbradford.nhs.uk/research-scientific/general-study-documentation-and-questionnaires-2/ (accessed 4 February 2016)].
Qualitative and objective methodologies were employed in subsamples to explore the lifestyles, behaviours and environments in this multiethnic population, including (1) food outlet mapping, (2) home food availability inventories, (3) a mealtime observation study of maternal feeding styles and (4) interviews with families. Further details of the methods and findings for each of these are provided in Investigation of social and environmental determinants of childhood obesity.
Out of 1916 eligible women, 1735 (91%) agreed to take part in the study. Of these, 28 mothers gave birth to twins. Descriptive statistics are provided here for singleton births only (n = 1707). In total, 77%, 75%, 74%, 70% and 70% of participants were followed up at 6, 12, 18, 24 and 36 months respectively; 47% of participants completed all of the assessments to date, with 17% (n = 294) formally withdrawing from the research. Participants who could not be contacted (or when the visit could not be scheduled) were not considered to be lost to follow-up unless a withdrawal form had been completed (i.e. withdrawal of consent, death or change of residence outside the area). Thus, in some instances, data are missing at one time point but are available at subsequent visits. The greatest factor that impacted on attrition rates was the inability to make contact with participants to book appointments.
The characteristics of the BIB1000 cohort were similar to those of the full BIB cohort,62 with a similar distribution of age, marital status and parity. Overall, 38% of women were of white British origin and 47% were of Pakistani origin; 41% of Pakistani women were born in the UK and, of the remainder who were born elsewhere, 24% moved to the UK before the age of 18 years. Around 20% of the sample questionnaires were administered in languages other than English, reflecting this migration pattern. Demographic differences by ethnicity within the BiB1000 cohort were also observed, with white British mothers tending to be younger, educated to a lower level and less likely to be married or cohabiting and having fewer children than mothers from other ethnic groups. More than 20% of Pakistani women had more than three children prior to the birth of the study infant. Correspondingly, household size for South Asian women, especially Pakistani women, was greater than that for other ethnicities. Infant gender, gestational age and proportion of preterm infants were similar between ethnic groups. Similarities were also observed for the mode of delivery and the proportion of stillbirths. Over 35% of white British women reported smoking during pregnancy compared with 4% and 3% of women of Pakistani and ‘other’ South Asian origins respectively. The proportion of women with gestational diabetes was greatest in the South Asian ethnic group, with a 10.5% prevalence in Pakistani women compared with a 5.5% prevalence in white British women.
Longitudinal data collection from the BiB1000 birth cohort has provided a sample for the NIHR programme to develop a deep and extensive understanding of the predictors and influences of health-related behaviours to help develop feasible and appropriate culturally specific intervention(s) for the prevention of childhood obesity. This was facilitated by experienced, enthusiastic, multilingual data collection staff. A unique quality of this cohort is its ethnic composition, with successful recruitment of approximately 50% of women from South Asian origin and a representative sample of women from across the socioeconomic groups within Bradford.
Modelling growth trajectories and obesity risk
Growth during infancy is an important indicator of health and well-being. 69 Evidence suggests that the obesity epidemic begins in early childhood and that the risk of obesity is greater in children who put on more weight in early life. Growth data for the BiB1000 cohort are available from two sources; the BiB1000 visits and the routine measurements recorded in health visitor records (Personal Child Health Record or ‘red book’). We assessed how reliable the data collected by health visitors in Bradford are by using a test–retest reliability study and investigated the agreement between data collected in the BiB1000 clinics and the routine data collected by health visitors. This work has been published in two separate papers. 70,71
We found that, in Bradford, following training, health workers can in general reliably measure child growth. The technical errors of measurements obtained in our study were comparable to those from other research studies and all coefficients of reliability were indicative of good quality control. We also found that there was good agreement between BiB1000 measurements and routine measurements, although wide limits of agreement between data sources may be observed.
The growth data collected as part of the BiB1000 study supplemented with routine measurements collected by health workers in the community have provided a comprehensive reliable data set to investigate growth in infancy. We have focused on investigating ethnic differences in growth trajectories and on the development of obesity risk in childhood. We used multilevel linear spline models with repeat measures of weight and length to describe growth trajectories for white British and Pakistani infants from birth to 2 years of age and to assess whether or not there are ethnic differences in these growth trajectories. Finally, we described the development of prediction equations to identify children at risk of obesity and integrate the equations into a novel user-friendly mobile phone application. This work has been published in two separate papers. 72,73
Modelling growth trajectories72
For the first time in the UK we estimated weight and length growth trajectories between birth and 2 years for Pakistani boys and girls and found that Pakistani boys and girls were lighter and had a shorter predicted mean length at birth than their white British counterparts but gained weight and length quicker in infancy. By age 2 years both ethnic groups had a similar weight, but Pakistani boys and girls were taller on average than white British boys and girls. Differences in maternal height explained some of the differences in weight and length at birth; however, adjustment for maternal height, smoking during pregnancy and gestational age did not explain the differences in postnatal growth rates.
Given the relationship of early postnatal growth to normal development and adult health, together with known anthropometric differences at birth in South Asian compared with white European infants, it is important to understand how size differs in this group in the postnatal period and what factors might explain these differences. The faster growth in South Asian children shown in our study could be beneficial for their early infant/childhood health as observed in low-income countries. 74 However, if the greater rate of weight gain in this population is driven by greater fat gain it may have adverse long-term consequences for cardiometabolic health75 and contribute to the increased risk of diabetes and CVD observed in South Asian adults. 76–78 South Asian children have been shown to be fatter for a given BMI than their European counterparts and markers of diabetes and CVD risk are increased in South Asian children and adolescents, suggesting that this faster early growth may indeed be contributing to adverse later cardiometabolic health. 24,79,80 We acknowledge that further replication of our findings by others and longer-term follow-up to examine associations with a range of early life and later outcomes will be required to clarify the importance of these ethnic differences in growth.
Development of a mobile phone app to predict childhood obesity73
Innovative strategies to identify infants at the greatest risk of childhood obesity are necessary for the prevention of obesity. We present the development of a practical mobile phone app (Figure 1) that can be used for a wide range of ages (4.5–13.5 months) in infancy when growth monitoring is part of routine health care. 81 The app requires information on a baby’s sex, date of birth, birthweight and current weight and users can optionally add maternal height and weight (to calculate BMI). We chose not to include ethnicity and gestational age because, although they were significant predictors, neither of these factors was significant in the internal and external validity analyses. Furthermore, ethnicity in our sample was restricted to white British and South Asian ethnicities and it was felt that this would not reflect the ethnic diversity (or lack thereof) in many areas. Maternal BMI was a significant predictor in the 6- and 9-month equations but, again, this information may not be available and so we developed two sets of prediction equations so that the app would work whether or not maternal BMI was available, with a negligible effect on the model fit.
FIGURE 1.
The Healthy Infant Weight? app.

In the future the app could be developed to incorporate any number of other functionalities, such as plotting of growth measurements on a growth chart, geospatial mapping of an infant’s obesity risk score compared with those of his or her peers and administration of an obesity prevention programme for those infants identified as being at high risk.
Ethnic differences in obesity risk factors
Epidemiological evidence has highlighted the importance of a number of exposures in pregnancy and early life that are associated with the development of obesity in childhood. In this study we investigated ethnic differences in five early-life risk factors for childhood obesity that are modifiable and can be targeted in future interventions. The risk factors considered were (1) breastfeeding, (2) infant diet, (3) infant sleep, (4) physical activity and (5) parenting style. The work on breastfeeding and parenting style has been published in two separate papers;82,83 the full reports for the other risk factors are presented in Appendix 1.
Ethnic differences in the initiation and duration of breastfeeding82
Compared with white British mothers, we found that mothers in all other ethnic groups examined were significantly more likely to initiate breastfeeding and continue any breastfeeding until their infant was 4 months of age, which is consistent with previously reported findings from the UK. 84,85 However, we found no significant differences by ethnicity after adjustment for covariates in the rates of exclusive breastfeeding at 4 months.
Ethnic differences in infant diet (see Appendix 1.1)
Analyses of dietary patterns found that, by 12 months of age, foods and drinks high in sugar and foods high in fat were consumed by infants. There was no fruit and vegetable consumption in 3% of infants; a higher intake of sweet commercial foods, fruit and high sugar drinks in Pakistani infants; and higher intakes of savoury baby foods and processed meat products in white British infants.
In comparison to intakes of key indicator food groups at 12 months, the 18-month data showed large statistically significant and nutritionally concerning increases in the consumption of unhealthier food items across the cohort. Large increases were observed in the intake of chips, processed meat products, savoury snacks and sugar-sweetened drinks. Encouragingly, the intake of fruit, vegetables and low-sugar drinks had also increased.
At 18 months Pakistani infants had a higher intake of chips, roast potatoes or potato shapes and consumed substantially less processed meat than white British infants. Pakistani children continued to drink more sugar-sweetened drinks and more pure fruit juice than their white British counterparts.
There were ethnic differences in the consumption of key nutrients and these also changed over time. These changes in diet may simply reflect different weaning strategies between the ethnic groups, with Pakistani babies breastfed for longer, reflected in lower protein and fibre intakes at 12 months, but patterns relating to the consumption of solid food becoming more established by 18 months.
This analysis contributes to the limited evidence on dietary patterns in early childhood and highlights ethnic differences in some consumption patterns. There was evidence of dietary patterns that emerged at 12 months tracking to 18 months and, once established, these may form the basis of an unhealthy diet that may become ingrained and difficult to shift. This information helps us to characterise early-life dietary patterns and will allow us to examine how early diet influences later outcomes. It can be used to inform the development of community-tailored and culturally appropriate obesity prevention interventions aimed at improving the nutritional health of infants, toddlers and children.
Infant sleep patterns (see Appendix 1.2)
We found ethnic differences in night-time sleeping patterns, with later sleep onset and wake times for Pakistani infants than for white British infants at both 18 and 36 months and with Pakistani infants experiencing a shorter maximum sleep duration. Ethnic differences in sleeping arrangements may be affecting infant sleep duration or maternal knowledge of infant sleep duration. For example, South Asian families tend to practise familial co-sleeping, with all children sharing a room with their parents for sleeping, whereas white British families practise separate sleeping arrangements, often with one child per room. Such differences may affect maternal knowledge of an infant’s sleep duration such that South Asian mothers may be more likely to be aware of night wakings. Sleep duration may also be affected if family members are more frequently disturbed by one another in the night.
Physical activity (see Appendix 1.3)
The majority of children in the BiB1000 cohort at age 2 years were meeting the Chief Medical Officer’s guideline of 180 minutes of physical activity each day. 86 There were no differences between the ethnic groups in total time spent on daily physical activity and, in addition, sedentary behaviour and television/DVD viewing were high for the whole group (on average 1.5 hours per day). There were, however, ethnic differences in the types of physical and sedentary activities that the children engaged in. White British children were reported to spend longer walking, in organised physical activity, playing outside and in proactive sedentary behaviours (e.g. being read to) than Pakistani children, who spent longer each day playing inside and in passive sedentary behaviour (watching television/DVDs). The differences in time spent in different types of activities may result in important lifestyle differences as the children grow up as observational studies have shown that time spent outdoors correlates with physical activity levels in school-aged children. 87,88 Time outdoors has also been associated with higher objectively measured physical activity levels89,90 and with a lower prevalence of overweight. 89 There were other marked differences between the ethnicities in possible determinants of physical activity and sedentary behaviour that may also contribute to the reported differences between ethnic groups later in childhood. 91 These included Pakistani children being less frequently restricted in their television viewing, having more barriers to physical activity and receiving less frequent support to be physically active from their parents.
Ethnic differences in parenting style83
There were no ethnic differences in parental self-efficacy and parental warmth; however, Pakistani mothers reported feeling more confident about their parenting abilities and were less likely to adopt a hostile approach to parenting. To our knowledge, no such data have been reported previously for UK-resident women and further work is needed to link these parenting styles with children’s current and future health. Women of both ethnic groups with more self-efficacious, warm and less hostile parenting styles reported significantly fewer problems with their infant’s temperament.
Understanding of these ethnic differences in modifiable risk factors has implications for the effective cultural adaptation of interventions to reduce childhood obesity.
Early risk factors for childhood obesity
In the last section we described ethnic differences in five early-life risk factors for childhood obesity. Here, we investigate the association between several early-life modifiable risk factors for childhood obesity and infant BMI at 3 years of age. This work has been published as a separate paper. 92
It is important to understand whether or not modifiable characteristics are related to BMI in infancy to ensure that appropriate interventions are developed to promote maintenance of healthy BMI levels into mid-childhood, when important relationships to future coronary heart disease risk emerge. Furthermore, knowing whether or not associations differ between South Asian- and white European-origin infants is important in knowing whether or not interventions should target different risk factors in these groups to reduce the ethnic differences in risk. In this section we describe the differences in the prevalence of potentially modifiable risk factors for childhood obesity between infants of white British origin and infants of Pakistani origin and investigate the association between these risk factors and childhood BMI measured at 3 years of age. We also examine possible ethnic differences in associations between the risk factors and child BMI.
We found that the prevalence of early-life risk factors for a higher BMI differed between mothers of white British ethnicity and mothers of Pakistani ethnicity. White British mothers were more likely to smoke during pregnancy (28% vs. 4%), have a higher BMI (obese: 24% vs. 16%), breastfeed for a shorter duration (> 4 months: 20% vs. 29%) and wean earlier, whereas Pakistani mothers had a higher rate of gestational diabetes (14% vs. 7%) and were less active (sufficiently active: 26% vs. 57%). There were consistent associations between BMI z-score and maternal smoking [mean difference in BMI z-score 0.33, 95% confidence interval (CI) 0.13 to 0.53], maternal obesity (0.37, 0.19 to 0.55), indulgent feeding style (0.15, −0.06 to 0.36), lower parental warmth scores (0.21, 0.05 to 0.36) and higher parental hostility scores (0.17, 0.01 to 0.33). Associations with mean BMI were the same for white British and Pakistani infants, with the exception of breastfeeding duration. Although we did not have sufficient statistical power to examine ethnic differences in the associations of risk factors with relative risks of overweight/obesity, the similarity in the associations with mean BMI between the two ethnic groups suggests that differences on a binary scale are unlikely.
Consistent with other studies we found that children of mothers who smoked during pregnancy were more likely to have a higher BMI SDS and a greater risk of being overweight,40,93,94 as were infants of overweight and obese mothers. 28,93,95
We found that certain aspects of feeding and parenting style were associated with a child’s BMI. Caregivers with an ’indulgent’ feeding style had infants with a higher BMI SDS and who were more likely to be overweight; this is consistent with other studies. 96,97 Children of parents with less warm and more hostile parenting styles were more likely to be overweight. Different measures and constructs of parenting styles have been previously studied; however, evidence linking the specific domains analysed in the current study to childhood BMI is scarce, although some studies have looked at associations with dietary and activity behaviours. 98,99 Evidence suggests that children raised by authoritative parents had lower BMI levels than children raised with other styles. 98
In this study we did not find strong evidence of an association between gestational diabetes, age at weaning, infant energy intake, infant protein intake and infant sleep duration and infant mean BMI or risk of overweight at age 3 years, despite evidence of associations between these risk factors and BMI in other studies. 40,93,100–104 However, many of these studies were conducted in older age groups and in non-UK populations with different ethnic compositions to that of the BiB study population.
The main strength of this analysis is that we have considered several key modifiable risk factors that have been collected longitudinally during pregnancy and infancy in a multiethnic cohort. To our knowledge this is the first time that these risk factors have been studied in early infancy in infants of Pakistani origin. The limitations of the study are that it was undertaken in a single centre and so may lack generalisability. The questionnaire relied on self-report to collect information on risk factors and there may have been reporting or social desirability bias.
This work adds to the literature on the role of the early life environment and later childhood obesity and is useful in identifying suitable targets for obesity prevention interventions in infancy. It has highlighted key differences in early-life risk factors between white British and Pakistani mothers and so has highlighted the importance of cultural adaptation of interventions. It has also helped identify key modifiable risk factors to target in pregnancy and postnatally.
Systematic review of diet and physical activity interventions to prevent or treat obesity in South Asian children and adults

The previous workstreams identified the important modifiable determinants of obesity to form targets for intervention and identified key differences in the patterns of these risk factors by ethnicity and socioeconomic status. These findings highlight the need for culturally sensitive interventions to be developed.
We performed a systematic review to identify evidence that could inform the development of an obesity prevention intervention for pregnant South Asian women and their children aged < 6 years. This systematic review has been published105 and is freely available at www.mdpi.com/1660-4601/12/1/566 (accessed 1 February 2016).
The metabolic risks associated with obesity are greater for South Asian populations than for white or other ethnic groups and levels of obesity in childhood are known to track into adulthood. Tackling obesity in South Asian populations is therefore a high priority. The rationale for this systematic review was the suggestion that there may be a differential effect of diet and physical activity interventions in South Asian populations compared with populations of other ethnicities. The research territory of the present review is an emergent rather than a mature field of enquiry, but it is urgently needed. Thus, the aim of this systematic review and meta-analysis was to assess the effectiveness of diet and physical activity interventions to prevent or treat obesity in South Asian populations living in or outside South Asia and to describe the characteristics of effective interventions.
Systematic reviews of any type of lifestyle intervention, of any length of follow-up that reported any anthropometric measure for children or adults of South Asian ethnicity were included. There was no restriction on the type of comparator and RCTs, controlled clinical trials and before-and-after studies were included. A comprehensive search strategy was implemented in five electronic databases: Applied Social Sciences Index and Abstracts (ASSIA), Cochrane Controlled Trials Register (CCTR), EMBASE, MEDLINE and Social Sciences Citation Index. The search was limited to English-language abstracts published between January 2006 and January 2014. References were screened and data extraction and quality assessment were carried out by two reviewers. The results were presented as a narrative synthesis and meta-analyses were carried out.
In total, 29 studies were included, seven in children, 21 in adults and one in a mixed-age population. No studies in children aged < 6 years were identified. Sixteen studies were conducted in South Asia, 10 in Europe and three in the USA. Effective or promising interventions included physical activity interventions in South Asian men in Norway and in South Asian schoolchildren in the UK. A home-based, family-orientated diet and physical activity intervention improved obesity outcomes in South Asian adults in the UK when adjusted for baseline differences. Meta-analyses of interventions in children showed no significant differences between intervention and control groups for BMI or waist circumference. Meta-analyses of adult interventions showed a significant improvement in weight in data from two trials when adjusted for baseline differences (mean difference −1.82 kg, 95% CI −2.48 to −1.16 kg) and in unadjusted data from three trials following sensitivity analysis (mean difference −1.20 kg, 95% CI −2.23 to −0.17 kg). Meta-analyses of adult interventions showed no significant differences between intervention and control groups for BMI and waist circumference. Twenty of 24 intervention groups showed improvements in adult BMI from baseline to follow-up; the average improvement in high-quality studies (n = 7) ranged from 0.31 kg/m2 to −0.8 kg/m2. There was no evidence that interventions were more or less effective according to whether or not the intervention was set in South Asia or by socioeconomic status.
Meta-analysis of a limited number of controlled trials found an unclear picture of the effects of interventions on BMI for South Asian children. Meta-analyses of a limited number of controlled trials showed significant improvements in weight for adults but no significant differences in BMI and waist circumference. One high-quality study in South Asian children found that a school-based physical activity intervention that was delivered within the normal school day and which was culturally sensitive was effective. There was also evidence of culturally appropriate approaches to, and characteristics of, effective interventions in adults that we believe could be transferred and used to develop effective interventions in children.
Investigation of social and environmental determinants of childhood obesity
To further explore the impact of social and environmental factors on health we conducted a range of further focused studies. The aim was to understand how these factors might constitute determinants of childhood obesity, how they might vary according to mothers’ ethnicity and how they might be modified, with a view to informing any subsequent intervention. Specific areas of focus were parental attitudes to eating and infant growth, interactions that accompany mealtimes and the availability of certain foods in the home and in the neighbourhood. The work on food availability in the home and in the neighbourhood has been published in two separate papers;106,107 the full reports for the other topics are presented in Appendix 1.
Investigation of social and environmental determinants of childhood obesity (see Appendix 1.4)
Fourteen mothers (n = 9 Pakistani and n = 5 white British mothers) were recruited and interviewed when their infant was aged between 3 and 5.5 months. Issues around perceptions of a ‘healthy baby’, breastfeeding and weaning and sources of support were explored. Transcripts and field notes were independently coded by two authors. Analysis sought to identify emerging themes using a thematic narrative approach;108 differences between ethnic groups were explored.
There was considerable shared ground between white and Pakistani mothers in relation to how they perceived a ‘healthy’ baby. Mothers expressed some anxiety about very underweight babies, but a concern about them being overweight was not strongly evident. For younger children who might be overweight the expectation (hope) was that ‘they will grow out of it’; for older children the problem was seen as being a cosmetic one rather than primarily a health concern.
At the time of interviewing, only three mothers were still breastfeeding. Approximately half of the remaining mothers had tried to breastfeed, averaging between 1 week and 10 days, and had then stopped. The most common reason why they had stopped was that the ‘baby was not getting enough food’. Most of the mothers interviewed were weaning already, often starting at around 4 months. Mothers were aware that there was guidance from health visitors about the correct time to wean. Some had heard advice from health visitors about baby-led weaning, but none reported trying this.
With regard to sources of advice and support there were two strong and inter-related themes: the importance of consistent advice and the many sources of advice that were available. Mothers received inconsistent advice from different professionals about breastfeeding and between professionals and family members in relation to weaning. Adding to this challenge was the wide range of sources used for advice (e.g. extended family, friends, midwives and health visitors).
In summary, the interviews provided data that were consistent with those previously reported in the literature. 59 Parental perceptions are developed through interactions with a range of sources of influence including family, friends and health professionals. The internet was of increasing prominence as a source of information. There was not a clear hierarchy of influence.
A mealtime observation study: obesity, ethnicity and observed maternal feeding styles (see Appendix 1.5)
Having identified the importance of parent and family beliefs in decisions to breastfeed and wean in early infancy, we sought to explore how feeding patterns were influenced by the shared family environment. Parents are key role models for their children, socialising children to their food choices, eating habits and feeding behaviours. Parenting styles have been shown to impact on eating behaviour and outcomes related to obesity. 98 General parenting styles have been summarised as having two dimensions: control/demandingness and warmth/responsiveness. 109,110 These independent dimensions yield four different parenting styles: authoritarian, authoritative, permissive and uninvolved parenting. Research has linked authoritative feeding styles to increased consumption of fruit and vegetable products. 111 However, many authors question whether these styles are invariant across different cultural groups. 112 There is an absence of research regarding parenting styles of social Asian families, especially those living in the UK. International studies regarding ethnicity and feeding practices are similarly limited.
The current study aimed to explore the influence of maternal weight and ethnicity on observed mealtime interactions. Twenty obese mothers (10 Asian and 10 non-Asian mothers) and 18 ‘healthy weight’ mothers (8 Asian and 10 non-Asian mothers) participating in the BiB1000 study consented to take part in the study along with their children. Children were aged between 18 months and 2 years, 24 were male and 14 were female.
Mothers were asked to prepare an ordinary meal for their child on the day of the observation. The mealtime was recorded and recordings were analysed using the Mealtime Observation Schedule (MOS). 113 The schedule codes parent behaviours as positive (e.g. praise, positive contact) or negative (e.g. negative eating comments) and child behaviours as positive (e.g. ‘self-bites’, appropriate verbal behaviour) or negative (e.g. refusing food, leaving the table). Validated questions assessing caregiver feeding style (authoritative, authoritarian, indulgent and uninvolved),114 parenting practices (self-efficacy, warmth and hostility66) and infant characteristics (adaptability, fussiness/difficultness, dullness and predictability)115 were administered at 6, 12 and 24 months as part of the standard schedule of measurement of the BiB1000 cohort. 63
Analyses found that South Asian mothers presented food more times to their child than non-Asian mothers. Meal duration was shortest for children whose mothers were South Asian and of healthy weight and longest for children whose mothers were non-Asian and of healthy weight.
South Asian mothers exhibited significantly less positive behaviours and significantly more negative behaviours during mealtimes than non-Asian mothers. Children with South Asian mothers demonstrated marginally greater levels of negative behaviours during mealtimes, with no difference in positive behaviours between the two ethnic groups. Children of South Asian, healthy-weight mothers spent more time ‘away from the table’ than children in the other groups. There were no effects of maternal weight on these measures.
In summary, there were no differences in parenting styles of feeding behaviours by maternal weight. Distinct ethnic differences were apparent, both in the physical organisation of mealtimes (more South Asian mothers did not sit their child in a chair or use a table for mealtimes) and in the types of interactions during mealtimes (with South Asian mothers showing slightly reduced positive behaviours and slightly increased negative behaviours). This is consistent with the observation that their children demonstrated less independent eating. Overall, the results indicate that South Asian mothers exert a different type of control during mealtimes with their children by giving a greater number of specific and clear direct instructions. This may be in response to more challenging behaviour of their children.
Researcher-conducted home food availability inventories106
For children, the home is a key environment as it serves as the primary physical and social context in which habits and norms are developed, including those specific to diet and physical activity. Home food availability/accessibility has been shown to relate to child food consumption,116–131 which is intuitive given that children’s food intake is largely dependent on what is provided to them by others. 124,127,132,133 The aim of this study, therefore, was to explore the home food availability of South Asian and white British participants in the BIB1000 study to describe what foods are available and to identify key differences by ethnicity or weight status.
Direct observations of food and drinks in the home were made for an opportunistic sample of 97 BiB1000 participants (n = 46 white British, n = 41 Pakistani, n = 10 ’other’ ethnicity) using a standardised protocol. 51 The inventory included counting portions of fruits (fresh, frozen, tinned, dried), vegetables (fresh, frozen, tinned), savoury snacks (crisps/tortillas, nuts), sweet snacks (cakes, biscuits, chocolate, sweets, ice cream) and beverages (sugar-sweetened drinks, diet drinks). See Appendix 2.3 for a copy of the home food availability inventory.
Findings from this exploratory study showed that all homes had some form of fruit and some form of vegetable available in them. Overall, the presence of foods and drinks was similar in all of the ethnic groups. More homes had fresh fruits and vegetables available than canned, frozen and dried fruits and vegetables. At least one type of snack food was also available in all of the included BiB1000 homes. Of these, crisps and biscuits were most likely to be available. Descriptive analysis compared differences by ethnicity and weight. Although no differences were found for the latter, unadjusted comparisons by ethnicity showed that homes of Pakistani mothers had approximately three times the quantity of sweetened beverages available in them. Although this finding may be dependent on confounding factors (a study within the USA found that household size, presence of the maternal grandmother and shopping habits all related to home food availability134), it does suggest that targeting these types of drinks would be useful within an intervention to prevent obesity, as these drinks offer no nutritive value.
Food outlet availability, deprivation and obesity in a multiethnic sample of pregnant women in Bradford, UK107
The final environmental factor influencing obesity addressed in the current workstream was the neighbour environment in which respondents lived. The conceptualisation of an obesogenic environment has changed the way that obesity is viewed and is key to national policy documents that address obesity. 13 The obesogenic environment operates on several levels and describes the changes in daily living, transport and access to recreational facilities, foods and food outlets that have contributed to positive energy balance and weight gain. It follows that the availability of, or people’s access to, food may be related to obesity. This could be through proximity to multiple fast-food outlets or the way that people shop at large out-of-town supermarkets and stockpile food at home. However, supportive evidence is far from compelling, even though there has been increasing attention paid to the location of food outlets, especially those selling fast foods.
There is equivocal evidence for a relationship between the location of fast-food outlets and weight status135–143 or fast-food consumption. 135,136,138,139,144 In contrast, the relationship between fast-food outlet density and deprivation is much clearer. Research from the UK, the USA and New Zealand has shown higher numbers of fast-food outlets in areas of high deprivation. 145–157 However, there has been relatively little attention paid to whether or not access to, and the consumption of, fast food are affected by ethnicity, outside the USA at least, and how this is related to obesity. 158
This study aimed to measure access to all food outlets and to investigate the relationship with body weight, obesity and deprivation in a biethnic sample of adult women using geographic information systems (GIS) methodology. It was hypothesised that food outlet availability would be related to deprivation and that availability would be greater for South Asian participants. In addition, obese women would have greater access to food outlets, especially those selling fast foods.
Our study population came from five inner wards in the Bradford Metropolitan District, chosen because they had a range of ethnic population mix (1.2–63.8% South Asian). We included data from 1198 women within the BiB1000 cohort who lived in the study area and who provided information on age, ethnicity, height, weight at booking of pregnancy and weight at 28 weeks of pregnancy.
To map food outlet availability, we increased the study area to a total of 16 wards (five wards in which participants lived and a further 11 wards immediately bounding those areas) in recognition that individuals would not necessarily stick to the ward boundaries for local shopping and eating patterns. This search area included 819 ‘output areas’ (OAs) (these are census geographical areas; an OA contains on average 125 households). Administrative information from the Bradford Metropolitan District Council (lists of food outlets held for health and hygiene purposes) and Bradford Yellow Pages (index of local businesses) was used to identify food outlets. A random selection of 90 OAs, stratified by deprivation, were visited to audit data collected from administrative sources.
A pool of 886 outlets was identified. These outlets were classified as ‘fast food’ (n = 364), other ‘eating out’ (restaurants, cafes; n = 247), supermarkets (n = 47), specialist food shops (e.g. butcher, bakery; n = 100) and smaller retail shops selling food (e.g. convenience stores; n = 128). Four measures of food access were used: the distance to the nearest food outlet (proximity) in each category for each participant, the number of outlets within each food outlet category in a 250-m, 500-m and 1000-m radius of each individual’s residential postcode, the number (density) of food outlets of each category in each super OA (containing four to six OAs) and proximity to clusters of three or more fast-food outlets. Univariable generalised estimating equation modelling, with obesity status as the outcome and maternal age, deprivation score and food access measure as the independent variables, was undertaken for both ethnic groups. The independent variables that were significant in the univariable analyses were combined in the multivariable analyses in a forced entry method. All statistical analyses were performed using Stata 10 (StataCorp LP, College Station, TX, USA) and statistical significance was set at p < 0.05.
Our results found increased food outlet availability within more deprived areas and for South Asian populations. However, the relationship between having fast-food outlet access or availability and weight status (BMI or being obese) in the South Asian group was opposite to what was hypothesised and in the non-Asian group was non-existent. This would seem to indicate that, in the current sample, increased access or availability is not related to increased consumption. Another important finding is that > 95% of participants lived within 500 m of a fast-food outlet. This degree of saturation has not been demonstrated previously but may be characteristic of UK inner cities.
This workstream aimed to explore the context and circumstances in which food choices are made. The results from these studies have the following implications for the development of a childhood obesity prevention intervention:
-
Understandings are arrived at, and choices are made, in the context of many interlinked systems of influence and these systems should be targeted in any intervention. Delivering interventions within a group setting may help to set up positive influences through peer support.
-
Intervention effectiveness will be enhanced if practitioners know which components of parenting to target within a culturally sensitive context. Parenting styles vary according to ethnicity and those practices that might constitute targets for intervention in one group would not be applicable to another, or at least would not be of equal salience.
-
Seeking to change food and drink consumption should focus on (a) promoting the availability and quantity of all types of fruits and vegetables (e.g. encouraging the purchase of tinned/frozen fruit in addition to the purchase of fresh fruit); (b) reducing the purchase of crisps and biscuits (which were both available in > 80% of homes); and (c) discouraging the purchase of sweetened beverages, especially within homes of Pakistani mothers (with 85% of these homes having at least one type of sweetened beverage available).
-
Living in close proximity to a fast-food outlet (within 500 m) was commonplace in the Bradford wards that were studied. This degree of proximity was observed in > 95% of participants. This should be considered when applications for further food outlets are made.
Using intervention mapping to develop a culturally appropriate intervention to prevent childhood obesity: development of the Healthy and Active Parenting Programme for Early Years intervention
The previous workstreams provided a wealth of epidemiological information about the risk factors for childhood obesity and the types of interpersonal, contextual and environmental factors that can influence eating behaviours. All of these are important targets for intervention. In addition, our work, including our systematic review, highlighted the importance of considering the cultural acceptability of interventions for different ethnicities and also the acceptability of interventions for low-income groups. In the current workstream we describe the development of a culturally acceptable childhood obesity prevention programme using a technique called intervention mapping. 159 This has been published as a separate paper. 160
Intervention mapping refers to a rigorous and systematic approach to developing evidence-based interventions. We followed the six key steps as follows: (1) needs assessment of parents, the wider community and practitioners and consideration of the evidence base, policy and practice; (2) identification of outcomes and change objectives following identification of barriers to behaviour change; (3) selection of theory-based methods and practical strategies to address barriers to behaviour change; (4) design of the intervention by developing evidence-based interactive activities and resources; (5) creating an adoption and implementation plan in which parenting practitioners were trained by health-care professionals to deliver the intervention within children’s centres; and (6) creating an evaluation plan.
A multidisciplinary intervention development team was convened that included experts in the areas of parenting, nutrition, breastfeeding and physical activity as well as a group of experienced community health practitioners. The group met every 6–8 weeks over the course of a 12-month period to develop the intervention. The intervention was informed by behavioural change principles161,162 and a typology of ways of ensuring the cultural adaptation of interventions informed the development of the intervention at each stage of the process. 163
The overall desired outcome of the intervention was to prevent childhood obesity. The intervention was targeted at overweight or obese pregnant mothers. Specifically, it aimed to (1) encourage mothers to make healthy food choices antenatally and maintain a healthy diet postnatally; (2) encourage mothers to increase their level of physical activity during pregnancy and meet the recommended guidelines for physical activity (150 minutes of moderate-intensity physical activity per week164) within 12 months of giving birth; (3) encourage breastfeeding (or appropriate bottle-feeding) until at least 6 months of age; (4) encourage infants to develop healthy food preferences and a healthy dietary intake; and (5) facilitate physical activity in infants and limit sedentary time.
Given that parenting skills were highlighted as an important predictor of later obesity (see Early risk factors for childhood obesity), it was agreed that the intervention should be developed in conjunction with an established community parenting programme: the Family Links Nurturing Programme (FLNP). The FLNP is one of the preferred parenting programmes in Bradford; its aims are to develop parents’ self-esteem and self-efficacy and their understanding of their own, and their children’s, emotional and physical needs. Qualitative research has demonstrated that parents value the programme and feel that it has had a positive impact on family relationships, their children’s behaviour, relationship quality and their own mental health. 165,166 This integration with the FLNP was key to ensure the sustainability of the intervention and represented a channel to ensure delivery as part of ’usual care’ that could continue without the involvement of the research team. The parenting aspects of the intervention developed by the FLNP aimed to reduce the risk of child abuse and neglect, improve couple relationships, reduce stress and perinatal depression and increase prospective parents’ understanding of child development. In recognition of this core component of the intervention, the intervention was designed to be delivered by facilitators trained and accredited by the FLNP [see https://familylinks.org.uk/train-with-us (accessed 8 March 2016) for details of the training].
The final intervention consisted of six group antenatal sessions and six group postnatal sessions and was named HAPPY (Healthy and Active Parenting Programme for early Years). It was planned that the antenatal sessions would take place weekly, starting when the mother was at 26–28 weeks’ gestation. Each session lasted approximately 2.5 hours. The postnatal sessions started when the infant was aged 4–6 weeks and continued at key developmental milestones (9 weeks, 12 weeks, 5 months, 7 months and 9 months). A summary of the intervention content for the antenatal sessions and the postnatal sessions can be found in Tables 1 and 2 respectively. Each session was detailed in a facilitator manual with step-by-step instructions on how to deliver the intervention. A 2-day training programme was developed to supplement the existing FLNP training that practitioners had already received. This included information on the background to the intervention mapping approach taken to develop the intervention; evidence-based practical education on the key messages of the intervention (nutrition, infant feeding and physical activity); time to explore the manual and practice delivering activities; and information on the importance of intervention fidelity, including how to record deviations in delivery.
| Session | Content |
|---|---|
| 1. Brain, science and bonding | Parent diet: healthy diet in pregnancy; links between what you eat when pregnant, you and your baby; links between maternal and childhood obesity; reflection on own diet and importance of food in the family |
| Parent physical activity: how the baby is developing in the womb and how physical activity can facilitate this | |
| Breastfeeding: identifying and overcoming barriers to breastfeeding | |
| 2. A celebration of birth | Parent diet: importance of eating well for the baby; dispel myths about weight gain in pregnancy and provide up-to-date information; Smart Snacks handout; food diaries |
| Parent physical activity: being active during pregnancy; discussion regarding myths about physical activity in pregnancy | |
| 3. Personal power, self-esteem and healthy choices about food | Parent diet: address barriers to healthy eating and plan for ways to overcome them; signpost to cooking information points; healthy foods can be convenient and inexpensive; impact of mother eating unhealthy foods; plan alternative cooking methods |
| Parent physical activity: list activities that women think they could do, work through from easy to difficult; gentle strengthening and conditioning exercises: demonstration by practitioners; worries about physical activity; visualise and positive self-talk; identify when activity can be freely integrated into normal life | |
| Breastfeeding: advantages/disadvantages of breastfeeding and bottle-feeding; the more you feed, the more milk is produced; encourage the identification of an influential family member, clarify likes and dislikes, talk with family members about these issues to enlist their support; learn more about breastfeeding skills; overcome stigma about breastfeeding in public, stories from other mothers | |
| 4. Boundaries, beliefs and values | Parent diet: additional information about snacks, food treats, swaps |
| Parent physical activity: back-up plan for physical activity at different times | |
| Breastfeeding: values and beliefs about bringing up children and linking this to breastfeeding | |
| 5. Feelings and how we communicate | Parent diet: food swaps and healthy meals feedback; identify vulnerable points in time and have contingencies for when want unhealthy foods |
| Parent physical activity: partners review their progress with regard to the collaborative plans made for physical activity in session 4; discussion about feelings relating to whether or not activity plans were fulfilled | |
| 6. Beyond labour day | Parent diet: identify someone at home/friend to discuss food habits with |
| Parent physical activity: pelvic floor exercises for immediately after pregnancy if uncomplicated; what activities are OK after pregnancy | |
| Breastfeeding: how to make up bottle correctly; signpost to health professionals; environmental changes: clothes that facilitate feeding; locations nearby; family members can do other things with the baby (than formula feed), e.g. bottle-feed using expressed milk; infant diet: planning ahead |
| Session | Content |
|---|---|
| 7. A celebration of birth (4 weeks) | Parent diet: information about what a healthy diet should consist of; food diaries; reflect on own diet and importance of food in the family |
| Parent physical activity: what activities are OK after pregnancy; gradually introduce more strenuous activity; leaflet with activity examples; physical activity for new mums quiz sheet; practitioner dispels myths | |
| Breastfeeding: reinforce that the more you feed, the more milk is produced; identifying someone to obtain support from; responsive feeding | |
| Infant physical activity: guidelines for baby activity; myths about physical activity for babies and infants; practitioner dispels myths; weekly age-appropriate activities; encourage structured and unstructured play | |
| 8. Bringing structure to your life (2 months) | Parent diet: healthy eating for parents vs. children; reflect on own eating patterns and provide ideas; balancing diet and avoiding takeaways |
| Parent physical activity: likes/dislikes about physical activity; activities for after pregnancy; identify barriers; integrating activity into normal life; small changes to family environment; structured activities in the house; the local area; self-talk and visualisation; choose a physical activity to learn or can already do | |
| Breastfeeding: identifying barriers; concerns about feeding baby; how to deal with life while trying to feed; encourage asking for help to enable breastfeeding to continue and other things to be accomplished | |
| Infant diet: introducing solids: why and when; follow signs of readiness for weaning | |
| Infant physical activity: structured play activities in the house without expensive toys; introducing games; recognising when baby wants to play; being flexible with playtime; making baby-active time a priority | |
| 9. Feeding and feelings (3 months) | Parent physical activity: identifying and addressing barriers; coping planning; the ’Pram Pedometer Challenge’ |
| Infant diet: what food and drinks to give; weaning: how to do it – texture and variety, developmental stages, equipment; repeated exposure and coping with food refusal; consequences of an unhealthy diet; facial expressions and tongue thrusting | |
| Infant physical activity: importance of other family members engaging the baby in activity; weekly age-appropriate activities for baby and mum; making home modifications to improve child physical activity and/or eating | |
| 10. Families and food (5 months) | Parent diet: feeding a family – what does it take; meal planning; shopping lists; healthy foods can be convenient and inexpensive; reading food labels; impact of mother eating unhealthy foods |
| Parent physical activity: review of group progress and setting goals for forthcoming weeks | |
| Infant diet: eating together; modelling behaviour and feeding role of family and parents; time issues with food planning and preparation | |
| Infant physical activity: discussion of television watching; entertaining baby/keeping baby safe when doing chores; doing activity as a family; weekly age-appropriate activities for baby and mum are demonstrated and practised; how to baby proof your house for safe physical activity | |
| 11. Making the most of your day (7 months) | Parent physical activity: review of group progress and setting goals for forthcoming weeks |
| Infant diet: weaning: how it’s going, introducing lumps | |
| Infant physical activity: visualisation and self-talk to build confidence; discussion of barriers and how to overcome them; planning for meal preparation, infant napping and active play; when can activity be integrated into normal life; environmental changes; weekly age-appropriate activities for baby and mum are demonstrated and practised; revisit discussion of sedentary behaviour and use of television | |
| 12. Continuing the HAPPY journey (9 months) | Parent physical activity: review of physical activity achievements; reflect on experiences; plan for physical activity in the future; include follow-up monitoring plan by practitioners; announce group winners |
| Infant diet: keeping motivated to feed family well | |
| Infant physical activity: structured play activities in the house; involving family and friends with infant play; what local area has to offer; baby proof your house in a physical activity-friendly way; weekly age-appropriate activities; planning for after the parenting programme; joining mum and baby activity groups; signposting and goal-setting |
The intervention mapping process, with its focus on multidisciplinary intervention development, resulted in the development of a multifaceted and evidence-based programme, capable of being integrated into existing health services within a multiethnic community in the UK. To our knowledge, this is the first childhood obesity prevention intervention of its kind with a focus on cultural appropriateness that integrates evidence based on physiological and psychosocial data collected from the local community.
The intervention mapping process was complex, time-consuming and not without challenges. These included managing competing interests from the stakeholder group and ensuring that the team understood enough about the technicalities of the process to ensure that appropriate intervention strategies were being highlighted.
Feasibility randomised controlled trial of the Healthy and Active Parenting Programme for Early Years intervention
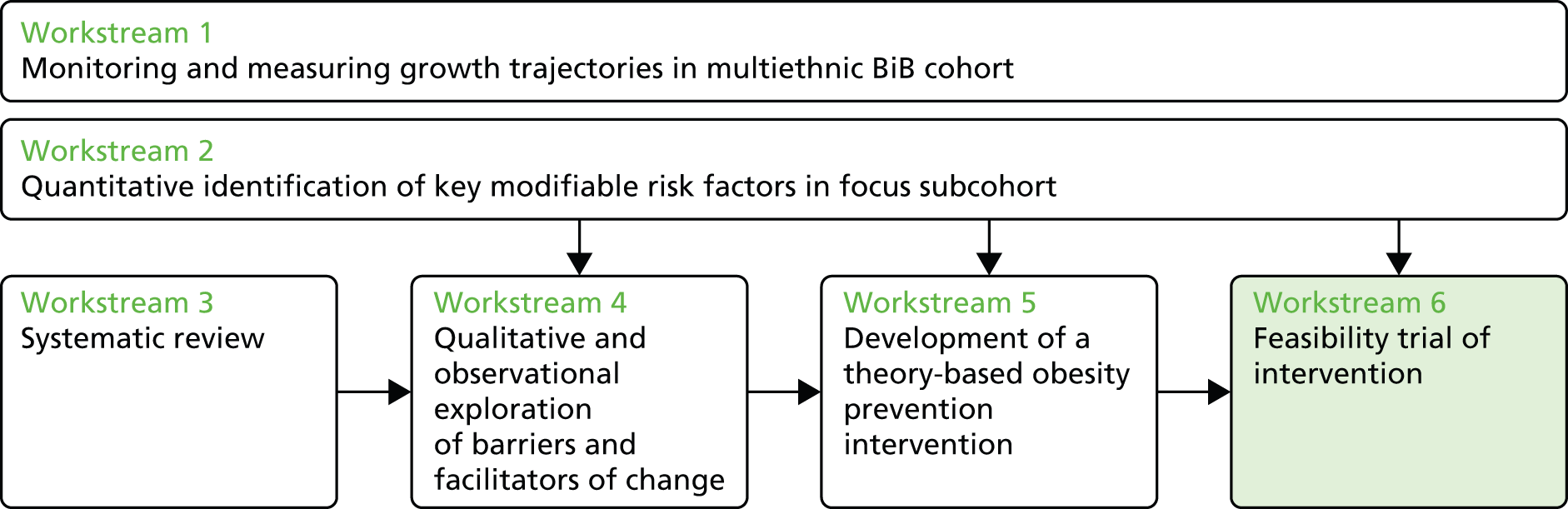
Having developed the HAPPY intervention, the current workstream aimed to test its feasibility and acceptability in a feasibility RCT (Phase II trial). We also aimed to provide information to inform the development of a full RCT (Phase III trial). The results of this feasibility RCT have been reported in a published article. 167
The specific objectives of the feasibility trial were to (1) establish the number of eligible participants in a maternity unit setting and an achievable recruitment rate; (2) establish the follow-up and attrition rates for the control and intervention groups; (3) assess the acceptability of the randomisation strategy and measurement tools; (4) determine whether or not data required for economic analysis can be collected reliably; (5) determine the primary outcome measure to estimate effect size and intraclass correlation coefficients to enable an accurate sample size calculation for a full trial; (6) assess the acceptability of the HAPPY intervention to parents and facilitators; (7) evaluate the fidelity of programme implementation and delivery by facilitators and (8) establish the capability and capacity of children’s service providers to deliver and incorporate the intervention into their programme of work.
An individually randomised controlled feasibility trial with blinded assessment was conducted. Inclusion criteria were being overweight or obese (having a BMI of ≥ 25 kg/m2 at the time of the pregnancy booking visit), being at least 18 years of age, able to attend intervention sessions and able to understand intervention sessions in the English language. Eligible participants were randomised to either an intervention group or a control group (usual care) in a 1 : 1 ratio stratified by maternal BMI (25–29.9 kg/m2/≥ 30 kg/m2), ethnicity (South Asian/other) and parity (first child/at least one other child). Participants completed questionnaires at baseline (T0, prior to randomisation, approximately 24 weeks’ gestation) in their home and again when their baby was 6 months old (T1, approximately 10 months after baseline, telephone interview) and 12 months old (T2, approximately 16 months after baseline, in person). Observations, qualitative interviews and structured questionnaires with facilitators were used to explore acceptability and fidelity. The trial was approved by the Bradford Research Ethics Committee (reference number 11/YH/0458) (trial registration number ISRCTN56735429).
The recruitment rate of those screened with a BMI of ≥ 25 kg/m2 was 30% (120/396). A Consolidated Standards of Reporting Trials (CONSORT) flow diagram can be found in Figure 2. Retention at 12 months was 66% for the intervention group and 75% for the control group. Of the 59 allocated to the intervention, 26 (44%) attended at least one antenatal appointment (attending on average 4.8 sessions) and 18 (31%) attended at least one postnatal session (average 4.6 sessions). Participants expressed some burden with regard to the baseline questionnaire assessment, particularly around the self-reported assessment of diet and physical activity. Responses to randomisation were mixed and there was some evidence that women were unsure of the reasons why they had been asked to take part, highlighting some problems with effective communication during the screening period. We found no problems with collecting economic data (service use and quality of life) at either the 6-month or the 12-month follow-up period.
FIGURE 2.
Consolidated Standards of Reporting Trials (CONSORT) flow diagram of study recruitment and retention. a, A small number of women ticked more than one reason, so totals add up to 129; b, recruitment target reached.

We explored a range of appropriate possible outcome measures: age- and sex-adjusted z-score at 12 months; conditional weight gain > 1 centile band; conditional weight gain > 2 centile bands; and weight > 85th centile at 12 months. Analysis indicated that any could be considered in a future Phase III trial. The adjusted effect size using age and standardised weight z-score at 12 months was 0.25 (95% CI –0.16 to 0.66, adjusted for maternal BMI, parity and ethnicity), favouring the intervention. After discussion with a range of clinical experts, with regard to the sample size calculation, we felt that it was important in the definitive trial to take into account the ideal minimum clinically important difference (MCID) and also ensure that the follow-up period would be long enough to give confidence in the sustained impact of the intervention. We selected a MCID of 0.3 BMI SDS at 24 months as the effect size for our Phase III trial.
Participant and facilitator reaction to the intervention content was positive overall. For those in the intervention group there were no associations between attendance at intervention sessions and maternal age, gestational age, parity, booking BMI or ethnicity. Reasons for non-attendance at intervention sessions were explored with seven mothers. Some mothers (3/7) knew from the start of the project (e.g. baseline visit) that they would not be able to attend sessions because of work commitments or other concerns. Others found attendance difficult because of the timing and locations of the sessions.
Fidelity as assessed by observations of sessions and facilitator logs was high. There were some issues with certain sessions with facilitators feeling that there was too much content to cover in the time allotted, but on the whole facilitators rated delivery as straightforward/easy. Facilitators expressed some disappointment at the low numbers of women attending the sessions (ranging between two and six respondents per session).
Each intervention session was delivered by two parenting programme facilitators and required 4.5 hours of facilitator time in total (2.5 hours delivery, 1.5 hours preparation, 30 minutes contacting families). This amounted to typical staff costs of £142 per session, assuming a mix of seniority. All rooms were provided free of charge in local children’s centres. Training time of 3 days per facilitator was required to allow them to deliver the intervention. One-off materials required to run the group (e.g. manuals for facilitators, reference books and DVD) cost £425 and materials for individual participants (e.g. parenting puzzle book, small gifts such as magnets, gift for child) cost £36 per participant. The total cost of staff time to deliver the training was £1163.
The feasibility trial suggests that recruitment and measurement for a definitive trial is feasible and that the HAPPY intervention is acceptable to parents and facilitators. Our experiences of recruitment are in line with those in other similar studies168–171 and our process evaluation has identified valuable areas to consider to improve intervention attendance. For example, participants allocated to the intervention who engaged early (i.e. came to the first session) were likely to continue to attend future sessions. However, there was a high overall attrition rate, with many participants lost early. This was largely because the team was unable to make contact with participants (after multiple attempts to call, visit homes and search GP records). It is clear that multiple methods of contact need to be collected at baseline and then during every subsequent assessment, including contacts for extended family members, friends and neighbours. One option that we plan to explore for a definitive full trial is the possibility of obtaining e-mail addresses and social media identities, which would be validated at recruitment. In addition, qualitative data from participants also indicated that not all of those recruited fully understood the requirements of being involved in the trial. As a consequence, some were not committed to being involved.
Based on our learning and other similar trials of complex interventions, we recommend a range of strategies to maximise intervention attendance and ensure optimal group sizes for the full trial. First, it is important for research midwives to provide more information at screening and recruitment about the nature of the trial and the expectations of participants. It is hoped that this will avoid the problem of recruiting individuals who are not committed or who are not likely to participate in the intervention should they be randomised. Second, post-randomisation home visits by facilitators should be planned to meet participants and set expectations about the intervention and to encourage attendance at the first intervention session.
We found that recruitment through research nurses is feasible and this has enabled us to set realistic recruitment targets for future centres who might be involved in a full trial. Within the current feasibility study we recruited an average of 13 participants per month despite a slowing of recruitment experienced during the month of Ramadan. Given that many larger maternity units recruit to competing trials, we believe that a realistic recruitment target of around nine women per month would be feasible.
This feasibility study has a number of important lessons for the planned definitive trial. We found that recruitment and study attrition rates were in line with those in other similar trials. On the whole, measurement tools and randomisation posed no major problems for study participants, although there were some issues with the assessment of potential secondary outcomes for physical activity. Participants, facilitators and service providers found the intervention to be useful and the fidelity of implementation was high. Although there was a high dropout rate for the initial intervention session, our findings suggest that those who attended the first session were likely to continue attending.
The current findings were considered sufficiently encouraging to develop a definitive Phase III trial. A funding application is currently under way.
One of the biggest challenges of the Phase II trial was setting up intervention groups of 8–10 women who were within 6 weeks’ gestation of each other and who lived in close proximity to one another. As a result, groups often did not run to capacity. This clearly impacted on costs and had an impact on the group dynamics. In response, we have changed the design so that, instead of conducting individual randomisation, clusters of 10 women will be allocated to the intervention or control together so that groups can be delivered to capacity (with individual randomisation, if it is feasible to recruit only 10 women within 6 weeks, there would not be enough to run a group after randomisation is considered). In addition, we plan to deliver the intervention in a central location with good transport links (similar to other antenatal classes) so that we do not have to wait for sufficient numbers of women to be recruited from a given postcode.
Conclusions and recommendations
Summary
This research programme has successfully achieved its principal aim of studying the patterns and aetiology of childhood obesity in a multiethnic population and has used this evidence to develop and pilot an obesity prevention intervention for early infancy. The programme completed almost all of its original objectives on time and on budget. A 9-month ’waiting period’ for 1-year weight outcomes was not factored in to the original grant timetable and so has created some no-cost delay with regard to the results of the feasibility trial.
The programme has promoted strong involvement of participants and practitioners. Almost 2000 families have been recruited into the study and they have been closely followed up for 3 years. Their enthusiasm for the research and altruism they have shown in providing information and participating in activities have been a constant source of motivation for the research team. These Bradford families have donated considerable amounts of time and shared their thoughts with the research team. This has enabled us to build up a detailed picture of the pattern of their lives and the interactions that characterise their families. This is an essential requirement if we are to understand the early risk factors for obesity.
Over 300 health visitors and 100 midwives were actively involved in the routine growth measurements for the study. Their role might be best described as co-producers of this research. This commitment to collect additional data and to engage with the possibility of changing established practices reflects a deep-rooted support for health research among this group of NHS staff. Both in this research programme and in the wider collaborations centred on the BiB birth cohort study it has been apparent that this willingness to engage in research and to consider changes in practice, both to facilitate research and to implement findings, is apparent in other groups of NHS staff. The importance of having the enthusiastic support of NHS staff and the potential for change that this produces was central to the research teams obtaining a major Collaboration for Leadership in Applied Health Research and Care (CLAHRC) grant from the NIHR. This implementation award allowed us to set up communities of practice for health visitors and midwives, providing time and space for clinicians to understand and harness the rich research and routine data that we were collecting in order to improve the quality of services. As a result of this close involvement, the redesign of services was achieved and improvements in services were implemented.
We have brought together national academic experts from Bradford, Leeds, York, Bristol, Edinburgh, Loughborough, Durham and London to establish a strong multidisciplinary research network. Over the course of 5 years we have pooled our experience to develop a robust but pragmatic approach to improving the understanding, monitoring and prevention of childhood obesity. This critical mass of academic experts has provided a strong partnership for further research capacity building. This has led to synergistic grant awards totalling over £4M from the NIHR, Medical Research Council, Diabetes UK, British Heart Foundation, Child Growth Foundation, Lullaby Trust (formally the Foundation for Sudden Infant Death Syndrome; FSID) and European Union covering a range of research from biomedical science to implementation science. In addition to the HAPPY feasibility trial we were successful in obtaining NIHR funding for another pilot trial of preschool play in the playground to increase physical activity in early life. The programme has provided a research platform for five Master’s students and five PhD students and has led to one Medical Research Council postdoctoral fellowship.
We are continuing to write up all of our new findings but so far > 16 papers have been accepted for peer-review publication and 36 abstracts have been published. Our Healthy Weight app is on iTunes and there is considerable interest from the children’s centres involved in the feasibility trial in terms of using the HAPPY intervention. Our results on South Asian cut-off levels for BMI have informed the latest National Institute for Health and Care Excellence (NICE) guidance on assessing BMI in minority ethnic groups (NICE PH46). 172 We have had strong media interest in our results with items on BBC television news and Radio 4 as well as on local radio stations and in local newspapers [see www.borninbradford.nhs.uk/the-biB-film-photography-and-poetry-gallery/ (accessed 16 March 2016)].
Conclusions from our research
The programme was successful in establishing a new childhood obesity cohort with longitudinal data collection in BiB1000. This cohort has provided a sample for the NIHR programme to develop an understanding of the predictors of and influences on health-related behaviours to help develop feasible and appropriate culturally specific intervention(s) for the prevention of childhood obesity. A unique quality of this cohort is its ethnic composition, with approximately 50% of women in the cohort being of South Asian origin, and the fact that it includes a representative sample of women from across socioeconomic groups within Bradford. Importantly, the cohort also provides a unique resource for the study of the long-term consequences of growth for childhood and later adult weight. Associations between growth and early weight and child health outcomes and educational attainment can be investigated at low cost because of the success of linkages that have been established in Bradford with primary care and education data.
There are a number of general limitations that should be considered as part of our overall conclusions. Our study was undertaken in one city and, although the results are likely to be generalisable to other large multiethnic cities in the UK, the particular white British/Pakistani composition of the BiB1000 cohort will be unique to Bradford. Prospective birth cohort studies are one of the most robust epidemiological study designs for investigating the aetiology of ill health. However, the observational nature of the design prevents any claims of causal attribution. Our qualitative studies have limitations in terms of the small sample sizes and generalisability and cannot provide quantitative predictions. Our pilot trial is by its nature preliminary and we found difficulties with recruitment and poor initial attendance.
The growth data collected as part of the BiB1000 study, supplemented with routine measurements collected by health workers in the community, provided a comprehensive and reliable data set to investigate growth in infancy and the development of obesity in childhood. For the first time in the UK we estimated weight and length growth trajectories between birth and 2 years for Pakistani boys and girls and found that they were lighter and had a shorter predicted mean length at birth than their white British counterparts, but gained weight and length more quickly in infancy. By age 2 years both ethnic groups had a similar weight but Pakistani boys and girls were taller on average than white British boys and girls. These differences in postnatal growth were not explained by maternal height, smoking during pregnancy or gestational age. We also developed data-driven prediction equations for risk of childhood obesity and incorporated them into a mobile phone app, thereby providing proof of concept that childhood obesity prediction research could be integrated with advancements in technology to deliver a clinically relevant tool to practitioners.
We found ethnic differences in breastfeeding, infant diet and sleeping patterns and in the types of physical and sedentary activities that the children engaged in. There was also evidence of dietary patterns that emerged at 12 months tracking to 18 months. Once established these patterns may become ingrained and difficult to change. There was little evidence that parenting styles differed between ethnic groups. It is important to understand ethnic differences in modifiable risk factors for childhood obesity so that interventions developed to reduce childhood obesity can be culturally adapted.
Linear and Poisson regression was used to determine the relative risk between risk factors and infant overweight. Smoking during pregnancy, maternal BMI, feeding style and parenting style were all associated with infants’ BMI at age 3 years. However, the associations between these risk factors and childhood BMI did not vary by ethnicity. Interventions to reduce childhood obesity should target smoking and maternal weight in the antenatal period and postnatally encourage the adoption of warmer, less hostile parenting styles and stricter approaches to feeding.
Our systematic review of diet and physical activity interventions to prevent or treat obesity in South Asian children and adults identified 29 studies, seven in children, 21 in adults and one in a mixed-age population. Meta-analysis of a limited number of controlled trials found an unclear picture of the effects of interventions on BMI for South Asian children. Meta-analyses of a limited number of controlled trials showed significant improvement in weight for adults but no significant differences in BMI and waist circumference. One high-quality study in South Asian children found that a school-based physical activity intervention that was delivered within the normal school day and which was culturally sensitive was effective. There was also evidence of culturally appropriate approaches to, and characteristics of, effective interventions in adults, which we believe could be transferred and used to develop effective interventions in children.
Our qualitative and observational studies exploring the influence of the family and neighbourhood settings identified a major gap in the cultural appropriateness of current measures and existing interventions for South Asian families living in the UK. Interventions need to consider how parents, in particular mothers, negotiate between the many factors that influence their behaviour, including cultural and family influences. That negotiation will be aided by interventions that support the development of self-efficacy and which offer support in how to evaluate the wide variety of advice that parents receive. Knowledge of the types and quantities of foods and drinks in family homes supports the development of intervention programmes that target an improvement in the foods available, both for obesity prevention or management and for overall diet improvement. Specifically, increasing the consumption of fruits and vegetables and reducing the consumption of sweetened drinks, crisps and biscuits should be a target. The stronger association between deprivation and fast-food density than obesity argues for more detailed accounts of the obesogenic environment that include measures of individual behaviour. The proliferation of fast-food outlets has public policy relevance and should be considered in planning applications.
Intervention mapping provided a feasible approach to developing a complex health behaviour change intervention (HAPPY). The approach was used to produce a transparent and replicable intervention whereby mechanisms of change can be investigated and identified and strategies used to manipulate them can be appropriately refined. Integration with the existing FLNP allowed the HAPPY intervention to access and utilise the expertise of existing parenting programme co-ordinators to deliver the intervention, thus increasing sustainability.
The HAPPY intervention was evaluated in a pilot RCT and was found to be feasible and acceptable. However, the recruitment rate was low and attrition between randomisation and intervention attendance was high. The full trial should address the importance of ensuring that women understand fully the nature of the research. To reduce attrition multiple methods of contact need to be collected at baseline and then during every subsequent assessment, including contacts for extended family members, friends and neighbours. A 24-month primary end point should be used to evaluate the longer-term effect of the intervention.
A proposal for a full multisite cluster RCT has incorporated these strategies and has been submitted for funding to evaluate the cost-effectiveness of the HAPPY intervention.
Recommendations for research
BiB1000: a cohort for the study of childhood obesity
-
Funding should be sought to support the follow-up of this unique multiethnic child growth cohort to investigate the associations between early life exposures and later child and adult obesity.
-
Data linkage to national child measurement data should be undertaken to describe growth trajectories of the children to reception year and year 6. This provides a low-cost method for capturing subsequent BMI data and an opportunity to rerun analyses of associations of modifiable risk factors with later outcomes.
Child growth
-
Reliability checks including external observation of intraobserver and interobserver error should be considered to measure the accuracy of routine growth data.
-
Further replication of our findings regarding ethnic differences in weight and length growth trajectories in infancy is needed.
-
Research is needed that explores longer-term follow-up of these growth trajectories and examines the associations with a range of anthropometric and clinical outcomes.
-
Further research is also needed to understand the genetic and environmental factors that might explain these differences.
-
Further validation of the mobile phone app in other populations is needed and qualitative work is needed to understand how the mobile phone app is received by health-care practitioners.
Ethnic differences in risk factors for childhood obesity
-
Despite higher rates of breastfeeding initiation and continuation to 4 months in minority ethnic groups, there is no evidence of ethnic differences in exclusive breastfeeding rates at 4 months. Therefore, interventions to increase exclusive breastfeeding rates need to target all ethnic groups.
-
In light of the introduction of inappropriate foods during infancy and evidence of tracking of dietary patterns between infancy and toddler age, healthy eating advice should be offered to parents before weaning begins to maximise the possibility of establishing healthy feeding patterns.
-
Obtaining data on 24-hour sleep patterns (not just night-time sleep) is vital for ethnic comparisons.
-
Future research on the impact of school times on constraining sleep duration of Pakistani children and its consequences in middle childhood should be explored.
-
Interventions in the early years should focus on parental behaviours and attitudes and barriers to their child’s physical activity.
-
Early years interventions should support parents to encourage their child’s physical activity; this is likely to include playing actively with their children and taking them to places where they can be physically active.
-
Further research is needed to investigate the association between early parenting and later childhood health, growth and behaviour.
Determinants of childhood obesity
-
Further research is needed to investigate differences between questionnaire responses and results from direct observation of child–feeding interactions.
-
More evidence on behaviour (purchase and consumption) and the use of transport for shopping is critical in developing our understanding about the role of fast-food outlets in the development of obesity.
-
GIS methods should be used to investigate the association of green space exposure with physical activity and childhood obesity.
Systematic review
-
We have described the types of interventions that show promise but we do not know which specific intervention components are effective. We recommend that more obesity interventions targeting South Asian populations are developed, particularly those targeting preschool children and their families. These studies should report (1) how interventions are culturally adapted; (2) the types of behaviour change techniques and theories that are used to underpin interventions; (3) anthropometric outcomes by measures of socioeconomic status; and (4) implementation and running costs. These recommendations would enable reviewers to assess how behaviour change techniques and theories moderate effectiveness, assess the equity impacts of interventions and examine explanations for heterogeneity between interventions.
-
The development of effective interventions may well require a great deal of qualitative and quantitative research on knowledge, attitudes, behaviours and perceptions.
-
More research is needed into the differential effects of lifestyle interventions in South Asian populations and other ethnic populations. The general approach so far has been to culturally adapt existing interventions; however, there may well be a need to develop new interventions from first principles.
Obesity intervention trial
-
Further research is needed to explore how to engage overweight mothers and motivate them to attend group-based intervention sessions and how to maintain attendance over time. Intervention sessions need to be planned in advance, allowing mothers a choice of dates and enabling facilitators to book protected time to run the sessions.
-
Future research should investigate the impact of different methods of recruitment (e.g. geographical vs. centralised) on intervention attendance and attrition.
-
A full-scale multisite cluster RCT should be conducted to examine the effectiveness and cost-effectiveness of the intervention. This should incorporate lessons from the pilot trial about recruitment and retention and include a longer-term primary end point.
-
Exploration of the best ways of translating knowledge and skills surrounding behaviour change to parenting practitioners would be beneficial to make maximum use of interactions surrounding lifestyle behaviour change. Further research is required to explore whether or not the HAPPY intervention materials can be adapted into other lower-cost means of dissemination (e.g. self-directed internet resources) and whether or not this offers an additional cost-effective means of intervention.
Acknowledgements
We are grateful to all of the families who took part in this study, the midwives for their help in recruiting them, the paediatricians and health visitors and the Born in Bradford team, which included interviewers, data managers, laboratory staff, clerical workers, research scientists, volunteers and managers.
We are particularly grateful to Pauline Raynor for her wonderful leadership and management in the recruitment of the BiB1000 cohort and to Derek Tuffnell for his clinical support. The development of the nutritional components of the HAPPY intervention owes much to the dedication and support of Jackie Loach and Judith Sargent and her team of Family Links facilitators, who were the driving force behind the successful implementation of the intervention. Ann Barratt helped to ensure that strong public engagement shaped the research from start to finish. Carolyn Clover and Lynn McVey provided indispensable administrative support.
The success of this programme is the result of the hard work and dedication of the following research staff: Dagmar Wailblinger, Sameera Ali, Kate Thompson, Samina Janjua, Sarah Ahmed, Zille Rabab, Jackie Bannister, Asma Hussain, Jo Stott, Rosalie Jozefek, Kerrie Jennings, Chrissie Bradley, Umar Toseeb, Aliyah Rizvi, Sameah Sabir, Emma Snowden, Julia Blackburn, Rihab Potrick, Syeda Ahmad, Natalie Baker and Julia Hackett.
We are grateful to completed and current PhD students who have worked on the BiB1000 study. These include Will Johnson, Jane West, Noortje Uphoff, Tom Norris, Daniel Bingham, Teumzghi Mebrahtu and Katy Shire (completed) and Hannah Roberts and Katie Marvin-Dowle (current).
Steering group members include John Wright, Carolyn Summerbell, Amanda Farrin, Diane Farrar, Emily Petherick, Gerry Richardson, Jackie Loach, Judith Sargent, Maria Bryant, Neil Small, Noel Cameron, Pinki Sahota, Raj Bhopal, Rosie McEachan, Sally E Barber and Shaheen Akhtar.
Contributions of authors
John Wright was responsible for the introduction to the report and the conclusions and recommendations.
Lesley Fairley, Emily Petherick, Gillian Santorelli, Debbie A Lawlor, Noel Cameron, Jane West and John Wright were responsible for modelling growth trajectories and obesity risk.
John Wright, Rosemary McEachan, Maria Bryant, Pinki Sahota, Gillian Santorelli, Sally Barber, Natalie Taylor, Amanda Farrin, Diane Farrar and Neil Small carried out the feasibility RCT of the HAPPY intervention.
John Wright, Maria Bryant, Gillian Santorelli and Jane West were responsible for recruitment and data collection for the BiB1000 study to investigate childhood obesity.
Lesley Fairley, Pinki Sahota, Gillian Santorelli, Sally Barber, Helen Ball and John Wright carried out the study on ethnic differences in obesity risk factors.
John Wright, Pinki Sahota and Natalie Taylor were responsible for using intervention mapping to develop a culturally appropriate intervention to prevent childhood obesity: development of the Healthy and Active Parenting Programme for Early Years intervention.
John Wright, Lesley Fairley, Maria Bryant, Emily Petherick, Pinki Sahota, Gillian Santorelli, Sally Barber, Debbie A Lawlor, Raj Bhopal, Noel Cameron, Andrew Hill, and Helen Ball carried out the study on early risk factors for childhood obesity.
Carolyn Summerbell and Tamara Brown carried out the systematic review of interventions to promote a healthy diet and physical activity in pregnant women and mothers with children under the age of 6 years with a focus on South Asian populations and low-income families.
Maria Bryant, Andrew Hill and Neil Small carried out the investigation of social and environmental determinants of childhood obesity.
Contributions of others
Will Johnson was involved in the study on modelling growth trajectories and obesity risk.
Stephanie Prady was involved in the study on ethnic differences in obesity risk factors.
Darren C Greenwood was involved in the study on early risk factors for childhood obesity.
Helen Moore, Sarah Smith, Wayne Douthwaite were involved in the systematic review of interventions to promote a healthy diet and physical activity in pregnant women and mothers with children under the age of 6 years with a focus on South Asian populations and low-income families.
Shaheen Akhtar, Sarah Wilson, Pauline Raynor, S Collins, LK Fraser, KL Edwards, M Tominitz and GP Clarke were involved in the investigation of social and environmental determinants of childhood obesity.
Shaheen Akhtar, Judith Sargent, Daniel Bingham, Sara Ahern and Gerry Richardson were involved in the feasibility RCT of the HAPPY intervention.
Publications
Recruitment and data collection for the BiB1000 cohort to investigate childhood obesity
Bryant M, Santorelli G, Raynor P, Fairley L, West J, Lawlor DA, et al. Born in Bradford 1000 (BIB1000): study design and cohort population characteristics. Longit Life Course Stud 2013;4:119–35.
Modelling growth trajectories and obesity risk
Johnson W, Cameron N, Dickson P, Emsley S, Raynor P, Seymour C, et al. The reliability of routine anthropometric data collected by health workers: a cross-sectional study. Int J Nurs Stud 2009;46:310–16. (Full-text article included in Appendix 3.)
Bryant M, Santorelli G, Fairley L, Petherick ES, Bhopal R, Lawlor DA, et al. Agreement between routine and research measurement of infant height and weight. Arch Dis Child 2015;100:24–9.
Fairley L, Petherick ES, Howe LD, Tilling K, Cameron N, Lawlor DA, et al. Describing differences in weight and length growth trajectories between white and Pakistani infants in the UK: analysis of the Born in Bradford birth cohort study using multilevel linear spline models. Arch Dis Child 2013;98:274–9.
Santorelli G, Petherick ES, Wright J, Wilson B, Samiei H, Cameron N, et al. Developing prediction equations and a mobile phone application to identify infants at risk of obesity. PLOS ONE 2013;8:e71183.
Ethnic differences in obesity risk factors
Santorelli G, Petherick ES, Waiblinger D, Fairley L. Ethnic differences in the initiation and duration of breastfeeding: evidence from the Born in Bradford cohort study. Paediatr Perinat Epidemiol 2013;27:388–92. (Full-text article included in Appendix 3.)
Prady SL, Kiernan K, Fairley L, Wilson S, Wright J. Self-reported maternal parenting style and confidence and infant temperament in a multi-ethnic community: results from the Born in Bradford cohort. J Child Health Care 2013;18:31–46. (Full-text article included in Appendix 3.)
Early risk factors for childhood obesity
Fairley L, Santorelli G, Lawlor DA, Bryant M, Bhopal R, Petherick ES, et al. The relationship between early life modifiable risk factors for childhood obesity, ethnicity and body mass index at age 3 years: findings from the Born in Bradford birth cohort study. BMC Obesity 2015;2:9.
Systematic review of diet and physical activity interventions to prevent or treat obesity in South Asian children and adults
Brown T, Smith S, Bhopal R, Kasim A, Summerbell C. Diet and physical activity interventions to prevent or treat obesity in South Asian children and adults: a systematic review and meta-analysis. Int J Environ Res Health 2015;12:566–94. URL: www.mdpi.com/1660-4601/12/1/566/htm#B40-ijerph-12-00566 (accessed 16 March 2016).
Investigation of social and environmental determinants of childhood obesity
Fraser LK, Edwards KL, Tominitz M, Clarke GP, Hill AJ. Food outlet availability, deprivation and obesity in a multi-ethnic sample of pregnant women in Bradford, UK. Soc Sci Med 2012;75:1048–56. (Full-text article included in Appendix 3.)
Bryant M, Sahota P, Santorelli G, Hill A, Wright J. An exploration and comparison of food and drink availability in homes in a sample family of white and Pakistani origin within the UK. Public Health Nutr 2015;18:1197–205. (Full-text article included in Appendix 3.)
Using intervention mapping to develop a culturally appropriate intervention to prevent childhood obesity: development of the Healthy and Active Parenting Programme for early Years intervention
Taylor N, Sahota P, Sargent J, Barber S, Loach J, Louch G, et al. Using intervention mapping to develop a culturally appropriate intervention to prevent childhood obesity: the HAPPY (Healthy and Active Parenting Programme for Early Years) study. Int J Behav Nutr Phys Act 2013;10:142.
Feasibility randomised controlled trial of the Healthy and Active Parenting Programme for early Years intervention
McEachan RRC, Santorelli G, Bryant M, Sahota P, Farrar D, Small N, et al. on behalf of the BiB Childhood Obesity Scientific Group. The HAPPY (Healthy and Active Parenting Programme for early Years) feasibility randomised control trial: acceptability and feasibility of an intervention to reduce infant obesity. BMC Public Health 2016;16:211. URL: http://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-016-2861-z (accessed 16 March 2016).
Other outputs from programme grant
Recruitment of the BiB1000 cohort to investigate childhood obesity
Journal articles
West J, Manchester B, Wright J, Lawlor DA, Waiblinger D. Reliability of routine clinical measurements of neonatal circumferences and research measurements of neonatal skinfold thicknesses: findings from the Born in Bradford study. Paediatr Perinat Epidemiol 2011;25:164–71.
Johnson W, Cameron N, Raynor P, Woffendin C, Wright J. Monitoring growth: the benefits and challenges of integrating the Born in Bradford research project with routine growth monitoring practice. Community Practitioner 2009;82:34–5.
Raynor P, Born in Bradford Collaborative Group. Born in Bradford, a cohort study of babies born in Bradford, and their parents: protocol for the recruitment phase. BMC Public Health 2008;8:327.
Bryant M, Santorelli G, Lawlor DA, Farrar D, Tuffnell D, Bhopal R, et al. A comparison of South Asian specific and established BMI thresholds for determining obesity prevalence in pregnancy and predicting pregnancy complications: findings from the Born in Bradford cohort. Int J Obes (Lond) 2013;38:444–50.
Conference presentations
Bryant M. Should the NHS use specific ethnic criteria to categorise South Asian women as ’obese’ during pregnancy? Oral presentation. Born in Bradford: Putting Research into Practice?, Annual Conference, Bradford Royal Infirmary, Bradford, UK, 28 June 2012.
Fairley L, Small N, Bhopal R, Leon DA, Wright J, Lawlor DA. Comparison of distributions of common indicators of socioeconomic position by ethnicity and migration: preliminary findings from the Born in Bradford birth cohort study. First CHICOS workshop, Barcelona, Spain, 11–12 April 2011.
Small N. Community and user involvement in BiB. Presentation at Born in Bradford Conference, Bradford Teaching Hospitals NHS Foundation Trust, Bradford, UK, 17 June 2010.
Raynor P, Small N, Wright J. Keeping in touch. European Child Cohort Network (EUCCONET) International Workshop, Tracking Sample Members in Longitudinal Studies, London, UK, 1–2 July 2010.
Fairley L, Small N, Lawlor D, West J, Wright J. Lifestyle and socioeconomic differences of Pakistani and white UK pregnant women: the Born in Bradford birth cohort. Society for Longitudinal and Lifecourse Studies, Cambridge, UK, 22–24 September 2010.
Fairley L, Small N, Lawlor DA, Wright J. Comparison of distribution of common indicators of socioeconomic position by ethnicity and migration: preliminary findings from the Born In Bradford birth cohort study. Society for Social Medicine Conference, Belfast, UK, 1 September 2010.
Lawlor D, Fairley L, West J, Raynor P, Wright J. Lifestyle and socioeconomic differences of Pakistani and white UK pregnant women: the Born in Bradford birth cohort. Annual Meeting, 6th World Congress on Developmental Origins of Health and Disease (DOHaD), Chile, November 2009.
Small N. Born in Bradford: public involvement in a large scale, long running study. Paper presented at 6th INVOLVE National Conference, Public Involvement in Research: Getting it Right and Making a Difference, Nottingham, UK, November 2008.
Small N, Raynor P. Community consent in the Born in Bradford birth cohort study. European Child Cohort Network (EUCCONET) Workshop on Consent, INED Paris, 17–18 February 2008.
Doctoral theses
Costa S. Measurement of Physical Activity and Sedentary Behaviour in Young Children and their Parents. PhD thesis. Loughborough: University of Loughborough; 2013.
Modelling growth trajectories and obesity risk
Journal articles
West J, Lawlor DA, Fairley L, Bhopal R, Cameron N, McKinney PA, et al. UK-born Pakistani-origin infants are relatively more adipose than white British infants: findings from 8704 mother–offspring pairs in the Born-in-Bradford prospective birth cohort. J Epidemiol Community Health 2013;67:544–51.
Conference presentations
Santorelli G, Wilson B. Developing a mobile phone application to predict the risk of childhood obesity. Oral presentation. Born in Bradford: Putting Research into Practice?, Annual Conference, Bradford Royal Infirmary, Bradford, UK, 28 June 2012.
Santorelli G. Developing a mobile phone application to predict the risk of childhood obesity. Oral presentation. Childhood Obesity Pandemic: Progress, Best Practices and Frameworks for Further Action Conference, Brussels, Belgium, October 2012.
Santorelli G. Developing a mobile phone application to predict the risk of childhood obesity. Oral presentation. Management of Obesity and its Complications Conference, London, UK, October 2012.
Fairley L, Petherick ES, Howe LD, Tilling K, Cameron N, Lawlor DA, et al. Differences in growth trajectories between white British and Pakistani infants in the UK: analysis of the Born in Bradford birth cohort study. Lancet 2012;380:S37.
Johnson W. Modelling of longitudinal data. Human Biology Association and American Association of Physical Anthropologists Meeting, Minneapolis, MN, USA, 11–16 April 2011.
Petherick E. Use of linear spline models to describe bi-ethnic differences in early childhood growth: findings from the Born in Bradford Birth cohort study. International Epidemiological Association (IEA) World Congress of Epidemiology, Edinburgh, UK, August 2011.
Cameron N. Growth trajectories and early life development of obesity. Presentation at Born in Bradford Conference, Bradford Teaching Hospitals NHS Foundation Trust, Bradford, UK, 16 June 2011.
Johnson W. Using routine anthropometric data to characterize infant growth and investigate risk for childhood obesity. Division of Epidemiology and Community Health, School of Public Health, University of Minnesota, USA, 2010.
Johnson W. Modelling the growth of Bradford infants. Royal Statistical Society Meeting, University of Leeds, Leeds, UK, 20 September 2010.
Johnson W, Cameron N. Using routine anthropometric data to characterize infant growth. International Society for the Advancement of Kinanthropometry Conference, Estoril, Portugal, November 2010.
West J. Differences in birth size between Pakistani and white babies. Oral presentation at Born in Bradford Conference, Bradford Teaching Hospitals NHS Foundation Trust, Bradford, UK, 17 June 2010.
Cameron N. Growth in the first year. Oral presentation at Born in Bradford Conference, Bradford Teaching Hospitals NHS Foundation Trust, Bradford, UK, 17 June 2010.
Johnson W, Cameron N. The growth of Pakistani and white infants, living in Bradford, UK, in comparison to WHO standards. Symposium of the Society for the Study of Human Biology, Frascati, Italy, June 2009.
Johnson W. The growth of Bradford infants. Child Growth Foundation Annual Meeting, Northampton, UK, 2009.
Doctoral theses
Johnson W. Born in Bradford (BiB): Examining the Birth Size and Postnatal Growth of Ethnic Minorities in Bradford. PhD thesis. Loughborough: University of Loughborough; 2010.
West J. Explaining Differences in Birth Size and Adiposity between Pakistani and White Babies. PhD thesis. Leeds: University of Leeds; 2012.
Ethnic differences in obesity risk factors
Journal articles
Traviss G, West R, House A. Maternal mental health and its association with infant growth at 6 months in ethnic groups: results from the Born-in-Bradford birth cohort study. PLOS ONE 2012;7:e30707.
Conference presentations
Lawlor D. Maternal pregnancy adiposity – a determinant of postnatal offspring adiposity and cardiometabolic outcomes? Plenary lecture. Developmental Origins of Health and Disease (DOHaD) 2012 Satellite Meeting: New Developments in Developmental Epidemiology, Rotterdam, Netherlands, 6 December 2012.
Lawlor D. Developmental overnutrition: an old hypothesis with new relevance? Keynote speaker. Special seminar sponsored by the Robinson Institute, University of Adelaide, Health Development Adelaide and the School of Population Health and Clinical Practice, University of Adelaide, SA, Australia, 24 January 2012.
Sahota P, Greenwood D. Ethnic differences in diets of 12 month old infants: BIB1000 study. Keynote speaker. MRC Human Nutrition Research Unit, Cambridge University, Cambridge, UK, 6 November 2012.
Prady S. Evidence about parenting in Bradford. Oral presentation. Born in Bradford: Putting Research into Practice?, Annual Conference, Bradford Royal Infirmary, Bradford, UK, 28 June 2012.
Prady S, Fairley L, Bloor K, Gilbody S, Kiernan K, Pickett K, et al. Risk factors for poor mental health during pregnancy from the Born in Bradford cohort: early results from a bi-ethnic sample. International Epidemiological Association (IEA) World Congress of Epidemiology, Edinburgh, UK, August 2011.
Petherick E. Association of prenatal and postanatal smoking and alcohol on birthweight. Oral presentation at Born in Bradford Conference, Bradford Teaching Hospitals NHS Foundation Trust, Bradford, UK, 17 June 2010.
Prady S, Miles J, Fairley L, Bloor K, Gilbody S, Kiernan K, et al. An examination of the psychometric properties of the GHQ-28 subscales in a bi-ethnic antenatal sample in the UK: preliminary results from the Born in Bradford cohort. International Epidemiological Association (IEA) World Congress of Epidemiology, Edinburgh, UK, August 2011.
Sheridan E. Consanguinity, biraderi and associations witth socio-economic position, mental health and birth weight. Oral presentation at Born in Bradford Conference, Bradford Teaching Hospitals NHS Foundation Trust, Bradford, UK, 17 June 2010.
Nieuwenhuijsen M, Smith R. Environmental exposures in pregnancy. Oral presentation at Born in Bradford Conference, Bradford Teaching Hospitals NHS Foundation Trust, Bradford, UK, 17 June 2010.
Small N. Infant mortality and migrant health in a Pakistani Muslim community in the UK. International Conference on Migration, Citizenship and Intercultural Relations, Deakin University, VIC, Australia, November 2009.
Small N. Infant mortality and morbidity in a migrant population of Pakistani origin in the UK. International Conference on Health for All: Opportunities and Challenges, International Sociological Association, Jaipur, India, September 2009.
Systematic review of interventions to promote a healthy diet and physical activity in pregnant women and mothers with children under the age of 6 years with a focus on South Asian populations and low-income families
Journal articles
Brown T, Smith S, Bhopal R, Kasim A, Summerbell C. Diet and physical activity interventions to prevent or treat obesity in South Asian children and adults: a systematic review and meta-analysis. Int J Environ Res Public Health 2015;12:566–94.
Investigation of social and environmental determinants of childhood obesity
Conference presentations
Small N, Akhtar S. Determinants of feeding practices and beliefs and attitudes about childhood obesity. Oral presentation at Born in Bradford Conference, Bradford Teaching Hospitals NHS Foundation Trust, Bradford, UK, 16 June 2011.
Doctoral theses
Mann R. Emotional Wellbeing in Motherhood: the Validity and Acceptability of Case Finding Questions to Identify Perinatal Depression. PhD thesis. York: University of York; 2012.
Nnadede K. Parenting Patterns in Families of Pakistani Origin. PhD thesis. York: University of York; 2013.
Development of an obesity prevention intervention
Conference presentations
Sahota P, Taylor N. A systematic, evidence-based and innovative approach to developing an intervention to prevent obesity. Oral presentation. Born in Bradford: Putting Research into Practice?, Annual Conference, Bradford Royal Infirmary, Bradford, UK, 28 June 2012.
McEachan R, Taylor N, Wright J, Lawton R, Raynor, P. Intervention mapping to develop two complex interventions: challenges and recommendations for future practice. Poster presentation. Population Health – Methods and Challenges, Birmingham, UK, April 2012.
Data sharing statement
Requests for data collected as part of the BiB1000 study can be made to the Born in Bradford executive group. Further information can be found here: www.borninbradford.nhs.uk/research-scientific/how-to-request-access-to-raw-bib-data/ (accessed 8 March 2016).
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, CCF, NETSCC, PGfAR or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the PGfAR programme or the Department of Health.
References
- Wang Y, Lobstein T. Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes 2006;1:11-25. http://dx.doi.org/10.1080/17477160600586747.
- Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the global burden of disease study 2013. Lancet 2014;384:766-81. http://dx.doi.org/10.1016/S0140-6736(14)60460-8.
- Rokholm B, Baker JL, Sorensen TI. The levelling off of the obesity epidemic since the year 1999 – a review of evidence and perspectives. Obes Rev 2010;11:835-46. http://dx.doi.org/10.1111/j.1467-789X.2010.00810.x.
- Kipping RR, Jago R, Lawlor DA. Obesity in children. Part 1: epidemiology, measurement, risk factors, and screening. BMJ 2008;337. http://dx.doi.org/10.1136/bmj.a1824.
- Health Survey for England 2012. Leeds: Health and Social Care Information Centre; 2013.
- Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ, et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet 2011;377:557-67. http://dx.doi.org/10.1016/S0140-6736(10)62037-5.
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014;311:806-14. http://dx.doi.org/10.1001/jama.2014.732.
- Bundred P, Kitchiner D, Buchan I. Prevalence of overweight and obese children between 1989 and 1998: population based series of cross sectional studies. BMJ 2001;322:326-8. http://dx.doi.org/10.1136/bmj.322.7282.326.
- Kimbro RT, Brooks-Gunn J, McLanahan S. Racial and ethnic differentials in overweight and obesity among 3-year-old children. Am J Public Health 2007;97:298-305. http://dx.doi.org/10.2105/AJPH.2005.080812.
- Lobstein T, Baur L, Uauy R. Obesity in children and young people: a crisis in public health. Obes Rev 2004;5:4-104. http://dx.doi.org/10.1111/j.1467-789X.2004.00133.x.
- Wright CM, Parker L, Lamont D, Craft AW. Implications of childhood obesity for adult health: findings from thousand families cohort study. BMJ 2001;323:1280-4. http://dx.doi.org/10.1136/bmj.323.7324.1280.
- Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet 2011;378:815-25. http://dx.doi.org/10.1016/S0140-6736(11)60814-3.
- Butland B, Jebb S, Kopelman P, McPherson K, Thomas S, Mardell J, et al. Foresight – Tackling Obesities: Future Choices – Project Report. London: Government Office for Science and Department of Health; 2007.
- Dietz WH. Childhood weight affects adult morbidity and mortality. J Nutr 1998;128:411-14S.
- Juonala M, Magnussen CG, Berenson GS, Venn A, Burns TL, Sabin MA, et al. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med 2011;365:1876-85. http://dx.doi.org/10.1056/NEJMoa1010112.
- Pulgarón ER. Childhood obesity: a review of increased risk for physical and psychological comorbidities. Clin Ther 2013;35:A18-32. http://dx.doi.org/10.1016/j.clinthera.2012.12.014.
- Reilly JJ, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J Obes (Lond) 2011;35:891-8. http://dx.doi.org/10.1038/ijo.2010.222.
- Friedlander SL, Larkin EK, Rosen CL, Palermo TM, Redline S. Decreased quality of life associated with obesity in school-aged children. Arch Pediatr Adolesc Med 2003;157:1206-11. http://dx.doi.org/10.1001/archpedi.157.12.1206.
- Han JC, Lawlor DA, Kimm SY. Childhood obesity. Lancet 2010;375:1737-48. http://dx.doi.org/10.1016/S0140-6736(10)60171-7.
- Nadeau KJ, Maahs DM, Daniels SR, Eckel RH. Childhood obesity and cardiovascular disease: links and prevention strategies. Nat Rev Cardiol 2011;8:513-25. http://dx.doi.org/10.1038/nrcardio.2011.86.
- Saxena S, Ambler G, Cole TJ, Majeed A. Ethnic group differences in overweight and obese children and young people in England: cross sectional survey. Arch Dis Child 2004;89:30-6.
- McKeigue PM, Shah B, Marmot MG. Relation of central obesity and insulin resistance with high diabetes prevalence and cardiovascular risk in South Asians. Lancet 1991;337:382-6. http://dx.doi.org/10.1016/0140-6736(91)91164-P.
- Yajnik CS, Lubree HG, Rege SS, Naik SS, Deshpande JA, Deshpande SS, et al. Adiposity and hyperinsulinemia in Indians are present at birth. J Clin Endocrinol Metab 2002;87:5575-80. http://dx.doi.org/10.1210/jc.2002-020434.
- Whincup PH, Gilg JA, Papacosta O, Seymour C, Miller GJ, Alberti KG, et al. Early evidence of ethnic differences in cardiovascular risk: cross sectional comparison of British South Asian and white children. BMJ 2002;324. http://dx.doi.org/10.1136/bmj.324.7338.635.
- West J, Lawlor DA, Fairley L, Bhopal R, Cameron N, McKinney PA, et al. UK-born Pakistani-origin infants are relatively more adipose than white British infants: findings from 8704 mother–offspring pairs in the Born-in-Bradford prospective birth cohort. J Epidemiol Community Health 2013;67:544-51. http://dx.doi.org/10.1136/jech-2012-201891.
- Jenum AK, Sommer C, Sletner L, Mørkrid K, Baerug A, Mosdøl A. Adiposity and hyperglycaemia in pregnancy and related health outcomes in European ethnic minorities of Asian and African origin: a review. Food Nutr Res 2013;57. http://dx.doi.org/10.3402/fnr.v57i0.18889.
- Ravelli AC, van Der Meulen JH, Osmond C, Barker DJ, Bleker OP. Obesity at the age of 50 y in men and women exposed to famine prenatally. Am J Clin Nutr 1999;70:811-16.
- Reilly JJ, Armstrong J, Dorosty AR, Emmett PM, Ness A, Rogers I, et al. Early life risk factors for obesity in childhood: cohort study. BMJ 2005;330. http://dx.doi.org/10.1136/bmj.38470.670903.E0.
- Parsons TJ, Power C, Manor O. Fetal and early life growth and body mass index from birth to early adulthood in 1958 British cohort: longitudinal study. BMJ 2001;323:1331-5. http://dx.doi.org/10.1136/bmj.323.7325.1331.
- Singhal A, Fewtrell M, Cole TJ, Lucas A. Low nutrient intake and early growth for later insulin resistance in adolescents born preterm. Lancet 2003;361:1089-97. http://dx.doi.org/10.1016/S0140-6736(03)12895-4.
- Lawlor DA, Chaturvedi N. Treatment and prevention of obesity – are there critical periods for intervention?. Int J Epidemiol 2006;35:3-9. http://dx.doi.org/10.1093/ije/dyi309.
- Lawlor DA, Lichtenstein P, Langstrom N. Association of maternal diabetes mellitus in pregnancy with offspring adiposity into early adulthood: sibling study in a prospective cohort of 280,866 men from 248,293 families. Circulation 2011;123:258-65. http://dx.doi.org/10.1161/CIRCULATIONAHA.110.980169.
- Druet C, Stettler N, Sharp S, Simmons RK, Cooper C, Smith GD, et al. Prediction of childhood obesity by infancy weight gain: an individual-level meta-analysis. Paediatr Perinat Epidemiol 2012;26:19-26. http://dx.doi.org/10.1111/j.1365-3016.2011.01213.x.
- Baird J, Fisher D, Lucas P, Kleijnen J, Roberts H, Law C. Being big or growing fast: systematic review of size and growth in infancy and later obesity. BMJ 2005;331. http://dx.doi.org/10.1136/bmj.38586.411273.E0.
- Faith MS, Kerns J. Infant and child feeding practices and childhood overweight: the role of restriction. Matern Child Nutr 2005;1:164-8. http://dx.doi.org/10.1111/j.1740-8709.2005.00024.x.
- Fox MK, Reidy K, Novak T, Ziegler P. Sources of energy and nutrients in the diets of infants and toddlers. J Am Diet Assoc 2006;106:28-42. http://dx.doi.org/10.1016/j.jada.2005.09.034.
- Millstone E, Lobstein T, Stirling A, Mohebati L. Policy Options for Responding to Obesity: Cross-National Report of the PorGrow Project. Brighton: SPRU, University of Sussex; 2006.
- Knutson KL. Sex differences in the association between sleep and body mass index in adolescents. J Pediatr 2005;147:830-4. http://dx.doi.org/10.1016/j.jpeds.2005.07.019.
- Monasta L, Batty GD, Cattaneo A, Lutje V, Ronfani L, Van Lenthe FJ, et al. Early-life determinants of overweight and obesity: a review of systematic reviews. Obes Rev 2010;11:695-708. http://dx.doi.org/10.1111/j.1467-789X.2010.00735.x.
- Kramer MS, Matush L, Vanilovich I, Platt RW, Bogdanovich N, Sevkovskaya Z, et al. Effects of prolonged and exclusive breastfeeding on child height, weight, adiposity, and blood pressure at age 6.5 y: evidence from a large randomized trial. Am J Clin Nutr 2007;86:1717-21.
- Oude LH, Baur L, Jansen H, Shrewsbury VA, O’Malley C, Stolk RP, et al. Interventions for treating obesity in children. Cochrane Database Syst Rev 2009;1.
- Summerbell CD, Waters E, Edmunds LD, Kelly S, Brown T, Campbell KJ. Interventions for preventing obesity in children. Cochrane Database Syst Rev 2005;3. http://dx.doi.org/10.1002/14651858.cd001871.pub2.
- van Sluijs EM, McMinn AM, Griffin SJ. Effectiveness of interventions to promote physical activity in children and adolescents: systematic review of controlled trials. BMJ 2007;335. http://dx.doi.org/10.1136/bmj.39320.843947.BE.
- Sharma M. International school-based interventions for preventing obesity in children. Obes Rev 2007;8:155-67. http://dx.doi.org/10.1111/j.1467-789X.2006.00268.x.
- Brown T, Kelly S, Summerbell C. Prevention of obesity: a review of interventions. Obes Rev 2007;8:127-30. http://dx.doi.org/10.1111/j.1467-789X.2007.00331.x.
- Campbell KJ, Hesketh KD. Strategies which aim to positively impact on weight, physical activity, diet and sedentary behaviours in children from zero to five years. A systematic review of the literature. Obes Rev 2007;8:327-38. http://dx.doi.org/10.1111/j.1467-789X.2006.00305.x.
- Waters E, de Silva-Sanigorski A, Hall BJ, Brown T, Campbell KJ, Gao Y, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev 2011;12. http://dx.doi.org/10.1002/14651858.cd001871.pub3.
- Bleich SN, Segal J, Wu Y, Wilson R, Wang Y. Systematic review of community-based childhood obesity prevention studies. Pediatrics 2013;132:e201-10. http://dx.doi.org/10.1542/peds.2013-0886.
- Hillier F, Pedley C, Summerbell C. Evidence base for primary prevention of obesity in children and adolescents. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2011;54:259-64. http://dx.doi.org/10.1007/s00103-010-1227-4.
- Barker DJ. Obesity and early life. Obes Rev 2007;8:45-9. http://dx.doi.org/10.1111/j.1467-789X.2007.00317.x.
- van der Horst K, Oenema A, Ferreira I, Wendel-Vos W, Giskes K, van Lenthe F, et al. A systematic review of environmental correlates of obesity-related dietary behaviors in youth. Health Educ Res 2007;22:203-26. http://dx.doi.org/10.1093/her/cyl069.
- Northstone K, Rogers I, Emmett P. Avon Longitudinal Study of Pregnancy and Childhood . Drinks consumed by 18-month-old children: are current recommendations being followed?. Eur J Clin Nutr 2002;56:236-44. http://dx.doi.org/10.1038/sj.ejcn.1601313.
- Reilly JJ, Jackson DM, Montgomery C, Kelly LA, Slater C, Grant S, et al. Total energy expenditure and physical activity in young Scottish children: mixed longitudinal study. Lancet 2004;363:211-12. http://dx.doi.org/10.1016/S0140-6736(03)15331-7.
- Etelson D, Brand DA, Patrick PA, Shirali A. Childhood obesity: do parents recognize this health risk?. Obes Res 2003;11:1362-8. http://dx.doi.org/10.1038/oby.2003.184.
- Ong KK, Loos RJ. Rapid infancy weight gain and subsequent obesity: systematic reviews and hopeful suggestions. Acta Paediatr 2006;95:904-8. http://dx.doi.org/10.1080/08035250600719754.
- Morandi A, Meyre D, Lobbens S, Kleinman K, Kaakinen M, Rifas-Shiman SL, et al. Estimation of newborn risk for child or adolescent obesity: lessons from longitudinal birth cohorts. PLOS ONE 2012;7. http://dx.doi.org/10.1371/journal.pone.0049919.
- Flynn MA, McNeil DA, Maloff B, Mutasingwa D, Wu M, Ford C, et al. Reducing obesity and related chronic disease risk in children and youth: a synthesis of evidence with ‘best practice’ recommendations. Obes Rev 2006;7:7-66. http://dx.doi.org/10.1111/j.1467-789X.2006.00242.x.
- Hesketh KD, Campbell KJ. Interventions to prevent obesity in 0–5 year olds: an updated systematic review of the literature. Obesity (Silver Spring) 2010;18:S27-35. http://dx.doi.org/10.1038/oby.2009.429.
- Pocock M, Trivedi D, Willis W, Bunn F, Magnusson J. Parental perceptions regarding healthy behaviours for preventing overweight and obesity in young children: a systematic review of qualitative studies. Obes Rev 2010;11:338-53. http://dx.doi.org/10.1111/j.1467-789X.2009.00648.x.
- Ward DS, Vaughn AE, Bangdiwala KI, Campbell M, Jones DJ, Panter AT, et al. Integrating a family-focused approach into child obesity prevention: rationale and design for the My Parenting SOS study randomized control trial. BMC Public Health 2011;11. http://dx.doi.org/10.1186/1471-2458-11-431.
- Harvey-Berino J, Rourke J. Obesity prevention in preschool native-american children: a pilot study using home visiting. Obes Res 2003;11:606-11. http://dx.doi.org/10.1038/oby.2003.87.
- Wright J, Small N, Raynor P, Tuffnell D, Bhopal R, Cameron N, et al. Cohort profile: the Born in Bradford multi-ethnic family cohort study. Int J Epidemiol 2013;42:978-91. http://dx.doi.org/10.1093/ije/dys112.
- Bryant M, Santorelli G, Fairley L, West J, Lawlor DA, Bhopal R, et al. Design and characteristics of a new birth cohort, beginning in pregnancy, to study the early origins and ethnic variation of childhood obesity: the BiB1000 study. Longit Life Course Stud 2013;4.
- Cole TJ, Freeman JV, Preece MA. Body mass index reference curves for the UK, 1990. Arch Dis Child 1995;73:25-9.
- Millenium Cohort First Study: CAPI Questionnaire Documentation. London: University College London; 2003.
- Australian Institute of Family Studies . Growing up in Australia: The Longitudinal Study of Australian Children: Wave I 2003. www.aifs.gov.au/growingup/pubs/discussion/dp2/index.html (accessed February 2012).
- Census 2001: General Report for England and Wales. London: ONS; 2005.
- Riboli E, Hunt K, Slimani N, Ferrari P, Norat T, Fahey M, et al. European Prospective Investigation into Cancer and Nutrition (EPIC): study populations and data collection. Public Health Nutr 2002;5:1113-24. http://dx.doi.org/10.1079/PHN2002394.
- Cameron N, Demerath E. Critical periods in human growth: relationships to chronic disease. Yearb Phys Anthropol 2002;45:159-84. http://dx.doi.org/10.1002/ajpa.10183.
- Johnson W, Cameron N, Dickson P, Emsley S, Raynor P, Seymour C, et al. The reliability of routine anthropometric data collected by health workers: a cross-sectional study. Int J Nurs Stud 2009;46:310-16.
- Bryant M, Santorelli G, Fairley L, Petherick ES, Bhopal R, Lawlor DA, et al. Agreement between routine and research measurement of infant height and weight. Arch Dis Child 2015;100:24-9.
- Fairley L, Petherick ES, Howe LD, Tilling K, Cameron N, Lawlor DA, et al. Describing differences in weight and length growth trajectories between white and Pakistani infants in the UK: analysis of the Born in Bradford birth cohort study using multilevel linear spline models. Arch Dis Child 2013;98:274-9.
- Santorelli G, Petherick ES, Wright J, Wilson B, Samiei H, Cameron N, et al. Developing prediction equations and a mobile phone application to identify infants at risk of obesity. PLOS ONE 2013;8.
- Victora CG, Adair L, Fall C, Hallal PC, Martorell R, Richter L, et al. Maternal and child undernutrition: consequences for adult health and human capital. Lancet 2008;371:340-57. http://dx.doi.org/10.1016/S0140-6736(07)61692-4.
- Singhal A, Lucas A. Early origins of cardiovascular disease: is there a unifying hypothesis?. Lancet 2004;363:1642-5. http://dx.doi.org/10.1016/S0140-6736(04)16210-7.
- Health Survey for England 1999: the Health of Minority Ethnic Groups. London: Department of Health; 2001.
- Barnett AH, Dixon AN, Bellary S, Hanif MW, O’Hare JP, Raymond NT, et al. Type 2 diabetes and cardiovascular risk in the UK south Asian community. Diabetologia 2006;49:2234-46. http://dx.doi.org/10.1007/s00125-006-0325-1.
- Balarajan R. Ethnicity and variations in mortality from coronary heart disease. Health Trends 1996;28:45-51.
- Whincup PH, Nightingale CM, Owen CG, Rudnicka AR, Gibb I, McKay CM, et al. Early emergence of ethnic differences in type 2 diabetes precursors in the UK: the Child Heart and Health Study in England (CHASE study). PLOS Med 2010;7. http://dx.doi.org/10.1371/journal.pmed.1000263.
- Ehtisham S, Crabtree N, Clark P, Shaw N, Barrett T. Ethnic differences in insulin resistance and body composition in United Kingdom adolescents. J Clin Endocrinol Metab 2005;90:3963-9. http://dx.doi.org/10.1210/jc.2004-2001.
- Healthy Weight, Healthy Lives: a Cross-Government Strategy for England. London: Department of Health; 2008.
- Santorelli G, Petherick ES, Waiblinger D, Fairley L. Ethnic differences in the initiation and duration of breastfeeding: evidence from the Born in Bradford cohort study. Paediatr Perinat Epidemiol 2013;27:388-92.
- Prady SL, Kiernan K, Fairley L, Wilson S, Wright J. Self-reported maternal parenting style and confidence and infant temperament in a multi-ethnic community: results from the Born in Bradford cohort. J Child Health Care 2013;18:31-46.
- Griffiths LJ, Tate AR, Dezateux C. The contribution of parental and community ethnicity to breastfeeding practices: evidence from the Millennium Cohort Study. Int J Epidemiol 2005;34:1378-86. http://dx.doi.org/10.1093/ije/dyi162.
- Hawkins SS, Lamb K, Cole TJ, Law C. Millennium Cohort Study Child Health Group . Influence of moving to the UK on maternal health behaviours: prospective cohort study. BMJ 2008;336:1052-5. http://dx.doi.org/10.1136/bmj.39532.688877.25.
- Physical Activity, Health Improvment and Protection. Start Active, Stay Active: Report on Physical Activity from the Four Home Countries’ Chief Medical Officers. London: Department of Health; 2011.
- Sallis JF, Prochaska JJ, Taylor WC. A review of correlates of physical activity of children and adolescents. Med Sci Sport Exerc 2000;32:963-75. http://dx.doi.org/10.1097/00005768-200005000-00014.
- Ferreira I, van der Horst K, Wendel-Vos W, Kremers S, van Lenthe FJ, Brug J. Environmental correlates of physical activity in youth – a review and update. Obes Rev 2007;8:129-54. http://dx.doi.org/10.1111/j.1467-789X.2006.00264.x.
- Cleland V, Crawford D, Baur LA, Hume C, Timperio A, Salmon J. A prospective examination of children’s time spent outdoors, objectively measured physical activity and overweight. Int J Obes (Lond) 2008;32:1685-93. http://dx.doi.org/10.1038/ijo.2008.171.
- Cooper AR, Page AS, Wheeler BW, Hillsdon M, Griew P, Jago R. Patterns of GPS measured time outdoors after school and objective physical activity in English children: the PEACH project. Int J Behav Nutr Phys Act 2010;7. http://dx.doi.org/10.1186/1479-5868-7-31.
- Owen CG, Nightingale CM, Rudnicka AR, Cook DG, Ekelund U, Whincup PH. Ethnic and gender differences in physical activity levels among 9–10-year-old children of white European, South Asian and African-Caribbean origin: the Child Heart Health Study in England (CHASE study). Int J Epidemiol 2009;38:1082-93. http://dx.doi.org/10.1093/ije/dyp176.
- Fairley L, Santorelli G, Lawlor DA, Bryant M, Bhopal R, Petherick ES, et al. The relationship between early life modifiable risk factors for childhood obesity, ethnicity and body mass index at age 3 years: findings from the Born in Bradford birth cohort study. BMC Obesity 2015;2.
- Weng SF, Redsell SA, Swift JA, Yang M, Glazebrook CP. Systematic review and meta-analyses of risk factors for childhood overweight identifiable during infancy. Arch Dis Child 2012;97:1019-26. http://dx.doi.org/10.1136/archdischild-2012-302263.
- Oken E, Levitan EB, Gillman MW. Maternal smoking during pregnancy and child overweight: systematic review and meta-analysis. Int J Obes (Lond) 2008;32:201-10. http://dx.doi.org/10.1038/sj.ijo.0803760.
- Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med 1997;337:869-73. http://dx.doi.org/10.1056/NEJM199709253371301.
- Hurley KM, Cross MB, Hughes SO. A systematic review of responsive feeding and child obesity in high-income countries. J Nutr 2011;141:495-501. http://dx.doi.org/10.3945/jn.110.130047.
- Hughes SO, Power TG, Orlet Fisher J, Mueller S, Nicklas TA. Revisiting a neglected construct: parenting styles in a child-feeding context. Appetite 2005;44:83-92. http://dx.doi.org/10.1016/j.appet.2004.08.007.
- Sleddens EF, Gerards SM, Thijs C, de Vries NK, Kremers SP. General parenting, childhood overweight and obesity-inducing behaviors: a review. Int J Pediatr Obes 2011;6:e12-27. http://dx.doi.org/10.3109/17477166.2011.566339.
- Campbell K, Hesketh K, Silverii A, Abbott G. Maternal self-efficacy regarding children’s eating and sedentary behaviours in the early years: associations with children’s food intake and sedentary behaviours. Int J Pediatr Obes 2010;5:501-8. http://dx.doi.org/10.3109/17477161003777425.
- Pearce J, Langley-Evans SC. The types of food introduced during complementary feeding and risk of childhood obesity: a systematic review. Int J Obes (Lond) 2013;37:477-85. http://dx.doi.org/10.1038/ijo.2013.8.
- Chen X, Beydoun MA, Wang Y. Is sleep duration associated with childhood obesity? A systematic review and meta-analysis. Obesity (Silver Spring) 2008;16:265-74. http://dx.doi.org/10.1038/oby.2007.63.
- Liu J, Zhang A, Li L. Sleep duration and overweight/obesity in children: review and implications for pediatric nursing. J Spec Pediatr Nurs 2012;17:193-204. http://dx.doi.org/10.1111/j.1744-6155.2012.00332.x.
- Philipps LH, Santhakumaran S, Gale C, Prior E, Logan KM, Hyde MJ, et al. The diabetic pregnancy and offspring BMI in childhood: a systematic review and meta-analysis. Diabetologia 2011;54:1957-66. http://dx.doi.org/10.1007/s00125-011-2180-y.
- Kim SY, England JL, Sharma JA, Njoroge T. Gestational diabetes mellitus and risk of childhood overweight and obesity in offspring: a systematic review. Exp Diabetes Res 2011;2011. http://dx.doi.org/10.1155/2011/541308.
- Brown T, Smith S, Bhopal R, Kasim A, Summerbell C. Diet and physical activity interventions to prevent or treat obesity in South Asian children and adults: a systematic review and meta-analysis. Int J Environ Res Public Health 2015;12:566-94. http://dx.doi.org/10.3390/ijerph120100566.
- Bryant M, Sahota P, Santorelli G, Hill A. An exploration and comparison of food and drink availability in homes in a sample of families of white and Pakistani origin within the UK. Public Health Nutr 2015;18:1197-205. http://dx.doi.org/10.1017/S1368980014000147.
- Fraser LK, Edwards KL, Tominitz M, Clarke GP, Hill AJ. Food outlet availability, deprivation and obesity in a multi-ethnic sample of pregnant women in Bradford, UK. Soc Sci Med 2012;75:1048-56. http://dx.doi.org/10.1016/j.socscimed.2012.04.041.
- Riessman CK. Narrative Analysis. London: Sage; 1993.
- Baumrind D. Current patterns of parental authority. Dev Psychol Monogr 1971;4:1-103. http://dx.doi.org/10.1037/h0030372.
- Maccoby EE, Martin JA, Hetherington EM. Handbook of Child Psychology: Socialization, Personality, and Social Development. New York, NY: Wiley; 1983.
- Blisset J. Relationships between parenting style, feeding style and feeding practices and fruit and vegetable consumption in early childhood. Appetite 2011;57. http://dx.doi.org/10.1016/j.appet.2011.05.318.
- Van Campen KS, Russell ST. Cultural Differences in Parenting Practices: What Asian American Families Can Teach Us (Vol. 2, No. 1). Tucson, AZ: Frances McClelland Institute for Children, Youth, and Families Research Link, University of Arizona; 2010.
- Wilson SL. A Mealtime Observation Study: Obesity, Ethnicity and Observed Maternal Feeding Styles 2011. http://etheses.whiterose.ac.uk/1739/1/Mealtime_Observation_Study_22nd_Sept_2011.pdf (accessed 2 February 2016).
- Cullen KW, Baranowski T, Rittenberry L, Cosart C, Hebert D, de Moor C. Child-reported family and peer influences on fruit, juice and vegetable consumption: reliability and validity of measures. Health Educ Res 2001;16:187-200. http://dx.doi.org/10.1093/her/16.2.187.
- Downs SM, Arnold A, Marshall D, McCargar LJ, Raine KD, Willows ND. Associations among the food environment, diet quality and weight status in Cree children in Quebec. Public Health Nutr 2009;12:1504-11. http://dx.doi.org/10.1017/S1368980008004515.
- Gable S, Lutz S. Household, parent, and child contributions to childhood obesity. Fam Relat 2000;49:293-300. http://dx.doi.org/10.1111/j.1741-3729.2000.00293.x.
- Gattshall ML, Shoup JA, Marshall JA, Crane LA, Estabrooks PA. Validation of a survey instrument to assess home environments for physical activity and healthy eating in overweight children. Int J Behav Nutr Phys Act 2008;5. http://dx.doi.org/10.1186/1479-5868-5-3.
- Hanson NI, Neumark-Sztainer D, Eisenberg ME, Story M, Wall M. Associations between parental report of the home food environment and adolescent intakes of fruits, vegetables and dairy foods. Public Health Nutr 2005;8:77-85. http://dx.doi.org/10.1079/PHN2005661.
- Hearn MD, Baranowski T, Baranowski J, Doyle C, Smith M, Lin L, et al. Environmental influences on dietary behavior among children: availability and accessibility of fruits and vegetables enable consumption. J Health Educ 1998;29:26-32. http://dx.doi.org/10.1080/10556699.1998.10603294.
- Kratt P, Reynolds K, Shewchuk R. The role of availability as a moderator of family fruit and vegetable consumption. Health Educ Behav 2000;27:471-82. http://dx.doi.org/10.1177/109019810002700409.
- Neumark-Sztainer D, Wall M, Perry C, Story M. Correlates of fruit and vegetable intake among adolescents. Findings from Project EAT. Prev Med 2003;37:198-20. http://dx.doi.org/10.1016/S0091-7435(03)00114-2.
- Patterson RE, Kristal AR, Shannon J, Hunt JR, White E. Using a brief household food inventory as an environmental indicator of individual dietary practices. Am J Public Health 1997;87:272-5. http://dx.doi.org/10.2105/AJPH.87.2.272.
- Pearson N, Biddle SJ, Gorely T. Family correlates of fruit and vegetable consumption in children and adolescents: a systematic review. Public Health Nutr 2009;12:267-83. http://dx.doi.org/10.1017/S1368980008002589.
- Raynor HA, Polley BA, Wing RR, Jeffery RW. Is dietary fat intake related to liking or household availability of high- and low-fat foods?. Obes Res 2004;12:816-23. http://dx.doi.org/10.1038/oby.2004.98.
- Reynolds KD, Hinton AW, Shewchuk R, Hickey CA. Social cognitive model of fruit and vegetable consumption in elementary school children. J Nutr Educ 1999;31:23-30. http://dx.doi.org/10.1016/S0022-3182(99)70381-X.
- Spurrier NJ, Magarey AA, Golley R, Curnow F, Sawyer MG. Relationships between the home environment and physical activity and dietary patterns of preschool children: a cross-sectional study. Int J Behav Nutr Phys Act 2008;5. http://dx.doi.org/10.1186/1479-5868-5-31.
- Baranowski T, Domel S, Gould R, Baranowski J, Leonard S, Treiber F, et al. Increasing fruit and vegetable consumption among 4th and 5th grade students – results form focus groups using reciprocal determinism. J Nutr Educ 1993;25:114-20. http://dx.doi.org/10.1016/S0022-3182(12)80567-X.
- Story M, Kaphingst KM, Robinson-O’Brien R, Glanz K. Creating healthy food and eating environments: policy and environmental approaches. Ann Rev Public Health 2008;29:253-72. http://dx.doi.org/10.1146/annurev.publhealth.29.020907.090926.
- Stevens J, Bryant M, Wang CH, Cai J, Bentley ME. Sample size and repeated measures required in studies of foods in the homes of African-American families. J Nutr 2012;142:1123-7. http://dx.doi.org/10.3945/jn.111.150060.
- Byrd-Bredbenner C, Abbot JM. Differences in food supplies of US households with and without overweight individuals. Appetite 2009;52:479-84. http://dx.doi.org/10.1016/j.appet.2008.12.011.
- Schefske SD, Bellows AC, Byrd-Bredbenner C, Cuite CL, Rapport H, Vivar T, et al. Nutrient analysis of varying socioeconomic status home food environments in New Jersey. Appetite 2010;54:384-9. http://dx.doi.org/10.1016/j.appet.2010.01.007.
- Fulkerson JA, Nelson MC, Lytle L, Moe S, Heitzler C, Pasch KE. The validation of a home food inventory. Int J Behav Nutr Phys Act 2008;5. http://dx.doi.org/10.1186/1479-5868-5-55.
- Schefske SD, Byrd-Bredbenner C, Cuite CL, Hallman WK. Using UPC Scanning Methods to Characterize Household Food Supplies of Multi-Ethnic Low Income Minorities 2010;110.
- Stevens J, Bryant M, Wang L, Borja J, Bentley ME. Exhaustive measurement of food items in the home using a universal product code scanner. Public Health Nutr 2011;14:314-18. http://dx.doi.org/10.1017/S1368980010001837.
- Davis B, Carpenter C. Proximity of fast-food restaurants to schools and adolescent obesity. Am J Public Health 2009;99:505-10. http://dx.doi.org/10.2105/AJPH.2008.137638.
- Jeffery RW, Baxter J, McGuire M, Linde J. Are fast food restaurants an environmental risk factor for obesity?. Int J Behav Nutr Phys Act 2006;3. http://dx.doi.org/10.1186/1479-5868-3-2.
- Mehta NK, Chang VW. Weight status and restaurant availability: a multilevel analysis. Am J Prev Med 2008;34:127-33. http://dx.doi.org/10.1016/j.amepre.2007.09.031.
- Morland KB, Evenson KR. Obesity prevalence and the local food environment. Health Place 2009;15:491-5. http://dx.doi.org/10.1016/j.healthplace.2008.09.004.
- Pearce J, Hiscock R, Blakely T, Witten K. A national study of the association between neighbourhood access to fast-food outlets and the diet and weight of local residents. Health Place 2009;15:193-7. http://dx.doi.org/10.1016/j.healthplace.2008.04.003.
- Burdette HL, Whitaker RC. Neighborhood playgrounds, fast food restaurants, and crime: relationships to overweight in low-income preschool children. Prev Med 2004;38:57-63. http://dx.doi.org/10.1016/j.ypmed.2003.09.029.
- Casey AA, Elliott M, Glanz K, Haire-Joshu D, Lovegreen SL, Saelens BE, et al. Impact of the food environment and physical activity environment on behaviors and weight status in rural US communities. Prev Med 2008;47:600-4. http://dx.doi.org/10.1016/j.ypmed.2008.10.001.
- Rundle A, Neckerman KM, Freeman L, Lovasi GS, Purciel M, Quinn J, et al. Neighborhood food environment and walkability predict obesity in New York City. Environ Health Perspect 2009;117:442-7. http://dx.doi.org/10.1289/ehp.11590.
- Wang MC, Cubbin C, Ahn D, Winkleby MA. Changes in neighbourhood food store environment, food behaviour and body mass index, 1981–1990. Public Health Nutr 2008;11:963-70. http://dx.doi.org/10.1017/S136898000700105X.
- Simmons D, McKenzie A, Eaton S, Cox N, Khan MA, Shaw J, et al. Choice and availability of takeaway and restaurant food is not related to the prevalence of adult obesity in rural communities in Australia. Int J Obes (Lond) 2005;29:703-10. http://dx.doi.org/10.1038/sj.ijo.0802941.
- Block JP, Scribner RA, DeSalvo KB. Fast food, race/ethnicity, and income: a geographic analysis. Am J Prev Med 2004;27:211-17. http://dx.doi.org/10.1016/j.amepre.2004.06.007.
- Burns CM, Inglis AD. Measuring food access in Melbourne: access to healthy and fast foods by car, bus and foot in an urban municipality in Melbourne. Health Place 2007;13:877-85. http://dx.doi.org/10.1016/j.healthplace.2007.02.005.
- Cummins SC, McKay L, MacIntyre S. McDonald’s restaurants and neighborhood deprivation in Scotland and England. Am J Prev Med 2005;29:308-10. http://dx.doi.org/10.1016/j.amepre.2005.06.011.
- Fraser LK, Edwards KL. The association between the geography of fast food outlets and childhood obesity rates in Leeds, UK. Health Place 2010;16:1124-8. http://dx.doi.org/10.1016/j.healthplace.2010.07.003.
- Lewis LB, Sloane DC, Nascimento LM, Diamant AL, Guinyard JJ, Yancey AK, et al. African Americans’ access to healthy food options in South Los Angeles restaurants. Am J Public Health 2005;95:668-73. http://dx.doi.org/10.2105/AJPH.2004.050260.
- Macdonald L, Cummins S, Macintyre S. Neighbourhood fast food environment and area deprivation – substitution or concentration?. Appetite 2007;49.
- Morland K, Wing S, Diez Roux A, Poole C. Neighborhood characteristics associated with the location of food stores and food service places. Am J Prev Med 2002;22:23-9. http://dx.doi.org/10.1016/S0749-3797(01)00403-2.
- Pearce J, Blakely T, Witten K, Bartie P. Neighborhood deprivation and access to fast-food retailing: a national study. Am J Prev Med 2007;32:375-82. http://dx.doi.org/10.1016/j.amepre.2007.01.009.
- Powell LM, Chaloupka FJ, Bao Y. The availability of fast-food and full-service restaurants in the United States: associations with neighborhood characteristics. Am J Prev Med 2007;33:S240-5. http://dx.doi.org/10.1016/j.amepre.2007.07.005.
- Reidpath DD, Burns C, Garrard J, Mahoney M, Townsend M. An ecological study of the relationship between social and environmental determinants of obesity. Health Place 2002;8:141-5. http://dx.doi.org/10.1016/S1353-8292(01)00028-4.
- Simon PA, Kwan D, Angelescu A, Shih M, Fielding JE. Proximity of fast food restaurants to schools: do neighborhood income and type of school matter?. Prev Med 2008;47:284-8. http://dx.doi.org/10.1016/j.ypmed.2008.02.021.
- Smoyer-Tomic KE, Spence JC, Raine KD, Amrhein C, Cameron N, Yasenovskiy V, et al. The association between neighborhood socioeconomic status and exposure to supermarkets and fast food outlets. Health Place 2008;14:740-54. http://dx.doi.org/10.1016/j.healthplace.2007.12.001.
- Zenk SN, Powell LM. US secondary schools and food outlets. Health Place 2008;14:336-46. http://dx.doi.org/10.1016/j.healthplace.2007.08.003.
- El-Sayed AM, Scarborough P, Galea S. Ethnic inequalities in obesity among children and adults in the UK: a systematic review of the literature. Obes Rev 2011;12:e516-34. http://dx.doi.org/10.1111/j.1467-789X.2010.00829.x.
- Bartholomew LK, Parcel GS, Kok G, Gottlieb NH. Planning Health Promotion Programs: An Intervention Mapping Approach. San Francisco, CA: Jossey-Bass; 2011.
- Taylor NJ, Sahota P, Sargent J, Barber S, Loach J, Louch G, et al. Using intervention mapping to develop a culturally appropriate intervention to prevent childhood obesity: the HAPPY (Healthy and Active Parenting Programme for Early Years) study. Int J Behav Nutr Phys Act 2013;10. http://dx.doi.org/10.1186/1479-5868-10-142.
- Michie S, Johnston M, Abraham C, Lawton R, Parker D, Walker A, et al. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Health Care 2005;14:26-33. http://dx.doi.org/10.1136/qshc.2004.011155.
- Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol 2008;27:379-87. http://dx.doi.org/10.1037/0278-6133.27.3.379.
- Liu J, Davidson E, Bhopal R, White M, Johnson M, Netto G, et al. Adapting health promotion interventions to meet the needs of ethnic minority groups: mixed-methods evidence synthesis. Health Technol Assess 2012;16. http://dx.doi.org/10.3310/hta16440.
- Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sport Exerc 2007;39:1423-34. http://dx.doi.org/10.1249/mss.0b013e3180616b27.
- Kirkpatrick S. Family Links Pilot Evaluation Study. Oxford: Oxford Health Services Research Unit; 2005.
- MacNeill V. The Family Links Nurturing Programme: a Report of a Qualitative Evaluation of Training and Implementation. Oxford: Family Links; 2005.
- McEachan RRC, Santorelli G, Bryant M, Sahota P, Farrar D, Small N, et al. on behalf of the BiB Childhood Obesity Scientific Group. The HAPPY (Healthy and Active Parenting Programme for early Years) feasibility randomised control trial: acceptability and feasibility of an intervention to reduce infant obesity. BMC Public Health 2016;16.
- Daniels LA, Mallan KM, Battistutta D, Nicholson JM, Perry R, Magarey A. Evaluation of an intervention to promote protective infant feeding practices to prevent childhood obesity: outcomes of the NOURISH RCT at 14 months of age and 6 months post the first of two intervention modules. Int J Obes (Lond) 2012;36:1292-8. http://dx.doi.org/10.1038/ijo.2012.96.
- Daniels LA, Magarey A, Battistutta D, Nicholson JM, Farrell A, Davidson G, et al. The NOURISH randomised control trial: Positive feeding practices and food preferences in early childhood – a primary prevention program for childhood obesity. BMC Public Health 2009;9. http://dx.doi.org/10.1186/1471-2458-9-387.
- Daniels LA, Wilson JL, Mallan KM, Mihrshahi S, Perry R, Nicholson JM, et al. Recruiting and engaging new mothers in nutrition research studies: lessons from the Australian NOURISH randomised controlled trial. Int J Behav Nutr Phys Act 2012;9. http://dx.doi.org/10.1186/1479-5868-9-129.
- Wen LM, Baur LA, Simpson JM, Rissel C, Wardle K, Flood VM. Effectiveness of home based early intervention on children’s BMI at age 2: randomised controlled trial. BMJ 2012;344. http://dx.doi.org/10.1136/bmj.e3732.
- BMI: Preventing Ill Health and Premature Death in Black, Asian and other Minority Ethnic Groups. London: NICE; 2013.
Appendix 1 Reports of studies not yet published
Appendix 2 Further details of data collection instruments
2.1: Interview schedule (social and environmental determinants of childhood obesity)
Ask about how baby’s development is going, is baby feeding and growing as she thought he/she should.
Ask about what goes on in a typical day in relation to baby’s feeding (if they say they can’t think of a typical day ask them to talk about yesterday).
Breastfeeding
Was baby ever breastfed?
-
If no: prompt – what made you decide not to breastfeed?
-
Is baby still being breastfed?
-
Does baby get anything else other than breast milk?
-
-
How old was baby when you stopped giving just breast milk?
-
What made you decide to stop just breastfeeding?
-
Feeding/weaning
-
What did/do you give baby? (details of food and drink)
-
How often/what amounts?
-
How did you decide what to give and how often and how much to give?
-
How has what is given changed as baby has got older?
-
Do you cook and prepare baby’s food yourself or buy pre-prepared food? (prompt for details of what is cooked and what is bought)
Other topics
-
How has the experience of baby been in relation to feeding?
-
Has baby been ’easy’ or difficult? [if they have had another child ask how this baby was compared with the previous one(s)]
-
Can you describe mealtimes in your house:
-
– Prompt: Eat at same times? Sit with family when eat?
-
– Does family eat together?
-
– Eat food prepared yourself or prepared food?
-
– Do different family members eat different foods?
-
-
Who does the food shopping in your family?
-
– Who decides what you will eat on any day?
-
– Who does the cooking?
-
– Does the regular shopper/cooker also buy and prepare baby’s food?
-
-
Is baby regularly looked after by someone else, either when you are at work or for any other reason? If yes then ask:
-
– Who looks after baby, where?
-
– Do they feed baby – if yes, what do they give baby (food and drink), how often and how much (this includes being looked after in the family home by extended family members)? Do you decide what baby gets to eat when he/she is away from you or do they?
-
-
Are you happy with how baby has been growing?
-
– Has baby been healthy or ’sickly’ – does baby sleep well?
-
– Do you think baby looks the right size for age (e.g. compared with others of the same age or with any previous children you have had)?
-
-
What do you think are the important things that need to happen to keep baby healthy (e.g. eating well, growing, sleeping well, somewhere warm and safe to be, lots of care and attention)?
-
If you are not sure what to do with baby or if you are worried about something who do you go to for advice (e.g. family members, friends, other mums, health professionals)?
-
Who do you think influences you when you are making decisions about bringing up baby? How strongly do they influence you? – you can choose as many as you like from this list.
-
Has there been one person in particular who has been a particular help/support with baby? If yes, who? (don’t need a name – just title, e.g. mother, health visitor).
Interviewer: Take some field notes just after you leave the house – that is, record details of where the interview took place, who was there (was baby there), what the room and the house and the street were like, whether there were toys around. How confident did you feel that mum was being open with you?
2.2: Mealtime observation schedule coding scheme
-
Praise.
-
Contact.
-
Specific instruction.
-
Vague instruction.
-
Prompt.
-
Eating comment.
-
Presentation of food.
-
Removal of food.
-
Social attention.
-
Aversive contact.
-
Aversive specific instruction.
-
Aversive vague instruction.
-
Aversive prompt.
-
Aversive eating comment.
-
Aversive social attention.
Source: Sanders MR, Le Grice B, Turner KMT. Mealtime Observation Schedule: an Observer’s Manual (rev. ed.). Unpublished technical manual. Brisbane: Behavior Research and Therapy Centre, University of Queensland; 1993.
-
Request for food.
-
Food preparation.
-
Self-bite.
-
Prompted bite.
-
Chew.
-
Appropriate verbal interaction.
-
Engaged activity.
-
Food refusal.
-
Vomit.
-
Playing with food.
-
Leaving the table.
-
Holding food.
-
Non-compliance.
-
Complaint.
-
Aversive demand.
-
Negative physical behaviours.
-
Oppositional behaviour.
-
Non-interaction.
Source: Sanders MR, Le Grice B, Turner KMT. Mealtime Observation Schedule: an Observer’s Manual (rev. ed.). Unpublished technical manual. Brisbane: Behavior Research and Therapy Centre, University of Queensland; 1993.
2.3: Home food availability inventory
Foods in your home
Please tell us whether you have had any of the following foods or drinks in your home over the past 7 days. Estimate the amount of food based on the greatest amount that you had in your home in that period.
Use the pictures on the guidance sheet to help you work out the sizes.
Tips for filling out this form:
-
Individual fruits are single pieces (e.g. one apple, one banana).
-
Individual tomatoes refer to regular-sized tomatoes. If you have cherry tomatoes, count each one as two.
-
A medium can of coke has 330 ml of coke.
-
One handful of crisps is about the same amount as a regular individual-sized bag of crisps.
-
Half a handful of salted nuts is about the same amount as a small individual-sized bag of peanuts.
There are also tips at the bottom of the table to help you decide how much you have of each item.
Remember: There are no wrong or right answers.
| Food/drink | Description | Size | Amount | |||
|---|---|---|---|---|---|---|
| Fruits | ||||||
| 1. Bananas | Fresh | Individual | 0 | 1–3 | 4–10 | > 10 |
| 2. Apples | Fresh | Individual | 0 | 1–3 | 4–10 | > 10 |
| 3. Melon | Fresh | Whole melon | 0 | 1/2 | 1 | > 1 |
| 4. Grapes | Fresh | Handful | 0 | I –3 | 4–10 | > 10 |
| 5. Oranges | Fresh | Individual | 0 | 1–3 | 4–10 | > 10 |
| 6. Pears | Fresh | Individual | 0 | 1–3 | 4–10 | > 10 |
| 7. Peaches | Fresh | Individual | 0 | 1–3 | 4–10 | > 10 |
| 8. Canned fruit in syrup | Any fruit | Medium-sized can | 0 | 1 can | 2–5 | > 5 |
| 9. Canned fruit in juice/water | Any fruit | Medium-sized can | 0 | 1 can | 2–5 | > 5 |
| 10. Plums | Fresh | Individual | 0 | 1–3 | 4–10 | > 10 |
| 11. Kiwis | Fresh | Individual | 0 | 1–3 | 4–10 | > 10 |
| 12. Pineapple | Fresh | Whole pineapple | 0 | 1/2 | 1 | > 1 |
| 13. Berries or cherries (including strawberries) | Fresh or frozen | Handful | 0 | 1 | 2 | > 2 |
| 14. Grapefruit | Fresh | Whole grapefruit | 0 | 1/2 | 1–3 | > 3 |
| 15. Fruit salad | Fresh | Cup/handful | 0 | 1–3 | 4–10 | > 10 |
| 16. Dried fruit | (e.g. raisins, apricots) | Cup/handful | 0 | 1 | 2 | > 2 |
| Vegetables | ||||||
| 17. Carrots | Fresh or frozen | Individual | 0 | 1–3 | 4–10 | > 10 |
| 18. Celery | Fresh | Individual stick | 0 | 1–3 | 4–10 | > 10 |
| 19. Greens/spinach | Fresh or frozen | Cup/handful | 0 | 1 | 2 | > 2 |
| 20. Lettuce | Fresh | Individual head or mixed bag | 0 | 1 | 2 | > 2 |
| 21. Sweet maize | Fresh or frozen | Cup/handful | 0 | 1 | 2 | > 2 |
| 22. Peas | Fresh or frozen | Cup/handful | 0 | 1 | 2 | > 2 |
| 23. Tomatoes | Fresh | Individual | 0 | 1–3 | 4–10 | > 10 |
| 24. Tomatoes | Canned | Medium can | 0 | 1 | 2–5 | > 5 |
| 25. Broccoli | Fresh or frozen | Florets/head | 0 | 1–3 | 4–10 | > 10 |
| 26. Green beans | Fresh or frozen | Cup/handful | 0 | 1 | 2 | > 2 |
| 27. Cabbage | Fresh | Whole cabbage | 0 | 1/2 | 1 | > 1 |
| 28. Other vegetables including aubergine, okra, etc. | Fresh | Cup/handful | 0 | 1/2 | 1 | > 1 |
| 29. Canned vegetables | Any vegetable | Medium-sized can | 0 | 1 can | 2–5 | > 5 |
| Snacks | ||||||
| 30. Crisps, tortilla chips | All varieties | Handful | 0 | 1–3 | 4–10 | > 10 |
| 31. Salted nuts | Including peanuts | Handful | 0 | ½ – 3 | 4–10 | > 10 |
| 32. Biscuits | All varieties | Medium-sized pack | 0 | 1–15 | 16–30 | > 30 |
| 33. Sweets | Hard and soft | Handful | 0 | 1 | 2–5 | > 5 |
| 34. Chocolate | All varieties | Medium-sized bar or handful | 0 | 1 | 2–5 | > 5 |
| 35. Cakes, muffins | All varieties | Medium portion | 0 | 1–3 | 4–10 | > 10 |
| 36. Ice cream | All varieties | Medium tub | 0 | 1 | 2 | > 2 |
| Drinks | ||||||
| 37. Fizzy drink (e.g. cola) | Not diet | Medium can/bottle | 0 | 1–5 | 6–10 | > 10 |
| 38. Fizzy drink (e.g. diet cola) | Diet | Medium can/bottle | 0 | 1–5 | 6–10 | > 10 |
| 39. Sports drink | All varieties | Medium bottle | 0 | 1–5 | 6–10 | > 10 |
| 40. Fruit drinks | Not 100% fresh | Medium can/bottle | 0 | 1–5 | 6–10 | > 10 |
Appendix 3 Full texts of publications that are not open access
The reliability of routine anthropometric data collected by health workers: a cross-sectional study
Reprinted from Int J Nurs Stud, vol. 46, Johnson W, Cameron N, Dickson P, Emsley S, Raynor P, Seymour C, Wright J. The reliability of routine anthropometric data collected by health workers: a cross-sectional study 2009,70 with permission from Elsevier.
Ethnic differences in the initiation and duration of breast feeding – results from the Born in Bradford birth cohort study
Reproduced with permission from Santorelli G, Petherick E, Waiblinger D, Cabieses B, Fairley L. Ethnic differences in the initiation and duration of breast feeding – results from the Born in Bradford birth cohort study. Paediatr Perinat Epidemiol 2013;27:388–92. 82 © John Wiley & Sons Ltd.
Self-reported maternal parenting style and confidence and infant temperament in a multi-ethnic community: results from the Born in Bradford cohort
Prady SL, Kiernan K, Fairley L, Wilson S, Wright J. Self-reported maternal parenting style and confidence and infant temperament in a multi-ethnic community: results from the Born in Bradford cohort. J Child Health Care 2013;18:31–46. 83 Reproduced with permission from SAGE.
An exploration and comparison of food and drink availability in homes in a sample family of White and Pakistani origin within the UK
Bryant M, Sahota P, Santorelli G, Hill A, Wright J. An exploration and comparison of food and drink availability in homes in a sample family of White and Pakistani origin within the UK. Public Health Nutr 2015;18:1197–205. 106 Reproduced with permission from Cambridge University Press.
Food outlet availability, deprivation and obesity in a multi-ethnic sample of pregnant women in Bradford, UK
Reprinted from Social Science & Medicine, vol. 75, Fraser LK, Edwards KL, Tominitz M, Clarke GP, Hill AJ, Food outlet availability, deprivation and obesity in a multi-ethnic sample of pregnant women in Bradford, UK, pp. 1048–56, 2012,107 with permission from Elsevier.
Appendix 4 Born in Bradford and the Twins Grow Up
Photographs Ian Beesley, poems Ian McMillan. Copyright permissions for the poems and photographs are held by Born in Bradford and permission to reproduce here has been granted. All photographs are used with the written consent of parents.
List of abbreviations
- BiB
- Born in Bradford
- BMI
- body mass index
- CI
- confidence interval
- CVD
- cardiovascular disease
- FLNP
- Family Links Nurturing Programme
- GIS
- geographic information systems
- HAPPY
- Healthy and Active Parenting Programme for early Years
- MCID
- minimum clinically important difference
- MOS
- Mealtime Observation Schedule
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- OA
- output area
- RCT
- randomised controlled trial
- SDS
- standard deviation score